Notes
Article history
The research reported in this issue of the journal was funded by the EME programme as project number 15/48/21. The contractual start date was in February 2017. The final report began editorial review in June 2020 and was accepted for publication in November 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The EME editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© 2021 Garety et al. This work was produced by Garety et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2021 Garety et al.
Chapter 1 The SlowMo blended digital therapy randomised controlled trial
Introduction
Paranoia, or fear of deliberate harm from others, is one of the most common symptoms of schizophrenia-spectrum disorders, and is associated with significant distress and disruption to the person’s life. 1 This results in increased service use, including inpatient admissions, and high costs to mental health-care providers. Developing effective interventions for paranoia is, thus, a clinical priority. The National Institute for Health and Care Excellence recommends cognitive–behavioural therapy (CBT) for psychosis, including paranoia. 2 Meta-analytical studies of first-generation CBT for psychosis have found small to medium sized beneficial effects for delusions (e.g. Turner et al. 3) and positive symptoms more broadly. 4 However, there remain significant challenges to access, engagement, adherence and effectiveness. 1,5
We approached developing the SlowMo therapy in two main ways: first, by adopting an interventionist causal approach6 to increase CBT for psychosis effectiveness and, second, by incorporating inclusive, human-centred design methods to improve the user experience of therapy and to enhance engagement and adherence. 7 The interventionist causal approach involves identifying mechanisms playing a causal role in paranoia (e.g. reasoning, worry and sleep dysfunction) and then developing tailored interventions. 8 SlowMo therapy focuses on reasoning processes that are robustly associated with paranoia: the highly replicated jumping to conclusions (JTC) bias (forming rapid judgements based on a small amount of information) and belief inflexibility bias (the metacognitive capacity for reflecting on one’s beliefs, changing them in the light of reflection and evidence, and generating and considering alternatives). 8,9 Meta-analyses have established that JTC is associated with psychosis, with some specificity for delusions. It also increases the risk of psychosis and predicts outcome in response to treatment. 10–12 Meta-analytic evidence supports an association between belief flexibility and delusions. 13 These thinking patterns are common: in 1800 patients with psychosis in NHS services, difficulties in slow, analytic thinking were present in 60.3% of patients with severe paranoia. 14 In summary, there is converging evidence for a causal role of JTC and belief flexibility in delusion development and maintenance, thereby providing a target for both prevention and treatment strategies. 15
Systematic attempts to ameliorate reasoning in people with psychosis to reduce positive symptoms have included group-based metacognitive training (MCT),16 with a focus on JTC as a causal reasoning bias. One meta-analysis of nine studies of MCT yielded small, non-significant, effects on reasoning, positive symptoms and delusions. 17 The most comprehensive meta-analysis included 15 studies and reported positive effects for delusion change. However, when restricted to studies at low risk of bias, the meta-analysis found small effect sizes for positive symptoms [g = −0.28, 95% confidence interval (CI) −0.50 to −0.06] and non-significant effects for delusions (g = −0.18, 95% CI −0.43 to 0.06). 18
Given the strong theoretical rationale and the mixed empirical findings, we built on this MCT research and on CBT for psychosis approaches for paranoia19 to develop a new cognitive–behavioural intervention. This intervention aims to enhance the impact on paranoia and reasoning, specifically by helping people to build awareness of their tendency to jump to conclusions and by intensively targeting belief flexibility. We have also used inclusive, human-centred design to address the needs of those for whom the content and process of standard therapy present barriers to engagement. The therapy redesign focused on improving its ease of use, enjoyment and perceived usefulness (known as the user experience) to support engagement and adherence for the widest possible range of people. 20,21 The SlowMo intervention is the first blended digital psychological therapy for paranoia [i.e. a face-to-face therapy supported by digital technology, for both in-session content and a tailored mobile telephone application (hereafter referred to as ‘mobile app’)]; it is the end point of a decade of development. 7,22–25 In proof-of-concept and feasibility studies, we found changes in reasoning and improvements in paranoia severity. 22–24 In an experimental study of 100 people with delusions, we compared a brief reasoning-focused digital intervention with an active control condition and found preliminary evidence that changes in belief flexibility mediated improvements in paranoia. 25 Further work validated the user experience of the digital interface for a diverse user population. 7 Over time, as we developed the intervention, we focused more on enhancing belief flexibility than on reducing JTC. We also adopted the term ‘fast and slow thinking’ to communicate the underlying reasoning concepts. 7,15,26 SlowMo therapy aims to assist people with paranoia by supporting them to identify their upsetting concerns and fast-thinking habits, then providing them with strategies to slow down for a moment to focus on new alternative information and develop ways of feeling safer. It aims to improve the appeal, ease of use and clinical effectiveness of CBT for paranoia. 7,27
The current study tested the SlowMo therapy in a fully powered, methodically rigorous, multisite randomised controlled trial (RCT). We aimed to test its clinical efficacy in reducing paranoia, to examine its acceptability, to determine the mechanisms through which it works and to identify participant characteristics that might moderate its effectiveness. We selected treatment as usual (TAU) as the comparator condition. This was because there is a low penetration of evidence-based psychological treatment in the NHS and, thus, the key efficacy question to address at this stage is whether or not SlowMo therapy confers benefits over and above standard care. We have previously established the superiority of an earlier brief version of the intervention against an active control intervention. We predicted that SlowMo therapy would improve paranoia and reasoning and might improve a number of other outcomes, such as self-concept, worry, quality of life and well-being.
An important secondary goal was to evaluate mechanisms of action; the trial hypotheses concern reasoning and are best tested where the control condition is inactive with respect to the targeted psychological processes. We hypothesised that SlowMo therapy would improve reasoning and that the primary mechanism for its treatment effects on paranoia would be mediated through reasoning, specifically belief flexibility and JTC. We also examined worry as a potential mediator, as it has previously been shown to mediate change in paranoia. 28 However, given that worry was not directly targeted by the treatment, we hypothesised that worry would not mediate the treatment effects of SlowMo on paranoia. The treatment effects of a previous version of our intervention were moderated adversely by negative symptoms and working memory. 25 We included hypotheses concerning these potential moderators to examine whether this study replicated these effects or if the redesign worked as intended and rendered the intervention equally accessible and effective across a wide range of users with different cognitive capacities and symptom profiles.
The research questions examined were as follows:
-
Is SlowMo efficacious in reducing paranoia severity over 24 weeks when added to TAU, compared with TAU alone?
-
Does SlowMo lead to changes in the following outcomes: reasoning, well-being, quality of life, self-schemas and others schemas, service use and worry?
-
Does SlowMo reduce paranoia severity by improving fast thinking (reducing belief inflexibility and JTC)?
-
Do participant characteristics (i.e. their cognitive capacities, specifically working memory and thinking habits; and their symptoms, specifically negative symptoms) moderate the effects of the intervention?
-
Does outcome differ by adherence to the intervention?
-
Is SlowMo therapy acceptable, as assessed by therapy uptake and adherence?
Primary hypotheses
-
The intervention will reduce paranoia severity over 24 weeks.
-
Fast thinking (belief inflexibility and JTC) will improve in response to the intervention.
-
Reductions in fast thinking will mediate positive change in paranoia severity.
Secondary hypotheses
-
Poorer working memory and more severe negative symptoms will negatively moderate treatment effects.
-
Therapy adherence will moderate the effects of treatment on outcome.
-
Worry will not mediate reductions in paranoia severity.
Methods
Study design
We conducted a parallel-arm RCT, with 1 : 1 allocation and blinded assessors, to test the efficacy of the SlowMo intervention in reducing paranoia severity when added to TAU, compared with TAU alone. Participants were recruited from mental health services with the same procedures across three main trial sites in England: South London and Maudsley NHS Foundation Trust, Sussex Partnership NHS Foundation Trust and Oxford Health NHS Foundation Trust. Additional patient identification centres, comprising NHS trusts near each of the three main recruitment NHS sites, were also employed. Participants were patients of secondary care community mental health services.
The trial received a favourable ethics opinion from Camberwell St. Giles Research Ethics Committee (REC) (REC reference 16/LO/1862; Integrated Research Administration System 206680). The trial protocol,29 including all study hypotheses, was published.
Participants
We sought referrals of patients with psychosis and distressing persecutory beliefs from community clinical teams in our NHS settings. The inclusion criteria were patients aged ≥ 18 years; with persistent (≥ 3 months) distressing paranoia [as assessed using the Schedules for Clinical Assessment in Neuropsychiatry30) and scoring > 29 on the Green Paranoid Thoughts Scales (GPTS), part B, persecutory subscale31]; with a diagnosis of schizophrenia-spectrum psychosis (F20–29, International Statistical Classification of Diseases and Related Health Problems, Tenth Revision32); with the capacity to provide informed consent; and with sufficient grasp of the English language to participate in trial processes. Exclusion criteria were profound visual and/or hearing impairment; the inability to engage in the assessment procedure; being currently in receipt of other psychological therapy for paranoia; and a primary diagnosis of substance abuse disorder, personality disorder, organic syndrome or learning disability. All participants gave written informed consent.
Randomisation and masking
After a baseline assessment, we randomly assigned (1 : 1) eligible patients to either eight sessions of the SlowMo intervention delivered within 12 weeks plus TAU (SlowMo group), or TAU alone (control group). Randomisation took place using a password-protected independent web-based service hosted at the King’s Clinical Trial Unit. The randomisation list was generated using randomly varying permuted blocks, stratified by site and baseline paranoia severity [median split of ≥ 62 (GPTS31 part B)].
Research assessors (all graduate psychologists) were masked to therapy allocation. Masking was supported by the site co-ordinators having responsibility for randomising and informing participants. If an allocation was revealed to the assessor, then re-masking occurred as far as was operationally feasible by the use of another rater. Where an allocation was revealed during an assessment session and re-allocation was not operationally feasible, these ratings were used. All breaks in masking were recorded.
Procedures
The SlowMo intervention
SlowMo therapy consisted of eight individual face-to-face sessions, with each module addressing a specific topic. Sessions typically lasted 60–90 minutes and were delivered within a 12-week time frame. The therapy delivery was assisted by a web-based application (hereafter referred to as ‘web app’) delivered using a touchscreen laptop (the ‘SlowMo web app’), with interactive features including information, animated vignettes, games and personalised content, which was synchronised with a native mobile app installed on a standard Android (Google Inc., Mountain View, CA, USA) smartphone that was provided to participants to assist therapy generalisation. Before therapy began, the clinician met the patient for an initial introduction and orientation to the approach. Delivery of SlowMo was flexible, with sessions added where helpful, for example the splitting of web app modules across separate meetings (tailored to individual preference and engagement), and ‘out of clinic’ behavioural work to promote mobile app use and therapy generalisation to the real world.
The intervention followed a clinical trial manual that was consistent during the trial. The only modifications to the therapy during the trial involved improvements to the digital interface of the web app and mobile app to further support the user experience.
Therapy sessions were delivered locally to the participant at convenient locations of their choosing, including team bases, patient’s homes, general practices or other local centres (e.g. community centres). Behavioural work was carried out in the participant’s local area and was guided by the participant’s goals. It typically involved testing out the SlowMo strategies and the mobile app in locations such as town centres, local cafes, pubs and markets.
Initial sessions involve building the metacognitive skill of noticing thoughts and thinking habits (visualised as bubbles spinning slow or fast). People learn the normalising message that fast thinking is part of human nature and can be useful at times. However, fast thinking can fuel worries and thinking slowly can be helpful in dealing with difficult situations and fears about other people. This key principle frames the sessions in which participants are supported to try out ways to slow down for a moment, for example by considering the impact of mood and past experiences on concerns, and by looking for safer alternative explanations. The web app structure is delivered consistently, but content is tailored throughout as participants interact with personalised worry bubbles, safer/positive alternative thought bubbles, key learning and messages for the week ahead (recorded by the person at the end of each session in text or audio form and then synchronised with the mobile app for day-to-day, out-of-session personal support). The SlowMo mobile app allows people to notice their fears and thinking habits as they occur in daily life, and supports them to slow down for a moment by accessing SlowMo strategies or personalised safer alternative bubbles, thereby finding other ways of managing distressing experiences (see Hardy et al. 7 and Garety et al. 29 for further detail).
The therapy was delivered by trained clinical or counselling psychologists who were experienced in CBT for psychosis. A total of 11 psychologists (10 doctoral-level clinical and one counselling) delivered therapy across the three sites. This comprised six main trial therapists delivering the majority of therapy and a further five local therapists. Weekly group supervision, including the use of therapy audio-recordings, was provided by the trial therapy lead (TW) to the main trial therapists (with regular consultation provided by PG and EK); supervisory arrangements for local trial therapists were provided by site therapy leads.
Uptake of the therapy delivery was assessed by the number and duration of sessions attended. Adherence to the treatment manual was assessed by the SlowMo therapy fidelity checklist that was completed by therapists at the end of each session; adherence to the manual was defined as no more than one web app component missed for any attended therapy session. Adherence to the mobile app was operationalised as at least one out-of-session interaction for a minimum of three of the therapy sessions.
Treatment-as-usual (standard care) was delivered in accordance with national and local service protocols and best practice guidelines. This usually consisted of prescription antipsychotic drugs, contact with a community mental health worker and regular outpatient appointments with a psychiatrist. Participation did not alter usual treatment decisions about medication or additional psychosocial interventions. The delivery of additional psychosocial treatments in both groups was recorded with the modified Client Service Receipt Inventory. 33
Follow-up intervals and assessments at each visit
The assessments of outcome measures were completed at 0 weeks (baseline), 12 weeks (end of therapy) and 24 weeks (follow-up). Research assessors did the enrolment and assessments in clinic settings or at the participant’s home. Participants were rewarded for their time and effort by a sum of £20 at each research visit. The primary outcome was self-rated.
Outcomes and other measures
The prespecified primary outcome was self-reported paranoia severity measured by the GPTS31 over 24 weeks. The GPTS31 comprises two scales that assess thinking relevant to paranoia and which are rated over the preceding month: ideas of social reference and persecution. Two 16-item subscales assess ideas of social reference (part A) and persecution (part B). We also assessed paranoia on two observer-rated scales: the Psychotic Symptom Rating Scales (PSYRATS) delusions scale,34 for which scores are expressed as a total and as two factors (conviction and distress35); and the persecutory delusions and ideas of reference items from the Scale for the Assessment of Positive Symptoms (SAPS36). In addition, we report outcomes on the Revised-Green Paranoid Thoughts Scale (R-GPTS) over 24 weeks using both total scores and subscale scores. The R-GPTS,37 which was published after publication of the trial protocol using data independent of the current study, reported improved psychometric properties for a revised scale constructed from a subset of the GPTS items. Inclusion of the R-GPTS as a secondary outcome measure was added to a revision of the statistical analysis plan (version 1.2) before statistical analysis commenced. It comprises two scales that assess thinking relevant to paranoia based on items from the original scale that are rated over the preceding month on a slightly modified scale: ideas of social reference (eight items) and persecution (10 items).
We collected other secondary outcomes using published and established measures of well-being [the Warwick–Edinburgh Mental Wellbeing Scale38 (WEMWBS)], quality of life [Manchester Short Assessment of Quality of Life (MANSA39)], self-schemas and other schemas [the Brief Core Schema Scales40 (BCSS)], service use (the Client Service Receipt Inventory33), and worry [Penn State Worry Questionnaire41 (PSWQ)].
Reasoning was assessed as both an outcome and a potential mediator by belief flexibility assessed by the possibility of being mistaken [self-rated and observer-rated per cent taken from the Maudsley Assessment of Delusions Schedule42 (MADS)], alternative explanations (from the Explanations of Experiences interview43) (both are commonly used published methods of assessing lack of belief flexibility relating to delusional beliefs) and by the JTC Beads Data-gathering Task9 versions 85 : 15 and 60 : 40. In addition, we have developed a self-reported measure, the Fast and Slow Thinking Questionnaire44 [previously named the Thinking About Paranoia Scale29 (TAPS)]. The Fast and Slow Thinking Questionnaire comprises 10 statements that are rated on a 5-point scale (1 = not at all, 5 = totally). There are two scales: one assessing fast (intuitive) thinking, reflecting a lack of information gathering, consideration of the possibility of being mistaken and generation of alternative explanations, and one measuring slow (analytical) thinking. We included the Fast and Slow Thinking Questionnaire as a reasoning outcome, but it was not prespecified in our hypotheses as a mediator.
We also used the following established measures of clinical and cognitive characteristics, which were assessed at baseline only, as potential moderators of treatment effects: Scales for Assessment of Positive Symptoms, a semistructured interview assessing positive symptoms of psychosis;36 Brief Negative Symptom Scale (BNSS), a semistructured interview designed to assess negative symptoms of psychosis;45 Beliefs about Problems Questionnaire (BAPQ), a self-reported questionnaire designed to assess illness perceptions, including secondary appraisals of the nature, cause, duration, consequences and management of illness/problems;46 Letter–Number Sequencing Test, a cognitive task that assesses working memory;47 Trail Making Test,48 a neuropsychological instrument assessing visual attention, psychomotor speed and shifting cognitive set; and Perception of Carer Criticism, which is a single self-reported item adapted from Hooley and Teasdale49 and used in other published studies,50 which assesses the person’s perception of criticism from a carer (where one is identified) over the previous month.
Data quality
Data quality was ensured by close monitoring and routine auditing for accuracy throughout the data collection period. To ensure the accuracy of the data entered into the database, the main outcome measure entry was checked for every participant’s baseline assessment by comparing the paper record with that on the database. An error rate of no more than 5% was deemed acceptable a priori (see trial protocol29). The data quality was confirmed to be acceptable, with error rates of 0.03%.
Inter-rater reliability
The inter-rater reliability analysis was conducted on the main observer-rated measure of paranoia, the PSYRATS, and both observer-rated belief flexibility items (possibility of being mistaken and alternative explanations) for 45 of the baseline assessments selected randomly (15 per site) from assessments conducted after an initial training and consensus period. The intraclass correlation coefficient (ICC) for the PSYRATS34 (absolute-agreement, two-way mixed-effects model, single measures) was 0.98 (95% CI 0.96 to 0.99), indicating excellent agreement. For alternative explanations, Cohen’s kappa was 0.96 (95% CI 0.87 to 1.00), in the ‘almost perfect’ range, and for possibility of being mistaken, Cohen’s kappa was 0.65 (95% CI –0.45 to 0.86), between the moderate and the substantial agreement ranges, according to Landis and Koch. 51 Table 1 lists all outcomes and other measures together with the schedule of assessments.
| Trial procedures | Time point | ||||
|---|---|---|---|---|---|
| Enrolment: completed within 4 weeks | Allocation: within 2 weeks of baseline (0 weeks) | Post allocation | Follow-up: 24 weeks | ||
| 0–12 weeks | 12 weeks | ||||
| Enrolment: routine eligibility screen | ✗ | ||||
| Informed consent | ✗ | ||||
| Allocation | ✗ | ||||
| Interventions | |||||
| SlowMo and TAU | ✗ | ||||
| TAU | ✗ | ||||
| Assessments: primary outcome | |||||
| Paranoia severity (GPTS total, scales A and B) | ✗ | ✗ | ✗ | ||
| Other paranoia outcomes | |||||
| PSYRATS delusions | ✗ | ✗ | ✗ | ||
| Delusions of persecution and reference items (SAPS) | ✗ | ✗ | ✗ | ||
| Hypothesised mediators | |||||
| Possibility of being mistaken (MADS) | ✗ | ✗ | ✗ | ||
| Alternative explanations (Explanations for Experiences) | ✗ | ✗ | ✗ | ||
| Jumping to conclusions reasoning | ✗ | ✗ | ✗ | ||
| Other problems and processes | |||||
| SAPS | ✗ | ||||
| BNSS | ✗ | ||||
| BAPQ | ✗ | ||||
| Letter–Number Sequencing Test | ✗ | ||||
| Trail Making Test | ✗ | ||||
| Fast and Slow Thinking Questionnaire (formally TAPS) | ✗ | ✗ | ✗ | ||
| PSWQ | ✗ | ✗ | ✗ | ||
| BCSS | ✗ | ✗ | ✗ | ||
| Perception of Carer Criticism | ✗ | ||||
| WEMWBS | ✗ | ✗ | ✗ | ||
| MANSA | ✗ | ✗ | ✗ | ||
| Client Service Receipt Inventory | ✗ | ✗ | |||
Adverse events
Information about possible adverse events was actively monitored, up to week 24 of follow-up. Possible adverse events included hospital admissions (owing to physical or mental health deterioration), crisis team involvement, self-harming behaviour and suicide attempts, and violent incidents necessitating police involvement. A standard method of reporting was employed, categorising events by severity (five grades: A–E). Any relatedness to trial participation was also recorded. All adverse events were reviewed by the chairperson of the Data Monitoring and Ethics Committee (DMEC) for ratings of relatedness to trial participation and seriousness, and were subsequently reviewed by the DMEC.
Statistical analysis
We powered the study to detect a clinically meaningful 10-point reduction in the GPTS total score with a standard deviation (SD) of 25 (effect size = 0.4). We accounted for the partial nested design because of clustering in the SlowMo group, assuming an ICC of 0.01 with 10 therapists, and for no clustering in the TAU group using the clsampsi command in Stata® version 16 (StataCorp LP, College Station, TX, USA). 52 With the 1 : 1 treatment allocation and the 0.05 significance level, a simple two-tailed t-test with 150 people per group had 90% power to detect an effect size of 0.4 and 80% power to detect an effect size of 0.35. To allow for a conservatively high 20% attrition, we aimed to recruit 360 patients at baseline split equally across three sites (120 per site, 60 per group per site).
We report data in line with the Consolidated Standards of Reporting Trials (CONSORT) 2018 Statement for Social and Psychological Interventions,53 showing attrition rates and loss to follow-up. All analyses are performed using the intention-to-treat population, incorporating data from all participants, including those who do not complete therapy. The statistical analysis plan was agreed with an independent DMEC before any inspection of post-randomisation data by the research team. Statisticians became unblinded following all data collection only, and the statistical analysis was performed unblinded owing to the need to account for therapist effects in the SlowMo group. No interim analysis was performed. All analysis was conducted in Stata version 16.0.
Descriptive statistics by randomised group are presented for baseline values, with no tests of statistical significance or CIs for differences between groups.
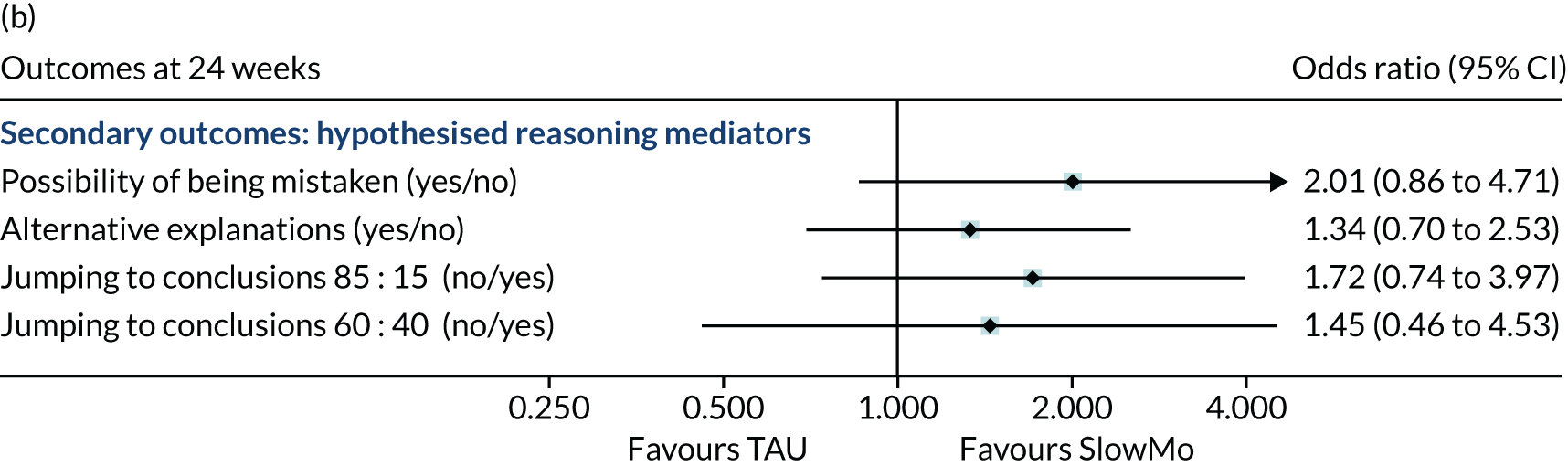
To test the primary hypothesis that the intervention would reduce paranoia severity over 12–24 weeks, we fitted a linear mixed model that allowed for clustering by both participants and therapists to the repeated measures of GPTS. 31 The model included the following as fixed effects: randomised group, time (coded as categorical), time by randomised group interaction, treatment site, baseline paranoia severity and the corresponding baseline assessment for the outcome under investigation. The treatment effect (adjusted between-group mean difference) was estimated from the model for each time point separately. All secondary outcome measures were analysed using the same modelling approach: linear mixed models for continuous outcomes and logistic mixed models for binary outcomes and reporting conditional odds ratios. Cohen’s d effect sizes at 12 and 24 weeks were calculated as the adjusted mean difference of the outcome divided by the sample SD of the outcome at baseline. These are displayed in a forest plot for all continuous outcomes and as odds ratios for binary outcomes (see Figures 2 and 3).
The moderation analyses investigated whether or not the effect of the SlowMo intervention on GPTS,31 R-GPTS37 and PSYRATS34 was moderated by the following:
-
the baseline measure of the outcomes
-
reasoning – belief flexibility (possibility of being mistaken42 and alternative explanations43) and JTC (beads task9 85 : 15: more than two beads drawn, yes/no)
-
negative symptoms (BNSS45)
-
BAPQ46
-
working memory (Letter–Number sequencing test47)
-
set-shifting [trail-making task48 (B–A)]
-
presence of a carer (yes/no)
-
perceived criticism of carer,49 if present.
For a continuous moderator, the difference in treatment effect between unit levels of the moderator can be interpreted as the difference in the estimated treatment effect between a participant with a moderator value at baseline of α + 1 and a participant with a moderator value at baseline of α. For a binary moderator (e.g. presence of a carer), the difference in treatment effect can be interpreted as the difference in the estimated treatment effect between participants with a carer and participants without a carer.
The mediation analyses examined the potential mechanisms underlying the effect of SlowMo plus TAU compared with TAU on clinical paranoia outcomes, GPTS,31 R-GPTS37 and PSYRATS. 34 Jumping to conclusions,9 belief flexibility (possibility of being mistaken42 and alternative explanations43) and worry41 at 12 weeks were individually considered as mediators of the effect on the outcomes at 12 weeks and 24 weeks separately. The analysis used causal mediation analysis based on parametric regression models. 54 This involved estimating a linear model for each mediator with random assignment, baseline outcome, baseline mediator, site and paranoia cut-off point at baseline as covariates, and separately estimating a linear model for each outcome with the mediator, group assignment, baseline outcome, baseline mediator, site and paranoid cut-off point as covariates. The effect of group assignment on the mediator is multiplied by the effect of the mediator on outcome to estimate the indirect effect, and the effect of SlowMo on outcome in the model including mediator is an estimate of the direct effect. The indirect and direct effects sum to the total effect, and bootstrapping with 500 replications was used to obtain valid standard errors (SEs) for the causal effects; 95% CIs are based on the percentile of the bootstrap distribution. The proportion mediated is the indirect effect divided by the total effect.
To account for departures from random allocation in the SlowMo group who received therapy, we performed two compliance-adjusted analyses for a binary compliance measure (attending at least one session of SlowMo therapy) and a continuous measure of the number of sessions received. Both analyses used a two-stage instrumental variables approach. The first stage involved regressing the treatment receipt measure on randomisation, baseline GPTS,31 site and paranoia, and saving the predicted value of the treatment receipt measure. In the second stage, this predicted value was included in the analysis models in place of the randomisation variable. Both models were estimated in a single bootstrap procedure to produce valid SEs for the effect of treatment received, with resampling at the participant level.
The first measure of compliance indicates anyone who receives at least one session of therapy. The treatment effect is interpreted as the complier-average causal effect, where complier is defined as those participants randomised to the SlowMo group who received at least one session of therapy and those participants randomised to the TAU group who would have received at least one session of therapy had they been randomised to the SlowMo group (a counterfactual, based on predictions from a model). The treatment effect is the adjusted mean difference between randomised groups within this subgroup of compliers.
The second measure of compliance is the number of sessions of therapy attended. This is observed for all participants in the SlowMo group (ranging from no sessions to eight sessions) and is fixed by design at zero in the TAU group. The treatment effect is the effect of one additional session of therapy on the outcome, assuming a linear effect, for example going from s sessions to s + 1 sessions for any s between 0 and 8. Details of the statistical approach for mediation analysis and departures from random allocation are outlined in Dunn et al. 55
Missing data on individual measures were prorated if > 90% of the items were completed; otherwise the measure was considered missing. We checked for differential predictors of missing outcomes by comparing responders to non-responders on key baseline variables. Maximum likelihood estimation in the mixed models accounts for missing outcome data under a missing-at-random assumption, conditional on the covariates included in the model.
The numbers of serious adverse events (SAEs) and adverse events are presented as the number of events and number of individuals with events for each randomised group.
Results
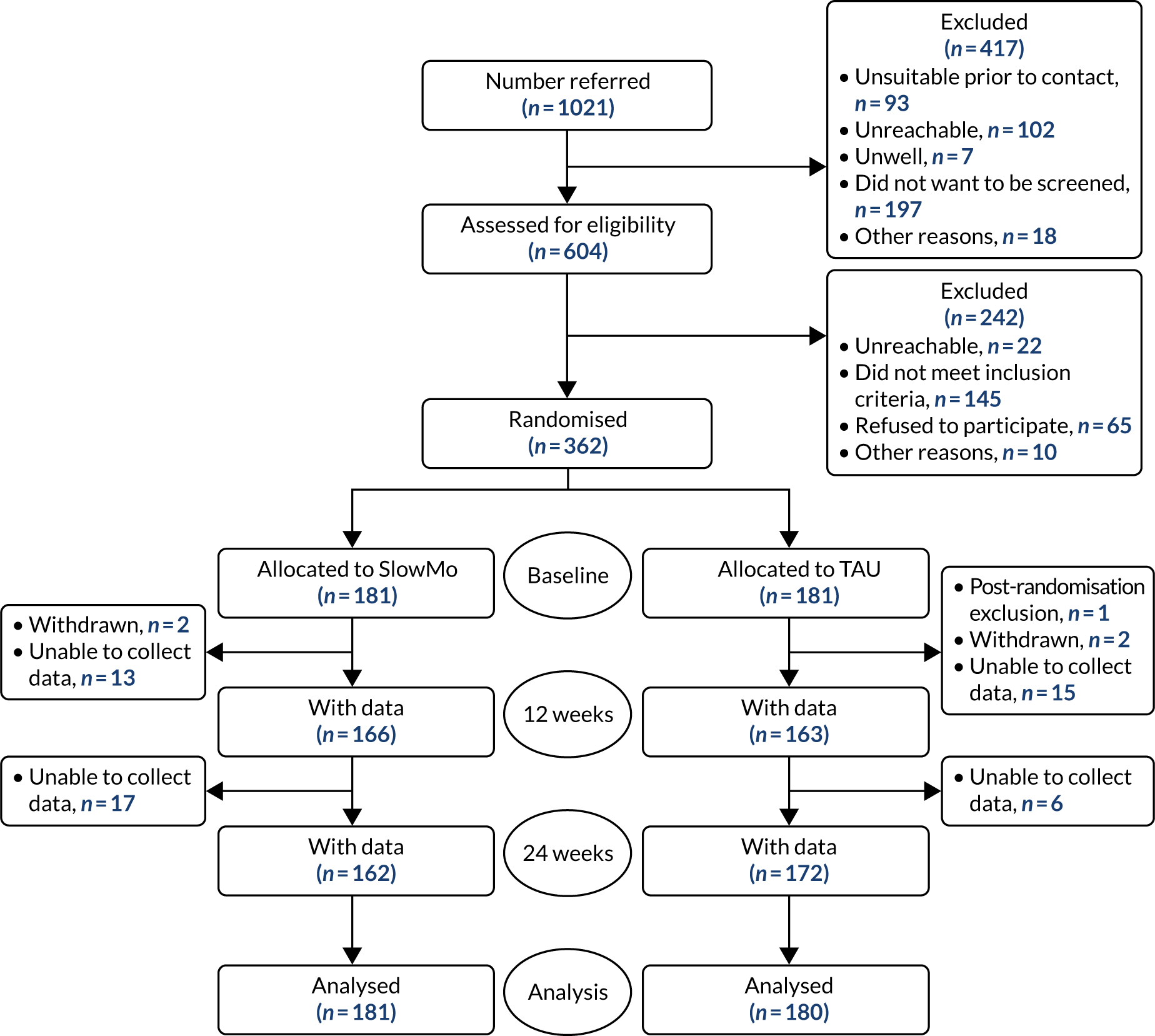
From 1 May 2017 to 14 May 2019, we assessed 604 people for eligibility and, of these, recruited 362 participants. In total, 181 participants were allocated to the SlowMo group and 181 participants were allocated to the treatment as usual group (Figure 1). There was one post-randomisation withdrawal: a participant in the control group who withdrew fully from the trial and requested that no data were included. The final sample was, therefore, 361 participants (Table 2 and see Figure 1).
FIGURE 1.
