Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 09/2001/09. The contractual start date was in October 2010. The final report began editorial review in November 2012 and was accepted for publication in February 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2013. This work was produced by Toye et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Aims
The aims of this study were to:
-
increase our understanding of patients’ experience of chronic non-malignant musculoskeletal (MSK) pain and therefore have an impact on quality of care
-
utilise existing research knowledge to improve understanding and, thus, best practice in patient care
-
contribute to the development of methods for qualitative research synthesis.
Chapter 2 Background
Chronic pain is common and universal; it occurs at all ages and in all populations and has been reported throughout recorded history.
p. 31
The alleviation of pain is a key aim of health care,2 yet pain can often remain a puzzle. 3 Chronic pain persists beyond the expected healing time and, by definition, is not amenable to routine treatments such as non-narcotic analgesia. 4 This is further complicated by the finding that pain is not always explained by a specific pathology and, even if a pathology is identified, the person will not necessarily develop pain. 3 Some suggest that chronic pain be acknowledged as a condition in its own right, rather than as a symptom of specific underlying disease. 3,5
Each year over 5 million people develop chronic pain. 6 Population estimates suggest that around 25% of adults around the world suffer with moderate or severe pain,1,7–10 and for between 6% and 14% of these adults the pain is severe and disabling. 3,11 We know that pain has a high impact on the individual’s physical, psychological and social well-being. 12 For example, 49% of patients with chronic pain experience depression, 25% lose their jobs and 16% feel that their chronic pain is so bad that they sometimes want to die. 6 Not only does pain have a major impact on participation in life, it also has an impact on ‘the economic balance-sheet of populations’ (p. 3). 1 Estimates suggest that the cost of chronic pain to the national economy may run into tens of billions of pounds each year. 2 Demographic changes leading to an increase in the older population are also likely to increase the need for appropriate health care. 3,13 MSK pain (notably back and joint pain) and headache are possibly the most predominant kinds of chronic pain. 3 MSK pain is pain associated with muscles, ligaments, tendons and bones. It can range from local pain (e.g. knee pain) to widespread bodily pain (e.g. fibromyalgia), making it difficult to accurately estimate how many people have chronic MSK pain. To further complicate this, those with severe MSK pain are also likely to suffer with pain in other parts of their body. 3,13 However, we know that the prevalence of MSK pain in the population is high and appears to be increasing,14 and this may have an impact on the provision of health care for those in pain. A greater understanding of patients’ experience of chronic pain could help to shape future health care for this group.
There are some signs that chronic pain is now being seen from a public health perspective. 1,15–17 The first English Pain Summit took place in November 2011, bringing together parliamentarians, health-care professionals, commissioners and patient groups to discuss chronic pain and pain services in the UK. 2 Chronic pain is also one of the four clinical priorities of the Royal College of General Practitioners for 2011–14. 18 The policy landscape suggests that access to effective pain relief is a fundamental human right that is often denied to those in chronic pain. However, there is a growing awareness that more could be done to support people in chronic pain to achieve the goal of living well with their pain. Recent policy published in England2 and further afield in the USA19 has begun to call for a cultural transformation in the way that people in chronic pain are viewed and treated and this meta-ethnography is set within this policy context.
One of the aims of qualitative research in health care is to understand the experience of illness and make sense of the complex processes involved. It aims to generate concepts that allow us to understand behaviour. 20 Qualitative interpretations allow us to ‘anticipate’ rather than predict what might happen in a particular situation. 20 It can thus lead to substantial improvements in health-care and policy decisions by enabling clinicians and policy-makers to understand the appropriateness and meaningfulness of interventions. The Cochrane Qualitative Research Methods Group acknowledges the importance of including qualitative findings within evidence-based health care and stresses that ‘evidence from qualitative studies can play an important role in adding value to systematic reviews for policy, practice and consumer decision-making’ (p. 571). 21 Syntheses of the existing body of qualitative research can also help to identify gaps in knowledge and to target these gaps. Insights from several meta-ethnographies in health care have contributed to a greater understanding of complex processes such as medicine taking,22 adherence to treatments for diabetes23 and use of antidepressants. 24 Excluding qualitative research from evidence-based practice may mean that we omit vital information from decisions related to policy and practice. 25
However, the proliferation of studies exploring the experience of chronic non-malignant MSK pain makes it difficult for clinicians and policy-makers to use this knowledge to inform practice and policy, and increases the danger that these findings are ‘doomed ultimately never to be visited’ (p. 786). 26 There is a growing body of qualitative research exploring patients’ experience of chronic MSK pain, yet there has been no attempt to systematically search the qualitative literature with the aim of increasing our conceptual understanding. The aim of qualitative synthesis is to systematically review and integrate the findings of qualitative research to increase our understanding.
Chapter 3 Methods
There are various methods for synthesising qualitative research. 27–30 Studies range from those aiming to describe qualitative findings to those that aim to be more interpretive and generate theory. As qualitative synthesis generally aims to move beyond description,31 it may be more useful to see these two approaches as two poles on a continuum. Meta-ethnography is an interpretive form of knowledge synthesis, proposed by Noblit and Hare,20 that aims to develop new conceptual understandings. As we aimed to produce a conceptual synthesis of qualitative findings related to chronic non-malignant MSK pain, we chose to use meta-ethnography as our method of qualitative synthesis. Some authors argue that meta-ethnography is more suited for synthesising a small number of studies. 23,32 Reviews of published qualitative syntheses show that, in the majority of syntheses using meta-ethnographic methods, the number of studies included ranges from 3 to 44. 25,28,32 There are only a very small number of meta-ethnographic syntheses that include a larger number of studies than this. 25,28 However, we knew that we were likely to find a large number of relevant studies and aimed to see if meta-ethnography could be used to synthesise when there is a large body of qualitative research.
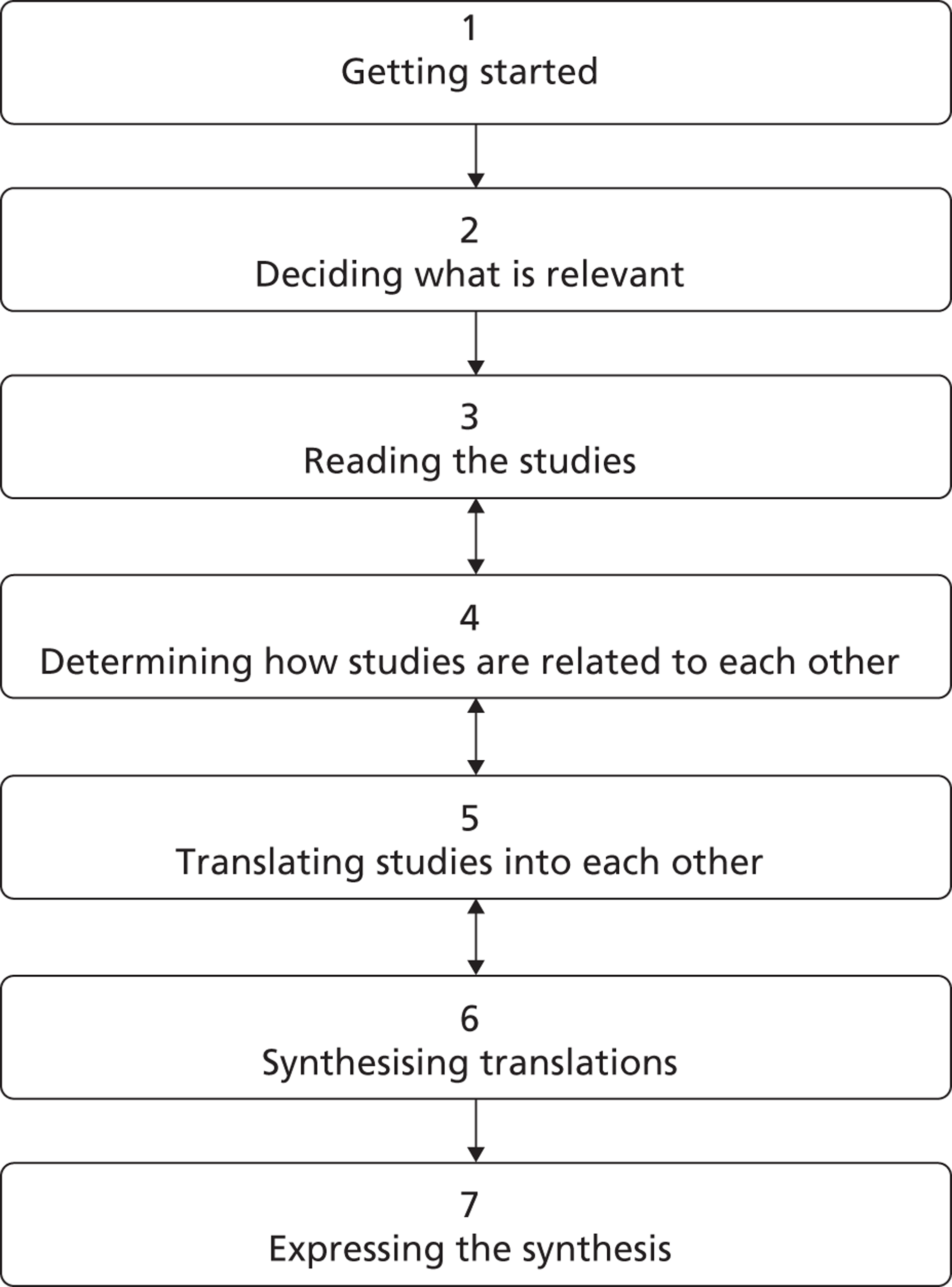
Meta-ethnography has been successfully used to synthesise qualitative studies in health care. In a recent Health Technology Assessment (HTA) report evaluating meta-ethnography, Campbell and colleagues28 identified 41 qualitative syntheses. Six of these explicitly employed meta-ethnography to synthesise findings and a further 16 described their method as meta-ethnographic. Other reviews of qualitative syntheses suggest that the number is much larger than this and increasing dramatically. 25,32 For example, Hannes and colleagues32 demonstrated that the number of qualitative syntheses in 2008 had doubled within 4 years, and that the most commonly used method of synthesis is meta-ethnography. We searched the medical databases [Allied and Complementary Medicine Database (AMED), EMBASE, Health Management Information Consortium (HMIC), MEDLINE, PsycINFO, British Nursing Index (BNI) and Cumulative Index to Nursing and Allied Health Literature (CINAHL)] using the terms meta AND ethnography (in title and abstract) and found 19 additional health-care studies published between 2009 and 2012 that explicitly used meta-ethnography. 24,33–50 This limited search may underestimate the number of qualitative syntheses now using meta-ethnography, but it seems clear that a growing number of researchers are using meta-ethnography to synthesise qualitative findings. Noblit and Hare20 propose seven stages to a meta-ethnography synthesis, which take the researcher from formulating a research idea to expressing the findings of research (Figure 1). These stages are not discrete but form part of an iterative research process.
1. Getting started
This stage of the research involves ‘finding something that is worthy of the synthesis effort’ (p. 27). 20 The decision to develop a conceptual synthesis of patients’ experience of chronic non-malignant MSK pain was an iterative process that was sparked at the British Pain Society Annual General Meeting in 2009 when two of the research team (FT and KS) first met. From here we approached other members of the team with a specific interest and expertise in chronic pain, qualitative research and research synthesis (Box 1). We began with informal meetings and telephone discussions, which culminated in a successful application to fund the project. The study protocol is provided in Appendix 1.
-
FT has a master’s degree in Archaeology and Anthropology and is also a qualified physiotherapist with an interest in chronic pain management. She has expertise in qualitative health research and methodology.
-
KS has a quantitative and qualitative health and pain research background and has used mixed methods in most of her research. She has experience of systematic reviews and qualitative research synthesis using meta-ethnography. Her professional background is in nursing.
-
NA is a doctoral-qualified nurse academic and practising pain nurse. He has completed syntheses of qualitative research using Joanna Briggs Institute Qualitative Assessment and Review Instrument (JBI-QARI) methodology.
-
MB has broad experience in systematic reviews. She has completed syntheses of qualitative research using JBI-QARI methodology. Her professional background is in nursing.
-
EC qualified as a nurse and throughout her 25-year research career has utilised mixed methods in her pain research.
-
KB is a qualified physiotherapist with 20 years of experience of running chronic pain management programmes. She is also an experienced researcher and uses mixed methods in most of her research.
The development of this meta-ethnography was both iterative and collaborative. Team members felt free to agree, disagree or change their mind within the safety of the group. The aim of considering alternative views within a team is not necessarily to agree on an interpretation but rather to enter into a dialectic process whereby our ideas are challenged and modified. This can lead to greater conceptual insight by challenging the boundaries of our own interpretations, just as a single word from another person can jog our memory or spark off insight when we had not expected it.
Throughout the project the project team met monthly either face-to-face or in Skype™ meetings (Skype Ltd Rives de Clausen, Luxembourg). We also met regularly with an advisory group that included two patient representatives and three NHS clinicians with experience in pain management (Box 2). The terms of reference for the advisory group are shown in Box 3.
-
A patient who has recent experience of treatment for non-malignant MSK pain from a NHS trust.
-
A patient with an interest in research from University/User Teaching and Research Action Partnership (UNTRAP) based at the University of Warwick. UNTRAP is a partnership between users of health and social care services and carers, the University of Warwick and the NHS. It aims to support the involvement of service users and carers in teaching and research.
-
A consultant in pain management who has been actively involved in policy decisions for chronic pain.
-
Two members of NHS staff working in chronic non-malignant pain.
-
To advise the project team and partner institutions on the project plans, including scope and range.
-
To review objectives and progress against plans and objectives.
-
To discuss and recommend any variations and developments.
-
To monitor the relationships between the current partners and any future additional institutions.
-
To review and discuss the quality of the research.
-
To help the researchers contribute to knowledge at a European and an international level.
2. Deciding what is relevant
This stage involved systematically searching for, screening and appraising potential studies to decide which to include in the synthesis. Qualitative syntheses do not aim to summarise the entire body of available knowledge, or make statistical inference from it. Qualitative syntheses are concerned with conceptual insight. Noblit and Hare20 strongly suggest that it is not necessary to include all published reports in a meta-ethnography: ‘Unless there is some substantive reason for an exhaustive search, generalizing from all studies of a particular setting yields trite conclusions’ (p. 28).
Campbell and colleagues28 also suggest that ‘omission of some papers is unlikely to have a dramatic effect on the results’ of qualitative synthesis (p. 35). However, for several reasons we decided to undertake a systematic search of published qualitative studies reporting patients’ experience of chronic MSK pain. Importantly, this project provided funding and the unique opportunity to identify the qualitative studies published in this area, and identify any gaps in knowledge. We wanted to produce a conceptual analysis with a weight of evidence that would have resonance with the health research community who were more used to quantitative systematic reviews. Finally, whereas previous meta-ethnographies in health care have included small numbers of studies,28 we knew that a systematic search in our chosen area would allow us to apply the methods of meta-ethnography to a large number of studies. Although Campbell and colleagues28 suggest that trying to include too many studies in a qualitative synthesis is unwieldy, we wanted the opportunity to see whether meta-ethnography could be useful in synthesising a large body of qualitative knowledge. With the ever-expanding body of qualitative research, qualitative syntheses are increasingly likely to identify large numbers of studies.
Scope of the search
-
Inclusions. Fully published reports of qualitative studies that explored adults’ experience of chronic non-malignant MSK pain. Chronic pain was defined as pain lasting for ≥ 3 months.
-
Exclusions. Cancer pain, neurological pain (e.g. stroke, multiple sclerosis), phantom pain, facial pain, head pain, dental/mouth pain, abdominal/visceral pain, menstrual/gynaecological pain, pelvic pain, samples in which the experience of the patient cannot be disentangled from that of others (e.g. carers, clinicians, partners), studies that explore chronic illness not explicitly chronic pain (e.g. rheumatoid arthritis studies that do not explicitly explore the experience of pain), samples that include conditions other than chronic MSK pain, auto-ethnography and studies that report individual case studies.
Search strategies
Strategies for identifying qualitative research may be unwieldy and often ‘trade-offs’ between recall and precision are necessary. 51 For this study we employed a qualified research librarian to help conduct the search. We chose several strategies:
Electronic databases
First, using a combination of free-text terms and thesaurus terms or subject headings we searched for relevant qualitative studies using six electronic bibliographic databases (MEDLINE, EMBASE, CINAHL, PsycINFO, AMED and HMIC). Studies were included up until the final search in February 2012 and there were no exclusions for dates. We used search terms available from the InterTASC Information Specialists’ Sub-Group (ISSG) Search Filter Resource (see www.york.ac.uk/inst/crd/intertasc/; accessed June 2013) to develop our search strategy. The ISSG is a group of information professionals supporting research groups producing technology assessments for the National Institute for Health and Care Excellence (NICE). The search was limited to studies of adults. As meta-ethnography relies on identifying and defining concepts within each study, we also chose to limit the search to English-language studies. The search syntax used for MEDLINE is shown as an example in Box 4 and the syntax for the other electronic databases is shown in Appendix 2.
Hand-searching
Hand-searching journals is an important strategy for comprehensively identifying relevant qualitative studies. 51–53 At an early team meeting we identified specific journals reporting significant numbers of qualitative research studies in full. These journals were Journal of Advanced Nursing, Social Science & Medicine, Qualitative Heath Research, Sociology of Health and Illness and Arthritis Care and Research. We subsequently added three additional journals for hand-searching (Disability and Rehabilitation, Scandinavian Journal of Caring Sciences and BMC Musculoskeletal Disorders) as these contributed the highest numbers of potential hits in the database searches (40, 20 and 15 studies respectively). We hand-searched the contents lists of these journals for 2001–11.
Reference lists
Finally, we searched the reference lists of all relevant qualitative studies for further potential studies. We did not specifically search the grey literature as we wanted to include fully published research reports only.
-
RESEARCH, QUALITATIVE/
-
ATTITUDE TO HEALTH/
-
INTERVIEWS AS TOPIC/
-
FOCUS GROUPS/
-
NURSING METHODOLOGY RESEARCH/
-
LIFE EXPERIENCES/
-
(qualitative OR ethno$OR emic OR etic OR phenomenolog).mp
-
(hermeneutic$OR heidegger$OR husserl$OR colaizzi$OR giorgi$OR glaser strauss).mp
-
(van AND kaam$OR van AND manen OR constant AND compar$).mp
-
(focus AND group$OR grounded AND theory OR narrative AND analysis OR lived AND experience$OR life).mp
-
(theoretical AND sampl$OR purposive AND sampl$OR ricoeur OR spiegelberg$OR merleau).mp
-
(field AND note$OR field AND record$OR fieldnote$OR field AND stud$).mp;
-
(participant$adj3 observ$).mp
-
(unstructured AND categor$OR structured AND categor$).mp
-
(maximum AND variation OR snowball).mp
-
(metasynthes$OR meta-synthes$OR metasummar$OR meta-summar$OR metastud$OR meta-stud$).mp
-
“action research”.mp
-
(audiorecord$OR taperecord$OR videorecord$OR videotap$).mp
-
exp PAIN/
-
exp ARTHRITIS, RHEUMATOID/
-
exp FIBROMYALGIA/
-
exp OSTEOARTHRITIS/
-
MUSCULOSKELETAL DISEASES/
-
exp ARTHRITIS/
-
1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 3 OR 14 OR 15 OR 16 OR 17 OR 18
-
19 or 20 or 21 or 22 or 23 or 24
-
25 AND 26
-
cancer.ti,ab
-
27 NOT 28
-
29 [Limit to: English Language and Humans and (Age Groups All Adult 19 plus years)];
Screening
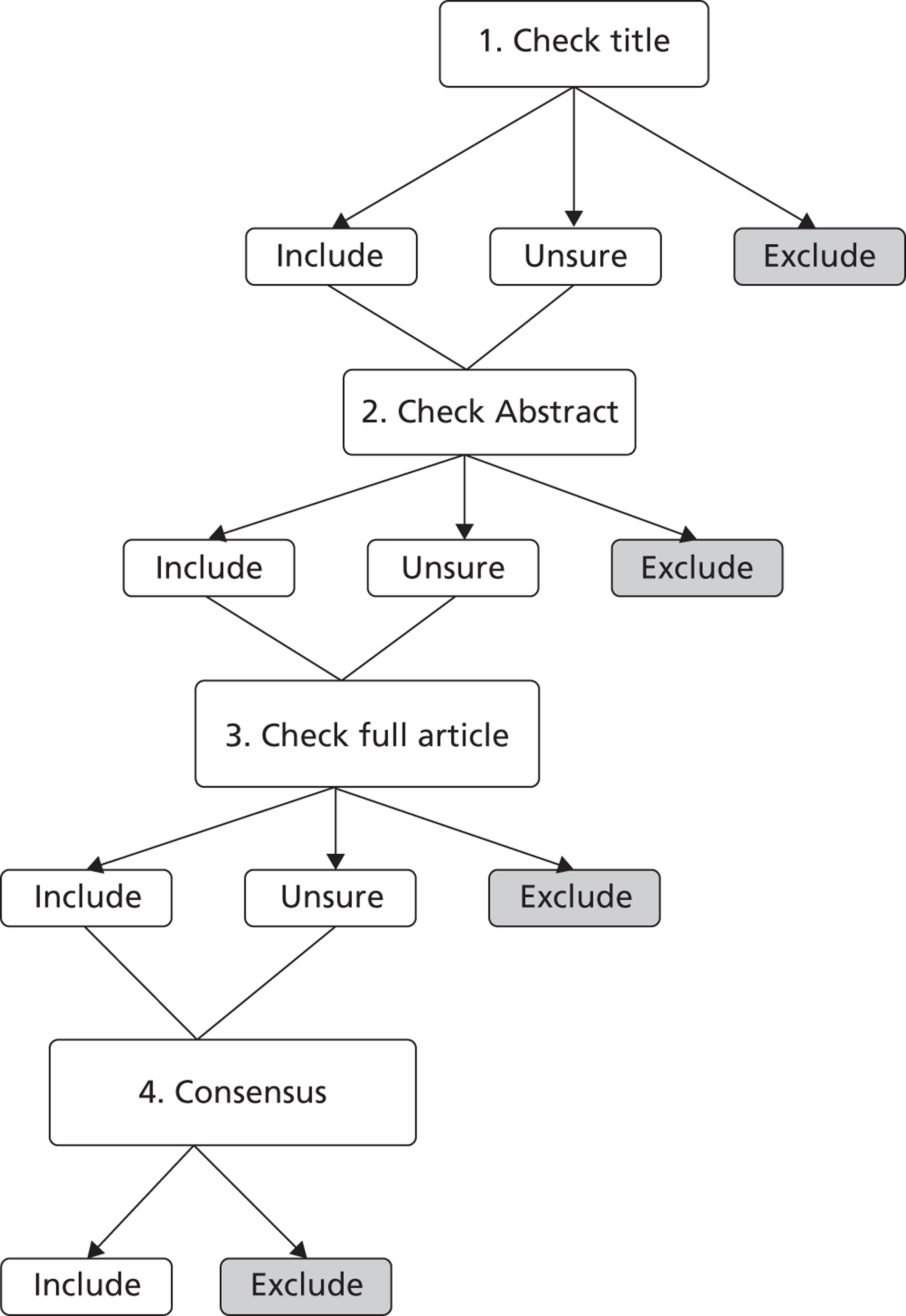
Once we had identified potential studies we adapted the process as outlined by Sandelowski and Barroso27 to exclude articles that did not meet the inclusion criteria. The stages of screening are shown in Figure 2. A research librarian and researcher (FT) screened the titles of the identified articles. If they were uncertain whether to include a study after reading the title, FT read the abstract. If she was still uncertain about inclusion, the full text was checked by two researchers. If they remained uncertain the article was sent to the full team for a consensus decision.
FIGURE 2.
Process for screening articles from the searches.
Quality appraisal
The use of quality criteria for qualitative research is widely debated. 54–58 There are now many suggested frameworks for appraising the quality of qualitative research, yet no consensus on what makes a qualitative study ‘good’ or ‘good enough’. 28,57 Although it is clear that structured checklists do not produce consistent judgements in qualitative research appraisal,57 these checklists may be useful in providing a focus for discussions. 28 Some researchers suggest that we attempt to distinguish ‘fatal’ methodological flaws in qualitative systematic reviews. 57,58 Others argue that quality appraisal should not be used at all to exclude studies from qualitative synthesis. 31 As appraisal tools tend to focus on method, some argue that excluding studies on this basis may mean that insightful studies are excluded. 28 However, although Campbell and colleagues28 suggest that studies should not be excluded on the grounds of quality, they do not recommend ‘abandoning appraisal’ altogether.
To be utilised within a meta-ethnography, a study must provide an adequate description of its concepts (Pope C, Britten N. Workshop on qualitative synthesis and meta-ethnography, course on meta-ethnography at Oxford Brookes University, June 2009, personal communication with FT, and references 20 and 28). We agreed that conceptual insight was fundamental to meta-ethnography, but also felt that papers should be reported ‘well enough’ methodologically to allow us to make a judgement about the inductiveness of the findings. In summary, we felt that we needed some assurances that a report was inductive and grounded in patients’ experience. To provide a focus for team discussion, the team decided to use checklists to assist quality appraisal. We did not intend to use a particular score as a cut-off point, but wanted to explore the utility of these scores for quality appraisal in qualitative synthesis. We used three methods of appraisal. First, we used the questions developed by the Critical Appraisal Skills Programme (CASP) for appraising qualitative research59 (Box 5), which have been used for appraising the quality of studies for meta-ethnography. 23,60,61 The CASP tool consists of 10 questions to consider when appraising qualitative research. Although it was not designed to provide a numerical score, we wanted to explore whether a score could be used to assist quality appraisal for meta-ethnography. After some discussion, the team agreed to assign a numerical score to each question to indicate whether we felt that the CASP question had (1) not been addressed, (2) been addressed partially or (3) been extensively addressed. This gave each paper a score ranging from 10 to 30.
