Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number 17/05/26. The contractual start date was in August 2019. The draft manuscript began editorial review in August 2022 and was accepted for publication in June 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Bellass et al. This work was produced by Bellass et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Bellass et al.
Chapter 1 Introduction
The prison population in England and Wales has almost doubled since 1990 to just under 80,000 people,1 with Government projections suggesting that this figure will continue to rise, reaching 98,700 by 2026. 2 People who enter prisons have often experienced multiple social and economic disadvantages which contribute to significantly higher levels of substance use, mental illness, infectious diseases and long-term conditions than in the population as a whole. 3,4 Although English prisons represent an opportunity to reduce these health inequalities,5 their failure to provide equivalent standards of care and achieve equivalent health outcomes – principles enshrined in international standards6 – has led to calls by the UK Government for the development of quality indicators to measure the extent of inequities between prison and community populations. 7
Multiple challenges exist, however. At the time of writing, performance measurement in prisons utilises the Health and Justice Indicators of Performance (HJIPs) framework, which somewhat increases the transparency of prison healthcare delivery8 and enables assessment of performance across prisons, but inhibits comparability with community primary care. Further, use of the quality and outcomes framework (QOF), which incentivises the achievement of evidence-based (EB) quality indicators through linked remuneration in community primary care,9 is not contractually mandated in prisons through commissioning frameworks. QOF monitoring activities are therefore reliant on individual clinicians’ motivation,10 leading to variability in performance measurement across the prison estate and constraints on the ability to compare community and prison populations. Finally, while the logistics of performance measurement and comparison are challenging in themselves, questions also remain about the interpretation of the principle of equivalence, and how the balance between measurement of care processes and health outcomes should be struck. Selecting sets of performance indicators requires rigorous and transparent consultative processes, yet little has been published on the prioritisation of prison healthcare indicators, and within this limited body of literature, selection processes are largely obscure.
Relatively little research has examined the quality of primary care provided in prisons11 to allow comparisons to the general population, or to explore ‘routine’ primary care rather than focusing on health issues commonly associated with the prison population, such as substance use or mental illness. Exceptions include Silverman-Retana et al. ,12 who found lower achievement on process of care indicators for a cohort of men with diabetes or hypertension in Mexico City compared to when they lived in the community, and McConnon et al. ,13 who found that people in Ontario who had been incarcerated were more likely than people who had not to be overdue for colorectal screening and breast cancer screening. As the UK prison population ages (the proportion of over 50s has risen from 7% in 2002 to just under 17% in 2021),2 reflected in the fact that non-communicable diseases (NCDs) have superseded suicide as the leading cause of mortality in English and Welsh prisons,3 a greater focus on routine primary care is warranted.
Similarly, there are limited data available on National Health Service (NHS) national screening or risk-assessment programmes in prison,14 yet prison leavers are more likely to be disproportionately affected by risk factors for NCDs,10,15,16 face barriers for care continuity across the prison–community interface10 and to have poorer health outcomes. 17,18 Further, there is limited evidence on factors affecting uptake of health care, although existing research suggests that the prison environment, patient gender, length of stay and ethnicity can all impact on patterns of utilisation. 19–21 Understanding variability across prisons, and how health care may perpetuate or exacerbate health inequalities, will provide important insights into how quality could be improved and inequalities reduced for this vulnerable population.
The Understanding and Improving the Quality of Primary Care in Prison (Qual-P) study was commissioned by the National Institute for Health and Care Research (NIHR) to explore gaps and variations in the quality of primary care for people in prison and identify quality-improvement interventions to promote high-quality prison care. The objectives were:
-
to identify candidate quality indicators based on current national guidance which can be assessed using routinely collected data through a stakeholder panel;
-
to explore perceptions of quality of care, including barriers to and enablers of recommended care and quality indicators, through qualitative interviews involving both ex-prisoners and prison healthcare providers;
-
to assess the quality of primary care provided to prisoners through quantitative analysis of anonymised and routinely held prison healthcare records;
-
to integrate the above findings within a stakeholder consensus process in order to prioritise and enhance quality-improvement interventions which can be monitored by our set of quality indicators.
In addition, the study team responded to a call from the NIHR for researchers to conduct further analyses of existing data pertaining to mental health (MH). The team was subsequently awarded an extension to the original project to conduct a secondary analysis of the qualitative interview data, and to compare achievement on physical health indicators for people diagnosed with mental illness and/or receiving psychotropic medication with achievement for people with no coded mental illness or prescription for psychotropic medication.
Structure of the report
Chapter 2 reports the findings of the scoping review of quality indicators in the prison setting.
Chapter 3 outlines an expert consultation process on indicator prioritisation.
Chapter 4 presents the findings from the qualitative work package (WP) (objective 2), exploring barriers and enablers to quality care from the perspectives of healthcare staff and people who have lived in prison.
Chapter 5 describes findings relating to the third objective, the quantitative analysis of healthcare records from 13 prisons in the North of England.
Chapter 6 integrates the findings from all prior WPs.
Chapter 7 describes the findings from the additional MH workstream, involving supplementary quantitative and qualitative analyses.
Chapter 8 brings the findings from across all WPs together and discusses what they mean on a higher level, with reference to the literature, and briefly concludes the whole report.
Chapter 2 Scoping review
Introduction
A scoping review was undertaken to identify and synthesise previous work conducted on quality indicators and performance measurement in the prison setting. The focus of the review was on the selection, development, implementation and review of quality indicators and performance measures. Our research question was: what is known from the research literature about the development and selection of quality indicators for primary health care in the prison setting?
Some material from this chapter has been reproduced from Bellass et al. (2022).
Bellass S, Canvin K, McLintock K, Wright N, Farragher T, Foy R, Sheard L. Quality indicators and performance measures for prison healthcare: a scoping review. Health Justice 2022;10(1):13. https://doi.org/10.1186/s40352-022-00175-9
This article is licensed under a Creative Commons Attribution 4.0 International License (CCBY 4.0) which permits use, sharing, adaptation, distribution and reproduction in any medium or format, provided the original work is properly cited. See http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Method
Scoping reviews are increasingly being used in health research to map the contours of knowledge on a particular topic. 22,23 However, in comparison to systematic reviews, which benefit from clearly articulated and replicable procedures, scoping review methodology has historically been less well-defined, resulting in considerable variability in approach and rigour. 23–27 In addressing the lack of consensus around scoping review methods, Arksey and O’Malley24 established a six-stage framework for conducting a scoping review, comprising identifying the research question, literature searching, selection of studies, charting the data, collating and reporting the results, and an optional stage of validating the review findings through stakeholder consultation. In comparison to systematic reviews, they suggest, scoping reviews typically have broader, more exploratory questions, are more inclusive in terms of study designs, and do not exclude studies based on an assessment of methodological rigour.
Other authors since have sought to expand Arksey and O’Malley’s work,24 offering further detail to the stages within the framework,25,27 for example, emphasising clarification of the focus of the question and the rationale of the study, and recommending a combination of independent reviews and team discussions to enhance the rigour of the process. Tricco et al. 26 called for standardised reporting of scoping reviews to increase transparency, which has resulted in the publication of the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews [PRISMA-ScR (www.prisma-statement.org/Extensions/ScopingReviews)],28 an adaptation of the PRISMA statement originally created for systematic reviews and meta-analyses (www.prisma-statement.org/). The PRISMA-ScR items were used to guide the scoping review reported here.
Eligibility criteria
The following criteria were developed to determine which sources would be eligible for inclusion in the review:
Inclusion criteria:
-
any type of literature that relates to the selection, development, implementation or review of quality indicators in the prison setting (either adult or juvenile);
-
in empirical papers, any research method employed;
-
any health condition;
-
published between January 2004 and December 2019;
-
English language only;
-
international literature.
As the specific focus of the review is performance measurement and the use of quality indicators in prisons, literature meeting the following criteria were excluded:
Exclusion criteria:
-
community criminal justice settings;
-
literature relating to the transition from prison to the community.
Information sources and search strategy
A published search strategy aimed at identifying primary care quality indicators for people with serious mental illness using three key concepts (primary care, quality indicators and serious mental illness)29 was adapted by an Information Specialist to include search terms relating to prison settings and exclude those relating specifically to serious mental illness. Hence, the search strategy (see Appendix 1 for the MEDLINE and CINAHL versions) was structured around three key concepts: quality indicators, primary care and prison. Boolean operators were used to combine synonyms in the concept groups with OR prior to combining the three groups of search results with AND.
It should be noted that in American literature, the term ‘prison’ is used differently to the UK context. In the USA, ‘prison’ typically refers to a confinement facility operated by the state or the Federal Bureau of Prisons, and usually houses people convicted of serious crimes. In contrast, jails in the USA are governed locally and accommodate people on remand or convicted of less serious crimes who are therefore likely to have short stays. The term ‘corrections’ is used in the USA to encompass both prisons and jails. The use of the term ‘prison’ in this review relates to the UK context and acts as an equivalent to the US word ‘corrections’.
Six databases were selected by the Information Specialist for their likelihood to index articles relating to quality indicators or to health quality in prisons: CINAHL, MEDLINE, Criminal Justice Abstracts, EMBASE, PsycINFO and Scopus. Searches were conducted separately for each database, using the Ebsco search for Criminal Justice Abstracts, the Ovid search for PsycInfo and EMBASE, and then adapting the search syntax for Scopus. Searches were conducted up to April 2021 by the Research Fellow (SB).
Additional methods of literature identification were conducted to augment the electronic search strategy. Four key journals (International Journal of Prisoner Health, Journal of Correctional Health Care, The Prison Journal and British Journal of General Practice) were hand-searched. In addition, the institutional profiles of seven key authors were examined for further relevant publications. Finally, forwards and backwards citation tracking was conducted on an initial group of 12 influential papers.
Search results were managed and de-duplicated in EndNote X9.
Study selection
The de-duplicated search results were divided equally between the Research Fellow (SB) and the Programme Manager (KC). Both researchers reviewed the abstracts of papers excluded by the other. As an additional check, a further search using the EndNote Quicksearch function was undertaken in the excluded groups using keyword/key phrase searches (e.g. performance measurement, quality indicators) to ensure that no papers containing these terms had been erroneously excluded.
Abstracts of literature that were identified from supplementary searches, that is, journal searches, author searches and citation tracking, were reviewed by both researchers. Where there was disagreement over the selection of sources, an inclusive approach was taken and the paper was put through to the full-text review stage. Both researchers reviewed the full-text articles, resolving any disagreements through consultation with a co-Principal Investigator (LS).
In accordance with the inclusive stance of scoping review methodology,23,24 and in contrast to systematic review methodology,30 papers were not excluded on the basis of a formal critical appraisal of study methodology, since the purpose of this review was to provide a descriptive overview of the literature on quality indicators in the prison setting, rather than to assess the robustness of clinical evidence underpinning the indicators.
Data charting and data items
A data charting table (see Appendix 2), was constructed using generic study features informed by the Joanna Briggs Institute Reviewer’s Manual https://wiki.joannabriggs.org/display/MANUAL/11.2.7+Data+extraction), and bespoke elements informed by detailed reading of six of the texts selected after full-text review. The chart was constructed by the Research Fellow and reviewed by the Programme Manager and a co-Principal Investigator (LS), and was adapted in an iterative process by the Research Fellow following further reading. The charting table facilitated comparison between studies.
Data items relating to the features of the study were extracted, such as the country of origin, the year, the study type and the funder. In addition, contextual elements relating to the development of quality indicators were charted, including drivers for the development of performance measurement, the challenges and constraints of the prison environment, issues relating to the transfer of performance measures from a community setting, and stakeholder engagement in decision-making processes.
Synthesis
Results were synthesised into the following groups, studies that: (1) reviewed quality indicators, (2) developed or recommended the use of explicit quality indicators or less explicit performance measures and (3) implemented quality indicators. Additionally, trends in performance measurement over time were synthesised.
Findings
Study selection
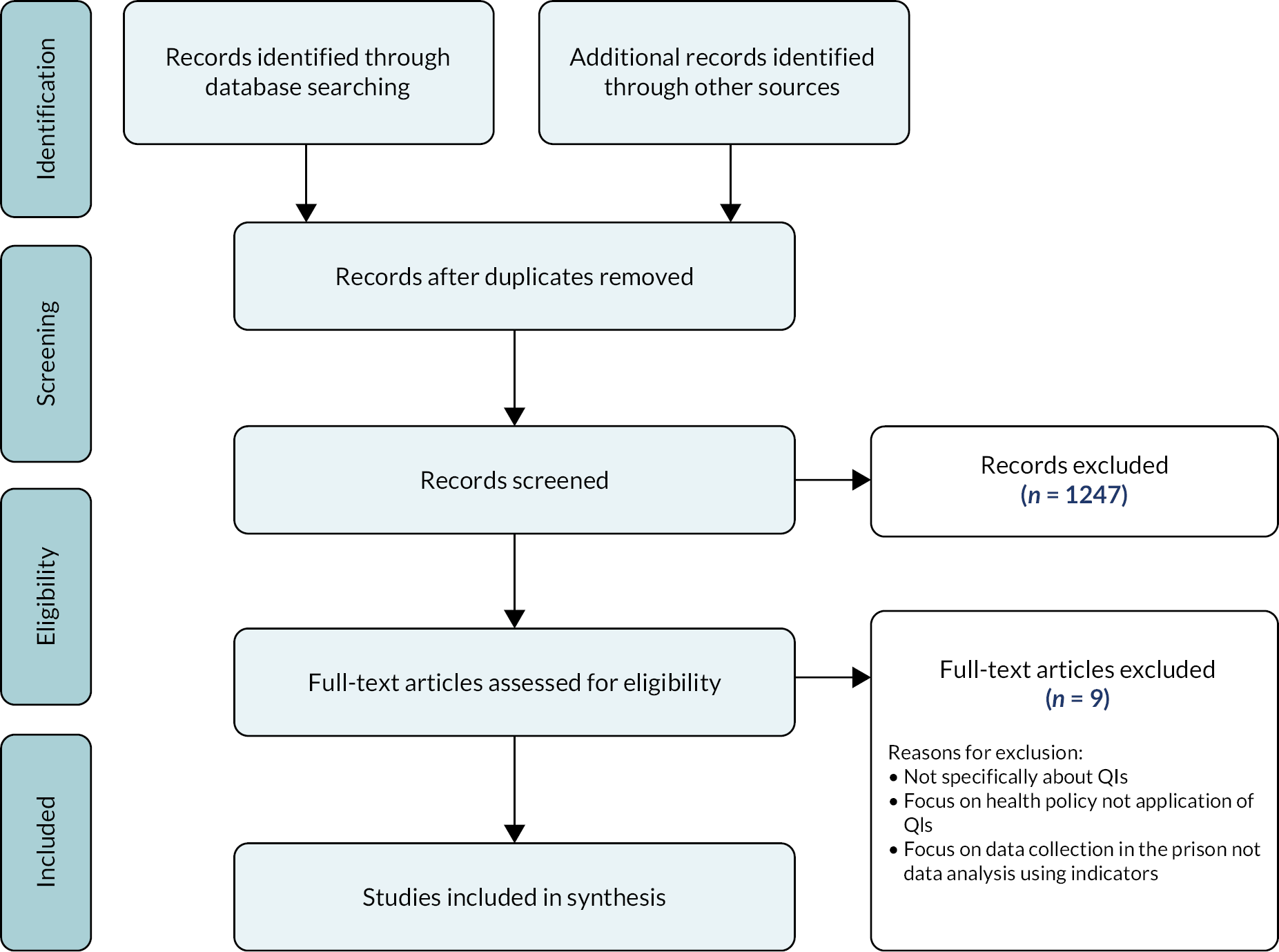
A PRISMA flow chart of the study selection process is shown in Figure 1. Of the 1271 sources identified from electronic searches and supplementary searches, 24 were assessed as eligible for full-text review following abstract screening. Nine of these were excluded due to lack of a focus on quality indicators, being policy- rather than care-oriented, or for focusing on data collection rather than analysis. Fifteen sources were included in the final synthesis.
FIGURE 1.
Selection of sources of evidence: Preferred Reporting Items for Systematic reviews and Meta-Analyses flow diagram. QI, quality indicator.
Study characteristics
The characteristics of the included studies are shown in Appendix 3, Table 14. All the studies were American in origin, bar one UK study. 31 Six studies developed quality indicators or performance measures,32–37 two sources reviewed indicators or approaches to performance measurement,38,39 while a further two described implementation,31,40 and one commentary paper advised on implementation. 41 One study developed and implemented indicators in a prison setting,42 while two described approaches to developing and testing indicators across US prisons,43,44 and one tested performance measurement of diabetes screening in one prison. 45
Three studies originated from the same research programme and were published in the same 2011 issue of the Journal of Correctional Health Care. The programme aim was to assess quality of healthcare measurement in California Department of Corrections and Rehabilitation (CDCR) and other prison systems and to recommend a portfolio of performance measures. The three studies were: an expert consultation process (reported in Asch et al. ,35 with the resulting list of indicators published by Teleki et al. 39) interviews, site visits and document reviews within CDCR,39 and a review of performance measurement activities in six correctional systems. 38
Types of quality indicators and performance measures
Most of the literature included quality indicators or performance measures, although the content varied widely from a few illustrative examples,32,35,40,41,43 to extensive lists. 33,34,36,39,44 Further variation was found in the format of measures, with some authors providing ‘explicit’ quality indicators33,35,39,40,44 – defined by Damberg et al. 38 as objective, EB measures that provide a standardised means of measuring quality across prisons – while others provided more broadly stated performance measures. 32,34,36,41,43 Explicit indicators, Damberg et al. 38 suggest, are distinguishable by their format; they have a clearly expressed denominator, that is, the number of people eligible for a particular measure, and a specified numerator, that is, the number of people from the denominator who satisfy the measure. Further parameters are often included, such as a reporting period, for example, the last 12 months, or particular diagnostic codes. The measure is then expressed as a percentage, calculated by dividing the numerator by the denominator and multiplying by 100. Explicit quality indicators are typically classified as ‘process’ indicators, that is, those focusing on care delivery, or outcome indicators, which measure the achievement of a particular health outcome, as demonstrated in Table 1.
| Process indicator | |
| Numerator | Number of prisoners from the denominator who received at least one serum potassium and either a serum creatinine (Cr) or a BUN therapeutic monitoring test in the measurement year |
| Denominator | Total number of prisoners who received at least a 180-day supply of ACE inhibitors, ARBs or diureticsa during the measurement year38 |
| Outcome indicator | |
| Numerator | Number of prisoners from the denominator having low-density lipoprotein < 100 on or between 60 and 365 days after discharge for an acute cardiovascular event |
| Denominator | Total number of prisoners aged 18–75 years as of 12/31 of the reporting year who were discharged alive in the year before the reporting year for acute MI38 |
In this body of literature, performance measures provided ways to assess prison healthcare quality, but the numerators, denominators and reporting periods were typically not specified, though often implied. For example, Greifinger36 appended a list of questions that could identify areas for clinical performance improvement through the interrogation of randomly selected small samples of healthcare records. For example, taking 10 records of people with positive tests for syphilis, gonorrhoea and chlamydia, Greifinger suggested that a measure of quality would be those who had received an appropriate prescription to treat their condition within 3 days. Similarly, Hoge et al. 34 suggested that people in prison who screen positive on a validated suicide risk assessment measure should ‘receive a referral to a MH staff member for evaluation. All inmates deemed to be an acute risk should be placed on suicide watch immediately and be immediately referred to the MH team’ (p. 643). Thus, the numerators and denominators are implicit in these measures of healthcare quality, but further work would be required to clarify the parameters of the metrics before they could be implemented in practice; clarifying denominators in the prison population, for instance, is particularly challenging given the transience of the population as people move between the community and the prison estate, or are transferred between prisons.
Studies focused on chronic care quality measurement
Four studies (Kountz and Orsetti,42 Castro,45 Booles31 and Kintz)37 were included in this review to give specific insights into quality assessment of chronic condition (CC) management in prison settings. Booles31 and Castro45 focused solely on diabetes, exploring, respectively, care processes and risk assessment. Booles31 conducted a survey of diabetes care quality in UK prisons, with 19 respondents, while Castro45 retrospectively analysed 50 health records of people diagnosed with diabetes during their prison term and held a consultation exercise to choose the most appropriate clinical guidelines for diabetes screening in prisons.
Kountz and Orsetti42 and Kintz37 explored quality of care for diabetes and other CCs [asthma and hypertension42 and asthma, human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS), hypertension/cardiovascular disease (CVD), lipid disorders, seizures, hepatitis, severe mental illness (SMI) and hepatic cirrhosis]. 37 Kountz and Orsetti42 developed and implemented a quality assessment tool, and Kintz,37 following Damberg et al. ,38 conducted a study of prison nurses’ perceptions of quality of care for chronic health conditions.
All of the authors identified the lack of standardised guidelines or their inconsistent application as causes of variability in care processes, which contributed to increased risks of sentinel events42 and diabetic complications. 31,45 Booles,31 for instance, in his survey of diabetes care in UK prisons, found that only 14 of the 19 prisons that responded were conducting routine monitoring of the diabetic patients, and only 37% of the sample had provided a mobile retinal screening service. Similarly, Kountz and Orsetti,42 when extracting a random sample of 10 medical charts, found that four people with diabetes were not receiving standard care. They also found that the lack of baseline data on CCs hampered efforts to identify high-risk patients and prevent sentinel events.
Castro,45 in her dissertation study on retrospectively identifying diabetes risk in 50 people subsequently diagnosed with diabetes in a US correctional facility (CF), found a lack of consistency in diabetes screening. For example, only 3 of 13 people with prediabetic impaired fasting glucose had subsequent HbA1c tests, although whether appointments were arranged but not attended is unclear.
Kintz,37 in her interview study with eight prison nurses, offered some insights into the barriers to quality health care for people in prison with CCs. Alongside confusion about which standards to apply, nurses reported that constrained resources resulted in acute care taking priority over long-term condition care. Inadequate data systems and poor levels of staff retention, education and appreciation of the value of performance measurement were other barriers that impeded efforts to provide quality of care. Kountz and Orsetti42 similarly found a reluctance among staff to employ the audit method they devised, with only two-thirds of the charts being completed on intake.
Methods of selecting performance measures or quality indicators
Several papers in the review described methods of selecting performance measures or quality indicators,32–36,44 with the quality indicators resulting from Asch et al. ’s35 consultation process being reported in the sister Teleki et al. 39 paper. There was noticeable variation in methodological rigour. For example, work that selected quality indicators varied significantly in the approach taken; there was a sharp contrast between the robust expert consensus processes employed by Asch et al. 35 and single individuals recommending indicators in Greifinger36 and Laffan. 41 None of the papers included in this review explicitly included the patient perspective, drawing instead on researcher, care provider or care manager input. However, it was noted by one group of authors, Asch et al. ,35 that people on the receiving end of care may have different priorities for performance measures, perhaps placing more value on outcome indicators which measure changes in health status, than those relating to care processes.
Non-rigorous approaches
Greifinger’s36 performance measures are oriented towards improving the safety of people in prison. Drawing on national and international prison healthcare standards, community patient safety standards relevant to prison settings, and his own experience of reviewing correctional health care, he compiled a guide of measures covering 30 domains of prison health care, including (but not limited to) access to care, chronic disease management, MH assessment and treatment, medical record-keeping, sexually transmitted infections (STIs) and mortality reviews.
Watts44 reports on the development of a quality indicator set based on the Healthcare Effectiveness Data and Information Set (HEDIS) metrics, the work conducted by the RAND organisation in 201135,38,39 and the Vermont Department of Corrections internal measurement system. However, very little information is given on the processes through which some of the measures were adapted for the prison setting. Similarly, Laffan,41 Bisset and Harrison43 and Raimer and Stobo40 provide short lists of measures but only minimal detail on the origin or development of the indicators.
Consensus approaches
Other authors described consensus approaches to select indicators. Asch et al. ,35 for instance, utilised a modified Delphi method, drawing on the expertise of a panel comprising nine senior people with clinical experience in correctional health care as well as relevant experience in other areas such as prison directorships, court-appointed monitorships and membership of clinical guideline committees. Following a review of health condition prevalence in prison populations, mortality statistics, and findings from qualitative interviews with healthcare providers and people responsible for quality measurement in correctional health,38,39 16 healthcare topics were chosen for further investigation. From accessing 29 community or correction-specific standards relating to the topics, and asking study participants to recommend indicators, 1731 indicators were identified. Of these, 662 were eliminated for being non-specific, leaving 1069 for further scrutiny. Following classification of indicators using the Donabedian structure–process–outcome taxonomy, content reviewers evaluated groups of indicators using criteria including importance to prison health care, scientific evidence base, implementability and interpretability. Indicators relating to specialist care were removed to retain a focus on primary care processes that were perceived to be within the jurisdiction of prison health care. As a result of this process, and a review of indicators rejected by the content reviewers, 111 indicators were presented to the panel for validity and feasibility assessment, with a 0–9 rating requested from panel members both before and during the meeting, and the level of agreement and disagreement being discussed at the meeting. Ultimately, 79 measures were retained, of which 62 were process indicators, 10 outcome indicators and 7 access indicators. The panel remarked that while these quantitative measures were a valuable means of assessing quality, they needed to be augmented by implicit quality measures such as mortality reviews and patient experience surveys.
While others have used similar consultation methods to identify quality indicators and performance measures, none match Asch et al. ’s35 rigorous multistaged approach. Stone et al. ,33 for instance, in their development of a quality indicator matrix for the Missouri Department of Corrections, appeared to rely only on the research team to identify the domains of healthcare delivery for which to identify standards and quality indicators, although administrators and medical staff were involved in selecting the final 32 indicators from an original list of 150. Where Stone et al. ’s33 work differed from Asch et al. ’s35 was in their attempts to select performance benchmarks (BMs) based on community BM data for similar indicators. This involved some modification of the indicators, for example, age range adjustments, to more closely align the prison population with the population as a whole.
Another study that sought to adapt community indicators for the prison setting was Hoge et al.’s34 selection of performance measures for MH care in prisons. Twenty-nine participants, including for-profit and independent MH practitioners and researchers, participated in a 6-hour roundtable discussion to reach consensus on meaningful indicators drawn from national standards. According to the authors, consensus was reached on nearly every subject.
Wright32 reports on the Association of State Correctional Administrators’ (ASCA) preliminary efforts to identify eight domains across the spectrum of activities in correctional systems that could be subject to a national performance measurement system that would enable a greater degree of transparency and accountability. Using seven comprehensive prison performance models, an ASCA subcommittee selected the eight most pertinent areas of correctional performance to assess, two of which were health-related: ‘substance abuse and MH’ and ‘health’. The subcommittee then selected three of the eight for their preliminary performance measurement system, including ‘substance abuse and MH’ but excluding ‘health’. Following some debate, the subcommittee decided upon performance indicators for each domain; for substance abuse and MH, they chose average daily rates of people receiving treatment for both conditions to be the indicators of performance.
Challenges and constraints of implementing quality assessment in the prison setting
Authors of papers in this review described a range of challenges to the implementation of performance measurement in prisons, including changing demographics of the prison population, the functionality of the data system, staffing and resourcing issues, and challenges to standardising quality of care measurement across different organisations.
Data system functionality
The inadequacies of existing data systems in prison settings were highlighted by most of the authors in this review, with key issues being poor co-ordination and a lack of functionality in key areas, such as capture and extraction of data,34,37,44,45 interface with other prison systems,38 prison pharmacies39,45 and community healthcare settings. 44 A lack of co-ordination with community healthcare settings leads to prison clinicians having to rely on patient self-report, which can compromise measures of prison healthcare quality. However, integrating prison health systems with those of community healthcare settings can be, as Bisset and Harrison43 noted, ‘unfamiliar and daunting territory’ (p. 3). Inconsistency in data input was also noted as a problem that could adversely affect the quality of analyses. 38,39,42,43
The absence of prison-specific BM data was cited as an inhibiting factor to quality assessment. 32,33,38 Additionally, the capacity of the data collection system was also perceived to be problematic, with requirements to collect data for legal purposes competing with the collection of data for quality-monitoring purposes:39,44 Teleki et al. 39 observed that there are ‘too many metrics being tracked for too many different purposes’ (p. 110), which can dilute performance measurement efforts. The same authors also identified difficulties clarifying the numerator and denominator, and a concern that the amount of data for some conditions would be too small to conduct a meaningful analysis. 39
Organisational issues
A few authors highlighted the difference in priorities between the medical staff and the prison administrators,31,34,41 noting that healthcare budgets may be managed by people lacking experience of healthcare delivery and that effective quality assessment of health care required collaboration between the two systems. 44
High staff turnover,34,37 under-staffing42 and the need to employ a data analyst to write and run queries38 were seen as difficulties that could jeopardise attempts to measure the quality of health care. In addition, the lack of a feedback loop for staff to gain insights into under-performing services can impede quality-improvement activities. 39
A further issue raised is whether standardisation should occur when institutions have varying mission statements, legal structures, and populations. 32 Standardisation can also be compromised by the lack of universal agreement on disease management for chronic health conditions. 37
Conclusion
While this review found limited evidence on the development and implementation of quality indicators and performance measurement in prison health care, and the evidence was virtually entirely restricted to the US context, a number of significant issues have been identified. These include the demographics of the prison population, the functionality of the data system, the format of quality indicators, stakeholder engagement, the choice of standards, target setting and staff engagement.
Chapter 3 Identification/development of quality indicators
Introduction
Measurement is a cornerstone of quality improvement in health care. Measures of the quality of care can be used to identify priorities for improvement, drive change through feedback to clinicians and healthcare organisations, and assess the impact of improvement strategies. In WP1, we set out to identify and select quality indicators that could be assessed using routinely collected data for use in the prison estate. We subsequently applied and analysed achievement of the selected indicators in our statistical analysis WP (see Chapter 5). This chapter describes the process by which we identified and developed the indicators.
Methods
Design
Our four-stage process comprised (1) identification and screening of candidate indicators from guidance and wider literature, (2) shortlisting and selection with a stakeholder consensus panel, (3) specifying eligible populations and criteria for achieving each indicator and (4) piloting data extraction to assess feasibility and refine indicators (Figure 2). We chose a modified RAND consensus process for shortlisting and selection to promote transparency in decision-making, and because it allowed interactions between participants which can help judgements requiring some degree of deliberation. 46
FIGURE 2.
Flow chart of the four-stage indicator selection and development process.
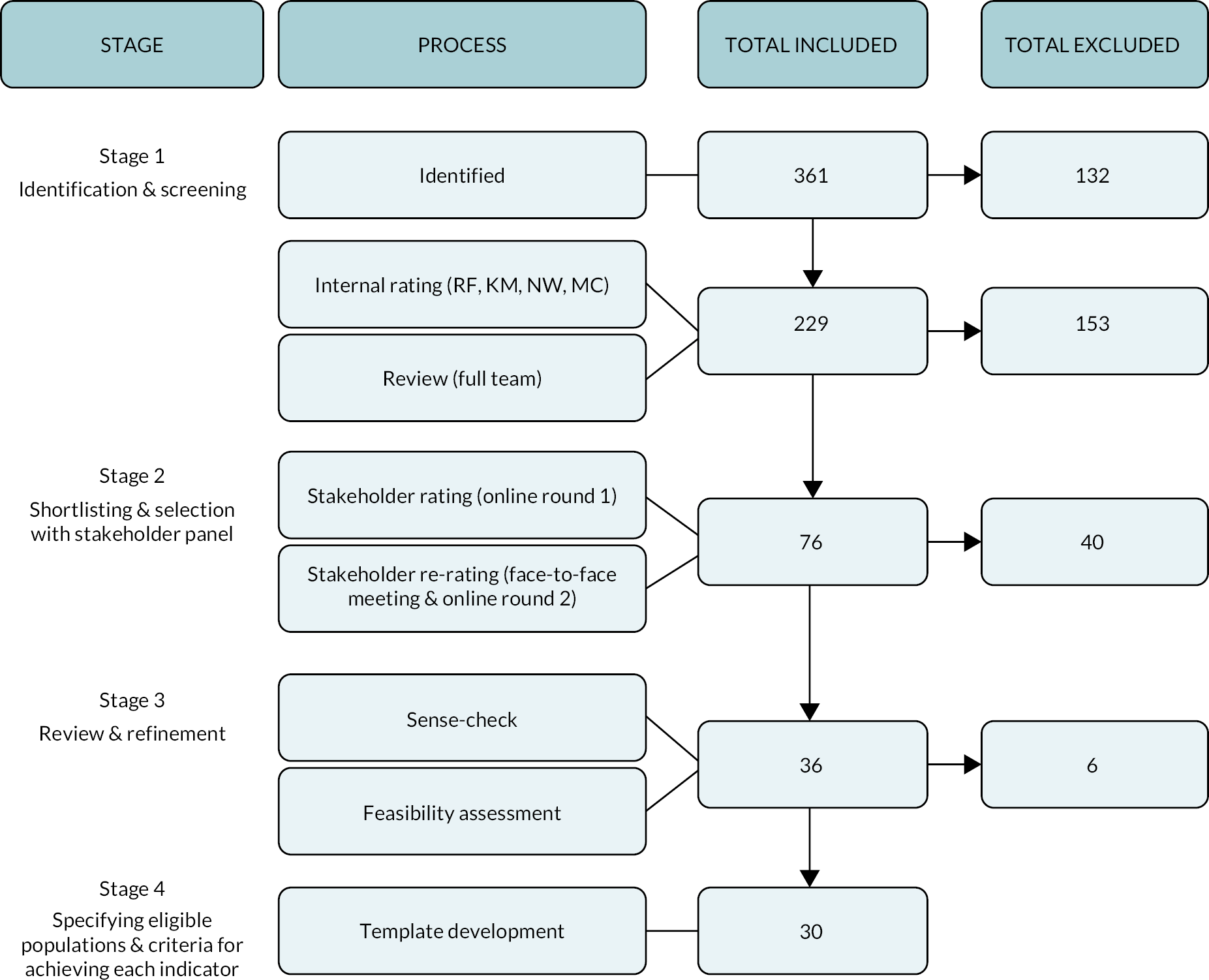
Stage 1: identification and screening of candidate indicators
We identified candidate indicators from guidance from the National Institute for Health and Care Excellence (NICE) including the QOF,47 clinical guidelines48–50 and the General Medical Service contract,51 and local quality indicators selected from local quality requirements from the NHS Standard Contract for prison health care 2019–20 for the North East, North West, and Yorkshire and Humber (set by the Commissioning Team under Schedule 4). We also drew on three studies that produced lists of indicators for use in primary care settings. 29,52,53 Our indicators were intended to measure individual-level care rather than organisational-level features and performance, which we allowed for in the analysis. Therefore, we did not draw upon Care Quality Commission (CQC) inspection standards.
We screened candidate indicators to prevent placing an excessive burden on the stakeholder consensus panel. An academic general practitioner (GP) (RF) conducted a preliminary screen of the full list of indicators and excluded those that were not relevant to primary care or had been superseded by new indicators. Four clinical team members, comprising RF, a former prison nurse and healthcare manager (MC), and two prison GPs (KM and NW), further screened the indicators. In an online survey, they independently screened according to two criteria: (1) likely amenability to measurement using routinely collected data and (2) potential for significant patient or population benefit. We collated the scores assigned by the clinical team members and then ranked the indicators. The full project team then systematically worked through the list of indicators during an internal workshop and discussed borderline indicators, discrepant ratings, and options for composite (combined) indicators.
Stage 2: shortlisting and selection with consensus panel
We had planned to recruit a panel of 11 participants, with a range of prison-specific, clinical and academic experience, recognising that consensus groups gain relatively little in reliability beyond this number. 46 We aimed to balance familiarity with day-to-day decision-making in community primary care with an appreciation of issues specific to the delivery of health care in the prison setting and the needs of the prison population. We invited several people with lived experience of prison to join the panel, but none accepted. Eight professionals from a range of criminal justice, health and MH backgrounds (including general practice, psychiatry, clinical psychology and nursing) accepted the invitation to participate.
We asked panellists to rate each candidate indicator independently online using a 1–9 Likert scale (where one is low and nine is high) according to the single criterion of ‘potential for significant patient benefit’. We provided instructions on rating and the list of indicators in a PDF by e-mail with a printed copy by post to use as a reference. To make the process accessible for panellists without relevant clinical training or former knowledge of quality indicators, we constructed a glossary of terms and plain-language descriptions of the indicators. We encouraged stakeholders to rate every indicator but provided a ‘don’t know’ option for all indicators. We piloted the functionality of the online survey with a project team member prior to sending to panellists. We also shared the original long list of indicators with the panel so they could highlight any indicators screened out earlier by the research team for reconsideration and asked them to suggest any indicators that we had not identified. We briefed the panel that we were ultimately aiming to provide a balanced suite of indicators which covered different aspects of primary care in prisons.
We calculated median scores for each rating using Microsoft Excel. We ordered indicators according to their median score for ‘potential for significant patient benefit’ and levels of discordance for presentation at a face-to-face panel meeting. We presented median ratings for each indicator. One of the authors (RF) facilitated a structured discussion which focused on indicators with the most discordant ratings. Low discordance was defined as all ratings for each indicator being three or fewer points apart, medium discordance at all ratings being between four and six points apart, and high discordance as at least two ratings between seven and nine points apart.
We gave panellists the opportunity to seek clarification about any aspects of indicators and to discuss their reasons for low or high ratings. Immediately after this discussion, panellists independently rated each indicator again. Five panellists completed both rounds, one of whom could not attend the face-to-face meeting and therefore completed ratings remotely. Our smaller than planned panel still collectively possessed a diverse range of perspectives,54 despite the difficulty in attracting busy clinicians and professionals to take part in this half-day exercise.
Stage 3: review and refinement
We reviewed and updated the list of indicators, considering them both individually and as a set. We disaggregated composite indicators and removed duplicates and low-rated indicators. We also conducted a sense-check to review face validity for individual indicators and as a set of indicators. Before moving to stage four, we conducted initial feasibility investigations; to be eligible for inclusion in our suite of indicators, data had to be routinely collected and coded in templates. If not, they could not be operationalised.
Stage 4: specifying eligible populations and criteria for achieving each indicator
We developed a template for each indicator which specified the eligible population (the denominator) and what criteria would need to be met for achieving the indicator (the numerator). The templates further included information on indicator sources and notes on development. We held several clinical team meetings (involving RF, KM and NW) to refine the indicators and monthly ‘troubleshooting’ meetings (involving RF, NW, KM, KC, PH, SR and TF) to develop and agree the data queries for each indicator. We designed data searches based upon existing algorithms, such as those used for QOF, wherever possible, to permit later comparisons with indicator achievement in community settings. The data specialist (SR) extracted anonymised individual patient-level data for the 13 prisons where health care was provided by Spectrum Community Health Community Interest Company (CIC) from SystmOne electronic health records. We reviewed descriptive summaries of the extracted data prepared by the statistician (TF) for apparent anomalies and discrepancies at the troubleshooting meetings. The data specialist subsequently refined searches until final versions were agreed.
Results
Stage 1: identification and screening of candidate indicators
We identified an initial ‘long-list’ of 361 candidate indicators (see Appendix 4) from the following sources:
-
55 from the NICE guideline for the physical health of people in prison;48
-
21 selected from local quality indicators from the NHS Standard Contract for prison health care 2019–20 for the North East, North West, and Yorkshire and Humber; and
-
17 opioid and related indicators from National Health Service England (NHSE) and Public Health England (PHE) guidance for prescribers55 and published work. 56
Preliminary screening excluded 132 indicators, including duplicates and indicators not relevant to primary care. Of the remaining 229 indicators, the clinical team rated 103 as measurable and of potential significant patient benefit: these indicators had full consensus for both criteria, or full consensus for one criterion and 75% consensus for the other (Table 2).
| Rated as measurable | Rated as of potential benefit to patient | Combined rating (%) | Number of indicators |
|---|---|---|---|
| 4 | 4 | 8 (100) | 43 |
| 4 | 3 | 7 (87.5) | 25 |
| 3 | 4 | 35 | |
| 3 | 3 | 6 (75) | 33 |
| 4 | 2 | 3a | |
| 2 | 4 | 19a | |
| 3 | 2 | 5 (62.5) | 9a |
| 2 | 3 | 49a | |
| 2 | 2 | 4 (50) | 13a |
| 229 | |||
Further review by the project team led to the promotion of 14 indicators from the 126 lower-rated indicators and their inclusion in Round 1 of the stakeholder survey. We also discarded 41 higher-rated indicators from the original 103, removing duplicates and indicators with substantial overlap. Following this internal rating and review process, we took forward a total 76 out of 229 indicators to the stakeholder panel.
Stage 2: shortlisting and selection with consensus panel
In the first round of online rating, seven of the eight stakeholder panel members rated 76 indicators. Panel discussions led to several single indicators around blood pressure control and lipid management being grouped into composites for the second round of rating, taking the number of indicators from 76 to 60. Five stakeholders then re-rated these 60 indicators. Discordance between ratings reduced following the face-to-face meeting (Table 3). In the first round, two (2.6%) indicators had low discordance (ratings ≤ 3 points apart), but this increased to 17 (28.3%) in the second round. Similarly, those with high discordance fell from 28 (36.8%) to 11 (18.3%).
| Level of discordance | Number of indicators | |
|---|---|---|
| Initial online rating (%) | Re-rating face-to-face and online (%) | |
| Low discordance Ratings are ≤3 points apart |
2 (2.6) | 17 (28.3) |
| Medium discordance Ratings are between 4 and 6 points apart |
46 (60.5) | 32 (53.3) |
| High discordance At least two panel members’ ratings were between 7 and 9 points apart |
28 (36.8) | 11 (18.3) |
| Total | 76 | 60 a |
The panel rated 31 (51.6%) indicators as having high potential for significant patient benefit (with median scores of 7–9), 22 (36.6%) as having medium potential (with median scores of 4–6), and seven (11.6%) as having low potential (with median scores of 1–3; Table 4).
| Potential for significant patient benefit measure (median scores) | Communicable disease | MH | Routine primary care | Prison-specific | Number of indicators (%) |
|---|---|---|---|---|---|
| High 7–9 | 3 | 4 | 17 | 7 | 31 (51.6) |
| Medium 4–6.5 | 4 | 2 | 15 | 1 | 22 (36.6) |
| Low 1–3.5 | 0 | 3 | 4 | 0 | 7 (11.6) |
| Total | 7 | 9 | 36 | 8 | 60 |
Stage 3: review and refinement
We discarded all seven of the lowest-rated indicators and 18 of the medium-rated indicators. We began indicator development with 31 indicators rated as having high potential for significant patient benefit but discarded nine of these because they could not be operationalised reliably, often because data were not routinely coded. This included various local quality indicators from the ‘prison-specific’ category relating to the number of individuals with complex mental or physical health problems or those on clinical substance-misuse pathways arriving without communication, and another regarding pre-release appointments with a nurse. Our enquiries suggested that staff typically used ‘free text’ rather than coded templates to enter data. Therefore, any search would significantly underestimate adherence to these indicators. Additionally, it was not possible to determine whether the denominator in the MH indicator should include anyone on the MH in-reach team caseload (i.e. the secondary care team) or only those who are subject to transfer to secure hospital. We also changed or discarded indicators where the additional complexity of devising and applying searches was likely to exceed the marginal benefits of measuring them in the prison population, such as one for chronic kidney disease (CKD) where recommended blood pressure control levels depended on the assessment of urinary albumin–creatinine ratios. The remainder were excluded as they overlapped with other indicators. We discarded a total of 34 indicators and were left with 26 (4 medium-rated and 22 high-rated).
We then disaggregated two composite indicators which would otherwise have added to the complexity of measurement and interpretation. We disaggregated one recommendation to offer equivalent health checks to those offered in the community, for example, the NHS health check programme, learning disabilities annual health check, relevant NHS screening programmes, such as those for abdominal aortic aneurysm (AAA) and bowel, breast and cervical cancer. This was to ensure that the three indicators taken forward (NHS screening for AAA and breast cancer respectively and the NHS health check programme) were specific to each programme. From these we constructed three separate indicators for AAA screening, breast screening and CVD risk assessment for the NHS health check programme.
We also disaggregated the indicator that we constructed for Round 2 of the stakeholder screening which comprised 10 separate blood pressure indicators to create two new composite indicators (each including four subindicators) covering blood pressure control in CVD, one for patients aged 79 and under and one for patients aged 80 and over.
We retained other composites, typically grouped together in planning and assessing care, such as measuring eight processes of care for type 2 diabetes (e.g. records of foot examination and smoking status). This resulted in a final total of 30 indicators, comprising 25 indicators rated by the panel as of high potential benefit to patients and 5 rated as of medium potential (after accounting for disaggregated indicators). A summary of ratings and refinements to the shortlist of 30 indicators can be found in Appendix 5.
Stage 4: specifying eligible populations and criteria for achieving each indicator
We took forward 30 candidate indicators. We made several decisions in defining the indicator denominators. First, we generally applied indicators over 12-month periods from 1 April to 31 March, so that we measured processes or outcomes of care over a year coinciding with the QOF reporting period. For certain indicators, such as those concerning opioid prescribing, our measurements were based upon an 8-week period up to 31 March. Both these approaches allowed us to make later, indirect comparisons with community data. Second, we generally disregarded any ‘exception reporting’ used for QOF. In the community, this allows practices to exclude eligible patients from the denominator of an indicator if patients refuse to attend for treatment or if the treatment covered by that indicator is likely to be inappropriate for an individual patient. There are concerns about ‘gaming’, whereby patients might be excluded to inflate apparent achievement, although this is unlikely to be widely misused. 57 QOF does not operate in prison general practice. We decided to include all eligible patients in denominators to ensure that we took a complete population perspective. Anecdotally, we had also learnt that patients in prison may miss healthcare appointments for reasons other than personal choice, such as unavailability of an escorting officer. Third, when considering care received over a given period, we measured the care received by an individual over that whole period whether or not she or he had been transferred to a different prison. In that way, our findings reflect care received by individuals rather than the care provided by individual prisons. However, we were unable to include any records of care provided in community general practice within the indicator period. Therefore, for example, an individual in prison for 6 months who had received appropriate diabetes checks in community primary care in the preceding 6 months would be coded as not meeting diabetes checks unless these also occurred in prison.
We resolved several queries after the research team sense-checked the emerging data. We made further decisions on how to operationalise and typically simplify indicators. For example, the original hepatitis B and C indicator was a complex composite that covered screening, vaccination and communication of results for hepatitis B and C, and which duplicated aspects of another indicator on screening for hepatitis B and C. We therefore focused on numbers of vaccinations given at prison population level and also for higher-risk groups (people coded as currently or recently using drugs). We also simplified a composite indicator on antipsychotic monitoring to focus on monitoring for risks of cardiometabolic disease [e.g. lipid levels, body mass index (BMI)].
In summary, we modified the wording of 7 indicators (simplified 3, expanded 4) out of our final list of 30 indicators (see Appendix 5). Our final list comprises:
-
nineteen indicators drawn from QOF;47
-
one indicator from advice for prescribers on the risk of the misuse of pregabalin and gabapentin;55
-
one from guidelines regarding the physical health of people in prison;48
-
three from guidance for the General Medical Services contract;51
-
one NICE Clinical Commissioning Group indicator;58
-
one from PHE Guidance. 61
The list encompassed the following domains: communicable disease; MH; prison-specific; diabetes, asthma and epilepsy care, screening and CVD.
Interpretation of findings
Our suite of indicators includes topics especially relevant to the prison population (MH, drug misuse and communicable diseases) and covers potentially overlooked ‘mundane’ aspects of primary care, such as the management of hypertension and asthma. Our indicators consider equity explicitly (e.g. in including those uniquely relevant to women and older people) and implicitly (e.g. analyses can examine differences in achievement according to age, coded ethnicity and sex). We recognise that the indicators cannot cover all aspects of care, including processes and outcomes which are not routinely captured and coded in electronic health records and important features of holistic care (such as communication skills). Therefore, their application needs to be complemented by other sources of data on quality of care.
We generally balanced three other characteristics of our indicators. First, we had a range of process and outcome indicators. Process indicators should ideally have a strong evidence base so that following the process predictably leads to improved outcomes [e.g. prescribing of secondary preventive treatment following myocardial infarction (MI)]. 62 The evidence base for several process indicators is less certain, but these can still be recognised as signals of good-quality care (e.g. processes of care for diabetes). 63 Indicators solely focusing on processes of care rather than health outcomes may not help overcome therapeutic inertia – the failure to intensify treatment in patients not meeting clinical goals of treatment (e.g. recommended blood pressure control in diabetes). 64 Outcome indicators are subject to higher ‘noise to signal’ ratios, whereby a range of factors beyond professional practice influence outcomes (e.g. varying patient concordance with blood pressure treatment). 65 Second, we included a range of single and composite indicators. We generally used composites for indicators assessing several, closely linked processes of care (e.g. for diabetes) and disaggregated them when considering outcomes (e.g. blood pressure control). Offering a battery of single, simpler indicators is more likely to be feasible in practice compared to more complex indicators and better direct specific actions to improve quality of care (e.g. in specifying gaps in attainment of specific aspects of diabetes care such as blood pressure control). 66 Third, most of our indicators focused on relatively common conditions or problems affecting people in prison (e.g. drug misuse). However, we recognised that solely focusing on common problems might marginalise rarer but clinically important needs. We therefore included some indicators that were important to the management of long-term conditions for older people (e.g. dementia, heart failure).
Summary of main findings
We have identified and developed a set of indicators, largely drawn from EB guidance, to assess the quality of primary care delivered in prisons. They are largely drawn from evidence-based guidance and, if followed, can deliver population benefits. The indicators cover both specific priorities for the prison population and core priorities of community primary care, thereby allowing assessments of care equivalence across settings. The indicators are based upon routinely collected data, thereby allowing efficient and scalable application beyond the research context to inform and drive quality-improvement strategies.
Chapter 4 Qualitative interview study with prison leavers and prison healthcare staff
Introduction
The qualitative study aimed to explore perceptions of the quality of prison health care from two perspectives: prison leavers (hereon referred to as patients) and prison healthcare staff. Specifically, the study aimed to identify barriers and facilitators of care delivery in prison, and to map these data to a multilayer theoretical framework to develop detailed understandings about prison healthcare quality.
Some material from this chapter has been reproduced from Sheard et al. (2023):
Sheard, L, Bellass S, McLintock K, Foy R, Canvin K. (2023) Understanding the organisational influences on the quality of and access to primary care in English prisons: A qualitative interview study. British Journal of General Practice, 100166
This article is licensed under a Creative Commons Attribution 4.0 International License (CCBY 4.0) which permits use, sharing, adaptation, distribution and reproduction in any medium or format, provided the original work is properly cited. See http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Methods
Ethics approval
We gained approval for the qualitative WP from the University of Leeds School of Medicine Research Ethics Committee (SoMREC) on 17 July 2019 (ref. no. 18-093), which permitted us to interview recently released people who were not on probation. Early engagement with agencies, however, identified that restricting eligibility to people not on probation would be likely to impede recruitment. We therefore sought approval from Her Majesty’s Prison and Probation Service (HMPPS) National Research Committee (NRC) to enable us to recruit people on probation. HMPPS NRC approved the study on 24 December 2019 (ref. no. 2019-383). As a result of the COVID-19 pandemic, HMPPS NRC suspended approval for all research studies on 20 March 2020. Fieldwork resumed in mid-July 2020.
Sample
Recruitment
We aimed to recruit around 15 participants in both of the participant groups, which was initially felt to be sufficient to ensure heterogeneity. Discussions with stakeholders resulted in a decision to extend the sample sizes in both groups to 20–25, to enable the inclusion of a wider range of healthcare professionals and a more diverse sample of patients. In particular, we were advised to ensure that women and those with chronic physical health conditions were represented in the patient sample. Ethical approval to increase the sample sizes was obtained. Prior to the pandemic, we had planned to conduct face-to-face recruitment of patients, and face-to-face interviewing of participants in both groups. Instead, virtually all recruitment and fieldwork were conducted using remote methods, that is, by telephone or video call.
Patient participants were recruited with the help of PPI consultants (n = 9), via local service providers (n = 6), Twitter (n = 3), a lived-experience panel (n = 2) and snowballing (n = 1). We monitored participant characteristics throughout recruitment. As the fieldwork progressed, we identified two key characteristics that were either absent or under-represented: women, and people with long-term physical health conditions. We made further recruitment efforts to address this limitation. Following advice from project team members, we contacted over 25 organisations, including hostels, third-sector organisations and theatre companies. Four women, two of whom had physical long-term conditions, were ultimately recruited to the sample, along with a further two men with long-term conditions.
Healthcare staff were recruited to the study via a range of routes. Facilitated by project team members, a global e-mail was circulated amongst Spectrum healthcare staff, which recruited 11 people, with a follow-up e-mail generating a further 3 participants. Heads of health care at another prison healthcare provider, Practice Plus Group, distributed information within teams, which resulted in two staff joining the study. A further two people responded to study promotion on Twitter, and one person was recruited via snowball sampling.
The sample was continuously monitored during the recruitment process, and project team members were asked to approach people performing prison healthcare roles that had not been included in the sample. A further three people participated in the study following approach by project team members.
Data collection
We interviewed 21 prison leavers and 22 prison healthcare staff. Data collection took place between November 2019 and March 2021. All interviews were conducted one-to-one, with two interviews conducted face-to-face before the pandemic, and the remaining 41 interviews conducted remotely via telephone or video call (staff), or by telephone (patients). Interviews with patients were between 18 and 73 minutes long (average = 35.4 minutes), and with prison healthcare staff between 31 and 61 minutes (average = 46.5 minutes).
Due to approximately all of the data collection being remote, and in line with guidance provided by SoMREC, most participants gave audio-recorded consent (n = 36), following discussion of the consent process with the researcher. The two patients who took part in pre-pandemic face-to-face interviews gave written consent, and five staff chose to e-mail completed consent forms which were then signed by the researcher and returned.
Although we informed participants that notes could be taken instead of audio-recording the interview, all participants consented to being recorded. Audio consent recordings and completed consent forms were stored on a separate server (or in a locked cabinet) to interview recordings. All audio recordings were stored in encrypted format, with the decryption key known to only three researchers (SB, KC and LS). Interview recordings were sent via a secure delivery service to a transcription company where they were stored on a secure server and deleted within 14 days of transcription.
Participants’ names were rarely mentioned in the interview recordings, but participants would frequently name prisons, NHS organisations, voluntary services, local areas or, very rarely, the names of prison staff. To ensure anonymity, names of individuals were deleted from the transcript, and the names of organisations or areas were replaced by codes stored in a password-protected spreadsheet, with the password known only to SB, KC and LS. A total of 48 prison establishments were mentioned in participant accounts, including open and closed female prisons (n = 8), adult male prisons (categories A–D, n = 38) and male young offenders’ institutions (n = 2).
Data analysis
Data from both groups have been mapped to a multilayer barriers and facilitators matrix which has been informed by Ferlie and Shortell’s67 approach to improving quality of care. In brief, Ferlie and Shortell67 argue that quality improvement in health care requires attention to four levels – the individual, the group or team, the organisation, and the larger system and environment within which the organisation is embedded. These layers are to some degree artificial due to myriad interdependencies: several issues operate at multiple levels. Nevertheless, it provides a useful heuristic to attempt to understand the complexity of care delivery and receipt in the prison setting.
It is important to outline how the model has been interpreted for the analysis. We have understood the individual level to pertain to psychological phenomena, including motivations, intentions, attitudes, beliefs and responsibilities. Examples include professional identity for staff, and a lack of autonomy or control for patients. These data account for a relatively small proportion of the full data set.
Data have been mapped to the group/team level where they relate explicitly to interpersonal processes within and between healthcare staff, prison officers and patients. Examples of data mapped to this level are intersubjective decision-making processes regarding care and the creation and maintenance of reputation. A substantial proportion of the data set was mapped to this level.
The organisational level accounts for most of the data collected. We understood this level to relate to perceptions of organisational culture, the organisation and delivery of health care as part of the prison regime (including access to health care), quality assurance, continuity of care as people move between prisons or in and out of prisons, material resources and contractual issues.
Finally, the larger environment/system level was understood to refer to forces beyond the prison environment, such as national or regional data infrastructure, clinical policies, standards and codes of conduct, national screening programmes and decisions made at national level regarding prison funding. Data mapped to this level were relatively sparse.
The data did not map in a straightforward way to the participant groups. Data presented here capture participants’ perceptions of barriers and facilitators and are not intended to represent factual accounts of policy or practice. A unique identifier is attached to each excerpt in the following format: gender, age, prison category(ies) (patients); healthcare professional (HCP)/prison category(ies) (staff).
Findings
Participant characteristics
Participant characteristics are presented in Table 5.
| Characteristics | Patients | Healthcare staff | |
|---|---|---|---|
| Gender | Male | 18 | 16 |
| Female | 4 | 6 | |
| Age group | 20s | 3 | 3 |
| 30s | 7 | 2 | |
| 40s | 10 | 9 | |
| 50s | 0 | 6 | |
| 60s | 1 | 1 | |
| Ethnicity | Black African | 1 | 0 |
| Black English | 1 | 0 | |
| British Asian | 3 | 0 | |
| White | 0 | 1 | |
| White British | 12 | 18 | |
| White English | 2 | 0 | |
| White Scottish | 0 | 1 | |
| White/Black Caribbean | 1 | 0 | |
| Arabic/English | 0 | 1 | |
| Not stated | 1 | 1 | |
| Male/female estate | Male | 18 | 18 |
| Female | 4 | 3 | |
| Both | – | 1 | |
| Prison category: male | A–D | 1 | 0 |
| A | 0 | 3 | |
| B | 4 | 5 | |
| C | 0 | 3 | |
| D | 0 | 2 | |
| A/B | 0 | 1 | |
| B, C | 10 | 1 | |
| B, C, D | 2 | 1 | |
| B, D | 0 | 1 | |
| C, D | 0 | 2 | |
| Prison category: female | Closed | 2 | 3 |
| Closed/semi-open | 2 | 0 | |
| No. of sentences in last 5 years | 1 (but many previously) | 1 | – |
| 1 | 10 | – | |
| 2 | 3 | – | |
| 3–4 | 2 | – | |
| Many | 2 | – | |
| Years in prison health care | 1–3 | – | 6 |
| 4–7 | – | 7 | |
| 8–10 | – | 2 | |
| More than 11 | – | 6 | |
| Not stated | – | 1 | |
| Profession | Administrator | – | 1 |
| Associate practitioner | – | 1 | |
| GP | – | 2 | |
| Health promotion worker | – | 1 | |
| MH nurse | – | 1 | |
| Nurse – band 5 | – | 2 | |
| Nurse prescriber | – | 1 | |
| Occupational therapist | – | 2 | |
| Pharmacy technician | – | 1 | |
| Physiotherapist | – | 1 | |
| Recovery worker | – | 1 | |
| Recovery/service development | – | 1 | |
| Senior clinical manager | – | 3 | |
| Senior nurse | – | 4 | |
| Years in current role | 1–3 | – | 9 |
| 4–7 | – | 7 | |
| 8–10 | – | 5 | |
| 11+ | – | 1 | |
Barriers and facilitators analysis
For a brief summary of the barriers and facilitators, see Table 6.
Individual level
Data that were mapped to the individual level related to psychological processes and internal attributes such as emotions, knowledge, autonomy, personal responsibilities and motivation. Barriers at this level relate to the impact of the system on autonomy and emotions that can hamper access to or delivery of care: facilitators to participants’ motivations or attitudes that enable them to work within or around the system.
Barriers
Lack of control
A recurring theme in the interviews with patients was a sense of lack of autonomy and control over their access to health care or to over-the-counter medications. Although some prisons have self-service kiosks where patients can request healthcare appointments and medication electronically, other prisons rely on a system involving paper applications (‘apps’), which patients complete and deposit in a box on the wing. Compared to care in the community, health care in prison was less likely to be viewed as something which could be influenced by individual agency, as one participant explained:
There might be a waiting time [in the community] but you know where you stand, you get to talk to the people that you want to talk to, you can speak to the doctor, they ring you within 24 hours … you can raise your concerns, you can get an emergency appointment.
M49/B
Furthermore, there was a sense that the more a patient tried to exercise control over access to care, the less likely it was to be successful. Several participants perceived that repeated requests for help could irritate officers and therefore be counterproductive, as one person explained: ‘You keep putting apps in and you will just piss the officers off. They will see an app and put it in the bin’ (M27/BC). This sense of a lack of control was more broadly embedded in the perception of not having equivalent human rights to people living in the community; participants described feeling like ‘second-class’ (M29a/BC) or ‘lower-class’ (M43b/BC) citizens. This could translate into demeaning or frustrating experiences such as not having the opportunity to shower before a healthcare appointment, having appointments cancelled with little warning, not having access to pain medication perceived to be commensurate with clinical need, or having complaints ignored.
Emotional responses
Experiencing frustration was not the sole province of patients: staff also described dealing with similar emotions caused by a range of factors including perceptions of laziness in other staff, inconsistency in the quality of nursing care and lack of co-operation from prison officers. In part, frustration could be caused by an inability to provide care in a manner consonant with their sense of professional identity. Recounting trying to deal with a very distressed patient without support from the MH team, one nurse working in a category C prison noted:
I felt useless, because we just couldn’t do anything for him. And it’s awful to watch, because I’d known him for years, known him since he was a sprog, been coming in and out since he was a juvie.
HCP-12/C
Wishing to support patients, but being constrained from doing so by lack of support, the regime, or occasionally by patients themselves: ‘you think, we’d just got that wound looking really nice, and then you got upset, and now it’s back to square one again’ (HCP-16/A), could lead to feelings of burnout.
Feelings of resignation were occasionally expressed by people in both participant groups – a perception that both staff and patients would have to manage the best they could in an enduring system. One patient, describing problems gaining access to his diabetic medication, observed that it was ‘literally just usual prison difficulties getting things you’re supposed to have’ (M36/B). Similarly, a GP noted that:
I’m so busy when I’m in there, I don’t feel that I have the time to report every little thing that is frustrating about the job …. So we let things go and I suppose eventually you’d develop a mentality of ‘Oh flip, nothing is ever going to happen, I’ll just cope with the way things are’.
HCP-05/CD
Patient knowledge and literacy
Several staff perceived patients to have minimal engagement with healthcare services outside prison, and to have limited knowledge of health conditions, which could impact their likelihood of accessing health care. This is potentially compounded by ‘invisible’ conditions, such as diabetes and by low levels of literacy. Low levels of literacy could not only hinder people from attending appointments, but could prevent them from using the application system altogether, as one GP explained: ‘first of all they have to put their problem in writing which is very difficult for some of them because they can’t write properly’ (HCP-05/CD).
Facilitators
Patients emphasised individual traits which could help them to obtain health care. Typically, participants in this group perceived that being assertive, persistent and articulate would facilitate their access to health care. One woman observed:
I am lucky in a way that I’m able to advocate for myself … I have a very good understanding of medical situations … and I can explain them … the time and the setting would make it difficult for people who didn’t have that ability … my overall experience is that health care is something you almost have to argue for and fight for and to a certain extent is associated to privileges.
F48/Closed
Despite the challenges of working in prison, several staff expressed their commitment to what was perceived to be a unique healthcare landscape, with some remarking that they would not wish to work elsewhere. One senior nurse, for instance, noted that:
I would just like to say that I absolutely love my job and I can’t see me going anywhere before retirement. I said they will take me out of there in a box … I don’t think I would fit anywhere else now.
HCP-18/C-D
This sense of the ‘specialness’ of working in prison health care led some participants to discuss the skills needed for clinical practice. The following were seen as skills particular to the prison environment:
-
Being able to cope with the constraints of working in a setting where security, rather than care, is given primacy.
-
The ability to adapt communication to people who may be distressed, abusive and disadvantaged.
Engaging with patients provided opportunities to make a difference to people’s lives, as the two quotes below exemplify:
I love working in prisons, I love it. I love working with prisoners, they are the most motivated, engaged, enthusiastic, grateful, everything that people wouldn’t think that they are. They are just the most endearing group of people … that I’ve ever worked with, so I stick with it because they are amazing. The rest of it is utterly hideous, to be honest.HCP-20/B
I feel it’s a place where I can really achieve things. It’s not like going into a well-run general practice where … patients are lovely and everything works perfectly. It is a place where you can really make changes and where you can, on an individual basis, you can really help these people.
HCP-09/BCD, Closed
The sense of fitting into the prison environment also required staff to present themselves in particular ways. One senior nurse, for example, stated that ‘if you are really, really soft and fluffy I think you would get walked on’ (HCP-18/C-D). Poor levels of staff retention were commonly attributed to individuals not being personally suited to working in prisons; in contrast, some staff who had intended to stay for a short time found high levels of job satisfaction.
The ability to provide care in the context of a strict regime was perceived by staff to be facilitated by individual proactivity and creativity. Identifying opportunities to improve care, being motivated and having confidence to make changes, and finding ways to work around the system were described by some of the staff. However, such innovative working could be vulnerable to being drawn away to perform other clinical tasks, as one recovery worker explained:
Our IDTS (Integrated Drug Treatment System) nurse is very good …. She has great plans for being proactive with the vulnerable population of men that also have substance misuse problems …. She will even do things like building a therapeutic alliance and run a detox group pre-COVID. She … receives no support for that. Although her role is part of health care, because she is a nurse she gets pulled to do an awful lot. She is just seen as an extra primary care person. She is not.
HCP-01/C
Group/team level
Data mapped to the group level relate to intersubjective processes between three groups: healthcare staff and patients, healthcare staff and prison officers, and prison officers and patients. Barriers at this level describe ways in which care quality is adversely affected by relational factors, while the facilitators are examples of ways in which positive relationships can benefit experiences of health care.
Barriers
Healthcare staff and patients
In general, patients reported positive interactions with healthcare staff, acknowledging the effect of under-resourcing on time available for interactions. Nevertheless, patients described some difficulties with the patient–clinician relationship. Some felt that nurses were more approachable than doctors, and that doctors were more likely to be condescending. However, such a narrative needs to be considered in the context of its being the doctor’s responsibility to conduct the challenging consultations of declining to prescribe analgesia (which has habit-forming potential) when there is no reasonable clinical indication. Indeed, requests for analgesic medications was the most frequently cited cause of tension in patient–staff relationships. While a few participants reported trying to acquire medication not related to their health conditions, it was more common for people to describe instances of having genuine need for which appropriate medication was not provided: ‘it’s very hard to be believed … a lot of the healthcare time is taken up deflecting’ (M45b/B-D); ‘instead of treating each person on their merit, they treat you the same across the board’ (M60/A-D). Several participants alluded to only paracetamol being available, even for a ‘snapped leg’ (M41/BC) or ‘broken arm’ (M45a/B). While recognising that some people would seek to acquire medication for recreational use or trading, patients felt this had the undeserved consequence of prescribers labelling all patients as drug-seekers. This sense of everyone being treated the same in prison, rather than as individuals, and that assumptions were made regarding medication, could be experienced as ‘quite demeaning and insulting’ (M35/BC). A few participants described feelings of dehumanisation and disrespect as a result of their interactions with healthcare staff. Participants suggested that while they deserved to be punished for crimes, the punishment should be incarceration, rather than receiving poor treatment or reduced access to health care.
Most of the healthcare staff participants suggested that their relationships with patients were positive; however, a few made negative observations about their colleagues’ relationships with patients. One person reported witnessing nurses tearing up application slips, while another noted that staff were not presenting a professional appearance to patients, by not wearing gloves or tying up their hair. These were believed to be manifestations of poor attitudes towards people in prison, as one recovery worker explained:
I find a lot of the nurses that I work with, their attitudes mostly are poor …. They are always ready on the back foot or the attack …. They have this negative view of, ‘You shouldn’t be in prison in the first place’. Some of them are trying their best to do as little as possible. They will take a two hour lunch break and then say, ‘I haven’t had time to look at the applications’ …. But you were sitting down for two hours chatting with the prison officers. It infuriates me.
HCP-01/C
The poor attitude towards patients was expressed in the dehumanising language used, according to a senior manager in the male estate, who recognised the need to encourage empathy among healthcare staff:
They would say … ‘Oh my god, this screeching man, this prisoner is a bit of a nightmare’, that’s just an example of the type of language …. And I would stop the conversation and say ‘Okay, so, can I just support you to reframe that? Are you saying this gentleman has learned some maladaptive behaviours that are very challenging, and we’re struggling to understand how we assist him with that?’ And initially it caused a bit of a titter across the team.
HCP-21/B-C
Healthcare staff and prison officers
Relationships with prison staff were variable, dependent on how accommodating officers were perceived to be. The most commonly cited barrier was the difficulty in persuading prison staff that a patient needed access to care. Staff reported that a patient may not be unlocked for an assessment, or, more typically, the need for a patient to attend Accident and Emergency could be challenged. Healthcare staff reported feeling dismayed that their clinical judgement could be brought into question by staff with little healthcare knowledge. Occasionally, combative terms would be used when describing trying to gain access to patients:
Sometimes you have to pull rank and say, ‘You bring this individual up to health care or I will send them out to hospital’. … I shouldn’t have to use that. I am not saying it is a threat, but I use it in the example of, ‘If they don’t come up and get reviewed here it is going to worsen; they will end up in hospital and they will end up as a bed watch’. Then all of a sudden you have staff everywhere crawling out of every nook and cranny. ‘You told me you didn’t have staff this morning, now I have eight officers stood in front of me?’
HCP-08/B
Importantly, established relationships between the prison staff and the healthcare team could make substantial differences to the numbers of people seen in a clinic. In one category C establishment, officers perceived as accommodating could improve the efficiency of the clinic by bringing patients one by one to the clinic, whereas those less willing to co-operate could make the service inefficient:
Some of the prison staff are brilliant; if it’s one of the ones we’ve known for a while, they’ll just say ‘Right [Name], who are we getting after this?’ And then as soon as they bring the first one over, he will then go back … to bring the next one over. So, it runs really smoothly, and I got to see about 16 on Sunday which is amazing …. On another day with different staff, I might be lucky if I see six, because they’ve got no … initiative. And you say to them ‘Can you just go to [wing name] and get me so and so ready for when we shout?’ They go ‘No, I’m going to stay here until you’re finished with the ones you’ve got’.