Trial profile and participant flow diagram (CONSORT).
| Site | Total referrals (n) | Excluded pre screening or awaiting screening (n) | Assessed for eligibility (n) | Screened: ineligible (n) | Screened: refused/unreachable/other (n) | Consented (n) | Randomised (n) | 12-week follow-up, n (%) | 24-week follow-up, n (%) |
|---|---|---|---|---|---|---|---|---|---|
| London | 339 | 128 | 211 | 33 | 47 | 131 | 131 | 114 (87) | 117 (90) |
| Oxford | 373 | 192 | 181 | 60 | 22 | 99 | 99 | 96 (97) | 94 (95) |
| Sussex | 309 | 97 | 212 | 52 | 28 | 132 | 132 | 118 (89) | 122 (92) |
| Total | 1021 | 417 | 604 | 145 | 97 | 362 | 362 | 328 (91) | 333 (92) |
Data were available for over 90% of the sample at each follow-up point (12 weeks: n = 328, 91%; 24 weeks: n = 333, 92%) (see Table 2). The 12-week assessments were conducted at a mean of 13.5 weeks (range 8.6–19.6 weeks) and the 24-week assessments were conducted at a mean of 25.2 weeks (range 12.9–38.3 weeks). Unmasking without replacement of an assessor occurred in 22 participants (6.7%) at 12 weeks and 19 participants (5.7%) at 24 weeks; however, in some instances unblinding occurred after a number of measures, including the primary outcome measure, had been collected: at 12 weeks, only 12 (3.6%) and, at 24 weeks, only 11 (3.3%) of the primary outcome GPTS data were collected unmasked (Table 3).
| Site | Participants for whom unblinding occurred, n (%) | 12-week follow-up, n (%) | 24-week follow-up, n (%) | ||
|---|---|---|---|---|---|
| Some data collected unblinded | GPTS collected unblinded | Some data collected unblinded | GPTS collected unblinded | ||
| London | 15 | 9 | 5 | 9 | 4 |
| Sussex | 18 | 8 | 4 | 3 | 2 |
| Oxford | 15 | 5 | 3 | 7 | 5 |
| Total | 48 (13.3) | 22 (6.7) | 12 (3.6) | 19 (5.7) | 11 (3.3) |
The baseline characteristics of the participants are shown in Table 4. As is typical of samples of people with persisting psychosis, there was a preponderance of male participants (70%) and there was an average age of 42.6 years. Other clinical characteristics (diagnosis, years in contact with services and medication equivalent dosages) were also typical. Eighty per cent of participants had clinical diagnoses of schizophrenia or schizoaffective disorder. Approximately 70% of the total participant sample were of white ethnicity, 58% lived alone and about 80% were unemployed. There were no marked demographic, diagnostic or clinical differences between the groups. Their paranoia was severe: 94.4% and 93.9% of the TAU and the SlowMo groups, respectively, met the criteria37 for likely presence of persecutory delusions on the GPTS31 (see Appendix 1, Table 17). Table 4 also shows the stratification factors (paranoia severity and site) and Table 5 shows the baseline values of negative symptoms, cognitive measures and carer characteristics examined as putative moderators.
| Characteristic | Treatment group | Overall (N = 361) | |
|---|---|---|---|
| SlowMo (N = 181) | TAU (N = 180) | ||
| Age (years), mean (SD) | 43.1 (11.7) | 42.2 (11.6) | 42.6 (11.6) |
| Sex, n (%) | |||
| Male | 132 (72.9) | 120 (66.7) | 252 (69.8) |
| Female | 49 (27.1) | 60 (33.3) | 109 (30.2) |
| Marital status, n (%) | |||
| Single | 145 (80.1) | 137 (76.1) | 282 (78.1) |
| Cohabiting | 6 (3.3) | 6 (3.3) | 12 (3.3) |
| Married or civil partnership | 22 (12.2) | 24 (13.3) | 46 (12.7) |
| Divorced | 7 (3.9) | 10 (5.6) | 17 (4.7) |
| Widowed | 1 (0.6) | 3 (1.7) | 4 (1.1) |
| Self-defined ethnicity, n (%) | |||
| White | 120 (66.3) | 129 (71.7) | 249 (69.0) |
| Black Caribbean | 9 (5.0) | 9 (5.0) | 18 (5.0) |
| Black African | 12 (6.6) | 10 (5.6) | 22 (6.1) |
| Black other | 16 (8.8) | 12 (6.7) | 28 (7.8) |
| Indian | 0 (0.0) | 3 (1.7) | 3 (0.8) |
| Pakistani | 4 (2.2) | 4 (2.2) | 8 (2.2) |
| Chinese | 1 (0.6) | 0 (0.0) | 1 (0.3) |
| Other | 19 (10.5) | 12 (6.7) | 31 (8.6) |
| Missing | 0 (0.0) | 1 (0.6) | 1 (0.3) |
| Highest level of schooling, n (%) | |||
| Primary school | 4 (2.2) | 3 (1.7) | 7 (1.9) |
| Secondary, no exams or qualifications | 30 (16.6) | 34 (18.9) | 64 (17.7) |
| Secondary O Level/CSE equivalent | 50 (27.6) | 51 (28.3) | 101 (28.0) |
| Secondary A Level equivalent | 23 (12.7) | 16 (8.9) | 39 (10.8) |
| Vocational education/college | 43 (23.8) | 44 (24.4) | 87 (24.1) |
| University degree/professional qualification | 31 (17.1) | 30 (16.7) | 61 (16.9) |
| Missing | 0 (0.0) | 2 (1.1) | 2 (0.6) |
| Current working status, n (%) | |||
| Unemployed | 141 (77.9) | 150 (83.3) | 291 (80.6) |
| Employed full time | 8 (4.4) | 8 (4.4) | 16 (4.4) |
| Employed part time | 15 (8.3) | 14 (7.8) | 29 (8.0) |
| Self-employed | 4 (2.2) | 2 (1.1) | 6 (1.7) |
| Retired | 10 (5.5) | 2 (1.1) | 12 (3.3) |
| Student | 1 (0.6) | 3 (1.7) | 4 (1.1) |
| Housewife/husband | 2 (1.1) | 1 (0.6) | 3 (0.8) |
| Normal living situation, n (%) | |||
| Living alone | 108 (59.7) | 103 (57.2) | 211 (58.4) |
| Living with partner | 19 (10.5) | 28 (15.6) | 47 (13.0) |
| Living with parents | 25 (13.8) | 30 (16.7) | 55 (15.2) |
| Living with other relatives | 4 (2.2) | 4 (2.2) | 8 (2.2) |
| Living with others | 25 (13.8) | 15 (8.3) | 40 (11.1) |
| Site, n (%) | |||
| London | 66 (36.5) | 64 (35.6) | 130 (36.0) |
| Oxford | 49 (27.1) | 50 (27.8) | 99 (27.4) |
| Sussex | 66 (36.5) | 66 (36.7) | 132 (36.6) |
| GPTS part B (stratification factor), n (%) | |||
| < 62 | 110 (60.8) | 109 (60.6) | 219 (60.7) |
| ≥ 62 | 71 (39.2) | 71 (39.4) | 142 (39.3) |
| Diagnosis, n (%) | |||
| Schizophrenia | 116 (64.1) | 109 (60.6) | 225 (62.3) |
| Schizoaffective | 30 (16.6) | 34 (18.9) | 64 (17.7) |
| Delusional disorder | 3 (1.7) | 3 (1.7) | 6 (1.7) |
| Psychosis (other) | 32 (17.7) | 34 (18.9) | 66 (18.3) |
| Time in contact with services (years), n (%) | |||
| < 1 | 7 (3.9) | 6 (3.3) | 13 (3.6) |
| 1–5 | 22 (12.2) | 33 (18.3) | 55 (15.2) |
| 6–10 | 40 (22.1) | 44 (24.4) | 84 (23.3) |
| 11–20 | 70 (38.7) | 70 (38.9) | 140 (38.8) |
| > 20 | 42 (23.2) | 27 (15.0) | 69 (19.1) |
| Chlorpromazine-equivalent dose of antipsychotic drug (mg/day), mean (SD) | 452.96 (399.45) | 519.97 (419.80) | 486.37 (410.53) |
| Moderator | Treatment group | Overall (N = 361) | |
|---|---|---|---|
| SlowMo (N = 181) | TAU (N = 180) | ||
| BNSS total, mean score (SD); n | 7.0 (8.4); 179 | 5.8 (8.1); 179 | 6.4 (8.2); 358 |
| BAPQ total, mean score (SD); n | 47.4 (6.4); 179 | 48.0 (5.5); 177 | 47.7 (6.0); 356 |
| Letter–Number Sequencing raw score, mean (SD); n | 7.6 (2.9); 176 | 8.2 (3.0); 171 | 7.9 (3.0); 347 |
| Trail-making task (B–A), mean score (SD); n | 69.7 (47.4); 157 | 63.3 (44.8); 160 | 66.5 (46.1); 317 |
| Trail-making part A, mean score (SD); n | 40.9 (16.9); 165 | 41.7 (20.2); 163 | 41.3 (18.6); 328 |
| Trail-making part B, mean score (SD); n | 110.6 (54.5); 165 | 105.0 (52.6); 163 | 107.8 (53.5); 328 |
| Carer, n (%) | |||
| No | 75 (41.9) | 72 (40.2) | 147 (41.1) |
| Yes | 104 (58.1) | 107 (59.8) | 211 (58.9) |
| How critical is your carer, n (%) | |||
| 0 (not at all) | 37 (35.6) | 30 (28.8) | 67 (32.2) |
| 1 | 11 (10.6) | 12 (11.5) | 23 (11.1) |
| 2 | 18 (17.3) | 17 (16.3) | 35 (16.8) |
| 3 | 19 (18.3) | 20 (19.2) | 39 (18.8) |
| 4 | 10 (9.6) | 18 (17.3) | 28 (13.5) |
| 5 (extremely) | 9 (8.7) | 7 (6.7) | 16 (7.7) |
In terms of treatment uptake, the average number of SlowMo sessions attended was 6.8 sessions (SD 2.6 sessions), rising to 7.3 sessions (SD 1.9 sessions) for those who attended at least one session. In total, 145 (80%) of those participants randomised to SlowMo (n = 181) completed all eight therapy sessions, 13 (7%) did not attend any sessions and a further 23 (14%) discontinued between session 1 and session 7. The mean session duration was 75 minutes (SD 29 minutes), including web app delivery and out-of-clinic work. Adherence to the delivery of the web app content was high, with each of the eight sessions reaching adherence ratings of at least 90%. Adherence to the mobile app was also high: of those who attended at least one therapy session and, therefore, were given a mobile telephone with the app installed, 71.4% met criteria for adherent use.
Both the descriptive statistics for all of the primary and secondary outcomes (Tables 6 and 7), and the effect estimates (Figures 2 and 3) show that SlowMo led to greater reductions in paranoia than TAU, as assessed by the total score of our primary outcome measure (GPTS31) post treatment [–8.06 (SE 2.85), 95% CI –13.64 to –2.48; p = 0.005] and at 24 weeks [–5.27 (SE 2.84, 95% CI –10.83 to 0.29; p = 0.063]. The reduction in paranoia on GPTS31 part B (persecutory) was significant at both time points, as was the R-GPTS37 total, PSYRATS34 delusions and SAPS36 persecutory delusion (see Figures 2 and 3). However, effects were less consistent for ideas of reference (as measured by GPTS31 part A, R-GPTS37 social reference and SAPS36 ideas/delusions of reference), with significant effects found either post treatment or at follow-up, but not at both time points (see Figure 2). See Appendix 1, Figure 9, for outcomes by group at three time points for the GPTS, R-GPTS and PSYRATS. Effect sizes were small (approximately Cohen’s d = 0.3) on the GPTS31 total, and moderate (Cohen’s d = 0.5) for PSYRATS34 total and SAPS36 persecutory delusions.
Treatment effects were found for some but not all of our reasoning measures: of the measures of belief flexibility, the possibility of being mistaken,42 both as a continuous rating and as a dichotomous rating, improved significantly, but alternative explanations43 did not improve. Jumping to conclusions9 showed little evidence of improvement (with only one significant finding: beads drawn at 12 weeks). The fast scale of the Fast and Slow Thinking Questionnaire44 showed improvements at both time points and the slow scale showed improvements at 24 weeks. Significant improvements, with a small effect size of approximately Cohen’s d = 0.3, were found for SlowMo in the following secondary outcome measures at either or both time points, and most consistently at 24-week follow-up: well-being (WEMWBS38), quality of life (MANSA39), worry (PSWQ41) and self-concept but not other-concept as measured on the BCSS40 (see Table 7 and Figure 2).
| Outcome | Treatment group, mean score (SD); n | Adjusted mean difference (SE) | 95% CI; p-value | |
|---|---|---|---|---|
| SlowMo | TAU | |||
| GPTS total | ||||
| Baseline | 104.7 (27.6); 180 | 105.9 (26.0); 179 | ||
| 12 weeks | 84.8 (30.8); 165 | 92.5 (33.1); 163 | –8.06 (2.85) | –13.64 to –2.48; 0.005 |
| 24 weeks | 81.7 (31.6); 161 | 86.3 (33.2); 171 | –5.27 (2.84) | –10.83 to 0.29; 0.063 |
| GPTS part A | ||||
| Baseline | 48.6 (15.9); 181 | 50.3 (15.1); 179 | ||
| 12 weeks | 40.2 (14.9); 165 | 44.2 (15.8); 163 | –3.49 (1.34) | –6.12 to –0.86; 0.009 |
| 24 weeks | 39.2 (15.0); 161 | 42.0 (15.8); 172 | –1.79 (1.34) | –4.41 to –0.83; 0.180 |
| GPTS part B | ||||
| Baseline | 56.2 (14.4); 180 | 55.9 (13.8); 180 | ||
| 12 weeks | 44.6 (18.1); 166 | 48.2 (18.7); 163 | –4.51 (1.71) | –7.87 to –1.15; 0.009 |
| 24 weeks | 42.2 (18.2); 161 | 45.1 (18.9); 171 | –3.53 (1.71) | –6.89 to –0.18; 0.039 |
| R-GPTS total | ||||
| Baseline | 40.7 (15.4); 179 | 41.5 (14.8); 180 | ||
| 12 weeks | 29.6 (17.2); 166 | 34.3 (18.6); 163 | –5.00 (1.61) | –8.16 to –1.86; 0.002 |
| 24 weeks | 27.5 (17.6); 160 | 31.1 (18.6); 169 | –3.42 (1.61) | –6.57 to –0.27; 0.034 |
| R-GPTS social reference | ||||
| Baseline | 16.0 (7.8); 180 | 17.1 (8.2); 180 | ||
| 12 weeks | 11.9 (7.6); 166 | 14.2 (8.1); 163 | –2.05 (0.70) | –3.42 to –0.68; 0.003 |
| 24 weeks | 11.3 (7.6); 160 | 13.1 (8.0); 172 | –1.15 (0.70) | –2.51 to 0.22; 0.099 |
| R-GPTS persecution | ||||
| Baseline | 24.7 (9.3); 180 | 24.4 (8.7); 180 | ||
| 12 weeks | 17.7 (11.1); 166 | 20.1 (11.7); 163 | –2.97 (1.07) | –5.07 to –0.88; 0.005 |
| 24 weeks | 16.3 (11.2); 161 | 18.0 (11.6); 169 | –2.25 (1.07) | –4.34 to –0.16; 0.035 |
| PSYRATS | ||||
| Baseline | 16.5 (3.3); 180 | 16.2 (3.1); 180 | ||
| 12 weeks | 13.2 (4.9); 166 | 14.5 (5.0); 162 | –1.53 (0.50) | –2.50 to –0.56; 0.002 |
| 24 weeks | 12.5 (5.2); 161 | 14.0 (5.5); 171 | –1.62 (0.49) | –2.59 to –0.65; 0.001 |
| PSYRATS distress | ||||
| Baseline | 8.1 (1.8); 181 | 7.9 (1.7); 180 | ||
| 12 weeks | 6.3 (2.8); 166 | 7.0 (2.8); 162 | –0.87 (0.29) | –1.44 to –0.30; 0.003 |
| 24 weeks | 6.0 (3.0); 161 | 6.8 (3.0); 171 | –0.76 (0.29) | –1.32 to –0.19; 0.009 |
| PSYRATS conviction | ||||
| Baseline | 8.4 (2.0); 180 | 8.3 (1.9); 180 | ||
| 12 weeks | 6.9 (2.5); 166 | 7.4 (2.6); 163 | –0.62 (0.25) | –1.11 to –0.13; 0.014 |
| 24 weeks | 6.4 (2.5); 161 | 7.2 (2.8); 172 | –0.84 (0.25) | –1.33 to –0.35; 0.001 |
| SAPS persecutory delusions | ||||
| Baseline | 3.5 (0.8); 181 | 3.4 (0.9); 180 | ||
| 12 weeks | 2.8 (1.3); 164 | 3.0 (1.3); 161 | –0.37 (0.18) | –0.71 to –0.03; 0.035 |
| 24 weeks | 2.5 (1.5); 161 | 2.8 (1.4); 171 | –0.46 (0.18) | –0.80 to –0.12; 0.009 |
| SAPS ideas and delusions of reference | ||||
| Baseline | 2.5 (1.8); 181 | 2.7 (1.7); 180 | ||
| 12 weeks | 2.2 (1.9); 165 | 2.4 (1.8); 161 | –0.18 (0.19) | –0.55 to 0.19; 0.350 |
| 24 weeks | 1.9 (1.9); 160 | 2.4 (1.9); 171 | –0.41 (0.19) | –0.79 to –0.04; 0.028 |
| Outcome | Treatment group | Effecta | 95% CI; p-value | |
|---|---|---|---|---|
| SlowMo | TAU | |||
| WEMWBS,b mean score (SD); n | ||||
| Baseline | 39.3 (9.1); 179 | 40.5 (8.7); 175 | ||
| 12 weeks | 42.2 (9.4); 164 | 41.6 (9.1); 157 | 1.56 (0.89) | –0.18 to 3.30; 0.079 |
| 24 weeks | 43.3 (11.0); 157 | 41.2 (9.6); 165 | 2.82 (0.89) | 1.08 to 4.56; 0.001 |
| PSWQ, mean score (SD); n | ||||
| Baseline | 56.9 (10.8); 179 | 56.6 (10.1); 175 | ||
| 12 weeks | 53.2 (11.6); 158 | 55.4 (11.5); 157 | –2.81 (0.90) | –4.57 to –1.04; 0.002 |
| 24 weeks | 52.2 (11.6); 154 | 54.5 (11.5); 163 | –2.24 (0.90) | –4.00 to –0.48; 0.013 |
| BCSS: negative self, mean score (SD); n | ||||
| Baseline | 9.9 (5.8); 181 | 10.3 (5.5); 178 | ||
| 12 weeks | 9.0 (6.0); 162 | 10.0 (6.0); 159 | –0.98 (0.48) | –1.92 to –0.04; 0.04 |
| 24 weeks | 8.4 (5.9); 160 | 9.7 (5.8); 167 | –1.19 (0.48) | –2.12 to –0.25; 0.013 |
| BCSS: positive self,b mean score (SD); n | ||||
| Baseline | 10.7 (5.6); 181 | 10.8 (5.4); 178 | ||
| 12 weeks | 11.5 (5.6); 164 | 11.5 (5.6); 159 | 0.33 (0.41) | –0.48 to 1.13; 0.427 |
| 24 weeks | 12.5 (5.5); 159 | 11.6 (5.8); 168 | 1.11 (0.41) | 0.31 to 1.92; 0.006 |
| BCSS: negative other, mean score (SD); n | ||||
| Baseline | 13.3 (6.1); 181 | 13.3 (5.8); 178 | ||
| 12 weeks | 12.9 (6.1); 163 | 13.0 (6.0); 159 | –0.21 (0.55) | –1.30 to 0.88; 0.703 |
| 24 weeks | 12.6 (6.2); 159 | 12.7 (6.3); 168 | –0.16 (0.55) | –1.25 to 0.92; 0.767 |
| BCSS: positive other,b mean score (SD); n | ||||
| Baseline | 11.6 (5.2); 180 | 11.1 (4.9); 177 | ||
| 12 weeks | 12.2 (5.1); 164 | 11.8 (4.8); 159 | 0.28 (0.42) | –0.55 to 1.12; 0.504 |
| 24 weeks | 12.4 (4.8); 158 | 12.1 (4.8); 168 | 0.34 (0.42) | –0.49 to 1.17; 0.420 |
| MANSA,b mean score (SD); n | ||||
| Baseline | 46.8 (9.9); 161 | 48.1 (10.2); 164 | ||
| 12 weeks | 48.1 (10.7); 145 | 48.9 (10.6); 146 | 0.76 (0.91) | –1.02 to 2.55; 0.401 |
| 24 weeks | 50.5 (11.7); 135 | 49.1 (9.5); 148 | 2.75 (0.92) | 0.94 to 4.55; 0.003 |
| Possibility of being mistaken (0–100),b mean score (SD); n | ||||
| Baseline | 34.6 (30.9); 181 | 35.1 (31.0); 180 | ||
| 12 weeks | 48.9 (32.2); 165 | 39.9 (33.2); 161 | 9.02 (3.16) | 2.83 to 15.21; 0.004 |
| 24 weeks | 45.3 (31.8); 161 | 37.7 (31.1); 172 | 8.88 (3.16) | 2.70 to 15.07; 0.005 |
| Possibility of being mistaken, yes/no (% yes/% no)b | ||||
| Baseline | 105/76 (58/42) | 106/74 (59/41) | ||
| 12 weeks | 124/41 (75/25) | 100/61 (62/38) | OR 3.83 | 1.53 to 9.59; 0.004 |
| 24 weeks | 105/56 (65/35) | 100/72 (58/42) | OR 2.01 | 0.86 to 4.70; 0.108 |
| Alternative explanations, yes/no (% yes/% no)b | ||||
| Baseline | 79/102 (44/56) | 85/94 (48/52) | ||
| 12 weeks | 90/74 (55/45) | 78/83 (48/52) | OR 1.74 | 0.90 to 3.36; 0.097 |
| 24 weeks | 87/73 (54/46) | 87/82 (52/48) | OR 1.33 | 0.70 to 2.55; 0.387 |
| JTC 85 : 15, yes/no (% yes/% no) | ||||
| Baseline | 103/77 (57/43) | 83/96 (46/54) | ||
| 12 weeks | 70/95 (42/58) | 68/91 (42/58) | OR 0.71 | 0.31 to 1.62; 0.422 |
| 24 weeks | 55/105 (34/66) | 62/107 (37/63) | OR 0.58 | 0.25 to 1.34; 0.204 |
| JTC 85 : 15 (number of beads drawn), mean (SD) | ||||
| Baseline | 3.8 (4.4) | 3.9 (4.0) | ||
| 12 weeks | 4.3 (4.3) | 4.1 (3.9) | 0.39 (0.43) | –0.45 to 1.22; 0.365 |
| 24 weeks | 5.2 (4.8) | 4.1 (3.3) | 0.99 (0.42) | 0.16 to 1.83; 0.019 |
| JTC 60 : 40, yes/no (% yes/% no) | ||||
| Baseline | 72/108 (40/60) | 59/120 (33/67) | ||
| 12 weeks | 47/118 (29/71) | 42/117 (26/74) | OR 0.82 | 0.26 to 2.51; 0.722 |
| 24 weeks | 43/117 (27/73) | 44/125 (26/74) | OR 0.69 | 0.22 to 2.18; 0.531 |
| JTC 60 : 40 (number of beads drawn), mean (SD) | ||||
| Baseline | 5.7 (5.4) | 5.7 (5.1) | ||
| 12 weeks | 7.0 (5.7) | 6.8 (5.4) | 0.28 (0.49) | –0.68 to 1.25; 0.563 |
| 24 weeks | 7.0 (5.2) | 6.5 (4.9) | 0.49 (0.49) | –0.47 to 1.45; 0.321 |
| FaST: fast scale, mean score (SD); n | ||||
| Baseline | 16.9 (4.7); 174 | 16.7 (4.3); 169 | ||
| 12 weeks | 15.3 (4.9); 165 | 16.2 (5.0); 160 | –1.07 (0.47) | –1.98 to –0.16; 0.022 |
| 24 weeks | 15.0 (4.4); 160 | 16.2 (5.1); 168 | –1.33 (0.46) | –2.23 to –0.42; 0.004 |
| FaST: slow scale,b mean score (SD); n | ||||
| Baseline | 19.9 (4.7); 174 | 19.7 (4.8); 169 | ||
| 12 weeks | 20.3 (4.8); 165 | 19.3 (4.8); 160 | 0.66 (0.45) | –0.22 to 1.55; 0.140 |
| 24 weeks | 20.3 (4.4); 160 | 19.3 (4.8); 168 | 1.00 (0.45) | 0.12 to 1.88; 0.027 |
FIGURE 2.
Forest plot of all continuous outcomes at (a) 12 weeks and (b) 24 weeks.
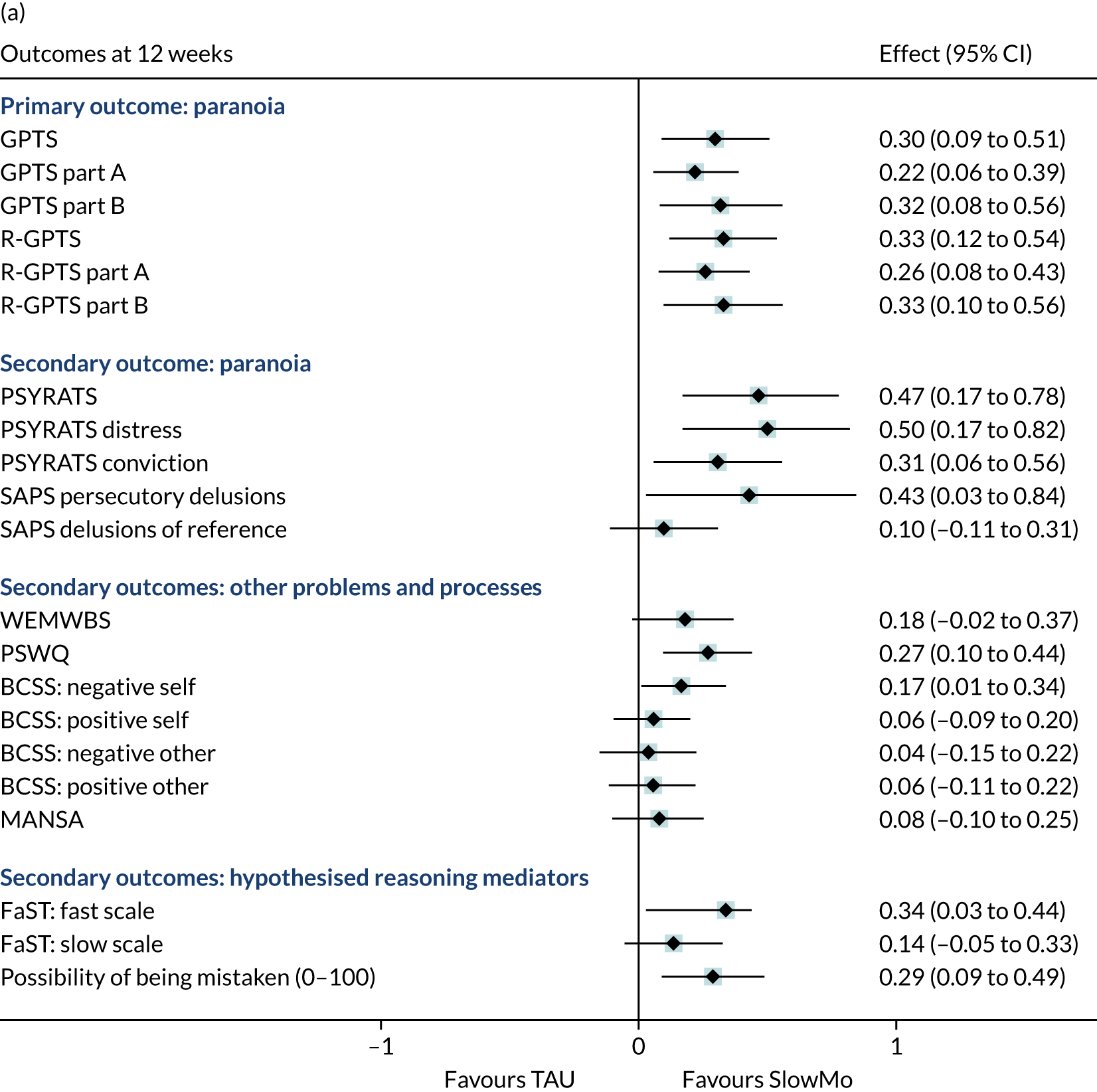
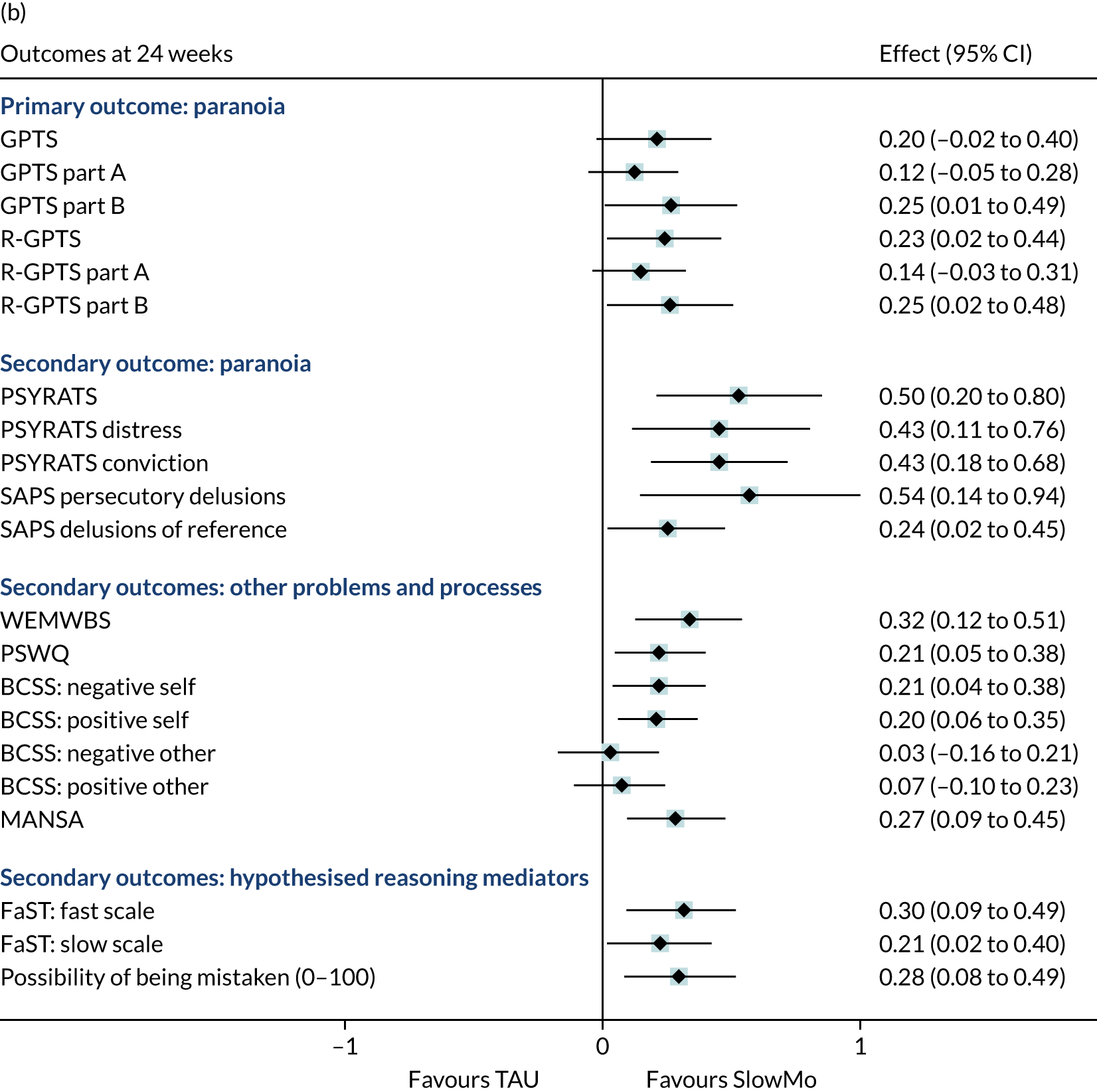
FIGURE 3.
Forest plot of binary outcomes at (a) 12 weeks and (b) 24 weeks.
The moderation analysis (Table 8) found no differential effects on the paranoia outcome as measured by the GPTS31 or the R-GPTS. 37 There was only one moderation effect, on the PSYRATS,34 with p < 0.05. However, given the number of tests conducted, this finding may have occurred by chance. These results show that the treatment is effective against paranoia at all levels of the moderators.
| Moderator | Outcome, difference in treatment effect (95% CI); p-value | ||
|---|---|---|---|
| GPTS | R-GPTS | PSYRATS | |
| Baseline outcome | |||
| 12 weeks | –0.08 (–0.28 to 0.13); 0.469 | –0.06 (–0.27 to 0.15); 0.568 | –0.31 (–0.62. to –0.01); 0.045 |
| 24 weeks | –0.12 (–0.32 to 0.09); 0.263 | –0.12 (–0.33 to 0.09); 0.271 | –0.24 (–0.54 to 0.07); 0.129 |
| BNSS | |||
| 12 weeks | 0.27 (–0.41 to 0.95); 0.439 | 0.02 (–0.37 to 0.42); 0.910 | –0.01 (–0.13 to 0.11); 0.922 |
| 24 weeks | –0.10 (–0.78 to 0.58); 0.777 | –0.07 (–0.47 to 0.32); 0.708 | 0.06 (–0.06 to 0.18); 0.317 |
| BAPQ | |||
| 12 weeks | 0.06 (–0.89 to 1.02); 0.896 | 0.08 (–0.46 to 0.62); 0.775 | 0.07 (–0.09 to 0.24); 0.383 |
| 24 weeks | 0.10 (–0.85 to 1.06); 0.833 | 0.02 (–0.52 to 0.56); 0.934 | 0.06 (–0.10 to 0.23); 0.452 |
| Letter–Number Sequencing raw score | |||
| 12 weeks | –0.44 (–2.31 to 1.42); 0.641 | –0.21 (–1.26 to 0.85); 0.697 | –0.21 (–0.54 to 0.12); 0.210 |
| 24 weeks | –0.21 (–2.06 to 1.63); 0.822 | –0.09 (–1.14 to 0.96); 0.867 | –0.30 (–0.62 to 0.03); 0.075 |
| Trail making task (B–A) | |||
| 12 weeks | 0.05 (–0.08 to 0.18); 0.436 | 0.03 (–0.04 to 0.10); 0.448 | 0.00 (–0.02 to 0.02); 0.889 |
| 24 weeks | 0.04 (–0.09 to 0.16); 0.574 | 0.01 (–0.06 to 0.09); 0.701 | 0.02 (0.00 to 0.04); 0.069 |
| Presence of a carer (yes/no) | |||
| 12 weeks | 7.71 (–3.56 to 18.98); 0.180 | 3.70 (–2.67 to 10.07); 0.255 | 1.12 (–0.85 to 3.08); 0.265 |
| 24 weeks | 1.23 (–10.01 to 12.46); 0.831 | 0.84 (–5.54 to 7.22); 0.796 | 0.48 (–1.47 to 2.44); 0.628 |
| Criticism of carer (only if carer present, n = 208) | |||
| 12 weeks | –0.28 (–4.73 to 4.17); 0.903 | –0.14 (–2.65 to 2.38); 0.915 | –0.62 (–1.41 to 0.17); 0.122 |
| 24 weeks | 2.48 (–1.93 to 6.88); 0.270 | 1.32 (–1.16 to 3.81); 0.297 | 0.14 (–0.64 to 0.92); 0.716 |
| Alternative explanations (yes/no) | |||
| 12 weeks | 2.62 (–8.50 to 13.75); 0.644 | 1.99 (–4.29 to 8.27); 0.534 | 1.15 (–0.79 to 3.09); 0.245 |
| 24 weeks | 4.39 (–6.69 to 15.46); 0.438 | 2.29 (–3.98 to 8.57); 0.474 | –0.12 (–2.05 to 1.81); 0.905 |
| Possibility of being mistaken (yes/no) | |||
| 12 weeks | 3.88 (–7.49 to 15.24); 0.504 | 3.07 (–3.36 to 9.51); 0.349 | 0.79 (–1.17 to 2.76); 0.429 |
| 24 weeks | 2.71 (–8.60 to 14.02); 0.639 | 1.67 (–4.76 to 8.10); 0.610 | 0.16 (–1.79 to 2.12); 0.871 |
| Jumping to conclusions (yes/no) | |||
| 12 weeks | –0.72 (–11.97 to 10.52); 0.90 | –0.75 (–7.10 to 5.60); 0.817 | –0.33 (–2.29 to 1.63); 0.744 |
| 24 weeks | 7.63 (–3.59 to 18.85); 0.183 | 5.76 (–0.60 to 12.11); 0.076 | 1.12 (–0.84 to 3.07); 0.264 |
The results of the mediation analysis on the GPTS31 at 12 and 24 weeks are shown in Table 9. The results for the R-GPTS37 and the PSYRATS34 are presented in Appendix 1 (see Tables 18 and 19). Only the possibility of being mistaken42 (whether measured as a binary variable or as a continuous measure) and worry41 mediated the effects of the treatment on all paranoia outcomes at 12 and 24 weeks. Approximately 40% of the total effect was mediated through each mediator at 12 weeks and 56% was mediated at 24 weeks.
| Mediator | Effect, causal mediation effect (bootstrap SE); 95% CI | Proportion mediated | ||
|---|---|---|---|---|
| Total | Direct | Indirect | ||
| Alternative explanations | ||||
| 12 weeks | –7.44 (2.98); –13.32 to –1.14 | –7.01 (2.94); –12.81 to –0.67 | –0.43 (0.44); –1.46 to 0.15 | 5.8 |
| 24 weeks | –4.86 (2.90); –10.74 to 0.92 | –4.55 (2.84); –10.12 to 1.03 | –0.31 (0.38); –1.33 to 0.26 | 6.4 |
| JTC 85 : 15 task | ||||
| 12 weeks | –7.24 (3.09); –13.03 to –0.64 | –6.89 (3.04); –12.80 to –0.83 | –0.34 (0.49); –1.27 to 0.58 | 4.7 |
| 24 weeks | –4.02 (2.94); –9.69 to 1.87 | –3.76 (2.92); –9.31 to 2.06 | –0.26 (0.41); –1.14 to 0.63 | 6.5 |
| JTC 60 : 40 task | ||||
| 12 weeks | –7.63 (3.05); –13.61 to –0.98 | –7.55 (3.04); –13.70 to –1.00 | –0.09 (0.44); –0.99 to 0.80 | 1.1 |
| 24 weeks | –4.60 (2.91); –10.14 to 1.29 | –4.57 (2.90); –10.12 to 1.42 | –0.03 (0.22); –0.48 to 0.44 | 0.7 |
| Possibility of being mistaken (yes/no) | ||||
| 12 weeks | –8.35 (2.99); –14.13 to –2.07 | –6.00 (2.93); –11.86 to 0.05 | –2.35 (1.08); –4.71 to –0.59 | 28.1 |
| 24 weeks | –5.26 (2.92); –11.14 to 0.53 | –3.55 (2.78); –8.67 to 1.96 | –1.71 (0.92); –3.93 to –0.39 | 32.5 |
| Possibility of being mistaken (1–100) | ||||
| 12 weeks | –7.58 (2.98); –13.44 to –1.01 | –4.86 (2.83); –10.21 to 0.97 | –2.72 (1.07); –5.04 to –0.91 | 35.9 |
| 24 weeks | –4.89 (2.89); –10.30 to 1.12 | –2.13 (2.69); –7.51 to 3.39 | –2.76 (1.02); –4.75 to –0.75 | 56.4 |
| Worry | ||||
| 12 weeks | –7.78 (3.00); –13.63 to –1.17 | –4.74 (2.96); –10.44 to 1.74 | –3.04 (1.10); –5.52 to –1.09 | 39.1 |
| 24 weeks | –4.46 (2.90); –10.42 to 1.12 | –1.95 (2.91); –7.48 to 4.02 | –2.51 (1.11); –5.13 to –0.97 | 56.3 |
The results of the compliance-adjusted analysis on the GPTS,31 R-GPTS37 and PSYRATS34 are shown in Table 10. Given that there is no access to SlowMo therapy for the TAU group, the complier-average causal effect is an adjustment to the intention-to-treat effect for each outcome divided by the predicted proportion of those in the SlowMo group who were observed to attend at least one session of therapy. The results show significant treatment effects of SlowMo therapy compared with TAU in the compliers at all time points. The dose–response effect shows that the treatment effect increases as the number of SlowMo sessions increases.
| Outcome | Compliance measure, treatment effect (bootstrap SE), 95% CI; p-value | |
|---|---|---|
| Any sessions (≥ 1) | Number of sessions | |
| GPTS | ||
| 12 weeks | –8.73 (2.52), –13.68 to –3.79; 0.001 | –1.19 (0.32), –1.83 to –0.56; < 0.001 |
| 24 weeks | –5.64 (2.47), –10.47 to –0.81; 0.022 | –0.77 (0.34), –1.44 to –0.10; 0.024 |
| R-GPTS | ||
| 12 weeks | –5.57 (1.40), –8.32 to –2.83; < 0.001 | –0.76 (0.19), –1.14 to –0.38; < 0.001 |
| 24 weeks | –3.79 (1.41), –6.56 to –1.02; 0.007 | –0.52 (0.20), –0.91 to –0.12; 0.010 |
| PSYRATS | ||
| 12 weeks | –1.64 (0.39), –2.41 to –0.87; < 0.001 | –0.22 (0.05), –0.33 to –0.12; < 0.001 |
| 24 weeks | –1.79 (0.42), –2.61 to –0.96; < 0.001 | –0.24 (0.06), –0.37 to –0.12; < 0.001 |
Fifty-four adverse events were reported over the course of the trial, of which 51 were serious events, occurring in 19 people in the SlowMo group and 21 in the TAU group (Table 11). There were no deaths recorded. More than half of the SAEs were mental health hospital admission or crisis referrals (SlowMo, n = 13; TAU, n = 16) or physical health crises (SlowMo, n = 8; TAU, n = 2), none of which was rated as being related to participation in the trial. One SAE in the TAU group was rated as ‘definitely related’ to trial involvement: it involved a complaint made when the research team shared information with the clinical team under a duty of care (confirmed as such by an independent ethics review). (The participant subsequently requested that their data be withdrawn and is, therefore, a ‘post-randomisation exclusion’ in the data analysis.)
| Adverse event | Treatment group, n (%) | |
|---|---|---|
| SlowMo | TAU | |
| Serious events (people) | ||
| Yes | 25 (19) | 26a (21) |
| No | 3 (3) | 0 (0) |
| Type of adverse events (people) | ||
| Physical | 8 (8) | 2 (2) |
| Self-harm | 1 (1) | 0 (0) |
| Serious violent incidents (victim) | 0 (0) | 1 (1) |
| Serious violent incidents (accused) | 1 (1) | 2 (2) |
| Referrals to crisis care | 5 (5) | 2 (2) |
| Admission to psychiatric hospital during follow-up | 8 (8) | 14 (10) |
| Deaths | 0 (0) | 0 (0) |
| Other | 5 (5) | 5 (4) |
| Intensity of events | ||
| Mild | 2 (7.1) | 0 (0.0) |
| Moderate | 11 (39.3) | 10 (38.5) |
| Severe | 15 (53.6) | 16 (61.5) |
| Relationship to trial participation (serious events) | ||
| Definitely related | 0 (0.0) | 1 (3.8) |
| Probably related | 0 (0.0) | 0 (0.0) |
| Possibly related | 1 (4.0) | 0 (0.0) |
| Unlikely related | 1 (4.0) | 0 (0.0) |
| Not related | 23 (92.0) | 25 (96.2) |
Concomitant treatments (psychosocial, psychological therapy and medications) and services (days in crisis care and in admission to hospital) that were provided to both groups as usual treatment were monitored from case note review and using a modified version of the Client Service Receipt Inventory33 (see Appendix 1, Tables 20 and 21).
