Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 08/1809/230. The contractual start date was in February 2009. The final report began editorial review in August 2012 and was accepted for publication in December 2012. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors' report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen's Printer and Controller of HMSO 2013. This work was produced by Senior et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Background
Older prisoners are the fastest growing subgroup in the prison estate in England and Wales. 1–4 In spite of the rapid increase in numbers and the complex and costly health and social care needs of older prisoners,5 their service provision is currently often suboptimal. 6 Emerging evidence has suggested that there are particular service provision and integration deficits at key transition points for older prisoners, such as on entry to and discharge from prison. 7
This programme of research examined the health and social care needs and current service provision for older male adults entering and leaving prison, and evaluated a model for systematic needs assessment and care planning for these groups. Women have been excluded from the study because of the low number of older female prisoners. In June 2011 there were only 63 female prisoners aged ≥ 60 years in England and Wales compared with 2952 male prisoners in this age group [National Offender Management Service (NOMS), 2011, personal communication].
Objectives
The specific objectives of the current study were:
-
to explore the lived experiences and needs of older people entering and leaving prison
-
to describe current provision of services, including integration between health care and social care services
-
to pilot and evaluate an intervention for identifying health and social care needs on reception into prison and ensuring that these are systematically addressed during older people's time in custody.
Methods
The research programmes was a mixed-methods study divided into four parts:
-
a study of all prisons in England and Wales housing adult men, establishing the current availability and degree of integration of health and social care services for older adults
-
establishing the health and social care needs of older men entering prison, including their experiences of reception into custody
-
the development, implementation and evaluation of an intervention to identify and manage the health care, social care and custodial needs of older men entering prison
-
exploration of the health and social care needs of older men released from prison into the community.
Ethical considerations
Ethical approval to conduct the study was obtained from South Staffordshire Local Research Ethics Committee (09/H1203/47) and the University of Manchester's Research Ethics Committee. To access Her Majesty's Prison Service (HMPS) establishments, governance approval was obtained from the NOMS National Research Committee and from individual prison governors/directors. For each establishment, site-specific approval was obtained from the relevant NHS primary care and mental health trusts. Research staff had NHS research passports and letters of access.
To ensure informed consent, all participants were provided with a participant information sheet (see Appendix 11). The information detailed on the sheet was also verbally imparted to ensure comprehension and allow for any literacy difficulties. Participants were provided with the opportunity to ask questions and were given at least 24 hours to consider their participation. Participants were frequently reminded of their right to withdraw from the study at any time. All written consent was obtained by researchers rather than prison or health care staff.
All participants had issues of confidentiality explained to them and were aware that the informationthey provided would be treated in confidence unless we were concerned for their immediate safety, or the safety of others. In such circumstances the appropriate individuals at prison establishments were informed. In some instances this led to the opening of Assessment, Care in Custody and Teamwork (ACCT) documents to ensure that prisoners who were at risk of self-harm were appropriately supported by prison and health care staff.
The safety of researchers was also prioritised and appropriate strategies were in place for conducting interviews in prison and in the community. Interviews were conducted in public places when possible. When this was not plausible because of interviewees' mobility difficulties, two researchers were present.
The University of Manchester and NHS protocols for data protection were strictly adhered to.
The authors have no competing interests to report.
Chapter 2 Background
The growing number of older prisoners
It has been well documented that the number of older prisoners is increasing rapidly in England and Wales. 1 In December 2012 there were 85 women in prison aged ≥ 60 years in England and Wales, compared with 3292 male prisoners in this age group (NOMS, 2013, personal communication). The proportion of male prisoners aged ≥ 60 years has steadily increased from 2% in 2002 to 4% in 2011 (NOMS, 2011, personal communication). This trend is also evident in both Canada and the USA. 8,9
There are a number of factors contributing to this increase, including changes to sentencing practices, for example an augmentation in mandatory sentencing, the pursuit of convictions in later life for historical offences, the use of indeterminate imprisonment for public protection and an increased number of life sentences. 7 Furthermore, the general population are living longer, thus there are a greater number of older people in society to commit crimes. 10–12
The Ministry of Justice projections (2011) estimate that the overall prison population may increase to 94,800 by June 2017 (NOMS, 2013, personal communication). Such projections take into account a number of factors, including the age of defendants entering the system. NOMS figures show that prisoners aged ≥ 50 years were the only age category subgroup to increase year on year since 2006 (NOMS, personal communication). The projected increase of this subgroup of prisoners will undoubtedly affect many aspects of the system, including creating increased pressure on prison-based health care provision as services attempt to address the complex health needs of older prisoners. 13 It has been argued that prisoners aged ≥ 50 years acquire age-related health problems 10 to 15 times faster than their peers in the general population. 14–16 As a consequence, the cost of health care for older prisoners is significantly higher than that for younger prisoners, with costs estimated to be between three- and eightfold higher. 13,16–18
Defining older prisoners
In the general population the definition of an older person is wholly socially constructed, with different age-dependent events, for example pension and benefit entitlements, occurring at different age points. Similarly, the age at which a person in custody is regarded as an older prisoner is, to some degree, arbitrary. Throughout this study the minimum cut-off age of 60 years is used to define an older person. This is in line with the lower cut-off age generally used by social services.
Policy and legislation
Currently, there is no national strategy for the care of older prisoners, despite repeated recommendations for one to be developed. 7,19 The provision of services for older prisoners across the English and Welsh prison estate has been under formal review since 2004, at which time an independent inspection of 15 prisons housing adult men by Her Majesty's Inspectorate of Prisons (HMIP) found that the physical design of establishments often restricted older people from accessing many areas of the prison. 19 Older prisoners were observed to be excluded from taking part in a full range of activities as a result. Some older prisoners reported feeling unsafe within establishments, and specific staff training to deal with issues affecting older prisoners was found to be sparse. 19 A follow-up inspection of 29 establishments in 2008 found that only three prisons had a policy specifically addressing the needs of older prisoners. The later inspection did, however, find that older prisoners were less fearful than had been identified previously and that the majority were happy with the care they received. 7 Her Majesty's Chief Inspectorate of Prisons' (HMCIP) review of older prisoner care raised grave concerns that older prisoners' needs were not planned or provided for after release. 7 Only four prisons could be identified as providing specific resettlement help for older prisoners. The recommendation from the previous review that the specific resettlement needs of older prisoners should be accurately assessed and provided for on release was thus reiterated. 7
Stemming from findings of the reviews of 2004 and 2008, and updates to the Disability Discrimination Act (now replaced by the Equality Act 2010), HMPS published Prison Service Order (PSO) 285520 relating to prisoners with disabilities, including reference to older prisoners. The overall standard stated that, ‘The Prison Service ensures that all prisoners are able, with reasonable adjustment, to participate equally in all aspects of prison life without discrimination’. 20 The PSO outlined the requirement for prisons to ensure that offending behaviour courses, work and education were accessible to older prisoners, and that prisons should consider having a lead member of staff for older prisoners. It also emphasised the need to have continuity in managing chronic physical health problems through effective multidisciplinary working and information sharing, reflective of the care of older people in the community. It is a well-established principle that prison-based health care provision should be equivalent in quality and range to health care provided in the community and that all national standards for health care apply equally in prison and community settings. 21 Thus, the National Service Framework for Older People22 applies in prison. The framework focuses on providing person-centred care to older people, whether in their own home or in a residential setting. It aims to diminish age discrimination and promote independence among older people as well as ensuring that care provided is relevant to older people's needs. It focuses particularly on health conditions relevant to older people, such as stroke and specific mental health problems associated with ageing. 22
The Department of Health produced a toolkit for good practice for older prisoner care in 2007. 23 The toolkit made specific recommendations aimed at bringing prison-based care into line with national policy and community practice. The document stipulated that older prisoners should be assessed using a health and social care assessment specifically designed for their needs and that this should be repeated every 6 months, with care plans made and reviewed accordingly. The Department of Health’s A Pathway to Care for Older Offenders23 emphasised the importance of comprehensive and systematic identification of the needs of older prisoners on entry into custody.
Currently, the provision of health care services in prison relies heavily on information elicited at reception from a generic screening instrument. 24 There are specific versions of the instrument for men and women; however, there are no specific questions relevant to assessing age-related needs, for example relating to memory, cognition or level of independence with daily living skills. Previous studies have shown that, if health problems are not elicited at reception, they are unlikely to be detected later during a person's detention;25 thus, it is appears unlikely that, without tools specifically designed to identify age-related health needs, such deficits would be routinely detected later during the custody period.
As part of A Pathway to Care for Older Offenders,23 the Department of Health has also made recommendations around preparation for release and follow-on support in the community, which are particularly pertinent to this study. The Department of Health stipulates that release planning for older prisoners should involve the following:
-
a health and social care needs assessment history being forwarded by the health care team to the offender manager
-
the conduction of a pre-release health and welfare assessment
-
an assessment by a social worker, conducted face-to-face
-
collaboration with external organisations
-
the organisation of a care package
-
formal arrangements for loans of occupational therapy equipment
-
a pre-release course specifically for older and retired prisoners. 23
In 2009, the National Association for the Care and Resettlement of Offenders (Nacro), in conjunction with the Department of Health, produced a training pack for prison staff working with older prisoners. 26 The purpose of this document was to raise awareness among staff of the common health difficulties experienced by older offenders. It intended to set out good practice guidelines and encourage the commencement of specialised activities for older prisoners such as older prisoner groups, in-cell work for those with mobility difficulties and appropriate exercise opportunities. Furthermore, it aimed to encourage staff working with older prisoners to contact community-based specialised agencies for older people to obtain information and support. 26 Throughout, the training pack attempted to pursue the principle of equivalent services for prisoners as for older people in the community.
The health and social care needs of older prisoners
Older prisoners have complex health needs. 27 The physical health needs of older prisoners are greater than those of both younger prisoners and those of a similar age living in the community. 14 Kingston et al.,3 in their UK sample of 121 prisoners aged ≥ 50 years in four prisons in and around Staffordshire, found that participants each had an average of 2.26 physical health problems. Approximately 85% of older prisoners have one or more major illness. The most frequently reported health conditions among older prisoners are cardiovascular diseases (35%), arthritis and/or back problems (41%), respiratory diseases (15%), endocrine disorders (21%) and sensory deficits (12%). 13,28
The mental health needs of older prisoners have been found to vary significantly from those of their younger counterparts in prison. 2 Older prisoners are at a greater risk of becoming isolated within the prison environment and are less likely to have social support, putting them at a greater risk of developing mental health difficulties. 29 In the aforementioned study by Kingston et al.,3 half of prisoners in the sample (n = 60) were identified as having a mental disorder, with depression being the most frequently diagnosed. Furthermore, 12% (n = 15) had symptoms of cognitive impairment. Strikingly, Fazel et al. 6 found that 86% of their sample showing signs of depression were not receiving antidepressant medication nor was depression documented in their medical records. In addition, alcohol is the most commonly misused substance among older prisoners. 30,31
There is a dearth of research regarding older prisoners' social care needs. Previous studies have shown that older prisoners have high levels of unmet need in the domains of accommodation release planning and daytime activities. 4 A comprehensive study carried out by Hayes et al. 32 in 2010 found that, of the sample of 262 prisoners aged ≥ 50 years, more than one-third had some level of functional need in activities of daily living and 14% had mobility difficulties. Nearly half were imprisoned far from their home area, which made contact with family and friends difficult; 15% had no contact at all with family or friends.
The provision of social care is an area often overlooked within the prison environment, largely because there is an apparent lack of understanding of what constitutes ‘social care need’ within a prison institutional setting. 33 The result is that the provision of social care becomes, by default and through a sense of necessity, the responsibility of health care services rather than being regarded as a wider, multi-agency responsibility. 7
There is currently very limited research focused on the specific issue of identifying and meeting the health and social care needs of older prisoners on entry into prison. It has been established that, within the general prison population, just over one-quarter of all self-inflicted deaths occur within 1 week of prison entry. 34 Furthermore, previous research conducted by Crawley35 suggested that older prisoners entering prison for the first time experience a number of distressing phenomena, labelled ‘entry shock’. Contributing factors included high levels of noise, lack of privacy, indigent facilities, claustrophobic conditions, perplexing rules and regulations and hostility from younger prisoners and uniformed staff. Within Crawley's study, many older prisoners reported that, in the absence of any support in prison, they were able to recall previous difficult experiences such as induction into the army or a childhood in care and that they used these as an, albeit imperfect, ‘blueprint’ for how to cope in the prison. 35
As well as the risks associated with reception into prison and the early weeks spent adapting to custody, some limited research has identified that the period post release is also risky in terms of prisoners' physical and mental health. 36 There have been a small number of studies that have explored, prior to discharge, older prisoners' concerns and issues about release,37–39 suggesting that older prisoners struggle disproportionately with community resettlement because of reduced support networks and the increased likelihood that they are suffering from health and mobility problems. 39 Crawley38 and Crawley and Sparks37 explored older prisoners' concerns regarding their release from prison, concluding that they often experienced intense anxieties about release and inadequately understood the resettlement process. Key concerns included where they were going to live and how they were going to get there; their physical safety on release (for those convicted of sexual offences in particular); loss of personal possessions and support networks; and access to health care for support with chronic illness. Their concerns prior to discharge were so intense that many of them felt that it would be better to stay in prison than be released into the community.
There is an increased risk of suicide among recently released prisoners in England and Wales, with the greatest elevation in risk identified in those aged ≥ 50 years. 40 Despite these increased needs, older prisoners' resettlement needs are often ignored; it has been suggested that, in spite of evidence to the contrary, this is because they are generally considered to be of lower risk than their younger peers,38 which is exacerbated by their being less assertive. 38 Crawley38 advocated the need for an emphasis on effective, proactive communication with older prisoners to reduce severe feelings of anxiety leading up to release. No studies have been published to date that have followed up older prisoners after their release to examine the barriers to and facilitators of successful community reintegration.
Assessing older prisoners' health and social care needs
There are challenges to effectively conducting health and social care assessments of older people in the community. 41 Problems have included the under-reporting of need, variations in assessments across disciplines and geographical areas and disagreement between different professionals. 41 The National Service Framework for Older People22 set out plans to improve the assessment of all older people's needs, including the introduction of the Single Assessment Process (SAP). The aims of the SAP were to standardise the assessment process across organisations and geographical areas, raise the standard of assessment, assist information sharing, prevent duplication of assessment processes and ensure holistic assessment of need. 22
Implementation of the SAP should result in an individual care plan that clearly describes the help to be provided and who should be contacted in case of emergency or should a person's needs change. 22 Additionally, the guidelines specify that care plans be agreed with the older person and that the older person should hold a copy of his or her own care plan. 22 Findings from an evaluation of the SAP suggested that its implementation had been uneven and that full implementation will be a long process. 42 Elsewhere, it has been suggested that statutory social services assessments have improved since the introduction of the SAP; however, the extent to which these improvements can be attributed to the SAP is unclear. 41
Health and social care services for older prisoners
The provision of services for older prisoners varies considerably between establishments. 7 HMCIP's 2008 review of 29 adult establishments7 found that few establishments had an older prisoner lead (OPL) responsible for co-ordinating the care of older prisoners. When in operation, the role was often given to the disability liaison officer (DLO), in addition to their already full workload. However, and more encouragingly, a further large-scale survey in 2010 of staff working in 92 establishments in England and Wales, conducted on behalf of the Prison Reform Trust,43 found that over one-third of prisons now had an older prisoner group/forum running at their establishment. It is also becoming evident that voluntary agencies are increasingly involved with older prisoners in some establishments, providing befriending services and help on release and running groups for older prisoners. 26 Specific older prisoner clinics were reportedly established in many prisons; however, the frequency of clinics varied considerably. Prison buddy schemes set up to help prisoners with tasks such as fetching meals or keeping cells tidy were also operational in some establishments. In certain prisons, older prisoners are housed together because of their differing psychosocial needs to those of their younger counterparts. 11 In summary, services available to older prisoners appear to be increasing, albeit in an ad hoc informal manner, lacking organisation or adherence to an overarching model of best practice but with some examples of apparent good practice. 44
Prisons are, for the most part, designed for younger, able-bodied prisoners. 7 Many prison establishments in England and Wales are of Victorian design and construction. Narrow staircases and cell doors and long corridors mean that those with mobility problems struggle to physically access many parts of prisons. 7 This frequently results in older prisoners with mobility problems being housed routinely in prison inpatient wards, simply because of a lack of appropriate facilities in other wing locations rather than because of a need for continuous nursing care. 7 It is noteworthy that, where adaptations have been made, such as the installation of chairlifts, equipment has often been found to be out of order. 7 Nacro and the Department of Health suggest that some simple adaptations should be made to care appropriately for older prisoners, for example doors and windows should be easily opened; less harsh lighting should be installed; radiators should be easily adjustable; special cutlery, plates, bowls and trays should be provided for older prisoners; and lower television shelves and appropriate seating should be made available in cells. 26
The commissioning of health and social care services
Historically, HMPS, through the existence of the Prison Medical Service, latterly renamed the Prison Health Service, was responsible for the provision of the majority of health care services for prisoners. Almost all services were provided ‘in house’, ranging from primary care for everyday physical complaints to inpatient care for those with severe mental health problems. HMPS directly employed doctors as prison medical officers, and part-time medical practitioners were also employed, usually local general practitioners (GPs). Other health care staff consisted largely of qualified nurses, usually with general or mental health qualifications, and prison health care officers, usually non-nurse-qualified personnel who undertook in-service training to assume duties traditionally associated with nursing staff.
Following sustained criticism of both standards of care provided to prisoners and the relative expense of such services, a clinical improvement partnership between the NHS and HMPS was established in 1999. 21 Initially, HMPS maintained control of the costs of health care services but, by 2006, budgetary control for health care provision in all public sector prisons was transferred to primary care trusts (PCTs).
The Health and Social Care Act 2012 heralded the transfer of the majority of NHS commissioning responsibilities across England from PCTs to clinical commissioning groups (CCGs), largely controlled by GPs. However, from April 2013, the responsibility for commissioning prison-based care will transfer from PCTs to the national NHS Commissioning Board, along with a number of other ‘specialist’ services. The national Commissioning Board will be supported across England by 27 local area teams (LATs) and it has been announced that 10 of the 27 LATs will develop specific expertise and lead on matters relating to the commissioning of offender health care including, but not limited to, prison-based services.
Although prison-based health care services within public sector prisons are now a fully integrated part of the wider NHS, the involvement of local authority social services with prisoners in need of social care remains underdeveloped. Anecdotally, particular issues seem to arise when requests are made to NHS services, and perhaps more markedly social services, to provide assessments or services for prisoner-patients not deemed to fall within the geographical boundaries of a particular area's service. For example, when a prisoner requires admission to secure mental health care, NHS commissioners for the prison where the person is housed may argue that they are not responsible for the care costs as the person's last known address outside custody is determined to be elsewhere in the country. Similarly, social services departments have frequently failed to accept that the populations of prisons within their geographical catchment area are ‘proper’ residents. Our study discusses these matters in detail throughout.
In future, again as part of the organisational changes contained within the Heath and Social Care Act 2012, a local health and well-being board (HWB) will be established in each of England's 152 upper-tier local or unitary authority areas, to co-ordinate commissioning across health, public health and social care. Each HWB will comprise representatives from the CCG, a director of public health, a director of children's services, a local Healthwatch England representative and other key stakeholders at the discretion of the local authority (Healthwatch England is the new independent ‘consumer champion’ for health and social care in England).
Each HWB is charged with co-ordinating a Joint Strategic Needs Assessment (JSNA) to identify the health and well-being needs of the local population, and producing an annual Joint Health and Wellbeing Strategy (JHWS) to outline how partners will address the needs of the local community through their commissioning of NHS, social care and public health provision. Most of the 152 local authorities in England have now formed shadow HWBs that are already developing the JSNAs and JHWSs for 2013–14. The need to undertake JSNAs for the whole of a local population may serve as a way of including prisoners' social care needs in a much more widespread and routine way than has previously been the case, although the success of this is currently unknown and will need to be reviewed when JSNAs and JHWSs are published and can be evaluated.
Integration between health care and social care services for older prisoners
The effective integration of health and social care services in the community has been a policy goal for over four decades. 45 The Department of Health's National Service Framework for Older People22 highlighted the importance of adequate integration between prison and community social care agencies to ensure that prisoners receive an adequate standard of care. 22 Successful integration between health care and social care services is challenging within prisons. 46 Accountability for the provision of social care services for older prisoners is a particular problem. 46 This is often because there is an overlap of service provision between prison, health and local authorities accompanied by high levels of uncertainty around which local authority is responsible for an older prisoner's care on release, particularly when older prisoners are discharged into different geographical areas from those of their prison establishment. 46 According to the Department of Health's recent publication entitled Caring for our Future; Reforming Care and Support,47 preparations are ongoing to address this dilemma. HMCIP's review in 20087 found little evidence of multidisciplinary working within prison environments, with particular deficits observed in the resettlement of older prisoners. In the main, prison staff considered the social care of older prisoners to be the responsibility of health care staff. In an overwhelming majority of cases, social care arrangements were found not to be in place for older prisoners. 7,44
Summary
The current study will identify whether or not any improvements have been made to service provision for older prisoners. It will also build on the existing literature to explore the barriers to and facilitators of integrative working between health care and social care services. Furthermore, it will aim to address the established deficit in systematically addressing the health and social care needs of older prisoners through the development, implementation and evaluation of a needs assessment and care-planning intervention for older prisoners.
Chapter 3 Determining the availability and integration of health care and social care services for older adults in prison
Introduction
Previous research suggests that provision of health and social care services specifically for older prisoners is ad hoc7,19 and that successfully integrating services is challenging. 7 The first part of this study aimed to establish current levels of service provision for older men in prison across England and Wales. It also aimed to ascertain how well health and social care services were integrating currently and identify common facilitators of and barriers to more effective integrative working.
Methods
Mixed methods were adopted in this part of the study, comprising a national questionnaire and semistructured interviews with a range of professional respondents.
Questionnaire
Development of the questionnaire
A questionnaire was designed to ascertain what health and social care services were available for older male prisoners in England and Wales and how well these services were currently integrated. A copy of the questionnaire is included in Appendix 2. The topics included in the questionnaire were drawn from the recommendations for good practice made in the Department of Health's older offender toolkit23 and HMCIP's review,7 supplemented by examination of additional key themes identified across the wider published literature base. The final version of the questionnaire examined the following areas:
-
details of staffing levels and training on issues related to ageing
-
absence/presence of an identified lead for older men
-
services available to older men
-
details of chronic disease and/or older adult clinics
-
details of work/activities and environmental adaptations for older men
-
access to, and engagement with, local social services departments and other specialist older adult services.
As part of the development process the questionnaire was piloted at 13 prisons. Findings from the pilot resulted in some minor alterations to the wording and structure of the questionnaire.
Distribution of the questionnaire
It was decided that, in the likely absence of an identified OPL in each prison, the health care manager at each establishment would be the most appropriate member of staff to complete the questionnaire, providing a consistent approach. An up-to-date list of names and contact details of all health care managers was obtained from the Offender Health Division at the Department of Health and cross-checked against records held by regional offender health leads.
A complete list of all prisons in England and Wales housing adult men (n = 97) at the time of the questionnaire distribution (October 2010) was created through HMPS sources, and questionnaires were distributed by post and email to the health care managers of all of these establishments. Sites were followed up by email 2 weeks after the initial distribution of questionnaires; by telephone after a further 2 weeks; and by letter after an additional 2 weeks for those still outstanding. If they wished, health care managers were given the option of completing the questionnaire by telephone interview with a member of research staff.
Questionnaire data analysis
Questionnaire data were entered into the Statistical Package for the Social Sciences (SPSS) version 19 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were generated from these data and analyses by prison type were conducted. Data were examined to identify whether or not there were any differences between geographical regions; none was observed and thus the data are presented here without any regional stratification.
Semistructured interviews
Semistructured interview sampling
Data from the questionnaire were used to identify prisons that reported particular successes or challenges in integrating health and social care services. A coding system was devised and responses to key questions about the integration of health and social care services were tallied. These questions identified whether or not contact with social care services occurred, by what means and how successful this contact was. Prisons that scored the highest and those that scored the lowest were identified and then approached for inclusion in the semistructured interview process.
In total, 32 staff members from the four highest-scoring and four lowest-scoring prisons, holding the following roles, were invited to participate in the semistructured interviews: health care manager, OPL, general nurse, health care assistant, offender manager, DLO, education employment and training officer, equalities/diversity officer, prison officer, social worker, social care worker, probation officer, specialist older adult worker, specialist older prisoner worker and housing worker.
Semistructured interview procedure
Staff members were approached in the first instance by the health care manager at each establishment to introduce the study and ask permission to pass their professional contact details on to the research team. A research assistant then contacted the prospective interviewees by telephone to discuss the study further. Information sheets and consent forms were sent electronically to all participants (see Appendix 11). Consent forms were signed by each participant and returned to the research assistant before interviews were conducted. All interviews were conducted between October 2011 and May 2012. Interviews were conducted over the telephone by a research assistant and recorded digitally. Interviews lasted approximately 30 minutes. Questions enquired about joined-up working, communication and information-sharing practices. At the end of the interview participants were thanked for their time and co-operation and informed of the next stages of the research and the timetable, outputs and methods of dissemination. The interview schedule is provided in Appendix 3.
Semistructured interview data analysis
Data from the interviews were transcribed verbatim and analysed using the constant comparison method. 48 Constant comparison analysis is one of the most widely used qualitative methods of analysis. 49 The method is rooted within the grounded theory approach developed by Glaser48 during the 1960s. Constant comparison ensures that theory stays rooted in the data,50 resulting in emerging theories developing from the data rather than already existent literature. 51 It is most appropriate for studies in which little is known about the topic or a new perspective is required and was therefore highly relevant to all aspects of this study.
Constant comparison methods involve both the fragmenting and the subsequent connecting of data. Pieces of data are coded and separated from their original interview transcript. Extracts are then compared and combined with other fragments until connections are made to help the researcher understand the overall picture of what the interviewee has said. 50 According to Glaser,48 there are four stages involved in the constant comparison method of analysis. For the purpose of our research these stages were followed in the context of our research questions. The first stage involved identifying provisional themes and comparing incidents that apply to such themes. The second stage involved comparisons between interviews. The third stage involved delimiting and integrating categories/concepts into themes. Overlapping categories/concepts or undefined categories/concepts were re-examined until final versions emerged. Stage four involved clarifying ideas, which leads to the formulation of a theory or multiple theories.
NVivo (version 8; QSR International, Southport, UK), a qualitative software package, was used to analyse transcripts. Such programs aid the researcher to store, sort and code qualitative data and increase the rigour of a qualitative study. 49 Two researchers conducted qualitative analysis for this study and there was therefore the opportunity for one researcher to take the role of a ‘peer debriefer’. This involved periodical discussions between the researcher conducting the analysis and the peer debriefer regarding matters of methodology and analytical procedures. This provided an opportunity to test emerging themes and increases the credibility of the findings. 49
Results
First, the questionnaire response rates and the numbers of older prisoners at establishments are presented. Second, questionnaire findings are presented under two broad topic areas: service availability and the integration of health and social care services. Third, findings from the semistructured interviews are presented to augment the questionnaire findings with more detailed information about key points.
Questionnaire response rates
The questionnaire was distributed to the health care managers of the 97 establishments housing adult males in England and Wales. Following rigorous follow-up processes, 78 health care managers returned a questionnaire, resulting in an overall response rate of 80%. Response rate by prison type ranged between 73% and 92% (Table 1). There was no difference in response rate between public sector prisons and private finance initiative prisons.
| Prison type | Adult male establishments in England and Wales, n | Adult male establishments that returned the health care questionnaire, n (%) |
|---|---|---|
| Local prisons | 36 | 33 (92) |
| Open prisons | 9 | 7 (78) |
| Training prisons | 52 | 38 (73) |
| Private prisons | 10 | 8 (80) |
| Public prisons | 87 | 70 (80) |
| Total sample | 97 | 78 (80) |
Numbers of older prisoners
Table 2 shows the total numbers of older prisoners across the 78 prisons and the proportion of the overall population that they constitute. Overall, older prisoners aged ≥ 60 years accounted for 4% of the population in the 78 establishments. These 78 establishments held 77% of the male prison population in June 2011. Prisons holding only sentenced prisoners had a higher proportion (5%) of older prisoners than local (3%) and open (3%) prisons. The private and public prisons had similar proportions of older prisoners.
| Prison type | Total number of prisoners held at establishments in this sample | Prisoners aged ≥ 60 years held at establishments in this sample | % of prisoners aged ≥ 60 years held at establishments in this sample |
|---|---|---|---|
| Local prisons | 27,779 | 824 | 3 |
| Open prisons | 3027 | 94 | 3 |
| Training prisons | 24,719 | 1265 | 5 |
| Private prisons | 7168 | 202 | 3 |
| Public prisons | 48,357 | 1981 | 4 |
| Total sample | 55,525 | 2183 | 4 |
A breakdown of older prisoners by specific age group and conviction status is shown in Table 3. Almost three-quarters (71%) were aged between 60 and 69 years. One-fifth (20%) of older prisoners were aged between 70 and 79 years and three (< 1%) prisoners were aged ≥ 90 years. Examination of the conviction status of older prisoners showed that the majority had been sentenced (84%) with fewer convicted but unsentenced (2%) or on remand (6%).
| Local prisons, n (%) | Open prisons, n (%) | Training prisons, n (%) | Private prisons, n (%) | Public prisons, n (%) | Total sample, n (%) | |
|---|---|---|---|---|---|---|
| Age group (years) | ||||||
| 60–69 | 603 (73) | 81 (86) | 974 (77) | 107 (53) | 1551 (78) | 1559 (71) |
| 70–79 | 167 (20) | 13 (14) | 252 (20) | 43 (21) | 389 (20) | 432 (20) |
| 80–89 | 30 (4) | 0 (0) | 18 (1) | 13 (6) | 35 (2) | 48 (2) |
| 90+ | 2 (0.02) | 0 (0) | 1 (0.1) | 0 (0) | 3 (0.2) | 3 (0.1) |
| Conviction status of total sample | ||||||
| Sentenced | 524 (64) | 76 (81) | 1219 (96) | 174 (88) | 1654 (85) | 1828 (84) |
| Convicted unsentenced | 39 (5) | 0 (0) | 0 (0) | 12 (6) | 27 (1) | 39 (2) |
| Remand prisoners | 121 (15) | 0 (0) | 0 (0) | 16 (8) | 105 (5) | 121 (6) |
Service availability for older prisoners
Questionnaire findings
Details of health care department staffing levels and training
The percentage of health care staff trained in the care and assessment of older prisoners within particular staff groups is shown in Table 4. Specific training in the care and assessment of older people was provided to health care staff in less than half of prisons in this sample (41%, 32).
In primary care and inpatient services, 8% (135) of health care staff had received training in the care and assessment of older people. A similar proportion of staff in mental health and in-reach services (7%, 28) had received training in this area.
