Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 16/52/23 . The contractual start date was in February 2018. The final report began editorial review in December 2020 and was accepted for publication in June 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Latter et al. This work was produced by Latter et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Latter et al.
Chapter 1 Introduction
Background and rationale
Patient/carer access to medicines at end of life (EoL) is critical for control of symptoms, including pain and distress, and recent evidence confirms that medicines optimisation at EoL is a research priority area for patients and carers. 1,2 The symptom of pain is a leading cause of concern among patients and the public in relation to EoL and dying, and analgesic use is a crucial part of effective symptom management. 3 Although, to the best of our knowledge, there are no detailed studies, research in related areas conducted over the last few years suggests that prescription, dispensing, supply and associated information given about medicines (see Glossary, Medicines access) are often considered difficult, complex, demanding, lacking co-ordination and involving a multiplicity of health-care professionals (HCPs) by patients using these services. 4,5 In one of the only few related studies,6 patients in the USA experienced barriers to accessing medicines, resulting in insufficient medication and delays in pain relief, or ‘diligent pain management efforts by multiple clinicians in multiple settings resulted in an oversupply of pain medications for some patients and raised issues related to communication, co-ordination, and safety’. In addition, we have accounts from community nurses (CNs) that they expend much effort in ensuring that patients on their caseloads are able to access medicines (e.g. by collecting prescriptions from general practices and delivering them to patients). 7 The British Medical Association (London, UK) highlighted three areas (i.e. system, professional and patient) where barriers specific to accessing pain relief at EoL can operate. 3 System barriers revolved around regulation and guidance, use of opioids and the nature of palliative care service provision. A review of UK cancer registry and primary care patient data by Ziegler et al. 8 highlighted EoL patients’ lack of access to opioids and suggested that this was strongly associated with hospital death. 8 The authors concluded that ‘to date no UK research has systematically charted and evaluated patient experience of medicines access during the last year of life’. 8
Internationally, research has repeatedly highlighted patients’ and carers’ needs for information regarding medicines in the EoL context,9,10 and a recent systematic review evaluating educational interventions to help carers manage medicines on behalf of patients in the home indicated that solutions remain elusive. 2 Recent work by this report’s authors focused on developing and testing education-focused interventions for pain and related medicines management in the home. 4,5,11 However, our experience during these studies has suggested that the information patients and carers receive about medicines at a key point earlier in the patient pathway (i.e. when medicines are prescribed, dispensed and supplied to them) has a critical influence on their ability to self-manage medicines in the home. Data generated from these studies suggested that, not just in relation to information given, these patients’ and carers’ experiences of prescribing, dispensing and supply were in themselves key influences on patient/carer medicines management, symptom control and subsequent unplanned use of out-of-hours (OOH) services and, yet, their experiences were problematic. In the UK context, little is known about this important aspect of patient and carer experience.
The delivery of EoL care is characterised by the involvement of a number of different professional groups and organisations. Typically, a patient’s care may include the involvement of palliative care specialists, along with generalists, and primary, secondary and community care specialists, as well as care from the voluntary sector (e.g. charity-funded hospice care). Although it is acknowledged that there may be patient and carer access problems with traditional systems, including general practitioner (GP) services (a significant provider of EoL care at home), little is known about these problems from the perspective of HCPs. Nurses take a lead role in providing community-based EoL care, but limited evidence suggests that here too there might be problems (e.g. nurses find it difficult to access GP services for EoL prescriptions8,12 and prescribing by palliative care nurses may not have been exploited to its full potential13,14). Moreover, community pharmacists’ (CPs) expertise in palliative care medicines optimisation remains underdeveloped. 15,16 There is a lack of in-depth research into the underlying context or causes of these issues, as well as their wider impact on patient experience of access to medicines. The National Institute for Health and Care Research’s (NIHR) themed review of EoL care research highlighted the need for innovative models of care. 17 Although there are some promising innovations in EoL care, such as pharmacist-attached palliative care teams, OOH support and community pharmacy-commissioned palliative care medicines services, the impact of these innovations on patient access to medicines, as well as their cost-effectiveness comparative to more traditional delivery models, remains largely unevaluated.
Our recent research suggests that the supply chain ‘upstream’ may be a contributing factor to the complexity and problems with access experienced by patients. 4,5 For example, patients and carers report a disconnection between prescriber choice of medicine/formulation/strength and pharmacy stocks, with prescriptions written without knowledge of currently available stock. Even when staff at a patient’s regular pharmacy make efforts to ensure stocks of a patient’s ‘usual’ medicine, rapid changes during EoL care may lead to newly prescribed medicines not being stocked. For medicines not in stock at the time the prescription is presented, the impact of a medicines wholesaler’s opening hours and delivery times OOH may block timely patient access. Previous research with wholesalers and distributors into the supply chain of medical products to patients concluded that ‘The consequences of supply disconnection revealed haphazard supply, unmet user needs and lack of information transfer between player groups’, including lack of patient feedback to wholesalers and distributors on the impact of their practices on patient access. 18 However, to our knowledge, the CP, wholesaler and distributor perspectives on the supply chain of EoL medicines have not been investigated. Therefore, they warrant examination to understand the contribution these different groups make to service delivery and the patient experience of medicines access.
A series of key reports has stressed the pressing need to improve EoL services because of unacceptable variation in access to, and experience of, care. 19,20 NIHR research has also identified poorly co-ordinated services and limited access to specialist palliative care. 17 Our recent research suggests that good access to, and information about, medicines at EoL remains a variable and often burdensome experience for many, affecting symptom control, quality of life and use of unplanned and OOH services. 4,5 At the same time, there are gaps in our knowledge about HCPs’ views on this, and why potential workforce solutions (e.g. use of nurses and pharmacists) to improving medicines access are apparently underutilised. Zeigler et al. ’s14 small survey found that there is potential to improve nurse prescribing in palliative care and recommended further research into patients’ views of this innovation in service delivery. Savage et al. 15 reported significant scope for improving access to, and interaction with, CPs for people with cancer pain and their families. The number of nurse and pharmacist prescribers is rising, with > 53,000 nurses21 and 880622 pharmacists now trained as independent prescribers. In addition, there are significant changes to community pharmacy services as the national integration agenda is driven forward, including commissioning of palliative care medicines access services, higher use of summary care records (SCRs) by community pharmacies, primary care-based pharmacists employed in general practices and community pharmacy-integrated urgent/emergency care services.
To the best of our knowledge, there are other innovations in EoL service provision emerging that offer the potential to improve medicines access experiences, but, to date, their impact on this important aspect of patient experience and their cost-effectiveness remains largely unexplored. Edwards et al. ’s23 study of patients with cancer showed that consultations about medicines provided by community pharmacy services, whether face to face or by telephone, were considered acceptable. Recent guidance from the National Institute for Health and Care Excellence (London, UK) addressed the delivery and organisation of EoL care services and detailed expectations around OOH pharmacy services, including access to medicines for symptom management in adults approaching the end of their life and effective mechanisms for care co-ordination among the community and primary care team. 24 Dedicated OOH EoL care advice lines have been developed for people in the last year of life and are now a recommended part of OOH service provision nationally. 24 From a Welsh perspective, in 2018, the Royal Pharmaceutical Society (RPS) (Cardiff, UK) issued a set of recommendations25 aimed at making sure patients who require palliative and EoL care can access a range of pharmacy expertise. Eleven recommendations, designed to strengthen pharmacy’s contribution to improved patient care, were made across four areas: (1) supporting and informing patients, (2) timely access, (3) workforce and (4) education and training. 25 At a time when EoL care remains a NHS delivery, professional and research priority, there is an urgent need to provide a systematic and detailed evaluation of these issues in the current national context to inform policy, service delivery and organisation, research and practice going forward.
We hypothesise that patients’ experiences of access are influenced by the characteristics of service provision. To better understand the influence of a range of different characteristics of service provision, a comparison of experiences across different service models would enable distillation of the features that lead to good- or poor-quality medicines access for patients. To the best of our knowledge, no research has systemically studied patient experience of medicines access against the backdrop of differing features of service delivery, such as GP-led care, community palliative care, specialist nurse team-led care and centralised OOH advice lines (currently operating in England), and/or the perspectives of HCPs and pharmaceutical wholesalers/distributors (WDs) involved in prescribing, dispensing, supplying and providing associated information about medicines.
National policy on EoL care has framed this study in that it examines a key issue (i.e. access to medicines) that exemplifies a current concern and imperative, including variation in service delivery and choice of care, as well as the principles outlined in Ambitions for Palliative and End of Life Care: A National Framework for Local Action 2015–202020 (i.e. fair access to services, maximising comfort and well-being, and co-ordination of care). 19,20 This research has aimed to contribute to the understanding of the effectiveness of recommendations and guidance for EoL service delivery that pertain to medicines access, by incorporating evaluation of models of care delivery that include care co-ordination, shared records and 24 hours per day, 7 days per week (24/7) cover, as well as other distinctive features.
Chapter 2 Methods
Study aim
We aimed to provide an evaluation of patient and carer access to medicines at EoL within the context of models of service delivery.
Objectives
-
To produce a critical overview of existing research on experiences and outcomes of medicines access within EoL models of service delivery through a systematic literature review (phase 1).
-
To undertake a large-scale survey to evaluate EoL care professionals’ current practices, as well as to:
-
identify factors influencing professionals’ contributions
-
assess the potential of the community-based nurse and pharmacist workforce to improve patient access to medicines at EoL
-
provide an overview of current models of service delivery (phase 2).
-
-
To evaluate and compare patient and carer experiences of medicines access within models of EoL service delivery, including those featuring innovations in care, through undertaking mixed-methods case studies of practice (phase 3).
-
To estimate the cost-effectiveness of service models (phase 3).
-
To map patient ‘access to medicines pathways’ at EoL, including timelines of problems, decisions, actions and use of services (phase 3).
-
To identify barriers to and facilitators of maximising the contribution of the nurse and pharmacist workforce to medicines access at EoL (phases 2 and 3).
-
To interview CPs, wholesalers and distributors to evaluate supply chain processes and identify challenges in providing access to EoL medicines (phase 4).
-
To convene an expert consensus-building workshop to review study findings and generate recommendations on key characteristics of EoL service delivery that support medicines access (phase 5).
Design and theoretical framework
The study used a multiphase mixed-methods design with sequential linked phases, where initial phases informed subsequent phases (Figure 1). 26 The study drew on systems thinking, acknowledging the complexity and multiplicity of actors, the ever-changing health-care context and that systems interact over time to create new patterns. 27 A whole-systems approach framed consideration of medicines access. This approach assumed that services are responsive to the needs of the individual patient/carer, stakeholders accept their interdependency and that action by any one stakeholder may have an impact on the whole system, those using the system do not experience gaps or duplication in provision, and relationships and partnerships are enhanced. 28 These theoretical assumptions informed data collection (e.g. sampling of multiple stakeholders and investigating issues of interdependency in data collection tools), as well as data analysis and interpretation (i.e. through frameworks derived from data collection tools, logic models and sensitivity to systems thinking and complexity).
FIGURE 1.
Study design and methods flow chart. CNS, clinical nurse specialist; TSL, telephone support line.
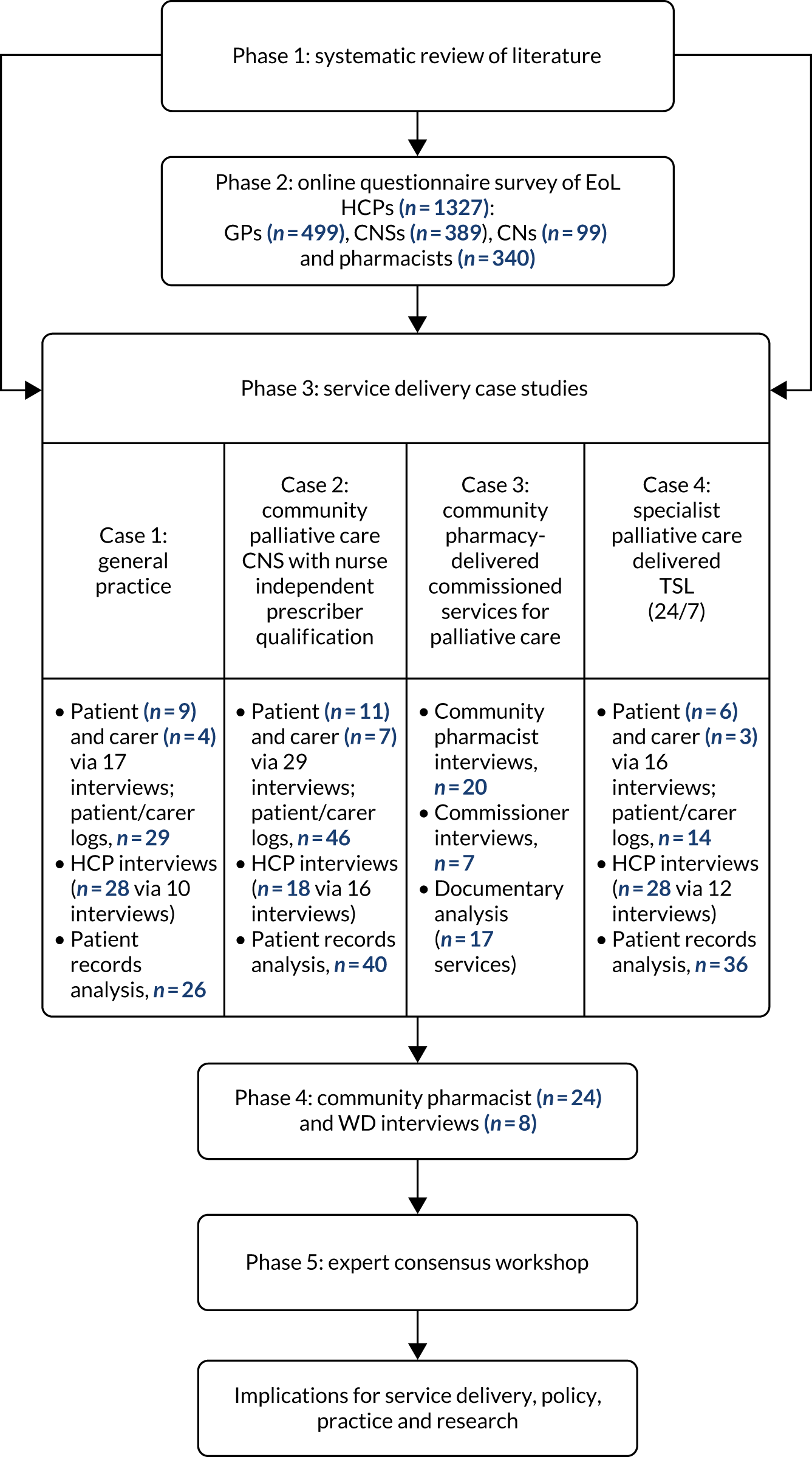
Research plan
Phase 1 (objective 1)
Phase 1 comprised a systematic review of research evaluating medicines access experiences, influences and outcomes across EoL service delivery models.
Phase 2 (objectives 2 and 6)
Phase 2 comprised an online questionnaire survey of GPs, community-based nurses and pharmacists practising in EoL care contexts.
Phase 3 (objectives 3–6)
Phase 3 involved an in-depth contextual evaluation of medicines access experiences, service costs and outcomes in EoL service delivery models, drawing on multiple stakeholder perspectives within multiple embedded mixed-method case studies (n = 4).
Phase 4 (objective 7)
Phase 4 comprised interviews with CPs and pharmaceutical WDs.
Phase 5 (objectives 8 and 9)
Phase 5 involved a stakeholder workshop with invited EoL care experts to review study findings and generate implications pertaining to EoL medicines access.
More detailed description of the methodology for each phase is provided in individual phase chapters. Standards for reporting qualitative research29 are used to report the qualitative elements of the study throughout.
Ethics
Phase 2 of the study was approved by the NHS Health Research Authority (IRAS reference 231837). Phases 3 and 4 were approved by the NHS Health Research Authority South Central – Hampshire A Research Ethics Committee (reference 18/SC/0675). All participants were informed that they were free to withdraw from the study at any time.
Patient and public involvement in the research
Patient and public involvement (PPI) was integral to the study. Three PPI participants acted as patient and carer representatives on the Study Steering Committee (SSC) and were recruited via the NIHR People in Research website [URL: www.peopleinresearch.org/ (accessed 8 November 2021)], one of whom (LR) was also a study co-applicant. The SSC met four times over the course of the study. In addition, PPI participants were supported before and after meetings by members of the research team, including the study PPI lead (AB). PPI participants were paid an honorarium per meeting for their time and contribution, and travel expenses were also paid. The SSC PPI participants contributed to all aspects of the research, commenting on study processes and findings, and ensured that the study focused on the issues of relevance to key stakeholders. In addition, two SSC PPI members presented their experiences of accessing medicines as part of the phase 5 workshop.
Chapter 3 Phase 1: systematic review and narrative synthesis of research evaluating medicines access experiences, influences and outcomes within end-of-life service delivery models
This chapter describes the first phase of the study (i.e. a systematic review and narrative synthesis of research).
Parts of this chapter have been reproduced with permission from Ogi et al. 30 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text includes minor additions and formatting changes to the original text.
Our aim was to systematically search for and critically review international research studies for evidence of (1) patient, carer and HCP experience of medicines access within the context of different models of EoL service delivery, and (2) patient and carer outcomes associated with medicines access experiences. Phase 1 addresses study objective 1. Key issues identified from the review were used to inform phases 2–4 of the study.
Method
The systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines. 31 A search of research, policy and grey literature was undertaken.
Information sources
Expert advice was sought from library specialists to generate relevant search terms and, in March 2019, four electronic databases (MEDLINE, PsycInfo, Cumulative Index to Nursing and Allied Health Literature and EMBASE) were searched for published literature from January 2006 to March 2019, using keywords, synonyms and Boolean operators. (As an example, the description and search terms for MEDLINE are shown in Appendix 1.) A citation search was conducted on the included articles for further relevant material. The Cochrane Library was searched to acquire relevant systematic reviews. PROSPERO (a database of international prospectively registered systematic reviews) was also searched to identify relevant ongoing systematic reviews. For information regarding relevant ongoing trials, ISRCTN and ClinicalTrials.gov were searched. Grey literature sources were searched for unpublished materials from January 2006 to June 2019. To obtain further relevant published or grey literature, members of the study’s SSC were asked for their top five references on this issue.
Study selection
Eligibility
The inclusion and exclusion criteria are summarised in Box 1. The search period began with 2006, as, at this point, nurses and pharmacists in the UK gained the legal ability to independently prescribe any medicine from the British National Formulary. 32
-
Studies evaluating patients’, carers’ and HCPs’ experiences and outcomes of medicine access processes specific to, or inclusive of, palliative and EoL care being provided to adult patients living in their own homes.
-
EoL: the last year of life.
-
Medicine access: prescribing, dispensing, supplying and providing associated information about medicines.
-
Prescribed medicines (excluding diagnostic tests, medical devices and materials).
-
Studies published in the English language.
-
Studies published between January 2006 and March 2019 (or June 2019 for The Cochrane Library and grey literature sources).
-
Services for, or related to, children.
-
Services for inpatients or not-at-home care (e.g. nursing home, hospital wards).
-
Services or support for medicines management at home.
-
Evaluation related to anticipatory, or ‘just-in-case’, medicines.
-
Geographical medicine access in low-economic countries not transferable to the UK.
-
Evaluation of professional capacities in medicines access processes.
Reproduced with permission from Ogi et al. 30 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The box includes minor additions and formatting changes to the original box.
Selection process
Studies were selected for inclusion using a two-step process. One researcher (MO) screened titles (and abstracts when necessary) to remove duplicates, using data management software (EndNote X8.2, Clarivate Analytics, Philadelphia, PA, USA). Following deduplication, titles and abstracts were screened to determine study eligibility. To ensure the validity of the process, two reviewers (MO and NC) each independently screened a random sample of 10% of abstracts and screening results were double-checked by a third reviewer (SL). After resolving disagreements and achieving consensus, screening proceeded by a single reviewer (MO). Following initial decisions on papers for inclusion, two reviewers (MO and SL) each independently reviewed full-text articles against all inclusion and exclusion criteria and resolved disagreements through discussion to achieve consensus.
Data extraction
Data extraction was conducted for each eligible study by a single reviewer (MO) and was checked against the original manuscript by another reviewer (SL). Quality appraisal using the mixed-methods appraisal tool, which is appropriate for systematic reviews that include qualitative, quantitative and mixed-method research studies,33 was undertaken by a single reviewer (MO), recorded on a data extraction sheet and then checked by another reviewer (SL). Data management software (EndNote) was used to organise the search results and references.
Synthesising and interpreting results
The search identified that studies included qualitative, quantitative, and mixed-methods research. Therefore, the framework for a mixed-studies review was utilised, with the thematic analysis of qualitative data within a data-based convergent synthesis design. 33 In this design, qualitative and quantitative data can be analysed and synthesised together. Overlaying this, however, and in keeping with the study focus, we structured the review according to models of service delivery that we found in the literature reviewed.
Findings
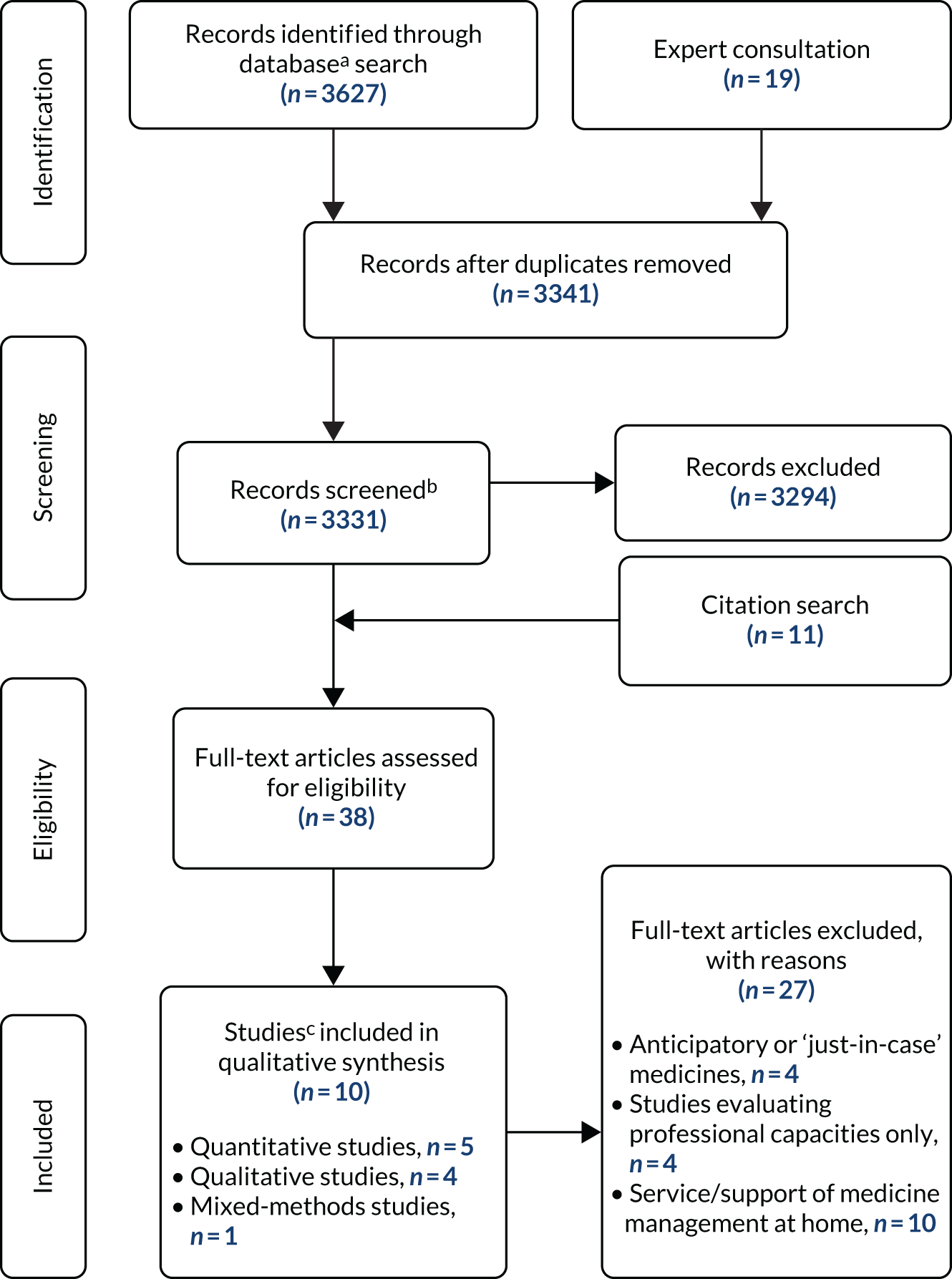
The electronic database search produced 3627 records and 19 records were identified through expert consultation, as shown in the PRISMA flow diagram in Figure 2. Ten studies (five quantitative studies, four qualitative studies and one mixed-methods study) were included in the review. There was one case of multiple reports of the same study,34,35 which were linked together for the purposes of the current review. The studies were from the UK (n = 4), the USA (n = 3), Ireland (n = 1), Australia (n = 1) and Japan (n = 1). Studies were predominantly inclusive of community pharmacy (n = 6), and other types of service delivery were specialist palliative home care medicines kits (n = 3), general practice (n = 1) and community-based clinical nurse specialist (CNS) prescribers (n = 1). In general, the quality of each study was rated as being moderate in terms of methodological rigour. Limitations included that samples were often insufficiently described, making conclusions about generalisability or transferability difficult; the development of data collection tools often lacked detail; and surveys had low response rates, making response bias difficult to rule out. There were no randomised controlled trials or large-scale studies.
FIGURE 2.
A PRISMA flow diagram for systematic reviews. 31 a, Databases: MEDLINE (n = 1306), Cumulative Index to Nursing and Allied Health Literature (n = 167), PsycInfo® (n = 968) and EMBASE (n = 1186); b, the reason for reduction: sources were not accessible (n = 10); and c, two papers34,35 reporting the same study were counted as one study. 34,35 Reproduced with permission from Ogi et al. 30 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
Medicines access and community pharmacy services
Four studies focused exclusively on investigating medicines access experiences related to community pharmacy,16,36–38 of which two studies16,38 included pharmacies providing commissioned palliative medicine services. Two further studies12,39 included evaluations of community pharmacy medicines access as part of investigating the broader model of community service provision for patients receiving home-based specialist palliative care. Two studies16,36 focused exclusively on the perspectives of CPs in providing access, whereas three other studies12,38,39 also included patients and other HCPs. Bennie et al. 37 focused solely on patients’ views of community pharmacy access. Overall, findings from all six studies12,16,36–39 revealed a picture of delays and problems with accessing medicines from community pharmacies.
Controlled drugs and pharmacy stock of palliative care medicines
Ise et al. 36 provide some quantitative data on access, with data indicating less than comprehensive provision. For example, in Ise et al. ’s36 nationwide survey in Japan, 77% of the 1036 community pharmacies reported holding a ‘narcotics’ (opioid) licence, but only 50% of the community pharmacies reported involvement in monthly provision of opioids. It is unclear why the other 23% of pharmacies did not hold a licence or how this affected the patient experience of accessing opioids, but Ise et al. 36 comment that a system whereby all community pharmacies can supply opioids to all patients who need them has clearly not been established. Certainly, lack of community pharmacy stock of palliative care medicines generally is also reported as problematic in other studies. 12,16,38 A study by Miller38 found that although 80% of 55 patients reported receiving palliative medicines on their first visit, one in five patients had to travel to more than one pharmacy before accessing their medicines, despite 73% of medicines being reported as ‘needed urgently’. In a study by Lucey et al.,12 although 54% of 22 patients (n = 22) reported medication changes during the study period were characterised by no delay, the numbers of patients were small (n = 12) and nurses reported 12 delays across 57 patients over a 12-week period, with the majority of these being a wait of > 48 hours. In 50% of cases, the main reason for delays was no stock in the community pharmacy. The proportion of all medicines acquisition episodes these nurse-reported delays represent is not clear. Although not measured quantitatively, CPs in Akram et al. ’s study16 of four localities in Scotland also reported delays in being able to provide palliative care medicines, and these pharmacies were part of an enhanced service and specialist network to provide these medicines to patients in the community.
Information provision
Data on community pharmacy information provision for patients is available in three studies36,37,39 and, again, these data show scope for improvement. Patients and carers in Bennie et al. ’s37 focus groups saw the pharmacist (as well as GPs) as a source of medicines information if they had a relationship with them. However, some patients and carers reported little contact with a CP and overall knowledge of services offered was poor, with patients often acquiring knowledge in an unplanned way through family and friends or when in a crisis situation. Patients and carers wanted a more proactive role from pharmacists, in particular information regarding prescription and supply processes of controlled drugs (CDs) or when a new medicine was prescribed. The sample in Bennie et al. ’s37 study was small, with 14 patients and 13 carers from one city in Scotland. Nevertheless, findings from Ise et al. ’s36 national survey also highlight gaps in information provision, with 50% of the 1036 pharmacists in the study reporting that they did not counsel patients about their palliative care medicines, primarily because they lacked information about the patient, and < 5% reporting that they had a room to counsel the patient privately. In an Australian study by Kuruvilla et al. ,39 carers and patients felt that sometimes the information provided was inadequate for them to manage their medications appropriately.
Influences on accessing medicines from community pharmacies
Four studies12,16,36,38 reported on influences that challenge or support the access process. Many of these influences can be classified as centrally concerned with communication between the pharmacist and other members of the health-care team. Communication into the pharmacy was reported as problematic, causing delays in supplying medicines, through a mismatch between prescriptions received and stocks held and/or a lack of information on the palliative care status of the patient. 16,36,38 The latter was due to either the pharmacist seeing unfamiliar patients who had been referred by another network pharmacist16 or HCPs’ reluctance to share information. 38 A finding reported by both studies that included enhanced or commissioned services also related to communication, that is medicines access was adversely affected by HCPs’ lack of knowledge about these services. 16,38 Miller38 concludes that this lack of knowledge found in her study resulted in patients and carers not always being able to access medicines promptly and that HCPs need to routinely be made aware of such services and their locations. Similarly, patients and carers in Bennie et al. ’s study37 also reported a lack of awareness of more general pharmacy services.
Further obstacles were also identified. For example, 33% (19/57) of pharmacists completing questionnaires in Lucey et al. ’s12 study reported difficulties in accessing stock and 49% reported that medicines not being on state reimbursement schemes caused delays. In addition, Lucey et al. 12 reported another factor that caused delays was having no one to courier prescriptions/medication to and from the GP, pharmacy and patient. The difficulty of patients or carers picking up medications from a community pharmacy was also noted by Miller. 38
Few data were available on factors supporting good access, related to the fact that studies highlighted poor access experiences. However, pharmacists in one study16 stated that pre-emptive communication from CNs about medicines likely to be required by patients was helpful, as well as being part of a network of pharmacists from whom medicines and advice could be accessed. Miller38 reported that the range of palliative medicines stocked was a key facilitating factor in access, although pharmacists reported practical difficulties keeping them in stock. Seventy per cent of pharmacists in Ise et al. ’s36 survey also said that being able to have a swift supply from, and ability to return opioids to, wholesalers would be useful, as well as being able to get stock from other local pharmacies. Akram et al. 16 also found that CPs wanted better training of counter staff and of locum pharmacists, as well as resources for pharmacists to support clinical practice. In a study by Kuruvilla et al. ,39 family involvement and delivery services seemed to be helpful, although the latter were not always available and, occasionally, there would be a financial burden for some patients when delivery was not free. In addition, patients and families receiving medicines in this way seldom interacted directly with pharmacists.
Outcomes of community pharmacy medicines access
There are few data on outcomes reported in the studies reviewed. One study38 reported that commissioned service pharmacies stocking an agreed list of palliative care medicines could shorten the time required to obtain urgently needed palliative medication compared with medication being provided by a non-commissioned service pharmacy. The median time taken for accessing urgent palliative care medicines was significantly longer for non-commissioned service pharmacies (5 hours) than for pharmacies commissioned to hold stock of palliative care medicines (10 minutes) (p = 0.002). In addition, compiling tailored lists of palliative care medications through communication between pharmacists and GPs resulted in a similar time-saving in commissioned pharmacies. 38 However, the impact of this on outcomes such as symptom control, patient and carer distress or use of emergency health services was not evaluated.
Overall, findings are suggestive of problems with accessing medicines from community pharmacies and a number of issues that delay access have been identified, many of which focus on either pharmacy stock or communication between the pharmacy and HCPs and patients. However, with the exception of one study,36 sample sizes were small and pertained to only a few localities, and there is a lack of data on outcomes of access experiences.
Medicines access and general practitioners
Only one study12 included data on GPs’ experiences of providing medicines access, focusing on delays and the causes of these. Questionnaires were sent to 268 GPs in one city, asking them to select the most common causes of delay from a prespecified list. A total of 111 questionnaires were returned (41% response rate). ‘No delay’ (the only ‘delay’-focused response option) was reported by only 34% of GPs. The most commonly cited factor causing delay was the need to clarify the advice given by the home care team (30.6%), followed by the inability of someone to collect the prescription (23.4%) and 18.9% of respondents reported the patient being unable to attend the surgery as a cause of delay.
Medicines access and community specialist nurse independent prescribers
One interpretive phenomenological study34,35 conducted interviews with six independent nurse prescribers employed as community palliative care CNSs. The study was conducted in one region in England and aimed to understand the lived experience of these nurses prescribing for palliative care patients in the community. The ‘most significant’ perceived benefit of nurse prescribing, reported by all six nurses, was that it enabled patients to access medication quickly, particularly ‘near the end of their life’, leading to effective symptom management. 34,35 The majority of the nurses also considered that it was during OOH that the ability to prescribe independently had the most impact, preventing delays by avoiding the need to call an OOH doctor, which could reportedly take many hours. The authors concluded that ‘[t]he ability of community palliative care CNSs to prescribe can facilitate rapid access to medicines, particularly during OOH periods’. 34,35
Medicines access and hospice emergency medication kits
Three studies40–42 from the USA evaluated the outcome of hospice emergency medication kits (HEMKs) with regard to use, impact and cost. Kits are typically ordered by a physician on referral to hospice care and are kept in the patient’s home. These kits allow the patient access to small quantities of medication that can be administered immediately on nurse instruction. Unlike just-in-case boxes, which are typically used in the UK to manage symptoms in the last few days of life, HEMKs are designed for potential use over a longer period of EoL care, including, for example, antibiotics. Emergency medication kits contain sufficient medications for 12–72 hours, thereby avoiding the immediate need for pharmacy and physician involvement after hours. 41 All studies included an evaluation of the perceived impact of HEMKs, which shed light on their effect on access to medicines. In all studies,40–42 clinicians providing care were asked about the impact of HEMKs on unplanned health-care resource use, with the majority of clinicians suggesting that kits averted use of other services. For example, 93% of the 78 home hospice nurses completing a questionnaire survey in one study42 reported that an emergency department visit or hospitalisation was avoided by having a kit in the home, with 26.1% of hospice nurses reporting that this was ‘often’ and 40.6% reporting that this was ‘very often’. Clinician views on helpfulness and patient satisfaction were also positive across the two studies41,42 measuring this, with 59% of nurses considering HEMKs to be helpful 100% of the time and 100% (n = 13) of the hospices using HEMKs in the other study reporting that it increased both patient and nurse satisfaction. In a comparison of a hospice using HEMKs for some patients with a hospice not using them, Walker and McPherson41 reported that after-hours nurses perceived that caller (i.e. patient/family) satisfaction was significantly higher in hospice patients with a kit than in both the non-kit hospice patients and the HEMK hospice patients without a kit (95%, 75% and 82%, respectively; p < 0.001). This study41 also measured the impact of HEMKs on perceived symptom relief time. Nurses in the hospice using HEMKs estimated that 56% of after-hours callers received symptom relief within 30 minutes, whereas nurses reported that none of their callers from the hospice without kits was treated satisfactorily in < 30 minutes.
Overall, although HEMKs were found to have a positive impact on a number of medicines access indicators in all three studies, including, perhaps notably, shorter time to symptom relief and reduced use of emergency services, all were small scale. Two studies40,41 were confined to a state-wide hospice survey and one study42 focused on a sample from one medical centre only, resulting in overall small numbers of hospices, clinicians and patient records included. In addition, the majority of the data from all studies were limited to clinicians’ perceptions only, with limited objective data and no patient or carer experiences captured.
Discussion
Our review found sparse research in this area. Nine16,34,35,37–42 of the 10 studies were small scale or pilot studies and local samples. Although it is difficult to generalise the results, this review identified several problems in current models and also highlighted potential approaches to improving medicine access.
Studies revealed that issues of medication stock availability at community pharmacies are likely to contribute to access problems. Pharmacies commissioned to provide stocks of locally agreed palliative medicines lists reduced these delays in medicine access. 38 However, the study by Miller38 evaluated only one local service and city area. This confirms that evaluation of these services on a wider scale is warranted. Alternatively, improvements upstream within the supply chain into community pharmacies might also be effective to avoid potential delays, and this is investigated further in Chapter 7. Studies also suggested that a number of problematic issues were linked to communication between pharmacists and patients (e.g. patients’ lack of awareness of services and of information provision about medicines) and/or between pharmacists and other HCPs (e.g. pharmacists’ lack of awareness of patients’ palliative care status and HCPs’ lack of awareness of commissioned pharmacy services).
Three studies40–42 in this review suggested that HEMKs, which comprise a number of palliative care medicines stored in the patient’s home that could be used in an emergency, can avert hospital admissions and emergency department visits and improve quality of care at home by providing timely access during OOH. HEMKs are not used in the UK at present, although the broad principle of anticipatory prescribing was explored in the study.
Community palliative care specialist nurse prescribers were also reported to provide OOH support and quicker medicine access in times of crisis. However, data were confined to one small-scale study34,35 and, therefore, further evidence, including larger-scale samples and insights of other stakeholders, is needed to endorse the value of nurse and pharmacist prescribing in this context.
Overall, conclusions are limited by the quantity and quality of the research conducted to date. Only a few models have been studied and only one study12 used a systems approach, studying different components of service delivery as a whole, with all other studies focussing on only one component. Medicines access provision by professionals such as a generalist CNs and GPs are understudied, as well as more recent initiatives such as specialist-delivered telephone support lines (TSLs) available OOH. Most studies focused on HCP self-report data and only four studies12,37–39 included views of patients. There was very few data on outcomes of medicine access experiences and so comparison between models in this respect was not possible.
Summary
Despite suggestions that accessing palliative care medicines to manage symptoms at home is problematic for patients, the review confirmed that there is very little large-scale or in-depth research into these experiences and how models of service delivery influence access. However, the review was useful in sensitising us to potential issues influencing access to medicines in different service delivery models. These issues are investigated further in phases 2–4, which also included evaluations of both established and more recent service delivery models, and patient and carer perspectives.
Chapter 4 Phase 2: online survey of health-care professionals
This chapter addresses objective 2 of the study. A large-scale online survey was conducted to evaluate professionals’ current practices, identify factors influencing professionals’ contributions and assess the potential of the community-based nurse and pharmacist workforce to improve patient access to medicines.
Parts of this chapter have been reproduced with permission from Latter et al. 43 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text includes minor additions and formatting changes to the original text.
Method
An online questionnaire survey was designed using the Checklist for Reporting Results of Internet E-Surveys. 44
Questionnaire design
The systematic narrative review (see Chapter 3) informed questionnaire design. Considering the limited research in this area, we also consulted with clinical and academic experts in the field to identify key issues. The final questionnaire, administered via Online Surveys [URL: www.onlinesurveys.ac.uk (accessed 9 November 2021)], comprised sections that included roles in access provision, in-hours and OOH medicines provision, interprofessional medicines communication, nurse and pharmacist prescribing and, to estimate service effectiveness, impact of access on pain control. Items (one to three per page) comprised closed-ended response formats, including Likert scales, and open-ended items. Questionnaire submission required completion of key filter questions, with descriptive responses optional.
Sample
The target sample comprised a convenience sample of representatives from the main professional (generalist and specialist) groups providing community-based EoL care in England, including GPs, pharmacists working in community pharmacies (i.e. CPs), pharmacists who are employed in general practices [i.e. primary care pharmacists (PCPs)], nurses who specialise in community palliative care (i.e. CNSs) and nurses delivering a range of care in patients’ homes, including palliative care (i.e. CNs).
Recruitment process and access
A survey website link was distributed via e-mail to GPs and pharmacists via research leads employed as part of NIHR Clinical Research Networks (CRNs). Based on estimated numbers of health professionals in a typical CRN, and our target response of 200 participants in each professional group, the link was distributed to GPs in registered research-active general practices in four CRNs (two in the north of England and two in the south of England) and to pharmacists in all 15 CRNs in England. Distribution to pharmacists occurred via various local pharmacist networks operating within the CRNs. Clinical leads for all hospices in England with teams of CNSs delivering community-based palliative care (146/167 hospices in England) distributed the survey via e-mail to their CNS teams, as did clinical leads in seven community trusts that employ CNSs directly. Based on estimated numbers of CNs in a typical community trust, local collaborators in four community trusts (two in the north of England, one in the south of England and one in the east of England) distributed the e-mail survey link to all CNs in the trust. In addition, the survey link was posted on relevant interest groups’ websites [e.g. Association of Supportive and Palliative Care Pharmacy (URL: www.aspcp.uk), ehospice (URL: https://ehospice.com) and the Association for Prescribers (Essex, UK) (URL: https://associationforprescribers.org.uk)] and distributed via newsletters [e.g. Hospice UK’s (London, UK) newsletter]. For general practices, community pharmacies and community trusts, organisational-level participation was captured via NIHR processes, which contributed to overall payments to the CRNs and to the general practices that participated.
Data collection
Data were collected from July to October 2018. Up to three reminders were distributed to maximise responses.
Analysis
Quantitative data were analysed using descriptive statistics. For the analysis of the pain control data, we conducted tests of differences in proportions, comparing question 1 (current pain levels) and question 2 (estimated pain levels with improvement to medicines access) responses. We also created a weighted estimate from question 1 data (i.e. pain level estimates across a typical 100 EoL patients who use the service) by multiplying the pain category (no = 0, mild = 1, moderate = 2 or severe = 3) by the proportion of individual respondents estimated would be in those categories (and, therefore, higher values represented higher levels of pain). We then conducted linear regression with the weighted variable as the dependent variable, controlling for the role of the respondent. Statistical analyses were conducted using Stata® (StataCorp LP, College Station, TX, USA). A directed content analysis approach was undertaken (by NC and JB) to analyse free-text responses, including quantification. 45
Results
Respondents
A total of 1327 responses from eligible HCPs were received [GPs, n = 499; CNSs, n = 389; CPs, n = 219; PCPs, n = 151; and CNs, n = 99 (note that 30 HCPs were employed as both CPs and PCPs)]. Missing data were very low (< 1% for most questions). All responses provided were used (i.e. there was no case-wise deletion) and no imputation was carried out. All percentages are calculated from responses provided (i.e. excluding missing data).
Medicines access practices
Methods of providing new prescriptions in-hours
Access routes to new prescriptions for palliative care medicines during working hours are shown in Table 1. (These medicines were defined as regular and as-necessary medicines, administered via all routes for symptom management during the last year of life, excluding ‘just-in-case’ boxes. 46) Most nurses and GPs were providing home visits for patients to issue new prescriptions. Large numbers of all professional groups were also providing consultations by telephone and a significant minority also reported using e-mail. Over 93% of all professional groups used referral to a GP as a route for patients to access medicines. Large proportions of all professionals also cited referral to a nurse prescriber. Table 1 also shows a relatively high level of engagement in helping to provide new scripts by PCPs. Fifty-two per cent (79/151) of the PCP sample also reported advising patients/carers about palliative care medicines [43% (65/151) did not] and 63% (95/151) reported engagement in systematically reviewing medicines prescribed for palliative care patients [32% (49/151) did not].
| Which of the following are you able to provide for patients to obtain new prescriptions during working hours? Please select all options you use: | Survey respondent, n (%) | ||||
|---|---|---|---|---|---|
| CNS | CN | GP | PCP | CP | |
| Personal home visits | 349 (92) | 82 (93) | 484 (98) | 52 (43) | 49 (35) |
| Telephone consultations | 335 (88) | 78 (91) | 498 (100) | 134 (96) | 147 (85) |
| E-mail consultations | 79 (24) | 8 (10) | 169 (35) | 32 (28) | 63 (43) |
| GP practice appointments | 168 (51) | 43 (56) | 496 (100) | 122 (91) | 44 (38) |
| Community pharmacy appointments | 37 (12) | 11 (15) | 118 (29) | 28 (29) | 131 (73) |
| Referral to nurse prescriber | 194 (58) | 69 (78) | 286 (65) | 102 (78) | 101 (62) |
| Referral to pharmacist prescriber | 64 (20) | 21 (26) | 149 (34) | 66 (65) | 81 (53) |
| Referral to GP | 375 (97) | 92 (96) | 351 (95) | 147 (100) | 185 (93) |
Overall, many respondents were satisfied with their ability to support patients to obtain new prescriptions during working hours. Fifty-seven per cent (762/1327) of respondents were extremely or very satisfied, especially GPs (386/499, 77%); however, 43% (567/1327) of the sample were somewhat, slightly or not at all satisfied.
Nurse and pharmacist prescribing
Of nurse and pharmacist respondents, 42% (160/386) of CNSs, 27% (27/99) of CNs, 76% (114/151) of PCPs and 16% (36/219) of CPs were qualified as independent prescribers. The most common reasons for not training as a prescriber were the cost of training (155/508, 31%), lack of employer/colleague support (122/508, 24%), no backfill of their post available while attending training (92/508, 18%) and no designated clinically based trainer available (80/508, 16%).
Of the nurse and pharmacist respondents, CNSs prescribed most frequently, with two-thirds (86/130, 66%) of CNSs prescribing at least two or three times per week, whereas two-thirds of the CNs (14/22, 64%), PCPs (60/87, 69%) and CPs (12/20, 60%) prescribed only once per month (or less). Analgesics, antiemetics and laxatives were identified as the most frequently prescribed medicines by all the nurse and pharmacist prescriber professional groups. For all respondent groups, the majority (206/244, 84%) prescribed CDs, ranging from 96% (125/130) of CNSs to 69% (60/87) of PCPs.
