Notes
Article history
The research reported in this issue of the journal was funded by the EME programme as project number 14/23/17. The contractual start date was in August 2016. The final report began editorial review in August 2020 and was accepted for publication in December 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The EME editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Asherson et al. This work was produced by Asherson et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Asherson et al.
Chapter 1 Introduction
Scientific background and rationale
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder that develops during childhood or early adolescence and frequently persists into adulthood. The disorder is defined by a persistent pattern of inattention and/or hyperactivity/impulsivity that interferes with or reduces the quality of functioning in daily life. 1 The impairments associated with ADHD are often severe and are well documented. They include educational and occupational failure, transport accidents, difficulty forming social and personal relationships, and the development of behavioural problems, including antisocial behaviour and criminality. 2–6 Many adults with ADHD struggle with mental health symptoms, such as a mental and physical restlessness, distractibility, emotional dysregulation, low self-esteem and sleep problems. 3 A further source of impairment is the high rate of coexisting disorders associated with ADHD. 7 These include general and specific learning difficulties, anxiety, depression, bipolar disorder, personality disorder and drug abuse disorders.
Attention deficit hyperactivity disorder affects around 5–7% of children. 8,9 Prevalence estimates for ADHD in adults range from 2.5% to 3.4%,10,11 with the most recent review reporting an average prevalence of 2.8% for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), ADHD. 7 Currently, there are no prevalence estimates for ADHD using Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria. These estimates are expected to be slightly larger than those for DSM-IV because of changes in symptom thresholds for adults and the age at onset criteria. The population prevalence contrasts considerably with the disproportionately high rate of people meeting ADHD diagnostic criteria in prison populations, which averages around 26%. 12 In this review and meta-analysis,12 studies using screening criteria for diagnosis had a significantly larger estimated ADHD prevalence (43%) than the subset of studies using a diagnostic clinical interview (26%), suggesting good sensitivity but a high rate of false positives when using screening tools. However, using clinical interview data,12 the rate of ADHD was estimated to be around 30% in male adolescents, 31% in male adults, 31% in female adolescents and 22% in female adults.
The National Institute for Health and Care Excellence (NICE) and the Scottish Intercollegiate Guidelines Network recommend stimulant medications, methylphenidate (MPH) or lisdexamfetamine, as first-line treatment for ADHD with significant impairment in children, adolescents and young adults. 13–15 These medications target the core symptoms of inattention and hyperactivity/impulsivity, and may also lead to reduced levels of emotional dysregulation. 16,17 Although psychoeducation and psychological interventions are also thought to be essential in the overall support provided for people with ADHD, they may not reduce core symptoms. Evidence for this conclusion comes from studies suggesting that psychological treatments may reduce coexisting problems (or enhance behaviours) relevant to the prison population, such as social skills, conduct problems and global mental health, but may not reduce core symptoms of the disorder. 18–20
Despite the recommendations from national guidelines, there is continued uncertainty about the value of diagnosing and treating ADHD in offender populations21 and in adults more generally. Raman et al. 22 reported that prevalence for medication use for ADHD averaged 0.03% in Western Europe (0.05% in the UK) among adults aged ≥ 19 years and 0.7% (0.64% in the UK) for children and adolescents. This is far below population prevalence for the disorder. The proportion of ADHD cases treated for ADHD in prisons is expected to be even smaller,21 yet clinical guidelines recommend the identification and treatment of ADHD at all ages, paying particular attention to the prison population, as well as those presenting with comorbid mental health disorders. 14 One potential reason for the low rate of treatment of ADHD in prisons is the lack of data on treatment effects in adolescents and adults presenting with complex coexisting mental health and behavioural disorders, and the limited research of the prison population. Concerns are expressed that the common occurrence of mental health, neurodevelopmental and psychosocial problems might provide a better explanation for impulsive, overactive and inattentive states in young offenders, or might interfere with the treatment response in cases of ADHD. For these reasons, NICE13 recommended that drug treatment efficacy trials are needed in offender populations (section 5.18.1.413) and repeated this recommendation in 2013. 23 The guideline13 stated that:
[T]here should be an assessment of efficacy in these groups (i.e. forensic and drug abuse populations) of the ADHD treatments already recommended for treatment in the community. Randomised controlled trial design is recommended.
Reproduced with permission from NICE. 13
There are two potential reasons why the response of ADHD symptoms to stimulant medications may be different for young adult offenders than for the samples of children, adolescents and adults involved in previous studies of ADHD in community settings. First, offenders present with an array of complex mental health problems that may better explain the states of inattentive, overactive, restless and impulsive behaviours used to define ADHD. This includes disorders commonly seen in offenders such as personality, anxiety, post-traumatic stress and substance abuse disorders. Second, nearly all previous trials of ADHD medications have been conducted in carefully selected samples with generally low levels of co-occurring psychosocial, behavioural and mental health problems. However, the co-occurrence of mental health disorders might modify the efficacy of drug treatments for ADHD.
One example is comorbid drug abuse. A meta-analysis24 of treatment trials found no effect of MPH on ADHD symptoms in ADHD cases with comorbid drug abuse [standardised mean difference (SMD) 0.08; p = 0.59], whereas there was a medium effect in samples without comorbid drug abuse (SMD 0.51; p < 0.00001). A review and meta-analysis25 of ADHD medications among patients with ADHD and drug dependency found only small reductions in the levels of ADHD symptoms following treatment (eight studies of MPH, three of atomoxetine, one of pemoline and one of bupropion), with an average SMD of around 0.30. When stratified by type of medication, significant reductions in ADHD symptoms were identified for MPH, with a mean dose of 62.2 mg per day across the eight MPH studies included in this review. Furthermore, an international consensus statement on treatment of ADHD with comorbid substance use disorder (SUD) concluded that several studies report lower effectiveness of standard-dose pharmacotherapy for the treatment of ADHD in patients with ADHD with comorbid SUD, and uptitration may be considered in patients who are unresponsive to standard doses. 26 Finally, two recent studies of MPH found that a low MPH dose (i.e. < 36 mg) was associated with treatment discontinuation,27 and that ADHD patients with a SUD were, on average, prescribed 40% larger doses than those without a SUD after 2 years of treatment. 28 These findings may be relevant to prison populations, for whom a history of drug abuse and ongoing access to drugs in prison is common.
Furthermore, concerns have been expressed about the potential for stimulant medications such as MPH to worsen coexisting conditions. The most recent research recommendations from NICE14 state that:
[N]o evidence was identified to justify different medication choices in people with ADHD and a history of psychosis, mania, or personality disorder. However, these groups are often excluded from trials. There are reasons (for example, mechanism of action of medication options, previous reports of adverse effects) to suspect that these groups may respond differently to different drugs, but a lack of trials to confirm this.
Reproduced with permission from NICE. 14
To address the questions raised, we have conducted a randomised controlled efficacy trial of osmotic releases oral system (OROS)-MPH, a sustained-release formulation of MPH, compared with placebo, in young male adult prisoners with ADHD who are aged 16–25 years.
Previous studies of methylphenidate in offenders with attention deficit hyperactivity disorder
This study followed on from an open-label study conducted by the chief investigator for this project that investigated the effects of OROS-MPH in 121 young male offenders in Her Majesty’s Prison and Young Offender Institution (HMP YOI) Isis in Southeast London, who met the criteria for DSM-5 ADHD. 29 The current study follows similar procedures to the open-label trial. This included screening all prisoners aged between 18 and 25 years admitted to the prison using a DSM-IV symptom checklist,30 with diagnosis confirmed using the Diagnostic Interview for ADHD in Adults 2.0 (DIVA 2.0),31 followed by medical review from consultant psychiatrists trained in the diagnosis of ADHD. Prevalence of ADHD in the prison was estimated to be 19%, of which 78% met criteria for the combined type presentation of ADHD. Large pre–post treatment reductions with SMDs of > 2, unadjusted for multiple outcome measures, were seen for investigator-rated ADHD symptoms using the Conners’ Adult ADHD Rating Scale-Observer (CAARS-O).
Previous community studies demonstrate the efficacy and cost-effectiveness of MPH in reducing ADHD symptoms in children, adolescents and adults with ADHD. 14 These conclusions are supported by a comprehensive review and meta-analysis of randomised controlled trials (RCTs) for MPH and other ADHD medications32 that, for MPH, found a large effect for children and adolescents [SMD –0.78, 95% confidence interval (CI) –0.93 to –0.62] and a moderate effect for adults (SMD –0.49, 95% CI –0.64 to –0.35). However, there are only limited trial data for the treatment of ADHD in young offenders presenting with a more complex mix of psychosocial, mental health and behavioural problems. One small RCT of MPH in a sample of 30 Swedish male prisoners with ADHD showed a very large effect (SMD 2.1) on ADHD symptom reduction. 33 Although this study supports the treatment of ADHD in offenders, it may not generalise to the young adult offenders in the UK with mainly short-term sentences investigated in this study because of the small sample size, older age group, selection of severe ADHD cases with long-term sentences and treatment on a special prison unit.
Pharmacoepidemiological studies provide another important source of information, particularly for longer-term benefits of treating ADHD and the impact on a broader range of important outcomes relevant to offenders with ADHD. 34 Unlike RCTs, these studies are representative of patients in real-world practice, include longer periods of follow-up and have large sample sizes. However, they are limited by confounding by indication, whereby patients may select treatments based on the nature or severity of their clinical condition. To account for this problem, these studies use within-individual designs, which compare periods of treatment with medication with periods of non-treatment. 34 A good example of this approach is suicidal behaviour, which was found to be more prevalent among adults treated for ADHD with stimulants than among those who had not been treated. However, there was a lower rate of suicidality when periods of treatment were compared with periods of non-treatment in the same individual. 35 These findings suggest that, although individuals with ADHD and suicidality may be more likely to be treated with MPH, during periods of treatment suicidality is likely to decrease. Using this approach, there is evidence for reductions in a range of outcomes relevant to offenders with ADHD, including serious transport accidents,36 depression,37 suicidality35 and SUDs. 38,39 In patients with ADHD and comorbid bipolar disorder, there was reduced relapse of mania when patients were also treated with mood stabilisers, but there was an increased risk of manic relapse when not taking mood stabilisers. 40 In patients with comorbid psychosis, there was no change in the risk of a psychotic relapse during periods of treatment and periods of non-treatment with MPH. 41
Of specific relevance to this application was a pharmacoepidemiological study using Swedish national registry data of 25,656 male patients with ADHD, which found a sixfold-higher rate of criminal convictions over a 4-year period among ADHD patients than among controls. 42 Regarding medication effects, they found a 32% reduction in the risk of criminal convictions using both ‘within’ and ‘between’ methods of analysis. Furthermore, these apparent protective effects on criminal convictions were seen for ADHD medications only (stimulants or atomoxetine), and not for commonly prescribed antidepressants, indicating the specificity of these findings to ADHD medications. Other important outcomes showing significant reductions during periods of treatment compared with periods of non-treatment included violent reoffending on release from prison43 and substance use. 38,39
Another area of interest is the potential for improving educational and behavioural outcomes for offenders with ADHD. 21 An initial descriptive study of ADHD in prisoners, conducted by co-applicant Susan Young, found a sixfold increase in critical incidents among prison inmates with high levels of ADHD symptoms, compared with inmates with low levels of ADHD symptoms. 44 The association of ADHD with behavioural problems in the prison remained significant, even after controlling for antisocial personality disorder (ASPD), suggesting that this is an important outcome for clinical trials in prison populations. Another important outcome is symptoms of emotional dysregulation, such as irritability, anger and aggression, which are commonly seen in offender populations. Although emotional dysregulation is commonly seen in young adults with ADHD, it is a transdiagnostic set of symptoms seen across a wide range of other common mental health disorders. 45–48 Meta-analyses of RCTs of ADHD medications found reductions in the symptoms of emotional dysregulation, including problems with temper control, mood lability and emotional over-reactivity. 16,17 Hence, treatment of offenders with ADHD might also lead to significant reductions in emotional dysregulation and, potentially, aggressive or violent behaviour. The symptoms of ADHD are also known to interfere with education and employment because of a combination of restlessness, reduced attention span, forgetfulness and problems with planning and organisation. 3 Treatment might therefore lead to greater positive engagement with prison education and rehabilitation programmes. In our open-label pilot study at HMP YOI Isis, we also found effects on all the secondary outcomes proposed for this study (all p < 0.001), including measures of emotional dysregulation, attitudes towards violence, the number of critical incidents and positive engagement with the education and rehabilitation programme. 29
Potential benefits and risks of the trial intervention
For many years, ADHD was thought to be a childhood-onset disorder that had limited impact on adult mental health. However, the symptoms and impairments that define ADHD often persist into adulthood, with similar responses to drug treatments, such as OROS-MPH, to those seen in children and adolescents. 3,32 Behavioural interventions can bring about further improvements in global clinical health, but only medication has been clearly shown to reduce the core symptoms of inattention and hyperactivity/impulsivity. For these reasons, clinical practice, expert consensus statements and national and international guidelines all indicate the need to diagnose and treat ADHD in adults using stimulants (MPH or lisdexamfetamine) as first-line treatments. 14
Currently, several pharmacological treatments for ADHD are recommended for use in adults in the UK. Among the most used in clinical practice is an extended-release formulation of OROS-MPH, which is thought to have clinical effects lasting up to 12 hours from a single dose. OROS-MPH is currently licensed for use in children and adolescents, and the subset of adults with ADHD who were diagnosed as children; however, it is not licensed in Europe for use de novo in adults who were not diagnosed with ADHD as children. This has been a source of concern for clinicians, who feel that there is no rationale for excluding treatments just because a diagnostic assessment was not performed in childhood, generating a considerable unmet need,4,5 particularly in the prison population for those aged > 18 years, among whom the prevalence of undiagnosed ADHD is high. 21,49 Furthermore, there is a risk that if ADHD is not included in adult mental health diagnostic assessments and treatment protocols, errors will be made, with patients put on antidepressants, antipsychotics or mood stabilisers for other conditions, while ADHD goes undiagnosed and untreated.
The potential value of treatment with OROS-MPH in young offenders with ADHD is that this is an established treatment with short- and long-term trial and post-marketing data to support the efficacy and safety of this medication in the treatment of ADHD. Potential benefits of treating young adult offenders with ADHD with OROS-MPH include improvements in clinical and behavioural outcomes. These include ADHD symptoms, emotional dysregulation, attitudes towards violence, critical incidents and engagement with educational and rehabilitation programmes. 29 Demonstrating the efficacy and safety of OROS-MPH on ADHD symptoms and associated impairments may provide the data required to develop effective health-care pathways, including the use of OROS-MPH for a substantial group of young offenders. Establishing efficacy of OROS-MPH in this population would provide the foundation needed to establish long-term effectiveness studies with the potential for demonstrating significant reductions in criminal behaviour and improved health economic outcomes.
One potential risk that is often raised is the risk of abuse or diversion, particularly in a population of offenders with ADHD and high rates of substance abuse. Stimulants can be abused by crushing short-acting formulations, such as immediate release MPH, which can then be insufflated (snorted) or dissolved in water for injection, leading to a rapid entry of drug into the brain and the experience of euphoria. The importance of the route of administration was demonstrated in a study that showed that, although there is a dose–response relationship between intravenous MPH and a feeling of euphoria, this is not the case with oral MPH. 50 This may not completely exclude the risk of abusing OROS-MPH in this way, but the evidence that this occurs is extremely limited; in addition, OROS-MPH is difficult to crush and it is difficult to extract MPH from OROS-MPH for injection. Risk of abuse was therefore reduced in this study by using this formulation of MPH. Furthermore, in the pilot study at HMP YOI Isis, we did not observe excessive drug-seeking behaviour for stimulant medication. 29 Indeed, the young adult offenders being treated for ADHD were noted to be generally cautious about increasing the dose of medication and were titrated to modest daily doses, compared with community samples: 18% used 18 mg, 37% used 36 mg, 14% used 54 mg, 26% used 72 mg and only 4% used 90 mg.
Related to dosing, the other potential risks are the usual range of common adverse effects observed when treating ADHD with OROS-MPH. In the pilot open trial, the low doses the participants were titrated to was thought to be related to a greater focus by prisoners on minor adverse effects such as appetite loss, headaches and sleep problems, compared with patients in the community. This potentially could be reflected in lower dosing, reducing the potential effects on reducing the core symptoms of ADHD. Other potential risks on heart and blood pressure are routinely monitored. Diversion for non-medical use is another potential problem, but has been mainly identified as a risk in higher education settings to enhance education performance. 51
Chapter 2 Methods
Trial objectives
The overall aim of the trial was to investigate the effects of OROS-MPH on reducing ADHD symptoms in young male prisoners aged 16–25 years who meet the DSM-5 diagnostic criteria for ADHD. The following study questions are addressed in three main objectives:
-
Primary objective – what is the efficacy of OROS-MPH in reducing inattention and hyperactivity/impulsivity in young male prisoners who meet the diagnostic criteria for DSM-5 ADHD?
-
Secondary objective: what is the efficacy of OROS-MPH in reducing secondary outcomes that are key indicators of behavioural and functional impairments used in the management of young male prisoners in the UK? These include emotional dysregulation, antisocial behaviour in the prison, violent attitudes (a measure linked to aggression) and reports of behaviour from prison staff.
-
Tertiary objective: are improvements in secondary behavioural outcomes mediated by improvements in ADHD symptoms or emotional dysregulation?
Trial design
Concerta in Adult Offenders with ADHD (CIAO)-II is a Phase IV, 8-week, parallel-arm, double-blinded, randomised, placebo-controlled trial of an extended-release formulation of MPH (OROS-MPH). ADHD symptoms, emotional dysregulation, attitudes towards violence, and behavioural outcomes were compared between the two trial arms.
Participants in the trial were young male prisoners aged 16–25 years who met the DSM-5 criteria for ADHD. Participants were randomised to 8 weeks of treatment with either OROS-MPH or placebo, titrated over the first 5 weeks to balance ADHD symptom improvement with adverse effects. A total of 200 participants were randomised and allocated in a 1 : 1 ratio to either the drug or placebo. By the end of the trial, 101 participants had been randomised to receive OROS-MPH and 99 had been randomised to the placebo arm. Randomisation was conducted by the King’s Clinical Trial Unit (KCTU), with blinding of investigators, including pharmacy staff, and participants. On completion of the 8-week trial, OROS-MPH or another medication for ADHD was offered to both the OROS-MPH and placebo groups as part of their ongoing clinical care.
Changes to protocol after trial commencement
A full list of all minor and substantial amendments to the protocol can be found (see Appendix 1, Table 31). Following the start of the trial, two minor amendments were made to the protocol, related to a clarification regarding the assessment of intelligence quotient (IQ), and to clarify that the Reactive–Proactive Aggression Questionnaire (RPQ) measure would be collected at baseline only. In addition, a substantial amendment was implemented on 18 December 2018. This amendment was approved by the Medicines and Healthcare products Regulatory Agency (MHRA), the Health Research Authority (HRA), Her Majesty’s Prison and Probation Service (HMPPS) (formerly known as the National Offender Management Service) and the Scottish Prison Service (SPS). Changes included an amendment to the timing of the database lock and clarifications to the wording describing the inclusion and exclusion criteria. The revised inclusion and exclusion criteria definitions had been applied from the start of the trial, but were not sufficiently well documented in the protocol. In addition, one of the secondary outcomes, the number of Incentive and Earned Privileges (IEPs) was dropped because these data are not recorded in Scottish prisons. No other outcomes were changed. A report on the final approved protocol is published in Trials. 52 This report refers to the final approved protocol.
Eligibility criteria for participants
Eligibility for the study was checked and recorded once a consent form (consent II: consent for the clinical trial) had been signed and baseline assessments had been completed, prior to randomisation. Using an algorithm that applied the DSM-5 criteria to the DIVA 2.0 interview data, cases were checked to ensure that they met the diagnostic criteria for DSM-5 ADHD. A clinical review by a psychiatrist trained in the diagnostic assessment of ADHD was then completed to check all of the inclusion and exclusion criteria. Mental capacity required for consent was evaluated by the clinician, including ability to understand all information, rating scale and interview questions, and to provide detailed descriptions of symptoms and behaviour.
The initial exclusion criteria of an IQ score of < 60 was based on the Wechsler Abbreviated Scale of Intelligence® Second Edition (WASI-II) estimates of IQ. This was later changed to include those with a WASI-II IQ estimate of < 60, for whom the score’s 95% CI spanned 60, and clinical assessment by the psychiatrist concluded that IQ was > 60 and that the participant had the mental capacity to provide informed consent. As there are no validated IQ tests for the visually impaired, including the WASI-II, this criterion was based on clinical judgement for participants with this impairment. This was also the procedure for anyone unable to complete the WASI-II assessment because of the severity of their ADHD symptoms or other mental health problems. This approach was applied to one participant with a low initial WASI-II test score.
Inclusion criteria
The inclusion criteria were as follows:
-
male
-
aged between 16 and 25 years at time of consent for screening
-
ability to speak English, defined as sufficient to complete study assessments
-
able to provide informed consent, defined as understanding the information sheet and being able to make an informed decision, taking into account pros and cons of trial participation
-
meeting clinical diagnostic criteria for DSM-5 ADHD.
Following the DSM-5,1 the diagnostic criteria for ADHD were defined as five or more symptoms of ADHD in either the inattentive or hyperactive–impulsive symptom domains, and six or more symptoms of ADHD in either the inattentive or hyperactive–impulsive symptom domains before the age of 12 years. When it was not possible to gain enough clinical information to score childhood symptoms of ADHD, the operational criteria applied were adapted to include evidence of several ADHD symptoms with impairment starting before the age of 12 years, and five or more symptoms in either domain currently, with moderate to severe impairment. This meets the requirement under DSM-5 for several symptoms starting before the age of 12 years.
In addition, we required a persistent non-episodic course of ADHD symptoms, impairments from the symptoms in two or more clinical or psychosocial domains, and that the symptoms were present in two or more settings.
Exclusion criteria
The exclusion criteria were as follows:
-
lacks capacity to give informed consent
-
moderate or severe learning disability, defined as IQ of < 60
-
serious risk of violence to the researcher
-
current major depression, psychosis, mania or hypomania
-
past history of bipolar disorder or schizophrenia, defined as those with episodic mania/hypomania or psychosis unrelated to acute drug intoxication, but not chronic emotional dysregulation (irritability, frustration, anger or emotional–mood instability)
-
medical contraindications to the use of stimulants, including glaucoma, hypertension, cardiovascular disease or structural heart problems
-
taking contraindicated medications during the 4 weeks prior to randomisation
-
showing drug-seeking behaviour or craving, defined as drug-seeking behaviour that was unusually severe and likely to affect the titration protocol because of unusual and excessive demands for drugs, or if there was a current withdrawal syndrome from an addiction disorder with drug dependency
-
receiving any ADHD medication between consent for screening and randomisation.
Trial setting
Participants were recruited from two prisons. HMP YOI Isis in London, England, opened in 2010 for sentenced young adults aged 18–25 years, but was later extended to include older prisoners. This is a category C prison, defined as suitable for prisoners who cannot be trusted in open conditions but who are unlikely to try to escape. There are two house blocks with four wings each, with mixed single and double cells, plus a segregation unit located between the house blocks. Operational capacity was 621 in January 2016. The prison focuses on rehabilitation and resettlement, and all prisoners are engaged with full-time education, occupation and rehabilitation programmes. There is a broad-based educational and vocational curriculum for young sentenced prisoners and available activities are, among others, mathematics, English, business studies, painting and decorating, waste management, mechanics and barbering.
Her Majesty’s Young Offender Institution (HM YOI) Polmont in Falkirk, Scotland, is a holding facility for young offenders in Scotland aged 16–21 years, with sentences ranging from 6 months to life. All participants were sentenced prisoners when screened for entry to the trial. It has the capacity to hold 760 prisoners and, since 2016, female prisoners have been housed in a separate wing. Individuals may stay in Polmont until age 23, depending on circumstances. In March 2019, Polmont had 370 male young offenders and 90 female young offenders. There are three house blocks and a segregation unit. Various activities are offered at Polmont, such as education and vocational training, and rehabilitation programmes such as Pathways, Moving Forward and Making Changes.
Recruitment procedure
Following consent to be screened for ADHD (consent I), screening questionnaire data were collected by the research teams using the Barkley DSM-IV ADHD symptom rating scale. 30 Prisoners who screened positive were invited to complete the DIVA 2.0. 31 This was followed by a clinical assessment by a psychiatrist trained in the diagnostic assessment of ADHD, including collateral information obtained from an informant whenever feasible. Participant’s expected release date could change at any time and additional convictions and charges could be added. Hence, it was not always possible to predict if a participant would be transferred, released or deported. For this reason, it is possible that some participants initially excluded because of a high risk of release could have taken part in the trial.
Following clinical review, prisoners who met the diagnostic criteria for ADHD and who met the other eligibility criteria for the trial were invited to take part in the clinical trial. Eligibility for the trial was further checked and recorded once the consent form for the clinical trial (consent II) had been signed and baseline assessments had been completed, prior to randomisation. Using an algorithm that applies the DSM-5 criteria to the DIVA 2.0 data, cases were checked to ensure that they met diagnostic criteria for DSM-5 ADHD. A clinical assessment and review by a psychiatrist trained in the diagnostic assessment of ADHD checked all inclusion and exclusion criteria prior to randomisation.
Intervention
Trial medication
The trial medication consisted of 18-mg capsules of OROS-MPH or placebo capsules.
Capsules were overencapsulated and packaged in bottles of 46. Each bottle was assigned a unique randomisation number and the randomisation system allocated the right bottle to each participant. Overencapsulation has been successfully adopted in previous studies to generate matched placebo to OROS-MPH, including the previous Swedish prison trial. 33 OROS-MPH was provided as commercial stock by Janssen-Cilag Ltd. Piramal Healthcare UK Ltd (Morpeth, UK) (arranged by Modepharma Ltd, Beckenham, UK) provided the trial kits by overencapsulating the OROS-MPH capsules and manufacturing the placebo to match, and by providing approved packaging and labelling, Qualified Person Certification and distribution for 220 patients. Janssen-Cilag Ltd provided the Summary of Product Characteristics (SmPC), which was updated throughout the trial.
The overencapsulated active capsules were repacked in high-density polyethylene (HDPE) plastic bottles without the need for a stability programme, as 18-mg OROS-MPH has marketing authorisation for both HDPE and blister packaging. Placebo capsules were manufactured once. Trial medication overencapsulation and packaging was undertaken in two campaigns to accommodate a trial duration of up to 3.5 years. OROS-MPH 18-mg capsules typically have a maximum shelf life of 3 years from the date of manufacture; however, by the time the product was repacked for the clinical trial, the remaining shelf life was likely to be < 2.5 years. Overencapsulation used DBcaps® (Capsugel, Inc., Morristown, NJ, USA) capsules, which are designed specifically for the blinding of clinical trial medication.
The reason for overencapsulating the OROS-MPH and placebo capsules, rather than manufacturing a matching placebo tablet, was because OROS-MPH capsules have printing on them and are of a distinct shape that would be difficult to manufacture and might have infringed copyright. We sought advice on this from previous investigators who used OROS-MPH, and from companies that provide drug and placebo supplies for studies. Studies on the use of DBcaps have shown that encapsulation of capsules results in a lag time of 2–3 minutes in disintegration, compared with the unencapsulated capsules. 53–55 The pharmacokinetic properties of 18-mg OROS-MPH prolonged-release capsules indicate release over several hours: following oral administration of OROS-MPH, the drug overcoat dissolves, providing an initial maximum drug concentration at about 1–2 hours. The MPH contained in the two internal drug layers is gradually released over the next several hours. Peak plasma concentrations are achieved at about 6–8 hours, after which plasma levels of MPH gradually decrease (section 5.2 of the SmPC56).
Prescribing procedure
All prescriptions were completed by the trial psychiatrists at each site. Each patient was allocated a kit consisting of a labelled carton containing four labelled bottles, each containing 46 of the 18-mg OROS-MPH capsules or 46 of the placebo capsules. Each kit and its bottles were labelled according to annex 13 of the European good manufacturing practice (GMP)57 and had their own unique treatment pack number. The centralised randomisation system allocated the correct treatment pack number to each participant during the trial. Trial medication was delivered as prescribed daily, with participants observed by prison health-care nursing staff to ensure that they swallowed the capsules. There is a daily record of how many capsules were given out and taken by the participants, recorded by the nursing staff.
Titration procedure
All trial medication was titrated in the same way. Treatment started at an initial dose of one capsule of trial medication for 1 week. The number of capsules was then increased weekly over the following 4 weeks, in increments of one capsule, to a maximum of four capsules. This reflected a dose range for the active medication of 18, 36, 54 and 72 mg. Titration upwards was stopped if all 18 ADHD symptoms were scored as negligible or absent (score of 0 or 1 on the CAARS-O) or if unacceptable adverse effects were reported. The trial medication could also be reduced by one capsule if there was a limiting adverse event (AE), in which case there were no further increases in dose for the duration of the trial or, potentially, the cessation of trial medication in some cases. Individual titration protocols are routinely used in clinical practice as they optimise the control of ADHD symptoms while minimising potential adverse effects, and have been used successfully in previous efficacy trials of OROS-MPH. 58,59
Medication was provided either once or twice daily, in the morning and/or at noon, up to the maximum daily dose. This provided flexibility to tailor the dose to the individual effects reported by participants and to maximise adherence to trial medication within the constraints of the prison system for delivery of controlled medications. A maximum dose of four capsules, equivalent to 72 mg of OROS-MPH, was included for this trial because previous trials and clinical consensus indicate that there is considerable individual variation in dosing to obtain the optimal balance of good control of ADHD symptoms while minimising common adverse effects. Although current licensing for OROS-MPH is up to 54 mg, this is based on dose levels for children and adolescents, rather than young adults, and NICE recommend a daily dose of MPH in adults to a maximum of 100 mg per day. 13,14 For OROS-MPH, the British National Formulary60 recommended doses up to a maximum of 108 mg in adults.
Unblinding
An emergency unblinding service was provided, but was not required at any stage of the trial. It was set up so that any health-care staff would be able to call an emergency number that was added to the labels for both the bottle and the box with the trial kit. In addition, code-breaking envelopes were printed and held at the company providing the unblinding service in case of an emergency, but were not used. Unblinding did not take place for any participants during the trial.
Adherence to trial medication
Based on experience from the pilot study, we envisaged that adherence to medication would present a challenge for around 20% of participants. This could be for several reasons. Some offenders may not feel motivated to take the trial medication if they experience adverse effects or do not feel that they are improving. They may also take medication intermittently because of strict prison regimes that allow only a brief time for leaving their cells to obtain medication or difficulty in getting to the location where medicines are dispensed. These cases were not expected to contribute to missing data, but could affect the overall outcome of the intention-to-treat (ITT) analyses.
In the pilot study at HMP YOI Isis, we accrued considerable experience in managing the expectations of offenders and providing the support needed to help participants adhere to the trial protocol. The following steps were therefore adopted to maximise adherence to medication:
-
In the pilot study, minor adverse effects were the most common reason for non-adherence to medication, affecting 13% of participants. This was linked to the observation that this population may be more sensitive to minor adverse effects, particularly changes in appetite, and sleep problems. To minimise this effect, we took care to identify the early signs of minor adverse effects such as appetite loss and to adjust the medication dose accordingly by systematic evaluation of ADHD symptoms and minor adverse effects during the titration phase of the trial.
-
Seven per cent of the pilot sample did not wish to take medication in the mornings and the protocol for the current trial was adjusted to allow for medication to be taken later in the day, until noon. This allowed for participants who got up later in the day, who worked mainly in the afternoons or who had a strong preference for mid-day dosing. This flexibility in dosing time reflects dosing decisions in non-trial patients and can provide a better match to participants’ daily routines.
-
During the pilot study, prison staff did not always let patients out of their cells to receive medication or remind participants to get up on time. To resolve this problem, we initiated the use of research staff, whenever possible, to assist in the delivery of medication by checking that prisoners were always out of their cells in time to receive trial medication.
-
In the pilot study, treatment was disrupted because of religious customs for several participants. We took care to check that participants were not randomised during periods when religious customs might interfere with adherence to the trial protocol.
-
In the pilot study, daily adherence to the trial medication reduced when participants were not reviewed weekly. One of the findings in the pilot study was the importance that prisoners gave to the weekly follow-up meetings during the titration process, during which they could discuss their symptoms and response to the treatment process in addition to completing trial assessments. We also provided brief support on an ad hoc basis or in the form of advice, if approached by prisoners when visiting the prison wings.
Concomitant treatments
All concomitant medications were recorded. Concomitant treatments were allowed with medications that are not contraindicated with MPH. Use of the following medications in the 4 weeks prior to the start of treatment with OROS-MPH was not permitted based on potential adverse drug interactions: clonidine, coumarins, monoamine oxidase inhibitors, moclobemide and rasagiline. There were no exclusions for this reason.
Measures
A schedule of trial assessments is provided in Table 1.
| Measure (description) | Rater | Baseline | Week (post randomisation) | |||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 8 | |||
| Demographic data | Health records | ✗ | ||||||
| DIVA 2.0 (ADHD assessment) | Investigator | ✗ | ||||||
| MINI 7.0.1 (comorbid mental health disorders) | Investigator | ✗ | ||||||
| WASI-II (IQ) | Investigator | ✗ | ||||||
| AUDIT-C (alcohol use) | Self-report | ✗ | ||||||
| NIDA Quick Screen (drug use) | Self-report | ✗ | ||||||
| CTQ (childhood trauma) | Self-report | ✗ | ||||||
| ZAN-BPD (borderline personality disorder) | Self-report | ✗ | ||||||
| RPQ (reactive–proactive aggression) | Self-report | ✗ | ||||||
| Weiss-CD (conduct disorder) | Self-report | ✗ | ||||||
| CAARS-O (ADHD symptoms) | Investigator | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| WRAADDS (emotional dysregulation) | Investigator | ✗ | ✗ | ✗ | ||||
| ARI-S (irritability) | Self-report | ✗ | ✗ | ✗ | ||||
| MEWS (spontaneous mind-wandering) | Self-report | ✗ | ✗ | ✗ | ||||
| BSI (general psychopathology) | Self-report | ✗ | ✗ | ✗ | ||||
| MINI checklist (MINI 7.0.1 symptom checklist) | Investigator | ✗ | ✗ | |||||
| CORE-OM (symptoms of psychological distress) | Self-report | ✗ | ✗ | |||||
| MVQ (attitudes towards violence) | Self-report | ✗ | ✗ | ✗ | ||||
| CGI scale | ||||||||
| Severity subscale | Investigator | ✗ | ✗ | ✗ | ||||
| Therapeutic outcome subscale | Investigator | ✗ | ✗ | |||||
| MOAS-Prison (prison officer-reported aggression) | Prison officer | ✗ | ✗ | |||||
| BRC-Prison (prison officer-reported behaviour) | Prison officer | ✗ | ✗ | |||||
| MOAS-Education (reported aggression in education) | Education staff | ✗ | ✗ | |||||
| BRC-Education (reported behaviour in education) | Education staff | ✗ | ✗ | |||||
| Critical incidents [number of behavioural incidents (adjudications) reported] | Prison records | ✗ | ✗ | |||||
| Education sessions | ||||||||
| Number scheduled | Prison records | ✗ | ✗ | |||||
| Number attended | Prison records | ✗ | ✗ | |||||
| Medication | ||||||||
| Dose prescribed | Health records | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| Number of capsules taken | Health records | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| AES (common adverse effects) | Investigator | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Heart rate/blood pressure | Investigator | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Height | Investigator | ✗ | ||||||
| Weight | Investigator | ✗ | ✗ | ✗ | ||||
Baseline-only measures were collected for all participants prior to randomisation, and included descriptors of the trial population and putative moderators of the treatment response. The primary outcome was the investigator-rated CAARS-O score at 8 weeks after the initial trial prescription. There were 13 secondary outcome measures (see Table 2) also assessed at 8 weeks. Baseline (pre-randomisation) values of the primary and secondary outcome measures were collected so that we could assess change. In addition, week-5 values were collected for variables that featured as putative mediators (see Table 2).
Once a participant had signed consent II for the RCT, baseline measures were obtained through face-to-face administration of the questionnaires. Help in reading or understanding questions was provided by research staff in most cases. Because of the large number of baseline measures, these were frequently collected across two sessions. All baseline measures were obtained prior to randomisation.
Data such as days incarcerated, release date, prison regime, adjudication, attendance at offender behaviour and educational programmes, demographic details and medical history were obtained by accessing prison and medical health records. The assessments were completed at baseline and at week 8 for the subset of outcome measures taken from prison records. Reports on the behaviour of participants were obtained from prison and education staff, reflecting behaviour at baseline and at week 8. Not all of the participants attended educational or rehabilitation programmes; hence, it was not possible to obtain measures from education staff for all participants. In addition, it was not always possible to obtain ratings from education staff because they did not always know the pupils or their names, and because of frequent staff changes and difficulties getting hold of teachers. The researchers tried to overcome these issues and found that the best option was to obtain the measure over the telephone.
Investigator-rated measures
These measures were completed by a trained psychiatrist or research assistant following interview assessments with participants:
-
The DIVA 2.0 – this is a semistructured diagnostic interview designed to capture the diagnostic symptoms and other criteria for DSM-IV ADHD. 31 It was used in this study as the main diagnostic instrument for the diagnosis of ADHD. Diagnoses were mainly based on descriptions of ADHD symptoms in daily life from the person being assessed, as well as other observations during the clinical assessment. In a few cases when it was not possible to obtain sufficiently clear descriptions of symptoms, particularly if there was no account of ADHD symptoms from before the age of 12 years, informants were contacted to further inform the DIVA 2.0 ratings. Since the start of the study, DIVA-5 has been published, which applies a different algorithm for DSM-5 criteria, although the individual items have not changed. The diagnostic algorithm applied to DIVA 2.0 was modified for the DSM-5 criteria, as defined in the inclusion criteria for this trial.
-
The Mini International Neuropsychiatric Interview (MINI) 7.0.1 – the MINI 7.0.1 is a semistructured interview assessment used to capture DSM-IV diagnostic criteria for common mental health disorders. 62 The sections completed included major depressive episode, suicidality, manic episode, hypomanic episode, panic disorder, agoraphobia, social anxiety disorder, obsessive–compulsive disorder, post-traumatic stress disorder (PTSD), psychotic disorder and mood disorder with psychotic features, generalised anxiety disorder, and ASPD.
-
The MINI checklist – in addition to diagnostic categories evaluated at baseline only, the MINI 7.0.1. includes a cross-disorder symptom checklist, with ratings from 0–10. We used this at baseline and also as an 8-week outcome assessment.
-
The Zanarini Rating Scale for Borderline Personality Disorder (ZAN-BPD) – the ZAN-BPD is a validated measure for the assessment of symptoms of borderline personality disorder (BPD). 63 We used this measure as a baseline moderator.
-
The CAARS-O64 – the 8-week CAARS-O assessment was the primary outcome measure for this study. The CAARS-O was also used as a secondary outcome at week 5, and to assist the psychiatrist in titrating participants to the optimal trial medication dose at weeks 1–4. The CAARS-O consists of the 18 DSM-IV ADHD symptoms, rated on a four-point Likert scale (0: not at all, never; 1: just a little, once in a while; 2: pretty much often; and 3: very much, frequently). This scale and other very similar scales have been extensively validated as outcome measures in previous clinical trials of adult ADHD.
-
The Wender–Reimherr Adult Attention Deficit Disorder Scale (WRAADDS) – we used the emotional dysregulation items from the WRAADDS. 65 We applied the emotional dysregulation items from an interview assessment of the WRAADS items, following previous publications on the treatment response of emotional symptoms in ADHD. 17,66
-
The Adverse Events Scale (AES)67 – this captures common known adverse effects associated with the use of MPH and other stimulant medications.
-
The Clinical Global Impression (CGI) scale68 – this was used by the research psychiatrist to give an overall rating of clinical severity, and a clinical impression of the clinical response and adverse effects of the trial medication. This was the only outcome obtained by the clinician (rather than the researcher) who was directly engaged in the titration of trial medication for each participant.
-
Physical health – body mass index (BMI), heart rate and blood pressure were measured to monitor the safety of the trial medication, as recommended. 14
Participant self-rating scales
Self-rating scales were given to the participants. The scale questions were usually read out to participants, who gave their response accordingly:
-
The RPQ69 – this scale is included as a baseline moderator capturing proactive and reactive forms of aggression.
-
The Weiss Conduct Disorder scale (Weiss-CD) – this scale was included to capture conduct disorder symptoms as a descriptor and baseline moderator.
-
The Alcohol Use Disorders Identification Test for Consumption (AUDIT-C) – this is validated as a quick screen for alcohol use problems. 70 This was used as a quick screen to capture alcohol use in the year prior to the current prison sentence.
-
The National Institute on Drug Abuse (NIDA) Quick Screen – this is a quick screen for drug use problems, adapted from the single-question screen for drug use in primary care by Saitz et al. 71
-
The Childhood Trauma Questionnaire (CTQ)72 – this was used to capture reports of childhood trauma that might moderate the clinical response to MPH.
-
The Barkley ADHD Self-Rating Scale for DSM-IV ADHD symptoms30 was used as an initial screening instrument. It is not reported as a baseline or outcome variable. Participants were considered to screen positive for ADHD if they scored two (often) or three (very often) for four or more symptoms in either the inattentive or hyperactive/impulsive symptom domains.
-
The Affective Reactivity Index-Self (ARI-S)73 – this is a self-rating scale for irritability.
-
The Mind Excessively Wandering Scale (MEWS)74 – this is a self-rating scale that captures excessive spontaneous mind-wandering, an aspect of psychopathology that is closely associated with ADHD and a good predictor of ADHD-associated impairment in daily life.