Comparatively, training prisons contained a higher percentage of trained staff, both in primary care and inpatient services (14%, 78) as well as in mental health and in-reach teams (15%, 22). The proportion of staff trained in open prisons was lower (2% and 0% respectively). There was a significant difference in the number of staff trained in primary care and inpatient services between private and public prisons [χ2 (1, n = 135) = 8.34, p = 0.004].
| Local prisons | Open prisons | Training prisons | Private prisons | Public prisons | Total sample | |
|---|---|---|---|---|---|---|
| Primary care and inpatient services | ||||||
| Staff employed, n | 1084 | 59 | 567 | 174 | 1536 | 1710 |
| Staff trained in the care and assessment of older people, n (%) | 56 (5) | 1 (2) | 78 (14) | 4 (2) | 131 (9) | 135 (8) |
| Specialist mental health/in-reach team | ||||||
| Staff employed, n | 224 | 12 | 143 | 33 | 346 | 379 |
| Staff trained in the care and assessment of older people, n (%) | 6 (3) | 0 (0) | 22 (15) | 2 (6) | 26 (8) | 28 (7) |
Older prisoner strategy and specific services for older prisoners
Table 5 outlines the specific services available to older prisoners across prison types. Overall, of the 78 establishments, 44 (56%) had a written older prisoner care policy. Only two of the seven open prisons (29%) had such a policy compared with 19/33 local prisons (58%). The majority of prisons (81%, 63/78) had an identified OPL in their health care department. The percentage of prisons with an identified OPL was higher within local prisons (88%, 29/33) than in open prisons (71%, 5/7). However, of the 63 designated OPLs, only 28/78 (36%) had received any specific training to support them in their role. In establishments where there was no identified OPL, 64% (n = 9) of health care managers stated that there was an intention to introduce one.
A prisoner helper/buddy/peer support scheme was most commonly found in training prisons, although they were not available in the majority of such establishments (45%, 17/38). None of the private prisons had an older prisoner helper/buddy scheme. The majority of prisons had a chronic disease clinic (89%, 69/78) but just over half operated a specific older adult clinic (53%, 41/78).
| Local prisons, n/N | Open prisons, n/N | Training prisons, n/N | Private prisons, n/N | Public prisons, n/N | Total sample, n/N | |
|---|---|---|---|---|---|---|
| Older prisoner strategy | ||||||
| Written older prisoner care policy | 19/33 | 2/7 | 23/38 | 5/8 | 39/70 | 44/78 |
| Identified lead for older prisoners within the health care department | 29/33 | 5/7 | 29/38 | 6/8 | 57/70 | 63/78 |
| OPL received training to support them in this role | 14/33 | 2/7 | 12/38 | 3/8 | 25/70 | 28/78 |
| Specific services available for older prisoners | ||||||
| Prisoner helper/buddy scheme | 9/33 | 1/7 | 17/38 | 0/8 | 27/70 | 27/78 |
| Reception screening tool for older prisoners at reception | 6/33 | 1/7 | 6/38 | 0/8 | 13/70 | 13/78 |
| Screening tool following transfer from another establishment | 12/33 | 1/7 | 15/38 | 2/8 | 26/70 | 28/78 |
| First night arrangements for older prisoners | 7/33 | 1/7 | 4/38 | 0/8 | 12/70 | 12/78 |
| Protocol for forwarding reception screening information to health care | 8/33 | 0/7 | 4/38 | 1/8 | 11/70 | 12/78 |
| Chronic disease and older adult clinics within prisons | ||||||
| Chronic disease clinic | 30/33 | 6/7 | 33/38 | 7/8 | 62/70 | 69/78 |
| Older adult clinic | 19/33 | 4/7 | 18/38 | 4/8 | 37/70 | 41/78 |
Specific activities for older prisoners
Just over half of the establishments (55%, 43/78) provided one or more activities specifically for, and accessed only by, older prisoners. Within these 43 establishments such services included social groups (26%, 11/43), gym and exercise sessions (42%, 18/43) and in-cell work (2%, 1/43). Activities specifically for older prisoners with mobility problems were provided by 33% (26/78) of prisons. Health care managers were asked what type of factors affected access to certain activities/areas for prisoners with mobility problems. Of those who responded, 64% (14/22) reported that there was a lack of lifts/ramps available where access to activities required prisoners to use stairs and 14% (3/22) stated that door dimensions were not large enough for wheelchairs. Where this was the case, two-thirds of respondents noted that no alternative activities were provided for those negatively affected.
The integration of health and social care services for older prisoners
Questionnaire findings
Over half of establishments (64%, 50/78) reported having some form of contact with external social care services. However, only 31% (24/78) of health care managers stated that there was a co-ordinated approach between their health care department and local social services, with only 15% (12/78) holding meetings to discuss older prisoner cases. Only 51% (40/78) had contact with other types of specialist older adult organisations (Table 6).
| Local prisons, n/N | Open prisons, n/N | Training prisons, n/N | Private prisons, n/N | Public prisons, n/N | Total prisons, n/N | |
|---|---|---|---|---|---|---|
| Contact with social care services | ||||||
| Establishment has contact with local social care services | 21/33 | 2/7 | 27/38 | 6/8 | 44/70 | 50/78 |
| Co-ordinated approach between health care and social services regarding older prisoners with social care needs | 11/33 | 2/7 | 11/38 | 2/8 | 22/70 | 24/78 |
| Sufficient communication from social services | 9/33 | 1/7 | 5/38 | 2/8 | 13/70 | 15/78 |
| Written protocol between health care and social services regarding older prisoners | 1/33 | 0/7 | 2/38 | 0/8 | 3/70 | 3/78 |
| Meetings held with staff from social services to discuss older prisoner cases | 7/33 | 0/7 | 5/38 | 3/8 | 9/70 | 12/78 |
| Contact with specialist older adult services | ||||||
| Contact with specialist older adult organisations | 18/33 | 5/7 | 17/38 | 3/8 | 37/70 | 40/78 |
| Co-ordinated approach between health care department and specialist older adult services | 11/33 | 1/7 | 10/38 | 2/8 | 20/70 | 22/78 |
| Specialist older adult services currently unavailable (but deemed necessary) | 7/33 | 1/7 | 9/38 | 2/8 | 15/70 | 17/78 |
Semistructured interview findings
Thirty-two interviews were conducted to investigate levels of integration between prison, prison health care and social care services staff. The overall aim of the interviews was to provide supplementary in-depth information to add context to the questionnaire findings, in particular to identify specific barriers to and facilitators of the integration of prison and community-based health and social care services.
Three overarching themes were identified and explored during the analysis. Themes and subthemes are shown in Table 7.
| Theme | Subtheme |
|---|---|
| 1. Responsibility and accountability | Ambiguity |
| Budget constraints | |
| Geographical limitations | |
| 2. Information sharing | Confidentiality of health care information |
| Focus on risk | |
| 3. Working practices | Staff attitudes |
| Restrictive prison regime |
Theme 1: responsibility and accountability
A prominent theme that emerged during interviews was the ambiguity that staff felt around who, or which disciplines/agencies, was properly responsible for providing social care to prisoners.
Problems around the integration of prison and community-based services was a recurring theme and integration was felt, in the majority of cases, to be non-existent. Even when they existed, relationships between prisons and social services were generally considered to be strained. One interviewee described how prison staff often considered the social care of older prisoners to be the responsibility of other prisoners rather than staff and therefore other prisoners would be left to assist older prisoners with their social care needs without adequate training to undertake such tasks:
‘Oh you [social care worker] shouldn’t have to do that [change incontinence pads]. Just leave . . . we’ll get the prisoners to do that.’ But it was giving our knowledge and expertise over to the prisoners to deal with the situations that they were dealing with in a safe manner, because they [other prisoners] were dealing with incontinence, and not dealing with it properly. So the spread of infection could have been quite high. So passing that knowledge over to them [other prisoners] from our point of view, we thought was quite . . . you know, it needed to be beneficial for them, because they [prisoners] were very much left by the prison officers [to care for older prisoners].
Social care worker, p1:32
Ambiguity over responsibility for social care was also evident among staff working within the prisons:
Because there is a social care aspect to some of it [care of older prisoners] there’s ambiguity over where that falls and who is responsible for delivering that. There is the belief by, I think a cultural belief, that older people, if they have a social care need or maybe need help with getting dressed or washed, that that should fall to health care because prison staff aren’t here to do that.
Health care manager, p1.9
Funding restrictions, in particular depleted local authority and social care service budgets, reportedly led to services not taking accountability for older prisoners' health and social care. This was reported by many interviewees as a major issue facing the sector as a whole:
Unfortunately, social services won’t get involved in prisons, because they say they don’t have the budget for it. And we’ve tried, even in cases where we’ve had people terminally ill, it’s been very difficult to get social services involved. We’ve had a chap who’s got quite . . . he’s quite disabled, mobility wise, and we had to pay for the assessment of that patient ourselves, whereas in the community he wouldn’t have to do that.
Health care manager, p1.23
Geographical limitations were highlighted as a significant barrier to effective integrative working. Many prisoners, particularly those serving long sentences, do not reside in prisons in their home area. Additionally, people are often routinely transferred between a number of establishments during their sentence and ongoing care from outside or prison-based agencies is often not considered to be a sufficient priority to keep an older person in one particular establishment. This can create tension between the prison and local social care services. A social worker in the mental health in-reach team illustrated this by detailing an experience of contacting a local authority on behalf of a prisoner, outside of the area in which his current prison was situated. He described a laborious process of trying to get staff in the person's home local authority area to accept that the prisoner was originally from their area. The local authority instead stated that the prisoner should be released to the area in which the prison was located, an area in which the prisoner had no home or family ties to help with successful community reintegration:
But certainly the local authority weren’t fully accepting of that individual and say, ‘yes this man’s from [our area] and therefore he can come back to us’.
Social worker, p1.31
One interviewee described a perverse situation whereby only by seemingly creating or allowing social care needs to arise through deliberate inaction could a prisoner be helped by social services:
[What the local authority says] He’s not a resident in our area – even though he may have been, it doesn’t matter. The usual thing – I’ve come across this several times when I visit [prison name]. The [local] authorities tend to say, okay, well, he’s in a residence already, he’s in prison. When he’s released and he’s homeless then we have a responsibility to pick him up. So they have to make themselves homeless before the local authority will respond.
Older prisoner organisation worker, p1.22
Theme 2: information sharing
Within the prison environment, as in the community, health care records are maintained in confidence; thus, information contained therein is not routinely shared with non-health care staff. With regard to meeting the social care needs of older men, this situation can have many repercussions, given that prisoners routinely live on residential wings under the day-to-day care of prison officers. Health care records can contain a wealth of information that would make the day-to-day support of older prisoners easier for prison discipline staff to manage, for example issues around incontinence management, mobility difficulties and maintaining personal and environmental cleanliness. Such information was generally not imparted to prison staff, and discipline staff in particular noted this as problematic:
Yes, giving information about people’s particular social needs, a lot of nursing staff will not give that information out because of medical confidence.
DLO, p1.4
A lack of adequate information sharing and effective integration was attributed to assessment and IT systems not being linked:
It’s integrating the assessment process but, at the moment, the IT systems just don’t talk.
Older prisoner organisation worker, p1.22
According to staff, information sharing was primarily focused on risk and public protection rather than the health and social care information needed to support individuals. Interviewees explained that appropriate links and communications were made when liaising with agencies involved in managing risk, for example the police and probation services; however, sharing around care issued was not considered to be of the same importance or as valuable an activity. It was evident that information-sharing practices were possible to develop and operate; however, to make progress integrating health and social care services to improve the meeting of individuals' needs, a greater importance needed to be placed on routine practices rather than on only higher-level risk-based information-sharing practices:
It’s not the health they look at, they look at the risks, it’s risk focused.
Older prisoner organisation worker, p1.22
We’re well aware, particularly in my department, of the need to protect the public. So we will always information share and contact the appropriate people.
Offender manager, p1.20
Theme 3: working practices
Staff were fully aware that the professional styles and attributes of individual staff directly affected how well staff worked together across professional and prison/community boundaries. Staff who adopted positive attitudes and proactively nurtured working relationships created an environment in which different agencies operated effectively together. Conversely, negative staff attitudes severely impeded the effective integration of health and social care services. A further barrier to integration and the meeting of individual needs was noted to be the time-bound and institutional fixed routines of all prisons, which frequently curtailed imaginative work and hampered new initiatives as they became caught up in, and were rendered inoperable by, overly burdensome security procedures.
A number of staff noted that forming positive working relationships improved integrative working. It resulted in staff having the ability to approach each other in an appropriate manner when seeking assistance:
But what oils the wheels if you like is the relationships, getting to know people, getting to know who you can ask about what and, if I say knowing how to approach them that’s perhaps not quite right, but if you know somebody and you’re able to just have a chat to them and they can put a face to the name and whatever, then it does make life a lot easier if you’re just talking to folk and trying to get what you want from them.
Probation officer, p1.30
The approach that a staff member takes when meeting the needs of older prisoners was seen to be an integral part of working. One interviewee emphasised that some prison staff had a very negative attitude towards the needs of less able prisoners:
Prison officers don’t really care about things like that [social care needs]. Prison officers felt that we [social care workers] shouldn’t have been in there [the prison] caring for the person that we were caring for.
Social care worker, p1.32
The prison regime was described as ‘time bound’. This caused problems as staff were continuously under pressure to maintain the strict prison regime. A social worker highlighted that it remains difficult for external agencies to gain access to prison establishments because of the limited time available to access prisoners. This inhibits effective integrative working, possibly leading to inequality of care provided to those in prison in comparison with older people in the community:
As a social worker, I have to work within the constraints of the prison regime, it’s difficult for outside agencies to gain access [to prisoners].
Social worker, p1.31
A lack of face-to-face contact between prison staff and staff working for external agencies was identified as a barrier to integrative working. There were limited opportunities for staff from outside agencies to meet with prison staff as a result of the strict prison regime. Face-to-face meetings were considered an essential part of multi-agency working but were held infrequently because of the practical difficulties faced:
I guess, the difficulty, again, that I’ve found is, you can make good links, with people, on the phone, but, ideally, it’s so much more effective, if you can go out and introduce yourself, to people, and they get to know a face and, you know, they put a face to a name, and vice versa.
Housing officer, p1.14
Summary
In this cross-sectional national survey an 80% response rate was achieved. Older prisoners represented 4% of the prison population within our sample; this is in line with national figures (4%; NOMS, 2012, personal communication).
Over half of the establishments had a written older prisoner policy and 80% of prisons had a designated OPL; however, only a minority of these staff had received any specialist training to undertake their role. An investigation of integration between health and social care services showed that 64% of establishments had contact with local social care services; however, only 33% believed that there was a co-ordinated approach between health care and social care services. Furthermore, only 16% of health care managers reported holding meetings with social services to discuss the care of older prisoners.
Qualitative interviews highlighted the nuanced institutional factors and working practices that facilitate the effective integration of health and social care services for older prisoners, and the barriers that staff face. Positive staff attitudes were highlighted as a prerequisite to effective working. Barriers to success included the lack of clarity felt by many staff regarding where responsibility and accountability for providing social care to prisoners actually lay. Locating people in prisons away from their home area impeded the ability, and indeed willingness, of social services to become involved in the very important tasks around resettling an older person in the community. Information sharing was felt to be successful only in terms of managing risks rather than in the equally important and, of course, very closely inter-related area of meeting individual need.
Chapter 4 Establishing the met compared with the unmet needs of older people entering prison
Introduction
Older prisoners' complex health and social care needs are often unmet. 4,6 The second part of this study aimed to establish the met and unmet needs of recently incarcerated older prisoners, as well as capture their experiences of being received into prison custody.
Methods
This part of the study employed mixed methods including structured and semistructured interviews with prisoners on entry into prison.
Sampling strategy
This part of the study involved ‘local prisons’ only. Local prisons hold people awaiting trial, those convicted of short sentences and those at the early stage of a long sentence. All local prison establishments in four geographical regions were approached to take part in this part of the study. The geographical regions were selected as a result of their close proximity to the research base and comprised North East England, Yorkshire and Humberside, the North West and the West Midlands.
Nine establishments out of 12 agreed to take part. The sample included three private prisons and six public prisons. Prisons were located in both rural and urban areas.
Inclusion criteria
Participants meeting the following criteria at the nine local prisons were invited to participate in this part of the study:
-
age ≥ 60 years
-
newly received into the prison (i.e. received from court rather than another prison establishment).
Participants
The overall sample was a consecutive sample of 100 prisoners aged ≥ 60 years received into the nine prisons between February 2010 and December 2011. The required sample size for the needs assessment phase of the study was discussed several times at the early steering group meetings. It was decided that a series of formal statistical sample size and power calculations would not be necessary, or appropriate, in the context of an exploratory descriptive needs assessment. The assessment tool [Camberwell Assessment of Need – Short Forensic Version (CANFOR-S52)] yields purely descriptive information regarding a series of met compared with unmet needs (expressed as percentage values) and from these data we felt that there was no purpose in generating inferential statistics such as confidence intervals or p-values. Therefore, we had no basis for making formal sample size and power calculations in relation to hypothesis-testing parameters or required levels of statistical precision. The CANFOR tool also assesses an array of widely different types of unmet need, some of which are fairly common and some of which are very rare. Given the novelty of our needs assessment work for this particular subgroup of prisoners, and the lack of prior knowledge on which to predict the levels of unmet need observed, we opted for a pragmatic sample size of 100 older male prisoners. It was felt that this would be sufficiently large for estimating levels of unmet need across most of the CANFOR domains, whilst also being of a manageable and feasible size in terms of what could be achieved given the resources available and the time scale.
Of those older prisoners approached, 18 refused to participate. The participation rate across all nine establishments was 85%. Twenty-seven of the 100 older prisoners (27%) were invited to participate in the semistructured interviews and all consented. Semistructured interviews were conducted until data saturation was reached and no new themes emerged. All interviews were conducted during the initial 10 weeks in prison custody.
Interview procedure
On a weekly basis a nominated member of prison staff identified prisoners aged ≥ 60 years entering the prison using the Computer – National Offender Management Information System (C-NOMIS). The research team at the University of Manchester contacted the named contact at each prison weekly or fortnightly (depending on the preference of the prison contact) to inquire about new receptions into the prison. The research assistant travelled to the prisons to inform potential participants of the study. Prisoners were given at least 24 hours to consider their participation and written informed consent was obtained. Interviews were conducted in interview rooms or cells in each prison. The structured and semistructured interviews lasted approximately half an hour each (a total of 1 hour combined). The semistructured interview was audio recorded when approval from the security department and the participant was obtained.
Structured interview tools
The following structured assessments were used:
-
CANFOR-S measures health and social need experienced over the last month across 25 domains. Each domain is scored as not applicable, no need, met need or unmet need. The CANFOR-S was specifically designed for use in forensic services and is appropriate for use in prison settings.
-
The Geriatric Depression Scale short form (GDS-15)53 contains 15 questions, which are answered yes or no. Items indicative of depression carry a score of 1. A total scale score of ≥ 5 is suggestive of mild depression and scale guidelines suggest that further investigation is warranted. A total score of ≥ 10 almost always indicates severe depression. In this study the GDS-15 had a Cronbach's alpha score of 0.85, suggesting good internal consistency.
-
The Brief Psychiatric Rating Scale (BPRS)54 consists of 24 seven-point ordered category rating scales. Items 1–14 are based on interviewees' answers to the interviewers' questions, while items 15–24 are based on the interviewers' observations of the participants' behaviour during the interview.
-
The UK minimum data set (MDS) for home resident assessment and care screening background (adapted version)55 recodes information from participants themselves and participants' health care records. The participant section collects information in 13 sections ranging from daily routine in the previous 12 months to psychological well-being in the previous 7 days. The staff section contains four sections collecting information on an older person's cognitive patterns, communication/hearing patterns, mood and behaviour patterns, mobility and activities of daily living. The final section records information contained in an older person's health care records. It contains seven subsections recording all aspects of an older person's health; it also details what medication is currently being prescribed and what external medical intervention was previously required. This was adapted by the research team for the prison environment.
-
Audit – A data sheet to collect information from prisoners' clinical records was designed by the research team. Information recorded during a prisoner's initial 4 weeks of custody was collected. Data were gathered from electronic and paper health care records. Data collected included details of the assessments that were carried out by health care staff on reception and subsequent follow-up assessments; what referrals or contacts with prison/health care/external agency staff were made; and individual interventions received.
Semistructured interview guide
The semistructured interview aimed to capture older prisoners' experiences of reception into custody (see Appendix 4). The interview ascertained the difficulties faced by older people entering prison, in particular how their health, social care and custodial needs were addressed. Participants were asked how their needs could have been more appropriately met and to comment on any additional services that they feel would have been beneficial.
Data analysis
Quantitative data analysis
Data were entered into SPSS version 19. Initial descriptive statistics were computed for all scales used. Missing data were treated by omitting cases for which data were incomplete (listwise deletion). Fourteen participants declined to complete the GDS-15 because this caused them distress and one participant's BPRS data were missing. Health care record data for 12 participants and audit data for 15 participants were unobtainable.
Results
Quantitative findings
Demographics
All demographic information is presented in Table 8. Participants' ages ranged between 60 and 81 years with a mean age of 65.5 years [standard deviation (SD) 5.35 years]. Prisoners were categorised into four age ranges with the majority aged between 60 and 69 years and only a small percentage aged > 75 years. The majority were white British (95%). Similar proportions of participants were single, married and divorced. In relation to offences committed, 19% were incarcerated for violent crimes, 28% for crimes of a sexual nature and 36% for other crimes, which varied from fraud to acquisitive crimes to drug offences, and 17% refused to disclose their offence. This is not dissimilar to national statistics of prisoners aged ≥ 60 years. In 2011, 20% of prisoners > 60 years were detained for violent crimes, 58% for crimes of a sexual nature and 22% for other crimes (NOMS, 2011, personal communication).
The majority of participants had their own private accommodation and lived independently of health/social service support before entering prison. In total, 25% of participants were serving sentences of < 12 months and 25% were serving sentences of between 1 and 5 years. Over half of the sample had not been in prison previously. The majority of interviews with participants took place during their initial 6 weeks in custody.
| Demographics | n (%) |
|---|---|
| Participant age (years) | |
| 60–64 | 59 (59) |
| 65–69 | 25 (25) |
| 70–74 | 8 (8) |
| 75+ | 8 (8) |
| Ethnicity | |
| White British | 95 (95) |
| Other mixed background | 1 (1) |
| Other Asian background | 1 (1) |
| Other background | 3 (3) |
| Marital status | |
| Single | 35 (35) |
| Married | 29 (29) |
| Divorced | 28 (28) |
| Separated | 5 (5) |
| Widowed | 3 (3) |
| Offence | |
| Violent | 19 (19) |
| Sexual | 28 (28) |
| Other | 36 (36) |
| Not disclosed | 17 (17) |
| Conviction status | |
| Convicted – sentenced | 58 (58) |
| Remand | 33 (33) |
| Licence recall | 6 (6) |
| Convicted – unsentenced | 2 (2) |
| Missing | 1 (1) |
| Sentence length | |
| < 12 months | 25 (25) |
| 1–5 years | 25 (25) |
| > 6 years | 10 (10) |
| Unsentenced | 40 (40) |
| Number of previous times in prison | |
| 0 | 51 (51) |
| 1–3 | 29 (29) |
| > 3 | 20 (20) |
| Length of time in prison at time of interview (weeks) | |
| 0–2 | 9 (9) |
| 3–4 | 38 (38) |
| 5–6 | 30 (30) |
| 7–8 | 15 (15) |
| 9–10 | 4 (4) |
| Missing | 4 (4) |
| Wing location | |
| Vulnerable prisoner unit | 43 (43) |
| Sentenced prisoners wing | 28 (28) |
| Remand/induction wing | 5 (5) |
| Health care | 14 (14) |
| Unknown | 5 (5) |
| Drug-free wing | 3 (3) |
| Detox wing | 2 (2) |
| Admitted from (at prison entry) | |
| Private home/flat with no health/personal social services | 72 (72) |
| Private home/flat with health/personal social services | 1 (1) |
| Sheltered housing | 8 (8) |
| Other | 19 (19) |
| Lived alone prior to entry | 40 (40) |
| College/apprenticeship | 39 (39) |
| University-level education | 10 (10) |
Camberwell Assessment of Need – Short Forensic Version
The CANFOR-S results are shown in Tables 9 and 10. Mean total need among this sample was 5.24 (SD 2.81) with a median of 5.00; mean met need was 2.51 (SD 1.51) and mean unmet need was 2.74 (SD 2.65), both with a median of 2.00.
The CANFOR-S contains five domains that can be scored as not applicable: accommodation, transport, childcare, sexual offending and arson. These items are not relevant to some respondents and are excluded when the scale is administered. Therefore, the number of cases analysed varies for these items. Table 10 shows that the highest proportions of unmet need were in the domains of information about condition and treatment (38%), psychological distress (34%), daytime activities (29%), benefits (28%) and food (22%).
| Met need | Unmet need | Total need | |
|---|---|---|---|
| Mean | 2.51 | 2.74 | 5.24 |
| SD | 1.51 | 2.65 | 2.81 |
| Median | 2.00 | 2.00 | 5.00 |
| Interquartile range | 1 | 3 | 4 |
| CANFOR-S domain | Cases analysed, N | Older prisoners with unmet need, n (%) | Older prisoners with met need, n (%) |
|---|---|---|---|
| Information about condition and treatment | 100 | 38 (38) | 12 (12) |
| Psychological distress | 100 | 34 (34) | 14 (14) |
| Daytime activities | 100 | 29 (29) | 28 (28) |
| Benefits | 100 | 28 (28) | 6 (6) |
| Food | 100 | 22 (22) | 65 (65) |
| Physical health | 100 | 21 (21) | 46 (46) |
| Telephone | 100 | 13 (13) | 5 (5) |
| Money | 100 | 13 (13) | 3 (3) |
| Company | 100 | 10 (10) | 0 (0) |
| Accommodationa | 57 | 9 (16) | 7 (12) |
| Looking after the living environment | 100 | 8 (8) | 14 (14) |
| Treatment | 100 | 8 (8) | 11 (11) |
| Alcohol | 100 | 7 (7) | 5 (5) |
| Self-care | 100 | 6 (6) | 9 (9) |
| Intimate relationships | 100 | 6 (6) | 4 (4) |
| Basic education | 100 | 5 (5) | 3 (3) |
| Transporta | 57 | 5 (9) | 2 (4) |
| Childcarea | 4 | 0 (0) | 4 (100) |
| Psychotic symptoms | 100 | 2 (2) | 3 (3) |
| Safety to self | 100 | 2 (2) | 6 (6) |
| Sexual expression | 100 | 1 (1) | 0 (0) |
| Sexual offendinga | 74 | 1 (1) | 4 (5) |
| Drugs | 100 | 0 (0) | 2 (2) |
| Arsona | 2 | 0 (0) | 2 (100) |
There was a significant association between unmet accommodation need and the type of offence that an offender committed [Fisher's exact test (n = 100) = 9.430, p = 0.007]. Those who committed ‘other’ offences, that is, not those of a sexual or violent nature, had greater unmet accommodation needs. There was also a significant association between unmet accommodation need and the location where an older prisoner was housed [Fisher's exact test (n = 100) = 9.676, p = 0.005]. Those housed in ‘other’ locations, that is, those not housed in health care or on the vulnerable prisoner wing, had a greater unmet accommodation need. There was a significant association between unmet psychological distress need and housing location [Fisher's exact test (n = 100) = 6.803, p = 0.03]. Those on the vulnerable prisoner wing were more likely to have unmet psychological distress than those in other wing locations. There was a significant association between unmet alcohol need and the number of times that an older prisoner had been in prison previously [Fisher's exact test (n = 100) = 6.243, p = 0.01]. Those who had been in prison three or more times were more likely to have an unmet alcohol need. There was also a significant association between the number of times that an older prisoner had previously been in prison and unmet safety to self need [Fisher's exact test (n = 100) = 5.019, p = 0.03]. All older prisoners with an unmet safety to self need had been in prison three or more times previously.
Geriatric Depression Scale short form
The mean GDS-15 score was 6.51 (SD 4.32). In total, 31.4% (n = 27) of the sample reached the cut-off on the GDS-15 indicating mild depression (> 5) and 23.3% (n = 20) of the sample reached the cut-off on the scale indicating severe depression (> 10); 45.3% (n = 39) had a score of ≤ 5 indicating no clinical signs of depression.
