Notes
Article history
The contractual start date for this research was in July 2017. This article began editorial review in July 2023 and was accepted for publication in February 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Global Health Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2025 Mytton et al. This work was produced by Mytton et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2025 Mytton et al.
Introduction
Injury is one of the world’s most preventable and important public health problems. Globally, unintentional and intentional injuries are estimated to take the lives of 4.4 million people every year, or 8% of all deaths. 1 For children and young people aged 5–29 years, road traffic injuries (RTIs), suicide and homicide are three of the top five causes of death. 1 Approximately 10% of disabilities are secondary to injuries and violence, and these injuries may have long-term consequences for individuals and their families. Injuries do not occur equitably across society: males are more likely to be injured than females, injury risk varies across the life course and by ethnic group, and people who live in greater disadvantage are more likely to be exposed to circumstances that place them at risk of being injured. Being injured can lead to loss of employment opportunities and income and may tip families into poverty. Over 90% of global injuries occur in low- and middle-income countries (LMICs). 2 One-third of the world’s morbidity and mortality due to injuries occurs in the 11 countries of the South-East Asia region. 3
Nepal appears in the lowest income category of countries globally and is on the Development Assistance Committee list as a country eligible to receive Official Development Assistance. The population of Nepal are at high risk of both unintentional and intentional harm from injuries. A major cause of fatal and non-fatal injuries in Nepal is road traffic crashes. 4 In the absence of rail infrastructure or commercial waterways, roads are the main method of transportation for goods and people in Nepal. A huge road-building programme over the last decade has seen 80,078 km of roads built and vehicle numbers increased by 800,000 in recent years. 4,5 Many new roads are not built with proven safety features and are poorly maintained. Nepal lacks an independent and fully functioning national road safety agency, vehicle safety standards are inadequate, and there is limited enforcement of existing traffic safety legislation. Rapid motorisation is leading to increased RTIs and deaths; however, without any injury surveillance, robust death registration or complete traffic police injury systems, the true numbers are unknown. RTI mortality was estimated at 15.95/100,000 population in 2018. 6 Sustainable Development Goal (SDG) 3 has a target to halve road traffic mortality by 2030. 7 A national Road Safety Action Plan8 was approved by the government in 2012, but in the absence of a functioning lead agency for road safety, action did not progress. A new road safety action plan for the second decade of action on road safety9 is awaited. Road injuries are more frequent and more severe in rural areas and in built-up areas alongside highways. 10
Most of the resident workforce is employed in agriculture. Household surveys and hospital data suggest that home injuries (e.g. falls, burns, poisoning), occupational injuries and animal-related injuries are significant,11–13 but true estimates are unclear. In addition, there are limited and variable emergency services,14 with little availability of effective prehospital care, so injured people often travel for hours to the nearest hospital without any stabilisation of their injuries, and they may deteriorate or die during the journey. Nepal is prone to natural disasters which lead to injuries. 15 In 2015, earthquakes killed almost 9000 and injured over 22,000 people. 16 The earthquake of April 2015 illustrated the fragility of the housing and road infrastructure, and the poor level of first aid skills and access to health care.
Tackling the burden of injuries in Nepal has the potential not only to save lives and prevent disability, but also to promote the economic and welfare development of the country. Nepal has experienced dramatic recent social, political and economic change. Democracy was established in 1990, but political instability held back development, with coalition governments changing on average once per year between 2007 and 2018. The constitution of Nepal, agreed in 2015 and enacted in 2018, has provided greater political stability and seen the implementation of a federalised system of government with decisions being made at national, provincial and local levels. The Nepal Ministry of Health and Population included the SDG aim of halving the burden of RTIs by 2020 in its Health Sector Strategy for 2015–20. 17 Other relevant recommendations stated in the strategy include the implementation of a surveillance system for RTIs (Outcome 7), strengthening the management of public health emergencies by mobilising trained human resources during emergencies (Outcome 8), and improving the availability and use of evidence in decision-making (Outcome 9).
Most injuries are the predictable outcome of specific circumstances. 18,19 By identifying those who are most likely to sustain injuries, and by establishing the personal, social, environmental, economic and political factors associated with injury events, society is able to intervene to prevent injuries from occurring. Research to establish effective and cost-effective interventions to prevent injuries has mostly occurred in high-income countries. Replicating an injury prevention intervention from a high-income country in a LMIC without adapting the intervention to the cultural and contextual norms of that setting means that it is unlikely to achieve its intended benefits.
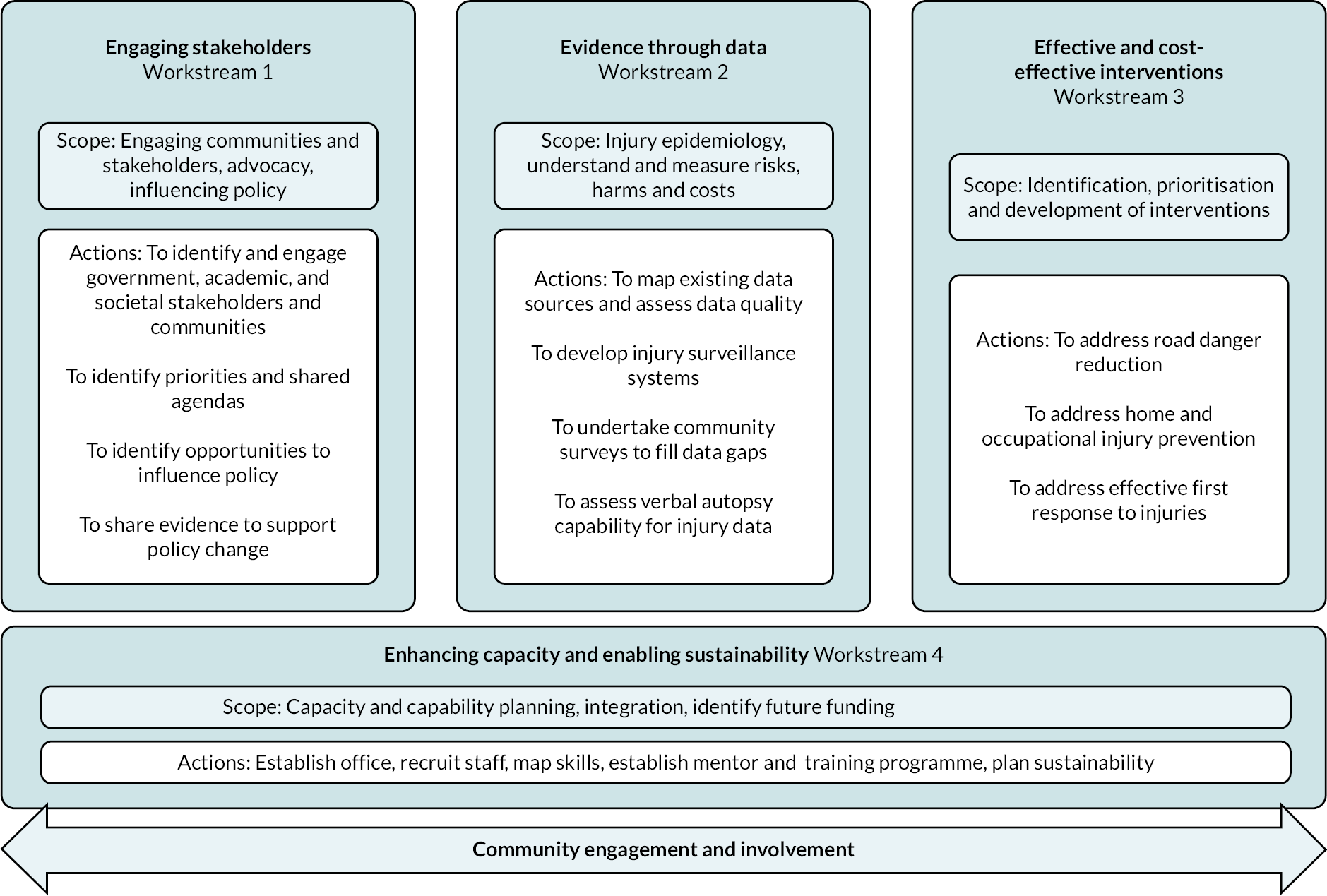
There was therefore a clear rationale for the proposal to develop the evidence base for injury prevention in Nepal. Funding from the National Institute for Health and Care Research (NIHR) enabled researchers at the University of the West of England (UWE), Bristol, to establish a partnership with Kathmandu Medical College (KMC) and establish there the Nepal Injury Research Centre (NIRC) with the dual aims of: (1) building capacity for injury prevention in Nepal and (2) establishing the epidemiology of injuries and identifying opportunities for intervention. The aim of the NIRC was to work with communities, advocacy groups, health organisations and the Government of Nepal to generate evidence to ultimately inform policies and change practice. Our research programme had three workstreams: (1) engaging stakeholders; (2) evidence through data; and (3) effective and cost-effective interventions. A fourth cross-cutting workstream focused on enhancing capacity and capability for injury prevention research and sustainability, and ran alongside a cross-cutting theme of community engagement and involvement.
Research pathway diagram
Each of the four workstreams was led by a member of the Nepal team with one or more UK advisers. Figure 1 illustrates the four workstreams delivered through the NIHR Global Health Research Group (GHRG) award.
FIGURE 1.
Overview of NIHR GHRG on Nepal Injury Research.
Summary of findings
Overview of outputs
The NIRC team completed 24 projects and publications through our NIHR GHRG award. In addition, a further three publications related to the engagement of stakeholders were generated through collaborations and additional funding consequent to the NIHR GHRG award. Workstream 4 (enhancing capacity and enabling sustainability) was designed to provide opportunities for training and development of the research team through engagement in the projects being delivered in workstreams 1–3. We did not formally evaluate the capacity-strengthening activities and therefore there are no publications from this workstream. An overview of these outputs, by workstream, is provided in Figures 2 and 3. Figure 2 summarises outputs by study design and participant number, and Figure 3 summarises outputs by topic.
FIGURE 2.
Overview of study designs and total participant engagement by workstream.
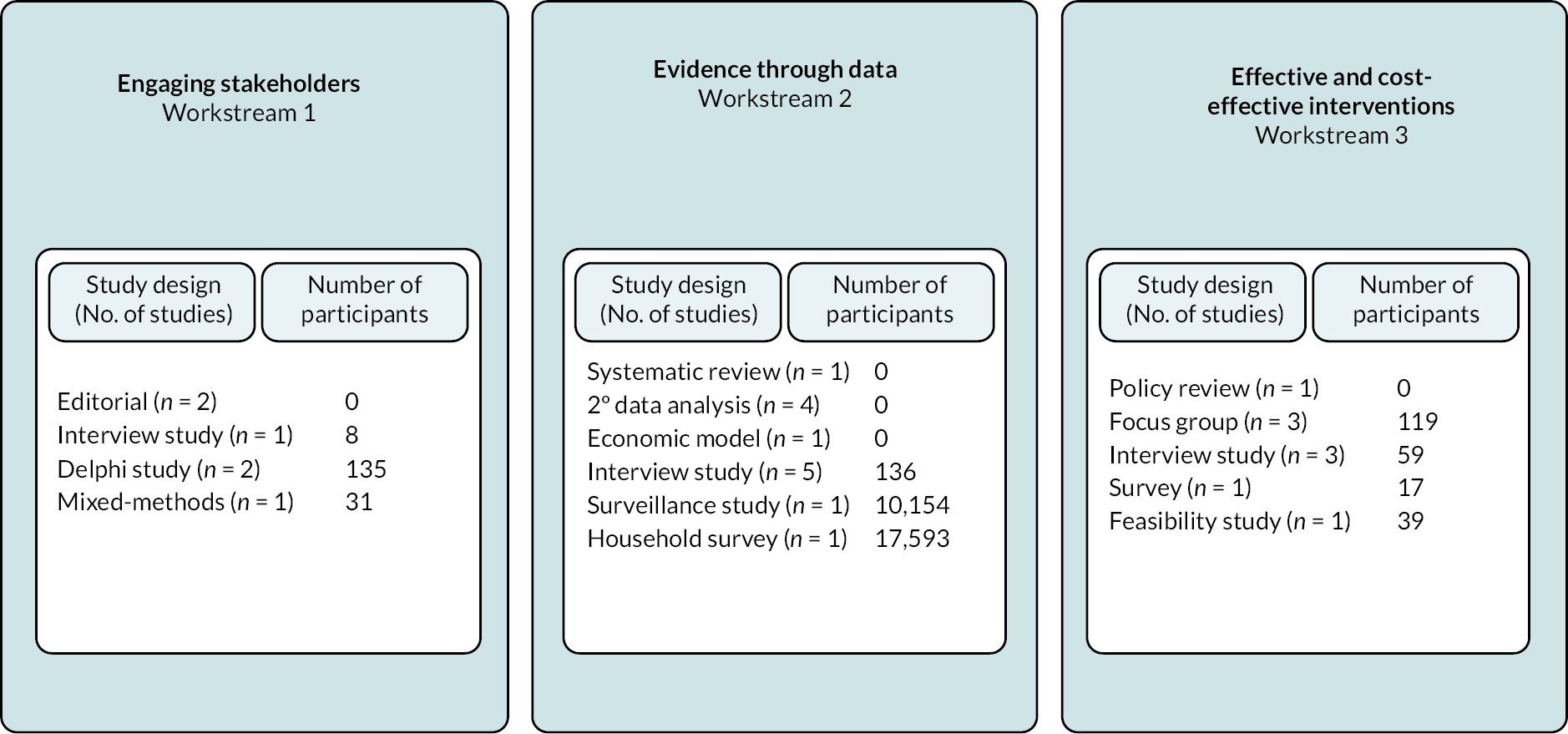
FIGURE 3.
Overview of publications arising from the NIHR GHRG on Nepal Injury Research, by workstream and topic. Footnote: Publications directly arising from the NIHR GHRG award are in black. Study titles may have been shortened for inclusion in this figure. Related publications funded through other sources are included in blue.