-
The Brief Symptom Inventory (BSI)75 – is a self-rating scale that captures comorbid symptoms reflecting common aspects of psychopathology. Subscales include nine symptom dimensions: somatisation, obsession–compulsion, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation and psychoticism.
-
The Maudsley Violence Questionnaire (MVQ)76 – this was designed to capture beliefs associated with violence. The machismo subscale relates to embarrassment over backing down and justification of violence in response to threat and attack. The acceptance subscale includes the overt enjoyment and acceptance of violence in everyday life. In previous research, the machismo subscale showed a greater relationship to actual violence76 and a greater reduction in the pilot study for this trial. 29 We report on the total scale in this trial.
-
The Clinical Outcomes in Routine Evaluation – Outcome Measure (CORE-OM)77 – this is a scale that captures subjective well-being, problems and symptoms, life-functioning, and risk and harm. It was designed to measure psychological distress before and after treatment.
Data from prison records and prison and education staff
Data were collected from prison records and prison and educational staff, relating to behaviour in the previous 56 days. For cases of individuals new to custody presenting with significant behavioural problems, the retrospective baseline reporting period was 56 days to allow for initial behavioural problems that may arise when people first enter prison. For 16 participants (nine in Isis and seven in Polmont), the time reported was shorter because they had not been in the prison for a sufficient length of time; this was reported as a protocol deviation. The following data were collected:
-
Critical incidents – critical incidents were taken from prison records for the period of 8 weeks prior to randomisation (baseline) and for the 8 weeks of the trial (8-week outcome). This item consisted of the number of adjudications for antisocial behaviour and reports of rule breaking at HMP YOI Isis and HM YOI Polmont.
-
Modified Overt Aggression Scale-Prison (MOAS-P) – ratings of aggressive behaviour by prison staff for the previous week were obtained using the Modified Overt Aggression Scale (MOAS). 78
-
Behaviour Report Card-Prison (BRC-P) – ratings of behaviour by prison staff for the previous week were obtained using behaviour report cards79 by prison officers.
-
Modified Overt Aggression Scale-Education (MOAS-E) – ratings of aggressive behaviour by education staff for the previous week were obtained using the MOAS. This item was optional, depending on whether or not prisoners attended education sessions.
-
Behaviour Report Card-Education (BRC-E) – classroom behaviour report cards scored by education staff were obtained for the previous week. This item is optional, depending on whether or not prisoners attended education sessions.
-
Incentives and earned privileges – the number of positive IEPs for positive engagement in education, occupational and rehabilitation programmes was obtained from prison records for the 2 months prior to randomisation, and after 8 weeks of the trial. IEPs were available at HMP YOI Isis only; for this reason, they were not included as an outcome in the statistical analysis plan (SAP).
Primary and secondary outcome measures
Details of the primary and secondary outcome measures at week 8 are listed in Table 2.
| Concept | Instrument (rater) | Information used in imputation step of MI analysis | Type of measure | Effect size |
|---|---|---|---|---|
| ADHD symptoms | CAARS-O (investigator rated) | Ma (B,4,5,8)b | Continuous scale | Mean difference |
| Emotional dysregulation | WRAADDS (investigator rated) | Ma (B,5,8)b | Continuous scale | Mean difference |
| Irritability | ARI-S (self-rated) | Ma (B,5,8)b | Continuous scale | Mean difference |
| Spontaneous mind-wandering | MEWS (self-rated) | Ma (B,5,8)b | Continuous scale | Mean difference |
| Attitudes towards violence | MVQ (self-rated) | Ma (B,5,8)b | Continuous scale | Mean difference |
| Common psychopathological symptoms | BSI (self-rated) | Ma (B,5,8)b | Continuous scale | Mean difference |
| Global impression of therapeutic effect | CGI scale-therapeutic (clinician rated) | Ma (B,5,8)b | Categorical | Mean difference |
| Behavioural problems recorded by prison officers as adjudications in prison records | Critical incidents (prison records) | Incident rate (B,8)b | Incident rate over 8-week period | Incidence rate ratio |
| Prison office ratings of aggressive behaviour | MOAS-P (prison officer rated) | Ma (B,8)b | Dichotomised (any aggressive event) | Odds ratio |
| Educational staff ratings of aggressive behaviour | MOAS-E (education staff rated) | Ma (B,8)b,c | Not analysed | Not analysed |
| Prison officer ratings of behaviour | BRC-P (prison officer rated) | Ma (B,8)b | Proxy count of incidents of inappropriate behaviour | Incidence rate ratio |
| Educational ratings of behaviour | BRC-E (education staff rated) | Ma (B,8)b,c | Not analysed | Not analysed |
| Engagement with the educational programme | Number of education sessions scheduled | Incident rate (B,8)b,c | Incident rate over 8-week period | Incidence rate ratio |
| Current psychological distress | CORE-OM (self-rated) | Ma (B,8)b | Continuous | Mean difference |
Primary outcome
The primary end point was the level of ADHD symptoms measured on the investigator-rated CAARS-O at 8 weeks post treatment initiation. This addresses the question of the efficacy of OROS-MPH on ADHD symptoms in young male adult offenders meeting the DSM-5 diagnostic criteria for ADHD. The investigator-rated CAARS-O score is a common outcome measure used in previous treatment trials of ADHD in the community, and measures the same list of 18 symptoms used as the primary outcome in nearly all other studies of adult ADHD. 32
Secondary outcomes
The secondary outcomes addressed important questions about the effects on comorbid symptoms and behavioural impairments that are commonly seen in offenders with ADHD. Ratings of behaviour from prison records and staff included the following: critical incidents recorded in the prison records for the 8-week period from initiation of the trial medication to the week 8 assessment, ratings of aggressive behaviour over the previous week by prison staff using the MOAS-P at 8 weeks, behaviour over the previous week reported using BRC-P from prison staff at 8 weeks, and engagement with educational activities (including the number of scheduled educational sessions, the proportion of scheduled educational sessions attended and reports of disruptive behaviour in education sessions reported at 8 weeks using the BRC-E and over the course of the trial using the MOAS-E). The reports from education staff were possible only for those participants who attended education or rehabilitation sessions. Ratings of symptoms and behaviour reported by participants included attitudes towards violence captured using the MVQ at 8 weeks; general distress and psychopathology captured using the CORE-OM and BSI at 8 weeks; excessive spontaneous mind-wandering captured using the MEWS at 5 and 8 weeks; symptoms of emotional dysregulation and irritability captured using the WRAADDS and ARI-S at 5 and 8 weeks; and the CGI scale at 5 and 8 weeks as a general measure of overall clinical improvement.
Mediator measures
To address the tertiary objectives, mediation hypotheses were tested using the following putative mediators and outcome variables: the CAARS-O hyperactive/impulsivity and inattention subscores, and the WRAADDS for emotional dysregulation at week 5 were considered as putative mediators. These measures were hypothesised to mediate treatment effects on secondary behavioural outcomes (critical incidents and BRC-P at week 8).
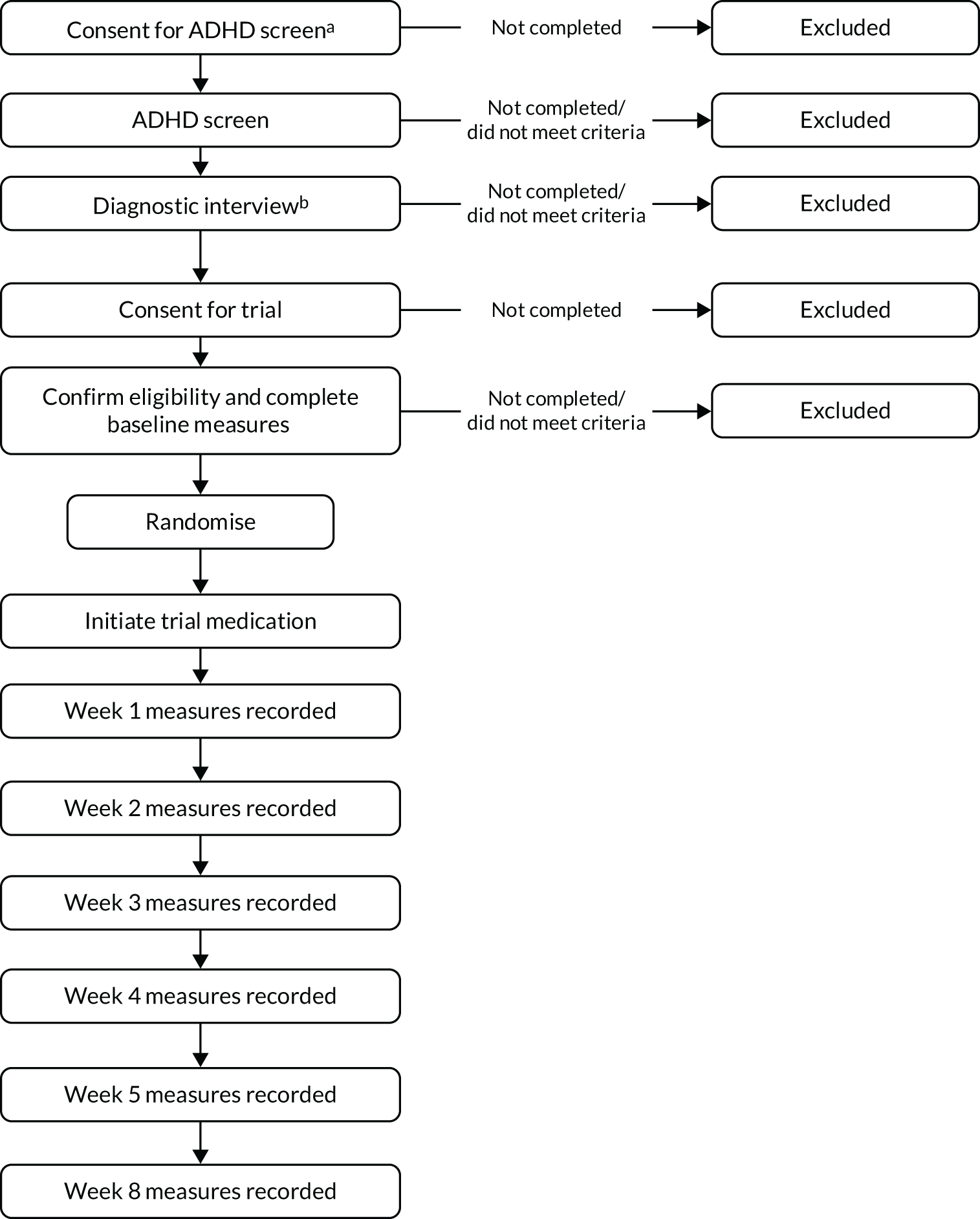
Participant timelines
A flow diagram of participant timelines is illustrated in Figure 1.
FIGURE 1.
Flow diagram of participant timelines. a, Prior to consent to be screened for ADHD, potential participants were provided with information about the trial. Initial consent (screening and diagnostic step) allowed for the use of screening questionnaires (Barkley ADHD self-rating scale for DSM-IV ADHD symptom); b, if ADHD was suspected, a diagnostic interview for ADHD was carried out, which included the DIVA interview for adult ADHD. Diagnosis of ADHD and suitability for the trial were then confirmed by a medical assessment prior to consent for the trial.
Consent
There were two stages of consent. Initial consent, consent I (screening and diagnostic step) allowed the use of the self-rated Barkley ADHD scale30 as a screening questionnaire for ADHD, followed by a diagnostic assessment using the DIVA 2.0 for adults. 31 This was followed by a review of the diagnosis by a trained psychiatrist. During these pre-trial steps, prisoners who failed to meet any of the eligibility criteria at any stage were not invited to continue in the trial. At HMP YOI Isis, routine screening was already in place using this scale and a pre cohort was identified before the start of the trial. These participants were asked to sign consent I at the time of the diagnostic interview. Routine screening did not take place at HM YOI Polmont before the start of this trial.
Following the pre-trial screening stage, individuals who met the diagnostic and eligibility criteria for the trial were invited to take part in the clinical trial, at which stage they were invited to take part in the RCT. Full information about the trial, and subsequent consent to participate (consent II), was completed with the trial psychiatrist after the diagnosis had been verified by clinical review. Participants completed baseline measures after signing consent II, to take part in the trial. Once the baseline measures had been completed, eligibility criteria were further checked, documented and entered into the trial database.
Research visits
Informed consent was divided into consent I, for diagnostic screening and identification of potential participants for the RCT, and consent II, required prior to obtaining baseline data and randomisation to OROS-MPH or placebo.
Following consent for screening (consent I) and confirmation of the diagnosis of ADHD and eligibility by a psychiatrist trained in the assessment of ADHD, information sheets and consent forms for the controlled trial (consent II) were provided to and discussed with potential participants (visit 1). Information sheets were reviewed and informed consent obtained for the clinical trial (visit 2). No limit was set for the time taken between visits 1 and 2 within the time frame of the project. Potential participants were encouraged to take as much time as they needed to reach a fully informed decision about participation in the trial.
Baseline data were then collected from participants (visit 3), prison and health-care records, and prison and educational staff. Once the patient baseline data had been collected and eligibility confirmed following medical review by one of the trial psychiatrists, participants were randomised to treatment with placebo or OROS-MPH (visit 4). Trial prescriptions were completed and given to the pharmacy. Medication was started within 1 week of randomisation, but usually within 2 or 3 days. At the end of week 1, participants were reviewed, and trial medication titrated according to their clinical response and adverse effect profile (visit 5, week 1 titration). Symptoms of ADHD were measured using the CAARS-O, AEs were checked using the AES, and heart rate and blood pressure were checked and recorded. This titration procedure was repeated at the end of weeks 2, 3 and 4 (visits 6–8) and was expected to remain unchanged. Five weeks after the start of the trial medication (visit 9, week-5 assessment), the maintenance prescription was checked and could be changed for a final time. The final dose was then maintained for the last 3 weeks of the trial, unless participants withdrew from ongoing treatment. At the week-5 assessment, outcome measures were completed by a research investigator (not the clinician who titrated the medication): the CAARS-O, WRAADDS and MEWS; heart rate and blood pressure; weight; and the AES. The CGI scale was completed by the psychiatrist who titrated the medication dose, as this measures a clinician’s view on the global clinical response to treatment; however, for 42 participants, the CGI scale was obtained by the researcher instead of the psychiatrist. The final visit, visit 10, was completed 3 weeks later, 8 weeks after the initiation of the trial medication. At this visit, all outcome measures were completed. As far as possible, the information on clinical response derived during the titration visits (weeks 1–4) was not shared with other members of the research team. Thus, potential unblinding based on the observed clinical response and AEs was minimised. Researchers who were engaged in generating outcome data also conducted data entry and undertook internal source data verification (SDV) checks, as well as checking data queries.
Sample size
The sample size of 200 young male offenders was determined as follows. The primary outcome was ADHD symptoms, measured using the CAARS-O, a total 18-item ADHD symptom score. The results of a single-arm open-label pilot study of young male prisoners with ADHD who were given MPH showed a mean decrease of 25.0 points with a standard deviation (SD) of 9.1. 29 This suggested a large standardised effect size of SMD 2.75. It could reasonably be assumed that at least 20% of this effect might be attributed to the effects of MPH. On this basis, this trial is powered to detect a standardised effect size of d = 0.55. Assuming a SD of 9.1, this would translate into a treatment difference of 5.0 points. This effect size is consistent with the results of a 2018 meta-regression analysis,32 which estimated the effect of treatment to be a SMD of 0.49 (95% CI 0.08 to 0.64). The sample size calculation used G*Power version 3 (Heinrich Heine University Düsseldorf, Germany)80 and was based on the use of a t-test to compare the means of the treatment groups. To have 90% power at the 5% significance level to detect a standardised effect of SMD 0.55, this trial would need to collect outcome data on 142 participants. Inflating for the expectation that loss to follow-up may be as high as 25%, a minimum of 190 participants are required, with the target for the trial set at 200. A 25% loss to follow-up was expected to be easily achieved, as, in the pilot study, 10% of participants left the prison as a result of unexpected transfers from the prison, whereas problems with adherence to trial medication were rarely followed by problems obtaining follow-up assessment data.
Interim analyses and stopping guidelines
No interim analyses were planned or performed. Stopping guidelines were based on recruitment rate and a review of feasibility for recruitment. All of the original recruitment targets were met. At milestone 3, the Data Monitoring Committee (DMC) reviewed progress with recruitment and safety, and recommended continuation of the trial.
The key milestones established before the start of the trial were as follows:
-
milestone 1 (3 months) – five participants recruited and trial medication initiated
-
milestone 2 (14 months) – 65 participants randomised and trial medication initiated
-
milestone 3 (24 months) – 120 participants randomised and trial medication initiated.
Milestone 1 was reached by the end of September 2017, with a total of 75 participants randomised (Isis, 47; Polmont, 28). By milestone 3, after the first 24 months of the trial, a total of 152 participants were randomised (Isis, 91; Polmont, 61). During this period, it was established that no other recruitment site was required.
Randomisation and blinding
Randomisation type and sequence generation
Randomisation to OROS-MPH or placebo was in a 1 : 1 ratio. Randomisation was at the participant level and was conducted using an online system set up by the KCTU, ensuring reliability and credibility in the randomisation process. Randomisation was stratified by prison, with variable block sizes to ensure that equal numbers of patients were allocated to the two arms in each prison stratum.
Randomisation allocation concealment mechanism and implementation
The randomisation process was conducted by trial psychiatrists, who entered the participant information (research identification number and participant name initials) into the KCTU randomisation system. The trial psychiatrists then completed initial trial prescriptions. Each participant was allocated a kit (labelled carton) containing four labelled bottles, each containing 46 OROS-MPH (18 mg) or placebo capsules. Each kit and its bottles were labelled according to annex 13 of the European GMP for investigational medicinal products (IMPs)57 and had their own pack number, which was matched to the randomisation number. The centralised randomisation system allocated the correct treatment kit number to each participant during the trial.
Blinding
Blinding was maintained for all trial investigators, including the on-site researchers, pharmacy staff and trial manager. The statistical team remained blinded to trial arm allocation until after the analyses laid out in the analysis plan were completed. Whenever possible, outcome measures were obtained by an assessor who was not involved in the titration procedures to minimise the potential for bias when rating outcome variables. This was possible for all assessments apart from 16 assessments when it was not possible because staff had to cover for each other, for example during sick leave. Researchers engaged in generating outcome data also entered the data into the trial database and conducted internal SDV checks, as well as resolving any data queries.
The main analysis data set did not include any trial medication dosage data to ensure that the trial statistician remained blinded. We did, however, conduct a sensitivity analysis to assess efficacy for those showing good compliance with the trial medication, as well as generating tables to describe the doses prescribed and taken over time by trial arm. The sensitivity analysis excluded those participants who took trial medication on < 75% of the days on which it was prescribed, which was thought to be a reasonable criterion for poor adherence to trial medication. These analyses were done last to minimise the risk of unblinding.
Withdrawal of subjects
Participants had the right to withdraw from the trial at any time for any reason. Health-care staff had the right to withdraw participants from the trial if they thought that the trial was having an adverse effect on the participants; this was not applied for any participant in the trial.
However, when participants discontinued trial medication, we invited them to remain in the trial to complete trial assessments, thereby minimising loss of data. When participants decided to withdraw from the trial, all efforts were made to report the reason for withdrawal as thoroughly as possible. Withdrawal from the trial was defined as withdrawal from taking the trial medication and from providing further follow-up assessment data. There was a significant group who continued to provide follow-up assessments, but who had withdrawn from taking trial medication.
Owing to potential concerns about the interaction of trial medication with unknown psychoactive substances, if a participant disclosed to any member of the research team that they had used ‘spice’ (synthetic cannabis or other unknown psychoactive substance) or there were suspicions of use reported by health-care or prison staff, while participating in the trial, a clinical evaluation was made. If this was current use (defined as within the previous 2 days), the trial medication was stopped. If this occurred earlier in the trial and was considered an isolated incident, the trial medication could continue. If the trial medication was stopped, the participant remained in the trial and was asked to complete trial assessments. A clinical assessment was made on a case-by-case basis to consider the safety of restarting trial medication 48 hours after stopping the trial medication.
Statistical analyses
A detailed SAP was developed by the trial statisticians in collaboration with the chief investigator, was reviewed by the DMC, and was reviewed and approved by the Trial Steering Committee (TSC) before the trial database was locked. Here we provide a summary of the statistical analysis approaches employed according to this plan. However, note that the decision of some analyses could be finalised only after having sight of the data, namely the necessity to employ multiple imputation (MI) to handle the missing data generating process and the distributional assumptions for some of the non-questionnaire secondary outcomes.
An ITT approach was used for all primary and secondary week-8 outcomes, that is participants were analysed in the groups to which they were randomised, irrespective of adherence to trial medication. The primary outcome measure, the CAARS-O, and the secondary outcome measures, MEWS, WRAADDS, ARI-S, CORE-OM, BSI, MVQ and CGI scale, were continuous variables. Their modelling relied on normal assumptions for error terms and the treatment effects were quantified by trial arm differences (and standardised differences). The MOAS-E, MOAS-P, BRC-P and BRC-E had also been expected to follow normal distributions and critical incidents had been expected to follow a Poisson distribution. However, on review, the residuals or all of the MOAS-P, MOAS-E, BRC-P, BRC-E and critical incidents were noticeably positive skewed, and possibly overdispersed or zero inflated, and so could not be modelled by a normal distribution (see Table 2).
The number of education sessions scheduled at 8 weeks was defined as being scheduled to attend any of offender training, vocational training or education sessions. We had intended to use logistic regression to analyse education as a binary variable of whether or not any education sessions were scheduled, but, at baseline, almost all (187/200) of the participants had some form of education session scheduled. At week 8, this increased to 191 out of 200 participants. Owing to this lack of variability in the binary education outcome, we instead analysed the underlying count variable ‘number of any form of education scheduled between baseline and week 8’ using a negative binomial distribution to allow for positive skewness and overdispersion of this variable. The proportion of education sessions attended out of those scheduled was also described by arm.
Education outcomes were considered for only the subpopulation of prisoners enrolled in education at baseline. A total of 187 trial participants were enrolled in some form of education at baseline. However, within this subpopulation, only 83 MOAS-E baseline forms were completed. Similarly, only 67 BRC-E forms were completed. We considered an actual sample size of less than half of the intended size at baseline to be too small to attempt meaningful formal inference. Thus, the education outcomes MOAS-E and BRC-E were summarised descriptively only.
The BRC-P was approximated by a negative binomial distribution, which is appropriate as, although not directly defined as a count of incidents, the questionnaire is a weighted proxy count of incidents of inappropriate behaviour. Thus, BRC-P was modelled in the same way as the number of education session scheduled.
The MOAS-P exhibited large zero inflation and too few remaining data points to allow modelling of the distribution (143/200 participants who were included in the trial were rated ‘0’ on the MOAS-P at 8 weeks). We therefore dichotomised this outcome to give a binary variable (1 = participant had any aggressive event, 0 = no aggression) and analysed it using logistic regression.
For critical incidents, which is a count of incidents, the data were positively skewed and zero inflated. However, the residuals were no longer zero inflated after baseline count of incidents was included in the analysis model. A negative binomial model, rather than a Poisson distribution, was employed to allow for overdispersion. In addition, the time in prison was included in the model as an offset to model the fact that the number of critical incidents reported at week 8 are proportional to the time spent in prison between randomisation and withdrawal from or the end of the 8-week trial.
Need for multiple imputation
Formal trial arm comparisons were carried out by MI, more specifically by using the flexible multivariate imputation by chained equations approach. 81 This was necessary because withdrawal from treatment was found to be predictive of missing primary outcomes (i.e. missing CAARS-O scores at 8 weeks). Withdrawal from treatment was defined as withdrawing completely from the trial through choice; through release, transfer or deportation; or withdrawing from treatment only. The association between treatment withdrawal during the trial and missing data in the primary outcome at 8 weeks was tested using Fisher’s exact test and found to be predictive (p < 0.001). Thus, a MI approach was pursued to allow for a missing data generating mechanism that was missing at random, with the observed variables allowed to drive missingness, including withdrawal from treatment.
We empirically assessed whether or not baseline variables were predictive of missing data using a forward logistic regression modelling approach. The following baseline variables were considered: all comorbidities as recorded using the MINI checklist, each individual MINI diagnosis, subscores of the WRAADDS (emotional over-reactivity, affective lability, temper), the MVQ, the CGI scale, the AES, IQ score, the CTQ, the number of days in prison prior to randomisation, the RPQ and the proactive and reactive subscales, the ZAN-BPD score, Weiss-CD, the MOAS as recorded by education staff (MOAS-E) and prison staff (MOAS-P), alcohol use, illicit drug use, ethnicity, their highest level of education, previous treatment for ADHD and employment. All baseline variables were considered unless one of the categories of the variable occurred too infrequently to expect to observe both missing and observed data (defined as < 21 observations). Variables were considered to be potentially important, and were later considered for inclusion in the imputation model, if they were statistically significant at a liberal 10% test level in a logistic regression of missingness at 8 weeks on the variable in question, trial arm and prison (the randomisation stratifier). A single potential predictor variable found that only employment prior to incarceration was predictive of providing CAARS-O data at 8 weeks, with those who were in employment, self-employed or in education being more likely to provide final outcomes (p = 0.075).
Multivariate imputation by chained equations was used with regression models for imputation of missing values in continuous variables, with logistic regression models for imputation of missing values in binary variables and with negative binomial models for imputation of missing values in counts.
Analysis model
The analysis models used to estimate treatment effects included the respective outcome variable as the dependent variable; and trial arm, baseline values of the outcome (if available) and randomisation stratifiers (prison sites) as explanatory variables. Depending on the distributional assumptions made for the various secondary outcomes, OROS-MPH effects were quantified by trial arm differences, odds ratios or incidence rate ratios (see Table 2).
Imputation model
For each outcome variable, the imputation model included (1) all of the variables of the analysis model, (2) measures of the outcome variable at baseline and at 4 and/or 5 weeks, if available, and (3) known predictors of missingness (withdrawal from treatment during the trial and employment prior to incarceration). List item 1 is stipulated by MI theory; item 2 was undertaken to improve the precision of the inferences and also to allow outcome measures at earlier time points to drive drop out at later time points; and item 3 accommodates identified predictors of missingness and allowed us to make a more realistic missing-at-random assumption.
Sensitivity analyses
Four sensitivity analyses were conducted. Sensitivity analyses were carried out for the primary outcome only (CAARS-O score at 8 weeks). The first sensitivity analysis assessed the assumption that the treatment effect is constant only within defined time windows. That is, only data recorded at the week-8 visit date ± 2 days were included in this sensitivity analysis. The second sensitivity analysis looked at the effect of delayed treatment initiation. Again, those who failed to start treatment within 7 days of randomisation were removed from the analysis of the primary outcome. The third sensitivity analysis evaluated the impact of IQ on the primary outcome. Those who did not record an IQ of > 60 on the WASI-II were excluded from this analysis. The fourth sensitivity analysis targeted the efficacy of OROS-MPH by considering the subgroup of trial participants who were considered to have complied with treatment. This was defined as taking any trial medication on at least 75% of the days on which it was prescribed. Those who withdrew or were released, transferred or deported were excluded.
Mechanisms analyses
Treatment effect modification by prespecified putative moderators CTQ, ZAN-BPD and reactive and proactive subscores of the RPQ was investigated for the primary outcome (i.e. CAARS-O score at 8 weeks). Moderators were investigated one at a time. For each putative moderator, the modelling for CAARS-O at week 8 was extended to include this variable and an interaction between the moderator and the trial arm. To accommodate these variables in the imputation step, the ‘just another variable’ approach to MI with interactions was used, that is both the fully observed moderator and the product term were simply added to the list of predictors variables available for imputation of missing values. The statistical significance of the interaction term then informs regarding treatment effect modification.
Treatment effect mediation of behavioural outcomes by 5-week improvements in ADHD symptoms or emotional dysregulation (measured using the WRAADDS) was assessed by fitting the following six single mediator models:
-
exposure – trial arm: mediator – CAARS-O hyperactivity/impulsivity subscore; outcome – BRC-P
-
exposure – trial arm: mediator – CAARS-O inattention subscore; outcome – BRC-P
-
exposure – trial arm: mediator – CAARS-O WRAADDS emotional dysregulation score; outcome – BRC-P
-
exposure – trial arm: mediator – CAARS-O hyperactivity/impulsivity subscore; outcome – critical incidents
-
exposure – trial arm: mediator – CAARS-O inattention subscore; outcome – critical incidents
-
exposure – trial arm: mediator – CAARS-O WRAADDS emotional dysregulation score; outcome – critical incidents
Based on complete cases only, causal mediation analyses were performed using the Stata® (StataCorp LP, College Station, TX, USA) command ‘paramed’. 81 To base this parametric mediation modelling on linear regression models, the respective outcome variables were log-transformed (BRC-P and critical incidents were count outcomes). Baseline values of the mediator and the outcome variable, prison, age, educational level and IQ were included as covariates in the mediator and outcome models because they were either hypothesised confounders of the mediator–outcome relationship or a randomisation stratifier (prison). The causal mediation analyses allowed for an interaction between trial arm and the respective mediator. To quantify mediation, we reported the estimated natural indirect effect and the natural direct effect. All analyses were carried out in Stata version 15.1.
Chapter 3 Trial management, procedures and timelines
Trial timelines
The project was planned to be delivered in 36 months, with the first 2 months for recruitment and training of research staff, and to ensure that all approvals were in place. A full-time trial manager was appointed before the formal start of the trial, funded from other resources, to ensure that all procedures and permissions were in place; this took an additional 10 months. The recruitment period was planned for 32 months, with 2 months for analysis and preparation of the final report. The recruitment target was met within this timeline despite HMP YOI Isis being told it could no longer randomise participants in February 2019 because the pharmacy had trial kits left for only one treatment arm. Therefore, the final participants were randomised at HM YOI Polmont to ensure that recruitment from the sites was more even and to avoid the need to transfer trial medication kits from one site to the other.
A 5-month no-cost extension was requested in February 2019 for two main reasons:
-
Extensive database checks were needed before the database lock and there was not sufficient time to complete these. The task was made more difficult because it was not possible to conduct all of the database checks outside of the prisons, and there were additional restrictions on access to medical and prison records dependent on whether a participant was still in prison, released, transferred to another prison or deported. These checks needed to be undertaken while research staff were still employed and on site.
-
The SAP for the project was very detailed and required 2–3 months of analysis. In addition, more time was needed to write the report and obtain feedback from co-applicants during the writing process.
Following database lock and review of the preliminary SAP, there was a planned meeting in November 2019 to discuss the trial findings with the DMC, TSC and Trial Management Group (TMG). This meeting led to a recommendation to conduct additional post hoc analyses that might provide an explanation for the main findings. As these further analyses were proposed after database lock and review of the main trial results, they should be regarded as exploratory in nature. The aim was to identify potential factors that might explain the trial findings and that could be considered in future research. These further analyses are reported in Chapter 5. These further analyses were acknowledged, but not formally reviewed, by the DMC and TSC chairpersons. To allow for this work, an additional no-cost extension was approved until 30 June 2020.
Trial set-up
The CIAO-II project started on 1 August 2016; within the first 3 months, it had received a favourable opinion from the East of England–Essex Research Ethics Committee (REC) (reference number 16/EE/0117, Integrated Research Application System project identifier: 179456), as well as HRA approval. The ethics application was submitted prior to the introduction of the HRA and approval was given for the trial to be processed through pre-HRA approval systems. Research and development (R&D) approvals were obtained from Oxleas NHS Foundation Trust and NHS Forth Valley (reference number FV908). In addition, permission was required from HMPPS (reference number 2016-129) and the SPS.
The KCTU provided the randomisation service, IMP management, and the clinical trial database system with full audit trail (InferMed MACRO, London, UK). These were set up in the 10 months before the trial started.
All research and pharmacy staff undertook good clinical practice (GCP) training. This was arranged by King’s Health Partners Clinical Trials Office (KHP CTO) or by NHS Forth Valley. Some pharmacy staff attended a GCP pharmacy training tailored for pharmacy staff and facilitated by KHP CTO. In addition, a GCP light training was provided by KHP CTO on site for health-care staff. Those health-care staff who were unable to attend the training owing to shift patterns were able to review GCP slides and complete a self-certificate. The GCP training was reviewed continuously throughout the trial to ensure that all new staff were trained and that they were added to the delegation log. All staff were retrained by KHP CTO or by NHS Forth Valley after 2 years. Curricula vitae for all health-care staff were collected and updated every 2 years, as per guidelines.
In September 2016, training was provided to all research staff on the standard operating procedure for the project and for the following measures: DIVA, MINI, ZAN-BPD, CAARS-O, CGI scale and WRAADDS. Subsequent new staff received in-house training or attended training events.
The trial was monitored by the KHP CTO on behalf of the sponsor. KHP CTO deemed the sites ready for recruitment with an e-mail confirming ‘green light’, which was obtained for HMP YOI Isis on 11 October 2016 and for HM YOI Polmont on 3 November 2016. An initial site initiation visit for Polmont took place on 13 October 2016, but there was a delay in obtaining ‘green light’ status because of major information technology (IT) issues in King’s College London, which caused a delay in accessing certain records required for the project. Seven participants had to be randomised ‘manually’ with the assistance of the KCTU as a result of the IT issues.
At HM YOI Polmont, there was no routine service for identifying young prisoners with ADHD. For this reason, a two-stage consent process was developed to avoid the situation of asking participants to sign consent for a trial for which they would not be eligible. The first consent (consent I) was for screening using the Barkley ADHD self-assessment form, followed by a DIVA 2.0 assessment for those who screened positive with the self-assessment form. Consent II was the main trial consent, required prior to collection of further baseline data and randomisation. At HMP YOI Isis, there was already an established ADHD service set up by the chief investigator, Philip Asherson. This site also ran the pilot study and screening for ADHD had been established as part of routine clinical care. This meant that, for this site, there was a pre cohort that had already been screened prior to trial commencement. The pre cohort participants who had already completed the Barkley ADHD self-assessment and had screened positive were invited to sign consent I (for the screening and diagnostic stage of the trial) if they attended a DIVA 2.0 assessment for ADHD.
In June 2015, the Scottish Government published a youth justice strategy82 with the aim of reducing the number of young people sent to prison by establishing an early and effective intervention that provided more community options. This meant that the prison population at HM YOI Polmont was less than half of its capacity at the start of the trial, thereby affecting the expected recruitment pool for the trial. This resulted in uneven recruitment between sites.
In March 2017, we were informed that the potential third site, Her Majesty’s Prison (HMP) Rochester, would close in November 2017 for refurbishment. It was therefore decided that this site would not be launched. Owing to the recruitment targets being met, it was decided not to set up an alternative third site. The planned refurbishment at HMP Rochester was later postponed.
Accountability for trial medication
All aspects of treatment and accountability for managing the medication storage and delivery were managed locally by the prison pharmacies and health-care teams, as per standard practice for this medication in the prisons. IMP accountability was recorded and verified. All aspects of treatment compliance and recording of treatment administration/refusal were managed by the prison mental health teams and locally by health-care staff, as per standard practice for these sites. Participants were observed when they were given medication and were checked to ensure that the capsules had been swallowed. This information was then recorded (signed off) by the nursing staff who had delivered the medication on prison pharmacy record sheets or digital records. Despite precautions taken by nurses with regards to seeing prisoners swallow medication, there are documented cases when prescribed medication was diverted. Although there were no such cases documented for the trial medication in this trial, it cannot be ruled out.
Safety checks
Participants were monitored daily by the prison mental health and health-care teams. Safety checks were conducted in line with NICE guidelines. 13
With regard to the research procedures of the trial, there was little risk to participant safety. Participants were aware that they could withdraw from the trial if they wished to do so. Participants who become upset or distressed were offered support by the research team and/or the prison mental health team.
The health-care team followed national guidelines on safety,13 which are predominantly related to the monitoring of cardiovascular function. More specifically, the clinical care followed the following procedures:
-
checks on heart rate and blood pressure before commencing treatments, and review of health-care records
-
potential cardiovascular abnormalities evaluated for risk
-
heart rate and blood pressure checked once a week for the first 5 weeks and at the end of the 8-week trial.
Other safety checks included the monitoring of AEs during assessments. In addition, participants were monitored daily by prison staff and any potential AEs were reported to the prison health-care team.
Procedures for recording and reporting adverse events
Safety remained the responsibility of the prison mental health care team. AEs of any medical or non-medical intervention were identified or recorded by the research team at each site, and were verified by the clinician who was part of the research team, an assigned medical colleague at specialist registrar grade or above who was a member of the prison health-care team, or the clinical lead for the project. The decision to stop treatment following an AE remained the responsibility of the clinical team. Minor AEs that did not fall under official reporting procedures were reported to the clinical team, for example sleep disturbance, minor levels of anxiety or dysthymia, small increases in heart rate and blood pressure, reduced appetite and other minor physical symptoms that did not endanger patients or cause more than minor distress. All other AEs from medication were recorded and reported in line with The Medicines for Human Use (Clinical Trials) Regulations 200483 and Amended Regulations 2006. 84
The research team, acting on behalf of King’s College London as sponsors, delegated the delivery of the sponsor’s responsibility for pharmacovigilance [as defined in Regulation 5 of the Medicines for Human Use (Clinical Trials) Regulations 200483] to the KHP CTO. Reporting of serious adverse events (SAEs) continued until the last participant’s final dose had been completed. For each participant, AEs were recorded from randomisation and reporting of AEs was from the time of first dose of the trial medication to the end of their involvement in the trial (last dose at the end of 8 weeks). All SAEs, serious adverse reactions (SARs), suspected unexpected serious adverse reactions (SUSARs) and important medical events (IMEs) (except those specified in the protocol as not requiring reporting) were reported immediately by the chief investigator or designated site investigators to the KHP CTO, in accordance with the current pharmacovigilance policy. Janssen-Cilag Ltd were notified at the same time.
The KHP CTO reported SUSARs and other SARs to the MHRA, who are competent authorities of other European Economic Area states in which the trial is taking place. The chief investigator reported to the relevant ethics committees. In this trial, there were no SUSARs or SARs, and only one SAE, identified as an IME.
Reporting timelines were as follows:
-
SUSARs that are fatal or life-threatening must be reported no later than 7 days after the sponsor is first aware of the reaction. Any additional relevant information must be reported within a further 8 days.
-
SUSARs that are not fatal or life-threatening must be reported within 15 days of the sponsor first becoming aware of the reaction.
The chief investigator and KHP CTO (on behalf of the co-sponsors) submitted a Development Safety Update Report relating to this trial IMP to the MHRA and REC annually.
Trial Steering Committee
A TSC was convened to provide overall supervision of the trial and ensure that the trial was conducted to the rigorous standards set out in the Medical Research Council guidelines for GCP. 85 The TSC monitored progress, adherence and safety. The TSC chairperson was Professor Jenny Shaw (Consultant Forensic Psychiatrist, University of Manchester); the other TSC members were Dr Ylva Ginsberg (Consultant Psychiatrist specialising in ADHD in prisoners, Stockholm, Sweden), Dr Peter Mason (Forensic Psychiatrist and specialist in ADHD, Cheshire and Wirral), Mr Anthony Davis (R&D Manager, Oxleas NHS Foundation Trust, London), Dr Ulrich Müller-Sedgwick (Barnet, Enfield and Haringey Mental Health NHS Trust, London) and Mrs Beverley Nolker (Prison Officers’ Association Learning, London, and user representative). Other user representatives were included, but had to be replaced during the trial. Non-independent members were lead applicants in London and Edinburgh (Philip Asherson and Lindsay Thomson). Other members of the TMG attended TSC meetings as observers and to report to the TSC. During the trial, four TSC meetings were conducted, all face to face, and all members of the TMG were able to attend these meetings.
Data Monitoring Committee
A DMC was convened to monitor the safety of participants, the ethical conduct of the trial and the quality of the data. The committee consisted of three members experienced in clinical trials, including an independent statistician. The DMC chairperson was Professor Seena Fazel, University of Oxford (an experienced Forensic Psychiatrist). Other members were Professor Chris Hollis, University of Nottingham (an expert on the Clinical Management of ADHD); and Adrian Cook (a trial statistician). DMC meetings were timed to occur prior to TSC meetings so that they could report to the TSC. There were four DMC meetings during the trial. The first two were face-to-face meetings, which the majority of members attended, and the last two were by telephone conference.
Trial management
The project was led by Professor Philip Asherson in London, supported by a trial manager. The trial manager liaised with the trial monitors and ethics board when required and supported the completion and ongoing management of the project. The research psychiatrist at HMP YOI Isis co-ordinated all daily activities on site. Principal investigator Lindsay Thomson led the project in Edinburgh and was supported by the local research assistant, who conducted similar day-to-day co-ordinating tasks in HM YOI Polmont. Weekly telephone conference calls were held throughout the trial with Philip Asherson, Lindsay Thomson, the trial manager and the on-site clinical research teams (psychiatrists and research assistants) to allow for discussions regarding recruitment, diagnosis and other procedures being followed by the clinical teams.
A TMG was established to review AEs and reporting, to review the progress of the trial, to review and report on file notes and potential protocol violations, and to discuss changes to the protocol. This group, led by the chief investigator, Philip Asherson, consisted of Lindsay Thomson, the statisticians, the trial manager and the clinical teams. Other co-applicants were invited to these meetings and occasionally attended. During the initial stages of the trial, the TMG met at the same time as the TSC. After the first two TMG meetings, the frequency of these meetings was increased to monthly (from December 2017, when 94 participants had been randomised to the trial) to facilitate a greater level of ongoing monitoring of the trial. Prior to these regular monthly TMG meetings, informal meetings between the trial manager (LJ) and, separately, with the trial statistician (RH) and with the clinical research associate (CRA) monitoring the trial on behalf of the sponsor were held, file notes were reviewed, and protocol deviations were discussed and documented as required.