Brief Psychiatric Rating Scale
Table 11 presents the mean and SD values for four scale items, as well as the percentage of cases reaching clinical significance. The mean total scale score was 28.9 (SD 4.176). The scale authors advise that a rating of 4–7 on any individual BPRS item indicates clinical significance of a symptom.
| BPRS item | Mean score (SD), n (%) reaching clinical significance |
|---|---|
| Somatic concern | 1.63 (1.09), 9 (9) |
| Anxiety | 2.10 (1.15), 11 (11) |
| Hallucinations | 1.00 (0.14), 0 (0) |
| Suicidality | 1.29 (0.67), 1 (1) |
UK minimum data set
This section provides the participants' responses to questions contained in the UK MDS. 55
Table 12 shows participants' daily routine before entering prison. Nearly half of the sample (49%) used tobacco products daily and 31% were involved in group activities with 15% usually attending religious services. Over 75% had daily contact with family/friends.
| Item | Yes, n (%) |
|---|---|
| Stays up late at night (after 2100) | 84 (85) |
| Naps regularly during the day (at least 1 hour) | 37 (37) |
| Goes out 1+ days a week | 90 (91a) |
| Stays busy with hobbies, reading or fixed daily routine | 86 (86) |
| Spends most of time alone or watching television | 42 (42) |
| Moves independently indoors (with appliances if used) | 77 (77) |
| Use of tobacco products at least daily | 49 (49) |
| Distinct food preferences (vegetarian, avoids certain foods for health reasons not just general dislike) | 24 (24) |
| Eats between meals all or most days | 41 (41) |
| Use of alcoholic beverages at least weekly | 58 (58) |
| In bedclothes most of the day | 17 (17) |
| Wakens to toilet all or most nights | 57 (57) |
| Has irregular bowel movement patterns (unpredictable/variable) | 17 (17) |
| Daily contact with relatives/close friends (visits/telephone calls but not letters) | 76 (76) |
| Usually attends church, chapel, synagogue, etc. | 15 (15) |
| Finds strength in faith | 31 (31) |
| Daily animal companion/presence | 51 (51) |
| Involved in group activities | 31 (31) |
Few participants had any short- or long-term memory problems (Table 13). A high proportion (97%) were able to recall the current season and where their cell was located on the wing (99%).
| Item | Yes, n (%) |
|---|---|
| Short-term memory | |
| Memory ok | 93 (93) |
| Memory problem | 7 (7) |
| Long-term memory | |
| Memory ok | 96 (96) |
| Memory problem | 4 (4) |
| Able to recall current season | 97 (97) |
| Able to remember where cell is on wing | 99 (99) |
| Normally able to remember names and faces of staff | 80 (80) |
| Able to recall name of prison and what kind of place it is | 97 (97) |
In total, 9% of older prisoners in this sample used a hearing aid. When questioned about their ability to understand others, 7% of participants reported some problems in this area (Table 14).
| Item | Yes, n (%) |
|---|---|
| Hearing aid present and used | 9 (9) |
| Hearing aid present and not used regularly | 3 (3) |
| Other receptive communication techniques used (e.g. lip reading/staff write messages) | 3 (3) |
| Ability to understand others | |
| Understands | 79 (79) |
| Usually understands | 14 (14) |
| Sometimes understands | 6 (6) |
| Rarely/never understands | 1 (1) |
The majority of older prisoners reported being able to read books and newspapers (83%). A high proportion (91%) had used glasses or contact lenses over the past 7 days (Table 15).
| Item | Yes, n (%) |
|---|---|
| Able to read books/newspapers | |
| Adequate | 83 (83) |
| Impaired | 16 (16) |
| Moderately impaired | 1 (1) |
| Side vision problems – decreased peripheral vision | 18 (18) |
| Sees halos or rings around light, sees flashes of light, sees curtain over eyes | 26 (26) |
| Used glasses, contact lenses or a magnifying glass over the last 7 days | 90 (91a) |
Nearly one-fifth of the sample (19%) used a stick, Zimmer frame or tripod to move around within the prison. A total of 3% used a wheelchair, which they either wheeled themselves or had another person wheel (Table 16).
| Item | Yes, n (%) |
|---|---|
| Stick/Zimmer frame/tripod | 18 (19a) |
| Wheelchair primary mode of locomotion | 3 (3) |
| Bedfast all or most of the time | 2 (2) |
| Bed rails used for bed mobility or transfer | 2 (2) |
| Lifted manually | 2 (2) |
| Lifted mechanically | 1 (1) |
| Transfer aid | 2 (2) |
| Potential for rehabilitation: participant believes he is capable of increased independence in at least some activities of daily living | 2 (2) |
Table 17 provides information on the psychological well-being of older prisoners within this sample. The majority (83%) reported interacting with others with ease. Under half (46%) reported pursuing involvement in prison life and 62% reported accepting invitations into group activities. Nearly one-fifth of prisoners (18%) were unhappy with their cellmates and 14% openly expressed anger with family or friends. A large proportion (38%) reported an absence of contact with family and friends.
| Item | Yes, n (%) |
|---|---|
| At ease interacting with others | 83 (83) |
| At ease doing planned or structured activities | 78 (79a) |
| At ease doing self-initiated activities | 98 (98) |
| Establishes own goals | 71 (72a) |
| Pursues involvement in prison life | 46 (46) |
| Accepts invitations into most group activities | 62 (62) |
| Unsettled relationships: covert/open conflict with or repeated criticism of staff | 8 (9a) |
| Unhappy with cellmate | 18 (18) |
| Unhappy with other prisoners | 9 (9) |
| Openly expresses conflict/anger with family/friends | 14 (14) |
| Absence of personal contact with family/friends | 38 (38) |
| Recent loss of close family member/friend | 31 (31) |
| Does not adjust easily to change of routines | 57 (58a) |
| Participant feels daily routine is very different from previous pattern in the community | 75 (86a) |
Nearly one-quarter of participants (24%) reported regularly feeling hungry and 25% reported having missed one or more meals in the previous 7 days (Table 18).
| Item | Yes, n (%) |
|---|---|
| Chewing problems | 11 (11) |
| Swallowing problems | 35 (35) |
| Mouth pain | 6 (6) |
| Doesn't like the taste of many foods in the prison | 22 (22) |
| Regularly feels hungry | 24 (24) |
| At most meals do you leave ≥ 25% of your food? | 30 (30) |
| In the last 7 days have you missed one or more meals? | 25 (25) |
| Dietary supplement between meals (e.g. high-calorie/protein shakes or diabetic snacks) | 44 (45a) |
| On a planned weight change programme | 1 (1) |
In total, 48% of older prisoners in this sample had dentures or a removable bridge and 11% reported having inflamed, swollen or bleeding gums (Table 19).
| Item | Yes, n (%) |
|---|---|
| Debris present in mouth prior to going to bed at night | 1 (1) |
| Has dentures or removable bridge | 48 (48) |
| Some/all natural teeth loss – does not have or use dentures (or partial plates) | 66 (66) |
| Broken, loose or carious teeth | 28 (28) |
| Inflamed gums, swollen or bleeding gums, oral abscesses, ulcers or rashes | 11 (11) |
| Daily cleaning of teeth/dentures or daily mouth care by participant or staff | 84 (84) |
For the most part older prisoners preferred to do activities in their own cell (82%). Over half of respondents (58%) reported a major change in the type of activities they were involved in since coming into prison; 55% reported that there was a major change in the amount of time spent doing activities since arriving in prison (Table 20).
| Item | Yes, n (%) |
|---|---|
| Do you nap in the morning, afternoon, evening? | |
| Morning | 4 (4) |
| Afternoon | 32 (32) |
| Evening | 3 (3) |
| Do you like to do activities in your own cell? | 81 (82) |
| Do you like to do activities on the wing/in the television room? | 55 (55) |
| Do you like to do activities outdoors? | 48 (48) |
| Have the types of activities you are involved in changed since coming to prison? | |
| No change | 25 (25) |
| Slight change | 15 (15) |
| Major change | 58 (58) |
| Has the amount of time you spend doing activities changed? | |
| No change | 23 (23) |
| Slight change | 18 (18) |
| Major change | 55 (55) |
Health problems
When asked about continence issues participants did not generally report any problems. Bowel patterns, however, were regular only in 37% of cases. A large proportion (38%) of participants experienced pain daily (Table 21).
| Item | Yes, n (%) |
|---|---|
| Continent | 93 (93) |
| Usually continent – bladder | 6 (6) |
| Occasionally incontinent – bladder | 1 (1) |
| Bowel elimination pattern regular | 37 (37) |
| Constipation | 14 (14) |
| Diarrhoea | 7 (7) |
| Faecal impaction | 3 (3) |
| Frequency with which participant experiences pain | |
| No pain | 46 (46) |
| Pain less than daily | 16 (16) |
| Pain daily | 38 (38) |
| Intensity of pain | |
| Mild pain | 20 (20) |
| Moderate pain | 22 (22) |
| Times when pain is horrible or excruciating | 16 (16) |
The intensity of pain experienced by participants varied from mild (20%) to excruciating (16%). Many older prisoners experienced pain in a number of locations, the most prominent being back pain (29%) and bone and hip pain (21%) (Table 22).
| Item | Yes, n (%) |
|---|---|
| Back pain | 29 (29) |
| Bone pain | 21 (21) |
| Chest pain while doing usual activity | 15 (15) |
| Headache | 14 (14) |
| Hip pain | 21 (21) |
| Incisional pain (recent operation) | 2 (2) |
| Joint pain | 25 (25) |
| Soft tissue pain | 15 (15) |
| Stomach pain | 9 (9) |
| Accidents – fell in past month | 11 (11) |
| Fracture in last month | 1 (1) |
Health care records
Health problems recorded in participants' health care notes are presented in Table 23. Information was recorded for 88 participants as some health care records were unavailable. A mental health problem or learning disability was recorded in over one-third of participants' health care notes. In total, 33% of older prisoners in this sample were diagnosed with high blood pressure and 18% had emphysema/chronic obstructive pulmonary disease (COPD) recorded in their records.
| Health problem | Yes, n (%) |
|---|---|
| Mental health history or learning disability | 33 (38) |
| Diabetes mellitus | 17 (19) |
| Arteriosclerotic heart disease | 4 (5) |
| High blood pressure | 29 (33) |
| Arthritis | 14 (16) |
| Depression | 12 (14) |
| Asthma | 13 (15) |
| Emphysema/COPD | 16 (18) |
| Cancer | 3 (3) |
Medications prescribed
Medications prescribed in the first 4 weeks of prison custody are presented in Table 24. The most common included cardiovascular system medication (48%) and central nervous system medication (42%).
| Item | Yes, n (%) |
|---|---|
| Gastrointestinal system medication | 35 (37) |
| Cardiovascular system medication | 46 (48) |
| Respiratory system medication | 23 (24) |
| Central nervous system medication | 40 (42) |
| Infections medication | 6 (6) |
| Endocrine system medication | 16 (17) |
| Obstetrics/gynaecology/urinary tract disorders medication | 6 (6) |
| Nutrition/blood medication | 6 (6) |
| Musculoskeletal/joint disease medication | 15 (16) |
| Eye medication | 3 (3) |
| Ear/nose/pharynx medication | 4 (4) |
| Skin medication | 9 (9) |
Audit of health care records
An audit of older prisoners' health care records (either electronic or paper based) was carried out for 85 older prisoner cases. A number of different records were examined. In some cases information from more than one source was used to complete the audit.
Reception health screening was documented in 81 cases (95%) and follow-up health screening was documented in 43 cases (51%). An older prisoner assessment was noted in records for 18 cases (21%) and a social care assessment was carried out in four cases (5%) (Table 25).
| Audit items | n (%) of completed audits |
|---|---|
| Health screening taken place at reception | 81 (95) |
| Participant has a GP in the community | 75 (88) |
| Medical information received from GP | 65 (76) |
| Follow-up health screening completed | 43 (51) |
| An older person assessment carried out | 18 (21) |
| Social care assessment carried out | 4 (5) |
Contact with services was examined for those presenting with symptoms of depression as measured by the GDS-15 (Table 26). A total of 47 (55%) had a GDS score clinically indicative of depression (> 5). Contact with prison and community services was analysed for 42 cases (five missing audits). Eight (19%) were receiving antidepressant medication and six (14%) had contact with a mental health nurse during the first 4 weeks of custody.
| Documented contact with prison staff/agency | n (%) |
|---|---|
| Seen by | |
| GP | 21 (50) |
| Mental health nurse | 6 (14) |
| Primary care mental health service | 1 (2) |
| Prison listener | 1 (2) |
| Individual interventions | |
| Opened ACCT | 7 (17) |
| Moved to safer cell | 1 (2) |
| Observation level specified | 3 (7) |
| Documented discussion of self-harm/suicide | 2 (5) |
| Care plan opened | 2 (5) |
Qualitative findings
A total of 27 of the 100 participants took part in semistructured interviews. These interviews were conducted until data saturation was reached and no new themes emerged. Demographic information for the 27 individuals who participated in the qualitative interviews is presented in Table 27. This subsample is representative compared with the total sample involved in this part of the study in terms of age, offence and sentence length (see Table 8).
| Demographics | n (%) |
|---|---|
| Participant age (years) | |
| 60–64 | 16 (59) |
| 65–69 | 5 (19) |
| 70–74 | 5 (19) |
| 75+ | 1 (3) |
| Offence | |
| Violent | 5 (19) |
| Sexual | 12 (44) |
| Other | 6 (22) |
| Not disclosed | 4 (15) |
| Sentence length | |
| < 12 months | 5 (22) |
| 1–5 years | 5 (15) |
| 6+ years | 6 (22) |
| Unsentenced | 11 (41) |
Table 28 shows the themes and subthemes identified with regard to older prisoners' health and social care needs on entry into prison.
| Main theme | Subtheme |
|---|---|
| Entry processes | ‘Entry shock’ |
| Lack of Information | |
| Dignity | |
| Mental health needs | Anxiety |
| Depression | |
| Physical health needs | Delays |
| Equivalent care to that in the community | |
| Social care needs | Benefits |
| Daytime activities | |
| Personal care needs | |
| The prison system | Prison officers |
| Prison facilities |
Theme 1: entry processes
Many interviewees found the process of entering prison daunting. They reported that the shock of entering a prison establishment led to reduced retention of information. Physical acts undertaken as part of the entry process were more likely to be remembered than the details of conversations and assessments conducted. Those who had experienced prison previously found the process less harrowing than first-time prisoners.
‘Entry shock’
The shock of entering prison in later life left some respondents feeling despairing and anxious. This was more apparent for those entering prison for the first time in later life than for repeat offenders:
Going in [to prison] is like a shock to the system isn’t it, when you come in prison at my age.
Prisoner, p2.17
Several respondents believed that the system was more amenable to those who had been incarcerated before because it was assumed that all prisoners knew what to expect:
Well yeah, because I’ve been here before so I know the score, you know what to watch out for.
Prisoner, p2.5
A number of interviewees struggled to remember what questions they were asked during their induction process. Memory loss concerning the entry process was a particular issue for first-time prisoners. It was attributed to the shock associated with the transition to prison life. Many reported that their initial days of custody were filled with feelings of uncertainty and worry. They were unable to retain information or recount what questions were asked during initial assessments:
I can’t remember, she [nurse] may have done, but I honestly can’t remember, it was, it’s pretty traumatic when you’re taken from one, as I say, one environment to another, which is alien to you, but she may have asked questions, I don’t know.
Prisoner, p2.6
Lack of information
A lack of awareness of the processes involved and a lack of information from staff caused high levels of anxiety among prisoners:
So we came on here [the prison wing] and they put us upstairs in that cell, and then we didn’t know, as I say, what was happening, we didn’t know – we had to ask everything, ‘Where do we go?, What do we do?’ And it was this what were getting us worried.
Prisoner, p2.65
Many first-time prisoners relied on other prisoners to provide them with information:
My pad mate, as we call them, not cell mates, pad mate, has been very helpful, he came in before Christmas and he showed me all, what I should do, and how to send out the application for the visit for my wife, and how to do this, and how you should write the letters, all the rest of it, which he was very helpful to me.
Prisoner, p2.34
Dignity
Older prisoners felt that some of the treatment they received on entry into prison was undignified. Many interviewees vividly recalled their belongings being taken and the strip-search being conducted when they entered prison. Many believed that, because of their age and physical deterioration, strip-searching was unnecessary:
Oh terrible, I felt degraded, cos they strip-search you, you’re stripped naked and you have to turn around in front of them, very, very degrading. They search for drugs, they search your clothing, I mean surely a man of my field who’s come in with two sticks I wouldn’t be doing all that.
Prisoner, p2.9
Theme 2: mental health needs
Older prisoners discussed their mental health and well-being on entry into prison. A number of prisoners discussed their low mood on prison entry. Many were anxious about their families on the outside and whether or not their finances would be dealt with appropriately. For the majority, these worries and concerns were not disclosed to staff.
Depression
Prisoners frequently disclosed that they felt depressed when they entered prison. This was attributed to the initial period of custody. These feelings were often not reported to staff:
Well, I felt depressed at the time. I mean, I’m all right now, but I was certainly in a bad way at the time when I came in.
Prisoner, p2.5
Anxiety
Interviewees repeatedly mentioned that they were anxious about their families outside prison. This was particularly relevant to some older prisoners who had not experienced separation from their partners previously. Some interviewees reported that their wives or partners were experiencing poor health and were now home alone. This caused them great concern:
No, I’m just worried about my wife being by herself at home, you know.
Prisoner, p2.34
A lack of available finances caused concern among older prisoners. This was particularly relevant as they depended on money being available in order to communicate with friends and relatives outside prison:
As long as my money’s there and if my money’s not there I’m stuck, I’m stuck if my money’s not there, cos I worry about communication.
Prisoner, p2.55
Theme 3: physical health needs
Older prisoners discussed delays in accessing health care services in prison and the differences between health care in prison and health care in the community.
Delays
Many reported delays in seeing a GP. They perceived there to be significantly more of a delay in accessing a GP in prison than in the community:
A week or something like that, about a week or a few weeks in, when I saw the doctor.
Prisoner, p2.9
Well I think it’s absolutely ridiculous that – three weeks, I mean if you have got a problem outside you don’t wait 3 weeks do you to see a doctor, you see them the next day.
Prisoner, p2.33
A delay in receiving medication on entry into prison was considered to be a major problem in prison establishments. Prisoners often had the medication they brought into prison confiscated on prison entry. Prescribed medication usually required verification by a prisoner's GP in the community. This led to significant delays in receiving medication. In one case the receipt of medication was reportedly delayed for 1 month after prison entry:
No, I think the main thing is my medical things. It’s why are your pills taken off you and then not given to you for a month, or nearly five weeks. And you think, are they wanting to cut the prison stock down or something, you know!
Prisoner, p2.33
Equivalent care to that in the community
Older prisoners perceived there to be differences between health care in prison and that in the community. Many believed that it was easier to get appropriate health care outside of prison. Prisoners explained that some medications were not available in prison:
I’ve seen the doctor, I told the tablets I’m on, what tablets I’m on, been on for 40 years. They said, ‘You can’t have them in here’.
Prisoner, p2.55
When you’re outside you can get treatment but when you’re in here [prison] you can’t, and if you don’t get treatment you die.
Prisoner, p2.31
Theme 4: social care needs
Many participants had unmet social care needs. These included a lack of help with benefits and daytime activities and a lack of support with activities of daily living.
Benefits
Financial problems were a cause of concern for many older prisoners. When asked to discuss how the prison was meeting their needs, many stated that help and information about pensions and benefits were sparse:
I don’t know, it’s just your money side of life . . . to sort your bank affairs out and all this and . . . There’s nothing.
Prisoner, p2.5
Daytime activities
Older prisoners reported that they would like to be employed in the prison; however, because of their mobility problems the available work was not suitable for them:
Would like very much, if I could just like just get out of my pad and do like maybe . . . well parade starts at eight-thirty of a morning, so they’re out till about eleven, they get back and then they’re out again from one o’clock to four o’clock. If I could just be out [of cell] for those hours oh it would be lovely, yeah.
Prisoner, p2.33
If available, many older prisoners attended the older prisoner group at their establishment. This was considered to be a welcome distraction from prison life:
Well, it’s [the older prisoner group] something to look forward to, they make you a drink of tea and biscuit, we have a talk, they were on about different things and they said like, you know, there is different things every week they do.
Prisoner, p2.17
Personal care needs
Older prisoners reported unmet social care needs. They struggled with activities of daily living such as washing and dressing. One prisoner felt that it was inappropriate to ask his male cellmate to help with such tasks, previously carried out by his wife:
I can’t get the towel round my back, I can’t get my arms round my back to dry myself and my wife helped me there, so you can’t ask a man to do that for you while you’re in there, it looks weird.
Prisoner, p2.21
One interviewee recounted that he had to ask his cellmate to apply medical cream to his legs as an appropriate member of staff did not come to assist him:
Since I’ve been here they gave me a tube and no-one came, on the second night my cellmate did it.
Prisoner, p2.33
Theme 5: the prison system
In the main, the prison system did not accommodate older prisoners' requirements. The design of many prison establishments was not appropriate for older prisoners. This caused anguish and distress among interviewees. Staff in the prison were considered unapproachable by some interviewees. Conversely, other prisoners commended them on their sense of humour.
Prison officers
Older prisoners' perceptions of prison officers emerged during interviews. Often they were commended for their sense of humour:
I mean they’re reasonably short staffed anyway, but their sense of humour is brilliant, some of them are absolutely hilarious you know.
Prisoner p2.10
Others interviewees believed that prison officers were not amenable and consequently did not approach them:
Yeah. Well, I don’t, I try and keep, I don’t mean my distance from them [prison officers], but I try not to approach them for anything. I try and work round it if you know what I mean.
Prisoner, p2.17
Reasons for this varied. Some respondents believed that prison officers were not willing to help them; others wanted to remain unnoticed:
They’re [prison officers] not interested. They just do their job, they don’t care if you’re alive or dead I’m telling you, they don’t care.
Participant, p2.45
One of the problems encountered by older prisoners was the staff's use of ‘prison slang’. The majority of older prisoners were unaware what was being referred to by different abbreviations, such as the use of ‘seg’ for segregation cells. This caused older prisoners much confusion and they became frustrated because of their lack of understanding:
I don’t know what seg is, you know, what’s seg, you know what I mean. I haven’t a clue what seg is. You’re on the CC or you’re on ID, I don’t know what this is. I haven’t a clue what all this is. They are expecting, they think that you know what it is.
Prisoner, p2.26
Prison facilities
A problem highlighted by older prisoners was the design of some prisons. A reliance on stairs meant that physical access to particular areas of the building was difficult for older prisoners with mobility problems:
Yeah, I should imagine it would, but it’s the total design of the place, you know, old people can’t walk up a set of steps, can they, basically.
Prisoner, p2.13
A startling example of inadequate arrangements for older prisoners is described below. Bunk beds were not accessible for older prisoners and this at times led to prisoners having to sleep on the floor:
No when I went in I were first in, so I said that’s my bunk, the bottom, I’m not getting up there [top bunk]. Anyway, the next chap that come in, he couldn’t get up, so he had to sleep on the floor.
Prisoner, p2.9
Older prisoners commented that the exercise facilities available were not suitable for their needs. One participant explained that he could not walk for long periods of time and would require frequent rests. There were no facilities available to support this request. When he suggested bringing a chair with him to the exercise yard he was reportedly met with resistance from prison officers:
If I could take a chair outside and sit down for say 5 minutes then start walking and when my back starts hurting sit down for another 5 minutes and then start walking, fine. So it’s just my back but they don’t allow you to do that.
Prisoner, p2.29
Summary
The second part of this study aimed to assess the unmet needs of recently incarcerated older prisoners, as well as capture their experiences of being received into prison custody. Results from the CANFOR-S showed that the highest proportions of unmet needs were in the domains of information about condition and treatment (38%), psychological distress (34%), daytime activities (29%), benefits (28%) and physical health (21%). Analysis of GDS-15 data found that 31% of the sample had a score indicative of mild depression and 23% of the sample had a score indicative of severe depression. Eight (19%) of those showing signs of depression were receiving antidepressant medication and six (14%) had contact with a mental health nurse during their initial 4 weeks in custody.
Semistructured interviews conducted during the initial period of prison custody highlighted that older prisoners entering prison for the first time suffered from ‘entry shock’, which was made worse by a lack of information received. Delays in accessing health care and receiving medication were a particular cause of concern. In the main, social care needs were not appropriately met. Furthermore, older prisoners considered some prison officers to be inapproachable and prison facilities to be largely inadequate.
Chapter 5 The development, implementation and evaluation of an intervention to identify and manage the health, social care and custodial needs of older people entering prison
Introduction
The Department of Health has emphasised the importance of regularly assessing older prisoners' health and social care needs using specialised assessments and care planning. 23 The present study has identified that only 19% of establishments currently use a specialised older prisoner assessment on entry into prison. This part of the study aimed to develop, pilot and evaluate an intervention for identifying the health and social care needs of older prisoners on reception into prison and ensuring that these are systematically addressed during older people's time in custody.
Method
This part of the study involved mixed methods including action research, documentary analysis and semistructured interviews with action-learning group members and older prisoners.
Action research
Action research involves cycles of planning, action and evaluation to conceptualise issues and generate solutions57 and enables practitioners and researchers to generate knowledge while simultaneously changing practice. 58 Action learning is ‘a continuous process of learning and reflection that happens with the support of a group or “set of colleagues”, working on real issues, with the intention of getting things done’ (p. 11). 59 Action learning has been used previously to develop practice in the prison setting and is known to be beneficial through simultaneously developing both staff and practice60–63 while taking into account the discrete social and cultural context of the prison.
Action-learning group meetings
Principles of action research were adopted to develop the Older prisoner Health and Social Care Assessment and Plan (OHSCAP) through the use of an action-learning group. An action-learning group comprising health care staff, prison staff and older prisoners was established at one adult male prison in England. The group was facilitated by an experienced action-learning group facilitator who was familiar with both prison culture and working practices. Action-learning group members were recruited following an initial open meeting at the prison when the aim of the project was explained and expressions of interest sought. At the first action-learning group meeting there were 14 members including two older prisoners, primary health care staff, a governor and prison officers from residential wings, the gym and the first-night centre. There was consistent representation from prison officers and prisoners throughout the life of the group; however, the involvement of health care staff reduced significantly as the project progressed.
Through a regular monthly action-learning group, cycles of planning, action and evaluation took place to support the development of the OHSCAP and its piloting in vivo. In developing the content of the OHSCAP, the action-learning group commenced by reflecting on current practice in their own prison, practice in other prisons using assessment tools currently being used elsewhere and provided to them by the wider project team, a HMCIP thematic review7 and a toolkit from the Department of Health. 23 Research publications pertaining to the needs assessments of older people in the community41,64,65 were also utilised to explore the nature of the SAP and other areas and types of assessment used in the wider community. Following reflection on the literature and existing practices, the action-learning group met monthly between November 2010 and September 2011 in a meeting room inside the prison where they developed the OHSCAP through iterative cycles of reflection and discussion, each of which underpinned the evolution of the tool.
The piloting of the OHSCAP by the prison's OPL took place between May 2011 and April 2012. This officer was deemed the most appropriate member of staff to undertake this work given his prison-wide lead responsibility for older offenders. During piloting the action-learning group met four times to receive feedback on the use of the tool and to agree amendments and changes in light of ongoing evaluation and reflection on practice. Feedback from the piloting phase centred on facilitated reflection by the OPL on a number of issues, including its ease of use, necessity, length of time to complete, referrals made, impact on role, influence on colleagues and prisoner response to assessment.
Figure 1 illustrates the action-learning group and piloting activity.
FIGURE 1.
Action-learning group and piloting activity.
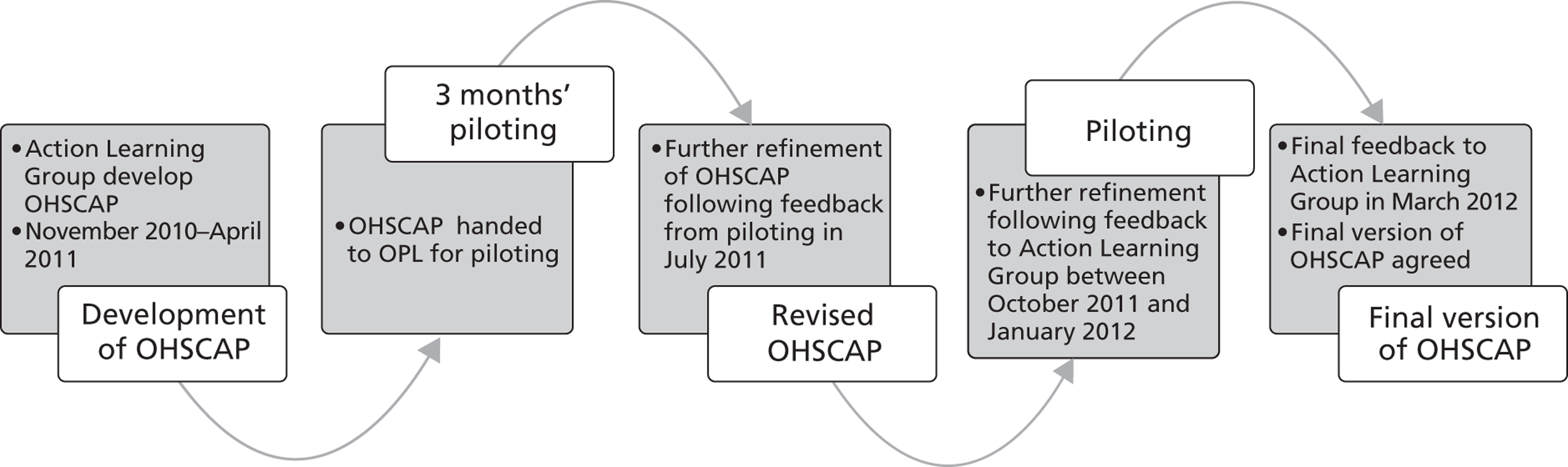
Data collection
Using an action research approach to developing practice requires an ongoing awareness of, and reflection on, various sources of data. 60 During the life of the action-learning group, data were collected from a number of sources to capture the activity of the group alongside the development of the OHSCAP and its evaluation.
Documentary analysis
Reflective notes from each action-learning group meeting were made by the facilitator to record group activity and OHSCAP development. It was envisaged that the development of individual action-learning group members and their perceptions of the value of action learning could be captured through individual reflective diaries. Unfortunately, but not unexpectedly, only one member of the action-learning group kept a reflective diary for 2 months. In addition to reflective notes and diaries, email conversations between the facilitator and the OPL pertaining to the piloting of the OHSCAP were captured as were the overarching project steering group-meeting notes, which were presented to the wider project team by the facilitator. All documentary data served to highlight the development of the action-learning group, the development of the OHSCAP and the progress of the piloting.
Semistructured interviews with action-learning group members
Semistructured interviews were conducted with action-learning group members (including the OPL) to ascertain their experiences of action learning and to evaluate the OHSCAP. Copies of the interview guides are included in Appendices 5 and 6. Six action-learning group members were interviewed including prison officers, health care staff and prisoners. Two of these interviews were held face-to-face and the remainder were held over the telephone. Interviews were audio recorded and lasted between 20 minutes and 1 hour.
Semistructured interviews with older prisoners
Semistructured interviews were conducted with older prisoners who received the OHSCAP (n = 24) to ascertain their opinions of the processes involved. The interview guide is included in Appendix 7. All prisoners aged ≥ 60 years who were newly received into the prison during the piloting time period were invited to receive the OHSCAP and participate in the interview. The interviews were conducted between 11 days (after they had received the OHSCAP) and 10 weeks after prison entry. These interviews lasted up to 90 minutes and were, on occasion, conducted across more than one session to fit around the prison regime. They were conducted in private interview rooms or offices on wings or in cells in the prison health care unit and were audio recorded.
Qualitative data analysis
Group facilitator reflective notes, action-learning group member reflective diaries, emails between the action-learning group facilitator and the OPL during piloting, steering group meeting reports and data from all semistructured interviews were analysed. Data from the interviews were audio recorded and transcribed verbatim. The constant comparison method of data analysis was adopted for all qualitative analysis conducted for the current study48 (see Chapter 3 for detailed information about this method of qualitative analysis). The computer software NVivo was used to conduct the analyses. Data were analysed until theoretical saturation was reached. Analysis of the data uncovered themes in two distinct areas of the work: the use of action learning in prison and the development and piloting of the OHSCAP.
Results
Demographic information for the 24 prisoners who participated in the semistructured interviews is presented in Table 29.
| Demographics | n (%) |
|---|---|
| Participant age (years) | |
| 60–64 | 14 (58) |
| 65–69 | 8 (33) |
| 70–74 | 0 (0) |
| 75+ | 1 (4) |
| Missing | 1 (4) |
| Offence | |
| Violent | 3 (13) |
| Sexual | 12 (50) |
| Other | 8 (33) |
| Not disclosed | 1 (4) |
| Sentence length | |
| < 12 months | 5 (21) |
| 1–5 years | 4 (17) |
| 6+ years | 4 (17) |
| Unsentenced | 7 (29) |
| Licence recall | 3 (13) |
| Missing | 1 (4) |
The findings are divided into two themes, namely the OHSCAP development and piloting and action learning in prison, as illustrated in Table 30.
| Theme | Subtheme |
|---|---|
| The OHSCAP – development and piloting | Content |
| Process | |
| Value | |
| Action learning in prison | Maintaining focus |
| Seeking clarity | |
| The importance of space | |
| Group composition |
Theme 1: the OHSCAP – development and piloting
Findings pertaining to the development and piloting of the OHSCAP are grouped into three themes: content, process and value.
The Older prisoner Health and Social Care Assessment and Plan content
Deciding the content of the OHSCAP was a key task for the action-learning group. Content was based on staff and prisoner experience (action-learning group members), information already collected elsewhere on the prisoner journey and literature/existing policies and practices in other prisons. The action-learning group designed the OHSACAP to include a series of open questions around relationships, activities, mobility, emotional well-being and physical well-being. In its initial stages the OHSCAP had two main sections, one relating to health care and the other to social care. Given the identified need for clear terminology that would resonate with prison officers, the action-learning group felt that the ‘health care’ section should be amended to refer to ‘well-being’. After the identification of issues among older prisoners pertaining to discharge from prison, a discharge planning section was also added. A care plan was also included that detailed any referrals and special arrangements to be made. A copy of the OHSCAP is included in Appendix 8.