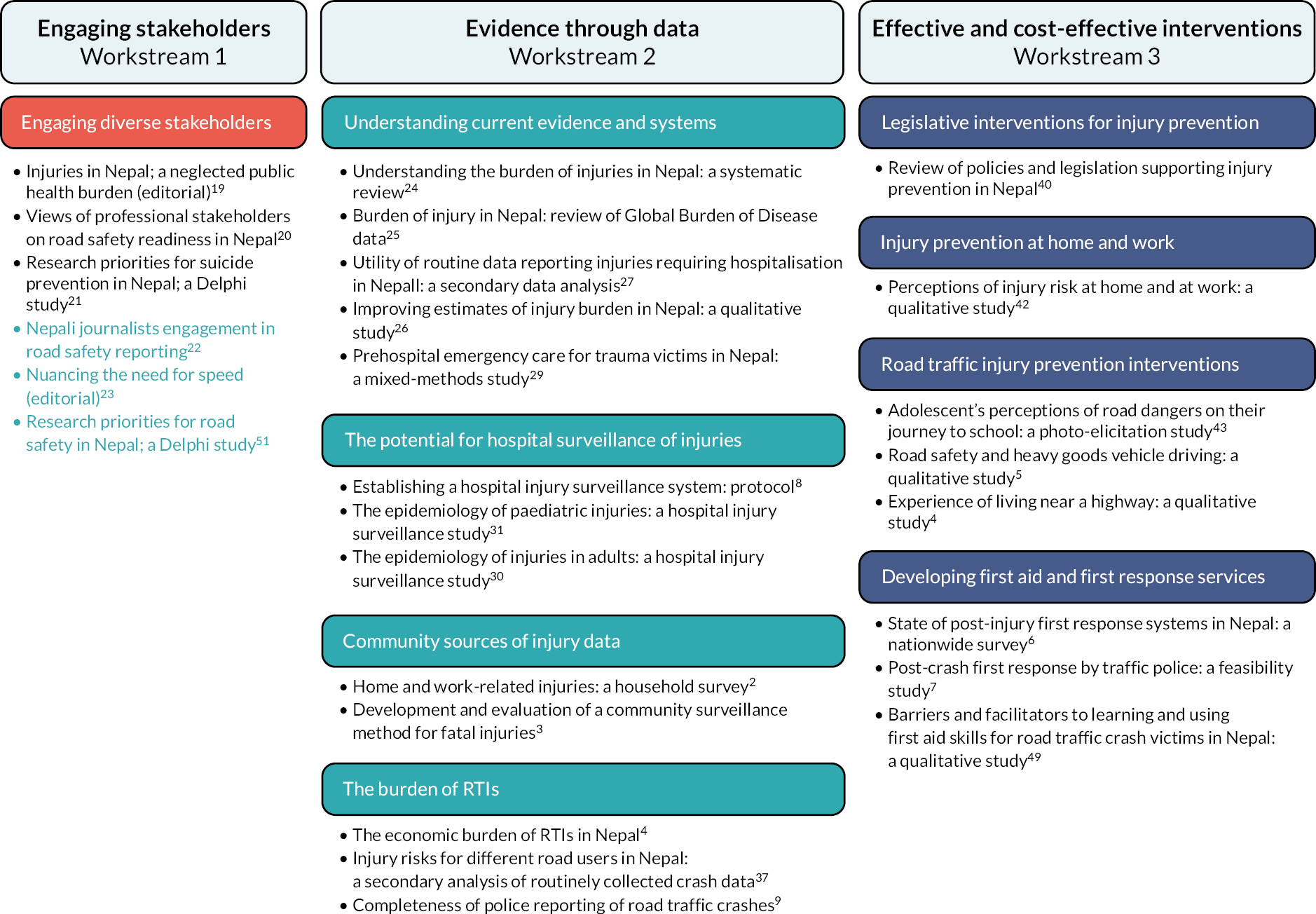
Early during the conduct of our NIHR GHRG award, through engagement with stakeholders from across different sectors, we became aware of concerns regarding the quality of routinely collected injury data in Nepal. This consequently became a significant focus of our work: to analyse these data to provide baseline estimates of injury burden, while identifying the strengths and limitations of the data systems and identifying opportunities to strengthen them. Consequently, 13 of the 24 primary publications relate to workstream 2. The absence of robust routinely collected injury data creates a barrier to the assessment of the impact of interventions unless bespoke outcome data collection systems are established. Activities in workstream 3 (effective and cost-effective interventions) focused primarily on the identification and prioritisation of areas for future injury prevention intervention development. The exception to this was the development of an intervention to train the traffic police in first aid for people injured in road traffic crashes, which was an intervention heavily promoted by stakeholders.
Project findings by workstream
Workstream 1 (engaging stakeholders)
Three primary publications and three related publications were produced under this workstream. A description of the aim and main findings of the three primary publications is followed by a description of the three related publications.
-
Injuries in Nepal: a neglected public health burden and ways forward 20
This editorial was published early in our award with the aim to inform other academics in Nepal that we had established the NIRC and that our intention was to strengthen the evidence available to inform policy and practice change. We highlighted the preventability of unintentional injuries, how injuries occur unequally across society and the current burden of injuries on the health-care system. To reach our intended audience, the editorial was published in one of the well-known Nepali medical journals.
-
Views of professional stakeholders on readiness for a safe road system in Nepal; an exploratory qualitative study 21
This study was completed early in our programme and designed to be small scale and exploratory in nature so that it could inform future road safety research activities. We aimed to explore the perspectives of diverse professionals whose jobs had the potential to influence the development of a safe road system in Nepal. Semistructured interviews with eight key informants were analysed thematically. The three themes identified were: the need to modify the behaviour of road users; the role of road planning, construction and maintenance; and the importance of good governance of roads. Areas for further inquiry and action were identified. Evidence from countries that have some of the lowest crash rates in the world indicates that creating a road system where the environment promotes safer driving and which is forgiving when drivers make mistakes is more effective in reducing road injuries and deaths than changing individual driver behaviour. 9 This illustrates the cultural shift necessary in Nepal from an assumption that individual behaviour change and improvements in an individual’s knowledge are more effective than environmental and legislative change. The participants acknowledged that there is already legislation in Nepal that could make the roads safer, but that this is often not implemented or enforced.
-
Identification of research priorities for suicide prevention in Nepal: a Delphi study 22
The initial 3-year funding for our NIHR GHRG award focused on unintentional injuries. During the first 2 years of our award, stakeholder feedback, secondary analysis of routine injury data and our own primary data collection indicated the significant and largely unacknowledged burden of suicide and self-harm in Nepal. When bidding for a further year of funding, we argued that a study to better understand the research priorities for suicide prevention in Nepal was justified. We conducted a Delphi study involving 42 participants including suicide prevention experts (psychiatrists, psychologists, psychiatric nurses, researchers and advocates) and individuals and families with experience of attempted suicide. Individual interviews yielded potential research questions which were then subjected to two rounds of ranking for importance. Prioritised research questions fell into three groups: studies to inform a better understanding of the epidemiology of suicide in Nepal; studies to strengthen evidence-based practice in prevention and response; and studies to better understand the needs of those at risk of self-harm and their families.
The related publications are summarised below.
-
Engaging Nepali journalists in good road safety reporting: evaluation of the impact of training workshops 23
In many low-income countries, Nepal included, media reports of road traffic crashes tend to be sensationalist, focusing on the number of dead or injured and frequently failing to provide information on their cause or preventability. Recognising journalists as stakeholders with the ability to influence public opinions and perceptions of safety, the World Health Organization (WHO) has developed two resources for journalists: a good reporting guide and a set of story ideas to encourage journalists to consider responsible reporting of crashes and injuries. Working with the WHO Nepal office, we were able to get these resources translated into Nepali and subsequently held three workshops for journalists from across a range of different media formats (print, radio, television and internet). Thirty-one journalists attended at least one of three workshops that were held over 9 months. Additional funding from UWE facilitated an evaluation of the workshops using a survey and a critical review of participating journalists’ outputs before and after participation. Participants responded positively to the opportunity to participate in the workshops, and there was an increase in the use of story ideas subsequent to attendance.
-
Nuancing the need for speed; temporal health system strengthening in low-income countries 24
This editorial was written by authors from NIHR GHRGs with a focus on injuries who met at a NIHR meeting early in 2019. The paper discusses the multiple factors that influence the ability to deliver timely quality care to patients experiencing trauma in low-resource settings. It describes how a robust understanding of the context (social, political, historical, cultural) is as important as an understanding of the underlying health-care system to generate improvements in health outcomes.
A third related publication reporting a Delphi study to identify the research priorities for road safety in Nepal is described in Related work.
Workstream 2: evidence through data
Understanding current evidence and systems
We completed five studies that utilised existing data to provide baseline epidemiological knowledge.
-
Understanding the burden of injuries in Nepal: a systematic review of published studies 25
This was the first study completed during our NIHR GHRG award. We systematically collated literature reporting numbers or rates of injuries sustained by people of any age who were residents in Nepal at the time of their injury and synthesised these data narratively. We excluded case series of fewer than 10 cases, studies reporting only the management of injuries or birth trauma, and secondary reports of previously published data. We identified 186 manuscripts published before September 2017 that reported 176 individual studies. Most (77%) publications were case series, frequently from one health-care provider. Thirty-six (19%) publications reported cross-sectional studies, mostly small surveys. Other than descriptive reporting by age and gender, there was very little exploration of inequalities in injury occurrence. We were surprised to find that only 22 (12%) publications reported RTIs, despite stakeholders advising us that this was the injury type causing the greatest concern in Nepal.
-
The burden of injuries in Nepal, 1990–2017: findings from the Global Burden of Disease Study 2017 (GBD 2017) 26
We analysed estimated data published in the GBD 2017 to explore injury-related deaths, years of life lost, incidence and disability-adjusted life-years in Nepal between 1990 and 2017. Over this period, injuries secondary to road traffic, falls and self-harm all increased in rank for cause of death, while injury-specific age-standardised mortality rates fell over the same period. GBD 2017 uses available routinely collected data on mortality, cause of death, incidence and prevalence to generate estimates suitable for international comparisons and to explore in-country trends over time. While the findings from our study indicate the increasing proportion of health burden and death due to injuries, we know that not all data sources were available to contribute to estimates for Nepal. Although GBD 2017 methods include modelling to adjust for under-reporting and misclassification of the cause of death, outputs may still underestimate the true health burden secondary to injuries in Nepal.
-
Utility of routine data reporting injuries requiring hospitalisation in Nepal 27
In the absence of national-level injury surveillance, routinely collected data from healthcare providers on attendance and admission to hospital can provide estimates of non-fatal injury burden. The Health Management Information System (HMIS) is used in healthcare settings across Nepal to record inpatient admissions and outpatient attendances, with monthly reports routinely submitted to the government. This study aimed to explore the utility of HMIS data to describe the burden of injuries in Nepal and to explore inequalities in injury admissions by age and sex. Published HMIS data on inpatient admissions between 2009–10 and 2016–7 were collated and analysed. Crude rates of total unintentional injury admissions increased over this period, while that for self-harm decreased. Analyses revealed how the rates of different types of injuries increased or decreased over time and how men and women, and people of different ages, experienced different injury rates. We noted variations in how different types of injuries were coded from year to year, suggesting that training and monitoring of data coders may be important to improve data quality, and how artefacts in data coding could account for apparently very low rates of some types of injuries.
-
Improving estimates of injury burden in Nepal: a qualitative study 28
This study built on the study analysing HMIS data reported above, and aimed to explore the strengths, and opportunities for improvement, of systems that routinely measured injury incidence. We evaluated four injury data systems: injury admissions and attendances captured through HMIS; the Road Accident Reporting system (recording traffic-related deaths and injuries captured by the traffic police); the Daily Incident Reporting system (recording unexplained deaths such as those secondary to drowning or self-harm, and captured by police departments); and deaths recorded through the civil registration system. Interviews were conducted with both front-line data collectors and strategic decision-makers across all four systems. We generated data flow diagrams to illustrate the data systems, and used framework analysis to identify and describe the strengths, limitations and opportunities of the four data systems. For all systems, opportunities were identified to improve the completeness of data collection and the accuracy and consistency of coding. Electronic data systems appeared to address some deficiencies; however, these were only likely to improve data validity with additional investment, training and monitoring.
-
Prehospital emergency care for trauma victims in Nepal: a mixed methods study 29
This study aimed to explore current knowledge and experience of providing prehospital care to people with injuries in Nepal. With no national ambulance service or emergency services phone number, the public tend to call any local hospital when seeking emergency help. Ambulances provided by local hospitals often only convey victims to healthcare facilities, and a professional trained to provide first aid (emergency medical technician, EMT) is not always available to travel with the patient. Working with the Nepal Ambulance Service, the largest prehospital care provider in Nepal, we completed a mixed-methods study including a secondary data analysis of 1 year of callout data and interviewed ambulance drivers, EMTs, dispatch officers and managers. Of 1408 trauma calls over 1 year, less than half involved the provision of care to patients either at the scene, en route to hospital or both. Cause of injury was not recorded in one-third of records. Interviews revealed the challenges of providing effective first response in an unco-ordinated system of largely private ambulance services. Heavy traffic, lack of prioritisation of emergency vehicles on the road and poor road quality often impeded arrival at the scene and delayed transport to hospital. At the scene, bystanders may not allow the EMTs to provide care but insist that the patient be immediately transferred to the hospital. Barriers to care and the opportunities for change identified indicate areas for future policy change and professional development. Promulgation of a ‘Good Samaritan’ law would support prehospital care providers to treat at the scene and en route without fear of future prosecution.
The potential for hospital surveillance of injuries
There is no current system of injury surveillance in Nepal to inform policy and practice. Therefore, working with one government hospital and one private hospital and their emergency department teams, we developed and implemented a hospital injury surveillance system in these two settings. We evaluated the feasibility of collecting data on every injury attendance in these two emergency departments over the course of 1 year and completed a process evaluation to understand the generalisability and sustainability of the model. The study resulted in three publications.
-
Establishing injury surveillance in emergency departments in Nepal: protocol for mixed methods prospective study 30
The first publication was a paper justifying the need for valid injury data to support the reduction of injury morbidity and mortality through improved prevention, policy development, and the allocation of resources and care. 30 The paper described our study protocol, the development of the injury surveillance system and the methods of the process evaluation.
-
The epidemiology of injuries in adults in Nepal: findings from a hospital-based injury surveillance study 31
-
Epidemiology of paediatric injuries in Nepal: evidence from emergency department injury surveillance 32
Two publications reported the results of the hospital surveillance study, one describing the epidemiology of injuries sustained by adults and the second describing the epidemiology of injuries sustained by children under the age of 18 years. 31,32 Over one-third of all attendances at these two emergency departments over 12 months were due to injuries. Of 7458 injuries in adults, the most common causes were road traffic collisions, falls and animal-related injuries. The impact on health services was significant, with 9.1% of adult injuries requiring admission and a further 8.1% transferred to another hospital for care. Of the 2696 children attending over the same period, two-thirds were male and over half were under 10 years of age. The three commonest causes of injury in children were falls, animal bites/stings and RTIs. Dog bites were a frequent cause of attendance, previously unreported in any literature on injuries in children in Nepal. We noted a surprisingly small proportion of attendances for some injury types, such as burns, suggesting that these may be treated at home. Limited staff in emergency departments meant that additional human resources were required for effective data collection. The hospital management teams valued the data that were fed back to them, and they recognised the potential of receiving such data on a routine basis.
Community sources of injury data
We completed two studies exploring community sources of injury data to improve our understanding of the epidemiology of injuries.
-
Home-related and work-related injuries in Makwanpur district, Nepal: a household survey 33
In this study we used a household survey to collect data to describe the epidemiology and burden of non-fatal injuries sustained at home and at work during the previous 3 months and fatal injuries occurring to household members in the previous 5 years. We surveyed almost 17,600 individuals from 3327 households across one district in Nepal and reported rates of non-fatal injuries sustained at home and at work. We explored the issue of inequalities in injury occurrence, which have rarely been reported in the published literature. We evidenced inequalities by sex, with more home injuries occurring to women and more work-related injuries occurring to men. Injury rates varied by ethnic group, illustrating a complex issue where the type of occupation is closely associated with an individual’s caste and ethnic group; often lower-caste individuals are employed in occupations with higher injury risks. Data collected on healthcare costs associated with injuries illustrated that households in the lowest income category sustained more home and work-related injuries than those in higher income categories, compounding health inequalities related to injury occurrence.