Ethics issues specific to this project
The trial was conducted in compliance with the principles of the Declaration of Helsinki (1996),86 the principles of GCP87 and in accordance with all applicable regulatory requirements, including but not limited to the Research Governance Framework and the Medicines for Human Use (Clinical Trials) Regulations 2004,83 as amended in 200684 and any subsequent amendments. The protocol and related documents were submitted for review to the East of England–Essex REC and to the MHRA for clinical trial authorisation. Annual progress and safety reports were completed, and a final report was submitted to the KHP CTO (on behalf of the sponsor), the REC and the MHRA within the timelines defined in the regulations.
Osmotic release oral system-MPH is licensed for first time use in young people with ADHD and severe impairment under aged 18 years only, although NICE also recommends OROS-MPH as a first-line treatment for ADHD in adults. The 8-week trial included a placebo group, so we were denying this group a recommended treatment for ADHD during this period. However, currently, prisoners with ADHD are rarely treated because of uncertainty regarding the validity of the ADHD diagnosis, efficacy of treatment, and concerns about potential drug abuse and diversion in prison populations. To address the issue of unequal access to treatment, we offered treatment to all participants once the trial was completed. Care was taken to ensure that no coercion was involved in recruiting prisoners to the trial. It was made clear that taking part in the trial would not have an effect in either a negative or positive way on their time in the prison or the prison regime.
Some participants might benefit from treatment that was offered as part of the clinical trial.
Participants were informed that their anonymised research data from this trial will be stored securely and may be shared with other scientists or research groups if this helps understanding of the trial findings. The data may also be used in combination with data from other similar studies. All personal information was stored in a secure place (a locked cabinet in a locked office in the prisons) and not allowed to leave the prison. Outside of the immediate health-care team involved in this research, no one will be able to match personal information (name and prison number) with the information gathered for research. Personal details were not linked to clinical or prison records in the research database. After completion of the trial, personal identifiable data relating to the trial will remain in the prison and be destroyed in accordance with GCP guidelines, and after authorisation from KHP CTO, on behalf of the sponsor. To achieve anonymity, each participant had an allocated identifiable number accessible to the local research team only.
Quality assurance
Monitoring of this trial to ensure compliance with GCP and scientific integrity was managed and oversight was retained by the KHP CTO Quality Team.
Data handling
The chief investigator, Philip Asherson, acts as custodian for the trial data. Data were stored on a database set up by KCTU. Patient data were pseudo-anonymised. All personal identification information and research identifier codes were stored on a password-protected computer by the clinical research teams. All data were stored, handled, processed and archived in line with the Data Protection Act 199888 and the Medicines for Human Use (Clinical Trials) Amended Regulations (2006). 84
Data management
Data were stored on a MACRO system trials database (Elsevier UK, London, UK), set up and managed by the KCTU. This allowed for full audit information and for checks on data entry that were used to ensure the integrity of the data collection and monitoring of the trial progress. At the end of the trial, all research records were transferred by secure courier service to the relevant NHS trust R&D department for archiving. The Trial Master File will be archived on behalf of the sponsor using Iron Mountain Inc. (Boston, MA, USA).
Researchers had unique log-in access to the trial database for their site. The system was designed to allow users to register participants and then collect and track data and manage their progress throughout the trial. The data entry system had restricted answer options, including values for ‘not applicable’, ‘not done’ and ‘unknown’. Any data field was tested for valid dates. The data entry system had pre-set minimum or maximum values on all questions requiring numerical values; anything outside of that range was flagged to the user to ensure that the value entered was correct. Data were collected on hard copies from various sources, such as participants’ records and prison and medical records. At the end of the trial, for each participant, the researcher conducted a SDV checklist to ensure that all the data entered had been entered correctly by double-checking the paper copies and any other source data, such as electronic medical and prison records. This was then signed and dated by the researcher and sent to the trial manager.
The trial manager and CRA had read-only access, but were able to raise SDV or discrepancies (data clarification request). The trial statistician conducted high-level checks after data extractions and any data checks needed were sent to the trial manager. The CRA monitored the trial on behalf of KHP CTO and 10% of participants had all of their research data checked against source data. In addition, the primary end point (CAARS-O score) was verified at 100% for all participants.
Patient and public involvement
Valuable feedback was given by participants in the pilot study and by prison staff. We also had positive feedback from Her Majesty’s Inspectorate of Prisons regarding the pilot trial. 89 Throughout the set-up and duration of the trial, we received advice from service users with ADHD or professionals working with prisoners. Special attention was paid to ensure that the information sheet and consent forms were written in appropriate language, as it was expected that there would be low levels of reading ability in this setting.
We lost contact with one service user member of the TSC during the trial, who was replaced by a service user with experience of both ADHD and prisons. Further insights were also given by Beverley Nolker, a service user who works for Prison Officers’ Association Learning. We had hoped to more directly include additional service users with both experience of ADHD and prisons; however, it was difficult to identify suitable individuals with the relevant experiences and to maintain their involvement and engagement.
We worked closely with Dr Kai Syng Tan, a King’s College London artist in residence with lived experience of ADHD. Kai visited HMP YOI Isis during the trial to understand the prison environment and what might motivate participants to engage in the trial. Following this, Kai generated images that emphasised choice, control, autonomy, self-care, self-respect, and, at the same time, was mindful of the stigma attached to ADHD. She designed an image that was used during the trial to remind participants of medication times for all their medications. The image was produced in the form of a flyer that prisoners could stick on the walls of their cells or use as a coaster.
At the end of the project dissemination took place at the Great Hall, Strand Campus, King’s College London. The event, attended by around 100 delegates, focused on the prevalence of ADHD in prisons, ADHD and comorbidities, what research has been done to further the management of ADHD in prisons and what ADHD services in prisons should look like. The event was free and open to the public, and generated a lot of interest from professionals in ADHD services and forensic settings and from members of the public.
Two consensus meetings, leading to publications, were organised and led by co-applicant Susan Young before and during the trial. 21,49 These included multidisciplinary groups of health-care and criminal justice system professionals and service users across sectors relevant to the management of children, adolescent and adult offenders. The initial meeting in November 2009 provided an overview of recommendations for ADHD services in the criminal justice system, and was the foundation for setting up the ADHD service at HMP YOI Isis, and the subsequent pilot study for this trial. The second meeting, in November 2016, provided an updated consensus opinion and recommendations for the identification and treatment of offenders with ADHD in the prison population.
Chapter 4 Results
Participant flow
The Consolidated Standards of Reporting Trials (CONSORT) diagram illustrates the recruitment process (Figure 2). A total of 200 participants were randomised to treatment with OROS-MPH or placebo.
FIGURE 2.
The CONSORT diagram. a, Two participants in the placebo arm were transferred to an accessible prison and the outcomes were collected from those persons. Outcomes not collected on other participants labeled as transferred, deported or released. Reproduced with permission from Asherson et al. 61 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
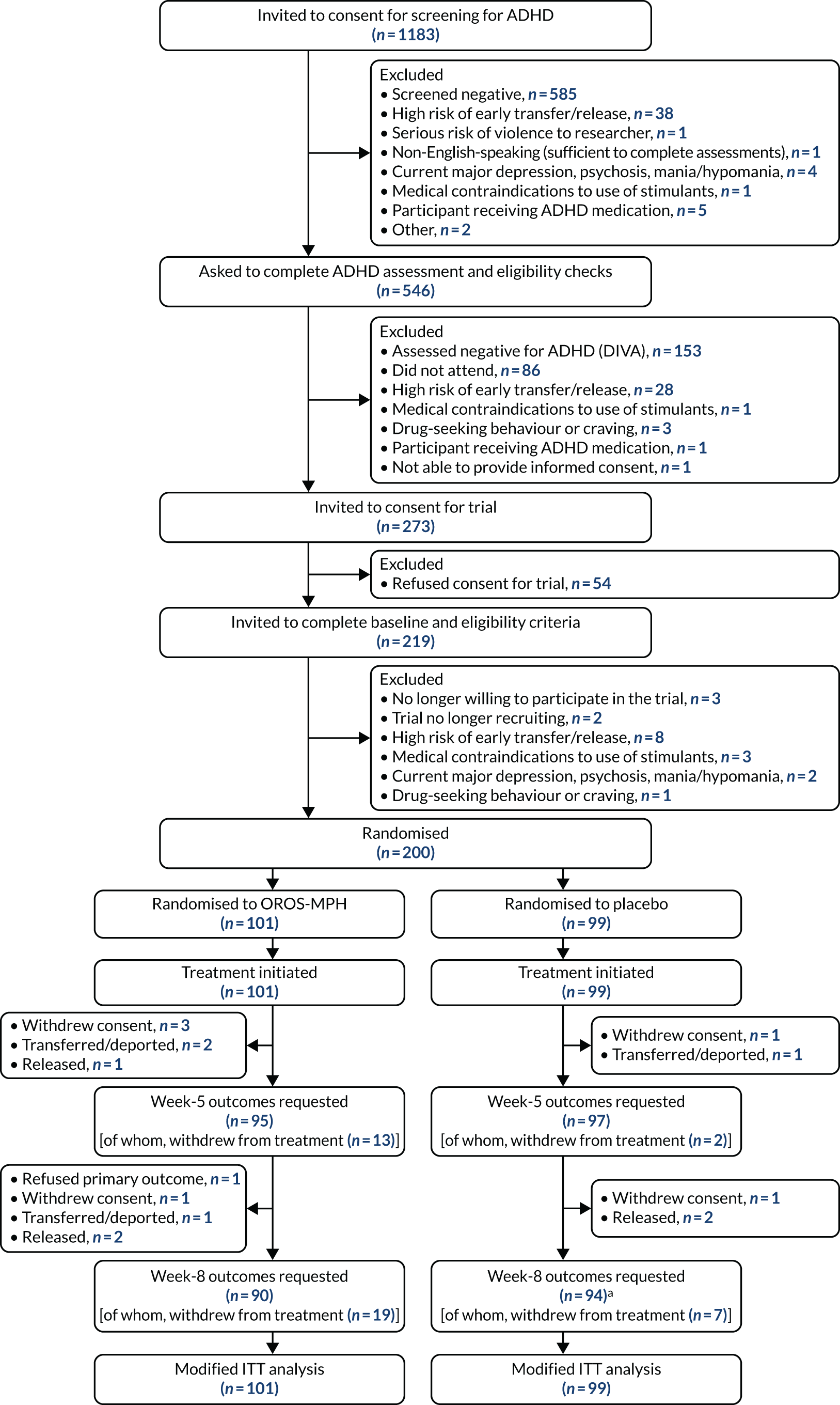
During trial recruitment, all male prisoners aged 16–25 years in HMP YOI Isis (London, Oxleas NHS Foundation Trust) and HM YOI Polmont (Scotland, NHS Forth Valley) were invited to be screened for ADHD. It was estimated that 1368 prisoners aged 16–25 years were asked to consent to screening for ADHD. Of these, around 185 (13.5%) declined to take part in the screening step and did not provide consent that would have allowed us to record this information. It is unknown whether or not those declining consent for screening differ from those participants who consented to be screened.
The CONSORT diagram shows that, of the 1183 prisoners who consented to be screened, 585 screened negative on the Barkley ADHD self-rating scale and a further 52 were excluded who were identified at this stage as not meeting eligibility criteria for the trial. The exclusions included 38 prisoners who were at high risk of early transfer or release during the trial period, one who posed a serious risk of violence towards researchers, one who was not an English speaker, five who were currently prescribed ADHD medication, four who had current major depression and one who had contraindications to the use of stimulants. Another individual was excluded due to low BMI (a clinical decision) and one was mistakenly excluded who was thought to be outside of the age range for the trial, despite being aged 25 years at the time of consent. This left 546 participants who were considered for a diagnostic assessment. Of these, 28 participants were excluded because they were thought to be at high risk of transfer or early release and 518 were invited for an ADHD assessment using the DIVA 2.0. Of these, 86 did not attend the assessment and 432 completed the DIVA 2.0 assessment. Of the 432 prisoners who completed DIVA 2.0 assessments, 279 were found to meet diagnostic criteria for DSM-5 ADHD, of which six did not meet one of the other eligibility criteria and were excluded. This left 273 prisoners who were invited to sign consent for the trial, of which 54 declined their consent. This left 219 prisoners who signed consent for the trial and were formally checked for eligibility. Of the 219 prisoners, three were no longer willing to participate, two were assessed after the trial had completed recruitment and 14 failed to meet eligibility criteria, leaving 200 participants who were randomised.
Post-randomisation losses to trial
At the primary outcome time point of 8 weeks, follow-up rates were good, with 90 and 94 participants completing final outcome measures in the OROS-MPH and placebo arms, respectively. Of these, 26 (OROS-MPH arm, n = 19; placebo arm, n = 7) had stopped medication, but provided 8-week outcome data, because they refused to take further medication during the trial (n = 24) or because they moved to an accessible prison where it was not possible to provide trial medication (n = 2). The other 16 participants had withdrawn from the trial (OROS-MPH arm, n = 4; placebo arm, n = 2); withdrawn from all aspects of the trial, but allowed prison record data to be used (OROS-MPH arm, n = 1); or had been released, deported or transferred to an inaccessible prison (OROS-MPH arm, n = 6; placebo arm, n = 3).
Eligibility violations
One participant was randomised despite scoring 51 on the WASI-II assessment for IQ. However, the clinical judgement was that the participant did in fact meet the trial criterion of IQ score of > 60, although the test result did not reflect this. Nevertheless, this was recorded as an eligibility violation on the basis of the test result. The participant was included in the target population because the low score was thought to reflect inattention on the day of the WASI-II assessment; WASI-II is not validated for people with ADHD and the eligibility criterion of 60 was within the 95% CI for the test result. This event led to a change in the protocol that clarified that the IQ assessment for the purpose of eligibility would be based on clinical judgement in addition to review of the WASI-II results owing to the limitations of the WASI-II test. A list of all protocol deviations is reported in Appendix 2, Table 32.
Baseline characteristics
Tables 3–6 summarise the baseline (pre-randomisation) characteristics of this sample. Site-specific baseline data are reported in Appendix 3, Tables 33–36, for HMP YOI Isis and in Appendix 4, Tables 37–40, for HM YOI Polmont. Table 3 summarises categorical demographic variables for each trial arm and overall. Table 4 summarises continuous baseline variables, including age, IQ, height and BMI; baseline values for clinical measures; and summaries of putative baseline moderators. Table 5 summarises coexisting mental health disorders defined by the MINI 7.0.1 assessment. Table 6 summarises prison behavioural reports from prison and educational staff, and the prison records. As expected from randomisation, these tables show that the two trial arms were well balanced with regard to clinical and demographic variables.
| Item name | Category name | Trial arm, n (%) | Total sample (N = 200), n (%) | |
|---|---|---|---|---|
| OROS-MPH (N = 101) | Placebo (N = 99) | |||
| Site | Isis | 58 (57.4) | 57 (57.6) | 115 (57.5) |
| Polmont | 43 (42.6) | 42 (42.4) | 85 (42.5) | |
| Ethnicity | White (white British, white Irish, white other) | 64 (63.4) | 61 (61.6) | 125 (62.5) |
| Other (Asian, other mixed, other, black African and white, black Caribbean and white) | 19 (18.8) | 10 (10.1) | 29 (14.5) | |
| Black (black African, black Caribbean, other black) | 18 (17.8) | 28 (28.3) | 46 (23.0) | |
| Education | No qualifications | 42 (41.6) | 37 (37.4) | 79 (39.5) |
| Any qualifications | 59 (58.4) | 62 (62.6) | 121 (60.5) | |
| Age (years) at leaving school | ≤ 14 | 26 (25.7) | 25 (25.3) | 51 (25.5) |
| 15 | 32 (31.7) | 22 (22.2) | 54 (27.0) | |
| ≥ 16 | 35 (34.7) | 43 (43.4) | 78 (39.0) | |
| Unknown | 8 (7.9) | 9 (9.1) | 17 (8.5) | |
| Employed (including in education) | Unemployed | 67 (66.3) | 66 (66.7) | 133 (66.5) |
| Employed | 34 (33.7) | 33 (33.3) | 67 (33.5) | |
| Offence category | Serious violence or sexual offence | 15 (14.9) | 14 (14.1) | 29 (14.5) |
| Assault | 25 (24.8) | 26 (26.3) | 51 (25.5) | |
| Drug related | 27 (26.7) | 30 (30.3) | 57 (28.5) | |
| Burglary or theft | 27 (26.7) | 20 (20.2) | 47 (23.5) | |
| Other, including possession of weapon, driving and wilful fire-raising | 7 (6.9) | 9 (9.1) | 16 (8.0) | |
| Previous ADHD treatment | Yes | 27 (26.7) | 20 (20.2) | 47 (23.5) |
| No or unknowna | 74 (73.3) | 79 (79.8) | 153 (76.5) | |
| Age (years) when ADHD medication last taken | ≤ 13 | 9 (8.9) | 3 (3.0) | 12 (6.0) |
| ≥ 14 | 18 (17.8) | 12 (12.1) | 30 (15.0) | |
| Unknown | 74 (73.3) | 84 (84.9) | 158 (79.0) | |
| Baseline characteristics | OROS-MPH arm | Placebo arm | Overall | |||
|---|---|---|---|---|---|---|
| Participants (n) | Mean (SD) | Participants (n) | Mean (SD) | Participants (n) | Mean (SD) | |
| Age, IQ, height and BMI | ||||||
| Age (years) (range 16–25) | 101 | 20.6 (1.9) | 99 | 20.8 (1.9) | 200 | 20.7 (1.9) |
| WASI-II score | 101 | 89.9 (13.5) | 99 | 88.9 (12.4) | 200 | 89.4 (13.0) |
| Height (cm) | 101 | 176.4 (7.2) | 99 | 177.2 (6.6) | 200 | 176.8 (6.9) |
| BMI (kg/m2) | 101 | 23.7 (3.4) | 99 | 23.7 (3.7) | 200 | 23.7 (3.5) |
| Clinical measures | ||||||
| CAARS-O score (range 0–54)a | 100 | 36.4 (9.8) | 99 | 37.2 (8.7) | 199 | 36.8 (9.2) |
| CAARS-O inattention score (range 0–27) | 101 | 17.9 (5.1) | 99 | 18.5 (4.7) | 200 | 18.2 (4.9) |
| CAARS-O hyperactivity/impulsivity score (range 0–27)a | 100 | 18.6 (5.7) | 99 | 18.7 (5.1) | 199 | 18.6 (5.4) |
| WRAADDS score (range 0–30) | 101 | 17.5 (5.7) | 99 | 18.1 (5.6) | 200 | 17.8 (5.7) |
| WRAADDS – temper subscale score (range 0–9) | 101 | 4.7 (2.5) | 99 | 5.2 (2.3) | 200 | 4.9 (2.4) |
| WRAADDS – lability subscale score (range 0–12) | 101 | 8.0 (2.3) | 99 | 8.1 (2.2) | 200 | 8.0 (2.2) |
| WRAADDS – over-reactivity subscale score (range 0–9) | 101 | 4.8 (2.2) | 99 | 4.8 (2.3) | 200 | 4.8 (2.2) |
| ARI-S score (range 0–14) | 101 | 9.3 (3.5) | 99 | 9.3 (3.7) | 200 | 9.3 (3.6) |
| MEWS score (range 0–36) | 101 | 25.7 (6.7) | 99 | 26.8 (6.2) | 200 | 26.3 (6.5) |
| CGI scale – severity score (range 1–7) | 101 | 4.0 (1.0) | 99 | 3.9 (1.1) | 200 | 3.9 (1.0) |
| CORE-OM score (range 0–136) | 101 | 43.5 (13.9) | 99 | 44.8 (15.3) | 200 | 44.2 (14.6) |
| MVQ score (range 0–75)b | 101 | 33.2 (9.4) | 99 | 34.6 (9.9) | 200 | 33.9 (9.6) |
| Weiss-CD score (range 0–45) | 101 | 17.9 (7.7) | 99 | 18.7 (7.8) | 200 | 18.3 (7.7) |
| Systolic blood pressure (mmHg) | 101 | 123.6 (11.2) | 99 | 124.1 (11.9) | 200 | 123.9 (11.5) |
| Diastolic blood pressure (mmHg) | 101 | 68.2 (9.9) | 99 | 68.1 (9.5) | 200 | 68.2 (9.7) |
| Heart rate (beats per minute) | 101 | 70.9 (10.7) | 99 | 70.0 (11.8) | 200 | 70.4 (11.2) |
| Putative moderator variables | ||||||
| RPQ-Proactive score (range 0–24)c | 101 | 6.8 (5.2) | 98 | 7.6 (5.6) | 199 | 7.2 (5.4) |
| RPQ-Reactive score (range 0–22)c | 101 | 14.1 (4.8) | 98 | 14.6 (5.0) | 199 | 14.4 (4.9) |
| RPQ total score (range 0–46)c | 101 | 20.9 (9.2) | 98 | 22.2 (9.7) | 199 | 21.5 (9.4) |
| CTQ score (range 28–140)d | 101 | 48.8 (18.8) | 99 | 48.9 (20.7) | 200 | 48.9 (20.7) |
| ZAN-BPD score (range 0–36) | 101 | 6.9 (5.1) | 99 | 6.3 (4.2) | 200 | 6.6 (4.6) |
| BSI score (range 0–212) | 101 | 52.5 (32.5) | 99 | 52.9 (35.9) | 200 | 52.7 (34.2) |
| Coexisting disorders | OROS-MPH arm participants | Placebo arm participants | Overall participants | |||
|---|---|---|---|---|---|---|
| Total (N) | With disorder, n (%) | Total (N) | With disorder, n (%) | Total (N) | With disorder, n (%) | |
| ASPD | 101 | 72 (71.3) | 99 | 77 (77.8) | 200 | 149 (74.5) |
| Mood disorder (major depression, suicidality, manic, hypomanic) | 101 | 30 (29.7) | 99 | 33 (33.3) | 200 | 63 (31.5) |
| Anxiety disorder (panic, agoraphobia, social anxiety, obsessive–compulsive disorder, PTSD) | 101 | 19 (18.8) | 99 | 19 (19.2) | 200 | 38 (19.0) |
| Potential problematic alcohol usea | 101 | 78 (77.2) | 99 | 71 (71.7) | 200 | 149 (74.5) |
| Illicit drug useb | 101 | 99 (98.0) | 99 | 95 (96.0) | 200 | 194 (97.0) |
| MINI checklist symptom scores (range 0–10 for each item) | ||||||
| Participants (n) | Minimum/median/maximum | Participants (n) | Minimum/median/maximum | Participants (n) | Minimum/median/maximum | |
| Depression | 101 | 0/1/7 | 99 | 0/1/8 | 200 | 0/1/8 |
| Anger | 101 | 0/4/9 | 99 | 0/5/9 | 200 | 0/4/9 |
| Mania | 101 | 0/0/6 | 99 | 0/0/3 | 200 | 0/0/6 |
| Anxiety | 101 | 0/1/8 | 99 | 0/1/8 | 200 | 0/1/8 |
| Physical symptoms | 101 | 0/0/6 | 99 | 0/0/5 | 200 | 0/0/6 |
| Suicidal thoughts | 101 | 0/0/3 | 99 | 0/0/3 | 200 | 0/0/3 |
| Psychosis | 101 | 0/0/1 | 99 | 0/0/3 | 200 | 0/0/3 |
| Sleep problems | 101 | 0/4/9 | 99 | 0/4/10 | 200 | 0/4/10 |
| Memory problems | 101 | 0/3/7 | 99 | 0/3/7 | 200 | 0/3/7 |
| Repetitive thoughts/behaviours | 101 | 0/0/7 | 99 | 0/0/7 | 200 | 0/0/7 |
| Dissociation | 101 | 0/0/0 | 99 | 0/0/5 | 200 | 0/0/5 |
| Personality function | 101 | 0/2/9 | 99 | 0/2/8 | 200 | 0/2/9 |
| Baseline behaviour report | OROS-MPH arm | Placebo arm | Overall | |||
|---|---|---|---|---|---|---|
| Participants (n) | Minimum/median/maximum | Participants (n) | Minimum/median/maximum | Participants (n) | Minimum/median/maximum | |
| MOAS-P score (range 0–40) | 101 | 0/0/15 | 99 | 0/0/19 | 200 | 0/0/19 |
| MOAS-E score (range 0–40) | 38 | 0/0/12 | 45 | 0/0/10 | 83 | 0/0/12 |
| BRC-P score | 101 | 6/8/24 | 99 | 6/8/21 | 200 | 6/8/24 |
| BRC-E score | 31 | 13/19/41 | 36 | 13/17/40 | 67 | 13/19/41 |
| Number of critical incidents | 101 | 0/0/6 | 99 | 0/0/10 | 200 | 0/0/10 |
| Number of days in prison out of the 56 days prior to randomisation | 101 | 24/56/56 | 99 | 27/56/56 | 200 | 24/56/56 |
| Number of education sessions (any type) scheduled | 94 | 0/21/123 | 93 | 0/25/126 | 187 | 0/23/126 |
| Number of education sessions (any type) attended | 94 | 0/15/112 | 93 | 0/19/126 | 187 | 0/17/126 |
| Proportion of scheduled education sessions (any type) attended | 94 | Mean 0.78 (SD 0.31) | 93 | Mean 0.82 (SD 0.26) | 187 | Mean 0.81 (SD 0.29) |
Participants had a mean age of 20.7 years at randomisation. A total of 62.5% were of white ethnicity and 37.5% were of black and minority ethnic backgrounds, which was representative of the prison population (see Chapter 6, Generalisability). General cognitive ability was below general populations norms, with an estimated mean IQ of 89.4 (SD 13.0). Regarding education, 39.5% had no qualifications and most participants left school before the age of 16 years or refused to give an age, with 39% leaving school aged ≥ 16 years. They were mostly unemployed: 66.5% unemployed, and 33.5% employed, self-employed or students. A large proportion of participants (76.5%) had not previously received ADHD medication.
Regarding mental health, participants in both trial arms were moderately ill according to the CGI severity scale, with a mean score of 3.9 (SD 1.0). Criteria for coexisting ASPD was met by 149 (74.5%) participants. Potential problem alcohol use was reported for 149 (74.5%) participants. Illicit drug use was reported by 194 (97%) of participants; however, in additional analyses, we found that around half of the sample met the criteria for high-risk problem use of alcohol, whereas few met the criteria for high risk of substance involvement, according to their self-reports (see Table 25).
Other mental health disorders recorded on the MINI were less frequent, including 38 cases with any type of anxiety disorder and 38% with any type of mood disorder. A total of 149 (74.5%) participants met diagnostic criteria for ASPD, but only 15 (7.5%) met criteria for BPD. High levels of childhood trauma were reported (see Table 24 for more details); however, only 13 (6.5%) participants met formal criteria for PTSD.
The mean baseline score for the primary outcome variable, the CAARS-O, was 36.8 (SD 9.2). Participants scored equally high in the inattentive and hyperactive symptom domains, with average symptom scores on the CAARS-O of 18.2 and 18.6, respectively.
Adherence to trial protocol and medication
Trial withdrawal
In this trial, we distinguished between formal withdrawal from the trial (withdrawal from all aspects of the trial); refusal to take further medication, but completion of outcomes; refusal to take further medication with partial completion of outcomes; transfer out of the prison with partial completion of outcomes; and transfer from the prison with no collection of outcomes. This information is summarised in the CONSORT diagram (see Figure 2).
Six participants formally withdrew (OROS-MPH arm, n = 4; placebo arm, n = 2). Four of these six participants withdrew by week 5 and two withdrew by week 8. The reason given by five of the participants was that they no longer wished to take part and one withdrew because the ‘medication didn’t work’.
Between randomisation and the start of week 5, 15 participants (OROS-MPH arm, n = 13; placebo arm, n = 2) had refused to take the trial medication, but were still providing outcome data, and four participants (OROS-MPH arm, n = 3; placebo arm, n = 1) had formally withdrawn. During this period, a further four participants (OROS-MPH arm, n = 3; placebo arm, n = 1) left the prison and were unable to provide further outcome data because they were released, transferred to an inaccessible prison or deported.
Between the start of week 5 and the end of week 8, a further nine participants (OROS-MPH arm, n = 6; placebo arm, n = 3) refused to take the trial medication, but continued to provide the primary outcome. In addition, two participants in the placebo arm had transferred to an accessible prison and were able to provide week-8 outcome data, but it was not possible to provide the trial medication once they had left the prisons taking part in the trial. Over the same period, two participants (OROS-MPH arm, n = 1; placebo arm, n = 1) formally withdrew, and one participant (in the OROS-MPH arm) allowed their prison records to be accessed, but did not provide primary outcome data. A further five participants (OROS-MPH arm, n = 3; placebo arm, n = 2) left the prison during this period because they were released, transferred to an inaccessible prison or deported.
Titration and prescribing of trial medication
All participants started on one capsule per day and were titrated weekly up to a maximum total of four capsules per day. A stable dose was prescribed for the final 3 weeks. The daily prescribed dose was recorded at the start of weeks 1, 2, 3, 4 and 5. From week 5 onwards, the dosage was stable for all participants, apart from 13 participants who had a dose increase at the start of week 6.
Participants were titrated by increasing the dose by one capsule per day up to a maximum of four capsules unless the ADHD symptoms reduced to negligible, there were limiting adverse effects or a participant objected. By the start of week 5, participants had been titrated to an average of 2.99 and 3.41 daily capsules in the OROS-MPH and placebo arms, respectively (Table 7). Concomitant medications were allowed during the trial and are listed in Appendix 6.
| Week (number of participants prescribed treatment at the start of the week) | OROS-MPH arm (N = 101) | Placebo arm (N = 99) | Overall (N = 200) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) number of capsules prescribed | Mean (SD) number of capsules taken | % of prescribed capsules taken | Mean (SD) number of capsules prescribed | Mean (SD) number of capsules taken | % of prescribed capsules taken | Mean (SD) number of capsules prescribed | Mean (SD) number of capsules taken | % of prescribed capsules taken | |
| 1 (200) | 1.00 (0.00) | 0.76 (0.32) | 76.0 | 1.00 (0.00) | 0.86 (0.23) | 86.0 | 1.00 (0.00) | 0.81 (0.28) | 81.0 |
| 2 (197) | 1.66 (0.50) | 1.23 (0.69) | 74.1 | 1.71 (0.46) | 1.35 (0.60) | 78.9 | 1.68 (0.48) | 1.29 (0.65) | 76.8 |
| 3 (191) | 2.20 (0.80) | 1.49 (0.98) | 67.7 | 2.44 (0.67) | 1.89 (0.88) | 77.5 | 2.32 (0.75) | 1.69 (0.95) | 72.8 |
| 4 (183) | 2.71 (1.08) | 1.55 (1.22) | 57.2 | 3.03 (1.00) | 2.22 (1.20) | 73.3 | 2.87 (1.05) | 1.88 (1.25) | 65.5 |
| 5 (177) | 2.99 (1.21) | 1.60 (1.38) | 53.5 | 3.41 (0.84) | 2.40 (1.27) | 70.4 | 3.21 (1.05) | 2.00 (1.38) | 62.3 |
| 6 (171) | 2.99 (1.21) | 1.57 (1.38) | 52.5 | 3.41 (0.84) | 2.33 (1.32) | 68.3 | 3.21 (1.05) | 1.95 (1.40) | 60.7 |
| 7 (171) | 2.99 (1.21) | 1.59 (1.38) | 53.2 | 3.41 (0.84) | 2.25 (1.43) | 66.0 | 3.21 (1.05) | 1.92 (1.44) | 59.8 |
| 8 (158) | 2.99 (1.21) | 1.41 (1.34) | 47.2 | 3.41 (0.84) | 1.99 (1.41) | 58.4 | 3.21 (1.05) | 1.70 (1.40) | 53.0 |
The dose of prescribed trial medication taken was recorded by the prison nurse on a daily basis (see Table 7). Participants received the medication directly from nursing staff each day, who then observed participants taking the medication. Although prescribed for daily use, participants did not always take the trial medication every day, which required them to attend the nursing station where the trial medication was dispensed. However, on the days when they did attend to take the trial medication, they took the full dose prescribed. By week 5, participants were taking an average of 1.60 and 2.40 capsules in the OROS-MPH and placebo arms, respectively. This dropped to 1.41 and 1.99 capsules per day for the OROS-MPH and placebo arms, respectively, by week 8. Participants in the OROS-MPH arm were less likely to take the medication each day (see Table 7) (Figure 3).
FIGURE 3.
Weekly mean number of capsules taken by trial arm.
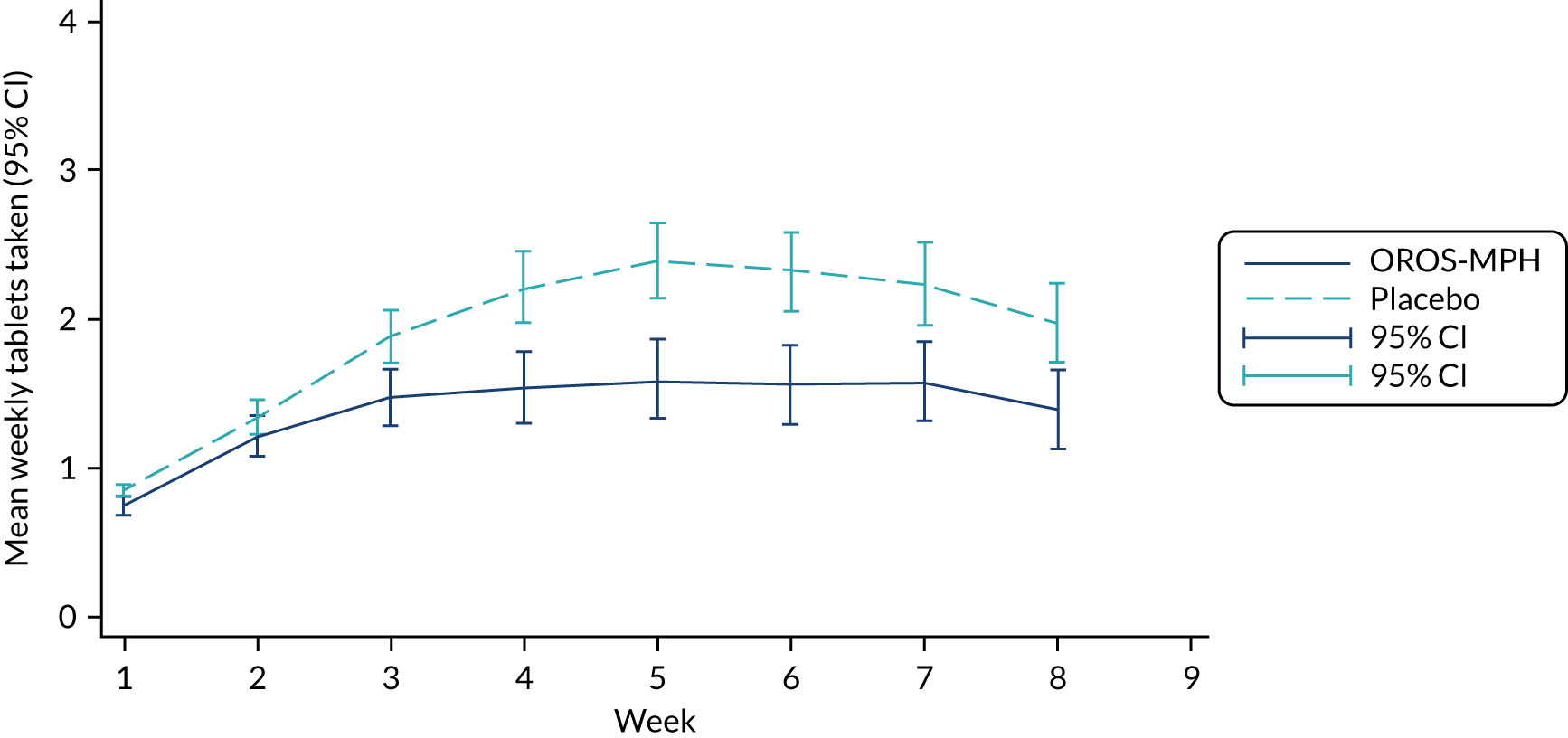
We defined compliance with the treatment regimen as taking one or more prescribed capsules on any given day in the trial, irrespective of the dose prescribed. Full compliance would mean taking one or more capsules on all 56 days, as this was the intended treatment regimen. By the end of week 4, 177 participants (82 in the OROS-MPH arm and 95 in the placebo arm) continued on treatment; by the end of week 8, 158 participants (71 in the OROS-MPH arm and 87 in the placebo arm) continued on treatment. The status of participants (ongoing; withdrawn from treatment, but not from the trial; withdrawn from trial; and released, deported or transferred) was recorded at weeks 1–5 and 8.
Table 7 reports on the number of capsules prescribed and the number of capsules taken each day for those whose status was reported as ‘ongoing’ at each trial visit. For this report, it was assumed that all participants who were ‘ongoing’ at the end of week 5 continued to take the same dose for the remainder of the trial. Of the 56 days of the trial, the mean number of days on which participants took treatment was 31.5 (SD 16.5) and 39.5 (SD 13.3) in the OROS-MPH and placebo arms, respectively, which is 56.3% and 70.5%, respectively, of the 56 days of the trial.
The assumption that the dose prescribed at the end of week 5 was continued to the end of the trial was made because a variable with prescribing information was included in the trial database at the start of weeks 1–5, but not at the start of week 6. In Chapter 5, we report additional analyses that account for 13 participants who increased the number of capsules at the start of week 6, estimated from the reports of dose taken each day throughout the trial (see Chapter 5, Could the trial outcome be affected by adherence to trial medication?).
Treatment arm prediction
Participants and researchers were asked at week 8 to which treatment arm they believed they had been assigned. In the OROS-MPH arm, 89 researchers and 88 participants reported their guess; in the placebo arm, 93 researchers and 92 participants reported their guess. In the OROS-MPH arm, 44 participants (50%) guessed correctly, and 47 researchers (52.8%) guessed correctly. In the placebo arm, 72 participants (78.3%) guessed correctly, and 68 researchers (73.1%) guessed correctly. Using a chi-squared test to compare the proportion of participants guessing that they were in the OROS-MPH arm between the trial arms, we found that the probability of guessing that a participant was assigned to the OROS-MPH arm was greater when a participant was randomised to OROS-MPH than when they were randomised to control for both participants’ (p = 0.001) and researchers’ guesses (p = 0.001). This may suggest that blinding was not adequately maintained.
Analysis of primary and secondary outcomes
Handling of missing data
Follow-up rates were high, so results should not be heavily affected by assumptions regarding the process of generating missing data. At week 8, 184 out of 200 participants completed the primary outcome, leaving 16 missing values. We found that withdrawal from treatment (p < 0.001) and employment status (p = 0.08) predicted missing primary outcome at 8 weeks. Thus, these two variables were included as predictors of missing values in the imputation step of our MI procedure (see Chapter 2, Need for multiple imputation). All results reported here are based on MI with k = 100 imputations to avoid missing data biases.
