Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 08/1808/238. The contractual start date was in January 2009. The final report began editorial review in July 2012 and was accepted for publication in January 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen's Printer and Controller of HMSO 2013. This work was produced by Buchanan et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Aims, background and methods
The subtitle of this project concerns ‘the realities of middle and front-line management work’. The problems of defining middle management, in any sector, and the ambiguities surrounding the location of front-line hospital managers, led to us drop ‘and front-line’ from this report. Role titles (ward sister, divisional nurse, operations manager), although not always accurate or consistent, offer a better guide to the nature of the work and responsibilities of post holders than ‘middle’ or ‘front-line’ designations
Things can only get different
You'll hear people say ‘management’ in inverted commas. And I'll say, but you all manage. I think that there's always been quite a hierarchy in the NHS. And I do not believe we've done as much as we can to break that down. I want everyone to take accountability and responsibility.
Modern matron, Netherby hospital
How do hospital managers in the NHS handle the demands of a constantly changing service? How do managers affect the quality of patient care and clinical outcomes? Patient safety is a national priority, but changing working practices following serious incidents can be problematic. Why? We know surprisingly little about the work experience, practices and attitudes of hospital managers, who are key to implementing local strategy and national initiatives. However, when things go wrong, this is the group that often takes the blame. This study seeks to build on what we know about management, change and leadership, and relate this to current trends.
This chapter describes the research questions and aims of this study, explains the background to the project and provides an overview of the research process and methods. This project began in 2009. By 2012, however, the service had changed in a number of significant ways. Two events in particular had an impact on acute hospital management roles during this period.
Economic crisis
The first of these events was the collapse of the investment bank Lehman Brothers, which filed for Chapter 11 bankruptcy protection in America on 15 September 2008. With debts of over US$600B, this was the largest corporate failure in American history, triggering a global financial crisis. This in turn led to massive government spending around the world to recapitalise other banks that were close to collapse because of their exposure to Lehman's debts.
In the UK, financial support for the banking sector increased UK public sector net debt to £845B by the end of 2009, prompting action to reduce government spending. Government policy was to ‘protect’ the NHS budget (> £100B a year). Nevertheless, cost inflation in the health service is historically higher than general inflation, and flat funding or small rises amounting to real decreases in annual NHS spending can generate deficits for individual provider organisations.
In 2010 the chief executive of the NHS, Sir David Nicholson, thus set the service the target of generating £20B of efficiency savings (one-fifth of annual spending) by 2014–15. Known as ‘the Nicholson challenge’ or ‘the NHS recession’, all health-care providers had to consider radical cost improvement programmes (CIPs) while maintaining the level, quality and safety of services.
New government
The second event was the election of a Conservative–Liberal Democrat coalition government following the general election in May 2010. The new Secretary of State for Health published his first White Paper in July 2010. 1 This set out proposals to abolish primary care trusts (PCTs) and strategic health authorities, give most of the NHS budget to clinical commissioning groups and create a National Commissioning Board. Trusts were also expected to achieve at least 3.5% cost improvements annually over 3–5 years while improving quality of care. The Secretary of State also proposed a 45% cut in the management costs of the service by 2014–15. Government ministers depicted health-care managers as ‘costly, pen-pushing bureaucrats’, and the service was now to be run by clinical staff: general practitioners, hospital doctors, and nurses.
These and other structural and regulatory changes were consolidated in a Health and Social Care Bill introduced to Parliament in January 2011. The lengthiest piece of legislation in British history, the bill's provisions were controversial. The uncertainties surrounding these proposals, how they would operate in practice and the implications for funding created a challenging management agenda. As one participant in this project observed:
Netherby is a £250 million hospital. Over the next three years, we're looking at inflated costs and deflated income. If we do nothing, in three years’ time, we will be losing up to £30 million a year, so we need to do something now. We have a transformation steering group whose remit is to design a programme to prevent the trust running up an annual £30 million loss. We want to avoid ‘slash and burn’, but we do need to lose staff and cut management layers. This means big change.
Director, Netherby hospital
Budget cuts, new structures, tighter regulation, fresh priorities, negative stereotyping – some participants in this study said that they ‘had seen it all before’. The NHS, which celebrated its 60th anniversary in 2008, has been subject to changes of this nature throughout its history. But for the majority of participants, this was new; one manager observed, ‘it feels different this time’. The scope of the structural and regulatory changes, the severity and pace of funding cuts, the need to improve quality and safety, and the job insecurities were unprecedented. Following Lehman's collapse and the shift in government policy, for health-care managers it was no longer ‘business as usual’. The acute hospital model was challenged with strategies for moving care into the community, focusing on prevention (alcohol abuse, obesity) and on self-management of long-term conditions (asthma, diabetes). From 2011, changes to tariffs meant that hospitals would no longer be remunerated in full for increases in emergency department attendances, and would be penalised for (among other breaches) emergency readmissions within 30 days. Management confidence in the ability of the service and individual provider trusts to deliver the necessary savings was low. 2
The NHS was thus passing through a further period of rapid and radical change during the life of this project. The context in which management work is carried out is crucial. The management implications of the changing institutional context are explored in Chapter 3. The local organisational contexts of the trusts participating in this project are discussed in Chapter 4. As institutional and organisational contexts change, management roles change too. As the chief executive of The King's Fund observed, ‘things can only get different’ (p. 14). 3
Research questions
Interviewer: What outputs would you like to see from this project?
Respondent: I want to understand what we can do to support and help those in increasingly challenging roles, because we need to get it right. Otherwise, they will do it badly or won't do it. I want to gain a better understanding of their motivation, so that we can help provide meaningful careers.
Senior executive, Greenhill hospital
This project addressed three sets of questions:
-
Realities: What are the pressures and demands facing middle managers in health care? What are the implications of these trends?
-
Changes: What roles do middle managers play in implementing changes? How are changes arising from serious incidents implemented, and how can this process be improved?
-
Contributions: How does management practice affect clinical and organisational outcomes? What factors influence management contributions to performance? How can the components of an ‘enabling environment’ for management work be assembled and sustained?
Realities
We can claim some understanding of the nature of general management roles,4 the realities of management work,5 rewards and pains6 and how managers spend their time. 7 Is that knowledge relevant to health care today? This project sought to understand how current pressures have affected the realities of middle management work in acute settings. Convention has managers running things as they are while leaders drive change. But managers at all levels in the NHS could be excused a cynical response to that distinction, having implemented a series of major changes affecting all aspects of the service – culture, structures, priorities, governance, working practices – and more.
Changes
There is a widespread perception that the management of change in health care is especially problematic. 8 This has led to a renewed emphasis on medical engagement in leadership and change. 9,10 Recent evidence suggests, however, that many radical changes are implemented, not by small groups of senior managers and doctors, but by distributed groups of middle managers and others, including clinical staff. 11 Several studies undermine the distinction between leaders who drive change and managers who maintain order, emphasising middle management roles in strategy, and in change ‘under the radar’. 12–14 The development of distributed change leadership, based on the spontaneous concertive action of staff at all levels, is evident in health care. 15,16 Clark et al. 17 note that ‘Enhanced clinical engagement should work towards a model of diffused leadership, where influence is exercised across a complex set of relationships, systems and cultures’ (p. 32, italics added for emphasis).
Change is thus a central aspect of middle management work. 18,19 Following serious incidents, the recommendations from investigations are sometimes adopted rapidly. However, despite efforts to ‘learn the lessons’, these recommendations often lead to little or no action. 20 Noting that the pace of change in improving patient safety had been slow, Donaldson21 cited the distinction between passive learning (identifying lessons) and active learning (implementing changes), noting that the latter does not follow automatically. This project thus explored the processes of change following serious incidents, to identify the conditions that respectively block and promote change in such contexts.
Contributions
One research tradition has sought to understand what managers do. 4,22 Another line of research concerns the contributions that middle managers make to clinical and wider organisational outcomes. This project sought to identify the conditions that enable, support and strengthen those contributions. Evidence suggests a systemic link between management practices and outcomes. 23–25 Management competencies are key, but organisational context is also crucial in determining receptiveness,26 setting priorities and incentives, focusing attention and energy and establishing an environment that either enables or stifles service improvement. What does an ‘enabling environment’ look like? How can the components of an enabling environment be assembled and sustained? One of the outcomes of this project (see Chapter 7) is a ‘contributions-based’ model of management work.
Why middle management?
The ward leaders – sisters and charge nurses – make or break the hospital's reputation. We have over fifty wards on two sites. Each has a team of twenty to thirty staff operating 24/7. It's where the costs arise, and where patients and visitors make judgements about standards, depending on staff approach and discipline. That's where the key business of patient care is.
Senior executive, Greenhill hospital
The NHS has since the mid-1980s focused attention on chief executives and trust boards. One manifestation of this was the Leadership Qualities Framework. 27 When it was first published, the principal investigator for the current project was working with a hospital in the Midlands. The human resources director was running management development sessions for new clinical directors and business managers – a group of ‘senior middle’ managers. She telephoned the Leadership Centre (part of the NHS Modernisation Agency) and requested 20 copies. She was asked about the use to which these would be put. When she explained, she was told that copies could not be provided. Why not? Because the framework was designed for board-level directors and not for less senior staff.
This anecdote is symptomatic of what appear to be deep-rooted attitudes towards leadership and management in the NHS. Since 2009 there has been a National Leadership Council. There was no National Management Council. There was an elite top leaders programme for those in roles deemed to be ‘business critical’. There was no top managers programme. The NHS had developed several leadership competency frameworks. There were no management competency frameworks. An NHS Leadership Academy was launched in November 2011. There was no Management Academy.
The updated version of the Leadership Qualities Framework28 does suggest that the framework applies to staff at all levels – except for two of the seven domains, ‘creating the vision’ and ‘implementing the strategy’, which are the preserve of ‘a relatively small group of people who hold designated positional roles, and are required to act as leaders in formal hierarchical positions. These two domains focus more on the contribution of individual leaders rather than the general leadership process’ (p. 8). If this ‘general leadership process’ means middle managers, then this implicit division of leadership labour ignores two decades of compelling research evidence. 29,30
One consequence of the focus on senior leadership is that less is known about the roles, experiences, contributions and motives of middle managers. 31 The presumption that their contributions are less ‘business critical’ has passed unchallenged. The Service Delivery and Organisation (SDO) research programme had funded previous studies on leadership, organisation cultures, performance management and service reconfiguration. Those studies, however, did not explore directly the work of middle managers. There was, therefore, a pressing need for research into the challenges facing management in health care and this was recognised as a priority theme for research. 32
Have conditions changed so dramatically since 2007 as to render the findings from this project obsolete? On the contrary. The impact of institutional and organisational context remains central to our understanding of management roles and contributions. For acute hospitals, change agendas are complex and challenging, and middle managers are key to implementation. Although other issues have surfaced and generated additional research questions, the challenges that the NHS has faced since 2007, and will face from 2012 onwards, have only reinforced the importance of this theme.
Research methods
This project used a multimethods collaborative design involving set-up interviews, focus groups, a management survey, documentation from participating sites, serious untoward incident narratives based on documentation and interviews, and management briefings (see details in Appendix 8). The aim throughout was to engage participants as co-researchers, in formulating the original proposal, in survey design and in selecting case incidents. The project stages are summarised in Table 1.
| Project stage | Timing | Description |
|---|---|---|
| Stage 1: set-up | January–October 2009 | Project launch, recruit research fellow, ethical approvals, advisory group, set-up interviews to gather background information on participating sites |
| Stage 2: management focus groups | January–October 2010 | Focus groups at each of six sites: identify motives, trends, contributions |
| Stage 3: management survey | August–October 2011 | Survey trust management populations: realities, changes, contributions |
| Stage 4: management briefings | June 2011–March 2012 | Feed back findings in briefing groups; explore implications for practice |
| Stage 5: managing extreme events | January 2010–March 2012 | Incident narratives, focusing on change following extreme or serious events |
| Stage 6: publication and dissemination | Ongoing, final report June 2012 | Final report, further dissemination |
Timescale and participating trusts
The project was based in six acute hospitals, selected to provide geographical spread and variation in size and status. To maintain anonymity and confidentiality, they were given pseudonyms. These hospitals are profiled in Table 2. A trust is a public sector corporation and is not a trust in the legal sense. This model was introduced in 1990 as part of the plan to develop an internal market in health services, with general practice fund holders buying care from independent providers. Trusts have a board with a chief executive and executive directors, and non-executive directors including a chairperson. Trusts are required to appoint an audit committee comprising non-executive directors (excluding chairpersons) to oversee finance and corporate governance.
Following controversy and trade union resistance, the ‘foundation trust’ concept was introduced in 2004. Foundation trusts have greater operational and financial autonomy, under a licence granted by the foundation trust regulator, Monitor. The organisation structures and governance arrangements of foundation trusts encouraged them to operate like businesses, with close links to local communities through boards of governors comprising members drawn from the populations that they served. All NHS trusts were expected to achieve foundation status by 2013–14. 33
| Trust | Sites | 2011–12 (£)a | Staffa | Bedsa | FTb | CEsc | Big issued |
|---|---|---|---|---|---|---|---|
| Burnside | 1 | 120M | 2400 | 400 | No | 2 | PCT relations |
| Clearview | 1 | 590M | 7000 | 1150 | Yes | 2 | Site development |
| Greenhill | 2 | 420M | 8000 | 1100 | Yes | 1 | Emergency targets |
| Netherby | 2 | 240M | 4200 | 600 | No | 5 | Ageing estate |
| South Netley | 2 | 490M | 9000 | 1150 | No | 2 | One site by 2014 |
| Wattle Park | 1 | 240M | 3400 | 700 | No | 2 | Merger plans |
In 2010–11 there were 258 hospitals in England,34 but only 172 acute trusts (of which around 140 had foundation status). The discrepancy is explained by the wave of mergers in the first decade of the 21st century, creating several trusts that combined more than one hospital, such as Greenhill, Netherby and South Netley, which each operated two hospitals at different locations.
The selection of those trusts cannot be seen as a representative sample in the traditional, statistical sense. However, the aims of developing theory and practical guidance rely on the more powerful concepts of analytical refinement and naturalistic generalisation, rather than on statistical generalisation. 35–37 With regard to understanding the problems of implementing change following serious incidents, statistical generalisation is irrelevant, but ‘isomorphic learning’ is important. 38 Sample size is not a concern in the context of these research and practice-related aims. Nevertheless, those six trusts can be regarded as broadly representative of the acute sector as they operate in the same policy, regulation and funding environment, facing the same government demands and public expectations, with similar internal structures, working conditions and terms of employment. Empirical support for a claim to representativeness comes from the observation that the middle management experience displayed broad similarities across those six trusts, despite their differences in size, structure, location, status and problems. There were differences, of course, but the similarities were more striking.
Collaborative research design
Collaborative research designs, although not without problems, have been shown to be effective in translating research into practice in health care. User engagement contributes to the development and dissemination of findings, and to building research capacity among those involved. 39 This project adopted a collaborative design, with five aspects. First, in negotiating access to participating trusts, the draft research proposal was circulated to chief executives and other board-level directors for comment. The draft was altered as a result of feedback received. Second, one of the questions asked in management set-up interviews concerned desirable outputs from this project. Recurring themes included the value of fresh evidence to support leadership and management development, managing a complex and contradictory agenda and implementing change to improve patient safety. Third, we ran a project launch event followed by three update workshops at which findings were fed back to participants for critical comment, focusing also on the implications for practice. Fourth, project findings were fed back to individual trusts in management briefings, triggering discussions around interpretation and emphasis and practical implications. Finally, this project was assisted by a SDO management fellow, on full-time secondment from Clearview for 8 months and attached to the project part-time over 2 years.
We also established an advisory group with eight members (see Appendix 2). Two were senior academics with experience of health-care management research. The other six included two in senior national NHS roles, an acute trust research and development manager, two freelance consultants specialising in health-care management development and our SDO management fellow who came from an operational management role at Clearview. The managers in this group outnumbered the academics. Together they provided a valuable sounding board and source of ideas and advice on project methods and focus, interpretation of findings and applications, and dissemination methods.
Data collection
Information came from five main sources: interviews, focus groups, survey, briefings and incident narratives. That information was complemented by documentation (annual plans, strategy documents, reports and accounts, board agendas and minutes, NHS staff survey results and trust newsletters), much of which was in the public domain and available from trust websites. Table 3 summarises the numbers of participants involved in each stage of the project, at each of the six acute trusts.
| Trust | Set-up interviews | Focus groupsa | Incident interviewsb | Survey | Briefingsc |
|---|---|---|---|---|---|
| Burnside | 10 | 47 (5) | 15 | 108 | 16 |
| Clearview | 24 | 52 (12) | 14 | 250 | 78 |
| Greenhill | 13 | 33 (7) | 2 | 77 | 85 |
| Netherby | 17 | 38 (9) | 6 | 86 | 40 |
| South Netley | 12 | 23 (2) | 0 | 90 | 2 |
| Wattle Park | 17 | 41 (5) | 9 | 0 | 0 |
| Total | 93 | 234 (40) | 46 | 611 | 221 |
| Total project participants | 1205 | ||||
The project stages involved the following activities.
Stage 1: set-up
-
Collection of background information on research sites through set-up interviews and internet downloads.
-
Recruiting, orienting and equipping research fellow.
-
Collating and reviewing literature on middle management, the management of ‘extreme’ change and management contributions to health-care organisation outcomes.
-
Ethical approvals, governance checks and research passports.
Set-up interviews had three objectives (see agenda in Appendix 2): first, to establish the key groups of middle and front-line managers with whom it would be appropriate to run focus group discussions; second, to gather background on each trust and its management agenda; and third, to establish logistical arrangements for distributing project information.
Stage 2: management focus groups
The original proposal was to run four focus groups at each participating site, involving around 100 managers in total. These discussions generated information concerning the changing nature of middle management work, and issues arising in those discussions also contributed to the design of the survey (see participant information and topic guide in Appendix 2). As Table 3 shows, however, over 230 managers participated in 40 focus group discussions. The main reason for exceeding the original target lay with replies to the interview question concerning the middle management groups to involve in this project and who would not be covered with only four focus groups. The widely distributed nature of the management population in an acute trust is explored in Chapter 2. At two trusts, South Netley and Wattle Park, arranging focus groups proved to be a logistical problem. Only two groups were run at South Netley and, although five were run at Wattle Park, one relied on interviews with clinical directors with whom we were never going to be able to meet as a group.
Stage 3: management survey
The aim of the management survey was to build on the qualitative information from interviews and focus groups, and to generate evidence from a larger sample on the nature of emerging pressures and demands, and the implications for management practice. The aim was to survey the entire middle management populations in the six participating trusts, but this was not possible. The plan was to use a ‘60–40’ design with around 60% of survey items common to all sites, for comparison and benchmarking purposes, and 40% tailored to local priorities. However, as the survey was being designed early in 2011, pressures on trust managers' time increased sharply, and three trusts decided not to complement the survey with their own questions. Findings are explored in Chapter 5 and full details of the survey design, administration and analysis are provided in Appendix 3.
Stage 4: management briefings
Starting in the second quarter of 2011, we offered management briefings to give participants an opportunity to assess the findings and their implications. These were also opportunities for respondent validation, to check interpretations and to explore implications for practice. The limited amounts of time that managers were able to give to these meetings meant that there was often little chance for extended discussion. However, the broadly favourable responses to these presentations did provide reassurance with regard to the main findings.
Stage 5: managing extreme events
This stage of the project focused on the management processes involved in implementing change following serious or ‘extreme’ incidents. 40 The aims included developing an understanding of processes that have rarely been investigated from a change management perspective, and developing frameworks of practical value in such settings. Patient safety and serious incident investigation are areas in which considerable amounts of work – theoretical and practical – already exist. However, the focus of that commentary concerns investigation methods to understand incident causality, and protocols to improve safe practice. The implementation of changes to practice is rarely automatic or straightforward, and there are gaps in our understanding of the potential problems. The aim, therefore, was to document narratives of successful and less successful attempts to implement change following serious incidents, to identify the conditions that shape the outcomes.
The incidents discussed in this report are listed in Table 4. The outcome in one of these incidents, concerning the handling of the Clostridium difficile outbreak at Burnside, was sustained success. Change following the other incidents, however, was problematic. Because of space constraints, four of these incidents are discussed in Chapter 6 and one is reported in Appendix 4.
| Serious incident | Trust |
|---|---|
| C. difficile outbreak | Burnside |
| Patient death, drugs interaction | Clearview |
| Mental health patient suicide | Clearview |
| Surgical patient misidentification | Clearview |
| Norovirus outbreak (see Appendix 4) | Wattle Park |
Stage 6: publication and knowledge transfer
Publication and dissemination traditionally follow project completion. In this case, however, the intent was to develop outputs from the project from an early stage, particularly when these had implications for management practice. We wanted to generate high-impact, readily accessible modes of communication, which nevertheless maintained the integrity and, where appropriate, the complexity of the issues at stake and implications for management practice. Outputs have included a series of research briefings, a podcast, a magazine article, a contribution to the Health Service Journal online resources section and conference and seminar presentations (see Appendix 5).
Data analysis
Table 5 summarises the approach to data analysis, linking information sources to the project themes.
| Stage, link to themes | Analysis, what this revealed |
|---|---|
| 1. Set-up interviews | Context profiling, of participating trusts |
| Managing realities | Outcomes: identify local priorities and management agenda, factors shaping management realities |
| 2. Focus groups | Content analysis, identifying recurring themes |
| Managing realities | Outcomes: identify pressures, trends affecting middle management, suggestions for strengthening management contribution |
| Managing change | |
| 3. 60–40 survey | Statistical analysis: descriptive statistics and frequency distributions; content analysis of open responses (one trust only) |
| Managing realities | Outcomes: sample characteristics, motives and values, incidence and experience of new challenges and trends, factors and practices impacting effectiveness, components of ‘enabling’ and ‘disabling’ environments for management work, changing patterns of management activity |
| Managing change | |
| Managing contribution | |
| 4. Briefing groups | Content analysis, identifying recurring themes |
| Managing contribution | Outcomes: respondent validation, practitioner check on analysis, interpretations, and implications for practice |
| 5. Extreme events | Visual mapping and event sequence analysis, of incident narratives |
| Managing change | Outcomes: identify recurring success and problem patterns in extreme change processes, contingency framework based on comparisons of incidents and contexts |
| Managing contribution |
Methodology assessment
This study has a number of limitations. First, data collection was uneven across the six participating trusts, mainly because of the growing pressures on hospital management and the difficulties in arranging meetings. Second, the extended time frame potentially jeopardises the relevance of information gathered towards the beginning of the project (although many of the pressures raised at that stage have intensified since). Third, coverage of this range of themes across six trusts has perhaps been achieved at the expense of depth; it was not possible to follow up many interesting issues because of time pressures on both researchers and participants. Fourth, this qualitative study of management contributions develops conclusions that would benefit from quantified support.
Problems arose more with regard to the context in which this project was conducted than with the project design. The context involved changes that were unprecedented in scale and pace, and which made exceptional demands on NHS staff time, particularly those with management responsibilities. We attempted to arrange 1-hour interviews with individuals and 1-hour focus group meetings with around half a dozen managers at a time, when operational pressures were already requiring them to work well beyond contract hours. It was also difficult to arrange for the distribution of, and encourage responses to, the survey because of pressure on resources. Although we were able to generate outputs from an early stage, the slower than expected accumulation of data delayed the data analysis process. Major outputs have thus also been delayed, and developing the publications stream further is a priority following the completion of this project report.
Nevertheless, the project design and methods allowed us to construct rich pictures of the changing realities of middle management work in acute settings and management contributions to organisational and clinical outcomes and how those contributions could be strengthened. The incident narratives have generated fresh insights, theoretical and practical, for streamlining change processes and contributing to patient safety. Participants saw this project as valuable and timely, and none refused to be interviewed. Focus groups invariably ran beyond their scheduled hour as participants wanted to continue discussion. We were invited to incorporate management briefings in trust leadership development programmes. We were asked to run additional management skills sessions, particularly with regard to the development of influencing and political skills, and on implementing change after serious incidents. Informal feedback from managers on project outputs has been highly favourable. We have also developed interesting and valuable suggestions for further research.
Chapter 2 The NHS management population
Names, ranks and numbers
We want to turn this into a great organisation, a great place to work. We need to engage people or lose talent, especially in general management roles. Retaining talent in management roles is going to be a problem. They could just walk away to other sectors.
Director, Greenhill
There is a widespread perception that the NHS is bureaucratic and overmanaged by ‘pen-pushers’ and ‘grey suits’. 31,41,42 Management costs were thus a popular target for politicians during the life of this project, particularly approaching the general election in May 2010. 43,44 In exploring the NHS management population, this chapter reaches four conclusions:
-
Evidence suggests that the NHS is undermanaged, despite claims about disproportionate increases in management numbers, and the composition of the NHS workforce is stable.
-
The proportion of staff with managerial responsibilities is much higher than suggested in official statistics, which do not recognise many middle managers or those whose roles combine clinical and managerial responsibilities.
-
Acute trust management includes ‘pure plays’ with managerial roles and ‘hybrids’ with combined clinical–managerial duties; hybrids outnumber pure plays by four to one.
-
The obsession with management numbers and costs overlooks more significant issues concerning management capacity and the contributions that middle and front-line management make to clinical and organisation outcomes.
Management numbers
The NHS Information Centre collates annual workforce census figures (www.ic.nhs.uk). The overview in March 2011 reported that, on 30 September 2010, as fieldwork for this study began, the NHS in England had nearly 1.2 million employees (full-time equivalent or FTE, Table 6), including 40,094 ‘managers and senior managers’ (Table 7).
| 2000 | 2010 | % increase | |
|---|---|---|---|
| Headcount | 1,118,958 | 1,431,557 | 28.0 |
| FTE | 892,620 | 1,186,571 | 32.9 |
| 2000 | 2010 | % increase | |
|---|---|---|---|
| Headcount | 25,256 | 41,962 | 66.1 |
| FTE | 24,253 | 40,094 | 65.3 |
Between 2000 and 2010, management numbers increased by 65%. The same calculation for 1999–2009 revealed a rise in management numbers of 84%. Total NHS employment rose by 30% over this period. Although the press made an issue of this ‘80–30’ disparity, basic arithmetic suggests a more prosaic conclusion. The disparity arises from the difference in the bases of the calculation, which is over a million in one case and around 20,000 in the other. Percentage calculations produce higher figures with smaller bases. For example, when team membership grows by only one person from two to three, that is a 50% increase. When team numbers swell to 101 from 100, that is a 1% increase.
The Information Centre figures (Table 8) show that managers represented just under 3% of the NHS workforce (FTEs) in 2000 and just over 3% in 2010 – hardly a dramatic increase. The census published in 2012 shows that total employment fell to 1,193,334 (headcount) by November 2011 and the number of managers and senior managers also fell to 3.2% of the total.
| 2000 | 2010 | |
|---|---|---|
| Headcount | 2.3 | 2.9 |
| FTE | 2.7 | 3.4 |
It is, however, appropriate to explain the increase in management numbers since 1999. Part of the explanation lies with the 30% increase in the numbers of staff requiring recruitment, selection, coaching, mentoring, supervision, appraisal, discipline, development – management. The increase was also likely to have arisen as a result of other demands:45
-
pursuit of foundation trust status, developing service-line management
-
waiting times and other targets, outcomes, performance standards
-
Quality, Innovation, Productivity and Prevention (QIPP) agenda
-
world-class commissioning, creation of clinical commissioning groups
-
patient choice, electronic booking, independent treatment centres
-
payment by results, changes to tariffs, fines
-
making £20B efficiency savings by 2015
-
constantly changing regulatory, auditing and accreditation regimes
-
serious incident and ‘never event’ investigation and reporting systems
-
Monitor and Care Quality Commission (CQC) compliance processes and quality accounting.
Drawing from Binley's Database of NHS Management, Walshe and Smith31 arrive at similar conclusions. Although using information gathered for commercial purposes, with different inclusion criteria, Binley's data have been collected in a consistent manner for a considerable period, and reveal trends similar to those in the Information Centre figures. According to Binley's Database, NHS management numbers in the UK rose by 28% between 1997 and 2010 (Table 9). Walshe and Smith note that NHS spending over this period increased by 105% in real terms, from £60B in 1996–7 to around £123B in 2010–11 (at 2011 prices). They conclude that the management workforce has not expanded disproportionately, having not only more staff, but also more money, to manage. Binley's Database also shows that management numbers in acute services (across the UK) have been relatively stable, with 14,810 in 1997, 12,642 in 2000 and 13,985 in 2010.
| Year | England | UK |
|---|---|---|
| 1997 | 20,029 | 24,822 |
| 2000 | 18,462 | 22,366 |
| 2010 | 27,413 | 31,871 |
How does the NHS compare with other sectors? The Office for National Statistics Labour Force Survey shows that around 15% of the total UK workforce are designated ‘managers and senior officials’. This proportion has changed little in the past decade, rising from 13.6% of all those in employment in 2001 to 15.6% in 2010 (www.statistics.gov.uk/statbase/product.asp?vlnk=14248). With only 3% of the workforce in management roles, the NHS may be short of management expertise.
Management costs
The question of management numbers is linked to costs, which, in a climate of global recession and domestic austerity, were the subject of debate. This debate was not new. In 2001, Appleby46 reported on ‘government's war on management costs (synonymous with managers/bureaucrats)’, asking, ‘what level of management costs should the NHS expect to bear in order to have a well-managed service?’ The ‘New Labour’ administration wanted to cut NHS management costs by £1B over 5 years from 1997. Appleby46 also noted that ‘Managers are not seen by most of the public as adding any value to the NHS or patient welfare. Indeed, most would like to see fewer managers and, yes, more doctors, more nurses, more beds.’ Reducing ‘bureaucracy’ is perennially popular.
McLellan47 noted that management costs were around 3% of the annual service budget in 2010. In comparison, US charities spend between 4% and 8% of revenue on management. The estimate for UK charities is between 5% and 13%. 48 McLellan47 cites these figures as evidence that the NHS is undermanaged, a situation that would be exacerbated, he argued, by the policy of cutting management costs by 45% by 2014–15, pointing to ‘the scale of the financial challenge facing the service and the potential lack of management capacity to deal with it’ (p. 3).
Drawing on an analysis by McKinsey, Santry43 reports that management accounted for 1.5% of the total NHS budget in 2009, putting the UK at number 18 in a list of 23 global health systems. Management in other countries consumed much higher proportions of their health-care budgets, including in Mexico (11.8%), the USA (7%) and France (6.8%). Santry was responding to a claim by the Secretary of State for Health that there was no comparative international evidence to show that the NHS had low management costs.
An undermanaged service?
The NHS Confederation49 argued that, as one of the largest employers on the planet, spending over £2B a week and meeting the health-care needs of around 60 million people, the proportion of managers in the NHS is low. The evidence indeed suggests that the NHS has ‘lean management’. The wisdom of policy to cut management numbers and costs is thus in doubt, as this weakens the motivation and commitment of managers, and dilutes the management capacity to implement change. The King's Fund42 commission on management in the NHS concluded that, ‘It might just as sensibly be asked, how can it be run effectively with only 45,000 managers?’ (p. 4).
Pure plays and hybrids
Other evidence shows that the official figures underestimate the numbers of those with either a ‘pure’ management role or a ‘hybrid’ role combining clinical duties with managerial responsibilities:
-
pure plays: roles that are wholly managerial
-
hybrids: roles that combine clinical and managerial responsibilities.
The NHS Information Centre data do not count as managers any clinical and scientific staff holding hybrid managerial roles; however, if hybrids as well as pure plays are counted, then the proportion of NHS staff in management positions is not 3% but around 30%.
Beyond the G matrix
Employment figures compiled by the NHS Information Centre50 were based on the Occupational Code Manual Version 9. Managers were covered in the ‘G matrix for administration and estates staff’. This included those with ‘overall responsibility for budgets, staff or assets, or who are held accountable for a significant area of work’. This included chief executives, board directors and deputies, and service managers reporting to them. However, managers who had to be qualified as doctors, nurses, therapists, scientists or ambulance personnel were coded in their professional area, such as clinical directors, modern matrons and ward sisters, and laboratory supervisors. Trust chairpersons and non-executive directors did not appear in the management numbers either. They were coded in the ‘Z matrix for general payments’ along with Macmillan and Marie Curie nurses.
Other line managers, team leaders and supervisors were coded as ‘clerical and administrative’. They were excluded from management numbers because they ‘do not have responsibility for a significant area of work/budget’, including ‘line managers for whom management is only a portion of their role who may also act as analysts or in some other administrative or clerical capacity’. This understates the significance of such roles – ward managers, outpatient department management, the management of diagnostic units and cleaning, catering and portering supervisors. Those staff can have a major impact on hospital performance and reputation.
Staff coded in the ‘clerical and administrative’ category in the G matrix, including those with managerial responsibilities, appeared in the census as ‘support to clinical staff’. In 2010, support staff accounted for 26.5% of all NHS employees in England, a proportion that had also been stable for a decade. The proportion of staff in ‘central functions’ – finance, personnel, information – was also relatively stable, at 8% of employees in 2010.
Who are these ‘uncoded middle managers’? One of the questions in the project set-up interviews was: ‘Who would you include in the middle management population of the trust – the key categories and/or groups to whom we should be speaking?’ Responses included hybrid roles (medical director, clinical director, senior/lead nurse, midwifery manager, modern matron, ward sister, specialty lead, laboratory team leader) as well as pure plays (deputy/assistant director, general manager and department head). Using an organisation's own definition of middle management is a strategy advocated by Currie and Procter,51 and adopted in this project.
The workforce information departments (who collate the census figures for the NHS Information Centre) in Clearview and Greenhill were asked to estimate the total management populations of their trusts, counting pure plays and hybrids. This was based on a briefing on the traditional definition of management in terms of planning, organising, supervising, directing, co-ordinating, reporting and budgeting, or POSDCoRB,52 and also taking responsibility for human resource management, and the implementation of service improvement, into account. If a role includes some or all of those activities then it is categorically a management role. The estimates are shown in Table 10. In both trusts, around one-third of staff had managerial roles, with pure plays accounting for 6% of the total. It is also important to note that hybrids in both cases outnumbered pure plays by four or five to one. The head of leadership and organisation development at Greenhill felt that these estimates were low. Asked to make an informed guess about the actual figure, she replied, ‘I think we're looking at 35 to 40 per cent’.
| Clearview | Greenhill | |
|---|---|---|
| Total staff (FTE; 2011a) | 7137 | 6254 |
| No. with management responsibilities | 2380 | 1940 |
| No. with management responsibilities as percentage of total staff | 33.3 | 31.0 |
| No. of pure plays | 398 | 405 |
| Pure plays as percentage of total staff | 5.6 | 6.5 |
| Pure plays as percentage of all management | 16.7 | 20.9 |
An overmanaged service?
The NHS may be viewed as undermanaged, with only 3% of its 1.4 million employees in management roles. Knowing that at least one-third of staff (in acute trusts) have managerial roles, can we conclude that the service is overmanaged? This raises the question of management capacity.
Management capacity can be defined as the ability of the function as a whole to respond effectively to the demands placed on it at any given time. The management agendas of the trusts collaborating in this study were lengthy, complex and fluid (see Chapter 4). Different profiles of pure plays and hybrids may be equally effective in the context of different local conditions, past histories and current agendas. It is not possible to assess capacity simply by comparing numbers. Fewer pure plays may mean lower management costs, but that could increase the burden on hybrids, reducing time for patients, professional development and innovative service improvements. That may in turn lead to the appointment of more clinical staff to compensate, cancelling the cost advantage of having fewer professional managers.
With regard to the ‘3% versus 30%’ question, at least four other factors impinge on the management capacity of an acute trust. First, ‘the other 30%’ are not all FTEs; most are hybrids. One senior hybrid asked about the mix of clinical and managerial responsibilities in nursing roles replied:
Head nurses are ‘50–50’. They're responsible for the managerial nursing aspects in their directorate. But I hold them accountable for nursing professional issues as well. For a matron, I would expect that to be very much more clinical. And probably it should be 75–25, clinical – managerial. For a ward sister, the ideal is that they should have two days a week where they can deal with the managerial elements of their role, but it's also about making sure standards are adhered to. So probably a 60–40 split.
In your judgement, are some of those staff spending more time on their management responsibilities than they should?
No. I would say it's the other way around. They don't get enough management time.
Director, Netherby
Interviews with modern matrons elsewhere suggest that this balance of responsibilities varies from trust to trust, and fluctuates over time, depending on the management agenda.
Second, despite our previous definition, some ‘pure plays’ have specialist non-managerial responsibilities and so they are not necessarily each a ‘full’ FTE. For example, one manager commented as follows about her managerial specialist responsibilities:
Question: Is my profession ‘manager’ or ‘trainer/coach’? Answer: Trainer/coach. Therefore, when answering what percentage do I ‘manage/lead’ versus what is ‘practical/specialist’, I'd say 70–30. I do have a practical/specialist role I fulfil that is not management. There is clear water between the two, and I suspect that many others will say the same. Few of them will see themselves as NHS managers wholly, rather a specialist first, in a management role, but their loyalties are often to the profession they trained hard in.
Senior manager, Greenhill
Thus, 100 pure plays does not necessarily equate to 100 FTE managers. Although no longer employed full-time in a clinical capacity, many pure plays have a clinical background (such as nursing) that they bring to their relationships with clinical staff, and use to inform decisions and judgements. Some maintain their registration, and ask their workforce information offices to code them with their profession in the annual census figures, and not in the G matrix as managers.
Third, most hybrids have had limited management education, beyond short courses. Pointing to the piecemeal ‘on the job’ management development of medical staff, Gillam53 argues that ‘the idea that all doctors can just “manage” is hopelessly naive’ (p. 1). Short courses include The King's Fund management and leadership for clinicians course, which runs over 5 days, and Leading an Empowered Organisation (LEO), which was a 3-day course (now discontinued) for staff (including nurses) in management and supervisory roles. A master’s degree in business administration takes a year of full-time study to complete; few clinical staff have the desire, time or financial resources to obtain this qualification. During this project, Clearview, Greenhill and South Netley implemented their own leadership and management development programmes. But these still amounted to more ‘short courses’, albeit intensive and tailored. The management capabilities of many hybrids are thus dependent on limited educational input and considerable on-the-job learning:
We don't have any managerial training and lots of work is left to us. I expect that in the future we will be left to make more decisions. There is more workload. You have to do appraisals, you are asked to create a new policy and deliver presentations and you are expected to do more.
Mixed focus group, Greenhill
I've been in post for three years, and I want promotion. Are they developing me into a matron's role? There is no ongoing development. Ward managers are just left to get on with it. You are left on your own. Find your own development. The one-to-one meetings that we have with more senior management are all about operations and finance.
Ward sister, Netherby
Fourth, many hybrids do not view themselves as managers or they use the label reluctantly. In 2010, ward managers at Netherby voted to change their job title – to ward sister. Other examples included:
I've been a consultant nephrologist since 2003, and I've been involved with the emergency department project since 2005. The role of clinical lead is managerial if you want to call it that. In the emergency department project, this has involved structure change. But ‘management’ has connotations among clinicians relating to stick not carrot. Managers are people who withhold resources rather than try to improve services. My role is more of a leadership and organisation development role, much wider than management.
Clinical director, Greenhill
I would describe my role as clinical leadership. I'm not nursing, not hands on. I am not at all managerial. My role is professional leadership. But this does influence behaviour, practice, change, service improvement, so managerial in those senses. The senior staff on the wards have managerial responsibility; ward sister, charge nurse are front-line managers. Matrons and head nurses are middle management. I have a manager role, but I have professional accountability, so the emphasis of my role is with professional leadership.
Senior nurse manager, Netherby
These participants were more comfortable describing themselves as ‘leaders’. Before fieldwork commenced, we were instructed by a senior manager at South Netley to change the subtitle on the project documentation, from ‘middle and front-line managers’, so that this would appear as a study of ‘managerial and clinical leads’. These views reflect a trend in the public sector to value and promote leadership at the expense of mere management. 54,55
Mintzberg4 offers a straightforward resolution to the ‘leadership versus management’ debate. Asking if one would like to be managed by someone who doesn't lead, or led by someone who doesn't manage, he concludes that, ‘We should be seeing managers as leaders, and leadership as management practiced well’ (p. 9, italics in original). With a similar view, and using ‘managers’ and ‘leaders’ interchangeably, Quinn et al. 56 argue that, ‘we want to distinguish between individuals who happen to have management positions and individuals who truly display leadership in their management of others’ (p. 333). The evidence from this project demonstrates that, if the distinguishing features of leadership concern designing, inspiring and driving change, then middle management roles in the NHS are indeed a blend of management and leadership.
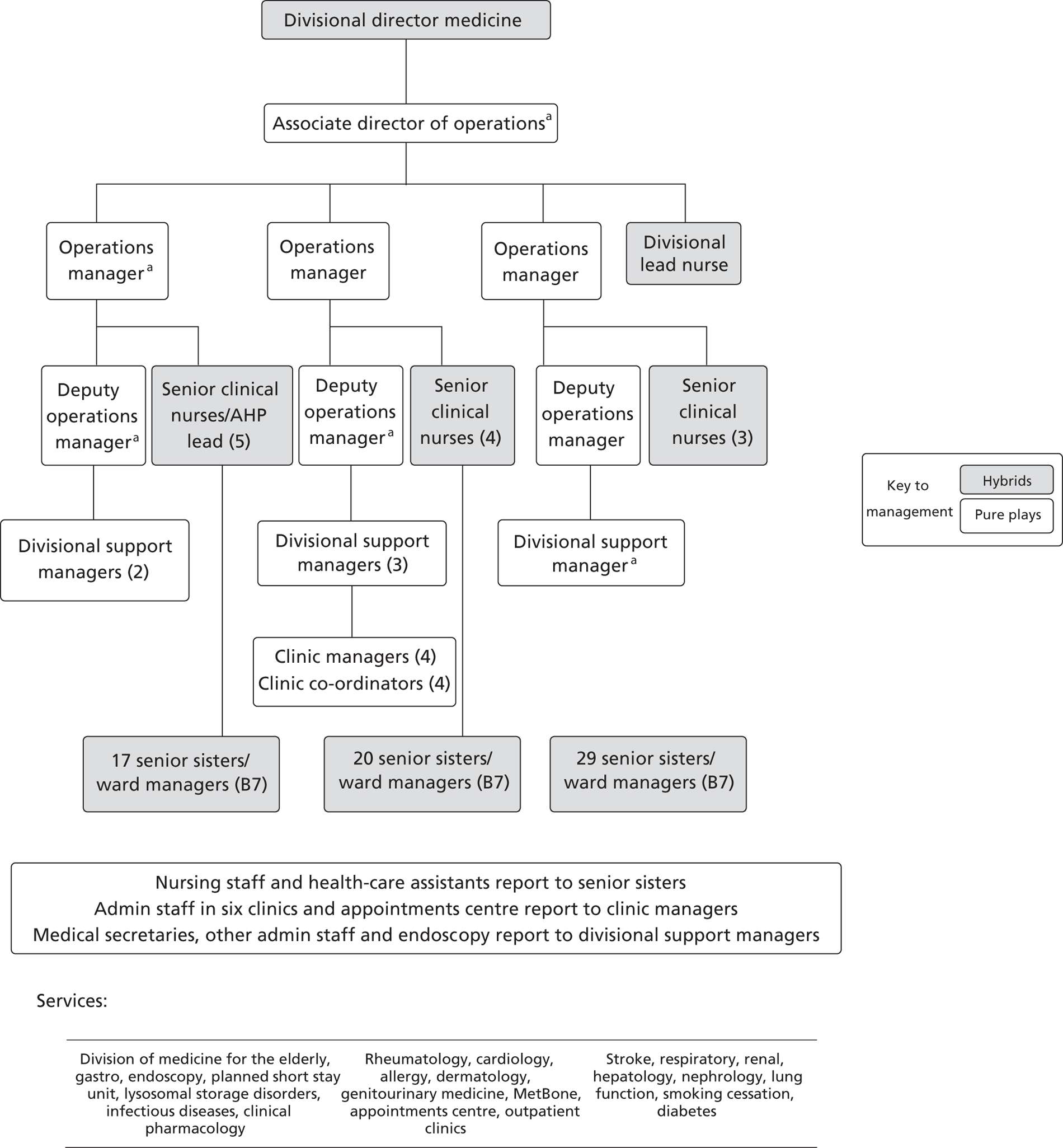
To illustrate how pure plays and hybrids populate a hospital management structure, Figure 1 shows the organisation chart for the medicine division at Clearview. This division had 350 beds in 16 wards, employing 1200 staff (headcount). The division's budget in 2010–11 was over £80M, with target savings of around £5M. The organisation chart identifies 21 pure plays and 80 hybrids. In other words, as indicated previously with regard to what appears to be the typical balance of roles at trust level, the ratio of hybrids to pure plays in this division was around 4 to 1.
FIGURE 1.
Clearview Hospital medicine division organisation chart (October 2011). a, Managers with clinical backgrounds. AHP, allied health professional.
Finding the front, defining the middle
For the purposes of this project it proved difficult to define unambiguously ‘the front line’ in relation to ‘the middle’. Definitions provided by various commentators suggest that this should not be a problem. However, three considerations apply. First, in acute care, the management ‘front line’ is mobile. Second, the hybrids who occupy this ‘fluidic space’ have onerous managerial responsibilities that influence quality of patient care, as well as organisational performance. Third, the distinctions between roles in this ambiguous zone are more important than whether they are defined as ‘middle’ or ‘front line’. We have thus dropped the phrase ‘front line’ from discussion. The term ‘middle management’ relates to anyone with managerial responsibilities who does not sit on a hospital board of directors. Distinctions between roles will be drawn with reference to specific job titles.
There are particular reasons for viewing ward sisters as middle, not front-line, managers. First, their roles are similar to those of matrons and senior nurses, to whom they report. Second, they are ‘mini-general managers’, controlling a budget, overseeing the development and morale of nursing staff, supporting medical staff, delivering service improvements and supporting and improving the patient experience. 57 Third, the ‘manager–subordinate’ relationship they have with other nurses is blurred, as staff nurses routinely ‘step up’ to cover for ward sisters in their absence. Fourth, with their operational experience, they act as intermediaries between senior management and day-to-day patient care. 58–60 Finally, it has been suggested that management regulation should not stop at board members, but should include ward managers. 61 The ward sister's experience is a middle management experience.
Conclusions and implications
Composition and capacity
The official census shows that around 3% of NHS employees are managers and senior managers. In contrast, when middle managers and those holding hybrid clinical-managerial roles are included, the actual proportion of staff in an acute trust with managerial responsibilities is around 30%. Management is a widely distributed function, not confined to a small cadre or elite.
There is little or no evidence to suggest that the NHS is overmanaged. The proportion of staff in management roles is (officially) much lower than the all-sector UK average. The (official) cost of management is similar to or lower than management costs in comparable settings, and is low on international comparisons. Support for the argument that the service is overmanaged relies on a flawed understanding of the arithmetic of percentage calculations. However, numbers and costs are less significant in relation to patient care, service improvement and overall performance than the management capacity of acute trusts.
NHS management has been equated with unnecessary bureaucracy. As later chapters reveal, this caricature is inaccurate. Cuts in the numbers of pure plays in acute settings could have serious consequences for the workloads of hybrids who would have to cover the resultant gaps, unless the scope of trust management agendas were to be reduced and simplified, and there is little sign of that happening. A policy of cutting management costs could thus jeopardise the effective implementation of other structural, regulatory and financial reforms, and could also jeopardise patient safety through increasing the management pressures and demands on those with hybrid responsibilities.
The denigration of NHS management, while resonating with public sentiment, damages the reputation, engagement, goodwill and motivation of a group that is key to implementing government policy, meeting national targets and maintaining the efficiency, quality and safety of day-to-day patient care. Although derogatory comments are presumably aimed at pure plays, the resultant image of management is a deterrent to clinical staff who may be invited to take on management roles. Potential candidates see through the ambiguous terminology of ‘leadership’, and have a clear understanding of the nature and perception of the management positions that they are being asked to assume. National rhetoric thus reinforces the perception of medical staff that colleagues who have taken management roles have ‘gone over to the dark side’. As it is government policy to encourage clinical staff to accept greater management responsibilities, this consequence is perverse.
Implications for practice
One implication for practice concerns the issue of management capacity, which in an acute trust, and based on the evidence from this project, can be seen as a product of:
-
management numbers
-
individual capabilities
-
engagement and motivation
-
organisational resources and infrastructure – the ‘enabling environment’
-
the quality of clinical-managerial collaboration
-
the ability to generate requisite variety.
Ashby's law of requisite variety62 argues that the management function must be able to generate at least the same levels of variety and complexity as the system being managed can adopt. Variety and complexity are required to deal effectively with variety and complexity; responses to complexity are often mistakenly aimed at simplification. The lack of multiple perspectives and diversity in thinking has been shown to reduce organisational resilience and contribute to system failures. 63 A management function whose members come from a range of different backgrounds should be able to generate greater diversity than a more homogeneous group; the quality of their collaboration is therefore a key factor. Echoing the notion of distributed leadership, forms of ‘management in the plural’, with multiple collaborators, can thus contribute significantly to capacity. 64 This issue will be explored further in Chapter 7.
This assessment assumes that it is possible to measure those factors, to operationalise the formula. This is problematic in practice, as each set of factors has multiple dimensions, and the understandings and definitions of those terms will differ from one setting to another. Nevertheless, in principle, this model – summarised in Figure 2, distinguishing individual and organisational dimensions – offers a starting point for exploring management capacity at system and trust levels.
FIGURE 2.
Dimensions of management capacity.
The management capacity six
| Individual dimensions | Organisational dimensions |
|---|---|
| Capabilities | Resources and infrastructure |
| Engagement and motivation | Clinical–managerial relationships |
| Numbers | Ability to generate requisite variety |
Most of the evidence from this study suggests either that acute trusts lacked management capacity or that available capacity was underutilised. Symptoms of undercapacity that were observed included problems arranging meetings due to busy diaries, meetings cancelled at short notice, regular evening and weekend working, managers saying that they could not cope with the workload, comments about ‘our firefighting culture’ and hiring external management consultants to help manage crises.
Symptoms suggesting that capacity was not being used effectively included the circulation of irrelevant and duplicated e-mails, staff performance issues not addressed, multiple unplanned interruptions throughout the day, minuted actions from meetings outstanding for months, frustration at bureaucracy impeding simple service improvements, managers criticised for decisions within their remit, experienced clinical and managerial staff carrying out basic administration, penalties for minor failures to achieve goals or targets and managers complaining, ‘just let me run my business’. Ideally, responses to an assessment suggesting that a trust or division is underutilising management capacity include:
-
redesign of cumbersome and dated systems and procedures
-
clear corporate e-mail policy to avoid duplication and overload
-
more preplanning, no ‘crisis of the day’, less ‘firefighting’
-
streamlined, simplified decision-making processes
-
increased autonomy for managers implementing service improvements
-
redesigned information technology (IT) systems to provide timely and useful information
-
shift senior management style away from ‘only blame, avoid praise’
-
shift senior management style to ‘high trust – high autonomy’.
Implications for research
Assessment of management capacity should be a fruitful area for further research, exploring the nature, source, assessment and implications of varying capacity levels. Improved understanding of capacity would provide a useful counterbalance to crude arguments about the value and contributions of management based on numbers and costs. As capacity is an organisational construct (incorporating individual dimensions), this suggests a shift in the research agenda with theoretical implications for health-care management, and with regard to management theory in general. This shift in emphasis is summarised in Table 11.
| Conventional approach | Complementary perspective |
|---|---|
| What individual managers do | What the management function contributes |
| Management roles | Management processes |
| Management numbers and costs | Management capacity |
These recommendations are not particularly novel. Management and organisation studies research has been working in these directions for some time. However, a more thorough exploration of management function, process and capacity in health care would have potential practical benefits for the service and the sector, as well as implications for the development of general management theory.
Chapter 3 The institutional context
The nature and significance of context
The NHS, like any other organisation, is embedded in a historical, sociocultural, economic and political context which shapes the norms, values and expectations that in turn influence the structures and processes of the health-care system. 65 The nature of, and relationships between, the dimensions of the institutional context are critical to understanding the demands that are placed on the management function, and the changing nature of managerial roles.
Context is not simply a stage on which action takes place. The context of an organisation is fluid and dynamic, influencing and in turn shaped by organisational events. 66 These inter-relationships do not necessarily generate a state of constant flux and indeterminacy. The institutional context is also responsible for reinforcing and perpetuating organisational characteristics, for maintaining patterns of continuity. For example, the so-called postmodern trend for flat, fluid, agile organic structures that was supposed to sweep away traditional, rigid, slow-moving bureaucratic structures has barely touched the NHS in its 60-year history. 67
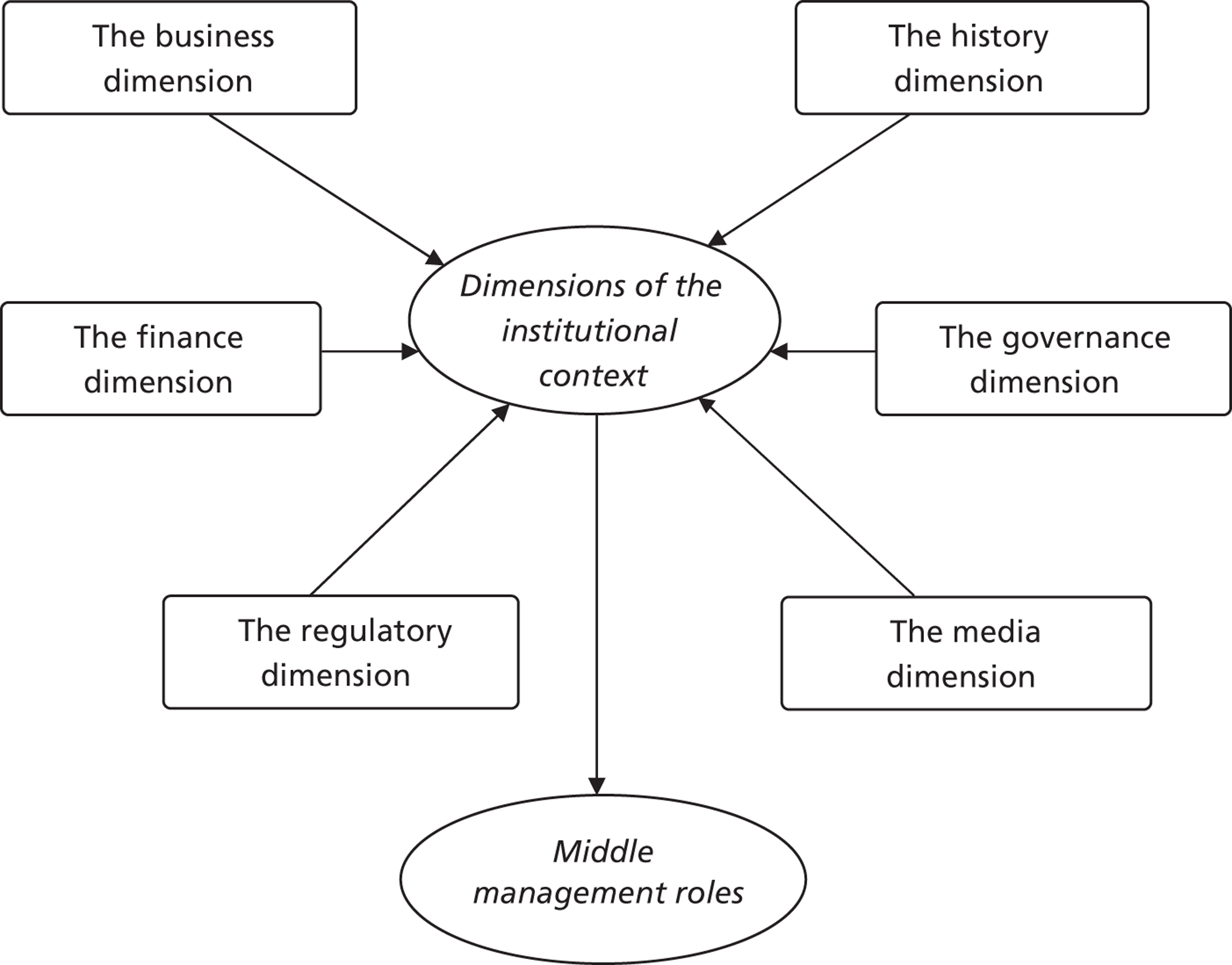
Six dimensions of the context in which the NHS operates are identified (Figure 3). These concern the history of the service, the contemporary business of health care, governance, regulation, finance and the role of the media. These dimensions overlap; discussion of regulatory regimes could equally belong with ‘governance’, and discussion of health care as a business with ‘finance’. The overarching aim of this discussion, however, is to explore relationships between the institutional context and middle management roles. The main conclusions from this analysis are:
-
History dimension. Although subject to constant reorganisations, core features of the hierarchical, centrally controlled professional bureaucracy appear to be relatively stable. Rules, regulations and slow decision processes can be beneficial, offering predictability and consistency, but can also impede innovation and rapid change. The current regulatory regime is a legacy from a series of ‘high-profile’ failures, the most recent concerning events at the Mid Staffordshire NHS Foundation Trust (‘Mid Staffs’). The global financial crisis that began in 2008 led to ongoing national austerity budgeting and to pressure on health care to make major efficiency savings, of approximately one-fifth of the annual spend of the service.