Discussion
To the best of our knowledge, the SlowMo trial is the largest trial to date of a psychological therapy focused on fear of harm from others (paranoia) undertaken in a clinical population. We recruited the target of 362 participants, with over 90% followed up at each time point. We addressed two main goals: to improve effectiveness and to overcome user experience barriers to engagement and adherence. The study results suggest that SlowMo therapy is clinically effective and supports the intended user experience.
We found consistent significant effects of SlowMo therapy on paranoia when added to routine treatment, compared with routine treatment alone, over and above the generally improving trajectory of both groups. Improvements were demonstrated on all paranoia and persecutory delusions outcomes across the 6 months (ranging from small to medium effect sizes). The effects were less consistent for ideas of reference, with significant effects at either post treatment or follow-up, but not both time points. There were also improvements in the reasoning targets of belief flexibility (possibility of being mistaken,42 but not alternative explanations43) and self-reported reasoning on the Fast and Slow Thinking Questionnaire44 (the fast subscale at both time points, and the slow subscale at 24 weeks). There was, however, little evidence of improvement in JTC9 (a single significant effect of the eight measured). There were treatment effects with small effect sizes on improving well-being, quality of life, self-concept and worry, with these important gains seen most consistently at the longer-term (6-month) follow-up. These represent sustained improvements in well-being and quality of life, and are highly valued by service users. 56
The therapy uptake and adherence were all in the upper range, suggesting that SlowMo therapy is highly acceptable. Furthermore, the effects were not moderated by hypothesised characteristics, indicating that it is beneficial regardless of cognitive capacity, baseline symptoms, the presence of a carer, or carer criticism. The treatment targeted reasoning to improve paranoia; we found that this outcome was, as hypothesised, mediated by improvement in a fundamental aspect of reasoning, belief flexibility (possibility of being mistaken42) and also, but not as hypothesised, reducing worry.
We found no evidence of the intervention being harmful. Both groups generally improved across the course of the trial and there were similar numbers of SAEs across the two groups. The most common SAEs of hospital crisis and inpatient admission were smaller in number of days at follow-up in both groups (see Appendix 1, Table 21). No SAE was considered definitely related to trial participation in the SlowMo group by the independent DMEC; the only SAE definitely related to trial involvement in the TAU group involved a complaint that information was shared under duty of care (see above). The relatedness of adverse events to the digital hardware and software supporting SlowMo therapy is reported in Chapter 3.
We used a range of measures of paranoia and a limitation of the study is that our primary outcome measure, the self-reported GPTS,31 was revised during the course of the trial. 37 Therefore, we report outcomes using both versions. These have similar results, but the newer, more psychometrically robust, revision37 yields slightly larger treatment effects and results in the follow-up effect for the total score moving into the range for conventional significance. SlowMo, although brief, at eight sessions, had a clinically worthwhile effect on delusions: using the new cut-off points provided by Freeman et al. 37 for the GPTS persecution, 38.5% of the SlowMo group (compared with 31.6% of the TAU group) no longer met the criteria for presence of a persecutory delusion at follow-up (increasing from 10% and 11%, respectively, at baseline) (see Appendix 1, Table 17). Furthermore, on observer-rated measures of paranoia (PSYRATS34 and SAPS36), the effect sizes were, in general, moderate and, for this reason, were greater than the rates reported in meta-analyses of longer courses of CBT for psychosis for delusions using these measures. 3,57 The clinically important target of distress associated with the delusion was reduced by the end of treatment with SlowMo compared with TAU, and sustained at follow-up.
SlowMo targets reasoning to improve paranoia. As intended, improvements were observed in belief flexibility and the possibility of being mistaken. 42 By contrast, JTC9 showed little evidence of change. On the tests of reasoning as a mechanism, the possibility of being mistaken mediated change in paranoia, explaining about 56% of the variance at follow-up. This is consistent with our earlier proof-of-concept study, which also found that the possibility of being mistaken mediated paranoia, but JTC did not mediate paranoia. 25 In the light of this and other meta-analytic evidence,10 we suggest that JTC (as assessed through the classic beads task9) may be best considered as trait like and relatively unresponsive to change over time, conferring vulnerability to persecutory beliefs, but with less evidence of a dynamic relationship with paranoia severity. This evolving understanding of reasoning biases and paranoia has resulted in our foregrounding of the promotion of ‘slow thinking’ and greater flexibility, with the aim of generating compensatory strategies for real-world fast thinking by encouraging the deliberative act of slowing down in the moment (see Ward and Garety15). Self-reported reductions in fast and slow thinking, as assessed by the Fast and Slow Thinking Questionnaire,44 suggest that the therapy may have changed awareness of and preferences for both unhelpful fast styles of thinking and useful slow styles of thinking, in keeping with the explicit and consistent SlowMo focus on building meta-cognitive awareness of thinking ‘habits’.
As Freeman58 has noted, persecutory delusions arise from a combination of causes, with each causal factor increasing the probability of such fears occurring. Another factor is worry. The Worry Intervention Trial28 demonstrated comparable changes in paranoia on PSYRATS delusions (Cohen’s d = 0.49) using a brief, six-session, cognitive–behavioural worry intervention and provided evidence that these changes were mediated through worry. 28 SlowMo showed a similar change in paranoia on the PSYRATS (Cohen’s d = 0.5) and, although not explicitly targeted in SlowMo, the observed changes in worry were also found to act as a mechanism of change in paranoia; paranoia improved as a consequence of reducing worry, with a similar proportion of the variance to that found for belief flexibility. This was not hypothesised. However, given that worry is a mechanism that clearly drives paranoia, which is described by participants as part of an emotional reaction to fast thinking, and SlowMo altered worry, we can conclude that worry reduction constitutes part of the treatment route for SlowMo.
We note that SlowMo shares features with worry reduction techniques. Both involve noticing one’s thoughts, consider approaches for decentring worrying thoughts and help with strategies to shift attention elsewhere, for example, in SlowMo, shifting from fast thoughts to alternative and safer (i.e. less worrying) thoughts. However, worry improved less in SlowMo than when it was directly targeted in the Worry Intervention Trial,28 as might be expected. Furthermore, we cannot tell from the current study how far worry and belief flexibility are independent routes to change, nor whether or not there might be other mechanisms for treatment effects, such as the parallel improvements in self-concepts and well-being that occurred.
Our original hypotheses, specified in our trial protocol, derived from a theory of change in which the primary process underpinning SlowMo was through reasoning. However, the evidence from this study suggests that there is the potential for other processes to also be involved in treatment effects. Indeed, our long-standing cognitive model of paranoia has proposed multifactorial causality, particularly highlighting both reasoning and emotional processes,59 and these findings are consistent with a multifactorial theory of change; future research should investigate the mechanisms to elucidate both the treatment effects of SlowMo and the causal mechanisms of paranoia. We intend to pursue these questions in future studies.
A limitation of the study is that the design did not control for the effects of time with a therapist. The choice of a TAU control was made because we wanted to test whether or not SlowMo confers benefits over and above standard care. In addition, we aimed to examine the mechanism of change and wished, therefore, to have a control condition which was, as far as possible, inert with respect to reasoning. Adjunctive treatments in TAU were closely monitored and were found to be similar across the groups: a few participants were given individual psychological therapy (albeit, as would be expected, slightly more in the TAU group). The types, dosage and frequency of antipsychotic and other medication were similar in each group.
Another limitation of the study is that when recruiting participants we focused on persecutory beliefs in the context of a clinical diagnosis of schizophrenia-spectrum psychosis and did not make an independent research diagnosis. The resulting clinical and demographic profile of participants appears to have been typical of a community sample of people with psychosis and long-standing delusions. The relatively high consent rate and low attrition rates indicate that our findings should be generalisable to this population; however, a fuller diagnostic and symptomatic assessment might have been more informative in terms of the generalisability of the findings to diagnostically selected participants.
Finally, we found that the effects of SlowMo are more consistent on persecutory delusions than ideas of reference. This was unanticipated. It may be that the persecutory beliefs, in improving, shifted down the hierarchy of paranoia60 to milder ideas of reference, but that therapy prevented such ideas and their experiential components from being actively elaborated into paranoid fears of intentional harm. Whether or not this was the case, we infer, however, that SlowMo should be developed to enhance work on referential ideas.
A central focus of developing SlowMo was to enhance the user experience of therapy to address implementation barriers. We used inclusive, human-centred design to create, to the best of our knowledge, the first blended digital therapy for paranoia, which sought to accommodate a diversity of needs. The impact of this on the service user’s experience is explored further in Chapter 3. We also worked with user research interviewers in a coproduction research model; this enabled us to evaluate the experience of participation in the trial and of therapy qualitatively, as reported in Chapter 4. We found that treatment effects were not moderated by baseline clinical or cognitive characteristics, or the presence of a carer. Thus, the SlowMo therapy design appears to be effective irrespective of these variations, something of crucial significance in relation to real-world implementation. Consistent with these findings, there was excellent uptake of face-to-face sessions and the mobile app. This suggests that the design achieved its aims of being trustworthy, enjoyable, memorable and easy to use. 7
A flexible approach to formulation aimed to ensure that the understanding of targeted processes (fast and slow thinking) was individualised and accessible. Out-of-clinic behavioural work modelled app use and promoted therapy generalisation. The mobile app enabled further personalisation of the therapy, using bubbles as visual metaphors to support learning, with step-by-step support to slow down in the moment, and immediate access to safer thoughts (that might otherwise be hindered by memory difficulties and threat-related arousal). The findings suggest that targeted CBT for psychosis, incorporating design and technology to improve people’s therapy experience and uptake, can facilitate a focus on the processes most likely to result in real-world change.
Conclusions
The SlowMo trial has demonstrated clinically worthwhile results, with consistent, sustained positive effects across a range of outcomes. These effects match or exceed those typically observed for standard CBT for psychosis, but were achieved in fewer sessions, which were accompanied by excellent engagement and retention, validating the therapy redesign. The results indicate that the treatment worked, in part, to help people to slow down their thinking, to be more flexible about their beliefs and to worry less, and was not moderated by baseline clinical severity, cognitive problems or the carer relationship. Further understanding of the mechanisms that mediate these improvements would be valuable. The trial results also argue for further implementation studies testing SlowMo’s real-world delivery within clinical pathways for persecutory delusions in a range of clinical settings.
Chapter 2 The impact of patient and public involvement in the SlowMo trial: reflections on peer innovation
Background
Definitions of patient and public involvement in research
The National Institute for Health Research INVOLVE guidance61 on patient and public involvement (PPI) defines PPI as ‘research being carried out “with” or “by” members of the public rather than “to”, “about” or “for” them’ (reproduced with permission from INVOLVE. 61 Copyright INVOLVE February 2012). Consultation is defined as one-off or regular advice that may or may not be acted on, whereas collaboration involves service users and researchers working in partnership with clearly agreed roles.
Theoretical rationale and influences
The theoretical rationale behind PPI in the SlowMo trial is the expectation of epistemic improvements in the rigour, relevance and reach (the three ‘Rs’) of the research. 62 Indeed, there is growing evidence of the impact of PPI on the processes and outcomes of mental health research through the increased reach of recruitment,63 the relevance of dissemination that involves service users,64,65 and the enhanced rigour, openness and honesty of responses when service user participants are interviewed by their peers. 66–68 The roles for PPI in the SlowMo trial were, thus, focused on support for recruitment, qualitative interview data collection and dissemination strategies. The identification of clear roles also served to minimise the risk of tokenism in the PPI contribution, wherein the absence of specific aims for PPI aims leads to a self-fulfilling prophecy of failure to demonstrate value and impact. 69
Consistent with the epistemic framework for PPI, the study incorporated a consideration of these three Rs on the impact of PPI; the PPI outcomes are reported in this paper with reference to the Guidance for Reporting Involvement of Patients and the Public 2 (GRIPP-2) reporting checklist for PPI in research. 70 This approach was influenced by the previous experiences of the PPI lead (KG) in collaborating with experts by experience, peer researchers and consultants,71,72 and by the research team’s interaction with service users in the development of the intervention and subsequent grant application (as outlined in Chapter 3 and elsewhere7).
Conceptual models and influences
Ives et al. 73 differentiate between PPI that is ‘consultation’ (by invitation, top-down, pragmatic and process-oriented, focused on rigour, relevance and reach) and PPI that is ‘partnership alliance’ or ‘collaboration’ (which is bottom-up, rights based and process oriented, representing community values, joint decision-making and the encouragement to offer new ideas). Consultation in the SlowMo trial built on the ‘critical friend’ model, in which a critical friend is a trusted person who asks provocative questions, provides data to be examined through another lens and offers a critique of a person’s work as a friend. The friend is an advocate for the success of the work. 74 The consultant role is, thus, objective and outside the immediate research team. 73 However, the SlowMo PPI approach also incorporated a ‘collaborative’ model of peer research, in which peer research is ‘research that is steered and conducted by people with lived experience of the issue being studied’. 75 The peer researcher role included co-design of the methodology, data collection and analysis of the SlowMo trial qualitative research, and, in this respect, overlapped to some extent with Ives et al. ’s73 partnership alliance.
Patient and public involvement in the grant application phase
Prior to the current project, an extensive research programme incorporating both a feasibility study and an interactive human-centred design approach was undertaken, as outlined in Chapter 3 and Hardy et al. 7 Revisions were made to the name and design of the intervention: the advice on pacing and personalising the intervention led to an extension from six to eight sessions, the language was made more accessible and the content was individualised.
Patient and public involvement input for the current project commenced with the grant application. The PPI consultants influenced the choice of primary outcome measure, which assesses distress and paranoia. They also advised that the intervention should address well-being, functioning and distress, such that these were incorporated into the outcome measures, alongside a secondary outcome measure of self-esteem. All of the PPI consultants felt strongly that there was a need to improve treatments and access to treatments for distressing paranoia.
Lay compared with expert patient and public involvement
One challenge in the identification of suitable PPI members lay in the well-documented tension between the recruitment of lay service users and the recruitment of professionalised ‘expert’ PPI members73 as a result of the incorporation of both lay consultant and peer researcher roles. Ives et al. 73 propose a paradox. Lay PPI consultants may struggle to contribute meaningfully in peer researcher roles involving research leadership, data collection or analysis owing to their lack of appropriate training. Yet, the provision of the training required for collaborative peer research roles produces ‘expert’ service users with a track record of PPI, who may then no longer hold their original critical friend perspective, but instead share the language and perspective of the researcher. Staley76 argues that there are different levels of involvement that require different levels of expertise and appropriately matched training. In the case of recruitment, for example, consultation with lay service users may be valuable, whereas qualitative data collection requires training and the development of expertise. 76 In the SlowMo trial, this tension was addressed by recruiting service users with a range of prior PPI expertise and by delivering training at 6-monthly intervals with each training session focusing on a different role, and progressing from consultant to peer researcher over the course of the project.
Aims of patient and public involvement in the SlowMo trial
The aims of PPI in the SlowMo trial were that the PPI team would be involved in three specific aspects of work:
-
assisting study recruitment by presenting the research to teams and participants and giving their perspective on the study, and helping with the development of materials, such as leaflets
-
conducting qualitative interviews on participants’ experiences of receiving SlowMo therapy
-
assisting in the future dissemination of findings.
Funding was secured to provide 8 hours of consultation per month. To assist in meeting these aims, the PPI team would receive training and supervision, meet as a group regionally and project-wide, and be involved in study management meetings.
Method
Identification of patient and public involvement members
Patient and public involvement members for the SlowMo PPI teams were identified through a combination of (1) recruitment from pre-existing PPI research and consultation groups; (2) identification of people who had themselves taken part in previous or current SlowMo research; and (3) direct expressions of interest in response to publicity. The PPI teams comprised nine people: two women and one man in Sussex; two women in Oxford; and two women and two men in London. PPI members were aged between 30 and 56 years and one woman and two men (all from London) were from a minority ethnic background, while all others were white British. All members had previous experience of using mental health services for a psychosis-spectrum condition.
Methods through which patient and public involvement members were involved
Involvement commenced with a whole PPI team introduction and training session, which was co-facilitated by the study PPI lead (KG) and local site leads. This was followed by a second training session 6 months later. Thereafter, regional teams met approximately every 1–3 months, with group discussion and activity facilitated by the site lead, and later by a designated PPI lead at the Sussex site as well. The PPI team planned to meet as a whole study group once or twice per year. Finally, PPI members were invited to key study meetings, including the study launch, study steering meetings and their results meeting.
Patient and public involvement induction and training
SlowMo PPI participants each received either an introductory session to demonstrate how the SlowMo intervention worked or a full course of SlowMo therapy prior to commencing their PPI role.
A whole-group introductory training programme was designed by the PPI lead (KG) based on previous training programmes that were co-produced with the service user involvement leads. The training focused on (1) an introduction to PPI and the critical friend model; (2) discussing, disclosing and using experiences; (3) an introduction to research methods, PPI and peer research in the SlowMo trial; and (4) supervision and safe guarding. Subsequent whole-group training was more consultative and PPI led, and included (1) site updates; (2) specific project work; (3) role-play practice and feedback in preparation for qualitative interview data collection; and (4) the development of personalised role boundaries, disclosure, keeping well and supervision plans. As recommended by Friesen et al. ,77 the PPI training prioritised the development of service users’ capacities. Additional training and practice also took place in regional small-group settings, facilitated by the site leads. As the study progressed, these training and consultation sessions were also attended by the research assistants, who worked closely with the PPI members on site-specific activities and interview data collection.
Planned patient and public involvement at different stages of the study
The core tasks for the PPI team, which were outlined at the start of the study, were to (1) support recruitment activity, (2) conduct qualitative interviews with service users regarding their experiences of SlowMo therapy and (3) support dissemination activity. Early PPI activity comprised consultation regarding recruitment materials and activities, and content of the qualitative interview topic guide. Subsequent input took a more formal, collaborative PPI model and involved PPI members acting as peer researchers to collect interview data, analyse sections of transcribed data and co-produce resulting themes from the qualitative substudy with the research team, as well as co-producing the Plain English summary and providing written project summaries for use in lay journals and future publications.
Measurement of the impact of patient and public involvement
The impact of PPI on the project was captured in a number of ways. First, a PPI log in the form of a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet was created in consultation with the PPI team. This log enabled the PPI team to create a written record of the recommendations that arose from site and whole-team meetings; the study team response to these recommendations; whether or not recommendations were implemented; and the PPI team perspective on the outcome. This log provided the opportunity for a quantitative record of recommendations made and the percentage of these that were adopted. Second, at various stages throughout the project, both early on, in relation to consultation, and later during the qualitative substudy, the PPI team provided written feedback on their qualitative subjective experiences of involvement. Third, PPI members attended study meetings and their impact was documented in meeting minutes. Finally, there were tangible impacts in the form of outputs produced by and as a result of the PPI group.
Results
Measurement of patient and public involvement input
The PPI team made substantial contributions to the SlowMo trial across all phases of the study, as captured through the measurement of PPI input. First, the PPI log (Table 12) revealed a total of 107 actions or recommendations arising from the PPI meetings, of which 87 (81%) were acted on. A number of actions were proposed that emerged out of the PPI discussions that were not part of or went beyond that which was expected of the PPI team. These actions are included in the actions recommended and acted on in the table, but examples are also listed in the footnote to Table 12 and in Wider impacts.
| Recommendation | Site, n (uncertain whether acted on) | Total (% acted on) | ||
|---|---|---|---|---|
| Sussex | Oxford | London | ||
| Recommendations regarding recruitment | 9 | 3 | 4 | 16 |
| Acted on | 7 | 2 | 4 | 13 (81)b |
| Recommendations regarding interviews | 9 | 4 | 4 | 17 |
| Acted on | 9 | 3 | 4 | 16 (94)b |
| Recommendations regarding disseminationa | 13 | 0 | 4 | 17 |
| Acted on | 8 | 0 | 2 (2 uncertain) | 10 (59)b |
| Emergent novel recommendationsc | 12 | 3 | 0 | 15 |
| Acted on | 9 | 0 (1 uncertain) | 0 | 9 (60)b |
| Organisational recommendations | 37 | 2 | 3 | 42 |
| Acted on | 35 | 1 (1 uncertain) | 3 | 39 (93)b |
Second, qualitative feedback from the PPI team revealed impacts on the study, the PPI participants themselves and the NHS more widely, the details of which are summarised in Boxes 1–3 and Appendix 2, Box 4.
Overall, my experience of delivering PPI Work for SlowMo has been empowering. In the sense that I feel I have gained knowledge and insight into growing an idea to help people with the same/similar experiences as myself. I felt being actively part of the team and process, working alongside the mental health professionals leading the project, was mutually beneficial and helped influence improvements/approaches to the way ideas were executed. Lastly, and most importantly, feeling that, hopefully, my opinions/thoughts/feedback voiced has helped to design and add what would have been missing input from a perspective of someone accessing it. The process of learning how to conduct the interviews and actually doing the interviews has been, overall, a rewarding experience. Especially as the interviews gave me the opportunity to hear first-hand positive accounts of the benefits doing SlowMo had provided. The main and most important one to me being improved quality of life in at least one area such as socially, self-care, mental health, accessing services/help etc. I also personally gained new transferable skills, improved on existing skills and built up my confidence.
Presenting the trials to teams was an interesting challenge at first. Mainly as I had to overcome my own worries, apprehensions and maintaining my mental health well-being to feel confident to do the presentations. After overcoming that hurdle with support from my team and lots of practice, I found actually doing the presentations to be a fantastic way of engaging with the teams in a way to fully show both the logistical and real-world application/lived experience for who the project is aimed for.
Being able to be there to answer questions of my experience of using SlowMo in an honest and simple way felt more of an authentic and involved representation of the project, in the sense that it’s good to be able to talk to someone who has experienced a product versus someone who only knows the information on what it is/instructions/how it helps. One person has a review based on research and another has a review on how it feels to use for its intended use/audience. Therefore, I felt I could add input to any questions based on first-hand experience which is more direct and I think feels more engaging and reassuring of its usability/benefits.
Being part of the interview panel was both eye opening and reassuring. Eye opening in the way that it’s surprising the things you notice, the way you think about what people say and how they say it. For example, hearing what I perceived to be both positive and negative statements/answers, which helped make me think of qualities/characteristics/skills/knowledge/experience etc., needed to work in mental health care. Reassuring in the sense when I was part of the process and I think the best candidate has been chosen in a fair and reasoned way. This is essential as I feel the mental health sector has to pick people who care, who can cope with the work (for their own self-care) and have the ability to help people with their care. It’s all centred and focused around care but also feasibility.
This work was very rewarding for a number of reasons: I have always wanted to work as a peer researcher with other people who suffer with psychosis and try to give hope based on my own experience of recovery. I also found that the work was very varied and, although it involved plenty of travelling to reach participants at different locations in the Sussex area, the benefits were that each interviewee was unique and had their own individual journeys with the intervention. It was especially good to record that most of the participants had also found the SlowMo therapy useful in some way. I found that participants seemed to appreciate being interviewed by Angie (who had personally undergone the therapy) and myself because we had ‘lived experience’ of psychosis. We were aided by an excellent team of research assistants, who organised the logistics of the interviews and, although I found it a bit daunting at first, I was well trained and rehearsed beforehand. Help was given in the early stages by doing mock run throughs with a list of questions and prompts, coproduced during monthly meetings by the PPI team and other research staff. I was also encouraged to write out my own ‘crib sheet’ to introduce myself in interviews and received useful tips and feedback throughout the entire process. It did take a while to get the first interview underway, but, after beginning this part of the study, I never felt overwhelmed or experienced any problems with participants despite occasionally touching on difficult subjects.
It was good to have the researchers working with us to develop some coding after transcribing the SlowMo post-therapy qualitative interviews that Angie and I carried out. I think it was perhaps an issue initially that we needed to have ‘respondents’ validity’ by going back to the interviewees to check their views had been captured properly, which didn’t turn out to be possible, but it was decided that Angie and I could do this on their behalf. The whole qualitative team, however, met to go through the transcripts and help develop themes to make sure everyone’s ideas were heard and give a balanced perspective, not just from service users. The researchers were very good at keeping everyone informed as the project progressed and sent out revisions of work for feedback on a number of occasions between meetings. They answered any queries I had and it was evident that the coding became clearer and more concise over time and I thought definitely reflected the key points that came out in the interviews. It was also nice to see a diagram of the process in the paper and that they had incorporated Angie’s and my contribution as a whole (including in the final submission).
When conducting the interviews, Angie thought that she and Dan had a good deal of time to rehearse the questions, but the experience of doing them for real gave confidence. Dan and Angie’s confidence helped the researchers to carry the research forward when the transcripts and coding came about. When carrying out the coding, Angie thought that it was important to recognise the relationship between the therapist and the participant. She also stressed that people on the SlowMo trial had not generally been offered any other therapies before and it was important to bring out these issues. Angie liked the way the researcher wrote the themes and made it easy to understand. Angie did say, however, that it was sometimes difficult to think of things off the top of her head, but, when the coding was done, she was happy to see that when participants were asked about the SlowMo therapy it was noted that it was clear that service users did not feel alone.
Third, minutes from study management meetings indicated that direct attendance and input of PPI members to these meetings occurred annually, despite an initial plan for at least 6-monthly attendance. In addition, one PPI member attended the launch meeting in 2018, two PPI members attended a study management meeting in 2018 and three members attended a study management meeting in 2019 that had a specific PPI focus and presentation.
Finally, there were numerous tangible products from the PPI input, the impacts of which are outlined in the following section, such as service user interviews, leaflets, press releases and British Broadcasting Corporation (BBC) coverage, that significantly enhanced the research, the experience of the PPI members themselves and the impacts on the NHS and wider community.
The impact of patient and public involvement
On the research
The positive impacts of PPI on the research study included the production of new recruitment leaflets and attendance at community team meetings to promote recruitment; the collection and analysis of interview data to explore service users’ experience of SlowMo therapy; and the co-production of the Plain English summary. The leaflet was produced by the team as additional patient-facing information to aid recruitment. It was also used by the PPI team as promotional material at team presentations, recovery college meetings and meetings of other such groups where service users were in attendance. For the qualitative interview study, which is reported in full in Chapter 4 of this report, the PPI team co-produced the focus group topic guide and conducted 22 qualitative interviews, all of which were led by either two PPI members or a PPI member supported by a research assistant. The data were analysed in two phases. In the first phase, the Sussex PPI team analysed a transcript collaboratively to produce a coding framework and held a series of meetings to reach consensus on initial themes. In the second phase, feedback was obtained through consultation with the London and Oxford PPI teams, and a further set of meetings led to a consensus on the final themes. In terms of study management, the PPI team co-produced regular summaries of PPI input to the steering committee and funding body. Dissemination outputs to date have included the co-produced Plain English summary, as well as a paper (currently in draft form) on the qualitative substudy of service users’ experiences of SlowMo therapy.
The major benefits of PPI on the trial were that the target recruitment was achieved with support from the PPI team; the qualitative substudy was co-produced and provided rich data concerning service users’ experiences of SlowMo therapy; and the Plain English summary of the results was co-produced: PPI members were provided with key method and results sections and were encouraged to write a lay summary in their own words. This was then drafted, shared and final feedback obtained before completion to produce the Plain English summary. A further impact of PPI input lay in the emergent outcomes that will be described in Wider impacts.
On the individual patient and public involvement members
There was a consistent core PPI group of five members throughout the 3-year study. PPI members worked well together and became more confident in their roles over time. Subjective qualitative feedback (see Boxes 1–3) revealed that PPI members felt that the PPI was well organised. Although PPI members found participation in the project daunting and challenging, as it involved a lot of travel, required them to overcome the hurdle of team presentations and was difficult to think on the spot, they felt well informed, well trained and encouraged, and were given time to understand and contribute such that everyone’s ideas were heard. PPI members reported impacts on their confidence, career aspirations, knowledge, insight and skills to support themselves in their roles. They felt that the work was varied, rewarding and empowering. There were no problems identified despite the difficult topics being discussed and the PPI input was valued, for example by service user participants, who appreciated being interviewed by service users who understood their experiences. The PPI members felt that there was a mutual benefit in helping to improve how ideas were executed and in providing authentic first-hand experience from someone at whom the therapy is aimed. However, not all PPI members provided subjective feedback; feedback was provided by PPI members who were more actively engaged.
Wider impacts
Importantly, in addition to the expected activities and resulting impacts, there were a variety of linked and ‘emergent’ activities and impacts. At a regional level, one of the PPI members produced an open letter reflecting their positive experiences of PPI membership and the importance of both PPI and research alongside front-line NHS work. This letter (see Appendix 2, Box 4) was used by the regional NHS PPI lead to promote and encourage more service users to take up PPI roles.
The PPI team developed the concept of the ‘SlowMo People’ website/page (Figure 4; see http://slowmotherapy.co.uk/slowmopeople/, accessed 26 May 2021) based on the Humans of New York website (www.humansofnewyork.com/). The website aimed to tell individual stories of how fast thinking can trip you up and how slowing down for a moment can be helpful. Drawing on both service users’ and researchers’ stories, the aim was to normalise the fast-thinking style while also presenting the real-life personal experiences of the impact of slowing down.
Finally, the Sussex PPI lead, team and therapist worked with one PPI member, the NHS communications team and a local newspaper to produce an article about the experience of paranoia and voice hearing, and the positive impact of receiving the SlowMo intervention. This was picked up nationally, resulting in a short film that was aired on prime-time television on the BBC’s The One Show in April 2018 (http://slowmotherapy.co.uk/news-2/, accessed 26 May 2021). The BBC’s The One Show has an audience of 5 million people. Feedback through Twitter suggested a major community value in providing a normalising portrayal and hopeful outcome for psychosis and voice hearing, for both general public and the people suffering with these experiences. The short film was also subsequently shown to people at the start of the therapy.
FIGURE 4.
The SlowMo People web page.
Factors that enabled or hindered the process or impact
The challenges to PPI involvement in the research included geography, travel, funding, regional PPI co-ordination and the well-being of the PPI team.
Contextual factors that enabled or hindered the process or impact
The PPI plan was led by Kathryn Greenwood, who has significant experience in co-leading PPI work from the Sussex site, which itself has a good track record in PPI. However, PPI should ideally be led or co-led by peer researchers. The study ran across three sites and an early decision was made to hold a small PPI group at each site to contribute meaningfully to local recruitment challenges and contribute to interview data collection. However, some PPI members struggled with travel on public transport, which created logistical challenges for attending meetings. PPI co-ordination was led from one site (Sussex) and all three sites did not have equal capacity to co-ordinate local PPI groups, given different staffing and logistical challenges. As a result, PPI meetings at one site were less frequent and the preparation and conduct of qualitative interviews were more challenging, with fewer interviews conducted. The study management meetings were in the central site (London), which involved significant time and travel for some PPI members to attend meetings. There was also variation in the confidence and capacity to use technology to join remotely. As a result, the PPI team members’ input was limited in study management meetings (although it was represented as a standing agenda item at each meeting by the PPI lead, KG) and was instead prioritised for collaborative discussion at a small number of specific study meetings that were well planned and co-ordinated in advance to enable attendance.