Outcome measures
Outcome measures are summarised by assessment time point and trial arm in Tables 8 and 9. Results of formal trial arm comparisons are provided in Tables 10–12. Figure 4 provides a graphical display of mean CAARS-O scores by trial arm. Table 8 and Figure 4 show that improvements over time were observed for the primary outcome, CAARS-O score, in both the OROS-MPH and placebo trial arms.
| Outcome measure | Time point | OROS-MPH arm | Placebo arm | Overall | |||
|---|---|---|---|---|---|---|---|
| Participants (n) | Score, mean (SD) | Participants (n) | Score, mean (SD) | Participants (n) | Score, mean (SD) | ||
| CAARS-O | Baseline | 100a | 36.4 (9.8) | 99 | 37.2 (8.7) | 199 | 36.8 (9.2) |
| Week 1 | 96 | 32.4 (9.9) | 98 | 31.2 (11.5) | 194 | 31.8 (10.7) | |
| Week 2 | 92 | 28.8 (11.2) | 97 | 29.6 (11.3) | 189 | 29.2 (11.3) | |
| Week 3 | 93 | 28.3 (11.3) | 94 | 30.3 (12.0) | 187 | 29.3 (11.7) | |
| Week 4 | 92 | 26.0 (12.5) | 96 | 29.1 (11.9) | 188 | 27.6 (12.3) | |
| Week 5 | 92 | 27.5 (12.7) | 95 | 28.8 (11.5) | 187 | 28.2 (12.1) | |
| Week 8 | 90 | 28.0 (11.9) | 94 | 29.3 (11.6) | 184 | 28.7 (11.7) | |
| MEWS | Baseline | 101 | 25.7 (6.7) | 99 | 26.8 (6.2) | 200 | 26.3 (6.5) |
| Week 5 | 92 | 20.5 (9.3) | 95 | 21.4 (9.4) | 187 | 21.0 (9.3) | |
| Week 8 | 90 | 19.8 (10.0) | 94 | 21.9 (9.2) | 184 | 20.9 (9.6) | |
| BSI | Baseline | 101 | 52.5 (32.5) | 99 | 52.9 (35.9) | 200 | 52.7 (34.2) |
| Week 5 | 92 | 38.4 (28.6) | 95 | 36.3 (25.3) | 187 | 37.4 (26.9) | |
| Week 8 | 88 | 35.0 (25.1) | 93 | 39.0 (34.1) | 181 | 37.1 (30.0) | |
| WRAADDS | Baseline | 101 | 17.5 (5.7) | 99 | 18.1 (5.6) | 200 | 17.8 (5.7) |
| Week 5 | 92 | 13.6 (5.8) | 95 | 14.3 (6.5) | 187 | 14.0 (6.2) | |
| Week 8 | 90 | 13.4 (6.1) | 94 | 14.5 (7.0) | 184 | 13.9 (6.6) | |
| ARI-S | Baseline | 101 | 9.3 (3.5) | 99 | 9.3 (3.7) | 200 | 9.3 (3.6) |
| Week 5 | 92 | 8.2 (3.7) | 95 | 7.6 (4.2) | 187 | 7.9 (3.9) | |
| Week 8 | 90 | 8.2 (4.1) | 94 | 8.0 (4.5) | 184 | 8.1 (4.3) | |
| CORE-OM | Baseline | 101 | 43.5 (13.9) | 99 | 44.8 (15.3) | 200 | 44.2 (14.6) |
| Week 8 | 89 | 38.0 (12.3) | 94 | 39.0 (13.4) | 183 | 38.6 (12.8) | |
| MVQ | Baseline | 101 | 33.2 (9.4) | 99 | 34.6 (9.9) | 200 | 33.9 (9.6) |
| Week 5 | 92 | 30.8 (11.2) | 94 | 32.4 (10.9) | 186 | 31.6 (11.0) | |
| Week 8 | 90 | 30.6 (12.5) | 94 | 33.1 (11.7) | 184 | 31.9 (12.1) | |
| CGI therapeutic effect | Week 5 | 84 | 10.0 (4.1) | 94 | 10.9 (3.0) | 178 | 10.5 (3.6) |
| Week 8 | 86 | 10.1 (4.2) | 93 | 10.9 (3.4) | 179 | 10.5 (3.8) | |
| Outcomes | Time point | OROS-MPH arm | Placebo arm | Overall | |||
|---|---|---|---|---|---|---|---|
| Participants (N) | Minimum/median/maximum | Participants (N) | Minimum/median/maximum | Participants (N) | Minimum/median/maximum | ||
| Prison officer-reported outcomes | |||||||
| MOAS-P score (range 0–40) | Baseline | 101 | 0/0/15 | 99 | 0/0/19 | 200 | 0/0/19 |
| Week 8 | 88 | 0/0/24 | 91 | 0/0/20 | 179 | 0/0/24 | |
| BRC-P score (range 6–30) | Baseline | 101 | 6/8/24 | 99 | 6/8/21 | 200 | 6/8/24 |
| Week 8 | 88 | 6/9/25 | 91 | 6/8/25 | 179 | 6/9/25 | |
| Number of critical incidents | Baseline | 101 | 0/0/6 | 99 | 0/0/10 | 200 | 0/0/10 |
| Week 8 | 97 | 0/0/8 | 97 | 0/0/8 | 194 | 0/0/8 | |
| Education staff-reported outcomes | |||||||
| n (%) | n (%) | n (%) | |||||
| Number of participants in any kind of education | Baseline | 101 | 94 (93.1) | 99 | 93 (94.0) | 200 | 187 (93.5) |
| Week 8 | 101 | 94 (93.1) | 99 | 97 (98.0) | 200 | 191 (95.5) | |
| Minimum/median/maximum | Minimum/median/maximum | Minimum/median/maximum | |||||
| MOAS-E score (range 0–40) | Baseline | 38 | 0/0/12 | 45 | 0/0/10 | 83 | 0/0/12 |
| Week 8 | 31 | 0/0/1 | 37 | 0/0/2 | 68 | 0/0/2 | |
| BRC-E score (range 6–30) | Baseline | 31 | 13/19/41 | 36 | 13/17/40 | 67 | 13/19/41 |
| Week 8 | 28 | 13/17/29 | 36 | 13/18/48 | 64 | 13/18/48 | |
| Number of education sessions scheduled | Baseline | 101 | 0/21/123 | 99 | 0/25/126 | 200 | 0/23/126 |
| Number of education sessions attended | Baseline | 101 | 0/15/112 | 99 | 0/19/126 | 200 | 0/17/126 |
| Number of education sessions scheduled | Week 8 | 94 | 0/34/146 | 97 | 1/32/142 | 191 | 0/32/146 |
| Number of education sessions attended | Week 8 | 94 | 0/23/143 | 97 | 0/22/142 | 191 | 0/23/143 |
| Mean (SD) | Mean (SD) | Mean (SD) | |||||
| Proportion of education sessions attendeda | Baseline | 101 | 0.78 (0.31) | 99 | 0.82 (0.26) | 200 | 0.81 (0.29) |
| Week 8 | 94 | 0.80 (0.28) | 97 | 0.82 (0.26) | 191 | 0.81 (0.27) | |
| Outcome measure | OROS-MPH arm vs. placebo arma | |||
|---|---|---|---|---|
| Estimated differenceb | 95% CI | Test (DF); p-value | Standardised differencec | |
| CAARS-O | 0.57 | –2.41 to 3.56 | t (183) = 0.38; 0.71 | 0.06 |
| MEWS | 1.06 | –1.39 to 3.52 | t (182) = 0.85; 0.39 | 0.16 |
| WRAADDS | 0.83 | –0.83 to 2.48 | t (175) = 0.98; 0.34 | 0.15 |
| ARI-S | –0.31 | –1.37 to 0.75 | t (176) = –0.58; 0.57 | –0.09 |
| CORE-OM | –0.18 | –3.46 to 3.10 | t (175) = –0.11; 0.91 | –0.01 |
| BSI | 2.46 | –4.81 to 9.74 | t (177) = 0.67; 0.51 | 0.07 |
| MVQ | 1.08 | –1.16 to 3.33 | t (179) = 0.95; 0.34 | 0.11 |
| CGI therapy effect | 0.65 | –0.46 to 1.76 | t (171) = 1.15; 0.25 | N/A |
| Outcome measure | OROS-MPH arm (N = 89) | Placebo arm (N = 94) | Overall (N = 183) |
|---|---|---|---|
| Reduction in CAARS-O score as percentage of baseline scores | |||
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Total scale | 21.2 (33.8) | 20.1 (29.7) | 20.7 (31.7) |
| Inattention subscale | 26.4 (36.9) | 22.1 (35.6) | 24.2 (36.1) |
| Hyperactivity/impulsivity subscale | 11.7 (59.3) | 16.3 (36.4) | 14.1 (48.8) |
| Responder rate at 8 weeks defined as 20% reduction from baseline CAARS-O score | |||
| n (%) | n (%) | n (%) | |
| Total scale | 43 (48.3) | 45 (47.9) | 88 (48.1) |
| Inattention subscale | 50 (55.6) | 51 (54.3) | 101 (54.9) |
| Hyperactivity/impulsivity subscale | 39 (44.3) | 44 (46.8) | 83 (45.6) |
| Measure | Description | OROS-MPH arm vs. placebo arma | |||
|---|---|---|---|---|---|
| Estimated OR [ln(OR)] | 95% CI for OR [95% CI for ln(OR)] | Test (z) | p-value | ||
| MOAS-P | Any act of aggression reported in the week prior to the week-8 time point (yes/no) | 0.57 [–0.56] | 0.28 to 1.15 [–1.26 to 0.14] | –1.56 | 0.12 |
| Estimated IRR [ln(IRR)] | 95% CI for IRR [95% CI ln(IRR)] | ||||
| BRC-P | Behavioural report score for the week prior to the week-8 time point | 0.95 [–0.06] | 0.85 to 1.06 [–0.16 to 0.06] | –0.98 | 0.33 |
| Critical incidents | Number of critical incidents recorded across the 8 weeks of the trial | 0.75 [–0.28] | 0.45 to 1.25 [–0.79 to 0.23] | 1.09 | 0.28 |
| Education sessions scheduled | Number of any type of education session scheduled across the 8 weeks of the trial | 0.98 [–0.02] | 0.84 to 1.14 [–0.17 to 0.13] | –0.28 | 0.78 |
FIGURE 4.
The CAARS-O mean scores and 95% CIs by trial arm.
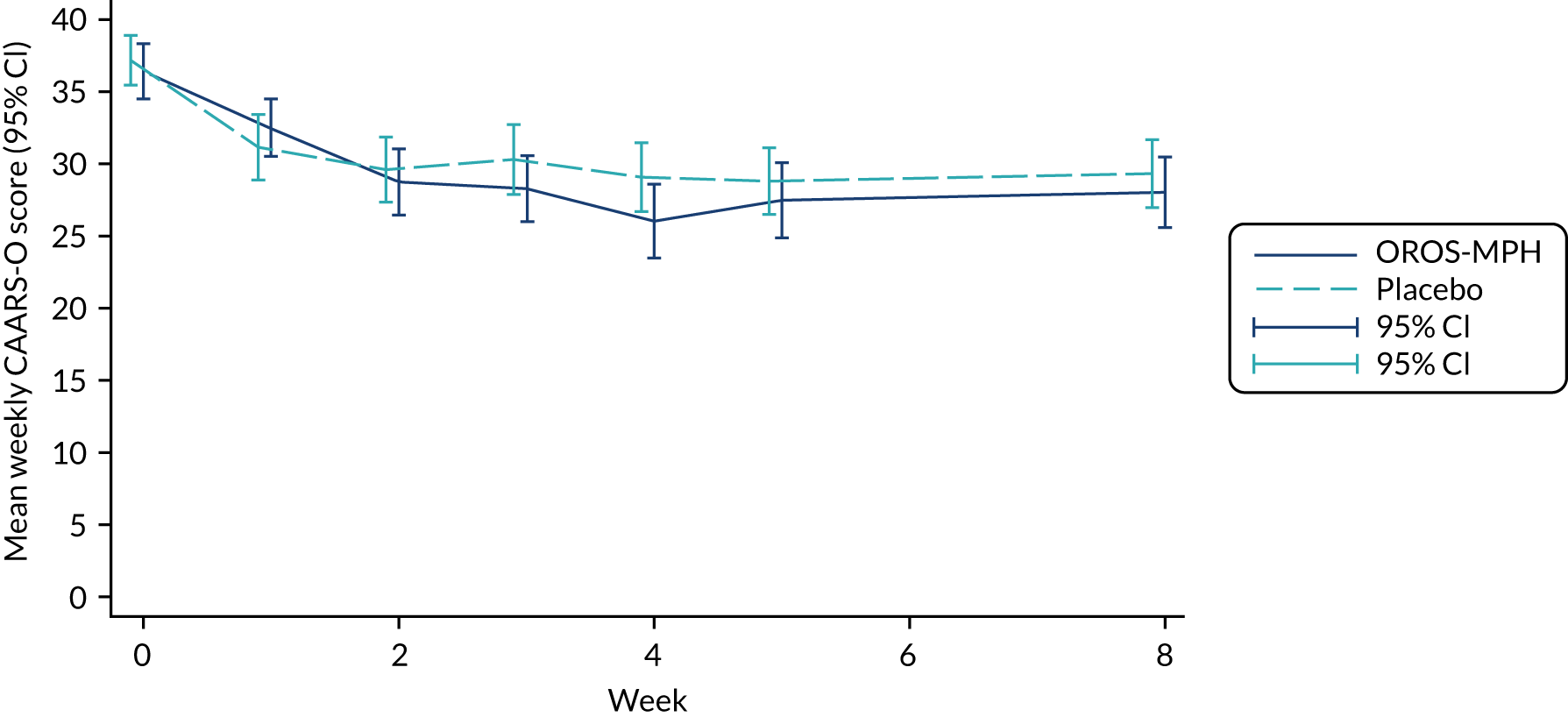
Primary outcome measure: CAARS-O score
The estimated score difference between the OROS-MPH and placebo arms for CAARS-O at 8 weeks was a reduction of 0.57 points (95% CI –2.41 to 3.56 points). This was an improvement in the OROS-MPH arm, but the effect on the CAARS-O score when standardised was very small, at 0.06 points. The difference was not statistically significant (see Table 10) and was smaller than the difference that the trial was powered to detect (minimum clinically important difference = 5 points, as per our sample size calculation).
Table 11 reports the change in CAARS-O scores relative to baseline for each subscale and the responder rate. To investigate the responder rate, we applied the operational definition of a responder applied by NICE14 of a 20% reduction in the baseline CAARS-O score. The percentage of responders was 48.3% for the OROS-MPH arm and 47.9% for the placebo arm.
Continuous secondary outcome measures
Small improvements between the active and placebo arms were seen for WRAADDS, MEWS, MVQ, BSI and CGI (therapeutic effects), but deterioration was seen for ARI-S and CORE-OM. However, none of the secondary outcomes showed statistically significant differences between the OROS-MPH and placebo arms (see Table 10). The continuous secondary outcomes had no defined clinically important score differences; however, in all cases, the standardised difference was very small (SMD < 0.2).
Education
At baseline, 187 out of 200 participants had some form of education scheduled. Only seven participants in the OROS-MPH arm and six participants in the placebo arm were not in any kind of education. The median number of sessions scheduled was 21 in the OROS-MPH arm and 25 in the placebo arm, and the median number of sessions attended was 15 and 19, respectively. The mean proportion of sessions attended in the 8 weeks prior to randomisation was 0.78 (SD 0.31) and 0.84 (SD 0.26) in the OROS-MPH and placebo arms, respectively. However, reports from education staff about behaviour in education sessions were difficult to obtain, with only 83 MOAS-E and 67 BRC-E forms completed at baseline.
The picture was similar at 8 weeks. Only seven participants in the OROS-MPH arm and two participants in the placebo arm were not in any kind of education, and the median number of sessions scheduled across the 8 weeks of the trial was 34 and 32 in the OROS-MPH and placebo arms, respectively. Of the sessions scheduled, the median number of sessions attended was 23 in the OROS-MPH arm and 22 in the placebo arm, giving mean proportions attended of 0.80 (SD 0.28) and 0.82 (SD 0.26), respectively.
Owing to the extreme lack of participants without any sessions scheduled, it was not possible to analyse education scheduled using logistic regression. As it was recorded as a count of sessions with noticeable skew, it was analysed as a negative binomial. The estimated incident rate ratio between the OROS-MPH and placebo arms was 0.98 (95% CI 0.84 to 1.14; p = 0.78), which is a very small and non-significant decrease in sessions scheduled in the active arm (see Table 12).
At baseline, the median MOAS-E score was 0 in both trial arms, with maximum scores of 12 and 10 in the OROS-MPH and placebo arms, respectively. At week 8, the median MOAS-E score was still 0 in both trial arms, with maximum scores of 1 and 2 in the OROS-MPH and placebo arms, respectively. The BRC-E median scores were 18 and 18 at baseline and 17 and 18 at week 8 in OROS-MPH and placebo arms, respectively.
Behavioural reports from prison officers
Reports of behaviour by prison officers are reported in Table 9. BRC-P and MOAS-P are prison officer reports of behaviour completed at baseline. Of 200 participants, 50 (25%) had the minimum score of 6 for the BRC-P at baseline and 143 out of 200 (71%) participants had a score of 0 for the MOAS-P at baseline. This means that they had zero incidents of aggression reported in the week before baseline.
For the BRC-P, the median score at baseline was 8 in both arms. At week 8, the median BRC-P score was 9 for the OROS-MPH arm and 8 for the placebo arm. The BRC-P was formally analysed using a negative binomial model, which estimated the incident rate ratio between the OROS-MPH and placebo arms as 0.95 (95% CI 0.85 to 1.06; p = 0.33) (see Table 12).
The median MOAS-P score at baseline was 0 in both arms, with 75 (74.3%) of the OROS-MPH arm participants and 68 (68.7%) of the placebo arm participants having zero incidents. At week 8, the median MOAS-P score was still 0 in both arms, with the majority (123/179) of participants having a score of 0, with a slightly larger percentage (68.7%) in the placebo arm than in the OROS-MPH arm (64.8%). Owing to the small size of the subpopulation with recorded numbers of events, this outcome variable was dichotomised (1 = yes, any aggressive events seen; 0 = no, no aggressive events) and analysed using logistic regression. At 8 weeks, the odds ratio between trial arms of any aggressive events as measured using MOAS-P was 0.57 (95% CI 0.28 to 1.15; p = 0.12), implying a non-significant improvement in the placebo arm (see Table 12). This surprisingly low odds ratio estimate is due to adjusting for the baseline level of events in the analysis model, which appears to be the driver of the aggressive events (MOAS-P) at week 8.
Critical incidents were prison records of negative behaviours noted in the 8 weeks immediately prior to baseline and before the final time point of 8 weeks. These records were partial at baseline for 11 participants who had not been in prison for 56 days prior to randomisation, and at week 8 for 16 participants who left the prison prior to the week-8 assessment. At baseline, this outcome was observed in all 200 participants; 125 (62.5%) participants had no negative behaviours reported. The number of reports at baseline of negative behaviours ranged from 0–10, with a median of 0 (see Table 9). Trial arms were very similar at baseline, with a median of 0 reported for both the OROS-MPH and placebo arms. By week 8, the trial arms were still very similar, with a median of 0 for both arms. The estimated incident rate ratio in critical incidents between the OROS-MPH and placebo arms at 8 weeks was 0.75 (95% CI –0.45 to 1.25; p = 0.28) (see Table 12).
Sensitivity analyses
Four sets of sensitivity analyses were conducted to check whether or not the results on the primary outcome were sensitive to collection of outcomes within the specified window, starting treatment within the specified time, sufficiently high IQ confirmed by a standardised test, or sufficient level of compliance with the treatment. In each case, the primary analysis, estimating the difference between trial arms in CAARS-O scores at 8 weeks, was repeated. The primary analysis was robust to all assumptions tested in these sensitivity analyses.
Sensitivity analysis 1: outcome window
As per protocol, the primary outcome time was at 8 weeks or 56 days, and not > 2 days before or after the expected date. Six participants had the primary outcome completed at > 58 days and 18 participants had the primary outcome completed before 54 days. Of 176 participants who completed the final outcomes on time, the estimated difference was 0.73 (95% CI –2.35 to 3.81; p = 0.64), which does not differ appreciably from that of the primary analysis.
Sensitivity analysis 2: acceptable treatment start time
Participants, once randomised, should have been prescribed a first dose and initiated treatment within no more than 7 days of randomisation. Fourteen of the 200 participants did not start treatment within the defined time. Of 186 participants who started treatment on time, the estimated difference was 0.65 (95% CI –2.47 to 3.78; p = 0.68), which does not differ appreciably from that of the primary analysis.
Sensitivity analysis 3: intelligence quotient
Attention deficit hyperactivity disorder symptoms can make IQ tests less reliable. Clinical judgement was used to assess IQ in addition to the use of the WASI-II IQ test. One participant was measured as having an IQ of < 60 on the test. This sensitivity analysis confirms that the result is valid if the sample is restricted to those who met the eligibility criterion relating to IQ test. The estimated difference was 0.51 (95% CI –2.51 to 3.53; p = 0.74).
Sensitivity analysis 4: compliance with treatment
A total of 83 participants complied with trial medication according to our definition of compliance of taking some or all of their prescribed trial medication on at least 75% of the days for which it was prescribed. In the OROS-MPH arm, 34 participants complied, compared with 49 in the placebo arm. The estimated trial arm difference in the compliers (–0.29) was a small difference in the opposite direction (a greater effect in the placebo arm), but was not statistically significant (95% CI –5.09 to 4.52; p = 0.91).
Moderator analyses
The following baseline variables were tested as putative moderators of the treatment effect: ZAN-BPD, CTQ, RPQ-Reactive and RPQ-Proactive. A term representing the interaction between trial arm and each potential moderator was included in the primary analysis model in addition to the moderator. No moderator had any significant effect either on its own or through interaction with trial arm (Table 13).
| Putative moderator | Estimated interaction effect | 95% CI | Test (DF); p-value |
|---|---|---|---|
| ZAN-BPD | 0.56 | –0.09 to 1.20 | t (181) = 1.70; 0.09 |
| CTQ | 0.10 | –0.06 to 0.25 | t (171) = 1.25; 0.21 |
| RPQ-Reactive | 0.23 | –0.37 to 0.83 | t (176) = 0.75; 0.45 |
| RPQ-Proactive | 0.28 | –0.26 to 0.82 | t (180) = 1.02; 0.11 |
Mediation analyses
We analysed the individual mediating effects of CAARS-O hyperactivity/impulsivity subscores, CAARS-O inattention subscores and WRAADDS emotional dysregulation, measured at 5 weeks, on BRC-P scores and the number of critical incidents measured at 8 weeks. The natural direct effect, natural indirect effect and total effect are shown in Table 14. The mediation observed was negligible (around zero) and no mediation test was statistically significant. All mediator effects were in the same direction as the total effect. The CIs shown are derived by bootstrapping (1000 replicates), with zero included in the respective interval, implying that an effect was not statistically significant.
| Mediator and outcome variables | Effect estimate (95% CI) | ||
|---|---|---|---|
| Natural direct | Natural indirect | Totala | |
| Mediator: CAARS-O hyperactivity/impulsivity subscore | |||
| Outcome: BRC-P score | –0.06 (–0.16 to 0.04) | 0.00 (–0.01 to 0.01) | –0.06 (–0.16 to 0.04) |
| Outcome: number of critical incidents | –0.66 (–1.36 to 0.05) | –0.01 (–0.008 to 0.06) | –0.67 (–1.37 to 0.03) |
| Mediator: CAARS-O inattention subscore | |||
| Outcome: BRC-P score | –0.06 (–0.15 to 0.05) | 0.00 (–0.01 to 0.03) | –0.06 (–0.15 to 0.05) |
| Outcome: number of critical incidents | –0.69 (–1.41 to 0.02) | 0.00 (–0.05 to 0.05) | –0.69 (–1.40 to 0.02) |
| Mediator: WRAADDS emotional dysregulation total score | |||
| Outcome: BRC-P score | –0.06 (–0.16 to 0.04) | 0.00 (–0.01 to 0.00) | –0.06 (–0.16 to 0.04) |
| Outcome: number of critical incidents | –0.67 (–1.37 to 0.03) | –0.03 (–0.06 to 0.12) | –0.64 (–1.34 to 0.06) |
Serious adverse events
One SAE took place during the trial. The SAE was classified as an IME after a participant tied a cord around his neck as a protest to a prison officer’s treatment. It was concluded that the participant did not intend to do any harm to himself, he did not require any treatment after the event, and it was not thought to be related to the trial medication. The blind was kept and the prisoner continued in the trial.
Adverse events
The numbers of AEs in a category are reported by person, rather than by number of events (Table 15). Of 336 AEs reported, 184 occurred in the OROS-MPH arm and 152 in the placebo arm. The numbers of participants reporting AEs were broadly similar across the two trial arms, with the exception of the High-Level Group Term categories for ‘appetite and general nutritional disorders’, ‘depressed mood disorders and disturbances’ and ‘dizziness’. This reflected appetite loss (13 participants in the OROS-MPH arm vs. 2 in the placebo arm), depressive symptoms (12 in the OROS-MPH arm vs. 4 in the placebo arm) and reports of dizziness (6 in the OROS-MPH arm vs. 0 in the placebo arm).
| SOC category | HLGT category | Trial arm, n (%) | Total sample (N = 200), n (%) | |
|---|---|---|---|---|
| OROS-MPH (N = 101) | Placebo (N = 99) | |||
| Blood and lymphatic system disorders | Blood and lymphatic system disorders | 1 (1.0) | 0 (0.0) | 1 (0.5) |
| Cardiac disorders | Cardiac signs and symptoms | 4 (4.0) | 1 (1.0) | 5 (2.5) |
| Ear and labyrinth disorders | External ear disorder | 3 (3.0) | 0 (0.0) | 3 (1.5) |
| Endocrine | Endocrine | 0 (0.0) | 1 (1.0) | 1 (0.5) |
| Eye disorders | Eye disorders NOS | 1 (1.0) | 0 (0.0) | 1 (0.5) |
| Ocular infection infestation, irritations and inflammation | 0 (0.0) | 2 (2.0) | 2 (1.0) | |
| Gastrointestinal disorders | Dental and gum disorders | 22 (21.8) | 15 (15.2) | 37 (18.5) |
| Gastrointestinal motility and defecation disorders | 11 (19.9) | 11 (11.1) | 22 (11.0) | |
| Gastrointestinal NOS | 0 (0.0) | 2 (2.0) | 2 (1.0) | |
| General disorders | General disorders NOS | 12 (11.9) | 7 (7.1) | 19 (9.5) |
| Immune system disorders | Allergic conditions | 5 (5.0) | 9 (9.1) | 14 (7.0) |
| Infections and infestations | Infections and infestations | 6 (5.9) | 12 (12.1) | 18 (9.0) |
| Injury, poisoning and procedural complications | Bone and joint injuries | 1 (1.0) | 5 (5.1) | 6 (3.0) |
| Soft-tissue injury | 11 (10.9) | 8 (8.1) | 19 (9.5) | |
| Metabolism and nutrition disorder | Appetite and general nutritional disorders | 13 (12.9) | 2 (2.0) | 15 (7.5) |
| Vitamin-related disorders | 1 (1.0) | 1 (1.0) | 2 (1.0) | |
| Musculoskeletal and connective tissue disorders | Musculoskeletal disorders | 15 (14.9) | 13 (13.1) | 28 (14.0) |
| Neoplasms benign, malignant and unspecified | Benign neoplasm | 1 (1.0) | 2 (2.0) | 3 (1.5) |
| Nervous system disorders | Dizziness | 6 (5.9) | 0 (0.0) | 6 (3.0) |
| Headache | 17 (16.8) | 14 (14.1) | 31 (15.5) | |
| Seizures | 1 (1.0) | 0 (0.0) | 1 (0.5) | |
| Psychiatric disorders | Conditions associated with drug abuse | 4 (4.0) | 9 (9.1) | 13 (6.5) |
| Depressed mood disorders and disturbances | 12 (11.9) | 4 (4.0) | 16 (8.0) | |
| Psychiatric and behavioural symptoms | 5 (5.0) | 5 (5.1) | 10 (5.0) | |
| Sleep disorders and disturbances | 11 (19.9) | 7 (7.1) | 18 (9.0) | |
| Somatic symptom and related disorders | 3 (3.0) | 0 (0.0) | 3 (1.5) | |
| Renal and urinary disorder | Urinary problem NOS | 1 (1.0) | 0 (0.0) | 1 (0.5) |
| Respiratory, thoracic and mediastinal disorders | Respiratory, thoracic and mediastinal disorders | 1 (1.0) | 0 (0.0) | 1 (0.5) |
| Skin and subcutaneous disorder | Epidermal and dermal conditions | 16 (15.8) | 22 (22.2) | 38 (19.0) |
Expected adverse effects were also followed-up systematically at each visit using the medication AES (Tables 16 and 17). Question 23 in the AES, ‘Feeling worse or different when the medication wears off (rebound)’, was not applicable, so we report on only 22 items. Each item on this scale is rated as follows: 0 = not at all, 1 = sometimes, 2 = often and 3 = all the time. The scale was dichotomised 0 (not at all or sometimes) and 1 (often or all the time) to reflect the absence or presence of the AE, respectively. The mean and SD of the total AES scores show that there was only a minor difference in total burden of AEs at 8 weeks in the OROS-MPH arm [mean 7.4 (SD 7.5)], compared with the placebo arm [mean 5.5 (SD 5.4)]. At baseline, these values were slightly larger [mean 10.3 (SD 7.5) for the OROS-MPH arm; mean 9.8 (SD 7.3) for the placebo arm], indicating that some reported AEs may reflect phenomena of the clinical condition that improved during the 8-week period of the trial.
| AES items | Trial arm, n (%) | Overall (N = 200), n (%) | |
|---|---|---|---|
| OROS-MPH (N = 101) | Placebo (N = 99) | ||
| Headache | 16 (15.8) | 15 (15.2) | 31 (15.5) |
| Dryness of the skin | 12 (11.9) | 17 (17.2) | 29 (14.5) |
| Dryness of the eyes | 1 (1.0) | 1 (0.0) | 2 (1.0) |
| Dryness of the mouth | 5 (5.0) | 7 (7.1) | 12 (6.0) |
| Thirst | 16 (15.8) | 16 (16.2) | 32 (16.0) |
| Sore throat | 5 (5.0) | 1 (1.0) | 6 (3.0) |
| Dizziness | 4 (4.0) | 1 (1.0) | 5 (2.5) |
| Nausea | 0 (0.0) | 2 (2.0) | 2 (1.0) |
| Stomach aches | 2 (2.0) | 3 (3.0) | 5 (2.5) |
| Vomiting | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Sweating | 9 (8.9) | 5 (5.1) | 14 (7.0) |
| Appetite reduction | 6 (5.9) | 8 (8.1) | 14 (7.0) |
| Diarrhoea | 2 (2.0) | 1 (1.0) | 3 (1.5) |
| Frequent urination | 4 (4.0) | 7 (7.1) | 11 (5.1) |
| Tics | 3 (3.0) | 6 (6.1) | 9 (4.5) |
| Sleep difficulties | 52 (51.5) | 50 (50.5) | 102 (51.0) |
| Mood instability | 32 (31.7) | 45 (45.5) | 77 (38.5) |
| Irritability | 38 (37.6) | 37 (37.4) | 75 (37.5) |
| Agitation/excitability | 38 (37.6) | 39 (39.4) | 77 (38.5) |
| Sadness | 9 (8.9) | 16 (16.2) | 25 (12.5) |
| Heart palpitations | 4 (4.0) | 4 (4.00) | 8 (4.0) |
| Sexual dysfunction | 2 (2.0) | 0 (0.0) | 2 (1.0) |
| AES items | Trial arm, n (%) | Overall (N = 200), n (%) | |
|---|---|---|---|
| OROS-MPH (N = 101) | Placebo (N = 99) | ||
| Headache | 18 (17.8) | 10 (10.1) | 28 (14.0) |
| Dryness of the skin | 14 (13.9) | 18 (18.2) | 32 (16.0) |
| Dryness of the eyes | 2 (2.0) | 4 (4.0) | 6 (3.0) |
| Dryness of the mouth | 20 (19.8) | 10 (10.1) | 30 (15.0) |
| Thirst | 22 (21.8) | 18 (18.2) | 40 (20.0) |
| Sore throat | 8 (7.9) | 6 (6.1) | 14 (7.0) |
| Dizziness | 6 (5.9) | 3 (3.0) | 9 (4.5) |
| Nausea | 8 (7.9) | 3 (3.0) | 11 (5.5) |
| Stomach aches | 7 (6.9) | 3 (3.0) | 10 (5.0) |
| Vomiting | 1 (1.0) | 1 (1.0) | 2 (1.0) |
| Sweating | 20 (19.8) | 8 (8.1) | 28 (14.0) |
| Appetite reduction | 35 (34.7) | 19 (19.2) | 54 (27.0) |
| Diarrhoea | 6 (5.9) | 1 (1.0) | 7 (3.5) |
| Frequent urination | 14 (13.9) | 11 (11.1) | 25 (12.5) |
| Tics | 3 (3.0) | 6 (6.1) | 9 (4.5) |
| Sleep difficulties | 56 (55.5) | 50 (50.5) | 106 (53.0) |
| Mood instability | 40 (39.6) | 46 (46.5) | 86 (43.0) |
| Irritability | 49 (48.5) | 49 (49.5) | 98 (49.0) |
| Agitation/excitability | 42 (41.6) | 43 (43.4) | 85 (42.5) |
| Sadness | 17 (16.8) | 19 (19.2) | 36 (18.0) |
| Heart palpitations | 6 (5.9) | 3 (3.0) | 9 (4.5) |
| Sexual dysfunction | 2 (2.0) | 0 (0.0) | 2 (1.0) |
The numbers and percentages of participants reporting each individual symptom are reported at baseline (see Table 16) and across the entire post-randomisation period between randomisation and week 8 (see Table 17). This shows that the most common adverse effects in the post-randomisation period that were related to the use of OROS-MPH, compared with the use of placebo, were headache (17.8% vs. 10.1%, respectively), dry mouth (19.8% vs. 10.1%, respectively), sweating (19.8% vs. 8.1%, respectively) and appetite reduction (34.7% vs. 19.2%, respectively).
Finally, blood pressure and heart rate were recorded at baseline, at each titration point during weeks 1–5 and at week 8. BMI (weight/height) was recorded at baseline, week 5 and week 8. The values overall and by trial arm are shown in Table 18. There was no noticeable difference between trial arms at any point in the trial.
| Vital signs | Time point | OROS-MPH arm | Placebo arm | Overall | |||
|---|---|---|---|---|---|---|---|
| Participants (n) | Mean (SD) | Participants (n) | Mean (SD) | Participants (n) | Mean (SD) | ||
| BMI (kg/m2) | Baseline | 101 | 23.7 (3.4) | 99 | 23.7 (3.7) | 200 | 23.7 (3.5) |
| Week 5 | 88 | 23.4 (3.5) | 88 | 24.2 (3.8) | 176 | 23.8 (3.7) | |
| Week 8 | 86 | 23.6 (3.4) | 87 | 24.2 (3.8) | 173 | 23.9 (3.6) | |
| Systolic blood pressure (mmHg) | Baseline | 101 | 123.6 (11.2) | 99 | 124.1 (11.9) | 200 | 123.9 (11.5) |
| Diastolic blood pressure (mmHg) | 101 | 68.2 (9.9) | 99 | 68.1 (9.5) | 200 | 68.2 (9.7) | |
| Heart rate (beats per minute) | 101 | 70.9 (10.7) | 99 | 70.0 (11.8) | 200 | 70.4 (11.2) | |
| Systolic blood pressure (mmHg) | Week 1 | 98 | 124.1 (10.3) | 98 | 125.2 (11.9) | 196 | 124.7 (11.0) |
| Diastolic blood pressure (mmHg) | 98 | 71.8 (9.7) | 98 | 70.8 (10.1) | 196 | 71.3 (9.9) | |
| Heart rate (beats per minute) | 98 | 76.5 (11.4) | 98 | 72.1 (10.4) | 196 | 74.3 (11.1) | |
| Systolic blood pressure (mmHg) | Week 2 | 92 | 124.5 (9.4) | 98 | 124.6 (12.1) | 190 | 124.5 (10.8) |
| Diastolic blood pressure (mmHg) | 92 | 70.9 (9.1) | 98 | 70.9 (10.0) | 190 | 70.9 (8.5) | |
| Heart rate (beats per minute) | 92 | 75.8 (11.7) | 98 | 74.4 (13.6) | 190 | 75.1 (12.7) | |
| Systolic blood pressure (mmHg) | Week 3 | 93 | 124.1 (12.3) | 95 | 122.5 (10.2) | 188 | 123.3 (11.3) |
| Diastolic blood pressure (mmHg) | 93 | 72.0 (10.0) | 95 | 69.8 (9.4) | 188 | 70.9 (9.7) | |
| Heart rate (beats per minute) | 93 | 75.7 (12.1) | 95 | 71.5 (10.8) | 188 | 73.6 (11.6) | |
| Systolic blood pressure (mmHg) | Week 4 | 92 | 124.1 (13.3) | 96 | 125.2 (14.6) | 188 | 124.6 (13.9) |
| Diastolic blood pressure (mmHg) | 92 | 72.5 (11.2) | 96 | 69.6 (9.0) | 188 | 71.0 (10.2) | |
| Heart rate (beats per minute) | 92 | 75.9 (12.7) | 96 | 73.5 (11.5) | 188 | 74.7 (12.1) | |
| Systolic blood pressure (mmHg) | Week 5 | 91 | 124.4 (11.5) | 93 | 124.7 (12.0) | 184 | 124.6 (11.8) |
| Diastolic blood pressure (mmHg) | 91 | 70.7 (10.3) | 93 | 69.9 (10.2) | 184 | 70.3 (10.2) | |
| Heart rate (beats per minute) | 91 | 75.0 (12.5) | 93 | 72.9 (10.6) | 184 | 73.9 (11.6) | |
| Systolic blood pressure (mmHg) | Week 8 | 89 | 125.0 (12.5) | 93 | 125.5 (14.0) | 182 | 125.2 (13.2) |
| Diastolic blood pressure (mmHg) | 89 | 70.9 (11.6) | 93 | 70.6 (9.3) | 182 | 70.8 (10.4) | |
| Heart rate (beats per minute) | 89 | 74.8 (11.2) | 93 | 71.9 (11.4) | 182 | 73.3 (11.3) | |
For a list of all concomitant medication, see Appendix 5, Tables 41 and 42.
Chapter 5 Additional analyses
Introduction
The findings from the primary trial analysis according to the prespecified SAP provide no evidence for a difference in effect between the placebo and treatment arms. Indeed, across all primary and secondary outcome variables, outcomes were remarkably similar in the trial arms at 8 weeks and do not indicate any advantage of OROS-MPH over placebo, even at trend level. Furthermore, findings from the per-protocol analyses, as laid out in the SAP, did not provide any evidence for efficacy of the OROS-MPH intervention either.
As outlined in the justification for this study, MPH has been investigated in adults with ADHD in community ADHD clinics in previous studies and was found to have an average SMD between-group effect of around 0.51. 24 A 2018 comprehensive network meta-analysis32 estimated an effect size from RCTs of MPH in reduction of ADHD symptoms in adults, with a SMD of 0.49 (95% CI 0.35 to 0.64). One of the key rationales for this study was to investigate whether or not OROS-MPH had a different effect in a young adult male prison population, compared with the previous studies. It was proposed that the symptoms of inattention and hyperactivity/impulsivity could potentially have a different meaning in this population, reflecting different comorbid mental health or neurodevelopmental disorders. It was further proposed that high levels of drug and alcohol use among offenders might modify the previously reported effects. Although a change in the effect size, compared with previous studies, was envisaged, the absence of even a small effect was unexpected (the estimated between-arm standardised effect is < 0.1).
Although there appeared to be no between-group effects, there was a change over the observation period indicating an apparent improvement in symptoms in both arms. The mean CAARS-O scores dropped from 36.4 points at baseline to 28.0 points at week 8 (a difference of 8.4 points) in the OROS-MPH arm of the trial and from 37.2 points to 29.3 points (a difference of 7.9 points) in the placebo arm (see Table 8). This is not unexpected as significant change has been observed in placebo arms of most RCTs for MPH in ADHD. However, we saw a much greater change in symptoms in the pilot study for this project at HMP YOI Isis, which included 121 participants in a single unblinded group receiving OROS-MPH. 29 The pilot study found the mean change over time for CAARS-O scores to be 22.6 points (decreasing from 37.6 to 15.0 points) using the primary outcome at week 12 and a last observation carried forward approach to deal with missing observations. For the week 8 secondary outcome data in the pilot using the last observation carried forward approach, the difference was even greater: 29.3 points (decreasing from 37.6 to 8.31 points). This is far larger than the change observed in either of the two treatment arms of the current trial.
For these reasons, we completed a set of further analyses to explore possible explanations for the unexpected findings in this trial. These further analyses were proposed after database lock and the review of the findings from the primary trial analyses according to the SAP. They are post hoc analyses and should be regarded as entirely exploratory in nature, with the aim of making suggestions for possible explanations of the trial findings.
Investigating differences between the open pilot study and the randomised controlled trial
We observed that the pre–post differences for both the treatment and placebo arms were smaller in this trial than in the previous open-label pilot study. To investigate the potential reasons for this we looked at differences in the conduct of the pilot study and the trial, and compared the estimated pre–post differences between the open-label pilot study (CIAO-I) and the RCT (CIAO-II) at the HMP YOI Isis site only (because the pilot was conducted at this site only).
Comparison of pre–post differences
To investigate whether or not the pre–post differences were of different sizes in the open-label pilot study (CIAO-I) and this RCT (CIAO-II), we applied similar inclusion and retention procedures across the two studies and restricted our attention to HMP YOI Isis only. Screening-level data are not available for the pilot study, but we confirmed that similar selection and inclusion criteria were applied across both studies. However, procedures for study retention differed between the two studies. A key difference is that, for the pilot study, participants were not retained in the study if they no longer wished to take the trial medication, whereas, in the current trial, an ITT approach was applied, with participants retained in the trial for outcome assessments regardless of whether or not they continued to take medication. To assess change over time under the same assumptions in both studies, we applied similar criteria for follow-up in the trial. In the pilot, participants left the study and provided no further outcome data after a period of non-compliance with trial medication. The criteria for compliance with medication and retention in the pilot were not clearly defined in the protocol and no medication log was obtained for the pilot study; however, we estimated this to be 10 days of continuously not taking the trial medication.
To illustrate this, we plot comparable data by applying similar compliance and follow-up rules to the OROS-MPH arm of the HMP YOI Isis data from this trial as those applied in the pilot study. To match the procedure followed in the pilot study as closely as possible, participant outcome data from the current trial were treated as missing following a continuous period of 10 days without taking trial medication. To match the outcome period in the current trial (baseline to week-8 assessment), we used the 8-week assessment data from the pilot study (rather than the 12-week data) and included only those participants who provided data at the 8-week time point.
A total of 58 participants were in the OROS-MPH arm and based in the HMP YOI Isis site. Of these, 41 participants were identified as having been in the OROS-MPH arm and not having a gap in taking study medication for more than 10 days at any time. The mean values for CAARS-O scores at baseline, week 5 and week 8 are presented in Table 19. The mean score change between baseline and week 8 was 11.1 points, and between baseline and week 5 it was 12.1 points. This compares with a score change of 25.0 points for the 8-week outcome and 25.1 points for the 5-week outcome in the pilot study.
| Time point | CIAO-I (open-label pilot study) | CIAO-II (current RCT) | ||||
|---|---|---|---|---|---|---|
| Participants (n) | Mean score (SD) | Change in score from baseline | Participants (n) | Mean score (SD) | Change in score from baseline | |
| Baseline | 81 | 36.5 (6.9) | 40a | 37.6 (11.0) | ||
| Week 5 | 81 | 11.4 (8.2) | 25.1 | 41 | 25.5 (14.6) | 12.1 |
| Week 8 | 81 | 11.5 (8.8) | 25.0 | 41 | 26.6 (13.9) | 11.1 |
In conclusion, even after ensuring that the same prison was assessed in both studies and change was estimated under the same assumptions, the observed difference over time remained much larger in the pilot study than in the trial.