In addition to the actual content, the way in which the OHSCAP was presented became very important to the group for a variety of reasons. It was decided that it needed to be clear, have a coloured cover to differentiate it from the ACCT assessment and include questions that promoted open discussion rather than requiring only a ‘yes/no’ response. Consequently, the OHSCAP had a format that aimed deliberately to facilitate discussion and exploration. This was considered imperative by the action-learning group to facilitate meaningful discussion between staff and prisoner, and to avoid the completion of the OHSCAP becoming a ‘tick box exercise’:
I don’t like tick box/questionnaires, they’re so impersonal, don’t always get the, I mean, when you’re just reeling off a question, yes, no, disagree, disagree strongly, tick boxes, yeah, I mean, that, to me, they’re a waste of time, statistically, but, yeah, the open questions that asks for some feedback were much better in my opinion, and we got quite a lot of information from doing that, rather than the tick boxes.
OPL, p3.26
The Older prisoner Health and Social Care Assessment and Plan process
The action-learning group considered the process of administering, formulating and reviewing the OHSCAP alongside the development of the tool's content. Although this dual focus could have been viewed as problematic, the nature of action learning lends itself well to the development of new initiatives in this way as group members can develop tools with a clear and simultaneous understanding of the current culture and practices. 58 It is suggested that this enables useful and effective tools to be developed that, from the outset, take account of local practices and are therefore less likely to fail.
In considering the overall aim of the OHSCAP, group members felt that developing an assessment tool that was based on the same operational principles as the ACCT process, which is well embedded and known in all prisons, would be useful. Figure 2 illustrates the OHSCAP process, which is explained further below.
FIGURE 2.
The OHSCAP process.
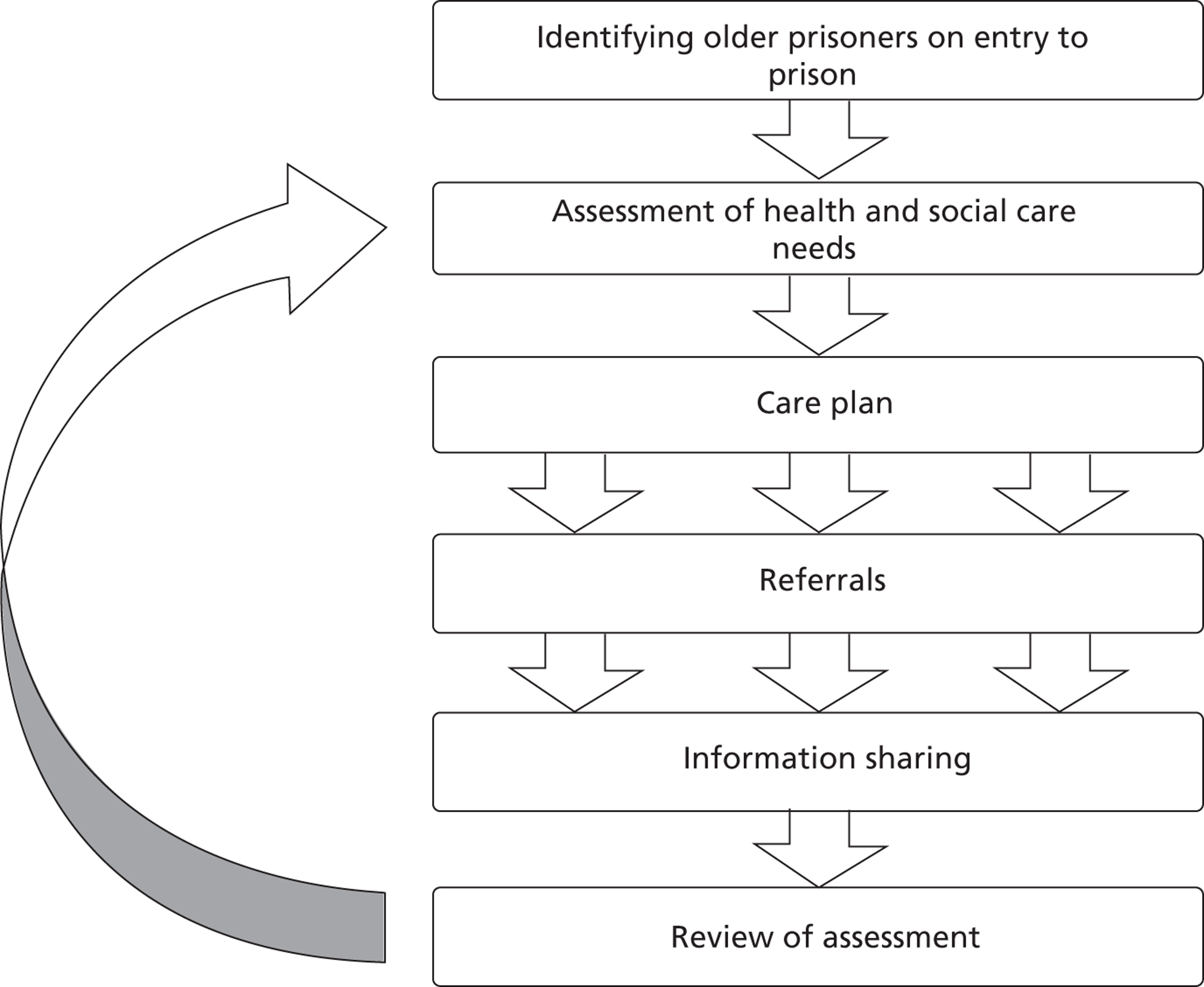
The OPL identified older prisoners entering the prison and conducted the assessments. Members of the action-learning group felt that he was the most appropriate person to conduct the assessments as his job description already included supporting older prisoners. The OPL stated that identifying older prisoners was a simple process and that they could be easily identified using the prison computer system C-NOMIS:
How we identified the older prisoners was, obviously, C-NOMIS, we ran a list of new admissions from the previous day, and any prisoner who showed up as an older prisoner by birth date we would highlight, and take some particular details off C-NOMIS to start his file.
OPL, p3.26
Prisoners considered the OPL to be helpful, professional and friendly and felt comfortable talking to him about their issues and concerns, as illustrated in the following quotes:
But the interview with [OPL], excellent, nice man, informed me of various things.
Prisoner, p3.8
I find him very understanding, he was very clear and concise when we went through the forms and the questions. You know, if everybody else was like [OPL], things would be alright.
Prisoner, p3.16
Older prisoners were very willing to discuss all issues with the OPL, including health care concerns:
No, I’ve had to speak to a lot of people about my health over the last, sort of 10 to 15 years so, quite used to it.
Prisoner, p3.16
The group decided initially that the health and social care nature of the assessment would necessitate a joint assessment by health care and discipline staff, with the latter taking the lead. Trialling this in practice identified some difficulties with health care staff availability; thus, it was decided that health care staff were not required at all assessments. Over time, it was decided by the group that it would be appropriate for the OPL to routinely conduct the assessment alone, with assistance from health care staff when deemed necessary:
Prisoners are happy to be assessed jointly [by a prison member of staff and healthcare member of staff], at the same time although there have been occasions when there has been no member of healthcare staff available. In those cases, the assessment has continued and healthcare been advised of any issues that were raised.
Facilitator notes, July 2011
It was decided that the OHSCAP would be best introduced between 7 and 10 days post reception into prison. This was based on discussion in the action-learning group around the wealth of information that is both asked for and provided to all prisoners, including older people, immediately after they arrive in prison. In particular, it was felt that older prisoners required a period to settle into the prison to be able to identify and articulate their needs effectively:
The prisoners in the group reported that their own experiences of reception had been ‘daunting’ and difficult, given that they did not know what questions to ask as they did not know what would be happening. They also said they had information overload during their first few hours in prison.
Facilitator notes, November 2010
Further evidence for the need to allow the older prisoners time to settle into prison before conducting the assessment was provided in the interviews with the older prisoners themselves, who often stated that they could not remember the details of what happened when they first came into prison because of ‘entry shock’, suggesting that it would therefore not be appropriate to conduct an assessment during the first few days after prison entry:
I did have an interview with someone [on entry into prison] . . . I can’t remember what it were for . . . I honestly couldn’t tell you.
Prisoner, p3.5
Prisoners were routinely offered a copy of their OHSCAP care plan but often declined it. The reasons for this are not clear. Further work is required to establish the advantages and disadvantages of the prisoner holding a copy of his care plan. For example, this may be advantageous when prisoners are discharged from prison, to avoid duplicating work and to allow professionals providing follow-on support to be able to easily identify what support has been provided to date. The care plan included space to detail any referrals made. As part of the OHSCAP, referrals were made to agencies such as Shelter, education, health care, solicitors and social services, illustrating the holistic nature of the assessment and planning undertaken. The OPL reported that such referrals were being made earlier as a result of the OHSCAP than would otherwise have happened. This has the potential to better prepare older prisoners for their release:
At least, we can get an early referral, then get details off the prisoner, and start making enquiries early, see what we can sort them out with, even if it’s just some temporary accommodation when they get out.
OPL, p3.26
The OHSCAP was designed by the action-learning group to be shared between appropriate agencies. Feedback during piloting indicated no perceived need to share the assessment itself. On reflection, during their interview the OPL felt that it would be useful to provide prisoners with a copy of their OHSCAP, write up a summary of the OHSCAP on the prison system C-NOMIS and also scan a copy of the OHSCAP onto SystmOne (the prison electronic primary health care records system). It was felt that this would save duplication of work when a prisoner moved on from the establishment and also allow other professionals in the establishment to be aware of the issues facing the older prisoner. It was, however, highlighted that prisoners would need to consent to health care information being shared.
The OPL conducted reviews of the care plans on an ad hoc basis. The action-learning group decided that it would be most appropriate for the OPL to decide when reviews were conducted, depending on the nature of an older prisoner's issues, rather than to have the process dictate fixed review periods. The OPL, however, stated that deciding when reviews should be timetabled was challenging. The OPL specified that a more structured time review period would be helpful. Training in case management may assist those conducting the OHSCAP to identify appropriate time periods for review, as this is a skill that is not currently routinely practised for other similar prison-based assessment processes:
Yeah, not having a set period, I mean, and it just being left open to doing a review was a bit difficult, I think if we had a set timescale for doing a review after doing the care plan, then it might have been more useful to me, because yeah, I did find it a little bit difficult when to revisit it.
OPL, p3.26
The Older prisoner Health and Social Care Assessment and Plan value
The OHSCAP allowed the OPL to identify older prisoners' health and social care issues. Key concerns identified were delays in receiving medication, problems using the telephone and homelessness/housing issues. A delay in receiving medication was a frequent concern of older prisoners, as it is in the wider prison population. 66 Prisoners discussed delays of up to 10 days for existing medication regimes to be re-established after prison entry. These delays caused them considerable distress. Some older prisoners even perceived these delays to be life-threatening:
To be without my medication for that length of time is not, it’s dangerous, it. I mean I’ve had a stroke, a slight stroke in past, but I’ve never gone to a full blown heart attack and doctor told me that any longer without this medication what I’ve got to have. It’s not a matter of just take it willy nilly, I’ve got to take it every day, which I’ve been doing since I got it like.
Prisoner, p3.1
Given an existing positive working relationship between the OPL and the health care team, effective liaison with health care staff appeared to speed up the prescription of medication:
Medication was something that I could probably resolve that day, or, certainly, get things moving, if they hadn’t already been resolved. I’d approach the wing nurse, and discuss the issue with her, and between us we’d come up with a plan as to what was the best way to approach, and sort out the problem, whether it was to book an appointment with the doctor straight away, or whether the nurse could contact the pharmacist, and sort it out that way.
OPL, p3.26
Use of the OHSCAP facilitated early resolution of day-to-day prison-based problems, as well as prompting early referral to other help agencies. Resolving such issues were considered to make life more tolerable for older prisoners who were deemed to be vulnerable by staff. Both staff and prisoners reported that older offenders tended not to complain about such issues but that the OHSCAP gave a structure through which to ‘legitimately’ discuss problems, even those of a sensitive nature:
I’ve only just come in [to prison], so I’m trying to keep a low profile. I don’t want to rock the boat.
Prisoner, p3.20
Because I think if I hadn’t asked them [older prisoners] outright about a particular issue they wouldn’t have mentioned it, that’s the impression I got.
OPL, p3.26
Prisoners appreciated the OPL's interest in their situation and enjoyed simply being listened to. The assessment therefore had additional therapeutic benefits for the older prisoners. There were also practical benefits of the OHSCAP for the OPL, who specified that the assessments created an easy record to refer back to when issues arose with specific prisoners. It also increased multi-agency working, with networking taking place as and when referrals were made.
Theme 2: action learning in prison
Four key themes emerged from the data that highlighted the challenges to and enablers of undertaking action learning in the prison setting. These were maintaining focus, seeking clarity, the importance of space and group composition.
Maintaining focus
Maintaining the focus of the action-learning group proved challenging. There was a tendency for the group to attempt to solve specific issues as they arose, rather than focus on the development of a system to manage them. On one level, this may have appeared to be problematic, given that the role of the action-learning group was to develop the OHSCAP; however, what was first regarded as challenging resulted in positive actions for older prisoners. Action-learning group members reported that the existence of the group assisted in the development of older prisoner representatives, the introduction of seating in exercise yards and the development of an increased awareness among staff of the needs of older prisoners:
I think it [the action-learning group] did raise the profile of the older prisoner, certainly on A Wing [vulnerable prisoner wing], in the fact that possibly their health needs were somewhat different to their more younger counterparts’.
Action-learning group staff member, p3.27
Seeking clarity
Part of the purpose of the action-learning group was to support professional development, alongside the actual production of the OHSCAP. In keeping with the action-learning approach to this work, the group required clear focused facilitation to allow exploration of particular issues and concepts that would underpin both the content and the process of the OHSCAP. For example, in discussing whose responsibility completing any assessment of older prisoners' needs would be, exploration of professional roles and responsibilities and the resultant conflict between prison officers' dual roles as social carer and custodian was apparent. Although this discussion was not directly related to the development of the OHSCAP initially, it provided room for consideration of each group member's role in caring for older prisoners. This led to fruitful discussion and the conclusion that it is the social care aspect of older prisoners' needs that is perhaps the most important area to consider in any assessment, as health needs have already been identified by health professionals through routine practices on reception to prison. However, this directed the group to consider the role of health care staff and that of prison officers:
[This] led to conversation about the barriers to caring for older prisoners e.g. cultural issues and the risks of [prison officers] being seen to be caring e.g. pushing wheelchairs, collecting meals, etc.
Facilitator notes, December 2010
In addition to seeking clarity around roles and responsibilities, the group also spent time reflecting on the information flow and the way in which information is shared across professional groups:
There appear to be key points along the process where information gathering takes place and where questions are replicated.
Facilitator notes, November 2010
Understanding the nature of information collected and its flow around the prison was central to the way in which the group assimilated and devised both the content of the OHSCAP and its process:
In some ways, much of the information we would expect to be collected regarding the older prisoner, is already collected. The group cannot see any huge gaps in the information. However, what they have decided is missing, is effective communication of the information.
Facilitator notes, January 2011
On a practical level, clarity around roles and information sharing needed to be gained by the group to enable it to move forward with both developing the OHSCAP and giving thought to the process of implementing it. However, on a more experiential level, reflection on these issues provided group members with useful understanding of other professional/service user perspectives.
The importance of space
Considering the space where action-learning groups meet is important in terms of group members feeling both physically and psychologically safe. 59 In light of the aims of this action-learning group being centred on developing the OHSCAP, a venue was also required that enabled creativity and open, honest sharing of thoughts. Given that the group membership included serving prisoners, utilising a venue outside of the prison was impossible. Initial meetings were held in a large open-plan area, with only seating and no tables. This was felt to stifle creativity and reduce the possibility of smaller group work as it promoted a more formal atmosphere:
We need to move the venue to somewhere that we can have tables and flip charts to get creative.
Facilitator notes, November 2010
Moving the venue to provide a more creative space was popular and supported a closer working group. In promoting a more informal, creative space, action-learning group members reported that they enjoyed opportunities to participate in group work and benefitted from inclusion in development:
The location of the meeting was better as we had tables to work on. I still think there is a lot of ground to cover but I really enjoyed the last meeting. I am glad to be part of the development of this assessment.
Reflective diary, November 2010
In addition, prisoner group members constructed an information sheet that they felt would be useful for new older prisoners coming into prison for the first time. Although this information sheet was not used directly in any process developed as part of the OHSCAP pathway, it provided action-learning group members with a clear understanding, from a prisoner perspective, of what was needed to support older prisoners who are new to prison. What could be viewed negatively as a lack of group focus not only enabled group members to identify solutions to specific issues but also was seen by the facilitator as useful in enabling members to use the action-learning space as a time for reflection and consideration of individual practices. This allowed for the explicit identification of tacit knowledge, which, when highlighted, provided group members with the realisation that, although they felt that there was nothing specific in place at the prison to manage older prisoners, there were processes that did address their needs:
After some general discussion about the venue and dates of subsequent meetings, the group began to consider current practices that occur in the prison as regards older prisoners. Although they initially stated that there were no specific processes in place for managing/assessing older prisoners on reception, it became clear that there were.
Facilitator notes, November 2010
It was good that after some discussion we have provisions in place for the over 55's.
Reflective diary, December 2010
This protected space for reflection through action learning allowed group members to step back from their day-to-day practice to view the processes in place at the prison, while input from service users in the group provided evidence of how processes felt for prisoners. This reflection on practice and experience proved useful to enable group members to identify and appreciate their work, thus providing a basis for further development.
Group composition
Attendance at the group wavered, particularly for health care and senior staff. However, this was not considered to be detrimental to the group's success. Indeed, the process of the group settling over time, with a reduced but consistent membership, was felt to be beneficial in terms of ‘getting things done’:
The meeting was small last month. I felt this helped and we were able to move forward more quickly with things.
Reflective diary, December 2010
Again, attendance was not ideal; however, those who are attending regularly, remain enthusiastic.
Facilitator notes, January 2011
Having prison officers, health care staff and prisoners in the action-learning group was very effective in terms of allowing potentially dissonant voices from all perspectives to be heard, and subsequently impacted on the development of the OHSCAP and group members:
Yeah, they [prisoner action-learning group members] didn’t feel as if they were intimidated in any way from the officers or from the members that were there at all, they were encouraged to voice their opinions.
Action-learning group prisoner member, p3.25
Summary
Overall, the content of and the process of delivering the OHSCAP was perceived by both staff and prisoners to be appropriate and beneficial. There is a need to effectively share the information collected among prison officers, offender managers and health care staff and to further develop the assessment review process.
The OHSCAP is valuable for assisting prison officers to address older prisoners' health and social care needs using a format that older prisoners found acceptable and empowering. It provides an opportunity to support older prisoners who have complex health and social care needs and are unlikely to otherwise raise their concerns.
It is possible to conduct multi-agency action learning within prisons and to involve both prisoners and prison staff effectively. There are, however, a multitude of challenges to overcome to facilitate action learning in prison, namely maintaining focus, clarifying key concepts and maintaining attendance at groups. Communication across prison departments must be improved to increase attendance at action-learning groups.
Overall, the use of action learning to facilitate the development of the OHSCAP was successful as a completed tool was developed and piloted, with encouraging results. In addition to producing the OHSCAP, group members benefitted professionally and the awareness, and provision, of care and support needs of older prisoners improved because of the extra activity that the action-learning group engaged in, be it consciously or subconsciously, for example raising awareness of the needs of older prisoners, arranging for extra seating and producing an information sheet for new prisoners.
The OHSCAP is a wholly original tool and is inherently protected by copyright.
Chapter 6 Exploring the health and social care needs of older male adults discharged from prison into the community
Introduction
We are aware that the post-release period is particularly risky for prisoners in terms of their physical and mental health. 40 Their anxieties about release prior to discharge from prison have also been documented;41 however, we are not aware of their issues and concerns after they have been released. This part of the study aimed to explore the health and social care needs of older male adults discharged from prison into the community.
Methodology
Qualitative interviews were conducted with participants approximately 4 weeks before and 4 weeks after their release from prison.
Qualitative data analysis
Qualitative interviews were carried out with prisoners in custody who had 4 weeks left to serve (see Appendix 9) with follow-up interviews in the community within 4 weeks of release (see Appendix 10). Unlike entry to prison when new prisoners are always received into ‘local prisons’, people can be discharged from any type of prison. Those serving short sentences or awaiting trial could be discharged from local prisons, but many of those serving a more substantial sentence could be released from ‘training prisons’, which concentrate on rehabilitation and training. Finally, ‘open prisons’ prepare prisoners nearing the end of their sentence for life in the community. All three types of prison were included to ensure representation from all prisoner groups.
Interviews took place in six local prisons, two training prisons and one open prison between May 2011 and June 2012. Prisoners were asked for contact details so that they could be interviewed again 1 month following release. Participants were identified through each prison site's named research contact through C-NOMIS. The research contact was able to identify those prisoners who were aged ≥ 60 years who had 4 weeks left to serve in custody. It was more difficult to identify the release date of prisoners who had received indeterminate sentences and had subsequently been moved to open conditions. These prisoners could be released with only a few days' notice. We therefore obtained consent from these prisoners to participate well in advance in case their release became imminent.
Once a potential prisoner participant was identified, an appropriate prison wing staff member checked whether or not the prisoner was willing to be approached by a member of the research team. If the prisoner agreed the researcher then approached the prisoner in a sensitive manner and at an appropriate time, introduced herself to the prisoner, explained who she was and also introduced and explained the study to the prisoner. A participant information sheet was provided (see Appendix 11) and the researcher explained the study verbally. If the participant agreed, the researcher arranged to come back another day to complete the interview.
During the data collection process it became apparent that we were reaching data saturation for those participants being released to reside in Probation Service-approved premises. We therefore ceased data collection for this group and attempted to recruit participants on short-term sentences who were not going to be residing in such accommodation. Recruiting these individuals was challenging because of the relatively small numbers involved and because they could be discharged from prison with minimal notice. However, we were able to successfully recruit individuals with such characteristics.
Sixty-two prisoners were interviewed in prison and 45 were followed up on release (73%). Six prisoners declined to participate in prison (10%). The majority of the prisoners had a probation worker in the community who was contacted on release to assist with follow-up. Follow-up interviews took place in probation offices, Probation Service-approved premises or over the telephone; one interview took place at the interviewee's home because of his mobility difficulties. Two researchers attended this interview for safety reasons. Interviews ranged from 10 to 90 minutes. The interviews were audio recorded and transcribed verbatim.
Qualitative interview guide
The initial qualitative interview covered prisoners' preparation for release in terms of their health and social care needs, including appropriateness of discharge accommodation and their awareness of health and social services that may be required for their continuing care. The follow-up interview focused on how well plans for release were put into action and what services prisoners subsequently accessed. During participants' second interviews they were asked about key issues that they had been concerned about in their initial interviews. Prisoners were also asked about contacts they had had with health and social services and any health problems, social care problems or suicidal thoughts they had had since discharge.
Qualitative data analysis
In line with the other parts of this study, qualitative analysis was conducted using the constant comparison method in the qualitative software package NVivo, as described in Chapter 3. Interview transcripts were linked to be able to identify participants' initial and follow-up interviews and track changes in perceptions. An overview of how participants' perceptions altered from before release from prison to after release from prison is presented in Tables 33 and 34. Key differences were identified in how perceptions changed between those who were and those who were not residing in Probation Service-approved premises.
Results
Qualitative interview findings
Table 31 displays participants' ages and whether or not they resided in Probation Service-approved premises immediately on release from prison. There was a higher percentage of participants in the follow-up sample than in the initial interview sample who were residing in Probation Service-approved premises.
| Demographics | Initial interview sample (N = 62), n (%) | Follow-up interview sample (N = 45), n (%) |
|---|---|---|
| Participant age (years) | ||
| 60–64 | 28 (45) | 22 (49) |
| 65–69 | 19 (31) | 15 (33) |
| 70–74 | 7 (11) | 2 (4) |
| 75+ | 6 (10) | 5 (11) |
| Missing | 2 (3) | 1 (2) |
| Probation Sevice-approved premises | ||
| Yes | 34 (55) | 28 (62) |
| No | 27 (44) | 17 (38) |
| Missing | 1 (2) | 0 (0) |
Table 32 displays the themes and subthemes identified with regard to the health and social care needs of older prisoners before discharge from prison and after release into the community.
| Main theme | Subthemes |
|---|---|
| Release planning processes | Lack of release planning |
| Courses | |
| Medication and medical records | |
| Communication | Lack of information formally received |
| Information received from other prisoners | |
| Uncomplaining | |
| The impact of sexual offending on release | Family conflict and absenteeism |
| Physical safety | |
| Mental health needs | Apprehension and anxiety |
| Depression | |
| Self-harm and suicide | |
| Guilt | |
| Loneliness | |
| ‘Sanity’ | |
| Social care needs | Accommodation |
| Finances | |
| Independence | |
| Physical health needs | Poor health |
| GP registration | |
| Community | Open environment |
| Media | |
| Socialising |
Theme 1: release planning processes
In general, interviewees perceived there to be a lack of planning for their release. Some release planning processes took place at certain prisons, although provision was ad hoc. One prison provided pre-release courses and some participants discussed how offender management courses assisted their preparation for release. Participants considered the prescription of medication on release to generally be satisfactory; however, not all prisoners were provided with a copy of their medical notes on release.
Lack of release planning
When asked about the plans for release prior to their discharge, the majority of prisoners simply stated that no plans had been made. It was their perception that their release was not being planned at all. This caused them a high level of anxiety in the months, weeks and days prior to release:
Nothing has been planned for my release, end of.
Prisoner, p4.19
It’s very, very strange feeling when you came out, they just threw you out . . . gates open and that were it.
Ex-prisoner, p4.9
Participants discussed the practical challenges of making plans for release while in prison. They described how they could not obtain telephone numbers or addresses to make contact with organisations about issues such as housing and hospital appointments. On occasions, participants knew the telephone number to call to obtain support but were unable to call it because they had only a limited number of telephone numbers approved for them to call within prison. Many of those residing in an open prison were unable to obtain day release to make plans for their discharge:
If I could, if I could get day release to go and find a place to stay that would be a good alternative, but that's just the pipe dream development.
Prisoner, p4.14
Courses
One prison participating in this part of the study offered a pre-release training course to prisoners; however, not all prisoners interviewed at this prison were aware of the course's existence. The few prisoners who attended a pre-release course reported that some aspects were informative but that the information imparted was not tailored to older prisoners' needs:
I mean, like getting jobs and what have you, that, that [part of the pre-release course] wasn’t for me because . . . with being long term sick . . . plus I was over sixty . . . well sixty-one and . . . I thought well that, that part and my insurance part [of the course] could be come in handy.
Prisoner, p4.16
Many of the participants had been convicted of sexual offences and discussed how the Sex Offender Treatment Programme prepared them for their release from prison. In particular, they described how it allowed them to consider in advance how they would deal with meeting children in the community (where applicable), their guilt and other individuals asking about where they had been during their prison sentence:
You see we learn that on course as well, if you are out on your own and somebody comes and someone comes and sits with you and they just say, ‘I know you’. ‘No you don’t’. ‘Yeah I do’, ‘You’re such a name you, you’ve been in prison for a sex offence’. ‘How would you cope with it?’ So we’ve to learn how to cope with that, you know and we know what to do with that, you know what to do, get up and walk away.
Prisoner, p4.9
Medication and medical records
Older prisoners were generally appropriately provided with medication on release from prison although they were often unaware what was going to happen about their medication until a few days before release. The provision of medication on release was generally not a concern for older prisoners as they had accumulated their own supply, thought that they would be provided with sufficient medication on release and felt able to access a GP quickly on release from prison:
No. They make sure you’ve got enough meds [medication] to come out with. Got to reception on the day of release and the meds what I’d ordered, which was the inhalers, they were there waiting for me, no problem.
Ex-prisoner, p4.27
Some prisoners were provided with a letter to be given to their GP on release, which summarised their medical records and current medication. However, this was the case only in a minority of participating prisons:
I did have a letter for my doctor, yeah. I did give that to my doctor, yes.
Prisoner, p4.54
Theme 2: communication
Communication was a key issue for release planning. Prisoners perceived there to be a lack of communication from formal channels (such as from probation workers and prison officers). They described how they received the majority of their information about release informally from other prisoners.
Lack of information formally received
Interviewees were frustrated by the lack of formal information they received. For many this caused a great deal of distress. In particular, they lacked information about where they were going to be living after their release. Frequently, participants would not know where they were going to be residing after discharge until a few days before their release:
I think it’s abysmal quite frankly . . . well you know the main thing is you don’t know where you’re going to go for a start . . . So you can’t even start planning.
Prisoner, p4.28
The frustration over the lack of contact with probation workers in the community and offender managers inside prisons was described by participants. Prisoners often did not know the name of their assigned probation worker in the community. Face-to-face meetings were held very rarely and many prisoners specified that they had received only one letter from their probation worker, very close to their release date. This letter would often simply state which Probation Service-approved premises they would be living in and at what time to meet on their day of release. Prisoners also experienced numerous changes in their assigned probation worker during their sentence. The following prisoner describes how he had seen his probation worker only once on entry to prison and was anxious to meet with her again now that his release was imminent:
I’ve got some questions I want . . . I’ve only seen her [Probation Worker] once while I’ve been in [prison]. I’ve been here 2 years. I saw her when I first came in and that’s it, I’ve not seen her since.
Prisoner, p4.12
Information received from other prisoners
Prisoners relied on those who had previously been released and recalled to prison for information about the release process. In particular, they relied on such prisoners for information about the conditions in Probation Service-approved premises. As a result, participants were extremely anxious about the prospect of going to Probation Service-approved premises as they believed that they would be full of young people who used drugs and that other residents would not tolerate living with those convicted of sexual offences. However, in general, prisoners were fairly satisfied with the Probation Service-approved premises when they actually arrived there:
Yeah, you get information off the other inmates saying they’re [Probation Service-approved premises] rough and this, that and the other, and don’t do this and don’t do that. But when you get there it’s totally different. It’s totally different to what I expected. I expected it to be a right rough place and fighting and all coming in drunk and whatnot.
Ex-prisoner, p4.27
Many of the prisoners stated that they felt that it would be useful to hear what the resettlement process was like from the perspectives of other prisoners; in particular, they were keen to receive further information about Probation Service-approved premises. Some of the interviewees had written to their peers in prison once they had been released to provide them with information. Ex-prisoners had decided to take this action because they felt that they would have appreciated such support themselves:
There’s a lot that could help me. I’ve actually written into prison to a couple of my old mates that are inside explaining to them what is expected of them when they get on the out, where they have to go, what they have to do . . . and I think if somebody had done that to me I would have been a lot better equipped to face the outside world. I wasn’t very well equipped, I must admit.
Ex-prisoner, p4.54
Uncomplaining
The older prisoners stated that in general they did not make complaints to health care staff or prison officers. This was because they did not want to create problems and they did not believe that their complaint would result in an action being taken:
I’ve never had put in complaints or anything in here, never, I just . . . take every day as it comes, you know . . . There’s things I could complain about but what’s the point? . . . They don’t do much about it.
Prisoner, p4.26
Older prisoners accepted their situation and did not feel that they needed to challenge it or obtain answers to key questions of concern. This was even the case for important issues such as release dates or where they were going to live on release from prison:
Interviewer: Okay, so do you think you’ll worry when, when you do get out?