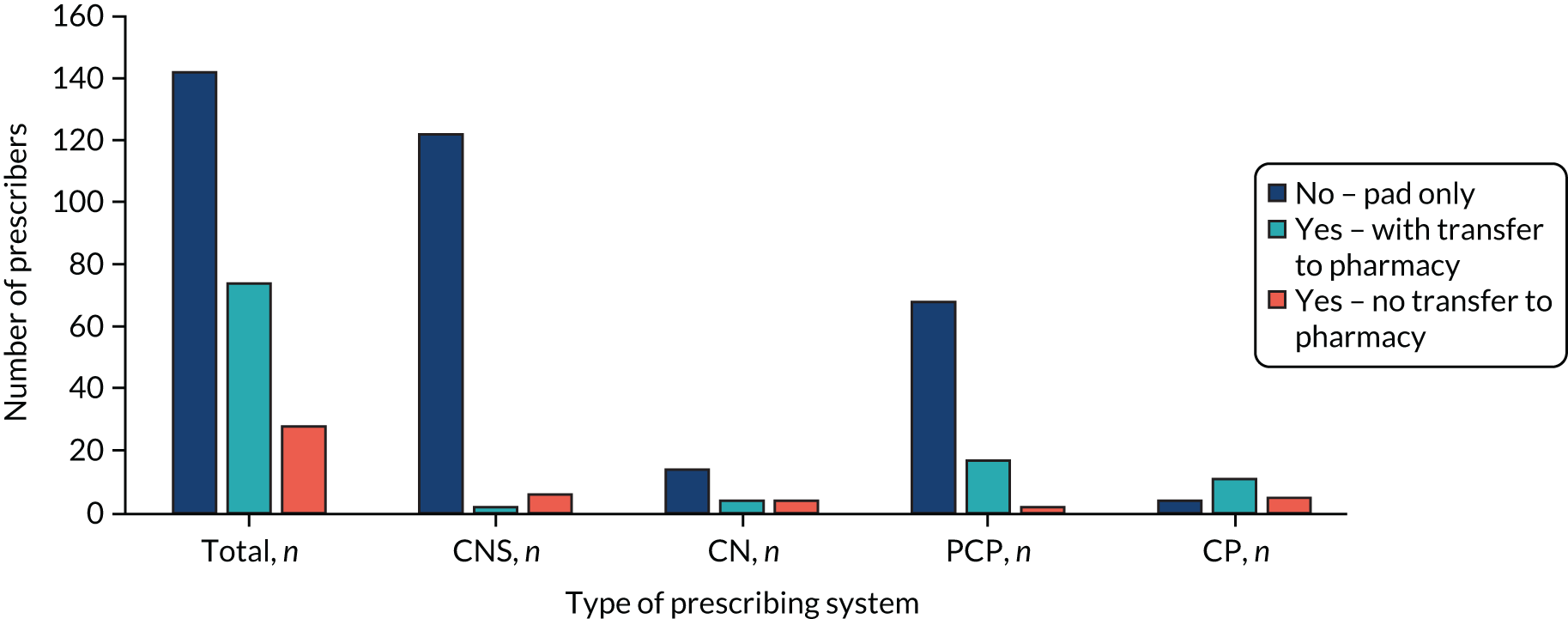
The majority (142/244, 58%) of prescribing nurses and pharmacists were not able to use an electronic prescribing system (Figure 3). Most CNS prescribers were restricted to writing prescriptions by hand via a paper prescription pad. Only a minority of all nurse and pharmacist respondent groups were able to prescribe electronically and transfer this electronically to the pharmacy.
FIGURE 3.
Nurses’ and pharmacists’ ability to prescribe electronically.
Out-of-hours services for medicines access
When asked if there was CNS service provision 7 days per week in their area, overall, 49% (656/1327) of respondents responded yes, 18% (239/1327) stated no provision and 33% (434/1327) were unaware whether or not there was provision. Of note, 76% (166/219) of CPs, 72% (109/151) of PCPs and 33% (167/499) of GPs were not aware. Twenty per cent (76/389) of CNS respondents reported covering 18.30 to 08.00 weekdays and 71% (276/389) reported covering weekends and bank holidays. For CNs, cover was 43% (43/99) and 67% (66/99), respectively.
Respondents were also asked how effective CNS 7 days per week cover was at facilitating OOH access to medicines for patients. Overall, 43% (280/656) of respondents rated CNS cover as extremely or very effective, 36% (235/656) reported cover as somewhat effective and 22% (141/656) reported cover as only slightly or not at all effective. Analysis of comments indicated that CNSs’ ability to prescribe medicines seemed to be critical in their perceived effectiveness, and, for some, this also interacted with access to pharmacy stocks to influence speed of access.
When asked about confidence in their ability to advise patients how to best access palliative care medicines OOH, nurses, particularly CNSs, tended to rate themselves as most confident. Seventy-nine per cent (307/389) of CNSs were extremely or very confident, as were 61% (61/99) of CNs. Pharmacists were less confident, with 30% (45/151) of PCPs and 39% (86/219) of CPs rating themselves as extremely or very confident. Although 47% (236/499) of GPs reported being extremely or very confident, 35% (177/499) were only somewhat confident and 18% (86/499) were slightly or not at all confident.
Community pharmacy-commissioned service provision
Table 2 shows the provision of commissioned palliative care medicines services by CP respondents (n = 219).
| If you are a CP in a community pharmacy, do you provide a commissioned service for palliative care (e.g. on-demand availability of specialist drugs)? | Yes, n (%) | No, n (%) |
|---|---|---|
| Commissioned servicea | 67 (31) | 148 (68) |
| Of those with a commissioned service | ||
| Stocking a locally agreed list of core palliative care medicines | 62 (93) | 5 (7.5) |
| OOH availability of palliative care medicines from your pharmacy | 32 (48) | 35 (52) |
| OOH availability of palliative care medicines from other linked pharmacies in your area | 19 (28) | 48 (72) |
| Provision of information on the service to other pharmacy contractors plus HCPs to signpost patients to the service | 47 (70) | 20 (30) |
| Provision of information on the service to patients plus carers directly | 41 (61) | 26 (39) |
Most services included stocking a core list of agreed palliative care medicines. A smaller proportion of services – approximately half – reported providing OOH medicines from their own pharmacy and 28% (19/67) via a linked pharmacy in their area. Around two-thirds of the sample reported providing information on the service to HCPs (47/67, 70%) and directly to patients and carers (41/67, 61%).
In contrast, when asked whether or not they were aware of commissioned services for palliative care medicines, overall, 39% (517/1327) of all HCPs stated yes, 9.2% (122/1327) reported no provision and 52% (690/1327) were unaware. GPs, especially, lacked awareness (340/499, 68%). However, when respondents were aware, the vast majority (433/517, 84%) considered that the service facilitates speed of access to medicines for patients.
Factors influencing medicines access service provision
Prescribing competence
Overall, just under two-thirds (518/819, 64%) of the sample reported feeling very competent (373/819, 46%) or extremely competent (145/819, 18%) in prescribing palliative care medicines, with 27% (217/819) feeling somewhat competent and 10% (84/819) reporting feeling slightly or not at all competent. CNS respondents reported greatest competence, with 84% (132/157) feeling very or extremely competent. Seventy per cent (347/498) of GPs reported feeling very or extremely competent, with almost one-third (142/498, 29%) rating themselves as somewhat competent. Over one-third (10/25, 40%) of CNs reported feeling very or extremely competent, with 48% (12/25) reporting that they were somewhat competent. Pharmacists reported less competence, with only 22% (24/109) of PCPs and 14% (7/49) of CPs reporting feeling extremely or very competent.
Access to patient records
Experience of access to shared patient records for communicating about medicines is shown in Table 3.
| Do you have access to shared patient records for communication about medicines access between health professionals? Tick all that you are able to access | Survey respondent | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CNS | CN | GP | PCP | CP | |||||||||||
| Paper, n (%) | Electronic, n (%) | None, n (%) | Paper, n (%) | Electronic, n (%) | None, n (%) | Paper, n (%) | Electronic, n (%) | None, n (%) | Paper, n (%) | Electronic, n (%) | None, n (%) | Paper, n (%) | Electronic, n (%) | None, n (%) | |
| GP records | 22 (5.7) | 203 (52) | 173 (44) | 5 (5.1) | 77 (78) | 18 (18) | 14 (9.3) | 145 (96) | 2 (1.3) | 10 (4.6) | 62 (28) | 149 (68) | |||
| GP OOH records | 8 (2.1) | 117 (30) | 264 (68) | 1 (1.0) | 60 (61) | 38 (38) | 72 (14) | 349 (70) | 86 (17) | 13 (8.6) | 100 (66) | 39 (26) | 6 (2.7) | 21 (9.6) | 192 (88) |
| CN records | 77 (20) | 218 (56) | 105 (27) | 39 (7.8) | 281 (56) | 186 (37) | 7 (4.6) | 97 (64) | 48 (32) | 1 (0.5) | 15 (6.9) | 203 (93) | |||
| Hospice/palliative care specialist records | 3 (3.0) | 66 (67) | 30 (30) | 46 (9.2) | 154 (31) | 304 (61) | 20 (13) | 58 (38) | 77 (51) | 3 (1.4) | 12 (5.5) | 204 (93) | |||
| CP records | 2 (0.5) | 18 (4.6) | 369 (95) | 1 (1.0) | 8 (8.1) | 90 (91) | 12 (2.4) | 29 (5.8) | 458 (92) | 4 (3.3)a | 9 (7.4)a | 108 (89) | |||
| SCRs | 23 (5.9) | 153 (39) | 219 (56) | 2 (2.0) | 60 (61) | 37 (37) | 26 (5.2) | 417 (84) | 59 (12) | 6 (4.0) | 138 (91) | 8 (5.3) | 13 (5.9) | 198 (90) | 8 (3.7) |
Data revealed a variable picture. Those based in general practice (i.e. GPs and PCPs) had relatively high levels of access. However, CNSs reported limited access to others’ records, whether paper or electronic, with 44% (173/389) reporting no access to GP records and 68% unable to access GP OOH records.
Satisfaction with access to shared records to facilitate medicines access reflected these results. Thirty-nine per cent (507/1327) of respondents, overall, were either not at all or only slightly satisfied. CNSs and CPs were especially likely to rate access as not at all satisfactory, with half (193/389, 50%) of all CNSs reporting that they were either not at all or only slightly satisfied.
Impact of nurse and pharmacist prescribing
Overall, just over half of respondents considered that prescribing by a nurse or pharmacist consistently had a beneficial impact on palliative care medicines access, with 21% (283/1327) and 34% (445/1327) of respondents considering prescribing by a nurse or pharmacist as always or often beneficial, respectively. However, one-quarter of GPs (124/499, 25%), 29% (44/151) of PCPs and 26% (58/219) of CPs reported that they did not know about the impact of this initiative on access to medicines, with comments reflecting their lack of, or limited experience of, these services.
Community pharmacy provision of palliative medicines
Table 4 shows the results of CP respondents’ opinions on issues identified in our review of the literature that may, potentially, have an impact on their ability to facilitate access to medicines, confirming that several issues were problematic in practice.
| How frequently do you | Never, n (%) | Rarely, n (%) | Sometimes, n (%) | Often, n (%) | Always, n (%) |
|---|---|---|---|---|---|
| Undertake medicines optimisation reviews for palliative care patients | 61 (28) | 65 (30) | 52 (24) | 26 (12) | 13 (6.0) |
| Feel that lack of awareness of patients’ palliative status influences your ability to help patients access medicines | 13 (6.0) | 22 (10) | 71 (33) | 87 (40) | 25 (11) |
| Encounter a discrepancy between palliative care medicines prescribed and the stock you hold | 12 (5.5) | 36 (17) | 76 (35) | 79 (36) | 14 (6.5) |
| Limit your stock of palliative care medicines because ‘use by’ dates are likely to expire | 27 (12) | 37 (17) | 47 (22) | 67 (31) | 40 (18) |
| Limit your stock of palliative care medicines because of lack of storage space | 63 (29) | 59 (27) | 38 (18) | 41 (19) | 15 (6.9) |
| Experience problems receiving Rx electronically from patients’ general practices | 28 (13) | 40 (18) | 65 (30) | 51 (23) | 34 (16) |
| Encounter carers not having satisfactory ID, seeking to collect CD prescriptions for patients | 16 (7.3) | 68 (31) | 73 (33) | 51 (23) | 10 (4.6) |
Service delivery solutions
A total of 909 (69%) respondents responded that there were solutions to problems with service delivery. Seven hundred and three of these respondents provided an analysable description of proposed solutions, with between one and six (mean 1.55; median 1) solutions in each response, generating 1087 ‘solutions’, which were thematically coded. Solutions were coded within 17 themes and ranged from 173 respondents (i.e. the most frequently cited) to four respondents (i.e. the least frequently cited). The top four themes (all cited by ≥ 145 respondents) are highlighted in Table 5 (note that the next most cited theme was notably lower with 96 respondents).
| Are there possible solutions to any gaps or problems with service delivery? | Number of respondents |
|---|---|
| Theme 1: improved pharmacy provision | 173 |
| Improved community pharmacy-delivered commissioned services for palliative care | |
| 24-hour community pharmacy provision, local availability, sufficient stocks and improved delivery from distributors | |
| Improved use of PCPs | |
| Theme 2: more non-medical prescribers | 162 |
| Palliative care specialist nurses, CNs and pharmacists (i.e. palliative care specialist pharmacists and PCPs) | |
| Increased funding, training places and support | |
| Greater availability OOH | |
| Systems to support non-medical prescribers to be active | |
| Theme 3: shared electronic records | 148 |
| Universal integrated systems and access, and timely updating | |
| Sharing across health-care providers (i.e. generalist and specialist palliative care, primary and secondary care, and in-hours and OOH) | |
| Theme 4: integrated HCP working | 145 |
| Between generalists (GPs, OOH GPs, CNs, PCPs, CPs) and specialist palliative care | |
| Between prescribers and CPs (regarding formularies and stock levels) | |
| Between CCGs/LPCs and community pharmacies and prescribers (regarding improved strategic management/guidance for medicine shortages) | |
| Signposting to community pharmacy OOH services |
A total of 173 respondents focused on the need for improved pharmacy provision to aid medicines access. Of these respondents’ solutions, 107 were specific to commissioned services for palliative care, including adequate incentives for provision (e.g. comprehensive reimbursement of costs), more pharmacies with this provision and related locality-based provision (e.g. one commissioned service pharmacy per locality), signposting of these services to HCPs and patients/carers (facilitating wider awareness of the services), improvements in stock availability (and related formularies to enable adequate stock levels), improved OOH access to services, audits of service provision and palliative care training of commissioned pharmacist service providers.
A total of 162 respondents addressed the need for greater numbers of palliative care specialist nurses, CNs and pharmacists to be prescribing. Responses from GPs appeared to demonstrate support for greater levels of nurse and pharmacist prescribing, particularly by palliative care specialist nurses. This was viewed as aiding faster access to medicines, as the prescription is provided as part of the patient assessment visit, while also improving care and prescribing safety through not having to relay messages about prescribing between different services.
A total of 148 respondents stated the need for access to shared electronic records to facilitate good practice in prescribing and informed patient assessment, as well as improved information-giving to patients/carers about medicines and related access. Record-sharing was key to providing timely access to medicines. Record-sharing was particularly important for CPs who desired shared electronic records access to be aware of an individual’s palliative status, enabling them to ‘answer quite a lot of the questions that can be raised’ by patients/carers about medicines and access to them.
Access to shared electronic records was also a crucial component of integrated HCP working (as stated by 145 respondents). Fragmented care delivery led respondents to state solutions that focused on the need for integrated working between all members of the multidisciplinary team (MDT) (including CPs), generalist and specialist palliative care providers (including methods of achieving this, such as joint patient visits and palliative care register-related meetings), prescribers and CPs (to ensure pharmacist awareness of local palliative care prescribing recommendations and appropriate stocks to meet needs), and Clinical Commissioning Groups (CCGs)/Local Pharmaceutical Committees (LPCs), community pharmacies and prescribers (to enable strategic management of medicine shortages).
Perceived effectiveness of service and impact of barriers
Respondents were asked to estimate the proportion of their patients who currently experienced no, mild, moderate and severe pain (question 1). Respondents were then asked to re-estimate these proportions following removal of barriers to medicines access (question 2). Figure 4 shows that there would be a significant perceived improvement in pain control with better medicines access (no pain, p = 0.0018; mild pain, p-value not significant; moderate pain, p = 0.026; severe pain, p = 0.047). However, missing data for these questions were higher than for other questions (18% and 23%, respectively) and a further 10% of respondents provided invalid answers to both questions (i.e. data that did not sum to 100).
FIGURE 4.
Mean proportions of responses across pain categories for the estimated effectiveness of current and improved medicines access. 43 Reproduced with permission from Latter et al. 43 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
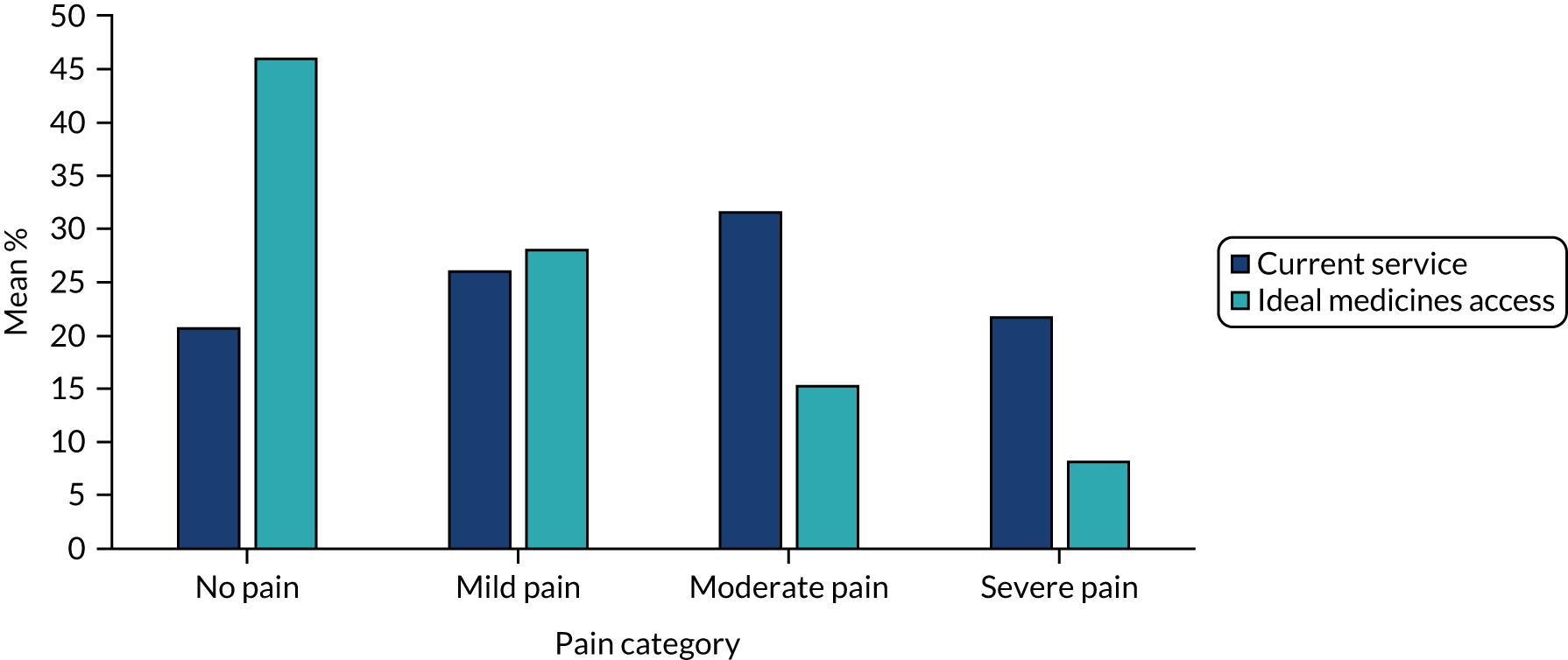
There was a clear impact of respondent role in data from questions 1 and 2, with pharmacists indicating that they see higher proportions of patients with poor pain control. This was likely an artefact of ‘case mix’ rather than service effectiveness. We tested the impact of various service factors on weighted question 1 response. After controlling for role, there were few statistically significant predictors of pain control outcomes. However, respondents within services with access to GP records or SCRs47 reported significantly lower pain estimates than respondents without access (p = 0.005 and p = 0.009, respectively).
Summary
Although only indicative, our results are suggestive of an impact of access to medicines on patient outcomes (e.g. level of pain control). The results also show that a range of HCPs and routes are currently being used to support patient access to palliative care medicines, but there is potential to increase the scale and effectiveness of these through addressing the barriers highlighted. These include training larger numbers of the nursing and pharmacist workforce to prescribe using electronic systems, as well as ensuring better access to shared electronic patient records across professional groups. This needs to take place alongside attention to tackling the impediments that currently reduce the effective provision of community pharmacy and community pharmacy-commissioned medicines services. Finally, greater team integration and communication, including improved awareness (among GPs and pharmacists in particular) of existing service provision, is warranted.
Chapter 5 Phase 3: case studies of service delivery models
Parts of this chapter are reproduced or adapted with permission from Campling et al. 48 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
This chapter addresses objectives 3–6, utilising comparative case study design with an analytic focus on service delivery models, specifically patient and carer experience of medicines access, cost-effectiveness, patient medicine access pathways, and barriers to and facilitators of maximising the contribution of the nursing and pharmacist workforce to medicine access. The chapter begins with an overview of the methods utilised across the sites, followed by a detailed description of each service delivery case study, together with the application of methods and the findings from each case.
Method
Sampling of case sites
Four service delivery models were purposively selected, informed by survey results:
-
general practice
-
community palliative care CNS with a nurse independent prescriber (NIP) qualification
-
community pharmacy-delivered commissioned services for palliative care
-
palliative care 24/7 TSL.
This ensured that a range of service delivery models were included, covering traditional models of service delivery (i.e. case 1) and those with more innovative characteristics (i.e. cases 2–4).
Sampling, data collection and analysis of subunits
Cases 1, 2 and 4
The sample size was determined by the goal of analytical, rather than statistical, generalisability and based on a requirement to achieve data saturation within the case (interviews) and pattern match data in the patient records. 49 Internal generalisability within each case was maximised by sampling patients/carers who were considered to be representative of others in the case. 50
The unit of analysis was the service delivery model, with embedded subunits of analysis.
Prospective data from up to 10 patients (and their carers, when appropriate) were sampled within each case study service model. The eligibility criteria for patients were as follows:
-
no longer receiving curative treatment (e.g. individuals listed as palliative on a palliative care register or CNS caseload)
-
in receipt of prescribed medicines for symptom management
-
living in their own home or in a home of a relative (but not a nursing or care home, or hostel, or individuals who are homeless)
-
survival could be reasonably anticipated to be no less than 12 weeks
-
able to give informed consent
-
able to speak and write English.
Patients/carers were asked to complete a structured log on medicines access experiences over an 8-week period from recruitment into the study. The logs collected data regarding obtaining prescriptions and medicines, plus supporting information, both in-hours and OOH. These logs supplemented and/or were an aide memoire to sequential interviews with patients/carers conducted at study entry and at 4 and 8 weeks. Interview guides and log data collection were informed by PPI feedback. Interview data were audio-recorded, transcribed and analysed using a framework analysis (see Appendix 2). 51 An initial coding framework was constructed from the interview guides and then developed inductively from the data to identify main themes (NC at site 1, JB at sites 2 and 4, and NC and ZE at site 3).
Health-care professionals who were providers of EoL care in the case study service model were purposively sampled and invited to take part in a semistructured interview, either individually or in a group. HCPs were asked about their experiences of facilitating access to medicines, including barriers and facilitating factors. Interviews were audio-recorded, transcribed and analysed using a framework analysis51 (see Appendix 2).
A retrospective convenience sample of up to 40 patient records (including patients taking part in recording logs and interviews) were reviewed. Data were extracted on medicines prescribed (including when and by whom) and services used (including OOH, unplanned or emergency services, and hospice or hospital admissions). For health economics analysis, see Chapter 6. Annotated timelines for each patient were also constructed when possible, with HCPs accessed, prescribing decisions and services used, to understand medicines access processes. 52
Case 3
Case 3 focused on community pharmacy-delivered commissioned services for palliative medicines. The data collection methods for this case differed from cases 1, 2 and 4. Data from phases 1 and 2 indicated that this was an important model to evaluate in more depth. However, scoping work highlighted that it was not feasible to identify and recruit patients using these services from general practices. For example, a palliative care patient from the typically small number registered with any one general practice is likely to use more than one community pharmacy, and/or patients using a particular commissioned service pharmacy are likely to be registered with a large number of general practices. In addition, our data suggested that CPs are often unaware which patients using their service are receiving palliative care. We were aware that documentary data on these services were publicly available, and that service commissioners were likely to have important insights into how these services have an impact on access to medicines. Therefore, this case focused on qualitative interviews across three sample groups, supplemented by documentary analysis. Sample groups were (1) CPs providing commissioned services, (2) commissioners of these services and (3) community-based HCPs [e.g. palliative care CNSs, CNs, CPs (not providing commissioned services) and GPs].
For details of the health economic evaluation, please see Chapter 6.
Case study data analysis
Data from within each case were triangulated (i.e. data source and method triangulation) to build in-depth contextual understanding of medicines access experiences in each delivery model. 53
Cross-case comparison
On completion of data analysis for each case, cross-case comparison was utilised for pattern matching and theory-building. 49 This comparative evaluation was developed through the construction of logic models for each case and against a framework of indicators characterising good practice in medicines access. This framework was informed by the phase 1 systematic review, the phase 2 survey, our PPI consultation and relevant national standards. 20,24 The framework included indicators such as speed of access to medicines; patient and carer burden (e.g. time, travel, cost, psychological distress) experienced in accessing medicines; number and type of contacts required before a medicine is supplied; accessibility, ease of use and comprehensiveness of information sources; and use of OOH, unplanned or emergency services. The framework was used to help evaluate each case and to enable systematic comparisons across service delivery types (see Appendices 8, 16, 19 and 24 for logic models for each case).
Case 1: general practice
Method
The case
The unit of analysis was services in which GPs were the main (usually sole) community-based prescriber. This unit of analysis was selected as representative of typical service delivery for community-based palliative patients.
Sampling
The case study was conducted in the south of England and included three general practices. Practices were sampled from 19 practices that were registered as the most research-active practices in the local CRN (i.e. those classified under the NIHR CRN’s Research Site Initiative scheme sessional level practices, recruiting to a minimum of seven studies per annum) and that were within reasonable travelling distance of the research team. The first three general practices approached agreed to participate in the study.
Patients and carers
Research staff in general practices searched the Gold Standards Framework (GSF) register (i.e. the palliative care register used by all the practices) for eligible individuals. Searches for new listings were repeated on a monthly basis.
Health-care professionals
General practitioners
All GPs (n = 31) practising in the three case study practices were invited to take part in an interview.
Community pharmacists
The lead pharmacists in six community pharmacies (identified via NHS Choices website54 as the nearest pharmacy to each of the general practices’ dual sites) were approached.
Community palliative care clinical nurse specialists
Team leads for each of the geographical areas covering the general practices were asked to attend a focus group, alongside one other nurse specialist from each team.
Community nurses
The head of nursing invited CNs from the community trust’s teams that covered the general practices to participate.
Findings
Sample
Table 6 displays participant recruitment by general practice and Appendix 3, Table 14, displays demographic data for the patient and carer sample.
| Practice number | Sample, n | ||
|---|---|---|---|
| Patients | Carers | HCPs | |
| 1 | 3 | 1 | 1 (GP) |
| 2 | 5 | 2 | 2 (GPs) |
| 3 | 1 | 1 | 1 (GP) |
| N/A | 2 (CPs) | ||
| N/A | 7 (community palliative care CNSs) | ||
| N/A | 15 (CNs) | ||
| Total | 9 | 4 | 28 |
| Overall total = 41 participants | |||
Data sources
Seventeen patient/carer interviews were conducted (by NC) (see Appendix 4, Table 15). Six patients deteriorated more quickly than their GP anticipated and so the numbers of interviews undertaken varied. This also affected the number of completed logs (n = 29) collected during the 8-week study period. After each patient/carer interview, field notes were completed (by NC), supplementing interviews as an additional data source.
Ten HCP interviews were undertaken (by NC) (see Appendix 5, Table 16). CPs and GPs were interviewed one to one. Three CN group interviews occurred, and a focus group was run with community palliative care CNSs.
Patient record data extraction forms were completed from electronic GP medical records (via EMIS Web, EMIS Health, Leeds, UK). Twenty-six forms were completed (for the nine recruited patients who took part in interviews, plus 17 other patients). The records-only data extraction was lower than the 30 sought for two reasons (reasons that also underpinned the recruitment of nine patients rather than the intended 10 patients, despite a lengthy recruitment period). First, palliative care patients were not proactively identified and added to the GSF and so smaller than anticipated numbers were listed as palliative care patients during the data collection period. Second, larger than anticipated numbers of patients identified as requiring palliative care were ineligible for study participation as they were living within nursing/care homes.
Description of the service delivery model
Appendix 6, Table 17, outlines key service delivery characteristics of the three general practices and associated community-delivered services in the area.
The general practices were all dual sites with large list sizes, ranging from 17,078 to 18,596. Two of the practices served urban populations and the third a semirural population. Of note were the deprivation index scores of either 9 (i.e. the second least deprived decile) or 10 (i.e. the least deprived decile) for the geographical areas the practices were in. 55
Community specialist palliative care service provision was predominantly provided by CNSs (led by a medical consultant) covering weekdays 08.30 to 16.30, but limited to on-call telephone advice at weekends. To ensure distinctiveness of the case, we identified, prior to site selection, that none of the community-based palliative care CNSs that covered the general practices was a NIP [with few in the service overall (2/17)].
General practices were all within the same CCG and commissioned a community pharmacy-delivered palliative care service. The service was offered by 11 pharmacies in the CCG region (out of 94 in total). The nearest commissioned pharmacy was between 1.5 and 8 miles of the general practice sites.
Patient and carer experience
Activities undertaken to access medicines
The activities that patients and carers undertook to access medicines, in their experience, frequently felt like work. These activities included getting prescriptions (both new and repeat), liaising with community pharmacies or practice dispensaries for medicines to be dispensed and then obtaining medicines via collection or arranging home delivery.
Patients accessed new prescriptions via their GP (requiring telephone consultations and/or practice/home visits), but often recommendations for new prescriptions came from other HCPs, such as palliative or secondary care specialists (e.g. hospital-based oncologists). When other HCPs advised new prescriptions, patients were reliant on these HCPs contacting the GP on their behalf, for example via hospital outpatient appointments letters, which meant a delay in the medicines being prescribed by the GP, or via a palliative care specialist nurse telephoning and e-mailing the GP with recommendations.
When medicines were achieving good symptom management, GPs often placed medicines onto repeat prescriptions for patients. To obtain these, patients and their carers utilised three different systems:
-
telephoning their community pharmacy (which acted on the patient’s behalf to request the repeat prescription from the general practice)
-
completing the back of their dispensed prescription slip (and dropping this into their general practice or practice dispensary)
-
utilising online repeat prescription request systems.
Patients and their families usually had to wait 2 working days following placing the repeat prescription request to obtain the medicines from their selected pharmacy, but others had to allow 7 days (and they this considered as unnecessarily lengthy). For some patients and their families, these varied systems to obtain repeat prescriptions were confusing:
My husband was getting very confused and I was getting confused. Every time we went down [to the general practice] you saw someone different who told you, you had to do something different. They were saying about doing it online and then they were saying ‘oh just drop it in the surgery’. ‘Oh, get it from the pharmacy’ . . .
P2003, practice 2, interview 1
Patients and their families communicated with their community pharmacy, general practice dispensary and, in some cases, hospital pharmacy (where patients were receiving palliative chemotherapy regimens). Community pharmacies often contacted the patient or their family once medicines were available for collection (via e-mail, text or telephone call), but, equally, some patients and families telephoned the pharmacies to check that medicines had been dispensed before making the journey to collect them. Most patients were reliant on family members to collect medicines from pharmacies on their behalf, and when this was not possible they arranged for home deliveries to be made. Patients and families selected pharmacies based on what was most convenient for them (usually the one closest to their general practice site).
The experiences of patients and their families were also framed by how they accessed medical devices (including wound dressings and catheter supplies), enteral feeds and home oxygen cylinders via other supply systems (see Appendix 7).
Who do they work with?
Patients and carers discussed working with different HCPs (e.g. their GP, palliative care CNSs, CNs and CPs), non-HCP staff at their general practice (e.g. receptionist/administrative staff) and family/friends to gain access to medicines.
After GPs, patients were most likely to refer to their palliative care CNS, if they had one (note that three patients did not). Contact with CNSs varied from once per week (either via telephone or a home visit) to occasional contact (or reliance on patient/carer-initiated contact when issues arose).
When contact was regular, CNSs were particularly valued by patients or carers for their specialist knowledge regarding palliative care medicines (as well as their ability to consult with a palliative medicine consultant). For more complex medicines-related or symptom management issues, carers would contact the nurse specialist rather than the GP. Patients appreciated that CNSs were easier to access than the GP and that they would do ‘the ringing round’ on behalf of the patient (i.e. contacting the consultant for complex advice and contacting the GP to advise medicine changes). When the nurse specialist advised medicine changes, the common experience was:
She informs the GP and we then pick the medication up that she’s suggested . . .
C2002, practice 2, interview 1
Community pharmacists were also mentioned often. Patients and carers valued feeling that their community pharmacy staff knew them:
I like them, and I go in there and say hello and they know what I need.
P2005, practice 2, interview 1
Such relationships were sometimes facilitated by the patient and their family having used the pharmacy for years:
I’ve known them all down there for years because we’ve lived here 34 years. So, whoever goes and gets my prescription they always say give her our love or they ask how I’m doing.
P2002, practice 2, interview 2
Community nurses were referred to occasionally, and this was usually in relation to the supply and potential administration of anticipatory medicines (i.e. just-in-case boxes delivered into the home).
Reception/administrative staff within general practices were also referred to. For example, one patient reported that the practice receptionist was the key source of information regarding how to access repeat prescriptions and had set up the ‘patient access’ to enable him to use the online repeat prescription request system.
Family members were key in patients’ ability to collect medicines. However, they played other roles, such as:
-
communicating with the general practice/GP to gain consultations and, therefore, prescriptions for medicines
-
taking the patient to all health-care appointments (both general practice and secondary care)
-
stock managing medicines (to work out what was required)
-
re-ordering repeat prescriptions
-
liaising with community pharmacies (and, on occasions, hospital pharmacies), as well as practice dispensaries.
Only one patient in the sample (at the time of data collection) was not reliant on his family to help with his access to medicines. Most patients highlighted how lucky they were to have family available to help.
Information provision
Information regarding medicines themselves, and how best to take them, came from the GP as prescriber, but also secondary care specialists and palliative care CNSs when they had recommended medicines to be prescribed by the GP. Palliative care CNSs were influential regarding patients’ understanding of medicines.
In relation to how to access medicines, patients and carers spoke of a lack of information provision. When a new prescription might be required, it was often difficult for patients and carers to decide which route to take, for example should they contact the GP or the specialist nurse. Patients and their families were left floundering over who to contact. As one carer simply said:
. . . it would just be useful if the GP said this is how you do it, if you want this, just do this.
C2001, practice 1, interview 3
For another carer, this was expressed as:
. . . nothing has really been clearly explained.
P2003, practice 2, interview 1
How best to access repeat prescriptions had often been worked out by patients and carers via trial and error or previous experiences (such as caring for others in the past). All patients and carers recognised that they should re-order medicines approximately 1 week in advance.
Patients and carers all referred to a desire to receive tailored face-to-face information regarding not only the medicines themselves but also how to access them.
Learning to navigate systems
Only two patients and one carer spoke of feeling confident using the various systems needed to access medicines. Despite a lack of expressed confidence in this, patients and carers referred to things that they had learnt themselves and to consequent behaviour changes, for example leaving as much time as possible when putting in a repeat prescription request ‘. . . not doing it the day before . . . trying to leave a lot of time’ (C2001, practice 2, interview 1) and telephoning the pharmacy to check that medicines were ready to be collected to prevent an unnecessary trip or having to wait in the pharmacy for the items to be dispensed. Patients and carers learnt about their community pharmacy operations, such as when in the day their pharmacy received deliveries (e.g. 11.00 and 15.00) and, therefore, when to contact the pharmacy regarding a prescription in case an order with a wholesaler needed to be placed. Patients and carers also learnt to use a system that worked for them to stock manage/keep track of their medicines and recognise when they were running low. Last, patients and carers learnt to check medicines dispensed for errors prior to leaving the pharmacy so that the items could be returned to stock if they already had enough of the medicine or if the medicine was not the correct dose or form (to prevent medicines wastage):
. . . What I know now which I didn’t know at the beginning is that once you walk out the pharmacy with it they can’t do anything with it so . . . we always check it before we leave . . .
P1002, practice 1, interview 1
Issues encountered
Patients and carers encountered an array of negative issues when accessing medicines, described below in order of frequency of occurrence.
Although the GP was the main community-based prescriber, GPs made prescribing decisions based on advice from multiple advisors, for example secondary care specialists (i.e. hospital-based specialists and, in some cases, these were specialists also acting in a private health-care capacity) and palliative care specialists (note that none in this case was a prescribing medic or nurse). This made for a complex web of prescribing decisions:
. . . As far as the blood pressure and paracetamols . . . the [private] oncologist said I’d need them. I definitely need the abiraterone [hormone modulator] and prednisone [corticosteroid]. He also e-mailed the doctor [GP] and said, I would need blood pressure tablets. The [hospice] e-mailed the doctor and said, I would need [opioid] painkillers. [Oncologist] also said, I would need Adcal [calcium supplement] . . .
P1003, practice 1, interview 1
Information transfer between secondary and primary care (reliant on outpatient appointment letters or discharge letters) limited the speed and appropriateness of prescribing by the GP following secondary care specialist advice:
When we went down to the GP surgery to get some medication, they didn’t have a note of anything I was on because the hospital hadn’t informed them . . . Eventually we went back to the hospital, got them to email it through . . . but it took a long time to get it . . .
P2003, practice 2, interview 1
Part of the issue encountered by patients relative to the GP being the main community-based prescriber was the difficulties they found in accessing their general practice:
Ringing up the surgery in order to speak to somebody about getting meds [medicines] is an absolute nightmare . . .
P1002, practice 1, interview 1
Patients spoke about having to listen to long recorded messages, needing to ring early enough in the day so that a doctor would be able to ring them back that same day, not being able to get through on the telephone (because of the overall number of calls and the system then cutting them off), waits of 20 minutes for calls to be answered and not being able to see a GP (i.e. having to see a practice nurse instead).
The issue appeared so severe that patients in one practice developed strategies to ‘circumnavigate’ the system. Patients did so by visiting the practice in person, ringing a direct telephone line for one of the reception staff (which the patient had been given) and using the mobile telephone number of the GP.
Collection of medicines from the community pharmacy (or practice dispensary) was invariably undertaken by the family of the patient and was the next most frequently cited issue. There were many collection-related difficulties, including:
-
medicines not being ready for collection (and having to return later in the day or a subsequent day)
-
medicines not being in stock (and being sent elsewhere to get them, e.g. an alternative pharmacy or practice dispensary)
-
finding practice dispensaries closed at lunchtime
-
the length of time between requesting the repeat prescription and it being available at the community pharmacy (e.g. up to 7 days)
-
the prescription itself not being available at the community pharmacy (despite the repeat prescription request having been made via the general practice)
-
having to wait at the pharmacy even when the medicine was in stock and the carer had left the requested length of time between prescription request and collection
-
having to leave the patient at home (to collect the medicines)
-
having to make a car trip to collect the medicines.
Patients and carers found themselves needing to purchase medicines. These medicines were not only supplements/vitamins that patients wished to take (e.g. multivitamins, coenzymes, turmeric, iron tablets, melatonin, vitamin B6, cannabidiol and tetrahydrocannabinol), but also medicines such as paracetamol (purchased over the counter) and medicines accessed via private specialists that were not covered by health insurance (e.g. low-dose naltrexone). Three patients were purchasing their own paracetamol. This was an issue as they were all taking 1 g four times a day (i.e. eight tablets per day) and their carers were purchasing them in supermarkets where the number of tablets per pack is 16 and only two packets can be purchased at a time. The issue was not the cost of the paracetamol (in comparison to the high costs of some supplements that patients were taking), but that buying two packets in the supermarket was only 4 days worth of supply. None of the patients and carers had asked for paracetamol to be added to the repeat prescription, and none knew that a packet in a pharmacy could have up to 32 tablets (as opposed to 16 tablets in a supermarket).
Facilitators of medicines access
The most important facilitator of medicines access for patients and carers was the availability of a key HCP who co-ordinated their access. For seven of the nine patient participants, they or their carers referred to a single community-based HCP (usually the GP) who took the lead role, acting as an available point of contact and co-ordinating systems to facilitate access to medicines.
These key HCPs were working to pull everything together, often going above and beyond for patients and their carers:
I think the perfect service that we’ve had has been generated by the GP to be honest because she’s on it . . . Because you can’t get an appointment at the surgery, you have to wait weeks and weeks when we’re in with that 3-week assessment Dr [name of GP] makes the appointment herself there so that mum comes in [again] in 3 weeks’ time . . . You could flag us up as the way the system really should work but it’s all about the GP . . .
C2002, practice 2, interview 1
When access experiences via a key HCP were deemed good by patients and carers, these experiences were based on long-standing relationships with their GPs (noted by two patients), with the GP caring for other members of the family too.
The second most important facilitator was having a family member, or the patient themselves, acting as a co-ordinator. Four patient participants had carers acting in this role. The carers brought expertise (through their own experiences or those gained supporting the patient) to the patients’ experience of accessing medicines. They knew what medicines the patient was on, ordered them, collected them and helped access prescribers/health-care consultations to gain new prescriptions. As a result, patients had great confidence in their carers’ ability to access medicines for them. One said that ‘it’s not easy for me, but . . . she can do anything!’ (P2002, practice 2, interview 1).
Three patients acted as co-ordinator of their own medicines access. They were masterful in this role, co-ordinating varied access routes to medicines (via both private and NHS care), as well as co-ordinating information transfer between secondary and primary care, and between multiple specialists and their GP prescriber.
The three remaining facilitators [all information technology (IT) related] were not as important, but were cited as beneficial.
For three of the nine patients, either they or their carer noted the value in being ‘flagged’ (i.e. identified as having EoL needs and requiring early access to a GP) on their general practice’s records system. This enabled faster access to their GP for issues that may have required changes in their medicines.
Patients and carers also referred to the value of electronic prescribing by their GP [i.e. the electronic prescription service (EPS)], which enabled the prescription to be transferred to the patients’ nominated community pharmacy. For the majority of patients who used this service, this cut out a link in the process (i.e. having to take the prescription to the pharmacy, enabling one trip rather than two to the pharmacy).
Most patients and carers used these systems and found them easy and quick to use:
I can watch telly, sit on my phone and think oh I need to order that and then I’ve ordered it rather than going down there [general practice] and ticking a form . . .
C2001, practice 2, interview 1
Health-care professional perspectives
Activities to aid access to medicines
Activities to aid access to medicines included:
-
CNSs and CNs advising the general practice prescriber of new medicines required or dose changes to existing medicines prescribing
-
CPs, and other HCPs (CNSs and CNs), checking whether medicines were in stock or could be ordered
-
community pharmacies helping to arrange home deliveries for patients who are housebound with no family to help with collection.
For both CNs and CNSs, much activity appeared to revolve around going ‘through the GP’ to ask the GP to prescribe the required medicine(s) and then following up with the GP to see if this had been actioned and if the medicine had been obtained by the patient. The work involved in this process (i.e. chasing to ensure that breaks in the medicines access process did not occur and that access was timely) was onerous:
We have to request it [prescribing of medicines] from the GP and that then is a process . . . If it’s an urgent medication . . . we would e-mail with a phone call to follow it up, so that it’s marked as urgent and then we spend a lot of time potentially chasing that to make sure that it’s been sorted out. Sent to the pharmacy and then delivered . . .
CN001–004
General practitioners undertaking prescribing (often following recommendations from other HCPs) expressed this as ensuring that ‘people have got access to the right medication for what they need now’ (GP301, practice 3).
Who do they work with? The family of the patient was frequently referred to by HCPs because of the ‘onus’ often placed on them to ‘go and collect’ medicines (CN001–004). This was reinforced by GPs, for example ‘a lot of the time it’s usually the relatives that will be involved in terms of collecting medication’ (GP202, practice 2), and CPs often referred to seeing carers and not the patients themselves. There was a perception among the CNs that because ‘engaging the families’ at EoL ‘is very difficult’ as ‘they [the family] feel very useless’ (CN001–004) families valued being given this task to ‘feel they’re really doing something’ (CN010–015). The reliance that HCPs placed on family members was summarised as follows:
Often you are dependent on the carer for the patient, a relative, picking up prescriptions and sorting things out . . . You are to some extent dependent on the carers to pick up issues, the wrong medicines, the wrong doses, have they been given enough for the weekend . . . Those sorts of things which if they’re not there you’d have to do yourself as a GP . . .
GP201, practice 2
General practitioners spoke of liaising with PCPs [who would review patients in the last year of life, ‘but not specifically palliative medication’ (GP101, practice 1)], CNs (e.g. in relation to setting up syringe drivers), local CPs (e.g. checking that specific medicines were in stock, checking doses and asking them to set up dosette boxes) and CNSs. CNs referred to working with GPs, CPs and CNSs (seeking to do joint visits when appropriate). CPs mainly referred to working with GPs. Palliative care CNSs referred to all other HCPs, as well as general practice reception staff (especially prescription clerks).
Issues of workload and under-resourcing of services (particularly among the community palliative care service) were discussed as precluding relationships, with staff turnover cited as an issue in relation to community nursing teams. Nevertheless, amid these service pressures, there were examples of effective HCP working relationships:
. . . I’ve got a very close working relationship with our palliative care CNS . . . she knows my mobile number, I know hers and we’ll text each other even if either of us is not working if it’s required about a patient . . .
GP101, practice 1
Information provision
All HCPs referred to providing information on medicines to patients/carers and some, particularly CPs and CNSs, reported providing information on how best to access them. The mainstay of information about medicines appeared to come from GPs as prescribers or from HCPs advising that specific medicines be started (or doses altered). GPs stated that they provided information such as the ‘pros and cons of each individual medicine, the potential side effects, the way that they’re titrated’ (GP101, practice 1):
. . . As a general rule when we prescribe we tell them this is what you do, this is what you take . . . if it’s a p.r.n. [as required] medication we have to give them specific instructions like how much to take and how often to take [it] and then if you are taking this much you may need to give us a call back in which case we may need to titrate up your background analgesia for example . . .
GP202, practice 2
In contrast, CNSs referred to the need to supplement information provided by the GP:
. . . Sometimes you find say the GP’s been out and prescribed . . . a new medication . . . you’ll go there [home visit] and they’ll [patient] say ‘oh, the GP prescribed this but, I didn’t really know what to do with it’ or ‘I was scared to take it because it’s morphine’ . . . and then you kind of explain . . . ‘you can take— take this much’ and, you know ‘this is when you take it’ . . . That happens quite often . . .
CNS001–007
Community pharmacists in the sample also referred to providing ‘extra additional information’ (CP001) about how to use medicines (i.e. when to take them, discussing concerns, what to expect, what to do when encountering side effects). They often found that family members were ‘quite well informed when they come in, they just want the reassurance that they’ve been given the right information’ (CP002). In contrast, CNs appeared to provide less-detailed information about medicines, for example in the words of one CN ‘we just say “this drug is for this, will alleviate this” but it’s not really much more than that’ (CN005–009).
Information regarding how best to access medicines fell to CNSs and CPs. The CNSs encountered the following scenario:
. . . What I’ve found with my patients, they don’t really know how to get their repeat supply . . .
CNS001–007
As a result, CNSs and CPs found that they needed to talk patients through the processes of how to get their medicines. CPs provided information on re-ordering medicines sufficiently in advance:
. . . we just say order 1 week before they run out or a few days, don’t allow for the medication to run out and then ring.
CP001
In contrast to patient and other HCP data, GPs believed that ‘most patients’ were ‘aware of’ the ‘mechanism for ordering’ medicines (GP101, practice 1).
Issues encountered
Although the GP was the main community-based prescriber, they were co-ordinating prescribing in response to requests from at least two other community-based HCP groups [i.e. specialist palliative care (usually CNSs) and CNs]:
We need to be communicating with the doctor [GP], the [specialist palliative care], because there are three different people putting input into this one prescription . . . there can be a bit of conflict . . .
CN005–009
The amount of work that HCPs other than GPs were doing to facilitate medicines access was substantial. These HCPs were also ensuring that medicines access worked for patients following prescriptions being generated by GPs.
Community nurses spoke of ‘taking on the problems’ for families (CN010–015), ‘going above and beyond’ and ‘picking up the pieces’ (CN005–009). Like CNSs, CNs were organising medicines for patients and carers, checking supplies in advance to ensure that these were enough, telephoning community pharmacies to source supplies and collecting medicines when needed:
The GP writes the prescription and he’ll write the medication [administration] chart [for subcutaneous administration] and that’s it. That’s his job done as far as he’s concerned . . . It’s joining up all that. The first thing my colleagues will do is ‘have you got this?’, ‘is this signed? ’. . . You do go above and beyond because . . . we want to give that patient the medication at the time that they need it for their symptom control. And if that means us thinking, like on twilight [until 22.00]: ‘I’ll just go to the chemist. We can’t let the family . . .’ I don’t think it enters our head not to go . . .