Baseline measures
To identify potential differences between participants in the two studies that could account for differences in treatment effects at HMP YOI Isis, we compared baseline measures for the participants who initiated trial medication in the two studies. Age and general cognitive ability (IQ) were similar between the two studies (Table 20) (see Appendices 3 and 4).
| Measure | CIAO-I (N = 121) | CIAOI-II (Isis only) (N = 115) |
|---|---|---|
| Age (years), mean (SD) | 21.1 (2.35) | 21.5 (1.9) |
| WASI-II IQ estimate, mean (SD) | 90.5 (11.8) | 88.8 (12.3) |
| Education, n (%) | ||
| Above GCSE | 2 (1.7) | 8 (7.0) |
| GCSE | 33 (27.3) | 76 (66.0) |
| Other | 69 (57.0) | 31 (27.0) |
| Missing data | 17 (14.0) | 0 (0.0) |
| Employment, n (%) | ||
| In paid employment | 12 (9.9) | 31 (27.0) |
| Self-employed | 1 (0.8) | 4 (3.5) |
| Unemployed | 103 (85.1) | 80 (70.0) |
| Missing data | 5 (4.1) | 0 (0.0) |
| Ethnicity, n (%) | ||
| White | 64 (52.9) | 40 (34.8) |
| Asian | 3 (2.5) | 2 (1.7) |
| Black | 33 (27.3) | 46 (40.0) |
| Mixed | 18 (14.9) | 22 (19.1) |
| Other | 3 (2.5) | 5 (4.3) |
| Baseline symptom scales, mean (SD) | ||
| CAARS-O | 37.6 (7.0) | 39.0 (9.1) |
| WRAADDS: emotional dysregulation | 18.7 (5.3) | 18.3 (6.4) |
| CGI | 4.4 (0.6) | 4.7 (0.6) |
| MVQ | 33.1 (10.0) | 32.1 (8.9) |
| Alcohol and drug use, n (%)a | ||
| Alcohol use | 92 (78.0) | 74 (64.3) |
| Cannabis use | 108 (91.5) | 109 (94.8) |
| Other drug use | 44 (37.3) | 48 (41.7) |
Ethnic background was slightly different; in the pilot and current trial, the proportions of white participants were 52.9% and 34.8% respectively, and the proportions of black participants were 27.3% and 40.0%, respectively. The current trial appears to be more representative of the ethnic mix of prisoners at HMP YOI Isis (see Chapter 6, Generalisability) than the pilot study. Potentially, there could be differences between ethnic groups in the way that ADHD symptoms are recognised and reported, and the different proportions of ethnic groups in the open-label pilot study, CIAO-I, and the CIAO-II RCT might lead to minor differences in pre–post differences. However, this seems an unlikely explanation as, in the current trial, outcomes between the OROS-MPH and placebo groups were similar between HMP YOI Isis and HM YOI Polmont, where 98% of participants came from predominantly white ethnic backgrounds.
There were also differences in the highest level of education achieved, with 29% obtaining an educational qualification up to General Certificate of Secondary Education (GCSE)/General National Vocational Qualification (GNVQ) level or higher in the pilot, compared with 73% in the current trial. This difference is thought to be largely due to a change in policy in August 2015, when mandatory assessments in English and mathematics were introduced, leading to a larger number of prisoners receiving qualifications within the prison system. However, it is also notable that the reported rate of unemployment prior to entering prison was 10% in the pilot study, compared with 27% in the current trial.
Overall, there is some evidence that participants in the current trial were functioning at a higher level than participants in the pilot study, potentially indicating a less impaired group. As impairment is a core component of ADHD, this may indicate greater uncertainty over the diagnosis of ADHD. Clinical measures of ADHD, emotional dysregulation, attitudes towards violence and overall global clinical severity were comparable between the two studies
Differences in the protocols or procedures for the pilot study and current trial
To establish whether or not there were any changes in the prison service over time that might have affected the trial outcomes, we reviewed with research staff any potential changes, such as mental health or nursing staff, age of inmates and change in the prison regime or length of sentences. Overall, there were few differences, although the health-care team at HMP YOI Isis during the pilot study had been run by Health Care UK, whereas the health-care team during the trial was run by Oxleas NHS Foundation Trust. However, this was unlikely to have had an impact because levels of training and experience appeared to be similar.
In HMP YOI Isis, the age range of prisoners was lower at the start of the pilot study, when all inmates were aged 18–25 years, and the age range was then later extended up to about aged 30 years. For the CIAO-II RCT, a subgroup of older prisoners, up to around 45 years of age, was introduced into the prison. It is not clear how this would have affected the results of the RCT, but this may have increased health-care staff workload because there are more general health issues with increasing age. Oxleas NHS Foundation Trust had also increased access to psychological treatments, although few of the trial participants were engaged in such programmes, making this unlikely to have contributed to differences between the two studies.
We also reviewed the study documentation to identify any potential differences. A key difference was the introduction of placebo in the current RCT, which affected the amount of documentation required for dispensing medication for each participant, with an increased involvement of the pharmacy and the health-care staff as a result of dispensing individual trial kits in the current trial.
We also estimated how much time researchers spent with participants in the two trials, and whether or not there were any changes in the level of support provided or the level of engagement with the research team. The main difference was that a single key research assistant was engaged throughout the pilot study, whereas, in the current RCT, there was greater turnover of key staff. There was also a higher rate of recruitment and more administrative tasks for the RCT, which might have reduced the contact time between participants and members of the research team. The larger number of measures in the RCT meant that more time was spent with individual participants, but that potentially less time was spent on follow-up and general support for participants. These changes in relation to research staff could potentially have reduced the combined effect of medication and staff attention in the current trial, compared with the pilot study. In addition, there may have been stronger rater bias effects, leading to lower investigator-rated CAARS-O scores in the pilot study, particularly as this was also an open trial.
Checking data integrity
To check for the possibility of a ‘hidden’ effect in the trial data for any reason, we investigated the possibility that there are two distinct clusters of outcomes. We would expect to see a bimodal distribution if there were any drug effects, reflecting the existence of two response groups. To achieve this, we checked the distribution in the change of CAARS-O scores from baseline to week 8 to see if there is any evidence for two clusters of the primary outcome data, by plotting the distribution of change scores from baseline to week 8. As shown in Figure 5, there is no evidence for two potential clusters.
FIGURE 5.
Distribution of change in CAARS-O scores from baseline to week 8.
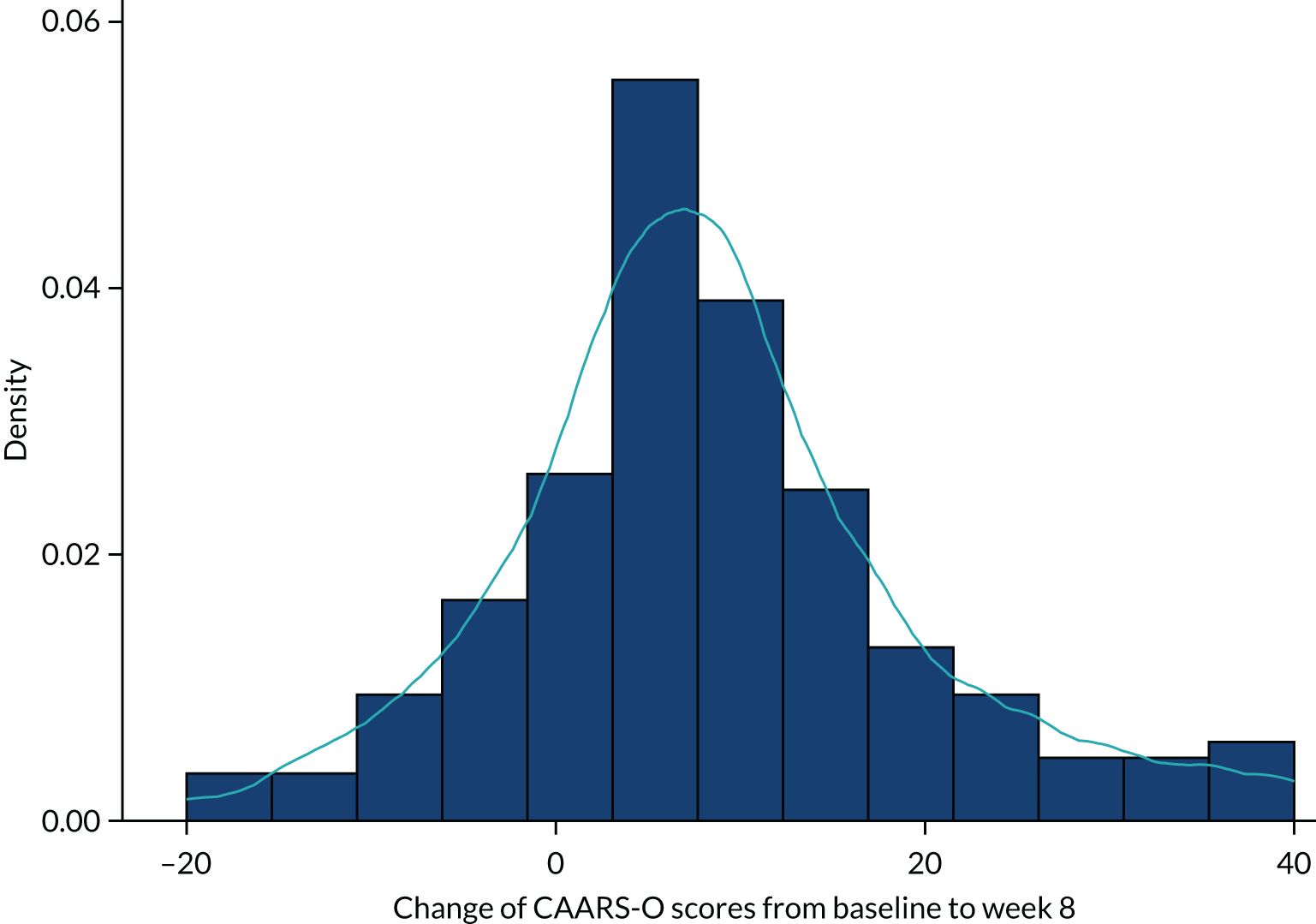
Investigating efficacy in specific populations (subgroup analyses for CAARS-O)
We conducted a series of subgroup analyses of the trial data to identify subgroups potentially showing a greater or smaller effect of the trial medication. These further analyses were designed to address specific questions that might explain the current findings and could form the basis for future studies. Subgroup analyses on very small subpopulations are unlikely to be informative; for this reason, we did not conduct analyses on subgroups of ≤ 30 participants.
Was the trial outcome effected by a systematic change to trial procedures?
To check whether or not a systematic change might have occurred during the trial (e.g. unidentified changes in the conduct of the trial procedures), we provide outcomes in order of randomisation to the trial. We provide outcome data by subgroups defined by order of recruitment: 1–50, 51–100, 101–150 and 151–200. As seen in Table 21, there is little evidence to suggest that CAARS-O scores (across trial arms) varied between the four groups at any assessment time point. In addition, the sizes of the estimated between-arm effects on OROS-MPH at 8 weeks did not show any OROS-MPH effects for any of the four subgroups. By definition, there are 50 participants in each subgroup, and the estimated treatment differences between the OROS-MPH and placebo arms, in groups 1–50, 51–100, 101–150 and 151–200, are as follows: 0.56 (95% CI –5.39 to 6.52), –0.001 (95% CI –6.41 to 6.41), 3.45 (95% CI –3.90 to 10.80) and –0.54 (95% CI –5.99 to 4.90), respectively.
| CAARS-O score at | Group, mean score (SD) | |||
|---|---|---|---|---|
| 1–50 | 51–100 | 101–150 | 151–200 | |
| Baseline | 34.4 (9.7) | 34.0 (9.78) | 38.7 (9.3) | 40.2 (6.4) |
| Week 5 | 24.6 (13.3) | 28.2 (10.1) | 30.4 (12.4) | 29.7 (11.6) |
| Week 8 | 26.0 (12.4) | 28.5 (11.0) | 29.5 (13.0) | 30.8 (10.0) |
Was the trial outcome affected by including less severe cases of attention deficit hyperactivity disorder in the trial?
To check whether or not only the most severe cases benefit from drug treatment, we assessed the treatment effects in high- and low-severity groups for ADHD symptoms at baseline. We provided a subgroup analysis for high severity based on the baseline CAARS-O score, defined as t-scores of 70 (equivalent to a raw score of ≥ 35 points). A total of 123 participants had a baseline CAARS-O score of ≥ 35 points. As shown in Table 22, this group show greater change in scores than the overall trial: 12.26 points for OROS-MPH and 9.35 points for placebo. This is an improvement in the OROS-MPH group, compared with the placebo group, of 2.81 points (95% CI –1.11 to 6.73 points; t = 1.42; p = 0.16), which is a larger difference than for the overall trial, but does not reach the effect size specified in the sample size calculation (5 points) and is not statistically significant
| CAARS-O score at | Trial arm, mean (SD) | Overall, mean (SD) | |
|---|---|---|---|
| OROS-MPH | Placebo | ||
| Baseline | 42.9 (4.9) | 42.6 (5.1) | 42.8 (5.0) |
| Week 5 | 30.4 (12.8) | 32.4 (11.1) | 31.4 (12.0) |
| Week 8 | 30.6 (11.9) | 33.3 (10.9) | 32.0 (11.4) |
Was the trial outcome affected by poor diagnostic accuracy in this prison population?
To investigate the potential effect of diagnostic accuracy, we provide outcome data for a subgroup with a more clearly defined cluster of ADHD symptoms, using the DIVA diagnostic instrument data. The rationale is that, by raising the usual symptom count thresholds for the diagnosis, we will enhance the specificity of the symptom count data to the diagnosis of ADHD, thereby enhancing the certainty of the diagnosis. This was achieved by defining the subgroup as individuals meeting combined type criteria for ADHD in both childhood and adulthood from the DIVA assessment using symptom thresholds of ≥ 7 for both symptoms of inattention and hyperactivity/impulsivity, in both childhood and adulthood.
From the total sample of 200 participants, 102 met these higher symptom thresholds. In this subgroup, the estimated score difference between the OROS-MPH and placebo arms was estimated to be 1.83 (95% CI –2.34 to 6.01; t = 0.87; p = 0.39). This was a non-significant improvement in the OROS-MPH arm.
Could the trial outcome be affected by including participants with different levels of emotional dysregulation?
Emotional dysregulation is known to be associated with ADHD and might reflect an index of severity of ADHD. However, symptoms of emotional dysregulation can also reflect the severity of other mental health disorders commonly seen in the prison population. It is therefore feasible that a group with high emotional dysregulation could show a greater effect of medication (if ADHD medication has greater effects in more severe cases), or might show a smaller effect of medication (if the symptoms of ADHD are better explained by a comorbid condition). We therefore investigated the outcomes by subgroups of high and low levels of emotional dysregulation, as measured by the WRAADDS at baseline (Table 23).
| CAARS-O score at | OROS-MPH arm, mean (SD) | Placebo arm, mean (SD) | ||
|---|---|---|---|---|
| Low level of emotional dysregulation | High level of emotional dysregulation | Low level of emotional dysregulation | High level of emotional dysregulation | |
| Baseline | 33.0 (10.4) | 39.8 (7.9) | 33.7 (8.0) | 39.3 (8.5) |
| Week 5 | 25.3 (11.9) | 29.6 (13.3) | 27.5 (11.3) | 29.6 (11.6) |
| Week 8 | 26.7 (12.3) | 29.3 (11.5) | 26.3 (10.5) | 31.0 (12.0) |
The median WRAADDS score at baseline was 17 in the the CIAO-II RCT sample. The participants were roughly evenly divided between low and high levels of emotional dysregulation, with 113 participants having high levels of emotional dysregulation. Table 23 shows summaries of the primary outcome variable by high or low level of emotional dysregulation and trial arm. The estimated score difference between the OROS-MPH and placebo arms in the subgroup with high emotional dysregulation was estimated to be 2.30 (95% CI –1.81 to 6.41; t = 1.11; p = 0.27). Although this is an improvement in the OROS-MPH arm, this is still below the difference stated in the sample size and is not statistically significant. There was also little observed difference between the two arms in the low level of emotional dysregulation subgroup, with an estimated score difference between the OROS-MPH and placebo arms of –0.85 (95% CI –5.54 to 3.84; t = 0.36; p = 0.72), which was an improvement in the OROS-MPH arm.
Could the trial outcome be affected by including participants with borderline personality disorder?
Symptoms of emotional dysregulation may also reflect the severity of other mental health disorders commonly seen in the prison population, such as BPD. It can be difficult to separate ADHD from BPD on clinical grounds alone. For example, in our recent research, we found that women meeting diagnostic criteria for BPD also show high levels of inattentiveness in their daily lives, in addition to shared symptoms such as emotional dysregulation. 46 To investigate the possibility that the subgroup meeting criteria for BPD might be reducing the overall effect of medication in the trial, we aimed to provide outcomes in a subgroup with and a subgroup without BPD. However, only 15 participants had a high risk of BPD, and 185 did not have BPD. These analyses were not performed as the BPD group was too small, and the small number of participants with BPD suggests that this was not an issue and was unlikely to provide an explanation.
Could the trial outcome be affected by including participants with high levels of childhood trauma?
The effect of childhood trauma has been widely discussed, but has rarely been investigated as a potential modifier of ADHD medication treatment effects. In clinical practice, some practitioners view childhood trauma as a potential cause of an ADHD-like syndrome that might not then show a typical response of ADHD symptoms to medication. To investigate the possibility that the subgroup with evidence of childhood trauma are reducing the overall effect of medication in the trial, we provide outcomes for a subgroup with and a subgroup without childhood trauma, defined as moderate to severe abuse according to the CTQ at baseline. The number of participants who reported abuse in the various categories are listed in Table 24. Out of 200 participants, 41 reported emotional abuse, 47 reported physical abuse, 12 reported sexual abuse, 167 reported emotional neglect and 197 reported physical neglect.
| CTQ subscales: type of abuse | OROS-MPH arm | Placebo arm | Total sample | |||
|---|---|---|---|---|---|---|
| n (%) | Mean (SD) | n (%) | Mean (SD) | n (%) | Mean (SD) | |
| Emotional | 22 (11.0) | 9.1 (4.8) | 19 (9.5) | 8.9 (5.1) | 41 (20.5) | 9.0 (4.9) |
| Physical | 27 (13.5) | 8.1 (4.5) | 20 (10.0) | 7.6 (4.6) | 47 (23.5) | 7.8 (4.5) |
| Sexual | 7 (3.5) | 5.7 (3.1) | 5 (2.5) | 5.5 (2.5) | 12 (6.0) | 5.6 (2.8) |
| Emotional neglect | 88 (44.0) | 20.2 (4.8) | 79 (39.5) | 20.0 (5.3) | 167 (83.5) | 20.1 (5.0) |
| Physical neglect | 101 (50.5) | 13.4 (1.9) | 96 (48.0) | 13.3 (1.9) | 197 (98.5) | 13.3 (1.9) |
Emotional abuse
The estimated score difference between the OROS-MPH and placebo arms in the subgroup with high levels of emotional abuse was 0.76 (95% CI –4.67 to 6.18; t = 0.03; p = 0.78). This is a small improvement in the OROS-MPH arm. The estimated score difference between the OROS-MPH and placebo arms in the subgroup without high levels of emotional abuse was 1.20 (95% CI –2.35 to 4.75; t = 0.67; p = 0.51): a small improvement in the OROS-MPH arm.
Physical abuse
The estimated score difference between the OROS-MPH and placebo arms in the subgroup with high levels of physical abuse was 1.62 (95% CI –4.82 to 8.07; t = 0.51; p = 0.61): a small improvement in the OROS-MPH arm. The estimated score difference between the OROS-MPH and placebo arms in the subgroup without high levels of physical abuse was 0.85 (95% CI –2.58 to 4.29; t = 0.49; p = 0.62): a small improvement in the OROS-MPH arm.
Sexual abuse
Owing to the extremely small numbers, this statistical analysis was not performed.
Emotional neglect
The estimated score difference between the OROS-MPH and placebo arms in the subgroup with high levels of emotional neglect was –0.22 (95% CI –3.13 to 3.57; t = 0.13; p = 0.90). This is a small improvement in the placebo arm.
Interestingly, but not significantly, for those without high levels of emotional neglect, the estimated score difference between the OROS-MPH and placebo arms was 3.71 (95% CI –3.26 to 10.69; t = 1.09; p = 0.29), which was an improvement in the OROS-MPH arm.
Physical neglect
This statistical analysis was not performed because 98.5% of the sample reported physical neglect.
Could the trial outcome be affected by including participants with comorbid disorders?
One question raised by the trial is the possibility that comorbid disorders may reflect a source of symptoms and impairments that might mimic ADHD in the young male prison population. Including cases with clearly defined ‘comorbid’ disorders might lead to reduction in the overall medication effect in the trial. To address this question, we provide subgroup data for those with and those without evidence of another mental health disorder according to the MINI for mental health disorders.
Overall comorbidity
Thirty-six participants had no comorbidity. This subgroup was estimated to have a very small improvement in the OROS-MPH arm, relative to the placebo arm, of 0.11 (95% CI –7.23 to 7.45; t = 0.03; p = 0.98). A total of 164 participants had at least one mental health comorbidity. The estimated score difference between the OROS-MPH and placebo arms for this subgroup was 0.98 (95% CI –2.38 to 4.34; t = 0.57; p = 0.57). This is an improvement in the OROS-MPH arm, but is not statistically significant and does not come close to the 5 points specified in the sample size calculation.
Anxiety
A total of 162 participants did not have anxiety. For this subgroup, the estimated score difference between the OROS-MPH and placebo arms was 0.39 (95% CI –2.82 to 3.60; t = 0.24; p = 0.81), which is a very small improvement in the OROS-MPH arm. Thirty-eight participants had an anxiety disorder. The estimated score difference between the OROS-MPH and placebo arms for this subgroup was 2.88 (95% CI –5.68 to 11.43; t = 0.69; p = 0.50). This was an improvement in the OROS-MPH arm that, although larger than that for the group without anxiety, is still not significant statistically.
Mood disorder
A total of 137 participants did not have a mood disorder. For this subgroup, the estimated score difference between the OROS-MPH and placebo arms was 0.32 (95% CI –3.53 to 4.17; t = 0.17; p = 0.87): a very small improvement in the OROS-MPH arm. Sixty-three participants had a mood disorder. The estimated score difference between the OROS-MPH and placebo arms for this subgroup was estimated to be larger, at 1.97 (95% CI –3.14 to 7.09; t = 0.77; p = 0.44). This was a small improvement in the OROS-MPH arm, but was not statistically significant.
Post-traumatic stress disorder
Thirteen participants had PTSD, eight had depersonalisation, four had derealisation and one was not assessed for PTSD. The subgroup analysis was not conducted because of the extremely small subsamples.
Antisocial personality disorder
Fifty-one participants did not have ASPD. The estimated score difference between the OROS-MPH and placebo arms in this subgroup was –0.98 (95%: CI –7.06 to 5.09; t = –0.33; p = 0.75), which was a small improvement in the placebo arm. A total of 149 participants had ASPD. The estimated score difference between the OROS-MPH and placebo arms for this subgroup was 1.40 (95% CI –2.18 to 4.98; t = 0.77; p = 0.44), which was a small improvement in the OROS-MPH arm. This was not statistically significant.
Could the trial outcome be affected by including participants with high levels of drug and alcohol usage?
Drug and alcohol use disorders are both associated with ADHD and might have an impact on the treatment response. This could arise because of brain damage as a long-term consequence of drug and alcohol use, either generating ADHD-like symptoms or reducing the potential effects of medication for ADHD. There could also be tolerance to OROS-MPH due to previous drug abuse, which only normalises after a period of time. Furthermore, a history of drug and alcohol abuse is likely to be an indicator for risk of ongoing (unmeasured) use of drugs in the prison during the trial, which might affect ADHD symptoms. To address this question, we used the AUDIT-C data to identify participants with high risk of alcohol abuse and the data from the NIDA screening tool to identify participants with high risk of drug abuse. We aimed to complete subgroup analyses for those with high risk and those with low risk of alcohol and drug abuse, to investigate whether or not including this group reduces the overall medication effects in the trial.
High risk of problem alcohol use
A total of 89 participants had potentially problematic alcohol use (defined as a score of ≥ 16 on the AUDIT-C). The estimated score difference between the OROS-MPH and placebo arms in this subgroup was 1.00 (95% CI –3.84 to 5.85; t = 0.41; p = 0.68): a small improvement in the OROS-MPH arm. For those who did not report problematic alcohol use, the estimated score difference between the OROS-MPH and placebo arms was 1.88 (95% CI –3.65 to 7.41; t = 0.68; p = 0.50): an improvement in the OROS-MPH arm.
High risk of problem drug abuse
Using the NIDA Quick Screen V1.0 criteria, we classified individuals as at low (none or minor use), medium and high risk for substance involvement (Table 25). We initially intended to apply the NIDA screening criteria for high risk of problematic drug use, namely a NIDA score of ≥ 27. However, although rates of reported drug use were high, the numbers meeting criteria for high risk of problem use were small; for this reason, these subgroup analyses were not conducted. Using the NIDA definition for high risk use, there were only:
-
Three problem users of opiates (street or prescription). The minimum, median and maximum usage scores were 0, 0 and 32, respectively.
-
Twelve problem users of cannabis. The minimum, median and maximum usage scores were 0, 7 and 39, respectively.
-
No problem users of ‘spice’. The minimum, median and maximum usage scores were 0, 0 and 17, respectively.
-
Four problem users of cocaine and methamphetamine. The minimum, median and maximum usage scores were 0, 0 and 39, respectively.
| Drug | NIDA risk group | Trial arm, n (%) | Overall, n (%) | |
|---|---|---|---|---|
| OROS-MPH | Placebo | |||
| Opiates | Lowa | 97 (96.0) | 96 (97.0) | 193 (96.5) |
| Medium | 2 (2.0) | 2 (2.0) | 4 (2.0) | |
| High | 2 (2.0) | 1 (1.0) | 3 (1.5) | |
| Cannabis | Lowa | 40 (39.6) | 41 (41.4) | 81 (40.5) |
| Medium | 55 (54.5 | 52 (52.5) | 107 (53.5) | |
| High | 6 (6.0) | 6 (6.0) | 12 (6.0) | |
| Spice | Lowa | 100 (99.0) | 95 (96.0) | 195 (97.5) |
| Medium | 1 (1.0) | 4 (4.0) | 5 (2.5) | |
| High | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Stimulants | Lowa | 81 (80.2) | 88 (88.9) | 169 (84.5) |
| Medium | 17 (16.8) | 10 (10.1) | 27 (13.5) | |
| High | 3 (3.0) | 1 (1.0) | 4 (2.0) | |
| Any of the above | Lowa | 39 (38.6) | 34 (34.3) | 73 (36.5) |
| Medium | 54 (53.5) | 57 (57.6) | 111 (55.5) | |
| High | 8 (7.9) | 8 (8.1) | 16 (8.0) | |
Because of the small numbers in the high-risk groups, we decided to complete an additional analysis regarding drug use to address the question of whether or not a group free of either moderate or severe use of any drug (score of ≥ 4 on the NIDA Quick Screen) showed a difference in the CAARS-O outcome at 8 weeks between the OROS-MPH and placebo arms.
A total of 73 participants had no or very low use of any of opiates, spice, cannabis or stimulants. In this subgroup, the estimated score difference between the OROS-MPH and placebo arms was –4.26 (95% CI –9.31 to 0.78; t = –1.69; p = 0.10). The placebo arm performed better than the OROS-MPH arm. For more information regarding drug use, see Appendix 6, Tables 43 and 44).
Could the trial outcome be affected by including participants with prior experience of stimulant medication, leading to biased reporting of the attention deficit hyperactivity disorder symptom response to medication?
Prior exposure to stimulant treatment for ADHD could change the reporting of symptoms because of prior experience of effects of medication on ADHD symptoms and adverse effects, leading to biased reporting. There is also the possibility that medication was stopped in these cases because of previous non-response or significant adverse effects. To investigate the possibility that these effects might reduce the overall effect of medication in the trial, we conducted subgroup analyses for a group with and a group without previous exposure to stimulant medication for ADHD.
A total of 153 participants had no previous treatment with stimulants for ADHD; one participant was not assessed. The subgroup that had not previously been treated with stimulants for ADHD had an estimated score difference between the OROS-MPH and placebo arms of 0.63 (95% CI –2.93 to 4.19; t = –0.35; p = 0.72) and the OROS-MPH arm performed better than the placebo arm. Forty-six participants had received stimulants for ADHD in the past, with the last dose taken at least 3 months previously. The estimated score difference between the OROS-MPH and placebo arms for this subgroup was 2.01 (95% CI –4.17 to 8.19; t = 0.66; p = 0.51): a small improvement in the OROS-MPH arm, which was not statistically significant.
Could the trial outcome be affected by underdosing of participants?
The optimal dose of MPH used in the treatment of adult ADHD is highly variable; hence, we adopted a titration procedure to individually titrate each participant to the optimal dose of trial medication. However, as noted in the CIAO-I open-label pilot study, this population was concerned by minor adverse effects and were titrated to relatively low average doses of the trial medication. This suggests that, in this population, the titration protocol might lead to underdosing of participants, potentially accounting for lesser effects of the drug, compared with placebo. To investigate this possibility, we compared the trial outcome for a subgroup titrated to a low dose with that of a subgroup titrated to a high dose, defined as subgroups titrated to one or two capsules for the low dose, and those titrated to three or four capsules for the high dose.
Table 26 shows the distribution of the prescribed dose at the start of week 5 and at the start of week 6 by trial arm (see Could the trial outcome be affected by adherence to trial medication? for an explanation of week-6 prescriptions) for those who were ongoing in the trial. As noted in the primary analyses, those allocated to OROS-MPH were titrated to lower doses than those in the placebo arm. For example, at the start of week 5, 74% were prescribed the higher dose (three or four capsules) in the OROS-MPH arm, compared with 86% in the placebo arm.
| Number of capsules prescribed per day | Trial arm, n (%) | Total sample, n (%) | |
|---|---|---|---|
| OROS-MPH | Placebo | ||
| Start of week 5 | |||
| 1 | 9 (11.0) | 3 (3.2) | 12 (6.8) |
| 2 | 11 (13.4) | 10 (10.5) | 21 (11.9) |
| 3 | 21 (25.6) | 25 (26.3) | 46 (26.0) |
| 4 | 40 (48.8) | 57 (60.0) | 97 (54.8) |
| Not prescribed | 1 (1.2) | 0 (0.0) | 1 (0.6) |
| Start of week 6 | |||
| 1 | 7 (9.0) | 2 (2.2) | 9 (5.3) |
| 2 | 10 (12.8) | 10 (10.8) | 20 (11.7) |
| 3 | 19 (24.4) | 19 (20.4) | 38 (22.2) |
| 4 | 42 (53.9) | 62 (66.7) | 104 (60.8) |
At the start of week 5, 143 participants were prescribed three or four capsules. The estimated score difference between the OROS-MPH and placebo arms in this subgroup was 0.47 (95% CI –3.03 to 3.97; t = –0.27; p = 0.79), which was an improvement in the OROS-MPH arm. Fifty-seven participants were prescribed one or two capsules at the start of week 5. The estimated difference between the OROS-MPH and placebo arms in this subgroup was 0.68 (95% CI –6.15 to 7.51; t = 0.20; p = 0.84), which is a small improvement in the OROS-MPH arm, but is not statistically significant.
Could the trial outcome be affected by adherence to trial medication?
Adherence to taking the trial medication on a daily basis was highly variable; this might have affected the assessment of efficacy by ITT. The high levels of poor adherence to medication was previously documented in the CIAO-I open-label pilot study, in which 40 out of 121 (33.9%) participants dropped out of treatment before the 8-week assessment; therefore, efforts were taken in the current trial to minimise this. 29 However, the per-protocol analysis, carried out according to the SAP-defined ‘compliance’ for the trial medication (i.e. having taken medication on 75% of the days during the trial period), did not show any different effect from the ITT analysis, suggesting that poor compliance is unlikely to explain the trial findings. Nevertheless, it is possible that our definition of compliance is not adequate to rule out all effects of adherence to the trial medication on the trial outcome. To address this problem, we investigated the impact of a set of alternative definitions of adherence with the trial medication on efficacy in this trial.
Summary of adherence to medication data
To provide an overview of the amount of drugs prescribed and taken, we produced descriptors of the dose prescribed and dose taken. This is already reported as part of the main results (see Chapter 4, Titration and prescribing of trial medication) for those ongoing on medication and uses the prescription data from the start of week 5 of the trial.
The protocol also allowed a final dose change at the start of week 6, prior to the final 3-week maintenance phase of the trial. Note that for weeks 1–5, the prescription was explicitly recorded in the database. For week 6, the prescription was not recorded, but is inferred from the maximum dosage taken by participants. In all cases, the nurses providing the prescriptions recorded a daily log of the dose taken. It is therefore reasonable to infer a prescription change for week 6 from the maximum dose taken on days 36–39, which is in line with the protocol for week-6 prescriptions. Using this approach, we describe the number of participants prescribed different doses of trial medication from the start of week 6 (see Table 26), which was maintained until the end of the trial. Table 27 shows the numbers recorded as prescriptions for weeks 1–5 and the inferred prescription for week 6.
| Week | Number (%) of participants prescribed trial medication | Mean (SD) numbers of capsules prescribed | ||
|---|---|---|---|---|
| OROS-MPH arm (N = 101) | Placebo arm (N = 99) | Overall (N = 200) | ||
| 1 | 200 (100.0) | 1.00 (0.00) | 1.00 (0.00) | 1.00 (0.00) |
| 2 | 197 (98.5) | 1.67 (0.47) | 1.71 (0.46) | 1.69 (0.46) |
| 3 | 191 (95.5) | 2.24 (0.74) | 2.44 (0.67) | 2.35 (0.71) |
| 4 | 183 (91.5) | 2.80 (0.98) | 3.06 (0.96) | 2.95 (0.97) |
| 5 | 177 (88.5) | 3.14 (1.03) | 3.41 (0.84) | 3.28 (0.94) |
| 6 | 171 (85.5) | 3.20 (1.03) | 3.49 (0.81) | 3.36 (0.92) |
To describe the overall adherence to prescribed trial medication, we describe the mean number of daily capsules taken by week and percentage of prescribed dosage taken (Table 28). Prescriptions for weeks 1–5 are based on the recorded prescription. The prescription for week 6 is inferred from the maximum number of capsules taken. The prescription for weeks 7 and 8 is identical to that of week 6. Note that, by the final week, the data are skewed; however, it is the percentage of medication taken of that prescribed (documented or inferred) that is of interest. Throughout the trial, the placebo group took a larger percentage of the capsules prescribed. By week 4, this difference had become more marked and remained more marked for the remaining weeks.
| Week | OROS-MPH arm (N = 101) | Placebo arm (N = 99) | Overall (N = 200) | |||
|---|---|---|---|---|---|---|
| Mean (SD) number of capsules taken by week | Percentage of prescribed medication | Mean (SD) number of capsules taken by week | Percentage of prescribed medication | Mean (SD) number of capsules taken by week | Percentage of prescribed medication | |
| 1 | 0.76 (0.32) | 76.0 | 0.86 (0.23) | 86.0 | 0.81 (0.28) | 81.0 |
| 2 | 1.23 (0.69) | 73.7 | 1.35 (0.60) | 78.9 | 1.29 (0.65) | 76.3 |
| 3 | 1.49 (0.98) | 66.5 | 1.89 (0.88) | 77.5 | 1.69 (0.95) | 71.9 |
| 4 | 1.55 (1.22) | 55.4 | 2.22 (1.20) | 72.5 | 1.88 (1.25) | 69.6 |
| 5 | 1.61 (1.38) | 51.3 | 2.40 (1.27) | 70.4 | 2.00 (1.38) | 61.0 |
| 6 | 1.57 (1.38) | 49.1 | 2.33 (1.32) | 66.8 | 1.95 (1.40) | 58.0 |
| 7 | 1.59 (1.38) | 49.7 | 2.25 (1.43) | 64.5 | 1.92 (1.44) | 57.1 |
| 8 | 1.41 (1.34) | 44.1 | 1.99 (1.41) | 57.0 | 1.70 (1.40) | 50.6 |
Figure 6 illustrates the mean adherence of participants by trial arm. The weekly adherence is defined as the number of days on which at least one tablet was taken, divided by seven. At the start of the trial, the mean adherence was 71.6% and 81.5% in the OROS-MPH and placebo arms, respectively. This dropped to 50.6% and 70.4% in week 5, and to 43.7% and 56.6% by week 8 for the OROS-MPH and placebo arms, respectively. The proportion of participants in the placebo group adhering was consistently larger throughout the trial, but adherence dropped off consistently throughout the trial in both arms.
FIGURE 6.
Mean adherence to prescribed trial medication.
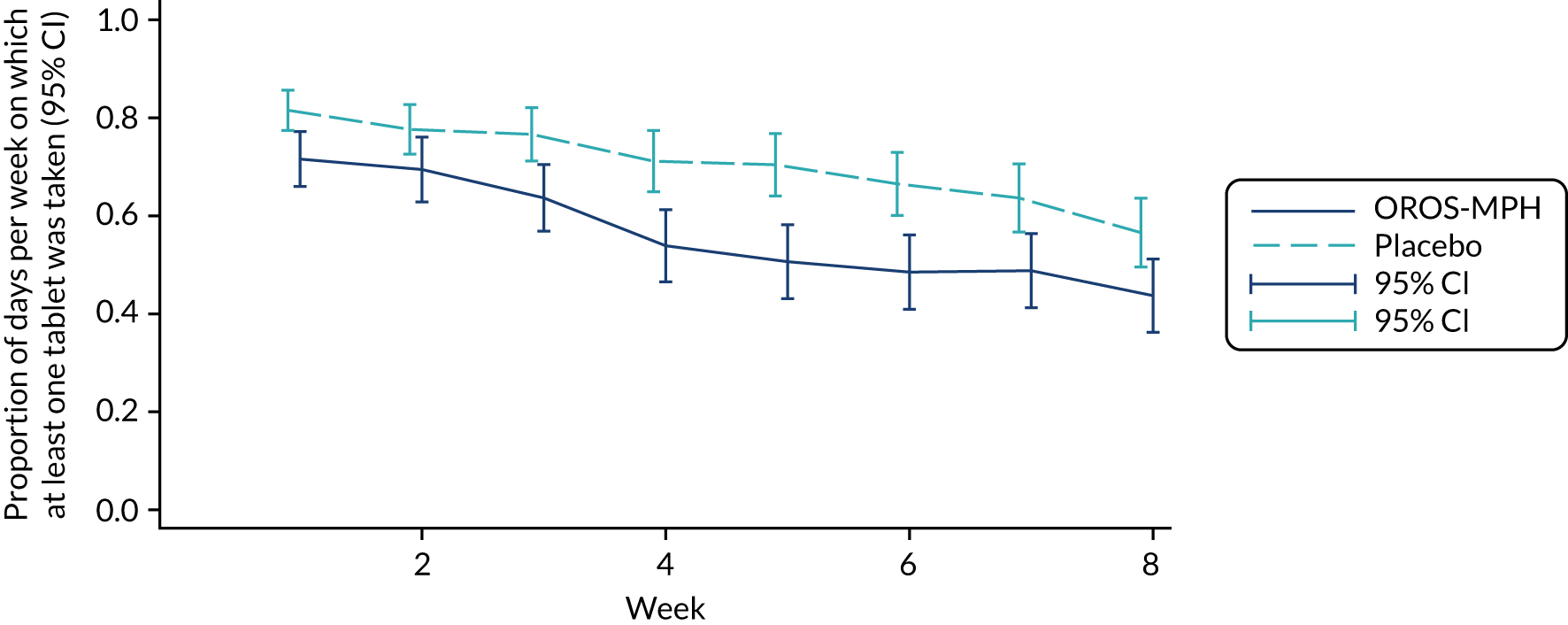
Effects of poor adherence
Adherence to trial medication might have been higher during the titration phase of the trial (when participants were visited every week) than during the maintenance phase. To investigate this, we conducted a per-protocol analysis of the effects of OROS-MPH, compared with placebo, on the CAARS-O outcome at week 5. Good compliance during this period was defined as those who had taken prescribed trial medication on 75% of the days before the end of week 5.
According to this definition, for the 88 participants who had complied with their allocated drug by week 5 (i.e. had taken at least one tablet on 75% of the days up to and including day 35), there was a between-arm difference in the CAARS-O score of –1.32 (95% CI –6.14 to 3.50; t = –0.54; p = 0.59), which is an improvement in the placebo arm. The mean and SD by trial arm in this group is shown in Table 29.
| CAARS-O score at | Trial arm, mean (SD) score | |
|---|---|---|
| OROS-MPH | Placebo | |
| Baseline | 35.8 (9.4) | 36.3 (8.4) |
| Week 5 | 28.3 (12.3) | 27.0 (11.6) |
Adherence to trial medication immediately prior to the outcome assessments might also affect the trial outcome, even if the active medication was significantly reducing ADHD symptoms on days when they did take the medication. This could occur because participants might report accurately on their level of ADHD symptoms on the day or the few days prior to the outcome assessment only. The short-term effects of OROS-MPH on reducing ADHD symptoms (for only 6–10 hours) means that participants in the active medication group might report high levels of symptoms if they had not taken medication in the period just prior to the outcome assessment, even among those who showed an effect on days when they did take the medication. To investigate the immediate effects of the trial medication, we conducted further per-protocol analyses on the week-5 and week-8 CAARS-O data. Adherence was defined as taking trial medication on the 2 days prior to the outcome assessment at week 5 and week 8, with those not taking medication on those days excluded from the analysis.