Prisoner: No . . . I’ll just take things as they come.
Prisoner, p4.20
The interviewees frequently referred to other individuals being in a worse situation than them:
I’ve got all my cups, plates, pots, pans, towels, everything. She’s [family member] got all sorts for me, you know, so I’m lucky in that sense, where some of these poor buggers don’t have anything, you know. Some don’t even get a letter or a visit. I feel sorry I do, I really do, so touch wood, at least there’s somebody always worse off than you isn’t there and that’s the way I look at it.
Prisoner, p4.9
The issue of independence was frequently referred to by participants. Many of the participants stressed that they did not want help or support and preferred to be as independent as possible:
Ideally I would like to be in my own house/flat but I will go along with it. I am an independent man.
Prisoner, p4.17
Theme 3: the impact of sexual offences on release
Several of the prisoners had been charged with sexual offences. They were not directly asked about their offences within this part of the current research project but would indirectly talk about their offences when discussing their plans for release. The impact of being charged with a sexual offence was highlighted when prisoners and ex-prisoners discussed their family conflicts or absence of family contact, their concerns about their physical safety, the restrictions placed on them for housing and employment and their inability to return to their home town.
Family conflict and absenteeism
Prisoners reluctantly discussed the conflict within their family and being ‘disowned’ by members of their family because of the sexual nature of their crime and the fact that family members were sometimes the victims:
Your family doesn’t want you. You know, they don’t want you near. There’s not so many families will take you back.
Prisoner, p4.9
A number of prisoners who had committed sexual offences did have one or two family members who were willing to support them on their release, with the proviso that they addressed their offending behaviour:
Well touch wood, touch wood, I’ve been, I got divorced, obviously my wife left me, wanted a divorce when I got done for this [committing a sexual offence] and that and I lost all my family, everything, not my family, I’ve lost all her family of her side, I’ve lost all my friends, I’ve still got a couple of friends who come to see me, who’s kept by me and everything and I’ve got my brothers and sisters who’s stood by me. They knew what happened, I told them the truth and they’ve said look we’ve always been a close family, blood’s thicker than water, we’re sticking by you, but you’re going to have to do something to help yourself.
Prisoner, p4.9
A number of prisoners and ex-prisoners did not want to make their families or friends feel uncomfortable and therefore chose not to contact them:
Well I’ve not spoken to any of my family, it’s my own choice, I was a bit too upset about all of that. I’ve not come to terms with that at all, because as I said I pleaded not guilty, I’m going to stay not guilty until I get something done about it, but with all this moving about at the moment I need to resettle somewhere where I can just say, right, I’ll not phone a solicitor up I’ll go and see him, because you’re better off speaking one to one than you are speaking over the phone, so that’s what I was thinking I might do.
Prisoner, p4.29
Physical safety
A number of the participants expressed concerns about their physical safety on their release from prison; however, in general, these concerns diminished once participants had been released into the community. Participants were largely appreciative of the police's efforts to reassure them of their safety on release from prison:
Well I’ve been told I’m going to [town], but as I, as I said to you last, yesterday was it, I’ve got concerns about my personal safety about going there, so I’m trying to get that changed.
Prisoner, p4.14
Well there there’s just, a little bit of over the top paranoia; I’ve come to realise that. I had, a couple of interviews with, the policemen who were on something to do with public protection. There was two policemen there and they were both very, very helpful . . . and assured me that, [local area] Police have really got misbehaviour well contained. And, another policeman came to see me . . . he’s another gentleman as well and he more or less gave me the same assurance and, I can I’ve walked into [town] with confidence. I don’t feel in danger of being attacked.
Ex-prisoner, p4.14
Theme 4: mental health needs
The older prisoners discussed their mental health and well-being prior to release and after discharge from prison. They described feelings of anxiety, depression, suicidal ideation, guilt and loneliness.
Apprehension and anxiety
Older prisoners described their apprehension about their release prior to discharge. The lack of information about where they would be living and therefore the lack of release planning created high levels of anxiety:
I told you I’m apprehensive . . . I don’t know what lies ahead and I’m not them type, I’ll always want to know what’s; and I like to plan my way ahead.
Prisoner, p4.11
The highest levels of anxiety were experienced prior to release; however, for a number of prisoners, this high level of anxiety was still present 4 weeks after their release. Those still experiencing anxiety 4 weeks after their release had difficulties readjusting to community life:
I said I’m just anxious, I’m just a bit frightened at the moment and a bit nervous and lonely.
Ex-prisoner, p4.9
Depression
Interviewees talked about their depression prior to committing their offences, experiencing depression in prison and their depression on release from prison. A number of the older prisoners considered their depression to have contributed to them committing their offences:
I was married for thirty-five years to one woman, five kids. She died of Huntington’s disease, right. A long time dying in hospital, then after that my eldest son about four months later, he committed suicide, because he lost his mum, we’re a close family and he loved her and everybody loved her . . . He committed suicide and all this was on my mind and I got a bit depressed, I got robbed, I got burgled, you know and robbed once . . . if that hadn’t have happened I’d have been still there and I’d have been still out, I wouldn’t have been in trouble, you know.
Prisoner, p4.12
Older prisoners also referred to their low mood while in prison:
I am up and down. The mornings are bad, I am very down in the morning. I have not spoken to anyone about it. I could talk to a nurse but I bottle things up. It’s my personality.
Prisoner, p4.62
Some of the participants perceived their depression to worsen on release from prison. Reasons for this included loneliness, a lack of information about future plans and boredom:
I felt low enough in there [prison] but because I was working and, and it wasn’t playing on my mind all the time . . . I was able to cope with it because all the time I’ve been in there I was working as a, a veg chef so I was working all the time. [Since release] I just sit and cry. I just sit and cry and once I get it out that’s it.
Ex-prisoner, p4.11
Self-harm and suicide
None of the participants included in this part of the current study stated that they were experiencing suicidal ideation once released; however, a number of participants expressed suicidal thoughts prior to discharge from prison. While being informed about the study, one participant stated that he was going to take his own life on release from prison. The researcher consequently opened an ACCT document. This participant (p4.1) stated that he had received no support prior to the opening of the ACCT:
Oh yeah they took a bit of notice of me then [after the researcher opened the ACCT document], and they said we're going to have to; I said I’ve been left alone, no one’s spoke to me, no one’s given me the time of day in any way, which is fair enough you know if someone’s just left there obviously there’s going to be problems isn’t there . . . I feel pleased, and I’m grateful for you because you’ve helped me so much because you spotted a problem that no one else did, if it weren’t for you I may not be here, you know that don’t you?
Prisoner, p4.1
Guilt
A minority of prisoners specified that they experienced feelings of guilt, which they struggled to deal with while in prison and after their release:
Well apart from, various matters of conscience related to my offence . . . I’ve been feeling okay. But sometimes I get ambushed by, you know, feelings I wish weren’t there. And, I’m sure they’re never going to go away. It’s something I’ve got to deal with, you know . . . It’s something I’ve got to deal with.
Ex-prisoner, p4.12
Loneliness
The concept of loneliness was a recurring theme throughout the interviews conducted in prison and in the community:
I still get . . . the feelings, I still get . . . them and I’m a bit lonely as well. Just a touch lonely sometimes when I’m on . . . my own.
Ex-prisoner, p4.9
‘Sanity’
When asked whether or not they required access to mental health services it became apparent that many of the older prisoners associated mental health services with sanity. For them, only those who were ‘insane’ or ‘mad’ would require mental health services. This has potential implications for older prisoners accessing support:
Interviewer: Do you feel you may require any mental health services when you are released?
Prisoner: No I’m all right I’m quite sane.
Prisoner, p4.27
Theme 5: social care needs
Older prisoners discussed the issue of accommodation, which was a key priority for them. They also highlighted their financial concerns that caused anxiety.
Accommodation
The lack of information about where prisoners would be residing on release caused them high levels of anxiety and frustration. This meant that they could not make any plans or emotionally prepare for their release:
Ex-prisoner: And then when they came they told me they had been to see me and they thought it was okay and then when the date of release was, they said this is where I was coming here [Probation Service-approved premises].
Interviewer: So you didn’t get confirmation of that until your day of release?
Ex-prisoner: Yes that’s right, because they don’t tell you until it’s time to go, they just say pack your things it’s you release date and that’s where we’re taking you to here.
Ex-prisoner, p4.29
A number of participants described how they became homeless on release from prison:
I ended up homeless, so I was put in emergency accommodation, er, and then the Council turned around and said, said well you, you are homeless but you’re homeless on your own volition sort of thing because you committed the offence so you made yourself homeless even though you had a, a secure accommodation as a victim.
Ex-prisoner, p4.11
Probation Service-approved premises, or ‘hostels’ as prisoners referred to them, were a frequent issue of concern for interviewees. The majority of participants (66%) were housed in such premises on their release from prison. Participants expressed concerns about the prospect of residing in Probation Service-approved premises. In particular, they were concerned about high levels of noise, sharing rooms with drug users and the potential for incidents of violence:
But it’s just the . . . hostel I’m concerned about, you know . . . Well they reckon it’s a terrible place, I don’t know, never been. You know, this is my first time in prison so . . . I wouldn’t know anything about that. But they say they’re [Probation Service-approved premises] not, not very good.
Prisoner, p4.26
I’m mixed with blooming smack-heads all day long, I don’t have any of that, I don’t do drugs.
Ex-prisoner, p4.1
Once they arrived at the approved premises, the participants generally found staff there to be helpful. They stated that staff members assisted them with housing applications, accessing a GP and emotional issues:
If you’re not sure of anything you can ask them [staff at Probation Service-approved premises] and they’ll put you right or they’ll go and get it for you or say ‘you need to go there’.
Ex-prisoner, p4.27
The town centre location of the majority of Probation Service-approved premises was considered to be convenient for accessing services such as health centres, banks and chemists. However, those with mobility difficulties expressed concerns about some Probation Service-approved premises that were located on hills:
Oh it was all right, it was all right, it wasn’t until I had got here [to Probation Service-approved premises] because it’s flat there [in prison] and as soon as I got out here on the hills my hips were burning like hell because it’s flat, it’s flat, oh I was in agony, the first week I was in agony walking around.
Ex-prisoner, p4.1
The Probation Service-approved premises were consistently compared to prisons. A number of prisoners stated that they would prefer to serve the whole of their sentence in prison rather than be released on licence to Probation Service-approved premises. The threat of recall to prison was unbearable for some older prisoners, to such an extent that they would prefer to remain in prison than live with the constant concern of being recalled:
Because I was 58, I’ve had my 59th, my 60th and it looks like I’m going to have my 61st in an institution [Probation Service-approved premises], I might as well have done all the time [in prison] as far as I’m concerned. You know, no one wants to be doing all that, I were only given 14 months so I could have done all the time and got the same as I’m getting now, so it makes no difference to me.
Prisoner, p4.1
There were examples of participants who had not been discharged into Probation Service-approved premises who were housed in inappropriate accommodation. One participant, who was awaiting a hip replacement, was unable to return home as a result of his licence conditions and was sleeping on a friend's couch for around 1 month. He stated that this sleeping arrangement caused him pain and that his probation worker was unwilling to help resolve the housing problem:
I slept on my friend’s sofa yeah . . . from the 13th until the 10th . . . [It was] bloody painful, embarrassing to say the least and she [probation worker] wouldn’t give a damn . . . ‘it’s not really my problem’, that’s what I got off that woman [probation worker].
Ex-prisoner, p4.5
One participant who used a wheelchair was placed in emergency accommodation on release. He was housed in a small house that had steps leading up to it. This meant that he was unable to enter or exit his home or use the kitchen or bathroom facilities independently. This caused him distress.
This house, it’s not equipped for me. I have a struggle getting everywhere, I can’t use the toilet because it’s too close to the wall. If you sit on the toilet your knees are up against the wall, there’s no safety rails round it . . . Getting in and out. It’s only narrow passageways. I have a job getting in and out. And I can’t get out there, out the front, I can’t get down them steps. If there was a fire in here I’d have to throw myself down them steps and probably break my other hip.
Ex-prisoner, p4.32
Finances
Finances were an area of considerable concern for older prisoners, particularly for those not being released into Probation Service-approved premises as they would be required to immediately start paying for items such as rent, telephone and electricity. In general, they felt that they lacked information and support to appropriately manage their finances on release from prison. A number of prisoners stated that they received information from a professional in prison about the reactivation of their pension credits on release from prison. Sometimes this information was received face-to-face and sometimes by letter. In a number of the prisons involved in the study, participants would be contacted about such matters prior to their release, and in some instances prisoners would have to put in an application to the relevant department for support with their finances. Frequently, prisoners were given a telephone number to call to activate their pension credits on the day that they were released from prison; however, they still experienced delays of up to 3 months in receiving their pension credit. Prisoners stressed how the reactivation of their pension credit on release from prison was considerably slower than the deactivation of their pension credit when they entered prison:
Before I went to prison I received my pension, I was saving for that, everything was under control. When I got to prison I got a letter off them – ‘Your pension’s stopped’, yeah okay obviously yeah it’s got to do, but it took me 2 months to get my pension back, now I’m released. So why all the trouble?
Ex-prisoner, p4.53
Many of the participants described how they were able to save money in prison in preparation for their release. They perceived this to be something only the older prisoners would have the foresight to do:
I don’t know what they will be doing to tell you the truth. When a prisoner leaves here with less than 50 pounds, alright when I leave here I have saved a bit of money since I have been here, I think I will be leaving here with about 400 pounds because I have not spent every penny like some clowns ha ha ha. Cos I came here [to prison] with just my wallet and a cheque card which is out of date so legally I will leave here with no money . . . That’s why I thought I better save some money, there is about 200 hundred in the bank, something like that, but at least it’s something more than a lot of these [other prisoners] will have.
Prisoner, p4.1
Older prisoners experienced difficulties with setting up bank accounts and accessing their bank accounts that had previously been created. None of the participants had experienced any support or advice in setting up a bank account while in prison. Some of the older prisoners experienced problems with adverse credit; others had difficulties because of a lack of formal identification documents:
So because I’ve got adverse credit they can’t give me a bank account because, because, I’m not creditworthy. And despite the fact they say ‘well look all I want is a standard bank account with a debit card on and with pin, pin and chip so I can go and pay my bills’. I said ‘I don’t want overdraft facilities’ . . . In fact you, you can set a, minimum credit balance I have to maintain all the time . . . But at the moment if I want to go shopping I have to go to a hole in the wall, take all my money out of my bank account that I’ve got in there, go and spend what I want to spend . . . And any money left I have to go back to the bank to pay it in.
Ex-prisoner, p4.16
Participants expressed concerns about insuring their home and car after release from prison. During pre-release courses, some participants had been informed about organisations willing to insure ex-offenders. Interviewees valued the provision of this information but were concerned about the high cost of insurance:
Now I’ve heard it’s [car insurance] like £1000, it could be £800, £900, you know, it’s a lot of money, it’s more than buying a car really, so there is that and I’ve only just found, somebody’s give me a name and I’ve looked at it and Unlock, it’s called Unlock and it’s an insurance company what’s set up for vulnerable prisoners and they work out an insurance what’s payable, affordable and everything, but on it there’ll be certain things you can’t claim for, what you could on a normal insurance, so there’s that to look into, ask how do I go about, can I have insurance and has it to be fully comp or third party when I ask the probation you know and see what she gives me the answer.
Prisoner, p4.9
Theme 6: physical health needs
Older prisoners described their physical health problems, which included heart conditions, breathing difficulties and mobility problems. None of the participants expressed concerns about registering with a GP.
Poor health
Older prisoners expressed concerns about their poor health; however, they did not seem to experience problems with accessing appropriate health care on release:
I am sick, I am part disabled long time now, first of all I was bad with asthma, go and come, go and come. After that I got arthritis, after that I become diabetic.
Prisoner, p4.57
GP registration
Participants felt able to easily register with a GP on release. Some expressed concerns about being unableto visit the GP they had previously been registered with (prior to incarceration) but in the main GP registration was not deemed problematic:
I have got a GP outside, but the thing is I won’t be living there, I don’t know if I will be in that area so that is the problem, so that’s the only thing I have got to contend with at the moment.
Prisoner, p4.1
Registering with a doctor will not be a problem.
Prisoner, P4.19
Theme 7: community
Older prisoners described how the ‘community’ outside of prison caused them anxiety. In particular, they discussed adjusting to an open environment, their appearance in the media and difficulties with socialising after release from prison.
Open environment
Many of the participants specified that they initially struggled with resettling into the community. In particular, they described difficulties acclimatising to being around lots of people and the speed at which people moved around and dealing with money:
The first week was pretty grotty. It took some getting used to, getting rid of the closed environment I was in, but once I was, you know, I’ve walked round town and the shops and things like that and once I got used to doing that amongst ordinary people again, yeah I’ve become a bit more relaxed . . . and we sort of get along and rub along, but once you lose those and you’re in the world on your own and you’re the offender, if you want, amongst ordinary people, you feel a little bit vulnerable at first.
Ex-prisoner, p4.54
Media
Appearing in the media (newspapers, television and radio) was a great concern for participants. Some had appeared in the local media and some in the national media. Participants who had committed a range of offences had appeared in the media, including those convicted of sexual offences and fraud. In some instances their appearance in the media led them to be concerned for their physical safety:
I have had no difficulties. My only concern is that my photo was in the paper. There was a headline saying ‘do not defraud the DWPs’ [Department for Work and Pensions]. Maybe they could have done this once but they did it seven times.
Prisoner, p4.10
When I was sentenced, it was front page news . . . It was on television and it was on the internet . . . Now that should explain everything . . . It was big in [local area], it wasn’t, it was just mentioned in the rest of England, south of England . . . My lawyer is in contact with [my probation worker] explaining to her that if they insist I go to [local area], and I am threatened, attacked, assaulted, harmed in any way, they will be held personally responsible.
Prisoner, p4.14
Socialising
Many older prisoners, particularly those convicted of sexual offences, explained that in general they did not socialise much on release and were often concerned about being rejected by their friends after discharge from prison:
No, I’m devoid of closeness with anybody now because of my offence and I don’t go and knock on people’s doors and say, ‘hello I’m back again, here I am, let’s have a cup of tea or a pint’. I don’t do that now because one, I don’t want to embarrass them telling me ‘no they don’t want to know me’ or embarrass myself by being rejected. So I leave it to chance and if I bump into people I will talk to them and be polite and see how they react . . . I’m frightened of some people’s reactions.
Ex-prisoner, p4.54
A number of the participants residing in Probation Service-approved premises stated that they had been advised by probation workers not to socialise with other individuals residing with them as they considered it to increase the possibility of reoffending. However, some of the older prisoners stated that they had made strong friendships with others living in the approved premises, which had supported them in their resettlement into the community:
Because we don’t know what people’s offences are in the hostel and the police and the hostel staff are quite definite about that, that you don’t hang around outside with people from the hostel because you don’t what they have, you know, what their crimes are and the, the hostel don’t want that sort of behaviour so, you know, if you meet them in the street you just sort of have an understanding that you, you don’t stop and talk.
Ex-prisoner, p4.6
A comparison of prisoners released to reside in Probation Service-approved premises and those released to other locations
Throughout the analysis it became apparent that there were distinct differences between those who were discharged to Probation Service-approved premises and those who were not. Table 33 displays illustrative quotes from a selection of participants who were released to reside in Probation Service-approved premises. The data illustrate participants' perspectives before and after release from prison. In general, participants who were released to Probation Service-approved premises were anxious about their release. However, when they were interviewed 4 weeks after release, they frequently reported that their immediate health and social care needs were largely well met. This contrasts with the data generated from participants who did not reside in Probation Service-approved premises immediately on release from prison. Illustrative quotes from these individuals are presented in Table 34. Such participants were more likely to perceive their health and social care needs to be unmet on release, even though they did not always anticipate that they would require support on release. Their unmet needs varied but included a lack of support with finances and employment and being inappropriately housed.
| Participant number | Prior to release from prison | After release from prison |
|---|---|---|
| p4.1 | ‘It's just I just don't know where I will be and everything like that . . . to an older one that's a big thing’ | ‘My needs have been met very well so far I would say, I'd honestly say they have been met well’ |
| p4.4 | ‘All I know is the last contact I had with him [probation worker] was for about 2 minutes. He came to the prison for a visit. He was supposed to be discussing my release plans, spoke to me for 2 minutes and left’ | ‘They've [Probation Service-approved premises staff] been very helpful, they've been very helpful, you know . . . they say if you've got a problem, go to them, I say well I would come to you anyway if I've got a problem’ |
| p4.14 | ‘Well I've been told I'm going to [town], but . . . I've got concerns about my personal safety about going there, so I'm trying to get that changed . . . Well I think, as I said yesterday, the standard response [from prison officers] is leave it with me, or I'll see what I can do and absolutely nothing is done at all’ | ‘As it turned out everything's alright . . . I had a couple of interviews with the policemen who were on something to do with public protection . . . they were both very, very helpful . . . and assured me that, they have really got misbehaviour well contained. I don't feel in danger of being attacked’ |
| p4.15 | ‘I'm a bit apprehensive and I mean, alright I'll go there [to Probation Service-approved premises] but I'd rather go to my lad [son's house]’ | ‘The staff [at Probation Service-approved premises] are okay . . . and everything is going fine . . . actually with, with the amenities around me . . . it's, it's alright’ |
| p4.22 | ‘Well to be honest, I don't really know, because as I say, I'm going to a hostel [Probation Service-approved premises]. I don't know what the hostel is. I'm apprehensive about the hostel’ | ‘Well, everything's worked out pretty well’ |
| Participant number | Prior to release from prison | After release from prison |
|---|---|---|
| p4.5 | ‘I'm not a liar but I'm not Al Capone, you know. I've been in prison once, you know, I'm not a habitual criminal, no, I can hack it and I know I can hack it, I don't need any help [on release] and that's not being belligerent’ | ‘I'm debating whether to have it [hip replacement] done or not . . . because there's no one there really to help me’ |
| p4.11 | ‘I am apprehensive. I don't know what's lies ahead and I'm not them type, I'll always want to know what's; and I like to plan my way ahead’ | ‘It's only emergency accommodation you only use it for emergency use only. So you don't put any furniture. I had no heating in there once, all I had was a little blow heater. I had no electric plug so I had to get them to do, put some plugs in there for my, my nebuliser. I feel like going outside and smacking a policeman or do something . . . Just to put me back inside’ |
| p4.19 | ‘Everywhere you go in here is a cul-de-sac . . . Nothing has been planned for my release end of’ | ‘There's nothing joined up, that's what I'm saying, the whole thing . . . Yes, I opened a bank account before I left prison . . . they sent me down to the bank . . . I phoned the bank they say they've sent all the stuff to prison. The prison haven't forwarded it to me, and I'm still stuck without a bank account’ |
| p4.20 | ‘I don't worry about it [release from prison]’ | ‘They have basically put [housed] me in this place, which is on the top floor where I can't get out in the wheelchair and there is no one to push me’ |
| p4.32 | ‘It [release from prison] can't come soon enough’ | ‘This house, it's not equipped for me. I have a struggle getting everywhere, I can't use the toilet because it's too close to the wall. If you sit on the toilet your knees are up against the wall, there's no safety rails round it’ |
Summary
In summary, planning for older prisoners' release was perceived to be inadequate by older prisoners. Indeed, the majority felt that their release had not been planned at all. A number of participants were unaware of where they were going to be living until a few days before their discharge from prison. This lack of information caused older prisoners high levels of anxiety prior to release and provided a key barrier for the older prisoner to plan his release. In particular, older prisoners were particularly anxious about the prospect of residing in Probation Service-approved premises. For those housed in Probation Service-approved premises, once they were released their anxiety levels were generally drastically reduced, largely as a result of having their key needs met. However, those residing in such locations considered themselves to be in a transitional period, not fully released into the community. Those who were not residing in Probation Service-approved premises had more unmet needs on release from prison.
The provision of pre-release courses was ad hoc and, when such courses were provided, information was not tailored to the needs of older prisoners. There was a perception that there had been minimal or no contact with probation workers and offender managers in preparation for release. Once released, older prisoners generally had appropriate access to a GP.
There appeared to be no real differences across types of prison in terms of release planning; it was perceived to be poor in all types of establishments. The majority of the participants who were not released into Probation Service-approved premises had been released from an open prison. Those who were not housed in Probation Service-approved premises were more likely to be concerned about financial matters. Those not released into Probation Service-approved premises who had social care needs were on occasion housed in inappropriate accommodation.
Chapter 7 Discussion
The overall aim of the study was to examine the health and social care needs and current service provision for older adults entering and leaving prison, and to evaluate a model for systematic needs assessment and care planning.
Current levels of service provision
The first part of this study aimed to establish current levels of service provision for older adults in prison across England and Wales. The Department of Health toolkit for good practice23 recommends that each prison should have an older prisoner policy, with a designated policy lead. This study found that only 56% of establishments had a written older prisoner policy. Previous research conducted by the Prison Reform Trust suggested that, when an older prisoner policy is in place, the needs of older prisoners have a higher profile within the prison system. 43 The lack of specific policies for older prisoners provides a possible explanation for why older prisoner service provision remains ad hoc across the prison estate. Consequently, findings from this study suggest that the development and effective implementation of an older prisoner policy at each establishment housing older males would be beneficial.
Since the last HMCIP report regarding older prisoners, there has been an increase in the number of designated leads for older prisoners within health care departments. 7 Within the current study, 88% of prisons had an OPL within their health care department compared with 38% in the latest HMCIP report in 2008. 7 However, only 36% of OPLs in the current study had received specific training to support them in this role, despite the Department of Health's recommendations that such training is essential. 23 Furthermore, although there was an increase in the number of assigned OPLs, there was a lack of evidence for the OPLs being active in their roles, despite this being a key theme of HMCIP's policy. 67 For example, only 35% of establishments had older prisoner/buddy schemes and only 53% had designated older adult clinics.
The integration of health and social care services
The first part of the current study also aimed to ascertain how well health and social care services were integrated and to identify facilitators of and barriers to effective integrative working. Only 33% of healthcare managers reported that there was a co-ordinated approach between their health care department and social services. This suggests that service provision for older prisoners is suboptimal and failing to meet the Department of Health's recommendation that there should be effective interagency co-operation between health care and social services. 26 Participants in the current study cited ambiguity concerning where responsibility for the social care of older prisoners lay as a key barrier to integrative working. This ambiguity, and the need for formal clarification of the responsibility of prisoners' social care needs, is well documented in the literature. 46,47 The current study has added to previous knowledge by illustrating that this ambiguity contributes to poor standards of social care for older prisoners.
Participants also referred to how the geographical organisation of social services accentuates the challenges of providing appropriate social care for older prisoners. This suggests that, where possible, it would be advantageous to locate older adults in prisons within the geographical area to which they will be released, to facilitate better co-ordination of their care. Furthermore, the development of local agreements between prisons and their local social services would assist in improving co-ordination of older prisoners' care. The findings of the current study further suggest that increased face-to-face networking between health and social care service staff would also improve co-ordinated care for this group.
The health and social care needs of older prisoners at prison entry
The second part of this study aimed to establish the unmet health and social care needs of older prisoners on entry to prison. We found that older prisoners have, on average, 2.74 unmet health and social care needs. A previous study conducted by Hayes et al. 4 on a cross-section of older prisoners found that they had, on average, two unmet needs. Our study focusing on reception only suggested that older prisoners have, on average, more unmet needs on entry to prison than at other stages of their sentence. Our findings further support the recommendation in the Department of Health toolkit23 that older prisoners' health and social care needs should be assessed appropriately on entry to prison. This is of particular importance because older prisoners have more complex health and social care needs than their younger counterparts and those of a similar age living in the community. 13
The current study found that 55% of participants had GDS-15 scores indicating symptoms of clinical depression on entry to prison, with 23% scoring in the range for severe depression. This was considerably higher than findings from a cross-sectional study by Hayes et al. 32 using the GDS, which found that 51% of older prisoners were showing symptoms of depression, with only 3% in the range for severe depression. Consequently, our findings suggest that symptoms of severe depression are more common on entry to prison than at other stages of the prison pathway. In addition, our findings illustrate that only 17% of participants showing symptoms of depression on prison entry were prescribed antidepressants within 4 weeks of entry into custody. These findings are similar to those of the cross-sectional study of Fazel et al. 6 conducted in 2004, which found that 14% of older prisoners presenting with depressive symptoms were prescribed antidepressants.
The development, implementation and evaluation of an intervention to identify and manage health, social and custodial needs of older people entering prison
The aim of the third part of the current study was to develop, pilot and evaluate an intervention for identifying the health and social care needs of older prisoners on reception into prison and ensuring that these are addressed systematically during older people's time in custody. This study successfully developed the OHSCAP through action learning with older prisoners, prison officers and health care staff. It was developed in line with the recommendations from the Department of Health's toolkit for good practice. 23 There is a dearth of research evaluating the use of older prisoner health and social care assessments. The OHSCAP was, however, perceived by both staff and prisoners to be acceptable, feasible and beneficial.
The Department of Health's toolkit emphasises the importance of regularly reviewing assessments and recommends that this should be conducted every 6 months. 23 During the piloting process the OHSCAP was reviewed as and when deemed appropriate by the prisoner and prison officer; however, making such decisions around flexible review intervals proved challenging. Consequently, training on case management may prove beneficial for prison officers administering and conducting the OHSCAP.
There is a need to effectively share the information collected from the OHSCAP among prison officers, offender managers and health care staff. This information was not adequately shared during the OHSCAP piloting process. The findings from this research suggest that it would be useful for the OPL to scan a copy of the OHSCAP onto SystmOne, write a summary of the key points from the OHSCAP onto C-NOMIS and provide a copy of the OHSCAP to the older prisoner. The Department of Health toolkit specifies that the older person should hold a copy of their own care plan. 23 However, older prisoners in the current study were reluctant to accept a copy of their OHSCAP. The reasons for this require further exploration.
Within the current study, both older prisoners and staff members stated that older prisoners normally avoid complaining. This finding is in line with the 2004 HMIP review,19 which found that older prisoners generally posed minimal problems for staff and, as a result, their own problems were often neglected. The OHSCAP proved a useful tool for supporting older prisoners who have complex health and social care needs and are unlikely to otherwise raise their concerns.
The action-learning approach taken to develop and implement the OHSCAP proved useful. To date, action learning has not been widely used in prison research; the involvement of prisoners in such an approach is particularly lacking. However, when it has been used, action learning has been proven to be an effective method for service and practice development in prisons, where there can be considerable resistance to change. 68,69
The health and social care needs of older prisoners discharged from prison into the community
The fourth part of the current study aimed to explore the health and social care needs of older male adults discharged from prison into the community. In the main, older prisoners perceived there to have been no planning for their release prior to their discharge from prison. This suggests that recommendations to assess the resettlement needs of prisoners on prison entry70 and to accurately assess and provide for older prisoners' needs on release7 are currently largely unmet. Those who are to be released to Probation Service-approved premises are often particularly anxious about this prior to their release; however, once they arrive there they generally have their health and social care needs fairly well met. Those who return home or who are housed in emergency accommodation were less likely to have their health and social care needs met on release.
In accordance with previous research conducted by Crawley,38 the current study found that the lack of information received by prisoners in preparation for their release caused high levels of anxiety. Many reported minimal or no contact from probation workers or offender managers. Crawley and Sparks37 had previously highlighted the need for more effective proactive communication with older prisoners to reduce severe feelings of anxiety leading up to their release; however, such improvements do not appear to have been made.