HCP-12/C
Prison officers and people in prison
Reports of relationships between prison officers and people in prison varied considerably. Generally, prison leavers reported that officers formed an opinion of them, and acted in accordance with that opinion. Two participants reported that new patients on the wing, unknown to officers, may not be unlocked for medication. Others perceived that officers violated their human rights by delaying or withholding access to health care, and felt that access to health care could be contingent upon their behaviour. One person, who described himself as not being an ‘angel’ in prison, felt that his access to health care was delayed for withholding information from officers about a fight on the wing:
There was a bit of an altercation on the wing. I snapped my tibia in two places and it took them 3 days to get me out to the hospital …. Possibly because I wasn’t prepared to speak about what was going on. It was quite serious. I fractured my eye socket. I was punished for not saying who it was. I believe that was why the health care was withdrawn.
M27/BC
Other participants reported similar impressions, with some reporting that officers could call healthcare staff to attend to a problem rather than asking the person to put an app in which could entail a lengthy wait. It was not uncommon for participants to state that those who were perceived to be less likely to cause difficulties could receive privileged access to care:
If you were a well-behaved prisoner and you went for work on time and didn’t cause the officers any trouble, but you went with a bad back, you seemed to get a new mattress within a week and painkillers the next day …. If you are a chronic self-harmer who takes his anger out on officers and is rude to healthcare staff, but you threaten to kill yourself tomorrow, you get to see health care in 2 weeks’ time. It seemed to be the back of the queue if you were not well-behaved and obnoxious and aggressive …. You could kill yourself tonight. The guy with a bad back is just waking up with a stiff back, but he doesn’t cause the officers any trouble and when he goes to health care …. He gets his new mattress and his painkillers by evening.
M29b/B
Officers broadcasting or publicising people’s reasons for visiting health care could be experienced as stigmatising, and may deter care-seeking. One person reported that a noticeboard indicated which people had an appointment with the sexual health team. Similarly, one member of staff reported that officers would ‘be banging on the door’ to inform people that they were due to attend a Hearing Voices group.
Facilitators
Healthcare staff and people in prison
Over half of the staff in the sample reported that having long-term relationships with patients facilitated the delivery of health care. Staff perceived that people in prison were more likely to trust healthcare staff – who were not seen as holding positions of authority in the prison regime – than prison officers. Familiarity with people in prison could inform decisions about in-possession (IP) medication and enabled observations of changes in a person’s general demeanour, noticing the ‘subtle differences’ (HCP-17/Closed) even when clinical observations did not indicate a problem. Aspects that promoted the development of trusting relationships appeared to be listening, involving patients in decision-making, and showing compassion and commitment to care. Communicating using visual aids for people with low levels of literacy, hand-delivering appointments for sensitive issues, such as cervical screening, and showing people clinical equipment in advance were also perceived to promote trust.
It’s just having manners and listening … because they are never listened to … throughout their lives, people haven’t often listened … I think sometimes I’ve noticed the element of touch … being in a prison as a nurse, if somebody is upset, just putting your hand on their arm.
HCP-15/Closed
Communication within healthcare teams
Many of the staff participants described good communication and working relationships with other healthcare staff, both within and beyond the prison, as key to providing quality health care to people in prison, and which, to some extent, could mitigate the problems caused by short-staffing. Managers feeding back positive care outcomes to staff was perceived to be helpful to motivate staff. Proximity was important: having different teams (e.g. primary care, MH, health promotion and substance-misuse teams) in the same building was reported to be beneficial, especially for dual diagnosis management, whereas communicating with teams off-site was perceived to be a barrier to healthcare delivery. The GPs in the sample praised nursing teams, remarking on the efficiency of care and the compassion with which nursing care was delivered. These informal relationships could promote workarounds, as one nurse observed:
We’re very lucky in some ways; the on-call doctor service that we’ve used, the 111, one of the doctors is a friend of mine and he did something he shouldn’t have done, he gave us a direct number to bypass 111 should we have an emergency.
HCP-12/C
Frequent multidisciplinary team (MDT) meetings were cited by two managerial staff as key to promoting change and improving standards of health care. These meetings were described as nurturing and supportive, subtly challenging outdated attitudes or practices. MDT meetings regarding planning of pain management for individuals were perceived to be a particularly useful way of sharing decision-making responsibility.
Organisational level
Data classified as organisational level, which formed the largest segment of the data set, related to the ways in which the culture within and across prisons, the organisation of services, resources, quality assurance and contractual issues could facilitate or hinder care quality.
Barriers
Staffing levels
Both participant groups reported the main barrier to delivering quality health care to be staffing levels. Difficulties attracting staff to the prison setting were perceived to be challenges of the environment and the population – ‘it’s like your most complex patients in a GP practice times 650’ (HCP-09/BCD, Closed) – but other barriers were mentioned, such as the time needed to clear security checks, and, compared to non-prison settings, inferior terms, conditions and career development opportunities.
Managerial staff described the impact of under-staffing on the ability to make innovations in the service. A senior manager in the male estate with a 50% backfill of agency staff found that service improvement was hampered. Similarly, a GP remarked upon the extensive use of locum GPs, noting that there was little incentive to become a substantive staff member because of the significantly higher pay that locums received. This impacted on longer-term service development:
It’s about … having clinicians who are interested in what they do and obviously with some of the locums you are not getting the buy-in that we do from your substantive staff, so not getting the people who are interested in creating new pathways, implementing new ideas.
HCP-09/BCD, Closed
Managerial-level staff also remarked upon the need to regularly review the skill mix in their teams, given trends in the prison population, such as the increase in older patients. One senior manager identified the need for more long-term-condition nurses, for instance, while a nurse noted that long-term-condition pathways were only just becoming established in her workplace (a remand prison), as historically residence had been viewed too short-term to implement chronic care management.
People in prison often remarked that healthcare staff were doing a good job, but in difficult circumstances. Reception appointments were sometimes described as ‘rushed’ (M41/BC), and people remarked on the length of queues to see the nurse. Queuing for medication was generally perceived to be an unpleasant experience or one that required making decisions how to spend time:
It was so much hassle, that in the end I just gave up taking the meds … it was just a fight all the time and sometimes you just don’t have that fight in you … it’s all people jumping in and fights going on and drug dealing going on around you … and you are getting involved in stuff that you don’t want to be involved in.
M45B/B-D
Lack of preventive care for mental illness and distress
Under-resourcing of health care led people in both participant groups to describe health care as reactive and crisis-led rather than preventive, particularly in relation to mental health care. We explore this issue in much greater detail in Chapter 7.
Unreliable communication pathways
Patients perceived the chain of communication for health care to be easily disrupted: ‘nine times out of ten it gets lost in transit … you get a slip through your door “your appointment was yesterday”’ (M60/A-D). Gaining access to appointments and test results was often described as depending upon a range of people including healthcare staff, prison officers, administrative staff and occasionally fellow patients who may be given the responsibility of delivering healthcare slips. Additionally, complaints were often reported as ignored. The resultant frustration among patients was reported by both participant groups.
Breakdowns in the chain of communication were perceived to be partly to blame for numbers of people not attending appointments, known as ‘did not attends’ (DNAs). People may not be aware they had an appointment, may not have received a movement slip enabling them to leave work or education to attend, or may not have their attempt to cancel an appointment recorded. However, issues from the security side of the prison could also impact on non-attendance, for example, incidents could result in wing lockdowns, people not being unlocked by officers, or, during COVID, officers not deeming the appointment necessary. People may have also moved wings, or, for remote appointments, the telephone in the cell may not be working. Other reasons for DNAs noted by staff were that the person may not realise the importance of the appointment, go on ‘walkabout’ (HCP-12/C), change their minds, fear a diagnosis, or dislike being in the waiting cell. One staff member reported that DNAs could be inaccurately coded as a refusal to attend:
Sometimes it isn’t their fault but it can be coded as a ‘failed to attend’ and that makes the figures look convenient. It’s easy to say they didn’t go, isn’t it?
HCP-15/Closed
There was some variation in what would happen following a DNA. The administrator, who worked in a remand prison, reported that the wing would be contacted to find out why the person hadn’t attended. Appointments were rebooked if the person had a ‘no access visit’ – a reason they hadn’t been able to attend such as court – but not rebooked if the person had refused to attend, unless the appointment was for a blood test, an electrocardiogram (ECG) or a dressing change. In other establishments, clinical staff would follow up with patients ad hoc if they had time, while in others the appointment would not be rebooked.
Difficulties with continuity of medication and care
Managing medication was regularly highlighted as an issue in relation to the administration of time-critical medications and the maintenance of medication for people arriving in prison. With regard to the latter, the timing of arrival was crucial. Urgent medication could be quickly arranged for people arriving Monday–Thursday, but Friday arrivals may necessitate a telephone call to out-of-hours GPs and a visit to a community pharmacy. In addition, out-of-area hospital appointments could cause a problem for the receiving prison, as one senior manager in the open estate noted:
You can bet your life on a Friday afternoon we’ll get a reception pitch-up who has got complex needs, who has got a hospital appointment in 2 days that he’s totally out of area, they’ve got no medication. All these things we are having to deal with.
HCP-03/D
Administering medications at certain times could also be difficult if it conflicted with the prison regime. Night sedation requires risk assessments, and some medications need to be taken at certain times of day. As one nurse noted, ‘we try and stick to the times as close as we can for those, but things happen’ (HCP-16/A). For one person with type 2 diabetes, not being known by prison staff during the start of his sentence meant that there were occasions during a short sentence (5.5 months) when he was not unlocked to receive metformin, a medication that should be taken at around the same time every day for optimal control of diabetes.
Sometimes the prison officers wouldn’t unlock me for my medication. I would press my bell and they would say, ‘You are not on the list’. I would say, ‘Go and ask the healthcare guys. They will tell you that I need to be unlocked’. A couple of times I didn’t get my metformin for those reasons …. Eventually health care gave me the metformin in-possession … I get that there are security issues and I was someone who hadn’t been in the prison very long, the prison staff didn’t know me, but at the end of the day if I am on the medication list then I should be getting my medication.
M36/B
Performance measurement
Staff participants were asked about the use of performance measures in prison health care. Junior staff and one of the GPs reported that, although aware of targets, they tended to have no involvement with audits, which were seen to be the province of healthcare managers. In general, managerial staff reported that the use of the QOF indicators, and, less commonly, the HJIPs (being phased out at the time of writing), routinely helped them to identify areas of performance that needed improving. The QOF was perceived to be more useful by the administrator, who noted that the HJIPs, based on monthly figures, may give a slightly misleading picture of current needs:
So, say you’ve got 300 patients eligible for an MMR vaccination at the end of the month …. But actually, a lot of those patients have been released or transferred but they’re still counted …. A lot of the patients don’t come into your custody until the last working day of the month, and they’re still on your eligible figures but you can’t actually do any interventions with them … the QOF’s a little bit better in that respect in that it only has the patients that are there on that day.
HCP-06/B
A criticism of quality indicators was that they were not always seen to be a true measure of performance, and were perceived to be limited in scope, such that some conditions received less focus. Others suggested that what was being measured was not necessarily indicative of care quality. A GP noted that ‘I think there’s focus sometimes on getting the tick in the box rather than actually improving people’s lives by what we are doing’ (HCP-09/BCD, Closed). In a similar vein, a senior nurse noted that performance measurement should assess ‘what we [are] actually doing that’s really real, not just you’ve done 10 ’flu vacs or 10 whatever’ (HCP-15/Closed). Other difficulties with quality indicators were that some staff argued that coding may be poor, that staff may not have received training, that the search function was limited and that there may be several templates for recording a single problem.
Some staff described complaint procedures and consultation with people in prison as other routes through which to assess performance, with some valuing the use of independent agencies, such as A Better Life. However, there was very little evidence of how complaints were used to inform or improve service delivery. One senior manager in the male estate noted that, prior to their tenure, ‘that pathway wasn’t working, so there could have been 400 complaints and we wouldn’t have known about it’ (HCP-21/B-C). Patients were generally disparaging about the complaint process. Although some people had received apologies as a result of complaints, or had managed to take complaints as far as the Ombudsman, it was not uncommon for people to report that they had received no feedback at all, and some doubted that the complaints had even reached their intended destination. One person stated:
The complaints go as far as you can throw them … I’ve put loads in, me, but you never hear anything back because the officers will get it and just bin it …. You have to hand them in to an officer …. But every other app, you put in a box. But for the complaints, you have to hand it to an officer, which is funny, isn’t it?
M29a/BC
The prison environment
Several participants remarked upon inadequacies in the environment which hampered the delivery of health care, or the maintenance of good health through adequate sanitation. As well as a greater use of telephone consultations, the COVID-19 pandemic had caused an increase in the delivery of care in wings and cells, with a corresponding impact on time for staff to travel around the prison. However, the physical spaces on the wings were described as poorly lit, cramped, and ill-equipped for clinical practice.
Providing spaces within health care for clinicians could also be challenging, particularly for allied health professionals (AHPs). A senior manager in a Category A prison, for example, struggled to find space for visiting AHPs, which impacted on waiting times for these services. Older prisons, built in the Victorian era, were perceived to be both more problematic than modern prisons and detrimental to the MH of people in prison:
[Modern prisons], it is a lot better on your mentality, yeah. One hundred per cent. A million times better in that kind of environment than in an environment like MB-02, which is … like I say, the whole environment, the building, the architecture made it to be domineering and to put you in a certain mind frame.
M38/BC
Racism
Three patients – two women and one man – referred to racism in prison. The man, who identified as black English, reported that healthcare staff of African ethnicity held racist attitudes: ‘a lot of the times the African women, men, are the ones you have problems with because … they just seem to have a bad attitude, like a superior attitude … they seem to have a chip on their shoulder’ (M45b/B-D). A female patient perceived white women to receive faster access to health care than women of colour, and observed the impact of the lack of interpreters on health care for people for whom English was a second language:
I felt like there was a lot of racism involved with health care. So if you are brown skinned, they don’t want to know you. It’s like you are at the bottom of the list …. So I could have put an application in to see the GP and somebody else would have put an application, both of us are low risk, both of us are asking for the same thing, yet I would have had no response forever and that other person would have got a response within a couple of days and been seen. And this was a regular occurrence with many women from a black and Asian background.
F39/Closed/semi-open
Facilitators
Continuity of care
Good communication between health care and pharmacies in sending and receiving prisons was perceived to facilitate continuity of care, and to assist healthcare departments to identify who was eligible for screening or vaccinations. One person with type 2 diabetes reported that all of his regular checks were carried out, including retinal screening, while a participant with HIV also reported regular viral load tests being conducted. Use of SystmOne and summary care records and direct communication between people in prison healthcare departments, or between prison and cancer screening hubs, were perceived to enable this.
Thorough and detailed screening at reception was seen to be beneficial to identifying health needs and referring to appropriate teams:
I have been here two and a half years and [reception] has changed about five times since I have been here. That is the main one we are always checking because if we can get a good reception process, that leads to a better standard of care. If the reception process is good then the right teams from the start are involved …. They put more options in for free text [where a member of staff can add ad-hoc comments providing further narrative] and you can’t really click off unless you free text now on some pages, which is good.
HCP-17/Closed
Safer prescribing
The creation of shared decision-making and medication reviews within pain-management pathways were regarded by staff as a useful way to respond to the challenges of medication diversion. Conservative management of pain using exercises, transcutaneous electrical nerve stimulation (TENS) machines and physiotherapy in one prison cluster involved extended individual appointments and a multidisciplinary approach to assess pain relief:
Everyone wants Gabapentinoids. Gabapentinoids are the bane of my life …. We now have a pain management pathway and we hold an MDT, so we have a process where the patient [has] a 20 minute to half an hour appointment to … thrash out their concerns and expectations … that information is brought along with a host of other information to our MDT, which we also have substance misuse, the doctors there, we have a report from the physios, we have a report from the wing staff because it’s not unusual for them to be doing cartwheels up and down the wing and then be crippled when they come in to see me, and then a decision is taken on what to do about their medication …. Because we have this appointment, patients are given the chance to actually tell us their views and people are going away from that appointment very pleased.
HCP-09/BCD, Closed
Service integration
Although some staff participants highlighted silo-working as an inhibitor to quality care, there were some examples of service integration, particularly where the provider was responsible for recovery and healthcare services. Having the MH team in reception in one remand prison also facilitated referral on entry. While a barrier to health care was that officers were not able to access patient information, in one inpatient unit patients were given an opt-out regarding information-sharing, which facilitated better care delivery.
Performance measurement
Although criticisms of performance measurement were identified in the previous section, managerial staff reported the ways in which the use of quality indicators helped them to monitor service delivery. One senior manager reported that reviewing waiting lists, for example, enabled him to plan for clinics from visiting clinicians, while other staff noted that audits assisted them to identify gaps, compare performance with national standards and improve services accordingly. Part of the process of assessing performance was perceived to be identifying meaningful clinical actions.
System level
Data relating to the system level, that is, that relates to the broader system in which prison health care is situated, were more sparse than for the other layers in the model. Nevertheless, both participant groups contributed some data on barriers and facilitators to care quality that were mapped to the system level.
Barriers
Prison–community general practice interface
Prisons in England and Wales use SystmOne to manage electronic healthcare records; however, only around a third of community general practices use the same system. Two patients reported that their medical records had gone missing in the prison setting. The administrator in the sample explained that even when community GPs use SystmOne, not all the records may be visible. Prison healthcare teams may therefore have to request summary care records from GP practices to ensure continuity of care, and some practices may not recognise the urgency of the request for information:
they [community general practices] think we can see everything, and at this stage – we will eventually – but at this stage we can’t, and to remind them that when we ask them for it, we need it soon …. Because without the confirmation, if we have nothing on the system, the patient will not be prescribed.
HCP-06/B
At the other end of the prison journey, some staff expressed concerns that care may not be continued when people are released. While some staff described efforts made to register leavers with a GP, others were concerned that the continuity would falter:
Going through the gates for our men is a nightmare; often the great care they get here ends because they don’t go anywhere or they can’t be signposted … I think the big pieces of work now are how do we join prison health into the mainstream? How do the community recognise us as part of their wider system? We have over 1000 men in prison. So, we need to join into those wider healthcare systems to be recognised more mainstream so that … when a man goes through the gate he doesn’t miss his last hepatitis injection because no one can find him and he doesn’t have a GP.
HCP-21/B-C
Community prescribing practices, particularly of medications that can be diverted, could cause difficulties in the prison environment. Some staff expressed the opinion that patients could pressurise community GPs to prescribe medication without clinical indication, which they expected to continue receiving in prison. As highlighted by one nurse who perceived that NICE guidelines could be applied inflexibly, there was potential for such requests to be an emotive issue and strain interdisciplinary staff relationships:
Sometimes you want to just shake the doctor and say ‘What are you doing?’ Yes, I get NICE guidelines … but we’ve got a lad who’s waiting to be seen in Gastro …. He was on 120 mg dihydrocodeine a day, he’s now on 15 twice a day. He didn’t get told he was being reduced. When it’s somebody with a genuine issue who is waiting to be seen, leave them on the analgesia until we find out what the cause of it is. But we don’t have a say in it. I think doctors in the community are a lot more flexible …. Ours, it’s straight down the line, ‘We’ve been told we have to do this, we have to do it’. And I think the lines can be wavy, they don’t have to be rigid.
HCP-12/C
Financial issues
Somewhat surprisingly, staff participants rarely referred to financial issues, with the exception of suggesting nurses’ posts should be advertised with higher pay to attract staff. Patients, however, did refer to finances. One participant, for example, perceived that prisons received money per resident and received funding for methadone, implying that prisons were incentivised to maintain or increase methadone doses. Additionally, others believed that certain preferable medications were not provided because of costs – for example, methadone instead of Subutex – or that hospital visits were delayed until transfer because of the cost of providing escorting officers and transportation. These were participant perceptions rather than the reality of healthcare delivery financing.
Facilitators
Professional standards and national screening programmes
Several staff members referred to national initiatives, such as NICE guidelines and the Nursing and Midwifery Council (NMC) code of conduct, as being useful standards to adhere to in attempts to provide equivalent healthcare provision to the community. All the women patients reported being offered cervical smears due during their sentence; however, none were old enough to receive routine breast screening. One woman perceived cervical screening to be driven by charities more than the healthcare department:‘there was a really big drive at [prison name] to get women to have their smear tests done … they were offering freebies … but I think that was because external agencies were or charities coming in and promoting things. I think if it was left to the prison I don’t really think they would have’.F39/Closed/semi-open
Impact of COVID-19
Most of the participants in this study had been released prior to the start of the COVID-19 pandemic. Staff talked about the difficulties in providing care when people had to be kept in wing cohorts, which one senior nurse described as a ‘logistical nightmare’ (HCP-18/C-D). Descriptions were given of the increased use of remote consultations (for both internal and external appointments) and a corresponding reduction in face-to-face interactions, a greater prioritisation of care for both primary and secondary care and longer delays waiting for specialist services, such as the dentist, the optician, or to receive physiotherapy equipment. Some areas of discontent emerged: one nurse expressed dismay that GPs were able to perform remote consultations, while nurses had to risk infection through face-to-face contact, while another reported that nurses had to absorb more of the GPs’ workload. Health promotion activities that included external providers coming into the prison and group-based health education were suspended. Because of the need to keep wings separate, staff reported that fewer people were able to attend clinics. This resulted in some staff trying to attend to multiple health issues in one appointment, for example, administering vaccinations when people were able to attend an appointment for another condition.
Suggestions for improvement
From the patients’ perspectives, suggested improvements fell into three categories: access to services and information, relationships with professionals and healthier lifestyles in prison.
In terms of access to services, patients suggested that waiting times for services could be reduced by greater provision. Participants also made suggestions to improve access to medications, including having different queues for one-off as opposed to repeat medications, and for staff to have greater access to the pharmacy. Longer appointments with healthcare professionals to perform a thorough clinical assessment was another suggestion, and greater provision of health information at reception and second screening.
Relationships between patients and healthcare staff were also an area identified for improvement, with several patients perceiving that they were treated with less respect than in the community. People wanted to be listened to, treated as individuals and to not be labelled as ‘drug-seeking’. While in general people appreciated the pressures staff were under, some did not feel that staff demonstrated empathy and commitment to the role.
Similarly to people who have lived in prison, staff called for a greater provision across a range of services including primary care, dentistry, mental health care and allied health services. Additionally, a greater degree of communication and integration with recovery services, security staff, community health services and other prisons were perceived to be beneficial to quality care. Improved terms and conditions for staff including better salaries, career trajectories for AHPs, targeted training and improved relationships between trust providers were thought to ameliorate difficulties with staff recruitment and retention. Upskilling staff and having greater specialisation – for instance, in long-term condition care – were identified as ways to respond to changing health needs of the prison population.
In terms of care provision, an increased use of telemedicine, daily drop-in clinics, along with improving clinic rooms and the functionality of IT systems, were perceived to have the potential to improve care. Finally, more health promotion and health education were identified as ways to support people to manage their own health.
Summary
| Sample | Barriers | Facilitators |
|---|---|---|
| Individual | ||
| Patients |
|
|
| Staff |
|
|
| Group | ||
| Patients |
|
|
| Staff |
|
|
| Organisation | ||
| Patients |
|
|
| Staff |
|
|
| System | ||
| Patients |
|
|
| Staff |
|
|
Chapter 5 An analysis of the quality of care using routinely collected data
Some material from this chapter has been reproduced from McLintock et al. (2023):McLintock K, Foy R, Canvin K, Bellass S, Hearty P, Wright N, Cunningham M, Seanor N, Sheard L, Farragher T. (2023) The quality of prison primary care: cross-sectional cluster-level analyses of prison healthcare data in the North of England. EClinicalMedicine. This article is licensed under a Creative Commons Attribution 4.0 International License (CCBY 4.0) which permits use, sharing, adaptation, distribution and reproduction in any medium or format, provided the original work is properly cited. See http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Introduction
It is accepted that people detained in prison are entitled to a standard of care at least equivalent to that available in the wider community,68 and that neglecting the health needs of people detained in prison has negative implications, not only for the individual, but also for society. 69,70 While the delivery of care may differ, with services tailored to meet the various requirements of the patient, level of security and prison regime, the principle of equivalence is intended to promote equitable health outcomes for this group of people. 68 Concerns raised about access and quality of health care in prisons suggest equivalence is not always achieved. 7,70
Recent research in prisons has focused on important issues such as public health, social care, dementia and mental health and neurodiversity,70–77 but less attention has been paid to the quality of ‘routine’ primary care provision. We aimed to assess the quality of primary care provided to prisoners through analysis of routinely collected healthcare data. We measured gaps between recommended and actual care, and analysed variations in adherence to recommended practice.
Methods
Study design and setting
We conducted repeated cross-sectional analyses of routinely collected, anonymised, electronic, primary care data from 13 prisons in the North of England, measuring achievement against 30 clinical quality indicators. All data were extracted remotely. The analysis included patient and prison characteristics to examine associations with quality indicators (QI) achievement. Data covered the period 1 April–31 March across 3 years (2017–8, 2018–9 and 2019–20), and were extracted between April and November 2020.
Of the 13 prisons, two were prisons and young offender institutions (YOIs) for women aged 18 years and over, one a prison and YOI for men aged 18 years and over, and 10 were prisons for adult males (two category A, three category B, three category C and two category D open prisons). At the time of data extraction, Spectrum Community Health Community Interest Company (Spectrum) was responsible for the majority of primary care provision for prisons included in the study. In five prisons, Spectrum provided GP and pharmacy services, with other services being provided by an alternative healthcare company.
Variables
We identified and applied a set of indicators to assess the quality of primary care in the prison population. We described this process in Chapter 3.
We designed extraction searches based on existing algorithms (e.g. the QOF indicators). This ensured data extraction was efficient and allowed indirect comparison of some indicator achievements with the community. For the same reason, we used a date range for searches that coincided with QOF years for 27 out of 30 indicators, covering 12-month periods ending 31 March for the years 2017–20 (Table 7). For indicators examining opioid, pregabalin and gabapentin prescribing, and prescribing of three or more psychotropic drugs, we used the 8-week period preceding 31 March for the years 2017–20.
| Indicators by group and name | Financial years | |
|---|---|---|
| Communicable disease | ||
| Dry blood spot testing | The proportion of new receptions to prison accepting opt out dry blood spot testing | 2017–8 2018–9 2019–20 |
| Hepatitis B vaccination (1) the whole prison population | The proportion of the prison population who have received one, two, three or four (course of three plus booster) hepatitis B vaccinations in the preceding 12 months | 2017–8 2018–9 2019–20 |
| Hepatitis B vaccination (2) people with a history of illicit drug use (a higher-risk group) | The proportion of people with a history of illicit drug use who have received one, two, three or four (course of three plus booster) hepatitis B vaccinations in the preceding 12 months | 2017–8 2018–9 2019–20 |
| Influenza immunisation | The proportion of people with one or more of CHD, stroke or transient ischaemic attack, diabetes or COPD who have received a flu vaccination between August and March | 2017–18 2018–19 2019–20 |
| MH | ||
| Antipsychotic monitoring | The proportion of people who have received three or more prescriptions for an antipsychotic in the preceding 12 months, and who have a record of blood testing (fasting glucose, HbA1c, lipid profile, urea and electrolytes, full blood count, liver function tests), BMI and blood pressure | 2017–8 2018–9 2019–20 |
| Polypharmacy | The proportion of the prison population prescribed three or more psychotropic drugs (antipsychotics, sedative antidepressants, hypnotics and anxiolytics, pregabalin or gabapentin, opioids) at the same time during an 8-week period | 2017–8 2018–9 2019–20 |
| Mental state examination | The proportion of people aged over 55 years in the prison population who have a record of one of the following assessments in the preceding 12 months; MMSE, 6-item CIT, GPCOG | 2017–8 2018–9 2019–20 |
| Diagnosis of dementia | The proportion of people with a new diagnosis of any form of dementia in the reporting year, and who have a record of the following blood tests between 12 months before and 6 months after the date of diagnosis: full blood count, calcium, glucose and/or HbA1c, urea and electrolytes, liver function, thyroid function, serum vitamin B12, folate levels | 2017–8 2018–9 2019–20 |
| Prison-specific | ||
| Consent to transfer medical records | The proportion of new receptions to prison who have been asked for consent to transfer medical records from GP to prison health care | 2017–8 2018–9 2019–20 |
| MR | The proportion of new receptions to prison with a code for a second-stage health assessment in the past 12 months, plus clinical codes for IP risk assessment and MR added in the week before the second-stage assessment | 2019–20a |
| Opioid and gabapentin prescribing |
All during an 8-week period |
2017–8 2018–9 2019–20 |
| Diabetes, asthma and epilepsy care | ||
| Blood pressure control in diabetes | The proportion of people with diabetes in whom the last blood pressure reading (measured in the preceding 12 months) is 140/80 mmHg or less | 2017–8 2018–9 2019–20 |
| Processes of care for diabetes | The proportion of people with diabetes who have had the following in the preceding 12 months: BMI, blood pressure, record of smoking status, foot examination, urine albumin–creatinine ratio, blood tests for HbA1c, cholesterol and serum creatinine | 2017–8 2018–9 2019–20 |
| Glycaemic control for diabetes | The proportion of people with diabetes without moderate or severe frailty, in whom the last HbA1c is 58 mmol/mol or less in the preceding 12 months | 2017–8 2018–9 2019–20 |
| Glycaemic control for diabetes with frailty | The proportion of people with diabetes and moderate or severe frailty, in whom the last HbA1c is 75 mmol/mol or less in the preceding 12 months | 2017–8 2018–9 2019–20 |
| Asthma review | The proportion of people with asthma who have had an asthma review in the preceding 12 months that includes an assessment of asthma control | 2017–8 2018–9 2019–20 |
| Epilepsy review and control | The proportion of people on drug treatment for epilepsy who have had an annual review and recorded as seizure-free in the preceding 12 months | 2017–8 2018–9 2019–20 |
| Screening | ||
| Cervical screening age 25–49 years | The proportion of women eligible for screening and aged 25–49 years who have had cervical screening in the preceding 5 years and 6 months | 2017–8 2018–9 2019–20 |
| Cervical screening age 50–64 years | The proportion of women eligible for screening and aged 50–64 years who have had cervical screening in the preceding 5 years and 6 months | 2017–8 2018–9 2019–20 |
| Breast screening | The proportion of women eligible for screening and aged 50–70 years who have had breast screening in the preceding 3 years | 2017–8 2018–9 2019–20 |
| AAA screening | The proportion of men eligible for screening and aged 65 years or over with a record of AAA screening | 2017–8 2018–9 2019–20 |
| CVD risk assessment | The proportion of people aged 45–74 years with a recorded CVD risk assessment in the preceding 5 years, and who do NOT have a diagnosis of: CHD, CKD, diabetes, hypertension, AF, transient ischaemic attack, familial hypercholesterolaemia, heart failure, peripheral arterial disease, stroke or previously documented 20% or higher 10-year CVD risk BEFORE the last 5 years | 2019–20a |
| CVD | ||
| Secondary prevention of stroke | The proportion of people with transient ischaemic attack or stroke, excluding those with haemorrhagic stroke, who have been prescribed an antiplatelet or anticoagulant in the preceding 12 months | 2017–8 2018–9 2019–20 |
| Anticoagulation for AF | The proportion of people with persistent or paroxysmal AF and a CHA2DS2-VASc score equal to two or more, with a prescription for warfarin or a direct-acting oral anticoagulant in the preceding 12 months | 2017–8 2018–9 2019–20 |
| Stroke risk assessment in AF | The proportion of people with persistent or paroxysmal AF and a CHA2DS2-VASc score in the preceding 12 months | 2017–8 2018–9 2019–20 |
| Blood pressure control in CVD (79 years or under) | The proportion of people aged 79 years or under, with CHD, hypertension, stroke, transient ischaemic attack or peripheral arterial disease, who have had a blood pressure of 140/90 mmHg or less in the preceding 12 months | 2017–8 2018–9 2019–20 |
| Blood pressure control in CVD (80 years or over) | The proportion of people aged 80 years or over, with CHD, hypertension, stroke, transient ischaemic attack or peripheral arterial disease, who have had a blood pressure of 150/90 mmHg or less in the preceding 12 months | 2017–8 2018–9 2019–20 |
| Secondary prevention of MI | The proportion of people who have had a MI and have received a prescription for an ACE-I or ARB, antiplatelet therapy, beta-blocker and a statin in the preceding 12 months | 2017–8 2018–9 2019–20 |
| Treatment of CHD | The proportion of people with CHD who have received a prescription for antiplatelet or anticoagulant therapy in the preceding 12 months | 2017–8 2018–9 2019–20 |
| Treatment of heart failure (1) | The proportion of people with heart failure who have been prescribed an ACE-I or ARB in the preceding 12 months | 2017–8 2018–9 2019–20 |
| Treatment of heart failure (2) | The proportion of people with heart failure who have been prescribed an ACE-I or ARB, and a beta-blocker, in the preceding 12 months | 2017–8 2018–9 2019–20 |
We defined variables about individuals and prisons that might explain variation in indicator achievement. These explanatory variables included prison name and category, age of individual (in decades), gender, length of stay (months in categories) and ethnic group [Office for National Statistics (ONS) categories]. We considered using sentence status but discarded it given a large number of missing records.
Data sources
SystmOne Prison is used in all prisons in England. This clinical system includes prisoner demographic data via integration with the Prison National Offender Management Information System (NOMIS), health screening data from the reception assessments, and data related to ongoing care including data on diagnoses (clinical codes), pathology results and prescribing. SystmOne Prison can be used by all healthcare services within a prison, displays all prison medical record data held for each person (including across multiple custodial sentences) and is transferable between prisons.
The data specialist (SR) extracted anonymised individual patient-level data for the 13 prisons from SystmOne Prison electronic health records. We reviewed a summary of the extracted data prepared by the statistician (TF) for apparent anomalies and discrepancies in team meetings. The data specialist iteratively refined searches until final versions were agreed.
Statistical analysis
Descriptive statistics for each indicator were produced by year for each of the explanatory variables. This permitted initial summaries of variation in attainment of each of the quality indicators and review for apparent anomalies and discrepancies.
For most indicators, higher proportions of achievement were desirable. For the indicators examining psychotropic, opioid and gabapentin prescribing, there was no specific criterion against which prescribing levels were compared; generally lower prescribing levels were desirable.
Multilevel mixed-effects logistic regression models were developed for each indicator to explore whether the explanatory variables were associated with achievement of the quality indicator. Achievement of the indicator was the outcome in each indicator model. Achievement was considered ‘met’ (i.e. coded 1 vs. 0 not met) whether it had occurred in an individual’s current prison or in a previous establishment within the time frame of the indicator. As we have repeated measures for people across and within years, for example, someone could have attended multiple prisons in the same year and different years, we had two levels – person identifier and year. Year was included in each of the QI models as both a random and fixed effect to account for the correlation between years and to explore the variation in achievement over the 3 years. In those QI indicator models with only one financial year of data, year was excluded, and for these QI indicators logistic regression models were used. Each of the explanatory variables was included univariately into the indicator models as fixed effects to explore its association with achievement of the indicator. Results from these univariate multilevel mixed-effects logistic regression models were presented as odds ratios (ORs) and accompanying 95% confidence intervals (CIs). No modelling was presented for seven indicators as the number of eligible patients and achievement was too small for meaningful analysis.
The explanatory variables were then included in multivariable multilevel mixed-effects logistic regression models to explore whether variation in achievement of the indicator remained after accounting for other explanatory variables, that is, other individual and prison-specific factors. Results from these multivariable multilevel mixed-effects logistic regression models were presented as ORs and probability of achievement of the indicator, with accompanying 95% CIs for both estimates. Prison category was not included in the multivariable models given close correlation between category and prison identity. Where numbers in subcategories were too small to produce robust estimates, or where the explanatory variable was removed from the model, these ORs and probabilities are not presented. These results from the univariate and multivariable multilevel mixed-effects logistic models were summarised (as outlined in the Results by quality indicator section) by the following themes: communicable disease, MH, prison-specific, diabetes, asthma and epilepsy care, screening and CVD.
All appropriate assumptions were checked and were met for each quality indicator (univariate and multivariable) multilevel mixed-effects logistic regression models:
-
There was no multicollinearity in the multivariable models. Prison category was not included in the multivariable models given close correlation between category and prison identity and so negated the potential issue of multicollinearity between these two explanatory variables.
-
Residuals were checked for normality, homoscedasticity and no outliers identified.
-
All individual and prison-specific factors were included as categorical variables and so checking for a linear relationship between continuous predictors was not applicable.
Generalised estimating equations (GEEs) might have been another modelling approach rather than multilevel mixed-effects and these are usually equivalent for linear models; this is not the case for binary outcomes. The fundamental difference between the two is in this interpretation of the (fixed) effects. GEEs produce population-averaged effects, while multilevel mixed-effects logistic regression models produce subject-specific effects. 78,79
We originally proposed to develop latent variable models. We hypothesised that there would likely be strong associations between the different indicators and these models could identify explanatory variables common across all indicators. This unifying model would have explored which factors are associated with quality in care in prisons as measured by all these indicators. However, from the development of the searches for each of the indicators, it became clear that eligibility often varied among indicators. Therefore, there was not a common eligible (denominator) population to include in the latent model and so conducting this analysis was not possible. These models would also have supported the estimation of the attainment false negative and positive rates using a Bayesian analysis framework. As no latent variable models were developed, the Bayesian analysis could not be done. All statistical analyses were carried out using Stata 16 software. 80
Ethical approval
We gained approval for this statistical WP from the University of Leeds SoMREC on 17 July 2019 (ref. no. 18-093). We approached HMPPS regarding approval for this WP and we were issued with an exemption notice dated 19 March 2019 which exempted us from applying for NRC approval as our quantitative analysis was based on routinely collected and anonymised data.
Results
Study population
Data from 13 prisons were examined. The study population increased in each year of the study, from 21,677 people in 2017–8 to 25,811 by 2019–20. Other demographic characteristics of the study population are summarised in Table 8. Of the study population, 92.2% were male and 42.7% were located in category B prisons. Around two-thirds of the study population were aged 20–40 years. Over half of the study population had short prison sentences, staying in prison for < 6 months. Data on ethnic group were missing for around 20% of the study population; most people included were white.
| Explanatory variables | Year and study population (%) | ||
|---|---|---|---|
| 2017–8 | 2018–9 | 2019–20 | |
| Total study population | |||
| 21,677 | 22,099 | 25,811 | |
| Gender | |||
| Male | 19,977 (92.2) | 20,295 (91.8) | 23,570 (91.3) |
| Female | 1699 (7.8) | 1802 (8.1) | 1376 (5.3) |
| Missing | < 10 (0.0001)a | < 10 (< 0.0001)a | 865 (3.4) |
| Prison category b | |||
| A | 1664 (7.7) | 1670 (7.6) | 1838 (7.1) |
| B | 9254 (42.7) | 9442 (42.7) | 11,904 (46.1) |
| C | 6035 (27.8) | 6204 (28.1) | 6870 (26.7) |
| Closed | 1720 (7.9) | 1802 (8.2) | 2245 (8.7) |
| D | 2189 (10.1) | 2189 (9.9) | 2149 (8.3) |
| YOI | 815 (3.8) | 792 (3.6) | 805 (3.1) |
| Age (years) b | |||
| 10 to <20 | 468 (2.2) | 436 (2.0) | 404 (1.6) |
| 20 to <30 | 6994 (32.3) | 7163 (32.4) | 8064 (31.2) |
| 30 to <40 | 7051 (32.5) | 7381 (33.4) | 9125 (35.4) |
| 40 to <50 | 4114 (19.0) | 4180 (18.9) | 4948 (19.2) |
| 50 to <60 | 2107 (9.7) | 1978 (9.0) | 2224 (8.6) |
| 60 to < 70 | 684 (3.2) | 701 (3.2) | 751 (2.9) |
| 70 to < 80 | 213 (1.0) | 209 (1.0) | 238 (0.9) |
| 80 to < 90 | 40 (0.2) | 45 (0.2) | 53 (0.2) |
| 90 to < 100 | < 10 (< 0.01)a | < 10 (< 0.01)a | < 10 (< 0.01)a |
| 100 to < 110 | < 10 (< 0.01)a | - | - |
| Length of stay (months) | |||
| < 1 | 4474 (20.6) | 4801 (21.7) | 6764 (26.2) |
| 1 to < 6 | 8075 (37.3) | 7742 (35.0) | 10,802 (41.9) |
| 6 to < 12 | 3672 (16.9) | 3616 (16.4) | 3893 (15.1) |
| 12 to < 24 | 2832 (13.1) | 3752 (17.0) | 2600 (10.1) |
| 24 + | 2624 (12.1) | 2188 (9.9) | 1752 (6.8) |
| Ethnic group b | |||
| White | 15,638 (72.1) | 14,911 (67.5) | 16,606 (64.3) |
| Mixed | 431 (2.0) | 371 (1.7) | 409 (1.6) |
| Asian or Asian British | 813 (3.8) | 726 (3.3) | 755 (2.9) |
| Black or Black British | 404 (2.0) | 364 (1.6) | 451 (1.7) |
| Chinese and other | 214 (1.0) | 167 (0.8) | 163 (0.6) |
| Unclassified | 372 (1.7) | 409 (1.9) | 387 (1.5) |
| Missing | 3805 (17.6) | 5151 (23.3) | 7040 (27.3) |
Results by quality indicator
All results are based upon a total study population of 25,811 people in 2019–20, unless otherwise stated. Variations in achievement between prisons were calculated as a ratio of the ORs for lowest and highest achievement (presented within brackets). Notable variations in achievement from multivariable multilevel logistic regression models are provided as ORs with 95% CIs (presented within brackets). The most recent comparisons in achievement from community settings are highlighted where available. These often came from QOF indicators. 81–84 It was not possible to use robust methods in this comparison (e.g. adjusting for demographic differences in the populations). Descriptive statistics pertaining to achievement for each quality indicator and comparisons with community populations where applicable are provided in Appendix 6, Table 16. The multilevel mixed-effects logistic regression models results are provided in Appendix 7, Table 17 and summaries of the model results by themes in Appendix 8, Tables 18–23.
Communicable disease
The proportion of new receptions to prison accepting opt out dry blood spot testing
Of 12,606 people (48.8%) eligible, less than half (44.8%) had the dry blood spot tests (DBST). Achievement increased 200-fold over 2017–20 (OR 2019–20: 212.3, 95% CI 170.4 to 264.1), after adjustment for other characteristics.
The likelihood that eligible people accepted dry blood spot testing varied 169-fold between 13 prisons, after adjustment for other characteristics (ORs 0.05–8.45). Compared to category A prisons, achievement was higher in all other categories (B, C, Closed, D, Young Offenders Institutes).
Compared to people with length of stay 1–6 months, those with a stay of <1 month were around half as likely to accept testing (OR 0.53, 0.48 to 0.58) and those with a stay over 6 months were more likely to accept testing (ORs for length of stay 6–12 months 1.36, 1.22 to 1.51, 12–24 months 1.3, 1.14 to 1.5 and over 24 months 10.15, 6.73 to 15.31).
The proportion of the prison population who have received one, two, three or four (course of three plus booster) hepatitis B vaccinations in the preceding 12 months: (1) the whole prison population, (2) people with a history of illicit drug use (a higher-risk group)
The whole prison population
Of 17,957 people (69.6%) who entered prison in the preceding 12 months, 8210 (45.7%) received one hepatitis B vaccination, 6676 (37.2%) two vaccinations, 5437 (30.3%) three vaccinations and 2212 (12.3%) all four vaccinations, while 410 (2.3%) declined vaccination. Achievement increased more than threefold over 2017–20 for all four vaccinations (OR 3.18, 2.89 to 3.49).
The likelihood of vaccination varied around fourfold between 13 prisons (ORs for one vaccination 0.52–2.04, two vaccinations 0.55–2.03, three vaccinations 0.55–2.14 and four vaccinations 0.48–1.59).
Compared to people staying 1–6 months, those staying less than a month were less likely to be vaccinated (ORs for one vaccination 0.76, 0.72 to 0.81, two vaccinations 0.72, 0.68 to 0.76, three vaccinations 0.69, 0.65 to 0.74 and four vaccinations 0.84, 0.77 to 0.92). People staying for over 24 months were more likely to be vaccinated (ORs for one vaccination 1.68, 1.43 to 1.98, two vaccinations 1.81, 1.53 to 2.14, three vaccinations 1.86, 1.56 to 2.21 and four vaccinations 2.13, 1.68 to 2.7). Compared to white people, black or Black British and Chinese and other people were less likely to be fully vaccinated (ORs for four vaccinations, black or Black British people 0.6, 0.45 to 0.8, Chinese and other people 0.55; 0.34 to 0.86), and Asian or Asian British people were less likely to receive one to three vaccinations (ORs for one vaccination 0.86; 0.77 to 0.97, two vaccinations 0.82; 0.73 to 0.93 and three vaccinations 0.84; 0.73 to 0.97).
People with a history of illicit drug use (a higher-risk group)
In 2019–20, 10,207 people had clinical codes indicating a history of illicit drug use (39.5% of the total study population, 57% of people who had entered prison in the preceding 12 months). Of this high-risk group, 5117 (50.1%) received one hepatitis B vaccination, 4176 (40.9%) two vaccinations, 3387 (33.2%) three vaccinations and 1493 (14.6%) all four vaccinations, while 2038 (20%) declined. Achievement improved more than twofold over 2017–20 for all four vaccinations (OR 2.89, 2.57 to 3.25).
The likelihood of vaccination varied 4 to almost 13-fold between prisons (ORs for one vaccination 0.64–6.99, two vaccinations 0.62–7.86, three vaccinations 0.64–3.11, and four vaccinations 0.52–2.34).
Compared to people staying 1–6 months, those staying less than a month were less likely to be vaccinated (ORs for one vaccination 0.83; 0.77 to 0.89, two vaccinations 0.8; 0.74 to 0.86, three vaccinations 0.76; 0.7 to 0.83 and four vaccinations 0.84, 0.75 to 0.94), while people staying 12–24 months were more likely to be vaccinated (ORs for four vaccinations 1.92, 1.64 to 2.24), as too were those staying over 24 months (ORs for four vaccinations 1.87,1.37 to 2.56). Compared to white people, black or Black British people were less likely to receive one, two or four vaccinations (ORs for one vaccination 0.75, 0.59 to 0.96, two vaccinations 0.77, 0.6 to 0.99 and four vaccinations 0.59, 0.38 to 0.9).
The proportion of people with one or more of coronary heart disease, stroke or transient ischaemic attack, diabetes or chronic obstructive pulmonary disease (COPD) who have received a flu vaccination between August and March
Of the 1752 people (6.8%) eligible, less than half (44.9%) were vaccinated. This compares unfavourably with community primary care, where over 70% with the same diagnoses were vaccinated in 2019–20. 81 Achievement slightly improved 1.2-fold over 2017–20 (OR 1.22; 1.02 to 1.45).
The likelihood of influenza vaccination varied 18-fold between prisons (ORs 0.13–2.36).
Compared to people staying 1–6 months, those staying less than a month were half as likely to be vaccinated (OR 0.46; 0.35 to 0.6), and those staying 6–24 months were around two to four times more likely to be vaccinated (ORs for length of stay 6–12 months 2.16; 1.74 to 2.69, 12–24 months 2.89; 2.29 to 3.65 and over 24 months 3.96; 3.09 to 5.07). Compared to white people, black or Black British and Chinese and other people were less likely to be vaccinated (ORs for black or Black British people 0.58; 0.34 to 0.99, Chinese and other people 0.40; 0.17 to 0.92).
Mental health
The proportion of people who have received three or more prescriptions for an antipsychotic in the preceding 12 months, and who have a record of blood testing (fasting glucose, HbA1c, lipid profile, urea and electrolytes, full blood count, liver function tests), BMI and blood pressure
We identified 463 people (1.8%) prescribed antipsychotics. Achievements for blood monitoring varied between 0% and 9.5% (0 (0%) fasting glucose, 25 (5.4%) lipid profile, 25 (5.4%) liver function test, 31 (6.7%) HbA1c%, 42 (9.1%) urea and electrolytes, 44 (9.5%) full blood count). For other measurements, 31 (6.7%) had BMI and 70 (15.1%) blood pressure recorded. These compare unfavourably with community primary care, where 74.4% of people had a BMI and 80.3% blood pressure recorded in 2019–20. 81 The likelihood of receiving any monitoring declined over 2017–20, for example, lipid measurement fell from 25% to 5% over 2017–20.
The likelihood of monitoring varied 3- to 127-fold between prisons, for example, 127-fold for fasting glucose (ORs 0.08–10.18) and 11-fold for blood pressure (ORs 0.47–5.23).
There were insufficient data for analyses on gender. Compared to white people, Asian or Asian British people were at least three times more likely to receive blood monitoring (OR for fasting glucose 196.3; 1.32 to 29,283.52, HbA1c% 6.69; 2.2 to 20.32, lipid profile 3.41; 1.06 to 11.02, urea and electrolytes 3.83; 1.28 to 11.46, full blood count 3.42; 1.13 to 10.38 and liver function tests 3.66; 1.2 to 11.16), but not BMI or blood pressure recording.
The proportion of the prison population prescribed three or more psychotropic drugs (antipsychotics, sedative antidepressants, hypnotics and anxiolytics, pregabalin or gabapentin, opioids) at the same time during an 8-week period
We identified 216 people (0.8%) prescribed three or more psychotropic drugs, and 103 people (0.4%) four or more. Over 2017–20, the likelihood of being prescribed three or more drugs increased nearly twofold (OR 1.76; 1.37 to 2.25) and four or more drugs over twofold (OR 2.30; 1.56 to 3.39).
We found an almost 12-fold difference in the likelihood of being prescribed threee or more psychotropic drugs (ORs 0.25–2.94) and a 33-fold difference in the likelihood of being prescribed four or more (ORs 0.10–3.30) between prisons. Compared to category A prisons, prescribing was higher in Closed prisons and lower in category D prisons for three or more and four or more psychotropic drugs.
Compared to people staying 1–6 months, people staying 12–24 months were twice as likely to be prescribed three or more and four or more psychotropic drugs (ORs for three or more 2.16; 1.64 to 2.85 and four or more drugs 2.82; 1.84 to 4.32). Compared to white people, Asian or Asian British people were almost five times less likely to be prescribed three or more drugs (OR 0.22; 0.07 to 0.69).
The proportion of people aged over 55 years in the prison population who have a record of one of the following assessments in the preceding 12 months; Mini Mental State Examination (MMSE), 6 item cognitive impairment test (6 CIT), General Practitioner Assessment of Cognition (GPCOG)
We identified 1884 people aged over 55 years (7.3% of the study population); 370 (19.6%) of these had a record of cognitive assessment. There was a 40-fold improvement in achievement over 2017–20 (OR 40.5; 25.3 to 64.6).
The likelihood of an assessment varied almost 169-fold between 13 prisons (ORs 0.65–109.76). The eligible population was otherwise too small for any further meaningful interpretation of the multivariable analysis.
The proportion of people with a new diagnosis of any form of dementia in the reporting year, and who have a record of the following blood tests between 12 months before and 6 months after the date of diagnosis: full blood count, calcium, glucose and/or HbA1c, urea and electrolytes, liver function, thyroid function, serum vitamin B12, folate levels
We identified 13 people (0.1%) who had a new diagnosis of dementia. Achievements for blood testing varied between 0% and 76.9% [0 (0%) had B12, six (46.2%) calcium, six (46.2%) folate, seven (53.8%) thyroid function, eight (61.5%) renal function, nine (69.2%) full blood count and 10 (76.9%) HbA1c% testing]. Composite achievement compared unfavourably with 70% in community primary care over 2018–9. 84
The eligible population was too small for any meaningful multivariable analysis.
Prison-specific
The proportion of new receptions to prison who have been asked for consent to transfer medical records from general practitioner (GP) to prison health care
Of the 17,957 people (69.6%) eligible, 12,639 (70.4%) were asked for consent to transfer medical records. A fourfold improvement in achievement was observed over 2017–20 (OR 4.28; 3.96 to 4.62).
The likelihood that people were asked for consent varied 337-fold between prisons (ORs 0.007–2.36). Compared to category A prisons, achievement was higher in category C, Closed and Young Offender Institute prisons, and lower in category B prisons.
Achievement was 10 times less likely in males (OR 0.1; 0.02 to 0.14). Compared to people aged 30–39 years, people aged 50–69 years were less likely to be asked for consent (OR 50–59 years 0.86; 0.76 to 0.97, 60–69 years 0.72; 0.58 to 0.89). Achievement increased with length of stay. Compared to people staying 1–6 months, those staying less than a month were less likely (OR 0.77; 0.71 to 0.83) and those staying over 6 months were more likely to be asked (ORs for length of stay 6–12 months 1.22; 1.11 to 1.34, 12–24 months 1.43; 1.25 to 1.63 and over 24 months 1.85; 1.47 to 2.31). Compared to white people, mixed, Asian or Asian British, black or Black British and Chinese and other people were less likely to be asked (ORs for mixed people 0.80; 0.65 to 0.99, Asian or Asian British people 0.80; 0.69 to 0.92, black or Black British people 0.75; 0.61 to 0.93 and Chinese and other people 0.70; 0.52 to 0.96).
The proportion of new receptions to prison with a code for a second-stage health assessment in the past 12 months, plus clinical codes for inpossession risk assessment and medicines reconciliation (MR) added in the week before the second-stage assessment
Of 8245 new receptions in 2019–20, 6173 people (74.9%) had a second-stage health assessment and were eligible. Of these, 2359 (38.2%) received both MR and IP risk assessment within 7 days. Three hundred and nineteen people (5.2%) received MR assessment alone, and 3810 (61.7%) IP risk assessment alone.
The likelihood that people received assessments within 7 days varied markedly between prisons. There was over 21,600-fold difference in the likelihood of receiving both assessments (ORs 0.45–9724.5), a 257-fold difference in receiving MR alone (ORs 0.86–221.59), and an almost 32,000-fold difference in receiving IP risk assessment alone (ORs 0.00007–2.23). While some of the ORs estimated are very large or small due to the relatively small numbers, they do indicate large variations between prisons.
Compared to people staying 1–6 months, people staying either less or more time were more likely to receive both assessments (e.g. OR < 1 month 3.02; 1.86 to 4.89; 24 months or more 1.54; 1.0 to 2.33).
-
The proportion of the prison population prescribed (1) any opioid, (2) any strong opioid, (3) benzodiazepines AND any opioid.
-
The proportion of people with any MH diagnosis prescribed any opioid.
-
The proportion of the prison population with NO coded diagnosis of neuropathic pain prescribed pregabalin or gabapentin during an 8-week period.
The prison population
Prescribed any opioid
During the 8 weeks preceding 31 March 2019–20, 2957 people (11.5%) were prescribed any opioid. Rates of prescribing are comparable to community primary care, where 12.8% of adults were prescribed opioids in 2011–2. 85 Unlike this analysis, the community study had excluded people with coded drug misuse and cancers.
The likelihood of opioid prescribing increased almost 1.5 times over 2017–20 (OR 1.47; 1.38 to 1.58). The likelihood of opioid prescribing varied fivefold between prisons (ORs 0.26–1.31).
Compared to people aged 30–39 years, people aged under 30 years were less than half as likely to be prescribed any opioid (ORs aged 10–19 years 0.14; 0.07 to 0.27 and 20–29 years 0.44; 0.41 to 0.48), and people aged 40–49 years more likely (OR 1.38; 1.29 to,1.48). Compared to people staying 1–6 months, those staying less than a month were less likely (OR 0.58; 0.50 to 0.64), and those staying over 6 months more likely to be prescribed any opioid (ORs for length of stay 6–12 months 1.59; 1.47 to 1.72, 12–24 months 1.82; 1.67 to 1.99 and over 24 months 1.85; 1.67 to 2.05). Compared to white people, mixed, Asian or Asian British, black or Black British, Chinese and other people were less likely to be prescribed any opioid (ORs for mixed people 0.55; 0.43 to 0.71, Asian or Asian British people 0.32; 0.25 to 0.4, black or Black British people 0.41; 0.31 to 0.54 and Chinese and other people 0.31; 0.2 to 0.48).
Prescribed any strong opioid
During the 8 weeks preceding 31 March 2019–20, 2257 people (8.7%) were prescribed any strong opioid. A 20% increase in strong opioid prescribing occurred over 2017–20 (OR 1.22; 1.14 to 1.32).
The likelihood of opioid prescribing varied almost fourfold between prisons (ORs 0.36–1.36). Prescribing patterns for strong opioids were broadly similar to those of any opioid.
Prescribed benzodiazepines AND any opioid
During the 8 weeks preceding 31 March 2019–20, 2257 people (8.7%) were prescribed benzodiazepines and any opioid. An 18% increase in this combination of prescribing occurred over 2017–20 (OR 1.18; 1.1 to 1.27).
The likelihood of prescribing benzodiazepines and any opioid varied 12-fold between prisons (ORs 0.39–4.68). Prescribing patterns were otherwise broadly similar to those of any opioid.
The proportion of people with any mental health diagnosis prescribed any opioid
Of 4054 people with any MH diagnosis, 770 (19.0%) were prescribed any opioid during the 8 weeks preceding 31 March. Opioid prescribing for people with any MH diagnosis increased by over 60% throughout 2017–20 (OR 1.64; 1.41 to 1.91).
The likelihood of opioid prescribing in people with a MH diagnosis varied 11-fold between prisons (ORs 0.27–3.0).
Compared to people aged 30–39 years, people aged under 30 years with any MH diagnosis were less likely to be prescribed opioids (ORs aged 10–19 years 0.24; 0.03 to 1.89 and 20–29 years 0.42; 0.35 to 0.51). People aged 40–59 years with any MH diagnosis were more likely to receive a prescription (ORs aged 40–49 years 1.4; 1.21 to 1.61 and 50–59 years 1.35; 1.11 to 1.63). Patterns of prescribing by length of stay were similar to those seen for any opioid. Compared to white people, mixed and Asian or Asian British people with any MH diagnosis were less likely to receive a prescription (ORs for mixed people 0.58; 0.36 to 0.95 and Asian or Asian British people 0.25; 0.13 to 0.48).
The proportion of the prison population with NO coded diagnosis of neuropathic pain prescribed pregabalin or gabapentin
Of 24,388 people (94.5%) with no coded diagnosis of neuropathic pain, 2014 people (0.8%) were prescribed pregabalin or gabapentin during the 8 weeks preceding 31 March. Prescribing modestly fell by around 10% over 2017–20 (OR 0.89; 0.71 to 1.1).
The likelihood of pregabalin or gabapentin prescribing in this group varied almost twofold between prisons (ORs 0.67–1.29). Other prescribing patterns were broadly similar to those for all opioids.
Diabetes, asthma and epilepsy care
The proportion of people with diabetes in whom the last blood pressure reading (measured in the preceding 12 months) is 140/80 mmHg or less
Of 770 people (3.0%) eligible for this indicator, a third (33.9%) had a blood pressure of 140/80 mmHg or less. This compared unfavourably with community primary care, where 68% of people with diabetes had a recorded BP in the target range in 2019–20. 81 There was no observed improvement over 2017–20 (OR 1.17; 0.9 to 1.51).
The likelihood that eligible people had a recorded blood pressure of 140/80 mmHg or less varied over threefold between prisons (ORs 0.95–3.42).
Achievement varied by age, length of stay and ethnic group. Compared to people on the diabetes register aged 50–59 years, younger people and those aged 80–89 years were more likely to have satisfactory blood pressure control (ORs aged 20–29 years 2.82; 1.87 to 4.3, 30–39 years 1.59; 1.13 to 2.2 and 80–89 years 2.15; 1.0 to 4.6). Compared to people staying 1–6 months, those staying over 24 months were almost twice as likely to have satisfactory blood pressure control (OR 1.95; 1.34 to 2.85). Compared to white people, Asian or Asian British people were less likely to have a blood pressure of 140/80 mmHg or less (OR 0.58; 0.36 to 0.95).
The proportion of people with diabetes who have had the following in the preceding 12 months: body mass index, blood pressure, record of smoking status, foot examination, urine albumin–creatinine ratio, blood tests for HbA1c, cholesterol and serum creatinine
We identified 770 people (3.0%) with diabetes. Achievements for monitoring varied between < 0.01% and 93.8%; < 5 (< 0.6%) serum creatinine, 194 (25.2%) urine albumin–creatinine ratio (ACR), 312 (40.5%) foot examination, 429 (55.7%) cholesterol, 502 (65.2%) HbA1c%, 642 (83.4%) smoking status, 666 (86.5%) BMI, and 722 (93.8%) blood pressure. Foot examination was the only subindicator directly comparable to community primary care, and achievement was around half that seen in the community (40.5% compared with 78.04%). 81 The likelihood of BMI, blood pressure and cholesterol monitoring increased over 2017–20; for example, blood pressure measurement increased 2.6-fold (OR 2.6; 1.7 to 4.0), and the odds of serum creatinine monitoring declined almost 80% over 2017–20 (OR 0.22; 0.06 to 0.86).
The likelihood of monitoring varied 2–20-fold between prisons; for example, 2-fold for blood pressure (ORs 0.66–1.68) and 20-fold variation for urine ACR (ORs 0.35–7.15).
Compared to the reference group of people aged 50–59 years, people aged 80–89 years were almost four times more likely to have BMI recorded (OR 3.83; 1.08 to 13.58), people aged 30–49 years were less likely to have HbA1c% (OR aged 30–39 years 0.5; 0.35 to 0.73 and 40–49 years 0.62; 0.45 to 0.86) or urine ACR monitoring (OR aged 30–39 years 0.57; 0.37 to 0.86 and 40–49 years 0.54; 0.38 to 0.77) and people aged 20–49 years were less likely to have cholesterol monitoring (OR aged 20–29 years 0.46; 0.28 to 0.76, 30–39 years 0.59; 0.41 to 0.85 and 40–49 years 0.7; 0.51 to 0.95).
Compared to people staying 1–6 months, people staying less than a month were less than half as likely, and those staying over 6 months more than twice as likely, to have HbA1c%, cholesterol, urine ACR monitoring or foot examination (e.g. ORs length of stay less than a month 0.32; 0.22 to 0.46, 6–12 months 2.47; 1.76, 3.47 to 12–24 months 2.76; 1.88 to 4.05 and over 24 months 4.91; 3.15 to 7.63). Compared to white people, Black or Black British people appeared almost eight times more likely to receive serum creatinine monitoring (OR 7.9; 1.07 to 58.26), and Chinese and other people were almost five times less likely to have blood pressure recorded (0.23; 0.08 to 0.66).
The proportion of people with diabetes without moderate or severe frailty, in whom the last HbA1c was 58 mmol/mol or less in the preceding 12 months
Out of 756 people (2.9%) with diabetes and without frailty, a third (34.4%) had a HbA1c of 58 mmol/mol or less. This compared unfavourably with community primary care, where 56.7% of people achieved satisfactory glycaemic control in 2019–20. 81 There was no evidence of improvement over 2017–20 (OR 2019–20 1.15; 0.88 to 1.51).
The likelihood that people with diabetes had a HbA1c of 58 mmol/mol or less varied sevenfold between prisons (ORs 0.34–2.39). Compared to category A prisons, achievement was lower in category B and Closed prisons.
Compared to people aged 50–59 years, people aged 30–39 years were around half as likely (OR 0.52; 0.35 to 0.76) and those aged 20–29 years less likely to achieve satisfactory glycaemic control (OR 0.31; 0.16 to 0.58). Compared to people staying 1–6 months, people staying less than a month were almost five times less likely (OR 0.21; 0.12 to 0.38) and those staying 6 months or more were at least twice as likely to have satisfactory glycaemic control (ORs for length of stay 6–12 months 2.58; 1.83 to 3.64, 12–24 months 2.07; 1.42 to 3.01 and over 24 months 2.47; 1.68 to 3.65). Compared to white people, black or Black British people were three times more likely to have satisfactory glycaemic control (OR 3.08; 1.6 to 5.91).
The proportion of people with diabetes and moderate or severe frailty, in whom the last HbA1c was 75 mmol/mol or less in the preceding 12 months
We identified 14 people (0.1%) with diabetes and moderate or severe frailty; over half (64.3%) had a HbA1c% of 75 mmol/mol or less in the preceding 12 months. This compared unfavourably with community primary care, where over 80% of people with moderate or severe frailty had a HbA1c% of 75 mmol/mol or less in 2019–20. 81
The eligible population was too small for any meaningful multivariable analysis.
The proportion of people with asthma who have had an asthma review in the preceding 12 months that included an assessment of asthma control
Out of 4459 people (17.3%) with coded asthma, 136 (3.1%) had had an asthma review in the preceding 12 months. This compared unfavourably with community primary care, where 67.1% of patients with asthma received a review in 2019–20. 81 The likelihood of asthma reviews declined 86% over 2017–20 (OR 2019–20 0.14; 0.11 to 0.17).
The likelihood of asthma reviews varied 11-fold between prisons (ORs 0.68–7.62). Compared to category A prisons, achievement was lower in all other categories. Achievement was particularly low in category B prisons, where people were 0.09 less likely to receive an asthma review (OR 0.09; 0.07 to 0.12).
Compared to people aged 30–39 years, achievement increased from age 40 to 79 years and peaked in people aged 70–79 years (OR aged 40–49 years 1.13; 0.91 to 1.39, 50–59 years 1.48; 1.15 to 1.9, 60–69 years 2.26; 1.57 to 3.25 and 70–79 years 4.11; 2.26 to 7.46). Compared to people staying 1–6 months, those staying less than a month were less likely to receive a review (OR 0.36; 0.24 to 0.53). Achievement increased with length of stay; people staying over 24 months were 11 times more likely to have reviews than those staying less than a month (ORs for length of stay less than a month 0.36; 0.24 to 0.53 and over 24 months 4.06; 3.14 to 5.24). Compared to white people, mixed, Asian or Asian British and Chinese and other people appeared more likely to have reviews (ORs for mixed people 1.05; 0.68 to 1.62, Asian or Asian British people 1.49; 1.04 to 2.14, and Chinese and other people 2.21; 1.03 to 4.75).
The proportion of people on drug treatment for epilepsy who have had an annual review and been recorded as seizure-free in the preceding 12 months
Out of 419 people (1.6%) prescribed drug treatment for epilepsy, 5 (1.2%) received an annual review and < 5 (< 1.00%) were coded as seizure-free in the preceding 12 months. This compared unfavourably with community primary care, where 57.5% of people were seizure-free in the preceding 12 months in 2013–4. 83
The eligible population was too small for any meaningful multivariable analysis.
Screening
The proportion of women eligible for screening and aged 25–49 years who have had cervical screening in the preceding 5 years and 6 months
Out of 1796 (7.0%) eligible women, 1145 (63.8%) had an adequate cervical screening test in the preceding 3 years and 6 months. Achievement was slightly lower than community primary care, where 71.5% of women aged 25–49 years had an adequate smear test in 2019–20. 81 The likelihood of cervical screening increased 1.6-fold over 2017–20 (OR 2019–20 1.61; 1.37 to 1.89).
Compared to women aged 30–39 years, women aged 20–29 were less likely (OR 0.6; 0.47 to 0.68) and those aged 40–49 years less likely to have cervical screening (OR 0.8; 0.72 to, 0.97). Compared to women staying 1–6 months, cervical screening was less likely for women staying less than a month (OR 0.7; 0.56 to 0.78), and around twice as likely for those staying 6 months or more (ORs for length of stay 6–12 months 1.9; 1.52 to 2.29, 12–24 months 2.0; 1.61 to 2.58 and over 24 months 2.6; 1.97 to 3.43). Compared with white women, Chinese or other women were less likely to have an adequate cervical screening test (OR 0.6; 0.33 to 0.95).
The proportion of women eligible for screening and aged 50–64 years who have had cervical screening in the preceding 5 years and 6 months
Out of 259 (1.0%) eligible women, 159 (61.4%) had an adequate cervical screening test performed in the preceding 5 years and 6 months. Achievement was slightly lower than community primary care where 77.6% of women aged 50–64 years had an adequate smear test in 2019–20. 81 The likelihood of cervical screening increased 1.5-fold over 2017–20 (OR 1.5; 1.01 to 2.24).
The eligible population was otherwise too small for any further meaningful multivariable analysis.
The proportion of women eligible for screening and aged 50–70 years who have had breast screening in the preceding 3 years
Out of 179 (0.7%) eligible women, 59 (33%) underwent breast screening. This compared unfavourably with data from NHS Digital, who reported an uptake of 70.5% in 2017–8. 86
The eligible population was otherwise too small for any further meaningful multivariable analysis.
The proportion of men eligible for screening and aged 65 years or over with a record of abdominal aortic aneurysm screening
Out of 540 (2.1%) eligible men, 241 (44.6%) underwent AAA screening. This compared unfavourably with data from PHE, who reported an initial uptake of AAA screening of 79.5% in 2014–5. 87 Achievement did not improve over 2017–20 (OR 1.32; 0.94 to 1.85).
The likelihood that eligible people received screening varied 14-fold between prisons (ORs 0.63–9.12). Compared to category A prisons, achievement was lower in category B, C and D prisons.
Compared to people staying 1–6 months, those staying less than a month were less likely to undergo screening (OR 0.27; 0.14–0.54). Achievement increased with length of stay; people staying over 24 months were almost 30-times more likely to undergo screening than people staying less than a month (ORs for length of stay less than a month 0.27; 0.14 to 0.54 and over 24 months 8.04; 4.53 to 14.26). Compared with white people, people of mixed ethnicity were almost four times less likely to undergo AAA screening (OR 0.26; 0.08 to 0.81).