For week 5, 97 participants had taken one or more capsules on both days immediately preceding the week-5 visit. In this subgroup, there was an estimated difference between the OROS-MPH and placebo arms of 2.30 (95% CI –2.28 to 6.88; t = 1.00; p = 0.32), which was an improvement in the OROS-MPH arm. For week 8, in the subgroup of 84 participants (one of whom did not provide an outcome) who had taken at least one capsule on both of the days preceding the week-8 visit, the estimated difference between the OROS-MPH and placebo arms was –0.22 (95% CI –4.87 to 4.44; t = –0.09; p = 0.93), which was a small improvement in the placebo arm.
Could adverse effects be driving adherence to the trial medication?
To investigate the potential association of adverse effects on adherence to trial medication, we investigated the proportion of prescribed medication taken by the presence or absence of the most commonly reported adverse effects of OROS-MPH, compared with placebo. We used the AES data from across the trial. As can be seen in Table 17, the common items from the AES showing the greatest difference between the two trial arms were sweating, headache, appetite loss and dry mouth. These were reported by 16%, 18%, 16% and 30% of participants, respectively, and 50% of participants reported one or more of these items.
For this analysis, we investigated the adherence to medication for each of these four AES items, as follows: (1) we measured adherence as the proportion of days on which any dose was taken divided by number of days medication was prescribed; (2) we calculated the mean proportion for groups reporting the presence or absence of each of the four AES items, and ran t-tests to compare the present with the absent groups; and (3) we considered an overall AES item measure of having at least one of the four items.
In Table 30, the mean adherence is shown by the group for which the AES items were present and the group for which they were not present. A difference in mean proportion of adherence by symptoms was tested using a t-test. There was no evidence to suggest that the adherence varied between those who did and those who did not display the most common adverse effects.
| AES item | Proportion of days, mean (SD) | Two-sided t-test p-value | |
|---|---|---|---|
| AE reported: yes | AE reported: no | ||
| Headache | 0.58 (0.24) | 0.67 (0.25) | 0.08 |
| Dry mouth | 0.68 (0.22) | 0.65 (0.26) | 0.44 |
| Sweating | 0.62 (0.25) | 0.66 (0.25) | 0.36 |
| Appetite loss | 0.66 (0.23) | 0.65 (0.26) | 0.88 |
| Any | 0.66 (0.23) | 0.65 (0.27) | 0.81 |
Chapter 6 Discussion (including interpretation, generalisability, overall evidence)
Generalisability
The trial targeted a sample that could be generalised to other prison populations of young males aged 16–25 years, meeting diagnostic criteria for ADHD, in the UK. To increase generalisability, a screening approach was taken to ensure that as many prisoners as possible who met diagnostic criteria were identified and invited to take part in the trial. Exclusion criteria were kept to a minimum and focused on excluding the minority of participants who posed a high risk to researchers, or who had coexisting disorders for which medical treatment of ADHD was a strong caution or contraindicated. Other criteria ensured that participants were able to understand the trial procedures and provide their own fully informed consent to the take part in the trial. The first step of the protocol was therefore a screening step in which all offenders entering the prisons were screened for ADHD, prior to being invited to complete detailed diagnostic assessments and review by a psychiatrist trained in the diagnosis of ADHD and other common mental health disorders. It is unknown if those prisoners who refused consent to be screened or did not attend the diagnostic interview for ADHD differ in any way from the trial participants.
The site HMP YOI Isis in London is a category C prison for sentenced prisoners, including male offenders aged 18–25 years deemed to be relatively low risk with short- to medium-length sentences. HM YOI Polmont in Scotland differs because it is the only prison in Scotland for young persons aged 16–21 years; therefore, there was no selection on type of crime, sentence or level of risk. Nevertheless, the range of crimes and sentencing was largely similar to HMP YOI Isis. The trial did not include any remand (pre-trial) or convicted but unsentenced prisoners, who generally show higher rates of comorbidity than sentenced prisoners. 90 The sample was all male, so these findings cannot be generalised to the female prison population.
The focus in this study and in the pilot study, as well as the previous Swedish study,33 was male prisoners; therefore, little is known about the efficacy of pharmacological treatments in treating female prisoners with ADHD. It is unknown whether or not there would be similar safety concerns and similar levels of behavioural problems, mental health disorders and substance misuse. It is expected that the profile of comorbid disorders might differ between male and female offenders, and their effects on pharmacological treatment in female offender populations remains largely unknown. The best evidence that similar effects may arise comes from pharmacoepidemiogical data from Sweden, although the number of females with ADHD at risk of committing criminal offences is far smaller. 91
Regarding ethnic background, at HMP YOI Isis, a clinical audit conducted in June 2019 found that ethnic minorities were approximately 70%, whereas the ADHD service had a case load of 38% ethnic minorities and 63% non-ethnic minority (white) prisoners. This indicated a considerable bias in the prisoners being referred for diagnosis and treatment by the health-care and prison staff within the London prison. These figures contrast with the proportion of people from ethnic minority backgrounds in London, reported in the 2011 UK National survey,92 of 59.8% from white, 18.4% from Asian, 13.3% from black and 8.5% from mixed and other backgrounds. This clearly demonstrates the well-established finding that ethnic minority groups are greatly over-represented in the prison population, which is an issue of general national and international concern. 93 The sample from which we recruited in London is representative of the prison population, but is not representative of the general population of youth with ADHD in the London area.
Regarding recruitment to the trial, we found that, at HMP YOI Isis, 34.8% of the participants came from white, 25.2% from other (including Asian and mixed background) and 40% from black backgrounds. The figure of 34.8% participants from a white background is close to the estimated proportion of 30% in the prison, indicating no bias in the selection for this trial based on ethnicity, in keeping with the screening approach we adopted for this trial. For Scotland, the 2011 survey reported a low rate of ethnic minority populations, of around 4%. At the time of writing, we had no information on the proportion of different ethnic groups residing at HM YOI Polmont, but, among participants in this trial, we found that > 98% were from white British backgrounds, providing a good representation of the ethnic mix in Scotland.
Previous research has also shown high rates of comorbidity in children, adolescents and adults diagnosed with ADHD in both clinical and epidemiological samples. A 2017 review7 of population surveys for adults with ADHD found that 52% met criteria for one or more comorbidities: oppositional defiant disorder (as children) or ASPD, 8%; intermittent explosive disorder, 13%; an anxiety disorder, 34%; a mood disorder, 22%; and a drug or alcohol problem, 11%. This compares with the findings in the current trial of 82% who had one or more comorbid mental health disorders: 19% with a mood disorder, 19% with an anxiety disorder, 75% with ASPD, 45% with problematic alcohol use (AUDIT-C score of ≥ 16) and 64% with moderate- to high-risk drug use (see Table 5 and Chapter 5, Could the trial outcome be affected by including participants with high levels of drug and alcohol usage?). This suggests that the prison population of young adults meeting diagnostic criteria for ADHD that we investigated here have a similar profile for anxiety and mood disorders, but higher rates of ASPD and problem alcohol and drug use. For the overall male convicted prison population, it would be expected that 7% had a psychosis, 40% a neurotic disorder, 63% a history of alcohol abuse, 43% a history of drug dependence and 63% a personality disorder. 90 Internationally, a meta-analysis of > 33,000 prisoners found that 3.6% of men had a psychosis and 10.2% had major depression. 94
Interpretation of primary and secondary outcomes
This report describes the results of a RCT of the short-term effects of OROS-MPH on ADHD symptoms and behavioural outcomes in young male prisoners aged 16–25 years with ADHD. The trial was completed within the planned time scale, meeting all recruitment targets at HMP YOI Isis (London, UK) and HM YOI Polmont (Falkirk, UK), with randomisation of 101 participants to the drug treatment arm and 99 to the placebo arm of the trial. The aim of the trial was to establish whether or not the efficacy of a long-acting formulation of MPH in this population was similar to the effects observed in comparable trials in non-prison (community) populations. The rationale for this trial consisted of arguments supporting both smaller and larger effects than previous studies in non–offender populations, reflecting the potential complexity of the diagnosis and response to ADHD drug treatments in young adult prisoners.
The primary and secondary outcomes of this trial failed to show statistically significant differences between the OROS-MPH and placebo treatment groups in the outcome assessment at 8 weeks. Any differences between the mean or median scores for the two arms were negligible for all of the outcome measures and are unlikely to be clinically meaningful even if found to be significant in a larger trial sample. To check for the possibility of a hidden effect in the trial data for any reason, we conducted a further analysis to look for two distinct clusters of outcomes in the data. We would expect to see a bimodal distribution if there were any drug effects, reflecting the existence of two response groups. We checked the distribution in the change of CAARS-O scores from baseline to week 8 by plotting the distribution of change scores, but found only a single smooth function that gave no hint of two distinct responder groups within the data (see Figure 5).
The lack of any benefit of the active drug against placebo was unexpected. MPH has been used in numerous previous RCTs of ADHD in children and adults, and shows a consistent moderate to large effect across the various studies using outcome measures that are the same or closely similar to the CAARS-O investigator-rated scale used in this trial. In a 2018 comprehensive network meta-analysis32 comparing the effects of different pharmacological treatments for ADHD, the data for MPH were found to have a SMD of 0.78 (95% CI 0.62 to 0.93) in children and 0.59 (95% CI 0.35 to 0.64) in adults with ADHD. We therefore need to consider possible reasons for seeing such robustly negative findings in this study of young male adult prisoners with ADHD.
Trial medication
To rule out any errors with the trial medication that could have affected the trial findings, a request was made to investigate this with Modepharma Ltd, which liaised with Piramal Healthcare UK Ltd regarding the trial kits. Batch records were reviewed and there was no evidence of any errors. Spot checks were also done on the randomisation data against the batch records. The trial kits were stored under temperature-controlled conditions by the manufacturer, during transit and in the pharmacy. Following randomisation, the trial medication was stored in the house block in the prisons, and, even though temperature was not controlled, there was no indication that temperature would have been > 30 °C, hence degradation of OROS-MPH is not expected. The decision not to monitor the temperature in the house block resulted from advice from the MHRA and was confirmed by the sponsor.
Adherence to medication
An important consideration is adherence to the trial medication, which was much poorer than completion of trial outcomes. For the ITT analysis of all randomised participants, we estimated a group difference for the primary outcome of 0.57 (95% CI –2.41 to 3.56; p = 0.71) (see Table 10). This is clearly not significant and shows a very small difference in change in CAARS-O score between the groups that is far from a clinically meaningful effect size. To address the potential effect of poor adherence to trial medication, a sensitivity analysis was repeated using only those participants who had complied with treatment, defined as taking prescribed trial medication on 75% of the days during which they were in the 8-week trial, and also not having withdrawn from treatment or the trial. Only 83 out of 200 (41.5%) participants met this criterion, of which 34 were taking OROS-MPH and 49 were taking placebo. The estimated group difference remained very small, at 0.29 (95% CI –2.90 to 7.01; p = 0.91) and was very similar to the ITT analysis. This finding, therefore, lends no support to the possibility that poor compliance with trial medication could explain the negative findings in this trial.
Given that MPH relative to placebo was shown to significantly reduce ADHD symptoms in previous trials of non-prison populations,32 the finding that the per-protocol and ITT analyses were so similar was itself surprising and emphasised the need to explore the effects of adherence to trial medication further. For example, it may be that adherence to trial medication was greater during the titration phase, with medication effects at 5 weeks that were lost by 8 weeks, or that the rapid onset and offset of symptom control with OROS-MPH led to differences in reporting of ADHD symptoms, depending on the proximity of taking trial medication to completion of the outcome measures. To explore this further, we conducted two additional subgroup analyses. First, we conducted an analysis of the effects of OROS-MPH versus placebo on the CAARS-O outcome at week 5, using a definition of good compliance as the group that had taken trial medication on 75% of the days before the end of week 5. Second, we investigated the possible impact of the short-term effects of medication influencing the accuracy of reports of ADHD symptoms by including only those who took trial medication on the 2 days prior to the outcome assessment at weeks 5 and 8, for the week-5 and week-8 outcomes, respectively. Of these additional analyses, the largest difference was seen for the week-5 outcome for a group of 97 participants who had taken one or more capsules on both days immediately preceding the assessment, with a difference in outcome between the trial arms of 2.30 (95% CI –2.28 to 6.88; t = 1.00; p = 0.32) (see Chapter 5, Effects of poor adherence).
Taken together, these analyses indicate that, although adherence to medication was poor, there was no apparent impact of adherence to trial medication on the trial outcomes from the initial sensitivity analyses or additional analyses.
Optimal dosing
The optimal dose of MPH used in the treatment of adult ADHD is highly variable; hence, we adopted a titration procedure to individually titrate each participant to the optimal dose of trial medication. A similar titration protocol using the same trial medication (OROS-MPH) in a previous community trial of adults with ADHD reported large drug/placebo differences for ADHD symptoms, although they titrated to higher doses, with a mean dose of 80.9 mg ± 31.8 mg. 59 However, as noted in the pilot study for this trial, the prison population titrated to relatively low average doses. 29 This means that the titration protocol we followed might lead to underdosing of participants, potentially accounting for smaller effects of the drug, compared with placebo. The reasons for such low dosing were not formally investigated in the previous study,29 but it might be due to high sensitivity to common adverse effects. For example, during the current trial, on the AES, 20 participants taking OROS-MPH, versus 10 taking placebo, reported dry mouth; 20 versus 8, respectively, reported sweating; and 35 versus 19, respectively, reported appetite loss. Although sleep disturbance is a common problem, reported by 51% of participants at baseline, differences between the OROS-MPH and placebo arms were small during the trial (56 vs. 50 participants, respectively).
To explore the potential effects of dose on the trial outcome, we completed subgroup analyses for low-dose (titrated to one or two capsules) and high-dose (titrated to three or four capsules) groups (see Chapter 5, Could the trial outcome be affected by underdosing of participants?). Around 19% were in the low-dose group and, overall, dosing seemed to be a reasonable reflection of standard clinical practice. However, the difference in ADHD symptoms between the OROS-MPH and placebo arms was slightly smaller in the high-dose group than the low-dose group; no clinically meaningful differences were seen between the two arms of the trial for either dosage group.
Overall, these findings do not suggest that low dosing could explain the lack of significant drug effects in this trial, compared with placebo. However, it remains possible that high levels of illicit drug use in this population might cause brain changes that reduce the effects of MPH. This was suggested by a 24-week randomised clinical trial95 of OROS-MPH in 54 released prisoners with ADHD and amphetamine dependence. In this trial,95 they titrated up to 180 mg per day, which is considerably higher than the dose range used in the current trial. They found that, compared with the placebo group, the OROS-MPH group showed significantly greater improvement in the CAARS self-report scale (ADHD symptoms) (95% CI −14.18 to −3.28; p = 0.002), with 17 out of 26 participants in the OROS-MPH group showing a symptoms reduction of at least 30%, compared with only 7 out of 26 in the placebo group. This trial95 therefore suggests that much higher doses of OROS-MPH than used in the current trial may be required to see clinically significant effects of OROS-MPH.
Another question that arises in the current trial is whether or not dosing during the titration procedure was driven by the experience of adverse effects of medication, rather than treatment effects. This was suggested by the finding of a lower average prescribed dose for OROS-MPH than for placebo (3.20 vs. 3.49, respectively) at the start of week 6 (see Table 27) and a smaller proportion of prescribed medication taken (44% vs. 57%, respectively) at week 8 (see Table 28), as well as a higher rate of common adverse effects in the OROS-MPH arm (see Chapter 4, Adverse events). To investigate this, we compared a measure of adherence to medication in a group with and a group without the most common side effects. However, no significant differences were identified, providing no evidence to support this explanation (see Chapter 5, Could adverse effects be driving adherence to the trial medication?). Nevertheless, no firm conclusions can be drawn from this analysis and sensitivity of prisoners to minor adverse effects remains a possibility.
We also asked participants and researchers at week 8 to which treatment arm they believed they had been assigned. In the OROS-MPH arm, 44 participants (50.0%) and 47 researchers (52.8%) guessed correctly, suggesting random guessing, whereas, for the placebo arm, 72 participants (78.3%) and 68 researchers (73.1%) guessed correctly. Overall, this indicated some ability for both researchers and participants to distinguish between the trial arms and suggests that participant blinding might not have been maintained (p = 0.001) (see Chapter 4, Treatment arm prediction).
Diagnostic accuracy and comorbidity
Another possible explanation could be poor accuracy for the diagnosis of ADHD in the population of young male adult prisoners who took part in this trial. This is a young male adult population, aged 16–25 years, with below average general cognitive ability, with comorbidities, and histories of childhood trauma and drug use, in which the diagnosis was based largely on self-report of symptoms and behaviours reflecting the diagnosis of ADHD. Assessment of ADHD was based on a face-to-face diagnostic interview with participants, and, in most cases, did not make use of more extensive investigations, such as informant report or school reports. This was different from the Swedish study,33 in which participants were extensively evaluated, which included neuropsychological testing; interviewing parents or significant others; and collecting information through school reports and previous medical records from child and adolescent psychiatry, adult psychiatry and forensic psychiatry, when applicable. This raises the possibility that participants over-reported ADHD symptoms, or that the symptoms they experienced might be better explained by alternative mental health, psychosocial or neurodevelopmental conditions.
A further complication could be the unmeasured use of drugs in the prison, such as spice, which could affect the mental state, producing ADHD-like symptoms at baseline. To explore the impact that diagnostic certainty might have on the trial outcome, we completed a subgroup analysis that used a high threshold of ADHD symptoms, derived from the DIVA 2.0 assessment. We considered that, the larger the number of symptoms of ADHD clustered together, both in middle childhood and currently, the more likely it was that they had the typical neurodevelopmental form of ADHD. We selected a group with seven or more symptoms in both the inattentive and hyperactive/impulsive symptom domains, in both childhood and adulthood. A total of 102 participants met these higher symptom thresholds, yet the improvement seen in the OROS-MPH versus placebo arms was no different from the sample overall (see Chapter 5, Was the trial outcome affected by poor diagnostic accuracy in this prison population?).
Further subgroup analyses investigated the potential role of comorbidities identified from the MINI. To ensure that mental health comorbidities were in sufficiently large numbers, specific mental health disorders were grouped into categories: mood disorders (major depression, suicidality, mania, hypomania), anxiety disorders (panic, agoraphobia, social anxiety, obsessive–compulsive disorder, PTSD) and ASPD. As expected, 164 (82%) participants in the sample had one or more comorbidities; only 36 (18%) had no comorbidities. Although the subgroup with no comorbidities was small, there was no evidence for a clinically significant difference in the primary outcome measure of ADHD symptoms, suggesting that it is unlikely that the presence of comorbidity could explain the lack of any significant effects in this trial. Further subgroup analyses investigated a group with and a group without anxiety and mood disorders, and found no evidence for any clinically meaningful effects in any of these subgroups. (see Chapter 5, Could the trial outcome be affected by including participants with comorbid disorders?)
Regarding comorbid drug and alcohol abuse, both are associated with ADHD and, as discussed in Chapter 1, Scientific background and rationale, might have an impact on the treatment response. Although RCTs do show effects on ADHD symptoms in patients with ADHD and drug dependency in previous studies, these use higher doses than the study reported here. For example, in the review from Cunill et al. ,25 the average dose of MPH used was 62.2 mg per day, and the overall consensus is that higher than standard doses may be required to see a clinical effect26,95 and to maintain compliance to taking MPH. 27 This could arise because of brain changes as a long-term consequence of drugs and/or alcohol, reducing the potential effects of medication for ADHD or requiring higher dosing. A history of drug and alcohol abuse is also likely to be an indicator of risk for ongoing (unmeasured) use of drugs in the prison during the trial, which might have a more direct impact on ADHD symptoms and the clinical response to OROS-MPH.
The availability of new psychoactive substances, particularly synthetic cannabis, known as spice, became highly prevalent in prisons during the preparation for this report and is now considered the most serious threat to the safety and security of the prison system as identified by prison inspectors. 96 Yet little is known about the effects of spice on ADHD symptoms and the treatment response to MPH, and, in our trial, very few participants reported using spice before the trial. Furthermore, although we did not include routine drug testing in this trial, available tests do not detect spice.
We attempted to account for drug use in additional subgroup analyses. According to the AUDIT-C data, 89 (44.5%) participants met criteria for problematic alcohol use, and neither the group at high risk nor the group at low risk showed significant differences in outcome between the two arms of the trial (see Chapter 5, Could the trial outcome be affected by including participants with high levels of drug and alcohol usage?). Similarly, there were no differences seen in outcome for the group with no or low risk of substance involvement according to the NIDA Quick Screen of SUD, although the subgroup analysis of 73 participants who had no or very low use of any of opiates, spice, cannabis or stimulants showed an estimated score difference between the OROS-MPH and placebo arms of 4.26 points (95% CI –9.31 to 0.78 points; t = –1.69; p = 0.10). This was below our threshold of 5 points and not statistically significant (see Chapter 5, Could the trial outcome be affected by including participants with high levels of drug and alcohol usage?).
Finally, it might be difficult to separate ADHD from BPD or ASPD on clinical grounds alone. 97 For example, in previous research,46 we found that women meeting diagnostic criteria for BPD also show high levels of inattentiveness in their daily lives, in addition to shared symptoms such as emotional dysregulation. Similar problems are also expected to arise for men with BPDs or ASPDs. The presence of personality disorder as a comorbidity might reduce the overall effect of medication, particularly if some of the symptoms of personality disorder mimic those of ADHD. To address this question, we investigated a group with and a group without ASPD and BPD, and found that 149 (74.5%) participants in the trial met ASPD criteria, but only 15 met BPD criteria. As the numbers of those with BPD and those without ASPD were so small, we did not investigate these groups further. For ASPD, we found only very small differences between those with and those without ASPD, suggesting that the presence of this comorbidity did not affect the trial findings (see Chapter 5, Could the trial outcome be affected by including participants with borderline personality disorder? and Could the trial outcome be affected by including participants with comorbid disorders?).
Overall, we found no evidence supporting the idea that removing (or including) specific comorbidities that might confound the diagnostic assessment, or the response of ADHD symptoms to OROS-MPH, played any role in explaining the outcome of this trial.
Other potential factors
We considered a number of additional factors that might explain the trial outcome.
Temporal effects might play a role if there was a systematic change at some time point during the trial, such as unidentified changes in conduct of the trial procedures. However, we are not aware of any potential changes during the trial procedures that could explain the lack of difference between the two trial arms and the analysis of groups of 50 participants divided by consecutive recruitment to the trial showed no temporal changes on differences in outcome between the trial arms (see Chapter 5, Was the trial outcome effected by a systematic change to trial procedures?).
Attention deficit hyperactivity disorder severity might also affect results if, in this population, only the most severe cases show a significant effect of medication, compared with placebo. This is possible, as the previous RCT of ADHD in a prison population in Sweden33 showed a very large effect with no observed change in the placebo arm. The cases in this study were a highly selective group of prisoners with severe ADHD, and lengthy sentences, who were kept in a special prison wing for the trial. In contrast, the cases in the CIAO-II RCT had relatively short-term sentences and were screened on entry to the prison, giving a population that included less severe cases regarding both their ADHD and criminal offences. It is feasible that the non-specific effects of the trial protocol could lead to similar improvements in both trial arms for less severe cases, but show greater drug versus placebo differences in more severe cases. To explore this question, we conducted a subgroup analysis that involved 123 participants who met the criteria for severe ADHD with a score on the baseline CAARS-O of ≥ 35, equivalent to a t-score of 70 (see Chapter 5, Was the trial outcome affected by including less severe cases of attention deficit hyperactivity disorder in the trial?). The results showed that there was a greater improvement in the OROS-MPH arm than in the placebo arm, but the difference of 2.81 (95% CI –1.11 to 6.73) was too small to be clinically meaningful, and was not significant even using the nominal significance value (p = 0.16).
Another index of severity could be emotional dysregulation, which varied across study participants. Emotional dysregulation is a transdiagnostic phenomenon that could reflect comorbid conditions, leading to an overall reduced effect of medication. Alternatively, emotional dysregulation could be an index of ADHD severity, predicting a larger effect in the group with higher levels of emotional dysregulation. Dividing the sample into a group with low and a group with high levels of emotional dysregulation, based on a median value for the WRAADDS, 113 (56.5%) participants in the sample had high levels of emotional dysregulation. However, the effect was again small and non-significant (see Chapter 5, Could the trial outcome be affected by including participants with different levels of emotional dysregulation?). Overall, there was no evidence that severity of ADHD or emotional dysregulation had a meaningful impact on the trial results.
Finally, we investigated the potential role of childhood trauma using findings from the baseline CTQ. The association of adverse childhood experiences (emotional abuse and neglect, physical abuse and neglect, and sexual abuse) is widely discussed in the literature,98 but has not been investigated as a potential confounder of ADHD medication treatment effects. However, the role of severe childhood trauma in ADHD and other mental health disorders, and its impact on response to pharmacological treatments is a frequent topic among clinicians. It is possible that severe childhood trauma might give rise to mental health disorders that overlap symptomatically with ADHD, may not respond to ADHD medications and require psychosocial treatment approaches. 99,100 In the trial sample, we did find high rates of reported childhood trauma. In particular, 21% reported childhood emotional abuse, 24% physical abuse, 84% emotional neglect and 98% physical neglect. Again, none of the subgroup analyses found differences between the arms that were of potential clinical significance, although we were greatly underpowered to investigate groups with low levels of childhood abuse. Therefore, it remains possible that high levels of childhood trauma and neglect might negate the effects of OROS-MPH in this population, requiring further studies in high-risk populations such as young offenders (see Chapter 5, Could the trial outcome be affected by including participants with high levels of childhood trauma?).
Comparison of pre–post effects from the pilot study
Prior to this trial, we conducted an open single-arm study to investigate the feasibility of diagnosing and treating young adult prisoners with ADHD. The pre–post findings from this trial were considerably greater than those from the RCT reported here. For the primary CAARS-O outcome measure in the pilot study, there was a mean difference from baseline to the 8-week outcome of 22.6 points in the ITT analysis,29 compared with 8.1 points in the current trial (OROS-MPH arm, 8.4 points; placebo arm, 7.9 points) (see Table 8). The pre–post effect in the pilot study was considerably larger than the pre–post effect for either the OROS-MPH or placebo arms in the current trial, which requires some explanation.
Overall, the pilot was conducted along closely similar lines to those of the current trial. Indeed, the protocol for this trial was based on the pilot study. Regarding selection criteria and outcome measures, these were similar for the screening and diagnostic step, subsequent titration of OROS-MPH, followed by outcome assessments after 8 and 12 weeks, including the primary CAARS-O outcome used the current study. There are, however, three key differences from the current study. First, the primary outcome was at 12 weeks for the pilot study, whereas it was at 8 weeks for the current trial. However, we also collected 8-week outcome data in the pilot study, enabling a direct comparison. Second, the titration protocol was to a higher value of 90 mg of OROS-MPH in the pilot study; however, as only 4% of the sample titrated to the highest dose, this had little impact on the results of the pilot study. Third, participants who did not comply with the trial medication left the pilot trial and did not provide follow-up data. Thus, the pre–post findings from this single-arm study can be considered equivalent to a per-protocol analysis of the current trial. Exclusion from follow-up usually followed a period of 3 consecutive days of not taking medication, after which this was discussed with the participant to try and identify why they had missed doses and problem-solve the difficulties. If participants then continued to be non-compliant for a further 7 days, their participation in the trial was stopped in most cases.
To provide a more accurate comparison of the two trials, we summarised the pre–post effects, using a similar definition for retention in the trial for the group treated with OROS-MPH at HMP YOI Isis (as the pilot was conducted at this site only). To achieve this, we report on the 8-week outcome data, and excluded those who did not take medication for a continuous period of 10 days from the current trial, to best match the pilot study data set. The comparison of the baseline data shows that the two studies were similar regarding the severity of ADHD: mean CAARS-O scores were 37.6 points for the subset from HMP YOI Isis that did not take trial medication for a continuous period of 10 days, compared with 36.5 points for the pilot study (see Table 19). Furthermore, the study samples were similar for other baseline measures, including age, IQ estimate, WRAADDS (emotional dysregulation) scores, number of critical incidents and the CGI global clinical severity score (see Table 20). Drug and alcohol use appeared to be broadly similar between the two studies, although different measures were used: cannabis use was 92% in the pilot study and 95% in the current trial, and other drug use was 37% in the pilot study and 42% in the current trial. One potential difference was in educational outcomes, although this is thought to be due to an increase in qualifications obtained while in prison in the current trial, compared with the pilot study.
However, despite the similarities in the patient populations in the two trials, the comparison of the CAARS-O outcome scores at 8 weeks showed considerable differences in the pre–post effects, with differences from baseline to the 8-week outcome of 8.1 points across the current trial overall (8.4 points in the OROS-MPH arm and 7.9 points in the placebo arm) and 11.08 points in the subset at HMP YOI Isis that did not take medication for a continuous period of 10 days, compared with 25.0 in the pilot study (see Table 19). This large difference is difficult to explain, but suggests that there were considerable differences in the rater bias effects when conducting the two trials of young adult prisoners with ADHD. We can only speculate what these might be, but would point towards the following potential factors. The pilot study was an open trial, so both the participants and investigator knew that participants were on an active medication. Furthermore, although similar diagnostic and selection procedures were involved in both the pilot study and this trial, there was only one research assistant throughout the pilot study, who also had a high degree of contact with participants and a vested interest in generating good outcomes. Potentially, this could have led to an informal source of supportive counselling or coaching, with a possible effect on reported ADHD symptoms. Together, these effects from both participants and the researcher might have generated much greater rater bias effects than envisaged, leading to the large difference in pre–post ADHD symptom scores between the two studies.
We further considered other aspects of the prison health-care setting that might have changed. For example, the responsibility and staffing at HMP YOI Isis changed because the service changed from being run by Health Care UK in the pilot study to being run by Oxleas NHS Foundation Trust in the current trial. However, the models of care were similar and we could not identify any significant differences in the nature or quality of the service delivered, particularly regarding the involvement of broader health care and the availability of specialist psychiatric care. Overall, we conclude that rater bias effects in prison studies of ADHD are far greater than we envisaged, with, potentially, a positive downwards bias (to lower CAARS-O outcome scores) in the open trial, and a positive upwards bias (to increase CAARS-O outcome scores) in the randomised clinical trial.
Comparison with Swedish study
The results of the current trial are also in marked contrast to those reported for the smaller Swedish prison study of OROS-MPH in 30 long-stay prisoners, which showed a very large effect on CAARS-O outcome scores, with a SMD for OROS-MPH versus placebo of 2.17 points. 33 Of particular note, unlike the current trial, and other trials of MPH compared with placebo in children and adults with ADHD, during the RCT there was a very small difference in the placebo group from baseline to the 5-week outcome measure, reflected in the large difference between the two arms of the trial at the 5-week outcome. The authors reported a large decrease from baseline to the 5-week outcome for the CAARS-O score of 19.6 points (95% CI 14.7 to 24.5 points; p < 0.001) in the OROS-MPH group, compared with a non-significant decrease of 1.9 points (95% CI –0.4 to 4.2 points) in the placebo group.
The Swedish study33 had a fixed titration protocol, starting at 36 mg per day for 3 days, 54 mg for 3 days, and then 72 mg for the remaining 4 weeks, potentially explaining the greater difference in ADHD symptom between OROS-MPH and placebo arms at the 5-week outcome. This view is further supported by the finding that, in the open-label extension of the Swedish study, the mean end-point dosage was a daily dose of 108 mg. The average dose achieved in the Swedish trial was therefore higher than that in the current trial, in which only 42 out of 101 participants randomised to the OROS-MPH arm reached the highest possible dose of 72 mg (see Table 26). The findings in the Swedish study, therefore, suggest that the overall large effect of medication versus placebo on ADHD symptoms may have been driven by the small response to placebo, as well as the use of a rapid fixed-dose titration to 72 mg of OROS-MPH.
There are some crucial differences in the trial designs that might explain this. The Swedish study33 was completed in Norrtälje prison, which is a high-security prison (highest security class A) hosting long-term convicts, a very different group to that of the current trial. Participants were drug free for at least 3 months prior to the trial and were drug tested at the start and throughout the trial. In the Swedish study, all participants who consented were moved to a mental health ward in the prison, which was rebranded as an ADHD ward for the duration of the trial. By staying on this wing, they were agreeing to limited contact with other inmates during the period of the RCT. Consequently, there were younger inmates who declined to participate since they prioritised other activities (e.g. playing football with other inmates instead of taking part in the trial). Participants on the ward were also much more closely monitored on a daily basis than participants in the current trial, and there were regular tests for drug abuse, thereby ensuring low or absent levels of drug use during the trial. This selection was entirely different from that of the current trial, in which participants were required to remain in prison only for the duration of the 8-week trial, and the large majority were on short-term sentences with an average of 14 months, with a subgroup being released early. The Swedish study33 also had participants that were older, with an average age of 34 years. There were also participant differences in the severity of ADHD. Although baseline CAARS-O scores were broadly similar to those of the current trial, averaging 40.0 points in the OROS-MPH arm and 39.9 points in the placebo arm, compared with 36.4 and 37.2 points in the OROS-MPH and placebo arms, respectively, of the current trial, the severity of the illness was markedly different. There was a CGI score in the Swedish sample of 5.9,33 compared with 3.9 in the current trial, and, in the Swedish study, there were higher rates of anxiety and mood disorders (73%), all 30 participants met criteria for ASPD, and just under one-quarter met criteria for autism spectrum disorder (not formally evaluated in the current trial).
The strong selection in the Swedish study33 was reflected in the high completion rate for the 5-week initial randomised placebo-controlled trial. All participants were told in advance that they would enter an open trial with flexible dosing only if they first completed the 5-week RCT, potentially leading to greater tolerance of short-term adverse effects and ensuring 72-mg dosing in all cases. Furthermore, by using forced titration over 1 week, participants did not have to wait long before experiencing effects from treatment if they were on MPH. The rapid titration to 72 mg in all cases had the potential to be more obvious to participants. By comparison, in the current trial, if participants received too low a dose for several weeks, any effects may be less obvious and less distinct from baseline.
These differences might have influenced participant reports of symptoms and behaviours. The absence of a treatment effect in the placebo arm is unusual in trials of MPH in ADHD, suggesting that general effects of being engaged in the trial had no role to play in the Swedish study. 33 This could arise, for example, if participants perceived no potential benefits of reporting change or they received no greater benefits from being in the trial than usual. In contrast, in the current trial, prisoners might have felt that reporting improved behaviour might lead to benefits such as a shorter time in prison or an increase in privileges, perhaps minimising differences in the reporting of ADHD symptoms in the two arms.
Another potential issue could be the suitability of the CAARS-O to detect changes in symptoms of ADHD in the UK prisons, compared with the Swedish prison, because of differences in the daily routine and rehabilitation programme. Some of the items, such as losing things necessary for tasks or activities or making mistakes during tasks because of a lack of attention, may have less relevance in an environment where prisoners are locked up for long periods, follow a monotonous routine and have low organisational demands, biasing the results in the UK prison environment towards a negative result. However, most participants were engaged in an active programme of education and training and were able to give examples of ADHD symptoms based on their daily experience, for example losing items in their cell because of untidiness, difficulties following conversations with inmates or teachers and forgetting to attend (for medication and other activities), as well as improvements in these and other functions, such as sustained focus when reading and writing, and feeling less restless.
Another difference was that there were no medication compliance issues in the Swedish sample, which is thought to be due to the small sample and very close monitoring in a specialised facility for the trial. However, as we have seen, in the current trial there is no evidence that adherence to medication had a significant impact on the trial findings, with similar effects in subgroups that showed good adherence to medication and the complete ITT sample. Although the majority of the inclusion and exclusion criteria were similar to those of the Swedish study, a higher level of ASPD and anxiety and mood disorders was noted in the Swedish study. It seems unlikely that this could explain the difference in the trial outcomes. Finally, in both studies, there were high levels of reported substance misuse, but in the Swedish study any evidence of substance misuse 3 months prior to baseline was an exclusion criterion. Furthermore, under the close monitoring in the ‘ADHD wing’ it would not be feasible for prisoners to access drugs such as spice and the Swedish prisoners had repeated supervised urine drug tests. This potentially had a significant impact in the current trial, but is an unmeasured risk, and experience and recent data suggest that higher dosages of MPH are required if there is ongoing substance misuse. 26–28
Limitations
There were a number of limitations that should be considered when interpreting the findings reported here.
Throughout the trial, the research teams had weekly telephone conference calls during which there was an opportunity to discuss the diagnosis of individual cases prior to randomisation. However, to reduce the potential for biasing outcome assessment data by the rater (who was part of the trial team in the prison), post-randomisation outcome assessments were not discussed. Initial training was provided for the primary outcome measure, but further training and evaluation throughout the trial to ensure that all staff continued to conduct the primary outcome assessments in a reliable way were not conducted. This might have led to a reduction in inter-rater reliability, although, in most cases, the same investigator conducted both the baseline and outcome assessments on the primary outcome measure, limiting the effects of using different raters on within-individual change in the primary outcome measure over the period of the trial.
Drug usage in prisons is a well-reported and documented problem. However, it was decided early on in the design phase of the protocol development that there would be no recording of drug usage during the trial because this would be unreliable if based on participants’ accounts of drug use in the prison. We considered the use of drug-testing as part of the trial, but one of the most common drugs found in the prison (spice) has no test, and we were concerned by the impact on recruitment and on patient selection that would be introduced, minimising the generalisability of the findings. During the trial, 18 participants were found to have been using drugs (cannabis or spice), or suspected to have been using drugs, by prison or health-care staff or disclosed drug use to the researchers during the trial, where it was recorded as an AE. However, there were probably other undetected cases. A high level of undetected drug use by participants might account, in part, for the lack of differences between the two trial arms, if, for example, drug use generates short-term effects that are similar to the ADHD symptoms captured in the primary and secondary outcome measures.
A potential confounder not measured in this trial was traumatic brain injury (TBI), which is seen in around 60% of prisoners. 101 In a study from co-applicant Susan Young,102 43% of prisoners were deemed to have suffered TBI using a strict definition, with a mean age at first head injury of 12.5 years. A further study103 reported that 60% of prisoners self-reported head injuries, with 16% reporting moderate to severe TBI. Adults with TBI were also younger when entering the criminal justice system. 103 Although there may be some clinical effects of MPH in ADHD secondary to TBI, this is not yet well established and the efficacy in this context remains uncertain. 104
Poor adherence to treatment in the current trial might be related to the aspects of the prison environment including a limited time window for receiving medication, safety concerns regarding gang relations exposing them to be targeted during dispensing, and inconsistent release of prisoners from cells to receive medication. These potential risks were not measured; however, in additional analyses we found no evidence for an effect in a subgroup with good adherence to treatment.
In addition to pharmacological treatments, some participants in this trial might also have received additional psychological therapies from prison health care or general practitioners (GPs), although this information was not recorded. Although such treatments could potentially reduce reported levels of ADHD symptoms, it is expected that these were evenly distributed across the two arms of the trial, and previous trials have found significant effects of MPH, but no effects of ADHD-tailored psychological interventions, compared with clinical management as usual. 105 Nevertheless, because this was not recorded, it is possible that psychological treatments were not evenly distributed between the two arms of the trial.
The number of behavioural problems recorded in the prison records were very small at baseline, and the prison officer ratings of aggression on the MOAS-P and BRC-R were both very low at baseline, meaning that these measures were largely uninformative. This could reflect a high level of tolerance by prison officers for minor to moderate levels of disruptive behaviour in this population.
The relationship between participants and research and prison staff might also play a key role in influencing participants’ reports of symptoms and behaviours, and could potentially have led to reported improvements in the placebo arm that swamped any potential effects of OROS-MPH. For this reason, we included information from prison records and behavioural reports from prison and education staff, although these were largely uninformative and lacked power to detect any potential differences. We also considered the use of more objective tests, such as QbTest, which measures both cognitive performance during a continuous performance task and motor activity, measured as head movement. However, in the pilot study, during which we did collect QbTest data, the data were found to be of too poor quality to report as a result of poor engagement with the test procedures by young prisoners with ADHD. Given the results of the present trial, it would be important to consider what other objective tests of clinical improvement could be used in future studies of young offenders with ADHD.
There are several potential sources of bias on ratings of the primary and secondary outcomes during the trial. For example, participants might have been very keen to please the researcher for a number of reasons. They may have looked forward to their assessments as a change from their usual prison routine, and a chance to discuss a broader range of problems related to their diagnosis and treatment in the prison. It should also be noted that the staff working on the trial at both sites were mostly female, potentially enhancing the motivation to appear to be doing well to please the research staff. This may have led to social desire bias,106 which might have had a similar impact on reporting of symptoms and behaviours in the two arms of the trial, thereby minimising potential differences in outcome.
Another potential bias could be the halo effect. These are young men on relatively short tariffs and quite a different sample to the older sample in Sweden who were on longer tariffs. They are likely to be aware that they might get a reduced tariff for good behaviour, and there may also be an expectation of greater privileges in the prison through participation in certain prison programmes. A further motivation might be the possibility that taking part in the trial and reporting good outcomes might increase the possibility of earlier release. This knowledge of the system might mean that they were highly motivated to communicate improved functioning or reduced impulsive or disruptive behaviours equally in the two arms of the trial. Although it was made clear that this was a research project that would have no influence on outcome, they may still have perceived that reporting good outcomes can only help their situation.
Another potential bias could be the Hawthorne effect,107 in which being aware that you are being observed can lead to changes in behaviour; this may have potentially affected both arms of the trial. This effect might be greatly exaggerated in prisons, where participants are aware that they are constantly watched by both health-care and prison staff, and intense relationships are formed.