-
Development and evaluation of a community surveillance method for estimating deaths due to injuries in rural Nepal 34
Although death registration is mandatory in Nepal, in practice, registration may not take place or may be significantly delayed, and cause of death is reported by relatives and not by health practitioners. This study was designed to explore the feasibility of collecting improved injury death data through existing community health systems. Female Community Health Volunteers (FCHVs) are women who support the health of their local communities and have proved essential in the development of primary health care in Nepal. We asked FCHVs in two rural areas of one district to report any deaths in the community they served over the course of 1 year. Families of individuals who appeared to have died following an injury were offered an interview to understand the circumstances of the injury event and the death. Feedback from the FCHVs and other healthcare staff involved in the study indicated that the surveillance system had been feasible and was potentially scalable. Of 427 deaths reported across these two communities, 67 were considered secondary to an injury. We were surprised to find that two-thirds of the injury deaths were due to self-harm or assault. Most injuries had occurred at home, only 10% of individuals received health care prior to death, and only one-quarter of deaths had been registered at the ward office. The study showed that collecting enhanced fatal injury data from communities was feasible and pointed to a previously unreported burden of fatal injuries in the community being due to self-harm and at risk of not being captured through vital registration systems.
The burden of road traffic injuries
We completed three studies exploring the epidemiology and impact of RTIs.
-
Economic burden of road traffic injuries in Nepal 35
Illustrating the economic burden of RTIs can engage policy-makers in understanding the need for change. The most recent evaluation of the economic impact of RTIs in Nepal used data from the fiscal year 2006–7 and was considered out of date due to the rapid increase in the use of motor vehicles in the subsequent 14 years. This study aimed to provide an up-to-date estimate of the economic burden of RTIs. An incidence-based cost-of-illness analysis was undertaken, seeking to identify all costs to society. RTI incidence data were from the Nepal Traffic Police with other variables taken from published studies. Costs included were medical and non-medical costs; productivity losses; and pain, grief and suffering costs. Analysis revealed that the total economic burden from RTIs in 2017 was US$122 million, with costs associated with productivity losses far exceeding those of medical care. We know that not all traffic crashes and injuries are reported to the traffic police and that the recording of minor or serious injuries is a matter of judgement by the police officer rather than a clinical opinion. 36 Some cost data were not available, such as those associated with the provision of emergency care. Therefore, this estimate of the economic burden is likely to underestimate the true cost.
-
Injury risks for different road users in Nepal – an analysis of routinely collected crash data 37
To inform road safety strategy, policy-makers need to understand which road users and which types of vehicles are most likely to be involved in road traffic crashes. These data have not been reported for Nepal in the last three World Status Reports on Road Safety. 6,38,39 In this study, we critically reviewed police crash data in one district over 2 years to better understand the strengths and limitations of police data and the feasibility of reporting crashes by road user and vehicle type. The number of crashes increased over the two periods studied and the data confirmed previous findings of casualty victims being mostly male and young adults. One-third of casualties reported in these data were the riders of motorised two- or three-wheelers, followed by passengers of four-wheeled vehicles, and drivers and passengers of buses. Powered two-wheelers (motorcycles and scooters) were the most frequent type of vehicle involved in collisions, followed by lorries and tipper trucks and cars. We found incomplete recording of data across most variables and found that the classification systems used were ambiguous or not designed to inform road safety monitoring or policy. Ongoing efforts by the Nepal Traffic Police to move to an electronic crash recording system have the potential to improve data quality.
-
Completeness of police reporting of traffic crashes in Nepal: evaluation using a community crash recording system 40
To further explore our concern that road traffic crashes were under-reported by the traffic police, we designed a study to validate police records. We recruited six shopkeepers whose premises faced a busy section of one of the main highways in Nepal and supported them to record every traffic crash occurring along the section of the road visible from their premises over the course of 1 year. We then compared their records against those of the traffic police for the same locations and over the same period. The shopkeepers reported 110 crashes, 70 of which involved injuries or fatalities. Over the same period, the traffic police recorded less than one-fifth of those recorded by shopkeepers. Crashes involving fatalities were more likely to be captured in police data than those resulting in minor injuries or vehicle damage only. The use of community record-keepers was an effective way to estimate the degree of under-reporting of road traffic crashes and provides evidence to argue for action to improve the proportion of crashes reported.
Workstream 3: effective and cost-effective interventions
Legislative interventions for injury prevention
-
The prevention of – and first response to – injuries in Nepal: a review of policies and legislation 41
The aim of this study was to identify and critically appraise all current policies and legislation in Nepal that had the potential to prevent injuries. We identified policies and legislation using our networks, stakeholder engagement and internet searches. Documents were critically appraised using the policy analytical framework published by the US Centers for Disease Control and Prevention. 42 Policies and legislation were mapped against recommendations for effective interventions for different types of injuries that had been published by the WHO. We identified 62 policies and legislation, of which almost two-fifths related to road injury and one-fifth to occupational injury. Of 127 strategic recommendations by the WHO, only 17% were adequately met by the policies and legislation available. Findings need to be viewed in the context of a changing governmental system in Nepal and the formation of the federalised system of government. While some supportive legislation exists, much is not implemented, and we identified frequent absences of delegated leadership, co-ordination across government departments or allocation of funding to support action.
Injury prevention at home and work
-
Perceptions of injury risk in the home and workplace in Nepal: a qualitative study 43
This study was designed to understand the perceptions of injury risk and injury prevention across a variety of settings in Nepal. Nine focus groups and nine individual interviews were held with participants across three local government areas in southern Nepal, and across a mixture of urban and rural settlements. The study identified six themes. Participants identified that living and working conditions were perceived as locations where injury hazards were present. Safety infrastructure and equipment were often absent, reported as due to a lack of financial resources. The occurrence of the injury was often reported to be due to chance or a normal consequence of their circumstances, with apparently little agency to keep themselves or others safe. Children and teenagers were specifically identified as being at risk of injuries. A perception that they would not be at risk, and that people who were injured were careless, was reported as a reason why safety was not given a high priority in the workplace. A lack of awareness of the risks and the focus on an individual’s responsibility to keep themselves safe led to many recommending that awareness programmes were necessary, with the government having responsibility to develop laws and enforce safety rules where these exist.
Road traffic injury prevention interventions
-
Adolescent’s perception of road risk on their routes to school in Makwanpur, Nepal; a qualitative study 44
This was one of a series of qualitative studies we completed to better understand how communities experienced road traffic in Nepal. We worked with communities living alongside the East–West Highway, one of the country’s main transport routes. Many schools are located directly next to the highway, and in this study we gained agreement from the headteacher of one school to recruit students who walked along the highway, to and from school. Using photovoice methodology, we provided students with a digital camera and asked them to take pictures as they walked to school of things they considered made their journey either safe or dangerous. Once at school, the researcher used the children’s photographs to facilitate an interview about their experience of the road, the traffic and the risk of injury. The children highlighted both environmental and behavioural factors that made them feel unsafe on their journeys, including lack of pavements, parked vehicles requiring children to walk in the road, and difficulties in crossing roads due to speeding and other inconsiderate driving. The method provided an opportunity for children’s voices to be heard, and the photographs provided supportive testimony of their concerns.
-
Experience of living near a highway in Nepal: community perceptions of road dangers in Makwanpur district 45
This qualitative study aimed to capture the views of people living alongside the East–West Highway. Members of four existing community groups were recruited and participated in focus groups exploring their experiences and perceptions of any risks posed by living in proximity to the highway. Five themes emerged from the analysis. Participants described how all road users, but particularly drivers of vehicles, behaved in ways that increased the likelihood of being injured or causing injuries to others. Lorry drivers were particularly highlighted as driving too fast, overtaking dangerously, and causing the deaths of pedestrians and other road users. Participants described how a lack of pavements, safe places to cross the road, designated parking areas and bus stops increased the risk of crashes and injuries. Some participants recognised that increasing the width of the roadway was likely to lead to increased speeds and thus make the road more dangerous. Many participants felt that most drivers were not worried about prosecution for failing to adhere to the traffic rules, as these were not enforced. Strict enforcement of traffic legislation and a public awareness campaign was felt to be needed.
-
Road safety and heavy goods vehicle driving in LMICs: qualitative evidence from Nepal 46
In response to public perceptions of the dangers posed by lorry drivers, we sought the views of 15 heavy goods vehicle (HGV) drivers in one-to-one interviews and conducted a focus group with 11 members of a transportation entrepreneurs association. Drivers and their professional representatives felt that HGV drivers were frequently inappropriately blamed for crashes and injuries. They described how the driver of the largest vehicle was usually assumed to be at fault and that crashes were seldom investigated to determine the cause of the event. They perceived that this led to more dangerous behaviour by pedestrians and the drivers of motorcycles and smaller vehicles, as these people did not fear prosecution. Most HGV drivers felt they had to belong to a transportation association, as they needed administrative and financial support if they were involved in a collision. Participants acknowledged a poor safety culture in the industry, with the profession attracting drivers with little education who learnt through an apprenticeship model and were given little formal training. Indeed, formal training was viewed negatively, as it did not involve training on the road, only in designated training areas. Wages for drivers were reported to be low and based on the number of trips made rather than hours driven, which encouraged speeding to maximise the trips completed in a day. While alcohol use was widely recognised as forbidden, drivers described how drugs were used to help them keep awake during long days and to cope with the pressured working environment. Poor road infrastructure – such as potholes, narrow roads without pavements for pedestrians, and inadequate truck parking spaces – was reported to increase the risk of crashes.
Developing first-aid and first-response services
-
State of post-injury first response systems in Nepal – a nationwide survey 47
This study provided us with an understanding of the status of post-injury first-response systems in Nepal as we commenced our NIHR GHRG award. An online survey, sent to academic and governmental organisations and non-governmental organisations (NGOs) sought to identify all the providers of post-injury first-response services in Nepal. These organisations were invited to complete a questionnaire to capture the breadth of services provided, their resources (staff, equipment etc.) and their training arrangements. Seventeen providers completed the questionnaire. Those who did not respond tended to be smaller-scale providers or those who provided temporary services following natural disasters (such as earthquakes or flooding). We identified a lack of co-ordination of first-response provider services, a lack of standardisation of care provided at the scene of an injury, and a lack of standardisation of training for first responders and first aiders.
-
Post-crash first response by traffic police in Nepal: a feasibility study 48
The Nepal Traffic Police are frequently called upon to provide care to road traffic crash victims and support their transfer to a health facility, but there is no standardised first aid training provided to them. In this study, we worked with one district traffic police unit, completing a first aid training needs survey which informed the development of a 3-day trauma-focused first-responder course, delivered in conjunction with the Nepal Red Cross Society. Pre- and post-course knowledge and confidence questionnaires showed improved scores after the course. Six months after the course, 44% of participants reported using at least one skill learnt, applying them on 92 occasions. Knowledge was better retained than confidence on repeat questionnaires. The study indicated that training traffic police in first aid skills was feasible and that these skills were being used. Further evaluation of effectiveness would be required prior to scaling up the training.
-
Barriers and facilitators to learning and using first aid skills for road traffic crash victims in Nepal: a qualitative study49)
In this qualitative study, we aimed to understand the barriers and facilitators to learning first aid and applying those skills to aid people injured in road traffic collisions. We conducted 30 semistructured interviews with: members of the public who had never learnt first aid; people who had previously been trained in first aid; and first aid trainers. Participants living close to busy roads had often witnessed road traffic crashes, recognised the need for care immediately after the crash and described a desire to help others. The main barrier reported to learning and using first aid skills for road traffic crash victims was the fear of being blamed and potentially prosecuted if the patient had a poor outcome following their care. An additional concern was that many people believed that the best thing to do to help a person injured in a crash was to get them to the hospital as quickly as possible, and consequently, providing first aid at the scene was perceived as delaying their access to care. Some participants described instances where offers of help had been declined in preference for transfer to hospital, or where financial costs (e.g. of transporting the victim) or limited equipment (e.g. lack of first aid materials) hindered their ability to provide care.
All publications synthesised in this manuscript are listed in Box 1.