Second, as two team members (NA and MB) were experienced in the use of the JBI-QARI in systematic reviews of evidence,62 we used this alongside the CASP tool as an alternative appraisal tool to stimulate discussion. The JBI-QARI also consists of 10 questions, which are rated as ‘yes’, ‘no’ or ‘unsure’ (Box 6). After rating each question the reviewer then makes the decision to include or exclude the paper. Early in the appraisal process we agreed that the JBI-QARI did not add anything further to the CASP tool with regard to the final decision on inclusion. However, for completeness we continued to grade each paper.
Finally, we categorised each paper as a key paper (conceptually rich and could potentially make an important contribution to the synthesis), a satisfactory paper, a paper that is irrelevant to the synthesis or a methodologically fatally flawed paper. 57 This method has also been used to determine inclusion of studies into meta-ethnography. 24 The concepts ‘fatally flawed’, ‘satisfactory’ and ‘key paper’ have not been defined but are global judgements made by a particular appraiser that comprise several unspecified factors.
-
Was there a clear statement of the aims of the research?
-
Is a qualitative methodology appropriate?
-
Was the research design appropriate to address the aims of the research?
-
Was the recruitment strategy appropriate to the aims of the research?
-
Were the data collected in a way that addressed the research issue?
-
Has the relationship between researcher and participants been adequately considered?
-
Have ethical issues been taken into consideration?
-
Was the data analysis sufficiently rigorous?
-
Is there a clear statement of findings?
-
How valuable is the research?
-
Is there congruity between the stated philosophical perspective and the research methodology?
-
Is there congruity between the research methodology and the research question or objectives?
-
Is there congruity between the research methodology and the methods used to collect data?
-
Is there congruity between the research methodology and the representation and analysis of data?
-
Is there congruity between the research methodology and the interpretation of results?
-
Is there a statement locating the researcher culturally or theoretically?
-
Is the influence of the researcher on the research, and vice versa, addressed?
-
Are participants, and their voices, adequately represented?
-
Is the research ethical according to current criteria or, for recent studies, is there evidence of ethical approval by an appropriate body?
-
Do the conclusions drawn in the research report flow from the analysis, or interpretation, of the data?
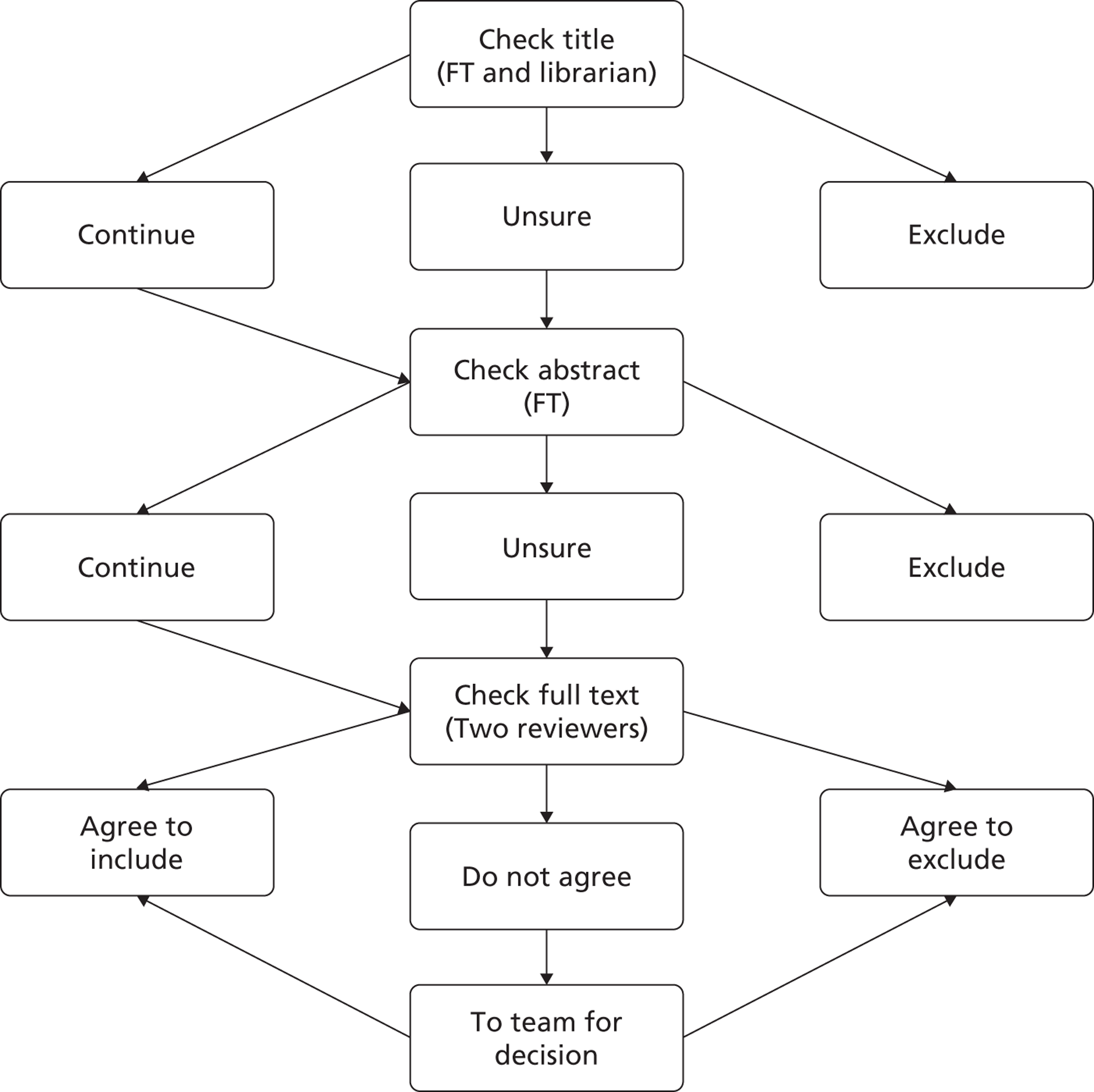
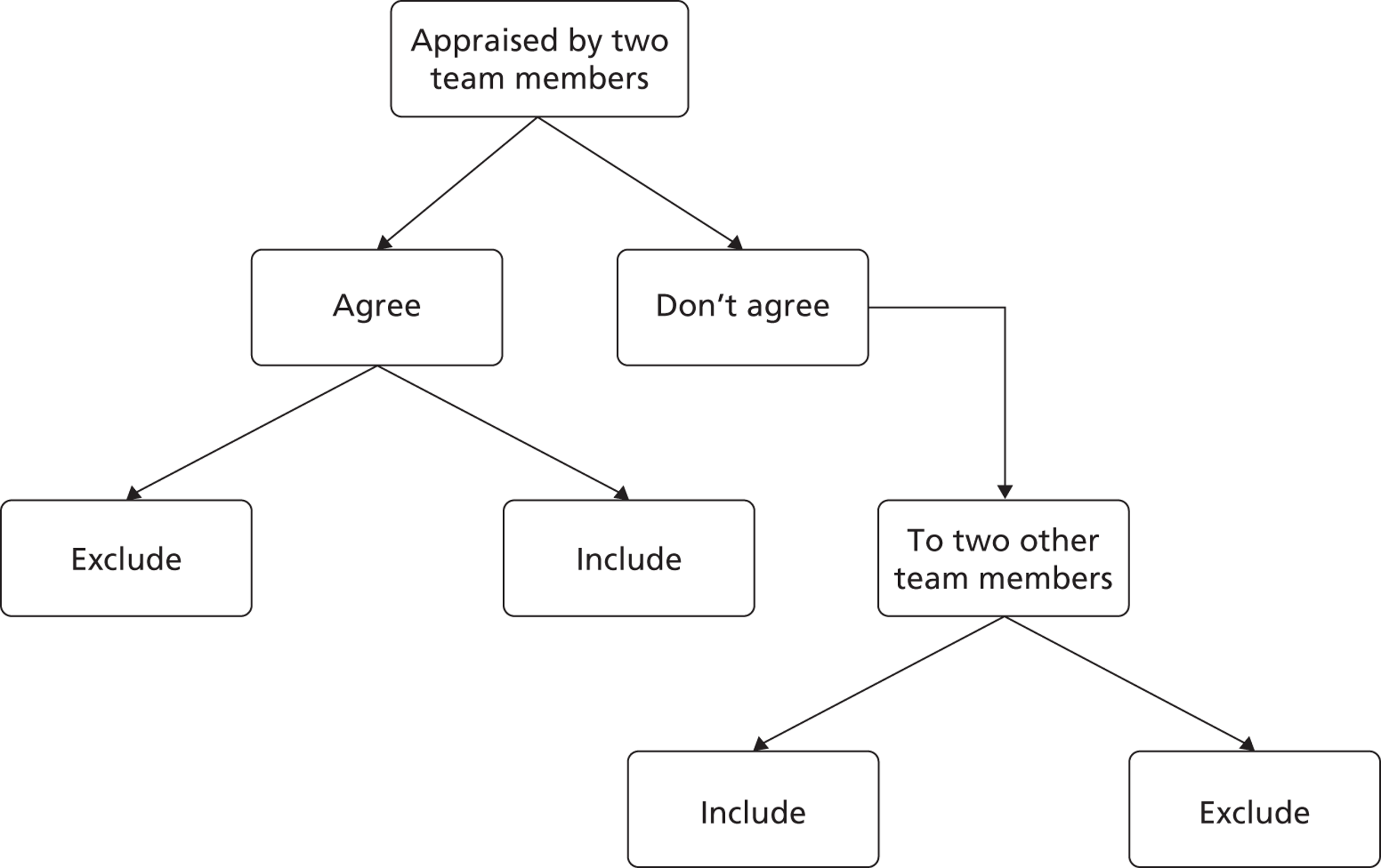
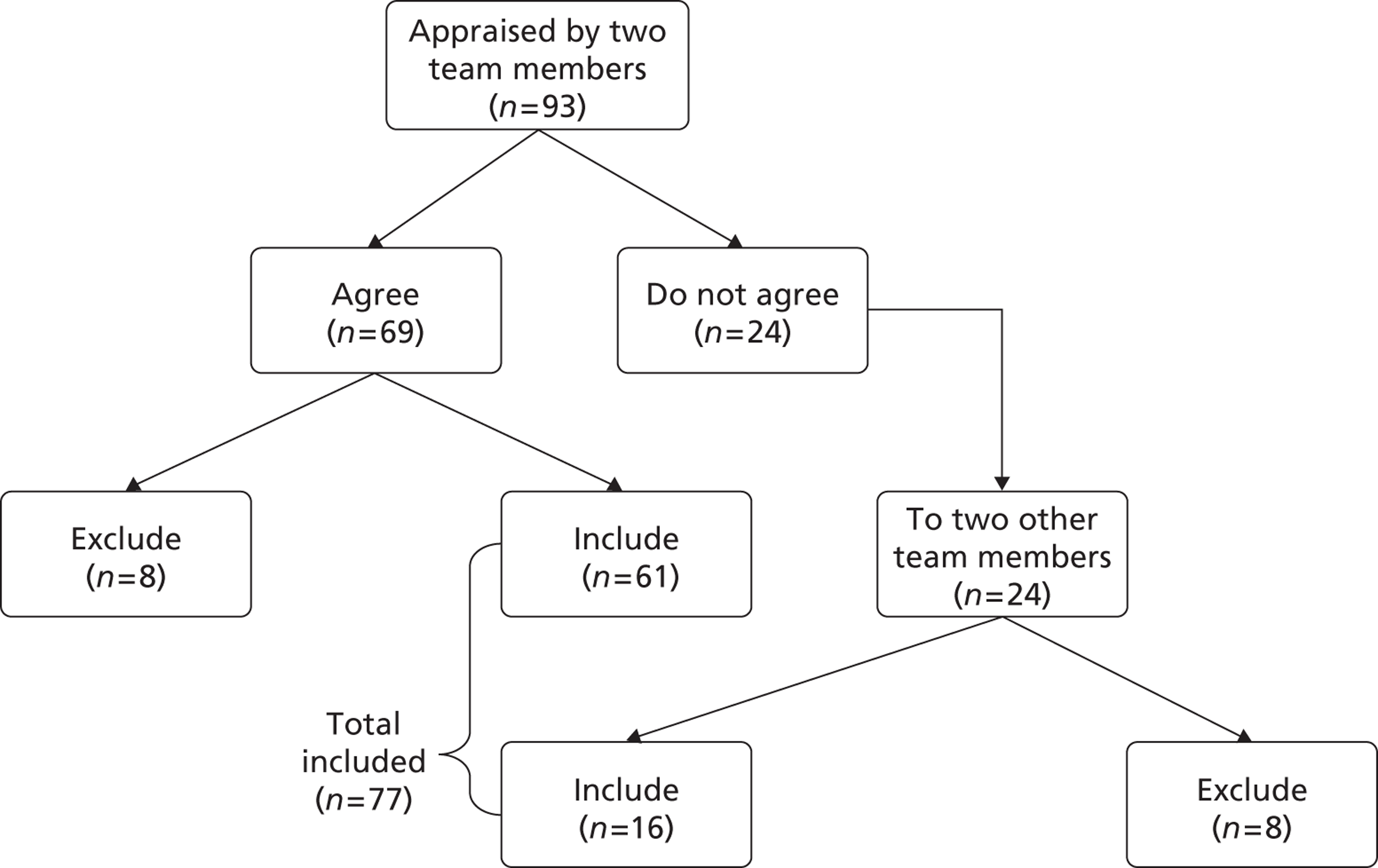
To test and refine the appraisal process each team member independently appraised the first 10 relevant studies identified and met to discuss their decisions. Two team members (FT and JA) appraised all subsequent papers and, if they were unable to reach an agreement, the paper was sent to two other team members to make a final decision (Figure 3). Team members were rotated so that they did not always appraise papers with the same person.
FIGURE 3.
Process for appraising papers.
3. Reading the studies
This stage of meta-ethnography involves thoroughly reading and rereading the studies to identify and describe the concepts. This requires ‘extensive attention to the details in the accounts’ (p. 28). 20 Thorough reading continues throughout all phases of meta-ethnography rather than being a discrete phase.
After the first reading, FT uploaded a PDF version of each complete study into NVivo 9 software (QSR International, Southport, UK) for analysing qualitative data. This allowed her to reread the primary research findings throughout all stages of analysis and compare the original interpretations to developing ideas. NVivo 9 allowed FT to collect, organise and analyse a large body of knowledge by ‘coding’ findings from the results and discussion sections of papers under ‘nodes’. Findings can be coded under several nodes simultaneously and the overlap between coding can be easily observed. This is particularly useful for team analysis as it allows the researcher to easily make a record of how each team member has coded data, whilst continuing to return to the original articles. NVivo 9 also allows researchers to write memos and link these memos to specific data to keep track of developing ideas and theories. FT classified each study on NVivo 9 so that the team could identify the following study characteristics: author, journal, year of publication, type of pain, number and age of participants, source and country of participants (e.g. pain clinic in UK), method of data collection (e.g. interviews) and methodological approach (e.g. grounded theory).
4. Determining how studies are related to each other
The purpose of careful reading in meta-ethnography is to identify and describe the ‘metaphors’ or concepts in studies and ‘translate’ or compare them with those in other studies. This is fundamental to meta-ethnography because concepts are the raw data of the synthesis. This stage involves creating ‘a list of key metaphors, phrases, ideas and/or concepts’ (p. 28). 20 However, although meta-ethnography requires clearly articulated concepts, it can sometimes be difficult to decipher these concepts through the description, in other words to see ‘the wood through the trees’. For example, the reader may find him- or herself attempting to recode findings or to condense them into higher conceptual categories to make sense of them. One of the aims of qualitative analysis is to develop conceptual categories that help us to understand an experience, rather than just describe that experience. 63 We describe a concept as a meaningful idea that develops by comparing particular instances. Fundamentally, concepts must explain not just describe the data.
However, as the act of description itself requires a level of interpretation, it can be difficult to decipher a concept; it may be more useful to understand ‘description’ and ‘concept’ as two poles on a spectrum. Campbell and colleagues28 recognise this difficulty: ‘It became apparent that the distinction between findings and concepts was neither simple to make nor useful, and because it was felt to be unnecessary it was abandoned’ (p. 55).
Sandelowski and Barroso27 also recognise the complexity of synthesising qualitative findings when levels of interpretation can range from thematic surveys, which make some effort to ‘move beyond a list’, to ‘fully integrated explanations’ of social phenomena (p. 145). Schütz’s64 concept of first- and second-order constructs is frequently used in meta-ethnography studies to distinguish the data of meta-ethnography. 28 Schütz makes a distinction between (1) first-order constructs (the participants’ ‘common sense’ interpretations in their own words) and (2) second-order constructs (the researchers’ interpretations based on first-order constructs). The ‘data’ of meta-ethnography are second-order constructs. In meta-ethnography, these second-order constructs are then further abstracted to develop third-order constructs (the researchers’ interpretations of the original authors’ interpretations). However, the distinction between first- and second-order constructs is somewhat ‘unclear’. 60 Importantly, although first-order constructs are often presented in meta-ethnographies to represent the patients’ ‘common sense’ interpretations in their own words, it is important to remember that these words are chosen by the researchers to illustrate their second-order interpretations. Our approach deviates from that of other meta-ethnographies in that we chose to base our synthesis entirely on second-order constructs. Specifically, we made the decision to only include concepts that we felt were clearly articulated. We did not attempt to ‘reorganise’ findings, but excluded data from analysis if we could not decipher a concept. We made this decision because of the methodological issues surrounding the reorganisation of data from qualitative research. The second-order interpretation is based on a body of knowledge accessed through fieldwork. Therefore, attempts to reorganise findings without access to the wider body of knowledge might not illuminate the conceptual interpretation originally intended. In other words, we could argue that attempts at reorganisation are not grounded in the body of knowledge. We therefore made the decision to define the second-order constructs and not to include findings for which we could not decipher a concept.
A collaborative approach to interpreting second-order constructs
A fundamental issue with deciphering second-order constructs is that readers interpret concepts in light of their own experience. Thus, different readers may suggest different interpretations. 20 Thus, a meaningful idea for one researcher may not be meaningful for another; one reader might see a concept whereas another might see no more than a description. The reader makes a personal judgement about whether there is a relevant concept and how to describe it. The unique methodological variance of our approach was to take a collaborative approach to interpreting second-order constructs and, thus, challenge our individual interpretations. In this way we aimed to consider alternative interpretations and ensure that interpretation of second-order constructs from the primary papers remained grounded in the originating studies. Paterson and colleagues65 advocate the benefits of collaborative endeavours for qualitative syntheses, as collaboration ‘requires that researchers be willing and able to risk voicing opinions not shared by everyone else in the group’ (p. 28). In short, the interpretation of each second-order construct entering the analysis was negotiated and constructed collaboratively.
To do this, three members of the team (FT, JA and one other team member selected on rotation) read each paper to identify and describe their interpretation of each construct. The team then discussed and developed a collaborative interpretation of each second-order construct. Because of the scale of the study and the potential number of second-order constructs, our interpretations needed to combine clarity and precision in as few words as possible. We therefore used a combination of the authors’ description of the second-order construct (when it briefly and clearly described the construct) and our interpretation of the original construct (if the original was unclear or lengthy). Our collaborative interpretations form the raw data of our synthesis in the same way that interview narrative forms the ‘data’ of qualitative analysis. This approach allowed us to compile an inventory of concise interpretations of second-order constructs that we felt confident were grounded in the primary studies.
Untranslatable concepts
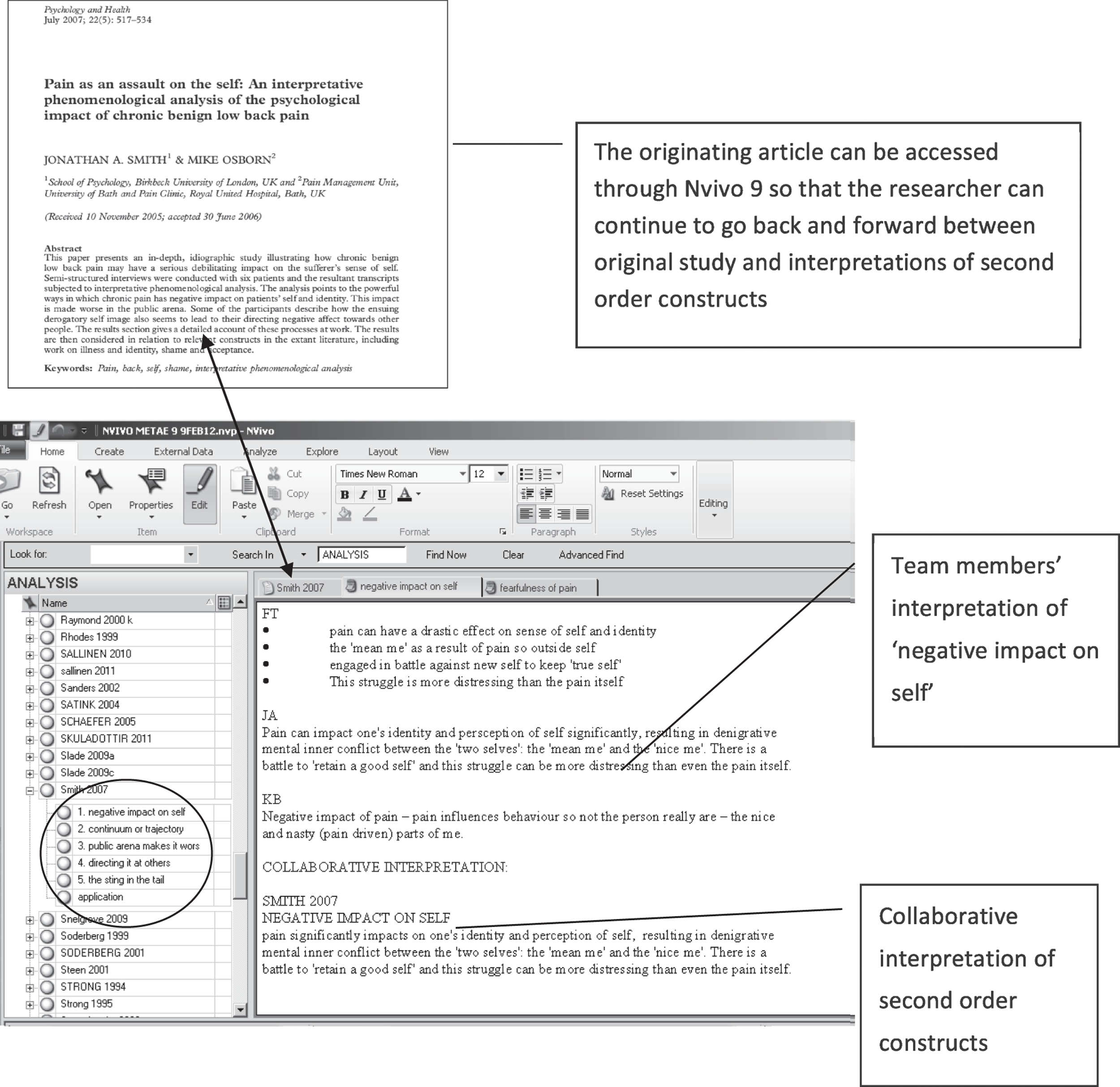
If team members agreed that there was no clear concept articulated, we labelled it ‘untranslatable’ and did not include it in the analysis. For example, in some cases the construct consisted of a descriptive account or list of items that we felt the urge to ‘recode’. In other words, there was no central idea pulling the description together. This did not mean that the study was rejected in its entirety; some studies combined clearly defined and ‘untranslatable’ concepts. If one team member deciphered a concept, we included it in the analysis, even if another member did not. Our aim was to challenge our interpretations, rather than reach consensus. Although this process was labour intensive, we wanted to be confident that the concepts were grounded in the original studies. We spent time reading and rereading the original papers to be certain that our interpretations were grounded in the original studies. The three individual interpretations and resulting collaborative interpretations were uploaded onto NVivo 9 (Figure 4). NVivo 9 allowed us to easily access the original studies whilst reading the attached memos and developing ideas.
FIGURE 4.
