Notes
Article history
The research reported in this issue of the journal was funded by the EME programme as project number 09/160/23. The contractual start date was in January 2011. The final report began editorial review in October 2013 and was accepted for publication in April 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The EME editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Paul Little is editor-in-chief of the Programme Grants for Applied Research journal.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Little et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Existing research
The lifetime prevalence of back pain has been estimated at between 59% and 90% and the annual incidence of back pain is approximately 5% of the population. 1 In the UK, 12.5% of all sick days are related to low back disorders (matched only by respiratory illness and mental illness), with very similar figures for other northern European countries. 2 Persistent or major recurrent back pain is one of the commonest chronic problems managed in primary care and has a poor long term prognosis. 3
Physiotherapy exercises
The literature supports the use of a course of supervised physiotherapy exercises tailored to patient expectations and with reinforcement in the management of chronic back pain. 4–6 Systematic reviews support strengthening, stretching and aerobic exercises; exercises tailored to the individual that can also be performed at home; 20 hours of contact time (10 group sessions); and exercise targeting the rehabilitation of deep abdominal and lumbar paraspinal muscles. 4,6,7 The National Institute for Health and Care Excellence (NICE) has reviewed the literature since the above systematic reviews and, although supervised and tailored exercises were supported by NICE as one option for patients,8 the advice was tempered by the results from the major UK back pain exercise and manipulation (BEAM) trial,9 which found modest effects of exercise alone or with manipulation. However, attendance at exercise sessions in the UK BEAM trial was poor and exercises in this trial did not target the rehabilitation of deep abdominal and lumbar paraspinal muscles, which are known to require specific rehabilitation,10,11 suggesting that further trials could helpfully address both of these issues.
Alexander technique
The NICE systematic review8 included the Medical Research Council (MRC) Alexander Technique Exercise and Massage (ATEAM) trial12 in the section on exercises, but the Alexander technique is not a form of physiotherapy exercise. It involves learning what not to do as a first priority, that is, learning to become aware of, release and avoid harmful habits of muscle use and improve co-ordination of movement, which sets it apart from specific exercises. 12 It can be used during simple activities of daily living, such as walking, sitting, standing and bending – all activities adversely affected by back pain. The technique aims to teach the correct use of the postural mechanisms that regulate upright support and locomotion. These mechanisms involve co-ordination of the trunk, head and limbs, and motor control of postural muscles, which can be poorly operating in individuals with chronic back pain. 13–16 Mostly habitual and unnoticed, an individual can be taught to become more aware of these mechanisms and make different choices about movement, co-ordination and locomotion. 14,15 In particular, the Alexander technique addresses the co-ordination of the trunk and head as a core relationship for good movement. It is taught by specialist gentle touch and verbal instruction and an individual learns self-help through the combination of these methods.
Although there is limited evidence on the mechanism of action, there is preliminary evidence of effectiveness: a small trial documented short-term benefit17 and more robust empirical proof of concept has come from a larger trial (the MRC ATEAM trial12) which documented that the Alexander technique is likely to be effective after 1 year for chronic and recurrent back pain. Massage was included as a comparison group in the ATEAM trial as it provided similar touch and attention to the Alexander technique, but did not provide similar training in self-management skills. There was a shorter-term effect of massage (at 3 months) but no longer-term effect; in contrast, the effect of the Alexander technique, which is designed to provide lifelong self-management skills, persisted for a year. This suggests that the effectiveness of the Alexander technique is unlikely to be due to the non-specific effects of touch and attention.
There is good reason to believe that the Alexander technique is distinct in principles, aims and practice from physiotherapy. Physiotherapy aims to strengthen, stretch, increase aerobic capacity and improve motor control and uses specific supervised exercises that are then practised at particular times. In contrast, the Alexander technique involves teaching the awareness of and release of harmful muscle tension; involves proprioceptive re-education; concentrates primarily on the key relationship of head–neck–back; uses the semi-supine position as a core technique; involves guiding and assessing movement and co-ordination; and is practised during activities of daily living. 12
Key issues in the evidence base that required clarification are:
-
Efficacy: the efficacy of an intermediate course of lessons in the Alexander technique. The relationship between number of lessons and outcome is not linear [half the benefit of 24 lessons (full course) was provided by a short course (six lessons)12]. The ATEAM trial12 demonstrated that receiving six lessons was highly cost-effective. However, although many patients having six lessons did achieve a clinically meaningful benefit, the average benefit was at the lower end of clinically meaningful efficacy [an average increment of 1.4 on the Roland–Morris Disability Questionnaire (RMDQ) after 1 year compared with normal care]. Thus, more information is needed for the lower/middle part of the response curve. The proposed full trial in the present study will provide key information in the range that is most likely to provide the most meaningful efficacy for patients (i.e. lessons required to achieve a RMDQ increment of ≥ 2.0–2.5). 12,18
-
Efficacy: the efficacy of adding physiotherapy group exercises. If exercises and the Alexander technique work by different mechanisms then it is plausible that they will have significant additive effects that might provide substantial improvement for chronic back pain. The only way to demonstrate this is to estimate the single and combined effects of the two interventions.
Mechanism and biomechanical/physiological markers of improvement
Alexander technique
The Alexander technique may work through the release of tension, decompression of the spine, more balanced muscle activity and improved flexibility (not necessarily an increased end range of motion), based on observations that poor trunk co-ordination, torsion, spinal compression and muscle asymmetry are associated with chronic back pain. 19 The focus of the Alexander technique on increasing awareness of movement would be expected to improve proprioception. Preliminary evidence suggests that the Alexander technique modifies muscle tone14–16,20 and increases flexibility,20 which requires confirmation.
Physiotherapy exercises
Weakness and wasting of the deep abdominal and lumbar paraspinal muscles, and altered recruitment of muscles (motor control), occur with low back pain and do not recover without specific rehabilitation exercises. 10,11,21,22 We predicted that indices of strength and changes in muscle architecture of the abdominal and posterior paraspinal muscles [thickness measured by ultrasound imaging (USI) as an indirect measure of strength and activity] are likely to be confirmed as important non-invasive markers and that these not only should improve with exercise but also will predict outcome. 10,23,24
The proposed study to follow the present feasibility study will also evaluate whether or not recovery of these muscles, and hence protection of the lumbar spine, occurs with the Alexander technique, to enhance our understanding of how back pain recovers and how to combine both the Alexander technique and physiotherapy, and will provide data that could help modify/target treatment in the future.
Risks and benefits
No adverse effects have been reported for the Alexander technique12 and adverse effects of physiotherapy exercises are also rare. 8 It is likely that the proposed full trial could provide evidence of benefit not only for individual interventions but also for the combined intervention, which will provide a range of useful information to inform choice for patients, clinicians and policy-makers.
Rationale for the full trial
There are two key efficacy questions that the study will answer, one related to phase 2-type evidence (whether or not an intermediate ‘dose’ of a 10-lesson course in the Alexander technique achieves important clinical benefit) and one related to additive benefit (whether or not exercises are additive to the Alexander technique). We also propose enhancing our understanding by investigating the likely mechanisms using several plausible intermediate biomechanical markers that could mediate improved health outcomes. This should increase our understanding of the causes and treatment of back pain and could also be used in monitoring and targeting of future treatment. However, before a full study can be justified a smaller feasibility study is necessary.
Chapter 2 Research objectives
The key objectives for the main trial will be to:
-
estimate whether or not an ‘intermediate’ course of 10 lessons in the Alexander technique achieves clinically meaningful efficacy
-
estimate the efficacy of combining the Alexander technique and physiotherapy
-
understand the possible mechanisms and mediators of improvement for both the Alexander technique and physiotherapy.
The key objectives for the feasibility study were to:
-
confirm the acceptability and attrition among individual and multiple groups in the proposed factorial trial, including the feasibility of multiple visits
-
assess the feasibility of all mechanistic measures and perform an exploratory analysis of these measures
-
provide provisional data on the likely effectiveness of 10 lessons in the Alexander technique
-
confirm whether or not/if the control group is stable, given the potential complexity of ‘normal care’ and the possible impact of the recent NICE guidelines
-
assess the implications of using both the invited (prevalent) population and opportunistically recruited (incident) populations
-
explore the sensitivity to change of different outcome measures in this population.
Chapter 3 Methods
Research design
This was a trial of two interventions, Alexander technique lessons and physiotherapy exercises. Clinical outcome and biomechanical/physiological measures were taken for all patients in this feasibility study (whereas if the main trial were to be funded the mechanistic measures will be taken on a subset of patients).
The study statistician supervised randomisation, blocked by group and stratified by history of previous pain (< 90 days and > 90 days). The board suggested stratification by previous history, which we accept is a very reasonable suggestion and which is supported by empirical evidence from a post hoc analysis of the ATEAM trial12 (those with a history of > 90 days of pain had the most improvement; furthermore, there was no evidence that making the criteria more stringent, for example > 180 days, increased apparent effectiveness).
When an eligible patient passed eligibility screening and consented to the study, randomisation was executed by the practice nurse in each practice ringing an external randomisation line.
Changes or additions to the protocol since application
The changes to the protocol since the application were:
-
The addition of the MyotonPRO (Myoton Ltd, London, UK) (see Addition to the biomechanical measurement protocol) as a reliable, non-invasive measure of muscle tone and mechanical properties (stiffness and elasticity).
-
Pilot testing of all measures included in the research proposal. This revealed that measures of spine length and curvature using the Vicon 3D motion analysis system (Vicon Motion Systems, Oxford, UK) were complex and too time-consuming to warrant inclusion, as they were not key measures.
-
Development of a second method of identifying participants who are currently seeing their general practitioner (GP) for care with back pain (see Chapter 4, Feasibility of recruitment).
-
The addition of a nested qualitative study with participants (see Appendix 3 for detailed methods and results).
-
Modification of physiotherapy classes: we estimated initially that 10 physiotherapy classes would be sufficient to provide sufficient input based on the existing evidence. On review of both the evidence and what timings were feasible in practice, LR proposed 12 classes of 90 minutes’ duration, which included a warm-up, stretches, a circuit of tailored exercises, a cool down, relaxation and a group discussion (‘tip of the day’).
Study population
Although definitions of acute (< 6 weeks), subacute (6–12 weeks) and chronic (> 12 weeks) have been used for back pain, NICE has pointed out that these are not very useful definitions in practice given the variable nature of chronic and recurrent back pain. 8 We initially proposed two methods of recruitment – a mailed invitation to patients who have attended their GP in the past with back pain and an invitation to patients opportunistically who attend surgery. Subsequently we added a mailed invitation to patients based on attendance in the last week. Patients who currently had a RMDQ score of ≥ 4 and a duration of pain of at least 3 weeks (i.e. patients with chronic or a non-trivial recurrent attack of pain) were eligible. Patients thus had chronic or recurrent back pain [had attended their GP previously (prevalent) or currently (incident) with back pain]. These were the key entry criteria that we used in our previous trial12 and were similar to those used in the UK BEAM trial,9 which has the great advantage of allowing a comparison with these trials. In the previous trial12 these criteria facilitated timely recruitment, were feasible and provided a population that had predominantly chronic pain and a control population that was relatively stable for a year despite having access to further care if needed (the control group reported on average 21 days of pain each month at the end of the year).
The exclusion criteria were similar to those in the ATEAM trial12 for comparability: previous experience of the Alexander technique; those aged > 65 years (serious spinal pathology more likely); clinical indicators of serious spinal pathology; previous spinal surgery (outcome may be very different and groups too small to analyse); history of psychosis or major alcohol abuse (difficulty completing outcomes); perceived inability to walk 100 m (exercise difficult); pregnancy; and pending litigation.
Planned interventions and proposed trial groups
Participants were randomised using computer-generated random numbers, stratified by history of previous pain (< 90 days and > 90 days), to one of four groups, by study staff ringing an external randomisation line (Table 1).
| Normal care | Normal care and 10 Alexander technique lessons | |
|---|---|---|
| Normal care | Group 1 | Group 2 |
| Physiotherapy group exercises | Group 3 | Group 4 |
There were two interventions:
-
Alexander technique. Patients were randomised to receive no lessons or to receive 10 lessons and a copy of a recommended book providing an introduction to the Alexander technique (see Appendix 1 for details of lessons). We already had information on the effects of six and 24 lessons;12 as six lessons had half the benefit of 24 lessons the dose response is likely to be steepest in the lower mid-range, hence the choice of 10 lessons (which are also likely to be both effective and the most cost-effective for a future pragmatic trial12). Ten lessons was a reasonable choice based on (1) consensus among senior teachers (CN and CC have consulted widely among their senior colleagues) and (2) the documentation of 25+ consecutive patients from four teachers (Carolyn Nicholls, Brighton Alexander Technique College, 2011, personal communication). After six lessons most people reported starting to see an improvement in pain, and after between nine and 12 lessons most patients reported being more confident in their skills to prevent and manage further episodes of pain.
-
Physiotherapy group exercises. Half of the patients in each of the two Alexander technique groups (no Alexander technique lessons and Alexander technique lessons) were randomised to receive supervised, tailored exercises in a group setting following an initial clinical assessment, thus making four groups. A group intervention, although not commonly used currently in the NHS, is supported by NICE8 as it is more likely to be cost-effective; hence, this package could have significant implications for future NHS care. We based the optimal exercise package on those developed previously, and this was consistent with current recommendations and systematic reviews;4,6,7,9,10,11,22,25–27 it included motor relearning, strengthening, stretching and aerobic exercises; exercises tailored to the individual that can also be performed at home; 20 hours of contact time (10–12 group sessions); and exercise targeting motor control of deep abdominal and lumbar paraspinal muscles. There was time to share success and encourage other group members in group sessions and group exercises, and we paid attention to negotiating agreement to attend most sessions, as poor attendance was an important issue in the UK BEAM trial. 9
Both the Alexander technique teachers and the physiotherapists were trained centrally to deliver sessions and to record process measures in a consistent manner; this helped reduce variability and monitor the quality control of the intervention.
Normal care
Patients were free to consult their GP as normal and GPs were free to prescribe analgesia or refer for further care according to NICE guidance as appropriate (including orthopaedic or routine physiotherapy assessment). This approach provided a stable control group in the ATEAM trial over the time course of a year. 12 As in the previous trial we aim to collect process information to monitor what additional NHS and non-NHS treatment patients receive in all groups, to be able to estimate the likely effect of such additional care. (We have not collected this information yet but will carry out a notes review in due course.)
For those offered both Alexander technique lessons and exercise classes, patients started Alexander lessons first so that when the exercise classes started they were best able to take advantage of the Alexander technique in facilitating exercise. We used a similar approach in our previous trial, which proved acceptable. 12
Outcome measures (at 3 and 6 months)
Clinical outcome measures
Key outcomes
The primary outcome was the RMDQ. Patients indicate the number of specified activities/functions limited by back pain. 28 The scale is designed for self-report, has been extensively validated and is the most widely used primary outcome in lower back pain. 29
Secondary outcomes (which were all used without logistic problems in the previous trial and which have been suggested as a basic data set for back pain research) comprised:
-
secondary measures for back pain28
-
number of days in pain reported during the last 4 weeks30 (a 4-week period facilitated recall) (this is distinct from pain intensity or disability30,31)
-
pain and disability (Von Korff pain and disability scale30)
-
Deyo ‘troublesomeness’ scale28
-
overall improvement (health transition29)
-
fear of activity (the short version of the Tampa Scale for Kinesiophobia32,33)
-
modified enablement scale. 12
We also measured health-related quality of life [European Quality of Life-5 Dimensions (EQ-5D)34] and will measure NHS resource use. Health service resource use will be quantified using data collected from GP notes after 1 year’s follow-up: the number of visits to the surgery, who was consulted (i.e. practice nurse or GP), the name, dose and duration of any drugs prescribed and all referrals (and who the patient was referred to plus the number of times he or she was seen). In addition, patients will be asked if they have self-referred to anyone for back pain (e.g. chiropractor, physiotherapist), the number of times they were seen and how much they paid per visit. The main emphasis of this study is not an economic analysis; however, in any pragmatic effectiveness trial to follow this trial, these data can be useful for a modelling exercise to help justify the trial groups.
Exploring other potential primary outcomes
Following the suggestion by the board, to allow us to explore sensitivity to change in this population, we also administered the Oswestry Disability Index and the Aberdeen pain and function scale35,36 at baseline and follow-up and compared these with the RMDQ and Von Korff measures, with a view to informing a definitive set of outcome measures for the main trial.
Laboratory-based biomechanical and neuromuscular physiological measures
Intermediate markers that we proposed might predict outcome were trunk flexibility/axial tone,14,16,20 trunk muscle strength,23,24 pelvic loading,37 spine length and curvature,38 proprioception, abdominal muscle recruitment patterns using surface electromyography (EMG)39 and trunk muscle size measurements on ultrasound images. 10,11 We hypothesised that graphical CHAIN models would help identify the key relationships.
We used valid and reliable measurement techniques. Flexibility to imposed torsion (axial tone) was measured with the participant standing on a rotating platform enclosed in a rigid frame (which we termed the trunk rotation device) that applies a small torsional strain and records the body’s resistance through load cells. 14,16,20 Isometric strength of the trunk flexors and extensors was measured using a Biodex dynamometer (Shirley, NY, USA). 23
The active straight leg raise (ASLR) test under load (applying manual compression to the pelvis) assesses the ability of the lumbopelvic region to effectively transfer load and is closely related to lumbar pelvic pain. It has good test–retest reliability. 37
Proprioception was tested using an inclinometer for the lumbar spine and a ‘cervical range of motion’ (CROM) device for the cervical spine to measure the angles between target and achieved movement, examining joint position sense of the lumbar spine and neck.