CN010–015
GPs’ completion of palliative care administration charts was raised by CNs. Some teams spoke of having ‘real problems with the doctors’ prescribing’ (CN010–015). A commonly encountered problem was the incorrect completion of administration charts. This precluded CNs being allowed to administer the medicines because of a lack of signatures, no stated route for medicine administration, no dates or insufficient ranges for the medicines prescribed.
The duality of the system, which required GPs to both write a prescription and complete administration charts for CNs, was perceived as unnecessary duplication by the GPs. It caused communication problems with CNs and affected patient access:
Our district [community] nurses obviously want a copy of the administration [chart] . . . and we have to do the prescription separately . . . I would say the communication between the district nursing team and the GPs . . . with regard to the documentation, was often problematic . . .
GP101, practice 1
In the words of one CN:
When you’re co-ordinating [the team] you literally spend hours back and forward [to the general practices] with these charts which is a waste of time . . . For us to actually administer it . . . it has to be dated . . . we have to follow these rules and I know that’s a bugbear for them and it must be a nightmare getting us ringing them up saying ‘Can you do it again?’ . . .
CN001–004
Another barrier related to the GP being the main community-based prescriber was the difficulties other HCPs found in trying to contact GPs and general practices owing to service pressures. Just as the patients and carers had experienced, HCPs also frequently encountered difficulties. CPs often sent physical notes to nearby general practices to prevent having to get through to the practice on telephone lines. CNs and CNSs referred to these problems and stated explicitly that patients complained ‘all the time’ about the length of time they spent trying to get through to their general practices. Furthermore, CNs and CNSs were often telephoned by patients to see if they could get through to the general practices/GPs on their behalf. The delays in the process below highlight the interruptions in medicines access for patients and what other HCPs needed to do to work the system:
You can wait on the phone, 20-plus minutes. So, you end up sending an e-mail . . . and then you end up trying to phone the surgery again to say ‘have you got the e-mail?’
Because you worry about it just sitting in a list somewhere . . .
Do you often e-mail the GPs direct?
Not for the palliative stuff. No.
You just can’t rely that it will be seen. I mean, you can put read receipts and make it important but, I just don’t bother anymore.
So, it’s reliant on [tele]phone calls?
Or just turn up, drive around there, and wait to be seen . . .
This was due to service pressures and raised by GPs and CNs. GPs were critical of the overall lack of specialist service-related input (rather than that provided by individual CNSs) and that the service was mainly weekday and advisory.
Community nurses spoke of not having met the palliative care CNSs because the specialist service was so ‘stretched’. Most CNs had communicated only with CNSs regarding patients over the telephone and although joint visits did occur they seemed rare. For some CNs, each time they rang the specialist palliative care service ‘you seem to have a new name’ (CN010–015). This was important in facilitating medicines access because although CNs found that CNSs could not always get to visit patients, when they did, they often worked behind the scenes to smooth patient experiences of medicines access and CNs often found them ‘more responsive than the GP’ (CN005–009). A lack of contact and, at times, a lack of professional relationships between these specialists and other HCPs precluded best access to medicines for patients.
When specialist palliative care was involved, GPs felt that the experience was one of them ‘advising in the background’. Furthermore, a series of circuitous processes occurred when specialist palliative care advised medicines to be prescribed, with potential for breaks at all points:
The palliative care team may decide they need to provide a medicine and they contact us . . . by telephone or e-mail, saying can we provide this medicine because of course they can’t prescribe it, which is a shame as they should be able to really . . . A duty doctor effectively takes that call, runs through it among all the other calls and gets it across to the pharmacy in time. Within that process you might have a problem with the e-mail getting through, processing the e-mail or processing the call or the duty doctor being busy . . . and then getting to the pharmacy with the script . . .
GP201, practice 2
None of the palliative care CNSs working across the general practices was a prescriber and only one of the two practices with PCP involvement had input from a PCP who could prescribe. Neither of the CPs interviewed were prescribers and although some of the community nursing teams included matrons or integrated care leads with both the V100 (community practitioner nurse prescribing course) and V300 (independent prescriber) prescribing qualifications, they were rarely used in EoL prescribing. This was because of reduced patient contact through managerial roles as service leads.
Reasons appeared to be lack of awareness regarding prescribing qualifications and options (e.g. some CNs were unaware that independent V300 prescribers could prescribe any medicines listed on the Drug Tariff, including CDs). In addition, lack of funding and distance to courses were cited as issues for CN participants. Nevertheless, HCP data demonstrated support for nurse and pharmacist independent prescribing, and some were considering undertaking the qualification:
I’m a huge advocate of nurse prescribing/pharmacist prescribing . . . They would probably do it rather better than doctors in some cases . . .
GP101, practice 1
To have more non-medical prescribers, will cut out some of those tiers of frustration and problems . . .
CNS001-007
Lack of access to shared records hindered medicines access (particularly best practice in relation to prescribing and associated interdisciplinary working). CPs were able to access only the SCR for patients, CNs had no access to palliative care nurse records (and vice versa) and the GPs could not view the community nursing or specialist palliative care records or GP OOH records.
HCPs, particularly CPs, cited legal issues around CD prescriptions allowing supplies of only 28 days and difficulties stocking CDs in community pharmacies (e.g. locked cabinet capacity and not knowing which CD or dose would be prescribed for patients) as precluding medicines access (both ease of supply and speed of access). CNSs spoke of community pharmacies not dispensing less-frequently used CDs (e.g. ketamine).
HCPs spoke of the frustrations of patients/carers if they needed to access GP OOH services via NHS 111. This specifically related to securing a supply of a newly prescribed medicine:
[Patients] may have suddenly deteriorated quicker than someone thought . . . it’s probably about 15 to 20 [tele]phone calls, sorting things out and some on-call pharmacists at the hospital are perhaps more willing [to dispense OOH] than others . . .
CNS001–007
Medicine shortages were raised by HCPs as barriers to medicines access. Shortages caused delays in speed of access and required changes to the medicine prescribed:
If we can’t find the item in stock [via distributors] then we call the prescriber to find an alternative . . . if it’s urgent like they need it now then, we do have a problem . . .
CP002
Although medicine shortage issues appeared to be related to all medicines, palliative care medicines reported to be in recent short supply were morphine, diamorphine and levomepromazine. Such situations delayed access and CNSs reported feeling that they were informed ‘late’ (e.g. via palliative care formulary alerts) and likely to hear via patients or CNs ‘struggling’ to get a particular medicine.
Although community pharmacy home delivery services were generally perceived as beneficial, CNs highlighted that some community pharmacies had started charging for home delivery. Home delivery also had an impact on information received by patients/carers because of reduced contact with a pharmacist:
Our [delivery] drivers aren’t trained . . . so if there is anything that the patient wants to know . . . then we have to ask them to ring the pharmacy . . .
CP002
Health-care professionals emphasised many issues to medicines access and related barriers, and majored on the facilitators outlined below as mechanisms to address these.
Facilitators of medicines access
Health-care professionals highlighted facilitators, both actual (i.e. already occurring in practice) and potential service-related improvements.
GPs, CNs and CNSs identified the value of proactively considering issues that might arise for patients in relation to their medicines and consequent prescribing needs. This was not only in relation to just-in-case (anticipatory) medicines that could be kept in the home for crisis situations but also pre-empting medicine needs OOH:
A lot of my time I’m trying to sort things out before the weekend . . . to make sure we’ve got enough medicines for the weekend . . .
GP201, practice 2
Similarly, the CNs spoke of how ‘in our heads we see a weekend coming’ (CN001–004) and proactively telephoned GPs if they thought that an increase in dosage was warranted.
EPS was cited by GPs and CPs as enabling faster medicines access. EPS removed a link in the access chain, and the addition of CDs to the system was viewed as a great improvement:
We get things [prescriptions] quicker, so it makes things easier for us if we have to order things in. Everything is quite clear, the dosage, I think it prompts doctors to make sure all the information is there . . .
CP002
CNs and GPs, as well as the team lead of the CNSs, referred to the need for CNSs to prescribe to facilitate medicines access for patients:
Our local hospice are looking at training the nurses up to be prescribers which would be a huge, huge benefit . . . that would save a lot of time and hassle for them and for us . . .
GP301, practice 3
Community nurses also emphasised how much of a facilitator this would be because of their ‘wealth of knowledge’ and because of their reviews of patients on their caseloads ‘they’re seeing them, often the GPs aren’t’ (CN001–004).
Continuing professional development (CPD) was highlighted as important for both CN and GP groups:
I don’t think we know enough . . . about all those different types of drugs, why you give certain things . . .
CN001–004
Integrated working both within and across HCP groups was viewed as another important facilitator of medicines access. HCPs referred to:
-
the need to include pharmacists (i.e. PCPs and CPs with professional scope of practice in palliative care) within future integration
-
improved use of palliative care registers (and related meetings)
-
availability of direct, professional-only telephone lines (for HCPs to use to contact general practices)
-
access to shared records.
Clinical nurse specialists were specific about the need for improved use of palliative care registers and associated regular MDT palliative care meetings to improve access to medicines. CNSs emphasised that for some general practices palliative care patients were ‘definitely on their radar’, yet for other practices such patients were ‘not on there [the register]’ (CNS001–007). Immense variability in the frequency and efficacy of meetings was noted. Despite these shortcomings, CNSs stated that such meetings ‘if everybody goes’ were key for ‘connection’ and HCP relationship-building, ultimately facilitating medicine access (CNS001-007).
Palliative care registers also facilitated the important issue of flagging palliative care patients on practice records. As highlighted by some patients and carers, HCPs recognised the impact this had when patients and carers contacted their general practice:
I suppose the most important routine from our point of view is when a patient is palliative . . . it’s entered on the records . . . We have a message screen which we enter the phrase GSF gold standard early access GP, and then we put the initials of the GP. So, they have access to me . . .
GP201, practice 2
Both CNSs and CNs argued for greater access to medicine stocks OOH. These nurses recognised that for CDs to be available the service provider would need to hold the required licenses and, therefore, acute trusts and pharmacies were deemed suitable options. Consequently, CNSs and CNs argued that available central stores of medicines for access OOH ‘would be very useful’ in facilitating medicines access (CN001–004).
Summary
Appendix 8, Table 18, summarises the general practice case service delivery characteristics, their mechanisms of action to influence medicines access, moderating and mediating factors, and the impacts on both patients/carers and on service outcomes. For patients and carers accessing medicines, this often felt like ‘work’. Medicines access involved gaining prescriptions (both new and repeat), liaising with community pharmacies or practice dispensaries for medicines to be dispensed and arranging for collection of medicines. Hurdles and delays were frequently encountered (see Appendix 9, Box 2), and so access was not a straightforward process but a set of burdensome activities. Patients had medicines supplied not just by community pharmacies (and general practice dispensaries), but also via hospital pharmacies and private health-care systems.
Health-care professionals were explicit about the impact of suboptimal access to medicines in the last year of life. For most HCPs, it was a critical issue, leading them to work around the system to avoid potential for distress for patients and their families. Most patients/carers referred to a single community-based HCP who took the lead role co-ordinating systems to facilitate access. This role was usually filled by the GP, except for two patients for whom this role was played by the palliative care nurse specialist. Not only were these lead HCPs working to facilitate access for patients, but, to circumvent poorly functioning, cumbersome access-related systems, other HCPs were also working to facilitate access, resulting in high levels of allied or duplicated activity (see Appendix 10, Box 3).
Case 2: community palliative care clinical nurse specialist with a nurse independent prescriber qualification (V300)
Method
The case
The unit of analysis in case 2 were patients registered on the caseloads of community palliative care CNSs who were independent prescribers.
Sampling
The case study was conducted in the north of England, centring on two CNS teams, each based in a city hospice. CNS teams were purposively selected because of the high proportion (> 80%) of independent prescribers (with V300 qualification) in the teams.
Patients and carers
Patients were required to be registered on a CNS caseload. Hospice research nurses searched CNS caseloads for eligible individuals and carried out repeated searches for new listings on a monthly basis.
Health-care professionals
GPs for two participants were invited to take part.
Specialist nurses were approached via the hospice research nurse.
CNs for two participants were approached via the hospice research nurse.
Pharmacists and doctors were approached via the hospice research nurse.
Findings
Sample
Table 7 displays participant recruitment and Appendix 11, Table 19, provides demographic data for the patient and carer sample.
| Sample | Total n |
|---|---|
| Patients | 11 |
| Carers | 7 |
| Total patients and carers | 18 |
| Community palliative care CNS nurse prescriber | 11 |
| CN leads | 2 |
| GP | 2 |
| Palliative care consultant | 1 |
| Palliative care doctor | 1 |
| Hospice pharmacist | 1 |
| Total HCPs | 18 |
| Overall total | 36 |
Data sources
Appendix 12, Table 20, displays the total number of patient/carer interviews across the sample (including the form of the interview). In total, 29 patient/carer interviews were undertaken (by JB). Three patients deteriorated more quickly than their CNS anticipated and so the numbers of interviews undertaken varied. This also affected the number of completed logs (n = 46) collected during the 8-week study period. Eighteen HCP interviews were undertaken (by JB) (see Appendix 13, Table 21).
Patient record data extraction forms were completed from electronic GP and hospice medical records [i.e. EMIS and SystmOne (The Phoenix Partnership, Leeds, UK)]. In total, data from 40 patients were collected (for 10 study patients who completed a minimum of two interviews and an additional 30 patients).
Description of the service delivery model
The service delivery model in case 2 was the CNS NIP. Key service delivery characteristics are outlined in Appendix 14, Table 22.
Patient and carer experience
Activities undertaken to access medicines
Accounts of the ease of the journey, from prescription through to receipt, varied within and between participants, and more difficult experiences were often due to reduced support (i.e. gaps in CNS service between staff changes) and the patient having a keen intention to manage this themselves. However, most patients/carers reported mainly positive experiences and were able to describe how CNS input simplified the prescription process for the patient/carer:
Yesterday I had a conversation with nurse [CNS] around at the hospice in relation to some medicines and she did it by way of e-mail to the practice and the practice then e-mailed me or text me to say that it had been done and it will be ready for collection this afternoon . . .
Dyad CNS08, interview 1
Some patients/carers described processes that required increased patient/carer input, such as calculating how frequently to re-order medication, setting reminders to re-order, keeping abreast of changes, prescription ordering methods and re-arranging collection and/or delivery times.
Most patients were contacted by their CNS at least once weekly. Patients appreciated that they could contact their CNS when they needed. CNSs were particularly valued by patients or carers for their specialist knowledge regarding palliative care medicines:
Definitely know more [about medicines] than what my doctor does . . . because they are having to deal with pain and patients constant all day . . .
Patient CNS03, interview 1
Many patients were able to say how working with the CNS NIP had been beneficial in accelerating access to repeat prescriptions when delays in the process had resulted in medicines being unavailable in patients’ usual pharmacy, when increased medicines were needed to cover holiday periods and when prescribed medicines (or doses) were not effective. Patients valued their CNS prescribing new medicines that they could collect that day. Patients also referred to other HCPs. For most patients, their regular GP was the HCP they accessed after the CNS (see Appendix 15). PCPs were referred to infrequently and usually in relation to adjusting doses. CPs dispensing patients’ medicines were chosen for convenience and had typically been used by patients prior to EoL care.
For several patients, their family was crucial as they undertook activities such as:
-
medicines stock management
-
communicating with HCPs (usually the CNS) to gain prescriptions
-
taking the patient to some health-care appointments or arranging home visits
-
telephoning contacts (e.g. the patient’s CNS and GP)
-
re-ordering repeat prescriptions
-
liaising/collecting medicines from community pharmacies (and, on occasions, hospital pharmacies).
Information provision
Patients reported that their CNSs provided sufficient information about their medicines regardless of who had prescribed it, including how and when to take it and what it was for. Patients said that they could ask their nurse for information about medicines at any time. CNSs anticipated problems with patients’ interpretation of medicines leaflets and so prepared the patient appropriately:
[CNS] said . . . when you read the leaflet don’t get a shock because it’s given for patients with schizophrenia . . . but in low doses it’s been found to be very beneficial in stopping you feeling sick.
Patient CNS04, interview 1
General practitioners and secondary care specialists were more likely to provide information for the medicines they initiated themselves or when asked to do so by the patients. CPs also provided medicines information when asked to do so by the patients. Accessing repeat prescriptions had often been worked out by patients and carers via previous experiences prior to their current diagnosis. CNS input had streamlined medicines experiences for patients who had persistently experienced issues, enabling speedier access. Patients valued being able to contact the CNS to prescribe medicines that were not ready when expected:
I wouldn’t say it’s been smooth . . . we’ve had a lot of times where nearly every time I went to the chemist it was like, oh guess what they haven’t got this I’ve got to go back . . . now we’re onto an equilibrium and it’s not too bad. Now we’ve got the CNS we can access it more quickly and more directly, so it has become better . . . We’ve had cases where we’ve done a repeat prescription and the stuff hasn’t come through and I’m thinking oramorph, something that you can’t really do without . . .
Dyad CNS10, interview 1
Learning to navigate systems
The CNS not only helped guide patients through systems, but also supported them in their self-management:
She’s very respectful so when she gives me the prescription and I say I’m going to deal with it she lets me deal with it. If I say I’m having trouble with something she’ll help me . . . she steps in when I need her to which is great . . .
Patient CNS02, interview 3
Patients and carers learned to prompt themselves to order medicines:
I’ve got reminders set up on my phone to do everything because otherwise I will just forget.
CNS02, interview 1
In addition, patients and carers learnt to leave enough time when putting in a repeat prescription request and would contact the pharmacy to check that the medicines were ready to be collected:
. . . you try and be organised so that you have got those 2 or 3 days but sometimes with controlled medicines they don’t like to give it you in advance.
Dyad CNS06, interview 1
Facilitators of medicines access
Having a designated CNS NIP with specialist palliative care knowledge who prescribed new medicines or requested GP prescriptions sped up access for the patient:
She’ll send it through to the GP practice who will then contact me and tell me that she’s been in touch with them and that they have on her behalf prescribed and it’s gone to the local chemist.
Dyad CNS08, interview 1
Clinical nurse specialists identified appropriate HCPs/teams and contacted these on behalf of the patient, speeding assessment and appropriate prescription:
I told her [CNS] what was wrong with me and she told me that two of the symptoms were for the GP, and in terms of the pain relief she speaks to the pain consultant and she did and she came back with the answer . . .
Dyad CNS01, interview 1
Clinical nurse specialists liaised with pharmacies to source medicines and provided information on how to obtain them, creating an access experience that is ‘seamless; she deals with it and it’s always ready the next day’ (dyad CNS12, interview 2).
In addition, CNSs facilitated access by using their knowledge of specialist EoL medicines and availability of local pharmacy services to liaise with pharmacies to source appropriate medicine and then re-prescribe for the patient in a timely manner. This was particularly valued when issues had occurred:
Three times, three prescriptions, they said they haven’t got it [pharmacy]. ‘When did you put it in?’ . . . We must have put it in last week and loads and loads of time and three times they said, ‘no we haven’t got it in yet, it’s not available yet’.
And I didn’t have any.
The chemist said, ‘oh well we’ll have to get another prescription it could take 4 or 5 hours for a doctor to phone you’. We came back and phoned [CNS] and within 20 minutes she had another prescription . . . and gave us a choice of places to go and collect it.
GP services were considered important in patient care; however, compared with the CNS, their prescribing role was almost exclusively to do with prescribing initial prescriptions (often at the request of the CNS) and taking responsibility for repeat prescriptions. Other HCPs mentioned were clinicians in hospital oncology departments (by two patients), PCPs (by one patient) and CNs (by one patient).
Issues encountered
Patients and carers encountered few negative issues. When these negative issues did exist, they related to initial, minor or infrequent problems that were often addressed by their CNS who also helped ensure that patients did not encounter subsequent issues.
-
medicines not being ready for collection (necessitating a return trip)
-
medicines not being in stock
-
the length of time between requesting the repeat prescription and it being available at the community pharmacy (up to 1 week for some)
-
the prescription itself not being available at the community pharmacy (after repeat prescription request made via the general practice)
-
not knowing when the home delivery would arrive and having to wait in or have a back-up plan should the medicine not be on this delivery (particularly if late or on a Friday).
Despite collection of medicines being the most frequently cited issue, the extent to which collection issues had an impact on the patient and carer varied. Examples given by nine patients/dyads referred to issues that were quickly resolved (e.g. initial prescriptions not usually stocked, alternative medicines and one-off or minor issues). However, one patient (CNS02) and another patient–carer dyad (CNS09) had experienced frequent issues with shortages, transfers of prescription to pharmacy or non-synchronised prescriptions, and both had, more recently, started to use their CNS to help solve these issues. CNSs typically addressed these issues by checking that the pharmacist had stock or delivery from suppliers before the patient’s next prescription was due. In addition, CNSs streamlined GP and pharmacist communication between each other and the patient. When collection of medicines was needed, most patients used their CNS to help; however, a few patients preferred to do this themselves if they were able.
Delays in information transfer between organisations with different electronic systems contributed to issues when there was more than one prescriber, and this limited the speed that GPs commenced repeat prescriptions. For example, for the patient below, poor synchronisation between multiple prescribers resulted in the patient not getting his medicine when re-prescribing followed de-prescribing over a 2-week period, but the CNS was able to correct this:
They’ve told me on the ward to put him back on to omeprazole . . . and it’s still not been done. That’s a fortnight ago . . . and it’s two doctors last week that I told . . . So that was going to be my job yesterday but the lady from the hospice [CNS] said I’ll sort it out . . .
Dyad CNS09, interview 1
This patient, who valued the expert care she received from her GP and palliative care team, described how the OOH GP complicated her medicines access:
This 111 doctor within about 3 minutes of seeing me decided that she should change my medication . . . ‘You should be taking twice the amount [sevredol] that they’ve prescribed, take 90 mgs not 40 mgs’ . . . I’ve been under the hospice’s care for 3 months and they’ve looked after me perfectly and I’m not listening to what you are going to say . . .
Dyad CNS01, interview 3
Few patients reported difficulties in accessing their GP, as CNSs were key to liaising with practices, requesting GP telephone, home or practice appointments. Two patients did report problems accessing GPs; however, experiences for one patient (CNS10) predated CNS involvement. The other patient (CNS02) described a preference to engage with the GP herself, allowing her to feel in control of her own care as much as she was able.
Health-care professional perspectives
Activities to aid access to medicines
Activities to aid access to medicines included:
-
CNSs requesting that GPs prescribe new medicines or alter dosage of existing medicines
-
GPs, palliative care doctors and CNSs prescribing
-
CNSs and CNs helping to obtain medicines (i.e. liaising with pharmacy to check stock, handing paper prescriptions to pharmacy and, occasionally, collecting medicines on behalf of patients).
Clinical nurse specialists’ activities followed a process. First, CNSs were tasked with assessing patients’ symptoms, existing treatment plans and what they could cope with to make a treatment plan. Then, CNSs checked patients’ nominated pharmacy for stock, provided information to the patient, wrote a prescription or sent an electronic request (or, in some cases, an e-mail or telephone call) to the GP to prescribe. CNSs’ decision to prescribe new medicines depended on how quickly the prescription was needed. (If there was no stock, CNSs would re-write the treatment plan for an alternative medicine or contact other local pharmacies.) If the medicines were needed urgently and a family member or friend was available to collect from a pharmacy with stock, then CNSs prescribed on a separate script for each item (to broaden choice of pharmacy). If no family member was available and the patient was able wait for a delivery and the medicines were available at the nominated pharmacy, then it was quicker for a GP to prescribe via electronic transfer. CNSs who reported more difficulty in accessing GPs than others typically undertook more independent prescribing, particularly if based in urban locations with a wide choice of pharmacies to collect from. This CNS described how her assessment considered factors that would enable the swiftest access:
Depending (1) on who the GP was, (2) what day of the week it was we’d make a decision whether I would ring the GP and discuss it with them and ask them to prescribe or whether I chose to prescribe it myself. So often the decision to prescribe it myself is usually speed of access so for instance yesterday I went to see a lady . . . she’d been vomiting all night, she was distressed so it was easier for me to do the prescription . . . I rang the chemist and they had it in so Dad kindly went and got it so she got her symptom relief really quickly . . .
CNS HP18
Although CNSs typically transferred responsibility for repeat prescriptions to the GP, they wrote repeat prescriptions when they judged that access would be speedier for the patient (e.g. exacerbation of symptoms, impending weekend/bank holiday, stock unavailable at usual pharmacy). GPs were satisfied with the medicines recommendations made by CNSs and were happy to prescribe these. One GP acknowledged that GPs in the practice rarely saw EoL patients and that they would often contact the palliative care team or refer to Electronic Palliative Care Co-ordination Systems (EPaCCSs) to prescribe themselves.
Much CN activity included contacting GP services (particularly OOH) to request a patient visit or recommend that they prescribe the required medicines. The district nurses (DNs) stated that most nurses in their teams did not prescribe; however, one DN said she:
. . . re-prescribe[d] for GPs when they prescribe incorrectly, and I will source the medication for them as well. There’s not many non-medical prescribers in the community district nursing integrated teams as they are now . . .
DN HP16
HCPs reported working with the patient themselves, their family and other HCPs.
The family of the patient was frequently referred to by all HCP groups because of their involvement in medicines access, including contacting prescribers, collecting medicines and keeping track of medicines. CNSs aimed to minimise burden on family by checking stock at local pharmacies before issuing prescriptions and, therefore, time spent collecting medicines was reduced, enabling family to focus on helping with medicines at home:
I’d often ring ahead to the chemist . . . she [daughter] didn’t want to be driving around and the patient didn’t want her driving around trying to find drugs . . . It was useful that I could just give her a script knowing that she could start something that day . . .
CNS HP10
CNSs spoke of engaging and liaising with:
-
GPs (e.g. providing advice, requesting prescriptions and appointments)
-
CPs (e.g. checking that specific medicines were in stock)
-
hospice doctors (e.g. requesting specialist advice and remote prescribing)
-
CNs (e.g. providing advice, carrying out prescription requests, and requesting visits and/or prescription if DN a prescriber).
District nurses acted on CNSs’ advice to prescribe and speed up access OOH:
So particularly at a weekend . . . we’ll give them [DNs] some advice on what to use and then they’ll prescribe it. So that’s really helpful otherwise it would mean either getting an OOH doctor or us going out, which would delay things . . .
CNS HP09
Clinical nurse specialists were able to enable dose changes for patients by requesting that hospice doctors access the electronic patient record to speed access to medicines for DNs to implement:
The doctors . . . can remote prescribe, so if we want to change syringe driver doses or something like that they can write it on the system so the district nurses can get out and get it done . . .
CNS HP08
When patients’ medicine needs were particularly complex or challenging, CNSs were able to consult with palliative care consultants ad hoc or at regular MDT meetings. This resource not only enabled CNSs to work with the patient in front of them, but it augmented their own specialist knowledge:
I . . . went to our MDT discussed the patient with our consultant who recommended how to manage his pain. So, I’ve been out today and prescribed something for his pain . . . Some meds [medicines] I think ‘oh can I prescribe that’ . . . We do pain, antisickness, the same kind of drugs all the time. So, there’s the odd time when it’s like ‘oh am I allowed to do that . . .’
CNS HP10
Information provision
General practitioners provided information about initial prescriptions and endeavoured to tailor the information given to the specific patient and avoided overwhelming them. One GP stated that he provided:
As much or as little as they ask . . . some patients don’t want to know very much at all . . . others want to know exactly what we use, when we use it, in what dose, how do they know that they’ve got enough, when it can be repeated again . . .
GP CNS02
Clinical nurse specialists introduced new medicines by ‘always explaining what we were thinking of trying, why . . . what the side effects, what we’re hoping to aim for with that’ (CNS HP18).
Clinical nurse specialists checked patients’ understanding of medicines prescribed by other HCPs and modified information previously given:
I had a patient last week who had come home from hospital with some lorazepam that he was meant to put under his tongue but it’s not generally used in that way, it will say swallow, and that’s what it said on the information . . .
CNS HP08
Clinical nurse specialists explained the rationale for HCPs’ prescribing choices:
A lot of patients . . . won’t want to take things . . . often I find explaining the action of the drugs and how they are working . . . helps them understand a bit better as to why they are needing them . . .
CNS HP09
Health-care professionals provided basic information about who to access for their prescription {e.g. ‘it’s calling us, it’s calling OOH [GP], the district nurses’ (GP HP07)}, what to do if barriers to repeats are encountered [e.g. ‘when I do a prescription I say it should go onto your repeat and you need to contact the GP, if you are having problems with that ring me’ (CNS Group2)] and where to access the medicines. Some patients had their own nominated pharmacy, whereas others needed help to:
. . . access the pharmacy itself . . . not all pharmacies are offering free delivery to housebound patients so it’s sometimes trying to guide them around that as well . . .
CNS HP07
In addition, CNSs provided ‘a leaflet . . . about the fact that we’re non-medical prescribers and what that means’ (CNS HP18).
Facilitators of medicines access
There were several facilitators of access to medicines and potential service-related improvements identified.
All HCP groups discussed the value of CNSs’ role in medicines access for patients. GPs valued CNSs’ engagement and close monitoring of patient and family in each step of the medicines access process, from assessment through to liaison with the pharmacist:
They’ll [CNSs] let us know . . . oh we’ve seen the patient; we’ve prescribed this are you happy with it . . . they’re really hands on and often they’ve dealt with everything . . .
GP HP07
Clinical nurse specialists described how their position within wider local services (with access to specialist knowledge and to shared records and networks with CNs and GPs in the community) supported their prescribing role. This facilitated speedy access to appropriate medicines and continuity of care for patients OOH, as it reduced the need for OOH GPs who were unfamiliar with the patients and their medicines:
[CNS nurse independent prescribing] is a need . . . we’re often in the best position because we know the patient, we know the GPs, we know the district nurses how they work and for that continuity and consistency with the plan . . . It’s certainly reduced the OOH contact to the GPs for the patients that are involved with us . . .
CNS HP18
Not only did CNS prescribing enable patients to obtain their medicines more speedily, it cut out the need for GP contact, therefore, saving both CNSs’ and GPs’ time:
Being able to initiate prescriptions it’s easier for patients that we can either give them the prescription there and then or get it sorted for them rather than having to go back to the GP, discuss with them and then get the drugs that way . . .
CNS HP03
Clinical nurse specialists were, typically, allocated more time to spend with their patients than other HCPs and this enabled them to assess patients’ capacity to safely access and administer their medicines, and then follow them up:
More time [than GPs] to spend with them [patients] before we make our prescribing decisions . . . I think as nurse prescribers we are really, really cautious and conscientious about our prescribing so if we’ve prescribed something, we’ll follow it up . . .
CNS HP17
Clinical nurse specialists were resourced to provide specialist medicines advice to other HCPs:
The GPs I work with are very reliant on the palliative care nurses and our services for advice on medicines . . . and symptom management . . .
CNS HP10
Integrated working (both within and across HCP groups) was perceived as an important facilitator and related not only to direct medicines access for specific patients, but also to indirect work for specialist advice about medicine stocks, suitability, interactions and CPD:
The CNS team, our medics are really supportive and then community GPs and pharmacists, that’s what helps you in your prescribing and decision making . . .
CNS HP17
Hospice pharmacists were readily accessible to CNSs:
For advice and also they’re very up on-again national shortages . . . We use them quite a lot even down to when we are prescribing if we are worried about interactions and . . . we want to check things.
CNS HP03
Integrated working was described by CNSs as being particularly helpful to patients ‘when there is one known GP who knows the patient well’ and with ‘all relevant services on board’ (CNS group 1). CNs felt supported by CNSs for advice and this was particularly valuable on weekends when GPs were not available. In addition, CNSs could advise the DN to prescribe for patients on their own caseload.
All HCPs highlighted the value of proactively considering potential symptom escalation and consequent prescribing needs (e.g. the pre-empting of medicine needs to cover OOH periods):
If the drug is in the kitchen cupboard it’s there. When the district nurse turns up at 18.00 and the patient is writhing in agony unexpectedly it’s there . . .
GP HP02
In addition, CNSs spoke of ‘planning in advance’ (CNS HP03).
Associated with MDT working was the importance of accessing shared records. CNS teams found the records useful when GPs used the same system:
A lot of my GPs are on SystmOne, which is the same computer system that we use so I can keep a track of their [patients’] medications, I can see what they’ve ordered when. So, if the patient is saying they’ve run out of some medication you can track back and find out why . . .
CNS HP08
District nurses were able to access and add to the city-wide shared patient records and this was crucial for them to act on CNS advice in prescribing for the patient:
It’s great that we can see the care record [city-wide shared patient record] and obviously we can see what the hospice are writing . . . if they’ve told me to prescribe something then I want them to document it on that before I prescribe it . . .
DN HP16
The final facilitator was access to medicines via an appropriately stocked pharmacy that was local, had a free delivery service and had a range of operating hours.
Issues encountered
Clinical nurse specialists’ knowledge and experience of specialist palliative care, local health services and medicines armed them with resources to pre-empt problems with medicines access, resolving them, in many cases, before they arose. Therefore, few issues were encountered.
When there were multiple prescribers, contemporaneous communication was key to ensure patient safety when prescribing. For patients with a high level of risk it was thought that the GP should be the sole prescriber to minimise this risk:
A lady recently who has clearly got an addiction issue was asking a number of people prescribing, we made a decision that one person, the GP, should be responsible for prescribing for that patient to ensure it’s safe . . .
CNS HP18
Health-care professionals discussed problems with dosing regimens for patients with multiple prescribers, when each prescriber increased the dose daily.
The electronic patient record did not have a function for nurses to prescribe electronically. This meant that nurses were not able to prescribe from their base and were only able to hand a paper prescription to the patient. Electronic prescribing would have enabled nurses to send the prescription directly to the pharmacy, speeding access to a delivery or collection of medicine. This was the most cited barrier to medicines access cited by CNs and CNSs. CNSs were typically saying:
Electronically . . . would be so much easier . . . handwriting a prescription is time consuming . . .
CNS HP08
Lack of access to shared records mostly affected medicines access when practices were not on SystmOne; however, SystmOne records were not always correct:
What it says on the record often bears no resemblance to what the patient is doing at home . . .
CNS HP18
Summary
Appendix 16, Table 23, summarises the CNS NIP case service delivery characteristics, their mechanisms of action to influence medicines access, moderating and mediating factors, and the impact on both patients/carers and on service outcomes. Access to medicines for patients/carers was considerably eased by their respective CNSs, which resulted in fewer barriers to, or delays experienced in, acquiring medicines. CNSs continually checked patients’ understanding of their medicines and provided information about how and where to access them and who and when to call for assistance and, therefore, problems that arose were minor, infrequent or quickly resolved. CNS NIP’s specialist knowledge of both medicines and local health-care services enabled them to facilitate solutions to immediate problems they encountered, but also improved ongoing access for patients and their families by removing obstacles in the process.
Patients benefited most from nurse prescribing when they had not been able to access their medicine via the usual route because of limitations (e.g. medicine stock, opening hours) of their nominated pharmacy and, instead, the nurse sourced medicines and wrote prescriptions for each item. In addition, patients benefited when GP services were difficult to access or when accessing a GP late in the day would result in late transfer of prescription to their nominated pharmacy. CNSs were clear that they prescribed for patients only when a CNS prescription would be speedier than a GP prescription (e.g. at the end of a week and when there was reduced access to GP services and/or pharmacy stock). This decision was due to their lack of access to EPS. Nonetheless, CNSs frequently contacted pharmacists to source medicines, discuss alternatives when necessary and reserve for collection or delivery. Therefore, patients (and their carers) referred to their CNS taking a leading role as an available point of contact and systems co-ordinator to facilitate their access to medicines.
Case 3: community pharmacy-delivered commissioned services for palliative care
Method
The case
The unit of analysis was community pharmacy-delivered commissioned services for palliative care (i.e. on-demand availability of specialist drugs). These community pharmacy-delivered commissioned are provided by community pharmacies that are funded by local CCGs or NHS England to provide locally or regionally determined stocks of ‘core’ lists of palliative care medicines and community pharmacy extended hours of opening, when possible. Further detail of the characteristics of these services is provided throughout the chapter.
Sampling
Community pharmacists providing commissioned services for palliative care
From 75 commissioned services schemes for palliative care across England, 37 CPs providing these services, who participated in the phase 2 survey, agreed to be contacted about phase 3 of the study. These CPs were initially approached, followed by 12 local CRNs that were active in community pharmacy research across England. Additional CPs providing this service interviewed for phase 4 (see Chapter 7), as well as research team contacts, were also approached.
Those interviewed were asked to provide details of their service commissioners and copies of service-related documents to inform commissioner sampling and documentary analysis.
Commissioners of community pharmacy-delivered services for palliative care
Commissioners were sampled via CP-provided information and publicly available data on CCG and NHS England websites. A mix of CCG and NHS England commissioners were sought.
Community-based health-care professionals in case sites
Nested sampling occurred, with community-based HCPs interviewed within the other case study sites asked for their views on these services.
Data collection
Qualitative interviews and analysis
Interviews with CPs and commissioners were performed via telephone. Semistructured interview guides were developed using phase 1 literature, phase 2 data and initial scoping of publicly available service-related documents. Guides incorporated questions on costs and resources to support service delivery and the relative effectiveness of the service. Interview data were audio-recorded, fully transcribed and analysed using framework analysis51 (by NC and ZE) (see Appendix 17).
Service-related documents as data sources and documentary analysis
Commissioner and pharmacist interviewees were asked to provide copies of all documents specific to current service provision. These documents acted as data sources and underwent documentary analysis. 56 The focus was on financial incentives (or otherwise) for providing the service, community pharmacy service locations, the numbers in relation to local/regional population demographics and need, the range of medicines on the stocked list (including whether or not there was a focus on just-in-case/anticipatory medicines alone) and any extended opening hours.
In addition, all LPC websites (circa n = 70) were searched via URL: https://lpc-online.org.uk/ (accessed 1 December 2021). If documents were current, they were added to documents obtained from interviewees.
Findings
The service delivery model
Across England, there were 75 commissioned services for palliative care commissioned by local CCGs (n = 48) or NHS England (n = 18). 57 For eight services there was no publicly available information on who commissions the service and one service was commissioned by a hospital trust. Services were funded to provide locally or regionally determined stocks of ‘core’ lists of palliative care medicines and community pharmacy extended hours of opening, when possible.
Documentary analysis
Not all information was available for every service, but a minimum documentary analysis consisted of one or more service specification documents and identification of medicines and pharmacies in a scheme.
Table 8 maps interviewees (and respective regions) to service-related documents obtained and documentary analysis. Documents were also obtained (via LPC websites) for three additional areas.
| Area | Documentary analysis | Participants, n | |
|---|---|---|---|
| CP | Commissioner | ||
| NHS England region 1 | Yes | 3 | 1 |
| NHS England region 2 | Yes | 1 | |
| NHS England region 3 | Unable to obtain documentsa | 1 | |
| CCG 1 | Yes | 1 | |
| CCG 2 | Yes | ||
| CCG 3 | Unable to obtain documentsb | 1 | |
| CCG 4 | Yes | 1 | |
| CCG 5 | Yes | 1 | |
| CCG 6 | Yes | 1 | |
| CCG 7 | Yes | 1 | |
| CCG 8 | Yes | 3 | |
| CCG 9 | Yes | ||
| CCG 10 | Yes | 1 | |
| CCG 11 | Yes | 1 | 1 |
| CCG 12 | Yes | 1 | |
| CCG 13 | Yes | 1 | |
| CCG 14 | Yes | 2 | 1 |
| CCG 15 | Unable to obtain documentsb | 1 | |
| CCG 16 | Yes | 2 | 1 |
| CCG 17 | Yes | ||
Description of services
Two of the 17 schemes were commissioned by NHS England regional teams and 15 were commissioned by CCGs. Two schemes were 24-hour (OOH) schemes to enable patients to access palliative care medicines when other pharmacies were closed (with a call-out mechanism). Fifteen schemes were more standard schemes that operated from several pharmacies in the area, requiring pharmacies to stock a specified list of palliative care medicines.
Service hours
Information on service hours was available for 12 of the 17 schemes, showing extended hours availability. Most schemes favoured 100-hour pharmacies or those with longer opening hours, including evenings and weekends. Two schemes were 24-hour (OOH) services and the remaining 10 schemes were extended-hour schemes, with opening times including 06.oo to 24.00 Monday to Friday, 06.30 to 22.30 on Saturday and 09.00 to 12.00 on Sunday.
Populations covered
Information about the number of pharmacies in the scheme was available for 12 of the 17 schemes. The number of pharmacies ranged from 1 to 57 per scheme (mean n = 15).
The population of patients per commissioned service pharmacy within each CCG or NHS England region was calculated utilising Office for National Statistics (2018) data. 58 Population per pharmacy ranged widely from 6740 to 612,764 (mean n = 133,454). Quality and Outcomes Framework (2019) data on the population of palliative care patients registered in each CCG indicated that the number or patients per pharmacy ranged from 21 to 2391 patients.
Independents versus multiples
Information on the use of multiple and independent pharmacies was available for 9 of the 17 schemes. All nine schemes used a mix of multiple and independent pharmacies, except one, which used only independents.
Medicines
Information on medicines was available for 13 of the 17 schemes. Several schemes had subschemes for different geographical areas, often using different medicines. Six schemes had a single medicines list and the largest scheme had eight lists within it.
There were 101 different medicines listed, including 17 different classes, with 593 medicines in total. The most common medicines listed were opioids (243/593, 41%). This included six different medicines (alfentanil, diamorphine, methadone, fentanyl, morphine and oxycodone) with between 1 and 11 forms and strengths (see Appendix 18, Table 24). Other common medicines were antisecretories, antiemetics, antipsychotics and diluents. Some schemes included medicines less commonly associated with palliative care, such as antidiarrhoeals, H2 antagonists and diuretics.
Payment
Two schemes were for 24-hour (OOH) services, with one scheme paying a weekly retainer of £150 (or £250 if the week contained a bank holiday). Both schemes paid call-out fees (one £133 and the other £150). Annual payments for the more standard service ranged from £150 to £775, with one scheme seeming to indicate no payment made.
Eleven of the 12 standard schemes (where information was available) included reimbursement for expired stock. Some standard schemes paid set-up costs, ranging from £50 to £500, but some did not disclose costs paid. One scheme offered to pay for additional CD storage if necessary.
Not all schemes indicated how payments were to be claimed. Two schemes required the pharmacy to invoice the CCG. Three schemes required quarterly claims or payments for as little as £37.
Audit
Only 8 of the 17 schemes mentioned audits. Four schemes indicated an annual audit, two schemes indicated a monthly audit, one scheme indicated that audits would be ‘periodic’ and one scheme said that audits could happen.
Continuing professional development as a requirement
Information on CPD was available for 13 of the 17 schemes. Six schemes had no CPD requirements, three schemes required that ‘relevant CPD should be carried out’ and four schemes asked for the Centre for Postgraduate Pharmacy Education (CPPE) palliative care package to be completed. However, it is important to note that the CPPE package is no longer available and only a small number of resources are now available from that provider, despite the requirements still ostensibly being in place.
Community pharmacist and commissioner views
Sample
Twenty CPs were interviewed (by JL) (eight interviews via CRNs, seven interviews via phase 2, three interviews via research team contacts and two interviews via phase 4), 17 of whom were operating services commissioned by CCGs (n = 13 services). Three CPs’ services were commissioned by the same NHS England region. Interviewees were employees in independent pharmacies (n = 14), large multiples (n = 5) and small multiples (n = 1). The total number of prescriptions issued per month in interviewees’ pharmacies ranged from 2645 to 25,796, with a median of 9158. Commissioner participants (interviewed by JL and ZE) were commissioners or commissioning staff of three NHS England regions and four CCG-commissioned services.
Types of pharmacy and service
Community pharmacists worked in a range of pharmacy types typical of community pharmacy service provision in England, including small independents in populated or city areas, chains (large multiples), pharmacies in or next to general practices, village pharmacies and 100-hour pharmacies in towns or hospitals. The service was available continuously during the opening hours of the pharmacy in 16 instances, with the remaining four pharmacies providing a rota service for 1 week in every 6 months (including on-call OOH provision, facilitating 24-hour service).
History of service and changes over time
Services had typically been operating for at least 5 years, ranging from 18 months to > 10 years, and many CPs had inherited a service that was operating in the pharmacy before their employment there. Most CPs suggested little or no changes over time, apart from medicines being removed or, more often, added to the list. Points raised included services considered to have been scaled back, with a lesser fee (possibly for financial reasons) to a service that no longer offered call-outs or an OOH arrangement (assumed to be through lack of demand or new extended-hour pharmacies being available in the area).
Most schemes were historically run by primary care trusts; however, when NHS England was later established, many CCGs then adopted these services. Other services were commissioned by NHS England regions, but, in some parts of the country, there was a reluctance by CCGs to commission, as there was little or no funding attached. Many schemes had been inherited by commissioner interviewees and interviewees recognised that an equitable service was not on offer across the area:
There were some areas that did the service, some areas they have no service, and some areas that are partial service . . . some pharmacies were paid for the service, some did it on a goodwill basis. [We] decided to put one service in place for all . . . no variation . . .
Commissioner F, NHS England
Often, commissioners were not fully aware of the history of their scheme before they came into post; however, they kept the same service and payment arrangements in place going forwards, with changes only to individual service providers leaving or joining the service, and to medicines.
Process of commissioning
When contracts were renewed, usually only minor changes were made in terms of processes, formularies and requirements. Service specifications and related documents on LPC websites were not always up to date. When an area needed service provision or a pharmacy dropped out (often when contracts were due for renewal), commissioners could ask for expressions of interest via the LPC. One commissioner described receiving more than 100 expressions of interest for the service and then using selection criteria (i.e. geography and opening hours) to identify contractors. Some commissioners tried to identify geographical gaps and then targeted pharmacies that had long opening hours to fill them.
Some commissioners were sole lead for the service, whereas others were part of a team. There were lengthy conversations to get service details agreed (which were usually in place for several years), often with the LPC.
Funding the service
The norm reported by the CPs was £150–350 per annum, either paid quarterly, 6-monthly or, often, annually. All services were reimbursed for out-of-date medicines, but services rarely needed to claim for this as medicines were generally used before expiry. The general feeling expressed was that funding was not an important factor in running the service, as the aim of the service was to provide a good service for patients/relatives at a stressful time. However, one CP, with a dual role in a pharmacy and CCG, considered funding to be meagre. Some commissioners commented on difficulties funding the service:
. . . we’re funding this at current but there is no budget to fund this service . . .
Commissioner E
I suppose the other main challenge would be the funding, restricted funding, you’ve only got a finite pot really to work with . . .
Commissioner F
Medicines stocked
All CPs reported being required to stock an ‘extensive’ list of medicines, ranging from 11 to 15, with different strengths and quantities. A handful pharmacies, mainly the 100-hour pharmacies, were also asked to keep an additional list of some more specialist medicines. Pharmacy staff mentioned that the main differences from standard medicines stocked in their pharmacy related to quantity and strength, rather than type.
Stock lists varied. The NHS England commissioner of the largest scheme aimed to have one list; however, because of local specialist palliative care prescribing variations, they had eight lists operating within six CCGs. Lists reportedly required regular review because of changes in prescribing habits. One CCG used a core list for all community pharmacies to stock and an additional list for four geographically dispersed pharmacies.
In the main, medicines stock availability at the time of data collection was not perceived to be an issue, although it had been in the past for some of the CPs for some CDs. Supply problems were experienced by CPs for a couple of EoL medicines. Some CPs reported being able to source medicines through wholesalers directly or by contacting the head office of their pharmacy chain. Other ways in which the occasional inability to dispense medicines was overcome included contacting other pharmacies locally to see if any had it in stock and either ‘signposting’ the patient, relative or nurse to such pharmacies or requisitioning/’transferring’ CDs from another pharmacy. If these ways were not fruitful, CPs contacted prescribers to see if an alternative medicine could be prescribed. This was not an issue with pharmacies that were co-located with surgeries, hospitals or hospices, but it could cause delays if the prescription had been issued OOH and/or by a locum GP that was unknown to the pharmacy.
