Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 16/01/24. The contractual start date was in September 2017. The final report began editorial review in August 2021 and was accepted for publication in February 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Hassiotis et al. This work was produced by Hassiotis et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Hassiotis et al.
Chapter 1 Background and study overview
Challenging behaviour and outcomes in adults with intellectual disabilities
Adults with intellectual disabilities (also known as learning disabilities in the UK) constitute around 1% of the population. 1 Substantial research shows that these adults have higher rates of mental ill-health,2 and many display challenging behaviour such as aggression towards others, property destruction and self-injury. 3–7 A whole-population epidemiological survey found that ≈ 18% of adults with intellectual disabilities living in the community present with new-onset or relapse of serious challenging behaviour. 8
Challenging behaviour may be the precursor to abuse and/or the implementation of restrictive practices by health-care staff looking after adults with intellectual disabilities. 9 The most recent examples of institutional abuse of adults with intellectual disabilities who display challenging behaviour came to light in 2011 at Winterbourne View hospital,10 followed by Whorlton Hall in 2018. 11 In England, the Transforming Care programme12 was published shortly after as a national response to the Winterbourne View scandal to improve the lives of adults with intellectual disabilities who display challenging behaviour by setting transparent monitoring procedures, conducting regular service audits, employing qualified health-care professionals and promoting advocacy. The interim government report published following the scandal emphasised that the quality of lives of adults with intellectual disabilities and their families improved following deinstitutionalisation. 12 However, the Learning Disability Census Report13 indicated minimal change over the years 2013–15 in relation to the number of inpatient admissions in England, length of inpatient stay, out-of-area placements and use of antipsychotic medication to manage challenging behaviour. This confirmed concerns about the pace of progress in the care provided for this population by community intellectual disability services (CIDSs) across the country. Similarly, data from inpatient services for adults with intellectual disabilities and/or autism showed a very gradual decrease in the number of admissions over time between March 2015 (admissions, n = 2895) and September 2020 (admissions, n = 2060). 14
Data collected by the Department of Health and Social Care indicated that 24,000 adults with intellectual disabilities would be at risk of being admitted to assessment and treatment units, which are often hundreds of miles away from their home, because of challenging behaviour. 6,15,16 These studies indicate that younger male adults with intellectual disabilities and history of previous admissions appear to be at an increased risk of re-admission, such that they should be a population of focus for intervention. 17 Previous concerns about the overprescription of medication were confirmed by a recent study that reported increased figures of psychotropic drug prescription by general practitioners (GPs) to adults with intellectual disabilities. 18,19 The ‘Stopping The Over-Medication of People with an intellectual disability, autism or both’ (STOMP) programme20 was launched by NHS England in 2016 to support adults with neurodevelopmental conditions (including intellectual disabilities) remain well and have a good quality of life. A recent study published by Public Health England reported changes that were in the desired direction over a 7-year period (January 2010–December 2017). 21 The study findings revealed that GPs’ prescription of psychotropic medication to adults with intellectual disabilities to manage challenging behaviour appeared to have decreased since the launch of the STOMP programme in June 2016,20 but it was too early to attribute any observations in prescribing trends to the programme. 21
Out-of-area prolonged hospitalisations and overprescription of psychotropic medication to adults with intellectual disabilities remain an excessive financial cost to the NHS, ranging from £96,000 to £222,000 per person annually, because of the need for more intensive support. 3,13,22 Failure to effectively address a display of challenging behaviour before it reaches a crisis point causes significant distress and burden to families and the consequent breakdown of placements. 23,24 Cumulative studies in Canada indicated that adults with intellectual disabilities were more likely to visit the emergency department,25 return to the emergency department within 30 days of discharge,26 have delayed discharge, be in long-term inpatient care and die prematurely. 27
The concept of intensive support teams in the UK
Specialist intensive services for adults with intellectual disabilities who display challenging behaviour appear to have operated internationally since 1985. 28 From as early as 1993, published literature from the UK has advocated for intensive support teams (ISTs) to support the effective management of challenging behaviour within the community and to prevent inpatient admissions. 29–31 In 1993, 65 specialist teams were operating in England and Wales. 32 ISTs were developed as specialist services that were expected to support people with intellectual disabilities who display challenging behaviour in their local communities following deinstitutionalisation. 32 A number of terms are used to describe ISTs, including ‘peripatetic teams’, ‘assertive outreach teams’ and ‘specialist behaviour teams’. 29,33
A recent survey29 identified 46 peripatetic services for people with intellectual disabilities who display challenging behaviour in England (teams, n = 40), Scotland (teams, n = 4), Wales (teams, n = 1) and Northern Ireland (team, n = 1). These teams aim to help carers manage such behaviours by delivering a range of multidisciplinary specialist support and interventions [e.g. positive behaviour support (PBS), positive psychology, behavioural, eclectic and proactive work) that aim to improve independence skills and mental and physical ill health; to reduce other risks; and, more recently, for those who are inpatients, to prompt timely discharge planning. 29 ISTs are seen as having a significant role in recovery and, therefore, as leading to a better quality of life and a reduction in the frequency and severity of further episodes of crisis.
Widespread concerns about the mental health, social and financial outcomes of inadequately supporting adults with intellectual disabilities who display challenging behaviour over the years were highlighted by NHS England in 2015 and 2017. 34,35 In Transforming Care: a National Response to Winterbourne View Hospital,12 ISTs were recommended to provide specialist, proactive and responsive care, aimed at avoiding unnecessary inpatient admissions, supporting adults within the community or reducing inpatient length of stay. In the main, ISTs are community-based, specialist, multidisciplinary (e.g. psychology, nursing, psychiatry) health-care teams that deliver interventions such as PBS or other support 24 hours per day, 7 days per week (24/7), when necessary, as part of their operation. 34,35
The announcement of the national ‘Building the Right Support’34 plan aimed to complement the previous policy initiative of 201212 by developing more community services to reduce the number of inpatient admissions for adults with intellectual disabilities who display challenging behaviour. 34 NHS England funded six services to act as pilot sites and reinvest any savings in enhancing their community services, including ISTs. In 2017, a total of 48 Transforming Care Partnerships were established in different areas of England to improve the quality of care and quality of life of adults with intellectual disabilities; they aimed to adapt their services in a way that would make a real difference to the lives of adults with intellectual disabilities. 35 Since 2015, the establishment of care and treatment reviews (CTRs) contributed to a sharp reduction in the number of unnecessary inpatient admissions. Data from inpatient services for adults with intellectual disabilities and/or autism showed that this resulted in a 30% decrease in the number of admissions between March 2015 (n = 2895) and September 2020 (n = 2060). 14 Similarly, > 70% (403/552) of CTRs for adults with intellectual disabilities and challenging behaviour were not admitted to hospital in 2016–17. 36
The Systemic, Therapeutic, Assessment, Resources, and Treatment (START) programme model was identified as best practice by the National Academy of Sciences Institute of Medicine in the USA. 37 It provides community-based, person-centred crisis intervention 24/7 for adults with intellectual disabilities who display challenging behaviour; this is delivered by a multidisciplinary team that collects outcome measures routinely and develops partnerships with local service providers. 38,39 Non-randomised research studies emphasised that adults with intellectual disabilities who received support from the intensive START clinical team reported less challenging behaviour, and fewer psychiatric emergency department visits and hospitalisations at 12 months. 38,39 Although the data suggest that the START programme has the potential to improve outcomes for adults with intellectual disabilities in crisis, a randomised controlled trial is yet to test if the START programme is effective for adults with intellectual disabilities who also experience a behavioural or mental health issue, especially as such issues often coexist with physical health comorbidities.
Different models of intensive support teams in the NHS
There is currently little evidence regarding the preferred IST model to meet the complex needs and challenging behaviour of adults with intellectual disabilities in the community. Previous research has demonstrated the positive contribution of standalone specialist behaviour support compared with standard treatment for adults with intellectual disabilities to improve the presentation of challenging behaviour over time (e.g. over 3 and 6 months). 40 On the other hand, Inchley-Mort et al. 41 reported that, at 6 and 12 months, the challenging behaviour of adults with intellectual disabilities who received standalone specialist behaviour support improved compared with the behaviour of those who received usual care from professionals based within a CIDS who were trained to deliver behavioural interventions.
Although there may be a rationale for standalone ISTs,40 there is currently no substantial evidence on long-term outcomes. This has led to scepticism about IST provision and concerns that devoting a large number of resources to specialist services will detract from offering good-quality care universally, especially as emerging evidence suggests that alternatives (e.g. embedded teams) may also be effective. 41 Furthermore, adults with intellectual disabilities and their carers may face disruption and discontinuity in care due to frequent changes in service provision and they may be dissatisfied with what they perceive as the less ‘expert’ service provided by CIDSs. 42 A pilot study found that placing IST staff within a CIDS for 6 months increased staff confidence and understanding of working with adults with intellectual disabilities who display challenging behaviour. 43 In addition, the findings of the service redesign pilot project reported that the CIDS team described the support from IST colleagues as beneficial to improving clinical outcomes for adults with intellectual disabilities, enhancing the IST’s visibility and providing clarity on the existing resources to manage challenging behaviour. 43
The national plan aspires to develop better community services for adults with intellectual disabilities who display challenging behaviour (and/or other complex needs) to reflect the diversity of this population. 34 The suggested service redesign focused on presenting adults with intellectual disabilities as living satisfying, valued lives and being treated with dignity and respect. 34 However, it does not distinguish between mental health and challenging behaviour functions, nor does it give any guidance on the duration of engagement with the individual with intellectual disability. This contrasts with the high-fidelity models that have been in operation in adult mental health, specifically home treatment teams, crisis teams and assertive outreach services. As a result, there is confusion about whether ISTs should follow the principles of operation found in mental health crisis resolution and home treatment teams or assertive case treatment teams. Clarification on these points is particularly important as it has direct consequences on how adults with intellectual disabilities who display challenging behaviour can be best supported in the short- and longer-term. Therefore, despite the roll-out of the Transforming Care programme,44 to the best of our knowledge, there has not been a systematic evaluation of ISTs in terms of characterisation, patient outcomes and relationships with other services in the areas in which they operate. Other potential challenges in establishing ISTs are the lack of a mandate to develop such services, the lack of specification of the approach to follow and the multiple configurations of CIDSs across England and other UK countries.
The literature from other populations (e.g. dementia care45) suggests that home treatment teams appear to offer effective management of crises and to reduce the number of admissions. Wheeler et al. 46 reported limited evidence of the clinical impact of crisis teams on hospital admissions in adults with acute mental health problems, but adults with acute mental health problems, carers and health-care professionals emphasised that accessibility, continuity of care, time to talk, practical help and treatment at home were valuable features of good practice by crisis resolution teams in adult mental health. Thus far, there has been limited reporting on stakeholder experiences of ISTs; however, two studies showed that adults with intellectual disabilities, family carers and care home (paid) carers find the involvement of IST staff and the frequency of contact helpful. 42,47
In addition, although the Building the Right Support34 plan was much needed, it was developed to improve care for adults with intellectual disabilities based on multiple-stakeholder consensus (including adults with intellectual disabilities, their families, service providers and clinicians), rather than on evidence-based information and high-quality research. However, NHS commissioners require robust information on the most efficient service model for adults with intellectual disabilities who display challenging behaviour to fund appropriate services. National Institute for Health and Care Excellence (NICE) guideline 11 on challenging behaviour3 reports the state of evidence thus:
It is widely recognised that locally accessible care settings could be beneficial and could reduce costs but there is no strong empirical evidence to support this.
NICE. 3
In short, an inquiry into ISTs’ characteristics and their ability to deliver positive outcomes to foster long-term investment in them is an important and pressing clinical question. In line with NHS England guidance15 for locally and effectively managing adults with intellectual disabilities who display challenging behaviour, this work will provide commissioners and clinicians with the evidence they need to deliver high-quality care to an underserved population. The project maps onto principles 7 (‘I can access specialist health and social care support in the community’) and 8 (‘If I need it, I get support to stay out of trouble’) of the plan outlined in the service model for commissioners of health and social care services in England. 34 This project is also in accordance with The NHS Long Term Plan,48 which aims to ‘improve community-based support so that adults can lead lives of their choosing in homes not hospitals; further reducing our reliance on specialist hospitals’ (Contains public sector information licensed under the Open Government Licence v3.0. URL: www.nationalarchives.gov.uk/doc/open-government-licence/version/3/).
Study aims and objectives
The overall aim of this study was to systematically examine the clinical and cost characteristics of different IST care models in England to ensure that ISTs are appropriately funded and implemented within the NHS.
The study objectives were to:
-
describe the geographical distribution and provision of IST services in England
-
create a typology of IST service operation in England
-
compare the clinical effectiveness of different IST models for service user outcomes, including challenging behaviour, mental health status, risk, satisfaction with care, quality of life and hospital admissions
-
estimate the costs of different IST models and investigate cost-effectiveness
-
understand how ISTs impact the lives of adults with intellectual disabilities who display challenging behaviour, their families and the local services
-
generate evidence to inform and support decision-making on commissioning ISTs for adults with intellectual disabilities who display challenging behaviour.
Our key research questions were:
-
What models of IST are currently in operation?
-
Which models perform better in achieving positive outcomes for service users?
-
What are the costs and cost-effectiveness of the different IST models and how do they compare?
-
How does the local service context support or hinder these processes?
-
What are service users’ and family carers’ experiences of ISTs and do they differ between models?
-
What are the views of multiple stakeholders on the strengths and limitations of ISTs and the processes that support or hinder their functioning?
Study design
A two-phase mixed-methods design was implemented to address these research questions. Figure 1 illustrates the overall design and flow of the study.
FIGURE 1.
Study overview.
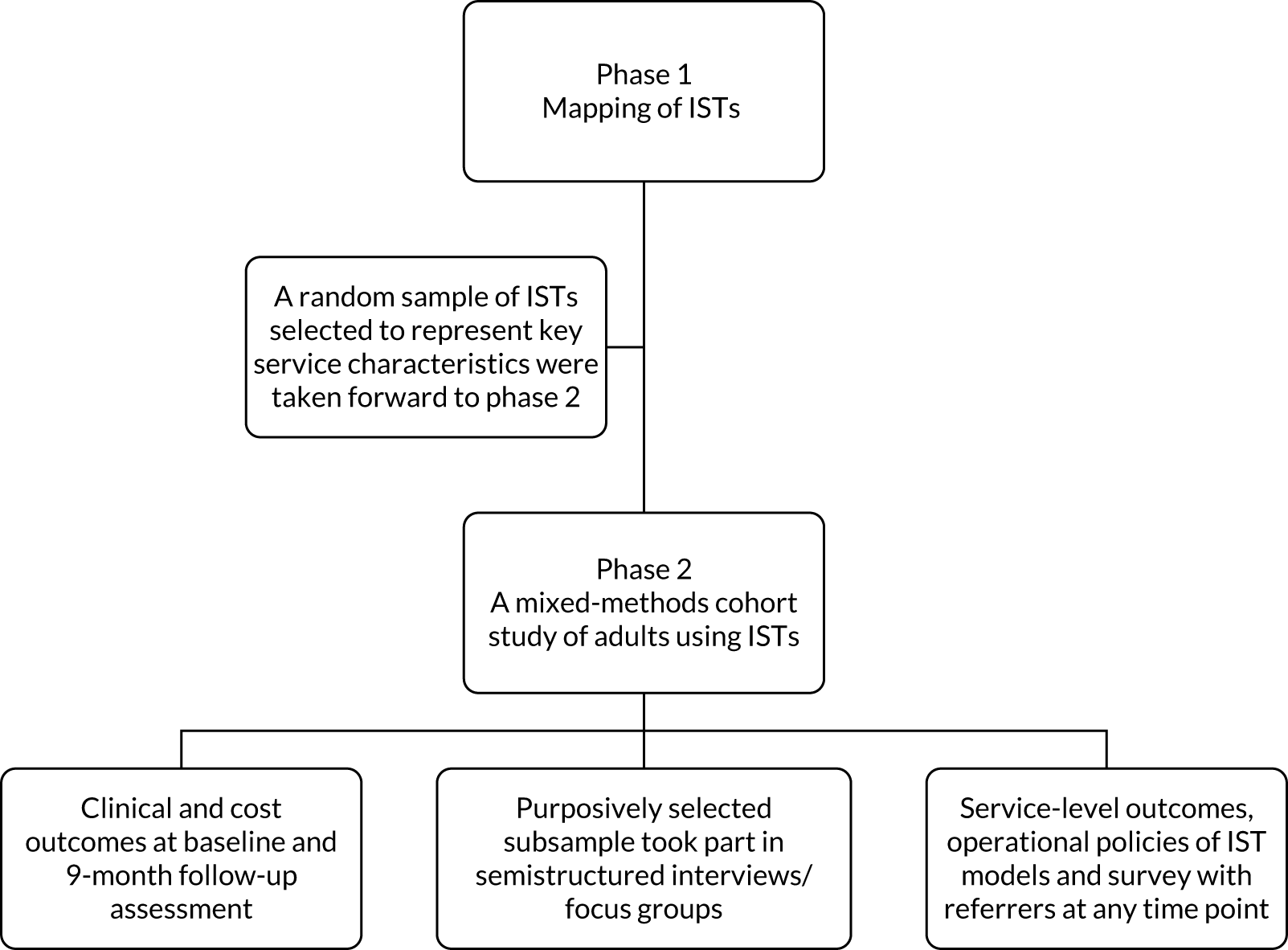
Phase 1 was a quantitative study that identified IST services in the 48 Transforming Care Partnerships in England, described their service characteristics and created a typology of different IST models.
Phase 2 was a mixed-methods cohort study that conducted a survey of health-care professionals’ experiences of the referral process to ISTs and investigated the:
-
clinical and cost outcomes of the identified IST models at 9 months from baseline
-
experiences of multiple stakeholders of ISTs
-
service-level outcomes and operational policies of the identified IST models.
Ethics approval
The Health Research Authority reviewed and approved the study and all amendments (substantial and non-substantial). The Research Ethics Committee reference number is 18/LO/0890.
Amendments to study protocol
The following changes were made to the original study protocol:
-
substantial amendments –
-
revised study exclusion criteria for phase 2
-
revised sample size and power calculations
-
additional information about qualitative interview transcriptions
-
number of teams changed from 16 to as many as needed to reach recruitment target; data collection for people who refer to ISTs extended to include self-completed survey (e-mail/online/paper or combination)
-
topic guide for adults with intellectual disabilities and relevant study documents [e.g. participant information sheets (PISs) and informed consent forms (ICFs)] updated to reflect staff changes.
-
-
non-substantial amendments –
-
addition of new research sites
-
addition of new research sites and revised GP letter
-
addition of new research site
-
withdrawal of research site and addition of new research site
-
change of local collaborator in one research site
-
addition of new research sites
-
updated study documents to reflect staff changes, use of digital platforms and telephone call to respond to the COVID-19 pandemic
-
costed study extension.
-
Deviation from the study protocol
The protocol for the study has been published. 49 The study diverged from the Health Research Authority-approved protocol to complete the qualitative evaluation of IST models, recruiting from 10 ISTs instead of seven ‘case study’ sites. The aim of conducting interviews in seven ‘case study’ sites was to link the perspectives of stakeholders to specific service context. Owing to problems recruiting from these seven sites during the COVID-19 pandemic, we extended our efforts to other sites with similar service characteristics.
Adverse events
No adverse events were reported to the study.
Data management
All aspects of data management of the study complied with the UK’s Data Protection Act 1998,50 good clinical practice and the General Data Protection Regulation. 51 Data from phase 1 were collected electronically using online survey software (Opinio; ObjectPlanet AS, Oslo, Norway) or on paper forms that did not contain identifiable information and were marked with an anonymised participant identification number only. The paper files from this project were stored on secure University College London (UCL) premises in a locked cupboard accessible to members of the UCL research team only. We followed all aspects of data protection as per research governance and social care and NHS policies. Any data stored at UCL was registered for data protection (Z6364106/2018/04/09) and participant records were anonymised. Identifiable data that constitutes the identification key to link consent forms to case report forms and audio-recordings of consent obtained by telephone/video were stored in the UCL secure platform Data Safe Haven.
Patient and public involvement
In the course of preparing the application, a number of consultations were carried out with two adults with intellectual disabilities and five family carers and paid carers of adults with intellectual disabilities who display challenging behaviour to select and discuss the topic of the funding proposal. They were unanimous in their praise for the accessibility and communication that they had with the IST and they stated that it should be a resource for all services for people with intellectual disabilities who are likely to display challenging behaviour. They emphasised the support that the IST provided in the community, at the person’s home and to the caregivers. They also talked about other aspects of the team, such as the teaching and training functions, that had been useful to them.
We were able to speak with two service users who had direct experience of working with the team; they mentioned that the professionals had helped them with ‘managing their anger’ and that they were very fond of them as they ‘visited often and could talk to staff’. All were supportive of the application because they thought that it was important to find out more about the teams and whether or not commissioners may be more interested in funding ISTs ‘if they know more about the benefits’. The feedback received from the adults with intellectual disabilities and the family carers was overwhelmingly positive and ISTs were seen as an important resource for reducing the number of admissions and maintaining these adults in the community.
In addition, a co-applicant gave a presentation on IST at an educational meeting for trainees and consultants in intellectual disability. The psychiatric audience considered issues such as evidence, the wider context of the teams and the need to have robust data on what works best, as they recognised that we need to improve the existing evidence base and value for money for CIDS practice.
Post award, we liaised with two London-based service user groups to decide the involvement of service users in the project. We enlisted interested adults who wished to be members of the Project Advisory Group. We conducted interviews to appoint people with a range of different experiences and carried out a 3-hour training session in research skills and tasks over the duration of the project using easy-read formats based on National Institute for Health and Care Research (NIHR) guidance. 52 The Project Advisory Group had two facilitators in case of illness or leave. We also sought input from family carers through local carer groups in co-applicants’ sites.
The Family Carer Advisory Group included four family carers recruited through the Challenging Behaviour Foundation (Chatham, UK), an independent charity of experts by experience.
The specific tasks of the service user and family carer advisors’ input to the Project Advisory Group were to (1) develop participant information resources and pilot instruments and topic guides; (2) contribute to the interpretation of the findings; (3) have an overview of the study processes, advise on recruitment and contact with potential participants and carers; and (4) report and disseminate the research findings.
Meetings with both expert-by-experience groups took place every 3 months. The Project Advisory Group remained actively engaged in all of the tasks listed above. In particular, their views during the qualitative coding and analysis of transcripts directed the final presentation of study findings. When physical or virtual presence in meetings was challenging, a telephone call was arranged to discuss the study progress and record each member’s comment.
Last, there was service user and family caregiver representation in the Study Steering Committee that oversaw the study. Thus, the interests of all parties and the views of those involved have been fully represented in the conduct of the study.
Chapter 2 Identification of intensive support models in England
Parts of this chapter have been reproduced with permission from Hassiotis et al. 53 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Introduction
Phase 1 of the study was required to proceed to the model evaluation phase and comprised a national survey that aimed to investigate the operation of ISTs in England.
The key objectives of the survey were to:
-
examine the geographical distribution and characteristics of ISTs in England
-
develop a typology of IST service models
-
describe the IST model profiles and contextual characteristics.
The phase 1 study has been published elsewhere. 53
Methods
A screening questionnaire (see additional files; www.journalslibrary.nihr.ac.uk/programmes/hsdr/160124/#/documentation; accessed 3 March 2022) was initially developed to identify the geographical distribution of ISTs, with reference to national guidance;30 it was sent to all specialist CIDSs in England. CIDSs were identified through multiple routes, including Clinical Commissioning Groups, online searches, previous research and the list of 48 Transforming Care Partnerships. The screening questionnaire included a list of the terms that are used to describe specialist intensive care in England (see Chapter 1).
The responses to the screening questionnaire were reviewed by members of the Project Management Group (PMG) to check whether or not the identified intensive teams fulfilled the IST criteria and should be contacted for the IST-specific survey. Any discrepancies regarding team assignment were resolved by discussion with all PMG members. The criteria were broad: (1) identification of IST function separate from CIDSs, (2) a referral pathway for challenging behaviour and/or (3) staff trained to deliver interventions for challenging behaviour.
The managers of all ISTs identified from the screening survey were invited to take part, and those who agreed to take part were sent a detailed online questionnaire using the Opinio platform (see additional files; www.journalslibrary.nihr.ac.uk/programmes/hsdr/160124/#/documentation; accessed 3 March 2022). The questionnaire was divided into 13 sections, including 62 open- and close-ended questions that covered information about service type and location, caseload and referral numbers, opening hours, response target times, staffing, management and funding, services provided by the IST, service user characteristics, use of outcome measures, interventions and assessments, and the intensity of support, as well as concluding questions. There were free-text questions that addressed the model and philosophy of IST care, suggested changes to the service, challenges faced by the IST and priorities for improving the service.
A number of strategies were adopted to achieve a high completion and return rate, such as having both an online and a hard-copy version of the survey, regular e-mail prompts and the option of completing the questionnaire by telephone. The survey response data were managed using the Opinio software.
Data analysis
The IST characteristics and geographical location of ISTs were summarised using descriptive statistics [i.e. count and percentage for categorical measures or median and interquartile ranges (IQRs) for continuous outcomes which were not normally distributed].
A hierarchical cluster analysis was performed using six grouping variables to develop a typology of ISTs and classify services on prespecified variables into a number of groups, with similar services being placed in the same group. These were:
-
setting of service
-
team composition
-
caseload
-
operating hours
-
type of referral permitted
-
use of outcome measures.
All factors were defined as binary measures for each of these variables. IST staff were grouped into professional categories such as nursing psychology, psychiatry, social work and other. The total number of health-care professionals was calculated for each team. Teams were defined as multiprofessional if they consisted of two or more professional staff categories. The caseload per team member was calculated as the number of service users per full-time equivalent (FTE) member of staff. A large caseload was defined as 2.5 or more clients per FTE staff member (excluding trainees), which is in line with guidance from the UK Department of Health and Social Care about mental health crisis teams. 54
The operating hours of ISTs were defined as extended hours of operation if they offered services outside working hours (09.00–17.00) on weekdays or offered any weekend services. Those ISTs that accepted referrals directly from service users eligible to receive specialist intellectual disability services, or from their family carers and paid carers, were defined as allowing self-referrals to their service. On the other hand, there were ISTs that accepted referrals exclusively from services such as GP services, mental health services or police or third-sector organisations, and not self-referrals. The remaining two grouping factors, setting (e.g. embedded within CIDSs or independent service separate from CIDSs) and whether or not the service used outcome measures, were based on direct responses to the relevant questions in the survey.
The six grouping variables were used to perform a hierarchical cluster analysis employing Ward’s method,55 with squared Euclidean distance as the dissimilarity measure. The accumulation of individual services into larger clusters was illustrated with a dendrogram. The dendrogram was carefully reviewed, taking into consideration the dissimilarity of measures for different clusters, a visual inspection of the dendrogram and a discussion about the clinical validity of the proposed models with the co-applicant experts. All analyses were carried out using Stata/IC, version 14.0 (StataCorp LP, College Station, TX, USA).
The qualitative data from free-text responses were analysed thematically. 56 Data were extracted into a Microsoft Excel® (Microsoft, Corporation, Redmond, WA, USA) spreadsheet to organise responses to each question into basic topic- and opinion-based themes. Two researchers independently conducted the initial coding and analysis under the supervision of a qualitative expert to ensure clarity and consistency among findings. Preliminary outputs were reviewed by all members of the research team.
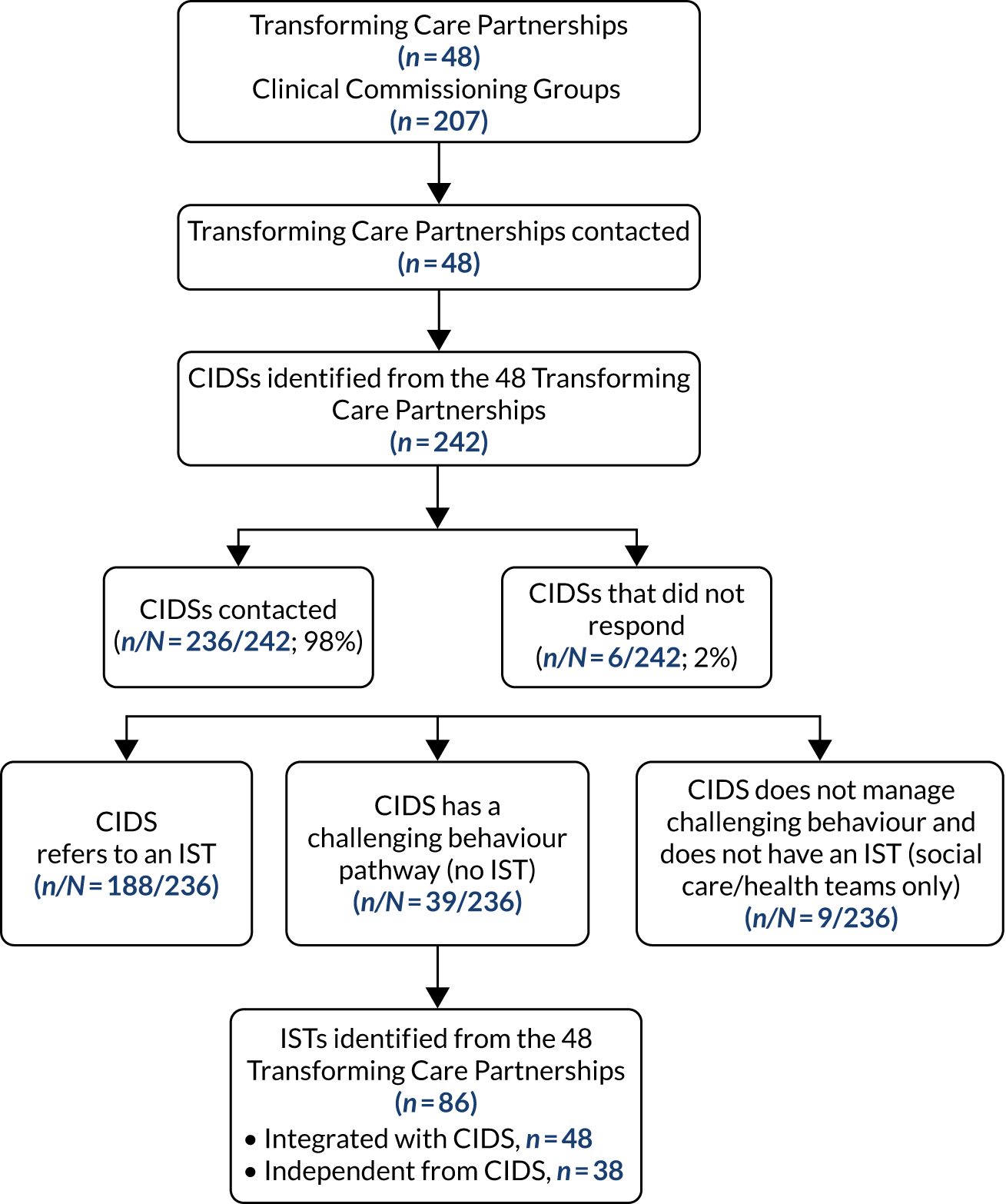
Results
Two-hundred and thirty-six out of 242 (98%) CIDSs completed and returned the screening questionnaire to identify ISTs. Of those, 188 CIDSs declared that they referred to 80 ISTs; the managers of these ISTs were sent a web link or hard copy of the detailed survey (Figure 2). In total, 73 (91%) IST managers returned their questionnaires.
FIGURE 2.
Flow diagram of the identification of ISTs during the screening survey with CIDSs. Reproduced with permission from Hassiotis et al. 53 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. This figure includes minor additions and formatting changes to the original figure.
Service characteristics of all intensive support teams
The main IST service domains are presented below.
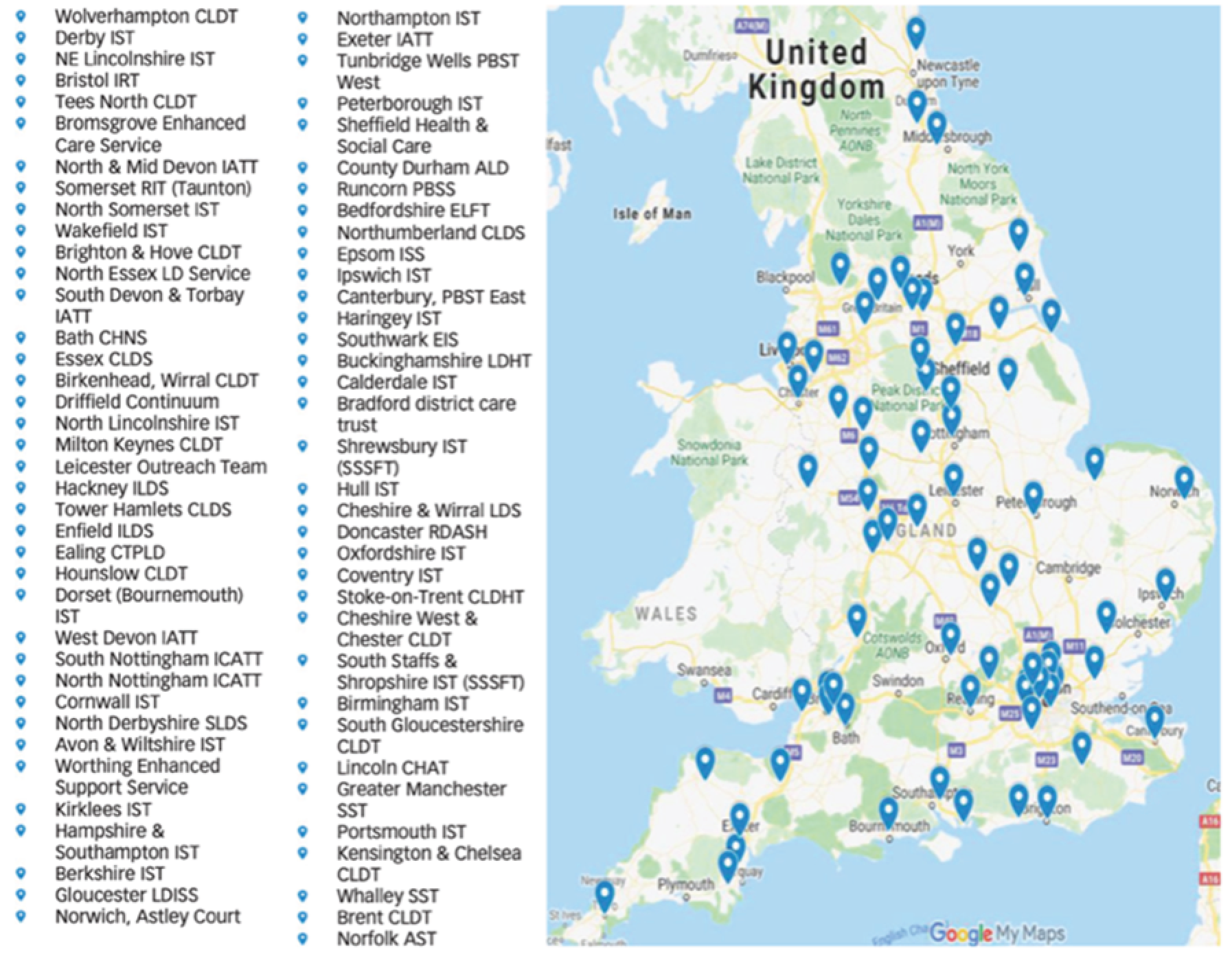
Service location and setting
The ISTs was equally distributed geographically throughout Northern England, the Midlands and Eastern England, and Southern England (Figure 3). The majority of the ISTs were funded by the NHS, although the lead organisation may have differed by area, including services that were funded by the local authority. Very few ISTs were part of social enterprises. Social enterprises are private businesses (usually registered as charities) that use their surplus money from selling/trading goods and/or providing services to reinvest in their services. They are autonomous from the NHS and financially viable, although they are considered part of the NHS by the public.
FIGURE 3.
Geographical location map of ISTs. ALD, Adult Learning Disability; AST, Adult Support Team; CHAT, Community Health Assessment Team; CHNS, Complex Health Needs Service; CLDHT, Community Learning Disability Health Team; CLDS, Community Learning Disability Service; CTPLD, Community Team for Adults with Learning Disabilities; CTPLS, Community Team for People with Learning Disabilities; EIS, Early Intervention Service; ELFT, East London Foundation Trust; IATT, Intensive Assessment and Treatment Team; ICATT, Intensive Community Assessment and Treatment Team; ILDS, Intensive Learning Disability Service; IRT, Intensive Response Team; ISS, Intensive Support Service; LD, Learning Disability; LDHT, Learning Disabilities Health Team; LDISS, Learning Disability Intensive Support Service; LDS, Learning Disability Service; NE, North East; PBSS, Positive Behaviour Support Service; PBST, Positive Behaviour Support Team; RDASH, Rotherham Doncaster and South Humber; RIT, Rapid Intervention Team; SLDS, Specialist Learning Disability Service; SSSFT, South Staffordshire and Shropshire Foundation Trust; SST, Specialist Support Team. Map data © 2019 Google (Google Inc., Mountain View, CA, USA). Reproduced from Hassiotis et al. 53 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. This figure includes minor additions and formatting changes to the original figure.