The relative latency (timing of onset) of muscle activation can be altered in people with back pain. 21,39 Surface EMG was recorded from the rectus abdominis, external oblique and internal oblique muscles while participants performed a clinically relevant manoeuvre; the ASLR test40 in supine was used for the abdominal muscles and an ipsilateral straight leg lift in prone was used for the paraspinal muscles. Improvement in muscle recruitment pattern (earlier onset) post intervention, if correlated with a reduction in symptoms, would suggest that better motor control contributed to the recovery mechanism.
Ultrasound imaging was used to measure muscle size (morphometry). A portable scanner with 5- to 7.5-MHz transducers was used to obtain images of the lateral abdominal (transversus abdominis and internal and external oblique muscles)10 and lumbar multifidus muscle. 11 Protocols followed international guidelines for obtaining images and measuring muscle thickness at rest and during functional manoeuvres to assess contractile ability. 10,11
Addition to the biomechanical measurement protocol
The MyotonPRO is a novel hand-held device that allows non-invasive, objective measurement of mechanical properties of muscles. 41 The device applies brief, gentle mechanical impulses to the skin over the muscle, which causes the muscle to oscillate, producing damped tissue oscillations, from which frequency (Hz; non-neural tone) and stiffness (N/m) are measured by automated analysis within the software. Elasticity is also measured by automated analysis and is characterised by the logarithmic (log) decrement of the dampened oscillations (dissipation of mechanical energy, i.e. how much energy is lost during one oscillation cycle), reflecting the ability of the tissue to recover its shape after being deformed.
Myoton technology has been shown to be valid42 and reliable in different muscles and age groups in the present investigators’ laboratory, both between days43 and between raters. 44 The lumbar multifidus muscle was tested with the participant resting in the prone lying and also in the upright sitting positions to examine the effects of change in posture on mechanical properties, which might provide a useful indicator of postural muscle activity.
A summary of the timings of the main groups of biomechanical and physiological measures is shown in Table 2.
| Measure | Time to perform measurement (minutes) |
|---|---|
| USI of multifidus muscle to measure muscle thickness at rest and contraction during straight leg lift into extension in prone | 15 |
| Recording surface EMG during straight leg lift to assess muscle onset (multifidus) | 10 |
| Muscle tone and mechanical properties (using hand-held MyotonPRO device) of multifidus in prone and sitting | 10 |
| Recording EMG during ASLR in supine to assess muscle onset (rectus abdominis, external oblique and internal oblique) | 10 |
| USI of muscle thickness of transversus abdominis, internal oblique and external oblique muscles at rest and during ASLR | 15 |
| Flexibility to imposed rotation to assess axial tone (trunk rotation test) | 20 |
| Proprioception of lumbar and cervical spine | 10 |
| Isometric trunk muscle flexion and extension strength using Biodex dynamometer | 10 |
| ASLR test with pelvic compression | 5 |
The measures took < 2 hours, allowing for setting up equipment and rest periods, and became shorter as the study progressed.
Table 3 provides a summary of what each of the laboratory tests measured, what direction of change would be beneficial and what the clinical implications are of such changes.
| Technique | What is being measured | Direction of change that is beneficial | Clinical implications of change |
|---|---|---|---|
| Proprioception testing of cervical and lumbar spine and of lumbar spine upright and in flexion | Ability to sense position of spine | Lower value (degrees) | Less error in finding original position |
| USI multifidus and transversus abdominis muscles | Thickness of muscles at rest | Greater thickness at rest (cm) | Increased force-generating capacity – muscle size relates to strength |
| Change in muscle thickness during leg lift. Measure of involuntary activity | Greater change in thickness during leg lift | Increased ability to recruit muscles automatically to protect lumbar spine | |
| EMG of transversus abdominis and multifidus muscles during leg lift | Timing (latency) of onset of muscle activation | Shorter time to muscle onset (ms) | Faster recruitment of muscles before leg lift to protect lumbar spine. Better motor control |
| Trunk rotation test | Flexibility to imposed torsion | Reduced values of axial stiffness (N/m) | Greater dynamic regulation of postural tone |
| Muscle tone and mechanical properties (Myoton device) | Clinically, abnormality can be low or high tone. Assume low | Note: Insufficient data to identify subgroups within treatment groups | |
| Tone | State of resting tension: non-neural tone | The higher the frequency (Hz) of oscillation, the greater the tone. Increase if low | Tone normalised |
| Stiffness | Muscle’s ability to resist force that modifies its shape | The higher the value (N/m), the greater the stiffness. Increase if low | Stiffness normalised |
| Elasticity | Muscle’s ability to recover its shape after being deformed | The lower the decrement (log), the greater elasticity. Decrease if high | Elasticity normalised |
| Lying to sitting to elicit postural muscle activity of the multifidus muscle | Postural activity of the three Myoton parameters | Higher Hz and N/m, lower log decrement | Muscle becomes more active in sitting position, with greater tone, stiffness and elasticity |
| Strength testing by dynamometry | Trunk flexor and extensor muscles | Greater force (N/m) | Increase in muscle strength |
| ASLR test with pelvic compression | Ability of lumbopelvic region to transfer load | Odds ratio < 1 | No pain on lifting leg |
Assessment and follow-up
Assessment of efficacy/effectiveness
All outcomes were measured at baseline and 3 and 6 months (for the main trial 12 months’ follow-up will be used but for the feasibility study 6 months sufficed).
We used well-validated self-completion postal questionnaires with up to two follow-up contacts for non-response. With this approach we anticipated that we were likely to achieve at least 80% follow-up. 12 There is little methodological advantage in independent researchers ringing patients to document answers to self-report questions instead of patients providing the answers to the same self-report questions themselves; furthermore, the questionnaire measures have been validated for self report. 18,45
The biomechanical and physiological assessments were performed by a research fellow. Although we asked patients not to reveal their exercises to the researcher, full blinding here was in practice difficult to enforce, given that patients in practice sometimes mentioned what exercises they had been doing.
Assessment of safety
We did not anticipate any safety issues but staff were encouraged to report any event on standardised forms. Patients were also able to report adverse events directly to the trial team.
Proposed sample size
We aimed to consent 20 patients per group from one centre to provide feasibility information (no formal sample size calculation was appropriate). For the exploratory analysis of mechanistic measures this sample should have been sufficient to detect a 0.66–0.75 standard deviation (SD) change in key intermediate outcomes (consistent with previous work).
Statistical analysis
For the feasibility and piloting elements (recruitment rates, attrition, adherence, characteristics of sample, acceptability, etc.), and for sensitivity to change of the outcomes, the analysis was descriptive. Regression models allowed a preliminary exploration of whether or not the intervention modifies intermediate biomechanical markers, the relationship between the intermediate markers and outcome (using graphical CHAIN models) and the relationship between teachers’ ratings and both intermediate markers and outcome. Although the analysis of effectiveness was underpowered, we performed an intention-to-treat analysis of covariance to estimate the main effects of the interventions, with no imputation of missing data. Although a factorial analysis is possible, we were particularly interested in the effect of combined compared with single interventions (i.e. four groups) on an intention-to-treat basis.
Ethical arrangements
We obtained multicentre research ethics committee approval and will facilitate data sharing on completion as appropriate (e.g. for individual patient data meta-analyses).
Research governance
The University of Southampton sponsored the study, which was subject to the normal conditions of research governance and was monitored by each participating primary care trust, and an independent trial steering committee supervised trial progress and management.
Patient and public involvement
The chair of the Southampton branch of BackCare, Colin Steel, agreed to be on the steering group as a service-user representative and has acted as a focal point for liaison with the larger patient group that he represents. Input was provided to the protocol when the ideas were being generated and there was regular liaison between Dr Roberts, Mr Steel and the local branch of BackCare. Unfortunately, Mr Steel suffered illness at the time of writing the report, which meant that he had to withdraw from the study and was unable to provide comments. We are very grateful to Mr Mike Price, also from the local BackCare group, for reading the report and providing comments. Mr Steel was not comfortable with e-mail and so liaison relied on the close relationship between the study team, represented by Dr Roberts, and Mr Steel. In retrospect, having more than one patient and public involvement representative and at least one patient and public involvement collaborator with e-mail would have facilitated communication.
Chapter 4 Results
Feasibility of recruitment
Several methods of recruitment were piloted and all proved to be feasible.
Invited recruitment for patient attending within the last 5 years
The easiest method of recruitment was to write to patients who had attended with back pain in the previous 5 years and, if they still had pain and fulfilled eligibility requirements, to then invite them to a recruitment appointment with the practice nurse; this was the method of recruitment used in the ATEAM trial. 12 A total of 1987 letters were sent from six practices. In total, 297 potentially eligible participants expressed an interest in participating and 170 replied that they were not interested; 68 were consented after receiving the invitation letter. This group included patients not currently seeking care for their back pain. However, in a significant number of cases this is likely to be because they felt that no further help was available. A typical comment from a patient to an Alexander technique teacher following the intervention was, ‘Why didn’t anyone tell me about this before?’ (also see qualitative report).
Opportunistic recruitment in surgery
Patients attending their GP with back pain were invited by the GP to participate during the consultation and were consented within the consultation. However, as might be expected, because of the time restrictions in an acute appointment, far fewer patients (n = 11) were recruited by this mechanism.
Invited recruitment based on attendance in the previous week
As already documented, the board was concerned that those who were not currently seeking care might be substantially different from those who are currently seeking care and so might not be a population relevant for policy-making in the NHS. It transpired that this might be an artificial distinction and a function of the lack of help perceived by patients (see comment above). Given the desire of the board for us to achieve meaningful recruitment at or near the time of presentation with an episode of care in the NHS, we also piloted a recruitment method based on a search of attendance with back pain in the previous week. This method of recruitment was piloted in two practices to demonstrate that the method was feasible. In one of the practices the yield from 6 weeks of brief searching was 57 invitations, with 10 patients replying that they were interested in participating and four patients consented, which suggests that the method is likely to be feasible and provide timely recruitment for any full trial, should a main trial be funded, based on recent presentation with back pain.
Feasibility of randomisation
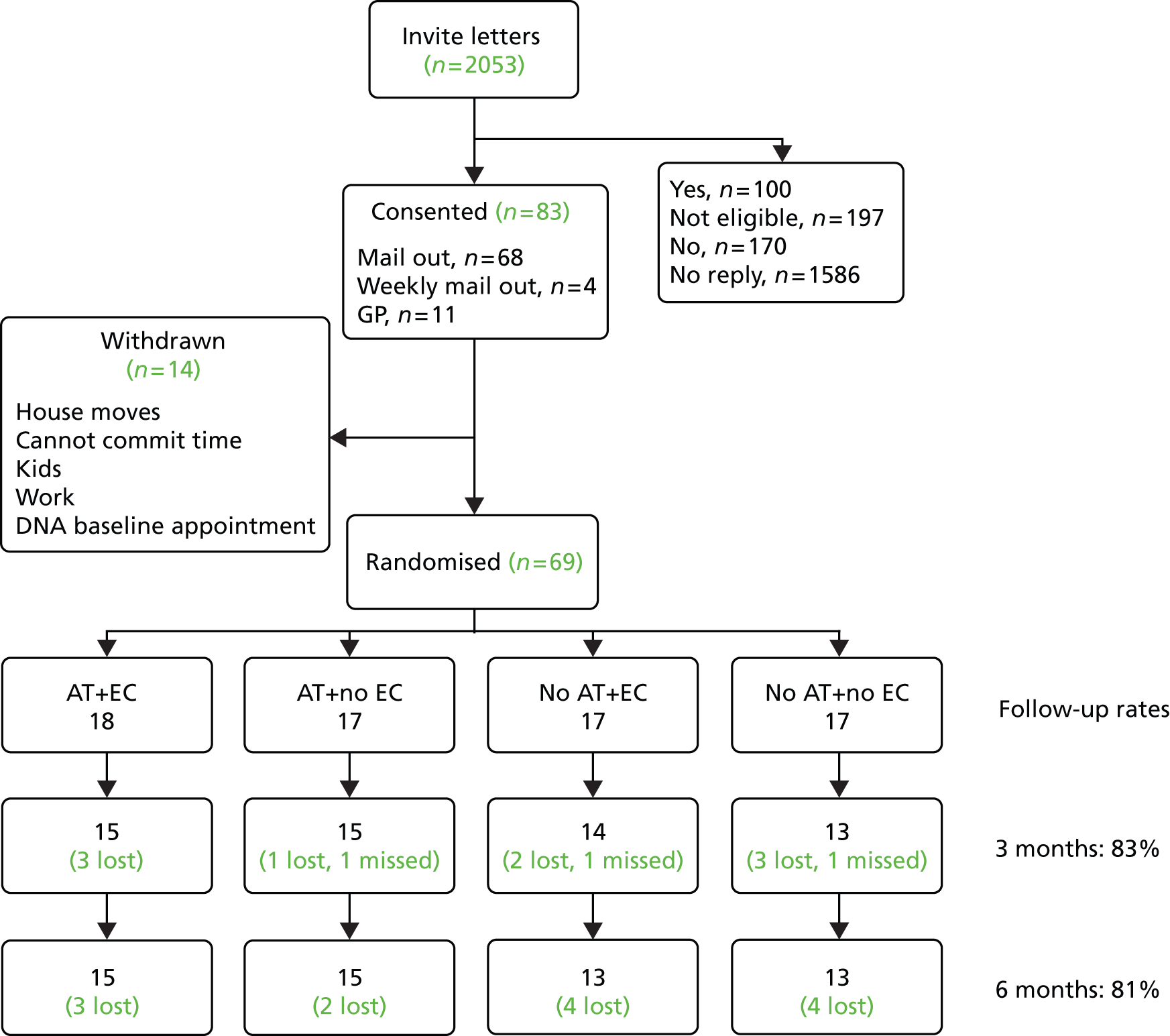
There were no issues here except that there was some dropout of participants (n = 14) between consent and randomisation, as shown in the CONsolidated Standards Of Reporting Trials (CONSORT) diagram (Figure 1), mainly because of time pressures.
FIGURE 1.
CONsolidated Standards Of Reporting Trials (CONSORT) diagram. AT, Alexander technique; DNA, did not attend; EC, exercise classes.
Even with the relatively small numbers, the groups were reasonably well balanced at baseline (Table 4).
| Characteristic | Control | Exercise classes only | Alexander technique only | Alexander technique + exercise classes |
|---|---|---|---|---|
| Sex (female), n/N (%) | 8/17 (47.1) | 13/17 (76.5) | 11/17 (64.7) | 11/18 (61.1) |
| Age (years), mean (SD) | 47.20 (11.57) (n = 16) | 47.93 (11.97) (n = 17) | 49.92 (10.11) (n = 17) | 56.45 (7.86) (n = 18) |
| Married, n/N (%) | 9/17 (52.9) | 9/17 (52.9) | 9/17 (52.9) | 10/18 (55.6) |
| Age left full-time education (years), mean (SD) | 18.5 (3.56) (n = 16) | 18.0 (2.40) (n = 17) | 19.63 (2.75) (n = 16) | 17.17 (2.68) |
| Prescription for back pain in last 3 months, n/N (%) | 8/16 (50.0) | 6/16 (37.5) | 7/15 (46.7) | 9/18 (50.0) |
| Taken non-prescription medication for back pain in last 3 months, n/N (%) | 9/17 (52.9) | 10/16 (62.5) | 10/15 (66.7) | 10/18 (55.6) |
| Days in pain (from patient registration), mean (SD) | 325.35 (111.95) (n = 17) | 308.35 (113.98) (n = 17) | 295.94 (130.55) (n = 17) | 348.17 (71.42) (n = 18) |
| Days pain interfered with activities in the last 4 weeks (from Von Korff pain and disability scale), mean (SD) | 4.25 (6.05) (n = 16) | 4.59 (5.60) (n = 16) | 3.88 (6.51) (n = 16) | 6.13 (9.43) (n = 16) |
| RMDQ score, mean (SD) | 9.24 (5.13) (n = 17) | 10.29 (5.45) (n = 17) | 10.06 (4.10) (n = 17) | 11.44 (3.91) (n = 18) |
| Von Korff pain and disability scale score, mean (SD) | 5.19 (2.23) (n = 17) | 5.21 (1.55) (n = 17) | 4.83 (1.99) (n = 17) | 5.68 (2.12) (n = 18) |
| Disability | 4.62 (2.67) | 4.53 (2.00) | 4.06 (2.03) | 5.13 (2.75) |
| Pain | 5.75 (2.04) | 5.88 (1.60) | 5.61 (2.13) | 6.22 (1.94) |
| Deyo troublesomeness scale score, mean (SD) | 2.75 (0.89) (n = 17) | 2.82 (0.89) (n = 17) | 2.86 (0.92) (n = 17) | 3.00 (0.82) (n = 18) |
| Tampa Scale for Kinesiophobia score, mean (SD) | 28.76 (6.98) (n = 17) | 25.29 (6.53) (n = 17) | 23.18 (5.07) (n = 17) | 28.75 (5.91) (n = 18) |
| Modified enablement scale score, mean (SD) | 17.29 (8.36) (n = 17) | 15.47 (10.06) (n = 16) | 13.35 (8.92) (n = 15) | 14.89 (6.45) (n = 16) |
| Oswestry Disability Index score, mean (SD) | 33.45 (15.67) (n = 17) | 30.43 (14.07) (n = 17) | 30.03 (13.95) (n = 17) | 32.55 (11.27) (n = 18) |
| Aberdeen pain and function scale score, mean (SD) | 25.17 (11.37) (n = 17) | 23.59 (10.27) (n = 17) | 23.24 (9.43) (n = 17) | 24.06 (5.60) (n = 18) |
| Overall improvement scale score, mean (SD) | 4.29 (0.92) (n = 17) | 3.94 (1.03) (n = 17) | 3.82 (0.95) (n = 17) | 4.22 (1.17) (n = 18) |
Feasibility of intervention lessons
Logistical issues
The Alexander technique lessons were implemented more easily than the exercise classes, as the Alexander technique teacher and the pupil arranged a mutually convenient time.
The exercise class intervention was more problematic logistically and some areas (e.g. Portsmouth practices) struggled to recruit and so the classes had few patients per group and were sometimes one-to-one rather than group sessions. There was a booking lag at one of the exercise class centres as patients could not get through on the telephone and so the study team took over the scheduling and the class administrators gave us slots to fill. There was a slight delay in starting classes while waiting for numbers to make a ‘group’. Patients found the limited flexibility in class times more difficult, but adherence was nevertheless reasonably good (> 50% attended ≥ 80% of classes; see the following section) compared with that seen in a previous large trial. 9 Transport to and from sessions was problematic for those without a car and so we arranged taxi collection and delivery when necessary (and so travel expenses for patients were a little more than anticipated). The time commitment for the classes, and particularly for the combined intervention, was a large burden, which suggests that, if the combined intervention is to be used, the intervention should be largely serially and flexibly organised rather than sessions being organised in parallel.
Feasibility of delivering the intervention: compliance with attending intervention classes
The previous ATEAM trial12 defined good adherence as attending five out of six lessons or 20 out of 24 lessons. This is attendance of just over 80%. We have followed this example and defined good adherence as the attendance of at least eight of the 10 Alexander technique lessons and 10 of the 12 exercise class lessons.
Of those randomised to receive Alexander technique lessons (either Alexander technique lessons only or both Alexander technique lessons and exercise classes), we have data from the lesson booklets (which were returned by practitioners) for 31 out of 35 participants. Only three out of the 31 participants did not complete all 10 lessons. One stopped at lesson 3, one at lesson 8 and one at lesson 9. Thus, 93.5% of participants for whom we have booklets returned by the practitioners (29/31) achieved ‘good adherence’ to the Alexander technique lessons. If we assume that those who did not return the booklets did not achieve good adherence, which is a conservative assumption, the figure would be 82.9% (29/35).
Of those randomised to receive exercise classes (either exercise classes or both exercise classes and Alexander technique lessons), we have data from the lesson booklets for 25 out of 35 participants. Of these, 19 completed all 12 lessons and ‘good adherence’ was achieved by 84.0% (21/25). If we assume that those who did not return the booklet did not achieve good adherence this figure would be 60.0% (21/35).
Table 5 provides a summary of the data on adherence.
| Group | Proportion achieving good adherence based on returned booklets, n/N (%) | Proportion achieving good adherence assuming that any who did not return the booklets did not achieve good adherence, n/N (%) |
|---|---|---|
| Alexander technique only | 15/16 (93.75) | 15/17 (88.24) |
| Both (at Alexander technique lessons) | 14/15 (93.33) | 14/18 (77.78) |
| Exercise classes only | 11/14 (78.57) | 11/17 (64.71) |
| Both (at exercise classes) | 10/11 (90.91) | 10/18 (55.56) |
In terms of harms, one patient who had been a little dizzy before starting the exercises (but who had not warned the staff) fell backwards in the exercise class group, grazing the underside of her arm.
Feasibility of retention
We followed up 57 of the 69 participants (83%) at 3 months and 56 out of 69 (81%) at 6 months. Those withdrawing mostly had other medical problems or problems with attending (Table 6). There was no significant difference in RMDQ score at baseline between those who withdrew and those who did not (10.25 vs. 10.28; p = 0.9836).
| ID | Comments | Group |
|---|---|---|
| 1009 | Patient diagnosed with cancer – due to have major hospital treatment | No AT + no EC |
| 1019 | Back pain now gone | No AT + no EC |
| 1036 | Been in hospital for 3 weeks – heart failure | No AT + no EC |
| 1072 | No reason given | No AT + no EC |
| 1071 | Being away for a couple of hours for exercise classes very difficult | No AT + EC |
| 1039 | In too much pain to attend physiotherapy classes | No AT + EC |
| 1071 | Being away for a couple of hours for exercise classes very difficult | No AT + EC |
| 1026 | Too busy to be able to make appointments | No AT + EC |
| 1028 | Transport no longer available | AT + no EC |
| 1029 | No reason given | AT + no EC |
| 1080 | Close relative and participant admitted to hospital | AT + EC |
| 1086 | No reason given | AT + EC |
| 1130 | Has other health problems and needs to sort these out and could not take any more time off work | AT + EC |
Feasibility of laboratory-based biomechanical and neuromuscular physiological measures
The board was concerned about the participant burden of the biomechanical measures. The feedback from patients was that this was one of the most interesting elements of the study, and follow-up rates for the measures were good despite the issues of time and transport. Pilot testing of all measures included in the research proposal revealed that measures of spine length and curvature using the Vicon 3D motion analysis system were complex and too time-consuming to warrant inclusion, as they were not key measures. Accurate alternative tools were not available.
All tests were well tolerated during the study, although a small number of participants (n = 14) reported mild sensations when standing in the trunk rotation testing device, including feeling nauseous, dizzy and unstable, but this did not prevent them being able to undergo testing. Surface EMG was used, which did not cause the discomfort that can occur with fine-wire EMG, but the drawback was poor-quality signals over the abdominal muscles, possibly because of subcutaneous fat. Data from the symptomatic side and during functional tasks (leg lifts for muscle thickness and EMG and changes in posture for Myoton measures) were more informative than data from the asymptomatic side and at rest. The duration of data collection sessions reduced as the study progressed (start approximately 120 minutes, end approximately 90–100 minutes) and proved to be acceptable to participants.
Sensitivity to change
Clinical outcome measures
Referees were keen to see a variety of potential major outcomes assessed as part of the feasibility trial (e.g. the Oswestry Disability Index and the Aberdeen pain and function scale). The standardised response mean has been calculated as the difference between the mean at follow-up and the mean at baseline divided by the SD of the difference. Most of the major questionnaire outcomes (RMDQ, Von Korff pain and disability scale, Oswestry Disability Index, Aberdeen pain and function scale) were equally sensitive to change (Table 7).