-
Business dimension. The private and public health-care sectors are now closely intertwined. In hospitals, clinical services are structured and run as ‘businesses within the business’. Clinical and managerial staff are encouraged to adopt a more commercial orientation and to develop new business models, managerial and process innovations, inventive uses of new technologies, public–private collaborations and competitive strategies. A key challenge concerns balancing efficiency and productivity with quality and safety of patient care. The NHS is also expected to generate revenue from innovations and exports.
-
Governance dimension. The government elected in 2010 embarked on a complex, rapid and controversial reorganisation of NHS structures. Some existing bodies were abolished (strategic health authorities and PCTs) and new ones were created, including a National Commissioning Board and local clinical commissioning groups. Policy to cut management costs generated considerable resentment. The promised liberation, autonomy and empowerment were difficult to spot, and ‘micromanagement’ continued.
-
Regulatory dimension. Providers answer to many regulators, auditors, inspectorates and accreditation agencies (RAIAs), whose information demands overlap and can be burdensome. Regulation has improved aspects of performance, but has not prevented systemic failures in care. The regulatory regime extends to innovation, where the call for a more creative, commercial approach is accompanied by a compliance framework, standardised efficiency measures, fines and an implementation board. In the wake of the Mid Staffs inquiry, some form of regulation of health-care management was expected to emerge during 2012–13.
-
Finance dimension. ‘The Nicholson challenge’ to find £20M efficiency savings between 2010–11 and 2014–15 was described as a ‘NHS recession’, a ‘funding ice age’ and a ‘perfect storm’. Trusts from 2010 had to implement CIPs generating recurrent savings of 3–4% per annum, raising anxiety about job security among all staff including management. Although cutting costs and improving productivity were over-riding issues, these actions had to be balanced with the priorities of improving the quality and safety of patient care. Middle managers in particular felt the need for financial management skills.
-
Media dimension. The press ‘rules of production’ mean that sensational, dramatic ‘bad news’ stories are more likely to be reported than good news. The constant ‘bad press’ influences public perceptions of the service and its staff, and also affects government policy. Commentary supportive of management is rare; poor management is typically blamed for system faults and failures, and a negative stereotype of managers as costly pen-pushing bureaucrats prevails, potentially inhibiting motivation and recruitment.
FIGURE 3.
Dimensions of the institutional context of the NHS.
The six dimensions
The history dimension
The history of the NHS is a history of change. An organisation of this size and cost is unlikely ever to be free from political intervention. As governments in the UK change at least every 5 years, the potential for turbulence is high. During this project, the service witnessed shifting government priorities, new organisational arrangements and regulatory systems and more ‘high-profile’ events including failures in care for the elderly,68 Winterbourne View69 and failures in care at Mid Staffs. 70
Subject to constant change, has the NHS now developed the agile, flexible, non-hierarchical, organic, responsive attributes of the post-bureaucratic archetype? Commentators have been predicting ‘the dinosaur scenario’, the extinction of bureaucracy, for a century. Buchanan and Fitzgerald67 argue that the NHS has become an ‘accessorised bureaucracy’. This has meant acquiring some fashionable new practices and private sector terminology while maintaining central control, complex structures, multiple regulatory bodies and the proliferation of performance metrics. This echoes a previous study which concluded that, although the ‘fur coat’ of structures had changed, the ‘knickers’ of the power relations that underpin the professional bureaucracy were intact. 71
The accessories, however, have improved access to and the quality of patient care and contributed to reductions in waiting times and infection rates. 72 Bureaucracy brings the benefits of unity, co-ordination, precision, predictability, consistency, impartiality, organisational memory and continuity across governments. 73,74 The accessorised bureaucracy provides a stable, predictable system that also features innovation and change, and may thus be a good hybrid solution.
In terms of recent history (2009–11), four sets of events were significant. First, Next Stage Review was published in June 2008,75 with a review 1 year later. 76 This review noted the challenges posed by demographic trends, rising public expectations and the rapid development of new technologies, and stressed the importance of improving the quality and safety of care, putting fresh emphasis on the role of clinical leadership.
Second, the financial crisis forced the UK government to support domestic banks, at considerable cost, leading to austerity measures to reduce the resultant deficit. The NHS was asked to find £20B of savings by 2014–15 through a quality, innovation, productivity and prevention programme. 77 Developing cost improvements to reduce spending on the required scale consumed considerable time and energy. Finding savings within one financial year was difficult; making recurring annual savings of 3–4% was a major challenge.
Third, the mortality rate at Mid Staffs since 2005 led to an investigation78 and then to an independent inquiry,70 followed by a public inquiry. Problems were attributed to failures in leadership and management, as well as to lapses in clinical care. This incident led to demands to regulate health-care managers. 61
Fourth, the general election in May 2010 returned a coalition government that proposed a radical reorganisation of the structure, funding and regulation of the service. New legislation was to scrap existing bodies – strategic health authorities, PCTs – and create others – a National Commissioning Board, clinical commissioning groups and Healthwatch England (a ‘consumers' champion’). The White Paper1 also indicated a 45% reduction in management costs. One participant in this study described the Department of Health as ‘a hyperactive child’, overloading staff with untested ideas disseminated in vast amounts of unco-ordinated documentation that nobody had time to read (clinical director, Netherby). Many commentators questioned the wisdom of introducing such a major reorganisation, accompanied by massive budget cuts, while reducing the numbers and costs of managers – within 4 years. 79
The business dimension
We need to learn better how to compete. We've got to run as a business now, we're beginning to get there, and pathology is at the forefront. We have a well equipped lab, we have senior management support, we deliver on targets, our finance is OK, half of our business is with the trust and other hospitals, and the other half of our business is with general practitioners. In 2009, microbiology and immunology started to offer fourteen new services. This is a growth business.
Clinical director, Netherby
Our future survival will depend on our ability to adopt a more business orientated way of thinking and working whilst being appraised for the quality of our patient services delivered through effective managerial practice.
Management development programme brochure, South Netley
When I speak to nurses and clinicians about ‘the business’, they physically recoil. It does not come naturally to doctors and nurses to see that they are part of a business when they have signed up for a vocation.
Operations manager, Clearview
Foundation trusts have greater autonomy than non-foundation trusts and are encouraged to operate as businesses. Payment by results was introduced in 2002 to promote competition, allowing low-cost providers to retain surpluses. Clinical services are now organised as autonomous ‘business units within the business’, which involves clinical staff in activity reviews, costing and budgeting, service improvement and developing business plans. The House of Commons Health Committee80 concluded that the foundation trust application process had ‘forced NHS organisations to operate in a more business-like way’ (p. 36). Commercial practices such as process redesign, quality improvement and ‘lean’ have become common practice across the service. 81–83
The private sector now plays a key role in public sector services. 84 The public services industry (PSI) involves private and third sector businesses providing services under government contract. The PSI in Britain employs 1.2 million people, generating annual revenues of around £80B, covering services such as maintenance and cleaning, computing and other business processes, social care facilities, services for the elderly, children and people with disabilities, custodial services, leisure services, waste management, and clinical care provided by independent treatment centres. Health is the largest component of government spending on the PSI, totalling £24B in 2007–8, followed by social protection (£18B), defence (£10B) and education (£7B). The Julius review84 concluded that subjecting providers to competition reduces costs without affecting quality, and advised that public service markets should be exposed to further competition.
The UK has several private health-care providers and insurance companies, with a market value of £6.1B in 2009–10. The second largest source of income for private providers, after medical cover, is the NHS, which accounts for one-quarter of the private sector's income. 85 The private company Circle was the first to be contracted to run a NHS hospital from 2012. In 2011, NHS Wirral became the first hospital to give expectant mothers the choice of either a NHS midwife or one employed by a private company. 86 From 2012, foundation trusts can earn up to half of their income from private work. 87
The NHS earns around £0.5B per annum treating private patients in NHS facilities; £1.6B was paid to doctors for private work in 2009. Britnell88 argues that a more entrepreneurial NHS could ‘make money for Britain’ by exporting construction and project management services, primary care expertise, education and training, health data management innovations and medical facilities to China, the Middle East and Africa, generating £50B in annual revenues.
These trends suggest that a ‘commercial mindset’ is required, to embrace new business models and strategies, organisational and managerial innovations, inventive uses of staff resources and new technologies, public–private sector collaborations and ways to involve patients in care management.
The governance dimension
National governance arrangements may seem remote from hospital management; however, these arrangements shape the expectations and demands placed on management and other staff, determine their goals and priorities and define the various other organisations with which acute trusts interact. Parliament has overall responsibility for the service. The Secretary of State for Health is assisted by five other health ministers, and oversight is conducted through three select committees, for health, public accounts and public administration. With an annual budget of £214M and 2200 staff, the Department of Health is responsible for strategic leadership and for achieving better health and well-being, better and safer care and better value for money. The department has three senior staff: permanent secretary (day-to-day running of the department), chief executive of the NHS (health service management and performance) and chief medical officer (medical adviser and professional head of medical staff in England). In addition to a departmental board (strategy) and a corporate management board (leadership and business planning), the NHS operations board oversees the day-to-day running of the service and the annual operating framework. The department also managed 20 ‘arm's-length bodies’, responsible for regulation, establishing standards and central services. A review in 2010 proposed to reduce their number to 10 by 2015. 89
The White Paper in 20101 set out a 5-year strategy, replacing the 5-year plan, From Good to Great, (2010–15), developed by the previous administration. 90 Promising to reduce micromanagement, the White Paper emphasised giving power to patients and clinicians. Policy thus concerned ‘liberating the NHS’, removing layers of bureaucracy, encouraging foundation trust autonomy and ‘empowering the front line’. The regulatory regime was to be strengthened. The CQC was to operate a joint licensing scheme with Monitor. The White Paper also promised ‘an NHS information revolution’, providing access to information on conditions, treatments, safety, effectiveness, lifestyle choices, outcomes, patient experience and national clinical audit information. Healthwatch England, a new ‘consumer champion’ body, was to advise other national bodies, and alert the CQC to concerns about quality of services. The new commissioning board would employ 3500 staff with a budget of £20B for direct commissioning.
Noting that reorganisations can have dysfunctional consequences, Edwards91 lists 69 changes in the NHS between 1974 and 2009, an average of two a year. Assessing these reforms, he comments:
This is like the television programme Scrap Heap Challenge where contestants have to construct complex projects out of a variety of different parts that don't fit together, were intended for another purpose and may be broken. Policies and incentives need bending, bolting together or otherwise adapting to make the local system work. But this is not an easy task. The definition of the right thing is often contested and the incentives and accountabilities are designed so that organisations, or departments have to look after their own interests. An optimal goal for a local system cannot be achieved by each of the participants trying to optimise their own position.
p. 1791
It is difficult to see, in this most recent reorganisation from 2010 onwards, the loosening of central control, relaxation of regulation or simplification of bureaucracy. The governance of the NHS is characterised by central command, complexity, bureaucracy, hierarchy and regulatory oversight, with control exercised through 5-year plans and annual operating frameworks.
The regulatory dimension
I've been inspected recently by the SHA [strategic health authority], OFSTED [Office for Standards in Education, Children’s Services and Skills], LINks [Local Involvement Networks], CQC, HOSC [Health Overview and Scrutiny Committee], HSE [Health and Safety Executive]. They all have different requirements, which overlap, but they have different parameters. And they all want information, reports, and action plans, which can contradict each other. And in all these bodies, I've yet to meet anyone who is an expert in health or emergency care. They'll ask about call bells in the toilets, and response times, and how often floors are cleaned. Nobody ever asks me how many lives we've saved, or how many people got better as a result of the treatment they received. I spend a lot of my time writing policies.
Lead nurse, Greenhill
NHS regulatory bodies have proliferated. This is frustrating when different bodies ask for similar information, and demotivating when the activity has no impact on the provision or improvement of patient care. Regulation in England appears to have reduced waiting times in comparison with Scotland. 92 Edwards and Lewis93 conclude that changes in regulation have encouraged a more businesslike approach and have also strengthened the focus on quality of patient care and safety. Nevertheless, a review by the NHS Confederation94 noted the ‘alarming overlap’ across 35 RAIAs in their focus on around 900 standards. Among those RAIAs, two bodies are key: Monitor and the CQC.
Monitor
Since 2004, Monitor has been the foundation trust regulator, responsible for establishing terms of authorisation and issuing licences. 95 In 2010–11, Monitor had 150 staff, with an annual budget of £15M, which was expected to rise to £50M as it assumed new ‘sector regulator’ powers from 2013. All providers of NHS services must now have a joint licence from Monitor and the CQC. Monitor's roles are to ensure financial viability and good governance. Assessment covers meeting national targets and standards, board roles and structures, monitoring of clinical quality and whether or not the trust is meeting its terms of authorisation. Trusts must provide annual plans, quarterly in-year submissions and exception reports. If a trust is found to be in breach, scrutiny becomes more intensive, leading to intervention in the case of a significant breach.
Care Quality Commission
Since 2009, the CQC has regulated the quality and safety of care in relation to national government standards. The CQC also registers providers who have to adhere to a compliance framework96,97 and meet the ‘essential standards of quality and safety’ set out in a 270-page document. 98 The CQC maintains a Quality and Risk Profile for each registered provider. It also operates an inspection regime, which has been controversial, particularly in failing to identify instances of poor-quality care that were later exposed through other routes. The CQC can launch responsive reviews if concerns are raised about quality and safety of care, with an ‘enforcement policy’ that includes warning notices, penalties, cautions and ultimately prosecution. The CQC has 2000 staff, and an annual budget of £140M, and in 2011 regulated 21,000 providers operating services from over 36,000 locations.
The operating framework for 2010–1199 relaxed the ‘transit time’ trigger for patients attending emergency departments, from 98% to 95% (of patients to be seen within a maximum of 4 hours). The maximum 18-week wait referral to treatment (RTT) target was dropped, but the framework indicated that commissioners should retain the RTT target in their contracts, and that median waiting times should be used as an additional measure. The National Clinical Director for Urgent and Emergency Care subsequently introduced in December 2010 eight new indicators on which emergency departments were to be assessed. In June 2011, the NHS Director of Performance announced that the 4-hour transit time target would continue to be performance managed after all, along with all of the new emergency department quality indicators.
The revised NHS Outcomes Framework for 2012–13100 proposed ‘one framework, five domains, 12 overarching indicators, 27 improvement areas and 60 indicators in total’ (p. 16). In December 2011, the Department of Health101 also decided to ‘bring about a major shift in culture within the NHS, and develop our people by “hard wiring” innovation into training and education for managers and clinicians’ (p. 13). This report identified six innovations for trusts to adopt. The ‘change in culture’ was to be driven by standardised efficiency measures and by fining providers and commissioners who did not implement National Institute for Health and Clinical Excellence (NICE) rules on best practice, in addition to a new central management ‘compliance regime’ supported by an Implementation Board with ‘task and finish’ groups that would lead changes in individual areas.
Senior managers themselves may become subject to regulation, arising from the public inquiry into Mid Staffs. 70 An advisory group has made recommendations including a statement of professional conduct, competency standards, strengthened appraisals and a professional accreditation scheme. 102 The Council for Healthcare Regulatory Excellence has produced a draft of the ethical, behavioural and technical standards that managers are expected to demonstrate. 103
The finance dimension
Every conversation about every activity – it's probably no exaggeration – and let's take training as an example, always begins with the question, ‘who's going to pay?’ Not ‘how does this benefit the organisation?’, ‘what's the need of the people working for us, and how does this fit with our objectives or our patients?’ It's always about, who pays, where's the money coming from.
Assistant director, Netherby
The NHS had been in deficit in 2006 but improved financial management produced a surplus by 2007–8. The operating framework for 2008–9 noted that, as financial difficulties were resolved, the service could focus attention on infection control, access, better health, inequalities, improving patient experience and staff satisfaction and emergency preparedness. 104 However, the impact of ‘the NHS recession’ became clear in 2009. By 2011, one commentator predicted ‘a funding ice age’ lasting at least until 2015. 105
The funding model has become increasingly complex and is subject to constant change as financial incentives and penalties are adjusted to encourage or discourage particular behaviours and activities. The core of the funding model is a payment by results system designed to ensure that funding follows patients, reinforcing the policy of patient choice. The main component of NHS spend (around 60%) provides for acute care. Acute trusts are thus paid for the activity that they undertake. Accurately recording and coding that activity is central to determining trust income.
From 2010–11, trusts were expected to make annual savings of 3.5%. For an acute trust with an annual turnover of £400M, that meant finding £14M in recurring annual savings. Small changes to the national funding model can thus have significant implications at local provider level. A survey of finance directors in 2010 found that, as well as recruitment freezes, 58% of finance directors in acute trusts predicted cuts in administrative and junior management roles, and 50% said that they expected the numbers of senior managers in their trust to fall. 106 In March 2011 the Health Service Journal published online the results of a survey of 279 chairpersons and chief executives, who reported that cutting costs and balancing their budgets was now their biggest challenge. The NHS operating framework for 2012–13 introduced a further 1.5% reduction in tariff (having been cut by that amount in the previous year), in addition to seeking 4% efficiency savings, and expressed the aim to drive the £20B savings programme ‘further and faster’, introducing penalties for poorly performing providers and for failures to provide accurate data. 107 Pressures on acute trusts from 2011 were substantially increased, leading providers to respond that these cost pressures were not sustainable and could result in unsafe working practices, and that the acute sector in 2012–13 was facing ‘a perfect storm’. 108
| Trust | Turnover 2010–11 | Target CIP | Actual CIP (%) |
|---|---|---|---|
| Burnside | £145M | £4.96M | £3.67M (76) |
| Clearview | £592M | £35M | £33M (94) |
| Greenhill | £422M | £30M | £30M (100) |
| Netherby | £236M | £10.4M | £10.52M (101) |
| South Netley | £450M | £24M | £28M (117) |
| Wattle Park | £244M | £13.8M | £15M (109) |
By mid-2011 it appeared that many acute trusts were missing the efficiency targets in their CIPs by significant margins. In addition, some trusts had made savings that were not recurrent, and increased emergency activity meant abandoning plans to close beds in some trusts. 109 Figures for the trusts participating in this project are shown in Table 12.
The media dimension
Managers are the jam in the sandwich. They don't like the negative stereotype. It's about the management of reputation. The NHS itself is not doing anything to curb ill feeling towards management. Even on Holby City [popular television programme] the manager is the bad guy; managers are the lowest of the low.
Operations manager, Clearview
The NHS operates in ‘a goldfish bowl of media scrutiny’ (p. 25). 42 Media reporting influences public perceptions of the service, and of its management and staff. For instance, in January 2012, the Health Service Journal reported the case of a London trust where the number of complaints had doubled over 9 months. An internal board report attributed this increase to adverse media coverage of the quality of care at the trust, the implication being that ‘bad news’ had sensitised the public to these issues and predisposed more patients to complain. By focusing on bad news, the media reinforce the view that the NHS is failing, and that its managers are costly bureaucrats. The press are in business to attract readers and make money. Davies110 sets out the ‘rules of production’ that shape the nature of reporting to achieve those ends:
-
run cheap stories – quick and safe to cover, no complex or contentious investigations
-
select safe facts – which can be attributed to official sources (spokespeople, reports)
-
avoid the electric fence – defer to anyone with power to do you damage
-
select safe ideas – use moral and political values and assumptions that are widely supported
-
always give both sides of the story – give ‘balance’ if you have to report something ‘unsafe’
-
print what they want – stories that increase readership – ‘if we can sell it, we'll tell it’
-
simplify – avoid context and ‘slow-burning tales’ in favour of short dramatic events
-
print what they want to believe – stories that are consistent with readers' values
-
go with the moral panic – in a crisis, sell the readership ‘a heightened version of its own emotional state in the crudest possible form’ (p. 142)
-
ninja turtle syndrome – run stories that are widely reported elsewhere, even if they lack merit (parents who prevented their children from watching the television series found themselves and their children isolated).
Hospitals that are meeting performance targets with balanced budgets, satisfied patients and capable staff are not good sources of sensational stories. Failures, crises, accidents, misconduct, mistreatment of patients and financial difficulties are more interesting. Sadly, the press and media in the UK do not have to work hard to find examples of the latter.
Following those rules of production, NHS managers get a bad press, although uncaring nurses and unregulated health-care assistants are not immune. The King's Fund report on leadership and management in the NHS began by observing that, ‘whenever politicians talk about management it is almost invariably a pejorative term. It is often equated sneeringly with bureaucracy’ (p. 1). 42 One opposition health spokesman spoke of the increasing number of ‘men in grey suits’ and a health minister derided primary care managers as ‘pen-pushers’ (p. 1). 42 The chairperson of the government's Future Forum on the NHS argued that ‘the government should stop slagging off managers’ (p. 9). 111
The King's Fund commission also observed that the negative stereotype was an insult to managers, and to clinical staff in managerial roles, arguing that clinicians are thus discouraged from taking on these roles. 42 In this latter respect, government ministerial rhetoric was seriously undermining the policy of encouraging greater clinical engagement in health-care management. The managers participating in this project were nevertheless committed to the service, and most (but not all) were more than happy to acknowledge their managerial responsibilities in research interviews and focus group discussions. However, many chose not to describe themselves as managers in public, and one observed that being labelled as a middle manager was ‘incredibly degrading’.
The management dilemma
The features of the institutional context of NHS management work are summarised in Table 13.
| History | Features of the (‘accessorised’) professional bureaucracy persist |
| Hierarchical, centrally funded, centrally controlled | |
| Constant reviews and disruptive reorganisations | |
| The legacy of ‘high-profile’ failures is a burdensome regulatory regime | |
| Global financial crisis – ongoing need to cut costs, find efficiencies | |
| Business | Public and private health-care sectors are now closely intertwined |
| Clinical services are structured and run as independent business streams | |
| Need to adopt an entrepreneurial, commercial mindset | |
| Must balance profitability with quality and safety of patient care | |
| Expected to generate revenue from innovation and exports | |
| Governance | New government introduces complex, rapid, controversial reorganisation |
| Powerful new central commissioning board | |
| Primary care to be responsible for £80B annual spending | |
| The policy of cutting management costs generates resentment | |
| Difficult to see the promised autonomy, empowerment and liberation | |
| Regulation | Many regulatory bodies (RAIAS), create significant administrative burden |
| Regulation has improved some aspects of performance | |
| Regulation has not prevented serious care failures | |
| Support for innovation comes with penalties and a compliance framework | |
| Regulation of managers expected from 2013 | |
| Finance | NHS recession, ‘funding ice age’, ‘perfect storm’ |
| ‘The Nicholson challenge’ – find £20B of savings | |
| Cutting costs – reorganising – increasing activity | |
| Uncertainties and anxieties over job security | |
| Need to balance savings with quality and safety of care | |
| Media | ‘Rules of production’ produce sensationally bad news |
| Media stories influence public perceptions and government policy | |
| Managers are typically blamed for problems and failures | |
| Commentary supportive of health-care management is rare | |
| The negative stereotype – ‘pen-pushing bureaucrats’ – prevails |
At the heart of this analysis sits a management dilemma. Providers are encouraged to operate as commercial enterprises, and to be entrepreneurial, innovative and revenue generating. But they are expected to do this in the face of a burdensome regulatory regime in which failure to comply with central controls can lead to financial penalties and senior staff job losses. This has not deterred many significant innovations. But this dilemma may be an insurmountable barrier to the ‘disruptive innovation’ that may be required by a traditional service in a rapidly changing world. 112
Chapter 4 The organisational context
The long ‘to do’ list
This chapter explores how the local organisational context shapes the nature of management work. First, the six acute trusts are profiled. Second, the implications of service-line management structures are considered. Third, the management agendas of two trusts are described. Finally, the implications for middle management are explored. The analysis of the institutional context in Chapter 3 exposed a tension between innovation and compliance. This chapter exposes a further tension, between policy to reduce management numbers and adding to management agendas. Information for this chapter comes from trust websites, other hospital information and set-up interviews. The conclusions are:
-
these are large, complex organisations, often one of the largest employers in their local area, some with histories reaching back to the 18th and 19th centuries
-
most have ‘legacy issues’ related to old buildings and computer systems, with the latter frequently being incompatible with one another and inadequately specified to provide appropriate and timely business information
-
clinical directorate structures, dating from the 1980s, were being replaced by service-line management, with divisions run as ‘businesses within a business’, bringing autonomy, transparency and accountability, but encouraging ‘silo’ working, discouraging information sharing, generating insecurity and creating a lack of clarity with regard to accountability
-
the scale of the financial and operational challenges was such that three trusts felt that it necessary to recruit external management consultancy support for their ‘transformation programmes’
-
those challenges focused attention on organisation culture and on leadership and management skills and styles
-
acute trust management agendas are long and complex, with most issues involving significant organisational change
-
middle managers are subjected to ‘multiloading’ (dealing with many different activities) and ‘perpetual loading’ (working at capacity, always economising), the standard responses to which (halt less essential activity, focus on a small number of key issues) are not available
-
capacity (see Chapter 2) is a critical management issue, and a priority for further research.
Trust profiles
To indicate the scale and complexity of the trusts participating in this study, and the scope of the hospital management task, Tables 14 and 15 profile the attributes of the two foundation and four non-foundation trusts respectively.
| Attributes | Clearview | Greenhill |
|---|---|---|
| Income 2010–11 | £577M | £430M |
| Population served | 500,000 | 612,000 |
| Outpatient visits | 460,000 | 430,000 |
| Day cases | 116,000 | 74,000 |
| Emergency attendances | 93,500 | 105,000 |
| Non-elective admissions | NA | 62,000 |
| Elective admissions | 67,800 (total) | 18,000 |
| Staff | 7100 | 8000 |
| Beds | 1000 | 600 |
| Wards | 40 | 52 |
| Sites | 1 | 2 |
Clearview
Established in the 18th century, Clearview moved to its current site in the 1960s. At the time of this project, this site was doubling in size, with new facilities to support existing services, provide new development opportunities and accommodate a specialist cardiothoracic hospital. Clearview was also the regional major trauma centre, had an international reputation for teaching and research and was one of the largest local employers. Between 2007 and 2009, most of the top team changed, and the average tenure of executive directors at December 2009 was 3 years.
Clearview had a £40M deficit for 2011–12, with activity levels outstripping funding, and with a need to work closely with commissioners. Meeting most performance targets, Clearview declared non-compliance with the emergency department transit time target in the final quarter of 2011–12, and did not meet the 62-day target for cancer patients in three out of four quarters, declaring ‘amber-red’ for governance. There were constant pressures on beds. Budget cuts included a vacancy freeze. The divisional structure established in 2009 created autonomous business units, but as divisional directors lacked managerial capabilities divisions were still subject to top team intervention. The IT infrastructure comprised ‘a hundred separate systems which were not linked to each other’ (assistant director operations). A new business intelligence system was designed to overcome this problem, with a performance ‘dashboard’ providing information on sickness, absenteeism and mandatory training making those aspects of staff management easier. An ‘eHospital’ was being planned.
Greenhill
Also established in the 18th century, Greenhill moved in 1960 to its current site where, in the 1940s, wooden huts had been erected to treat war wounded. Greenhill merged again in 2002 with another hospital and was the second largest employer in the area. A service-line management structure was introduced in 2009, with each of the four clinical divisions managed by a triumvirate including chief of service, divisional nursing director and divisional director of service delivery. The average tenure of executive directors at December 2009 was 3 years.
In 2009–10, Greenhill saved £24M, and planned savings of £30M for 2010–11 were achieved. The operating framework requirements of December 2011 meant that a further £18M savings had to be found, involving the potential loss of several hundred posts. In 2009, Greenhill failed to meet emergency department targets and decided to redesign radically the care of emergency patients. Greenhill had an ambitious organisation development programme, launched in 2007 and driven by an organisation development task group, to develop a ‘high-performing organisation’. The trust had its own leadership development framework. Objectives for 2011–12 were to generate a surplus of 0.5% for reinvestment, achieve a financial risk rating of 4, develop service-line management and patient-level costing and develop a plan for the optimal distribution of services across the two sites. This last item was an ongoing source of tension, as there was still a ‘divide’ between the sites.
Burnside
Established in the early 19th century, Burnside had 60 departments that were organised in 2011–12 into five clinical business units: women and children, acute medicine, specialty medicine, surgery and clinical support. Activity levels were rising, particularly emergency attendances and non-elective treatment. Staff numbers in 2011 were the same, however, as in 2007. The average tenure of executive directors at December 2009 was 3.5 years.
Management at the time of this study faced several issues. The foundation status bid was paused by Monitor in 2009 for financial reasons. The trust had a CIP, supported by external management consultants, to save £24M over 2 years to 2013–14. Burnside was also involved in a regional acute services review designed to improve efficiencies across five hospitals. The workforce was local and stable, but with some recruitment difficulties, and the commitment of consultants to the trust was questioned. Some performance targets were not being met – cancellations, recalls, waiting times – and maintaining care quality with financial constraints was perceived to be difficult. Relationships with commissioners were poor because of disagreements over funding. A ‘lean’ programme was launched in 2008, to find efficiencies and generate savings. Welcomed by most staff, but resisted by ‘slippery pigs’ and ‘dinosaurs’, this programme generated £6M in savings. Burnside was seen as a hospital that was ‘busy being busy’, without time for reflection.
| Attributes | Burnside | Netherby | South Netley | Wattle Park |
|---|---|---|---|---|
| Income 2010–11 | £121.2M | £230M | £495M | £244M |
| Population | 270,000 | 880,000 | 900,000 | 480,000 |
| Emergency attendances | 66,000 | 80,000 | 90,000 | 95,000 |
| Elective admissions | 23,500 | 50,000 | 21,000 | 81,000 |
| Non-elective admissions | 22,000 | 40,000 | 59,000 | 30,000 |
| Staff | 2100 | 4200 | 9500 | 3400 |
| Beds | 400 | 600 | 1100 | 650 |
| Wards | 19 | 30 | 95 | 24 |
| Sites | 2 | 2 | 2 | 1 |
Netherby
Netherby's history dated from the 18th century, some of the original buildings were still in use and the hospital launched a modernisation programme from 2008. A teaching hospital, Netherby was also a designated cancer centre, operated a satellite day surgery service at a community hospital and was the regional designated primary stroke centre. It was one of the largest local employers but had recruitment problems. Although staff turnover was low, this meant ‘no new blood’ and maintained ‘a family atmosphere with a no-challenge culture’. Netherby had five chief executives during this project. The average tenure of executive directors at December 2009 (excluding one particularly long-serving director) was 2 years.
Management challenges included the ageing estate and rising levels of non-elective activity. The pressure on beds was constant, but a reduction in bed numbers to 500 was planned for 2012. A deficit of £30M was forecast for 2013–14 and a transformation programme was launched supported by external management consultants who established reviews of services based on profitability. The service improvement team had much success with ‘lean’ projects, improving care quality and saving time, but came under pressure to reduce costs. The workstreams of the transformation programme explored length of stay, outpatient department productivity, administration and secretarial processes, and staffing. Management posts, ‘back office’ functions and corporate services were also reviewed in 2011. An overall reduction in posts by around 600 was expected, and a service-line management structure would reduce the number of directorates, and cut management layers, numbers and costs.
South Netley
The headquarters site at South Netley opened in the 1920s as a tuberculosis hospital and expanded during the Second World War in the expectation of high casualty rates from bombing. Many wartime buildings were still in use at the time of this project. South Netley's second site was opened in the early 20th century as a workhouse, was used as an army hospital during the First World War and a new hospital was built on the expanded site in the 1920s. South Netley was building a £430M ‘state of the art’ hospital on its second site, due to open in 2014, with the headquarters site becoming a community hospital. Funding the new build put the foundation trust bid on hold until 2012. The average tenure of executive directors in post in December 2009 was 5 years, making this the most stable board of the six trusts participating in this study.
One challenge was to develop ‘new hospital working’, with new practices, culture, behaviours, systems and structures. The hospital was consistently meeting performance targets and had among the lowest mortality rates in the country. Nevertheless, South Netley also had to make savings of £28M in 2011–12. Financial targets had been met since 2006–7, but relationships with commissioners were described as ‘a battle’ and ‘fraught’. Senior management regarded the results of the 2010 annual staff survey as disappointing, with low scores concerning satisfaction with quality of patient care that staff were able to deliver, pressures of work and stress. Staff engagement was thus a priority. South Netley had developed its own leadership development programme aiming ‘to adopt a more business orientated way of thinking and working’. This programme was designed for the ‘172 mission critical leaders’ and would eventually cover ‘the top 600’ staff. This programme focused on five ‘core leadership behaviours’: understanding and managing context, working in partnership to drive improvement, tackling difficult issues, empowering others and emotional intelligence.
Wattle Park
Formerly a 19th-century workhouse, Wattle Park was established on its current site after the First World War, inheriting a collection of elderly buildings. Because of financial pressures, the trust was discussing a merger with two other hospitals, which was agreed in December 2011. An independent bid for foundation status was abandoned and redevelopment plans were deferred. There was only one change of chief executive during this project, but the hospital had a history of instability at board level, and trust between the top team and middle management had been weakened. The average tenure of executive directors in post at December 2009 was 2 years.
In 2006, Wattle Park had a deficit of £40M and launched a turnaround programme. Financial problems persisted, however, contributing to the urgency of merger discussions, with savings of £14M required in 2011–12. In October 2011, considering ‘extraordinary financial measures’, staff were asked to ‘sacrifice’ part of their annual leave, take unpaid leave or perform additional unpaid sessional duties. The executive team gave up 2 days' holiday entitlement. At the end of 2011, the Department of Health designated Wattle Park as financially ‘unsustainable’ and further savings of £28M were to be achieved by March 2012. Senior staff felt that management competency gaps were not addressed, as training and development budgets were frozen along with cuts in middle management posts, which had weakened management capacity. IT systems were seen as unable to provide appropriate management information. Wattle Park was well rated by the CQC but a review in 2011 raised concerns about cleanliness, infection control and staffing levels. The use of ‘lean’ methods had been successful, and a ‘patient experience revolution’ beginning with ‘in your shoes’ workshops involved over 5000 patients and staff in developing quality initiatives. All staff were given customer service training and nurse-led ‘hourly rounding’ on wards was introduced.
Wattle Park also had to deal with a high volume of referrals, weak demand management, a growing and ageing local population and attempts to move care into the community that were problematic because of a lack of facilities and because anticipated savings did not materialise. A senior manager said, ‘So we're left with a very difficult management agenda, in terms of trying to balance all these priorities.’
Changing structures
The regulator, Monitor, was encouraging established and aspiring foundation trusts to adopt service-line management methods,113 and hospitals were introducing new organisation structures, with new management roles and responsibilities. This involved establishing autonomous clinical divisions operating ‘businesses within a business’, with clinical staff taking the lead on service development. Each business unit thus had clearly identified resources, including staff and support services.
In 2009, for example, Netherby had a traditional clinical directorate structure, with a separate management team for each of the 18 directorates. The 10 clinical directorates were each managed by a triumvirate including a clinical director, directorate manager and head nurse. An external management consultant working with Netherby in 2011 was asked about the strengths of this structure: ‘I'm struggling to think of any strengths of the current organisation. Managers seem to be dedicated and the pay is good.’ Turning to weaknesses, he observed:
The hierarchies are too deep. There are no clear lines of responsibility and accountability. The information to inform decisions is poor. Business cases are based on selective information. There's a lot of flag waving around ‘clinical standards’ and ‘patient safety’. One-third of the staff are in the ‘administrative and secretarial’ category. How much energy do we need in those areas? There's a lot of bureaucracy. We need to understand non-value-adding activities. What are the consequences of not doing some of these things? Do we know how much this is costing? At the moment it's all anecdotal; we need evidence. We're short of change agents who possess ‘Rottweiler tenacity’. And there's too much politics.
One director observed that issues were ‘passed up the tree’ and escalated unnecessarily. Accountability and performance management were lacking. There were too many directorate managers and management layers, and structures were not consistent across services. In 2011, Netherby introduced a service-line management structure. Two care groups – medicine and surgery – were created, each with a group director, lead nurse and two general managers. The clinical directors became medical service leads, each supported by a service manager. This management reorganisation would generate savings of between £2M and £3M per annum.
For Monitor, the benefits of this approach included the empowerment of clinicians, efficiency and productivity, local ownership of budgets, ‘seeing the big picture’ and accurate patient-level costing. According to matrons at Greenhill, however, these structures were problematic.
Greenhill introduced a service-line structure just before this project began, and the matrons argued that the new ‘independent’ divisions had entrenched the trust's ‘silo mentality’. An operations manager at Clearview described the now hostile resource discussions between their divisions as ‘Reservoir Dogs’ moments (from the movie in which leading characters threateningly point their guns at each other). The Greenhill matrons argued that divisional silos had other problems:
We used to know what was going on in the other areas or divisions. And we used to share good practice. But not now. As modern matrons, we have to take on the role of duty lead nurse (DLN) once or twice a week. This involves a shift from seven in the morning until three in the afternoon. And we also do this once a month on a weekend. The nature of this role hasn't changed much, but we are now being asked to do this more often. As the organisation structure has become more ‘silo’ based, this means that we don't have such a good understanding of what happens in other areas as we did before. So that makes the DLN role more difficult because you're always having to ask about things, to get the information.
If duty nurses do not fully understand the issues they face, and spend time gathering information, this may adversely affect the quality and safety of care. The advantages and drawbacks of service-line management structures in acute settings have not been well researched.
Management agendas
A central feature of the organisational context concerns the nature of the agendas that management had to deal with. In set-up interviews, middle and senior managers were asked to identify the main issues on the management agendas of their trusts. Given space constraints, this section explores the agendas of two trusts, Netherby and Greenhill: one foundation, the other not.
The Netherby management agenda
At Netherby, a picture of the management agenda was constructed from the responses of 17 managers, including four board members, seven hybrids and six managers. They identified 86 items, which were content analysed to identify themes. This revealed an agenda with 16 main themes and two other issues concerning uncertainty and competing priorities. Many of the main items were inter-related, but their separation serves an analytical purpose in establishing an overview of the nature of the agenda. Content analysis assumes that an issue that is mentioned more frequently may be more significant than those which are mentioned infrequently. However, that is not necessarily the case, and Table 16 does not indicate relative priorities. Management attention to communications and serious incidents can be as strategically significant as that to targets and finance.
| Item (count) | Substance | Illustration |
|---|---|---|
| Targets (17) | Multiple targets, distraction | Targets – hundreds of them; easy to get distracted from the daily running of the trust |
| Finance (12) | Find savings, generate income, increase productivity | It's an obsession – every conversation is about money, need to increase productivity; we've implemented lean; where do we find another £0.75M this year? |
| Relationships (9) | PCT, other hospitals, community health, ambulance service | Collaboration is difficult; competition is the norm; we need to work with our PCT to make sure that systems and processes are in place in the community |
| Change (8) | Changes to culture, structure, work practice | Need to work differently; change the culture from apathy to one in which people take responsibility; too many directorates |
| Activity (6) | Growth in demand, winter pressures | Volume of work is increasing; 20% rise in one area with the same team; capacity and demand for next winter |
| Regulation (6) | Workload involved in responding to guidelines | Monitor and CQC compliance; increasing burden of regulation; the pressures are getting stronger; the governance agenda is massive |
| Facilities (5) | Buildings, layouts, space | Ageing estate; need to ensure that patients feel comfortable and safe; the environment has to be right; financial restrictions mean that it will be challenging to maintain standards |
| Information systems (4) | IT infrastructure, clinical and managerial information | Inadequate IT; we need good market information and internal costing and management systems; challenge is to develop live information on activity and costs |
| Clinical engagement (3) | National policy for clinical leadership | Clinical directors don't see themselves as leaders; clinical engagement; we must get it right, get key players on board |
| Business orientation (3) | Development of a more commercial approach | We need to be more business orientated; we've got to run as a business now; we need to learn better how to compete |
| Management changes (3) | Top team instability | Lack of job stability among senior management; changes to our senior team have been destabilising |
| Leadership development (3) | Leadership and management skills | Assessment centres and personal development for directorate managers; training for those in leadership roles |
| Patient and public expectations (2) | PPI agenda | Managing public expectations; the pressure to do other things means that there's a danger we lose patient focus |
| HR issues (2) | Turnover, development | Low staff turnover has advantages but it means ‘no new blood’; staff development once in post |
| Learning from SUIs (2) | Learning in general and following Mid Staffs | We have experienced SUIs, which have been subject to SHA investigation; pressure following Mid Staffs |
| Communications (1) | Information flow down the organisation | Managers don't pass on information; sister said, ‘I don't know where the chief executive's office is’ |
Of the two other items the first concerned ‘competing priorities’, based on comments such as ‘it's increasingly difficult to strike a balance across these different demands, balancing the budget while improving productivity’ and ‘effectiveness, patient experience, safety; managing these multiple demands is tricky’. The second concerned ‘uncertainty’, based on comments such as ‘the uncertainty that we are facing’, ‘managers are working in an extremely uncertain and unstable environment’ and ‘how to construct a sustainable 5-year plan in this context?’.
Thus, this management agenda had five properties:
-
length: this is a big ‘to do’ list
-
complexity: the items are individually complex and they are intertwined
-
strategic: all of these issues are strategic, in terms of contribution to long-term performance and survival, and they are all always important
-
change: all of these items involve significant ongoing organisational changes
-
typical: this list reflects who we spoke to and when; a different sample at a different time would produce a different result, but we would nevertheless expect to see a similar pattern, and we do see this at other participating sites.
Table 16 is based on information from 2009–10. Were this question to be revisited in 2015, say, a different set of items would probably emerge. However, given the continuities in the institutional context (see Chapter 3), it is highly likely that, although specific themes may become more or less salient, those properties of the acute trust management agenda are relatively durable.
The Greenhill management agenda
Content analysis of replies to the ‘management agenda’ question at Greenhill is shown in Table 17, based on responses from 12 participants, including two board members, four hybrids and six managers, who identified 57 agenda items, coded under nine theme headings and a ‘regulation and other issues’ category.
| Item (count) | Substance | Illustrative quotes |
|---|---|---|
| Finance (11) | New environment; find savings, less resource, increasing demand | The trust historically is not good at saving money; we're expecting a cut of £60M over the next 3 years; this is the hardest we've ever faced |
| Change (11) | Improvement, redesign, learning from SUIs, change culture and style | We want to instil continuous improvement; redesign, productivity, right first time; how do we get real change?; how do we get learning from incidents and complaints? |
| Targets (9) | RTT, quality, safety, A&E waits | Priority to make services safe and high quality; financial constraints; we have not met the transit time target for 2 years; why crunch numbers to make government look good |
| Clinical engagement (6) | Style, culture, clinical leadership, teamwork, development | Who leads and manages the divisions – that's confused; medical leadership is a challenge; management got results by pushing harder, not by changing anything; engaging doctors might be right, but we don't want to disengage managers |
| Activity (5) | Rising workload, same staff, productivity, increasing pace of care | Increasing levels of activity is a key issue; we need to improve productivity; worrying increase in emergency admissions; meeting standards with an increasing workload |
| Staff engagement (4) | Communication issues; lack of corporate perspective; need to develop teamwork | We're not good at engaging people in solutions; I'm not sure our doctors are engaged with the trust; some can and won't, some can't, others are willing and flexible; challenge to use the skills and knowledge we have in teams |
| Staffing (3) | Shortages in some areas; recruitment and retention problems | We do not have ideal staff levels in midwifery; difficulties in paediatrics too; qualified children's nurses are scarce; not enough emergency department consultants |
| Relationships (3) | Challenging relations with PCT, SHA, Monitor | Relationships with PCT inhibit change; to achieve savings radical changes rather than marginal improvements are required; climate of mistrust; PCT is a bully; ‘world-class commissioning’ means ‘being a stronger bully’ |
| Patient and public expectations (3) | Increasing public expectations | Rising patient expectations of the NHS; doing what patients want and not what we want to do; being accountable to the public and staff but without being punitive |
| Regulation and other issues (2) | Burden of bureaucracy, accreditation demands, risk management | More explicit bureaucracy; regulatory demands, need to register with CQC; three suicides over 8 months – questions around safe management of self-harm patients |
This displays the same items and properties as the Netherby agenda – lengthy, complex, strategic and change orientated.
Much doing to be done
If NHS managers are struggling it is because of the size of the agenda and the lack of respect for the management task involved; and the systematic lack of investment in learning – it is hard to learn together when there is so much ‘doing’ to be done.
p. 19114
What are the management implications of this analysis of organisational context and management agendas? From an operational management perspective, there is a daily challenge to match patient demand with clinical, physical and financial resources. Patient numbers are high and unpredictable, and reduced length of stay means that patient flows are faster paced. Demand has increased in many services while resources have been cut. Management has also had to address radical changes flowing from national, regional and local reorganisations, higher public expectations, an increasingly burdensome regulatory regime and the need to reduce costs, year on year, potentially affecting job security. In this context it is not possible to focus on, say, two or three issues in 1 year and on another set of issues the next. This is an agenda on which all of the items are always priorities, which compete with each other for attention and resources, and which change frequently.
From research in commercial organisations, Bruch and Menges115 describe a similar pattern: increasing market pressures and speed of activities, raised performance goals, new technologies and systems and attempts ‘to make this furious pace the new normal’ (p. 82). This leads to what they call ‘the acceleration trap’, in which focus is scattered, staff are demotivated and customers become confused. In the ‘fully trapped’ companies that they studied, 60% of employees agreed or strongly agreed that they lacked sufficient resources to get their work done.
Are NHS managers experiencing a similar ‘acceleration trap’? Our management survey (see Appendix 3) included two items relevant to this question. One concerned having sufficient resources (reverse wording from that of Bruch and Menges115) and the other concerned improving the service with fewer resources. Responses to those items are summarised in Table 18.
| Burnside | Clearview | Greenhill | Netherby | South Netley | Whole sample | |
|---|---|---|---|---|---|---|
| Question: ‘I have sufficient resources to carry out my management responsibilities effectively’ | ||||||
| % agree | 39 | 28 | 42 | 19 | 24 | 30 |
| % disagree | 49 | 53 | 38 | 66 | 54 | 52 |
| % disagree and neutral | 62 | 72 | 58 | 81 | 76 | 70 |
| Question: ‘I am expected to improve the service we provide despite resources being cut’ | ||||||
| % agree | 92 | 92 | 94 | 91 | 95 | 93 |
The percentage of managers agreeing or strongly agreeing that they possessed sufficient resources ranged from 19% at Netherby to 42% at Greenhill. The ‘% disagree’ figures are more comparable with the Bruch Menges question, and range from 66% at Netherby to 38% at Greenhill. Experience of the acceleration trap thus appears to be mixed. However, only 30% of the whole sample agreed or strongly agreed that they had sufficient resources, with 70% disagreeing or neutral. Turning to the second of the items, a more consistent picture emerges. In all five trusts, > 90% of respondents agreed or strongly agreed that they were expected to improve the service despite resource cuts.
Having to cover many different kinds of activity simultaneously is what Bruch and Menges115 call ‘multiloading’. An associated pattern is ‘perpetual loading’, in which the organisation operates close to capacity, drives employees hard and deprives them of any hope of retreat: ‘when is the economising going to come to an end?’ (p. 83). The solutions for breaking out of this trap are to prioritise projects, halt less important work and clarify strategy. They cite the chief executive who allowed managers to name only three ‘must win battles’ to focus attention, energy and action.
The evidence from this project suggests that many health-care managers are subjected to multiloading and perpetual loading. The institutional and organisational contexts, however, make it difficult to follow the obvious advice. Recent experience suggests, for example, that an acute trust focusing its management attention on, say, addressing financial problems and the demands of regulatory bodies may find that less attention is paid to the quality and safety of patient care, with disastrous results. This appears to have been part of the explanation for events at Mid Staffs. 70,78
A further answer to the problems of multiloading and perpetual loading lies with management capacity. Our evidence indicates that middle managers are highly motivated and deeply committed, but that they are overstretched and under-resourced. National policy has been to treat health-care managers as wasteful bureaucrats and to reduce management numbers and costs. This has been accompanied by other policies, directives and initiatives that have added to the management agendas of acute trusts, stretching capacity even further. Management capacity should perhaps be a priority issue for further research.
Chapter 5 The realities of middle management
Introduction
One of the main aims of this study was to gain a better understanding of the realities of middle management work in acute health-care settings and, in particular, to understand:
-
the motives and rewards for middle managers
-
the pressures and demands that they face
-
how middle management work is changing.
This chapter first reviews published research evidence relating to the nature of middle management work in general and then reviews evidence relating to the nature of middle management work in health care. The evidence from this study concerning motivation, demands and trends in the nature of management work is then summarised, drawing on survey results along with interviews and focus groups. The main conclusions from this analysis are that:
-
Middle managers in general hold a wide range of responsibilities, from ‘keeping the show on the road’ to contributing to strategy, innovation and change, with a profile that sharply contradicts the ‘pen-pushing bureaucrats’ imagery.
-
Middle managers, since at least the start of the 21st century, have seen their jobs enlarged, their responsibilities widened, the pace and intensity of their work increased, their working hours lengthened and their performance monitored more closely.
-
Managers in health care face trends and pressures similar to those affecting middle management elsewhere, but also face the challenges of driving change in a professional bureaucracy, dealing with a negative image and a perceived absence of adequate support for hybrids with managerial responsibilities.
-
Surprising survey findings concern the absence of the negative management stereotype (the majority were happy to be seen as managers), the prevalence of ‘extreme job’ characteristics and low levels of both job and organisational satisfaction.
-
Survey findings triggering concern relate to unsustainable workloads, inadequate resources, poor work–life balance, the small but significant proportion considering leaving the service and the view that financial pressures have compromised patient safety.
-
The primary motivations and rewards for middle managers include making a difference, driving innovation and change, doing a good job, feeling valued, developing others, working in high-performing teams, and personal development.
-
A small number said that rewards were lacking, that contributions were not being recognised and that leadership styles were demotivating, and 42% of survey respondents agreed or strongly agreed with the item, ‘I sometimes feel like leaving this employment for good’.
-
Many middle managers in health care appear to have jobs with a profile that can be described as ‘extreme’ in terms of pace, intensity, scope, conflicting priorities, long working hours and other characteristics – a pattern that is exciting and fulfilling for some.
-
Extreme jobs are also associated with stress, fatigue and poor work–life balance, can generate organisational and domestic difficulties, may not be sustainable and may be especially problematic for those in hybrid managerial roles in which rapid and intense context switching between different kinds of complex tasks could increase human error.
-
Given the multiple roles of middle managers in ‘keeping the show on the road’, mediating between the front line and top team and driving change and innovation, it may be useful to consider strategies for ‘releasing time to manage’ in the face of increasing workloads and decreasing resources.
-
One research priority arising from this analysis concerns the development of a better theoretical and practical understanding of the concept of management capacity, and of how capacity can be assessed and strengthened in a context of financial constraints.
-
A second research priority concerns understanding the nature, incidence and implications of extreme jobs among health-care managers, along with ways to redesign such roles, and/or provide better forms of support for those who hold extreme jobs, including resilience training.
Studying management roles in the 1980s, Scase and Goffee116 described a context in which (conservative) government policies were increasing pressure on all organisations to be more cost-effective and efficient, with corporate restructuring reducing management job security. Expectations of personal development and opportunities to exercise independent judgement were not being met, and middle managers were being asked to achieve goals with limited resources, and with tighter monitoring of standards. Scase and Goffee116 reported that the ‘reluctant managers’ in their study were ‘able to adapt by investing very little of themselves in their work and merely performing their jobs to an acceptable minimum standard’, particularly in bureaucratic settings with more rules and constraints, and with more scope for minimalist role playing (p. 51).
These observations concerning cost pressures, insecurity, regulation and diminishing resources apply to health care in the second decade of the 21st century. However, rather than respond by decreasing personal investment in work, for many health-care middle managers in the current study the issue concerned potentially excessive personal investment, in the form of ‘extreme jobs’.
The management role
Interest in management work dates from 1956 and Whyte's The Organization Man,117 which created the stereotype of the compliant, risk-averse bureaucrat, an image that survives into the 21st century in characters such as David Brent, the manager in the television comedy series The Office. Whyte's account was followed by numerous other studies of management roles. From observation in a chemical plant in the American Midwest, Dalton118 noted that departures from formal organisation processes were required to make the plant run smoothly, emphasising the role of informal networks, office politics and personal influence. Following in Dalton's ethnographic footsteps, Watson6 documents the rewarding and painful realities of managing from his study of a telecommunications factory in the British Midlands. The subtitle of Watson's book is ‘culture, chaos and control’, highlighting dimensions of the management work that he observed.
Mintzberg4,119,120 describes the activities of management on the ‘planes’ of information (communicating, controlling), people (leading, linking) and action (doing, dealing). He also describes the pace, brevity, variety, fragmentation and discontinuity of management work, and the preference for action and informal and oral communication. Defining management as ‘deciding what should be done then getting other people to do it’ (p. 6), Stewart5 is also concerned with management activities – planning, organising, motivating, controlling, co-ordinating, staff development – noting the variation in management roles, and the fragmented, chaotic and hectic nature of the work. From his study of general managers, Kotter7 notes the long working hours (60–90 a week) and the considerable time spent in conversation, asking questions, joking and persuading – but this is intelligence gathering, not time-wasting.
Hales22 portrays the variety in management work, which typically involves activities such as acting as figurehead, monitoring and disseminating information, networking, negotiating, scheduling and monitoring work, allocating resources, human resource management, problem-solving, innovating, and technical tasks relating to professional or functional specialisms. Management thus involves an ‘inescapable preoccupation with routine . . . keeping the show on the road’ (p. 51), reacting to events, focusing on the urgent and unforeseen, accompanied by tension, pressure and conflict in juggling competing demands. There is also considerable choice and negotiation over the nature and boundaries of the management job and how it is done.
Hales22 notes that the focus on what managers do overlooks the impact of those activities. The management contribution is explored in the following chapter. However, it is important to note that evidence concerning middle management contributions to organisational effectiveness departs from the stereotype of bureaucratic blockers. It is now recognised that middle managers play a key intermediating role between front-line operations and senior management. 30,121 Middle managers have also been identified as key change agents,122 leading change ‘quietly’14,123 and ‘below the radar’,124,125 as ‘ideas practitioners’,126 as well as implementing, synthesising, championing and facilitating strategic organisational change. 12,29
How are middle management roles themselves changing? From their study of eight public and private sector organisations in six Western European countries, Dopson and Stewart127 challenged the image of middle managers as frustrated, powerless and disillusioned with dreary jobs in rigid hierarchies. They found middle managers responding to complex and changing pressures, with increased workloads and responsibility, with accountability for a wider range of duties, seen by senior management as pivotal to implementing change. Middle managers had to become more flexible and generalist, and shorter hierarchies had put them closer to the top team.