Related to these potential effects of the participant–rater interactions, participation in the trial may also have increased the sense of self-worth of participants, as some commented that they had never been asked to consent to anything before. They liked the idea that they were given a free choice whether or not to participate. Because of our screening procedure, many of the participants diagnosed with ADHD for this trial may not otherwise have engaged with the mental health team at all and the constant contact with the researchers, who had more time to spend than the health-care staff, may also have had a positive effect on participants’ well-being. It is also feasible that improvements in a general sense of well-being as a result of the research procedures might have led to lower clinical and behavioural ratings in both arms equally. Although the research staff were trained to enquire about specific examples of current symptoms and behaviours to minimise these potential effects on the primary outcome, it would not be difficult for participants to report symptom improvements when they are asked the same questions at each research assessment because they would come to understand, to an extent, the questions they were being asked.
Regarding the recording of prison record data, it was discovered early on during the trial that, at HMP YOI Isis, the prison record data for participants who were transferred, released or deported would no longer be accessible to the research team. These were accessible with assistance from HMPPS. It was also found that the adjudication data may not be a true reflection of all of the critical incidents that took place, as only issues that had been witnessed were logged by prison officers. There has also been a reduction in prison officers and increased staff turnover during the preceding few years that might have led to an overall lack of sensitivity to reporting critical incidents. This reduction was considerable. The HMPPS budget was reduced from £3.47B in 2010/11 to £2.71B in 2016/17; as a consequence, there was a 30% reduction in front-line prison officers. 108–110
At HM YOI Polmont, it was discovered during the data-checking stage at the end of the trial that the educational, vocational training sessions scheduled and attended were different on the trial database (using data collected at the time) from the prison database (using data at the end of the trial, which had changed from the time the data had been collected). This issue was explored and it was discovered that there was no audit trail on this information within the prison system, and that the prison database could have been entered or modified at any stage. This was discussed between the chief investigator, statistician, sponsor representative and the trial manager, and it was agreed that the data obtained at the time of data-gathering at baseline and week 8 should be used, as these were records of the prison database at those times.
The system in place to give IEPs for negative and positive behaviour was abandoned at HM YOI Polmont just before the start of the project, meaning that these data were available at the HMP YOI Isis site only. For this reason, IEPs were dropped from the SAP.
No pre tests were completed to compare the placebo with the active medication in relation to shape, size, colour, taste or smell. Even though the outer shell between the placebo and active medication was identical, once opened, there is a slight visible difference in size, with the distinctive black ink mark on the active medication that was not possible to replicate on the placebo capsules. This means that a participant who hid the medication in his mouth while being observed to swallow it could potentially open the shell and then establish whether or not he had received OROS-MPH. However, it is not likely that this had a significant impact on the trial outcome because adherence to treatment and dosing was lower in the OROS-MPH arm, guessing of trial medication arm was similar for participants and researchers (for OROS-MPH guessing was close to 50%, indicating random awareness for the active medication) and dosing might have been driven by the presence of adverse effects.
General considerations
General considerations that arise from the conduct of the trial protocol are useful to consider for future trials of mental health and behavioural problems in prison settings.
In the trial protocol, we indicated that, based on experience from the pilot study, we envisaged that adherence to the treatment regime would be challenging for around 20% of participants. However, in the current trial, adherence in terms of the percentage of prescribed tablets taken was around 50% overall by week 8, suggesting that the likely adherence rate was overestimated in the trial protocol. Apart from patient choice, several factors affected adherence to medication that were specific to the prison setting. The participants were able to receive the medication during set times only, and one of the prisons required the participants to remember to bring their identification cards with them. At times, there were issues with participants not being let out of their cells to receive trial (or any other) medication. We were able to manage some of these difficulties by using research staff to support the process of delivering trial medication, and adherence did appear to be greater when research staff were present during the dispensing times. For example, they were able to remind participants about the medication, to remind them to bring their identification cards and to ensure that prison officers let participants out of their cells to get to the medication dispending hatch. At HMP YOI Isis, this approach was implemented a few months into the trial to increase compliance and researchers made themselves available 4 days a week during the dispensing times in the morning. This indicates that, when working with prisoners with ADHD, there needs to be additional support from both prison and health-care staff to ensure that prisoners receive their required medication.
Compliance with some other medications appears to be greater than for the trial medication, but this level of information is not routinely collected in the prison setting. As a snapshot, during a week at HM YOI Polmont, five prisoners prescribed ADHD medication adhered to the treatment 40% of the time, in contrast with 77% adherence to daily general medication by 13 prisoners. Related to this, there were concerns about the type and use of mental health medications being prescribed. Pharmacy staff were particularly concerned by the high rate of prescribing and high doses requested for sedative medications such as mirtazapine and sedative antipsychotics. These drugs are likely to have an internal market in the prison that relates to the high demand for sedation among prisoners, as well as high levels of irritable and aggressive behaviour and sleep problems being managed in this way. The Inspectorate of Prisons report96 states that prisoners are more likely to use depressants than stimulants to counter the boredom and stress of prison life. In contrast, as seen in both our trial data and from the treatment of non-trial patients, there was generally intermittent use of OROS-MPH and dosing was low, indicating that participants were not pushing for higher doses in the same way they do for sedative medications. This also indicates a low abuse potential for OROS-MPH, which is difficult to use in a way that gets you ‘high’, and the potential internal market among prisoners for this medication appears to be low.
More generally, although procedures were in place for the delivery of critical medications to prisoners, the health-care staff often reported difficulties in delivering pharmacological treatments to prisoners. For example, Inspectorate of Prisons reports state that the clinical rooms (for dispensing of medication) were very crowded, which made the risk of error more likely,111 and lack of effective supervision of medicine queues compromised patient confidentiality and increased the potential for medication diversion. 112 Therefore, it is worth considering the processes and procedures around dispensing medication in the prison setting to fully be able to evaluate the efficacy of a medication. It may be that mental health well-being is not considered high priority, and there needs to be greater support around the dispensing of medication by prison staff. Regarding the prescribing of stimulant medications for ADHD, because these are controlled medications, they require two people to issue the medication to prisoners, unlike other psychotropic medications. This needs to be explored further to be able to generalise these findings and consider the support needed for the delivery to prisoners of effective treatments for mental health problems.
The majority of the participants had short-term sentences and many probably faced unknown arrangements once released, such as no fixed abode and not being signed up with a GP, which would be required for any future medication. Therefore, many faced the serious prospect of having no follow-up procedures in place following release and, in the absence of an agreed clinical pathway, jeopardising their future ADHD treatment. This might have affected the participants and made them feel as if it would be pointless and not make any difference to their lives to engage fully with treatments offered in the prison setting. This contrasted with the Swedish study,33 in which there was a much longer period for planning treatment following the trial and continued treatment was assured either with the regular prison psychiatrists or by direct referral to an outpatient clinic. Future studies could focus not only on outcomes in prisons, but, critically, on wider clinical and social care pathways, including the support given in the community around housing and employment, as well as the focus on treating mental health disorders.
There was a noticeable difference in compliance with medication between the Swedish study33 and the current trial, reflecting a different approach in relation to the dispensing between the prison settings. In the Swedish study, participants could receive their medication at any point until lunchtime, and it was dispensed by the prison officers. In the CIAO-II RCT, the dispensing was by health-care staff during heavily restricted time slots, which was also affected by the prison regime tactics such as ‘lock down’ and ‘split regimes’. This flexible approach in the Swedish study was considered to be a major factor that contributed to the excellent adherence to medication and the direct involvement of prison officers in delivering mental health treatments may also have played a critical role. These factors could be explored further in future studies to evaluate the full impact that strict dispensing practice has, not only on treatment of ADHD, but on mental health disorders more generally.
It would be beneficial to look at the effect of prisoners attending behaviour programmes, both individually or in a group, on recidivism and critical incidents to fully understand the impact such measures can have and to contrast outcomes in prisoners who meet criteria for ADHD with those of prisoners who do not meet criteria for ADHD. For example, an evaluation of one prison programme found a statistically significant reduction of 6 per cent in the 1-year reconviction rate, compared with the reconviction rate of a matched comparison group, and a statistically significant reduction in the frequency of reoffending of 60 recordable offences per 100 released prisoners. 113
It would also be useful for future studies of ADHD among prisoners if they had controls in the prison setting who did not meet the ADHD criteria to evaluate the effects of alcohol and substance misuse, childhood trauma and other factors in the prison setting on this group, compared with those diagnosed with ADHD.
Prison services for ADHD are thought to be highly underdeveloped. 21 For example, there was no access to ADHD diagnosis and treatment prior to the current trials at HMP YOI Isis. A basic survey of existing services for prisoners with ADHD would be useful to understand what provision currently looks like nationally. Prisoners are meant to receive the same services as they would in the community, in accordance with the principle of equivalence. 114
Conclusions and recommendations for future research
In conclusion, the trial is robustly neutral and does not support the routine treatment of young adult offenders with MPH.
Although this conclusion is disappointing, there are several lessons to be considered for future research and clinical practice. We divide these into the following: two recommendations with the highest priority, questions that address limitations of the current trial, general considerations for mental health research in prisons, and the future of clinical care for ADHD among prisoners.
High-priority research
Following the findings of this trial, there are two main objectives we recommend as having the highest priority: dosing and community studies.
Dosing
We cannot rule out the potential effects of poor adherence to trial medication and inappropriate dose titration. Overdosing, resulting in intolerable side effects, and underdosing, resulting in limited efficacy, are both common reasons for poor adherence and may have affected the results of this trial. Future studies of prisoners with ADHD should consider using a fixed-dose titration and ensuring that adequate doses are maintained.
Community studies
We cannot rule out the potential impact of the prison environment and trial procedures in this context on the reporting of ADHD symptoms. Future studies are, therefore, still required to investigate the treatment of ADHD in offenders in community settings.
Addressing limitations of the current trial
Multimodal treatment
The poor response to medication in this trial might reflect high levels of coexisting mental health disorders and exposure to high levels of trauma. Future studies could investigate the impact of a more comprehensive multimodal approach to treatment, including psychosocial and psychological treatments alongside medication for ADHD.
Early detection and prevention
The poor response in this trial might reflect the severity of ADHD and entrenched behaviours that have developed over many years. Future research should focus on early detection and prevention of ADHD, and the associated development of conduct disorder and ASPD.
Informant and use of objective measures
The possibility that participants exaggerated their symptoms in the ADHD screening test and DIVA might have led to a dilution of the number of participants with ADHD, leading to a negative result. One way to counteract this in future studies would be to require greater reliance on collateral history or past school reports in making the diagnosis, the use of tests of cognitive performance for deficits associated with ADHD such as sustained attention and response inhibition deficits, and measurement of motor restlessness.
General recommendation for investigations of mental health disorders and neurodevelopmental disabilities in prisoners
Effects of substance abuse
Active misuse of substances is a persisting issue in the two prisons that took part in this trial, as in others in the UK and elsewhere. The substances used by prisoners, such as spice, may be of lower cost and quality than in the community, and the effects of the use of such substances on this trial are essentially unknown. Future research needs to investigate the impact of spice and other drug use on ADHD symptoms, related conditions and the response to medication. We also need to understand whether or not, and how, the endemic use of substances in our prisons can be improved, given what is known about the adverse mental state effects of widespread uncontrolled substance misuse.
Models of care for individuals with complex and multiple conditions
A model is required (and should be subsequently evaluated) for the multidisciplinary and multiagency review of people who present with complex and multiple clinical conditions, including ADHD (e.g. the coexistence of ADHD, substance misuse and head injury). Although this framework is already meant to exist for those with serious mental illnesses through the Care Programme Approach in England and Wales,115 a wider framework including health and social care components may be useful for all prisoners who present with one or more conditions.
Future management of attention deficit hyperactivity disorder in prisoners
Clinical services for attention deficit hyperactivity disorder
Although the findings of this trial do not support the routine treatment of ADHD with OROS-MPH in prisoners, given the existing literature on treatment of ADHD, these findings should not exclude a role for health-care services in managing prisoners with ADHD. This may be particularly important for cases with greater severity and diagnostic certainty. In line with developments in community psychiatry, services for ADHD should ideally be integrated within existing prison mental health inreach teams, and considered alongside the treatment of substance abuse, and comorbid mental health and neurodevelopmental conditions. Examination of clinical pathways for ADHD is still indicated, with a focus on community mental health team engagement and onward GP registration for those with severe disorders, a good response to treatment of ADHD, and consideration of suitable options for employment and accommodation.
Barriers to treatment
Qualitative research is needed to find out from the prisoners what barriers there are to the management of ADHD in the community and in prisons. Qualitative research is also needed to find out what mental health and prison staff think about the diagnosis and management of ADHD. Given that few community or prison services currently include ADHD treatment components, it is likely that those who would benefit from the diagnosis and treatment of ADHD will not be receiving the assessment, care or treatment that they require.
Acknowledgements
We thank all of the trial participants and the health-care, pharmacy and prison staff at HMP YOI Isis and HM YOI Polmont, as well as pharmacy staff at Forth Valley Royal Hospital, and the staff at King’s Health Partners Clinical Trial Office and the King's Clinical Trial Unit.
Philip Asherson is supported by the National Institute for Health and Care Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London, and by a NIHR Senior Investigator award (NF-SI-0616-10040).
Research teams
A huge thank you to all the fantastic research staff who have worked with us over the years: Craig Marsh, Megan Bedding, Laura Giannulli, Megan Mansfield, Caroline Kelly, Lauren Wilson, Clare McCafferty, Grace Williamson, Khuram Khan, Donnie McPherson, Sharon Jakobowitz, Lydia Carter-Mackie and Prajakta Patil.
Contributions of authors
Philip Asherson (https://orcid.org/0000-0003-2667-2254) (Chief Investigator) had overall responsibility for the trial design and trial management.
Lena Johansson (https://orcid.org/0000-0002-4473-1134) (Clinical Trial Manager) co-ordinated the implementation of the trial and day-to-day management, and contributed to the interpretation of the trial findings.
Rachel Holland (https://orcid.org/0000-0002-8630-2821) (Trial Statistician) developed the SAP, prepared DMC reports, completed all analyses and contributed to the interpretation of the trial findings.
Megan Bedding (https://orcid.org/0000-0002-5256-0021) (Research Worker) contributed to data collection, was a TMG member and contributed to the the interpretation of the trial findings.
Andrew Forrester (https://orcid.org/0000-0003-2510-1249) (Co-applicant) contributed to the design and interpretation of the trial findings, and dissemination activities.
Laura Giannulli (https://orcid.org/0000-0002-4182-1820) (Research Worker) contributed to data collection, was a TMG member and contributed to the interpretation of the trial findings.
Ylva Ginsberg (https://orcid.org/0000-0003-1934-376X) (TSC member) contributed to the interpretation of the trial and writing of the final report.
Sheila Howitt (https://orcid.org/0000-0002-2489-2440) (Co-applicant, Research Psychiatrist) contributed to the design, data collection and interpretation of the trial findings.
Imogen Kretzschmar (https://orcid.org/0000-0002-4615-7754) (Research Psychiatrist) was a TMG member and contributed to data collection and the interpretation of the trial findings.
Stephen Lawrie (https://orcid.org/0000-0002-2444-5675) (Co-applicant) contributed to the design and interpretation of the trial findings.
Craig Marsh (https://orcid.org/0000-0003-2149-8189) (Research Psychiatrist), Caroline Kelly (https://orcid.org/0000-0003-4349-5915) (Research Worker), Megan Mansfield (https://orcid.org/0000-0003-2896-3119) (Research Worker), Clare McCafferty (https://orcid.org/0000-0002-3633-2686) (Research Nurse) and Khuram Khan (Research Psychiatrist) contributed to data collection, were TMG members and contributed to the interpretation of the trial findings.
Ulrich Müller-Sedgwick (https://orcid.org/0000-0002-5499-4077) (TSC member) contributed to the interpretation of the trial findings.
John Strang (https://orcid.org/0000-0002-5413-2725) (Co-applicant) contributed to the design and interpretation of the trial findings.
Grace Williamson (https://orcid.org/0000-0002-4618-5819) (Research Placement Student) and Lauren Wilson (https://orcid.org/0000-0001-8817-6788) (Research Placement Student) contributed to data collection, were TMG members and contributed to the interpretation of the trial findings.
Susan Young (https://orcid.org/0000-0002-8494-6949) (Co-applicant) contributed to the design and interpretation of the trial findings and dissemination activities.
Sabine Landau (https://orcid.org/0000-0002-3615-8075) (Statistician and Co-applicant) provided senior statistical support throughout the trial.
Lindsay Thomson (https://orcid.org/0000-0002-0748-6547) (Principle Investigator and Co-applicant) was instrumental in the development of the trial, led the group in Scotland and contributed to analysis and interpretation of the trial findings.
All authors contributed to the writing of the report and had the opportunity to revise it prior to submission.
Publications
Asherson P, Johansson L, Holland R, Fahy T, Forester A, Howitt S, et al. Randomised controlled trial of the short-term effects of OROS-methylphenidate on ADHD symptoms and behavioural outcomes in young male prisoners with attention-deficit/hyperactivity disorder (CIAO-II). Trials 2019;20:663.
Asherson P, Johansson L, Holland R, Bedding M, Forrester A, Giannulli L, et al. Randomised controlled trial of the short-term effects of osmotic-release oral system methylphenidate on symptoms and behavioural outcomes in young male prisoners with attention deficit hyperactivity disorder: CIAO-II study [published online ahead of print June 3 2022]. Br J Psychiatry 2022.
Data-sharing statement
All data-sharing requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted, following review. The data set that will be shared will be a pseudo-anonymised data set and will not include date of birth, initials or prison name.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research. The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the MRC, the EME programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the EME programme or the Department of Health and Social Care.
References
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition 2013. https://doi.org/10.1176/appi.books.9780890425596.
- Asherson P. Clinical assessment and treatment of attention deficit hyperactivity disorder in adults. Expert Rev Neurother 2005;5:525-39. https://doi.org/10.1586/14737175.5.4.525.
- Asherson P, Buitelaar J, Faraone SV, Rohde LA. Adult attention-deficit hyperactivity disorder: key conceptual issues. Lancet Psychiatry 2016;3:568-78. https://doi.org/10.1016/S2215-0366(16)30032-3.
- Kooij SJ, Bejerot S, Blackwell A, Caci H, Casas-Brugué M, Carpentier PJ, et al. European consensus statement on diagnosis and treatment of adult ADHD: the European Network Adult ADHD. BMC Psychiatry 2010;10. https://doi.org/10.1186/1471-244X-10-67.
- Kooij JJS, Bijlenga D, Salerno L, Jaeschke R, Bitter I, Balázs J, et al. Updated European consensus statement on diagnosis and treatment of adult ADHD. Eur Psychiatry 2019;56:14-3. https://doi.org/10.1016/j.eurpsy.2018.11.001.
- Faraone SV, Asherson P, Banaschewski T, Biederman J, Buitelaar JK, Romos-Quiroga JA, et al. Attention-deficit/hyperactivity disorder. Nat Rev Dis Primers 2015;1. https://doi.org/10.1038/nrdp.2015.20.
- Fayyad J, Sampson NA, Hwang I, Adamowski T, Aguilar-Gaxiola S, Al-Hamzawi A, et al. The descriptive epidemiology of DSM-IV Adult ADHD in the World Health Organization World Mental Health Surveys. Atten Defic Hyperact Disord 2017;9:47-65. https://doi.org/10.1007/s12402-016-0208-3.
- Polanczyk G, Rohde LA. Epidemiology of attention-deficit/hyperactivity disorder across the lifespan. Curr Opin Psychiatry 2007;20:386-92. https://doi.org/10.1097/YCO.0b013e3281568d7a.
- Polanczyk GV, Willcutt EG, Salum GA, Kieling C, Rohde LA. ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. Int J Epidemiol 2014;43:434-42. https://doi.org/10.1093/ije/dyt261.
- Fayyad J, De Graaf R, Kessler R, Alonso J, Angermeyer M, Demyttenaere K, et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry 2007;190:402-9. https://doi.org/10.1192/bjp.bp.106.034389.
- Simon V, Czobor P, Bálint S, Mészáros A, Bitter I. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br J Psychiatry 2009;194:204-11. https://doi.org/10.1192/bjp.bp.107.048827.
- Young S, Moss D, Sedgwick O, Fridman M, Hodgkins P. A meta-analysis of the prevalence of attention deficit hyperactivity disorder in incarcerated populations. Psychol Med 2015;45:247-58. https://doi.org/10.1017/S0033291714000762.
- National Institute for Health and Care Excellence (NICE) . Attention Deficit Hyperactivity Disorder: Diagnosis and Management. Clinical Guideline [CG72] 2008.
- National Institute for Health and Care Excellence (NICE) . Attention Deficit Hyperactivity Disorder: Diagnosis and Management. NICE Guideline [NG87] 2018.
- Scottish Intercollegiate Guidelines Network . Management of Attention Deficit Hyperactivity and Hyperkinetic Disorders in Children and Young People: A National Clinical Guideline 2009.
- Lenzi F, Cortese S, Harris J, Masi G. Pharmacotherapy of emotional dysregulation in adults with ADHD: a systematic review and meta-analysis. Neurosci Biobehav Rev 2018;84:359-67. https://doi.org/10.1016/j.neubiorev.2017.08.010.
- Moukhtarian TR, Cooper RE, Vassos E, Moran P, Asherson P. Effects of stimulants and atomoxetine on emotional lability in adults: a systematic review and meta-analysis. Eur Psychiatry 2017;44:198-207. https://doi.org/10.1016/j.eurpsy.2017.05.021.
- Sonuga-Barke EJ, Brandeis D, Cortese S, Daley D, Ferrin M, Holtmann M, et al. Nonpharmacological interventions for ADHD: systematic review and meta-analyses of randomized controlled trials of dietary and psychological treatments. Am J Psychiatry 2013;170:275-89. https://doi.org/10.1176/appi.ajp.2012.12070991.
- Daley D, Van Der Oord S, Ferrin M, Cortese S, Danckaerts M, Doepfner M, et al. Practitioner review: current best practice in the use of parent training and other behavioural interventions in the treatment of children and adolescents with attention deficit hyperactivity disorder. J Child Psychol Psychiatry 2018;59:932-47. https://doi.org/10.1111/jcpp.12825.
- Retz W, Rösler M, Ose C, Scherag A, Alm B, Philipsen A, et al. Multiscale assessment of treatment efficacy in adults with ADHD: a randomized placebo-controlled, multi-centre study with extended-release methylphenidate. World J Biol Psychiatry 2012;13:48-59. https://doi.org/10.3109/15622975.2010.540257.
- Young S, Gudjonsson G, Chitsabesan P, Colley B, Farrag E, Forrester A, et al. Identification and treatment of offenders with attention-deficit/hyperactivity disorder in the prison population: a practical approach based upon expert consensus. BMC Psychiatry 2018;18. https://doi.org/10.1186/s12888-018-1858-9.
- Raman SR, Man KKC, Bahmanyar S, Berard A, Bilder S, Boukhris T, et al. Trends in attention-deficit hyperactivity disorder medication use: a retrospective observational study using population-based databases. Lancet Psychiatry 2018;5:824-35. https://doi.org/10.1016/S2215-0366(18)30293-1.
- National Institute for Health and Care Excellence (NICE) . Attention Deficit Hyperactivity Disorder: Evidence Update 45 2013. http://arms.evidence.nhs.uk/resources/hub/1027558/attachment (accessed November 2020).
- Koesters M, Becker T, Kilian R, Fegert JM, Weinmann S. Limits of meta-analysis: methylphenidate in the treatment of adult attention-deficit hyperactivity disorder. J Psychopharmacol 2009;23:733-44. https://doi.org/10.1177/0269881108092338.
- Cunill R, Castells X, Tobias A, Capellà D. Pharmacological treatment of attention deficit hyperactivity disorder with co-morbid drug dependence. J Psychopharmacol 2015;29:15-23. https://doi.org/10.1177/0269881114544777.
- Crunelle CL, van den Brink W, Moggi F, Konstenius M, Franck J, Levin FR, et al. International consensus statement on screening, diagnosis and treatment of substance use disorder patients with comorbid attention deficit/hyperactivity disorder. Eur Addict Res 2018;24:43-51. https://doi.org/10.1159/000487767.
- Skoglund C, Brandt L, Almqvist C, D’Onofrio BM, Konstenius M, Franck J, et al. Factors associated with adherence to methylphenidate treatment in adult patients with attention-deficit/hyperactivity disorder and substance use disorders. J Clin Psychopharmacol 2016;36:222-8. https://doi.org/10.1097/JCP.0000000000000501.
- Skoglund C, Brandt L, D’Onofrio B, Larsson H, Franck J. Methylphenidate doses in attention deficit/hyperactivity disorder and comorbid substance use disorders. Eur Neuropsychopharmacol 2017;27:1144-52. https://doi.org/10.1016/j.euroneuro.2017.08.435.
- Asherson P, Evans C, Young S. A Pilot Study of Concerta XL in Adult Offenders With ADHD 2018. www.clinicaltrialsregister.eu/ctr-search/trial/2012-000517-37/results (accessed 18 January 2021).
- Barkley R, Murphy K. A Clinical Workbook: Attention-Deficit Hyperactivity Disorder. New York, NY: Guilford; 1998.
- Kooij JJ, Kooij JJ. Diagnostic Assessment and Treatment. Amsterdam: Pearson Assessment and Information BV; 2010.
- Cortese S, Adamo N, Del Giovane C, Mohr-Jensen C, Hayes AJ, Carucci S, et al. Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: a systematic review and network meta-analysis. Lancet Psychiatry 2018;5:727-38. https://doi.org/10.1016/S2215-0366(18)30269-4.
- Ginsberg Y, Lindefors N. Methylphenidate treatment of adult male prison inmates with attention-deficit hyperactivity disorder: randomised double-blind placebo-controlled trial with open-label extension. Br J Psychiatry 2012;200:68-73. https://doi.org/10.1192/bjp.bp.111.092940.
- Chang Z, Ghirardi L, Quinn PD, Asherson P, D’Onofrio BM, Larsson H. Risks and benefits of attention-deficit/hyperactivity disorder medication on behavioral and neuropsychiatric outcomes: a qualitative review of pharmacoepidemiology studies using linked prescription databases. Biol Psychiatry 2019;86:335-43. https://doi.org/10.1016/j.biopsych.2019.04.009.
- Chen Q, Sjölander A, Runeson B, D’Onofrio BM, Lichtenstein P, Larsson H. Drug treatment for attention-deficit/hyperactivity disorder and suicidal behaviour: register based study. BMJ 2014;348. https://doi.org/10.1136/bmj.g3769.
- Chang Z, Lichtenstein P, D’Onofrio BM, Sjölander A, Larsson H. Serious transport accidents in adults with attention-deficit/hyperactivity disorder and the effect of medication: a population-based study. JAMA Psychiatry 2014;71:319-25. https://doi.org/10.1001/jamapsychiatry.2013.4174.
- Chang Z, D’Onofrio BM, Quinn PD, Lichtenstein P, Larsson H. Medication for attention-deficit/hyperactivity disorder and risk for depression: a nationwide longitudinal cohort study. Biol Psychiatry 2016;80:916-22. https://doi.org/10.1016/j.biopsych.2016.02.018.
- Quinn PD, Chang Z, Hur K, Gibbons RD, Lahey B, Rickert ME, et al. ADHD medication and substance-related problems. Am J Psychiatry 2017;174:877-85. https://doi.org/10.1176/appi.ajp.2017.16060686.
- Chang Z, Lichtenstein P, Halldner L, D’Onofrio B, Serlachius E, Fazel S, et al. Stimulant ADHD medication and risk for substance abuse. J Child Psychol Psychiatry 2014;55:878-85. https://doi.org/10.1111/jcpp.12164.
- Viktorin A, Rydén E, Thase ME, Chang Z, Lundholm C, D’Onofrio BM, et al. The risk of treatment-emergent mania with methylphenidate in bipolar disorder. Am J Psychiatry 2017;174:341-8. https://doi.org/10.1176/appi.ajp.2016.16040467.
- Hollis C, Chen Q, Chang Z, Quinn PD, Viktorin A, Lichtenstein P, et al. Methylphenidate and the risk of psychosis in adolescents and young adults: a population-based cohort study. Lancet Psychiatry 2019;6:651-8. https://doi.org/10.1016/S2215-0366(19)30189-0.
- Lichtenstein P, Larsson H. Medication for attention deficit-hyperactivity disorder and criminality. N Engl J Med 2013;368. https://doi.org/10.1056/NEJMc1215531.
- Chang Z, Lichtenstein P, Långström N, Larsson H, Fazel S. Association between prescription of major psychotropic medications and violent reoffending after prison release. JAMA 2016;316:1798-807. https://doi.org/10.1001/jama.2016.15380.
- Young S, Gudjonsson GH, Wells J, Asherson P, Theobald D, Oliver B, et al. Attention deficit hyperactivity disorder and critical incidents in a Scottish prison population. Pers Individ Differ 2009;46:265-9. https://doi.org/10.1016/j.paid.2008.10.003.
- Skirrow C, McLoughlin G, Kuntsi J, Asherson P. Behavioral, neurocognitive and treatment overlap between attention-deficit/hyperactivity disorder and mood instability. Expert Rev Neurother 2009;9:489-503. https://doi.org/10.1586/ern.09.2.
- Moukhtarian TR. Investigation in the Overlap of ADHD and Borderline Personality Disorder: A Multi-Modal Approach 2019.
- Kockler TD, Santangelo PS, Limberger MF, Bohus M, Ebner-Priemer UW. Specific or transdiagnostic? The occurrence of emotions and their association with distress in the daily life of patients with borderline personality disorder compared to clinical and healthy controls. Psychiatry Res 2020;284. https://doi.org/10.1016/j.psychres.2019.112692.
- Kockler TD, Tschacher W, Santangelo PS, Limberger MF, Ebner-Priemer UW. Specificity of emotion sequences in borderline personality disorder compared to posttraumatic stress disorder, bulimia nervosa, and healthy controls: an e-diary study. Borderline Personal Disord Emot Dysregul 2017;4. https://doi.org/10.1186/s40479-017-0077-1.
- Young SJ, Adamou M, Bolea B, Gudjonsson G, Müller U, Pitts M, et al. The identification and management of ADHD offenders within the criminal justice system: a consensus statement from the UK Adult ADHD Network and criminal justice agencies. BMC Psychiatry 2011;11. https://doi.org/10.1186/1471-244X-11-32.
- Swanson JM, Volkow ND. Serum and brain concentrations of methylphenidate: implications for use and abuse. Neurosci Biobehav Rev 2003;27:615-21. https://doi.org/10.1016/j.neubiorev.2003.08.013.
- Faraone SV, Hess J, Wilens T. Prevalence and Consequences of the nonmedical use of amphetamine among persons calling poison control centers. J Atten Disord 2019;23:1219-28. https://doi.org/10.1177/1087054719843182.
- Asherson P, Johansson L, Holland R, Fahy T, Forester A, Howitt S, et al. Randomised controlled trial of the short-term effects of OROS-methylphenidate on ADHD symptoms and behavioural outcomes in young male prisoners with attention-deficit/hyperactivity disorder (CIAO-II). Trials 2019;20. https://doi.org/10.1186/s13063-019-3705-9.
- Wilding IR, Clark D, Wray H, Alderman J, Muirhead N, Sikes CR. In vivo disintegration profiles of encapsulated and nonencapsulated sumatriptan: gamma scintigraphy in healthy volunteers. J Clin Pharmacol 2005;45:101-5. https://doi.org/10.1177/0091270004270560.
- Faust MB. Effect of variations in backfill on dissolution for an overencapsulated comparator product. Pharm Eng 1999;19:48-54.
- Esseku F, Lesher M, Bijlani V, Adeyeye MC. Overencapsulation and Drug Product Performance of Selected Drugs Using Hard Gelatin DBcaps Capsules n.d.
- Electronic Medicines Compendium . Concerta XL 18 mg Prolonged-Release Tablets n.d. www.medicines.org.uk/emc/product/6872/smpc (accessed 21 January 2021).
- European Medicines Agency . Good Manufacturing Practice. n.d. www.ema.europa.eu/en/human-regulatory/research-development/compliance/good-manufacturing-practice (accessed 21 January 2021).
- Newcorn JH, Nagy P, Childress AC, Frick G, Yan B, Pliszka S. Randomized, double-blind, placebo-controlled acute comparator trials of lisdexamfetamine and extended-release methylphenidate in adolescents with attention-deficit/hyperactivity disorder. CNS Drugs 2017;31:999-1014. https://doi.org/10.1007/s40263-017-0468-2.
- Biederman J, Mick E, Surman C, Doyle R, Hammerness P, Harpold T, et al. A randomized, placebo-controlled trial of OROS methylphenidate in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry 2006;59:829-35. https://doi.org/10.1016/j.biopsych.2005.09.011.
- Joint Formulary Committee . British National Formulary 2011.
- Asherson P, Johansson L, Holland R, Bedding M, Forrester A, Giannulli L, et al. Randomised controlled trial of the short-term effects of osmotic-release oral system methylphenidate on symptoms and behavioural outcomes in young male prisoners with attention deficit hyperactivity disorder: CIAO-II study. Br J Psychiatry 2022. https://doi.org/10.1192/bjp.2022.77.
- Black DW, Arndt S, Hale N, Rogerson R. Use of the Mini International Neuropsychiatric Interview (MINI) as a screening tool in prisons: results of a preliminary study. J Am Acad Psychiatry Law 2004;32:158-62.
- Zanarini MC, Vujanovic AA, Parachini EA, Boulanger JL, Frankenburg FR, Hennen J. Zanarini Rating Scale for Borderline Personality Disorder (ZAN-BPD): a continuous measure of DSM-IV borderline psychopathology. J Pers Disord 2003;17:233-42. https://doi.org/10.1521/pedi.17.3.233.22147.
- Conners CK, Erhardt D, Sparrow E. Adult ADHD Rating Scales (CAARS). Technical Manual. New York, NY: Multi Health Systems Inc.; 1999.
- Reimherr FW, Marchant BK, Strong RE, Hedges DW, Adler L, Spencer TJ, et al. Emotional dysregulation in adult ADHD and response to atomoxetine. Biol Psychiatry 2005;58:125-31. https://doi.org/10.1016/j.biopsych.2005.04.040.
- Rösler M, Retz W, Fischer R, Ose C, Alm B, Deckert J, et al. Twenty-four-week treatment with extended release methylphenidate improves emotional symptoms in adult ADHD. World J Biol Psychiatry 2010;11:709-18. https://doi.org/10.3109/15622971003624197.
- Canadian ADHD Resource Alliance . CADDRA Patient ADHD Medication Form n.d. www.caddra.ca/wp-content/uploads/CADDRA-Patient-ADHD-Medication-Form.pdf (accessed 2015).
- Guy W, Rush JA. Task Force for the Handbook of Psychiatric Measures Handbook of Psychiatric Measures. Washington, DC: American Psychiatric Association; 2000.
- Raine A, Dodge K, Loeber R, Gatzke-Kopp L, Lynam D, Reynolds C, et al. The Reactive–Proactive Aggression Questionnaire: differential correlates of reactive and proactive aggression in adolescent boys. Aggress Behav 2006;32:159-71. https://doi.org/10.1002/ab.20115.
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med 1998;158:1789-95. https://doi.org/10.1001/archinte.158.16.1789.
- Saitz R, Palfai TP, Cheng DM, Alford DP, Bernstein JA, Lloyd-Travaglini CA, et al. Screening and brief intervention for drug use in primary care: the ASPIRE randomized clinical trial. JAMA 2014;312:502-13. https://doi.org/10.1001/jama.2014.7862.
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl 2003;27:169-90. https://doi.org/10.1016/S0145-2134(02)00541-0.
- Stringaris A, Goodman R, Ferdinando S, Razdan V, Muhrer E, Leibenluft E, et al. The Affective Reactivity Index: a concise irritability scale for clinical and research settings. J Child Psychol Psychiatry 2012;53:1109-17. https://doi.org/10.1111/j.1469-7610.2012.02561.x.
- Mowlem FD, Skirrow C, Reid P, Maltezos S, Nijjar SK, Merwood A, et al. Validation of the Mind Excessively Wandering Scale and the relationship of mind wandering to impairment in adult ADHD. J Atten Disord 2016. https://doi.org/10.1177/1087054716651927.
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med 1983;13:595-60. https://doi.org/10.1017/S0033291700048017.
- Walker J, Bowes N. The evaluation of violent thinking in adult offenders and non-offenders using the Maudsley Violence Questionnaire. Crim Behav Ment Health 2013;23:113-23. https://doi.org/10.1002/cbm.1861.
- Evans C, Connell J, Barkham M, Margison F, McGrath G, Mellor-Clark J, et al. Towards a standardised brief outcome measure: psychometric properties and utility of the CORE-OM. Br J Psychiatry 2002;180:51-60. https://doi.org/10.1192/bjp.180.1.51.
- Knoedler DW. The Modified Overt Aggression Scale. Am J Psychiatry 1989;146:1081-2. https://doi.org/10.1176/ajp.146.8.1081b.
- Wright J. Classroom Behaviour Report Card Resource Book 2003. www.interventioncentral.org (accessed 18 January 2021).
- Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39:175-91. https://doi.org/10.3758/BF03193146.
- Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychol Methods 2010;15:309-34. https://doi.org/10.1037/a0020761.
- The Scottish Government . Preventing Offending: Getting It Right for Children and Young People 2015.
- Great Britain . The Medicines for Human Use (Clinical Trials) Regulations 2004 2004.
- Great Britain . The Medicines for Human Use (Clinical Trials) Amendment Regulations 2006 2006.
- Medical Research Council . MRC Clinical Trials Series: MRC Guidelines for Good Clinical Practice in Clinical Trials n.d. https://mrc.ukri.org/documents/pdf/good-clinical-practice-in-clinical-trials/ (accessed 4 February 2021).
- World Medical Association . Declaration of Helsinki 1996 n.d. www.wma.net/what-we-do/medical-ethics/declaration-of-helsinki/doh-oct1996/ (accessed 4 February 2021).
- Good Clinical Practice Network . ICH Harmonised Guideline Integrated Addendum to ICH E6(R1): Guideline for Good Clinical Practice ICH E6(R2) ICH Consensus Guideline n.d. https://ichgcp.net/# (accessed 4 February 2021).
- Great Britain . Data Protection Act 1998 1998.
- Independent Monitoring Boards . Report of the Independent Monitoring Board: January–December 2013 n.d. www.imb.org.uk/app/uploads/2015/01/isis-2013.pdf (accessed 18 January 2021).
- Singleton N, Meltzer H, Gatward R, Coid J, Deasy D. Psychiatric Morbidity Among Prisoners in England and Wales. Newport: Office for National Statistics; 1998.
- Lichtenstein P, Halldner L, Zetterqvist J, Sjölander A, Serlachius E, Fazel S, et al. Medication for attention deficit-hyperactivity disorder and criminality. N Engl J Med 2012;367:2006-14. https://doi.org/10.1056/NEJMoa1203241.
- Office for National Statistics . 2011 Census. Who We Are. How We Live. What We Do n.d. https://webarchive.nationalarchives.gov.uk/20160129062745/http://www.ons.gov.uk/ons/guide-method/census/2011/index.html (accessed 4 February 2021).
- Uhrig N. Black, Asian and Minority Ethnic Disproportionality in the Criminal Justice System in England and Wales. London: Ministry of Justice; 2016.
- Fazel S, Seewald K. Severe mental illness in 33,588 prisoners worldwide: systematic review and meta-regression analysis. Br J Psychiatry 2012;200:364-73. https://doi.org/10.1192/bjp.bp.111.096370.
- Konstenius M, Jayaram-Lindström N, Guterstam J, Beck O, Philips B, Franck J. Methylphenidate for attention deficit hyperactivity disorder and drug relapse in criminal offenders with substance dependence: a 24-week randomized placebo-controlled trial. Addiction 2014;109:440-9. https://doi.org/10.1111/add.12369.
- HM Inspectorate of Prisons . Changing Patterns of Substance Misuse in Adult Prisons and Service Responses 2015.
- Moukhtarian TR, Mintah RS, Moran P, Asherson P. Emotion dysregulation in attention-deficit/hyperactivity disorder and borderline personality disorder. Borderline Personal Disord Emot Dysregul 2018;5. https://doi.org/10.1186/s40479-018-0086-8.
- Brown NM, Brown SN, Briggs RD, Germán M, Belamarich PF, Oyeku SO. Associations between adverse childhood experiences and ADHD diagnosis and severity. Acad Pediatr 2017;17:349-55. https://doi.org/10.1016/j.acap.2016.08.013.
- Forneris CA, Gartlehner G, Brownley KA, Gaynes BN, Sonis J, Coker-Schwimmer E, et al. Interventions to prevent post-traumatic stress disorder: a systematic review. Am J Prev Med 2013;44:635-50. https://doi.org/10.1016/j.amepre.2013.02.013.
- Szymanski K, Sapanski L, Conway F. Trauma and ADHD — association or diagnostic confusion? A clinical perspective. J Infant Child Adolesc Psychother 2011;10:51-9. https://doi.org/10.1080/15289168.2011.575704.
- Shiroma EJ, Ferguson PL, Pickelsimer EE. Prevalence of traumatic brain injury in an offender population: a meta-analysis. J Correct Health Care 2010;16:147-59. https://doi.org/10.1177/1078345809356538.
- Young S, González RA, Fridman M, Hodgkins P, Kim K, Gudjonsson GH. Health-related quality of life in prisoners with attention-deficit hyperactivity disorder and head injury. BMC Psychiatry 2018;18. https://doi.org/10.1186/s12888-018-1785-9.
- Chitsabesan P, Lennox C, Williams H, Tariq O, Shaw J. Traumatic brain injury in juvenile offenders: findings from the comprehensive health assessment tool study and the development of a specialist linkworker service. J Head Trauma Rehabil 2015;30:106-15. https://doi.org/10.1097/HTR.0000000000000129.
- Huang CH, Huang CC, Sun CK, Lin GH, Hou WH. Methylphenidate on cognitive improvement in patients with traumatic brain injury: a meta-analysis. Curr Neuropharmacol 2016;14:272-81. https://doi.org/10.2174/1570159X13666150514233033.