Workstream 1 (engaging stakeholders)
-
Injuries in Nepal – a neglected public health burden and ways forward (Joshi SK, Pant PR, Banstola A, Bhatta S, Mytton J. Kathmandu Univ Med J 2017;15:269–70. https://doi.org/10.17613/9fw0-ta32)
-
Views of professional stakeholders on readiness for a safe road system in Nepal; an exploratory qualitative study (Pandey B, Khadka A, Joshi E, Joshi SK, Parkin J, Pilkington P, Mytton J. Int J Inj Contr Saf Promot 2022;29:217–25. https://doi.org/10.1080/17457300.2021.1983845)
-
Identification of research priorities for suicide prevention in Nepal: a Delphi study (Joshi E, Bhatta S, Joshi SK, Mytton J. BMC Psychiatry 2022;22:429. https://doi.org/10.1186/s12888-022-04074-z)
-
Engaging Nepali journalists in good road safety reporting: evaluation of the impact of training workshops (Pant PR, Dahal S, Joshi SK, Mytton J. SAGE Open. https://doi.org/10.1177/21582440231204161)
-
Nuancing the need for speed: temporal health system strengthening in low-income countries (Bashford T, Joannides A, Phuyal K, Bhatta S, Mytton J, Harrison R, Hutchinson P. BMJ Glob Health 2019;4:e001816. https://doi.org/10.1136/bmjgh-2019-001816)
Workstream 2: evidence through data
Understanding current evidence and systems
-
Understanding the burden of injuries in Nepal: a systematic review of published studies (Mytton JA, Bhatta S, Thorne M, Pant PR. Cogent Med 2019;6:1673654. https://doi.org/10.1080/2331205X.2019.1673654)
-
The burden of injuries in Nepal, 1990–2017: findings from the Global Burden of Disease Study 2017 (Pant PR, Banstola A, Bhatta S, Mytton JA, Acharya D, Bhattarai S, et al. Inj Prev 2020;26: i57–66. https://doi.org/10.1136/injuryprev-2019-043309)
-
Utility of routine data reporting injuries requiring hospitalisation in Nepal: a secondary data analysis (Pandey B, Bray I, Joshi SK, Mytton JA. Global Health Res 2024. https://doi.org/10.3310/ATAE3098)
-
Improving estimates of injury burden in Nepal: a qualitative study (Bhatta S, Bhatta S, Mytton J, Joshi SK. J Nepal Health Res Counc 2022;20:339–46. https://doi.org/10.33314/jnhrc.v20i02.3929)
-
Prehospital emergency care for trauma victims in Nepal: a mixed-methods study (Banstola A, Gautam P, Smart G, Joshi SK, and Mytton J. Global Health Res 2024. https://doi.org/10.3310/TMTG2437)
The potential for hospital surveillance of injuries
-
Establishing injury surveillance in emergency departments in Nepal: protocol for mixed methods prospective study (Magnus D, Bhatta S, Mytton J, Joshi E, Bird EL, Bhatta S, et al. BMC Health Serv Res 2020;20:433. https://doi.org/10.1186/s12913-020-05280-9)
-
The epidemiology of injuries in adults in Nepal: findings from a hospital-based injury surveillance study (Bhatta S, Magnus D, Mytton J, Joshi E, Bhatta S, Adhikari D, et al. Int J Environ Res Public Health 2021;18:12701. https://doi.org/10.3390/ijerph182312701)
-
Epidemiology of paediatric injuries in Nepal: evidence from emergency department injury surveillance (Magnus D, Bhatta S, Mytton J, Joshi E, Bhatta S, Manandhar S, Joshi S. Arch Dis Child 2021;106:1050–5. https://doi.org/10.1136/archdischild-2020-321198)
Community sources of injury data
-
Home-related and work-related injuries in Makwanpur district, Nepal: a household survey (Pant PR, Deave T, Banstola A, Bhatta S, Joshi E, Adhikari D, et al. Inj Prev 2021;27:450–5. https://doi.org/10.1136/injuryprev-2020-043986)
-
Development and evaluation of a community surveillance method for estimating deaths due to injuries in rural Nepal (Bhatta S, Mytton J, Joshi E, Bhatta S, Adhikari D, Manandhar SR, Joshi SK. Int J Environ Res Public Health 2021;18:8912. https://doi.org/10.3390/ijerph18178912)
The burden of RTIs
-
Economic burden of road traffic injuries in Nepal (Banstola A, Kigozi J, Barton P, Mytton J. Int J Environ Res Public Health 2020;17:4571. https://doi.org/10.3390/ijerph17124571)
-
Injury risks for different road users in Nepal: a secondary analysis of routinely collected crash data Bhatta S, Pathak P, Khadka A, Parkin J, Pilkington P, Joshi SK, Mytton J. Global Health Res 2024. https://doi.org/10.3310/DWTR9883)
-
Completeness of police reporting of traffic crashes in Nepal: evaluation using a community crash recording system (Khadka A, Parkin J, Pilkington P, Joshi SK, Mytton J. Traffic Inj Prev 2022;23:79–84. https://doi.org/10.1080/15389588.2021.2012766)
Workstream 3: effective and cost-effective interventions
Legislative interventions for injury prevention
-
The prevention of – and first response to – injuries in Nepal: a review of policies and legislation (Pant PR, Mytton J, Dharel MR, Dangi A, Rai WB, Joshi SK. Health Res Policy Syst 2021;19:65. https://doi.org/10.1186/s12961-021-00686-1)
Injury prevention at home and work
-
Perceptions of injury risk in the home and workplace in Nepal: a qualitative study (Joshi E, Bhatta S, Deave T, Mytton J, Adhikari D, Manandhar SR, Joshi SK. BMJ Open 2021;11:e044273. https://doi.org/10.1136/bmjopen-2020-044273)
Road traffic injury prevention interventions
-
Adolescent’s perception of road risk on their routes to school in Makwanpur, Nepal; a qualitative study (Gautam P, Mytton JA, Joshi SK, Pilkington P. J Transp Health 2021;20:101009. Accepted for publication 8 January 2021 https://doi.org/10.1016/j.jth.2021.101009)
-
Experience of living near a highway in Nepal: community perceptions of road dangers in Makwanpur district (Joshi E, Gautam P, Khadka A, Pilkington P, Parkin J, Joshi SK, Mytton J. J Transp Health 2022;24:101337. https://doi.org/10.1016/j.jth.2022.101337)
-
Road safety and heavy goods vehicle driving in LMICs: qualitative evidence from Nepal (Khadka A, Gautam P, Joshi E, Pilkington P, Parkin J, Joshi SK, Mytton J. J Transp Health 2021;23:101247. https://doi.org/10.1016/j.jth.2021.101247)
Developing first aid and first-response services
-
State of post-injury first response systems in Nepal – a nationwide survey (Banstola A, Smart G, Raut R, Ghimire KP, Pant PR, Joshi P, et al. Front Public Health 2021;9:607127. https://doi.org/10.3389/fpubh.2021.607127)
-
Post‐crash first response by traffic police in Nepal: a feasibility study (Smart G, Banstola A, Raut R, Ghimire K, Mytton J, Joshi E, Joshi S. Int J Environ Res Public Health 2022;19:8481. https://doi.org/10.3390/ijerph19148481)
-
Barriers and facilitators to learning and using first aid skills for road traffic crash victims in Nepal: a qualitative study (Pandey B, Banstola A, Smart G, Joshi SK, Mytton J. Global Health Res 2024. https://doi.org/10.3310/UTKW7640)
Discussion/interpretation
Principal findings by injury type
Injuries on the road
Our research found that the current evidence base for road safety in Nepal is poor,25 with much of the evidence based on small or single-hospital case series or on traffic police data. A review of policy and legislation supporting injury prevention in Nepal41 showed that only a proportion of WHO-recommended interventions are currently supported by legislation and that even where legislation exists, it is frequently not fully implemented. An analysis of the economic burden of RTIs found that the costs to the country had increased by more than threefold between 2007 and 2016. 35 Typically, road safety decision-making in Nepal depends on data from the traffic police. Our studies have shown that, while valuable to indicate which types of road users are at greatest risk of being involved in a collision,37 by engaging local shopkeepers to record road crashes in their community, we illustrated the potential degree of under-reporting of crashes to the police40 and that the current systems do not facilitate accurate coding. 28 Our qualitative studies showed that communities,45 commercial drivers46 and adolescents44 all perceive their road environment to be dangerous and want action to address this. Interviews with professionals with the authority to improve road safety21 indicated a tendency to blame individuals’ road behaviour, rather than recognising that environmental and legislative change to promote a road system that is forgiving of individual error has been shown to lead to the greatest reductions in RTIs and deaths.
First response to injuries
Our studies exploring the post-crash care system in Nepal showed that there is a lack of co-ordination of first-response provider services, together with poor standardisation of training for first responders and first aiders, resulting in variable care provided at the scene of a crash. 47 Training the traffic police in first response to RTIs is feasible,48 as is training members of the public to provide first aid to crash victims,49 but a major barrier is the lack of a Good Samaritan Law which protects first aiders, first responders and emergency department staff from blame or prosecution should the injured patient have a poor outcome. Interviews with current ambulance staff highlighted significant challenges when trying to handover RTI patients to hospital emergency department staff. Issues included an apparent lack of understanding of each other’s roles, differing expectations of care provision, and reluctance to accept patients when ability to pay cannot be clarified. 29
Injuries at home and work
Our studies enhance our understanding of the epidemiology of injuries sustained at home and work. Our systematic review of publications reporting injuries in Nepal25 illustrated how current evidence reporting the epidemiology of injuries was dependent on studies at high risk of bias (predominantly case series). We also observed that inequalities in injury occurrence were seldom reported except to report injuries by age and sex. Case series reporting episodes of suicide and of poisoning were relatively common but may have just reflected researcher interests rather than reflecting the true burden of harm. We conducted a household survey33 covering over 17,500 residents which illustrated inequalities by income level (those in the lowest income categories experiencing greater numbers of injuries) and by ethnic group. A concurrent qualitative study43 showed that injuries were largely seen as occurring by chance and that individuals had little agency or access to safety equipment or systems to keep themselves safe. While there was a tendency to blame individuals for being ‘careless’, there was also an acknowledgement that the government had a responsibility to enact and enforce safety legislation. A hospital surveillance study illustrated that collecting injury surveillance data via emergency departments was feasible with adequate staffing and that such systems were perceived as valuable to clinicians and managers as well as epidemiologists. Over the course of a year, more than 30% of attendances were due to injuries, predominantly falls, RTIs and animal-related injuries (often bites by dogs). 31,32 We noted that 5.5% of attendances were for self-harm, particularly pesticide/insecticide/rodenticide self-poisoning or hanging. This finding, together with our study showing that two-thirds of community-based fatal injuries were due to suicide,34 led us to complete a Delphi study of research priorities for suicide prevention. 22 This study identified that future self-harm research should focus on a better understanding of the epidemiology of suicide in Nepal, evidence-based practice in prevention and response, and research to understand the needs of those at risk of suicide and the needs of their families.
Injury data collection systems
A qualitative study that mapped injury data across four routine data systems improved our understanding of the strengths and limitations of routinely available injury data. 28 This study reinforced our concerns regarding the completeness and coding of injury data that had been suggested through our analysis of HMIS data27 and hospital31,32 and community32 surveillance studies. At present, any intervention studies to reduce injuries are going to need to include their own data collection systems, as routine data are not accurate or complete enough to monitor the effectiveness of any intervention.
Strengths and weaknesses of the studies/in relation to other studies
The outputs described in this synopsis represent the most comprehensive assessment to date of the status of injury occurrence in Nepal and provide clear indications of the extent of the burden of preventable harm. Unlike the findings of our systematic review of publications reporting injuries in Nepal, the study designs we used were much less at risk of bias, and the limitations of our studies were clearly described in each of our publications. Our qualitative studies showed that injuries were frequently perceived to be an inevitable consequence of life. Participants showed only limited agency to reduce their injury risks, suggesting that awareness-raising of the preventability of injury would be helpful. Our policy review indicated that the Government of Nepal has a clear role to play in developing legislation based on evidence-based policies recommended by the WHO and to implement such legislation fully.
We chose to conduct a large number of studies across a wide range of injury types. To achieve this, we focused our fieldwork in Makwanpur district of Bagmati Province. While a smaller number of studies recruiting participants from across the country would have resulted in nationally representative samples, the breadth of evidence gained would not have been feasible in the time available. We chose Makwanpur district as it includes three of the four topographies of Nepal (the plains, low hills and mid hills). The findings arising from studies in Makwanpur district have the potential to be generalisable across a wide range of districts in Nepal with similar topographies.
Reflections on the project and what could have been done differently/major or significant changes
We were ambitious in the number and breadth of the studies we conducted within the NIHR GHRG award. The limited evidence supporting effective injury prevention identified through our systematic review at the beginning of the award encouraged us to maximise the scope of the research delivered; however, the number of concurrent projects led to additional logistical and administrative challenges.
We conducted all our data collection in Nepali, with Nepali researchers advising the wider research team on how to maximise the value of the data obtained by considering Nepali culture and context. Qualitative data collected in Nepali were translated into English prior to analysis. We considered trying to conduct our analyses in Nepali but translation into English was necessary because the qualitative analysis software NVivo (QSR International, Warrington, UK) does not support Nepali script. This decision also enabled English-speaking members of the research team to better support the capacity-strengthening of Nepali early-career researchers with qualitative analysis skills. Translations were checked by a second bilingual researcher to minimise the likelihood that nuance and meaning were distorted during translation.
One of the unexpected findings emerging from our studies was how differently the word ‘injury’ was conceptualised in Nepali society. In academic injury prevention circles, the term ‘injury’ is widely understood by its definition as being harm sustained when the body is exposed to forces outside its tolerance. In the Nepali language, there is no direct translation of the word ‘injury’; rather it is a ‘loan word’ adopted into the Nepali language from English. We therefore conducted additional research to explore this issue (see Related work). As our understanding of this issue became clearer, we adopted the language we used in participant information sheets and during data collection to ensure that the full range of injuries we were interested in was being captured by the researchers.
Challenges faced
Changes of government/federalisation
During our NIHR GHRG award (2017–21), there was significant reform to the structures of government in Nepal. The constitution of Nepal was enacted in 2018, 9 months after our award commenced. The constitution facilitated a move away from a unitary government to a federalised republic with three levels: a single federal government, 7 provincial governments and 753 local governments. 50 Provinces now have their own legislature, and local governments have their own elected representatives and governing body. Devolution of power and budgets to provinces and local governments, and appointments of representatives to posts, have been incremental since 2018. Delegation of responsibilities has been slow, though the priority area was the delivery of universal health coverage and the provision of basic health care services. The impact on our studies has been modest. We have engaged with local government where appropriate and feasible, particularly to gain permission for studies at the local level. Most legislation with the potential to impact on injury prevention was written during the period of unitary government and has yet to be updated to reflect the federalised system. Therefore, our advocacy to date has primarily been at the federal level of government. Budgets and remits are now more clearly understood. In the future, we will work more closely with local governments to facilitate local change and develop evidence and guidance with the potential to be rolled out widely across local government areas. We will continue to advocate centrally, specifically for legislative change and enforcement of existing legislation.
Ethnic groups
Nepal is a country with many ethnic groups, including those descended from Chinese and Indian heritage. The epidemiology of injuries is known to be socially patterned, and through our systematic review of studies reporting injuries in Nepal25 we found no reporting of injury occurrence by ethnic group. During our studies we captured ethnic group when collecting demographic data, though this required us to include 102 ethnic groups on our data collection form. Analysis of so many ethnic groups required collation of groups into categories. We identified different classification systems used by different organisations, and through discussion agreed to report our ethnic group data using the six-category system used by the Ministry of Health and Population in its guidelines for the reporting of HMIS data. We were able to show that injury occurrence was more frequent in the ethnic group categories with the lowest socioeconomic status. We also noted that the classification system used included a mixture of castes, ethnic groups and religions. In Nepal, some ethnic groups are associated with specific occupations, and different occupations are associated with different levels of income and risk of injury. Therefore, a comprehensive understanding of the association between ethnicity and injury is complex and fell outside the scope of our award.
COVID-19
The COVID-19 pandemic hit when we were 2 years 8 months into our 4-year programme of research. We were fortunate that most of the data for studies agreed in our original 3-year award had already been collected and were being analysed. Our hospital surveillance study was required to close early, 1 week before the completion of a year of injury surveillance, and the collection of the second year of traffic police RTI data needed to be delayed until the initial lockdowns were over. Following a period of transition, as all researchers started to work from home, we were able to continue with our analyses remotely. We were fortunate that our researchers had access to good internet connections, making remote working feasible. At the time the pandemic started, we were preparing protocols and ethics applications for four studies to be conducted during a 1-year extension period. One of these new studies was no longer feasible; therefore, it was replaced with an alternative study. The other three studies were all qualitative and we redesigned them so that focus groups were replaced by one-to-one interviews that could occur remotely (by phone or video call) rather than face to face. Dissemination activities were significantly delayed until late in 2021 when it was feasible to travel to present findings to communities, practitioners and decision-makers.
Engagement with partners and stakeholders
Effective engagement with our collaborating partners and with external stakeholders has been essential for the effective delivery of our programme of research.
Partner engagement
The primary strategic partner in the NIHR GHRG award was KMC. We worked towards an equitable partnership with KMC and created a team culture where individual voices could be heard and respected. Strategic decisions were made together and discussed at monthly Project Delivery Group meetings which were chaired by one of the co-directors. Online meetings took place at 15 or 45 minutes past the hour in the UK, so they occurred on the hour or half hour in Nepal. We developed the NIRC website so that content was in both Nepali and in English where feasible. To develop stronger links between UWE and KMC, Professor Sunil Kumar Joshi was invited to be a Visiting Professor at UWE, Bristol and Professor Julie Mytton was made a Visiting Professor at KMC. All component studies in our programme of research had a Nepali lead who was based either in Kathmandu or in the UK. Mother and Infant Research Activities (MIRA), a research NGO, were a partner who facilitated much of our field research. We worked with two other NGOs: the Nepal Red Cross Society and Swatantrata Abhiyan. In the spirit of working in equitable partnerships, we invited them to join our programme as research partners. Neither organisation had previously worked as a research partner, and this generated additional work for both parties that did not necessarily enhance the outputs. Engaging them as stakeholders in future collaborations may enable them to contribute in a way that they are more used to and may be less onerous administratively.
Stakeholder engagement
To establish our stakeholder network, we held a launch event on 6 September 2018 attended by over 100 stakeholders, including representatives of the Ministry of Health and Population, the Parliamentary Committee for Health and Education, the National Planning Commission, Department of Health Sciences, WHO Nepal Office, Department for International Development Nepal, KMC and Kathmandu University. We held two injury research events to raise awareness of the burden of injuries and the potential for prevention and to disseminate findings of our research. The first event, in April 2019, was attended by 135 participants and was opened with keynote speakers from the Health Emergency and Disaster Management Unit of the Ministry of Health and Population and the Department of Roads. It was attended by six members of our International Steering Committee. The second event, held online due to the COVID-19 pandemic, was in September 2021 and attended by 76 participants. Ministers from the Ministries of Health and Transport in the Government of Nepal attended both events, together with representatives of NGOs and advocacy organisations.