Interventions used
Intensive support teams offer a range of interventions, including PBS, psychoeducation and other psychosocial interventions. A detailed summary of all of the key IST characteristics is shown in Table 1. 53
| Characteristic | ISTs (N = 73), n (%) |
|---|---|
| Location and setting | |
| Region | |
| Northern England | 19 (26) |
| Midlands and Eastern England | 22 (30) |
| Southern England | 23 (32) |
| London | 9 (12) |
| Setting | |
| Mainly funded by NHS (Clinical Commissioning Groups) | 67 (92) |
| Mixed funding, including from local authority | 20 (27) |
| In social enterprise | 3 (4) |
| Standalone service | 25 (34) |
| Length of time in operation (months), median (IQR) | 48 (24–96) |
| Service users | |
| Size of current caseload, median (IQR) | 25 (15–50) |
| Number of service users on at-risk register, median (IQR) | 6 (2–15) |
| Average visit duration | |
| 30–60 minutes | 25 (35) |
| 60–120 minutes | 43 (60) |
| > 120 minutes | 4 (6) |
| Extended working hours | 48 (66) |
| IST operates a duty/crisis line | 38 (52) |
| Outcome measures used | 55 (75) |
| Staffing, training and skills | |
| Multiprofessional staff team | 65 (89) |
| Intellectual (learning) disability nurses | 62 (85) |
| Clinical psychologists | 57 (78) |
| Speech and language therapists | 38 (52) |
| Occupational therapists | 33 (45) |
| Psychiatrists | 31 (42) |
| Social workers | 59 (81) |
| Trainee staff (e.g. student nurses, trainee associate practitioners) | 38 (52) |
| One or more team members trained as an approved mental health practitioner | 6 (8) |
| Perceived need for additional training or skills (e.g. additional professional roles or additional skills such as intervention and prevention strategies) | 50 (68) |
| Eligibility and referrals | |
| Lower age limit | |
| IST accepts adults only (people aged ≥ 18 years) | 59 (81) |
| IST accepts young people (aged 14–17 years) | 12 (16) |
| No lower age limit | 2 (3) |
| Upper age limit | |
| None | 71 (97) |
| IST accepts patients in contact with the criminal justice system | 65 (89) |
| IST accepts patients experiencing mental health problems | 71 (97) |
| IST accepts patients with intellectual disabilities and challenging behaviour who are not in crisis but who need support | 64 (88) |
| IST provides early hospital discharge support | 72 (99) |
| IST accepts self-referrals | 41 (56) |
| IST accepts referrals without further assessment from trusted assessors | 14 (19) |
| Target time to respond to referrer (days), median (IQR) | 5 (1–14) |
| Target time to commence assessment (days), median (IQR) | 5 (1.5–14) |
| Target time to complete assessment (days), median (IQR) | 7 (3–28) |
| IST operates a waiting list | 7 (10) |
| Interventions used | |
| PBS | 72 (99) |
| Psychoeducational interventions with service users’ family carers or paid carers | 68 (94) |
| Other evidence-based psychosocial therapies (e.g. anger management, mindfulness, counselling, cognitive behavioural therapy) | 68 (94) |
Caseload
The ISTs’ median caseload was 25 (range 15–50) adults with intellectual disabilities who display challenging behaviour, whereas the median number of adults considered to be at risk of admission was 6 (range 2–15). The average duration of an IST staff member’s visit to a service user was usually 1–2 hours. In total, 66% of the ISTs reported working extended hours and 52% operated a duty/crisis line.
Staffing, training and skills
A common feature of ISTs was their multidisciplinary nature. A number of health and care professionals worked together in ISTs; the most common type of professional was nursing staff, followed by social workers. More than 65% of IST managers described a perceived need for additional training or skills in their service.
Referrals and eligibility
Most ISTs operated with few or no limitations on accepting referrals for adults with intellectual disabilities relating to challenging behaviours, or for mental ill health either in the acute phase or for ongoing care. Self-referral was accepted by 41 ISTs. The IST managers reported that assessments take place within 5 days and are completed within 7 days. In total, 19% of ISTs accepted referrals for young people aged 14–17 years, ensuring a smooth transition to adult specialist services, with 3% of those ISTs indicating that they had no lower age limit and worked across the lifespan.
Cluster analysis
The cluster analysis included data from 71 ISTs because we were unable to obtain data on FTEs from the IST managers of two teams. A two-cluster typology was preferred over a three-cluster typology on the basis of distance dissimilarity statistics from the cluster analysis and discussion among experts. The three-cluster typology split the independent provision cluster into two clusters of fairly equal size (n = 27 and n = 19, respectively). These two subclusters were differentiated most strongly on whether or not they were a standalone service, whether or not they had a large caseload, and whether or not self-referral was permitted. Information about the factor clustering is shown in the dendrogram (Figure 4), which illustrates the agglomeration of individual services into ever-larger clusters. Horizontal lines at zero indicate clusters of services that are identical in relation to the grouping factors. Horizontal lines nearer the bottom of the dendrogram represent the merging of clusters that are similar to each other. Horizontal lines nearer the top of the dendrogram represent the merging of more heterogeneous clusters, with larger distance values. Long vertical lines indicate that two clusters that are dissimilar to each other are being combined and suggest that the clusters represent distinct types of services.
FIGURE 4.
Dendrogram illustrating cluster agglomeration. Reproduced from Hassiotis et al. 53 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. This figure includes minor additions and formatting changes to the original figure.
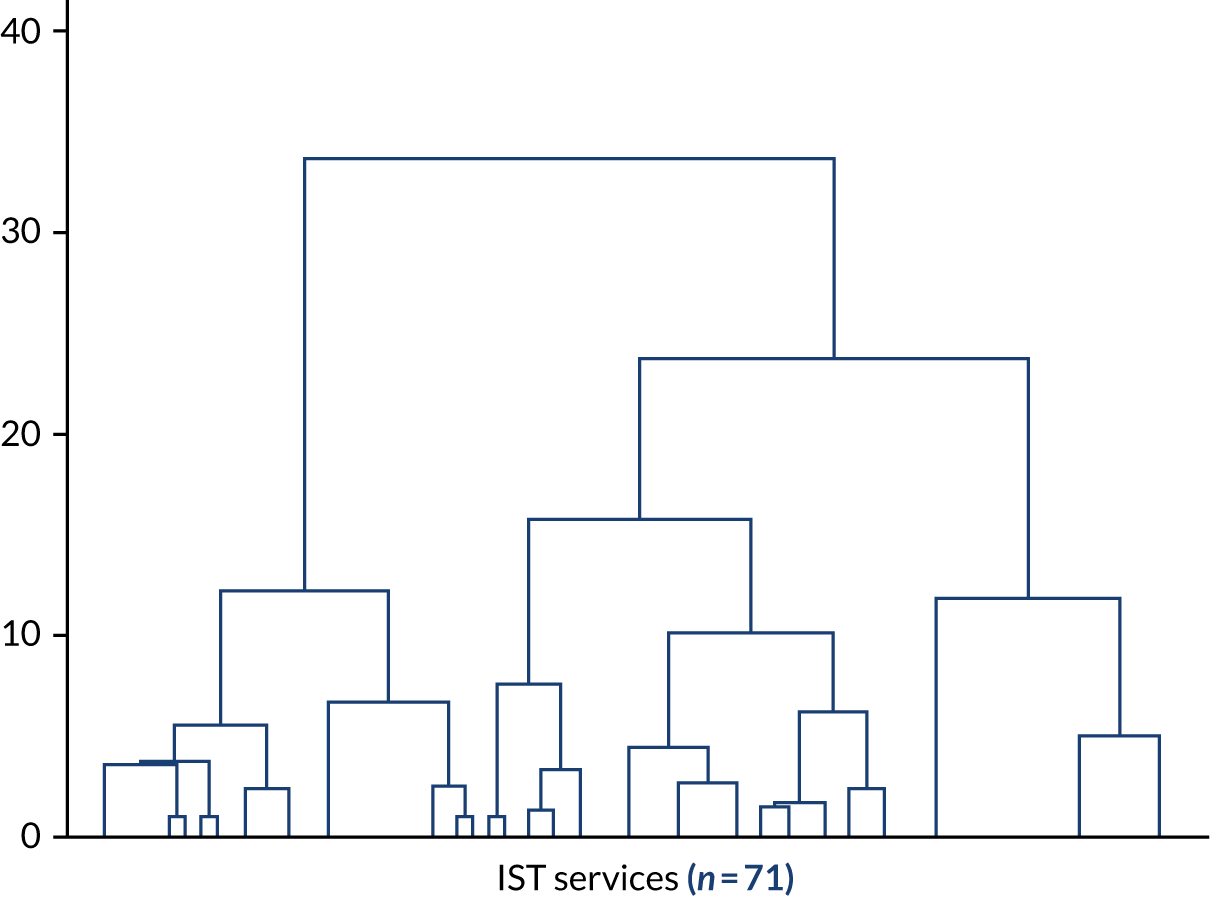
We named the two models the enhanced model and the independent model. Enhanced ISTs were more likely to (1) accept self-referrals, (2) have a large caseload, (3) be integrated with the CIDS function and (4) provide longer-term support than independent ISTs. Enhanced ISTs were less likely to use outcome measures than independent ISTs. A detailed presentation of the characteristics of each IST model is shown in Table 2. Based on the data, there is limited evidence that service models were sufficiently distinguished by whether or not they employ a mix of health and social care professionals (i.e. multidisciplinary teams) or if they operate extended opening hours.
| Characteristic | Model, n (%) | |
|---|---|---|
| Enhanced (N = 25) | Independent (N = 46) | |
| Self-referral permitted | 25 (100) | 16 (35) |
| Large caseload | 23 (92) | 15 (33) |
| Outcome measures used | 13 (52) | 41 (89) |
| Standalone service | 3 (12) | 21 (46) |
| Multiprofessional staff team | 21 (84) | 43 (93) |
| Extended working hours | 16 (64) | 31 (67) |
| Other service characteristics | ||
| Working hours | ||
| Monday–Friday only, 7–8 hours | 9 (36) | 15 (33) |
| Monday–Friday only, ≥ 8 hours | 9 (36) | 8 (17) |
| Monday–Friday, ≥ 7 hours, and weekends | 5 (20) | 13 (28) |
| Monday–Friday, 24 hours, and weekends | 2 (8) | 10 (22) |
| Staffing (FTE), median (IQR) | 5.6 (3.6–9.6) | 10.2 (6.8–15.0) |
| Level of intellectual disability | ||
| All levels (mild/moderate/severe/profound) | 18 (72) | 38 (83) |
| All except profound | 2 (8) | 4 (9) |
| All except mild | 4 (16) | 2 (4) |
| Other combination | 1 (4) | 2 (4) |
| Clients with a neurodevelopmental disorder, mean (SD) | 62.1 (21.5) | 51.1 (22.5) |
| Frequency of contact with clients | ||
| Less than once per week | 1 (4) | 2 (4) |
| Once per week | 8 (33) | 9 (20) |
| Twice per week | 5 (21) | 6 (13) |
| Three or more times per week | 6 (25) | 14 (30) |
| Other | 4 (17) | 15 (33) |
| Duration of contact with clients | ||
| 1–3 months | 0 | 7 (15) |
| 3–6 months | 7 (29) | 20 (33) |
| 6–12 months | 13 (54) | 20 (43) |
| ≥ 12 months | 4 (17) | 4 (9) |
Philosophy of care, perceived challenges and priorities for improvement for intensive support teams
Respondents mentioned that the intervention model they used was pivotal to the success of their approach:
The service advocates a PBS approach to supporting service users. The evidence from the team supports that early identification of service user difficulties significantly reduces the likelihood of placement breakdown.
Team manager, independent IST
Others referred to the care the service provides as:
Person-centred, holistic ethos, use of positive behaviour support.
Team manager, enhanced IST
Intensive support team managers’ responses suggested that specialist care from the IST was valued, leading to plans to expand the skill mix of the IST staff. In addition, recruiting qualified and/or experienced health-care professionals to ISTs was described as a positive development:
Restructuring of joint LD [learning development] services and appointment of PBS specialist to lead internal and external support staff.
Clinical nurse specialist, independent IST
We are going to be enhancing the team and increasing working hours.
Lead behaviour nurse, enhanced IST
A lack of resources, high staff turnover, variable expectations from accommodation providers and the quality of care provided to adults with intellectual disabilities who display challenging behaviour were the most commonly identified challenges:
Clinical demands high – team have not been fully resourced since its start date. Retention of staff and recruitment problematic. Long periods without team manager in place. Difficult to function as an ‘intensive’ support team and meet referral needs and manage risks and trust targets/expectations.
Team manager, independent IST
Working with specialist residential providers who do not obviously have the degree of specialism that they advertise in winning support contracts (e.g. little to no specialist training for staff around autism, communication, challenging behaviour and/or mental health), who then become reliant on our team for longer than we are able to lead on all aspects of mental health/behavioural assessment and support.
Team manager, independent IST
Intensive support team managers reported that the service priorities were the implementation of national policies, a provision of intensive care outside of usual working hours and liaison with other local agencies to improve communication and referral procedures:
Improving links with mainstream services and inputting on reasonable adjustments. Improving awareness in out-of-hours services to avoid hospital admissions out of hours.
Team manager, independent IST
. . . addressing the STOMP (overmedication with antipsychotics) agenda, develop service user involvement in the IST work and improving risk management.
Team manager, enhanced IST
Clinical pathways were noted as areas requiring improvement for some ISTs, as were enhancement of IST workforce skills through specialist training and adopting evidence-based practice. Staff training in PBS was identified as an important part of delivering person-centred care:
Increase up-skilling of staff teams to reduce ongoing reliance on service (e.g. skills, etc.).
Team manager, enhanced IST
Expanding the IST function to work with an all-age service user population, particularly those aged ≤ 18 years, or patients with autism and other populations, such as those with borderline intellectual functioning, were identified as potential future additions to ISTs.
Summary
Phase 1 was a comprehensive description of the geographical distribution, characteristics and service models of IST care in England. Specialist services for adults with intellectual disabilities who display challenging behaviour appeared to be operational across England, although London had the smallest number of ISTs. Following careful consideration of the clinical utility of the findings from the cluster analysis, we found that there were two IST models (enhanced and independent). The role of ISTs encompassed many different components of care, from the management of challenging behaviour in adults with intellectual disabilities to the facilitation of the discharge of inpatients with intellectual disabilities, the assessment and treatment of adults with intellectual disabilities, autism diagnostic assessments and often the support of adults with intellectual disabilities involved in the criminal justice system. Just over half of ISTs (52%) reported operating a daily help line (also called a duty line) staffed by health professionals with the capacity to respond immediately to crises, and one-third of the ISTs provided 24-hour and weekend support to adults with intellectual disabilities and families in distress. However, IST managers across the two models reported that the system appeared to lack flexibility when an individual was in crisis because of the limited/lack of alternative services to avoid admission and the small number of skilled social care providers.
Chapter 3 Clinical evaluation of intensive support team models
Introduction
There is currently little evidence about whether different models of ISTs for challenging behaviour (i.e. dedicated vs. alternative) achieve better clinical outcomes for adults with intellectual disabilities who display challenging behaviour. There is a need for a systematic evaluation of whether or not a specific model of IST is optimal for treating and managing challenging behaviour in local communities, and able to deliver positive outcomes for patients and their families. For more information, please see the published protocol. 49
Methods
We conducted a cohort study of adults with intellectual disabilities, with a nested case–control comparison of two IST models. We included a random selection of 21 ISTs in England representing one of two models: enhanced or independent (Table 3). Random sampling ensured representation of different sizes of teams/caseloads, and both rural and urban services (where possible) for the second stage of the study.
| Grouping variable | Model | |
|---|---|---|
| Enhanced | Independent | |
| Design | Embedded with CIDS | Standalone teams |
| Support length | > 6 months | 3–12 months |
| Referrals | Self-referral | Professional referral only |
| Caseload | ≥ 20 service users | ≈ 15 service users |
| Outcome measures | Limited use of outcome measures | Outcome measure use |
Inclusion criteria
Service
The inclusion criteria for services were as follows: the IST adheres to one of the identified models, it has been operational for ≥ 12 months, there is commitment to fund it for the study duration, and it has the capacity and capability to recruit the required number of participants.
Service users
The inclusion criteria for service users were as follows: participants were adults with mild to profound intellectual disabilities based on clinical diagnosis, aged ≥ 18 years and eligible to receive support from an IST service.
Exclusion criteria
Service
The exclusion criteria for services were as follows: the IST has been operational for < 12 months at selection or there are plans to dissolve it.
Service users
The exclusion criteria for service users were as follows: a primary clinical diagnosis of personality disorder or substance misuse, or a decision by the clinical team that a referral to the study would be inappropriate (e.g. because of ongoing legal challenges to the service or because the person was acutely unwell).
Procedures
Participant consent and enrolment
Potential participants were identified by each IST professional either at the first clinical assessment or from the IST services’ caseloads. IST professionals gave potential participants brief verbal information about the study and those agreeing to speak to the researcher had their contact details shared with the researcher. For those who were referred to the study but who did not have the mental capacity to consent, consent was sought from their family and paid carers, who acted as (family/nominated) consultees. For service users with decision-making capacity, the researcher spoke to the potential participant over the telephone or in person, and sent or gave the service user the PIS (in easy-read format) to inform them of the reasons for undertaking the study, the kind of questions we would be asking their carer, and that we would ask for information from their notes to check details, such as the number of service contacts, which we would undertake twice (first at baseline and then at the 9-month follow-up).
If the service user agreed to take part in the study, they completed a written consent form or consent was taken by telephone/video call and audio-recorded for purposes of verifying consent. The researcher then repeated the above process (using the carer PIS) with the service user’s paid carer or family carer to seek their consent to take part and complete the study questionnaires. At the time of referral and/or treatment, some participants did not have the decision-making capacity to consider participation. For those service users lacking decision-making capacity, the researcher approached their personal or nominated consultee (using the consultee PIS) and sought written or audio-recorded (by telephone/video) assent to include the service user in the study. Reasons for ineligibility and/or exclusion of eligible service users were documented. Participants were allowed to withdraw from the study at any point. (The service user, paid carer and family carer, and personal consultee PISs and ICFs can be accessed at URL: www.fundingawards.nihr.ac.uk/award/16/01/24.)
Outcome measures
Participants were either new referrals or existing IST cases. A baseline assessment was carried out, with follow-up at 9 months (± 4 weeks) after the baseline. The follow-up assessment time point reflected the period of involvement of the IST, which lasted ≥ 12 months and was a pragmatic reflection of clinical practice. At the time of completion, the country was in the first COVID-19 lockdown and in-person assessments were not allowed. The end of the study was the date of the last video/telephone follow-up with the last participant.
Primary outcome
The primary outcome was change in challenging behaviour as measured by the Aberrant Behaviour Checklist-Community, version 2 (ABC-C). 57 This is an established and internationally used carer-administered measure of challenging behaviour that measures psychiatric symptoms and behaviour across five domains: irritability, lethargy, stereotypic behaviour, hyperactivity and inappropriate speech. It was adopted as the primary outcome measure as reduction in challenging behaviour is the main remit of ISTs.
Secondary outcomes
-
Mental health comorbidity: the carer-reported Psychiatric Assessment Schedule for Adults with Developmental Disabilities (PAS-ADD) Clinical Interview58 is used for screening for a mental disorder, but it is not diagnostic.
-
Clinical risk: the Threshold Assessment Grid (TAG)59 measures clinical risk and previous research has found associations between perceived risk and hospital admission. 60
-
The Quality of Life Questionnaire (QoL-Q). 61 This is a widely used measure with good psychometric properties that has been developed specifically for adults with intellectual disabilities and can be proxy completed.
-
Health-related quality of life: the EuroQol-5 Dimensions, five-level version (EQ-5D-5L),62 is a standard measure for health economic evaluations and it is used to generate quality-adjusted life-years (QALYs) as a result of IST input. Two versions were administered where possible. If the service user had capacity, a self-report version of the EQ-5D-5L was utilised. If the service user lacked capacity, the proxy version of the measure was completed by their carer. In the case of the service user having capacity, the carer was also asked to complete the proxy version and the responses were compared.
-
Service use: the Client Service Receipt Inventory (CSRI)63 (adapted for the study, 6-month retrospective service use at each assessment point) is a widely used service use questionnaire and has been validated for use in mental health and intellectual disabilities services research.
We collected sociodemographic information, the number of hospital admissions and maintenance of accommodation at follow-up.
Sample size
Assuming two IST models, detecting a difference of 0.45 standard deviations (SDs) in primary outcome score would require 96 participants per group (192 in total) with 5% significance (two-sided) and 80% power and an interclass correlation coefficient of 0.02. 40,64 After inflation for 15% loss to follow-up, the estimated sample size was 113 participants per model (226 participants in total).
Statistical analysis
The data analysis plan follows an a priori developed statistical analysis plan (see additional files; www.journalslibrary.nihr.ac.uk/programmes/hsdr/160124/#/documentation; accessed 3 March 2022).
Data cleaning
Prior to performing analyses, basic checks were performed by the statistician (LM) to ensure the quality of the data. Each outcome (primary and secondary) variable was checked for the following: missing values, values outside an acceptable range and other inconsistencies. If missing values or other inconsistencies were found, the data in question were sent to the study manager for checking and were confirmed as correct and left unchanged, corrected or deemed to be missing, as appropriate.
Baseline characteristics
The baseline characteristics of participants are summarised separately for the two types of service identified in phase 1 of the study. Categorical variables are reported as counts and percentages, whereas continuous variables are summarised as means and SDs or medians and IQRs as appropriate, depending on the distribution of the data.
Primary outcome analysis
All analyses were conducted using Stata, version 16. The primary outcome was the change in challenging behaviour, as measured by a change in ABC-C score between baseline and the 9-month follow-up. Change in ABC-C total score from baseline to the 9-month follow-up was calculated for each participant. The mean difference in ABC-C change score between the two IST models identified in phase 1 of the study was estimated using a mixed-effects linear regression model with change in ABC-C score as the outcome, a fixed effect of service type as the main exposure, and a random effect of IST to account for clustering within services. For ABC-C and the domains, a positive coefficient denotes improvement.
The potential confounders identified were age; sex; accommodation type; level of intellectual disability [i.e. Short Adaptive Behaviour Scale (SABS) score]; level of risk (baseline TAG); presence of autism and/or attention deficit hyperactivity disorder (ADHD); number of physical comorbidities; and PAS-ADD Clinical Interview organic condition, affective or neurotic disorder and psychotic disorder scores. These were specified as covariates in the adjusted multilevel linear regression models, which were similar to the unadjusted model described above. The estimated difference in change in ABC-C total score from both unadjusted and adjusted models was reported with accompanying 95% confidence interval (CI), and the p-value was reported for the unadjusted model only.
Owing to the data collection window of 9 months ± 4 weeks, the length of time between the baseline and 9-month follow-up measures may vary between participants. To ensure that effect sizes were not biased as a result of this, we performed a sensitivity analysis by adding a fixed effect for the length of follow-up to the above models.
Model checking
The statistical model for the primary outcome analysis included an assumption that the residuals were normally distributed. This assumption was checked through the construction of appropriate histograms and normal quantile plots.
Missing data
The potential for bias due to missing data was assessed by exploring the number of missing observations in key variables and considering potential missingness mechanisms. Predictors of missingness analysis was carried out, in which the outcome was presence or absence of ABC-C at 9 months. Each baseline characteristic was univariately included as a fixed effect in mixed-effects logistic regression models, with a random effect for IST. The only variable accounting for missing data was ‘physical health problems’ (see Appendix 1, Table 20).
Secondary analyses
The secondary outcomes detailed above were analysed using statistical models analogous to those used for the primary outcome. Where change in TAG was the outcome, TAG at baseline was not included as a covariate. For TAG scores, a positive coefficient indicates improvement, and for QoL-Q scores, a negative coefficient indicates improvement. Binary outcomes were analysed using mixed-effects logistic regression models and were not adjusted for covariates owing to limited power. The p-values are not reported for secondary outcomes. The analyses of secondary outcomes are considered exploratory, and these outcomes were analysed using available data only.
Results
Intensive support team recruitment
Twenty-one ISTs across England agreed to participate in the study; 11 were enhanced ISTs and 10 were independent ISTs.
Participant enrolment
Recruitment of participants began in September 2018 and was completed in May 2020 (19 months). In total, 724 participants were screened, with 306 not meeting the inclusion criteria. Following review of the inclusion/exclusion criteria, 418 adults with intellectual disabilities were eligible to participate in the study and were approached by the IST or research team of each research sites and/or us. Just over one-quarter (n = 108) of eligible adults with intellectual disabilities declined participation and 310 adults with intellectual disabilities expressed an interest in the study. From this, a further 84 adults with intellectual disabilities declined involvement because of an inability to commit, lack of interest, health problems, or discharge by the time the researchers contacted them (Figure 5). In total, 226 participants were recruited to the study, with 115 adults with intellectual disabilities in the enhanced model and 111 in the independent model.
FIGURE 5.
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) diagram.
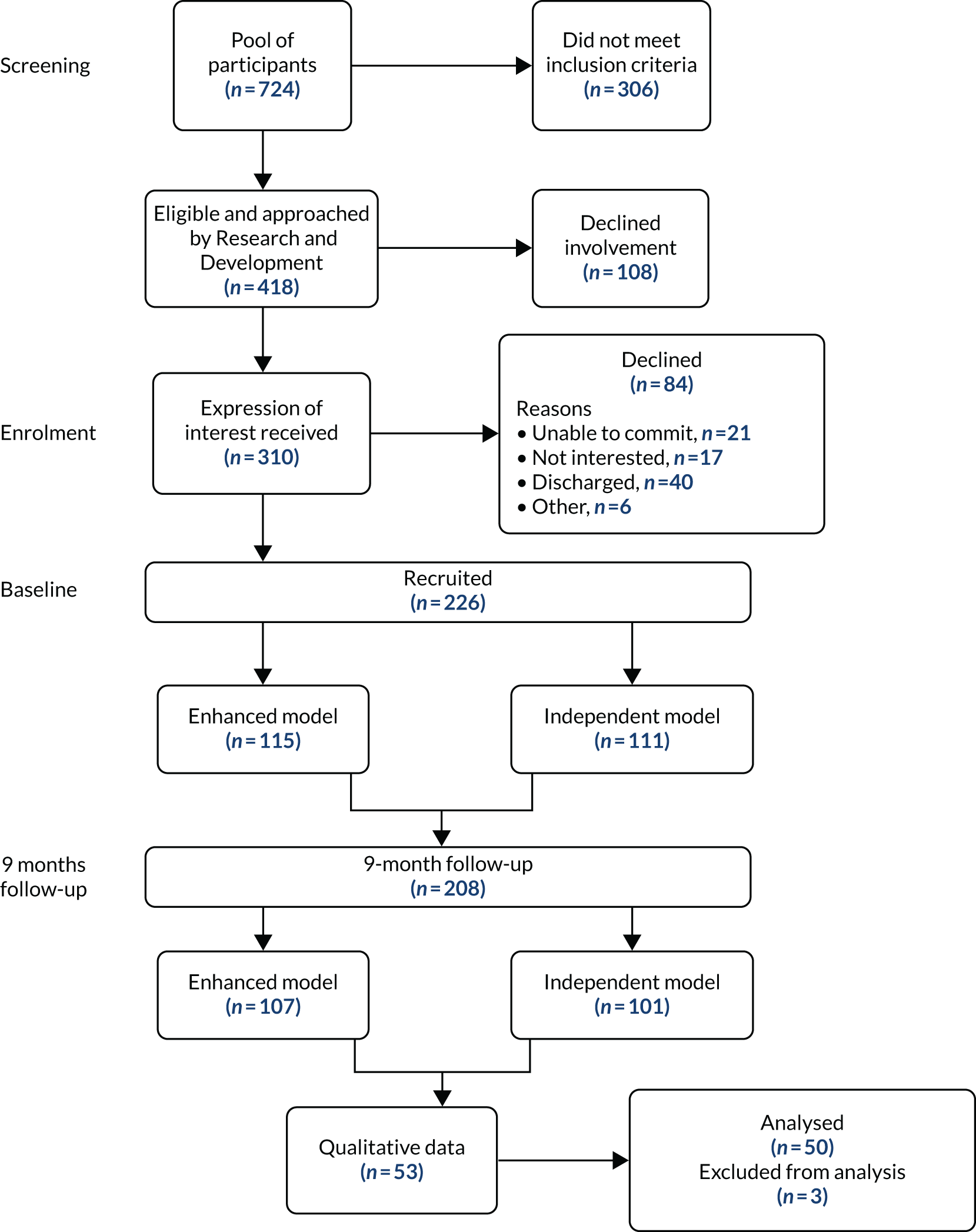
Follow-up
Follow-up data collection took place 9 months post baseline data collection for each participant and was conducted between May 2019 and January 2021 (20 months). In total, 18 participants were lost to follow-up (attrition rate 8%). The reasons for loss to follow-up were as follows: declined follow-up assessment, for example because of hospitalisation, imprisonment, change of care provider, excessive stress during the pandemic, or because they had withdrawn since the first assessment (n = 9); participants were non-contactable (n = 5); the follow-up assessment window was breached (n = 2); or death (n = 2). In total, 208 (92%) adults with intellectual disabilities completed the follow-up assessment (enhanced, n = 107; independent, n = 101). See Figure 5 for the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) diagram.
Characteristics of participants
The baseline demographic characteristics of the entire sample are shown in Table 4 by IST model. The median age of the overall sample was 29 years. Most participants were male, of white ethnicity and single. A larger percentage was in education, day centre, looking after family or ‘other’ in the enhanced model than in the independent model (45% vs. 32%, respectively; p = 0.035). A larger percentage of adults had sensory problems in the independent model than in the enhanced model (68% vs. 52%, respectively; p = 0.018; Table 5). There were no other significant differences between models. The characteristics at the 9-month follow-up can be found in Appendix 1, Tables 18 and 19.
| Characteristic | Total (N = 226) | Model | p-value | ||||
|---|---|---|---|---|---|---|---|
| Enhanced (N = 115) | Independent (N = 111) | ||||||
| n/N | % | n/N | % | n/N | % | ||
| Age (years) | |||||||
| Median (IQR) | 29 (23–39) | 30 (24–41) | 28 (22–38) | 0.183 | |||
| Aged ≥ 25 | 151/226 | 67 | 81/115 | 70 | 70/111 | 63 | 0.239 |
| Sex | |||||||
| Male | 155/226 | 69 | 80/115 | 70 | 75/111 | 68 | 0.746 |
| Female | 71/226 | 31 | |||||
| Ethnicity | 0.382 | ||||||
| White | 181/226 | 80 | 90/115 | 78 | 91/111 | 82 | |
| Black | 23/226 | 10 | 11/115 | 10 | 12/111 | 11 | |
| Asian | 17/226 | 8 | 12/115 | 10 | 5/111 | 5 | |
| Other | 5/226 | 2 | 2/115 | 2 | 3/111 | 3 | |
| Marital status | 0.498 | ||||||
| Single | 224/226 | 99 | 113/115 | 98 | 111/111 | 100 | |
| Married | 2/226 | 1 | |||||
| Living situation | 0.354 | ||||||
| Alone or with partner (with or without children) | 45/226 | 20 | 23/115 | 20 | 22/111 | 20 | |
| With parents or relatives | 58/226 | 26 | 34/115 | 30 | 24/111 | 22 | |
| Other (e.g. sheltered accommodation, group living, hospital) | 123/226 | 54 | 58/115 | 58 | 65/111 | 59 | |
| Accommodation | 0.279 | ||||||
| Median (IQR) (months) | 47 (12–144) | 48 (12–132) | 36 (11–146) | ||||
| Family home | 68/225 | 30 | 38/114 | 33 | 30/111 | 27 | |
| Supported living | 81/225 | 36 | 34/114 | 30 | 47/111 | 42 | |
| Residential | 60/225 | 27 | 33/114 | 29 | 27/111 | 24 | |
| Independent | 16/225 | 7 | 9/114 | 8 | 7/111 | 6 | |
| Length of time in current accommodation < 6 months | 32/226 | 11 | 13/115 | 11 | 19/111 | 17 | |
| Main source of income | |||||||
| Salary/wage | 1/226 | 0.4 | 0/115 | 0 | 1/111 | 1 | 0.491 |
| Family support | 62/226 | 27 | 35/115 | 30 | 27/111 | 24 | 0.303 |
| State benefits | 226/226 | 100 | 115/115 | 100 | 111/111 | 100 | a |
| Occupational status | |||||||
| None | 140/226 | 62 | 67/115 | 58 | 73/111 | 66 | 0.245 |
| Any employment | 4/226 | 2 | 2/115 | 2 | 2/111 | 2 | 0.972 |
| Education, day centre, looking after family, other | 87/226 | 38 | 52/115 | 45 | 35/111 | 32 | 0.035 |
| Voluntary work | 12/226 | 5 | 6/115 | 5 | 6/111 | 5 | 0.950 |
| Characteristic | Total (N = 226) | Model | p-value | ||||
|---|---|---|---|---|---|---|---|
| Enhanced (N = 115) | Independent (N = 111) | ||||||
| Mean or n/N | SD or % | Mean or n/N | SD or % | Mean or n/N | SD or % | ||
| Neurodevelopmental disorder | |||||||
| Neither ASD nor ADHD | 66/226 | 29% | 33/115 | 29% | 33/111 | 30% | 0.628 |
| ASD or ADHD | 144/226 | 64% | 72/115 | 63% | 72/111 | 65% | |
| Both ASD and ADHD | 16/226 | 7% | 10/115 | 9% | 6/111 | 5% | |
| Ability level (SABS) | 52 | 24 | 50 | 25 | 56 | 22 | 0.079 |
| Aetiology of intellectual disability | 0.385 | ||||||
| Down syndrome | 10/225 | 4% | 6/114 | 5% | 4/111 | 4% | |
| Fragile X syndrome | 2/225 | 1% | 1/114 | 1% | 1/111 | 1% | |
| Unknown | 181/225 | 80% | 95/114 | 83% | 86/111 | 77% | |
| Other | 32/225 | 14% | 12/114 | 11% | 20/111 | 18% | |
| Physical health problems | 197/226 | 87% | 99/115 | 86% | 98/111 | 88% | 0.621 |
| Mobility problems | 85/226 | 38% | 45/115 | 39% | 40/111 | 36% | 0.631 |
| Sensory problems | 135/226 | 60% | 60/115 | 52% | 75/111 | 68% | 0.018 |
| Epilepsy | 58/226 | 26% | 33/115 | 29% | 25/111 | 23% | 0.288 |
| Incontinence | 76/226 | 34% | 41/115 | 36% | 35/111 | 32% | 0.512 |
| Cancer | 2/226 | 1% | 0/115 | 0% | 2/111 | 2% | 0.240 |
| Overweight | 18/226 | 8% | 7/115 | 6% | 11/111 | 10% | 0.289 |
| Diabetes | 13/226 | 6% | 6/115 | 5% | 7/111 | 6% | 0.725 |
| Overweight or diabetes | 27/226 | 12% | 12/115 | 10% | 15/111 | 14% | 0.476 |
| Cardiovascular related | 7/226 | 3% | 4/115 | 3% | 3/111 | 3% | > 0.999 |
| Respiratory related | 11/226 | 5% | 6/115 | 5% | 5/111 | 5% | 0.803 |
| Other physical health problem(s) | 68/226 | 30% | 33/115 | 29% | 35/111 | 32% | 0.642 |
| ABC-C total | 63 | 33 | 64 | 34 | 62 | 32 | 0.607 |
| Irritability | 20 | 11 | 21 | 11 | 20 | 11 | 0.660 |
| Lethargy | 14 | 9 | 14 | 9 | 14 | 10 | 0.784 |
| Stereotypic behaviour | 5 | 5 | 6 | 6 | 5 | 5 | 0.116 |
| Hyperactivity | 19 | 12 | 19 | 13 | 18 | 11 | 0.363 |
| Inappropriate speech | 5 | 4 | 4 | 4 | 5 | 4 | 0.288 |
| PAS-ADD Clinical Interview | |||||||
| Organic condition | 30/226 | 13% | 14/115 | 12% | 16/111 | 14% | 0.620 |
| Affective or neurotic disorder | 48/226 | 21% | 22/115 | 19% | 26/111 | 23% | 0.430 |
| Psychotic disorder | 15/226 | 7% | 4/115 | 3% | 11/111 | 10% | 0.063 |
| TAG | 14 | 5 | 14 | 5 | 13 | 5 | 0.307 |
| QoL-Q | 70 | 10 | 70 | 11 | 69 | 8 | 0.581 |
Primary outcome
The primary outcome was a change in ABC-C score between baseline and the 9-month follow-up. The results can be seen in Table 6. All primary outcome analyses showed a positive outcome (i.e. improvement) in change in ABC-C total score from baseline to 9 months. However, unadjusted analyses found no difference between the IST models for change in the ABC-C total score from baseline to 9 months (β 3.08, 95% CI –7.32 to 13.48; p = 0.561). This held true for adjusted analyses (β 4.27, 95% CI –6.34 to 14.87; p = 0.430), and time between baseline and 9-month data collection and other covariate-adjusted analyses (β 3.62, 95% CI –6.99 to 14.22). The only predictors of missingness were physical health conditions (see Table 20). The adjusted models included the number of physical health problems.
| Outcome | Model | |||||
|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | |||||
| Number | Coefficient | 95% CI | Number | Coefficient | 95% CI | |
| Change in ABC-C total | 208 | 3.08 | –7.32 to 13.48 | 163 | 4.27 | –6.34 to 14.87 |
| Adjusted for length of follow-up | 204 | 2.75 | –7.56 to 13.06 | 160 | 3.62 | –6.99 to 14.22 |
| Change in ABC-C | ||||||
| Irritability | 208 | 1.14 | –2.41 to 4.69 | 163 | 2.09 | –1.67 to 5.86 |
| Lethargy | 208 | 1.40 | –1.77 to 4.58 | 163 | 1.31 | –1.82 to 4.44 |
| Stereotypic behaviour | 208 | –0.05 | –1.44 to 1.34 | 163 | 0.69 | –0.77 to 2.14 |
| Hyperactivity | 208 | –0.07 | –3.54 to 3.39 | 163 | –0.11 | –3.68 to 3.45 |
| Inappropriate speech | 208 | 0.83 | –0.10 to 1.77 | 163 | 0.37 | –0.86 to 1.60 |
Secondary outcomes
Secondary outcomes are presented in Table 7. No significant differences were found between the IST models for any secondary outcomes from baseline to 9 months. No significant differences were found between the IST models for the subscores of the PAS-ADD Clinical Interview scale [organic condition (odds ratio 1.09, 95% CI 0.39 to 3.02), affective or neurotic disorder (odds ratio 0.91, 95% CI 0.32 to 2.59), psychotic disorder (odds ratio 1.08, 95% CI 0.21 to 5.50)], change in TAG score (adjusted β 1.12, 95% CI –0.44 to 2.68) or change in QoL-Q score (adjusted β –2.63, 95% CI –5.65 to 0.40) from baseline to 9 months.
| Outcome | Model | |||
|---|---|---|---|---|
| Unadjusted | Adjusted | |||
| Estimate | 95% CI | Estimate | 95% CI | |
| PAS-ADD Clinical Interview (odds ratio) | ||||
| Organic condition | 1.09 | 0.39 to 3.02 | ||
| Affective or neurotic disorder | 0.91 | 0.32 to 2.59 | ||
| Psychotic disorder | 1.08 | 0.21 to 5.50 | ||
| Change in TAG score between baseline and 9 months (β) | 1.11 | –0.35 to 2.57 | 1.12 | –0.44 to 2.68 |
| Change in QoL-Q score between baseline and 9 months (β) | –0.75 | –3.62 to 2.11 | –2.63 | –5.65 to 0.40 |
Summary
Overall, analyses showed an improvement in ABC-C score from baseline to 9 months. However, unadjusted and adjusted analyses found that there was no significant difference between the IST models in ABC-C score at 9 months. In addition, there were no significant differences between IST models for any of the secondary outcomes at 9 months. It is possible that the function of the two models overlapped, including patient profiles and treatments delivered.