Developing collaborative interpretations of second-order constructs using NVivo 9. Published with permission from QSR International. The left window shows how each study was set up as a ‘node’ on NVivo 9, with each of its concepts as subnodes. For example, Smith 2007 contains the concepts ‘negative impact on self’, ‘continuum or hierarchy’, ‘public arena makes it worse’, ‘directing it at others’ and ‘the sting in the tail’. The right window shows a memo attached to the concept ‘negative impact on self’. This memo shows three team members’ interpretations of the concept and the final interpretation of this concept used in the analysis. Reproduced with permission from Taylor & Francis Ltd, URL: www.tandfonline.com: Smith JA, Osborn M. Pain as an assault on the self: an interpretative phenomenological analysis of the psychological impact of chronic benign low back pain. Psychol Health 2007;22 :517–35. 66
5. Translating studies into each other
The next stage in meta-ethnography involves exploring how the second-order constructs are related to each other, thus translating studies into each other. 20 This is achieved through the constant comparative method of grounded theory. 67 By constantly comparing constructs we begin to see similarities and differences between them and organise them into further abstracted conceptual categories with shared meanings. In other meta-ethnographies, for example those of Campbell and colleagues,28 researchers have used an index paper as a way of orienting the synthesis. 68 In these examples, concepts from an early or ‘index’ paper are compared with concepts from subsequent studies. However, there are methodological issues with using an index paper to begin analysis. One could argue that using an index paper is comparable to being constrained by a priori concepts. There is also the problem of how to decide which paper to use as an index paper. The chosen index paper can potentially have a dramatic effect on the resulting interpretation. How do we define a ‘classic’ paper? There is no consensus about what makes a study ‘good’,28,57 and suggested criteria for appraising quality vary considerably. 69 We also need to consider that we will not necessarily find the conceptually rich papers first. Qualitative analysis does not start when the full body of data is collected but continues alongside data collection; the process of searching and analysing is iterative. The decision to use an index paper may rest on the number of studies to be synthesised. We knew that this meta-ethnography would include a large number of studies and comparing concepts across studies from an index paper in this way was likely to be unwieldy.
All team members were given the full list of second-order constructs and asked to organise them, through constant comparison, into categories or ‘piles’ that shared meaning. Each team member wrote a description for each category or ‘pile’. This process of categorisation using constant comparison is integral to qualitative research. The team met to discuss their categories and definitions. We did not aim to reach consensus, but to collaboratively develop our interpretations over time. At team meetings members broke into separate groups and then regrouped to discuss findings. Conceptual categories were written up on a whiteboard and discussed. Although team members gave different labels to their categories, it became clear through discussion that there was an encouraging overlap in the definitions of categories. Table 1 gives the team categories for the MSK second-order constructs and illustrates the overlap in team categories. For example, the concept that later developed as ‘struggling to affirm self’ was labelled as ‘self and body’, ‘body in pain’, ‘body is alien’, ‘pain as alien’, ‘altered body’ and ‘body self’. If we found that second-order constructs did not ‘fit’ our developing conceptual categories, we went back to the original studies to challenge our interpretations and discussed the constructs within the group. We also went back to the original studies after the final model was developed to check for fit. If we still felt that a construct did not ‘fit’, we did not include it in the analysis.
| Conceptual categories for MSK | |||||
|---|---|---|---|---|---|
| FT | JA | KB | KS | NA | EC |
| Health-care professionals The system Medication |
The medical system | Expectations of health-care professionals | The system Health-care professionals Medication |
Health care as barrier | Health-care professionals |
| Self and body I am not me Relationship to body |
Body in pain Perceptions of self |
Body is alien Mind body image esteem Normal vs. abnormal |
Pain as alien Altered body Loss of self Normalising |
Body self Dualism |
Striving to be normal Who am I – sense of self |
| Thinking about future | Challenges of pain | Hope vs. despair | Hope vs. resignation Unpredictability |
Unpredictability and fear emotions | Impediments (various) |
| Making sense of pain | Patient explanations for pain | Medical model | Cause and treatment medical model Make sense of pain |
Making sense of pain | |
| Negotiating reciprocity and capability | Impact on relationships | Community Family Communication |
Relationships Social disruption |
Relationships Dependence Social withdrawal Isolation |
|
| Proving credibility | Perceptions of others | Stigma Acceptance |
Proving credibility Moral narrative |
Lack of understanding Validation and representation |
|
| Work benefits | Dealing with benefits system | Work and benefits | Work Benefits |
Work | Work |
| Trusting myself – becoming expert | Community Pain management Road to accepting new self |
Acceptance and self-management | Being with others is supportive Do it despite pain Moving forward |
Being strong Competence Learning to cope |
Managing self and moving forward Living alongside pain |
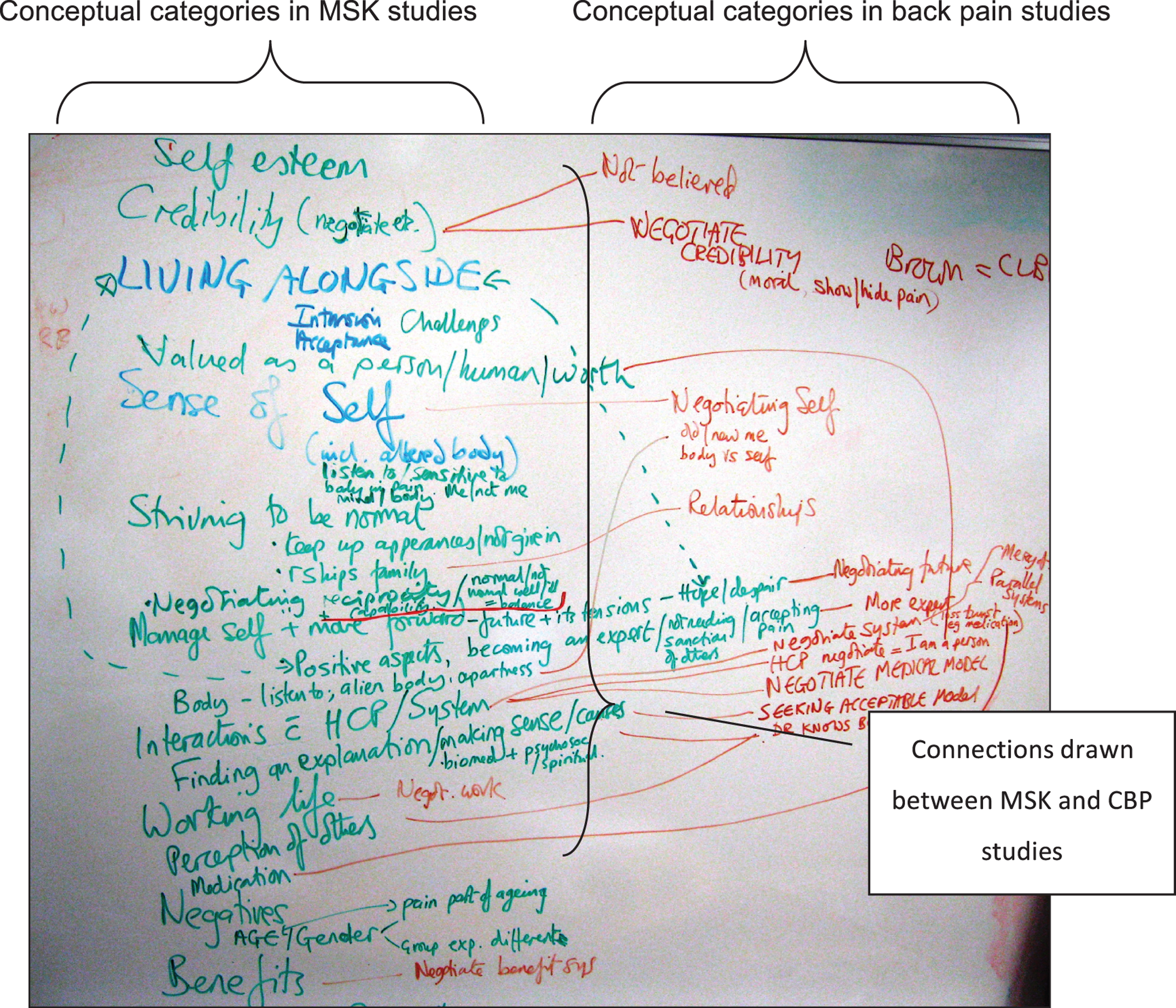
We kept the second-order constructs for fibromyalgia, chronic back pain (CBP) and all other MSK studies separate from each other so that we could explore any differences in conceptual categories between these groups. The process of categorising second-order constructs was repeated for MSK, fibromyalgia and CBP. After several team meetings we agreed to amalgamate MSK and CBP studies as the categories overlapped considerably. However, we decided to keep the fibromyalgia studies separate in the analysis as there were some differences in categorisation. Figure 5 shows how we compared and contrasted categories for MSK and CBP using a whiteboard. The same process was repeated for MSK and fibromyalgia.
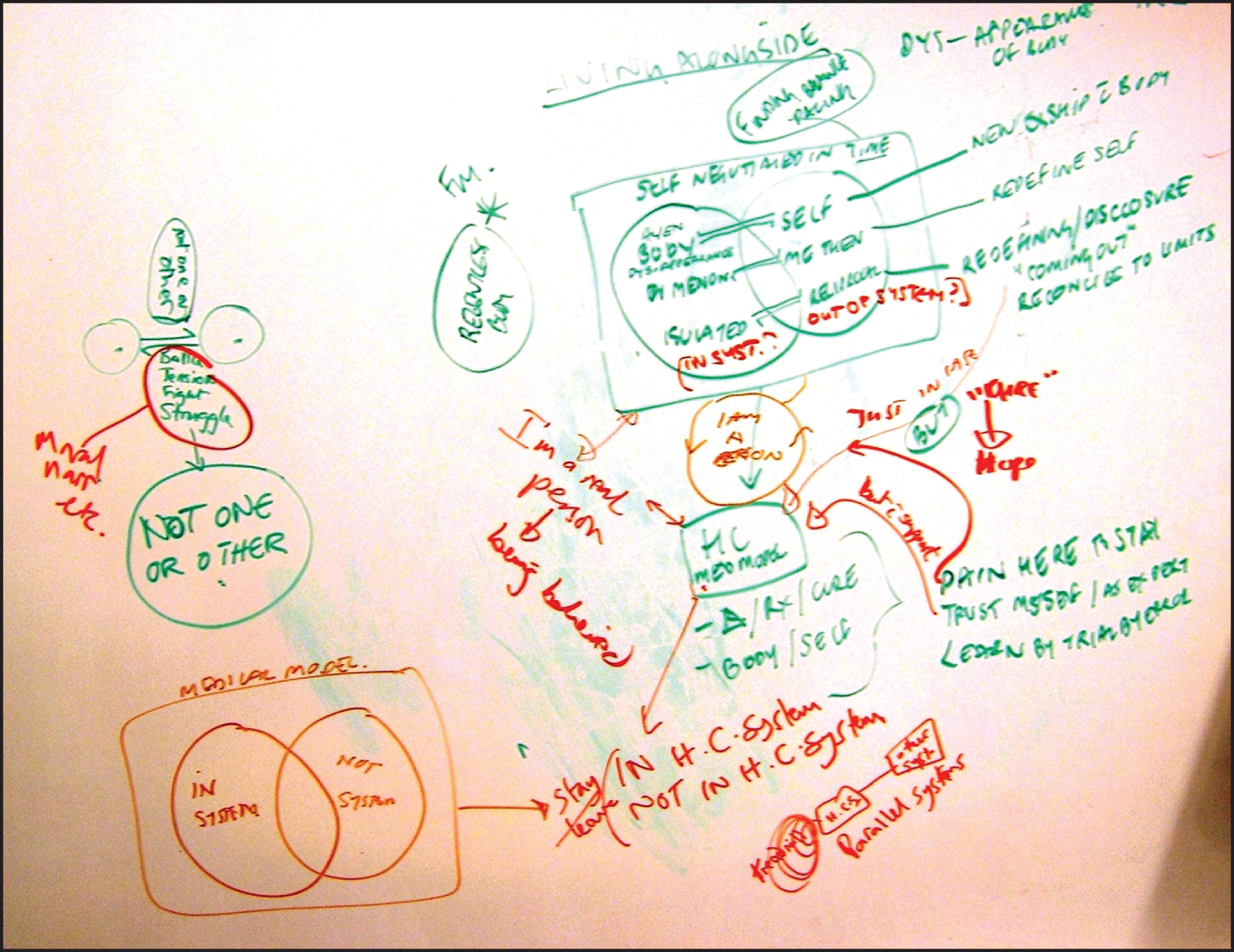
FIGURE 5.
Comparing the conceptual categories from CBP and MSK studies during team meetings using a whiteboard. This shows how the team compared categories that were developed from MSK and CBP second-order constructs. MSK categories are shown on the left and CBP categories are shown on the right. Connecting lines show links between categories.
Using NVivo 9 to assist analysis
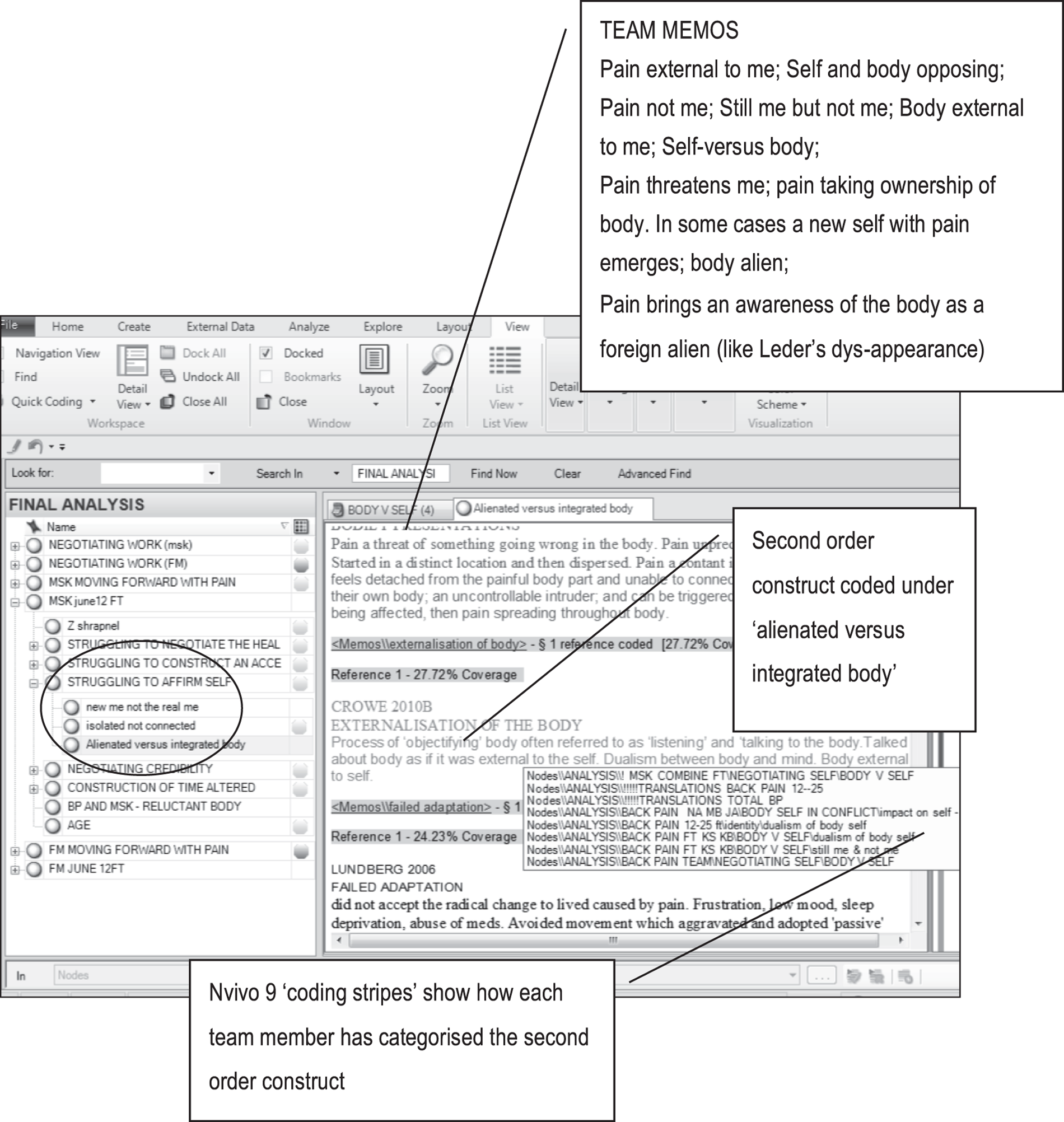
We combined the benefits of face-to-face team discussions with the benefits of using NVivo 9 software for qualitative analysis. NVivo is commonly used by qualitative researchers to assist analysis. However, not all qualitative researchers would choose to use computer software to organise their thoughts. We do not advocate a ‘right’ way of doing this, as it is a matter of personal preference. Some researchers prefer to use a more ‘hands-on’ approach with pen, paper and scissors; we also needed to consider that not all team or advisory group members had access to the computer software. Although NVivo 9 has the capacity to allow multiple researchers to simultaneously code onto a single database, we felt that because of the scale of the study this would be unwieldy, and therefore the principal investigator (FT) maintained and organised the NVivo 9 database. FT found it useful to code and organise the second-order constructs using NVivo 9. After each team meeting FT transferred the coding, categorising and supporting definitions and notes for each team member onto the NVivo 9 database (Figure 6). This allowed her to compare how each team member had categorised and defined conceptual categories and to return to the original article. Although the software has the capacity to produce models and graphics to support analysis, we found it more useful for team analysis to use a whiteboard when developing our conceptual models.
FIGURE 6.
Transferring team coding and team memos onto a NVivo 9 database. Published with permission from QSR International. The left screen shows the developing team categories for MSK second-order constructs. For example, the category ‘struggling to affirm self’ incorporates ‘new me not the real me’, ‘isolated not connected’ and ‘alienated vs. integrated body’. The right screen shows how NVivo 9 ‘coding stripes’ are used to identify how each team member has coded a particular second-order construct. In this example the construct ‘externalisation of the body’ has been coded by team members as ‘body vs. self’, ‘body–self in conflict’, ‘dualism of body–self’, ‘still me but not me’ and ‘negotiating body–self’. The team categories were brought together into the conceptual category ‘alienated vs. integrated body’.
6. Synthesising translations
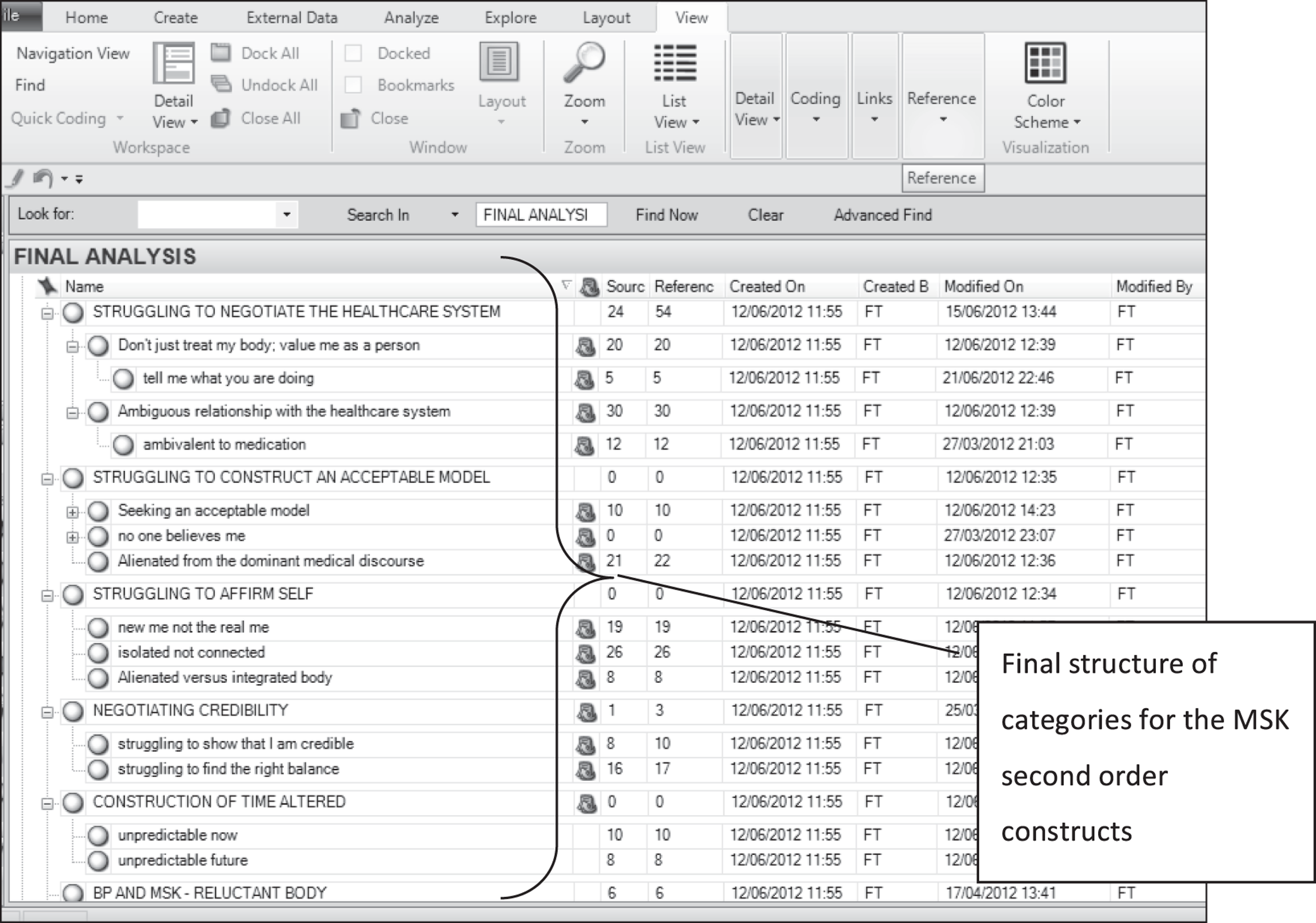
The next stage of meta-ethnography is to synthesise or make sense of the process of translation. Noblit and Hare20 suggest three genres of synthesis for meta-ethnography: (1) refutational (in which findings contradict each other), (2) reciprocal (in which findings are directly comparable) and (3) findings are taken together and interpreted as a line of argument. This third type of synthesis involves ‘making a whole into something more than the parts alone imply’ (p. 28). We intended to develop a line of argument synthesis. This is achieved by constantly comparing concepts and suggesting an interpretive order. In the words of Noblit and Hare:20 ‘We first translate the studies into one another. Then we develop a grounded theory that puts the similarities and differences between studies into interpretive order’ (p. 64).
Drawing on team discussions, and using NVivo 9 to continually compare concepts, categories and team memos, we developed a structure of categories that ‘made sense’ of the developing team analysis. Each team member then considered whether or not the structure reflected the discussions that had taken place. If a team member did not think that a particular second-order construct fit, we discussed this in meetings and made any necessary changes. Figure 7 shows how the final list of categories was developed using NVivo 9.
FIGURE 7.
Team coding structure for MSK using NVivo 9. Published with permission from QSR International. This illustrates the final structure of categories for the MSK second-order constructs on NVivo 9.
We found it useful to construct a diagram to develop and refine our line of argument. This diagram was developed collaboratively over time and was the focus for team discussions during this phase. Figure 8 illustrates the development of this model in team meetings using a whiteboard. Several amended versions of this diagram were created until we arrived at a model that reflected our final interpretation.
FIGURE 8.
Developing a line of argument using a whiteboard.
7. Expressing the synthesis
This phase concerns the dissemination of the research findings to maximise their impact.
Chapter 4 Results
Deciding what is relevant
Search and screening
The results of the systematic search are shown in Figure 9. We screened the full text of 321 potentially relevant studies and excluded 228 for the following reasons:
-
chronicity of pain was not explicit in the sample description82–122
-
did not explicitly state that it was specifically about MSK pain173–209
-
included perceptions of others such as family members, carers, clinicians210–243
-
did not meet the specific scope, for example explored perceptions of fatigue or exercise266–280
-
explored the experience of chronic disease rather than chronic pain. 281–295
FIGURE 9.
Results of the search strategy.