The proportion of people aged 45–74 years with a recorded cardiovascular disease risk assessment in the preceding 5 years, and who do NOT have a diagnosis of: coronary heart disease, chronic kidney disease, diabetes, hypertension, atrial fibrillation (AF), transient ischaemic attack, familial hypercholesterolaemia, heart failure, peripheral arterial disease, stroke or previously documented 20% or higher 10-year cardiovascular disease risk BEFORE the last 5 years
Out of 1183 (14.4%) eligible people, 353 (29.8%) received CVD risk assessment. This compares unfavourably with data from PHE, who reported community uptake of 43.7% in 2019–20. 88
The likelihood that eligible people received screening varied almost 15-fold between prisons (ORs 0.69–10.04). Compared to category A prisons, achievement was higher in category D, and lower in category B, C and Closed prisons.
Compared to those staying 1–6 months, people staying 6–24 months were around 1.8 times more likely to receive CVD risk assessment (ORs for length of stay 6–12 months 1.88; 1.19 to 2.97 and 12–24 months 1.78; 1.12 to 2.82).
Cardiovascular disease
The proportion of people with transient ischaemic attack or stroke, excluding those with hemorrhagic stroke, who have been prescribed an antiplatelet or anticoagulant in the preceding 12 months
Out of 86 (0.3%) people with a diagnosis of transient ischaemic attack (TIA) or ischaemic stroke, 51 (59.3%) received a prescription for antiplatelet or anticoagulant medication in the preceding 12 months. This compared unfavourably with community primary care, where 91% of eligible patients were prescribed antiplatelet or anticoagulant medication in 2019–20. 81 There was no change in achievement over 2017–20 (OR 0.84; 0.22 to 3.16).
The likelihood of antiplatelet or anticoagulant prescriptions varied 43-fold between prisons (ORs 0.03–1.29). Compared to category A prisons, achievement was higher in category B, C and D prisons.
The eligible population was otherwise too small for any further meaningful multivariable analysis.
The proportion of people with persistent or paroxysmal atrial fibrillation and a CHA2DS2-VASc score equal to two or more, with a prescription for warfarin or a direct-acting oral anticoagulant in the preceding 12 months
Out of 54 (0.2%) people with AF and a CHA2DS2-VASc score of 2 or more, 45 (83.3%) were prescribed anticoagulant drug therapy. This was comparable to community primary care, where 87.26% of eligible people were prescribed anticoagulants in 2019–20. 81
The eligible population was too small for any meaningful multivariable analysis.
The proportion of people with persistent or paroxysmal atrial fibrillation and a CHA2DS2-VASc score in the preceding 12 months
Out of 25 (0.1%) people with AF, 15 (60%) had been assessed for stroke risk using the CHA2DS2-VASc scoring system in the preceding 12 months. This compared unfavourably with community primary care, where 93.4% of patients had been assessed in 2019–20. 81 The likelihood of assessment increased five-fold over 2017–20.
The likelihood of assessment varied 34-fold between prisons (ORs 0.15–5.14). The eligible population was otherwise too small for any further meaningful multivariable analysis.
The proportion of people aged 79 years or under, with coronary heart disease, hypertension, stroke, transient ischaemic attack or peripheral arterial disease, who have had a blood pressure of 140/90 mmHg or less in the preceding 12 months
Out of 1311 (5.1%) eligible people, less than half (44.7%) had a recorded blood pressure of 140/90 mmHg or less in the preceding 12 months. This compared unfavourably with 70% in community primary care during 2019–20. 81 Achievement did not improve over 2017–20 (OR 2019–20 0.94; 0.78 to 1.13).
The likelihood of satisfactory blood pressure control varied over sixfold between prisons (ORs 0.52–3.42).
Compared to people aged 50–59 years, people aged 20–39 years were more likely to have satisfactory blood pressure control (ORs aged 20–29 years 1.88; 1.23 to 2.86 and 30–39 years 1.36; 1.06 to 1.74). Compared to people staying 1–6 months, those staying over 24 months were 1.4 times more likely to achieve blood pressure control (OR 1.42; 1.08 to 1.87). Compared to white people, Asian or Asian British people were more likely to have satisfactory blood pressure control (OR 1.76; 1.09 to 2.84).
The proportion of people aged 80 years or over, with coronary heart disease, hypertension, stroke, transient ischaemic attack or peripheral arterial disease, who have had a blood pressure of 150/90 mmHg or less in the preceding 12 months
Out of 19 (0.1%) eligible people, over half (52.6%) had a recorded blood pressure of 150/90 mmHg or less. This compared unfavourably with over 80% achievement in community primary care during 2019–20. 81
The eligible population was too small for any meaningful multivariable analysis.
The proportion of people who have had a myocardial infarction and have received a prescription for an angiotensin-converting enzyme-inhibitor or angiotensin receptor blocker, antiplatelet therapy, beta-blocker and a statin in the preceding 12 months
Out of 492 (1.9%) people with a record of MI, none achieved the composite indicator of prescription for ACE-inhibitor (ACE-I) or ARB, antiplatelet, beta-blocker and statin. Achievements for prescribing of individual drugs varied between 0% and 70.3% [there were no prescriptions for an ARB licensed for use following MI; 207 people (42.1%) were prescribed an ACE-I, 300 (61.0%) an antiplatelet, 280 (56.9%) a beta-blocker and 346 (70.3%) a statin]. Levels of statin prescribing were comparable to community primary care, where 70.6% of people received a prescription in 2014–5. 82 The likelihood of being prescribed an ACE-I increased 1.5-fold over 2017–20 (OR 2019–20 1.47; 1.07 to 2.02); there was no change in prescribing of any other drugs.
Patterns of prescribing were similar for ACE-Is, antiplatelets, beta-blockers, and statins. The likelihood of prescriptions varied widely between prisons. While the ORs estimated are very large due to the relatively small numbers, they do indicate large variations between prisons, for example, 74,000-fold for statin prescribing (ORs 0.63–46,751.94) to over 13 million-fold for ACE-I prescribing (ORs 0.17–2,270,222.54).
Compared to people aged 50–59 years, those aged 20–49 years were less likely to receive treatment (example ORs for ACE-I prescribing aged 20–29 years 0.15; 0.03 to 0.66, 30–39 years 0.36; 0.2 to 0.65 and 40–49 years 0.64; 0.44 to 0.96). For antiplatelet drugs, those aged 70–79 years were less likely to receive treatment (OR 0.63; 0.4 to 0.99). Compared to people staying 1–6 months, those staying less than a month were at least half as likely to receive treatment (ORs for prescribing for people with length of stay less than a month: ACE-I 0.45; 0.27 to 0.75, antiplatelet 0.42; 0.26 to 0.68, beta-blocker 0.41; 0.26 to 0.66 and statin 0.48; 0.3 to 0.79).
The proportion of people with coronary heart disease who have received a prescription for antiplatelet or anticoagulant therapy in the preceding 12 months
Out of 494 (1.9%) people with coronary heart disease (CHD), 360 (72.9%) had a prescription for aspirin, an alternative antiplatelet therapy, or an anticoagulant in the last 12 months. This compared unfavourably with 90.8% in community primary care during 2019–20. 81 Achievement did not change over 2017–20 (OR 2019–20 1.13; 0.78 to 1.64).
The likelihood of treatment varied twofold between prisons (ORs 0.86–2.10). Compared to category A prisons, achievement was lower in category B and Closed prisons.
People aged under 50 years were less than half as likely to be prescribed aspirin, an alternative antiplatelet therapy, or an anticoagulant (ORs aged 20–29 years 0.15; 0.05 to 0.4, 30–39 years 0.11; 0.06 to 0.19, 40–49 years 0.40; 0.26 to 0.6). Compared to people staying 1–6 months, people staying less than a month were less likely to receive treatment (OR 0.41; 0.25 to 0.67).
The proportion of people with heart failure who have been prescribed an angiotensin-converting enzyme-inhibitor or angiotensin receptor blocker in the preceding 12 months
Out of 98 (0.4%) people with heart failure, 62 (63.3%) were prescribed an ACE-I or ARB in the last 12 months. This compared unfavourably with 82% in community primary care over 2019–20. 81 The likelihood of prescribing declined by almost 70% over 2017–20.
The likelihood that eligible people received treatment varied almost sevenfold between prisons (ORs 0.6–3.94). The eligible population was otherwise too small for any further meaningful analyses.
The proportion of people with heart failure who have been prescribed an angiotensin-converting enzyme-inhibitor or angiotensin receptor blocker, and a beta-blocker, in the preceding 12 months
Out of 61 (0.2%) people with heart failure, 49 (80.3%) were treated with an ACE-I or ARB and a beta-blocker. This achievement was similar to 82% in community primary care during 2019–20. 81 The likelihood of receiving a prescription declined by over 10% over 2017–20 (OR 2019–20 0.87; 0.27 to 2.76).
The eligible population was otherwise too small for any meaningful analyses.
Interpretation of findings
Principal findings
We found significant scope for improvement and marked variations in the quality of primary care, as measured by a suite of indicators using routinely collected data, examining a total of 25,811 records from 13 prisons in the North of England. These gaps and variations in care spanned different domains of care, both for indicators that reflected particular needs of the prison population and those reflecting more general primary care needs, for example, MR and processes of care for diabetes. The extent of variations between prisons was incompletely explained by differences in available prison population characteristics, suggesting that much of the variation is attributable to differences in how health care is organised and delivered locally.
We found encouraging trends suggesting improvement over time for several indicators, such as influenza immunisation, improving hepatitis B vaccination and falling gabapentinoid prescribing, and strengths in performance, such as for secondary prevention of stroke. However, we identified areas of concern, where overall achievement had declined over a 3-year period, notably declining antipsychotic monitoring and rising opioid prescribing.
The scope for improvement we identified can be seen in two ways. First, overall achievement was clearly low for some indicators, such as epilepsy review and control. Second, overall achievement in prisons appeared low relative to community general practice, for example, glycaemic control for diabetes. However, we also found strengths in performance, such as secondary prevention of stroke.
Associations with achievement
Overall achievement varied widely across indicators, with no clear pattern by type of indicator or clinical domain. For example, achievement in processes of care varied from 1.2% of eligible patients receiving an annual epilepsy review, to 93.8% of people on the diabetes register receiving a blood pressure check in the preceding 12 months. We observed similar variations in achievement of intermediate outcomes of care; for example, 0.2% of people with a diagnosis of epilepsy were coded as seizure free in the last 12 months, and 33.9% of people with a diagnosis of diabetes had a blood pressure in the target range of 140/80 mmHg or less. When indicators were reviewed by pre-defined domains of care (communicable disease, MH, prison-specific, diabetes, asthma and epilepsy care, screening and CVD), no clear pattern in achievement was seen.
Associations between indicator achievement and demographic characteristics were also considered. Short length of stay (< 1 month) was frequently associated with lower achievement across prison-specific, diabetes, asthma and epilepsy care, CVD and screening domains. Shorter stays could represent missed opportunities for health intervention and may accompany recidivism, reflecting the negative health impact of repeated incarceration.
Longer length of stay (typically over 6 months) was associated with higher achievement in some diabetes, asthma and epilepsy care, CVD and screening domains, and lower achievement in the prison-specific indicator concerning MR and IP risk assessment. The higher levels of achievement in some long-term conditions and screening domains may suggest the circumstances of longer stays facilitate delivery of these aspects of care. The reasons for this are not known, though individuals may spend longer periods in a single prison, increasing familiarity with healthcare professionals, systems and access to care.
No clear, overall trends were seen for achievement by gender, age, prison category or ethnic group.
Achievement over time varied within and between pre-defined domains. There was improvement in performance for eight indicators, for example dry blood spot testing, mental state examination, consent to transfer medical records and cervical screening (both age groups). There was deterioration in five indicators, for example antipsychotic monitoring and asthma review. No change or insufficient data for multivariable analysis in 14 indicators, for example blood pressure control in CVD (both age groups), AAA screening, diagnosis of dementia, were found. Achievements were mixed in three composite indicators, for example opioid and gabapentin prescribing, where all opioid prescribing increased, and gabapentin or pregabalin prescribing decreased over the study period.
Conclusion
To the best of our knowledge, this is the first study to examine the quality of primary care across multiple prisons and a range of indicators. We found substantial scope for improvement and marked variations in the quality of primary care, as measured using routinely collected data, examining a total of 25,811 records from 13 prisons in the North of England. Gaps and variations in care spanned different domains, both for indicators that reflected particular needs of the prison population (e.g. MR) and those reflecting more general primary care needs (e.g. diabetes care).
The extent of variations between prisons was not accounted for by differences in available prison population characteristics, though length of stay and ethnic group were associated with some differences in indicator achievement. This suggests that much variation is attributable to local differences in healthcare organisation and delivery.
We found encouraging trends suggesting improvement over time for several indicators, such as improving hepatitis B vaccination and falling gabapentinoid prescribing, and strengths in performance, such as for secondary prevention of stroke. However, we identified areas of concern, where overall achievement had declined over a 3-year period, notably declining antipsychotic monitoring and rising opioid prescribing.
Relatively short lengths of stay were frequently associated with lower achievement across prison-specific, long-term conditions and screening domains. Shorter stays could represent missed opportunities for health intervention and may accompany recidivism, reflecting the negative health impact of repeated incarceration.
Chapter 6 Integration and identification of interventions to improve the health of people in prison
Introduction
In earlier WPs, we identified a suite of quality indicators which could be applied using routinely collected data, assessed adherence to these indicators across 13 prisons, and explored barriers to and enablers of high-quality care. This WP aimed to integrate these findings through structured stakeholder deliberations to prioritise quality indicators and quality-improvement interventions that are likely to be relevant and feasible to deliver in prison settings and can be monitored by our suite of indicators.
Methods
We convened a three-part stakeholder panel, inviting people involved in commissioning and delivering primary care in prisons, as well as advocates for people in prisons.
Participant identification and engagement
We identified stakeholders through professional networks of project team members and oversight committee members. Invited stakeholders were those responsible for commissioning or delivering prison healthcare services in England (Table 9). We e-mailed an invitation to our first workshop to all on the list, with recipients encouraged to cascade it to other interested parties. We also promoted our first workshop at relevant dissemination events, including the Royal College of General Practitioners Secure Environments Group meeting (September 2021) and the Health and Justice Summit (October 2021).
| Type of role or organisation | Name of organisation |
|---|---|
| Prison healthcare provider | Spectrum CIC Hanham Secure Health Practice Plus Group |
| Commissioners | NHSE |
| Prison group director/prison governor | HMPPS |
| Health and Justice Leads | PHE |
| Public Health Registrars | S7a Assurance Group |
| Prison health researchers | Nuffield Trust |
| Voluntary sector | A Better Life Revolving Doors |
| Practitioner committees | Forensic and secure environments group Royal College of General Practitioners Secure Environments Group |
Procedure
We took the panel through the following steps:
-
Reviewing findings from WP3 (statistical results) to identify priorities for improvement based on scope for improvement for each indicator, that is, low performance; groups of prisoners associated with lower achievement of indicators, such as older people, longer- or shorter-term prisoners.
-
Considering findings from WP2 (qualitative findings) to understand barriers to and enablers of good quality of care, considering levers for change at individual, team, organisational and wider system levels.
-
A briefing summarising the range of approaches (interventions) potentially available to support the implementation of quality indicators, drawn from a broad overview of systematic reviews89–94 and a scoping review.
-
Mapping of implementation interventions to identified barriers and enablers. For example, if clinical staff or teams were unaware of their poorer performance relative to other clinical staff and teams, then audit and feedback comparing data on performance can help identify erroneous perceptions and use social comparisons and goal-setting to motivate change.
-
Application of APEASE criteria (affordability, practicability, effectiveness, acceptability, safety and equity),95 in considering the likely intervention adaptability to and sustainability within the prison healthcare environment.
We had originally planned to cover these steps over three face-to-face workshops, each lasting 4–6 hours, to allow sufficient time for discussion and consensus. However, we shifted to online meetings because of the COVID-19 pandemic. We redesigned the workshops to take place using Microsoft Teams. In light of recent empirical research, which has identified sustaining attention as a major contributor to videoconferencing fatigue,96 we restricted the duration of Teams meetings to a maximum of 2 hours each. We therefore had to focus and limit some of the aforementioned steps for the panel. Regrettably, the expert-by-experience (FB) was unable to attend the online workshops as planned. We therefore devised an alternative way to include him and to incorporate his views and comments.
Figure 3 summarises our modified approach. Steps 1–6 outline the process for stakeholder involvement, and steps A–F outline the process via which we involved the expert-by-experience. In short, we recorded all three workshops, capturing the presentations and subsequent discussions and the expert-by-experience watched the recordings at his own pace, pausing to audio-record ‘voice notes’ on his smartphone. His comments and observations are integrated into the discussion reported below. For ease of reading, we will further detail some of our procedures in Results.
FIGURE 3.
Stakeholder engagement workflow.
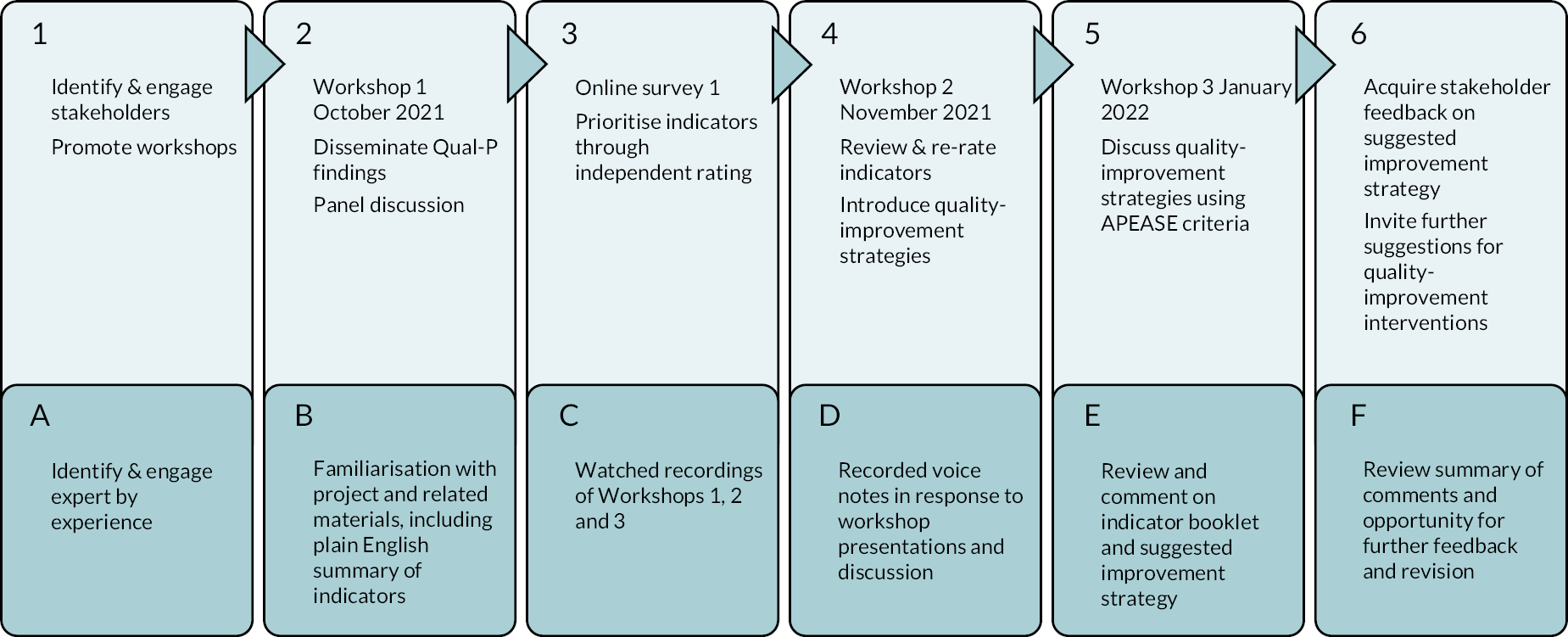
Results
Workshop 1
The first workshop took place on 27 October 2021 and aimed to disseminate the findings from the qualitative and quantitative WPs to stakeholders, to invite comments and feedback, and to encourage engagement with the remaining workshops and activities in WP4. We sent all participants a briefing document prior to the workshop which provided an overview of the study, an agenda for the workshop and the list of indicators used in the quantitative analysis.
Participants
Twenty-eight stakeholders joined the workshop. Represented organisations included healthcare providers (Spectrum, Practice Plus Group and Hanham Secure Health), commissioners (North of England Commissioning support unit), HMPPS, The Royal College of General Practitioners Secure Environments Group, NHSE and Improvement, S7a Assurance Group, PHE, A Better Life and the Nuffield Trust.
Presentations
Following an overview of the study rationale and aim, we presented key findings from the qualitative and quantitative WPs. From the qualitative study, we described barriers to and facilitators of high-quality care at individual, group, organisation and systems levels. From the quantitative study, we presented results for nine indicators within three categories: scope for improvement, variations across prisons, and variations by personal characteristics (Table 10).
| Indicator data presented |
|---|
| Scope for improvement |
| The percentage of people with CHD, stroke or transient ischaemic attack, diabetes and/or COPD who have had influenza immunisation in the preceding 1 August and 31 March |
| The percentage of people on the diabetes register (1) who have had a blood pressure reading recorded in the last 12 months and (2) in whom the last blood pressure reading (measured in the preceding 12 months) was 140/80 mmHg or less |
| The percentage of people on the asthma register who have had an asthma review in the preceding 12 months that included an assessment of asthma control using the three Royal College of Physicians (RCP) questions |
| The percentage of people with a coded diagnosis of epilepsy and who have been prescribed drug treatment for epilepsy (1) who have had an epilepsy annual review in the past 12 months and (2) been coded as seizure-free in the last 12 months |
| Variations across prisons |
| The percentage of people with a record of a MI who are prescribed an ACE-I, ARB, antiplatelet therapy, beta-blocker or a statin |
| The percentage of people (1) out of the whole prison population prescribed (a) any opioid, (b) any strong opioid, (c) benzodiazepines AND any opioid; (2) with any MH diagnosis prescribed any opioid; (3) out of the whole prison population with NO coded diagnosis of neuropathic pain prescribed pregabalin or gabapentin, during an 8-week period |
| Variations by personal characteristics |
| The percentage of new receptions who have been asked for consent to transfer medical records from their GP to the prison healthcare service in the past 12 months |
| The percentage of people prescribed three or more psychotropic drugs (antipsychotics, sedative antidepressants, hypnotics and anxiolytics, pregabalin or gabapentin, opioids) at the same time during an 8-week period |
| The percentage of new receptions who have had dried blood spot testing in the past 12 months |
Indicator selection also reflected a range of domains, including prevention, prescribing, long-term condition and prison-specific care. Where available, we presented corresponding QOF data from community primary care; however, we emphasised that demographic differences between community and prison populations limited comparability.
Discussion points
Most comments concerned opioid prescribing across the prison–community primary care interface. Participants suggested that opioid prescribing might be initiated in the community, reduced in prison, and then increased or restarted in the community. Therefore, opioid prescribing could be a more significant problem for people moving regularly between the community and the prison estate. Participants acknowledged prescribing pressures in both settings; in prison, prescribing decisions may be hurried due to pressure of time, while in the community GPs may feel unsupported in managing opioid requests during challenging consultations. Feedback on prescribing in prison and better communication channels between prisons and community GPs were suggested as possible ways of reducing opioid prescribing. Finally, achieving consistency in the workforce may promote better prescribing practices; current regular use of locum and agency prescribing staff limited clinician accountability. The expert-by-experience also recognised the implications of the tradability of drugs such as opioids but questioned the blanket interpretation of the data. He emphasised the importance of asking patients about opioid reduction, not least because prisoners interpret the refusal of medication as mistreatment or second-rate care, especially if medication was originally prescribed by their community GP. He also suggested caution when focusing solely on prescribing rates given the interrelationship with, for example, MH and self-harm.
Participants also raised quality of care in the women’s estate, with a particular focus on the need for gender-specific indicators and polypharmacy. Polypharmacy was highlighted as a challenge arising from a higher prevalence of psychosocial needs amongst the female prison population. One participant recognised the established role of QOF indicators for long-term conditions in community general practice. The absence of such a scheme for prison primary care means that there is no incentive to use QOF coding templates consistently across prisons, which hinders assessment of care equivalence. The expert-by-experience noted that while data from prisons and the community might not be comparable, this is often invoked to close down conversations about prisoners’ experiences of differences in care.
Following the discussion, we informed participants of the two remaining planned workshops and invited them to complete an online survey to rate our suite of indicators before the second workshop. All participants were sent a booklet containing the quantitative data analyses for the entire set of quality indicators after the workshop. The indicator booklet presented these analyses in the same simplified infographic format as the slides presented in the workshops but with explanatory text below. Appendix 9 shows an illustrative excerpt from the booklet, including the key to the infographic.
Inter-workshop activity: quality indicator prioritisation online survey (Round 1)
After the first workshop, participants were invited to take part in an online survey (Round 1 survey). We made the survey available immediately after the first workshop for a period of 2 weeks. We recognised that it would not be feasible for prison providers to target improvement on all 30 indicators simultaneously. We further anticipated that there would be insufficient time within the second workshop to allow any meaningful discussion of all indicators. Accordingly, this survey differed to the rating exercises in the stakeholder consensus exercise conducted in WP1 (see Chapter 3) in several ways. Rather than aiming to discard indicators, the purpose of this rating exercise was to identify a manageable number of indicators from our final suite of 30 for discussion in workshops 2 and 3 and to prioritise one or two for subsequent development as illustrative quality-improvement strategies. This time participants were asked to rate our suite of indicators on a scale of 1–9 (where 1 indicated strongest disagreement, and 9 strongest agreement) according to two criteria: the importance of the indicator, and the feasibility of achieving change. As detailed above, participants who had attended workshop one, viewed the recording or read the indicator booklet (see Appendix 9) were apprised of the findings from our analysis, which may have informed their views about importance and feasibility and subsequently their ratings.
Twelve stakeholders participated in this survey, including representation from prison healthcare providers and clinical leads, healthcare commissioners, PHE and Health and Justice leads. We collated and summarised scores for each indicator. We assessed levels of discordance between participants, with the intention of focusing later discussion on those with maximal discordance, defined as at least two participants rating an indicator feature 1–3 and at least three rating 7–9. Appendix 10, Table 24 summarises Round 1 findings. We therefore developed rulesets (see Appendix 11, Table 25) to exempt indicators from further workshop discussions based on Round 1 ratings. We applied a ruleset which exempted indicators with median scores of < 8 for importance regardless of perceived feasibility. This led to the exclusion of six indicators: hepatitis B vaccination; antipsychotic monitoring; cognitive testing in over 55s; laboratory tests in diagnosis of dementia; prescribing of an ACE-I or ARB for heart failure; and prescribing of an ACE-I or ARB and a beta-blocker for heart failure.
Workshop 2
We held the second workshop on 23 November 2021. We invited participants to re-rate the quality indicators during the workshop based on feedback and a discussion of the Round 1 survey ratings.
Participants
Ten external stakeholders participated, from prison healthcare provider and commissioning organisations, PHE and the Nuffield Trust. We recognised attrition in participation from the first workshop, partly given the demands of managing the COVID-19 pandemic in prisons at that time.
Presentations
Project team members gave three presentations: the results of the indicator ratings from Round 1 of the survey; findings from an international scoping review of interventions to implement EB health care in prisons; and an overview of quality-improvement strategies to change professional and organisational practice.
Discussion points
Participants reviewed exempted indicators from Round 1 of the survey (see Appendix 10). Antipsychotic monitoring was considered important (even with lower levels of obesity amongst people taking antipsychotics in prison compared to people in secure hospitals) given the high prevalence of antipsychotic prescribing in prisons and current poor performance around this indicator. Participants also suggested that CITs deserved more attention because early signs of impairment may be masked by the prison regime, and that cognitive testing was not routinely performed in prison.
For other indicators, data availability was highlighted as a potential problem. Connectivity between public health screening databases and SystmOne for national screening programmes (including cervical screening) was poor, although steps to improve the interface and resolve this constraint were under way. Further, limitations with summary care records from GPs may affect the interpretation of all indicators with a 12-month time period for transient prison populations, since the average duration of a remand stay was 13 weeks.
The indicator measuring epilepsy care was considered problematic given the frequency of pseudoseizures in the prison setting, which affects the assessment of eligibility for this indicator. The expert-by-experience did not dispute this but noted that he was unaware of this phenomenon. For complex long-term condition indicators, such as those relating to cardiovascular conditions, lower achievement was suggested as being related to coding limitations from existing template structures and skills deficits amongst staff.
Organisational logistics contributed to variable achievement for some indicators. Achievement of mammography screening, for example, depended on whether women had to leave the prison estate or whether a screening van could be situated on site. Health checks, such as the CVD risk assessment, tended to be targeted at people in prison for at least 2 years, excluding those spending less time in prison.
A query was raised concerning the high level of discordance on the feasibility of improving performance on consent to transfer medical records. Busy reception clinics, and the fact that people entering the prison estate may be withdrawing from substances, and therefore not in a position to give consent, may hinder achievement of the indicator. Solutions suggested included recommending an opt-out rather than opt-in, or requesting health-record information on a different lawful basis according to General Data Protection Regulation (GDPR). Participants noted inconsistencies in community GPs’ requirements for consent, and a lack of nationally agreed interpretation of, and guidance regarding, GDPR legislation. System-level change would therefore be required to improve achievement on this indicator. The expert-by-experience noted that even when patients did provide their consent, many reported that their records were not transferred.
Re-ratings of indicators
Seven people participated in the live re-rating of indicators during the workshop (see Appendix 10). No indicators retained a maximum importance score of 9. The median dropped to 8 for all these indicators.
Most median scores remained unchanged, but changes to the median Importance rating promoted or demoted five indicators to or from the exclusions group when applying Ruleset 4. Two were promoted: antipsychotic laboratory tests and cognitive tests for the over 55s, and three were demoted: epilepsy, aortic abdominal aneurysm screening, and HbA1c control in people with diabetes and without frailty.
Only one indicator (consent to transfer medical records) had been included with median Importance of < 8 (because of high discordance). Discordance for that indicator decreased to moderate but Importance increased to 8, retaining that indicator in the inclusions group. Several other indicators moved to another discordance category based on the re-ratings, yet remained in the inclusions group.
Interventions to improve the implementation of evidence-based health care in prison
There is a growing body of literature evaluating interventions to promote the implementation of EB practice, but the extent and rigour of such evaluations in prison settings are unknown. We therefore conducted a scoping review to identify and describe evaluations of implementation interventions in the prison setting. We searched EMBASE, MEDLINE, CINAHL Plus, Scopus and grey literature up to August 2021, supplemented by hand searching. We identified 15 studies from 17 papers, including one randomised controlled trial, one controlled interrupted time series analysis and 13 uncontrolled before-and-after studies. Eight studies took place in US settings and four in the UK. Ten studies evaluated combined (multifaceted) interventions, typically including education for staff or patients. Most interventions targeted communicable diseases, MH and screening uptake. Thirteen studies reported outcomes of testing, prescribing and referrals.
Overall, we found there was a lack of high-quality evidence to inform strategies to improve the implementation of EB health care in prisons, and an over-reliance on weak evaluation designs. While most evaluations had focused on recognised priorities for the prison population, relatively little attention had been paid to long-term conditions which are also core to primary care delivery, such as hypertension or asthma. We therefore considered the evidence base from a wider range of contexts.
Overview of implementation interventions
We introduced participants to systematic reviews of interventions to promote the uptake of evidence-based practice, mainly taken from Cochrane reviews. 89–94 These reviews covered educational meetings, financial incentives, inter-professional collaboration, patient-mediated interventions, local opinion leadership, computerised clinical decision support systems (CDSSs), and audit and feedback. Workshop 3 revisited these interventions in more depth. We also included a description based on our own published work of how routinely collected data could be harnessed within audit and feedback to reduce potentially harmful opioid prescribing. 56
Discussion points
The central issue raised concerned how the current prison healthcare tendering processes create a competitive, rather than collaborative, relationship between prison healthcare providers. While participants reported examples of local collaborative and partnership working with healthcare trusts and community services, prison health care was described as provider-specific; the subsequent lack of transparency across providers undermined consistency and continuity at a national level. Changing prison healthcare providers, combined with low levels of staff retention, can lead to attritions of organisational memory and inefficient reinvention of pre-existing effective practices.
The potential for using routine data to improve health care was recognised, with one suggestion to explore ways in which secondary care routine data could inform primary care within prison estates. Participants expressed an interest in using audit and feedback to reduce opioid prescribing in prison estates.
Workshop 3
The third and final workshop considered the applicability of six candidate implementation interventions identified by high-quality systematic reviews89–94 to the prison setting. Our deliberations were guided by the APEASE framework, which considers Affordability, Practicability, Effectiveness, Acceptability, Safety and Equity. 95 We asked for suggestions for further interventions and levers for change, and presented a suggested illustrative strategy for one indicator.
Participants
Three external stakeholders attended the workshop, with representation from Spectrum CIC and the Royal College of General Practitioners (RCGP) Secure Environments Group, along with several project team members.
Candidate implementation interventions
We now set these out in more detail with summaries of the workshop discussions.
Educational meetings
Definition
Educational meetings include interactive forms of continuing medical education which aim to facilitate improvements in professional practice through improving clinician skills and knowledge.
Evidence base
A systematic review of 81 randomised trials found that educational meetings make modest improvements in processes of care (6%) and achievement of treatment goals (3%). 89 Education meetings were found to have larger effects on quality improvement when attendance was higher and meetings more interactive in format, and smaller effects on improvement when changing complex clinical behaviours or addressing challenging conditions. Education meetings are commonly used and generally feasible, but have an associated cost of releasing professionals from clinical duties.
Discussion summary
Participants acknowledged the importance of education to improve care quality but recognised issues with practicability and equity. Limited resources and lack of protected time for education mean other tasks may take priority, leading to low levels of attendance or meetings being deferred. The expert-by-experience commented that given workloads (especially in the aftermath of the pandemic), staff did not have time for education. Reaching all staff with this strategy – and hence disseminating key messages across the whole service – is challenging due to shift patterns and high levels of part-time, agency and locum staff, which affects quality of care and staff–patient relationships. Further, educational approaches may encompass a range of effective and ineffective techniques, which may undermine their reliability as an effective strategy.
Facilitators of staff education meetings included a supportive organisational ethos and line management structure, Incentivisation (e.g. including attendance at education meetings in staff contracts), embedding education within individual clinical supervision and team briefings, and offering flexible learning options such as webinars. Education meetings may be more effective when used strategically, for example to educate staff about a forthcoming quality-improvement initiative, rather than as a sole strategy to improve care quality. Specific educational topics identified by staff in the Qual-P qualitative study included long-term condition care, trauma-informed care and improving signposting during the reception process.
Interprofessional collaboration
Definition
Inter-professional collaboration describes a range of structured activities whereby prison primary care staff can communicate with other specialist healthcare teams either across the prison estate or beyond the prison setting to optimise patient care.
Evidence base
A review of nine randomised trials found small improvements in patient outcomes, adherence to recommended practice and use of healthcare resources. 90 However, this body of evidence was classified as ‘low certainty’, meaning it may not be robust enough to base recommendations on.
Discussion summary
Inter-professional collaboration within and beyond prisons was seen as an effective strategy to improve care quality and patient safety, with current efforts including nationally mandated governance structures97 (with variability in local implementation), established concordats and pathways with local trusts, and patient safety huddles with prison and healthcare staff to manage risk for challenging patients. However, shared care may be inequitably distributed across the prison estate as a consequence of commissioning arrangements or individual initiatives. Sustaining collaboration requires consistent input of resources; therefore, practicability and affordability may be considerations, which could again vary according to local priorities.
There may be particular patient groups whose care is undermined by insufficient inter-professional collaboration, and for whom specific recommendations could be made. Where there is limited collaboration with secondary care MH, for example, and a lack of clarity about the relative responsibilities of primary and secondary care teams, people with severe and enduring mental illness may not be adequately supported in prison. Local statutory commissioned health needs assessments can identify priority patient groups within local populations.
Staff in the Qual-P qualitative study suggested several areas that could benefit from improved inter-professional collaboration. These included collaborative care involving: primary care and MH teams for people on Assessment, Care in Custody and Teamwork (ACCT) care orders; MH and substance-misuse teams to improve care for dual diagnoses; primary care and substance misuse for teams to integrate clinical and psychosocial care; prison and community primary care to share best practice and improve care continuity; and primary care and security staff when arranging access to emergency departments or escorting patients to clinics.
Patient-mediated interventions
Definition
Patient-mediated interventions incorporate three broad categories of activities: patient-reported health information, which uses information collected from patients (e.g. psychometric tests) prior to a clinical consultation; patient information, which informs or reminds patients about recommended care; and patient education, which aims to increase knowledge about their health condition and available care options, and improve self-management practices.
Evidence base
Evidence from 25 randomised trials indicates moderate positive effects of patient-mediated interventions on clinical practice:91 9% for patient-reported health information; 12% for patient information; and 11% for patient education. However, evidence for patient information was less robust than for the other two categories.
Discussion summary
A constraint on practicability in the prison setting is that some types of patient education – for example, supported self-management programmes for people with or at risk of diabetes – cannot be delivered in the same way as for people in the community. Questions were raised about the validity of patient-completed psychometric test scores (e.g. for depression or anxiety) in advance of clinical appointments; more accurate assessments could be gained during appointments. Online sources of information and education (e.g. for MH and well-being) are inaccessible for people in prison; however, better use could be made of screens in holding cells as people often have considerable waits for appointments. Video content, possibly made by patients, to communicate key messages may help to modify help-seeking behaviour and manage patient expectations. Staff in the Qual-P qualitative study suggested patients may benefit from group education sessions on long-term condition self-management.
Local opinion leaders
Definition
Opinion leaders are individuals recognised as having both expertise in a particular issue and sufficient credibility to influence others in a network. The role of opinion leaders in quality-improvement campaigns may include offering support and guidance, encouraging collaboration, and delivering feedback and advice on the results of clinical audits. Through their position as respected colleagues embedded in local networks, opinion leaders can act as catalysts for change.
Evidence base
A systematic review of 24 randomised trials suggested that use of local opinion leaders led to an absolute improvement of 10.8% in healthcare professionals’ compliance with recommended EB practice. 92
Discussion summary
Participants highlighted effective examples of local opinion leadership – healthcare support workers promoting the change to smoke-free establishments and senior clinicians discussing concerning data with clinical teams, for example cancelled bowel cancer screenings. There was general support for local opinion leaders, with the panel acknowledging the importance of experience or understanding of secure settings for local opinion leaders to be acceptable as credible agents of change. The expert-by-experience highlighted the need to consider the prison regime and how it is prioritised over everything, regardless of implications. He commented that it is apparent to patients where there are gaps in leadership, a lack of team spirit and no ownership of problems.
Computerised clinical decision support systems
Definition
A feature of electronic health records, CDSSs prompt healthcare professionals to deliver evidence-based care during clinical consultations. CDSSs can vary in levels of sophistication from simple alerts to clinical prediction rules which estimate probabilities of developing a disease or clinical outcomes.
Evidence base
A systematic review of 94 randomised and 14 quasi-randomised trials found that most CDSSs lead to a small to moderate increase in patients receiving desired care (5.8%) and a slight increase (0.3%) in the achievement of clinical outcomes. 93 Larger effects occur when there is low adherence prior to the intervention. While CDSSs can be useful in clinical practice, large numbers or less relevant alerts may be counterproductive, leading to alert fatigue and reduced clinician receptivity.
Discussion summary
While it was noted that computerised alerts on the prison data system (SystmOne) were less frequent than on other electronic health-record systems, for example EMIS Web, the drawbacks – alert fatigue, disruption to the flow of clinical consultations, limited patient specificity – may reduce acceptability. Targeted prompts, however, such as for overdue screenings or over-prescribing, could be effective to guide clinicians towards appropriate care. Where there is a clear link between the recommended action and patient outcomes then prompts may be a useful initiative. Identifying and decommissioning prompts where there is no link to outcome improvement may reduce alert fatigue and hence increase overall utility and effectiveness of CDSSs.
Audit and feedback
Definition
Audit and feedback involve comparing individual performance data with professional standards of care and providing feedback to encourage clinicians to adhere to care guidelines.
Evidence base
A review of 140 randomised trials found that audit and feedback improved processes of care by 4.3% on average (interquartile range 0.5–16%). 94 The review identified five key features which improve effectiveness: low baseline performance, delivery by a supervisor or colleague rather than a manager, repeated cycles, combined verbal and written delivery, and including a target and action plan. The feasibility of audits depends on access to meaningful routine data and analytic capability.
Discussion summary
Participants identified challenges to the effectiveness and acceptability of audits, noting limited observed improvements following some audits and that the range of audits requested could add to the pressures faced by COVID-fatigued staff. Practicability could vary across the estate, largely dependent on whether establishments had dedicated staff to extract and analyse audit data. Data quality can also be variable and affect accuracy of feedback.
Challenges notwithstanding, participants acknowledged the potential effectiveness of audit and feedback to improve clinical care, through making audits more streamlined, collaborative and meaningful to frontline staff, and using data to identify priorities for improvement. An offender health audit plan, driven by commissioners, could offer a consistent vehicle for conducting audit and feedback. Other suggestions included a central resource for analytic support to increase practicability and ensure equity across the estate, and a recommendation that prison healthcare systems are subject to the same performance feedback loops as community general practice with regard to prescribing data. Qual-P has demonstrated the feasibility of conducting meaningful and targeted audit of specific indicators, and the evidence base recommends repeated and goal-setting audit processes as a foundation for improvement strategies.
Further suggestions for implementation interventions and levers
We noted that many interventions tended to target teams or individuals rather than promote organisational or system-level change. We therefore particularly welcomed additional participant suggestions for the latter categories. Suggestions included:
-
Improving linkage of prison and community primary care records to enable continuity of care, especially for long-term conditions and managing problematic prescribing.
-
Review of the specialist MH workforce for secure environments with the possibility of joint posts across prisons and secure hospitals.
-
Use of standard electronic health-record templates for priority populations (e.g. people with learning disabilities) to prompt recommended care and to enable population management.
Further consultation following the workshops
We shared a summary of Workshop 3 with all stakeholders who had previously expressed interest in our work. We continued to seek suggestions for implementation interventions and levers. We also drafted and sought opinions on an illustrative strategy to reduce opioid and gabapentinoid prescribing (see Appendix 12). We recognised that no one intervention by itself is likely to bring about a significant reduction in opioid or gabapentinoid prescribing. Any improvement strategy needs to target key influences on practice that are amenable to change. We therefore suggested a combination of approaches.
We shared this illustrative strategy to demonstrate how different interventions and levers for change can be combined for any of the 30 quality indicators we identified and assessed in earlier WPs. We subsequently outlined a further strategy for improving the management of hypertension (see Appendix 13). One of our workshop objectives had been to prioritise indicators for targeted improvement. We only managed to exempt six indicators that were perceived as less important and less feasible to change performance for. However, we have demonstrated the value of indicators that make efficient use of routinely collected data in highlighting scope for improvement across and between prisons, and hence guiding the targeting of future improvement strategies.
Chapter 7 Mental health analysis
Introduction
In our analysis of routinely collected healthcare data (reported in Chapter 5), we found variation in the quality of primary care for physical health problems between prisons. In this chapter, we focus our attention on mental illness. It is widely accepted that both people in prison and people with mental illness experience health inequalities. In the general population, there exists a ‘mortality gap’ for people with SMI or a history of substance misuse. 98 This gap is associated with increased rates of suicide, accidental or violent death, increased prevalence of risk factors such as smoking and obesity and consequent comorbid physical health problems (which are associated with diagnoses and drug treatments for mental illness), reduced uptake of physical health care and screening, and ‘diagnostic overshadowing’ (misattribution of symptoms of physical illness to mental illness). 99 The prevalence of long-term physical and mental illness and disability is higher in the prison population compared to equivalent community populations. 100–103 In prison, rates of mental illness, including psychosis, depression, personality disorder and drug and alcohol dependency, are higher than in the community. 104–106 As with physical illness, people in prison present with multiple and complex conditions, with reportedly 70% of prisoners meeting the criteria for two or more psychiatric diagnoses. 107 The prison setting, however, is not conducive to mental healthcare provision108 and may even exacerbate mental distress. 109 Self-injurious behaviours are common in prison110 and suicide rates are higher than those in the community. 111 Unsurprisingly, people in prison are higher users of healthcare services, which may be linked to reduced physical activity, the quality of nutrition, and access to over-the-counter medications, social care and self-directed support. 112,113
In this chapter we report secondary analyses undertaken with a focus on mental health. Our aim was twofold: (1) to deepen our understanding of mental illness and mental health care in prison by revisiting the qualitative data from interviews with healthcare professionals and prison leavers, and (2) to analyse quality of care for subgroups of people in prison with a diagnosed mental illness compared to those without.
Qualitative analysis
Methods
The qualitative data reported in this analysis were collected using the same methods described in Chapter 4. The original data set comprises 21 interviews with prison leavers and 22 with prison healthcare staff. Five healthcare professionals and two prison leavers did not mention MH and the interviewer (SB) did not ask about it. Transcripts with mental health-related content were included in this analysis (i.e. 19 prison leaver transcripts and 17 healthcare professional transcripts). We conducted an inductive, reflexive thematic analysis. 114 The interviews and original analysis were undertaken by one of the authors (SB). The analysis reported here was undertaken by another author (KC). This process involved reading the transcripts in full, reviewing existing extracts coded by SB as related to MH, and then development of a thematic schema to organise the data.
Findings
Most participants (patients and staff) spoke spontaneously during interviews about their experiences and observations of mental distress and its causes and consequences. Of these, 17 were healthcare professionals and 19 were prison leavers, comprising 77% and 90% of the original samples, respectively (see Appendix 14, Table 28). Just one of the healthcare professionals interviewed was a MH professional (a MH nurse). Of the 19 prison leavers who mentioned MH in their interview, 15 (11 men and 4 women) had personally experienced mental distress and/or had a diagnosed MH condition. Participants described experiencing a wide range of conditions and expressions of mental distress, including psychosis, post-traumatic stress disorder (PTSD), schizophrenia, bipolar disorder, personality disorder, anxiety, depression, self-harm acts and thoughts, and drug and alcohol misuse. Of those who had accessed MH services in prison, just two reported that their needs had been met. There were no discernible differences between the characteristics of the two groups. The characteristics of the full sample are described in Chapter 4.
Mental distress as an inseparable and inevitable feature of imprisonment
The participants in this study portrayed mental distress as a ‘big issue’ and ‘huge problem’ in prison. Both staff and prison leavers remarked on the disproportionately high rates of mental ill-health, describing their perception of MH crises as having reached ‘epidemic scale’ (PL09 male, 43) and mental illness at rates of ‘90 per cent’ in one female prison (HCP17 MH Nurse, female estate) and anxiety and depression comprising ‘a good 25%’ of consultations (HCP09 GP, male and female estate). It was recognised that the prison population were a very vulnerable group with multiple and complex health and social problems. Accordingly, participants presented mental distress, imprisonment, physical health and behaviour as ‘part and parcel of everything’:
Whenever you have an interaction with someone that’s ostensibly about a physical problem, it’s quite likely that a mental health problem will come up in that conversation because they’ll bring something up with you that they might not have otherwise brought up. Or it might be directly related; obviously self-harm, self-neglect, the choices that people are making are often related to their mental health.
HCP16 Nurse, male estate
Participants also made links between mental distress and legal and illegal substance use, describing how ‘they always cross over pretty much’ (PL13 male, 38) and how prisons are ‘flooded’ with drug misuse and individuals prescribed ‘a lot of medication’ (PL18 female, 30s). This concept of inseparability gave rise to the notion that experiencing mental distress in prison is inevitable given the everyday reality of imprisonment which involves the loss of privacy and autonomy and separation from family:
As an individual, a human on this planet, you are going to have some kind of mental health issues being incarcerated in that environment.
PL18 female, 30s
Individual vulnerability and ability to adjust to imprisonment also played a part: ‘a lot of people can’t handle that’ (PL04 male, 41). One participant conveyed her sense of fragility in the context of being separated from her family combined with the fallout from substance use:
You’re an empty shell, do you know what I mean? I felt like if you’d tapped me, I’d just crumble.
PL15 female, 40
Both staff and prison leavers thought that people with mental illness ‘shouldn’t be in prison’ (PL03 45m), describing the prison environment as inappropriate and ‘not therapeutic for them at all’ (HCP16 Nurse, male estate):
I’ve seen women with dreadful mental health problems who have had to … for their own safety and safety of others have had to be in the segregation unit and it hasn’t been the appropriate …. They ought to have been in a mental hospital and had mental health care.
HCP15 Nurse, female estate
One participant reflected on the incompatibility of the prison environment with symptoms of distress: ‘it’s a horrible place to be anxious’ (PL09 male, 43); especially in the absence of support mechanisms, ‘in a prison environment, who do you turn to?’ (PL21 female, 30). Thus, while the numbers of individuals experiencing distress was considered disproportionate, the distress itself was not.
There are quite a lot of people who don’t have a realistic hope of ever being released, and so it’s difficult to say ‘Well, they have depression’, as such, because it’s almost an understandable reaction to the situation, it’s not a disproportionate reaction as such.
HCP16 Nurse, male estate
Prison leavers not only conveyed an acute sense of the risks associated with mental distress: ‘they could harm themselves, they could hang themselves, they could slash their wrists’ (PL10 male, 44); they also viewed these outcomes as highly likely: ‘There is every chance someone in that mind frame might self-harm’ (PL12 male, 29). This accompanied the encroaching sense of the inevitability of self-harm and suicide attempts, given credence by participants’ observations of the frequency of these behaviours. Self-harm was described as a ‘daily’ event (HCP12 Nurse, male estate) that had increased during the pandemic. The perceived inevitability of self-harm was both driven and confirmed by the belief that ‘doing something quite drastic’ (PL12 male, 29) was the only way to secure medical attention.
P: If you threaten it, that’s not enough, you’d have to actually attempt to do it.
I: Right, so to say that you’re thinking of it, –
P: That wouldn’t be enough to see a mental health worker, no way.
PL09 male, 43
Professionals confirmed the view that accessing MH support is more likely, and quicker, for those experiencing ‘a crisis situation’ (HCP04 Nurse, male estate) or ‘if they have self-harmed or tried to self-harm’ (HCP11 Associate practitioner, male estate):
You find that the people who shout the loudest, bang the drums the loudest, who use blades for attention, sometimes it’s attention-seeking and other times it’s because you find nobody is listening, that is the only way you get the attention you need, because you are ignored.
PL16 male, 46
Prison mental health care as a low priority
Mental health care was described as ‘really bad’ (PL09 male, 43; PL08 male, 29) and inadequate given the demand: ‘three nurses for 1500 people is a bit of a joke’ (PL05 male, 27). Staff shortages, ‘phenomenal’ caseloads (HCP15 Nurse, female estate) and the consequently ‘really stretched’ (HCP05 GP, male estate) and ‘overworked’ (PL05 male, 27) workforce was acknowledged as a contributory factor by staff and prison leavers.
Mental health within the prison from the prisoners has deteriorated so much to the point it makes me question how are they going to pick up the pieces, because anyone that you speak to is suffering with some form of mental health problem and they are not providing the service. You can’t even talk to an officer, let alone speak to someone from mental health.
PL21 female, 30
Prison leavers also reported difficulties accessing prescribed medication for MH issues which caused ‘distress’ and ‘worry’ (PL16 male, 46) as well as recurrence of symptoms:
I kept asking for my medication … you are stood in the queue for about twenty minutes half an hour so yeah I used to dread them queues and then I think this happened about six days on the trot erm they didn’t have my prescribed medication.
PL01 male, 30
Many participants expressed the view that MH was not a priority in the prison setting and that prisons ‘don’t cater for that kind of thing’ (PL08 male, 29).
The mental health team are really bad in the prison service. You’re locked behind your door and they just let you get on with it. That’s my personal opinion; the mental health issues are never, ever dealt with.
PL03 male, 45
Relatedly, they viewed the response to mental distress as perfunctory and dismissive:
If I wasn’t going home, you would have not seen me. That is the truth of it, you would have not bothered, but because I am going home and you need to make sure that your paperwork is in place, you are seeing me.
PL21 female, 30
One staff participant described the lack of recognition of the importance of MH training:
They are a general nurse, a lot of the time in the prison environment it is, ‘Can you assess their mental health while you are there?’ Maybe they are not trained or competent enough to do that. It is allowed to do a skimming over rather than an in-depth specialist going to see them.
HCP17 MH nurse, female estate
Expressing and seeking help for mental distress as risky
Risk of being ignored
In expressing their mental distress or seeking help, prison leavers risked being ‘ignored’ (PL21 female, 30) or ‘palmed-off’ (PL05 male, 27).
Myself, I suffer with PTSD and it’s just, ‘Deal with it, son’.
PL03 male, 45
Some described their own experiences of this, but also witnessed others not receiving care for apparent distress. Observing others being treated this way could impact their expectations for assistance with their own mental distress:
You are trying to convince yourself that everything is going to be okay, but really it’s not okay as we just really need to speak to somebody and that makes it even worse because you are like, god, the woman that’s next door to me, she’s screaming in her sleep and she’s banging on the door and she needs help, she is screaming for help, but she’s just being ignored. So if they are not dealing with me and they are definitely not dealing with her, what luck do we have?
PL21 female, 30
Similarly, prison leavers also referred to the risk of suspicions around false claims of distress in order to access tradeable medications:
‘He’s just trying to blag this out of us, just trying to blag that out of us’, when that’s not always the case. Especially for mental health, do you know what I mean? Some people actually need antipsychotic drugs, some people actually need sleepers. But because those drugs have been abused, there’s very much a ‘no-no’ attitude.
PL03 male, 45
This attitude was in turn interpreted as meaningful, purposeful and intentionally punitive – and confirming assumptions about the provision of care and the uncaring environment.
They need to treat people with a bit more respect. Some people have deep underlying issues, but the way they treat them is like dirt, like filth. That is why these people try and harm themselves.
PL10 male, 44
As described above, prison leavers were acutely aware of the potential consequences of ignoring individuals seeking help for mental distress:
Some people go crazy, they hang themselves, they do daft things because they are not getting the attention they need.
PL10 male, 44
Risk of unmet needs and unwanted consequences
Although participants described the difficulties accessing MH services in prison, both staff and prison leavers identified the risks of patients’ needs remaining unmet and intervention having other unwanted consequences. Even when patients did access services, they did not necessarily get the help they wanted or needed, and in some cases they might not get any help at all. One participant thought that asking for help and not getting any was particularly risky to mental health:
The value in them reaching out is quite strong – how much it took for that individual to reach out and ask for help. Some people don’t like asking for help, so when they surrender and say, ‘I need some help’, and it doesn’t come, that can make your position 1000 times worse.
PL05 male, 27
Prison leavers’ expression of dissatisfaction with services was sometimes due to the outcome not meeting their expectations (and expectations varied between participants). One participant who was eventually diagnosed with attention deficit hyperactivity disorder (ADHD), anxiety and depression said he felt ‘let down’ after originally seeing a psychiatrist who ‘just wrote it off as psychosis’. While some wanted medication, others perceived that: ‘They just ply you with medication that you don’t need and that makes you even worse’ (PL08 male, 29).
Staff also perceived an ‘over-reliance’ on medication, in lieu of other forms of treatment and support, because ‘we have nothing else but medication’ (HCP09 GP, male and female estate):
There are a lot of people who really need somebody to talk to. They don’t need medication, they don’t need high-level mental health input, but they do need somebody to talk to, and because the mental health team are so busy, that comes to us, whereas really we’re not counsellors, or not very good counsellors. There’s a bit of a gap in provision, so we end up giving them medication when really what they’d benefit from more is a course of counselling or more access to talking therapies.
HCP05 GP, male estate
Furthermore, displaying distress or seeking help could lead to other unwanted outcomes. One healthcare staff participant in an open prison believed that residents would avoid seeking support for their MH out of fear that they would be transferred back to a closed prison, while a prison leaver described being told that he could be transferred to a psychiatric hospital:
A psychiatrist came in and gave me an assessment …. An outside psychiatrist, very smart, looked like a city sort of fellow really, very smart, very slick hair …. And he said, ‘If anything like this happens again, you will be in … you will go into a mental home, a psych ward and it is a lot worse in there’, he said.
PL13 male, 38
Summary of main findings
Both healthcare professionals and prison leavers described mental distress as common in prison, partly due to people entering with pre-existing mental illness, but also because prison would cause mental distress to those without and exacerbate it in those with. In this way, mental distress was portrayed as omnipresent, inseparable from the experience of imprisonment.
Mental distress and mental crises (expressed in the form of self-harm or suicide attempts) were also considered inevitable (especially by prison leavers). This belief was linked to their inseparability from imprisonment per se, but also to (1) the unsuitability of the prison environment to people experiencing distress, (2) the fragility of the individuals in question, (3) the difficulty accessing MH support and (4) the perception that MH support could only be accessed in urgent or crisis situations (such as self-harm).
Finally, we found that experiencing mental distress in prison involves high stakes. Seeking support for mental distress was portrayed as involving multiple risks, including failing to access support, exacerbating existing negative feelings, and dissatisfaction and disappointment with any eventual contact with or treatment from the MH team.
Analysis of electronic health records
Our analysis of routinely collected data (detailed in Chapter 5) found that the quality of primary care varied between prisons. The data also provide an opportunity to understand variations related to mental illness. This additional analysis aimed to investigate whether achievement of the quality indicators assessed in Chapter 5 are associated with MH groups, and explore the degree to which any variations can be accounted for by recorded prison and population characteristics.
Methods
We identified three MH groups based on the two indicators related to the MH diagnosis subgroup of the opioid prescription indicator and the antipsychotic prescription indicator, as outlined in Table 11.
| MH group | Description of identification of group |
|---|---|
| No MH diagnosis | People with NO MH diagnosis based on the subgroup of the indicator of opioid prescription in the preceding 8 weeks from 31 March OR DID NOT receive three or more prescriptions for an antipsychotic in the preceding 12 months. |
| MH diagnosis with psychotropic drugs | People with a MH diagnosis based on the subgroup of the indicator of opioid prescription in the preceding 8 weeks from 31 March AND have received three or more prescriptions for an antipsychotic in the preceding 12 months. |
| MH diagnosis without psychotropic drugs | People with a MH diagnosis based on the subgroup of the indicator of opioid prescription in the preceding 8 weeks from 31 March AND DID NOT receive three or more prescriptions for an antipsychotic in the preceding 12 months. |
To explore the associations between the indicators and the MH groups, multilevel logistic regression models were developed. Separate models for each indicator were developed with achievement of each indicator as the outcome and year included as fixed and random effects to account for the correlation between people with multiple stays across the 3 years. Inclusion of the MH group variable as a fixed effect provided ORs (and accompanying 95% CIs) with No MH as the comparator group. The models were developed further by inclusion of the other characteristics to explore whether any associations between the MH group and achievement of the indicators were accounted for by other individual and prison factors. The resultant adjusted ORs and 95% CIs are presented.
Results
Of the 69,587 prison stays over the 3 years, 13.7% of stays had a MH diagnosis while 1.5% had a psychotropic drug prescription (see Appendix 15, Table 29). In the first 2 years, the patterns of the distribution between the MH groups are similar. However, in the third year, more stays (16.8%) had a coded MH diagnosis than in the previous 2 years (12% in 2017–8).
There were differences in the proportions with a MH diagnosis (with and without psychotropic drugs) between prisons, prison category, gender, age, length of stay and ethnic group. For example, 36.4% of stays by women have a MH diagnosis compared to 11.9% of stays by men, while MH diagnoses were most common in white ethnic group stays (17%) compared with other ethnic groups. These differences in proportions by MH groups and the characteristics indicated that these factors might account for any differences in achievement of the indicators by MH groups. Therefore, we adjusted for these factors in the subsequent models.
From the summary of the proportions of achievement of each indicator by MH group, there is an indication of variation in MH and the indicators (Table 12), which was better explored in the multi-level logistic models (see Appendix 16).
| Variable | All prison stays | No. of stays (% of all) – by MH groupa | ||
|---|---|---|---|---|
| No mental health | MH with psychotropic drugs | MH without psychotropic drugs | ||
| All prison stays | 69,587 | 60,064 (86.3) | 1033 (1.5) | 8490 (12.2) |
| Year | ||||
| 2017–8 | 21,677 | 19,085 (88.0) | 244 (1.1) | 2348 (10.8) |
| 2018–9 | 22,099 | 19,510 (88.3) | 326 (1.5) | 2263 (10.2) |
| 2019–20 | 25,811 | 21,469 (83.2) | 463 (1.8) | 3879 (15.0) |
| Prison | ||||
| Prison 1 | 4066 | 3153 (77.5) | 43 (1.1) | 870 (21.4) |
| Prison 2 | 8945 | 6449 (72.1) | 122 (1.4) | 2374 (26.5) |
| Prison 3 | 7954 | 7193 (90.4) | 127 (1.6) | 634 (8.0) |
| Prison 4 | 7089 | 6641 (93.7) | 94 (1.3) | 354 (5.0) |
| Prison 5 | 1929 | 1737 (90.0) | 5 (0.3) | 187 (9.7) |
| Prison 6 | 4598 | 4580 (99.6) | 18 (0.4) | 0 (0.0) |
| Prison 7 | 2149 | 1855 (86.3) | 135 (6.3) | 159 (7.4) |
| Prison 8 | 3618 | 1976 (54.6) | 95 (2.6) | 1547 (42.8) |
| Prison 9 | 3069 | 2795 (91.1) | 87 (2.8) | 187 (6.1) |
| Prison 10 | 8817 | 7582 (86.0) | 57 (0.6) | 1178 (13.4) |
| Prison 11 | 12,838 | 12,146 (94.6) | 193 (1.5) | 499 (3.9) |
| Prison 12 | 2412 | 2408 (99.8) | 4 (0.2) | 0 (0.0) |
| Prison 13 | 2103 | 1549 (73.7) | 53 (2.5) | 501 (23.8) |
| Prison category | ||||
| A | 5172 | 4344 (84.0) | 140 (2.7) | 688 (13.3) |
| B | 30,600 | 26,177 (85.5) | 372 (1.2) | 4051 (13.2) |
| C | 19,109 | 16,987 (88.9) | 264 (1.4) | 1858 (9.7) |
| Closed | 5767 | 3831 (66.4) | 230 (4.0) | 1706 (29.6) |
| D | 6527 | 6317 (96.8) | 23 (0.4) | 187 (2.9) |
| YOI | 2412 | 2408 (99.8) | 4 (0.2) | 0 (0.0) |
| Gender | ||||
| Female | 4877 | 3101 (63.6) | 155 (3.2) | 1621 (33.2) |
| Male | 63,842 | 56,252 (88.1) | 803 (1.3) | 6787 (10.6) |
| Missing | 868 | 711 (81.9) | 75 (8.6) | 82 (9.4) |
| Age – years | ||||
| 10 to <20 | 1308 | 1275 (97.5) | 8 (0.6) | 25 (1.9) |
| 20 to <30 | 22,221 | 20,098 (90.4) | 197 (0.9) | 1926 (8.7) |
| 30 to <40 | 23,557 | 20,009 (84.9) | 406 (1.7) | 3142 (13.3) |
| 40 to <50 | 13,242 | 10,795 (81.5) | 275 (2.1) | 2172 (16.4) |
| 50 to <60 | 6309 | 5319 (84.3) | 101 (1.6) | 889 (14.1) |
| 60 to <70 | 2136 | 1845 (86.4) | 24 (1.1) | 267 (12.5) |
| 70 to <80 | 660 | 585 (88.6) | 16 (2.4) | 59 (8.9) |
| 80 to <90 | 138 | 126 (91.3) | 4 (2.9) | 8 (5.8) |
| 90 to <100 | 7 | 4 (57.1) | 2 (28.6) | 1 (14.3) |
| 100 to <110 | 2 | 1 (50.0) | 0 (0.0) | 1 (50.0) |
| Missing | 7 | 7 (100.0) | 0 (0.0) | 0 (0.0) |
| Length of stay (months) | ||||
| <1 | 16,039 | 14,162 (88.3) | 156 (1.0) | 1721 (10.7) |
| 1 to <6 | 26,619 | 22,820 (85.7) | 387 (1.5) | 3412 (12.8) |
| 6 to <12 | 11,181 | 9568 (85.6) | 191 (1.7) | 1422 (12.7) |
| 12 to <24 | 9184 | 8029 (87.4) | 145 (1.6) | 1010 (11.0) |
| 24+ | 6564 | 5485 (83.6) | 154 (2.3) | 925 (14.1) |
| Ethnic group | ||||
| White | 47,155 | 39,116 (83.0) | 822 (1.7) | 7217 (15.3) |
| Mixed | 1211 | 1055 (87.1) | 14 (1.2) | 142 (11.7) |
| Asian or Asian British | 2294 | 2100 (91.5) | 19 (0.8) | 175 (7.6) |
| Black or Black British | 1219 | 1081 (88.7) | 19 (1.6) | 119 (9.8) |
| Chinese and other | 544 | 476 (87.5) | 13 (2.4) | 55 (10.1) |
| Unclassified | 1168 | 1050 (89.9) | 15 (1.3) | 103 (8.8) |
| Missing | 15,996 | 15,186 (94.9) | 131 (0.8) | 679 (4.2) |
Most communicable disease, MH and prison-specific indicators were associated with MH (see Appendix 16). Generally, the odds of achievement of these indicators were higher in those with a MH diagnosis (with and without psychotropic drugs) compared to those with no MH diagnosis, even with adjustment for other factors (see Appendix 16, Table 30). For example, the odds of receiving one hepatitis B vaccination in the preceding 12 months was 90% higher for those with a MH diagnosis without psychotropic drugs compared to those with no MH diagnosis, adjusting for other factors (OR 1.90; 95% CI 1.78 to 2.02), and 65% higher in those with MH diagnosis with psychotropic drugs (1.65; 1.41 to 1.94).
Few of the Diabetes, Asthma and Epilepsy Care, Screening and CVD indicators were associated with mental health. Where associations existed, the odds of achievement of these indicators were generally higher in those with a MH diagnosis without psychotropic drugs compared to those with no MH diagnosis, even with adjustment for other factors. For example, the odds of people aged 79 years or under, with CHD, hypertension, stroke, transient ischaemic attack or peripheral arterial disease, having a blood pressure of 140/90 mmHg or less in the preceding 12 months was 25% higher in those with a MH diagnosis without psychotropic drugs compared to those with no MH diagnosis, adjusting for other factors (1.25; 1.02 to 1.53), and 68% higher in those with MH diagnosis with psychotropic drugs (1.68; 0.96 to 2.96). In only one of these indicators is the association in those with MH with psychotropic drugs. In those with a MH diagnosis and psychotropic drugs, the odds of the last HbA1c being 58 mmol/mol or less in the preceding 12 months in people with diabetes without moderate or severe frailty were 2.2 times higher than those with no MH diagnosis (2.18; 1.32 to 3.59).
In two indicators, the odds of achievement of the indicators were lower in those with a MH diagnosis without psychotropic drugs compared to those with no MH diagnosis, even with adjustment for other factors. Firstly, in those with a MH diagnosis and without psychotropic drugs, the odds of people who had had a MI being prescribed three cardiovascular medicines (out of the following: ACE-Is or ARBs, antiplatelet therapy, beta-blockers and statins) was 47% lower than those with no MH diagnosis (0.53; 0.37 to 0.74). Secondly, the odds of eligible women aged 50–70 having a breast screen in the preceding 3 years was 53% lower for those with MH diagnosis and not prescribed psychotropic drugs than those with no MH diagnosis (0.47; 0.28 to 0.79).
Interpretation
Across most indicators, achievement was generally higher for stays of prisoners with coded mental illness than for those without. Achievement also tended to be higher for stays of prisoners with coded mental illness and prescribed antipsychotics. At face value, these findings may appear counterintuitive considering there is a significant evidence base highlighting how people living with severe and enduring mental illness in the community have poorer physical health outcomes. 115 However, people in prison with mental illness are more likely to experience comorbidities and have more frequent encounters with health care, which in turn provides more opportunities for delivering and recording processes of care. What we cannot tell from our data is to what extent actual individual needs were met and whether care delivered improved outcomes.
Nevertheless, we still identified examples where prisoners with coded mental illness were less likely to experience recommended care than those without, namely breast screening for women aged 50–70 years and drug treatment following MI. Furthermore, we found increased likelihoods of opioid prescribing, gabapentinoid prescribing and psychotropic polypharmacy for stays of prisoners with coded mental illness compared to those without. Although such patterns might broadly be expected, the magnitude of such risks was striking, with a more than 17-fold likelihood of being prescribed four or more psychotropic drugs for people prescribed antipsychotics and a more than 4-fold likelihood for other people with coded mental illness.
Chapter 8 Discussion
Some material from this chapter has been reproduced from Sheard et al. (2023):Sheard, L, Bellass S, McLintock K, Foy R, Canvin K. (2023) Understanding the organisational influences on the quality of and access to primary care in English prisons: A qualitative interview study. British Journal of General Practice, 100166
This article is licensed under a Creative Commons Attribution 4.0 International License (CCBY 4.0) which permits use, sharing, adaptation, distribution and reproduction in any medium or format, provided the original work is properly cited. See http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
What have we learnt about the quality of prison health care?
In this section, we draw together the high-level take-home messages from across all WPs to provide an overall account about the quality of prison health care grounded in the empirical data. In doing so, we have derived five broad headline discursive-level ideas of interest which comment on the state of play regarding prison health care. As our empirical chapters focus on data sets which are UK-specific, we use this section to mostly comment on ideas of interest which are context-bound to the UK setting. While our scoping review (see Chapter 2) predominantly identified work from the USA, we will include findings from this WP as and when applicable. The five ideas of interest are:
-
measurement and monitoring
-
variability
-
health inequalities
-
prison organisation and system
-
prison–community interface.