| Measure | Mean (SD) difference baseline to 6 months | Standardised response mean |
|---|---|---|
| RMDQ | 3.93 (5.32) | 0.737 |
| Von Korff pain and disability scale | 1.68 (2.11) | 0.796 |
| Deyo troublesomeness scale | 0.55 (0.80) | 0.688 |
| Tampa Scale for Kinesiophobia | 4.04 (6.53) | 0.619 |
| Modified enablement scale | 4.48 (9.47) | 0.473 |
| Oswestry Oswestry Disability Index | 7.55 (10.22) | 0.739 |
| Aberdeen pain and function scale | 5.23 (7.41) | 0.706 |
| Overall improvement scale | 0.63 (1.51) | 0.414 |
Change in laboratory-based measures
All laboratory-based biomechanical and neurophysiological tests showed changes at 6 months at the 5% level of significance in at least one of the intervention groups, apart from lumbar proprioception, which was significant only at the 10% level (Table 8). When changes were not significant they were nearly always in a beneficial direction, reducing the likelihood of type 1 errors.
| Measure | Control | Exercise classes only | Alexander technique only | Alexander technique + exercise classes | ||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) score at baseline | Change in mean score (95% CI; p-value) | Mean (SD) score at baseline | Change in mean score (95% CI; p-value) | Mean (SD) score at baseline | Change in mean score (95% CI; p-value) | Mean (SD) score at baseline | Change in mean score (95% CI; p-value) | |
| Proprioception – cervical (degrees) | (n = 12) | (n = 13) | (n = 15) | (n = 15) | ||||
| X | 2.06 (1.99) | −0.33 (−2.47 to 1.60; 0.738) | 2.06 (1.70) | 0.28 (−1.56 to 2.12; 0.744) | 3.14 (2.82) | −1.71 (−3.62 to 0.20; 0.075) | 2.17 (1.81) | −0.49 (−1.98 to 1.00; 0.492) |
| Y | 2.04 (1.74) | −0.31 (−1.57 to 0.96; 607) | 2.59 (2.09) | 0.72 (−2.37 to 0.93; 0.361) | 4.67 (2.77) | −2.62 (−4.66 to −0.59; 0.015) | 3.15 (2.17) | −1.49 (−3.03 to 0.05; 0.057) |
| Z | 0.57 (0.75) | 0.39 (−0.69 to 1.47; 0.445) | 0.88 (0.94) | −0.10 (−0.85 to 0.66; 0.790) | 1.10 (1.74) | −0.38 (−0.96 to 0.21; 0.193) | 0.81 (1.11) | 0.53 (0.06 to 1.01; 0.031) |
| Proprioception – lumbar | (n = 12) | (n = 13) | (n = 14) | (n = 15) | ||||
| From ‘upright/zero’ position | 1.88 (1.51) | −0.64 (−1.68 to 0.40; 0.205) | 2.12 (1.67) | −0.79 (−1.80 to 0.21; 0.110) | 1.85 (1.91) | −0.14 (−1.04 to 0.75; 0.735) | 1.65 (1.59) | −0.78 (−1.96 to 0.40; 0.179) |
| From ‘20° flexion’ position | 2.45 (1.98) | 0.61 (−1.17 to 2.39; 0.466) | 3.16 (3.98) | −0.85 (−3.28 to 1.59; 0.463) | 4.35 (2.82) | −1.71 (−3.69 to 0.26; 0.084) | 3.28 (2.30) | −1.64 (−3.37 to 0.08; 0.061) |
| USI – multifidus thickness (cm) symptomatic side | (n = 13) | (n = 12) | (n = 13) | (n = 13) | ||||
| Relaxed | 2.78 (0.26) | 0.07 (−0.01 to 0.15; 0.087) | 2.84 (0.51) | 0.23 (0.06 to 0.40; 0.011) | 2.93 (0.37) | 0.08 (−0.10 to 0.26; 0.351) | 2.98 (0.44) | 0.18 (0.09 to 0.27; 0.001) |
| Contracted [change in thickness (cm) during leg lift] | 3.14 (0.33) | 0.12 (−0.04 to 0.28; 0.126) | 3.05 (0.41) | 0.35 (0.23 to 0.46; < 0.001) | 3.27 (0.37) | 0.25 (0.11 to 0.37; 0.002) | 3.30 (0.44) | 0.24 (0.05 to 0.42; 0.015) |
| USI – transversus abdominis thickness (cm) symptomatic side | (n = 13) | (n = 12) | (n = 14) | (n = 14) | ||||
| Relaxed | 0.37 (0.15) | 0.03 (0.01 to 0.05; 0.017) | 0.36 (0.13) | 0.01 (−0.05 to 0.03; 0.626) | 0.38 (0.15) | 0.02 (−0.03 to 0.07; 0.345) | 0.38 (0.14) | 0.05 (0.02 to 0.09; 0.008) |
| Contracted | 0.40 (0.16) | 0.04 (−0.01 to 0.10; 0.093) | 0.38 (0.13) | 0.02 (−0.02 to 0.07; 0.284) | 0.40 (0.17) | 0.07 (0.00 to 0.12; 0.047) | 0.41 (0.14) | 0.05 (0.01 to 0.10; 0.031) |
| Myoton measures – symptomatic side | (n = 13) | (n = 12) | (n = 12) | (n = 14) | ||||
| Tone (frequency: Hz) | ||||||||
| Prone | 16.55 (2.71) | 1.69 (0.47 to 2.91; 0.011) | 16.06 (3.43) | 0.51 (−0.98 to 2.00; 0.467) | 16.06 (1.81) | 1.68 (0.11 to 3.26; 0.038) | 16.87 (2.90) | 0.28 (−0.20 to 0.77; 0.230) |
| Seated | 21.13 (5.38) | 1.32 (−1.29 to 3.93; 0.292) | 18.24 (4.05) | 2.85 (0.87 to 4.83; 0.009) | 18.25 (4.35) | 2.88 (0.09 to 5.66; 0.044) | 19.02 (5.26) | 2.52 (0.75 to 4.29; 0.009) |
| Stiffness (N/m) | ||||||||
| Prone | 343.52 (82.28) | 35.56 (−22.35 to 93.48; 0.206) | 331.0 (108.0) | 26.86 (−76.90 to 123.18; 0.262) | 326.9 (77.6) | 45.70 (9.71 to 81.60; 0.017) | 359.8 (96.9) | 11.90 (−10.91 to 34.00; 0.265) |
| Seated | 533.7 (173.68) | 49.0 (−36.8 to 134.9; 0.237) | 444.9 (160.1) | 96.1 (19.2 to 172.9; 0.019) | 447.7 (162.1) | 82.29 (−18.40 to 183.00; 0.101) | 464.8 (169.3) | 74.3 (12.4 to 136.1; 0.022) |
| Elasticity (log decrement) | ||||||||
| Prone | 1.34 (0.26) | 0.05 (−0.03 to 0.13; 0.221) | 1.35 (0.29) | 0.10 (−0.05 to 0.26; 0.155) | 1.37 (0.24) | 0.12 (0.03 to 0.22; 0.017) | 1.57 (0.29) | 0.14 (0.02 to 0.27; 0.028) |
| Seated | 1.24 (0.51) | 0.05 (−0.22 to 0.13; 0.572) | 1.08 (0.15) | 0.05 (−0.13 to 0.02; 0.156) | 1.26 (0.42) | 0.180 (0.003 to 0.360; 0.046) | 1.35 (0.31) | 0.06 (−0.25 to 0.12; 0.467) |
| EMG | (n = 9) | (n = 9) | (n = 11) | (n = 12) | ||||
| Multifidus latency (ms) | 0.44 (0.20) | 0.08 (−0.13 to 0.29; 0.430) | 0.38 (0.25) | 0.11 (−0.12 to 0.35; 0.306) | 0.37 (0.09) | 0.17 (0.03 to 0.32; 0.025) | 0.32 (0.11) | 0.03 (−0.05 to 0.10; 0.431) |
| Trunk muscle strength (N/m; Biodex) | (n =11) | (n = 13) | (n = 14) | (n = 14) | ||||
| Flexion | 50.06 (26.44) | 10.90 (2.74 to 19.10; 0.014) | 51.77 (31.86) | 15.00 (1.27 to 28.80; 0.035) | 62.7 (28.7) | 13.5 (−5.2 to 32.3; 0.141) | 49.4 (18.6) | 15.20 (0.54 to 29.90; 0.043) |
| Extension | 125.4 (84.3) | 23.10 (−2.29 to 48.40; 0.070) | 125.9 (84.2) | 28.0 (−9.4 to 65.3; 0.128) | 114.6 (49.8) | 39.40 (5.24 to 73.50; 0.028) | 106.5 (65.7) | 32.50 (7.36 to 57.70; 0.015) |
Exploratory analyses of effectiveness
Main clinical results
All analyses are based on a linear regression model and control for baseline score on the scale being tested. The models were tested to assure adherence to the linear regression assumptions, that the residuals were normally distributed and that there was no significant heteroskedasticity. As expected given the very limited power, most outcomes did not reach significance at the 5% level and so the lack of significance should be interpreted very cautiously; some reached significance at the 10% level by 3 and 6 months, particularly in the combined group (Tables 9 and 10 respectively), and when changes were not significant they were nearly always in a beneficial direction, suggesting that type 1 errors are unlikely. The estimates suggest that clinically important improvements were probably occurring [e.g. the RMDQ documented clinically important changes (> 2.59) by 6 months]; of the other two major questionnaire outcomes assessed (Aberdeen pain and function scale and Oswestry Disability Index), the Aberdeen instrument perhaps differentiated between groups a little better and performed close to significance at both 3 and 6 months for the combined group.
| Measure | Control | Exercise classes only | Alexander technique only | Alexander technique + exercise classes |
|---|---|---|---|---|
| Mean (SD) score at 3 months | Difference in mean score from control at 3 months (95% CI; p-value) | Difference in mean score from control at 3 months (95% CI; p-value) | Difference in mean score from control at 3 months (95% CI; p-value) | |
| RMDQ (n = 57) | 7.46 (4.77) | −1.90 (−5.41 to 1.60; 0.281) | −1.37 (−4.82 to 2.07; 0.427) | −0.75 (−4.21 to 2.72; 0.667) |
| Von Korff pain and disability scale (n = 57) | 4.50 (0.50) | −1.06 (−2.48 to 0.36; 0.139) | −0.51 (−1.91 to 0.90; 0.472) | −1.25 (−2.64 to 0.15; 0.080) |
| Disability (n = 57) | 3.85 (3.00) | −1.30 (−2.97 to 0.37; 0.124) | −0.52 (−2.18 to 1.14; 0.534) | −1.18 (−2.82 to 0.47; 0.157) |
| Pain (n = 57) | 5.15 (2.18) | −0.88 (−2.26 to 0.50; 0.208) | −0.63 (−1.99 to 0.73; 0.358) | −1.27 (−2.63 to 0.10; 0.068) |
| Days pain inhibited activities in the last 4 weeks (Von Korff pain and disability scale Q4) (n = 50) | 3.33 (6.54) | −1.07 (−5.08 to 2.93; 0.592) | −0.78 (−4.78 to 3.23; 0.698) | −3.07 (−7.09 to 0.95; 0.131) |
| Deyo troublesomeness scale (n = 57) | 2.73 (0.96) | −0.36 (−0.93 to 0.22; 0.215) | −0.41 (−0.97 to 0.16; 0.154) | −0.42 (−0.98 to 0.14; 0.142) |
| Tampa Scale for Kinesiophobia (fear avoidance) (n = 57) | 27.62 (6.44) | −0.58 (−5.09 to 3.92; 0.796) | 2.27 (−2.43 to 6.99; 0.336) | −2.80 (−7.11 to 1.51; 0.199) |
| Modified enablement scale (n = 57) | 14.54 (10.10) | −5.19 (−10.55 to 0.17; 0.058) | −4.23 (−9.60 to 1.15; 0.121) | −4.13 (−9.40 to 1.13; 0.121) |
| Oswestry Disability Index (n = 57) | 32.85 (18.60) | −0.42 (−5.63 to 4.80; 0.874) | 0.67 (−4.45 to 5.81; 0.793) | −4.09 (−9.15 to 0.97; 0.111) |
| Aberdeen pain and function scale (n = 57) | 26.31 (16.70) | −3.24 (−8.42 to 1.94; 0.215) | −3.88 (−8.99 to 1.22; 0.133) | −4.88 (−9.96 to 0.19; 0.059) |
| Overall improvement (health transition) (n = 57) | 4.15 (0.99) | −1.37 (−2.15 to −0.59; 0.001) | −1.09 (−1.87 to −0.31; 0.007) | −1.22 (−1.97 to −0.47; 0.002) |
| Measure | Control | Exercise classes only | Alexander technique only | Alexander technique + exercise classes |
|---|---|---|---|---|
| Mean (SD) score at 6 months | Difference in mean score from control at 6 months (95% CI; p-value) | Difference in mean score from control at 6 months (95% CI; p-value) | Difference in mean score from control at 6 months (95% CI; p-value) | |
| RMDQ (n = 54) | 8.17 (4.34) | −3.00 (−6.88 to 0.88; 0.126) | −2.86 (−6.53 to 0.81; 0.124) | −2.51 (−6.21 to 1.19; 0.179) |
| Von Korff pain and disability scale (n = 55) | 3.61 (1.80) | 0.31 (−1.21 to 1.83; 0.686) | −0.14 (−1.61 to 1.34; 0.852) | −0.90 (−2.39 to 0.58; 0.228) |
| Disability (n = 55) | 3.03 (1.95) | 0.45 (−1.36 to 2.26; 0.620) | −0.41 (−2.16 to 1.35; 0.642) | −1.10 (−2.87 to 0.66; 0.216) |
| Pain (n = 55) | 4.19 (1.98) | 0.15 (−1.34 to 1.63; 0.841) | 0.09 (−1.35 to 1.52; 0.906) | −0.59 (−2.04 to 0.86; 0.415) |
| Days pain inhibited activities in last 4 weeks (Von Korff pain and disability scale Q4) (n = 47) | 2.70 (5.03) | −0.40 (−4.55 to 3.75; 0.847) | 0.81 (−3.35 to 4.97; 0.697) | −3.06 (−7.17 to 1.06; 0.141) |
| Deyo troublesomeness scale (n = 56) | 2.59 (0.93) | −0.30 (−0.88 to 0.29; 0.318) | −0.28 (−0.85 to 0.29; 0.325) | −0.63 (−1.19 to −0.06; 0.030) |
| Tampa Scale for Kinesiophobia (n = 56) | 25.46 (6.65) | −2.44 (−7.19 to 2.32; 0.308) | −1.47 (−6.23 to 3.29; 0.537) | −3.31 (−7.87 to 1.24; 0.150) |
| Modified enablement scale (n = 56) | 14.92 (11.32) | −5.23 (−11.26 to 0.81; 0.088) | −5.99 (−11.89 to −0.09; 0.047) | −5.06 (−10.88 to 0.75; 0.086) |
| Oswestry Disability Index (n = 56) | 29.03 (16.59) | −0.71 (−8.92 to 7.50; 0.863) | −2.65 (−10.52 to 5.21; 0.501) | −3.55 (−11.30 to 4.20; 0.362) |
| Aberdeen pain and function scale (n = 56) | 23.31 (11.31) | −0.81 (−6.69 to 5.07; 0.784) | −2.34 (−8.02 to 3.35; 0.413) | −5.21 (−10.71 to 0.36, 0.066) |
| Overall improvement (n = 56) | 3.77 (1.01) | −0.22 (−1.16 to 0.71; 0.637) | −0.49 (−1.40 to 0.42; 0.282) | −0.63 (−1.50 to 0.24; 0.151) |
The concern that the NICE guidance8 would result in an unstable control group was not borne out. The control group improved only a little (change in RMDQ score from 9 to 8 at 6 months), which was entirely consistent with the level of change observed in the control group (pre NICE guidance) in our previous trial. 12
‘Dose response’: rating of pain and function by participants at Alexander technique lessons and exercise classes
The justification for assuming that we might be able to observe a ‘dosing’ effect (i.e. that the benefit apparent after lessons is maintained) was that after six lessons in the previous Alexander technique trial12 the benefit remained stable over at least 9 months, that is, the impact of the intervention was achieved quickly and was relatively stable. The weekly changes in RMDQ score are shown in Table 11 for participants receiving Alexander technique lessons.
| Week | All Alexander technique participants | Alexander technique only | Alexander technique + exercise classes |
|---|---|---|---|
| 1 | 10.26 (5.12) | 10.06 (5.27) | 10.47 (5.14) |
| 2 | 9.61 (4.98) | 9.25 (5.08) | 10.00 (5.03) |
| 3 | 8.77 (4.88) | 7.81 (4.90) | 9.80 (4.80) |
| 4 | 8.53 (4.93) | 8.13 (5.04) | 8.93 (4.95) |
| 5 | 8.27 (5.05) | 8.27 (5.44) | 8.27 (4.82) |
| 6 | 7.93 (4.76) | 7.73 (4.79) | 8.13 (4.90) |
| 7 | 7.33 (5.11) | 7.60 (4.84) | 7.07 (5.52) |
| 8 | 7.17 (5.07) | 6.67 (5.07) | 7.71 (5.21) |
| 9 | 6.57 (5.17) | 5.86 (5.05) | 7.29 (5.38) |
| 10 | 6.19 (5.61) | 5.57 (4.97) | 6.85 (6.36) |
Accepting that the time in between lessons was not exactly the same for all participants, then treating this as panel data shows a significant effect of an increased number of lessons over time. For all Alexander technique participants, for each additional lesson, the RMDQ score decreases by a mean of 0.48 points (p < 0.001). This relationship is very similar regardless of the randomisation group (0.47 for the Alexander technique-only group and 0.48 for the Alexander technique + exercise class group; p < 0.0001 for both). There seems to be no levelling off of effectiveness after six lessons (the briefer intervention in the ATEAM trial12) and up to 10 lessons at least is likely to provide consistent improvement.
For exercise classes, for all exercise class participants, the RMDQ score decreases significantly over time, by a mean of 0.26 points for each additional lesson (p < 0.001) (Table 12). Here, the effect is significant in both randomisation groups but is slightly higher in the exercise class-only group (a mean decrease of 0.31 points compared with a mean decrease of 0.21 points in the Alexander technique + exercise class group). Once again, there seems to be no levelling off of effect, suggesting that 12 weeks of classes is likely to be beneficial.
| Week | All exercise class participants | Exercise classes only | Alexander technique + exercise classes |
|---|---|---|---|
| 1 | 8.20 (4.97) | 8.43 (5.00) | 7.91 (5.17) |
| 2 | 8.88 (5.63) | 9.57 (6.21) | 8.00 (4.94) |
| 3 | 7.80 (4.86) | 7.93 (4.75) | 7.64 (5.22) |
| 4 | 7.42 (4.79) | 7.23 (4.49) | 7.64 (5.33) |
| 5 | 8.20 (5.48) | 8.86 (5.65) | 7.36 (5.41) |
| 6 | 7.36 (5.04) | 7.79 (4.54) | 6.82 (5.79) |
| 7 | 6.91 (4.94) | 7.08 (4.03) | 6.70 (6.17) |
| 8 | 6.83 (5.17) | 6.62 (4.39) | 7.10 (6.28) |
| 9 | 6.39 (5.28) | 6.46 (4.54) | 6.30 (6.38) |
| 10 | 5.67 (5.14) | 5.45 (3.72) | 5.90 (6.57) |
| 11 | 5.38 (5.00) | 4.82 (3.16) | 6.00 (6.62) |
| 12 | 5.24 (5.37) | 4.73 (4.20) | 5.80 (6.61) |
We also assessed the ‘dose–response’ relationship for days in pain recorded in the Alexander technique diaries (Table 13) and the exercise class diaries (Table 14) by those who completed them. Overall, for Alexander technique lessons, for all Alexander technique participants, there was a decrease in the mean number of days in pain of 0.15 per lesson [95% confidence interval (CI) 0.09 to 0.21; p < 0.0001]. The corresponding figure was 0.14 in the Alexander technique-only group (95% CI 0.05 to 0.22; p = 0.002) and 0.15 in the Alexander technique plus exercise class group (95% CI 0.07 to 0.24; p < 0.0001). Similarly, for all exercise class participants, each additional exercise class resulted in a reduction in mean number of days in pain of 0.10 (95% CI 0.05 to 0.15; p < 0.0001). The corresponding figure was 0.09 in the exercise class-only group (95% CI 0.02 to 0.17; p = 0.018) and 0.11 in the exercise class pus Alexander technique group (95% CI 0.06 to 0.16; p < 0.0001).
| Week | All Alexander technique participants | Alexander technique only | Alexander technique + exercise classes |
|---|---|---|---|
| 1 | 5.48 (2.38) | 5.25 (2.41) | 5.73 (2.40) |
| 2 | 5.32 (2.40) | 5.00 (2.45) | 5.67 (2.38) |
| 3 | 4.63 (2.67) | 4.19 (2.69) | 5.14 (2.65) |
| 4 | 4.27 (2.79) | 3.87 (3.02) | 4.67 (2.58) |
| 5 | 4.82 (2.82) | 4.14 (2.96) | 5.50 (2.59) |
| 6 | 4.73 (2.79) | 4.80 (2.62) | 4.67 (3.04) |
| 7 | 4.86 (2.49) | 4.80 (2.34) | 4.93 (2.73) |
| 8 | 4.93 (2.69) | 4.53 (3.07) | 5.36 (2.24) |
| 9 | 4.29 (2.92) | 3.93 (3.08) | 4.64 (2.82) |
| 10 | 4.04 (2.80) | 3.71 (2.70) | 4.36 (2.95) |
| Week | All exercise class participants | Exercise classes only | Alexander technique + exercise classes |
|---|---|---|---|
| 1 | 4.48 (2.58) | 4.64 (2.73) | 4.27 (2.49) |
| 2 | 4.48 (2.45) | 4.57 (2.44) | 4.35 (2.58) |
| 3 | 3.72 (2.57) | 3.36 (2.62) | 4.18 (2.56) |
| 4 | 4.04 (2.40) | 3.92 (2.47) | 4.18 (2.44) |
| 5 | 4.12 (2.43) | 4.50 (2.21) | 3.63 (2.73) |
| 6 | 4.33 (2.43) | 4.79 (2.33) | 3.70 (2.54) |
| 7 | 3.78 (2.45) | 4.15 (2.44) | 3.30 (2.50) |
| 8 | 3.52 (2.68) | 3.36 (2.73) | 3.70 (2.75) |
| 9 | 3.36 (2.57) | 3.50 (2.50) | 3.20 (2.78) |
| 10 | 3.43 (2.42) | 3.64 (2.16) | 3.20 (2.78) |
| 11 | 3.19 (2.48) | 3.27 (2.24) | 3.10 (2.85) |
| 12 | 3.19 (2.40) | 2.91 (2.39) | 3.50 (2.51) |
Exploratory analyses of intermediate markers (laboratory-based tests)
As with the clinical outcomes the analysis of intermediate measures is underpowered and so it is not very useful to comment on negative findings. Similarly, although we will briefly comment here on results significant at the 10% and 5% levels, extreme caution in the interpretation is needed given the danger of type 1 errors because of the number of intermediate markers present. The results should be viewed conservatively in the context of the hypothesised changes (Table 15) and the CHAIN model (see Figure 2 and Tables 19 and 20). The danger of type 1 errors is reduced by the fact that most biomarker and clinical changes, even if not significant, changed in a beneficial direction.
| Function | Hypothesised expected findings | Actual findings | ||
|---|---|---|---|---|
| AT lessons | ECs | 3 months | 6 months | |
| Proprioception – lumbar | Improve? | Improve | Yes – AT, AT + EC | |
| Trunk muscle strength (Biodex) | Increase | Yes – EC extension | ||
| Paraspinal muscle size and contractility (ultrasound) | Increase | Yes – EC | ||
| Paraspinal muscle recruitment (EMG) | Improve? | Increase | Yes – AT | |
| Abdominal muscle size and contractility (ultrasound) | Increase | |||
| Abdominal muscle recruitment (EMG) | Improve? | Improve motor control | ||
| Pelvic loading ability (ASLR) | Improve | Yes – AT | ||
| Trunk flexibility/axial tone | Improve | N/A | ||
| Muscle tone and mechanical properties | Improve (tone) | Improve (stiffness and tone) | Partially – AT, EC | Partially – AT, AT + EC |
Differences between randomised groups at 3 months
Significant differences between randomised groups at 3 months were observed for lumbar proprioception and trunk extension strength (see Appendix 2, Table 16, for baseline measures and Appendix 2, Table 17, for 3-month measures).
For lumbar proprioception at 20° flexion, the Alexander technique and the Alexander technique plus exercise class groups had significantly lower errors (between the target position and the achieved position) than the control group (p = 0.026 and p = 0.035 respectively) after controlling for their baseline scores. The change in level of error for the exercise class group was in the same direction as for the other two groups and was significant at the 10% level (p = 0.08).
Trunk extension strength (measured using the Biodex system) in the exercise class-only group was significantly stronger (by 36 N/m; p = 0.027) than in the control group at 3 months. The changes in the other two groups were in the same direction.
The ASLR compression test was the only binary measure and so the odds of scoring a 1 on this test were compared by group. At 3 months the odds ratio was 1.03 (95% CI 0.18 to 5.82; p = 0.973) in the exercise class-only group, 2.10 (95% CI 0.24 to 17.78; p = 0.496) in the Alexander technique-only group and 0.59 (95% CI 0.10 to 3.40; p = 0.554) in the combined Alexander technique plus exercise class group.
Differences between randomised groups at 6 months (see Appendix 2, Table 18)
There were no longer any significant differences between randomised groups at 6 months for lumbar proprioception or trunk extension strength. There were additional differences that had not been seen at 3 months for multifidus muscle thickness at rest and contracted, the Myoton measurements of multifidus muscle mechanical properties, EMG onset of the lumbar paraspinal muscles and the ASLR test. The axial rotation testing device failed to function for a period (a replacement part had to be obtained from abroad) and so too few participants completed this test to enable reliable results to be obtained (n = 16 at 6 months, n = 9 at 3 months). The EMG recordings over the abdominal muscles were also too few to analyse because of difficulties in obtaining acceptable recordings.
Lumbar multifidus muscle thickness measured using USI was significantly greater in the exercise class-only group than in the control group in the relaxed and contracted muscle. These two variables were also significantly greater at the 10% level for the combined Alexander technique plus exercise class group. These observations were as expected for the exercise intervention, which included activities to improve the strength (and thus size) of the multifidus muscle as well as automatic activity of the muscle during functional tasks.
Multifidus muscle tone and mechanical properties were measured using the MyotonPRO device. There was lower elasticity (higher decrement values) in the treatment groups than in the control group, which reached significance below the 5% level only in the Alexander technique plus exercise class group in the prone lying position. The treatment groups had lower values than the control group for tone (frequency) and stiffness (N/m) and the difference reached significance at the 10% level for frequency in the prone position (p = 0.076). The mechanical properties of muscles measured by the MyotonPRO device differ according to the physiological composition and habitual activity of the muscle. 41 Few muscles have been characterised at this relatively early stage in the use of Myoton technology to allow definitive interpretation of these findings for the multifidus muscle. A fully powered study would help elucidate the relationships between Myoton parameters and other measures of muscle characteristics and behaviours. It is known, however, that Myoton technology can detect subtle changes in muscle stiffness42 and that the changes in parameters during muscle contraction include increases in stiffness and tone (frequency) and reduction in elasticity (increase in decrement). The present observations suggest that the combined Alexander technique plus exercise class group had less muscle tension than the control group.
Compared with the control group, earlier onset of EMG activity of paraspinal muscles occurred on the symptomatic side during an ipsilateral leg lift in the Alexander technique-only group for the multifidus muscle, indicating better motor control.