- Philipsen A, Jans T, Graf E, Matthies S, Borel P, Colla M, et al. Effects of group psychotherapy, individual counseling, methylphenidate, and placebo in the treatment of adult attention-deficit/hyperactivity disorder: a randomized clinical trial. JAMA Psychiatry 2015;72:1199-210. https://doi.org/10.1001/jamapsychiatry.2015.2146.
- Krumpal I. Determinants of social desirability bias in sensitive surveys: a literature review. Qual Quant 2013;47:2025-47. https://doi.org/10.1007/s11135-011-9640-9.
- Morberg BM, Malling AS, Jensen BR, Gredal O, Wermuth L, Bech P. The Hawthorne effect as a pre-placebo expectation in Parkinsons disease patients participating in a randomized placebo-controlled clinical study. Nord J Psychiatry 2018;72:442-6. https://doi.org/10.1080/08039488.2018.1468480.
- Piper M, Forrester A, Shaw J. Prison healthcare services: the need for political courage. Br J Psychiatry 2019;215:579-81. https://doi.org/10.1192/bjp.2019.43.
- Ismail N. The politics of austerity, imprisonment and ignorance: a case study of English prisons. Med Sci Law 2020;60:89-92. https://doi.org/10.1177/0025802419899744.
- House of Commons Justice Select Committee . Prisons: Planning and Policies 2015.
- HM Chief Inspector of Prisons . Report on an Unannounced Inspection of HMP YOI Isis: 17–28 February 2014 n.d. www.justiceinspectorates.gov.uk/hmiprisons/wp-content/uploads/sites/4/2014/08/Isis-Web-2014.pdf (accessed 4 February 2021).
- HM Chief Inspector of Prisons . Report on an Unannounced Inspection of HMP YOI Isis: 23 July–2 August 2018 n.d. www.justiceinspectorates.gov.uk/hmiprisons/wp-content/uploads/sites/4/2018/12/HMP-YOI-Isis-Web-2018.pdf (accessed 4 February 2021).
- Sadlier G. Evaluation of the Impact of the HM Prison Service Enhanced Thinking Skills Programme on Reoffending Outcomes of the Surveying Prisoner Crime Reduction (SPCR) Sample. London: Ministry of Justice; 2010.
- Till A, Forrester A, Exworthy T. The development of equivalence as a mechanism to improve prison healthcare. J R Soc Med 2014;107:179-82. https://doi.org/10.1177/0141076814523949.
- Goodwin N, Lawton-Smith S. Integrating care for people with mental illness: the Care Programme Approach in England and its implications for long-term conditions management. Int J Integr Care 2010;10. https://doi.org/10.5334/ijic.516.
Appendix 1 Protocol amendments
| Version and date | Minor/substantial amendment | Approved date | Reason for change |
|---|---|---|---|
| Version 1.1, 22 March 2016 | N/A |
|
First approved version |
| Version 1.2, 5 July 2016 | Substantial amendment 1 (prior to project start) |
|
Remove Gough Socialization Scale (protocol section 6.1) |
| Version 1.3, 29 March 2017 | Minor amendment 3 | HRA: 6 April 2017 |
|
| Version 1.4, 3 May 2017 | Minor amendment 4 | HRA: 26 May 2017 | Remove RPQ from week 5 and week 8 table and text as it is a baseline measure only (protocol sections 6.1 and 7.1.2) |
| Version 2.0, 30 August 2018 | Substantial amendment 2 |
|
|
Appendix 2 Protocol deviations
| File note number | Treatment arm obtained after formal unblinding following database lock: OROS-MPH/Placebo | Description | Action |
|---|---|---|---|
| TMF 1 | 2 Placebo | Unblinding information given to trial manager by Modepharma Ltd in error | This was reported to KCTU using the incident reporting form and a note was added on the randomisation system |
| TMF 9 | N/A | Database design error in Trial Medication Log 2 | This was reported to KCTU using the incident reporting form |
| Isis 2 | OROS-MPH | Researcher took consent II because psychiatrist not available and did baseline measures before the psychiatrist countersigned consent | N/A |
| Isis 4 | OROS-MPH | Prescription not reviewed properly, hence no medication last week | N/A |
| Isis 5 | Placebo | Did not meet the IQ exclusion criterion, but test re-done and met the exclusion criterion, which prompted a protocol amendment to clarify regarding IQ test with ADHD participants | This was reported to KCTU using the incident reporting form and a note was added on the randomisation system |
| Isis 6 |
3 Placebo 1 OROS-MPH |
Consent II obtained by researcher rather than psychiatrist | This was reported to KCTU and no further action taken |
| Isis 7 | OROS-MPH | Week 2 visit missed | N/A |
| Isis 8 | Placebo | Destruction of medication on house block before authorisation | KHP CTO made a note of this and reminded pharmacy staff that the trial kits have to be authorised for destruction first |
| Isis 9 |
3 Placebo 1 OROS-MPH |
Consent I was signed rather than consent II | N/A |
| Isis 13 |
15 Placebo 15 OROS-MPH |
The CGI measure was obtained by researcher rather than by psychiatrist | N/A |
| Isis 14 | OROS-MPH | Week 8 measures obtained late | N/A |
| Isis 15 | OROS-MPH | Missing capsule | Reported on NHS Datix (Datix Ltd, London, UK) reporting system |
| Isis 16 | OROS-MPH | Week 5 measures obtained late | N/A |
| Isis 18 | OROS-MPH | Amended start date because participants unable to access medication | N/A |
| Isis 19 | Placebo | Medication stopped in error by a member of health-care staff | N/A |
| Isis 20 | Placebo | Participant transferred to another prison and week-8 measures were obtained at other prison | N/A |
| Isis 21 | Placebo | Participant transferred; no week-5 measures and week-8 measures obtained at other prison | N/A |
| Isis 22 | OROS-MPH | Amended start date as participant unable to access medication | N/A |
| Isis 23 |
1 Placebo 3 OROS-MPH |
Missing consent I because participants part of the pre cohort | N/A |
| Isis 24 | Placebo | Amended trial start date, and week-3 and week-8 measures collected 1 day early | N/A |
| Isis 25 | OROS-MPH | Consent I was signed rather than consent II | N/A |
| Isis 26 |
1 Placebo 1 OROS-MPH |
Researcher obtained measure rather than psychiatrist | N/A |
| Isis 27 | OROS-MPH | Wrong date of birth entered into the randomisation system | This was reported to KCTU using the incident reporting form and a note was added on the randomisation system |
| Isis 28 | 2 Placebo | Medication error | Reported on NHS Datix reporting system. This was reported to MHRA as a notification of serious breach of GCP or trial protocol, but it was confirmed not to be a serious breach |
| Isis 30 | OROS-MPH | Prescription stopped owing to a system administration error | N/A |
| Isis 31 | Placebo | Prescription not active for 1 day | N/A |
| Isis 32 |
8 Placebo 6 OROS-MPH |
Titration measures completed by researcher rather than psychiatrist | N/A |
| Isis 36 | Placebo | Amended trial start date and week-1 measures obtained 1 day early | N/A |
| Isis 39 | OROS-MPH | Medication stopped for 1 day because of suspected spice use | N/A |
| Isis 40 | Placebo | Medication administration error | Reported on NHS Datix reporting system. This was reported to MHRA as a notification of serious breach of GCP or trial protocol, but it was confirmed not to be a serious breach |
| Isis 41 | N/A | Participant was excluded because of his age, but he should have been considered for the trial as he was 25 years at the time of signing consent I, as per protocol | N/A |
| Isis 42 | OROS-MPH | Participant in segregation and week-8 measures obtained later as a result of prison restrictions in access | N/A |
| Isis 43 | Placebo | Participant deported; week-5 and week-8 measures could not be obtained | N/A |
| Isis 46 | OROS-MPH | The WASI-II was completed prior to consent II because there were queries regarding participant’s IQ and it was needed for medical assessment | N/A |
| Isis 48 |
43 Placebo 38 OROS-MPH |
No week-5 note was added in the medical records by psychiatrist confirming that the prescription was reviewed | N/A |
| Isis 49 | OROS-MPH | Medication inaccessible to participant for 1 day because of house block move | N/A |
| Isis 54 | 2 OROS-MPH | Prescription ended 1 day early | N/A |
| Isis 59 | Placebo | Week-8 vital measures were completed outside of the time frame because of lack of access to participant | N/A |
| Isis 64 | OROS-MPH | Participant was in segregation because of safety concerns and was not always escorted to receive his medication, hence he had lack of access to his medication | N/A |
| Isis 68 | Placebo | Prescription written by non-GCP-trained doctor owing to system failure and the prescription being deleted | N/A |
| Isis 74 | OROS-MPH | Participant’s week 2–4 measures were not completed and participant refused trial medication | N/A |
| Isis 75 | OROS-MPH | Missing BSI and CORE-OM scores at week 8 | N/A |
| Isis 77 |
3 Placebo 6 OROS-MPH |
Data from prison records for those who had been at the prison for less than 56 days when baseline measure obtained | N/A |
| Isis 78 | Placebo | Missing RPQ score at baseline | N/A |
| Isis 79 |
2 Placebo 1 OROS-MPH |
Missing WRAADS question in pack at baseline | N/A |
| Isis 80 |
4 Placebo 3 OROS-MPH |
Missing MVQ questions in pack at baseline | N/A |
| Isis 81 |
2 Placebo 1 OROS-MPH |
Weight missing as a result of being in segregation | N/A |
| Isis 82 | OROS-MPH | Participant refused week-2 titration assessment | N/A |
| Isis 83 | Placebo | Missing MVQ measure at week 5 | N/A |
| Isis 88 | Placebo | Missing remaining capsules at the end of the trial | Reported on NHS Datix reporting system |
| Isis 93 |
9 Placebo 9 OROS-MPH |
Missing Ward Controlled Drugs books from the prison house blocks | This was discussed with CRA Meeraa Benedict, and it was confirmed by Helen Critchley and Hannah Mason at KHP CTO, that is, it was not regarded as a serious breach that would require reporting to the MHRA |
| Polmont 1 | OROS-MPH | More than 1 week from randomisation to starting medication | N/A |
| Polmont 3 | Placebo | IMP start date modified because of prescription issue | N/A |
| Polmont 4 | OROS-MPH | IMP start date modified because participant undergoing an investigation for a medical condition | N/A |
| Polmont 7 | Placebo | IMP start date modified because participant initially refused medication but then changed his mind | N/A |
| Polmont 9 | N/A | Duplication of screening | As per advice from KCTU, the duplicated personal identification number for the participant who was screened twice was used for another participant |
| Polmont 11 | OROS-MPH | Medication error: participant given a Concerta 18-mg capsule from stock medication rather than the allocated trial medication | N/A |
| Polmont 12 | OROS-MPH | Partly missing week-5 measures as participant only wanted to see the psychiatrist for the titration appointment | N/A |
| Polmont 13 |
1 Placebo 1 OROS-MPH |
Week-2 measures not done because of adverse weather conditions and staff advised not to travel | N/A |
| Polmont 14 | Placebo | Incorrect medication count; new counting protocol introduced | This was reported to Modepharma Ltd and investigated by Piramal Healthcare UK Ltd |
| Polmont 15 |
4 Placebo 4 OROS-MPH 2 N/A |
Signature in incorrect place on consent form | N/A |
| Polmont 16 | Placebo | Week-8 measures obtained late | N/A |
| Polmont 17 | 3 OROS-MPH | IMP destroyed at the end of trial prior to authorisation by the CRA | KHP CTO made a note of this and reminded pharmacy staff that the trial kits have to be authorised for destruction first |
| Polmont 20 | OROS-MPH | Missing some of the week-8 measures | N/A |
| Polmont 21 | Placebo | Missing some of the week-8 measures | N/A |
| Polmont 23 | Placebo | Medication not offered to participant | N/A |
| Polmont 25 | OROS-MPH | The WASI-II was completed prior to consent II as there were queries regarding participant’s IQ and it was needed for medical assessment | N/A |
| Polmont 26 | Placebo | Incorrect number of capsules in bottle | This was reported to Modepharma Ltd and investigated by Piramal Healthcare UK Ltd |
| Polmont 27 | N/A | Excluded by clinician because of low weight | N/A |
| Polmont 33 | Placebo | Incorrect trial medication given | Reported on NHS IR1 reporting system |
| Polmont 38 | Placebo | Medication started > 7 days after randomisation | N/A |
| Polmont 40 | Placebo | Week-8 measures completed late | N/A |
| Polmont 41 | OROS-MPH | Week-5 measures completed late | N/A |
| Polmont 42 | Placebo | Some baseline measures were repeated because of spice use, which delayed enrolment | N/A |
| Polmont 44 | OROS-MPH | Week-8 measures not all completed | N/A |
| Polmont 47 | OROS-MPH | Medication not withheld pending substance misuse review | N/A |
| Polmont 52 | Placebo | Mirtazapine prescribed mid-trial; trial medication stopped | N/A |
| Polmont 54 | OROS-MPH | Medication started > 7 days after randomisation | N/A |
| Polmont 56 |
10 Placebo 7 OROS-MPH |
Trial medication taken for > 56 days | N/A |
| Polmont 60 | OROS-MPH | Medication error during Controlled Drugs checks; participant had been administrated two capsules rather than one prior to being titrated | N/A |
| Polmont 63 |
10 Placebo 11 OROS-MPH |
Medication guess not recorded | N/A |
| Polmont 64 | OROS-MPH | Week-5 measures partially completed | N/A |
| Polmont 65 | Placebo | Week-8 measures obtained late | N/A |
| Polmont 67 |
2 Placebo 5 OROS-MPH |
Data from prison records for those who had been at the prison for less than 56 days when baseline measure obtained | N/A |
| Polmont 68 |
5 Placebo 7 OROS-MPH |
Participants refused appointments | N/A |
| Polmont 70 |
8 Placebo 5 OROS-MPH |
Titrated at week-5 appointment | N/A |
| Polmont 72 |
10 Placebo 12 OROS-MPH |
Concomitant medication source data not available | N/A |
| Polmont 74 |
3 Placebo 3 OROS-MPH |
CGI measure not completed by psychiatrist | N/A |
| Polmont 75 |
6 Placebo 2 OROS-MPH |
Missing weight and vital signs data | N/A |
| Polmont 76 | Placebo | Week-8 BSI measure not completed | N/A |
| Polmont 77 | OROS-MPH | Week-5 CGI measure completed incorrectly by psychiatrist | N/A |
| Polmont 83 | 3 OROS-MPH | CGI question missing answer | N/A |
Appendix 3 Her Majesty’s Prison and Young Offender Institution Isis baseline data
| Item name | Category name | OROS-MPH arm participants | Placebo arm participants | Total sample | |||
|---|---|---|---|---|---|---|---|
| N | n (%) | N | n (%) | N | n (%) | ||
| Ethnicity | White (white British, white Irish, white other) | 58 | 21 (36.2) | 57 | 19 (33.3) | 200 | 40 (34.8) |
| Other (Asian, other mixed, other, black African and white, black Caribbean and white) | 19 (32.8) | 10 (17.5) | 29 (25.2) | ||||
| Black (black African, black Caribbean, other black) | 18 (31.0) | 28 (49.2) | 46 (40.0) | ||||
| Education | No qualifications | 58 | 18 (31.0) | 57 | 13 (22.8) | 115 | 31 (27.0) |
| Any qualifications | 40 (69.0) | 44 (77.2) | 84 (73.0) | ||||
| Age (years) at leaving school | ≤ 14 | 58 | 14 (24.1) | 57 | 11 (19.3) | 115 | 25 (21.7) |
| 15 | 16 (27.6) | 13 (22.8) | 29 (25.2) | ||||
| ≥ 16 | 20 (34.5) | 24 (42.1) | 44 (38.3) | ||||
| Unknown | 8 (13.8) | 9 (15.8) | 17 (14.8) | ||||
| Employed (including in education) | Unemployed | 58 | 40 (69.0) | 57 | 40 (70.2) | 115 | 80 (69.6) |
| Employed | 18 (31.0) | 17 (29.8) | 35 (30.4) | ||||
| Offence category | Serious violence or sexual offence | 58 | 6 (10.3) | 57 | 9 (15.3) | 115 | 15 (13.0) |
| Assault | 2 (3.5) | 3 (5.3) | 5 (4.3) | ||||
| Drug related | 23 (39.7) | 30 (52.6) | 53 (46.1) | ||||
| Burglary or theft | 22 (37.9) | 12 (21.0) | 34 (29.6) | ||||
| Other, including possession of weapon, driving and wilful fire-raising | 5 (8.6) | 3 (5.3) | 8 (7.0) | ||||
| Previous ADHD treatment | Yes | 58 | 17 (29.3) | 57 | 9 (15.8) | 115 | 26 (22.6) |
| No or unknowna | 41 (70.7) | 48 (84.2) | 89 (77.4) | ||||
| Age (years) when ADHD medication last taken | ≤ 13 | 17 | 6 (35.3) | 9 | 2 (22.2) | 26 | 8 (30.8) |
| ≥ 14 | 11 (64.7) | 7 (77.8) | 18 (69.2) | ||||
| Baseline characteristics | OROS-MPH arm | Placebo arm | Overall | |||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| Age (years) (range 16–25) | 58 | 21.4 (1.9) | 57 | 21.6 (2.0) | 115 | 21.5 (1.9) |
| IQ (WASI-IIa score) | 58 | 89 (13.0) | 57 | 88.5 (11.3) | 115 | 88.8 (12.3) |
| Height (cm) | 58 | 177.2 (6.9) | 57 | 178.3 (7.1) | 115 | 177.8 (7.0) |
| BMI (kg/m2) | 58 | 24.3 (3.1) | 57 | 24.2 (3.9) | 115 | 24.2 (3.5) |
| Clinical measures | ||||||
| CAARS-O score (range 0–54)b | 57 | 38.1 (9.9) | 57 | 39.9 (8.2) | 114 | 39.0 (9.1) |
| CAARS-O hyperactivity score (range 0–27)b | 57 | 19.5 (5.7) | 57 | 20.0 (4.8) | 114 | 19.8 (5.3) |
| CAARS-O inattention score (range 0–27) | 58 | 18.6 (5.1) | 57 | 19.8 (4.6) | 115 | 19.2 (4.9) |
| WRAADDS score (range 0–30) | 58 | 18.4 (6.5) | 57 | 18.2 (6.4) | 115 | 18.3 (6.4) |
| WRAADDS – temper subscale score (range 0–9) | 58 | 4.9 (2.7) | 57 | 5.1 (2.5) | 115 | 5.0 (2.6) |
| WRAADDS – lability subscale score (range 0–12) | 58 | 8.6 (2.4) | 57 | 8.2 (2.5) | 115 | 8.4 (2.5) |
| WRAADDS – over-reactivity subscale score (range 0–9) | 58 | 5.0 (2.5) | 57 | 4.8 (2.5) | 115 | 4.9 (2.5) |
| ARI-S score (range 0–14) | 58 | 9.8 (3.5) | 57 | 9.5 (3.9) | 115 | 9.7 (3.7) |
| MEWS score (range 0–36) | 58 | 25.5 (7.8) | 57 | 26.4 (7.1) | 115 | 26.0 (7.5) |
| CGI-severity score (range 1–7) | 58 | 4.7 (0.7) | 57 | 4.6 (0.6) | 115 | 4.7 (0.6) |
| CORE-OM score (range 0–136) | 58 | 44.5 (14.9) | 57 | 46.1 (17.7) | 115 | 45.3 (16.3) |
| MVQ score (range 0–75)c | 58 | 32.4 (8.6) | 57 | 31.7 (9.2) | 115 | 32.1 (8.9) |
| Weiss-CD score (range 0–45) | 58 | 19.4 (8.2) | 57 | 18.6 (8.4) | 115 | 19.0 (8.3) |
| Systolic blood pressure (mmHg) | 58 | 124.5 (11.4) | 57 | 126.4 (11.9) | 115 | 125.4 (11.6) |
| Diastolic blood pressure (mmHg) | 58 | 67.2 (10.0) | 57 | 68.4 (9.1) | 115 | 67.8 (9.6) |
| Heart rate (beats per minute) | 58 | 70.0 (10.7) | 57 | 68.6 (11.7) | 115 | 69.3 (11.1) |
| Putative moderator variables | ||||||
| RPQ-Proactive score (range 0–24)d | 58 | 6.3 (5.2) | 56 | 7.4 (5.8) | 114 | 6.8 (5.5) |
| RPQ-Reactive score (range 0–22)d | 58 | 13.7 (5.0) | 56 | 14.8 (4.8) | 114 | 14.3 (4.9) |
| RPQ total (range 0–46)d | 58 | 20.0 (9.3) | 56 | 22.3 (9.8) | 114 | 21.1 (9.6) |
| CTQ score (range 28–140)e | 58 | 50.0 (18.5) | 57 | 50.6 (20.6) | 115 | 50.3 (19.5) |
| ZAN-BPD score (range 0–36) | 58 | 8.1 (5.1) | 57 | 7.7 (4.8) | 115 | 7.9 (4.9) |
| BSI score (range 0–212) | 58 | 53.3 (31.8) | 57 | 58.2 (38.1) | 115 | 55.7 (35.0) |
| Coexisting disorders | Trial arm, n (%) | Overall (N = 115), n (%) | |
|---|---|---|---|
| OROS-MPH (N = 58) | Placebo (N = 57) | ||
| ASPD | 51 (87.9) | 48 (84.2) | 99 (86.1) |
| Mood disorder (major depression, suicidality, manic, hypomanic) | 10 (17.2) | 13 (22.8) | 23 (20.0) |
| Anxiety disorder (panic, agoraphobia, social anxiety, obsessive–compulsive disorder, PTSD) | 15 (25.9) | 16 (28.1) | 31 (27.0) |
| Potential problematic alcohol usea | 40 (69.0) | 34 (59.7) | 74 (64.4) |
| Illicit drug useb | 56 (96.6) | 53 (93.0) | 109 (94.8) |
| MINI checklist symptom scores (range 0–10 for each item) | Minimum/median/maximum | Minimum/median/maximum | Minimum/median/maximum |
| Depression | 0/2/7 | 0/1/8 | 0/2/8 |
| Anger | 0/6/9 | 0/5/9 | 0/5/9 |
| Mania | 0/0/6 | 0/0/3 | 0/0/6 |
| Anxiety | 0/2/8 | 0/2/8 | 0/2/8 |
| Physical symptoms | 0/0/6 | 0/0/5 | 0/0/6 |
| Suicidal thoughts | 0/0/3 | 0/0/3 | 0/0/3 |
| Psychosis | 0/0/0 | 0/0/3 | 0/0/3 |
| Sleep problems | 0/5/9 | 0/3/10 | 0/4/10 |
| Memory problems | 0/4/7 | 0/3/7 | 0/4/7 |
| Repetitive thoughts/behaviours | 0/0/7 | 0/0/7 | 0/0/7 |
| Dissociation | 0/0/0 | 0/0/5 | 0/0/5 |
| Personality function | 0/6/9 | 0/5/8 | 0/5/9 |
| Baseline behaviour report | OROS-MPH arm | Placebo arm | Overall | |||
|---|---|---|---|---|---|---|
| Participants (n) | Minimum/median/maximum | Participants (n) | Minimum/median/maximum | Participants (n) | Minimum/median/maximum | |
| MOAS-P score (range 0–40) | 58 | 0/0/15 | 57 | 0/0/17 | 115 | 0/0/17 |
| MOAS-E score (range 0–40) | 21 | 0/0/12 | 28 | 0/0/10 | 49 | 0/0/12 |
| BRC-P score | 58 | 6/8/19 | 57 | 6/8/21 | 115 | 6/8/21 |
| BRC-E score | 21 | 13/20/39 | 28 | 13/17/27 | 49 | 13/17/39 |
| Number of critical incidents | 58 | 0/0/4 | 57 | 0/0/4 | 115 | 0/0/4 |
| Number of days in prison out of the 56 days prior to randomisation, mean (SD) | 58 | 55.2 (3.6) | 57 | 55.0 (4.6) | 115 | 55.1 (4.1) |
| Number of education sessions (any type) scheduled | 58 | 0/12/55 | 57 | 0/16/69 | 115 | 0/14/69 |
| Number of education sessions (any type) attended | 58 | 0/12/55 | 57 | 0/14/69 | 115 | 0/12/69 |
| Proportion of scheduled education sessions (any type) attended, mean (SD) | 58 | 0.90 (0.18) | 57 | 0.92 (0.12) | 115 | 0.91 (0.15) |
Appendix 4 Her Majesty’s Young Offender Institution Polmont baseline data
| Item name | Category name | OROS-MPH arm participants | Placebo arm participants | Total sample | |||
|---|---|---|---|---|---|---|---|
| N | n (%) | N | n (%) | N | n (%) | ||
| Ethnicity | White (white British, white Irish, white other) | 43 | 43 (100.0) | 42 | 42 (100.0) | 85 | 85 (100.0) |
| Education | No qualifications | 43 | 24 (55.8) | 42 | 24 (57.1) | 85 | 48 (56.5) |
| Any qualifications | 19 (44.2) | 18 (42.9) | 37 (43.5) | ||||
| Age (years) at leaving school | ≤ 14 | 43 | 12 (27.9) | 42 | 14 (33.3) | 85 | 26 (30.6) |
| 15 | 16 (37.2) | 9 (21.4) | 25 (29.4) | ||||
| ≥ 16 | 15 (34.9) | 19 (45.2) | 34 (40.0) | ||||
| Employed (including in education) | Unemployed | 43 | 27 (62.8) | 42 | 26 (61.9) | 85 | 53 (62.3) |
| Employed | 16 (37.2) | 16 (38.1) | 32 (37.7) | ||||
| Offence category | Serious violence or sexual offence | 43 | 9 (20.9) | 42 | 5 (11.9) | 85 | 14 (16.5) |
| Assault | 23 (53.5) | 23 (54.8) | 46 (54.1) | ||||
| Other, including possession of weapon, driving and wilful fire-raising, burglary or theft or drug related | 11 (25.6) | 14 (33.4) | 25 (29.4) | ||||
| Had previous ADHD treatment | Yes | 43 | 10 (23.3) | 42 | 11 (26.2) | 85 | 21 (24.7) |
| No or unknowna | 33 (76.7) | 31 (73.8) | 64 (75.3) | ||||
| Age (years) when ADHD medication last taken | ≤ 13 | 10 | 3 (30.0) | 11 | 1 (9.0) | 21 | 4 (19.1) |
| ≥ 14 | 7 (70.0) | 5 (45.5) | 12 (57.1) | ||||
| Unknown | 0 (0.0) | 5 (45.5) | 5 (23.8) | ||||
| Baseline characteristics | OROS-MPH arm | Placebo arm | Overall | |||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| Age (years) (range 16–25) | 43 | 19.4 (1.1) | 42 | 19.7 (1.2) | 85 | 19.6 (1.2) |
| IQ (WASI-II score) | 43 | 91.0 (14.0) | 42 | 89.4 (13.9) | 85 | 90.2 (13.9) |
| Height (cm) | 43 | 175.3 (7.5) | 42 | 175.7 (5.5) | 85 | 175.5 (6.6) |
| BMI (kg/m2) | 43 | 23.0 (3.8) | 42 | 23.0 (3.3) | 85 | 23.0 (3.5) |
| Clinical measures | ||||||
| CAARS-O score (range 0–54) | 43 | 34.2 (9.2) | 42 | 33.5 (8.1) | 85 | 33.9 (8.6) |
| CAARS-O hyperactivity score (range 0–27) | 43 | 17.3 (5.5) | 42 | 16.8 (5.1) | 85 | 17.1 (5.2) |
| CAARS-O inattention score (range 0–27) | 43 | 16.9 (4.9) | 42 | 16.7 (4.1) | 85 | 16.8 (4.5) |
| WRAADDS score (range 0–30) | 43 | 16.2 (4.3) | 42 | 17.9 (4.4) | 85 | 17.1 (4.4) |
| WRAADDS – temper subscale score (range 0–9) | 43 | 4.4 (2.1) | 42 | 5.2 (2.0) | 85 | 4.8 (2.1) |
| WRAADDS – lability subscale score (range 0–12) | 43 | 7.3 (1.8) | 42 | 7.9 (1.8) | 85 | 7.6 (1.8) |
| WRAADDS – over-reactivity subscale score (range 0–9) | 43 | 4.6 (1.8) | 42 | 4.9 (1.8) | 85 | 4.7 (1.8) |
| ARI-S score (range 0–14) | 43 | 8.6 (3.4) | 42 | 9.1 (3.4) | 85 | 8.8 (3.4) |
| MEWS score (range 0–36) | 43 | 25.9 (4.8) | 42 | 27.4 (4.8) | 85 | 26.6 (4.8) |
| CGI-severity score (range 1–7) | 43 | 3.1 (0.5) | 42 | 2.9 (0.6) | 85 | 3.0 (0.5) |
| CORE-OM score (range 0–136) | 43 | 42.3 (12.4) | 42 | 43.0 (11.3) | 85 | 42.6 (11.8) |
| MVQ score (range 0–75)a | 43 | 34.3 (10.3) | 42 | 38.5 (9.4) | 85 | 36.4 (10.0) |
| Weiss-CD score (range 0–45) | 43 | 15.8 (6.5) | 42 | 18.9 (6.9) | 85 | 3.0 (0.5) |
| Systolic blood pressure (mmHg) | 43 | 122.5 (11.0) | 42 | 121.1 (11.3) | 85 | 121.8 (11.1) |
| Diastolic blood pressure (mmHg) | 43 | 69.7 (9.7) | 42 | 67.6 (10.1) | 85 | 68.7 (9.9) |
| Heart rate (beats per minute) | 43 | 72.2 (10.8) | 42 | 71.8 (11.8) | 85 | 72 (11.2) |
| Putative moderator variables | ||||||
| RPQ-Proactive score (range 0–24) | 43 | 7.5 (5.2) | 42 | 7.8 (5.3) | 85 | 7.6 (5.2) |
| RPQ-Reactive score (range 0–22) | 43 | 14.6 (4.4) | 42 | 14.4 (5.4) | 85 | 14.5 (4.9) |
| RPQ total (range 0–46) | 43 | 22.1 (8.9) | 42 | 22.1 (9.5) | 85 | 22.1 (9.2) |
| CTQ score (range 28–140)b | 43 | 47.3 (19.2) | 42 | 46.6 (20.9) | 85 | 46.9 (20.9) |
| ZAN-BPD score (range 0–36) | 43 | 5.3 (4.6) | 42 | 4.5 (2.2) | 85 | 4.9 (3.6) |
| BSI score (range 0–212) | 43 | 51.5 (33.9) | 42 | 45.8 (31.7) | 85 | 48.7 (32.8) |
| Coexisting disorders | Trial arm, n (%) | Overall (N = 85), n (%) | |
|---|---|---|---|
| OROS-MPH (N = 43) | Placebo (N = 42) | ||
| ASPD | 21 (48.8) | 29 (69.0) | 50 (74.5) |
| Mood disorder (major depression, suicidality, manic, hypomanic) | 20 (46.5) | 20 (47.6) | 40 (47.1) |
| Anxiety disorder (panic, agoraphobia, social anxiety, obsessive–compulsive disorder, PTSD) | 4 (9.3) | 3 (7.1) | 7 (8.2) |
| Potential problematic alcohol usea | 43 (100.0) | 42 (100.0) | 85 (100.0) |
| Illicit drug useb | 38 (88.4) | 37 (88.1) | 75 (88.2) |
| MINI checklist symptom scores (range 0–10 for each item) | Minimum/median/maximum | Minimum/median/maximum | Minimum/median/maximum |
| Depression | 0/1/3 | 0/1/4 | 0/1/4 |
| Anger | 0/3/7 | 0/4/7 | 0/4/7 |
| Mania | 0/0/3 | 0/0/3 | 0/0/3 |
| Anxiety | 0/1/5 | 0/1/6 | 0/1/6 |
| Physical symptoms | 0/0/5 | 0/0/2 | 0/0/5 |
| Suicidal thoughts | 0/0/2 | 0/0/3 | 0/0/3 |
| Psychosis | 0/0/1 | 0/0/1 | 0/0/1 |
| Sleep problems | 0/2/7 | 0/4/9 | 0/4/9 |
| Memory problems | 0/2/6 | 0/3/7 | 0/2/7 |
| Repetitive thoughts/behaviours | 0/0/4 | 0/0/4 | 0/0/4 |
| Dissociation | 0/0/0 | 0/0/1 | 0/0/1 |
| Personality function | 0/0/4 | 0/1/5 | 0/0/5 |
| Baseline behaviour report | OROS-MPH arm | Placebo arm | Overall | |||
|---|---|---|---|---|---|---|
| Participants (n) | Minimum/median/maximum | Participants (n) | Minimum/median/maximum | Participants (n) | Minimum/median/maximum | |
| MOAS-P score (range 0–40) | 43 | 0/0/15 | 42 | 0/0/19 | 85 | 0/0/19 |
| MOAS-E score (range 0–40) | 17 | 0/0/1 | 17 | 0/0/6 | 34 | 0/0/6 |
| BRC-P score | 43 | 6/9/24 | 42 | 6/10/21 | 85 | 6/9/24 |
| BRC-E score | 17 | 13/18/41 | 17 | 13/21/40 | 34 | 13/19/41 |
| Number of critical incidents | 43 | 0/0/6 | 42 | 0/0/10 | 85 | 0/0/10 |
| Number of days in prison out of the 56 days prior to randomisation, mean (SD) | 43 | 53.7 (7.2) | 42 | 55.8 (1.1) | 85 | 54.7 (5.2) |
| Number of education sessions (any type) scheduled | 43 | 0/54/123 | 42 | 0/62/126 | 85 | 0/57/126 |
| Number of education sessions (any type) attended | 43 | 0/31/112 | 42 | 0/34/126 | 85 | 0/34/126 |
| Proportion of scheduled education sessions (any type) attended, mean (SD) | 43 | 0.65 (0.38) | 42 | 0.73 (0.33) | 85 | 0.69 (0.36) |
Appendix 5 Concomitant medication at baseline and during the trial
Concomitant medication at baseline
A total of 60 participants (33 in the OROS-MPH arm and 27 in placebo arm) had no concomitant medication at baseline. Note that paracetamol was not logged at HM YOI Polmont, as such medication was dispensed by prison officers.
| Class of drug | Trial arm, n (%) | Overall, n (%) | |
|---|---|---|---|
| OROS-MPH | Placebo | ||
| Antidepressant | 13 (12.9) | 10 (10.1) | 23 (11.5) |
| Antihistamine | 1 (1.0) | 1 (1.0) | 2 (1.0) |
| Antipsychotic | 2 (2.0) | 4 (4.0) | 6 (3.0) |
| Methadone | 0 (0.0) | 1 (1.0) | 1 (0.5) |
| OROS-MPH | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Herbal sedative | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Melatonin | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Nicotine | 5 (5.0) | 3 (3.0) | 8 (4.0) |
| Non-psychotropic | 18 (17.8) | 25 (25.3) | 43 (21.5) |
| Propanolol | 4 (4.0) | 1 (1.0) | 5 (2.5) |
| Sodium valproate | 1 (1.0) | 0 (0.0) | 1 (0.5) |
Concomitant medication during the trial
A participant was given a standard dose of OROS-MPH from commercial stock in error.
| Class of drug | Trial arm, n (%) | Overall, n (%) | |
|---|---|---|---|
| OROS-MPH | Placebo | ||
| Antidepressant | 1 (1.0) | 2 (2.0) | 3 (1.5) |
| Antihistamine | 7 (6.9) | 6 (6.1) | 13 (6.5) |
| Antipsychotic | 1 (1.0) | 0 (0.0) | 1 (0.5) |
| OROS-MPH | 1 (1.0) | 0 (0.0) | 1 (0.5) |
| Herbal sedative | 1 (1.0) | 0 (0.0) | 1 (0.5) |
| Melatonin | 0 (0.0) | 1 (1.0) | 1 (0.5) |
| Nicotine | 6 (5.9) | 5 (5.1) | 11 (5.5) |
| Non-psychotropic | 36 (35.6) | 41 (41.4) | 77 (38.5) |
| Propanolol | 0 (0.0) | 1 (1.0) | 1 (0.5) |
| Sodium valproate | 1 (1.0) | 0 (0.0) | 1 (0.5) |
Appendix 6 Additional information regarding illicit drug use prior to incarceration
Of the 200 trial participants, 194 reported using drugs of one or more types in the year prior to incarceration. The number of drugs used by an individual is shown in Table 43. As would be expected from randomisation, the two trial arms were balanced in terms of illicit drug use.
| Class of drug | Trial arm, n (%) | Overall, n (%) | |
|---|---|---|---|
| OROS-MPH | Placebo | ||
| Cannabis | 97 (96.0) | 93 (93.9) | 190 (95.0) |
| Cocaine | 53 (51.5) | 48 (48.5) | 101 (50.5) |
| Methamphetamine | 28 (27.7) | 21 (21.2) | 49 (24.5) |
| Inhalants | 4 (4.0) | 5 (5.1) | 9 (4.5) |
| Sedatives or sleeping pills | 22 (21.8) | 21 (21.2) | 43 (21.5) |
| Hallucinogens | 38 (37.6) | 28 (28.3) | 66 (33.0) |
| Street opioids | 5 (5.0) | 4 (4.0) | 9 (4.5) |
| Prescription opioids | 10 (9.9) | 16 (16.2) | 26 (23.0) |
| Spice | 12 (11.9) | 21 (21.2) | 33 (16.5) |
| Other | 30 (10.0) | 25 (8.7) | 55 (9.4) |
| None | 2 (0.7) | 4 (1.4) | 6 (1.0) |
| Total number of drugs used | Trial arm, n (%) | Overall, n (%) | |
|---|---|---|---|
| OROS-MPH | Placebo | ||
| 0 | 2 (2.0) | 4 (4.0) | 6 (3.0) |
| 1 | 35 (34.7) | 39 (39.4) | 74 (37.0) |
| 2 | 13 (12.9) | 13 (13.1) | 26 (13.0) |
| 3 | 21 (20.8) | 10 (10.1) | 31 (16.0) |
| 4 | 8 (7.9) | 11 (11.1) | 19 (10.0) |
| 5 | 6 (5.9) | 6 (6.1) | 12 (6.0) |
| 6 | 9 (8.9) | 7 (7.1) | 16 (8.0) |
| 7 | 7 (6.9) | 9 (9.1) | 16 (8.0) |
List of abbreviations
- ADHD
- attention deficit hyperactivity disorder
- AE
- adverse event
- AES
- Adverse Events Scale
- ARI-S
- Affective Reactivity Index-Self
- ASPD
- antisocial personality disorder
- AUDIT-C
- Alcohol Use Disorders Identification Test for Consumption
- BMI
- body mass index
- BPD
- borderline personality disorder
- BRC-E
- Behaviour Report Card-Education
- BRC-P
- Behaviour Report Card-Prison
- BSI
- Brief Symptom Inventory
- CAARS-O
- Conners’ Adult Attention deficit hyperactivity disorder Rating Scale-Observer
- CGI
- Clinical Global Impression
- CI
- confidence interval
- CIAO
- Concerta in Adult Offenders with ADHD
- CONSORT
- Consolidated Standards of Reporting Trials
- CORE-OM
- Clinical Outcomes in Routine Evaluation – Outcome Measure
- CRA
- clinical research associate
- CTQ
- Childhood Trauma Questionnaire
- DIVA 2.0
- Diagnostic Interview for ADHD in Adults 2.0
- DMC
- Data Monitoring Committee
- DSM-5
- Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- DSM-IV
- Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition
- GCP
- good clinical practice
- GMP
- good manufacturing practice
- GP
- general practitioner
- HDPE
- high-density polyethylene
- HM YOI
- Her Majesty’s Young Offender Institution
- HMP
- Her Majesty’s Prison
- HMP YOI
- Her Majesty’s Prison and Young Offender Institution
- HMPPS
- Her Majesty’s Prison and Probation Service
- HRA
- Health Research Authority
- IEP
- Incentive and Earned Privilege
- IME
- important medical event
- IMP
- investigational medicinal product
- IQ
- intelligence quotient
- IT
- information technology
- ITT
- intention to treat
- KCTU
- King’s Clinical Trials Unit
- KHP CTO
- King’s Health Partners Clinical Trials Office
- MEWS
- Mind Excessively Wandering Scale
- MHRA
- Medicines and Healthcare products Regulatory Agency
- MI
- multiple imputation
- MINI
- Mini International Neuropsychiatric Interview
- MOAS
- Modified Overt Aggression Scale
- MOAS-E
- Modified Overt Aggression Scale-Education
- MOAS-P
- Modified Overt Aggression Scale-Prison
- MPH
- methylphenidate
- MVQ
- Maudsley Violence Questionnaire
- NICE
- National Institute for Health and Care Excellence
- NIDA
- National Institute on Drug Abuse
- OROS
- osmotic release oral system
- PTSD
- post-traumatic stress disorder
- R&D
- research and development
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- RPQ
- Reactive–Proactive Aggression Questionnaire
- SAE
- serious adverse event
- SAP
- statistical analysis plan
- SAR
- serious adverse reaction
- SD
- standard deviation
- SDV
- source data verification
- SMD
- standardised mean difference
- SmPC
- Summary of Product Characteristics
- SPS
- Scottish Prison Service
- SUD
- substance use disorder
- SUSAR
- suspected unexpected serious adverse reaction
- TBI
- traumatic brain injury
- TMG
- Trial Management Group
- TSC
- Trial Steering Committee
- WASI-II
- Wechsler Abbreviated Scale of Intelligence® Second Edition
- Weiss-CD
- Weiss Conduct Disorder scale
- WRAADDS
- Wender–Reimherr Adult Attention Deficit Disorder Scale
- ZAN-BPD
- Zanarini Rating Scale for Borderline Personality Disorder