Chapter 4 Cost evaluation of intensive support team models
Introduction
The Transforming Care programme12 is aimed at enabling adults with intellectual disabilities and/or autism who display challenging behaviour to remain in their local communities, access the right support and reduce the number of costly inpatient admissions. Intensive community support, such as that provided by ISTs, is seen as a way to mitigate these challenges; however, there are a number of models of provision and, despite the prioritisation of ISTs and substantial financial backing by the government, no available economic evidence exists on the value for money for these services. The aim of the health economics component of the study was to derive and report the costs of each IST model and to investigate the cost-effectiveness of the IST care models (using two outcome measures in turn). The health economic component was carried out alongside the clinical evaluation. For more information, see the published protocol. 49
Methods
The inclusion/exclusion criteria for the IST service models and service users are described in Chapter 3. The study procedures, including recruitment, consent and outcome measures, were the same as those described in Chapter 3.
Economic analysis
The data analysis plan follows an a priori developed health economics analysis plan (HEAP) (see additional files; www.journalslibrary.nihr.ac.uk/programmes/hsdr/160124/#/documentation; accessed 3 March 2022).
Economic perspective
The economic evaluation adopted two perspectives. In the first instance, the analysis took a health and social care perspective that covered hospital and community health and social care services. Other voluntary-sector provision was also included, as most support from outside the family is funded by social services and provided by not-for-profit organisations. In addition, as family members and carers provide the majority of support for most people with intellectual disabilities, a wider societal perspective was also considered, one that included not only the cost to health and social care, but also the cost of unpaid support to the study participant from family and friends.
Cost of intensive support teams
The costs of each IST service model were calculated using established approaches to service costing. 63 Informed by this approach, the research team obtained a description of each IST model (phase 1 of the study) and collected financial information from the service managers in each of the IST models that took part in the evaluation phase (defined in Chapter 2). In addition, service managers were asked to record details on staffing by Agenda for Change (AfC) band, working hours of staff in different professions, the average percentage of time spent with clients (face to face and non-face to face), whether or not the role involved travel, the number of sessions with clients per case, and the size of the caseload and the number of referrals over 12 months. These data were combined to give an overall average annual cost per study participant for each IST model. The annualised average cost per study participant for each model was then weighted to derive a cost per study participant for each IST model over 9 months.
The costing relates to all care functions or activities provided by the IST, as it was not possible to carry out microcosting by function or activity (e.g. assessment, postassessment activities within the ISTs) because all ISTs were unable to provide such detailed activity-based information. Adopting this approach to costing the IST models, which covered all care activities by each service, was less intrusive. In cases where the numeric data required from service managers were missing, median imputation was adopted to avoid distributional concerns from using the mean values.
Costing service and support external to intensive support teams
The calculation of service and support costs was separated into the identification, measurement and valuation of relevant resources. All unit costs are for the financial year 2020/21, uprated when necessary using the NHS Cost Inflation Index (NHSCII). 65 No discounting was necessary as the analytical period was < 12 months.
Identification of services and support use
We collected resource use in the following categories:
-
use of health and social care services –
-
hospital care services:
-
overnight inpatient stays (psychiatric intensive care ward, acute psychiatric ward, psychiatric rehabilitation ward, general medical elective/planned inpatient admission, general medical non-elective/unplanned inpatient admission, general medical intensive care/high-dependency unit)
-
accident and emergency (A&E) attendances (physical health-related, mental health-related), including whether the participant was then (1) admitted to hospital or (2) not admitted to hospital
-
outpatient appointments (psychiatric outpatient appointment, day patient procedure/test, general medical outpatient appointment)
-
-
primary/community care services (including health and social care and voluntary-sector services):
-
GP (surgery/home/telephone consultation)
-
community/district nurse
-
community psychiatric nurse
-
learning disability nurse (looks after physical health)
-
psychiatrist
-
psychologist
-
care manager/social worker
-
occupational therapist
-
art/drama/music therapist
-
alternative therapist (e.g. reflexologist)
-
counsellor
-
physiotherapy
-
dentist
-
speech and language therapist
-
community support worker
-
extra 1 : 1 paid support to access a day centre
-
1 : 1 paid support for day opportunity (as part of 24-hour support package)
-
1 : 1 paid support for day opportunity (separate from support package at home)
-
unpaid care.
-
-
Measurement of health, social care services and support
Data on the use of services outside the IST were collected using the CSRI. 66 The CSRI is a widely used service use questionnaire, has been validated for use in mental health and intellectual disability services research and was adapted specifically for this study. Information about the study participants’ use of services was collected from a family member or paid carer during interviews with a researcher at baseline and 9 months, covering a retrospective period of 6 months. The CSRI asked study participants for the number and duration of contacts with various professionals and support services. There was the need to balance potential recall bias when relying on patient self-reporting against the cost, time burden and completeness of information obtained using other methods. We adopted a retrospective period of 6 months to minimise the potential bias with recall over a longer period and the researcher time involved in collecting data over shorter time frames that fell outside the data collection period for other reasons.
Valuation of services and support use
A unit cost was applied to CSRI data on contacts made with professionals and services to calculate the cost of health and social care (including voluntary-sector) services used by each participant in the study. The unit costs used in the cost analysis are summarised in Table 8. For all health and social care (including voluntary-sector) services data, nationally applicable unit costs were attached using 2020/21 prices to reflect the long-run marginal opportunity costs drawn from available public-sector sources. The cost per unit of measurement for each service type was taken from the Personal Social Services Research Unit (PSSRU) Unit Costs of Health and Social Care 2018,73 which is produced annually. The National Schedule of Reference Costs74 was used for inpatient and outpatient attendances and for community-based services that were not included in the PSSRU compendium of unit costs. Unit costs of services not obtained from these two sources were derived using the salary of the professional, employer on-costs (superannuation and national insurance), overhead costs (administrative managerial, capital), the costs of supervision and any equipment or consumables costs. Costs older than the chosen financial year were inflated using the NHSCII, reported by the PSSRU Unit Costs of Health and Social Care 2020. 65
| Service | Unit cost (£) | Source |
|---|---|---|
| Community-based service | ||
| GP (minutes) | ||
| Surgery | 4.35 | a |
| Home | 6.88 | b |
| Telephone | 3.97 | a |
| Nurse (minutes) | ||
| Community | 0.98 | b |
| Psychiatric community | 1.36 | b |
| District | 1.36 | b |
| Psychiatrist (minutes) | 2.57 | c |
| Psychologist (minutes) | 1.98 | c |
| Care manager (minutes) | 1.36 | b |
| Occupational therapist (minutes) | 0.83 | a |
| Art therapist (sessions) | 18.5 | d |
| Alternative therapist (minutes) | 0.53 | a |
| Counsellor (minutes) | 1.98 | c |
| Physiotherapist (minutes) | 0.84 | a |
| Dentist (visits) | 135.94 | a |
| Speech therapist (minutes) | 0.69 | b |
| Support worker (minutes) | 0.92 | b |
| Day centre (sessions) | 30.35 | b |
| Day opportunity (days) | 123.04 | b |
| Hospital-based care | ||
| Psychiatric (bed-days) | ||
| Intensive care unit | 1570.17 | e |
| Acute hospital | 236.1 | e |
| Rehabilitation | 376.09 | e |
| General (bed-days) | ||
| Elective/non-elective admission | 4260.24/3440.16 | e |
| General high-dependency unit | 1272.43 | e |
| A&E: admitted/not admitted (attendances) | 174.46/145.21 | f |
| Outpatient (appointments) | ||
| Psychiatry | 262.8 | f |
| General | 206.85 | f |
| Day hospital (attendances) | 785.61 | f |
| Paid/unpaid carer (hours) | 9.00/15.00 | g |
Unpaid care
Respondents who were not in paid employment found it challenging to give an estimate of the time that they spent providing care to study participants. We assumed that a minimum of 8 hours of care was provided by family or friends, for which they did not receive any monetary payment. The costs of unpaid care were valued at the wage rate for carers in paid employment or, for those not in paid employment, at the hourly cost of a home care worker. We extrapolated the 6-monthly costs over the 9 months for use in the economic evaluation.
Data cleaning and missing data
The data analysis follows a HEAP developed before data analysis commenced. Prior to data analysis, all data relevant to the economic evaluation, including data collected from the CSRI questionnaire and EQ-5D-5L questionnaire, were checked and cleaned. The clinical team provided cleaned ABC-C data and demographic data for the study participants and caregivers for use in the economic analysis. We used the same approach as the statistical analysis to deal with missing data, that is if there were any participants for whom data were not collected within this period, their data were considered missing for the purpose of the economic analysis.
Because the estimation of QALYs requires data at each time point, only the complete cases were included in the cost-effectiveness analysis. No imputation was conducted for QALYs.
Prior to performing analyses, we adopted an approach that was consistent with that used for the statistical analysis. The health economics team performed checks on the data to ensure accuracy. Each service and support use variable were checked for:
-
missing values
-
values outside an acceptable range.
If missing values or values out of an acceptable range were found, the data in question were queried with the study manager and confirmed as correct and left unchanged, corrected or deemed to be missing, as appropriate.
Analysis of outcomes
Two outcome measures were used in the economic evaluation in turn: the ABC-C and QALYs. For the purposes of the economic analysis, the primary outcome was challenging behaviour, measured as the total score on the ABC-C at baseline and at the 9-month time point.
The secondary measures of outcome, QALYs, were calculated from the EQ-5D-5L scores at baseline and 9 months (± 4 weeks). Two versions were administered, where possible. If the service user had the capacity, a self-report version of the EQ-5D-5L was used; if the service user lacked capacity, the proxy version of the measure was completed by their carer.
The EQ-5D-5L consists of five domains: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. 75 Each domain can receive a score of 1, 2, 3, 4 or 5, corresponding to no, slight, moderate, severe or extreme problems, respectively. QALY gains will be derived by developing value sets from the EQ-5D-5L by means of a crosswalk to the EQ-5D-5L value sets76 at each time point, with appropriate adjustments for the time involved and linear interpolation to calculate the area under the QALY curve. At the time of writing this report, population weights to derive QALYs from the EQ-5D-5L were not available.
The mean difference in ABC-C at 9 months and the mean difference in QALYs over 9 months were compared, in turn, between the two IST models using a multilevel regression model. For the ABC-C analysis, we adjusted for baseline ABC-C score, age, sex, living arrangements, level of intellectual disability, presence of autism and clinical comorbidities, and other variables identified a priori. For the QALY analyses, we adjusted for the same baseline variables, except for substituting QALYs for ABC-C. Non-parametric bootstrapping was used to estimate 95% CIs for the mean outcome. Values were judged to be significant (p < 0.05) if the bias-corrected CIs of between-group costs excluded zero was also repeated in the section from which the query arose.
Analysis of service use and costs
For each type of service included in the CSRI questionnaire, participants’ use was reported as the mean by group and as the percentage of the group who had at least one contact. Differences in the number of individuals with intellectual disabilities who use the service and the mean number of contacts were summarised for each IST model at baseline and at 9 months’ follow-up. We analysed differences in mean health and social care and wider societal cost at 9 months between the IST models by regressing the total cost from each perspective based on IST model, baseline costs, baseline ABC-C score, baseline health-related quality of life (EQ-5D-5L tariffs), and a range of clinical and sociodemographic indicators. Non-parametric bootstrapping was used to estimate 95% CIs for mean costs. Values were judged to be significant (p < 0.05) if the bias-corrected CIs of between-group costs excluded zero.
Cost-effectiveness analysis
The cost-effectiveness analyses focused on comparing the two IST models identified in Chapter 2. The primary cost-effectiveness analysis assessed cost-effectiveness in terms of the primary measure of outcome (ABC-C score) and a secondary cost–utility analysis was undertaken using QALYs, calculated from the EQ-5D-5L measure of health-related quality of life. The cost-effectiveness analyses were conducted from a health and social care perspective and a wider societal perspective, in turn. The incremental cost-effectiveness ratio (ICER) was calculated as the difference in the cost of the two IST models divided by the outcome (measured using the ABC-C score or QALYs).
Cost-effectiveness acceptability curves (CEACs) were plotted to locate the findings of the economic evaluation in their wider decision-making context. The CEAC illustrates the probability that one of the IST models is cost-effective compared with another across a range of hypothesised values placed on incremental outcome improvements (i.e. willingness to pay by health and social care system decision-makers). Each CEAC77 was derived using a net-benefit approach. The monetary values of incremental effects and incremental costs for each case were combined, and the net monetary benefit was derived as:
where λ is the willingness to pay for a one-point difference in the outcome measure (ABC-C or QALYs), and subscripts a and b denote IST model a and IST model b, respectively. We explored a range of willingness-to-pay values for each outcome in turn.
Sensitivity analyses
Sensitivity analyses were used to assess the robustness of our results. In the sensitivity analyses, we examined the extent to which individuals with missing outcome data varied by baseline characteristics. This was investigated separately for each outcome (ABC-C score and QALYs) using logistic regression. The first step was to model a binary variable (missing vs. not missing) in logistic regression with each baseline demographic variable. Those variables identified as significantly associated with missingness were input in multivariable logistic regression to determine which variables remained significant. The main analyses were then repeated, adjusting for those factors found to be associated with ‘missingness’ on each outcome.
The Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist78 is presented in Appendix 1.
Results
Staffing intensive support team models
Service managers from eight enhanced ISTs and eight independent ISTs returned the data collection pro forma. Service managers provided information on staff job titles by AfC bands, working time, and the average percentage of time spent with the actual client (e.g. face-to-face contact or on the telephone with the client) or completing tasks related to the client (e.g. telephone calls to book appointments, team discussions, writing up patient notes and caseload information).
Service managers who returned IST data collection pro formas provided skills mix data on the job title and AfC bands. In total, 81% of professionals were in AfC bands 3–7 in the enhanced model, whereas 87% of professionals were in AfC bands 3–7 in the independent model. The number of senior staff was 18 compared with 12 (enhanced model vs. independent model); thus, it is worth considering the differing skill mix and seniority between the IST models. The list of professionals by AfC bands is shown in Table 9.
| Enhanced | Independent | ||||
|---|---|---|---|---|---|
| Job title | Number | Current AfC band | Job title | Number | Current AfC band |
| Assistant practitioner | 9 | 4 | Assistant psychologist | 7 | 4 |
| Assistant psychologist | 5 | 4 | Behaviour specialist | 2 | 6 |
| Behaviour nurse specialist | 3 | 7 | Charge nurse | 2 | 6 |
| Behaviour support worker | 2 | 4 | Clinical nurse practitioner | 6 | 6 |
| Clinical psychologist | 13 | 8a | Clinical psychologist | 8 | 8a |
| Clinical support worker | 3 | 3 | Clinical service manager | 1 | 8a |
| Clinical team manager | 2 | 7 | Clinical support worker | 3 | 3 |
| Consultant psychiatrist | 3 | 8d | Community nurse | 20 | 6 |
| Health-care assistant | 4 | 4 | Community support worker | 3 | 3 |
| Intensive assessment and treatment team practitioner | 1 | 5 | Consultant psychiatrist | 3 | 8d |
| Intensive support nurse | 5 | 6 | Health-care assistant | 2 | 3 |
| Intensive support practitioner | 2 | 5 | IST practitioner | 1 | 4 |
| Learning disability nurse | 1 | 8a | Learning disability community nurse | 2 | 5 |
| Nurse practitioner | 12 | 5 | Nurse | 5 | 7 |
| Occupational therapist | 8 | 7 | Nurse practitioner | 2 | 7 |
| Occupational therapy technical instructor | 3 | 3 | Occupational therapist | 7 | 6 |
| PBS specialist | 1 | 6 | Outreach worker | 3 | 4 |
| Physiotherapist | 8 | 6 | Speech and language therapist | 9 | 6 |
| Specialty doctor | 1 | 8b | Therapy assistant | 1 | 4 |
| Speech and language therapist | 7 | 7 | Trainee nurse associate | 1 | 3 |
| Trainee nurse associate | 2 | 4 | Trainee psychiatrist | 1 | 6 |
Caseload and referrals
The caseload data did not consistently reflect a 12-month period and, in some cases, reflected the total caseload at the time of data collection. Referral data collected at both 6 and 12 months for 20 out of 21 teams were used to provide a proxy measure of caseload for each model over 12 months. Referral data over 6 months were available for 20 out of 21 teams (enhanced, n/N = 10/11; independent, n/N = 10/10) and at 12 months for 15 out of 21 teams (enhanced, n/N = 5/11; independent, n/N = 10/10).
Missing referral data for teams with data at 6 months but not at 12 months were imputed using a multiplication factor obtained from teams with referral data at both 6 and 12 months. Using this approach, we derived a total annual caseload that was then divided by the number of teams in each model to calculate an average caseload by model by team over 12 months as 64 for independent model and 123 cases for the enhanced model.
Intensive support team model costs
The calculation of the unit cost of the IST models was based on the approach developed by the PSSRU at the University of Kent (Kent, UK). For both models, the unit costs were based on the skills mix and median salaries for AfC bands. Weighted average salaries for each type of worker were multiplied by the proportion of that type of worker in the team to produce a generic IST worker’s salary.
The salary on-costs were based on the NHS contribution rate of 20.6% of pensionable pay,79 and 13.8% employer national insurance rates. 80 Expenditure data to assist with identifying managerial overheads and capital overheads were poorly completed. Therefore, managerial and non-care staff overheads were calculated based on values taken from the 2013/14 financial accounts for 10 community trusts, reported in the Unit Costs of Health and Social Care 202065 as 24.5% of direct salary costs. Non-staff overheads, which include the cost to the provider for office, travel/transport, publishing, training courses, supplies and clinical and general services, and utilities such as water gas and electricity were calculated at 38.2% of direct salary costs.
The capital overheads were based on capital overheads for scientific and professional staff. Sixteen out of the participating 21 teams returned the costing pro forma (enhanced, n/N = 8/11; independent, n/N = 8/10) and, at 12 months, referral data were available for 15 out of 21 teams (enhanced, n/N = 5/11; independent, n/N = 10/10). ISTs with both 12-month referral data and staffing data were used to derive a mean annual cost per case for the cost-effectiveness analyses. The average annual cost per case was calculated as the average annual cost per team member multiplied by the average number of professionals on a team, divided by the proxy measure of caseload over 12 months.
In the enhanced model, 63% of contact with clients was face to face. In this model, there were on average 12 professionals (minimum 1, maximum 21) working in each team. We therefore calculated the average annual cost per team in the enhanced model to be £612,612 (Table 10). The annual costs are likely to be higher or lower than this, depending on the number of professionals in each team and the proportion of professionals in higher AfC bands. The average annual cost per case was £4980 (over 9 months, the cost was £3735).
| Cost category | 2020/21 (£ per year) |
|---|---|
| Salary | 23,401 |
| Salary oncosts, including employers’ National Insurance and superannuation contributions | 8050 |
| Overheads | |
| Management and other non-care staff | 5733 |
| Non-staff | 8939 |
| Capital overheads | 5353 |
| Ratio of direct face-to-face time to indirect time | 1 : 0.58 |
| Working time | 33 weeks per annum and 30 hours per week |
| Caseload per teama | 985 |
| Team members (mean) | 12 |
| Averages | |
| Per hour | 51.57 |
| Per hour of face-to-face patient contact | 81.48 |
| Annual cost of team member | 51,051 |
| Annual cost per case | 4980 |
In the independent model, 64.2% of contact with clients was face to face. In this model type, there were on average 11 professionals (minimum 6, maximum 21) working in each team. We therefore calculated the average annual cost per team in the independent model to be £647,812 (Table 11). The annual costs are likely to be higher or lower than this, depending on the number of professionals in each team and the proportion of professionals in higher AfC bands. The average annual cost per case was £10,122 (over 9 months, the cost was £7591.50).
| Cost category | 2020/21 (£ per year) |
|---|---|
| Salary | 27,477 |
| Salary oncosts, including employers’ national insurance and superannuation contributions | 9452 |
| Overheads | |
| Management and other non-care staff | 6732 |
| Non-staff | 10,496 |
| Capital overheads | 5353 |
| Ratio of direct face-to-face time to indirect time | 1 : 0.56 |
| Working time | 35 weeks per annum and 32 hours per week |
| Caseload per teama | 511 |
| Team members (mean) | 11 |
| Averages | |
| Per hour | 52.58 |
| Per hour of face-to-face patient contact | 82.02 |
| Annual cost of team member | 58,892 |
| Annual cost per case | 10,122 |
Baseline comparisons of service use and support data collection
At baseline, full-service use data were available for 210 study participants (enhanced, n = 107; independent, n = 103).
Service use and support
Resource use differences were not compared statistically. There were two main reasons for this: first, the economic evaluation was focused on costs and cost-effectiveness and, second, to avoid problems associated with multiple testing. Therefore, resource use patterns are described without statistical comparisons.
The number of nights in hospital was broadly similar in the two IST models (see Appendix 1, Table 22). Notably, service users in the independent model spent marginally longer in a psychiatric ward on average than those in the enhanced model [mean 8.63 (SD 39.98) vs. mean 5.26 (SD 28.10) bed-days, respectively]. Community-based health and social care service use appeared broadly comparable between the two models at baseline (see Appendix 1, Table 22).
The mean use of inpatient, outpatient and day-patient health services over the 9-month follow-up period are reported in Appendix 1, Table 21. The pattern of general outpatient attendances, day hospital contacts and A&E attendance was broadly similar for both models. However, on average, service users in the independent model had marginally more contacts with their GP than those in the enhanced model [mean 4.88 (SD 14.20) vs. mean 3.47 (SD 3.96) attendances, respectively].
Costs
The total costs, including a breakdown of costs by service-providing sector but excluding intervention costs, are summarised in Appendix 1, Table 23. To calculate the costs for 9 months, we extrapolated the costs for 6 months to 9 months.
From a NHS/Personal Social Services perspective, the mean total health and social care cost over 9 months’ follow-up was £15,324.18 in the independent model and £15,302.66 in the enhanced model; the adjusted mean difference in costs was not statistically significant (£3409.95, 95% CI –£9957.92 to £4039.89).
From a societal perspective, the mean total cost over 9 months’ follow-up was £26,117.84 in the enhanced model and £24,259.33 in the independent model; the adjusted mean difference in costs was not statistically significant (–£4712.30, 95% CI –£11,124.85 to £2106.36).
Outcomes
Primary and secondary outcomes at baseline and the 9-month follow-up for the two IST models used in the economic evaluation are shown in Appendix 1, Table 24. The table distinguishes the IST models and reports the difference in baseline and 9-month ABC-C scores. The EQ-5D-5L was used to report health-related quality of life, focusing on the utility scores for the person with intellectual disabilities, and the QALYs from baseline to 9 months. The EQ-5D-5L proxy measure was used to report proxy utility scores for the person with intellectual disabilities and QALYs from baseline to 9 months.
Challenging behaviour
As shown in Appendix 1, Table 24, we found no evidence of a difference in baseline ABC-C score between the enhanced and independent models (mean difference 0.15, 95% CI –7.46 to 7.76; p = 0.97). In the same table, we see that a similar pattern was observed at 9 months (mean difference –5.07, 95% CI –14.93 to 2.14; p = 0.31). At follow-up, the observed ABC-C score reduced by 13% for the enhanced model and by 21% for the independent model. A lower ABC-C score is considered an improvement in ABC-C score.
Health-related quality of life
At baseline, self-report EQ-5D-5L utility data were available for 18 out of 111 study participants in the independent model and 22 out of 115 study participants in the enhanced model. The self-report mean utility score at baseline was 0.8123 (SD 0.2086) for the independent model and 0.6381 (SD 0.2734) for the enhanced model. At 9 months’ follow-up, self-report utility data were available for 2 out of 111 participants in the independent model and 8 out of 115 participants in the enhanced model. Using self-report data, the mean utility score at 9 months was 0.4675 (SD 0.2015) for the independent model and 0.5320 (SD 0.3081) for the enhanced model. Owing to limited utility score data for adults with intellectual disabilities, we were unable to explore differences in the models at baseline and 9-month follow-up, or QALYs from baseline to follow-up.
Carer-reported utility scores of adults with intellectual disabilities are shown in Appendix 1, Table 24. We found that the mean health utilities score, measured using the EQ-5D-5L (proxy), was slightly higher in the independent model than in the enhanced model across the entire follow-up period, with the resultant QALYs also being higher for the independent model, but the QALY mean difference (0.0158) was not significant (p = 0.273) following adjustment for baseline demographic and clinical characteristics, including risk (TAG score).
Medication
As shown in Table 12, the type of medication prescribed to adults with intellectual disabilities who display challenging behaviour was relatively similar in the enhanced and independent models at baseline and 9-month follow-up. The mean number of prescribed medications was the same for both models at baseline (n = 5). At follow-up, the mean number of prescribed medications was smaller in the independent model (enhanced, n = 5; independent, n = 4).
| Medication | Baseline | 9-month follow-up | ||||||
|---|---|---|---|---|---|---|---|---|
| Enhanced (N = 115; valid n = 97) | Independent (N = 111; valid n = 91) | Enhanced (N = 107; valid n = 94) | Independent (N = 101; valid n = 91) | |||||
| Mean (SD) | Range | Mean (SD) | Range | Mean (SD) | Range | Mean (SD) | Range | |
| Number per participant | 4.97 (3.28) | 1–17 | 5.10 (3.51) | 1–17 | 5 (3.22) | 1–21 | 4.06 (3.32) | 1–17 |
| Medication type | Frequency | Per cent | Frequency | Per cent | Frequency | Per cent | Frequency | Per cent |
| Antipsychotic | 81 | 17.16 | 88 | 17.78 | 86 | 18.3 | 83 | 19.81 |
| Other psychotropic | 166 | 35.17 | 146 | 29.49 | 148 | 31.49 | 136 | 32.46 |
| Sedatives | 60 | 12.71 | 50 | 10.1 | 54 | 11.49 | 48 | 11.46 |
| Antidepressant | 45 | 9.53 | 53 | 10.71 | 33 | 7.02 | 41 | 9.79 |
| Antiepileptic/mood stabiliser | 60 | 12.71 | 41 | 8.28 | 60 | 12.77 | 41 | 9.79 |
| Stimulant | 1 | 0.21 | 2 | 0.4 | 1 | 0.21 | 6 | 1.43 |
| Non-psychotropic | 225 | 47.67 | 261 | 52.73 | 236 | 50.21 | 200 | 47.73 |
| Psychotropic | 247 | 52.33 | 234 | 47.27 | 234 | 49.79 | 219 | 52.27 |
| Only one psychotropic | 17 | 17.89 | 21 | 21.65 | 15 | 15.96 | 23 | 25.27 |
| More than one psychotropic | 68 | 71.58 | 67 | 69.07 | 67 | 71.28 | 61 | 67.03 |
More adults with intellectual disabilities who display challenging behaviour were prescribed other psychotropic medication at baseline in the enhanced model (≈ 35%) than in the independent model (≈ 30%). Other psychotropic medication includes sedatives, antidepressants, antiepileptic medication/mood stabiliser and stimulants. They were also prescribed more non-psychotropic medication in the enhanced model (≈ 50%) than in the independent model (≈ 48%) at the 9-month follow-up.
More adults with intellectual disabilities were prescribed non-psychotropic medication at baseline in the independent model (≈ 53%) than in the enhanced model (≈ 48%). Similarly, we observed that more adults with intellectual disabilities were prescribed only one psychotropic medication in the independent model (≈ 22% at baseline, ≈ 25% at follow-up) than in the enhanced model (≈ 18% at baseline, ≈ 16% at follow-up). Last, we observed that more adults with intellectual disabilities who display challenging behaviour were prescribed stimulants in the independent model (≈ 2%) than in the enhanced model (< 0.5%) at the 9-month follow-up.
Cost-effectiveness (over 9 months)
Results from the net-benefit regression using the two outcome measures (ABC-C total score and QALYs) examined in the economic evaluation in turn from a health and social care and societal perspective are summarised in Appendix 1, Table 25, and the ICERs are reported in Appendix 1, Table 26. The cost and outcome differences for each outcome were obtained (after adjustment for baseline demographic and clinical characteristics, and risk score) for those adults with no missing data.
Health and social care perspective
Health and social care costs were slightly higher for study participants in the independent model than the enhanced model, but the difference was not statistically significant and the service users in the independent model enjoyed better outcomes, whether they were measured in terms of challenging behaviour (ABC-C score) or in terms of health-related quality of life (QALYs). However, the difference for both outcomes was not statistically significant. Whether or not these results imply that the independent model is cost-effective compared with the enhanced model depends on the decision-maker’s willingness to pay for these improvements in challenging behaviour or gains in health-related quality of life. To aid discussion of willingness to pay, we computed the ICERs. We also plotted the associated CEACs.
Looking first at the ABC-C total score (see Appendix 1, Table 26), the mean cost per one-point improvement on the ABC-C was £88.08. The scatterplot is shown in Appendix 1, Figure 10, and the CEAC for this outcome measure is shown in Appendix 1, Figure 11. We are not aware of any previously suggested monetary thresholds for gauging cost-effectiveness on the ABC-C. However, if we assumed a willingness to pay of £500, the probability that the independent model would be seen as cost-effective compared with the enhanced model would be 68.6%.
For the other outcome, the mean cost per QALY gained was £28,262. The scatter plot is shown in Appendix 1, Figure 12, and the CEAC shown in Appendix 1, Figure 13, illustrates the probability of cost-effectiveness for a number of hypothesised values of willingness to pay. At the £20,000-per-QALY threshold associated with NICE recommendations,81 the probability that the independent model would be seen as cost-effective compared with the enhanced model was 61%; at the higher NICE threshold of £30,000, the probability was 63%.
Societal perspective
A wider societal perspective that included not only the IST model cost, but also the cost to health and social care and the cost of unpaid support to the study participant provided by family and friends, was considered against outcomes. Under the societal perspective, the adjusted societal costs were lower (mean difference –£855.80, 95% CI –£8342.54 to £6059.69) and the ABC-C outcomes were better in the independent model than in the enhanced model (mean difference –5.07, 95% CI –14.93 to 2.14), but the differences in costs and outcomes were not statistically significant. This generated an ICER (the additional cost of one intervention compared with another, divided by the additional effects) of –£168.79 (ABC-C score) and –£54,164.56 (QALYs), suggesting that the independent model dominates the enhanced model (i.e. the independent model is both cheaper and more effective).
The scatterplots of the bootstrapped cost and effectiveness pairs for the independent model compared with the enhanced model (see Appendix 1, Figures 14 and 16) illustrate that point estimates are dispersed across the four quadrants of the cost-effectiveness plane, with a larger proportion and the majority of the scatter points falling in the south-east quadrant of the cost-effectiveness plane, indicating that the independent model replications are cheaper and more effective than those of the enhanced model. Considering the reduction in the ABC-C score when comparing the two models, the probability that the independent model is cost-effective is > 60% even when the decision maker is not willing to pay for any point improvement in the ABC-C score. (see Appendix 1, Figure 15); the probability does not fall below 50% and is closer to 52% at the standard NICE-preferred willingness-to-pay levels of £20,000–30,000 per QALY (see Appendix 1, Figure 17).
Sensitivity analysis
We investigated the extent to which adjusting for the factors contributing to missing outcome data for both outcome measures (ABC-C and QALYs) and total costs at 9 months had an impact on the main results. We focused on QALYs (proxy report), as baseline self-report EQ-5D-5L utility data were available for only 18 out of 111 participants in the independent model and 22 out of 115 participants in the enhanced model. For the sensitivity analysis, we modelled the binary variable missing versus not missing in logistic regression, with each baseline demographic variable as the dependent variable. The variables identified as significantly associated with missingness were then used as alternatives to the baseline covariates used in the main analyses. All other variables used in the main analyses did not change and a new ICER was estimated.
We conducted four independent sensitivity analyses from each perspective, using the ABC-C and the QALY in turn, to assess the robustness of our results. The sensitivity analyses are shown in Appendix 1, Table 27:
-
We investigated the factors contributing to missing health and social care cost data at 9 months and, following adjustment for those factors, we derived a new adjusted mean difference in health and social care cost between the two IST models. The factors found to be associated with missing health and social care data were the number of physical conditions, reason for intellectual disability and living situation. We used the new adjusted incremental health and social care cost at 9 months, and compared it with the incremental ABC-C score at 9 months and QALYs over 9 months in turn.
-
We investigated the factors contributing to missing societal cost data at 9 months and, following adjustment for those factors, derived a new adjusted mean difference in societal costs between the two IST models. The factors found to be associated with missing societal cost data were the same as those found to be associated with missing health and social care data: the number of physical conditions, reason for intellectual disability and living situation. We used the new adjusted incremental societal care cost at 9 months, and compared it with the incremental ABC-C score at 9 months and QALYs over 9 months in turn.
-
We investigated the factors contributing to missing QALYs data over 9 months and, following adjustment for those factors, derived a new adjusted mean difference in QALYs (EQ-5D-5L proxy) between the two IST models. The factors found to be associated with missing QALY data were number of physical conditions and gross personal income. We used the new adjusted incremental QALY over 9 months, and compared it with the total health and social care cost and societal costs at 9 months in turn.
Adjusting for factors associated with missing data in narrower perspectives, focusing on the cost of the interventions and the health and social care costs only, did not alter the findings in the main analyses (see Appendix 1, Figures 18 and 20).
Adjusting for factors associated with missing societal cost data at 9 months and leaving the outcomes for ABC-C and QALYs unchanged increased the overall mean difference in total cost between the two IST models, making the independent model costlier than the enhanced model and improving the challenging behaviour and health-related quality-of-life outcomes. For the additional costs, there is likely to be a lower net benefit to society.
Given that there were higher costs and better outcomes, we explored the probability of the independent model being cost-effective. The CEAC showed that, following adjustment for missing societal costs, the probability of the independent model being cost-effective compared with the enhanced model fell by 20% to 39% (considering the outcome as challenging behaviour, measured using the total ABC-C score) if society was not willing to pay for a unit improvement in the challenging behaviour score. There is a small chance that the independent model would be cost-effective relative to the enhanced model, as there is only a 42% probability of cost-effectiveness at the standard NICE-preferred willingness-to-pay levels of £20,000–30,000 per QALY and a 39% probability at £0 per QALY (see Appendix 1, Figures 19 and 21).
Summary
We found no statistically significant difference in societal costs between the models. We found no statistically significant difference in health and social care costs between the models. However, the independent model was more costly to operate per case than the enhanced model. This is because of the smaller caseload and the larger proportion of band 6 professionals in the independent model than the enhanced model. The marginally higher observed hospital-based care costs in the independent model were offset by higher community-based care costs and unpaid carer costs for those in the enhanced model at our primary economic end point of 9 months. Although observed health-related quality of life was slightly higher in the independent model than in the enhanced model across the entire follow-up period, with the resultant QALYs also higher for the independent model, the QALY difference did not reach statistical significance. Given this uncertainty in the results, with the lack of statistically significant differences in costs and outcomes, we looked at the likelihood that the independent model would provide better value for money than the enhanced model.