Process factors that enabled or hindered the process or impact
The study team welcomed PPI involvement in the study and responded creatively and flexibly to ideas and challenges as they arose. The PPI team remained relatively stable, with five PPI members contributing for the entire project. There was variation in attendance at the whole-site PPI training and consultation sessions, which was related to factors such as mental well-being. Funding was comparatively limited for PPI co-ordination and input at the multisite level. This may have affected the robustness of data collection for the PPI log. However, redistribution of funds across sites based on activity level ameliorated other impacts. There was also a potential challenge identified with respect to the aim for meaningful PPI input to dissemination activities occurring beyond the funding window. These included the Plain English summary, other dissemination materials, qualitative project publication, website updates and a presentation at the stakeholder event. An agreement was reached to fund costed service user consultants’ time for specific dissemination activities beyond the end of funding. Finally, there were understandable fluctuations in the life situation, health and well-being of PPI members at all sites, which affected participation in meetings and other PPI activities. Where this occurred, flexible individual plans were put in place to support meaningful contributions. One PPI member decided to stop attending PPI meetings before the end of the study. Another PPI member sadly passed away, which naturally had a significant impact on the team and was discussed both individually within the local site and as a wider team in the subsequent all-site meeting.
Discussion
How patient and public involvement influenced the whole study
The main impacts of PPI within and beyond the SlowMo trial were in the qualitative substudy (see Chapter 4) and the emergent innovations that were identified as wider community impacts. The qualitative substudy was a planned part of the research project that aimed to investigate participants’ experiences of the SlowMo intervention and the associated blended digital approach, including use of the in-session web app and mobile app. This was a strength of the planned PPI input, as the substudy was fully collaborative, from the development of the topic guide to the PPI facilitation in all interviews across all three sites, the whole PPI group involvement in the thematic analysis and the final summary of the results. This substudy is reported in detail in Chapter 4 and in an upcoming paper. The contribution of PPI to the recruitment of participants in one site was highly impactful and completely opened up responses to the study from some teams, for which referrals went from zero across two different trials to recruitment of 15–20 people from the same team. PPI was also central to recruitment of excellent research staff, with a PPI member taking an active role on the interview panel.
The most significant emergent innovations included the BBC’s The One Show broadcast and SlowMo people page that, although consistent with planned dissemination activity, were highly innovative and creative, and went well beyond the initial expectations of producing patient leaflets, lay summaries, presentations, and co-produced, peer-reviewed and service user journals.
Limitations of the patient and public involvement contribution in the SlowMo trial
Overall, the PPI contribution to the SlowMo trial was well supported, with clear impacts on the research and wider society, and positive experiences for individual PPI members, who felt that they were valued, supported, empowered, rewarded and understood, and that their contributions mattered. They also described positive personal growth in knowledge, skills and confidence. The PPI in the SlowMo trial met five out of the six UK standards for PPI:78 being inclusive, working together, supporting learning, employing plain-language communication and evaluating impact. The only standard not explicitly met related to involvement in research governance, which was less relevant to this specific project. However, although many aspects of PPI in the SlowMo trial went exceptionally well, there were a number of challenges. The funding requested for PPI was lower than INVOLVE recommendations,78 there was no service user PPI co-lead and there were challenges to managing PPI across geographies and sites. Although some peer-led suggestions and innovations were adopted, others were only partially taken forward or were not supported owing to lack of capacity in the PPI and research teams, or the need to deliver specific a priori trial objectives.
The evaluation of the patient and public involvement impact in the SlowMo trial
There are many advocates of the need to evaluate the impact of PPI in research (e.g. Gillard et al. 79 and Barber et al. 80). However, a common criticism of PPI is that it is difficult to demonstrate its unique contribution and its added value to a research project. Some studies81 have evaluated PPI systematically using questionnaires, and semistructured and qualitative interviews repeated longitudinally. However, this approach may in and of itself be couched in empirical research methodology. 82,83 Indeed, Friesen et al. ,77 have argued that involvement is more than what is captured by a singular epistemic focus on research impact. 84
In the SlowMo trial, we planned to evaluate the impact both quantitively, in terms of the proportion of PPI recommendations that were adopted of those that were recorded in the log, and qualitatively, in terms of subjective feedback and study group document review. The log was relatively well maintained; however, owing to resourcing issues and the challenges of updating across multiple sites, it is possible that some entries were omitted. In addition, subjective experiences were limited to PPI members who were more engaged, thus being open to the criticism levied by Petit-Zeman and Locock85 that perhaps diverse voices are not being heard. It is also acknowledged that the proportion of recommendations that were adopted is a blunt measure of impact, being dependent on the number and nature of the recommendations made and the ease with which they could be achieved. Some recommendations had greater potential impact and value than others, and a future log might also consider the nature and relative weight of recommendations adopted and the reasons for them not being enacted.
The PPI team collaborated on and were heavily involved in the qualitative substudy of service users’ experiences of the SlowMo intervention. This study produced new knowledge in the form of a richer understanding of the service users’ experiences of the trial, intervention content, blended therapy approach, service users’ recommendations to improve the technological experience and contribution to outcomes. However, it could be argued that the plan for this substudy was developed by the research team and that, although co-production was really strong, the added value of the PPI collaboration cannot be fully disentangled.
Perhaps the clearest and most tangible impacts were not those that emerged from the narrow epistemic focus on enhanced research quality, but those that arose as unique outcomes with added value from the PPI, such as the BBC’s The One Show film and the SlowMo people webpage. There is often limited scope for these emergent community-based impacts within a funded research study, and several other such innovations, such as the use of thunderclaps, Twibbons and a public Facebook page, which were also proposed by the PPI team were not taken forward. Although a variety of factors affected these decisions, funded research studies may necessarily be forced to limit unanticipated innovation.
Theoretical-conceptual developments in the definition of patient and public involvement roles
Traditional PPI roles that were utilised in the SlowMo PPI included the critical friend model of consultation and the peer researcher model of collaboration. These roles had an impact across the research aims, design, ethics, delivery and implementation of research, as well as on the public, researchers, participants, organisations and wider community. 64,67 However, as highlighted by Friesen et al. ,77 PPI should perhaps focus not only on the impact of PPI on research knowledge, but on the way that power and decision-making are shared in the knowledge-making process.
An important and novel role for PPI in research is that of an emergent peer innovator. Experience in the SlowMo trial and other studies72 has identified that an added value of PPI in research is the unexpected, emergent outcomes that arise when a group of enthusiastic service users come together within a collaborative framework linked to a specific study. There is significant potential for impact arising from the freedom and desire to extend this impact to aid service users and communities beyond the specific, predesignated constraints of the research study. In the current study, there were numerous emergent ideas and outcomes, including the newspaper article (www.theargus.co.uk/news/15963698.innovative-app-help-patients-schizophrenia-launched-sussex/, accessed 26 May 2021) and the BBC’s The One Show coverage (available on the SlowMo website) and the SlowMo people website. By taking these ideas forward, the SlowMo PPI collaboration enabled power-sharing in the knowledge-making process, as recommended by Friesen et al. ,77 to produce a response to community-level ignorance and stigma: the BBC’s The One Show was aired on prime-time TV to over 5 million viewers. These ideas have the potential for widespread impact, but not all of these ideas can be supported within a specific research study and budget. A challenge for future PPI in research will be how to ensure cost-effective study delivery while providing space and support for peer innovation where it emerges.
Future recommendations
Future projects should have a comprehensive and detailed PPI plan, akin to the detailed project plan and costed with reference to INVOLVE guidance,78 at the grant application stage. Arguably, PPI input to grants would benefit from the requirement for a detailed PPI plan at the submission stage, alongside the detailed project plan, flow chart and Gantt chart. We recommend that grant-funding bodies permit or make available a proportion of the funded PPI plan to facilitate and support emergent peer innovation, and to allow for the development of important creative products and impacts that arise from this PPI collaboration. The enhanced community impact and higher national profile for PPI roles and recruitment might encourage more service users to take up this role, which would in turn create a larger and more diverse pool of peer researchers from whom PPI leads would emerge. Finally, to harness this interest and diversity of representation would require proactive outreach and flexibility in opportunity for engagement.
Chapter 3 The user experience of SlowMo therapy in the trial: mobile app adherence, participant survey and technical problems
Background
SlowMo therapy is, to the best of our knowledge, the first digital therapeutic for psychosis developed using inclusive human-centred design. 20,21 The design aimed to support adherence by improving the user experience of a targeted CBT for paranoia for the widest possible range of people. This chapter will describe the digital literacy of the therapy sample; the adherence to the SlowMo mobile app based on self-reported and system analytics; a survey evaluating the enjoyment, usefulness and ease of use of the SlowMo mobile app; and the technical issues related to the SlowMo therapy software and hardware.
Why focus on the user experience of psychological therapy?
User experience reflects the extent to which an intervention is perceived by a person as useful in meeting their needs and is enjoyable and easy to use. 21 Ease of use, or usability, has been defined as ‘a quality attribute that assesses how easy interfaces are to use’. 86 It relates to the ease with which a person can become competent in using a product or service, achieve their objectives for use and recall how to use the product or service during future interactions. User experience, therefore, determines how likely people are to engage with a design and continue to use it. This has been relatively neglected in psychological therapy, for which the focus has instead been on efficacy by developing interventions that target evidence-based mechanisms to improve mental health outcomes. 87 These interventionist-causal approaches have shown promise over traditional psychological therapies for psychosis. 88
However, there are significant barriers to the effective implementation of these targeted therapies for psychosis and efficacious interventions will be limited in their impact if stakeholders are not sufficiently willing and able to use them in routine care. 1 Obstacles include therapy being difficult to access owing to resource constraints, uptake being low even when therapy is offered, and people struggling to adhere to therapy and apply it to their problems in daily life. 5,89–91 Optimising the user experience of therapy provides a means of addressing implementation barriers and improving uptake and adherence. Psychological concepts and techniques can be ‘reframed’ by redesigning conventional means of supporting behaviour change. 92,93 Digital technology affords unique opportunities to address the user experience of therapy because the user interface (i.e. the digital artefacts through which therapy is delivered) can be modified and personalised to meet people’s needs. 94
Digital therapeutics for psychosis
Digital therapeutics for psychosis are in their infancy, with encouraging findings for mobile apps, virtual reality and web-based support. 95–102 The use of digital therapeutics requires access, willingness to engage with technology and sufficient competency or support. Promisingly, people with psychosis appear to have comparable access and use of technology to the general population. 103–106 However, people with psychosis have higher rates of digital exclusion if they are older, are from an ethnic minortiy background, experience cognitive difficulties or experience persisting symptoms, resulting in a ‘digital divide’. 104,107,108 Being female and of white ethnicity is associated with a higher rate of digital therapy completion. 109 Nonetheless, digitally excluded people with psychosis are willing to access technology. 107,110 Torous et al. 111 found that an interest in mental health apps does not translate to high use, as only 10% of outpatients had a mental health app downloaded on their telephone, and privacy and economic concerns were common. This is consistent with findings across digital health, for which the level of implementation of therapeutics in real-world settings is poor and rates of attrition are high, especially in the absence of interpersonal support. 112–114
Poor user experience has been highlighted as a critical barrier to engagement with digital therapeutics, particularly for marginalised groups. 115,116 Digital designs are often ‘skeuomorphic’, replicating analogue versions of therapy artefacts and, therefore, failing to address barriers to use. 117 For example, a commonly used tool for identifying and modifying distressing cognitions in CBT, a thought record, is often digitally reproduced with the same interface as paper versions: usually text prompts and response boxes presented as a form. A skeuomorphic digital thought record does not address obstacles to its use, for example being cognitively demanding and having an unappealing interface. Graham et al. 94 propose that human-centred design should underpin the development of digital therapeutics because improved user experience is expected to mediate better clinical outcomes. Human-centred design involves developing a rich understanding of the problem area and its context, from a range of stakeholder perspectives, to identify valued outcomes. 92–94,118,119 Therefore, participatory design, or co-design, is inherent to this approach and entails direct user involvement. 120,121 However, participatory design in digital mental health has tended to neglect design-thinking methodology, which can constrain innovation so that new designs are variations of the status quo. 92,122 In addition, a risk inherent in participatory design is that the most willing, able and vocal users are more likely to be involved, neglecting the needs of the marginalised people, whom the design should address. To reduce health inequalities, attention needs to be paid to a diverse range of people with psychosis, particularly those who are from a minority ethnic background, have cognitive difficulties and who experience severe symptoms. 109,123–127
The development of SlowMo therapy: inclusive human-centred design
The SlowMo therapy is an exemplar of an inclusive human-centred design approach to developing digital therapeutics for psychosis. 7 Prior to the SlowMo trial, a multidisciplinary team of people with lived experience, clinicians, researchers, industrial designers and software developers integrated the best practice principles of design thinking and participatory design to create the therapy. The Design Council’s128 double-diamond method was used, which consisted of ethnographic investigation of the problem context (the discover phase), and using insights from this phase to reframe the problem and generate a design brief (the define phase). Solutions to the brief were generated and iteratively tested with users (the develop phase), with feedback determining the optimal design for development (the deliver phase). Our strategy for involving people in the design process, inclusive human-centred design, was different from conventional human-centred design. It involved purposive sampling of people from the extreme ends of the distributions of relevant variables (i.e. gender, age, ethnicity, cognitive abilities, use of technology and attitudes to therapy) to increase the likelihood that the design met the needs of the widest range of people. 20 The inclusive, human-centred design research identified the importance of therapy being usable, trustworthy, enjoyable, personalised and normalising, and of it offering flexible interpersonal support, in line with other recommendations for improving implementation of digital therapeutics for psychosis. 129–131
This iterative process and feedback led to the development of the SlowMo therapy, a blended digital therapy consisting of an intuitive web app to augment the experience of face-to-face individual therapy sessions, which is synchronised with a native mobile app for use in daily life. SlowMo therapy is presented as a journey that supports people to notice the large, fast-spinning and grey worry bubbles that fuel distress, and to make use of the slow-spinning and coloured bubbles to shrink fears and feel safer. The use of personalisation, ambient information and, particularly, visual rather than verbal metaphors aimed to provide a step change in therapy delivery by enhancing appeal and reducing cognitive demands.
The mobile app consisted of a redesigned CBT thought record for managing paranoia that attempted to overcome the aforementioned limitations of paper versions. This incorporated an attractive visual representation of thoughts and their attributes; simple interactions to support monitoring and modifying thoughts; easy access to previously identified helpful suggestions and thoughts; positive reinforcement for engaging in slowing down; and a flexible interface that afforded several ways of slowing down fast thoughts, depending on a person’s needs and preference (e.g. quick access to safer thoughts on the home screen or working through all stages of slowing down a thought over multiple screens). Concerns about privacy were addressed by developing a native app with opt-in data transfer. The mobile app also relied on user-initiated interaction and optional push notifications to accommodate those who might find notifications intrusive. 95,132
The SlowMo therapy design has now been tested in a large sample of people with psychosis in a multicentre RCT, as described in Chapter 1. Therefore, it provides an opportunity to validate the inclusive, human-centred design of our digital therapeutic for psychosis and to evaluate whether or not the design was successful in achieving its aims.
Evaluating user experience: validation of the SlowMo therapy design
Evaluating the user experience of digital therapeutics requires moving beyond the usual focus on efficacy and effectiveness outcomes in intervention research. User experience assessment can include subjective measures of usefulness, usability and satisfaction, as well as objective means, such as system analytics of passive or active interactions with technology. 94 However, there is little consensus regarding how best to define and measure user experience, and studies often have no theory or data to support the criteria employed. 133 A recent review of studies evaluating the usage of digital therapy found that more frequent and prolonged use was assumed to be desirable. This assumption risks conflating engagement with adherence and not recognising that disengagement may reflect e-attainment [i.e. technology-assisted achievement of goal(s)] of personal goals if skills acquisition has been sufficiently supported. 115,134 Therefore, adopting multiple metrices of engagement, reflecting the goals of both the technology and the individual, is recommended.
A further concern is whether or not digital therapeutic use is impeded by technical problems with the hardware or software, and whether or not adverse events that are related to technology occur. 135,136 This chapter will describe a multidimensional assessment of the SlowMo therapy user experience to evaluate whether or not its inclusive, human-centred design is likely to support implementation for a diverse range of people. 7,94,118 Excellent adherence rates for the SlowMo web app sessions and therapy fidelity have been reported in Chapter 1; therefore, the mobile app adherence will be the focus here. The therapy sample will be characterised in relation to their digital literacy, followed by presentation of the SlowMo mobile app adherence based on self-reported and system analytics, a survey evaluation of user experience, and rates of technical problems and technology-related adverse events. Chapter 4 will build on this with a co-produced qualitative study of the trial participants’ verbal accounts of their experience of SlowMo therapy.
Research questions
The research questions are as follows:
-
What is the digital literacy of the therapy sample and is this impacted by service users’ characteristics (i.e. gender, age, ethnicity and paranoia severity)?
-
Does the SlowMo mobile app have acceptable rates of self-reported and system analytics adherence, and are they impacted by service users’ characteristics (i.e. age, gender, ethnicity and paranoia severity)?
-
What are the self-reported rates of usefulness, enjoyment and usability for the SlowMo mobile app, and are they affected by service users’ characteristics (i.e. age, gender, ethnicity and paranoia severity)?
-
How prevalent are technical problems associated with use of the SlowMo web app and mobile app?
-
How prevalent are adverse events associated with use of the SlowMo web app and mobile app?
Methods and measures
Digital literacy
Digital literacy was investigated at the beginning of therapy for all participants who attended at least one session in relation to (1) self-reported ownership of smartphones or access to a computer, (2) frequency of use of smartphones (excluding telephone calls) and computers, and (3) confidence in using smartphones and computers. Frequency and confidence of use were assessed on scales from 0 to 100, with the anchors of ‘never’ and ‘all the time’, and ‘not at all’ and ‘totally’ for frequency and confidence, respectively. These digital literacy variables were selected because they were the most relevant to the user experience of SlowMo therapy, given that the therapy involved using a laptop computer (in sessions) and a smartphone (outside sessions). Given that reported health inequalities related to demographic factors, we planned to examine digital literacy in relation to gender, age and ethnicity.
Self-reported and system analytics of adherence to the SlowMo mobile app
Adherence to the SlowMo mobile app was assessed subjectively and objectively to validate whether or not the design had the intended effects on the user experience and subsequent usage. Participants were asked to report at the end of therapy how much they were using the mobile app and if they intended to use it in the future (rated from ‘0 – never’ to ‘100 – all the time’). Objective adherence was assessed according to analytic data for mobile app use. We operationalised adherence as at least one out-of-session interaction for a minimum of three of the therapy sessions. This was based on seven therapy sessions because session eight data were not valid; mobile app data syncing did not occur following the end of therapy (the mobile app was a native app and we did not have informed consent for ongoing data collection after therapy had ended). The adherence criteria were based on the assumption that engagement with the mobile app would be indicative of its usefulness, usability and appeal; however, sustained use throughout therapy was not necessary given that the aim was to support internalisation of the skill of slowing down in response to fast thinking. 15,115 Home screen views were selected as the target interaction given that slowing down with the mobile app is undertaken through viewing the home screen (to access safer thoughts) or subsequent screens that provide multiple routes to slowing down.
User experience survey for the SlowMo mobile app
User experience was assessed by a 12-item user experience survey (UES) (see Appendix 3) that was adapted from a 26-item self-reported measure employed by Ben-Zeev et al. ,137 in a study of a mobile app, FOCUS, that supports self-management of psychosis. The UES consisted of four items assessing usefulness, four items assessing usability and four items assessing enjoyment. Each item was rated on a scale from 0 to 100, with anchors of ‘totally disagree’ and ‘totally agree’. Ratings for each item were summed (with four items reverse scored) (range from 0 to 400 for each category) and a percentage score calculated. This exercise was undertaken at the end of therapy for participants who had completed all eight therapy sessions. We also examined the impact of service users’ characteristics on self-reported user experience on the survey.
Technical problems related to the SlowMo web app and mobile app
The therapists completed a survey at the end of each therapy session to document whether or not in the sessions there were any technical problems with internet connectivity, any technical problems with the web app software, any technical problems with data syncing between the web app and the mobile app and any other participant-reported technical problems. These were all recorded as ‘yes’ or ‘no’, with a brief description of the nature of the problem, if any.
Adverse events related to the SlowMo therapy hardware and software
As noted in Chapter 1, adverse events were actively monitored for the duration of the trial and were categorised by severity and relatedness to trial participation recorded. In addition, for any adverse events related to trial procedures in the therapy group, it was documented whether or not there was any evidence indicating that the event was related to the SlowMo software (i.e. the web app and mobile app) and hardware (i.e. the mobile phone provided to participants). Any events were rated from 1 to 5: 1, definitely related; 2, probably related; 3, possibly related; 4, unlikely to be related; and 5, not related. This information was then reviewed by the chairperson of the DMEC and the DMEC.
Statistical methods
Summary statistics were calculated for all variables for the entire SlowMo therapy group and split by site. To investigate the impact of participant characteristics on user experience, we performed independent group t-tests (gender and GPTS paranoia severity) or one-way analyses of variance (ethnicity and age) for the continuous dependent variables of digital literacy, self-reported app adherence and the UES, and chi-squared tests for smartphone ownership, computer access and system analytics app adherence (rated adherent/non-adherent). Independent group t-tests were also conducted to examine the association between system analytics adherence and pre-therapy smartphone literacy. Categories for the participant characteristics were gender (male and female), age (< 35, 35–49 and ≥ 50 years), ethnicity (white, black and other ethnicity – consisting of Asian people and people from other ethnic backgrounds) and paranoia severity (low and high, dichotomised by a median split of < 61 and ≥ 62 on the GPTS).
Results
Digital literacy
Smartphone ownership and computer access in the SlowMo therapy group among those participants who attended at least one session, together with the frequency of use and confidence, are displayed in Table 13 by site and overall. This indicates that just over three-quarters of the sample owned a smartphone, which was consistent across all sites. For smartphone owners, the frequency of use was comparable in Sussex and Oxford and lower in London. A similar pattern was found for smartphone confidence. Computer access, frequency of use and confidence were the highest in Sussex, followed by Oxford, and then London. The impact of gender, age, ethnicity and paranoia severity on smartphone and computer ownership and on smartphone use and confidence is shown in Figures 5 and 6, respectively, with inferential statistics presented in Appendix 3, Table 22. There were significant age differences in smartphone literacy, with older people being less likely to report ownership and confidence in using a smartphone. Older people and women were also significantly less confident in using computers. Ethnicity had a significant impact on computer access and smartphone and computer confidence, with people from a black ethnic group reporting less access and less confidence than those from white and other ethnic groups. Paranoia severity did not have a significant relationship to digital literacy.
| Variable | Site | Overall | ||
|---|---|---|---|---|
| Sussex | Oxford | London | ||
| Smartphone ownership reported, n (%)a | 44 (77.2) | 30 (76.9) | 48 (77.4) | 122 (77.2) |
| Computer access reported, n (%)b | 42 (77.8) | 26 (66.7) | 34 (56.7) | 102 (66.7) |
| Smartphone use, mean (SD) | 63 (37) | 61 (38) | 57 (35) | 60 (36) |
| Smartphone confidence, mean (SD) | 65 (32) | 62 (31) | 55 (36) | 60 (33) |
| Computer use, mean (SD) | 51 (38) | 46 (34) | 43 (33) | 47 (35) |
| Computer confidence, mean (SD) | 63 (32) | 57 (26) | 50 (32) | 56 (31) |
FIGURE 5.
Smartphone ownership and computer access among people attending at least one therapy session (n = 168). (a) Smartphone ownership by gender, (b) computer access by gender, (c) smartphone ownership by age, (d) computer access by age, (e) smartphone ownership by ethnicity, (f) computer access by ethnicity, (g) smartphone ownership by paranoia severity and (h) computer access by paranoia severity.
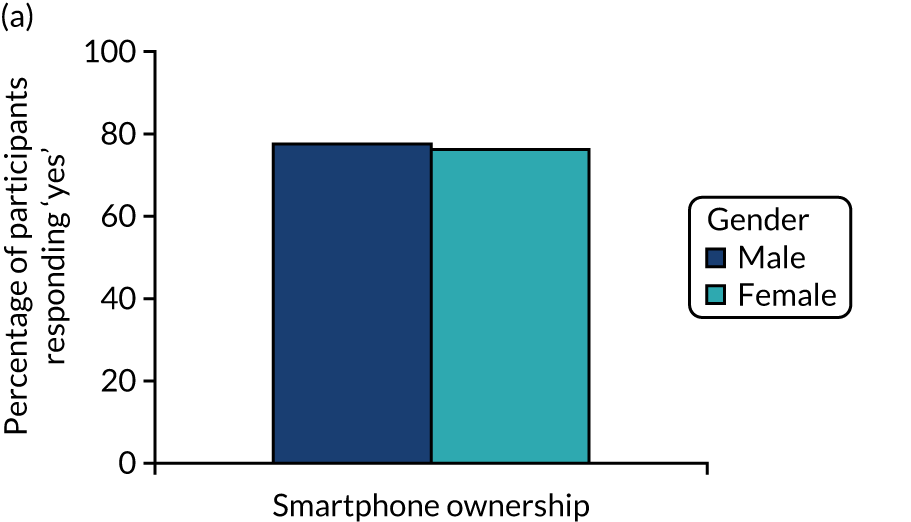
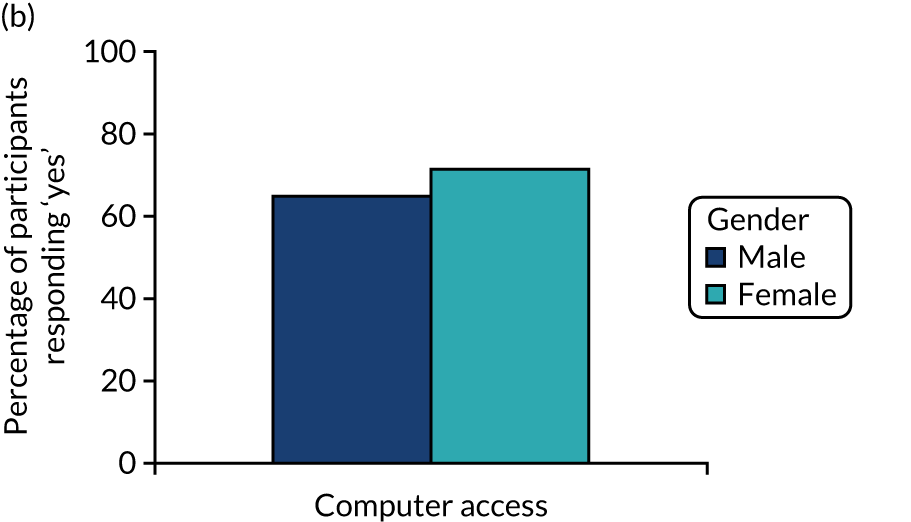
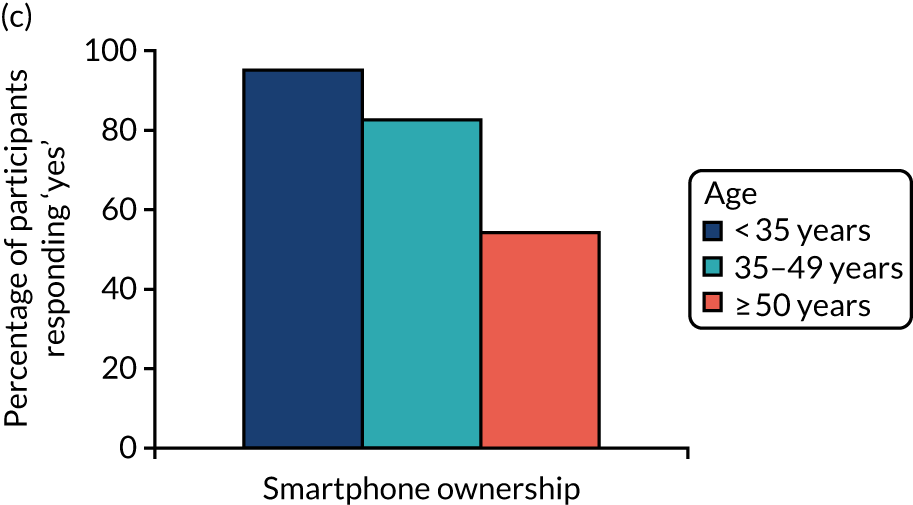
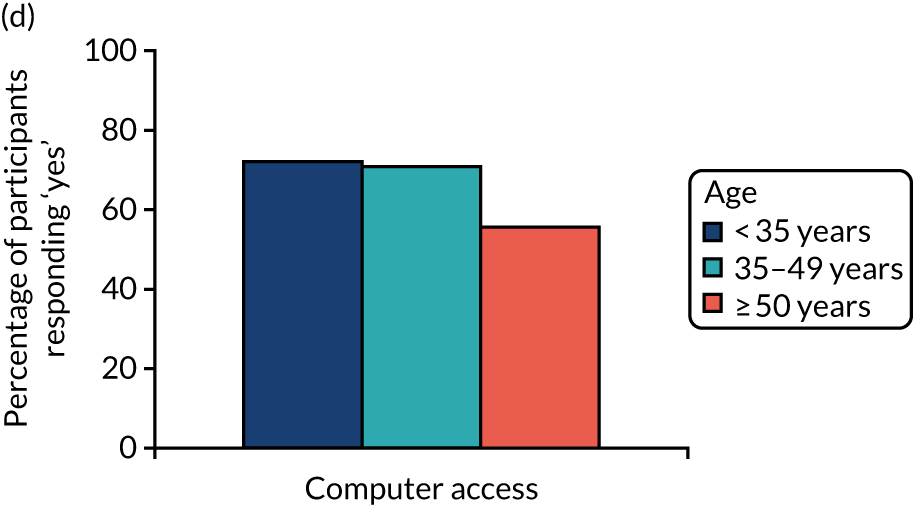
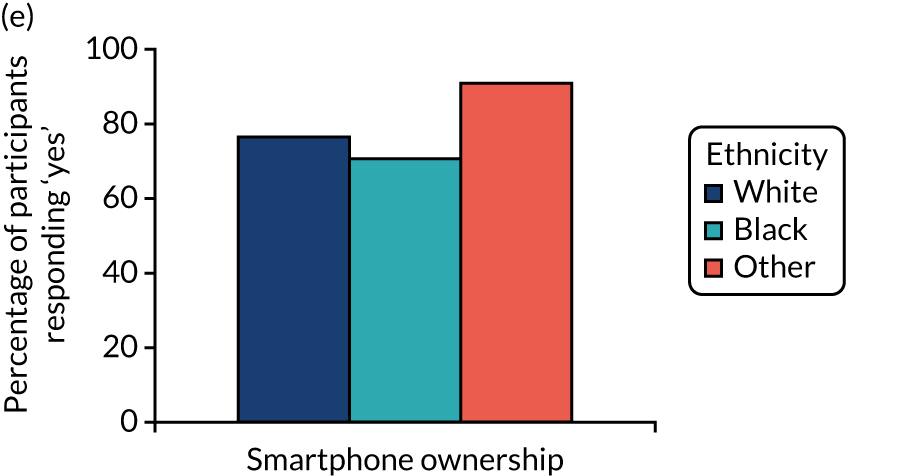
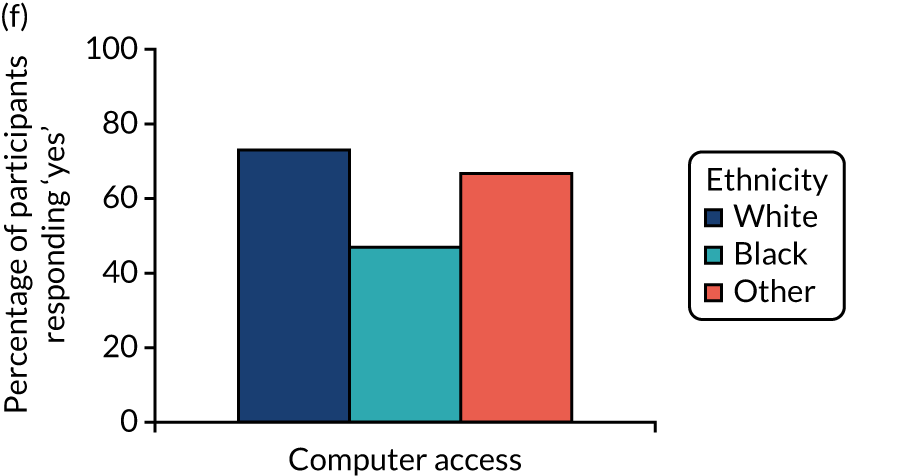
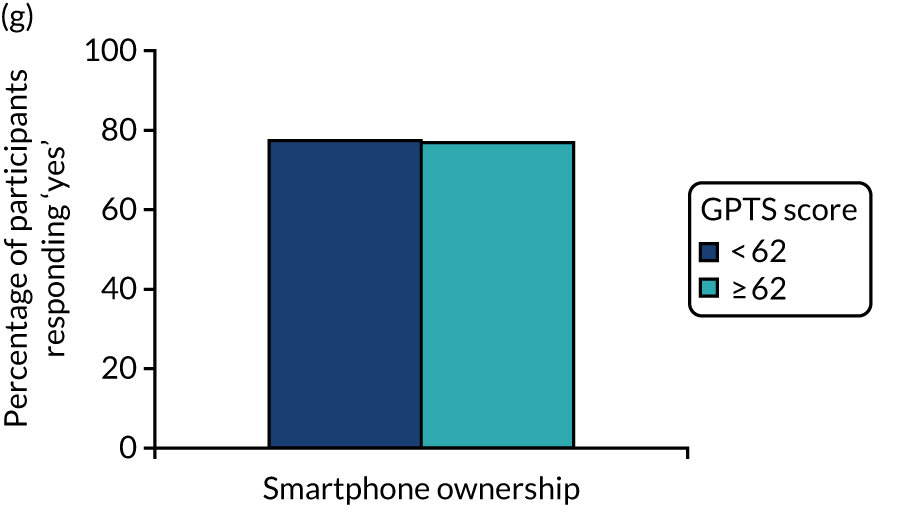
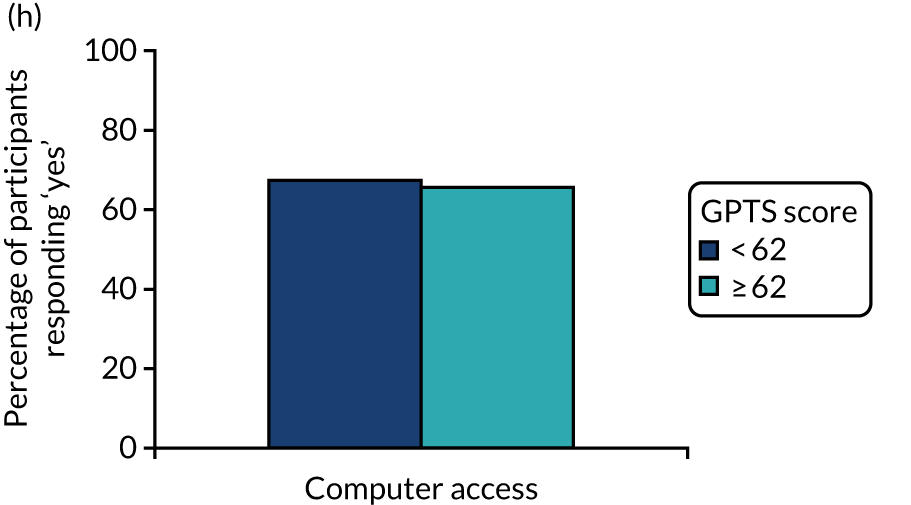
FIGURE 6.
Smartphone and computer use and confidence among people attending at least one therapy session (n = 168). (a) Smartphone and computer use by gender, (b) smartphone and computer confidence by gender, (c) smartphone and computer use by age, (d) smartphone and computer confidence by age, (e) smartphone and computer frequency by ethnicity, (f) smartphone and computer confidence by ethnicity, (g) smartphone and computer use by paranoia severity and (h) smartphone and computer confidence by paranoia severity.