Measurement and monitoring
The bedrock of any strive towards improvement for healthcare providers and services is to have a robust system of measurement and monitoring in place within an organisation, and an ability to BM between similar organisations or services. There are several important facets of measurement and monitoring that are necessary to provide high-quality health care. 116 Clinicians and managers need to know if the safety, effectiveness and quality of care are better or worse than they were previously. They also need to know if patients are receiving ‘reliably delivered’ health care: that is, health care that is timely and appropriate care relevant to their health condition and its severity.
Measurement and monitoring of the acute hospital sector and primary care are formally incentivised with Commissioning for Quality and Innovation (CQUIN) payments to secondary care and the QOF payments to general practice respectively. CQUIN and QOF financially incentivise hospitals and general practice to meet targets concerning certain standards of care for patients. For general practice, the indicators span clinical domains, public health and quality improvement. QOF allows practices to compare their performance with previous years and also compare themselves with other practices. QOF participation rates are high, with 96% of general practices taking part in 2019–20. 81
This study suggested that the absence of formal incentives for prison healthcare measurement and monitoring undermines the motivation of individuals and teams working in health care to spend time and effort in non-mandated recording in a pressured system. Wright et al. 117 have previously discussed how the opportunity to improve clinical outcomes associated with long-term conditions is being missed while QOF monitoring in prisons remains non-incentivised. Our interview study revealed that healthcare staff were aware of performance measures within prison health care, including both QOF and the Health and Justice Performance Indicators. However, there was a personal lack of involvement with this area of work and it was viewed as the province of management. Where QOF was used to plan care, it was criticised as being unreliable when applied to the prison population. Local audits were referred to as sometimes being useful, but management participants put forward the need not to simply implement measurement tools or scales (either local or national) without the ability to understand the whole patient journey. Additionally, clinical coding was said to be poor in prison health care, which further hampers the ability to measure and monitor change over time and between prisons.
Our stakeholder consensus process in WP1B recognised a preference for simple, single (non-composite) indicators, which help ensure feasibility in practice and enhance transparency of measurement. 118 This is because the final working list of 30 indicators taken forward to be tested contained some bespoke indicators that are not routinely applied to prison health care. We were conscious from the outset of not developing indicators through this research study that would, going forwards, be minimally operationalised (or even not at all) if they were prohibitively complex and required input from specialist performance management personnel. Our statistical analysis of routinely collected data in WP3 involved a lengthy process of data extraction, undertaken by a data specialist at Spectrum CIC. While we were able to base many of the extractions for the 30 indicators on existing QOF template algorithms, several required modifications to ensure necessary data could be extracted. We intend to develop an open-source codebook which we will make freely available to prison healthcare providers’ data and performance teams to apply to their own routinely collected data. This will explicate some of the background work involved in the development of an effective method of measuring and monitoring the quality of prison health care.
The findings of WP3 demonstrated high variability in quality of care between different prisons, which is not solely attributable to differences in prisoner demographics. This denotes that measurement and monitoring across the prison estate – and specifically between different healthcare providers – is a problematic task as variation is likely to be attributable to the local organisation of prison health care. The heterogeneity of the local organisation of care across the prison estate makes comparison difficult and deters a standardised approach to measurement and monitoring. This brings us onto our next high-level message: variability.
Variability
Variability in quality of health care could be viewed as a fundamental problem of health inequality. Comparable healthcare organisations, such as hospitals of a similar size, patient turnover and level of resource/expenditure, can have highly variable outcomes for patients. Dixon-Woods et al. 119 highlight four areas of variability which have the most impact on a healthcare organisation’s outcomes. These are: goals, intelligence, systems, culture and behaviour, with considerable inconsistency in these domains across NHS organisations. Intelligence is said to be critical, with healthcare organisations needing to know how well they are performing and most critically where they need to improve. 119 Marked variability can be seen even between two services in a similar geographic area that deliver the same defined treatment pathway to patients. Hughes et al. 120 compared two services which had significantly differing outcomes for elective hip and knee replacement surgery and found distributed leadership, clinical autonomy, a sense of team resilience and strong communication between all levels of staff were critical factors that enabled excellent care to be delivered. Such variations are also common in primary care. For example, Willis et al. 53 found variations in levels of adherence to a set of EB process and outcome indicators, which were not explained by routinely collected patient or practice variables.
Our analysis of routinely collected data shows that such variations are also present in prison primary care and cannot be solely attributed to differences in recorded prison population characteristics. Many of these variations are likely to be attributable to differences in organisational and clinical behaviours.
We observed few particular patterns of achievement when, for example, we grouped indicators by domains (e.g. diabetes, asthma, communicable disease). The most notable pattern we observed across several domains, particularly those related to long-term condition management, was lower achievement associated with shorter lengths of stay. This undoubtedly reflects the challenges of delivering primary care to a population with a high turnover but might also be seen as a missed opportunity to intervene.
There is little previous work examining variations of care in prison settings. A study conducted in Germany across prisons in 11 federal states looked at prescribing for tuberculosis (TB), HIV, hepatitis C (HCV) and opiate substitution treatment (OST). 121 The authors found TB and HIV treatment to be adequate, but HCV treatment was considered low and OST treatment highly variable. Furthermore, there were high levels of variations in treatment. This study adds to the literature by deliberately including a focus on the ‘mundane’ conditions which are commonly managed in community primary care (e.g. hypertension, type 2 diabetes).
Notably, we examined primary care delivery in all 13 prisons delivered almost entirely by the same healthcare third-sector, non-profit healthcare provider (Spectrum CIC), which has high-quality care as a core organisational goal. Additionally, all 13 prisons were located within the North of England. To find such variability of achievement for healthcare indicators across 13 prisons delivered by a single care provider suggests that behavioural and cultural factors inside the prison gates have a large role in influencing outcomes. This is consistent with what staff and patient participants told us in the qualitative interviews.
Variability as described by our participants in the qualitative interviews provides a different perspective on what we mean by this concept. People in prison talked about variability in relation to their access to health care. They told us that this depended on how accommodating and efficient the prison officers were at facilitating a patient’s request for a healthcare appointment and/or then unlocking the patient from their cell in time to attend a healthcare appointment. This was often perceived as being contingent on a prisoner’s behaviour and whether they were considered ‘trouble’. Given these explicit barriers, whether a patient even got through to a clinician was seen as highly variable, with many prisons having a high ‘DNA’ appointment rate, as expressed by staff participants in our interviews. This is reinforced by the literature. Davies et al. 122 demonstrated that 40% of hospital outpatient appointments made for people in prison are not attended. Grey evidence from the Independent Monitoring Boards gives a figure of 20–30% ‘DNA’ level for in-prison healthcare appointments. 123 The variability in access to health care for patients in prison seems to be largely dependent on factors outside the control of the healthcare provider and healthcare department. This brings us back to the beginning of this section in considering the pertinence of Dixon-Woods et al. ’s119 four areas of variability, where it is clear that, certainly, the goals of the prison regime differ from the healthcare goals, alongside having disaggregated models of culture and behaviour between the two spheres.
Health inequalities
While ethnic minority populations are over-represented in prison, the prison population in the UK is pictured as predominantly being made up of young, white men mostly sentenced for non-severe crimes or on remand. It is known that women, older prisoners and those from minority ethnic groups have distinct health needs compared to the prison population as a whole. 124 In this section, we discuss where health inequalities may lie. Our analyses showed no clear overall trend for indicator achievement by age, gender or ethnicity.
Age
The prison population is changing, with the most striking demographic change being that of age. The percentage of over 50s in the UK prison estate has increased by from 7% to 17% in a little under 20 years. 2 This situation is not unique to the UK, with this demographic shift occurring in many countries across the world. 125 Older people are now entering prison more often, due to being sentenced for historical crimes; the prison population in general is ageing. Older male prisoners on remand have been found to have high rates of alcohol use, psychotic illness and self-harm when compared with younger male remand prisoners. 125 A Swiss study found that the average number of diseases reported by older prisoners over the age of 50 was 2.26 times higher than for those aged under 50. 126 Our international scoping review (undertaken as part of WP1) found that the ageing prison population represents a major challenge regarding performance measurement in the prison system. This is often related to an increase in the prevalence of chronic, long-term conditions, with 85% of over 50s in prison reported to have three or more long-term health conditions. This is a particularly acute situation in the USA, which has the highest number of incarcerated individuals per capita in the world.
In our quality indicator selection in WP1, we were conscious of selecting indicators which are more likely to be relevant for older prisoners, such as hypertension, heart disease and dementia. One interesting indicator is that of the proportion of men who are aged 65 years and older and are eligible for AAA screening (a condition more likely to occur with increasing age). We found that 2.1% of male prisoners were eligible for this screening but only around 45% of them had received it. This does not compare favourably with the community setting, where screening for the same group reaches around 80%. 87 High variation (14-fold) was seen between individual prisons, and men staying in prison longer than 24 months increased the likelihood of undergoing this screening (30-fold). This important screening test for older men is therefore not being universally received by all those who need it. In our qualitative interviews, we found that the major issues about health care which were raised by staff and patients generally applied to all prisoners regardless of age. Staff participants at management level highlighted the importance of adequate skill mix amongst clinical staff to ensure older prisoners were provided for, particularly related to long-term condition management. We did not specifically sample staff participants who worked primarily with older prisoners and our oldest patient participant was 60, with most being in their 30s or early 40s.
Gender
Women constitute around 4–5% of the UK prison population and this figure has been consistent for several decades. 127 A primary focus regarding women and incarceration in the UK is to prevent women from entering the prison estate in the first place and also to reduce the number of women who are serving sentences for petty crimes. 128 Indeed, 39% of all female prisoners are serving a sentence for theft or a petty crime. 129 While the vast majority of prisoners are male, female prisoners have specific and important health needs. 130 Literature on female imprisonment and health conditions has tended to focus on MH, self-harm, pregnancy and childbirth, with much less attention paid to long-term conditions and prevention. A notable exception is a qualitative paper from 2008 by Plugge et al. ,131 which looked at female prisoners’ experiences of primary care in prison. We were conscious of this when selecting indicators in WP1 and included two indicators related to cervical screening and one to breast screening. Our scoping review found that breast and cervical screening quality indicators had been considered in three previous USA studies, with reproductive health (pregnancy testing, pre-natal care, post-natal care and caesarean section rates) also considered by these same three studies. 33,39,44 It is useful to take a closer look at one particular female-specific indicator that we tested in our statistical WP: that of cervical screening uptake among women aged 25–49 years. We found that women aged 30–39 were most likely to have had cervical screening as opposed to other age groups and that achievement for women aged 25–49 was around 64%, which is slightly lower than that achieved in a comparable community sample (71%). 81 Importantly, there was improvement over time seen in this indicator between 2017 and 2020. While it is disappointing that cervical screening achievement is not on a par with community rates, it is reassuring to see that gains are being made over time in this female-specific area of health.
In our qualitative study, we interviewed four women (out of 21 patient participants) and gained useful information about cervical screening, which was said to be driven and organised by external charities rather than the prison healthcare department itself. The overt and major healthcare issues identified from the qualitative fieldwork seemed to apply as significantly to women as they did to men, and we did not come across female-specific elements of health care that were considered profound. This could be because the study focused on everyday aspects of primary care delivery as opposed to the areas more traditionally researched and/or aligned with the health of female prisoners. Delegates in our WP4 workshops highlighted the importance of gender-specific indicators and noted the challenge of polypharmacy due to the greater psycho-social needs of women in prison.
Ethnicity
Around 26% of people in prison identify themselves as belonging to an ethnic minority group,129 which is double the number of people from an ethnic minority group in the UK general population. Further, over half (51%) of all people in YOIs in the UK are from a black or minority ethnic background, which David Lammy MP has said represents ‘an American scale of disproportionality’. 132 The Prison Reform Trust has drawn attention to the fact that black and minority ethnic people are more likely to be sent to prison from court than their white peers, and black and Asian people are more likely to be serving longer sentences than other ethnic groups. 133 Little academic literature focuses on prison health care and the experiences of people in prison from an ethnic minority background engaging with and receiving health care in the UK. Our international scoping review did not find any quality indicators or performance measures which were specific to ethnic minority populations in US prisons. A paper contained within the review36 proposed an indicator called ‘provisions of interpreters needed … and patient education in other languages’ but this relates to people whose first language is not English rather than specifically to ethnic minority health provision. In our stakeholder consensus process in WP1, the shortlist of chosen indicators to take forward for testing included many which could analyse differences in achievement by ethnicity. It is important to note here that ethnicity must be coded in the prison healthcare clinical system for this to be a viable exercise.
Our WP3 statistical analysis specifically assessed achievement of indicators by the stated ethnicity of people in prison. However, there were no clear trends seen across indicators for achievement by ethnic group. Individual indicators showed divergent findings. For example, regarding hepatitis B vaccination, white people were more likely to be fully vaccinated as compared to other ethnic groups. Regarding diabetes care, white people were more likely than Asian people to have a normal blood pressure reading. For cervical cancer screening, white women were more likely to have cervical screening than women from a Chinese or other ethnic minority. Conversely, we found that black people were three times more likely to have satisfactory glycaemic control regarding their diabetes than white people. Therefore, even in the same healthcare domain of diabetes care, we can see divergent achievement by ethnic groups that cannot be readily explained. A US study found that health disparities between black and white prisoners varied as pertaining to health condition,134 with the main consistent finding being that prisoners have worse health than what the authors call ‘their noninstitutionalized counterparts’. It is useful to see that international literature can confirm our results, which at first may appear contrary.
Moving onto our qualitative WP2, we ensured that our sample of people who had been in prison was ethnically diverse, with 6 out of the 21 participants self-identifying as being from a non-white background. This represents 28% of the sample from an ethnic minority background, which is on a par with the national figure of 26% of the prison population. We were told by people in prison about direct instances of racism they had witnessed in a healthcare setting. One woman noted that white women seemed to gain faster access to health care than women from black and Asian backgrounds. Language barriers for prisoners whose first language was not English were said to inhibit healthcare communication and access. Similarly to the gender-specific section above, the major healthcare issues discussed during the qualitative interviews seemed to apply significantly to all participants regardless of their ethnic background. In WP4, participants did not discuss indicators in relation to the needs of prisoners from an ethnic minority background despite being sensitised to gender, as previously noted above.
Prison organisation and system
The entire healthcare system in the UK, both inside and outside the prison gates, is under extreme pressure. Hospitals and community primary care are struggling to meet demand from a growing and ageing population. While demand for health care has risen significantly in the past 15 years, since 2010 it has been coupled with a prolonged squeeze on funding which has seen the system straining to meet increased demand with fewer resources. 135 This is coupled with a loss of medical and nursing staff from the NHS due to burnout and stress, with a national GP vacancy rate at 14%136 and a 96% reduction of European Union (EU) nurses joining the UK nursing register after the UK left the EU. 137 The prison system faces similar problems in workforce recruitment and retention, but these are exacerbated by prisons being perceived as an unattractive environment to work in, given the complexity of the patient population and the constraints of the physical conditions in which clinicians deliver care. The Royal College of Nursing (RCN) found that two-thirds of prison nurses who took part in a survey said the care they provided on their last shift was compromised and that the quality of care was poor. 138 The RCN has called for better investment in the prison nursing workforce to raise standards of care delivery and patient safety. A recent academic study from the USA found the main challenges as described by the prison healthcare workforce in one State were constraints around being able to deliver care effectively and safely. 139 This was mainly attributed to understaffing, high numbers of vacant positions and lack of resources. Ismail129 had noted that funding for prison healthcare services in the UK have been ring-fenced by the NHS, but day-to-day delivery has been compromised by a 22% reduction in funding for the prison service itself between 2010 and 2017. This has created a severe staffing deficiency in the prison officer workforce which has then led to deteriorating conditions in healthcare provision. A prominent issue of note here is missed medical appointments (‘DNA’) inside the prison ranging from 20% to 30% of all primary care appointments. 123 This is often attributed to a lack of prison officers to unlock prisoners from their cells and escort them to the healthcare wing, demonstrating a system-wide access problem attributable to workforce outside the healthcare department. Additionally, the extent to which the priorities of the prison regime heavily influence aspects of the delivery of health care must not be underestimated. There is an over-riding concern with security issues which have no equivalent comparison with health care delivered in the community. Edge et al. 140 in their qualitative study with people in prison in England found that security concerns over-rode healthcare needs and created humiliation and fear alongside delayed access to health care and reduced patient autonomy.
Our qualitative work offered the most useful insights about how the prison system and workforce issues influence quality of health care. In our qualitative findings chapter, we present the descriptive findings under four levels: individual, team, organisation and system. In this current section, we take a deeper, more discursive look at the importance of organisational-level factors. We found what could be described as a compounded problem, with the main umbrella issue of understaffing of the healthcare workforce causing knock-on effects and unintended consequences, creating a vicious circle through which the workforce was further depleted (Figure 4). There was a clear acknowledgement by healthcare staff participants of there not being enough staff on the ground on a day-to-day basis and a significant amount of the workforce being locums or from agencies. Understaffing had a demonstrable impact on both patients and staff. Patients described healthcare appointments as being ‘rushed’, not feeling they were getting the time or attention they needed and having to stand in lengthy, unpleasant queues to obtain medication at the medication hatch. We were told in one instance of a patient who had decided to stop taking his medication as he did not want to get involved in the fighting and drug-dealing which was occurring on a daily basis in the medication queue. Healthcare staff spoke about the impact that a sizable locum workforce had on the service, with minimal ability to deliver service improvement or development when substantive and permanent staff were lacking.
FIGURE 4.
Diagram of organisational-level factors.
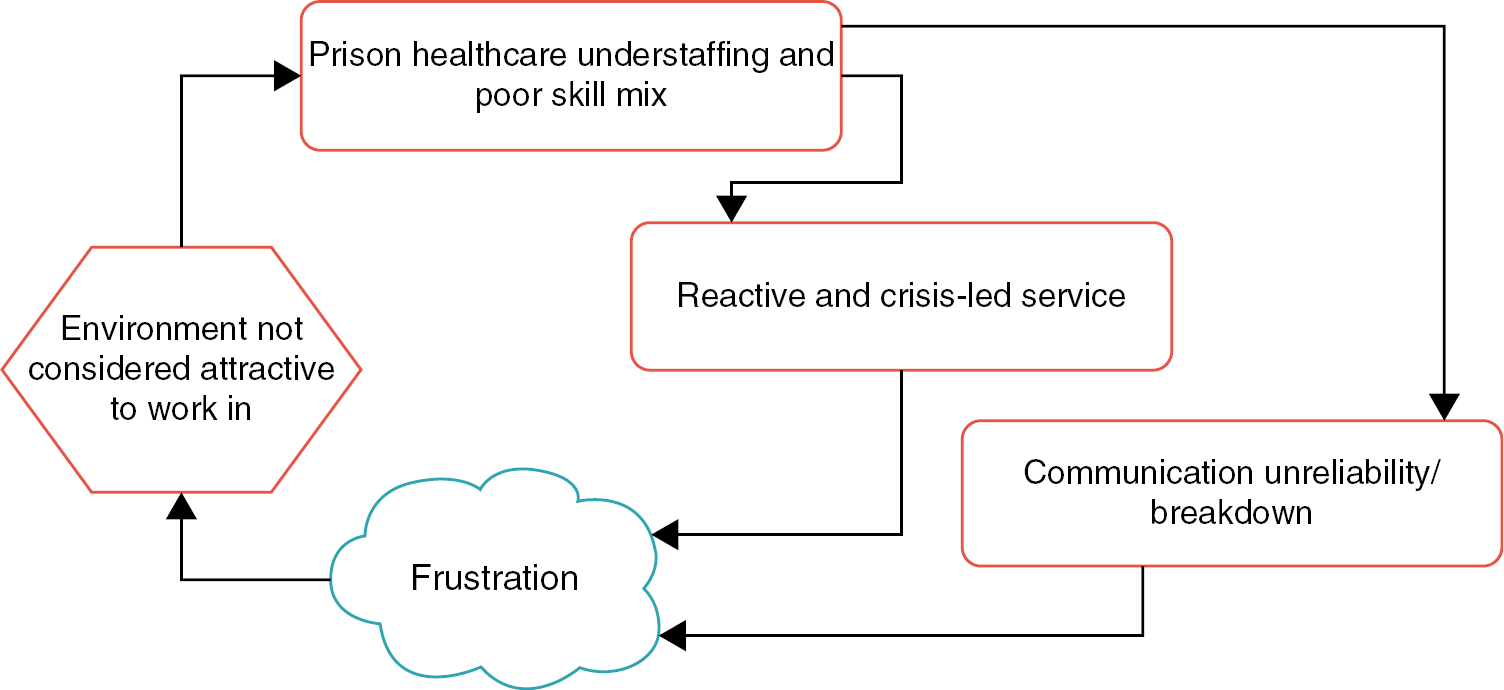
Related to the above, healthcare delivery was implicitly critiqued by both groups as being reactive and crisis-led. This took varying forms. As staff were often firefighting their way through a large and complex caseload, patients’ perceived minor problems were sometimes put off or ignored until they became major issues which staff were then forced to deal with in an urgent manner. A pertinent example of this is medication continuity. We found that patients who had long-term health conditions but were in prison on short sentences sometimes fared worse than similar patients who were serving a long-term sentence. Those with short-term sentences often had to advocate for themselves and continually remind staff and officers about their condition and required medicines, as they were not well known to healthcare staff or the healthcare department.
We also found there was a lack of responsibility for effective communication, often leading to breakdowns in communication about health care. A prime example of this was the poor communication mechanisms for patients being informed of healthcare appointment times and dates. After requesting a healthcare appointment, some patients did not receive a date but were never told why. A recurrent problem we were told about is an appointment being booked for a patient with the healthcare department but the patient never being reliably informed of this outcome and therefore erroneously missing the appointment as they were unaware of it. Frustratingly, some patients knew they had an appointment but were not unlocked from their cell in time by an officer in order to make the scheduled appointment (this issue represents a significant number of healthcare ‘DNAs’ and is a national-level problem, as described above). The above-described organisational-level communication issues were a persistent source of tension which led to patients, healthcare staff and prison officers becoming angry and frustrated with each other.
It is useful to understand the findings from our other WPs regarding the prison setting as an organisation and system in relation to quality of care. Our scoping review found that prison quality indicators in the USA focused on process rather than structure. Where organisational issues were considered, this constituted only a small number of published papers, with only one research team drawing attention to the fact that high staff turnover may jeopardise measurement of the quality of health care. 34 As a result of our stakeholder consensus process in WP1B, we realised that most of the shortlisted indicators focused on healthcare conditions and processes rather than indicators pertaining to structure or organisation. This could be due to various reasons: a facet of structural indicators is that they are much lower in volume when compared to process or outcome indicators, structural indicators may generate ‘noise’ (disputable findings) that is not considered useful or valuable for clinicians or managers to work with, and the notion that indicators need to be based on information that is concretely and routinely coded, which is likely to be less the case for structural level aspects of health care. In our analysis of routinely collected data (WP3), one of the most interesting findings in relation to organisational-level factors was the substantial variation between different prisons for certain indicators, even when prison population characteristics were adjusted for. This suggests that variation is largely attributable to the local delivery and organisation of health care at the level of the individual prison. Factors outside the healthcare department may be important here, as for the most part it was one healthcare provider that served all 13 prisons whose data was interrogated in WP3. The findings of WP3 alerted us to a lower achievement in indicators for those people in prison with shorter sentences (< 1 month). This is reinforced in the qualitative findings, where patients had to be vocal about making themselves and their medical needs known to the healthcare department. Given that understaffing is one of the major organisational issues flagged by participants in our qualitative study, it is interesting that there is not a quality indicator in our shortlist regarding this. However, this could relate to England having no legal minimum staffing levels (for hospital, community or prison health care) but rather suggested ratio levels which are often discounted given persistent staffing shortages. In the WP4 workshops, participants discussed workforce issues when examining indicators related to prescribing. This was interesting as participants voiced how achieving consistency in the workforce may promote better prescribing practices, and how regular use of a large locum workforce limits clinician accountability. A system-level issue raised was the competitive tendering process for prison healthcare contracts and how this served to inhibit a collaborative relationship between providers, alongside an inefficient reinvention of clinical practices with each new contract cycle. However, this landscape is changing with the creation of Integrated Care Systems, which may reduce the need for competition in this manner.
Prison–community interface
The health of people in prison depends on many other factors outside of the health care delivered to them in this setting. It depends heavily on the health care they have received in the community before entering prison, their health status throughout their life and health care received after release. The period of time immediately after release is known to be particularly challenging for the health of people who have been in prison. There is a much higher risk of hospitalisation within the first 7 days of release from prison when compared to the general population. 141 Responsibility for the care of most patients regularly passes between prison and community healthcare staff and clinicians, given the high rate of recidivism in the UK prison population. 142 Continuity of health care between these settings has been identified as a core objective by NHS England and the UK government97 but there are several key barriers which impact on high-quality continuity of care. These could be factors that are influenced by the ‘prison–community interface’ and which we saw represented in our data and the literature in this area. First, there is limited interoperability between clinical IT systems, with prisons in England and Wales using SystmOne but only a third of community general practices using this system. 143 Second, prescribing – particularly opioid prescribing – exists on a carousel whereby prison clinicians are advised to reduce opioid prescribing to minimise the risk of diversion inside the prison, only for community GPs to be approached by the patient for opioids to be re-prescribed upon release. 142 Third, the management of long-term conditions is often disrupted by the patient moving between community and prison, and this subsequently has an impact on the continuation of community prescriptions and therefore important medication. 10 Fourth, as described above, QOF is not incentivised in prison health care, which has hindered comparisons of performance between the two settings.
Our scoping review found that research teams in the USA had paid attention to several of the above issues, most notably the lack of data-system functionality between prisons and community health care. Prison clinicians were said to have to rely on patient self-report due to system inoperability, which sometimes compromised the quality of care. 44 Several jails in the USA have tried to integrate prison and community healthcare systems but have found this a challenging and daunting task. 43 While a UK-specific factor is the non-incentivisation of QOF in prisons, several studies from the USA have remarked upon an absence of prison-specific healthcare benchmarking (BMing) data. 32,33,38 It is interesting to see that prison–community interface problems in the UK seem to exist substantively also in the USA and this demonstrates that this effect on healthcare quality in prisons is most likely an international problem. In our stakeholder consensus process in WP1, we ensured that we included indicators relating to opioid prescribing due to its importance for overall quality of care. We based our measurements for opioid indicators on an 8-week period in order to enable indirect comparisons with community data.
Moving onto our analysis of routinely collected data, we measured achievement of one indicator which was highly specific to the prison–community interface. This indicator focused on ‘the proportion of new receptions to prison who have been asked for consent to transfer medical records from GP to prison health care’. In this case, ‘new receptions’ means people newly entering the prison. We found that of the people who were eligible, 70% were asked for consent to transfer medical records and this represented a fourfold improvement over 2017–20. However, this indicator had one of the highest variations between prisons that we found in our data set: a 337-fold difference. An interpretation of this finding is that whether people entering prison are asked for consent to transfer their community medical records is likely to be dependent upon individual prison policies. Regarding the opioid indicator, we measured the proportion of the prison population prescribed opioids during an 8-week period. Compared to the most recent community general practice estimate of 12.8% being prescribed any opioid, the finding that 11.5% of people in prison were prescribed any opioid using the same indicator appears favourable, given the prevalence of drug-seeking behaviour in prison populations. 85 However, any comparisons need to be undertaken with caution given the differences in population characteristics and measurement at different time points. Two of our further findings highlight the need for closer attention to such prescribing. First, compared to 2018, the likelihood of opioid prescribing was almost 1.5 times higher in 2020. Second, prescribing of strong opioids was markedly higher, at 8.7% in prison compared to 0.85% in the community. In our first workshop for WP4, participants pointed to one of the most pressing issues for quality of prison health care being opioid prescribing between prison and community primary care (the specific issue of: initiation in the community, reduction or cessation in prison and then increase or reinstatement in the community again). Participants thought there needed to be better communication channels between community and prison GPs to overcome this challenge. One participant emphasised the importance of asking and involving patients in opioid reduction. In the second WP4 workshop, connectivity between public health screening programmes and SystmOne was noted as an important issue by participants in addition to the limitations of summary care records provided by community primary care. Further, the indicator related to consent for transfer of medical records was thought to be difficult to improve upon unless this consent process was made opt-out rather than opt-in. A large amount of discussion in the WP4 workshops about the prison–community interface was generated by expert participants who work clinically and managerially (or had lived experience) in prison health care on a daily basis. This further reinforces the importance of this distinct topic area.
We gained rich information about the prison–community interface from our qualitative WP findings. Again, the issue of opioid prescribing was discussed, with both groups of participants noting it as a cause of tension between healthcare staff and people in prison. Some patients perceived that they were being unfairly labelled as a drug-seeker and not being treated as an individual. It was the view of one nurse participant that some prescribing practices were inflexible and could be detrimental to patients who genuinely needed medicines. Continuity of medicines from community to prison was highlighted as a big issue; people entering the prison on a Friday often encountered problems in this regard. Despite the interoperability between prison and community data systems, staff participants discussed how a thorough and detailed screening at the reception clinic was beneficial to identifying the health needs of a newly received prisoner. Staff participants talked about the need to request a patient’s summary care record from their community GP and how some practices may not recognise the urgency contained within this request. At the other end of the patient journey, some staff expressed concerns that care for medical conditions simply ends when patients leave the prison gates if they are not already registered with a community GP.
Strengths and limitations
Here, we bring together the strengths and limitations from each of the WPs to provide a summative account.
Strengths
Overall, a significant strength of our research project was its mixed-methods approach, which allowed for an examination of the phenomena of quality of prison health care from different epistemologies, perspectives and angles. We generated, developed (WP1), measured (WP3) and prioritised (WP4) 30 quality indicators through a robust process to ensure clinical relevance and population impact, basing them around data we judged would be recorded with reasonable reliability. The 30 indicators were largely drawn from EB guidance. This was an intensive and multistaged approach moving from a long list of 371 indicators through to our final chosen 30, and has been described in detail throughout the rest of this report. We consider reaching a final shortlist of 30 and then being able to measure them as a key study strength. Our 30 indicators may have significant population benefits, if prison healthcare teams and providers are able to apply them to relevant data sets. Further, our use of routinely recorded and coded data means that these indicators can be applied at modest costs and integrated within quality-improvement strategies.
Our qualitative WP provided a broader context in which we could understand the results from our analysis of routine data alongside the generation of findings which illuminated the whole prison healthcare milieu. This provided a wider picture than conducting either of these WPs in isolation. We interviewed prison leavers and prison healthcare staff and we were able to integrate the findings from these two groups to produce a higher-order account which was able to pinpoint the most important issues relating to quality of prison health care. The diversity of our sample is evident with the overt inclusion of women, people from ethnic minority groups and those living with long-term health conditions. Further, we gained the collective experience of participants across many prisons in the North of England, and we did not place any restrictions on where people had been in prison or which prisons they worked in. Our qualitative study asked people in general terms what they thought about prison health care and probed deeper to understand perceptions of routine aspects of primary care. This is a unique strength because the prison healthcare literature tends to focus on MH or substance use or specific health conditions rather than the general experience of healthcare provision in the round.
Our entire programme of research was designed to minimise any undue burdens on the prison estate; we did not wish to occupy valuable prison officer time for escorting research staff around a prison. This meant that we chose to speak to people who had been released from prison about their reflective healthcare experiences; we interviewed healthcare staff over the phone and we were able to access anonymised and routinely collected data from prison healthcare records via Spectrum CIC (our healthcare provider co-applicant) without physically entering any prisons. We designed the study between 2016 and 2018, but our conservative design which ensured no burden on the prison estate proved to be an unintended significant benefit when the COVID-19 pandemic hit the UK. Indeed, the prison service suspended our qualitative research for 6 months under a national ban on any previously approved research study. We were fortunate that we could re-start our qualitative fieldwork as soon as the national ban was lifted, as we were not entering the prison estate. Some prison-located research studies took upwards of 12 months to resume, as conditions of lockdown in prisons extended much further in duration than in community settings.
Limitations
A major limitation of the study was the impact that COVID-19 had on our ability to undertake timely elements of some WPs. Foremost, our qualitative work was badly affected by the formal pause in fieldwork which the prison service instigated. Our statistical work was also delayed as members of the data team at Spectrum CIC were redeployed onto higher-priority COVID-19 studies.
It is useful to look in detail at some specific limitations per WP. In WP1, which was our first stakeholder consensus process and development of indicators, we highlight three main limitations. First, we were not able to seek representation from people with lived experience of imprisonment on our stakeholder panel despite extensive invitations. Those we approached said they were willing to tell us their story but did not wish to take part in the panel. This could be because the topic is considered dry and potentially academic/uninteresting. Second, our indicators were only developed within one electronic health-record system (SystmOne) which is widely used for prison health care in the UK. While the codes we used are likely to be applicable to other electronic health records, there may be differences in data recording (e.g. use of templates) which may affect feasibility of measurement. Third, we measured only coded clinical data. Coding is not mandatory and can be inconsistent, driven by ease and individual clinicians’ familiarity. 142 Our indicators may therefore underestimate true adherence to indicators. However, we generally discarded indicators which would have mainly relied on free-text entries and focused on those judged to be coded with reasonable reliability or which measured objective data (e.g. prescribing).
In our international scoping review, the major limitation was that only literature from the US context was identified across 15 papers that we included in the review. We were surprised that no peer-reviewed literature existed about quality indicators or performance measurement outside the USA, albeit we only had the resources to access abstracts published in the English language. Additionally, we did not perform a critical appraisal of the studies reported in the 15 papers as our review was scoping in nature rather than systematic.
In our qualitative work (WP2) and our targeted MH qualitative analysis (WP5), we interviewed people who had left prison, obviating the need to enter the prison estate. We used a four-level barriers and levers matrix to analyse our original qualitative data, of which the four levels were: individual, group/team, system, organisation. 67 We paid equal attention in the matrix analysis on barriers and levers for all four levels and incorporated the perspectives of both participant groups (where appropriate). It could be that a differing type of analysis, such as an inductive or interpretive approach, may have produced slightly different findings and led us to focus on the issues that were most prevalent for each participant group. We acknowledge that qualitative findings are not readily generalisable to the experience of all people in prison or prison healthcare staff and we urge caution when thinking about how these findings might apply to prison healthcare services outside of England. However, we do believe that our findings are credible and dependable and have made a distinct contribution to the research on this topic.
Moving onto WP3, our analysis of routinely collected data, there are a number of limitations related to both the technicality of our research and also the coding of clinical data. First, as previously stated, we accessed the data from one provider who was confined to 13 prisons in the North of England. This meant we were not able to examine outcomes between providers, which could have generated insights into the impact of different approaches to the organisation and delivery of care. Further, ways of working outside of the North of England could be different to other regions of England. However, the consistent use of SystmOne Prison in all sites also negated concerns about differences in performance associated with the choice of clinical computing system. Second, the generalisability of our results is applicable to the wider prison population in the UK but potentially not internationally for prison populations in other countries which may have a different demography. While the age and gender profile of our data was broadly consistent with recent national-level statistics,1,127 we found lower proportions of ethnic groups when compared to national statistics for England. This is likely to be attributable to suboptimal recording of ethnicity in computerised medical records, which is a known problem. 144 Third, our indicators were limited to routinely collected data and only assessed measurable features of care. This approach is relatively efficient, transparent and scalable but it is difficult to improve quality without being able to establish a baseline and assess progress. Fourth, we were unable to assess the care delivered in community general practice, before incarceration. This was in part due to limitations on data sharing, and meant the influence of care delivered in the community on prescribing and ongoing management was not explored. The importance of data-sharing between partners to support continuity of care and aid development of effective outcome measures is acknowledged,97 and the initiative in England to connect the prison estate with the NHS Spine is intended to eventually link with lifelong patient electronic records held by community general practice. Fifth, our community comparisons do not really compare like with like; for example, they cannot account for differences in demography. Rates of strong opioid prescribing appeared higher in the prison population than in a community population. This may be due to differences in the denominator in the community study, where people with diagnoses of drug misuse and cancer were excluded from analysis. 85 We advise caution when interpreting such differences in achievement.
A key limitation, in response to the COVID-19 pandemic, in our stakeholder deliberation process (WP4) was that we had to change from face-to-face workshops of planned 4–6-hour durations to online workshops averaging 2-hour durations. We shortened the workshop durations because we judged that participants would struggle to maintain engagement for longer time periods. This meant that we were unable to consider our findings and discuss implications in as much depth as we would have preferred. We attempted to compensate for this by consulting participants in between workshops but levels of engagement transpired to be relatively limited. It is also worth highlighting that our subsequent suggested quality-improvement approaches are based upon a combination of evidence and consensus but have yet to be operationalised and evaluated in a prison setting.
Limitations exist for our MH quantitative analysis (WP5). Our identification of the MH groups in this analysis is based on the two indicators related to the MH diagnosis subgroup of the opioid prescription indicator and the antipsychotic prescription indicator. A MH diagnosis relies on accurate and reliable coding and as such there may be people with mental illness who were not coded. This under-coding could result in underestimating the likelihood of the achievement of the indicators in the MH groups, thus underestimating association between the indicator achievement and mental health. Furthermore, differentiating between those with MH with and without psychotropic drugs could be problematic, as this is based on whether they receive three or more prescriptions for an antipsychotic in the preceding 12 months. Those on one or two psychotropics would be classified as being without psychotropics based on the available data, and so associations in this group could be overestimated. Therefore, while we were able to assess measurable features of care for people with MH diagnoses from routinely collected data which are relatively efficient, transparent and scalable, further work is required to better understand and implement clinical coding systems across prison health care.
Patient and public involvement
Given the stigma and exclusion faced by individuals with experience of imprisonment, the primary aim of our PPI strategy was to ensure that experts-by-experience would be involved in meaningful ways at various levels of the project, in different roles and making various types of contribution. Our intention was that involvement would be of mutual benefit to them and the project. To achieve this, we set out to make involvement as accessible as possible by devising a multifaceted, flexible PPI strategy that could be adapted to the needs of the project and those wishing to be involved. To facilitate the involvement of experts-by-experience, we offered support (e.g. training, mentoring, signposting, advice, co-facilitation) and payment. We produced an information sheet featuring an overview of the project, the members of the team and the role of PPI. We also produced a plain-English list of the quality indicator shortlist. We made these materials available to everyone involved in the project and freely accessible copies were hosted on our website and promoted via the project Twitter account (@Qual_P). The website has a dedicated section for ‘community’ posts which invites people to make comments and suggestions and to ask questions. All recruitment efforts emphasised that there were a range of ways to get involved, each involving different levels of commitment.
A total of seven experts-by-experience were involved in the project in different roles. People with lived experience of prison were involved at all stages, from development to dissemination, to governance. We developed the initial project application with input from two people with lived-experience of imprisonment. We also engaged three experts-by-experience (MB, MC, PP) to collaborate with us on the development of recruitment materials, the recruitment and sampling strategy and the qualitative interview schedule, to facilitate recruitment and interviewing (see Chapter 4) and another (FD) to contribute to the workshops in the integration WP (see Chapter 6). We also had lived experience representation on our Oversight Committee from Paula Harriott, PPI lead for the Prison Reform Trust. We had intermittent representation at our bi-monthly research team meetings where an expert-by-experience participated in discussions about the quantitative analysis WP (see Chapter 5), the integration WP (see Chapter 6) and dissemination. We also invited comments, questions and suggestions from the prisoner policy network (PPN) led by Paula Harriott. The PPN brings together people with lived experience of prison who wish to get involved in policy work, from those who want to be kept informed to those who want to develop a more active role.
As anticipated, PPI activity evolved over the course of the project, not least in response to the pandemic and other challenges relating to the recruitment and retention of experts-by-experience. Prior to the commencement of the project, both experts-by-experience who contributed to the development of the project had to withdraw from their formal roles as co-applicant and nominated PPI representative, respectively. Despite trying different routes and methods, we found it difficult to engage individuals who were willing to perform an ongoing PPI role in the study. Some individuals that we approached told us that they would be prepared to make a one-off contribution as interview participants but were not willing to get involved in a medium- to long-term PPI capacity, such as attending research meetings. Although we engaged two individuals (MB, MC) to advise on the qualitative WP, they were only involved in discrete activities. A further expert-by-experience (PP) who had multiple roles in the study and contributed to several WPs was unable to continue his role in the project. These challenges had two main consequences: first, we completed the stakeholder consensus process with minimal input from people with lived experience and, second, we had intermittent input from people with lived experience of imprisonment at our research team meetings. Furthermore, despite the opportunities for individuals to provide feedback or to volunteer to contribute to the project as an expert-by-experience, we did not receive any comments via the website or PPN network. Our plans were also limited by the pandemic: we considered it would be inappropriate, unethical, and logistically difficult to approach new contacts during this time. We are cognisant of the fact that prison leavers may face multiple challenges upon release ranging from homelessness, health problems, unemployment, disrupted personal relationships and financial difficulties, and that these may have been barriers to their involvement in PPI activities, especially those requiring long-term or regular commitment. Other issues may have also deterred people from getting involved, such as wishing to move on after imprisonment. We found that the individuals who did get involved were those who were working in paid roles that drew on their experiential expertise.
In response to these challenges, we developed ways to maximise the PPI input we did have. To partly compensate for these gaps, we drew on the expertise of the head of a local charity (BG) with over 20 years’ experience of public involvement, who attended Project Team meetings and performed the role of ‘critical friend’. Although she did not purport to speak on behalf of people with lived experience, she brought a wealth of experience of working in the sector and put us in touch with an expert-by-experience (PP). This provided the continuity that was missing in the absence of a permanent expert-by-experience team member. Instead of convening a lay stakeholder panel during the pandemic, we sought feedback on the quality indicator selection process from Paula Harriott, who provided a non-research, lived-experience perspective.
Despite the challenges we faced, it is a strength of our approach that we responded flexibly to overcome these challenges by ensuring that the lived-experience voice was incorporated throughout the project and particularly at key stages, including the initial development of the study, in participant-facing materials and alongside other stakeholders in the final integration WP. It is also a strength of our approach that we involved people with lived experience of prison at all stages of the project, including at the crucial stage of project development. Experts-by-experience were also involved in various levels and roles, contributing to the governance (via the Oversight Committee and the research team meetings) and strategic discussions and decision-making. Several experts-by-experience were involved in practical ways by contributing to the development of accessible and appropriate participant-facing materials and assisting with recruitment. The contribution of one expert-by-experience (PP) was pivotal, as he liaised with services and individuals at a time when we were unable to physically visit potential recruitment sites due to pandemic-related restrictions. Using his existing networks, he brokered relationships between academia and some of the most vulnerable and marginalised groups in society, something that we could not have achieved in his absence. We also utilised a range of different approaches to engage with the community, including the use of Twitter and our website, and the PPN network. Although we did not receive comments on the study via the website or PPN network, we did receive some interest (including retweets and likes) on our Twitter account. It is important to provide opportunities for individuals to access information about the project without facilitation by a third party and also to create an open, safe environment where people can engage with and scrutinise research on their own terms. This involves ensuring they have access to research and opportunities to be aware of current debates and to contribute (or not) if they wish. We also developed the innovative ‘voice memo’ approach (see Chapter 6) in partnership with the expert-by-experience (FB), partly because he could not attend the workshops, but also as a ‘reasonable adjustment’ to accommodate his neurodiverse needs. This approach had strengths and limitations. It was a limitation that the lived-experience consultant could not attend the events and did not complete the survey. This meant that the contributions he made could not influence the discussion or inform other stakeholders’ thoughts and comments. This also meant that we were unable to respond to his questions. It is, however, a strength of the approach that the lived-experience consultant was able to contribute in a flexible manner and to comment freely and without interruption or contradiction. To reduce written communication and partially offset the absence of interaction between the lived-experience consultant and the other stakeholders, we held several meetings to discuss and reflect on both the process and the workshop content.
In conclusion, the impact of PPI in this project was substantial. The attendance of experts-by-experience at meetings and, by extension, as members of the research team enhanced the team’s self-awareness around use of language, patient-versus-clinician perspectives and the day-to-day reality of living in prison. The involvement of Paula Harriott from an early stage of the project (post-funding) instigated the emphasis on a two-way exchange of information with prison leavers and experts-by-experience. Accordingly, alongside quantifiable impact such as assistance with recruitment, all the experts-by-experience brought extensive knowledge and a wealth of insight to the project.
Equality and diversity
Participant representation
Participant representation in the qualitative work package (see Chapter 4)
Prison leaver participants
This study has been undertaken with one of the most marginalised and vulnerable groups in society. Various groups are over-represented in the prison population, including people from ethnic minority backgrounds, people with addiction issues, care leavers, people with learning disabilities, people with chronic health conditions, those with multiple and complex health and social problems and those experiencing digital inequality.
The qualitative WP (see Chapter 4) involved sampling and recruitment of prison leaver participants. Our sampling and recruitment strategy was designed to include a range of individuals with experience of imprisonment. To this end, we liaised with various organisations and individuals (including one of our lived-experience advisers) to identify and access individuals who could be approached about participating.
People in prison have lower levels of literacy and some have limited ability to communicate in English. For these reasons, we relied on the assistance of individuals to personally approach potential participants and verbally introduce the study. We also produced all written materials (such as the information sheet and consent form) in plain English in a large plain font. Care was taken throughout the study to use non-stigmatising language (such as prison leaver). Prior to commencing an interview (all interviews were conducted by video or telephone), the interviewer (SB) read aloud the information sheet and guided the participant through the consent form and recorded their verbal consent. In addition, we made audio-recordings of the information sheet which we stored on our website and we encouraged people to access this. We also produced a plain-English summary of the whole study and a plain-English description of the quality indicators (also available on the website). We used other strategies to recruit individuals not in contact with organisations, including employing recruiters who drew on their personal networks, snowballing, and by promoting the study via our dedicated Twitter account.
We did not set out to specifically include or exclude people who were not fluent in English, and in the event none of our recruitment partners identified a potential participant who could not speak English. On reflection, our reliance on English-speaking recruiters and organisations may account for this and could have been overcome by a dedicated strategy.
We had to make changes to our original recruitment and data-collection strategy due to COVID-related restrictions. This necessitated the use of remote recruitment and data-collection methods such as e-mail and tele- and video-conferencing. Attempts to engage prison leavers who often had no e-mail address and limited or no access to a mobile phone, data or minutes, however, exposed the digital inequalities experienced by this group. The risk here was that only those with access to digital resources would have the opportunity to participate. Accordingly, we negotiated with service staff for access to agency landlines for participants without any access to a mobile phone. Our lived-experience adviser’s practical assistance with recruitment and facilitating interviews was crucial in overcoming this barrier.
Overall, the final qualitative sample of prison leavers featured men and women of different ages and ethnic backgrounds, with varying experience of imprisonment, and a range of health conditions and experiences of health care in prison.
Healthcare staff participants
Some aspects of our recruitment strategy for healthcare staff differed, notably that we circulated promotion e-mails via healthcare providers’ global staff e-mail lists. Similar to the prison leaver recruitment strategy we promoted the study via Twitter and via our personal and professional networks and used snowballing. The resulting sample varied in terms of ethnic background, age, professional training and job description, and length of service.
Participant representation in the quantitative work package (see Chapter 5)
Healthcare records for a sample of ~25,811 people in prison, 2018–21
The sample of prisoner health records used for the analyses in the statistical analysis (see Chapter 5) was determined by the composition of the prison population during March 2018–March 2021 at the 13 prisons included in the sample and thus was beyond our control. Data on ethnic group were missing for around 20% of the study population; most people included were white. Other characteristics of the sample are reported in Chapter 5.
Analyses
In our analyses, we examined the impact of ethnicity, gender and age on achievement of the quality indicators. We also examined achievement for the underserved subgroup of those with a mental illness diagnosis (see Chapter 7). Additionally, examining achievement for some indicators required attention to other vulnerable groups, such as those prescribed opioids.
Participant representation amongst stakeholders in the consensus and integration work packages (see Chapters 3 and 6)
This part of the study also relied heavily on the involvement of (professional) stakeholders.
Consensus process participants
We engaged stakeholders in the consensus process to prioritise quality indicators for data extraction in WP1 (see Chapter 3). We identified a selection of stakeholders via our networks who would be able to assess and rate the quality indicators for potential for patient benefit. Accordingly, we approached individuals with professional experience of the criminal justice system (CJS), prison health care or expertise in quality indicators or delivery of primary care to underserved groups. Our priority here was to identify individuals from a range of professional backgrounds with the knowledge and expertise required to engage with and undertake the rating process. It is possible that this resulted in limited diversity (other than gender) in this stakeholder group. We did, however, attempt to simplify the consensus process and to make it accessible for individuals without clinical backgrounds by only asking participants to rate the quality indicators according to one and not two criteria (potential for patient benefit) as originally planned and by providing a booklet containing plain-English descriptions of each of the quality indicators we were asking stakeholders to rate.
Integration process participants
We also involved stakeholders in a series of workshops to consider the findings from the various elements of Qual-P plus existing evidence about implementing quality-improvement strategies in WP4 (see Chapter 6). The strategy here was to promote the study and its findings to a much wider professional audience. This led to attendance and engagement of a much more diverse group (although limited to professionals working in health and justice).
Representation in the research team
The research comprises a range of experts who vary in professional background, experience and areas of expertise. The team includes prison GPs, an academic (community) GP, a statistician, commissioners, qualitative methodologists, junior researchers, charity management, and lived experience (described under Patient and Public Involvement and Engagement activities). Together, the team combined community and prison-specific healthcare expertise and clinical and academic experience, perspectives from the frontline, management and commissioning, and a range of healthcare providers and prisons.
Junior members received support and supervision from more senior members of the team via regular one-to-one meetings. Junior members attended conferences and other meetings to present findings, attended courses, were supported to produce peer-reviewed articles and other outputs and were involved in the development of new grants.
Representation in patient and public involvement and engagement activities
Individuals with lived experience of prison from across the country were involved in the study, aided by the use of telephone and video calls as opposed to the resource-heavy demands of face-to-face meetings.
Implications for practice
There is a loss of informational continuity between community and prison primary care, which undermines individual patient care as well as the ability to measure and improve whole-system care. Improved linkage of individual electronic health records at this interface may deliver benefits for patient care and system-level improvement.
Our work has demonstrated marked gaps and variations in achievement of quality indicators across 13 prisons served by one primary care provider which are incompletely explained by population characteristics. Such gaps and variations are likely to be a more widespread phenomenon affecting other prisons and warrant attention.
Our suite of indicators, based on routinely collected data, may serve as a foundation for an efficient and EB audit and feedback intervention, which could be scaled up and applied across the prison sector. As they are based on routinely collected data, it should be feasible for healthcare providers to adopt or adapt our data-collection templates. There is now a well-established and evolving evidence base to guide effective feedback methods, such as providing repeated rather than one-off feedback and incorporating action planning into feedback.
Suggestions for action from our briefing on opioid and gabapentinoid prescribing:
-
Initiate multidisciplinary care plans for prisoner patients prescribed three or more psychotropic medicines, which include involvement from primary care, the drug and alcohol recovery team (DART), MH and the prison service.
-
Adopt regular prescribing audits using routinely collected data and EB comparative feedback to prison healthcare teams that includes persuasive messaging and action plans directed at prescribers.
-
Support clinicians to change prescribing practice through nationally recognised training courses, such as the RCGP courses in the management of substance misuse.
-
Escalate details for the small number of prisoner patients who show intimidating behaviour towards clinicians in seeking prescribed drugs to the prison service through an agreed pathway so that ‘safe haven’ support can be provided in individual consultations.
-
Potentially stigmatising attitudes and behaviours vary between individual staff members and so there is merit in tailoring current statutory and mandatory training in equality and diversity for prison staff to reduce the likelihood of such staff delivering (or withholding) treatment in a punitive fashion.
-
There would be merit in providing confidentiality and wider information governance training to discipline staff so that a patient’s sensitive health information is not (either intentionally or inadvertently) made available to their peers.
-
Prisons represent an ideal environment in which to encourage uptake of national screening and immunisation interventions yet uptake is variable, thus presenting an opportunity for awareness-raising amongst both staff and patients.
-
Some prison-based clinical staff are deskilled in the area of long-term condition management; there is merit in reviving historical models of clinical quality whereby healthcare staff are encouraged to work part of the week in community primary care settings.
-
Variation in prison healthcare performance could be addressed by providing anonymised feedback to healthcare teams for a range of indicators to enable an individual team’s performance to be gauged against their peers.
-
Monitoring the reason why patients ‘did not attend’ healthcare appointments (individual choice or system constraint) should be undertaken in order to improve attendance rates and patient experience while making recommendations for resource allocation.
-
Incentivising attainment of national agreed outcomes (i.e. the QOF) has enhanced the standard of community long-term condition monitoring, thus presenting an opportunity to review commissioning frameworks and key performance indicators in this regard for prison healthcare teams.
Recommendations for research
Quantitative research: We identified no consistent pattern by ethnicity in achievement of indicators. However, we noted that Asian and Asian British people were less likely to experience psychotropic polypharmacy and, along with black and Black British and Chinese people, less likely to be prescribed opioids. Does this occur because of discrimination at the point of assessing needs and prescribing or are there other factors that protect people from different ethnicities from potentially harmful prescribing?
We identified no rigorous evaluations of strategies to improve the quality of primary care in prisons. A range of single or combined improvement strategies, informed by a wider evidence base, are promising and amenable to evaluation through randomised trial or rigorous quasi-experimental evaluation designs.
We have demonstrated the feasibility of using routinely collected data to measure quality of care at scale in prison primary care. This would form an ideal platform for an audit and feedback programme to improve care. While we have specifically suggested audit and feedback as an improvement strategy for prisons, given its known effectiveness in improving the quality of health care across different settings it would be useful to establish its effectiveness in this setting.
Qualitative research: One of the main issues identified through our qualitative research findings which requires more in-depth and further understanding is that of healthcare access for people in prison. We came across the issue of DNAs for primary care appointments inside the prison. Further qualitative research, most likely ethnographic in nature, is needed to understand why DNA rates are so high and what solutions can be implemented to reduce DNAs in order to ensure people in prison have timely access to health care. Our research consciously focused on contributing aspects of health inequalities and we were mindful to examine indicators related to age and gender. However, there is a distinct lack of qualitative research about the racialised experience of receiving/accessing health care while in prison. While research exists about being an ethnic minority prisoner in general, there is virtually nothing about the healthcare needs and experiences of ethnic minority prisoners. Lastly, staffing levels in prison came out strongly through our qualitative interviews. While the acute and community sector has research evidence about safer staffing, there is scant evidence about its impacts on the delivery of health care in the prison setting.
Additional information
Contributions of authors
Sue Bellass (https://orcid.org/0000-0001-9383-4116) (Research Fellow, qualitative researcher) undertook all fieldwork and analysis for the qualitative work package and was the lead for the scoping review. She also supported both stakeholder consensus processes. Sue wrote Chapters 1, 2, 4 and co-wrote Chapter 6.
Krysia Canvin (https://orcid.org/0000-0001-6571-6411) (Programme Manager, qualitative researcher) managed the programme of research throughout and worked in all work packages but most significantly the qualitative research. She conducted the secondary qualitative analysis focusing on mental health. Krysia co-wrote Chapters 3, 6 and 7.
Tracey Farragher (https://orcid.org/0000-0002-1968-6378) (Senior Lecturer, epidemiologist) led the routinely collected data work package and the quantitative part of the mental health analysis. She conducted all statistical analyses. Tracey co-wrote Chapters 5 and 7.
Kate McLintock (https://orcid.org/0000-0002-9479-263X) (Clinical Academic and Prison GP) provided clinical interpretation to all work packages and worked on the routinely collected data work package. Kate co-wrote Chapter 5.
Nat Wright (https://orcid.org/0000-0003-3547-3724) (Clinical Research Lead and Prison GP) provided clinical interpretation to all work packages and facilitated access to the routinely collected data.
Pip Hearty (https://orcid.org/0000-0002-0172-505X) (Research Fellow, mixed methods researcher) worked on data extraction in the routinely collected data work package and facilitated access to participants in the qualitative work package.
Nicola Seanor (https://orcid.org/0000-0001-5651-2177) (Joint Lead for Health and Justice Commissioning Support) provided a commissioner and policy interpretation to all work packages.
Marie Cunningham (https://orcid.org/0000-0002-1871-4728) (Joint Lead for Health and Justice Commissioning Support) provided a commissioner, policy and clinical interpretation to all work packages.
Robbie Foy (https://orcid.org/0000-0003-0605-7713) (Clinical Professor of Primary Care) was joint Principal Investigator programme of research and worked most significantly on both stakeholder consensus work packages and the routinely collected data work package. He co-wrote Chapters 3, 5 and 6.
Laura Sheard (https://orcid.org/0000-0002-9241-8361) (Associate Professor, qualitative methodologist) was joint Principal Investigator of the programme of research and worked most significantly on the qualitative work package. She wrote Chapter 8.
All authors reviewed the contents of this final report as a whole and provided revisions and comments.
Acknowledgements
We thank all of the people who participated in interviews for the qualitative work package and the many individuals and organisations who assisted with participant recruitment but cannot be named here to protect participants’ anonymity.
We are sincerely grateful to Stephen Roddis for his substantial efforts in ensuring a comprehensive data extract at Spectrum CIC and Stephen Graham for facilitating this process. Our thanks also to Bridget Gill from Spectrum People for attending research team meetings and acting as a ‘critical friend’. We are grateful to the members of the project Oversight Committee who provided invaluable guidance and support and facilitated the dissemination of emerging findings: James Woodall (chair), Paula Harriott, Eamonn O’Moore, Tim Doran, Richard Keers, Maria Panagioti, Tim Kirkpatrick, Sarah Bromley and Kathryn Waldegrave.
We also thank Wendy Hobson and Anna Halliday and other staff from the University of Leeds and Sharon Medley and George Charlesworth at Spectrum CIC for their administrative support, alongside Paul Eckhart for his proofreading and editorial work. Martin Simpson-Scott at NIHR made our lives easier with his swift and helpful responses to all our queries.
We especially wish to thank everyone with lived experience of prison who contributed their considerable expertise and undoubtedly improved the quality of the project: Fabien Decodts, Phil Pearce, Michaela Booth and Marc Conway, and the two individuals originally involved (not named to protect their identity).
Data-sharing statement
All data generated that can be shared are contained within the report. All data queries and requests should be submitted to the corresponding author for consideration.
Ethics statement
The whole programme of research was granted ethical approval by University of Leeds School of Medicine Research Ethics Committee on 17 July 2019 (Ref: 18-093).
Permission from the prison service was required to interview people in the community who were on probation at the time of the interview. This was granted by HMPPS National Research Committee on 24 December 2019 (Ref: 2019-383). The routinely collected data work package was exempted from requiring ethical review by HMPPS NRC and we were issued with a letter of exemption on 19 March 2019.
Information governance statement
University of Leeds is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under Data Protection legislation University of Leeds is the Data Processor and Data Controller, and we process personal data in accordance with their instructions. You can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for DHSC’s Data Protection Officer: dpo@leeds.ac.uk.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/GRFV4068.
Primary conflicts of interest: Sue Bellass: None declared.
Krysia Canvin reports that she has received funding from UKRI ESRC (2021–2) and is a member of an independent oversight committee: The Prevention Of Suicide Behaviour in Prison: Enhancing Access to Therapy (PROSPECT) Programme (NIHR Programme Grants for Applied Research -RP-PG-0218-20006, 2020–present).
Tracey Farragher reports that she is Chair of MBRC (NIHR Manchester Biomedical Research Centre) Health Inequalities Steering Group (HISG). She was also a board member for HS&DR commissioned calls panel.
Kate McLintock reports that she was in paid employment with Spectrum Community Health Community Interest Company (April 2019–October 2021).
Nat Wright reports that he is the NIHR Yorkshire and Humber primary care specialty lead and is a co-applicant on a recently successfully funded NIHR programme grant. He also sits on the Royal College of General Practitioners Secure Environments Group and also the NHSE England Secure Environments Clinical Reference Group. Previously, he was a panel member for two HTA committees. In the last year, he has received honoraria from Camurus and Indivior pharmaceutical companies for training and writing and activities.
Pip Hearty: None declared.
Nicola Seanor reports that she is Non-Executive Director at Calderdale and Huddersfield Foundation Trust and Lead for Health and Justice at NECS.
Marie Cunningham: None declared.
Robbie Foy reports that he is in receipt of several grants from National Institute for Health and Care Research and receives grant funding from Yorkshire Cancer Research (YCR). He is Chair of three independent oversight committees: Implementing improved asthma self-management as routine (IMP2ART, PGfAR, 2018–present); Acne Care Online (ACO; PGfAR, 2022–present); and Social Influence Interventions for Clinical Behaviour Change Among Health Professionals (SOCIAL, HS&DR 2018–20). He is also Chair of the Data Monitoring Committee At-Risk Registers Integrated into primary care to Stop Asthma crises (ARRISA-UK, HTA, 2015–present) and Co-chair of the Implementation Strategy Group, National Institute for Health and Care Excellence. Previously, he was a member of the Dissemination Centre Advisory Group. He also reports that he is a member of the primary care-led post diagnostic Dementia care (PriDem; Alzheimer’s Society; 2019–present).
Laura Sheard reports that she is in receipt of several grants from ESRC, UKPRP, NIHR (PGfAR, HS&DR, PHR, HTA) and has recently sat as a guest committee member on several funding boards (RfPB mental health, MRC Qualitative methods, SBRI Implementation). She is associate editor for Implementation Science.
Publications
Bellass S, Canvin K, McLintock K, Wright N. Integrating primary care across the prison and community interface. Br J Gen Pract 2021;71(703):56–7. https://doi.org/10.3399/bjgp21X714653
Bellass S, Canvin K, McLintock K, Wright N, Farragher T, Foy R, Sheard L. Quality indicators and performance measures for prison healthcare: a scoping review. Health Justice 2022;10(13). https://doi.org/10.1186/s40352-022-00175-9
https://doi.org/10.3399/bjgp21X714653
Bellass S, Canvin K, Sheard L. ‘Trying to battle a very slow version of the system that exists outside’: experiences of waiting for healthcare in English prisons (in review with Health).
Blackaby J, Byrne J, Bellass S, Canvin K, Foy R. Interventions to improve the implementation of evidence-based healthcare in prisons: a scoping review (in review with BMC Health and Justice).
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Ministry of Justice, HM Prison Service, and Her Majesty’s Prison and Probation Service . Prison Population Figures: 2022 2022. www.gov.uk/government/statistics/prison-population-figures-2022 (accessed 8 August 2022).
- Sturge G, Tunnicliffe R. UK Prison Population Statistics 2021. https://commonslibrary.parliament.uk/research-briefings/sn04334/ (accessed 8 August 2022).
- Stürup-Toft KA, O’Moore EJ, Plugge EH. Looking behind the bars: emerging health issues for people in prison. Br Med Bull 2018;125:15-23. https://doi.org/10.1093/bmb/ldx052.
- Kinner SA, Young JT. Understanding and improving the health of people who experience incarceration: an overview and synthesis. Epidemiol Rev 2018;40:4-11. https://doi.org/10.1093/epirev/mxx018.
- Baybutt M, Khadoudja C. Health-promoting prisons: theory to practice. Glob Health Promot 2016;23:66-74. https://doi.org/10.1177/1757975915614182.
- United Nations Office on Drugs and Crime . The United Nations Standard Minimum Rules for the Treatment of Prisoners (the Nelson Mandela Rules) 2015. www.unodc.org/documents/justice-and-prison-reform/Nelson_Mandela_Rules-E-ebook.pdf (accessed 8 August 2022).
- House of Commons Health and Social Care Committee . Prison Health: Twelfth Report of Session 2017–2019 2018. https://publications.parliament.uk/pa/cm201719/cmselect/cmhealth/963/963.pdf (accessed 8 August 2022).
- Leaman J, Richards AA, Emslie L, O’Moore EJ. Improving health in prisons – from evidence to policy to implementation – experiences from the UK. Int J Prison Health 2017;13:139-67. https://doi.org/10.1108/IJPH-09-2016-0056.
- Dawda P, Jenkins R, Varnam R. Quality Improvement in General Practice: The King’s Fund Discussion Paper. London: The King’s Fund; 2011.
- Wright NMJ, Hankins F, Hearty P. Long-term condition management for prisoners: improving the processes between community and prison. BMC Fam Pract 2021;22. https://doi.org/10.1186/s12875-021-01417-9.
- La Cerra C, Sorrentino M, Franconi I, Notarnicola I, Petrucci C, Lancia L. Primary care program in prison: a review of the literature. J Correct Health Care 2017;23:147-56. https://doi.org/10.1177/1078345817699801.
- Silverman-Retana O, Servan-Mori E, Lopez-Ridaura R, Bautista-Arredondo S. Diabetes and hypertension care among male prisoners in Mexico City: exploring transition of care and the equivalence principle. Int J Public Health 2016;61:651-9. https://doi.org/10.1007/s00038-016-0812-1.
- McConnon A, Fung K, Lofters A, Hwang SW, Kouyoumdjian FG. Colorectal and breast cancer screening status for people in Ontario provincial correctional facilities. Am J Prev Med 2019;56:487-93. https://doi.org/10.1016/j.amepre.2018.11.011.
- Williams M, Thomson L, Butcher E, Morriss R, Khunti K, Packham C. NHS health check programme: a qualitative study of prison experience. J Public Health 2020;44:174-83. https://doi.org/10.1093/pubmed/fdaa189.
- Thomas EH, Wang EA, Curry LA, Chen PG. Patients’ experiences managing cardiovascular disease and risk factors in prison. BMC Health Justice 2016;4. https://doi.org/10.1186/s40352-016-0035-9.
- Wangmo T, Hauri S, Meyer AH, Elger BS. Patterns of older and younger prisoners’ primary healthcare utilization in Switzerland. Int J Prison Health 2016;12:173-84. https://doi.org/10.1108/IJPH-03-2016-0006.
- Binswanger IA, Krueger PM, Steiner JF. Prevalence of chronic medical conditions among jail and prison inmates in the USA compared with the general population. J Epidemiol Community Health 2009;63:912-9. https://doi.org/10.1136/jech.2009.090662.
- Wilper AP, Woolhandler S, Boyd JW, Lasser KE, McCormick D, Bor DH, et al. The health and health care of US prisoners: results of a nationwide survey. Am J Public Health 2009;99:666-72. https://doi.org/10.2105/AJPH.2008.144279.
- Nowotny KM. Health care needs and service use among male prison inmates in the United States: a multi-level behavioral model of prison health service utilization. BMC Health Justice 2017;5. https://doi.org/10.1186/s40352-017-0052-3.
- Spycher J, Dusheiko M, Beaupère P, Gravier B, Moschetti K. Healthcare in a pure gatekeeping system: utilization of primary, mental and emergency care in the prison population over time. BMC Health Justice 2021;9. https://doi.org/10.1186/s40352-021-00136-8.
- Forrester A, Exworthy T, Chao O, Slade K, Parrott J. Influencing the care pathway for prisoners with acute mental illness. Crim Behav Ment Health 2013;23:217-26. https://doi.org/10.1002/cbm.1870.
- Peterson J, Pearce PF, Ferguson LA, Langford CA. Understanding scoping reviews: definition, purpose, and process. J Am Assoc Nurse Pract 2017;29:12-6. https://doi.org/10.1002/2327-6924.12380.
- Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods 2014;5:371-85. https://doi.org/10.1002/jrsm.1123.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19-32. https://doi.org/10.1080/1364557032000119616.
- Colquhoun HL, Levac D, O’Brien KK, Straus S, Tricco AC, Perrier L, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol 2014;67:1291-4. https://doi.org/10.1016/j.jclinepi.2014.03.013.
- Tricco AC, Lillie E, Zarin W, O’Brien K, Colquhoun H, Kastner M, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol 2016;16. https://doi.org/10.1186/s12874-016-0116-4.
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5. https://doi.org/10.1186/1748-5908-5-69.
- Tricco AC, Lille E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467-73. https://doi.org/10.7326/M18-0850.
- Kronenberg C, Doran T, Goddard M, Kendrick T, Gilbody S, Dare CR, et al. Identifying primary care quality indicators for people with serious mental illness: a systematic review. Br J Gen Pract 2017;67:e519-30. https://doi.org/10.3399/bjgp17X691721.
- Munn Z, Stern C, Aromataris E, Lockwood C, Jordan Z. What kind of systematic review should I conduct? A proposed typology and guidance for systematic reviewers in the medical and health sciences. BMC Med Res Methodol 2018;18. https://doi.org/10.1186/s12874-017-0468-4.
- Booles K. Survey on the quality of diabetes care in prison settings across the UK. J Diabetes Nurs 2011;15:168-76.
- Wright KN. Designing a national performance measurement system. Prison J 2005;85:368-93. https://doi.org/10.1177/0032885505279389.
- Stone TT, Kaiser RM, Mantese A. Health care quality in prisons: a comprehensive matrix for evaluation. J Correct Health Care 2006;12:89-103. https://doi.org/10.1177/1078345806288948.
- Hoge SK, Greifinger RB, Lundquist T, Mellow J. Mental health performance measurement in corrections. Int J Offender Ther Comp Criminol 2009;53:634-47. https://doi.org/10.1177/0306624X08322692.
- Asch SM, Damberg CL, Hiatt L, Teleki SS, Shaw R, Hill TE, et al. Selecting performance indicators for prison health care. J Correct Health Care 2011;17:138-49. https://doi.org/10.1177/1078345810397712.
- Greifinger RB. Independent review of clinical health services for prisoners. Int J Prison Health 2012;8:141-50. https://doi.org/10.1108/17449201211285012.
- Kintz KE. Quality Measures in Correctional Health Care. Scholar Archive, 990. Oregon Health and Science University.; 2013.