Our analyses suggest that there is a 50 : 50 chance that the independent model is cost-effective compared with the enhanced model. The probability of the independent model being cost-effective compared with the enhanced model does not fall below 50% and is closer to 52% at the standard NICE-preferred willingness-to-pay levels of £20,000–30,000 per QALY. It is therefore unlikely that there are any economic gains from choosing one model of care over the other. The main analyses are, on the whole, consistent with the sensitivity analyses using both broader and narrower cost perspectives. However, these findings should be treated with caution given the observational study design and the fact that, at the time of writing the analysis plan, we were unable to assess or adjust for the impact that COVID-19 would have had on the patterns and intensity of service use and support (costs) in both of these models.
Chapter 5 Service-level processes and outcomes of intensive support team models
Introduction
This chapter provides a comprehensive description of additional elements relating to the function of ISTs. These are service-specific data from the 21 ISTs that took part in the clinical effectiveness and cost-effectiveness study (Chapters 3 and 4). The key objective was to obtain an understanding of the IST role in the wider local care network of services for adults with intellectual disabilities who display challenging behaviour.
Methods
Patient throughput
The managers of the 21 participating ISTs were approached by e-mail between June 2020 and August 2020 to report on the following items: (1) current total caseload, (2) referral numbers over the past 12 months, (3) level of service user engagement with the service, (4) time from assessment to delivery of management plan (in days), (5) other IST scope (e.g. training provided) and (6) engagement with other services.
Operational policies
An up-to-date copy of the operational policy documents of the IST was retrieved and the latest version confirmed with the IST manager. Each policy document was scrutinised regarding whether or not it contained information about the IST objectives, organisational characteristics and skill mix, and included reference to national guidelines relating to the treatment of people with intellectual disabilities.
Referrers’ survey
Originally, we had considered the IST as having a presence within the crisis care landscape. However, having investigated the pathway to ISTs, we discovered that the ISTs were exclusively associated with CIDSs, not other services, for the purpose of receiving referrals. Therefore, we developed a brief survey of health-care practitioners from CIDSs who had experience of referring to a participating IST. The survey is available at URL: www.fundingawards.nihr.ac.uk/award/16/01/24.
The questionnaire included 22 open- and close-ended questions that covered information about the number of referrals to the IST, outcome of referral, time from referral until first assessment, level of satisfaction with the referral process, interventions offered to service users, and length of time open to the IST. There were free-text questions that addressed health-care professionals’ views of the way that an IST compares or fits with other services, and the IST’s limitations. The survey was administered online in April–June 2020 and was managed via the Opinio software. The IST managers liaised with the researchers in distributing the survey.
Data analysis
Descriptive data were summarised in tables and graphs, reporting percentages and/or ranges, where appropriate. We received 12-month referral data for 20 out of 21 teams (enhanced, n/N = 10/11; independent, n/N = 10/10). All qualitative information from the operational policy documents and the additional comments from the service-level data and referrers’ survey were analysed thematically. 56
Results
Patient throughput
The responses related to 20 ISTs. One IST manager was newly appointed to the role and was unable to extract information about the service as it coincided with the first lockdown of the COVID-19 pandemic.
The mean caseload of enhanced ISTs was 51 adults with intellectual disabilities. The mean number of referrals to ISTs in the enhanced model was 101 adults with intellectual disabilities at 12 months. Moreover, it was evident that ISTs in the enhanced model required a few weeks to respond to referrals, arranging assessments within 18 days (range 14–22 days) on average, with the management plan finalised within 7 weeks (mean 52 days, range 48–54 days). The engagement of adults with intellectual disabilities and their carers with the IST, as reported by IST managers and the NHS care note system, was high in both models (enhanced, 94%; independent, 95%) (Table 13).
| Service characteristic | Model, mean (range) | |
|---|---|---|
| Enhanced (ISTs, n = 10) | Independent (ISTs, n = 10) | |
| Caseload (number of patients) | 51 (10–126) | 30 (7–67) |
| Referrals per 12 months (number of patients) | 101 (16–256) | 80 (12–144) |
| Percentage of patients engaged | 94 (80–100) | 95 (92–100) |
| Days from referral to assessment | 18 (14–22) | 5 (4–7) |
| Days from assessment to delivery of management plan | 52 (48–54) | 33 (22–44) |
Comparatively, the independent ISTs included a mean caseload of 30 adults with intellectual disabilities and received a mean number of 80 referrals in a 12-month period. In addition, ISTs in the independent model responded quicker to referrals than the enhanced model, arranging assessments within 5 days (range 4–7 days) on average, with the management plan finalised within 1 month (range 22–44 days) (see Table 13).
Responses regarding other IST roles, particularly training and engagement with other services, are reported in the subsequent sections.
Training of carers
Most sites (16/20) from both IST models reported that they provided training to carers that was focused on individual needs, taking into consideration additional diagnoses and including psychoeducation, raising awareness about intensive interaction for improving communication and recording (e.g. using the ABC-C chart, incident reports) of challenging behaviour, or sharing knowledge (e.g. dysphagia, attachment difficulties, sensory integration, active listening) to understand and implement the care plan to better support adults with intellectual disabilities who display challenging behaviour. The IST provided ongoing support to ensure evidence-based interventions, such as PBS, were embedded before they progressively reduced their input.
Engagement with other services
Intensive support team professionals from both models reported collaborations with a range of local services, such as mental health (n = 9), social care (n = 9), crisis teams (n = 9), forensic outreach and liaison services (n = 9), Clinical Commissioning Groups (n = 5), acute liaison nurses (n = 3), home treatment teams (n = 3) and other boroughs (n = 1) (Figure 6). Furthermore, ISTs supported transitions through working with educational placements and/or children services, and primary care to facilitate health checks and physical health investigations. ISTs were also committed to joint assessments with other agencies to identify suitable placements, or to determine a hospital placement if all else failed.
One independent IST stated that they had an on-call service between 20.00 and 08.00 for urgent advice or crisis management. This service was available to participants in their current caseload, but could extend to those who found themselves in crisis and adults with intellectual impairment who were not on the caseload. Therefore, they received calls from multiple sources, such as service providers, family carers, CIDSs, GPs and adults with intellectual disabilities. In a 6-month period (1 March–31 August 2020), this independent IST logged 343 calls in relation to the on-call service.
FIGURE 6.
The ISTs’ engagement with other services.
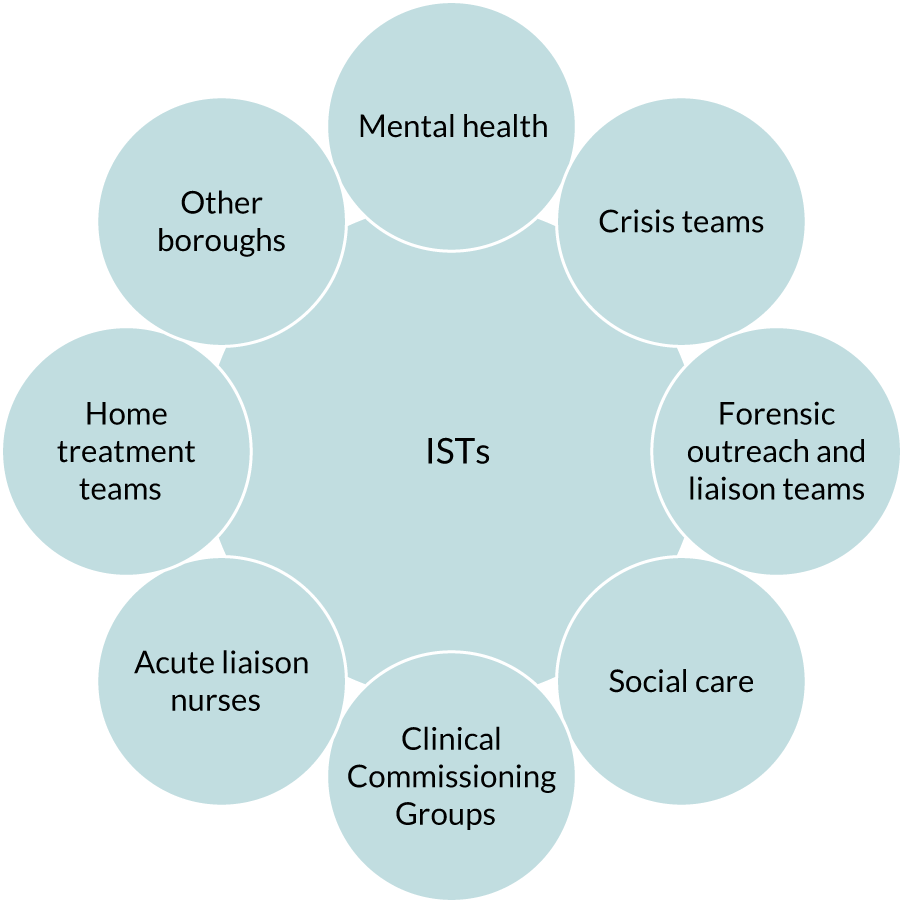
Operational policy documents
Intensive support team managers from 16 sites shared the latest operational policy document, which covered 19 ISTs. In a few instances, when there was more than one IST at a site, the ISTs shared the same operational framework. Two ISTs in the independent model did not have an operational policy. Each policy document was scrutinised regarding whether or not it contained information about the IST objectives, organisational characteristics and skill mix, and included reference to national guidelines.
Aims of intensive support teams
The core aims of ISTs in both models were to reduce placement breakdown (total ISTs, N = 15; enhanced, n = 9; independent, n = 6) and the number of hospital admissions (total ISTs, N = 14; enhanced, n = 8; independent, n = 6). Ten ISTs (enhanced, n = 5; independent, n = 5) explicitly referred to the management of challenging behaviour and 11 teams (enhanced, n = 6; independent, n = 5) referred to maintaining long-term placement integration of the adult with intellectual disability in the local community to improve their well-being and quality of life. Two independent ISTs referred to assertive outreach to support people with complex and enduring needs within the community. All 16 ISTs had crisis care plans in their operational policy documents regarding placement breakdown and hospital admissions because of significant mental illness and/or challenging behaviours. Three ISTs specified that they were not crisis intervention services, but supported and advised those services, offering guidance where appropriate. Last, one independent IST mentioned that they had a waiting list and mentioned plans regarding handling adults with intellectual disabilities being on the waiting list.
Organisational characteristics of intensive support teams
The vast majority of ISTs (n = 18) were set up almost exclusively for the care of adults with intellectual disabilities who display challenging behaviour, but, even so, IST will liaise with other services such as forensic services (n = 1). Only one independent IST stated that the IST remit included adults with autism spectrum disorder (ASD) in the absence of intellectual disabilities. Nine teams (enhanced, n = 5; independent, n = 4) mentioned involvement with family and friends. Three independent ISTs had guidelines for transitions between care providers. Enhanced (n = 7) and independent (n = 6) ISTs specified their working hours to be flexible, even working out-of-office hours on a 24-hour basis, when needed, but a minority of ISTs from both IST models (n = 5) did not offer out-of-hours crisis care.
Skill mix in intensive support teams
According to the operational framework, ISTs were predominantly set up to be led by nurses (total ISTs, N = 11; enhanced, n = 4; independent, n = 7) and psychologists (total ISTs, N = 9; enhanced, n = 5; independent, n = 4), although one independent IST was led by a speech and language therapist. All ISTs suggested that they were multidisciplinary services. The majority of ISTs (n = 18) mentioned that they had access to mental health services or other teams within the CIDS in their operational policies. Furthermore, 12 teams (enhanced, n = 6; independent, n = 5) had a consultant psychiatrist, 16 (enhanced, n = 7; independent, n = 9) had a speech and language therapist, 14 (enhanced, n = 5; independent, n = 9) had an occupational therapist, nine (enhanced, n = 5; independent, n = 4) had a physiotherapist, three (enhanced, n = 1; independent, n = 2) had an art therapist, six (enhanced, n = 4; independent, n = 2) had a social worker and three (enhanced, n = 1 ISTs; independent, n = 2) had a dietitian. Further details are shown in Table 14.
| Role | Model (number of ISTs) | |
|---|---|---|
| Enhanced (N = 10) | Independent (N = 11) | |
| Clinical lead | ||
| Intellectual disability nurse | 4 | 7 |
| Psychologist | 5 | 4 |
| Speech and language therapist | 1 | 0 |
| Group of professionals in the IST | ||
| Clinical psychologist/assistant psychologist | 9 | 10 |
| Community or intellectual disability nurse | 9 | 10 |
| Consultant psychiatrist | 6 | 5 |
| Occupational therapist | 5 | 9 |
| Speech and language therapist | 7 | 9 |
| Physiotherapist | 5 | 4 |
| Art therapist | 1 | 1 |
| Social worker | 4 | 2 |
| Dietitian | 1 | 2 |
National guidelines
The Transforming Care programme12 was referenced in the operational policies of 14 enhanced ISTs and eight independent ISTs. The Valuing People strategy82 was acknowledged in six operational policy documents (ISTs: enhanced, n = 3; independent, n = 3); similarly, the Care Programme Approach83 was mentioned as a process for complex mental health care in two enhanced ISTs’ operational policies and one independent IST’s operational policy. Last, the STOMP3 initiative was referenced in two enhanced ISTs’ operational policies. The STOMP project is a national programme that aims to stop the unnecessary prescription of psychotropic medication to adults with intellectual disabilities (with or without autism). 20
Referrers’ survey
The survey was completed by 31 CIDS health-care professionals who referred adults with intellectual disabilities to ISTs. Health-care professionals in CIDSs are described as ‘referrers’ in this chapter. The findings are not presented per IST model because the survey was directed to CIDSs, aiming to explore the levels of satisfaction of current IST procedures and practices, irrespective of the operational models.
Reason for referral to the intensive support team
A broad range of reasons for referral were reported and are listed below, ranked in order from most to least common (Figure 7):
-
to develop better understanding and support the management of challenging behaviour (e.g. risk of harm to self or others) in adults with intellectual disabilities
-
to support complex health-care needs
-
to provide care following involvement with the criminal justice system
-
to prevent placement breakdown and risk of psychiatric inpatient admission
-
to guide the transition to adult services for young adults presenting with challenging behaviour
-
to support the training needs of staff regarding PBS or Challenging Behaviour frameworks.
FIGURE 7.
Reasons for referral to the IST.

A few (n = 3; 10%) referrers specifically mentioned referral to ISTs for functional analyses with regards to challenging behaviour. A small number (n = 2; 7%) of referrers mentioned the Dynamic Support Database (DSD) tool. The DSD is a screening tool that is used by referrers to monitor adults with intellectual disabilities, autism or both who are at risk of a hospital admission. The overall rating of the tool (i.e. red, amber or green) reflects the level of risk of admission to inpatient services. If the individual’s score was amber or red, they were referred to the IST. 84
Referral process
According to referrers, ISTs responded to referrals in 0–6 days. A few (n = 3; 10%) referrers stated that referrals were discussed with the IST lead prior to making the referral to ensure that the person was eligible for specialist support. Such informal conversations were seen as helpful because they provided a swift response at a point of crisis. Only one referrer described the referral process as part of the CIDS weekly meetings, to which the IST lead was invited and at which they could discuss urgent cases.
Referrers (n = 28; 90%) expressed their satisfaction with the referral process, which they believed contributed to the prevention of inpatient psychiatric admissions. Five (16%) referrers thought that the enhanced model facilitated proactive and rapid work between professionals, providing better quality care to adults with intellectual disabilities who display challenging behaviour. The vast majority of referrers (n = 29; 94%) would recommend the IST to other colleagues, describing IST staff as very understanding, skilled, helpful and responsive.
Delivery of intensive support team care
The 31 referrers accounted for 130 referrals to ISTs, of which over 112 (86%) had been accepted for IST support. The mean number of referrals per IST professional was 5 (range 1–30) over the preceding 12 months. Adults with intellectual disabilities who display challenging behaviour received IST support for a period ranging from 3 to ≥ 12 months (Figure 8), although a small minority were seen for up to a month, which is likely to be a period of assessing eligibility for the service or resolution of the original reason for referral. Twenty-six referrers (84%) stated that the length of time of support given by ISTs was appropriate.
FIGURE 8.
How long adults with intellectual disabilities were under IST care.
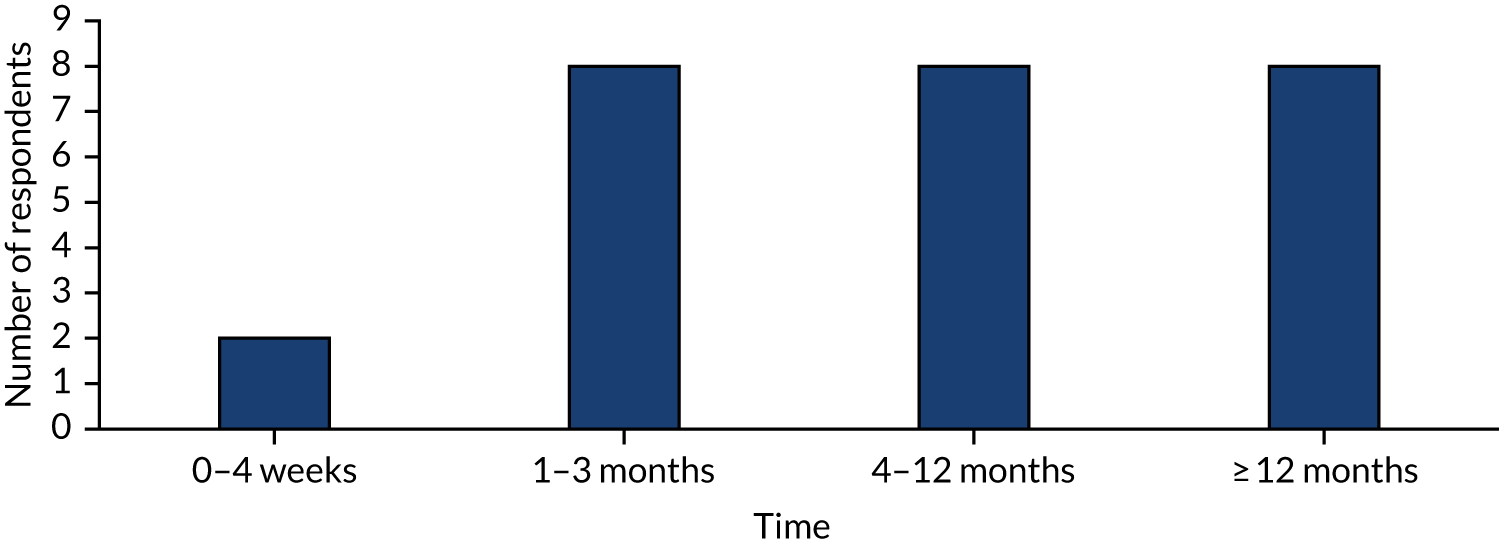
Free-text questions addressed the support offered to adults with intellectual disabilities, family carers, paid carers and other professionals by ISTs; the way that the IST compares or fits with other services; and the ISTs limitations.
Support offered by intensive support teams
Adults with intellectual disabilities
The IST co-ordinated the care plan of the adult with intellectual disability. The IST conducted home visits to assess and manage challenging behaviour, complete risk assessments and monitor medication.
Family carers
Referrers stated that the IST liaised with family carers on a weekly basis through telephone calls and home visits to monitor progress and provide emotional support to family carers. In addition, the IST staff signposted family carers to relevant services if needed, and provided a dialogue regarding sourcing appropriate care provision.
Paid carers
The IST worked with paid carers to enable them to follow and implement the PBS plan. The IST outlined the functions of behaviours to paid carers (i.e. helping them to understand behaviour triggers), offered additional skill training (e.g. anxiety management, understanding autism, modelling of specific behavioural strategies), and carried out periodic service reviews, including revision of the PBS plan. The IST would consider staff well-being and debriefing after episodes of challenging behaviour to ensure that paid carers were able to maintain good practice.
Other professionals
The IST dedicated time to helping referrers understand the IST role and promoting multidisciplinary work with CIDSs. They worked collaboratively with other services/teams during inpatient admission and discharge planning to create and review care plans and risk assessments, facilitated CTR36 and contributed to service development projects, such as developing pathways for challenging behaviour.
How the intensive support team compares or fits with other services
Fits well with the community intellectual disability service
Referrers stated that the IST had a good knowledge of the networks and relationships between different support teams. Overall, it was highlighted that working within (or closely with) the CIDS enabled the IST to respond to the crisis more effectively, demonstrating a proactive approach, and they were jointly commissioned, with health and social care input. One referrer reported that they were currently working to embed the IST in the CIDS so that the services were not separate.
Comparison to other services
Referrers reported that ISTs were able to provide more accessible, responsive and intensive input to crisis situations as the main service for this client group. In addition, the outreach service was described as ‘great, as it is an opportunity to discuss and reflect on individual case studies’, with the commissioners (managers responsible for service development and care prioritisation) holding positive views of the IST. It was also mentioned that referrals are limited to challenging behaviour, which may be a narrow remit. There were some contradictory views: one respondent stated that the IST was specialist in their field; another stated that the IST had lost some degree of specialism in recent years, had become slightly less cohesive and was in need of a clinical lead.
Limitations of the intensive support team
Twenty-seven referrers (87%) reported a number of limitations related to the IST’s function, including resources, focus on PBS plans, and lack of leadership and service clarity.
Core functions
A number of referrers (n = 11; 35%) were concerned about the IST’s access to resources, including funding, staffing and flexible working hours. The responsibility of responding to crises may detract from more therapy-based work, such as functional assessments or staff and carer support and training. There is significant variation by locality and some roles may be under-represented, despite potentially being central to the implementation of behavioural interventions (e.g. specialist support workers). One referrer suggested that support workers could complement the service and assist with face-to-face contact when needed.
Other issues included the fact that sometimes ISTs focused too much on PBS when many placement breakdowns were due to mental illness and some behaviours still need to be managed by medication. Following this, a referrer emphasised that sometimes there can be underlying unmet health needs that may not have been identified by referrers. As a result, the IST invests resources and time in inappropriate referrals. A number of referrers (n = 8; 26%) reported that the boundaries between services were unclear, which caused confusion regarding the way in which the CIDS and IST can work collaboratively (e.g. who is in charge of a case, which parts of the care plan are delivered by whom); a lack of clarity surrounding who was in charge of care co-ordination; and unclear referral criteria, which may prevent individuals from gaining help from the appropriate services.
Minimises engagement with mainstream services
A few (n = 4; 13%) referrers stated that ISTs appear distinct from CIDSs and do not utilise all the expertise that may be available in a locality, including strong liaison with mental health services. This results in services being isolated, which, in turn, produces unrealistic expectations from CIDSs. One referrer considered the potential that having independent ISTs deskills professionals in the community services with regard to responding effectively to challenging behaviour. A cascade of expertise, rather than a narrowly focused service, might be a better approach.
Summary
Patient throughput data from the two IST models indicated that the operation of ISTs varied somewhat between models, with enhanced ISTs having a 41% larger caseload and 21% more referrals than the independent ISTs over 1 year. The increased size of the caseload and flow of referrals in enhanced ISTs compared with those of independent ISTs, whose caseload and number of referrals were less demanding, were associated with delays in responding to the needs of adults with intellectual disabilities who display challenging behaviour.
However, some of these data were estimates provided by IST managers during the first lockdown of the COVID-19 pandemic and, therefore, they were not fully reflective of the total work undertaken by both CIDSs and ISTs during that time. Therefore, we advise that these data should be interpreted with caution.
We found that teams in the independent model had smaller caseloads. This is one of the characteristics of the intensive case management model in adult mental health services. 85 However, our present work does not support a choice of IST model based on caseload size only.
Referrers expressed their satisfaction with the referral process; acknowledged the support provided to adults with intellectual disabilities, carers and other services to be regarded as suitable; and recommended the future use of ISTs. Regardless of the positive comments about the contribution of ISTs to the care of adults with intellectual disabilities, referrers mentioned a number of limitations of the operation and functioning of ISTs that should be addressed to improve care provision. However, in our study, referrers from CIDSs valued the ISTs’ input and, on the whole, the IST response was considered prompt and collaborative. Limitations to the model were also reported in terms of its role and focus within the wider provision of community specialist services to a vulnerable, complex and underserved population.
Chapter 6 Stakeholder perspectives on intensive support teams
Introduction
This chapter focuses on the qualitative investigation into multiple stakeholders’ views and experiences of IST care. Specifically, we interviewed IST managers, IST professionals, family carers, care home (paid) carers and adult users of ISTs with mild to moderate intellectual disabilities. We have used the Consolidated Criteria for Reporting Qualitative Studies,86 a 32-item checklist, to guide the reporting of this study (see Appendix 2).
Methods
We carried out individual semistructured interviews and focus groups to explore stakeholder experiences and perspectives of ISTs in England in urban and rural areas (see Appendix 2). Purposive sampling aimed to achieve variation in age, work experience, sex, ethnicity, professional background, carer roles and relationship to the person with intellectual disability in both IST models.
Five trained and experienced female researchers, employed as either study managers (doctoral researcher, n = 1; Doctor of Philosophy student, n = 1) or research assistants (Master of Science graduates, n = 3), interviewed IST managers from 14 of the 21 participating ISTs who took part in the phase 2 evaluation (see Chapters 3 and 4) throughout the study period.
We intended to concentrate the remaining interviews with IST professionals, family carers and paid carers, and adults with intellectual disabilities on seven ‘case study’ sites. ‘Case study’ sites were selected to represent service variability within each IST model (enhanced and independent) identified from our previous survey data analysis (see Chapter 2). In addition, these services were selected to capture the service variability within each model, including location in urban and rural areas, size of caseload, operational procedures, funding arrangements and length of service’s existence. Further details of these seven sites are provided in Appendix 2. This part of the project coincided with the COVID-19 pandemic and consequent lockdown, leading to significant difficulty in recruiting and remotely interviewing a sufficient numbers of adults with mild to moderate intellectual disabilities. Therefore, we carried out some of the interviews at different sites from those originally chosen (Table 15).
| Study site | Model | Stakeholder groups | |||
|---|---|---|---|---|---|
| IST professionals (n = 14) | Family carers (n = 9) | Paid carers (n = 7) | Service users (n = 6) | ||
| IST 1a | Enhanced | ✗ | |||
| IST 2a | Enhanced | ✗✗✗✗ | ✗ | ✗ | |
| IST 3a | Enhanced | ✗ | ✗✗ | ✗✗ | ✗✗✗ |
| IST Aa | Independent | ✗✗✗✗✗ | ✗ | ||
| IST Ba | Independent | ✗ | ✗✗ | ✗ | |
| IST Ca | Independent | ✗ | ✗ | ✗ | |
| IST Da | Independent | ✗ | ✗ | ✗✗ | |
| Additional IST E | Independent | ✗ | |||
| Additional IST 4 | Enhanced | ✗✗ | |||
| Additional IST 5 | Enhanced | ✗ | |||
Recruitment took place over a 12-month period between October 2019 and October 2020. Focus groups lasted ≈ 60–80 minutes; individual interviews lasted ≈ 25–35 minutes. IST managers and professionals from all sites participating at the time were interviewed relatively early in phase 2. Adults with intellectual disabilities, family carer and paid carer participants who expressed an interest in taking part in the qualitative phase of the study were interviewed near the time of the patient’s discharge or around the 9-month follow-up, whichever was sooner. We had to adapt the in-person interviews to remote contact because of the lockdowns necessitated by the COVID-19 health emergency. Therefore, we offered a range of remote options to adults with intellectual disabilities and to their family carers or paid carers. These included a range of digital platforms and telephone calls, ensuring that, for all stakeholder interviews, we followed the research sponsor governance about confidentiality that was available at the time.
All semistructured interview schedules for each stakeholder group were developed with the help of the PMG, and the Service User and Family Carer Advisory Group. They covered views on current IST practices, access to the IST, aspects of IST care that were perceived as important, barriers to IST care and suggestions for good practice. For the study topic guides (with prompts) for each stakeholder member, see additional files (www.journalslibrary.nihr.ac.uk/programmes/hsdr/160124/#/documentation; accessed 3 March 2022).
Data analysis
Interviews and focus group discussions were audio-recorded and transcribed verbatim by an external UCL-approved agency. All identifiable information was removed at this phase, following review of the transcripts for quality assurance by the research team. Transcripts were not shared with study participants. Data were analysed using thematic analysis56 conducted using NVivo (QSR International, Warrington, UK) specialist software for data handling. This included familiarisation of the data; generating of initial codes; generating themes; reviewing, defining and naming themes; and compiling this report.
A staged, collaborative and primarily inductive analytic approach was adopted, allowing us to iteratively develop a set of themes that captured key concerns and topics, and more abstract or underlying issues. Two researchers (AK and LH) familiarised themselves with the data independently, developed themes and subthemes, and liaised with the qualitative expert (NM) and the chief investigator (AH) several times to resolve any discrepancies and discuss the final definitions of themes and subthemes.
Although the numbers in the stakeholder subgroups that linked to each IST were relatively small, triangulation of the various stakeholder perspectives allowed us to obtain a broad picture. Thus, we were able to compare the two IST models and different stakeholders’ perspectives, and analyse the data set as a whole to understand broadly common views and experiences of ISTs. The analysis involved close collaboration between the qualitative researcher, the qualitative lead and other key members of the study team. The Service User and Family Carer Advisory Group were also consulted to provide their views on emerging themes and findings.
Results
Setting and interviewee characteristics
We approached 101 potentially eligible participants half of whom agreed to be interviewed (n = 50). We conducted 40 individual interviews and two focus groups of 5 participants each. Interviewees included n = 14 IST managers, n = 14 IST professionals, n = 9 family carers, n = 7 paid carers and n = 6 adults with mild to moderate intellectual disabilities who were still on IST caseloads. See Table 15 for the IST characteristics; for more detailed descriptions of the seven IST sites that were originally identified for data collection (see Table 13 and Appendix 2.)
Intensive support team managers and non-managerial staff
Intensive support team managers were drawn from four professional backgrounds: nursing, psychology, speech and language therapy, and social care. Practitioners from three professions [psychologists (early career and post qualifications), assistant practitioners (i.e. nursing or social care), and specialist nurses] took part in the interviews or focus group discussions. Detailed characteristics of the IST managers and professionals are shown in Table 16.
| Characteristic | IST managers (N = 14) | IST professionals (N = 14) |
|---|---|---|
| Sex (n) | ||
| Female | 10 | 12 |
| Male | 4 | 2 |
| Age (years) | ||
| Median | 41 | 28 |
| Median (IQR) | 6 (40–46) | 13 (27–40) |
| Ethnicity (n) | ||
| White British | 12 | 7a |
| White Irish | 0 | 2a |
| Other white | 1 | – |
| Asian Indian | 1 | – |
| Number of years in service | ||
| Median | 5 | 3 |
| Median (IQR) | 9 (4–13) | 2 (1–3) |
| Number of years’ experience in intellectual disabilities | ||
| Median | 20 | 5 |
| Median (IQR) | 19 (11–30) | 5 (2–7) |
| Professional background (n) | ||
| Nursing | 10 | 4 |
| Psychology | 3 | 5 |
| Speech and language therapist | 1 | 5 |
| Social work/other | – | – |
| Model (n) | ||
| Enhanced | 7 | 6 |
| Independent | 7 | 8 |
Service users and carers
On average, service users were aged 28 years, and all identified as white British. Five (out of six) had an additional diagnosis and had been receiving specialist support from the IST for > 1 year. The family and paid carers had a mean age of 65 years and 37 years, respectively, were of white British ethnicity and were predominantly female. Detailed characteristics of the carers are shown in Table 17.
| Characteristic | Service users (N = 6) | Family carers (N = 9) | Paid carers (N = 7) |
|---|---|---|---|
| Sex (n) | |||
| Female | 2 | 6 | 4 |
| Male | 4 | 3 | 3 |
| Age (years) | |||
| Median | 28 | 6 | 37 |
| Median (IQR) | 14 (26–40) | 9 (61–70) | 9 (34–43) |
| Ethnicity (n) | |||
| White British | 6 | 7 | 6 |
| Black African | – | 1 | 1 |
| Asian Indian | – | 1 | – |
| Number of years in current role | |||
| Median | Not applicable | Not applicable | 8 |
| Median (IQR) | – | – | 8.25 (4.75–13) |
| Number of years’ experience in intellectual disabilities | |||
| Median | Not applicable | Not applicable | 9 |
| Median (IQR) | – | – | 6 (7–13) |
| Relationship to service user | |||
| Parent | Not applicable | 7 | Not applicable |
| Brother | – | 1 | – |
| Aunt | – | 1 | – |
| Comorbid mental health condition | |||
| ASD | 1 | Not applicable | Not applicable |
| ASD and Ehlers–Danlos syndrome | 1 | – | – |
| ASD and ADHD | 2 | – | – |
| Cerebral palsy | 1 | – | – |
| Model | |||
| Enhanced | 5 | 4 | 3 |
| Independent | 1 | 5 | 4 |
Qualitative findings
We present our qualitative findings below in three sections. Section 1 draws on data from all stakeholder groups (i.e. family carers, paid carers, adults with intellectual disabilities, IST managers and professionals) to synthesise common views regarding what is valued about the care that ISTs provide and the aspects of this care that are seen as problematic. IST managers and professionals had additional and often more detailed views on the role, functioning and organisation of ISTs. Section 2 focuses on these views, structuring this material in terms of professionals’ views on the facilitators and barriers to implementing IST care. Section 3 considers suggestions for how ISTs could be improved.
In general, we did not find differences in respondents’ views according to whether they were commenting on ISTs classified as enhanced or independent. We therefore present data pooled from all the study sites. Some differences in stakeholder perspectives are elaborated on in more detail in the subsequent sections, together with illustrative interview extracts.
Section 1: valued features of intensive support team care – multistakeholder views
Service accessibility and flexibility
Service accessibility and flexibility were highlighted as important features of good IST care by IST managers and professionals. They reported these to be core characteristics of their service response, and they included conducting late home visits and observations, as needed. In addition, they promoted and supported joint work with other NHS services, in particular when the IST signposted adults with intellectual disabilities to a different service (e.g. CIDSs, community mental health teams). Last, they highlighted the importance of IST practitioners being not only responsive, but also approachable and friendly towards service users:
I’ve been stood in gardens at 10, 11 o’clock at night . . . You don’t finish there. So, there’s flexibility.
IST manager, enhanced IST
We work so well . . . and we’re all quite friendly, jolly adults that I think we’re quite welcoming and adults tend to react well.
IST professional, independent IST
The perception of an accessible service was comforting to many participants with intellectual disabilities and their family or paid carers. They said the IST staff responded to telephone calls and conducted visits when carers and adults with intellectual disabilities got worried or felt upset, and also that the IST remained present in their lives by telephoning them regularly to monitor how they were coping during the COVID-19 pandemic. Carers described feeling confident in liaising with the IST professionals any time they or those they care for need additional support because they are familiar with the service users and, therefore, are able to advocate on their behalf and access services for care or treatments:
. . . when we have needed something very urgent, the IATT team [intensive assessment and treatment team] have been really responsive, they’ve been brilliant.
Adult with intellectual disability, enhanced IST
Person-centred care
All stakeholders highlighted the importance of person-centred care. In particular, IST managers and IST practitioners provided examples of how they involve carers and adults with intellectual disabilities in care or review meetings, including making any adjustments that they deem necessary:
The letters that we send out, they’re already always written to the adults, where possible. We have the provision here, so if adults are anxious about coming into the room they can sit on the sofas outside. We have the door open so they can hear what’s being talked about, so that they can come and join the meeting if they want to.
IST manager, enhanced IST
When possible, the person with intellectual disability was consulted about their behaviour support plan and what they would like to happen if they were in a mental health crisis:
. . . when I’ve got a problem or something happens, you know, I can tell her . . . ‘this is what I want to speak to you about,’ and then, obviously, we can discuss what to do next, what’s the next step . . . and then at least someone can come back and say ‘yeah, OK’ . . . ‘we’ll do that now’, they’ll do things for me.
Adult with intellectual disability, enhanced IST
Intensive support team professionals served as a conduit for addressing several needs for the people on their caseload, extending to supporting requests for social or other services (e.g. respite care, obtaining a wheelchair aid) and identifying ways to help the service user be more connected to their local community, such as accessing activities and education. In particular, family carers valued the support provided to adults with intellectual disabilities for making arrangements regarding the person’s transportation and helping with school activities or courses:
It was the first time that she was going to school and that was with the help of them. They helped her with all the things. Take her to drop her to activities and all the things.
Family carer, enhanced IST
Family carers described being reassured by the ISTs’ approach to supporting and training care home staff, especially during a crisis that they feared might affect the placement’s security. For example, regular visits to service providers from IST practitioners meant that their loved ones received quality assurance. In addition, paid carers and adults with intellectual disabilities agreed that developing a PBS plan that takes into consideration the day-to-day needs of the individual with intellectual disabilities (e.g. monitoring medication, accessing activities, practising social skills through social stories to reduce social isolation) benefits adults with intellectual disabilities, who then feel happier and able to enjoy life more:
I liked colouring . . . did some playing . . . like arts and crafts . . . I like to do some playing.