Extended opening hours
Thirteen of the community pharmacies routinely operated extended opening hours (outside standard weekday hours and Saturday mornings). No CPs had to change their opening hours as a result of participating in the scheme.
Network of pharmacies
Apart from two CPs, most were in and around a city or town with other participating pharmacies. Two exceptions were pharmacies in village settings with no other pharmacies nearby. The majority of CPs claimed to be familiar with which pharmacies were offering the service in their areas and communicated with others (e.g. to source medicines not in their stock).
Awareness-raising to health-care professionals and patients/carers
Most CPs considered that HCPs (usually nurses), patients and carers were aware that their pharmacy was one that offered a commissioned service. Typically, one CP suggested:
[HCPs are more aware now] as they’re given a list of the pharmacies in the area who can supply palliative care. What I do find, quite a lot of them will actually phone up first and just double-check with us if we either have items in stock or we are available to do it. I’m seeing a lot more of this now than I was a few years ago . . .
CP 13
Most CPs suggested that if the prescriber knew which pharmacies were on the list, then they could convey this to patients/carers. However, one CP had found that changes in staff (notably CNs) necessitated the development of a method to keep them up to date and used a laminated copy of pharmacies/opening hours (as an ‘aide memoire’) for nurses to carry in their cars.
No service was advertised directly to the public and commissioners felt that this was something that patients should be directed to by HCPs:
We just didn’t want patients turning up willy nilly, we wanted it to be a more targeted approach . . .
Commissioner E, NHS England
Commissioners were of the view that information from most services was disseminated to multiple HCPs:
. . . so that goes to all pharmacies, GPs, dentists, I presume optometrists, councils, community providers, hospices, on-call people . . . and then [we] ask people to disseminate accordingly . . .
Commissioner E, NHS England
One commissioner acknowledged that there could be more information-sharing about the service, and this was something they were addressing in their next iteration of the service:
We admit that there probably hasn’t been enough publicity and sharing of that information across not only the community pharmacy network and the LPC but also the professionals trying to access those services, and the public . . .
Commissioner C, CCG
Some commissioners communicated information, but this information could get lost or mislaid, especially with staff turnover. Communication between the commissioning team and the pharmacies was also important for timely awareness of changes to the formulary or shortages.
Promoting the service to HCPs may not have occurred because commissioners did not wish reliance on the service, but would rather see HCPs plan ahead:
. . . but we try not to promote it too much because if we promote it . . . we don’t want people to think this is a service that means you don’t have to think ahead . . .
Commissioner A, CCG
Commissioner engagement with the service
Engagement was dependent on the individual commissioners and pharmacists, but there were some examples of good practice where education events were held (at a hospice) and twice-yearly visits to pharmacies performed to promote engagement in the service, undertake stock checks/audits and/or communicate medicine shortages. This type of engagement was not demonstrated by the larger schemes and one commissioner had very little involvement or understanding of their service. Owing to larger services being commissioned by NHS England, other responsibilities and medicine shortages, there may increasingly have been less time for commissioners to engage with services. With larger services commissioned by NHS England, other responsibilities and medicine shortages, there may increasingly have been less time for commissioners to engage with services.
Audit requirements
Few CPs suggested that auditing was required of them. However, of those CPs who had experience of any form of auditing, two indicated that they had to submit a self-‘audit’ report quarterly to obtain payment through PharmOutcomes (Pinnacle Systems Management Ltd, Isle of Wight, UK) (i.e. the system used for claiming payment in some areas). This report included service usage and recording of expired medicines.
According to commissioners, a varied amount of auditing took place and they expressed a wish to do more. Barriers included restricted time of both commissioning teams and community pharmacies. Some commissioners conducted visits for audits and one LPC had requested that any audit should be carried out by the commissioners, as pharmacies were already overstretched. Audits included questions on stock, prescribing patterns and barriers, as well as some quality assurance issues, such as appropriate claims, out-of-stocks and opening hours. Requests to pharmacies for quarterly stocktakes were sometimes made and some commissioners requested evidence of completion of a CPPE module.
Three commissioners conducted no audits, relying on complaints to tell them whether or not the service was working:
. . . and we have to take it that if we don’t hear about the service, we’re assuming that it’s working . . .
Commissioner E, NHS England
Several commissioners looked at whether or not appropriate claims were being received as a form of audit. When an audit was carried out (in the minority of cases), it was reportedly used for refining services and ensuring that pharmacies were providing the service. Commissioners were keen to ensure value for money through processes such as stock rotation.
Scale of usage
The number of calls on the service varied widely, ranging from ‘hardly ever at all’ in pharmacies on the on-call rota, to three or four per month in standard-hour pharmacies, to four or five per week (including more at weekends) in 100-hour pharmacies in, or co-located, with hospitals.
Views on the impact of the service
All CPs considered that their service worked well in relation to aims and by comparison with access prior to being in a commissioned service. Reasons for this improvement included the following:
-
The service works well at difficult times (e.g. when planning is insufficient or with unanticipated deterioration/worsening of symptom control).
-
The service provided is much needed, especially in the last few hours of life. Extended hours means not having to wait for a pharmacist to get into the pharmacy or having to wait until the next day when the pharmacy is open.
-
The service has improved on pre-commissioned services in which the range of medicines was not easily accessible to CPs and which necessitated people having to go into hospital/hospice.
-
A visible, one-trip service for patients’ relatives is provided. It was claimed that relatives know where to go to get medicines dispensed via such services. As one CP said:
CP 5
In the past [prior to the service] I had a patient for which we didn’t have [the correct injection] and the relatives were so frustrated with us because we didn’t and they had to go to a different pharmacy . . . So, yes, I think having your daily local pharmacist helping you with this kind of service . . . it’s a great benefit for the whole community . . .
-
The service is both an emergency service, preventing unnecessary hospice/hospital admission, and one to support ‘managed’ palliative care at home when patients had been prescribed anticipatory medicines.
-
The location of the service (e.g. near or next door to a general practice) was of benefit, with patients/carers and HCPs knowing about the service.
For commissioners, the scheme and medicines included were a back-up or emergency response for when things could not be, or had not been, planned for. Most commissioners thought that the scheme helped access to medicines for patients at the EoL and all who answered the question (four/seven) ‘Is the service better at enabling patient/carer access to medicines’ thought that this was the case.
Resources required
Most CPs experienced no specialist training other than online CPD (which, for many, was completed quite a long time ago). An exception was one group of commissioned pharmacies with links to a hospice, and a further referred to the availability of ‘in-house training’ for new medicines and/or new members of staff.
Most pharmacies had enough space for stock. Commonly, part of a drawer or shelf was dedicated to the medicines that did not need to go into the CD cabinet.
Challenges to improving medicines access through commissioned service provision
Challenges were infrequently cited by the CPs and included fulfilling prescriptions when there was a medicines shortage, incomplete prescriptions necessitating the pharmacist to contact the prescriber and difficulty reading the prescription if written by hand (less common with electronic prescribing).
Many CPs considered the list to be too long, with medicines/doses that were not prescribed. This, in conjunction with medicines being dispensed but not necessarily used, led to a concern about the wastage of medicines.
In contrast, challenges were commonly stated by commissioners. The most frequently cited challenge was staff turnover and use of locums, leading to poor communication or knowledge about the service and lack of continuity:
One of our big issues is reminding the guys that actually they are in the service . . .
Commissioner A, CCG
Medicine shortages, including when items had been recently dispensed without time for re-stocking, were also challenging for commissioners, particularly for some CDs. Another challenge was the lack of patient, carer or HCP feedback, meaning that pharmacy staff were unaware of whether or not the service was adequate or useful.
Commissioners spent a range of their time managing this service, ranging from 2 hours per month to 7 hours per week. Remuneration and budget concerns were also discussed by several commissioners:
. . . they feel like their funding’s been cut and they’re asked to do more for less . . .
Commissioner D, CCG
Medicines lists and their variations took much time and effort to agree across stakeholders and often required review after considering medicines shortages. Challenges with identifying and maintaining commissioners’ relationships with key stakeholders, such as LPCs, hospices and CD-accountable officers, were also discussed, as well as ensuring that individuals were working with a common goal when agreeing specifications, namely the medicines to be supplied:
So, when we initially started the group everyone came with their own agenda . . . the challenge is getting all the stakeholders on the same page . . .
Commissioner G, NHS England
Facilitators of improving medicines access through commissioned service provision
Local pharmaceutical committees were perceived by commissioners as helpful, acting as a point of contact for pharmacies and an information resource. When staff in pharmacies were dedicated to service provision, services were seen a pleasure to commission. Views of commissioners varied in where they thought this service should be commissioned from; however, most agreed that a single national service would prevent unnecessary duplication of time and effort:
. . . but it doesn’t make a lot of sense for every single CCG to have a slightly different service. And things like the list of drugs, you know. The amount of effort that goes into deciding that and there’s no reason. A patient being treated with palliative care is the same in any part of the country, aren’t they . . . ?
Commissioner A, CCG
Against a context of, overall, positive CP evaluation of the service, improvement suggestions from CPs included the provision of periodic training, extended roles for pharmacists with prescribing, greater communication and integration within the MDT, and mechanisms (e.g. administration, stock and supply) to enhance the efficiency of the service.
Feedback from service users
No commissioned service had any formal route for service user feedback. Some informal HCP negative feedback about medicines supply was investigated by a NHS England commissioner, but as another commissioner recognised:
Probably at that time of a patient’s life you are not going to then write to me and complain, you just want to get the drug and there are different priorities, aren’t there . . .
Commissioner E, NHS England
Health-care professionals’ views
Views expressed by the 74 HCPs interviewed often contrasted markedly to those involved in the delivery, or commissioning, of such services. The similarity in views across the cases means that they are presented as a whole here, with exceptions cited.
Awareness and knowledge of the service
Across cases, there was a lack of awareness of commissioned services. The exception was among the TSL case staff who all knew of the services and how to access a list of pharmacies and their opening hours. Overall, however, when there was HCP awareness of the existence of this service, there was a notable lack of knowledge of which local pharmacies provided this service, opening hours, medicines commissioned and stock levels that pharmacies should hold.
Nurses (particularly CNSs) generally knew where to locate a list of commissioned pharmacies, but some were unsure how current these were. GPs, if they knew of the services’ existence, were not aware which local pharmacies were commissioned services and neither were CPs who did not provide a commissioned service themselves.
Impact on patient/carer experience of access
When HCPs were aware of the service, CNs and CNSs spoke positively of its utility for patients and carers accessing medicines. The HCPs perceived the service as able to make ‘such a big difference’ for patients, preventing escalation via unnecessary visits to accident and emergency (A&E) departments and hospital admissions. For both groups of nurses (i.e. CNs and CNSs), the service had the potential to prevent families ‘struggling to get the drugs and going from pharmacy to pharmacy and feeling really distressed and upset’ and wasting ‘precious time’ that could be spent with the patient (palliative care CNSs 001–007).
Perceived issues with service delivery
Community nurses highlighted that commissioned pharmacies were ‘not always’ able to dispense what they needed from the service list. One CN said that ‘you ring them up and say “oh, you’re the nominated chemist” . . . they’ll say “oh, we’ve got that, but we haven’t got that”’ (CNs 005–009). Palliative care CNSs expressed similar insights, perhaps because both groups were the most likely to utilise the service on behalf of patients and their families, noting that service effectiveness depended on how well the medicines were actively stocked:
I’ve found that they’re the ones that are meant to help, things still need to be ordered and actually the other local pharmacy has been much more helpful and been able to get it quicker.
CNS, HPGroup1, Case 2
Telephone support line staff, such as palliative care CNSs and CNs, spent a great deal of time telephoning around pharmacies to source stock and had not necessarily experienced better levels of stock in commissioned pharmacies.
Furthermore, many HCPs (in cases 2 and 4) reported few or no services in their area, and because of this the more local and well-known pharmacies were used instead.
Awareness-raising of the service
Awareness-raising appeared to be hampered by commissioner concerns regarding the CD stock and, therefore, security of the pharmacies, and so knowledge levels of the service among HCPs were low. Unsurprisingly, given the low levels of awareness and understanding of the service provided, signposting to these pharmacies was not often referred to, apart from by CNSs and some CNs. These CNSs and CNs discussed signposting patients and their families to the commissioned service pharmacies nearest them (but only if they had already checked that required medicines were in stock). Such signposting was further complicated by some HCPs questioning the ethics of advertising one pharmacy over another, with HCPs stating that they would do so only if the pharmacy was known to have medicine unobtainable elsewhere:
We’re not supposed to recommend a pharmacy actually. It’s got to be patient choice and we’re not supposed to influence but having said that if it’s in the best interests of a patient who needs medication and they can’t get hold of it then yes I would . . .
CN HP06, Case 2
Summary
Appendix 19, Table 25, summarises community pharmacy-delivered commissioned services for palliative care case service delivery characteristics, their mechanisms of action to influence medicines access, moderating and mediating factors, and the impacts on both patients/carers and on service outcomes. There were high levels of variation between the commissioned services. The nature of each service (including level of extended hours), number of community pharmacies involved (per head of population) and range of medicines stocked all varied. Publicly available information about services was often incomplete or out of date. There was evidence that the service commissioned was not always available in terms of pharmacies having required medicines in stock and, in some instances, non-commissioned pharmacies appeared to offer an equivalent service. CPs and commissioners often inherited a service that had been in operation for several years and some commissioners revised little about the service, whereas others had taken a more strategic approach to changes. Audits and CPD were usually not performed in practice, even when cited in service documents.
Services covered different purposes, including to support managed palliative care through higher stock levels and an increased range of stock, thereby offering alternatives to other pharmacies where stock was out, in potentially avoidable urgent situations in which pre-emptive prescribing had not been adequate and in unavoidable urgent situations (i.e. unpredictable symptom escalation).
Although for most CPs the service was merely an extension of their existing stock (and did not require additional opening hours), there was arguably a lack of financial incentive to provide the service. CPs appeared to be predominantly providing services out of goodwill, as they recognised this to be an important and stressful time for patients/carers. However, CPs and other HCPs generally thought that the service was valuable in several ways and, when functioning effectively, very definitely increased speed and ease of access to medicines, with outcomes including preventing unnecessary hospital and hospice admissions and patient/carer distress.
Nonetheless, levels of awareness of the service were low across HCP groups. Awareness was greatest among specialist palliative care nurses, although even among this group knowledge levels were variable, with the latter also true of CNs. Very low levels of awareness of these services were encountered across GPs and CPs not providing services; consequently, services were not visible to patients (in contrast to what CPs providing the service assumed). Information regarding services was not relayed to patients/carers routinely, although in practice it was often nurses who were doing the work of liaising with, and at times going to, the pharmacy for patients. Although most CPs did not see lack of stock as a problem, nurses tended to view this as a challenge, adding physical and emotional burdens to a family by asking them to visit another pharmacy or return the next day. Finally, there was no formal feedback from service users to commissioners.
Case 4: palliative care 24 hours per day, 7 days per week telephone support line
Method
The case
The unit of analysis in case 4 was a 24/7 palliative care TSL, which was based within an acute NHS hospital trust. It was embedded within wider services (i.e. primary care, GP OOH and teams working in the community, hospice and hospital) and provided video support/telemedicine services, with staff including experienced NHS nurses. Those providing the TSL service were supported by education, training, coaching and facilitation by specialists in palliative care, EoL facilitators and GP EoL leads.
Sampling
The case study centred on a single TSL that was selected because it represented an innovative model of service delivery.
Patients and carers
In addition to the eligibility criteria in other case sites, patients were registered with the TSL service and had contacted this service at least twice.
Health-care professionals
Health-care professionals who were working with EoL patients in the TSL and wider services (e.g. community teams, hospices) in a geographical area commissioned by a single CCG. HCPs were identified by patients (as being key in their care) and by snowball sampling and networking.
Findings
Sample
Thirty-nine participants consented to take part (Table 9). We were unable to recruit the target number of 10 patients because it was more difficult than expected for TSL staff to anticipate that patients would live for 12 weeks. Appendix 20, Table 26, displays the demographic data for the patient and carer sample.
| Sample | Total n |
|---|---|
| Patients | 6 |
| Carers | 3 |
| Total patients and carers | 9 |
| Digital hub staff | 14a |
| DN leads | 7 |
| Community palliative care CNSs | 4b |
| CNs | 3 |
| Palliative care support team: lead nurse | 1 |
| Palliative care consultant | 1 |
| Total HCPs | 30 |
| Overall total participants | 39 |
Data sources
Appendix 21, Table 27, displays the total number of patient/carer interviews across the sample (including the form of the interview). In total, 16 patient/carer interviews were undertaken (by JB). One patient deteriorated more quickly than anticipated and another was not available for a final interview and so the number of interviews undertaken varied. This also affected the number of completed logs (n = 14) collected during the 8-week study period. Patients were registered at four general practices. Twelve HCP interviews were undertaken (by JB) (see Appendix 22, Table 28).
Data extraction forms were completed from electronic GP and hospice medical records. In total, data from 36 patients were collected in this case study (for six study patients who completed a minimum of two interviews and an additional 30 patients). The additional 30 patients were selected using the same search strategy as the interview patients; however, speaking and writing English and the ability to consent eligibility criteria were not included.
The service delivery model
Key service delivery characteristics of services provided by 24/7 TSL and associated community-delivered services in the area (in-hours and OOH) are outlined in Appendix 23, Table 29.
The TSL is one of three specialist services in a digital care hub operating 24/7, 365 days of the year. The digital care hub is staffed by a highly experienced MDT, comprising nurses, therapists and paramedics from a variety of backgrounds and able to flex across all three services in response to peak demands. Incoming telephone calls from TSL patients are prioritised. The TSL was developed by palliative care consultants for patients (registered on the GSF) and their families to deliver a single point of access (SPA) to expert clinical and social assessments, diagnoses, advice and support. The aim of the TSL is to help GSF patients live as well as possible in their place of choice. Typically, around 50% of patients have cancer and the other 50% of patients have other progressive diseases. The TSL is part of wider specialist palliative care services that are supported by local community services.
The TSL typically handles > 1000 calls per month and around two-thirds of these are received during OOH (i.e. evening, night or weekend). Eight per cent of calls are from patients in the last 3 months of life (or their carer). Around 40% of patients’ calls are resolved by the TSL service. The remainder of calls result in an onward referral to another service by the TSL. CNs receive the most (almost 60%) referrals. The OOH GP service and patients’ usual GP receive the next highest proportion (19% and 14%, respectively) and the remainder are for specialist palliative care services. Medicines queries account for approximately half of all calls and these issues are usually resolved by providing information about medicines, telephoning pharmacies to source medicines and arranging access to a prescriber.
The digital care hub is commissioned by the CCG and is a joint venture (50 : 50) between the acute NHS trust providing the clinical staff and an independent telemedicine organisation (combining clinical and technical knowledge and expertise). The hub provides technical design, delivery and support.
Health-care professional and patient perspectives
Activities to aid access to medicines
The TSL team worked with community, hospital and hospice services to resolve issues that patients contacted them about. Activities of the TSL team typically related to accessing medicines and included:
-
co-ordinating a prescriber home visit (or request to a GP/NIP/hospital medic to write a prescription)
-
liaising with community pharmacies and hospital dispensaries to source and reserve medicines
-
arranging home deliveries from community pharmacies.
The TSL team selected a route to a prescription that was the fastest and most convenient route for each patient, considering their clinical record, the issue, availability of carers, time and day, geographical location and availability of services.
In addition, TSL staff were able to work proactively with patients who were vulnerable or isolated, reminding them to take medicines:
He was saying he had too much pain . . . because he’d not been taking his medication . . . so then we were prompting him to make sure he took his pain relief . . .
TSL group 1
Patients used the TSL to obtain a home visit or practice appointment, resulting in the diagnosis of symptoms and ensuing prescriptions. Few patients had used the TSL more than once for medicines access, but envisaged further use nearer the end of their life. Patients said that they felt confident in navigating systems to access medicines or that HCPs would do this on their behalf. In addition, patients expressed confidence that the TSL would navigate services for them when the need arose.
The TSL team made onward referrals to GPs and nursing teams working in the community to request patient appointments, telephone calls or visits. In addition, the team worked with community pharmacies to check and reserve stock and request a prescriber either transferred the prescription to the pharmacy or wrote paper prescriptions for families to hand in. If medicines were not available in the community (e.g. unusual medicines or OOH), then the TSL liaised with most appropriate prescribers and pharmacies close to patients’ homes (e.g. hospital emergency department doctors re-prescribed medicines for collection from hospital pharmacies). The TSL team also promoted interdisciplinary working by accessing CNSs for enquiries regarding specific patients and specialist advice.
A community nursing and health-care assistant palliative care support team worked until 22.00 and were, therefore, more likely than other services to work with the TSL team OOH.
The TSL team worked with patients and families. Family members often phoned on patients’ behalf. The team considered which pharmacies were convenient for patients/families when telephoning around to source medicines.
Community HCPs provided patients with the TSL telephone number to contact them with any concern 24/7.
The TSL team’s palliative care knowledge meant that they could provide a rationale for prescribers’ choices and instruct on effective use:
You had that call in about that man with oxycodone and paracetamol and you’d explained to them about taking paracetamol and how it can help your other medicines work . . .
TSL HCP group1
Although the TSL team were able to provide information about who to access for prescriptions, and where to obtain medicines, they typically accessed the relevant service on behalf of the patient.
Patients’ contact with the TSL was usually OOH and infrequent and, therefore, their usual HCPs were the main source of information about medicines. Some patients had telephoned the service with questions about new medicines when they were unable to access their usual HCP. Information regarding how best to access the medicines had also been gained from their previous experience of doing so.
Facilitators of medicines access
HCPs reported that patients valued fast, simple and consistent 24-hour access to the TSL. The single number also meant that community HCPs needed to provide just one number, with the advice that patients should phone this number when they needed help accessing medicines.
The TSL team co-ordinated the most appropriate service to address each individual issue on behalf of the patient/family, releasing them from the often immense work of navigating these services themselves and taking ‘away the hassle for them, they’re not having to chase up GPs themselves they’re just making this one call’ (TSL nurse HP01).
The TSL team’s co-ordination was particularly valuable OOH when patients’ usual services were closed. HCPs appreciated the difficulties patients experienced in navigating services, particularly OOH, and the TSL removed this burden by contacting appropriate services on their behalf:
If people run out of medicines out of hours then [TSL] will be able to help them because it’s hard for patients to navigate the system isn’t it, and to know who to ring if their surgery is closed . . . that was one of the principles that patients could ring . . . and [TSL] would support them without asking them to phone multiple other people . . .
PC Cons HP02
When medicines had not been received, the TSL liaised with pharmacies to rectify problems and ensure that the patient would obtain their medicines in the speediest and most convenient way:
We can . . . find out which pharmacies are open, which ones are staying open late, which ones are the closest and then arrange for it [prescription] to be sent . . .
TSL nurse HP01
The TSL team arranged access to usual or OOH GPs for new or repeat prescriptions when patients telephoned with escalating symptoms, and provided advice about how to best utilise existing medicines while waiting for the prescriber:
Well say a patient was ringing [TSL] they can see on the SystmOne all the medicines they’re on and all the repeats they’re on so they could give advice on medicines. They probably just do what we do [CNS team] but they can be there for out-of-hours as well and get hold of GPs . . .
CNS HP28
Patients valued the TSL team for its ability to identify and contact an appropriate and accessible service to assess symptoms and issue a prescription. Calls related to shortness of breath (n = 3) and increasing pain (n = 4) were all seen soon after by CNs or OOH doctors (resulting in a new prescription) or immediately by an ambulance or paramedic. Most patients (n = 4) lived in rural locations and the remaining two patients were not within walking distance of their usual HCP or pharmacy and so the TSL team’s co-ordination of services provided the fastest access to a prescriber.
Telephone support line HCPs were qualified and experienced in patient-facing roles. TSL HCPs’ training enabled them to identify which callers required regular follow-up calls:
If you are concerned about somebody . . . I’ll just give them a quick call and see what they’re like . . . We do get some frequent callers, so you do get to know why people are calling and some behaviours and I think we’ve had some people who are a bit more rural who are, they’re quite isolated. So, I think there will be a call about something whether it’s them in pain or they’ve dropped their tablets, or they’ve run out of prescription . . .
TSL OT HP25
The TSL team reported that they provided an overarching service that joined up other services that patients accessed so that it would feel ‘seamless [to patients] like you’ve been expecting their call’ (TSL OT HP25) and all part of the same service. The TSL team said that they addressed patients’ issues calmly and with confidence to reduce patient distress:
I do think we sort of shield the patients from the issue because like I say if you’ve got a carer or a patient themselves who is exhibiting symptoms the last thing you want to hear is somebody go, ‘oh you haven’t got any medication, well I don’t know what we’re going to do’. So literally it’s, ‘leave it with me and I’ll give you a call back and we’ll see what we can do’ . . . And then there will be lots of work done in the background . . . There’s a mad scrabble that goes on. And literally we’ve had where one member of staff for the day has been dealing with a medication issue. So that’s taken one member of staff out all day because of trying to literally co-ordinate that . . .
TSL nurse HP01
Non-clinical TSL call handling staff supported the team by undertaking work delegated by the HCPs (e.g. background work contacting other HCPs for prescriptions and visits, setting up video calls) and, therefore, freed up clinician time for direct patient work.
The CPD and governance requirements of the HCPs operating the TSL were led by palliative care medical consultants. The TSL team were trained to a level of competence that enabled them not only to provide information about palliative care medicines and how to access them, but also to communicate with EoL patients appropriate to the context:
Everybody who works in the hub and picks up a [TSL] call is all trained to the same level so they know exactly what the person needs or how they can get what the person needs in their own home. The consultant and the other palliative care consultants are very integral to the training . . . so that we can provide a really good service . . .
TSL nurse HP30
Where integrated working between community and secondary services was in place and these services had a strong knowledge of palliative care, co-ordination of medicines was smoother for patients:
We’re [TSL] only as good as the community services so it’s not just [us] it’s about the community pharmacy on board, it’s about knowing what drugs are there, it’s about having MAR [medicines administration] charts in place for when it’s social care carers going in, what can they give, what do you need your DNs to go and give. It’s just a complete system approach . . .
TSL OT HP25
The TSL team’s knowledge of health-care services provided in the whole CCG area was enhanced by their clinical leadership, provided by three palliative care consultants:
. . . who rotate every 2 years, one in hospital, one in community and one in the local hospice . . . they are seeing the full breadth of palliative care . . .
HCP group1
Community HCPs handed responsibility to the TSL team to arrange a GP to prescribe, speeding access when the CN identified a medicine need during a home visit:
So I can just ring up [TSL] and say, ‘hiya it’s [name] palliative care support team, you get me a GP for such and such,’ and they’ll say, ‘yes what for’ . . . so [TSL] will ring the GP and the GP will then ring us and say what do you need and I’ll say, ‘I just need some buscopan that’s all I need . . .’
CN HP21
The palliative care support team often telephoned the TSL to enable them to continue to patient visits and this was particularly useful OOH when there were fewer HCPs working:
They have all the information in front of them and instead of sitting and waiting on hold [for a GP] when we’re out . . . it’s easier just to ring [TSL] and say will you get me an out-of-hours GP for this patient . . . they’ll say yes I’ll sort it. And they do they sort it for us . . .
CN HP21
Palliative care CNSs were reported to support the TSL, as their specialist knowledge about a wider range of palliative care medicines meant that they could provide advice to the team and were also available at weekends to do so. The CNSs with a NIP qualification were also valued for being able to write a new prescription or correct a GP prescription.
All services shared updates about opening hours, shortages and stockists of typical medicines and/or unusual medicines, as well as a list of community pharmacies commissioned to hold specific palliative care medicines.
The TSL team was able to access patients’ medical records for each service where the patient was registered. These records were essential for recording and checking relevant clinical history (e.g. types and dosages of medicines prescribed, comorbidities and allergies, carer information and services accessed) and allowed HCPs to plan the next steps in co-ordinating services to access medicines:
We’ve got SystmOne right across secondary care, community, the hospice use it, the GPs, the out-of-hours GPs. So, we’ve truly got a single record. And everything is in the EPaCCS, so all the care planning, so we know where to look and everybody is contributing to that same record and that same care plan . . .
TSL HCP group1
The TSL team used the ‘task’ instant messaging feature of the patient record to request input from other services (e.g. requesting a GP prescription or home visit) and also from other TSL staff (e.g. nurse tasks a non-clinical call handler to delegate an appropriate duty related to that patient). Tasks became part of patients’ clinical records and provided details of what work needed doing and what had already been carried out, with specific patients and aided planning, co-ordination and follow-up of medicines issues.
Patients had agreed that their clinical records for each service be shared so each of the TSL team, hospital, hospice and community services had sight of it and could enter information. Patients were aware that this enabled the TSL team to consider the complexity of their condition to co-ordinate the best service to meet their needs. In addition, it reduced the need for a lengthy explanation of the patient’s condition, reducing patient/carer distress. This also meant more timely and accurate communication of information between patients, families and HCPs:
You don’t have to go through the rigmarole of explaining everything. They’ve got your records there; they can see clearly what’s going on. So, yes, it’s a really good service for somebody in my position . . .
Patient T01, interview 1
Issues encountered
The TSL worked well at facilitating access to medicines when patients’ GPs had a good understanding of the EoL context and were able to adapt GP services to patients’ needs. On the other hand, ‘a poor GP, a locum who perhaps doesn’t understand it [palliative medicines] very well then that hinders it’ (TSL nurse HP30).
Some GPs had limited experience in palliative care and often nurses working in the community detected and corrected dosage errors caused by:
. . . [GPs] just printing off the EoL anticipatory template, it comes up populated doesn’t it? They might have 50 mgs of diamorphine or morphine sulfate in the driver and they are still writing them up 2.5 [breakthrough pro re nata dose] . . . So, I spend hours going back to my GPs saying this is not right . . .
DN leads group 2
Some interviewees reported that general practices were not always responsive to, or did not have capacity to, adapt systems to accommodate patients’ needs:
GP surgeries can be quite resistant to them [patients] getting drugs if they don’t follow the correct process . . . they’re having a hard time anyway and they need someone to be on their side and not say you should have rung up yesterday . . .
PC Cons HP02
There was a lack of nurse independent prescribing in the more rural areas of the region. When the hospice provided the CNS service, only two were prescribers. The TSL team reported that having more prescribers in community teams (i.e. CNs and specialist nurses) would provide wider access to prescribers, reducing waiting times for a GP, particularly in remote areas.
There were three independent prescribers within the TSL team; however, they could not prescribe directly to patients. CNSs could prescribe via paper, but not EPS. For both CNSs and TSL staff, access to EPS would have facilitated faster access to medicines for patients:
If [telephone service] had the facility [electronic prescribing] as well [as us] because like I say some of them are starting . . . to do the prescribing that would make it a lot better. I could do that in the house because I can get on remotely, if I could send that remotely to the chemist in somebody’s house knowing that it’s going to get delivered that day . . .
CNS HP26
The TSL service experienced challenges in meeting the needs of patients living in remote areas. CNs, GPs, OOH GPs and pharmacy services were sparse in this region of the CCG. Only one CN was available to visit patients OOH, which had an impact on patients in terms of delay in pain relief:
Just the other day it was a 2-hour wait for a nurse to go out. If your relative is in pain waiting for a nurse to go and administer an injection 2 hours is a long time . . . they’re so stretched . . . It’s a huge [geographical] area . . .
TSL HCP group 1
Access to all NHS care trust community nursing teams (except for the palliative care support team, which could be contacted directly) by HCPs and patients was by a SPA that was not operated by trained HCPs and that had no triage or prioritisation system in place. The TSL team often needed to request CN visits and often queued up to 20 minutes for a SPA operator to connect with the relevant service. In addition, SPA operators sometimes failed to pass on the messages they received. This delay in communication reduced the effectiveness of the TSL team at enabling patients in the city and town areas in accessing a nurse who could prescribe or contact a GP for a prescription:
[I] could see that [patient] rung [TSL] at 9.05 but I didn’t actually get the call until 10.45 from SPA . . . because they hadn’t passed it through . . . [TSL] type we’ll speak to district nurses and we’ll visit as soon as possible. So, then your family are looking at you, they say where have you been . . .?
DN leads, group 2
Summary
Appendix 24, Table 30, summarises palliative care 24/7 TSL service delivery characteristics, their mechanisms of action to influence medicines access, moderating and mediating factors, and the impacts on both patients/carers and on service outcomes. Patients were generally accessing their medicines themselves and had gained confidence to do so from their own experience navigating systems. Patients used the TSL when their symptoms exacerbated to gain access to an appropriate service (e.g. OOH GP, CN or paramedic followed by a prescription or hospital admission).
All patients referred to the TSL as a useful SPA in addition to their usual HCP. HCPs discussed patients’ use of the TSL to access medicines, particularly in the last few weeks of life. The TSL team emphasised the importance of their service co-ordinating local community and primary care services, particularly when unexpected issues occurred for patients that resulted in difficulties accessing their medicines. The TSL team stressed the importance of resolving medicines issues in a calm and timely manner to prevent distress to patients who were often unaware of the complex background work required to resolve these issues.
The work undertaken by patients, carers and HCPs to access medicines in a timely fashion was described by the HCPs as challenging at times; however, the 24/7 TSL team’s use of trained and experienced staff aided its effectiveness in responding to patients’ concerns by providing advice about medicines, where to obtain them and/or co-ordinating local appropriate community services on patients’ behalf. Furthermore, the TSL team’s base within a digital care hub enabled the use of a secure communication system and an electronic shared health records system that was central to using contemporaneous patient information to co-ordinate services.
Chapter 6 Costs and cost-effectiveness of medicines access services
The health economic workstream in the study aimed to estimate the relative value of services for providing access to medicines at EoL. The services evaluated were limited to the four case studies included in Chapter 5.
This workstream first estimated the health-care costs associated with each of the services. It then made use of the care record data to estimate the health-care resources typically used by patients receiving three of the four services and to explore whether or not these data could be used as proxies for effectiveness. Using information from these two analyses, expert input and an adaptation of an existing decision model, we sought to provide estimates of cost-effectiveness for the four medicines access services. Given the scarcity of evidence on the effectiveness of these services, the results presented here are reliant on many assumptions and should be considered preliminary and indicative only.
Method
Service costs
We outline the costs for the provision of each of the four case study service types. We do this by first describing the typical pathways in those services by which patients seek and receive prescription medicines and then attaching unit costs to HCP type and time. We acknowledge that the pathways can vary considerably across different individuals and centres, but our aim was to describe the most likely scenario and cost on that basis. All costs excluded cost of the medication, as this is variable between observations and is assumed to be equal across service types. We also excluded pharmacy delivery service costs, as we assumed that this is applied to all services in relatively equal measure and there is little evidence available as to the patient pick-up : pharmacy delivery ratio.
We conducted targeted literature searches to identify evidence relating to resources expended in the provision of services. Very little empirical data (e.g. from time and motion studies) were available to inform this work and, therefore, we relied heavily on the experts within the research team who provided plausible estimates.
When the pathway and resources had been agreed with the team, we applied unit costs to derive a total cost for both new and repeat prescriptions. Most unit costs came from NHS reference costs59 or Personal Social Services Research Unit (PSSRU) reports. 60 All costs were inflated to 2020/21 prices (GBP) using health inflation assumptions. 61
To illustrate the budget impact of each service, we estimated total annual costs (at 1 and 5 years) if all eligible patients in England were to receive the service. Discounting at 3.5% was applied to costs beyond 1 year.
Sample
We analysed data from retrospective samples (target n = 40) of GP patient/specialist palliative care provider records for case study services 1, 2 and 4. The purpose of this was to capture typical resource use for each service, including resources that are part of the planned pathway and unplanned service use, and to provide the associated costs of these resources.
Data collection
A standardised data extraction form was developed and refined with the team to capture the resource use for each patient (see Appendix 25) over a period of 8 weeks. The captured resources were across three broad categories: (1) secondary care (e.g. hospital stays, hospital ward type, length of stay, hospital visits), (2) hospice care (e.g. inpatient, outpatient, length of stay) and (3) primary care (e.g. GP visits, pharmacist contacts, DN visits). When it made sense to do so, for each of these, additional information was gathered on whether the resource use was planned or unplanned, was OOH or not and whether or not the contact was related to symptom management (as opposed to disease treatment, e.g. chemotherapy receipt).
Analysis
For case study services 1, 2 and 4, we present health-care resource use and costs (see Appendix 26) across three categories: (1) secondary care, (2) hospice and (3) community/primary care. We present descriptive statistics in the form of means, standard deviations (SDs) and ranges for resource use items and cost categories. We ran regression analyses, predicting costs using a generalised linear model (GLM) that accounts for the skewed nature of the data to estimate whether or not there were significant differences in costs according to service type.
We were not able to capture some data that may have helped to control for imbalance/different case mixes across service sites. Consequently, there is a risk that any resource use or cost differential observed is not due to the resource expenditure or effectiveness of the service, but due to other reasons (e.g. a particular site having more severely ill patients). Unfortunately, time on register, which we believed was a rough proxy for proximity to death/disease severity, was not completed in a uniform way across case sites. In case sites 1 and 4, this variable represented time on the GSF register, whereas in case site 2 this represented time on CNS caseload. These variables were thought to be incompatible and, therefore, ruled out the use of time on register as a control variable in the primary analysis.
We tested whether or not the patient’s diagnosis (cancer vs. non-cancer) had an impact on costs and found that there was no significant relationship between the two. However, we did retain this in the main analysis. We used the margins command to estimate marginal effects (i.e. mean costs per study site) from the models. We generated bootstrapped GLM estimates to help deal with the skewed nature of the cost data and to generate more robust confidence intervals (CIs) around mean values. 62 We used 500 bootstrapped samples with replacements for all analyses. The exception was that predicting hospice costs, which, because of the small number of non-zero costs, took much longer to converge and meant that a much smaller number of simulations was implemented (n = 10).
To provide an idea of the budget impact of introducing these services given the subsequent resource use, we multiplied the mean resource use costs by the population who may receive the services. We assumed the typical survival of those whose records were included in the analysis to be 12 months.
Therefore, the calculation was:
with 52 being the number of weeks in a year and 8 (weeks) the time horizon of the collected data. We identified the population who could receive the services as 239,822 individuals based on CCG prevalence estimates. 63 We also assumed that this is the annual incidence on the basis that, within a 12-month period, those receiving palliative care would have died.
Missing data
Missing data on length of hospital stay were estimated using simple mean imputation and taking the average of existing data. There was no other imputation of missing data. When responses were entirely missed, we interpreted this as zero resource use.
Analysis
We explored whether or not the resource use data could provide a proxy measure of service effectiveness. For each service type, we estimated the average:
-
planned/unplanned visits to a hospital or hospice (including inpatient, A&E visit or outpatient attendance) required for symptom management
-
OOH GP visits (in surgery or at home) required.
We did this using simple mean estimates (e.g. the number experiencing an event/sample). We also explored the use of Poisson regression (for count data) and logistic regression (for binary data) to predict emergency/unplanned health-care use, adjusting for diagnosis.
Cost-effectiveness
A preliminary economic evaluation that compared the case study services following the National Institute for Health and Care Excellence reference case was conducted. Standard care was defined as GP provision of medicines (case site 1). The analysis was conducted from the perspective of the health-care service provider and the main outcome was cost per incremental quality-adjusted life-year (QALY). A wider cost perspective was considered, but during the service costing exercise it was unclear whether a patient or carer cost (e.g. for travel) differential would exist between services.
A decision-analytic model, which had been developed in a previously funded NIHR research programme,64 was used. The Markov model was adapted to capture the impact of uncontrolled symptoms. The standard care arm of the original model was retained and updated with costs and effectiveness from the current research (see Appendix 26, Table 31, for parameter values). Effectiveness of the services was based on the probability of requiring unplanned hospice or hospital contact for symptom management, as this was considered a suitable proxy for the effectiveness of medicines access services. The a priori hypothesis being that better access to medicines would reduce unplanned visits. Data for this were taken from the care record analysis. Unplanned care and secondary care receipt was associated with a cost (again, taken from the record analysis) and a health-related quality-of-life decrement that was assumed to last 1 week. Model structure and survival data from the original model were retained. Data were not available on the effectiveness of case site 3 and this was assumed to be the same as the GP-led service, with additional threshold analyses conducted. The model had weekly cycles over a 12-month horizon and, therefore, discounting was not required. An initial new prescription fee was used for all services, followed by a repeat prescription every 4 weeks.
Incremental cost-effectiveness ratios (ICERs) were estimated, with uncertainty explored in deterministic and probabilistic sensitivity analyses. Net monetary benefit (NMB) is reported (QALY × QALY threshold – costs) and the willingness-to-pay threshold per QALY gained was assumed to equal £20,000. We also estimated the expected value of perfect information, which attributes a cost to the parameter uncertainty in the model. Parameter values for the model are included in Appendix 26. We have followed reporting in accordance with the Consolidated Health Economic Evaluation Reporting Standards guideline. 65
Results
Service costs
The unit costs for each service are presented in Appendix 26 and total costs are presented in Table 12.
Case 1: general practice prescribers
New prescription resource elements were assumed to be:
-
an initial GP appointment
-
GP time for writing a new prescription
-
CNS time for contacting pharmacy
-
dispensing time of a CP.
Based on information from the phase 3 sites, repeat prescriptions are generally processed by the practice administrative staff/receptionists. However, these processing costs have not been included in the four case study services, as the costs are likely to be minimal. Therefore, the costing of repeat prescriptions included pharmacist dispensing time costs only (see Appendix 26, Table 32).
Case 2: clinical nurse specialist prescribers
Although the level of CNS involvement for accessing medicines is higher in the CNS case study, our data suggest that GPs are still most likely to prescribe a new prescription. This is usually based on a CNS recommendation, once the patient is referred to the CNS team, that visit the patient at home or see them following patient attendance at an outpatient appointment in a hospice. The CNS then requested a prescription from a GP, usually via SystmOne. Therefore, resources used in case 2 were assumed to be:
-
an initial CNS consultation
-
time required to request a prescription via SystmOne
-
GP/nurse prescriber time for writing a prescription
-
CNS time for contacting the pharmacy
-
dispensing time of a CP.
Repeat prescriptions were the responsibility of the general practice and so will have the same costs associated as case 1 (see Appendix 26, Table 33).
Case 3: community pharmacy-delivered commissioned services for palliative care
New prescriptions for case 3 include the average cost to provide commissioned services for palliative care medicines at pharmacies, after which the patient pathway will follow either scenario described in cases 1 or 2. As patients could follow either pathway, we decided to take the weighted average of two-thirds of the case 1 costs and one-third of the case 2 costs, based on phase 2 survey responses. Repeat prescriptions would follow the same procedure as cases 1 and 2.
Average cost per patient per pharmacy providing commissioned services
The commissioned services cost per pharmacy was estimated using the service-level agreement retainer fees from a convenience sample of nine CCGs across England. The population that each CCG is expected to cover was also recorded alongside the number of patients registered to receive palliative care support and proportion of pharmacies offering the services. We used this information to estimate the average retainer fee cost per prescription. Set-up fees and reimbursement costs for expired stock were not included (see Appendix 26, Table 34).
Case 4: palliative care 24/7 telephone support line
Patients who call the TSL concerning prescriptions are usually referred on by a nurse to a GP and, therefore, case 4 has a very similar pathway to case 1. The costs are likely to include an initial GP consultation for new prescriptions with the inclusion of a cost per call to the TSL. Costs increase for the TSL for OOH, as nurses are given unsocial hours payments for any weekday after 20.00 and before 06.00. There is also a mixed skill set of staff operating this service, with band 3 nursing assistants accounting for 20% and band 6 nursing assistants for accounting for 80%, which we used to weight the staff costs. Repeat prescriptions include the same costs as cases 1–3, but we also assume an additional call to the TSL is made. We have not included a cost for referring patients to the TSL (see Appendix 26, Table 35).
Budget impact analysis
We estimated the number of patients requiring palliative care services to be 239,822 based on the CCG prevalence estimates. 63 The total number (n = 1,591,156) of prescriptions required by this population was taken from Ziegler et al. 66 The Handbook of Practice Management67 states that 80% of all prescriptions are repeats and we assumed that this would apply to a palliative care context. From this information, we estimated that there are 318,231 new prescriptions and 1,272,925 repeat prescriptions per annum. Multiplying these figures by the total service costs from the previous tables gave us estimates for the total cost of providing each service to the palliative care population for 1 and 5 years (Table 10).
| Case | Total cost (£) per prescription | 1-year cost (£) for patient population | 5-year cost (£) for patient population |
|---|---|---|---|
| Case 1 | |||
| New prescription | 79.50 | 25,299,140 | |
| Repeat prescription | 19.00 | 24,184,610 | |
| Total cost | 49,483,750 | 231,241,485 | |
| Case 2 | |||
| New prescription | 59.97 | 19,083,024 | |
| Repeat prescription | 19.00 | 24,184,610 | |
| Total cost | 43,267,634 | 202,193,082 | |
| Case 3 | |||
| New prescription | 76.41 | 24,315,452 | |
| Repeat prescription | 19.00 | 24,184,610 | |
| Total cost | 48,500,062 | 223,736,106 | |
| Case 4 | |||
| New prescription | 91.05 | 28,975,661 | |
| Repeat prescription | 24.43 | 31,099,641 | |
| Total cost | 60,075,302 | 277,133,957 | |
Resource use analysis
Cost analysis
The unit costs for the resource use valuation are included in Appendix 26, Table 36, and the available sample detail is included in Appendix 26, Table 37. There are clear imbalances between case sites, with a much higher proportion of the case study 4 site patients having a non-cancer diagnosis. There was a broad range of time on the palliative care register and large differences between case study sites in this regard, with case site 2 contributing patients with a much lower average time in palliative care, highlighting that these data are likely to be incomparable across sites.
Unadjusted resource use across key categories and by case study site are included in Appendix 26, Table 38. Hospice outpatient visits were noticeably higher in site 2 than in the other sites. The number of inpatient stays, and length of stay, appeared to be larger in case study site 1 than in the other sites. Hospice use appeared higher in site 2 and the number of GP visits were noticeably larger in case 4 than in the other sites. Unadjusted descriptive statistics by case study site for the main cost categories are included in Table 11. Total costs are similar for case sites 1 and 2 and these are notably higher than costs for case site 4. Hospital costs are higher for site 1 than the other services, but incur much lower primary care costs. Hospice costs are notably higher for case site 2 than in the other sites. There are several statistically significant differences observed as denoted in the table.
| Case study | Variable | n | Mean cost (£) | SD (£) | Minimum cost (£) | Maximum cost (£) |
|---|---|---|---|---|---|---|
| 1 | Hospital costs | 26 | 2214.06a | 3498.06 | 0.00 | 12,236.00 |
| Hospice costs | 26 | 357.50 | 985.81 | 0.00 | 3998.00 | |
| Primary and community costs | 26 | 193.52b | 174.50 | 0.00 | 672.49 | |
| Total | 26 | 2765.08c | 3526.64 | 0.00 | 12,698.87 | |
| 2 | Hospital costs | 40 | 716.90 | 1027.26 | 0.00 | 5177.00 |
| Hospice costs | 40 | 679.15 | 2752.73 | 0.00 | 15,958.00 | |
| Primary and community costs | 40 | 1066.19d | 981.60 | 46.68 | 3132.64 | |
| Total | 40 | 2462.24 | 2830.04 | 490.08 | 17,284.90 | |
| 4 | Hospital costs | 36 | 612.61 | 1745.86 | 0.00 | 7866.00 |
| Hospice costs | 36 | 135.11 | 793.53 | 0.00 | 4763.00 | |
| Primary and community costs | 36 | 629.01 | 687.75 | 39.00 | 2773.35 | |
| Total | 36 | 1376.73 | 2224.85 | 58.74 | 10,317.70 |
Table 12 includes the adjusted GLM bootstrapped estimates of costs with CIs for the total and category costs across the case study sites. These values represent mean estimated health-care resource use costs over 8 weeks for patients receiving each type of service. The values may be useful in estimating the costs of the alternative service types over longer periods. The values do not include the cost of the service provision itself. The hospice costs were not estimable because the model did not converge and this is possibly because of the small number of non-zero costs, especially in case site 4. The values in the adjusted model are not substantially different from that generated in the unadjusted model. Again, hospital costs are significantly higher in case 1 than in case 2 (with p = 0.067 vs. case 4). Primary care costs are significantly higher in case 2 than in cases 1 and 4. Total costs are similar for cases 1 and 2. Case 4 total costs are significantly lower than case 1 total costs (with p = 0.058 vs. case 2).
| Cost | Case study | Mean cost (£) | SE (£) | 95% CI (£) |
|---|---|---|---|---|
| Hospital costs | 1 | 2208a | 829 | 583 to 3833 |
| 2 | 730 | 233 | 273 to 1188 | |
| 4 | 601 | 353 | 0b to 1292 | |
| Hospice costs | 1 | Model did not converge | ||
| 2 | ||||
| 4 | ||||
| Primary care | 1 | 195c | 37 | 121 to 268 |
| 2 | 1095 | 175 | 752 to 1439 | |
| 4 | 608d | 117 | 379 to 838 | |
| Total cost | 1 | 2782 | 713 | 1385 to 4178 |
| 2 | 2592 | 560 | 1495 to 3688 | |
| 4 | 1299e | 366 | 582 to 2016 | |
Budget impact
Appendix 26, Table 39, includes the budget impact estimates for each of the three service types, which shows the cost of health-care resource use per service, per year, multiplied by the total number of patients eligible to receive the service. These do not include the initial cost of the service, but resulting patient health-care use costs. These figures do not incorporate uncertainty. The population figures assume that all patients in England would receive that service.