- Damberg CL, Shaw R, Teleki SS, Hiatt L, Asch SM. A review of quality measures used by state and federal prisons. J Correct Health Care 2011;17:122-37. https://doi.org/10.1177/1078345810397605.
- Teleki SS, Damberg CL, Shaw R, Hiatt L, Williams B, Hill TE, et al. The current state of quality of care measurement in the California Department of Corrections and Rehabilitation. J Correct Health Care 2011;17:100-21. https://doi.org/10.1177/1078345810397498.
- Raimer BG, Stobo JD. Health care delivery in the Texas prison system: the role of academic medicine. JAMA 2004;292:485-9. https://doi.org/10.1001/jama.292.4.485.
- Laffan S. Evaluation of your medical department. Am Jails 2016;30:62-4.
- Kountz DS, Orsetti M. Reducing variability in chronic disease management: utility of chart audit tools with medical director oversight. J Correct Health Care 2007;13:180-95. https://doi.org/10.1177/1078345807303095.
- Bisset MM, Harrison EA. Health Outcomes in Corrections: Health Information Technology and the Correctional Health Outcome and Resource Data Set (CHORDS) 2012. https://cochs.org/files/health-it-hie/chords-ncchc.pdf (accessed 8 August 2022).
- Watts B. Development of a Performance-Based RFP for Correctional Health Care Services in Vermont 2015. https://cochs.org/files/jurisdiction/pay-for-performance.pdf (accessed 8 August 2022).
- Castro ME. Diabetes Screening in Inmates: A Quality Improvement Pilot Project. Connecticut: University of Connecticut; 2014.
- Murphy E, Black N, Lamping D, Mckee C, Sanderson C. Consensus development methods, and their use in clinical guideline development: a review. Health Technol Assess 1998;2. https://doi.org/10.3310/hta2030.
- National Institute for Health and Care Excellence . NICE Quality and Outcomes Framework (QOF) Indicator n.d. www.nice.org.uk/standards-and-indicators/qofindicators/ (accessed 8 August 2022).
- National Institute for Health and Care Excellence (NICE) . Physical Health of People in Prison 2016. www.nice.org.uk/guidance/ng57/chapter/recommendations (accessed 8 August 2022).
- National Institute for Health and Care Excellence (NICE) . Dementia: Supporting People With Dementia and Their Carers in Health and Social Care 2006. https://dementiapartnerships.com/wp-content/uploads/sites/2/nice-cg42.pdf (accessed 8 August 2022).
- National Institute for Health and Care Excellence (NICE) . Psychosis and Schizophrenia in Adults. Treatment and Management 2014. www.nice.org.uk/guidance/cg178/evidence/full-guideline-490503565 (accessed 8 August 2022).
- British Medical Association (BMA) and NHS England . 2019/20/General/Medical/Services/(GMS)/Contract/Quality/and/Outcomes/Framework/(QOF)/Guidance/for/GMS/Contract/2019/20/in/England 2019. www.england.nhs.uk/wp-content/uploads/2019/05/gms-contract-qof-guidance-april-2019.pdf (accessed 8 August 2022).
- Rushforth B, Stokes T, Andrews E, Willis TA, McEachan R, Faulkner S, et al. Developing ‘high impact’ guideline-based quality indicators for UK primary care: a multi-stage consensus process. BMC Fam Pract 2015;16. https://doi.org/10.1186/s12875-015-0350-6.
- Willis TA, West R, Rushforth B, Stokes T, Glidewell L, Carder P, et al. ASPIRE Programme Team . Variations in achievement of evidence-based, high-impact quality indicators in general practice: an observational study. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0177949.
- Thangaratinam S, Redman CWE. The Delphi technique. Obstet Gynaecol 2011;7:120-5. https://doi.org/10.1576/toag.7.2.120.27071.
- Public Health England (PHE) and NHS England . Advice for Prescribers on the Risk of the Misuse of Pregabalin and Gabapentin 2014. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/385791/PHE-NHS_England_pregabalin_and_gabapentin_advice_Dec_2014.pdf#:~:text=Practitioners%20should%20prescribe%20pregabalin%20and%20gabapentin%20appropriately%20to,drugs%20will%20use%20their%20medicines%20appropriately%20without%20misuse (accessed 8 August 2022).
- Alderson SL, Farragher TM, Willis TA, Carder P, Johnson S, Foy R. The effects of an evidence- and theory-informed feedback intervention on opioid prescribing for non-cancer pain in primary care: a controlled interrupted time series analysis. PLOS Med 2021;18. https://doi.org/10.1371/journal.pmed.1003796.
- Campbell S, Hannon K, Lester H. Exception reporting in the quality and outcomes framework: views of practice staff – a qualitative study. Br J Gen Pract 2011;61:e183-9. https://doi.org/10.3399/bjgp11X567117.
- National Institute for Health and Care Excellence (NICE) . The Proportion of Women Aged 50–70 Years Whose Record Shows a Breast Screening Test Has Been Performed Within the Last 3 Years 2017. www.nice.org.uk/standards-and-indicators/ccgoisindicators/ (accessed 8 August 2022).
- National Institute for Clinical Excellence (NICE) . GP Quality Improvement Indicator 2010. www.nice.org.uk/standards-and-indicators/gpqualityimprovements/the-percentage-of-patients-with-a-new-diagnosis-of-dementia-recorded-in-the-preceding-1-april-to-31-march-with-a-record-of-fbc-calcium-glucose-renal-and-liver-function-thyroid-function-tests-serum-vitamin-b12-and-folate-levels-recorded-between-6-months-be (accessed 8 August 2022).
- National Institute for Clinical Excellence (NICE) . GP Quality Improvement Indicator 2014. www.nice.org.uk/Standards-and-Indicators/GPQualityImprovements/the-percentage-of-patients-who-had-a-myocardial-infarction-in-the-preceding-1-april-to-31-march-and-who-are-currently-being-treated-with-ace-i-or-arb-if-ace-i-intolerant-dual-anti-platelet-therapy-a-statin-and-a-beta-blocker-for-those-patients-with-left-v (accessed 8 August 2022).
- Public Health England (PHE) . Abdominal Aortic Aneurysm Screening: Programme Overview. Public Health England Guidance 2021. www.gov.uk/guidance/abdominal-aortic-aneurysm-screening-programme-overview (accessed 8 August 2022).
- Chassin MR, Loeb JM, Schmaltz SP, Wachter RM. Accountability measures – using measurement to promote quality improvement. N Engl J Med 2010;363:683-8. https://doi.org/10.1056/NEJMsb1002320.
- National Diabetes Audit . National Diabetes Audit: Are Services Providing Good Quality Diabetes Care? A Summary Report of the National Diabetes Audit: Care Processes and Treatment Targets 2016–2017 n.d. www.diabetes.org.uk/resources-s3/2018-06/NDA_%20Summary_v8.pdf (accessed 8 August 2022).
- Guthrie B, Inkster M, Fahey T. Tackling therapeutic inertia: role of treatment data in quality indicators. BMJ 2007;335:542-4. https://doi.org/10.1136/bmj.39259.400069.AD.
- Brown C, Hofer T, Johal A, Thomson R, Nicholl J, Franklin BD, et al. An epistemology of patient safety research: a framework for study design and interpretation – part 3: end points and measurement. Qual Saf Health Care 2008;17:170-7. https://doi.org/10.1136/qshc.2007.023655.
- Guthrie B. Measuring the quality of healthcare systems using composites. BMJ 2008;337. https://doi.org/10.1136/bmj.a639.
- Ferlie EB, Shortell SM. Improving the quality of healthcare in the United Kingdom and the United States: a framework for change. Milbank Q 2001;79:281-315. https://doi.org/10.1111/1468-0009.00206.
- Royal College of General Practitioners Secure Environments Group . Equivalence of Care in Secure Environments in the UK. Position Statement 2018. www.rcgp.org.uk/getmedia/c9ff1b91-4673-4f7e-9bea-ded1c9674adb/RGCP-secure-group-report-july-2018.pdf (accessed 8 August 2022).
- Leaman J. Rapid Review of Evidence of the Impact on Health Outcomes of NHS Commissioned Health Services for People in Secure and Detained Settings to Inform Future Health Interventions and Prioritisation in England. Public Health England; 2016.
- The Lancet Public Health . Living in detention: a matter of health justice. Lancet Public Health 2020;5:e71-e126. https://doi.org/10.1016/S2468-2667(20)30008-6.
- Brooker C, Coid J. Mental health services are failing the criminal justice system. BMJ 2022;26. https://doi.org/10.1136/bmj-2021-069776.
- Senior J, Forsyth K, Walsh E, O’Hara K, Stevenson C, Hayes A, et al. Health and social care services for older male adults in prison: the identification of current service provision and piloting of an assessment and care planning model. Health Serv Deliv Res 2013;1:1-138. https://doi.org/10.3310/hsdr01050.
- Kirkpatrick T, Lennox C, Taylor R, Anderson R, Maguire M, Haddad M, et al. Evaluation of a complex intervention (Engager) for prisoners with common mental health problems, near to and after release: study protocol for a randomised controlled trial. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-017931.
- Shaw J, Conover S, Herman D, Jarrett M, Leese M, McCrone P, et al. Critical time Intervention for Severely mentally ill Prisoners (CrISP): a randomised controlled trial. Health Serv Deliv Res 2017;5:1-138. https://doi.org/10.3310/hsdr05080.
- Morrissey C, Geach N, Alexander R, Chester V, Devapriam J, Duggan C, et al. Researching outcomes from forensic services for people with intellectual or developmental disabilities: a systematic review, evidence synthesis and expert and patient/carer consultation. Health Serv Deliv Res 2017;5:1-102. https://doi.org/10.3310/hsdr05030.
- Asherson P, Johansson L, Holland R, Fahy T, Forester A, Howitt S, et al. Randomised controlled trial of the short-term effects of OROS-methylphenidate on ADHD symptoms and behavioural outcomes in young male prisoners with attention-deficit/hyperactivity disorder (CIAO-II). Trials 2019;20. https://doi.org/10.1186/s13063-019-3705-9.
- Demou E, Dobson R, Sweeting H, Brown A, Sidwell S, O’Donnell R, et al. From smoking-permitted to smokefree prisons: a 3-year evaluation of the changes in occupational exposure to second-hand smoke across a national prison system. Ann Work Exp Health 2020;64:959-69. https://doi.org/10.1093/annweh/wxaa073.
- Molenberghs G, Verbeke G. Models for Discrete Longitudinal Data. New York: Springer; 2005.
- Diggle PJ, Liang KY, Zeger SL. Analysis of Longitudinal Data. New York: Oxford University Press; 1994.
- StataCorp . Stata Statistical Software: Release 16 2019.
- National Health Service Digital . Quality and Outcomes Framework (QOF), 2019–2020 Official Statistics 2020. https://digital.nhs.uk/data-and-information/publications/statistical/quality-and-outcomes-framework-achievement-prevalence-and-exceptions-data/2019–20 (accessed 8 August 2022).
- National Health Service Digital . Quality and Outcomes Framework (QOF), 2014–15 Official Statistics 2015. https://digital.nhs.uk/data-and-information/publications/statistical/quality-and-outcomes-framework-achievement-prevalence-and-exceptions-data/quality-and-outcomes-framework-qof-2014-15 (accessed 8 August 2022).
- National Health Service Digital . Quality and Outcomes Framework (QOF), 2013–14. Official Statistics 2014. https://digital.nhs.uk/data-and-information/publications/statistical/quality-and-outcomes-framework-achievement-prevalence-and-exceptions-data/quality-and-outcomes-framework-qof-2013-14 (accessed 8 August 2022).
- National Health Service Digital . Quality and Outcomes Framework (QOF), Achievement, Prevalence and Exceptions. Official Statistics 2019. https://digital.nhs.uk/data-and-information/publications/statistical/quality-and-outcomes-framework-achievement-prevalence-and-exceptions-data/2018-19-pas (accessed 8 August 2022).
- Foy R, Leaman B, McCroriePetty D, House A, Bennett M, . Prescribed opioids in primary care: cross-sectional and longitudinal analyses of influence of patient and practice characteristics. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010276.
- National Health Service Digital . Breast Screening Programme, England 2017–18. National Statistics, Official Statistics 2019. https://digital.nhs.uk/data-and-information/publications/statistical/breast-screening-programme/england-2017-18 (accessed 8 August 2022).
- Public Health England . Research and Analysis. Abdominal Aortic Aneurysm Screening: 2014 to 2015 Data 2015. www.gov.uk/government/publications/abdominal-aortic-aneurysm-screening-2014-to-2015-data (accessed 8 August 2022).
- Public Health England . NHS Health Check 2020. https://fingertips.phe.org.uk/profile/nhs-health-check-detailed (accessed 8 August 2022).
- Forsetlund L, Bjørndal A, Rashidian A, Jamtvedt G, O’Brien MA, Wolf FM, et al. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2009;2. https://doi.org/10.1002/14651858.CD003030.pub2.
- Reeves S, Pelone F, Harrison R, Goldman J, Zwarenstein M. Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Syst Rev 2017;6. https://doi.org/10.1002/14651858.CD000072.pub3.
- Fønhus MS, Dalsbø TK, Johansen M, Fretheim A, Skirbekk H, Flottorp SA. Patient-mediated interventions to improve professional practice. Cochrane Database Syst Rev 2018;9. https://doi.org/10.1002/14651858.CD012472.pub2.
- Flodgren G, O’Brien MA, Parmelli E, Grimshaw JM. Local opinion leaders: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2019;6. https://doi.org/10.1002/14651858.CD000125.pub5.
- Kwan JL, Lo L, Ferguson J, Goldberg H, Diaz-Martinez JP, Tomlinson G, et al. Computerised clinical decision support systems and absolute improvements in care: meta-analysis of controlled clinical trials. BMJ 2020;370. https://doi.org/10.1136/bmj.m3216.
- Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2012;6. https://doi.org/10.1002/14651858.CD000259.pub3.
- Michie S, Atkins L, West R. The Behaviour Change Wheel: A Guide to Designing Interventions. London: Silverback; 2014.
- Bennett AA, Campion ED, Keeler KR, Keener SK. Videoconference fatigue? Exploring changes in fatigue after videoconference meetings during COVID-19. J Appl Psychol 2021;106:330-44. https://doi.org/10.1037/apl0000906.
- Ministry of Justice . National Partnership Agreement for Prison Healthcare in England 2018–2021 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/767832/6.4289_MoJ_National_health_partnership_A4-L_v10_web.pdf (accessed 8 August 2022).
- Chang CK, Hayes RD, Perera G, Broadbent MTM, Fernandes AC, Lee WE, et al. Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLOS ONE 2011;6. https://doi.org/10.1371/journal.pone.0019590.
- Ashworth M, Schofield P, Das-Munshi J. Physical health in severe mental illness. Br J Gen Pract 2017;67:436-7. https://doi.org/10.3399/bjgp17X692621.
- Bridgwood A, Malbon G. Survey of the Physical Health of Prisoners 1994: A Survey of Sentenced Male Prisoners in England and Wales. London: Stationery Office Books; 1995.
- Condon L, Gill H, Harris F. A review of prison health and its implications for primary care nursing in England and Wales: the research evidence. J Clin Nurs 2007;16:1201-9. https://doi.org/10.1111/j.1365-2702.2007.01799.x.
- Plugge E, Douglas N, Fitzpatrick R. The Health of Women in Prison: Study Findings. Oxford: The University of Oxford; 2006.
- Rennie C, Senior J, Shaw J. The future is offender health: evidencing mainstream health services throughout the offender pathway. Crim Behav Ment Health 2009;19:1-8. https://doi.org/10.1002/cbm.723.
- Durcan G. The Future of Prison Mental Health Care in England: A National Consultation and Review. London: Centre for Mental Health; 2021.
- Durcan G. Mental Health and Criminal Justice: Views from Consultation Across England and Wales. London: Centre for Mental Health; 2016.
- Singleton N, Meltzer H, Gatward R. Psychiatric Morbidity Among Prisoners in England and Wales. London: Stationery Office; 1998.
- Bebbington P, Jakobowitz S, McKenzie N, Killaspy H, Iveson R, Duffield G, et al. Assessing needs for psychiatric treatment in prisoners: 1. Prevalence of disorder. Soc Psychiatry Psychiatr Epidemiol 2017;52:221-9. https://doi.org/10.1007/s00127-016-1311-7.
- Jordan M. Embracing the notion that context is crucial in prison mental health care. Br J Forensic Pract 2010;12:26-35. https://doi.org/10.5042/bjfp.2010.0612.
- Department of Health . The Bradley Report: Lord Bradley’s Review of People With Mental Health Problems or Learning Disabilities in the Criminal Justice System 2009.
- Hewson T, Gutridge K, Bernard Z, Kay K, Robinson L. A systematic review and mixed-methods synthesis of the experiences, perceptions and attitudes of prison staff regarding adult prisoners who self-harm. BJPsych Open 2022;8. https://doi.org/10.1192/bjo.2022.70.
- Brooker C, Tocque K, West G, Norman-Taylor A, Fowler J. Suicide in probation: towards the ideation-to-action model. Probat J 2021;70:6-18. https://doi.org/10.1177/02645505211041581.
- Marshall T, Simpson S, Stevens A. Use of health services by prison inmates: comparisons with the community. J Epidemiol Community Health 2001;55:364-5. https://doi.org/10.1136/jech.55.5.364.
- Her Majesty’s Inspectorate of Prisons . Life in Prison: Food 2016. www.justiceinspectorates.gov.uk/hmiprisons/wp-content/uploads/sites/4/2016/09/Life-in-prison-Food-Web-2016.pdf (accessed 8 August 2022).
- Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health 2019;11:589-97. https://doi.org/10.1080/2159676X.2019.1628806.
- Public Health England . Severe Mental Illness (SMI) and Physical Health Inequalities: Briefing 2018. www.gov.uk/government/publications/severe-mental-illness-smi-physical-health-inequalities/severe-mental-illness-and-physical-health-inequalities-briefing (accessed 8 August 2022).
- Vincent C, Burnett S, Carthey J. The Measurement and Monitoring of Safety. Drawing Together Academic Evidence and Practical Experience to Produce a Framework for Safety Measurement and Monitoring. The Health Foundation; 2013.
- Wright N, Hankins F, Hearty P, Allot D, Allgar V. Long-Term Condition Management for Prisoners: Exploring Prevalence and Compliance With QOF Monitoring. Foursquare 2020. https://doi.org/10.21203/rs.3.rs-45365/v1.
- Barclay M, DixonWoods M, Lyratzopoulos G. The problem with composite indicators. BMJ Qual Saf 2019;28:338-44. https://doi.org/10.1136/bmjqs-2018-007798.
- Dixon-Woods M, Baker R, Charles K, Dawson J, Jerzembek G, Martin G, et al. Culture and behaviour in the English National Health Service: overview of lessons from a large multimethod study. BMJ Qual Saf 2014;23:106-15. https://doi.org/10.1136/bmjqs-2013-001947.
- Hughes L, Sheard L, Pinkney L, Lawton RL. Excellence in elective hip and knee surgery: what does it look like? A positive deviance approach. J Health Serv Res Policy 2019;25:5-12. https://doi.org/10.1177/1355819619867350.
- Müller J, Schmidt D, Kollan C, Lehmann M, Bremer V, Zimmermann R. High variability of TB, HIV, hepatitis C treatment and opioid substitution therapy among prisoners in Germany. BMC Public Health 2017;17. https://doi.org/10.1186/s12889-017-4840-4.
- Davies M, Rolewicz L, Schlepper L, Fagunwa F. Locked out? Prisoners’ Use of Hospital Care. Nuffield Trust; 2020.
- Association of Members of Independent Monitoring Boards . Written Evidence from AMIMB (Association of Members of Independent Monitoring Boards). PRH0043 2018. http://data.parliament.uk/writtenevidence/committeeevidence.svc/evidencedocument/health-and-social-care-committee/prison-health/written/85961.html (accessed 8 August 2022).
- Harris F, Hek G, Condon L. Health needs of prisoners in England and Wales: the implications for prison healthcare of gender, age and ethnicity. Health Soc Care Community 2007;15. https://doi.org/10.1111/j.1365-2524.2006.00662.x.
- Davoren M, Fitzpatrick M, Caddow F, Caddow M, O’Neill C, O’Neill H, et al. Older men and older women remand prisoners: mental illness, physical illness, offending patterns and needs. Int Psychogeriatr 2015;27:747-55. https://doi.org/10.1017/S1041610214002348.
- Wangmo T, Meyer AH, Bretschneider W, Handtke V, Kressig RW, Gravier B, et al. Ageing prisoners’ disease burden: is being old a better predictor than time served in prison?. Gerontology 2015;61:116-23. https://doi.org/10.1159/000363766.
- Ministry of Justice . Statistics on Women and the Criminal Justice System 2019. A Ministry of Justice Publication Under Section 95 of the Criminal Justice Act 1991 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/938360/statistics-on-women-and-the-criminal-justice-system-2019.pdf (accessed 8 August 2022).
- All Party Parliamentary Group on Women in the Penal System . Inquiry into Women’s Health and Well-Being in Prisons 2022. https://howardleague.org/wp-content/uploads/2022/04/APPG-womens-health-and-well-being-FINAL.pdf (accessed 8 August 2022).
- Ismail N. Rolling back the prison estate: the pervasive impact of macroeconomic austerity on prisoner health in England. J Public Health 2020;42:625-32. https://doi.org/10.1093/pubmed/fdz058.
- Prisons and Health. World Health Organisation; 2014.
- Plugge E, Douglas N, Fitzpatrick R. Patients, prisoners, or people? Women prisoners’ experiences of primary care in prison: a qualitative study. Br J Gen Pract 2008;58:630-6. https://doi.org/10.3399/bjgp08X330771.
- Grierson J. More than half of young people in jail are of BME background. Guardian 2019. www.theguardian.com/society/2019/jan/29/more-than-half-young-people-jail-are-of-bme-background (accessed 8 August 2022).
- Prison Reform Trust . Race n.d. https://prisonreformtrust.org.uk/project/race/ (accessed 8 August 2022).
- Nowotny KM, Rogers RG, Boardman JD. Racial disparities in health conditions among prisoners compared with the general population. SSM Popul Health 2017;3:487-96. https://doi.org/10.1016/j.ssmph.2017.05.011.
- Maguire D, Dunn P, McKenna H. How Hospital Activity in the NHS in England Has Changed Over Time. The King’s Fund; 2016.
- Osborne S. One in Seven GP Posts Empty As Vacancy Rates Remain High. Pulse 2021. www.pulsetoday.co.uk/news/workforce/one-in-seven-gp-posts-empty-as-vacancy-rates-remain-high/#:~:text=The%20high%20vacancy%20rate%20%E2%80%93%20at,vacancies%20from%20across%20the%20UK (accessed 8 August 2022).
- Murray R. Falling Number of Nurses in the NHS Paints a Worrying Picture. The King’s Fund Blog; 2017.
- Royal College of Nursing . RCN Warns Failure to Invest in Prison Healthcare Staff Will Jeopardise Safety. Press Release 2018. www.rcn.org.uk/news-and-events/press-releases/rcn-warns-failure-to-invest-in-prison-healthcare-staff-will-jeopardise-safety (accessed 8 August 2022).
- Stephenson AL, Bell N. Finding meaningful work in difficult circumstances: a study of prison healthcare workers. Health Serv Manage Res 2019;32:69-77. https://doi.org/10.1177/0951484818787698.
- Edge C, Stockley MR, Swabey ML, King ME, Decodts MF, Hard DJ, et al. Secondary care clinicians and staff have a key role in delivering equivalence of care for prisoners: a qualitative study of prisoners’ experiences. EClinicalMedicine 2020;24. https://doi.org/10.1016/j.eclinm.2020.100416.
- Wang EA, Wang Y, Krumholz HM. A high risk of hospitalization following release from correctional facilities in Medicare beneficiaries: a retrospective matched cohort study, 2002 to 2010. JAMA Intern Med 2013;173:1621-8. https://doi.org/10.1001/jamainternmed.2013.9008.
- Bellass S, Canvin K, McLintock K, Wright N. Integrating primary care across the prison and community interface. Br J Gen Pract 2021;71:56-7. https://doi.org/10.3399/bjgp21X714653.
- Kontopantelis E, Stevens RJ, Helms PJ, Edwards D, Doran T, Ashcroft DM. Spatial distribution of clinical computer systems in primary care in England in 2016 and implications for primary care electronic medical record databases: a cross-sectional population study. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-020738.
- Tippu Z, Correa A, Liyanage H, Burleigh D, McGovern A, Van Vlymen J, et al. Ethnicity recording in primary care computerised medical record systems: an ontological approach. J Innov Health Inform 2017;23. https://doi.org/10.14236/jhi.v23i4.920.
- Nayrouz S, Ploumaki S, Farooq R, Stock D, Lim H. Physical health problems in patients with severe mental illness: relationship between antipsychotic treatment and physical health. Eur Neuropsychopharmacol 2011;21:S480-1.
- NHS Health Check Programme n.d. www.nhs.uk/conditions/nhs-health-check/ (accessed 11 August 2022).
- Wood S, Foy R, Willis TA, Carder P, Johnson S, Alderson S. General practice responses to opioid prescribing feedback: a qualitative process evaluation. Br J Gen Pract 2021;71:e788-96. https://doi.org/10.3399/BJGP.2020.1117.
- Lawton R, Heyhoe J, Louch G, Ingleson E, Glidewell L, Willis TA, et al. ASPIRE Programme . ASPIRE programme. Using the Theoretical Domains Framework (TDF) to understand adherence to multiple evidence-based indicators in primary care: a qualitative study. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0479-2.
- Glidewell L, Willis TA, Petty D, Lawton R, McEachan RRC, Ingleson E, et al. ASPIRE Programme Team . To what extent can behaviour change techniques be identified within an adaptable implementation package for primary care? A prospective directed content analysis. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0704-7.
- Glidewell L, Hunter C, Ward V, McEachan RRC, Lawton R, Willis TA, et al. ASPIRE Programme Team . Explaining variable effects of an adaptable implementation package to promote evidence-based practice in primary care: a longitudinal process evaluation. Implement Sci 2022;17. https://doi.org/10.1186/s13012-021-01166-4.
Appendix 1 MEDLINE and CINAHL search strategies
Database: Ovid MEDLINE® 1946 to November 2019 Week 5
-
exp Primary Health Care/ (152443)
-
general practitioners/ (7345)
-
physicians, primary care/ (3186)
-
general practice/ (12767)
-
Family Practice/ (64847)
-
Community Health Services/ (31036)
-
Community Health Nursing/ (19450)
-
((general or family) adj (practice* or practitioner* or physician* or doctor* or nurs* or dentist*)).tw. (97053)
-
GP*.tw. (147573)
-
(primary adj4 (care or health* or service* or center* or centre* or practice*)).tw. (132583)
-
Nurse Clinicians/ (8148)
-
Nurse Practitioners/ (17345)
-
nurse*.tw. (237289)
-
Pharmacists/ (16002)
-
pharmacist*.tw. (25202)
-
Physical Therapists/ (1617)
-
physio*.tw. (639357)
-
(physical adj4 therapist*).tw. (5093)
-
or/1-18 [Primary care] (1368966)
-
exp Quality Indicators, Health Care/ (20382)
-
(quality adj4 (indicat* or measure* or criteria* or indicat* or assurance* or improv*)).tw. (197196)
-
((clinical or performance or safety or process or outcome or prescribing or prevent*) adj4 indicator*).tw. (16607)
-
benchmarking.tw. (5691)
-
(performance adj4 (evaluat* or measur*)).tw. (73351)
-
(performance adj4 (evaluat* or measur* or criteria* or indicat*)).tw. (85879)
-
(incentive* adj4 (scheme* or assess* or measure* or outcome*)).tw. (1039)
-
“Standard of Care”/ (2338)
-
(standard* adj2 (healthcare or care)).tw. (37628)
-
Quality Indicators, Health Care/ (15100)
-
“Quality of Health Care”/ (71001)
-
(quality adj2 (healthcare or care)).tw. (50933)
-
patient outcome assessment/ (4401)
-
(patient adj3 outcome adj (measure* or assessment*)).tw. (3957)
-
proms.tw. (1010)
-
patient satisfaction/ (79149)
-
patient preference/ (7735)
-
(patient* adj3 (experience* or satisf* or preference*)).tw. (163042)
-
or/20-37 [Quality indicators] (613621)
-
Prisons/ (9351)
-
Prisoners/ (16143)
-
((Secure or correctional) adj2 (unit or units or facility or institution* or facilities or centre* or center*)).tw. (1772)
-
(Prison* or jail* or offender* or reoffend* or convict* or inmate* or detainee* or cellmate* or incarcerat* or felon).tw. (30054)
-
(Penal or penitentiary or gaol or reformator*).tw. (2009)
-
or/39-43 [Prison] (39961)
-
19 and 38 and 44 (191)
CINAHL
| # | Query | Results |
|---|---|---|
| S42 | S17 AND S35 AND S41 | 152 |
| S41 | S36 OR S37 OR S38 OR S39 OR S40 | 21,444 |
| S40 | TI ((Penal or penitentiary or gaol or reformator*)) OR AB ((Penal or penitentiary or gaol or reformator*)) | 400 |
| S39 | TI ((Prison* or jail* or offender* or reoffend* or convict* or inmate* or detainee* or cellmate* or incarcerat* or felon)) OR AB ((Prison* or jail* or offender* or reoffend* or convict* or inmate* or detainee* or cellmate* or incarcerat* or felon)) | 16,322 |
| S38 | TI (((Secure or correctional) N2 (unit or units or facility or institution* or facilities or centre* or center*))) OR AB (((Secure or correctional) N2 (unit or units or facility or institution* or facilities or centre* or center*))) | 1231 |
| S37 | (MH “Prisoners”) | 8,228 |
| S36 | (MH “Correctional Facilities”) | 5342 |
| S35 | S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 | 357,910 |
| S34 | TI ((patient* N3 (experience* or satisf* or preference*))) OR AB ((patient* N3 (experience* or satisf* or preference*))) | 73,878 |
| S33 | (MH “Patient Preference”) | 487 |
| S32 | (MH “Patient Satisfaction”) | 50,036 |
| S31 | TI PROMS OR AB PROMS | 1362 |
| S30 | TI ((patient N3 outcome N (measure* or assessment*))) OR AB ((patient N3 outcome N (measure* or assessment*))) | 141 |
| S29 | (MH “Outcome Assessment”) | 40,393 |
| S28 | TI ((quality N2 (healthcare or care))) OR AB ((quality N2 (healthcare or care))) | 48,427 |
| S27 | (MH “Quality of Health Care”) | 67,174 |
| S26 | TI ((standard* N2 (healthcare or care))) OR AB ((standard* N2 (healthcare or care))) | 22,931 |
| S25 | TI ((incentive* N4 (scheme* or assess* or measure* or outcome*))) OR AB ((incentive* N4 (scheme* or assess* or measure* or outcome*))) | 752 |
| S24 | TI ((performance N4 (evaluat* or measur* or criteria* or indicat*))) OR AB ((performance N4 (evaluat* or measur* or criteria* or indicat*))) | 30,546 |
| S23 | TI ((performance N4 (evaluat* or measur*))) OR AB ((performance N4 (evaluat* or measur*))) | 26,278 |
| S22 | TI benchmarking OR AB benchmarking | 2896 |
| S21 | (MH “Benchmarking”) | 6726 |
| S20 | TI (((clinical or performance or safety or process or outcome or prescribing or prevent*) N4 indicator*)) OR AB (((clinical or performance or safety or process or outcome or prescribing or prevent*) N4 indicator*)) | 8353 |
| S19 | TI ((quality N4 (indicat* or measure* or criteria* or indicat* or assurance* or improv*))) OR AB ((quality N4 (indicat* or measure* or criteria* or indicat* or assurance* or improv*))) | 95,762 |
| S18 | (MH “Clinical Indicators”) | 11,455 |
| S17 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 | 567,168 |
| S16 | TI (physical n4 therapist*) OR AB (physical n4 therapist*) | 6763 |
| S15 | TI physio* OR AB physio* | 83,023 |
| S14 | (MH “Physical Therapists”) | 10,688 |
| S13 | TI pharmacist* OR AB pharmacist* | 15,763 |
| S12 | (MH “Pharmacists”) | 13,357 |
| S11 | TI Nurse* OR AB Nurse* | 296,782 |
| S10 | (MH “Practical Nurses”) | 5280 |
| S9 | (MH “Clinical Nurse Specialists”) | 6744 |
| S8 | TI ((primary N4 (care or health* or service* or center* or centre* or practice*)) OR AB ((primary N4 (care or health* or service* or center* or centre* or practice*)) | 85,435 |
| S7 | TI GP* OR AB GP* | 25,055 |
| S6 | TI (((general or family) N (practice* or practitioner* or physician* or doctor* or nurs* or dentist*))) OR AB (((general or family) N (practice* or practitioner* or physician* or doctor* or nurs* or dentist*))) | 760 |
| S5 | (MH “Community Health Nursing”) | 24,624 |
| S4 | (MH “Community Health Services”) | 18,960 |
| S3 | (MH “Family Practice”) | 22,818 |
| S2 | (MH “Physicians, Family”) | 17,702 |
| S1 | (MH “Primary Health Care”) | 57,007 |
Appendix 2
| Sources included (author, year) | Stone et al.33 | Booles31 | Greifinger36 | |
|---|---|---|---|---|
| Hoge et al.34 | Damberg et al.38 | Kintz37 | Wright32 | |
| Asch et al.35 | Teleki et al.39 | Watts44 | Raimer and Stobo40 | |
| Kountz and Orsetti42 | Bisset and Harrison43 | Castro45 | Laffan41 | |
| Country of origin | – All USA33–35,42 | – USA38,39,43 – UK31 |
– All USA36,37,44,45 | – All USA32,40,41 |
| Adult/juvenile | – All adult33–35,42 | All adult31,38,39,43 | All adult36,37,44,45 | Not specified32,40,41 |
| Condition-specific | – No33,35 – 3 CCs – asthma, diabetes, hypertension42 – MH34 |
– No38,39 – Diabetes31 – Gives examples of diabetes measures43 |
– No36,44 – 9 CCs: asthma/respiratory, diabetes, HIV/AIDS, hypertension/CVD, lipid disorders, seizure disorders, HCV/chronic hepatitis, hepatic cirrhosis, severe mental illness37 – Diabetes45 |
– No41 – Substance abuse and MH32 – CCs: hypertension, diabetes, psychiatric disorders, hepatitis, HIV40 |
| Develops, implements, tests or refines QIs | – Develops33–35 – Implements (chart audit)42 |
– Reviews38,39 – Surveys31 – Develops and tests43 |
– Develops36,37 – Tests45 – Develops and tests44 |
– Advises on implementation41 – Develops32 – Implements40 |
| Are lists of QIs or performance measures (PMs) provided? | – Yes33,34 – No42 – Only examples; full list provided in Teleki et al.35 |
– Gives key domains/clinical areas38 – Yes39 – No31,43 |
– Yes36,44,45 – No37 |
– Yes41 – Yes (very brief)32 – Some outcome QIs are listed in the text, not in numerator/denominator format40 |
| Related to other studies | – Asch et al.35 is related to Damberg et al.38 and Teleki et al.39 | – Asch et al.35 is related to Damberg et al.38 and Teleki et al.39 | – Kintz37 frames study in relation to Damberg et al.39 | – Asch et al.35 cite Raimer and Stobo40 |
| Drivers/broader context | – Large numbers of people dying because of medical errors; increased public awareness/expectation motivating health care (HC) organisations to minimise errors and improve outcomes.33 – External audit identified variability in CC management. Occurrence of sentinel event (at least 1 every 3 months) often first indication of CC, inability to stratify patients according to risk. Increasing public expectation of high standard of care. Attorney inmate complaint about lack of medication for diabetes led to inspection of 10 random charts where 4 patients not receiving standard of care. Responsibility of HC providers to provide ‘smooth road’ for maintaining health of inmates. Provider compensation decisions can be guided by objective feedback from chart audit system. Mandate for equivalency of care.42 – HC settings increasingly turning to EB practice, i.e. care based on scientific/clinical evidence. Standard of care in correctional facilities (CFs) ‘widely regarded as inadequate’; report that CFs don’t conform to guidelines for MH care. More recent evidence suggests quality of MH care declining. Legal case in 1970s kick-started attempts to improve CF HC (Estelle v Gamble–prisoners’ 8th amendment rights violated). Courts articulate principles, e.g. requirement for inmates to have greater access to care; but leave the implementation to others. It is unclear what standards are being applied by civil rights investigations and that the standards are ‘vague’. For-profit HCPs provide substantial share of HC in USA CFs. CF administrators lack expertise in managing HC and contract out to for-profit HCPs, expect costs and quality to be improved by them. For-profit HCPs have divisions charged with monitoring and improving quality.Care more heavily regulated in the community; those who pay for care understand HC delivery, and wield power and require adherence to standards; stakeholders in correctional care don’t yet have enough power to demand adherence. In some places administrators set standards but lack experience to do so. Expectations for HC may be a combination of correctional administrators, local legislative leadership and private vendors. Funding constraints may drive officials to lowest-cost provider: ‘quality of care becomes an afterthought’. Correctional agencies need strong commitment to quality, PM and accreditation.34 – Prisoners have higher rates of disease than ‘FW’ population and studies have found HC deficiencies. FW initiated PM to improve quality; some evidence correlates better care with PM. Need to standardise quality-measurement systems.35 |
– Part of Asch et al.’s35 project. Prisons facing litigation due to inadequacy of HC; in 2005 239 CFs under court orders or consent decrees. Notes FW has turned to PM to improve accountability and identify areas for improvement. Little known about extent to which PMs used in CFSs. Interest in achieving accreditation encourages development of PM.38 – Part of Asch and Damberg work. California Department Of Corrections (DOC) ‘in midst of extreme legal remedy’ to address access and quality of HC, plus deficiencies relating to disability, MH and dental health. Although a large DOC, other systems could start to face similar problems. Prisoners’ health worse than FW population, and prison population ageing, more people with CCs. 17% of deaths in 2007 deemed preventable/possibly preventable (poor clinician management, delays in access to care/medication). Deficits in FW HC too, which has led to greater interest in PM generally. Receiver put forward turnaround plan of action to improve quality of HC. Clinical Operations Branch formed by receiver to oversee quality. OIG also conducts audits to track compliance with court requirements.39– RCN published guidance for nursing care in the Criminal Justice System (CJS)in 2009 outlining need for focus on CCs. Potential of prison as opportunity to provide services to ‘hard-to-reach’ people with diabetes. RCN identified care and management of diabetes as an issue that needed addressing.31 – Many jails don’t have access to electronic health-record systems or sometimes even the internet. National Commission On Correctional Health Care (NCCHC) is developing CHORDS for uniform approach to quality and BMing and disease surveillance. Belief that having the data set will in itself acclimate prisons to PM. CHORDS not resource-intensive or technology-dependent. BMing considered most effective way to use data to improve performance to allow for comparative analysis. Currently no national outcome data sets; IT able to support PM in CFs is costly. Authors suggest electronic health-record system improves efficiencies in medication administration and nursing, CC management, reduces duplication, supports research, and publicly available outcome data contribute to patient decision-making (in the community). 2002 Congress report recommended surveillance of infectious diseases, CCs and MH as well as use of national EB guidelines.43 |
– Prisoners have a right to equivalent care, but CF HC does not always meet these expectations. Quality of HC defined as ‘degree to which health services for individuals and populations increase the likelihood of desired health outcomes’. Patient safety (part of concept of quality) = avoidance of errors of commission or omission. Most of standards related to patient safety. Many CFs look at structure and process not quality of clinical care. Clinical PM should help evaluators focus on quality-improvement (Qim) opportunities.36 – Development of standards in correctional HC patchy. Providers challenged to provide quality care with limited resources. Demographics of prison population have changed with ageing population and longer sentences leading to rise in CCs; estimated that 85% of >50s have three or more CCs, 79% of ≥65-year-olds have a CC that causes decreased physical function.37 – Diabetes prevalence in CFs set to increase because of ageing population. Poor lifestyles/limited HC access before prison may mean people entering prison have undiagnosed diabetes. Impact of diabetes on correctional budgets – significant. Delayed diagnosis and treatment can lead to development of costly comorbid conditions. T2D screening of inmates recommended but not fully implemented, which risks litigation. Lack of standardisation and availability of different guidelines may mean practitioners unsure which to follow, and people may be excluded who could benefit. Objectives for care – primary (improving healthy behaviours in people at risk), secondary (enrolling in diabetic screening medical education), tertiary (improving glucose control, trying to reduce complications).45 – Act 41 passed by Vermont state in 2011 authorised study to improve quality of HC in Vermont DOC at less cost. Study suggested that alternative contracting model could achieve these aims. Didn’t specify model. DOC HC system viewed as provider network with standards commensurate with the community. PM in Vermont also influenced by emergence of ACO (network of providers delivering co-ordinated care), Act 48, State Innovation Grant and movement towards accountability based on performance. ACOs include finance measures and incentivised care. DOC looked to develop a system that means HC is EB, cost-effective, high-quality, co-ordinated. Data recording practices had to change so correctional data aligned with ‘big data’ collected in the community. DOC offered financial rewards to contractors if performed well on outcome measures.Interest in developing request for proposals (RFPs) with PMs integrated, focusing on particularities of correctional environment while reflecting community health reforms and priorities. References Estelle and Gamble case and violation of 8th amendment. Constitutional requirement relates to care access not health outcomes or equivalency of care (although this is part of DOC mandate). Those with access to high-quality treatment less likely to reoffend. Performance-based structure is needed to protect state from accusations of indifference.44 |
– Compliance is needed with local, state and federal laws. Equivalence of care. Notes differing priorities of correctional and medical staff. Person responsible for co-ordinating medical department should be aware of clinical standards, laws, health needs and staffing/budget issues.41 – Highest priority of ASCA is to develop PM system for CFs across all CF functions (not just health). Early report showed lack of standardisation of data collection and availability. Prisons used to have low accountability, being managed by individual wardens with the emphasis on maintaining the status quo. In late 60s/early 70s courts started to find prison care unconstitutional. Prison population expanded dramatically and status of prisons heightened, and there was a general move towards accountability in public sector; agencies expected to be efficient and open to scrutiny. PM one of techniques for ‘continuous assessment of internal capabilities’. PM from early 80s means that high and low performing CFs can be identified and ‘resources could be tied to performance’ BM ‘at the heart’ of PM and allows for comparison. Agencies have to liaise to set BMs. Sees PM as move from ‘operational management’ system to strategic decision-based management32 – Notes ‘several independent factors’ at play. Argues health needs of inmates not given attention until 1970s, then first standards published in 1976 by American Public Health Association. American Medical Association (AMA) then published standards. Then – impact of court findings of constitutional violations had 25 states under court order by early 1980s, accompanied by huge increase in prison population due to less judicial discretion on sentencing, including higher numbers of women and elderly. Increasing CCs, increasing costs, diminishing budgets. Managed HC model implemented in Texas in 1994 to deliver HC while reducing costs.40 |
| Study design | – QI selection with consultation.33 – Implementation of chart audit.42 – Development of MH PMs.34 – QI selection with expert consensus.35 |
– Review of PM in 6 correctional systems38 – Qualitative interview study of California DOC staff + document review + site visits39 – Audit (survey) of all UK prisons and detention centres31 – Pilot study of CHORDS with several leading correctional systems focusing on care for diabetes43 |
– Collation of PMs for external review of quality36 – Dissertation: literature review and qualitative interviews with nurses37 – Dissertation: literature review and retrospective review of health records of 50 inmates to describe number and frequency of T2D major risk factors in inmates with T2D and expert consultation to select guideline to address T2D risk45 |
–Not a study but a recommendation for how to assess medical care in CFs, which conditions, and how frequently.41 –Collaboration between ASCA members to BM performance.32 –Not a study as such; this is a report on a HC delivery model in Texas prisons which provides some data on prevalence and outcomes.40 |
| – Creation of performance metrics for the DOC. Describes policy environment in which RFPs aligned with reforms developed. Nearly 200 key informant interviews fed into definition of professional standards.44 | ||||
| Funder | – Missouri DOC.33 – Not stated.34,42 – CDCR.35 |
– CDCR.38,39 – RCN Diabetes Nursing Forum and Prison Nurses Forum.31 – NCCHC.43 |
– Not stated.36,37,44,45 | – Not stated.41 – Correctional Program Office, Bureau of Justice Statistics and National Institute of Justice.32 – HC delivery system based on contracts between Correctional Managed Health Care Committee, Texas Department of Criminal Justice and two medical schools.40 |
| Aim | – To develop comprehensive model of performance evaluation; matrix of QIs to demonstrate performance against benchmarked QIs in community; recommend processes to improve management and treatment.33 – Examine challenges to CC management of asthma, diabetes and hypertension; research tools to reduce variability; introduction of chart audit tool; data generated and 6m post-implementation review.42– To develop set of performance measures for MH care through consensus process.34 – To ask national experts to review existing FW and CF QIs.35 |
– To review QI sets used in CFs.38 – Assessment of California DOC clinical quality-management approaches.39 – To determine expertise and knowledge of clinicians to help identify level of diabetes service; to identify strengths and limitations of care management strategies.31– To establish standard PMs; balance the current emphasis on policy and court compliance with patient outcome data; standardise performance expectations; support implementation of primary care and Qim in CFs; contribute to public health and health services research; support correctional health care’s involvement with national reform efforts.43 |
– Focus on PM of HC that has greatest potential to improve patient safety. Aim not stated explicitly but is to provide set of QIs that can be used in correctional HC.36 – To create a roadmap to improve quality of care for Oregon’s DOC, looking particularly at 9 CCs: asthma/respiratory, diabetes, HIV/AIDS, hypertension/CVD, lipid disorders, seizure disorders, HCV/chronic hepatitis, hepatic cirrhosis, severe mental illness.37– To facilitate standardised T2D screening in a correctional system, to describe T2D risk factors in inmates diagnosed with T2D.45 – To design a performance-based contract for CF health service delivery.44 |
– To describe metrics that should be measured monthly and discussed in a meeting with correctional and medical staff.41 – To design empirical outcome-oriented measures (across CF functions, not just health) that can be uniformly applied, so specifying numerator/denominator. To identify 8 measures, specify 4, choose QIs for 4, set rules for measuring QIs to enable comparison across institutions.32– To explore changes in health outcomes since managed HC model implemented.40 |
| Question(s) | – Can community QIs be used in CFs? Which QIs describe CF HC services? Can the QIs be used to systematically assess quality of HC for offenders?33 – Can use of chart audit minimise variability in care for patients with one or more chronic diseases (asthma, diabetes, hypertension)?42– Not explicitly stated, but seems to be largely about the method and whether consensus could be reached on PMs for MH.34 – Not explicitly stated; would be about whether a list of valid and feasible QIs could be created through an expert consultation process.35 |
– What PMs are being used by CFs? What dimensions/domains are the focus, and where do gaps exist? What are the barriers and facilitators to PM?38 – What quality of care measures are already being used in California DOC?What are the areas of greatest need/gaps that should inform selection of QIs given resource constraints? What barriers or facilitators affect ability to construct QIs?39 – Not explicitly formulated as a question; would be: what is the current status of diabetes care and management in UK jails and detention centres?31 – Not explicitly stated.43 |
– Not explicitly stated.36 – How did Oregon DOC measure HC outcomes? How did QIs compare to Damberg et al.’s (2011) work?37 – What’s the number and frequency of T2D risk factors in adult male inmates diagnosed with T2D? Which screening guideline best targets these risk factors?45 |
– N/a.41 – Not stated.32,40 |
| Site/setting | – Missouri DOC.33 – Somerset County Jail, New Jersey (high turnover; average stay 8 days but up to 2 years).42 – 1-day meeting at John Jay College.34 – 1 day meeting at RAND corporation.35 |
– Study conducted for the California DOC and Rehabilitation. Purposive sample: 6 of the 51 correctional systems in the USA: Bureau of Prisons (BoP), Missouri, New York, Ohio, Texas and Washington DOCs, selected because of being large systems which have active PM programmes.38 | – N/a.36 – Oregon DOC.37 – One CF, doesn’t appear to be named. Research conducted for University of Connecticut.45 – Vermont DOC (8 CFs).44 |
– Not stated. The paper offers general advice to all CFs.41 – ASCA members.32 – Texas Department of Criminal Justice.40 |
| – California DOC (33 jails).39 – All UK prisons and detention centres.31 – ‘Several’ prison systems – number/identity not specified.43 |
||||
| Methodology | Reviewed existing QIs. BM data collected to compare to other HC orgs. Compared CF/community demographic and cause of death data.33– Constructed pen and paper chart audit tool in collaboration with internal medical colleagues using NCCHC standards.42 – Roundtable discussion regarding the creation of MH PMs for CFs based on nationally accepted standards (n = 29). 17 for-profit HC providers, 6 psychiatrists, 1 psychologist (+research team?). Discussion over a day, consensus reached on ‘nearly every’ PM.34– RAND corporation collated and surveyed QIs from prisons/FW for review/recommendation by prison and quality-measurement experts using modified Delphi method. Content reviewers assessed and eliminated QIs |
– MEDLINE and Google search for published articles on PM in CFs. Key informant interviews (telephone) and documentary reviews of 6 systems.38– Reviews of 45 documents (Google search plus acquisition from receiver’s office); 20 interviews (administrative staff from HQ, and admin and clinical staff from prisons); site visits in 4 prisons (3 because of focus on Qim, 1 women’s). Snowball sampling. Respondents asked to consider strengths and weaknesses of current system, how quality was measured, barriers and facilitators to quality, gaps and current initiatives. Thematic analysis on interviews and visits performed by three researchers and discussed with other researchers and receiver staff. Data from documents extracted to a template.39 | – Selection of QIs by author, based on standards and his experience as external reviewer; notes that some PMs are based unreliably on ‘wisdom and experience’.36– Literature review and qualitative interviews with 8 nurses (convenience sample). Literature review, health-record review of 50 inmates with T2D diagnosed in incarceration; expert consultation to select guideline.45 – Three-phase analysis of HC provider models according to 8 variables: continuity of care, care planning, staffing, capacity for data sharing, procedures for prior approval, quality assurance and utilisation management, data collection and metrics, governance, finance.200 interviews with executives and other key informants on how care |
– N/a, not a research paper.41 – ASCA members collaborated to BM prison performance. Reviewed PM models and selected 8 performance domains, one of which was ‘health’ and one ‘substance abuse and MH’. The others were not health related. Offender profile and costs were also included as contextual measures. Selected public safety, institutional safety, substance abuse and MH and offender profile as ones to specify.32– Operational performance evaluation system used to monitor > 100 clinical performance and outcomes for 8 conditions including access to care, clinician intervention, disease monitoring, preventative care, chart documentation and patient outcomes. Retrospective analysis of management for 6 diseases: asthma, coronary artery disease, type |
| prior to expert panel meeting. 97 went to panel. 14 reinstated from longlist; 111 reviewed by panel in numerator/denominator format. Panellists rated on 1–9 scale for validity and feasibility before and during meeting. ≥ 7 median score for validity was threshold, and ≥ 4 for feasibility (difficult for panel members to assess future data environment). 79 QIs put forward by panel.35 | – Questionnaire developed by RCN Diabetes Nursing Forum, based on RCN Qim Hub (a web-based data-management system) and piloted with unknown number of members of the Forum and prison service representatives. 19 responded (16 male prisons).31– Pilot study using correctional institutions. Short-stay measures used. Patients whose data are included must not be incarcerated 45 days prior to study period as QIs do not include filter for new patients. Data submitted using excel spreadsheets to central site where they would be organised and a confidential report generated with BM data on similar facilities.43 | planning, continuity of care, staffing etc. managed. Align QA with HEDIS (used in the community), but adapt for correctional environment.44 | 1 diabetes, hypertension, hyperlipidaemia and seizure disorders.40 | |
| Results | – Inpatient beds: half of the responding prisons had inpatient beds; it was unclear how other prisons would manage diabetes crises. All but one prison had a register of people with diabetes. 14/19 reported screening for diabetes using HbA1c, urinalysis, weight and blood pressure. 14 prisons had lead person for diabetes care, 12 had written guidelines/policies. 11 prisons referred to local and DoH guidelines.Findings showed that type 1 diabetes relatively uncommon in the prison environment. 12 had specific diabetes clinics, but less than two-thirds of the prisons surveyed identified specific diabetes care as being important. 8/12 had attending specialist nurse. GPs and podiatrists also involved in care but diabetes consultant and dietician were less frequent visitors. Only seven | – Key issues from literature review: legal obligation to provide HC; ethical considerations re conducting research with prison inmates; increasing prevalence of CCs; limited knowledge of QIs. Barriers to measuring quality of HC outcomes: pressure to address acute issues may distract from attention to CCs; staff retention; insufficient staff education that is timely; lack of managerial encouragement; lack of electronic health record means too much time spent looking for charts.37 | – N/a.32,41 – Considerable improvement in mean level of compliance with indicators for all 6 conditions. Mean glucose level decreased for T1DM patients, mean lipoprotein level decreased, blood pressure improved in people with hypertension. Rates of HIV- and asthma-related deaths declined. Costs also reduced by $215 million in first 6 years.40 |
|
| institutions had been visited by mobile eye screening even though the standard is for everyone with diabetes to be offered an annual check.Regular treatment reviews (3- or 6-monthly) took place in 89% of responding institutions, the other two did annual reviews. Prisoners were seen annually by podiatrists in 13 prisons, and as | – Mean age at time of T2D diagnosis 45.64 years; mean BMI prior to diagnosis 30.54. Four most common risk factors – BMI ≥ 25, belonging to high-risk ethnic group, age ≥ 45, history of hypertension. Incidence of T2D diagnosed during incarceration could be significant.45 – List of 53 metrics appended.44 |
|||
| necessary in the other prisons. All had dietary regimens agreed within 7 days, and 17/19 reported that prisoners with diabetes were able to access food outside meal times, including glucose tablets or biscuits to avoid hypoglycaemia. | ||||
| All but one of the prisons reported that diabetic prisoners were encouraged to self-manage. The results for blood glucose monitoring were not fully in line with national recommendations. In addition, there was no standard approach to managing at-risk patients. Only 5 institutions offered education to prison staff and only 1 had been trained in dealing with a hypoglycaemic event. Diabetes education on diet, education and monitoring was offered to prisoners in 12 prisons.31 | ||||
| Link to community QIs | – Community QIs modified for CFs.33 – Notes that NCCHC guidelines based on clinical guidelines from national organisations e.g. American Diabetes Association.42 – Not stated.34 – Notes that prisons frequently adapt FW QIs. Both FW and CF sources used for QIs.35 |
– Found prisons were using FW QIs and home-grown measures, generally strove for equivalency of care; one uses FW BM data. One system queried the external validity of FW QIs.38 – Interviewees noted challenge in applying FW measures to CFs, e.g. lack of phone access, need to arrange escorts for prisoners.39 |
– Meaningful outcome measurement difficult in small populations, and there are high-risk situations unique to CFs, e.g. hunger strikes, suicide risk assessment, timely urgent care. Expected performance – 90%, 100% on some, e.g. continuity of ARV, follow-up on consultant recommendations.36 | –Not stated.32,40,41 |
| – N/a.31 – CHORDS data set modelled after HEDIS, a PM system in the community. Standard HC measures in the community typically anticipate longer periods of care, so short-stay measures used.43 |
– Aligns QA with HEDIS. COCHS developed a performance-based incentive calculator using threshold and BM to calculate incentive. Author notes that quality standards had more rigorous thresholds and BMs.44 | |||
| Criteria for QI inclusion | – Represent CF population; address HC problems amenable to change; EB; relevant to org Qim; relevant to health policy; measurable; multilevel data available; balanced and coherent set.33 – N/a42 – ‘Meaningful’ PMs that are quantitative so can be tracked over time, clearly defined so feasible to extract reliable data, based on nationally accepted standards.34– Had to have been tested/deployed in existing HC system. Used 4 criteria of relevance to prison population, scientific soundness, implementable and interpretable. Focus on primary care as specialist care not usually under jurisdiction of CFs.35 |
– Particular interest in ‘explicit’ QIs, defined as: implementable in standardised reproducible way. Well defined numerator/denominator and definitions for components, e.g. time frames, diagnostic codes. Focus on processes and outcomes substantiated by evidence.Implicit measures, e.g. death, reviews involve subjective judgements. Draws distinction between explicit QIs and guidelines, prevalence measures, policies and standards which do not provide means of assessing outcomes of HC delivery. One system noted measures have to be amenable to change, EB, available/reliable data sources, appropriate periodicity.38 | – 30 areas of correctional health where risk of most serious harm to inmates. Measures that can be used to assess performance quantitatively, by CF, and allows comparative analysis of aggregated data. Focus on quality and timeliness.36 – Major risk factors named in one or more guidelines, routinely documented and retrievable by the researcher.45 |
– Not stated. The author has described a range of measurements which are largely counts of service uptake, e.g. number of MH encounters, number of hospitalisations.41 – Manageable – opted for small number of indicators, and ones that are a priority for correctional staff.32– Not discussed in detail, but they included indicators relating to access of care, clinician intervention, disease monitoring and prevention, chart documentation and health outcomes.40 |
| – N/a.31 – From national guidelines (NQF). Short-stay measures (continuous incarceration for 120 days); longer-term measures adapted from community (e.g. 365 days) may not be appropriate for CFs.43 |
||||
| QI sources | – National Committee For Quality Assurance (ACA) Healthy People 2010 NCCHC and ACA standards.33 – NCCHC and ‘other national sources’ such as American Diabetes Association.42– NCCHC publication Standards for Health Services offer guidance for structural and policy facets but not detailed clinical guidance on treatment and management; NCCHC used expert panels to adapt clinical guidelines – one exists for schizophrenia.34 – 29 sources – USA, UK and Canada. CF and FW, some disease-specific.35 |
–Documentary analysis of 6 correctional systems; key informant interviews.38 – Author made judgements about the quality of the service on the basis of adherence to national standards including NICE guidelines, and NSF.31– Federal agency for healthcare research and quality, National Committee for QualityAssurance, National Quality Forum.43 |
– Cites a range of sources, including UN, WHO, World Medical Association, NCCHC, American Psychiatric Association (APA), ACA, American Public Health Association.36– Guidelines: diabetes management in correctional institutions, NCCHC diabetes guideline, Federal Bureau of Prisons guideline – all recommend screening high risk but vary on major risk factors.45 | – Cites NCCHC, ACA and ANA.41 Cite performance indicator models: Logan’s PMs, BoP staff management, Council of Juvenile Correctional Administrators’ PMs, Florida DOC, Powell’s PMs, North Carolina PMs, ASCA issue areas/information categories.32– AMA, NCCHC, accredited by Joint Commission on Accreditation of Healthcare Organisations (JCAHO).42 |
| Who reviewed and no. of indicators | – Research team (2 university; 1 DOC) generated 150 indicators; consulted with administrators and physicians (number unstated) to reduce number of QIs to 50; further reduced to those with BM data from comparable population (n = 32). QIs in numerator/denominator format appended.33 – N/a42 – For-profit HC providers, 6 psychiatrists, 1 psychologist, research team. 4 core PMs for medication adherence, with a further 16 for monitoring side effects and toxicity; 4 for suicide prevention, 2 for treatment planning, and 3 for sleep medication. Some PMs had subsections.34 |
– Research team reviewed PMs. Numbers of QIs not given, but broad spectrum of health conditions covered including screening, prevention and access. Variation regarding how systems addressed CC (not specified).38 – Not specified; probably NCCHC.43 |
– Author created list of ~140 PMs and appended to article.36 – Medical directors of correctional system and contracted HC provider; community-based diabetes educator with expertise in treating inmates.45 – Not entirely clear – members of COCHS and Vermont DOC.44 |
– The author has outlined the measures that she thinks should be reviewed every month.41 – Author + subcommittee members + practitioner and academic advisory group. Members and expertise not specified. Decision made to ‘start small’ in order to achieve success, with plan to add other QIs later. Health-related QIs were: ADR of inmates receiving substance abuse treatment and ADR of inmates receiving MH treatment.32 – Appears that they used the standards accredited for.40 |
| –1731 initial number following review of public sources of QIs in 16 topic areas. First screen to remove vague QIs reduced number to 1069. Ninety-seven QIs submitted for panel review after content review.35 | ||||
| Modifications to QIs | – Several had age adjusted to mirror offender population.33 – N/a42 – Detail not given – topics were discussed and published guidelines looked at during the meeting.34 – Notes that FW access and structural QIs are difficult to translate to prison population.35 |
– Different systems utilised different time periods for standards, possibly due to lack of consensus on appropriate time frame or taking into account real-world challenges.38 – Shorter time periods, e.g. 120 days compared to 365 days.43 |
– No evidence of QI modification.41 – Noted that QIs should be presented as rates per 1000 to allow for comparisons across larger/smaller CFs.32 – Not stated.40 |
|
| Reasons for elimination of QIs | – Intensive data collection/too time consuming; inconsistent/unavailable data; required judgement (i.e. introducing subjectivity); lack of availability of BM data (although some QIs were retained without BM if seen to be particularly relevant).33 – N/a34,42 – Too vague, insufficient detail. Content reviewers assessed for importance, scientific soundness, implementability and interpretability. Particular focus – relevance to prison population and good evidence base.35 |
– Structure and process issues relating to a range of areas including sanitation, nutrition, CC guidelines, restraints, policies etc.36 –Female-specific risk factors for diabetes. Risk factors not retrievable by researcher. Panel rejected BoP guideline because targeted screening was low risk; only 8% of people with T2D would have been screened. Using American diabetes guideline, 84% would have been screened. NCCHC criteria – 98% would have been screened.45 |
–Elimination of QIs not discussed.41 – Opted to select key priority areas, recognising that to be successful.32 – Not stated.40 |
|
| QI taxonomy employed | – Clinical outcomes, clinical processes, function/QoL, patient satisfaction; seven HC areas: acute, subacute, ambulatory, behavioural, nursing, rehab, hospice care. Not all 7 were included in final matrix. Final 32 indicators covered 11 health categories: women’s health, heart disease, infectious disease, pulmonary disease, wellness, prevention, asthma, diabetes, medication administration, screening, behavioural health.33 | – Explicit numerator/denominator QIs vs. implicit review QIs; QIs relating to policies, standards, prevalence and guidelines acknowledged but not part of the review. Found correctional systems had mix of explicit QIs, prevalence measures and standards. Found nearly all systems had facilities accredited by NCCHC and ACA, which have standards, prevalence measures and process measures but not outcome measures. | – Uses notion of structure–process–quality of clinical care; argues structure and process important for evaluation but do not provide comprehensive picture.36 | – No taxonomy employed. QIs are HC process-oriented, apart from an additional set including grievances, policies and procedures, staff education.41 – Not enough detail given.32 – Used access to care, clinician intervention, disease monitoring and prevention, chart documentation and health outcomes.40 |
| – N/a42 – PMs developed in four domains: medication adherence, suicide prevention, MH treatment planning, sleep medication usage.34 – 16 topics chosen following review of CF morbidity and mortality and qualitative interviews. 4 QI types: access to care; structure; process and outcome. Process indicators further divided into screening, diagnosis, treatment, follow-up.35 |
Completeness of documentation was a QI in one system. Few prison systems took account of patient experience; only 2 of 6 had done surveys, only one of these perceived it to be useful. Doubts cast on utility of subjective information. All conduct death reviews; no standard definition of preventability.38 – Structure, process, outcome. Explicit/implicit. Authors focused on explicit replicable measures. Counts (e.g. of deaths, suicides) and policies/standards of care used more than explicit indicators. Death reviews have led to Qim.39 |
|||
| Data sources/systems | – Electronic medical record system and custodial info system; patient satisfaction survey designed and implemented (9 questions with 5-point Likert plus free-text)33 – Hand-written charts for individual patients. Summary data produced 6 months post implementation on each of three CCs give an overview of prevalence, treatment and comorbidities.42 – N/a – PMs not implemented.34 – Project staff collated information on potential data sources for the QIs that were put forward by the panel, e.g. medical, laboratory, pharmacy, grievance rates. Notes FW data sources more well-developed than CFs.35 |
– Different systems at various stages in PM, with differing functionality of data systems. System-wide electronic data most useful for population-based audits.38 – Data collected using Excel spreadsheet and submitted to central site.43 |
– Notes that calculation of overall score on the QIs should not be aggregated as poor performance on any single one creates risk.36 – Prison healthcare records of 50 inmates.45 |
– Author does not refer to data infrastructure, just notes that capturing data monthly will allow for analysis of trends.41 – Adjusted data for number of prisoners, and chose a particular date (30 June) as proxy for average daily population.32 – UTMB houses prison hospital with telehealth and electronic medical record system accessible by prisons and the hub site.40 |
| Assumptions | – Using community BMs suggest CFs can be held to same standards. That QI implementation results in better care, especially in correctional setting. That patient satisfaction survey the best way to elicit patient views of quality.33 –That chart audit encourages staff to think systematically and at a population rather than an individual-patient level.42 |
– That correctional systems of a similar size will be the most useful, which has some weight; however smaller systems may also have made useful contributions.38 – Staff assume patients may have unrealistic expectations or are exasperated (study participants not authors).39– That standardised protocols are most beneficial.31 |
– Unclear on origin of 90% as good BM, could be arbitrary.36 – That nurses were best placed to answer questions on HC quality measurement.37–That standardising by choosing one guideline can reduce risk of inappropriate screening; that standardised screening leads to reduction in costs.45 |
|
| – That clinician view has primacy; no weight given to patient perspective in any of the PMs.34 – Stated evidence that PM creates better care but evidence not critiqued. Should QIs be ‘real-world’ or not?35 |
– That presence of data set in itself would encourage prisons to focus on PM. No information given on implementation of system; perhaps assumptions that it would be straightforward?43 |
– That incentivising performance will lead to an improvement. That it’s feasible to raise thresholds every year over years 1–3.44 | ||
| Challenges and constraints | – CFs not able to engage in Qim because lack of quality models, established QIs and BMs. Lack of BM data to create standards; lack of standardised data entry; lack of standardised query language; manual chart review required.33 – Overworked nursing staff, rapid turnover so need CC assessment at intake; high levels of non-insurance so CCs may not be identified or treated in the community. Medical staff failing to seek/record information on intake leads to inability to recognise change in CC; baseline measurements needed. Pharmacists raised concerns about costs, nursing staff under-resourced in terms of time; only some nurses fully compliant with chart completion; some physicians defensive. Chart audits can improve quality of care, but need consistent completion; a tool not fully implemented may increase institution’s vulnerability.42 |
– Functionality of data system. May take some time to achieve data capture. Absence of comparable data from prison systems – prison-specific BMs could be helpful. Data may be inconsistently input into system. Data systems without built-in reporting capabilities require programmers to write specific queries. If data system not linked across facilities, it could be difficult to populate some measures. Free-text language could be unstandardised. Competing priorities for resources. System has to allow for evolution of PM; measures may be dropped when standards successfully met or medical evidence changes.38 | – Many CFs don’t address quality of clinical care and focus on structural/processual issues instead.36 – Notes lack of universal agreement on disease management for CCs leading to inconsistent application of standards, lack of standardised measure to deliver HC ethically, implementation of HC model that meets legal requirements. Lack of electronic health records.37 – Limitations of data system meant data for some risk factors (e.g. lifestyle, first-degree relative with diabetes) could not be extracted.45 |
– The differing priorities between CF staff and medical staff.41 – Difficult to standardise across CFs because of varying missions, legal structures, and organisational arrangements – describes cross-CF measuring as ‘highly complex’. Notes Florida DOC, BOP and Minnesota DOC took 10 years to develop a PM system with integral data system.32 – No single HC delivery system is optional in all correctional settings. Challenges include huge growth in prison population, legal mandate to improve care, financial limitations.40 |
| – Challenge to achieve compliance to any measures established: recruitment/retention of staff, implementation of quality-management programmes, creation of adequate IT systems, funding, the relationship between correctional staff and HC providers.34– CF resource constraints mean need structured process to prioritise QIs. Panel felt explicit quantitative measures needed to be balanced by implicit measures that are more subjective, e.g. death reviews and peer reviews. Panel concerned that data systems would not be adequate for rigorous PM. | – Data system needed to enable more co-ordinated and efficient care, integrated with a pharmacy management system. Significant amount of data generated for legal requirements but not helpful for Qim. Data stop being collected when standard met consistently. Lack of feedback loop to HC providers. OIG audits rely on too small a number of cases to be deemed useful. Data also collected for disciplinary purposes. Gaps in the following areas: infectious disease, MH, CC and preventive screening/assessment at reception centres. | – Data system inadequate to collect, track and report data. DOC had to develop workarounds to track data. Large volumes of data may be collected but may not be relatable to QA activities. Financial incentives needed as motivation. HC services in CFs traditionally have little connection to HC systems in community; two systems need to have a bidirectional interface for results-based accountability.44 | ||
| Manual chart reviews would also be needed. Also noted important gaps in QIs, e.g. for methicillin-resistant Staphylococcus aureus. Number of QIs could be too many. PM system needed to be implemented with Qim initiative so deficits revealed could be addressed.35 | Requests for care need to be triaged to avoid under- or over-utilisation. Minimal measurement/assessment of patient perspective – grievance tracking is most systematic means. Efforts to survey patients can focus on satisfaction rather than experience. Lack of disease registry across California DOC is difficult; difficult to identify numerator/denominator populations. Volume overload of court requirements threatens measurement – ‘too many metrics … for too many different purposes’. Lack of accessible pharmacy data hampers PM. Diagnostic codes aren’t tracked systematically, medical charts may be inconsistently completed or misplaced. Staff would need education on QIs and Qim.39 – Lack of a consistent approach to staff training impacts quality of diabetes care.31 |
|||
| – Barriers to implementing electronic health records include data security and patient confidentiality, plus competing for limited resources. IT able to support PM in CFs is costly, and implementation time-consuming. Practitioners have to alter the way they practise and ensure data entry is consistent. ‘Daunting and unfamiliar territory’ for prisons to integrate IT and to use community health information exchanges.43 | ||||
| Power dynamics | – Research team appear to control process. Consultation process with others not explicated in any detail. No evidence of PPI. Evidence of patient satisfaction survey though results due to be published elsewhere (article not found).33 – Lead author is CF’s medical director; he seems to have instigated and implemented this initiative. Chart audit done in collaboration with other internal staff. No evidence of any external consultation processes. Two-thirds of audits not completed on intake despite being mandated, because of pressures in correctional setting or temporary staff.42 – Not clear what the relationship would have been between the for-profit HC providers and others. No PPI involvement.34– Nominating committee of prominent CF personnel identified 9 panel members with broad-ranging expertise and experience in CFs or PM. Process measures proliferate because of accountability channels for HC providers, but outcome measures are more important to patients. No PPI involvement in consultation. Notes that most QIs are ones which are used in monitoring CF court cases.35 |
– Court cases, though punitive, have often served as an impetus to increase resources.38 –Data collected to comply with court requirements, by OIG as part of regular audit and for disciplinary purposes. More local control wanted in death reviews although HQ need to be involved. Qim efforts improved under receiver’s leadership.39 – CHORDS is a commercial product/service that CFs would pay for, but the suggestion is that it would shift the focus of data collection from court/legal requirements to improving outcomes and quality of care.43 |
– Author had selected PMs; no evidence of consultation processes.36 | – Author seems to have selected PMs, no evidence of consultation processes.41 – Agency executives form performance partnerships to choose QIs/outcomes, allows for comparison across organisations. Suggests that corrections setting the agenda about what’s important wrest power away from the media, who can misinterpret comparisons, and politicians (and maybe legal system?)32 |
| Flow charts/processes | – QIs identify best processes and outcomes and create standards for orgs to meet/exceed. Orgs can set BMs from QIs.33 –Chart audits devised from standards and seen as a mechanism through which to implement guidelines to minimise variability in HC. Clinical practice guidelines provide summary of treatment/disease management, clinical pathways structure decision-making process, PMs provide method to assess outcomes.42 – Not stated.34 |
– Standards and BMs arise from interviews with key informants. Financial incentives given on basis of performance calculations. Standard increased by 5% each year over years 1–3.44 | – Agency executives collaborate to identify outcomes, select desirable outcomes, choose QIs, develop data collection procedures.32 | |
| Conclusions/recommendations/areas for future study or work | – External validity of community HC standards not established, few BMs available; establish consistent education protocols and data documentation practices.33 – Chart audits facilitate avoidance of sentinel events by alerting medical director to needs and care required to meet standards, and educational needs of staff. Future work includes planning ways to improve compliance and consider how to use chart audit to save money by reviewing specific medication usage.42 – Notes that system needs to be changed to shift the focus from cost to quality; correctional stakeholders need more power to require adherence to standards.34– Process measures dominate because of control and accountability for HC providers, but outcome measures are of more concern to patients. Data |
– Recommends further adoption of explicit QIs that address highest-priority health concerns.38 – Need for explicit QIs that are not vague, and that are based on latest medical evidence. Data system has to be adequate, and data inputted consistently with diagnostic codes. Data systems need to be linked together to include pharmacy. Important for metrics to be embedded in the data system. Need regular review of the number of metrics so don’t reach overload, and feedback loop needs to be in place for data to reach frontline staff.39– Policies and procedures should be in place for screening, management and care of people with diabetes. There should be a diabetes register and a standardised approach to screening. Reviews should be equivalent to diabetes care in the community. Glucose monitoring should be individualised not |
– Recommends sampling 10–12 records, and increasing the sample size to 20 or 25 if problems are identified. Recommended measures are for external review; author suggests PM should also be internally assessed.36 – Larger sample size, greater number of CFFs. Exploration of factors that may be specific to correctional population. Use of electronic health-record system linked to pharmacy records would be helpful, plus guidelines on monitoring people just below levels for screening.45– Data management system facilitates communication between corrections and other HC providers; high level of commitment from legislature, governors’ office and state agencies crucial to drive through reforms to CF HC; community HC providers have a role in serving offenders; performance-based contracting structures can improve health and reduce costs.44 |
– Recommends that monthly meetings enable timely review of measures to identify trends, problems and solutions.41 – Exact definitions and counting rules needed for uniform approach across prisons. Review of data-collecting practices ‘imperative’ to ensure validity and reliability. 5 remaining tasks: create data platform for data to be entered; develop PM capacity in prisons; assess fidelity to counting rules; devise analytic methods to take into account population differences among systems; develop new standards and QIs.Suggests a danger is that the focus will be on data production rather than moving to a PM culture. Capacity development needed to shift from rule-based to results-based system, requires organisational transformation. Argues that health records ‘must evolve into PM databases’. Staff training needed |
| systems need to be able to produce PM data. Authors recommend phased approach to implementation. Gaps in health conditions need to be addressed and way to update QIs needs to be incorporated as medical evidence changes standards/recommendations for care.35 | standardised. Roles and responsibilities should be clarified, and staff training and prisoner education reviewed. Teamwork needed between HC staff and prison staff.31– Anticipate that CHORDS will establish national outcome-oriented data set, will encourage correctional systems to adopt IT.43 | to use and analyse PM data. When agency can produce PM data internally, should be able to join a national PM system. Researchers able to use sophisticated analyses will be needed to ensure cross-system analyses are appropriate.32– Concludes by challenging suggestions that managed care model can’t be applied to CFs, stating that success involves use of standard guidelines, education programmes, common formulary, CC clinics, electronic medical records and telemedicine.40 | ||
| Critique | – Doesn’t cite evidence to show that implementation of QIs does improve performance. Consultation method is opaque; it’s not clear how many people were involved or why they were selected. No evidence of PPI involvement. Patient satisfaction results don’t appear to have been published elsewhere. Knowledge of other similar work appears limited. No attention paid to health inequalities; i.e. should screening BMs be different for people where ethnicity is associated with greater risk?33 | – Would have been useful to include poorly performing prisons in site visits. Document searches limited to Google.39 Limited sample; potentially only the prisons more confident in their approach to diabetes care/management responded. Results ambiguous or lacking detail in places, it’s not clear how the questionnaire was developed and how well it was tested.31– Some evidence presented about effectiveness of IT and improvements to outcomes, but still sketchy. |
– Recommends refining toolkit for individual CFs, but then it would be difficult to standardise and BM against other organisations. No justification given for the 90% BM, or for the sample size of records. PMs not ‘explicit’; no numerator/denominator given.36 – Researcher had pre-existing relationship with the DOC which may have influenced data collection and interpretation of findings. Descriptive analysis.37 |
– Type of indicators seems largely limited to process, with some relating more to organisation rather than patient care. There do not appear to be any outcome indicators. The author appears to have selected indicators without consultation, and the number and range of indicators are limited. No PPI, clinician or quality-measurement specialist included in selection process.41 |
| –Provides information at an individual level rather than population level. No evidence of consultation about using this approach. Cites one other similar use of chart audit approach. Vague on other sources of care standards. Review process sounds labour-intensive, which may have impeded uptake. Authors pay some attention to health inequalities. Note two-thirds of audits not completed on intake, then state that two-thirds are completed.42 | There are a number of unknowns in this paper – what the QIs are (only a few are given, and not in numerator/denominator format), who is inputting data into the spreadsheet, how that will be implemented and managed, and therefore how reliable those data are, how scalable it is to use numerous QIs for different conditions.43 | – Small sample size (n = 50) to base decisions regarding guideline selection on? Drawn from one system, may be difficult to generalise/extrapolate to other areas. Reliant on data-recording accuracy. First 50 records selected – didn’t appear to be randomisation processes – sampling bias. Only 3 people on expert panel. No mention of severe mental illness (SMI) or antipsychotic medication, which is a risk factor for T2D.45 | ||
| – Again there is no evidence of any PPI involvement in the process. Although they stated that they wanted quantitative measures that could be tracked over time, and therefore implied objectivity and standardisation, some of the ‘measures’ are written more as standards that could not easily be operationalised in the way suggested. For example, staff should be trained to deal with suicidal individuals, with no mention of the extent of the training and skillset targeted. The PMs are not presented in numerator/denominator format. Not clear what the next step would be now PMs developed.34 | – Process of feeding data from ~200 interviews into the 53 appended performance metrics lacks transparency. Very little information given on participants and their areas of expertise. Helpful insights into influences of overlapping spheres of law, policy and reform.44 | |||
| – Used only US/UK and Canadian QI sources – no reason given for international approach only reaching as far as UK and Canada. Mentions that each QI represents minimum not optimal standard of care, but no BM data given in the QI examples. Patient perspective only given briefest of mentions in conclusion – seems an afterthought. Again next steps not clear – not sure how this work will be disseminated and utilised by CFs. Gaps in areas not covered by QIs are not fully articulated.35 |
Appendix 3
| Source and year (in chronological order) | Design/source type and setting | Process reported | Key findings |
|---|---|---|---|
| Raimer and Stobo, 2004. Health care delivery in the Texas prison system: the role of academic medicine. Journal of the American Medical Association.40 | Report Texas, USA |
Implementation of managed care programme | -Improved care for six CCs and health outcomes (e.g. blood glucose in diabetes, low-density lipoprotein levels in hyperlipidaemia) -Includes list |
| Wright, 2005. Designing a national performance measurement system. The Prison Journal.32 | Consensus process USA |
Development of correctional measures | -Identified eight domains as priorities, including ‘health’, ‘substance abuse and mental health’ -Includes list |
| Stone et al., 2006. Health care quality in prisons: a comprehensive matrix for evaluation. Journal of Correctional Health Care.33 | Selection by team Missouri Department of Corrections, USA |
Development of a quality indicator matrix | -Identified 32 quality indicators across 11 health domains, including women’s health, infectious disease, long-term conditions -Includes list |
| Kountz and Orsetti, 2007. Reducing variability in chronic disease management: utility of chart audit tools with medical director oversight. Journal of Correctional Health Care.42 | Clinical performance review USA |
Development and implementation of a chart audit tool | -Chart audit tool enabled risk stratification of prisoners and identification of required follow-ups, reducing the risk of sentinel events |
| Hoge et al., 2009. Mental health performance measurement in corrections. International Journal of Offender Therapy and Comparative Criminology.34 | Consensus panel USA |
Development of MH performance measures | -Identified four key areas as priorities: medication adherence, suicide prevention, MH treatment planning and sleep medication usage -Recommended standards-based performance measures for each -Includes list |
| Asch et al., 2011. Selecting performance indicators for prison health care. Journal of Correctional Health Care.35 | Modified Delphi USA |
Development of quality indicators |
-Retained 79 quality indicators for, e.g. medication monitoring, infectious disease, psychiatric disorders, substance use and metabolic diseases -Includes list |
| Damberg et al., 2011. A review of quality measures used by state and federal prisons. Journal of Correctional Health Care.38 | Review Six US correctional health systems |
Review of quality indicators | -Identified considerable variation in performance measurement portfolios and data system functionality -All systems included explicit quality indicators, prevalence measures and standards covering a range of health conditions |
| Teleki et al., 2011. The current state of quality of care measurement in the California Department of Corrections and Rehabilitation. Journal of Correctional Health Care.39 | Review California Department of Corrections, USA |
Review of approaches to performance measurement | -Identified gaps in measurement of, e.g. access, clinical quality, experience of care provision -Includes list |
| Booles, 2011. Survey on the quality of diabetes care in prison settings across the UK. Journal of Diabetes Nursing.31 | Survey Diabetes care in UK prisons |
Surveys implementation of guidelines | -Identified good-quality diabetes care, e.g. prompt follow-ups after admission -Found that dietary assessment, screening and hypoglycaemic-event management lacked standardisation |
| Bisset and Harrison, 2012. Health outcomes in corrections: health information technology and the correctional health outcome and resource data set. Community Oriented Correctional Health Services.43 | Pilot study USA |
Development and testing of national data set to monitor quality | -Identified potential for a national US data set with standardised quality indicators to enable BMing and facilities to assess and compare their performance -Includes list |
| Greifinger, 2012. Independent review of clinical health services for prisoners. International Journal of Prisoner Health.36 | Independent review Prison health care, USA |
Development of systematic method for assessing quality of clinical care | -Identified potential for care to be assessed using performance measures covering a range of health domains (e.g. suicide prevention, medication management, chronic health conditions) -Includes list |
| Kintz, 2013. Quality Measures in Correctional Health Care. Dissertation.37 | Qualitative interviews exploring performance management with prison nurses Oregon prison system, USA |
Development of quality measures | -Identified a need for health outcomes to be measured explicitly |
| Castro, 2014. Diabetes Screening in Inmates: A Quality-Improvement Pilot Project. Dissertation.45 | Expert consultation USA |
Testing of diabetes screening guideline | -Identified a guideline that facilitated performance measurement of diabetes screening |
| Watts, 2015. Development of a performance-based RFP for Correctional Health Care Services in Vermont. Community Oriented Correctional Health Services.44 | Design not reported Vermont Department of Corrections, USA |
Development and testing of performance metrics | -Evidence-based performance measures permit BMing both within prison systems and between prisons and the community -Includes list |
| Laffan, 2016. Evaluation of your medical department. American Jails.41 | Commentary Prison healthcare departments, USA |
Advises implementation of quality assessment | -Effective performance measurement depends on the working relationship between medical teams and correctional administrators -Includes list |
Appendix 4 Longlist of quality indicators and clinical practice recommendations (before de-duplication)
NICE quality and outcomes framework indicators47,51
-
The contractor establishes and maintains a register of patients with AF. AF001.