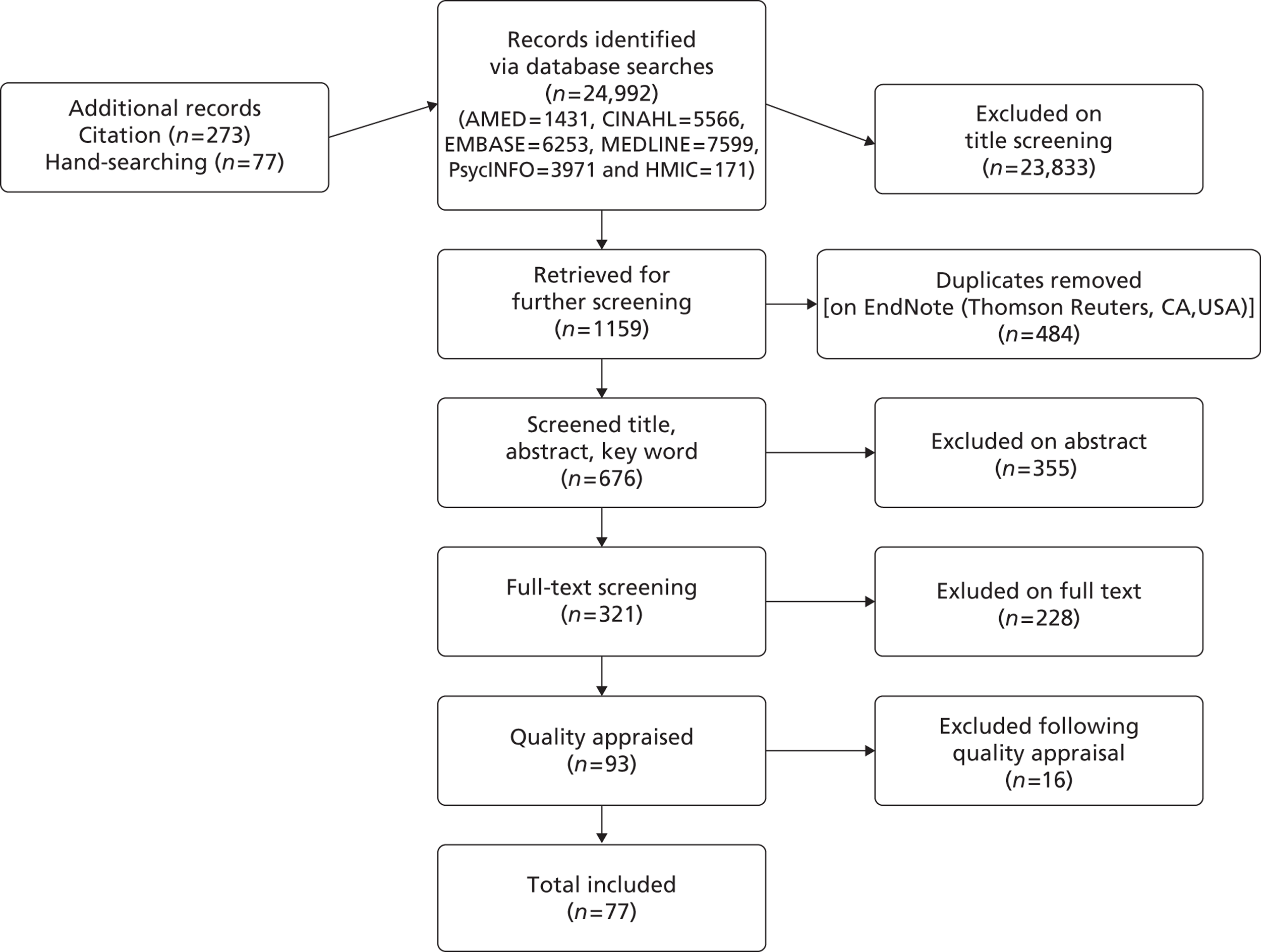
Ninety-three studies66,296–387 met the study scope and were appraised (see Figure 9).
Quality appraisal
Figure 10 shows that we appraised 93 studies and excluded 16,296–311 meaning that we included 77 studies66,312–387 in the meta-ethnography. There was a wide range in CASP scores between FT and JA, from –12 to 5. Table 2 shows the scores and ranks given to all papers appraised by the team.
FIGURE 10.
Results of quality appraisal by the team.
| Study | FT CASP score | FT rank | JA CASP score | JA rank | Difference in CASP score | Agree | Final decision |
|---|---|---|---|---|---|---|---|
| Aegler 2009312 | 26 | SAT | 25 | SAT | 1 | Yes | In |
| Allegreti 2010313 | 21 | SAT | 20 | SAT | 1 | Yes | In |
| Bair 2009314 | 22 | SAT | 24 | SAT | – 2 | Yes | In |
| Campbell 2007315 | 23 | SAT | 24 | SAT | – 1 | Yes | In |
| Campbell 2008316 | 25 | SAT | 23 | SAT | 2 | Yes | In |
| Cook 2000317 | 20 | SAT | 25 | SAT | – 5 | Yes | In |
| Coole 2010318 | 22 | SAT | 21 | SAT | 1 | Yes | In |
| Coole 2010319 | 24 | SAT | 22 | SAT | 2 | Yes | In |
| Coole 2010320 | 23 | SAT | 21 | SAT | 2 | Yes | In |
| Cooper 2009321 | 21 | SAT | 22 | SAT | – 1 | Yes | In |
| Cooper 2008322 | 21 | SAT | 23 | SAT | – 2 | Yes | In |
| Crowe 2010323 | 21 | SAT | 24 | SAT | – 3 | Yes | In |
| De Vries 2011324 | 23 | SAT | 27 | KP | – 4 | Yes | In |
| Dickson 2003325 | 23 | SAT | 23 | SAT | 0 | Yes | In |
| Dragesund 2008326 | 22 | SAT | 23 | SAT | – 1 | Yes | In |
| Gustaffson 2004327 | 23 | SAT | 23 | SAT | 0 | Yes | In |
| Hallberg 1998328 | 22 | SAT | 20 | SAT | 2 | Yes | In |
| Hallberg 2000329 | 23 | SAT | 20 | SAT | 3 | Yes | In |
| Harding 2005330 | 25 | SAT | 25 | KP | 0 | Yes | In |
| Hunhammar 2009331 | 21 | SAT | 21a | SAT | 0 | Yes | In |
| Johansson 1996332 | 23 | SAT | 21 | SAT | 2 | Yes | In |
| Johansson 1997333 | 20 | SAT | 21 | SAT | – 1 | Yes | In |
| Johansson 1999334 | 20 | SAT | 21 | SAT | – 1 | Yes | In |
| Lachapelle 2008335 | 24 | SAT | 22 | SAT | 2 | Yes | In |
| Liddle 2007336 | 22 | SAT | 27 | SAT | – 5 | Yes | In |
| Lofgren 2006337 | 21 | SAT | 24 | SAT | – 3 | Yes | In |
| Lundberg 2007338 | 24 | SAT | 25a | SAT | – 1 | Yes | In |
| Madden 2006339 | 22 | SAT | 22 | SAT | 0 | Yes | In |
| Mannerkorpi 1999340 | 22 | SAT | 22a | SAT | 0 | Yes | In |
| Mengshoel 2004341 | 23 | KP | 25 | KP | – 2 | Yes | In |
| Osborn 1998342 | 28 | KP | 24 | KP | 4 | Yes | In |
| Osborn 2006343 | 25 | KP | 22 | SAT | 3 | Yes | In |
| Osborn 2008344 | 27 | SAT | 27a | KP | 0 | Yes | In |
| Patel 2007345 | 20 | SAT | 20 | SAT | 0 | Yes | In |
| Paulson 2002346 | 26 | SAT | 27 | KP | – 1 | Yes | In |
| Paulson 2002347 | 20 | SAT | 23 | SAT | – 3 | Yes | In |
| Raheim 2006348 | 24 | SAT | 23 | SAT | 1 | Yes | In |
| Raymond 2000349 | 20 | SAT | 24 | SAT | – 4 | Yes | In |
| Rhodes 1999350 | 20 | KP | 22 | KP | – 2 | Yes | In |
| Sallinen 2010351 | 22 | SAT | 24 | SAT | – 2 | Yes | In |
| Sallinen 2011352 | 22 | SAT | 24 | SAT | – 2 | Yes | In |
| Sanders 2002353 | 24 | KP | 23 | SAT | 1 | Yes | In |
| Satink 2004354 | 19b | SAT | 25 | SAT | – 6 | Yes | In |
| Skuladottir 2011355 | 20 | SAT | 22a | SAT | – 2 | Yes | In |
| Slade 2009356 | 21 | SAT | 24 | SAT | – 3 | Yes | In |
| Slade 2009357 | 22 | SAT | 24 | SAT | – 2 | Yes | In |
| Smith 200766 | 28 | KP | 24 | KP | 4 | Yes | In |
| Snelgrove 2009358 | 25 | KP | 23 | KP | 2 | Yes | In |
| Soderberg 1999359 | 20 | SAT | 23 | SAT | – 3 | Yes | In |
| Soderberg 2001360 | 20 | SAT | 23 | SAT | – 3 | Yes | In |
| Sturge-Jacobs 2002361 | 22 | SAT | 24 | KP | – 2 | Yes | In |
| Teh 2009362 | 22 | SAT | 25 | SAT | – 3 | Yes | In |
| Toye 2010363 | 23 | SAT | 22 | SAT | 1 | Yes | In |
| Toye 2012364 | 23 | SAT | 22 | SAT | 1 | Yes | In |
| Toye 2012365 | 23 | SAT | 22 | SAT | 1 | Yes | In |
| Undeland 2007366 | 22 | SAT | 20 | SAT | 2 | Yes | In |
| Walker 1999367 | 22 | SAT | 26 | KP | – 4 | Yes | In |
| Walker 2006368 | 21 | SAT | 21 | SAT | 0 | Yes | In |
| Werner 2003369 | 24 | KP | 22 | SAT | 2 | Yes | In |
| Werner 2003370 | 24 | KP | 22 | SAT | 2 | Yes | In |
| Werner 2004371 | 21 | KP | 21 | SAT | 0 | Yes | In |
| Afrell 2007372 | 19 | FF | 20 | SAT | – 1 | No | In |
| Arnold 2008373 | 18 | FF | 22 | SAT | – 4 | No | In |
| Crowe 2010374 | 18 | FF | 24 | SAT | – 6 | No | In |
| Cunningham 2006375 | 19 | FF | 20 | SAT | – 1 | No | In |
| De Souza 2011376 | 18 | FF | 23 | SAT | – 5 | No | In |
| Gullacksen 2004377 | 18 | FF | 19 | SAT | – 1 | No | In |
| Hellström 1999378 | 22 | SAT | 19 | FF | 3 | No | In |
| Holloway 2007379 | 22 | SAT | 17 | FF | 5 | No | In |
| Kelley 1997380 | 14 | FF | 18 | SAT | – 4 | No | In |
| Lempp 2009381 | 18 | FF | 21 | SAT | – 3 | No | In |
| Liedberg 2002382 | 18 | FF | 22 | SAT | – 4 | No | In |
| Paulson 2001383 | 18 | FF | 25 | SAT | – 7 | No | In |
| Schaefer 2005384 | 14 | FF | 22 | SAT | – 8 | No | In |
| Steen 2001385 | 18 | FF | 21 | SAT | – 3 | No | In |
| Strong 1994386 | 17 | FF | 23 | SAT | – 6 | No | In |
| Strong 1995387 | 17 | FF | 20 | SAT | – 3 | No | In |
| Busch 2005296 | 19 | FF | 19 | FF | 0 | Yes | Out |
| Chew 1997297 | 16 | FF | 19 | FF | – 3 | Yes | Out |
| De Souza 2007299 | 17 | FF | 19 | FF | – 2 | Yes | Out |
| Holloway 2000310 | 16b | FF | 14 | FF | 2 | Yes | Out |
| May 2000309 | 13 | FF | 19 | FF | – 6 | Yes | Out |
| Morone 2008301 | 17 | FF | 19 | FF | – 2 | Yes | Out |
| Silva 2011305 | 17b | FF | 19 | FF | – 2 | Yes | Out |
| Sokunbi 2010306 | 19 | FF | 19 | FF | 0 | Yes | Out |
| Cudney 2002298 | 18 | FF | 21a | SAT | – 3 | No | Out |
| Liedberg 2006300 | 19 | FF | 22 | SAT | – 3 | No | Out |
| Raak 2006302 | 16 | FF | 20 | SAT | – 4 | No | Out |
| Reid 1991303 | 16 | FF | 22 | KP | – 6 | No | Out |
| Schaefer 1995304 | 12 | FF | 24 | SAT | – 12 | No | Out |
| Schaefer 1997311 | 17 | FF | 20 | SAT | – 3 | No | Out |
| Tavafian 2008307 | 14b | FF | 20 | SAT | – 6 | No | Out |
| Wade 2003308 | 18 | FF | 25 | SAT | – 7 | No | Out |
Following study appraisal, FT and JA agreed on 69 of the 93 studies (61 included, eight excluded). We did not use a cut-off score for inclusion. FT and JA did not agree on 24 studies and these were sent to be appraised by two other members of the team (16 included, eight excluded). Table 3 shows the percentage agreement between FT and JA for each method of appraisal. Agreement between FT and JA ranged from 52% to 74% for the CASP questions and from 29% to 82% for the JBI-QARI questions. Agreement for the rankings ‘fatally flawed’, ‘satisfactory’ or ‘key paper’ was 62%. The median (range) scores for papers rated as ‘fatally flawed’, ‘satisfactory’ and ‘key paper’ are shown in Table 4. FT and JA agreed that five studies were key papers; FT graded a further five as key papers and JA graded a further seven as key papers (Table 5). Because of this low level of agreement, the category ‘key paper’ was not useful for the purpose of analysis. Although we had discussed the possibility of performing a form of ‘sensitivity analysis’ to determine whether or not our findings were altered if we included only key papers, lack of agreement over what a key paper was made this impossible; we also could not use the other scores to determine any particular level of evidence.
| Appraisal tool questions | % agreement between reviewers 1 and 2 |
|---|---|
| CASP 1 | 59 |
| CASP 2 | 74 |
| CASP 3 | 52 |
| CASP 4 | 57 |
| CASP 5 | 65 |
| CASP 6 | 67 |
| CASP 7 | 52 |
| CASP 8 | 60 |
| CASP 9 | 63 |
| CASP 10 | 55 |
| FF, SAT, KP ranking | 62 |
| JBI-QARI 1 | 50 |
| JBI-QARI 2 | 78 |
| JBI-QARI 3 | 82 |
| JBI-QARI 4 | 61 |
| JBI-QARI 5 | 57 |
| JBI-QARI 6 | 61 |
| JBI-QARI 7 | 29 |
| JBI-QARI 8 | 42 |
| JBI-QARI 9 | 66 |
| JBI-QARI 10 | 60 |
| JBI-QARI final decision | 74 |
| Rating | FT | JA |
|---|---|---|
| Fatally flawed | 17 (12–19) | 18 (14–19) |
| Satisfactory | 22 (19–27) | 22 (18–27) |
| Key paper | 24 (20–28) | 25 (22–27) |
Included studies
We included 77 papers in the meta-ethnography reporting 60 individual qualitative studies. The studies that produced more than one paper are indicated in Tables 6 and 7. Forty-nine papers (37 individual studies) explored the experience of people with chronic MSK pain. 66,312,323,325,326,330–334,336,338,342–345,350,353–358,362–365,367,372,374,376,379,385–387 Twenty-eight papers (23 individual studies) explored the experience of people with fibromyalgia. 324,327–329,335,337,339–341,346,349,351,352,359–361,366,373,375,377,378,380–384 A description of these studies is provided in Tables 6 and 7, showing for each study the age range and source of participants, the country where the study was carried out, the method of data collection and the methodology used.
| Study | Age range (years) | Source of participants | Condition | Country | n | Male, n | Data collection | Methodologya |
|---|---|---|---|---|---|---|---|---|
| Aegler 2009312 | 29–61 | PMP | MSK | Switzerland | 8 | 3 | Semistructured interviews | Thematic analysis |
| Afrell 2007372 | 30–72 | PC, PMP, pain clinic | MSK | Sweden | 20 | 7 | Semistructured interviews | Phenomenology |
| Allegreti 2010313 | 28–72 | PC | CBP | USA | 23 | 12 | Semistructured interviews | Thematic analysis |
| Bair 2009314 | 27–84 | RCT | MSK | USA | 18 | 7 | Focus groups | Thematic analysis |
| Campbell 2007315 | 34–78 | PMP | CBP | UK | 16 | NK | Focus groups | Thematic analysis |
| Campbell 2008316 | 36–66 | Non-service users | MSK | UK | 12 | 3 | Interviews | Thematic analysis |
| Cook 2000317 | 22–63 | Back pain rehab | CBP | UK | 7 | 3 | Semistructured interviews | Thematic analysis |
| bCoole 2010318 | 22–58 | Back pain rehab | CBP | UK | 25 | 12 | Semistructured interviews | Thematic analysis |
| bCoole 2010319 | 22–58 | Back pain rehab | CBP | UK | 25 | 12 | Semistructured interviews | Thematic analysis |
| bCoole 2010320 | 22–58 | Back pain rehab | CBP | UK | 25 | 12 | Semistructured interviews | Thematic analysis |
| bCooper 2009321 | 18–65 | PT | CBP | UK | 25 | 5 | Semistructured interviews | Framework analysis |
| bCooper 2008322 | 18–65 | PT | CBP | UK | 25 | 5 | Semistructured interviews | Framework analysis |
| bCrowe 2010374 | 25–80 | Adverts and PT | CBP | New Zealand | 64 | 33 | Semistructured interviews | Thematic analysis |
| bCrowe 2010323 | 25–80 | Adverts | CBP | UK | 64 | 33 | Semistructured interviews | Thematic analysis |
| De Souza 2011376 | 27–79 | Rheumatology | CBP | UK | 11 | 5 | Unstructured interviews | Thematic analysis |
| Dickson 2003325 | 63–80 | PC | MSK | USA | 7 | 0 | Interviews and observation | Thematic analysis |
| Dragesund 2008326 | 26–68 | PT | MSK | Norway | 13 | 5 | Focus groups | Thematic analysis |
| Harding 2005330 | 29–71 | PMP | MSK | UK | 15 | 3 | In-depth interviews | Framework analysis |
| Holloway 2007379 | 28–62 | pain clinic | CBP | UK | 18 | 12 | Semistructured interviews | IPA |
| Hunhammar 2009331 | 19–58 | PC | MSK | Sweden | 15 | 6 | In-depth interviews | Grounded theory |
| bJohansson 1996332 | 21–60 | PC | MSK | Sweden | 20 | 0 | Semistructured interviews | Grounded theory |
| bJohansson 1997333 | 21–60 | PC | MSK | Sweden | 20 | 0 | Semistructured interviews | Grounded theory |
| bJohansson 1999334 | 21–60 | PC | MSK | Sweden | 20 | 0 | Semistructured interviews | Grounded theory |
| Liddle 2007336 | 20–65 | University | CBP | Northern Ireland | 18 | 4 | Focus groups | Thematic analysis |
| Lundberg 2007338 | 30–64 | PT | MSK | Sweden | 10 | 5 | In-depth interviews | Phenomenology |
| Osborn 1998342 | 25–55 | Back pain rehab | CBP | UK | 9 | 0 | Semistructured interviews | IPA |
| bOsborn 2006343 | 36–52 | Pain clinic | CBP | UK | 6 | 4 | Semistructured interviews | IPA |
| Osborn 2008344 | 36–52 | Pain clinic | CBP | UK | 10 | 5 | Semistructured interviews | IPA |
| Patel 2007345 | 29–62 | Benefits office | MSK | UK | 38 | 15 | Semistructured interviews | Thematic analysis |
| Rhodes 1999350 | 25–65 | Health-care plan | CBP | USA | 54 | 20 | In-depth interviews | Thematic analysis |
| Sanders 2002353 | 51–91 | Survey | MSK | UK | 27 | 10 | In-depth interviews | Grounded theory |
| Satink 2004354 | 42–70 | PMP | CBP | Netherlands | 7 | 3 | Narrative interview | Phenomenology |
| Skuladottir 2011355 | 35–55 | Adverts | MSK | Iceland | 5 | 0 | In-depth interviews | Grounded theory |
| bSlade 2009356 | 26–64 | Adverts and university | CBP | Australia | 18 | 2 | Focus groups | Grounded theory |
| bSlade 2009357 | 26–65 | Adverts and university | CBP | Australia | 18 | 2 | Focus groups | Grounded theory |
| bSmith 200766 | 36–52 | Pain clinic | CBP | UK | 6 | 4 | Semistructured interviews | IPA |
| Snelgrove 2009358 | 39–66 | Pain clinic | CBP | UK | 10 | 3 | Semistructured interviews | IPA |
| Steen 2001385 | Adults | RCT | MSK | Norway | 48 | NK | Semistructured interviews | Phenomenology |
| Strong 1994386 | 30–75 | Adverts | CBP | Australia | 7 | 3 | Focus groups | Thematic analysis |
| Strong 1995387 | 30–75 | Adverts | CBP | New Zealand | 15 | 4 | Focus groups | Thematic analysis |
| Teh 2009362 | 63–86 | Pain clinic | CBP | USA | 15 | 5 | In-depth interviews | Grounded theory |
| bToye 2010363 | 29–67 | PMP | CBP | UK | 20 | 7 | Semistructured interviews | Grounded theory |
| bToye 2012364 | 29–67 | PMP | CBP | UK | 20 | 7 | Semistructured interviews | Grounded theory |
| bToye 2012365 | 29–67 | PMP | CBP | UK | 20 | 7 | Semistructured interviews | Grounded theory |
| bWalker 1999367 | 28–80 | Pain clinic | CBP | UK | 20 | 12 | In-depth interviews | Phenomenology |
| bWalker 2006368 | 28–80 | Pain clinic | CBP | UK | 20 | 12 | In-depth interviews | Phenomenology |
| bWerner 2003369 | 26–58 | PC and PMP | MSK | Norway | 10 | 0 | In-depth interviews | Phenomenology |
| bWerner 2004371 | 26–58 | PC and PMP | MSK | Norway | 10 | 0 | In-depth interviews | Phenomenology |
| Werner 2003370 | 31–53 | PMP | MSK | Norway | 6 | 0 | In-depth interviews | Phenomenology |
| Study | Age range (years) | Source of participants | Condition | Country | n | Male, n | Data collection | Methodologya |
|---|---|---|---|---|---|---|---|---|
| Arnold 2008373 | 31–72 | Rheumatology | FM | USA | 48 | 0 | Focus groups | Grounded theory |
| Cunningham 2006375 | 30–70 | University | FM | Canada | 8 | 1 | Semistructured interviews | Thematic analysis |
| bHallberg 1998328 | 22–60 | Insurance hospital | FM | Sweden | 22 | 0 | Semistructured interviews | Grounded theory |
| bHallberg 2000329 | 22–60 | Insurance hospital | FM | Sweden | 22 | 0 | Semistructured interviews | Grounded theory |
| Hellström 1999378 | 32–50 | FM group | FM | Sweden | 10 | 1 | In-depth interviews | Phenomenology |
| Kelley 1997380 | Mean 50 | PMP | FM | USA | 22 | 0 | In-depth interviews | Narrative analysis |
| Lempp 2009381 | 20–69 | Rheumatology | FM | UK | 12 | 1 | Semistructured interviews | Thematic analysis |
| Liedberg 2002382 | 26–64 | Questionnaire survey | FM | Sweden | 39 | 0 | In-depth interviews | Thematic analysis |
| Lofgren 2006337 | 30–63 | PMP | FM | Sweden | 12 | 0 | Diaries, focus groups, interviews | Grounded theory |
| Madden 2006339 | 25–55 | Hospital databases | FM | UK | 17 | 1 | Semistructured interviews | Induction/abduction |
| Mannerkorpi 1999340 | 29–59 | FM group | FM | Sweden | 11 | 0 | In-depth interviews | Phenomenology |
| Mengshoel 2004341 | 37–49 | PMP | FM | Norway | 5 | 0 | Semistructured interviews | Thematic analysis |
| bPaulson 2001383 | 41–56 | Rheumatology | FM | Sweden | 14 | 14 | Narrative interviews | Phenomenology |
| bPaulson 2002346 | 41–56 | Rheumatology | FM | Sweden | 14 | 14 | Narrative interviews | Phenomenology |
| bPaulson 2002347 | 41–56 | Rheumatology | FM | Sweden | 14 | 14 | Narrative interviews | Phenomenology |
| Raheim 2006348 | 34–51 | PC, PT, FM group | FM | Norway | 12 | 0 | Life-form interviews | Phenomenology |
| Raymond 2000349 | 38–47 | FM association | FM | Canada | 7 | 1 | Semistructured interviews | Thematic analysis |
| bSallinen 2010351 | 34–65 | PMP | FM | Finland | 20 | 0 | Narrative interviews | Thematic analysis |
| bSallinen 2011352 | 34–65 | PMP | FM | Finland | 20 | 0 | Narrative interviews | Thematic analysis |
| Schaefer 2005384 | 37–59 | Adverts | FM | USA | 10 | 0 | In-depth interviews | Phenomenology |
| bSoderberg 1999359 | 35–50 | Rheumatology | FM | Sweden | 14 | 0 | In-depth interviews | Phenomenology |
| bSoderberg 2001360 | 35–60 | Rheumatology | FM | Sweden | 25 | 0 | In-depth interviews | Thematic analysis |
| Sturge-Jacobs 2002361 | 20–57 | PMP | FM | Canada | 9 | 0 | Unstructured interviews | Phenomenology |
| Undeland 2007366 | 42–67 | FM group | FM | Norway | 11 | 0 | Focus groups | Thematic analysis |
| De Vries 2011324 | 31–60 | Adverts and FM website | FM and MSK | Netherlands | 21 | 9 | Semistructured interviews | Thematic analysis |
| Gullacksen 2004377 | 23–55 | PMP | FM and MSK | Sweden | 18 | 0 | In-depth interviews | Phenomenology |
| Gustaffson 2004327 | 23–59 | Pain management | FM and MSK | Sweden | 18 | 0 | Semistructured interviews | Grounded theory |
| Lachapelle 2008335 | 23–75 | Adverts | FM and MSK | Canada | 45 | 0 | Ethnography and focus groups | Ethnography |
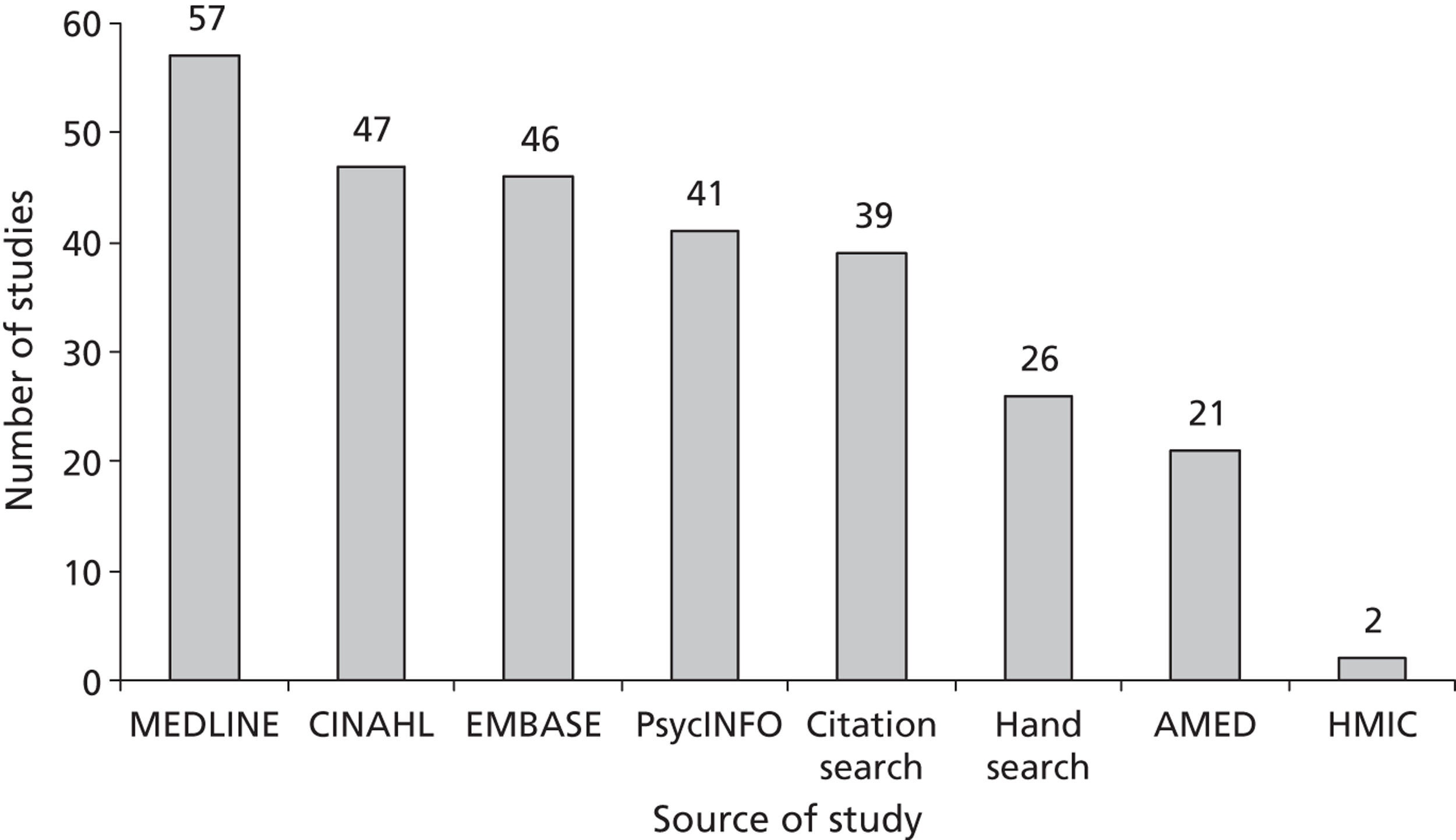
Figure 11 shows the sources of the included studies. In total, 74% of the included studies (n = 57) were identified from MEDLINE and 95% of the studies (n = 73) were identified by combining MEDLINE, CINAHL and PsycINFO. EMBASE and AMED added only one additional study each and HMIC added no extra studies. Hand-searching and citation searching added three additional studies. Included studies came from 40 different journals (Table 8). The highest contributors were Disability and Rehabilitation (7), Scandinavian Journal of Caring Sciences (7), Social Science & Medicine (5) and Qualitative Health Research (5).