Effectiveness proxy analysis
Appendix 26, Table 40, includes the unadjusted means for hospital and hospice visits for symptom management and OOH GP visits.
The Poisson regression did not yield any statistically significant differences between case sites after controlling for diagnosis. The most noticeable difference observed was the lower average number of unplanned hospital or hospice visits for symptom management for case 2 than for case 1. However, this was not found to be statistically significant (p = 0.08).
The logistic regression indicated that case site 4 patients were statistically significantly (p = 0.03) less likely than case site 1 patients to require an unplanned hospital or hospice visit for symptom management. This trend was apparent for case site 2 (vs. case site 1), but did not reach statistical significance (p = 0.06). Using the margins command, the probabilities of requiring an unplanned hospital or hospice visit for symptom management were estimated as 0.33, 0.14 and 0.07 for case sites 1, 2 and 4, respectively.
Cost-effectiveness
The expected 12-month costs and QALYs per service and ICERs (deterministic and sensitivity analyses) are included in Table 13. The NMB figures indicate that the TSL service has the highest value and the GP prescriber service the lowest value. Both CP and TSL services dominate (i.e. are cheaper and more effective) than the GP service. Figure 5 is a cost-effectiveness plane and shows the 10,000 simulations from the probabilistic sensitivity analysis for the pairwise comparisons of services compared with GP prescribers. Most of the TSL simulations are in the south-east quadrant, indicating dominance over the GP prescriber service. Figure 6 is a cost-effectiveness acceptability curve, which shows that TSL is the optimal choice (with an 85% chance of being cost-effective) at a £20,000 per QALY threshold, followed by CNS prescribers (with an 15% chance of being cost-effective). The population expected value of perfect information over 1 year was estimated to be £49,670,413, indicating a substantial cost of uncertainty. This suggests that further research investment (e.g. a trial) is warranted to reduce decision uncertainty.
| Service | Cost (£) | QALY | NMB (£) | Pairwise ICER vs. GP | Pairwise INMB vs. GP |
|---|---|---|---|---|---|
| Deterministic base case | |||||
| GP | 4083 | 4.669 | 89,289 | ||
| CNS | 3329 | 5.000 | 96,670 | Dominates | 7381 |
| CP | 4079 | 4.669 | 89,292 | Dominates | 3 |
| TSL | 3180 | 5.112 | 99,059 | Dominates | 9770 |
| Sensitivity analyses | |||||
| 50% reduction in utility decrement for unplanned hospital/hospice care | |||||
| GP | 4083 | 4.940 | 94,710 | ||
| CNS | 3329 | 5.106 | 98,785 | Dominates | 4075 |
| CP | 4079 | 4.940 | 94,713 | Dominates | 3 |
| TSL | 3180 | 5.162 | 100,057 | Dominates | 5347 |
| Additional new prescription every 3 months | |||||
| GP | 4401 | 4.669 | 88,971 | ||
| CNS | 3569 | 5.000 | 96,430 | Dominates | 7459 |
| CP | 4385 | 4.669 | 88,987 | Dominates | 15 |
| TSL | 3544 | 5.112 | 98,695 | Dominates | 9724 |
| Additional new prescription every 3 months except in GP service | |||||
| GP | 4083 | 4.669 | 89,289 | ||
| CNS | 3569 | 5.000 | 96,430 | Dominates | 7141 |
| CP | 4385 | 4.669 | 88,987 | Dominated | –303 |
| TSL | 3544 | 5.112 | 98,695 | Dominates | 9406 |
| 50% reduction in unplanned hospital/hospice use for GP/CP services | |||||
| GP | 3481 | 4.940 | 95,324 | ||
| CNS | 3329 | 5.000 | 96,670 | Dominates | 1345 |
| CP | 3478 | 4.940 | 95,328 | Dominates | 3 |
| TSL | 3180 | 5.112 | 99,059 | Dominates | 3735 |
FIGURE 5.
Cost-effectiveness plane for case studies vs. GP-led service.
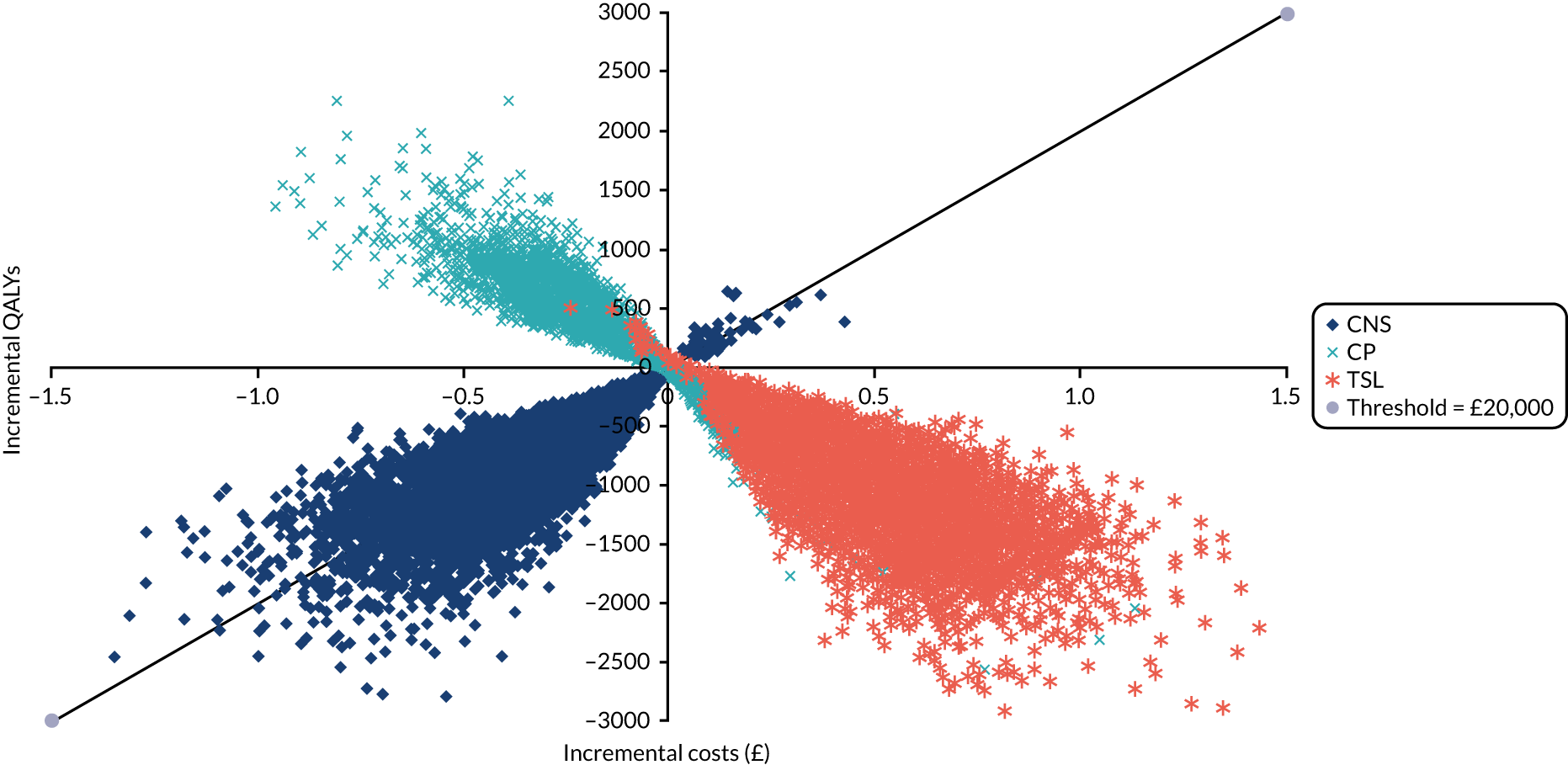
FIGURE 6.
Cost-effectiveness acceptability curve. WTP, willingness to pay.
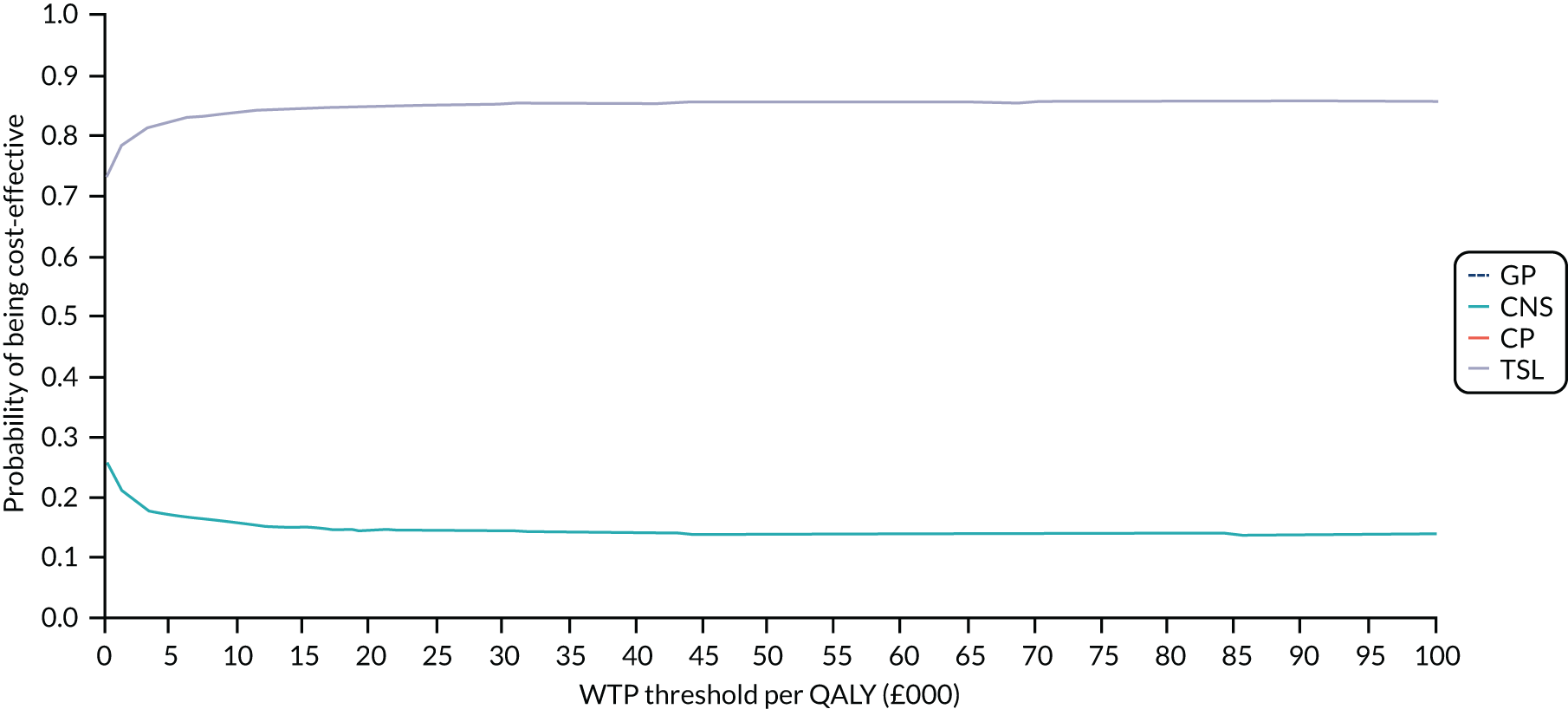
Discussion
This analysis sought to estimate the cost of medicines access services and health-care resource use costs associated with three of the four case site services investigated. We used this information and a previous decision model to estimate cost-effectiveness.
There was very few data on which to base the service costing and, therefore, several assumptions were required. Costs for new prescriptions ranged from £60 to £91 and were more or less equivalent for repeat prescriptions. These costs represent substantial differences when accounting for the eligible population over a 5-year period, with a £70M differential between cheapest (i.e. case 2) and most expensive (i.e. case 4) services. There was around a £30M difference between standard care (i.e. case 1) and the cheapest service (i.e. case 2) over 5 years.
The resource use analysis was possible for only case study services 1, 2 and 4. The samples available were small and we were not in a position to identify and control for potential imbalance across case sites. Consequently, there is significant uncertainty around the presented results. However, while acknowledging the shortcomings of the data, aside from the much larger proportion of patients with a non-cancer diagnosis in case site 4, we were not aware of any systematic differences between case sites. Despite the small sample size, we did observe some statistically significant differences in costs between case sites. Reasonably robust findings are that the case 1 site (i.e. GP service) is associated with significantly higher hospital costs than case 2 and, notably (although not statistically significantly), higher hospital costs than case 4. Conversely, cases 2 and 4 had significantly higher primary and community care costs than case 1. Case 2 also had notably higher hospice costs than the other case sites; however, this was based on a small sample of non-zero costs. Case 4 had significantly lower total costs than observed in case 1 and, notably, lower costs than case site 2.
An interpretation of the cost differentials observed is that GP-led services are poor at preventing (or, indeed, rely on) secondary care use, whereas case site services 2 and 4 make better use of community services, obviating the need for secondary care. The costs for case sites 1 and 2 are similar, suggesting that for the latter there may be a transfer of care from secondary to primary/community care of relatively equal magnitude (i.e. in cost terms). However, costs for case site 4, even after controlling for the high proportion of non-cancer patients, are still much lower, suggesting that this full transfer does not occur.
The budget impact analysis provides a scaled-up representation of the case site costs. These are substantial, with total costs estimated to be > £2B, even for the lowest cost service. Annual hospital costs for case site 1 were estimated to be > £2B higher than for case 2 or 4. There is a £2B difference in costs between case 1 and case 4. Therefore, if we were confident in the cost results, by shifting all patients to case site 4 services, cost savings of £2B per annum might be expected (i.e. £10B over 5 years, without discounting). What we can say is that, given the magnitude of these figures and potential for cost savings, further research is warranted on this topic to identify the best value for money strategies.
The proxy effectiveness analysis indicated clear differences in the probability that patients from each case site would require unplanned health (hospital/hospice) care to deal with symptoms. In addition to the caveats already placed around the sample size and data quality, we should note that these results do not allow us to comment on the quality of life of patients receiving each type of service. Nor do these results provide insight into the resource use or effectiveness of case site 3 services, which could not be included in the data collection strategy.
We used a previous model as the analytical tool to estimate cost-effectiveness. The results indicated that the highest value service was the TSL, which had an 85% chance of being the optimal choice. Both CNS prescriber and TSL services were both cheaper and more effective than the GP prescriber service. There are several limitations to the analysis. The original model was created for a cancer setting and, as not all patients eligible for the services evaluated will have a cancer diagnosis, not all inputs will be perfectly suited (e.g. utility estimates and survival). The results are largely driven by the probability of an unplanned hospital/hospice visit and, therefore, the caveats around data quality outlined above apply. These data also do not allow us to say much about the value of the community pharmacy service. However, the budget impact of these services is substantial, as is the cost of uncertainty relating to optimal service configuration and this indicates that additional research in this area is justified.
Chapter 7 Phase 4: supply into community pharmacy
Parts of this chapter are reproduced or adapted with permission from Campling et al. 48 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
This chapter addresses objective 7 (i.e. evaluating supply chain processes into community pharmacy and identifying challenges in providing medicines access in the last year of life).
A whole-system perspective underpinning this phase of the study encompassed examining how groups within the supply chain inter-relate (i.e. how they are influenced by relationships, information flows and professional perspectives).
Method
A qualitative approach was utilised. Telephone interviews were sought with 20 CPs and circa 10 pharmaceutical WDs.
Sampling
Pharmacists
Community pharmacists were purposively sampled via all 15 CRNs in England, CPs who participated in case 3 (in phase 3) and snowball sampling from interviewees.
Pharmaceutical WDs
A range of sampling approaches was utilised to purposively sample ‘elites’ (i.e. those with decision-making responsibility at senior management and board level). 68 Four routes to sampling were used to target participants in full-line wholesalers (FLs) and short-line wholesalers (SLs) and members of the Healthcare Distribution Association (HDA) (London, UK) (i.e. the trade association representing pharmaceutical WDs) with a distribution or wholesale role within large multiple community pharmacies (i.e. chains):
-
WDs (approximately 15) were sent an invitation by the HDA.
-
Members of the SSC were approached to discuss purposive sampling within their own organisation or in other organisations.
-
Snowball sampling from interviewees was utilised.
-
SL wholesalers were identified via CP participants.
Data collection
Semistructured interviews were conducted. Interview guides were developed by five members of the research team (NC, AB, SL, EM and LB) and were informed by phase 1, emergent findings from phases 2 and 3, and SSC meeting discussions.
Data analysis
Following informed consent, all interviews were audio-recorded, fully transcribed and analysed using a framework analysis (see Appendices 27 and 28). 51 Two initial coding frameworks (one for the CP data and another for the WD data) were developed from the interview guides (NC) and then further developed inductively from the data (NC and EM). Interviews with CPs and WDs were analysed separately (NC and EM, respectively) and then triangulated (NC).
Findings
Twenty-four interviews with CPs (NC) and eight interviews with WDs (EM) were undertaken.
Community pharmacist sample
Twenty-one CPs were recruited via CRNs, one CP was recruited from phase 3, one CP was referred from a CP interviewee and one CP was recruited via sampling pharmacy chains for the WD sample. Appendix 29, Table 41, displays the CP sample. Participants represented 11 CRN regions across England, dominated by the north-west of London and the south. The largest proportion of participants (n = 11, 45.8%) was working within independents, seven (29.1%) within large multiples and six (25%) within small multiples. The number of prescriptions dispensed per month ranged from 1469 to 16,918 prescriptions, with a median of 7169 prescriptions. Between one and three FLs were reported to be utilised by participants (with a median of three FLs). Some pharmacies (large multiples) used no SLs, whereas others used up to 14 (median three) SLs. For others, this was difficult to estimate, as they utilised the services of a third party to place orders via SLs. Fifteen SLs were named by participants as being used. Overall, between 2 and 16 (median five) wholesalers (both FLs and SLs) were used.
Wholesaler/distributor sample
Eight WD interviews were undertaken, utilising purposive sampling across a range of FL (n = 5), SL (n = 2) and large multiple chain (n = 1) wholesalers. Participants had experiential knowledge of pharmaceutical supply into community pharmacies, including of palliative medicines.
Participants were identified through the HDA and snowballing; however, recruitment proved challenging and so additional approaches were made via university networks, LinkedIn (URL: https://uk.linkedin.com; LinkedIn Corporation, Sunnyvale, CA, USA) and e-mails/telephone calls to WD customer services. SL contacts provided by CPs were also approached. Eighteen wholesaler customer service teams and 26 representatives were contacted (from a total of 26 companies), resulting in eight participants from six WDs. Three individuals were excluded/declined (written consent not provided, n = 1; too busy, n = 1, distribution business recently sold, n = 1).
Supply chain routes
All interviews informed a diagrammatic representation of supply routes and distribution channels into community pharmacy (Figure 7).
FIGURE 7.
Supply chain routes into community pharmacy (from study data). Reproduced with permission from Campling et al. 48 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
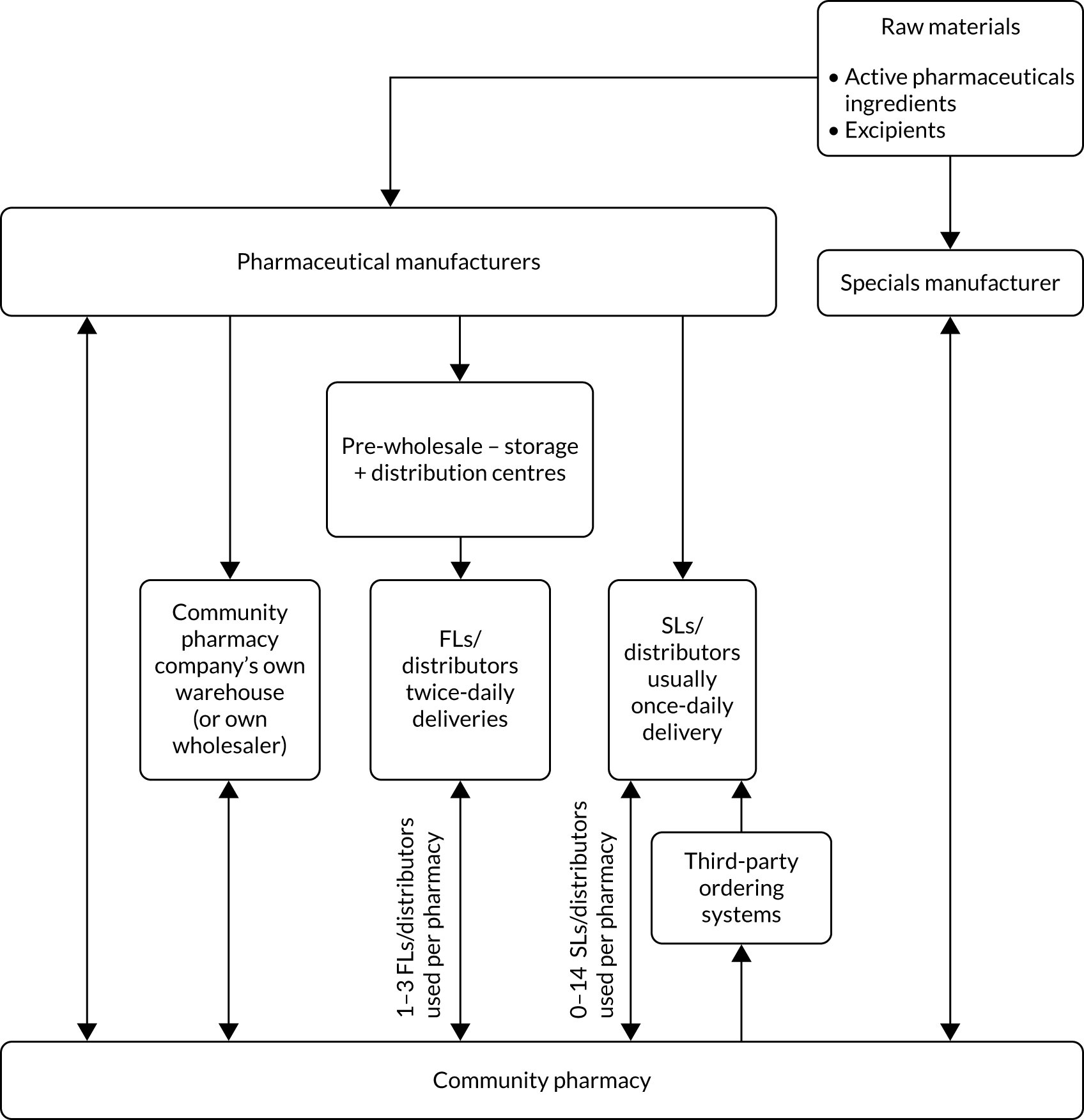
Community pharmacist findings
Role played facilitating medicines access: service provision
Community pharmacists’ role encompassed stock management within their pharmacy or, at scale, across numerous pharmacies; anticipating and/or triaging prescriptions for patients; dispensing of medicines to a patient/family member; providing information about medicines and how to access them to patients/family members; provision of home delivery; and, where commissioned, provision of a palliative medicines service.
Pharmacist roles were helped by experiential knowledge (with some CPs practising for over 20 years and holding senior positions), which grew incrementally with time:
You learn as you do it . . . it’s a maze out there . . . there are so many different products . . . experience helps to navigate through this [supply] process . . .
CP22, independent
Community pharmacists perceived medicine supply to those in the last year of life to be central to their role. It was often an emotive issue for them:
These are the most vulnerable people at the most vulnerable time looking to spend time [together] at the end of their life and a prescription [without the medicine] is no use to them nor their family . . .
CP16, independent
Stock management
To ensure continuity of medication supply to patients, some participants pre-emptively engaged with their stock management:
We generally take a proactive approach to medicine stock holding. So, I suppose the phrase is we’d rather be looking at it than looking for it . . . we carry a significant range of controlled drug medicines and medicines that might be required in end-of-life situations . . .
CP10, independent
For others, a more traditional approach to stock management was taken, reducing pharmacy stock levels (and overall stock value) while maintaining enough stocks to meet anticipated local need (derived from prescribing data).
Anticipating and/or triaging of prescriptions
Some CPs discussed how, on occasion, they anticipated prescriptions being sent electronically (via EPS) to the pharmacy to facilitate supply at the weekend for patients, whereas others discussed how they triaged (and prioritised) prescriptions for patients they knew to be in the last year of their life:
It’s a very community-based pharmacy so we tend to know who is poorly and who is getting worse and we might look for scripts and certainly if I see their names, I will immediately pull them out . . . so you are triaging constantly . . .
CP09, large multiple
Role played facilitating medicines access: relationship-building
All CPs emphasised that to fulfil their role facilitating medicines access, they were reliant on building relationships with patients, families and HCPs.
Patients and families
Often embedded in respective communities via well-established businesses, CPs sought to facilitate seamless care through the provision of medicines to their local EoL populations. Some CPs had developed relationships with patients and their families over numerous years:
I know all the patients by first name, I’ve been here for many years . . .
CP11, independent
Other health-care professionals
To provide care and medicines access, some CPs worked to develop and maintain relationships with a myriad of relevant HCPs (e.g. local GPs, palliative care CNSs, CNs and other pharmacists) with varying levels of success:
. . . specialist nurses, community nurses, community matrons . . . all call in to us, we supply them, we help them, we deliver, we call out. We do as much as we can to help them . . . There are strong relationships with those people . . .
CP16, independent
The lines of communication are nowhere near as good [as in the past]. But this again is because people are going around chasing their tails . . .
CP15 independent
Relationships with local general practices, and GPs, were unanimously viewed as crucial. This was particularly the case when prescriptions needed to be changed by the GP prescriber, with the pharmacist recommending available medicines options or requesting a review of the medicines:
We’d often contact the GP on their [patients’] behalf and just try and bridge communication gaps so that patients are not left frustrated without medication . . .
CP07, independent
Despite this need for relationships, contact with general practices and GPs could be problematic. For many, speaking to the GP directly was a lengthy process and so most either e-mailed or sent a note to the receptionists at the practice to pass to the GPs. This meant that messages were not received until GPs were out of surgeries. Relationship-building appeared easier for CPs co-located next door to a general practice, as staff within the pharmacy could physically take the prescription request to the practice.
Facilitators of access and supply into community pharmacy
Use of key wholesalers/distributors
All CPs spoke of using key WDs for supply into their pharmacies (usually one, occasionally two, as first-line options). The use of key WDs could also facilitate communication and relationships between the pharmacy and WD:
[Where] a medication has been out of stock and it comes back in stock and the suppliers tend to give us a call letting us know that this is back in stock ‘would you like to take an order before the stock runs out?’ Which is very helpful . . . You can only get this when you do have a good relationship with them . . .
CP03, independent
Decisions about which WDs were used hinged on cost, availability and speed of supply, and some CPs explicitly referred to using a protocol-based decision-making system.
Information technology systems
Supply was facilitated by pharmacy IT systems for stock management and/or for placing orders with WDs. The extent to which pharmacies used IT systems to manage their stocks varied, but all pharmacies placed orders with WDs via online systems. Only a few SLs did not provide any online ordering platform. In general, online ordering systems were perceived to facilitate supply:
The online ordering systems are very good. Send an order, instant reply, yes it’s in stock or no it’s not . . .
CP21, large multiple
Time to delivery
Community pharmacists were generally satisfied with the time to delivery offered by WDs. All FLs were able to provide twice-daily deliveries and SLs provided once-daily delivery (with some also able to provide twice-daily deliveries).
Community pharmacists emphasised that when orders needed to be placed to fill a prescription, if WDs had their own stocks then delivery could be that same day for orders placed before the respective cut-off time:
It just depends on whether we order it in time before our cut off. For one of the wholesalers I think it’s 11.30, one it’s 12.15. So, if you order it before then then it will come in a few hours . . .
CP24, small multiple
Once the cut-off time had been crossed, then delivery into the pharmacy would be for the following day. Ability of the WDs to provide same- or following-day delivery was perceived to be as good as possible, considering the need for supplies to be transported from distribution centres/warehouses. When third parties were used to place orders, then generally supply would be for the following day.
Sourcing stock from other pharmacies
When pharmacies did not hold stocks of the required medicines, or could not source them via WDs, most CPs contacted other pharmacies on behalf of patients. CPs spoke of contacting nearby pharmacies that were part of large multiples because of their likelihood of holding more extensive stocks and their ability to contact other chain branches. In addition, most CPs referred to the use of community pharmacy networks, often run via instant messaging applications:
If anything goes short . . . we now WhatsApp [Facebook, Inc., Menlo Park, CA, USA] . . . it’s a big group of 20 of us . . . somebody has got them in stock, and they [pharmacy staff with the product in stock] bring it to us. That way . . . we can help each other . . .
CP11, I
Barriers to access and supply into community pharmacy
Barriers to supply into community pharmacy, and ultimately medicines access, outnumbered facilitating factors. For CPs, this did not mean that patients necessarily had poor experiences of community pharmacy-related medicines access, rather that there were numerous hurdles to supply needing to be overcome and CPs worked tirelessly to overcome these.
Medicine shortages
Medicine shortages were, generally, a universal challenge experienced by CPs, potentially exacerbated by Brexit (i.e. the UK’s exit from Europe). A lack of information surrounding medicines shortages was problematic, with CPs having to seek information via various sources, such as professional organisations, rather than from WDs and manufacturers. This contributed to the pharmacists’ workload and to further delays in accessing medicines:
If I give them, the wholesalers, a call . . . they just say, ‘we’re not getting it back until this date’ and that’s it. They don’t really tell you what’s going on. Really what I have to do is search online through the PSNC [Pharmaceutical Services Negotiating Committee] and obviously various pharmacy channels to see what’s happening, if it’s a manufacturing problem, if it’s a licensing problem or there’s another issue . . .
CP05, small multiple
In relation to palliative medicines specifically, CPs reported varying difficulties related to shortages, ‘which is more distressing . . .’ (CP07, independent), but ‘. . . we haven’t experienced the problems that we’ve seen in other parts of our business with non-availability of drugs generally . . .’ (CP12, small multiple). It appeared that some CPs had successfully weathered palliative medicines shortages because of the efforts they and their pharmacies put into sourcing medicines, sometimes from all over the world.
Medicine shortages led to quotas being imposed by the WDs and/or manufacturers. These quotas were perceived as a hurdle that the CPs had to navigate to gain supplies, and were often harshly viewed as creating additional work and causing a delay in supplying to patients:
Often we’re having to fax anonymised prescriptions to a quota team which has been set up by the mainline wholesalers who then ration out stocks . . . We’ve had a patient on phenytoin suspension, in the last year of her life . . . It’s been a challenge to get hold of that for her family. So, we’ve had to contact [named manufacturer] directly to get supplies issued . . .
CP07, independent
Community pharmacists highlighted that any shortage in the market would drive up the price of the respective medicine. This was a key issue because of professional obligations to supply the medicines, but prices frequently exceeded the monthly stated Drug Tariff price (i.e. purchase cost to the pharmacy exceeds reimbursement price). In addition, at the time of purchase, CPs did not know whether or not a price concession would be granted retrospectively and at what price. This led to profound consequences, with pharmacies dispensing such medicines at a loss, contributing to some pharmacies operating at a loss overall. Alternatively, medicines were returned to the WD because the purchase price was deemed too far in excess of the Drug Tariff price, leading to delays in patient access:
As soon as something becomes short in the market the prices go sky-high . . . Sometimes we’re getting reimbursed £1 for it and we paid £20 . . . you’ve got patients who need their medication, so you take a gamble and order it in and hand it out and just hope for the best . . .
CP19, independent
When medicine shortages occurred, CPs perceived placing a request for a prescription change via the prescriber as a ‘last resort’ once they had exhausted all avenues for supply. It was apparent that getting a prescription changed via the prescriber contributed to delay in medicines access for the patient.
Need to use multiple wholesalers/distributors
Although utilising key WDs was a facilitator to supply, conversely, the need to use multiple WDs (range 2–16, median 5) acted as a barrier, with CPs endlessly having to shop around ‘from one to another’ (CP14, independent). This precluded straightforward supply, adding complexity to supply chain routes into pharmacies and contributed to the onerous workload of CPs. The necessity to use multiple WDs was part of the context of medicine shortages:
. . . so, over the last year we’ve increased it by three wholesalers . . . short-liners, just to give us extra options if we can’t get hold of things . . .
CP19, independent
Community pharmacists also perceived that Solus agreements (i.e. when the manufacturer uses a sole/single WD to distribute their products) contributed to their need to use numerous WDs. They were often critical of such practices, describing them as monopolies or restrictive practices:
It annoys me intensely that something like midazolam we seem to only be able to get through one particular wholesaler . . . The fact that we have restrictive practices in what wholesalers can supply seems to fly in the face of all logic to me . . .
CP15, independent
For some CPs, mainly those in independents, it was only their pharmacies’ use of numerous WDs that enabled them to accommodate such Solus agreements and access the full range of medicines prescribed for patients during the last year of life.
Lack of communication and relationships with wholesalers/distributors and manufacturers
Another barrier to supply was the lack of meaningful communication (two-way information transfer underpinned by trust) with WDs and manufacturers, and the consequent lack of relationships. CPs highlighted that when they needed to speak to WDs, particularly regarding medicine shortages, they did so by telephoning the respective company’s customer services team. It was relatively rare (according to CPs) for WDs to contact CPs and so communication was generally pharmacist initiated. Telephoning service centres was time-consuming and like telephoning a ‘call centre’, not knowing who they were talking to:
It’s always the telesales consultants . . . There’s no clinical knowledge there at all . . . that’s just how it works, you just phone up, have you got so and so, and they’ll say yes or no . . .
CP17, large multiple
The lack of clinical insight held by those answering the telephones at WDs was an issue for some CPs because they did not appear to understand the urgency of palliative medicine supply:
It used to be quite some time ago that when you’d speak to someone, they’d have more of an awareness about the medication . . . Now there’s less . . . so, they may not understand how urgent it is . . .
CP23, large multiple
Furthermore, a lack of understanding could preclude the WDs’ sales staff searching for alternative options and a total reliance on their IT systems:
We look at the product and go right eight different manufacturers they all come with their own seven-digit PIP [Pharmacy Interface Product] code and we’ve been in situations where we’ve read each code out on the phone and they’ve gone ‘no, no, no, no, oh the fifth one is in’, brilliant. ‘Is your software not searching for it’ . . .?
CP06, independent
This lack of meaningful communication and information exchange precluded relationship development between CPs and WDs, and this was a fundamental barrier to supply:
I don’t think you do have a relationship with them, not like you used to. There are no reps that come round. I wouldn’t even know who my account managers were anymore with these big companies [FLs]. Never see them. Never ring up or anything . . .
CP14, independent
This appeared to be underpinned by mistrust on the part of the CPs towards WDs and manufacturers, triggered by conflicting cultures and priorities. The CPs argued that they were primarily focused on patient care and needs (and accountability to the patient), whereas CPs perceived the WDs and manufacturers to be focused entirely on commercial priorities:
[To get access to medicines] . . . I have to jump through hoops, spend time which equals money, takes me away from looking after patients and all of my staff away from looking after patients to try and source medication or products . . . they’re commercial operations looking to make the most that they can out of what they’re doing . . .
CP16, independent
Shortcomings of ordering systems
Despite IT ordering systems being a facilitator of supply, many CPs identified shortcomings of online systems:
A lot of times I’ve given [named FL] a call and I’ve said ‘oh yes I placed the order online’ and it said it went through and they were like ‘oh well yes we only had this reserve amount and you are number 40 something and you will be waiting for it’.
CP02, small multiple
Community pharmacists stated that the majority of orders could be dealt with solely online, but as soon as there was an issue (e.g. the product being identified as out of stock), then they would need to ring the WD (e.g. to find out if there was a date the product would be back in stock). Other reasons for needing to telephone the WDs were to find out about specific brand availability, expiration dates of the product, the price of the product (as prices altered daily), where a product was low in stock if they actually had it, if the product was a switch line (i.e. switched to supply from a different warehouse/distribution centre and, therefore, how long it would take to be delivered), and where a third-party order platform was used to ascertain availability (as in such cases availability of products was not stated on the platform system). The telephoning round WDs, although it did not occur for most ordering, was perceived as hugely time-consuming to gain ‘definitive answers’ and source product for the patient.
Disincentives to stocking palliative medicines
Pharmacies from which the CPs operated varied widely in the number of prescriptions dispensed per month (see Appendix 29, Table 41) and so, for some CPs, a lack of stock turnover of palliative medicines was a strong disincentive for stocking such medicines:
The hurdle is that the medication are usually high value, so pharmacists don’t tend to keep them in stock. They’re also not commonly prescribed, you don’t know which strength they’re going to be . . .
CP17, large multiple
Related to this were the associated costs of the medicines and the lack of a long shelf life for some medicines. CPs could also be concerned of the risk of the medicines not being collected by patients or their families:
Some of these medicines are not very long dated, like midazolam and stuff aren’t. And then you get some stuff that you are never going to use, like . . . glycopyrronium injections . . . if they’ve not collected it . . . one or two of these injections can be £70/£80 . . . a lot of small businesses they’re marginalised as it is at the moment and with small operating margins can they afford to do these medicines . . .
CP08, independent
Some CPs discussed disincentives specific to stocking CDs often used in palliative care, including legal requirement to store the medicines in locked cupboards, the inability to return CDs to the WD when the medicines were not collected by the patient/family and the requirements around the destruction of out-of-date Schedule 2 CDs (subject to full CD requirements). In the main, disincentives revolved around the implications (e.g. cost) of medicines not being collected.
Lack of weekend ordering and Sunday deliveries
Community pharmacists who worked at weekends and worked in stores with Sunday (or bank holiday) opening emphasised that supply into community pharmacies over weekends could be an issue for patients:
I’ve had occasions where you might get the prescription on the Saturday and obviously because wholesalers are closed weekends you can’t get a supply in until Monday . . .
CP04, small multiple
Although pharmacies usually had one delivery (per WD) on a Saturday, the inability to place orders over the weekend and the requirement to wait for Monday’s deliveries was a barrier to supply into pharmacies and, ultimately, medicines access over the weekend.
Issues with wholesaler/distributor deliveries
Some CPs referred to occasional issues with deliveries into their community pharmacies:
Traffic jams and snow. They’re very rare. Usually the wholesalers are decent enough to phone us and say look the M25 there’s been a crash your delivery won’t be there, or your delivery will be in at 17.00 today.
CP06, independent
However, for others, delivery issues appeared more frequent, particularly in relation to missing products from orders that that goes unnoticed until a delivery arrives.
Wholesaler/distributor findings
Role played facilitating medicines access
Wholesalers/distributors discussed strategic elements in supplying palliative medicines to community pharmacies. Strategic elements, such as commercial and quality drivers, were articulated as ‘value-added’ services and helped WDs set themselves apart from their competitors by providing benefit to the manufacturer and/or community pharmacy.
Commercial and quality drivers
Most WDs discussed commercial and quality drivers as important in gaining community pharmacy business. Three large national wholesalers provided a FL service of all pharmaceuticals, including palliative medicines, in contrast to SLs that provided a limited range and usually at a competitive price. Competition in the branded medicines market was more limited, with three FLs mainly competing for manufacturers’ business. Competition was based on winning business from their competitors, as they all serviced the same customer group. Some participants discussed Solus or dual arrangements, which, according to interviewees, assured continuity of supply from the WD:
. . . If we’ve got one source of supply that goes through to one distributor and then to the end-user we can keep a much tighter rein on where that stock is, how is it supplied, control of that stock, control of purchasing . . . There’s a lot of benefits of having a very tight and secure supply chain, assured supply chain . . .
WD05, FL
Solus or dual arrangements were, therefore, perceived to generate more secure business:
Commercially it’s better for us to get all of the volume where you get 100% market share [Solus contract]. We’re in a volume-based business so this brings us volume.
WD03, FL
Despite this perception, the Solus contract could increase the risk of supply failure, as the product could not be accessed by pharmacies via other WDs.
Commercial drivers also dictated the discount awarded to pharmacies based on the volume of stock purchased from WDs. Within the Solus contract there was less of a need to be competitive, being the sole supplier, and so any discounts applied were based on commercial decisions.
Inability to secure sufficient stock levels was considered a commercial ‘faux pas’, as it had a negative impact for the business as a commercial enterprise (i.e. not having assets to sell) and also resulted in not being able to offer the expected service to patients. WDs struggled to differentiate within the market, offering very similar services:
I suppose we don’t really compete on availability we compete on other services for pharmacies so I suppose healthy competition between wholesalers will improve the availability of product if product is available in the market . . .
WD01, FL
Quality improvement of service, facilities and infrastructure was one of the key means to maintain a WD’s competitive position and increase the volume of stock sold.
Facilitators of access and supply into community pharmacy
Relationship-building
All WDs noted the importance of relationship-building in facilitating medicines access, whether through formal agreements or contracting arrangements with manufacturers, day-to-day relationships with community pharmacies (via sales and customer service teams) or informal communications and networks. Relationships were stated to support regular dialogue, with a two-way flow of information and feedback on problems and issues up and down the supply chain:
I think ultimately it’s about good communication and good dialogue between all of the people that sit in the supply chain . . .
WD04, FL
Upstream relationships with manufacturers/suppliers
Contracts or agreements with manufacturers/suppliers could provide assurance of inbound stock to WDs; however, formal contracts were not universally used because of manufacturers/suppliers not being able to guarantee to supply against an order (e.g. owing to adverse weather, shortage of raw materials or quality audit failure). When supply disruptions were envisaged, manufacturers were responsible for informing and communicating this information to the Department of Health and Social Care (DHSC):
What does work very well is when the manufacturers help us and let us know when they’ve got a [shortage] problem because that allows us to make alternative arrangements . . . from time to time it could be better and that’s always something we’d work together with.
WD03, FL
Downstream relationships with pharmacies
Wholesalers/distributors reported that community pharmacies accessed information on medicines shortages from online ordering systems and customer services teams. This was viewed as a two-way conversation through telesales or sales representatives providing feedback to WDs and manufacturers. WDs reported that they had a strategic role to put pressure on manufacturers when shortages were identified by pharmacies. WDs argued that they benefited from their role in this triad by transferring information (e.g. regarding changes in prescribing patterns) from pharmacies upstream to manufacturers. This could instigate proactive responses from manufacturers regarding production plans/stock level holding:
We will inform them [pharmacies] of supply chain issues from our side in terms of procurement from manufacturers and likewise they will communicate back if they have again noticed any changes in prescribing habit or difficulties that other suppliers in the UK supply chain are experiencing.
WD08, SL
Collaborative relationships
A few WDs discussed good practice in supply chain management when severe medicines shortages, such as with diamorphine injection, had been co-ordinated nationally via the DHSC Medicines Supply Team and NHS England and NHS Improvement (NHSE&I) Commercial Medicines Unit. There was a willingness to work collaboratively to get medicines to patients, setting aside competitive relations in response to the shortage:
I think that . . . where there has been a problem where we’ve seen collaboration across the commercial medicines unit the DHSC and the manufacturer and ourselves as wholesalers in the middle I think it’s probably when we see best practice.
WD03, FL
Relationships between WDs, manufacturers and community pharmacies were viewed as extremely important in supplying palliative medicines, and WDs reported acting as a point of mediation in the supply chain.
Investment in logistics infrastructure
All WDs identified logistical issues in the pharmaceutical supply chain as critical in ensuring medicines access at EoL. There was emphasis on the requirement for WDs to deliver on time and in full so that they could be responsive to community pharmacies’ and patients’ needs. This was facilitated by contracting with reputable haulage firms familiar with regulatory governance, investing in logistics infrastructure and by having a clear visibility of stock levels:
We’ve invested a lot into the logistics side of things to ensure that they get to the patient in every bit as good condition as they arrived into us . . .
WD08, SL
Wholesalers/distributors reported that high-quality logistics infrastructure ensured that stock could be delivered with increased certainty and that orders would be delivered on the same or next day, on time and complete.
Demand and stock management
Wholesalers/distributors sought to ensure supply continuity into community pharmacies, with a key element being access to stock within the UK market and, if there was a shortage, their ability to source an alternative product outside the UK. If the product was generic, then there tended to be a greater source of alternative suppliers. If a product could not be sourced, then it was because it could not be found (as opposed to no attempt made):
. . . majority of time that shortages occur are about not having the product available for supply and that’s down to maybe raw material, maybe choice and allocations to different countries, maybe production issues . . .
WD05, FL
If we can’t get hold of one drug, we’d probably work with another company that had got a competitor drug . . .
WD02, FL
Wholesalers/distributors advised that they shared their demand profile and activity with manufacturers to inform manufacturing capacity management. This information transfer aimed to ensure that stock levels were as needed and that medicines shortages did not develop.
The majority of WDs described complex systems for managing stock in response to forecasted demand.
Transparency regarding customer demand patterns, stock holding levels and locations of stock meant that WDs could adjust stock levels throughout the country in distribution centres to respond to spikes in demand.
Buffer stock availability
Most participants discussed how buffer stocks (i.e. stocks within the UK and Europe) had an important role in adding resilience into the supply chain to facilitate medicines access. Holding buffer stock could be recommended by the manufacturer to the pre-wholesaler if they expected a product shortage or it could involve the WD transferring stock between distribution centres (ensuring quicker response times for orders and equitable distribution):
They [pre-wholesaler] hold a buffer [stock] which normally means that there is strong supply into the market .
WD01, FL
Wholesalers/distributors reported that stock availability was always dependent on manufacturer production schedule and lead time for distribution. SLs were noted to fill a gap when FLs were devoid of stock to maintain supplies into community pharmacies.
Barriers to access and supply into community pharmacy
Wholesalers/distributors discussed barriers to the supply of palliative medicines, which were often outside their control.
Supply chain disruptions
Manufacturers’ commercial decisions on where to send their product worldwide (influenced by UK regulations, medicines pricing and the value of sterling) had an impact on supply. These commercial decisions, together with globalisation of manufacturing sites, meant that WDs could have limited supplies of medicines, leaving them unable to meet customer demand:
A manufacturer . . . producing products on a global basis has many choices to make . . . in terms of how many places around the world is that product manufactured . . . if that is only one or two units . . . and those units have problems then that has a worldwide implication of non-availability of stock.