-
The contractor establishes and maintains a register of patients with asthma, excluding patients with asthma who have been prescribed no asthma-related drugs in the preceding 12 months. AST001.
-
The contractor establishes and maintains a register of all cancer patients defined as a ‘register of patients with a diagnosis of cancer excluding non-melanotic skin cancers diagnosed on or after 1 April 2003’. CAN001.
-
The percentage of patients aged 79 years or under, with CHD, in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less. CHD008.
-
The percentage of patients aged 80 years or over, with CHD, in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. CHD009.
-
The contractor establishes and maintains a register of patients with CHD. CHD01.
-
The contractor establishes and maintains a register of patients with COPD. COPD001.
-
The percentage of patients with COPD and Medical Research Council (MRC) dyspnoea scale ≥ 3 at any time in the preceding 12 months, with a subsequent record of an offer of referral to a pulmonary rehabilitation programme. COPD008.
-
The proportion of women eligible for screening and aged 25–49 years at the end of reporting period whose notes record than an adequate cervical screening test has been performed in the preceding 3 years and 6 months. CS005.
-
The proportion of women eligible for screening and aged 50–64 years and the end of reporting period whose notes record that an adequate cervical screening test has been performed in the previous 5 years and 6 months. CS006.
-
In those patients with a new diagnosis of hypertension aged 30 or over and who have not attained the age of 75, recorded between the preceding 1 April and 31 March (excluding those with pre-existing CHD, diabetes, stroke and/or TIA), who have a recorded CVD risk assessment score [using an assessment tool agreed with NHS Commissioning Board (CB)] of ≥ 20% in the preceding 12 months: the percentage who are currently treated with statins. CVD-PP001.
-
The contractor establishes and maintains a register of patients diagnosed with dementia. DEM001.
-
The percentage of patients with diabetes, on the register, without moderate or severe frailty, on the register, in whom the last blood pressure reading (measured in the preceding 12 months) is 140/80 mmHg or less. DM019.
-
The percentage of patients with diabetes, on the register, with moderate or severe frailty, on the register, in whom the last International Federation of Clinical Chemistry (IFCC)-HbA1c is 75 mmol/mol or less in the preceding 12 months. DM021.
-
The percentage of patients with diabetes, on the register, aged 40 years and over, with no history of CVD and without moderate or severe frailty, who are currently treated with a statin (excluding patients with type 2 diabetes and a CVD risk score of < 10% recorded in the preceding 3 years). DM022.
-
The percentage of patients with diabetes, on the register, and a history of CVD (excluding haemorrhagic stroke) who are currently treated with a statin. DM023.
-
The percentage of patients with diabetes, on the register, without moderate or severe frailty, on the register, in whom the last IFCC-HbA1c is 58 mmol/mol or less in the preceding 12 months. NM157.
-
The contractor establishes and maintains a register of patients aged 18 or over receiving drug treatment for epilepsy. EP001.
-
The contractor establishes and maintains a register of patients with heart failure. HF001.
-
The contractor establishes and maintains a register of patients with established hypertension. HYP001.
-
The percentage of patients aged 79 years or under, with hypertension, in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less. HYP003.
-
The percentage of patients aged 80 years and over, with hypertension, in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. HYP007.
-
The contactor establishes and maintains a register of patients with schizophrenia, bipolar affective disorder and other psychoses and other patients on lithium therapy. MH001.
-
The percentage of patients with schizophrenia, bipolar affective disorder and other psychoses who have a record of BMI in the preceding 12 months. MH006.
-
The contractor establishes and maintains a register of patients aged 18 years or over with a BMI ≥ 30 in the preceding 12 months. OB001.
-
The contractor establishes and maintains a register of all patients in need of palliative care/support irrespective of age. PC001.
-
The contractor can demonstrate continuous quality-improvement activity focused upon prescribing safety as specified in the QOF guidance. QI001.
-
The contractor has participated in network activity to regularly share and discuss learning from quality-improvement activity as specified in the QOF guidance. This would usually include participating in a minimum of two peer-review meetings. QI002.
-
The contractor can demonstrate continuous quality-improvement activity focused on end-of-life care as specified in the QOF guidance. QI003.
-
The contractor has participated in network activity to regularly share and discuss learning from quality-improvement activity as specified in the QOF guidance. This would usually include participating in a minimum of two network peer-review meetings. QI004.
-
The percentage of patients aged 80 years or over, with a history of stroke or TIA, in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. STAI011.
-
The contractor establishes and maintains a register of patients with stroke or TIA. STIA001.
-
The percentage of patients aged 79 years or under, with a history of stroke or TIA, in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less. STIA010.
-
The percentage of patients with CHD in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. CHD002.
-
The percentage of patients with CHD whose last measured cholesterol (measured in the preceding 12 months) is 5 mmol/l or less. CHD003.
-
The percentage of patients on the CKD register in whom the last blood pressure reading (measured in the preceding 12 months) is 140/85 mmHg or less. CKD002.
-
The percentage of patients on the CKD register whose notes have a record of a urine ACR [or protein : creatinine ratio (PCR)] test in the preceding 12 months. CKD004.
-
The contractor establishes and maintains a register of women aged 54 or under who have been prescribed any method of contraception at least once in the last year, or other clinically appropriate interval, for example last 5 years for an intrauterine system (IUS). CON001.
-
The percentage of women, on the register, prescribed emergency hormonal contraception one or more times in the preceding 12 months by the contractor who have received information from the contractor about long-acting reversible contraception at the time or within 1 month of the prescription. CON003.
-
The percentage of patients with COPD with a record of FEV1 in the preceding 12 months. COPD004.
-
The percentage of patients with COPD and MRC dyspnoea grade ≥ 3 at any time in the preceding 12 months, with a record of oxygen saturation value within the preceding 12 months. COPD005.
-
The contractor has a protocol that is in line with national guidance agreed with the NHS CB for the management of cervical screening, which includes staff training, management of patient call/recall, exception reporting and the regular monitoring of inadequate sample rates. CS001.
-
The percentage of women aged 25 or over and who have not attained the age of 65 whose notes record that a cervical screening test has been performed in the preceding 5 years. CS002.
-
The contractor has a policy for auditing its cervical screening service and performs an audit of inadequate cervical screening tests in relation to individual sample-takers at least every 2 years. CS004.
-
The percentage of patients diagnosed with hypertension (diagnosed after or on 1 April 2009) who are given lifestyle advice in the preceding 12 months for: smoking cessation, safe alcohol consumption and healthy diet. CVD-PP002.
-
The percentage of patients with a new diagnosis of dementia recorded in the preceding 1 April to 31 March with a record of FBC, calcium, glucose, renal and liver function, thyroid function tests, serum vitamin B12 and folate levels recorded between 12 months before or 6 months after entering on to the register. DEM005.
-
The percentage of patients with diabetes, on the register, whose last measured total cholesterol (measured within the preceding 12 months) is 5 mmol/l or less. DM004.
-
The percentage of patients with diabetes, on the register, who have a record of an ACR test in the preceding 12 months. DM005
-
The percentage of patients with diabetes, on the register, in whom the last IFCC-HbA1c is 59 mmol/mol or less in the preceding 12 months. DM007.
-
The percentage of patients with diabetes, on the register, in whom the last IFCC-HbA1c is 64 mmol/mol or less in the preceding 12 months. DM008.
-
The percentage of patients with diabetes, on the register, in whom the last IFCC-HbA1c is 75 mmol/mol or less in the preceding 12 months. DM009.
-
The percentage of patients with diabetes, on the register, who have a record of retinal screening in the preceding 12 months. DM011.
-
The percentage of patients 18 or over on drug treatment for epilepsy who have been seizure-free for the last 12 months recorded in the preceding 12 months. EP002.
-
The percentage of women aged 18 or over and who have not attained the age of 55 who are taking antiepileptic drugs who have a record of information and counselling about contraception, conception and pregnancy in the preceding 12 months. EP003.
-
The percentage of patients with hypertension in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. HYP006.
-
The percentage of patients on the learning disability register with Down syndrome aged 18 or over who have a record of blood thyroid-stimulating hormone (TSH) in the preceding 12 months. LD002.
-
The percentage of patients aged 40 or over with schizophrenia, bipolar affective disorder and other psychoses who have a record of total cholesterol–HDL ratio in the preceding 12 months. MH004.
-
The percentage of patients aged 40 or over with schizophrenia, bipolar affective disorder and other psychoses who have a record of blood glucose or HbA1c in the preceding 12 months. MH005.
-
The percentage of patients with schizophrenia, bipolar affective disorder and other psychoses who have a record of alcohol consumption in the preceding 12 months. MH007.
-
The percentage of women aged 25 or over and who have not attained the age of 65 with schizophrenia, bipolar affective disorder and other psychoses whose notes record that a cervical screening test has been performed in the preceding 5 years. MH008.
-
The percentage of women aged 25 or over and who have not attained the age of 65 with schizophrenia, bipolar affective disorder and other psychoses whose notes record that a cervical screening test has been performed in the preceding 5 years. MH008.
-
The percentage of patients on lithium therapy with a record of serum creatinine and TSH in the preceding 9 months. MH009.
-
The percentage of patients on lithium therapy with lithium levels in the therapeutic range in the preceding 4 months. MH010.
-
The percentage of patients on the CKD register with hypertension and proteinuria who are currently treated with renin–angiotensin system antagonists. NM84.
-
The percentage of patients aged 50 or over, and who have not attained the age of 75, with a fragility fracture on or after 1 April 2012, in whom osteoporosis is confirmed on a dual-energy X-ray absorptiometry (DEXA) scan, who are currently treated with an appropriate bone-sparing agent. OST002.
-
The percentage of patients aged 75 or over with a record of a fragility fracture on or after 1 April 2014 and a diagnosis of osteoporosis, who are currently treated with a bone-sparing agent. OST005.
-
The percentage of patients with peripheral arterial disease (PAD) in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. PAD002.
-
The percentage of patients with peripheral arterial disease in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. PAD002.
-
The percentage of patients with peripheral arterial disease in whom the last measured total cholesterol (measured in the preceding 12 months) is 5 mmol/l or less. PAD003.
-
The percentage of patients with peripheral arterial disease with a record in the preceding 12 months that aspirin or an alternative antiplatelet is being taken. PAD004.
-
The contractor has regular (at least 3 monthly) multidisciplinary case-review meetings where all patients on the palliative care register are discussed. PC002.
-
The percentage of patients with rheumatoid arthritis aged 30 or over and who have not attained the age of 85 who have had a cardiovascular risk assessment using a CVD risk-assessment tool adjusted for RA in the preceding 12 months. RA003.
-
The percentage of patients aged 50 or over and who have not attained the age of 91 with rheumatoid arthritis who have had an assessment of fracture risk using a risk-assessment toll adjusted for RA in the preceding 24 months. RA004.
-
The percentage of patients aged 15 or over whose notes record smoking status in the preceding 24 months. SMOK001.
-
The contractor supports patients who smoke in stopping smoking by a strategy which includes providing literature and offering appropriate therapy. SMOK003.
-
The percentage of patients with a stroke shown to be non-haemorrhagic, or a history of TIA whose last measured total cholesterol (measured in the preceding 12 months) is 5 mmol/l or less. STAI005.
-
The percentage of patients with a history of a stroke or TIA in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. STIA003.
-
The percentage of patients with a stroke or TIA (diagnosed on or after 1 April 2014) who have a record of a referral for further investigation between 3 months before or 1 month after the date of the latest recorded or stroke or the first TIA. STIA008.
-
The contractor establishes and maintains a register of patients with hypothyroidism who are currently treated with levothyroxine. THY001.
-
The percentage of patients with hypothyroidism, on the register, with thyroid function tests recorded in the preceding 12 months. THY002.
-
In those patients with AF whose latest record of a CHADS2 score is > 1, the percentage of patients who are currently treated with anticoagulation therapy. AF004.
-
In those patients with AF in whom there is record of a CHADS2 score of 1 the percentage of patients who are currently treated with anticoagulation drug therapy or antiplatelet therapy. AF005.
-
The percentage of patients with a history of MI (on or after 1 April 2011) currently treated with an ACE-I (or ARB if ACE-I-intolerant), aspirin or an alternative antiplatelet therapy, beta-blocker and statin. CHD006.
-
The percentage of patients on the CKD register with hypertension and proteinuria who are currently treated with an ACE-I or ARB. CKD003.
-
The percentage of patients with diabetes, on the register, in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. NM01.
-
The percentage of patients with diabetes, on the register, in whom the last blood pressure reading (measured in the preceding 12 months) is 140/80 mmHg or less. NM02.
-
The percentage of women under the age of 55 years who are taking antiepileptic drugs who have a record of information and counselling about contraception, conception and pregnancy in the preceding 15 months. NM03.
-
Percentage of patients on the Learning Disability register with Down syndrome aged 18 and over who have a record of blood TSH in the previous 15 months (excluding those who are on the thyroid disease register). NM04.
-
The percentage of patients with a new diagnosis of dementia recorded in the preceding 1 April to 31 March with a record of FBC, calcium, glucose, renal and liver function, thyroid function tests, serum vitamin B12 and folate levels recorded between 6 months before or after entering on to the register. NM09.
-
The percentage of patients with hypothyroidism, on the register, with thyroid function tests recorded in the preceding 12 months (Inherited). NM100.
-
The percentage of patients aged 8 or over with asthma (diagnosed on or after 1 April 2006), on the register, with measures of variability or reversibility recorded between 3 months before or any time after diagnosis (Inherited). NM101.
-
The percentage of patients with asthma aged 14 or over and who have not attained the age of 20, on the register, in whom there is a record of smoking status in the preceding 12 months (Inherited). NM102.
-
The percentage of patients with COPD (diagnosed on or after 1 April 2011) in whom the diagnosis has been confirmed by post-bronchodilator spirometry between 3 months before and 12 months after entering on to the register (Inherited). NM103.
-
The percentage of patients with COPD who have had a review, undertaken by a healthcare professional, including an assessment of breathlessness using the MRC dyspnoea scale in the preceding 12 months (Inherited). NM104.
-
The percentage of patients with COPD with a record of FEV1 in the preceding 12 months (Inherited). NM105.
-
The percentage of patients with COPD who have had influenza immunisation in the preceding 1 August to 31 March (Inherited). NM106.
-
The percentage of patients diagnosed with dementia whose care plan has been reviewed in a face-to-face review in the preceding 12 months (Inherited). NM107.
-
The percentage of patients with schizophrenia, bipolar affective disorder and other psychoses who have a comprehensive care plan documented in the record, in the preceding 12 months, agreed between individuals, their family and/or carers as appropriate (Inherited). NM108.
-
The percentage of patients on the CKD register whose notes have a record of a urine ACR (or PCR) test in the preceding 12 months (Inherited). NM109.
-
The percentage of patients aged 18 or over on drug treatment for epilepsy who have been seizure-free for the last 12 months recorded in the preceding 12 months (Inherited). NM110.
-
The contractor supports patients who smoke in stopping smoking by a strategy which includes providing literature and offering appropriate therapy (Inherited). NM113.
-
The percentage of women, on the register, prescribed an oral or patch contraceptive method in the preceding 12 months who have also received information from the contractor about long-acting reversible methods of contraception in the preceding 12 months (Inherited). NM114.
-
The percentage of patients on the CKD register in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less (Inherited). NM117.
-
The percentage of patients with CHD whose last measured total cholesterol (measured in the preceding 12 months) is 5 mmol/l or less (Inherited). NM118.
-
The percentage of patients with schizophrenia, bipolar affective disorder and other psychoses aged 25–84 (excluding those with pre-existing CHD, diabetes, stroke and/or TIA) who have had a CVD risk assessment performed in the preceding 12 months (using an assessment tool agreed with NHS England). NM120.
-
The percentage of patients with CHD, stroke or TIA, diabetes, hypertension, peripheral arterial disease, heart failure, COPD, asthma and/or rheumatoid arthritis who have had a BMI recorded in the preceding 12 months. NM121.
-
The percentage of patients with CHD, stroke or transient ischaemic attack, diabetes and/or COPD who have influenza immunisation in the preceding 1 August and 31 March. NM122.
-
The percentage of patients with a new diagnosis of depression and/or anxiety disorder in the preceding 1 April to 31 March, whose notes record an offer of referral for psychological treatment within 3 months of the date of diagnosis (Inherited). NM123.
-
The percentage of patients with schizophrenia, bipolar affective disorder or other psychoses whose notes record smoking status in the preceding 12 months. NM124.
-
The percentage of patients with schizophrenia, bipolar affective disorder or other psychoses who are recorded as current smokers who have a record of an offer of support and treatment within the preceding 12 months. NM125.
-
The percentage of patients with any or any combination of the following conditions: CHD, PAD, stroke or TIA, hypertension, diabetes, COPD, CKD or asthma, whose notes record smoking status in the preceding 12 months. NM126.
-
The percentage of patients with any or any combination of the following conditions: CHD, PAD, stroke or TIA, hypertension, diabetes, COPD, CKD, asthma, who are recorded as current smokers who have a record of an offer of support and treatment within the preceding 12 months. NM127.
-
The contractor establishes and maintains a register of patients aged 18 or over with a BMI ≥ 25 in the preceding 12 months. NM128.
-
The percentage of patients aged 18 and over with schizophrenia, bipolar affective disorder and other psychoses who have a record of total cholesterol:HDL ratio in the preceding 12 months. NM129.
-
The percentage of patients with diabetes with a record of a foot examination and risk classification: (1) low risk (normal sensation, palpable pulses), (2) increased risk (neuropathy or absent pulses), (3) high risk (neuropathy or absent pulses plus deformity or skin changes or previous ulcer) or (4) ulcerated foot within the preceding 15 months. NM13.
-
The percentage of patients aged 18 years and over with schizophrenia, bipolar affective disorder and other psychoses who have a record of blood glucose or HbA1c in the preceding 12 months. NM130.
-
The percentage of patients with diabetes with a record of testing of foot sensation using a 10 g monofilament within the preceding 12 months. NM131.
-
The percentage of patients aged 25–84 years with a new diagnosis of hypertension or type 2 diabetes, recorded between the preceding 1 April and 31 March (excluding those with pre-existing CHD, stroke and/or TIA) who have had a consultation for cardiovascular risk assessment using the QRISK2 risk assessment tool between 3 months before and 3 months after date of diagnosis (Inherited). NM132.
-
In those patients with a new diagnosis of hypertension or type 2 diabetes aged 25–84 years, recorded between the preceding 1 April and 31 March (excluding those with pre-existing CHD, stroke and/or TIA), who have a recorded CVD risk-assessment score (using the QRISK2 assessment tool) of > 20% in the preceding 12 months: the percentage who are currently treated with statins (unless there is a contraindication). NM133.
-
The percentage of patients with diabetes, on the register, who have had influenza immunisation in the preceding 1 August to 31 March (Inherited). NM139.
-
The percentage of patients with stroke or TIA who have had influenza immunisation in the preceding 1 August to 31 March (Inherited). NM140.
-
The percentage of patients with schizophrenia, bipolar affective disorder and other psychoses who have a record of alcohol consumption in the preceding 15 months. NM15.
-
The percentage of patients with a diagnosis of heart failure (diagnosed on or after 1 April 2006) which has been confirmed by an echocardiogram or by specialist assessment 3 months before or 12 months after entering on to the register (Inherited). NM16.
-
The percentage of patients with schizophrenia, bipolar affective disorder and other psychoses who have a record of BMI in the preceding 15 months. NM16.
-
The percentage of patients with schizophrenia, bipolar affective disorder and other psychoses who have a record of blood pressure in the preceding 15 months. NM17.
-
The percentage of patients with asthma, on the register, who have had an asthma review in the preceding 12 months that includes an assessment of asthma control using the three RCP questions. NM23.
-
The percentage of patients newly diagnosed with diabetes, on the register, in the preceding 1 April to 31 March who have a record of being referred to a structured education programme within 9 months after entry on to the diabetes register. NM27.
-
The percentage of patients with diabetes who have a record of a dietary review by a suitably competent professional in the preceding 15 months. NM28.
-
The contractor establishes and maintains a register of patients: (1) aged 50 or over and who have not attained the age of 75 with a record of a fragility fracture on or after 1 April 2012 and a diagnosis of osteoporosis confirmed on DEXA scan, and (2) aged 75 or over with a record of a fragility fracture on or after 1 April 2014 and a diagnosis of osteoporosis. NM29.
-
The contractor establishes and maintains a register of patients with peripheral arterial disease. NM32.
-
The percentage of patients with peripheral arterial disease with a record in the preceding 15 months that aspirin or an alternative antiplatelet is being taken. NM33.
-
The percentage of patients with peripheral arterial disease in whom the last measured total cholesterol (measured in preceding 15 months) is 5.0 mmol/l or less. NM35.
-
The percentage of patients with hypertension aged 16–74 years in whom there is an annual assessment of physical activity, using the General Practice Physical Activity Questionnaire (GPPAQ), in the preceding 15 months. NM36.
-
The percentage of patients with hypertension aged 16–74 years who score ‘less than active’ on the GPPAQ in the preceding 15 months, who also have a record of a brief intervention in the preceding 15 months. NM37.
-
The percentage of patients with any or any combination of the following conditions: CHD, PAD, stroke or TIA, hypertension, diabetes, COPD, CKD, asthma, schizophrenia, bipolar affective disorder or other psychoses who are recorded as current smokers who have a record of an offer of support and treatment within the preceding 12 months. NM38.
-
The percentage of patients with any or any combination of the following conditions: CHD, PAD, stroke or TIA, hypertension, diabetes, COPD, CKD, asthma, schizophrenia, bipolar affective disorder or other psychoses who smoke whose notes contain a record of an offer of support and treatment within the preceding 15 months. NM39.
-
The percentage of patients aged 15 years and over who are recorded as current smokers who have a record of an offer of support and treatment within the preceding 24 months. NM40.
-
The contractor establishes and maintains a register of all patients aged 17 or over with diabetes mellitus, which specifies the type of diabetes where a diagnosis has been confirmed. NM41.
-
The percentage of patients with COPD and MRC Dyspnoea Scale ≥ 3 at any time in the preceding 15 months, with a subsequent record of an offer of referral to a pulmonary rehabilitation programme. NM47.
-
The percentage of patients with heart failure diagnosed within the preceding 15 months with a subsequent record of an offer of referral for an exercise-based rehabilitation programme within the preceding 15 months. NM48.
-
The percentage of patients with a new diagnosis of depression in the preceding 1 April to 31 March who have had a bio-psychosocial assessment by the point of diagnosis. NM49.
-
The percentage of patients with a new diagnosis of depression in the preceding 1 April to 31 March who have been reviewed within 10–35 days of the date of diagnosis. NM50.
-
The percentage of male patients with diabetes with a record of being asked about erectile dysfunction in the preceding 15 months. NM51.
-
The percentage of male patients with diabetes who have a record of erectile dysfunction with a record of advice and assessment of contributory factors and treatment options in the preceding 15 months. NM52.
-
The percentage of patients under 80 years old with hypertension in whom the last recorded blood pressure (measured in the preceding 9 months) is 140/90 or less. NM53.
-
The percentage of patients aged 80 years and over with hypertension in whom the last recorded blood pressure (measured in the preceding 9 months) is 150/90 or less. NM54.
-
The practice can produce a register of all patients aged 16 years and over with rheumatoid arthritis. NM55.
-
The percentage of patients with rheumatoid arthritis aged 30–84 years who have had a cardiovascular risk assessment using a CVD risk assessment tool adjusted for RA in the preceding 15 months. NM56.
-
The percentage of patients aged 50–90 years with rheumatoid arthritis who have had an assessment of fracture risk using a risk-assessment tool adjusted for RA in the preceding 27 months. NM57.
-
The percentage of patients with rheumatoid arthritis, on the register, who have had a face-to-face review in the preceding 12 months. NM58.
-
The percentage of patients with diabetes who have a record of an ACR test in the preceding 15 months. NM59.
-
The percentage of patients with a stroke shown to be non-haemorrhagic or a history of TIA whose last measured total cholesterol (measured in the preceding 15 months) is 5 mmol/l or less. NM60.
-
The percentage of patients aged 40 years and over with a blood pressure measurement recorded in the preceding 5 years. NM61.
-
The percentage of patients with cancer diagnosed within the preceding 15 months who have a review recorded as occurring within 3 months of the practice receiving confirmation of the diagnosis. NM61.
-
The percentage of patients with dementia with the contact details of a named carer on their record. NM64.
-
The percentage of patients with dementia (diagnosed on or after 1 April 2014) who have a record of attendance at a memory-assessment service up to 12 months before entering on to the register. NM65.
-
The percentage of patients with a new diagnosis of hypertension (diagnosed on or after 1 April 2014) which has been confirmed by ambulatory blood pressure monitoring (ABPM) or home blood pressure monitoring (HBPM) in the 3 months before entering on to the register. NM66.
-
The percentage of patients aged 79 or under with peripheral arterial disease in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less. NM67.
-
The percentage of patients aged 79 or under with CHD in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less. NM68.
-
The percentage of patients aged 79 or under with stroke or TIA in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less. NM69.
-
The percentage of women with diabetes aged 17 or over and who have not attained the age of 45 who have a record of being given information and advice about pregnancy or conception or contraception tailored to their pregnancy and contraceptive intentions recorded in the preceding 12 months. NM70.
-
The percentage of women with epilepsy aged 18 or over and who have not attained the age of 45 who are taking antiepileptic drugs who have a record of being given information and advice about pregnancy or conception or contraception tailored to their pregnancy and contraceptive intentions recorded in the preceding 12 months. NM71.
-
The contractor establishes and maintains a register of patients with learning disabilities. NM73.
-
The percentage of patients with diabetes who have had the following care processes performed in the preceding 12 months: BMI measurement; BP measurement; HbA1c measurement; cholesterol measurement; record of smoking status; foot examination; albumin–creatinine ratio; serum creatinine measurement. NM74.
-
The percentage of patients with a new diagnosis of hypertension in the preceding 1 April to 31 March who have a record of urinary albumin–creatinine ratio test in the 3 months before or after the date of entry to the hypertension register. NM75.
-
The percentage of patients with a new diagnosis of hypertension in the preceding 1 April to 31 March who have a record of a test for haematuria in the 3 months before or after the date of entry to the hypertension register. NM76.
-
The percentage of patients with a new diagnosis of hypertension in the preceding 1 April to 31 March who have a record of a 12-lead electrocardiogram (ECG) performed in the 3 months before or after the date of entry to the hypertension register. NM77.
-
The percentage of women with schizophrenia, bipolar affective disorder or other psychoses under the age of 45 years who have been given information and advice about pregnancy, conception or contraception tailored to their pregnancy and contraceptive intentions recorded in the preceding 12 months. NM78.
-
The percentage of patients who had a MI in the preceding 1 April to 31 March and who are currently being treated with ACE-I (or ARB if ACE-I-intolerant), dual antiplatelet therapy, beta-blocker and a statin. NM79.
-
The percentage of patients with a history of MI (more than 12 months ago) who are currently being treated with an ACE-I (or ARB if ACE-I intolerant), aspirin (or clopidogrel) (or anticoagulant drug therapy) and a statin and a beta-blocker for those patients with left ventricular systolic dysfunction. NM80.
-
The percentage of patients with AF in whom stroke risk has been assessed using the CHA2DS2-VASc score risk stratification scoring system in the preceding 12 months (excluding those patients with a previous CHADS2 or CHA2DS2-VASc score of 2 or more). NM81.
-
In those patients with AF with a record of a CHA2DS2-VASc score of 2 or more, the percentage of patients who are currently treated with anticoagulation drug therapy. [Patients with a previous score of 2 or above using CHADS2, recorded prior to (implementation date) should be included in the denominator.] NM82.
-
The contractor establishes and maintains a register of patients aged 18 years or over with CKD with classification of categories G3a to G5 (previously stage 3–5). NM83.
-
The percentage of patients on the CKD register who have hypertension and proteinuria and who are currently being treated with renin–angiotensin system antagonists. NM84.
-
The percentage of patients with CHD who have had influenza immunisation in the preceding 1 August to 31 March (Inherited). NM87.
-
The percentage of patients with CHD with a record in the preceding 12 months that aspirin, an alternative antiplatelet therapy, or an anticoagulant is being taken (Inherited). NM88.
-
In those patients with a current diagnosis of heart failure due to left ventricular systolic dysfunction, the percentage of patients who are currently treated with an ACE-I or ARB (Inherited). NM172.
-
In those patients with a current diagnosis of heart failure due to left ventricular systolic dysfunction who are currently treated with an ACE-I or ARB, the percentage of patients who are additionally currently treated with a beta-blocker licensed for heart failure (Inherited). NM173.
-
The percentage of patients with a stroke shown to be non-haemorrhagic, or a history of TIA, who have a record in the preceding 12 months that an antiplatelet agent or an anticoagulant is being taken (Inherited). NM94.
-
The percentage of patients with diabetes, on the register, with a diagnosis of nephropathy (clinical proteinuria) or micro-albuminuria who are currently treated with an ACE-I (or ARBs) (Inherited). NM95.
-
The percentage of patients with diabetes, on the register, in whom the last IFCC-HbA1c is 64 mmol/mol or less in the preceding 12 months (Inherited). NM96.
-
The percentage of patients with diabetes, on the register, in whom the last IFCC-HbA1c is 75 mmol/mol or less in the preceding 12 months (Inherited). NM97.
-
The percentage of patients with diabetes, on the register, who have a record of retinal screening in the preceding 12 months (Inherited). NM98.
-
The contractor establishes and maintains a register of patients with hypothyroidism who are currently treated with levothyroxine (Inherited). NM99.
-
The contractor establishes and maintains a register of patients with AF. AF001.
-
The contractor establishes and maintains a register of patients with asthma, excluding patients with asthma who have been prescribed no asthma-related drugs in the preceding 12 months. AST001.
-
The contractor establishes and maintains a register of all cancer patients defined as a ‘register of patients with a diagnosis of cancer excluding non-melanotic skin cancers diagnosed on or after 1 April 2003’. CAN001.
-
The percentage of patients aged 79 years or under, with CHD, in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less. CHD008.
-
The percentage of patients aged 80 years or over, with CHD, in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. CHD009.
-
The contractor establishes and maintains a register of patients with CHD. CHD01.
-
The contractor establishes and maintains a register of patients with COPD. COPD001.
-
The percentage of patients with COPD and MRC dyspnoea scale ≥ 3 at any time in the preceding 12 months, with a subsequent record of an offer of referral to a pulmonary rehabilitation programme. COPD008.
-
The proportion of women eligible for screening and aged 25–49 years at the end of reporting period whose notes record that an adequate cervical screening test has been performed in the preceding 3 years and 6 months. CS005.
-
The proportion of women eligible for screening and aged 50–64 years and the end of reporting period whose notes record that an adequate cervical screening test has been performed in the previous 5 years and 6 months. CS006.
-
In those patients with a new diagnosis of hypertension aged 30 or over and who have not attained the age of 75, recorded between the preceding 1 April to 31 March (excluding those with pre-existing CHD, diabetes, stroke and/or TIA), who have a recorded CVD risk assessment score (using an assessment tool agreed with NHS CB) of ≥ 20% in the preceding 12 months: the percentage who are currently treated with statins. CVD-PP001.
-
The contractor establishes and maintains a register of patients diagnosed with dementia. DEM001.
-
The percentage of patients with diabetes, on the register, without moderate or severe frailty, on the register, in whom the last blood pressure reading (measured in the preceding 12 months) is 140/80 mmHg or less. DM019.
-
The percentage of patients with diabetes, on the register, with moderate or severe frailty, on the register, in whom the last IFCC-HbA1c is 75 mmol/mol or less in the preceding 12 months. DM021.
-
The percentage of patients with diabetes, on the register, aged 40 years and over, with no history of CVD and without moderate or severe frailty, who are currently treated with a statin. (excluding patients with type 2 diabetes and a CVD risk score of < 10% recorded in the preceding 3 years). DM022.
-
The percentage of patients with diabetes, on the register, and a history of CVD (excluding haemorrhagic stroke) who are currently treated with a statin. DM023.
-
The percentage of patients with diabetes, on the register, without moderate or severe frailty, on the register, in whom the last IFCC-HbA1c is 58 mmol/mol or less in the preceding 12 months. NM157.
-
The contractor establishes and maintains a register of patients aged 18 or over receiving drug treatment for epilepsy. EP001.
-
The contractor establishes and maintains a register of patients with heart failure. HF001.
-
The contractor establishes and maintains a register of patients with established hypertension. HYP001.
-
The percentage of patients aged 79 years or under, with hypertension, in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less. HYP003.
-
The percentage of patients aged 80 years and over, with hypertension, in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. HYP007.
-
The contactor establishes and maintains a register of patients with schizophrenia, bipolar affective disorder and other psychoses and other patients on lithium therapy. MH001.
-
The percentage of patients with schizophrenia, bipolar affective disorder and other psychoses who have a record of BMI in the preceding 12 months. MH006
-
The contractor establishes and maintains a register of patients aged 18 years or over with a BMI ≥ 30 in the preceding 12 months. OB001.
-
The contractor establishes and maintains a register of all patients in need of palliative care/support irrespective of age. PC001.
-
The contractor can demonstrate continuous quality-improvement activity focused upon prescribing safety as specified in the QOF guidance. QI001.
-
The contractor has participated in network activity to regularly share and discuss learning from quality-improvement activity as specified in the QOF guidance. This would usually include participating in a minimum of two peer-review meetings. QI002.
-
The contractor can demonstrate continuous quality-improvement activity focused on end-of-life care as specified in the QOF guidance. QI003.
-
The contractor has participated in network activity to regularly share and discuss learning from quality-improvement activity as specified in the QOF guidance. This would usually include participating in a minimum of two network peer-review meetings. QI004.
-
The percentage of patients aged 80 years or over, with a history of stroke or TIA, in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. STAI011.
-
The contractor establishes and maintains a register of patients with stroke or TIA. STIA001.
-
The percentage of patients aged 79 years or under, with a history of stroke or TIA, in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less. STIA010.
-
The percentage of patients with CHD in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. CHD002.
-
The percentage of patients with CHD whose last measured cholesterol (measured in the preceding 12 months) is 5 mmol/l or less. CHD003.
-
The percentage of patients on the CKD register in whom the last blood pressure reading (measured in the preceding 12 months) is 140/85 mmHg or less. CKD002.
-
The percentage of patients on the CKD register whose notes have a record of a urine ACR (or PCR) test in the preceding 12 months. CKD004.
-
The contractor establishes and maintains a register of women aged 54 or under who have been prescribed any method of contraception at least once in the last year, or other clinically appropriate interval, for example last 5 years for an IUS. CON001.
-
The percentage of women, on the register, prescribed emergency hormonal contraception one or more times in the preceding 12 months by the contractor who have received information from the contractor about long-acting reversible contraception at the time or within 1 month of the prescription. CON003.
-
The percentage of patients with COPD with a record of FEV1 in the preceding 12 months. COPD004.
-
The percentage of patients with COPD and MRC dyspnoea grade ≥ 3 at any time in the preceding 12 months, with a record of oxygen saturation value within the preceding 12 months. COPD005.
-
The contractor has a protocol that is in line with national guidance agreed with the NHS CB for the management of cervical screening, which includes staff training, management of patient call/recall, exception reporting and the regular monitoring of inadequate sample rates. CS001.
-
The percentage of women aged 25 or over and who have not attained the age of 65 whose notes record that a cervical screening test has been performed in the preceding 5 years. CS002.
-
The contractor has a policy for auditing its cervical screening service and performs an audit of inadequate cervical screening tests in relation to individual sample-takers at least every 2 years. CS004.
-
The percentage of patients diagnosed with hypertension (diagnosed after or on 1 April 2009) who are given lifestyle advice in the preceding 12 months for: smoking cessation, safe alcohol consumption and healthy diet. CVD-PP002.
-
The percentage of patients with a new diagnosis of dementia recorded in the preceding 1 April to 31 March with a record of FBC, calcium, glucose, renal and liver function, thyroid function tests, serum vitamin B12 and folate levels recorded between 12 months before or 6 months after entering on to the register. DEM005.
-
The percentage of patients with diabetes, on the register, whose last measured total cholesterol (measured within the preceding 12 months) is 5 mmol/l or less. DM004.
-
The percentage of patients with diabetes, on the register, who have a record of an ACR test in the preceding 12 months. DM005.
-
The percentage of patients with diabetes, on the register, in whom the last IFCC-HbA1c is 59 mmol/mol or less in the preceding 12 months. DM007.
-
The percentage of patients with diabetes, on the register, in whom the last IFCC-HbA1c is 64 mmol/mol or less in the preceding 12 months. DM008.
-
The percentage of patients with diabetes, on the register, in whom the last IFCC-HbA1c is 75 mmol/mol or less in the preceding 12 months. DM009.
-
The percentage of patients with diabetes, on the register, who have a record of retinal screening in the preceding 12 months. DM011.
-
The percentage of patients 18 or over on drug treatment for epilepsy who have been seizure-free for the last 12 months recorded in the preceding 12 months. EP002.
-
The percentage of women aged 18 or over and who have not attained the age of 55 who are taking antiepileptic drugs who have a record of information and counselling about contraception, conception and pregnancy in the preceding 12 months. EP003.
-
The percentage of patients with hypertension in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. HYP006.
-
The percentage of patients on the learning disability register with Down syndrome aged 18 or over who have a record of blood TSH in the preceding 12 months. LD002.
-
The percentage of patients aged 40 or over with schizophrenia, bipolar affective disorder and other psychoses who have a record of total cholesterol-HDL ratio in the preceding 12 months. MH004.
-
The percentage of patients aged 40 or over with schizophrenia, bipolar affective disorder and other psychoses who have a record of blood glucose or HbA1c in the preceding 12 months MH005.
-
The percentage of patients with schizophrenia, bipolar affective disorder and other psychoses who have a record of alcohol consumption in the preceding 12 months. MH007.
-
The percentage of women aged 25 or over and who have not attained the age of 65 with schizophrenia, bipolar affective disorder and other psychoses whose notes record that a cervical screening test has been performed in the preceding 5 years. MH008.
-
The percentage of women aged 25 or over and who have not attained the age of 65 with schizophrenia, bipolar affective disorder and other psychoses whose notes record that a cervical screening test has been performed in the preceding 5 years. MH008.
-
The percentage of patients on lithium therapy with a record of serum creatinine and TSH in the preceding 9 months. MH009.
-
The percentage of patients on lithium therapy with lithium levels in the therapeutic range in the preceding 4 months. MH010.
-
The percentage of patients on the CKD register with hypertension and proteinuria who are currently treated with renin–angiotensin system antagonists. NM84.
-
The percentage of patients aged 50 or over, and who have not attained the age of 75, with a fragility fracture on or after 1 April 2012, in whom osteoporosis is confirmed on DEXA scan, who are currently treated with an appropriate bone-sparing agent. OST002.
-
The percentage of patients aged 75 or over with a record of a fragility fracture on or after 1 April 2014 and a diagnosis of osteoporosis, who are currently treated with a bone-sparing agent. OST005.
-
The percentage of patients with peripheral arterial disease in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. PAD002.
-
The percentage of patients with peripheral arterial disease in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. PAD002.
-
The percentage of patients with peripheral arterial disease in whom the last measured total cholesterol (measured in the preceding 12 months) is 5 mmol/l or less. PAD003.
-
The percentage of patients with peripheral arterial disease with a record in the preceding 12 months that aspirin or an alternative antiplatelet is being taken. PAD004.
-
The contractor has regular (at least 3 monthly) multidisciplinary case-review meetings where all patients on the palliative care register are discussed. PC002.
-
The percentage of patients with rheumatoid arthritis aged 30 or over and who have not attained the age of 85 who have had a cardiovascular risk assessment using a CVD risk-assessment tool adjusted for RA in the preceding 12 months. RA003.
-
The percentage of patients aged 50 or over and who have not attained the age of 91 with rheumatoid arthritis who have had an assessment of fracture risk using a risk-assessment tool adjusted for RA in the preceding 24 months. RA004.
-
The percentage of patients aged 15 or over whose notes record smoking status in the preceding 24 months. SMOK001.
-
The contractor supports patients who smoke in stopping smoking by a strategy which includes providing literature and offering appropriate therapy. SMOK003.
-
The percentage of patients with a stroke shown to be non-haemorrhagic or a history of TIA whose last measured total cholesterol (measured in the preceding 12 months) is 5 mmol/l or less. STAI005.
-
The percentage of patients with a history of a stroke or TIA in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. STIA003.
-
The percentage of patients with a stroke or TIA (diagnosed on or after 1 April 2014) who have a record of a referral for further investigation between 3 months before and 1 month after the date of the latest recorded or stroke or the first TIA. STIA008.
-
The contractor establishes and maintains a register of patients with hypothyroidism who are currently treated with levothyroxine. THY001.
-
The percentage of patients with hypothyroidism, on the register, with thyroid function tests recorded in the preceding 12 months. THY002.
-
In those patients with AF whose latest record of a CHADS2 score is >1, the percentage of patients who are currently treated with anticoagulation therapy. AF004.
-
In those patients with AF in whom there is record of a CHADS2 score of 1 the percentage of patients who are currently treated with anticoagulation drug therapy or antiplatelet therapy. AF005.
-
The percentage of patients with a history of MI (on or after 1 April 2011) currently treated with an ACE-I (or ARB if ACE-I-intolerant), aspirin or an alternative antiplatelet therapy, beta-blocker and statin. CHD006.
-
The percentage of patients on the CKD register with hypertension and proteinuria who are currently treated with an ACE-I or ARB. CKD003.
-
The percentage of patients with diabetes, on the register, in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. NM01.
-
The percentage of patients with diabetes, on the register, in whom the last blood pressure reading (measured in the preceding 12 months) is 140/80 mmHg or less. NM02.
-
The percentage of women under the age of 55 years who are taking antiepileptic drugs who have a record of information and counselling about contraception, conception and pregnancy in the preceding 15 months. NM03.
-
Percentage of patients on the Learning Disability register with Down syndrome aged 18 and over who have a record of blood TSH in the previous 15 months (excluding those who are on the thyroid disease register). NM04.
-
The percentage of patients with a new diagnosis of dementia recorded in the preceding 1 April to 31 March with a record of FBC, calcium, glucose, renal and liver function, thyroid function tests, serum vitamin B12 and folate levels recorded between 6 months before and after entering on to the register NM09.
-
The percentage of patients with hypothyroidism, on the register, with thyroid function tests recorded in the preceding 12 months (Inherited). NM100.
-
The percentage of patients aged 8 or over with asthma (diagnosed on or after 1 April 2006), on the register, with measures of variability or reversibility recorded between 3 months before and any time after diagnosis (Inherited). NM101.
-
The percentage of patients with asthma aged 14 or over and who have not attained the age of 20, on the register, in whom there is a record of smoking status in the preceding 12 months (Inherited). NM102.
-
The percentage of patients with COPD (diagnosed on or after 1 April 2011) in whom the diagnosis has been confirmed by post bronchodilator spirometry between 3 months before and 12 months after entering on to the register (Inherited). NM103.
-
The percentage of patients with COPD who have had a review, undertaken by a healthcare professional, including an assessment of breathlessness using the MRC dyspnoea scale in the preceding 12 months (Inherited). NM104.
-
The percentage of patients with COPD with a record of FEV1 in the preceding 12 months (Inherited). NM105.
-
The percentage of patients with COPD who have had influenza immunisation in the preceding 1 August to 31 March (Inherited). NM106.
-
The percentage of patients diagnosed with dementia whose care plan has been reviewed in a face-to-face review in the preceding 12 months (Inherited). NM107.
-
The percentage of patients with schizophrenia, bipolar affective disorder and other psychoses who have a comprehensive care plan documented in the record, in the preceding 12 months, agreed between individuals, their family and/or carers as appropriate (Inherited). NM108.
-
The percentage of patients on the CKD register whose notes have a record of a urine ACR (or protein–creatinine ratio) test in the preceding 12 months (Inherited). NM109.
-
The percentage of patients aged 18 or over on drug treatment for epilepsy who have been seizure-free for the last 12 months recorded in the preceding 12 months (Inherited). NM110.
-
The contractor supports patients who smoke in stopping smoking by a strategy which includes providing literature and offering appropriate therapy (Inherited). NM113.
-
The percentage of women, on the register, prescribed an oral or patch contraceptive method in the preceding 12 months who have also received information from the contractor about long-acting reversible methods of contraception in the preceding 12 months (Inherited). NM114.
-
The percentage of patients on the CKD register in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less (Inherited). NM117.
-
The percentage of patients with CHD whose last measured total cholesterol (measured in the preceding 12 months) is 5 mmol/l or less. (Inherited). NM118.
-
The percentage of patients with schizophrenia, bipolar affective disorder and other psychoses aged 25–84 (excluding those with pre-existing CHD, diabetes, stroke and/or TIA) who have had a CVD risk assessment performed in the preceding 12 months (using an assessment tool agreed with NHS England). NM120.
-
The percentage of patients with CHD, stroke or TIA, diabetes, hypertension, peripheral arterial disease, heart failure, COPD, asthma and/or rheumatoid arthritis who have had a BMI recorded in the preceding 12 months. NM121.
-
The percentage of patients with CHD, stroke or transient ischaemic attack, diabetes and/or COPD who have influenza immunisation in the preceding 1 August and 31 March. NM122.
-
The percentage of patients with a new diagnosis of depression and/or anxiety disorder in the preceding 1 April to 31 March, whose notes record an offer of referral for psychological treatment within 3 months of the date of diagnosis (Inherited). NM123.
-
The percentage of patients with schizophrenia, bipolar affective disorder or other psychoses whose notes record smoking status in the preceding 12 months. NM124.
-
The percentage of patients with schizophrenia, bipolar affective disorder or other psychoses who are recorded as current smokers who have a record of an offer of support and treatment within the preceding 12 months. NM125.
-
The percentage of patients with any or any combination of the following conditions: CHD, PAD, stroke or TIA, hypertension, diabetes, COPD, CKD or asthma, whose notes record smoking status in the preceding 12 months. NM126.
-
The percentage of patients with any or any combination of the following conditions: CHD, PAD, stroke or TIA, hypertension, diabetes, COPD, CKD, asthma who are recorded as current smokers who have a record of an offer of support and treatment within the preceding 12 months. NM127.
-
The contractor establishes and maintains a register of patients aged 18 or over with a BMI ≥ 25 in the preceding 12 months. NM128.
-
The percentage of patients aged 18 and over with schizophrenia, bipolar affective disorder and other psychoses who have a record of total cholesterol–HDL ratio in the preceding 12 months. NM129.
-
The percentage of patients with diabetes with a record of a foot examination and risk classification: (1) low risk (normal sensation, palpable pulses), (2) increased risk (neuropathy or absent pulses), (3) high risk (neuropathy or absent pulses plus deformity or skin changes or previous ulcer) or (4) ulcerated foot within the preceding 15 months. NM13.
-
The percentage of patients aged 18 years and over with schizophrenia, bipolar affective disorder and other psychoses who have a record of blood glucose or HbA1c in the preceding 12 months. NM130.
-
The percentage of patients with diabetes with a record of testing of foot sensation using a 10-g monofilament within the preceding 12 months. NM131.
-
The percentage of patients aged 25–84, years with a new diagnosis of hypertension or type 2 diabetes, recorded between the preceding 1 April and 31 March (excluding those with pre-existing CHD, stroke and/or TIA) who have had a consultation for cardiovascular risk assessment using the QRISK2 risk-assessment tool between 3 months before and 3 months after date of diagnosis (Inherited). NM132.
-
In those patients with a new diagnosis of hypertension or type 2 diabetes aged 25–84 years, recorded between the preceding 1 April and 31 March (excluding those with pre-existing CHD, stroke and/or TIA), who have a recorded CVD risk-assessment score (using the QRISK2 assessment tool) of > 20% in the preceding 12 months: the percentage who are currently treated with statins (unless there is a contraindication). NM133.
-
The percentage of patients with diabetes, on the register, who have had influenza immunisation in the preceding 1 August to 31 March (Inherited). NM139.
-
The percentage of patients with stroke or TIA who have had influenza immunisation in the preceding 1 August to 31 March (Inherited). NM140.
-
The percentage of patients with schizophrenia, bipolar affective disorder and other psychoses who have a record of alcohol consumption in the preceding 15 months. NM15.
-
The percentage of patients with a diagnosis of heart failure (diagnosed on or after 1 April 2006) which has been confirmed by an echocardiogram or by specialist assessment 3 months before or 12 months after entering on to the register (Inherited). NM16.
-
The percentage of patients with schizophrenia, bipolar affective disorder and other psychoses who have a record of BMI in the preceding 15 months. NM16.
-
The percentage of patients with schizophrenia, bipolar affective disorder and other psychoses who have a record of blood pressure in the preceding 15 months. NM17.
-
The percentage of patients with asthma, on the register, who have had an asthma review in the preceding 12 months that includes an assessment of asthma control using the three RCP questions. NM23.
-
The percentage of patients newly diagnosed with diabetes, on the register, in the preceding 1 April to 31 March who have a record of being referred to a structured education programme within 9 months after entry on to the diabetes register. NM27.
-
The percentage of patients with diabetes who have a record of a dietary review by a suitably competent professional in the preceding 15 months. NM28.
-
The contractor establishes and maintains a register of patients: (1) aged 50 or over and who have not attained the age of 75 with a record of a fragility fracture on or after 1 April 2012 and a diagnosis of osteoporosis confirmed on DEXA scan, and (2) aged 75 or over with a record of a fragility fracture on or after 1 April 2014 and a diagnosis of osteoporosis. NM29.
-
The contractor establishes and maintains a register of patients with peripheral arterial disease. NM32.
-
The percentage of patients with peripheral arterial disease with a record in the preceding 15 months that aspirin or an alternative antiplatelet is being taken. NM33.
-
The percentage of patients with peripheral arterial disease in whom the last measured total cholesterol (measured in preceding 15 months) is 5.0 mmol/l or less. NM35.
-
The percentage of patients with hypertension aged 16 to 74 years in whom there is an annual assessment of physical activity, using GPPAQ, in the preceding 15 months. NM36.
-
The percentage of patients with hypertension aged 16–74 years who score ‘less than active’ on GPPAQ in the preceding 15 months, who also have a record of a brief intervention in the preceding 15 months. NM37.
-
The percentage of patients with any or any combination of the following conditions: CHD, PAD, stroke or TIA, hypertension, diabetes, COPD, CKD, asthma, schizophrenia, bipolar affective disorder or other psychoses who are recorded as current smokers who have a record of an offer of support and treatment within the preceding 12 months. NM38.
-
The percentage of patients with any or any combination of the following conditions: CHD, PAD, stroke or TIA, hypertension, diabetes, COPD, CKD, asthma, schizophrenia, bipolar affective disorder or other psychoses who smoke whose notes contain a record of an offer of support and treatment within the preceding 15 months. NM39.
-
The percentage of patients aged 15 years and over who are recorded as current smokers who have a record of an offer of support and treatment within the preceding 24 months. NM40.
-
The contractor establishes and maintains a register of all patients aged 17 or over with diabetes mellitus which specifies the type of diabetes where a diagnosis has been confirmed. NM41.
-
The percentage of patients with COPD and MRC Dyspnoea Scale ≥ 3 at any time in the preceding 15 months, with a subsequent record of an offer of referral to a pulmonary rehabilitation programme. NM47.
-
The percentage of patients with heart failure diagnosed within the preceding 15 months with a subsequent record of an offer of referral for an exercise-based rehabilitation programme within the preceding 15 months. NM48.
-
The percentage of patients with a new diagnosis of depression in the preceding 1 April to 31 March who have had a bio-psychosocial assessment by the point of diagnosis. NM49.
-
The percentage of patients with a new diagnosis of depression in the preceding 1 April to 31 March who have been reviewed within 10–35 days of the date of diagnosis. NM50.
-
The percentage of male patients with diabetes with a record of being asked about erectile dysfunction in the preceding 15 months. NM51.
-
The percentage of male patients with diabetes who have a record of erectile dysfunction with a record of advice and assessment of contributory factors and treatment options in the preceding 15 months. NM52.
-
The percentage of patients under 80 years old with hypertension in whom the last recorded blood pressure (measured in the preceding 9 months) is 140/90 or less. NM53.
-
The percentage of patients aged 80 years and over with hypertension in whom the last recorded blood pressure (measured in the preceding 9 months) is 150/90 or less. NM54.
-
The practice can produce a register of all patients aged 16 years and over with rheumatoid arthritis. NM55.
-
The percentage of patients with rheumatoid arthritis aged 30–84 years who have had a cardiovascular risk assessment using a CVD risk-assessment tool adjusted for RA in the preceding 15 months. NM56.
-
The percentage of patients aged 50–90 years with rheumatoid arthritis who have had an assessment of fracture risk using a risk-assessment tool adjusted for RA in the preceding 27 months. NM57.
-
The percentage of patients with rheumatoid arthritis, on the register, who have had a face-to-face review in the preceding 12 months. NM58.
-
The percentage of patients with diabetes who have a record of an ACR test in the preceding 15 months. NM59.
-
The percentage of patients with a stroke shown to be non-haemorrhagic or a history of TIA whose last measured total cholesterol (measured in the preceding 15 months) is 5 mmol/l or less. NM60.
-
The percentage of patients aged 40 years and over with a blood pressure measurement recorded in the preceding 5 years. NM61.
-
The percentage of patients with cancer diagnosed within the preceding 15 months who have a review recorded as occurring within 3 months of the practice receiving confirmation of the diagnosis. NM61.
-
The percentage of patients with dementia with the contact details of a named carer on their record. NM64.
-
The percentage of patients with dementia (diagnosed on or after 1 April 2014) who have a record of attendance at a memory-assessment service up to 12 months before entering on to the register. NM65.
-
The percentage of patients with a new diagnosis of hypertension (diagnosed on or after 1 April 2014) which has been confirmed by ABPM or HBPM in the 3 months before entering on to the register. NM66.
-
The percentage of patients aged 79 or under with peripheral arterial disease in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less. NM67.
-
The percentage of patients aged 79 or under with CHD in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less. NM68.
-
The percentage of patients aged 79 or under with stroke or TIA in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less. NM69.
-
The percentage of women with diabetes aged 17 or over and who have not attained the age of 45 who have a record of being given information and advice about pregnancy or conception or contraception tailored to their pregnancy and contraceptive intentions recorded in the preceding 12 months. NM70.
-
The percentage of women with epilepsy aged 18 or over and who have not attained the age of 45 who are taking antiepileptic drugs who have a record of being given information and advice about pregnancy or conception or contraception tailored to their pregnancy and contraceptive intentions recorded in the preceding 12 months. NM71.
-
The contractor establishes and maintains a register of patients with learning disabilities. NM73.
-
The percentage of patients with diabetes who have had the following care processes performed in the preceding 12 months: BMI measurement; BP measurement; HbA1c measurement; cholesterol measurement; record of smoking status; foot examination; albumin–creatinine ratio; serum creatinine measurement. NM74.
-
The percentage of patients with a new diagnosis of hypertension in the preceding 1 April to 31 March who have a record of urinary albumin–creatinine ratio test in the 3 months before or after the date of entry to the hypertension register. NM75.
-
The percentage of patients with a new diagnosis of hypertension in the preceding 1 April to 31 March who have a record of a test for haematuria in the 3 months before or after the date of entry to the hypertension register. NM76.
-
The percentage of patients with a new diagnosis of hypertension in the preceding 1 April to 31 March who have a record of a 12-lead ECG performed in the 3 months before or after the date of entry to the hypertension register. NM77.
-
The percentage of women with schizophrenia, bipolar affective disorder or other psychoses under the age of 45 years who have been given information and advice about pregnancy, conception or contraception tailored to their pregnancy and contraceptive intentions recorded in the preceding 12 months. NM78.
-
The percentage of patients who had a MI in the preceding 1 April to 31 March and who are currently being treated with ACE-I (or ARB if ACE-I-intolerant), dual antiplatelet therapy, beta-blocker and a statin. NM79.
-
The percentage of patients with a history of MI (more than 12 months ago) who are currently being treated with an ACE-I (or ARB if ACE-I-intolerant), aspirin (or clopidogrel) (or anticoagulant drug therapy) and a statin and a beta-blocker for those patients with left ventricular systolic dysfunction. NM80.
-
The percentage of patients with AF in whom stroke risk has been assessed using the CHA2DS2-VASc score risk stratification scoring system in the preceding 12 months (excluding those patients with a previous CHADS2 or CHA2DS2-VASc score of 2 or more). NM81.