During the ASLR compression test, all three intervention groups showed an odds ratio of < 1 and this was highly statistically significant in the Alexander technique group (p = 0.007), indicating a better ability to transfer load through the pelvis.
Graphical CHAIN model
The graphical CHAIN model (Figure 2 and see Appendix 2, Table 19) demonstrates that the only significant predictor at baseline of RMDQ score at 6 months was number of days in pain. Three laboratory measurement variables at 6 months were associated with RMDQ score at 6 months. These were lumbar proprioception at 20° flexion (beta coefficient 1.48°, 95% CI 0.83° to 2.12°; p < 0.001) and the lumbar multifidus mechanical properties measured using the MyotonPRO of tone (frequency) (0.94 Hz, 95% CI 0.48 Hz to 1.40 Hz; p < 0.0001) and difference in elasticity (log decrement) from lying to sitting, that is, altered activity with change in posture (−4.86, 95% CI −0.01 to −9.72; p < 0.05). Even with the small number of participants, the Alexander technique was shown to influence the mechanical property of elasticity at 6 months, suggesting that this may be a key element of the effectiveness of the Alexander technique. Likewise, exercise classes were shown to influence change in muscle tone from lying to sitting, suggesting that improvement in postural tone is a key element in the effectiveness of physiotherapy.
FIGURE 2.
Graphical CHAIN model illustrating biomechanical and physiological variables associated with outcome 6 months after the intervention. AT, Alexander technique; TrA, transversus abdominus; US, ultrasound.
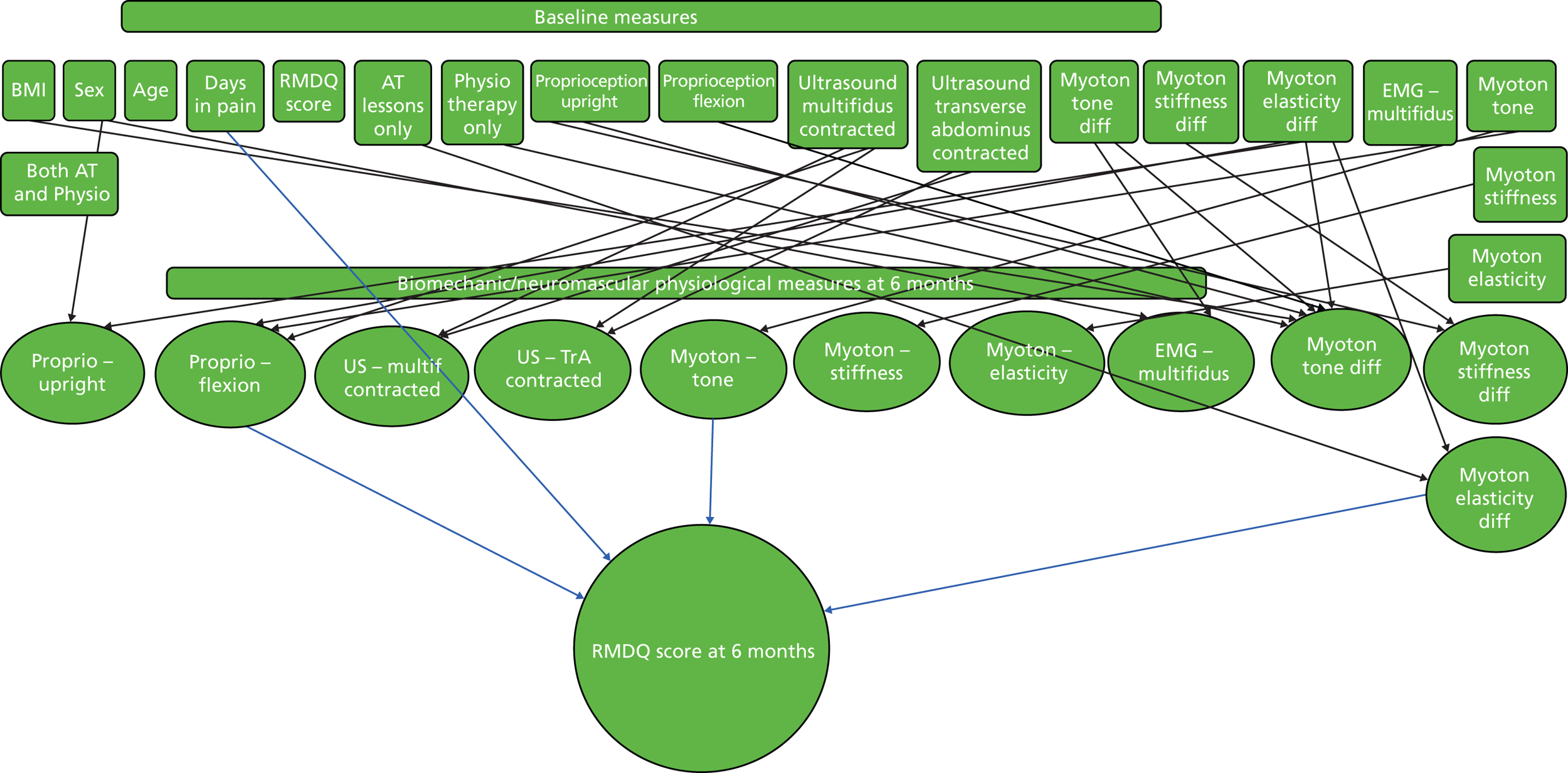
The baseline variables that were predictive of 6-month variables were laboratory measures, mainly proprioception, and multifidus muscle mechanical properties (using the MyotonPRO) and thickness (from USI). Of these baseline variables, multifidus muscle elasticity (difference in decrement values from prone to sitting measured using the MyotonPRO device) predicted four variables at 6 months: itself, proprioception in upright and flexion postures and multifidus muscle tone (change in Myoton frequency with posture). Multifidus thickness (when contracted during a straight leg lift, measured using USI) predicted itself, the thickness of the transversus abdominus muscle when contracted (which was reciprocally predictive of the thickness of the multifidus muscle when contracted) and proprioception in flexion. Five baseline variables were predictive of two variables each at 6 months. Going from left to right in the top row of Figure 2, the upright proprioception test predicted the Myoton measures of postural changes in tone (frequency) and stiffness. Contracted transversus abdominis muscle thickness predicted itself and contracted multifidus muscle thickness. Change in multifidus tone (frequency) with posture predicted itself and recruitment of the multifidus muscle (EMG onset). Multifidus tone at rest predicted itself and proprioception in flexion.
At 6 months, multifidus tone difference (i.e. change in frequency between lying and sitting) was associated with itself at baseline, body mass index, lumbar proprioception in the upright and 20° flexion positions, difference in multifidus tone (frequency) from prone to sitting and the exercise class-only intervention. The only other variable with more than two associations was proprioception in flexion, which was associated with multifidus thickness (contracted), multifidus tone at rest (Myoton frequency) and multifidus elasticity with change in posture (difference in decrement).
Understanding key issues in the trial: qualitative substudy
The qualitative substudy is reported in Appendix 3. This substudy documented the need for the provision of more information about the Alexander technique prior to consent (given its limited penetration in care to date), the low expectations of care for chronic back pain in the NHS and the low expectations of tailored physiotherapy classes (participants perceived that they were getting something that they had already tried and were pleasantly surprised by the group sessions). Time commitments for the interventions were a problem for some patients, but mostly there were very positive comments about both Alexander technique lessons and exercise classes and surprisingly positive comments about the biomechanical measurements.
Feedback from Alexander technique teachers
Carolyn Nicholls asked for feedback from all of the teachers involved in the study and their comments are shown in detail in Appendix 4. Most teachers reported observing significant benefits from the Alexander technique but commented on difficulties that participants had in arranging appointments, especially those receiving both Alexander technique lessons and exercise classes. For those who were working and looking after a family, keeping the appointments was doable but challenging. Retired people fared better in this respect. Several teachers commented that participants who received both Alexander technique lessons and exercise classes found the exercise classes easier, and this had also been noted by the physiotherapists.
Chapter 5 Discussion
The study focused on feasibility and demonstrated that the trial procedures were feasible, including retention and follow-up, different participant recruitment mechanisms and combining interventions (although care must be taken with running both Alexander technique lessons and exercise classes in parallel and with the scheduling of appointments). The study confirmed both that the main outcome was suitable, being sensitive to change, and that other outcomes might also be considered (particularly the Aberdeen pain and function scale). The exploratory analysis of clinical outcomes suggests that the estimates of treatment effects are likely to be clinically important and of a similar order to those seen with more intensive treatment regimes, in particular 10 Alexander technique lessons appeared to provide the same order of benefit as 24 Alexander technique lessons did in the ATEAM trial. 12 The exploratory analysis of biomechanical markers suggests that improved proprioception and modified muscle mechanical properties are likely to be associated with better outcomes.
Strengths and limitations
This study is the first to assess a 10-week course of Alexander technique lessons, to provide some comparison with a tailored group physiotherapy exercise class regime, to explore both the possible benefits of combining Alexander technique lessons and physiotherapy exercises and also possible biomechanical markers of recovery. The study was able to assess a number of areas of feasibility successfully, but being a feasibility study it was not powered to assess clinical or biomechanical outcomes and so it is particularly difficult to interpret negative findings and all estimates are very imprecise.
Nevertheless, the effects observed are in the range seen previously for a much more intensive Alexander technique intervention, and some were significant at the 5% or 10% level, even with such small numbers of participants. The ability to demonstrate changes in both clinical outcomes and biomechanical markers will be affected by adherence, which was mostly good or very good, but the impact of the physiotherapy exercise classes has probably been underestimated given the difficulties faced by some participants in attending classes. The number of intermediate biomechanical markers makes type 1 errors very likely but the risk of this is lessened by reference to our previous hypotheses and by the highly significant changes seen in key biomarkers in the CHAIN model, which cannot sensibly be explained by chance as they would be highly significant even if a Bonferroni correction was used. Interpretation of the inter-relationships between these variables will be more secure in a fully powered trial. We have shown that collection of heath-related quality of life data is feasible. It is very likely that both interventions are highly cost-effective, as the clinical outcomes are similar to those seen with previous more intensive and cost-effective interventions but the resource input is less;46 however, at this stage no formal economic modelling has been undertaken.
Feasibility outcomes
Several methods of recruitment were piloted: opportunistic recruitment in surgery (i.e. patient seen by the GP or nurse for an acute problem and then referred to the study), invited recruitment based on attendance with back pain in the last 5 years (as used in the ATEAM trial12) and invited recruitment based on very recent attendance with back pain. All of these methods proved to be feasible. The reason for exploring different methods was concern at the application stage that using invited recruitment for patients attending within the last 5 years (as in the ATEAM trial12) would target patients who might not be receiving current care in the NHS (and who would therefore be a non-attending population who were unlikely to use NHS resources); the board therefore requested that we also use opportunistic recruitment. Opportunistic recruitment in surgeries certainly provided some participants but the rate of recruitment was very slow and, if this method was used as the only method of recruitment, it would make the study much more expensive. As a result, we also piloted invited recruitment of patients who had been seen in the past week; this worked well and could provide an important mechanism for identifying eligible patients currently receiving care. Qualitative work documented that some patients who were not currently receiving care were not avoiding care but were not attending because they felt that, as a result of their past experiences of the NHS, the NHS had little to offer. Arguably, such patients should not be excluded from access to the interventions based on such past experiences.
The board had other major concerns. The first was about whether or not multiple intervention groups would be acceptable, given the number of sessions required to attend. This was certainly a problem for some patients, although even in the most intensive group most patients achieved good adherence for exercise classes (and better than in a previous large UK trial9) and, although patients clearly found it challenging based on both Alexander technique teachers’ comments and the qualitative study, adherence was excellent for Alexander technique lessons. However, the study highlights the need for a clearer explanation to be given about time commitments at the point of consent. One of the issues for patients was the time taken to travel to exercise classes and the fact that classes were at fixed times, which interfered with work and other commitments; there were similar issues for some patients with regard to Alexander technique lessons. Qualitative work suggested that for some patients the group environment was helpful and so abandoning the classes as a format for physiotherapy intervention would be premature.
A second concern was whether or not the RMDQ score was likely to be stable in the control group in the context of recent national guidance and, if not stable, whether or not this reflected higher referrals than previously. As we demonstrated the stability of the control group (a decrease in RMDQ score of only 1 point in 6 months) we did not investigate this further at this stage, although clearly in any future trial we would be able to document all referrals fully, as we did in the ATEAM trial12 by follow-up notes review.
Feasibility of laboratory biomechanical tests
All tests proved feasible although we had limited data from the axial tone testing device as it broke down and required a new part. To our surprise, many patients commented on how interesting the various tests were. There is currently no reason based on patient informal reports or the quantitative or qualitative data to significantly modify the measurement regimes, with the exception of EMG of the abdominal muscles, for which poor-quality signals were obtained; we would therefore not envisage using this measure in a larger trial.
Clinical outcomes
As expected, most outcomes did not reach significance at the 5% level, although some reached significance at the 10% level by 3 and 6 months, particularly in the combined group, and nearly all outcomes changed in a beneficial direction compared with the control group, which suggests that type 1 errors are not likely. Even with such small group numbers it seems likely that clinically important improvements were probably occurring [e.g. the RMDQ documented clinically important changes (> 2.5) by 6 months]. There was no clear evidence that the treatment effects were bottoming out by the end of 10 Alexander technique lessons or 12 exercise classes but, as the magnitude of the effects seems likely to be of the order of that seen with more intensive interventions, it will be difficult to justify more lessons or more classes in a future trial. Although in principle it might be possible to vary the numbers of lessons/sessions, to have more than four groups in any future trial (e.g. both 10 and 18 Alexander technique lessons and 12 and 18 exercise classes) would complicate and significantly increase the costs of the trial. There was good evidence of sensitivity to change of both the RMDQ and also the other main potential outcomes (Aberdeen pain and function scale, Oswestry Disability Index), and even the enlarged battery of questionnaires was acceptable to patients. Of the additional measures, the Aberdeen instrument seemed to differentiate between groups a little better than other outcomes and so would perhaps be the choice of additional instrument for any future main trial.
Effects of the interventions on laboratory measures at 3 months’ follow-up
The hypothesised relative effects of the Alexander technique and exercise classes on laboratory measures were summarised in the results section (see Table 15). The Alexander technique intervention was expected to improve trunk flexibility to imposed torsion (trunk rotation test); muscle tone (measured using the MyotonPRO device), proprioception of the cervical and lumbar areas; abdominal muscle recruitment (indicating improved motor control); and multifidus recruitment, muscle size and contractile ability. Of these measures, lumbar proprioception significantly improved comparison with the control group at 3 months.
The physiotherapy exercise class intervention was hypothesised to improve muscle stiffness and tone (measured using the MyotonPRO device); trunk muscle strength; pelvic loading ability (ASLR); proprioception of the lumbar spine; abdominal muscle recruitment; and multifidus muscle size and contractility. Of these measures, lumbar proprioception and trunk extension strength were improved compared with the control group.
Given the low power of the study, the significant findings at the 10% level for the different measures at 3 months may have reached significance at the 5% level with larger numbers of participants. It might be expected that the effects of the interventions may take 6 months to manifest for some of the biomechanical and neuromuscular function measures (see the following section).
Effects of the interventions on laboratory measures at 6 months’ follow-up
Alexander technique lessons resulted in improvements in multifidus muscle recruitment and mechanical properties (measured using the MyotonPRO device), which were predicted, as well as in pelvic loading ability, which had not been predicted. The expected effects on trunk flexibility and proprioception were not found, although there were very limited data to test the former (because of axial trunk rotation equipment failure).
The exercise class group showed expected improvements in multifidus muscle thickness, contractile ability and mechanical properties but not in muscle strength, recruitment or proprioception.
As already mentioned, it is likely that any negative results are due to the small group numbers (i.e. type 2 error) in this preliminary study and so they should be interpreted very cautiously; there could also be limitations because of the lack of sensitivity of the tests.
Mechanisms of treatment effects during recovery
The hypothesised effects of treatment were related to proposed mechanisms. The mechanism of action of the Alexander technique technique was proposed to be through improved muscle tone, proprioception (position sense) and motor control of spinal movements (indicated by earlier onset of EMG), and the importance of these was supported by the graphical CHAIN model. The physiotherapy exercise classes involved activities that would be expected to improve muscle strength, proprioception and motor control. These mechanisms were partially confirmed by this preliminary study, but confirmation and fuller exploration of the likely mechanisms requires a larger study.
Sensitivity and predictive value of assessment tools for later studies
The graphical CHAIN model at 6 months (see Figure 2 and Tables 19 and 20) indicates that the most predictive measures of the primary outcome at 6 months and other laboratory measures were proprioception, parameters of muscle mechanical properties (measured using the MyotonPRO device) and muscle thickness measurements (using USI). These were more predictive than EMG, which is a gold standard laboratory technique used in back pain research. 21,39
It is important to stress here that the relationship between clinical outcomes and biomechanical and neurophysiological markers commonly used in back pain research has yet to be clarified. It is widely reported that lower back pain is associated with abnormal muscle morphometry (thickness at rest and change during contraction) and motor control. Measurements of these two parameters (using USI and EMG) are often used to target interventions but baseline tests are not predictive of outcome47 and changes in muscle parameters pre–post intervention may not correlate with clinical outcomes, although limited evidence exists for change in multifidus thickness. 48 A possible explanation for this lack of correlation may be that the tests used are not relevant to the impairment being targeted. In previous studies on which these observations of abdominal and lumbar spine muscles were based, the tasks used to elicit involuntary contraction of trunk muscles were mainly arm lifts (some used voluntary abdominal muscle contraction, which is not as functional as automatic contraction). We therefore used leg lifts to see whether or not correlation with clinical measures could be improved, as leg lifts might be more functionally relevant to the lumbopelvic muscles than arm lifts. 49 The present preliminary findings showed that most of the laboratory techniques used were sensitive to change pre to post intervention at 6 months (see Table 8), although these measures were not well correlated with clinical outcomes (see Figure 2 and Table 19). We also used novel tests of muscle characteristics that would be relevant to altering muscle tone, which the Alexander technique aims to influence. These novel tests were (1) the trunk rotation test, which was recently found to be sensitive to a reduction in resistance to rotation immediately after an Alexander technique session in people with lower back pain,20 and (2) MyotonPRO technology for testing non-neural tone and mechanical properties of muscle, including stiffness and elasticity.
Another important point to highlight is that lack of correlation between the clinical measures and the laboratory measures does not necessarily mean that the muscle tests are insensitive to change; it could indicate that, although an intervention has been clinically beneficial in reducing symptoms and improving function, it may not have been effective at treating the muscle impairment. An example of this possibility was demonstrated by a study of targeted multifidus exercises compared with medical treatment in acute lower back pain, which found that muscle wasting did not recover without exercises but that symptoms resolved in both the treatment group and the control group. 22 Importantly, when patients were followed up at 1 and 3 years, there was a significantly greater recurrence of lower back pain in the control group. 50 The findings suggest that the dissociation between muscle measurements and clinical outcomes indicated that the spine was at risk of further injury.
The multifidus and abdominal muscle thickness measures were related (see Figure 2), as expected from the literature,47 but there is very limited evidence available on the predictive value of ultrasound muscle thickness measurements. 47,48,51
The Myoton and axial trunk rotation devices both provide indications of muscle tone (state of tension) and so might be expected to show similar findings. However, there were insufficient data from the trunk rotation device to enable their comparison at this stage. The Myoton observations are novel as research on the technology is in the relatively early stages. Myoton parameters relate to proprioception and muscle thickness measures. The axial rotation test is also relatively new, with limited existing literature on the test. 14–16,20
Muscle strength gives an indication of functional capacity and testing is commonly used in back pain studies but relies on volition. Maximal effort can be affected by pain or fear of pain and so the lack of effect of interventions on trunk muscle strength may have been influenced by the methodology. Furthermore, maximal effort was not confirmed by twitch interpolation electrical stimulation, for practical reasons. 52
Chapter 6 Conclusion
With modest modifications a full trial is likely to be feasible. There is encouraging evidence that both interventions may provide clinically important benefits, particularly the combined intervention. Novel biomechanical markers that could be targets for interventions have been identified; a better outcome was associated with changes in muscle tone, elasticity and proprioception. There is also preliminary evidence that, in turn, these markers were modified by the interventions. As well as shedding light on the mechanisms of action of the Alexander technique intervention, the proposed study has the potential to provide further insight into predictive laboratory-based biomechanical and neuromuscular physiological markers and their relationship to clinical outcomes in lower back pain research.
Recommendations for a future trial
We propose that any future full trial should ideally:
-
include all three participant recruitment strategies with the same inclusion criteria but aim to include at least half of those who have been identified as having care recently (i.e. opportunistic or invited based on attendance in the last week) to be able to explore possible differences in effectiveness.