FIGURE 11.
Sources of included studies.
| Journal | Papers, n |
|---|---|
|
|
Determining how studies are related
A glossary of all of the collaborative interpretations of each second-order construct is given in Appendix 3. These represent the raw data of our meta-ethnography.
Table 9 shows findings that were not included in the meta-ethnography because the team agreed that they were ‘untranslatable’. In other words, we felt that there was no central idea that pulled together the original findings. We did not attempt to reorganise these findings to include them in our analysis.
| Study | Author descriptor of theme used in primary study |
|---|---|
| Allegretti 2010313 | Convergence with physician |
| Arnold 2008373 | Other |
| Bair 2009314 | Barriers to self-management – ‘other’ |
| Cook 2000317 | Cognitive perceptual factors |
| Cook 2000317 | Patient experiences |
| Cook 2000317 | Quality of life |
| Cook 2000317 | Relationship with health-care professional |
| Cook 2000317 | Experience of active rehabilitation |
| Coole 2010320 | Assistance from employer |
| Coole 2010320 | Fewer options if working alone |
| Coole 2010320 | Pros and cons of working for oneself |
| Cooper 2009321 | Not self-managing, awaiting further investigation |
| Crowe 2010323 | Low-impact exercise |
| Cunningham 2006375 | Ongoing process of managing fibromyalgia |
| De Souza 2011376 | Friends and family |
| Dragesund 2008326 | Associations about body |
| Dragesund 2008326 | Aware of body |
| Dragesund 2008326 | Feeling for the body |
| Hallberg 2000329 | Diverse pain coping |
| Hallberg 2000329 | Subjective pain language |
| Kelley 1997380 | Depression |
| Kelley 1997380 | Feeling good |
| Kelley 1997380 | Needs |
| Lachapelle 2008335 | It could be worse |
| Lachapelle 2008335 | Realising no cure |
| Lachapelle 2008335 | Receiving a diagnosis |
| Lempp 2009381 | Life before and after diagnosis |
| Liddle 2007336 | Effect on individual |
| Liddle 2007336 | Limitations to recovery |
| Liddle 2007336 | Physiotherapy recommendations |
| Patel 2007345 | Painful condition |
| Schaefer 2005384 | Coming to grips and making changes |
| Schaefer 2005384 | Managing symptoms |
| Slade 2009357 | Participant suggestions |
| Snelgrove 2009358 | Painful body and self |
| Snelgrove 2009358 | Physical coping strategies |
| Strong 1994386 | Domestic |
| Strong 1994386 | Mobility |
| Strong 1994386 | Negative emotions |
| Strong 1994386 | Positive emotions |
| Strong 1994386 | Relationships |
| Strong 1994386 | Treatment |
| Strong 1995387 | What do you do when in pain |
| Teh 2009362 | Involved in quality of care |
| Walker 1999367 | Challenging the medical model |
Translating studies into each other: developing the conceptual categories
This section describes the team’s final conceptual categories, illustrated by examples of second-order constructs. We have chosen particular second-order constructs to illustrate our conceptual categories in the same way that primary qualitative research studies use narratives as exemplars of concepts or themes. The second-order constructs supporting each conceptual category are presented in Appendix 4. These tables show the team memos describing each category. Table 10 shows an example of the team memos and second-order constructs supporting one conceptual category (‘alienated vs. integrated body’).
| Team memos: pain external to me; self and body opposing; pain not me; still me but not me; body external to me; self vs. body; pain threatens me; pain taking ownership of body; in some cases a new self with pain emerges; body alien; pain brings an awareness of the body as a foreign alien (like Leder’s dys-appearance of body388) | |
| MSK | Fibromyalgia |
|---|---|
| Osborn 2008:344
fearfulness of pain Rhodes 1999:350 anatomical body Johansson 1999:334 bodily presentations Crowe 2010:323 externalisation of the body Lundberg 2007:338 failed adaptation Osborn 2006:343 living with body separate from self Snelgrove 2009:358 crucial nature of pain – body/self/pain as a threat Afrell 2007:372 acceptance typologies – rejecting the body |
Raheim 2006:348
theoretical interpretation – lived body Raheim 2006:348 typologies – powerlessness Paulson 2002:346 body as obstruction – reluctant body Sturge-Jacobs 2002:361 thinking in a fog Raheim 2006:348 typologies – coping |
Fundamental to the patients’ experience of chronic MSK pain is a constant struggle: (1) struggle to affirm myself; (2) struggle to reconstruct myself in time; (3) struggle to construct an explanation for suffering; (4) struggle to negotiate the health-care system; and (5) struggle to prove legitimacy. The over-riding theme of these categories is adversarial, giving a sense of being guilty until proven innocent. However, in spite of this constant struggle there is also a sense of (6) moving forward alongside my pain. We discuss differences in category descriptions for fibromyalgia and MSK studies throughout the following sections.
1. Struggling to affirm myself
The category ‘struggling to affirm myself’ describes a struggle to hold on to the ‘real self’, which is threatened by continuing pain. It incorporates three concepts: (a) alienated versus integrated body, (b) the ‘new me’ is not the ‘real me’ and (c) isolated not connected me.
1(a) Alienated versus integrated body
The alienated body describes how a person with chronic pain experiences a fragmentation of body and self. Chronic pain makes a person become aware of their body when before they were not. Body and self are no longer integrated, and the painful body becomes it, as opposed to me. Pain takes ownership of the body and is experienced as a malevolent presence. 343 Crowe and colleagues323 describe this as the ‘externalisation of the body’, in which self and body come apart and the body becomes external to the self.
Second-order construct: Osborn and Smith 2006:343 living with body separate from self
Pain has made me aware of my body now. Separation of painful body from self. Self and body opposing entities. Painful part not me. Unpleasant and relentless presence of a body that is ‘not me’. Living with pain affects who I am [self]. New body alien. I feel powerless against an alien body. Dysfunctional part of body not me. Distinction made between the original self and that self which had emerged due to pain.
Paulson and colleagues346 describe the body in pain as ‘a reluctant body’ that is unresponsive to the demands of meaningful participation. This altered relationship with the body, if antagonistic, can make a person feel ‘homeless’ in his or her own body.
Second-order construct: Raheim 2006:348 theoretical interpretation – lived body
Participants describe dualism of body in pain with a distinction between self and body. No longer unconscious of the body but more aware of it, while paradoxically feeling ‘homeless in one’s own body’, and wanting to escape from it. Some do not report feelings of disintegration, but rather view the body in pain as a ‘problematic friend’ with which they can cope. Dialogue between self and body is either positive or negative: (a) impossible enemy – antagonistic (parasitic) dualism; homeless in body, (b) friendly dialogue – symbiotic dualism; at home in my body
Negotiating an unrelenting body
The category ‘unrelenting body’ is linked to the change in the way that the person experiences his or her own body. This category developed from the fibromyalgia studies. The unrelenting body overwhelms and drains a person’s resources. This concept includes second-order constructs that describe the tangible bodily presence of chronic pain and its wide-reaching effects. Chronic pain is physically ‘agonising’ and its impact goes beyond the physical body to become emotionally unrelenting. The concept describes the powerlessness of the person in pain against an unrelenting body.
Second-order construct: Lachapelle 2008:335 barriers to acceptance – unrelenting pain and fatigue
Unrelenting pain and fatigue – women drained of physical and emotional resources.
Second-order construct: Lempp 2009:381 change in health identity
Illness became increasingly intrusive in life and began to undermine their confidence and sense of self. Self-esteem undermined. Fear of not being able to rely on body and the unpredictability of the illness.
Integral to the unrelenting bodily experience of fibromyalgia pain is an engulfing and insurmountable fatigue.
Second-order construct: Sturge-Jacobs 2002:361 fatigue invisible foe
Fatigue engulfing, insurmountable and overwhelming, insidious, unseen and uncontrollable. Affects all aspects of life. Activities had to be avoided or prioritised. Fear of becoming a burden on friends and family (i.e. non-reciprocal relationships). Always receiving help and not giving.
Fibromyalgia studies also describe the cognitive effects of unrelenting pain, a ‘fibro-fog’. Living in this fog a person becomes forgetful, lacks motivation and finds it difficult to focus or to articulate his or her thoughts. 373
Second-order construct: Sturge-Jacobs 2002:361 thinking in a fog
Brain ‘in a fog’; unable to concentrate or think clearly. Difficulties with problem solving, abstract thinking, and the inability to make appropriate judgement calls or on-the-spot decisions were areas of concern for all participants. Mind and body ‘constantly at odds’. Sense of being in a dark place. Could affect ability to continue meaningful employment.
As we were surprised not to find this concept developed in the MSK papers, we searched for second-order constructs that supported this category in the MSK papers and found only three papers. 331,358,368 In short, there was more focus on the experience of the body in pain in fibromyalgia studies.
1(b) ‘New me’ not the ‘real me’
This describes the discrepancy and ensuing struggle between a past ‘real me’ and a present ‘not real me’ with pain. A person in pain struggles to balance this deficit and to prevent the erosion of the real self. The new me is described as ‘not real’ and the old me as ‘real’. There is now a chasm between what other people think that I am (the new me in pain) and what I think I am (the past me). In this way Osborn and Smith342 describe how a person compares their self now with a past self. A person in pain looks back nostalgically to the ‘real me’ of the past.
Second-order construct: Osborn and Smith 1998:342 comparing this self with other selves
Compared self with others and past/future self.
a. I am not like the old me who was fit and able to work hard. Some defined themselves as bereaved. Grieved for the old self. I am not my happy previous self – look back nostalgically. Painful reminder of loss. Past self considered to represent the real self replaced by new false persona. Pain denies me my right to be me.
b. Fear what future will bring. Feelings of uncertainty.
c. Constantly comparing to others and put emphasis on disability. Took refuge in thinking of those who were worse off, but this could make them think of a possibly worse future (also this does not compensate for my loss).
Second-order construct: Paulson 2002:346 being a different man – not being the same
No longer feel like a ‘whole man’. Had lived life at high tempo, cheerful, kind, offered help. Not the same – could no longer manage multiple activities due to failing strength and inability to concentrate (compounded by feelings of sorrow for lost abilities; isolation when not treated like others at work; irritability that affected relationships; and suicidal thoughts due to these). Anger often directed towards family. Over time came to accept and worry less what people felt.
This struggle to hold onto the old me is experienced as mourning and can be as distressing as the pain itself.
Second-order construct: Werner 2003:369 for better or worse – sorrow at loss
Negative effects due to the increased level of awareness which leads to sorrow at loss of aspects of self. An increased feeling of despair is caused by having to realise that you might never be restored to your former healthy state. Sorrow and bitterness at having to revise the picture of self.
It also describes a fight to keep hold of the old me and to appear normal; being changed by pain is interpreted as ‘giving in’.
Second-order construct: Lachapelle 2008:335 barriers to acceptance – fight to be normal
Mounting losses and fight to be normal – struggle to maintain pre-pain identity. Felt they had let the pain ‘win’. Struggled to maintain normalcy; ‘put on a play’, ‘cover it up’. Acceptance meant you had to take on changes and accept changed identity (sometimes felt guilty for this, e.g. gender roles).
Second-order construct: Harding 2005:330 spoiled identity
The reductions required by the chronic pain have an impact on sense of identity and cause people to perceive themselves as different from others. There is a tension between outward appearance remaining ‘normal’ and internal changed identities. Some felt that they had ‘given in’ to pain; others grudgingly accommodated the changes and lowered expectations.
However, although fighting to be my old self, at the same time I acknowledge that I am irreparably altered. Toye and Barker363 suggest that continuing to fight to be me and accepting my loss are not mutually exclusive, and both concepts are upheld by strong cultural rhetoric that values both fighting and acceptance.
Second-order construct: Toye and Barker 2010:363 I am still me but not me
Paradox: a. You must learn to live with it [use of cultural rhetoric]; b. I am still me and I will fight to be [use of cultural rhetoric]. These are not mutually exclusive; can accept defeat but still fight on [lose battle; win war].
1(c) Isolated not connected me
This captures the changes in a person’s relationships with others (partners, family, friends, colleagues and community) and the impact of this on self. It describes the isolating effect of chronic pain and the battle to retain balanced reciprocal relationships. Former roles are entrenched in my ‘old self’, and my new self in pain challenges these roles. Pain can irreparably disconnect and isolate the person from others. However, there is also a sense that for some it is possible to move forward and redefine relationships more positively in spite of pain.
Second-order construct: Raheim 2006:348 theoretical interpretation – lived relations
Chronic pain alters the relationships we have and can either destroy (detached/dissociated relationship/destroy) or allow us to build new relationships (mutuality/reciprocal relationship/build up) as we redefine who we are.
Although help from family and friends is valued, this help can change the dynamic of the relationship, in particular towards dependency, and can therefore cause distress. Thus, pain can be the tipping point of some relationships. In some cases it can reinforce relationships by affirming who is important. Emotional support from friends is valued, but this is counterbalanced by concern over not overburdening others and creating a deficit in reciprocity. A person struggles to find a balance between having the benefits of support yet retaining independence. Change in family roles can undermine a person’s self-worth, resulting in feelings of guilt from being unable to meet the needs of family or work. There is also the sense that some find it possible to strengthen bonds in the face of a common enemy.
Second-order construct: De Souza 2011:376 spouses and partners
Help and support from spouse/partner valued but also caused feelings distress and helplessness. Strain on marital relationships due to both stress and reluctance to have a sexual relationship due to pain. Additional stress of chronic pain can be tipping point for weak relationship, but in other relationships there was closeness and support to deal with the pain together.
Second-order construct: Lachapelle 2008:335 facilitators to acceptance – perceived social support.
Emotional support from friends was counterbalanced by a concern over not overburdening. Limited by a lack of understanding on the part of supporters and fears the possible onset of supporter fatigue. Support groups ambiguous; some offered a safe haven whilst others perceived as discouraging and designed to force on participants a particular agenda. Professional counselling could help to mourn loss of old self and redefine new identity.
Isolation is exacerbated by a person’s attempts to appear normal to others and hide pain. However, striving for normalcy and attempting to meet the expectations of others can be a double-edged sword as people might not believe that a person has pain. The invisibility of pain discredits and others interpret complaints of pain as an excuse for non-participation in expected roles.
Second-order construct: Slade 2009:357 stigma – community, friends, family
Judgement extended to family, friends and community. People see back pain as an excuse for non-participation and poor performance. The invisibility of pain is a barrier to legitimacy.
Isolation is further exacerbated by the negative effect of pain on my emotions and desired personality. Anger and low mood is projected out to those around me and I am no longer feel that I am the person that I was. This can lead to the further breakdown of intimate, family, social and community relations.
Second-order construct: Walker 2006:368 loss – relationships
Irritability, need to be alone, loss of trust and disbelief, lead to breakdown of physical and emotional relationships with partners. Also became isolated from friends and work. Came to know who to trust and who true friends were. For older people, dependence might increase contact with the family.
2. Construction of time altered: unpredictable now and in the future
This concept describes an alteration in a person’s perceptions of their self through time: their plans, expectations and dreams for the future. In this way pain disrupts a person’s teleological construct, the perception that we move towards a purpose. In pain, both (a) the present and (b) the future become unpredictable, disrupting a sense of purpose.
2(a) Unpredictable now
The unpredictability of pain means that a person in pain cannot plan but lives in an endless timeless present; time shrinks to now. This concept describes the unpredictable nature of chronic pain and the need to be constantly vigilant of the body. Life becomes dominated by caution and spontaneity is lost. Mengshoel and Heggen341 describe this as ‘living life on a knife edge’ (p. 49). It becomes necessary to meticulously plan daily schedules to maintain participation in daily routines.
Second-order construct: Crowe 2010:323 need for vigilance
Because it is unpredictable you need to be constantly vigilant about what you were doing and how you move. People became cautious to attempt things they had always taken for granted. Related to body differently; loss of spontaneity even for previously routine activities.
Second-order construct: Snelgrove 2009:358 crucial nature of pain – loss of spontaneity
Loss of ability to do even most mundane and taken for granted activities of daily living. Loss of spontaneity; need to plan everything I do.
Second-order construct: Paulson 2002:346 body as obstruction – living day by day
Fluctuations in pain mean you have to live by the moment, not plan for future. Need to live life at your own speed so you can maintain participation.
2(b) Unpredictable future
This describes the change in a person’s expected timeline: things are not going to be how I thought they would be; my purpose is altered. On balance, the future is interpreted as bleak, and people with chronic pain anticipate both progression of symptoms and further dependence. Osborn and Smith342 describe how a person in pain compares themself now with a future perceived self and fears what the future might bring. The sense of certainty for the future rooted in a past ‘real self’ had diminished. This brings anxiety about what the future holds.
Second-order construct: Walker 2006:368 loss – hope
Turmoil, chaos, turbulence. Patient wrestles powerful emotions of uncertainty about the future, fears of potential worsening of illness, and feelings of vulnerability and helplessness. Inability to make plans; need to live each day as it comes; not knowing what the future holds; fear of getting worse. Like Frank’s chaos narrative389 – ‘being shipwrecked by the storm of disease’. Describe life as imprisoned by pain with no knowledge of release.
Second-order construct: Coole 2010:319 concerns about future at work
Perceived condition as progressive and had concerns about maintaining work or life quality after work. May be unable to enjoy leisure or retirement. Also considered effect of ageing on ongoing pain.
Although the person’s construction of a future self has been altered by pain, there is an expressed need to keep hopeful in the face of adversity; a struggle between hopelessness and hope. Lachapelle and colleagues335 describes how acceptance of loss is not incompatible with retaining hope for the future. Madden and Sim339 suggests that some degree of clinical uncertainty may allow a person to hold onto some hope when no cure has been found.
Second-order construct: Lachapelle 2008:335 meaning of acceptance
Meaning of acceptance ambiguous; implies giving in/resignation. Patients preferred ‘dealing with, managing, coming to terms with, embracing’. Means pursuing life activities in spite of pain [activity engagement]. I am willing to engage rather than avoid. Hope for improvement in pain and symptoms not incompatible with acceptance of current state. Retained hope for reduced pain at the same time as accepting chronicity of pain and that there was no cure for pain [acceptance begins with giving up hope of cure].
3. Struggling to construct an explanation for suffering
This describes the fundamental need to find an acceptable explanation for suffering. It incorporates three related concepts:
-
(a) alienated from the dominant medical discourse
-
(b) no one believes me
-
(c) seeking alternative explanations.
3(a) Alienated from the dominant medical discourse
This describes the cultural (thus rhetorical) power of the biomedical model, which has the power to give or take credibility. The biomedical model takes disease to be an objective biomedical category that can be accounted for by a specific aetiology, a category that is not influenced by psychosocial factors, or judgements about moral worthiness. The medical model of illness also implies an illness trajectory in which, following diagnosis and treatment, a person’s health is restored. 390 It demonstrates the persisting polarity inherent in the biomedical model (real/unreal, physical/mental, medical/psychological, body/mind). The person in pain needs to attribute a biomedical cause to experience it as legitimate. People describe how they have failed the medical test and find themselves betwixt and between,391 being neither credibly ‘ill’ nor symptomatically ‘well’. Paradoxically, although a person does not want to be ill, a medical diagnosis is necessary to validate their experience. Rhodes and colleagues350 describe the experience of pain as either ‘aligned’ or ‘alienated’ from the medical model. Thus, although a person is certain of their experience of pain, they have no proof and the experience becomes invalid. Existing outside the dominant discourse can sometimes mean that they begin to doubt the reality of their own pain.
Second-order construct: Rhodes 1999:350 aligned or alienated
Aligned – tests fit the anatomical model. For some patients diagnostic tests produce ‘results’ (‘black and white’ X-rays, tests) for which the visual image corresponds exactly with their experience of pain. Tests seem so positively transparent and simplistic – give proof. Deviation should show up and be susceptible to repair.
Alienated – don’t fit – guilty, disillusioned. Other patients found a discrepancy between their own ‘inner’ experience of pain and the diagnosis and needed to legitimise what they felt. This can lead to feelings of guilt, disillusionment with medicine, doubts about the tests and frustration. I am certain (I think) but I have no proof.
Second-order construct: Slade 2009:357 stigma – pathology-driven validation
Medical validation valued for credibility. Lack of this a barrier to participation that is physiologically, psychologically and socially disabling. Patients felt validity of illness in question as imaging tests revealed no cause/evidence of pain. Expressed relief or an easier pathway when an X-ray or MRI demonstrated pathology. Compounded by misdiagnosis or change in imaging findings. Feel need to legitimise self as not ‘mad’ or ‘bad’.
Second-order construct: Campbell 2007:315 unmet expectations
Patients expect an explanation, diagnosis, treatment and cure but this is not forthcoming. Leads to frustration and anger at impotence of medical system. Feel that they are not believed because of invisibility of pain; seek to make invisible visible in order to legitimise pain. They have failed a medical test. Anger and frustration at the perceived ineptitude of the medical profession was evident. Leads to engendering personal remedies.
Fibromyalgia: an ambiguous diagnosis
Patients with fibromyalgia also experience alienation from the biomedical model in spite of having a diagnosis. At first the diagnosis of fibromyalgia is experienced as a relief and can provide a springboard to living alongside the pain. Diagnosis shows them that they do not have a fatal illness, and also legitimises their experiences. However, over time the diagnosis can become a burden; they come to realise that, rather than identifying a specific organic pathology, fibromyalgia describes a spectrum of symptoms. This model of diagnosis does not fit the medical model, which requires a specific aetiology.
Second-order construct: Undeland 2007:366 relief of name but diagnosis becomes a burden
Relief at diagnosis followed by conflict (what is the cause, no cure, fear of stigma, meant inevitable disability, disbelief by others, or not taken seriously, ‘just a bit of fibromyalgia’). Diagnosis brought no understanding or appreciation. Despair and sorrow when they realised the impact of fibromyalgia on their lives. This process was lonely. Some people expected improvement after diagnosis and it was difficult for the women to explain the lack of progress. Some women remarked that their doctors felt that fibromyalgia was just a word associated with hysterical women. This turmoil leads some to continue to search for a diagnosis.