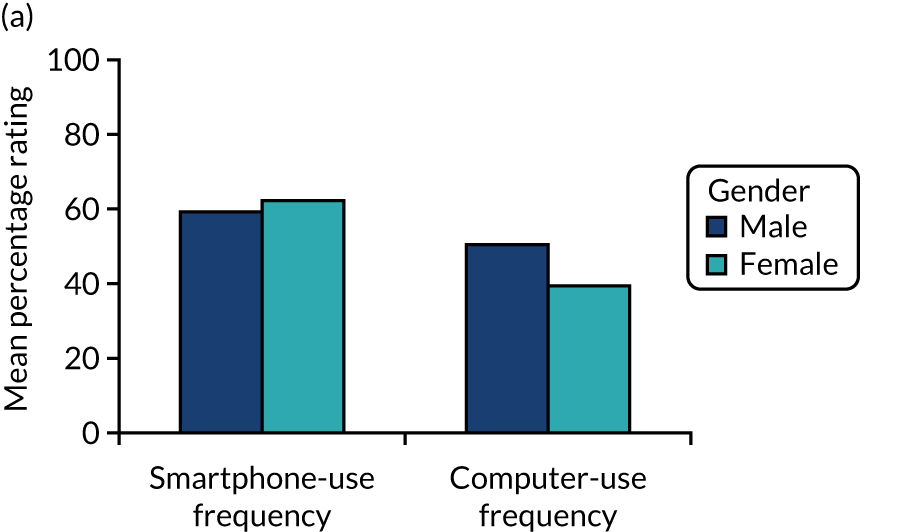
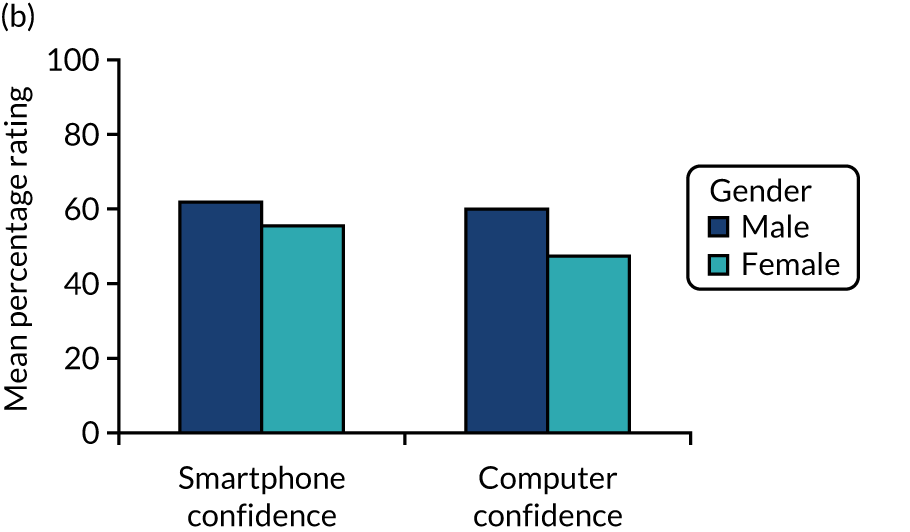
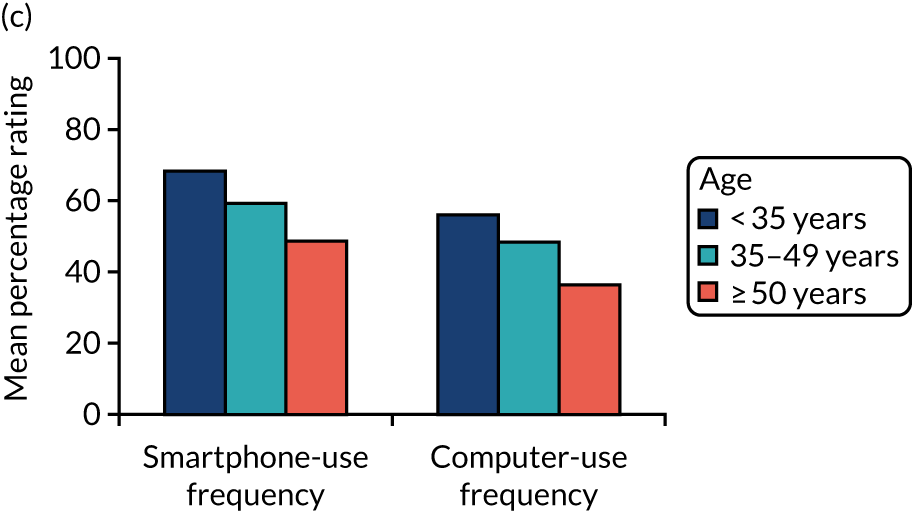
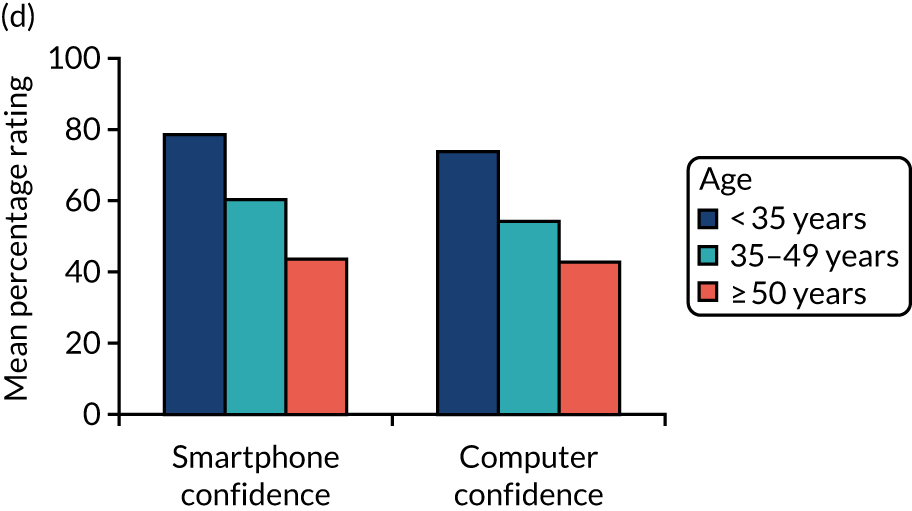
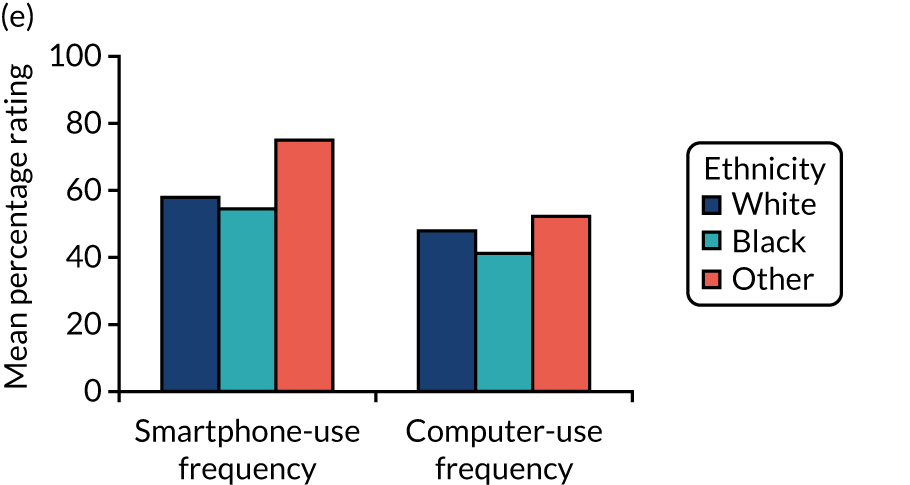
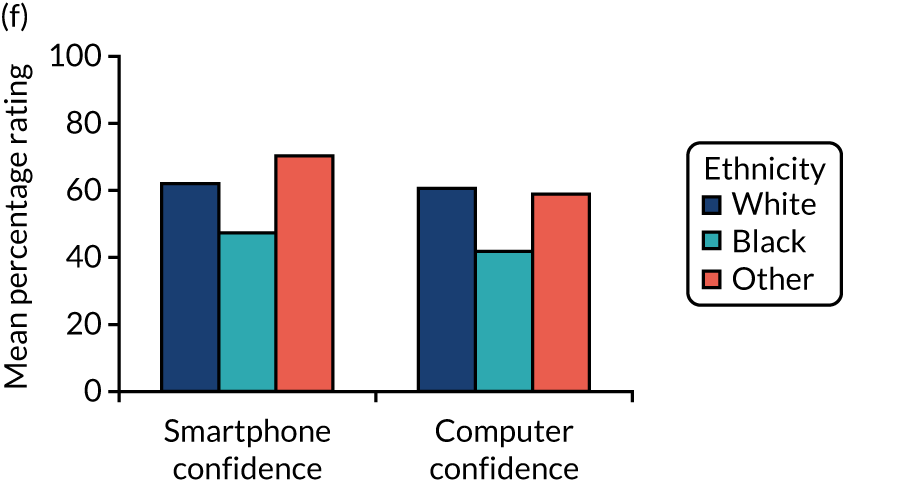
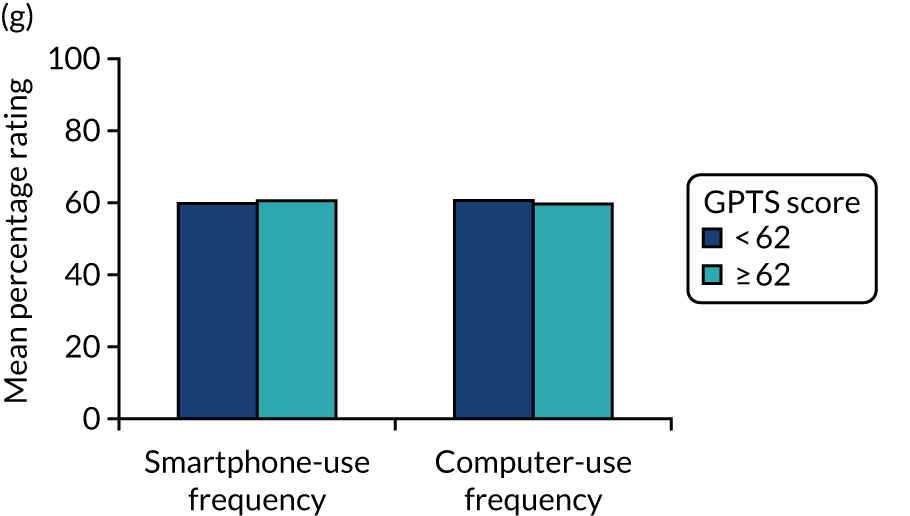
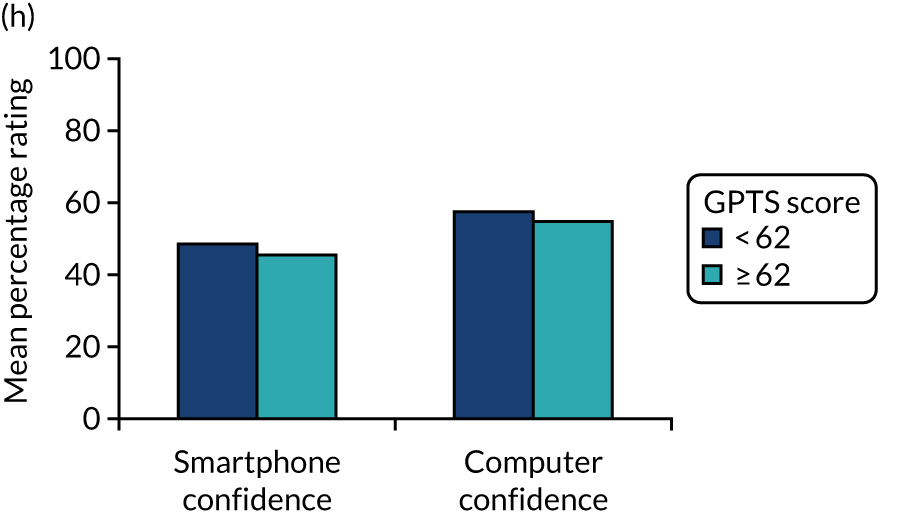
Self-reported and system analytics adherence to the SlowMo mobile app
Self-reported current and intended future use of the mobile app are reported in Table 14. This assessment was not offered to the first 45 therapy cases, and completion rates were 80% and 78% for current and intended future use, respectively, for the remaining cases. The data indicate that the rate of current use varied from never to all of the time, with participants, on average, reporting using the mobile app just under half of the time. The current reported use was highest in Oxford and lowest in Sussex. By contrast, all participants reported at least some intention to use the mobile app again in the future, and the average frequency of intended use was also higher than current use, at just over half of the time. Self-reported adherence was compared with participants’ characteristics of age, gender, ethnicity and paranoia severity, as shown in Appendix 3, Table 23. Female participants reported significantly higher current and future intended use of the mobile app than male participants. There were no significant differences in current and intended use for age, ethnicity or paranoia severity.
| Site | Mean (SD) | Range |
|---|---|---|
| How much have you been using the mobile app? | ||
| Sussex (n = 28) | 37.07 (25.94) | 0–90 |
| Oxford (n = 15) | 55.33 (25.67) | 0–100 |
| London (n = 37) | 46.32 (24.35) | 0–100 |
| Total (N = 80) | 44.77 (25.69) | 0–100 |
| Will I use the mobile app in the future? | ||
| Sussex (n = 26) | 56.96 (23.14) | 10–100 |
| Oxford (n = 15) | 68.20 (24.42) | 30–100 |
| London (n = 37) | 63.43 (22.17) | 10–100 |
| Total (N = 78) | 62.19 (23.00) | 10–100 |
The system analytics adherence for the mobile app had some data lost at the beginning of the trial owing to a bug in the code. Once rectified, analytics data were stored when the participant had the version of the mobile app with the analytics coded installed; for individuals in therapy when the analytics issue was resolved, the mobile app could be updated to this version at any stage of therapy (sessions 1–8). Participants were defined as having missing analytics when there were insufficient data points to determine mobile app adherence according to our a priori criterion of at least one home screen view for at least three sessions.
For participants in the therapy group, 65.4% met the mobile app adherence criterion. This increased to 71.4% for participants who attended at least one session (and were, therefore, provided with a mobile phone with the mobile app installed). Among those participants attending all eight sessions, the adherence rate was 80.7%, suggesting a high rate of adherence. One-fifth of participants (21.4%) used the mobile app outside every recorded session. System analytics adherence was compared with participants’ characteristics of age, gender, ethnicity and paranoia severity, as well as pre-therapy smartphone use and confidence, as shown in Appendix 3, Table 24. There were no significant differences in the analytics adherence to the mobile app according to age, gender, ethnicity or paranoia severity. However, adherence rates were higher among those who attended all eight sessions, reported using smartphones more frequently and were confident in smartphone use prior to therapy.
User experience scale for the SlowMo mobile app
The UES findings for each subscale and the total score are presented in Table 15. The UES was not offered to the participants who completed therapy at the beginning of the trial (n = 45). A further three participants were not eligible to complete the UES, as they declined any engagement with the SlowMo mobile app. For the remaining sample, the completion rate was 85%. UES ratings were comparable across all subscales, with the majority of people providing positive ratings for enjoyment, usability and usefulness. However, there was a large range of scores, suggesting that the mobile app was positively received by most but not all participants. Figure 7 shows the UES ratings in relation to gender, age, ethnicity and paranoia severity.
| UES variable | Site | Total | ||
|---|---|---|---|---|
| Sussex | Oxford | London | ||
| Enjoyment (%) | ||||
| Mean (SD) | 72.08 (17.70) | 73.32 (20.32) | 75.19 (19.04) | 73.75 (18.64) |
| Range | 31–98 | 45–100 | 35–100 | 31–100 |
| Usability (%) | ||||
| Mean (SD) | 73.71 (19.73) | 74.32 (24.12) | 73.86 (22.12) | 73.89 (21.42) |
| Range | 33–100 | 23–100 | 35–100 | 23–100 |
| Usefulness (%) | ||||
| Mean (SD) | 76.32 (17.80) | 79.10 (14.43) | 77.44 (19.11) | 77.35 (17.70) |
| Range | 25–100 | 60–100 | 20–100 | 20–100 |
| Total UES (%) | ||||
| Mean (SD) | 74.03 (16.84) | 75.58 (17.61) | 75.50 (17.44) | 74.99 (17.06) |
| Range | 30–99 | 46–100 | 42–100 | 30–100 |
FIGURE 7.
User experience survey subscales and total scores among therapy completers (n = 82). (a) Gender, (b) age, (c) ethnicity and (d) paranoia severity.
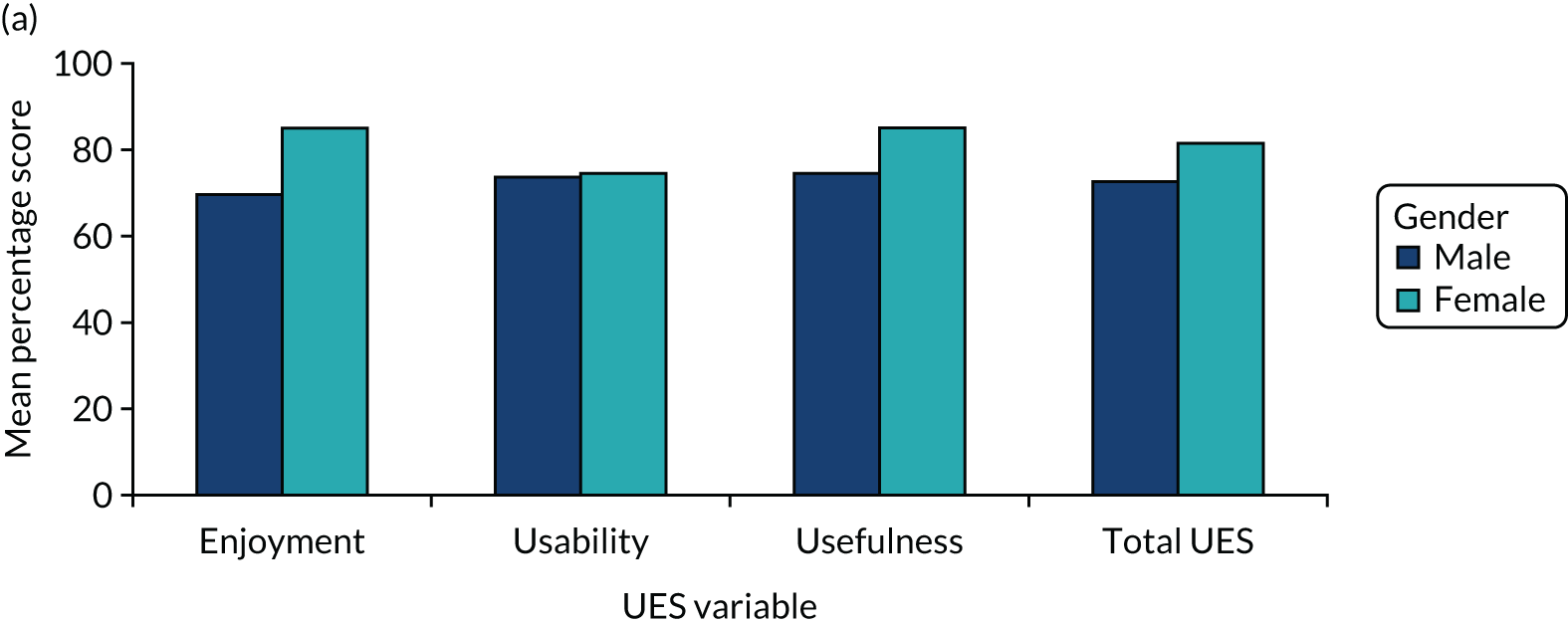
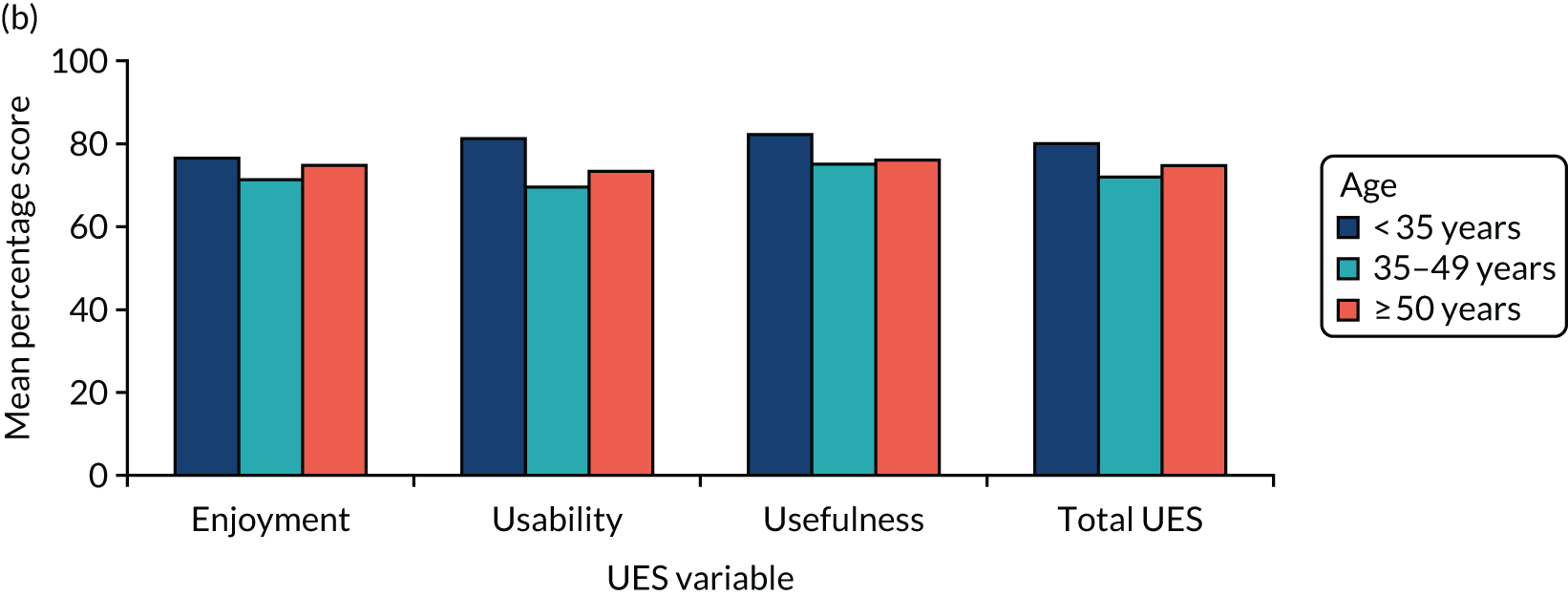
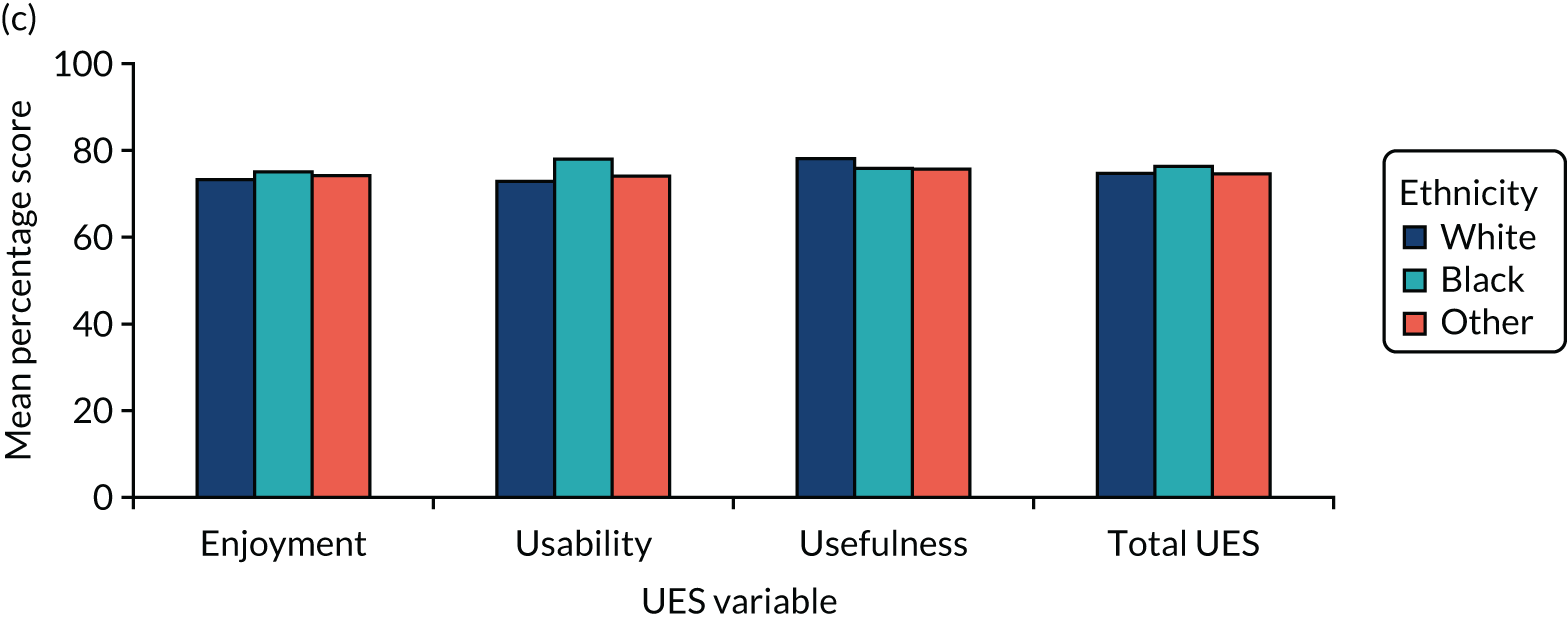
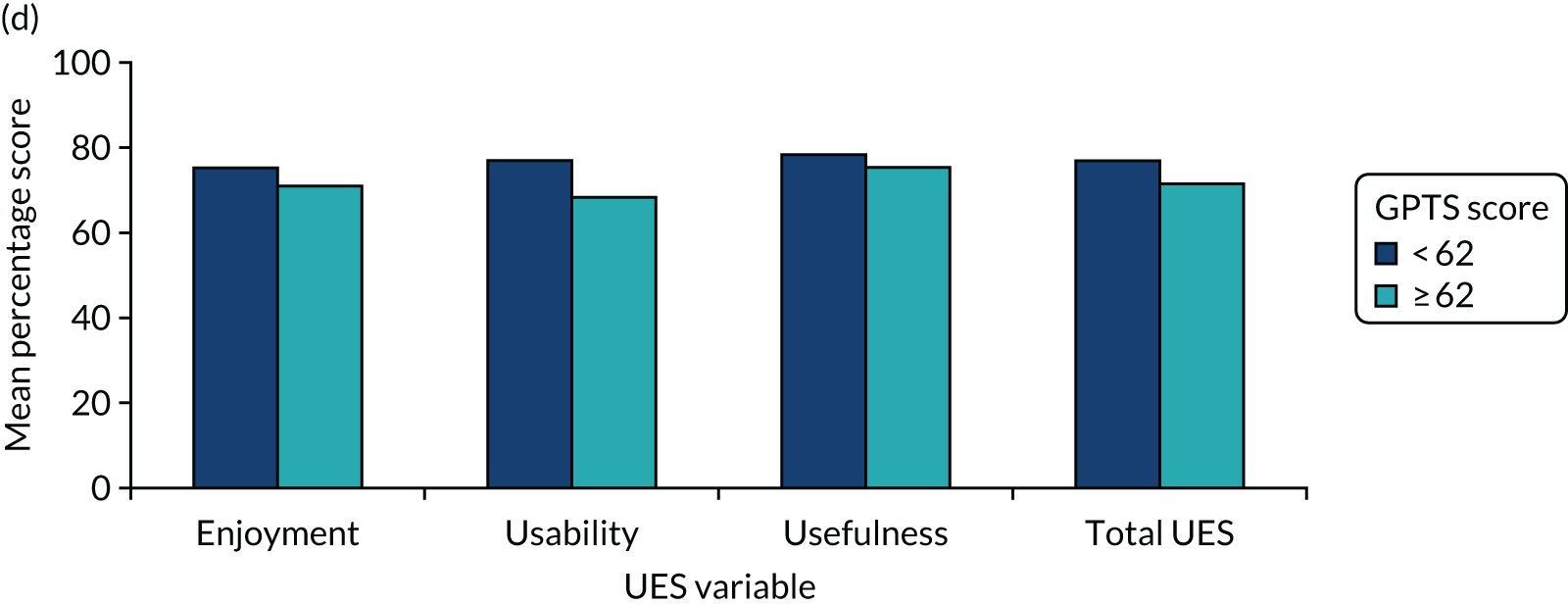
The UES ratings were compared with participant characteristics, as shown in Appendix 3, Table 25. There were significant differences depending on gender, with women reporting higher rates of enjoyment and usefulness; however, rates of usability were similar for male and female participants. The significant differences in smartphone confidence prior to therapy did not appear to affect the self-reported user experience, as there were no significant differences depending on age and ethnicity. There were also no differences in UES ratings in relation to paranoia severity.
Technical problems
The technical problems with the SlowMo therapy connectivity, data syncing and software are shown in Appendix 3, Table 26. This demonstrates that technical problems occurred, although these were for a minority of sessions only. The most common technical problems were internet connectivity and data syncing.
Adverse events related to the SlowMo software (web app and mobile app) and hardware (mobile phone)
None of the 54 adverse events reported over the course of the trial was assessed as being related to the SlowMo mobile app software. There was one non-serious adverse events that was judged as ‘definitely’ related to the mobile phone that was provided to a participant so that they could access the mobile app. This involved a concern raised by a carer that the participant was using the SlowMo mobile phone to access a dating site using the internet connection at their home, which they viewed as inappropriate and reported to the trial therapist.
Discussion
This chapter evaluated the user experience of the SlowMo mobile app. The data provide a validation of the inclusive, human-centred design of the SlowMo therapy, as excellent rates of self-reported and system analytics mobile app adherence were found. The a priori criterion for mobile app adherence was met by 80.7% of participants who completed all eight sessions and 26.1% of people used the mobile app at least once outside every session. The UES ratings further suggest that most people perceived the mobile app as easy to use, enjoyable and useful. Alongside the high rates of therapy session attendance and therapy fidelity reported in Chapter 1, the results suggest that the SlowMo design did enhance the user experience as intended, to support engagement and adherence. The ‘digital divide’ previously identified in psychosis research and evidenced in our digital literacy data did not appear to affect user experience, as age, ethnicity and paranoia severity did not influence self-reported adherence, system analytics adherence or UES findings. 107,108 The exception was that female participants were significantly more likely than male participants to be adherent to the mobile app and reported higher rates of usefulness and enjoyment, with comparable usability ratings. This is consistent with previous findings that women with psychosis are more likely to engage in digital therapeutics and suggests that development of SlowMo should focus on optimising the interface for men’s needs. 109 Unsurprisingly, people who reported being more confident and frequent users of smartphones prior to starting the therapy were more likely to be adherent to the mobile app. This insight emphasises the importance of digital literacy assessments so that individualised technical support can be provided; we plan to continue improving the SlowMo design to further enhance accessibility for those who are less familiar with technology.
The mobile app adherence rates were high, especially as mobile app use was encouraged only if it was in line with the person’s preferences, suggesting that this form of therapy was perceived as useful by participants. In contrast to other research investigating mobile apps for psychosis,96,98,130 the software did not provide regular prompts nor was use incentivised as part of the trial design. People were able to access some paper therapy resources, if they wished, for use outside sessions, and therapists reported that a blend of modalities was often valued. A further strength of the study is that we conducted multidimensional assessment of user experience using self-reported and objective measures, and specified adherence criteria a priori, in line with recommendations for assessing the user experience of digital therapeutics. 133,138 The findings reported here provide an initial validation of the SlowMo therapy design and we plan to conduct further analyses of digital usage of the mobile app. Important issues include granular examination of the functions used and the types of interactions, how usage varies over the course of therapy and how patterns of use relate to mental health outcomes. This work will help to elucidate whether reduced use reflects disengagement or e-attainment, and what constitutes a sufficient ‘dose’ of the mobile app for people to internalise the skill of slowing down, as well as potential detrimental patterns of use, such as excessive engagement. 111,115,139
Technical problems were assessed, consistent with reporting recommendations for digital therapeutic trials, and were infrequent. 135 They were mainly attributable to connectivity issues, emphasising the infrastructure challenges to scaling up digital therapeutics in the NHS. The technical problems with the SlowMo software were mostly because of issues in syncing the web app and mobile app data, and these issues reduced as the code was updated during the trial. The research tested a minimum viable product that had not yet been fully optimised. The trial context meant that therapists were willing and able to resolve technical issues. However, additional software development and maintenance will be required to minimise the need for technical support in the future.
A limitation of the work is that mobile app analytics were lost for 18 people in the therapy sample owing to a bug in the code; however, we do not anticipate that these analytic data would have differed from the rest of the sample. Another limitation is that we are in the process of developing an implementation strategy. This will be the focus for the next stage of our work and is critical given that most health technologies fail to be adopted, scaled up, spread and sustained, even where they are efficacious in RCTs. 140 Nonetheless, the tailoring of the SlowMo design to its specific target problem, a range of intended users, and the delivery context may support initial adoption, together with a strong value proposition to stakeholders that it has high rates of engagement and impact across a range of clinically meaningful outcomes. Further work will need to consider integration within existing care pathways and service design to support uptake. We intend to expand our inclusive, human-centred design participation beyond people with lived experience of psychosis, and intend to include a range of front-line therapists, service managers and commissioners. A health economic evaluation will be a necessary component of this research. Given the impact of SlowMo on a range of outcomes, we plan to build on this by incorporating other therapeutic targets and techniques. Our aim is to develop a modular digital therapy for psychosis, in line with the principles of agile science. 141 The SlowMo mobile app is currently user initiated, and some people may benefit from more responsive technology to deliver context-based interventions when they are needed. 142 We have already tested the feasibility of integrating wearable technology for stress monitoring into the SlowMo mobile app and intend to further explore this technology.
In conclusion, the findings suggest that the inclusive, human-centred design of SlowMo therapy supported the user experience of the intervention and resulted in excellent rates of adherence among a wide range of people. This comprehensive evaluation of the user experience of SlowMo therapy is in line with a recent coproduced call for digital therapeutic research to focus on how we can optimise existing interventions, the impact of psychosis on engagement, and whether or not digital therapies can improve reach and access for marginalised groups. 143 We further investigate the user experience of SlowMo therapy in the next chapter, with a coproduced qualitative study of the therapy experience. Together with the clinical efficacy and moderation results reported in Chapter 1, this work supports the further development of SlowMo therapy and testing in the NHS, with the ultimate aim to scale up, spread and sustain national and international implementation. Our approach underscores the need to focus on both effectiveness and user experience when developing digital therapeutics, and we strongly advocate adoption of this strategy to improve therapy outcomes for people with psychosis.
Chapter 4 The user experience of SlowMo therapy: a co-produced thematic analysis of service users’ subjective experience
Introduction
I’m trying to do what the lady did, he showed me a video of this lady, she has the same problem as me and now when I was watching it she goes out and comes in and don’t let her neighbours worry her and I’m trying to do the same, I’m trying.
Paranoia, or fear of deliberate harm from others, is common and has a severe impact on mental health and quality of life,144,145 yet there are issues with both delivery and uptake of psychological therapies for paranoia and psychosis. 72 Large effect sizes have recently been found for the impact of brief causal-interventionist therapy approaches on paranoia that target sleep, worry and positive self-schema. 28,146–148 SlowMo therapy is a related causal-interventionist approach and is the first blended digital therapy for paranoia. It targets ‘fast-thinking’ habits or reasoning biases that are thought to underlie distressing fears of harm from others. 29 It is brief, with the potential to be delivered to large numbers of service users, and was designed in line with recommendations for improving implementation of digital therapies for psychosis. 129,131,149 The blended approach reduces the risk of therapist drift150 and the inclusive, human-centred design in the development of the intervention7 aimed to ensure that the therapy was usable, trustworthy, enjoyable, personalised and normalising, and offered flexible interpersonal support.