-
include the RMDQ as the primary outcome
-
include secondary outcomes – the battery of secondary outcomes recommended for back pain research and included in this and the previous trial (days in pain, Von Korff pain and disability scale, Deyo troublesomeness scale, overall improvement, enablement, fear of activity), but also the Aberdeen instrument
-
include biomechanical/neuromuscular physiological measures – include the same range of laboratory markers included in the feasibility study, except for EMG of abdominal muscles
-
maintain 10 lessons of Alexander technique and 12 classes of physiotherapy, but explore ways of improving the flexibility and accessibility of the interventions when possible
-
include a more extensive discussion of trial commitments at the time of consent.
Acknowledgements
Mrs Julie Hooper provided administrative support to the study and co-ordinated patient contact and telephone follow-up for those not returning the questionnaires.
Mr Colin Steel, in liaison with the Southampton branch of BackCare, provided comments on the protocol, study procedures and outcomes. Mr Mike Price from the Southampton branch of BackCare commented on the final report.
The authors thank the participants and the Alexander technique teachers and physiotherapists in participating practices. We also thank Myoton Ltd (London) for loan of the MyotonPRO device and Aleko Peipsi Myoton (CEO, Myoton AS, Estonia) for providing training in its use.
Contributions of authors
Professor Paul Little had the original idea for the study, led the development of the protocol and the grant application, provided overall co-ordination and drafted the first version of the report.
Dr Beth Stuart developed the analysis protocol with Professor Peter Smith and performed the analysis of the quantitative measures and commented on drafts of the report.
Professor Maria Stokes helped develop the overall protocol and grant application, developed the biomechanical protocols, provided co-ordination of the biochemical measures, drafted the report of the biomechanical measures and commented on drafts of the report.
Mrs Carolyn Nicholls helped develop the overall protocol and grant application, developed the structure of the training, lessons and outcomes for Alexander technique teachers, co-ordinated the Alexander technique teachers and delivery of the Alexander technique lessons and commented on drafts of the report.
Dr Lisa Roberts helped develop the overall protocol and grant application, helped develop the biomechanical protocols, developed the physiotherapy exercise class intervention and co-ordinated the classes and commented on drafts of the report.
Dr Stephen Preece helped develop the overall protocol and grant application, developed the biomechanical protocols with Professor Maria Stokes and commented on drafts of the report.
Dr Tim Cacciatore helped develop the overall protocol and grant application, developed the biomechanical protocols with MS, advised on the purchase, construction and use of the torsion device and commented on drafts of the report.
Mr Simon Brown developed the protocol for the biomechanical measures with Professor Maria Stokes and performed the measures and analysed the output and contributed to drafting of the report.
Professor George Lewith developed the original idea of the study with Professor Paul Little, contributed to the development of the protocol and the grant application and commented on the draft report.
Dr Adam Geraghty helped develop the overall protocol and grant application, commented on drafts of the report and supervised the qualitative study.
Professor Lucy Yardley helped develop the overall protocol and grant application, commented on drafts of the report and with Dr Adam Geraghty supervised the qualitative study.
Mrs Gilly O’Reilly helped develop the overall protocol, co-ordinated the study on a day-to-day basis and commented on drafts of the report.
Mrs Caroline Chalk helped develop the overall protocol and grant application and developed the structure of training, lessons and outcomes for Alexander technique teachers.
Professor Debbie Sharp developed the original idea of the study with Professor Paul Little, contributed to the development of the protocol and the grant application and commented on the draft report.
Professor Peter Smith helped develop the overall protocol and grant application, developed the analysis protocol, co-ordinated the statistical analysis and commented on drafts of the report.
Disclaimers
This report presents independent research. The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NETSCC, the EME programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the EME programme or the Department of Health.
References
- Hermans V. Research on Work-Related Low Back Disorders. Brussels: Institute for Occupational Safety and Health; 2000.
- Andersson G. Epidemiological features of chronic low-back pain. Lancet 1999;354:581-5. http://dx.doi.org/10.1016/S0140-6736(99)01312-4.
- Croft P, MacFarlane G, Papageorgiou A, Thomas E, Silman A. Outcome of low back pain in general practice: a prospective study. BMJ 1998;316:1356-9. http://dx.doi.org/10.1136/bmj.316.7141.1356.
- Hayden J, van Tulder M, Malmivaara A, Koes B. Meta-analysis: exercise therapy for non-specific low back pain. Ann Intern Med 2005;142:765-75. http://dx.doi.org/10.7326/0003-4819-142-9-200505030-00013.
- van Tulder M. Conservative non-pharmacological treatment for chronic low back pain. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a974.
- Clinical Guidelines for the Physiotherapy Management of Persistent Low Back Pain. London: Chartered Society of Physiotherapy; 2006.
- Hayden J, van Tulder M, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med 2005;142:776-85. http://dx.doi.org/10.7326/0003-4819-142-9-200505030-00014.
- Low Back Pain: Early Management of Persistent Non-Specific Low Back Pain. London: NICE; 2009.
- UK BEAM trial team . United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: effectiveness of physical treatments for back pain in primary care. BMJ 2004;329. http://dx.doi.org/10.1136/bmj.38282.669225.AE.
- Stokes M, Hides J, Elliott J, Kiesel K, Hodges P. Rehabilitative ultrasound imaging of the posterior paraspinal muscles. J Orthop Sports Phys Ther 2007;37:581-95. http://dx.doi.org/10.2519/jospt.2007.2599.
- Teyhen D, Gill S, Whittaker J, Henry S, Hides A, Hodges P. Rehabilitative ultrasound imaging of the abdominal muscles. J Orthop Sports Phys Ther 2007;37:450-66. http://dx.doi.org/10.2519/jospt.2007.2558.
- Little P, Lewith G, Webley F, Evans M, Beattie A, Middleton K, et al. Randomised controlled trial of Alexander technique lessons, exercise, and massage (ATEAM) for chronic and recurrent back pain. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a884.
- Ferreira P, Ferreira M, Hodges P. Changes in recruitment of the abdominal muscles in people with low back pain: ultrasound measurement of muscle activity. Spine 2004;29:2560-6. http://dx.doi.org/10.1097/01.brs.0000144410.89182.f9.
- Cacciatore T, Gurfinkel V, Horak F, Cordo P, Ames K. Increased dynamic regulation of postural tone through Alexander Technique training. Hum Mov Sci 2011;30:74-89. http://dx.doi.org/10.1016/j.humov.2010.10.002.
- Cacciatore T, Horak F, Henry S. Improvement in automatic postural coordination following Alexander technique lessons in a person with low back pain. Phys Ther 2005;85:565-78.
- Gurfinkel V, Cacciatore T, Cordo P, Horak F, Nutt J, Skoss R. Postural muscle tone in the body axis of healthy humans. J Neurophysiol 2006;96:2678-87. http://dx.doi.org/10.1152/jn.00406.2006.
- Ernst E, Canter P. The Alexander technique: a systematic review of controlled clinical trials. Forsch Komplementarmed Klass Naturheilkd 2003;10:325-9. http://dx.doi.org/10.1159/000075886.
- Jordan K, Dunn K, Lewis M, Croft P. A minimal clinically important difference was derived for the Roland–Morris Disability Questionnaire for low back pain. J Clin Epidemiol 2006;59:45-52. http://dx.doi.org/10.1016/j.jclinepi.2005.03.018.
- Lamoth C, Meijer O, Wuisman J, van Dieen J, Levin M, Beek P. Pelvis–thorax coordination in the transverse plane during walking in persons with nonspecific low back pain. Spine 2002;27:E92-9. http://dx.doi.org/10.1097/00007632-200202150-00016.
- Cacciatore T, Gurfinkel V, Horak F, Ames K. Increased dynamic regulation of postural tone through Alexander technique training. Hum Mov Sci 2011;30:74-89. http://dx.doi.org/10.1016/j.humov.2010.10.002.
- Hodges P, Moseley G. Pain and motor control of the lumbopelvic region: effect and possible mechamisms. J Electromyogr Kinesiol 2003;13:361-70. http://dx.doi.org/10.1016/S1050-6411(03)00042-7.
- Hides J, Richardson C, Jull G. Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine 1996;21:2763-9. http://dx.doi.org/10.1097/00007632-199612010-00011.
- Bayramoglu M, Akman M, Kilinc S, Cetin N, Ozker R. Isokinetic measurement of trunk muscle strength in women with chronic low-back pain. Am J Phys Med Rehabil 2001;80:650-5. http://dx.doi.org/10.1097/00002060-200109000-00004.
- Lee J, Hoshino Y, Nakamura K, Kariya K, Saita K, Ito K. Trunk muscle weakness as a risk factor for low back pain: a 5-year prospective study. Spine 1999;24:54-7. http://dx.doi.org/10.1097/00007632-199901010-00013.
- Teyhen D, Riegler J, Westrick B, Miller A, Molloy J, Childs J. Changes in deep abdominal muscle thickness during common trunk-strengthening exercises using ultrasound imaging. J Orthop Sports Phys Ther 2008;38:596-605. http://dx.doi.org/10.2519/jospt.2008.2897.
- Frost H, Klaber-Moffett J, Moser JS, Fairbank JCT. Randomised controlled trial for evaluation of fitness programme for patients with chronic low back pain. BMJ 1995;310:151-4. http://dx.doi.org/10.1136/bmj.310.6973.151.
- Slade S, Keating J. Trunk-strengthening exercises for chronic low back pain: a systematic review. J Manipulative Physiol Ther 2006;29:163-73. http://dx.doi.org/10.1016/j.jmpt.2005.12.011.
- Deyo RA, Battie M, Beurskens AJH, Bombardier C, Croft P, Koes B, et al. Outcome measures for low back pain research: a proposal for standardized use. Spine 1998;23:2003-13. http://dx.doi.org/10.1097/00007632-199809150-00018.
- Beurskens A, de Vet H, Koke A. Reponsiveness of functional status in low back pain: a comparison of different instruments. Pain 1996;65:71-6. http://dx.doi.org/10.1016/0304-3959(95)00149-2.
- Von Korff M, Ormel J, Keefe M, Dworkin S. Grading the severity of chronic pain. Pain 1992;50:133-49. http://dx.doi.org/10.1016/0304-3959(92)90154-4.
- Von Korff M, Deyo R, Cherkin D, Barlow W. Back pain in primary care. Spine 1993;18:855-62. http://dx.doi.org/10.1097/00007632-199306000-00008.
- Woby S. Psychometric properties of the TSK-11: a shortened version of the Tampa Scale for Kinesiophobia. Pain 2009;117:137-44. http://dx.doi.org/10.1016/j.pain.2005.05.029.
- Kori S, Miller R, Todd D. Kinesiophobia: a new view of chronic pain behaviour. Pain Manag 1990;3:35-43.
- Johnsen LG, Hellum C, Nygaard OP, Storheim K, Brox JI, Rossvoll I, et al. Comparison of the SF6D, the EQ5D, and the Oswestry Disability Index in patients with chronic low back pain and degenerative disc disease. BMC Musculoskelet Disord 2013;14. http://dx.doi.org/10.1186/1471-2474-14-148.
- Bombardier C. Outcome assessments in the evaluation of treatment of spinal disorders: summary and general recommendations. Spine 2000;25:3100-3. http://dx.doi.org/10.1097/00007632-200012150-00003.
- Ruta D, Garratt A, Wardlaw D, Russell I. Developing a valid and reliable measure for health outcome for patients with low back pain. Spine 1994;19:1887-96. http://dx.doi.org/10.1097/00007632-199409000-00004.
- Mens J, Vleeming A, Snidjers CJ, Koes B, Stam H. Reliability and validity of the active straight leg raise test in posterior pelvic pain since pregnancy. Spine 2001;26:1167-71. http://dx.doi.org/10.1097/00007632-200105150-00015.
- Lovell F, Rothstein J, Personius W. Reliability of clinical measurements of lumbar lordosis taken with a flexible rule. Phys Ther 1989;69:96-105.
- Williams J, Haq I, Lee R. An investigation into the onset, pattern, and effects of pain relief on lumbar extensor electromyography in people with acute and chronic low back pain. J Manipulative Physiol Ther 2013;36:91-100. http://dx.doi.org/10.1016/j.jmpt.2012.12.006.
- Mens J, Vleeming A, Snidjers CJ, Stam H, Ginai A. The active straight leg raising test and mobility of the pelvic joints. Eur Spine J 1999;8:468-73. http://dx.doi.org/10.1007/s005860050206.
- Gavronski G, Veraksits A, Vasar E, Maaross J. Evaluation of viscoelastic parameters of the skeletal muscles in junior triathletes. Physiol Meas 2007;28:625-37. http://dx.doi.org/10.1088/0967-3334/28/6/002.
- Ditroilo M, Hunter A, Haslam S, DeVito G. The effectiveness of two novel techniques in establishing the mechanical and contractile responses of biceps femoris. Physiol Meas 2011;32:1315-26. http://dx.doi.org/10.1088/0967-3334/32/8/020.
- Bailey L, Samuel D, Warner M, Stokes M. Parameters representing muscle tone, elasticity and stiffness of biceps brachii in healthy older males: symmetry and within-session reliability using the MyotonPRO. J Neurol Disord 2013;1:1-7. http://dx.doi.org/10.4172/2329-6895.1000116.
- Agyapong-Badu S, Aird L, Bailey L, Mooney K, Mullix J, Warner M, et al. Interrater reliability of muscle tone, stiffness and elasticity measurements of rectus femoris and biceps brachii in healthy young and older males. Working Papers Health Sci 2013;1:1-11.
- Roland M, Morris R. A study of the natural history of low back pain. 1: development of a reliable and sensitive measure of of disability in low back pain. Spine 1983;8:141-4. http://dx.doi.org/10.1097/00007632-198303000-00004.
- Hollinghurst S, Sharp D, Ballard K, Barnett J, Beattie A, Evans M, et al. Randomised controlled trial of Alexander technique lessons, exercise, and massage (ATEAM) for chronic and recurrent back pain: economic evaluation. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a2656.
- Wong A, Parent E, Funabashi M, Stanton T, Kawchuk G. Do various baseline characteristics of transversus abdominis and lumbar multifidus predict clinical outcomes in non-specific low back pain?. Pain 2013. http://dx.doi.org/10.1016/j.pain.2013.07.010.
- Koppenhaver S, Fritz J, Herbert J, Kawchuk G, Childs J, Parent E, et al. Association between changes in abdominal and lumbar multifidus. J Orthop Sports Phys Ther 2011;41:389-99. http://dx.doi.org/10.2519/jospt.2011.3632.
- Hides J, Richardson C, Jull G. Use of realtime ultrasound imaging for feedback in rehabilitation. Man Ther 1998;3:125-31. http://dx.doi.org/10.1016/S1356-689X(98)80002-7.
- Hides J, Jull G, Richardson C. Long-term effects of specific stabilizing exercises for first-episode low back pain. Spine 2001;26:E243-8. http://dx.doi.org/10.1097/00007632-200106010-00004.
- Mannion A, Caporaso F, Pulkovski N, Sprott H. Spine stabilisation exercises in the treatment of chronic low back pain: a good clinical outcome is not associated with improved abdominal muscle function. Eur Spine J 2012;21:1301-10. http://dx.doi.org/10.1007/s00586-012-2155-9.
- Gandevia S. Twitch interoloation: a valid measure with misinterpreted meaning. J Appl Physiol 2009;107:363-4.
- Nicholls C. Body Breath and Being. Hove: D&B Publishing; 2008.
- Macdonald G. Illustrated Elements of Alexander Technique. Shaftesbury: Element Books (UK); 2002.
- Gelb M. Body Learning. London: Aurum Press; 2004.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. http://dx.doi.org/10.1191/1478088706qp063oa.
Appendix 1 Alexander technique lessons and physiotherapy exercise classes
Appendix 1.1: Detailed description of the Alexander technique and lessons
The Alexander technique is a taught approach. Anyone taking Alexander technique lessons is regarded as learning the technique, not as a patient; lessons are not a form of passive therapy or treatment.
The teachers’ aim was to teach the Alexander technique and how to make use of it to reduce the intensity and frequency of poor habits and facilitate improvements in co-ordination, muscle tone and musculoskeletal use.
Teachers first investigated whether or not there was something – perhaps a particular habitual way of standing, sitting or moving – that was underlying or exacerbating the problem. Habits that restrict freedom of movement of the head and neck and that cause stiffening and shortening of the spine and commonly result in pain were given priority and were progressively reduced.
How is the Alexander technique taught?
During lessons, teachers used frequent hand contact to observe and interpret subtle changes in muscle tone and co-ordination and also to convey non-verbal information. This was integrated with oral and written advice and information.
Hand contact was also used to:
-
clarify the meaning of verbal explanations and advice
-
help people:
-
direct their attention where needed
-
become aware of and release unwanted head, neck and spine muscle tension
-
gain immediate feedback
-
allow lengthening of the spine
-
improve axial muscle tone and co-ordination
-
facilitate the dynamic inter-relationships of the head, neck and back
-
improve musculoskeletal use
-
maintain improvements during activity.
-
Other teaching aids included diagrams, models and the example of the teachers’ own manner of use.
The Alexander technique was taught through practical application of the technique in carrying out simple activities:
-
initially quiet standing, quiet sitting, then moving from one to the other, or lying semi-supine on a firm surface
-
preparation for and carrying out activities such as walking, crawling, turning, raising a hand or speaking
-
later, other activities of general value or of particular interest, such as playing a musical instrument, writing or using a computer.
Difficulties were discussed and resolved.
The content of each lesson varied according to the observed and reported needs and limitations of each individual. All were encouraged to spend some time each day (15–20 minutes) practising the Alexander technique while in a semi-supine position (lying on the back with head supported, knees bent and feet flat on supporting surface) and to use the Alexander technique in their everyday activities.
Lesson pattern
All lessons were one-to-one. Participants were usually asked to remove shoes but otherwise remained fully clothed. Lessons lasted for 30–40 minutes and each participant was encouraged to record the time between lessons dedicated to practising the Alexander technique. Participants were provided with a book on the technique – either Body Breath and Being,53 Illustrated Elements of Alexander Technique54 or Body Learning. 55
The first four lessons were planned at twice-weekly intervals and subsequent lessons were weekly.
In practice, the schedule could be difficult to achieve in exactly the above format and it was negotiated flexibly with patients, as in the ATEAM trial. 12 The practical activities used, what was taught and the pupils’ progress and difficulties encountered were recorded on forms designed for the trial.
Alexander technique teachers
All Alexander technique teachers in the trial had successfully undergone 3 years of training on a Society of Teachers of the Alexander Technique (STAT)-approved course; were currently registered members of STAT; and had at least 3 years’ post-qualification experience. Lessons took place at the teachers’ normal place of work, either their home or in a private clinic.
Appendix 1.2: Physiotherapy exercise class content
Overview
As for other ‘back to fitness’ programmes, the format of the physiotherapy exercise classes was based on the biopsychosocial model, aiming to help participants overcome any fears and avoidance of movement and enable them to return to normal activities.
The content of the exercise package was based on those developed previously and is consistent with current recommendations and systematic reviews. 4,6,7,9–11,22,25–27 It included:
-
stretching and mobilising
-
motor relearning, balance and co-ordination
-
strengthening
-
activity modification exercises
-
cardiovascular exercises
-
exercise targeting the rehabilitation of deep abdominal and lumbar paraspinal muscles
-
exercises tailored to the individual that may be performed at home
-
around 20 hours of contact time (one initial assessment, one individual follow-up session to tailor the exercise programme and 12 group sessions lasting for 90 minutes each).
There was time to share success and encourage other group members in the group sessions and particular attention was paid, both at initial consenting and at each group session, to gaining robust agreement from every individual to attend every session – as attendance was an important issue in the UK BEAM trial. 9 Help and training was provided for this.
Principles of cognitive–behavioural management were incorporated into the classes whereby health behaviour was praised and pain behaviour was not.
Each session comprised:
-
a 5-minute cardiovascular warm-up
-
stretches for the major muscle groups
-
a circuit with 10 different tailored exercises (chosen by the referring physiotherapist from those in this manual); 2 minutes will be spent on each exercise
-
‘cool-down’ time comprising additional stretching and 5 minutes of light aerobic exercise
-
a period of relaxation
-
group discussion – ‘tip of the day’.
At all stages, class participants were encouraged to think of themselves as ‘sports people’ who need to improve their fitness rather than as disabled patients, and to aim to work at a perceived physical exertion level of ‘somewhat hard’. They were also advised that this type of activity can cause some discomfort if they are unaccustomed to such activities.
Participants were advised not to compete with each other and that repetitions and progression of exercises are on a personal basis, with each person recording their own progress during the circuit exercises. They were also encouraged to continue these activities outside the sessions and to think about other activities to return to, or try for the first time, as their fitness improved.
Session content
Warm-up and stretching (10 minutes)
This is important to prepare the body for the activities ahead. It included:
-
General warm-up: light physical activity that results in a light sweat. Examples include:
-
trampette
-
cycling using static pedals
-
exercise bike
-
treadmill
-
-
Stretches: major muscle groups including:
-
hamstrings
-
quadriceps
-
calf (gastrocnemius and soleus)
-
Iliopsoas
-
cervical spine extension
-
cervical spine side flexion
-
shoulder rolls
-
triceps
-
horizontal flexion
-
thoracic spine rotation
-
lumbar side flexion.
-
Possible circuit activities
| Stretching and mobilising | |||
|---|---|---|---|
| 1 |