Adult with intellectual disability, independent IST
Carer involvement
The active engagement of all relevant parties involved in the care of an adult with intellectual disability who was being supported by the IST was identified as an important element of good IST care across the stakeholder groups. IST managers and practitioners agreed that the contribution of carers (i.e. family or paid) was important in meetings in which professionals formulated, assessed and developed a management plan to support the individual with intellectual disabilities. Such meetings function as multidisciplinary focal points at which current challenges are discussed, the functioning of the ISTs and its role in the care of the individual are clarified, support needs are evaluated, and allocation of roles among professionals take place. The involvement of family or paid carers in multidisciplinary review meetings was seen as positive in promoting thinking about an individual’s needs more broadly. Working collaboratively and having regular contact with paid carers regarding risk assessment, updates on progress and incident reporting were seen as particularly helpful in managing challenging behaviour:
Everybody is involved in decision-making right from the beginning, from the point of referral. We have psychiatry, nurse, prescribers, behaviour support workers, and everybody has an equal voice, alongside the individual where possible. The families, carers, support workers and other professionals like social worker and anybody else that’s involved in their care and that. So we all make decisions together, and that’s the real strength, I think, is the multidisciplinary formulation, assessment and planning, really, in terms of who’s going to do what, why we’re doing it, how, how long we’re going to do that for.
IST manager and professional in focus group, enhanced IST
The majority of paid and family carers viewed the IST staff’s effort to involve them in the care plan as a positive aspect. Most family carers and all paid carers reported being listened to and being an integral part of the individual’s care plan and treatment decision-making processes. They appreciated that the IST offered practical suggestions to handle challenging behaviours, and carers agreed that they coped better with the individual with intellectual disability as a result of the IST input, even when there were setbacks:
They disclosed that care plan with us, especially because it’s working because Z has settled with a view to the care plan. They did the care plan, came to us first, they asked our opinion, and we went through that before. We discussed, whenever they came after we debriefed each other. I think that overall, I can say they did support us very well.
Paid carer, independent IST
Section 1.1: what can be improved?
Although they were a minority, some family carers described liaising with the IST as problematic at the start of the IST’s involvement, regardless of the IST model. These family carers had either made unsuccessful attempts to connect to professionals (i.e. telephone calls) or not received updates from the IST professionals for long periods. In particular, families of adults with intellectual disabilities in supported living or residential care were not fully informed of the IST’s involvement until they were invited to meetings. Similarly, one adult with intellectual disability found it difficult to contact the IST at the beginning of the allocation process:
Lack of communication to start with, as took long time to get appointment.
Adult with intellectual disability, enhanced IST
In addition, family carers noted their perception that IST professionals did not always acknowledge the challenges of living with an adult with intellectual disability and, consequently, the full extent of family carers’ needs:
I don’t think they quite understand everything. I think, sometimes, they haven’t a clue what it’s like to live with it.
Family carer, independent IST
The regular meetings have stopped. The big problem is the communication with everybody. So we’re constantly having to chase around, phoning adults, saying ‘what is happening and what are you doing about this?’. And it just feels like you can never get an answer. Nobody ever phones you back. They’re not available, they never phone back.
Family carer, enhanced IST
Three adults with intellectual disabilities reported that they valued feeling independent. Adults with intellectual disabilities found it difficult to communicate their wishes because of a speech impediment or because they were unable to fully understand the IST’s involvement in care. As a result, they relied on carers (family or paid) to support communication with IST health-care professionals. This was described by one service user as ‘a bit confusing at times’:
. . . sometimes they have been difficult, because of my spoke [sic] and on the phone, so my parents have to come help me.
Adult with intellectual disability, enhanced IST
A few carer interviewees thought that some aspects could be better accomplished or delivered by having easier access to social workers. They suggested that social workers could be part of the ISTs, rather than liaising with duty social workers during an emergency. A social worker integrated into an IST would be able to access information rapidly through clinical records, rather than family carers repeatedly sharing personal information with different professionals each time. IST managers and family carers emphasised that social workers could also support the identification of meaningful opportunities (e.g. employment, activities) for adults with mild intellectual disabilities to integrate them in the community. Last, IST managers acknowledged that tailored interventions (e.g. family therapy) should be offered to family carers:
I just sometimes feel frustrated when there’s nobody there for him. Because, years ago, there was something every day. The services, the activities. I mean, he’s gone at odd times to the allotment, but he won’t go a lot. I can’t believe the things he used to do and there’s just nothing for them, is there?
Family carer, independent IST
Section 2: the role and organisation of intensive support teams
Intensive support team managers and professionals focused explicitly on IST functioning and its relationship to other health and social care services.
Section 2.1: facilitators of intensive support team care
The majority of IST service managers and professionals stressed the benefits of developing and retaining trustworthy relationships with other teams and/or building good liaison with internal and external agencies (i.e. GPs, community mental health, social workers, forensic teams, police), with the aim of providing better care to adults with intellectual disabilities in a timely manner. In particular, IST managers and professionals valued collaboration with CIDSs and social workers to complete joint assessments:
We are really well resourced. We work alongside primary care nurses and daily GPs if there are any issues. We also work alongside our CHC [Continuing Healthcare Commissioning] colleagues. They are the ones that go and do the health assessments to see if adults meet the Continuing Healthcare Funding criteria. The fact that we are multidisciplinary definitely helps us.
IST manager, enhanced IST
In addition, IST practitioners highlighted the importance of (informal and formal) consultation among professionals, often referred to as ‘corridor conversations’, which were perceived as helpful in managing ongoing cases that require support. Working well with other teams can take different forms, including making informal arrangements with practitioners to share a day with the IST, offering consultation to other multidisciplinary teams and liaising with practitioners (e.g. occupational therapist, social worker) to support the delivery of care for adults with intellectual disabilities:
We’ve been through a bit of a ping-pong situation. ‘This isn’t for us, send that there.’ But to be in explaining what reasonable adjustment means and what you can do, that’s fine, you can have a bit of help here at my doors. I’m just helping out.
IST manager, enhanced IST
Among the positive features of IST care was the ongoing review of service provision, which was exclusively referenced by IST staff. Stakeholders from both integrated and enhanced ISTs described how a combination of mechanisms (e.g. verbal feedback) and system outcomes (e.g. admission rates, clinical records) define the success of their work. For example, IST professionals reported that regular contact with commissioners who compare inpatient admission rates every year, the use of outcome measures [e.g. Health of the Nation Outcome Scales for People with Learning Disabilities (HoNOS-LD), Challenging Behaviour Inventory], reviews of clinical records, and regular feedback from carers about the support received were indicative of the quality of IST care for adults with intellectual disabilities and their families:
We try to collect service user feedback where that’s possible . . . we would always ask that in sessions anyway. So, hopefully, we’re getting that feedback and can use that live . . . We do also use outcome measures as well that will help us evidence change.
IST professional, enhanced IST
Intensive support team staff from both IST models recognised the value of continuous professional development for members of the IST [i.e. foundation degree (e.g. combined academic and vocational qualification), PBS training]. In addition, they reported that the development of a network of champions with family carers and/or paid carers was among the positive features of IST care. IST staff highlighted the value of supporting carers (family and paid) and offering one-to-one training to upskill them to recognise triggers of challenging behaviour before an incident occurs, with the aim of preventing a crisis, placement breakdown or hospital admission. The ‘training the carer’ model appears to be an efficient way of forming a relationship with other carers in informal meetings or support groups in which they share their experiences, learn from each other and develop knowledge following supervision from the IST:
We talk about support the supporter. Walk the walk. We go out with somebody on a one to one. If adults are a bit unsure about going somewhere new, we talk them through it, and increase their confidence that way. It’s like modelling on an individual level.
IST manager, enhanced IST
Section 2.2: barriers to intensive support team care
Intensive support team managers reported that the challenge of recruiting and retaining qualified staff was a common concern. In particular, ISTs that operated 24/7 and were based in rural areas faced challenges in attracting qualified professionals. In addition, concerns were raised about how the termination of the degree in intellectual disability nursing in local universities would affect the future of local NHS staffing levels owing to the potential shortage of qualified professionals:
We really struggle, which is why we can’t recruit into nursing posts. Our registered professionals have quite a high turnover because of the on-call hours.
IST manager, independent IST
You’re not going to get lots of adults applying. The area is definitely a hindrance to recruitment. It’s a vast area. It looks really small but it’s not. From one end to the other you’re talking a good hour and a half to go across.
IST manager, enhanced IST
Intensive support team professionals described small ISTs or part-time working arrangements as problematic during periods when referrals are expected to increase (e.g. at Christmas), which affects caseload and time management. One service emphasised the intensity of working in the IST, which entails not only offering daily support but also managing the flow of referrals and establishing the safety of colleagues during out-of-office-hours assessments (e.g. work in pairs). In addition, IST managers were under pressure to justify the IST service to commissioners, who expected ISTs to respond quickly to referrals, have large caseloads and be available 24 hours per day:
The teams have been a bit battered . . . Being 24/7 as well is quite a challenge for me because I really don’t get to switch off, because, ultimately, even if I’m not on call, because I take my turn on call the same as anyone else in the team . . . But at 02.00 in the morning if someone doesn’t know what to do, then they’re on my phone. And then commissioners, my manager quite regularly at 07.00 in the morning they’re on the phone . . . That is intense. You’re kind of answerable to so many adults all the time.
IST manager, independent IST
A few IST staff highlighted the challenge of working with accommodation providers owing to the high staff turnover, which may affect the care that adults with intellectual disabilities receive and have an emotional impact on them. Furthermore, the IST invests time to upskill paid carers to better support adults with intellectual disabilities and work with complex cases; therefore, the ISTs must frequently roll out training for new staff:
We don’t have a huge abundance of skilled providers. We’re often engaging with providers who are either overwhelmed because they’re the only provider in that particular area [or] are underskilled.
IST manager, independent IST
Intensive support team managers expressed frustration at what they saw as broad eligibility criteria for IST care. As a result, referrals included adults with intellectual disabilities whose mental health needs were a priority (i.e. psychosis) and those with ASD without intellectual disability, who have limited access to other community facilities. This is a recognised ongoing challenge for services that refer to these adults as ‘exemptions’. They are not eligible to access services for adults with intellectual disabilities, but these are the only available resources seen as relevant or appropriate to fill a care gap in services that needs to be addressed:
There is a significant black hole at the moment for adults who have autism but don’t have a learning disability to fall into. Our trust will assess if they’ve received their diagnosis. They may not be eligible for our service, but some of our PBS approach[es] are highly relevant. So, literally, at the moment, we are recording those adults in our risk management system in order to evidence to the CCG, to the Clinical Commissioning Group, very clearly what the identified need is.
IST manager, enhanced IST
Service boundaries often involve limiting the referrals by strict criteria, for example prioritising high-risk cases only. This may, however, lead to the exclusion of adults with intellectual disabilities with less challenging presentation, who would equally benefit from additional support:
There’s a whole layer of adults who still might have significant difficulties because of their learning disability, but don’t meet our really high threshold criteria. They won’t get a service because they’re not at risk of placement breakdown.
IST manager, enhanced IST
Managing individuals with intellectual disabilities during a mental health crisis was seen as incompatible with IST care, which was described as ‘proactive’ and possibly starting before the crisis arises:
We’ve got no bed management team to find beds at times when adults are in crisis. If we’re left to get on and do our job, everything’s fine, it’s having to do all the other little bits . . . It took 4 days to actually find a bed. I spent 6 hours one day ringing different services just to say ‘have you got a bed anywhere?’.
IST manager, enhanced IST
Last, ISTs often support adults with intellectual disabilities for long periods owing to the waiting lists in CIDSs, or difficulty in identifying an alternative placement or care home service provider:
We’ll see it through from beginning to end, which can, sometimes, be labour intensive because we might have done all the work but recognise that we need an alternative placement. And you could be 6 months looking for an alternative placement to then support them through the transition. So, depending on where they are and how adults are, we might close and then reopen them, or keep them open.
IST manager, independent IST
It was predominantly IST managers who raised the impact of financial austerity and the consequent limited funding for IST care. IST managers from both models reported that fiscal constraints to social care cause distress and potentially exacerbate challenging behaviour in adults with intellectual disabilities whose care packages have been reduced, with potential detriment to their well-being:
The repercussions of austerity and the cuts that social care has experienced over a relatively long period of time have really impacted on adults with learning disabilities. Our social care colleagues are often involved in reviewing packages of care and reducing them. We have felt the repercussions of reduced packages of support, reduced amount of community enabling in the last 2 years.
IST manager, enhanced IST
Concerns about costs included impacted funding decisions about increases in IST personnel or lack of training resources to upskill IST professionals. Managers had to make pragmatic decisions (i.e. recruit inexperienced professionals with significant development needs), which had potential consequences for the quality of care being delivered to service users. Last, increased supervision needs were a source of additional work for already overstretched professionals in the IST:
We’re a small team of four. Our work is intensive and the assessment’s very intensive, you’ve got two adults. We generally work as a pair, obviously for safety as well. That’s two adults that are left in our intensive support. So, unfortunately, at the moment, we are what we are but we need to expand.
IST manager, independent IST
Section 3: suggestions for improving intensive support teams
Wider training
Intensive support team staff agreed that upskilling and supporting paid carers and providers is an important element of their work. In addition, in areas where funding is available to support service providers, it was noted that it could be used to enhance the skills of paid carers to enable them to support a population with increasingly complex needs and multimorbidity:
We’ve got a lot of providers popping up all over the place at the moment that have all lovely brochures telling us all the amazing things they can do. And then people move in and, and it doesn’t quite work out that way and we find that we have to come in and pick up the pieces.
IST manager, independent IST
I personally think that we have to provide the training to, to the top managers for it to be cascaded down to the bottom. So, the expectation from there . . . You know, the, the, the supporters have that expectation and they have to meet those goals. So, if we were a wider team, we’d be able to go out and start doing some education within social care, within the managers of these services, and say ‘right, this is what your care team needs to do to enable . . . to give somebody a really good community present life’, you know, and we’re not . . .
IST manager, independent IST
Visibility of the intensive support team and collaborative approach
The need to promote the existence of the IST was unanimously referenced by all stakeholders. Each locality should be better informed about the breadth of services available to support adults with intellectual disabilities who display challenging behaviour. Developing better knowledge about NHS services that support people with intellectual disabilities is useful not only for service users, but also for professionals:
I don’t think for one moment that the social worker who was involved with C at that time really knew of their existence or what they could provide. I think it’s the agencies that are involved in supporting adults like C, perhaps themselves need to better informed about what other agencies and organisations are capable of providing.
Family carer, independent IST
Intensive support team professionals highlighted the need to establish better links with mental health services. Having a partnership with community mental health teams would enhance opportunities to review cases early, support peer supervision, decrease inappropriate referrals and consolidate the preventative role of ISTs. ISTs should promote their work to professionals and external agencies, including social care providers, police, etc.:
If you think someone might need to ring us but you’re not sure, um, don’t wait to put a referral in. If there’s an MDT [multidisciplinary team], invite us to it. So we don’t need a referral to come to an MDT. Invite us. We’ll open them on the system for that day and close them again. Just invite us. We’ve also put in over the last year a duty work system, so that there’s someone around that can speak to you.
IST manager, independent IST
User-friendly intensive support teams
Intensive support team managers and family carers from both IST models highlighted that PBS plans need to be more easily accessible. For example, lengthy PBS plans could be substituted with brief easy-read documents that are manageable to read and comprehend. It is common for paid carers or care home managers to lack the time to review the full PBS plan owing to a heavy workload, but, most importantly, the use of academic language discourages support workers from fully engaging:
Why do we produce 40-page PBSs for adults who need an easy-read grab sheet, positive behavioural support?
IST manager, independent IST
Summary
This chapter described multiple stakeholders’ experiences and views of ISTs in England. Overall, there were common issues in both IST models, with no major differences detected in the experiences of stakeholders. Although recruitment difficulties meant that the qualitative study included a smaller than intended number of respondents in some stakeholder groups, findings suggest that families, paid carers and adults with intellectual disabilities value elements of IST care, find it supportive, and value staff making efforts to implement reasonable adjustments and being involved in care planning.
However, there appear to be tensions regarding expectations of what good care looks like, whether or not it is sufficiently tailored to individual needs and how the role of the IST is evolving. The IST staff responses allude to IST services having a rather narrow remit and therefore other patient groups (i.e. people with mental ill health or people with autism but without intellectual disabilities) may be disadvantaged owing to a lack of appropriate services. There are clear concerns about paid carer turnover and IST professional recruitment and retention, especially as many such teams are led by nurses or psychologists. IST managers appear to be weary of financial constraints and the need to justify the existence of ISTs in the absence of key performance indicators. Training is seen as a core function of IST staff, who often work with support workers or family carers to implement behaviour support plans. We understood the stakeholders to indicate that ISTs are not part of a wider crisis service network; they may lack the range of relationships with such services, especially those provided by adult mental health, and may not be visible enough to their own client base and their carers.
These findings are limited by the smaller-than-anticipated number of interviews that we were able to conduct. The recruitment difficulties coincided with the start of the COVID-19 pandemic and the first national lockdown, and particularly affected family carers, paid carers and adults with mild to moderate intellectual disabilities. Despite NIHR advice on adaptations to facilitate research studies during the COVID-19 pandemic (e.g. remote data collection, use of digital technology), we were unable to overcome some of the challenges associated with the abrupt move to remote working and data collection. Detailed information about the impact of COVID-19 on the study is presented in Chapter 7.
Chapter 7 Recruitment challenges and COVID-19’s impact
Recruitment challenges
Collaborating NHS sites took much longer than expected (≈ 2–3 months) to provide local approvals, confirm capacity and capability, and provide a letter of access for the researchers to recruit participants locally. Most NHS sites had limited to no Clinical Research Network support; when such input was available, it took time to allocate a clinical study officer to support participant recruitment to a national portfolio study. Furthermore, clinical teams had very few new referrals, as service users were on IST caseloads for long periods. A further challenge was the turnover of clinical studies officers/research nurses who were also leaving their posts, which contributed to the unstable flow of referrals for weeks until a new person was employed, set up and trained to support screening and recruitment. Last, conversations with research and development departments that had expressed an interest in joining the study stalled for a variety of reasons, for example being unable to identify a principal investigator or meet the local recruitment target.
Despite the capacity and capability assessment that led to the service taking part in the study, we found that there was some resistance from service managers to share information about adults with intellectual disabilities with no capacity or a next of kin who would take responsibility for their participation in research. As is often mentioned, adults with intellectual disabilities are hard to engage in research owing to numerous gatekeepers such as support staff, professionals and families, especially for those who lack capacity. Researchers have to continuously educate them on the legitimacy of study and its governance. The project manager had to contact four professionals (i.e. care home worker, care home manager, IST manager and clinical practitioner) to obtain permission to visit a participant. Usually, care home managers/social workers were verbally in agreement to join the study, but they would request a best-interests meeting before a final decision could be made. Care home providers also requested to receive consent from family members, although care home providers were the main carer for the person with intellectual disability. Other problems related to obtaining updated contact details of carers of potential participants. There had been instances in which 2.5 months elapsed from first contact to baseline. Figure 9 presents phase 2 participant recruitment from June 2018 to May 2020.
FIGURE 9.
Participant recruitment graph.
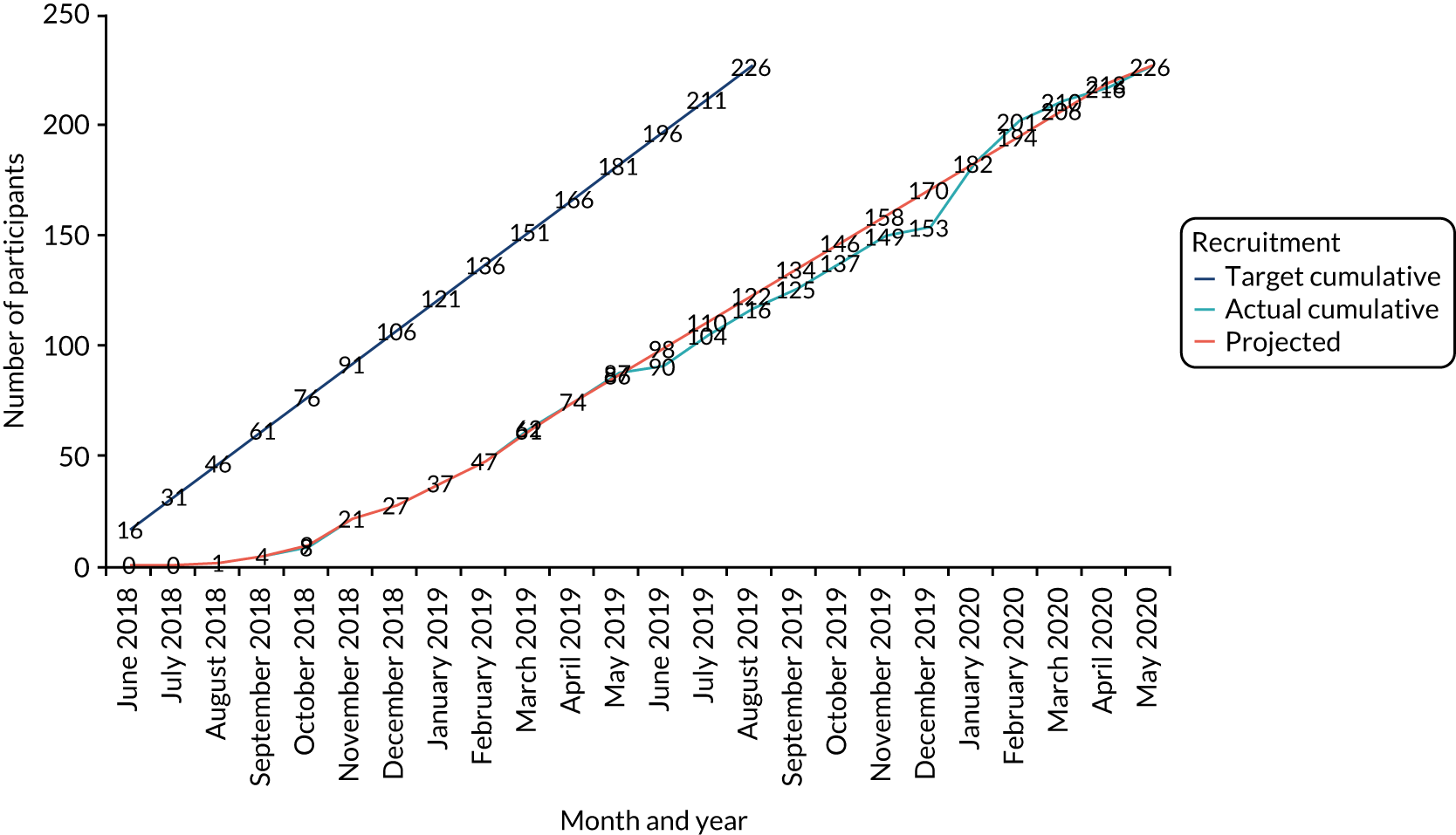
COVID-19’s impact and adaptations
Three NHS sites withdrew their interest in supporting the study when NIHR suspended all non-COVID related research in March 2020. There were five new referrals from all sites up to the end of May 2020. Following review of all referrals to the study, including those previously uncontactable, 32 potential participants were identified, of whom 14 were still eligible to take part. The research team received ethics approval to complete the consent process and research assessments remotely using digital tools [e.g. through Zoom calls (Zoom Video Communications, San Jose, CA, USA), telephone calls, scanned copies via e-mail] to complete recruitment. However, conducting interviews with family carers, paid carers and adults with (mild to moderate) intellectual disabilities, although mainly feasible, also presented difficulties for several reasons:
-
Digital poverty (e.g. lack of computer, smartphone, WiFi). Family carers reported having no access to a computer, laptop, tablet or smartphone and, in a few instances, no access to a WiFi network to conduct the interview remotely using digital technology platforms.
-
Insufficient support and knowledge of digital platforms (e.g. Zoom, e-mail, scanning) during the first national lockdown when all of these processes were implemented at pace. Family carers described not being confident users of digital platforms, including accessing e-mails and/or logging into Zoom/Microsoft Teams®. As a result, sharing PISs and ICFs to be signed and returned electronically was difficult for family carers.
-
Changes as a result of COVID-19 (e.g. service user’s return to family home, change of care provider, move to a new house) had an impact on the 9-month follow-up assessments. Families, new service managers or providers were not previously informed of the study and did not commit to completing the study during the COVID-19 pandemic.
-
Obtaining consent from adults with intellectual disabilities with mild to moderate intellectual disabilities who did not have sufficient verbal ability to provide informed consent or who had a hearing impairment had an impact on the screening and identification of potentially interested participants from both the participating ‘case study’ sites and the remaining ISTs. Carers (family and paid) were also hesitant to attempt to discuss the PIS and complete a ICF with the adult with intellectual disability at the time and to facilitate the interview. Many were concerned that additional changes to routines could trigger more challenging behaviour.
-
The emotional burden (e.g. increased anxiety, challenging behaviour, carer responsibilities) and change of priorities (e.g. family bereavement, limited interest in research) during the first national lockdown had an impact on the overall number of recruited family and paid carers in addition to that of adults with intellectual disabilities. Some stakeholders who were previously interested in taking part in the qualitative work cancelled the interview because of additional caring responsibilities. Adults with intellectual disabilities were also stressed, and carers reported being exhausted owing to the change in daily routine. In addition, paid carers at care homes were separated from their family homes to take care of vulnerable adults with intellectual disabilities and minimise the transmission of COVID-19 by staying in care homes between shifts or covering colleagues who were on sick leave at the time. Therefore, priorities shifted during the COVID-19 pandemic, leading to lower recruitment rates in the qualitative work than in the published study protocol,49 particularly for adults with intellectual disabilities. Participating in interviews was less important to family carers and paid carers, whose responsibilities changed within a week when the national lockdown was announced in March 2020. Overall, the COVID-19 pandemic had an impact on the screening and recruitment of family and paid carers and adults with intellectual disabilities to a significant extent during the first national lockdown, resulting in a smaller sample size than anticipated.
Our related paper on how to enhance participation of people with intellectual disabilities in research has been published elsewhere. 87
Chapter 8 Discussion
Introduction
In this chapter, we present the main study findings, placing them within the context of existing evidence; discuss the strengths and limitations of the study; and make recommendations for future research.
Main findings
There appears to be clinical and statistical support for two models of intensive support services: independent and enhanced. Although they have distinct characteristics, they also have several overlapping functions and there is little to distinguish them in terms of medium-term service user clinical outcomes. The profile of the caseload and the pattern of service use costs and health-related quality of life are similar for both models. Based on health-related quality of life, the two models are equally effective at the NICE threshold for treatments of £20,000–30,000. The care provided is mainly to adults with intellectual disabilities who display challenging behaviour, but we found limited evidence for an expansion of the remit to supporting discharge from psychiatric hospitals and intervening in mental health crises. The services are well liked by service users and their carers and are seen as essential in complementing the work of professionals in the specialist CIDSs, as reported by referrers from those services. There are suggested areas for improvement, including a clearer role in the wider range of services available during a crisis and the need for interventions beyond behavioural approaches. As expected, the majority of the participants in both models were receiving multiple other medications in addition to a psychotropic medication.
Strengths and limitations
This is the first study, to our knowledge, that has systematically investigated the models and function of ISTs in England. The present study went further than previous evaluations of such teams in single sites, encompassing many parts of England in real-world practice. We were able to establish a comprehensive picture of those services and of the outcomes that they achieve in the medium term for adults with intellectual disabilities who display challenging behaviour. The study was fully powered, with very good retention of participants (< 10% attrition) and low data missingness. We randomly selected ISTs in both urban and rural areas as research sites, and study participants were representative of the population in IST caseloads; therefore, we believe that there is a reduced risk of bias.
The findings from this study are highly relevant to the support of very vulnerable individuals with intellectual disabilities in the community and are potentially applicable to other UK countries that have a similar health and care structure.
The study also had its limitations:
-
It might be subject to possible respondent social desirability bias.
-
We may have omitted other elements of functions relating to ISTs that could be of importance but that were not captured in the survey during the mapping phase of IST (phase 1). For example, we did not ask specifically about integration with other local mental health services, gatekeeping roles, information sharing or record keeping.
-
We may have over/underascertained the number of ISTs and therefore the typology may lack precision. However, we argue that the resulting typology has an empirical basis and face validity based on clinician experience of such services and self-identification by ISTs. We accept that the typology has no theoretical basis in literature relating to intellectual disability, but it has largely adopted functions and indicators from publications on mental health crisis care, which itself suffers from limited evidence of quantifiable functions of home treatment and intensive case management.
-
This was a cohort study with a nested case–control comparison, not a randomised controlled trial; therefore, it is subject to selection bias, although there were no differences between the participants in each IST model at baseline.
-
The turnover of paid carers may have affected the reporting of challenging behaviour if the carer had not known the person with intellectual disability well enough.
-
The lack of statistical significance in clinical outcomes between models may be an indication that adults who are referred during a crisis will recover substantially in the short to medium term (regression to the mean), especially in cases where the disorder is remitting/relapsing, as is the case with challenging behaviour. Although both models appeared to produce reductions in challenging behaviour, we cannot say with any certainty that the models were both effective as we did not include a usual-care comparator.
-
It is likely that there has been some impact of the COVID-19 pandemic, but we were unable to fully adjust for it on the patterns and intensity of service use and support (costs) in both models. For example, service-level data were lacking in some instances because managers at the research sites were unable to access data during the first and subsequent lockdowns as most were working from home. Furthermore, we found that we were not able to access interviewees with intellectual disabilities as many participants, including their caregivers, were mentally distressed or did not have access to digital platforms and support to enable them to participate in an interview. Therefore, although we used a sampling frame to ensure representation of seven case study sites to enable us to gain a deeper understanding of stakeholder views of IST support, we had to include three further research sites from the same IST model to increase the number of interviewees.
Findings in the context of existing literature
The care and support of adults with intellectual disabilities who display challenging behaviour remains a policy priority, and there is a long-term commitment to improve provision. 34,44,88 At this time, there is no specific guidance or indication of expected outcomes from ISTs, such as duration of engagement or size of caseload, beyond a reduction in inpatient bed-days. However, this reduction is not operationalised and appears to be left to the discretion of the clinicians involved in each case. One potentially useful indicator might be the difference between estimated and actual discharge date. Findings from crisis care in adult mental health indicate that compulsory admissions are not reduced in the 2 months following a crisis;89 therefore, the role and skills of the staff and of the IST model in the crisis pathway for adults with intellectual disabilities requires further elucidation. The fidelity of the IST model is not well conceptualised compared with the fidelity of the adult mental health crisis resolution model, and the breadth and delivery of interventions should be expanded beyond that of Positive Behaviour Support.
We found that ISTs were more common than previous investigations had suggested, and this growth may in part be driven by the national Transforming Care programme. 44 Davison et al. 29 explored the provision of specialist support teams (called peripatetic support teams in their study) a decade ago (in 2012) within the overall UK landscape of services for people with intellectual disabilities across the lifespan who display challenging behaviour. The authors identified 46 specialist teams in the UK, 40 of which were in England. However, only half of the teams that were sent a survey completed it, resulting in a much lower response rate than the 90% response rate in the present study. The authors concluded that the IST provision had reduced, in contrast to our findings, which have shown an increase in such services, at least in England. Since then, 34 new ISTs have been established in England alone,53 which underscores the belief in the usefulness of ISTs in the management of adults with intellectual disabilities who display challenging behaviour.
Our findings are broadly in agreement with the findings from Davison et al. 29 in that therapeutic approaches are mainly behavioural (the majority explicitly mentioned PBS); may offer a range of other interventions, although they were poorly defined; and few operate extended hours or have a remit to work with children.
Previous evidence suggested that embedded teams may be effective,41 whereas other studies have demonstrated the positive contribution of standalone specialist behaviour support over standard treatment for adults with intellectual disabilities to reduce challenging behaviour. 40 However, these were single-site studies, and they evaluated services that had a clear operational remit. It is telling that neither of these evaluated services exist today. The findings that there is no difference in clinical effectiveness between the two models, but that overall they both appear to be beneficial and are well liked by service users, their family carers and referrers could help the potential roll out to all UK countries based on local need and available resources. The majority of independent ISTs regularly used outcome measures. Our findings were consistent with previous research33,90 indicating that outcome measures varied widely across services. However, the HoNOS-LD91 was the most consistent and often the only outcome measure used.
Iemmi et al. 92 reported on the economic evaluation of one IST delivering PBS to five patients. Their study claimed that the IST contributed to improved outcomes in challenging behaviour and increased community participation at a total cost to health and social care services of £2296 per week. Hassiotis et al. 40 highlighted that the IST was cost neutral when service use was taken into consideration. Our present economic evaluation highlighted that the service costs of enhanced ISTs are not significantly different from those of independent ISTs, and nor are the health-related quality-of-life gains. As the clinical and cost findings align, we suggest that neither IST model has an advantage over the other. However, as the burden of challenging behaviour in terms of out-of-area prolonged hospitalisations and overprescription of psychotropic medication to adults with intellectual disabilities remains substantial,3,13,22 it is likely that costs could be offset by the establishment of an IST with a cost per case of between £4980 and £10,122 for the enhanced and independent models, respectively, which is significantly cheaper than current costs and well within the NICE cost-acceptability threshold. However, given that these are not strictly novel services, they must work harder to justify their work beyond and above usual care.
Legislation and policy encourage professionals to work with carers in ways that complement and enhance their roles to maximise their capacity to care for a vulnerable adult. 44,78 Family carers are recognised as a valuable resource for their relatives, community, services and governments. A systematic review explored the formal support received by family carers of an adult with intellectual disability who display challenging behaviour. 93 James93 concluded that family carers need to ‘fight’ for psychological support and psychoeducation from different service systems. Carers, however, reported being satisfied with professionals once they accessed services. Another study94 suggested that easy access to services and approachable professionals, practical guidance and psychological support are imperative features of future service development for family carers of adults with severe intellectual disabilities who display challenging behaviour. The views and experiences of our carer and service user stakeholders confirmed that the three valued features of IST care were accessible and flexible services, person-centred care and carer involvement. Although we found examples of good practice in the implementation of reasonable adjustments, we identified a need to strengthen consistent communication with adults with intellectual disabilities who display challenging behaviour, and a need to empower them to be more in charge of their treatment and self-management.
Hemmings et al. 95 reported on findings from three UK studies on the essential elements of community care for adults with intellectual disabilities from the perspective of professionals working in those services. Although the review was focused on people with mental health problems, it mentions interface with mental health services as a particular challenge and area for development. The studies also indicated that there was no support for mental health intensive care services for people with intellectual disabilities, but there was a desire to establish the presence of workers with knowledge of intellectual disability within existing structures. Our professional respondents found the role of the IST within the local service landscape a challenge and acknowledged issues with the access and flow of referrals. Often, ISTs were seen as the last resort when a patient could not be referred to other generic mental health services.
A report by the Royal College of Psychiatrists96 summarised the range of services available to people with intellectual disabilities with mental ill-health. ISTs have been described as being single- or multiprofessional, as offering specialist assessment and treatment or signposting to other services and as having defined staff roles,97 but also as often being difficult to access. 98 However, this literature is not directly relevant as it does not include stakeholder experience and is mostly focused on mental health services distinct from those related to challenging behaviour.
The Transforming Care programme44 set out its intent of improving community services for people with intellectual disabilities in the Building the Right Support34 plan, an evaluation published in 2018 based on 10 case studies and other information. Many areas saw the establishment of ISTs as part of their local quality improvement of services for people with intellectual disabilities, but these were only a small part of the overall evaluation of a policy programme. However, the findings indicated that significant gaps remained in the community support for a range of issues, including care of young people, mental health and care of autistic individuals, and attention to prevention. A consultation with stakeholders addressed the whole of the programme and it was not possible to disaggregate the stakeholder findings that related specifically to ISTs.
A particular concern, in our opinion, is the lack of a clear remit of ISTs that corresponds to a model of care and includes specific active ingredients and key performance indicators. Research on Crisis Resolutions Teams46 indicates that longer hours and the presence of a psychiatrist in the team may be associated with fewer admissions, and that stakeholders value integration with other services, home-based care and a core team around an individual. Medical prescribing and staff training were also seen as important and supported by guidelines. Findings from this study also indicate that eligibility for care may be a significant barrier for certain patient groups, for example where there is no confirmed diagnosis of intellectual disability, and these individuals are likely to be left unsupported. Clarity regarding which service can provide care is essential, especially as it is shown that contact with crisis care in the first 12 months of discharge leads to re-admission. 17
Implications for practice
The Building the Right Support34 plan proposed nine pillars central to the improvement of community support for people with intellectual disabilities who also display challenging behaviour, are autistic or have mental ill-health. Several pillars (e.g. a good and meaningful everyday life; person-centred, planned, proactive and co-ordinated care; choice and control) are value statements and some (e.g. mainstream NHS services, specialist health and social care support in the community, support to stay out of trouble) point towards specific services or interventions that could prevent challenging behaviour or effectively support those individuals to remain in their communities.
Although ISTs are mentioned, their role in contributing to the overall objectives of the Building the Right Support34 plan is unclear and not stated in recently released documents. An issue also remains regarding the profile of service users eligible for IST care compared with other services that cover offenders with intellectual disabilities, who have very different needs from the majority of people who display challenging behaviour. In the course of the present research, we found that a minority of ISTs were asked to change their role in response to local changes in service provision or other factors. As ISTs become more embedded in the discourse of community support for adults with intellectual disabilities whose behaviours challenge, the anxiety around their funding continuing may lessen if they are recognised as essential in maintaining those individuals in their local communities. Clearly, this was a concern voiced by IST managers.