Service-user experiences of therapy are critical. Therapeutic alliance can have a causal impact on the effectiveness of treatments in psychosis,91 and alliance with online digital interventions may promote engagement. 151 Historically, therapeutic alliance is defined as the quality of the working relationship between the service user and the therapist in terms of shared goals and tasks, and a bond characterised by interest, warmth, empathy, authenticity, genuine concern, understanding and hope. 152–154 In blended therapies, this working relationship is extended to a ‘triangle of alliance’ between the service user, the clinician and the digital platform. 155,156 The traditional therapeutic alliance is potentially enhanced by the incorporation of technology, evidenced by greater commitment to goals and tasks. 157 The alliance is likely to vary across different platforms and levels of therapist involvement, and, in SlowMo therapy, this alliance is extended further to incorporate the service-user’s relationship with the mobile app.
However, evidence of user experiences of using a mobile app is only recently emerging. In a recent study,149 service users with psychosis reported that they felt a sense of autonomy and control while using an app to manage their symptoms. A proof-of-concept trial130 found high feasibility and acceptability as well as large treatment effect sizes for users of the Actissist app compared with a comparative symptom-tracking app. However, another app (FOCUS) offering cognitive interventions for psychosis found that, although usability rates were high, with 87% of users finding it easy to use and helpful for their symptoms, a small group of participants reported difficulties in engaging with the technology and expressed the need for more technical support. 137
The SlowMo trial, which we have reported in Chapter 1, found that the therapy had a positive impact on a range of mental health outcomes. In validating the aims of the design we have also demonstrated, in Chapters 1 and 3, excellent rates of adherence to the sessions and mobile app, and of self-reported ease of use, usefulness and enjoyment, that did not appear to be impacted by demographics; however, people who were less confident in using smartphones were less likely to make use of the mobile app. Given recommendations to employ multidimensional objective and subjective assessments of user experience133 to support implementation, this analysis will evaluate service users’ subjective qualitative experience of and alliance with the therapy, including the therapist, digital elements and their interaction. Qualitative feedback will thus be gathered to provide a detailed evaluation of the design, and be used to support further development of the intervention, in preparation for evaluation in an implementation trial context. There is much still to be understood about the implementation of digital interventions for psychosis and paranoia and, although progress has been made and implementation frameworks created,129 no study has so far evaluated a blended therapy with both digital input and therapist sessions.
The initial research questions related, therefore, to the uptake of the digital platform, therapy concepts and blended therapy approach, and how these were perceived and experienced by service users. The methods, data collection and analysis were coproduced with peer researchers. This approach enhances the rigour of qualitative methods because service users may be more forthcoming and open when interviewed by their peers. 66 Peer researcher involvement in the analysis may also lead to the identification of novel themes and critical reflections on the process. 79,158 The collaboration with peer researchers in the evaluation of the service user experiences of the blended SlowMo therapy thus adds methodological rigour to this approach and provides a rich subjective perspective.
Aim
The study, using a coproduced collaborative approach with peer researcher involvement in the design, delivery and evaluation, aimed to explore the subjective service user experience of the:
-
SlowMo therapy content and concepts
-
blended therapy approach (the triangle of alliance)
-
digital aspects of the intervention.
In addition, there was a specific aim to undertake a detailed evaluation of the product design and the technological challenges to inform improvements prior to future implementation.
Method
Participants
For this study, the participants recruited to the main study (see Chapter 1) at each site were subsequently invited to take part in the qualitative substudy on completion of the 24-week follow-up, commencing once the PPI researchers were trained and with an aim to recruit 20 participants across the three sites. Inclusion criteria were the same as for the main trial, with the exception that participants also needed to have completed at least one SlowMo therapy session and the 24-week follow-up assessment.
Procedure
A topic guide for the qualitative interviews was initially developed by the research team to provide a detailed evaluation of the design brief. This was then revised and coproduced in collaboration with the SlowMo PPI team over a series of meetings (see Appendix 1). PPI team members had all received either the SlowMo therapy or an introduction to the therapy and materials. They received comprehensive training in peer researcher roles, and role-play practice in conducting qualitative interviews using the topic guide. Supervision was provided by the PPI lead (Sussex) or trial/site co-ordinators (London/Oxford) throughout the process. All interview data were then collected by either two peer researchers working together (Sussex), or one peer worker and a graduate researcher (London and Oxford). Participants were reimbursed £20 for their time. All interviews were audio-recorded, with the exception of one (see Results), and transcribed verbatim.
Epistemological position
The study’s theoretical perspective and methodology are underpinned by the epistemological position of critical realism,159,160 which recognises that, although reality exists, all knowledge is socially produced and is influenced by the observer’s context and worldview. 160,161 The potential for thematic analysis to lack consistency and coherence162 can be reduced by the transparent application of an epistemological position that can coherently underpin the study findings. 163 Multiple equally valid accounts of the same phenomenon are always available164 and the reality is only imperfectly known. 165,166 Multiple approaches were, therefore, taken to capture the reality of participant perspectives, including data collection by peer researchers, multiple coding, triangulation, validation and transparency with respect to stance and experience.
Analysis
A reflexive thematic analysis approach was applied to the transcribed data using a constructionist framework in six steps: familiarisation, initial coding, searching for themes, reviewing themes, defining and naming themes, and producing the report. 167 Data were analysed in two phases, each comprising 11 transcripts (50% of the data), using multiple coding and triangulation to reach consensus on the theme structure. In the first phase, the lead author, peer researchers, graduate psychologists and site co-ordinator/trial therapist in Sussex independently coded an initial transcript and met to discuss and agree the initial coding framework. Further transcripts were then coded by the graduate psychologist and clinical researcher. Codes were summarised and reviewed by the wider group to define the candidate theme structure, after which the graduate psychologist and clinical researchers then coded the remaining transcripts to produce the phase 1 theme structure, with supporting quotations. A third wider-group consultation with the PPI peer researchers who had conducted the interviews and collected the data clarified and validated the theme structure and provided provisional names. The second phase was conducted independently on the remaining 11 transcripts, but mirroring the approach with multiple coding and triangulation. The coding frames of the two phases were then combined and presented, with supporting quotations, in a meeting with the whole PPI team across all three sites. All discrepancies between phase 1 and phase 2 coding were discussed, quotations were reviewed and consensus reached on the language used to describe each theme.
Experiences and stance of the patient and public involvement peer researchers
The peer researchers were part of the SlowMo PPI team. As presented in Chapter 2, in terms of their experience, peer researchers found it rewarding to hear participants’ unique journeys, to realise that their roles as peer researchers were appreciated by participants and to find that most participants had found the SlowMo therapy helpful in some way. They grew in confidence, despite experiencing challenges at times. They noted that the coding became clearer and more concise over time, that everyone’s ideas were heard and that the themes definitely reflected the key points that came out in the interviews (see the upcoming PPI paper for more detail).
In terms of stance, for the most part, the peer researchers were inexperienced in qualitative data collection and analysis prior to this study, and, in this respect, they brought a novel ‘lay’ perspective. However, all of the peer researchers had worked with the SlowMo trial for approximately 1.5 years before they commenced data collection, and two out of the four peer researchers had previously received the SlowMo intervention as part of a previous version of the therapy or during piloting for the current trial. Although this enabled them to engage and empathise with participants’ experiences of the therapy, it may also have contributed to some bias in their interpretations of the results.
Stance of the graduate coders
To reduce the risk of bias, the primary coder in phase 1 was independent of the SlowMo trial, which enabled greater objectivity and reduced the risk of bias in initial coding; however, at times, this hampered the understanding of the nuances of participants, responses to the intervention, which then required discussion with the broader study team. The primary coder in phase 2 was a SlowMo graduate research psychologist who was familiar with the intervention and the phase 1 coding, but undertook the second phase coding independently with a critical reflective stance.
Results
Out of the 28 eligible participants who were approached in Sussex and London, five declined to participate and three were unreachable. One London participant did not consent to the audio-recording of their interview; therefore, field notes that were taken during their interview were included. Twenty-two participants took part, constituting 12.2% of the total SlowMo therapy sample. Their demographic details are provided in Table 16. Eighteen of the participants were male (82%), 18 were white British (82%), 19 were single (86%), 17 were unemployed (77%) and 14 lived alone (64%). Only three participants (14%) had received higher education beyond A Levels (Advanced Levels). The mean age for the whole sample was 44.9 years (range 20–64 years) and their mean GPTS part B score was 51.8 (range 29–79).
| Participant ID | Demographic | ||||||
|---|---|---|---|---|---|---|---|
| Age (years) | Gender | Ethnicity | Marital status | Highest education | Working status | Living situation | |
| Sussex | |||||||
| S1 | 20 | Male | Pakistani | Single | Secondary (O Level/CSE) | Unemployed | Parents |
| S2 | 61 | Male | White British | Married | Secondary, no examinations | Unemployed | Others |
| S3 | 57 | Male | White British | Single | Secondary, no examinations | Unemployed | Alone |
| S4 | 46 | Female | White British | Single | Higher education | Unemployed | Alone |
| S5 | 42 | Male | White British | Single | Higher education | Volunteer | Parents |
| S6 | 30 | Male | White British | Single | Secondary, no examinations | Unemployed | Alone |
| S7 | 27 | Male | White British | Single | Vocational/college | Unemployed | Alone |
| S8 | 53 | Male | White British | Single | Secondary (O Level/CSE) | Unemployed | Alone |
| S9 | 39 | Male | White British | Single | Secondary (A Level) | Part time | Alone |
| S10 | 58 | Male | White British | Single | Secondary (O Level/CSE) | Unemployed | Alone |
| S11 | 64 | Male | White British | Divorced | Secondary, no examinations | Unemployed | Alone |
| S12 | 49 | Male | White British | Single | Secondary (O Level/CSE) | Volunteer | Alone |
| Oxford | |||||||
| O13 | 34 | Female | White British | Single | Higher education | Part time | Others |
| O14 | 47 | Male | White British | Single | Secondary (O Level/CSE) | Unemployed | Alone |
| London | |||||||
| L15 | 24 | Male | Black African | Single | Secondary (O Level/CSE) | Unemployed | Parents |
| L16 | 43 | Male | White British | Single | Secondary (O Level/CSE) | Unemployed | Others |
| L17 | 56 | Female | White British | Single | Primary school | Unemployed | Alone |
| L18 | 35 | Male | Other | Single | Secondary (O Level/CSE) | Volunteer | Parents |
| L19 | 54 | Male | White British | Single | Vocational/college | Unemployed | Alone |
| L20 | 31 | Male | White British | Single | Vocational/college | Unemployed | Relatives |
| L21 | 63 | Female | White British | Widowed | Secondary (O Level/CSE) | Unemployed | Alone |
| L22 | 54 | Male | Black other | Single | Secondary (O Level/CSE) | Unemployed | Alone |
The qualitative sample demographics were similar to those of the main study reported in Chapter 1, in which participants were largely male (70%), of white ethnicity (70%), unemployed (80%) and living alone (58%), with a slightly lower average age of 42.6 years and a slightly higher GPTS part B score of 56.2 (SlowMo group).
Development and validation of theme structure
The final theme structure comprised six core themes and 20 subthemes. In terms of the six core themes, between phase 1 and phase 2, two themes remained unchanged (slowing things down, and improvements in paranoia and well-being). There was a slight change in wording of one theme, from ‘a new step on the recovery journey’ to ‘starting the SlowMo journey’, and a slight change of wording and focus of another, from ‘challenges in use of the SlowMo app’ to ‘approaches and challenges of technology’. The final two themes became more distinct: ‘feeling connected and understood’ became ‘value and learning from social connections’ and ‘drivers of progress’ was determined to reflect more specifically ‘the central role of the supportive therapist relationship’. Of the final 20 subthemes, six were identical from phase 1 to phase 2, five were new subthemes from phase 2, three changed wording slightly, three technical subthemes were expanded in focus, two learning subthemes were collapsed into one and another learning subtheme was expanded into two. All members of the qualitative team, including all PPI members, agreed the final structure (Figure 8).
FIGURE 8.
The structure of the qualitative experiences of SlowMo.
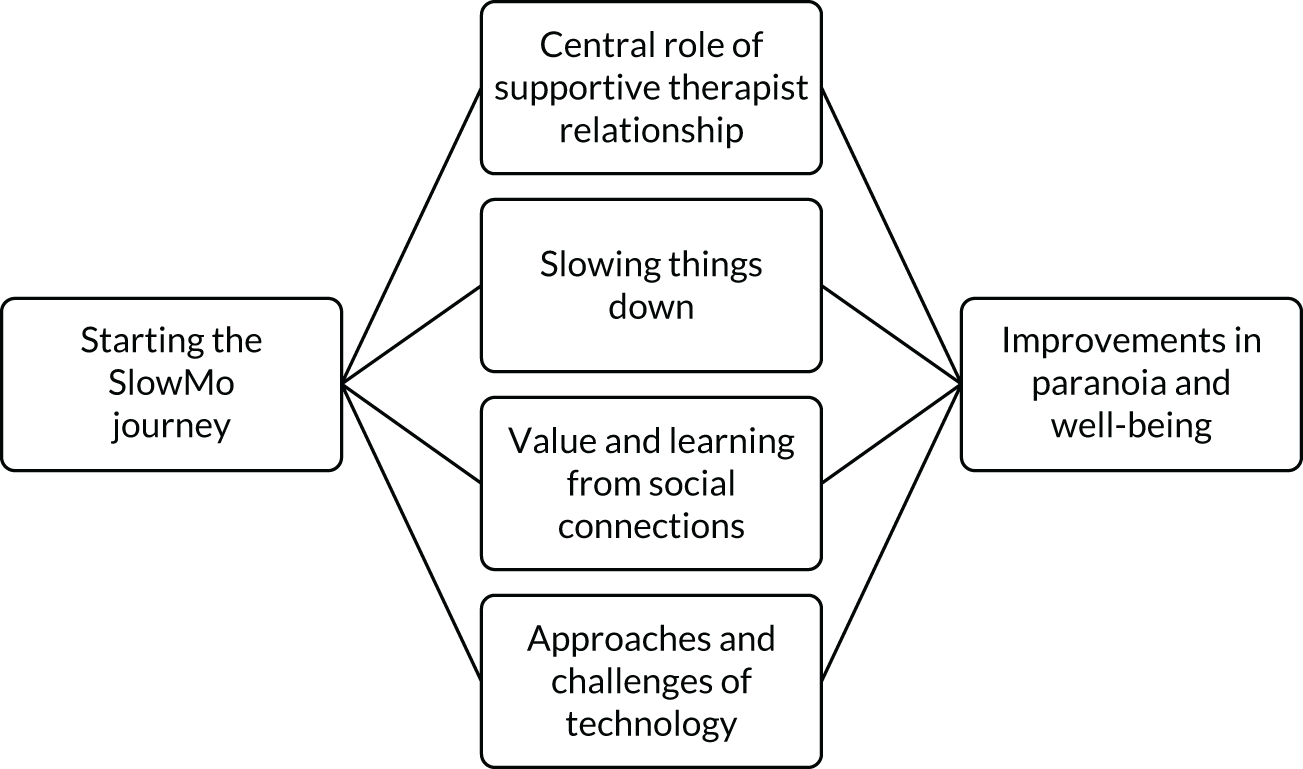
Starting the SlowMo journey
This theme captured the reasons for starting the SlowMo therapy, feelings before starting and the symptom barriers to engagement.
Reasons for starting the SlowMo therapy
Reasons for starting the SlowMo therapy included an opportunity offered and not sought, an opportunity for help, feeling stuck and a desire to take part in research:L17:S8:
It was [CPN] that got me to do it, she came to my house then she showed me this leaflet, she said, ‘You’ve got a 50/50 chance of doing it, would you like to do it?’. I said, ‘I’ll try, I’ll have a go’.
Oh mainly, ‘cause I wasn’t getting anywhere, my illness or whatever, has been on the same tablets for a long time. And I wasn’t getting anywhere so I thought I might try something.
Feelings before starting
Service users in all sites described feeling nervous and uncertain, but also open, willing and ready for new experiences:L21:O14:O13:
I was nervous, very nervous. I didn’t have no confidence, so I have now . . .
Apprehensive. Meeting with people I didn’t know.
I am eager to explore new opportunities as well, so that kind of made me go for it as well.
Voices and anxiety as barriers
Symptoms of voice hearing and anxiety were highlighted as specific barriers to starting SlowMo therapy:S10:
It was daunting at first, ‘cause it was the first time I’d actually spoken about them yeah. The way I felt with my voices. Basically it took me a good 10 minutes to listen to what she was saying because my voices were telling me not to listen and she was going to do this to me, she was going to do that to me yeah.
Central role of supportive therapist relationship
Importance of talking and being listened to
[what made the most difference?] Just being able to talk about my problems and focus on them and just come up with genuine ideas.
I found the talks we had, I found most invaluable. I thought that was amazing . . . actually having someone to talk to when we were going through it, I found amazing.
A positive therapist relationship
He made me really relaxed and any problems I had I could talk to him, which I don’t usually . . . So things came out that I haven’t told anybody.
Therapist as a supportive guide
The therapist’s approach to supporting both the therapy and the use of technology was described. The therapists were described as flexible, providing clear explanations, and their positive support promoted engagement and use of technology, while the computer content also supported the therapist:
I trusted her and felt comfortable with her. She explained everything very clearly . . . she was very sensitive towards my feelings, erm, when I was struggling. Erm, and with the computer she just helped me to see things more clearly.
I think if it was just the computer, then again it wouldn’t work; I think you need that interaction as well . . . I had one bad day where I just couldn’t focus and that was just really bad. But then I had someone who was really understanding about that and that made all the difference, and I didn’t feel, like, too pressured. I could learn at my own pace.
Never used a computer, but I learnt with [therapist].
I thought the computer was really there to support the, uhm, face-to-face talk. Uhm. It seemed to me that the therapy had been done so that it gave equal problems to the face-to-face therapy and computer therapy . . . I preferred in some ways more emphasis on the face to face perhaps . . . if it’s more psychological therapy which involves emotions . . . having a computer may sort of negate that, make it feel bland. Uhm. But in the way it’s done with [therapist], erm, it seemed to work quite well.
Slowing things down
This theme revealed how service users identified with the important central message from the SlowMo therapy. They found the concepts of slow and fast thinking to be helpful and valued the learning of this new skill, which importantly became more integrated into their thinking style over time with practice. However, some participants felt that progress through the sessions themselves was too slow and that the speed of delivery should be adapted to the participant. We aimed to address cognitive barriers to use; therefore, it is understandable that the intervention seemed insufficiently fast for more able participants. We have now integrated these insights into an updated product specification and will develop this ahead of an implementation research study:
It was very introductory kind of thing. I felt, maybe quite appropriately, it was quite slow actually to get to the juicy part, if you like. And [therapist] often would say I was often ahead of the project, ahead of the sessions, because I was thinking of things that were going to be introduced later on. So . . . for someone who is sort of getting to grips with it a bit quicker it could be condensed or you could introduce sort of the more advanced part of the earlier on.
Slow and fast thinking are relevant and helpful
I don’t worry so much, it’s my neighbours, they make me stressed and then I’ll say ‘No, I’ve got to slow down’. You have to because if not, if you carry on, you make yourself ill and you’ll land up in hospital.
I always insisted on going on . . . it might be a split-second decision . . . which is basically fast thinking. I was trained to always look out for the worst-case scenario . . . SlowMo slow thinking wasn’t difficult, but it was different . . . I found that using that where I live, all those idiots in the other blocks, if you think through possible other scenarios and then think ‘I don’t actually know those people and they don’t know me, so they can’t be talking about me’, whereas prior to SlowMo I would think ‘Why are they talking about me? What is going on?’ and that would stress me out really badly.
Oh the helpful bits were slowing up the thinking, thinking about other things that could be happening rather than just going to your first point.
Learning a new thinking skill set
It was very hard because me, I think quickly, but I slowed it down and I’ve learnt how to do that now.
Practice integrates the slow-thinking style
. . . my feelings are quite strong sometimes. And you have to keep on repeating about the other[thought], it could be something else. Sometimes you have to do it three or four times. It takes a while to get off what you are thinking cause the feelings are quite strong.
Instead of just believing and trusting in that fast-thinking conclusion that I have arrived at, there’s been more of an interaction on my part to counteract it with slow thinking . . . It was much closer to the end of therapy, I was quite actively engaging in slow thinking and quite often.
Value and learning from social connections
Vignettes and videos help to feel less isolated
Participants described how they related to the SlowMo vignettes and learnt that they were not alone:
I was hearing other people’s like feedback and . . . some of what they said sort of related to me a little bit . . . it was just helpful because some of the stuff they were saying sort of, it happened to me before . . . so, yeah it was, I just kind of relate to it, sort of.
Well just watching the videos and, erm, seeing like the people, I wasn’t alone, because young people like myself or younger than me or older than me does, err, have mental health, like I’m not the only one.
Learning and support through vignettes and peers
Participants described learning from and being inspired by the SlowMo vignettes and promotional videos, and liking the recommendations to learn from and be supported by others with the same lived experiences, although some people wanted a greater range of vignettes:
I’m trying to do what the lady did, he showed me a video of this lady, she has the same problem as me and now when I was watching it she goes out and comes in and don’t let her neighbours worry her and I’m trying to do the same, I’m trying.
[What made the most difference?] Erm I think the voices of real people thing. As soon as I left therapy every time, it’s stuck in my head you know. So if I get into that situation I try to rethink it the way that SlowMo taught me really, how to, how to do it.
Yeah, so what I said with the three people, it is a bit limited with what happened to them, and I think there is an awful lot more situations that people undergoing problems are confronted with and maybe you could actually put those into the software . . . like expanding it, make it sort of like a broader selection of situations and scenarios.
Approaches and challenges of technology
Personal relationship with the mobile app
Initially, people described that paranoia and self-consciousness were sometimes barriers to the use of the mobile app in public. Participants described viewing the mobile app as like a best friend, but also that they gradually moved from the mobile app to instilling responses in memory. However, the mobile app alone did not seem sufficient at the end of therapy and several participants expressed a desire for more sessions or even to take part again:
It’s difficult for me . . . yeah I always felt a bit of conscious somebody might be coming along and looking over your shoulder.
That’s right, that is my best friend.
I’m not sure if my condition has improved, but I don’t find I need to use it so much now.
I didn’t feel the need to get it [the mobile app] out of the pocket. Nothing to do with anybody else. But for me I just remembered it anyway.
Even though I don’t look at the phone, I just remember about slowing down.
It’s a shame that the therapy can’t carry on for longer. Once I stopped I felt there was something a bit missing. Which is why I am looking into taking up something now.
Use of technology to support positive outcomes
The mobile app was seen by participants as a tool to aid connectedness in daily life, the thought bubbles were seen as a guide and the computer scenarios and games were seen as learning tools:
The phone actually helps when you’re on the bus . . . if I start getting agitated about who’s looking at me and who’s not looking at me yeah, I just start playing with the bubble.
Every day if I go out, I always do what I need to do on it, like take my deep breaths and get me encouraged to go out . . . But that phone is always with me when I’m out. And if I stop, I use it as well.
Before I go out, check phone, then leave, pop the bubbles, slow down. I used it every day, not using it now. The tips helpful and personal message when have worries and message come up, worked as reminder.
Challenges to using technology
In some cases, the lack of interest in technology or the limits of the mobile app interface were a barrier to use and, as expected, technical issues with the minimum viable product were described. Recommended improvements included having larger fonts, animations in colour, a ‘check-in’ rating for how you’re feeling on the phone and written instructions on how to use the phone (onboarding), which is a priority for the next iteration:
. . . technology, and trying to keep up with it. I mean yesterday I tried to look up a few apps on the SlowMo and sometimes I was trying to find something, erm, something about err feeling insecure about something and I tried to find the answer that I gave myself, but I found that a little bit difficult.
I have bought things like iPods [Apple Inc., Cupertino, CA, USA] and Nintendo [Kyoto, Japan], but I know the main thing is the smartphone, but it’s too much technology for me. I can’t really be bothered to take the phone out with me.
. . . umm I did find when I wrote things for the bubbles, the type was a bit big and when the bubbles got smaller I couldn’t read everything it said.
. . . I had my own phone and I didn’t want to go around carrying two phones.
Cognitive demands of blended therapy as therapeutic or overwhelming
Some participants described the experience of a blended therapy approach as therapeutic, whereas others found it cognitively demanding:
You have got someone who is caring and understanding, but then you have got the visual and the video. And the things that might be passing through your mind . . . you need to sort of hit as many as possible to try and calm me down, so if you have got all of those stimulated by like looking and feeling, and then you are almost touching as well, it’s very engaging.
. . . just looking at the computer and, erm, and, also listening to [therapist], I mean, erm, it was quite, it was understanding what was on the computer with like all the cases they had, of the different [scenarios] . . . probably nearer to the end, my brain just totally, you know, shut down.
Improvements in paranoia and well-being
Participants at all sites reported multiple impacts on their mental health and well-being.
Decreases in paranoid thinking and in worry
Participants described a reduction in paranoia and worries and that the interventions supported people to have clearer thoughts:
Well the paranoia has dropped quite a bit, yeah. I’m not as extremely paranoid as I used to be.
I’m a worrier, but now I’m not a worrier as much as I was . . . it slowed me down quite a lot.
. . . you do think everybody is talking about you; I mean that was the big thing that I took from it. It just made me think ‘Hang on a minute, get a grip, it’s not like that at all’. That was the biggest thing that I took from it: just seeing things a bit more clearly.
Increased engagement with social life
I never used to go out, you see, and I go out on my scooter now with confidence. Before I wouldn’t; I always thought people were going to attack me and I don’t feel like that now.
I was not going out, not taking bus, at home all the time, walking. After 2/3 months, took the bus. Bike made me feel better and I start working.
I started up my art classes. I used to do a lot on my own, but now I go to other people for more structured art classes.
I suppose my social life has improved. It’s made me more comfortable around people I think. I have met more people and done more things I would say. Like just going to the movies, chilling or playing video games.
Increased confidence and perseverance
I am more confident, if I hear something I just brush it under the water; slow thinking for me, you know.
When I do my housework and they bellow at me ‘Stop doing, stop doing, we didn’t tell you to do it’, I just carry on doing it. I thought ‘No, I’m going to carry on doing it’.
Support with other mental health difficulties
Participants described support for a range of other mental health difficulties, including anxiety, stress, panic attacks, voice-hearing experiences and depression:
It’s teaching me to not sort of stress so much. Not, you know, not to get over anxious about stuff.
This is the first time in 5 years as I haven’t been in hospital with my depression and psychosis. So I think it’s really made a difference. Normally I am sort of in hospital 3 or 4 months a year.
Positive view of the future
Before SlowMo I was doomed, yeah, but now I’ve got a bit more positive outlook; yeah, I can actually live a bit of life.
I was like ‘I’m a weirdo, a nutter’, all that kind of thing, and then you realise that there is a lot of people in the same boat and there is a lot of nice people out there. It just gives you a more positive outlook.
Discussion
This chapter provided an in-depth exploration of the user experience of the SlowMo therapy design, generating insights for further development work and to support implementation. The six core themes captured the nerves and experiences of starting the SlowMo journey; the central role of the supportive therapist, who acted as a guide to accessing the therapy and the technology; and the relationships, approaches and challenges experienced in the use of the technology. Key features of the therapy from the participants’ perspectives were the concept of slowing things down, which was learnt and internalised through time and practice, and the value and learning achieved through social connections with the vignette characters that helped to normalise experiences and model coping strategies. As expected for a minimal viable product, technical difficulties were reported and recommendations were made for improvements. Positive impacts of the SlowMo therapy that were reported directly by participants included the impact on paranoia and other mental health difficulties, enhanced engagement with social and daily life, increased confidence and a positive outlook for the future.
Participants’ primary reasons for starting the SlowMo therapy were often a sense of feeling stuck and the opportunity to get help. Indeed, one of the peer researchers ‘stressed that people on the SlowMo trial had not generally been offered any other therapies before and it was important to bring out these issues’ (see Box 3) and some of the quotations make it clear that these issues had never been discussed before. As therapy progressed, participants expressed that the interactive multimedia feature of the vignettes made them feel connected, understood and less isolated in their experiences. Studies have also shown that participants enjoy digital platforms that are tailored, personalised and communicative. 149 Participants learned and retained their therapy skills better by observing the vignettes and several participants requested more characters dealing with different worries that often occur in paranoia. This experience of viewing others coping with similar experiences is an important factor that affects acceptability and engagement. 168 Participants recognised the importance of slowing down and focused on changing their thinking style by being more flexible in their thoughts and seeking more information, as discussed in Chapter 1. The thought bubbles helped participants to develop their skills to slow down their thinking and were an accessible resource that offered coping ideas and strategies (also discussed in Chapter 1).
A qualitative study on views of psychosis users reported that digital health interventions are seen as providing immediate and direct access to health care, reducing the pressure of waiting time. 169 A systematic review170 also found that ‘at-risk’ or first episode of psychosis individuals use the internet and mobile technologies for their mental health difficulties more frequently than those with longer-term psychosis, although this may have been related to users’ age and familiarity with technology. We found that participants were more likely to use the app earlier in the therapy, when paranoia was arguably more acute, and that the use of the app appeared to reduce as participants’ mental state improved and the thinking processes became internalised. This is consistent with the concept of e-attainment, as outlined in Chapter 3.
The presence of the therapist during the session was viewed as central to the process. The therapist was seen as critical in bridging the gap between the participant and the technical features of the mobile app, which in turn led to more favourable experiences of the technology. In the present study, the majority opinion was that the digital component of the therapy augmented the rich therapeutic relationship, in contrast to a stand-alone digital intervention. 171 This is supported by a recent systematic review168 that found that, when peer-to-peer interactions on mobile health (mHealth) apps were not moderated by clinicians or researchers, the retention rates slipped from very high (94.5%) to very low (14%), highlighting the role of the therapist in improving adherence. Importantly, however, in the current study, the participants also described a form of relationship that developed with the mobile app itself as an emerging experience. The mobile app reminded participants of the learning gained in therapy and was referred to as a ‘best friend’ in some cases.
Participants noted technical challenges, as expected given that the trial tested a minimal viable product of SlowMo therapy. 7 Technical recommendations have now been integrated into a product specification for an updated version of the SlowMo therapy, including improving the synching of content from the computer app to the mobile app, increasing font size, providing additional onboarding (written instructions) for use of the mobile app and coding the apps for cross-platform use. A study109 looking at factors affecting implementation of digital health interventions reported that interventions that are user friendly, adaptable to users’ needs and available on the participants’ own phone lead to better engagement. The participants who were recruited in previous qualitative studies by Aref-Adib et al. 171 and Bucci et al. 169 were mostly young, digital natives with a mean age of 28 years and 26 years, respectively. In the present study, the mean age of the participants was 45 years and, thus, a strength of this study was the broadly positive experience of blended therapy in this older age group. 109 Stigma surrounding mental health continued to be a barrier, especially for people suffering from paranoia, who, on occasion, felt self-conscious when using the mobile app in public. Although the SlowMo platform offers a normalising, supportive platform for participants, suspiciousness and pre-existing views towards technology might also affect participants’ usage. 109 Indeed, Chapter 3 has already shown that, although age, ethnicity and paranoia did not, in general, impact the use of the mobile app, pre-therapy confidence in technology did play a part.
Finally, participants reported improvements in paranoia, worry, confidence, distress, outlook and social life, mirroring the quantitative results from Chapter 1. These findings support the efficacy results of the SlowMo trial, which showed positive impacts of the therapy on paranoia and worry, alongside impacts on belief flexibility, fast and slow thinking, and other well-being, self-concept and quality-of-life outcomes. The therapy proved to have far-reaching impacts, as participants mentioned improvements in their social life and co-existing conditions in keeping with the broad pattern of improvements across secondary outcomes reported in Chapter 1. Participants reported increased self-confidence and better management of other stresses, which is consistent with the use of technology to promote a sense of autonomy and for mobile apps to offer real-time help. 169
To conclude, participants of the SlowMo therapy had a positive experience with the digital blended therapy. There were reductions in paranoia and improved overall well-being as a result of feeling understood, relating to vignettes, accepting and learning a new thinking style of slow thinking through interactive thought bubbles, and being supported by a therapist to reinforce their learning through the use of out-of-clinic sessions and the mobile app.
Strengths and limitations
This is one of the first studies to gather detailed personal and contextual information to understand the factors influencing user experience of a specific digital blended therapy for paranoia. Data were gathered from a reasonably representative sample of > 10% of those participants randomised to receive SlowMo therapy. Service user researchers co-delivered the study by supporting recruitment, conducting all interviews with the participants and co-producing the final thematic analysis, which enhanced the robustness of the results. A number of steps were taken during the course of the analysis to enhance the overall rigour of the study and limit sources of bias. The initial coding was conducted by an independent researcher, with multiple coding and triangulation to reach a consensus on the theme structure. Regular meetings involving a diverse mix of professional and peer researchers ensured that participants’ responses were considered from a variety of viewpoints.
Limitations included the limited sampling of the Oxford participants and the limited ethnic diversity, especially from the black ethnic group with lower smartphone use and lower confidence prior to therapy. The diversity of the sample with respect to digital literacy, cognitive abilities and paranoia severity is not known. Furthermore, although participants were invited sequentially, it is unclear if those who agreed to take part were also those who were more positive about the therapy.
Conclusions
These findings offer valuable insights into participants’ experiences with SlowMo therapy. Importantly, many participants described feeling stuck prior to starting the therapy. They valued the central role of the supportive therapist, who guided them through the therapy and the use of the technology. Participants stated that key concepts of slow and fast thinking were helpful and that they valued learning from the social connections with the vignette characters. The personal relationship with the mobile app was experienced positively, and the integration of the slow-thinking style over time in a form of e-attainment was accompanied by improvements in paranoia, well-being and social integration, and reductions in worry, stress and depression. In this respect, the ‘triangle of alliance’ between the service user, the therapist and the digital platforms was highly effective, and there was a clear sense of a shared bond, goals and tasks to support improved paranoia and mental well-being. Important consideration was given to the less visible personal and social barriers that affect uptake of digital therapy, such as lack of instructions on how to use a mobile app, preference for using the mobile app on one’s own phone and the impact on usage pattern when symptoms become acute. This study, in combination with Chapter 3, provides critical information to support the development of the next iteration of the SlowMo blended therapy for future practice and implementation.
Acknowledgements
We acknowledge the contribution to the study of Dr Mar Rus-Calafell, Dr Nicola Collett, Dr Alison McGourty and Dr Catarina Sacadura, who were main trial therapists and supervised local therapists and the research workers. Dr Helen Harding (née Waller) contributed to the early development of the SlowMo intervention, before this study commenced, and to the design of the trial. Ms Kirsty James provided input to the statistical analysis.
We thank the nine PPI team members who acted as peer researchers and service user consultants during the study (as reported in Chapters 2 and 4). Those who have given permission to use their names were Alice Hicks, (first names only) Angie, Dan, Amy, Helen and Natalie, and (pseudonyms) Anthony and Alex. One PPI team member sadly died during the study; they made an important early contribution (but permission to name them in this report was not granted before their death). They cared passionately about improving the lives of people with mental health problems and dedicated their time and energy to making a positive difference. We would like to acknowledge their kindness and warmth as a person and the intelligence and wisdom that they brought to the project. We also thank Megha Gurnani and Daniel Michelson, both of the University of Sussex, who contributed to the qualitative interview study reported in Chapter 4: Megha Gurnani was the graduate coder and Daniel Michelson co-supervised Megha Gurnani.
We would like to acknowledge the contribution of the research workers in the trial: Ujala Ilyas, Elâ Örücü, Valerija Lvova, Phoebe Marple-Horvat, Rikesh Halkoree, Evelin Vogel, Eva Tolmeijer, Claire Vella, Vicci Smallman, Anna East, Catherine Belton and Michaela Rea. We also acknowledge Dr Sam Fraser, Dr Katherine Pugh, Dr Simone Farrelly, Dr Annabel Irwins, Dr Katherine Laws and Dr Emma Černis for their contribution as local trial therapists.
The Helen Hamlyn Centre for Design, Royal College of Art collaborated on the therapy design prior to the trial. Evolyst (Birmingham, UK) carried out the software development and provided software maintenance during the trial.