In addition to having them attend our launch event and injury research showcase events, we engaged with policy-makers through multiple routes. We established two stakeholder engagement groups: a Road Danger Reduction Forum and a First Response Reference Group. The purpose of these groups was to gain understanding of the local and national context, to provide a forum for advice to improve the ability to deliver our studies and to feed back after study completion to improve the likelihood of impact. At the first meeting of these two fora, we completed a rapid prioritisation process to identify a ranked list of issues to inform the development of our studies. We invited policy-makers and those with awareness of the provider landscape to participate. We successfully advocated for the establishment of a cross-governmental National Advisory Committee for Injury Prevention and Control at the end of 2018. In February 2020, Mytton, Joshi and Pant attended the WHO third Global Ministerial Conference on Road Safety in Stockholm and supported the Minister for Transport from Nepal and his delegation. Swatantrata Abhiyan organised a preconference briefing event in Nepal on 6 February 2020, which NIRC supported and to which government officials participating in the conference were invited. At a local level, we engaged with municipality mayors in the areas where we conducted fieldwork. Mayors gave us permission to conduct our studies within their jurisdiction, and we disseminated findings back to them at the end of the studies to support them to make strategic decisions at a local government level.
In 2020, Khadka attended a workshop on road safety organised by the World Bank, and Gautam participated in the second Kathmandu Road Safety Film Festival organised by Safe School Zone Nepal, the National Road Safety Alliance and the Nepal Automobiles Association. In May 2020, Pant was a panellist in an online event organised by the Brain Gain Centre, the Nepal Government’s initiative for diaspora engagement, and in June 2020 moderated a webinar hosted by the Nepal Road Safety Alliance on safer mobility during COVID-19, involving a Member of the Nepal National Assembly. The NIRC participated in a consultation event to identify research gaps and views on the theme of ‘disability and safety’ that was attended by the Spinal Injury Rehabilitation Centre, the National Federation of the Disabled Nepal (NFDN) and government officials working on disability from the Department of Health Services (Ministry of Health and Population).
We collaborated with educational institutions in Nepal throughout the award. We developed and ran two interprofessional short courses on road safety, where we invited students from different disciplines and different higher education institutions across Kathmandu to develop their knowledge and skills in road safety together, emphasising the necessity for cross-sector collaboration. We developed a collaboration with the Kathmandu School of Arts (Kathmandu University) to develop injury prevention messages for the public. Dr Sudhamshu Dahal and a mass communication student at the School of Arts supported the delivery and evaluation of the workshops with journalists and our subsequent publication. 23 We collaborated with Professor Subedi at Tribhuvan University to develop a workshop and qualitative study to explore the conceptualisation of injuries in Nepali society.
Individual training and capacity-strengthening activities
The NIHR GHRG award funded the establishment of a new research centre in KMC to focus on injury prevention. Our approach to individual capacity-strengthening involved offering each early-career researcher the opportunity to complete a research training needs self-assessment, followed by a one-to-one interview with our UK training lead. This provided the early-career researcher with facilitated time to consider their own career ambitions and trajectory and to consider how they could develop their knowledge and skills. We emphasised learning by doing, providing each early-career researcher with the opportunity to lead a study, prepare ethics and study documentation, collect and analyse data, and lead the writing of one or more publications.
We identified six NIHR Academy Members in our award. Three completed Master’s-level courses at UWE; two completed a Master’s in Public Health at UWE, one of whom achieved the best international student award, and both gained distinctions; one Academy Member completed a Master’s in Health Economics and Health Policy at the University of Birmingham and achieved a merit grade. Our data manager achieved a merit grade in the MSc in Data Science at UWE. One researcher already held a Master’s degree, and two postdoctoral Academy Members had individual training plans. One was awarded a scholarship to attend the Johns Hopkins Global Road Safety Leadership Course in Baltimore in September 2019. One attended a qualitative research methods short course at the University of Bristol. Three NIHR Academy Members were successful with applications to the WHO Violence and Injury Prevention Mentorship programme. Two benefited from having an expert injury prevention mentor over the course of 1 year, to support them in their preferred area of learning. The WHO were unable to identify a mentor with the appropriate expertise for the third successful applicant.
In addition to the individually tailored capacity-strengthening programme, we provided training for all members of the NIRC through regular large group learning events. Early in our award, we identified the need to develop capacity in research governance, data governance and financial governance, and we provided courses on these topics in 2018, delivered by UK experts. Our activities on good data governance were led by Professor Felix Ritchie at UWE, who had previously developed Good Data Governance training for the UK Office of National Statistics. These materials were adapted for the Nepal context and have gone on to inform the delivery of Good Data Governance training for researchers from other LMICs, funded by the NIHR. Additional training provided in-house by UK researchers included courses on data management using REDCap (Research Electronic Data Capture software, Vanderbilt University, Nashville, TN, USA), community engagement and involvement, knowledge mobilisation and research impact, qualitative research methods, Delphi methods, advocacy and team dynamics. We provided training in writing publications and policy briefs, preparing conference abstracts, oral presentation skills and grant writing. Some training was delivered by a junior member of the team supported by a senior colleague. About halfway through our award, we established monthly ‘educational meetings’ where we facilitated peer learning on issues that were topical at that point in the award.
We improved local knowledge of injury prevention by developing the injury prevention curriculum for community medicine students at KMC, and running an injury prevention research course in 2019, delivered in person to researchers in Nepal with video contributions from the Nepali academic diaspora in Qatar and from the UK. Tackling road safety requires a multiagency approach; therefore, we developed an interprofessional short course to enable participants to learn how disciplines can collaborate to reduce road risks.
Institutional capacity-strengthening
The NIHR GHRG award was the first of this scale for KMC from a UK funder. Therefore, the early institutional capacity-strengthening focused on enabling KMC to understand and comply with the contractual requirements of the award. We supported all our Nepali collaborators to complete a Good Financial Grants Practice self-assessment prior to signing the UWE-collaborator contracts. We successfully applied to the NIHR Financial Assurance Fund and subsequently ran a series of workshops on good financial governance face-to-face with the financial officers of our collaborating organisations in 2018. Training in good research governance, good data governance and REDCap software were made available to the professional services staff in addition to the research team to support institutional capacity-strengthening. We developed standard operating procedures to enable the research team in Nepal to understand the processes requiring compliance.
Kathmandu Medical College had recently completed construction of a new teaching and clinical facility in Duwakot, several miles outside central Kathmandu. Professor Joshi negotiated office space there to establish the NIRC. This space needed to be equipped with desks, chairs, computers, a printer, internet, video-conferencing technology and a portable projector. The award enabled the NIRC to establish and maintain a website (www.nirc.org.np, accessed 29 May 2024) and obtain a licence to host a REDCap database. A full-time data manager supported the set-up of the database, a backup server with two hard drives and tablet computers preloaded with REDCap forms. This infrastructure was intended to become self-sustaining, by providing a database resource that KMC could offer to other researchers in KMC and Kathmandu University for a fee. We funded software licences for reference management [EndNote; Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA], qualitative data analysis (NVivo), quantitative data analysis [SPSS; IBM Corporation, Armonk, NY, USA] as well as Microsoft Office® 365 (Microsoft Corporation, Redmond, WA, USA). Originally recognised nationally as a clinical and teaching institution, KMC is now recognised as a research institution, having attracted other grants since our award was made. This change is reflected in KMC’s new website (https://kmc.edu.np, accessed 29 May 2024). In addition to the main office in Kathmandu, we also supported the establishment of a field office in Hetauda, the main town in Makwanpur district, where most of our fieldwork took place. This office was provided with a computer, printer, modem and furniture (e.g. tables, chairs, cupboard).
Community engagement and involvement
Community engagement and involvement underpinned each of our projects and workstreams. Through community engagement and involvement, we identified the following groups at increased risk of injury: (1) in road environments – children, young people, novice drivers, cyclists/motorcyclists, people with disabilities, passengers; (2) those with under-reported minor/moderate injuries less visible to policy-makers – particularly in domestic and workplace settings; (3) secondary to social inequity – women/girls (sexual/domestic violence), lower castes/ethnicities, people with lower incomes or disabilities, and geographically isolated communities.
Examples of community involvement in research design and delivery include:
-
In February 2019, we worked with the head teacher and staff at a school in Makwanpur to identify feasible ways to enable children to engage in a study exploring road dangers on their journey to school. 44 In the same area, we worked with existing community organisations (mothers’ groups and neighbourhood development committees) to explore residents’ experience of living next to a busy highway. 45
-
Community consultation in October 2019 on road safety reached 27 people (road crash victims, traffic police, driving professionals, students, shopkeepers and roadside residents). This involvement helped identify sites at high risk for crashes in which to conduct road safety studies. We engaged six shopkeepers at these sites as community data collectors in our study to validate the frequency of RTIs recorded by the traffic police. 40 These participants stated that the experience had changed their view of road safety, with some motivated to begin advocacy.
-
Engagement meetings in October 2019 (five meetings, six participants, involving government/health service provider senior staff) identified that the injuries most ‘visible’ to policy-makers, and thus likely to be prioritised when allocating resources, were those recorded for hospital inpatients. Those seeking alternative care could be missed.
-
We worked with the Makwanpur traffic police to inform delivery of two studies,37,48 The traffic police advised us on under what circumstances data could be accessed and helped us to develop data extraction materials and processes.
Practitioner engagement was essential for the successful delivery of some studies. We worked with FCHVs and staff in 10 health posts in Makwanpur to establish a feasible method to identify and log deaths in their local community as part of our fatal injury enquiry study. 35 We also worked closely with the emergency department clinicians and the hospital management boards at two hospitals in Hetauda, Makwanpur for our hospital injury surveillance study. 30–32
Community engagement and involvement substantively shaped the work included in our costed extension. We held a full-day engagement workshop in December 2019 involving 36 participants – civil society/community groups, teachers, health professionals and social science students/academics. With no direct translation for the word ‘injury’ in the Nepali language, this workshop informed how we communicate about injury research and prevention in Nepal, and also stimulated reflection on how well international, professionalised concepts of injury translate to local contexts.
Engagement with communities was essential for dissemination of study outputs. We worked with students at the School of Arts at Kathmandu University to develop creative ways to expand the reach and accessibility of our injury prevention messages for target groups. Students helped us develop posters and visual outputs to disseminate key messages arising from our research. Published outputs led to further engagement with the public: Banstola’s publication on the economic burden of traffic injuries in Nepal35 generated considerable media interest, and an interview with Rastriya Samachar Samiti (the largest news agency in Nepal) led to 34 mentions in online news outlets.
Equality, diversity and inclusion
Participant representation
Injuries are known to be socially patterned. Globally, most types of injuries are more common in males than females, except for burns and scalds, which are typically associated with cooking activities traditionally undertaken by women. Different types of injuries affect people of different ages; children may be particularly vulnerable due to their level of developmental awareness and ability to manage injury risks, and the elderly are particularly vulnerable to fall injuries. Through our hospital surveillance study,30–32 community surveillance of fatal injuries study,34 household survey,33 analysis of HMIS data27 and road crash monitoring studies,37 we have explored the incidence of injuries by age and gender. We found a predominance of self-harm injuries in women in the hospital injury surveillance study, which provided justification for including a study to identify the research priorities for suicide prevention in our extension application. 22 We know that injuries are frequently inequitably distributed by ethnic group, yet we found there is almost no literature from Nepal on the incidence of injuries by ethnic group. 25 We therefore included over 100 different ethnic group options in the demographic data collected in our hospital surveillance study,30 our community fatal injury surveillance study34 and the household survey,33 and have consequently illustrated inequalities in injury occurrence by ethnicity. There is no standardised way to cluster and present data by ethnic group, and we are yet to identify robust, timely national data on ethnic group, broken down by region and age and sex to enable disaggregated rates to be determined. Sustaining an injury can cause significant financial hardship and can tip families into poverty. We found that the distribution of injuries by income level was also seldom reported in the existing literature. We explored the financial impact of injuries on families in our community fatal injury surveillance study34 and in the household survey of home and work injuries. 33 At a societal level, we have published research on the modelled economic burden of RTIs. 35 We have found that marginalised groups have welcomed the opportunity to engage in our studies. By adapting our methods, we have been able to explore how seldom-heard groups are vulnerable to road injuries. For example, we used photovoice methods to enable adolescents to record features of their journeys to school that increased or decreased their safety. 44 We worked with mothers’ groups to hear the voice of women raising families alongside a busy highway. 45 Truck drivers are often vilified as the cause of road traffic crashes, but no one has previously given them a voice. Through a qualitative study, we heard of their concerns for their own safety every day they are on the road, their fear of being blamed and physically hurt if a crash happens irrespective of whether it is their fault, and the pressures they work under. 46 All of our data collection was done by Nepali researchers using the local language, to facilitate engagement.
Research team
We started our GHRG award with three male Nepali early-career researchers with whom we had worked previously. We were pleased to recruit three female early-career researchers to the Kathmandu team in 2018. Through additional grants, we grew the team to include an additional two male and two female researchers from diverse disciplines. The team included those from different castes, ethnic groups and from both within and outside the Kathmandu Valley. None of our team disclosed a disability.
Impact and learning
What difference has been made already?
Our award has helped raise awareness of injuries and the opportunities for injury prevention with the public, with NGOs, with the Nepal and SE Asia office of the WHO and with the Government of Nepal. Over 4 years the NIRC team have become known locally for their work on injury prevention, with invitations to speak on Nepali television and at national health conferences. Professor Joshi has been invited to contribute as an expert adviser for meetings at the Ministry of Health and Population [including, e.g. meetings to discuss the development of injury surveillance in Nepal (May 2022), the development of a national injury prevention strategy and 5-year action plan (July 2022), a policy dialogue on road safety (July 2022), and drafting the national response to the second decade of action on road safety (July 2022)]. He has also been invited to contribute to a national policy dialogue on developing a national approach to research, led by the Policy Research Institute in Nepal. In February 2020, following support to the Nepali Minister for Transport to participate in the Global Ministerial Conference on Road Safety in Sweden, the minister committed to improving road safety education in schools and to reviewing current road safety laws. Countries that have made the best progress with reducing RTIs have done so by getting different agencies to work together on the challenge. We therefore advocated for the establishment of a cross-governmental National Advisory Committee on Injury Prevention and Control, which was established in 2018. Unfortunately, the COVID-19 pandemic resulted in this committee failing to sit during the latter years of our award.
We have helped train the next generation of injury prevention researchers and raised awareness of injury prevention in different professional groups. Three researchers working at the NIRC – one funded through our GHRG award, one funded through our Health Policy and Systems Research Development Award and one funded through Global Challenges Research Fund quality-related research (GCRF QR) funding from UWE – were successful in securing PhD studentships in the UK, Australia and New Zealand, respectively, following completion of our GHRG award.
We worked with students at Kathmandu University School of Arts to develop injury prevention messages based on the findings of our studies which were disseminated to the communities and to health posts in Makwanpur district where our fieldwork was conducted. Presentations to the health-care staff in these locations at the end of our award were well attended and received positive feedback. Our follow-up of journalists who attended a series of media workshops shows they are starting to discuss prevention in their reports of road traffic crashes, and our evaluation23 suggests that attendance at the workshops has influenced how the journalists report road crash events.
What longer-term impact might there be?
There is potential for significant longer-term impact from our GHRG award, in terms of economy, efficiency, effectiveness, equity and environmental impact.