Our study cannot draw definitive conclusions about the critical care components of ISTs, but it is clear that these are valued services that have been considered for many years now as central to the effective management of people with intellectual disabilities who display challenging behaviour. However, utilising the service appropriately and mandating its establishment within a modernised approach to managing challenging behaviour and supporting people locally requires a revised definition of the role that is informed by stakeholders’ views and research findings. In particular, we have found several commonalities with relevant research from Crisis Resolution Teams and those lessons must be heeded regarding the content of the IST’s involvement, the fidelity of its approach and its position in the acute care system,99 regardless of the type of IST model. Recently, there has been interest in creating a stratified approach to the care of service users with intellectual disabilities who are at risk of admission. Bohen and Woodrow100 and Mottershead and Woodrow84 have published some initial findings from the development of the Dynamic Support Database. Although such work is in its early stages, it may be promising in refining the profile of service users requiring intensive support to avoid admission, pointing towards prevention and intervention strategies, and contributing to the specification of ISTs.
We argue that ISTs cannot remain outside any discussions about a national service model for people with intellectual disabilities, nor be an afterthought that depends on changing commissioning priorities. They must be a serious contender for managing acute crisis care, in addition to a host of other functions that must be fully operationalised and agreed between a variety of stakeholders.
Research recommendations
Following the guidance from NICE and the Transforming Care programme,12 working in partnership with adults with intellectual disabilities, their families and carers would help ensure any investment is well managed. Based on the findings of the study and taking into consideration the evidence-base required by commissioners and professionals responsible for the care and support of adults with intellectual disabilities, we make the following recommendations for future research:
-
A randomised controlled evaluation of ISTs against treatment as usual. Treatment as usual will have to be redefined (i.e. not solely understood as lack of ISTs) because of several policy changes and the likely expansion of ISTs across all areas in England.
-
Identification of the key elements of good intensive support and its role in the crisis pathway for adults with intellectual disabilities who display challenging behaviour across all levels of intellectual disability.
-
Examination of wider system challenges that impact staff turnover and well-being and whether or not these may affect patient care.
-
Further analysis of the data set generated by this study.
-
Development of service model fidelity.
Chapter 9 Conclusions
Summary of findings and implications
This study is, to our knowledge, the first to systematically evaluate ISTs in England. The findings suggest that there has been progress, for example in the number of ISTs available across the country, which are broadly well received by stakeholders who use the services and also by referrers. In recent years there has been a paucity of research around mental health crisis support for people with intellectual disabilities who may also display challenging behaviour. At the same time, there is ongoing concern regarding people with intellectual disabilities across the lifespan who remain inpatients in mostly out-of-area private assessment and treatment units. ISTs appear to have little to do in supporting repatriation and, in the main, are local services supporting specialist community intellectual disability teams. An approach that is better integrated with other provision, encompasses well-defined intensive support and has a clearer remit of ISTs’ role in the crisis pathway may be required.
In our study, we had a rather small number of admissions over 20 months of recruitment, about one or two per month for all areas, and 40 discharges. Therefore, for the majority of participants, it is possible to support them in their localities, but a rethink of utilising services and care models will need to be considered for those who display severe challenging behaviour and aggression. Although, overall, stakeholders were pleased with the IST offer regardless of the model, it is of some concern that the care provided lacks fidelity beyond a behavioural framework. There are clearly a number of unmet needs to do with family carer burden or paid carer attitudes and support that also need to be addressed. It would appear that the core role of ISTs as traditionally conceived has not changed much in the past 40 years, despite our better understanding of the mental health needs and emerging multimorbidity of people with intellectual disabilities. We argue that the service model to support adults with intellectual disabilities who display challenging behaviour is less important, but that there are imperatives for the development of a high-fidelity acute-care framework that is part of all discussions around improving support for people with intellectual disabilities.
Acknowledgements
The research team would like to thank the study participants for their support and contributions.
We are very grateful to the Project Advisory Group of experts by experience for their support and commitment to the study over time. In particular, we acknowledge the support and contribution of Narender Kaur, Lorna Bryan, Janet Seamer, Sandy Smith and Brendan Leahy from Synergy (Camden, UK).
We would also like to thank the Study Steering Committee, chaired by Professor Nora Grace, for its oversight of the study.
We are grateful to the IST research team of Amy Walsh, Isobel Harrison, Dr Victoria Ratti, Jessica Budgett and Peiayo Tang for their contribution to delivering the intensive support teams for adults with intellectual disabilities displaying challenging behaviour (IST-ID) study.
Contributions of authors
Angela Hassiotis (https://orcid.org/0000-0002-9800-3909) (Professor of Psychiatry of Intellectual Disability) was the lead applicant and principal investigator. She oversaw delivery of the project, led all aspects of the work, and supervised the research team, except for the health economic team.
Athanasia Kouroupa (https://orcid.org/0000-0003-3659-160X) (Research Fellow) contributed to recruitment of the phase 2 research sites, study set-up, data collection, database management, and qualitative coding and analysis. She also led the write-up of this report and supported the work of the Project Advisory Group.
Leila Hamza (https://orcid.org/0000-0003-3439-6800) (Research Assistant) was responsible for participant recruitment, formulation of quantitative data and analysis of qualitative transcripts of interviews with adults with intellectual disabilities.
Nicola Morant (https://orcid.org/0000-0003-4022-8133) (Associate Professor) was a co-applicant. She developed an analytical framework, supervised the qualitative analysis and contributed to the write-up of qualitative data.
Ian Hall (https://orcid.org/0000-0002-5669-1571) (Consultant Psychiatrist) was a co-applicant. He supported the interpretation of the phase 1 and 2 study findings.
Louise Marston (https://orcid.org/0000-0002-9973-1131) (Associate Professor in Statistics) conducted the quantitative analysis of clinical outcomes in phase 2 and supported the write-up of the quantitative evaluation.
Renee Romeo (https://orcid.org/0000-0003-3871-9697) (Reader in Health Economics) was a co-applicant. She led all aspects of the economic evaluation and supervised the researchers working on the economic evaluation.
Nahel Yaziji (https://orcid.org/0000-0002-2273-7957) (Research Associate in Health Economics) conducted the health economic evaluation analysis.
Rebecca Jones (https://orcid.org/0000-0001-6924-0924) (Principal Research Fellow) conducted the quantitative analysis of outcomes in phase 1.
Ken Courtenay (https://orcid.org/0000-0002-1098-271X) (Consultant Psychiatrist) was a co-applicant. He supported the interpretation of the phase 1 and 2 study findings.
Peter Langdon (https://orcid.org/0000-0002-7745-1825) (Professor in the Centre for Educational Development, Appraisal and Research) was a co-applicant. He supported the interpretation of the phase 1 and 2 study findings.
Laurence Taggart (https://orcid.org/0000-0002-0954-2127) (Reader in Nursing and Health Research) was a co-applicant. He supported the interpretation of the phase 1 and 2 study findings.
Vicky Crossey (https://orcid.org/0000-0003-4354-8853) (Consultant Psychiatrist) was a co-applicant. She supported the interpretation of the phase 1 and 2 study findings.
Brynmor Lloyd-Evans (https://orcid.org/0000-0001-9866-788X) (Senior Lecturer) was a co-applicant. He supported the interpretation of the phase 1 and 2 study findings.
Publications
Hassiotis A, Walsh A, Budgett J, Harrison I, Jones R, Morant N, et al. Intensive support for adults with intellectual disability and behaviours that challenge: a survey of provision and service typologies in England. BJPsych Open 2020;6:e20.
Hassiotis A, Langdon P, Courtenay K, Hall I, Lloyd-Evans B, Romeo R, et al. Expanding capacity in mental health research in intellectual disabilities. BJPsych Bulletin 2020;7:1–4.
Hassiotis A, Kouroupa A, Jones R, Morant N, Courtenay K, Hall I, et al. Clinical and cost evaluation of intensive support team (IST) models for adults with intellectual disabilities who display challenging behaviour: a comparative cohort study protocol. BMJ Open 2021;11:e043358.
Other dissemination
Flippable infographic booklets communicating the study findings can be found here:
-
The IST-ID Study Quantitative Results. URL: https://issuu.com/angelahassiotis_ist/docs/ist_quan_magazine (accessed 2 March 2022).
-
The IST-ID Study – Qualitative Results. URL: https://issuu.com/angelahassiotis_ist/docs/ist_qual_magazine (accessed 2 March 2022).
Data-sharing statement
All data set requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Maulik PK, Mascarenhas MN, Mathers CD, Dua T, Saxena S. Prevalence of intellectual disability: a meta-analysis of population-based studies. Res Dev Disabil 2011;32:419-36. https://doi.org/10.1016/j.ridd.2010.12.018.
- Cooper SA, Smiley E, Morrison J, Williamson A, Allan L. Mental ill-health in adults with intellectual disabilities: prevalence and associated factors. Br J Psychiatry 2007;190:27-35. https://doi.org/10.1192/bjp.bp.106.022483.
- National Institute for Health and Care Excellence (NICE) . Challenging Behaviour and Learning Disabilities: Prevention and Interventions for People With Learning Disabilities Whose Behaviour Challenges 2015. www.nice.org.uk/guidance/NG11/chapter/1-recommendations (accessed June 2021).
- Cooper SA, Smiley E, Allan LM, Jackson A, Finlayson J, Mantry D, et al. Adults with intellectual disabilities: prevalence, incidence and remission of self-injurious behaviour, and related factors. J Intellect Disabil Res 2009;53:200-16. https://doi.org/10.1111/j.1365-2788.2008.01060.x.
- Jones S, Cooper SA, Smiley E, Allan L, Williamson A, Morrison J. Prevalence of, and factors associated with, problem behaviors in adults with intellectual disabilities. J Nerv Ment Dis 2008;196:678-86. https://doi.org/10.1097/NMD.0b013e318183f85c.
- Lowe K, Allen D, Jones E, Brophy S, Moore K, James W. Challenging behaviours: prevalence and topographies. J Intellect Disabil Res 2007;51:625-36. https://doi.org/10.1111/j.1365-2788.2006.00948.x.
- Totsika V, Hastings RP. Persistent challenging behaviour in people with an intellectual disability. Curr Opin Psychiatry 2009;22:437-41. https://doi.org/10.1097/YCO.0b013e32832cd9b8.
- Bowring DL, Totsika V, Hastings RP, Toogood S, McMahon M. Prevalence of psychotropic medication use and association with challenging behaviour in adults with an intellectual disability. A total population study. J Intellect Disabil Res 2017;61:604-17. https://doi.org/10.1111/jir.12359.
- Heaton S, Whitaker S. The attitudes of trained and untrained staff in coping with challenging behaviour in secure and community settings. Br J Dev Disabil 2012;58:40-7. https://doi.org/10.1179/2047387711Y.0000000006.
- Flynn M, Hollins S. Acting on the lessons of Winterbourne View Hospital. BMJ 2013;346. https://doi.org/10.1136/bmj.f18.
- Murphy G. Whorlton Hall: a predictable tragedy?. BMJ 2019;366. https://doi.org/10.1136/bmj.l4705.
- Department of Health and Social Care . Transforming Care: A National Response to Winterbourne View Hospital 2012. www.gov.uk/government/uploads/system/uploads/attachment_data/file/213215/final-report.pdf (accessed May 2021).
- NHS Digital . Learning Disability Census Report 2015. https://files.digital.nhs.uk/publicationimport/pub19xxx/pub19428/ld-census-initial-sep15-rep.pdf (accessed 2 March 2022).
- NHS England . Patient Trends and Change Over Time 2020. www.england.nhs.uk/wp-content/uploads/2020/12/learning-disability-and-autism-patient-trends-and-change-over-time-sept-2020.pdf (accessed May 2021).
- NHS England . Supporting People With a Learning Disability and Or Autism Who Have a Mental Health Condition or Display Behaviour That Challenges 2015. www.england.nhs.uk/wp-content/uploads/2015/07/ld-draft-serv-mod.pdf (accessed January 2022).
- Perry DW, Shervington T, Mungur N, Marston G, Martin D, Brown G. Why are people with intellectual disability moved ‘out-of-area’?. J Policy Pract Intellect Disabil 2007;4:203-9. https://doi.org/10.1111/j.1741-1130.2007.00119.x.
- Sheehan R, Mutch J, Marston L, Osborn D, Hassiotis A. Risk factors for in-patient admission among adults with intellectual disability and autism: investigation of electronic clinical records. BJPsych Open 2020;7. https://doi.org/10.1192/bjo.2020.135.
- Glover G, Williams R, Branford D, Avery R, Chauhan U, Hoghton M, et al. Prescribing of Psychotropic Drugs to People With Learning Disabilities and Or Autism by General Practitioners in England 2015. https://webarchive.nationalarchives.gov.uk/20160704152031/www.improvinghealthandlives.org.uk/gsf.php5?f=313881&fv=21599 (accessed December 2021).
- Sheehan R, Hassiotis A, Walters K, Osborn D, Strydom A, Horsfall L. Mental illness, challenging behaviour, and psychotropic drug prescribing in people with intellectual disability: UK population based cohort study. BMJ 2015;351. https://doi.org/10.1136/bmj.h4326.
- NHS England . STOMP and STAMP: Stopping The Over-Medication of Children and Young People With a Learning Disability, Autism or Both (STOMP) and Supporting Treatment and Appropriate Medication in Paediatrics (STAMP) n.d. www.england.nhs.uk/wp-content/uploads/2019/02/STOMP-STAMP-a5-leaflet.pdf (accessed 2 March 2022).
- Mehta H, Glover G. Psychotropic Drugs and People with Learning Disabilities or Autism. London: Public Health England; 2019.
- Hassiotis A, Parkes C, Jones L, Fitzgerald B, Romeo R. Individual characteristics and service expenditure on challenging behaviour for adults with intellectual disabilities. J Appl Res Intellect Disabil 2008;21:438-45. https://doi.org/10.1111/j.1468-3148.2007.00413.x.
- Taggart L, McMillan R, Lawson A. Predictors of hospital admission for women with learning disabilities and psychiatric disorders compared with women maintained in community settings. Adv Ment Heal Learn Disabil 2009;3:30-41. https://doi.org/10.1108/17530180200900007.
- Painter J, Ingham B, Trevithick L, Hastings RP, Roy A. Correlates for the risk of specialist ID hospital admission for people with intellectual disabilities: development of the LDNAT inpatient index. Tizard Learn Disabil Rev 2018;23:42-50. https://doi.org/10.1108/TLDR-04-2017-0015.
- Durbin A, Balogh R, Lin E, Wilton AS, Lunsky Y. Emergency department use: common presenting issues and continuity of care for individuals with and without intellectual and developmental disabilities. J Autism Dev Disord 2018;48:3542-50. https://doi.org/10.1007/s10803-018-3615-9.
- Durbin A, Balogh R, Lin E, Wilton AS, Selick A, Dobranowski KM, et al. Repeat emergency department visits for individuals with intellectual and developmental disabilities and psychiatric disorders. Am J Intellect Dev Disabil 2019;124:206-19. https://doi.org/10.1352/1944-7558-124.3.206.
- Lin E, Balogh R, Chung H, Dobranowski K, Durbin A, Volpe T, et al. Looking across health and healthcare outcomes for people with intellectual and developmental disabilities and psychiatric disorders: population-based longitudinal study. Br J Psychiatry 2021;218:51-7. https://doi.org/10.1192/bjp.2020.202.
- Donnellan AM, LaVigna GW, Zambito J, Thvedt J. A time-limited intensive intervention program model to support community placement for persons with severe behavior problems. J Assoc Pers Sev Handicap 1985;10:123-31. https://doi.org/10.1177/154079698501000301.
- Davison S, Mcgill P, Baker P, Allen D. A national UK survey of periopatetic support teams for children and adults with intellectual and developmental disability who display challenging behaviour. Int J Posit Behav Support 2015;5:26-33.
- Mansell JL. Services for People with Learning Disabilities and Challenging Behaviour or Mental Health Needs. London: Department of Health and Social Care; 2007.
- Hassiotis A. Community mental health services for individuals with intellectual disabilities. Dis Manag Health Outcomes 2002;10:409-17. https://doi.org/10.2165/00115677-200210070-00002.
- Emerson E, Forrest J, Cambridge P, Mansell J. Community support teams for people with learning disabilities and challenging behaviours: results of a national survey. J Ment Health 1996;5:396-40. https://doi.org/10.1080/09638239619301.
- Guinn A, Jaydeokar S, McCarthy J, Roy A, Hassiotis A. A survey of consultant psychiatrists in intellectual disability based in England. Adv Ment Health Intellect Disabil 2016;10:258-70. https://doi.org/10.1108/AMHID-03-2015-0012.
- NHS England . Building the Right Support: A National Plan to Develop Community Services and Close Inpatient Facilities for People With a Learning Disability and Or Autism Who Display Behaviour That Challenges, Including Those With a Mental Health Condition 2015. www.england.nhs.uk/wp-content/uploads/2015/10/ld-nat-imp-plan-oct15.pdf (accessed May 2021).
- NHS England . Mapping of Clinical Commissioning Groups to Transforming Care Partnerships 2017. www.england.nhs.uk/learning-disabilities/tcp/ (accessed December 2021).
- NHS England . Care and Treatment Reviews (CTRs): Policy and Guidance. Including Policy and Guidance on Care, Education and Treatment Reviews (CETRs) for Children and Young People 2017. www.england.nhs.uk/wp-content/uploads/2017/03/ctr-policy-v2.pdf (accessed March 2022).
- National Center for START Services, Institute on Disability/ICED, University of New Hampshire . National Center for START Services n.d. https://centerforstartservices.org (accessed 3 March 2022).
- Beasley JB, Kalb L, Klein A. Improving mental health outcomes for individuals with intellectual disability through the Iowa START (I-START) program. J Ment Health Res Intellect Disabil 2018;11:287-300. https://doi.org/10.1080/19315864.2018.1504362.
- Kalb LG, Beasley J, Caoili A, Klein A. Improvement in mental health outcomes and caregiver service experiences associated with the START program. Am J Intellect Dev Disabil 2019;124:25-34. https://doi.org/10.1352/1944-7558-124.1.25.
- Hassiotis A, Robotham D, Canagasabey A, Romeo R, Langridge D, Blizard R, et al. Randomized, single-blind, controlled trial of a specialist behavior therapy team for challenging behavior in adults with intellectual disabilities. Am J Psychiatry 2009;166:1278-85. https://doi.org/10.1176/appi.ajp.2009.08111747.
- Inchley-Mort S, Rantell K, Wahlich C, Hassiotis A. Complex behaviour service: enhanced model for challenging behaviour. Adv Ment Health Intellect Disabil 2014;8:219-27. https://doi.org/10.1108/AMHID-08-2013-0056.
- Robotham D, King M, Canagasabey A, Inchley-Mort S, Hassiotis A. Social validity of randomised controlled trials in health services research and intellectual disabilities: a qualitative exploration of stakeholder views. Trials 2011;12. https://doi.org/10.1186/1745-6215-12-144.
- White J, Symes M, Pearce C. Redesigning a community-based challenging behaviour intensive support service. Adv Ment Health Intellect Disabil 2019;13:123-32. https://doi.org/10.1108/AMHID-11-2018-0047.
- Association of Directors of Adult Social Services, Care Quality Commission, Department of Health and Social Care, Health Education England, Local Government Association, NHS England . Transforming Care for People With Learning Disabilities – Next Steps 2015. www.england.nhs.uk/wp-content/uploads/2015/01/transform-care-nxt-stps.pdf (accessed 2 March 2022).
- Toot S, Devine M, Orrell M. The effectiveness of crisis resolution/home treatment teams for older people with mental health problems: a systematic review and scoping exercise. Int J Geriatr Psychiatry 2011;26:1221-30. https://doi.org/10.1002/gps.2686.
- Wheeler C, Lloyd-Evans B, Churchard A, Fitzgerald C, Fullarton K, Mosse L, et al. Implementation of the Crisis Resolution Team model in adult mental health settings: a systematic review. BMC Psychiatry 2015;15. https://doi.org/10.1186/s12888-015-0441-x.
- Inchley-Mort S, Hassiotis A. Complex behaviour service: content analysis of stakeholder opinions. Adv Ment Health Intellect Disabil 2014;8:228-36. https://doi.org/10.1108/AMHID-08-2013-0057.
- NHS England . The NHS Long Term Plan 2019. www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf (accessed January 2022).
- Hassiotis A, Kouroupa A, Jones R, Morant N, Courtenay K, Hall I, et al. Clinical and cost evaluation of intensive support teams (IST) models for adults with intellectual disabilities who display challenging behaviour: a comparative cohort study protocol. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2020-043358.
- Great Britain . Data Protection Act 1998 1998.
- European Parliament and Council of the European Union . Regulation (EU) 2016 679 of the European Parliament and of the Council of 27 April 2016 on the Protection of Natural Persons With Regard to the Processing of Personal Data and on the Free Movement of Such Data, and Repealing Directive 95 46 EC (General Data Protection Regulation) n.d.
- National Institute for Health and Care Research . User Carer Researcher Guidelines 2014. www.nihr.ac.uk/nihr-in-your-area/mental-health/documents/UserCarerResearcherGuidelinesMay2014_FINAL.pdf (accessed August 2021).
- Hassiotis A, Walsh A, Budgett J, Harrison I, Jones R, Morant N, et al. Intensive support for adults with intellectual disability and behaviours that challenge: a survey of provision and service typologies in England. BJPsych Open 2020;6. https://doi.org/10.1192/bjo.2020.2.
- Department of Health and Social Care . The Mental Health Policy Implementation Guide 2001. webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4009350 (accessed May 2021).
- Ward JH. Hierarchical grouping to optimize an objective function. Am Stat Assoc 1963;58:236-44. https://doi.org/10.1080/01621459.1963.10500845.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Aman MG, Singh NN, Stewart AW, Field CJ. The aberrant behavior checklist: a behavior rating scale for the assessment of treatment effects. Am J Ment Defic 1985;89:485-91. https://doi.org/10.1037/t10453-000.
- Prosser H, Moss S, Costello H, Simpson N, Patel P, Rowe S. Reliability and validity of the Mini PAS-ADD for assessing psychiatric disorders in adults with intellectual disability. J Intellect Disabil Res 1998;42:264-72. https://doi.org/10.1046/j.1365-2788.1998.00146.x.
- Slade M, Powell R, Rosen A, Strathdee G. Threshold Assessment Grid (TAG): the development of a valid and brief scale to assess the severity of mental illness. Soc Psychiatry Psychiatr Epidemiol 2000;35:78-85. https://doi.org/10.1007/s001270050011.
- Hall I, Parkes C, Samuels S, Hassiotis A. Working across boundaries: clinical outcomes for an integrated mental health service for people with intellectual disabilities. J Intellect Disabil Res 2006;50:598-607. https://doi.org/10.1111/j.1365-2788.2006.00821.x.
- Shalock RL, Keith KD. Quality of Life Questionnaire Manual. Worthington, OH: IDS Publishing Corporation; 1993.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- Beecham J, Knapp MRJ. The Economic Evaluation of Mental Health Care. Aldershot: Ashgate Publishing Limited; 1995.
- Hassiotis A, Poppe M, Strydom A, Vickerstaff V, Hall IS, Crabtree J, et al. Clinical outcomes of staff training in positive behaviour support to reduce challenging behaviour in adults with intellectual disability: cluster randomised controlled trial. Br J Psychiatry 2018;212:161-8. https://doi.org/10.1192/bjp.2017.34.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2020. Canterbury: Personal Social Services Research Unit, University of Kent; 2020.
- Beecham J, Knapp M, Thornicroft G. Measuring Mental Health Needs. London: Gaskell; 2001.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2015 n.d. www.pssru.ac.uk/project-pages/unit-costs/unit-costs-2015/[0] (accessed 2 March 2022).
- Curtis L. Unit Costs of Health and Social Care 2014 n.d. www.pssru.ac.uk/project-pages/unit-costs/unit-costs-2014/ (accessed 2 March 2022).
- Uttley L, Stevenson M, Scope A, Rawdin A, Sutton A. The clinical and cost effectiveness of group art therapy for people with non-psychotic mental health disorders: a systematic review and cost-effectiveness analysis. BMC Psychiatry 2015;15. https://doi.org/10.1186/s12888-015-0528-4.
- NHS . National Schedule of NHS Costs 2018 19 n.d. https://www.england.nhs.uk/publication/2018-19-national-cost-collection-data-publication/ (accessed April 2021).
- Department of Health and Social Care . 2020/21/National/Tariff/Payment/System 2020.
- Office for National Statistics . Average Household Income, UK: Financial Year Ending 2020 2020. www.ons.gov.uk/peoplepopulationandcommunity/personalandhouseholdfinances/incomeandwealth/bulletins/householddisposableincomeandinequality/financialyearending2020provisional (accessed April 2021).
- Curtis L, Burns A. Unit Costs of Health and Social Care 2018. Canterbury: Personal Social Services Research Unit, University of Kent; 2018.
- Department of Health and Social Care . National Schedule of Reference Costs 2018. https://improvement.nhs.uk/resources/reference-costs/ (accessed 25 February 2022).
- Van Reenen M, Janssen B. EQ-5D-5L User Guide, Basic Information on How to Use the EQ-5D-5L Instrument. Version 2.1 2015. https://euroqol.org/wp-content/uploads/2016/09/EQ-5D-5L_UserGuide_2015.pdf (accessed April 2021).
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15. https://doi.org/10.1016/j.jval.2012.02.008.
- van Hout BA, Al MJ, Gordon GS, Rutten FF. Costs, effects and C/E-ratios alongside a clinical trial. Health Econ 1994;3:309-19. https://doi.org/10.1002/hec.4730030505.
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. Int J Technol Assess Health Care 2013;29:117-22. https://doi.org/10.1017/S0266462313000160.
- NHS Employers . Pension Contributions and Tax Relief n.d. https://www.nhsemployers.org/articles/pension-contributions-and-tax-relief#:~:text=Employer%20contributions%20and%20administration%20levy,known%20as%20the%20scheme%20valuation (accessed April 2021).
- gov.uk . National Insurance Rates and Categories n.d. https://www.gov.uk/national-insurance-rates-letters (accessed April 2021).
- National Institute for Health and Care Excellence (NICE) . The Guidelines Manual. Process and Methods [PMG6] n.d. www.nice.org.uk/process/pmg6/chapter/assessing-cost-effectiveness (accessed 30 March 2022).
- Department of Health and Social Care . A New Strategy for Learning Disability for the 21st Century 2001. www.gov.uk/government/uploads/system/uploads/attachment_data/file/250877/5086.pdf (accessed May 2021).
- Department of Health and Social Care . Refocusing the Care Programme Approach 2008. www.dh.gov.uk/publications%0Ahttp://webarchive.nationalarchives.gov.uk/20130107105354/http:/www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_083649.pdf (accessed May 2021).
- Mottershead T, Woodrow C. Practicality, utility and face-validity of the dynamic support database. Adv Ment Health Intellect Disabil 2019;13:228-36. https://doi.org/10.1108/AMHID-04-2019-0009.
- Burns T, Fiander M, Kent A, Ukoumunne OC, Byford S, Fahy T, et al. Effects of case-load size on the process of care of patients with severe psychotic illness. Report from the UK700 trial. Br J Psychiatry 2000;177:427-33. https://doi.org/10.1017/S0007125000227359.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349-57. https://doi.org/10.1093/intqhc/mzm042.
- Hassiotis A, Langdon P, Courtenay K, Hall I, Lloyd-Evans B, Romeo R, et al. Expanding capacity in mental health research in intellectual disabilities. BJPsych Bulletin 2020;7:1-4. https://doi.org/10.1192/bjb.2020.117.
- National Institute for Health and Care Excellence (NICE) . Learning Disabilities and Behaviour That Challenges: Service Design and Delivery. 2018. www.nice.org.uk/guidance/ng93/resources/learning-disabilities-and-behaviour-that-challenges-service-design-and-delivery-pdf-1837753480645 (accessed May 2021).
- Bone JK, McCloud T, Scott HR, Machin K, Markham S, Persaud K, et al. Psychosocial interventions to reduce compulsory psychiatric admissions: a rapid evidence synthesis. E Clinical Medicine 2019;10:58-67. https://doi.org/10.1016/j.eclinm.2019.03.017.
- Chaplin R. General psychiatric services for adults with intellectual disability and mental illness. J Intellect Disabil Res 2004;48:1-10. https://doi.org/10.1111/j.1365-2788.2004.00580.x.
- Roy A, Matthews H, Clifford P, Fowler V, Martin DM. Health of the Nation Outcome Scales for People with Learning Disabilities (HoNOS-LD): glossary for HoNOS-LD score sheet. Br J Psychiatry 2002;180:67-70. https://doi.org/10.1192/bjp.180.1.67.
- Iemmi V, Knapp M, Saville M, McWade P, McLennan K, Toogood S. Positive behavioural support for adults with intellectual disabilities and behaviour that challenges: an initial exploration of the economic case. Int J Posit Behav Support 2015;5:16-25.
- James N. The formal support experiences of family carers of people with an intellectual disability who also display challenging behaviour and/or mental health issues: what do carers say?. J Intellect Disabil 2013;17:6-23. https://doi.org/10.1177/1744629512472610.
- Hubert J. ‘My heart is always where he is’. Perspectives of mothers of young people with severe intellectual disabilities and challenging behaviour living at home. Br J Learn Disabil 2011;39:216-24. https://doi.org/10.1111/j.1468-3156.2010.00658.x.
- Hemmings C, Bouras N, Craig T. How should community mental health of intellectual disability services evolve?. Int J Environ Res Public Health 2014;11:8624-31. https://doi.org/10.3390/ijerph110908624.
- Royal College of Psychiatrists . Community-Based Services for People With Intellectual Disability and Mental Health Problems: Literature Review and Survey Results 2015. www.rcpsych.ac.uk/docs/default-source/members/faculties/intellectual-disability/id-fr-id-06.pdf?sfvrsn=5a230b9c_2 (accessed December 2021).
- Sheehan R, Paschos D. A comparison of different models to meet the mental health needs of adults with intellectual disabilities. Adv Ment Heal Intellect Disabil 2013;7:161-8. https://doi.org/10.1108/20441281311320747.
- Chaplin E, O’Hara J, Holt G, Bouras N. Mental health services for people with intellectual disability: challenges to care delivery. Br J Learn Disabil 2009;37:157-64. https://doi.org/10.1111/j.1468-3156.2008.00540.x.
- Morant N, Lloyd-Evans B, Lamb D, Fullarton K, Brown E, Paterson B, et al. Crisis resolution and home treatment: stakeholders’ views on critical ingredients and implementation in England. BMC Psychiatry 2017;17. https://doi.org/10.1186/s12888-017-1421-0.
- Bohen F, Woodrow C. Dynamic support database clinical support tool: inter-rater reliability. Adv Ment Heal Intellect Disabil 2020;14:25-32. https://doi.org/10.1108/AMHID-09-2019-0027.
- Royal College of Psychiatrists, The British Psychological Society, Royal College of Speech and Language Therapists . Challenging Behaviour: A Unified Approach 2007.