|
One-legged knee curl
|
Alternate knee to chest |
| 2 |

|
Two-legged knee curl
|
Supine knee curls |
| 3 |

|
Prone back stretch
|
Spinal extension |
| 4 |

|
Kneeling back stretch
|
Spinal flexion in kneeling or child pose with shoulder elevation |
| 5 |

|
Log roll
|
Log roll |
| 6 |

|
Knee drops
|
Lumbar rotation |
| 7 |

|
Supine back stretch
|
Lumbar rotation with knee extension |
| 8 |

|
Pelvic tilting on hands and knees
|
Pelvic tilting in four-point kneeling |
| 9 |

|
Pelvic tilting with towel
|
Crook lying pelvic tilt with towel |
| 10 |

|
Standing rotation
|
Thoracic rotation |
| 11 |

|
Sitting side bend
|
Thoracic side flexion |
| 12 |

|
Thigh stretch
|
Hamstring |
| 13 |


|
Sitting leg swing
|
Neurodynamic slider in slump sitting |
| Motor relearning, balance and co-ordination exercises | |||
| 14 |

|
Gym ball – sitting
|
Gym ball – sitting |
| 15 |

|
Gym ball – arms
|
Gym ball sitting with 90° shoulder abduction |
| 16 |

|
Gym ball – sitting rock
|
Gym ball – pelvic tilting in sitting |
| 17 |

|
Gym ball – foot lift
|
Gym ball – hip flexion |
| 18 |

|
Kneeling without one arm
|
Four-point balance arm extension |
| 19 |

|
Kneeling without one leg
|
Four-point balance leg extension |
| 20 |

|
Kneeling without one arm or leg
|
Four-point balance alternate arm and leg extension |
| Strengthening | |||
| 21 |