Second-order construct: Mengshoel 2004:341 ambivalence about diagnosis
Patients still want a biomedical diagnosis and are unhappy to have a diagnosis based on subjective criteria. Diagnosis of fibromyalgia a relief (as not a fatal disease) as well as a burden (not rooted in treatable biological signs and viewed with scepticism).
Second-order construct: Madden 2006:339 discovering a disease – fibromyalgia an empty diagnosis
Participants felt that they had received an empty diagnosis; difficult to explain to others as not really understood by patient.
The uncertainty of having no diagnosis is replaced by a new kind of uncertainty as fibromyalgia is regarded by others with varying levels of scepticism. The diagnosis of fibromyalgia can also come to gain ‘master status’ whereby every bodily symptom is explained away by fibromyalgia and is not taken seriously by others.
Second-order construct: Madden 2006:339 seeking answers – biomedical ambiguity
Fibromyalgia symptoms wide ranging and ambiguous; difficulty of locating specific symptoms with the illness. This led to confusion over definition of diagnosis; feeling that no one really knows what it is. ‘The diagnosis is seemingly adapted to suit the presentation of the illness, rather than the illness fitting within a predefined diagnostic framework’
p. 2971
3(b) No one believes me
This concept describes the experience of the discredited person standing outside the dominant biomedical model. This cultural model seeks tangible, physical evidence. If nobody can see pain, and there is no legitimising medical diagnosis, credibility is lost.
Second-order construct: Holloway 2007:379 stigma in everyday life
Patients felt stigmatised socially for having an invisible illness; people don’t believe that there is anything wrong at all. Provoked by media reports of benefit fraud.
Second-order construct: Lachapelle 2008:335 barriers to acceptance – support and belief of others
Lack of support and belief from others a barrier to acceptance. It was important to have a concrete diagnosis to feel legitimate and get support from others. friends, colleagues and families began to treat them the same as the health-care professionals did. Delays in diagnosis damaging to fibromyalgia women’s social (support) networks.
As a result of residing outside the dominant model, the person experiences overwhelming doubt from people around them. This doubt permeates a person’s experiences at work, in their social life, in health care and among family, altering the fabric of experience. At times a person can come to doubt their own experiences. 363,370,371
Second-order construct: Osborn and Smith 1998:342 not being believed
No visible sign of suffering. Uncertainty about pain made them vulnerable to judgements of those around them. Continual need to justify self. It is real; I am not mad or bad. Faced threat of rejection even by nearest and dearest. Pain has caused a shift in familial reciprocal roles. I am a burden but also people don’t believe me. Lack of credible evidence made them feel guilty of the burden they were placing on their families. Uncomfortable about not being able to reciprocate but becoming the one that is cared for. Appearing too healthy or mobile threatened credibility. Forced to appear ill but this meant bearing burden of not being seen as self by others (e.g. I’m not a cripple). Denied opportunity to relate to others in a world free of the influence of pain.
Second-order construct: Slade 2009:357 stigma – community, friends, family
Judgement extended to family, friends and community. People see back pain as an excuse for non-participation and poor performance. The invisibility of pain is a barrier to legitimacy.
Soderberg and colleagues359 describe the discrediting experience as a threat to human dignity. It threatens a fundamental quality of life, which involves being recognised as a credible human being.
Second-order construct: Soderberg 1999:359 threat to integrity – credibility and invisibility
Lack of belief from others; not taken seriously; others felt it imaginary or psychological. Naming the illness meant that it existed. If you don’t look sick you are not sick. Diagnosis and participation in research increased credibility. Felt lucky to be believed. Lack of belief and a threat to their human dignity, thus depriving opportunity to be a whole human being. Engagement implies ‘fraternity’, i.e. treat someone like your brother.
3(c) In Striving for an alternative acceptable explanation
This describes a tenacious approach towards finding an explanation for pain in the absence of a medical diagnosis. It illustrates that those in pain do not necessarily subscribe uniquely to medical interpretations, and are open to alternatives. For example, they may consider that age, certain activities, life events, emotional turmoil or genetic predisposition may all contribute to a person’s pain. It describes an active struggle to find an explanation for suffering and to search for an alternative remedy if a medical explanation is not achievable.
Second-order construct: Soderberg 1999:359 struggles for understanding – seeking explanations
To be stricken with illness without understanding why is the classic dilemma of Job. An explanation does more than identify biological process. Explanation and understanding give relief. Diagnosis positive because you know the illness is not grave. Also makes unbelievable acceptable. Also makes it easier to accept and know you are not alone. Understanding through experience gives relief. An explanation can contribute to living a life of dignity
Second-order construct: Harding 2005:330 making sense of pain
Tried to make sense of the cause of pain by locating it in the context of their lives (e.g. cancer, bereavement, diabetes, etc.). Used diverse explanations to explain their pain. Doctors were perceived as not helping them make sense of their pain but only providing a medical interpretation for it. For most, there was a consistent tendency to not wholly subscribe to the medical interpretation.
Second-order construct: Dickson 2003:325 reconstructing meaning of pain – managing and tolerating
Continued to seek out traditional means to manage their symptoms, alongside search for cure. Shift from pain being symptom of disease to being part of ageing [positive view of aging in Korean culture]. Women gained control over their pain and began to interpret their experience as part of growing older.
Alternative explanations may help a person to come to terms with pain. Dickson and Kim325 describe how some Korean women with osteoarthritis found it helpful to shift from a medical interpretation to an interpretation that explained symptoms as the normal result of ageing. Toye and Barker365 suggest that there may be a link between recovery and successfully constructing an acceptable explanatory model for pain.
Second-order construct: Mengshoel 2004:341 a new interpretation
Come to understand that diagnosis fibromyalgia had its limits and only a label for pain in muscles. No longer preoccupied with seeking biomedical explanation. They talked about strategies to end the pain which involved listening to their body and take things slowly when needed. Realise there is a close link with pain and life events. Cause of symptoms sought in everyday life. They described living life on a knife edge and they need to take precautions to stay healthy. Learned to slow down and assess situation to avoid relapse. New strategy of analysing life events.
Second-order construct: Toye and Barker 2012:365 restoring hope – constructing an acceptable explanatory model
Successful patients had accepted a link between mind and body and embraced psychological interventions. However, physical explanations were still important, and they constructed a model, which saw the body as out of balance rather than broken, thus being able to retain legitimacy in spite of having no diagnosis. Unsuccessful patients held onto medical model.
4. Struggling to negotiate the health-care system
This category describes the person’s struggle to negotiate the health-care system when they have chronic MSK pain. It includes two categories: (a) the ambivalent relationship with the health-care system and (b) value me as a person, don’t just treat my body.
4(a) Ambivalent relationship with the health-care system
This describes the person’s ambivalent relationship with the health-care system. Although reticent to engage with a system that is failing their needs, at the same time they feel compelled to engage. There remains a continuing faith in a system that is failing. Although this faith is tested, the person retains hope for a future cure. There is also a sense of being ‘trapped in the system’.
Second-order construct: Campbell 2007:315 back to square one
Feel entrapped in a medical system where GP is gatekeeper to other treatments. Reticent to re-engage with a system that previously had little to offer, but things may have moved on now. Feel that a cure (for something so simple) is now possible and should be made available. Tenacity rather than acquiescence evident (versus Illich392).
Second-order construct: Walker 1999:367 being in the system – losing faith
Felt health-care professionals had given up on finding a diagnosis and cure, and blamed the patient for their own condition. Patients lost faith in doctors who did not understand their world.
This relationship with health care is described as tenacious not acquiescent, with a feeling that the individual has a personal responsibility to do something for their pain. However, despite this, the person remains at the mercy of the system. Attempts to understand their suffering are continually thwarted as the person continues to be referred on to yet another health professional ‘like a shuttlecock’. Some start to doubt the existence of an expert, or that anything can actually be done. This can lead to anger at the impotence of the system.
Second-order construct: Harding 2005:330 unmet expectations
A person needs their doctors to bear witness to their pain experience. This has a profound effect on their functioning as individuals. Expectations of medical system are not met. Loss of faith in medical system due to GPs’ inability to diagnose and treat; their lack of time to listen and understand patient condition; disbelief of patient descriptions and lack of concern; not being taken seriously. Could receive a range of different sometimes contradictory opinions from medical professionals as to the cause pain and way to treat it. Search for an alternative remedy is taken up.
Second-order construct: Walker 1999:367 being in the system – waiting
Feeling like a ‘shuttlecock’ long periods of waiting and being sent back and forth for non-productive treatments. All patients felt too much time wasted waiting in vain for ‘productive’ assistance in the medical system.
This ambivalent relationship towards the health-care system is less evident in fibromyalgia studies, in which the concept describes doctors’ reluctance to use the diagnosis of fibromyalgia or being uncertain about effective treatment options.
Second-order construct: Undeland 2007:366 diagnostic uncertainty
Patients search for a diagnosis impeded by GPs reluctance to use a diagnosis of fibromyalgia. Patients saw doctors hoping for relief and explanations but had difficulty explaining their symptoms. Several participants described doctors who were hesitant or dismissive, claiming fibromyalgia was a fashion tag.
Medication: demonstrating the ambivalent relationship to health care
The experience of medication illustrates the ambivalent relationship to health care. It is described as treating the symptoms of pain rather than curing it, and therefore as not fitting the expectations of the medical model. Patients describe medication as a means of being kept quiet by medical professionals who are uncertain of what else to do for them.
Second-order construct: Liddle 2007:336 treatment received
Disappointment at unmet expectations of treatment. Frustration at inability of medical system to relieve pain, and diversity of attempts to resolve the problem. GPs over-emphasised use of medication. Participants were concerned that this was treating the symptom without addressing the source of their condition.
However, although people are concerned about the side effects of medication they continue to take it, but describe how they will alter their prescribed doses and use supplements without consulting their doctor. This illustrates the proactive rather than acquiescent approach to health care.
Second-order construct: Teh 2009:362 participation in pain treatment – working outside health-care professional relationship
Patients sometimes changed pain medications without consulting health-care professional, due to dislike of pain medications and fear of reliance on these. Working on own to manage pain – change own medication, taking supplements or exploring alternative remedies. Patients resourceful in accessing alternative health strategies.
Second-order construct: Lempp 2009:381 quality of care – interventions
Ambivalence to medication; concern over dependence and that it might mask symptoms but not ‘cure’ the disease. Drugs ineffective for pain relief and most ‘followed their own intuition rather than medical advice.’ Physiotherapy whilst positive for some, on the whole brought up negative memories. Many tried alternative medicine/therapy, again with little relief apart from use of heat.
4(b) Value me as a person, don’t just treat my body
This category describes the experience of not feeling valued as a person by the health-care professional. It describes a fundamental need to feel cared for; to be listened to, valued, heard and believed. It describes a person’s need for their health-care professional to believe and bear witness to their suffering, particularly as credibility is threatened by the invisibility of pain. There is a paradox inherent in this experience of health care: I want my physical body to be treated, but at same time I need to be valued as integrated body–self. This need is described as central to the therapeutic relationship, not as an adjunct.
Second-order construct: Teh 2009:362 importance of relationship with health-care professional
Relationship with health-care professional valued: being understood, seeing them as a person, being remembered and continuity of care means feel known, safe, legitimate. Being unknown, not heard or understood means isolation and de-legitimacy.
Second-order construct: Harding 2005:330 unmet expectations
A person needs their doctors to bear witness to their pain experience. This has a profound effect on their functioning as individuals. Expectations of medical system are not met. Loss of faith in medical system due to GPs’ inability to diagnose and treat; their lack of time to listen and understand patient condition; disbelief of patient descriptions and lack of concern; not being taken seriously. Could receive a range of different sometimes contradictory opinions from medical professionals as to the cause pain and way to treat it. Search for an alternative remedy is taken up.
Osborn and Smith344 illustrate the benefits of therapeutic alliance and the importance of having a health-care professional sharing the experience.
Second-order construct: Osborn and Smith 2008:344 containing fear through social connection
Pain remained unchanged as an object of thought but they felt better able to manage the fear it evoked. Their pain possessed the same meanings and was no different in its threatening potential and unpleasantness: Each participant felt more able to manage his or her pain, They reported an increase in the degree of self-confidence they felt in the face of their on-going pain and a reduction in the level of fear and worry. Therapeutic alliance eased sense of isolation, vulnerability, and fear. Someone else is part of the experience.
Slade and colleagues356 describe how patients valued a therapeutic alliance based on mutual information and enquiry. They wanted to be informed and consulted about care decisions: I am a person so tell me what you are doing.
Second-order construct: Slade 2009:356 engagement with health care – partnership
All participants expressed the need for mutual enquiry, problem-solving, negotiation and re-negotiation between care-provider and care-seeker to establish mutual therapeutic goals’. Patients wanting to feel that their opinions are sought and considered through every part of their care pathway.
5. Struggling to prove legitimacy
This category focuses on the adversarial and contested quality of the chronic pain experience, which may distinguish it from other types of bodily pain. It incorporates the shame and stigma of not fitting the dominant medical narrative and describes the way that people struggle to prove to others that they are credible. The category incorporates the performative dimension of pain: (a) struggling to find the right balance between hiding or showing pain, between appearing ‘sick’ or ‘well’ and (b) struggling to prove that I am a ‘good’ and valued person.
5(a) Struggling to find the right balance: do I hide or show my pain; am I sick or well?
The absence of a medical diagnosis means that a person must attempt to perform their credibility to others. This concept describes the struggle to find the right balance between hiding and showing pain to others. It describes an etiquette, or ‘right way’, of performing pain. If I appear too sick or not sick enough then others don’t believe me.
Second-order construct: Toye and Barker 2010:363 mustn’t look too ill
Face the paradox – Patients had to negotiate a balance between not looking ‘too ill’ and yet looking ill enough, and resolved this by hiding their illness even from those close to them.
a. Consistency or persistence of pain behaviour an important dimension of judging whether or not someone was genuine.
b. but don’t look too ill or people won’t believe you. There is a ‘right way to be in pain’.
There is a strong pull to hide pain from others and to appear ‘normal’. This pull is increased by a sense of shame and stigma at having medically unexplained pain. 66 Although there is a sense that I want others to know that I have pain, there is also a sense that I don’t want to appear as if I am unable to cope or that I am not my old self.
Second-order construct: Skuladottir 2011:355 quest for normalcy – avoid sick role and maintain dignity
Took trouble to maintain appearance which meant that some did not realise or understand how they felt. Some tried to hide pain or conceal that there was anything wrong. Wanted to appear normal and maintain a sense of dignity. Felt this was respectable and made them more like ‘normal’ people. If you look too good it doesn’t look like you are suffering.
Second-order construct: Paulson 2002:347 not being a whiner
Most of the men seemed to have remained with pain until a point of (near) collapse before seeking medical help (often persuaded by their partner) as they did not wish to appear as whiners. Even when sick leave was recommended by physician and allowed by employer the men insisted on getting back to work as soon as possible. Were aware of lack of credibility of fibromyalgia and were reluctant to divulge all symptoms or anxiety there were causing.
Second-order construct: Smith and Osborn 2007:66 public arena makes it worse
Social isolation appealing as less pressure to hide ‘miserable self’. Patients felt reduced to ‘a bit of a person’ as unable to fulfil (familial) roles to their ideal standards; felt vulnerable to ridicule or punishment from others; and felt perceived as a ‘burden’ and without ‘value’ by society. Sense of shame.
Paradoxically, the performative dimension of pain, which incorporates striving for normal participation and hiding pain, can further threaten a person’s credibility, particularly in the absence of medical proof. A person with chronic pain faces the continuing dilemma: do I struggle to participate as I used to (thus being ‘well’) or remain exempt from participation (thus being ‘sick’). If I am not altered, then am I actually ill at all?
Second-order construct: Johansson 1999:334 self-perception
Invisibility of symptoms damaging to one’s reputation as it evoked disbelief on the part of others. Being at home could increase expectations about household duties. At the same time, if she managed this, then neighbours were suspicious – why can’t she work! Can affect a woman’s very sense of being a capable woman (wife, mother, sexual partner). Uncertain about how to deal with limitations imposed by illness on work capacity, especially as many patients felt that going out to work improved their image socially despite their perpetual struggle with the physical pain.
5(b) Struggling to prove that I am a ‘good’ and valuable person
This describes how a person with chronic pain strives to present a picture of themselves as a ‘good’ person who is not culpable for their condition. Narratives often appeal to the ‘real me’ before pain; I am not really like this. Narratives of a previous life are used to emphasise the ‘good me’. Bury393 describes this as performing ‘moral narratives’. These narratives are less evident in the fibromyalgia second-order constructs and this fits with the view that they become more important when a medical diagnosis is absent.
Second-order construct: Snelgrove 2009:358 maintaining integrity – cause of pain
Explanation for pain physical not psychological; often described as caused when doing something virtuous. Patients explanations couched in a previously virtuous life and they are therefore blameless.
Second-order construct: Werner 2004:371 some people pour out their troubles
Narrative of strength. Important to be strong and fighter not weak and complaining. On the one hand I am like those other women (because I have pain) but I am different (not one of those whingers). I am strong, I have a positive attitude, I don’t whine, I am never sick, I don’t go to the doctors. Women work to appear credible and distance themselves from ‘the others’. I am not to blame.
Part of this struggle to prove that I am a good and valuable person involves a comparison with other people. Although being amongst other people with pain can legitimise experience (I am not the only one who has it), people take care to emphasise the ‘good’ qualities that are unique.
Second-order construct: Toye and Barker 2010:363 I am not like the others
Paradox.
Meeting others with pain confirmed legitimacy.
But I am not like the others. Patients were ambivalent in their relationships with other patients, and also stressed how they were ‘not like them’.
Social comparison and moral narrative used to rank self and confirm legitimacy.
Struggling to negotiate the workplace: demonstrating the adversarial experience of chronic pain
This section provides an example of the adversarial experience of chronic MSK pain as the person with chronic pain struggles to negotiate their position at work. We categorised second-order constructs related to work experience as:
-
struggle to affirm my ‘working’ self
-
hostility at work isolating
-
unpredictability of symptoms and the need for flexible work
-
battling the system to stay in work (benefits and health care).
This describes the losses to self that accompany changes in work role. Work is described as adding value to self; it can be a place where a person feels respected and valued. There is a sense that work makes us what we are.
Second-order construct: de Vries 2011:324 motivators for staying at work – work as value
Work gave recognition, approval, self-realisation and self-respect. Work gives status and offers opportunity to be valued by peers. Work provides a mission to life. Gave link to society and value to life. Work is the ‘normal’ thing to do.
Second-order construct: Liedberg 2002:382 values and norms – meaning of work
Work valued by respondents as it made them feel useful members of society, appreciated by others and able to socialise. Many mourned over their lost professional identity [you are what you do at work]. Experience great loss of work role and social contacts that go with it.
Employees were therefore concerned not to be seen as ‘bad workers’ or as letting everyone else down at work. This meant that some people left work, worked through pain or took annual leave rather than be off sick.
Second-order construct: Patel 2007:345 perceptions at work – fear of letting employer down
Letting people down was expressed in terms of a threat to the patient’s own self-image as a worker: Some left work voluntarily for fear of letting employers down or not being seen as a good worker.
Second-order construct: de Vries 2011:324 motivators for staying at work – work as responsibility
A few perceived their work role as indispensable and that others relied on them. Therefore felt their absence impacted on work productivity as they could not be substituted, therefore worked through pain to meet work responsibilities and to not place a burden on their colleagues.
Loss of work was associated with feelings of personal betrayal if employers did not support them. Whereas they had felt that they were integral to the workplace before their pain, they now felt that they were easily dispensable, as if they were being ‘treated like a number’. They feared that employers saw them as too risky to keep on.
Second-order construct: Walker 2006:368 loss – employment
Sense of loss related to work exacerbated by lack of understanding from employers, particularly if employment had been longstanding. Felt a sense of betrayal by employer as pressure felt to leave work. Feel like they are treated ‘just like a number’ even when work had been valued prior to pain. Patients went to great lengths to find employment and often hid back pain from their employers (e.g. by taking holiday instead of sick leave). Guilt and resentment at losing/not finding suitable employment.
Second-order construct: Patel 2007:345 perceptions at work – employers’ limited understanding
Employer support and understanding limited due to a lack of awareness, negative perceptions (that the ill person will frequently be off work) and, perhaps, lack of personal experience. Patients feel that use of walking aids may make their case appear more plausible to employers; however, employers may also see such persons as more ‘risky’ to employ.
For those who managed to stay in work, relationships with colleagues could become hostile. They did not feel understood by others and worried about gaining a reputation for being ‘work-shy’. This feeling was exacerbated by a culture of judgement regarding pain.
Second-order construct: Holloway 2007:379 stigma at work
All described struggle to stay at work and stories of unsympathetic encounters with colleagues who could be hostile. This created an environment of mistrust. Media reports of back pain being do not help.
Second-order construct: Slade 2009:357 stigma – workplace
Many felt responsible for back injuries despite poor workplace policies. This guilt compounded by judgements by colleagues. Culture of judgement exacerbated by compensable bodies. Reputation for being ‘workshy’ despite attempts to stay in work.
The unpredictability of symptoms and fear of symptom progression made people feel that they could not continue at work. This was exacerbated by the fear that employers no longer valued them.
Second-order construct: Coole 2010:319 difficulty coping with flare-ups
Uncertainty at the unpredictable nature of their pain which made them unable to work at times. Effect on consistency of ability to work. Loss of confidence. Concerned that employers would not tolerate this unpredictability.
Second-order construct: Patel 2007:345 uncertainty – pain and health
The unpredictability of the severity of pain and limitation, and the duration of a flare-up made it very difficult for patients to foresee how they would cope with returning to and remaining in work: inability to cope with fluctuating nature of pain makes return to work less possible (as flexible working patterns not very common). Disadvantage in competitive working market.
They struggled to balance work commitments with other essential roles, as well as leisure and social activities. Work took its toll. Some were forced out of work because they found it impossible to find this balance. This could mean periods of time in and out of work.
Second-order construct: Sallinen 2010:351 being in-between
Refers to the process of moving back and forth between full work ability and work disability.
a. working in poor health and exceeding capacity
b. forced out of work into long term sick yet access to benefits denied = stress and financial difficulties.
Second-order construct: de Vries 2011:324 consequences of staying at work
Patients generally felt staying in work had many benefits. Dis-benefits included reduced opportunities for a social life and to pursue hobbies. Diminished capacity for leisure and pleasurable activities; increased pain and fatigue.
Although it was possible to maintain this balance with some flexibility in working arrangements, this flexibility was not generally forthcoming and there was a limit to the support that they could expect from colleagues.
Second-order construct: Coole 2010:320 employers’ help depends on managers
Some received help from managers and colleagues to adjust their work so they could maintain reciprocal working. Short term flexibility allowed them to feel valued at work. If work was reduced indefinitely then they felt a burden that they were not part of team and that colleagues would not support them indefinitely. Exacerbated by lack of belief and cuts to workforce.
Second-order construct: de Vries 2011:324 success factors (work) – adjustment latitude
Involves a range of crucial adaptation strategies around prioritising work, being flexible in execution of tasks (e.g. using a mobile phone that allowed one to not be confined to a desk), adapting ways of working with colleagues (delegation of tasks and accepting assistance) and working in partnership with families (i.e. accepting support as may be necessary). Not everyone at work experiences this latitude at work.
This category illustrates the adversarial nature of chronic pain in relation to work and benefits and was described only in MSK studies. It includes two subcategories: battling for benefits and a health-care system that does not facilitate return to work.
The person with chronic pain struggles to prove that they are sick in order to gain access to benefits.
Second-order construct: Holloway 2007:379 stigmatisation in health-care systems
Often disbelieved by health professionals and told pain was ‘all in the head’. This has an impact on benefits and compensation as patients perceived as malingerers.
Second-order construct: Walker 1999:367 being in the system – your life is not your own
Deservingness of benefits payment out of the hands of patients, resting solely on the opinion of medical professionals/benefits officers.
Leaving benefits is seen as risky because it is so hard to access them in the first place.
Second-order construct: Walker 1999:367 being in the system – battling for benefits
Forced to stay IN benefit system; no perceived advantage of coming out of it, although DID want to work. This concept underscores the challenges generated by the state.
Second-order construct: Patel 2007:345 uncertainty – benefits
Patients not only perceive leaving benefits as risky but also returning back to benefits as time consuming and bureaucratic. Feared leaving benefits but saw employment as making them better off. Return to benefits within 1 year of coping unsuccessfully with work (government initiative) perceived as daunting and as not offering financial stability.
This is exacerbated by a sense that benefits officers lack the skills and understanding to help them get back to the right job, or that they were stuck in a low-income job with no opportunity for retraining.
Second-order construct: Patel 2007:345 benefits organisation – (limited)
Limited support on advice from benefits officer about return to work. Felt jobs offered were inappropriate to their condition.
Second-order construct: Patel 2007:345 personal obstacles – qualifications and experience
High-level skills could be a barrier for return to work as applicants did not want to be trapped in a job that was not commensurate with their level of training. Those with low-level skills thought lack of training was also a barrier to return to work.
Although there are benefits from gaining access to certification of sick leave (e.g. it legitimises pain), this can be a double-edged sword. For example, it may affect access to future employment and opportunities, or alienate a person from work colleagues. It also may force a person to enter the health-care system to seek the legitimisation of diagnosis.