Hassard et al. 128 interviewed 250 managers in 30 organisations in the USA, the UK and Japan, concluding that middle management roles have become more challenging, with longer working hours, increased performance pressures, expectations of rapid results and a blurring of work–domestic boundaries. This may be offset by higher salaries, greater responsibilities and more interesting work, ‘but the overall feeling of being overwhelmed in work while the traditional promotional ladder has been largely removed was a major and widespread finding’ (p. 228). However, this study also found that middle managers were highly motivated despite the pressures, and they argue that performance could be improved if the pressures were released. In addition, ‘authoritarianism and top-down rule were alive and well’ (p. 13); there was not much sign of the ‘post-bureaucratic’ organisation.
The evidence thus shows that middle managers have an increasingly varied range of responsibilities, with long working hours and rising performance expectations, playing key roles in operational and human resource management, mediating between the front line and top team, contributing to strategy, innovation and change. These features also apply to middle management work in health care, as explained below.
Middle management in health care
Over the past decade, layers of national and regional organisations have accumulated, resulting in excessive bureaucracy, inefficiency and duplication. The Government will therefore impose the largest reduction in administrative costs in NHS history. Over the next four years we will reduce the NHS's management costs by more than 45%.
p. 431
Despite evidence confirming the significance of middle management, the stereotype of the ‘petty bureaucrat’ prevails in health care, where management costs are associated with wasteful bureaucracy. Hyde et al. 129 argue that denigration of the function obscures vital strategic and co-ordinating work, that ‘middle management’ is an identity that nobody wants and that middle managers have become ‘a lost health service tribe’. However, Currie and Procter51 stress the importance of the ‘diplomat’ role of middle managers in a professional bureaucracy, mediating between medical and corporate goals. Carney130 and Pappas et al. 131 argue that ‘the strategic middle manager’ has become more, not less important in health care. National policy has rejected those perspectives.
Hyde et al. 129 observe that ‘little is known about the realities of health management and middle management work in the NHS is obscured’ (p. 18). One reason for the lack of evidence perhaps concerns the distributed nature of the function, which does not comprise a well-defined group;132 literature reviews must rely on search terms such as ‘lead nurse’, ‘ward sister’, ‘modern matron’, ‘service lead’, ‘clinical director’ (see Chapter 2). A second plausible reason relates to the stigma attached to middle management, making this group difficult to identify. In addition, a search for relevant literature reveals more commentary than research, which is more likely to be published in sector- and occupation-specific journals than in general organisation and management studies journals. The current study thus seeks to contribute to our understanding of those management realities.
A review of published evidence leads to eight observations. First, research focuses on nurse management roles and clinical directors, with less attention to other middle managerial levels and non-clinical management roles. Second, hybridisation has meant changing job titles, from ward sister to ward manager (in the UK133), from charge nurse to nurse unit manager (in New Zealand134), reflecting expanding roles, covering larger areas and more staff, and increasing workloads with longer working hours. 135–138 Third, hybridisation involves clinical staff in budgeting, human resource management, planning, change and administration. 139–144 Fourth, middle managers (pure plays and hybrids) have been subjected to increased monitoring and accountability. 145–147 Fifth, the significance of the bridging role of middle management, between front line and top team, has increased. 148 Sixth, these changes have taken place in the absence of adequate preparation for those moving from clinical to hybrid roles. 149 Seventh, hybrid middle managers have problems balancing clinical and organisational priorities and resource allocations. 150,151 Finally, the emphasis in middle management roles has shifted towards change agency and leadership. 152–154
Research also suggests that middle managers face several problems in addition to workload and competing stakeholders. They are often excluded from decision-making and feel isolated and controlled. 141,155,156 They have difficulty influencing and challenging doctors51,157 and work with ambiguous lines of responsibility. 158 Hybrids report tensions between clinical and operational priorities,159,160 along with difficulty balancing professional development with work objectives,161 and the transition from a clinical to a hybrid managerial role raises identity issues. 156,162 Hybrids are also concerned about isolation from their professional peers. 157 Many feel that they lack support and are unprepared for handling human resource management issues. 163 They are also acutely aware of the negative stereotype devaluing management and threatening job security. 1,145,152,164
In sum, middle managers in health care face a range of pressures similar to those in other sectors, including widening roles, increasing responsibility, longer working hours, work intensification and more intrusive performance management. However, the management population of the NHS comprises a heterogeneous combination of pure plays and hybrids, who also have to contend with the challenges of driving change in a professional bureaucracy, a negative stereotype and, for hybrids in particular, a perceived lack of preparation for, and subsequent support in, managerial roles.
Management survey findings
This section summarises findings from our survey, conducted in 2011. Using 5-point Likert-scaled items, the survey had five sections: realities, job characteristics, organisational outcomes, job satisfaction and personal experience. Items also included a widely adopted organisational commitment scale165 and a similarly well-recognised set of stress indicators. 166 The survey was distributed by e-mail at five trusts, covering staff with managerial and hybrid roles. The response rate varied from 77% at Greenhill (distribution was confined to the trust's ‘100 leaders’), to 19% at Clearview and Netherby. The overall response rate was 24%, generating 611 usable responses. Of those, 18% had management roles and 51% had hybrid roles; 31% did not answer this question. Of the total, 42% were female and 19% were male; 39% did not answer this question. Over two-thirds of responses fell into five categories of work: management, administrative and clerical, project management, nursing and finance. Further details of the survey administration, along with sample properties, response rates, frequency distributions for the whole sample and responses for each trust, are reported in Appendix 3.
Some findings were anticipated, others were surprising and some are cause for concern (percentages cited here are the aggregates of either ‘agree and strongly agree’ or ‘disagree and strongly disagree’; Appendix 3 reports the detailed breakdown of responses across the full scale).
Anticipated: motivation, commitment, change orientation, unclear responsibilities
Interviews and focus groups revealed middle managers to be highly motivated and deeply committed and survey responses confirmed this: 75% indicated that they were motivated by making a difference to patient well-being, 90% were motivated by developing others and 94% felt that their work made an organisational contribution. The shift in the focus of management work towards change was also confirmed: 65% said that they exercised influence in their areas, 70% got a ‘buzz’ from the challenge in the job and almost 80% agreed that they had become more businesslike in their approach to managing.
All of the trusts in this study had recently undergone, or were about to experience, internal reorganisations in addition to changes to national governance, regulatory and commissioning structures. Thus, although 70% agreed that they were clear about their own roles, 56% said that it was often unclear who was responsible for what.
Surprising: absent stereotyping, extreme jobs, low satisfaction
There was little sign of the negative management stereotype or of the traditional animosity between clinical and managerial professions: 60% said that clinical staff valued their management contribution, 70% did not resent reducing clinical duties to carry out management work and 76% were happy to be seen as a manager. This was surprising as some interviewees had denied having managerial responsibilities (although in the judgement of the interviewer they clearly did); one operations manager explained that he never described himself as a ‘health-care manager’ at social events, another described the favourite catchphrase of a senior consultant with whom he worked closely as ‘those wretched managers’ and one trust asked that the project subtitle, which appeared on participant information, be changed from ‘middle and front-line management work’ to a study of ‘managerial and clinical leads’. ‘Happy to be a manager’ was broadly consistent across all five trusts.
Interviews and focus groups suggested that some middle managers had ‘extreme jobs’, with fast pace, intense effort and long hours. 167 A health-care variant on the original model was thus developed. Responses to those survey items suggest that this phenomenon is more widespread than anticipated. The implications are discussed in Extreme jobs, resilience and job crafting.
Also surprising was the low proportion – 28% – indicating satisfaction with their organisation, with only 50% expressing satisfaction with their job. Commitment to patients, colleagues and the work clearly does not translate into satisfaction with the job or the organisation.
Cause for concern: workloads, safety, personal costs, disaffection
The managers responding to this survey appear to have been pressured by heavy workloads and to have had inadequate resources: only 30% thought that resources were sufficient for their role, 58% said that their role was unmanageable, 68% said that they did not have enough time for their management duties, 80% said that pressure to meet targets had risen and 90% said that the focus on cost-effectiveness had increased.
A second cause for concern relates to the possibility that patient safety is compromised by financial pressures: 51% agreed that trade-offs were made between safety, quality and finance, and 54% agreed that financial pressures put patients at risk (22% strongly).
A third source of concern relates to the high personal costs of the pressures in management roles, with only 30% indicating that they could maintain a satisfactory work–life balance and 50% worrying about problems, having difficulty unwinding and feeling used up and exhausted after work.
Finally, three items indicate a degree of disillusionment: 26% said that an offer of more money would tempt them to leave, 42% said that they sometimes felt like leaving for good and 44% felt that they had relevant capabilities that were not being used in their role.
These results are broadly consistent with the findings from the study of trends in middle management work by Hassard et al. 128 discussed earlier, and have potentially significant implications. First, at an individual level, those kinds of pressures are not sustainable and can be expected to affect stress, burnout, performance and the ability to retain capable staff. Second, this context is hardly conducive to the commercial, entrepreneurial, innovative approach to service redesign and delivery improvement that health-care managers in the acute sector have been encouraged to adopt. Finally, and perhaps most seriously, is the observation that patient safety is being compromised. Patient safety was a national priority during the life of this project, but national policies appear to have been contributing to creating an environment in which that priority was undermined.
Motives and rewards
The stereotype suggests that middle managers are motivated by bureaucratic rules, organisational stability and administrative order. The reality is different. Survey responses suggest that middle managers have other motives and information from set-up interviews supports this observation. Here, findings from two trusts elaborate this point, and evidence from others is briefly presented.
Netherby
At Netherby, 17 set-up interviews were conducted with four board members, seven hybrids and six managers. In response to the question, ‘what in your opinion are the motives and rewards for middle managers in this trust?’, interviewees generated 40 responses; content analysis suggested the six main themes (and an ‘other’ category) summarised in Table 19.
| Theme | Item count | Illustrative comments |
|---|---|---|
| Making a difference | 13 | ‘Make things better for patients’; ‘see improvement, give it a go’ |
| ‘Buzz from innovation’; ‘take risks, think beyond the current setting’ | ||
| ‘Motivating to learn from incidents and implement changes’ | ||
| ‘Setting up projects to improve things can be highly motivational’ | ||
| ‘We want to be performing better, encouraging improvement’ | ||
| Doing a good job | 9 | ‘Managers get a buzz from things coming together’ |
| ‘Job satisfaction, see things through’; ‘help deliver high quality care’ | ||
| ‘If the organisation is successful, that is satisfying’ | ||
| ‘Motivated by delivering care that compares with what our peers are doing’ | ||
| Hygiene factors | 9 | ‘Good employer’; ‘pensions, terms and conditions, good retention’ |
| ‘Career routes, always somewhere to go’ | ||
| ‘Reward package, holidays and sickness benefits good’ | ||
| ‘Security, important in this sector, now challenged’ | ||
| Feeling valued | 4 | ‘Feeling valued’; ‘done a good job, somebody just saying “well done” ’ |
| ‘Feedback from patients and colleagues is satisfying’ | ||
| Personal development | 2 | ‘Keeping up to date with the latest developments’ |
| ‘Build up specialist knowledge and expertise’ | ||
| Public sector values | 1 | ‘Public service, you don't join to make money as a middle manager’ |
| Other | 2 | ‘At the exec level, the motivations are to see the hospital improve and taking the hospital forward; middle managers’ motivation is not making mistakes and keeping within budgets' (board member) |
Analysis of answers to this question from 12 interviewees at Greenhill (two board members, four hybrids, six managers) is shown in Table 20. This group identified 42 items divided into nine themes.
| Theme | Item count | Illustrative comments |
|---|---|---|
| Making a difference | 8 | ‘It's rewarding for managers who can try out new ideas’ |
| ‘We are trying to change, there's a lot of innovative work going on’ | ||
| ‘Rewarding to work on a concern, to make a difference to patients’ | ||
| ‘The opportunity to develop the service as a whole is exciting’ | ||
| Hygiene factors | 7 | ‘The pay is good’; ‘we treat people well’; ‘so far jobs are safe’ |
| ‘Leave and sick pay and pensions are generous’ | ||
| ‘Lots of development opportunities’ | ||
| Doing a good job | 5 | ‘On the front line, when they get it right, that's very rewarding’ |
| ‘The vast majority of patients are happy with the services we provide’ | ||
| ‘Our rewards strategy relies on professionalism and integrity’ | ||
| Feeling valued | 3 | ‘Most people respond to having their work acknowledged’ |
| ‘The little “thank you's”, which aren't often, a letter saying “well done” ’ | ||
| Colleagues | 3 | ‘I work with an amazing team; people who love their jobs, good humour’ |
| ‘Everybody values other professions’; ‘people take pride in their division’ | ||
| Public sector values | 3 | ‘A lot of NHS managers believe in the NHS – I care passionately’ |
| Developing others | 3 | ‘Seeing people turn themselves around and become more supportive’ |
| ‘Rewarding to hear someone say, “I think I could chair that meeting now” ’ | ||
| Inside track | 2 | ‘My position gives me inside knowledge, strategic understanding’ |
| ‘Voyeuristic, working with different groups, global view of the service’ | ||
| Struggling to answer | 8 | ‘I'm struggling to think of motivation and rewards’ |
| ‘This is a tough place to work at the moment; managers are having to fight through difficulties and fix them, and this is an ongoing struggle’ | ||
| ‘Do you get through the first few years, or get destroyed in the first year?’ |
The analysis reveals a combination of professional (making a difference), intrinsic (feeling valued) and ideological (public sector commitment) motivations. However, one-quarter of items for both trusts concerned pay, conditions and job security. In the financial climate prevailing during this project, the role of hygiene factors is not surprising.
This pattern was echoed across all six trusts. For example, nine interviewees at Burnside identified improving patient care, recognition, doing a good job, personal and career development and the hospital's convenient location. Seven interviewees at Clearview identified making a difference, overcoming challenges, improving patient care and safety, personal accomplishment and working with exceptional and inspirational people. Motives from a mixed focus group at South Netley included making a difference, improving the patient experience, seeing the impact, being inspired and energised by colleagues, progression, lean efficient work, personal flexibility, seeing others enjoying their work and taking pride in the job, recognition, and sharing ideas and practice. A general manager at South Netley added, ‘The intellectual challenge of dealing with “wicked problems”. You get a tremendous kick when you pull it off’, and ‘Massive peer support, working together, common goals.’
Despite mentions of hygiene factors, comments such as ‘It's not about money’ were also common. However, the ‘other’ and ‘struggling to answer’ themes at Netherby and Greenhill, respectively, confirm the disaffection revealed in survey responses:
There are no rewards for middle managers.
Deputy director, Netherby
The experience of middle managers is, they only get beaten up. It is rare for middle managers to participate in an interesting improvement project. There are just not so many opportunities to take risks and introduce innovations in the current climate.
Medical director, Netherby
There are few or no rewards, either financial or in terms of appreciation.
Clinical director, Greenhill
We're bad at recognition, and people say, ‘we don't feel valued’. We don't make best use of non-pay benefits.
Associate director, Greenhill
I have to admit that I struggle sometimes to remain motivated. I'm not always enthused from above. I've been working today with a junior nurse, and we had the patients singing; it was great. I work on a short stay acute medical ward. We need to keep asking, what do our patients want, what do they expect – that motivates me, and I love my job. But being summoned by management, being challenged constantly, that's not motivating.
Ward sister, Netherby
The motivations and rewards for middle managers thus include making a difference, driving innovation and change, doing a good job, feeling valued, developing others, working in high-performing teams and personal development. There was also a view that rewards were lacking, that contributions were not being recognised and that senior leadership styles were demotivating. Although this was a minority position, 42% of survey respondents agreed or strongly agreed with the item, ‘I sometimes feel like leaving this employment for good’. At three trusts, Greenhill, Netherby and South Netley, that proportion was around 50%.
How is the role changing?
I manage the PALS [Patient Advice and Liaison Service] team of three officers across the two sites, four complaints officers, and staff in patient and public involvement who I have also picked up. I have just got them organised and they are working well. My aim is to value and nurture my staff and I've put a lot of emotional investment into developing the team. Now I have to find £27,000 savings over two years; £12,000 last year, which I didn't achieve, and £15,000 this year. Starting from January 2010. I have just got them organised, and now this. I want to weep.
Senior manager, Greenhill
Middle managers in general have seen their jobs enlarged, their responsibilities widened, the pace and intensity of work increased, working hours lengthened and performance monitored more closely. Middle managers in health care face broadly similar issues. From survey data, Table 21 shows the proportions who agreed/agreed strongly with 14 items that sought to capture these trends.
| Item | % agree |
|---|---|
| 1. The need for me to focus on cost-effectiveness has increased | 88 |
| 2. The pressure for my department to meet targets has increased | 83 |
| 3. The need for me to be more businesslike and commercial has increased | 78 |
| 4. The amount of bureaucracy that I need to deal with has increased | 78 |
| 5. I have enough time to complete all of my management duties | 21 |
| 6. I have sufficient resources to carry out my management responsibilities effectively | 30 |
| 7. My overall workload is usually manageable | 31 |
| 8. I am able to maintain a satisfactory work–life balance | 34 |
| 9. As the pressure on me increases, I have to pass the pressure on to the staff for whom I am responsible | 51 |
| 10. It is becoming harder to motivate staff in the current cost-cutting climate | 71 |
| 11. The expectation that clinical staff will take on managerial roles has increased | 71 |
| 12. I often struggle to balance the priorities of both my managerial and my clinical roles | 53 |
| 13. I have had to reduce my clinical work to fulfil my management duties | 44 |
| 14. I resent having to reduce clinical responsibilities to undertake managerial work | 29 |
For the first four items, around 80% or more agreed, reflecting pressures stemming from the government policies being pursued during this project, concerning cost-effectiveness, targets, commercial orientation and performance monitoring and regulation. Responses to the next four items capture the consequences for individual management roles: lack of time, insufficient resources, unmanageable workload and unsatisfactory work–life balance. Only one-third or less did not rate those issues as problems. Items 9 and 10 concern the human resource management implications, passing pressure down the organisation, and finding it more difficult to motivate staff respectively.
The last four items apply to hybrid roles, with clinical staff increasingly taking on managerial roles. However, although just over half of respondents agreed that they had problems balancing managerial and clinical responsibilities and > 40% said that they had reduced clinical duties accordingly, given the pressures on all middle managers it might have been anticipated that the proportion of hybrids experiencing this clash of priorities would have been much higher. Also surprising is the low proportion – less than one-third – expressing resentment at having to reduce clinical responsibilities in favour of managerial work. This again contradicts the negative stereotype of health-care management and is also at odds with the image of health-care professionals who are supposed to place a low value on the management role. This suggests that the traditional tension between ‘white coats and grey suits’ may be eroding, with recognition of the need for closer interprofessional collaboration in the face of the range of complex challenges facing the sector.
Details behind those responses can be seen in the focus group discussion with three lead nurses at Greenhill. Their insights, summarised in Table 22, reflect dimensions of the management agenda discussed earlier and were typical of responses from other groups about changes in management roles.
This is a bleak picture, suggesting that managers lack the time, resources and support to fulfil their responsibilities effectively. The threats and blame, bureaucracy, inspections, tension, firefighting, increasing workloads and lack of trust and autonomy are likely to work against pressures to be more adaptive, creative, innovative and commercially orientated. Nevertheless, focus group participants invariably expressed their commitment to the service, to their profession and to patients. The bleak picture must be set in the context of positive responses under other headings, particularly with regard to motives and contributions. One conclusion is that, if the trends captured in Table 22 were to be reversed, the resultant effect on motivation, commitment and contribution could enhance individual, divisional and corporate effectiveness considerably. This set of issues is discussed in Chapter 6, in terms of building and sustaining an enabling environment for management work, in which most of the appropriate actions are cost neutral, requiring changes in attitudes, behaviours and processes.
| There's more . . . | There's less . . . |
|---|---|
| Uncertainty: ‘it's not clear, to which master do I answer?’; ‘new structure, unclear management roles’ | Trust: ‘we're not trusted to manage’; ‘we're not allowed to use our experience’ |
| Patients: ‘under pressure from growing patient numbers’; ‘no evidence of care moving into the community’ | Autonomy: ‘it's not your own workload any more’; ‘everybody has a say in running my business’ |
| Tension: ‘between us and managers who're paid more’; ‘arguments over finance rules and allowances’ | Money: ‘there's no money to improve things’; ‘can't backfill to support training’ |
| Threats and blame: ‘weekly performance management threats’; ‘when things go wrong, it comes back to me’ | Support: ‘support services don't do either’; ‘limited administrative support’ |
| Bureaucracy: ‘our hands are tied with micromanagement’; ‘red tape; layers and layers of policies’ | Management development: ‘division head has no management training’; ‘you get put in post then given training’ |
| Inspections: ‘overlapping and contradictory’; ‘information, reports, action plans’ | Time: ‘we're plate-spinning all the time’; ‘there's no such thing as “out of hours” here’ |
| Loading responsibility onto me: ‘get this done’; ‘the nurses will do it’; ‘what do you want me to stop doing?’ | And there's also more . . . |
| Panic, knee-jerk, firefighting: ‘we're always firefighting, knee-jerk responses’; ‘what are we going to panic about this week?’ | E-mails: ‘e-mails copied to everyone by people who need to cover their backs; it's dog eat dog’ |
These changes appear to have taken some management roles in a different direction, creating for some what have been described as ‘extreme jobs’, which are the subject of the following section.
Extreme jobs, resilience and job crafting
Are the dimensions of the changing roles of health-care managers undesirable? This section offers a more nuanced response, based on the concept of the ‘extreme job’, identified by Hewlett and Luce167 among high-earning professionals in law, finance and consultancy. They identified 10 dimensions of such roles, but four appear to be less relevant in health care: direct reports, entertaining clients out of hours, profit and loss responsibility and international travel. From the preceding discussion of how management roles are changing, the other six dimensions that may apply are:
-
unpredictable work patterns
-
fast pace with tight deadlines
-
broad scope of responsibility
-
‘24/7 availability’
-
mentoring and coaching other staff
-
long working hours.
Our focus group evidence suggested a further six ‘extreme’ health-care dimensions, which are illustrated here with candid quotes from participants (the sources of the following quotes are omitted to preserve anonymity):
-
7. Making life or death decisions:
-
‘We were on the unit while the alarms were going off, and the patient kept going into cardiac arrest. It was disturbing from my perspective, because I'm a nurse by background and I've worked in ITU [Intensive Therapy Unit], and they were flying around, the arrest button was going, alarms were going and it was very hard.’
-
-
8. Dealing with conflicting and changing priorities:
-
‘It's a case of, “what are we going to panic about this week?” We have more to deal with. There are so many competing priorities and edicts, it's easy to get swamped and forget why you're here.’
-
‘There will be a big push on something, because we're having a visit, or we're non-compliant in an area, so we do that, then forget it, and move on. We're having a visit about safeguarding, so that's in vogue.’
-
-
9. Doing more with fewer resources:
-
‘I was told to “get that racking off the floor”, by screwing it to the wall. But I can't do that; it costs too much. I can't spend £400 on a bit of equipment, an ophthalmoscope, but we could be sued if a symptom is missed. Medical engineering want £35 a year for the maintenance contract. So, no new equipment.’
-
‘We're facing greater demands. It's hamsters on the wheel. We need head space. It's like Winnie-the-Pooh being dragged backwards down the stairs by Christopher Robin; there must be a better way to come downstairs, if only I could stop bumping and think about it.’
-
-
10. Responding to audit, compliance, regulation and inspection agencies:
-
‘Responding to regulatory bodies, all coming at it from different angles. I spent last week just filling in forms, responding to request for information. I had no time to do anything that would make a difference.’
-
‘I've been inspected by the SHA, OFSTED, LINKS, CQC, HOSC, HSE. They have different requirements, which overlap, but they have different parameters. They all want information, reports, and action plans, which contradict each other.’
-
-
11. ‘Big tent problem-solving’; the need to get many people to agree:
-
‘I think I'm creative at finding innovative solutions. But implementing anything new takes massive amounts of energy, and you are ground down. You get doors closed in your face repeatedly.’
-
‘There's so much red tape. Our hands are tied. I have to get four sign-offs before I can recruit a nurse. We're not trusted to manage.’
-
-
12. The floggings will stop when morale improves:
-
‘There are no meetings where you are given credit for success. It doesn't matter what we do, it's never good enough.’
-
‘My general manager is like “the grim reaper”. No positives, all negatives. We never get any thanks or positives, even when we have made our targets.’
-
This 12-component profile was used to design a simple diagnostic with items such as, ‘I never know what's going to happen next in this job’ (unpredictable work patterns), ‘I'm always trying to meet another deadline’ (fast pace, tight deadlines) and so on. This was completed by six members of an operations management team at Clearview, who were asked to respond ‘yes’ or ‘no’ to each item on the premise that ‘yes’ to six or more items implied an extreme job. The group commented:
I answered all but one of the questions with a ‘yes’. I have tried to stick to my working hours (minus lunch) and have just seen the work pile up.
Directorate support manager
I can answer yes to all the questions. Some parts I love, but there are many days where I would like space to think. This is becoming more precious. We have made errors through firefighting, but we applaud ourselves when we go ‘phew that was a lucky escape’.
Operations manager
Answers are a mix of yes, no, and sometimes.
Operations manager
This is reasonably balanced, not exaggerated or understated. The greatest frustration in medical management is the challenge of producing change in an environment that is very resistant.
Consultant
The adrenalin rush can occur without the need to rush around. Great colleagues are even greater if you don't get so tired that you snap at them.
Discharge planning manager
There is a great deal to be said for people who manage their workload in a way that means that they work their hours (plus some extra when necessary). They shouldn't feel bad about working their contracted hours.
Deputy operations manager
This pilot suggested that the concept of an extreme job profile for health-care management had face validity, judging by the first four responses, and that jobs vary in substance and over time on those dimensions. Some feel that extreme jobs should not be necessary. This diagnostic became the ‘job characteristics’ section of the survey. Responses to the 12 items are shown in Table 23.
| Item | % agree |
|---|---|
| I never know what's going to happen next in this job | 54 |
| I'm always trying to meet another deadline | 81 |
| My management responsibilities just seem to keep expanding | 68 |
| I am constantly expected to respond instantly | 77 |
| I am responsible for showing less experienced staff how to perform effectively | 78 |
| I frequently arrive earlier and/or leave later than my contract requires | 83 |
| I make decisions that directly affect the lives of patients | 76 |
| My priorities change every week | 58 |
| I am expected to improve the service we provide despite resources being cut | 93 |
| A lot of my time is spent responding to requests for information, reports and action plans | 76 |
| I have to get large numbers of people to agree even to make small changes | 66 |
| It doesn't matter what I do, it is never good enough | 32 |
With one exception, agreement with the items was high, ranging from 54% (relating to unpredictability) to > 90% (doing more with less). This response pattern suggests that the incidence of extreme jobs (as defined by these items) in health-care management is widespread. Only around 30% agreed with the last item, a result inconsistent with focus group comments. Either those comments were misinterpreted, or this item was badly worded; an item reading ‘it is never good enough for senior management’ may have produced different results.
As expected, those with high extreme jobs scores also indicated higher stress levels and poorer work–life balance. Interestingly, the positive relationship between having an extreme job and being under stress was stronger in men, despite the fact that women were more stressed generally. There was no relationship between extreme jobs and commitment, the latter being more closely associated with influence, recognition and ‘buzz’.
Hewlett and Luce167 found that ‘extreme jobbers’ were attracted by the challenge, enjoyed the work and felt fulfilled by it. Asked, ‘why do you do it?’, they mentioned adrenaline rush, great colleagues, good pay, power and status and recognition for achievement. Those items were added to our survey design and responses are summarised in Table 24. We know that health-care managers are motivated by the challenge and the ‘buzz’ that make extreme jobs attractive. We also know that working with colleagues in high-performing teams is another key motivator. However, less than half thought that they were well paid, and recognition, power and status appear not to be experienced by around two-thirds of this sample. Other evidence shows that health-care managers are also motivated by making a difference, driving change and innovation, doing a good job and developing others. The health-care variant of the extreme job profile proposed here may thus be accompanied by a health care-specific motivational profile relying at least in part on professional and public sector values and purpose, which may offset or buffer or compensate for the negative aspects of extreme jobs.
| Item | % agree |
|---|---|
| I get a ‘buzz’ from the stimulation and challenge in my job | 71 |
| In my job I get to work with high-calibre colleagues | 68 |
| I am well paid for what I do | 48 |
| I get recognition for my achievements in this job | 40 |
| I enjoy the power and status that I have in my role | 36 |
The subtitle of the article by Hewlett and Luce is ‘the dangerous allure of the 70-hour workweek’. High-performing ‘adrenaline junkies’, in particular, appear to enjoy this kind of work,168 so where is the danger? Multitasking for long hours across complex roles can lead to fatigue, burnout and mistakes. 169 In such circumstances, family life may also be adversely affected. In a health-care context, patient safety and care quality could potentially be compromised. In addition, working constantly at this pace may not be sustainable. 170 Only one-third of survey respondents said that they were able to maintain a satisfactory work–life balance. But an improved work–life balance could create a climate that is not challenging enough for the ‘A players’, who then become more difficult to recruit and retain.
A varied, intense, fast-paced role with responsibility and long hours can be rewarding. The fact that such jobs can be attractive, however, could be a problem. The original research found extreme jobs among high-earning professionals. This study suggests that some middle and senior managers in acute health care may also have jobs that are extreme, in terms of the profile suggested here. Most hospital managers are ‘hybrids’, covering managerial and clinical responsibilities. If the management component of their roles has become more extreme, this may affect the time and energy that they devote to patients, could increase the potential for errors and may also discourage clinical staff from taking on such jobs in the first place. In addition, some of the extreme health-care job dimensions are potentially demotivating: competing priorities, having to do more with less, the burden of regulation, bureaucratic barriers, a climate of negativity. The assumption that all extreme jobs are exhilarating and motivating is misleading; some are exhausting and frustrating.
There are substantial research traditions with regard to ‘heavy work investment’ topics such as long hours, work intensification and ‘workaholism’. However, research into extreme jobs has been limited, perhaps because of the non-academic source of this concept. A literature search identified only two other studies,171,172 which found that longer hours were associated with higher satisfaction, better career prospects and higher salary, but with higher levels of stress, more psychosomatic symptoms, lower family satisfaction and poorer emotional health.
Developing resilience
This suggests that survival in an extreme job requires a degree of mental toughness and personal resilience, in addition to an ability to manage stress. Discussing senior executive roles in the NHS, Sergeant173 observes that, although there are numerous leadership development programmes available, ‘it is much more difficult to teach the political skills, attitude, resilience and the robustness required to survive in a high pressure environment’ (p. 13). Defining individual resilience in terms of ‘rebounding despite adversity or change’ (p. 3), Lewis et al. 174 review research in this area, and explore a range of strategies, tools and resources for developing individual, team and organisational resilience. The US Army, with around 1.1 million members, and thus similar in size to the NHS, has developed a Comprehensive Soldier Fitness (CSF) programme, the aim of which is ‘to increase psychological strength and positive performance and to reduce the incidence of maladaptive responses’ (p. 4). 175 The subtitle of this reference is ‘building resilience in a challenging institutional context’, and the potential relevance of this approach in health-care settings should thus not be dismissed. Another aim of the CSF is to instil post-traumatic growth, with ‘universal resilience training’. The experience of adversity is thus a potential source of meaning and personal growth, and post-traumatic stress does not become a problem. The authors of this programme suggest that, although relevant to US Army members, resilience training may be relevant to other large institutions.
The design of work is not static. Individual-level alternatives to extreme jobs may be found in ‘job crafting’, which involves proactive adjustments to activities, time and work intensity,176 and in ‘i-deals’,177 in which individuals negotiate their own idiosyncratic terms with an employer. Work can also be redesigned at a group level, to calibrate the efforts of those who wish to limit their hours in an extreme jobs culture. 178 This study did not aim to explore the nature and consequences of either job crafting or i-deals. However, aspects of both of these perspectives were apparent in the information provided by some respondents, and are discussed here briefly for the purposes of illustration. Given the potential impact of extreme jobs on individual and organisational effectiveness, and on quality and safety of patient care, this is an area where further research would be valuable.
To illustrate the nature of job crafting, Table 25 summarises the dimensions of the role of one modern matron in one of the trusts participating in this study (trust not named to preserve anonymity). In practice, these dimensions are closely inter-related and are separated here for analytical purposes. This profile is based on an extended interview during which this matron described how the role reflected her professional training and personal preferences, as well as the formal job description. This is a senior nurse hybrid role, which in this case included five areas of clinical responsibility and 20 leadership, organisational and managerial areas, indicating where the emphasis of this role lay.
| Clinical roles | Nursing: work clinically twice a week, check patient needs and moods |
| Clinical problem-solving: problem patients, falls, concerns | |
| Customer relations: working with and reassuring relatives | |
| Liaison: with PALS, acting on issues where appropriate | |
| Change agent – service improvement: infection control, patient experience | |
| Leadership roles | Head nurse cover: head nurse is monitor, controller, co-ordinator |
| Leader: on the shop floor, ‘living, breathing’, hands-on but detached | |
| Change agent – process innovation: ward efficiency, lean, developing ideas | |
| Role model: for less experienced nurses | |
| Enforcer: dress code, infection control regulations | |
| Organisational roles | Linking pin: shop floor to top team, share good practice |
| Team player: work with ward sisters – partners not disempowered | |
| Fixer: explore nursing issues and provide support and resources | |
| Complaints handler: resolve issues from patients, relatives, doctors | |
| Management roles | Operations manager: oversee three wards (100 beds), monitor patient flow |
| Performance manager: weekly reviews and budget meetings | |
| Safety manager: safe ward staffing, infection control | |
| Quality manager: ‘saving lives’ audit tool, achieve quality standards | |
| Training and development manager: develop staff, customer care for nurses | |
| Support roles | Supervisor: giving voice to health-care assistants |
| Morale officer: enthusing, motivating, valuing, praising staff | |
| Thermometer: walk the floor at 0700, speak to all patients and staff | |
| Supportive ear: matron's clinic twice weekly – anyone can raise anything | |
| Coach and mentor: for junior nurses | |
| Human shield: buffer against senior management criticisms |
This is someone who is deeply committed to nursing and to the role of modern matron, who enjoys her work thoroughly and who is enthusiastic about sharing her views and experiences with others. Describing her approach to her role, she said:
How often do I work a thirty-seven and a half-hour week? Never. I've got a good directorate manager who in the end kicks me out. But I normally work from seven till five or six, most days. And I don't have to work that. It's just, I feel, if I'm not in early I don't see my night staff, and I like to be there for them. And I need to know that each of my shifts is OK, is fine. So my time management could be better.
OK, I'm a ‘feely’ person. And you have to feel it. If you don't feel it, we don't want you in this directorate. If you don't feel that pain, if you don't feel that upset – and I'm really passionate – I walk on my wards and I want . . . boom, boom, boom . . . and they understand that, and at seven in the morning, bless them, they are saying, ‘C, we don't need your boom, boom, boom’. But I do; I want boom, boom, boom . . . it's a blue sky out there. And I know that everybody's not like that. And I don't expect it of other people. But I also don't want someone to . . . which some of the new nurses feel . . . that we should feel grateful that they are here, that they are on a five-day stretch and they haven't had a day off yet, yeah, and – chopped liver. Nurses get paid a good salary now. We're a bit like farmers; we'll always cry poverty. But if we're paying good salaries we need something back. We need them to have a bit of ownership, accountability, responsibility.
Given the hours, the scope of responsibility and the multitasking, this can be described as an extreme job. However, those properties of the role have either been chosen or emphasised by this individual. Not everyone holding a modern matron position will wish to carry out – to craft – this role in this manner. To explore those variations, a senior clinical nurse (modern matron) at one of the other five trusts participating in this project was asked to compare this profile with her own role. For the purposes of this discussion, her response had two main components. First, this profile was recognisable, being broadly similar to her own role. Second, she observed that her role was different in a small number of significant ways. She devoted less time to direct patient-facing clinical activities (she did not work clinical shifts), she did not spend time socialising with patients and getting to know them or their backgrounds and she did not work extended hours. Her summary comments were:
I found this very stressful, and wonder, is this person an adrenaline junkie? She is very caring, but I would question her need to be at work six days a week, twelve hours a day. It feels like she is holding onto a runaway horse by the mane rather than trying to tether and train it. The NHS is hard, and life on the wards is hard, but she is taking all the responsibility. We have staff like her at this trust, too, and their wards fail when they are away. That is not good management. Sorry to be critical. She is obviously working her socks off but there is an easier way.
It is significant that this second matron was critical of the approach of the first, as well as pointing out differences in the way they had each crafted their respective roles.
A matron's role is flexible and senior enough to allow for this degree of individual job crafting. Clearly this is not possible in all roles, but is likely to be the case for many hybrids. Not noted in this discussion is the way in which a matron's role overlaps considerably with that of a ward sister, whose profile will share many of the characteristics shown in Table 25. Many if not all of the non-clinical dimensions of a matron's role also overlap with those of an operations or a general manager. Job crafting may address individual motives and preferences while creating role overlaps and potential confusion. Finally, the second matron's criticisms reflect earlier discussion concerning the desirability of and necessity for extreme jobs. This appears to be an under-researched area.
Conclusions and implications: releasing time to manage
There's no time for extra projects and that sort of thing, which is a shame. So you're just doing your day job, there's no time . . . you don't get a chance on any working parties for progression and that sort of thing. I don't think we do enough forward planning. Because we haven't got the time to do that. While you recognise that, yes, this is a firefighting type of job, and it is reactive as opposed to proactive, I'm sure, well, in fact I know, that if we had more time to plan, we would do things differently, and a bit more efficiently.
Operations manager, Clearview
The combined weight of evidence from past research and from this project suggests that middle managers play key roles in maintaining operations, mediating between the front line and top team, developing innovative service improvements and helping both to shape and to implement strategy. Further evidence concerning middle management contributions is explored in the following chapter. Middle managers appear to be deeply committed to the service and its patients, and highly motivated to make a difference. The motivational profile includes hygiene factors but is dominated by themes that would be cost neutral to strengthen, such as teamwork, recognition and autonomy. However, the evidence also portrays a group that is facing increasing workloads, decreasing resources, tighter regulation and more onerous performance expectations. Although having the ideas, this group lacks not only the resources but also the authority, senior management support and the time to develop them.
One initiative that has seen widespread application in acute trusts is ‘the Productive Ward’, an initiative designed by the NHS Institute for Innovation and Improvement. The aim of this initiative, with regard to nursing staff, concerns ‘releasing time to care’. It would therefore be useful to consider ways of ‘releasing time to manage’. Asked in focus group discussions to identify steps to achieve this, middle managers offered the following suggestions:
-
What can I do?
-
walk the floor, talk to people, don't be driven by e-mails
-
make time for reflection, create space where problems or issues can ‘sit’, for example on a whiteboard in an office – people can visit and offer thoughts and suggestions.
-
-
What can we do at directorate level?
-
ensure that staff are prepared in advance for performance review meetings; rehearse
-
rapid improvement events, step back, time out to reflect on what we are doing
-
release time at the mid-levels, ‘office days’, fewer and shorter meetings.
-
-
What corporate actions would help?
-
clinical director and directorate manager make a powerful team – develop this potential
-
give managers timely and understandable financial information
-
empower ward sisters to manage their wards effectively
-
we have potential at all levels that we need to tap into
-
make it safe to challenge; the attitude, ‘I'm only a porter’, needs to be replaced.
-
These suggestions are offered here for three reasons. First, they demonstrate that the constraints on middle managers are widely recognised. Second, they indicate that there are many, simple, practical steps that could begin to address this issue. Third, they serve to introduce the concept of an ‘enabling environment’ – a supportive context for management work – and this concept is explored in more detail in Chapter 4.
The NHS has a motivated and committed middle management population. Given the motivational profile, most of the actions necessary to sustain and to strengthen motivation and commitment are cost neutral. Middle managers are a key source of new ideas and innovations for service improvement and development. The workload, time and other organisational constraints under which they operate stifle their ability to implement those ideas. The middle management population is thus in danger of becoming an underutilised, misused, wasted and potentially wasting asset.
Research priorities
Management capacity
This analysis of the realities of middle management indicates two research priorities. One concerns the question of management capacity, which was discussed in Chapter 2. The expectations and demands placed on middle managers in the acute sector – pure plays and hybrids – have increased, and in the context of current health-care policies those expectations and demands are likely to continue to increase. Were the traditional acute trust model to come under more pressure, triggering a wave of mergers, takeovers and accompanying service reconfigurations,179 and if the regulatory regime were to become stricter and more invasive,180 middle managers would once again be in the front line of responding to those challenges – in addition to the existing management agenda. During this project, as indicated previously, the managerial resources available to acute trusts were themselves being reorganised, streamlined and reduced. This was increasing the managerial responsibilities of hybrids, many of whom had little or limited managerial experience or education.
Urgent research questions thus include:
-
How should management capacity be understood, defined and assessed?
-
How can an acute trust determine whether or not management capacity is adequate in relation to the agenda that it faces?
-
How can management capacity be sustained and strengthened in the context of long-term financial and regulatory pressures?
Extreme jobs
The concept of extreme health-care management jobs has face validity and has a degree of support from the qualitative and survey evidence generated by this project. The motivational profile that accompanies extreme jobs in acute settings also seems to have distinct properties. Extreme jobs may not be problematic. Many high performers enjoy the pace and challenge and are attracted by the intrinsic and extrinsic rewards that such roles can provide. But the long hours that extreme jobs entail have predictable consequences for stress and work–life balance, and can reduce individual performance and increase the incidence of mistakes. In particular, for a hybrid who combines managerial and clinical responsibilities, the negative implications of an extreme job could potentially jeopardise patient safety as well as personal well-being. These observations are speculative, extrapolating from the preliminary conclusions of this project, and are not stated here as firm claims. However, given what we know about other trends affecting middle managers, a further speculation is that some extreme jobs are likely to become even more extreme.
Urgent research (and practical management) questions thus include:
-
Is there a distinct ‘extreme jobs’ pattern among middle (and senior) managers in health care in general, and in the acute sector in particular, with an accompanying motivational profile?
-
How widespread is this pattern among pure plays and hybrids, and how does the balance of advantages and drawbacks influence individual and unit performance?
-
If the incidence and consequences of extreme jobs are on balance problematic, how can such roles be redesigned (job crafting and i-deals) so that they are less extreme, or are ‘positively extreme’, and what additional supports can be provided for those in extreme jobs, and for hybrids in particular?
Chapter 6 Managing change following extreme events
‘Making change happen is challenging when people do not have any sense of having been part of the problem’
(Chief executive, acute trust)
What's the problem?
Managing serious incidents
What are we good at?
The hospital investigates thoroughly. It is good at identifying incidents, and beginning investigations quickly.
Assistant director, Burnside
If the issue is clinical, and confined to a specific area, we handle it well. We had a ‘never event’ recently, where a nasogastric tube was inserted incorrectly into a patient's lung, and this wasn't picked up on the x-ray. This incident led to a complete change in process, and we've sorted this now to the extent that the probability of this happening again is very low.
General manager, South Netley
Rigorous analysis – all staff are trained in root cause analysis techniques; excellent systems and templates to ask the correct questions and a team approach to problem solving. And no blame; people can learn without the fear of being blamed. However this does not suggest that people are not held to account.
Operations manager, Clearview
What are we not good at?
Good at finding out what happened, but slippage then follows. The hospital needs to learn how to manage the long tail of the process.
Medical director, Burnside
We're not effective at cascading the learning. Investigations are handled at a high level, and things don't always get back to the front line. Matrons and ward managers are involved in the incident, but the root cause analysis is ‘lifted out’ of their area. Someone will come and say, ‘we need a statement from you’. Nursing staff feel terrible about this because they're made to feel guilty, and the process isn't explained to them.
General manager, South Netley
We are less good at follow-up action. We are great at putting out the fire. I don't think that we are as good at finding out what caused the fire – we are great at producing an action plan that says what the issues are and what we are going to do, but we are less good at keeping hold of it, not letting it drop off the agenda.
Assistant director, Clearview
Serious untoward incidents and ‘never events’ are typically followed by an investigation to establish root causes and to recommend actions to prevent further incidents. However, receptiveness to change cannot be guaranteed, and recommendations are often ignored. One example of such failure to change concerns the death of 17-month-old Peter Connelly in 2007. 181,182 Previously, in 2000, 8-year-old Victoria Climbié had been killed by her guardians in the same London borough, Haringey, where Peter lived. In a 400-page report with 108 recommendations, the public inquiry (chaired by Lord Laming) into Victoria's death had previously blamed systemic failures among the agencies responsible for monitoring vulnerable children: the local authority, social services, the NHS, the police. 183 In 2008, Laming noted that many child protection agencies had ignored his recommendations,184 saying that, ‘I despair about the organisations that have not put in place the recommendations which I judged to be little more than good basic practice’. Inquiry recommendations typically establish ‘defensive’ change agendas, aimed at preventing particular behaviours and events. Defensive agendas are less interesting and more challenging to implement than progressive agendas, which focus on making things happen. 185
Terminology surrounding events such as these is varied: accident, adverse event, catastrophe, crisis, critical event, deviance, disaster, error, failure, misconduct, mistake, near miss, never event, non-conformity, sentinel event, serious incident, violation. For the purposes of this report, we will use the term ‘extreme event’ as the category label. We will consider four extreme events. Case selection criteria included management recommendations and access to staff and documentation. Interviews were based on a topic guide (see Appendix 2) and, despite the sensitive nature of these issues, participants welcomed the opportunity to discuss their experiences with a researcher.
Donaldson21 distinguishes between passive learning (identifying lessons) and active learning (implementing changes). The interview quotes opening this chapter indicate strengths in the former and weaknesses in the latter. Given our limited understanding of the factors that impede ‘active learning’, this study sought to understand:
-
the conditions that respectively enable and constrain the diffusion, implementation and embedding of changes following extreme events
-
the support, tools, frameworks and guidelines that would strengthen change management capability in such contexts.
The main conclusions from this chapter are that:
-
Extreme events proceed through broadly comparable phases. The weight of research and commentary lies with the pre-crisis, event and crisis management phases. The post-crisis phase – implementing change – has attracted less attention.
-
Following an incident, three inter-related issues become significant: causality (why did this happen?), agenda (organisational learning and recommendations for change) and process (change implementation).
-
The causality of extreme events is usually complex, involving the combination and interaction of numerous factors, at different levels of analysis, over time. There is a need for multilevel, sociotechnical explanations of extreme events, leading to multilevel systemic agendas for organisational change.
-
The context for change following an extreme event can be described as a ‘wicked situation’, dealing with several inter-related contributory factors, in the absence of stakeholder consensus, and in which the ‘rules’ of participative change management no longer apply.
-
The effective management of sustainable post-event change involves the development of context-sensitive approaches that address systemic organisational issues, with a progressive agenda, engaging staff involved and addressing conflicting perspectives.
-
In addition to evaluating complementary methods of incident investigation, research should seek to evaluate applications of high-reliability organisation concepts in acute care settings.
The management of extreme events
Figures published yesterday by the National Patient Safety Agency show that more than 5,000 patients died or were seriously injured as a result of NHS safety incidents in the six months to March 2011. A total of 1,313 people in England and 78 in Wales died as a result of medical errors involving the care they received from hospitals, mental health trusts and ambulance services. A further 3,699 patients in England suffered ‘severe harm’ – permanent harm, including disability and scarring.
NHS Confederation press summaries, 14 September 2011; www.nhs.confed.org
Following a number of ‘high-profile’ service failures, patient safety has become a national priority. 99 From 2003, a voluntary reporting scheme, the National Reporting and Learning System (NRLS), operated by the National Patient Safety Agency (NPSA) has been in place. This invited health-care organisations to report serious untoward incidents. Serious untoward incidents are events likely to cause significant harm to patients, members of the public or staff and that could also cause disruption to the service and damage the reputation of the organisation and/or its employees. ‘Never events’ (25 are designated) are a category of serious incidents that should not occur if preventative measures are in place (e.g. wrong site surgery, misidentification of patient). In April 2010, reporting became mandatory. The increase in the number of incidents submitted to the NRLS between 2003 and 2010 can be explained by the growing percentage of health-care providers submitting monthly reports (1% in 2004; 81% in 2009); around one million incidents are now reported annually. In 2009, although most incidents caused no harm, 3735 were reported to have caused death (NPSA Quarterly Data Workbook: www.nrls.npsa.nhs.uk/resources). Walshe and Higgins186 date the increase in inquiries into major service failures from the Ely Hospital scandal in 1967. Recent events at Mid Staffs have also been subject to several investigations. 70
Some of these serious untoward incidents lead to compensation claims. Established in 1995, the NHS Litigation Authority (NHSLA) handles claims against the NHS, administering the Clinical Negligence Scheme for Trusts (CNST) and managing non-clinical claims and the ‘liabilities to third parties’ scheme. Table 26 shows the numbers of claims received since 2004 and the payments made against them. 187
| Year | CNST claims received | Payments on clinical claims (£000s) | Payments on non-clinical claims (£000s) |
|---|---|---|---|
| 2004–5 | 5609 | 329,412 | 25,119 |
| 2005–6 | 5697 | 384,390 | 31,278 |
| 2006–7 | 5426 | 424,351 | 33,883 |
| 2007–8 | 5470 | 456,301 | 27,715 |
| 2008–9 | 6088 | 614,342 | 37,890 |
| 2009–10 | 6652 | 650,973 | 40,376 |
| 2010–11 | 8655 | 729,100 | 42,400 |
The total cost of claims was almost £800M in 2010–11, more than double the cost in 2004–5. By 2012, a typical settlement for a catastrophic injury claim was £6M. The NHLSA attributed these rising costs to the ‘no win no fee’ market whereby claimants can litigate with no financial risk, and to lawyers and agencies ‘farming’ complaints against NHS organisations. 188
Serious incidents and never events harm patients, disrupt services, damage organisational reputations and individual careers and can generate heavy costs. There is now a substantial body of work in this area, triggered by the landmark publication by the US Institute of Medicine, To Err is Human,189 which estimated the annual cost of health-care errors (in the USA) to be between $17B and $29B. That literature is rich in terms of guidelines, diagnostics, protocols, checklists and alerts. The main problem, however, appears to lie not with guidance, but with implementation.
Much is already known about the causes and management of extreme events. Crisis management research has mirrored the stages of the event sequence narrative. This typically begins with the ‘incubation period’190 and associated ‘resident pathogens’,191 followed by a focus on risk management and emergency planning. 192,193 There is practical crisis management advice,194 along with accounts of individual events: the Mann Gulch disaster;195 the loss of the Challenger space shuttle;196 Snook's account of a fatal friendly fire incident;197 Perrow's studies of ‘normal accidents’. 198 Inquiry reports can be seen as proxy research data. 199,200 The development and application of safety cultures,201 ‘resilience engineering’202 and ‘high-reliability organisation’203 have been advocated as ways to reduce the incidence and impact of extreme events.
The dominant perspective in the post-event period views what happens to inquiry recommendations in terms of organisational learning. 204 A number of commentators have noted the absence of a change management perspective,40,205 and this is the lens – focusing on the design and implementation of a change agenda – through which the extreme events summarised in this chapter are viewed.
Root cause analysis (RCA) is the main approach to health-care incident investigation. RCA tends to focus on immediate and well-understood causes, and can overlook wider systemic, contextual and temporal factors. Carroll199 explores the logics driving incident review teams in nuclear power and chemical processing settings, concluding that RCA leads to ‘root cause seduction’, by which he means a reassuring preference for simple and rapid solutions, potentially overlooking the less obvious and more challenging systemic roots of failures. Leveson206 argues that ‘the emphasis in accident analysis needs to shift from “cause” (which has a limiting, blame orientation) to understanding accidents in terms of reasons, i.e., why the events and errors occurred’ (p. 241). Although based on research in other sectors, the advice of these commentators appears useful in examining the reasons behind and the aftermath of the health-care incidents discussed later in this chapter.
Current approaches to accident modelling also rely on systems-theoretical perspectives,207,208 rather than ‘domino’ and ‘Swiss cheese’ models. Rasmussen209,210 observes that, although incidents may be caused by loss of control of work processes, other factors are involved in safety control. Figure 4 depicts what Rasmussen209 calls ‘the problem space’ (p. 185), identifying the multiple layers of control that are often implicated in accident causation, the disciplines associated with their respective study and ‘environmental stressors’ such as changing political climate, public expectations, financial pressures, changes in education and competencies and the pace of technological change.
FIGURE 4.
The problem space: sociotechnical system risk management hierarchy. Based on Rasmussen, 1997. 209
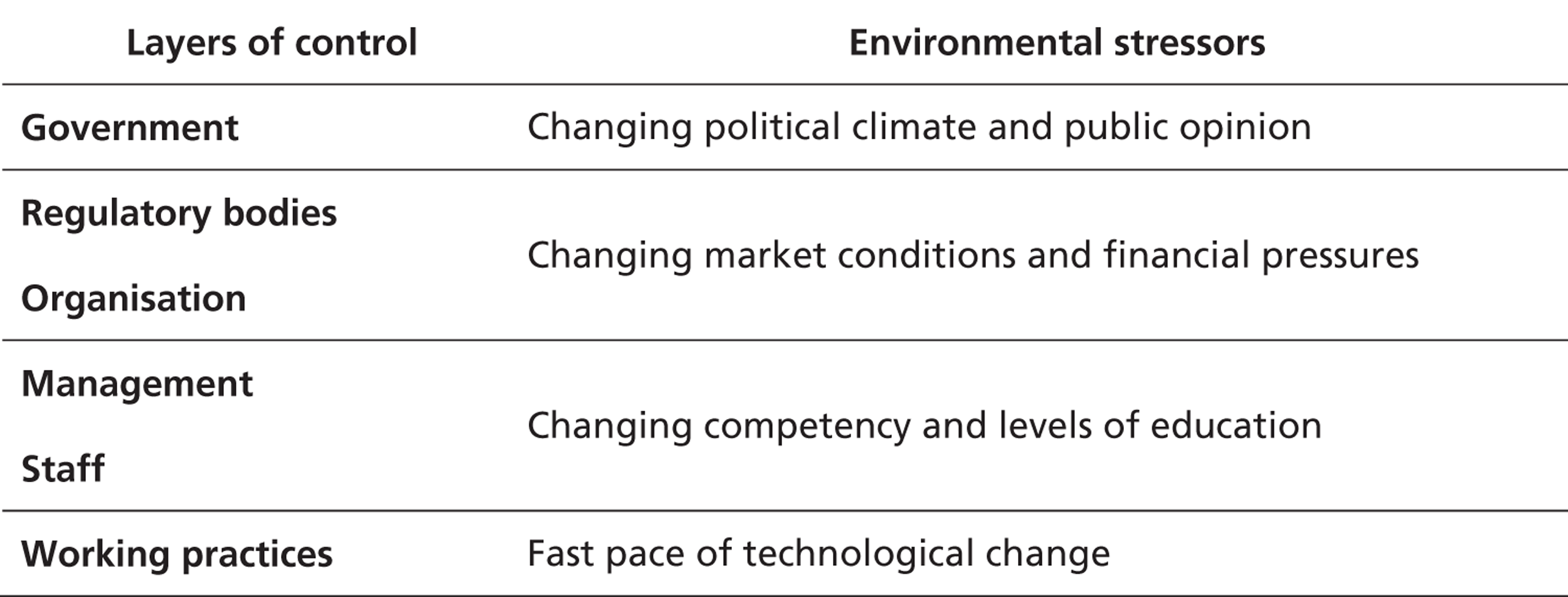
This generic model seems to be relevant to UK health care, particularly with regard to system layers and environmental stressors. An accident scenario can be represented by an ‘accimap’ showing how events and conditions interact, revealing the pattern of antecedents, causality and consequences. Figure 5 shows an accimap for the case of Mrs Mayland (discussed later). Although difficult to read in this format, this illustrates the complex causality behind this patient's death, and the links between different layers of analysis over time. Although this patient died from a prescribing error, the accimap also captures the roles of regulatory bodies, organisation and management, infrastructure and processes and procedures. Rasmussen209 argues that such incidents ‘have not been caused by a coincidence of independent failures and human errors, but by a systemic migration of organisational behaviour toward accident under the influence of pressure toward cost-effectiveness in an aggressive, competitive environment’ (p. 189). Individual decision-makers don't see ‘the complete picture’ and are not able to judge the state of defences, which depend on decisions taken by others elsewhere.