Appendix 1 Chapter 4 Consolidated Health Economic Evaluation Reporting Standards checklist, tables and figures
Tables
| Characteristic | Mean or n/N | SD or % |
|---|---|---|
| Marital status | ||
| Single | 204/206 | 99% |
| Living situation | ||
| Alone or with partner (with or without children) | 49/206 | 24% |
| With parents | 56/206 | 27% |
| With relatives | 4/206 | 2% |
| Other | 97/206 | 47% |
| Accommodation | ||
| Family home | 62/201 | 31% |
| Supported living | 70/201 | 35% |
| Residential | 59/201 | 29% |
| Independent | 10/201 | 5% |
| Physical health problems | 172/206 | 84% |
| Mobility problems | 68/206 | 33% |
| Sensory problems | 101/206 | 49% |
| Epilepsy | 56/206 | 27% |
| Incontinence | 80/206 | 39% |
| Other physical health problem(s) | 98/206 | 48% |
| Main source of income | ||
| Salary/wage | 1/206 | 0.5% |
| Family support | 56/206 | 27% |
| State benefits | 206/206 | 100% |
| Other | 1/206 | 0.5% |
| Occupational status | ||
| None | 152/206 | 74% |
| Part-time paid employment (≥ 30 hours per week) | 1/206 | 0.5% |
| Employed, but only paid up to the subscribed limit | 1/206 | 0.5% |
| Voluntary work | 8/206 | 4% |
| College | 17/206 | 8% |
| Day centre | 31/206 | 15% |
| School | 2/206 | 1% |
| Other | 4/206 | 2% |
| Have an unpaid carer | 135/206 | 66% |
| Carer receives carer’s allowance | 52/135 | 39% |
| Relationship to carer | ||
| Parent | 115/135 | 85% |
| Sibling | 13/135 | 10% |
| Spouse | 2/135 | 1% |
| Other relative | 2/135 | 1% |
| Other | 3/135 | 2% |
| Carer’s employment status | ||
| Paid employment | 54/135 | 40% |
| Unemployed | 29/135 | 21% |
| Housewife/husband | 14/135 | 10% |
| Retired | 38/135 | 28% |
| Still seeing the IST team | 123/206 | 60% |
| ABC-C | ||
| Total | 52 | 33 |
| Irritability | 16 | 11 |
| Lethargy | 11 | 9 |
| Stereotypic behaviour | 5 | 5 |
| Hyperactivity | 16 | 11 |
| Inappropriate speech | 4 | 4 |
| PAS-ADD Clinical Interview | ||
| Organic condition | 16/204 | 8% |
| Affective or neurotic disorder | 22/204 | 11% |
| Psychotic disorder | 6/204 | 3% |
| TAG | 13 | 5 |
| QoL-Q | 74 | 10 |
| Characteristic | Model | p-value | |||
|---|---|---|---|---|---|
| Enhanced (N = 106) | Independent (N = 100) | ||||
| Mean or n/N | SD or % | Mean or n/N | SD or % | ||
| Marital status | > 0.999 | ||||
| Single | 104/106 | 98% | 100/100 | 100% | |
| Married | 1/106 | 1% | 0/100 | 0% | |
| Divorced | 1/106 | 1% | 0/100 | 0% | |
| Living situation | 0.213 | ||||
| Alone or with partner +/– children | 25/106 | 24% | 24/100 | 24% | |
| With parents | 31/106 | 29% | 25/100 | 25% | |
| With relatives | 4/106 | 4% | 0/100 | 0% | |
| Other | 46/106 | 43% | 51/100 | 51% | |
| Accommodation | 0.546 | ||||
| Median (months) (IQR) | 45 (15–128) | 45 (19–154) | |||
| Family home | 34/103 | 33% | 28/98 | 29% | |
| Supported living | 36/103 | 35% | 34/98 | 35% | |
| Residential | 30/103 | 29% | 29/98 | 30% | |
| Independent | 3/103 | 3% | 7/98 | 7% | |
| Length of time (< 6 months) in current accommodation | 8/106 | 8% | 7/100 | 7% | |
| Physical health problems | 88/106 | 83% | 84/100 | 84% | 0.850 |
| Mobility problems | 39/106 | 37% | 29/100 | 29% | 0.235 |
| Sensory problems | 47/106 | 44% | 54/100 | 54% | 0.166 |
| Epilepsy | 32/106 | 30% | 24/100 | 24% | 0.318 |
| Incontinence | 43/106 | 41% | 37/100 | 37% | 0.600 |
| Other physical health problem(s) | 49/106 | 46% | 49/100 | 49% | 0.690 |
| Main source of income | |||||
| Salary/wage | 0/106 | 0% | 1/100 | 1% | 0.485 |
| Family support | 31/106 | 29% | 25/100 | 25% | 0.494 |
| State benefits | 106/106 | 100% | 100/100 | 100% | a |
| Occupational status | |||||
| None | 75/106 | 71% | 77/100 | 77% | 0.308 |
| Part-time paid employment (≤ 30 hours per week) | 0/106 | 0% | 1/100 | 1% | 0.485 |
| Employed, but only paid up to the subscribed limit | 0/106 | 0% | 1/100 | 1% | 0.485 |
| Voluntary work | 6/106 | 6% | 2/100 | 2% | 0.281 |
| College | 9/106 | 8% | 8/100 | 8% | 0.898 |
| Day centre | 16/106 | 15% | 15/100 | 15% | 0.985 |
| School | 256 (/106 | 2% | 0/100 | 0% | 0.498 |
| Other | 3/106 | 3% | 1/100 | 1% | 0.622 |
| Have an unpaid carer | 75/106 | 71% | 60/100 | 60% | 0.105 |
| Carer receives carer’s allowance | 27/75 | 36% | 25/60 | 42% | 0.501 |
| Relationship to carer | 0.871 | ||||
| Parent | 62/75 | 83% | 53/60 | 88% | |
| Sibling | 9/75 | 12% | 4/60 | 7% | |
| Spouse | 1/75 | 1% | 1/60 | 2% | |
| Other relative | 1/75 | 1% | 1/60 | 2% | |
| Other | 2/75 | 3% | 1/60 | 2% | |
| Carer’s employment status | 0.816 | ||||
| Paid employment | 32/75 | 43% | 22/60 | 37% | |
| Unemployed | 14/75 | 19% | 15/60 | 25% | |
| Housewife/husband | 8/75 | 11% | 6/60 | 10% | |
| Retired | 21/75 | 28% | 17/60 | 28% | |
| Still seeing the IST team | 78/106 | 74% | 45/100 | 45% | < 0.001 |
| ABC-C | |||||
| Total | 56 | 34 | 49 | 32 | 0.123 |
| Irritability | 17 | 11 | 15 | 10 | 0.161 |
| Lethargy | 12 | 9 | 11 | 9 | 0.266 |
| Stereotypic behaviour | 6 | 5 | 5 | 5 | 0.130 |
| Hyperactivity | 17 | 11 | 14 | 11 | 0.188 |
| Inappropriate speech | 4 | 4 | 4 | 4 | 0.328 |
| PAS-ADD Clinical Interview | |||||
| Organic condition | 8/106 | 8% | 8/98 | 8% | 0.870 |
| Affective or neurotic disorder | 12/106 | 11% | 10/98 | 10% | 0.797 |
| Psychotic disorder | 3/106 | 3% | 3/98 | 3% | > 0.999 |
| TAG | 14 | 5 | 12 | 5 | 0.019 |
| QoL-Q | 73 | 10 | 74 | 10 | 0.929 |
| Characteristic | Odds ratio | 95% CI |
|---|---|---|
| IST type 2 (independent model) | 1.32 | 0.50 to 3.49 |
| Age (years) | 1.00 | 0.96 to 1.04 |
| Age ≥ 25 | 0.99 | 0.36 to 2.76 |
| Sex | ||
| Male | 1.10 | 0.40 to 3.06 |
| Ethnicity | ||
| White | Reference | |
| Non-white | 0.22 | 0.03 to 1.69 |
| Marital status | ||
| Single | a | |
| Living situation | ||
| Alone or with partner (with or without children) | Reference | |
| With parents | 1.72 | 0.30 to 9.85 |
| With relatives | 7.17 | 0.50 to 103.55 |
| Other | 2.11 | 0.45 to 9.92 |
| Accommodation | ||
| Family home | Reference | |
| Supported living | 1.19 | 0.36 to 3.94 |
| Residential | 1.15 | 0.31 to 4.17 |
| Independent | 0.84 | 0.09 to 7.73 |
| ASD | 2.54 | 0.71 to 9.05 |
| ADHD | 0.50 | 0.06 to 3.92 |
| Neither ASD nor ADHD | Reference | |
| ASD or ADHD | 2.26 | 0.63 to 8.16 |
| Both ASD and ADHD | 1.40 | 0.14 to 14.42 |
| SABS | 0.99 | 0.96 to 1.01 |
| Reason for intellectual disability | ||
| Down syndrome | Reference | |
| Fragile X syndrome | a | |
| Unknown | ||
| Other | ||
| Physical health problems | a | |
| Mobility problems | 2.85 | 1.06 to 7.65 |
| Sensory problems | 5.98 | 1.34 to 26.69 |
| Epilepsy | 1.12 | 0.38 to 3.30 |
| Incontinence | 2.10 | 0.80 to 5.54 |
| Overweight | 2.57 | 0.67 to 9.89 |
| Diabetes | b | |
| Overweight or diabetes | 2.30 | 0.70 to 7.57 |
| Cardiovascular related | 10.20 | 2.09 to 49.82 |
| Respiratory related | a | |
| Other physical health problem(s) | 0.89 | 0.30 to 2.58 |
| Number of physical health problems of those above | 1.67 | 1.20 to 2.34 |
| At least two physical health problems of those above | 5.75 | 1.29 to 25.62 |
| Main source of income | ||
| Salary/wage | a | |
| Family support | 0.51 | 0.14 to 1.81 |
| State benefits | a | |
| Other | a | |
| Occupational status | ||
| None | 1.25 | 0.45 to 3.46 |
| Part-time paid employment (≤ 30 hours per week) | a | |
| Employed, but only paid up to the subscribed limit | a | |
| Voluntary work | a | |
| College | 1.18 | 0.25 to 5.48 |
| Day centre | 0.98 | 0.31 to 3.11 |
| Looking after family | a | |
| School | 2.39 | 0.26 to 21.63 |
| Other | a | |
| Have an unpaid carer | 0.93 | 0.33 to 2.58 |
| Carer receives carer’s allowance | 0.98 | 0.28 to 3.42 |
| Relationship to carer | ||
| Parent | Reference | |
| Sibling | ||
| Spouse | ||
| Other | ||
| PAS-ADD Clinical Interview | ||
| Organic condition | a | |
| Affective or neurotic disorder | 1.06 | 0.33 to 3.40 |
| Psychotic disorder | 1.88 | 0.39 to 9.04 |
| TAG | 0.96 | 0.87 to 1.07 |
| QoL-Q | 1.00 | 0.95 to 1.06 |
| Service use | Model | |||||||
|---|---|---|---|---|---|---|---|---|
| Independent | Enhanced | |||||||
| Valid n | Mean | SD | Percentage using at least once | Valid n | Mean | SD | Percentage using at least once | |
| Hospital-based care | ||||||||
| Psychiatric inpatient (bed-days) | 109 | 6.94 | 29.00 | 10.1 | 114 | 4.04 | 20.20 | 7.0 |
| General inpatient (bed-days) | 109 | 0.27 | 1.25 | 7.3 | 114 | 0.08 | 0.75 | 1.8 |
| Psychiatric outpatient (attendances) | 109 | 0.07 | 0.35 | 4.6 | 114 | 0.15 | 0.57 | 8.8 |
| General outpatient (attendances) | 109 | 0.41 | 1.23 | 16.5 | 114 | 0.78 | 2.19 | 33.1 |
| Day hospital (attendances) | 109 | 0.20 | 0.62 | 11.9 | 114 | 0.23 | 1.23 | 7.0 |
| A&E psychiatric: admitted (attendances) | 109 | 0.04 | 0.19 | 3.7 | 114 | 0.03 | 0.16 | 2.6 |
| A&E psychiatric: not admitted (attendances) | 109 | 0.14 | 1.16 | 3.7 | 114 | 0.07 | 0.37 | 5.3 |
| A&E physical: admitted (attendances) | 109 | 0.17 | 0.99 | 9.2 | 114 | 0.08 | 0.50 | 2.6 |
| A&E physical: not admitted (attendances) | 109 | 0.13 | 0.46 | 10.1 | 114 | 0.47 | 1.98 | 20.2 |
| Community-based health and social care services | ||||||||
| General practice (contacts) | 109 | 4.30 | 5.90 | 97.2 | 114 | 4.63 | 7.16 | 86.8 |
| Other health and social care services (contacts)a | 103 | 82.9 | 82.9 | 100 | 108 | 71.0 | 100.3 | 98.2 |
| Informal support | ||||||||
| Paid carer (%) | 71 | 28 | 39.44 | 81 | 30 | 37 | ||
| Service use | Model | |||||||
|---|---|---|---|---|---|---|---|---|
| Independent | Enhanced | |||||||
| Valid n | Mean | SD | Percentage using at least once | Valid n | Mean | SD | Percentage using at least once | |
| Hospital-based care | ||||||||
| Psychiatric inpatient (bed-days) | 100 | 8.63 | 39.98 | 6.0 | 104 | 5.26 | 28.05 | 4.8 |
| General inpatient (bed-days) | 100 | 0.35 | 2.08 | 4.0 | 104 | 0.22 | 1.17 | 5.8 |
| Psychiatric outpatient (attendances) | 100 | 0.08 | 0.44 | 4.0 | 104 | 0.23 | 0.99 | 8.7 |
| General outpatient (attendances) | 100 | 0.26 | 0.69 | 16.0 | 104 | 0.40 | 0.94 | 22.1 |
| Day hospital (attendances) | 100 | 0.07 | 0.36 | 5.0 | 104 | 0.03 | 0.17 | 2.9 |
| A&E psychiatric: admitted (attendances) | 100 | 0.03 | 0.17 | 3.0 | 104 | 0.02 | 0.14 | 1.9 |
| A&E psychiatric: not admitted (attendances) | 100 | 0.01 | 0.10 | 1.0 | 104 | 0.04 | 0.24 | 2.9 |
| A&E physical: admitted (attendances) | 100 | 0.04 | 0.24 | 3.0 | 104 | 0.07 | 0.42 | 3.9 |
| A&E physical: not admitted (attendances) | 100 | 0.03 | 0.17 | 3.0 | 104 | 0.07 | 0.32 | 4.8 |
| Community-based health and social care services | ||||||||
| General practice (contacts) | 100 | 4.8 | 14.20 | 88.0 | 104 | 3.47 | 3.96 | 87.5 |
| Other health and social care services (contacts)a | 100 | 71.0 | 100.40 | 95.0 | 102 | 82.19 | 109.80 | 96.1 |
| Informal care | ||||||||
| Paid carer (yes) | 60 | 22 | 36.67 | 73 | 30 | 41.10 | ||
| Costs (£, 2020/21 prices) | Model | Independent – enhanced | ||||||
|---|---|---|---|---|---|---|---|---|
| Independent | Enhanced | |||||||
| Valid n | Mean | SD | Valid n | Mean | SD | Adjusted mean differencea,b | 95% CI | |
| Hospital-based care | ||||||||
| Baseline | 109 | 3699.30 | 10,195.30 | 114 | 2423.90 | 8735.09 | 983.10 | –1867.14 to 5025.82 |
| 9 months | 104 | 6388.0 | 22,417.80 | 100 | 4545.60 | 18,439.40 | –538.89 | –9957.92 to 4039.89 |
| Community-based health and social care services | ||||||||
| Baseline | 103 | 6213.36 | 8965.26 | 107 | 5058.19 | 7924.25 | 702.89 | –1782.60 to 2894.75 |
| 9 months | 98 | 8817.90 | 14,787.10 | 102 | 10,670.40 | 15,960.8 | –2287.15 | –6755.61 to 1446.98 |
| Total health and social care | ||||||||
| Baseline | 103 | 9224.64 | 13,007.3 | 107 | 7275.35 | 13,211.5 | 1223.20 | –1867.14 to 5025.82 |
| 9 months | 98 | 15,324.18 | 30,301.5 | 102 | 15,302.66 | 25,786.9 | –3409.95 | –9957.92 to 4039.89 |
| Informal care | ||||||||
| Baseline | 110 | 6550.5 | 5366.91 | 115 | 7104.59 | 4982.9 | –464.49 | –1836.84 to 847.21 |
| 9 months | 100 | 8963.4 | 8010 | 106 | 10,520.8 | 7450.8 | –1123.01 | –2727.50 to 621.51 |
| Total societal | ||||||||
| Baseline | 103 | 15,774.18 | 13,706.4 | 107 | 14,481.63 | 13,835.8 | 643.48 | –3141.41 to 4214.73 |
| 9-months | 98 | 24,259.33 | 31,385.1 | 102 | 26,117.84 | 26,754.9 | –4712.30 | –11,124.85 to 2106.36 |
| Outcome measure | Model | Adjusted mean difference | 95% CI | p-value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Independent (N = 111) | Enhanced (N = 115) | ||||||||
| Valid n | Mean | SD | Valid n | Mean | SD | ||||
| Primary outcome | |||||||||
| ABC-C score | |||||||||
| Baseline | 110 | 62 | 32 | 115 | 64 | 34 | 0.15a | –7.51 to 9.31 | 0.969 |
| 9 months | 101 | 49 | 32 | 107 | 56 | 34 | –5.07b | –14.93 to 2.14 | 0.306 |
| Secondary outcome | |||||||||
| Proxy utility scores | |||||||||
| Baseline | 106 | 0.6737 | 0.2431 | 112 | 0.6141 | 0.2776 | 0.0118 | –0.0548 to 0.0893 | 0.742 |
| 9 months | 100 | 0.6827 | 0.2493 | 103 | 00.6142 | 0.2854 | 0.0421 | –0.0232 to 0.1250 | 0.273 |
| Proxy QALYs | |||||||||
| 9 months | 98 | 0.5049 | 0.1574 | 101 | 0.4637 | 0.1907 | 0.0158 | –0.0088 to 0.0508 | 0.273 |
| Costs (£, 2020/21 prices) | Model | Independent – enhanced | ||||||
|---|---|---|---|---|---|---|---|---|
| Independent (N = 111) | Enhanced (N = 115) | |||||||
| Valid n | Mean | SD | Valid n | Mean | SD | Adjusted mean difference | 95% CI | |
| a: IST model cost | 110 | 7591.5 | – | 115 | 3735 | – | ||
| b: health and social care costs | 98 | 15,324.18 | 30,301.5 | 102 | 15,302.66 | 25,786.9 | –3409.95 | –9957.92 to 4039.89 |
| c: unpaid carer costs | 100 | 8963.4 | 8010 | 106 | 10,520.8 | 7450.8 | –1123.01 | –2727.50 to 621.51 |
| Total health and social care costs, excluding informal care (a + b) | 98 | 22,915.6 | 30,301.5 | 102 | 19,037.6 | 25,786.9 | 446.55 | –5637.60 to 7519.30 |
| Total health and social care costs, including informal care (a + b + c) | 98 | 31,850.8 | 31,385.1 | 102 | 29,852.8 | 26,754.9 | –855.80 | –8342.54 to 6059.69 |
| Challenging behaviour score (ABC-C) at 9 months | 101 | 49 | 32 | 107 | 56 | 34 | –5.07 | –14.93 to 2.14 |
| QALYs (EQ-5D-5L proxy) at 9 months | 98 | 0.5049 | 0.1574 | 101 | 0.4637 | 0.1907 | 0.0158 | –0.0088 to 0.0508 |
| Perspective | ||
|---|---|---|
| Health and social care | Societal | |
| Incremental costs (£), mean (95% CI)a | 446.55 (–5637.60 to 7519.30) | –855.80 (–8342.54 to 6059.69) |
| Incremental effect, mean (95% CI) | ||
| Points improvement in ABC-C score | –5.07 (–14.93 to 2.14) | –5.07 (–14.93 to 2.14) |
| QALY EQ-5D-5L, proxy score | 0.0158 (–0.0088 to 0.0508) | 0.0158 (–0.0088 to 0.0508) |
| ICERs | ||
| Additional cost per additional point improvement in the ABC-C scale (£) | 88.08 | –168.79 |
| Additional cost per additional QALY (£) | 28,262.66 | –54,164.56 |
| Perspective | ||
|---|---|---|
| Health and social care | Societal | |
| Sensitivity analyses | ||
| Using new adjusted incremental costs, mean (95% CI)a | 2997.14 (–4191.248 to 11,461.4) | 1167.53 (–7528.34 to 9816.40) |
| Using new adjusted incremental outcome (ABC-C score)b | –5.96 (–17.79 to 3.78) | –5.96 (–17.79 to 3.78) |
| Using new adjusted incremental outcome (QALY EQ-5D-5L proxy score)c | 0.0704 (0.0064 to 0.1498) | 0.0704 (0.0064 to 0.1498) |
| ICERs | ||
| ICER using new adjusted incremental costs | ||
| Incremental outcome (ABC-C) unchanged: incremental cost per outcome (ABC-C score) | 591.15 | 230.28 |
| Incremental outcome QALYs EQ-5D-5L proxy unchanged: incremental cost per outcome (QALY EQ-5D-5L proxy score) | 189,692.41 | 73,894.30 |
| ICER using new adjusted incremental outcome (ABC-C) | ||
| Incremental cost unchanged: incremental cost per outcome (ABC-C score) | 74.92 | –143.59 |
| ICER using new adjusted incremental QALYs EQ-5D-5L proxy score | ||
| Incremental costs unchanged: incremental cost per outcome (QALY EQ-5D-5L proxy score) | 6343.04 | –12,156.25 |
Figures
FIGURE 10.
Scatterplot showing the bootstrapped mean differences in health and social care costs and effects (ABC-C total score) of the independent model compared with the enhanced model.
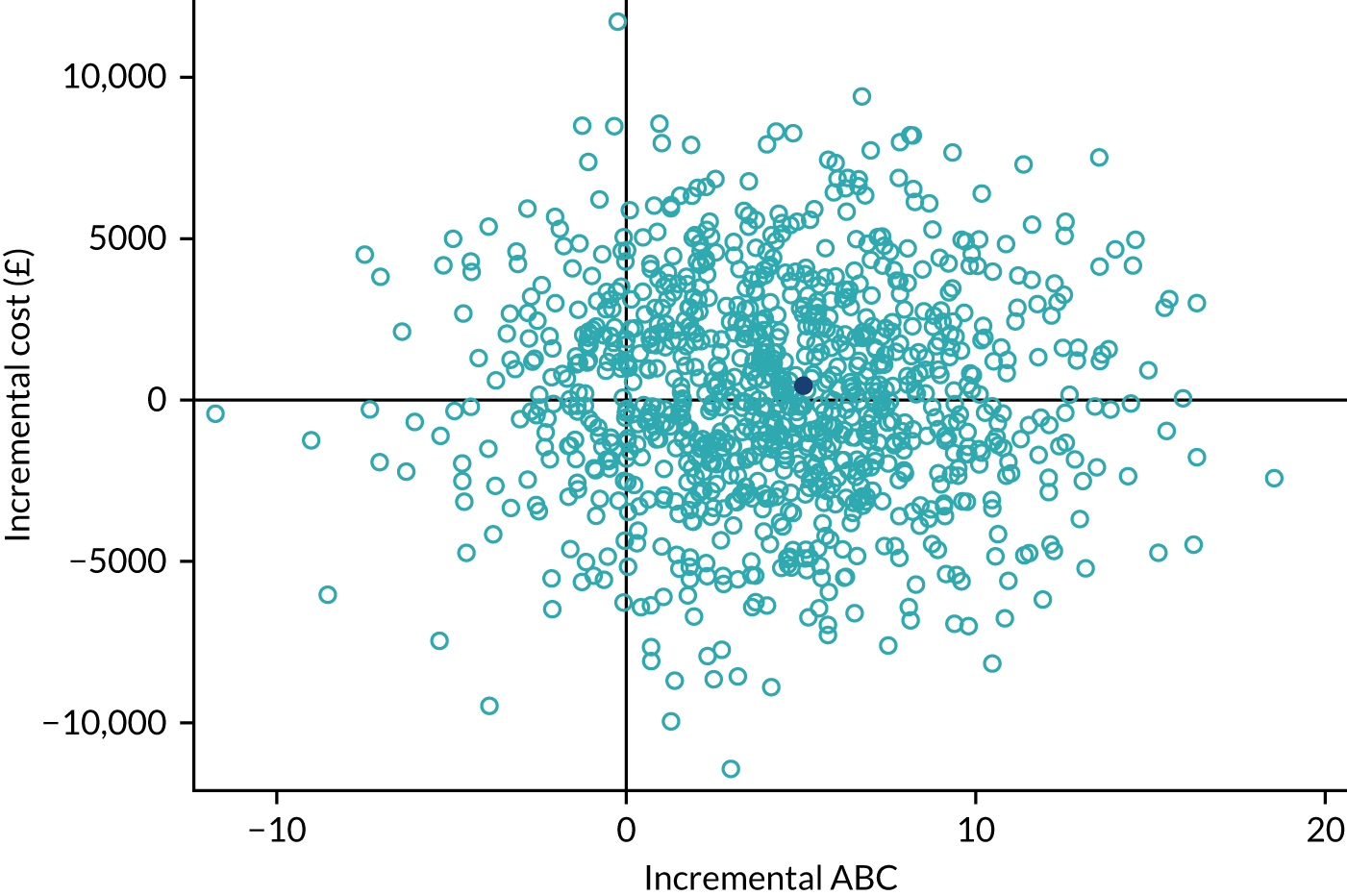
FIGURE 11.
The CEAC showing the probability that the independent model is cost-effective compared with the enhanced model: health and social care perspective, with cost-effectiveness measured by ABC-C score at 9 months. The dashed line indicates a willingness-to-pay threshold of £500.
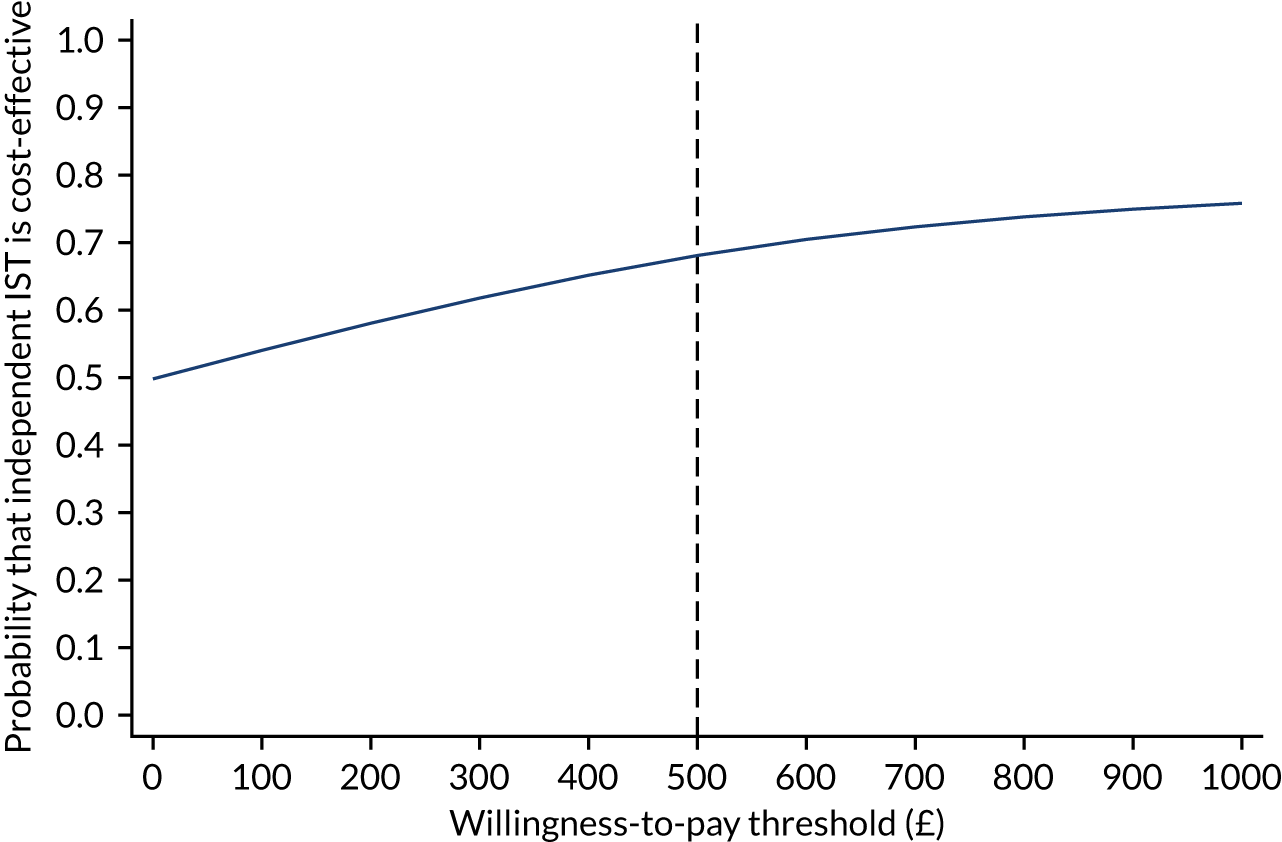
FIGURE 12.
Scatterplot showing the bootstrapped mean differences in health and social care costs and effects (QALYs) of the independent model compared with the enhanced model.
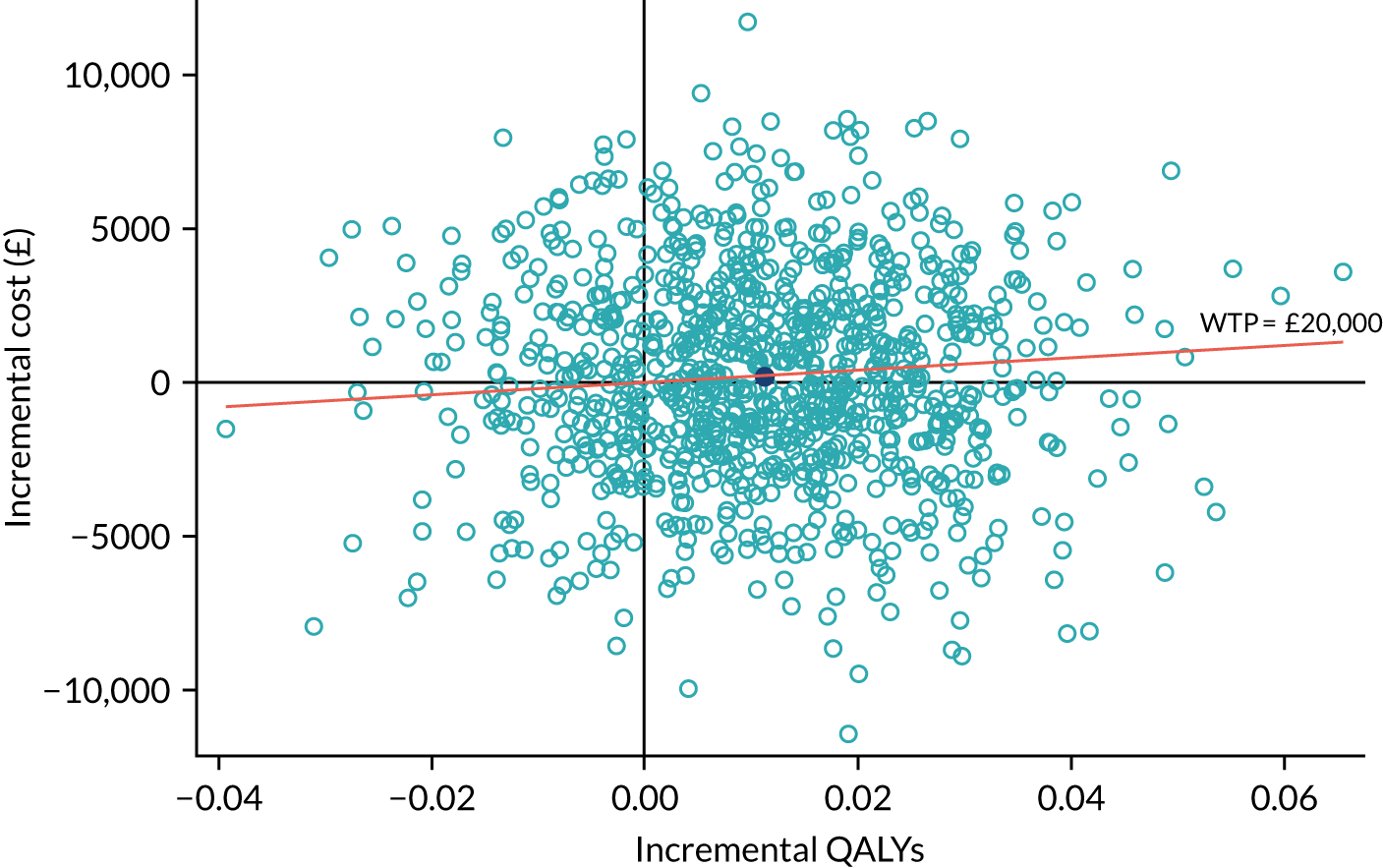
FIGURE 13.
The CEAC showing the probability that the independent model is cost-effective compared with the enhanced model: health and social care perspective, with cost-effectiveness measured in QALYs over 9 months. The dashed lines indicate the NICE-preferred willingness-to-pay levels of £20,000–30,000.
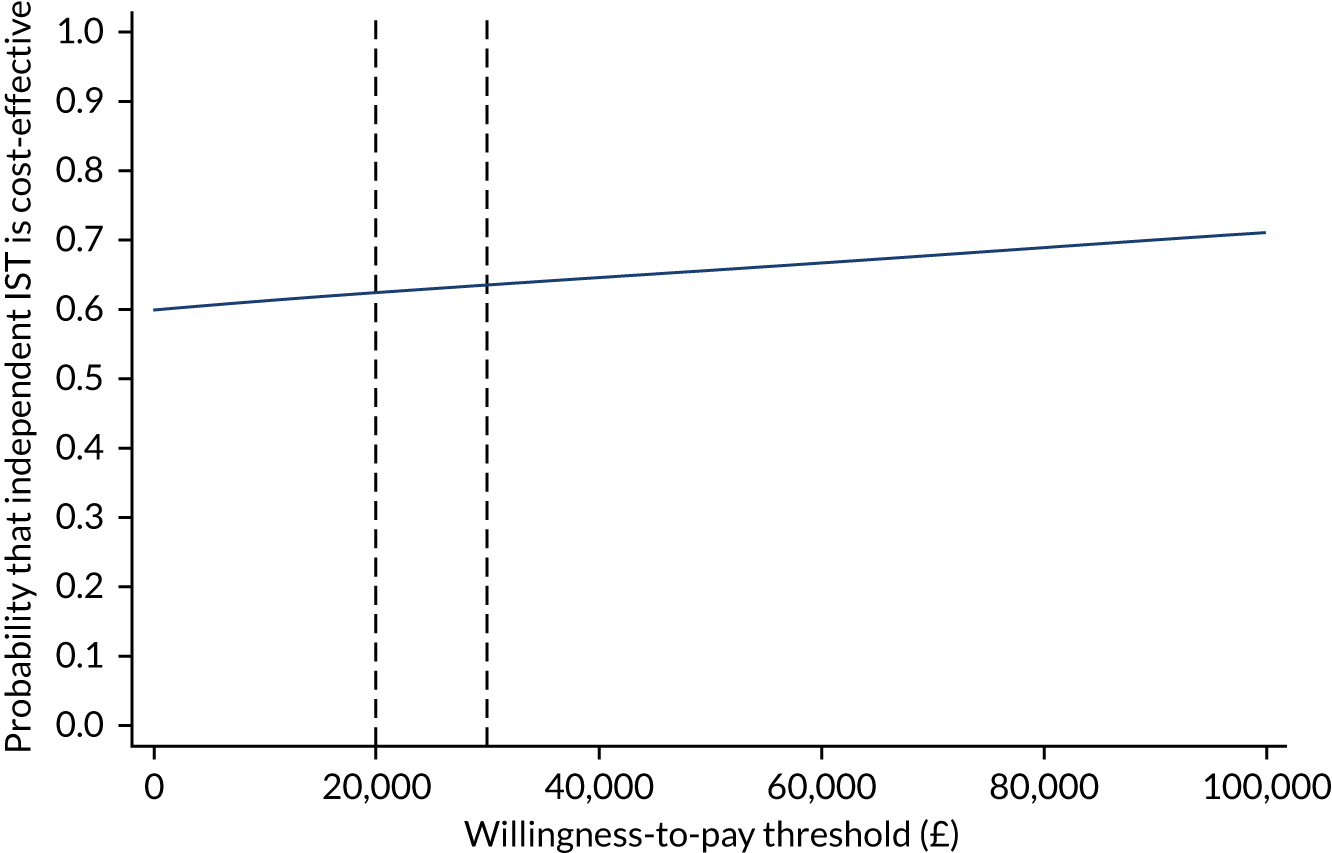
FIGURE 14.
Scatterplot showing the bootstrapped mean differences in societal costs and effects (ABC-C total score) of the independent model compared with the enhanced model.
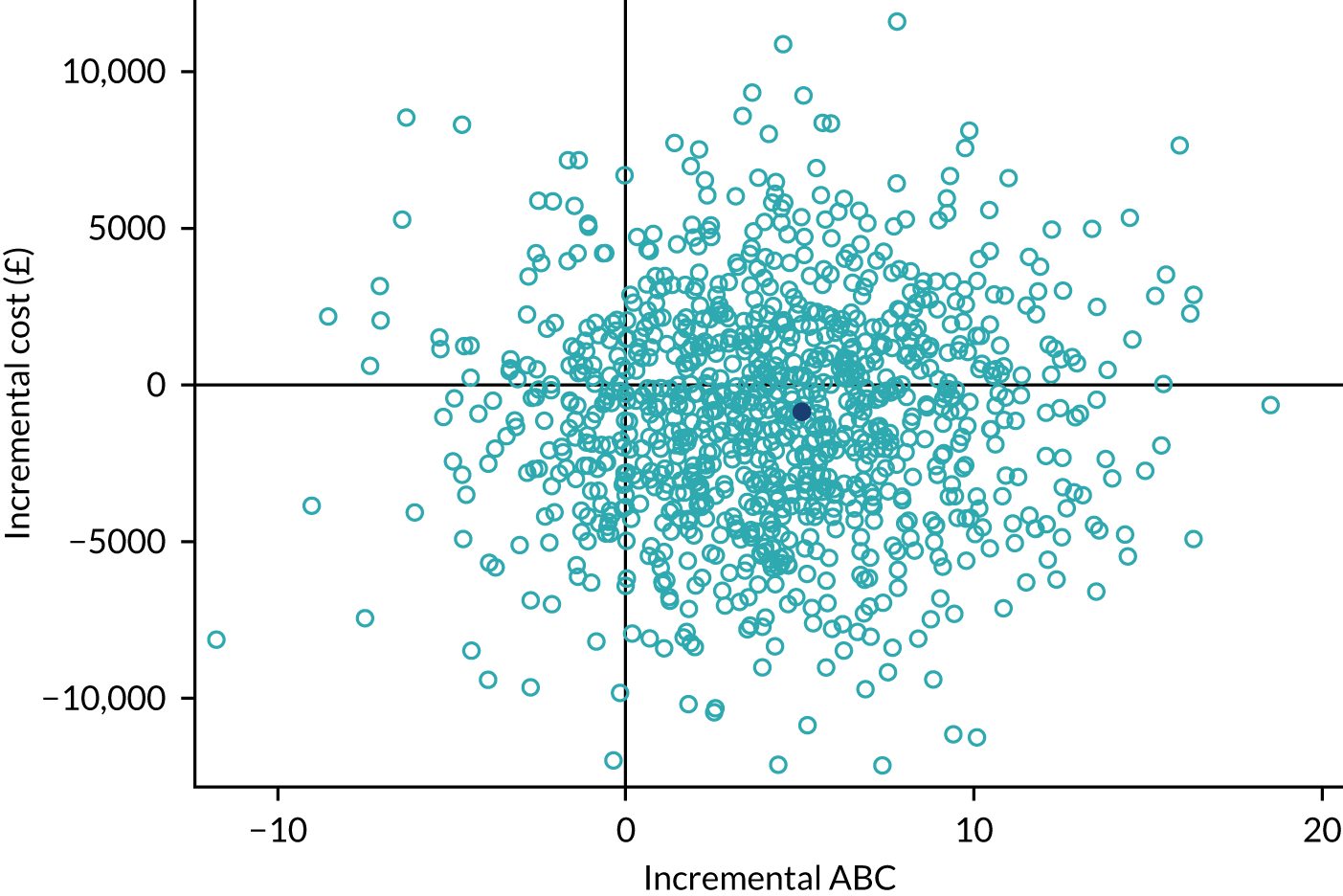
FIGURE 15.
The CEAC showing the probability that the independent model is cost-effective compared with the enhanced model: societal perspective, with cost-effectiveness measured by ABC-C score at 9 months. The dashed line indicates a willingness-to-pay threshold of £500.
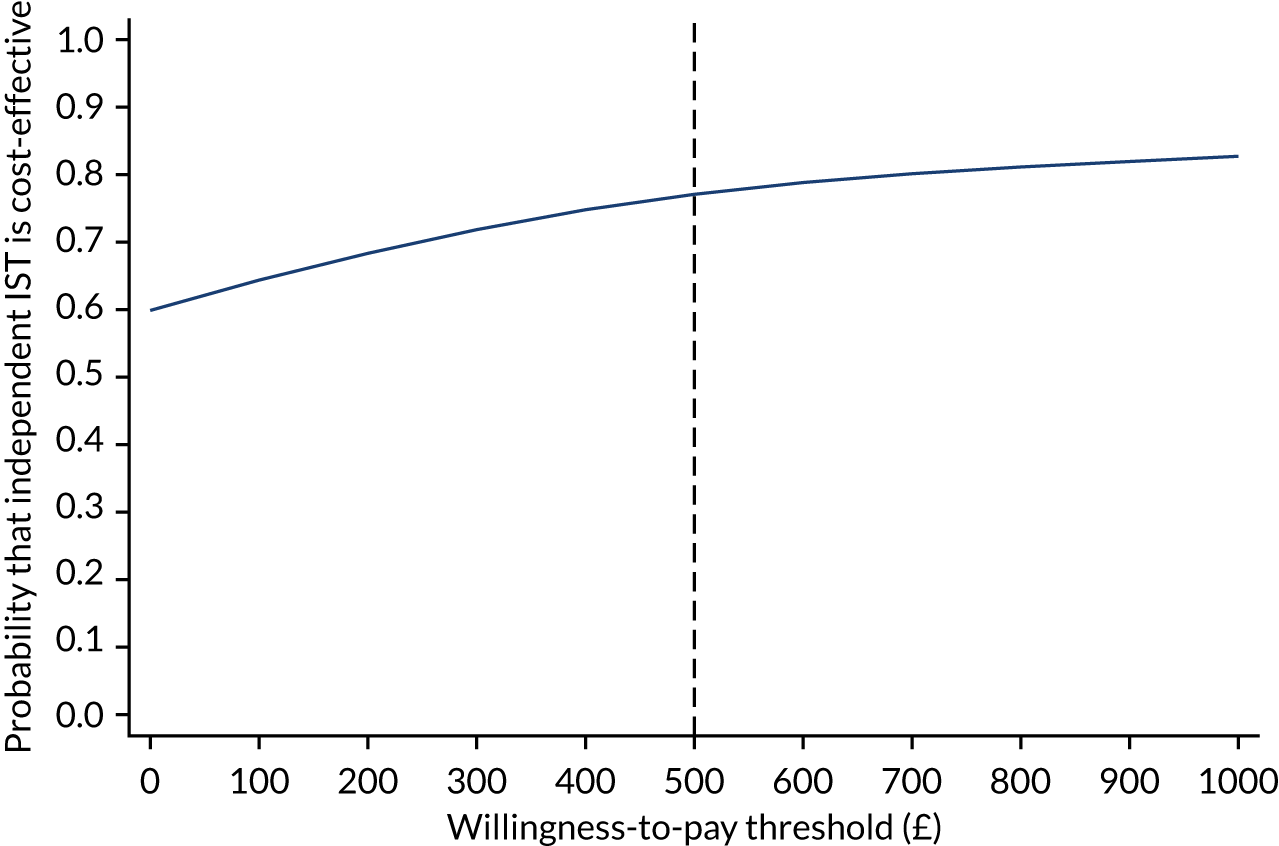
FIGURE 16.