Pre-release courses are one means of providing information to older prisoners prior to discharge. Within the current study, a pre-release course was reportedly provided at only one of the nine establishments involved, and not all participants residing in that establishment were aware of the existence of the course. Additionally, the pre-release course identified was not designed with older prisoners' needs in mind. Consequently, it appears that establishments are currently largely failing to adhere to the Department of Health's23 recommendation to provide older prisoners with pre-release courses that are tailored to their needs.
Methodological strengths and limitations
Within this study, 60 years was used as the lower cut-off age for older prisoners. For a number of reasons, since this study began, there has been a shift towards using 50 years as the minimum age for defining older prisoners. Collins and Bird71 found similar rates of illness in male and female prisoners aged ≥ 50 years as in those in the community who were aged ≥ 60 years. Furthermore, Hayes et al.,4 investigating the physical, mental and social care needs of older male prisoners in England, found similarities in health needs in those aged 50–59 years and those aged ≥ 60 years. Much prison-based literature suggests that 50 years is an appropriate cut-off by which to delineate older prisoners, as lifestyle choices common among offenders, including substance misuse, risky sexual behaviour and a lack of preventative health care, have also been shown to accelerate ageing. 10,72 Prison-related factors, including the stress of prison life, increased anxiety, isolation and separation from family and friends, the threat of victimisation and the prospect of living one's life in detention, may also be associated with lower life expectancy and premature ageing. 72
Thus, current evidence suggests that adopting a cut-off age of 50 years is most appropriate when designing services for this group and this is reflected in the fact that, at the time of writing, both in the USA and the UK, the most frequently used cut-off age for defining ‘older’ prisoners is 50 or 55 years. 73 However, when the current study commenced in 2009 the age of 60 years was the most commonly applied minimum age used to define older prisoners in forensic mental health literature74 and this was reflected in our study. Fifty years should therefore be used as the minimum cut-off age for older prisoner studies in the future. This study did not include women because of the low number of female prisoners aged ≥ 60 years in England and Wales.
The questionnaire was a national survey distributed to all establishments housing adult males in England and Wales and achieved an 80% response rate. The main reason for this favourable response rate was the comprehensive follow-up strategy that was employed, involving telephone calls, letters and emails. Good response rates were received for all types of prisons. Furthermore, there was no difference in response rate between private and public prisons. Interviews were conducted with staff regarding the levels of integration between health and social care services. Staff from eight prisons undertaking various professional roles were interviewed. We selected prisons that reported particular successes or challenges in integrating health and social care services to ascertain a range of barriers and facilitators. We did, however, experience considerable difficulties in identifying social care workers to interview within the selected prisons, reflecting the relative shortage of this profession within establishments.
The research study involved interviewing 100 older prisoners on entry to prison. Local prisons were selected that were within reasonable geographical reach of the research base. The findings suggest that the sample was not dissimilar to national statistics in relation to offences. In total, 95% of the sample were White British; this is similar to the 92% of white British prisoners aged ≥ 60 years in England and Wales (NOMS, 2012, personal communication). Audits of health care records took place on entry into prison. This aspect of the study was reliant on accurate records being made by health care staff and the quality and availability of such information was found to vary across establishments.
It would have been beneficial to compare findings from those who received the OHSCAP with findings from those who had received treatment as usual. However, only a small number of older prisoners entered the prison where the OHSCAP was piloted and this proved not to be possible. The data obtained from participants who received the OHSCAP can, however, be used to inform and power a future randomised controlled trial to assess the effectiveness of the OHSCAP in reducing older prisoners' unmet health and social care needs. Furthermore, the qualitative data obtained have illustrated the feasibility of delivering the OHSCAP as part of the prison regime, and its acceptability to both prisoners and staff.
Action learning provided a successful means of developing and implementing the OHSCAP within the prison environment. There were, however, some challenges to overcome when adopting such an approach. The involvement of health care and senior staff reduced as time elapsed. This was not, however, detrimental to the development or implementation of the OHSCAP. It is possible that a lack of senior staff involvement in the groups actually allowed other members to speak freely. Furthermore, senior staff were very supportive of the implementation of the OHSCAP and were instrumental in establishing the action-learning groups. We do not have any evidence for the reasons behind the reduction in health care staff involvement and therefore speculation would be inappropriate.
Semistructured interviews were conducted with older prisoners released from prison into the community. We successfully followed up 73% of participants in the community. This was a far higher proportion than anticipated initially and was largely because the majority of older prisoners were assigned a probation worker in the community who could facilitate the follow-up interview. The interviews were conducted approximately 4 weeks after discharge, when the majority of participants were residing in Probation Service-approved premises. Additional follow-up interviews would provide an understanding of how well older prisoners' health and social care needs are met once they are residing in private premises, without the close links to services that are present in Probation Service-approved premises.
Chapter 8 Conclusion
The number of OPLs in health care departments has increased in recent years but they do not all appear to be fully active in their roles in tailoring and improving services for older prisoners. Furthermore, 44% of establishments do not have a specific policy to ensure that older prisoners' needs are considered throughout the prisoner pathway. There is a lack of integration between health and social care services because of ambiguity regarding the responsibility for older prisoners' social care. Furthermore, the geographical organisation of social services can result in the responsible social service being located a considerable distance from where prisoners are being held. In such instances, local social services do notco-ordinate their care. Older prisoners have on average 2.74 unmet health and social care needs on entry to prison. The most frequent unmet need was in relation to the provision of information about their care and treatment. The OHSCAP has provided a feasible and acceptable means of identifying and systematically addressing older prisoners' health and social care needs. Release planning for older prisoners was frequently non-existent. Those who did not reside in Probation Service-approved premises immediately on release from prison often had unmet health and social care needs.
Implications for the management of policy and practice
The evidence from the current study suggests the following:
-
Fundamental adaptations to prison buildings are still required to allow older prisoners with mobility difficulties physical access to services and facilities fully in accordance with the Equality Act 2010.
-
There has been an increase in the number of assigned OPLs in health care departments; however, they are still not present in all establishments and a large proportion are not active in their roles. Each prison should identify an OPL within their health care department who should lead on the development of specialist services such as older prisoner/buddy schemes and designated older adult clinics.
-
A large proportion of establishments are failing to adhere to the Department of Health's recommendation23 that they should have an older prisoner policy in place. Each establishment should develop such a policy.
-
Establishments and their partners are, in the main, failing to meet the Department of Health's recommendation23 that there should be effective interagency co-operation between health care and social services. An identified social care lead may well assist with these difficulties and help to actively support and address older prisoners' social care needs.
-
The ambiguity regarding the responsibility of social care for older prisoners requires clarification to improve integrative working.
-
An increase in face-to-face networking opportunities would improve effective integrative working between health and social care staff.
-
It would be beneficial to house older prisoners in close proximity to their planned location on release from prison to improve the co-ordination of their care.
-
Comprehensive local agreements between prisons and social services should ensure that local social services effectively co-ordinate care for all prisoners.
-
The Department of Health's recommendation23 to provide an older person with a specific health and social care assessment on entry is largely unmet. Evidence suggests that such specialised assessments are required because older prisoners have more complex health and social care needs than their younger counterparts and those of a similar age living in the community.
-
The OHSCAP is feasible, acceptable and of value to older prisoners and staff. Furthermore, it has been developed with service user input through action learning.
-
It would be beneficial for OPLs to receive training in the use of the OHSCAP and case management.
-
Release planning for older prisoners requires improvement. There was no evidence to suggest that Nacro's recommendation26 to start planning for prisoners' release from prison entry was being met. Furthermore, HMCIP's recommendations7 around involving older prisoners and health care, social care and prison staff in the release planning process were generally not adhered to, causing high levels of anxiety for older prisoners.
-
The Department of Health's recommendation23 that prisons provide pre-release courses specifically designed for older prisoners was not adhered to. Each establishment should regularly provide such courses.
Recommendations for further research
-
The effectiveness of the OHSCAP in reducing older prisoners' unmet health and social care needs should be evaluated using a randomised controlled trial design. Studies should evaluate its effectiveness at prison entry, throughout custody and on release into the community and include investigation of the longer-term outcomes of the OHSCAP.
-
Future evaluations of the OHSCAP should include a review of assessments and care plans to ascertain the precise processes involved and the quality of care plans produced.
-
Methods of effectively sharing the information obtained using the OHSCAP should be explored.
-
Appropriate social care services for older prisoners should be modelled, commissioned and evaluated to ascertain their effectiveness in appropriately caring for older prisoners.
-
The delays that older prisoners experienced in receiving their medication on entry into prison should be further investigated.
-
Future prison health research should attempt to involve all relevant groups, including older prisoners, when appropriate.
-
In-depth qualitative interviews with professionals involved in planning older prisoners' release would help to ascertain the challengers to and enablers of effective release planning for older prisoners.
-
In-depth qualitative interviews with older prisoners after they leave Probation Service-approved premises were beyond the scope of this research. Such work would help to ascertain whether or not they receive appropriate health and social care services when access to services may be reduced.
Acknowledgements
We would like to thank all of the staff and prisoners who participated in this research and assisted in its organisation. Their contribution was highly valuable and we are very grateful to them for giving up their time to be involved.
Contribution of authors
| Author | Job title | Area of speciality | Role |
|---|---|---|---|
| Dr Jane Senior | Research Fellow | Prison mental health care and nursing | Conception and design, drafting report and supervision |
| Ms Katrina Forsyth | Research Assistant | Research methodology | Data collection, data analysis and drafting report |
| Dr Elizabeth Walsh | Senior Lecturer in Offender Health | Offender prison health and clinical supervision | Conception and design, data collection, data analysis and drafting report |
| Ms Kate O'Hara | Research Assistant | Forensic psychology | Data collection, data analysis and drafting report |
| Ms Caroline Stevenson | Research Assistant | Forensic psychology | Data collection and revision of report |
| Dr Adrian Hayes | Researcher | Offender health | Conception and design and revision of report |
| Ms Vicky Short | Research Assistant | Offender health | Data collection and revision of report |
| Dr Roger Webb | Senior Research Fellow | Psychiatric epidemiology | Interpretation of data and revision of report |
| Professor David Challis | Professor of Community Care Research | Community care research and Director of Personal Social Services Research Unit | Conception and design and revision of report |
| Dr Seena Fazel | Clinical Senior Lecturer in Forensic Psychiatry and Honorary Consultant Forensic Psychiatrist | Forensic psychiatry | Conception and design and revision of report |
| Professor Alistair Burns | Professor of Forensic Psychiatry and Deputy Dean (Clinical Affairs) | Older people's mental health | Conception and design and revision of report |
| Professor Jenny Shaw | Professor of Forensic Psychiatry | Forensic psychiatry offender health | Principal investigator, conception and design, revision of report and supervision |
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
The views expressed in this publication are those of the authors and not necessarily those of the PHR programme or the Department of Health.
References
- Williams J. Fifty – the new sixty? The health and social care of older prisoners. Qual Ageing 2010;11:16-24. http://dx.doi.org/10.5042/qiaoa.2010.0525.
- Kakoullis A, Le Mesurier N, Kingston P. The mental health of older prisoners. Int Psychogeriatr 2010;22:693-701. http://dx.doi.org/10.1017/S1041610210000359.
- Kingston P, Le Mesurier N, Yorston G, Wardle S, Heath L. Psychiatric morbidity in older prisoners: unrecognized and undertreated. Int Psychogeriatr 2011;1:1-7.
- Hayes A, Burns A, Turnbull P, Shaw J. The health and social needs of older male prisoners. Int J Geriatr Psychiatry 2012;27:1155-62. http://dx.doi.org/10.1002/gps.3761.
- Fazel S, Hope T, O’Donnell I, Jacoby R. Hidden psychiatric morbidity in elderly prisoners. Br J Psychiatry 2001;179:535-9. http://dx.doi.org/10.1192/bjp.179.6.535.
- Fazel S, Hope T, O’Donnell I, Jacoby R. Unmet treatment needs of older prisoners: a primary care survey. Age Ageing 2004;4:396-8. http://dx.doi.org/10.1093/ageing/afh113.
- Older prisoners in England and Wales: a follow-up to the 2004 thematic review. London: HM Inspectorate of Prisons; 2008.
- Gallagher EM. Elders in prison: health and well-being of older inmates. Int J Law Psychiatry 2001;24:325-33. http://dx.doi.org/10.1016/S0160-2527(00)00080-7.
- Loeb S, AbuDagga A. Health-related research on older inmates: an integrative review. Res Nurs Health 2006;29:556-65. http://dx.doi.org/10.1002/nur.20177.
- Williams JL, Edwards T. The aging inmate population: Southern states outlook. Alabama: Council of State Governments Southern Legislative; 2006.
- Howse K. Growing old in prison. A scoping study on older prisoners. London: Prison Reform Trust; 2003.
- Wheeler M, Connelly M, Wheeler B. Aging prison populations: directions for Oklahoma. J Okla Crim Just Res Consortium 1995;2:72-9.
- Fazel S, Hope T, O’Donnell I, Piper M, Jacoby R. Health of elderly male prisoners: worse than the general population, worse than younger prisoners. Age Ageing 2001;30:403-7. http://dx.doi.org/10.1093/ageing/30.5.403.
- Uzoaba J. Managing older offenders: where do we stand?. Ottawa, ON: Correctional Services of Canada; 1998.
- Mitka M. Aging prisoners stressing health care system. J Am Med Assoc 2004;292:423-4. http://dx.doi.org/10.1001/jama.292.4.423.
- Old behind bars. The aging prison population in the United States. New York: Human Rights Watch; 2012.
- Dubler NN. The collision of confinement and care: end of life care in prisons and jails. J Law Med Ethics 1998;26:149-56. http://dx.doi.org/10.1111/j.1748-720X.1998.tb01670.x.
- Ornduff JS. Releasing the elderly inmate: a solution to prison overcrowding. Elder Law J 1996;4:173-200.
- No problems – old and quiet: older prisoners in England and Wales. A thematic review by HM Chief Inspector of Prisons. London: HMIP; 2004.
- Prison Service Order (PSO) 2855. Prisoners with disabilities. London: HMPS; 2008.
- The future organisation of prison health care. London: Department of Health; 1999.
- National service framework for older people. London: Department of Health; 2001.
- A pathway to care for older offenders. A toolkit for good practice. London: Department of Health; 2007.
- Grubin D, Carson D, Parsons S. Report on new reception health screening arrangements: the result of a pilot study in 10 prisons. Newcastle: University of Newcastle; 2002.
- Birmingham L, Mason D, Grubin D. Health screening at first reception into prison. J Forensic Psychiatr 1997;8:435-9. http://dx.doi.org/10.1080/09585189708412022.
- A resource pack for working with older prisoners. London: Nacro; 2009.
- Fazel S, Baillargeon J. The health of prisoners. Lancet 2011;377:956-65. http://dx.doi.org/10.1016/S0140-6736(10)61053-7.
- Loeb S, Steffensmeier D. Older male prisoners: health status, self-efficacy beliefs, and health-promoting behaviors. J Correct Health Care 2006;12:269-78. http://dx.doi.org/10.1177/1078345806296031.
- Bond GD, Thompson LA, Malloy DM. Lifespan differences in the social networks of prison inmates. Int J Aging Hum Dev 2005;61:161-78. http://dx.doi.org/10.2190/7H5P-2AHJ-L34Q-GW9U.
- Colsher P, Wallace R, Loeffelholz P, Sales M. Health status of older male prisoners – a comprehensive survey. Am J Public Health 1992;82:881-4. http://dx.doi.org/10.2105/AJPH.82.6.881.
- Arndt S, Turvey C, Flaum M. Older offenders, substance abuse, and treatment. Am J Geriatr Psychiatry 2002;10:733-9.
- Hayes AJ, Burns A, Shaw J. Health, social and custodial needs of older men in prison. Manchester: University of Manchester; 2010.
- Frazer L. Ageing inside. Bristol: University of Bristol, School for Policy Studies; 2003.
- Shaw J, Appleby L. A national study of self-inflicted deaths in prison Custody in England and Wales from 1999 to 2007. Manchester: University of Manchester; 2011.
- Crawley E. Surviving the prison experience? Imprisonment and elderly men. Prison Serv J 2005;160:3-8.
- Williamson M. Improving the health and social outcomes of people recently released from prisons in the UK: a perspective from primary care. London: Sainsbury Centre for Mental Health; 2006.
- Crawley E, Sparks R. Is there life after imprisonment? How elderly men talk about imprisonment and release. Criminol Crim Justice 2006;6:63-82. http://dx.doi.org/10.1177/1748895806060667.
- Crawley E. Release and resettlement: the perspectives of older prisoners. Crim Justice Matters 2004;56:32-3. http://dx.doi.org/10.1080/09627250408552945.
- Davies M. The reintegration of elderly prisoners: an exploration of services provided in England and Wales. Internet J Criminol 2012:2045-673.
- Pratt D, Appleby L, Piper N, Webb R, Shaw J. Suicide in recently released prisoners: a case–control study. Psychol Med 2010;40:827-35. http://dx.doi.org/10.1017/S0033291709991048.
- Clarkson P, Abendstern M, Stutcliffe C, Hughes J, Challis D. Reliability of needs assessment in the community care of older people: impact of the single assessment process in England. J Public Health 2009;31:521-9. http://dx.doi.org/10.1093/pubmed/fdp035.
- Abendstern M, Clarkson P. A systematic evaluation of the development and impact of the single assessment process in England. Manchester: University of Manchester, Personal Social Services Research Unit; 2008.
- Cooney F, Braggins J. Good practice with older people in prison – the views of prison staff. London: Prison Reform Trust; 2010.
- Doing time: the experiences and needs of older people in prison. London: Prison Reform Trust; 2008.
- Humphries R, Curry N. Integrating health and social care. London: The King's Fund; 2011.
- Law Commission . Adult Social Care Consultation Analysis 2011. http://lawcommission.justice.gov.uk/docs/ASC_Consultation_Analysis_full-version.pdf (accessed March 2013).
- White Paper: caring for our future; reforming care and support. London: Department of Health; 2012.
- Glaser B. The constant comparison method of qualitative analysis. Soc Probl 1965;12:436-45. http://dx.doi.org/10.2307/798843.
- Leech NL, Onwuegbuzie AJ. Beyond constant comparison qualitative data analysis: using NVivo. School Psychol Q 2011;26:70-84. http://dx.doi.org/10.1037/a0022711.
- Boeije H. A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Qual Quant 2002;36:391-409. http://dx.doi.org/10.1023/A:1020909529486.
- Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. London: Sage Publications; 2006.
- Thomas S, Harty M, Parrott J, McCrone P, Slade M, Thornicroft G. The Forensic CAN (CANFOR). A needs assessment for forensic mental health service users. London: Gaskell; 2003.
- Sheikh R, Yesavage J. Geriatric Depression Scale (GDS). Recent evidence and development of a shorter version. Clin Gerontol 1986;5:165-73. http://dx.doi.org/10.1300/J018v05n01_09.
- Overall J, Gorham D. The Brief Psychiatric Rating Scale. Psychol Rep 1962;10:799-812. http://dx.doi.org/10.2466/pr0.1962.10.3.799.
- Challis D, Stewart K, Sturdy D, Worden A. UK long term care resident assessment instrument user's manual, MDS/RAI UK. York: InterRAI UK; 2000.
- British national formulary. BMA and RPS; 2012.
- Sanders J, Waterman H. Using action research to improve and understand professional practice. Work Base Learn Prim Care 2005;3:294-30.
- Bucknall T, Kent B, Manley K, Manley K, McCormack B, Wilson V. International practice development in nursing and healthcare. Oxford: Blackwell; 2008.
- McGill I, Brockbank A. The action learning handbook. London: Routledge Falmer; 2004.
- Walsh E, Dilworth S, Freshwater D. Establishing clinical supervision in prison health care settings: phase three. Bournemouth: Department of Health; 2007.
- Walsh E, Freshwater D. The mental health awareness of prison staff in England and Wales. J Correct Healthcare 2009;15:302-9. http://dx.doi.org/10.1177/1078345809341532.
- Walsh E, Freshwater D. The mental wellbeing of prison nurses in England and Wales. J Res Nurs 2009;14:553-64. http://dx.doi.org/10.1177/1744987109346762.
- Walsh E. Partnership work with health professionals in segregation units. Prison Serv J 2009;181:34-6.
- Powell J, Robison J, Roberts H, Thomas G. The single assessment process in primary care: older people's accounts of the process. Br J Soc Work 2007;37:1043-58. http://dx.doi.org/10.1093/bjsw/bcl032.
- Dickinson A. Implementing the single assessment process: opportunities and challenges. J Interprof Care 2006;20:365-79. http://dx.doi.org/10.1080/13561820600807270.
- Shaw J, Senior J, Hayes AJ, Davies L, Appleby L. Evaluation of the Care of At Risk Prisoners Project. Manchester: University of Manchester; 2006.
- Prison Service Order 3050: continuity of health care for prisoners. London: HMPS; 2006.
- Freshwater D, Cahill J, Walsh E, Muncey T, Esterhuizen P. Art and science in health care research: pushing at open doors or locked in institutions?. Qual Health Res 2012;22:1-8. http://dx.doi.org/10.1177/1049732312449206.
- Bennett C, Perry J, Lapworth T, Davies J, Preece V. Supporting prison nurses: an action research approach to education. Br J Nurs 2010;19:782-6.
- Integrated resettlement: putting the pieces together. London: Nacro; 2005.
- Collins D, Bird R. The penitentiary visit – a new role for geriatricians?. Age Ageing 2007;1:11-3.
- Anno BJ. Correctional health care: addressing the needs of elderly, chronically ill, and terminally ill inmates. Washington, DC: National Institute of Corrections; 2004.
- Wahidin A, Aday R. The needs of older men and women in the criminal justice system: an international perspective. Prison Serv J 2005;160:13-2.
- Fazel S, Jacoby R, Jacoby R, Oppenheimer C. Psychiatry in the elderly. Oxford: Oxford University Press; 2002.
Appendix 1 Project protocol
Aims/Objectives
This programme of research aims to establish the efficacy of services for older people entering and leaving prison, and to explore how a targeted intervention can improve pathways to care at key transitional times.
The specific objectives of the proposed project are:
-
To explore the lived experience and needs of older people entering and leaving prison;
-
To describe current provision of services, including integration between health and social services, and;
-
To pilot and evaluate a mechanism for identifying heath and social care needs on reception into prison, ensuring these are systematically addressed during older people's time in custody.
Background
Population
Prisoners aged 60 and over are the fastest-growing age group in the England and Wales prison estate, their numbers having trebled over the last decade. On the 30th June 2009 there were 2538 prisoners in England and Wales aged 60 and over and, with movement towards longer sentencing and higher rates of conviction for historical offences, numbers have been projected to rise even further (Department of Health (DoH), 2007; Prison Reform Trust, 2010). It has been estimated that the cost of keeping older people in custody is six times higher than for younger prisoners (unpublished internal report, HMP Wymott), largely due to the poorer physical health of older prisoners, with, for example, an increased need to transfer prisoners to hospital for emergency treatment.
Needs in Prison
Older prisoners have been described as suffering from ‘institutional neglect’ (Hayes & Fazel, 2008), according to DoH definitions (Home Office & DoH, 2000). A study of 203 sentenced men aged over 60 showed elevated levels of physical and mental illness (particularly chronic diseases), with rates of depression five times higher than either younger prisoners or older adults in the community (Fazelet al, 2001a,b). The most common chronic conditions were psychiatric (45%), cardiovascular (35%) and musculoskeletal (24%) disorders. Suicide rates in older prisoners are five times those of the age-matched general population (Fazelet al, 2005). Results from a PhD conducted by one of the applicants (Hayes, 2008) show that 38% of older prisoners have unmet physical health needs according to the CANFOR-S (Thomaset al, 2003), compared to 17% in a random prison sample (Senioret al, 2007). Similarly, a minority of those with mental health problems receive appropriate medication; Fazelet al(2004) found that only 18 percent of older prisoners with diagnosed depression were prescribed antidepressant medication. HM Inspectorate of Prisons (2004) noted that prison mental health services are geared towards younger people, with little access to specialist geriatric or old age psychiatry services (Collins & Bird, 2007).
Social care needs of older offenders have not been systematically assessed to date, but data from HMP Wymott showed that 29% of older prisoners had some daily living skills needs, most commonly mobility, and keeping their cell clean (Hayes, 2008). Sixty percent were rated as being at risk of exploitation, abuse or manipulation from other, more able, prisoners. Furthermore, 60% had a problem with social interaction, and 74% had a need for established daily routines.
Several high-profile policy and guidance documents are directly applicable to older prisoners, (e.g. HM Inspectorate of Prisons Thematic Review (2004); DoH Pathway to Care for Older Offenders (2007), NHS National Service Frameworks (DoH, 2001) and the Disability Discrimination Act (2004)). A review of individual Prison Inspectorate reports (Hayes, 2008) shows little evidence to suggest that they have been implemented.
Entry to Prison
The DoH (2007) Pathway to Care for Older Offenders emphasised the importance of comprehensive and systematic identification of the needs of older prisoners on entry into custody. Currently, the provision of health care services in prison relies heavily on information elicited by a screening instrument on reception (Grubinet al, 2002). However, there are no specific questions for older adults, for example relating to memory, cognition or level of independence with daily living skills. Previous studies have shown that if health problems are not elicited at reception, they are unlikely to be detected later (Birminghamet al, 1997). Therefore it is highly unlikely that a subsequent assessment of these age specific needs will be conducted routinely later during the custody period.
DoH (2007) stated that needs assessments for older people in prison should include physical and mental health, mobility and activities of daily living, as well as medication management. The document also stated that such assessments should be carried out when prisoners reach the age of 60, and be reviewed at minimum every six months. Although not specifically mentioned, it is logical that this should also apply to all people who are over 60 when they first enter prison.
Pathways to Care for Older Offenders (DoH, 2007) emphasised the requirement for older prisoners to receive the same range and quality of health care services as are available in the community. However, no specific references were made to a recent policy to improve and standardise needs assessment for older people in the wider community, introduced in the National Service Framework for Older People (DoH, 2001). The Single Assessment Process (SAP) was developed following criticisms of the content of assessments of health and social care need for older people, particularly on entry to institutional care (e.g. Stewartet al, 1999). SAP aimed to operationalise the promotion of person-centred care by formalising an assessment integrating different professional groups across a variety of settings. The SAP was fully implemented in 2004 and comprised assessment of the following areas: users' perspectives; clinical background; disease prevention; personal care and physical wellbeing; senses; mental health; relationships; safety; and immediate environment and resources. A national evaluation of SAP has been undertaken involving one of the applicants (DC).
This approach to needs assessment has clear benefits for older prisoners where no comprehensive or specialist assessment is currently in place. However, it is important to consider issues beyond assessment, including how services will be offered on the basis of identified need. The intervention will also need to be tailored to prisoners in view of the differences in needs between prisoners and older people in the general population and the nature of the prison environment.
Exit from Prison
Discharge from psychiatric hospital is associated with both an exacerbation of symptoms and an increased risk of suicide (e.g. Farhallet al, 2003; Applebyet al, 1999). Prattet al(2006) showed that recently released prisoners were at significantly increased risk of suicide after release, and older offenders had a higher relative risk in relation to younger offenders for completing suicide within twelve months of release. International studies have highlighted similar concerns (e.g. Binswangeret al, 2007; Kariminiaet al, 2007).
Almost all prisoners will leave custody in their lifetime. Contact with family and friends, and finding employment or permanent accommodation have been cited by younger prisoners as their priorities upon release with these issues taking precedence over establishing contact with community mental health services (Senioret al, 2005; Shaw & Thornicroft, 2007).
Many older people leaving custody will need to re-engage with health and social care services for treatment of chronic illnesses, and most will not be expected to work after discharge and will need to establish their entitlement to state pension and other benefits. In addition, those identified as being a continued risk to others may need to relocate and begin their lives in a new area. However, currently prisoners with health problems are often released without any attempt to provide continuity of care (Nacro, 2005).
To date, there has been little research on problems faced by older prisoners on release from prison. Two UK qualitative studies have focussed on older prisoners' fears for release but did not follow these people into the community to establish the problems actually experienced: Parrish (2003) described perceptions of helplessness with regard to accessing community health services. In Crawley and Sparks (2006), many older prisoners described having lost their home and possessions whilst in custody, having limited assistance from probation services before release, and being forced to live in hostels with young people perceived to be dangerous drug addicts. Older people, particularly those convicted of sexual offences, felt at risk from these younger offenders, and also from people in their neighbourhoods.
Frazer (2003) interviewed staff working with older prisoners, and reported difficulties in resettlement. Staff noted a ‘significant strategic gap in this area’ [p68], and felt many elderly offenders did not have their needs met by current service provision.
HM Inspectorate of Prisons' thematic review of older prisoners (HMIP, 2004) featured heavy criticism of resettlement and reintegration. They surveyed 442 men aged 60 and over, noting that 28% would be at least aged 70 on release. Resettlement services provided by prisons were strongly geared towards younger offenders with no evidence that consideration had been given to issues surrounding retirement, management of chronic illness, or social isolation. Few prisoners knew who to contact for their resettlement needs, including claiming benefits, finding accommodation or continuity of health care on release.
Thus, the limited evidence available suggests complex needs for older people leaving prison, but which are largely unmet. However, the lack of research into the experiences of recently-released prisoners must first be addressed before an attempt can be made to improve continuity of care.
Need
Prisoners aged 60 and over are the fastest growing age group in the England and Wales prison system. It has been established they have much more complex health and social needs than younger prisoners, and that these are often unmet. The cost of housing older prisoners has been estimated at six times that of younger prisoners. Despite this, there is no national strategy for the care and management of older prisoners, and few prisons provide any specialist services for their different needs.
Transition in and out of prison is particularly difficult for older people, in particular the provision of relevant services for their increased health and social needs.
This project aims: to determine what health and social services are currently available for older prisoners; to explore the main issues of entering and leaving prison; and to design a new system of assessment and care planning for older people newly received into custody.
Policy states that prison health services should be equivalent in scope and quality to those available in the community. However, social services departments rarely provide any input to prisons, meaning many older prisoners' mobility and functional needs are not addressed. We will establish, by questionnaire, current specialist service provision for older people at all prisons in England and Wales; examine the integration between health and social services in each; and, by qualitative interview, establish factors that promote and inhibit effective integration.
Transitions between health services and other institutions are problematic for older people, and this is particularly true for older people entering prison.
We will conduct interviews with up to 100 people aged 60 plus received into eleven prisons in order to explore the difficulties faced by this group, and what may improve their care. We will also review their clinical records to determine what contact they have with the various prison agencies and departments.
There is currently no specialist assessment for older people on reception to prison, which means that many of their health and social needs are not routinely identified or addressed. We will facilitate an Action-learning group to design, implement and evaluate a new system of assessment and care planning in one prison, based on principles of the Single Assessment Process already established in the community.
The needs of older people on discharge from prison have yet to be established. We will conduct qualitative interviews with up to 60 prisoners immediately before release, and again in the community. These will cover what problems they expected on release, and how these were dealt with in the community.