We thank all of the trial participants; the independent members of the Trial Steering Committee [Professor Richard Bentall (chairperson), Dr Robert Dudley, Mr Maurice Arbuthnot, Professor Richard Hooper, and Dr Alison Brabban] and the DMEC [Professor Andrew Gumley (chairperson), Professor John Norrie and Professor David Kingdon]; and the clinical teams in South London and Maudsley NHS Foundation Trust, Oxford Health NHS Foundation Trust and Sussex Partnership NHS Foundation Trust for their support of the trial.
Contributions of authors
Philippa Garety (https://orcid.org/0000-0002-5637-1340) (Professor of Clinical Psychology) designed the trial, took main responsibility for the first draft of the study report, was the main lead for the trial, led the investigation in London, and provided input for the training and supervision in the therapy and digital platform.
Thomas Ward (https://orcid.org/0000-0002-7608-5755) (Research Clinical Psychologist, Trial Co-ordinator) provided input on the first draft of the study report, was the trial co-ordinator and therapy lead, and provided training and supervision in the therapy and digital platform.
Richard Emsley (https://orcid.org/0000-0002-1218-675X) (Professor of Medical Statistics and Trials Methodology) designed the trial, provided input on the first draft of the study report and carried out the statistical analysis.
Kathryn Greenwood (https://orcid.org/0000-0001-7899-8980) (Professor in Clinical Psychology) designed the trial, provided input on the first draft of the study report, was the PPI lead and led the investigation in Sussex.
Daniel Freeman (https://orcid.org/0000-0002-2541-2197) (Professor of Clinical Psychology) designed the trial and led the investigation in Oxford.
David Fowler (https://orcid.org/0000-0001-5806-2659) (Professor in Psychology) designed the trial and led the investigation in Sussex.
Elizabeth Kuipers (https://orcid.org/0000-0002-0041-7338) (Professor Emerita of Clinical Psychology) designed the trial, and provided input on the training and supervision in the therapy and digital platform.
Paul Bebbington (https://orcid.org/0000-0002-6030-7456) (Professor Emeritus of Psychiatry) designed the trial.
Graham Dunn (https://orcid.org/0000-0001-7091-3161) (Professor of Biostatistics) designed the trial.
Amy Hardy (https://orcid.org/0000-0002-6044-6093) (Research Clinical Psychologist) designed the trial, provided input on the first draft of the study report, was the digital lead, and provided training in and supervision on the therapy and digital platform.
All authors contributed to, read and approved the final report.
Graham Dunn died in 2019 before the study was completed. He was a leading statistician and trials methodologist, with particular expertise in mediation analysis. He worked with and influenced other members of the team over decades. His contribution to the design and conduct of the study was outstanding.
Publication
Garety P, Ward T, Emsley R, Greenwood K, Freeman D, Fowler D, et al. Effects of SlowMo, a blended digital therapy targeting reasoning, on paranoia among people with psychosis: a randomized clinical trial. [published online ahead of print 7 April 2021] JAMA Psychiatry 2021.
Data-sharing statement
The data sets generated and/or analysed during the current study will be available in anonymised form from the corresponding author (Philippa Garety) on reasonable request, subject to review, following the publication of results.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research. The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the MRC, NETSCC, the EME programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the EME programme or the Department of Health and Social Care.
References
- The Schizophrenia Commission . The Abandoned Illness: A Report from the Schizophrenia Commission 2012.
- National Institute for Health and Care Excellence (NICE) . Psychosis and Schizophrenia: Treatment and Management. 2014.
- Turner DT, Burger S, Smit F, Valmaggia LR, van der Gaag M. What constitutes sufficient evidence for case formulation-driven CBT for psychosis? Cumulative meta-analysis of the effect on hallucinations and delusions. Schizophr Bull 2020;46:1072-85. https://doi.org/10.1093/schbul/sbaa045.
- Bighelli I, Salanti G, Huhn M, Schneider-Thoma J, Krause M, Reitmeir C, et al. Psychological interventions to reduce positive symptoms in schizophrenia: systematic review and network meta-analysis. World Psychiatry 2018;17:316-29. https://doi.org/10.1002/wps.20577.
- Freeman D, Dunn G, Garety P, Weinman J, Kuipers E, Fowler D, et al. Patients’ beliefs about the causes, persistence and control of psychotic experiences predict take-up of effective cognitive behaviour therapy for psychosis. Psychol Med 2013;43:269-77. https://doi.org/10.1017/S0033291712001225.
- Kendler KS, Campbell J. Interventionist causal models in psychiatry: repositioning the mind-body problem. Psychol Med 2009;39:881-7. https://doi.org/10.1017/S0033291708004467.
- Hardy A, Wojdecka A, West J, Matthews E, Golby C, Ward T, et al. How inclusive, user-centered design research can improve psychological therapies for psychosis: development of SlowMo. JMIR Ment Health 2018;5. https://doi.org/10.2196/11222.
- Garety PA, Freeman D. The past and future of delusions research: from the inexplicable to the treatable. Br J Psychiatry 2013;203:327-33. https://doi.org/10.1192/bjp.bp.113.126953.
- Garety PA, Freeman D, Jolley S, Dunn G, Bebbington PE, Fowler DG, et al. Reasoning, emotions, and delusional conviction in psychosis. J Abnorm Psychol 2005;114:373-84. https://doi.org/10.1037/0021-843X.114.3.373.
- Dudley R, Taylor P, Wickham S, Hutton P. Psychosis, delusions and the ‘jumping to conclusions’ reasoning bias: a systematic review and meta-analysis. Schizophr Bull 2016;42:652-65. https://doi.org/10.1093/schbul/sbv150.
- McLean BF, Mattiske JK, Balzan RP. Association of the jumping to conclusions and evidence integration biases with delusions in psychosis: a detailed meta-analysis. Schizophr Bull 2016;11. https://doi.org/10.1093/schbul/sbw056.
- So SH, Siu NY, Wong HL, Chan W, Garety PA. ‘Jumping to conclusions’ data-gathering bias in psychosis and other psychiatric disorders – two meta-analyses of comparisons between patients and healthy individuals. Clin Psychol Rev 2016;46:151-67. https://doi.org/10.1016/j.cpr.2016.05.001.
- Zhu C, Sun X, So SH. Associations between belief inflexibility and dimensions of delusions: a meta-analytic review of two approaches to assessing belief flexibility. Br J Clin Psychol 2018;57:59-81. https://doi.org/10.1111/bjc.12154.
- Freeman D, Taylor KM, Molodynski A, Waite F. Treatable clinical intervention targets for patients with schizophrenia. Schizophr Res 2019;211:44-50. https://doi.org/10.1016/j.schres.2019.07.016.
- Ward T, Garety PA. Fast and slow thinking in distressing delusions: a review of the literature and implications for targeted therapy. Schizophr Res 2019;203:80-7. https://doi.org/10.1016/j.schres.2017.08.045.
- Moritz S, Andreou C, Schneider BC, Wittekind CE, Menon M, Balzan RP, et al. Sowing the seeds of doubt: a narrative review on metacognitive training in schizophrenia. Clin Psychol Rev 2014;34:358-66. https://doi.org/10.1016/j.cpr.2014.04.004.
- van Oosterhout B, Smit F, Krabbendam L, Castelein S, Staring AB, van der Gaag M. Metacognitive training for schizophrenia spectrum patients: a meta-analysis on outcome studies. Psychol Med 2016;46:47-5. https://doi.org/10.1017/S0033291715001105.
- Eichner C, Berna F. Acceptance and efficacy of metacognitive training (MCT) on positive symptoms and delusions in patients with schizophrenia: a meta-analysis taking into account important moderators. Schizophr Bull 2016;42:952-62. https://doi.org/10.1093/schbul/sbv225.
- Freeman D, Garety P. Advances in understanding and treating persecutory delusions: a review. Soc Psychiatry Psychiatr Epidemiol 2014;49:1179-89. https://doi.org/10.1007/s00127-014-0928-7.
- Clarkson PJ, Coleman R. History of inclusive design in the UK. Appl Ergon 2015;46:235-47. https://doi.org/10.1016/j.apergo.2013.03.002.
- Norman D. The Design of Everyday Things: Revised and Expanded Edition. New York, NY: Basic Books; 2013.
- Ross K, Freeman D, Dunn G, Garety P. A randomized experimental investigation of reasoning training for people with delusions. Schizophr Bull 2011;37:324-33. https://doi.org/10.1093/schbul/sbn165.
- Waller H, Freeman D, Jolley S, Dunn G, Garety P. Targeting reasoning biases in delusions: a pilot study of the Maudsley Review Training Programme for individuals with persistent, high conviction delusions. J Behav Ther Exp Psychiatry 2011;42:414-21. https://doi.org/10.1016/j.jbtep.2011.03.001.
- Waller H, Emsley R, Freeman D, Bebbington P, Dunn G, Fowler D, et al. Thinking well: a randomised controlled feasibility study of a new CBT therapy targeting reasoning biases in people with distressing persecutory delusional beliefs. J Behav Ther Exp Psychiatry 2015;48:82-9. https://doi.org/10.1016/j.jbtep.2015.02.007.
- Garety P, Waller H, Emsley R, Jolley S, Kuipers E, Bebbington P, et al. Cognitive mechanisms of change in delusions: an experimental investigation targeting reasoning to effect change in paranoia. Schizophr Bull 2015;41:400-10. https://doi.org/10.1093/schbul/sbu103.
- Kahneman D. Thinking, Fast and Slow. New York, NY: Farrar, Straus and Giroux; 2011.
- Garety PA, Hardy A. The clinical relevance of appraisals of psychotic experiences. World Psychiatry 2017;16:140-1. https://doi.org/10.1002/wps.20408.
- Freeman D, Dunn G, Startup H, Pugh K, Cordwell J, Mander H, et al. Effects of cognitive behaviour therapy for worry on persecutory delusions in patients with psychosis (WIT): a parallel, single-blind, randomised controlled trial with a mediation analysis. Lancet Psychiatry 2015;2:305-13. https://doi.org/10.1016/S2215-0366(15)00039-5.
- Garety PA, Ward T, Freeman D, Fowler D, Emsley R, Dunn G, et al. SlowMo, a digital therapy targeting reasoning in paranoia, versus treatment as usual in the treatment of people who fear harm from others: study protocol for a randomised controlled trial. Trials 2017;18. https://doi.org/10.1186/s13063-017-2242-7.
- World Health Organization (WHO) . SCAN Schedules for Clinical Assessment in Neuropsychiatry, Version 1.0. 1992.
- Green CE, Freeman D, Kuipers E, Bebbington P, Fowler D, Dunn G, et al. Measuring ideas of persecution and social reference: the Green et al. Paranoid Thought Scales (GPTS). Psychol Med 2008;38:101-11. https://doi.org/10.1017/S0033291707001638.
- World Health Organization (WHO) . The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research 2010.
- Beecham J, Knapp M. The Economic Evaluation of Mental Health Care. Aldershot: Arena; 1995.
- Haddock G, McCarron J, Tarrier N, Faragher EB. Scales to measure dimensions of hallucinations and delusions: the psychotic symptom rating scales (PSYRATS). Psychol Med 1999;29:879-89. https://doi.org/10.1017/s0033291799008661.
- Steel C, Garety PA, Freeman D, Craig E, Kuipers E, Bebbington P, et al. The multidimensional measurement of the positive symptoms of psychosis. Int J Methods Psychiatr Res 2007;16:88-96. https://doi.org/10.1002/Mpr.203.
- Andreasen NC. The Scale of the Assessment of Positive Symptoms (SAPS). Iowa City, IA: University of Iowa; 1984.
- Freeman D, Loe BS, Kingdon D, Startup H, Molodynski A, Rosebrock L, et al. The revised Green et al., Paranoid Thoughts Scale (R-GPTS): psychometric properties, severity ranges, and clinical cut-offs. Psychol Med 2019;51:1-10. https://doi.org/10.1017/S0033291719003155.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-63.
- Priebe S, Huxley P, Knight S, Evans S. Application and results of the Manchester Short Assessment of Quality of Life (MANSA). Int J Soc Psychiatry 1999;45:7-12. https://doi.org/10.1177/002076409904500102.
- Fowler D, Freeman D, Smith B, Kuipers E, Bebbington P, Bashforth H, et al. The Brief Core Schema Scales (BCSS): psychometric properties and associations with paranoia and grandiosity in non-clinical and psychosis samples. Psychol Med 2006;36:749-59. https://doi.org/10.1017/S0033291706007355.
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther 1990;28:487-95. https://doi.org/10.1016/0005-7967(90)90135-6.
- Wessely S, Buchanan A, Reed A, Cutting J, Everitt B, Garety P, et al. Acting on delusions. I: prevalence. Br J Psychiatry 1993;163:69-76. https://doi.org/10.1192/bjp.163.1.69.
- Freeman D, Garety PA, Fowler D, Kuipers E, Bebbington PE, Dunn G. Why do people with delusions fail to choose more realistic explanations for their experiences? An empirical investigation. J Consult Clin Psychol 2004;72:671-80. https://doi.org/10.1037/0022-006X.72.4.671.
- Hardy A, Tolmeijer E, Edwards V, Ward T, Freeman D, Emsley R, et al. Measuring reasoning in paranoia: development of the Fast and Slow Thinking Questionnaire. Schizophr Bull 2020;1. https://doi.org/10.1093/schizbullopen/sgaa035.
- Kirkpatrick B, Strauss GP, Nguyen L, Fischer BA, Daniel DG, Cienfuegos A, et al. The brief negative symptom scale: psychometric properties. Schizophr Bull 2011;37:300-5. https://doi.org/10.1093/schbul/sbq059.
- Marcus E, Garety P, Weinman J, Emsley R, Dunn G, Bebbington P, et al. A pilot validation of a modified Illness Perceptions Questionnaire designed to predict response to cognitive therapy for psychosis. J Behav Ther Exp Psychiatry 2014;45:459-66. https://doi.org/10.1016/j.jbtep.2014.06.003.
- Wechsler DW. Wechsler Adult Intelligence Scale – Third Edition (WAIS III). San Antonio, TX: The Psychological Corporation; 1997.
- Lezak MD, Howieson DB, Loring DW, Fischer JS. Neuropsychological Assessment. Oxford: Oxford University Press; 2004.
- Hooley JM, Teasdale JD. Predictors of relapse in unipolar depressives: expressed emotion, marital distress, and perceived criticism. J Abnorm Psychol 1989;98:229-35. https://doi.org/10.1037//0021-843x.98.3.229.
- Onwumere J, Kuipers E, Bebbington P, Dunn G, Freeman D, Fowler D, et al. Patient perceptions of caregiver criticism in psychosis: links with patient and caregiver functioning. J Nerv Ment Dis 2009;197:85-91. https://doi.org/10.1097/NMD.0b013e3181960e57.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74. https://doi.org/10.2307/2529310.
- Batistatou E, Roberts C, Roberts S. Sample size and power calculations for trials and quasi-experimental studies with clustering. Stata J 2014;14:159-75. https://doi.org/10.1177/1536867X1401400111.
- Montgomery P, Grant S, Mayo-Wilson E, Macdonald G, Michie S, Hopewell S, et al. Reporting randomised trials of social and psychological interventions: the CONSORT-SPI 2018 Extension. Trials 2018;19. https://doi.org/10.1186/s13063-018-2733-1.
- Landau S, Emsley R, Dunn G. Beyond total treatment effects in randomised controlled trials: baseline measurement of intermediate outcomes needed to reduce confounding in mediation investigations. Clin Trials 2018;15:247-56. https://doi.org/10.1177/1740774518760300.
- Dunn G, Emsley R, Liu H, Landau S, Green J, White I, et al. Evaluation and validation of social and psychological markers in randomised trials of complex interventions in mental health: a methodological research programme. Health Technol Assess 2015;19. https://doi.org/10.3310/hta19930.
- The Lancet Psychiatry . Measuring success: the problem with primary outcomes. Lancet Psychiatry 2020;7. https://doi.org/10.1016/S2215-0366(19)30483-3.
- Mehl S, Werner D, Lincoln TM. Corrigendum: does Cognitive Behavior Therapy for psychosis (CBTp) show a sustainable effect on delusions? A meta-analysis. Front Psychol 2019;10. https://doi.org/10.3389/fpsyg.2019.01868.
- Freeman D. Persecutory delusions: a cognitive perspective on understanding and treatment. Lancet Psychiatry 2016;3:685-92. https://doi.org/10.1016/S2215-0366(16)00066-3.
- Freeman D, Garety PA, Kuipers E, Fowler D, Bebbington PE. A cognitive model of persecutory delusions. Br J Clin Psychol 2002;41:331-47. https://doi.org/10.1348/014466502760387461.
- Freeman D, Garety PA, Bebbington PE, Smith B, Rollinson R, Fowler D, et al. Psychological investigation of the structure of paranoia in a non-clinical population. Br J Psychiatry 2005;186:427-35. https://doi.org/10.1192/bjp.186.5.427.
- INVOLVE . Definition of PPI n.d. www.invo.org.uk/wp-content/uploads/2019/11/UK-standards-for-public-involvement-v6.pdf (accessed 26 May 2021).
- Chalmers I. What do I want from health research and researchers when I am a patient?. BMJ 1995;310:1315-18. https://doi.org/10.1136/bmj.310.6990.1315.
- Crocker JC, Ricci-Cabello I, Parker A, Hirst JA, Chant A, Petit-Zeman S, et al. Impact of patient and public involvement on enrolment and retention in clinical trials: systematic review and meta-analysis. BMJ 2018;363. https://doi.org/10.1136/bmj.k4738.
- Staley K. Exploring Impact: Public Involvement in NHS Public Health and Social Care Research. Eastleigh: INVOLVE; 2009.
- Crocker JC, Boylan AM, Bostock J, Locock L. Is it worth it? Patient and public views on the impact of their involvement in health research and its assessment: a UK-based qualitative interview study. Health Expect 2017;20:519-28. https://doi.org/10.1111/hex.12479.
- Simpson EL, House AO. Involving users in the delivery and evaluation of mental health services: systematic review. BMJ 2002;325. https://doi.org/10.1136/bmj.325.7375.1265.
- Brett J, Staniszewska S, Mockford C, Herron-Marx S, Hughes J, Tysall C, et al. Mapping the impact of patient and public involvement on health and social care research: a systematic review. Health Expect 2014;17:637-50. https://doi.org/10.1111/j.1369-7625.2012.00795.x.
- Brett J, Staniszewska S, Mockford C, Herron-Marx S, Hughes J, Tysall C, et al. A systematic review of the impact of patient and public involvement on service users, researchers and communities. Patient 2014;7:387-95. https://doi.org/10.1007/s40271-014-0065-0.
- Snape D, Kirkham J, Britten N, Froggatt K, Gradinger F, Lobban F, et al. Exploring perceived barriers, drivers, impacts and the need for evaluation of public involvement in health and social care research: a modified Delphi study. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-004943.
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. Res Involv Engagem 2017;3. https://doi.org/10.1186/s40900-017-0062-2.
- Sweeney A, Greenwood KE, Williams S, Wykes T, Rose DS. Hearing the voices of service user researchers in collaborative qualitative data analysis: the case for multiple coding. Health Expect 2013;16:e89-99. https://doi.org/10.1111/j.1369-7625.2012.00810.x.
- Greenwood K, Alford K, O’Leary I, Peters E, Hardy A, Cavanagh K, et al. The U.I study: study protocol for a feasibility randomised controlled trial of a pre-cognitive behavioural therapy digital ‘informed choice’ intervention to improve attitudes towards uptake and implementation of CBT for psychosis. Trials 2018;19. https://doi.org/10.1186/s13063-018-3023-7.
- Ives J, Damery S, Redwod S. PPI, paradoxes and Plato: who’s sailing the ship?. J Med Ethics 2013;39:181-5. https://doi.org/10.1136/medethics-2011-100150.
- Costa AL, Kallick B. Through the lens of a critical friend. Educ Leadersh 1993;51:49-51. https://doi.org/10.1007/BF03341507.
- McPin Foundation n.d. http://mcpin.org/get-involved/become-a-peer-researcher/ (accessed 2015).
- Staley K. There is no paradox with PPI in research. J Med Ethics 2013;39:186-7. https://doi.org/10.1136/medethics-2012-100512.
- Friesen P, Lignou S, Sheehan M, Singh I. Measuring the impact of participatory research in psychiatry: how the search for epistemic justifications obscures ethical considerations [published online ahead of print December 18 2019]. Health Expect 2019. https://doi.org/10.1111/hex.12988.
- INVOLVE . UK Standards for Public Involvement n.d. www.invo.org.uk/wp-content/uploads/2019/11/UK-standards-for-public-involvement-v6.pdf (accessed 6 May 2020).
- Gillard S, Borschmann R, Turner K, Goodrich-Purnell N, Lovell K, Chambers M. ‘What difference does it make?’ Finding evidence of the impact of mental health service user researchers on research into the experiences of detained psychiatric patients. Health Expect 2010;13:185-94. https://doi.org/10.1111/j.1369-7625.2010.00596.x.
- Barber R, Boote JD, Parry GD, Cooper CL, Yeeles P, Cook S. Can the impact of public involvement on research be evaluated? A mixed methods study. Health Expect 2012;15:229-41. https://doi.org/10.1111/j.1369-7625.2010.00660.x.
- Littlewood DL, Quinlivan L, Steeg S, Bennett C, Bickley H, Rodway C, et al. Evaluating the impact of patient and carer involvement in suicide and self-harm research: a mixed-methods, longitudinal study protocol [published online ahead of print December 5 2019]. Health Expect 2019. https://doi.org/10.1111/hex.13000.
- Staley K, Barron D. Learning as an outcome of involvement in research: what are the implications for practice, reporting and evaluation?. Res Involv Engagem 2019;5. https://doi.org/10.1186/s40900-019-0147-1.
- Staley K. Changing what researchers’ think and do’: is this how involvement impacts on research?. Res All 2017;1:158-67. https://doi.org/10.18546/RFA.01.1.13.
- Staley K. ‘Is it worth doing?’ Measuring the impact of patient and public involvement in research. Res Involv Engagem 2015;1. https://doi.org/10.1186/s40900-015-0008-5.
- Petit-Zeman S, Locock L. Health care: bring on the evidence. Nature 2013;501:160-1. https://doi.org/10.1038/501160a.
- Nielsen J. Usability Engineering. Burlington, MA: Morgan Kaufmann; 1994.
- Holmes EA, Ghaderi A, Harmer CJ, Ramchandani PG, Cuijpers P, Morrison AP, et al. The Lancet Psychiatry Commission on psychological treatments research in tomorrow’s science. Lancet Psychiatry 2018;5:237-86. https://doi.org/10.1016/S2215-0366(17)30513-8.
- Lincoln TM, Peters E. A systematic review and discussion of symptom specific cognitive behavioural approaches to delusions and hallucinations. Schizophr Res 2019;203:66-79. https://doi.org/10.1016/j.schres.2017.12.014.
- Colling C, Evans L, Broadbent M, Chandran D, Craig TJ, Kolliakou A, et al. Identification of the delivery of cognitive behavioural therapy for psychosis (CBTp) using a cross-sectional sample from electronic health records and open-text information in a large UK-based mental health case register. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-015297.
- Haddock G, Eisner E, Boone C, Davies G, Coogan C, Barrowclough C. An investigation of the implementation of NICE-recommended CBT interventions for people with schizophrenia. J Ment Health 2014;23:162-5. https://doi.org/10.3109/09638237.2013.869571.
- Goldsmith LP, Lewis SW, Dunn G, Bentall RP. Psychological treatments for early psychosis can be beneficial or harmful, depending on the therapeutic alliance: an instrumental variable analysis. Psychol Med 2015;45:2365-73. https://doi.org/10.1017/S003329171500032X.
- Dorst K. Design beyond design. She Ji 2019;5:117-27. https://doi.org/10.1016/j.sheji.2019.05.001.
- Dorst K. Frame innovation: create new thinking by design. Cambridge, MA: The MIT Press; 2015.
- Graham AK, Lattie EG, Mohr DC. Experimental therapeutics for digital mental health. JAMA Psychiatry 2019;76:1223-4. https://doi.org/10.1001/jamapsychiatry.2019.2075.
- Bell IH, Rossell SL, Farhall J, Hayward M, Lim MH, Fielding-Smith SF, et al. Pilot randomised controlled trial of a brief coping-focused intervention for hearing voices blended with smartphone-based ecological momentary assessment and intervention (SAVVy): feasibility, acceptability and preliminary clinical outcomes. Schizophr Res 2020;216:479-87. https://doi.org/10.1016/j.schres.2019.10.026.
- Ben-Zeev D, Brian RM, Jonathan G, Razzano L, Pashka N, Carpenter-Song E, et al. Mobile Health (mHealth) versus clinic-based group intervention for people with serious mental illness: a randomized controlled trial. Psychiatr Serv 2018;69:978-85. https://doi.org/10.1176/appi.ps.201800063.
- Bucci S, Barrowclough C, Ainsworth J, Machin M, Morris R, Berry K, et al. Actissist: proof-of-concept trial of a theory-driven digital intervention for psychosis. Schizophr Bull 2018;44:1070-80. https://doi.org/10.1093/schbul/sby032.
- Depp CA, Perivoliotis D, Holden J, Dorr J, Granholm EL. Single-session mobile-augmented intervention in serious mental illness: a three-arm randomized controlled trial. Schizophr Bull 2019;45:752-62. https://doi.org/10.1093/schbul/sby135.
- Freeman D, Bradley J, Antley A, Bourke E, DeWeever N, Evans N, et al. Virtual reality in the treatment of persecutory delusions: randomised controlled experimental study testing how to reduce delusional conviction. Br J Psychiatry 2016;209:62-7. https://doi.org/10.1192/bjp.bp.115.176438.
- Gumley A, Bradstreet S, Ainsworth J, Allan S, Alvarez-Jimenez M, Beattie L, et al. Early signs monitoring to prevent relapse in psychosis and promote well-being, engagement, and recovery: protocol for a feasibility cluster randomized controlled trial harnessing mobile phone technology blended with peer support. JMIR Res Protoc 2020;9. https://doi.org/10.2196/15058.
- Pot-Kolder RMCA, Geraets CNW, Veling W, van Beilen M, Staring ABP, Gijsman HJ, et al. Virtual-reality-based cognitive behavioural therapy versus waiting list control for paranoid ideation and social avoidance in patients with psychotic disorders: a single-blind randomised controlled trial. Lancet Psychiatry 2018;5:217-26. https://doi.org/10.1016/S2215-0366(18)30053-1.
- Schlosser DA, Campellone TR, Truong B, Etter K, Vergani S, Komaiko K, et al. Efficacy of PRIME, a mobile app intervention designed to improve motivation in young people with schizophrenia. Schizophr Bull 2018;44:1010-20. https://doi.org/10.1093/schbul/sby078.
- Baumel A, Muench F, Edan S, Kane JM. Objective user engagement with mental health apps: systematic search and panel-based usage analysis. J Med Internet Res 2019;21. https://doi.org/10.2196/14567.
- Bonet L, Llácer B, Hernandez-Viadel M, Arce D, Blanquer I, Cañete C, et al. Differences in the use and opinions about new eHealth technologies among patients with psychosis: structured questionnaire. JMIR Ment Health 2018;5. https://doi.org/10.2196/mental.9950.
- Firth J, Cotter J, Torous J, Bucci S, Firth JA, Yung AR. Mobile phone ownership and endorsement of ‘mHealth’ among people with psychosis: a meta-analysis of cross-sectional studies. Schizophr Bull 2016;42:448-55. https://doi.org/10.1093/schbul/sbv132.
- Pew Research Center Internet & Technology . Mobile Fact Sheet 2019. www.pewinternet.org/fact-sheet/mobile/ (accessed 27 May 2020).
- Greer B, Robotham D, Simblett S, Curtis H, Griffiths H, Wykes T. Digital exclusion among mental health service users: qualitative investigation. J Med Internet Res 2019;21. https://doi.org/10.2196/11696.
- Robotham D, Satkunanathan S, Doughty L, Wykes T. Do we still have a digital divide in mental health? A five-year survey follow-up. J Med Internet Res 2016;18. https://doi.org/10.2196/jmir.6511.
- Aref-Adib G, McCloud T, Ross J, O’Hanlon P, Appleton V, Rowe S, et al. Factors affecting implementation of digital health interventions for people with psychosis or bipolar disorder, and their family and friends: a systematic review. Lancet Psychiatry 2019;6:257-66. https://doi.org/10.1016/S2215-0366(18)30302-X.
- Gilster P. Digital Literacy. Hoboken, NJ: John Wiley & Sons Inc.; 1997.
- Torous J, Wisniewski H, Liu G, Keshavan M. Mental health mobile phone app usage, concerns, and benefits among psychiatric outpatients: comparative survey study. JMIR Ment Health 2018;5. https://doi.org/10.2196/11715.
- Elliott JH, Turner T, Clavisi O, Thomas J, Higgins JP, Mavergames C, et al. Living systematic reviews: an emerging opportunity to narrow the evidence-practice gap. PLOS Med 2014;11. https://doi.org/10.1371/journal.pmed.1001603.
- Peiris D, Miranda JJ, Mohr DC. Going beyond killer apps: building a better mHealth evidence base. BMJ Glob Health 2018;3. https://doi.org/10.1136/bmjgh-2017-000676.
- World Health Organization (WHO) . Knowledge Translation in Global Health 2011.
- Sanatkar S, Baldwin PA, Huckvale K, Clarke J, Christensen H, Harvey S, et al. Using cluster analysis to explore engagement and e-attainment as emergent behavior in electronic mental health. J Med Internet Res 2019;21. https://doi.org/10.2196/14728.
- Torous J, Nicholas J, Larsen ME, Firth J, Christensen H. Clinical review of user engagement with mental health smartphone apps: evidence, theory and improvements. Evid Based Ment Health 2018;21:116-19. https://doi.org/10.1136/eb-2018-102891.
- Schueller SM, Muñoz RF, Mohr DC. Realizing the potential of behavioral intervention technologies. Curr Dir Psychol Sci 2013;22:478-83. https://doi.org/10.1177/0963721413495872.
- Mohr DC, Riper H, Schueller SM. A solution-focused research approach to achieve an implementable revolution in digital mental health. JAMA Psychiatry 2018;75:113-14. https://doi.org/10.1001/jamapsychiatry.2017.3838.
- Yardley L, Morrison L, Bradbury K, Muller I. The person-based approach to intervention development: application to digital health-related behavior change interventions. J Med Internet Res 2015;17. https://doi.org/10.2196/jmir.4055.
- de Beurs D, van Bruinessen I, Noordman J, Friele R, van Dulmen S. Active involvement of end users when developing web-based mental health interventions. Front Psychiatry 2017;8. https://doi.org/10.3389/fpsyt.2017.00072.
- Orlowski S, Matthews B, Bidargaddi N, Jones G, Lawn S, Venning A, et al. Mental health technologies: designing with consumers. JMIR Hum Factors 2016;3. https://doi.org/10.2196/humanfactors.4336.
- Altman M, Huang TTK, Breland JY. Design thinking in health care. Prev Chronic Dis 2018;15. https://doi.org/10.5888/pcd15.180128.
- Alvarez-Jimenez M, Alcazar-Corcoles MA, González-Blanch C, Bendall S, McGorry PD, Gleeson JF. Online, social media and mobile technologies for psychosis treatment: a systematic review on novel user-led interventions. Schizophr Res 2014;156:96-106. https://doi.org/10.1016/j.schres.2014.03.021.
- Ludden GD, van Rompay TJ, Kelders SM, van Gemert-Pijnen JE. How to increase reach and adherence of web-based interventions: a design research viewpoint. J Med Internet Res 2015;17. https://doi.org/10.2196/jmir.4201.
- Kreyenbuhl J, Buchanan RW, Dickerson FB, Dixon LB. Schizophrenia Patient Outcomes Research Team (PORT) . The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2009. Schizophr Bull 2010;36:94-103. https://doi.org/10.1093/schbul/sbp130.
- Rotondi AJ, Sinkule J, Haas GL, Spring MB, Litschge CM, Newhill CE, et al. Designing websites for persons with cognitive deficits: design and usability of a psychoeducational intervention for persons with severe mental illness. Psychol Serv 2007;4:202-24. https://doi.org/10.1037/1541-1559.4.3.202.
- Young JW, Geyer MA. Developing treatments for cognitive deficits in schizophrenia: the challenge of translation. J Psychopharmacol 2015;29:178-96. https://doi.org/10.1177/0269881114555252.
- Design Council . 11 Lessons: Managing Design in 11 Global Brands: A Study of the Design Process 2005.
- Allan S, Bradstreet S, Mcleod H, Farhall J, Lambrou M, Gleeson J, et al. Developing a hypothetical implementation framework of expectations for monitoring early signs of psychosis relapse using a mobile app: qualitative study. J Med Internet Res 2019;21. https://doi.org/10.2196/14366.
- Bucci S, Schwannauer M, Berry N. The digital revolution and its impact on mental health care. Psychol Psychother 2019;92:277-97. https://doi.org/10.1111/papt.12222.
- Sarkar U, Gourley GI, Lyles CR, Tieu L, Clarity C, Newmark L, et al. Usability of commercially available mobile applications for diverse patients. J Gen Intern Med 2016;31:1417-26. https://doi.org/10.1007/s11606-016-3771-6.
- Vachon H, Viechtbauer W, Rintala A, Myin-Germeys I. Compliance and retention with the experience sampling method over the continuum of severe mental disorders: meta-analysis and recommendations. J Med Internet Res 2019;21. https://doi.org/10.2196/14475.
- Ng MM, Firth J, Minen M, Torous J. User engagement in mental health apps: a review of measurement, reporting, and validity. Psychiatr Serv 2019;70:538-44. https://doi.org/10.1176/appi.ps.201800519.
- Sieverink F, Kelders SM, van Gemert-Pijnen JE. Clarifying the concept of adherence to ehealth technology: systematic review on when usage becomes adherence. J Med Internet Res 2017;19. https://doi.org/10.2196/jmir.8578.
- Agarwal S, LeFevre AE, Lee J, L’Engle K, Mehl G, Sinha C, et al. Guidelines for reporting of health interventions using mobile phones: mobile health (mHealth) evidence reporting and assessment (mERA) checklist. BMJ 2016;352. https://doi.org/10.1136/bmj.i1174.
- Bradstreet S, Allan S, Gumley A. Adverse event monitoring in mHealth for psychosis interventions provides an important opportunity for learning. J Ment Health 2019;28:461-6. https://doi.org/10.1080/09638237.2019.1630727.
- Ben-Zeev D, Brenner CJ, Begale M, Duffecy J, Mohr DC, Mueser KT. Feasibility, acceptability, and preliminary efficacy of a smartphone intervention for schizophrenia. Schizophr Bull 2014;40:1244-53. https://doi.org/10.1093/schbul/sbu033.
- Flett JAM, Fletcher BD, Riordan BC, Patterson T, Hayne H, Conner TS. The peril of self-reported adherence in digital interventions: a brief example. Internet Interv 2019;18. https://doi.org/10.1016/j.invent.2019.100267.
- Pham Q, Graham G, Carrion C, Morita PP, Seto E, Stinson JN, et al. A library of analytic indicators to evaluate effective engagement with consumer mhealth apps for chronic conditions: scoping review. JMIR Mhealth Uhealth 2019;7. https://doi.org/10.2196/11941.
- Greenhalgh T, Wherton J, Papoutsi C, Lynch J, Hughes G, A’Court C, et al. Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J Med Internet Res 2017;19. https://doi.org/10.2196/jmir.8775.
- Hekler EB, Klasnja P, Riley WT, Buman MP, Huberty J, Rivera DE, et al. Agile science: creating useful products for behavior change in the real world. Transl Behav Med 2016;6:317-28. https://doi.org/10.1007/s13142-016-0395-7.
- Nahum-Shani I, Smith SN, Spring BJ, Collins LM, Witkiewitz K, Tewari A, et al. Just-in-Time Adaptive Interventions (JITAIs) in mobile health: key components and design principles for ongoing health behavior support. Ann Behav Med 2018;52:446-62. https://doi.org/10.1007/s12160-016-9830-8.
- Hollis C, Sampson S, Simons L, Davies EB, Churchill R, Betton V, et al. Identifying research priorities for digital technology in mental health care: results of the James Lind Alliance Priority Setting Partnership. Lancet Psychiatry 2018;5:845-54. https://doi.org/10.1016/S2215-0366(18)30296-7.