|
Prone hold
|
Isometric back extensors |
| 22 |

|
Side lying leg lift
|
Hip abduction in side lying |
| 23 |

|
Side lying bent leg lift
|
Hip abduction with knee flexion in side lying |
| 24 |

|
Kneeling leg lift
|
Four-point kneeling hip extension with knee flexion |
| 25 |

|
Wall squats
|
90° squats against the wall |
| 26 |

|
Chair squats
|
90° squats with chair support |
| 27 |

|
Ball squats
|
90° gym ball squats against the wall |
| 28 |

|
Standing on one leg
|
Alternate leg lifts |
| 29 |

|
Toe raises
|
Isometric calf |
| 30 |

|
Bridging
|
Bridging |
| 31 |

|
Bridging on one leg
|
Bridging with leg extension |
| 32 |

|
Wall press-up
|
Wall press-up |
| 33 |

|
Gym ball with weights
|
Gym ball – 90° flexion with hand weights |
| 34 |


|
Lunges
|
Alternate forward lunges in standing |
| Activity modification | |||
| 35 |

|
Touching your toes
|
Flexion in standing |
| 36 |

|
Sitting and standing
|
Sit to stand |
| Cardiovascular | |||
| 37 |

|
Exercise bike
|
Exercise bike |
| 38 |

|
Treadmill
|
Treadmill |
| 39 |

|
Step-ups
|
Step-ups |
| 40 |

|
Trampette
|
Trampette |
| 41 |

|
Cross-trainer
|
Cross-trainer |
Cool down
Light, physical activity that results in a light sweat. Examples included:
-
trampette
-
cycling using static pedals
-
exercise bike
-
treadmill.
Stretches
As per the warm-up. Major muscle groups include:
-
hamstrings
-
quadriceps
-
calf (gastrocnemius and soleus)
-
iliopsoas
-
cervical spine extension
-
cervical spine side flexion
-
shoulder rolls
-
triceps
-
horizontal flexion
-
thoracic spine rotation
-
lumbar side flexion.
Dr Lisa Roberts, December 2011
Appendix 2 Laboratory measures
See Table 3 for a summary of the tests and variables measured.
| Characteristic/measure | Control, mean (SD) | Exercise classes only, mean (SD) | Alexander technique only, mean (SD) | Alexander technique + exercise classes, mean (SD) |
|---|---|---|---|---|
| Number of participants | 17 | 17 | 17 | 18 |
| Sex (female), n/N (%) | 8/17 (47.1) | 13/17 (76.5) | 11/17 (64.7) | 11/18 (61.1) |
| Age (years) | 47.20 (11.57) | 47.93 (11.97) | 49.92 (10.11) | 56.45 (7.86) |
| Body mass index (kg/m2) | 25.48 (3.49) | 26.71 (5.59) | 25.98 (4.75) | 28.44 (4.33) |
| Proprioception – cervical (degrees) | ||||
| X | 2.06 (1.99) | 2.06 (1.70) | 3.14 (2.82) | 2.17 (1.81) |
| Y | 2.04 (1.74) | 2.59 (2.09) | 4.67 (2.77) | 3.15 (2.17) |
| Z | 0.57 (0.75) | 0.88 (0.94) | 1.10 (1.74) | 0.81 (1.11) |
| Proprioception – lumbar (degrees) | ||||
| From ‘upright/zero’ position | 1.88 (1.51) | 2.12 (1.67) | 1.85 (1.91) | 1.65 (1.59) |
| From ’20° flexion’ position | 2.45 (1.98) | 3.16 (3.98) | 4.35 (2.82) | 3.28 (2.30) |
| USI – multifidus thickness (cm) | ||||
| Symptomatic side | ||||
| Relaxed | 2.78 (0.15) | 2.84 (0.51) | 2.93 (0.37) | 2.98 (0.44) |
| Contracted | 3.14 (0.33) | 3.05 (0.41) | 3.27 (0.37) | 3.30 (0.44) |
| Non-symptomatic side | ||||
| Relaxed | 2.74 (0.30) | 2.87 (0.50) | 2.92 (0.34) | 3.05 (0.34) |
| Contracted | 3.03 (0.36) | 3.16 (0.53) | 3.24 (0.40) | 3.40 (0.38) |
| USI – transversus abdominis thickness (cm) | ||||
| Symptomatic side | ||||
| Relaxed | 0.37 (0.15) | 0.36 (0.13) | 0.38 (0.15) | 0.38 (0.14) |
| Contracted | 0.40 (0.16) | 0.38 (0.13) | 0.40 (0.17) | 0.41 (0.14) |
| Non-symptomatic side | ||||
| Relaxed | 0.38 (0.13) | 0.36 (0.15) | 0.39 (0.12) | 0.36 (0.13) |
| Contracted | 0.42 (0.13) | 0.37 (0.16) | 0.44 (0.16) | 0.41 (0.14) |
| ASLR compression test (response of 1a), n/N (%) | 6/15 (40.00) | 8/17 (47.06) | 6/12 (50.00) | 7/17 (41.18) |
| Multifidus mechanical properties (MyotonPRO device) | ||||
| Symptomatic side | ||||
| Tone (frequency; Hz) | ||||
| Prone | 16.55 (2.71) | 16.06 (3.43) | 16.06 (1.81) | 16.87 (2.90) |
| Seated | 21.13 (5.38) | 18.24 (4.05) | 18.25 (4.35) | 19.02 (5.26) |
| Stiffness (N/m) | ||||
| Prone | 343.52 (82.28) | 331.03 (108.00) | 326.93 (77.56) | 359.82 (96.90) |
| Seated | 533.73 (173.68) | 444.94 (160.10) | 447.65 (162.07) | 464.84 (169.30) |
| Elasticity (log decrement) | ||||
| Prone | 1.34 (0.26) | 1.35 (0.29) | 1.37 (0.24) | 1.57 (0.29) |
| Seated | 1.24 (0.51) | 1.08 (0.15) | 1.26 (0.42) | 1.35 (0.31) |
| Non-symptomatic side | ||||
| Tone (frequency; Hz) | ||||
| Prone | 16.55 (2.81) | 15.41 (2.20) | 16.39 (2.81) | 16.72 (3.29) |
| Seated | 20.36 (5.04) | 18.08 (4.59) | 19.47 (5.35) | 18.91 (5.26) |
| Stiffness (N/m) | ||||
| Prone | 350.07 (86.20) | 313.95 (86.86) | 329.33 (88.34) | 350.39 (109.61) |
| Seated | 520.02 (175.46) | 438.04 (175.89) | 477.78 (190.18) | 452.88 (184.86) |
| Elasticity (log decrement) | ||||
| Prone | 1.37 (0.32) | 1.33 (0.27) | 1.41 (0.34) | 1.52 (0.26) |
| Seated | 1.22 (0.52) | 1.12 (0.18) | 1.14 (0.27) | 1.31 (0.26) |
| EMG (onset of muscle activation) (ms) | ||||
| Rectus abdominis | ||||
| Symptomatic | −0.16 (0.17) | −0.19 (0.12) | N/A (only one observation) | −0.18 (0.27) |
| Non-symptomatic | −0.16 (0.14) | −0.22 (0.14) | N/A (only one observation) | N/A (only one observation) |
| Internal oblique | ||||
| Symptomatic | −0.24 (0.12) | −0.21 (0.12) | −0.25 (0.10) | −0.18 (0.09) |
| Non-symptomatic | −0.22 (0.08) | −0.21 (0.08) | −0.29 (0.07) | −0.28 (0.17) |
| Multifidus | ||||
| Symptomatic | −0.44 (0.20) | −0.38 (0.25) | −0.37 (0.09) | −0.32 (0.11) |
| Non-symptomatic | −0.38 (0.23) | −0.31 (0.13) | −0.41 (0.16) | −0.32 (0.08) |
| Trunk axial rotation test (N/m) | ||||
| Back peak to peakb | 3.05 (0.74) | 3.10 (1.08) | 3.04 (0.77) | 3.48 (1.05) |
| Back phase advance | 4.78 (3.17) | 5.33 (1.87) | 7.34 (3.58) | 5.31 (2.88) |
| Hip peak to peakb | 2.27 (0.48) | 2.44 (1.37) | 2.50 (0.89) | 2.89 (1.14) |
| Hip phase advance | 6.65 (1.74) | 6.55 (2.56) | 5.70 (4.69) | 6.49 (6.01) |
| Trunk muscle strength (Biodex) (N/m) | ||||
| Flexion | 50.06 (26.44) | 51.77 (31.86) | 62.65 (28.65) | 49.38 (18.63) |
| Extension | 125.44 (84.28) | 125.86 (84.23) | 114.58 (49.83) | 106.52 (65.66) |
| Measure | Control, mean (SD) | Exercise classes only, mean difference from control (95% CI; p-value) | Alexander technique only, mean difference from control (95% CI; p-value) | Alexander technique + exercise classes, mean difference from control (95% CI; p-value) |
|---|---|---|---|---|
| Proprioception – cervical (degrees) | ||||
| X (n = 57) | 1.38 (1.63) | 0.05 (−1.38 to 1.48; 0.943) | 0.24 (−1.18 to 1.66; 0.737) | 1.05 (−0.35 to 2.46; 0.142) |
| Y (n = 57) | 3.05 (3.46) | −0.67 (−2.51 to 1.18; 0.472) | −0.29 (−2.27 to 1.69; 0.771) | −1.47 (−3.31 to 0.37; 0.117) |
| Z (n = 57) | 0.49 (0.65) | 0.01 (−0.66 to 0.68; 0.981) | 0.13 (−0.54 to 0.79; 0.707) | 0.27 (−0.38 to 0.92; 0.407) |
| Proprioception – lumbar (degrees) | ||||
| From ‘upright/zero’ position (n = 56) | 1.21 (1.07) | −0.16 (−1.02 to 0.70; 0.705) | 0.04 (−0.82 to 0.90; 0.926) | 0.23 (−0.61 to 1.08; 0.585) |
| From ‘20° flexion’ position | 4.26 (3.35) | −1.75 (−3.71 to 0.21; 0.08) | −2.37 (−4.45 to −0.30; 0.026) | −2.15 (−4.14 to −0.16; 0.035) |
| USI – multifidus thickness (symptomatic side) (cm) | ||||
| Relaxed (n = 53) | 3.25 (0.26) | 0.002 (−0.110 to 0.120; 0.960) | 0.02 (−0.09 to 0.14; 0.699) | −0.02 (−0.13 to 0.10; 0.762) |
| Contracted (n = 52) | 2.86 (0.34) | −0.06 (−0.20 to 0.08; 0.397) | −0.02 (−0.16 to 0.12; 0.763) | −0.11 (−0.24 to 0.03; 0.120) |
| USI – transversus abdominis thickness (symptomatic side) (cm) | ||||
| Relaxed (n = 52) | 0.36 (0.13) | −0.01 (−0.05 to 0.04; 0.710) | −0.02 (−0.06 to 0.02; 0.360) | 0.01 (−0.04 to 0.05) |
| Contracted (n = 53) | 0.41 (0.20) | −0.02 (−0.10 to 0.06; 0.581) | −0.03 (−0.10 to 0.05; 0.472) | −0.01 (−0.09 to 0.06; 0.691) |
| Multifidus mechanical properties (MyotonPRO device) (symptomatic side) | ||||
| Tone (frequency; Hz) | ||||
| Prone (n = 54) | 17.88 (4.08) | −0.56 (−2.07 to 0.96; 0.465) | −0.29 (−1.79 to 1.21; 0.699) | −0.68 (−2.17 to 0.81; 0.363) |
| Seated (n = 54) | 21.95 (3.11) | 1.45 (−0.90 to 3.80; 0.220) | 1.41 (−0.91 to 3.72; 0.228) | 1.28 (−1.02 to 3.58; 0.269) |
| Stiffness (N/m) | ||||
| Prone (n = 54) | 407.17 (128.78) | −35.86 (−87.90 to 16.18; 0.172) | −26.43 (−77.89 to 25.03; 0.307) | −31.90 (−82.98 to 19.19; 0.215) |
| Seated (n = 54) | 537.26 (111.53) | 51.51 (−35.18 to 123.19; 0.238) | 45.43 (−39.80 to 130.66; 0.289) | 69.82 (−15.60 to 155.30; 0.107) |
| Elasticity (log decrement) | ||||
| Prone (n = 54) | 1.53 (0.45) | −0.13 (−0.33 to 0.07; 0.199) | 0.05 (−0.14 to 0.25; 0.588) | −0.01 (−0.21 to 0.19; 0.925) |
| Seated (n = 54) | 1.31 (0.66) | −0.12 (−0.34 to 0.11; 0.314) | −0.05 (−0.27 to 0.17; 0.643) | 0.04 (−0.18 to 0.26; 0.739) |
| EMG (onset of muscle activation) (symptomatic side during leg lift on symptomatic side) (ms) | ||||
| Internal oblique (n = 29) | −0.38 (0.17) | 0.05 (−0.15 to 0.26; 0.593) | 0.01 (−0.21 to 0.23; 0.915) | 0.140 (−0.080 to 0.366; 0.204) |
| Multifidus (n = 40) | −0.48 (0.25) | 0.10 (−0.06 to 0.26; 0.208) | 0.10 (−0.06 to 0.26; 0.229) | −0.02 (−0.18 to 0.14; 0.831) |
| Trunk axial rotation test (N/m) | ||||
| Back peak to peaka (n = 16) | 3.28 (0.99) | −0.44 (−1.74 to 0.86; 0.469) | −0.63 (−2.10 to 0.84; 0.363) | −0.42 (−2.03 to 1.19; 0.575) |
| Back phase advance (n = 16) | 4.58 (3.83) | −1.03 (−6.23 to 4.18; 0.672) | −4.36 (−10.17 to 1.45; 0.127) | 1.79 (−3.38 to 6.98; 0.462) |
| Hip peak to peaka (n = 10) | 2.57 (1.06) | 0.22 (−1.29 to 1.72; 0.727) | −0.51 (−1.91 to 0.89; 0.390) | −0.39 (−2.30 to 1.52; 0.623) |
| Hip phase advance (n = 9) | 9.19 (2.84) | 2.19 (−5.21 to 9.59; 0.458) | −2.08 (−9.52 to 5.37; 0.482) | −1.46 (−8.22 to 5.30; 0.581) |
| Trunk muscle strength (Biodex) (N/m) | ||||
| Flexion (n = 53) | 51.98 (20.56) | 5.60 (−8.13 to 19.33; 0.416) | −2.74 (−17.08 to 11.60; 0.702) | −2.26 (−15.87 to 11.35; 0.740) |
| Extension (n = 53) | 104.56 (56.18) | 35.87 (4.28 to 67.46; 0.027) | 19.58 (−12.43 to 51.58; 0.225) | 6.65 (−24.82 to 38.12; 0.673) |
| Measure | Control, mean (SD) | Exercise classes only, mean difference from control (95% CI; p-value) | Alexander technique only, mean difference from control (95% CI; p-value) | Alexander technique + exercise classes, mean difference from control (95% CI; p-value) |
|---|---|---|---|---|
| Proprioception – cervical (degrees) | ||||
| X (n = 55) | 2.28 (2.53) | −0.07 (−1.67 to 1.54; 0.935) | −0.52 (−2.08 to 1.03; 0.503) | −0.76 (−2.31 to 0.79; 0.329) |
| Y (n = 55) | 1.31 (1.49) | 0.81 (−0.59 to 2.21; 0.249) | 0.55 (−0.91 to 2.01; 0.452) | 0.39 (−0.98 to 1.77; 0.567) |
| Z (n = 57) | 0.81 (1.61) | −0.27 (−1.14 to 0.60; 0.540) | −0.38 (−1.24 to 0.47; 0.372) | 0.18 (−0.67 to 1.03; 0.666) |
| Proprioception – lumbar (degrees) | ||||
| From ‘upright/zero’ position (n = 56) | 1.08 (0.70) | −0.11 (−0.92 to 0.70; 0.786) | 0.23 (−0.57 to 1.03; 0.563) | 0.03 (−0.76 to 0.81; 0.949) |
| From ‘20° flexion’ position | 2.50 (2.44) | −0.21 (−1.82 to 1.40; 0.793) | −0.10 (−1.73 to 1.53; 0.904) | −0.70 (−2.27 to 0.87; 0.377) |
| USI – multifidus thickness (symptomatic side) (cm) | ||||
| Relaxed (n = 53) | 2.86 (0.23) | 0.18 (0.02 to 0.34; 0.033) | 0.06 (−0.11 to 0.22; 0.494) | 0.15 (−0.01 to 0.31; 0.066) |
| Contracted (n = 52) | 3.20 (0.22) | 0.22 (0.04 to 0.41; 0.021) | 0.15 (−0.04 to 0.35; 0.116) | 0.16 (−0.03 to 0.35; 0.092) |
| USI – transversus abdominis thickness (symptomatic side) (cm) | ||||
| Relaxed (n = 51) | 0.38 (0.14) | −0.02 (−0.07 to 0.03; 0.415) | −0.006 (−0.050 to 0.040; 0.814) | 0.03 (−0.02 to 0.07; 0.306) |
| Contracted (n = 53) | 0.42 (0.16) | −0.02 (−0.09 to 0.05; 0.562) | 0.02 (−0.05 to 0.08; 0.612) | 0.01 (−0.06 to 0.08; 0.745) |
| Multifidus mechanical properties (MyotonPRO device) (symptomatic side) | ||||
| Tone (frequency; Hz) | ||||
| Prone (n = 53) | 18.71 (3.28) | −1.32 (−2.97 to 0.32; 0.113) | −0.17 (−1.75 to 1.42; 0.834) | −1.43 (−3.00 to 0.15; 0.076) |
| Seated (n = 53) | 22.77 (4.72) | 0.66 (−2.57 to 3.89; 0.682) | 0.91 (−2.14 to 3.96; 0.551) | 0.58 (−2.47 to 3.62; 0.704) |
| Stiffness (N/m) | ||||
| Prone (n = 53) | 395.33 (81.87) | −16.69 (−68.84 to 35.46; 0.523) | 1.51 (−48.72 to 51.74; 0.952) | −23.87 (−73.84 to 26.10; 0.342) |
| Seated (n = 53) | 614.69 (143.76) | 2.77 (−106.70 to 112.24; 0.960) | 0.94 (−102.51 to 104.37; 0.986) | −10.31 (−114.29 to 93.67; 0.843) |
| Elasticity (log decrement) | ||||
| Prone (n = 53) | 1.43 (0.24) | 0.05 (−0.09 to 0.19; 0.494) | 0.07 (−0.06 to 0.21; 0.287) | 0.15 (0.01 to 0.29; 0.039) |
| Seated (n = 53) | 1.13 (0.23) | −0.07 (−0.22 to 0.07; 0.324) | −0.07 (−0.21 to 0.07; 0.335) | 0.10 (−0.04 to 0.24; 0.161) |
| EMG (onset of muscle activation) (symptomatic side during leg lift on symptomatic side) (ms) | ||||
| Internal oblique (n = 25) | −0.13 (0.13) | 0.00 (−0.22 to 0.22; 0.998) | −0.16 (−0.39 to 0.07; 0.167) | 0.03 (−0.18 to 0.24; 0.762) |
| Multifidus (n = 39) | −0.42 (0.20) | 0.08 (−0.07 to 0.24; 0.291) | 0.17 (0.01 to 0.33; 0.039) | 0.11 (−0.05 to 0.27; 0.171) |
| Trunk axial rotation test (N/m) | ||||
| Back peak to peaka (n = 12) | 2.94 (1.03) | 0.09 (−1.56 to 1.74; 0.899) | 0.51 (−1.26 to 2.29; 0.517) | 0.12 (−2.16 to 2.41; 0.903) |
| Back phase advance (n = 12) | 5.74 (2.12) | −1.76 (−4.97 to 1.44; 0.234) | −1.35 (−5.16 to 2.46; 0.430) | 1.89 (−1.78 to 5.55; 0.263) |
| Hip peak to peaka (n = 7) | 2.04 (0.90) | 0.74 (−1.55 to 3.03; 0.380) | −0.22 (−1.55 to 1.12; 0.639) | N/A |
| Hip phase advance (n = 7) | 10.17 (2.18) | −6.71 (−19.55 to 6.12; 0.195) | −6.26 (−12.40 to −0.12; 0.048) | N/A |
| Trunk muscle strength (Biodex) (N/m) | ||||
| Flexion (n = 50) | 51.81 (24.84) | 4.32 (−15.73 to 24.36; 0.667) | 2.88 (−17.97 to 23.73; 0.782) | 4.37 (−15.08 to 23.81; 0.653) |
| Extension (n = 50) | 118.28 (80.02) | 7.20 (−35.17 to 49.58; 0.734) | 16.73 (−25.87 to 59.33; 0.433) | 10.20 (−30.96 to 51.36; 0.620) |
| ASLR compression test (OR)b | 1.00 | 0.60 (0.09 to 3.80; 0.584) | 0.02 (0.00 to 0.35; 0.007) | 0.39 (0.06 to 2.41; 0.312) |
| Measure | Coefficient (95% CI; p-value) |
|---|---|
| Lumbar proprioception (degrees) – upright at 6 months | |
|
−0.73 (−1.38 to −0.08; 0.029) |
|
−1.07 (−2.06 to −0.09; 0.034) |
| Lumbar proprioception (degrees) – flexion at 6 months | |
|
−2.19 (−4.13 to −0.26; 0.028) |
|
−0.32 (−0.57 to −0.07; 0.013) |
|
2.30 (0.24 to 4.37; 0.030) |
| USI – multifidus thickness (cm) contracted at 6 months | |
|
0.68 (0.43 to 0.94; < 0.0001) |
|
0.09 (0.01 to 0.18; 0.026) |
| USI – transversus abdominis thickness (cm) contracted at 6 months | |
|
0.71 (0.49 to 0.94; < 0.0001) |
|
−0.01 (−0.01 to −0.002; 0.006) |
| Myoton – tone (frequency; Hz) prone at 6 months | |
|
0.94 (0.66 to 1.23; < 0.0001) |
| Myoton – stiffness (N/m) prone at 6 months | |
|
0.63 (0.37 to 0.90; < 0.0001) |
| Myoton – elasticity (decrement) prone at 6 months | |
|
0.80 (0.59 to 1.01; < 0.0001) |
| Myoton – tone (frequency; Hz) difference prone to seated at 6 months | |
|
0.37 (0.14 to 0.59; 0.002) |
|
−0.39 (−0.65 to −0.14; 0.004) |
|
0.55 (0.16 to 0.95; 0.008) |
|
0.17 (0.01 to 0.33; 0.037) |
|
−1.80 (−3.34 to −0.27; 0.023) |
|
4.11 (1.98 to 6.23; < 0.0001) |
| Myoton – stiffness (N/m) difference prone to seated at 6 months | |
|
0.51 (0.17 to 0.85; 0.005) |
|
28.54 (4.32 to 52.76; 0.022) |
| Myoton – elasticity (decrement) difference prone to seated at 6 months | |
|
0.37 (0.10 to 0.64; 0.009) |
|
0.22 (0.02 to 0.42; 0.030) |
| EMG | |
|
−0.16 (−0.27 to −0.04; 0.008) |
|
0.03 (0.01 to 0.05; 0.001) |
| Measure | Coefficient (95% CI; p-value) |
|---|---|
| Myoton – elasticity (decrement) difference prone to seated at 6 months | −4.86 (−9.72 to −0.01; 0.050) |
| Myoton – tone (frequency; Hz) prone at 6 months | 0.94 (0.48 to 1.40; < 0.0001) |
| Proprioception (degrees) – flexion at 6 months | 1.48 (0.83 to 2.12; < 0.0001) |
| Days in pain at baseline | 0.01 (0.00 to 0.22; 0.049) |
Appendix 3 Qualitative study
This qualitative study was performed by two medical students (Andrew Deans and Zak Taylor) who were trained in interview techniques as part of an undergraduate research project; they were supervised by Dr Adam Geraghty and Professor Paul Little.
Aim
The aim of this study was to assess patients’ expectations, experiences and views of the treatment groups available as part of the Alexander technique and Supervised Physiotherapy Exercises in back paiN (ASPEN) trial.
Methods
Participants who were already part of the ASPEN trial were recruited to the study by written consent. The sample was a convenience sample of participants in the trial. Participants who responded were contacted by telephone to arrange a suitable time for their interview. Data collection was performed using semistructured qualitative interviews.
Interview process
Interviews were conducted by telephone at a time that was convenient to the participant. The interviews followed an interview schedule that is shown later in this appendix (see Interview schedule). The interviews explored participants’ expectations and views of treatment options at the start of the trial and looked at how these views had changed during its course. Another important part of the interviews discussed measurements of the participants that were taken as part of the ASPEN trial. This aimed to explore whether or not these measurements made sense to the participants and to assess if they caused any problems.