Methods
Part 1
A questionnaire will be developed and sent to the healthcare managers of all prisons housing adult males in England and Wales, after first being piloted at the sites already involved in Parts 2, 3 and 4 of the project. The questionnaire will establish current service provision for older prisoners, and ascertain how well health and social services are integrated at each site. The following issues will be included in the questionnaire, in accordance with recommendations made in the DoH's (2007) older offender pathway toolkit for good practice:
-
number and proportion of prisoners aged 60 and over;
-
details of staffing levels and training in healthcare departments;
-
identified lead for older prisoners;
-
access to and engagement with local social services departments;
-
access to and engagement with specialist older adult health services;
-
details of chronic disease and/or older adult clinics, and;
-
details of activities available for older prisoners with mobility problems.
The results will be analysed using SPSS, with presentation of findings by type of establishment and by region. From questionnaire responses, two sites with good integration and two sites with poor integration between health and social services will be selected. Individuals working at these establishments will be approached to take part in semi-structured telephone interviews to identify factors which promote or inhibit collaborative working. Interviews will be with prison healthcare managers, as well as representatives from local Primary Care Trusts and Social Services departments to ensure all perspectives are included.
Interviews will be transcribed and will be analysed thematically using a constant comparison method (Glaser, 1965; Merriam, 1998). Under this method, newly gathered data are compared with all previously gathered data that might be similar or different, in order to develop conceptualizations of possible relationships. Categories of data are constructed which cut across the preponderance of data, capturing recurrent patterns and themes. The categories are developed intuitively, but are systematic, informed by the purpose of the study, the investigator's orientation, and the knowledge and meanings made explicit by participants themselves (Glaser, 1965; Merriam, 1998).
Part 2
This part of the study aims to establish the met versus unmet needs of older people entering prison and to capture experiences of reception into custody. It will take place in ‘local prisons’ which hold; people awaiting trial, those convicted of short sentences and those at the early stage of a longer sentence.
For the quantitative element, a demographics sheet, the CANFOR (Thomaset al., 2003), the Geriatric Depression Scale (Yesavageet al., 1983) the Brief Psychiatric Rating Scale (Overall & Gorham, 1962) and the Minimum Data Set Residential Assessment Instrument (Challiset al., 2000) will be used to determine unmet health and social needs, and the clinical and discipline records of participating prisoners will be examined. Specifically, the following will be audited for the first four weeks of custody:
-
the presence of any needs or risk assessment;
-
documented contact with any prison staff group or agency;
-
any individual interventions provided.
We aim to use these quantitative tools to interview up to 100 participants. Quantitative data will be analysed using frequencies and descriptive statistics.
To add to the quantitative data, qualitative interviews will be carried out with newly-received prisoners aged 60 and over, in the participating prisons. They will be interviewed approximately four weeks after arrival into prison. The interview will ascertain the difficulties faced by older people entering prison, in particular how their health, social and custodial needs were addressed. Participants will be asked how their needs could be more appropriately met and to comment on any additional services they feel would have been beneficial.
These qualitative interviews will be conducted with up to 60 of the participants or until data saturation is reached.
Part 3
This part of the study aims to introduce to one prison a relevant and comprehensive assessment of need for older people entering prison, including a pathway of care for identified needs. The assessment will be based on core principles of the Single Assessment Process and the subsequent Common Assessment Framework, implemented in the community following the National Service Framework for Older Adults (DoH, 2001). Thus, a battery of appropriate needs and risk assessments will be combined, based on current practice in the local areas. Actual content will be determined with the participating prison and local health/social services, but is likely to include:
-
physical and mental health needs;
-
suicidal ideation;
-
language and communication;
-
activities of daily living;
-
mobility and environmental needs;
-
contact with family and friends;
-
religious/cultural needs;
-
cognitive impairment;
-
security needs;
-
financial needs and benefit entitlement;
-
access to information about treatment and services;
-
medication management, and;
-
dietary needs.
The development of the assessment must include specific information about what is to happen should needs in any of these areas be present. A care pathway will be established in tandem with the assessment to illustrate what should be provided for each identified domain of need. Once finalised, the assessment will be implemented for all newly-received prisoners aged 60 and over in the designated prison.
Principles of action research will be used to develop both the assessment and care pathway so that all relevant stakeholders are included and to facilitate adaptation based on experience. Thus, an Action-learning group will be convened at the participating site with input from appropriate staff groups within the prison and older prisoners themselves. The group will meet to define the content of the assessment and care pathway as well as the time needed to conduct the extra work and how this can be managed practically. Meeting will continue for the first three months of use, when changes can be made to the process. As part of the action research, staff delivering the assessment and older prisoners receiving it, will be interviewed as to their views and experiences. In addition, staff will be asked to keep diaries detailing the extra time taken to conduct the assessment.
The quantitative and qualitative interviews described in part 2 will be held with newly received older prisoners before and after the implementation of the assessment tool and care pathway. In addition, once the assessment has been agreed and used for three months, qualitative interviews will be conducted with staff regarding the effectiveness of the newly implemented tool and care pathway.
Part 4
The final part of the study will examine transitions out of prison back into the community. Qualitative interviews will be carried out with prisoners having approximately four weeks left to serve, with follow-up interviews within four weeks of release. Unlike entry to prison where new prisoners are always received into ‘local prisons’, people can be discharged from any type of prison. Those serving short sentences, or awaiting trial could be discharged from local prisons, but many of those serving a more substantial sentence could be released from ‘training prisons’ which concentrate on rehabilitation and training. Finally, open prisons prepare prisoners nearing the end of their sentence for life in the community. All three types of prison will be included to ensure representation from all prisoner groups. Thus, interviews will take place in two local prisons, two training prisons and one open prison. We aim to interview approximately 60 participants but will recruit until data saturation is reached.
The qualitative interview will cover their preparation for release in terms of their health and social care needs, including appropriateness of discharge accommodation and their awareness of health and social services which may be required for their continuing care. Prisoners will also be asked for contact details so they can be interviewed again one month following release. This interview will focus on how well plans for release were put into action, and what services they subsequently accessed. Clinical and offender management records will be audited for the presence and quality of any discharge care plans. Prisoners will also be asked about contacts they have had with health and social care services and any suicidal behaviour since discharge. Qualitative analysis will be conducted using the constant comparison method, described above, while descriptive quantitative data will be presented.
Contribution to existing research
This project will build on the existing continuity of care literature both in prison and community environment. This group of older adults has specific and complex needs not currently addressed by existing service provision. The proposed research will directly improve the care of older people entering prison, and provide useful data on which to base future interventions.
Plan of Investigation
The overall programme will examine health and social care needs and current health and social care provision for older adults entering and leaving prison, and evaluate a model for systematic needs assessment and care planning for these groups. The project is split into four parts, taking place in a variety of sites across the prison estate in England and Wales.
Part 1 – Determining the availability and integration of health and social care services for older adults in prison across England and Wales.
Part 1 (months)
12–22: Develop and pilot questionnaire
17–18: Governance Approval
22: Send out questionnaires
22–28: Chase up questionnaires
26–31: Analysis of questionnaires
32–34: Conduct qualitative interviews
34–35: Transcription
35–37: Analysis of interviews
38–39: Write Up
Part 2 – Establishing met versus unmet health and social needs for older people entering prison, including their experiences of reception into custody.
Part 2 (months)
1–4: Recruit sites (on-going as necessary)
1–4: Develop interview schedule
4–6: Staff training
5–12: Governance Approval
13–39: Quantitative and qualitative interviews
16–21: Develop audit proforma
22–40: Transcription of interviews
38–40: Analysis of interviews
40–42: Write up
Part 3 – The development, implementation and evaluation of an intervention to identify and manage health, social and custodial needs of older people entering prison.
Part 3 (months)
7–18: Recruit site to develop and implement assessment tool
7–18: Obtain governance approvals
21–26: Develop assessment tool
27–29: Further development and implementation of assessment tool
31–32: Post-assessment implementation qualitative interviews
32–33: Write up
Part 4 – Exploring the health and social needs of older adults discharged from prison into the community.
Part 4 (months)
1–16: Recruit sites and develop interview schedule
2–16: Governance approval
16–30: Qualitative interviews
17–32: Follow-up interviews and transcription
22–34: Analysis of interviews
35–37: Write Up
Project Management
Two research assistants will be employed for the duration of the project, one of which will act as project manager and the other will concentrate on data collection. The researchers will hold monthly meetings with the Chief Investigator and bi-annual meetings with the project steering committee.
Service users/public involvement
HMP Wymott houses the largest number of older offenders in the North West and runs a club for prisoners aged 60 or over. The team has accessed this group several times to introduce, discuss, and disseminate research relevant to older prisoners. The idea for this study came from comments made by this group during discussion of a previous project.
During the cross-sectional study of the health and social needs of older prisoners (Hayes, 2008), prison staff were asked about health and social services available to older prisoners. Their views demonstrated a specific interest in meeting the needs of older prisoners and meeting published guidelines from the DoH and HM Chief Inspector of Prisons.
Part 3 of the project incorporates service user involvement. The Action-learning group convened will include prisoners as well as staff from various prison departments. Their views will therefore be taken into account during the development of the assessment tool and care pathway for older prisoners.
References
- Appleby L, Shaw J, Amos T, McDonnell R, Harris C, . Suicide within 12 months of contact with mental health services: National Clinical Survey. British Medical Journal 1999;318:1235-9.
- Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, . Release from Prison – A High Risk of Death for Former Inmates. New England Journal of Medicine 2007;356:157-65.
- Birmingham L, Mason D, Grubin D. Health screening at first reception into prison. Journal of Forensic Psychiatry 1997;8:435-9.
- Challis D, Stewart K, Sturdy D, . UK Long Term Care Resident Assessment Instrument: Users' Manual. York: Inter RAI UK; 2000.
- Collins DR, Bird R. The Penitentiary visit – a new role for geriatricians?. Age and Ageing 2007;36:11-3.
- Crawley E, Sparks R. Hidden Injuries? Researching the Experiences of Older Men in English Prisons. Howard Journal of Criminal Justice 2005;44:345-56.
- Crawley E, Sparks R. Is there life after imprisonment? How elderly men talk about imprisonment and release. Criminology and Criminal Justice 2006;6:63-82.
- National Service Framework for older people. London: Department of Health; 2001.
- A pathway to care for older offenders: a toolkit for good practice. London: DoH; 2007.
- Farhall J, Trauer T, Newton R, Cheung P. Minimizing adverse effects on patients of involuntary relation from long-stay wards to community residences. Psychiatric Services 2003;54:1022-7.
- Fazel S, Benning R, Danesh J. Suicides in male prisoners in England and Wales, 1978–2003. Lancet 2005;366:1301-2.
- Fazel S, Hope T, O’Donnell I, Jacoby R. Hidden psychiatric morbidity in elderly prisoners. British Journal of Psychiatry 2001;179:535-9.
- Fazel S, Hope T, O’Donnell I, Jacoby R. Unmet Treatment Needs of Older Prisoners: a Primary Care Survey. Age and Aging 2004;33:396-8.
- Fazel S, Hope T, O’Donnell I, Piper M, Jacoby R. Health of elderly male prisoners: worse than the general population, worse than younger prisoners. Age and Ageing 2001;30:403-7.
- Frazer L. Ageing Inside: School for Policy Studies Working Paper Series, Paper Number 1. Bristol: School for Policy Studies; 2003.
- Glaser BG. The Constant Comparative Method of Qualitative Analysis. Social Problems 1965;12:436-45.
- Grubin D, Carson, D, Parsons S. Report on New Reception Health Screening Arrangements: The Result of a Pilot Study in 10 Prisons. London: DoH; 2002.
- Hayes AJ. The Needs of Older Adults in Prison 2008.
- Hayes AJ, Fazel S, Pritchard J. Good Practice in Safeguarding Adults: Working Effectively in Adult Protection. London: Jessica Kingsley Publishers; 2008.
- ‘No problems – old and quiet': Older prisoners in England and Wales. London: HMIP; 2004.
- No Secrets: Guidance on developing and implementing multi-agency policies and procedures to protect vulnerable adults from abuse. London: DoH; 2000.
- Kariminia A, Law MG, Butler TG, Levy MH, Corben SP, Kaldor JM, et al. Suicide risk among recently released prisoners in New South Wales, Australia. Medical Journal of Australia 2007;187:387-90.
- Merriam S. Qualitative Research and Case Study Applications in Education. San Francisco: Jassey-Bass Publishers; 1998.
- Integrated resettlement: putting the pieces together. London: NACRO; 2005.
- Parrish A. Reaching behind the bars. Nursing Older People 2003;15:10-3.
- Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychological Reports 1962;10:790-812.
- Pratt D, Piper M, Appleby L, Webb R, Shaw J. Suicide in recently released prisoners: a population-based cohort study. Lancet 2006;368:119-23.
- Bromley Briefings Prison Fact file, July 2010. London: Prison Reform Trust; 2010.
- Senior J, Hayes AJ, Bowen A, Foster K, Clayton R, . Evaluation of the ‘Care of At-Risk Prisoners Project' 2005.
- Senior J, Hayes AJ, Pratt D, Thomas SD, Fahy T, . The identification and management of suicide risk in local prisons. Journal of Forensic Psychiatry &Amp; Psychology 2007;18:368-80.
- Shaw J, Thornicroft G. Management for Released Prisoners With Severe and Enduring Mental Illness 2007.
- Stewart K, Challis D, Carpenter I, . Assessment approaches for older people receiving social care: content and coverage. International Journal of Geriatric Psychiatry 1999;14:147-56.
- Thomas S, Harty MA, Parrott J, McCrone P, Slade M, . CANFOR: Camberwell Assessment of Need – Forensic Version. Gaskell: London; 2003.
- Yesavage JA, Brink TL, Rose TL, . Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatric Research 1983;17:37-49.
Appendix 2 Questionnaire
SECTION 1: NUMBER AND PROPORTION OF PRISONERS AGED 60 YEARS AND OVER
1.1 What is the name of your establishment? (If you work at more than one establishment, please complete a separate questionnaire for each)
………………………………………………………………………………………………………………………
1.2 How many prisoners are currently located in your establishment? □
1.3 How many prisoners in your establishment are aged 60 years and over? □
1.4 Of those prisoners aged 60 years and over, how many are aged between:
60–69 years □
70–79 years □
80–89 years □
90 years and above □
1.5 Of those prisoners aged 60 years and over, how many are:
Sentenced prisoners □
Convicted, un-sentenced prisoners □
Remand prisoners □
SECTION 2: DETAILS OF STAFFING LEVELS IN HEALTHCARE DEPARTMENTS
2.1 How many staff are currently employed within your primary care and in-patient services (excluding specialist mental health/in-reach workers)? □
2.2 How many staff are currently employed within your specialist mental health/in-reach team (excluding primary care and in-patient services)? □
SECTION 3: NUMBER OF HEALTHCARE STAFF TRAINED IN THE CARE OF OLDER PEOPLE
3.1 Is any training (internal or external) in the assessment and care of older people offered to staff working within your establishment (if no, please go to question 3.12)?
No = 0 Yes = 1 □
3.2 If yes, who delivers this training (e.g. healthcare staff, in-reach staff, discipline staff, external agency – please specify)?
………………………………………………………………………………………………………………………
3.3 Please describe what training is offered to staff working within your establishment regarding the assessment and care of older people (i.e. title of course, how often is it held, how long does it last etc.).
………………………………………………………………………………………………………………………
3.4 What specific topic areas does this training cover?
………………………………………………………………………………………………………………………
3.5 How many staff within your primary care and in-patient services have received training in the assessment and care of older people during the last 12 months (excluding specialist mental health/in-reach team)? □
3.6 How many staff within your specialist mental health/in-reach team have received training in the assessment and care of older people in the last 12 months (excluding primary care and in-patient services)? □
3.7 Do all your healthcare staff have the opportunity to be trained in the assessment and care of older people (if yes, please go to question 3.9)?
No = 0 Yes = 1 □
3.8 If no, who is the training available to?
………………………………………………………………………………………………………………………
3.9 Is refresher training offered for those healthcare staff trained in the assessment and care of older people (if no, please go to question 3.11)?
No = 0 Yes = 1 □
3.10 If yes, how often is this refresher training offered to healthcare staff?
………………………………………………………………………………………………………………………
3.11 Do you consider training in the assessment and care of older people to be sufficient at your establishment?
No = 0 Yes = 1 □
3.12 Please explain why you consider training in the assessment and care of older people to be/not to be sufficient at your establishment?
………………………………………………………………………………………………………………………
SECTION 4: IDENTIFIED LEAD FOR OLDER PRISONERS
4.1 Do you have a written older prisoner care policy at your establishment? If so, please enclose a copy with your questionnaire.
No = 0 Yes = 1 □
4.2 Do you have an identified lead for older prisoners within your Healthcare Department (if no, please go to question 4.9)?
No = 0 Yes = 1 □
4.3 If yes, how long has there been an identified lead for older prisoners within your Healthcare Department?
□ years and □ months.
4.4 Please explain what duties the older person lead at your establishment is responsible for.
………………………………………………………………………………………………………………………
4.5 Has the older prisoners lead received training to support them in this role (if no, please go to question 4.12)?
No = 0 Yes = 1 □
4.6 If yes, please specify what training the older prisoners lead has received and which organisation/s provided the training?
………………………………………………………………………………………………………………………
4.7 Is the older prisoner lead offered refresher training (if no, please go to question 4.12)?
No = 0 Yes = 1 □
4.8 If yes, at what time intervals? (please now go to question 4.12)
□ years and □ months.
4.9 If your Healthcare Department does not have an identified lead for older prisoners, does your establishment have any existing plans to introduce one (if no, please go to question 4.11)?
No = 0 Yes = 1 □
4.10 If yes, when will a lead for older prisoners be established?
………………………………………………………………………………………………………………………
4.11 If your establishment does not have an identified lead for older prisoners, do you consider that one is required?
No = 0 Yes = 1 □
4.12 Please explain what you consider to be the benefits of having an older prisoner lead (Please answer this question whether or not your establishment has an older prisoner lead).
………………………………………………………………………………………………………………………
4.13 Do you have a prisoner helper/buddy scheme specifically for older prisoners?
No = 0 Yes = 1 □
SECTION 5: RECEPTION PROCEDURES FOR OLDER PRISONERS
5.1 Does your establishment currently use a reception screening assessment tool specifically designed for older prisoners?
at initial reception □
following transfer into the prison □
No = 0 Yes = 1 □
5.2 If you answered yes to either of the above, how long has this older prisoner specific reception screening assessment been used at your establishment?
□ years and □ months.
5.3 If an older prisoner is transferred from another prison into your establishment, do you receive their care plan from their previous prison?
Never = 0 Rarely = 1 Sometimes = 2 Always = 3 □
5.4 Does your establishment have any specific first night arrangements for older prisoners?
No = 0 Yes = 1 □
5.5 Do you have a written protocol regarding the forwarding of older prisoners' reception screening information to healthcare? If so, please enclose it with this questionnaire.
No = 0 Yes = 1 □
SECTION 6: ACCESS TO AND ENGAGEMENT WITH LOCAL SOCIAL SERVICES DEPARTMENTS
6.1 Which local social care services does your establishment have contact with?
………………………………………………………………………………………………………………………
6.2 Do you consider there to be a coordinated approach between your Healthcare Department and social services regarding older prisoners with social care needs?
No = 0 Yes = 1 □
6.3 Please explain your response to question 6.2.
………………………………………………………………………………………………………………………
………………………………………………………………………………………………………………………
6.4 Is there a written protocol between your Healthcare Department and social services regarding older prisoners with social care needs? If so, please enclose it with this questionnaire.
No = 0 Yes = 1 □
6.5 Do you hold meetings with staff from social services to discuss individual case management for older prisoners (if no, please go to question 6.7)?
No = 0 Yes = 1 □
6.6 If yes, on average, how often do these meetings occur?
Annually = 1 Bi-annually = 2 Quarterly = 3 Monthly = 4 Weekly = 5 Daily = 6 □
6.7 Does your establishment experience sufficient communication from social services?
No = 0 Yes = 1 □
6.8 Please explain your response to question 6.7.
………………………………………………………………………………………………………………………
………………………………………………………………………………………………………………………
SECTION 7: ACCESS TO AND ENGAGEMENT WITH SPECIALIST OLDER ADULT SERVICES
7.1 Does your establishment have contact with specialist older adult organisations/services (e.g. Age Concern/Help the Aged/Age UK) (if no, please go to question 7.7)?
No = 0 Yes = 1 □
7.2 If yes, please state which specialist older adult organisations/services are available to older people at your establishment?
………………………………………………………………………………………………………………………
7.3 Please state what services these organisations provide for older prisoners at your establishment?
………………………………………………………………………………………………………………………
7.4 Do you consider there to be a coordinated approach between your Healthcare Department and these specialist older adult organisations/services?
No = 0 Yes = 1 □
7.5 Please explain your response to question 7.4.
……………………………………………………………………………………..…………………………………
7.6 Do you have an Age Concern Coordinator working in your establishment?
No = 0 Yes = 1 □
7.7 If your establishment does not have contact with any specialist older adult organisations/services, do you consider that contact is needed (if no, please go to question 8.1)?
No = 0 Yes = 1 □
7.8 If yes, please state which specialist older adult services would be useful to older people at your establishment AND why.
………………………………………………………………………………………………………………………
SECTION 8: DETAILS OF CHRONIC DISEASE OR OLDER ADULT CLINICS
8.1 Does your establishment offer a chronic disease clinic (if no, please go to question 8.5)?
No = 0 Yes = 1 □
8.2 If yes, please specify what services the chronic disease clinic offers?
………………………………………………………………………………………………………………………
8.3 How often is the chronic disease clinic run at your establishment?
………………………………………………………………………………………………………………………
8.4 How long has the chronic disease clinic been running at your establishment?
………………………………………………………………………………………………………………………
8.5 If your establishment does not have a chronic disease clinic, do you think one is needed?
No = 0 Yes = 1 □
8.6 Does your establishment offer an older adult clinic (if no, please go to question 8.10)?
No = 0 Yes = 1 □
8.7 If yes, please specify what services the older adult clinic offers?
………………………………………………………………………………………………………………………
8.8 How often is the older adult clinic run at your establishment?
………………………………………………………………………………………………………………………
8.9 How long has the older adult clinic been running at your establishment?
………………………………………………………………………………………………………………………
8.10 If your establishment does not have an older adult clinic, do you think one is needed?
No = 0 Yes = 1 □
SECTION 9: DETAILS OF ACTIVITIES AVAILABLE FOR OLDER PRISONERS WITH MOBILITY PROBLEMS
9.1 Does your establishment provide any activities designed specifically for and accessed only by older prisoners (if no, please go to question 9.3)
No = 0 Yes = 1 □
9.2 If yes, please specify what activities are provided?
………………………………………………………………………………………………………………………
9.3 Does your establishment provide any activities specifically for older prisoners with mobility problems (if no, please go to question 9.5)?
No = 0 Yes = 1 □
9.4 If yes, please specify what activities are provided?
………………………………………………………………………………………………………………………
9.5 Can older prisoners with mobility problems access the following services/activities at your establishment (if your establishment does not provide a service/activity please mark N/A)?
No = 0 Yes = 1 Not applicable = N/A
Education □
Library □
Gym □
Workshops □
Healthcare □
Canteen □
Television room □
Association areas (inside) □
Association areas (outside) □
Visiting areas □
Chaplaincy □
Exercise areas (inside) □
Exercise (outside) □
Other service/activity (please state)…………………………………………………………………………………
Other service/activity (please state)…………………………………………………………………………………
9.6 In addition, please specify WHY they are unable to access some of the above activities/services (if applicable).
………………………………………………………………………………………………………………………
9.6.1 When activities are not accessible to older prisoners with mobility problems, does your establishment offer alternatives for this group (if no, please go to question 9.9)?
No = 0 Yes = 1 □
9.7 If yes, please specify what alternatives are provided for older prisoners with mobility problems?
………………………………………………………………………………………………………………………
9.8 Are there opportunities for older prisoners with mobility problems to work (If yes, please specify what types of work opportunities are available)?
No = 0 Yes = 1 □
Please specify:
………………………………………………………………………………………………………………………
9.9 Are the mobility problems of older prisoners taken into account when work is allocated to them?
No = 0 Yes = 1 □
9.10 Are walking frames routinely provided when needed?
No = 0 Yes = 1 □
9.11 Is age taken into account when cells are allocated to prisoners?
No = 0 Yes = 1 □
9.12 Is disability taken into account when cells are allocated to prisoners?
No = 0 Yes = 1 □
9.13 Are age-suitable arrangements made when allocating beds to prisoners?
No = 0 Yes = 1 □
9.14 Is disability taken into account when beds are allocated to prisoners?
No = 0 Yes = 1 □
9.15 Is seating in association areas suitable for older prisoners with mobility problems?
No = 0 Yes = 1 □
9.16 Is seating in cells suitable for older prisoners with mobility problems?
No = 0 Yes = 1 □
9.17 Are cells which have the necessary adaptations to accommodate less mobile and disabled prisoners routinely provided when needed?
No = 0 Yes = 1 □
9.18 Are washing facilities which have the necessary adaptations to accommodate less mobile and disabled prisoners routinely provided when needed?
No = 0 Yes = 1 □
9.19 Do toilet facilities have the necessary adaptations to accommodate less mobile and disabled prisoners?
No = 0 Yes = 1 □
SECTION 10: ADDITIONAL INFORMATION
10.1 Please use this space for comments and/or additional information you feel is not covered in this questionnaire, with specific reference to any difficulties your establishment faces in the care and management of older prisoners and/or suggestions for improvements.
10.2 Please use this space to provide any feedback about the questionnaire.
Many thanks for completing this questionnaire. Please enclose the following information if applicable:
-
written policy regarding older prisoners
-
written protocol regarding the forwarding of older prisoners' reception screening information to healthcare
-
written protocol between your Healthcare Department and social services regarding older prisoners with social care needs
Appendix 3 Staff interview guide
Key objective: investigate integration between health, prison and social care services.
Introduction
-
1.1 Could you tell me a little bit about your role?
-
1.2 What specific duties/involvement do you have regarding/with older offenders?
-
1.3 Are these official or unofficial duties?
Entry into prison
-
2.1 Who gathers information regarding older offenders?
-
2.2 When is this information collected?
-
2.3 What information do you receive about older offenders?
-
2.4 Do you get the information you need? Too much information? Irrelevant information?
-
2.5 Are there problems with obtaining information?
-
2.6 What happens to the information gathered at the assessment/induction phase?
Joined-up working within the prison
-
3.1 Do you have a lead for older offenders within the establishment?
-
3.2 Is this a prison or health care member of staff, or is there one in each department?
-
3.3 Does the lead/leads link in with other departments in the prison and with outside agencies? If so, in what ways?
-
3.4 What inhibits/facilitates this liaison function?
-
3.5 Is there anything that could be improved concerning this role?
-
3.6 If no older lead present, are you aware of such a role?
-
3.7 Do you think there is a need to have such a role?
-
3.8 In what ways do you and your colleagues work with other departments to support older offenders?
-
3.9 What facilitates this joined-up working?
-
3.10 What blocks such work?
-
3.11 How could this be improved?
Communication/information sharing
-
4.1 How do you share information between departments within the prison? Make referrals? Seek advice? Written means, informal meetings?
-
4.2 How appropriate are these systems of communication? How could they be improved? Quantity of information received?
Internal staff working with external agencies
-
5.1 What services do you link up with to support older offenders?
-
5.2 What services do you think need to be involved with older offenders?
-
5.3 What assists joined-up working?
-
5.4 What are the barriers to joined-up working?
-
5.5 What aspects of joined-up working could be improved?
-
5.6 Are there any other services available that you think should be involved?
-
5.7 How do you and your colleagues communicate with external agencies? To make referrals? In seeking advice?
-
5.8 What are the problems you face working with external agencies?
-
5.9 What would be a way of improving the communication/information gathering/referral process?
Discharge from prison/support in the community
-
6.1 What is your role in the release of an ‘older’ offender?
-
6.2 How far in advance does this take place?
-
6.3 When is the offender notified about this process?
-
6.4 How do you work with external agencies to support the release of ‘older’ offenders?
-
6.5 What departments work with agencies to support the release of an older offender?
-
6.6 What works well during this?
-
6.7 How could this be improved?
-
6.8 What communication takes place between you, your colleagues and external agencies involved in the release of ‘older’ offenders?
-
6.9 What works well in this process?
-
6.10 What doesn't work well in this process?
Summary
-
7.1 What ways do you feel your establishment is successful in supporting ‘older’ offenders?
-
7.2 How does your establishment support joined-up working between departments?
-
7.3 How does your establishment support collaborative working with other agencies/services?
-
7.4 What ways do you feel your establishment is successful at exchanging information?
-
7.5 What are the barriers to appropriately supporting ‘older’ offenders?
-
7.6 Is there anything else you would like to add about health and social care services for ‘older’ offenders at this establishment?
Appendix 4 Interview guide for prisoners entering prison
-
How long have you been in this prison?
-
Can you describe your experience of arriving into this prison?
-
How have any issues that were raised upon your reception into prison been dealt with? Is there anything you would have liked to have happen instead?
-
What services are you aware of, and have you been in contact with any since arriving into prison? What support and for what are you currently getting from this prison? Is there anything that prevents you getting the help/support you need? Are you aware of this prison offering any specialist services for older prisoners? If so, what services?
-
Do you think you have any needs that are different from those of younger prisoners? If so, what are they? Do you consider you need different services from other prisoners because of your age? If so, why, if not, why not?
-
How have you settled into this prison? Has it been easy or difficult? Why?
-
Have you raised any concerns after you went through the initial reception process? If so, what were these concerns and how were they dealt with?
-
Do you have any current concerns or issues about being in prison? What are they? Do you know how to resolve them?
-
I've come to the end of my questions now, is there anything else you would like to discuss?
Appendix 5 Interview guide for action-learning group members
-
How did you find being a member of the action-learning group?
-
To what extent was the membership of the group appropriate? (health care staff/prison staff/prisoners)
-
To what extent did you feel able to discuss your views in the action-learning group?
-
Did anything happen as a result of the action-learning group being in existence? If so, what changes were made? How did these changes come about?
-
Did being a member of the action-learning group benefit you personally? If so, how?
-
Is there anything else you would like to add about being a member of the action-learning group?
Appendix 6 Interview guide for older prisoner lead
Before the implementation of the intervention
-
What was your role in supporting older prisoners before you became involved in this research?
-
How did you identify older prisoners before you became involved in this research?
-
What assessments were in place for older prisoners' health and social needs before this research started?
-
How were older prisoners supported before this research was started?
-
What worked well about the process for supporting older prisoners before the research started?
-
What required improvements to allow you and your colleagues to successfully support older prisoners before this research started?
After the implementation of the intervention
-
How did you identify older prisoners to participate in the assessment?
-
Can you describe how you conduct the assessments? (Where did you conduct them? Was a member of health care staff present?)
-
What were the common issues raised by older prisoners during the assessments?
-
What types of referrals were you making as a result of the intervention?
-
Is there anything you would change about the intervention?
-
How well did conducting the assessment and reviews fit into your job role?
-
How much of your time did you spend conducting the assessments and reviews?
-
How well equipped did you feel to conduct the assessment and reviews?
-
To what extent has the way you support older prisoners changed as a result of this research?
-
Is there anything else you would like to add about conducting the assessment and review process?
Appendix 7 Interview guide for prisoners who received the Older prisoner Health and Social Care Assessment and Plan
-
How long have you been in this prison?