FIGURE 5.
Accimap of the Mrs Mayland incident. BNF, British National Formulary; CT, computed tomography; GCSF, granulocyte colony-stimulating factor.
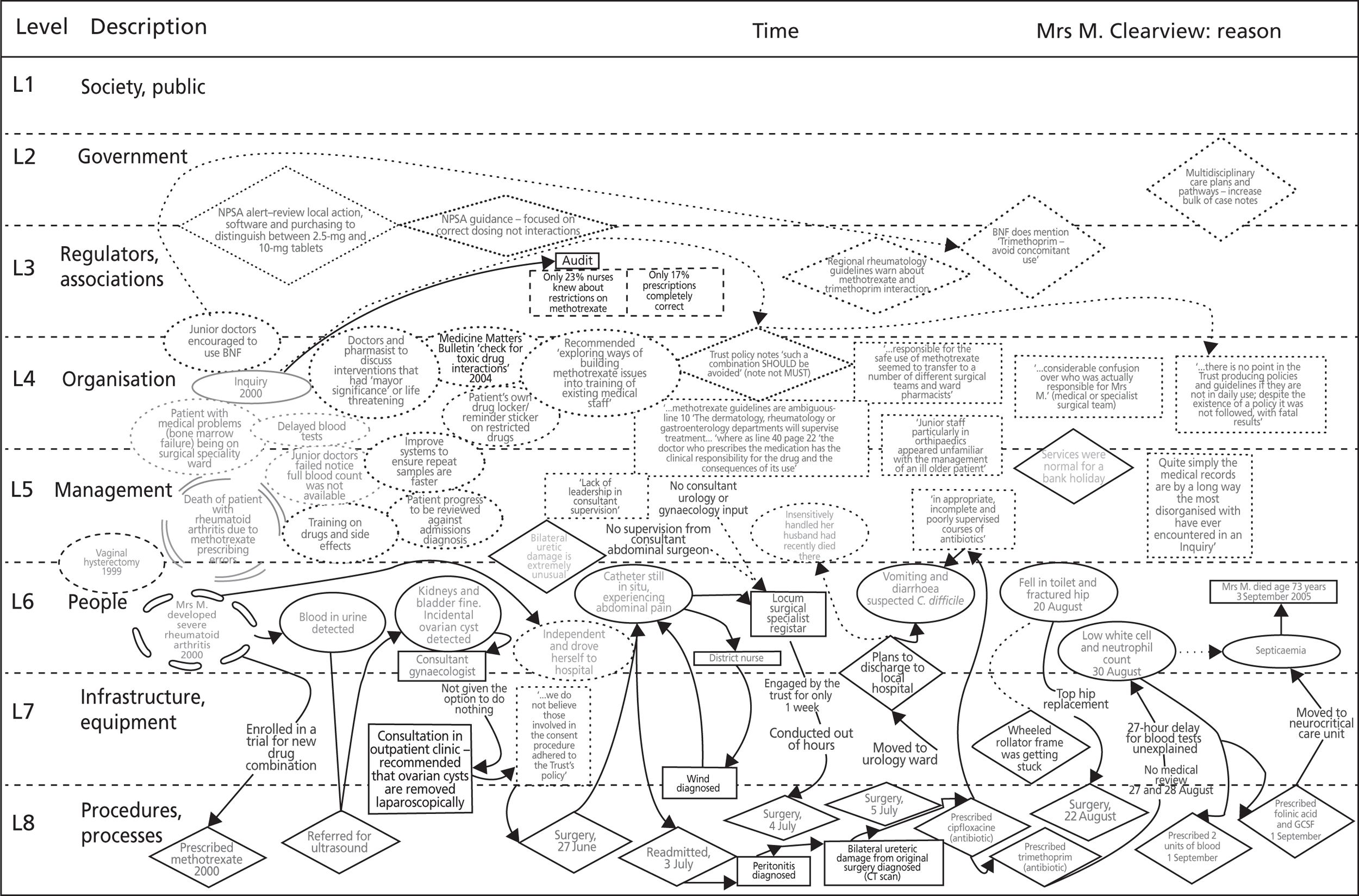
The systemic nature of serious incidents in health care is reflected in ‘the London protocol’, which identifies the hierarchy of factors influencing clinical practice: institutional context, organisation and management factors, work environment, team factors, individual (staff) factors, task factors and patient characteristics. 211,212 Although this protocol underpins RCA training, the process and outcomes of investigations based on this approach do not always reflect a systems perspective.
Nicolini et al. 213,214 identify barriers to learning from RCA investigations. Investigations are conducted by staff who were not involved in the incident and who continue with their full-time roles. Interrogating witnesses, collating and analysing evidence and drafting recommendations can be a complex and protracted process. Outcomes are often influenced by time constraints and lack of expertise. Tensions are generated by the need to make service improvements in the face of limited resources, competing priorities and conflicting views. They found that investigation reports often focused on local clinical practices and context, and they also note that ‘many potential root causes were discounted in the analytical process, often based upon the assumption that such latent factors were not easily resolved or because the complexity and ambiguity of the issue would not allow it to be resolved with a single, clearly containable countermeasure’ (p. 37). 213 Patterns and trends in incidents were rarely considered and the investigation report was often seen as an end in itself. The need to produce an acceptable plan focused attention on available solutions and minor improvements, rather than on organisational changes with substantial resource implications. This study concluded that risk managers and investigation teams lacked ‘a coherent orientation towards managing change’ (p. 39), for which the typical strategy meant designating a clinician responsible for the action plan, and checking progress some months later. Implementation issues such as facilitating change, addressing resistance and linking to other initiatives were rarely considered.
The four incidents that follow illustrate many of these issues, confirming aspects of the nature of investigation processes and reinforcing the barriers identified by Nicolini et al. This analysis also points to ways in which RCA methods could be complemented by other tools and perspectives, to increase the probability of effective and more rapid changes flowing from such events.
Clostridium difficile at Burnside
In contrast to the incidents that follow, the way in which Burnside managed a serious outbreak of C. difficile was a success. This incident was explored, at the chief executive's suggestion, to explain that success. The resultant approach is termed a ‘maintenance model’, because the actions necessary to prevent a recurrence of a crisis such as this are quite different in nature and timescale from those actions that were required to contain the crisis in the first instance. In other words, the maintenance phase of the event sequence, after the immediate crisis was over, was as important as the initial crisis management and emergency response. How did this incident arise? The factors contributing to the outbreak are summarised in Table 27, which, although not following precisely the model in Figure 4, illustrates the multilayered nature of the problem.
| Factor | Nature | Implications |
|---|---|---|
| Environment | C. difficile strains vary by location | Local variation in infection |
| Government targets | Focus attention on monitored activities | |
| Technical | Development of broad-spectrum antibiotics | Reduce health risks by prescribing bacterial infection control drugs – no need for targeted prescriptions |
| Low-grade paper towels | Increased possibility of antibiotic-resistant microbials | |
| Inconvenient location of basins | Ineffective hand washing | |
| Organisational | Functional silos | Incidence of C. difficile not communicated |
| Weak reporting lines of infection control team | No corporate awareness of C. difficile rates | |
| Poor governance structures | Low awareness and poor auditing of responses | |
| Managerial | No monitoring or communication of HCAIs | No ownership of HCAI issues |
| No comparison with other hospitals | ||
| Limited resource for infection control team – HCAIs given low priority | ||
| Processes | Unco-ordinated patient movement and infected patients not isolated | Increased potential for cross-infection |
| Limited patient screening | Risk of cross-infection | |
| Liberal use of broad-spectrum antibiotics | Lack of awareness of carriers | |
| Inappropriate dress code | Development of antibiotic resistance | |
| Variable hand-washing regime | Impede effective hand washing |
Table 28 extends that pre-crisis context, identifying the subsequent main phases in the event sequence narrative for this incident, and tracking the impact on C. difficile infection rates.
| Phase | Key features | C. difficile rate |
|---|---|---|
| Pre-crisis | Problem understood but tolerated | 20–30 cases a month |
| No sense of crisis | Perceived normal | |
| Limited action – isolation unit opened 2007 | Increases to 47: November 2006 | |
| Crisis | Rated one of the worst hospitals in England | ‘Bloody hell we're in the bottom ten’: June 2007 |
| SHA ‘support team’ offer advice | ||
| Emergency response | CEO signals top priority | Rate reduced to 15 cases a month: August 2007 |
| Powerful turnaround team established | ||
| Prescribing policy changed | ||
| Additional resources and facilities | ||
| Corporate reporting for infection control | ||
| Maintenance | Team continues to meet | ‘Spectacular improvement’: June 2008; consistently 0–5 cases a month: October 2009– |
| New procedures, screening programme | ||
| New facilities, improved environment | ||
| Staff training, dress code | ||
| Patient tracking software developed | ||
| Creative change agenda | ||
| SHA visits in 2008 note improvements |
During the pre-crisis ‘incubation period’ the infection rate of up to 30 a month was perceived as ‘normal’ and, although this was a known problem, this did not trigger any special action. This changed when, in June 2007, national tables identified Burnside as having one of the worst C. difficile infection rates in England; as one staff member noted, ‘bloody hell we're in the bottom ten’. This observation did then trigger a rapid emergency response, the details of which are shown in Table 29. The hospital's success appeared to be due to the impact of a combination of actions managed as an evolving programme, constituting a ‘package deal’, in contrast with traditional ‘stepwise’ change implementation guidelines. This six main components of this ‘package’ included:
-
A turnaround team: a cross-departmental clinical and managerial group with authority to act without further permission from senior managers.
-
Appraise and prioritise: rapid decisions on immediate actions, delayed action on more difficult and sensitive issues.
-
Emergency response: quick demonstration that the problem was understood and was being addressed; autocratic, ‘no questions – no negotiations’ style; ‘political fix’ to reassure external stakeholders as well as ‘real fixes’ to resolve the problem.
-
Systemic solution: systemic problems need systemic solutions, including individual, team, organisational, financial, infrastructural and other factors; in addition to many changes in working practice, communications were frequent, authoritative and appealed to professional values rather than external targets.
-
Measure and report progress: infection rates were monitored and published; all staff were made constantly aware of performance on key metrics; continuing success motivated staff to maintain the trajectory.
-
Plan for continuity: crisis over, is the turnaround team redundant? No; the team continues to work, maintain focus on the agenda, maintain and improve reduction in infection rates – the shift from emergency response to maintenance phase was critical to success.
The number of new cases fell below 15 a month in August 2007, and by the end of 2009 the rate was between zero and five new cases a month; that rate has been maintained since (Figure 6).
FIGURE 6.
Clostridium difficile infection rates at Burnside, December 2005–September 2011.
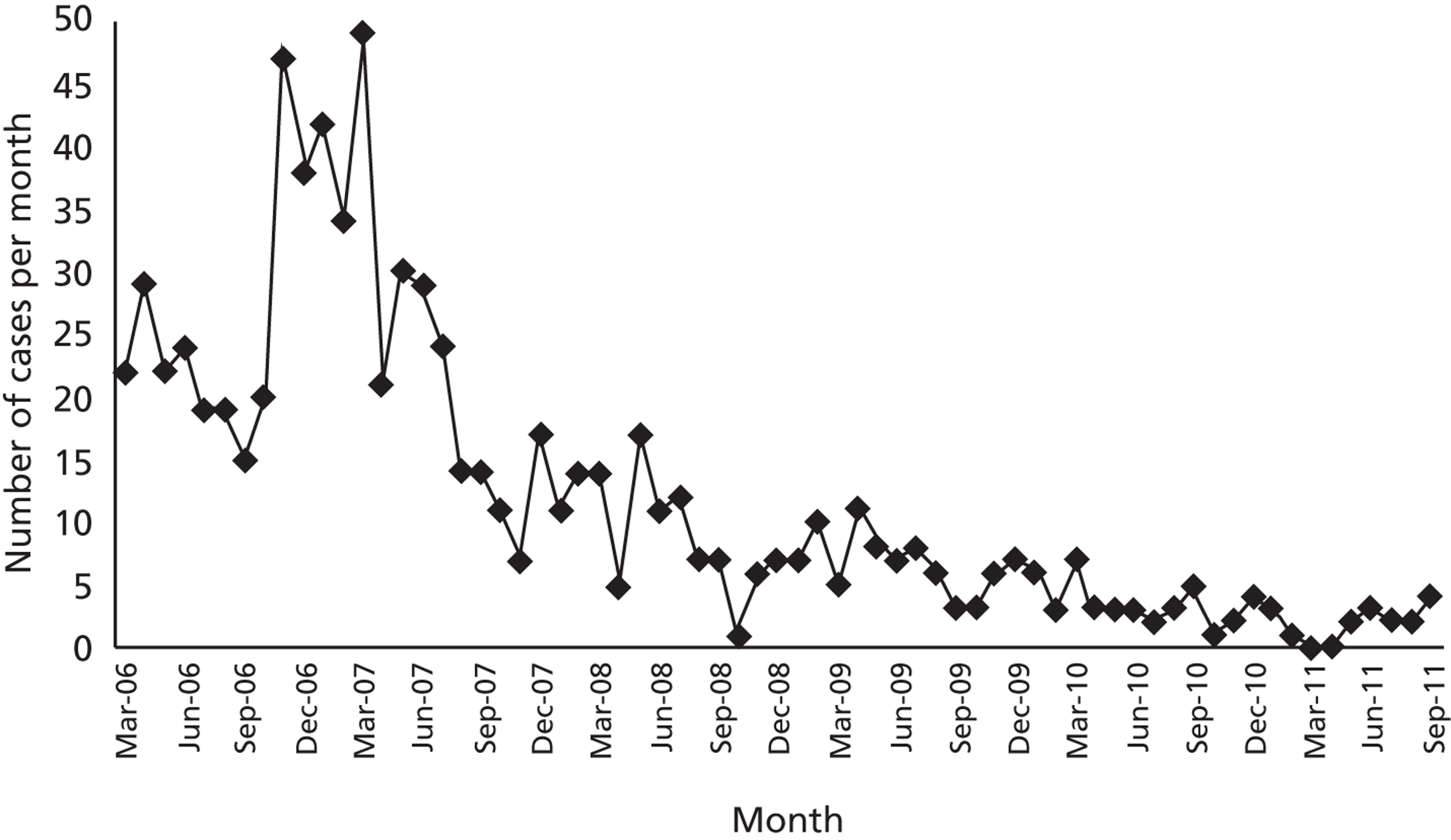
What works in one setting will not always work elsewhere. However, this analysis suggests that changes can be implemented rapidly through a combination of compelling evidence, autocratic management (where appropriate), a powerful cross-functional management team and innovative communications that encourage behaviour change by addressing beliefs and values rather than focusing on externally imposed targets. This combination of actions, including a constantly changing change agenda (to combat the ‘infection control fatigue’ identified by an infection control nurse), accompanied by attention to sustainability was successful both in the short term and in the long run. This was not a ‘quick fix’ approach to crisis management. The Burnside ‘maintenance model’ is consistent with the systems approach outlined above, and offers a practical framework that could be adapted by other provider organisations faced with similar difficulties.
| Factor | Actions | Consequences |
|---|---|---|
| Environment | Similar incident had occurred in a nearby hospital | Management aware of wider problem and implications |
| National league tables show comparatively poor performance | Seriousness of problem exposed – seen as ‘at crisis level’ | |
| SHA sends team to investigate and support | Guidance, support, legitimacy for radical actions and investment | |
| Financial | Immediate additional funding | New isolation unit |
| Increased recurring budget | More resource for infection control | |
| Isolation bays in wards | ||
| Increased space between beds | ||
| Technical | Upgrade hand towels | Improved hand hygiene |
| Upgrade hand-washing facilities | Increased rates of hand washing | |
| Organisational | Create C. difficile turnaround team | Integrated cross-functional working-focused activities |
| Change reporting lines for infection control to director of nursing and chief executive | Direct access to executive management group and board | |
| Double the size of infection control team | Highlight importance of HCAIs | |
| Create and staff dedicated C. difficile isolation unit | Skilled staff caring for patients; patients segregated to reduce cross-infections | |
| Managerial | Chief executive and board ‘own’ HCAI rates | Collective hospital-wide ownership of HCAIs |
| Communication appeals to personal and professional values | Significance of HCAIs widely understood | |
| Challenge behaviours (e.g. hand hygiene); confront resistance to change (e.g. prescribing practices) | Commitment to change | |
| Process | Amend dress code | All lead to reduced cross-infection |
| Training increased | ||
| Develop manual of practice | ||
| Daily ward rounds by infection control nurse and pharmacy staff | ||
| Routine patient screening | ||
| Individual | Choice of autocratic change agent | Direction and energy |
Mrs Mayland
The incident involved the death of a patient . . . a catalogue of errors, but the final element that caused her death was being prescribed two drugs that interact with each other, and the results weren't picked up quickly enough and then acted upon. She died just over a week after the drugs were administered. A catalogue of errors up to that point with people not knowing who's in charge and not being clear. But as with all of the most serious untoward incidents, there was a sort of an opportunity, almost up until the last few hours when it could have been turned around.
Associate director, Clearview
Mrs Mayland attended Clearview for a hysterectomy in 1999 – which will be taken as the starting point for this incident timeline. In 2000, she developed severe rheumatoid arthritis and was enrolled in a trial for a new treatment regime that included methotrexate, a ‘high-risk’ drug. In 2000, another arthritic patient at Clearview died as a result of a methotrexate prescribing error. The inquiry noted that this was a medical patient on a surgical specialty ward, blood tests had been delayed and junior doctors did not notice that a full blood count test result was not available. An audit found that only 23% of nurses knew about restrictions on the use of methotrexate, and only 17% of prescriptions were completely accurate. Training and drugs policy were to be revised.
While Mrs Mayland was taking part in the trial, blood was detected in her urine, and an ultrasound scan detected a large ovarian cyst. In spite of her arthritis, she drove herself to Clearview for elective surgery on 26 June 2005. She never left the hospital alive. She was referred to a consultant gynaecologist who removed the cyst laparosopically. Shortly after that procedure she suffered abdominal pain and failure to pass urine. Bilateral ureteric damage from the surgery was identified and corrected. She was then to be discharged to another hospital, which caused distress as her husband had recently died there, so she remained at Clearview. The subsequent inquiry suggested that she should have been given the option to return home, and one interviewee noted that, at this point, ‘she nearly escaped us’. However, she contracted a C. difficile infection from which her recovery was slow. She was then given a faulty rollator (a wheeled walking frame) and fell and fractured her hip; a total hip replacement had to be performed. For this procedure she received the antibiotic trimethoprim, which interacted with the methotrexate. Her blood count began to show a low white cell and neutrophil count. Clinical and nursing records show delays in conducting blood tests and lack of attention to her deteriorating condition. Mrs Mayland died on 3 September 2005. The incident timeline ran for 11 years, from 1999 to 2010, when a final review of the original inquiry recommendations was conducted.
The post-event segment of the incident timeline lasted for 5 years and is summarised in Table 30. This incident had a profound effect on the trust. It led to the establishment of a Patient Safety Executive and the development of a Patient Safety Unit reporting to the trust quality committee, a ‘safety first’ programme with a new patient safety strategy and a more proactive approach to safety issues with Clinical Area Safety Assessments (CASAs) of clinical processes. Patient safety became an important board agenda item, along with patient stories. One of the roles of the Patient Safety Unit was to pursue recommendations that had not been fully resolved.
| Date | Event |
|---|---|
| 3 September 2005 | Mrs Mayland dies, age 73 years – causes of death included septicaemia and bone marrow failure due to the interaction of methotrexate and trimethoprim, complications arising from previous surgery and failure to act on an abnormal blood test result |
| 27 September 2005 | Assistant director of risk meets with family; seven members of inquiry panel agreed – chairperson, chief nurse, associate director pharmacy, consultant obstetrician, consultant histopathologist, non-executive director, family representative with background in health care (and advice from pharmacology professor); 30 members of staff are interviewed and statements taken |
| Immediate changes | Structured daily shift report instituted, training on medical early warning system formalised on wards, review of safe prescribing of methotrexate, role of senior clinical nurse altered to ensure greater clinical profile |
| January 2006 | New methotrexate policy and procedure |
| July 2006 | Inquiry report published – 122 pages, 46 recommendations; steering group established with acting chief executive, director of operations, director of administration, chief nurse, medical director and governance manager |
| September 2006 | Trust response to inquiry report published; steering group's remit is to oversee implementation of inquiry recommendations: report is widely disseminated to staff; recommendations allocated to four working groups: medical records and documentation, medicines management, inpatient care and requesting and reporting blood tests – other recommendations addressed by key individuals |
| March 2007 | Inquiry recommendations progress report: 30 pages |
| January 2008 | Inquiry recommendations final report: 17 pages |
| September 2010 | Inquiry recommendations final report: 21 pages |
The inquiry report in 2006 made 46 recommendations. By the end of the first quarter of 2010, 4.5 years after Mrs Mayland's death, 31 of those recommendations had been ‘completed and closed’, six were ‘completed but with remaining issues’ and nine were ‘unresolved and open’. In other words, two-thirds of the recommendations were considered to have been implemented in full, with one-third outstanding or requiring further work. What is the explanation for that ‘tail’ of issues?
Table 31 summarises the 31 recommendations ‘completed’ by September 2010. Organisational changes often generate problems, but in this instance creating a new unit, hiring more staff, streamlining processes, providing more training and nominating ‘methotrexate days’ could be regarded as ‘low hanging fruit’, and hardly likely to trigger resistance. One interpretation, therefore, is that recommendations that were simpler and quicker to implement were tackled first.
| Theme | Number of recommendations |
|---|---|
| Guidelines, policy document, information sheets, forms: revised methotrexate ALERT sheet, guidelines for inpatient management, policy on drug interactions, information sheets, prescription charts | 17 |
| Organisational changes: new elderly trauma unit with two extra consultants, new consultant microbiologist, breast surgeons removed from general surgery on-call rota, revised pharmacy system for urgent requests, medicines management formalised in nursing handover, improved nursing leadership on one ward, more frequent collection system for urgent blood tests, Monday and Tuesday are designated ‘methotrexate days’ | 8 |
| Patient monitoring systems: identifying and monitoring methotrexate patients | 3 |
| Training: dealing with abnormal blood test results and ALERT and ALS for junior doctors | 2 |
| IT: new computer system indicating location of drugs not held centrally | 1 |
| Total | 31 |
Do the recommendations that had not been implemented fully display any common properties? The six items identified as ‘completed but with issues’ were:
-
despite review, the content and structure of medical records were still unsatisfactory
-
despite development of new nursing care plans, new forms and plans that were ‘outside the agreed process’ were being added to notes
-
the ALERT (acute life-threatening events recognition and treatment) sheet had been revised and, although this was in use for 90% of patients, only 10% of these were completed accurately
-
despite the introduction of standardised patient observation charts, there were many different charts in use across the trust, with some areas using an electronic system
-
procedures for requesting repeat test samples had been defined but results were not recorded appropriately, and many results were not recorded in the medical records at all
-
the management of deteriorating patients was part of the medical early warning system (MEWS) with which the trust was 85% compliant, but care of deteriorating patients on general wards was still a cause for concern.
These items appear to concern the reluctance of staff to abandon the old variety of systems, procedures and working practices in favour of new standardised processes.
There were a further nine items – one-fifth of the recommendations – still ‘open’ at the time of the review in 2010, summarised in Table 32. With the exception of the ward pharmacists' issue, the ‘open’ items concern the non-compliance of clinical (mainly medical) staff with new systems, procedures and other working practices, and with what appear to be attempts to standardise procedures in the interests of consistency and predictability.
| Recommendation | Status |
|---|---|
| Review consultant gynaecologists' operations | High standard of care but no database to record outcomes and complications; unresolved |
| Improve cross-referral between specialities | Not implemented, ‘work to be done’ to improve quality and consistency of handovers |
| Families should be offered choice on discharge | Disagreement regarding discharge location dealt with in case conference; ‘the perfect discharge’ not in place |
| Those ordering tests should ensure that a fail-safe mechanism is in place for reviewing results | Revised procedure introduced but not being used, handover of clinical information ‘remains a concern’ and ‘medical records are often of a poor quality’ |
| Better medical handover at nights, weekends and bank holidays | New guidelines in medicine division but handover takes a different form with different IT support in each area |
| Communicate abnormal blood results directly to doctor in charge | Revised procedure introduced but not fully used, with only one-quarter of results recorded in abnormal results book |
| Ensure that posts are training posts and not ‘clinical fellow’ posts | Still a mixture of training and non-training posts, and difficulties recruiting and retaining medical staff |
| Regular ward rounds and cover for surgical patients with complex conditions | Medicine directorate guidance on ward rounds in place, guidance on complex care under development; increase in number of consultant-led ward rounds, but impact is indeterminate because of inadequate note keeping |
| Review ward pharmacist role to focus more on clinical activity | Teamwork supporting inexperienced staff, but ward pharmacists still have non-clinical duties and do not work a 7-day week |
The progress pattern can thus be explained as follows:
-
issues resolved: ‘easy to implement’ changes such as revised guidelines
-
issues partially resolved: staff using old systems and practices rather than switching to new
-
issues unresolved: medical staff reluctant to adopt standardised procedures.
There had been considerable progress. The management of patients on methotrexate and multidisciplinary teamworking had been improved, and education packages for doctors in training had been revised. Nevertheless, in 2010, prescribing errors were being reported at a rate of 150 a month, and between January 2005 and May 2012 the trust logged 210 incidents (none serious) specifically involving methotrexate, with some of those incidents also involving trimethoprim. At around £10M for a trust-wide system, the cost of electronic prescribing was prohibitive. The 2010 review noted that, although one feature of Mrs Mayland's case was failure to act on a blood test result, ‘resolving abnormal results has been far more challenging than originally anticipated and recent incidents identify that this remains a significant issue’. It thus appears that the ‘completed with issues’ and ‘open’ recommendations concerned actions that had been mandated, but not managed – managed in the sense of establishing the benefits to staff, gaining agreement and commitment, involving those affected in implementation, tackling resistance, regularly monitoring progress and preventing or inhibiting the use of the previous systems and practices that were being replaced. In sum, an ‘orientation towards managing change’ seems to have been absent in this instance. 213
Mr Torrens
Mr Torrens came to the emergency department at Clearview late in the evening of 30 December 2010 having taken an overdose of co-codamol tablets earlier in the day. A young man, with a long history of depression and anxiety attacks, he had attempted suicide in 2005 with an overdose of paracetamol, and had stopped taking antidepressants 2 months before this latest incident. He was admitted to the Clinical Decisions Unit (CDU). He was co-operative during his initial assessment, based on a ‘prompt for mental health/suicidal patients’ form, which informs clinical judgement but does not provide a risk score. Mr Torrens also said that, although he had left a suicide note, this was an impulsive act which he now regretted. By 0530 the following morning he was considered to be medically stable and was referred for psychiatric assessment. This assessment did not take place. The on-call psychiatrist was working at another hospital and his car broke down at 0800. He decided to hand Mr Torrens over to the liaison psychiatry nurse who was due to arrive in the CDU at 0900.
Mr Torrens tried twice to leave the CDU. On the first attempt the nurse in charge took him back to bed and the on-call emergency department doctor noted in the medical record that security should be called if he attempted to leave again. On his second attempt, security was not called. At 0905 the ward housekeeper noticed that Mr Torrens was not on the ward and informed the nurse in charge who initiated a missing persons search. Attempts were made to contact Mr Torrens by mobile telephone, his parents were advised that he was missing and security and police were informed. However, at 0915, Mr Torrens was struck by a train on the railway line close to the hospital and died from his injuries. The liaison psychiatry nurse had arrived at 0910; she was able to access Mr Torrens' detailed mental health records from a ward terminal, which acute trust staff were unable to do.
The investigation into this incident identified three root causes:
-
The mental health assessment performed by emergency department staff did not assess fully the risks associated with patients liable to self-harm.
-
Training to recognise the triggers and behaviours of self-harming patients was inadequate.
-
Support for patients with mental health needs in the emergency department was insufficient.
Training for emergency department staff in recognising and managing patients with mental health issues was subsequently implemented. However, emergency departments can be busy, frenetic environments, unsuitable for patients who are agitated and suffering from mental health disorders. However, the third recommendation here was key. Clearview did not employ on-site psychiatric cover. Psychiatric support was based at another site, with support on call out of hours. Acute trust emergency department staff did not have electronic access to mental health records, and also lacked skills for dealing with mental health patients. In addition, many patients presenting in an emergency department are inebriated or have taken drugs, and mental health staff will not assess under those conditions, waiting until patients are sober and/or the drugs have cleared their system. This meant that psychiatric assessments were often delayed and patients could be moved to another unit, with staff less skilled in managing mental health patients, in order to meet the emergency department 4-hour target. These delayed assessments may have come to be seen as normal:
I think it was an accepted part of the emergency department and the CDU. I think it was probably the thinking – oh, it has always been done this way, always come here, always been accepted to keep the mental health patients, and there has always been a delay in getting them reviewed or moved to a more appropriate environment. That's how it has been.
Senior nurse, Clearview
The provision of out-of-hours psychiatric support was a long-standing concern, with studies suggesting that at least 5% of patients arriving in emergency departments have mental health problems. Acute hospital patients are coded according to medical condition and not mental state, so that figure may be inaccurate. One interviewee commented:
We have had a massive increase, with 18 per cent of people who self-harm through drugs mainly because of the climate we are living in. People are coming in losing their jobs, so mental health is definitely on the increase. And as a department, we don't really have that infrastructure. The other problem is [psychiatric support] not being on site.
Operations manager, Clearview
There had been a similar incident earlier that year, in July, when a male patient in the emergency department became increasingly agitated but his mental condition was not assessed. At nine o'clock in the evening, the patient tried to abscond, stabbed a member of staff with a pen and injured 11 others before the police arrested him (the mental health trust having refused to admit him to their unit). He was assessed the following morning at the police station and then moved to a secure mental health unit. This incident had also prompted discussion between acute and mental health trust management, but without progress.
Following this more recent incident, the management teams from the acute and mental health trusts met to explore appropriate actions. However, at the time of writing, little had been achieved:
I suppose it was the incident on New Year's Eve that was the absolute organisational wake-up call. Having said that, it has been painfully slow to do anything. I think we have a different view on mental health to the mental health trust. Things that cause us angst they do not see as an issue, and I don't think they understand why we see it as an issue sometimes. So getting an understanding of what the problems are hasn't been easy because, actually, what are problems to them are not problems to us, and vice versa.
Senior nurse, Clearview
There was a shared desire to resolve these issues, but no project lead had taken responsibility. In 2012, the mental health trust funded a new facility on the Clearview site, ‘a better environment’ where their staff could undertake assessments, but no changes were made to staff numbers or other working arrangements. One solution concerned the appointment of a mental health nurse or specialist social worker based at Clearview. From the acute trust's perspective, however, this involved covering a staff shortage for the mental health trust. It was proposed to fund a ‘pilot’ mental health nurse cover in the emergency department during twilight hours, along with a new rapid assessment model. The provision of on-site consultant psychiatric cover was considered to be more difficult to achieve.
The main impediments to further change in this case thus appear to concern:
-
two organisations with differing views on the conditions that should trigger a psychiatric assessment and the circumstances under which such an assessment should take place
-
lack of funding for additional staff and the unwillingness of one organisation to contribute to the staff costs of the other
-
mental health trust concern about triggering conflict were they to suggest evening and weekend rotas to staff
-
two organisations with different information systems and separate secure access codes.
Patients requiring psychiatric assessment continued to present in the emergency department at Clearview. In 2012, another incident similar to the case of Mr Torrens occurred, but this was still under investigation at the time of writing.
Mr Mitcham
I hate walking the floor now. I see bombs waiting to explode everywhere.
Extreme events workshop participant, Clearview
Mr Mitcham, 66 years old, came to the Clearview eye unit in October 2011 for cataract treatment involving the implant of an intraocular lens under local anaesthetic. He was the last patient having this treatment on the afternoon theatre list and he was patient number 7. However, patient number 6 arrived late and was not ready for surgery. Mr Mitcham was thus taken into the theatre by the anaesthetic practitioner as the sixth patient. The operating surgeon was not made aware of this change in running order. Believing that she was operating on patient six, she implanted in Mr Mitcham the lens for that patient, only realising the error when completing the operation note after the procedure. The consultant was informed immediately and Mr Mitcham was taken back into theatre where the incorrect lens was replaced without problem. He was discharged that day and suffered no permanent harm. The hospital serious incident management group decided that this met the criteria for a ‘never event’ and an investigation was conducted.
Why did this happen? The anaesthetic practitioner (senior nurse and team leader) had arrived in the theatre half-way through the list and had missed the team brief at the start. Although aware that patient number 6 was not ready, she did not explain the change in the running order to the other theatre staff. The operating surgeon then failed to check the patient's wristband, assuming that she had the correct patient. The surgeon addressed Mr Mitcham as patient number 6 when he arrived in theatre, but he did not correct her. It had become normal practice for operating surgeons to identify patients on the ward, at the consent stage, and not to repeat this identity check in theatre. However, patients listed for cataract surgery were placed on a generic list, which meant that the operating surgeon may not have seen a particular patient before the day of surgery, which is what happened in Mr Mitcham's case.
The investigation concluded that the root cause of the incident was a failure to follow normal checking procedures, which included the World Health Organization (WHO) theatre checklist. The surgeon was experienced but had been working at Clearview only since the beginning of that week, and this was her second full theatre list. During her induction, guidance on the use of the WHO checklist, and Clearview theatre procedures, had not been clear (hospitals apply this checklist in different ways). The first five patients on the list that afternoon were operated on without incident.
The main recommendation following this incident concerned the correct use of the WHO checklist. Induction processes in ophthalmology were reviewed and the importance of following checking and handover procedures was reinforced. As normal, to provide an impartial assessment, the incident investigation was conducted by the hospital's assistant director of risk and patient safety and a patient safety manager. They were advised by a Serious Incident Management Group, which included a consultant ophthalmologist, the ophthalmology unit leader, two operations managers, a divisional lead nurse, the head of medical staffing and the Patient Advice and Liaison Service (PALS) manager.
There had been four ‘never events’ in Clearview theatres over as many weeks in 2011: a retained clamp in a patient's neck following surgery, cardiac arrest during sight-saving surgery leading to an adverse neurological outcome, a retained ‘fish’ following abdominal surgery and the wrong implant for Mr Mitcham. Following a long period in which no such incidents had occurred, the theatre teams had a ‘high performance – high reliability’ reputation and were surprised and shocked that these events had occurred and were concerned that this should not happen again. Three members of the research team were thus invited to run a workshop in March 2012 on ‘managing change after extreme events’ for 11 members of the theatre management group. The workshop aim was to provide fresh perspectives and tools to help participants develop solutions. One of these tools concerned the development of ‘mess maps’ to help explain why these events occurred. 215
Workshop participants were asked to develop a mess map for each of the four never events, using flip charts and ‘Post-it’ notes, identifying immediate causes, along with the role of underpinning issues and contributory factors, the external context, local conditions and other reasons. 206 The mess map for Mr Mitcham is shown in Figure 7. This echoes the findings of the investigation: new surgeon, inadequate induction, poor communications, lax checking procedures. The mess map also identifies four other sets of contributory factors, not picked up by the incident investigation:
-
External pressures. The map notes the 18-week RTT target and the need for external reporting of never events, even though in this case no patient was harmed.
-
Internal pressures. The morning clinic was busy, surgeons were under pressure ‘to get a move on’, surgeons arrived late, staff missed their lunch break, surgeons had complained that afternoon lists were too long.
-
Personal preferences. Medical staff behaviour could be idiosyncratic, ‘everybody does their own thing’, the new surgeon had a different lens-matching practice, the consultant was doing paperwork at the time.
-
Smooth running. Paradoxically, this incident may have occurred in part because things were going well – Friday afternoon, experienced staff, mundane process, five cases routine, changing list order is commonplace; did a successful theatre team ‘drop their guard’ under these conditions?
FIGURE 7.
Mess map of the Mr Mitcham never event. EPR, electronic patient record.

This mess map, produced relatively quickly during a workshop by staff who were involved in the incident, appears to offer a richer explanation for the incident than the carefully researched investigation report, and reflects more closely the systems-theoretical model of incident causality explained earlier.
In the aftermath of future incidents of this kind, one option would therefore be to complement impartial RCA with a mess mapping process involving the staff concerned, to develop action plans to which those staff have themselves contributed. There was further internal support for the conclusions of this mess mapping exercise. The trust had formed a Never Events Group, to identify actions to prevent further incidents and to give staff ‘the opportunity to comment on their view of life in the theatres and any factors which might impact on their ability to deliver the highest standards of care to our patients’. This second aim was achieved through ‘listening events’ in November 2011, with 10 senior staff acting as facilitators and which involved over 100 staff, who welcomed this opportunity to share their views. The listening events report categorised the feedback as follows:
-
procedures and systems: not enough time to spend with patients
-
culture in theatre: bullying, racism, spinning out procedures to fill the time
-
communication and team interaction issues: inconsistent and contradictory messages
-
leadership: lack of engagement with staff, watching not experiencing
-
training: non-existent induction processes, people moving too quickly
-
staffing issues: lack of porters, ratio of trained to untrained staff cut to critical
-
time pressures: many issues only apparent on morning of operation, WHO checklist
-
equipment and instrumentation: no systematic review of sets, wrong instruments
-
other: incident handling criticised, safety events held at times when most cannot attend.
Despite evidence pointing to organisational conditions and system properties, the report concluded:
It should be remembered that the four never events were, to varying degrees, the result of individuals failing to follow procedures and good practice. However, if any of the factors identified in the listening events acted as contributory factors then action needs to be taken to address these issues.
Individual human failures were thus seen as the primary explanation for these never events. This conclusion makes ‘the fundamental attribution error’ of blaming individuals and overlooking the context in which they work. 216 The conclusion also overlooks the trust's own evidence concerning ‘life in the theatres’. A more comprehensive approach to understanding why this incident happened is illustrated in Table 33, which locates the combined findings from the investigation, the theatre team's mess map and the listening exercise in Rasmussen's ‘problem space’. 209
| System layer | Causal and contributory factors |
|---|---|
| Government | 18-week RTT target |
| Regulators | Need to report never events to external regulators |
| Organisation | Culture in theatre: bullying, racism, filling time |
| Busy morning clinic | |
| Non-existent induction processes, people moving too quickly | |
| Staffing, lack of porters, ratio of trained to untrained staff critical | |
| Time pressures, not enough time to spend with patients | |
| Management | Leadership, lack of engagement with staff, watching not experiencing |
| Pressure on surgeons to get a move on | |
| Surgeons complain that afternoon lists are too long | |
| Surgeon did not have adequate WHO checklist training on induction | |
| Incident handling problems, safety events run when most cannot attend | |
| Staff | Experienced staff, adequate numbers |
| Everyone has their own way of doing things | |
| Consultant doing paperwork | |
| Surgeons arrive late | |
| Anaesthetic practitioner takes patient 7 to save time | |
| Surgeon selects lens without reference to patient's notes | |
| Infrastructure and equipment | Two systems for patient notes: hard copy and electronic record |
| No systematic reviews of surgical sets, wrong instruments | |
| Processes and procedures | Failure to follow checking procedures; sign in, sign out not completed |
| WHO-advised final preoperative pause not conducted correctly | |
| Unclear guidance on theatre practice during induction | |
| Doctor sees patient independently of consultant | |
| Friday afternoon, mundane process, five cases completed without problems | |
| Changing list order is commonplace | |
| Did staff get a lunch break? | |
| Nurses do not inform doctor of changed running order | |
| Patient ID not checked when local anaesthetic given |
Although thorough induction training and verification processes are important, to reduce the future incidence of never events in theatres this analysis points to a wider change agenda, addressing organisation, management, staff, infrastructure and process issues (some of which were subsequently addressed). Viewed from a systemic perspective, it is also possible to reach beyond one incident, and consider what can be learned from incidents like this.
Managing change in wicked situations
We are good at reporting, we're good at investigating, we're good at making recommendations. But it all falls apart in the implementation. Either things don't get implemented at all, or they get implemented, and if you go back one year, two years, three years later, it's slowly tailed off, to a point where nobody quite knew why we were doing it anyway, and something else has come along.
Assistant director, Clearview
The aim of this ‘small-n’ analysis of four idiosyncratic cases is not to generalise to the population of such events, but to inform theory and practice, particularly with regard to the implementation of changes aimed at preventing or reducing the incidence and impact of such events in the future. This involves a combination of analytical refinement and naturalistic generalisation. 35,37 The former concerns developing understanding of theory, refining current assumptions and concepts, whereas the latter concerns the transference of ideas and solutions to similar contexts. (A fifth case, a norovirus outbreak at Wattle Park in which the incident definition was ambiguous, is described in Appendix 4.)
The management of extreme events concerns the linkages between an understanding of why an event happened (causality), the changes that need to be implemented to defend against a recurrence (agenda) and the implementation of those changes (process). Table 34 outlines the findings from the four events reported here with regard to those issues and to the outcomes.
| Incident | Causality | Agenda | Process | Outcomes |
|---|---|---|---|---|
| Burnside | Systemic, multilayered problem | Systemic multilayered solution | Powerful and enduring team | Change successful and sustained |
| Mayland | Systemic, multilayered problem with long timeline | 46 items for pharmacy, patient care, education and training, medical records and communication | Steering group, working groups, changes mandated but not managed | New policy, structures, processes and documentation, but working practices unchanged |
| Torrens | Inadequate patient assessment, staff training and patient support | Closer collaboration between acute and mental health trusts | Management meetings, difference of views, no project lead responsible | Unresolved, ongoing, minor changes to facilities |
| Mitcham | Theatre guidelines not followed (staff identify other issues) | Improve induction, use guidelines | None: dissemination of investigation report | Too early to judge (no further never events to date) |
Managing change in such settings is problematic. In breach of conventional change management guidelines, staff who are to be affected are excluded from contributing to the change agenda, other than as witnesses giving evidence, and the implementation process is more likely to be directive than participative. Borrowing the concept of ‘wicked problems’,217 this could be seen as managing change in ‘wicked situations’ with the properties outlined in Table 35.
| Causes | The trigger event has a complex, multilayered explanation |
| Immediate causes are combined with latent or underlying factors | |
| The event timeline reaches deep into the past and can extend long into the future | |
| Some of the basic assumptions of those involved have been challenged | |
| Stakeholders are arguing about what caused this; some do not think it is a problem | |
| Agenda | The ‘defensive’ agenda comes from the recommendations of an investigation |
| Gaps and flaws in organisation and management processes have been revealed | |
| There is an expectation of quick fixes, to ‘close’ the incident | |
| Stakeholders disagree about what changes, if any, are appropriate | |
| There is no ‘correct’ solution, and it cannot be guarantee that the changes will work | |
| Process | Change has been delayed pending the investigation |
| The urgency has gone, but other emotions linger – disbelief, anger, guilt, apathy | |
| The normal rules of change implementation do not apply | |
| Those who will implement were excluded from developing the agenda | |
| Changes to work, organisation and management practices will be resisted |
This can become a ‘super wicked situation’ if:
-
There is more than one organisation involved and their perspectives differ.
-
This was a repeat of at least one previous incident, so past solutions have not worked.
-
The media picked up the story; they are looking for a scapegoat and demanding action.
None of the events reported here attracted significant media attention. The death of Mr Torrens appears to have created a super wicked situation, given the organisational tensions involved. Drawing on the successes and problems arising in those incidents, the management of change in wicked situations may involve developing context-sensitive approaches with these properties:
-
Agenda. Go beyond quick fixes and address underlying system issues; use this as an opportunity to address long-standing organisational problems; develop a progressive change agenda, linked if necessary to a defensive one; restore the sense of urgency that accompanied the incident in the first place; receptiveness to change may not be high, and may require stimulation; establish meaningful metrics to track progress.
-
Process. Secure long-term senior management support and resourcing; structure a project team, steering group or board that can act on their decisions; engage colleagues who were excluded by the investigation process; resolve competing views of event causality and appropriate responses; address resistance to the ‘difficult’ changes to roles and working practices; design a communication strategy that will inspire as well as inform; aim to sustain changes beyond initial implementation and success.
Two environmental issues may also be important in some settings. One concerns handling the media reporting the story, who can influence the change agenda. The other, as in Mr Torrens' case, concerns managing interorganisational tensions and differences of perspective. In wicked situations such as those found here, it may therefore not be adequate, as some commentators have suggested,205,213 simply to provide risk management personnel with development in change management capabilities, or to have change management specialists on investigation teams. Investigation processes are currently driven by specially formed, impartial groups, using prescribed templates, aiming to produce a ‘quality report’, including practical recommendations, within a set timescale. What may also be helpful, instead of or perhaps in parallel with that formal approach, is a process driven by the staff involved in an incident, using relatively simple and flexible ‘mess mapping’ and other appropriate tools, to identify immediate and systemic changes that will have a sustainable impact.
Serious incidents, never events and other types of accident and failure can be regarded as inevitable features of complex systems. Appropriate responses to this observation thus include constant scanning for warning signs, developing flexible, context-sensitive working practices and helping those involved to deal with ambiguity and to make decisions that are often based on unclear and evolving information. Is it possible to organise in ways that allow problems to be anticipated and caught before they become crises, and to develop systems for containment as well as for effective responses? These are the goals of researchers and commentators advocating high-reliability organisation characteristics. 203,218
Given the complex, systemic, organisation-wide antecedents of these kinds of incidents, it is perhaps not surprising that it has already been suggested that high-reliability concepts can be adapted to health-care contexts. 219 Originally based on studies of aircraft carriers and nuclear power installations, the qualities of high-reliability organisations include mindful preoccupation with failure, reluctance to simplify interpretations, sensitivity to operations, commitment to resilience and deference to expertise. Expertise often resides with front-line staff who are close to the flow of events, and more senior staff must be prepared, when appropriate, to relinquish command. Developing a high-reliability approach requires a sustained organisation-wide programme, rather than managed fixes following specific incidents. With the priority attached to improving the quality and safety of patient care while reducing costs, the systematic tailoring and evaluation of high-reliability methods in acute health-care settings would constitute a valuable research agenda.
Chapter 7 Management contributions
Introduction
The focus of my role lies with clinical and managerial strategy and service business plans. The aim is to clarify thinking for the future. I work closely with the medical staff, to bring another set of skills. A lot of my work is commissioned in the corridor. Every service has to develop a formal vision and strategy, with investment objectives. They are my customers, and I help them to develop these plans. With new developments, I ask them, ‘what's the story?’. Often it's about bringing people into the room, exploring their positions, and reconciling these. With one of our services, it took a year to get a consensual story; there were big issues on which different people had different views. So this is a mediating and facilitating role. Sometimes this even involves ‘proximity talks’ when relationships are poor. I'm a quiet spoken pushy bastard. One consultant calls me ‘the spin doctor’. I'm good with words, reframing, convincing. I like getting results. It doesn't always work.
Assistant director, Clearview
This study sought to develop a profile of middle management contributions and to understand:
-
how management work affects clinical and organisational outcomes
-
factors impeding management contributions to performance
-
how an ‘enabling environment’ for management work can be assembled and sustained.
This chapter first reviews past research concerning middle management contributions in general and in health care, before exploring the combined evidence from this project. The main conclusions are:
-
Previous research shows middle managers in general contributing to organisation strategy and performance, through mediating, boundary spanning, innovating, championing, influencing and change implementation roles. Past research offers a similar account of middle managers in health care, with human resource, operational and performance management practices being linked to improved patient outcomes and organisational performance.
-
From this study, the profile of middle management contributions includes maintaining day-to-day performance, firefighting, ensuring a focus on the patient experience, identifying and ‘selling’ new ideas, translating ideas into working initiatives, process and pathway redesign, facilitating change, troubleshooting, leveraging targets to improve performance, developing infrastructure, developing others and managing external partnerships.
-
Past research indicates that supportive cultures combine flexible roles and structures, freedom to innovate, resources and senior management support. Conditions that constrain middle managers include systems and policies that encourage conservative behaviour, complex approval cycles, micromanagement, lack of autonomy and unclear direction from the top.
-
The components of an ‘enabling environment’ for management work include top team communications, business intelligence, cutting non-value-adding activity, autonomy to innovate, organisation structures, organisational norms, performance management, interprofessional work, support services, personal development, teamwork and resources; investment in information systems, management development and additional resources can be costly, but action to improve the enabling environment under other headings is cost neutral.
-
Evidence from this study also indicates that encouraging co-management – shared leadership of change – by clinical and managerial staff working collaboratively could have major benefits for clinical and organisational outcomes. Several other low-cost, low-risk, high-impact suggestions for building an enabling environment were generated. At a time of rising demand and diminishing resources, it is not clear why these were not more common in practice.
The strategic middle manager
Managers make a huge contribution to patient care, developing services, measuring quality. One of the key things that I find myself doing is drawing ideas together and implementing them. I go to all the clinical meetings, and I'm heavily involved. I also attend consultants' meetings. I act as a linchpin. If I'm not there, the discussion and outcomes can become more fragmented.
General manager, South Netley
Middle managers at large
There is research evidence to support the negative stereotype of middle managers, regardless of sector. National political and media commentary during this project also pictured health-care managers whose main contributions to the service included bureaucracy and overheads (see Chapter 3). From an analysis of the interventions of 90 middle managers in the decision processes of their firms, Guth and MacMillan220 concluded that those who felt that their self-interest was compromised could sabotage, delay or damage the implementation of strategic initiatives. Meyer221 showed how middle managers subverted a merger process that was not in their interests. Emphasising the role of personal goals, Sillince and Mueller222 note that middle managers reframe directives and ‘talk down’ expectations when strategy is seen to be failing, and when they are likely to be blamed.
However, the weight of research indicates that these findings do not generalise to the management population as a whole, and evidence from this project indicates that the negative portrayal of middle managers in health care is inaccurate. Bower223 was one of the first to recognise the importance of middle managers as change agents, with upwards influence on strategy based on knowledge of the organisational context, nurturing, testing and championing initiatives and contributing flexibility by deviating from formal expectations. From her study of 165 middle managers, Kanter224 concluded that ‘a company's productivity depends to a great degree on how innovative its middle managers are’ (p. 95). Context, however, is important. Kanter found innovation flourishing in companies in which territories overlapped, with frequent cross-functional contact, free flows of information and excess in budgets, and in which many managers had loosely defined roles and assignments (‘solve problems’). Multiple reporting relationships and overlapping territories, Kanter argues, encourage managers to develop their own ideas and sell them to their peers.
Middle managers' contributions to innovation and change are widely recognised, partly because of the work of Wooldridge and Floyd225 who argued that middle management involvement in shaping strategy led to better decisions, higher degrees of consensus, improved implementation and better organisational performance. They developed a typology of middle management contributions to strategy: (1) gathering and synthesising information, (2) justifying and championing alternatives, (3) facilitating organisational adaptability (relaxing rules, ‘buying time’) and (4) translating goals into action and selling initiatives to staff. 12,29,226 They also emphasise the co-ordinating, mediating, interpreting and negotiating roles of middle managers, arguing that it is difficult to isolate an individual's role because it is the pattern of strategic influence of middle managers that affects performance. The ‘boundary spanners’ are more influential, and senior managers wishing middle managers to be more innovative are advised to consider ‘putting more managers into regular contact with the environment’ (p. 482). 226 Research continues to emphasise middle managers' roles in shaping, mediating and implementing strategic change. 58,227 Boyett and Currie228 report how middle managers in an Irish telecommunications firm designed an alternative strategy that was more profitable than the one that senior management had intended. Mair229 also argues that middle managers can influence organisational performance through the way in which strategy is enacted. She found that superior unit performance in a financial services firm was associated with middle managers whose actions were aligned with corporate strategy. She also found that middle managers with many role moves performed better than those who stayed put (experiencing no new challenges).
Managers may not always be free to exercise these strategic roles. Kuratko and Goldsby230 identify conditions that discourage ‘the entrepreneurial middle manager’ from taking risks and innovating:
-
systems and policies that encourage consistent, safe, conservative behaviour
-
complex approval cycles with elaborate documentation
-
controls that encourage micromanagement
-
top-down management and lack of delegated authority.
Middle managers combine access to top management with knowledge of operational capabilities. Wooldridge et al. 30 conclude that a middle management perspective is valuable, partly due to that mediating role, and as a counter to the ‘upper echelons’ view of strategic choice. They also note that ‘complex geographically dispersed organisations cannot be managed by single actors or even small groups but require distributed and interactive leadership throughout the organisation, with middle managers as important mediators between levels and units’ (p. 1191). Balogun231 argues that, even when middle managers are ‘change recipients’, the way in which directives are interpreted and implemented may differ from (and improve on) senior management intentions.
Middle managers in health care
Previous research has found middle managers playing similar strategic roles in health care. The impact of management practices on patient outcomes is illustrated by West et al. 23 Their survey of 61 English hospitals found that mortality rates following emergency and elective surgery were significantly lower in hospitals with human resource practices concerning staff appraisal, training and teamwork. This relationship was stronger when the human resource director was a full voting member of the hospital management board. Suspicious of those results, medical staff asked how management practices could affect patient mortality. The researchers' response232 was:
Our answer is simple, though it may seem strange to those who deal with individuals rather than organisations. If you have HR practices that focus on effort and skill; develop people's skills; encourage co-operation, collaboration, innovation and synergy in teams for most, if not all, employees, the whole system functions and performs better. If the receptionists, porters, ancillary staff, secretaries, nurses, managers and, yes, the doctors are working effectively, the system as a whole will function effectively.
p. 3522
A study in the Health Service Journal found that trusts rated ‘weak’ on service quality in 2009 had increased middle management numbers by only 5% between 2004 and 2008; trusts rated ‘excellent’, in contrast, had increased management numbers by 46%. 233 This implies that ‘weak’ trusts were undermanaged and that cutting management could adversely affect service quality. From their survey of 50 senior NHS managers, Hutton and Callow234 observe that the service is slow to adopt new ideas because of rigid structures, poor communication channels, inadequate decision processes and lack of knowledge management skills. Even when a new approach is agreed, implementation can be poor, and managerial intervention, they argue, is essential to drive innovation to improve quality, productivity and safety.
Management practices in general, and human resource practices in particular, affect individual, team and organisational performance. ‘High-performance’ human resource practices affect work design, training and development, performance appraisal, teamwork, involvement, autonomy, and leadership style, with the aim of improving skill, motivation and commitment and thus performance outcomes. 235,236 Dorgan et al. 25 developed an assessment covering three sets of practices: operational management, performance and targets management and talent management. First applied to manufacturing and retail organisations,237 this was used to compare management practices in 1200 acute hospitals in seven countries, including 184 hospitals in the UK. Hospitals were given a ‘management score’ (1 = ‘weak’, 5 = ‘strong’) that could then be compared with performance measures.
To score ‘5’ for talent management, hospitals have to operate systems for managing high and poor performers, training and development, recruitment and retention. A top score for operations management is based on layout and patient flows, pathway management, standardisation of clinical processes and protocols and effective use of staff. The top score for performance management considers how process improvements are addressed, how quality indicators are used for performance tracking, conduct of performance reviews and consequences when agreed plans are not enacted. Five sets of factors were found to influence management practice scores:
-
competition: hospitals facing more competition had higher scores than those facing little or none
-
skills: hospitals with clinically qualified senior managers had higher scores, presumably because those managers were better able to communicate with clinical staff (the UK had the lowest proportion of clinical managers, 56%, compared with 93% in Sweden)
-
autonomy: hospitals that gave managers higher levels of autonomy scored more highly
-
scale: larger hospitals had higher management scores than smaller units
-
ownership: private hospitals scored more highly than public hospitals.