-
In those patients with AF with a record of a CHA2DS2-VASc score of 2 or more, the percentage of patients who are currently treated with anticoagulation drug therapy. [Patients with a previous score of 2 or above using CHADS2 recorded prior to (implementation date) should be included in the denominator.] NM82.
-
The contractor establishes and maintains a register of patients aged 18 years or over with CKD with classification of categories G3a to G5 (previously stage 3–5). NM83.
-
The percentage of patients on the CKD register who have hypertension and proteinuria and who are currently being treated with renin–angiotensin system antagonists. NM84.
-
The percentage of patients with CHD who have had influenza immunisation in the preceding 1 August to 31 March (Inherited). NM87.
-
The percentage of patients with CHD with a record in the preceding 12 months that aspirin, an alternative antiplatelet therapy, or an anticoagulant is being taken (Inherited). NM88.
-
In those patients with a current diagnosis of heart failure due to left ventricular systolic dysfunction, the percentage of patients who are currently treated with an ACE-I or ARB (Inherited). NM172.
-
In those patients with a current diagnosis of heart failure due to left ventricular systolic dysfunction who are currently treated with an ACE-I or ARB, the percentage of patients who are additionally currently treated with a beta-blocker licensed for heart failure (Inherited). NM173.
-
The percentage of patients with a stroke shown to be non-haemorrhagic or a history of TIA who have a record in the preceding 12 months that an antiplatelet agent or an anticoagulant is being taken (Inherited). NM94.
-
The percentage of patients with diabetes, on the register, with a diagnosis of nephropathy (clinical proteinuria) or micro-albuminuria who are currently treated with an ACE-I (or ARBs) (Inherited). NM95.
-
The percentage of patients with diabetes, on the register, in whom the last IFCC-HbA1c is 64 mmol/mol or less in the preceding 12 months (Inherited). NM96.
-
The percentage of patients with diabetes, on the register, in whom the last IFCC-HbA1c is 75 mmol/mol or less in the preceding 12 months (Inherited). NM97.
-
The percentage of patients with diabetes, on the register, who have a record of retinal screening in the preceding 12 months (Inherited). NM98.
-
The contractor establishes and maintains a register of patients with hypothyroidism who are currently treated with levothyroxine (Inherited). NM99.
Primary care quality indicators for people with serious mental illness29
-
Co-ordinated care – identify key worker (social worker or community psychiatric nurse) – Routine data.
-
Staff continuity – good communication between staff and infrequent staff changes – Routine data.
-
Continuity: CONNECT is a patient questionnaire with 72 items, each rated on a five-point scale, with 13 scales and one single-item indicator: General co-ordination – ‘Overall, is your MH treatment well co-ordinated?’ Primary care scales – ‘How often is psychiatrist in contact with your primary care doctor?’ (Never, Rarely, Sometimes, Often, Always) – Primary data.
-
Total number of follow-up contacts during treatment episode after initial evaluation – Routine data.
-
Patients with SMI who smoke who are offered tobacco counselling/help to stop smoking – Routine data.
-
Alcohol-misuse screening – Routine data.
-
Screening for illicit drug use, type, quantity and frequency – Routine data.
-
Referral to substance-misuse disorder specialty care, if appropriate – Routine data.
-
HIV screening with co-occurring substance misuse for SMI service users – Routine data.
-
Practice can produce register of all SMI patients – Routine data.
-
Service user registration with a primary health organisation – Routine data.
-
Service user registration with markers of care recorded: contact with secondary health services, written care plans, 6-month MH review, identified care co-ordinator, evidence of physical examination – Routine data.
-
Patients who do not attend the practice for their annual review who are identified and followed up by the practice team – Routine data.
-
System contact: number of patients in contact with the treatment system – Routine data.
-
Surveillance to prevent relapse – Routine data.
-
Crisis management and out-of-hours services – Routine data.
-
Access to services and range of services – Routine data.
-
Family care – record of families living with person with schizophrenia – Primary data.
-
Duration of untreated psychosis: number of recently diagnosed patients – Routine data.
-
Waiting time between registration and start of treatment – Routine data.
-
All current medication clearly available at all consultations – known drug dosages, frequencies, history of side effects, review date – Primary data.
-
Monitor patients suffering extrapyramidal effects, check compliance – Routine data.
-
Assess weight gain, use of concomitant medication – Routine data.
-
Use of lithium: plasma lithium levels monitored regularly – Routine data.
-
Percentages of bipolar service users prescribed antidepressants and anxiolytics – Routine data.
-
Proportion of patients who are receiving depot antipsychotics who have appropriate laboratory screening tests – Routine data.
-
Patients have their antipsychotic medication reviewed regularly, considering symptoms and side effects: appropriate referral to specialist – Routine data.
-
Polypharmacy: reduce number of patients using more than four psychotropic drugs at the same time – Routine data.
-
Monitoring patients with neurological, sexual, sleeping and sedation side effects – Routine data.
-
Percentage of patients given annual MH review by GP – Routine data.
-
Comprehensive mental status examination and history conducted in patients with a new treatment episode – Routine data.
-
Referral for specialist MH assessment – Routine data.
-
Comprehensive assessment of comorbid psychiatric conditions and response to treatment – Routine data.
-
Reassess severity of symptoms – Routine data.
-
Examined for duration of untreated psychosis – Primary data.
-
Delayed diagnosis – Primary data.
-
Informal carer contacts – Primary data.
-
Information on employment status – Primary data.
-
Diabetes monitoring for people with diabetes and schizophrenia – Routine data.
-
Diabetes and cholesterol monitoring for people with schizophrenia and diabetes – Routine data.
-
Diabetes screening for people who are using antipsychotic medications – Routine data.
-
Blood pressure screening for patients with diabetes – Routine data.
-
Weight management/BMI monitoring – Routine data.
-
Proportion with increased BMI/abdominal waistline – Routine data.
-
Patients with diabetes who received education about diabetes, nutrition, cooking, physical activity, or exercise – Routine data.
-
Counselling on physical activity and/or nutrition for those with documented elevated BMI – Routine data.
-
Retinal exam for patients with SMI who have diabetes – Routine data.
-
Foot exam for patients with SMI who have diabetes – Routine data.
-
Hypertension counselling: patients with hypertension who received education services related to hypertension, nutrition, cooking, physical activity or exercise – Routine data.
-
Hypertension: recording and monitoring patients with hypertension and high blood cholesterol [low-density lipoprotein (LDL)] – Routine data.
-
Breast cancer screening for women – Routine data.
-
Colorectal cancer screening – Routine data.
-
Proportion of patients who have an increased blood pressure – Routine data.
-
Proportion of patients who have an increased blood glucose level – Routine data.
-
Proportion of patients who have low levels of glycosylated haemoglobin – Routine data.
-
Proportion of patients who have increased level of blood lipids – Routine data.
-
Comprehensive physical health assessment with appropriate advice – Routine data.
-
Patients with diabetes who received psychoeducation related to weight (BMI), diabetes (blood glucose levels) – Routine data.
-
Medical attention for nephropathy – Routine data.
High-impact quality indicators in general practice53
-
Diabetes: composite indicator recording the proportion of eligible patients receiving all nine recommended processes of care:
-
blood pressure measurement;
-
HbA1c measurement;
-
cholesterol measurement;
-
urine ACR/PCR testing or proteinuria code;
-
estimated glomerular filtration rate (eGFR) or serum creatinine testing;
-
foot review;
-
retinal screening;
-
BMI recording;
-
smoking status.
-
-
Set of 9 indicators focusing on avoiding adverse effects of non-steroidal antiinflammatory drugs (NSAIDs) and antiplatelet drugs:
-
Prescribing a traditional oral NSAID or low-dose aspirin in patients with a history of peptic ulceration without co-prescription of gastroprotection.
-
Prescribing a traditional oral NSAID in patients aged 75 years or over without co-prescription of gastroprotection.
-
Prescribing of a traditional oral NSAID and aspirin in patients aged 65 years or over without co-prescription of gastroprotection.
-
Prescribing of aspirin and clopidogrel in patients aged 65 years or over without co-prescription of gastroprotection.
-
Prescribing of warfarin and a traditional oral NSAID without co-prescription of gastroprotection.
-
Prescribing of warfarin and low dose aspirin or clopidogrel without co-prescription of gastroprotection.
-
Prescribing an oral NSAID in patients with heart failure.
-
Prescribing an oral NSAID in patients prescribed both a diuretic and an angiotensin-converting-enzyme inhibitor (ACE inhibitor) or ARB.
-
Prescribing an oral NSAID in patients with CKD.
-
-
The proportion of patients with a record of AF and a score of two or higher on the CHADS2 risk tool who have a current prescription for anticoagulation therapy.
-
The proportion of patients with a lifetime record of MI who are receiving the recommended four drugs: ACE inhibitor or ARB, aspirin or antiplatelet, beta-blocker and statin.
-
The proportion of patients with type 2 diabetes that achieve each of the three recommended target levels: BP < 140/80 mmHg (or < 130/80 mmHg if kidney, eye or cerebrovascular damage), HbA1c ≤ 59 mmol/mol, and cholesterol ≤ 5 mmol/l.
-
Blood pressure control in hypertension: the proportion of patients achieving individual, age-dependent targets in the previous 9 month: BP < 140/90 mmHg if aged under 80 years, or < 150/90 mmHg if aged 80 years or more.
-
Blood pressure control in CKD: a combination of two indicators assessing the achievement of recommended BP targets in specific patient groups: < 140/85 mmHg, or < 130/80 mmHg if record of diabetes or proteinuria.
High-impact guideline-based quality indicators for United Kingdom primary care52
-
Smoking: the percentage of patients in high-risk groups whose notes record smoking status and the offer of support and treatment within preceding 15 months (composite).
-
COPD: diagnosis of COPD, through use of spirometry and chest radiograph (composite).
-
CKD: the percentage of patients on the CKD register with hypertension and proteinuria who are treated with an ACE-I or ARB.
-
CKD: measurement of blood pressure, urinary protein excretion and lifestyle advice (composite).
-
CKD: blood pressure and urinary protein excretion targets, and appropriate drug therapy (composite).
-
MI: all patients who have had an acute MI should be offered specific combination drug treatment.
-
Chronic heart failure: measurement of serum natriuretic peptides and referral where appropriate (composite).
-
AF: recommendations concerning use of anticoagulants in AF (composite).
-
Hypertension: blood pressure targets in those under/over 80 years of age (composite).
-
Hypertension: lifestyle advice and monitoring of cholesterol and urinary protein excretion (composite).
-
Type 2 diabetes: nine annual processes of care: that is, measurement of blood pressure, lipids, renal function, urine ACR, glycaemic control, BMI, smoking status, plus foot and eye checks (composite).
-
Type 2 diabetes: integrate dietary advice with a personalised diabetes management plan.
-
Type 2 diabetes: cardiovascular risk assessment and subsequent statin therapy where indicated.
-
Type 2 diabetes: achievement of target levels for blood pressure, cholesterol and glycaemic control (composite).
-
Type 2 diabetes: for a person on dual therapy who is markedly hyperglycaemic, consider starting insulin therapy in preference to adding other drugs to control blood glucose.
-
Diabetes mellitus: the percentage of patients with diabetes in whom the last blood pressure is ≤140/80 mmHg.
-
NSAIDs: use of NSAIDs and monitoring of potential side effects (composite).
-
Depression in adults: recommendations concerning severity-appropriate treatment of depression (composite).
Guidelines for the physical health of people in prison48
-
At first reception into prison, a healthcare professional (or trained healthcare assistant under the supervision of a registered nurse) should carry out a health assessment for every person. Do this before the person is allocated to their cell. As part of the assessment, identify any issues that may affect the person’s immediate health and safety before the second-stage health assessment priority health needs to be addressed at the next clinical opportunity.
-
Ensure continuity of care for people transferring from one custodial setting to another (including court, the receiving prison or during escort periods) by, for example: accessing relevant information from the patient clinical record, prisoner escort record and cell-sharing risk assessment, checking medicines and any outstanding medical appointments.
-
Take into account any communication needs or difficulties the person has (including reading and writing ability), and follow the principles in NICE’s guideline on patient experience in adult NHS services.
-
The first-stage health assessment should include the questions and actions in table 1. It should cover: physical health, alcohol use, substance misuse, MH, self-harm and suicide risk.
-
Give the person advice about how to contact prison health services and book GP appointments in the future.
-
Ask the person for consent to transfer their medical records from their GP to the prison healthcare service (see recommendations 1.7.1 and 1.7.2 for more information about transfer of medical records).
-
Enter in the person’s medical record: all answers to the reception health assessment questions; health-related observations, including those about behaviour and mental state (including eye contact, body language, rapid, slow or strange speech, poor hygiene, strange thoughts); details of any action taken.
-
Carry out a MR (in line with NICE’s guideline on medicines optimisation) before the second-stage health assessment. See also recommendations 1.4.1 and 1.7.10 for recommendations on risk assessments for IP medicines and ensuring continuity of medicine.
-
Healthcare professionals in prisons should ensure people coming into prison are screened for TB within 48 hours of arrival.
-
Report all suspected and confirmed TB cases to the local multidisciplinary TB team within 1 working day.
-
If a case of TB is confirmed: arrange for the local multidisciplinary TB team to visit within 5 working days. Contact the local PHE unit and multidisciplinary TB team to arrange a contact investigations exercise. They should also consider using mobile X-ray to check for further cases.
-
Put contingency, liaison and handover plans in place to ensure continuity of care before a person being treated for TB is transferred between prisons or released. Any other agencies working with the person should also be involved in this planning.
-
A healthcare professional (e.g. a registered general nurse) should carry out a second-stage health assessment for every person in prison. Do this within 7 days of the first-stage health assessment, and include as a minimum:
-
reviewing the actions and outcomes from the first-stage health assessment;
-
asking the person about any previous misuse of alcohol, use of drugs or improper use of prescription medicine; if they have ever suffered a head injury or lost consciousness, and, if so: how many times this has happened, whether they have ever been unconscious for more than 20 minutes, whether they have any problems with their memory or concentration; smoking history; the date of their last sexual health screen; any history of serious illness in their family (e.g. heart disease, diabetes, epilepsy, cancer or CCs); their expected release date, and if < 1 month plan a pre-release health assessment: see recommendation 1.7.5; whether they have ever had a screening test (e.g. a cervical screening test or mammogram); whether they have, or have had, any gynaecological problems;
-
measuring and recording the person’s height, weight, pulse, blood pressure and temperature, and carrying out a urinalysis.
-
-
Review the person’s first- and second-stage health-assessment records, medical history, GP and vaccination records and refer the person to the GP or a relevant clinic if further assessment is needed. See, for example, NICE’s guidelines on CVD (recommendations on identifying people for full formal risk assessment) or type 2 diabetes (the recommendation on risk assessment). Arrange a follow-up appointment if needed.
-
Consider using the Correctional Mental Health Screen for Men (CMHS-M) or Women (CMHS-W) to identify possible MH problems if: the person’s history, presentation or behaviour suggests they may have a MH problem; the person’s responses to the first-stage health assessment suggest they may have a MH problem; the person has a chronic physical health problem with associated functional impairment; concerns have been raised by other agencies about the person’s abilities to participate in the criminal justice process.
-
When using the CMHS-M or CMHS-W with a transgender person, use the measure that is in line with their preferred gender identity.
-
If there is other evidence supporting the likelihood of MH problems, or a man scores 6 or more on the CMHS-M, or a woman scores 4 or more on the CMHS-W: a practitioner who is trained to perform an assessment of MH problems should conduct further assessment or a practitioner who is not trained to perform an assessment of MH problems should refer the person to an appropriately trained professional for further assessment.
-
Offer people tailored health advice based on their responses to the assessment questions. This should be in a variety of formats (including face-to-face). It should include advice on: alcohol (see NICE’s guideline on alcohol-use disorders), substance misuse (see NICE’s guideline on drug misuse in over 16s), exercise (see recommendations 1.3.3 and 1.3.4), diet (see recommendation 1.3.5), stopping smoking (see recommendation 1.3.6), sexual health (see recommendations 1.3.7 and 1.3.8).
-
Offer the person advice, with supporting literature if appropriate, on: how to contact prison health services and book GP appointments or other clinics, for example, dental, optician, chiropodist, substance-misuse and recovery services; where to find health information that is accessible and understandable; how to attend or get a referral to attend any health-promoting activities in the future (see recommendations 1.3.1–1.3.8); medicines adherence (see recommendation 1.4.7).
-
Enter in the person’s medical record: all answers to the second-stage health assessment questions; health-related observations; details of any action taken.
-
Plan a follow-up healthcare review at a suitable time based on clinical judgement, taking into account the age of the person and length of their sentence. For people who may be in prison for < 1 month, see recommendation 1.7.5.
-
Hepatitis B and C – the recommendations in this section have been adapted from the NICE guideline on hepatitis B. Prison healthcare services (working with the NHS lead for hepatitis) should ensure that: all people are offered a hepatitis B vaccination when entering prison (for the vaccination schedule, refer to the Green Book); all people are offered access to confidential testing for hepatitis B and C when entering prison and during their detention; people who test for hepatitis B or C receive the results of the test, regardless of their location, when they become available; results from hepatitis B and C testing are provided to the person’s community-based GP, if consent is given.
-
HIV – the recommendations in this section have been adapted from the NICE guideline on HIV testing.
-
- Offer all people HIV testing when entering prison.
-
- Primary care providers should ensure annual HIV testing is part of the integrated health care offered to men who are known to have sex with men.
-
- Provide information on HIV testing and discuss why it is recommended (including to those who indicate that they may wish to decline the test).
-
- Conduct post-test discussions, including giving positive test results and delivering post-test and general health-promotion interventions.
-
- Recognise illnesses that may signify primary HIV infection and clinical indicator diseases that often coexist with HIV.
-
-
STIs – identify people at high risk of STIs using their sexual history. Opportunities for risk assessment may arise during consultations on contraception, pregnancy or abortion, and when carrying out a cervical smear test or offering an STI test. Risk assessment could also be carried out during routine care or when a new patient registers; have structured, one-to-one discussions with people at high risk of STIs (if trained in sexual health), or arrange for these discussions to take place with a trained practitioner.
-
Other health checks and screening – offer people equivalent health checks to those offered in the community, for example: the NHS health check programme; learning disabilities; annual health check; relevant NHS screening programmes, such as those for AAA and bowel, breast and cervical cancer.
-
Ensure that the different teams (including prison staff) that manage a person’s care in prison communicate with one another to co-ordinate care.
-
Share information with other health and social care staff, offender supervisors and probation providers who are involved in the person’s care in prison if necessary for the person’s care.
-
Ensure that people with complex health and social care needs have a lead care co-ordinator responsible for managing their care. Ensure that the person and all healthcare and prison staff know who this is.
-
Share relevant information about people with complex needs with prison staff using prison record systems in line with legislation and national guidance. This should include information about any high-level risks, such as: risk of self-harm, risk to others, communicable diseases, epilepsy, diabetes, allergies, deteriorating health conditions, learning disabilities.
-
Review people in prison with complex health and social care needs. Ensure that if a person is supported by a multidisciplinary team, the teams meet regularly to plan and co-ordinate ongoing management. These should be facilitated by primary care.
-
Document all health and social care patient interactions and any information related to health and social care in the person’s primary care patient record.
-
Consider using peer support and mentoring to help promote a healthy lifestyle while in prison.
-
Offer people in prison tailored health information in a variety of formats, including face-to-face. Include advice about: exercise, diet, stopping smoking, sexual health, personal hygiene, including oral hygiene.
-
Encourage people to be physically active. Offer them information about: the benefits of exercise, what exercise facilities are provided, where they are and how they can use them; for example: going to the gym, using the exercise yard, exercises that can be done in the cell.
-
Offer people information and advice in line with recommendations in the NICE guidelines on: physical activity: brief advice for adults in primary care, physical activity: exercise referral schemes, preventing excess weight gain, obesity: identification, assessment and management (section 1.6 on physical activity).
-
Offer people information about: the benefits of a healthy diet and healthier food options available in the prison. See section 1.7 on dietary advice in NICE’s guideline on obesity: identification, assessment and management.
-
Offer people in prison information about the risks of smoking and support available to stop as part of smoking-cessation services (e.g. nicotine patches and motivational support). See the NICE pathway on smoking.
-
Offer people in prison information about STIs and available sexual health services.
-
Ensure that people in prison have discreet access to condoms, dental dams and water-based lubricants without the need to ask for them.
-
Carry out an individual risk assessment to determine if the person can hold their medicines IP. Allow people in prison to hold all medicine IP unless the person does not pass the risk assessment.
-
Directly observe the administration of all schedule 2 and 3 medicines (also see NICE’s guideline on controlled drugs) and medicines for tuberculosis (see NICE’s guideline on tuberculosis).
-
Directly observe the administration of any medicine that is not IP.
-
Work with prison staff to ensure a system is in place to supervise the administering of medicines not held IP to maximise adherence allow timings of medicines doses to align with the prescribed dose regime, reduce diversion (passing medicines on to other people) and protect confidentiality; see the section on supporting adherence in NICE’s guideline on medicines adherence.
-
Review and (if necessary) repeat a person’s risk assessment for IP medicine if the person’s circumstances change. Involve a multidisciplinary team if needed, including prison staff and the person. Examples of when the risk assessment should be repeated include: if carrying out a medicines review if a person is considered able to manage their own medicines after a period of having medicines not IP; if there is a medicine safety incident, including evidence of self-harm if someone has raised security concerns (e.g. about bullying, diversion or hoarding); if the person has not been taking their prescribed medicines; if there is concern about the person’s ability to self-medicate when following the ACCT care planning approach; if the person is transferred to or from a segregation unit.
-
Consider providing storage for IP medicine in prison cells, for example, a lockable cupboard.
-
Give people in prison information and education about medicine adherence (see the section on patient involvement in decisions about medicines in NICE’s guideline on medicine adherence).
Monitor people with CCs in accordance with the following NICE guidelines:
-
Chronic heart failure www.nice.org.uk/guidance/ng106.
-
Epilepsy www.nice.org.uk/guidance/cg137.
-
Hypertension www.nice.org.uk/guidance/ng136.
-
Secondary prevention of MI www.nice.org.uk/guidance/cg172.
-
Diabetes (Type 1) www.nice.org.uk/guidance/ng17.
-
Diabetes (Type 2) www.nice.org.uk/guidance/ng28.
-
Asthma www.nice.org.uk/guidance/qs25.
Local quality indicators
Selected from local quality requirements from the NHS Standard Contract for prison healthcare 2019/2020 for the North East, North West, and Yorkshire and Humber (set by the Commissioning Team under schedule 4) www.england.nhs.uk/nhs-standard-contract/previous-nhs-standard-contracts/19-20/.
-
Number and percentage of patients over the age of 55 who have received an examination/assessment of their attention and concentration, orientation, short- and long-term memory, praxis, language and executive function using a validated tool such as MMSE, six-item Cognitive Impairment Test (6–CIT), or the GPCOG, in accordance with NICE CG42.
-
Number of patients who have been appropriately referred to Memory Assessment Services.
-
Number of patients who have been diagnosed with dementia and what type of dementia: that is vascular, Lewy body etc.
-
Number of patients who are taking acetylcholinesterase inhibitors (donepezil, galantamine, rivastigmine) for mild to moderate disease, or memantine for moderate disease.
-
Detailed ‘How am I Driving Report’ from SystmOne to be submitted with improvement plan for areas that are recording a red indicator.
-
Transfers should be in accordance with NICE NG57, NG66 and Substance Misuse clinical guidance (Orange book). Transfers between Prisons and Courts:
-
Number and percentage of patients with ongoing health needs and/or on prescribed medication seen by a nurse prior to transfer to another establishment.
-
Number and percentage of patients on prescribed medication who are transferred with 7 days' worth of medication.
-
Number and percentage of patients seen by a nurse and declared unfit for transfer.
-
-
The provider to provide a narrative report detailing the total numbers of transfers arriving in the prison, broken down to each month in the time period with the following fields:
-
Arriving without medication – sending prison to be identified.
-
Individuals on clinical substance-misuse pathways arriving without communication with Substance-Misuse Team – sending prison to be identified.
-
Complex MH patients arriving without communication with MH team – sending prison to be identified.
-
Individuals with complex physical health problems arriving without communication with physical health team.
-
Details of reports/concerns received from prisons where it has been highlighted that a patient has been transferred unsafely – containing remedial actions to prevent reoccurrence.
-
-
Released from prison:
-
Number and percentage of patients seen by a nurse prior to release from custody.
-
Number and percentage of patients released from custody with 7 days' worth of medication.
-
-
A pathway is in place with secondary care specialist services and clearly details:
-
The process for blood-borne virus (BBV) screening within the healthcare service in the prison, including screening at reception/second reception and opportunistic screening.
-
How DBSTs are ordered.
-
Where the tests are sent for testing.
-
How results are received back in health care.
-
How patients are informed of the results.
-
The process for referrals to specialist services for those patients with positive results.
-
-
Data to be provided per prison via opt-out method to include amount of DBST, aiming for a target uptake rate of 70%:
-
Number of new receptions per month.
-
Number and percentage of new receptions offered DBST.
-
Number and percentage of new receptions accepting the opt-out DBST.
-
-
Tetanus, diphtheria and inactivated polio vaccine (Td/IPV) – numbers eligible as per National Immunisation Schedule and number received as per National Immunisation Schedule and % who have received.
-
Hep A – numbers eligible as per National Immunisation Schedule and number received as per National Immunisation Schedule – and % received.
-
Pneumococcal (PPV) – numbers eligible as per National Immunisation Schedule and number received as per National Immunisation Schedule, then they can provide % received.
-
The providers have developed a detailed multiagency seasonal flu plan for the implementation and delivery of a vaccination programme for patients, and demonstrate the preparation required for an anticipated outbreak of seasonal flu. The plan must be agreed with PHE.
-
The providers have developed a detailed multiagency Outbreak Plan per prison which has been submitted and agreed with PHE.
-
The provider has in place Patient Group Directions to support both flu vaccination and antiviral medication – there should be no gap in compliance with the antiviral medication, and the flu vaccine patient group direction should be fully authorised before 1 September 2019.
-
The provider to provide a standard operating procedure (SOP) for the management of people with end-of-life care needs within the establishment. SOP to include, but not limited to, access to specialist palliative care advice and support, and suitably trained personnel for administration of syringe driver.
-
Re-audit of Dying Well In Custody against the Ambitions Standards.
-
Submission of Dying Well In Custody audit indicating full compliance against the Dying Well In Custody Ambition standards.
-
Quarterly analysis of numbers of the following medication supported by logs and graphs indicating reduction and improvement plan for reduction: tramadol; pregabalin; gabapentin; benzodiazepines; codeine; zopiclone.
-
An up-to-date Medicines Management Strategy, which includes the reduction of tradeable medication.
Opioid, gabapentin and benzodiazepine prescribing55,56
-
Prescribed pregabalin/gabapentin but no diagnosis of neuropathic pain in clinical record. Current evidence suggests that the risk of misuse may be greater with pregabalin than gabapentin. Consider changing patients to gabapentin who have never previously tried gabapentin for neuropathic pain rather than continuing with pregabalin. It is important for prescribers to have a complete list of medications (including any over-the-counter products or illicit drugs) that patients are taking so that hazardous drug interactions can be minimised or avoided. If dependence on pregabalin or gabapentin, or other misuse or diversion, is suspected or identified the patient should be reviewed and the concerns of the prescriber should be discussed sensitively and documented clearly.
-
Pregabalin/gabapentin prescription and at CKD stage 3–5. Currently, pregabalin appears to be more sought-after for misuse than gabapentin. There is a growing illegal market, and these drugs are also being bought through online pharmacies. Prescribers should evaluate the risks of continued prescribing and make appropriate decisions regarding quantity of drugs prescribed and the intervals at which the patient should be reviewed. If dependence on prescribed medication is suspected or confirmed, the problem may require specialist advice on managing the dependence. It may simply require agreement on suitable controls on access to, and maximum daily use, of the drugs being misused (when it is felt the medication is still needed for the management of the original indication). Careful reassessment of the patient may lead to an appropriate decision to offer a planned withdrawal of the medication, particularly if the medication does not appear any longer to be required for the main clinical indication.
-
Over 65 years and prescribed pregabalin/gabapentin in last 8 weeks. In 2013, the total use in England of both these medicines was 8.2 million prescriptions. This represents a 46% rise in prescribing of gabapentin and 53% rise in pregabalin prescribing since 2011. Prescribers should set realistic expectations and treatment goals. Achieving pain-free status is not always achievable. Reduction in pain by 50% is a commonly used end point in clinical trials. If completely inappropriate use is confirmed (e.g. if there is unequivocal objective evidence that the drugs are simply being diverted), the drugs should be stopped. However, in some cases, patients may have diverted a portion of their treatment, such as to a family member, and so adequate assessment is needed to try and determine the most suitable approach in each case and context.
-
Diagnosis of depression and MH and prescribed pregabalin/gabapentin in last 8 weeks. Gabapentin and pregabalin have been mentioned on death certificates as adjunctive substances in patients dying of drug poisoning.
-
Patient issued at least two of gabapentin/pregabalin/duloxetine/amitriptyline in last 8 weeks. Between 2013 and 2015 in the UK, deaths reported to involve gabapentinoids increased by almost 400%.
-
Pregabalin/gabapentin and an opioid in last 8 weeks.
-
Any issue of lidocaine patch in last 8 weeks.
-
Lidocaine patch and no diagnosis of post-herpetic neuralgia.
-
Lidocaine patch on repeat for last 6 months.
-
Prescribed strong opioids.
Overcoming barriers to self-management of chronic pain in primary care.
Self-management is a recommended intervention for chronic pain and can improve patients’ quality of life and reduce impact on NHS services. This study found a number of barriers to self-management. Many patients felt the initial discussion about self-management came too late or not at all. Consider discussing self-management of pain much earlier in the patient pathway for those at risk of developing chronic non-cancer pain.
-
Men aged under 50 years and prescribed strong opioids.
Initial starting dose and the first refill of an opioid prescription increase risk of chronic use.
This retrospective cohort study followed opioid-naïve patients after their first prescription. Those who received more than one prescription within the first month of taking opioids and those given a higher morphine equivalent dose of opioid were more likely to become long-term users of opioids. Could we reduce the number of people becoming long-term users by thinking twice about that first repeat prescription?
-
Patients aged over 75 and prescribed strong or weak opioids.
Tramadol kills more people than heroin and cocaine.
Professor Jack Crane, State Pathologist of Northern Ireland, says tramadol is now claiming more lives than any other drug. Reclassification to a class C drug last year has made it illegal to use without a prescription, but many are obtaining it via the black market. He is campaigning for it to be reclassified to a Class A drug. In 2014, 240 deaths in Britain were linked to tramadol. Perhaps we need to think carefully before prescribing?
-
Women aged over 65 years and prescribed strong or weak opioids.
-
Polypharmacy (on 10 or more repeat prescriptions) and prescribed strong or weak opioids.
-
Any MH diagnoses and prescribed strong or weak opioids.
-
Taking antidepressant and a strong or weak opioid.
-
Taking benzodiazepines and a strong or weak opioid.
Appendix 5
| Unique identifier | Original wording | Final wording | Substantial refinements | Potential for patient benefit |
|---|---|---|---|---|
| Communicable disease | ||||
| Dry blood spot testing | Data to be provided per prison via opt-out method to include amount of DBST aiming for a target uptake rate of 70%: (1) number of new receptions per month; (2) number and percentage of new receptions offered DBST; (3) number and percentage of new receptions accepting the opt out DBST. (Local quality indicator, selected from local quality requirements from the NHS Standard Contract for prison healthcare 2019/20 for the North East, North West, and Yorkshire and Humber set by the Commissioning Team under schedule 4. www.england.nhs.uk/nhs-standard-contract/previous-nhs-standard-contracts/19-20/) | The proportion of new receptions to prison accepting opt out dry blood spot testing | Simplified | High potential |
| Hepatitis B vaccination | Prison healthcare services (working with the NHS lead for hepatitis) should ensure that: (1) all people are offered a hepatitis B vaccination when entering prison (for the vaccination schedule, refer to the Green Book); (2) all people are offered access to confidential testing for hepatitis B and C when entering prison and during their detention; (3) people who test for hepatitis B or C receive the results of the test, regardless of their location, when they become available; (4) results from hepatitis B and C testing are provided to the person’s community-based GP, if consent is given. NICE identity code: NG57. Date of Publication: 2 November 2016.48 | The proportion of the prison population who have received one, two, three or four (course of three plus booster). The proportion of people with a history of illicit drug use who have received one, two, three or four (course of three plus booster). Hepatitis B vaccinations in the preceding 12 months. Hepatitis B vaccinations in the preceding 12 months | Simplified | High potential |
| Influenza immunisation | The percentage of patients with CHD, stroke or transient ischemic attack, diabetes and/or COPD who have influenza immunisation in the preceding 1 August and 31 March. NICE identity code: NM122. Date of publication: 3 August 2015.47 | The proportion of people with one or more of CHD, stroke or transient ischaemic attack, diabetes or COPD who have received a flu vaccination between August and March | None | High potential |
| Mental health | ||||
| Antipsychotic monitoring | Patients have their antipsychotic medication reviewed regularly, considering symptoms and side effects. NICE identity code: CG178. Date of publication: 2014.29,50 | The proportion of people who have received three or more prescriptions for an antipsychotic in the preceding 12 months, and who have a record of blood testing (fasting glucose, HbA1c, lipid profile, urea and electrolytes, full blood count, liver function tests), BMI and blood pressure | Details added | High potential |
| Polypharmacy | Polypharmacy: reduce number of patients using more than four psychotropic drugs at the same time.29,145 | The proportion of the prison population prescribed three or more psychotropic drugs (antipsychotics, sedative antidepressants, hypnotics and anxiolytics, pregabalin or gabapentin, opioids) at the same time during an 8-week period | Details added | High potential |
| Mental state examination | Number and percentage of patients over the age of 55 who have received an examination/assessment of their attention and concentration, orientation, short and long-term memory, praxis, language and executive function using a validated tool such as MMSE, 6-item CIT, or the GPCOG, in accordance with NICE CG42. NICE identity code: CG42. Date of publication: 2006.49 | The proportion of people aged over 55 years in the prison population who have a record of one of the following assessments in the preceding 12 months; MMSE, 6-item CIT, GPCOG | None | High potential |
| Diagnosis of dementia | The percentage of patients with a new diagnosis of dementia recorded in the preceding 1 April to 31 March with a record of FBC, calcium, glucose, renal and liver function, thyroid function tests, serum vitamin B12 and folate levels recorded between 6 months before or after entering on to the register. NICE identity code: NM09. Date of publication: 3 August 2010.59 | The proportion of people with a new diagnosis of any form of dementia in the reporting year, and who have a record of the following blood tests between 12 months before and 6 months after the date of diagnosis: full blood count, calcium, glucose and/or HbA1c, urea and electrolytes, liver function, thyroid function, serum vitamin B12, folate levels | None | High potential |
| Prison-specific | ||||
| Consent to transfer medical records | Ask the person for consent to transfer their medical records from their GP to the prison healthcare service. NICE identity code: NG57. Date of publication: 2 November 2016.48 | The proportion of new receptions to prison who have been asked for consent to transfer medical records from GP to prison health care | None | High potential |
| MR | Carry out a MR (in line with NICE’s guideline 6 on medicine optimisation) before the second-stage health assessment. NICE identity code: NG57. Date of publication: 2 November 2016.48 | The proportion of new receptions to prison with a code for a second-stage health assessment in the past 12 months, plus clinical codes for IP risk assessment and MR added in the week before the second-stage assessment | Details added | High potential |
| Opioid and gabapentin prescribing | Careful consideration of first repeat opioid prescription for strong opioids (to avoid the long-term opioid use that is associated with > 1 prescriptions in the first month of treatment for men < 50 years)55,56 | (1) The proportion of the prison population prescribed: (i) any opioid, (ii) any strong opioid, (iii) benzodiazepines AND any opioid (2) the proportion of people with any MH diagnosis prescribed any opioid (3) the proportion of the prison population with NO coded diagnosis of neuropathic pain prescribed pregabalin or gabapentin … during an 8-week period |
Details added | High potential |
| Diabetes, asthma and epilepsy care | ||||
| Blood pressure control in diabetes | The percentage of patients with diabetes, on the register, without moderate or severe frailty, on the register, in whom the last blood pressure reading (measured in the preceding 12 months) is 140/80 mmHg or less. NICE identity code: NM02. Date of publication: 3 August 2010.47 | The proportion of people with diabetes in whom the last blood pressure reading (measured in the preceding 12 months) is 140/80 mmHg or less | Simplified (removed ‘without frailty’ wording) | Medium potential |
| Processes of care for diabetes | The percentage of patients with diabetes who have had the following care processes performed in the preceding 12 months: BMI measurement; BP measurement; HbA1c measurement; cholesterol measurement; record of smoking status; foot examination; albumin–creatinine ratio; serum creatinine measurement. NICE identity code: NM74. Date of publication: 1 August 2014.47 | The proportion of people with diabetes who have had the following in the preceding 12 months: BMI, blood pressure, record of smoking status, foot examination, urine albumin–creatinine ratio; blood tests for HbA1c, cholesterol and serum creatinine | None | High potential |
| Glycaemic control for diabetes | The percentage of patients with diabetes without moderate or severe frailty, on the register, in whom the last IFCC-HbA1c is 58 mmol/mol or less in the preceding 12 months. NICE identity code: NM157. Date of publication: 16 October 2018. Last update: August 2022.47 | The proportion of people with diabetes without moderate or severe frailty, in whom the last HbA1c is 58 mmol/mol or less in the preceding 12 months | None | Medium potential |
| Glycaemic control for diabetes with frailty | The percentage of patients with diabetes with moderate or severe frailty, on the register, in whom the last IFCC-HbA1c is 75 mmol/mol or less in the preceding 12 months. NICE identity code: NM158. Date of publication: 17 October 2018.47 | The proportion of people with diabetes and moderate or severe frailty, in whom the last HbA1c is 75 mmol/mol or less in the preceding 12 months | None | Medium potential |
| Asthma review | The percentage of patients with asthma, on the register, who have had an asthma review in the preceding 12 months that includes an assessment of asthma control using the 3 RCP questions. Identity code: AST003. Last revised in May 2021.51 | The proportion of people with asthma who have had an asthma review in the preceding 12 months that includes an assessment of asthma control | None | Medium potential |
| Epilepsy review and control | The percentage of patients aged 18 or over on drug treatment for epilepsy who have been seizure-free for the last 12 months recorded in the preceding 12 months. NICE identity code: NM110. Date of publication: 3 August 2015.47 | The proportion of people on drug treatment for epilepsy who have had an annual review and recorded as seizure-free in the preceding 12 months | None | Medium potential |
| Screening | ||||
| Cervical screening age 25–49 years | The proportion of patients eligible for cervical screening and aged 25–49 years at end of period reported whose notes record that an adequate cervical screening test has been performed in the previous 3.5 years. NICE identity code: NM154. Date of publication: 31 July 2017.47 | The proportion of women eligible for screening and aged 25–49 years who have had cervical screening in the preceding 5 years and 6 months | None | High potential |
| Cervical screening age 50–64 years | The proportion of patients eligible for cervical screening and aged 50–64 years at end of period reported whose notes record that an adequate cervical screening test has been performed in the previous 5.5 years. NICE identity code: NM155. Date of publication: 31 July 2017.47 | The proportion of women eligible for screening and aged 50–64 years who have had cervical screening in the preceding 5 years and 6 months | None | High potential |
| Breast screening | Offer people equivalent health checks to those offered in the community, for example: relevant NHS screening programmes, such as those for breast cancer.48 Refers to: The proportion of women aged 50–70 years whose record shows a breast screening test has been performed within the last 3 years. NICE identity code: CCG84. Date of publication: 17 November 2017.58 |
The proportion of women eligible for screening and aged 50–70 years who have had breast screening in the preceding 3 years | None but disaggregated from composite screening indicator | High potential |
| AAA screening | Offer people equivalent health checks to those offered in the community, for example: relevant NHS screening programmes, such as those for AAA.48 Refers to: AAA screening is offered to men during the screening year (1 April to 31 March) that they turn 65. Date of publication: 2 January 2015.61 |
The proportion of men eligible for screening and aged 65 years or over with a record of AAA screening | None but disaggregated from composite screening indicator | High potential |
| CVD risk assessment | Offer people equivalent health checks to those offered in the community, for example: the NHS health check programme.48 Refers to: the NHS health check programme.146 |
The proportion of people aged 45–74 years with a recorded CVD risk assessment in the preceding 5 years, and who do NOT have a diagnosis of: CHD, CKD, diabetes, hypertension, AF, transient ischaemic attack, familial hypercholesterolaemia, heart failure, peripheral arterial disease, stroke or previously documented 20% or higher 10-year CVD risk BEFORE the last 5 years | High potential | |
| CVD | ||||
| Secondary prevention of stroke | The percentage of patients with a stroke shown to be non-haemorrhagic, or a history of TIA, who have a record in the preceding 12 months that an antiplatelet agent or an anticoagulant is being taken. NICE identity code: NM94. Date of publication: 3 August 2015.47 | The proportion of people with transient ischaemic attack or stroke, excluding those with haemorrhagic stroke, who have been prescribed an antiplatelet or anticoagulant in the preceding 12 months | None | High potential |
| Anticoagulation for AF | In those patients with AF with a record of a CHA2DS2-VASc score of 2 or more, the percentage of patients who are currently treated with anticoagulation drug therapy. NICE identity code: NM82. Date of publication: 1 August 2014.47 | The proportion of people with persistent or paroxysmal AF and a CHA2DS2-VASc score equal to 2 or more, with a prescription for warfarin or a direct-acting oral anticoagulant in the preceding 12 months | None | High potential |
| Stroke risk assessment in AF | The percentage of patients with AF in whom stroke risk has been assessed using the CHA2DS2-VASc score risk stratification scoring system in the preceding 12 months (excluding those patients with a previous CHADS2 or CHA2DS2-VASc score of 2 or more). NICE identity code: NM81. Date of publication: 1 August 2014.47 | The proportion of people with persistent or paroxysmal AF and a CHA2DS2-VASc score in the preceding 12 months | None | High potential |
| Blood pressure control in CVD (79 years or under) | – The percentage of patients aged 79 or under with peripheral arterial disease in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less. NICE identity code: NM67. Date of publication: 1 August 2013. (NICE 2013)47 – The percentage of patients aged 79 years or under, with CHD, in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less. NICE identity code: NM68. Date of publication: 1 August 2013. (NICE 2013)48 |
The proportion of people aged 79 years or under, with CHD, hypertension, stroke, transient ischaemic attack or peripheral arterial disease, who have had a blood pressure of 140/90 mmHg or less in the preceding 12 months | Disaggregated from BP summary then four of those single indicators combined into a composite | High potential |
| – The percentage of patients aged 79 or under with stroke or TIA in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less. NICE identity code: NM69. Date of publication: 1 August 2013.47 – The percentage of patients aged 79 years or under, with hypertension, in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less. Identity code: HYP003. Date of publication: 2019.51 |
||||
| Blood pressure control in CVD (80 years or over) | – The percentage of patients aged 80 years and over, with hypertension, in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. NICE identity code: NM54. Date of publication: 1 August 2012.47 – The percentage of patients aged 80 years or over, with a history of stroke or TIA, in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. Identity code: STIA011. Date of publication: 2019.51 |
The proportion of people aged 80 years or over, with CHD, hypertension, stroke, transient ischaemic attack or peripheral arterial disease, who have had a blood pressure of 150/90 mmHg or less in the preceding 12 months | Disaggregated from BP summary then four of those single indicators combined into a composite | High potential |
| – The percentage of patients aged 80 years or over, with CHD, in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. Identity code: CHD009. Date of publication: 2019.51 – The percentage of patients with peripheral arterial disease in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less. NICE identity code: NM193. Date of publication: 31 July 2019.47 |
||||
| Secondary prevention of MI | The percentage of patients who had a MI in the preceding 1 April to 31 March and who are currently being treated with ACE-I (or ARB if ACE-I intolerant), dual antiplatelet therapy, a statin and a beta-blocker for those patients with left ventricular systolic dysfunction. NICE identity code: NM79. Date of publication: 1 August 2014.60 | The proportion of people who have had a MI and have received a prescription for an ACE-I or ARB, antiplatelet therapy, beta-blocker and a statin in the preceding 12 months | None | High potential |
| Treatment of CHD | The percentage of patients with CHD with a record in the preceding 12 months that aspirin, an alternative antiplatelet therapy, or an anticoagulant is being taken. NICE identity code: NM88. Date of publication: 3 August 2015.47 | The proportion of people with CHD who have received a prescription for antiplatelet or anticoagulant therapy in the preceding 12 months | None | High potential |
| Treatment of heart failure (1) | In those patients with a current diagnosis of heart failure due to left ventricular systolic dysfunction who are currently treated with an ACE-I or ARB, the percentage of patients who are additionally currently treated with a beta-blocker licensed for heart failure. Identity code: NM173. Date of publication: 31 July 2019.47 | The proportion of people with heart failure who have been prescribed an ACE-I or ARB in the preceding 12 months | None | High potential |
| Treatment of heart failure (2) | The percentage of patients with a current diagnosis of heart failure due to left ventricular systolic dysfunction, who are currently treated with an ACE-I or ARB. NICE identity code: NM172. Date of publication: 31 July 2019.47 | The proportion of people with heart failure who have been prescribed an ACE-I or ARB, and a beta-blocker, in the preceding 12 months | None | High potential |
Appendix 6
| Indicator | Achievement (%) | Comparison with community (%) |
|---|---|---|
| Communicable disease | ||
| The percentage of new receptions who have had dried blood spot testing in the past 12 months | 44.8 | |
| The percentage of people with a record of hepatitis B vaccination in the past 12 months | ||
| (1) out of the whole prison population | ||
| 1 vaccination | 45.7 | |
| 2 vaccinations | 37.2 | |
| 3 vaccinations | 30.3 | |
| 4 vaccinations | 12.3 | |
| (2) out of people with clinical code indicating a history of illicit drug use | ||
| 1 vaccination | 0.1 | |
| 2 vaccinations | 40.9 | |
| 3 vaccinations | 33.2 | |
| 4 vaccinations | 14.6 | |
| The percentage of people with CHD, stroke or transient ischaemic attack, diabetes and/or COPD who have had flu vaccination in the preceding 1 August and 31 March | 44.9 | 70.0 |
| Mental health | ||
| The percentage of people prescribed antipsychotics who have had appropriate laboratory screening tests (fasting glucose, HbA1c, lipid profile, urea and electrolytes, full blood count, liver function tests, BMI, blood pressure) in the past 12 months | ||
| Blood monitoring | 0–9.5 | |
| Blood pressure | 15.1 | 80.3 |
| The proportion of people prescribed three or more psychotropic drugs (antipsychotics, sedative antidepressants, hypnotics and anxiolytics, pregabalin or gabapentin, opioids) at the same time during an 8-week period | ||
| Three or more | 0.8 | |
| Four or more | 0.4 | |
| The percentage of patients aged over 55 years in the preceding 1 April to 31 March who have a record of MMSE, 6-item CIT, or the GPCOG in the past 12 months | 19.6 | |
| The percentage of people with a new clinical code for any forms of dementia recorded in the preceding 1 April to 31 March with a record of full blood count, calcium, glucose and/or HbA1c, renal and liver function, thyroid function tests, serum vitamin B12 and folate levels recorded between 12 months before or 6 months after entering onto the register | 0–76.9 | 70.01 |
| Prison-specific | ||
| The percentage of new receptions who have been asked for consent to transfer medical records from their GP to the prison healthcare service in the past 12 months | 70.4 | |
| The percentage of new receptions in the past 12 months who have had an IP risk assessment and MR added in the 7 days before their second reception screening | 38.2 (both) | |
| The percentage of people prescribed, during an 8-week period | ||
| (1) out of the whole prison population (i) any opioid | 11.5 | 12.8 (est) |
| (1) out of the whole prison population (ii) any strong opioid | 8.7 | 0.85 |
| (1) out of the whole prison population (iii) benzodiazepines AND any opioid | 8.7 | |
| (2) with any MH diagnosis prescribed any opioid | 19 | |
| (3) out of the whole prison population with NO coded diagnosis of neuropathic pain prescribed pregabalin or gabapentin | 0.8 | |
| Diabetes, asthma and epilepsy care | ||
| The percentage of people on the diabetes register who have had the following care processes performed in the preceding 12 months: BMI measurement; BP measurement; HbA1c measurement; cholesterol measurement; record of smoking status; foot examination; albumin–creatinine ratio; serum creatinine measurement | 0.01–93.8 | |
| Foot examination | 40.5 | 78 |
| The percentage of people on the diabetes register, (1) who have had a blood pressure reading recorded in the last 12 months, and (2) in whom the last blood pressure reading (measured in the preceding 12 months) is 140/80 mmHg or less | 33.9 | 68 |
| The percentage of people on the diabetes register, without moderate or severe frailty, (1) who have had their IFCC-HbA1c recorded in the preceding 12 months, and (2) in whom their last IFCC-HbA1c (recorded in the preceding 12 months) is 58 mmol/mol or less | 34.4 | 56.7 |
| The percentage of people on the diabetes register, with moderate or severe frailty, (1) who have had their IFCC-HbA1c recorded in the preceding 12 months, and (2) in whom their last IFCC-HbA1c (recorded in the preceding 12 months) is 75 mmol/mol or less | 64.3 | 80 |
| The percentage of people on the asthma register who have had an asthma review in the preceding 12 months that includes an assessment of asthma control using the 3 RCP questions | 3.1 | 67.14 |
| The percentage of people with a coded diagnosis of epilepsy and who have been prescribed drug treatment for epilepsy | ||
| (1) who have had an epilepsy annual review in the past 12 months | 1.2 | |
| (2) been coded as seizure-free in the last 12 months | 0.2 | 57.5 |
| Screening | ||
| The percentage of women eligible for screening and aged 25–49 years at the end of reporting period whose notes record that an adequate cervical screening test has been performed in the preceding 3 years and 6 months | 63.8 | 71.48 |
| The percentage of women eligible for screening and aged 50–64 years at the end of the reporting period whose notes record that an adequate cervical screening test has been performed in the previous 5 years and 6 months | 61.4 | 77.64 |
| The percentage of women aged 53–70 years with a record of mammography in the preceding 3 years | 33 | 70.5 |
| The percentage of men aged 65 years or over with a record of AAA screening | 44.6 | 79.5 |
| The percentage of people aged 45–74 years who do NOT have a current diagnosis of any of the following: CHD, CKD, diabetes, hypertension, AF, TIA, familial hypercholesterolaemia, heart failure, peripheral arterial disease, or stroke, or have a previously documented 20% or higher 10-year CVD risk BEFORE the last 5 years, who have a recorded CVD risk assessment score in the preceding 5 years | 29.8 | 43.7 |
| CVD | ||
| The percentage of people with a record of a MI who are prescribed an ACE-I, ARB, antiplatelet therapy, beta-blocker or a statin | ||
| statin | 70.3 | 70.6 |
| ACE-I | 42.1 | |
| ARB | 0 | |
| The percentage of people with a clinical code for persistent or paroxysmal AF and whose most recent CHA2DS2-VASc score is 2 or more, with a current acute or repeat prescription for anticoagulation drug therapy | 83.2 | 87.3 |
| The percentage of people with a clinical code for persistent or paroxysmal AF in whom stroke risk has been assessed using the CHA2DS2-VASc in the preceding 12 months | 60 | 93.4 |
| The percentage of people with a clinical code for TIA, stroke or ischaemic stroke (not haemorrhagic stroke) prescribed any antiplatelet or anticoagulant in the preceding 12 months | 59.3 | 91 |
| The percentage of people aged 79 or under, with CHD OR hypertension OR stroke/TIA OR peripheral arterial disease (but NOT diabetes or CKD), (1) who have had a blood pressure reading recorded in the last 12 months and (2) in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less | 44.7 | 70 |
| The percentage of people aged 80 years or over, with CHD OR hypertension OR stroke/TIA OR peripheral arterial disease (but NOT diabetes or CKD), (1) who have had a blood pressure reading recorded in the last 12 months and (2) in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less | 52.6 | 80 |
| The percentage of people with a record of CHD who are prescribed aspirin, alternative antiplatelet therapy or anticoagulant in the last 12 months | 72.9 | 90.8 |
| The percentage of people with a record of heart failure due to left ventricular systolic dysfunction, who are prescribed an ACE-I or ARB in the last 12 months | 63.3 | 82 |
| The percentage of people with a record of heart failure due to left ventricular systolic dysfunction and who are currently treated with an ACE-I or ARB, who are additionally prescribed a beta-blocker | 80.3 | 82 |
Appendix 7
Appendix 8 Summaries of the model results by themes
Tables 18–23: Quality indicators and results. Searches covered the 12-month period ending 31 March for the years 2017–20 except for indicators examining opioid, gabapentinoid and psychotropic prescribing, which used an 8-week period preceding 31 March for the years 2017–20.