-
What happened when you did the older prisoner assessment with the older prisoner lead?
-
Can you describe your experience of arriving into this prison?
-
How have any issues that were raised upon your reception into prison been dealt with? Is there anything you would have liked to have happen instead?
-
What services are you aware of, and have you been in contact with any since arriving into prison? What support and for what are you currently getting from this prison? Is there anything that prevents you getting the help/support you need? Are you aware of this prison offering any specialist services for older prisoners? If so, what services?
-
Do you think you have any needs that are different from those of younger prisoners? If so, what are they? Do you consider you need different services from other prisoners because of your age? If so, why, if not, why not?
-
How have you settled into this prison? Has it been easy or difficult? Why?
-
Have you raised any concerns after you went through the initial reception process? If so, what were these concerns and how were they dealt with?
-
Do you have any current concerns or issues about being in prison? What are they? Do you know how to resolve them?
-
I've come to the end of my questions now, is there anything else you would like to discuss?
Appendix 8 Older prisoner Health and Social Care Assessment and Plan (OHSCAP)
General information
-
This assessment tool is divided into three areas: wellbeing, social care and discharge from prison. It revisits information that may already have been provided on initial reception, and identifies new information that has come to light following a few days in custody. It then explores any issues relevant to ensuring appropriate discharge from prison.
-
It is to be completed 7–10 days after the prisoner has arrived in the prison.
-
Ideally it will be completed by both health care and discipline staff together, jointly interviewing the prisoner. This is provided he is happy to discuss his health issues in front of the discipline officer. However, it may be more appropriate for the discipline officer to take the lead and refer to health care if necessary.
-
The assessment will be reviewed at a time deemed appropriate by staff completing it, and the prisoner.
-
A care plan must be completed by the staff conducting the assessment, and agreed with the prisoner. The prisoner may retain a copy of the care plan if they want to.
Social assessment
The aim of this part of the assessment is to discuss any issues with the prisoner that might be affecting his ability to settle into prison life and feel safe. The questions are divided into three sections: relationships, activities and mobility. There is space in the assessment to record discussion on any other areas that might be important to the prisoner.
Wellbeing assessment
This part of the assessment revisits the information gathered during medical reception a week earlier to see if there have been any changes, and to identify if the prisoner requires further health/wellbeing assessment following the first week of settling into custody.
Discharge from prison
This part of the assessment explores the issues that require addressing prior to the prisoner being discharged from prison.
SECTION 1: SOCIAL ASSESSMENT
| Name | Date of Birth | ||
| Age | NOMS Number |
A: Relationships
Ask the person if they have been able to maintain their social and family relationships whilst they have been in prison. Is anyone looking after their finances/benefits, etc.? How are they getting along with other prisoners? Do they feel safe?
B: Activities
What is the prisoner doing with their time? What are their interests/hobbies? Are they aware of what is available to them, e.g. gym, over 60s club, library? Do they want to work? Are they going out on exercise? If not, why not?
C: Mobility
Is the prisoner managing to get around safely? Can they collect their own meals, get in/out of bed, get to/from their cell to association, and in/out of shower? Can they walk to visits/healthcare/treatment room, etc.?
SECTION 2: WELLBEING ASSESSMENT
D. Emotional wellbeing
Is the prisoner coping OK with being in prison? How are they feeling in general? Are they feeling supported? Are they getting on with other prisoners – feeling safe? Are they sleeping? Do they have any concerns?
E. Physical wellbeing
Are there any physical problems that have arisen since first reception in to prison? Can they think of anything they might have forgotten to mention when they first arrived? For example, have they got their reading glasses/contact lens solution, etc.? Does the prisoner know how to access health care? Are they able to attend to their own personal hygiene needs effectively?
F. Medications and treatment
Does the prisoner take any medication? If so, have they been getting it at the right times? Are there any problems with getting their medication, e.g. ability to attend treatment room, pressured into giving it to other prisoners?
G. Any other concerns that have not already been mentioned?
SECTION 3: DISCHARGE FROM PRISON
H. Discharge from prison
When is the person being discharged from prison? Where do they plan to go? Will they be welcome there? Do they have finances in place to support themselves? Are there any health care/social care needs that need to be considered?
| ______________________________ | _________________________ | _________________ |
| Healthcare staff (sign) (IF PRESENT) | (Print Name) | Date |
| ______________________________ | _________________________ | _________________ |
| Discipline staff (sign) | (Print Name) | Date |
| ______________________________ | _________________________ | _________________ |
| Prisoner (sign) | (Print Name) | Date |
Care plan
To be completed in conjunction with prisoner
| Number | Issue raised from assessment | Aim of action | Action (including by whom and when) | Date to be reviewed and rationale | Status of action |
|---|---|---|---|---|---|
| 1 | |||||
| 2 | |||||
| 3 | |||||
| 4 |
Review
Date:
Reviewer(s):
| Number | Progress since last review | Action planned | Next review with rationale |
|---|---|---|---|
| 1 | |||
| 2 | |||
| 3 | |||
| 4 |
Review
Date:
Reviewer(s):
| Number | Progress since last review | Action planned | Next review with rationale |
|---|---|---|---|
© 2012 The University of Manchester and University of Leeds all rights reserved.
Appendix 9 Interview guide for prisoners approaching release from prison
-
Can you tell me when you are going to be released from this prison? How long have you been in prison?
-
Have any plans been made for your release? If so, can you describe what plans have been made? How do you feel about these plans?
-
Is there anything you feel that is not planned for yet regarding your release? If so, can you describe what you feel has not been planned for?
-
Do you know where you are staying after your release? If so, do you feel this accommodation is appropriate for you? If so, why? If not, why not?
-
Is there anything that concerns you about your release?
-
Once being released do you feel you may face any difficulties?
-
Do you feel you may face any difficulties that are different to those of younger prisoners who are released? If so, what do you anticipate these difficulties to be and why? If not, why not?
-
Is there anything you feel is important for your successful resettlement back into the community? Is there anything you need?
-
How do you feel about being released?
-
Are you aware of any services that exist in the community that can help you after you have been released?
-
I've come to the end of my questions now, is there anything else you would like to discuss?
Appendix 10 Interview guide for prisoners released from prison
-
How long have you been released from prison?
-
How have things been going for you since you have been released?
-
When I spoke to you before you said that ______ was planned for? How has this worked out?
-
When I spoke to you before you said ______ was not planned for? Has this been resolved? If so, how? If not, how would you have liked it to have been resolved?
-
Have you accessed any services since being released? Have they helped you? How did you find out about them/access them?
-
When I spoke to you before you said you were staying at ______. How has this been?
-
How well do you think your release was planned?
-
How well do you feel your needs have been met since being released?
-
Is there anything you have found difficult since being released?
-
How have you been feeling since being released? How settled do you feel at present?
-
Is there anything else you feel you need for your continued resettlement?
-
I've come to the end of my questions now, is there anything else you would like to discuss?
Appendix 11 Participant information sheets and consent forms
Staff interview participant information sheet (see Chapter 3)
The University of Manchester
Health and Social Care Services for Older Male Adults in Prison
Staff Information Sheet
Introduction
My name is _____________, I am a researcher working at the University of Manchester, School of Community Based Medicine. We would like to invite you to take part in a research study about the needs of older adults in prison.
What is the purpose of the study?
The purpose of this study is to investigate what current services are available to older prisoners, and ascertain how health and social services for older offenders are integrated. A questionnaire has been sent to the healthcare managers of all prisons housing adult males in England and Wales. Interviews will now take place with individuals working at a selection of establishments to find out more information. Representatives from external agencies working with older offenders will also be involved in interviews.
What will I have to do if I take part?
If you agree to take part in the study, you will be asked to take part in a telephone interview at a time which is convenient to you. Questions will cover what services are available for older prisoners, as well as, integration between health and social service agencies working with older offenders. This will take approximately 30 minutes of your time.
What happens if I don't want to take part?
Taking part in this study is voluntary. If you would prefer not to take part you do not have to give a reason and no pressure will be put on you to try and change your mind. You can change your mind about taking part at any time.
Will my taking part in this study be kept confidential?
Yes. All the information you give us will be kept confidential within the research team, and used for the purposes of this study only. The only exception to this would be if you tell us something that raises concerns about your safety, or the safety of others. Should this occur, we would have to inform the appropriate organisations. All information will be used in a way that will not allow you or your establishment/agency to be identified individually.
What happens with my information?
This will be kept in a locked filing cabinet for no longer than 5 years. Only the research team will have access to these. The research team hope to publish the results in academic journals and provide best practice booklets. This may include anonymous quotes from the interviews, with any identifying information removed.
Who is organising and funding the research?
Staff employed by Manchester University are conducting the research. The project is funded by NHS National Institute for Health Research Service Delivery and Organisation Programme. If you would like to make a complaint about the research, please contact a member of the research team, who will give you the relevant contact details in order to make your complaint.
What do I do now?
Think about the information on this sheet. A member of the research team will be contacting you shortly to answer any questions you may have and ask you if you are interested in participating in the study. After your questions have been answered, if you agree to participate please sign the consent form and return it by email, fax or by post. Please do not hesitate to contact me at any time, if you have any questions regarding any aspect of this process.
THANK YOU FOR READING THIS
Version 1, 14 October 2011. Part 1: staff information form
Older prisoner participant information sheet (see Chapter 4)
The University of Manchester
Health and Social Care Services for Older Male Adults in Prison
Participant Information Sheet
Introduction
My name is ______________________, I am a researcher working at the University of Manchester, School of Community Based Medicine. We would like to invite you to take part in a research study about the needs of older adults entering prison. Before you decide whether to take part, please read the following information carefully and discuss it with others if you wish.
What is the purpose of the study?
The purpose of this study is to explore the experiences and needs of older male adults entering and leaving prison, and to find out how the prison is able to meet these needs. We are interested in trying to improve services by asking people who have experienced services for their opinions. With the results of this study, we hope to be able to plan better care for those older adults entering and leaving prison.
Why have you been contacted?
You have been contacted as you have recently entered prison and you are aged 60 years or over.
What will I have to do if I take part?
If you agree to take part in the study, I will ask you to fill in a questionnaire which will ask about your healthcare and social needs in prison. I will also ask you some further detailed questions about any difficulties you may have faced when you entered prison, how your health, social and custodial needs have been met and whether any additional services would have been beneficial to you on entering prison. This will take approximately 1 hour of your time, but this can be spread over several sessions if you wish. The interview will take place at a time that is convenient to you. I may ask to access your medical and discipline records to see what has been documented about your care whilst you have been in prison. I may also ask your Personal Officer or a member of your Healthcare team for further information regarding your health and social care needs.
What happens if I don't want to take part?
Taking part in this study is voluntary. If you would prefer not to take part you do not have to give a reason and no pressure will be put on you to try and change your mind. You can change your mind about taking part at any time. If you decide not to take part, or withdraw at any stage, your legal and parole rights and your access to medical care will not be affected.
Will my taking part in this study be kept confidential?
Yes. All the information you give us will be kept confidential within the research team, and used for the purposes of this study only. The information will be used in a way that will not allow you to be identified individually. The only exception to this is if, after interview, we feel your health or safety, or that of others around you is at immediate risk because of something you have told us about how you are feeling. In that case, we will have to pass that information on to the prison healthcare staff, so that they can help you further. We would like to record the interview using a dictaphone, and in this case you will be asked for your permission. The recording will be kept confidential, and will not have your name on it. If you decide that you do not want the interview recorded, you can still take part.
What happens with my information?
This will be kept in a locked filing cabinet for no longer than 5 years. Only the research team will have access to these. The research team hope to publish the results in academic journals and provide best practice booklets. This may include anonymous quotes from the interviews, with any identifying information removed.
What are the possible drawbacks to taking part?
We are interested in hearing about your experience. The study does not involve any treatment or counselling. You may find talking about parts of your experience stressful or upsetting. If this happens, you can choose not to talk about these parts of your experience or stop the interview at any time without giving a reason.
What are the possible benefits to taking part?
Your views and opinions will allow us to develop recommendations to improve services for older adults entering and leaving prison. This may not benefit you personally, but may help other older adults entering and leaving prison in the future.
Who is organising and funding the research?
Staff employed by Manchester University are conducting the research. The project is funded by NHS National Institute for Health Research Service Delivery and Organisation Programme. If you would like to make a complaint about the research, please contact a member of the research team, or get a member of staff to contact the research team on your behalf, who will give you the relevant contact details in order to make your complaint.
What do I do now?
Think about the information on this sheet and ask me about anything that you are not sure about. If you agree to take part, we will go ahead.
If, after taking part in the research, you want further information or have any more questions about the study, tell your personal officer who will then contact me and I will come back to see you.
But if after taking part, you become upset and need help immediately to deal with your feelings without hurting yourself, it is very important that you talk to someone straight away.
Any member of staff in the prison will be able to help you, all you need to do is speak to someone.
Please do this as soon as you start feeling upset, it will help.
THANK YOU FOR READING THIS
Version 4, 31 March 2010. Part 2: older adults
Older prisoner participant information sheet (see Chapter 5)
The University of Manchester
Health and Social Care Services for Older Male Adults in Prison
Participant Information Sheet
Introduction
My name is ______________________, I am a researcher working at the University of Manchester, School of Community Based Medicine. We would like to invite you to take part in a research study about the needs of older adults in prison. Before you decide whether to take part, please read the following information carefully and discuss it with others if you wish.
What is the purpose of the study?
The purpose of this study is to design and use a questionnaire exploring the needs of older male adults in prison, so that a plan of care can be then be developed to meet these needs.
Why have you been contacted?
You have been contacted as you have recently entered prison and you are aged 60 years or over.
What will I have to do if I take part?
If you agree to take part in the study, a trained prison staff member will ask you a series of questions about your needs in prison. This will include questions about your physical and mental health needs, thoughts of suicide, communication needs, daily living needs, contact with family and friends, mobility needs, religious/cultural needs, financial needs and benefit entitlement, access to services, medication management and dietary needs. This will take approximately 1 hour of your time. From this questionnaire prison staff will identify your needs and a plan of care will be developed in order to help meet your needs. At a later date a researcher will conduct a short 30 minute interview with you to ask your opinions about your experience of the questionnaire and the plan of care that was developed for you. The interview will take place at a time that is convenient to you. I may ask to access your medical and discipline records to see what has been documented about your care whilst you have been in prison.
What happens if I don't want to take part?
Taking part in this study is voluntary. If you would prefer not to take part you do not have to give a reason and no pressure will be put on you to try and change your mind. You can change your mind about taking part at any time. If you decide not to take part, or withdraw at any stage, your legal and parole rights and your access to medical care will not be affected.
Will my taking part in this study be kept confidential?
Yes. All the information you give us will be kept confidential within the research team, and used for the purposes of this study only. The information will be used in a way that will not allow you to be identified individually. The only exception to this is if we feel your health or safety, or that of others around you is at immediate risk because of something you have told us about how you are feeling. In that case, we will have to pass that information on to the prison healthcare staff, so that they can help you further. We would like to record the 30 minute interview using a dictaphone, and in this case you will be asked for your permission. The recording will be kept confidential, and will not have your name on it. If you decide that you do not want the interview recorded, you can still take part.
What happens with my information?
This will be kept in a locked filing cabinet for no longer than 5 years. Only the research team will have access to these. The research team hope to publish the results in academic journals and provide best practice booklets. This may include anonymous quotes from the 30 minute interview, with any identifying information removed.
What are the possible drawbacks to taking part?
You may find talking about some aspects of your needs stressful or upsetting. If this happens, you can choose not to talk about these aspects or stop the interviews at any time without giving a reason.
What are the possible benefits to taking part?
Your participation will allow us to develop recommendations to improve services for older adults in prison, as well as help us identify and care plan for your own needs whilst in prison.
Who is organising and funding the research?
Staff employed by Manchester University are conducting the research. The project is funded by NHS National Institute for Health Research Service Delivery and Organisation Programme. If you would like to make a complaint about the research, please contact a member of the research team, or get a member of staff to contact the research team on your behalf, who will give you the relevant contact details in order to make your complaint.
What do I do now?
Think about the information on this sheet and ask me about anything that you are not sure about. If you agree to take part, we will go ahead.
If, after taking part in the research, you want further information or have any more questions about the study, tell your personal officer who will then contact me and I will come back to see you.
But if after taking part, you become upset and need help immediately to deal with your feelings without hurting yourself, it is very important that you talk to someone straight away.
Any member of staff in the prison will be able to help you, all you need to do is speak to someone.
Please do this as soon as you start feeling upset, it will help.
THANK YOU FOR READING THIS
Version 3, 31 March 2010. Part 3: older adults
Action-learning group member (prisoner) participant information sheet (see Chapter 5)
The University of Manchester
Health and Social Care Services for Older Male Adults in Prison
Participant Information Sheet
Introduction
My name is ______________________, I am a researcher working at the University of Manchester, School of Community Based Medicine. We would like to invite you to take part in a research study about the needs of older adults entering prison. Before you decide whether to take part, please read the following information carefully and discuss it with others if you wish.
What is the purpose of the study?
The purpose of this study is to develop a needs assessment and pathway of care for older male adults (those aged 60 years and over) entering prison. This needs assessment and care pathway will then be put into action at HMP Leeds and evaluated.
Why have you been contacted?
You have been contacted because you are 60 or over and have experienced the process of entering HMP Leeds.
What will I have to do if I take part?
If you agree to take part in the study, I will invite you to a number of meetings being held over a nine month period. During these meeting, you will be given the chance to express your views about the process of older prisoners entering HMP Leeds and their care. You will also be invited to express your view on how this process could be improved, where relevant.
What happens if I don't want to take part?
Taking part in this study is voluntary. If you would prefer not to take part you do not have to give a reason and no pressure will be put on you to try and change your mind. You can change your mind about taking part at any time. If you decide not to take part, or withdraw at any stage, your legal and parole rights and your access to medical care will not be affected.
Will my taking part in this study be kept confidential?
Yes. All the information you give us will be kept confidential within the research team, and used for the purposes of this study only. The information will be used in a way that will not allow you to be identified individually. The only exception to this is if, after interview, we feel your health or safety, or that of others around you is at immediate risk because of something you have told us about how you are feeling. In that case, we will have to pass that information on to the prison healthcare staff, so that they can help you further. We would like to record the interview using a dictaphone, and in this case you will be asked for your permission. The recording will be kept confidential, and will not have your name on it. If you decide that you do not want the interview recorded, you can still take part.
What happens with my information?
This will be kept in a locked filing cabinet for no longer than 5 years. Only the research team will have access to these. The research team hope to publish the results in academic journals and provide best practice booklets.
What are the possible drawbacks to taking part?
We are interested in hearing about your experience. The study does not involve any treatment or counselling. You may find talking about parts of your experience stressful or upsetting. If this happens, you can choose not to talk about these parts of your experience
What are the possible benefits to taking part?
Your views and opinions will allow us to develop recommendations to improve services for older adults entering and leaving prison. This may not benefit you personally, but may help other older adults entering and leaving prison in the future.
Who is organising and funding the research?
Staff employed by Manchester University are conducting the research. The project is funded by NHS National Institute for Health Research Service Delivery and Organisation Programme. If you would like to make a complaint about the research, please contact a member of the research team, or get a member of staff to contact the research team on your behalf, who will give you the relevant contact details in order to make your complaint.
What do I do now?
Think about the information on this sheet and ask me about anything that you are not sure about. If you agree to take part, we will go ahead.
If, after taking part in the research, you want further information or have any more questions about the study, tell your personal officer who will then contact me and I will come back to see you.
But if after taking part, you become upset and need help immediately to deal with your feelings without hurting yourself, it is very important that you talk to someone straight away.
Any member of staff in the prison will be able to help you, all you need to do is speak to someone.
Please do this as soon as you start feeling upset, it will help.
THANK YOU FOR READING THIS
Version 1, 29 September 2010. Part 3: prisoner action-learning group member
Action-learning group member (staff) participant information sheet (see Chapter 5)
The University of Manchester
Health and Social Care Services for Older Male Adults in Prison
Staff Information Sheet
Introduction
My name is ______________________, I am a researcher working at the University of Manchester, School of Community Based Medicine. We would like to invite you to take part in a research study about the needs of older adults in prison.
What is the purpose of the study?
The purpose of this study is to design, develop and implement a comprehensive assessment of need for older male adults (those aged 60 years and over) entering prison, including a pathway of care for identified needs.
What will I have to do if I take part?
If you agree to take part in the study, you may be asked to contribute to monthly meetings, over a nine month period, to inform the development and implementation of the assessment and care pathway. You may also be asked to complete a diary detailing your experience of implementing the assessment and care pathway. At a later date a researcher may conduct an interview with you about your views and experiences of the assessment. The interview will take place at a time that is convenient to you and will last approximately 30 minutes.
What happens if I don't want to take part?
Taking part in this study is voluntary. If you would prefer not to take part you do not have to give a reason and no pressure will be put on you to try and change your mind. You can change your mind about taking part at any time.
Will my taking part in this study be kept confidential?
Yes. All the information you give us will be kept confidential within the research team, and used for the purposes of this study only. The information will be used in a way that will not allow you to be identified individually.
What happens with my information?
This will be kept in a locked filing cabinet for no longer than 5 years. Only the research team will have access to these. The research team hope to publish the results in academic journals and provide best practice booklets. This may include anonymous quotes from the interview, with any identifying information removed.
Who is organising and funding the research?
Staff employed by Manchester University are conducting the research. The project is funded by NHS National Institute for Health Research Service Delivery and Organisation Programme. If you would like to make a complaint about the research, please contact a member of the research team, who will give you the relevant contact details in order to make your complaint.
What do I do now?
Think about the information on this sheet and ask me about anything that you are not sure about. If you agree to take part, we will go ahead.
THANK YOU FOR READING THIS
Version 1, 29 September 2010. Part 3: staff (action-learning group members)
Older prisoner participant information sheet (see Chapter 6)
The University of Manchester
Health and Social Care Services for Older Male Adults in Prison
Participant Information Sheet
Introduction
My name is _______________________, I am a researcher working at the University of Manchester, School of Community Based Medicine. At the moment we are working on a project to look at the needs of older male adults leaving prison and entering the community. We would like to invite you to take part in this study. Before you decide whether to take part, please read the following information carefully and discuss it with others if you wish.
What is the purpose of the study?
The purpose of this study is to explore the experiences and needs of older male adults entering and leaving prison, and to find out how the prison is able to meet these needs. We are interested in trying to improve services by asking people who have experienced services for their opinions. With the results of this study, we hope to be able to plan better care for those older adults entering and leaving prison.
Why have you been contacted?
You have been contacted as you are shortly due to be released from prison and you are aged 60 years or over.
What will I have to do if I take part?
If you agree to take part in the study, I will ask you to take part in two interviews of approximately 45 minutes each. The first interview will take place in prison, four weeks before you are about to be released. I will ask you questions about your preparation for release, including your awareness of the health and social services required for your continuing care. I may ask to access your medical and discipline records to see what has been documented about your preparation for release.
The second interview will take place approximately four weeks after you have been released. I will ask for your contact details after the first interview so I can arrange for the second interview to take place in the community, via a relevant agency. In the second interview I will ask you questions about any contact you have had with health and social care services since being released and how you have been feeling in terms of your mental health since being released. Any travel expenses you incur for the second interview will be reimbursed.
What happens if I don't want to take part?
Taking part in this study is voluntary. If you would prefer not to take part you do not have to give a reason and no pressure will be put on you to try and change your mind. You can change your mind about taking part at any time. If you decide not to take part, or withdraw at any stage, your legal and parole rights and your access to medical care will not be affected.
Will my taking part in this study be kept confidential?
Yes. All the information you give us will be confidential and used for the purposes of this study only. The information will be used in a way that will not allow you to be identified individually. The only exception to this is if, after interview, we feel your health or safety, or that of others around you is at immediate risk because of something you have told us about how you are feeling. In that case, we will have to pass that information on to the prison healthcare staff, so that they can help you further. We would like to record the interview using a dictaphone, and in this case you will be asked for your permission. The recording will be kept confidential, and will not have your name on it. If you decide that you do not want the interview recorded, you can still take part.
What happens with my information?
This will be kept in a locked filing cabinet for no longer than 5 years. Only the research team will have access to these. The research team hope to publish the results in academic journals and provide best practice booklets. This may include anonymous quotes from the interviews, with any identifying information removed.
What are the possible drawbacks to taking part?
We are interested in hearing about your experience. The study does not involve any treatment or counselling. You may find talking about parts of your experience stressful or upsetting. If this happens, you can choose not to talk about these parts of your experience or stop the interview at any time without giving a reason.
What are the possible benefits of taking part?
Your views and opinions will allow us to develop recommendations to improve services for older adults entering and leaving prison. This may not benefit you personally, but may help other adults entering and leaving prison in the future.
Who is organising and funding the research?
Staff employed by Manchester University are conducting the research. The project is funded by NHS National Institute for Health Research Service Delivery and Organisation Programme. If you would like to make a complaint about the research, please contact a member of the research team, or get a member of staff to contact the research team on your behalf, who will give you the relevant contact details in order to make your complaint.
What do I do now?
Think about the information on this sheet and ask me about anything that you are not sure about. If you agree to take part, we will go ahead.
If, after taking part in the first interview, you want further information or have any more questions about the study, tell your personal officer who will then contact me and I will come back to see you.
But if after taking part, you become upset and need help immediately to deal with your feelings without hurting yourself, it is very important that you talk to someone straight away.
Any member of staff in the prison will be able to help you, all you need to do is speak to someone. Please do this as soon as you start feeling upset, it will help.
After your second interview I will provide you with an information sheet with the contact details of relevant community agencies you can contact for support if needed. If I have concerns about your mental health after the interview I will have to contact appropriate persons/agencies.
THANK YOU FOR READING THIS
Version 3, 31 March 2010. Part 4: older adults
Staff interview consent form (see Chapter 3)
The University of Manchester
Health and Social Care Services for Older Male Adults in Prison
CONSENT FORM
Name _____________________________________________________________________________________
Research ID Number _________________ (please leave blank)
PLEASE INITIAL THE BOXES IF YOU AGREE WITH EACH SECTION:
Version 1, 14 October 2011. Part 1: staff consent form.
Older prisoner consent form (see Chapter 4)
The University of Manchester
Health and Social Care Services for Older Male Adults in Prison
CONSENT FORM
Name _____________________________________________________________________________________
Research ID Number _________________ (please leave blank)
Version 4, 2 December 2009. Part 2: older adults
Older prisoner consent form (see Chapter 5)
The University of Manchester
Health and Social Care Services for Older Male Adults in Prison
CONSENT FORM
Name _____________________________________________________________________________________
Research ID Number _________________ (please leave blank)
Version 3, 8 June 2009. Part 3: older adults
Action-learning group member (prisoner) consent form (see Chapter 5)
The University of Manchester
Health and Social Care Services for Older Male Adults in Prison
CONSENT FORM
Name _____________________________________________________________________________________
Research ID Number _________________ (please leave blank)
Version 1, 29 September 2010. Part 3: prisoner action-learning group member
Action-learning group member (staff) consent form (see Chapter 5)
The University of Manchester
Health and Social Care Services for Older Male Adults in Prison
CONSENT FORM
Name _____________________________________________________________________________________
Research ID Number _________________ (please leave blank)
Version 1, 29 September 2010. Part 3: staff action-learning group member
Older prisoner consent form (see Chapter 6)
The University of Manchester
Health and Social Care Services for Older Male Adults in Prison
CONSENT FORM
Name _____________________________________________________________________________________
Research ID Number _________________ (please leave blank)
Version 3, 8 June 2009. Part 4: older adults
Glossary
- Assessment, Care in Custody and Teamwork
- The care management system currently in operation across the England and Wales prison estate to assess, risk manage and care for prisoners identified as being at risk of suicide or self-harm.
- Action-learning group
- A collection of individuals who participate in a process of learning and reflection with the intention of getting things done.
- Action research
- Cycles of planning, action and evaluation to conceptualise issues and generate solutions and enable practitioners and researchers to generate knowledge while simultaneously changing practice.
- Clinical commissioning group
- The health commissioning organisations that will replace primary care trusts by April 2013. Commissioning organisations are responsible for planning and purchasing health care across local areas.
- First night centre
- A specific unit where those newly arrived in custody are located for the first few nights in prison, before being moved onto a normal residential wing. They are designed to offer higher levels of support and supervision to both orientate prisoners to the prison's regime and expectations and better protect against the increased risk of suicide and/or self-harm in this period.
- Health and well-being boards
- These are being established as part of the Health and Social Care Act 2012 as a forum for key leaders across health and social care sectors to enable them to work together to improve the health and well-being of their local population.
- In-patient services
- Twenty-four-hour nursing care available in a residential prison unit.
- Joint Strategic Needs Assessment
- This is a process for identifying current and future health and well-being needs to inform future services.
- Local prison
- A type of prison that contains those awaiting trial, convicted of short sentences and at the beginning of longer sentences.
- Mental health and in-reach services
- The service in prison that identifies and treats mental disorders among prisoners.
- Open prison
- A type of prison that has no perimeter security and trusts those contained, usually prisoners at the end of long sentences or those on very short sentences, not to abscond.
- Private prison
- A prison operated by a third party contracted by a government agency.
- Public prison
- A prison operated by Her Majesty's Prison Service.
- Primary care
- Health care services provided to prisoners that are similar to those provided by a general practitioner in the community.
- Social care
- All forms of personal care and other practical assistance for individuals who by reason of age, illness, disability, pregnancy, childbirth or dependence on alcohol or drugs, or for any other similar circumstances, are in need of such care or assistance.
- Segregation cell/unit
- A separate part of a prison where prisoners are kept away from the general prison population in more restrictive conditions for their own safety or the safety of others.
- SystmOne
- A centralised clinical system that provides health care professionals with a complete management system including electronic patient records.
- Training prison
- A type of prison that holds only sentenced prisoners, usually transferred from local prisons.
- Vulnerable prisoner wing
- A section of a prison that houses certain categories of prisoner considered to be at risk of harm from the general prison population.
List of abbreviations
- ACCT
- Assessment, Care in Custody and Teamwork
- BPRS
- Brief Psychiatric Rating Scale
- CANFOR-S
- Camberwell Assessment of Need – Short Forensic Version
- CCG
- clinical commissioning group
- C-NOMIS
- Computer – National Offender Management Information System
- COPD
- chronic obstructive pulmonary disease
- DLO
- disability liaison officer
- GDS
- Geriatric Depression Scale
- GDS-15
- Geriatric Depression Scale short form
- GP
- general practitioner
- HMCIP
- Her Majesty's Chief Inspectorate of Prisons
- HMIP
- Her Majesty's Inspectorate of Prisons
- HMPS
- Her Majesty's Prison Service
- HWB
- health and well-being board
- JHWS
- Joint Health and Wellbeing Strategy
- JSNA
- Joint Strategic Needs Assessment
- LAT
- local area team
- MDS
- minimum data set
- Nacro
- National Association for the Care and Resettlement of Offenders
- NOMS
- National Offender Management Service
- OHSCAP
- Older prisoner Health and Social Care Assessment and Plan
- OPL
- older prisoner lead
- PCT
- primary care trust
- PSO
- Prison Service Order
- SAP
- Single Assessment Process
- SD
- standard deviation
- SPSS
- Statistical Package for the Social Sciences
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.