Careful not to claim causality, the researchers suggest that these findings confirm that management really does contribute to patient well-being – a claim supported by the observation25 that, in the UK, a 1-point increase in management practice score was associated with:
-
a 6.5% reduction in death rates for emergency patients with heart attacks (30-day risk-adjusted acute myocardial infarction mortality rate)
-
a 33% increase in income per bed
-
a 20% increase in probability that a hospital is above average for patient satisfaction.
From their analysis of NHS staff survey data from 2006 to 2009, West et al. 238 conclude that management practices that offer a positive experience for staff lead to positive outcomes for staff and patients, influencing patient satisfaction, mortality, infection rates, absenteeism and turnover (NHS staff are absent, on average, 10.7 days a year, costing £1.75B). Factors that increase engagement include good management and leadership, a safe work environment, meaningful roles, support for personal development and involvement in decision-making. Echoing the previous study by West et al.,239 one predictor of patient mortality rates was the percentage of staff working in well-structured teams with clear objectives, meeting regularly to review and improve performance.
The notion that health-care managers contribute only to red tape and costs appears to be inaccurate. Middle managers mediate between the front line and the top team, shaping and championing innovations, influencing others to support change and implementing service improvements. ‘High-performance’ practices are associated with staff engagement, patient satisfaction, mortality rates and other positive clinical outcomes. One study even showed that trusts that had achieved better service quality ratings had increased management numbers.
Evidence from this study
This section first explores the pressures and demands on middle management and then considers contributions to clinical and organisational outcomes.
Pressures and demands
Drawing on survey evidence, Chapter 5 explored the pressures and demands facing middle managers. A similar picture emerged from content analysis of set-up interviews, reflecting the ‘multiloaded’ nature of the management agenda and the ways in which middle management roles are changing. These pressures are revisited in brief here. The pattern of themes was broadly similar across all six trusts, except for local issues such as the merger at Wattle Park, relocation at South Netley and serious incidents at Netherby. The main pressures and demands on middle management included:
-
finance: pressure to cut costs, an increasingly complex funding model
-
workload: increasing, no headspace, need broad shoulders and thick skin
-
regulation: burdensome bureaucracy, daily pressure to meet targets
-
systems: dated IT system, inadequate information, fighting with systems that do not work
-
external relations: overcoming boundaries, acute and primary care not ‘joined up’
-
change: no resources to implement new ideas, change is extremely slow
-
staffing: staff shortages and recruitment problems, insecurity, fatigue
-
other: public expectations, taking patients seriously, learning from serious incidents.
Rising public expectations, increasing workloads, financial challenges, burdensome regulation (external and internal), staffing problems, poor information systems, the difficulties of implementing change, and relationships with external agencies such as commissioning bodies were common themes. Once ‘contributions’ have been explored, we will turn to participants' suggestions with regard to dealing with those pressures and to developing an enabling environment for management work.
Management contributions
This study focused on middle management contributions to clinical outcomes and to organisational performance in general. These contributions are multifaceted, and evidence has been drawn together from several sources, formal and informal, including access meetings with senior hospital staff, interviews, focus groups and feedback from participants during project update and briefing meetings. Table 36 summarises the contributions profile developed from that evidence.
| Contribution | Explanation |
|---|---|
| Maintaining day-to-day performance | Keeping the show on the road, risk assessment, staffing/workforce/human resource management issues, oversight of links with other headings |
| Firefighting | Listening, problem spotting, rapid response |
| Patient experience focus | Ensuring that patients' voices are heard when business decisions are being made |
| Identifying and ‘selling’ | Spotting, designing and implementing service improvement initiatives, persuading others, working across internal boundaries |
| Translating ideas into working initiatives | Shaping ideas from colleagues and external sources |
| Process and pathway redesign | Lean methods, productive ward initiatives |
| Facilitating change | Taking risks, working with clinicians, running rapid improvement events |
| Troubleshooting | Dealing with underperforming areas, finding and delivering cost savings, solving ‘wicked problems’ |
| Leveraging targets to improve performance | Dashboards, benchmarking |
| Developing infrastructure | IT, equipment, physical facilities |
| Developing others | Skills development, ‘getting people on board’, picking up devolved human resource issues |
| Managing external partnerships | Working with local authorities, police, PCTs |
This profile was initially derived from content analysis of set-up interviews in which respondents were asked to cite ‘examples that illustrate the role that middle managers have played in this trust to improve clinical outcomes and quality of care’. This was one question in a 1-hour interview schedule and response patterns varied. Most participants cited a small number of recent examples with which they were familiar. Table 35 is thus based on aggregated responses, producing a stereotypical profile. Although portraying middle management contributions in general, this profile will clearly not be consistent with the activities of any one individual or group, and patterns of contributions will vary over time and with setting and circumstances.
To explain how this profile was constructed, Table 37 provides a selective summary of the content analysis of responses of 17 managers at Netherby (four board members, seven hybrids and six managers) who generated 34 examples of management contributions in five categories. Table 38 summarises the analysis of responses from 13 managers at Greenhill (two board members, five hybrids and six managers) who generated 21 examples in four categories.
| Contribution | Item count | Illustrative quotes |
|---|---|---|
| Process redesign | 13 | ‘lean methods in pathology to take waste out of the system and save time’ |
| ‘process mapping to become more effective with less resources’ | ||
| ‘new heart centre with redesigned process, reduced waiting time and patient visits and increased capacity’ | ||
| Developing infrastructure | 9 | ‘making sure all doctors and nurses have wireless LAN access’ |
| ‘middle management implemented our digital X-ray system’ | ||
| ‘facilities worked with oncology to install the new linac machine’a | ||
| Translating and implementing ideas | 5 | ‘managers saw business opportunity for new ophthalmology treatments and developed proposals to enable clinical staff to realise this’ |
| ‘managers contribute to solving clinical governance problems’ | ||
| ‘managers make the business case for funding’ | ||
| Developing others | 4 | ‘deliver nurse practice development’ |
| ‘training in standard work practices’ | ||
| ‘training all staff in blood handling across the patient pathway’ | ||
| Leveraging targets to improve performance | 3 | ‘management benchmarking against other trusts has led to new working practices and governance arrangements’ |
| ‘targets for infection control have sharply reduced MRSA and C. diff’ |
| Contribution | Item count | Illustrative quotes |
|---|---|---|
| Facilitating change | 14 | ‘running corporate rapid improvement events, get whole departments involved in reengineering’ |
| ‘importing new ideas from outside and piloting’ | ||
| ‘working with clinicians to implement changes’ | ||
| Process redesign | 5 | ‘process redesign of emergency patient pathway’ |
| ‘implementation of revised discharge procedures’ | ||
| ‘midwifery managers developed a new triage system for maternity care’ | ||
| Developing others | 1 | ‘bring leadership and development into the organisation to act as a driver for a change of culture’ |
| Translating and implementing ideas | 1 | ‘helping clinical staff with good ideas to translate, shape and implement them’ |
Two dimensions of the management contribution that did not arise directly from formal interviews and focus groups concerned ‘maintaining day-to-day performance’ and ‘firefighting’. Focusing on specific examples, interview answers overlooked what might appear to be the more mundane aspects of the management role. During a project update event, the medical director from Burnside observed that managers' contributions to operational management were missing: dealing with staff absence, handling devolved human resource management issues, managing beds and patient flows, locating lost records, acquiring missing equipment, handling complaints, fixing budget problems. The project focus on ‘big and dramatic’ overlooked the routine but no less important roles that middle managers play. Also, discussing how ‘extreme jobs’ focus attention on immediate problems at the expense of system changes, an operations manager at Clearview defended the ‘firefighting’ aspect of her role. She observed that many of the ‘routine’ problems that arose could have adverse consequences for patients if not resolved quickly, and that clinical staff were not always aware of those issues, nor would they have the time or the capability to deal with them.
One respondent at Clearview highlighted the work of their Patient Experience Support Team (PEST), which had attracted national interest as well as local support for its work in ensuring that patients' voices were represented when business decisions were being taken:
We take our survey data and complaint data, and a senior team including the assistant director of nursing and my director look at it and decide where we are going to go. This period, our department of medicine for the elderly had an increase in complaints. Rather than go in and do one ward, we are going in to do a whole department; twenty-two sessions with 108 staff over a two-week period, based on the problems that they are having. Sometimes you forget that you are trailblazing, but we probably are, it says a lot about the organisation that you are allowed to, you are enabled to go off and do some of this stuff differently. You don't always know it when you are doing it that it is so different. I was asked to present at a conference a couple of months ago. My first event where people had actually paid to come and listen to me and the response was just overwhelming, people saying ‘oh my god this is what we want to do’. You just don't realise. For you it is just everyday. You know that some things have worked well and other things not so well, but you don't realise just how ahead of the game you are. It is good to do that. When I came back I was enthused and wanted to keep it going.
Assistant director, Clearview
The same respondent at Clearview gave an example of ‘troubleshooting’ in an underperforming area:
The emergency department had a high volume of complaints. So we lifted about fifty harsh quotes and ran a day on the quotes; the group owned it completely, and challenged each other, worried about their reputation. The quarter following the training, they didn't have a single complaint. It hasn't been entirely maintained but it has improved.
Assistant director, Clearview
Another Clearview respondent cited this example of process redesign:
We have so many project-based examples using lean tools. Our recovery team, for example, wanted to redesign the area around the bedspace, make it more streamlined, easier to clean, to get the team around the patient. They then moved on to the canteen area. We have many of these – hundreds of small examples. We've also done a lot of clinical pathway work, for example coordination of the paediatric pathway. Can we measure the impact? It's not hard to measure quality – ‘I feel better’, and ‘the patients are happy’.
Senior manager, Clearview
Several interviewees described successful clinical–managerial collaborations, a theme that also arose in focus group discussions. One (who said that ‘being called a middle manager is incredibly degrading’) described the following initiative:
Creation of the emergency assessment unit, which encompasses A&E [accident and emergency]. Typically in A&E you go get triaged. If you are sick, you get admitted and get seen by a consultant, twelve, twenty-four, thirty-six hours later. Do we ‘see and treat’ and send home, or admit then decide what to do with them? We brought the senior consultant review [of each patient] into the first four hours. A challenging, revolutionary idea, buggers up the four hour target, but is much better long term; diagnostics are done much faster. Two people drove that forward, one clinician, and one manager. The two working together was really important. Neither could have done it without the other.
Assistant director, Clearview
The following manager gave this example of co-ordinating external partnerships to implement changes suggested by a doctor:
One of my successes, which I'm pleased about, concerned a doctor in the accident and emergency department who wanted to introduce an initiative to reduce the incidence of alcohol-related crime. This contributes to between five and ten hospital deaths per annum. It was a good idea, but he couldn't make it happen. Well, I made it happen. This involved bringing together the hospital, the local authority, and police, getting senior staff interested. We organised a large conference in a local club with about eighty people. All agencies were represented at senior level – we had the top brass, bouncers, the trust chair. We had to be bullish with the police, but we developed an action plan, and those agencies now all meet regularly every month to work through the plan and its implementation. We had a ‘recall conference’ last week to review progress, and to draft a plan for next year. The level of these incidents is down 7 per cent.
Assistant director, Clearview
This general manager at South Netley offered two examples of contributions to patient care quality in circumstances in which clinical staff either would not have attempted to solve the problem or would not have been able to deal with it on their own:
Ambulance delays. Shift coordinators in accident and emergency focus on the patients in the department. They don't see the queues outside. They are ‘not their patients’. Delays of an hour were being tolerated. So the assistant general manager [AGM] worked with the shift coordinators and the matron to convince them that this mattered. The consultants are still blinkered in this regard. The AGM got one shift coordinator to lead on this, and to find ways to unload patients more quickly. We now have fewer patients waiting for transfer from ambulance to emergency department. This has multiple benefits. They are in a more congenial and safe environment, with better facilities and staff should things go wrong. And the ambulance and crew are free to return to duties.
Length of stay in care for the elderly. Benchmarking showed that any HRG [Healthcare Resource Group]with ‘complex elderly’ in the name was problematic; chest pain with or without complications, over or under seventy-five, and so on. We have a lot with urinary infections. Our turnaround averages eighteen days, while other hospitals are five or six days. We have discussed what needs to change with the clinicians. This is work in progress, and we haven't got there yet. One suggestion is that a consultant and specialty nurse review each patient on day of admission. Currently, this initiative has a lower priority. If I can shift that, I will be well pleased.
General manager, South Netley
Finally, another respondent at South Netley described the management role in bringing clinical and other stakeholders together to work collaboratively on an infection control problem:
Another example is in infection control and how we have handled this. The infection control team reports to the director of nursing. The recently appointed deputy director of nursing is an individual who can pull things together. Previously, the infection control team was disparate, poorly managed and poorly led. So we had poor infection control. The new deputy has given them direction and engaged everybody, and this has made a huge difference to infection control. She's not the DIPC [Director of Infection Prevention and Control]; that used to be a microbiologist, who failed to do that (and is now on maternity leave). Our new medical director is the DIPC. The new deputy director got everyone involved; doctors, nurses, nurses challenging doctors, she got the facilities people involved. Our rates of MRSA [methicillin-resistant Staphylococcus aureus] and C. diff are now very low.
General manager, South Netley
Middle managers were making a major impact on quality of care, clinical outcomes and organisational performance, and taking pride in the results. Many of these service improvements involved issues that clinical staff were unable or unwilling to address by themselves. Collaborative working, combining different perspectives on problems, was often cited as making a difference. This evidence complements accounts of ‘strategic/entrepreneurial middle managers’, demonstrating the wider-ranging contributions to operations management, firefighting and problem-solving, maintaining patient focus, managing external relationships, improving infrastructure (IT, equipment, estate) and initiating and implementing process, pathway and other changes. This profile was constructed in a context of increasing demands and diminishing resources, with many managers observing that they lacked the time, autonomy, resources and top management support to develop further ideas. This supports the case for ‘releasing time to manage’, allowing middle managers to make an even greater impact on the design, running and quality of the service.
Sweat the small stuff
During this project, the management emphasis understandably lay with large-scale changes to the organisation, delivery, funding and regulation of the service. In this context, solving minor, annoying problems would appear to be unimportant. However, interviews with consultants at Clearview revealed not only their support for management, but also their frustration with minor problems that were not being addressed. This led to the design of an initiative, ‘sweat the small stuff’, which asked staff in the gastroenterology service to nominate minor problems, which were then rapidly solved by a small project team at minimal cost within 5 days, generating benefits for patients, staff and hospital performance. These outcomes strengthened clinical–managerial relationships, which are key to implementing larger-scale changes, and which had suffered because ‘the small stuff’ was not being fixed. This project won an innovation award at Clearview and was applied in other services. The conference paper reporting this initiative is provided in Appendix 7.
Wicked problems
Two management contributions – troubleshooting and firefighting – concern problem-solving. Management problems can be categorised as either ‘tame’ or ‘wicked’. Tame problems are well defined with clear ‘stopping points’, solutions can be objectively seen as right or wrong and possible solutions can be tried and abandoned. ‘Wicked’ problems have no definitive problem statement as different stakeholders have conflicting views. They have no stopping point; the search for better solutions continues. There are no correct answers, only better or worse solutions, and wicked problems tend to be unique, without precedents. Learning by trial and error is hard because every attempt counts. 217 Problems become ‘super wicked’ when time is short, there is no central authority and those who are trying to solve the problem are also creating it. Many of the problems that middle managers in acute settings have to deal with are ‘wicked’ or ‘super wicked’ problems. Examples include organisation culture change, developing service-line management structures, complex patient discharge procedures and staff performance management. Wicked problems cannot be addressed with logical, reductionist analyses – with which clinical staff are familiar. The combination of managerial and clinical perspectives can thus be key to addressing these problems. This project experimented with visual tools such as mess mapping. 215 Wicked problems represent a further dimension of the management contribution, finding solutions by combining stakeholder views.
What has to change?
Interviewer: Red tape, not allowed to use your experience, not trusted to manage – I thought the trust was developing a culture that encouraged engagement and empowerment?
Respondent: Well it's the usual kind of conflict between the two. Politically correct, and good management processes, encouraging empowerment, engagement, and so on. But, when money is tight, you start getting micro-managed. So things like duty rosters – I can't trust my ward managers now, my ward sisters, to do a duty roster. It's got to come from me, and I've got to sign it off. Because I'm told that I must sign off rotas.
Lead nurse, Greenhill
As organisational problems mount, and new ideas and rapid solutions are at a premium, the senior management reflex is often to centralise decisions, to tighten controls, to limit autonomy. As an associate director at Greenhill observed, ‘We need to “let go”, and that's incredibly difficult at a time when we feel the need to tighten the reins’. However, those responses stifle innovation and demotivate those who are close to the problems but who are constrained in the actions they can take. In this ‘disabling’ setting, middle managers in this study were asked how their contributions to clinical and organisational outcomes could be strengthened. There was no shortage of answers. This section summarises those answers and outlines a model of the ‘enabling environment’ (Table 39).
| Properties | In practice . . . |
|---|---|
| Top team communications | Clear, consistent, two way, listening |
| Business intelligence | IT systems that provide appropriate and timely information, easily |
| Zero non-value adding | Streamlined governance, simplified audit and compliance systems |
| Autonomy to innovate | Fixing problems on own initiative without sign-off delays |
| Organisation structures | No silos, information-sharing, cross-service collaboration |
| Organisational norms | Patients not targets, engagement, management valued, risk-taking |
| Performance management | Hold managers to account, provide support for performance problems |
| Interprofessional work | Mutual respect between clinical and managerial staff |
| Support services | Rapid, appropriate advice, action and problem-solving |
| Personal development | Leadership and management training and development |
| Teamwork | Collaboration, information-sharing, consider wider impact of decisions |
| Resources | Staffing, investing to save, granting decision rights within budget |
Most actions to support an enabling environment for management work are cost neutral. Only three of these dimensions are cost generating: business intelligence, personal development and resources.
To represent the richness of the evidence, we will first summarise the content analyses of interview responses from two trusts and then present typical responses from focus group discussions. Suggestions for strengthening management contributions displayed similar patterns irrespective of trust or respondents' roles. So, for example, content analysis of responses from 17 interviewees at Netherby generated 45 ideas, highlighting suggestions for appropriate action. Most suggestions concerned top team communications, autonomy to innovate, organisational norms and performance management. Table 40 shows an illustrative selection.
| Theme | Suggestions and areas for attention (selective) |
|---|---|
| Top team communications | ‘stability and direction from top team please’ |
| ‘senior managers not listening to middle and front line’ | |
| ‘executive team should be more inclusive, listen to front-line managers’ | |
| Business intelligence | ‘real-time information that identifies the “hot spots” we need to influence’ |
| ‘better information systems technology to exploit real-time information’ | |
| Autonomy to innovate | ‘let's not have all decisions made on the executive directors' corridor’ |
| ‘empower middle and front-line managers to make decisions’ | |
| ‘shape the service without having to jump through hoops and be knocked back’ | |
| Organisation norms | ‘balance the pressure on targets with focus on quality of patient care’ |
| ‘we don't steal ideas from others often enough’ | |
| ‘address the managerial–medical silos and mindsets’ | |
| Performance management | ‘provide support to tackle performance management issues’ |
| ‘we reward bad practice by giving additional resources’ | |
| ‘you don't need to do much to be seen as doing a good job’ | |
| Interprofessional work | ‘too much time devoted to interprofessional power and status struggles’ |
| ‘training for doctors and nurses funded differently – perpetuates barriers’ | |
| Support services | ‘provide support, don't dampen enthusiasm’ |
| ‘good, consistent HR support’ | |
| Personal development | ‘management development processes’ |
| ‘allow managers to go visit other places, do research, trial things’ | |
| Resources | ‘enough money to make things happen’ |
The 12 interviewees at Greenhill generated 56 ideas. Similar to the Netherby responses, this pattern is illustrated in Table 41, again emphasising the importance of top team communications, autonomy to innovate, organisation norms, performance management, organisation structure, personal development and adequate resources.
| Theme | Suggestions and areas for attention (selective) |
|---|---|
| Top team communications | ‘do directors know what it's like to work on an understaffed ward?’ |
| Business intelligence | ‘change the IT’ |
| Zero non-value adding | ‘general managers doing administration, burdened with dross’ |
| Autonomy to innovate | ‘allow middle managers to think about and develop ideas’ |
| Organisation structures | ‘divisional structure is divisive – traditional professional silos’ |
| Organisation norms | ‘we do fixes and patches – we need to rethink, look outwards’ |
| Performance management | ‘we have no performance management, hold people to account’ |
| Interprofessional work | ‘few consultants comfortable with multiprofessional programmes’ |
| Support services | ‘what can we do to support those in increasingly challenging roles?’ |
| Personal development | ‘leadership development – for a management role, there is no training’ |
| Teamwork | ‘use the skills and knowledge and innovation we have in teams’ |
| Resources | ‘people are on their knees – inspirational people who are weary’ |
Focus group participants were asked the same question: ‘what would have to change in order to strengthen the contributions that you as a manager can make to quality of patient care, and to clinical and organisational outcomes?’ The pattern of responses was consistent with those from interviews. Here are just three examples from the 40 focus groups that were conducted during this project.
One focus group at South Netley included matron neurosciences, assistant general manager medicine, quality manager, human resources partner, assistant general manager, physiotherapy team lead trauma and orthopaedics, neurosciences physiotherapy team lead, assistant general manager surgical services, advanced nurse practitioner neuroscience, physiotherapy manager and leadership development consultant. From a long list of ideas for strengthening their contributions, their priority areas were:
-
‘clarity and priority around goals; clear strategic direction’
-
‘senior management speak transformational then act transactional’
-
‘give us space to achieve; freedom to try things out, without the bureaucracy’
-
‘clarifying expectations for ward staff, particularly responsibilities of band 5 nurses’
-
‘norms and culture get in the way, but we know these are hard to change’
-
‘performance management – the NHS is not accustomed to this – so when people don't deliver, there is little or no accountability; but performance management can be supportive’
-
‘human resource policies for proper sickness, absenteeism and performance management’
-
‘need to develop coping strategies, survival skills’.
Once again, top team communication, autonomy to innovate, organisation norms, performance management and personal development were significant. This focus group also suggested ‘more information, fewer rumours’, ‘less whizzing around operationally’, ‘change in culture away from command and control’ and ‘less struggling to understand the analytical information we're given’. They also suggested that senior management ‘come and work with us, to understand what's going on’, and wanted to see the ‘executive team modelling the behaviour that we are expected to demonstrate’ (they were no longer allowed to use bank staff whereas the executive team hired external management consultants). Reinforcing earlier discussion of clinical–managerial collaboration, this focus group also expressed the desire for ‘an increased culture of clinical–managerial joint working’.
A second example concerns a focus group with four modern matrons at Greenhill who identified the suggestions in Figure 8, indicating what they felt there should be more of and less of. Supporting the final comment in Figure 8, a ward sister in another Greenhill focus group said:
I tackled the CEO in the meeting and got nothing. I e-mailed him, and I got a wishy-washy response. And when I challenged him on the issue he was rude to me. Communication from the top down has to improve. It's almost as if they have a hidden agenda.
FIGURE 8.
What has to change: modern matrons at Greenhill.
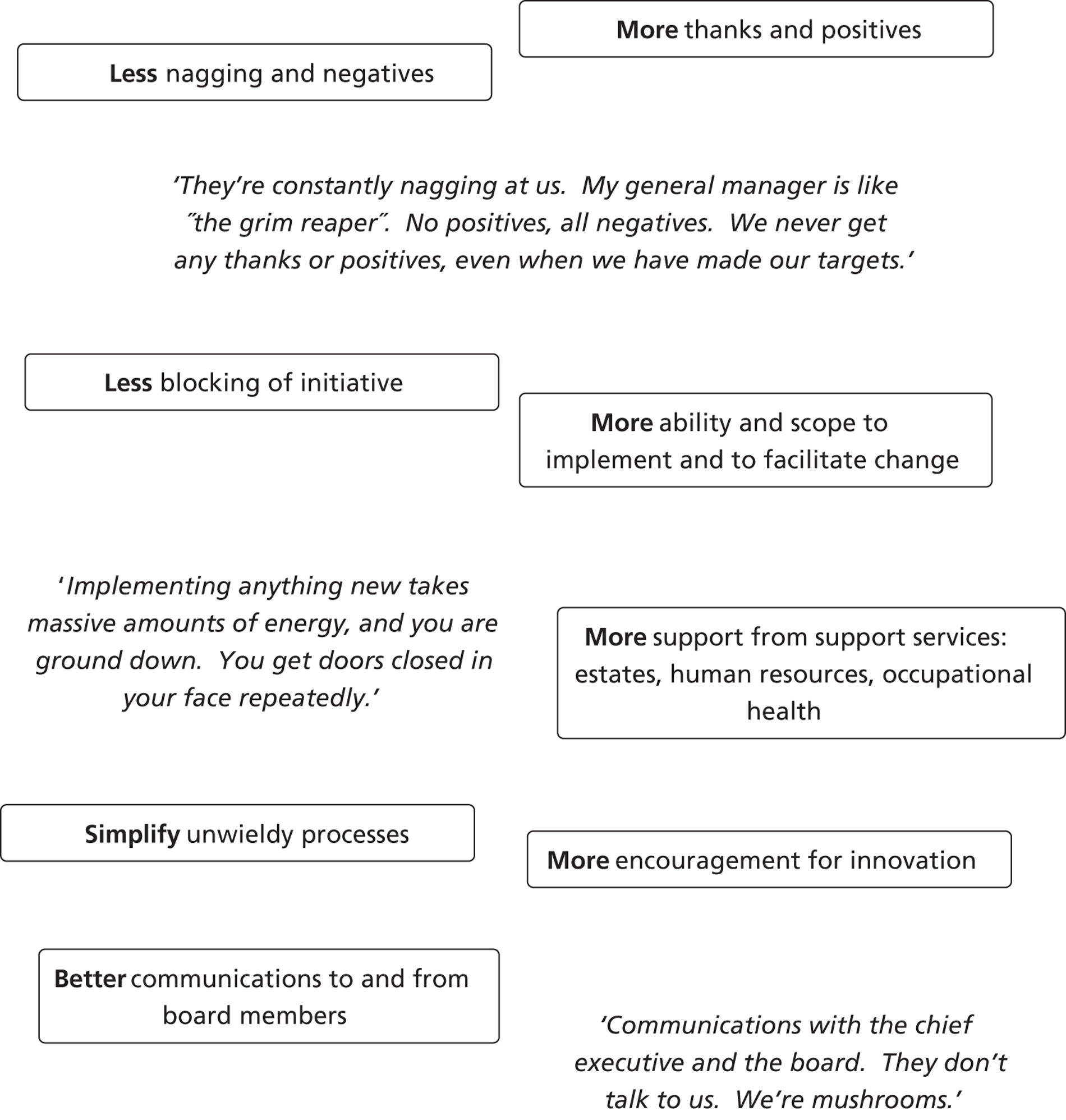
Our third focus group example concerns the 10-member operations management team in the medicine division at Clearview, including operations managers, deputy operations managers, division support managers, divisional lead nurse and senior clinical nurses. Their suggestions for strengthening the management contribution covered individual, divisional and corporate actions.
At an individual level, time management, developing self and others, ‘being in the know’, role clarity and being more proactive and risk-taking were seen as important actions: ‘I get involved in the nitty gritty, I should not have to’, ‘more time with line manager to emulate skills’, ‘keep up with new programmes, be aware’, ‘review job roles and tasks and how they need to change’ and ‘move from being reactive to proactive and take more risks, more power to act with patients, use judgement’.
At a divisional level, ‘being in the know’ was again important, along with meetings management, role clarity, learning and sharing practice, and human resource policies: ‘we should all take responsibility to stay informed’, ‘ensure that groups, forums, workstreams have consistent attendance from the same people, not different people each time, which reduces engagement’, ‘clear roles and responsibilities; understanding of roles of others’, ‘learn from the firefighting incidents, and share best practice more across the division’ and ‘enable staff to do the job and tighten up human resources processes’.
Corporate actions recommended by this focus group included improved central human resource support for recruitment, more opportunities for formal and informal networking with peers, better communications between divisions, better clarity of roles, the celebration of errors as learning opportunities rather than a blame culture, support services with a ‘customer orientation’, dissemination of best practice – a ‘learning and sharing organisation’ – stronger trust values with regard to respect for and engagement of staff, and reduced conflict between finance and patient safety.
It is significant to note that these ideas concern aspects of personal style, approach to the job, time allocation, the clarity with which roles are defined and understood, responsibilities, communications, sharing, learning, support, networking, values. None of these suggestions imply the need for additional resources. Other than the potential opportunity costs involved in acting differently, these suggestions for strengthening management contributions would be free to implement, and would have potentially significant positive implications for clinical and organisational outcomes.
Space limitations do not allow a full reporting of the responses from all 40 focus groups, which raised similar themes and issues. Shown against the same 12 themes, Table 42 lists the 24 ‘ways to strengthen the management contribution’ codes from the combined focus group content analysis. Translating this information from interviews and focus groups into guidelines for management practice, corporate issues that appear to be of particular significance and concern include:
-
clarity and consistency with regard to trust goals and priorities
-
clear and consistent communications that keep staff well informed
-
support services with a customer orientation providing effective and timely support
-
updated IT systems that provide appropriate financial and other management information
-
strengthened performance management systems
-
investment in leadership and management development
-
encouragement and support for clinical–managerial collaboration.
| Theme | Focus group content analysis codes |
|---|---|
| Top team communications | Better leadership, planning and stability |
| Clarity of strategy | |
| Better support and leadership from senior managers | |
| Improve communication and recognition | |
| Business intelligence | Measures, metrics and data |
| Zero non-value adding | Reduce targets and bureaucracy |
| Standardisation of processes | |
| Autonomy to innovate | Increase authority, ownership and accountability |
| Focus on change management and new ideas | |
| Organisation structures | Change structure, systems and processes |
| Organisation norms | Culture/climate |
| Increased patient and clinical focus | |
| More learning from others and improved links | |
| Focus on outputs and achievements | |
| Become more businesslike | |
| Performance management | Improved performance management |
| Interprofessional work | Relationships with doctors |
| Support services | Better selection of staff |
| Improved support systems | |
| Personal development | Training and development |
| Develop resilience, manage expectations | |
| Teamwork | Teamwork mentality and staff engagement |
| Resources | More staff |
| More time and space |
Board-level executives may in addition wish to consider:
-
not interfering in operations; focus instead on planning and prioritising
-
avoiding a ‘panic of the week’ approach
-
listening to middle managers who have a better understanding of operational issues
-
involving middle managers in key decisions
-
empowering middle managers to make decisions, giving them ‘space to achieve’
-
emphasising positives rather than negatives.
Steps that individual managers said that they found useful included ‘get out and about’, ‘make time for reflection’, ‘look at what processes and practices could be done differently to reduce the pressure’, ‘avoid perfectionism’, ‘find support in colleagues’ and ‘develop persistence, political skill and a thick skin’. In sum, be more proactive, reflective, self-aware and resilient.
A contributions-based model of management
This study aimed to develop a profile of middle management contributions, to understand how clinical and organisational outcomes are affected, to identify factors impeding management contributions and to establish the dimensions of an ‘enabling environment’ for management work. In this field, one research tradition focuses on management roles and activities. A second tradition concentrates on linking aspects of management work to organisational outcomes. In other words, an interest in what managers do sits alongside a focus on what managers achieve – the added value. This study aimed to contribute in particular to the latter tradition, not by attempting to correlate specific management practices with performance metrics, but by profiling the contributions of the middle management function, and demonstrating how these are shaped by institutional and organisational contexts.
Figure 9 summarises the overall argument of this project, drawing as indicated on the conclusions of previous chapters. This is loosely based on the model developed by Wooldridge et al. 30 Their ‘organising framework’ is designed to inform research rather than to explain how the management contribution is enabled and constrained, and indicates the significance of institutional and organisational contexts without detailing their properties. Figure 9 in contrast shows how middle management contributions in health care are shaped by national institutional and local organisational contexts, by the composition of the management function and by the enabling (or disabling) properties of the environment in which middle managers operate.
Previous cross-sector research portrays middle managers contributing to organisational outcomes through influencing strategy, by nurturing and championing initiatives and through co-ordinating, mediating, interpreting and negotiating roles. The advantages that middle managers have in driving innovation and change are based on the combination of access to top management and knowledge of operational capabilities. Research also indicates that middle management involvement in strategy leads to improved decision-making, higher degrees of consensus, improved implementation and better organisational performance. There is no reason why these observations concerning middle management work in general should not apply in health-care settings.
Factors inhibiting ‘entrepreneurial’ middle managers include policies that encourage conservative behaviour, complex approval cycles, micromanagement and lack of delegated authority – all of which were observed in this study. Factors fostering innovation include overlapping territories, cross-functional contacts, free flows of information, excess in budgets, loosely defined roles and contact with other organisations. These ‘propellants’ were less evident, and their absence may be sustained by the divisional silos that accompany service-line management structures.
FIGURE 9.
A contributions-based model of the acute trust middle management function. The arrows between the components of this model indicate influence and dependencies (one way or mutual) and are not intended to represent causal relationships.
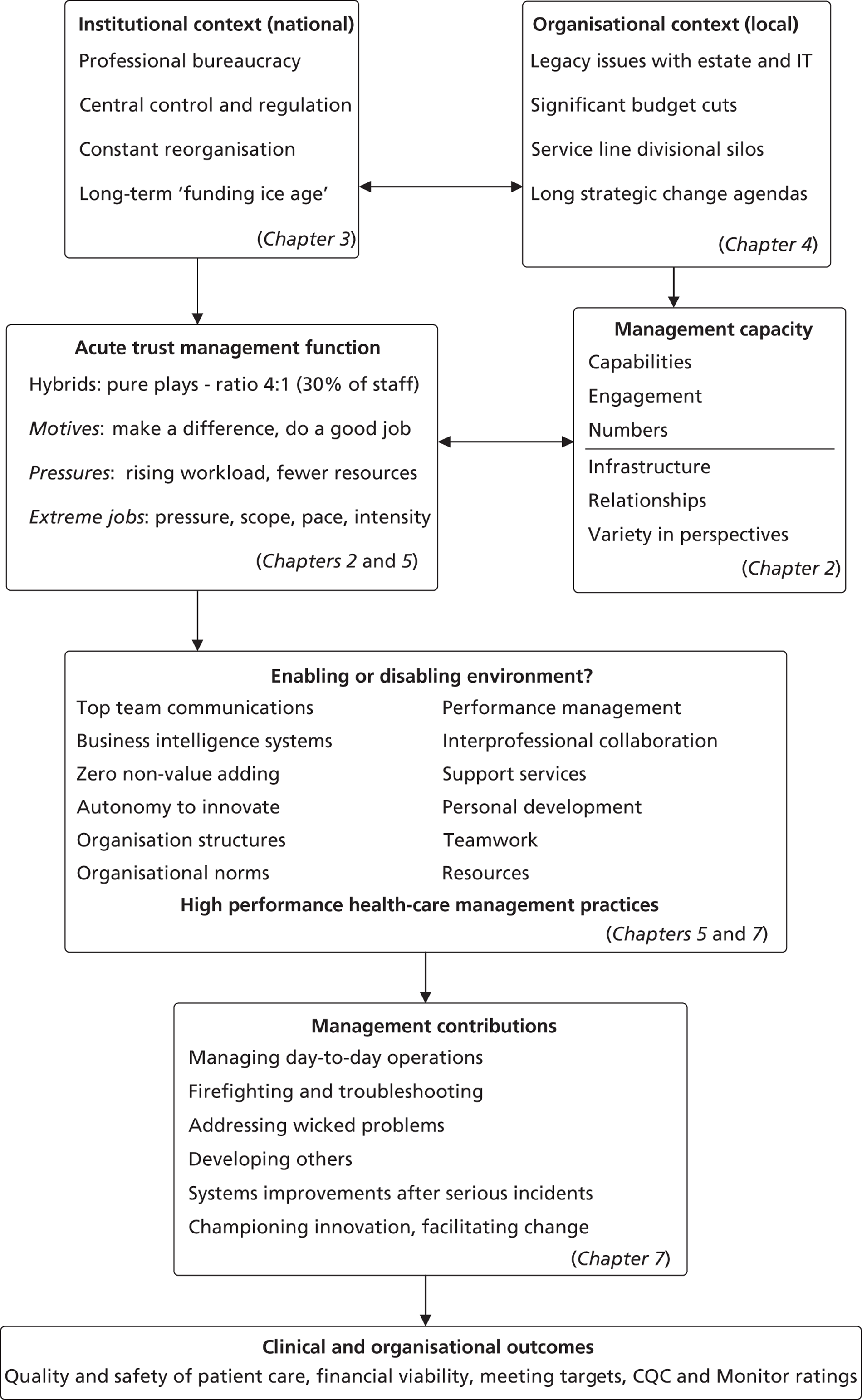
The concept of the enabling environment is not novel. For example, Burns and Stalker240 showed that ‘organic management systems’ operated more effectively in turbulent environments than bureaucratic or ‘mechanistic’ systems. Kanter241 argued that ‘integrative’ cultures encouraged innovation and adaptability, whereas ‘segmentalist’ (bureaucratic) cultures did not.
Several commentators have examined the related concept of ‘high-performance’ work systems,242,243 which involve clusters of practices designed to increase capabilities, commitment, motivation and individual and organisational performance. Huselid244 linked high-performance work practices to higher productivity, lower staff turnover and higher corporate financial performance, such practices contributing US$18,500 per employee in shareholder value and $4000 per employee in additional profits. Pfeffer245 claimed that high-performance practices could raise an organisation's stock market value by US$20,000–40,000 per employee through policies such as job security, careful recruitment, decentralisation and self-managing teams, remuneration linked to organisational performance, investment in training, reduced status differentials, and information sharing across the organisation. Popular in textbooks, high-performance practices have been less common in practice. 246
High-performance perspectives have been applied mainly to shop floor operatives in manufacturing. Thorlby and Mabin247 ask whether or not the NHS has become a high-performing system and, although pointing to improvements, their analysis focuses on conditions and metrics (cancer, cardiovascular disease, drug costs, survival rates) and not on the organisation conditions and management practices that produce those results. However, Michie and West236 develop a ‘high-performance’ framework for health care, linking patient outcomes and organisational performance to people management practices that include job design, teamwork, involvement, control over work, leadership, and training and development. The ‘enabling environment’ concept is also related to the notion of organisation culture. The latter has attracted multiple definitions and is typically operationalised in terms of organisational properties. In contrast, the notion of enabling environment in the context of this discussion is grounded in specific policies, behaviours and practices. From their study of organisation cultures in the NHS, Mannion et al. 248 found that the service was becoming more hierarchical and competitive, but that the links between culture and performance were difficult to disentangle. Haq249 reports the results of a survey of 132 managers attending NHS leadership programmes, concluding that only 9% were creating a high-performance environment in which teams felt motivated and focused, whereas 77% were creating a ‘tolerable or demotivating’ climate, resulting in disengagement, minimal discretionary effort and underperformance.
Davenport and Harding250 argue that a key senior management responsibility concerns the creation and maintenance of conditions in which others can be successful, establishing ‘the context for performance’. Pointing to ‘the competitive advantage in the middle of your organisation’, they argue that middle managers are repositories of experience, insight and influence, with accumulated operational and organisational knowledge, managing operations, developing others, keeping the show on the road, energising change – consistent with middle management roles in health care. Our concern in this project lies with an organisational environment that enables middle managers to carry out those operational, problem-solving, service improvement and change leadership roles more effectively. The evidence indicates that organisational environments in acute trusts could be more enabling and supportive. Many of the actions required to strengthen those environments are cost neutral, which is significant given the expectation that the service faces a continuing ‘funding ice age’. Hurst and Williams251 therefore ask if NHS hospitals can do more with less, pointing to the importance of leadership, management, staff engagement, improved operational processes and new technology adoption. The ‘enabling environment’ in Table 39, therefore, can be read as a ‘high-performance profile’ for middle management work. To strengthen contributions to clinical and organisational outcomes, senior executives may wish to consider the performance dividend that would result from implementing cost-neutral policies and practices such as:
-
‘high-visibility’ board members setting and communicating clear goals and priorities
-
listening to and acting on ideas from staff at all levels
-
remembering to praise the positives
-
ensuring that management roles are seen to be recognised and valued
-
streamlining internal governance arrangements and information requirements
-
where possible simplifying the provision of information to external bodies
-
providing appropriate and timely business and management information (activity levels, capacity, costs, outcomes), perhaps exploring simple low-cost IT solutions
-
granting middle managers authority to fix problems within their own budgets
-
allowing middle managers to act on their own initiative to pilot innovations
-
creating opportunities for the exchange of information and ideas with other organisations
-
eliminating or at least reducing the sign-offs, which generate frustration and delays
-
designing a rigorous and supportive performance management system with appropriate professional support for managers who operate the system
-
ensuring cross-divisional information-sharing and improvement initiatives
-
encouraging clinical–managerial collaboration, to foster trust, respect and mutual understanding, and to drive major change initiatives
-
insisting that support services – human resources, finance, IT, estates – adopt a customer orientation
-
opening up opportunities for leadership and management development for those with or aspiring to hold managerial responsibilities
-
implementing team-building activities; good teamwork does not always develop naturally
-
considering ‘invest to save’ projects in which spending will improve future cost-effectiveness.
These are surely ‘common sense’ actions, but the evidence suggests that they are not common in practice. In a context of rapid, radical and ongoing change, with demand rising and funding falling, in which new ways of working are at a premium, why would an organisation not consider taking such low-cost, low-risk, high-return steps? Senior managers, perhaps, in restricting the autonomy and voice of middle managers, are simply passing on down the hierarchy the pressures that they experience from national bodies. Another explanation perhaps rests with the composition of the middle management function, dominated by hybrids with little management training, and who may not be trusted by more experienced executives to make appropriate management decisions.
As well as building an enabling environment, these suggestions have other benefits. First, capable, motivated and committed managers are more likely to stay with an organisation that listens to their ideas, allows them to be innovative, to make a difference. In other words, these guidelines constitute an effective retention strategy. Second, these steps generate low-cost, in-house, tailored development opportunities. Many middle managers participating in this project indicated that their development opportunities had been curtailed by budget cuts that prevented attendance on generic external programmes. Third, clinical staff may be more willing to assume managerial responsibilities, and to discharge these enthusiastically, if they know that they will be allowed ‘space to achieve’. Finally, all of these factors contribute to management capacity, an issue raised in Chapter 2 and a research priority arising from this study. Building and sustaining an environment that enables management work contributes to capacity, motivation, retention and development, and increases the attractiveness of pure and hybrid middle managerial roles.
Management in the plural
Our board-level contact at one trust was asked to comment on the enabling environment concept. He replied that this model was helpful, but requested a simpler, more focused approach. His executive team would want to know ‘the two or three things that would make a big difference, the small number of high-impact changes’. In considering how to respond to that request, one theme appears to be particularly prominent: the comanagement, or shared leadership of change, by clinical and managerial staff, hybrids and pure plays, working in collaboration.
Management, as with leadership, can be defined as a solution to the problem of collective effort. 252 As we have seen, hospital management is a widely distributed function, dominated by hybrids who outnumber pure plays by four to one. The capacity of that function to address effectively the multitude of operational and strategic demands placed on it is therefore crucial. This appears to require what might be termed ‘management in the plural’, drawing on the collective resources of managers with different backgrounds, skills and views.
The concept of distributed leadership, or ‘leadership in the plural’,64 recognises that leadership behaviours can be seen at all levels of an organisation. The traditional concept of focused leadership emphasises the attributes and capabilities of senior individuals. Distributed leadership concerns the achievement of goals through collective action, which may be formally designated, but can also develop spontaneously. 253–255 The notion of distributed leadership is endorsed in the NHS Leadership Framework28 and in the review of leadership and management conducted by The King's Fund. 42 Denis et al. 256 argue that a ‘plurality of leaders’ may be necessary, as no one individual acting alone can combine the influence, expertise and legitimacy needed to drive change in complex social systems. In their review of research in this area, Denis et al. 64 also explore the merits of conceptualising leadership as a collective phenomenon:
It is the common experience of life within and beyond organisations that leadership and leaders are to be found in many places. In a shared power world, plural forms of leadership where different people bring different resources, capabilities, and sources of legitimacy (and yes, followers) to the table offer a path to getting things done: not an idealized path, and not a path that always succeeds, but a key component of organising nonetheless that needs attention from organisational scholars.
p. 6464
Terminology in this field is also distributed. Fitzsimons et al. 257 identify shared, distributed, dispersed, devolved, democratic, distributive, collaborative, collective, co-operative, concurrent, co-ordinated, relational and coleadership, and then distinguish between leadership that is shared (among those holding formal leadership roles) and leadership that is distributed (performed by many across the organisation). Martin et al. 258 distinguish between ‘quiet distributed’ and ‘quiet dispersed’ forms of leadership, the former being within the control of the project in hand, the latter being more diffuse. Currie and Lockett259 explore concertive, conjoint and collective forms of distributed leadership, identifying a spectrum between top team models at one extreme and the spontaneous collaboration of actors pooling their expertise and skills at the other.
What of shared or distributed management? Mintzberg4 introduces these terms in a section on ‘managing beyond the manager’ (p. 147). By ‘shared managing’, he means ‘one managerial job shared among several people’, which is not how the concept of shared leadership is understood. ‘Distributed managing’ concerns the diffusion of responsibility for some managerial roles to various non-managers in a unit (p. 152). Both concepts appear to work more closely with formal organisational positions and hierarchies, and do not address the more fluid, relational, interactional and processual ‘leadership relays’ with which Denis et al. 64 and others have been concerned.
Denis et al. 64 cite examples of distributed leadership, including in health care. 11 They note that these cases ‘do not provide evidence that such forms necessarily lead to positive outcomes or that success might not have been obtained in other ways’ (p. 39). We have reported in this chapter, however, several instances in which change and service improvements may not have occurred, or would not have been implemented so rapidly, had some form of shared leadership – or shared management – not been invoked to make that happen.
Management in the plural is a ‘high-impact, high-performance’ response to our executive. This concerns two components of the capacity model: requisite variety and clinical–managerial relationships. Pure plays and hybrids bring contrasting views to the complex problems that they face and share. There have been several reported experiments in joint working. These include the NHS Institute Duality Leadership Programme,260 the NHS London Prepare to Lead scheme, the North Western Deanery leadership development programme and the London Paired Learning initiative. 53,261 Can shared management, in different forms, develop from isolated examples to widespread norm? Collaborative approaches, particularly in the context of diminishing resources, may be key to identifying, designing, establishing consensus for and implementing the more innovative SDO changes necessary to improve effectiveness, quality and safety.
This discussion points to a challenging research agenda. Currie et al. 262 show how distributed leadership is diluted by bureaucracy, power differentials and a centralised performance management regime focusing on a small number of individuals. Denis et al. 64 note that distributed leadership may have negative outcomes, and research has not explored the discord, conflict and rivalries that might arise. Gronn254 recognises the continuing importance of hierarchical leadership alongside distributed forms. Currie and Lockett259 also argue that enthusiasm for distributed leadership may dilute the role of hierarchy. We therefore need to develop a better understanding of management in the plural. In which health-care contexts are such approaches appropriate? Which models make the biggest difference, to those involved, to organisational outcomes and to patients?
Acknowledgements
We would like to dedicate this report to the memory of our colleague, Joe Jaina. Joe was instrumental in helping to establish this project in terms of concept and design, co-authoring the proposals and negotiating access with two of the six participating trusts. However, Joe tragically died from cancer before he could see those efforts rewarded. He remains a co-author of this report in recognition of his irreplaceable contributions.
We wish to thank all of the NHS staff who have contributed so much to this project by so generously giving us their time. Staff at all levels have been willing to share with us their experiences and ideas, despite the many pressures that the service faced as this project unfolded, and for this we are exceptionally grateful. We would also like to thank a number of members of our project team who, although not involved in authoring this final report, made other valuable contributions to the project. Jayne Ashley, our project administrator, handled the many demands that we placed on her with a calm professionalism; thanks Jayne. Catherine Bailey and Janice Osbourne made valuable contributions to data collection and literature reviews, and Janet Price, Kim Turnbull James and Charles Wainwright provided ongoing advice on different aspects of the project. We are also grateful for the support from our advisory group members who supplied us with reassurance and awkward but helpful questions throughout: David Grantham, Kathleen Hunter, Valerie Iles, Simone Jordan, Neil Offley, Graeme Currie and Jacky Holloway. We would also like to thank Dianne Bown-Wilson, Elena Doldor, Marcus Durand, Charlotte Gascoigne and Paula Higson for their contributions to reviewing sections of the literature, data analysis and interpretation and case study development.
Contribution of authors
Publications
See Appendix 5 for project outputs and Appendix 6 for related publications.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
References
- Equity and excellence: liberating the NHS. London: Her Majesty's Stationery Office; 2010.
- Carlisle D. Managers' big worries over £20 billion target. Health Serv J 2011:19-22.
- Ham C. More of the same is not an option. Health Serv J 2010:14-5.
- Mintzberg H. Managing. Harlow, Essex: Financial Times Prentice Hall; 2009.
- Stewart R. The reality of management. London: Pan/Heinemann; 1997.
- Watson TJ. In search of management: culture, chaos and control in managerial work. London: Routledge; 1994.
- Kotter JP. What effective general managers really do. Harv Bus Rev 1999;77:145-59.
- Øvretveit J, Aslaksen A. The quality journeys of six Norwegian hospitals: an action evaluation. Oslo: Norwegian Medical Association; 1999.
- Medical leadership competency framework. London: NHS Institute for Innovation and Improvement; 2008.
- Hamilton P, Spurgeon P, Clark J, Dent J, Armit K. Engaging doctors: can doctors influence organisational performance?. London: NHS Institute for Innovation and Improvement; 2008.
- Buchanan DA, Addicott R, Fitzgerald L, Ferlie E, Baeza J. Nobody in charge: distributed change agency in healthcare. Hum Relat 2007;60:1065-90. http://dx.doi.org/10.1177/0018726707081158.
- Floyd SW, Wooldridge BJ. The strategic middle manager. San Francisco, CA: Jossey-Bass; 1996.
- Huy QN. Emotional balancing of organizational continuity and radical change: the contribution of middle managers. Admin Sci Q 2002;47:31-69. http://dx.doi.org/10.2307/3094890.
- Badaracco JL. Leading quietly: an unorthodox guide to doing the right thing. Boston, MA: Harvard Business School Press; 2002.
- Brooks I. Leadership of a cultural change process. Leadership Org Dev J 1996;17:31-7. http://dx.doi.org/10.1108/01437739610127496.
- Lüscher LS, Lewis MW. Organizational change and managerial sense making: working through paradox. Acad Manag J 2008;51:221-40. http://dx.doi.org/10.5465/AMJ.2008.31767217.
- Clark J, Spurgeon P, Dent J. Surrender to progress. Health Serv J 2008:32-3.
- Locock L. Maps and journeys: redesign in the NHS. Birmingham: University of Birmingham, Health Services Management Centre; 2001.
- Iles V, Sutherland K. Organisational change: a review for health care managers, professionals and researchers. London: National Co-ordinating Centre for NHS Service Delivery and Organisation Research and Development; 2001.
- Learning from investigations. London: Commission for Health Audit and Inspection; 2008.
- Donaldson L. An organisation with a memory. London: Department of Health/The Stationery Office; 2000.
- Hales C. Does it matter what managers do?. Bus Strat Rev 2001;12:50-8. http://dx.doi.org/10.1111/1467-8616.00174.
- West MA, Borrill C, Dawson J, Scully J, Carter M, Anelay S, et al. The link between the management of employees and patient mortality in acute hospitals. Int J Hum Resource Manag 2002;13:1299-310. http://dx.doi.org/10.1080/09585190210156521.
- Boyne GA, Meier KJ, O’Toole LJ, Walker RM. Public service performance: perspectives on measurement and management. Cambridge: Cambridge University Press; 2006.
- Dorgan S, Layton D, Bloom N, Homkes R, Sadun R, Van Reenen J. Management in healthcare: why good practice really matters. London: McKinsey & Company and London School of Economics and Political Science; 2010.
- Pettigrew AM, Ferlie E, McKee L. Shaping strategic change: making change in large organizations – the case of the National Health Service. London: Sage Publications; 1992.
- NHS leadership qualities framework. London: NHS Modernisation Agency Leadership Centre; 2002.
- NHS leadership framework. London: National Leadership Council; 2011.
- Floyd SW, Wooldridge B. Middle management involvement in strategy and its association with strategic type: a research note. Strat Manag J 1992;13:153-67. http://dx.doi.org/10.1002/smj.4250131012.
- Wooldridge B, Schmid T, Floyd SW. The middle management perspective on strategy process: contributions, synthesis, and future research. J Manag 2008;34:1190-221. http://dx.doi.org/10.1177/0149206308324326.
- Walshe K, Smith L. The NHS management workforce. London: The King's Fund; 2011.
- Christian S, Anderson S. Review of research needs and priorities 2007. London: NHS National Institute for Health Research; 2007.
- The operating framework for the NHS in England 2008/09. London: Department of Health; 2007.
- Davies P. The NHS handbook 2010/11. London: NHS Confederation; 2010.
- Tsoukas H. A dialogical approach to the creation of new knowledge in organizations. Organ Sci 2009;20:941-57. http://dx.doi.org/10.1287/orsc.1090.0435.
- Stake RE, Denzin NK, Lincoln YS. Handbook of qualitative research. Thousand Oaks, CA: Sage Publications; 2000.
- Buchanan DA, Symon G, Cassell C. Qualitative organizational research: core methods and current challenges. London: Sage Publications; 2012.
- Toft B, Reynolds S. Learning from disasters: a management approach. Houndmills, Basingstoke: Palgrave Macmillan; 2005.
- Denis J-L, Lomas J. Convergent evolution: the academic and policy roots of collaborative research. J Health Serv Res Pol 2003;8:1-5. http://dx.doi.org/10.1258/135581903322405108.
- Buchanan DA. Good practice, not rocket science: understanding failures to change after extreme events. J Change Manag 2011;11:273-88. http://dx.doi.org/10.1080/14697017.2011.597571.
- Edwards N. Managers: can the NHS manage without them?. London: Social Market Foundation; 2004.
- The future of leadership and management in the NHS: no more heroes. London: The King's Fund; 2011.
- Santry C. Abolishing targets will reduce the need for managers, David Cameron says. Health Serv J 2010.
- Commissioning: fourth report of session 2009–10. London: The Stationery Office; 2010.
- Ham C. NHS managers are the wrong targets for cuts. The Guardian 2012.
- Appleby J. Cut and run. Health Serv J 2001. www.hsj.co.uk/cut-and-run/24493.article (accessed accessed 22 February 2012).
- McLellan A. We need NHS managers to tackle the first financial crisis since 1987. Health Serv J 2010.
- Ham C. It makes a welcome change to hear praise for NHS managers. Health Serv J 2011. www.hsj.co.uk/comment/opinion/it-makes-a-welcome-change-to-hear-praise (accessed accessed 22 February 2012).
- Management in the NHS: the facts. London: NHS Confederation; 2007.
- NHS Information Centre . NHS Occupation Code Manual Version 9 n.d. www.ic.nhs.uk/article/2268/NHS-Occupation-Codes (accessed accessed 28 February 2012).
- Currie G, Procter SJ. The antecedents of middle managers' strategic contribution: the case of a professional bureaucracy. J Manag Stud 2005;42:1325-56. http://dx.doi.org/10.1111/j.1467-6486.2005.00546.x.
- Gulick L, Urwick L. Papers on the science of administration. New York, NY: Institute of Public Administration; 1937.
- Gillam S. Teaching doctors in training about management and leadership. BMJ 2011;343:1-2. http://dx.doi.org/10.1136/bmj.d5672.
- Learmonth M. Doing things with words: the case of ‘management' and ‘administration'. Publ Admin 2005;83:617-37. http://dx.doi.org/10.1111/j.0033-3298.2005.00465.x.
- O’Reilly D, Reed M. Leaderism: an evolution of managerialism in UK public service reform. Publ Admin 2010;88:960-78. http://dx.doi.org/10.1111/j.1467-9299.2010.01864.x.