WD05, FL
Many of the WDs referred to shortages that had an impact on their ability to supply customers, requiring WDs to source alternatives and increase stockholdings of other products. WDs expressed concern about supply assurance regarding palliative medicines:
We’re concerned . . . that manufacturers will . . . choose not to supply the drugs to the UK because they will be able to make more money supplying it elsewhere in the EU [European Union]. So . . . the supply chain . . . is a really big worry and for palliative care medicines that’s especially important. This isn’t something where you can order something in and wait 2 months . . . it’s being ordered because it is needed there and then and once you’ve missed that chance to support the patient at that crucial moment in their lives that moment has gone.
WD06, large multiple
Strategic drivers
Strategic supply influences that acted as barriers included generic medicines, quotas and storage capacity, all of which influenced WDs’ decision-making.
Downstream issues
Participants reported instances of downstream issues that affected the supply chain. These issues included export trading by pharmacies, product switches, geographical differences in palliative medicines lists, speculative stockholding by pharmacies, changes in prescribing habits and stockpiling by patients due to a lack of understanding about the supply chain.
Upstream issues
The inability of manufacturers to adequately predict operational issues or forecast demand led to production issues and shortages of manufactured stock. WDs considered the notice period and delay in release of information from manufacturers/DHSC problematic, reportedly due to commercial sensitivity of information. WDs considered that there was not always enough time to make alternative arrangements (e.g. ordering in alternative products) to maintain supplies into pharmacies, and worked closely with manufacturer account managers to try to assure product availability.
Conceptual model of supply into community pharmacy
A conceptual model representing supply into community pharmacy was developed from the data (Figure 8). The ‘whole system’ of supply was influenced by macro-level systems (i.e. structural, legal, regulatory and economic external conditions nationally and internationally), meso-level systems (i.e. local organisational factors and influences, such as organisational culture and incentives) and micro-level systems (i.e. individual attributes and interaction, both of which were helped and hindered by IT). Effective relationship-building and maintenance, meaningful information transfer, effective stock management and robust logistics infrastructure were key to a more responsive supply chain, enabling faster medicines access for patients at EoL. Conversely, the opposite of these, or more limited application of them, led to a less robust supply chain and slower medicines access.
FIGURE 8.
Conceptual model of supply into community pharmacies. Reproduced with permission from Campling et al. 48 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
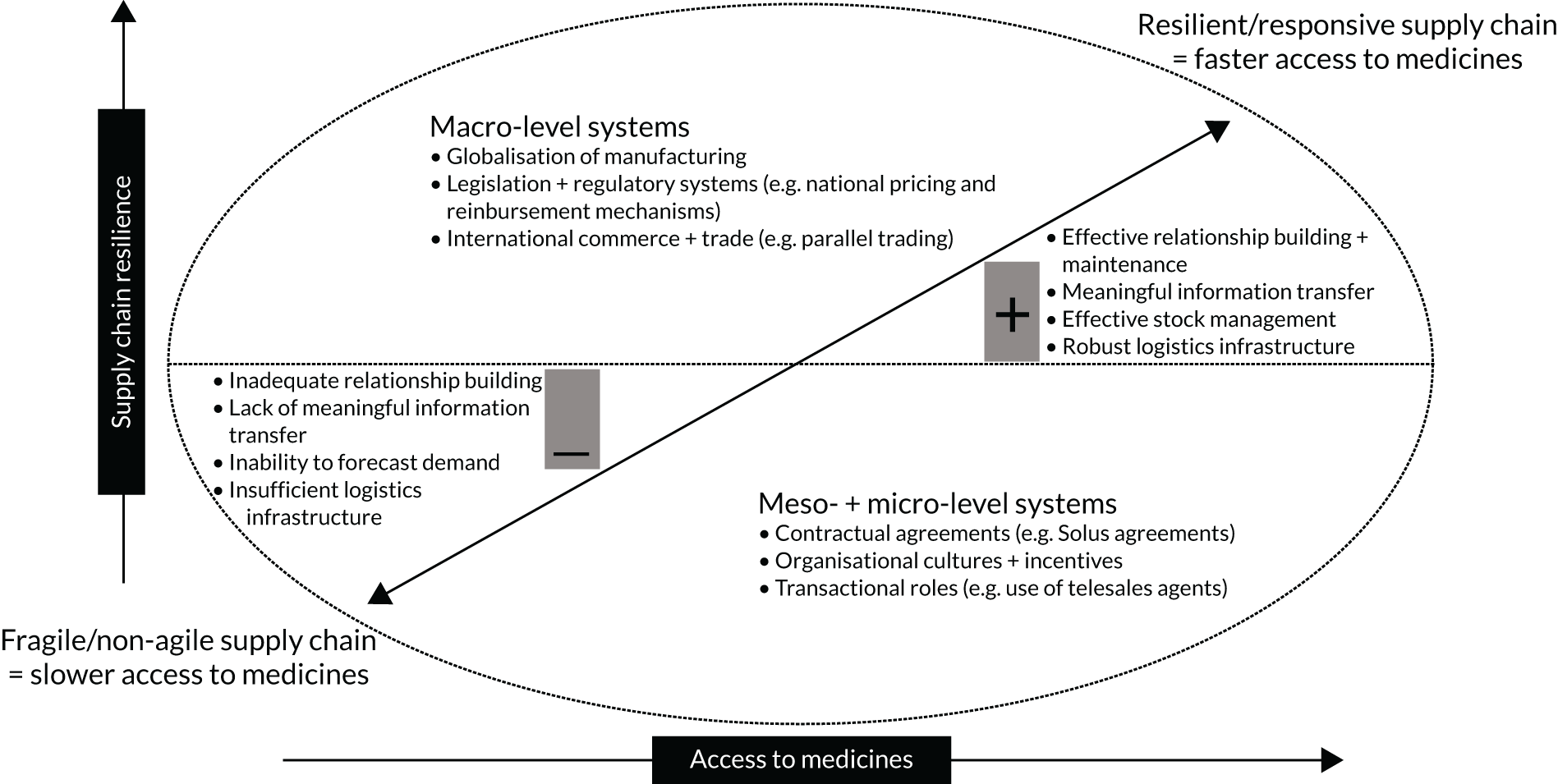
Appendix 30, Table 42, summarises macro-, meso- and micro-level systems influencing supply, their mechanisms of action, associated mediating factors and the ultimate impact on the responsiveness of the supply chain.
Summary
The findings highlight issues affecting access to palliative medicines as relayed by two major stakeholders in the pharmaceutical supply chain (i.e. CPs and WDs).
Community pharmacists sought to do everything they could to supply medicines to people at EoL and for these CPs it was a priority. For CPs, supply into their pharmacies was aided by using key WDs (one or two as first-line options) and all perceived time to delivery to be as good as possible, considering the need to transport medicines from storage facilities. However, CPs were often challenged by deficiencies in the supply chain and having to ‘work around’ the system so that medicines could be sourced and supplied to patients in a timely manner. The significant hurdles that CPs needed to circumnavigate were medicines shortages, the need to use multiple WDs, the lack of communication and relationships with WDs and manufacturers, shortcomings of ordering systems, disincentives to stocking palliative medicines, and the lack of weekend ordering and Sunday deliveries.
Wholesalers/distributors described distribution management and continuing improvement of logistics infrastructure as critical to ensuring that stock could be located and moved to respond to community pharmacy orders rapidly. Nevertheless, WDs were aware of challenges in the supply chain, particularly meeting unexpected demand, and claimed to act as a point of liaison in the triadic relationship between manufacturer, WD and community pharmacy. WDs felt that they managed relationships with manufacturers on behalf of CPs, as well as on their own behalf. One of the main problems reported by WDs (like CPs) was medicines shortages from manufacturers perceived to be outside the WDs’ control, despite sharing information on product demand. It was argued that manufacturers’ commercial decisions had an impact on supply. Despite having sophisticated materials management systems to secure stock and fulfil customer orders, WDs reported commonplace downstream issues, such as trading by pharmacies, product switches by CCGs and stockpiling of drugs (by pharmacies and patients), causing problems. These issues led to the enforcement of stock restrictions via quotas to ration medicines supplies and restrict these activities, limiting access to medicines.
Perspectives between sample groups were widely divergent. WDs appeared to view relationships with CPs as effective, enabling a two-way information transfer. In contrast, CPs argued that when contact did occur with WDs (via telesales staff) it was not productive or satisfactory, nor two way, as the information transfer from WDs was only as good as the information on the IT system and telesales staff lacked clinical insight. WDs perceived that they were conduits for relationships with manufacturers on behalf of CPs, despite CPs doubting the motivations and actions of WDs. Pivotally, conflicting cultures and incentives between WDs (i.e. commercial priorities) and CPs (i.e. patient focus and accountability) contributed to disconnections between groups, precluding effective information transfer necessary to make improvements in medicines access.
Chapter 8 Phase 5: expert workshop
This chapter describes the final phase of the study, which was an expert workshop. This chapter addresses objectives 8 and 9, which focus on an expert review of preliminary study findings and expert-generated implications pertaining to EoL service delivery model characteristics needed to support medicines access.
Method
Sampling
We aimed to capture national and local expertise in EoL and/or EoL medicines access, including policy, service delivery, research, education and PPI perspectives. We also aimed to include representation from a range of service delivery constituents (e.g. specialist, generalist, primary, community and acute care), as well as the different HCP groups engaged in supporting access.
Potential participants for the workshop were identified through purposive and snowball sampling, including using the study teams’ and SSC members’ networks. All members of the SSC were invited to attend the workshop. Invitations were sent to 42 individuals, representing 40 organisations, including NHS England, NHS Wales, Macmillan Cancer Support (London, UK), Marie Curie (London, UK), Association for Prescribers, Hospice UK, Royal College of Nursing (London, UK), Royal College of General Practitioners (London, UK), the Association of Palliative Medicine (Fareham, UK), the Association of Supportive and Palliative Care Pharmacy, eight hospices, six higher education institutions (HEIs), four hospital trusts, two NHS community trusts, two community pharmacies, five general practices and CCGs, and three PPI representatives.
Data collection
It was originally planned that the workshop would be run as a face-to-face event, with a plenary opening speaker and an external chairperson. Although 38 participants had confirmed attendance at this event, which was scheduled for March 2020, this was required to be postponed because of the COVID-19 pandemic. The workshop was, therefore, first rescheduled to another face-to-face event in September 2020. However, the continued enforcement of COVID-19 pandemic restrictions meant that the workshop needed to be converted to an online event.
Participants who had previously confirmed attendance for the March event were invited to the September online workshop. A summary of the study and the findings were prepared as a PowerPoint® (Microsoft Corporation, Redmond, WA, USA) slide set. The workshop was held using Microsoft Teams (Microsoft Corporation, Redmond, WA, USA) and was audio- and video-recorded, with a transcript made of the audio-recording and participants’ ‘chat’ comments to aid analysis of key discussion points.
Findings
Twenty-four participants accepted an invitation to attend the rescheduled workshop (plus nine research team members). In total, 28 participants (external expert participants, n = 19; research team members, n = 9) took part in the online event. Participants represented NHS England, NHS Wales, Association of Palliative Medicine, Marie Curie, the Association of Supportive and Palliative Care Pharmacy, hospices, community pharmacy, general practices, LPCs, acute NHS trusts and HEIs. Professions represented were inclusive of medicine, nursing, pharmacy and radiography. Three PPI representatives also participated.
A summary of key points from PPI representatives’ presentations and key discussion points for each service delivery model are presented below.
Patient and public involvement experiences
In their roles as previous carers for a family member at EoL, PPI presenters highlighted the following.
The benefits of timely access to appropriate medicines included effective symptom control, enabling home care as opposed to admissions to hospital and/or hospice.
Barriers encountered included accessibility of prescriptions being ‘process-heavy’ [e.g. getting prescriptions, liaising with the pharmacy and obtaining the medicines (both collection and delivery) was all very time-consuming], information provision was mixed [e.g. service providers sometimes assuming that some things do not need to be said (such as if the syringe driver bleeps, do not panic), especially when carers are not listening because they are anxious and tired] and acting as a co-ordinator was time-consuming and difficult because EoL care of a family member is difficult.
Facilitators of medicines access included good information provision; availability and accessibility of information OOH; a MDT approach and MDT communication; accessibility of prescriptions through online repeat prescription request systems and EPS; HCPs understanding the unique circumstances of the patient and family and knowing the patient and family cannot be overestimated; and a pharmacist being accessible on the telephone, including OOH, and being able to give support for the logistics of ordering and responsibility for delivery of medicines to the home, as well as for advice, expectations, reassurance (i.e. that what is happening is normal) and finding the right HCP who fits for the situation.
General practice model
Key findings that formed the focus of discussion were as follows:
-
It is sometimes difficult to access GPs/general practices and the GP workforce numbers are declining.
-
The need for CPs to be able to recognise palliative care scripts to prioritise and ensure their speedy delivery to patients. Participants endorsed our finding that palliative care scripts were not always recognisable by pharmacists who do not have access to patient records. It was suggested that ways of identifying these scripts are needed. A participant was able to give a local example in Scotland of GP records being shared with pharmacies, and the initiative of patient-held e-records was also suggested. During the COVID-19 pandemic, pharmacists have been given enhanced access to the SCR, which has been reported as helpful.
-
A need for HCPs to be aware of the services that other HCPs in the MDT offer. Participants recognised our finding that there is a lack of awareness on the part of HCPs of other HCPs’ EoL services. In respect of GP–pharmacy communication, participants considered that co-location of the pharmacy with the general practice greatly aided communication.
-
The value of a specialist link or facilitator pharmacist to educate HCPs across a range of care settings and attend general practice-based MDT palliative care meetings was raised.
-
It was suggested that the commissioning of new HCP services should include a dissemination plan to inform all HCP groups, as well as patients and carers.
-
Participants considered that both integrated care pathways and Primary Care Networks (PCNs) could help to improve interprofessional communication. For example, PCN pharmacists have an obligation to communicate with GPs and their teams as part of quality assurance. The COVID-19 pandemic led to good practice in this area, with, for example, daily interprofessional calls helping to create greater awareness of each other’s’ services. The use of remote online communication, such as through Zoom (Zoom Video Communications, San Jose, CA, USA) or Teams, used during the pandemic had also made interprofessional communication easier. This should be continued and could also be used for interprofessional teaching and education purposes.
Clinical nurse specialist prescribing model
Key findings that formed the focus of discussion were as follows:
-
Participants recognised the study findings on the need to upskill more of the CNS workforce to be prescribers, where there was local need, and community CNSs finding it difficult to access prescribing training courses (because of competition for places with other specialties and being a non-NHS provider).
-
The time costs of CNS prescribers resorting to handwritten scripts and not being able to use EPS, as well as the necessity of, and the significant challenges of not being able to, access shared electronic records, with IT systems not being joined up across the hospice (i.e. NHS interface).
-
COVID-19 had increased general practice-based nurse prescribers’, as well as GPs’, use of EPS. Now that the EPS includes CDs, it was recognised as working well from general practices, although it was noted that other community settings had much less EPS access.
-
Skilling up the CP workforce to be prescribers was a strategic plan nationally.
-
CNSs prescribing in the home might need support and communication systems with the GP/a medic to share prescribing responsibility.
-
Hospice-based CNSs may not be expected to take on responsibility for repeat prescribing, but may do for new and acute symptoms.
-
In the light of local needs and the different contexts and settings in which EoL HCPs prescribe medicines, participants suggested the idea of right person and right place for prescribing rather than a one size fits all approach.
Community pharmacy model
Key findings that formed the focus of discussion were as follows:
-
A need for more commissioned service pharmacies keeping a stock of EoL medicines, using a small national formulary across all pharmacies. This would promote consistency and fairness of access to core medicines, keep accessibility local to patients and services would capitalise on existing local relationships between patients and pharmacists. Area- or PCN-specific medicines could then also be added as a second level.
-
A universal, local scheme could help to increase awareness of other HCPs of the service.
-
It was noted that during the COVID-19 pandemic extra pharmacies had been commissioned (i.e. added to existing service provision) to keep stocks of EoL medicines.
-
Adding information to the SCR and pharmacists’ access was seen as a helpful solution.
Telephone support line model
Key findings that formed the focus of discussion were as follows:
-
The importance of remote telephone support was endorsed.
-
The work of co-ordination in accessing medicines was seen as necessary, to some degree, for individualised care and because EoL care is not simple. The issues raised with regard to this was who does this, how and the cost. It was also noted that carers’ costs are not built in.
-
A national standard mini-formulary of the most commonly used EoL medicines, would get over the work of telephoning around numerous pharmacies to source medicines. There would then be an onus on pharmacies to manage stocks so that they have always got those medicines in (and it was thought such an initiative should smooth things out significantly).
-
Participants noted that there is always the issue of out-of-stock medicines. Therefore, its important to use the PCN and practice pharmacies within PCNs to communicate up-to-date information (i.e. if something on the core list is out of stock, then GPs and nurses need to know).
-
Any consideration of the costs of the service need be balanced against less use of other services as a consequence of having the TSL in place.
-
From a PPI point of view, it was raised that carers and patients may be more inclined to use a service that they perceive as cheaper (e.g. if a service is sited in a community pharmacy and not a general practice).
Summary
A workshop of expert participants reviewed the study findings on service delivery models, the characteristics and costs of these, and how these have an impact on medicines access. Participants recognised and endorsed many of the study findings. Implications were generated through debate of key issues, which included interprofessional integration, communication and awareness; access to shared records, particularly across the community, hospice and NHS interface; the need for a multiprofessional prescriber workforce, with universal access to electronic prescribing systems; and greater and swifter access to community pharmacies’ stocks of palliative care medicines.
Chapter 9 Discussion
Parts of this chapter are reproduced or adapted with permission from Campling et al. 48 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
This chapter draws together the findings from the study phases. The chapter will highlight key features associated with service models that influence patients’ and carers’ ability to swiftly and efficiently access medicines at home during the last year of life. A number of overarching influential issues will be discussed, drawing out where and how these are problematic and what needs to be considered by policy-makers, commissioners, health service managers and practitioners to improve medicines access.
Synthesis of findings: characteristics of service delivery models
The study was framed with reference to systems thinking, a perspective that acknowledges complexity and recognises the multiplicity of actors, the ever-changing context and that systems interact over time to create new patterns. 28 We recognised that the process of accessing a medicine (defined as prescribing, dispensing, supplying and providing associated information about medicines) necessarily involves a number of components, stages, processes and different HCPs.
Systems thinking operates to make a system explicit, including charting the relationships and connections between system components. Understanding a system is a prerequisite to identifying where to intervene to strengthen it and will aid understanding of interventions’ knock-on effects elsewhere in the system, as well as the intended and unintended consequences. The study design has enabled us to provide an overall description of the system of accessing palliative care medicines in the community, and the relationships between service delivery models and system components (see Appendix 31, Table 43). Data about these different components and relationships drew on the perspectives of all the actors (i.e. GPs, specialist palliative care nurses, CNs, CPs, patients and carers, and commissioners) across different sectors of the health economy (i.e. primary care, community care, community pharmacy and hospice care), as well as WDs engaged in the supply chain of medicines into community pharmacies. Our findings confirmed that accessing medicines is a process characterised by complexity, not only because of the various stages, processes and actors involved, but also because these cross the boundaries of private–public health-care provision (i.e. non-NHS hospice care, community pharmacies and the commercial sector in the supply chain). Furthermore, our data showed that patients were also accessing medicines and medical supplies from other sources, not just primary care, but secondary and private paid-for care too. Systems are also characterised by interdependency. 28 In the medicines access process, this was observed in the inter-relationships of HCP team members and service delivery sectors. For example, if a GP prescriber was unaware of the community pharmacy stock of particular palliative medicines, a mismatch between a prescription and stock sometimes occurred, leading to a delay in dispensing at the community pharmacy. HCPs rated integrated working highly as a solution to some of the current problems with access, further reinforcing the interdependency of components of this system. This is played out against a clinical context of rapidly changing symptoms and often pain and emotional distress, creating an urgent need for the supply of medicines into the home. Therefore, this distinguishes the system of palliative medicines access from other systems of medicines supply, such as those required to support the management of long-term illnesses. Although it shares some components (e.g. the request for a prescription or re-prescription from a prescriber and dispensing of the medicine from a community pharmacy) the system of palliative medicines supply is underpinned by less stable symptoms than those typically experienced in long-term illnesses, such as hypertension or asthma. The time frame of illness experience is also more compressed and the physical and emotional distress of managing palliative care is arguably greater, particularly as pain is a common symptom. At the same time, palliative care service provision is somewhat uniquely characterised by a complexity not seen in medicines supply systems for long-term illnesses, that is care delivery by charity-funded hospice-employed HCPs is a more prominent feature, creating extra interorganisational communication difficulties, as exemplified in disparate IT systems. Those employed by charity-funded hospices also have less access to DHSC-resourced training and development, despite making a significant contribution to care delivery to NHS patients. The CD nature of some palliative medicines also shapes the distinctiveness of this system of access, which is comparative to medicines supply for long-term illnesses or non-pharmaceutical provision at EoL. For example, we found that the limited shelf life of CDs inhibited some CPs from keeping them in stock. The systems complexity of the medicines access process is associated with a number of key features in our findings, which are discussed further below, together with their implications for policy and practice.
Systems thinking deploys explicit models, with assumptions laid out that can be calibrated to data and repeated by others. 27 There are a number of tools that can be used to map events and/or processes and how these are connected, and these tools illustrate and analyse connections between people and processes. 27 In Chapter 5 we referenced logic models to show the mechanisms of actions arising from the characteristics of each service delivery model studied and highlighted how these are shaped by moderating and mediating factors to produce patient and service outcomes. To synthesise our overall study findings and draw together features of service delivery and how these influence the system of medicines access, we constructed an overarching logic model using stages and components of the access process experienced by patients (see Appendix 31, Table 43).
Appendix 31, Table 43, shows how the service delivery models we studied are associated with factors that operate to support or impede the system components of the access process. It can be seen that some models appear to be operating better than others to support timely patient access to medicines. The traditional model of GP services as the main prescription provider has limitations and needs to be seen in the context of this being an overstretched service, with declining GP numbers and rising demand. We also found that GP services were associated with higher service (prescription) costs than a CNS prescriber service and higher total resource use costs than the TSL. CNS prescribers appeared to reduce the burden of access work on patients and carers and provide good information about EoL medicines and services, with fewer apparent delays experienced in acquiring medicines. Nevertheless, this model was not operating to its full potential because of CNS prescribers’ lack of access to electronic prescribing systems and deficiencies in the community pharmacy service. The TSL model also appeared to offer advantages by being available as a single point of contact at times of need, particularly OOH, shifting the work of access off patients and carers and using shared records and access to a local network of HCPs’ services to speed the access process. Although the TSL service had the greatest service costs, our data suggested that it may in fact be the most cost-effective. However, it should be noted that patient data in this site were limited and further research is required on similar OOH telephone support services to support these findings. In addition, our findings also show that community pharmacy services, in general, as well as community pharmacy-delivered commissioned services for palliative care, currently operate with a number of limitations that will need to be rectified if they are to deliver their potential.
Although our foci have been on ‘service delivery models’ and studying these in-depth has enabled a comprehensive understanding of each to emerge, in reality these may be combined as components experienced by patients as parts of a medicines access system. All patients will continue to receive medicines services from a general practice with whom they are registered. Our data suggest that combining this GP service with a CNS prescriber service delivery element, where the CNS may work in conjunction with or replace the GP service as the main prescriber, is likely to be advantageous in supporting medicines access and is likely to be less costly. Our data also suggest that the addition of a TSL service alongside GP services for patients receiving palliative care is likely to reduce burden on patients and carers, speed medicines access and may also be cost-effective. However, even with a shift to develop greater nurse prescriber and TSL services, all patients will continue to need to use a community pharmacy service as part of the access process. Therefore, the factors that currently work to limit the effectiveness of community pharmacy will need addressing to fully maximise the potential of any new services. In addition, in keeping with a systems thinking approach, consideration will need to be given to the impact of any intervention on each of the persons and processes in the system that we have described here.
Medicines access: key issues
Health-care professional survey respondents considered that pain levels of patients on their caseloads would be significantly better if access to medicines was improved. In addition, many HCPs in our study told us that accessing medicines at EoL is a critically important issue and one that they worked hard to try to address. Study findings highlight a number of overarching key issues operating to influence the access process and HCPs’ ability to support it.
Increased points of access through diversifying the prescriber workforce
Our data highlighted that, for many, GP services remain the dominant model for EoL patients to access new scripts and, yet, this is a service that can be characterised by burdensome and delayed access, as well as being more costly relative to other community-based services. In the context of a declining GP workforce and rising patient demand, the policy drive to diversify primary care service skill mix is already under way, with initiatives such as advanced clinical practitioner roles, GP practice-employed paramedics and PCN-attached pharmacists all increasingly part of primary and community care service delivery. 69 Our findings suggest that a more distributed model of prescribing is also required, rather than one in which prescribing authority is invested in a single professional group (i.e. GPs). Enabling more specialist palliative care nurses to prescribe would benefit patients seeking to access medicines in the last year of life. Most specialist nurse prescribers in our survey considered themselves competent and prescribed frequently for patients, and in the CNS prescriber case site they offered good information and facilitated the co-ordination of services for patients. However, fewer than a half of CNS participants in our survey were trained as prescribers. CNSs are often employed by part or wholly charity-funded hospices. Although CNSs are a vital part of EoL care delivery, if they are less able to access NHS funding for prescribing training courses and backfill, then this limits their potential contribution to faster access to medicines for patients.
Community nurses also form a key component of EoL care delivery and further research is required to understand the potential of the CN workforce to prescribe palliative care medicines and the impact that this might have on the access process. Relatively large numbers of PCPs in our study were qualified as prescribers and also had good access to shared patient records. Although many PCPs were engaged in advising palliative care patients about medicines and/or undertaking medicines reviews, most reported that they did not feel highly competent prescribing in this area and were not prescribing often. Greater consideration could be given to further developing the role of PCPs who are interested in specialising in this area, with consideration of PCN population care needs.
Streamlined co-ordination required to access medicines
The often significant degree of co-ordination required to access medicines was apparent within all elements of service delivery that we studied. Characterised as a complex systems process inherent in the logistics of accessing medicines was the need to communicate with numerous different HCPs who are operating in different sectors of health-care delivery against a backdrop of urgent medicines need. Co-ordinating access was undertaken by HCPs and/or patients and carers. Some degree of co-ordination and liaison will inevitably be required across interfaces of health-care and delivery systems, and for some patients and carers this may be a desired part of self-management. However, the work of co-ordination was often overly lengthy and burdensome, and sometimes caused distress. Access points and processes for obtaining new or repeat medicines were not always clear to patients, and HCPs sometimes lacked awareness of services available to support access. Co-ordination was also often hidden work. At the TSL service site, staff reported that the work required to supply an EoL medicine to a patient was often deliberately hidden to reduce patient distress. We found considerable unseen work undertaken by CPs to support the supply chain of medicines into their pharmacies. The work of co-ordination appeared to be compensating for deficiencies in the access chain elsewhere, notably accessibility of GP services when they were the main prescribing service and community pharmacies when stock of EoL medicines was unreliable. The hidden work of co-ordination has been observed in hospital contexts. Allen70 observed the invisible work of nurses as focal actors, creating a myriad of processes to sustain networks through which care was organised and often acting as a countervailing force to very loosely organised health systems. 70 The effort and time spent in co-ordinating access could be streamlined if more nurses were able to prescribe directly to patients, if all HCPs were able to access shared electronic records and if community pharmacy stocks were more reliable. Many HCPs in the study survey also recommended better integration of the MDT as one of their top solutions to medicines access problems. Combined with a more streamlined process, the use of a named responsible clinician or care co-ordinator, in line with national recommendations,24 might work to shift the focus of access away from reliance on GP services, reduce duplication of work across HCPs, and make a single point of contact for patients and HCPs, as well as make the work of co-ordination more evident. However, named care co-ordinators are only likely to be effective with improved interprofessional communication systems and, in particular, shared access to electronic records, including in the home. The TSL also appeared to offer a good service for EoL patients, providing an accessible single point of contact, particularly OOH, which functioned to offer the information-giving and co-ordination role that CNSs undertake in the home. However, the limited data collected on this service model, as well as its distinct features (i.e. being part of a larger digital hub with shared access to electronic records), mean that further research is required to evaluate the impact and cost-effectiveness of TSL services more generally.
Any recommendations for named care co-ordinators or single points of access need to be taken forward with cognisance of the often complex current organisational context in which EoL care is delivered. In keeping with our description of its complexity highlighted above, others71,72 have also illuminated the particular multiplicity of professional groups operating across different domains, sectors and levels of care in this context. The task of co-ordination might also be made more difficult by contested decisions about who should take on these roles. Although interprofessional rivalries were not an overt finding in this study, this has been found to be a feature of care delivery in the EoL context elsewhere,71,73 and this may, therefore, influence the feasibility, legitimacy and effectiveness of any appointed care co-ordinator roles. It may also constrain the development and contribution of nurse and pharmacist prescribing in this context. The reluctance of the medical profession to relinquish the authority associated with its long-held, unique prescribing role has been noted. 74 However, as we move increasingly to a multiprofessional primary care and prescriber workforce, we might expect any such attitudes to be diminishing and to be less of a constraint.
The importance of patient–professional and interprofessional relationships
Underpinning the co-ordination work required to access medicines were pre-existing relationships between HCPs and patients and carers, and between HCPs in a locality. Where relationships existed, this exerted traction on the access process, generating commitment to action and speeding up the processes involved. Such relationships were evident in that some GPs (case 1) spent effort working outside usual systems to enable patients to stay in contact with them, CNSs and TSL support staff contacted other known HCPs in their local networks to initiate scripts or check stock and, in community pharmacy relationships with local HCPs, helped ensure the availability of stock. In contrast, where relationships were absent, this hindered elements of the access process. For example, commissioners of community pharmacy-delivered palliative care reported difficulties with awareness and continuity of services as a result of CP staff turnover and locums, and some CPs expressed the difficulty that they no longer had relationships with WDs.
The importance of continuity of care for patients is widely recognised, including at EoL. 75,76 We have found that relationships formed when care is continuous support access to medicines. As demands on the health-care system increase, and in the face of staff turnover, there is great potential for discontinuity and further fragmentation of care, which will likely increase the effort and length of medicines access processes.
The study also found that there is potential for greater awareness by some HCPs of other HCPs’ services. HCPs’ lack of awareness means that signposting patients to such services, as well as HCPs’ own use of them, may be less than optimal. Attention to opportunities for interprofessional communication is warranted. Workshop participants told us that management of care delivery during the COVID-19 pandemic had forged ways of doing this, for example daily general practice–CP calls, including using video technology. This is an example of a more widespread trend in the increase in, and ease of, staff–staff interaction supported by digital technology noted to have occurred during the pandemic. 77
Systems to support fast, electronic communication and information transfer
Access to shared patient records was a key area of HCP dissatisfaction to emerge from the study. CNSs, in particular, were dissatisfied with their current access, but all professional groups expressed relatively high levels of dissatisfaction about this. Respondents also identified shared records access as one of the top four solutions to problems with current service delivery. In addition, survey data suggested that HCPs’ access to shared records was a significant determinant of pain levels of patients on their caseload. The TSL service operated with full access to shared records, which was an important factor in its apparent success.
Health-care professional access to records when faced with a patient needing a medicine is essential for safe and accurate prescribing, which needs to be based on full knowledge of clinical and medicines history. Universal access across community service delivery interfaces (i.e. primary, community and hospice care), as well as with secondary care and between in-hours and OOH service delivery, is warranted. This access is also required in the home setting. The potential of CNS prescribers will only be unleashed if they are able to access patient records to support prescribing. Hospices are external to mainstream NHS IT systems, but during the study we did identify examples of localities where hospice-based CNSs were sharing patient records with other HCPs. Workshop participants also suggested patient-held records as a solution, a practice that has been more widely endorsed. 78 Changes ushered in by the COVID-19 pandemic may also offer important learning here. Research77 has highlighted that the increased sharing of patient data enabled during this time was welcomed, and was supported by a streamlining of bureaucracy, increased tolerance of risk and responsiveness of digital suppliers to meet local needs. Urgent attention needs to be given to ways of integrating current and future IT systems to support shared access, not least because movement to a more multiprofessional prescriber workforce will result in an even greater need for interprofessional communication and co-ordination. Reflecting on the scale and pace of digital change in general practice during the pandemic, The King’s Fund77 recommend a review of procurement processes and a focus on the interoperability of systems by suppliers and national bodies.
The study also highlighted current inequity in access to EPS, with a majority of current nurse and PCP prescribers able to issue handwritten scripts only. The impact of this was apparent, with CNSs often needing to refer back to GPs to prescribe as a mechanism of transfer of scripts to pharmacy and, therefore, delaying patient access to medicines.
Given the multiple system components involved in the medicines access process, streamlined cross-system communication through both interprofessional access to electronic shared patient records and EPS available to all is critical to support timely access to EoL medicines.
Community pharmacy: community pharmacist integration and reliable medicines stock
Study findings highlighted a number of problems with the current community pharmacy service delivery to support access to EoL medicines. Some of these problems appear to emanate from CPs’ lack of integration within primary and community care MDTs and, therefore, within the patient palliative care pathway, from identification of EoL status through to death. For example, many pharmacists reported that they lacked awareness of patients’ palliative care status, which influenced their ability to help patients access medicines. In addition, prescriptions from GPs did not always match medicines in stock, which sometimes created a need to source medicines from other pharmacies. Calls have repeatedly been made for greater integration of CPs within health-care teams. 79 In palliative care, RPS Wales25 recommend that CPs have greater access to patient records. In addition, workshop participants cited examples of improved collaboration with CPs through daily COVID-19-related interprofessional calls and CPs’ enhanced access to SCRs during this time. Study findings suggest that encouragement could be given to sustaining such innovations beyond the pandemic in the interests of hastening access to medicines and enabling CPs to fulfil a greater information-giving role to palliative care patients. This will need to be considered alongside redesigns in supply chain systems to free up CPs from the current onerous work they are doing to source medicines, especially in times of shortages.
Lack of reliable stock of the right medicines in community pharmacies was also a key finding, even sometimes at pharmacies commissioned to provide stocks of palliative care medicines. This caused work for both patients/carers and HCPs trying to source stock from other pharmacies and, thereby, delayed access and increased potential for distress. CNSs pre-empted problems caused by lack of stock by handwriting individual scripts for medicines so that patients could use different pharmacies for dispensing different items. Many CPs reported that they limited their stock of palliative care medicines because of medicines’ expiry dates. Mismatches between scripts received and medicines held, as well as CPs being unable to anticipate patient need, also contributed to this problem.
Additional problems with community pharmacy-commissioned services were an insufficient number of pharmacies in some areas, low HCP awareness of services, medicines’ lists were sometimes long and varied between and within services, not all pharmacies offered OOH services and pharmacies were not usually evenly geographically spread. Consequently, community pharmacy-commissioned services were often not local to EoL patients who could not, therefore, take advantage of them. Workshop participants endorsed the idea of a new commissioned service entailing a small and standardised core list of palliative care medicines universally held by all community pharmacies. Participants were also clear that many more pharmacies had been commissioned to provide stocks of palliative care medicines since the pandemic, and an evaluation of this will be of value. Other practices developed during the COVID-19 pandemic may also offer solutions. In the light of the demand for palliative care medicines and community-based care, workshop participants gave examples of localities where community medicines hubs (e.g. at local hospitals) were available 24/7 together with minimum delivery times and medicines couriered to patients’ homes. Furthermore, any learning from the legislation permitting reuse of CDs in care homes during the pandemic could be applied to CD reuse in other settings to offset wastage and speed access in some instances.
Even with greater diversification and expansion of the prescriber workforce, supported by streamlined systems for better communication and co-ordination, ease and speed of medicines access in all service delivery models will depend, in part, on community pharmacies functioning more effectively.
Consideration of the above may result in what we see as a gold-standard service delivery (i.e. patients who are well informed in managing their medicines and who know who their single point of contact is and how to contact them when new or repeat medicines are required). This gold-standard service delivery would allow for the right HCP to be easily and quickly contactable, patient records to be accessible (and checked) and medicines to be safely prescribed for a patient using electronic systems, including remotely in patients’ homes. Subsequently, the prescription would be smoothly transferred to the community pharmacy, which immediately dispenses the medicines from stock held and medicines would be delivered swiftly to the patient’s home, a process that is inclusive of OOH needs for medicines.
Strengths and limitations
A key strength of the study was its utilisation of a mixed-methods and multiple-phase design, as well as its use of views of multiple stakeholders, to produce a comprehensive and multifaceted evaluation of a complex health service and delivery issue. The use of integrated phases allowed us to investigate further key issues that emerged in previous phases as the study progressed. The online survey enabled us to gather large-scale data on HCPs’ current practices and influences in operation, and case studies provided complementary in-depth data, including the perspectives of patients and carers from an often hard-to-reach group, as well as illustrations of causal mechanisms at work. The study also included a health economics evaluation to enable assessments of costs and resource use of the different models. The study was designed to enable us to capture the views of all actors in the access process, from upstream WDs and service commissioners to CPs, other HCPs and patients/carers managing medicines in the home.
Our target numbers of HCPs completing the online survey were significantly exceeded in all but the CN group, despite extra recruitment efforts focused on the latter. Nevertheless, because of the survey method of distribution, response rates were not able to be calculated and respondents may not be representative of these HCP groups more generally. It is possible that some GPs, CPs, PCPs and CNs who participated were more likely to have had an interest in EoL care and, therefore, higher than typical levels of EoL medicines access activity and competence might have been reported.
In phase 3, patient recruitment was slightly lower than targeted in two case sites because of the lack of regular identification of patients on EoL registers and many not being cared for at home. In addition, at all sites, details of medicines prescribed recorded in patient records were not sufficiently comprehensive to enable timelines of medicines access actions and influences to be drawn up for all patients as we envisaged.
Despite CP recruitment challenges in phases 3 and 4, we spent time following up respondents, using snowballing, as well as local and national pharmacist networks, to overcome these challenges. This meant that, together with the CP and PCP sample size in the survey, the study captured the views of this important but often hard-to-reach and under-researched group. Commissioners and WDs were also hard to reach and recruit and, despite much time and effort spent in following up WD leads in particular, sample sizes for these groups were undertarget. Data were collected in the build-up to Brexit, which may have influenced recruitment. Insights were gained from interviews with these under-researched groups. It is acknowledged, however, that the interviewees recruited may not have represented the full range of views of the groups they represent.
The study included self-report measures to capture professionals’ and patients’ experiences. We applied methodological principles to reduce bias and enhance rigour, including the use of multiple methods and triangulation. The use of CRNs to recruit GPs and some CPs may have resulted in participants and/or service delivery configurations that differed from those operating outside these networks.
We did not include the views of pharmaceutical manufacturers in seeking to understand the supply chain of medicines into community pharmacies. Experience in this study suggests that pharmaceutical manufacturers may have proved time-consuming and difficult to recruit, requiring a longer and more costly study. It may also have been useful to have included more specialist HCPs, in particular those in the secondary sector, to further understand their contribution and influences on access experiences, as well as other actors now playing a part in community EoL medicines provision, such as paramedic prescribers.
Conclusions
To the best of our knowledge, the ActMed study is the first study to undertake a large-scale, in-depth evaluation of medicines access through the lens of service delivery models that form components of an often complex system. A mixed-methods design was used and multistakeholder views investigated to reveal current practice, as well as factors operating to support or impede the access process. We have highlighted where good practice is in operation, as well as components of the service system that are currently delaying access, causing unnecessary effort for many HCPs and increasing the potential for patient and carer distress when they are unable to obtain medicines in good time and with minimal effort.
Implications for policy, service development and practice
Study findings on the operation of service delivery models, influences on HCPs’ contributions and the current contribution of the nurse and pharmacist workforce to accessing EoL medicines in the community point to the following implications:
-
Greater consideration should be given by service delivery commissioners and managers to implementing named EoL care co-ordinators, in line with current EoL recommendations,20,24 who would act as single points of contact for patients to initiate new or repeat prescriptions.
-
Strategic prioritisation by service delivery organisations of training for more CNSs to enable them to prescribe medicines independently to patients is needed. Funding also needs to be made available from Health Education England to hospices for the costs of HEI courses, as well as backfill costs, given hospice-employed CNSs’ important contributions to patient care and the potential benefits and cost-effectiveness of this model of service delivery compared with a GP services-prescribing model.
-
Consideration should also be given by Health Education England and community trusts to prioritising upskilling of larger numbers of the CN workforce to enable them to independently prescribe palliative care medicines and to support patients and their carers to manage these.
-
NHS Digital and local IT system suppliers need to work together to ensure that there is greater harmonisation of local IT systems so that all HCPs have access to shared electronic patient records across organisational interfaces.
-
NHS Digital and local IT system suppliers also need to work together to reduce current inequities in professionals’ access to EPS and ensure that all prescribing nurses and pharmacists working in the community have access to electronic prescribing systems, including in patients’ homes.
-
Commissioning TSL services might offer single-point-of-contact, cost-effective models of provision that work both in-hours and OOH to locally co-ordinate medicines access systems and processes, as well as acting as information-giving hubs about EoL medicines and services for patients and carers.
-
NHSE&I and other national policy-making bodies, such as RPS, as well as local CCGs and PCNs, should continue to drive the integration of CPs within the wider community and primary health-care teams and facilitate pharmacist embeddedness in the patient palliative care pathway, with access to information about patients’ palliative care status, with patient consent, via enhanced SCR or patient record access.
-
NHSE&I should consider a new model of commissioning community pharmacy services for palliative care, one that involves a smaller, rationalised, commonly agreed and widely recognised core list of medicines. National and local commissioners also need to ensure larger numbers of, and a more even distribution of, pharmacies or other community hubs holding a stock of palliative medicines, which is also accessible OOH and able to be delivered swiftly and free of charge to patients’ homes.
-
At a local level, primary, community and specialist palliative care service commissioners and managers should promote interprofessional awareness of EoL services, in particular those available OOH, in commissioned pharmacy services and those provided by specialist palliative care providers, including CNS prescribing.
-
Pharmaceutical WDs and their trade association should engage with CPs both individually and collectively for two-way communication about practices that best support efficient and equitable distribution of stock. In particular, both parties should consider more efficient and effective methods of sourcing medicines in short supply to free up pharmacist time to fulfil their potential in their professional, patient-facing role.
As above, given the complex system of medicines access as we have characterised it, action on any of these implications needs to be planned and consequences for each component of the system modelled to achieve maximum benefit. Similarly, a systems approach to further research (see Further research) is also recommended.
Further research
Potential areas for further research include:
-
a study to understand the feasibility, processes and impact of introducing and formalising a named EoL care co-ordinator role
-
further evaluation of the impact and cost-effectiveness of TSL and other similar OOH services on EoL medicines access, given the promising signals that were evidenced in this study
-
an evaluation of the impact on medicines access experiences, costs and outcomes of increasing the numbers of nurses and pharmacists prescribing for EoL patients being cared for at home
-
an evaluation of the impact and cost-effectiveness of new commissioned community pharmacy-delivered palliative medicines services
-
a full economic evaluation of service models in the light of their substantial budget impact over the eligible patient population
-
an evaluation of the impact on medicines access of good practice models in electronic shared records access, including the service requirements necessary to support greater shared access and how these might best be rolled out across health system interfaces.
Acknowledgements
We extend our grateful thanks to all patients, carers and staff who participated in the study, as well as attendees at the stakeholder workshop. We are also grateful to members of the SSC, in particular to Alison Allam and Mari James, our PPI members, who, together with Lesley Roberts, generously gave their time and shared their experiences of accessing medicines for family members at EoL.
We also thank Mize Ogi for undertaking the systematic search, review and data extraction, and contributing to the write up of the review; organisations who supported the advertisement and distribution of the online survey, in particular Hospice UK; and Judith Lathlean (independent consultant) for data collection and analysis in the community pharmacy case study site.
We are grateful to Lynn Auty for study support throughout and to Amy Thomas for report formatting.
Contributions of authors
Sue Latter (https://orcid.org/0000-0003-0973-0512) (Professor of Health Services Research) led the writing of the protocol, provided overall direction, contributed to data analysis and drafted sections of the report.
Natasha Campling (https://orcid.org/0000-0002-4158-7894) (Senior Research Fellow) contributed to the writing of the protocol, led the study management, led data collection and analysis of all study phases, and drafted sections of the report.
Jacqueline Birtwistle (https://orcid.org/0000-0002-6083-589X) (Research Fellow) undertook data collection and analysis for the online survey and case studies, and drafted sections of the report.
Alison Richardson (https://orcid.org/0000-0003-3127-5755) (Professor of Cancer Nursing and EoL Care) contributed to the writing of the protocol, study management and data analysis, and drafted sections of the report.
Michael I Bennett (https://orcid.org/0000-0002-8369-8349) (St Gemma’s Professor of Palliative Medicine) contributed to the writing of the protocol, study management and data analysis, and reviewed sections of the report.
David Meads (https://orcid.org/0000-0003-1369-2483) (Associate Professor, Health Economics) contributed to the writing of the protocol, contributed to study management, led the health economics components of the data collection and data analysis, and drafted sections of the report.
Alison Blenkinsopp (https://orcid.org/0000-0001-8872-2769) (Professor of the Practice of Pharmacy) contributed to the writing of the protocol, study management and data analysis.
Liz Breen (https://orcid.org/0000-0001-5204-1187) (Reader in Health Service Operations) contributed to study management and to data analysis of supply chain interviews, and drafted supply chain sections of the report.
Zoe Edwards (https://orcid.org/0000-0001-6525-8190) (Senior Research Fellow in Medicines Optimisation) undertook data collection and analysis for the community pharmacy case study, and drafted case study sections of the report.
Claire Sloan (https://orcid.org/0000-0002-5324-8275) (Research Assistant, Health Economics) undertook data collection and analysis for the health economics components, and drafted health economics sections of the report.
Elizabeth Miller (https://orcid.org/0000-0003-2008-6764) (Advanced Clinical Pharmacist, Palliative Care) undertook data collection and analysis for the supply chain interviews, and drafted supply chain sections of the report.
Sean Ewings (https://orcid.org/0000-0001-7214-4917) (Associate Professor of Medical Statistics) contributed to the writing of the protocol and to data collection, and led data analysis of the online survey.
Miriam Santer (https://orcid.org/0000-0001-7264-5260) (Associate Professor in Primary Care Research) contributed to the writing of the protocol and to data analysis and reviewed sections of the report.
Lesley Roberts (https://orcid.org/0000-0002-2353-2240) (PPI representative) contributed to the writing of the protocol, design of data collection tools, and data analysis and interpretation.
Publications
Latter S, Campling N, Birtwistle J, Richardson A, Bennett MI, Ewings S, et al. Supporting patient access to medicines in community palliative care: online survey of health professionals’ practice, perceived effectiveness and influencing factors. BMC Palliative Care 2020;19:148.
Ogi M, Campling N, Birtwistle J, Richardson A, Bennett MI, Santer M, Latter S. Community access to palliative care medicines – patient and professional experience: systematic review and narrative synthesis [published online ahead of print 28 March 2021]. BMJ Support Palliat Care 2021.
Campling N, Birtwistle J, Richardson A, Bennett MI, Meads D, Santer M, Latter S. Access to palliative care medicines in the community: an evaluation of practice and costs using case studies of service models in England. Int J Nurs Stud 2022;132:104275.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review. Exclusive use will be retained until the publication of major outputs.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Palliative and End of Life Care Priority Setting Partnership, James Lind Alliance . Putting Patients, Carers and Clinicians at the Heart of Palliative and End of Life Care Research 2015. www.mariecurie.org.uk/globalassets/media/documents/research/PeolcPSP_Final_Report.pdf (accessed January 2020).
- Latter S, Hopkinson JB, Richardson A, Hughes JA, Lowson E, Edwards D. How can we help family carers manage pain medicines for patients with advanced cancer? A systematic review of intervention studies. BMJ Support Palliat Care 2016;6:263-75. https://doi.org/10.1136/bmjspcare-2015-000958.