Economy
Through funding from the NIHR GHRG award, supplemented by other external grant income, we grew the team of researchers at the NIRC. All appointments were considered successful, and we retained all staff through to the end of the award. Rates of pay for the research team were relatively good for Nepal, and this was reflected in the high-calibre candidates who applied for our advertised positions.
Our study of the economic burden of RTIs in Nepal35 showed the increasing and significant financial impact of these injuries on the Nepali economy. This impact has increased in real terms since the previous estimates were published using data from the 2006 to 2007 financial year. The modelling used to underpin the new published estimate needed to use proxy measures for several variables and therefore may underestimate the true impact of RTIs on the country.
Efficiency
The cultural norm for evidence dissemination in Nepal would be through face-to-face meetings and events; failure to do so may risk being considered disrespectful to those in decision-making positions. The COVID-19 pandemic significantly limited our ability to meet with people, and a shift to online dissemination was both necessary and swift. We worked hard to establish and extend networks of stakeholders and senior decision-makers and to share with them, primarily electronically, the evidence we have generated. This appears to have been largely successful, as evidenced by the fact that Professor Joshi is now quite frequently invited to attend meetings with decision-makers and offer his expertise.
Effectiveness
Our research has been epidemiological, qualitative or policy-focused, and our programme has not included the evaluation of effectiveness or cost-effectiveness of interventions. Our outputs are enabling Professor Joshi to have conversations with decision-makers regarding evidence-based policy, the need for complete and well-coded data and multiagency approaches to injury prevention. We completed a study to examine the feasibility of delivering first aid training to traffic police officers which indicated that this intervention could potentially be formally evaluated using an experimental design in the future.
Equity
We demonstrated the ability to recruit a gender-balanced team of early-career researchers through this award (see also Equality, diversity and inclusion). We showed that previously published literature on injuries in Nepal had rarely explored inequalities in injury occurrence and we therefore prioritised this during the epidemiological studies we completed, particularly with regard to inequalities by ethnic group.
Environmental impact
Our GHRG award did not have any direct impacts upon the environment. The rapidly increasing vehicle fleet is significantly contributing to deteriorating air quality, particularly in Kathmandu Valley, where Kathmandu City is now considered to have some of the highest air pollution levels in the world. Interventions to reduce the risk of RTIs – such as improved traffic management, legislation to improve the roadworthiness of vehicles and road infrastructure changes that separate vehicles from other road users – all have the potential to contribute to improved air quality.
Areas for future research
We identified the following areas for future research.
Road safety
-
Research to address the gap in translating evidence into legislation that is then effectively implemented. Examples include the lack of enforcement of the use of helmets for pillion passengers on motorcycles or of seatbelts for passengers in vehicles.
-
Research to reduce the risk of injury for those most vulnerable on the roads, including pedestrians, those using public transport and those travelling by motorcycle.
First response to injury
-
Research to support the development of an effective first-response system across Nepal.
-
Research that leads to the standardisation of effective first-response care. Examples include the development of effective interprofessional working between prehospital and emergency department care providers, and the establishment of legislation that protects from prosecution those trying to support injured patients.
Staying safe at home and work
-
Research that further describes the epidemiology of injuries occurring at home and at work and identification of the risk factors that could be addressed. Examples include reducing the incidence of dog bites, and consequent rabies risk.
-
The development of either targeted or universal interventions that address risk factors for injuries at home or at work.
Injury data systems
-
The establishment of injury surveillance, either through surveillance systems or through improved recording of routine health care use, to better understand injury trends and enable the monitoring of interventions to prevent injuries.
-
Research to understand the association between ethnic group and injury incidence, exploring the interplay of caste and occupation, thereby identifying vulnerable groups suitable for targeted action.
Suicide and self-harm
-
Research to understand the needs of those at risk of self-harm and their families.
-
Research to understand the epidemiology of suicide in Nepal.
-
Studies to strengthen culturally competent and evidence-based approaches to suicide prevention and response.
Related work
This section discusses activities that were not directly funded by NIHR, but arose from the work funded.
The scale and complexity of the challenge to improve road safety indicated that the next step should be to complete a Delphi study to establish agreed priorities for road safety research in Nepal. We successfully applied for a NIHR Global Health Systems and Policy Research Development Award (ref: NIHR129877) which ran concurrently with the NIHR GHRG award. The WHO has described five ‘pillars’ of road safety: road safety management, safer roads, safer vehicles, safer road users and effective post-crash response. 51 In our Delphi study, we recruited and interviewed 93 experts from across the 5 pillars of road safety and generated a series of potential research questions relating to each pillar. These questions were then subjected to two rounds of ranking for importance and a further ranking for urgency. This resulted in six research questions considered important and urgent. 52
As a consequence of securing the NIHR GHRG award, we were eligible to apply for GCRF QR funding from UWE, Bristol. We secured £207,000 over a total of 3 years. This award funded additional researchers to our team in Nepal and additional capacity to manage the studies from the UK. Two studies and one capacity-strengthening activity were completed. The first study explored the experience of safe mobility around Kathmandu for people living with disabilities. We worked with an advocacy NGO, the NFDN, to design the study and identify potential participants. Participants were invited to use a body-worn camera to record a typical journey they made across the city. They were interviewed about their experiences, the hazards they encountered and their strategies for managing those hazards. We showed the videos of their journeys to people in decision-making positions across the road management system in Kathmandu, which provided stimulating prompts for a subsequent interview. 53
A second study explored the conceptualisation of the term ‘injury’ in Nepali society. Through a series of interviews with members of the public from different walks of life, we explored the language they used to describe different types of injuries and their understanding of the term ‘injury’. We discovered that there was marked variation in how the term was interpreted. Particularly of note was the expectation that an injury would result in a visible wound to the body, and that trauma that does not leave visible consequences (e.g. drowning, suffocation, or poisoning) may not be considered an injury. We produced a short video to explain how researchers need to take care when communicating with the public about injuries (www.youtube.com/watch?v=LLMmQ4xoKEA, accessed 12 September 2023).
As a capacity-strengthening activity, we developed a multidisciplinary online training course on road safety. In June 2020 we ran a 5-day course bringing together 33 postgraduate community medicine and transport engineering students to learn together. The students learnt about the causes of road traffic collisions and how to reduce the risk of crashes. By undertaking group activities together, students learnt how different professional groups can contribute collaboratively towards reducing the number of road traffic collisions, injuries and deaths. Following the success of the first course, the training materials were refined and a second 4-day course was delivered in May 2021, this time with students from four disciplines: community medicine, transport engineering, public health and town planning. The course was well evaluated with positive feedback relating to both the content and the opportunity to learn collaboratively. A post-course meeting with the programme leads from all four disciplines in June 2021 confirmed that all perceived the benefit of the interprofessional learning experience and agreed to continuing such interdisciplinary learning in future.
Collaborations/further funding/future work
The findings from the NIHR GHRG award, together with the outputs from the NIHR GHR Health Policy and Systems Research Development Award, enabled us to successfully bid for a NIHR GHR Health Policy and Systems Research programme award (ref: NIHR150089) to develop the road safety system in Nepal using the ‘safe systems’ approach endorsed by the WHO and the United Nations in their second Decade of Action for Road Safety 2021–30. 9 This 4-year award commenced in November 2022 and includes three work packages: (i) closing the evidence-policy-practice gap, (ii) improving the safety of public transport, and (iii) improving post-crash care.
Aspirational/pre-planned dissemination or discussions to ensure the outcomes of the research are taken forward for implementation by key stakeholders, partners and target audiences
We have continued to work closely with the Ministry of Health and Population in Nepal, particularly the Department of Health Services and the Health Emergency Operations Centre, and with the Ministry of Physical Infrastructure and Transport. Securing the NIHR GHR Health Policy and Systems Research award has led us to have a continuing dialogue with senior decision-makers over a prolonged period and beyond the lifetime of the GHRG award. This dialogue has continued through civil servants where ministers have changed roles following elections. Professor Joshi has been invited to advise the Government of Nepal on developments in road safety, surveillance and the development of first-response systems, and draws on the evidence generated through the GHRG award when possible and appropriate.
Implications for decision-makers
Our studies exploring the strength and utility of existing routine data systems to monitor injury occurrence suggest that it is not currently possible to use these systems for effective surveillance to monitor either trends or the impact of policy or intervention changes. Either a bespoke sentinel surveillance system or strengthening existing systems to capture healthcare service use following an injury could address this gap.
The Government of Nepal does not currently have legislation that addresses all evidence-based recommendations for policy for road safety. Where legislation exists, it is frequently not implemented, or only partially implemented. Examples, where the implementation of existing policy could make a difference, would be the enforcement of crash helmets for pillion passengers on motorcycles and the enforcement of seatbelt wearing where these are available in vehicles. Recent enforcement to monitor the use of alcohol by drivers within Kathmandu Valley indicates that enhanced enforcement is possible when prioritised by the government.
The Government of Nepal has recently introduced the National Ambulance Guideline 2078 which describes the actions required to establish prehospital services in Nepal and describes standards for ambulances and EMTs. Our research can inform the implementation of these standards. Decision-makers should continue to evaluate the roll-out of this guideline to ensure it is delivering the effective service it intends.
Research recommendations
Future research calls should prioritise:
-
Road safety interventions in Nepal, including those leading to the implementation and enforcement of culturally competent and evidence-based legislation for road safety, and interventions that reduce the risk of injury and death for road users.
-
The development of injury data systems and the ability to monitor trends in injury incidence by key demographic variables such as ethnic group, and the application and use of such data systems to inform where interventions should be targeted and to determine the effectiveness of such systems.
-
Research to support the establishment of effective first-response systems in Nepal and the ability to integrate these with existing healthcare infrastructure.
-
A greater understanding of the drivers of self-harm in Nepal and actions that can be taken to identify and support those at risk of suicide.
Conclusions
Through a series of quantitative and qualitative studies, we have strengthened the evidence available on the epidemiology of injuries in Nepal and highlighted the significant impact of injuries, and risk of injury, on communities. Our data have shown the important and increasing burden of RTIs on society, including the impact on the economy of the country. In addition, previously poorly reported injuries, such as those occurring at home, at work and as a consequence of self-harm, have been highlighted. Injuries are largely preventable. Our critical review of legislation supporting injury prevention has highlighted gaps that need to be filled and indicated where there is a need to fully implement existing policies. The absence of a co-ordinated national first-response service and the lack of standardisation of training in first response compounds the burden of injuries in Nepal. Recent policy to address these issues in the first-response system is welcomed. Lack of legislation to protect first responders and emergency care providers is impacting on care practices and needs to be addressed. The ability to routinely monitor injury trends and inequalities in injury occurrence is essential. Current injury data collection systems are at high risk of being incomplete and inaccurately coded and hinder the ability to monitor progress with injury prevention initiatives. The potential to reduce the burden of preventable injuries in Nepal is significant, and the opportunities to strengthen data systems and legislation to prevent injuries are achievable with social and political will.
Additional information
CRediT contribution statement
Julie Mytton (https://orcid.org/0000-0002-0306-4750): Conceptualisation, Formal analysis, Funding acquisition, Methodology, Project administration, Supervision, Writing – original draft, Writing – editing and reviewing.
Sunil Kumar Joshi (https://orcid.org/0000-0002-2704-5060): Conceptualisation, Funding acquisition, Methodology, Project administration, Supervision, Writing – original draft, Writing – editing and reviewing.
Amrit Banstola (https://orcid.org/0000-0003-3185-9638): Formal analysis, Investigation, Methodology, Project administration, Resources, Writing – original draft, Writing – editing and reviewing.
Santosh Bhatta (https://orcid.org/0000-0001-6393-2495): Formal Analysis, Investigation, Methodology, Project administration, Resources, Writing – original draft, Writing – editing and reviewing.
Sumiksha Bhatta (https://orcid.org/0000-0001-9969-1494): Formal analysis, Investigation, Methodology, Writing – original draft, Writing – editing and reviewing.
Toity Deave (https://orcid.org/0000-0001-9966-8948): Methodology, Supervision, Writing – original draft, Writing – editing and reviewing.
Preeti Gautam (https://orcid.org/0000-0002-2040-5000): Formal analysis, Investigation, Methodology, Project administration, Resources, writing – original draft, Writing – editing and reviewing.
Elisha Joshi (https://orcid.org/0000-0002-3534-276X): Formal analysis, Investigation, Methodology, Project administration, Resources, Writing – original draft, Writing – editing and reviewing.
Prerita Joshi (https://orcid.org/0009-0001-9436-1768): Formal analysis, Investigation, Project administration, Writing – original draft, Writing – editing and reviewing.
Anish Khadka (https://orcid.org/0000-0003-4432-7198): Formal analysis, Investigation, Methodology, Project administration, Resources, Writing – original draft, Writing – editing and reviewing.
Dan Magnus (https://orcid.org/0000-0001-7801-8401): Formal analysis, Methodology, Supervision, Writing – original draft, Writing – editing and reviewing.
Sunil Raja Manandhar (https://orcid.org/0000-0002-6583-3973): Investigation, Project administration, Writing – editing and reviewing.
Bidhya Pandey (https://orcid.org/0000-0002-6222-9383): Formal analysis, Investigation, Methodology, Project administration, Resources, Writing – original draft, Writing – editing and reviewing.
Puspa Raj Pant (https://orcid.org/0000-0002-8827-0018): Formal analysis, Investigation, Methodology, Project administration, Resources, Writing – original draft, Writing – editing and reviewing.
John Parkin (https://orcid.org/0000-0002-6084-4569): Formal analysis, Methodology, Writing – original draft, Writing – editing and reviewing.
Paul Pilkington (https://orcid.org/0000-0002-5408-361X): Investigation, Methodology, Writing – original draft, Writing – editing and reviewing.
Gary Smart (https://orcid.org/0000-0002-8578-0661): Formal analysis, Investigation, Methodology, Writing – original draft, Writing – editing and reviewing.
Isabelle Bray (https://orcid.org/0000-0002-5353-3287): Formal analysis, Methodology, Writing – original draft, Writing – editing and reviewing.
Pratiksha Pathak (https://orcid.org/0000-0002-3582-147X): Formal analysis, Writing – original draft, Writing – editing and reviewing.
Acknowledgements
We acknowledge the support of our colleagues at MIRA who expertly facilitated the delivery of fieldwork conducted in Makwanpur district. Their established networks and reputation as a trusted partner in the local community greatly aided the engagement of communities and stakeholders. We acknowledge the support of Swatantrata Abhiyan, a human rights NGO, who were particularly helpful when completing our review of policies and legislation supporting injury prevention in Nepal. We also acknowledge the contribution of colleagues at the Nepal Red Cross Society who greatly aided delivery of our studies exploring the delivery of first-response services. In particular, we would like to acknowledge Writu Bhatta Rai, Milan Raj Dharel, Amrit Dangi, Krishna Prasad Ghimire and Raju Raut for being non-academic co-authors on scientific publications. We acknowledge the contribution of Furba Sherpa for his support in accessing and processing data for studies with the Nepal Ambulance Service and for his support in drafting publications. We acknowledge Emer Brangan for her support with supervision and methodological guidance to the research team. We would like to thank all the members of the public, community representatives, advocates, clinicians, managers, senior decision-makers, stakeholders, students and academics who contributed to our studies as participants, advisory group members, or community engagement and involvement contributors, without whom our programme of research would not have been completed.