- Freeman D, McManus S, Brugha T, Meltzer H, Jenkins R, Bebbington P. Concomitants of paranoia in the general population. Psychol Med 2011;41:923-36. https://doi.org/10.1017/S0033291710001546.
- Freeman D, Garety P. Helping patients with paranoid and suspicious thoughts: a cognitive–behavioural approach. Adv Psychiat Treat 2006;12:404-15. https://doi.org/10.1192/apt.12.6.404.
- Freeman D. Improving cognitive treatments for delusions. Schizophr Res 2011;132:135-9. https://doi.org/10.1016/j.schres.2011.08.012.
- Freeman D, Pugh K, Dunn G, Evans N, Sheaves B, Waite F, et al. An early Phase II randomised controlled trial testing the effect on persecutory delusions of using CBT to reduce negative cognitions about the self: the potential benefits of enhancing self confidence. Schizophr Res 2014;160:186-92. https://doi.org/10.1016/j.schres.2014.10.038.
- Freeman D, Waite F, Startup H, Myers E, Lister R, McInerney J, et al. Efficacy of cognitive behavioural therapy for sleep improvement in patients with persistent delusions and hallucinations (BEST): a prospective, assessor-blind, randomised controlled pilot trial. Lancet Psychiatry 2015;2:975-83. https://doi.org/10.1016/S2215-0366(15)00314-4.
- Berry N, Lobban F, Emsley R, Bucci S. Acceptability of interventions delivered online and through mobile phones for people who experience severe mental health problems: a systematic review. J Med Internet Res 2016;18. https://doi.org/10.2196/jmir.5250.
- Kooistra LC, Ruwaard J, Wiersma JE, van Oppen P, van der Vaart R, van Gemert-Pijnen JEWC, et al. Development and initial evaluation of blended cognitive behavioural treatment for major depression in routine specialized mental health care. Internet Interv 2016;4:61-7. https://doi.org/10.1016/j.invent.2016.01.003.
- Clarke J, Proudfoot J, Whitton A, Birch MR, Boyd M, Parker G, et al. Therapeutic alliance with a fully automated mobile phone and web-based intervention: secondary analysis of a randomized controlled trial. JMIR Ment Health 2016;3. https://doi.org/10.2196/mental.4656.
- Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy 1979;16. https://doi.org/10.1037/h0085885.
- Lopez A, Schwenk S, Schneck CD, Griffin RJ, Mishkind MC. Technology-based mental health treatment and the impact on the therapeutic alliance. Curr Psychiatry Rep 2019;21. https://doi.org/10.1007/s11920-019-1055-7.
- Henson P, Wisniewski H, Hollis C, Keshavan M, Torous J. Digital mental health apps and the therapeutic alliance: initial review. BJPsych Open 2019;5. https://doi.org/10.1192/bjo.2018.86.
- Cavanagh K, Bennett-Levy J, Richards DA, Farrand P, Christensen H, Griffiths KM, et al. Oxford Guides in Cognitive Behavioural Therapy. Oxford Guide to Low Intensity CBT Interventions. Oxford: Oxford University Press; 2010.
- Cavanagh K, Millings A. (Inter) personal computing: the role of the therapeutic relationship in e-mental health. J Contemp Psychother 2013;43:197-206. https://doi.org/10.1007/s10879-013-9242-z.
- Lopez A. An investigation of the use of internet based resources in support of the therapeutic alliance. Clin Soc Work 2015;43:189-200. https://doi.org/10.1007/s10615-014-0509-y.
- Gillard S, Simons L, Turner K, Lucock M, Edwards C. Patient and public involvement in the coproduction of knowledge: reflection on the analysis of qualitative data in a mental health study. Qual Health Res 2012;22:1126-37. https://doi.org/10.1177/1049732312448541.
- Collier A. Critical Realism: An Introduction to Roy Bhaskar’s Philosophy. London: Verso; 1994.
- Bhaskar R. Scientific Realism and Human Emancipation. New York, NY: Routledge; 2009.
- Ponterotto JG. Qualitative research training in counseling psychology: a survey of directors of training. Teach Psychol 2005;32:60-2.
- Holloway I, Todres L. The status of method: flexibility, consistency and coherence. Qual 2003;3:345-57. https://doi.org/10.1177/1468794103033004.
- Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods 2017;16:1-13. https://doi.org/10.1177/1609406917733847.
- Hammersley M. Action research: a contradiction in terms?. Oxf Rev Educ 2004;30:165-81. https://doi.org/10.1080/0305498042000215502.
- Porter S. Validity, trustworthiness and rigour: reasserting realism in qualitative research. J Adv Nurs 2007;60:79-86. https://doi.org/10.1111/j.1365-2648.2007.04360.x.
- Letourneau G, Allen M, Cody WK. Philosophical and Theoretical Perspectives for Advanced Nursing Practice. Boston, MA: Jones and Bartlett Publishers; 2006.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Biagianti B, Quraishi SH, Schlosser DA. Potential benefits of incorporating peer-to-peer interactions into digital interventions for psychotic disorders: a systematic review. Psychiatr Serv 2018;69:377-88. https://doi.org/10.1176/appi.ps.201700283.
- Bucci S, Morris R, Berry K, Berry N, Haddock G, Barrowclough C, et al. Early psychosis service user views on digital technology: qualitative analysis. JMIR Ment Health 2018;5. https://doi.org/10.2196/10091.
- Killikelly C, He Z, Reeder C, Wykes T. Improving adherence to web-based and mobile technologies for people with psychosis: systematic review of new potential predictors of adherence. JMIR Mhealth Uhealth 2017;5. https://doi.org/10.2196/mhealth.7088.
- Aref-Adib G, O’Hanlon P, Fullarton K, Morant N, Sommerlad A, Johnson S, et al. A qualitative study of online mental health information seeking behaviour by those with psychosis. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-0952-0.
Appendix 1 Chapter 1 supplementary tables and figure
| Time point | Treatment group | GPTS part B persecution, n (%) | R-GPTS part B, n (%) | ||
|---|---|---|---|---|---|
| < 35 | ≥ 35 | < 18 | ≥ 18 | ||
| Baseline | TAU | 10 (5.6) | 170 (94.4) | 45 (25.0) | 135 (75.0) |
| SlowMo | 11 (6.1) | 169 (93.9) | 54 (30.0) | 126 (70.0) | |
| 12 weeks | TAU | 45 (27.6) | 118 (72.4) | 68 (41.7) | 95 (58.3) |
| SlowMo | 57 (34.3) | 109 (65.7) | 87 (52.4) | 79 (47.6) | |
| 24 weeks | TAU | 54 (31.6) | 117 (68.4) | 85 (50.3) | 84 (49.7) |
| SlowMo | 62 (38.5) | 99 (61.5) | 91 (56.5) | 70 (43.5) | |
| Mediator | Effect, causal mediation effect (bootstrap SE); (95% CI) | Proportion mediated | ||
|---|---|---|---|---|
| Total | Direct | Indirect | ||
| Alternative explanations | ||||
| 12 weeks | –1.52 (0.49); (–2.49 to –0.62) | –1.47 (0.48); (–2.40 to –0.56) | –0.04 (0.06); (–0.19 to 0.05) | 2.6 |
| 24 weeks | –4.12 (1.69); (–7.39 to –0.44) | –3.82 (1.71); (–7.12 to 0.04) | –0.30 (0.28); (–0.99 to 0.09) | 7.3 |
| JTC 85 : 15 task | ||||
| 12 weeks | –1.45 (0.50); (–2.42 to –0.50) | –1.40 (0.48); (–2.32 to –0.48) | –0.05 (0.08); (–0.24 to 0.08) | 3.4 |
| 24 weeks | –3.77 (1.72); (–6.81 to 0.11) | –3.61 (1.73); (–6.66 to 0.21) | –0.17 (0.24); (–0.64 to 0.38) | 4.5 |
| JTC 60 : 40 task | ||||
| 12 weeks | –1.50 (0.50); (–2.49 to –0.51) | –1.49 (0.49); (–2.47 to –0.49) | –0.01 (0.05); (–0.12 to 0.09) | 0.7 |
| 24 weeks | –4.14 (1.69); (–7.32 to –0.61) | –4.12 (1.71); (–7.42 to –0.56) | –0.03 (0.16); (–0.35 to 0.39) | 0.7 |
| Possibility of being mistaken (yes/no) | ||||
| 12 weeks | –1.64 (0.49); (–2.56 to –0.65) | –1.34 (0.47); (–2.21 to –0.43) | –0.30 (0.14); (–0.60 to –0.07) | 18.3 |
| 24 weeks | –4.49 (1.67); (–7.64 to –0.98) | –3.57 (1.65); (–6.77 to –0.35) | –0.92 (0.52); (–2.24 to –0.16) | 20.5 |
| Possibility of being mistaken (1–100) | ||||
| 12 weeks | –1.52 (0.48); (–2.43 to –0.59) | –1.08 (0.45); (–1.98 to –0.22) | –0.44 (0.17); (–0.81 to –0.12) | 28.9 |
| 24 weeks | –4.04 (1.68); –7.21 to –0.30 | –2.69 (1.67); (–5.96 to 0.71) | –1.35 (0.58); (–2.64 to –0.34) | 33.4 |
| Worry | ||||
| 12 weeks | –1.55 (0.50); (–2.49 to –0.63) | –1.10 (0.48); (–1.97 to –0.18) | –0.45 (0.16); (–0.83 to –0.16) | 29.0 |
| 24 weeks | –3.77 (1.65); (–6.97 to –0.40) | –2.57 (1.66); (–5.80 to 0.85) | –1.20 (0.52); (–2.35 to –0.32) | 31.8 |
| Mediator | Effect, causal mediation effect (bootstrap SE); (95% CI) | Proportion mediated | ||
|---|---|---|---|---|
| Total | Direct | Indirect | ||
| Alternative explanations | ||||
| 12 weeks | –4.63 (1.68); (–8.10 to –1.48) | –4.38 (1.67); (–7.65 to –1.19) | –0.25 (0.25); (–0.86 to 0.09) | 5.4 |
| 24 weeks | –3.42 (1.71); (–6.61 to –0.10) | –3.18 (1.70); (–6.40 to 0.13) | –0.25 (0.25); (–0.83 to 0.11) | 7.3 |
| JTC 85 : 15 task | ||||
| 12 weeks | –4.61 (1.73); (–7.91 to –1.31) | –4.44 (1.72); (–7.72 to –1.17) | –0.17 (0.28); (–0.83 to 0.32) | 3.7 |
| 24 weeks | –3.01 (1.75); (–6.07 to 0.51) | –2.85 (1.75); (–5.97 to 0.79) | –0.15 (0.25); (–0.63 to 0.39) | 5.0 |
| JTC 60 : 40 task | ||||
| 12 weeks | –4.72 (1.72); (–7.98 to –1.44) | –4.70 (1.68); (–7.88 to –1.50) | –0.03 (0.25); (–0.57 to 0.43) | 0.6 |
| 24 weeks | –3.32 (1.72); (–6.74 to 0.17) | –3.31 (1.73); (–6.71 to 0.08) | –0.01 (0.15); (–0.31 to 0.38) | 0.3 |
| Possibility of being mistaken (yes/no) | ||||
| 12 weeks | –5.14 (1.70); (–8.48 to –1.88) | –3.80 (1.65); (–7.17 to –0.58) | –1.34 (0.60); (–2.73 to –0.36) | 26.1 |
| 24 weeks | –3.65 (1.71); (–6.80 to –0.26) | –2.63 (1.68); (–5.84 to 0.70) | –1.02 (0.54); (–2.37 to –0.26) | 27.9 |
| Possibility of being mistaken (1–100) | ||||
| 12 weeks | –4.76 (1.67); (–8.03 to –1.62) | –3.20 (1.57); (–6.28 to –0.37) | –1.55 (0.62); (–2.86 to –0.39) | 32.6 |
| 24 weeks | –3.28 (1.70); (–6.50 to 0.16) | –1.70 (1.61); (–4.80 to 1.46) | –1.58 (0.61); (–2.78 to –0.43) | 48.2 |
| Worry | ||||
| 12 weeks | –4.87 (1.63); (–8.10 to –1.84) | –3.17 (1.60); (–6.18 to 0.01) | –1.71 (0.62); (–2.95 to –0.58) | 35.1 |
| 24 weeks | –3.14 (1.67); (–6.39 to 0.10) | –1.75 (1.66); (–4.74 to 1.46) | –1.39 (0.57); (–2.64 to –0.52) | 44.3 |
| Concomitant therapy | Treatment group | |
|---|---|---|
| SlowMo | TAU | |
| Therapy | ||
| One-to-one CBT (paranoia focus) | 7 (7) | 12 (11) |
| Sessions | 7.6 (10.0) | 7.0 (5.4) |
| One-to-one psychology (non-paranoia focus) | 8 (8) | 26 (25) |
| Sessions | 4.7 (3.5) | 9.1 (6.2) |
| Psychology groups (paranoia) | 2 (2) | 2 (2) |
| Sessions | 3.5 (2.1) | 1.0 (0.0) |
| Psychology group (non-paranoia) | 6 (6) | 7 (7) |
| Sessions | 7.0 (8.6) | 7.3 (7.9) |
| Family intervention | 2 (2) | 4 (4) |
| Sessions | 2.5 (2.1) | 6.5 (3.4) |
| Health and well-being groups | 3 (3) | 8 (6) |
| Sessions | 7.7 (10.7) | 4.5 (2.1) |
| One-to-one therapy (non-psychology) | 1 (1) | 2 (2) |
| Sessions | 3.0 (–) | 14.0 (4.2) |
| Art therapy | 1 (1) | 2 (2) |
| Sessions | 11.0 (–) | 21.5 (0.7) |
| Other | 1 (1) | 7 (7) |
| Sessions | 6.0 (–) | 8.4 (10.0) |
| Medication | ||
| Typical antipsychotic | 29 (20) | 25 (22) |
| Atypical antipsychotic | 225 (142) | 198 (141) |
| Clozapine (Clozaril®, Novartis Pharmaceuticals Corporation, East Hanover, NJ) | 27 (23) | 39 (31) |
| Mood stabiliser | 26 (23) | 26 (23) |
| Antidepressant | 74 (67) | 82 (70) |
| Antianxiety/hypnotic | 24 (20) | 28 (26) |
| Other psychiatric | 34 (28) | 21 (15) |
| Reported non-psychiatric | 13 (8) | 23 (15) |
| Service | Baseline, n (%) | Follow-up, n (%) | ||||
|---|---|---|---|---|---|---|
| Treatment group | Overall | Treatment group | Overall | |||
| SlowMo | TAU | SlowMo | TAU | |||
| Home treatment (days), n (%) | ||||||
| 0 | 150 (82.9) | 149 (83.7) | 299 (83.3) | 151 (89.3) | 162 (92.0) | 313 (90.7) |
| 1 | 6 (3.3) | 3 (1.7) | 9 (2.5) | 7 (4.1) | 1 (0.6) | 8 (2.3) |
| 2 | 13 (7.2) | 19 (10.7) | 32 (8.9) | 11 (6.5) | 11 (6.2) | 22 (6.4) |
| 3 | 3 (1.7) | 2 (1.1) | 5 (1.4) | 0 (0.0) | 1 (0.6) | 1 (0.3) |
| 4 | 7 (3.9) | 4 (2.2) | 11 (3.1) | 0 (0.0) | 1 (0.6) | 1 (0.3) |
| 6 | 1 (0.6) | 0 (0.0) | 1 (0.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| 7 | 0 (0.0) | 1 (0.6) | 1 (0.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| 8 | 1 (0.6) | 0 (0.0) | 1 (0.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Total days, n | 83 | 70 | 153 | 29 | 30 | 59 |
| Hospital admission (days) | ||||||
| 0–10 | 162 (89.5) | 155 (87.1) | 317 (88.3) | 159 (94.1) | 166 (94.3) | 325 (94.2) |
| Total days | 47 | 14 | 61 | 32 | 10 | 42 |
| 11–50 | 11 (6.1) | 17 (9.6) | 28 (7.8) | 5 (3.0) | 3 (1.7) | 8 (2.3) |
| Total days | 294 | 424 | 718 | 133 | 45 | 178 |
| 51–100 | 3 (1.7) | 3 (1.7) | 6 (1.7) | 2 (1.2) | 4 (2.3) | 6 (1.7) |
| Total days | 225 | 233 | 458 | 132 | 236 | 368 |
| > 100, n (%) | 5 (2.8) | 3 (1.7) | 8 (2.2) | 3 (1.8) | 3 (1.7) | 6 (1.7) |
| Total days | 856 | 414 | 1270 | 502 | 385 | 887 |
| Total days over all categories | 1422 | 1085 | 2507 | 799 | 676 | 1475 |
FIGURE 9.
Plots of mean outcomes over time in each group for (a) GPTS, (b) R-GPTS and (c) PSYRATS.
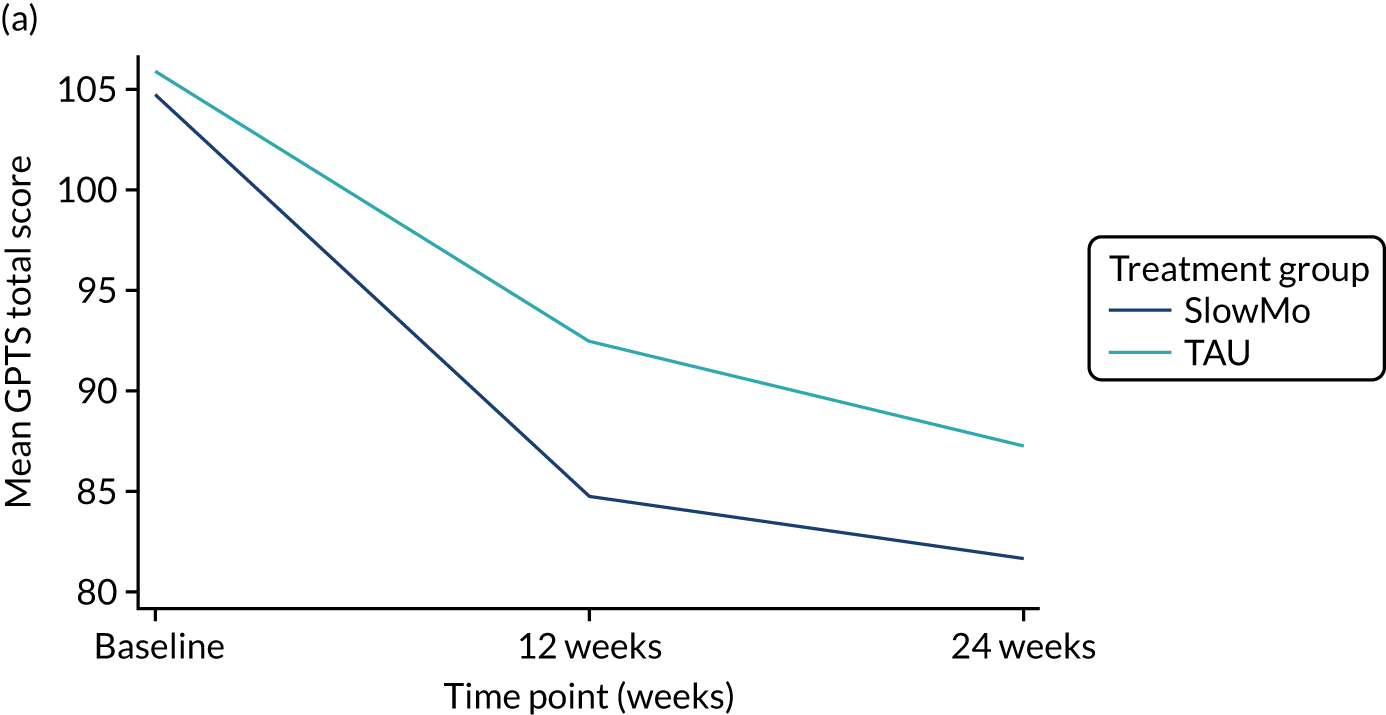
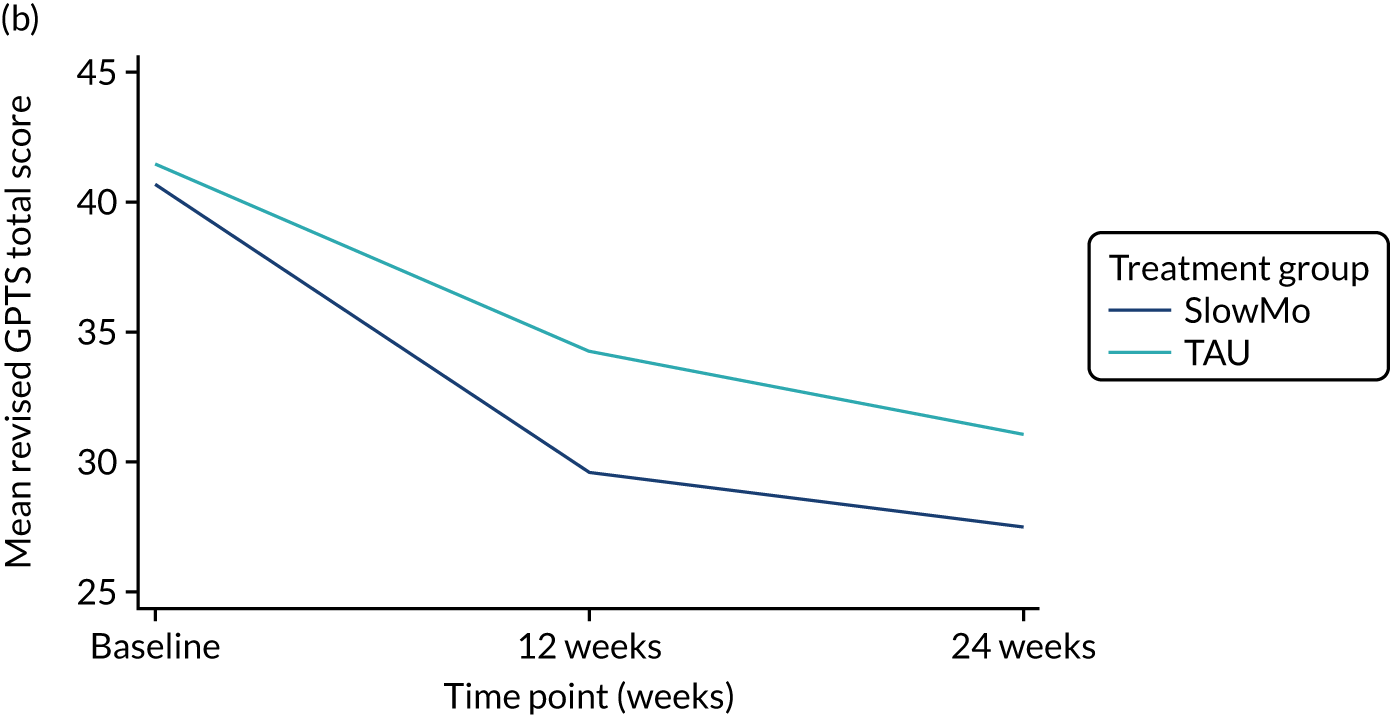
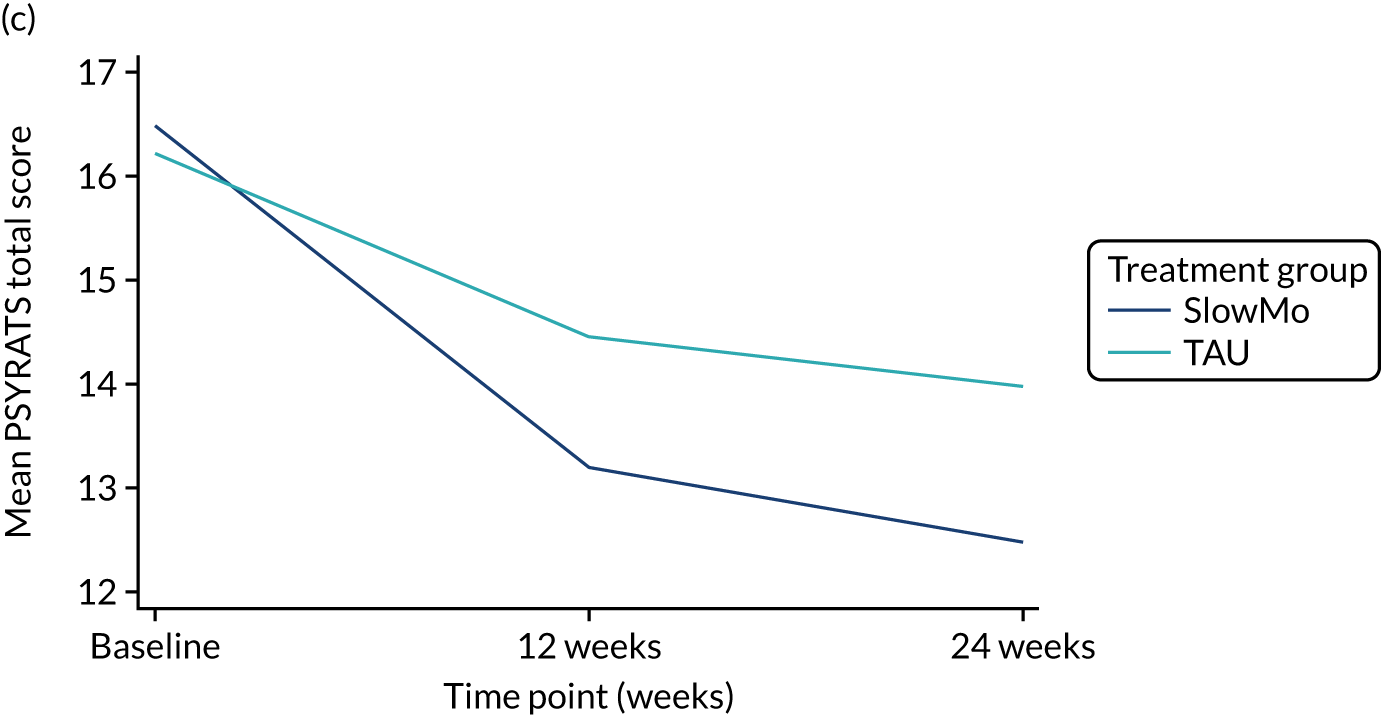
Appendix 2 Chapter 2 supplementary material
My name is Dan and I am a regular visitor to your Depot Clinic for my treatment as I am a psychosis sufferer. I was put onto the Research Network for service users with the help of my care co-ordinator in 2012 and have worked on a number of research studies since then as a ‘Lived Experience’ consultant. I was initially referred to take part in a study as a participant, but explained to the Research Assistant that I didn’t think I’d be suitable. I was then interviewed and offered other work and my experience went from there. Unfortunately, I don’t often have the time or opportunity to talk to the Community Mental Health Teams about the work I have done, so have been encouraged by colleagues to write this letter.
I have been involved with several PhD students over the years and have given feedback to make sure their research is relevant to patients in the long term. My work is understandably centred on the psychosis theme within the trust and my experience as a service user in this area helps to make sure PPI is implemented. At the moment I am working on two studies (‘SlowMo’, which aims to alleviate anxiety and fear of harm in sufferers, and a second study, for which I am on a steering committee as a ‘Lived Experience’ representative).
My personal opinion is that the research work done by myself and academics/clinicians doesn’t always get the recognition it deserves and perhaps isn’t translated into ‘real-world’ practice for various reasons, not least the crippling pressures of the current economic climate! PPI though, is becoming more and more important and rightly so, as it is critical to develop even better patient-centred treatments and make sure all the relevant parties’ views are clearly heard. However, thanks to the many dedicated people I have met in the field of mental health, I can now appreciate the roles played by not just researchers, but also the frontline staff I have come into contact with. I would also recommend (if possible) that more service users are referred to do the type of work I do, as it is very rewarding, including financially, and would aid with their recovery.
Thank you for all your help over the years and I hope you might be interested in my perspective. Feel free to contact me if you would like to find out more . . .
Appendix 3 Chapter 3 supplementary material
User experience survey
We are interested in your experience of using the SlowMo mobile app. Your feedback is very important for helping us to improve the app, so please be as honest as possible.
Please rate each of the items below on a scale of 0 = ‘totally disagree’ to 10 = ‘totally agree’.
Rating
(0–10)
1. I enjoyed using the app. _______
2. The app was too complicated to be helpful to me. _______
3. The app was easy to use. _______
4. The app was boring. _______
5. The app helped me to manage my difficulties better. _______
6. I would recommend the app to people with similar difficulties to me. _______
7. I couldn’t get used to the app. _______
8. The app felt relevant to me and my problems. _______
9. I felt frustrated using the app. _______
10. The information on the app was easy to understand. _______
11. The app was fun. ______
12. The app was not useful for managing my problems. ______
1, 4*, 9*, 11 – enjoyment
2*, 3, 7, 11 – usability
5, 6, 8, 12* – usefulness/acceptability
* reverse score
| Digital literacy variable | Participant variable | Test (df) | Value | p-value | Mean difference 95% CI |
|---|---|---|---|---|---|
| Smartphone ownership | Age | χ2(2) | 23.11 | < 0.001** | – |
| Gender | χ2(1) | 0.03 | 0.853 | – | |
| Ethnicity | χ2(2) | 3.23 | 0.199 | – | |
| Paranoia severity | χ2(1) | 0.01 | 0.942 | – | |
| Smartphone use: frequency | Age | F(2,124) | 2.50 | 0.086 | – |
| Gender | t(125) | 0.41 | 0.683 | –11.55 to 17.59 | |
| Ethnicity | F(2,124) | 2.14 | 0.122 | – | |
| Paranoia severity | t(125) | –0.10 | 0.920 | –13.80 to 12.47 | |
| Smartphone use: confidence | Age | F(2,154) | 14.10 | < 0.001** | – |
| Gender | t(155) | –1.06 | 0.293 | –18.21 to 5.53 | |
| Ethnicity | F(2,154) | 3.74 | 0.026* | – | |
| Paranoia severity | t(155) | 0.18 | 0.855 | –9.73 to 11.73 | |
| Computer access | Age | χ2(2) | 3.56 | 0.168 | – |
| Gender | χ2(1) | 0.59 | 0.442 | – | |
| Ethnicity | χ2(2) | 7.44 | 0.024* | – | |
| Paranoia severity | χ2(1) | 0.05 | 0.815 | – | |
| Computer use: frequency | Age | F(2,122) | 2.89 | 0.059 | – |
| Gender | t(76) | –1.75 | 0.085 | –23.55 to 1.54 | |
| Ethnicity | F(2,122) | 0.49 | 0.614 | – | |
| Paranoia severity | t(123) | 0.49 | 0.628 | –9.64 to 15.92 | |
| Computer use: confidence | Age | F(2,154) | 13.08 | < 0.001** | – |
| Gender | t(155) | –2.30 | 0.023* | –23.40 to –1.80 | |
| Ethnicity | F(2,154) | 4.86 | 0.009** | – | |
| Paranoia severity | t(104) | 0.51 | 0.615 | –8.01 to 13.48 |
| Self-reported adherence variable | Participant variable | Test (df) | Value | p-value | Mean difference 95% CI |
|---|---|---|---|---|---|
| Self-reported current use of mobile app | Age | F(2,77) | 1.53 | 0.222 | – |
| Gender | t(78) | –3.26 | 0.002** | –31.9 to –7.72 | |
| Ethnicity | F(2,77) | 0.04 | 0.957 | – | |
| Paranoia severity | t(78) | –0.99 | 0.325 | –17.82 to 5.97 | |
| Self-reported intended future use of mobile app | Age | F(2,75) | 1.13 | 0.327 | – |
| Gender | t(76) | –2.99 | 0.004** | –27.48 to –5.53 | |
| Ethnicity | F(2,75) | 0.55 | 0.582 | – | |
| Paranoia severity | t(76) | –0.43 | 0.669 | –13.11 to 8.46 |
| Participant variable | Attended at least one session | Attended all eight sessions | ||||||
|---|---|---|---|---|---|---|---|---|
| Test (df) | Value | p-value | Mean difference 95% CI | Test (df) | Value | p-value | Mean difference 95% CI | |
| Age | χ2(2) | 4.65 | 0.098 | – | χ2(2) | 2.32 | 0.314 | – |
| Gender | χ2(1) | 1.01 | 0.315 | – | χ2(1) | 0.65 | 0.419 | – |
| Ethnicity | χ2(2) | 1.19 | 0.549 | – | χ2(2) | 0.96 | 0.863 | – |
| Paranoia severity | χ2(1) | 0.37 | 0.541 | – | χ2(1) | 0.01 | 0.954 | – |
| Smartphone use: frequency | t(101) | –1.17 | 0.244 | –27.49 to 7.07 | t(90) | –2.48 | 0.015* | –46.33 to –5.13 |
| Smartphone use: confidence | t(124) | –1.58 | 0.115 | –23.19 to 2.55 | t(108) | –2.17 | 0.032* | –32.16 to –1.45 |
| User experience variable | Participant variable | Test (df) | Value | p–value | Mean difference 95% CI |
|---|---|---|---|---|---|
| Enjoyment | Age | F(2,79) | 0.58 | 0.588 | – |
| Gender | t(80) | –3.52 | 0.001** | –23.00 to –6.00 | |
| Ethnicity | F(2,79) | 0.53 | 0.949 | – | |
| Paranoia severity | t(80) | 1.01 | 0.315 | –4.54 to 13.18 | |
| Usability | Age | F(2,79) | 2.15 | 0.123 | – |
| Gender | t(80) | –0.16 | 0.875 | –12.05 to 9.84 | |
| Ethnicity | F(2,79) | 0.28 | 0.754 | – | |
| Paranoia severity | t(80) | 1.79 | 0.078 | –1.00 to –18.30 | |
| Usefulness | Age | F(2,79) | 1.26 | 0.290 | – |
| Gender | t(80) | 2.45 | 0.016* | –19.02 to –2.98 | |
| Ethnicity | F(2,79) | 0.16 | 0.855 | – | |
| Paranoia severity | t(80) | 0.75 | 0.456 | –5.1 to 11.14 | |
| Total UES | Age | F(2,79) | 1.58 | 0.212 | – |
| Gender | t(80) | –2.14 | 0.036* | –17.17 to –1.15 | |
| Ethnicity | F(2,79) | 0.05 | 0.956 | – | |
| Paranoia severity | t(80) | 1.37 | 0.174 | –2.40 to 13.08 |
| Technical problem | Session, n (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| One (N = 149) | Two (N = 140) | Three (N = 133) | Four (N = 129) | Five (N = 125) | Six (N = 123) | Seven (N = 119) | Eight (N = 118) | |
| Internet connection | 12 (8.1) | 6 (4.3) | 4 (3.0) | 5 (3.9) | 3 (2.4) | 2 (1.6) | 3 (2.5) | 0 (0.0) |
| Data synching | 14 (9.4) | 31 (22.1) | 22 (16.5) | 15 (11.6) | 19 (15.2) | 16 (13.0) | 13 (10.9) | 9 (7.6) |
| Software | 12 (8.1) | 26 (18.6) | 9 (6.8) | 4 (3.1) | 6 (4.8) | 7 (5.7) | 9 (7.6) | 8 (6.8) |
List of abbreviations
- BAPQ
- Beliefs about Problems Questionnaire
- BBC
- British Broadcasting Corporation
- BCSS
- Brief Core Schema Scales
- BNSS
- Brief Negative Symptom Scale
- CBT
- cognitive–behavioural therapy
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- DMEC
- Data Monitoring and Ethics Committee
- GPTS
- Green Paranoid Thoughts Scale
- ICC
- intraclass correlation coefficient
- JTC
- jumping to conclusions
- MADS
- Maudsley Assessment of Delusions Schedule
- MANSA
- Manchester Short Assessment of Quality of Life
- MCT
- metacognitive training
- PPI
- patient and public involvement
- PSWQ
- Penn State Worry Questionnaire
- PSYRATS
- Psychotic Symptom Rating Scales
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- R-GPTS
- Revised-Green Paranoid Thoughts Scale
- SAE
- serious adverse event
- SAPS
- Scale for the Assessment of Positive Symptoms
- SD
- standard deviation
- SE
- standard error
- TAPS
- Thinking About Paranoia Scale
- TAU
- treatment as usual
- UES
- user experience survey
- WEMWBS
- Warwick–Edinburgh Mental Wellbeing Scale