- British Medical Association . Improving Analgesic Use to Support Pain Management at the End of Life 2017. www.bma.org.uk/media/2102/analgesics-end-of-life-1.pdf (accessed 15 June 2020).
- Latter S, Hopkinson J, Richardson A, Lowson E, Hughes J, Hughes J, et al. A Phase I-II Feasibility Trial of Cancer Carer Medicines Management (CCMM): An Educational Intervention for Carer Management of Pain Medication in Cancer Patients at End of Life. Final Report 2015. https://doi.org/10.1136/bmjspcare-2014-000838.9.
- Bennett MI, Mulvey MR, Campling N, Latter S, Richardson A, Bekker H, et al. Self-management toolkit and delivery strategy for end-of-life pain: the mixed-methods feasibility study. Health Technol Assess 2017;21. https://doi.org/10.3310/hta21760.
- Schumacher KL, Plano Clark VL, West CM, Dodd MJ, Rabow MW, Miaskowski C. Pain medication management processes used by oncology outpatients and family caregivers part II: home and lifestyle contexts. J Pain Symptom Manage 2014;48:784-96. https://doi.org/10.1016/j.jpainsymman.2013.12.247.
- Herklots A, Baileff A, Latter S. Community matrons’ experience as independent prescribers. Br J Community Nurs 2015;20. https://doi.org/10.12968/bjcn.2015.20.5.217.
- Ziegler L, Mulvey M, Blenkinsopp A, Petty D, Bennett MI. Opioid prescribing for patients with cancer in the last year of life: a longitudinal population cohort study. Pain 2016;157:2445-51. https://doi.org/10.1097/j.pain.0000000000000656.
- Bennett MI, Bagnall AM, Closs JS. How effective are patient-based educational interventions in the management of cancer pain? Systematic review and meta-analysis. Pain 2009;143:192-9. https://doi.org/10.1016/j.pain.2009.01.016.
- Bee PE, Barnes P, Luker KA. A systematic review of informal caregivers’ needs in providing home-based end-of-life care to people with cancer. J Clin Nurs 2009;18:1379-93. https://doi.org/10.1111/j.1365-2702.2008.02405.x.
- Bennett MI, Allsop MJ, Allen P, Allmark C, Bewick BM, Black K, et al. Pain self-management interventions for community-based patients with advanced cancer: a research programme including the IMPACCT RCT. Programme Grants Appl Res 2021;9. https://doi.org/10.3310/pgfar09150.
- Lucey M, McQuillan R, MacCallion A, Corrigan M, Flynn J, Connaire K. Access to medications in the community by patients in a palliative setting. A systems analysis. Palliat Med 2008;22:185-9. https://doi.org/10.1177/0269216307085722.
- Mason B, Epiphaniou E, Nanton V, Donaldson A, Shipman C, Daveson BA, et al. Coordination of care for individuals with advanced progressive conditions: a multi-site ethnographic and serial interview study. Br J Gen Pract 2013;63:e580-8. https://doi.org/10.3399/bjgp13X670714.
- Ziegler L, Bennett M, Blenkinsopp A, Coppock S. Non-medical prescribing in palliative care: a regional survey. Palliat Med 2015;29:177-81. https://doi.org/10.1177/0269216314557346.
- Savage I, Blenkinsopp A, Closs SJ, Bennett MI. ‘Like doing a jigsaw with half the parts missing’: community pharmacists and the management of cancer pain in the community. Int J Pharm Practice 2013;21:151-60. https://doi.org/10.1111/j.2042-7174.2012.00245.x.
- Akram G, Bennie M, McKellar S, Michels S, Hudson S, Trundle J. Effective delivery of pharmaceutical palliative care: challenges in the community pharmacy setting. J Palliat Med 2012;15:317-21. https://doi.org/10.1089/jpm.2011.0262.
- National Institute for Health and Care Research . Themed Review: Better Endings – Right Care, Right Place, Right Time 2015. https://content.nihr.ac.uk/nihrdc/themedreview-000826-BE/Better-endings-FINAL-WEB.pdf (accessed 15 June 2020).
- Campling N, Grocott P, Cowley S. Disconnection: the user voice within the wound dressing supply chain. J Nurs Manag 2008;16:204-13. https://doi.org/10.1111/j.1365-2834.2007.00818.x.
- Department of Health and Social Care . What’s Important to Me: A Review of Choice in End of Life Care 2015. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/407244/CHOICE_REVIEW_FINAL_for_web.pdf (accessed 15 June 2020).
- National Palliative and End of Life Care Partnership . Ambitions for Palliative and End of Life Care: A National Framework for Local Action 2015–2020 2015. https://www.nationalvoices.org.uk/sites/default/files/public/publications/ambitions-for-palliative-and-end-of-life-care.pdf (accessed 15 June 2020).
- i5 Health . Non-Medical Prescribing (NMP): An Economic Evaluation 2015.
- Wickware C. Pharmacist Independent Prescriber Workforce Has More Than Tripled Since 2016 2021. https://pharmaceutical-journal.com/article/news/pharmacist-independent-prescriber-workforce-has-more-than-tripled-since-2016 (accessed 17 February 2022).
- Edwards Z, Blenkinsopp A, Ziegler L, Bennett MI. How do patients with cancer pain view community pharmacy services? An interview study. Health Soc Care Community 2018;26:507-18. https://doi.org/10.1111/hsc.12549.
- National Institute for Health and Care Excellence . End of Life Care for Adults. Quality Standard [QS13] 2011. www.nice.org.uk/guidance/qs13 (accessed 15 June 2020).
- Royal Pharmaceutical Society Wales . Palliative and End of Life Care: Pharmacy’s Contribution to Improved Patient Care 2018. www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Policy/RPS%20Wales%20Palliative%20and%20End%20of%20Life%20Care%20Policy%20WEB.pdf?ver=2019-06-17-120534-630 (accessed 15 June 2020).
- Creswell J, Plano Clark VW. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA: SAGE Publications Ltd; 2011.
- Peters DH. The application of systems thinking in health: why use systems thinking?. Health Res Policy Syst 2014;12. https://doi.org/10.1186/1478-4505-12-51.
- Department of Health and Social Care . Developing a ‘Whole System Approach’ 2009. https://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/Browsable/DH_4923908 (accessed 15 June 2020).
- O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad 2014;89:1245-51. https://doi.org/10.1097/ACM.0000000000000388.
- Ogi M, Campling N, Birtwistle J, Richardson A, Bennett MI, Santer M, et al. Community access to palliative care medicines – patient and professional experience: systematic review and narrative synthesis. BMJ Support Palliat Care 2021. https://doi.org/10.1136/bmjspcare-2020-002761.
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred Reporting Items for Systematic Review and Meta-analysis Protocols (PRISMA-P) 2015 statement. Sys Rev 2015;4. https://doi.org/10.1186/2046-4053-4-1.
- Joint Formulary Committee . British National Formulary (Online) n.d. www.medicinescomplete.com (accessed 9 December 2021).
- Hong QN, Fabregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inf 2018;34:285-91. https://doi.org/10.3233/EFI-180221.
- Latham K, Nyatanga B. Community palliative care clinical nurse specialists as independent prescribers: part 1. Br J Community Nurs 2018;23:94-8. https://doi.org/10.12968/bjcn.2018.23.2.94.
- Latham K, Nyatanga B. Community palliative care clinical nurse specialists as independent prescribers: part 2. Br J Community Nurs 2018;23:126-33. https://doi.org/10.12968/bjcn.2018.23.3.126.
- Ise Y, Morita T, Maehori N, Kutsuwa M, Shiokawa M, Kizawa Y. Role of the community pharmacy in palliative care: a nationwide survey in Japan. J Palliat Med 2010;13:733-7. https://doi.org/10.1089/jpm.2009.0362.
- Bennie M, Cocoran E, Trundle J, Mackay C, Akram G. How community pharmacists could improve their role as providers of medicines information. Eur J Palliat Care 2013;4:188-91.
- Miller EJ. A Mixed Methods Study Investigating the Community Pharmacist’s Role in Palliative Care 2017.
- Kuruvilla L, Weeks G, Eastman P, George J. Medication management for community palliative care patients and the role of a specialist palliative care pharmacist: a qualitative exploration of consumer and health care professional perspectives. Palliat Med 2018;32:1369-77. https://doi.org/10.1177/0269216318777390.
- Bishop MF, Stephens L, Goodrich M, Byock I. Medication kits for managing symptomatic emergencies in the home: a survey of common hospice practice. J Palliat Med 2009;12:37-44. https://doi.org/10.1089/jpm.2008.0193.
- Walker KA, McPherson ML. Perceived value and cost of providing emergency medication kits to home hospice patients in Maryland. Am J Hosp Palliat Care 2010;27:254-60. https://doi.org/10.1177/1049909109350178.
- Leigh AE, Burgio KL, Williams BR, Kvale E, Bailey FA. Hospice emergency kit for veterans: a pilot study. J Palliat Med 2013;16:356-61. https://doi.org/10.1089/jpm.2012.0304.
- Latter S, Campling N, Birtwistle J, Richardson A, Bennett MI, Ewings S, et al. Supporting patient access to medicines in community palliative care: online survey of health professionals’ practice, perceived effectiveness and influencing factors. BMC Palliat Care 2020;19. https://doi.org/10.1186/s12904-020-00649-3.
- Eysenbach G. Improving the quality of web surveys: the Checklist for Reporting Results of Internet E Surveys (CHERRIES). J Med Internet Res 2004;6. https://doi.org/10.2196/jmir.6.3.e34.
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277-88. https://doi.org/10.1177/1049732305276687.
- Johnstone L. Facilitating anticipatory prescribing in end-of-life care. Pharm J 2017;289:301-4.
- NHS Digital . Summary Care Record (SCR) in Community Pharmacy 2020. https://digital.nhs.uk/services/summary-care-records-scr/summary-care-record-scr-in-community-pharmacy (accessed 22 January 2020).
- Campling N, Birtwistle J, Richardson A, Bennett MI, Meads D, Santer M, et al. Access to palliative care medicines in the community: an evaluation of practice and costs using case studies of service models in England. Int J Nurs Stud 2022;132. https://doi.org/10.1016/j.ijnurstu.2022.104275.
- Yin RK. Case Study Research: Design and Method. Thousand Oaks, CA: SAGE Publications Ltd; 2014.
- Gomm R, Hammersley M, Forster P. Case Study Method. London: SAGE Publications Ltd; 2000.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analysing Qualitative Data. London: Routledge; 1994.
- Trebble TM, Hansi N, Hydes T, Smith MA, Baker M. Process mapping the patient journey: an introduction. BMJ 2010;341. https://doi.org/10.1136/bmj.c4078.
- Denzin NK. The Research Act: A Theoretical Introduction to Sociological Methods. Piscataway, NJ: Transaction Publishers; 1973.
- NHS . Find a Pharmacy n.d. www.nhs.uk/service-search/pharmacy/find-a-pharmacy (accessed 16 February 2022).
- Public Health England . National General Practice Profiles Index of Multiple Deprivation 2019. https://fingertips.phe.org.uk/profile/general-practice/ (accessed 26 March 2020).
- Coffey A, Flick U. The SAGE Handbook of Qualitative Data Analysis. London: SAGE Publications Ltd; 2014.
- Pharmaceutical Services Negotiating Committee . About Community Pharmacy 2019. http://psnc.org.uk/psncs-work/about-community-pharmacy/ (accessed 26 March 2020).
- Office for National Statistics . Population Estimates for the UK, England, Wales, Scotland and Northern Ireland: Mid-2018 National and Subnational Mid-Year Population Estimates for the UK and Its Constituent Countries by Administrative Area, Age, Sex and Components of Population Change 2019. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/annualmidyearpopulationestimates/mid2018 (accessed 22 May 2020).
- NHS England . National Cost Collection for the NHS 2020. www.england.nhs.uk/national-cost-collection/ (accessed 1 November 2020).
- Curtis LA, Burns A. Units Costs of Health and Social Care 2019. Canterbury: PSSRU, University of Kent; 2019.
- UK Government . Economic Assumptions 2016 17 to 2020 21 n.d. www.gov.uk/government/publications/economic-assumptions-201617-to-202021/economic-assumptions-201617-to-202021 (accessed 22 February 2022).
- Mihaylova B, Briggs A, O’Hagan A, Thompson SG. Review of statistical methods for analysing healthcare resources and costs. Health Econ 2011;20:897-916. https://doi.org/10.1002/hec.1653.
- NHS Digital . Quality and Outcomes Framework, Achievement, Prevalence and Exceptions Data 2018–19 2019. https://digital.nhs.uk/data-and-information/publications/statistical/quality-and-outcomes-framework-achievement-prevalence-and-exceptions-data/2018-19-pas (accessed 6 December 2021).
- Meads DM, O’Dwyer JL, Hulme CT, Lopez RR, Bennett MI. Cost-effectiveness of pain management strategies in advanced cancer. Int J Technol Assess Health Care 2019;35:141-9. https://doi.org/10.1017/S0266462319000114.
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) – explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Health 2013;16:231-50. https://doi.org/10.1016/j.jval.2013.02.002.
- Ziegler L, Bennett MI, Mulvey M, Hamilton T, Blenkinsopp A. Characterising the growth in palliative care prescribing 2011–2015: analysis of national medical and non-medical activity. Palliat Med 2018;32:767-74. https://doi.org/10.1177/0269216317739805.
- Bajwa J, Patel N, Ali M. Managing drugs in the practice. Handb Pract Manage 2016;100:1-44. https://doi.org/10.1177/0962144X16642942.
- Harvey WS. Strategies for conducting elite interviews. Qual Res 2011;11:431-41. https://doi.org/10.1177/1468794111404329.
- NHS England . The NHS Long Term Plan 2019. www.longtermplan.nhs.uk (accessed 15 June 2020).
- Allen D. The Invisible Work of Nurses: Hospitals, Organisation and Healthcare. London: Routledge; 2014.
- Bailey S, Hodgson D, Lennie SJ, Bresnen M, Hyde P. Managing death: navigating divergent logics in end-of-life care. Sociol Health Illn 2020;42:1277-95. https://doi.org/10.1111/1467-9566.13095.
- Barker R, Wilson P, Butler C. Does national policy in England help deliver better and more consistent care for those at the end of life?. J Health Serv Res Policy 2020;25:238-45. https://doi.org/10.1177/1355819620914939.
- Nancarrow SA, Borthwick AM. Dynamic professional boundaries in the healthcare workforce. Sociol Health Illn 2005;27:897-919. https://doi.org/10.1111/j.1467-9566.2005.00463.x.
- Britten N. Prescribing and the defence of clinical autonomy. Sociol Health Illn 2001;23:478-96. https://doi.org/10.1111/1467-9566.00261.
- NHS Scotland . Continuity and Care Coordination in Palliative and End-of-Life Care: Evidence for What Works 2019. https://ihub.scot/media/5909/continuity-and-care-coordination-in-palliative-and-end-of-life-care.pdf (accessed 1 November 2020).
- Hudson BF, Best S, Stone P, Noble TB. Impact of informational and relational continuity for people with palliative care needs: a mixed methods rapid review. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-027323.
- Baird B, Maguire D. Understanding Factors That Enabled Digital Service Change in General Practice During the Covid-19 Pandemic 2020. www.kingsfund.org.uk/publications/digital-service-change-general-practice-during-covid-19 (accessed 22 April 2021).
- Williams H, Donaldson SL, Noble S, Hibbert P, Watson R, Kenkre J, et al. Quality improvement priorities for safer out-of-hours palliative care: lessons from a mixed-methods analysis of a national incident-reporting database. Palliat Med 2019;33:346-56. https://doi.org/10.1177/0269216318817692.
- Pharmaceutical Services Negotiating Committee and Pharmacy Voice . Community Pharmacy Forward View 2016.
- Meads DM, O’Dwyer JL, Hulme CT, Chintakayala P, Vinall-Collier K, Bennett MI. Patient preferences for pain management in advanced cancer: results from a discrete choice experiment. Patient 2017;10:643-51. https://doi.org/10.1007/s40271-017-0236-x.
- NHS Digital . Quality and Outcomes Framework, Achievement, Prevalence and Exceptions Data 2018–19 [PAS] n.d. https://digital.nhs.uk/pubs/qof1819 (accessed 7 December 2021).
- Curtis L, Burns A. Units Costs of Health and Social Care 2018. Canterbury: PSSRU, University of Kent; 2018.
- Monitor, NHS Trust Development Authority . Economic Assumptions 2016 17 to 2020 21 2016. www.gov.uk/government/publications/economic-assumptions-201617-to-202021/economic-assumptions-201617-to-202021 (accessed 2 June 2020).
- Jenkins A, Eckel SF. Analysing methods for improved management of workflow in an outpatient pharmacy setting. Am J Health Syst Pharm 2012;69:966-71. https://doi.org/10.2146/ajhp110389.
- NHS England . NHS Standard Contract 2021 22: Particulars (Full Length) n.d. https://www.cpsc.org.uk/download_file/1722/273 (accessed 14 January 2022).
- NHS England . Local Enhanced Service Contract 2018–2019. Supply of Drugs for Use in Palliative Care by Community Pharmacies in Nene CCG and Corby CCG n.d. https://psnc.org.uk/northamptonshire-and-milton-keynes-lpc/wp-content/uploads/sites/102/2018/04/Palliative-Care-LES-Contract-2018-19.pdf (accessed 14 January 2022).
- Community Pharmacy Liverpool . Palliative Care Service n.d. https://liverpool-lpc.org.uk/commissioned-services/liverpool-ccg/palliative-care-service/ (accessed 14 January 2022).
- Community Pharmacy Sefton . Palliative Care Service Spec. n.d. https://psnc.org.uk/sefton-lpc/public-health-campaigns/ccg-commissioned/pallative-care-pgd/ (accessed 14 January 2022).
- Great Yarmouth and Waveney Clinical Commissioning Group . Palliative Care Specialist Drug Scheme n.d. https://psnc.org.uk/suffolk-lpc/wp-content/uploads/sites/108/2015/04/SLA-Palliative-Drugs_Apr15-Mar16-TEMPLATE.doc (accessed 14 January 2022).
- Swift A. Locally Commissioned Pharmacy Service – Palliative Care n.d. https://psnc.org.uk/greater-manchester-lpc/wp-content/uploads/sites/118/2019/05/NHS-Contract-Palliative-Care-Service-Specification-March-2019.pdf (accessed 14 January 2022).
- Office for National Statistics . Clinical Commissioning Group Population Estimates (National Statistics) n.d. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/clinicalcommissioninggroupmidyearpopulationestimates (accessed 14 January 2022).
- Office for Health Improvement & Disparities . Palliative and End of Life Care Profiles n.d. https://fingertips.phe.org.uk/profile/end-of-life/data#page/6/gid/1938133060/pat/46/par/E39000048/ati/165/are/E38000001/iid/294/age/1/sex/4 (accessed 14 January 2022).
- Curtis L, Burns A. Units Costs of Health and Social Care 2014. Canterbury: PSSRU, University of Kent; 2014.
- NHS Employers . Unsocial Hours Payments 2019. www.nhsemployers.org/pay-pensions-and-reward/agenda-for-change/nhs-terms-and-conditions-of-service-handbook/unsocial-hours-payments (accessed 1 November 2020).
- Livingstone H, Wilson L. Goldline Service Year End Report 1st April 2017 to 31st March 2018 2018. www.airedale-trust.nhs.uk/wp/wp-content/uploads/2018/08/Goldline-Annual-Report-2017-2018.pdf (accessed 1 November 2020).
- GOV UK . End of Life Care Economic Tool n.d. www.gov.uk/government/publications/end-of-life-care-economic-tool (accessed 8 December 2021).
- Curtis L, Burns A. Units Costs of Health and Social Care 2015. Canterbury: PSSRU, University of Kent; 2015.
- Curtis L, Burns A. Units Costs of Health and Social Care 2017. Canterbury: PSSRU, University of Kent; 2017.
- Curtis L, Burns A. Units Costs of Health and Social Care 2010. Canterbury: PSSRU, University of Kent; 2010.
- Curtis L, Burns A. Units Costs of Health and Social Care 2012. Canterbury: PSSRU, University of Kent; 2012.
- NHS Digital . GP Workload Survey n.d. https://digital.nhs.uk/data-and-information/areas-of-interest/workforce/gp-workload-survey (accessed 8 December 2021).
- Pope C, Turnbull J, Jones J, Prichard J, Rowsell A, Halford S. Has the NHS 111 urgent care telephone service been a success? Case study and secondary data analysis in England. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-014815.
Appendix 1 Systematic review: search terms for MEDLINE (EBSCOhost)
MEDLINE (EBSCOhost)
Date searched: March 2019
Date range searched: January 2006 to March 2019
Search strategy
| S1 | (MH “Palliative Care”) |
| S2 | (MH “Terminal Care”) |
| S3 | palliative n3 care |
| S4 | terminal N3 care |
| S5 | “end of life” or EOL |
| S6 | palliat* |
| S7 | terminal and patients |
| S8 | medicat* |
| S9 | medicine* |
| S10 | drug* |
| S11 | (MH “Pharmacies”) |
| S12 | (MH “Community Pharmacy Services”) |
| S13 | access* |
| S14 | suppl* |
| S15 | dispens* |
| S16 | distribut* |
| S17 | availab* |
| S18 | deliver* |
| S19 | administ* |
| S20 | “out of hours” |
| S21 | prescri* |
| S22 | pharmac* |
| S23 | primary N3 care |
| S24 | primary health care |
| S25 | home |
| S26 | communit* |
| S27 | general practice |
| S28 | (MH “General Practice”) |
| S29 | “Family practice” |
| S30 | local N3 Pharmac* |
| S31 | “Community practice” |
| S32 | Community N3 Pharmac* |
| S33 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 |
| S34 | S8 OR S9 OR S10 |
| S35 | S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 |
| S36 | S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 |
| S37 | S33 AND S34 AND S35 AND S36 |
| Limiters - Date of Publication: 20060101-20180331; English Language; Human; Age Related: All Adult: 19+ years |
Appendix 2 Framework analysis cases 1, 2 and 4: patient/carer and health-care professional data
Patient and carer interview data
-
Activities to access medicines.
-
Getting prescriptions (new).
-
Getting prescriptions (repeat).
-
Dispensing.
-
– Liaison with CP/dispensary.
-
-
Obtaining the medicines.
-
– Collection/delivery.
-
– Hospital pharmacy supply.
-
-
OOH.
-
-
Issues encountered.
-
CD access.
-
OOH access.
-
Lack of non-medical prescribers.
-
Collection of medicines.
-
Incorrect/duplicate dispensing.
-
Wastage.
-
Self-purchase.
-
Multiple prescribers.
-
Work involved.
-
Implications of home delivery.
-
-
What is beneficial?
-
Key HCP.
-
– Single point of contact plus availability.
-
– System co-ordination.
-
– Non-medical prescribers.
-
-
Online repeat prescription request systems.
-
-
Who do you work with?
-
HCPs.
-
– CNSs.
-
– GPs.
-
– CPs.
-
-
Family and friends.
-
– Issues encountered.
-
– Collection related.
-
– Not ready.
-
– Incorrect/duplicate medicines.
-
-
– Those with no family.
-
-
-
-
Information provision.
-
Understanding.
-
– Medicines.
-
– How to access.
-
-
Level and format.
-
– Too much.
-
– Too little/missing.
-
– Format.
-
-
What would help.
-
-
Navigating systems.
-
Confidence.
-
Learning (what have you learnt).
-
Behaviour change (what are you doing differently).
-
-
Impact on symptoms.
-
Impact on unplanned use of health-care services/resources.
Health-care professional interview data
-
Activities to support patient access to medicines.
-
Prescribing.
-
Providing prescriptions (new).
-
Providing prescriptions (repeat).
-
Dispensing.
-
– Liaison with CP/dispensary.
-
-
Enabling medicine supply.
-
– Collection/delivery.
-
-
OOH.
-
-
Issues encountered.
-
Providing CD access.
-
Providing OOH access.
-
Lack of non-medical prescribers.
-
Collection of medicines.
-
Incorrect/duplicate dispensing.
-
Wastage.
-
Multiple prescribers.
-
Work involved.
-
Shared records.
-
– Not knowing patient’s palliative status.
-
-
Barriers to stocking palliative care medications.
-
Implications of home delivery.
-
Electronic prescribing and transfer.
-
Competence in palliative care.
-
Specialist palliative care input.
-
-
What is beneficial?
-
Facilitators: good practice.
-
Facilitators: practice transformation.
-
-
Who do you work with?
-
HCPs.
-
– Facilitators.
-
– Issues encountered.
-
– CNSs.
-
– GPs.
-
– CPs.
-
-
Patient and family.
-
– Facilitators.
-
– Issues encountered.
-
– Those with no family.
-
-
-
Information provision.
-
Medicines.
-
How to access.
-
-
Overall service delivery.
-
Facilitators.
-
Barriers.
-
Solutions.
-
-
Awareness of community pharmacy-delivered commissioned services for palliative care.
-
Understanding of the service.
-
Use by patients.
-
Impact on patient experience of access.
-
Impact on pain.
-
Impact on prevention of admissions.
-
Awareness-raising of the service.
-
Resources required.
-
Cost reduction.
-
Main challenges.
-
– Solutions.
-
-
Appendix 3 General practice: patient and carer sample
| Sample group | Sex | Age range (median) (years) | Main diagnosis | Highest educational attainment | Relationship to patient |
|---|---|---|---|---|---|
| Patients |
Males, n = 3 Females, n = 6 |
51–97 (65) |
Cancer, n = 8 Motor neurone disease, n = 1 |
Left school aged 14 years, n = 1 School level, n = 5 Undergraduate degree, n = 2 Master’s degree, n = 1 |
|
| Carers | Females, n = 4 | 33–74 (52) |
School level, n = 2 Undergraduate degree, n = 1 Master’s degree, n = 1 |
Spouse, n = 2 Child, n = 1 Grandchild, n = 1 |
Appendix 4 General practice: patient/carer interviews and log completion
| Patient/carer ID code | Interview form | Time point | Number of interviewsa | Number of logsb |
|---|---|---|---|---|
| P1001; C1001 | Dyad interviews (patient + carer), face to face | Study entry and week 4 interviews (patient died week 6) | 2 | 1 (patient completed) |
| P1002 | Patient interview, face to face | Study entry interview (patient died week 7) | 1 | None |
| P1003 | Patient interviews, 2 × face to face (study entry and week 8) and 1 × telephone (week 4) | Study entry, week 4 and week 8 interviews | 3 | 7 (patient completed) |
| P2001; C2001 | Carer interviews, face to face | Study entry, week 4 and week 8 interviews | 3 | 9 (carer completed) |
| P2002; C2002 | Dyad interviews (patient + carer), face-to-face | Study entry, week 4 and week 8 interviews | 3 | 8 (carer completed) |
| P2003 | Patient interviews, face to face | Study entry and week 4 interviews (patient not well enough for week 8 interview) | 2 | 4 (carer completed) |
| P2004 | Patient interview, face to face | Study entry interview (patient died week 3) | 1 | None |
| P2005 | Patient interview, face to face | Study entry interview (patient not well enough for subsequent interviews) | 1 | None |
| P3001; C3001 | Dyad interview (patient + carer), face to face | Study entry interview (patient died week 6) | 1 | None |
Appendix 5 General practice: health-care professional interviews
| Professional group | ID code | Interview form | Number of interviewsa |
|---|---|---|---|
| CNs | CN001–004; CN005–009; CN010–015 | Group interviews, face to face (four, five and six participants, respectively) | 3 |
| CPs | CP001; CP002 | 1 : 1 interviews, 1 × face to face and 1 × telephone | 2 |
| GPs | GP101; GP201; GP202; GP301 | 1 : 1 interviews, telephone | 4 |
| Community palliative care CNSs | CNS001–007 | Focus group, face to face (seven participants) | 1 |
Appendix 6 General practice: key service delivery descriptors
| Service provision | Description |
|---|---|
| General practice specific |
Practice 1: service and hours Eight GPs List size: 18,596 08.30–18.00 Monday–Friday Dual site practice, both dispensing sites PCP involvement (4 days/week), not a prescriber Semi-rural population Records access EMIS Web IT system (not able to view community nursing, specialist palliative care or GP OOH records) Practice 2: service and hours Ten GPs plus two GP registrars List size: 17,078 08.00–18.30, Monday–Friday Dual site practice, neither dispensing sites PCP involvement (1 day/week), prescriber Urban population Deprivation decile 10 Records access EMIS Web IT system (not able to view community nursing, specialist palliative care or GP OOH records) Practice 3: service and hours Thirteen GPs List size: 17,400 08.00–19.00, Monday–Friday Dual site practice, neither dispensing sites No PCP involvement Urban population Deprivation decile 10 Records access EMIS Web IT system (not able to view community nursing, specialist palliative care or GP OOH records) |
| GP OOH |
Service and hours Regional service 18.30–08.00 and 18.30 Friday–08.00 Monday Covers all BHs Provision includes patient call backs from GPs to establish condition and appropriate intervention (e.g. home visit by a GP or advanced nurse practitioner, or patient seen at nearest of 10 primary care centres) Access/referral Via 111 service, operated by regional ambulance service. Call triage by non-clinical staff Prescribing 150 GPs (predominantly locums) and 20 advanced nurse practitioners offer direct services to patients (including prescribing) via call back Location The nearest primary care centre to the three general practices is 6–9 miles Records access Service providers cannot view patient records. Summary of the call sent to patient’s GP |
| Community nursing |
Service and hours Integrated care teams (i.e. nurses and support workers) provide community nursing support and EoL care in the home 08.30–18.00 and twilight coverage until 22.00 Access/referral Referrals via patient’s GP, hospital services and palliative care CNSs Prescribing Teams include matrons/integrated care leads with V100 and V300 prescribing qualifications, but rarely used in EoL prescribing Location Service provided by a NHS foundation trust. Four separate teams working from three community hospital/care home bases cover the three general practices. Practice 1 refers to base X (team A), practice 2 refers to base Y (teams B and C) and practice 3 refers to base Z (team D). Bases are 0.5–4 miles from the three general practices Records access Care teams can view GP records, but not GP OOH records nor specialist palliative care records |
| Community specialist palliative care |
Service and hours Led by a medical consultant in palliative care, alongside 17 CNSs 08.30–16.00, Monday–Friday service for patients and contact details provided to patients by their own CNS. A CNS gives telephone advice to HCPs at weekends/BHs. Admission to the inpatient unit of local hospice possible for uncontrolled symptoms or care while dying. Each general practice has one CNS attached to it. CNSs attend monthly general practice palliative care (GSF meetings) as able (i.e. workload dependent). CNSs provide an advice-based service and recommendations/changes to a patient’s medicines sent to the general practice via e-mail for prescribing (either via the individual’s GP or duty doctor). CNSs liaise with CN teams as required Access/referral Referrals by patient’s GP or hospital teams Prescribing Two of 17 CNS team are nurse prescribers (with V300 qualifications). Neither nurse prescribers cover the three general practices Location Based within local hospice and this is 4–14 miles from the three general practices Records access Service staff can view GP records, but not GP OOH records nor community nursing records |
| Community pharmacy-commissioned palliative care |
Service and hours Eleven community pharmacies deliver a service for palliative care, commissioned by local CCG (which covers the three general practices). All are open Monday–Saturday (often with late opening), five are open for 6 hours on Sunday (the closest three are 6–13 miles from the three general practices) Access/referral Self-access but depends on patients/carers being signposted to the pharmacies Prescribing None of the CPs within the pharmacies was prescribers Location Nearest is 1.5–8 miles from the three practices Records access CPs can view patient’s SCR (if the patient has consented) |
Appendix 7 Annotated timeline exemplar: case 1 general practice
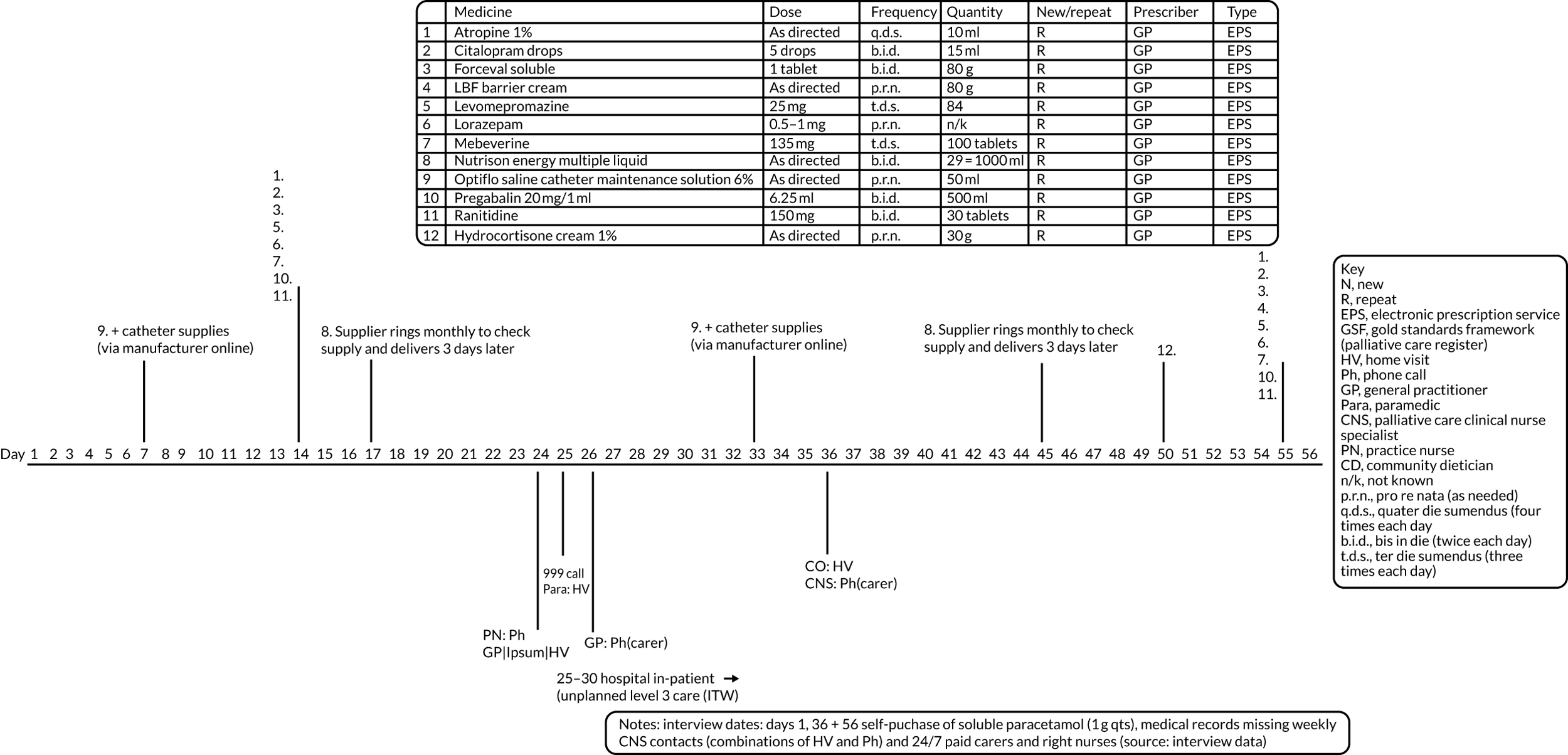
Appendix 8 Logic model: general practice case
| Service delivery characteristic | Mechanism of action | Moderating and mediating factor | Patient and carer impact | Service outcome |
|---|---|---|---|---|
|
|
Positive:
|
Positive:
|
Positive:
|
Negative:
|
Negative:
|
Negative:
|
||
|
|
Positive:
|
Positive:
|
Negative:
|
|
|
Positive:
|
Negative:
|
Positive:
|
|
|
Positive:
|
Positive:
|
Positive:
|
Negative:
|
Negative:
|
Negative:
|
||
|
|
Positive:
|
Positive:
|
Positive:
|
Negative:
|
Negative:
|
|||
|
|
Positive:
|
Positive:
|
Positive:
|
|
|
Positive:
|
Positive:
|
Positive:
|
|
|
Positive:
|
Positive:
|
Positive:
|
Appendix 9 Patient/carer frequently encountered hurdles and delays in medicines access
-
Difficulties accessing general practices (and GP appointments) to gain new prescriptions.
-
Difficulties accessing GP appointments caused other HCPs to be accessed instead (e.g. palliative care CNSs were often telephoned by the patient/carer and asked to contact the GP on the patient’s behalf).
-
Medicines not put onto repeat prescriptions routinely. Patients usually needed to ask for this to be carried out.
-
Patients/carers not knowing how to re-order repeat prescriptions or which system they should use (e.g. via completing the back of their dispensed prescription slip vs. utilising online repeat prescription request systems).
-
Patients/carers having to register to use online repeat prescription request systems (via ‘patient access’ on their general practice’s website).
-
Patients/carers having to stock check their medicines supplies to know what is needed to be re-ordered and when (medicines were often not in sync, especially when both as-required and regular medicines were taken).
-
The prescription itself not being available at the community pharmacy despite the repeat prescription request having been made via the general practice.
-
Patients/carers having to leave up to 1 week between repeat prescription request and the medicines being ready for collection at the community pharmacy or general practice dispensary.
-
Patients being reliant on family members collecting medicines on their behalf (who may not know what should be dispensed) or on community pharmacy-arranged home delivery services (with no specified time for delivery and some services charging).
-
General practice dispensaries and community pharmacies not having the medicines in stock and needing to order the medicines in or being sent elsewhere to get them (e.g. another pharmacy).
-
General practice dispensaries being closed at lunchtimes.
-
Patients/carers having to wait at the pharmacy for the medicines to be dispensed even when the medicine was in stock and the patient/carer had left the requested length of time between prescription request and collection.
-
Patients/carers having to make a car trip to collect the medicines as most patients/carers used community pharmacies near their general practice rather than near their home.
-
Possibility of dispensing errors (e.g. medicines dispensed that had not been requested, ones that had been requested could be missing or in a form not expected, such as tablets not liquid, tablets not capsules).
Appendix 10 Activity by other health-care professionals when the general practitioner is the main community-based prescriber
-
Prescribing new and repeat prescriptions (frequently based on recommendations by palliative and secondary care specialists).
-
Making patient referrals for specialist palliative care and community nursing services.
-
Some GPs were proactive in their care of their patients [e.g. ringing/texting patients to see how they were (without prompts), thinking about and initiating alternative medicines and options, and setting up regular patient visits (both at home or in the practice), all of which were key to underpinning effective/best medicines access]; however, this was far from the experience for all (demonstrated by both the HCP and patient/carer data).
-
Advising patients/carers on the medicines themselves.
-
Specialist assessment of the patient, often on a regular basis.
-
Recommending medicines/changes to the GP for prescribing (required e-mail and follow-up telephone call).
-
E-mailing/telephoning GPs with updates on patients and contacting GPs when patients/carers had been unable to get through to general practices/gain GP appointments.
-
Stock checking medicines for patients when needed.
-
Ringing community pharmacies to source supplies of relevant medicines for patients (then asking family carers to collect them from the respective pharmacy).
-
Advising patients/carers on the medicines themselves and how best to access medicines.
-
Advising carers if they were collecting medicines from community pharmacies on the patients’ behalf.
-
Contacting GP prescribers when there were difficulties in gaining supplies/medicine shortages and recommending alternatives to be prescribed, or when the medicines had been incorrectly prescribed.
-
Requesting repeat prescriptions from general practices on behalf of patients (when patients called the pharmacy directly).
-
Advising carers on the medicines themselves and how to access them.
-
Contacting GPs when nursing administration charts were incorrectly completed and insufficient ranges prescribed.
-
Stock checking medicines to ensure that syringe driver supplies and STAT doses (i.e. doses to be given statim, or immediately) were enough to cover OOH periods.
-
Contacting community pharmacies to source supplies of medicines for syringe drivers and just-in-case/anticipatory medicines for patients (e.g. collecting supplies themselves from pharmacies when urgently required to cover OOH periods).
-
Advising carers if they were collecting CDs on the patients’ behalf (e.g. to take identification and to take the medicines straight home and not leave them in their car).
Reproduced with permission from Campling et al. 48 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The box includes minor additions and formatting changes to the original box.
Appendix 11 Clinical nurse specialist site: patient and carer sample
| Sample group | Sex | Age range (median) (years) | Main diagnosis | Highest educational attainment | Relationship to patient |
|---|---|---|---|---|---|
| Patients (from nine general practices) |
Males, n = 4 Females, n = 7 |
35–74 (71) | Cancer, n = 11 |
School level, n = 9 Undergraduate degree, n = 1 Master’s degree, n = 1 |
|
| Carers |
Males, n = 2 Females, n = 5 |
38–70 (70) |
School level, n = 5 Undergraduate, n = 2 |
Spouse, n = 5 Child, n = 2 |
Appendix 12 Clinical nurse specialist site: patient/carer interviews and log completion
| ID code | Interview form | Time point of interviews | Number of interviewsa | Number of logsb |
|---|---|---|---|---|
| Patient01; carers01a + 01b | Dyad interviews (patient + 2 carers), study entry face to face and 1 × telephone (week 4) | Study entry and weeks 4 and 8 | 3 | 3 (patient completed) |
| Patient02 | Patient interviews, face to face | Study entry and weeks 4 and 8 | 3 | 10 (patient completed) |
| Patient03 | Patient interviews, face to face | Study entry (patient died week 3) | 1 | 0 |
| Patient04 | Patient interviews, face to face | Study entry and weeks 4 and 8 | 3 | 4 (patient completed) |
| Patient06; carer06 | Dyad interviews (patient + carer), face to face | Study entry and week 4 (patient unwell at week 8) | 2 | 0 |
| Patient07 | Patient interviews, face to face | Study entry and weeks 4 and 8 | 3 | 4 (patient completed) |
| Patient08 | Dyad interviews (patient + carer), face to face | Study entry and weeks 4 and 8 | 3 | 1 (patient completed) |
| Patient09; carer09 | Dyad interviews (patient + carer), face to face | Study entry and week 4 (patient died week 6) | 2 | 8 (carer completed) |
| Patient10; carer10 | Dyad interviews (patient + carer), face-to-face (study entry, 2 × telephone patient only (week 4 + 8) | Study entry and weeks 4 and 8 | 3 | 3 (patient completed) |
| Patient11 | Patient interviews, face to face | Study entry and weeks 4 and 8 | 3 | 7 (patient completed) |
| Patient12; carer12 | Dyad interviews (patient + carer), face to face | Study entry and weeks 4 and 8 | 3 | 6 (carer completed) |
Appendix 13 Clinical nurse specialist site: health-care professional interviews
| Professional group | ID code | Interview form | Number of interviewsa |
|---|---|---|---|
| Palliative care consultant | HP01 | 1 : 1 interview, face to face | 1 |
| GP | HP02; HP07 | 1 : 1 interviews, 1 × face to face and 1 × telephone | 2 |
| Hospice pharmacist | HP04 | 1 : 1 interview, face to face | 1 |
| Palliative care doctor | HP05 | 1 : 1 interview, face to face | 1 |
| CN lead | HP06; HP16 | 1 : 1 interviews, 1 × face to face and 1 × telephone | 2 |
| Community palliative care CNS | HP03; HP08; HP09; HP10; HP11; HP12; HP13; HP14; HP15; HP17; HP18 |
1 : 1 interviews, face to face (n = 6) Focus group, face to face (two groups, one with two participants and the other with three participants) |
8 |
Appendix 14 Clinical nurse specialist site: services provided by clinical nurse specialists, nurse independent practitioners and associated community-delivered services
| Service provision | Description |
|---|---|
| CNS team |
Two teams each based in a city hospice 10 or 11 WTE in each team Team A: 11 CNS (9 NIP) Team B: 12 CNS (10 NIP) Each CNS covers between 2 and 11 (mean 5) general practices (depending on their working hours and managerial responsibilities) Palliative care CNSs A total of 240 on CNS caseloads (26–30 per full-time CNS) Core hours: 08.30–17.00 OOH: duty CNS, one in each team Monday–Friday 07.30–08.00, 17.30–18.00 and weekends 08.00–17.30 for telephone advice to patients and HCPs, and urgent visits CNS team attend every GSF meeting Referral criteria Specialist palliative care needs Referrals From a HCP via e-mail form Records access SystmOne EPaCCS City-wide shared patient record: a bespoke digital shared records system enabling HCPs to view real-time health and care information across care providers and between different systems. Brings together certain important information about patients registered at GP, hospital, community health-care, social services or mental health teams settings Each hospice has a one WTE pharmacist and one WTE pharmacy technician |
| General practice service |
Three CCGs Urban and rural mix Total city-wide population: 784,846 101 general practices (city wide) Deprivation deciles 1–10 Records access Most SystmOne Some EMIS EPaCCS City-wide shared patient record |
| GP OOH cover |
OOH cover: 18.00 until 07.30 (patients) Two urgent treatment walk-in centres GP extended access service Monday–Friday 06.30–20.00 and weekend and BH mornings NHS 111 |
| Community nursing service |
13 teams provided by a community trust service whole city area supporting EoL patients at home Matrons and CNs Some matrons or integrated care team leads (DNs) with V300 prescribing qualification Limited access to SystmOne and EMIS records, but can access the city-wide shared patient record OOH weekends and evenings: one nurse OOH to cover whole city |
| Commissioned palliative medicines service: pharmacy |
City centre One CP in the city centre. Closes at midnight every day and opens at 06.00 on weekdays, 07.00 on Saturdays and 09.00 on Sundays Outer city (within 6 miles of the city centre) Thirteen outer-city CPs within 6 miles of the city centre Monday to Saturday: all open, most from 07.00 to 09.00 (with one from 10.00) until 18.30–20.30, with four staying open until 22.00 or midnight on weekdays and until 23.00 on Saturdays Sundays: most open for 6–8 hours and one for 12 hours Towns (more than 6 miles from the city centre) Three CPs in towns more than 6 miles outside the city Monday to Saturday: all are open from 07.00–08.30 until 18.15–20.00, with one staying open until 23.00 on weekdays and another closed on Saturdays Sundays: two open for 7 and 9 hours Patients self-access the service |
Appendix 15 Annotated timeline exemplar: case 2 clinical nurse specialist site
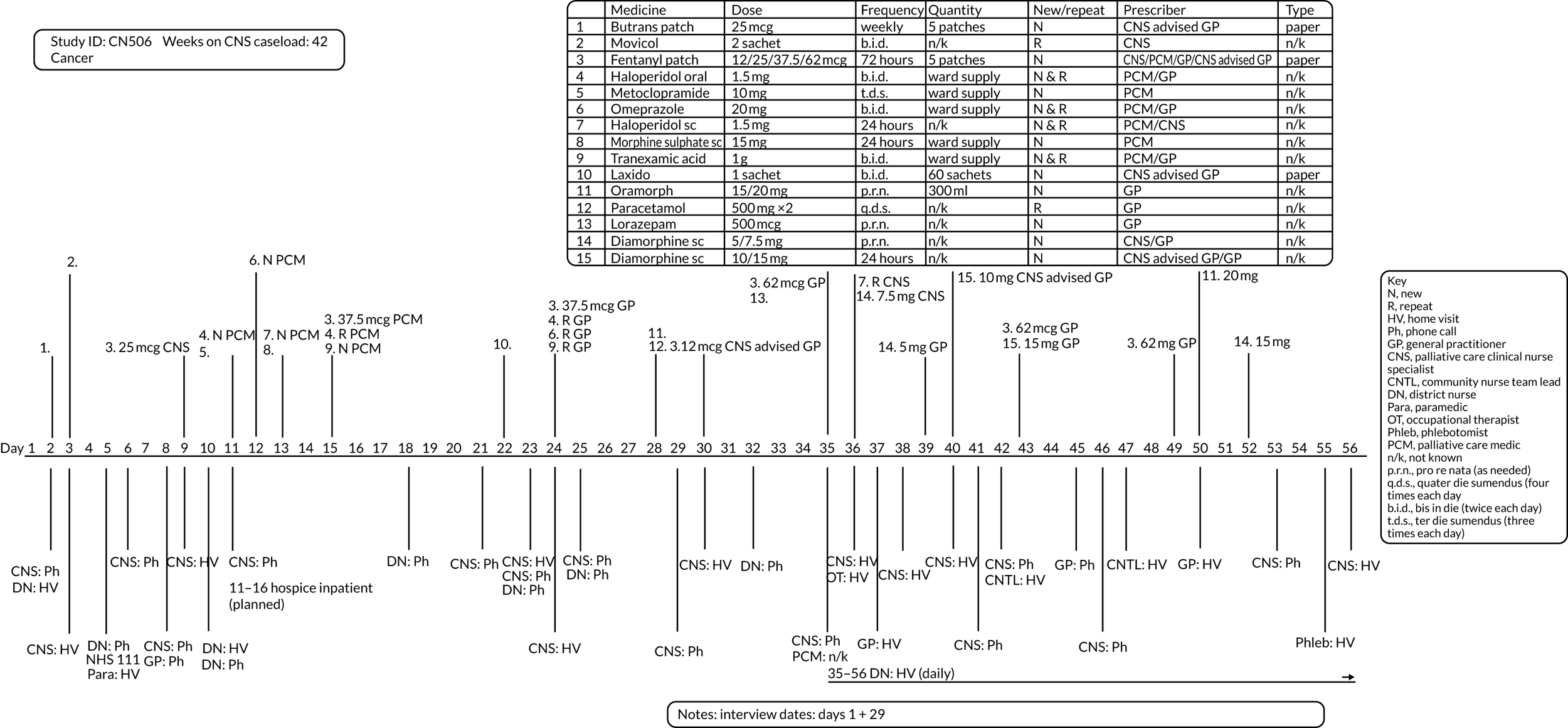
Appendix 16 Logic model: community palliative care clinical nurse specialist independent prescriber case
| Service delivery characteristic | Mechanism of action | Moderating and mediating factor | Patient and carer impact | Service outcome |
|---|---|---|---|---|
|
|
Positive:
|
Positive:
|
Positive:
|
Negative:
|
||||
|
|
Positive:
|
Positive:
|
Positive:
|
|
|
Positive:
|
Positive:
|
Positive:
|
|
|
Positive:
|
Positive:
|
|
|
|
Positive:
|
Positive:
|
|
|
|
Positive:
|
Positive:
|
Appendix 17 Framework analysis case 3: community pharmacy-delivered commissioned services for palliative care
Community pharmacists
-
Service details (local or regional commissioner service).