- Quinn RE, Faerman SR, Thompson MP, McGrath MR, St Clair LS. Becoming a master manager: a competing values approach. New York, NY: John Wiley; 2011.
- Hales C. Moving down the line?: the shifting boundary between middle and first-line management. J Gen Manag 2006;32:31-55.
- Balogun J. From blaming the middle to harnessing its potential: creating change intermediaries. Br J Manag 2003;14:69-83. http://dx.doi.org/10.1111/1467-8551.00266.
- Shi WS, Markoczy L, Dess GG. The role of middle management in the strategy process: group affiliation, structural holes, and tertius iungens. J Manag 2009;35:1453-80. http://dx.doi.org/10.1177/0149206309346338.
- Inamdar SN, Osland A, Wells P. Restructuring with the middle-management advantage. Health Care Manag 2010;29:305-17.
- Moore A. A license to manage?. Health Serv J Regul Suppl 2011:1-7.
- Ashby WR. An introduction to cybernetics. London: Chapman & Hall; 1956.
- Shrivastava S, Sonpar K, Pazzaglia F. Normal accident theory versus high reliability theory: a resolution and call for an open systems view of accidents. Hum Relat 2009;62:1357-90. http://dx.doi.org/10.1177/0018726709339117.
- Denis J-L, Langley A, Sergi V. Leadership in the plural. Acad Manag Ann 2012;6:1-73.
- Suddaby R, Elsbach KD, Greenwood R, Meyer JW, Zilber TB. Organizations and their institutional environments: bringing meaning, values and culture back in. Acad Manag J 2010;53:1234-40. http://dx.doi.org/10.5465/AMJ.2010.57317486.
- Dopson S, Fitzgerald L, Dopson S, Fitzgerald L. Knowledge to action: evidence-based health care in context. Oxford: Oxford University Press; 2005.
- Buchanan DA, Fitzgerald L, Clegg S, Harris M, Höpfl H. Managing modernity: beyond bureaucracy?. Oxford: Oxford University Press; 2011.
- Abraham A. Care and compassion: report of the health service ombudsman on ten investigations into NHS care of older people. London: The Stationery Office; 2011.
- Review of compliance: Castlebeck Care (Teesdale) Ltd. Newcastle upon Tyne: Care Quality Commission; 2011.
- Francis R. Independent inquiry into care provided by Mid Staffordshire NHS Foundation Trust January 2005 – March 2009 (two volumes). London: The Stationery Office; 2010.
- Kitchener M, Brock DM, Powell MJ, Hinings CR. Restructuring the Professional organization: accounting, health care and law. London: Routledge; 1999.
- Nicholson D. The year: NHS chief executive's annual report 2008/09. London: Department of Health; 2009.
- Olsen JP. Maybe it is time to rediscover bureaucracy. J Publ Admin Res Theor 2006;16:1-24. http://dx.doi.org/10.1093/jopart/mui027.
- Leavitt HJ. Top down: why hierarchies are here to stay and how to manage them more effectively. Boston, MA: Harvard Business School Press; 2005.
- High quality care for all: NHS next stage review final report. London: Department of Health; 2008.
- High quality care for all: our journey so far. London: Department of Health; 2009.
- The operating framework for the NHS in England 2010/11. London: Department of Health; 2009.
- Investigation into Mid Staffordshire NHS Foundation Trust. London: Commission for Health Audit and Inspection; 2009.
- West D. MPs: NHS white paper lacked credible plan. Health Serv J 2011.
- Foundation trusts and Monitor. London: The Stationery Office; 2008.
- Jones D, Mitchell A. Lean thinking for the NHS. London: NHS Confederation; 2006.
- Powell AE, Rushmer RK, Davies HTO. A systematic narrative review of quality improvement models in healthcare. Edinburgh: NHS Quality Improvement Scotland; 2009.
- Stanley S, Eaton M. Powerful change for pathology. Health Serv J 2011:28-9.
- Julius D. Understanding the public services industry: how big, how good, where next?. London: Department for Business, Enterprise and Regulatory Reform; 2008.
- Boyle C, Lewis C. Competition check-up for private care. The Times 2010:38-9.
- Barrow M, Smyth C. Lives at risk as hospitals run into cash crisis. The Times 2011.
- Smyth C, Asthana A. Expansion of private care in NHS hospitals. The Times 2011:1-6.
- Britnell M. How the NHS could make money for Britain. The Times 2011.
- Liberating the NHS: report of the arm's-length bodies review. London: Department of Health; 2010.
- NHS 2010–2015: from good to great. London: The Stationery Office; 2009.
- Edwards N. Only our best can solve this puzzle. Health Serv J 2011:16-7.
- Propper C, Sutton M, Whitnall C, Windmeijer F. Did ‘targets and terror' reduce waiting times in England for hospital care?. B.E. J Econ Anal Poli 2008;8:1-25. http://dx.doi.org/10.2202/1935-1682.1863.
- Edwards N, Lewis R. Balancing external requirements and a positive internal culture. London: The King's Fund; 2011.
- What's it all for?: removing unnecessary bureaucracy in regulation. London: NHS Confederation and Independent Healthcare Advisory Services; 2009.
- Compliance framework 2011–12. London: Monitor; 2011.
- Guidance about compliance with the Health and Social Care Act 2008 (registration requirements) regulations 2009. London: Care Quality Commission; 2009.
- How we monitor compliance. London: Care Quality Commission; 2011.
- Essential standards of quality and safety. London: Care Quality Commission; 2010.
- Revision to the operating framework for the NHS in England 2010/11. London: Department of Health; 2010.
- The NHS outcomes framework 2012/13. London: Department of Health; 2011.
- Innovation, health and wealth: accelerating adoption and diffusion in the NHS. Leeds: Department of Health; 2011.
- Santry C. Weak managers could be struck off. Health Serv J 2010:4-5.
- Standards for members of NHS boards and governing bodies in England. London: Council for Healthcare Regulatory Excellence; 2012.
- The operating framework for the NHS in England 2008/09. London: Department of Health; 2007.
- Appleby J. An NHS ice age may have only just begun. Health Serv J 2011.
- Gainsbury S. Financial directors feel a distinct nip in the air. Health Serv J 2010:12-3.
- The operating framework for the NHS in England 2012/13. London: Department of Health; 2011.
- Dowler C, Clover B. Pressure piles up on acute hospital sector. Health Serv J 2011:4-5.
- Clover B. Dozens of trusts missed savings target in 2010–11. Health Serv J 2011:6-7.
- Davies N. Flat Earth News. London: Vintage Books; 2009.
- West D. Future Forum demands end to manager bashing. Health Serv J 2011.
- Christensen CM, Bohmer R, Kenagy J. Will disruptive innovations cure health care?. Harv Bus Rev 2000;78:102-12.
- Service-line management: an overview. London: Monitor; 2009.
- Malby B. Suited must not mean booted. Health Serv J 2011:18-9.
- Bruch H, Menges JI. The acceleration trap. Harv Bus Rev 2010;88:80-6.
- Scase R, Goffee R. Reluctant managers: their work and lifestyles. London: Routledge; 1989.
- Whyte WH. The organization man. Harmondsworth, Middlesex: Penguin Books; 1956.
- Dalton M. Men who manage. New York, NY: Wiley; 1959.
- Mintzberg H. The nature of managerial work. London: Harper Collins; 1973.
- Mintzberg H. Rounding out the managerial job. Sloan Manag Rev 1994;36:11-26.
- Hassan F. The frontline advantage. Harv Bus Rev 2011;89:106-14.
- Huy QN. In praise of middle managers. Harv Bus Rev 2001;79:72-9.
- Badaracco JL. We don't need another hero. Harv Bus Rev 2001;79:121-6.
- Meyerson DE. Radical change, the quiet way. Harv Bus Rev 2001;79:92-100.
- Meyerson DE. Tempered radicals: how people use difference to inspire change at work. Boston, MA: Harvard Business School Press; 2001.
- Davenport TH, Prusak L, Wilson HJ. Who's bringing you hot ideas and how are you responding?. Harv Bus Rev 2003;81:58-64.
- Dopson S, Stewart R. What is happening to middle management?. Br J Manag 1990;1:3-16. http://dx.doi.org/10.1111/j.1467-8551.1990.tb00151.x.
- Hassard J, McCann L, Morris J. Managing in the modern corporation: the intensification of managerial work in the USA, UK and Japan. Cambridge: Cambridge University Press; 2009.
- Hyde P, Granter E, McCann L, Hassard J, Dickinson H, Mannion R. The reform of health care: shaping, adapting and resisting policy developments. Houndmills, Basingstoke: Palgrave Macmillan; 2012.
- Carney M. Middle manager involvement in strategy development in not-for-profit organizations: the director of nursing perspective. J Nurs Manag 2004;12:13-21. http://dx.doi.org/10.1111/j.1365-2834.2004.00388.x.
- Pappas JM, Flaherty KE, Wooldridge B. Tapping into hospital champions: strategic middle managers. Health Care Manag Rev 2004;29:8-16. http://dx.doi.org/10.1097/00004010-200401000-00003.
- Currie G. Reluctant but resourceful middle managers: the case of nurses in the NHS. J Nurs Manag 2006;14:5-12. http://dx.doi.org/10.1111/j.1365-2934.2005.00613.x.
- Bolton SC. Multiple roles?: nurses as managers in the NHS. Int J Publ Sector Manag 2003;16:122-30. http://dx.doi.org/10.1108/09513550310467975.
- Gough R, Fitzpatrick M. Reluctant managers: nurses surviving despite the bottom line. N Z J Employ Relat 2004;29:49-66.
- Thorpe K, Loo R. Balancing professional and personal satisfaction of nurse managers: current and future perspectives in a changing health care system. J Nurs Manag 2003;22:400-15.
- Loo R, Thorpe K. Making female first-line nurse managers more effective: a Delphi study of occupational stress. Women Manag Rev 2004;19:88-96. http://dx.doi.org/10.1108/09649420410525298.
- Wise S. Wanted: the next generation of nurse and midwifery managers. Int J Publ Sector Manag 2007;20:473-83. http://dx.doi.org/10.1108/09513550710818368.
- Bergin E. On becoming a manager and attaining managerial integrity. Leader Health Serv 2009;22:58-75. http://dx.doi.org/10.1108/17511870910928029.
- Llewellyn S. ‘Two-way windows': clinicians as medical managers. Organ Stud 2001;22:593-62. http://dx.doi.org/10.1177/0170840601224003.
- Savage J, Scott C. The modern matron: a hybrid management role with implications for continuous quality improvement. J Nurs Manag 2004;12:419-26. http://dx.doi.org/10.1111/j.1365-2834.2004.00511.x.
- Forbes T, Hallier J, Kelly L. Doctors as managers: investors and reluctants in a dual role. Health Serv Manag Res 2004;17:167-76. http://dx.doi.org/10.1258/0951484041485638.
- Sargent P, Pickard S, Sheaff R, Boaden R. Patient and carer perceptions of case management for long term conditions. Health Soc Care Community 2007;15:511-19. http://dx.doi.org/10.1111/j.1365-2524.2007.00708.x.
- Currie G, Koteyko N, Nerlich B. The dynamics of professions and development of new roles in public services organizations: the case of modern matrons in the English NHS. Publ Admin 2009;87:295-311. http://dx.doi.org/10.1111/j.1467-9299.2009.01755.x.
- Wikström E, Dellve L. Contemporary leadership in healthcare organizations: fragmented or concurrent leadership. J Health Organ Manag 2009;23:411-28. http://dx.doi.org/10.1108/14777260910979308.
- Preston D, Loan-Clarke J. The NHS manager: a view from the bridge. J Manag Med 2000;14:100-8. http://dx.doi.org/10.1108/02689230010346411.
- Elina V, Juhani L, Tiina T, Kari M, Irma V, Mauri I, et al. Doctor-managers as decision makers in hospitals and health centres. J Health Organ Manag 2006;20:85-94. http://dx.doi.org/10.1108/14777260610661493.
- Valentino CL. The role of middle managers in the transmission and integration of organizational culture. J Healthc Manag 2004;49:393-404.
- Embertson MK. The importance of middle managers in healthcare organizations. J Healthc Manag 2006;51:223-32.
- Porter S, Anderson L, Chetty A, Dyker S, Murphy F, Cheyne H, et al. Operational competency development in E and F grade nursing staff: preparation for management. J Nurs Manag 2006;14:384-90. http://dx.doi.org/10.1111/j.1365-2934.2006.00628.x.
- Waters D, Clarke M, Ingall A, Dean-Jones M. Evaluation of a pilot mentoring programme for nurse managers. J Adv Nurs 2003;42:516-26. http://dx.doi.org/10.1046/j.1365-2648.2003.02651.x.
- Palfrey C, Thomas P, Phillips C. Health services management: what are the ethical dimensions?. Int J Publ Sector Manag 2006;19:57-66. http://dx.doi.org/10.1108/09513550610640393.
- Merali F. NHS managers' views of their culture and their public image: the implications for NHS reforms. Int J Publ Sector Manag 2003;16:549-63. http://dx.doi.org/10.1108/09513550310500409.
- Management matters: how NHS managers are making a difference. London: NHS Confederation; 2003.
- Crawford P, Brown B. Soft authority: ecologies of infection management in the working lives of modern matrons and infection control staff. Sociol Health Illn 2008;30:756-71. http://dx.doi.org/10.1111/j.1467-9566.2008.01086.x.
- Scott J. Management retention in the NHS. J Manag Med 2002;6:292-30.
- Forbes T, Hallier J. Social identify and self-enactment strategies: adapting to change in professional–manager relationships in the NHS. J Nurs Manag 2006;14:34-42. http://dx.doi.org/10.1111/j.1365-2934.2005.00614.x.
- Carney M. Health service management: culture, consensus and the middle manager. Cork: Oak Tree Press; 2006.
- Dopson S, Fitzgerald L. The role of the middle manager in the implementation of evidence-based health care. J Nurs Manag 2006;14:43-51. http://dx.doi.org/10.1111/j.1365-2934.2005.00612.x.
- Hewison A. Managerial values and rationality in the UK National Health Service. Publ Manag Rev 2002;44:549-79. http://dx.doi.org/10.1080/14616670210164762.
- Cathcart EB, Greenspan M, Quin M. The making of a nurse manager: the role of experiential learning in leadership development. J Nurs Manag 2010;18:440-7. http://dx.doi.org/10.1111/j.1365-2834.2010.01082.x.
- Gould D. The matron's role in acute National Health Service trusts. J Nurs Manag 2008;16:804-12. http://dx.doi.org/10.1111/j.1365-2834.2008.00880.x.
- Doherty C. A qualitative study of health service reform on nurses' working lives: learning from the UK National Health Service. Int J Nurs Stud 2009;46:1134-42. http://dx.doi.org/10.1016/j.ijnurstu.2009.01.014.
- Hallier J, Forbes T. The role of social identity in doctors' experiences of clinical managing. Employee Relat 2005;27:47-70. http://dx.doi.org/10.1108/01425450510569300.
- Cameron D. The NHS will sicken unless we modernise. The Times 2011.
- Cook J, Wall T. New work attitude measures of trust, organisational commitment and personal need non-fulfilment. J Occup Psychol 1980;53:39-52. http://dx.doi.org/10.1111/j.2044-8325.1980.tb00005.x.
- Rose M, Houston DM. Work–life balance in the 21st century. Houndmills, Basingstoke: Palgrave Macmillan; 2005.
- Hewlett SA, Luce CB. Extreme jobs: the dangerous allure of the 70-hour workweek. Harv Bus Rev 2006;84:49-5.
- Making part-time work. London: Medical Women's Federation; 2008.
- Ng TWH, Feldman DC. Long work hours: a social identity perspective on meta-analysis data. J Organ Behav 2008;29:853-80. http://dx.doi.org/10.1002/job.536.
- Pfeffer J. Building sustainable organizations: the human factor. Acad Manag Perspect 2010;24:34-45. http://dx.doi.org/10.5465/AMP.2010.50304415.
- Burke RJ, Fiksenbaum L. Managerial and professional women in ‘extreme jobs': benefits and costs. Equal Opportun Int 2000;28:432-42. http://dx.doi.org/10.1108/02610150910964277.
- Burke RJ, Fiksenbaum L. Are managerial women in ‘extreme jobs' disadvantaged?. Gender Manag 2009;24:5-13. http://dx.doi.org/10.1108/17542410910930716.
- Sergeant A. NHS chief executives: bold and old. London: Hoggett Bowers; 2009.
- Lewis R, Donaldson-Feilder E, Pangallo A. Developing resilience. London: Chartered Institute for Personnel and Development; 2011.
- Cornum R, Matthews MD, Seligman MEP. Comprehensive soldier fitness: building resilience in a challenging institutional context. Am Psychol 2011;66:4-9. http://dx.doi.org/10.1037/a0021420.
- Wrzesniewski A, Dutton JE. Crafting a job: revisioning employees as active crafters of their work. Acad Manag Rev 2001;26:179-201.
- Rousseau DM, Ho VT, Greenberg J. I-deals: idiosyncratic terms in employment relationships. Acad Manag Rev 2006;31:977-94. http://dx.doi.org/10.5465/AMR.2006.22527470.
- Perlow LA. Time to coordinate: toward an understanding of work-time standards and norms in a multicountry study of software engineers. Work Occup 2001;28:91-111. http://dx.doi.org/10.1177/0730888401028001006.
- Clover B. Acute sector faces unprecedented shake-up. Health Serv J 2012:6-7.
- Dowler C. Monitor chair admits it must get tougher. Health Serv J 2012:4-5.
- Review of the involvement and action taken by health bodies in relation to the case of Baby P. London: Care Quality Commission; 2009.
- Laming W. The protection of children in England: a progress report. London: The Stationery Office; 2009.
- Laming W. The Victoria Climbié inquiry. Norwich: Her Majesty's Stationery Office; 2003.
- File on 4: child protection policies. London; 2008.
- Keller S, Meaney M, Pung C. What successful transformations share. Chicago, IL: McKinsey; 2010.
- Walshe K, Higgins J. The use and impact of inquiries in the NHS. BMJ 2002;325:895-900. http://dx.doi.org/10.1136/bmj.325.7369.895.
- Report and accounts 2010. London: The Stationery Office; n.d.
- Sherman J. NHS forced into bailout as damage claims soar. The Times 2012:1-10.
- Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington, DC: Institute of Medicine, National Academy Press; 2000.
- Turner B, Pidgeon N. Man-made disasters. London: Butterworth Heinemann; 1997.
- Reason J. Managing the risks of organizational accidents. Aldershot: Ashgate Publishing; 1997.
- Gardner D. Risk: the science and politics of fear. London: Virgin Books/Random House; 2008.
- McGraw AP, Todorov A, Kunreuther H. A policy maker's dilemma: preventing terrorism or preventing blame. Organ Behav Hum Dec 2011;115:25-34. http://dx.doi.org/10.1016/j.obhdp.2011.01.004.
- Elliott D, Swartz E, Herbane B. Business continuity management: a crisis management approach. London: Routledge; 2010.
- Weick KE. The collapse of sensemaking in organizations: the Mann Gulch disaster. Admin Sci Q 1993;38:628-52. http://dx.doi.org/10.2307/2393339.
- Vaughan D. The Challenger launch decision: risky technology, culture, and deviance at NASA. Chicago, IL: University of Chicago Press; 1996.
- Snook SA. Friendly fire: the accidental shootdown of US Black Hawks over Northern Iraq. Princeton, NJ: Princeton University Press; 2000.
- Perrow C. Normal accidents: living with high-risk technologies. Princeton, NJ: Princeton University Press; 1999.
- Carroll JS. Organizational learning activities in high-hazard industries: the logics underlying self-analysis. J Manag Stud 1998;35:699-717. http://dx.doi.org/10.1111/1467-6486.00116.
- Brown AD. Authoritative sensemaking in a public inquiry report. Organ Stud 2003;25:95-112. http://dx.doi.org/10.1177/0170840604038182.
- Vogus TJ, Sutcliffe KM, Weick KE. Doing no harm: enabling, enacting, and elaborating a culture of safety in health care. Acad Manag Perspect 2010;24:60-77. http://dx.doi.org/10.5465/AMP.2010.55206385.
- Hollnagel E, Woods DD, Leveson N. Resilience engineering: concepts and precepts. Aldershot, Hampshire: Ashgate Publishing; 2006.
- Weick KE, Sutcliffe KM. Managing the unexpected: resilient performance in an age of uncertainty. San Francisco, CA: Jossey-Bass; 2007.
- Mahler JG, Casamayou MH. Organizational learning at NASA: the Challenger and Columbia accidents. Washington, DC: Georgetown University Press; 2009.
- Elliott D. The failure of organisational learning from crisis: a matter of life and death?. J Conting Crisis Manag 2009;17:157-68. http://dx.doi.org/10.1111/j.1468-5973.2009.00576.x.
- Leveson N. A new accident model for engineering safer systems. Saf Sci 2004;42:237-70. http://dx.doi.org/10.1016/S0925-7535(03)00047-X.
- Reason J. Human error: models and management. BMJ 2000;320:768-70. http://dx.doi.org/10.1136/bmj.320.7237.768.
- Qureshi ZH. A review of accident modelling approaches for complex critical sociotechnical systems. Edinburgh, South Australia: Defence Science and Technology Organisation; 2008.
- Rasmussen J. Risk management in a dynamic society: a modelling problem. Saf Sci 1997;27:183-21. http://dx.doi.org/10.1016/S0925-7535(97)00052-0.
- Rasmussen J, Svedung I. Proactive risk management in a dynamic society. Karlstad: Swedish Rescue Services Agency; 2000.
- Vincent C, Taylor-Adams S, Stanhope N. Framework for analysing risk and safety in clinical medicine. BMJ 1998;316:1154-7. http://dx.doi.org/10.1136/bmj.316.7138.1154.
- How safe are clinical systems?. London: The Health Foundation; 2011.
- Nicolini D, Waring J, Mengis J. The challenges of undertaking root cause analysis in health care: a qualitative study. J Health Serv Res Pol 2011;16:34-41. http://dx.doi.org/10.1258/jhsrp.2010.010092.
- Nicolini D, Waring J, Mengis J. Policy and practice in the use of root cause analysis to investigate clinical adverse events: mind the gap. Soc Sci Med 2011;73:217-25. http://dx.doi.org/10.1016/j.socscimed.2011.05.010.
- Horn RE, Weber RP. New tools for resolving wicked problems: mess mapping and resolution mapping processes. San Francisco, CA: Stanford University, Macro VU(r) and Strategy Kinetics; 2007.
- Ross L, Berkowitz L. Advances in experimental social psychology. New York: Academic Press; 1977.
- Rittel HWJ, Webber MM. Dilemmas in a general theory of planning. Pol Sci 1973;4:155-69. http://dx.doi.org/10.1007/BF01405730.
- Weick KE, Roberts KH. Collective mind in organizations: heedful interrelating on flight decks. Admin Sci Q 2003;38:357-81. http://dx.doi.org/10.2307/2393372.
- Vincent C, Benn J, Hanna G. High reliability in healthcare. BMJ 2010;340:225-6. http://dx.doi.org/10.1136/bmj.c84.
- Guth WD, MacMillan IC. Strategy implementation versus middle manager self-interest. Strat Manag J 1986;7:313-27. http://dx.doi.org/10.1002/smj.4250070403.
- Meyer CB. Destructive dynamics of middle management intervention in postmerger processes. J Appl Behav Sci 2006;42:397-419. http://dx.doi.org/10.1177/0021886306289420.
- Sillince J, Mueller F. Switching strategic perspective: the reframing of accounts of responsibility. Organ Stud 2007;28:155-76. http://dx.doi.org/10.1177/0170840606067989.
- Bower JL. Managing the resource allocation process. Boston, MA: Graduate School of Business Administration, Harvard University; 1970.
- Kanter RM. The middle manager as innovator. Harv Bus Rev 1982;60:95-105.
- Wooldridge BJ, Floyd SW. The strategy process, middle management involvement, and organizational performance. Strat Manag J 1990;11:231-41. http://dx.doi.org/10.1002/smj.4250110305.
- Floyd SW, Wooldridge B. Middle managers' strategic influence and organizational performance. J Manag Stud 1997;34:465-85. http://dx.doi.org/10.1111/1467-6486.00059.
- Rouleau L, Balogun J. Middle managers, strategic sensemaking, and discursive competence. J Manag Stud 2011;48:953-83. http://dx.doi.org/10.1111/j.1467-6486.2010.00941.x.
- Boyett I, Currie G. Middle managers moulding international strategy: an Irish start-up in Jamaican telecoms. Long Range Plann 2004;37:51-66. http://dx.doi.org/10.1016/j.lrp.2003.11.009.
- Mair J. Exploring the determinants of unit performance: the role of middle managers in stimulating profit growth. Group Organ Manag 2005;30:263-88. http://dx.doi.org/10.1177/1059601104269113.
- Kuratko DF, Goldsby MG. Corporate entrepreneurs or rogue middle managers?: a framework for ethical corporate entrepreneurship. J Bus Ethics 2004;55:13-30. http://dx.doi.org/10.1007/s10551-004-1775-3.
- Balogun J. When organisations change: a middle management perspective on getting it right. London: Advanced Institute of Management Research; 2008.
- West M, Johnson R. A matter of life and death. People Manag 2002;8:30-6.
- Santry C. Quality strongly linked to increase in managers. Health Serv J 2010:4-5.
- Hutton J, Callow C. NHS leaders are key to innovation. Health Serv J 2010.
- Purcell J, Kinnie N, Hutchinson S, Rayton B, Stuart J. Understanding the people and performance link: unlocking the black box. London: Chartered Institute for Personnel and Development; 2003.
- Michie S, West M. Managing people and performance: an evidence based framework applied to health service organizations. Int J Manag Rev n.d. http://dx.doi.org/10.1111/j.1460-8545.2004.00098.x.
- Bloom N, Van Reenen J. Why do management practices differ across firms and countries?. J Econ Perspect 2010;24:203-24. http://dx.doi.org/10.1257/jep.24.1.203.
- West M, Dawson J, Admasachew L, Topakas A. NHS staff management and health service quality. London: Department of Health; 2011.
- West M, Guthrie JP, Dawson AF, Carter M. Reducing patient mortality in hospitals: the role of human resource management. J Organ Behav 2006;27:983-1002. http://dx.doi.org/10.1002/job.396.
- Burns T, Stalker GM. The management of innovation. London: Tavistock Publications; 1961.
- Kanter RM. The change masters: corporate entrepreneurs at work. London: George Allen & Unwin; 1983.
- Buchanan DA, McCalman J. High performance work systems: the digital experience. London: Routledge; 1989.
- Lawler EE, Mohrman SA, Ledford GE. Strategies for high performance organizations. San Francisco, CA: Jossey-Bass; 1998.
- Huselid MA. The impact of human resource management practices on turnover, productivity, and corporate financial performance. Acad Manag J 1995;38:635-72. http://dx.doi.org/10.2307/256741.
- Pfeffer J. The human equation: building profits by putting people first. Boston, MA: Harvard Business School Press; 1998.
- Guest D, King Z. Personnel's paradox. People Manag 2001;7:24-9.
- Thorlby R, Mabin J. A high performing NHS?: a review of progress 1997–2010. London: The King's Fund; 2010.
- Mannion R, Davies H, Harrison S, Konteh F, Greener I, McDonald R, et al. Changing management cultures and organizational performance in the NHS. London: Queen's Printer and Controller of HMSO; 2010.
- Haq L. Lead from the middle. Health Serv J 2011:23-5.
- Davenport TO, Harding SD. The manager redefined: the competitive advantage in the middle of your organization. San Francisco, CA: Jossey-Bass; 2010.
- Hurst J, Williams S. Can NHS hospitals do more with less?. London: Nuffield Trust; 2012.
- Kaiser RB, Hogan R, Craig SB. Leadership and the fate of organizations. Am Psychol 2008;63:96-110. http://dx.doi.org/10.1037/0003-066X.63.2.96.
- Gronn P. Distributed leadership as a unit of analysis. Leader Q 2002;13:423-51. http://dx.doi.org/10.1016/S1048-9843(02)00120-0.
- Gronn P. Leadership configurations. Leadership 2009;5:381-94. http://dx.doi.org/10.1177/1742715009337770.
- Hernandez M, Eberly MB, Avolio BJ, Johnson MD. The loci and mechanisms of leadership: exploring a more comprehensive view of leadership theory. Leader Q 2011;22:1165-85. http://dx.doi.org/10.1016/j.leaqua.2011.09.009.
- Denis J-L, Langley A, Rouleau L. Strategizing in pluralistic contexts: rethinking theoretical frames. Hum Relat 2007;60:179-215. http://dx.doi.org/10.1177/0018726707075288.
- Fitzsimons D, James KT, Denyer D. Alternative approaches for studying shared and distributed leadership. Int J Manag Rev 2011;13:313-28. http://dx.doi.org/10.1111/j.1468-2370.2011.00312.x.
- Martin GP, Currie G, Finn R. Leadership, service reform, and public–service networks: the case of cancer-genetics pilots in the English NHS. J Publ Admin Res Theor 2009;19:769-94. http://dx.doi.org/10.1093/jopart/mun016.
- Currie G, Lockett A. Distributing leadership in health and social care: concertive, conjoint or collective?. Int J Manag Rev 2011;13:286-300. http://dx.doi.org/10.1111/j.1468-2370.2011.00308.x.
- Atkinson S, Spurgeon P, Clark J, Armit K. Engaging doctors: what can we learn from trusts with high levels of medical engagement?. Coventry: NHS Institute for Innovation and Improvement; 2011.
- Klaber B, Lee J, Abraham R, Lemer C, Smith L. How pairing clinicians with managers could speed up clinical excellence. Health Serv J 2011:21-3.
- Currie G, Grubnic S, Hodges R. Leadership in public services networks: antecedents, process and outcome. Publ Admin 2011;89:242-60. http://dx.doi.org/10.1111/j.1467-9299.2011.01931.x.
Appendix 1 Research protocol
Research protocol Version 1: 09.02.2009
Cranfield University
School of Management and Cranfield Health
NHS National Institute for Health Research Service Delivery and Organization Research Programme
241 Management Practice in Healthcare Organizations: proposal #0001926
How do they manage?: research protocol
A study of the realities of middle and front line management work in healthcare
Three and a half years, starting January 2009
Research team:
Professor David A. Buchanan
Dr Catherine Bailey
Dr David Denyer
Dr Clare Kelliher
Ms Cíara Moore
Dr Janice Osbourne
Dr Emma Parry
Dr Colin Pilbeam
Dr Janet Price
Professor Kim Turnbull-James
Dr Charles Wainwright
Scientific summary
Managers constitute 3 per cent of the NHS workforce. That figure underestimates the impact of management practice on clinical outcomes, quality of patient care, and organizational performance. The NHS has concentrated on senior leadership, and less is known about the experience and attitudes of middle and front line managers in acute care, who are the focus of this project. Exploring the realities of management work, their role in change, and links between practice and performance, this study has four aims.
The first is to contribute to the practice and theory of healthcare management in order to improve patient care and organizational performance. The second is to provide evidence-based guidance for management development, strengthening the impact of management practices on hospital performance, streamlining the implementation of changes following adverse events in the interests of patient safety.
These first two aims will be achieved with new perspectives, approaches, frameworks, diagnostics, methods, tools, and processes based on new evidence. We will identify the organizational features that support managers in contributing to clinical and corporate performance, building an ‘enabling environment’.
Our third aim is to engage stakeholders as co-researchers through our collaborative research design. In addition to respondent validation, this approach will develop ‘high impact’ channels for communicating the implications of findings. Our final aim is to develop the theory of managing, synthesizing current models, theories of distributed leadership, and processual-contextual perspectives on change.
Our collaborative research design involves six acute trusts over six stages: (1) set up (research assistant, background information, literature review, ethical approval), (2) management focus groups, (3) management survey concentrating on the themes of realities, changes, and contributions, with 60 per cent of items common for all sites for comparison, and 40 per cent based on local trust issues and priorities, (4) management briefings to check findings, explore implications, consider diffusion mechanisms, and identify cases for the next stage, (5) case studies of change following adverse incidents, and (6) publication and knowledge transfer. We will also track changes in the management role in one PCT, linked to one of the acute sites, exploring through interviews with a small number of key informants (middle and senior managers) the implications for inter-organizational relationships, and the impact on acute management roles. Research methods thus include document analysis, focus groups, self-report survey questionnaires, interviews, and case studies of ‘extreme change’. Analysis methods include context profiling, content analysis, statistical analysis, visual mapping, event sequence analysis, and ideas capture from briefing groups.
Outcomes can be measured in terms of service impact. For patients and service users, this concerns management practices that will improve quality of care and clinical outcomes, and rapid changes following ‘extreme’ events leading to improved patient safety. For middle and front line managers, this means a better understanding of how the role is evolving, new competency requirements, methods for influencing clinical and organizational outcomes, and techniques for managing ‘extreme’ change. For senior managers, we will provide guidance on management development and support needs, and advice on developing an ‘enabling context’ for the management impact on clinical, organizational outcomes, and change. For policy makers, this research will deliver a model of management work, explaining the demands and pressures, the new competencies required, the contributions to change and performance outcomes, and the implications of extending clinical engagement in management.
Lay summary
How do hospital managers handle the pressures and demands of a constantly changing health service? What effect do managers have on the quality of patient care and the outcomes of treatment? We know little about the work experience and attitudes of hospital managers, but when things go wrong, this is the group which usually takes the blame. Patient safety is a national priority, and we particularly want to find out how changes to working practices are managed after serious incidents. This can be a problem, as the advice of enquiries, in health and elsewhere, can often sit on the shelf. This study will build on what we already know about the realities of middle and front line management work and organizational change. We will collect the information we need using focus groups, a survey, and interviews which will enable us to develop case studies of serious incidents and the changes to which they lead. We will also ask the middle and front line managers involved in this study to help us with the design of the survey, and with choosing examples of serious incidents. As participating managers are among the main users of the findings from this project, we will ask them to check our understanding of the data, and to help us to develop novel ways to communicate the implications, so that this work does have an impact on management practice. The study will do this through advice on management support and development based on a better understanding of how managers work and of the factors that are shaping their roles. We will look at how managers can contribute more effectively to the quality and outcomes of patient care as well as to overall hospital performance. And we will develop guidelines for effectively implementing changes to healthcare working practices.
Details of research proposal
Introduction, aims and objectives
This project will address three related sets of questions:
-
Realities: What are the new pressures and demands facing middle and front line managers in healthcare? What are the implications of these trends? How do managers cope with shifting priorities and expectations?
-
Changes: What roles do middle and front line managers play in implementing changes? How are changes arising from adverse events implemented, and how can this process be improved?
-
Contributions: How does management practice affect clinical and organizational outcomes? What factors influence the management contribution to performance? How can the components of an ‘enabling environment’ for the management contribution be assembled and sustained?
What we don't know
The service has invested in senior management (Department of Health, 2002). We know less about the working lives of middle and front line managers; the motives and rewards, the challenges and tensions, how the job is changing, and new capabilities required. But when things go wrong, here is the group which often attracts most of the criticism.
Managing realities: we don't know whether or how today's novel pressures and demands are affecting the realities of middle and front line management work in acute settings, or the nature of the attributes and competencies required in these roles. But we do seem to understand the main components of traditional general management roles (Mintzberg, 1994).
Managing change: we don't know why, following ‘extreme’ or adverse events, inquiry recommendations sit on a shelf, but are sometimes adopted rapidly. But implementing change is a key aspect of middle and front line management work, and we do seem to understand many aspects of ‘normal’ change in healthcare (Locock, 2001).
Managing contribution: we don't know how middle and front line managers influence organizational and clinical outcomes, through change implementation and other dimensions of the role, or what would reinforce that contribution. But we assume that management practice is fundamental (Christian and Anderson, 2007).
We will thus follow ‘the chain of evidence’ from management realities, through change, to outcomes, focusing on middle and front line managers in acute care. ‘Middle and front line’ refers to management posts below trust board level, including career managers, clinical staff in ‘hybrid’ managerial roles, and medical staff who perform management and leadership functions (Department of Health, 2008). This embraces ward sisters, consultants, general managers, and clinical directors. While management in primary care is important, this is not a major theme in this project. PCT managers now focus on commissioning rather than delivering care, and SDO is funding separate research into commissioning. However, we are considering a PCT case study, proposed by a participating acute trust, focusing on changes in the primary care management role, implications for inter-organizational relationships, and the impact on management in acute settings.
Objective and aims
Our overarching objective is to make a difference, contributing to the practice and theory of healthcare management to improve patient care and organizational performance. Our first aim is to generate fresh evidence, concerning managing realities, changes, and contributions. Our second aim is to develop evidence-based guidance (tools, perspectives, frameworks, diagnostics, methods, approaches, processes), informing management development, identifying factors jeopardizing and facilitating change, and enhancing the links from management practice to organizational and clinical outcomes. Our third aim is to engage stakeholders in the development of actionable knowledge, through our collaborative research design, disseminating implications by using our advisory board structure and participants to develop innovative communication modes and channels. Our fourth aim is to contribute to the theory of managing, by synthesizing and building on current thinking with regard to models of the management role, theories of distributed leadership and change agency, and processual-contextual perspectives on organizational change and service improvement.
Managing realities
Middle and front line managers face new pressures and demands; what are the implications? Managers, the textbook says, keep things running as they are, while leaders drive change; administrators versus innovators. Managers at all levels in the NHS may be excused a cynical response to this distinction, having implemented a series of major changes affecting all aspects of the service – culture, structures, priorities, governance, working practices – and more. The NHS Operating Framework for 2008/09 and the Next Stage Review continue the theme of transformation (Department of Health 2007; 2008). Following Next Stage, medical training will include management and leadership skills as a matter of routine. How do healthcare managers – professional and clinical – cope with a broad, diverse, and shifting agenda of competing priorities and expectations, and serial change generating ‘reform fatigue’ (Leatherman and Sutherland, 2008)? How do middle and front line managers cope with this challenging and sometimes contradictory context?
Managing changes
There is a perception that healthcare is ‘different’, and that the management of change is problematic (Øvretveit and Aslaksen, 1999). This has led to a renewed emphasis on medical engagement in leadership and change (NHS Institute, 2008; Hamiltonet al., 2008). Nevertheless, many of the goals of The NHS Plan have been achieved, switching priorities away from finance and waiting times to quality of care, access, patient and public involvement, and patient safety (Department of Health, 2007). Recent studies show that many radical changes are implemented, not by small groups of senior managers and doctors, but by middle managers and other staff. With the emphasis on patient safety (a core standard; Healthcare Commission, 2007), we will explore the processes of change which follow extreme, adverse, or ‘sentinel’ events, such as accidents, misconduct, and other serious untoward incidents. Considerable efforts are often expended to learn the lessons from such incidents, but those lessons are not always implemented (Donaldson, 2000; Healthcare Commission, 2008). These issues have rarely been investigated from a change management perspective. We will remedy this oversight, linked to a separate cross-sectoral Cranfield project in this area. This is an area in which improved understanding will significantly benefit practice and patients (Shortellet al., 2007).
Managing contributions
How does management practice influence clinical and organizational outcomes? Managerial effectiveness is a slippery concept, stakeholders have competing views (Micheli and Neely, 2006), and assessing the impact of single practices on specific results is problematic. Nevertheless, research suggests a systemic link to outcomes (Westet al., 2002; Boyneet al., 2006). While management competencies and practices are key, organizational context is also crucial, in determining receptiveness (Pettigrewet al., 1992), setting priorities and incentives, focusing attention and energy, and establishing an environment that either enables or stifles service improvement. What does an ‘enabling environment’ look like, and how can the components of this environment be assembled and sustained?
Relevance to SDO call for proposals
Our project focuses on the ‘realities of management’ theme (iii); ‘work life, roles and behaviours’, addressing priorities identified by Christian and Anderson (2007, p. 19) who concluded that, ‘Management issues were seen as a fundamental determinant of organizational performance: in particular the importance of different management practices; the competency of managers to fulfil their roles; the ability to link in with front-line staff; and involving key figures in proposed changes’. We will explore related themes, such as clinical–managerial relationships, decision-making, and knowledge utilization (Rousseau, Manning and Denyer, 2008; David Denyer, is a member of the American evidence-based management collaborative established by Denise Rousseau). But a better understanding of managing realities, changes, and contributions are where this research will have the most significant impact on organizational performance, and quality and outcomes of patient care.
A second intent of this call for proposals is to promote exchange between academic and practitioner communities. Our project engages participating managers throughout the research process, from developing this proposal, through advising on the collection and interpretation of data, to developing implications for practice, and disseminating findings.
Background; NHS context and relevant literature
Of the 1.3 million employees in the NHS in England, there are approximately 36,500 managers, less than 3 per cent of the total (The Information Centre, 2007). That probably underestimates the number of staff who as part of their role perform management functions. And that percentage understates the significance of management contributions to performance. The desire to engage medical staff in management and leadership dates from the 1980s, and has achieved new urgency in current proposals, such as the ‘medical leadership competency framework’ approved by the Academy of Medical Royal Colleges (NHS Institute, 2008; Hamiltonet al., 2008). In the context of the theoretical underpinning explained shortly, it is interesting to note that John Clark (Clarket al., 2008, p. 33), director of the Enhancing Engagement in Medical Leadership project observes that, ‘Enhanced clinical engagement should work towards a model of diffused leadership, where influence is exercised across a complex set of relationships, systems and cultures. It is a set of behaviours that should apply to all rather than a few’.
Although the Next Stage Review promises ‘no new targets’, the change agenda is sustained. Lord Darzi focuses management attention on accelerating the pace of change with regard to quality of care (linked to funding), patient choice, personalized budgets and care plans, and integrated care, complemented by clinical and board leadership programmes (Department of Health, 2008). The Operating Framework for 2008/09, noting a shift in emphasis away from finance and waiting times, declares an ‘ambitious new chapter’ in the transformation of the NHS, focusing on other issues including patient safety, access, better health and reduced inequalities, improving the patient experience and staff satisfaction, and enhanced emergency preparedness; not a recipe for stability (Department of Health, 2007). These aspirations will be achieved by empowering local management and staff to deliver with less central direction.
The Operating Framework also makes clear (p. 32) that the status of Foundation Trust is no longer an aspiration, but an expectation for all. The governance arrangements of Foundation Trusts, particularly with service line reporting, mean that trusts, and their clinical services, run like businesses. Plans and decisions are now commonly couched in commercial discourse; business units, customers, competitors, marketing (‘promotion of services’), cost allocations, profitability, portfolio analysis, mergers and acquisitions, business development (e.g., Shepherd, 2008). This reflects values different from those that have inspired a publicly funded healthcare system for the past 60 years. Our anecdotal evidence indicates that managers generally welcome these developments, but that many clinical staff remain sceptical. There is evidence to suggest that these changes are creating new tensions (Sambrook, 2005). It is in this dynamic context of the ongoing – accelerating – transformation of healthcare that this study is positioned.
Realities
Broadly, we think we understand what managers do; roles (Mintzberg, 1973; 1994), realities (Stewart, 1997), rewards and pains (Watson, 1994), how they spend their time (Kotter, 1999). But is that knowledge relevant to healthcare management today? Previous research into management roles is mainly ethnographic, using observational methods. Hales (1999) criticizes work which describes management without a theory of managing. Our aim is to understand the links between the realities and the contributions of management work. This will take the form of a multilevel perspective synthesizing three theoretical lenses (Watson, 1997). First, frameworks such as Mintzberg (1994) are a useful starting point, highlighting the interaction between values, competencies and style, role purpose, managing information, people and action, and the wider context. This model assumes a manager responsible for a single unit, a situation that does not always apply in the collaborative, process-driven, network organizational forms common in healthcare, where managing across internal and external boundaries is increasingly important. This model is silent concerning the links from management practices to outcomes; the ‘well rounded’ manager is presumably effective. Second, theories of distributed leadership (Gronn, 2002) draw attention to the fluid contributions to change at all levels (Bailey and Burr, 2005; Buchananet al., 2007a). Third, process explanations consider how factors at different levels of analysis interact over time to shape outcomes (Langley, 2009). This perspective views ‘context’ not as a neutral stage on which action unfolds, but as shaping conditions, events, interactions, and outcomes by enabling, constraining, and predisposing (Fitzgeraldet al., 2002).
Changes
Recent studies undermine the distinction between leaders who drive change and managers who maintain order, portraying middle management roles in strategy, and in change ‘by stealth’ and ‘under the radar’ (Floyd and Wooldridge, 1996; Huy, 2002; Badaracco, 2002). The development of distributed change leadership, based on the spontaneous concertive action of staff at all levels, is evident in healthcare (Brooks, 1996; Lüscher and Lewis, 2008). From a recent SDO project, Buchananet al. (2007b) describe a distributed approach to service improvement in the treatment of prostate cancer involving large numbers of staff across the cancer network organizations. Contradictory anecdotal evidence suggests that middle managers follow directions, and have little input into the design of change, focusing on the immediate and the tactical, but there is no robust evidence concerning middle and front line management experience and perceptions. Implementing change following extreme, adverse or ‘sentinel’ events, such as accidents, misconduct, and other serious incidents, is often problematic. We don't know why this is so, although this affects patient safety. Consequently, we will focus on these events, rather than develop yet another ‘n-step guide’ to ‘normal’ change (Collins, 1998). Donaldson (2000) recognized the gap between passive learning (establishing the lessons) and active learning (embedding new practices). But in a recent report, he observes that ‘the pace of change has been too slow’ and that ‘we need to redouble our efforts to implement systems and interventions that actively and continuously reduce risk to patients’ (Department of Health, 2006, p. 4).
Our preliminary working definition of an ‘extreme event’ is an incident that suggests the need for significant organizational changes in order to prevent or to reduce the probability of a recurrence. When extreme events occur, the focus tends to lie with establishing cause, attributing blame, and remedy. Once recommendations from an enquiry are published, attention fades. Research has mirrored this profile of concern. There are studies of the ‘incubation phase’, (Turner and Pidgeon, 1997), the causes of ‘normal accidents’ (Perrow, 1999; Vaughan, 1999), the ‘critical period’ (Stein, 2004), sensemaking in crises (Weick, 1993), crisis management (Lagadec, 1997; Lalonde, 2007), ‘high reliability organizations’ (Weick and Roberts, 2003), and the role of public inquiries (Brown, 2000; 2003). The implementation phase has attracted less attention, and studies of extreme events from a change management perspective are lacking (although much can be learned from outliers; Pettigrew, 1990). Research on avoiding wrong site surgery is instructive, Rogerset al. (2004) noting that guidelines are inconsistently implemented because of the failure to account for the complex operating theatre environment. Linked to a separately funded cross-sectoral study with overlapping project team membership, we will explore the conditions that respectively block and promote ‘active learning’ and change in such contexts.
Contributions
Building on the concept of the ‘receptive context’ for change (Pettigrew et al., 2002), we will identify the clusters of factors that respectively stifle and strengthen the contributions of middle and front line managers to clinical and organizational outcomes. We will identify the features of an ‘enabling environment’, and explore how these differ within and across acute care settings. Identifying the impact of management practices and changes on organizational performance is problematic (Iles and Sutherland, 2001). This is due to the systemic nature of the links between actions and outcomes (Westet al., 2002), to the multiplicity of stakeholders, and to the socially constructed nature of ‘effectiveness’. Understanding these links requires a process perspective, in contrast with traditional variance explanations (Mohr, 1982; Langley 1999 and 2009; Van de Ven and Poole, 2002; Buchanan and Dawson, 2007). Process explanations demonstrate how antecedents lead, in particular contexts, to outcomes over time. The concept of ‘conjunctural causality’ involves identifying the clusters, combinations, or configurations of factors that explain the consequences of interest (Armenakis and Bedeian, 1999; Goldstone, 2003; Walkeret al., 2007; Fitzgerald and Buchanan, 2007). A recent review of research concerning contributions to service improvement through medical engagement in management revealed little positive impact, but demonstrated how lack of such engagement is problematic (Ham and Dickinson, 2007).
Plan of investigation
Research design
Collaborative research designs, although not without problems, have been shown to be effective in translating research into practice in healthcare (Denis and Lomas, 2003), and allow for local tailoring of data collection. User engagement contributes to the development and dissemination of findings, and to building research capacity among those involved. This design combines quantitative and rich idiographic data, enabling within-organization, cross-organization, cross-occupation and other comparisons. Outputs will be generated at each stage, not just at the end of the project. This is a six-stage multi-methods collaborative design involving six hospitals and one primary care trust. The acute sites display geographical spread, including Foundation and non-Foundation Trusts. We may add trusts with wider variance in financial challenge, population characteristics, and local competition, for the survey described in the methods section.
Advisory groups
We require a sounding board involving concerned and passionate individuals who will learn with us while contributing their ideas and insights. So, we will establish a two-tier advisory group. Tier one includes four healthcare managers and two independent academics, meeting quarterly. Tier two is a virtual group, with 20 managers and clinical staff drawn from our national, regional, and local networks, and with whom contact will be maintained by telephone, e-mail, WebEx, and our project website. These two groups will advise on project methods and focus, access to stakeholder networks, interpretation of findings, applications, and dissemination. The combination of Operating Framework priorities, SHA visions, Local Area Agreements, Next Stage Review, and other national initiatives implies that management structures and roles in place as this research unfolds may differ from configurations at the proposal stage. Management practice in healthcare is a moving target, and our sounding board will ensure that this study sits at the cutting edge of practice and theory.
Research methods
This is a multi-methods collaborative project using local participation, focus groups, surveys, documentation, performance data, case exemplars based on documentation and interviews, and management briefings. We will engage participants as co-researchers, in survey questionnaire design, case selection, data analysis and interpretation, exploring implications for management practice, and developing innovative methods for disseminating findings.
Stage 1a (3 months) pre-research administration activity
The first three months of this project will involve:
-
obtaining multi-centre and trust ethical approvals – we will seek approval for the study as a whole, then submit the questionnaire design as an amendment;
-
recruiting, orienting, and equipping our research assistant;
-
conducting a systematic review of the literature on middle and front line healthcare management, the management of ‘extreme’ change in healthcare, and models of management contributions to healthcare organization outcomes;
-
recruiting members of our advisory groups;
-
establishing links with other research teams working on similar questions;
-
designing and establishing the project website.
Stage 1b (three months) site briefing and set-up processes
The second three months of this project will involve:
-
the collection of background information on our research sites through internet downloads and informal meetings;
-
acute trust liaison and briefing meetings with senior management to establish working contacts along with administrative and logistical arrangements;
-
setting up the primary care case study, identifying up to five key informants (middle and senior managers), collating background documentation, arranging site visits (four to six over two and a half years), linking with other SDO research in this domain.
Stage 2 (6 months) Management focus groups
We will run three or four focus groups at each of the six acute trusts. Aiming for attendance of around 8 at each focus group meeting, this procedure will involve between 150 and 200 managers who will help us to understand new and emerging themes, pressures, trends and developments affecting middle and front line management in general, and in particular with regard to local management needs, issues, and priorities. The findings from these focus groups, at each site, in aggregate, and considering cross-site comparisons, will thus inform the subsequent survey design, and will constitute data in their own right, on the changing nature of middle and front line management work.
Stage 3 (9 months) The 60-40 Survey
This survey questionnaire will generate evidence on the nature of new and emerging management pressures and demands, and the implications for management practice, for management development and support, and for a theory of managing. Capturing experiences and attitudes, we will survey the middle and front line management populations (around 1,500 total) in our participating acute trusts. We will use a ‘60-40’ design, in which approximately 60 per cent of survey items will be common to all sites, for comparison and benchmarking purposes, and 40 per cent will be tailored to local priorities following the advice of the management focus groups. As well as the content, the percentages of common and tailored items are likely to vary between sites, and these variations will in turn provide further useful insights. The time allocated to this stage of the project reflects the workload involved in administering the survey, and then collecting, coding, and analysing the data. Subject to participant input and local tailoring, indicative themes are likely to include:
Biodata
-
survey responses will be anonymous and the data confidential
-
standard biodata to permit a range of within-sample comparisons
-
background; healthcare, other public sector, commercial, clinical, armed forces
-
and current role; managerial, hybrid, clinical with management duties
Managing realities
-
values, attitudes, motives, priorities
-
new pressures, demands, patterns of activity, and fresh emphases shaping the work
-
changing personal attributes and competency requirements
-
the management support and development implications of current trends
Managing changes
-
effect of professional barriers and multidisciplinary teams on service improvement
-
management attitudes to innovation, growth, and risk
-
what factors block effective implementation of service improvement
-
change issues arising in implementing the lessons from extreme events
Managing contributions
-
is there a medical–managerial divide over what constitutes ‘performance’
-
which practices, methods, perspectives make a difference
-
what barriers must be removed to strengthen the impact of management practices
-
does an ‘audit and compliance’ context stifle innovation
These themes will be elaborated through participant collaboration in focus groups, to ensure that the survey addresses local needs and priorities as well as the overall research objectives.
Stage 4 (3 months) Management briefings
It is important that research participants have an early opportunity to assess the findings and their implications. At this stage, findings will be presented to volunteer management focus groups at each site, with five objectives. First, for respondent validation. Second, to check interpretations. Third, to develop practical implications. Fourth, to explore innovative modes of dissemination. Fifth, to identify exemplars case studies for stage 5.
Stage 5 (6 months) Managing extreme events
These case examples will improve our understanding of change processes following adverse or ‘extreme’ incidents, and help develop practical diagnostics and frameworks. We will ask briefing groups to identify six incidents, nominally one in each acute trust. The main case selection criterion concerns opportunity to learn about the conditions in which changes following an extreme incident are either straightforward, or problematic, respectively. Through interviews and documentation, we will identify factors contributing to the outcomes. Although a small sample, we will develop moderatum generalizations (Williams, 2000), and contribute to theory through analytical refinement (Tsoukas, 2009). Recognizing the sensitivities and emotions potentially surrounding such events, discussions with potential study sites suggest that research in this area is less problematic than might appear, for several reasons. First, significant relevant information is often already in the public domain. Second, our focus lies with the subsequent management of change, and not with conducting fresh investigations. Third, the desire for individual and organizational learning is often strong and unmet. Fourth, those who have been involved often welcome an opportunity confidentially and anonymously to share their thoughts and experiences. Fifth, we will include successful examples of change following extreme incidents, as equally valuable learning opportunities. Finally, events may have occurred in the past, allowing emotions and sensitivities to subside.
Stage 6 (6 months) publication and knowledge transfer
We will engage our advisory groups and the management participants in this project – the end users of the results – in a series of informal exchanges and where possible face to face meetings, to help develop innovative modes of dissemination (beyond professional journals, academic articles, and lengthy reports). We recognize the need to develop high impact, readily accessible modes of communication, which retain the integrity, and where appropriate the complexity, of the issues at stake and the implications for practice. The main analytical approaches and techniques that we will deploy at each stage, what we will be looking for, and the anticipated contributions to each of the project's three main themes – realities, changes, and contributions – are summarized in Table 1. In addition to this structured approach, we will be looking for the surprising, the unexpected, the ‘outliers’ in these data streams, and we will be considering what fresh insights – practical and theoretical – these are likely to reveal.
| Stage, link to themes | Analysis, what will this tell us |
|---|---|
| 1. Set-up | Context profiling, of participating trusts based on background documentation, key organizational and environmental factors |
| Managing realities | Outcomes: identify local priorities, dimensions of within- and cross-site variations, factors potentially shaping management realities |
| Primary care case | Thematic case report documenting two-year period |
| Outcomes: changes in management role in primary care, implications for inter-organizational relationships, impact on acute management | |
| 2. Focus groups | Content analysis, of discussion and key themes |
| Managing realities | Outcomes: identify recurring patterns of emerging themes, pressures, trends, emphases, and developments affecting middle and front line management; deeper understanding of local needs and priorities, identify idiosyncratic, unexpected, ‘outlier’ themes |
| Managing change | |
| 3. 60-40 survey | Statistical analysis, frequency distributions and crosstabs (ordinal and nominal data); coding and content analysis of open responses |
| Managing realities | Outcomes: sample characteristics, motives and values, incidence and experience of new challenges and trends, factors and practices impacting effectiveness, components of ‘enabling’ and ‘disabling’ environments for management work, changing patterns of management activity, comparisons of attitudes and experience controlling for age, experience, gender, current role, background, service area and/or function, cross-site comparisons, cross-occupational (e.g., medical-managerial) perceptions and relationships, site-specific findings, unexpected ‘outlier’ results |
| Managing change | |
| Managing contribution | |
| 4. Briefing groups | Content analysis, of discussion and key themes |
| Managing contribution | Outcomes: respondent validation, practitioner check on analysis and interpretations, explore management implications, capture dissemination ideas, identify case exemplars for next stage |
| 5. Extreme events | Visual mapping and event sequence analysis, of incident narratives |
| Managing change | Outcomes: identify recurring success and problem patterns in extreme change processes, development of conjunctural explanations, contingency management framework based on cross-case comparisons of incidents and following contexts |
| Managing contribution | |
| 6. Knowledge transfer | Ideas capture |
| Managing contribution | Outcomes: clarify and strengthen implications for management practice, develop high impact communications methods, range of publications, briefing seminars and documents, management development and support programmes |
Data collection and management procedures
This section explains the project data collection and handling arrangements, explaining how ethical issues arising from this study will be addressed.