Second-order construct: Coole 2010:319 concern about sickness record
Concerns that sick leave perceived negatively and had an impact on employment record and job security. Use holiday leave rather than sick leave. Paradox – only seen as legitimate if they have a sick note, not self-certified – damned if I do and damned if I don’t! i.e. need sick record to be legitimate but don’t want a sick record.
Second-order construct: Walker 1999:367 being in the system – damned if you do and damned if you don’t
Compensation claims could alienate you from colleagues at work OR force you to seek medical diagnosis and treatment. Negative consequences of applying for compensation and apportioning blame. This describes being alienated because of legal process but if you don’t then you won’t get compensation [note – Marx; system covertly suppresses claims for what you deserve].
This describes the negative impact of the health-care system and occupational health services on return to work. It describes the lack of dialogue between employers, occupational health and health services.
Second-order construct: Coole 2010:318 no employment help from GP – lack of dialogue between GPs, health-care professionals and employers
Any joined up dialogue and action missing. This need is therefore undertaken by the patient who then worries whether his explanations will be accepted as valid by the employer.
Second-order construct: Coole 2010:318 no employment help from GP – GPs write sick notes
GPs wrote sick notes rather than suggesting modifications to work duties. Most of the advice about returning to work did not follow the occupational guidelines and many either did not return to work or had to request additional information on their certificates to permit them adjusted work duties. Some patients felt they simply had to comply with what the GP said. Others signed off work while awaiting tests and results
Contact with health-care professionals was not experienced as facilitating a graded return to work. Patients are told to ‘take care’ or avoid certain tasks, or may be issued sick notes whilst they wait for test results, thus becoming trapped in the system of medical consultation.
Second-order construct: Coole 2010:318 no employment help from GP – clinicians increase concerns
Advice from health-care practitioners often negative. Warnings linked harm to duties at work and increased concerns about staying in work; ‘be careful’; ‘take is steady’. Did not contact employers or advise on temporary modifications.
Second-order construct: Patel 2007:345 health-care barriers
Trapped in a cycle of repeated consultations that stopped return to work. Long waits and not being taken seriously by health-care professionals exacerbated this. Some had been classified unsuitable to work by benefits medical officers. This assessment for work eligibility became a deterrent to taking on rehab to return to work
6. Moving forward alongside my pain
Despite the constant struggle to appear credible, studies also reveal that some people with chronic MSK pain find ways of moving forward alongside their pain. This section presents categories that are described by people who are moving forward with pain. These categories describe a more positive existence alongside chronic pain:
-
(a) listening to and integrating my painful body
-
(b) redefining normal and focusing less on loss
-
(c) being part of a community of other people with pain
-
(d) being open about my pain
-
(e) realising that there is no cure
-
(f) becoming expert through experimentation.
6(a) Listening to and integrating my painful body
This describes a new relationship of trust and co-operation with the body. The alienated body becomes integrated by listening to and respecting it. It becomes a speaking partner and teacher. The person in pain is no longer at mercy of the body but a co-expert.
Second-order construct: Dragesund 2008:326 associations about the body
Body a limitation AND a possibility for some; unpredictable body limits opportunities – body has an existence of its own. Become more present in the body. New opportunities for participation connected to an increased ability to prevent pain from dominating. Not about controlling body but listening to it. No longer at mercy of the body.
Second-order construct: Afrell 2007:372 acceptance typologies – active process of change
Pro-active decision to make adaptations. Integrating the aching body takes a trusting and hopeful co-operation between self and body. The subject learns from the body and finds a new relation to his or her body in the same process. the body is looked upon as a speaking partner and a teacher. In this interplay, the subjects have grown as individuals and have begun to look at their future with optimism, although they know it will require great effort.
A person learns to balance his or her personal resources through co-operation with the body.
Second-order construct: Dragesund 2008:326 aware of body
Greater sensitivity to body and symptoms; different to previous pain free experience of detachment from one’s body. Physical exercise and knowledge of bodily symptoms gave a sense of control over pain and tiredness. Need to respect limits on body (and life) imposed by pain.
Second-order construct: Raheim 2006:348 typologies – coping
A dialogue between the body and self creates a caring relationship despite its treachery. Dialogue with partner and family about pain and needs appears integral to adjustment and gaining the support of others. Working with the body and not against it.
6(b) Redefining normal and less focus on lost self
This describes the person in pain who no longer focuses on losses but on reconstructing an acceptable new self. It describes an acceptance of change and a sense of repairing existence; I have changed but I am still me, and can enjoy life.
Second-order construct: Lachapelle 2008:335 process of acceptance – redefining normal
Letting go of pre-pain self-expectations and shifting their focus to what they could accomplish now, despite the pain, was an important next step. The knowledge that no return to pain-free status possible. Followed by a grieving of losses and a redefinition of goals, although conscious of having the power to also choose a path of giving in to negative emotions.
Second-order construct: Skuladottir 2011:355 quest for normalcy
Retain optimism hope positive thinking goals at same time be realistic. Although pain has changed me I am still a strong person. Gaining a sense of achievement from the things I can do. More of a focus here on positive thinking and seeking meaningful activities to occupy time and focus in order to maintain good mood and optimism.
New patterns and routines are developed and the focus is on accomplishment in spite of pain.
Second-order construct: Werner 2003:369 applying the competence – focusing on resources (not pain)
Learnt to be less focused on pain and more on personal resources and enhancement, i.e. what can I actually do rather than how do I feel; simply to ‘treat’ oneself or enjoy a pleasurable activity and mobility; making adjustments to amount of tasks to be undertaken in relation to bodily capacity and letting others know about this work capacity.
Second-order construct: Gullacksen 2004:377 stage 3 – maintenance (handling future changes)
Normalising life in spite of pain demands skilful strategies of coping. Increased self-knowledge gained through this (hidden) struggle.
This process is experienced alongside a sense of grieving for the old ‘real self’.
Second-order construct: Lofgren 2006:337 grieving
The sense of loss of a previous life but also the time when the process of grieving allows a turning point and new opportunities. Entailed working through loss of former self and body to reach a point of finding new ways to live life. Work through feelings of disappointment, self-blame, sadness, despair, regret. Grieving process important to rehabilitation.
6(c) Being part of a community of others with pain
This describes the positive impact of being part of a community of others with pain. It brings a sense of sharing, being valued and becoming credible; there are others who understand, believe and respect me.
Second-order construct: Gustaffson 2004:327 shame to respect
Started rehabilitation with feelings of shame and self-doubt. Felt disbelieved by health professionals and misunderstood by family. The group interaction realised a change from these negative emotions to a greater sense of respect and self-worth with more positive relations with others.
Second-order construct: Werner 2003:369 for better or worse – recognition gives strength
Recognition and respect demonstrated within groups strengthened participants’ self-confidence and self-esteem while diminishing feelings of guilt for not being restored to full health. The participants described the strength, confidence, and awareness gained from the treatment programme as being useful bodily and emotionally, and gave social competence outside the group context.
Second-order construct: Sallinen 2011:352 permission to talk
Permission to talk – peer encounters often a turning point after wrestling with disbelief for a long time. Had kept feelings to themselves so as not to jeopardise existing relationships. Now had ‘permission to talk’ with genuinely interested peers and valued this. It captures the relief and joy of feeling free to unburden the experiences of pain with those who did not judge.
However, despite the benefits of being recognised within a group of others with pain, this concept incorporates a sense of ambivalence: I am like the others but at the same time I am not like them, and do not want to ‘celebrate illness’. This was reinforced by narratives of the self as a ‘good’ person, with the possible implication that I am better than the others.
Second-order construct: Mengshoel 2004:341 unwilling to celebrate illness
The women actively resisted the sick role through participation in the fibromyalgia patients’ association and non-disclosure to employers, for example; did not want to ‘celebrate illness’ with other sufferers; described it as a fellowship designed to endure a hopeless fate. Keep it quiet.
6(d) Telling others about my pain
This describes the release that comes with no longer having to hide pain from others and the benefits of letting others know about my limitations. It shows how a person begins to limit the demands of others and manage resources.
Second-order construct: Werner 2003:369 applying the competence – informing others
Women now let others know of their limitations and capabilities. Being outspoken about personal needs and desires was said to be a constantly on-going internal and external process of work.
Second-order construct: Gustaffson 2004:327 setting limits – telling others
Programme has taught them to tell others about their condition and thus reduce demands on themselves [learn to say no].
There is a sense that the person no longer needs to gain the approval of others.
Second-order construct: Werner 2003:369 applying the competence – encountering others
With renewed self-esteem following the programme patients were less reactive to and concerned about what others felt about their chronic pain, and less preoccupied with gaining approval.
6(e) Realising that there is no cure for my pain
This describes the realisation that pain is here to stay. The person in pain becomes liberated from the ceaseless search for a cure, which has previously limited the possibility of moving forward.
Second-order construct: Gullacksen 2004:377 stage 1 – acknowledgement
Acknowledging that pain was not temporary was crucial to adjustment. Necessary to give up the aspiration to return to life as ‘normal’. This grew as an ‘inner certainty’. no longer possible to hide situation. Now turned toward the future, although this did create anxiety about what future holds. Stopped waiting for a cure to be found and turned to own resources. Hope for recovery maintained but no longer an obstacle to alternative possibilities. Change begun.
Second-order construct: Harding 2005:330 living with and planning for the future
With time there came a sense of resignation to the pain and accepting it as a part of life for the foreseeable future. Acceptance of pain and whether it would ever eventually end dominated this theme. Some reported the notion of an increased pain threshold to accommodate the pain. This acceptance marked a significant point of the patients pain career and was characterised by a sense of active adaptation.
For some, this ‘acceptance’ marked a new phase in moving forward into a new life alongside pain.
Second-order construct: Paulson 2002:346 striving to endure – nurturing hope
The men had come to terms with a future that may not be pain free. This seemed to help them to be hopeful for the future. Keep courage.
There is a sense that recovery is about becoming someone new rather than returning to what you were before.
Second-order construct: Sallinen 2010:351 coping with fluctuating symptoms
Process of learning to live with fluctuating symptoms by adopting strategies of prioritising, pacing and work adjustments. Others experienced release from work an amnesty, as it allowed them to break down tasks and listen to their body. Able to maintain role with some compromises. Coping was expressed as an acceptable goal of recovery, thus recognising that full remission might not be possible.
6(f) Becoming an expert
This describes the process of becoming an expert: becoming less reliant on a health-care professional to know and meet my needs. It describes how the person comes to know their own body and gains the confidence to experiment and choose to change their behaviour.
Second-order construct: Steen 2001:385 experimenting
Narrative of discovery [learning to trust own opinions?]. This seemed to capture how the group and leaders gave them permission to explore, be curious and be creative. The feeling generated to be celebrated and not hidden. A respect for patient opinions about illness and exercise choices although they may have limited experience of these processes. Also seems to be about patients valuing freedom to try things out, such as different methodological approaches (and make mistakes), rather than only following the instructions from health professionals.
Second-order construct: Skuladottir 2011:355 quest for normalcy – involved in decision-making
Women felt they were the experts in their own pain and valued participation in decision-making surrounding pain. Realised the limitations of health-care professionals and that I am the expert of my pain. I am in charge.
For those with fibromyalgia, this could be triggered by obtaining a ‘name’ for a condition that they could now seek to understand.
Second-order construct: Lofgren 2006:337 constant struggle – being knowledgeable
Described as learning everything there is to know about fibromyalgia. They read the journals and the Internet and/or discussed with others. The knowledge gave them both self-esteem and respect for others similarly placed. It helped them find new ways to cope and encouraged them in thinking about their pain as not dangerous.’
Second-order construct: Lachapelle 2008:335 facilitators to acceptance – self-management education
Having a diagnosis was a key turning point for them to seek out information about their condition. Effective self-management linked to the undertaking of non-medical strategies that improved ability to perform activities desired despite pain, empowering patients to take control of their lives. Women with fibromyalgia more self-reliant in educating themselves about illness compared to women with arthritis who received greater access to information for health and specialist organisational sources.
Constructs that did not fit our team categories
Although there are always data that do not ‘fit’ in qualitative analysis, we found relatively few second-order constructs (six MSK and four fibromyalgia) that we did not think fit into our conceptual categories. These are shown in Box 7. We did not want to ‘shoehorn’ constructs into categories if we did not think that they ‘fit’.
Aegler 2009:312 challenge to finish performance.
Frequently not able to finish a performance and needed strong intent. However, occupations completed even if body racked by pain as this brought a sense of satisfaction. Sometimes completed task in spite of potential consequences and increased pain.
Bair 2009:314 to self-management – fear of hurt.
Fear of increased pain – acute fear of aggravated pain if one exercises.
Bair 2009:314 barriers to self-management – strategies don’t work.
Difficulty in doing the exercises and experiencing exercises as ineffective also a barrier. Why do it if it does not work?
Coole 2010:320 employers – managers with back pain.
Perceived managers who had had back pain were more supportive.
Gullacksen 2004:377 stage 1 – prelude.
Slow to change as pain often regarded as temporary at first. As sick periods got longer and effected life – reached a critical point.
Hunhammar 2009:331 striving to master variable pain – space for health.
The experience of chronic non-specific pain added an additional burden to life which required a space to meet these demands such as physiotherapists’ appointments or time to keep fit. Gender differences emerged with childcare a main consideration for women.
Paulson 2001:383 local to spread-out pain.
Localised pain can spread out over all of body. Exercise helped only in early stages, and then it became too painful to use this strategy to relieve pain. Frustrating.
Paulson 2001383 worrying and not worrying pain.
Single areas of the body that ached but were mobile were less worrying than a situation where multiple areas experienced intense pain.
Paulson 2002:346 striving to endure – search for alleviation.
Felt lives could be different if pain went. Searched for ways to lessen pain and improve quality of life. May include medication, or trying to work through pain or even periods alone. Peace of mind found from gaining access to disability pensions as no longer had to explain invisible symptoms.
Toye 2012:365 restoring hope – deconstructing fear of specific movements.
Prior to pain management, fear of moving had made them avoid specific movements. Several factors helped to deconstruct fear: learning that hurt does not mean harm, seeing other in group do feared movement, performing feared movements, working through flare-ups under supervision.
Synthesising translations: line of argument
Our findings revealed the new concept of an adversarial struggle that explained what chronic MSK pain was like. The following describes our line of argument or conceptual model, which explains the categories described above.
The constant struggle of chronic musculoskeletal pain
Figure 12 illustrates the constant struggle to affirm the self; to reconstruct a sense of self in time; to find an explanation for suffering; to negotiate the health-care system; to prove legitimacy. These over-riding themes are adversarial, giving a sense of being guilty until proven innocent. The person is pulled in different directions; between an integrated or an alienated body; between the ‘real me’ or the ‘not real me’; between a connected me or an isolated me. Amidst this struggle, their present and future have become unpredictable. The way that the person constructed their self in time prior to pain (their hopes, expectations and aspirations) is now altered.
FIGURE 12.
Conceptual model – struggling with chronic pain.
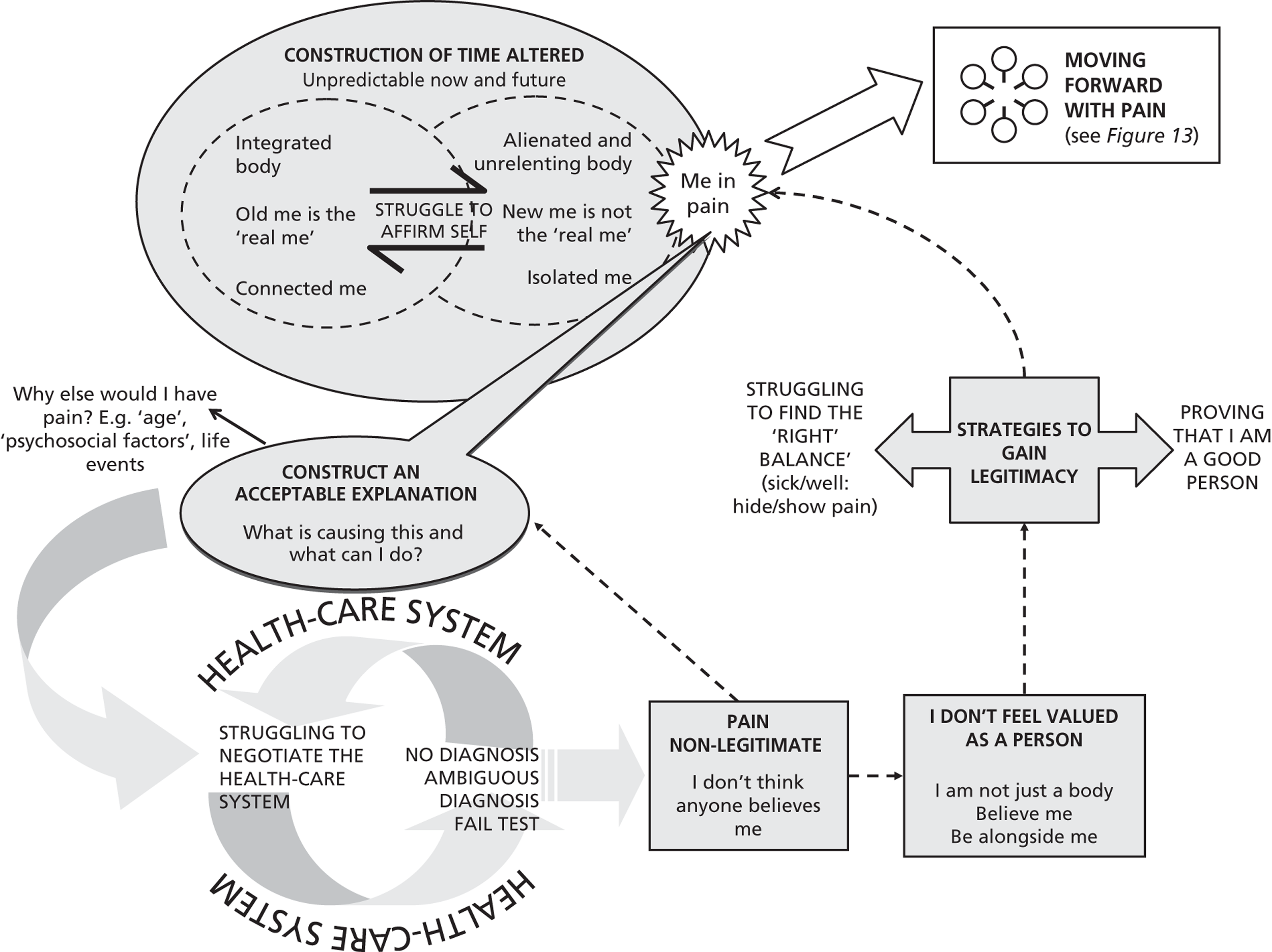
On a different front, the person battles to attain an acceptable explanation for their suffering. The person looks towards the health-care system where the medical model prevails. This model takes disease to be an objective biomedical category that can be accounted for by a specific aetiology; it implies an illness trajectory whereby a cure naturally follows diagnosis and treatment. The person with chronic MSK pain does not fit this model and they become alienated from it. This is experienced as ‘failing’ the medical test. In spite of this, the person feels compelled to re-enter the system: if I pass the test then there must be a cure; if I pass the test then it must be true and everyone will believe me. Thus, the person continues to struggle to negotiate the health-care system despite their ambivalence towards it, knowing that it is failing to meet their expectations as being in the system legitimates their pain. Our interpretations suggest that people with chronic pain also explore alternative explanations for their suffering: age, psychosocial factors or life events. In their struggle to negotiate the health-care system, they do not feel that they are believed or valued by health-care professionals. Despite the mind–body dualism inherent in the medical model, the person in pain needs to feel that they are more than just a body; to feel that the medical professional is alongside them as another human being. There is a sense that this is fundamental to the therapeutic encounter rather than just an adjunct.
Alienation from the medical model means that pain itself is experienced as non-legitimate. The person with chronic pain uses strategies to gain legitimacy. First, they use narratives to prove to those around them that they are a good and valued member of society. Second, they struggle to find the right balance between hiding and showing others that they are in pain, or between appearing ‘too ill’ or appearing ‘too well’. The outcome of this struggle has an impact on the struggle to affirm self. If I am ‘too well’ or hide my pain completely then I do not appear legitimately ill. If I am ‘too ill’ or show my pain ‘too much’ then I cannot be me.
Moving forward alongside pain
Figure 13 illustrates categories linked to moving forward alongside pain. Through listening to and integrating the painful body (1), the person moves away from an alienated and unrelenting body. Although the body is still experienced as apart from self, there is a sense of co-operation that enables the person to move forward. Living alongside pain also involves redefining a sense of ‘normal self’ and focusing less on loss (2). Although this may follow a period of grief and loss, some discover that the new person is as real. Telling others about my pain and not feeling compelled to hide it or gain approval (3) can affirm reciprocal relationships with others, and a feeling of being connected again. Meeting other people with chronic pain (4) also brings a sense of being connected, despite feelings of ambivalence (I am not completely like the others). Finally, realising that there is no cure for pain (5) and becoming an expert (6) may provide a resolution to the struggle to negotiate the health-care system and their alienation from the medical model. As the ceaseless struggle to find a diagnosis and cure ends, a person becomes open to other possibilities. By gaining knowledge of their body, the person gains the confidence to experiment and change their behaviour, without the sanction of the health-care professional. There is a sense that I am now the expert of my own body.
FIGURE 13.
Conceptual model – moving forward with pain.
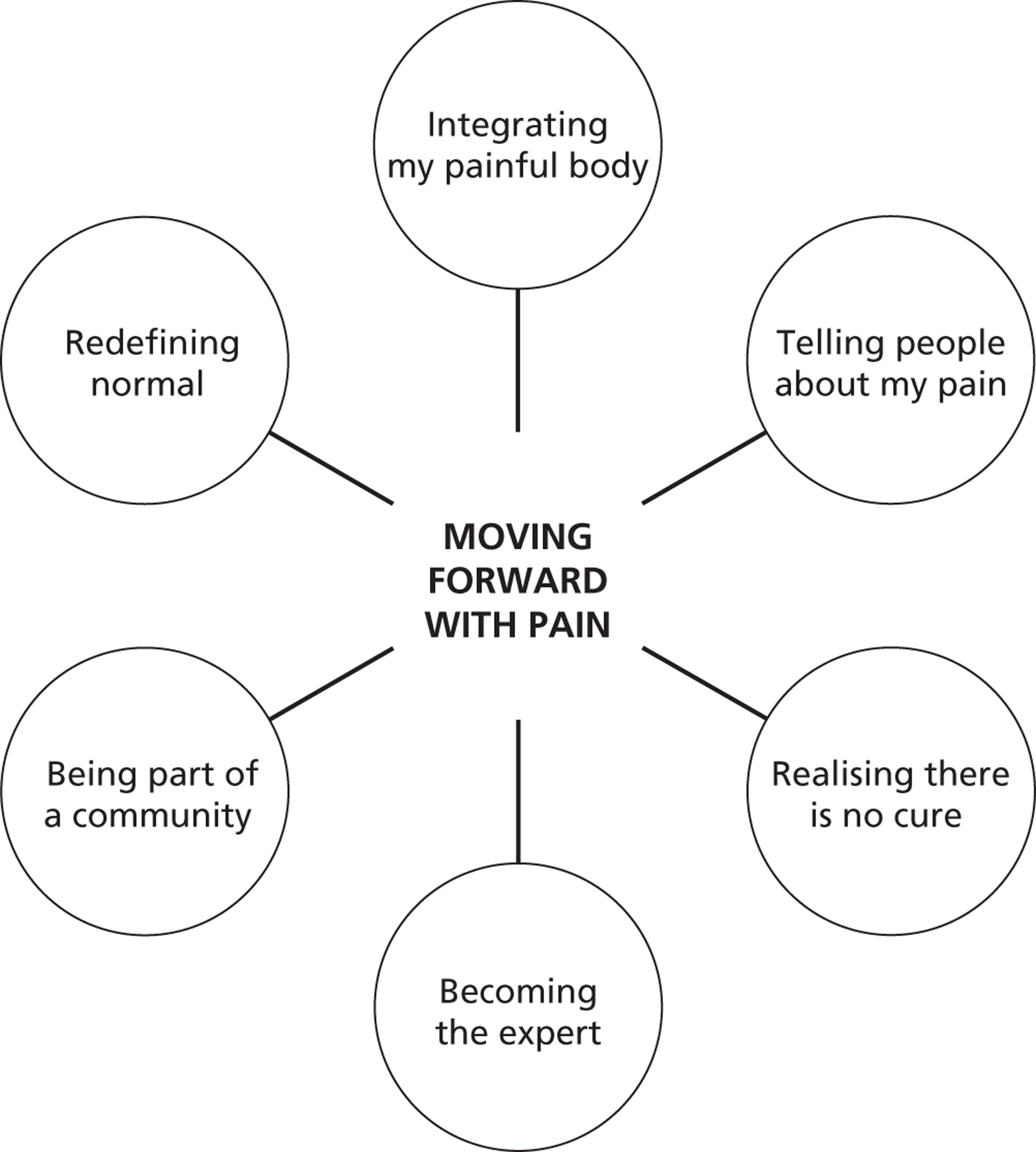
Chapter 5 Discussion
We have used the methods of meta-ethnography to produce a conceptual synthesis of studies exploring patients’ experience of chronic non-malignant MSK pain. Our model presents a line of argument that highlights the adversarial experience of people with chronic MSK pain but which also offers an understanding of how some aspects can be surmounted. Although facets of this struggle are evident in the primary studies, our innovation is to show that struggle pervades multiple levels of the person’s lived experience: their sense of body and self; their biographical trajectory, their reciprocal relationships at home and in the wider community; and their experience of health-care services. We described the person’s struggle to keep hold of a sense of self whilst feeling misunderstood and misbelieved. This adversarial experience is central to our model and may distinguish it from other types of chronic pain. For example, a person who suffers pain from cancer may not face the same struggle of proving their credibility to others. Fundamental to this adversarial experience is the cultural value placed on the biomedical model. This model has deep roots and can have a large impact on the experience of suffering. In spite of this struggle, our model offers an understanding of how a person with chronic MSK pain can move forward alongside their pain. This involves a process of integrating the painful body, redefining a self that you want to live with, feeling valued as a worthy human being with unique experiences and participating in valued reciprocal roles. It also involves realising that a medical cure is unlikely and moving away from the focus on the health-care professional as expert. We now discuss our findings focusing on implications for health care and possible areas for future research.