Questions were designed to be open to gain the most in-depth understanding of the research questions. Each of the interviews lasted 20–35 minutes and was audio taped; the recordings were then sent for transcription.
Analysis
A thematic analysis was performed, as described by Braun and Clarke,56 starting with familiarisation with the data. A coding manual was created, enabling each code to be defined. As the analysis continued the coding manual was constantly reviewed and altered as new codes emerged. As this was a joint project, with two of the researchers being relatively inexperienced, the initial transcripts were coded together to ensure that both researchers could become clear on the coding process. Transcripts were then analysed separately by the researchers and, as the coding process developed, we met to evaluate, discuss and refine our coding manual. The coding process and manual were reviewed by Dr Adam Geraghty and Professor Paul Little.
Results
In total, 59 consent forms were posted to participants in the ASPEN trial; 28 consent forms were returned and 20 participants were available to contact for an interview. One further participant was excluded because of an upcoming medical procedure and therefore 19 interviews were performed. In total, 13 of the patients were female and six were male. The youngest participant was aged 20 years and the oldest (and modal) age was 66 years. The average age of participants in the data set was 53.8 years. All of the participants described their ethnicity as white. Of the participants interviewed, six came from the physiotherapy exercises group, five from the Alexander technique group, five from the combined therapy group and three from the normal care group; perhaps the most instructive group were the combined group, and the themes that came from this group were largely replicated in the other groups.
The themes and subthemes that were identified are shown in Table 21.
| Theme | Subtheme |
|---|---|
| Preconceptions of treatment | Approach to treatment |
| Expectations of treatment | |
| Time commitments of treatment | |
| Group environment | Teachers/group leaders |
| Benefits of treatment to the patient | |
| Participants’ views on measurements | Feedback of results |
Preconceptions of treatment
Participants who undertook Alexander technique lessons had a very limited knowledge of the treatment other than what they had learned from a brief internet search. Physiotherapy was better understood as it is more ‘common knowledge’; however, it was frequently mentioned that the physiotherapy exercises in this trial were not what was expected initially.
| Participant 1000 (combined) |
|
| Participant 1104 (Alexander technique) |
|
The Alexander technique was approached with initial scepticism by some participants. One of the participants noted that he did not believe that the treatment would work but would try it anyway, but most were willing to commence the treatment with an ‘open mind’ as it was believed that this would be a way to gain benefit from the trial.
| Participant 1024 (Alexander technique) |
|
| Participant 1048 (Alexander technique) |
|
| Participant 1082 (Alexander technique) |
|
Expectations of treatment from the participants’ perspectives were varied. Expectations of the Alexander technique were higher than expectations of physiotherapy, but the majority of participants were realistic about what the treatment could offer them. Only one of the participants was expecting to be completely cured; most expected some level of improvement but not a complete cure. Some in the normal care group were very disappointed not to be offered either intervention, but considerable altruism was evident. There were commonly poor expectations about what could be provided in the NHS for chronic back pain.
| Participant 1024 (Alexander technique) |
|
| Participant 1082 (Alexander technique) |
|
| Participant 1055 (normal care) |
|
| Participant 1012 (normal care) |
|
| Participants 1055 (normal care) |
|
Time commitments
One of the issues raised was the time commitments engendered by the trial, in terms of having to both practise exercises and travel and attend physiotherapy classes at fixed times or attend Alexander technique lessons during work hours.
| Participant 1000 (combined) |
|
| Participant 1006 (combined) |
|
| Participant 1048 (Alexander technique) |
|
| Participant 1034 (exercise classes) |
|
Group environment
The group environment in the physiotherapy classes was mostly seen as positive, with participants suggesting that it helped to increase motivation and satisfaction.
| Participant 1000 (combined) |
|
| Participant 1006 (combined) |
|
| Participants 1085 (exercise classes) |
|
The feedback from the interviewees regarding the skills, manner and knowledge of the group leaders was universally positive. In most cases the leaders of the physiotherapy group sessions were the same throughout the trial, which helped provide a sense of continuity of care and helped with the development of relationships between the leaders and participants, which in turn led to a more rewarding experience. It was noted that when group leaders were changed the treatment became disjointed.
| Participant 1023 (combined) |
|
| Participant 1048 (Alexander technique) |
|
| Participant 1133 (combined) |
|
Benefits of treatment to participants
During the interview process several of the participants suggested that the benefits of the treatment were exceptional. Overall, the responses to both the Alexander technique lessons and the physiotherapy exercises as treatments were very positive. In the combined treatment group the techniques learnt as part of the Alexander technique were seen as most effective in the self-management of back pain. This was because the Alexander technique could be applied to all aspects of daily life and was therefore a very effective management tool. Physiotherapy exercises were also seen to be beneficial to patients, but some commented that it was seen as more of a short-term fix.
| Participant 1023 (combined – talking about the Alexander technique) |
|
| Participant 1088 (Alexander technique) |
|
| Participant 1094 (combined – talking about the Alexander technique) |
|
Participants’ views on measurements
| Participant 1024 (Alexander technique) |
|
| Participant 1094 (combined) |
|
The qualitative data collected explored whether or not the biomechanical measurements made sense and were helpful and whether or not there were any problems. Feedback about the measurements was mixed. Many found the process fascinating although some were not really interested. The measurements were well explained and time was taken to ensure that the processes involved made sense. Understandably, there was a curiosity amongst the cohort about what the measurements were assessing and whether or not they were showing an improvement during the course of the trial. Some suggested that the results of the measurements provided reassurance that they were improving during the course of the trial. Other participants noted in the interview process that feedback on their measurements throughout the trial would have been beneficial.
Interview schedule
I am interested in your expectations, experiences and views of the ASPEN trial. Your interview will be confidential and you will not be identified in the write-up of the study. However, quotes from the interview may be used in the write-up, but again you will not be identified. Are you happy to continue with the interview?
I’d like to talk to you about [intervention]-
Could you please tell me about your feelings when you started the intervention?
Prompts: That’s really interesting, could you tell me more about that
-
Now that you have had a chance to try it, how do you feel about doing [intervention]?
Prompts: What have been the good things about doing [intervention]? What have been the bad things about doing [intervention]?
-
How do you think other people feel about [intervention]?
Prompts: Family, friends, health-care professionals. How does their opinion alter how you feel?
-
How easy has it been to fit the [intervention] into your daily life?
Prompts: Can you tell me about any problems you have had carrying out [intervention]? Can you tell me about any ways you have been able to overcome these problems? Can you tell me about anything that has helped you to carry out [intervention]?
Patients’ expectations about what the trial would deliver for them-
Can you tell me about your expectations of the intervention at the start of the trial?
Prompts: Have you done anything similar before? Can you tell me about that? As you have now tried the intervention how have your expectations changed?
Patients’ experiences of their Alexander technique teacher or the physiotherapy group leader-
Could you tell me about how you have found working with the Alexander technique teacher?
Prompts: That’s very interesting, could you tell me more?
-
Could you tell me about how you have found working with the physiotherapy group leader?
Prompts: That’s very interesting, could you tell me more?
Patients’ enjoyment (or lack of) of the process-
Can you tell me about things you might have enjoyed learning about the Alexander technique?
-
Can you tell me about things you might have enjoyed about taking part in the physiotherapy group sessions?
Prompts: Which bits have been the most enjoyable/helpful?
-
Can you tell me about what you have not enjoyed about the Alexander technique?
-
Can you tell me what you have not enjoyed about taking part in the physiotherapy group sessions?
-
Can you tell me what you thought about the measurements taken during the intervention?
Prompts: Did you feel as though these measurements made sense? Could you tell me about any ways that these measurements were helpful?
-
Could you tell me about any problems that these measurements caused?
-
Could you tell me whether these measurements were interesting to you?
Prompts: Did you feel like the measurements affected how you felt about doing the intervention? That’s very interesting to me; could you tell me more about that?
Thank you for your time. Is there anything else that you wish to add?
Appendix 4 Comments from teachers fed back to Carolyn Nicholls
Teacher 1
I had one pupil, who managed both Alexander technique and physiotherapy exercise, she found Alexander technique useful to a degree within her habitual limitation whilst exercising. The pupil was attentive during her lesson and found it helped her mobility when applying the technique to her use.
I was allocated three pupils all of whom came from an area that took two buses and a ten minute uphill walk to reach me, the one pupil that actually managed to complete the course, after a few lessons was provided with a taxi to and from the lesson (I had spoken to the office regarding the surgery location initially), but somehow they were convinced it was the nearest one to myself.
The other two pupils with whom I made contact, made lesson appointments but did not turn up, having varying excuses from, they’d forgotten, to having to collect their benefit or not answering the phone at all. Unfortunately the surgery covered an area of benefits and unemployment that did not lend itself to commitment.
Teacher 2
I had four people and all of them finished the trial and were very appreciative of the Alexander technique lessons. In all four cases their back pain reduced significantly, I think actually it went completely in every case. One, who had a number of other problems, has carried on having lessons with me and another sent his wife who brought her daughter and her friend for lessons. Two of the four were also supposed to have physiotherapy sessions and one completed them together with her Alexander technique lessons satisfactorily. The other opted out of the physiotherapy because he couldn’t get enough time off from work to attend the sessions.
Teacher 3
It was generally easier for the older people to engage with the project and adhere to their commitments. Working people, particularly with children, found the amount of hours of the commitment difficult. The times for physiotherapy (morning or afternoon) was difficult for working people. Nobody dropped out.
Teacher 4
The two with Alexander technique and physio were both retired and were able to fit both types of disciplines in without a problem. They both showed positive signs of freedom of movement with all the aspects of the Alexander technique that I taught them, with a noticeable difference in being able to bend down to put on their shoes and generally to be able to walk about without as much pain as they had previous to their Alexander technique lessons.
Both enjoyed their physio exercises and found that once they had had one or two physio sessions and then came back to the Alexander technique after, they could see the benefit that having six Alexander technique lessons first before starting physio made a difference. They both reported that it would have been quite difficult to carry out some of the exercises as easily without the knowledge of the Alexander technique. One pupil remarked that the physiotherapist was quite amazed in their ability and suppleness and ease to be able to sit and stand as well as they did and was interested to know (and HOW) what the Alexander technique lessons entailed and what the Alexander technique was doing for them. The third person (male) regrettably dropped out at lesson 9 due to work commitments and sent to work in Scotland. All three pupils had a significant drop in pain over their course of lessons from most days with pain to only occasional pain, but they reported that the level of pain became less especially with the Semi Supine which they practised each day.
Teacher 5
I had one person pull out, in fact she never started, she said she was doing ‘lots‘ to help her back and didn’t want anything else. She sounded very worried on the phone, as if I was going to try and force her. Case 1 was completely changed by the sessions realising her attitude wasn’t helping her back pain, as well as making some postural change, her back pain was considerably reduced. Case 2 I could see the Alexander technique was helping her and she admitted the sessions had helped her in how she went about her day.
Teacher 6
Generally the lessons were very well received. I had one drop out after two lessons. Her reason was that the two lessons had totally cured her back pain! She was also struggling to juggle work/family commitments so did not want to put more time in when she felt she had what she needed. The only pupil that I feel did not respond had diagnosed Parkinson’s disease (and I don’t think that he should have been accepted on to the trial). One lady had back pain particularly first thing in the morning. She apparently had an old bed so I do wonder just how much this held back her progress.
Teacher 7
I had one pupil who declined the physio sessions because she had four children and it meant she would not be able to pick up from school but she did complete the Alexander technique lessons with much reduced pain by the end. I had one pupil who had both the Alexander technique and physio, she was most impressed with the obvious very apparent difference, between herself and others who had had Alexander technique lessons. All the pupils I had seemed impressed with how they felt when they remembered to direct and the reduction in pain and discomfort, however none signed up for private lessons. Could this be because at the end of 10 lessons they felt they could manage? It would be interesting to know how they feel a year on.
One pupil who had a heart op after nine lessons did not return to take up the 10th but wrote a letter to say how helpful the Alexander technique directions had been in the recovery process but was unable to make the journey out to me.
Teacher 8
Two of my pupils from the trial did physio plus the Alexander technique and found the both most helpful. They both mentioned how well the physios worked with the technique, and lying down after the exercises. One in particular continued lessons for quite a while after the study but has since drifted off. He did manage to reduce the amount of painkillers he took, of which he was taking a great deal. The second one thought she had learned enough with the Alexander technique and the physio exercises to manage on her own. Her physio continued after her lessons ended, so I don’t know how she ended the trial.
List of abbreviations
- ASLR
- active straight leg raise
- ASPEN
- Alexander technique and Supervised Physiotherapy Exercises in back paiN
- ATEAM
- Alexander Technique Exercise and Massage
- BEAM
- back pain exercise and manipulation
- CI
- confidence interval
- EMG
- electromyography
- GP
- general practitioner
- MRC
- Medical Research Council
- NICE
- National Institute for Health and Care Excellence
- RMDQ
- Roland–Morris Disability Questionnaire
- SD
- standard deviation
- STAT
- Society of Teachers of the Alexander Technique
- USI
- ultrasound imaging