Informed consent, confidentiality, and right to withdraw
The methods used for data collection in this study involve a combination of focus groups, self-report survey, and qualitative case studies based on interviews and document analysis. These are standard organizational research methods, which are appropriate to the research aims, organizational context, and participants. The participants are all middle and front line hospital managers, with a small number of senior managers serving as gatekeepers to the study in their respective organizations. There is no direct or indirect patient involvement. The primary ethical issues thus concern informed consent, anonymity and confidentiality, and the right to withdraw from the study at any time without question.
Informed consent will be addressed in two ways. First, all potential participants will be given detailed participant information sheets. Given the duration of the project, and the different methods that will be used, separate information sheets will be distributed prior to the different stages of the project, explaining both the aims and methods of the project as a whole, and the specific purpose and nature of the focus groups, survey, briefing groups, and case interviews respectively (appended). Where possible and appropriate, distribution of information sheets will be prefaced by a question-and-answer briefing, organized by the management gatekeepers at each site, and delivered by a member of the research team, explaining the aims and methods of the study, guaranteeing anonymity and confidentiality, and explaining the right to withdraw. Second, participation in this study is voluntary, at the discretion of individual managers. The time that will elapse between receipt of the participant information and the scheduling of the corresponding data collection will be a minimum of one week.
Individuals taking part in focus and briefing groups and in interviews in the course of this project will sign consent forms; appropriately amended versions of these consent forms will be used (appended). Signed consent will be obtained by the research team member on the day of each meeting, prior to which potential participants will have already seen the project participant information sheet. The first question that members of the research team will always ask will concern further questions about the project which participants may have before data collection begins. As consent forms will disclose individual identities, these will be stored in a locked drawer in an administrative office which is permanently staffed during working hours (two staff members take breaks in turn), and which is locked outside working hours (and is also locked if for some reason both members of staff need to be absent at the same time). Consent forms will be destroyed at the end of the project.
Anonymity and confidentiality will be guaranteed in two ways. First, data will be reported in aggregate. The organizations involved in the study will be give pseudonyms (‘Loamshire NHS Trust’) unless permission is granted in writing to use the organization's real name. Where verbatim quotes from individuals are used to illustrate findings, these will be anonymised (‘a manager said’) and identity cues will be omitted. Second, project data will be stored on password-protected Cranfield University computers, and individual comments will not be stored in electronic files with attributable names. Transcripts of group meetings and interviews, and files containing other sensitive information, will be stored in a password-secured project folder on the School of Management server, which itself can only be accessed (locally or remotely) with a separate username and password. There will therefore be no need for research team members to exchange files by e-mail or to store files on usb memory, both of which pose potential data security risks.
Cranfield School of Management carries professional indemnity insurance for research staff, giving participants in this study a legal remedy should breach of confidence occur. The right to withdraw is explained clearly and unambiguously in the participant information sheets, and decisions to withdraw will be respected without question.
Participants’ time commitment
Focus group meetings will each last around one hour. Self-report survey questionnaire completion will take approximately thirty minutes. Briefing group meetings will each last around one hour. Case study interviews will each last around one hour; depending on how each case study develops, we may ask a small number of participants for a follow-up interview (conducted under the same conditions as the first interview), again lasting for up to an hour. Interviews for the primary care study will last from half an hour to one hour each. A small number of participants may be involved in focus groups, survey, briefing groups, and case study interviews; for those participants, the total time commitment to this project over three years would be approximately three and a half hours (four and a half hours if a re-interview were requested and consent given). For most participants, however, participation in this study is likely to involve one procedure only, lasting from half an hour to one hour. For the primary care study, the time commitments of interviewees will total six hours over three years.
Sensitive topics
As this project will explore a range of different aspects of middle and front line management roles, it is possible that some participants may find themselves being sharing information about work experiences that they may have found difficult and/or distressing. Such disclosure, which will be voluntary, could nevertheless lead to personal discomfort. This might include, for example, management plans and actions that were not successful, or serious incidents affecting staff and/or patients where the participant was involved in some manner. This possibility will be addressed in the first instance through paragraphs in the participant information sheets for focus and briefing groups and case interviews indicating that this situation could arise, and that participants should take this into account when deciding whether or not to contribute to this project. Should this situation then arise during a group discussion or interview, the researcher present will terminate the conversation immediately. If the participant would find it helpful, the research team member will then offer the participant an opportunity to discuss the matter further, in a private debriefing, off the record. Should such a situation arise, the associated information will not be recorded, will not be discussed with other members of the research team, and will not be added to the data stream for this project.
Participant identification
We will rely on senior management gatekeepers to identify the middle and front line management population at each acute trust, to communicate the project information to them, and to invite them to consider attending our focus group meetings in stage 2, to take part in the survey in stage 3, to attend the briefing sessions in stage 4, and to contact us for interview in stage 5. As the criterion for inclusion in this study concerns holding a middle or front line management position in an acute trust, potential participants will be screened by job title, and where necessary by job description (job titles do not always clearly indicate whether or not a particular role is a managerial one, or has a managerial component). There is, however, no requirement for members of the research team to have sight of any personal records of the staff involved. For the primary care case study, we will again rely on a senior management gatekeeper to identify potential informants, to communicate the project to them, and to ask them to consider contacting the research team either for interview, and/or to discuss the project further before making a final decision with regard to participation.
Members of the research team will not have sight of any personal records relating to any trust management staff, the identification of participants and direct communication with potential participants being facilitated by a senior management gatekeeper nominated by the chief executive in each participating trust. Where it may be necessary to inspect a job description, a generic description for a post of that kind will suffice, and there will be no need for members of the research team to see job descriptions for specific individuals. For the purposes of this study, only job titles will be used as identifiers for data storage and analysis purposes.
For stage 5 of the project, interviewees will be identified on a ‘key informant’ basis depending on their roles in relation to the incidents chosen for study. As these incidents will be identified by participants in briefing groups in stage 4, these key informants cannot be identified until the case incidents have been determined. We anticipate that some key informants will be briefing group participants who will thus be self-nominating, but whose informed consent to participate in this stage of the project will still be sought.
Contacting participants
Participants at each participating trust will first be informed of this study through a general internal mailing to all potential participants from the trust chief executive, or from her or his nominee. This will be accompanied by the focus group participant information sheet describing the aims and methods of the study, and the nature of the participation required at this stage. This information sheet explains our procedures for guaranteeing anonymity and confidentiality, and also explains the right to withdraw from the study at any time without question. The information sheet carries contact information for the research team members who can be contacted directly by potential participants who may have questions or concerns about the study. Following circulation of the information sheet, focus group meetings will be scheduled in each participating trust, and middle and front line managers will be invited to attend these, again through an internal mailing circulated by the chief executive's nominee. Similar central mailing procedures will then be deployed at subsequent stages of the project for the purposes of the self-report survey and briefing groups.
With regard to the case study incidents that will form the focus of stage 5 of this project, these will be nominated by participants in the briefing group discussions during stage 4. We will therefore also ask participants to identify the colleagues who are likely to be key informants in relation to those incidents – which in many cases will probably include themselves – and to speak to them on behalf of the research team, inviting them to approach us for interview. Given the project timescale, it may be appropriate at the start of this stage to circulate the project information sheet again to potential informants.
For stage 5 we will ask briefing group participants who suggest particular incidents for further study, or the appropriate senior management gatekeeper at each site, to pass the relevant participant information sheet to potential key informants, asking them to contact the designated member of the research team if they would be willing to share their experience of that incident. Should key informants in relation to a nominated incident not be forthcoming, we will not pursue that case further, but instead seek identify a substitute incident. (Experience in other sectors with similar issues suggests that we are likely to be presented with more such incidents than it will be possible to follow up given the time and resources available to the project.)
Data storage and retention
Survey and interview data will be stored electronically in appropriate computer files. All Cranfield computers, PCs and laptops, are configured with password-protected access. Data will be stored on the School of Management server which can only be accessed by users with assigned usernames and passwords, and in a project folder that can only be accessed with a further password. This procedure restricts access to project data to member of the research team, and obviates the need to exchange files by e-mail or to store files on usb memory. No data from this project will be stored on NHS computers or on computers belonging to any other organizations. We will use digital recorders to record interviews – where permission is granted – and digital files (which can take up considerable disk storage space) will be deleted following transcription. Files recording focus group discussions and interview transcripts will be labelled anonymously to avoid disclosing identities. Direct quotations from participants may be used in a fully anonymised manner in reports and publications, and this usage is explained in the project participant information sheet. We will not, without permission, use the actual name of any of the Trusts involved in this study; given the research aims and objectives, this will not be necessary. For reporting purposes, therefore, trusts will be allocated pseudonyms (e.g., ‘Norwood NHS Trust’, ‘Grange NHS Trust’). Senior managers who have acted as gatekeepers for this project will be asked to check reports prior to submission for publication in order to ensure that identity cues have been omitted.
Only members of the research team will have access to participant data relating to this study. These data will relate only to what participants have said in conversation (focus and briefing groups and interviews) and to self-report survey responses, and will not include any other personal data beyond the basic biodata requested in the survey instrument. Data will be analysed by members of the research team, either on the Cranfield campus, or in researchers' home offices. Computer files including transcripts of group discussions and interviews will contain no personal identifiers.
This study will generate a significant amount of quantitative and qualitative data, which can be analysed and written up in a range of different ways, for different purposes. In order to maximize the contribution of this study, to theory and to NHS management practice, our aim is to disseminate the findings and their implications widely, in a range of traditional and innovative styles (publications and teaching materials, for example). That process is unlikely to be completed within twelve months following the official end-date of the project. However, there will be no need to store data for more than five years as we expect that our aims in this regard will have been accomplished by then. Data will continue to be stored after the project in the same manner as during the project, on password protected Cranfield University computers to which only members of the research team have access. If the data custodian, Professor David Buchanan, were to leave the institution during this period, this responsibility will pass to another member of the research team, in the first instance to Dr Catherine Bailey, then if necessary to other team members in alphabetical sequence.
Benefits to the NHS
For patients and service users, although not involved directly in project fieldwork, this research will deliver:
-
management practices and organizational features that have been demonstrated to contribute to improved quality of care and clinical outcomes;
-
rapid changes to working practices following ‘extreme’ events, thus leading to improved patient safety.
For middle and front line managers, this research will deliver:
-
knowledge of how middle and front line management work is evolving, and why;
-
new competency requirements, and how these are acquired and can be best supported;
-
new practices, tools, diagnostics, and frameworks for influencing clinical outcomes, care quality, and organizational performance;
-
approaches and techniques for managing both ‘extreme’ and ‘normal’ organizational change.
For senior managers, this research will deliver new information on management development priorities and support needs, and a practical guide to the construction and maintenance of an ‘enabling context’ for maximizing the impact of management practices on clinical, care-related, organizational, and change-related outcomes.
For policy makers, this research will deliver a model of healthcare management work, explaining the demands and pressures which these roles generate, the competencies required, the contributions of management practices to change and performance outcomes, and the implications for extending clinical engagement in management and leadership roles.
This project will thus deliver fresh evidence about the realities of middle and front line management work, new perspectives on the implementation of change in atypical circumstances, and a better understanding of the effects of management practices. While evidence, perspectives, and understanding are intangible outcomes, they are nevertheless valuable to the extent that they redirect attention and energy, shape our understanding of problems and the settings in which they arise, and help to guide practical action.
The involvement of stakeholders
Our research design has the advantage of involving significant numbers of individuals with experience of and commitment to the service. Stakeholders will have multiple opportunities to contribute insights and to challenge. This project has several national, regional, and local stakeholders including policy makers, managers, clinical staff, and patients. These groups are not remote entities to be considered when the study is over. On the contrary, one role of our virtual advisory group is to help us to capture the views of those groups from the start.
Cranfield's mission is to improve management practice through research that generates ‘near to market’ actionable knowledge. Our collaborative design, advisory groups, the involvement of management participants, focus and briefing groups, and dissemination mechanisms, are intended to ensure continuing stakeholder involvement, particularly in the co-production of implications for practice, and innovative ideas for dissemination.
Dissemination plans
Researcher: ‘In what form would you like to see our findings presented?’ Chief executive: ‘Not another report.’ Our staged and collaborative research design means that outputs will develop throughout the project, and data streams will be ultimately combined into a series of publications, including academic journals and a book. Our final report will be complemented by briefs summarizing practical guidance, and we will publish in practitioner journals. We will also use Cranfield open and customized programmes, and our Public Sector Performance Roundtable. The project will feature on our School website, and WebEx will be used as an interactive dissemination tool. We will also contribute to practitioner workshops and conferences. But those are all relatively conventional outcomes. We are sensitive to the need to develop ‘high impact’ communication and dissemination media and channels for this project. To help us to develop more innovative methods for disseminating findings, propelling the research-into-practice process, we will be driven by ideas from our project advisory and management briefing groups. We will be seeking their ideas in this respect throughout the project, and not just towards the end.
Project timetable*
This project will run over 42 months, from 1 January 2009 to 30 June 2012:
Stage 1a Pre-research administration activity: January to October 2009
Stage 1b Site briefing and set-up processes: April to December 2009
Stage 2 Management focus groups: January 2010 to December 2010
Stage 3 The 60–40 survey: January to September 2011
Stage 4 Management briefings: June to December 2011
Stage 5 Managing extreme events: January 2010 to December 2011
Stage 6 Publication and dissemination: ongoing
* These timings are approximate, affected by delays generated by ethical approvals process, and pressures on service managers
Interim reports
We will submit interim reports during the first month following the completion of each stage of the project – in July 2009, January 2010, October 2010, January 2011, July 2011, and January 2012. These reports will summarize progress, key findings, theoretical developments, practical implications, problems arising and how these will be addressed, and will highlight any unusual, unanticipated, and particularly significant issues and outcomes.
References
- Armenakis A.A., Bedeian A.G. Organizational change: a review of theory and research in the 1990s. Journal of Management 1999;25:293-315.
- Badaracco J.L. Leading Quietly: An Unorthodox Guide to Doing the Right Thing. Boston, MA: Harvard Business School Press; 2002.
- Bailey C., Burr J. Luck, Legacy, or Leadership: The Contribution of Leadership to Sustained Organizational Success in NHS Trusts. Cranfield: The NHS Leadership Centre and Cranfield School of Management; 2005.
- Boyne G.A., Meier K.J., O’Toole L.J, and Walker R.M. Public Service Performance: Perspectives on Measurement and Management. Cambridge: Cambridge University Press; 2006.
- Brooks I. Leadership of a cultural change process. Leadership and Organization Development Journal 1996;17:31-7.
- Brown A.D. Making sense of inquiry sensemaking. Journal of Management Studies 2000;37:45-7.
- Brown A.D. Authoritative sensemaking in a public inquiry report. Organization Studies 2003;25:95-112.
- Buchanan D.A., Dawson P. Discourse and audience: organizational change as multi-story process. Journal of Management Studies 2007;44:669-86.
- Buchanan D.A., Caldwell R., Meyer J., Storey J., Wainwright C. Leadership transmission: a muddled metaphor?. Journal of Health Organization and Management 2007;21:246-58.
- Buchanan D.A., Addicott R., Fitzgerald L., Ferlie E., Baeza J. Nobody in charge: distributed change agency in healthcare. Human Relations 2007;60:1065-90.
- Christian S., Anderson S. Review of Research Needs and Priorities 2007. London: NHS National Institute for Health Research; 2007.
- Clark J., Spurgeon P., Dent J. Surrender to progress. Health Service Journal 2008:32-3.
- Collins D. Organizational Change: Sociological Perspectives. London: Routledge; 1998.
- Denis J.-L., Lomas J. Convergent evolution: the academic and policy roots of collaborative research. Journal of Health Services Research and Policy 2003;8:1-5.
- NHS Leadership Qualities Framework. London: NHS Modernisation Agency Leadership Centre; 2002.
- Safety First: A Report for Patients, Clinicians and Healthcare Managers. London: Department of Health; 2006.
- The Operating Framework for the NHS in England 2008/09. London: Department of Health; 2007.
- High Quality Care For All: NHS Next Stage Review Final Report. London: Department of Health, cmnd 7432; 2008.
- Donaldson L. An Organization With a Memory. London: Department of Health/The Stationery Office; 2000.
- Fitzgerald L., Buchanan D.A., Buchanan David A., Fitzgerald Louise, Ketley Diane. The Sustainability and Spread of Organizational Change: Modernizing Healthcare. Abingdon, Oxon: Routledge; 2007.
- Fitzgerald L., Ferlie E., Wood M., Hawkins C. Interlocking interactions, the diffusion of innovations in healthcare. Human Relations 2002;55:1429-49.
- Floyd S.W., Wooldridge B.J. The Strategic Middle Manager. San Francisco: Jossey-Bass; 1996.
- Goldstone J.A., Mahoney James, Rueschemeyer Dietrich. Comparative Historical Analysis in the Social Sciences. Cambridge: Cambridge University Press; 2003.
- Gronn P. Distributed leadership as a unit of analysis. Leadership Quarterly 2002;13:423-51.
- Hales C. Why do managers to what they do?: reconciling evidence and theory in accounts of managerial work. British Journal of Management 1999;10:335-50.
- Ham C., Dickinson H. Engaging Doctors in Leadership: A Review of the Literature. Coventry: The NHS Institute for Innovation and Improvement; 2007.
- Hamilton P., Spurgeon P., Clark J., Dent J., Armit K. Engaging Doctors: Can Doctors Influence Organisational Performance. London: Academy of Medical Royal Colleges and NHS Institute for Innovation and Improvement; 2008.
- Criteria for Assessing Core Standards in 2007/2008: Acute Trusts. London: Commission for Health Audit and Inspection; 2007.
- Learning From Investigations. London: Commission for Health Audit and Inspection; 2008.
- Huy Q.N. Emotional balancing of organizational continuity and radical change: the contribution of middle managers. Administrative Science Quarterly 2002;47:31-69.
- Iles V., Sutherland K. Organizational Change: A Review for Health Care Managers, Professionals and Researchers. London: National Co-ordinating Centre for NHS Service Delivery and Organization Research and Development; 2001.
- Kotter J.P. What effective general managers really do. Harvard Business Review 1999;77:145-59.
- Lagadec P. Learning processes for crisis management in complex organizations. Journal of Contingencies &Amp; Crisis Management 1997;5:24-31.
- Lalonde C. The potential contribution of the field of organizational development to crisis management. Journal of Contingencies &Amp; Crisis Management 2007;15:95-104.
- Leatherman S., Sutherland K. The Quest for Quality in the NHS: A Mid-Term Evaluation of the Ten-Year Quality Agenda. London: Nuffield Trust; 2008.
- Langley A., Buchanan David A., Bryman Alan. The Sage Handbook of Organizational Research Methods. London: Sage Publications; 2009.
- Lüscher L.S., Lewis M.W. Organizational change and managerial sensemaking: working through paradox. Academy of Management Journal 2008;51:221-40.
- Micheli P., Neely A. 2006.
- Mintzberg H. The Nature of Managerial Work. London: Harper Collins; 1973.
- Mintzberg H. Rounding out the managerial job. Sloan Management Review 1994;36:11-26.
- Mohr L.B. Explaining Organizational Behaviour: The Limits and Possibilities of Theory and Research. San Francisco: Jossey-Bass Publishers; 1982.
- Medical Leadership Competency Framework. Warwick: NHS Institute for Innovation and Improvement; 2008.
- Øvretveit J., Aslaksen A. The Quality Journeys of Six Norwegian Hospitals: An Action Evaluation. Oslo: Norwegian Medical Association; 1999.
- Perrow C. Normal Accidents: Living With High-Risk Technologies. New Jersey: Princeton University Press; 1999.
- Pettigrew A.M. Longitudinal field research on change: theory and practice. Organization Science 1990;1:267-92.
- Pettigrew A.M., Ferlie E., McKee L. Shaping Strategic Change: Making Change in Large Organizations – The Case of the National Health Service. London: Sage Publications; 1992.
- Rogers M.L., Cook R.I., Bower R., Molloy M., Render M.L. Barriers to implementing wrong site surgery guidelines: a cognitive work analysis. IEEE Transactions on Systems, Man &Amp; Cybernetics: Part A 2004;34:757-63.
- Rousseau D.M., Manning J., Denyer D. Evidence in management and organizational science: assembling the field's full weight of scientific knowledge through syntheses. The Academy of Management Annals 2008;2:475-51.
- Rueschemeyer D., Mahoney James, Rueschemeyer Dietrich. Comparative Historical Analysis in the Social Sciences. Cambridge: Cambridge University Press; 2003.
- Sambrook S. Management development in the NHS: nurses and managers, discourses and identities. Journal of European Industrial Training 2005;30:48-64.
- Shepherd A. Finance: make your business boom. Health Services Journal 2008. URL: www.hsj.co.uk/printpage.html?pageid=1767141.
- Shortell S.M., Rundall T.G., Hsu J. Improving patient care by linking evidence-based medicine and evidence-based management. Journal of the American Medical Association 2007;298:673-76.
- Stein M. The critical period of disasters: insights from sense-making and psychoanalytic theory. Human Relations 2004;57:1243-61.
- Stewart R. The Reality of Management. London: Pan/Heinemann (third edn); 1997.
- Staff in the NHS 1997. London: The Information Centre; 2007.
- Tsoukas H., Buchanan David A., Bryman Alan. The Sage Handbook of Organizational Research Methods. London: Sage Publications; 2009.
- Turner B., Pidgeon N. Man-Made Disasters. London: Butterworth Heinemann; 1997.
- Van de Ven A.H., Poole M.S., Baum Joel A.C. The Blackwell Companion to Organizations. Malden, MA and Oxford: Blackwell Publishing; 2002.
- Vaughan D. The dark side of organizations: mistake, misconduct, and disaster. Annual Review of Sociology 1999;25:271-305.
- Walker H.J., Armenakis A.A., Bernerth J.B. Factors influencing organizational change efforts. Journal of Organizational Change Management 2007;20:761-73.
- Watson T.J. In Search of Management: Culture, Chaos and Control in Managerial Work. London: Routledge; 1994.
- Watson T.J. Theorizing managerial work: a pragmatic pluralist approach to interdisciplinary research. British Journal of Management 1997;8:3-8.
- Weick K.E. The collapse of sensemaking in organizations: the Mann Gulch disaster. Administrative Science Quarterly 1993;38:628-52.
- Weick K.E., Roberts K.H. Collective mind in organizations: heedful interrelating on flight decks. Administrative Science Quarterly 2003;38:357-81.
- West M.A., Borrill C., Dawson J., Scully J., Carter M., Anelay S., et al. The link between the management of employees and patient mortality in acute hospitals. International Journal of Human Resource Management 2002;13:1299-310.
- Williams M. Interpretivism and generalization. Sociology 2000;34:209-24.
Appendix 2 Project documentation
Information sheets, topic guides and consent forms are version 1 (9 February 2009) with the exception of the research interview consent form, which is version 2 (4 April 2009).
Appendix 3 Management survey
Appendix 4 Managing the norovirus outbreak at Wattle Park
Main conclusions
-
Wattle Park had previous experience of norovirus (the winter vomiting bug), but this incident was on a much larger scale and the hospital appears to have been unprepared to handle it.
-
As this incident was different in scale and consequences from previous outbreaks, this was a significant learning opportunity with regard to future infection management procedures.
-
The involvement of two external agencies potentially exacerbated the impact of this outbreak, hastening decisions to close wards and to withdraw service provision.
-
Initially defined as a serious outbreak of norovirus, this incident quickly morphed to become a serious interruption of emergency and elective services.
-
Changes in the aftermath of this incident focused on hygiene procedures that were not picked up in the recommendations of the external review; these procedures were within the control of middle management, whereas costly changes to ageing facilities were not.
-
Changes in the aftermath of incidents like this are shaped by the context in which the incident occurred, and in this case by the financial and local political conditions facing this hospital, and by the differing views and priorities of the two external agencies involved.
Introduction
In January 2010 there was a major outbreak of norovirus (the winter vomiting bug) at Wattle Park. Unlike previous outbreaks, the number of cases rose rapidly, and within a few weeks all but four of the hospital's 33 wards were closed to new admissions. The hospital was also closed to emergency admissions for 96 hours, and inpatient elective surgery was cancelled for 5 weeks. Once the outbreak was under control, an external review into the causes was commissioned. This review identified a number of contributory factors concerning infection control procedures, ward cleaning and the layout and condition of the hospital estate. Recommendations thus involved changes to infection control procedures, most notably ward closure, and isolation of suspected cases; the cleaning arrangements following a ward closure; increase in size and skill mix of the infection control team; and more rapid confirmation of cases through on-site testing. One year later, several changes had been made. However, in a number of areas, recommendations had not been implemented. No changes had been made to the infection control team and, because of financial constraints, only limited changes had been made to the premises, thereby limiting the opportunity for isolation of suspected cases. There had also been considerable focus on hand hygiene following the outbreak, although this had not been mentioned in the report, and the hospital had a good record in relation to MRSA and C. difficile. Senior managers also questioned the definition of this incident: was this the control of the virus, or the inability to provide emergency and other services? This case report concludes that the focus of activity following the outbreak was influenced in part by the hospital's context, and in particular the financial position, and the political context in which the external review was received. After an event like this, there is a perception of the need for urgent change. But what takes place in the aftermath needs to be seen in the context in which the incident occurred, the investigation took place and the report was received, particularly in relation to directing energy for change.
Assessing the progress in implementing the recommendations from the review 1 year after the outbreak, some of the focus for change was on activities not mentioned in the recommendations, notably on hand hygiene and clinical practice. This is puzzling. Given the serious nature and consequences of the outbreak, attention might have been expected to focus on the recommendations, particularly as the report was completed rapidly following containment of the outbreak. However, the focus of activity and the widening of the discourse concerning necessary change were shaped by contextual factors, including the financial position of the trust, how the report was disseminated and perceptions of the findings.
The report was not widely circulated to hospital staff. Several senior nursing staff said that they had not seen it. This was in part because the initial draft was not well received by the executive team and modifications were requested. The outbreak and its consequences generated strong emotional responses from staff, particularly nurses. It may have been the case that managers, not fully aware of the recommendations, focused efforts on general infection control, even though this had not been specifically highlighted by the review.
The trust's severely constrained financial situation meant that it was difficult to respond fully in the short term to recommendations involving investment. Faced with this constraint, and the pressures to be seen to be doing something following an incident of this nature, the result may have been a focus on activity overtly linked to infection control, involving little or no cost. Furthermore, decisions concerning the allocation of resources in this area were beyond the control of managers such as lead nurses, who could not authorise the creation of isolation bays, but were able to persuade colleagues to wash their hands between each patient episode.
The outbreak
At the beginning of 2010, Wattle Park experienced a serious outbreak of norovirus. This spread quickly, affecting many inpatient wards over several weeks. At the peak of the outbreak, all but four of the hospital's wards were closed to new admissions for about 1 month. This situation compromised the hospital's ability to provide services to the local community. Scheduled elective in-patient procedures were cancelled over 5 weeks, resulting in an estimated loss of income of around £6M. Emergency admissions were also closed for 96 hours and the hospital was in ‘major incident mode’ for 5 weeks. For some of this time, to reduce the likelihood of the virus being brought in from the community, access to the hospital was controlled by security guards and inpatients were not allowed visitors for a period of 3 weeks.
There had been several previous outbreaks of norovirus at this hospital, but none had been as serious as this. In the past, the procedures in place successfully controlled the spread of infection, with minor impact on service delivery. However, the experience on this occasion was different, and the Director of Infection Prevention and Control (DIPC) admitted that, in spite of the external investigation, it was not entirely clear why the virus had spread so rapidly this time.
Information sources
The information for this case study was collected in early 2011, around 12 months after the start of the outbreak. This involved semistructured interviews with eight hospital staff and access to hospital board papers, including the investigation report. Local press reports were also consulted. Interviewees reflected different roles and levels of seniority, including two board directors, two operational managers, two clinical staff and two staff with infection control responsibilities. Interviews lasted around 1 hour and were conducted in the hospital, in working time. With prior permission, interviews were audio recorded and subsequently transcribed for analysis. Board papers and press reports were subject to content analysis.
Organisational context
Wattle Park is a teaching hospital offering a full range of services, with an emergency department and urgent care centre, with 700 beds, 3400 staff and a budget of £240M in 2010–11. The trust had faced financial difficulties for several years. In 2006–7, a survival strategy was designed to address a deficit of £25M, and over 250 posts were lost following a recruitment freeze. Training budgets were also reduced. Many managers described the rather crude approach that was used at that time as ‘slash and burn’, some indicating that they felt that the trust had ‘thrown the baby out with the bathwater’. Several managers said that the hospital was still suffering from the remaining scars.
Wattle Park was still facing cost pressures at the time of this study, compounded by deficits among local commissioners. Although the position became more secure in 2011, staff were ‘battle weary’. There was uncertainty over the hospital's future role with proposals to reorganise services in the area, and Wattle Park was considering merging with other nearby trusts. It was felt that the hospital would survive, and continue to provide emergency, maternity and related services, but it was unclear which other services the hospital would retain.
Much of the hospital was housed in Victorian buildings that had been altered over the years. Most of the medical wards were in the older areas and were traditional ‘Nightingale wards’. Less than 10% of the hospital's beds were in single rooms, and none of those rooms on the medical wards had en suite facilities. There was an isolation unit with nine single rooms and two bays with three and four beds each respectively. Only one single room in this unit had en suite facilities.
Incident background
The symptoms of norovirus include nausea, projectile vomiting and diarrhoea. The virus is easily spread from one person to another by the aerosols of projectile vomit and through faecal–oral contamination. The infectious dose of the virus is low and immunity tends to last for only a few weeks. People of all ages are susceptible. Not all of those who are infected, however, exhibit all of the symptoms and, without testing, accurate diagnosis is difficult. Furthermore, the symptoms of norovirus are common to some other conditions. Although this virus is not considered to be serious in healthy individuals, and recovery typically takes only 2 or 3 days, it may be more serious for those with existing conditions who may take much longer to recover. The virus is excreted for 48 hours after symptoms have stopped, but may linger for several weeks.
The outbreak began on Friday 8 January 2010 when a case of diarrhoea and vomiting (D&V) was reported to the infection control team in one of the medical wards. The team then found that six patients on this ward had symptoms. Given the conditions of these patients, the DIPC thought that some of these symptoms might derive from other non-infectious causes and decided to place this ward ‘under surveillance’. Restrictions were placed on moving patients out of this ward, but not on new admissions. The ward was reviewed over the weekend, when further cases of D&V were identified, but the ward remained ‘under surveillance’ and was not closed to new admissions.
On Sunday 10 January, two more medical wards reported patients with D&V symptoms. One of these wards was subsequently closed to new admissions while the other was placed under surveillance, as it was felt that the symptoms were unlikely to be caused by a norovirus infection. On Monday 11 January, the hospital formally declared a norovirus outbreak and informed the Health Protection Agency (HPA) and commissioners. The wards under surveillance were closed to new admissions and daily outbreak meetings were instituted to control the spread of the virus. Over the following 5 days, more wards reported patients with symptoms, and these were assessed by the infection control team. More wards were closed to new admissions until all patients in the ward had been symptom free for at least 48 hours.
On Tuesday 12 January, the hospital declared a Sustained Ongoing Internal Major Incident, and from Wednesday 13 January, for 5 weeks, all elective inpatient admissions were cancelled. From 25 to 29 January the hospital closed to emergency admissions for 96 hours to avoid admitting any more infected patients from the community. From 26 January, the ‘Bronze Control Team’ was based in the hospital boardroom, dealing with operational decision-making and communications and providing support to the infection control team. Additional specialist infection control nurses were seconded from neighbouring hospitals.
Following a meeting of hospital management with their commissioners and the HPA, a more risk-averse approach to closing wards to new admissions was adopted. It was agreed that reported cases would be assumed to be norovirus unless proven otherwise, and wards would be closed to new admissions when ward staff reported two or more patients with D&V symptoms. Previously, the policy had been to reopen wards 48 hours after the last symptoms had been observed. This was now changed to 72 hours, in line with HPA guidelines.
There was conflicting opinion about the progress of the outbreak. The DIPC said that he believed that the outbreak was coming to an end by 18 January, when the number of new cases reported was only three, although there was a high number of ongoing cases. This was in line with the hospital's previous experience of albeit more limited outbreaks.
Investigation
Following the incident, an external review was jointly commissioned by the hospital and its main commissioning body. The investigation report was delivered in a relatively short period of time and a first draft was available in February 2010.
The review was conducted by an infection control professional from a hospital in another area. This review largely involved conversations with senior managers and the infection control team. The resultant report highlighted a number of shortcomings. Overall, there had been a failure on the wards to recognise the symptoms of the virus and to report these to the infection control team at an early stage. This, it was felt, had resulted in the spread of infection both within and between wards. The review also pointed to the failure of the infection control team to close wards to new admissions quickly enough, as opposed to placing them ‘under surveillance’, a status that was, as became evident, poorly understood by other staff. These factors had increased the infection rate.
The report focused on the infection control and outbreak management aspects of the incident. However, there was controversy at board level, in part because views of the causes of the outbreak were subject to some considerable variation. It is also noteworthy that the report did not appear to have been widely circulated or the recommendations discussed with staff. Several interviewees said that they had not had sight of the final report and were thus not familiar with the recommendations. Furthermore, although there were some post-incident workshops run by the emergency planning team designed to learn lessons from how the outbreak was handled, one lead nurse indicated that, because of the intense pressures experienced by ward staff, some found it hard to go back and relive their experiences of those weeks:
Our emergency planning officer carried out some workshops where various people across the organisation came together to discuss the good things, the bad things, what we needed to do differently. The workshop I went to wasn't particularly well attended. I think by that time people had . . . it was such . . . and I can't explain how stressful a time it was, and people were just kind of like, ‘Oh no, no, I can't revisit that. I don't think people could really. I don't think because they didn't want to. I just don't think people could relive it.
The review also identified the following issues:
-
Failure to close wards at the start of the outbreak contributed to the spread of infection.
-
Staff were not clear what ‘under surveillance’ meant with regard to the movement of patients.
-
Contractual arrangements for ward cleaning were not adequate to deal with the outbreak, not allowing for enhanced levels of cleaning or for terminal cleaning before reopening a ward.
-
There had been debate over whether or not to cohort infected patients in the same ward (and many wards had empty beds, being closed to new patients). Cohorting also allows empty wards to be cleaned and reopened for emergency admissions. However, the cohorting process involves moving infected patients around the hospital, thus increasing the risk of further infection. It was decided during the outbreak, in agreement with commissioners, to cohort patients, allowing 10 wards to be cleaned and reopened. If one of the primary purposes of an acute hospital is to provide emergency health care to the local population, then anything which compromises that is of major significance. The decision to close emergency admissions was made when there were many empty beds in the hospital, because affected patients were not cohorted. The review noted that, had cohorting taken place earlier, the emergency pathway would not have been compromised.
-
Infection control was not helped by the old Victorian buildings and the hospital layout. The Nightingale wards also made the hospital vulnerable to the spread of infection.
-
The layout meant that it was not possible to admit new patients to single rooms, allowing them to be assessed for infection. In some cases, patients displaying symptoms were moved to another ward to give them a single room, thus increasing the risk of spreading the infection during transfer, and spreading infection to that other ward.
-
Assessment for D&V symptoms in the emergency department was not routine, and patients infected in the community were bringing the infection with them when admitted to wards.
-
Keeping potentially affected patients in the admissions area also meant that there was an ongoing source of infection which could be transferred to other wards.
-
At the time of the outbreak, rapid testing for the virus was not available on site. The delay in getting test results meant that patient management decisions were also delayed.
The recommendations
The external review made the following eight recommendations:
-
Wards should be closed at an early stage, rather than designated ‘under surveillance’, which only prevents patients being moved out of a ward.
-
An area should be designated for suspected and confirmed cases that are admitted, to cohort them and to protect other patients. Bays should be provided for confirmed cases and single rooms for suspected cases.
-
The infection control team should assess risks and clinically review cases, to inform isolation and ward closure decisions.
-
The size and skill mix of the infection control team should be reviewed given the size of the hospital and the age and nature of its facilities.
-
The provision of on-site testing facilities for the virus should be considered, to inform decisions about outbreak management at an earlier stage.
-
Cleaning contracts should be revised to include provisions for enhanced cleaning levels (e.g. frequent cleaning of touch surfaces) and terminal cleaning in the case of outbreaks.
-
A process of inspection and sign-off should be introduced for cleaning clinical areas before they are reopened.
-
HPA guidance on hospital viral outbreaks of this nature needs to be updated.
Change following the incident
There was a difference of opinion among those interviewed concerning what constituted ‘the incident’. One definition concerned the outbreak and spread of norovirus resulting in ward closures. The incident generated significant management challenges, with an incident command team being established in the boardroom and the infection control team playing a central role. The outbreak also resulted in negative reporting in the local press, probably causing long-term damage to the trust's reputation. However, some staff, particularly senior managers, began to see this incident in the wider context of the trust's ability to fulfil its role as a district hospital and to provide services to the local population. As such, managing the outbreak, at least as it progressed, was positioned against the ability to carry on delivering elective and emergency services. This was felt particularly strongly following the 96-hour closure of the emergency pathway and prompted the decision to cohort infected patients to allow for wards to be reopened. A senior manager observed:
The strategic objective was to reduce the chance of cross infection [but] became a situation where we had to switch the strategic objective to protect an emergency pathway. At a certain point, ninety-six hours into having the A&E shut to emergency admissions, the nature of the incident changed.
Overall, there was a need to balance the consequences of controlling the virus with maintaining emergency services. The same senior manager commented:
So, our strategic objective then changed to maintaining the integrity of the emergency pathway, and the board had an open conversation about this, knowing that we might as a consequence of this, expose some patients to norovirus who otherwise wouldn't have been. But the relative risk of norovirus, which is unpleasant, it's a forty-eight- to seventy-two-hour self-limiting condition, whereas driving patients round in the back of ambulances, looking for hospitals who can take them, is a much higher risk, and will affect many more people than potential exposure to norovirus.
Elective surgery was cancelled for 5 weeks. However, the considerable loss of income which this entailed (around £6M) was felt to be less crucial to the trust, because cancelling surgery had other significant non-financial consequences. For example, recovering from these cancellations took much longer than recovery from the closure of emergency services in relation to the rescheduling of operations. A shared notion of what constitutes an incident is likely to have implications for how an organisation responds, and the types of changes that are planned to avoid further similar incidents.
A year after the outbreak, a number of changes were reported to have taken place to avoid a further similar situation. Nevertheless, it was acknowledged that norovirus would remain in the community and that measures were required to prevent the infection spreading and limit the damage that an outbreak would inflict on the hospital's ability to continue to provide services. Interviewees also reported issues that had not changed, or changes that had not been sustained.
The nature of the hospital estate was seen to be a major factor in the spread of the outbreak. This was not only because of the predominance of Nightingale wards and the lack of single and side rooms, which would have enabled infected patients to be isolated, but also because of the fabric of the building and the age and quality of the furnishings. One senior manager remarked, ‘If you wash a porous wall, it is still porous’. In addition, in some parts of the hospital, the doors were not wide enough to allow the type of bed used for elderly patients to pass through, and isolation and cohorting thus became more problematic. There was widespread agreement that there was limited scope to deal with these problems. One senior manager commented that, ‘In truth, the place should be razed to the ground and something built that's fit for the 21st, not the 19th century’.
The lack of single rooms meant that it was difficult to isolate patients who were displaying symptoms of the virus before they were sent to a ward. Single rooms would allow time for patients to be isolated, to check if they were infected or whether or not their symptoms had other causes. Many felt that this was a main reason for the rapid spread of the virus in the hospital. Nightingale wards were seen as problematic because, if there was an infected patient on the ward, this exposed around 20 other patients to the virus. However, there were some differing views about the extent to which Nightingale wards really were the problem. One lead nurse indicated that good hygiene practices could minimise cross-infection irrespective of layout. It was noted that, if patients were in four- or six-bed bays, with one nurse in each bay, then cross-infection was likely to be restricted to the other three or five patients in that bay. Nightingale wards also meant that, when restrictions were placed on patients moving out of wards where there had been an infection, a larger number of beds were affected rather than the small number in a bay. If admissions were restricted because of infection, this could result in large numbers of empty beds, unavailable for emergency admissions or elective surgery patients.
At the time that the research was conducted, progress had been made in providing side rooms so that patients admitted through the emergency department displaying symptoms of infection could be isolated and their condition monitored. A ward refurbishment programme was also in place, which included reconfiguring the Nightingale wards into bays. However, these plans resulted in an overall loss of beds, as bays require more space. It was estimated that, following refurbishment, 85 beds would have been lost across the hospital. Progress on the refurbishment was slow because, in an already financially challenged trust, resources to fund this were limited. One board member indicated that they had put some money aside each year to fund this. In addition, there had been unforeseen problems, such as the discovery of asbestos, which had to be removed first and which delayed building work. At the same time, however, an increase in the number of side rooms and single rooms would allow the trust to make progress on achieving its targets for single-sex wards.
The report highlighted ward cleaning as an area for attention with regard to the additional cleaning required during a virus outbreak and procedures for ensuring that cleaning had been carried out to an acceptable standard. Those interviewed said that good progress had been made and that they had established a new set of arrangements in collaboration with the cleaning company.
The reporting of suspected cases to the infection control team and the timing of the decision to close wards were also identified as contributing to the speed of the outbreak. Several respondents said that they felt that wards were not closed early enough and that this had contributed to the spread of the virus. Following the outbreak, staff were encouraged to send specimens for testing early on, so that suspected cases could be confirmed and the appropriate steps taken as soon as possible. This was reported to be generally improved, with staff being more vigilant. However, it was acknowledged that, for example, a patient who did not need assistance to go to the toilet could have symptoms and not report them initially, but that by the time they did report symptoms several other patients might have gone to the toilet and been exposed to the virus on touch surfaces such as door handles or taps. Although rapid reporting of suspected cases was seen to have improved, the infection control team indicated that this was an area where staff needed constant reminders to remain vigilant, and that over-reporting was preferable to under-reporting.
The report also noted that the infection control team was small for a trust of this size, and at the time of the outbreak one staff member was on long-term sick leave. At the time of this study there had been no changes to the size or composition of the team, but there was no indication that this lack of resource had impacted on the spread of the outbreak. Additional resources were brought in from neighbouring trusts when the outbreak escalated. The lack of in-house resources may have affected the executive's decision to call in the HPA at an early stage. Some comments were made by staff about the clarity of the advice given by the infection control team and how in some instances this conflicted with the advice from the HPA.
Interestingly, following the outbreak, hand hygiene attracted a lot of attention. Hand hygiene was not identified in the report as a contributory factor in the spread of the virus and the trust had a good record of controlling MRSA and C. difficile infections, indicating that hand hygiene had not historically been a problem. However, at the time of the research, hand hygiene was mentioned as a contributory factor by many interviewees, who also noted that ward layouts meant that hand washing was not made easy for staff. In many Nightingale wards, for example, there might be two basins in the middle of the ward, requiring staff to walk up and down the ward frequently to wash hands between patients. Alcohol gel was provided by each bed, but this is not effective against norovirus. An operational manager argued that there was a need to be more proactive, that portable sinks should be placed at the entrance to wards, that ward staff should take responsibility to ensure that they were replenished regularly and that hand-drying materials were available and disposed of safely. It was noted that the provision of washbasins was to be addressed in the refurbishment of wards.
It was also observed that there was some misunderstanding in this area among staff. For example, some thought that, if they wore gloves, frequent hand washing was less necessary. The infection control team had run many training and awareness programmes about hand hygiene and dress codes since the outbreak, but there was a general view that this remained a problem. Interviewees indicated that good progress had been made initially following the outbreak, but that this was difficult to sustain. It was acknowledged that staff were busy and there was a need for constant reminders to be vigilant. Trust management had made it clear that they would use disciplinary procedures against members of staff not adhering to hand hygiene practices. The director of operations said:
Fair enough, you know, there may be a situation where, for whatever reason, you've had a mental aberration and you're reminded to wash your hands and you do it. The second time, you get a letter saying, ‘You still haven't got this as a normal part of your daily business.’ And on the third occasion you are then disciplined.
There were, however, no reports of any disciplinary action being taken against members of staff, and some interviewees felt that senior management were not serious about this. One executive team member defended the lack of disciplinary action, noting that it was recognised that staff worked under very difficult circumstances and that failure to wash hands was not see as deliberate but as human error. Other senior managers indicated that a lesson learned here was that ‘you cannot drop your guard’ on hygiene and that there was a need for constant reinforcement.
Although improved hand hygiene is always likely to be beneficial in a hospital, it is interesting to observe that, 1 year on from the outbreak, this remained a major focus of attention and was deemed by many interviewees to have contributed to the spread of the virus. This is particularly interesting as it was not mentioned in the investigation report and the trust had a good record in controlling other infections. This outbreak had a traumatic impact on staff, many of whom had never experienced anything as widespread as this. Only senior managers were able to control the refurbishment of buildings and to increase the size of the infection control team, so hand hygiene may have become the focus of activity as this was in the control of all members of staff. Hand hygiene is also an issue over which responsibility is widespread – doctors, nurses, cleaners – and that crosses specialties and levels in the organisation hierarchy. Moreover, a number of those interviewed, from different areas, felt that there was a ‘blame culture’ in the hospital, and that blame for the norovirus outbreak was attributed to ward staff, which had been demoralising.
A number of general lessons were also learned:
-
it is necessary to limit the number of people who move between wards during an outbreak, including non-clinical staff, such as the newspaper seller
-
to prevent cross-contamination, domestic staff should work only on either infected or non-infected wards
-
agency nursing staff (the use of which was common) should not work shifts in both infected and non-infected wards.
One operational manager indicated that, when it happened, the hospital did not publicise the outbreak widely until measures such as preventing visitors from coming to the hospital and closing the emergency pathway had already been taken. She indicated that the trust had become more confident and assertive in publishing information about infections and communicating to visitors the need to be vigilant, especially with regard to hand washing. This research was carried out approximately 1 year after the outbreak, at which time the hospital had a small number of cases of norovirus, having closed five wards. It was felt that this was a good test of its ability to manage the outbreak effectively, and to protect emergency and elective pathways.
Managing the outbreak
The infection control team believed that the outbreak could have been managed differently, with less impact on service delivery. Team members felt that, when the decision was made to bring in the HPA, measures were put into place which resulted in a greater degree of ward closure than was necessary. They also felt that, once the outbreak had started to develop, there was a degree of over-reporting (although it was desirable that staff notified the infection control team of suspected cases) and that, for some patients, their symptoms had other causes. Their view was that the outbreak had been contained in about 2 weeks but that, as a result of the involvement of external bodies (commissioners and the HPA), it was prolonged. Team members suggested that the HPA had been cautious and that the management of the outbreak was taken over by people more experienced in managing infection control in the community rather than in a hospital. It was argued that, had this approach not been taken, hospital services may not have been compromised.
Several interviewees observed that, when the outbreak team was set up in the boardroom, too many people became involved and noise levels were high, with lots of mini-meetings taking place. Because the boardroom was located on the main hospital corridor, it was easy for people to ‘drop by’ and ‘see how things were going’. This was felt to have been unhelpful, and with this volume of traffic through the boardroom, some from infected wards, this could have been a source of cross-contamination.
It was also felt that one of the problems that the outbreak team faced was dealing with conflicting advice from different sources. In particular, there were differences of opinion between the infection control team and the HPA. The HPA was felt to be cautious in its approach and this inhibited the ability to deliver services. However, it was acknowledged that the HPA had to be involved, for the hospital's own protection, and as a result the hospital was faced with comparing different forms of risk. By contrast, the commissioners were concerned with the political implications associated with the reduction in service provision and as a result were keen to see actions that would allow services to be resumed.
Appendix 5 Project outputs
Buchanan DA. Healthcare managers: the other front line? A 6-minute television interview, based on this project, available on the Cranfield School of Management website and on the Cranfield section on YouTube from mid-July 2010, accompanied by a PDF transcript. Also published in the September 2010 issue of Think Cranfield, a quarterly online newsletter reporting on topical issues and Cranfield research.
Buchanan DA. Two years from now, I don't just want to be doing what we do today more efficiently: CIP, QIPP, and strategic change in healthcare. Paper presented at the British Academy of Management Annual Conference, Symposium on Strategic Management and Performance in Changing Times, Sheffield, September 2010.
Buchanan DA. NHS managers: the other front line? Think Cranfield, September 2010. URL: www.som.cranfield.ac.uk/som/p15286/Think-Cranfield/2010/September-2010/NHS-Managers-The-Other-Frontline (accessed 22 February 2012).
Buchanan DA. Leading and implementing change: recognizing the other NHS front line. Health Service Journal Seventh Annual Leadership Forum, Cavendish Centre, London, 29 November 2010.
Buchanan DA, Bailey C, Osbourne J. Up to our shoulders in concrete: how the need for radical change inhibits radical change. Poster presentation to Delivering Better Health Services, Health Services Research Network and Service Delivery and Organisation Network Joint Annual Conference, Manchester, June 2010.
Denyer D, Buchanan DA, Parry E, Osbourne JA. My job is wicked: the pressures and demands on middle management in the NHS. Developmental paper, British Academy of Management Annual Conference, Aston University Birmingham, Healthcare Organization and Management track, September 2011.
Moore C, Buchanan DA. Sweat the small stuff: minor problems, rapid fixes, major gains. Paper presented to the 8th International Conference on Organisational Behaviour in Healthcare, Dublin, April 2012.
Osbourne JA, Parry E. We’re struggling with the sense of victim in the middle: the emotional labour of management in healthcare. Developmental paper, British Academy of Management Annual Conference, Aston University, Birmingham, Healthcare Organization and Management track, September 2011.
Parry E, Buchanan DA. Releasing time to manage. Manag Focus, Spring 2011, pp. 10–13.
Pilbeam CJ, Buchanan DA. A very unpleasant disease: the rapid reform and maintenance of infection. Paper presented to the Seventh Biennial International Conference in Organisational Behaviour in Healthcare, University of Birmingham, April 2010.
Pilbeam CJ, Buchanan DA. After the crisis: the maintenance model of effective change. Health Serv J Online Resource Centre, 16 August 2010. URL (available to HSJ subscribers): www.hsj.co.uk/resource-centre/your-ideas-and-suggestions/changes-in-patient-safety/5017551.article (accessed 22 February 2012).
Pilbeam C, Moore C. Are you talkin’ to me?: a social network analysis of a change agent’s interactions. Developmental paper, British Academy of Management Annual Conference, Aston University, Birmingham, Healthcare Organization and Management track, September 2011.
Pilbeam CJ, Buchanan DA. A very unpleasant disease: successful post-crisis management in a hospital setting. In Dickinson H, Mannion R, editors. The reform of health care: shaping, adapting and resisting policy developments. Houndmills, Basingstoke: Palgrave Macmillan; 2011 pp. 211–26.
Research briefings
We also published a series of short (four-page) research briefings. These each addressed a single topic or theme and they were written for our end-user management audience. They were available in hard copy (colour printed A4 card) and also as PDF web downloads.
Buchanan DA. Releasing time to manage: what stops middle and front line managers from doing their jobs more effectively, and what can you do about it? Cranfield Healthcare Management Group Research Briefing 1, September 2010.
Buchanan DA. Names, ranks, and numbers: how many managers does the NHS have, and is that enough? Cranfield Healthcare Management Group Research Briefing 4, October 2010.
Buchanan DA. Spot the manager: how to identify middle and front line managers in the NHS. Cranfield Healthcare Management Group Research Briefing 5, November 2010.
Buchanan DA. Are healthcare management jobs becoming extreme jobs: and what are the implications of this trend? Cranfield Healthcare Management Group Research Briefing 7, February 2011.
Buchanan DA. Elsenham crossing: a wholly avoidable accident. Cranfield Healthcare Management Group Research Briefing 9, May 2011.
Buchanan DA. Reinforcing the management contribution. Cranfield Healthcare Management Group Research Briefing 10, May 2011.
Buchanan DA, Moore C. Management capacity: framework and assessment guidelines. Cranfield Healthcare Management Group Research Briefing 14, October 2011.
Buchanan DA. Grandmother’s footsteps: the institutional context of management work. Cranfield Healthcare Management Group Research Briefing 18, February 2012.
Gascoigne C. A review of research on extreme jobs: long hours, intense effort, high challenge. Cranfield Healthcare Management Group Research Briefing 19, May 2012.
Moore C. Knowing me, knowing you: interpersonal relationships between managers and hospital consultants. Cranfield Healthcare Management Group Research Briefing 11, May 2011.
Moore C. You are what you email: how do you manage your relationship with your inbox. Cranfield Healthcare Management Group Research Briefing 12, May 2011.
Moore C. Sticking plasters over big problems: are you managing your wicked problems or using sticking plasters? Cranfield Healthcare Management Group Research Briefing 13, September 2011.
Moore C. Mental toughness: applying sports and navy principles to healthcare. Cranfield Healthcare Management Group Research Briefing 16, December 2011.
Moore C. Sweat the small stuff: minor problems, rapid fixes, major gains. Cranfield Healthcare Management Group Research Briefing 17, January 2012.
Osbourne J. What motivates NHS managers?: is it just money? Cranfield Healthcare Management Group Research Briefing 3, December 2010.
Osbourne J. Challenges facing healthcare managers: what past research reveals. Cranfield Healthcare Management Group Research Briefing 6, January 2011.
Osbourne J. Managers have feelings too: emotions of healthcare managers. Cranfield Healthcare Management Group Research Briefing 8, April 2011.
Pilbeam CJ, Buchanan DA. After the crisis: the maintenance model of effective change. Cranfield Healthcare Management Group Research Briefing 2, September 2010.
Turnbull James K. What leadership practices are needed in complex healthcare organizations? Cranfield Healthcare Management Group Research Briefing 15, November 2011.
Appendix 6 Related publications
This appendix lists publications that, although not drawing directly from the fieldwork of this project, are authored or co-authored by members of the project team and address issues closely related to the aims of the project. These publications thus form part of the overall dissemination of findings arising from and related to the project.
Adams R, Tranfield D, Denyer D. A taxonomy of innovation: configurations of attributes in healthcare innovations. Int J Innov Manag 2011;15:359–92.
Adams R, Tranfield DR, Denyer D. Process antecedents of challenging, under-cover and readily-adopted innovations. J Health Organ Manag 2013;in press.
Briner RB, Denyer D, Rousseau DR. Evidence-based management: concept clean-up time? Acad Manag Perspect 2009;23:19–32.
Buchanan DA. Good practice, not rocket science: understanding failures to change after extreme events. J Change Manag 2011;11:273–88.
Buchanan DA, Storey J. Don’t stop the clock: manipulating hospital waiting lists. J Health Organ Manag 2010;24:343–60.
Buchanan DA, Fitzgerald L. New lock, new stock, new barrel, same gun: the accessorized bureaucracy of healthcare. In Clegg S, Harris M, Höpfl H, editors. Managing modernity: beyond bureaucracy? Oxford: Oxford University Press; 2011. pp. 56–80.