Data-sharing statement
Quantitative data are available on reasonable request. Data associated with the studies summarised in this synopsis paper are included in the published articles and the related supplementary information. All data requests should be submitted to the corresponding author for consideration.
Ethics statement
All publications summarised in this synopsis paper gained ethical approval in Nepal either through the Nepal Health Research Council or Kathmandu Medical College Institutional Review Committee. These approvals were then ratified by the Faculty Research Ethics Committee at the University of the West of England, Bristol prior to data collection. All publications describe the ethical approvals obtained for that study. Dates of approvals are shown in the table below.
| Study name (reference for associated publications) | Date of ethical approval | Approved by | Date of ratification by the Faculty REC at UWE Bristol |
|---|---|---|---|
| Workstream 1 (engaging stakeholders) | |||
| Injuries in Nepal: a neglected public health burden (editorial)20 | N/R | N/R | N/R |
| Perceptions of road dangers by professional stakeholders21 | 31 May 2019 | KMC Institutional Review Committee | 4 June 2019 |
| Research priorities for suicide prevention in Nepal22 | 25 November 2020 | Nepal Health Research Council | 9 December 2020 |
| Nepali journalists’ engagement in road safety reporting23 | N/R | N/R | N/R |
| Nuancing the need for speed (editorial)24 | N/R | N/R | N/R |
| Research priorities for road safety in Nepal52 | 9 June 2020 | KMC Institutional Review Committee | 18 June 2020 |
| Workstream 2 (evidence through data) | |||
| Understanding the burden of injuries in Nepal: a systematic review25 | N/R | N/R | N/R |
| Burden of injuries in Nepal: a review of GBD data26 | N/R | N/R | N/R |
| Utility of routine data reporting injuries requiring hospitalisation27 | 6 June 2019 | UWE, Bristol | N/R |
| Improving estimates of injury burden in Nepal27 | 10 September 2020 | Nepal Health Research Council | 23 September 2020 |
| Prehospital emergency care for trauma victims29 | 13 January 2020 | Nepal Health Research Council | 26 January 2021 |
| Surveillance of hospital-attended injury in Nepal 30–32 | 16 January 2019 | Nepal Health Research Council | 11 February 2019 |
| Household survey of home and work-related injuries33 | 30 January 2019 | Nepal Health Research Council | 21 February 2019 |
| Development of a community surveillance method for fatal injuries34 | 16 January 2019 | Nepal Health Research Council | 23 January 2019 |
| Economic burden of RTIs in Nepal35 | N/R | N/R | N/R |
| Injury risks for different road users: a secondary analysis37 | 10 May 2018 | Nepal Health Research Council | 30 May 2018 |
| Completeness of police reporting of road traffic crashes40 | 15 April 2019 | KMC Institutional Review Committee | 30 May 2019 |
| Workstream 3 (effective and cost-effective interventions) | |||
| Review of policies and legislation supporting injury prevention in Nepal41 | N/R | N/R | N/R |
| Perception of injury risk at home and at work43 | 16 January 2019 | Nepal Health Research Council | 5 April 2019 |
| Perceptions of road dangers by communities and stakeholders44–46 | 31 May 2019 | KMC Institutional Review Committee | 4 June 2019 |
| State of post-injury first response systems in Nepal47 | 10 October 2018 | Nepal Health Research Council | 25 October 2018 |
| Post-crash first response by traffic police: a feasibility study48 | 16 January 2019 | Nepal Health Research Council | 11 February 2019 |
| Barriers and facilitators to first aid after a RTC49 | 16 December 2020 | Nepal Health Research Council | 5 January 2021 |
Information governance statement
The data governance and management strategy applied to each of the studies completed through this award used the ‘five safes’ framework. 54 This is a systematic approach to good data governance, commonly used in government data management systems. The framework breaks data management and governance into five broad issues which need to be addressed: (1) safe projects, (2) safe people and (3) safe settings (which are all amenable to managerial controls); and (4) safe data and (5) safe outputs (which are amenable to statistical controls). The secure use of data within each project is determined by the system created by the five safes framework such that not every dimension needs to be as safe as another. Each study summarised in this synopsis paper had its own data management plan prepared as part of the application for ethical approval.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/GTJY4911.
Primary conflicts of interest: None of the authors have competing interests to declare, apart from Julie Mytton who was a member of the HTA MNCH Panel from 2008 to 2015 and Sunil Kumar Joshi who is an Editorial Board Member for BMJ Injury Prevention.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the GHR programme or the Department of Health and Social Care.
This synopsis was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
List of publications
Publications
Joshi SK, Pant PR, Banstola A, Bhatta S, Mytton J. Injuries in Nepal: a neglected public health burden and ways forward. Kathmandu Univ Med J 2018;15. https://doi.org/10.17613/9fw0-ta32
Bashford T, Joannides A, Phuyal K, Bhatta S, Mytton J, Harrison R, et al. Nuancing the need for speed: temporal health system strengthening in low-income countries. BMJ Glob Health 2019;4(4):e001816. https://doi.org/10.1136/bmjgh-2019-001816
Mytton JA, Bhatta S, Thorne M, Pant PR. Understanding the burden of injuries in Nepal: a systematic review of published studies. Cogent Med 2019;6(1):1673654. https://doi.org/10.1080/2331205X.2019.1673654
Banstola A, Kigozi J, Barton P, Mytton J. Economic burden of road traffic injuries in Nepal. Int J Environ Res Public Health 2020;17(12):4571. https://doi.org/10.3390/ijerph17124571
Magnus D, Bhatta S, Mytton J, Joshi E, Bird EL, Bhatta S, et al. Establishing injury surveillance in emergency departments in Nepal: protocol for mixed methods prospective study. BMC Health Serv Res 2020;20(1):433. https://doi.org/10.1186/s12913-020-05280-9
Pant PR, Banstola A, Bhatta S, Mytton JA, Acharya D, Bhattarai S, et al. Burden of injuries in Nepal, 1990–2017: findings from the Global Burden of Disease Study 2017. Inj Prev 2020;26(Suppl. 2):i57–66. https://doi.org/10.1136/injuryprev-2019-043309
Banstola A, Smart G, Raut R, Ghimire KP, Pant PR, Joshi P, et al. State of post-injury first response systems in Nepal – a nationwide survey. Front Publ Health 2021;9. https://doi.org/10.3389/fpubh.2021.607127
Bhatta S, Magnus D, Mytton J, Joshi E, Bhatta S, Adhikari D, et al. The epidemiology of injuries in adults in Nepal: findings from a hospital-based injury surveillance study. Int J Environ Res Publ Health 2021;18(23):12701. https://doi.org/10.3390/ijerph182312701
Bhatta S, Mytton J, Joshi E, Bhatta S, Adhikari D, Manandhar SR, et al. Development and evaluation of a community surveillance method for estimating deaths due to injuries in rural Nepal. Int J Environ Res Public Health 2021;18(17):8912. https://doi.org/10.3390/ijerph18178912
Gautam P, Mytton JA, Joshi SK, Pilkington P. Adolescent’s perception of road risk on their routes to school in Makwanpur, Nepal; a qualitative study. J Transp Health 2021;20:101009. https://doi.org/10.1016/j.jth.2021.101009
Joshi E, Bhatta S, Deave T, Mytton J, Adhikari D, Manandhar SR, et al. Perceptions of injury risk in the home and workplace in Nepal: a qualitative study. BMJ Open 2021;11(3):e044273. https://doi.org/10.1136/bmjopen-2020-044273
Khadka A, Gautam P, Joshi E, Pilkington P, Parkin J, Joshi SK, et al. Road safety and heavy goods vehicle driving in LMICs: qualitative evidence from Nepal. J Transp Health 2021;23:101247. https://doi.org/10.1016/j.jth.2021.101247
Magnus D, Bhatta S, Mytton J, Joshi E, Bhatta S, Manandhar S, et al. Epidemiology of paediatric injuries in Nepal: evidence from emergency department injury surveillance. Arch Dis Child 2021;106(11):1050–5. https://doi.org/10.1136/archdischild-2020-321198
Pant PR, Deave T, Banstola A, Bhatta S, Joshi E, Adhikari D, et al. Home-related and work-related injuries in Makwanpur district, Nepal: a household survey. Inj Prev 2021;27(5):450–5. https://doi.org/10.1136/injuryprev-2020-043986
Pant PR, Mytton J, Dharel MR, Dangi A, Rai WB, Joshi SK. The prevention of – and first response to – injuries in Nepal: a review of policies and legislation. Health Research Policy and Systems [Internet]. 2021 Apr 14 [cited 2023 May 19];19(1):65. Available from: https://doi.org/10.1186/s12961-021-00686-1
Bhatta S, Bhatta S, Mytton J, Joshi SK. Improving estimates of injury burden in Nepal: a qualitative study. J Nepal Health Res Council 2022;20(2). https://doi.org/10.33314/jnhrc.v20i02.3929
Joshi E, Bhatta S, Joshi SK, Mytton J. Identification of research priorities for suicide prevention in Nepal: a Delphi study. BMC Psychiatr 2022;22(1):429. https://doi.org/10.1186/s12888-022-04074-z
Joshi E, Gautam P, Khadka A, Pilkington P, Parkin J, Joshi SK, et al. Experience of living near a highway in Nepal: community perceptions of road dangers in Makwanpur district. J Transp Health 2022;24:101337. https://doi.org/10.1016/j.jth.2022.101337
Khadka A, Parkin J, Pilkington P, Joshi SK, Mytton J. Completeness of police reporting of traffic crashes in Nepal: evaluation using a community crash recording system. Traff Inj Prev 2022;23(2):79–84. https://doi.org/10.1080/15389588.2021.2012766
Pandey B, Khadka A, Joshi E, Joshi SK, Parkin J, Pilkington P, et al. Views of professional stakeholders on readiness for a safe road system in Nepal; an exploratory qualitative study. Int J Inj Contr Safe Promot 2022;29(2):217–25. https://doi.org/10.1080/17457300.2021.1983845
Pant PR, Rana P, Pradhan K, Joshi SK, Mytton J. Identifying research priorities for road safety in Nepal: a Delphi study. BMJ Open 2022;12(4):e059312. https://doi.org/10.1136/bmjopen-2021-059312
Smart G, Banstola A, Raut R, Ghimire K, Mytton J, Joshi E, et al. Post-crash first response by traffic police in Nepal: a feasibility study. Int J Environ Res Public Health 2022;19(14):8481. https://doi.org/10.3390/ijerph19148481
Pandey B, Banstola A, Smart G, Joshi SK, Mytton J. Barriers and facilitators to learning and using first aid skills for road traffic crash victims in Nepal: a qualitative study [published online ahead of print XXXX XX 2024] Global Health Res 2024. https://doi.org/10.3310/UTKW7640
Bhatta S, Pathak P, Khadka A, Parkin J, Pilkington P, Joshi SK, Mytton J. Injury risks for different road users in Nepal: a secondary analysis of routinely collected crash data [published online ahead of print XXXX XX 2024] Global Health Res 2024. https://doi.org/10.3310/DWTR9883
Amrit Banstola, Preeti Gautam, Gary Smart, Sunil Kumar Joshi and Julie Mytton.Banstola A, Gautam P, Smart G, Joshi SK, and Mytton J. Prehospital emergency care for trauma victims in Nepal: a mixed-methods study [published online ahead of print July 10 2024]. Global Health Res 2024. https://doi.org/10.3310/TMTG2437
Pandey B, Bray I, Joshi SK, Mytton JA. Utility of routine data reporting injuries requiring hospitalisation in Nepal: a secondary data analysis [published online ahead of print May 22 2024]. Global Health Res 2024. https://doi.org/10.3310/ATAE3098
Conference papers
Mytton J, Pant P, Ellis M, Baset K ul, Joshi SK. PW 1641 Establishing an injury research centre in Nepal; challenges and opportunities. Inj Prev 2018;24(Suppl. 2):A178–9. URL: https://injuryprevention.bmj.com/content/24/Suppl_2/A178.3 (accessed 19 May 2023).
Bhatta S, Magnus D, Mytton J, Adhikari D, Manandhar SR, Joshi E, et al. 5E.002 Feasibility of hospital-based injury surveillance in Nepal: a prospective study. Inj Prev 2021;27(Suppl. 2):A44–5. URL: https://injuryprevention.bmj.com/content/27/Suppl_2/A44.3 (accessed 19 May 2023).
Bhatta S, Mytton J, Adhikari D, Manandhar SR, Joshi E, Bhatta S, et al. P4.011 Community-level estimates of death due to injuries in Makwanpur district, Nepal. Inj Prev 2021;27(Suppl. 2):A70. URL: https://injuryprevention.bmj.com/content/27/Suppl_2/A70.2 (accessed 19 May 2023).
Deave T, Pant P, Manandhar SR, Adhikari D, Joshi E, Joshi S, et al. 3F.005 The epidemiology of home and workplace injuries in Nepal: a household survey. Inj Prev 2021;27(Suppl. 2):A28–9. URL: https://injuryprevention.bmj.com/content/27/Suppl_2/A28.4 (accessed 19 May 2023).
Gautam P, Mytton J, Pilkington P, Joshi S. 7A.001 Adolescent’s perception of road risk on their routes to school in Makwanpur, Nepal; a qualitative study. Inj Prev 2021;27(Suppl. 2):A55–6. URL: https://injuryprevention.bmj.com/content/27/Suppl_2/A55.3 (accessed 19 May 2023).
Khadka A, Gautam P, Joshi E, Pilkington P, Parkin J, Joshi S, et al. 3F.006 Truck drivers’ perception of road danger in Nepal: a qualitative study. Inj Prev 2021;27(Suppl. 2):A29. URL: https://injuryprevention.bmj.com/content/27/Suppl_2/A29.1 (accessed 19 May 2023).
Mytton J, Ellis M, Manhandar S, Joshi SK. 6C.004 Using capacity strengthening to enable effective injury prevention in Nepal. Inj Prev 2021;27(Suppl. 2):A52. URL: https://injuryprevention.bmj.com/content/27/Suppl_2/A52.3 (accessed 19 May 2023).
Mytton J, Joshi SK. Identification of research priorities for a safe systems approach to road safety in Nepal. Sixth Global Symposium on Health Systems Research. 13 January 2021 URL: www.youtube.com/watch?v=7gvi43STDi8&list=PL3-x3r4b6RFHOQPRTDPLzBCR2OMJ0CGN3&index=7 (accessed 14 December 2023).
Pandey B, Mytton J, Bray I, Joshi S. 5E.003 Epidemiology of injuries among in-patients in Nepal: a secondary data analysis. Inj Prev 2021;27(Suppl. 2):A45. URL: https://injuryprevention.bmj.com/content/27/Suppl_2/A45.1 (accessed 19 May 2023).
Pant PR, Dahal S, Krishnaswamy K, Joshi SK, Mytton J. 3C.006 Enabling journalists to contribute to the road safety system: experience from Nepal. Inj Prev 2021;27(Suppl. 2):A25. URL: https://injuryprevention.bmj.com/content/27/Suppl_2/A25.2 (accessed 23 May 2023).
Pant PR, Dangi A, Dharel M, Bhatta W, Joshi SK, Mytton J. 4C.003 Status of Nepal’s legislation for injury prevention and control: a critical review. Inj Prev 2021;27(Suppl. 2):A35. URL: https://injuryprevention.bmj.com/content/27/Suppl_2/A35.2 (accessed 19 May 2023).