Scatterplot showing the bootstrapped mean differences in societal costs and effects (QALYs) of the independent model compared with the enhanced model.
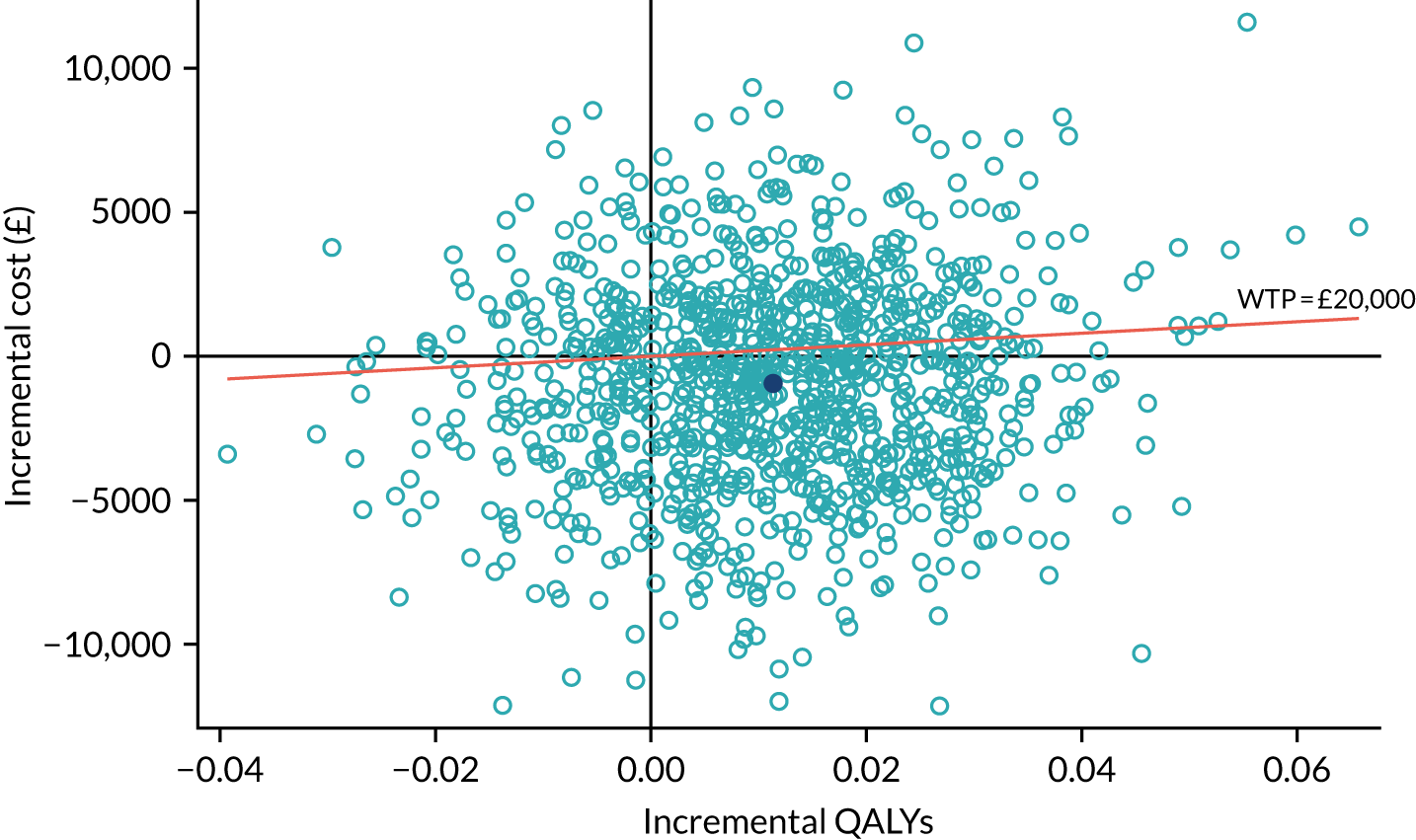
FIGURE 17.
The CEAC showing the probability that the independent model is cost-effective compared with the enhanced model: societal perspective, with cost-effectiveness measured in QALYs over 9 months. The dashed lines indicate the NICE-preferred willingness-to-pay levels of £20,000–30,000.
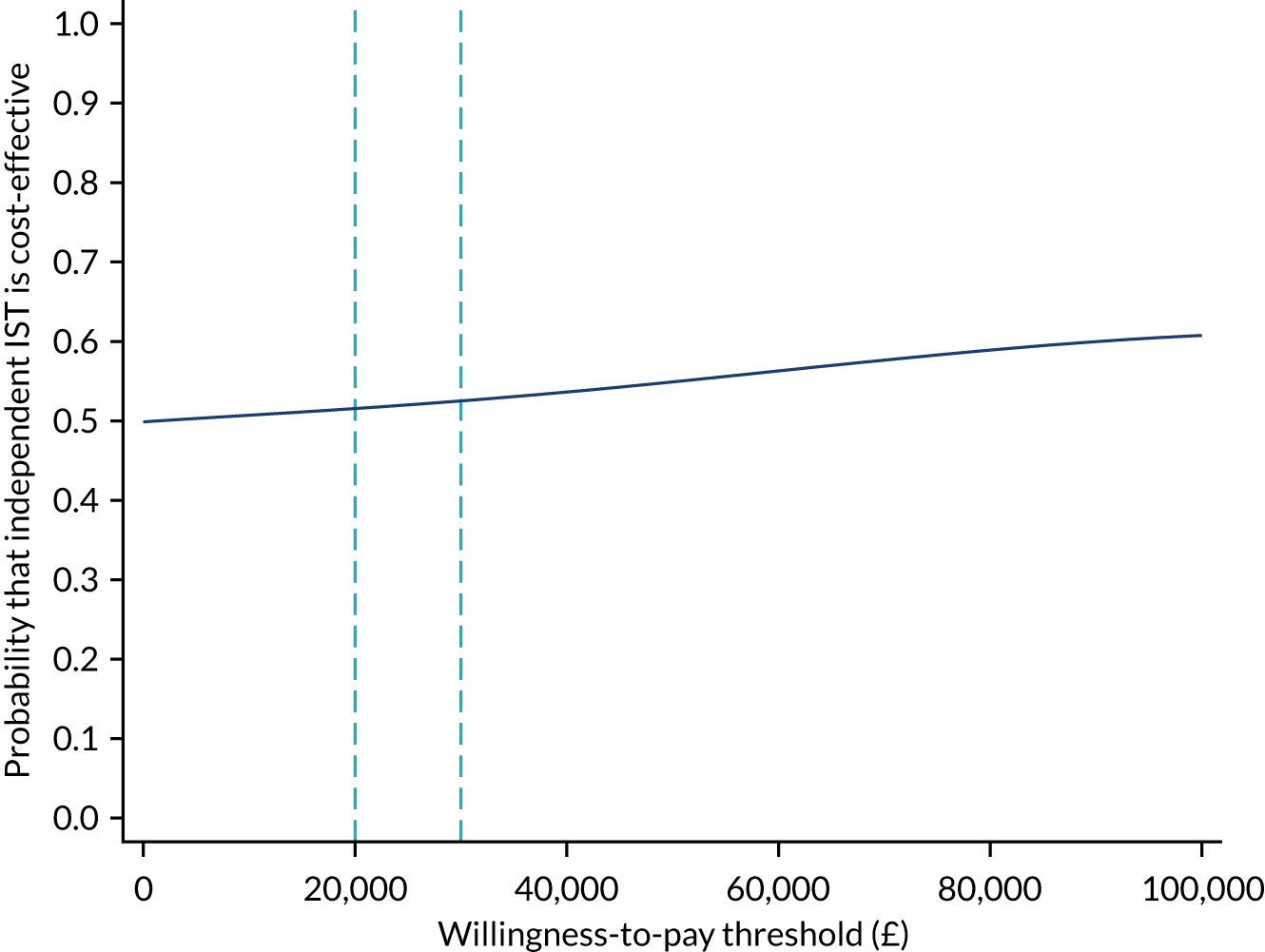
FIGURE 18.
Sensitivity analysis: CEAC showing the probability that the independent model is cost-effective compared with enhanced model – health and social care perspective, with cost-effectiveness measured by ABC-C score at 9 months and health and social care costs adjusted. The dashed line indicates a willingness-to-pay threshold of £500.
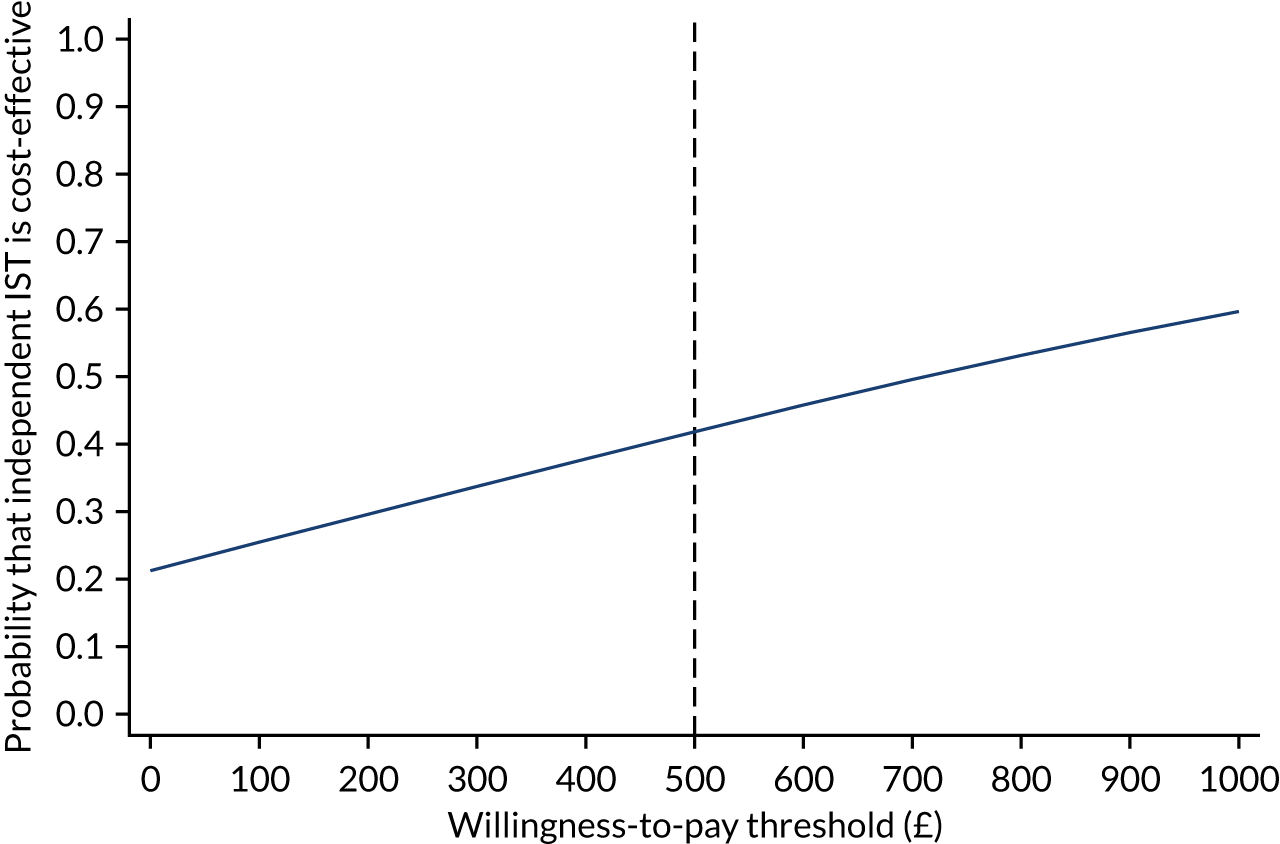
FIGURE 19.
Sensitivity analysis: CEAC showing the probability that the independent model is cost-effective compared with the enhanced model – societal perspective, with cost-effectiveness measured by ABC-C score at 9 months and societal costs adjusted. The dashed line indicates a willingness-to-pay threshold of £500.
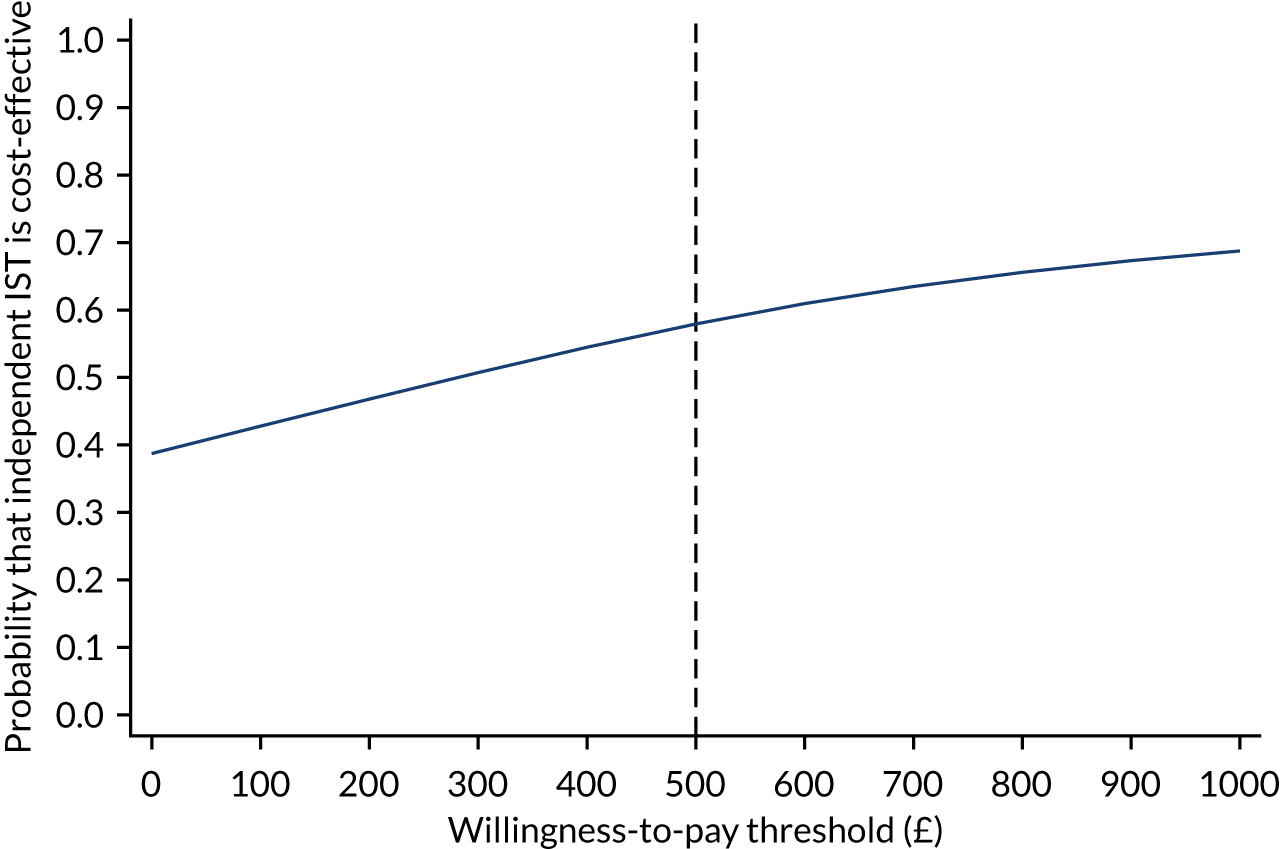
FIGURE 20.
Sensitivity analysis: CEAC showing the probability that the independent model is cost-effective compared with the enhanced model – health and social care perspective, with cost-effectiveness measured in QALYs at 9 months and health and social care costs adjusted. The dashed lines indicate the NICE-preferred willingness-to-pay levels of £20,000–30,000.
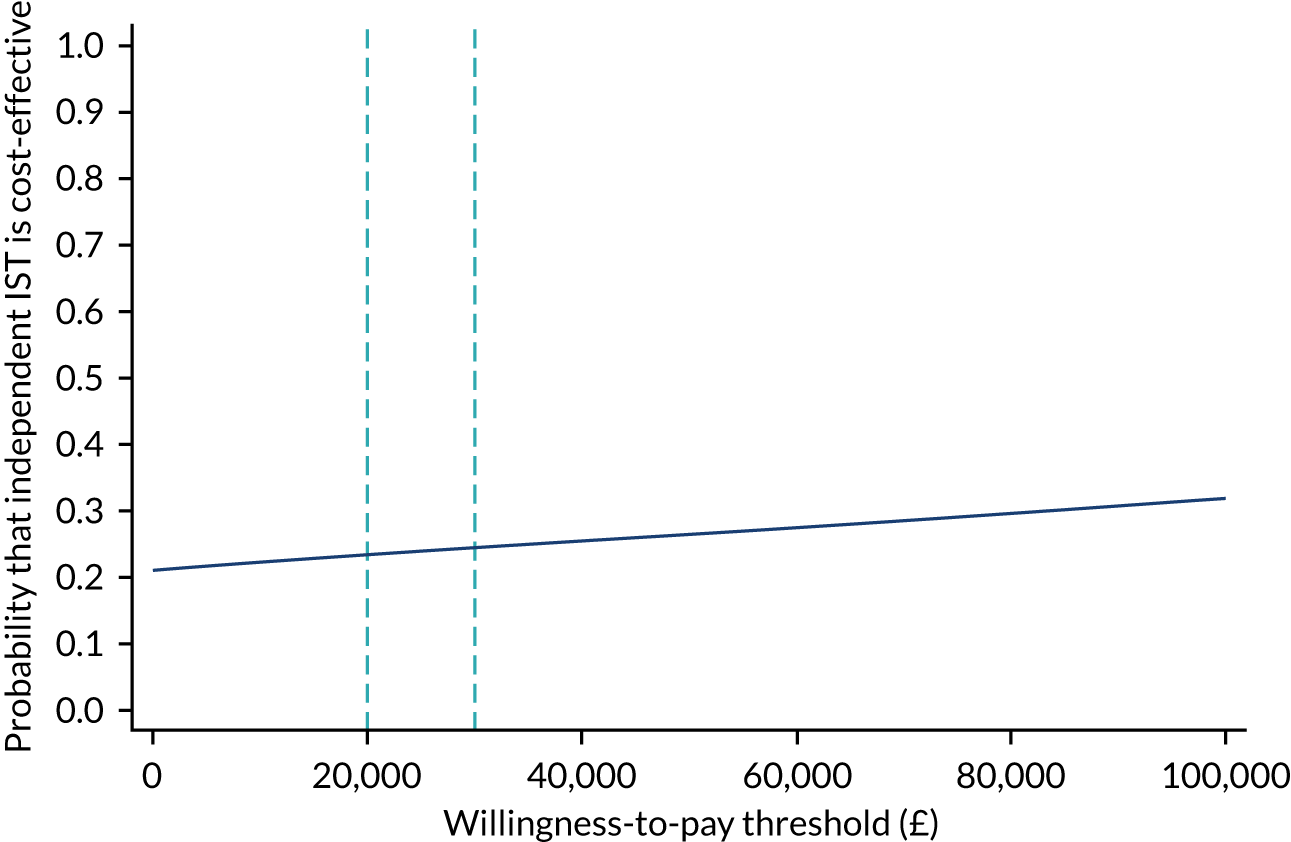
FIGURE 21.
Sensitivity analysis: CEAC showing the probability that the independent model is cost-effective compared with the enhanced model – societal perspective, with cost-effectiveness measured in QALYs over 9 months and societal costs adjusted. The dashed lines indicate the NICE-preferred willingness-to-pay levels of £20,000–30,000.
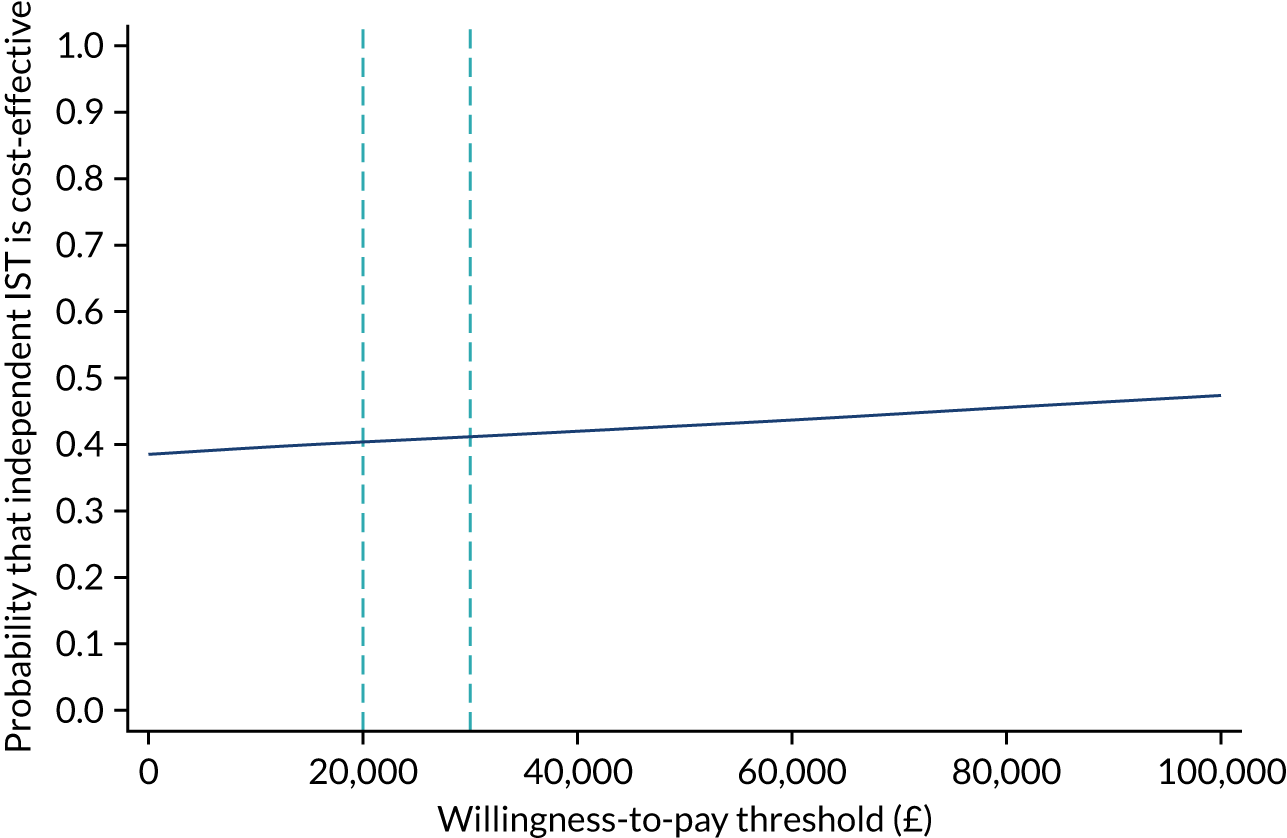
Appendix 2 Chapter 6 documents
The intensive support teams for adults with intellectual disabilities and challenging behaviour study: qualitative ‘case study’ sites selection
Three ISTs were selected from the enhanced model.
IST 1
Summary
-
Location: urban.
-
Caseload: 17 patients.
-
Setup: integrated, operates as a separate ‘Challenging Needs pathway’ within the community learning disability team (CLDT) (integrated health and social care).
-
NHS funded.
-
Multidisciplinary team.
-
Operating hours: community team can provide emergency social care support 24/7, pathway input extended hours Monday–Friday.
-
IST intensity: no specific response time target, typically input twice per week, average time of support > 12 months.
-
Team established: Community Team for People with Learning Disabilities (CTPLD) 2010; new ‘Challenging Needs pathway’ finalised in January 2019.
-
Outcome measures: Challenging Behaviour Interview, HoNOS-LD, quality-of-life measures and Frenchay Activities Index.
The IST 1 care pathway for people with learning disabilities who present with challenging needs is a pathway that has been created within the wider integrated health and social care team: the IST 1 adult CTPLD. The CTPLD offers support for adults aged ≥ 18 who have a diagnosis of a learning disability. The pathway does not manage patients with a learning disability and mental health problem.
All of the CTPLD are co-located and the CTPLD includes health and social care professionals, for example social workers, speech and language therapists, physiotherapists, learning disability nurses, clinical psychologists, a consultant psychiatrist, advanced nurse practitioners and PBS practitioners.
Eligibility to receive services is based on being registered with a local GP and living in the borough. Referrals can be either made by other professionals or self-referrals. Referrals are often made by the duty support worker. There is no specified response time target. The service estimates that 90% of their referrals have a neurodevelopmental disorder diagnosis.
The CTPLD emergency duty team provides social care support 24/7; however, the health support is currently available Monday–Friday, 09.00–17.00 only. Support needs are identified through a holistic assessment and support-planning process. An assessment can be offered to an adult with needs, a carer with needs arising from caring for another adult, young people with care needs, and young carers who are moving towards adulthood.
IST 2
Summary
-
Location: rural.
-
Caseload: > 200 patients.
-
Setup: standalone team on the same site as the CLDT.
-
Social enterprise.
-
Multidisciplinary team.
-
Operating hours: normal working hours, Monday–Friday.
-
IST intensity: not a crisis service, no specific response time target, intensity depends on individual needs, normally input for > 12 months.
-
Team established: 2010.
-
Outcome measures: none.
The IST is a fully integrated health and social care provider, and is part of an employee-owned social enterprise that is a community benefit society. It is part of the Adult Learning Disability Team, which consists of the IST, CLDT, Adult Learning Disability Psychology Service and the Carers Support Service. More recently, a new team for Adults with Autism has been added.
The IST consists of two clinical psychologists (FTE), a speech and language therapist (0.2 FTE), a consultant psychiatrist (0.2 FTE), a behaviour nurse therapist (FTE) and four behaviour support workers. The team leader is one of the consultant clinical psychologists and also manages the CLDT and the high-functioning autism service. The IST has retained the same staff from when it was established in 2010 and all posts are filled. The manager would like to develop a role for a prescribing nurse in the team to address the STOMP agenda;20 they would also like to develop and review their managing of risk and develop user involvement in the IST.
They accept referrals (including self-referrals) from adults aged ≥ 18 years with any severity of learning disability and will support people with specific mental health problems as well. The team will also work to support the families and paid carers who work with the service user.
IST 3
Summary
-
Location: rural.
-
Caseload: > 250 patients.
-
Setup: standalone team (no community team support) split over two sites.
-
NHS funded.
-
Multidisciplinary team.
-
Operating hours: normal working hours, Monday–Friday.
-
IST intensity: operates a waiting list (normally < 1 month), operates a duty line on weekdays 09.00–17.00 that rotates with band 6+ staff, intensity based on risk and intervention needed, average input 6–12 months.
-
Team established: 2016.
-
Outcome measures: none.
The role of IATTs is to support families, paid carers and other services in their delivery of health-related interventions for people with a learning disability who are experiencing or causing others high levels of distress. The North and Mid team are split into two teams. The team covers a very large geographical area. They are standalone teams that do not have an additional layer of community support.
Combined, the two teams consist of six learning disability nurses (0.4 FTE), one psychiatrist (FTE), one staff-grade doctor (FTE), four clinical psychologists (FTE), two occupational therapists (FTE), four speech and language therapists (FTE), one social worker (post not filled), five assistant practitioners (FTE), two trainee nurses (posts not filled) and one trainee psychologist (post not filled).
The team operates a duty line that operates 09.00–17.00 on weekdays and the telephone rotates between band 6+ staff, who act as professional advisors. All referrals have to be made through this line. The team adapted to an IST/IATT model from a CLDT model in about 2016. Some challenges appear to be arising because they have a high threshold for their referral criteria (potential placement breakdown and evidence of moderate to severe learning disability), which means that a lot of the populations who need additional support do not currently receive it owing to the lack of a CLDT.
Intensive support team 3 has two defined pathways of care and intervention (challenging behaviour and mental health and complex health) and a further pathway is in development for adults with learning disabilities and dementia. It is a very large team to manage and is split over two bases, which makes cohesiveness more challenging. IST 3 appears to be very stretched in terms of meeting the needs of their very large caseload and is also faced with the challenges of the county, that is shortages of specialist social care and service providers. The manager of the team also felt that there was a gap in autism provision for individuals with challenging behaviour but borderline learning disability.
Four ISTs were selected from the independent model.
IST A
Summary
-
Location: urban.
-
Caseload: 15 patients.
-
Setup: IST embedded within the community HLDP.
-
NHS funded.
-
Multidisciplinary team.
-
Operating hours: normal working hours, Monday–Friday.
-
IST intensity: no specific targets, average input time > 12 months but meant to be maximum of 12 months.
-
Team established: 2012.
-
Outcome measures: HoNOS-LD.
Intensive support team A is embedded within the local CLDT and is based within the same building. It was established as an alternative to inpatient hospital care. The team consists of one dedicated assessment intervention team nurse (FTE), one consultant psychiatrist (0.2 FTE), one psychologist (0.4 FTE), three community nurses and two assistant psychologists (FTE).
Intensive support team A adheres to the Challenging Behaviour: A Unified Approach101 model as a template for best practice. Its aim is to support adults with intellectual disabilities whose placements are at risk of breaking down because of a significant mental illness and/or challenging behaviour, and who require intensive multidisciplinary support to maintain them in the community. Once the team receives a referral (through the CLDT only, using a referral form) they will make pre-assessment contact within 5 working days. The team does not work with people presenting for the first time in a crisis; this work is undertaken by the community team before referring to the IST if considered necessary. The team will work with those who are on the IST caseload who present in a crisis while under their care. Some challenges picked up by the survey include recruiting to vacant posts, especially learning disability nursing posts, discharging people from the caseload and the management of team data.
IST B
Summary
-
Location: urban.
-
Caseload: 37 patients.
-
Setup: standalone team.
-
NHS funded.
-
Multidisciplinary team.
-
Operating hours: 7 days per week, extended hours.
-
IST intensity: responds quickly within 24 hours. Input can range from daily to once per fortnight depending on need, mode frequency 1–2 times per week. Average input is for 3–6 months.
-
Team established: 2015.
-
Outcome measures: HoNOS-LD and Maslow Assessment of Needs Scale – Learning Disabilities.
There are two standalone ISTs in the area. They work in close partnership with the CLDTs. IST B accepts referrals from health and social care colleagues. It operates 7 days per week, during which referrals can be made and received at any time and will be responded to within 24 hours. Every accepted referral receives an initial assessment, which may conclude that another team/service is best placed to handle the referral.
The team consists of six learning disability nurses (FTE), one psychiatrist (0.15 FTE), one clinical psychologist (0.5 FTE), one assistant psychologist (0.5 FTE), one behaviour specialist (FTE), one occupational therapist (FTE), two speech and language therapists (0.4 FTE), one doctor (0.4 FTE) and one support worker (FTE). The team is nurse-led, and the nurse also manages the community learning disability nurses across 4–5 CLDTs.
The team are currently piloting a programme called the ‘Asperger’s group’ locally, in which the team accepts referrals for individuals with autism but no learning disability who present with a challenging behaviour, unless that behaviour is better understood as a symptom of a mental health condition. This came into place because this population was falling through the net and not being seen by mental health or learning disability services. Working with individuals they have not previously been familiar with is presenting some challenges. The team are also starting to reduce the minimum age from 18 years to 17.5 years to help the transition from child to adult services if required.
IST C
Summary
-
Location: rural.
-
Caseload: 4 patients.
-
Setup: IST embedded within the CLDT.
-
NHS funded.
-
Multidisciplinary team.
-
Operating hours: 7 days per week, extended hours (can work 24/7 hours if required).
-
IST intensity: responds quickly within 24 hours and completes assessment within 48 hours. Input is initially daily and then ≥ 3 times per week. Average input is for 3–6 months.
-
Team established: 2017.
-
Outcome measures: Behaviour Problems Inventory and Health Equalities Framework.
The IST C is a small team embedded within the CLDT that works very intensively with its small caseload and a highly person-centred approach. The IST operates between 08.00 and 20.00, but can work 24/7 if needed. The IST struggles to recruit to their posts (mainly because of their rural location) and also covers a very large area. The IST only takes referrals from the CLDT via e-mailed referral forms. The team feel like they need to expand in staff numbers to be more effective and enable them to provide more training throughout the area.
The IST consists of five learning disability nurses (3 FTE), one clinical psychologist (0.2 FTE), one occupational therapist (0.5 FTE), one speech and language therapist (FTE) and one support worker (FTE). Some of the staff are rotated between two ISTs. The service manager also manages another local IST. The manager is also discussing developing a new forensic IST.
The IST feels that there is a real lack of appropriate placements in the area and not enough social care resources, so the IST spend a lot of their time providing bespoke training for service providers. The manager would like a dedicated social worker within the team but one can be pooled from a neighbouring IST when needed. The IST may also get involved with people who are currently in hospital to help plan transitions into placements.
IST D
Summary
-
Location: rural.
-
Caseload: 28 patients.
-
Setup: standalone IST.
-
NHS funded.
-
Multidisciplinary team.
-
Operating hours: 08.00–20.00 on weekdays, 09.00–17.00 at weekends, and a 24/7 line operating on shifts.
-
IST intensity: can respond to ‘then and there’ crisis resolution. For planned referrals, it will respond within 7 days and complete initial assessment within 7 days. Input ≥ 3 times per week. Average input is for 6–12 months.
-
Team established: 2003, but restructured in 2018.
-
Outcome measures: Life Star.
The IST has been through recent changes, starting in January 2018. The IST has had a change of service specification and a redesign; it also now accept referrals for people with autism in some forms without learning disabilities, and adults aged ≥ 16 years. They have also changed their working hours and now offer a 24/7 service by working in shifts. They are a standalone team based in the city centre.
The team consists of seven learning disability nurses (FTE), two clinical psychologists (0.8 FTE), one occupational therapist (FTE), two speech and language therapists (1.8 FTE) and 10 support workers (9.2 FTE). The manager is a speech and language therapist by background. The manager would like to add an assistant psychologist and an art therapist to the team.
The IST feels that it is very commissioner facing and it catches up with commissioners once per month about which patients are in beds. All professions are operationally managed via the manager of the IST. The manager feels that having assistant practitioners really helps them as it means they can put the hours in to implement the treatment plan; however, this is perhaps still not to the extent that commissioners want in terms of ‘wrap around support’. They have found it much more difficult to recruit into nursing posts. The entire team sits in the same building and has a weekly meeting together. The IST also has reflective practice sessions led by a clinical psychologist, which are very well attended and necessary. The IST has a formal meeting for each service user every 2 weeks.
Now that the IST is offering support for individuals with autism without learning disabilities that are at risk of hospital admission and adults aged ≥ 16 years old, the IST has a lot more work providing support to additional teams. They began to provide an on-call service 24/7 in January 2019. Team members on shift will take the on-call telephone home with them. In the office, hours are 08.00–20.00 on weekdays and 09.00–17.00 at the weekend. IST D used to be a much larger team but felt that it was not very effective at that size.
List of abbreviations
- 24/7
- 24 hours per day, 7 days per week
- ABC-C
- Aberrant Behaviour Checklist-Community, version 2
- ADHD
- attention deficit hyperactivity disorder
- A&E
- accident and emergency
- AfC
- Agenda for Change
- ASD
- autism spectrum disorder
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CIDS
- community intellectual disability service
- CLDT
- community learning disability team
- CSRI
- Client Service Receipt Inventory
- CTPLD
- community team for people with learning disabilities
- CTR
- care and treatment review
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- FTE
- full-time equivalent
- GP
- general practitioner
- HEAP
- health economics analysis plan
- HoNOS-LD
- Health of the Nation Outcome Scales for People with Learning Disabilities
- IATT
- intensive assessment and treatment team
- ICER
- incremental cost-effectiveness ratio
- ICF
- informed consent form
- IQR
- interquartile range
- IST
- intensive support team
- IST-ID
- intensive support teams for adults with intellectual disabilities and challenging behaviour
- NHSCII
- NHS Cost Inflation Index
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- PAS-ADD
- Psychiatric Assessment Schedule for Adults with Developmental Disabilities
- PBS
- positive behaviour support
- PIS
- participant information sheet
- PMG
- Project Management Group
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- QoL-Q
- Quality of Life Questionnaire
- SABS
- Short Adaptive Behaviour Scale
- SD
- standard deviation
- START
- Systemic, Therapeutic, Assessment, Resources, and Treatment
- STOMP
- Stopping The Over-Medication of People with an intellectual disability, autism or both
- TAG
- Threshold Assessment Grid
- UCL
- University College London