Fitzsimons D, Turnbull James K, Denyer D. Alternative approaches for studying shared and distributed leadership. Int J Manag Rev 2011;13:313–28.
Turnbull-James K. Leadership in context: lessons from new leadership theory and current leadership development practice. Paper commissioned by The King’s Fund to inform the Commission on Leadership and Management. London: The King’s Fund; 2011.
Submitted and under review
Buchanan DA, Denyer D. Researching tomorrow's crisis: methodological innovations and wider implications [published online ahead of print 13 November 2012]. Int J Manag Rev 2012. doi:10.1111/ijmr.12002. (Submitted on invitation from guest editors for special issue on management research methods and practice.)
Appendix 7 Sweating the small stuff: minor problems, rapid fixes, major gains
Paper presented to the Eighth International Organizational Behaviour in Healthcare Conference, Trinity College Dublin, Ireland, 15–18 April 2012
Cíara Moore, SDO Management Fellow, and David A. Buchanan, Professor of Organizational Behaviour, Cranfield University School of Management
Corresponding author:
David A. Buchanan
Professor of Organizational Behaviour
Cranfield University School of Management
Cranfield, Bedfordshire, MK43 0AL, UK
T: + 44 (0) 1234 751122 x 3481
F: + 44 (0) 1234 751806
E: David.Buchanan@Cranfield.ac.uk
M: + 44 (0) 7850 143 602
Abstract
Solving small, annoying problems may appear to be unimportant in a political and economic climate that focuses attention on radical long-term changes to the organization, delivery, funding, and regulation of the healthcare system. However, as the initiative reported here suggests, small changes can generate major benefits for patients, staff, and hospital performance. This approach can also strengthen clinical–managerial relationships, which are key to larger scale initiatives, and which can suffer when ‘the small stuff’ is not fixed. The success of this initiative is explained with reference to a process model of change combining context, content, process, and individual dispositions. This model could also identify other settings where this approach is likely to be effective. On the basis of this experience, healthcare managers may be advised to be alert to what appear to be minor unresolved issues, and to address these in addition to undertaking larger scale, longer term projects.
Acknowledgements: The research on which this paper is based was funded by the National Institute for Health Research Service Delivery and Organisation programme (award number SDO/08/1808/238, ‘How do they manage?: a study of the realities of middle and front line management work in healthcare’).
Disclaimer: This paper is based on independent research commissioned by the National Institute for Health Research. The views expressed in this presentation are those of the authors, and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
For want of a nail . . .
For many middle managers, they can see the problem and know how to fix it, but it's easy to let it drop. Will I pick up the coding battle today? Maybe not.
Operations manager, Clearview hospital
Very slow, very frustrating, and quite often not enough progress in an acceptable time, and the base problem remains. And after some time it becomes embedded and accepted because the middle manager concludes it's too hard to address.
Interim director, North Somerton hospital
The aim of this paper is to explore the potential benefits to patients, staff, and overall organizational performance, of addressing minor problems in an acute hospital setting – unanswered e-mails, delayed equipment orders. These issues can be overlooked in a context where major change is at a premium. However, a small-scale initiative designed to address such issues reveals the potential to generate savings, increase staff morale, improve quality of patient care, expose underlying problems, and strengthen clinical–managerial relationships. The success of this initiative set the foundation for further improvements, in this and other services. The change continuum from ‘fine tuning’ to ‘transformational’ implies the relative superiority of the latter (Stace and Dunphy, 2001; Kotter, 2008), which may be misleading.
In the current economic climate, attention focuses on radical changes to the ways in which healthcare is funded, organized, delivered and regulated (Department of Health, 2010). For the National Health Service (NHS) in England, meeting ‘the Nicholson challenge’ to cut the annual budget by £20 billion by 2014–15 involves implementing major cost improvement programmes (CIPs), which have meant cutting tens of millions of pounds from hospital budgets. National policy means that these reductions in spend must be accompanied by plans to maintain Quality, encourage Innovation, increase Productivity, and strengthen Prevention (of incidents which jeopardize patient safety); the so-called QIPP agenda. This implies ‘disruptive innovation’ (Christensenet al., 2000), not ‘tinkering’ (Abrahamson, 2004).
These policy-driven changes accompany the challenges facing all modern healthcare systems: rising patient expectations; ageing society; wider information availability; changing nature of disease; advances in treatments; changing workforce (Department of Health, 2009). The traditional model of the acute hospital is thus now in question, with the advent of polyclinics, care in the community, improved management of long-term conditions, and the integration of services in further attempts to reduce costs and streamline care (Edwards, 2010a).
Aims and methods
This initiative was part of a wider study of management contributions to change to improve clinical and organizational outcomes. Clinical/medical managerial relationships are a component of the ‘receptive context’ for change (Pettigrewet al., 1992), and evidence shows that initiatives that are clinically led are more likely to succeed (Locock, 2001). In addition, change in a large, complex, public sector, professional bureaucracy is (allegedly) intrinsically problematic (Øvretveit and Aslaksen, 1999; Edwards, 2010b). But the NHS is expected to undergo radical change (Department of Health, 2009): ‘the productivity challenge’, ‘the scale of the challenge before us’ (p. 3), ‘change on an unprecedented scale’ (p. 7). This agenda does not imply fine-tuning. How are clinical/medical–managerial relationships developing in this context? Are small changes of little or no value in the face of this ‘unprecedented challenge’?
At Clearview hospital (pseudonym), to explore medical–managerial relationships, pilot interviews were conducted with seven consultants – senior doctors who were leading specialists with international reputations in their respective fields of medicine. Contrary to expectations, and to traditional stereotypes (McCarthyet al., 1993), these doctors recognized and welcomed the value of management support (Moore, 2011). However, they also noted that management workload pressures meant that small problems were often not resolved. For example, one consultant had waited eight months for a connection to allow a colleague to share the printer in his office. A source of daily frustration, such problems contributed to a perceived lack of management action, and damaged managerial credibility.
The aims of this initiative, therefore, were to identify the small problems in one clinical service, to understand why these had not been tackled, to fix these quickly, to establish the benefits, and to assess the applicability of this initiative to other clinical services.
The Clearview context
When the computer on the ward was bust, I said to the ward manager, we need a new one, and she said we need to ask the operations manager. When I asked the operations manager, she said the ward manager could do it. So it takes ages to just sort out the computer. It's this inefficiency which is irksome.
Consultant, medicine division, Clearview hospital
Clearview is an acute hospital with an annual budget of around £600 million, 7,000 staff, and 1,000 beds. Clearview was implementing cost improvement projects (CIPs) to reduce a projected £10 million deficit in 2011/12, and it was predicted that further savings of over £18 million would be required to reach break even, given the rising costs of pay and medical supplies. Clearview had seven divisions: cancer; women and children's and; emergency and perioperative care; diagnostics; medicine; neurosciences; surgery. The medicine division had CIPs totalling £9 million at the time of this initiative.
The initiative reported in this paper involved the gastroenterology service, which was part of the medicine division, with an annual budget of around £4.5 million, 70 staff, 6 consultants, a 22 ‘single-rooms’ ward, a five-room endoscopy suite, and daily outpatient clinics. This was a high volume service with a team that was receptive to change, and this initiative had the support of one of the consultants who encouraged his colleagues to participate.
Sweat the small stuff
Normally, if I need a computer, I phone the shop, or get online, and say ‘printer’ – and it arrives the next day. Here you have to fill in several forms. They go to someone who e-mails back to say you've filled in the wrong forms. You send it back again, they take several weeks, and then they procure what seems like the most expensive computer in Christendom. And eight weeks later, if you are lucky, something that looks like a computer arrives, but isn't the one you ordered.
Consultant, medicine division, Clearview hospital
This initiative, called Sweat the small stuff, was implemented by a three-person team, who first agreed a project charter, which was then approved by the medicine division's budget holder and associate director. The team implemented a five-day process; could minor problems be identified, explored, and resolved in such a short time? Why had those small issues not been resolved previously? And what impact would solving these issues have on the staff concerned and patient care? The three team members' roles were:
The animateur
In the arts world, the animateur is a driving force, a facilitator, a promoter who inspires others and gets them engaged in a project. This management role has also recently been recognized as key in healthcare commissioning settings (Checklandet al., 2011, forthcoming). For this initiative, the animateur was the division operations manager, who designed and coordinated the project, invited the head of the gastroenterology service to trial this approach with his staff, and recruited the other two members of the project team.
The consultant champion
It was important for the team's membership to include one of the consultants who had expressed frustration with management's perceived inability to fix small problems. His membership signalled that this was a medical–managerial collaboration which he was championing. The consultant sent the project's trigger e-mail to his team, including doctors, nurses, management and administrative staff, inviting them to identify appropriate issues.
The ‘who knows who knows what’ role
This team member, personal assistant to the assistant operations director and operations managers, had worked at Clearview for several years in an administrative capacity, had developed an extensive network, had a small team with its own networks, and understood the short cuts through which issues could be resolved quickly. Katz and Lazer (2003, p. 20) describe this as the ‘who knows who knows what’ team role. Her detailed tacit operational knowledge of the hospital was thus a key ingredient of the success of this initiative. The first task that she and her team undertook involved listing their contacts in support areas – people who they knew and trusted, and who could be called upon to help resolve issues quickly.
Customer service
One of the themes emerging from the pilot interviews concerned customer service. Hospital staff who place orders or requests through internal systems expect a response similar to that which they receive when shopping online at home. Amazon and Tesco, for example, process orders rapidly, and e-mail customers to advise of delays, offering discounts when things go badly wrong. But hospital staff note that, when they order equipment, or request that issues be resolved, they often do not know whether or not their request has been received, if it is receiving attention, or what stage their request has reached. This initiative, therefore, sought to ensure that the responses from the project team were rapid, and that staff were kept up to date with regard to progress on the issues they raised. Those staff members were thus seen as clients, and the aim was to treat them as such, by giving them one, three and five day updates.
Day 1: 24 hours – All clients were contacted within 24 hours of registering their issue with the project team. They each received an e-mail thanking them for registering their issue, and they were advised that a further update would follow on day three. In most cases, a brief conversation ensured that background information was captured concerning the nature or frequency of the issue raised, and its impact. This information allowed assessment of how successfully the issue had been resolved, in terms of time, money and other benefits.
Day 3: update – On the third working day of the initiative, all clients were updated on progress with their issue. Of five issues, one had been resolved at this point, and the others all had actions in progress. Clients were delighted that their issues were resolved or were close to resolution.
Day 5: closure – The final step; workable solutions had been identified for all issues, three had been completed, and two required some further work (explained below). Those who had contributed issues to the initiative were thanked and invited to provide feedback on the process.
A form was designed with which to register issues, but most came through informal requests to the project champion. It was expected that ‘we need more staff’ would be a common theme, but this was not so. The clients who raised the issues for fixing are shown in Table 1, and were a mix of administrative, nursing, managerial and medical staff.
| Issue | Raised by |
|---|---|
| The patient pathways fix | Deputy operations manager |
| The coding fix (1) | Specialist nurse and consultant gastroenterologist |
| The coding fix (2) | Specialist nurse |
| The scanner fix | Medical secretary |
| The patient safety fix | Consultant gastroenterologist |
Problems and fixes
Five ‘small problems’ were raised, involving patient pathways, two separate issues related to coding, a scanner, and patient safety. What were these problems, why had they not previously been resolved, how were they fixed, and what were the outcomes?
The patient pathways fix
For one gastroenterology manager, the issue concerned the lack of knowledge among administrative and clerical staff in the hospital appointments centre, and in the clinic and endoscopy suite, concerning patient pathways. This led to overbooked and underbooked clinics, to patients being booked outside waiting times targets (18 weeks, or 2 weeks for cancer patients), to booking with the wrong clinician, or booking onto the wrong endoscopy list. She felt that this problem related not just to understanding targets, but more importantly concerned understanding the needs of the specialty and its patients. The gastroenterology management team had requested that a link be established between the clinic and the service – a member of the clinic team who would act as ‘expert’ on gastroenterology patients. Staff numbers, and the movements of staff between clinic areas, prevented this.
This problem had a significant impact on how efficiently the clinics would run. If a patient was placed in the wrong clinic, consultant time would be wasted, and the patient would have to be allocated to the correct consultant, involving a further hospital visit. This was occurring in every clinic, wasting up to half an hour each time. The costs are shown in Table 2. Overbooked clinics often ran late, and incorrect patient bookings added to the frustration. Fixing this issue would thus release time which consultants could spend with patients.
| Number of clinics | Time lost | Value |
|---|---|---|
| 20 a week | 30 minutes per clinic | £56 consultant's time |
| Annual savings if fixed: | 420 hours (42 working weeks) | £47,040 |
A discussion with the deputy operations manager revealed that many administrative staff did not understand the patient pathways. As these pathways had not been mapped, the operational lead for this initiative and the deputy operations manager decided to create a visual map (on one page) of patients' pathways based on a ‘condition of the week’ template; for example, coeliac disease, the patient journey, correct placement, symptoms and causes, and lead consultants for the specialist area. These maps were the presented at one of the daily facilitated meetings, for clinic, endoscopy suite and administrative staff, with the aim of accumulating a manual of pictorial representations of all the main pathways.
The coding fix (1)
‘Key point is the code for immunosuppression monitoring in clinic – we have been waiting for MONTHS/YEARS for this. I have no idea why, but it drives us all nuts.’ (consultant gastroenterologist, Clearview hospital: capitals in original e-mail)
Coding is the process of recording the treatments that patients receive; the accuracy of the coding thus affects the payments that the hospital receives from its healthcare commissioners. There were two issues related to coding. The first concerned immunosuppression monitoring, for which a code was required to enable the clinic to be set up and registered on the hospital information system, and then to allow data to be collected on this nurse-led service.
This problem took ten minutes to fix. The normal process for setting up codes is to create a ‘change in methodology recording’ form (CMR). The information on this form was used by the information services team to allocate a code. When first asked why this code had not been set up, the directorate support manager said that they were waiting for the information services team to respond. Ten minutes later, the manager realized that the code had already been allocated, about a month earlier, and was sitting in her inbox.
Why had this not been actioned? The manager had been overwhelmed with work. She had taken on an additional role of booking patients into specialist procedures, and was juggling this with managing a team, with multiple pathways and targets. It was also ascertained that her inbox was full; she may have seen the message and acknowledged it, but with managing her extended workload, she had not actioned this. Within a day of the initiative she agreed to meet with the specialist nurse who would run the clinic, and together they finalized the clinic times and numbers and the clinic was set up. From the moment this clinic is set up the team will be able to count their activity more accurately and generate income (see Table 3).
| Number of patients | Income | |
|---|---|---|
| 5 per week | £95 per patient | |
| Annual total redeemed | Based on a 42 week year | £19,995 |
The coding fix (2)
The second coding issue was more complex. The gastroenterology team had been asked to trial a new telephone clinic for patients with chronic inflammatory bowel disease. The aim was to establish an open access advice line for patients, but a code was required to capture the activity of this service. This would ensure safe medication for those using highly toxic and expensive drugs; promote self-management of the condition by providing expert advice; avoid unnecessary admissions; and facilitate early discharge. The advice line would be funded by reducing the need for a nurse follow-up. The team had piloted this as a ‘ghost service’ expecting commissioners eventually to fund it. However, the lack of a telephone clinic code meant that nurses were manually collecting the data, and forwarding this information to the finance department to cost on a monthly basis, thus reducing the benefits from reduced nurse input, and adding administrative time of two hours a month compiling that information.
The deputy operations manager had set up this telephone clinic, and was advised by the assistant director of commissioning not to set up a code, as this was not required for this ‘ghost service’, for which payment from commissioners may not be forthcoming. However, she was given different advice by the information services manager who she should have approached first. This illustrates the problems of understanding the roles and responsibilities of others in a complex organization, where problems may not be resolved through lack of such basic information. A CMR form was completed and the service was set up on the hospital information system, reducing the need to capture data manually. The main benefits for patients included admission avoidance, and reduced number of hospital visits.
The scanner fix
A team of three medical secretaries suggested that a barcode scanner would reduce the time spent tracking the location of patients' medical records (which are bar-coded for identification purposes), and manually logging this information on the hospital information system. The team had used a scanner several years ago, but it was not replaced when it broke down. One option was to use a spare scanner from another department, but that turned out to be incompatible with their computers. When asked why a new scanner had not been acquired, the team responded that they had ‘assumed at the time it was due to funding issues’.
It normally took 30 minutes a day to manually enter patient records, and this time could be halved with a scanner. An appropriate scanner cost £89, and was bought within three working days. This was made possible in part due to the preparatory work for this initiative, as the budget holder had been alerted to the possibility of such costs arising. She had agreed that, as long as the expenditure was justified, she would support such purchases. In addition, the ‘who knows who knows what’ member of the team knew that it was possible to procure urgent goods for next day delivery by using a hospital credit card. Standard processes can take weeks to unfold. The scanner arrived on Day 5, but had to be processed by ‘goods inwards’, the hospital's central delivery point where orders are checked before internal delivery. The medical secretaries got their scanner on Day 6. One responded, ‘Fantastic; we are enjoying having one less task for sure. Such a small, inexpensive item has saved us time and is making a boring job much less of a chore’.
The original scanner had not been replaced for over five years (see Table 4). The accumulated cost of 95 lost working days over those five years was estimated to be £11,340.
| Time lost with manual input | Annual time lost | Total annual hours lost | Working days lost |
|---|---|---|---|
| Time saved with scanner | Annual time saved | Total annual hours saved | Working days saved |
| 90 minutes lost per day | 18,900 minutes, based on 42 weeks | 315 | 39 |
| 45 minutes a day | 9450 minutes saved, based on 42 weeks | 157 | 19 |
The patient safety fix
One of the great frustrations in hospital medicine is dealing with enquiries or the results of investigations for patients under someone else's care. With a triage system, patients would often be admitted on the day I was on call for general medicine, but would be triaged to another specialty, so I would never see them. The way patients were allocated in the morning meant that they were not correctly re-allocated to the new consultant on the hospital patient administration system. As a consequence, the results of every investigation performed during the admission, and questions from GP surgeries, would continue to come to me, generating significant amounts of wasted time for me and my secretary. The same would apply in reverse for many of my patients. This was rectified simply by educating those responsible for patient allocation, and will save enormous amounts of time across the division over the course of the year.
Consultant gastroenterologist, Clearview hospital
One gastroenterology consultant had observed that, following his on-call days, he often found that patients who had been admitted were still registered in his name on the hospital system. He was thus spending around two hours each month dealing with the administration related to patients who were no longer under his care, and this incorrect allocation could pose patient safety issues. This issue affected the team of six consultants – and perhaps the medicine division as a whole. This was an important issue, so it was important to resolve it.
The hospital information system was limited in terms of visual presentation and reporting. Some years ago, a separate web-based system was developed, ‘patient monitor’, which captured patient details and allowed consulting teams to collate these by medical ‘firm’ and make patient notes or action lists. This also allowed them to print out patient lists with notes which made handovers easier. The main hospital system did not have this function, but ‘patient monitor’ could ensure that patient changes were recorded in the main system.
At the medicine division daily morning report, all patients admitted the previous day were discussed and, if necessary, allocated to the correct speciality. For example, a patient admitted by the on call gastroenterologist may have a cardiology problem, and so would be allocated to the cardiology team at morning report. The administrative team who attended this meeting had to enter the required changes, to clinical team and consultant, live onto ‘patient monitor’. However, at this stage of the process, the administrative team occasionally overlooked the change of consultant. The patient flow manager agreed to ensure that his administrative team were aware of the need to complete these allocations fully and correctly.
Patients could also be moved to the care of a different consultant some time after admission, and the ward clerks had to be aware of this problem, too. The deputy operations manager agreed to put this item onto the agenda of the ward clerks' forum. While the solution to this problem was clear, given the education requirement, it would take time for these changes to become sustainable, requiring ongoing monitoring, audit, and training. The consultants were pleased with this change. Although this would reduce the time they spent on unnecessary administration, the main benefit here concerned patient safety. A subsequent audit showed that all patients were being allocated correctly (Table 5).
| Number of hours | Value | |
|---|---|---|
| 2 hours per on call duty | £224 for 2 hours | |
| 6 consultants, 8 on call sessions per annum | ||
| Total annual savings | 96 hours | £10,752 |
Much doing to be done
If NHS managers are struggling it is because of the size of the agenda and the lack of respect for the management task involved; and the systematic lack of investment in learning – it is hard to learn together when there is so much ‘doing’ to be done.
Malby, 2011, p. 19
Table 6 summarizes the five problems, the nature of each issue, why it had not been resolved, how it was resolved, the cost of the fix, and the benefits – which fall into five categories:
-
financial: income generation
-
processual: safer patient allocation
-
temporal: tasks performed more quickly; less waiting time
-
emotional: reduced annoyance, boredom, frustration
-
relational: improved inter-professional relationships
| Problem | Why was this not fixed? | The fix | Cost of fix | Benefits of fix |
|---|---|---|---|---|
| Patient pathways | Obvious solution – a dedicated liaison person – not possible due to staff shortage and budget restrictions | A manual of visual process maps to explain pathways to endoscopy clinic and administrative staff; built up gradually and presented at weekly meetings | None | Less consultant time wasted, patients spared further hospital visit, £47,000 consultants' time |
| Multiple, complex pathways not clear to staff booking patients into wrong clinics | ||||
| Coding (1) | Code was set up, but directorate support manager overlooked e-mail due to pressure of work | Code registered; short conversation with specialist nurse who would run the clinic to agree clinic times and patient numbers | None | £20,000 new annual revenue |
| Clinic code not organized, unable to claim income | ||||
| Coding (2) | Senior commissioning management advice that a code was not required | Information services manager gives different advice, code is set up | None | Less administration for specialist nurses, reduced admissions and fewer hospital clinic visits for patients, improved service demand management |
| Telephone advice line code not set; manual data entry | ||||
| Scanner | Spare barcode scanner in another department did not work; assumed no budget for replacement | New scanner costed and acquired in five days (plus one day's delay in the ‘goods inward’ department) | £89.00 | 157 FTE secretarial hours saved pa, lost time over five years cost £11,000, £2,500 secretarial time saved pa |
| Broken, not replaced for five years | ||||
| Patient safety | Mechanism in place, but not used consistently due to poor understanding | Issue brought daily to medicine division morning report, where patients are reallocated to correct clinical team following on call admission | None | Reduced time spent on administration, audit shows patient safety improved, £11,000 consultants' time saved |
| Incorrect patient allocation to medical teams |
The benefits to patients concern safety, reduced hospital visits and waiting times, and clinical staff who have more time to spend with them. The benefits to staff relate to reductions in routine manual work, and considerably less frustration. Corporate benefits include income generation, improvements in quality of care and safety, and improved relationships, thus contributing to the implementation of more radical initiatives in future.
The small issues underpinning this initiative had not previously been addressed due to:
-
workload
-
budget and logistical problems
-
incorrect advice
-
lack of understanding.
It is interesting that, in only one case, the failure to have fixed the issue was due to lack of finance (for an additional staff member), and that was resolved with the creative and cost-neutral development of visual process maps. Only one fix involved minor expenditure.
Informal feedback from the gastroenterology team was positive. The opportunity to be involved in solving those issues was welcomed, although two gastroenterology managers (deputy operations and directorate support), the animateur, and the ‘who knows who knows what’, did most of the work. However, the work involved was hardly burdensome: the animateur kept a log and calculated that, in helping to resolve those issues, she had spent 40 minutes in conversations over five days. Although it is managers who often leave those small issues unresolved, they typically have a better understanding of how to fix them. Clinical and medical staff often lack, and may have little time or desire to develop, the networks and the organisational knowledge that contributed to this initiative. Administrative staff were also a valuable source of potentially untapped knowledge, particularly with regard to negotiating the bureaucracy and finding short cuts.
Drawing on findings from the wider project, middle managers in acute hospitals are confronted with long and complex change agendas, with many conflicting priorities, all of which are always urgent. This has been described as ‘multiloading’ (Bruch and Menges, 2010; Malby, 2011), and was a feature of management work at Clearview. In this context, it is perhaps not surprising that ‘big change’ attracted attention, and ‘small stuff’ was overlooked. And as is often the case in healthcare, the solutions to these small problems saved expensive staff time, but were not ‘cash releasing’, but one would generate income.
From a theoretical standpoint, how can the success of this initiative be explained? Drawing on an influential processual perspective (Pettigrewet al., 2001; Dawson, 2003), Walkeret al. (2007) argue that change outcomes are shaped by the ‘integrative influence’ of context, content, process, and individual dispositions. Context refers to forces in the external and internal environments. Content concerns the changes being implemented, whether they are fundamental or incremental, changing the organization's character or fine tuning, episodic or continuous. Process relates to the actions of change agents. Significant individual factors include dispositions, behaviours, and reactions to change. Table 7 summarizes the nature of these four sets of factors in this case. First, there were many external and internal pressures for change. Second, the change agenda was driven by the staff of the clinical service, and was not externally imposed. In addition, the changes were not radical, but involved fine-tuning that was perceived to be important. Third, the three-person team – animateur, consultant champion, ‘who knows who knows what’ – appears to have been particularly effective, in launching the initiative, and in bringing it rapidly to a successful conclusion. Finally, the frustrations, and the ambitions of those involved were key to creating and sustaining interest in and commitment to the project.
| Factor | Sweat the small stuff |
|---|---|
| Context: factors in external and internal environment | External: demands for productivity, efficiency, cost savings, improved care quality and safety |
| Internal: high volume service, high performance team, ambitious to improve, small, known, but frustrating unsolved problems | |
| Content: the changes being implemented | Small problems, incremental change, fine tuning, ‘tinkering’, episodic, not ongoing fundamental, radical or strategic change |
| Sourced from mix of team members – ‘clients’ – their issues, their priorities, not externally imposed | |
| Process: actions taken by the change agents | Established project team with three members: animateur, clinical champion, and ‘who knows who knows what’ member |
| Initial groundwork with powerbrokers; rapid process with five-day deadline, constant feedback to ‘clients’ | |
| Individual dispositions: attitudes, behaviours, reactions to change | High performance, high aspiration team receptive to change; enthusiastic medical support; ambitious project lead |
| Frustration with bureaucracy, inefficiencies, and slow pace of change, especially with apparently minor issues |
From a managerial standpoint, it would appear to be a simple matter to extend this small-scale initiative to another clinical service. However, it also seems reasonable to assume that the probability of success elsewhere may depend on the extent to which the configuration of context, content, process, and individual dispositions broadly mirror those encountered in the, perhaps ‘ideal’, setting of this particular gastroenterology service. Where conditions may not appear to be ideal, this model can also act as a guide to remedial action.
Finally, considering the processual, temporal, emotional and relational benefits, what is the significance of an initiative focusing on minor issues in a climate of ‘unprecedented challenge’? Was this of value, or was this a diversion from the main transformational agenda? This initiative can be considered to have value in at least three respects.
First, several issues were resolved quickly, to the satisfaction of staff involved, at little cost other than small amounts of time and a £90 scanner. For those faced with the daily frustrations of those minor annoyances, those quick and permanent fixes were welcome. One of the consultants involved subsequently used the ‘quick fix’ developed in one of these instances to resolve another, similar problem just as rapidly. And it was planned to extend this initiative to other divisions and services.
Second, ‘tinkering’ has a recognized place in the toolkit of change management. Abrahamson (2000; 2004) describes tinkering as ‘fiddling with the nuts and bolts’, of what already exists in order to generate inspired solutions to current problems, rather than trying to create something new from scratch. He argues that tinkering is typically inexpensive and rapid, is not as destabilizing as large-scale radical change can often be, and is more likely to succeed (or to have lower opportunity costs of failure).
Third, previous research has suggested that one predictor of the success of the next change initiative concerns an organisation's past experience (Walkeret al., 2007). A track record of successful change encourages a predisposition to support further initiatives. Commentary in this field thus recommends achieving ‘quick wins’ (for a healthcare example, see Klaberet al., 2011). Sweat the small stuff achieved several welcome and visible quick wins, with possible medium and long term benefits beyond the five day programme. As previously indicated, another healthcare-specific predictor of the success of change lies with the quality of clinical/managerial relationships. This initiative served to strengthen relationships which were positive at the start, albeit weakened by those ongoing unresolved problems.
In other words, the cluster of ‘soft’ benefits that emerged from this small-scale initiative may contribute in significant ways to the support for, and the implementation and success of, the more radical, transformational, disruptive change agenda facing healthcare. This initiative also helped to cement the mutual interprofessional trust, respect, and collaboration on which those larger-scale challenges are likely to depend.
References
- Abrahamson E. Change without pain. Harvard Business Review 2000;78:75-9.
- Abrahamson E. Change Without Pain: How Managers Can Overcome Initiative Overload, Organizational Chaos, and Employee Burnout. Boston, MA: Harvard Business School Press; 2004.
- Bruch H., Menges J.I. The acceleration trap. Harvard Business Review 2010;88:80-6.
- Checkland K., Snow S., McDermott I., Harrison S., Coleman A. Animateurs and animation: what makes a good commissioning manager?. Journal of Health Services Research &Amp; Policy 2011.
- Christensen C.M., Bohmer R., Kenagy J. Will disruptive innovations cure health care?. Harvard Business Review 2000;78:102-12.
- Dawson P. Reshaping Change: A Processual Approach. London: Routledge; 2003.
- NHS 2010. London: The Stationery Office; 2009.
- Equity and Excellence: Liberating the NHS. London: Her Majesty's Stationery Office; 2010.
- Edwards N. Dealing with the Downturn: Using the Evidence. London: The NHS Confederation; 2010.
- Edwards N. The Triumph of Hope Over Experience: Lessons from the History of Reorganization. London: The NHS Confederation; 2010.
- Katz N., Lazer D. Kennedy School of Government. Harvard University; 2003.
- Klaber B., Lee J., Abraham R., Lemer C., Smith L. How pairing clinicians with managers could speed up clinical excellence. Health Service Journal 2011:21-3.
- Kotter J.P. A Sense of Urgency. Boston, MA: Harvard Business School Press; 2008.
- Locock L. Maps and Journeys: Redesign in the NHS. Birmingham: The University of Birmingham, Health Services Management Centre; 2001.
- McCarthy S., Berman R., Bell L. Professionals in healthcare: perceptions of managers. Journal of Management in Medicine 1993;7:48-55.
- Moore C. Knowing me, knowing you: interpersonal relationships between managers and hospital consultants. Cranfield Healthcare Management Group Research Briefing 11 2011.
- Stace D., Dunphy D. Beyond the Boundaries: Leading and Re-creating the Successful Enterprise. Sydney: McGraw Hill; 2001.
- Malby B. Suited must not mean booted. Health Service Journal 2011:18-9.
- Øvretveit J., Aslaksen A. The Quality Journeys of Six Norwegian Hospitals: An Action Evaluation. Oslo: Norwegian Medical Association; 1999.
- Pettigrew A.M., Ferlie E., McKee L. Shaping Strategic Change: Making Change in Large Organizations – The Case of the National Health Service. London: Sage Publications; 1992.
- Pettigrew A.M., Woodman R.W., Cameron K.S. Studying organizational change and development: challenges for future research. Academy of Management Journal 2001;44:697-713.
- Walker H.J., Armenakis A.A., Bernerth J.B. Factors influencing organizational change efforts. Journal of Organizational Change Management 2007;20:761-73.
Appendix 8 Research methods
Aims and backdrop
The main aim of this appendix is to provide further details concerning the data collection and analysis methods used in this project. A further aim is to explore the wider lessons from this experience for future studies of this nature. The research methods are outlined briefly in Chapter 1. In this appendix we go ‘behind the scenes’ of the fieldwork and analysis process in more detail.
The backdrop to this project is explained in Chapter 1 with regard to the economic crisis from 2008 and the change of government in 2010. Both of those events have had a continuing impact on the funding and governance of the service as a whole, and on the management agendas of acute trusts. Chapter 3 outlines the dimensions of the institutional context in which NHS providers operate. The emphasis in those accounts lies with the challenges facing middle management in acute hospitals. But those trends and developments also affected significantly the conduct of this research, for which funding was secured in late 2008, with the aim of commencing fieldwork in 2009. This appendix thus also considers how those contextual conditions influenced the collection and analysis of data.
It was the best of times, it was the worst of times, to be conducting a study of middle management roles in acute trusts. On the one hand, managers were faced with new agendas and priorities, creating ideal conditions for exploring responses to these challenges and how managerial roles and structures were being reshaped, and identifying the new capabilities and processes that might be required. On the other hand, those new agendas and priorities generated considerable pressures, increasing demands on managers' time and reducing their availability for research meetings. The original project timetable was thus abandoned from an early stage and a 6-month extension was subsequently required, taking this project up to the end of June 2012, rather than to December 2011 as planned.
This appendix is structured in terms of the main project stages (see Table 1), considering the details of data collection and analysis, and also exploring how the wider context of this study shaped those processes, and the lessons for future research that can be drawn from this experience. We will thus return first to the recruitment of the six participating sites, followed by the set-up meetings, the focus groups, the management survey and finally the case incidents.
To secure a measure of respondent validation, we also invited participants at the six trusts to a project launch event in 2009, to project update workshops in 2010 and 2011 and to an end-of-project conference in June 2012, as well as to a series of management briefing sessions from mid-2011 onwards. As those various events were part of the verification process with regard to the analysis and interpretation of interview and focus group information in particular, their contributions in this regard will be discussed under those headings. It should also be noted, however, that those events were also offered to project participants at no cost as a courtesy, to say ‘thank you’ for contributing to this study, and to maintain the relationship for future research, should that be appropriate.
Site recruitment
A call for proposals in the area of ‘management practice’ was published in April 2008. Recognising that we could contribute to this theme, we began to pull together a project team and to approach potential participating trusts, while developing the outline proposal. As Chapter 1 indicates, the aim was to establish a collaborative research design, and this was adopted from this stage. With a combination of corporate and personal links with the six participating trusts, each was approached in 2008 through either their chief executive or an executive board member, who were each then asked to comment – critically – on the outline proposal. This step confirmed the interest in principle of those trusts in this project, and provided reassurance that the proposal was addressing themes and issues that they considered to be significant. One issue from an early draft, concerning teamwork, was rejected as having attracted enough research and practical attention already.
The outline proposal was accepted by SDO, as was the subsequent full research proposal, and January 2009 was the formal project start date. Each trust was thus revisited early in 2009 to identify key contacts through whom the research team would work, and to establish the project logistics in terms of distributing participant information and arranging interviews and focus groups. To gather background information about each trust, and to establish the management groups that would be involved in focus group discussions and the management survey, key contacts were asked to assist in arranging a small number of set-up interviews, as described in the following section.
The original project plan allowed 6 months for gaining ethical approval and for completing governance checks through the Integrated Research Application System (IRAS). A favourable ethical approval was granted in April 2009, by Cambridgeshire 3 Research Ethics Committee. The governance checks, however, were not completed until the end of October that year; the processes applied by the Coordinated System for gaining NHS Permission – CSP – were cumbersome and time-consuming. National Institute for Health Research guidelines at that time stated that project team members did not require research passports, given the levels of access required to hospital staff and information. One of the Comprehensive Local Research Networks implicated in this project insisted that passports were required, again contributing to delay.
A process that was expected to last 6 months thus took 10 months, consuming considerably more time and effort than anticipated, particularly on the part of the principal investigator. The research governance framework has since been revised and studies such as this, involving NHS staff in their professional capacities, no longer require the approvals that were necessary for this study.
This delay was to have three consequences for data collection and analysis. First, it was not possible to start arranging focus group meetings with middle managers (many of whom have ‘hybrid’ clinical responsibilities) during the final quarter of calendar 2009, at the point when annual ‘winter pressures’ start to mount. This meant that focus group arrangements could not be activated until well into 2010.
Second, this had a predictable ‘knock-on’ effect on the rest of the project with regard to the timing of data collection in subsequent phases. Although steps were taken to limit the damage, a 6-month extension was eventually required at the end of the project. This early delay also affected data analysis. It is more straightforward to analyse information, and especially qualitative information, that has been gathered, complete, within a defined period than it is to handle information that accumulates more slowly, in an unpredictable manner, in which the end point is unclear.
Third, a degree of momentum had been lost. Having stimulated the interest of senior hospital staff through 2008 and early 2009, having arranged interviews to gather background information and having agreed the focus group logistics, core data collection would not begin until well into 2010. Some key staff had left or changed roles in that time, one trust had appointed a new chief executive and the site recruitment process thus had to be repeated, requiring further investments of time.
Set-up interviews
As explained in Chapter 1, the set-up interviews (see agenda in Appendix 2) had three objectives: first, to identify the management groups who would be involved in the project; second, to gather background information about the trust and its management agenda; and, third, to establish the logistical arrangements at each site for distributing project information. In preparation for the subsequent focus groups and management survey, interviewees were also asked about the pressures and demands facing middle managers, about their motivations and rewards and for examples of management contributions to clinical outcomes and care quality. A final question was, ‘what has to change to allow middle managers to make an even stronger contribution?’. These interviews were relatively informal, lasting up to 1 hour, with the researcher taking notes that were subsequently transcribed (no recording took place at this stage).
These interviews began with each site's lead contact, who was then asked to nominate colleagues who would be able to provide further background information. This process had several benefits. First, it stimulated interest in the project among those approached. Second, the management contributions of ‘hybrids’ were reinforced. Third, it confirmed the scope and challenge of acute trust management agendas, which, apart from specific local issues, were similar across all six sites. Consequently, this programme was extended, eventually covering 93 interviewees (see Table 3).
The transcribed interview notes were subjected to content analysis, question by question. Content analysis is a data reduction method, commonly applied to qualitative information, and is based on identifying and categorising (coding) recurring themes. For example, answers to the ‘motives and rewards’ question from 13 interviewees at Greenhill were coded in nine categories (Table 43).
| Category label | Illustrative quote |
|---|---|
| Make a difference | ‘It's rewarding to work with staff groups on a concern – what can we learn, what will make a difference to patients?’ |
| Colleagues | ‘I work with an amazing team; delightful people who enjoy their jobs’ |
| Hygiene factors | ‘Leave and sick pay and pensions are generous; pay is competitive’ |
Similar analyses were conducted for ‘pressures’, ‘contributions’ and ‘what has to change’. These analyses were first carried out by the lead researcher for each site, and then checked by the principal investigator. The project research fellow collated and further checked these analyses. There is clearly a degree of subjectivity involved in categorising and labelling interview comments such as these, and content analysis can be controversial for that reason. However, in this case, and as the above illustrations suggest, only minor disputes arose over category labels, and the tables in the main report allow readers to check whether or not the categories make sense to them. The number of items coded in each category was also recorded, simply to provide a rough indication of the weight of evidence being gathered; for example, the 13 interviewees at Greenhill identified a total of 42 ‘motivation’ items.
How confident are we that this analysis has captured accurately the information that interviewees provided? In addition to discussion within the project team, these analyses were presented to a group of management participants from the six participating trusts at the first project update workshop in June 2010. Participants were asked whether or not they ‘recognised’ these analyses as an accurate portrayal of the issues; no challenges were launched. This step is sometimes called ‘respondent validation’, a term suggesting degrees of rigour and finality that are rarely present. However, these findings were also presented at the second update workshop in June 2011, in 16 management-briefing sessions and at the final project conference in June 2012, where they invariably met with agreement.
Focus groups
As explained previously, the focus group programme was delayed by more than 6 months because of delays created first by the ethical approvals and governance checks and then by the onset of ‘winter pressures’. Following the comments from set-up interviews, the aim was to involve four groups in particular at each participating site: clinical directors, directorate managers, ward sisters and matrons. However, where possible, it was also decided to involve the heads of support services departments, non-executive directors, service managers, clinical leads with service improvement responsibilities and staff in leadership and management development roles. Focus group discussions followed a topic guide (see Appendix 2) with three issues concerning motives and rewards, how management roles were changing and what would have to change to strengthen management contributions. Group discussions were each facilitated by two members of the project team, with one guiding the discussion and the other taking notes that were subsequently transcribed. Focus group discussions were not recorded (transcribing group conversations can be extremely difficult).
Focus group discussion transcripts were subjected to the same content analysis procedures as set-up interviews. The researchers involved produced a first analysis (see, for example, Figure 8), which was scrutinised by the principal investigator, with all focus group analyses being collated by the project research fellow. All of the focus group transcripts were then recoded by an independent researcher (using a NVivo database, version 9; QSR International, Southport, UK), whose choice of categories proved to be almost identical (see Table 42). As with the set-up interviews, the results of these analyses were also presented at the update workshop in 2011 and at the final project conference in 2012, thus increasing confidence that this analytical approach had accurately captured the issues raised by project participants.
The logistics of arranging focus group discussions proved to be more challenging than anticipated. The intent was to use existing meetings where possible, rather than arranging separate meetings and rooms. However, this involved, for each group, identifying a meeting that an appropriate number would be attending, at which the agenda was short enough to accommodate an additional discussion, and where the duration of the meeting permitted this. This arrangement worked well in many instances. Some staff did not appear to meet regularly with peers (support department heads at Netherby; assistant general managers at South Netley) and special meetings with mixed occupational groups thus had to be arranged. Where it was possible to use existing meeting schedules, the research often had to wait for two or more meeting cycles to occur before an appropriately ‘light’ agenda would arise, and ≥ 2 months would then elapse before that meeting could take place. At some sites it proved impossible to meet with particular groups at all during the life of the project – clinical directors and consultants at Burnside, divisional directors at Greenhill – not because of lack of interest in the study, but because of lack of diary space. A similar difficulty at Wattle Park was resolved by the research team member meeting individually with five clinical directors whose respective diaries appeared never to share empty spaces. We have no systematic evidence but many anecdotes of middle and senior managers deliberately and routinely double- and treble-booking diary slots, then hoping that one or more of those meetings would be cancelled for some reason, or making a judgement on the day as to which was the most important. One focus group meeting (Clearview) was cancelled 10 minutes after it had started as participants (an operations management team) were called to help resolve a beds crisis.
These logistical problems meant that the focus group programme, which was originally scheduled to run over 6 months, actually ran over an 18-month period. As explained above, this delayed a systematic analysis of the collected focus group information, which was one reason for involving an independent researcher to recode the transcripts towards the end of the project, in 2012. Nevertheless, 40 focus groups were conducted over 18 months with over 200 participants – around double the original number of targets. The main report does not explore the contrasts across the six participating trusts with regard to the findings from either the set-up interviews or the focus groups. This is because the conclusions – the motives, pressures, contributions, and desirable changes – were similar in each hospital.
Management survey
Details of the survey design and administration are provided in Appendix 3, along with an analysis of the sample characteristics. The majority of survey items were based on findings from set-up interviews and focus groups, and were designed to test those items with a larger sample. As explained in Chapter 5, the survey also incorporated a widely adopted organisational commitment scale, and a recognised set of stress indicators. A novel ‘extreme jobs’ scale was also built into the design, based on focus group discussions and on a ‘proof of concept’ pilot, facilitated by the project's SDO management fellow at one of the six participating trusts. The original plan was to use a ‘60–40’ design in which 60% of the survey items would be common to all sites, with 40% tailored (by local management) to local issues and priorities. Only two sites, Burnside and South Netley, took the opportunity to add a small number of additional items to the core survey; management at the other participating trusts were too busy in the second half of 2011 to contemplate this level of involvement.
The survey design passed through numerous iterations, within the project team, in discussion with the project advisory group and with the project's SDO management fellow (an operations manager) and following a (hard copy) pilot at one participating trust. Drafts of the design were also circulated to the lead management contacts at each site for comment. In addition to overall item coverage and detailed wording, one of the main problems was length: initial designs were too long and this would almost certainly have reduced the response rate. The final design thus reflects a series of compromises, resulting in a short instrument (70 items) that could be completed in less than 15 minutes.
The pattern of survey responses varied widely across the five trusts that were able and willing to participate. Wattle Park was engaged in merger discussions during the second half of 2011 when the survey was administered and did not want the distraction of an internal management survey. Senior management at Greenhill decided, without prior consultation with the research team, to restrict the survey distribution to their ‘100 leaders’ (as part of an internal development programme) rather than to the trust management population as a whole. Different administration methods were considered, including hard copy mailing and group administration, which would be complex and costly. The participating trusts all expressed a preference for online administration. In some respects this was relatively straightforward. Once the survey design had stabilised, it was uploaded to the Cranfield secure server and a unique link was created for each of the five trusts that would participate. That link was to be distributed at each trust in an e-mail from a senior manager (preferably our lead contact at each site). Through this route, the research team would know which trust the responses had come from but would have no personal details of respondents, other than in the replies that they provided. This approach, however, was not straightforward.
Two problems arose. First, the lead contacts who were to distribute the e-mail were those same busy managers who were double- and treble-booking their diaries by the second half of 2011. Inevitably, most delegated this task to a secretary, or to a colleague with little knowledge of this project, but who had work priorities of their own to deal with. The research team was not always informed of these delegations. This generated delays, and some errors, in the survey distribution. Second, the issue of directing the survey to the middle management population of ‘pure plays’ and ‘hybrids’ was dependent on the e-mail distribution lists at each hospital. Those lists use other staff categories and differ from one trust to another. The mailing strategy thus had to be determined separately at each trust, often by someone who, as just indicated, was not familiar with the project or its objectives.
Despite these problems, over 600 useable responses were received, with an overall response rate of 24%. (The annual NHS Staff Satisfaction Survey has a response rate of around 50%.) Descriptive statistics only are included in the main report, for two reasons. First, the sample size is small for inferential investigation; average cell values fall sharply and conclusions become meaningless. Second, the pattern of responses is similar across all five participating trusts and supports the qualitative findings, despite differences in local conditions.
Case incidents
The incidents reported in Chapter 6 were based in each case on interviews with relatively small numbers of staff who had been directly or indirectly involved in the incidents and on the associated documentation including statements, RCAs and timelines, investigation reports and, when available, progress reports. The evidence with respect to each incident varied significantly. The case of Mrs Mayland dated from 2005 and the Burnside C. difficile case dated from 2006, so there was consequently a greater volume of information available concerning those two incidents (both of which had been nominated by the respective trust chief executives as incidents that it would be useful to study). The case of Mr Torrens occurred at the end of 2010 and events relating to that incident were still unfolding during this project. The case of Mr Mitcham, a ‘never event’, occurred in late 2011, as the fieldwork for this project drew to a close. The collection of evidence concerning the latter two incidents was facilitated by the SDO management fellow seconded to this project, but nevertheless, given the sensitivity and recency of those incidents, less information was available in those cases than in the other two. As discussed previously in this appendix, it was once again not possible to gather precisely comparable evidence relating to each case.
Establishing access to the staff involved in these incidents was not problematic. On the contrary, those who were involved mostly welcomed the opportunity to share their experiences with external researchers (anonymously, and in confidence). As a further indication of this willingness to share information, the operating theatre team involved in the Mr Mitcham case asked two members of the project team, Buchanan and Denyer, to facilitate a workshop for them on the theme of ‘managing change in the aftermath of serious incidents’. These two project team members had already conducted workshops on this theme for several other audiences, and Denyer had previous experience with this topic in other sectors including nuclear reprocessing, fire and rescue services and high-security mental health care. The arrangements were once again brokered by our SDO management fellow and a 1-day (invitation only) workshop was designed to cover three main issues: using a ‘mess mapping’ tool to explore incident causality, helping the team to establish their own change agenda and identifying and tackling the barriers to post-incident change implementation. The ‘mess map’ for the Mr Mitcham incident appears in Chapter 6 (see Figure 7), along with information from a report produced by the trust's Never Events Group, which was provided to the two researcher-presenters as background to inform the running of the workshop.
This was not an action research intervention, but rather an attempt to provide assistance and support on request. Feedback from the event indicated that it was seen as valuable, and we were invited to repeat the workshop for another theatre's team. It was understood that information collected through this process would contribute to this project, appropriately anonymised. We are aware, however, that the risk management team at that trust have since been considering other systems-based approaches to the overall management of serious incidents and never events. With funding for this project coming to an end, the opportunity to follow its progress in that regard has not been available.
These kinds of incidents typically unfold over prolonged periods. The case of Mrs Mayland is a good example of this, with events and outcomes being shaped by a combination of factors at different levels of analysis interacting over time. This suggests a narrative-based processual approach to analysis. This has been started in Chapter 6, based on an ‘ideal narrative’: an understanding of incident causality should inform a change agenda, which should in turn trigger an appropriate change process. It appears, however, that this narrative is often ‘edited’ by events and circumstances such that the change process does not occur (or is partial or delayed) and a further similar incident occurs. The aim is to explain how and why this ‘editing’ takes place, and if possible how to prevent this in the interests of more rapid and effective change. It proved difficult within the length constraint of the project report to present the evidence (typically rich and interesting) surrounding the four cases along with more comprehensive theoretical development. The weight of treatment in the report, therefore, lies with the evidence, and theory development will feature in follow-on publications.
Limitations
As indicated in Chapter 1 of the main report, this study has several limitations.
First, data collection was uneven across the six participating trusts because of the mounting pressures and challenges facing hospital management at the time of this study, and the consequent difficulties in arranging and rearranging meetings (especially from late 2010 onwards). Initial plans for a ‘common data set’ to be collected from each trust had to be abandoned. The information that was gathered, however, demonstrates a mutually reinforcing internal consistency across the different data streams, which indicates that, had it been possible to gather a more standardised set of information, the conclusions would not have been much different. Nevertheless, the lack of a common data set for each participating trust does inhibit cross-site comparisons and contrasts.
Second, the extended time frame of this project potentially jeopardises the relevance of the findings. The SDO scoping study that led to the funding of this research was conducted in 2007–8. Publication of the final project report is in 2013. The NHS at the end of that period is a different organisation from the one that presented in 2007–8, in numerous respects, and particularly from an organisational and managerial perspective. However, the pressures and challenges facing hospital managers over this period appear not to have abated, but are continuing, and may escalate. Economic recovery in the UK is proving to be slower than anticipated, the government is still attempting to run down a budget deficit, in part by cutting government expenditure, and as a major contributor to that expenditure the NHS is being required to continue to make efficiency savings. It is possible that the findings and implications of this study may become more and not less relevant in this unfolding context. Nevertheless, the timeline of this project must be a cause for concern, and this is addressed in the concluding section of this appendix.
Third, coverage of the range of themes in this project – realities, contributions, changes following serious incidents – has been achieved at the expense of depth. It was not possible to follow up many interesting lines of enquiry because of the time pressures facing both researchers and participants. This was particularly the case with regard to some of the serious incidents, which were identified as valuable learning opportunities in the context of the research objectives, but which would have taken considerably more time to document effectively. This was also the case with many accounts of management contributions to clinical outcomes, especially in collaboration with clinical and/or medical colleagues, a theme that is developed in Chapter 7 but which merits closer attention. Nevertheless, we feel that this study has generated findings with useful implications for organisation and management, as well as identifying a number of interesting and valuable further research priorities.
Fourth, the quantitative support provided by the management survey for the findings from the qualitative components of this study will not satisfy a number of readers. Qualitative research in general still attracts suspicion (an appearance of lack of rigour is inevitable) and is often discounted by those with scientific and medical backgrounds who are more readily convinced by double-blind randomised control trials. There are a number of areas where quantitative methods would strengthen this study. One topic, for example, concerns the broad range of management contributions to clinical and organisational outcomes, with past studies tending to focus on single metrics and assuming a more linear causal model. Another area concerns the costs of not implementing, rapidly and effectively, the findings from investigations into serious incidents and never events. Those costs appear to be rising, and this research has proposed more effective approaches to change implementation in such conditions.
A study of this nature will always display imperfections. Nevertheless, we hope that the conclusions from this research will inform leadership and management development and contributions, and organisational change following extreme events, in useful, innovative and productive ways.
Lessons from this project
This experience suggests the following four lessons to inform future studies.
1. Collaborative research designs
This research adopted a collaborative design that began with drafting the outline research proposal – long before funding was secured or fieldwork would begin. This necessitated a series of additional meetings with senior hospital staff, arranging project workshops and other events, responding to requests to run tailored development sessions for staff groups and holding management briefing sessions to feed back project findings. The recruitment of a SDO management fellow was also a key component of this strategy. It must be recognised that collaborative designs such as this consume considerably more (preparation, travel and meeting) time and energy on the part of researchers than traditional ‘neutral observer’ designs. Nevertheless, the benefits significantly outweigh the drawbacks. These benefits include a better understanding of ‘end-user’ needs, perceptions and presenting problems; the engagement of participants as co-researchers and co-producers of findings; access to information that may not have appeared significant to the research team, or the existence of which the team may have been unaware; and rapid feedback on the suitability of materials for practitioner audiences. In addition, the NHS is a complex organisation experiencing broad and rapid changes that can be difficult for ‘outsiders’ to follow. Collaborative relationships are thus valuable in this regard, too, providing researches with ‘insider’ briefings. In sum, the efforts involved in setting up and maintaining a collaborative research design carry multiple valuable rewards.
2. Data collection in a high-pressure context
With hindsight, it would have been useful to have maintained a log of the research meetings that were cancelled and rearranged, only to be cancelled and rearranged again during this project. Many meetings had to be set up several weeks, and in some cases months, in advance, and some of those were cancelled and rearranged too. As pressures on management mounted in 2011 in particular, availability for research was curtailed. It proved impossible to arrange more than a single meeting with a single person on each site research visit, thus involving considerably more travel costs and time than had been anticipated. It was possible in a small number of instances to gather information through e-mail and telephone calls but, given the substance of this study, personal interviews were preferable. The pressured nature of the context is beyond the control of the research team. However, these predictable delays should be built into a project schedule in advance.
3. Online survey administration
Online administration may sound like an ‘easy option’ for the busy researcher, avoiding the costs of copying and mailing, and capturing data into a statistics package. This is also a preferred model for most research participants. However, as explained above, logistical problems arise. Were we to repeat this exercise, we would (1) seek to brief in person the individuals delegated to send the e-mails and (2) arrange to be present when e-mailing took place, to monitor when and to whom the survey was sent. Sadly, this ‘low-trust – high-control’ approach seems advisable in a high-pressure context.
4. Matching the pace of research to the pace of change
Research projects unfolding over 3 years, with large teams, can have benefits in terms of the depth with which issues can be explored and the ability to cover a range of settings. The main disadvantage concerns the time that elapses between framing questions and publishing answers. In a rapidly changing service, there is also a place for ‘agile research’, with shorter time frames and smaller teams, focusing on current and emerging themes and problems and producing actionable knowledge quickly. Agile research need not be limited to narrowly defined issues. On the contrary, it is with the more strategic developments and challenges that answers and solutions are most pressing.
List of abbreviations
- A&E
- accident and emergency
- AGM
- assistant general manager
- ALERT
- acute life-threatening events recognition and treatment
- CDU
- Clinical Decisions Unit
- CIP
- cost improvement programme
- CNST
- Clinical Negligence Scheme for Trusts
- CQC
- Care Quality Commission
- CSF
- Comprehensive Soldier Fitness
- D&V
- diarrhoea and vomiting (norovirus symptoms)
- DIPC
- Director of Infection Prevention and Control
- FTE
- full-time equivalent (employees)
- HOSC
- Health Overview and Scrutiny Committee
- HPA
- Health Protection Agency
- HSE
- Health and Safety Executive
- IT
- information technology
- LINks
- Local Involvement Networks
- Mid Staffs
- Mid Staffordshire NHS Foundation Trust
- MRSA
- methicillin-resistant Staphylococcus aureus (health care-associated infection)
- NPSA
- National Patient Safety Agency
- NRLS
- National Reporting and Learning System
- OFSTED
- Office for Standards in Education, Children's Services and Skills
- PALS
- Patient Advice and Liaison Service
- PCT
- primary care trust
- PSI
- public services industry
- RAIAs
- regulators, auditors, inspectorates and accreditation agencies
- RCA
- root cause analysis
- RTT
- referral to treatment (18-week target maximum waiting time)
- SDO
- Service Delivery and Organisation
- SHA
- strategic health authority
- WHO
- World Health Organization
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices in which case the abbreviation is defined in the figure legend or at the end of the table.