| Indicator | Achievement | Variation in ORs between prisons (range of ORs) | Association between explanatory variables and achievement (OR; 95% CI) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019–20 (%)a | 2019–20 compared to 2017–18 (OR; 95% CI) | Prison categoryb (comparator category A) | Genderc (comparator female) | Agec (comparator 30–39 years) | Length of stay (months)c (comparator 1–<6 months) | Ethnic groupc (comparator white people) | |||||||
| Higher | Lower | Higher | Lower | Higher | Lower | Higher | Lower | Higher | Lower | ||||
| Blood pressure control in diabetes: proportion of the prison population with diabetes whose most recent blood pressure was ≤140/80 mmHg in the last 12 months | 261 of 770 eligible people (33.9%) | No change (1.17; 0.9 to 1.51) | 3.6-fold (0.95 to 3.42) | C (1.94; 1.47 to 2.57) Closed (2.94; 2.05 to 4.22) D (1.61; 1.14 to 2.27) |
d | d | d | 20–29 (2.82; 1.86526 to 4.3) 30–39 (1.59; 1.13148 to 2.2) 80–89 (2.15; 1.00321 to 4.6) (comparator 50–59 years) |
d | >24 (1.95; 1.34 to 2.85) | d | d | Asian/Asian British (0.58; 0.36 to 0.95) |
| Processes of care for diabetes: proportion of the prison population with diabetes who have had ≥5 of these measurements in the preceding 12 months: BMI, blood pressure, record of smoking status, foot examination, urine albumin–creatinine ratio, blood tests for HbA1c, cholesterol, creatinine | 426 of 770 eligible people (55.3%) | Increase (1.51; 1.15 to 1.99) | 5.7-fold (0.78 to 4.46) | d | B (0.10; 0.07 to 0.13) C (0.30; 0.22 to 0.4) Closed (0.12; 0.08 to 0.18) D (0.37; 0.26 to 0.54) |
d | d | 50–59 (1.76; 1.23 to 2.54) | d | 6–12 (2.29; 1.65 to 3.19) 12–24 (2.39; 1.67 to 3.42) >24 (3.41; 2.32 to 5.03) |
<1 (0.38; 0.25 to 0.58) | d | d |
| Glycaemic control for diabetes: proportion of the prison population with diabetes and without moderate or severe frailty, whose most recent HbA1c was ≤58 mmol/mol in the last 12 months | 260 of 756 eligible people (34.4%) | No change (1.15; 0.88 to 1.51) | 7-fold (0.34 to 2.39) | d | B (0.36; 0.28 to 0.47) Closed (0.60; 0.41 to 0.86) |
d | d | d | 20–29 (0.31; 0.16 to 0.58) 30–39 (0.52; 0.35 to 0.76) (comparator 50–59 years) |
6–12 (2.58; 1.83 to 3.64) 12–24 (2.07; 1.42 to 3.01) >24 (2.47; 1.68 to 3.65) |
<1 (0.21; 0.12 to 0.38) | Black/Black British (3.08; 1.6 to 5.91) | d |
| Glycaemic control for diabetes with frailty: proportion of the prison population with diabetes and moderate or severe frailty, whose most recent HbA1c was ≤75 mmol/mol in the last 12 months | 9 of 14 eligible people (64.3%) | e | e | e | e | e | e | e | e | e | e | e | e |
| Asthma review: proportion of the prison population with asthma who had an asthma review in the last 12 months that included an assessment of asthma control | 136 of 4459 eligible people (3.1%) | Decrease (0.14; 0.11 to 0.17) | 11.2-fold (0.68 to 7.62) | d | B (0.09; 0.07 to 0.12) C (0.20; 0.16 to 0.25) Closed (0.25; 0.19 to 0.32) D (0.18; 0.14 to 0.24) YOI (0.31; 0.22 to 0.43) |
d | d | 50–59 (1.48; 1.15 to 1.9) 60–69 (2.26; 1.57 to 3.25) 70–79 (4.11; 2.26 to 7.46) |
d | 6–12 (1.78; 1.4 to 2.25) 12–24 (2.58; 2.04 to 3.27) >24 (4.06; 3.14 to 5.24) |
<1 (0.36; 0.24 to 0.53) | Asian/Asian British (1.49; 1.04 to 2.14) Chinese/other (2.21; 1.03 to 4.75) |
d |
| Epilepsy review and control: proportion of the prison population with epilepsy and prescribed antiepileptic drug(s), who had an annual review and were seizure-free in the last 12 months | Annual review: 5 of 419 eligible people (1.2%) Seizure-free: 1 of 419 eligible people (<1.00%) |
e | e | e | e | e | e | e | e | e | e | e | e |
| Secondary prevention of stroke: proportion of the prison population with transient ischaemic attack or stroke (excluding haemorrhagic stroke), prescribed an antiplatelet/anticoagulant in the last 12 months | 51 of 86 eligible people (59.3%) | No change (0.84; 0.22 to 3.16) | 43-fold (0.03 to 1.29) | B (14.65; 5.32 to 40.38) C (8.23; 3.94 to 17.2) D (23.96; 5.08 to 113.02) |
d | d | d | d | d | d | d | d | d |
| Anticoagulation for AF: proportion of the prison population with persistent/paroxysmal AF and CHA2DS2-VASc score ≥2, with a prescription for warfarin/direct-acting oral anticoagulant in the last 12 months | 45 of 54 eligible people (83.3%) | e | e | e | e | e | e | e | e | e | e | e | e |
| Stroke risk assessment in AF: proportion of the prison population with persistent/paroxysmal AF, and a CHA2DS2-VASc score in the last 12 months | 15 of 25 eligible people (60%) | Increase (5.17; 1.02 to 26.2) | 34.3-fold (0.15 to 5.14) | d | C (0.19; 0.05 to 0.74) | d | d | d | d | d | d | d | d |
| Blood pressure control in people 79 years or under with CVD: proportion of the prison population aged ≤79 years with CHD, hypertension, stroke, transient ischaemic attack or peripheral arterial disease, and without diabetes or CKD, with blood pressure ≤ 140/90 mmHg in the last 12 months | 586 of 1311 eligible people (44.7%) | No change (0.94; 0.78 to 1.13) | 6.6-fold (0.52 to 3.42) | C (1.32; 1.08 to 1.62) Closed (2.31; 1.74 to 3.06) D (2.06; 1.58 to 2.68) |
d | d | d | 20–29 (1.88; 1.23 to 2.86) 30–39 (1.36; 1.06 to 1.74) (comparator 50–59 years) |
d | >24 (1.42; 1.08 to 1.87) | d | Asian/Asian British (1.76; 1.09 to 2.84) | d |
| Blood pressure control in people 80 years or over with CVD: proportion of the prison population aged ≥80 years with CHD, hypertension, stroke, transient ischaemic attack or peripheral arterial disease, and without diabetes or CKD, with blood pressure ≤ 150/90 mmHg in the last 12 months | 10 of 19 eligible people (52.6%) | e | e | e | e | e | e | e | e | e | e | e | e |
| Secondary prevention of MI: proportion of the prison population with MI, prescribed all of the following in the last 12 months: ACE-I/ARB, antiplatelet, beta-blocker and statin | 0 of 492 eligible people (0%) | d | d | d | d | d | d | d | d | d | d | d | d |
| Treatment of CHD: proportion of the prison population with CHD prescribed antiplatelet/anticoagulant therapy in the last 12 months | 360 of 494 eligible people (72.9%) | No change (1.13; 0.78 to 1.64) | 2.4-fold (0.86 to 2.10) | d | B (0.46; 0.32 to 0.66) Closed (0.23; 0.14 to 0.4) |
d | d | d | 20–29 (0.15; 0.05 to 0.4) 30–39 (0.11; 0.06 to 0.19) 40–49 (0.40; 0.26 to 0.6) (comparator 50–59 years) |
d | <1 (0.41; 0.25 to 0.67) | d | d |
| Treatment of heart failure: proportion of the prison population with heart failure, prescribed an ACE-I/ARB in the last 12 months | 62 of 98 eligible people (63.3%) | Decrease (0.32; 0.12 to 0.82) | 6.6-fold (0.6 to 3.94) | B (2.36; 1.02 to 5.49) C (3.21; 1.4 to 7.36) D (5.74; 1.42 to 23.28) |
d | d | d | d | d | d | d | d | d |
| Treatment of heart failure: proportion of the prison population with heart failure, prescribed an ACE-I/ARB and beta-blocker, in the last 12 months | 49 of 61 eligible people (80.3%) | Decrease (0.87; 0.27 to 2.76) | d | d | d | d | d | d | d | d | d | d | d |
| Indicator | Achievement | Variation in ORs between prisons (range of ORs) | Association between explanatory variables and achievement (OR; 95% CI) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019–20 (%) | 2019–20 compared to 2017–18 (OR; 95% CI) | Prison categorya (comparator category A) | Genderb (comparator female) | Ageb (comparator 30–39 years) | Length of stay (months)b (comparator 1–<6 months) | Ethnic groupb (comparator white people) | |||||||
| Higher | Lower | Higher | Lower | Higher | Lower | Higher | Lower | Higher | Lower | ||||
| Cervical screening age 25–49 years: proportion of women in prison eligible for cervical screening, aged 25–49 years who had the test in the last 3 years and 6 months | 1145 of 1796 eligible people (63.8%) | Increase (1.61; 1.37 to 1.89) | c | c | c | c | c | c | 20–29 (0.6; 0.47 to 0.68) 40–49 (0.8; 0.72 to 0.97 |
6–12 (1.9; 1.52 to 2.29) 12–24 (2.0; 1.61 to 2.58) >24 (2.6; 1.97 to 3.43) |
<1 (0.7; 0.56 to 0.78) | c | Chinese/other (0.6; 0.33 to 0.95) |
| Cervical screening age 50–64 years: proportion of women in prison eligible for cervical screening, aged 50–64 years who had the test in the last 5 years and 6 months | 159 of 259 eligible people (61.4%) | Increase (1.5; 1.01 to 2.24) | c | c | c | c | c | c | c | c | c | c | c |
| Breast screening: proportion of women in prison eligible for breast screening, aged 50–70 years, who had the test in the last 3 years | 59 of 179 eligible people (33%) | Increase (1.69; 0.88 to 3.21) | c | c | c | c | c | c | c | c | c | c | c |
| AAA screening: proportion of men in prison eligible for AAA screening, aged ≥65 years who have had the test | 241 of 540 eligible people (44.6%) | No change (1.32; 0.94 to 1.85) | 14.5-fold (0.63 to 9.12) | c | B (0.29; 0.22 to 0.38) C (0.51; 0.39 to 0.68) D (0.66; 0.44 to 0.99) |
c | c | c | c | 12–24 (5.04; 2.98 to 8.54) >24 (8.04; 4.53 to 14.26) |
<1 (0.27; 0.14 to 0.54) | Mixed (3.59; 1 to 12.89) | c |
| CVD risk assessment: proportion of the prison population aged 45–74 years with CVD risk assessment in the last 5 years. People with diagnoses of CHD, CKD, diabetes, hypertension, AF, transient ischaemic attack, familial hypercholesterolaemia, heart failure, peripheral arterial disease, stroke or ≥20% 10-year CVD risk before the last 5 years were excluded | 353 of 1183 eligible people (29.8%) | d | 14.6-fold (0.69 to 10.04) | D (1.82; 1.17 to 2.84) | B (0.44; 0.3 to 0.63) C (0.56; 0.41 to 0.78) Closed (0.48; 0.29 to 0.8) |
c | c | c | c | 6–12 (1.88; 1.19 to 2.97) 12–24 (1.78; 1.12 to 2.82) |
c | c | c |
| Indicator | Achievement | Variation in ORs between prisons (range of ORs) | Association between explanatory variables and achievement (OR; 95% CI) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019–20 (%) | 2019–20 compared to 2017–18 (OR; 95% CI) | Prison categorya (comparator category A) | Genderb (comparator female) | Age (comparator 30–39 years)b | Length of stay (months)b (comparator 1–<6 months) | Ethnic groupb (comparator white people) | |||||||
| Higher | Lower | Higher | Lower | Higher | Lower | Higher | Lower | Higher | Lower | ||||
| Antipsychotic monitoring: proportion of the prison population with ≥3 prescriptions for a first- or second-generation antipsychotic drug, and ≥5 of these measurements in the preceding 12 months: BMI, blood pressure, blood tests for fasting glucose and/or HbA1c, lipid profile, renal and liver function, full blood count | 24 of 463 eligible people (5.2%) | Decrease (0.13; 0.07 to 0.24) | 12.57-fold (0.68 to 8.55) | c | B (0.07; 0.04 to 0.13) C (0.14; 0.08 to 0.24) Closed (0.21; 0.12 to 0.36) |
c | c | c | c | >24 (3.48; 1.66 to 7.31) | c | Asian/Asian British (5.67; 1.84 to 17.46) Black/Black British (4.04; 1.12 to 14.54) |
c |
| Polypharmacy, prescribed three or more psychotropic drugs: proportion of the prison population prescribed ≥3 psychotropic drugs (antipsychotics, sedative antidepressants, hypnotics and anxiolytics, pregabalin or gabapentin, opioids) at the same time during an 8-week period | 216 of 25,811 eligible people (0.8%) | Increase (1.76; 1.37 to 2.25) | 11.9-fold (0.25 to 2.94) | Closed (3.33; 2.3 to 4.82) | D (0.35; 0.2 to 0.64) | c | c | c | 20–29 (0.51; 0.38 to 0.69) | 6-–2 (1.64; 1.26 to 2.14) 12–24 (2.16; 1.64 to 2.85) |
<1 (0.43; 0.31 to 0.62) | c | Asian/Asian British (0.22; 0.07 to 0.69) |
| Polypharmacy, prescribed four or more psychotropic drugs: proportion of the prison population prescribed ≥4 psychotropic drugs at the same time during an 8-week period | 103 of 25,811 eligible people (0.4%) | Increase (2.30; 1.56 to 3.39) |
33-fold (0.10 to 3.30) | Closed (6.22; 3.3 to 11.72) | D (0.07; 0.01 to 0.57) | c | c | c | 20–29 (0.56; 0.36 to 0.87) | 6–12 (2.19; 1.48 to 3.24) 12–24 (2.82; 1.84 to 4.32) >24 (1.92; 1.07 to 3.42) |
<1 (0.38; 0.21 to 0.67) | c | c |
| Mental state examination: proportion of the prison population over 55 years with a record of one of these assessments in the preceding 12 months: MMSE, 6-item CIT, GPCOG | 370 of 1884 eligible people (19.6%) | Increase (40.47; 25.34 to 64.64) | 168.9-fold (0.65 to 109.76) | B (8.41; 5.79 to 12.2) Closed (2.52; 1.48 to 4.3) D (6.87; 4.44 to 10.64) |
c | c | c | c | c | c | c | c | c |
| Diagnosis of dementia: proportion of the prison population with a new diagnosis of any form of dementia, and a record of ≥5 of these blood tests 12 months before to 6 months after date of diagnosis: full blood count, calcium, glucose and/or HbA1c, renal and liver function, thyroid function, vitamin B12, folate | 6 of 13 eligible people (46.2%) | d | d | d | d | d | d | d | d | d | d | d | d |
| Indicator | Achievement | Variation in ORs between prisons (range of ORs) | Association between explanatory variables and achievement (OR; 95% CI) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019–20 (%) | 2019–20 compared to 2017–8 (OR; 95% CI) | Prison categorya (comparator category A) | Genderb (comparator female) | Age (comparator 30–39 years)b | Length of stay (months)b (comparator 1–<6 months) | Ethnic groupb (comparator white people) | |||||||
| Higher | Lower | Higher | Lower | Higher | Lower | Higher | Lower | Higher | Lower | ||||
| Dried blood spot testing: proportion of new receptions to prison accepting opt out dried blood spot testing for hepatitis B, HCV and HIV | 5653 of 12,606 (44.8%) | Increase (212.13; 170.37 to 264.13) | 169-fold (0.05 to 8.45) | B (1.31; 1.1 to 1.55) C (2.95; 2.48 to 3.51) Closed (8.09; 6.68 to 9.79) D (2.94; 2.45 to 3.54) YOI (3.87; 3.1 to 4.83) |
c | c | c | c | c | 6–12 (1.36; 1.22 to 1.51) 12–24 (1.30; 1.14 to 1.5) >24 (10.15; 6.73 to 15.31) |
<1 (0.53; 0.48 to 0.58) | c | c |
| Hepatitis B vaccination for the those entering prison in the last 12 months: proportion of those entering prison in the last 12 months who have received at least one hepatitis B vaccination in the preceding 12 months | 8210 of 17,957 eligible people (45.7%) | Increase (2.45; 2.32 to 2.6) | 3.9-fold (0.52 to 2.04) | Closed (1.47; 1.29 to 1.67) D (1.20; 1.05 to 1.36) YOI (1.63; 1.4 to 1.91) |
B (0.63; 0.56 to 0.7) | c | c | c | 10–19 (0.55; 0.46 to 0.66) 40–49 (0.92; 0.86 to 0.98) 50–59 (0.84; 0.76 to 0.91) 60–69 (0.75; 0.64 to 0.88) 70–79 (0.58; 0.42 to 0.79) 80–89 (0.48; 0.25 to 0.92) |
6–12 (1.14; 1.06 to 1.22) 12–24 (1.65; 1.5 to 1.8) >24 (1.68; 1.43 to 1.98) |
<1 (0.76; 0.72 to 0.81) | c | Asian/Asian British (0.86; 0.77 to 0.97) Black/Black British (0.76; 0.65 to 0.9) Chinese/other (0.72; 0.57 to 0.92) |
| Hepatitis B vaccination for people with a history of illicit drug use: proportion of the prison population with a history of illicit drug use who have received at least one hepatitis B vaccination in the preceding 12 months | 5117 of 10,207 eligible people (50.1%) | Increase (3.64; 3.37 to 3.93) | 10.9-fold (0.64 to 6.99) | Closed (1.76; 1.47 to 2.12) YOI (1.50; 1.21 to 1.86) |
B (0.67; 0.57 to 0.8) | c | c | c | 10–19 (0.6; 0.47 to 0.76) 40–49 (0.89; 0.82 to 0.96) 50–59 (0.86; 0.76 to 0.99) 60–69 (0.55; 0.39 to 0.78) |
6–12 (1.12; 1.03 to 1.23) 12–24 (1.53; 1.36 to 1.73) >24 (1.46; 1.15 to 1.85) |
<1 (0.83; 0.77 to 0.89) | c | Black/Black British (0.75; 0.59 to 0.96) |
| Influenza immunisation: proportion of the prison population with one or more of: CHD, stroke, transient ischaemic attack, diabetes or COPD, who received an influenza vaccination August–March | 787 of 1752 eligible people (44.9%) | Increase (1.22; 1.02 to 1.45) | 18.2-fold (0.13 to 2.36) | c | B (0.26; 0.22 to 0.31) C (0.82; 0.68 to 0.99) Closed (0.42; 0.34 to 0.52) D (0.60; 0.47 to 0.76) YOI (0.12; 0.03 to 0.56) |
c | c | c | c | 6–12 (2.16; 1.74 to 2.69) 12–24 (2.89; 2.29 to 3.65) >24 (3.96; 3.09 to 5.07) |
<1 (0.46; 0.35 to 0.6) | c | Black/Black British (0.58; 0.34 to 0.99) Chinese/other (0.40; 0.17 to 0.92) |
| Indicator | Achievement | Variation in ORs between prisons (range of ORs) | Association between explanatory variables and achievement (OR; 95% CI) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019–20 (%) | 2019–20 compared to 2017–18 (OR; 95% CI) | Prison categorya (comparator category A) |
Gender b (comparator female) | Ageb (comparator 30–39 years) | Length of stay (months)b (comparator 1–<6 months) | Ethnic groupb (comparator white people) | |||||||
| Higher | Lower | Higher | Lower | Higher | Lower | Higher | Lower | Higher | Lower | ||||
| Prescribed any opioid: proportion of the prison population prescribed any opioid during an 8-week period | 2957 of 25,811 eligible people (11.5%) | Increase (1.47; 1.38 to 1.58) | 5-fold (0.26 to 1.31) | C (1.30; 1.19 to 1.43) Closed (1.47; 1.32 to 1.64) |
B (0.73; 0.66 to 0.8) D (0.14; 0.11 to 0.17) |
c | c | 40–49 (1.38; 1.29 to 1.48) | 10–19 (0.14; 0.07 to 0.27) 20–29 (0.44; 0.41 to 0.48) 60–69 (0.83; 0.71 to 0.97) |
6–12 (1.59; 1.47 to 1.72) 12–24 (1.82; 1.67 to 1.99) >24 (1.85; 1.67 to 2.05) |
<1 (0.58; 0.53 to 0.64) | c | Mixed (0.55; 0.43 to 0.71) Asian/Asian British (0.32; 0.25 to 0.4) Black/Black British (0.41; 0.31 to 0.54) Chinese/other (0.31; 0.2 to 0.48) |
| Prescribed any strong opioid: proportion of the prison population prescribed any strong opioid during an 8-week period | 2257 of 25,811 eligible people (8.7%) | Increase (1.22; 1.14 to 1.32) | 3.8-fold (0.36 to 1.36) | Closed (1.21; 1.09 to 1.35) | B (0.47; 0.43 to 0.52) D (0.14; 0.11 to 0.17) |
c | c | 40–49 (1.39; 1.3 to 1.49) 50–59 (1.22; 1.11 to 1.34) |
10–19 (0.06; 0.02 to 0.18) 20–29 (0.38; 0.34 to 0.41) |
6–12 (1.44; 1.32 to 1.57) 12–24 (1.75; 1.59 to 1.91) >24 (1.92; 1.73 to 2.13) |
<1 (0.79; 0.72 to 0.87) | c | Mixed (0.51; 0.39 to 0.67) Asian/Asian British (0.34; 0.26 to 0.43) Black/Black British (0.37; 0.28 to 0.5) Chinese/other (0.33; 0.21 to 0.51) |
| Prescribed any opioid with benzodiazepines: proportion of the prison population prescribed any opioid and benzodiazepines during an 8-week period | 2257 of 25,811 eligible people (8.7%) | Increase (1.18; 1.1 to 1.27) | 12-fold (0.39 to 4.68) | B (1.20; 1.1 to 1.32) Closed (1.24; 1.11 to 1.38) |
D (0.13; 0.11 to 0.16) | c | c | 40–49 (1.32; 1.24 to 1.42) 50–59 (1.19; 1.09 to 1.31) |
10–19 (0.46; 0.34 to 0.61) 20–29 (0.5; 0.47 to 0.54) |
6–12 (1.36; 1.26 to 1.47) 12–24 (1.6; 1.47 to 1.75) >24 (1.82; 1.64 to 2.02) |
<1 (0.85; 0.78 to 0.92) | c | Mixed (0.62; 0.5 to 0.78) Asian/Asian British (0.56; 0.48 to 0.65) Black/Black British (0.47; 0.37 to 0.6) Chinese/other (0.48; 0.35 to 0.66) |
| People with any mental illness prescribed any opioid: proportion of the prison population with any mental illness prescribed any opioid during an 8-week period | 770 of 4054 eligible people (19.0%) | Increase (1.64; 1.41 to 1.91) | 11.1-fold (0.27 to 3.0) | C (2.04; 1.62 to 2.58) Closed (1.60; 1.26 to 2.03) |
c | c | c | 40–49 (1.4; 1.21 to 1.61) 50–59 (1.35; 1.11 to 1.63) |
10–19 (0.24; 0.03 to 1.89) 20–29 (0.42; 0.35 to 0.51) 70–79 (0.47; 0.23 to 0.95) |
6–12 (1.71; 1.46 to 2.02) 12–24 (2.01; 1.67 to 2.42) >24 (1.95; 1.56 to 2.43) |
<1 (0.66; 0.54 to 0.81) | c | Mixed (0.58; 0.36 to 0.95) Asian/Asian British (0.25; 0.13 to 0.48) |
| No diagnosis of neuropathic pain and prescribed a gabapentinoid: proportion of the prison population with no coded diagnosis of neuropathic pain prescribed pregabalin or gabapentin during an 8-week period | 204 of 24,388 eligible people (0.8%) | Decrease (0.89; 0.71 to 1.1) | 1.93-fold (0.67 to 1.29) | c | B (0.40; 0.32 to 0.5) C (0.27; 0.21 to 0.35) D (0.18; 0.12 to 0.28) |
c | c | 40–49 (1.77; 1.43 to 2.19) 50–59 (1.7; 1.31 to 2.21) 60–69 (1.54; 1.02 to 2.31) 90–99 (12.22; 1.41 to 105.56) |
20–29 (0.25; 0.17 to 0.36) | 6–12 (1.77; 1.38 to 2.29) 12–24 (1.91; 1.43 to 2.54) >24 (1.91; 1.36 to 2.67) |
<1 (0.51; 0.37 to 0.7) | c | Mixed (0.33; 0.12 to 0.9) Asian/Asian British (0.18; 0.07 to 0.48) Black/Black British (0.22; 0.07 to 0.69) |
| Indicator | Achievement | Variation in ORs between prisons (range of ORs) | Association between explanatory variables and achievement (OR; 95% CI) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019–20 (%) | 2019–20 compared to 2017–18 (OR; 95% CI) | Prison categorya (comparator category A) |
Genderb (comparator female) | Age (comparator 30–39 years)b | Length of stay (months)b (comparator 1–<6 months) | Ethnic groupb (comparator white people) | |||||||
| Higher | Lower | Higher | Lower | Higher | Lower | Higher | Lower | Higher | Lower | ||||
| Consent to transfer medical records: proportion of new receptions to prison who have been asked for consent to transfer medical records from community primary care to prison health care | 12,639 of 17,957 eligible people (70.4%) | Increase (4.28; 3.96 to 4.62) | 337.1-fold (0.007 to 2.36) | C (1.43; 1.26 to 1.64) Closed (2.86; 2.44 to 3.35) YOI (3.88; 3.08 to 4.89) |
B (0.38; 0.33 to 0.43) | c | Men (0.1; 0.02 to 0.14) | c | 50–59 (0.86; 0.76 to 0.97) 60–69 (0.72; 0.58 to 0.89) |
6–12 (1.22; 1.11 to 1.34) 12–24 (1.43; 1.25 to 1.63) >24 (1.85; 1.47 to 2.31) |
<1 (0.77; 0.71 to 0.83) | c | Mixed (0.80; 0.65 to 0.99) Asian/Asian British (0.80; 0.69 to 0.92) Black/Black British (0.75; 0.61 to 0.93) Chinese/other (0.70; 0.52 to 0.96) |
| MR and IP risk assessment: proportion of new receptions to prison who had a second-stage health assessment, plus IP risk assessmentf and MRg accurately communicated in the week before that assessment. | 2359 of 6173 eligible people (38.2%) | d | 21,610-fold (0.45 to 9724.5) | B (5.91; 4.81 to 7.25) D (1.70; 1.33 to 2.16) |
C (0.43; 0.35 to 0.52) YOI (0.02; 0.01 to 0.06) |
c | c | c | c | <1 (3.02; 1.86 to 4.89) 6–12 (3.17; 2.26 to 4.44) >24 (1.54; 1.01 to 2.33) |
c | c | c |
Appendix 9 Excerpt from indicator booklet
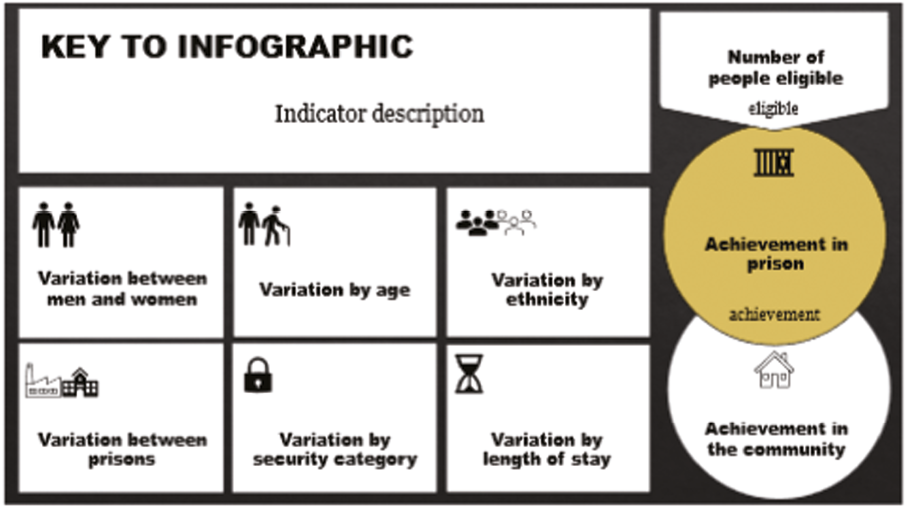
|
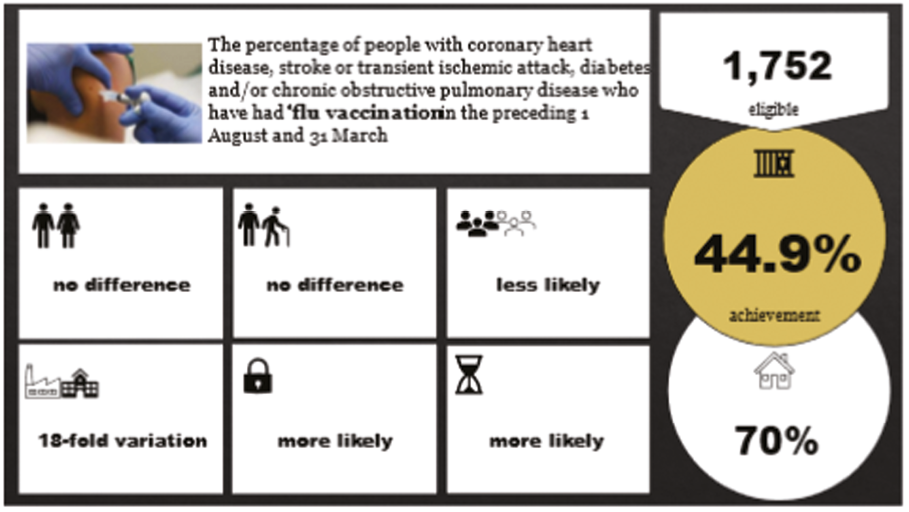
|
| Each indicator is presented in the same format: a simplified infographic-style illustration at the top of the page and a more detailed narrative below. The key to the symbols in the infographic can be seen above. Where a whole square is greyed out, this means no data were available. |
Of the 1752 people (6.8%) eligible for this indicator, less than half (44.9%) were vaccinated. This compares unfavourably with community primary care where over 70% with the same diagnoses were vaccinated in 2019–20. Achievement did improve over 2017–20. The likelihood of influenza vaccination varied 18-fold between prisons (ORs 0.13–2.36). We found no differences by gender or age. Compared to people staying 1–6 months, those staying less than a month were half as likely to be vaccinated and those staying 6–24 months were two to four times more likely to be vaccinated. Compared to white people, black or Black British and Chinese and other people were less likely to be vaccinated. |
Appendix 10
| Indicator | Criterion | Round 1 | Round 2 | |||
|---|---|---|---|---|---|---|
| Median and range | Outcome | Median and range | Change to median | Outcome | ||
| Communicable disease | ||||||
| The percentage of new receptions who have had dried blood spot testing in the past 12 months | Importance | 8 (6–9a) | Moderate discordance | 8 (5–9a) | 0 | |
| Feasibility | 7 (6–9a) | 8 (5–9a) | +1 | |||
| The percentage of people with a record of hepatitis B vaccination in the past 12 months, (1) out of the whole prison population and (2) out of people with clinical code indicating a history of illicit drug use | Importance | 7.5 (5–9a) | Exempt | 7 (5–9a) | – 0.5 | |
| Feasibility | 6 (5–9a) | 7 (5–9a) | +1 | |||
| The percentage of people with CHD, stroke or transient ischaemic attack, diabetes and/or COPD who have had flu vaccination in the preceding 1 August and 31 March | Importance | 8 (4–9a) | Moderate discordance | 8 (5–9a) | 0 | |
| Feasibility | 7.5 (5–9a) | 8 (5–9a) | +0.5 | |||
| Mental health | ||||||
| The percentage of people prescribed antipsychotics who have had appropriate laboratory screening tests (fasting glucose, HbA1c, lipid profile, urea and electrolytes, full blood count, liver function tests, BMI, blood pressure) in the past 12 months | Importance | 7.5 (7–9) | Exempt | 8.5 (7–9) | +1 | Promoted to inclusion |
| Feasibility | 6.5 (5–9a) | 8 (7–9) | +1.5 | |||
| The percentage of people prescribed three or more psychotropic drugs (antipsychotics, sedative antidepressants, hypnotics and anxiolytics, pregabalin or gabapentin, opioids) at the same time during an 8-week period | Importance | 8.5 (5–9a) | Moderate discordance | 8 (5–9a) | –0.5 | |
| Feasibility | 7 (5–9a) | 7 (5–8) | 0 | |||
| The percentage of patients aged over 55 years in the preceding 1 April to 31 March who have a record of MMSE, 6-item CIT, or the GPCOG in the past 12 months | Importance | 7 (5–9a) | Exempt | 8 (5–9a) | +1 | Promoted to inclusion |
| Feasibility | 6 (2–9b) | 7 (4–8a) | +1 | |||
| The percentage of people with a new clinical code for any forms of dementia recorded in the preceding 1 April to 31 March with a record of FBC, calcium, glucose and/or HbA1c, renal and liver function, thyroid function tests, serum vitamin B12 and folate levels recorded between 12 months before and 6 months after entering on to the register | Importance | 7 (5–9a) | Exempt | 7 (5–9a) | 0 | |
| Feasibility | 6 (2–8b) | 7 (7–9) | +1 | |||
| Prison-specific | ||||||
| The percentage of new receptions who have been asked for consent to transfer medical records from their GP to the prison health care service in the past 12 months | Importance | 7 (2–9b) | High discordance | 8a (4–9) | +1 | |
| Feasibility | 6 (1–9b) | 7a (5–9a) | +1 | |||
| The percentage of new receptions in the past 12 months who have had an IP risk assessment and MR added in the 7 days before their second reception screening | Importance | 9 (7–9) | Maximum importance | 8 (4–9a) | –1 | Demoted from maximum importance category |
| Feasibility | 8 (5–9a) | 7.5 (6–9a) | – 0.5 | |||
| The percentage of people (1) out of the whole prison population prescribed (a) any opioid, (b) any strong opioid, (3) benzodiazepines AND any opioid; (2) with any MH diagnosis prescribed any opioid; (3) out of the whole prison population with NO coded diagnosis of neuropathic pain prescribed pregabalin or gabapentin, during an 8-week period | Importance | 9 (7–9) | Maximum Importance | 8 (5–9a) | –1 | Demoted from maximum importance |
| Feasibility | 7 (5–8) | 6.5 (5–8) | –0.5 | |||
| Diabetes, asthma and epilepsy care | ||||||
| The percentage of people on the diabetes register (1) who have had a blood pressure reading recorded in the last 12 months and (2) in whom the last blood pressure reading (measured in the preceding 12 months) is 140/80 mmHg or less | Importance | 8 (7–9) | Low discordance | 8.5 (6–9a) | +0.5 | |
| Feasibility | 8 (5–9a) | Moderate discordance | 8 (7–9) | 0 | ||
| The percentage of people on the diabetes register who have had the following care processes performed in the preceding 12 months: BMI measurement; BP measurement; HbA1c measurement; cholesterol measurement; record of smoking status; foot examination; albumin–creatinine ratio; serum creatinine measurement | Importance | 8 (7–9) | Low discordance | 8.5 (6–9a) | +0.5 | |
| Feasibility | 7 (4–9a) | Moderate discordance | 7.5 (7–9) | +0.5 | ||
| The percentage of people on the diabetes register, without moderate or severe frailty, (1) who have had their IFCC-HbA1c recorded in the preceding 12 months and (2) in whom their last IFCC-HbA1c (recorded in the preceding 12 months) is 58 mmol/mol or less | Importance | 8 (5–9a) | Moderate discordance | 7 (6–9a) | –1 | Exempt |
| Feasibility | 7 (4–9a) | 7 (5–9a) | 0 | |||
| The percentage of people on the diabetes register, with moderate or severe frailty, (1) who have had their IFCC-HbA1c recorded in the preceding 12 months and (2) in whom their last IFCC-HbA1c (recorded in the preceding 12 months) is 75 mmol/mol or less | Importance | 8 (7–9) | Low discordance | 8.5 (6–9a) | +0.5 | |
| Feasibility | 7 (4–9a) | Moderate discordance | 7 (7–9) | 0 | ||
| The percentage of people on the asthma register who have had an asthma review in the preceding 12 months that includes an assessment of asthma control using the 3 RCP questions | Importance | 8 (7–9) | Low discordance | 8.5 (5–9a) | +0.5 | |
| Feasibility | 7 (5–9) | Moderate discordance | 7.5 (7–9) | +0.5 | ||
| The percentage of people with a coded diagnosis of epilepsy and who have been prescribed drug treatment for epilepsy (1) who have had an epilepsy annual review in the past 12 months and (2) been coded as seizure-free in the last 12 months | Importance | 8 (7–9) | Low discordance | 7.5 (7–9) | –0.5 | Exempt |
| Feasibility | 7 (4–9a) | Moderate discordance | 7 (6–9a) | 0 | ||
| Screening | ||||||
| The percentage of women eligible for screening and aged 25–49 years at the end of reporting period whose notes record that an adequate cervical screening test has been performed in the preceding 3 years and 6 months | Importance | 9 (7–9) | Maximum importance | 8 (6–9a) | –1 | Demoted from maximum importance category |
| Feasibility | 7.5 (2–9b) | 7 (6–9a) | –0.5 | |||
| The percentage of women eligible for screening and aged 50–64 years at the end of the reporting period whose notes record that an adequate cervical screening test has been performed in the previous 5 years and 6 months | Importance | 9 (7–9) | Maximum importance | 8 (6–9a) | –1 | Demoted from maximum importance category |
| Feasibility | 7.5 (2–9b) | 7 (6–9a) | –0.5 | |||
| The percentage of women aged 53–70 years with a record of mammography in the preceding 3 years | Importance | 8 (6–9a) | Moderate discordance | 8a (6–9a) | 0 | |
| Feasibility | 7 (2–9b) | High discordance | 7 (5–9a) | 0 | ||
| The percentage of men aged 65 years or over with a record of AAA screening | Importance | 8 (6–9a) | Moderate discordance | 7 (7–9) | –1 | Exempt |
| Feasibility | 7 (6–9a) | 7 (6–9a) | 0 | |||
| The percentage of people aged 45–74 years who do NOT have a current diagnosis of any of the following: CHD, CKD, diabetes, hypertension, AF, TIA, familial hypercholesterolaemia, heart failure, peripheral arterial disease, or stroke, or have a previously documented 20% or higher 10-year CVD risk BEFORE the last 5 years, who have a recorded CVD risk assessment score in the preceding 5 years | Importance | 8 (6–9a) | Moderate discordance | 8a (6–9a) | 0 | |
| Feasibility | 7 (2–9b) | High discordance | 7 (6–8) | 0 | ||
| CVD | ||||||
| The percentage of people with a clinical code for TIA, stroke or ischaemic stroke (not haemorrhagic stroke) prescribed any antiplatelet or anticoagulant in the preceding 12 months | Importance | 8 (5–9) | Moderate discordance | 8a (6–9a) | 0 | |
| Feasibility | 7 (4–9) | 7a (6–9a) | 0 | |||
| The percentage of people with a clinical code for persistent or paroxysmal AF and whose most recent CHA2DS2-VASc score is 2 or more, with a current acute or repeat prescription for anticoagulation drug therapy | Importance | 8 (5–9a) | Moderate discordance | 8 (6–9a) | 0 | |
| Feasibility | 7 (5–9) | 7 (5–9a) | 0 | |||
| The percentage of people with a clinical code for persistent or paroxysmal AF in whom stroke risk has been assessed using the CHA2DS2-VASc in the preceding 12 months | Importance | 8 (5–9a) | Moderate discordance | 8 (6–9a) | 0 | |
| Feasibility | 7 (4–9a) | 7 (7–9) | 0 | |||
| The percentage of people aged 79 or under, with CHD OR hypertension OR stroke/TIA OR peripheral arterial disease (but NOT diabetes or CKD), (1) who have had a blood pressure reading recorded in the last 12 months, and (2) in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less | Importance | 8 (6–9a) | Moderate discordance | 8a (6–9a) | 0 | |
| Feasibility | 7 (3–9b) | High discordance | 7a (6–9a) | 0 | ||
| The percentage of people aged 80 years or over, with CHD OR hypertension OR stroke/TIA OR peripheral arterial disease (but NOT diabetes or CKD), (1) who have had a blood pressure reading recorded in the last 12 months, and (2) in whom the last blood pressure reading (measured in the preceding 12 months) is 150/90 mmHg or less | Importance | 8 (6–9a) | Moderate discordance | 8a (6–9a) | 0 | |
| Feasibility | 7 (3–8a) | 7a (6–9a) | 0 | |||
| The percentage of people with a record of a MI who are prescribed an ACE-I, ARB, antiplatelet therapy, beta-blocker or a statin | Importance | 8 (5–9a) | Moderate discordance | 8 (6–9) | 0 | |
| Feasibility | 7.5 (4–9a) | 8 (6–9) | +0.5 | |||
| The percentage of people with a record of CHD who are prescribed aspirin, alternative antiplatelet therapy, or anticoagulant in the last 12 months | Importance | 8 (6–9a) | Moderate discordance | 8a (6–9a) | 0 | |
| Feasibility | 7 (3–9b) | High discordance | 7a (6–9a) | 0 | ||
| The percentage of people with a record of heart failure due to left ventricular systolic dysfunction, who are prescribed an ACE-I or ARB in the last 12 months | Importance | 7 (6–9a) | Exempt | 7 (5–9a) | 0 | |
| Feasibility | 7 (3–9b) | 6 (6–7) | –1 | |||
| The percentage of people with a record of heart failure due to left ventricular systolic dysfunction and who are currently treated with an ACE-I or ARB, who are additionally prescribed a beta-blocker | Importance | 7.5 (6–9a) | Exempt | 7.5 (5–9a) | 0 | |
| Feasibility | 6 (3–9b) | 6.5 (6–7) | +0.5 | |||
Appendix 11
| Ruleset for excluding indicators | Number of indicators exempt if ruleset applied | |
|---|---|---|
| 1 | Moderate or low discordance AND median score < 7 for importance Regardless of feasibility |
0 |
| 2 | Moderate or low discordance AND median score < 7 for importance OR Moderate or low discordance AND median score < 7 for feasibility |
2 |
| 3 | Moderate or low discordance AND median score < 7 for importance OR Median score < 7 for feasibility regardless of discordance |
5 |
| 4 | Moderate or low discordance AND median score < 8 for importance Regardless of feasibility |
6 |
| 5 | Moderate or low discordance AND median score < 8 for importance AND Moderate or low discordance AND median score < 7 for feasibility |
2 |
| 6 | Moderate or low discordance AND median score < 8 for importance OR Moderate or low discordance AND median score < 7 for feasibility |
5 |
| 7 | Moderate or low discordance AND median score < 8 for importance AND Moderate or low discordance AND median score < 8 for feasibility |
2 |
| 8 | Moderate or low discordance AND median score < 8 for importance OR Moderate or low discordance AND median score < 8 for feasibility |
20 |
Appendix 12 Quality-improvement strategy for reducing opioid and gabapentinoid prescribing in the prison estate
Indicators
-
The percentage of people out of the whole prison population during the preceding 8 weeks prescribed (1) any opioid, (2) any strong opioid and (3) benzodiazepines AND any opioid.
-
The percentage of people with any MH diagnosis prescribed any opioid during the preceding 8 weeks.
-
The percentage of people out of the whole prison population with NO coded diagnosis of neuropathic pain, prescribed pregabalin or gabapentin during the preceding 8 weeks.
Rationale
Opioids are commonly prescribed for acute and long-term pain. However, prescribing for long-term pain is discouraged given the absence of evidence of effectiveness and recognised risks of dependence and other harms (e.g. falls in older people). Gabapentinoids are also discouraged for similar reasons unless there is documented evidence of neuropathic (nerve) pain.
Key findings from an analysis of 13 prisons
-
11.5% of people (2957 out of 25,811) had been prescribed any opioid during the preceding 8 weeks in March 2020. Compared to 2018, the likelihood of opioid prescribing was almost 1.5 times higher in 2020. The likelihood of any opioid prescribing varied fivefold between prisons.
-
People aged 40–50 years were more likely to be prescribed any opioid compared to other age groups.
-
Compared to people spending 1–6 months in prison, those in prison for longer periods were over 1.5 times more likely to be prescribed any opioid.
-
People with any of black, Asian or Asian British, black or Black British, and Chinese or other ethnicities were around half as likely to be prescribed any opioids than people with coded white ethnicity.
-
8.7% (2257) were prescribed any strong opioid, with a fourfold variation between prisons.
-
8.7% (2257) were prescribed benzodiazepines AND any opioid, with an over eightfold variation between prisons.
-
19% (770) of people with any MH diagnosis were prescribed any opioid.
-
Of people with no documented code of neuropathic pain, 0.8% (204) were prescribed pregabalin or gabapentin, with a threefold variation between prisons.
-
Males were under half as likely to be prescribed gabapentinoids as females.
Key considerations from an analysis of interviews with staff and people in prison and from stakeholder workshops
Enablers of quality improvement
-
Staff: Experienced prescribers; proficiency in use of templates and clinical coding; administrative staff able to do regular prescribing analyses; collaborative working between primary care staff, substance-misuse staff, physiotherapists and security staff; communication with community prescribers to promote consistent prescribing across prison–community interface.
-
Leadership: Supportive organisational ethos and line management; embedding education and performance feedback within existing supervisory and team briefing structures; managerial staff able to interpret performance data and lead improvement work.
-
Monitoring: Inclusion of the indicators in the contracting quality schedule
-
Care provision: Longer scheduled appointments to discuss concerns, expectations, harms and coping strategies.
-
Patient education: Peer group support and information; involvement of voluntary sector agencies.
Barriers to quality improvement
-
Staff: High staff turnover and over-reliance on locum staff; lack of protected time for education, including shift patterns that reduce opportunities for face-to-face training; negative attitudes to performance measurement; inconsistent record-keeping.
-
Data systems: Limited speed and functionality of electronic health-record systems.
-
Care provision: Limited alternatives for pain management in the prison setting; patient perceptions that staff are making decisions based on assumptions of medication diversion rather than genuine clinical need.
-
Patient education: Perceptions of not being listened to and treated as ‘lower class’; limited literacy or language; lack of access to web-based materials; existing educational programmes or materials not adapted for prison settings; attendance at face-to-face education sessions dependent on security staff availability.
Interventions and levers for change
No one approach by itself is likely to bring about a significant reduction in opioid or gabapentinoid prescribing. Any improvement strategy needs to target key influences on practice that are amenable to change. We suggest a combination of approaches (Table 26), partly based upon a community primary care campaign to reduce opioid prescribing. 56,147
| Intervention | Goal | Content | Resources |
|---|---|---|---|
| Brief educational webinar | Raise awareness | Harms associated with prescribing Measures planned to help reduce prescribing, including a ‘Whole prison approach’ |
Production time Staff time in viewing |
| Training courses | Improve knowledge and skills | Nationally recognised training courses for clinical staff, e.g. RCGP courses in the management of substance misuse Training for wider prison staff on substance misuse and pain management |
Participation fees Staff release time |
| Audit and feedback | Highlight any discrepancies between perceived and actual clinical practice Motivate change through comparisons over time or between prisons Promote action planning |
Repeated comparative feedback Supportive and non-judgmental messaging Highlight patient groups at higher risk of prescribing (e.g. longer stays) and from prescribing (e.g. mental illness) Evidence bites on harms and ineffectiveness of opioid prescribing for long-term pain Key messages |
Searches and collation based on routinely collected data Feedback design and production |
Action planning template with practical suggestions |
|||
| Opinion leaders | Peer-group influence by clinicians perceived as credible and educationally influential | Reinforcement of feedback and key messages | Protected time for training and work of opinion leaders |
| Patient education and support | Educate patients about harms and limitations of prescribing Promote alternative coping strategies for long-term pain |
Use of MH therapies to support symptom management, e.g. pain, insomnia Existing patient support websites and printed information Engage with peer supporters in the prison Highlighting risks using opioids for other, non-indicated reasons, e.g. bench pressing more under the influence of opioids |
Time sourcing and checking support materials Online access Support time for less literate patients |
| Inter-professional collaboration | Support or share clinical management through enhanced communication between specialist and primary care teams | Provision of general and patient-specific advice, e.g.
|
Time of specialist and prison primary care teams |
| Escalation pathways | Provide additional support for selected patients and their clinicians | ‘Safe haven’ consultation support for the small number of prisoner patients who show intimidating behaviour towards clinicians in seeking prescribed drugs Highlighting to the prison those who have become threatening or abusive, including use of security reports Managing the risk of those who are potentially trading medicines |
Design and provision of ‘safe haven’ arrangements Risk-management process for staff and patients |
Appendix 13 Quality-improvement strategy for the management of hypertension in the prison estate
Relevant indicators
-
The proportion of people aged 79 years or under, with CHD, hypertension, stroke, transient ischaemic attack or peripheral arterial disease, in whom the last blood pressure reading (measured in the preceding 12 months) is 140/90 mmHg or less.
-
The proportion of people with diabetes in whom the last blood pressure reading (measured in the preceding 12 months) is 140/80 mmHg or less.
Rationale
Hypertension increases the risk of a number of conditions, including heart failure, coronary artery disease, stroke, CKD, peripheral arterial disease and vascular dementia. There is a strong evidence base and well-established pathways for the management of hypertension.
Key findings from an analysis of 13 prisons
-
Around 5% of people in prison are under 80 years old and have a known history of CHD, hypertension, stroke, transient ischaemic attack or peripheral arterial disease. Of these, less than half (44.7%) had a last recorded blood pressure of 140/90 mmHg or less in the preceding 12 months.
-
Around 3% of people in prison have diabetes. Of these, a third (33.9%) had a last recorded blood pressure of 140/80 mmHg or less.
-
These compare unfavourably with around 70% achievement community primary care.
-
The likelihood of satisfactory blood pressure control varied up to sixfold between prisons, even after accounting for prison and demographic characteristics.
-
Blood pressure control was generally better in people aged 20–39 years and in people staying over 24 months.
-
Compared to white people, Asian or Asian British people were generally more likely to have satisfactory blood pressure control but had poorer control if they had diabetes.
Key considerations from an analysis of interviews with staff and people in prison and from stakeholder workshops
Enablers of quality improvement
-
Staff: Clinical staff with interest in long-term conditions and proficient in using associated electronic health-record templates; administrative staff able to do regular analyses of clinical performance.
-
Training: Availability of online courses.
-
Leadership: Supportive organisational ethos and line management; embedding education and performance feedback within existing supervisory and team briefing structures; managerial staff able to interpret performance data and lead improvement work.
-
Monitoring: Inclusion of hypertension indicators in the contracting quality schedule.
-
Care provision: Wing-based nursing care or drop-in clinics to review blood pressure; recognised care and referral pathways.
-
Patient education: Peer group support and information; involvement of voluntary sector agencies.
Barriers to quality improvement
-
Staff: High staff turnover and over-reliance on locum staff; lack of protected time for education, including shift patterns that reduce opportunities for face-to-face training; negative attitudes to performance measurement; inconsistent record keeping.
-
Data systems: Limited speed and functionality of electronic health-record systems.
-
Patient education: Perceptions of not being listened to and treated as ‘lower class’; limited literacy or language; lack of access to web-based materials; existing educational programmes or materials not adapted for prison settings; attendance at face-to-face education sessions dependent on security staff availability.
-
Care provision: Wing-based rooms not designed as clinical spaces and often poorly equipped.
Interventions and levers for change
No one approach by itself is likely to bring about a significant improvement in the management of hypertension. Any improvement strategy needs to target key influences on practice that are amenable to change. We suggest a combination of approaches (Table 27), drawing upon earlier research exploring influences on blood pressure control in community primary care and lessons learnt from the evaluation of an improvement strategy. 148–150 Given the high prevalence of people with poorly controlled blood pressure, it is worth considering focusing efforts on specific patient groups (e.g. those with diabetes) to increase the likelihood that clinical staff can observe improvements from their efforts. 150
| Intervention | Goal | Content | Resources |
|---|---|---|---|
| Brief educational webinar | Raise awareness | Benefits of blood pressure control Measures planned to improve blood pressure control |
Production time Staff time in viewing Availability of computers |
| Training courses | Improve clinical management knowledge and skills | Clinical pathways for blood pressure control Individualising treatment plans and targets |
Participation fees Staff release time |
| Audit and feedback | Highlight any discrepancies between perceived and actual clinical practice Motivate change through comparisons over time or between prisons Promote action planning |
Repeated feedback comparing performance over time, between prisons, and with community performance Supportive and non-judgmental messaging Highlight patient groups at higher risk of missing targets, e.g. Asian or Asian British people with diabetes, people with shorter stays |
Searches and collation based on routinely collected data Feedback design and production |
| Evidence bites on benefits of blood pressure control Action planning template with practical suggestions |
|||
| Computerised alerts | Prompt clinicians to address specific care needs | Automated alerts when blood pressure is above target levels | Programming support |
| Opinion leaders | Peer-group influence by clinicians perceived as credible and educationally influential | Reinforcement of feedback and key messages | Protected time for training and work of opinion leaders |
| Patient education | Educate patients about harms of untreated raised blood pressure | Existing patient support websites and printed information Health and well-being peers and events, e.g. including blood pressure checks |
Time sourcing and checking support materials Support time for less literate patients |
| Organisational resources | Ensuring availability of basic equipment in all clinical areas, e.g. validated sphygmomanometers | Standards for and regular checks of room equipment | Equipment |
Appendix 14
| Characteristics | Prison leavers who mentioned mental health | Prison leavers who did not mention mental health | HCPs who mentioned mental health | HCPs who did not mention mental health | |||
|---|---|---|---|---|---|---|---|
| Personal experience | Observer | Total | Healthcare staff | ||||
| Gender | Male | 11 | 4 | 15 | 2 | 12 | 4 |
| Female | 4 | 0 | 4 | 0 | 5 | 1 | |
| Age group | 20s | 1 | 2 | 3 | 0 | 3 | 0 |
| 30s | 5 | 0 | 5 | 2 | 1 | 1 | |
| 40s | 9 | 1 | 10 | 0 | 5 | 4 | |
| 50s | 0 | 0 | 0 | 0 | 6 | 0 | |
| 60s | 0 | 1 | 1 | 0 | 1 | 0 | |
| Ethnicity | Black African | 0 | 0 | 0 | 1 | 0 | 0 |
| Black English | 0 | 1 | 1 | 1 | 0 | 0 | |
| British Asian | 2 | 1 | 3 | 0 | 0 | 0 | |
| White | 0 | 0 | 0 | 0 | 1 | 0 | |
| White British | 10 | 1 | 11 | 1 | 14 | 4 | |
| White English | 1 | 1 | 2 | 0 | 0 | 0 | |
| White Scottish | 0 | 0 | 0 | 0 | 1 | 0 | |
| White/Black Caribbean | 1 | 1 | 1 | 0 | 0 | 0 | |
| Arabic/English | 0 | 0 | 0 | 0 | 0 | 1 | |
| Not stated | 1 | 0 | 1 | 0 | 1 | 0 | |
| Male/female estate | Male | 11 | 4 | 15 | 2 | 13 | 5 |
| Female | 4 | 0 | 4 | 0 | 3 | 0 | |
| Both | – | – | – | – | 1 | 0 | |
| Prison category: Male | A–D | – | – | 1 | 0 | 0 | 0 |
| A | – | – | 0 | 0 | 2 | 1 | |
| B | – | – | 3 | 1 | 4 | 1 | |
| C | – | – | 0 | 0 | 2 | 1 | |
| D | – | – | 0 | 0 | 1 | 1 | |
| A/B | – | – | 0 | 0 | 1 | 0 | |
| B, C | – | – | 9 | 1 | 1 | 0 | |
| B, C, D | – | – | 2 | 0 | 0 | 1 | |
| B, D | – | – | 0 | 0 | 1 | 0 | |
| C, D | – | – | 0 | 0 | 2 | 0 | |
| Prison category: Female | Closed | – | – | 2 | 0 | 0 | 0 |
| Closed/semi-open | – | – | 2 | 0 | 0 | 0 | |
| No. of sentences in last 5 years | 0 | – | – | 3 | 0 | – | – |
| 1 (but many previously) | – | – | 1 | 0 | – | – | |
| 1 | – | – | 8 | 2 | – | – | |
| 2 | – | – | 3 | 0 | – | – | |
| 3–4 | – | – | 2 | 0 | – | – | |
| Many | – | – | 2 | 0 | – | – | |
| Years in prison health care | 1–3 | – | – | – | – | 4 | 2 |
| 4–7 | – | – | – | – | 6 | 1 | |
| 8–10 | – | – | – | – | 2 | 0 | |
| More than 11 | – | – | – | – | 4 | 2 | |
| Not stated | – | 1 | 0 | ||||
| Profession | Administrator | – | – | – | – | 0 | 1 |
| Associate practitioner | – | – | – | – | 1 | 0 | |
| GP | – | – | – | – | 2 | 0 | |
| Health promotion worker | – | – | – | – | 1 | 0 | |
| MH nurse | – | – | – | – | 1 | 0 | |
| Nurse – band 5 | – | – | – | – | 2 | 0 | |
| Nurse prescriber | – | – | – | – | 1 | 0 | |
| Occupational therapist | – | – | – | – | 2 | 0 | |
| Pharmacy technician | – | – | – | – | 0 | 1 | |
| Physiotherapist | – | – | – | – | 0 | 1 | |
| Recovery worker | – | – | – | – | 1 | 0 | |
| Recovery/service development | – | – | – | – | 0 | 1 | |
| Senior clinical manager | – | – | – | – | 2 | 1 | |
| Senior nurse | – | – | – | – | 4 | 0 | |
| Years in current role | 1–3 | – | – | – | – | 7 | 2 |
| 4–7 | – | – | – | – | 5 | 2 | |
| 8–10 | – | – | – | – | 4 | 1 | |
| 11+ | – | – | – | – | 1 | 0 | |
Appendix 15
| Indicator | All eligible stays | Number eligible stays (% All) | Number achieving indicator (% eligible stays) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No MHa | MH with psychotropic drugsa | MH without psychotropic drugsa | No MHa | MH with psychotropic drugsa | MH without psychotropic drugsa | ||||||||||
| Communicable disease | |||||||||||||||
| New receptions to prison accepting opt-out dry blood spot testing | 38,079 | 33,682 | (88.5) | 465 | (1.2) | 3932 | (10.3) | 8008 | (83.7) | 159 | (1.7) | 1404 | (14.7) | ||
| Prison population who have received one, two, three or four (course of three plus booster) hepatitis B vaccinations in the preceding 12 months | |||||||||||||||
| Hepatitis B vaccines of the population who entered in the last 12 months | 1st Hep B | 47,948 | 41,496 | (86.5) | 716 | (1.5) | 5736 | (12.0) | 13,774 | (82.0) | 358 | (2.1) | 2660 | (15.8) | |
| 1st and 2nd Hep B | 10,818 | (81.5) | 300 | (2.3) | 2157 | (16.2) | |||||||||
| 1st, 2nd and 3rd Hep B | 7342 | (80.1) | 215 | (2.3) | 1605 | (17.5) | |||||||||
| 1st, 2nd, 3rd and 4th Hep B | 3325 | (77.6) | 119 | (2.8) | 842 | (19.6) | |||||||||
| In prison in the last 12 months with a clinical code added at any time indicating a history of any illicit drug use | 1st Hep B | 26,130 | 21,811 | (83.5) | 488 | (1.9) | 3831 | (14.7) | 8077 | (78.7) | 267 | (2.6) | 1924 | (18.7) | |
| 1st and 2nd Hep B | 6712 | (78.5) | 233 | (2.7) | 1606 | (18.8) | |||||||||
| 1st, 2nd and 3rd Hep B | 5334 | (78.1) | 187 | (2.7) | 1311 | (19.2) | |||||||||
| 1st, 2nd, 3rd and 4th Hep B | 2133 | (75.1) | 88 | (3.1) | 619 | (21.8) | |||||||||
| People with one or more of CHD, stroke or transient ischaemic attack, diabetes or COPD who have received a flu vaccination between August and March | 4586 | 3559 | (77.6) | 137 | (3.0) | 890 | (19.4) | 1525 | (76.9) | 61 | (3.1) | 397 | (20.0) | ||
| Mental health | |||||||||||||||
| Prison population prescribed three or more psychotropic drugs (antipsychotics, sedative antidepressants, hypnotics and anxiolytics, pregabalin or gabapentin, opioids) at the same time during an 8-week period | |||||||||||||||
| Three or more | 69,587 | 60,064 | (86.3) | 1033 | (1.5) | 8490 | (12.2) | 227 | (46.5) | 61 | (12.5) | 200 | (41.0) | ||
| Four or more | 69 | (34.5) | 33 | (16.5) | 98 | (49.0) | |||||||||
| People who have received three or more prescriptions for an antipsychotic in the preceding 12 months, and who have a record of blood testing (fasting glucose, HbA1c, lipid profile, urea and electrolytes, full blood count, liver function tests), BMI and blood pressure | |||||||||||||||
| Fasting glucose | 1033 | – | 1033 | (100.0) | – | – | 9 | (100.0) | – | ||||||
| HbA1c | – | 135 | (100.0) | – | |||||||||||
| Lipid profile | – | 107 | (100.0) | – | |||||||||||
| Urea and electrolytes | – | 193 | (100.0) | – | |||||||||||
| Full blood count | – | 202 | (100.0) | – | |||||||||||
| Liver function | – | 164 | (100.0) | – | |||||||||||
| BMI | – | 294 | (100.0) | – | |||||||||||
| Blood pressure | – | 366 | (100.0) | – | |||||||||||
| Four of the six blood tests | – | 157 | (100.0) | – | |||||||||||
| People aged over 55 years in the prison population who have a record of one of the following assessments in the preceding 12 months; MMSE, 6-item CIT, GPCOG | 5359 | 4636 | (86.5) | 81 | (1.5) | 642 | (12.0) | 397 | (76.6) | 10 | (1.9) | 111 | (21.4) | ||
| People with a new diagnosis of any form of dementia in the reporting year, and who have a record of the following blood tests between 12 months before and 6 months after the date of diagnosis: | |||||||||||||||
| Full blood count | 33 | 25 | (75.8) | 1 | (3.0) | 7 | (21.2) | 18 | (75.0) | 1 | (4.2) | 5 | (20.8) | ||
| Calcium | 14 | (87.5) | 1 | (6.3) | 1 | (6.3) | |||||||||
| HbA1c | 17 | (73.9) | 1 | (4.3) | 5 | (21.7) | |||||||||
| Renal | 17 | (81.0) | 1 | (4.8) | 3 | (14.3) | |||||||||
| Thyroid | 11 | (64.7) | 1 | (5.9) | 5 | (29.4) | |||||||||
| Serum | – | – | – | ||||||||||||
| Folate | 9 | (69.2) | 1 | (7.7) | 3 | (23.1) | |||||||||
| Five of the eight blood tests | 9 | (60.0) | 1 | (6.7) | 5 | (33.3) | |||||||||
| Prison-specific | |||||||||||||||
| New receptions to prison who have been asked for consent to transfer medical records from GP to prison health care | 47,112 | 40,680 | (86.3) | 719 | (1.5) | 5713 | (12.1) | 27,476 | (87.4) | 577 | (1.8) | 3368 | (10.7) | ||
| New receptions to prison with a code for a second-stage health assessment in the past 12 months, plus clinical codes for IP risk assessment and MR added in the week before the second-stage assessment | |||||||||||||||
| Both MR and IP assessment within 7 days | 5821 | 4954 | (85.1) | 110 | (1.9) | 757 | (13.0) | 1743 | (77.8) | 28 | (1.3) | 468 | (20.9) | ||
| Had MR during stay, but did not satisfy both within 7 days | 217 | (71.6) | 10 | (3.3) | 76 | (25.1) | |||||||||
| Had IP during stay, but did not satisfy both within 7 days | 3207 | (89.6) | 82 | (2.3) | 289 | (8.1) | |||||||||
| Prison population prescribed opioids in the preceding 8 weeks from 31 March | |||||||||||||||
| All prison population | Prescribed any opioid in the preceding 8 weeks from 31 March | 69,587 | 60,064 | (86.3) | 1033 | (1.5) | 8490 | (12.2) | 5530 | (75.9) | 294 | (4.0) | 1463 | (20.1) | |
| Prescribed any strong opioid in the preceding 8 weeks from 31 March | 4771 | (74.7) | 219 | (3.4) | 1395 | (21.8) | |||||||||
| Prescribed benzodiazepines AND any opioid in preceding 8 weeks from 31 March | 7340 | (81.8) | 219 | (2.4) | 1414 | (15.8) | |||||||||
| Any MH diagnosis | Prescribed any opioid in the preceding 8 weeks from 31 March | 8918 | – | 428 | (4.8) | 8490 | (95.2) | – | 86 | (5.6) | 1456 | (94.4) | |||
| All prison population AND NO coded diagnosis of neuropathic pain | Prescribed pregabalin OR gabapentin in the preceding 8 weeks from 31 March | 66,075 | 57,513 | (87.0) | 934 | (1.4) | 7628 | (11.5) | 399 | (65.2) | 32 | (5.2) | 181 | (29.6) | |
| Diabetes, asthma and epilepsy care | |||||||||||||||
| People with diabetes in whom the last blood pressure reading (measured in the preceding 12 months) is 140/80 mmHg or less | 2158 | 1735 | (80.4) | 84 | (3.9) | 339 | (15.7) | 570 | (77.8) | 33 | (4.5) | 130 | (17.7) | ||
| People with diabetes who have had the following in the preceding 12 months: | BMI | 2158 | 1715 | (79.5) | 87 | (4.0) | 356 | (16.5) | 1380 | (79.4) | 75 | (4.3) | 282 | (16.2) | |
| Blood pressure | 1487 | (78.7) | 81 | (4.3) | 322 | (17.0) | |||||||||
| HbA1c | 1007 | (78.2) | 63 | (4.9) | 217 | (16.9) | |||||||||
| Cholesterol | 850 | (78.4) | 48 | (4.4) | 186 | (17.2) | |||||||||
| Smoke status | 1388 | (78.9) | 76 | (4.3) | 295 | (16.8) | |||||||||
| Foot exam | 608 | (79.7) | 29 | (3.8) | 126 | (16.5) | |||||||||
| ACR | 407 | (80.0) | 19 | (3.7) | 83 | (16.3) | |||||||||
| Serum creatinine | 12 | (92.3) | 1 | (7.7) | – | ||||||||||
| Five of the eight items/tests | 892 | (77.7) | 51 | (4.4) | 205 | (17.9) | |||||||||
| People with diabetes without moderate or severe frailty, in whom the last HbA1c is 58 mmol/mol or less in the preceding 12 months | 2128 | 1696 | (79.7) | 84 | (3.9) | 348 | (16.4) | 572 | (77.2) | 42 | (5.7) | 127 | (17.1) | ||
| People with diabetes and moderate or severe frailty, in whom the last HbA1c is 75 mmol/mol or less in the preceding 12 months | 30 | 19 | (63.3) | 3 | (10.0) | 8 | (26.7) | 13 | (76.5) | 1 | (5.9) | 3 | (17.6) | ||
| People with asthma who have had an asthma review in the preceding 12 months that includes an assessment of asthma control | 11,406 | 9002 | (78.9) | 272 | (2.4) | 2132 | (18.7) | 754 | (79.9) | 29 | (3.1) | 161 | (17.1) | ||
| People on drug treatment for epilepsy who have had an annual review and recorded as seizure-free in the preceding 12 months | |||||||||||||||
| Annual review | 1009 | 743 | (73.6) | 46 | (4.6) | 220 | (21.8) | 23 | (95.8) | – | 1 | (4.2) | |||
| Seizure-free | 6 | (100.0) | – | – | |||||||||||
| Screening | |||||||||||||||
| Women eligible for screening and aged 25–49 years who have had cervical screening in the preceding 5 years and 6 months | 4501 | 2928 | (65.1) | 197 | (4.4) | 1376 | (30.6) | 1711 | (61.5) | 126 | (4.5) | 947 | (34.0) | ||
| Women eligible for screening and aged 50–64 years who have had cervical screening in the preceding 5 years and 6 months | 717 | 473 | (66.0) | 14 | (2.0) | 230 | (32.1) | 254 | (61.4) | 9 | (2.2) | 151 | (36.5) | ||
| Women eligible for screening and aged 50–70 years who have had breast screening in the preceding 3 years | 498 | 334 | (67.1) | 8 | (1.6) | 156 | (31.3) | 124 | (80.0) | 2 | (1.3) | 29 | (18.7) | ||
| Men eligible for screening and aged 65 years or over with a record of AAA screening | 1519 | 1339 | (88.2) | 26 | (1.7) | 154 | (10.1) | 607 | (88.9) | 6 | (0.9) | 70 | (10.2) | ||
| People aged 45–74 years with a recorded CVD risk assessment in the preceding 5 years, and who do NOT have a diagnosis of: CHD, CKD, diabetes, hypertension, AF, transient ischaemic attack, familial hypercholesterolaemia, heart failure, peripheral arterial disease, stroke or previously documented 20% or higher 10-year CVD risk BEFORE the last 5 years | 1138 | 969 | (85.1) | 21 | (1.8) | 148 | (13.0) | 276 | (80.5) | 10 | (2.9) | 57 | (16.6) | ||
| CVD | |||||||||||||||
| People with transient ischaemic attack or stroke, excluding those with haemorrhagic stroke, who have been prescribed an antiplatelet or anticoagulant in the preceding 12 months | 231 | 178 | (77.1) | 9 | (3.9) | 44 | (19.0) | 114 | (75.0) | 4 | (2.6) | 34 | (22.4) | ||
| People with persistent or paroxysmal AF and a CHA2DS2-VASc score equal to 2 or more, with a prescription for warfarin or a direct-acting oral anticoagulant in the preceding 12 months | 147 | 108 | (73.5) | 3 | (2.0) | 36 | (24.5) | 88 | (73.3) | 2 | (1.7) | 30 | (25.0) | ||
| People with persistent or paroxysmal AF and a CHA2DS2-VASc score in the preceding 12 months | 70 | 53 | (75.7) | 1 | (1.4) | 16 | (22.9) | 22 | (64.7) | 1 | (2.9) | 11 | (32.4) | ||
| People aged 79 years or under, with CHD, hypertension, stroke, transient ischaemic attack or peripheral arterial disease, who have had a blood pressure of 140/90 mmHg or less in the preceding 12 months | 3403 | 2762 | (81.2) | 55 | (1.6) | 586 | (17.2) | 1231 | (78.9) | 30 | (1.9) | 300 | (19.2) | ||
| People aged 80 years or over, with CHD, hypertension, stroke, transient ischaemic attack or peripheral arterial disease, who have had a blood pressure of 150/90 mmHg or less in the preceding 12 months | 39 | 37 | (94.9) | 2 | (5.1) | – | 25 | (96.2) | 1 | (3.8) | – | ||||
| People who have had a MI and have received a prescription for an ACE-I or ARB, antiplatelet therapy, beta-blocker and a statin in the preceding 12 months | |||||||||||||||
| All classes of drugs | 1264 | 991 | (78.4) | 36 | (2.8) | 237 | (18.8) | – | – | – | |||||
| ACE-I | 432 | (84.9) | 9 | (1.8) | 68 | (13.4) | |||||||||
| ARB | 1 | (100.0) | – | – | |||||||||||
| Antiplatelet therapy | 605 | (80.0) | 21 | (2.8) | 130 | (17.2) | |||||||||
| Beta-blocker | 588 | (82.6) | 13 | (1.8) | 111 | (15.6) | |||||||||
| Statin | 710 | (79.6) | 25 | (2.8) | 157 | (17.6) | |||||||||
| Three out of the four classes of drugs | 541 | (82.7) | 12 | (1.8) | 101 | (15.4) | |||||||||
| People with CHD who have received a prescription for antiplatelet or anticoagulant therapy in the preceding 12 months | 1290 | 1015 | (78.7) | 36 | (2.8) | 239 | (18.5) | 747 | (80.1) | 27 | (2.9) | 159 | (17.0) | ||
| People with heart failure who have been prescribed an ACE-I or ARB in the preceding 12 months | 234 | 186 | (79.5) | 1 | (0.4) | 47 | (20.1) | 131 | (81.9) | – | 29 | (18.1) | |||
| People with heart failure who have been prescribed an ACE-I or ARB, and a beta-blocker, in the preceding 12 months | 155 | 126 | (81.3) | – | 29 | (18.7) | 105 | (82.7) | – | 22 | (17.3) | ||||
Appendix 16
| Indicator | OR of achieving indicator (95% CI) – unadjusteda | OR of achieving indicator (95% CI) – adjustedb | ||||||
|---|---|---|---|---|---|---|---|---|
| No MHc | MH with psychotropic drugsc | MH without psychotropic drugsc | No MHc | MH with psychotropic drugsc | MH without psychotropic drugsc | |||
| Communicable disease | ||||||||
| New receptions to prison accepting opt-out dry blood spot testing | 1.0 | 1.54 (1.24 to 1.91) | 1.89 (1.74 to 2.05) | 1.0 | 1.06 (0.82 to 1.37) | 1.16 (1.04 to 1.28) | ||
| Prison population who have received one hepatitis B vaccination in the preceding 12 months | ||||||||
| Of the population who entered in the last 12 months | 1.0 | 1.88 (1.62 to 2.18) | 1.63 (1.54 to 1.72) | 1.0 | 1.65 (1.41 to 1.94) | 1.9 (1.78 to 2.02) | ||
| Of patients resident in the study prison in the last 12 months with a clinical code added at any time indicating a history of any illicit drug use | 1.0 | 1.82 (1.51 to 2.19) | 1.57 (1.46 to 1.68) | 1.0 | 1.58 (1.29 to 1.92) | 1.79 (1.65 to 1.94) | ||
| People with one or more of CHD, stroke or transient ischaemic attack, diabetes or COPD who have received a flu vaccination between August and March | 1.0 | 1.07 (0.76 to 1.51) | 1.06 (0.92 to 1.23) | 1.0 | 1.09 (0.73 to 1.61) | 1.16 (0.97 to 1.39) | ||
| Mental health | ||||||||
| Prison population prescribed three or more psychotropic drugs (antipsychotics, sedative antidepressants, hypnotics and anxiolytics, pregabalin or gabapentin, opioids) at the same time during an 8-week period | ||||||||
| Three or more | 1.0 | 16.18 (12.1 to 21.63) | 6.29 (5.19 to 7.62) | 1.0 | 11.13 (8.19 to 15.11) | 3.72 (2.99 to 4.63) | ||
| Four or more | 1.0 | 27.42 (18.01 to 41.75) | 9.79 (7.18 to 13.35) | 1.0 | 17.53 (11.26 to 27.29) | 4.47 (3.15 to 6.33) | ||
| People aged over 55 years in the prison population who have a record of one of the following assessments in the preceding 12 months; MMSE, 6-item CIT, GPCOG | 1.0 | 1.41 (0.7 to 2.82) | 2.21 (1.74 to 2.82) | 1.0 | 1.88 (0.76 to 4.61) | 1.47 (1.07 to 2.04) | ||
| Prison-specific | ||||||||
| New receptions to prison who have been asked for consent to transfer medical records from GP to prison health care | 1.0 | 1.84 (1.53 to 2.22) | 0.67 (0.63 to 0.71) | 1.0 | 2.3 (1.75 to 3.02) | 1.9 (1.73 to 2.07) | ||
| New receptions to prison with a code for a second-stage health assessment in the past 12 months, plus clinical codes for IP risk assessment and MR added in the week before the 2nd-stage assessment | ||||||||
| Had MR during stay, but did not satisfy both within 7 days | 1.0 | 2.18 (1.12 to 4.24) | 2.44 (1.85 to 3.2) | 1.0 | 3.73 (1.64 to 8.5) | 2.04 (1.4 to 2.98) | ||
| Had IP during stay, but did not satisfy both within 7 days | 1.0 | 1.6 (1.03 to 2.46) | 0.34 (0.29 to 0.39) | 1.0 | 1.21 (0.54 to 2.69) | 1.34 (0.99 to 1.82) | ||
| Prison population prescribed opioids in the preceding 8 weeks from 31 March | ||||||||
| All prison population | Prescribed any opioid in the preceding 8 weeks from 31 March | 1.0 | 3.85 (3.35 to 4.42) | 2.04 (1.91 to 2.17) | 1.0 | 2.74 (2.35 to 3.2) | 1.95 (1.81 to 2.09) | |
| Prescribed any strong opioid in the preceding 8 weeks from 31 March | 1.0 | 3.14 (2.69 to 3.65) | 2.32 (2.17 to 2.47) | 1.0 | 2.07 (1.75 to 2.45) | 2.36 (2.19 to 2.55) | ||
| Prescribed benzodiazepines AND any opioid in preceding 8 weeks from 31 March | 1.0 | 2.01 (1.72 to 2.35) | 1.57 (1.47 to 1.67) | 1.0 | 1.72 (1.45 to 2.05) | 1.57 (1.46 to 1.69) | ||
| Any MH diagnosis | Prescribed any opioid in the preceding 8 weeks from 31 March | 1.0 | 1.22 (0.96 to 1.56) | - | 1.0 | 1.01 (0.77 to 1.31) | - | |
| All prison population AND NO coded diagnosis of neuropathic pain | Prescribed pregabalin OR gabapentin in the preceding 8 weeks from 31 March | 1.0 | 5.23 (3.62 to 7.54) | 3.56 (2.98 to 4.25) | 1.0 | 3.72 (2.55 to 5.42) | 2.71 (2.22 to 3.31) | |
| Diabetes, asthma and epilepsy care | ||||||||
| People with diabetes in whom the last blood pressure reading (measured in the preceding 12 months) is 140/80 mmHg or less | 1.0 | 1.36 (0.87 to 2.13) | 1.27 (1 to 1.62) | 1.0 | 1.51 (0.93 to 2.45) | 1.08 (0.82 to 1.42) | ||
| People with diabetes who have had the following in the preceding 12 months: BMI, blood pressure, record of smoking status, foot examination, urine albumin–creatinine ratio blood tests for HbA1c, cholesterol and serum creatinine | ||||||||
| Five of the eight items/tests | 1.0 | 1.29 (0.84 to 2.01) | 1.24 (0.99 to 1.57) | 1.0 | 1.15 (0.67 to 1.96) | 1.33 (1 to 1.77) | ||
| People with diabetes without moderate or severe frailty, in whom the last HbA1c is 58 mmol/mol or less in the preceding 12 months | 1.0 | 1.97 (1.27 to 3.06) | 1.13 (0.89 to 1.44) | 1.0 | 2.18 (1.32 to 3.59) | 1.12 (0.85 to 1.48) | ||
| People with asthma who have had an asthma review in the preceding 12 months that includes an assessment of asthma control | 1.0 | 1.73 (1.15 to 2.61) | 1.01 (0.84 to 1.21) | 1.0 | 1.29 (0.81 to 2.06) | 0.95 (0.76 to 1.18) | ||
| Screening | ||||||||
| Women eligible for screening and aged 25–49 years who have had cervical screening in the preceding 5 years and 6 months | 1.0 | 1.21 (0.9 to 1.64) | 1.58 (1.38 to 1.81) | 1.0 | 1.03 (0.76 to 1.41) | 1.55 (1.33 to 1.8) | ||
| Women eligible for screening and aged 50–64 years who have had cervical screening in the preceding 5 years and 6 months | 1.0 | 1.57 (0.52 to 4.76) | 1.7 (1.22 to 2.37) | 1.0 | 1.45 (0.47 to 4.45) | 1.73 (1.21 to 2.48) | ||
| Women eligible for screening and aged 50–70 years who have had breast screening in the preceding 3 years | 1.0 | 0.56 (0.11 to 2.83) | 0.39 (0.25 to 0.62) | 1.0 | 0.44 (0.09 to 2.27) | 0.47 (0.28 to 0.79) | ||
| Men eligible for screening and aged 65 years or over with a record of AAA screening | 1.0 | 0.36 (0.14 to 0.9) | 1.01 (0.72 to 1.41) | 1.0 | 0.33 (0.1 to 1.07) | 1.47 (0.91 to 2.35) | ||
| People aged 45–74 years with a recorded CVD risk assessment in the preceding 5 years, and who do NOT have a diagnosis of: CHD, CKD, diabetes, hypertension, AF, transient ischaemic attack, familial hypercholesterolaemia, heart failure, peripheral arterial disease, stroke or previously documented 20% or higher 10-year CVD risk BEFORE the last 5 years | 1.0 | 2.28 (0.96 to 5.44) | 1.57 (1.1 to 2.25) | 1.0 | 2.27 (0.9 to 5.71) | 1.12 (0.75 to 1.68) | ||
| CVD | ||||||||
| People with transient ischaemic attack or stroke, excluding those with haemorrhagic stroke, who have been prescribed an antiplatelet or anticoagulant in the preceding 12 months | 1.0 | 0.48 (0.12 to 1.87) | 1.91 (0.88 to 4.14) | 1.0 | 0.13 (0.01 to 1.08) | 1.02 (0.25 to 4.11) | ||
| People with persistent or paroxysmal AF and a CHA2DS2-VASc score equal to 2 or more, with a prescription for warfarin or a direct-acting oral anticoagulant in the preceding 12 months | 1.0 | 0.44 (0.04 to 5.19) | 1.13 (0.41 to 3.1) | 1.0 | - | - | ||
| People with persistent or paroxysmal AF and a CHA2DS2-VASc score in the preceding 12 months | 1.0 | 1 (0 to 0) | 2.73 (0.81 to 9.23) | 1.0 | - | 0.79 (0.11 to 5.68) | ||
| People aged 79 years or under, with CHD, hypertension, stroke, transient ischaemic attack or peripheral arterial disease, who have had a blood pressure of 140/90 mmHg or less in the preceding 12 months | 1.0 | 1.5 (0.88 to 2.56) | 1.31 (1.09 to 1.56) | 1.0 | 1.68 (0.96 to 2.96) | 1.25 (1.02 to 1.53) | ||
| People who have had a MI and have received a prescription for an ACE-I or ARB, antiplatelet therapy, beta-blocker and a statin in the preceding 12 months | ||||||||
| Three out of the four classes of drugs | 1.0 | 0.42 (0.21 to 0.84) | 0.62 (0.46 to 0.82) | 1.0 | 0.48 (0.22 to 1.05) | 0.53 (0.37 to 0.74) | ||
| People with CHD who have received a prescription for antiplatelet or anticoagulant therapy in the preceding 12 months | 1.0 | 1.07 (0.5 to 2.32) | 0.71 (0.53 to 0.96) | 1.0 | 1.78 (0.69 to 4.59) | 0.8 (0.55 to 1.16) | ||
| People with heart failure who have been prescribed an ACE-I or ARB in the preceding 12 months | 1.0 | 1 (0 to 0) | 0.71 (0.36 to 1.39) | 1.0 | - | 0.48 (0.18 to 1.27) | ||
| People with heart failure who have been prescribed an ACE-I or ARB, and a beta-blocker in the preceding 12 months | 1.0 | 1 (0 to 0) | 0.63 (0.24 to 1.68) | 1.0 | - | 0.65 (0.17 to 2.59) | ||
List of abbreviations
- AAA
- abdominal aortic aneurysm
- ACA
- American Correctional Association
- ACE
- angiotensin-converting enzyme
- ACR
- albumin–creatinine ratio
- ADHD
- attention deficit hyperactivity disorder
- AF
- atrial fibrillation
- AHP
- allied health professional
- AIDS
- acquired immunodeficiency syndrome
- AMA
- American Medical Association
- ARB
- angiotensin receptor blocker
- ASCA
- Association of State Correctional Administrators’
- BM
- benchmark
- BMing
- benchmarking
- BMI
- body mass index
- BoP
- Bureau of Prisons
- CB
- commissioning board
- CC
- chronic condition
- CDCR
- California Department of Corrections and Rehabilitation
- CDSSs
- clinical decision support systems
- CF
- correctional facility
- CHA2DS2-VASc
- congestive heart failure, hypertension, age ≥75 (doubled), diabetes, stroke (doubled), vascular disease, age 65–74, and sex (female)
- CHD
- coronary heart disease
- CI
- confidence interval
- CIC
- Community Interest Company
- CIT
- cognitive impairment test
- CJS
- Criminal Justice System
- CMHS
- Correctional Mental Health Screen
- COPD
- chronic obstructive pulmonary disease
- CVD
- cardiovascular disease
- DBST
- dry blood spot tests
- DNA
- did not attend
- DOC
- Department Of Corrections
- DEXA
- dual-energy X-ray absorptiometry
- EB
- evidence-based
- ECG
- electrocardiogram
- GP
- general practitioner
- GPCOG
- General Practitioner Assessment of Cognition
- HC
- health care
- HCP
- healthcare professional
- HCV
- hepatitis C virus
- HEDIS
- Healthcare Effectiveness Data and Information Set
- HIV
- human immunodeficiency virus
- HMPPS
- Her Majesty’s Prison and Probation Service
- IFCC
- International Federation of Clinical Chemistry
- IP
- in possession
- MDT
- multidisciplinary team
- MH
- mental health
- MI
- myocardial infarction
- MMR
- measles, mumps and rubella
- MMSE
- Mini Mental State Examination
- MR
- medicines reconciliation
- MRC
- Medical Research Council
- NCCHC
- National Commission on Correctional Health Care
- NHS
- National Health Service
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- NRC
- National Research Committee
- ONS
- Office for National Statistics
- OR
- odds ratio
- OST
- opiate substitution treatment
- PAD
- peripheral arterial disease
- PCR
- protein–creatinine ratio
- PHE
- Public Health England
- PPI
- patient and public involvement
- PPN
- prisoner policy network
- PRISMA-ScR
- Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews
- PTSD
- post-traumatic stress disorder
- QI
- quality indicator
- Qim
- quality improvement
- QOF
- quality and outcomes framework
- RCGP
- Royal College of General Practitioners
- RCN
- Royal College of Nursing
- RCP
- Royal College of Physicians
- RFP
- request for proposals
- SMI
- severe mental illness
- SoMREC
- School of Medicine Research Ethics Committee
- STIs
- sexually transmitted infections
- TB
- tuberculosis
- TIA
- transient ischaemic attack
- TSH
- thyroid-stimulating hormone
- WP
- work packages
- YOIs
- young offender institutions