Paudel S, Subedi M, Brangan E, Mytton J, Joshi S. 4C.001 Conceptualising ‘injury’ in Nepal: building shared understandings as a foundation for engagement. Inj Prev 2021;27(Suppl. 2):A34–5. URL: https://injuryprevention.bmj.com/content/27/Suppl_2/A34.3 (accessed 19 May 2023).
Smart G, Banstola A, Raut R, Ghimire K, Joshi E, Joshi SK, et al. 3D.001 Post-crash trauma care: first-responder training for the traffic police in Makwanpur, Nepal. Inj Prev 2021;27(Suppl. 2):A25. URL: https://injuryprevention.bmj.com/content/27/Suppl_2/A25.3 (accessed 19 May 2023).
Joshi E, Mytton J, Bhatta S, Joshi SK. 204 Service-user, clinician, advocate and academic priorities for suicide prevention research in Nepal. Inj Prev 2022;28(Suppl. 2):A31. URL: https://injuryprevention.bmj.com/content/28/Suppl_2/A31.3 (accessed 19 May 2023).
Mytton J, Pant P, Rana P, Pradhan K, Joshi SK. 201 Interagency collaboration for the identification of road safety research priorities in Nepal. Inj Prev 2022;28(Suppl. 2):A31. URL: https://injuryprevention.bmj.com/content/28/Suppl_2/A31.1 (accessed 19 May 2023).
Funding
This research was funded by the National Institute for Health and Care Research (NIHR) Global Health Research programme (NIHR award ref: 16/137/49) using UK aid from the UK Government to support global health research. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the UK government.
This synopsis provides an overview of the research award The burden of injuries in Nepal: findings from the NIHR Global Health Research Group. Other articles published as part of this thread are: [LINKS to other articles]. For more information about this research please view the award page [https://www.fundingawards.nihr.ac.uk/award/16/137/49])
About this synopsis
The contractual start date for this research was in July 2017. This article began editorial review in July 2023 and was accepted for publication in February 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Global Health Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Copyright
Copyright © 2025 Mytton et al. This work was produced by Mytton et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://doi.org/10.1001/jamapsychiatry.2014.2502. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
List of abbreviations
- EMT
- Emergency Medical Technician
- FCHV
- Female Community Health Volunteer
- GBD
- Global Burden of Disease
- GCRF
- Global Challenges Research Fund
- GHR
- Global Health Research
- GHRG
- Global Health Research Group
- HGV
- heavy goods vehicle
- HMIS
- Health Management Information System
- KMC
- Kathmandu Medical College
- LMIC
- low- and middle- income country
- MIRA
- Mother and Infant Research Activities
- NFDN
- National Federation of the Disabled Nepal
- NGO
- non-governmental organisation
- NIHR
- National Institute for Health and Care Research
- NIRC
- Nepal Injury Research Centre
- QR
- quality-related research
- RTI
- road traffic injury
- SDG
- Sustainable Development Goal
- UWE
- University of the West of England
- WHO
- World Health Organization
References
- World Health Organization . Injuries and Violence 2023. https://www.who.int/news-room/fact-sheets/detail/injuries-and-violence (accessed 1 July 2024).
- Gosselin RA, Spiegel DA, Coughlin R, Zirkle LG. Injuries: the neglected burden in developing countries. Bull World Health Organ 2009;87. https://doi.org/10.2471/blt.08.052290.
- Dhillon PK, Jeemon P, Arora NK, Mathur P, Maskey M, Sukirna RD, et al. Status of epidemiology in the WHO South-East Asia region: burden of disease, determinants of health and epidemiological research, workforce and training capacity. Int J Epidemiol 2012;41:847-60. https://doi.org/10.1093/ije/dys046.
- Karkee R, Lee AH. Epidemiology of road traffic injuries in Nepal, 2001–2013: systematic review and secondary data analysis. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010757.
- Government of Nepal . Nepal Economic Survey (Fiscal Year 2015 2016) 2016. https://mof.gov.np/site/publication-detail/1129 (accessed 14 December 2023).
- World Health Organization . Global Status Report on Road Safety 2018 2018. https://apps.who.int/iris/handle/10665/276462 (accessed 14 December 2023).
- UN General Assembly . Transforming Our World : The 2030 Agenda for Sustainable Development, A RES 70 1. 21 October 2015 n.d. www.refworld.org/legal/resolution/unga/2015/en/111816 (accessed 08 April 2024).
- Government of Nepal . Nepal Road Safety Action Plan (2013–2020) 2013. www.dor.gov.np/home/publication/traffic-safety/force/road-safety-action-plan-english (accessed 12 September 2023).
- World Health Organization . Global Plan for the Second Decade of Action for Road Safety 2021. www.who.int/teams/social-determinants-of-health/safety-and-mobility/decade-of-action-for-road-safety-2021-2030 (accessed 14 December 2023).
- Thapa AJ. Status Paper on Road Safety in Nepal. Kathmandu, Nepal: Department of Roads, Government of Nepal; 2013.
- Pant PR, Towner E, Ellis M, Manandhar D, Pilkington P, Mytton J. Epidemiology of unintentional child injuries in the Makwanpur district of Nepal: a household survey. Int J Environ Res Public Health 2015;12:15118-28. https://doi.org/10.3390/ijerph121214967.
- Bhattarai D, Singh SB, Baral D, Sah RB, Budhathoki SS, Pokharel PK. Work-related injuries among farmers: a cross-sectional study from rural Nepal. J Occup Med Toxicol 2016;11. https://doi.org/10.1186/s12995-016-0137-2.
- Bhatta S, Pant PR, Mytton J. Usefulness of hospital emergency department records to explore access to injury care in Nepal. Int J Emerg Med 2016;9. https://doi.org/10.1186/s12245-016-0120-9.
- Pandey NR. Emergency medicine in Nepal: present practice and direction for future. Int J Emerg Med 2016;9. https://doi.org/10.1186/s12245-016-0118-3.
- Sharma DC. Nepal earthquake exposes gaps in disaster preparedness. Lancet 2015;385:1819-20. https://doi.org/10.1016/S0140-6736(15)60913-8.
- Shrestha B, Pathranarakul P. Nepal Government’s emergency response to the 2015 earthquake: a case study. Soc Sci 2018;7. https://doi.org/10.3390/socsci7080127.
- UNFPA Nepal . Nepal Health Sector Strategy 2015–2020 2018. https://nepal.unfpa.org/en/publications/nepal-health-sector-strategy-2015-2020 (accessed 14 December 2023).
- Peden M, Oyegbite K, Ozanne-Smith J, Hyder A. World Report on Child Injury Prevention. Geneva: World Health Organization; 2004.
- Peden M, Scurfield R, Sleet D, Mohan D. World Report on Road Traffic Injury Prevention. Geneva: World Health Organization; 2010.
- Joshi SK, Pant P, Banstola A, Bhatta S, Mytton J. Injuries in Nepal: a neglected public health burden and ways forward. Kathmandu Univ Med J 2017;15:269-70. https://doi.org/10.17613/9fw0-ta32.
- Pandey B, Khadka A, Joshi E, Joshi SK, Parkin J, Pilkington P, et al. Views of professional stakeholders on readiness for a safe road system in Nepal; an exploratory qualitative study. Int J Inj Contr Saf Promot 2022;29:217-25. https://doi.org/10.1080/17457300.2021.1983845.
- Joshi E, Bhatta S, Joshi SK, Mytton J. Identification of research priorities for suicide prevention in Nepal: a Delphi study. BMC Psychiatry 2022;22. https://doi.org/10.1186/s12888-022-04074-z.
- Pant PR, Dahal S, Joshi SK, Mytton J. Engaging Nepali journalists in good road safety reporting: evaluation of the impact of training workshops. SAGE Open 2023;13. https://doi.org/10.1177/21582440231204161.
- Bashford T, Joannides A, Phuyal K, Bhatta S, Mytton J, Harrison R, et al. Nuancing the need for speed: temporal health system strengthening in low-income countries. BMJ Glob Health 2019;4. https://doi.org/10.1136/bmjgh-2019-001816.
- Mytton JA, Bhatta S, Thorne M, Pant PR. Understanding the burden of injuries in Nepal: a systematic review of published studies. Cogent Med 2019;6. https://doi.org/10.1080/2331205X.2019.1673654.
- Pant PR, Banstola A, Bhatta S, Mytton JA, Acharya D, Bhattarai S, et al. Burden of injuries in Nepal, 1990–2017: findings from the Global Burden of Disease Study 2017. Inj Prev 2020;26:i57-66. https://doi.org/10.1136/injuryprev-2019-043309.
- Pandey B, Bray I, Joshi SK, Mytton JA. Utility of routine data reporting injuries requiring hospitalisation in Nepal: a secondary data analysis [published online ahead of print May 22 2024]. Global Health Res 2024. https://doi.org/10.3310/ATAE3098.
- Bhatta S, Bhatta S, Mytton J, Joshi SK. Improving estimates of injury burden in Nepal: a qualitative study. J Nepal Health Res Counc 2022;20:339-46. https://doi.org/10.33314/jnhrc.v20i02.3929.
- Magnus D, Bhatta S, Mytton J, Joshi E, Bird EL, Bhatta S, et al. Establishing injury surveillance in emergency departments in Nepal: protocol for mixed methods prospective study. BMC Health Serv Res 2020;20. https://doi.org/10.1186/s12913-020-05280-9.
- Banstola A, Gautam P, Smart G, Joshi SK, Mytton J. Prehospital emergency care for trauma victims in Nepal: a mixed-methods study [published online ahead of print July 10 2024]. Global Health Res 2024. https://doi.org/10.3310/TMTG2437.
- Bhatta S, Magnus D, Mytton J, Joshi E, Bhatta S, Adhikari D, et al. The epidemiology of injuries in adults in Nepal: findings from a hospital-based injury surveillance study. Int J Environ Res Public Health 2021;18. https://doi.org/10.3390/ijerph182312701.
- Magnus D, Bhatta S, Mytton J, Joshi E, Bhatta S, Manandhar S, et al. Epidemiology of paediatric injuries in Nepal: evidence from emergency department injury surveillance. Arch Dis Child 2021;106:1050-5. https://doi.org/10.1136/archdischild-2020-321198.
- Pant PR, Deave T, Banstola A, Bhatta S, Joshi E, Adhikari D, et al. Home-related and work-related injuries in Makwanpur district, Nepal: a household survey. Inj Prev 2021;27:450-5. https://doi.org/10.1136/injuryprev-2020-043986.
- Bhatta S, Mytton J, Joshi E, Bhatta S, Adhikari D, Manandhar SR, et al. Development and evaluation of a community surveillance method for estimating deaths due to injuries in rural Nepal. Int J Environ Res Public Health 2021;18. https://doi.org/10.3390/ijerph18178912.
- Banstola A, Kigozi J, Barton P, Mytton J. Economic burden of road traffic injuries in Nepal. Int J Environ Res Public Health 2020;17. https://doi.org/10.3390/ijerph17124571.
- Khadka A, Parkin J, Pilkington P, Joshi SK, Mytton J. Completeness of police reporting of traffic crashes in Nepal: evaluation using a community crash recording system. Traffic Inj Prev 2022;23:79-84. https://doi.org/10.1080/15389588.2021.2012766.
- Bhatta S, Pathak P, Khadka A, Parkin J, Pilkington P, Joshi SK, et al. Injury risks for different road users in Nepal: a secondary analysis of routinely collected crash data [published online ahead of print XXXX XX 2024]. Global Health Res 2024. https://doi.org/10.3310/DWTR9883.
- World Health Organization . WHO Global Status Report on Road Safety 2013: Supporting a Decade of Action 2013. https://apps.who.int/iris/handle/10665/78256 (accessed 14 December 2023).
- World Health Organization . Global Status Report on Road Safety 2015 2015. https://apps.who.int/iris/handle/10665/189242 (accessed 14 December 2023).
- Khadka A, Parkin J, Pilkington P, Joshi SK, Mytton J. Completeness of police reporting of traffic crashes in Nepal: evaluation using a community crash recording system. Traffic Inj Prev 2022;23:79-84. https://doi.org/10.1080/15389588.2021.2012766.
- Pant PR, Mytton J, Dharel MR, Dangi A, Rai WB, Joshi SK. The prevention of – and first response to – injuries in Nepal: a review of policies and legislation. Health Res Policy Syst 2021;19. https://doi.org/10.1186/s12961-021-00686-1.
- Centers for Disease Control and Prevention: Office of the Associate Director for Policy . CDC’s Policy Analytical Framework n.d. https://stacks.cdc.gov/view/cdc/25335 (accessed 14 December 2023).
- Joshi E, Bhatta S, Deave T, Mytton J, Adhikari D, Manandhar SR, et al. Perceptions of injury risk in the home and workplace in Nepal: a qualitative study. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2020-044273.
- Gautam P, Mytton JA, Joshi SK, Pilkington P. Adolescent’s perception of road risk on their routes to school in Makwanpur, Nepal; a qualitative study. J Transp Health 2021;20. https://doi.org/10.1016/j.jth.2021.101009.
- Joshi E, Gautam P, Khadka A, Pilkington P, Parkin J, Joshi SK, et al. Experience of living near a highway in Nepal: community perceptions of road dangers in Makwanpur district. J Transp Health 2022;24. https://doi.org/10.1016/j.jth.2022.101337.
- Khadka A, Gautam P, Joshi E, Pilkington P, Parkin J, Joshi SK, et al. Road safety and heavy goods vehicle driving in LMICs: qualitative evidence from Nepal. J Transp Health 2021;23. https://doi.org/10.1016/j.jth.2021.101247.
- Banstola A, Smart G, Raut R, Ghimire KP, Pant PR, Joshi P, et al. State of post-injury first response systems in Nepal – a nationwide survey. Front Public Health 2021;9. https://doi.org/10.3389/fpubh.2021.607127.
- Smart G, Banstola A, Raut R, Ghimire K, Mytton J, Joshi E, et al. Post-crash first response by traffic police in Nepal: a feasibility study. Int J Environ Res Public Health 2022;19. https://doi.org/10.3390/ijerph19148481.
- Pandey B, Banstola A, Smart G, Joshi SK, Mytton J. Barriers and facilitators to learning and using first aid skills for road traffic crash victims in Nepal: a qualitative study [published online ahead of print XXXX XX 2024]. Global Health Res 2024. https://doi.org/10.3310/UTKW7640.
- Vaidya A, Simkhada P, Simkhada B. The impact of federalization on health sector in Nepal: new opportunities and challenges. J Nepal Health Res Counc 2019;17:558-9. https://doi.org/10.33314/jnhrc.v17i4.2217.
- World Health Organization . Global Plan for the Decade of Action on Road Safety 2011–2020 2011. www.who.int/publications/m/item/global-plan-for-the-decade-of-action-for-road-safety-2011-2020 (accessed 14 December 2023).
- Pant PR, Rana P, Pradhan K, Joshi SK, Mytton J. Identifying research priorities for road safety in Nepal: a Delphi study. BMJ Open 2022;12. https://doi.org/10.1136/bmjopen-2021-059312.
- Gautam P, Khadka A, Chand OB, Prasai M, Paudel S, Joshi SK, et al. Facilitators and barriers to inclusive and safe mobility on urban roads in Kathmandu, Nepal: a participatory research study. Disabil Soc 2024:1-22. https://doi.org/10.1080/09687599.2024.2331728.
- Desai T, Ritchie F, Whelpton R. The Five Safes: Designing Data Access for Research. Bristol: University of the West of England; 2016.