-
History.
-
How long in operation.
-
Changes over time.
-
Funding (£ per annum), including payments and reimbursement for out-of-date medicines.
-
Types of medicines stocked.
-
Extended opening hours.
-
Network of pharmacies.
-
Awareness-raising to patients/carers/HCPs.
-
Audit requirements.
-
-
Role of pharmacist.
-
What is your role in the service?
-
What happens?
-
What do you do?
-
-
Scale of usage.
-
How often do patients use it (i.e. medicines on the list and/or extended hours)?
-
How many patients in a typical week make use of it?
-
-
Service functioning.
-
How well does it work in relation to the aims of the service?
-
– Extra stock.
-
– Extended hours.
-
– Networking.
-
-
What are the difficulties?
-
– Funding incentives.
-
– Limits due to space.
-
– Expiry dates.
-
– Local prescribing versus stock.
-
-
-
Comparison with normal care (vs. a CP without commissioned service).
-
Is it better at enabling patients and carers to access medicines?
-
– Quantify (%).
-
-
Is it better at managing pain?
-
– Quantify (%).
-
-
Is it better at preventing admissions?
-
– Quantify (%).
-
-
-
Awareness-raising regarding service.
-
Experience of raising awareness to patients/carers.
-
Experience of raising awareness to HCPs.
-
Main barriers.
-
Main facilitators.
-
-
Resources required.
-
Training (one-off/ongoing).
-
Stock management time.
-
Time for provision of extended hours.
-
Resources associated with extra stock.
-
CP networking/communication.
-
Resources associated with raising awareness.
-
-
Barriers and facilitators.
-
Challenges to improving access via commissioned services.
-
Solutions needed to improve service.
-
Clinical Commissioning Group and NHS England commissioners
-
Service details (local or regional commissioner service).
-
What is the commissioned service?
-
– Costs/reimbursements.
-
– Stock.
-
– Extended hours.
-
– Service information for patients/carers.
-
– Service information for HCP.
-
-
-
Size.
-
Number of CPs commissioned.
-
Coverage.
-
Opt-in/opt-out opportunities.
-
How are CPs selected?
-
-
How was the service-level agreement decided?
-
History: original incentive.
-
Changes over time.
-
-
Process of commissioning.
-
Who leads it?
-
How is it led?
-
Time frame.
-
Cycle.
-
-
Commissioner involvement.
-
Commissioner engagement with service.
-
-
Evaluation.
-
Audit/service review/evaluation.
-
– Results and actions of this audit/service review/evaluation.
-
-
Feedback from service users (patients/carers/HCPs).
-
– Results and actions of feedback.
-
-
-
Comparison with normal care (vs. a CP without commissioned service).
-
Is it better at enabling patients and carers to access medicines?
-
– Quantify (%).
-
-
Is it better at managing pain?
-
– Quantify (%).
-
-
Is it better at preventing admissions?
-
– Quantify (%).
-
-
-
Commissioning resource.
-
Time in planning commissioning.
-
Ongoing engagement.
-
Evaluation.
-
Staff resource.
-
Time.
-
Facilities.
-
-
Barriers and facilitators.
-
Challenges to commissioning effective service.
-
Solutions needed to improve service.
-
Appendix 18 Medicines included in community pharmacy palliative care medicines schemes
| Drug | Inclusion in lists, n (%) |
|---|---|
| Opioid | 243 (41) |
| Antisecretory | 65 (11) |
| Antiemetic (including somatostatin analogue) | 61 (10) |
| Antipsychotic | 57 (10) |
| Benzodiazepine | 45 (8) |
| Diluent | 41 (7) |
| Steroid | 29 (5) |
| Heparin | 18 (3) |
| Antibacterial | 14 (2) |
| Vitamin K | 6 (1) |
| Antiepileptic | 4 (< 1) |
| Analgesic (simple) | 2 (< 1) |
| Antifibrinolytic | 2 (< 1) |
| Diuretic | 2 (< 1) |
| H2 antagonist | 2 (< 1) |
| Antidiarrhoeal | 1 (< 1) |
| Saline (hydration) | 1 (< 1) |
Appendix 19 Logic model: community pharmacy-delivered commissioned services for palliative care case
| Service delivery characteristic | Mechanism of action | Moderating and mediating factor | Patient and carer impact | Service outcome |
|---|---|---|---|---|
|
|
Positive:
|
Positive:
|
Positive:
|
Negative:
|
Negative:
|
Negative:
|
||
|
|
Positive:
|
||
Negative:
|
Negative:
|
Negative:
|
||
|
|
Positive:
|
Appendix 20 Telephone support line site: patient and carer sample
| Sample group | Sex | Age range (median) (years) | Main diagnosis | Highest educational attainment | Relationship to patient |
|---|---|---|---|---|---|
| Patients |
Male, n = 3 Female, n = 3 |
61–75 (68.5) |
Cancer, n = 3 Non-cancer, n = 3 |
School level, n = 4 College, n = 1 Undergraduate degree, n = 1 |
|
| Carers |
Male, n = 1 Female, n = 2 |
60–72 (72) |
School level, n = 2 Postgraduate, n = 1 |
Spouse, n = 3 |
Appendix 21 Telephone support line site: patient/carer interviews and log completion
| ID code | Interview form | Time point of interviews | Number of interviewsa | Number of logsb |
|---|---|---|---|---|
| T01 | Patient interviews, face to face (study entry) and telephone (week 4) | Study entry and week 4 (patient died week 8) | 2 | 2 (patient completed) |
| T02 | Patient interviews, face to face | Study entry and week 4 (could not contact patient at week 8) | 2 | 1 (patient completed) |
| T03 and Carer 03 | Dyad interviews, face to face | Study entry and weeks 4 and 8 | 3 | 2 (patient completed) |
| T04 and Carer 04 | Dyad interviews, face to face | Study entry and weeks 4 and 8 | 3 | 3 (patient completed) |
| T05 | Patient interviews, face to face, (study entry + week 4) and telephone (week 8) | Study entry and weeks 4 and 8 | 3 | 3 (patient completed) |
| T06 and Carer 06 | Dyad interviews, face to face (study entry + week 4) and telephone (week 8) | Study entry and weeks 4 and 8 | 3 | 3 (patient completed) |
Appendix 22 Telephone support line site: health-care professional interviews
| Professional group | ID code | Interview form | Number of interviewsa |
|---|---|---|---|
| Palliative care consultant (acute trust) | HP02 | 1 : 1 interview, face to face | 1 |
| Digital hub staff (acute trust) (n = 14) | |||
| Nurses (n = 2) and OT (n = 1) | HP01, HP25, HP30 | 1 : 1 interview, face to face | 3 |
| Nurses (n = 8), OT (n = 1), call handler (n = 1) and manager (n = 1) | HP03–HP13 | Focus group, face to face | 1 |
| DN leads (care NHS trust) (n = 7) | HP14–HP20 | Focus group, face to face | 1 |
| CN palliative care support team (care NHS trust) lead | HP21 | 1 : 1 interview, face to face | 1 |
| CNs (acute trust) (n = 3) | HP22–HP24 | Focus group, face to face | 1 |
| Community palliative care CNSs (hospice) (n = 4) | HP26–HP29 | 1 : 1 interview, face to face | 4 |
Appendix 23 Telephone support line site: key service delivery descriptors
| Service provision | Description |
|---|---|
| TSL service |
Commissioned by a single CCG and provided by an acute hospital trust A palliative care-specific service: one of three telephone services provided by an overarching digital hub. Staff (described below) work on all three telephone services, with TSL calls prioritised Eight triage stations, enabling any combination of up to eight video/telephone calls simultaneously Twenty-six band 6 HCPs (22 WTE) Six (WTE) of these 26 HCPs specifically commissioned for the TSL Nurses (including 3 × NIP) and OTs Three clinical band 3 HCSWs/non-clinical call handlers Daytime shift: 08.00–20.00 with eight operators (bands 3 and 6) Overnight shift: 20.00–08.00 with three operators (band 6) Referrals are from community and acute health-care services via EPaCCS on SystmOne Access to all health services’ electronic patient records (with patient consent) |
| CCG area and general practices |
Population of 600,000 Incorporates significant deprivation and some affluence, urban, rural and city living One of the most diverse CCG areas nationally and significant health inequalities exist across the different localities within the district Two distinct regions The northern part of the region has two main (urban) towns and two (rural) market towns and it is geographically approximately seven times larger (population approximately 165,000) than the southern part of the region The southern part of the region (population approximately 435,000) covers a city centre and surrounding urban area with high levels of ethnic minorities, social housing and deprivation General practices Seventy-three GP OOH cover NHS 111 service commissioned by the CCG Evening, weekends and bank holidays: home visits and telephone advice or referral to another service |
| CNS service |
Palliative care CNSs Two services Hospice A Covers northern part of the region Eight CNSs (2 × NIP) Core hours: Monday–Friday, 08.30–17.00; weekends, one duty CNS for telephone advice to patients and consultancy to HCPs NHS care trust Covers the city part of the southern region Six CNSs (all NIP) Core hours: Monday–Friday, 08.30–17.00 Other community CNS teams: provided by acute hospital trust. Working with (heart failure, neurology, cardiac, respiratory) outpatients in the community |
| Community nursing service |
Two services Acute hospital trust CNs One team of covers the northern part (two market towns, rural and most remote) of the northern area NHS care trust CNs Teams are attached to general practices and cover the southern city area and two towns in the northern area CNs are supported by the palliative care support team (12 nurses and 10 HCSWs). The palliative care support team works closely with GPs and CNs, providing care to patients in their home in last 6 weeks of life, 08.00–22.00, 7 days per week |
| Community pharmacy-commissioned palliative care service |
In the northern area there are five CPs in four towns/villages, approximately 10 miles apart All are open Monday–Saturday between 07.30 and 09.00, two close at 22.00 everyday and one closes at mid-day on Saturdays. Three are open on Sundays (for 5, 6 and 13 hours) In the southern area, there are five CPs within 2 miles of the city centre and another four in nearby towns/villages approximately 3–5 miles apart The city CPs all open Monday–Saturday between 07.00 and 09.00 and close between 18.30 and 20.30, with one closing at midnight. All open on Sundays (for 6, 7 and 13 hours) The outer-city CPs open Monday–Saturday between 07.00 and 09.00 and close between 20.00 and 23.00. Three are open on Sundays (for 6, 10 and 12 hours) |
Appendix 24 Logic model: palliative care 24 hours per day, 7 days per week telephone support line
| Service delivery characteristic | Mechanism of action | Moderating and mediating factors | Patient and carer impact | Service outcome |
|---|---|---|---|---|
|
|
Positive:
|
Positive:
|
Positive:
|
Appendix 25 Phase 3: data extraction form
Appendix 26 Additional cost and cost-effectiveness tables
| Parametera | Mean | SE | Distribution for PSA | Source |
|---|---|---|---|---|
| Weekly probability of unplanned hospital/hospice visit for symptom management | ||||
| GP | 0.049 | 0.013 | Beta | ActMed data records (see Appendix 25) |
| CNS | 0.019 | 0.008 | Beta | ActMed data records (see Appendix 25) |
| Community pharmacy | 0.049 | 0.013 | Beta | Assumed same as GP |
| TSL | 0.009 | 0.006 | Beta | ActMed data records (see Appendix 25) |
| Weekly cost (£) of palliative care | 224.80 | 36.04 | Log-normal | ActMed data records (see Appendix 25) |
| Cost (£) of unplanned hospital/hospice visit for symptom management | 452.98 | 89.31 | Log-normal | ActMed data records (see Appendix 25) |
| Prescription costs (£) | ||||
| GP: new | 79.50 | Fixed | ActMed service costing (all) | |
| GP: repeat | 19.00 | Fixed | ||
| CNS: new | 59.97 | Fixed | ||
| CNS: repeat | 19.00 | Fixed | ||
| Community pharmacy: new | 76.41 | Fixed | ||
| Community pharmacy: repeat | 19.00 | Fixed | ||
| TSL: new | 91.05 | Fixed | ||
| TSL: repeat | 24.43 | Fixed | ||
| Utility | ||||
| Utility value for all patients | 0.457 | 0.025 | Beta | IMPACCT survey data80 |
| Utility decrement for unplanned hospital/hospice visit for symptom management | 0.205 | 0.045 | Beta | IMPACCT survey data80 |
| Duration of decrement | 1 week | Fixed | Assumption | |
| Annual eligible patient population | 239,822 | Fixed | NHS Digital81 | |
| Service/resource | Mean value (£) | Source/notes |
|---|---|---|
| Initial GP consultation | 39.00 | PSSRU (p. 120).60 Unit cost per patient contact lasting 9.22 minutes, including direct care staff costs with qualification |
| GP time for new prescription | 21.50 | Based on team discussions. GP assumed to take 5 minutes to write a prescription (considering tasks such as finding the patient’s medical record, NHS number, address, etc.) at £4.30 per minute of patient contact (PSSRU, p. 12060) |
| GP contacts community pharmacy | 13.00 | PSSRU (p. 120).60 Assumed as £156 per hour of GP activity. Based on team discussions. Duration assumed to be 5 minutes |
| CP dispensing time | 19.00 | PSSRU (p. 184).82 £71 per hour of patient-related activities was inflated to 2018/19 prices (£77.39)83 to find a cost per minute of £1.29. Duration was taken from PSSRU60 as 14.73 minutes |
| Total costs per patient: new prescription | 92.50 | Includes GP consultation, new prescription written, GP contact to pharmacy and pharmacy dispensing time |
| Total cost per patient: repeat prescription | 19.00 | Includes pharmacy dispensing time |
| Service/resource | Mean value (£) | Source/notes |
|---|---|---|
| Initial CNS consultation | 11.50 | PSSRU (p. 117).60 Band 6 nurse costing £46 per hour (£0.77 per minute) lasting 15 minutes based on PSSRU (p. 175)82 |
| CNS new prescription request to GP | 7.67 | PSSRU (p. 118).60 Band 6 nurse costing £46 per hour (£0.77 per minute). Based on team discussions, CNS requests are assumed to take 5 minutes and are carried out using a number of methods, such as SystmOne, telephone or SMS. An additional 5 minutes was added as the requesting nurse will check the record later or follow-up with a telephone call to check that the prescription has been processed |
| GP/nurse prescriber time for new prescription | 19.73 | Based on team discussions. GP assumed to take 5 minutes to write a prescription (considering tasks such as finding the patient’s medical record, NHS number, address, etc.) at £4.30 per minute patient contact (PSSRU pp. 118 and 12060). Band 6 nurse costing £46 per hour (£0.77 per minute). Weighted average of 90% GP : 10% CNS prescription times |
| CNS contacts community pharmacy | 3.83 | PSSRU (p. 118).60 Band 6 nurse costing £46 per hour. Based on team discussions, duration assumed to be 5 minutes |
| CP dispensing time | 19.00 | PSSRU 2014 (p. 184). £71 per hour of patient-related activities was inflated to 2018/19 prices (£77.39) to find a cost per minute of £1.29. Duration was taken as 14.73 minutes84 |
| Total costs per patient: new prescription | 61.73 | Includes nurse consultation, CNS contact with GP, new prescription written by a GP or CNS, CNS contact to pharmacy and pharmacy dispensing time |
| Total costs per patient: repeat prescription | 19.00 | Includes pharmacy dispensing time |
| Service/resource | Mean value (£) | Source/notes |
|---|---|---|
| Average cost to provide commissioned palliative care services per pharmacy | 3.42 | Based on retainer fees provided in service-level agreements and estimates,85–92 from the Quality of Outcomes Framework and Office for National Statistics |
| Weighted average of cases 1 and 2 new prescription costs | 82.24 | 67% were case 1 and 33% were case 2 |
| CP dispensing time | 19.00 | PSSRU 2014 (p. 184).93 £71 per hour of patient-related activities was inflated to 2018/19 prices (£77.39) to find a cost per minute of £1.29. Duration was taken as 14.73 minutes84 |
| Total costs per patient: new prescription | 87.22 | Includes average cost to provide commissioned services and the weighted average of costs from cases 1 and 2, with two-thirds of the costs from case 1 and one-third of the costs from case 2 |
| Total costs per patient: repeat prescription | 19.00 | Includes pharmacist dispensing time |
| Service/resource | Mean value (£) | Source/notes |
|---|---|---|
| In-hours cost per call | 3.05 | PSSRU (pp. 118 and 157).60 Band 3 nursing assistant (£26.68 per hour) for 20% of calls and band 6 nurse (£46 per hour) for 80%, which was then divided by length of call, based on team discussions, assumed to be 6 minutes for advanced nurse telephone consultations |
| OOH cost per call | 4.10 | Only band 6 at time plus 30%94 |
| Weighted average cost per call | 3.77 | Calculated using weighted average of the two cost per calls above and an audit,95 which stated that 69% of calls (out of 12,118 calls) were received OOH |
| Referral from TSL nurse to GP prescriber | 2.75 | Referral assumed to be an e-mail that took 3 minutes to write |
| Weighted average onward referral | 42.07 | Out of the 12,118 calls to the TSL, 7218 were referred on to a DN (n = 4450), OOH GP (n = 1414), in-hours GP (n = 1083) or palliative care CNS (n = 271).95 This figure is the weighted average of these based on their cost per hour from PSSRU60 |
| Initial GP consultations | 39.00 | PSSRU (p. 120).60 Unit cost per patient contact lasting 9.22 minutes, including direct care staff costs with qualification |
| GP/nurse prescriber time for new prescription | 19.73 | Based on team discussions. GP assumed to take 5 minutes to write a prescription (considering tasks such as finding the patient’s medical record, NHS number, address, etc.) at £4.30 per minute patient contact (PSSRU pp. 118 and 120).60 Band 6 nurse costing £46 per hour (£0.77 per minute). Weighted average of 90% GP : 10% CNS prescription times |
| Nurse contacts community pharmacy | 3.83 | PSSRU (p. 118).60 Band 6 nurse costing £46 per hour. Based on team discussions, duration assumed to be 5 minutes |
| CP dispensing time | 19.00 | PSSRU 2014 (p. 184).93 £71 per hour of patient-related activities was inflated to 2018/19 prices (£77.39) to find a cost per minute of £1.29. Duration was taken as 14.73 minutes84 |
| Total cost per patient: new prescription | 130.16 | Includes average cost per call, referral time from TSL nurse, weighted average onward referral, initial GP consultation, new prescription by GP/CNS and pharmacist dispensing time |
| Total cost per patient: repeat prescription | 22.77 | Includes average cost per call and pharmacist dispensing time |
| Type of service | Cost (£, 2018/19 prices) | NHS reference code | Source (page number/code) | Inflated from year | Notes |
|---|---|---|---|---|---|
| Hospital care | |||||
| Hospital A&E visit | 144.00 | TO1–TO4NA | NHS reference costs.59 A&E non-admitted | N/A | Weighted average of TO1NA–TO4NA |
| Inpatient, specialist palliative care | 437.00 | SD01A | NHS reference costs.59 Inpatient specialist palliative care, 19 years and over | N/A | |
| Outpatient, medical specialist palliative care attendance | 185.00 | SD04A | Medical specialist palliative care attendance, 19 years and over | N/A | |
| ICU cost per day | 933.00 | CCU01 | Non-specific, general adult critical care patients predominate | N/A | |
| Hospice care | |||||
| Hospice inpatient stay, per day | 433.00 | End of Life Care Economic Tool 96 | 2017 | Inpatient hospice cost of approximately £425 per person per day | |
| Hospice outpatient appointment | 185.00 | SD04A | Medical specialist palliative care attendance, 19 years and over | N/A | |
| Day hospice visit | 101.00 | SD05A | Non-medical specialist palliative care attendance, 19 years and over | N/A | Assumed same as non-medical outpatient attendance |
| Primary and community care | |||||
| GP, surgery visit | 39.00 | PSSRU (p. 120).60 Unit cost per patient contact lasting 9.22 minutes, including direct care staff costs with qualification | N/A | Per surgery consultation lasting 9.22 minutes | |
| GP, home visit | 95.47 | PSSRU (p. 176);97 PSSRU (p. 162)98 | 2017 | PSSRU98 (2017) estimates for costs/minute and PSSRU97 (2015) estimates for duration. Inflated using the UK Government Economic Assumptions 2016/17 to 2020/21 guidance61 | |
| GP, telephone consultation | 28.97 | PSSRU (p. 176);97 PSSRU (p. 162)98 | 2017 | PSSRU98 (2017) estimates for costs/minute and PSSRU97 (2015) estimates for duration | |
| GP, OOH, GP base visit | 50.68 | PSSRU (p. 120).60 Unit cost per patient contact lasting 9.22 minutes, including direct care staff costs with qualification. PSSRU (p. 176);97 PSSRU (p. 162)98 | N/A | Estimated using the ratio of GP surgery visits to GP home visits | |
| GP, OOH, home visit | 124.06 | PSSRU98 estimates for costs/minute and PSSRU97 estimates for duration estimates for OOH consultations | 2015/2017 | ||
| GP, OOH, telephone consultation | 37.65 | PSSRU (p. 120).60 Unit cost per patient contact lasting 9.22 minutes, including direct care staff costs with qualification. PSSRU (p. 176);97 PSSRU (p. 162)98 | N/A | Estimated using the ratio of GP surgery visits to GP telephone costs | |
| PCP (practice based), surgery visit | 11.89 | PSSRU (p. 184)93 | 2014 | £71 per hour of patient-related activities was inflated to 2018/19 prices (£77.39) to find a cost per minute of £1.29. Length of consultation was assumed equal to GP face-to-face appointment duration | |
| PCP (practice based), home visit | 29.11 | PSSRU (p. 184)93 | 2014 | Estimated using the ratio of GP surgery visits to GP home visits | |
| PCP (practice based), telephone consultation | 9.16 | PSSRU (p. 184)93 | 2014 | £71 per hour of patient-related activities was inflated to 2018/19 prices (£77.39) to find a cost per minute of £1.29. Length of consultation was assumed equal to GP telephone appointment duration of 7.1 minutes from PSSRU93 | |
| Nurse practitioner, surgery visit | 28.00 | PSSRU (p. 117);60 PSSRU (p. 165)99 | N/A | Band 7 nurse costing £112 per hour of patient-related activities. 15 minutes per consultation from PSSRU99 | |
| Nurse practitioner, telephone consultation | 11.20 | PSSRU (p. 117);60 PSSRU (p. 165)99 | N/A | Band 7 nurse costing £112 per hour of patient-related activities. Assumed to be 6 minutes based on nurse practitioner telephone duration (PSSRU99) | |
| DN, home visit | 41.00 | PSSRU (p. 175);100 PSSRU (p. 159)99 | 2012 | £70 per hour of home visiting (including travel) for DNs was inflated to £77, duration of 20 minutes per home visit from PSSRU99 plus 12 minutes of travel101 | |
| DN, telephone consultation | 17.74 | PSSRU (p. 175);100 PSSRU (p. 165)99 | 2012 | £58 per hour of patient-related work was inflated to £63.80. Assumed to be 6 minutes based on nurse practitioner telephone duration (PSSRU99) | |
| Palliative care CNS, home visit | 58.67 | PSSRU (p. 117);60 PSSRU (p. 165)99 | N/A | Band 7 nurse costing £112 per hour of patient-related activities. 25-minute consultation from PSSRU99 plus 12 minutes of travel101 | |
| Palliative care CNS, telephone consultation | 11.20 | PSSRU (p. 117);60 PSSRU (p. 165)99 | N/A | Band 7 nurse costing £112 per hour of patient-related activities. Assumed to be 6 minutes based on nurse practitioner telephone duration (PSSRU99) | |
| Other costs | |||||
| Gold Line telephone contact | 9.79 | PSSRU (p. 117);60 PSSRU (p. 165)99 | N/A | Weighted average of day and night telephone calls to Gold Line | |
| NHS 111, telephone call | 13.49 | Pope et al.102 | 2017 | Based on four clinics and cost-per-call could differ depending on demand | |
| 999 ambulance service, telephone call | 7.00 | ASC1 | PSSRU (p. 82)60 | N/A | |
| Paramedic, home visit | 196.00 | ASS01 | PSSRU (p. 82)60 | 2018 | Defined as ‘see and treat and refer’ |
| Case | Sample | Diagnosis (%)a | Time (weeks) on palliative care registerb | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | Cancer | Non-cancer | n | Mean | SD | Minimum | Maximum | |
| Combined | 104 | 74.50 | 25.50 | 82 | 51.9 | 55 | 5 | 350 | |
| By service type | |||||||||
| 1 | 28 | 26.90 | 84.60 | 15.40 | 24 | 50 | 74.5 | 8 | 350 |
| 2 | 40 | 38.50 | 97.50 | 2.50 | 22 | 20.8 | 13.1 | 5 | 45 |
| 4 | 36 | 34.60 | 41.70 | 58.30 | 36 | 72.3 | 47.1 | 16 | 196 |
| Case study | Variable | n | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|---|
| 1 | Outpatient visits | 26 | 0.88 | 1.18 | 0 | 4 |
| A&E visits | 26 | 0.23 | 0.51 | 0 | 2 | |
| Inpatient stays | 26 | 0.73 | 0.92 | 0 | 3 | |
| Total hospital length of stay (days) | 26 | 4.22 | 7.23 | 0 | 28 | |
| Hospice outpatient visits | 26 | 0.15 | 0.37 | 0 | 1 | |
| Hospice inpatient stays | 26 | 0.00 | 0.00 | 0 | 0 | |
| Hospice day centre visits | 26 | 0.08 | 0.27 | 0 | 1 | |
| Total hospice length of stay (days) | 26 | 0.81 | 2.25 | 0 | 9 | |
| GP visits | 26 | 1.31 | 1.41 | 0 | 6 | |
| 2 | Outpatient visits | 40 | 2.03 | 2.24 | 0 | 8 |
| A&E visits | 40 | 0.03 | 0.16 | 0 | 1 | |
| Inpatient stays | 40 | 0.23 | 0.48 | 0 | 2 | |
| Total hospital length of stay (days) | 40 | 0.78 | 2.15 | 0 | 11 | |
| Hospice outpatient visits | 40 | 0.13 | 0.46 | 0 | 2 | |
| Hospice inpatient stays | 40 | 0.25 | 0.67 | 0 | 3 | |
| Hospice day centre visits | 40 | 0.05 | 0.22 | 0 | 1 | |
| Total hospice length of stay (days) | 40 | 1.45 | 6.21 | 0 | 36 | |
| GP visits | 40 | 1.25 | 1.46 | 0 | 5 | |
| 4 | Outpatient visits | 36 | 0.67 | 1.24 | 0 | 4 |
| A&E visits | 36 | 0.19 | 0.58 | 0 | 2 | |
| Inpatient stays | 36 | 0.14 | 0.42 | 0 | 2 | |
| Total hospital length of stay (days) | 36 | 1.06 | 3.80 | 0 | 18 | |
| Hospice outpatient visits | 36 | 0.03 | 0.17 | 0 | 1 | |
| Hospice inpatient stays | 36 | 0.00 | 0.00 | 0 | 0 | |
| Hospice day centre visits | 36 | 0.03 | 0.17 | 0 | 1 | |
| Total hospice length of stay (days) | 36 | 0.31 | 1.83 | 0 | 11 | |
| GP visits | 36 | 2.61 | 2.87 | 0 | 12 |
| Cost | Case study | Annual cost (£) | |
|---|---|---|---|
| Patient | Population | ||
| Hospital costs | 1 | 14,352 | 3,441,878,579 |
| 2 | 4748 | 1,138,705,973 | |
| 4 | 3909 | 937,465,889 | |
| Hospice costsa | 1 | 2324 | 557,286,373 |
| 2 | 4414 | 1,058,688,223 | |
| 4 | 878 | 210,616,992 | |
| Primary care | 1 | 1265 | 303,476,958 |
| 2 | 7120 | 1,707,640,800 | |
| 4 | 3954 | 948,295,171 | |
| Total cost | 1 | 18,080 | 4,336,048,071 |
| 2 | 16,846 | 4,040,104,845 | |
| 4 | 8444 | 2,025,007,205 | |
| Case study | Variable | n | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|---|
| 1 | GP OOH visit | 26 | 0.00 | 0.00 | 0 | 0 |
| Hospital or hospice visit for symptom management | 26 | 0.92 | 1.26 | 0 | 4 | |
| Unplanned hospital or hospice visit for symptom management | 26 | 0.50 | 0.86 | 0 | 4 | |
| 2 | GP OOH visit | 40 | 0.08 | 0.27 | 0 | 1 |
| Hospital or hospice visit for symptom management | 40 | 0.83 | 1.38 | 0 | 5 | |
| Unplanned hospital or hospice visit for symptom management | 40 | 0.28 | 0.64 | 0 | 3 | |
| 4 | GP OOH visit | 36 | 0.17 | 0.56 | 0 | 3 |
| Hospital or hospice visit for symptom management | 36 | 0.50 | 0.91 | 0 | 3 | |
| Unplanned hospital or hospice visit for symptom management | 36 | 0.11 | 0.46 | 0 | 2 |
Appendix 27 Phase 4: coding framework for community pharmacist data
-
Role played facilitating access (service provision).
-
Stock management.
-
Anticipation and triaging of prescriptions.
-
Ordering.
-
Dispensing.
-
Information provision to patients/family members.
-
Home delivery service.
-
Commissioned ‘palliative care pharmacy’.
-
-
Role played facilitating access (relationship-building).
-
Patients/family members.
-
Other HCPs.
-
– GPs.
-
– CNs.
-
– Palliative care specialists/nurses.
-
– Pharmacists.
-
-
-
Facilitators of supply chain processes.
-
EPS.
-
– Recent change of EPS for CDs.
-
-
Standardised prescribing (formularies).
-
– Hold stocks of commonly used medicines.
-
-
Supply into the pharmacy.
-
– Use of key wholesalers.
-
– Relationship development/improved communication.
-
– Prioritisation of wholesalers (cascade system).
-
– Pharmacy having own wholesaler.
-
-
– IT systems (stock management and/or ordering).
-
– Time to delivery from distributor.
-
– Two deliveries per day for FLs.
-
– Predominantly one delivery per day for SLs.
-
-
– Sourcing stock from other pharmacies.
-
– Other pharmacies using alternative wholesalers.
-
– Chains versus independents.
-
– Use of pharmacy networks.
-
-
-
-
Barriers to supply chain processes.
-
Disincentives to stocking palliative care medicines.
-
– Disincentives to stocking CDs.
-
– Implications if not collected.
-
– Unable to return to wholesaler.
-
– Process of destruction when medicines expire.
-
-
-
Lack of communication/relationships.
-
– With distributors.
-
– With manufacturers.
-
-
Shortcomings of online ordering systems.
-
– Not sufficiently live.
-
– Switch lines.
-
– Third party.
-
– System breakdowns.
-
-
Lack of weekend ordering and Sunday deliveries.
-
Issues with wholesaler deliveries.
-
– Missing parts of order.
-
– Delivery does not arrive.
-
-
Medicines shortages/problems in supply.
-
– Out of stock at wholesalers.
-
– Stock quotas.
-
– Drive up prices.
-
– Prioritise hospital supply.
-
– Request for prescription change.
-
-
Need to use multiple distributors.
-
– Solus agreements.
-
-
Appendix 28 Phase 4: coding framework for wholesaler/distributor data
-
Role in facilitating access (wholesaler services).
-
Logistics/distribution/warehousing.
-
Deliveries.
-
Demand/stock management.
-
Pre-wholesale.
-
Product/inventory management.
-
Commercial drivers.
-
Quality drivers.
-
-
Role in facilitating access (relationships).
-
Contracting with manufacturers/upstream.
-
– Due diligence in contracting to assure availability.
-
– Pressure on manufacturer to come back into stock.
-
-
Client services: key accounts/customer services.
-
– Information on stock shortages.
-
– Acting on feedback.
-
-
Interorganisational collaboration/commercial medicines unit (NHS team): two-way communications – set restrictions in the supply chain based on risk.
-
Trade association.
-
-
Facilitators of supply chain processes.
-
Stock available in the market.
-
Alternative product/supplier: same license.
-
IT systems integration: manufacturer can see supply/predict demand.
-
– IT restriction rules.
-
-
Buffer stocks: how many weeks?
-
UK/close European Union pre-wholesale.
-
-
Barriers to supply chain processes in community.
-
Supply chain disruptions.
-
– Manufacturing issues.
-
– Predicting patterns and inability for manufacturer to increase capacity.
-
-
– Shortages.
-
– Number of shortages.
-
– Information from manufacturer on shortage and commercial sensitivity.
-
-
– Notice periods of shortages/size of shortage/length of shortage/degree of problem/amount remaining in stock.
-
– Fragility of supply chain.
-
-
– Quality assurance: recalls, Falsified Medicines Directive, supply assurance.
-
– Drug recalls: effect on pharmacies/patients, decrease of stock in marketplace.
-
-
-
Globalisation.
-
– Parallel import/export market/UK policy/UK pricing/value of pound/manufacturers decision on where to send stock across world.
-
-
Strategic drivers.
-
– Generic medicines as a commodity.
-
– Quotas.
-
– Pharmacy quotas: knowledge of quota being there and need for prescription validation.
-
– Wholesaler quotas.
-
– Quotas in other countries.
-
-
– Fridge line capacity/CD storage capacity/size of warehouse.
-
– Downstream: trading, switches, geographical differences in formularies across country/speculative stockholding (e.g. Brexit).
-
-
Appendix 29 Phase 4: characteristics of community pharmacist sample
| ID number | CRN region | Pharmacy size | Total number of prescriptions (September 2019) | WD usage |
|---|---|---|---|---|
|
Ph4CP0-1Ph4CP24 (inclusive) Participants: n = 24 Five participants providing commissioned services for palliative care [locally commissioned service (via CCG), n = 4; enhanced service (commissioned via NHS England area team), n = 1] |
North West London, n = 7 Eastern, n = 4 North West Coast, n = 3 Kent, Surrey and Sussex, n = 2 East Midlands, n = 2 Greater Manchester, n = 2 South London, n = 1 North East and North Cumbria, n = 1 Thames Valley and South Midlands, n = 1 Yorkshire and the Humber, n = 1 CRN regions, n = 11 |
Independent, n = 11 Large multiple, n = 7 Small multiple, n = 6 |
Range: 1469–16,918 Median: 7169 |
FL: range 1–3, median 3 SL: range 0–14, median 3 Overall: range 2–16, median 5 |
Appendix 30 Logic model of supply into community pharmacy: macro-, meso- and micro-level systems
| System | Mechanism of action | Mediating factor (+/–) | Impact on supply chain (+/–) |
|---|---|---|---|
| Macro-level systems | |||
| Globalisation of manufacturing |
A: increased outsourcing of manufacturing and resulting increases in global supply routes B: finite active ingredients/raw materials globally may limit production and manufactured stocks |
A: skilled management of remote operations required (+/–) A: robust logistics and pre-wholesale infrastructure required (+/–) B: global medicines shortages may be induced by limited active ingredients/raw materials (–) B: insufficient capacity for manufacture via limited raw materials leads to shortages, and/or affects production schedule and lead times for production (–) |
Complex interaction of mediating factors:
|
| Legislation and regulatory systems |
A: national pricing and reimbursement mechanisms via the Drug Tariff in England B: price concessions via the DHSC in England – increase reimbursement prices for certain medicines (for the month in which they are granted) C: influence of the DHSC in the case of severe shortages D: legislation surrounding supply of CDs (e.g. requirements for locked storage, inability to return CDs to WDs, requirements around destruction of out-of-date CDs) E: medicines regulatory agency ensures compliance with regulations |
A: national retrospective reimbursement system may limit products entering the UK marketplace (–) B: price concession levels not known at time of stock procurement by CPs, products returned to WD if price deemed too high or CPs accommodate a potential loss between purchase price and price concession (–) C: any marketplace shortage drives up price of medicine (–) C: lack of national-level guidance on managing shortages, except in the case of severe shortages (–) C: general willingness of WDs to work collaboratively in the case of severe shortages (+) C: potential prioritisation of hospital supply over community supply in the case of severe shortages (–) D: CD-related legislation acts as disincentive to stocking these medicines by CPs and limits storage capacity at WDs (–) E: auditing of manufacturers by regulators and WDs must maintain regulatory compliance (+) |
Complex interaction of mediating factors:
|
| International commerce and trade |
A: global competition for medicines supply at competitive prices B: parallel trading across countries C: withdrawal from the European Union (Brexit) D: quotas may be implemented by governments in other countries |
A: difficulty forecasting demand for WDs and manufacturers (–) A: insufficient product to meet overall global demand (–) A: global low demand for generics leads to products being withdrawn from the marketplace (–) B: WDs’ ability to source products outside the UK (+) C: establishment of national stockpiles of key medicines for European Union withdrawal (+/–) D: international trade limited by quotas imposed abroad (–) |
Complex interaction of mediating factors:
|
| Meso-level systems | |||
| Contractual agreements |
A: contracting agreements between WDs and manufacturers B: contracting agreements between WDs and haulage/logistics firms C: Solus agreements – sole WD for some manufacturers D: prioritisation of WDs by community pharmacies – one WD used as first line, another as second line and so on E: WD discount agreements made with CPs based on volume of stock purchased |
A: provide assurance of inbound stock to WDs (+) B: helps to ensure delivery to CPs, with twice-daily deliveries by FLs (+) C: increased security and less fragmented supply chain (+) C: risk of supply failure as products cannot be accessed via other WDs (–) C: CPs required to use multiple WDs to accommodate Solus agreements and, therefore, adds complexity to supply chain routes (–) D: cascade protocols for CPs of which WDs to use and, therefore, adds complexity to supply chain routes (–) E: price discounts encourage larger pharmacies to bulk purchase and hold warehouse stocks of medicines (+/–) |
Complex interaction of mediating factors:
|
| Organisational cultures and incentives |
A: contrasting cultures between WDs and CPs B: commercial priorities of WDs C: patient-facing focus of CPs (accountability to the patient), but underlying commercial incentives for CPs |
A, B + C: lack of meaningful two-way communication (–) A, B + C: lack of relationship-building (–) A, B + C: mistrust on part of CPs of WDs’ motivations and actions (–) |
|
| IT stock management and ordering systems |
A: IT systems facilitate sophisticated stock management by WDs (accounting for demand patterns, stock holding levels and locations of stock) B: IT systems generally facilitate CP ordering and time to delivery |
A: stock volumes at WDs managed across distribution centres/warehouses (+) A: liaison with manufacturers based on recent demand (+/–) B: CP orders Monday–Friday only (–) and WD deliveries Monday–Saturday (+) B: cut-off times for CP ordering must be met for same or next day delivery (–) B: ordering systems may be insufficiently live or be limited in functionality (–) |
Complex interaction of mediating factors:
|
| Micro-level systems | |||
| Transactional roles |
A: use of telesales agents (lack of clinical insight/understanding of palliative care medicines) B: delegation of customer service interaction with WDs to dispensers in community pharmacy C: information transfer from WD customer centres to CPs limited to that contained within the IT system |
A + B: lack of relationship development between CPs and WDs (–) A + B: lack of feedback received by WDs from patients + carers/CPs (–) A, B + C: lack of meaningful two-way information transfer between CPs and WDs (–) |
|
Appendix 31 Logic model integration of study findings across stages of the patient access pathway
| Stage of access process | Mechanism of impact | Moderating and mediating factors | Model and evidence source | Patient and carer impact |
|---|---|---|---|---|
| Patient recognition of need for a new or repeat medicine | Swift and accurate recognition of symptoms, symptom control and side effects initiates timely access process |
|
|
|
|
|
|||
|
|
|
||
| Patient communication of need | Swift contact with the most appropriate person speeds the access process |
|
|
|
|
|
|||
|
|
|||
|
|
|
||
|
|
|||
|
|
|||
| HCP assessment of patient need | Accurate assessment leads to the right medicine, dose and formulation of medicine(s) being prescribed |
|
|
|
|
|
|||
|
|
|||
|
|
|||
|
|
|||
|
|
|||
|
|
|
||
|
|
|||
| Appropriate prescription issued | Clinically appropriate prescription results in the patient being able to safely take medicine(s) for effective symptom control |
|
|
|
|
|
|||
|
|
|
||
|
|
|||
|
|
|||
| Transfer of script to pharmacy | CP is notified that the prescribed medicine is required |
|
|
|
|
|
|
||
| Dispensing | CP is able to dispense the medicine(s) prescribed, including OOH |
|
|
|
|
|
|||
|
|
|||
|
|
|
||
|
|
|||
|
|
|||
|
|
|||
|
|
|||
|
|
|||
| Supply to the patient | The right medicine is supplied swiftly to the patient or carer |
|
|
|
|
|
|||
|
|
|||
|
|
|||
|
|
|||
|
|
Glossary
- Anticipatory medicines (‘just-in-case’ medicines)
- Palliative care medicines prescribed and dispensed to be kept in the home in anticipation of crisis situations during the last few days or weeks of life.
- Community pharmacies (types)
- Pharmacies in the community range from large multiples (i.e. > 100 pharmacies) with shops on many high streets or within supermarkets, through to small multiples (i.e. 6–99 pharmacies) to individually owned pharmacies (i.e. independents with one to five pharmacies) in small communities, often in suburbs of towns or cities, deprived areas or rural settings. According to the latest figures for general pharmaceutical services, in 2018/19 there were 11,539 community pharmacies in England and the average number of items dispensed by each community pharmacy was 87,212, 64.9% of which were via the electronic prescribing service.
- Community pharmacy-delivered commissioned services for palliative care
- Services are funded to provide locally or regionally determined stocks of ‘core’ palliative care medicines and community pharmacies are required to provide extended hours of opening, when possible.
- Drug Tariff
- A tariff produced monthly by NHS Prescription Services on behalf of the Department of Health and Social Care. The Drug Tariff outlines the prices that will be paid to pharmacy contractors (e.g. community pharmacies) for the reimbursement or remuneration of services, including for medicines and dispensing fees.
- Electronic prescription service
- A service that enables the prescriber to generate electronic prescriptions and transfer the prescription electronically to a patient’s nominated pharmacy.
- End of life
- Pertaining to the last year of life.
- Full-line wholesalers/distributors
- Wholesalers and distributors that carry and distribute a wide variety of, or complete range of, pharmaceutical products. Wholesalers and distributors handle large sales volumes and can provide a broad range of services, such as stocking inventories, warehouse operations, extended financing services (supplying credit) and employing telesales staff.
- Independent prescribing
- Prescribing by nurses and pharmacists in the UK who have completed a prescribing course. This includes prescribing of any medicine, provided it is within their competence to do so.
- Medicines access
- In this study, ‘access’ is defined as the prescription, dispensing and supply of medicines and the provision of associated information about medicines. The focus is patient and/or carer ability to obtain medicines from a prescriber and a dispenser, together with the acquisition of any information and skills about medicines given at that point.
- Parallel importing
- Branded medicines that are bought in one European country (at a cheaper price) and are sold at a higher price in the purchasing country.
- Pharmaceutical distributors
- Distributors that purchase prescription medicines and other medical products directly from pharmaceutical manufacturers for storage in warehouses and distribution centres. Community pharmacies place orders with distributors for the medicines they need. Distributors are often logistics experts, providing transport and haulage, and typically offering next-day delivery (except Sundays), but do not manufacture, prescribe or promote medicines.
- Pre-emptive prescribing
- Prescribing based on proactive consideration of symptoms/issues that may arise for patients and in anticipation of need.
- Quotas
- Maximum levels of product that can be supplied to pharmacies. These levels can be imposed by wholesalers and/or manufacturers (as well as countries).
- Short-line wholesalers/distributors
- Wholesalers and distributors that offer a limited range of products, mainly generics and some parallel imports, cutting costs by limiting the medicines available and supplying only those medicines that offer sufficient margins. As a result, community pharmacies (i.e. independents and small multiples) often use short-line wholesalers to obtain generics if a short-line wholesaler is offering a better price than the full-line wholesalers.
- Solus agreements
- Contracts in which one party is linked only to the other party (e.g. a pharmaceutical manufacturer solely using one distributor).
- Summary care record
- An electronic record of patient information created from general practitioner medical records. Community pharmacy staff can access core information on medicines, allergies and adverse reactions.
List of abbreviations
- 24/7
- 24 hours per day, 7 days per week
- A&E
- accident and emergency
- CCG
- Clinical Commissioning Group
- CD
- controlled drug
- CI
- confidence interval
- CN
- community nurse
- CNS
- clinical nurse specialist
- CP
- community pharmacist
- CPD
- continuing professional development
- CPPE
- Centre for Postgraduate Pharmacy Education
- CRN
- Clinical Research Network
- DHSC
- Department of Health and Social Care
- DN
- district nurse
- EoL
- end of life
- EPaCCS
- Electronic Palliative Care Co-ordination System
- EPS
- electronic prescription service
- FL
- full-line wholesaler
- GLM
- generalised linear model
- GP
- general practitioner
- GSF
- Gold Standards Framework
- HCP
- health-care professional
- HDA
- Healthcare Distribution Association
- HEI
- higher education institution
- HEMK
- hospice emergency medication kit
- ICER
- incremental cost-effectiveness ratio
- IT
- information technology
- LPC
- Local Pharmaceutical Committee
- MDT
- multidisciplinary team
- NHSE&I
- NHS England and NHS Improvement
- NIHR
- National Institute for Health and Care Research
- NIP
- nurse independent prescriber
- NMB
- net monetary benefit
- OOH
- out of hours
- PCN
- Primary Care Network
- PCP
- primary care pharmacist
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- RPS
- Royal Pharmaceutical Society
- SCR
- summary care record
- SD
- standard deviation
- SL
- short-line wholesaler
- SPA
- single point of access
- SSC
- Study Steering Committee
- TSL
- telephone support line
- WD
- wholesaler/distributor