Integrating my body
Our model suggests that dualistic therapeutic approaches do not encourage a person to move forward, and that a more embodied approach to illness might help. A theory of embodiment has its philosophical roots in the writings of Merleau-Ponty,394 who breaks down the dualism of mind and body to focus on the central place of the body in constructing our experience of the world. Embodiment theory emphasises bodily experience and the way in which we construct this experience. 388,395–398 This embodied approach in no way denies the existence of disease, but shifts the ‘level of analysis’397 to the individual’s understanding of the experience. Thus, Frank’s397 ‘medicalised body’ and Kleinmnan’s conceptualisation of the biomedical model as a culturally specific ‘explanatory model’ demonstrate that, although we are bodies, the conditions through which we experience our bodies are constrained by culture. Our model supports the suggestion that, because chronic illness is constructed in a certain way, it is experienced as ‘failure’:
The dilemma of the ill . . . is that they are constructed as responsible for their health and thus feel guilty, and simultaneously understand themselves as having less and less control over their bodies . . . while patients feel responsible, professional medicine places the cause of their disease beyond their control.
p. 138397
Our model also suggests that the way in which we experience our own body has an impact on the way that we construct disease. As part of a person’s struggle we described the fragmentation of body and self, and suggested that moving forward with pain involves a process of reintegrating the painful body. In his classic work, The Absent Body, Leder388 explores reasons for this fragmentation, which he argues explain the prevalence of Cartesian dualism (see http://plato.stanford.edu/entries/dualism/#MinBod; accessed 2 July 2013) in the development of Western scientific thought and modern medicine. Cartesian dualism conceptualises mind and body as separate entities. Leder388 argues that, before the onset of pain, our bodies are ‘essentially characterised by absence’ (p. 73). Under conditions of health, we perform actions automatically and remain unaware of our body until something goes wrong with it. Health presupposes that we remain unaware of our bodies. 396 When in pain, the body emerges as an ‘alien presence’; it ‘dys-appears’. I no longer am a body but have a body,388 and my body becomes an ‘it’ as opposed to an ‘I’. Wall399 describes this dualism as epitomised by the expression ‘my foot hurts me’ as if in some way the foot is apart from myself (p. 23). It is because ‘the body seizes our awareness particularly at times of disturbance, [that] it can come to appear “other” and opposed to the self’ (p. 70). 388 This fragmentation of ‘mind trapped inside an alien body’ means that our bodies become mistrusted and ‘forgotten as a ground of knowledge’ (p. 86). 388 Our concept ‘integrating my painful body’ implies an altered therapeutic relationship with the body in which the dualism of mind and body are broken down.
Our model opens up possibilities for therapies that aim to change the way that we experience our own body when we are in pain. For example, mindfulness-based therapies encourage those with pain to learn a ‘particular kind of attention characterized by a non-judgmental awareness, openness, curiosity, and acceptance of . . . experiences’ such as pain (p. 83). 400 Qualitative research focusing on the way that we experience our own body when it goes wrong, a phenomenology of the body, would be useful to help understand the efficacy of therapeutic approaches such as mindfulness. This research would help us to understand the impact of these approaches on recovery from illness.
Accepting pain and redefining my self
Our model shows how threats to self-identity are fundamental to the experience of chronic pain401 and suggests that moving forward with pain involves redefining self. Patients struggle to reconcile the new self in pain with an old self-rooted in the past or a hoped-for-self in the future. This is supported by Campbell and colleagues’28 meta-ethnography of rheumatoid arthritis, which describes a loss of ‘life definition’ (p. 111). Our model links to developing psychological theories utilised in pain management. In particular, it supports studies showing that an individual’s capacity to redefine their self, their psychological flexibility, may help people move forward with pain and reduce its impact. 402,403 A new wave of acceptance and commitment therapies (ACTs) focusing on psychological flexibility is showing promise in the treatment of those with chronic pain. These therapies construct acceptance as moving towards goals that define self alongside a ‘willingness to continue to actively experience pain along with related thoughts and feeling’ (p. 145). 404 Although moving towards self-defining goals is integral to ACT, acceptance might mean different things to different patients (and their clinicians). For example, for some the term ‘acceptance’ might imply giving up404,405 and this may have an impact on their willingness to engage in ACT. Qualitative research exploring the meaning of acceptance for both patients and clinicians might help us to understand the efficacy of these approaches.
We do not know why certain patients can accept and redefine their sense of self and others cannot. It may be related to the degree of disruption to self that is caused by pain. The enmeshment model developed by Pincus and Morley406 proposes that, if a person regards their ideal self as unobtainable in the presence of pain, they are less likely to accept chronic pain. The enmeshment model incorporates self-discrepancy theory,407 which proposes that the extent to which pain disrupts our lives depends on the meaning that it holds for us. In self-discrepancy theory meaning incorporates three constructs: (1) actual self – ‘your representation of the attributes that someone (yourself or another) believes you actually possess’; (2) ideal self – ‘your representation of the attributes that someone (yourself or another) would like you, ideally, to possess’; and (3) ought self – ‘your representation of the attributes that someone (yourself or another) believes you should or ought to possess’ (p. 320–1). 407 Our ideal and ought selves act as guides that we strive to achieve. Discrepancies between these guides and our actual self can lead to powerful emotions such as shame, dejection, embarrassment or even fear. Ideally, these powerful emotions drive us to actions that will ultimately reduce the discrepancy. The enmeshment model extends self-discrepancy theory by suggesting that the degree to which certain goals are integral or ‘enmeshed’ with my self-concept will determine the degree of emotional consequences. 406 For example, if the desire to be independent or to interact with others is highly valued, this is likely to lead to greater distress if it is threatened. 401 Self-discrepancy theory incorporates the importance of what another person thinks about me. In other words, any discrepancy between what people think I am and what they hoped or expected can have a powerful effect on how I feel and behave. These psychological models are useful as they acknowledge that we cannot understand the impact of pain unless we try to understand personal meanings. Therapeutic approaches aimed at helping a person to move forward with pain need to focus on facilitating redefinition of valued self.
Redefining self in space and time
Our model shows how a person’s construct of self now and in the future is altered. We described how the unpredictability of pain creates an endless present in which the person in pain becomes constantly vigilant of the body. Thus, the person in pain becomes focused on the here and now. Leder388,408 describes this as the ‘centripetal mode’ in which a person focuses in towards the body rather than out towards the world and future. When we have pain we no longer engage in the world as we once did. Our usual sense of time and space is replaced by constant bodily vigilance; ‘the oppressive nearness of coenaesthesia’ (p. 75). 388 ‘Our sensory experience, normally directed ecstatically upon the world, is now forced inward in a centripetal fashion. We no longer see hear, feel the world through our bodies: instead the body itself becomes what we feel’ (p. 255). 408
Our model supports approaches that empower a person to live outwards towards the world, rather than in towards the body. In other words, therapeutic approaches that empower participation, defined as ‘involvement in life situations’ (p. 10). 409 This means trying to live as a reciprocating person with meaningful social roles, setting goals and making plans for the future. For example, pain management may aim to empower a person to remain in or return to work, or to continue to move towards family or educational goals. Our model illustrates the impact that not feeling that anyone believes you has on participation. The International Classification of Functioning, Disability and Health410 regard ‘stigma’, ‘stereotypes’, ‘people’s reactions’ and ‘prejudice’ as key factors limiting participation, factors that go beyond the activity limitations resulting from physical impairment. Our model shows that a sense of not feeling believed causes social isolation and limits participation. As participation is integral to a return to health, research is needed on the factors, beyond physical impairment, that limit participation for those with chronic pain. This opens up possibilities for therapies that aim to empower participation.
We described how a person’s construction of time is altered. Leder’s388 centripetal mode incorporates this altered relationship with time; ‘pain seizes [us] back to the present’ and we are no longer at ease to ‘roam the future’ (p. 75). Although our model supports this pull towards the moment now, we also found that people in pain simultaneously looked towards the future with a sense of misgiving. Before pain our construct of self-in-the-future remains dynamic; none of us is likely to turn out precisely as we plan. However, in conditions of health, we do not remain focused on this discrepancy. In contrast, for those with chronic pain, the discrepancy between what we had planned and what is now felt to be likely is brought starkly to the foreground. The life that we, or others, planned is irreparably altered. The future ‘dys-appears’ giving a sense of hopelessness. This altered regard towards the future has an impact on a person’s self-perception. Patients and their clinicians therefore face the challenge of reconciling a sense of hope with the realisation that pain is here to stay. Research focusing on how a person can reconcile hope with an acceptance that pain is here to stay would help us to understand outcomes for people with chronic MSK pain.
Patient as subject not object
We describe relationships with health-care professionals that do not necessarily empower patients to move forward. We show that patients with chronic MSK pain do not feel heard, believed or understood as living subjects. This clinical relationship focusing on the patient as an object is historically and culturally embedded: ‘The post-Cartesian world has very successfully out-descarted Descartes. It has perfected a pain so stripped down that it has almost no meaning’ (p. 274). 411
Foucault412 described the paradoxical position of the clinical encounter, in which the doctor aims to diagnose a disease rather than understand the person’s experience: ‘If one wishes to know the illness from which he is suffering, one must subtract the individual, with his [or her] particular qualities’ (p. 15).
However, it is ‘pathos’, the feeling of suffering and powerlessness, of ‘life going wrong’, that precedes a person’s visit to the doctor (p. 137). 396 Our model suggests that central to the therapeutic relationship is the recognition of ‘pathos’; the patient is a subject rather than an ‘object’ of investigation. This concept is central to models of patient-centred care. 413 Leder388 argues that, when treated as the object, the person becomes conscious of themselves as an alien thing, thus reinforcing dualist metaphysics. Our model supports a therapeutic relationship that challenges the dualism of mind and body, and meets the patient as an embodied individual: ‘When the patient is not treated as a living, desiring, suffering being, compliance is reduced, evidence is overlooked, inappropriate treatments are prescribed, genuine healing gives way to “fixing the machine” ’ (p. 97). 388
We described a need for a person in pain to feel that the health-care professional is alongside them with their pain. Affirming a person’s experience and allowing an empathetic interpretation of their story is not an adjunct, but integral to health care. 395 This is far away from the clinical encounter described by Foucault,412 in which patients’ meanings are stripped away by the health professional in their well-intentioned efforts to diagnose a disease. People construct the meaning of illness through their stories, and it is only by listening to these stories that we understand their response to illness. For example, narratives can tell us about discrepancies between a person’s actual, ideal and ought selves: what am I like compared with what I used to be and what I wanted to be? Narratives also reveal underlying tensions. Bury393 describes moral narratives in which people make efforts so show themselves as worthy human beings, which our model supports. These narratives are particularly important when there is no explanation for their suffering, and a person feels alienated from the biomedical model. 123,393,389 Illness narratives emphasise the cultural context of illness and how it impacts on suffering. This therapeutic need to be heard and valued may have implications for education, for example the use of arts and humanities in clinical education to help health professionals develop skills of empathy and compassion. 414
Towards a culturally embodied model of pain
Our model supports anthropological studies that have shown that suffering gives rise to a search for an explanation. 415 An explanation allows us to do something to relieve our suffering, to take reparatory action. The way that we explain illness is embedded in our culture and we learn this from those around us. Our findings show that cultural models used to explain illness are integral to personal meanings, and therefore the experience of illness. The medical model is an example of a culturally specific model for explaining suffering. 395 However, this model has certain characteristics that are fundamentally antagonistic to the experience of those with chronic MSK pain: the dualism of mind and body; specific aetiology and curability of disease. 415–417 The biomedical model does not fit the experience of those with chronic MSK pain yet still remains highly valued and integral to credibility, even though we know that biological findings do not fully explain pain. Biomedical approaches based on a dualism of body and mind are ‘ill-equipped to resolve the problem of pain’ (p. 41). 418 Many health-care professionals may not feel that they adhere to a biomedical model, and may indeed be surprised by the finding that is it highly valued. However, cultural expectations of diagnosis and cure still have a powerful effect on the experience of pain: ‘society itself is changed by its belief in medicine and surgery’ (p. 162). 399 The Cartesian dualism of mind and body integral to the development of Western scientific thinking (erroneously) presupposes that, if something cannot be found in my body, it must be in my mind. We describe how people struggle to achieve a diagnosis and ‘pass the medical test’ so that people will believe them. Importantly, although qualitative studies have consistently shown that people with chronic pain feel that health-care professionals (and others) do not believe them, this disbelief is still deeply felt. This finding has implications for health-care practice.
Taking an anthropological perspective, Csordas419 proposes that healing is a cultural process that involves altering the meaning of suffering in order to generate possibilities for the future. Croft and colleagues3 suggest that a change in model would improve the outcome for patients with MSK pain, in particular moving away from the focus on pathology and towards the experience of symptoms. In other words, treat symptoms rather than defined pathological conditions. This requires a shift away from the prevailing explanatory model. It can be extremely difficult to challenge cultural models as they are inherently stable and have a logic grounded in culture. 123 We have described how patients feel compelled, yet at the same time reticent, to engage in a health-care system that is failing their needs. There is a sense of being ‘trapped in the system’. This compulsion may be fuelled by the value placed on a cultural model in which diagnosis, treatment and cure are culturally expected norms. The compulsion is further fuelled by a person’s need to legitimise pain. However, although difficult to challenge, static cultural models do shift if they continue to be challenged by lived experience. 420 Our analysis shows that cultural models can hide deep underlying tensions. 391 The biopsychosocial model is an alternative cultural model that has been successfully used for some years in therapeutic approaches for chronic pain. It aims to focus on the ‘human experience’ of illness and suggests that illness experience is the result of a complex relationship between biological factors and psychosocial factors. 390 Although the biopsychosocial model goes a long way towards incorporating experience into our understanding of pain, it faces criticisms in that it is still ‘dualistic’ at its core. For example, Grace418 argues that psychological factors tend to be ‘grafted onto the somatic’ (p. 44). Our interpretation supports a truly ‘integrative’ model’ that treats pain as an embodied experience. 418,421,422 Embodiment focuses on meaning, which can be understood only in the context of the individual’s social, cultural and historical context. Meaning is vital to an individual’s emotional response and actions; it is ‘never external to pain, never something “added on” ‘ (p. 48). 418 This fits with the International Association for the Study of Pain definition of pain as a sensory and emotional experience: ‘Pain is always accompanied by emotion and meaning so that each pain is unique to the individual’ (p. 38). 399
Culture gives meaning to experience by providing a system for ordering and categorising experience. 415 In her classic texts, Susan Sontag uses the examples of cancer and tuberculosis423 and later acquired immunodeficiency syndrome424 to show how cultural meanings are attributed to illness, even if illness has a specific pathology. In short, imaginative or ‘metaphoric thinking’ regarding illness is integral to the experience of suffering. Discrepancies between cultural categories and our experience can result in powerful emotions that cannot be understood outside the cultural context. For example, the mismatch between the experience of chronic pain and the biomedical model can produce feelings of worthlessness, fear, agitation, shame and guilt. Explanations that focus on culturally embedded meaning might provide a useful link between culture and physiology. 418,421,422
The performative aspects of pain experience
Our model also suggests that performance is integral to the experience of chronic MSK pain. The struggle to successfully perform pain has important implications for chronic pain management. First, we describe the person’s struggle to balance whether or not to show or hide their pain; to appear well or ill. In this way their experience of pain is scripted to present a particular impression. This should not in any way imply that pain is not real; Goffman425 suggests that performance is integral to social life. Through performance we make things happen by presenting a certain picture of ourselves.
When an individual appears in the presence of others, there will usually be some reason for them to mobilise their activity so that it will convey an impression to others which it is in their interests to convey (p. 3). 425 Our model also resonates with Turner’s391 influential anthropological work on performing cultures. Like Goffman,425 he supports a theatrical paradigm for culture. 426 Turner’s work is important because he observes the dynamic and dramatic process maintaining cultural life. He describes how cultural norms are not static but continually re-enacted through a performative process whereby (1) cultural rules are breached, (2) there is a period of crisis when the person remains outside or ‘liminal’ to culture, (3) redressive action is taken and (4) there is a resolution of crisis through reintegration or schism with culture. This resonates with facets of our model: I don’t fit the medical model (breach); nobody believes me (crisis); I am struggling to prove legitimacy, to negotiate the health-care system and to construct an explanation for my suffering (redressive action). However, our model demonstrates that, for many people with chronic MSK pain, there is no resolution and they remain culturally liminal. From the Greek word limen, meaning harbour, liminality refers to a person or thing that is neither wholly one thing nor the other; a person who resides in-between categories. Some argue that a person with unexplained symptoms may be stigmatised because they are culturally liminal. 123,427 We also show how a person with MSK pain uses moral narrative to perform their credibility by presenting a certain ‘virtuous’ picture of themselves. 393,428 These moral narratives may be particularly important when medical explanations are absent and a person finds themselves standing outside culture. 393
Qualitative syntheses in musculoskeletal pain
There is already an insightful qualitative synthesis exploring the experience of rheumatoid arthritis. 28 Campbell and colleagues’28 meta-ethnography of rheumatoid arthritis supports important areas of our conceptual analysis. For example, their model highlights the person’s need to explain elusive symptoms; the unpredictability and unrelenting nature of rheumatoid arthritis; the loss of ‘life definition’ and disruption to self; a dread of the future; and the loss of reciprocal roles and social isolation. Unlike Campbell and colleagues, we identified concepts that describe patients’ experience of health care, although these were less evident in the fibromyalgia studies. This may highlight the relative importance and impact of patients’ experience of health care, particularly for people with MSK pain for whom a diagnosis is often absent. In short, the experience of health care is integral to a person’s experience of pain, and was more prevalent in the second-order constructs from primary studies than the experience of pain itself. We did not identify a qualitative synthesis that explored the experience of osteoarthritis and this might be a useful future synthesis.
There is a previous qualitative synthesis of fibromyalgia studies429 and, as the condition incorporates symptoms other than MSK pain, we discussed with the advisory group whether or not to include fibromyalgia studies in our meta-ethnography. We decided to include fibromyalgia on the basis that chronic MSK pain was central to the experience, and that the studies were therefore likely to be insightful. We also wanted to be able to compare fibromyalgia and MSK concepts arising from our analysis. Our synthesis includes 19 of the 28 papers incorporated in Sim and Madden’s429 fibromyalgia synthesis. We did not include papers that did not meet our criteria for inclusion, and included an additional nine fibromyalgia studies. 324,327,335,351,352,366,373,377,381 Their synthesis supports important areas of our conceptual analysis, for example the ‘conscious awareness’ of the body in pain; the unrelenting nature of fibromyalgia; isolation and loneliness; the search for an diagnosis; the ambiguity of diagnosis and loss of legitimacy. It also supports concepts related to moving forward with pain, including listening to the body, accepting loses and re-evaluating life. This overlap in themes is encouraging and supports the integrity and usefulness of qualitative syntheses in health research.
In another systematic review of qualitative studies, Parsons and colleagues430 explored the influence of patients’ and primary care practitioners’ beliefs and expectations about chronic MSK pain on the process of care. Their finding that clear communication and trust is integral resonates with our model. Their review also supports the finding that the biomedical model does not fit the experience of those with chronic MSK. In particular, although they suggest that the causation of pain was grounded in the biomedical model by practitioners and in personal experience by patients, there was conflict in both patients and practitioners about the balance of these two causal explanations.
Methodological issues
We have discussed our conceptual model and some of the health-care and research implications. The following section explores methodological issues specific to meta-ethnography. Campbell and colleagues28 acknowledge that there are different ways of carrying out meta-ethnography and that it is not useful to be rigid in one’s approach. There are both epistemological and practical challenges involved when synthesising qualitative research. A useful description of some of these challenges is given in a HTA report by Murphy and colleagues. 69 We will focus on challenges specific to meta-ethnography.
Does qualitative synthesis remove us too far from the participant’s experience?
Of particular relevance to meta-ethnography is the qualitative research emphasis on the idiographic origin of knowledge. In other words, qualitative research focuses on the unique experience of the individual within a particular context. However, qualitative synthesis is an interpretation (third-order construct) of an interpretation (second-order construct) of an interpretation (first-order construct). 27 Does qualitative synthesis then remove us too far from the primary experience to reveal any truth? The capacity of qualitative research to say something that is transferable outside its context has roots in the qualitative research tradition, notably grounded theory. 67 You could argue that qualitative research aims to develop ideas that help us to anticipate the decisions that a person might make beyond the specific context. However, it is important that the interpretations of qualitative research remain grounded in experience. We took great care to make sure that our concepts were grounded in the primary studies by collaboratively challenging our individual interpretations of second-order constructs. Although we recognise that this adds another level of interpretation, it gave us confidence that we were holding true to the meaning of the original author. We also emphasise that our final analysis is an interpretation by using our second-order constructs rather than participants’ own words to illustrate our concepts. To allow readers to challenge our interpretations, we remain transparent by presenting all second-order constructs (see Appendix 3), including those that did not fit the developing theory (see Box 7) and findings that we judged were ‘untranslatable’ (Table 9). In summary, we share the view that the construction of knowledge always involves a level of abstraction beyond the primary experience, and that transferable knowledge can be gained from qualitative research and its syntheses. However, this knowledge should be grounded in participants’ experience.
Do I need to carry out an exhaustive literature search or could this time be better spent?
Both researchers and funders should consider whether or not an exhaustive search of the literature is necessary for qualitative syntheses. It could be argued that we have spent a disproportionate amount of time searching for relevant studies and that this time could have been better spent. In their original text on meta-ethnography, Noblit and Hare20 do not advocate an exhaustive literature search and their examples of meta-ethnography include syntheses of between two and six papers. Qualitative syntheses do not aim to summarise the entire body of available knowledge or make statistical inference. Qualitative research uses small samples, either to develop conceptual insight67 or to gain insight into the particular and unique. 431 Including too many studies might therefore make conceptual analysis ‘unwieldy’ or make it difficult to maintain insight or ‘sufficient familiarity’. 28 Campbell and colleagues28 suggest that 38 studies is around the maximum number in meta-ethnography that will allow ‘sufficient familiarity’.
The extent of any search will depend partly on the area of study and on the time and funding available. For example, if very little is published about a topic it may be necessary to expand the search more widely. We knew from the outset that we would find many studies exploring the experience of chronic pain. Our systematic search was therefore time-consuming and, although 95% of the studies were found using three databases (MEDLINE, CINAHL and PsycINFO), it took > 6 months of a 2-year study to complete the search. However, we wanted to produce a conceptual analysis with a weight of evidence that would have resonance with the health research community. The Cochrane Collaboration has a major role in providing systematic reviews of high-quality research. Its approach includes a systematic search for all of the evidence on a topic. We felt that it was important to follow this approach to ensure that our findings were not dismissed as lacking rigour by failing to search for all studies.
Do I include everything that fits the inclusion criteria?
To limit the number of studies included, we applied strict inclusion criteria, excluding > 200 studies because they did not meet our specific scope. Specific information about the study sample was often not in the study abstract, meaning that we had to retrieve the full text of > 300 studies. A clearer description of the study sample in the abstract would facilitate more cost-effective research syntheses. There are good arguments for using homogeneous samples in qualitative research431 and we specifically focused on the experience of people with chronic non-malignant MSK pain. This might mean that we excluded some insightful, arguably ‘classic’ papers (e.g. references 98, 145, 176, 432 and 433). It also meant that we excluded papers that explored the experience of people with chronic MSK diseases such as osteoarthritis and rheumatoid arthritis. Although we know that pain is often integral to the experience of people with MSK diseases, we excluded those papers that we agreed explored the experience of the disease, rather than chronic pain. It also meant that we excluded papers in which the study sample included those with chronic pain from other sites (e.g. visceral pain or headache).
The issue with deciding not to include all of the studies that match the inclusion criteria is how to decide what to include. Some qualitative researchers suggest a more targeted approach to sampling data, for example stop searching for new data when ‘theoretical saturation’ is reached, that is, when collecting additional data seems to add no more insight. 67 This is more comparable with the sampling strategies commonly used in qualitative research. Qualitative analysis does not aim to achieve statistical representation but to develop ideas by exploring a particular experience. In contrast to quantitative analysis, qualitative analysis does not begin when all of the data are collected. Analysis and data collection occur simultaneously and analysis is ongoing throughout data collection. One option might therefore be to start searching a particular database and expand the search as analysis proceeds. For example, in their synthesis Dixon-Woods and colleagues29 began with a purposive sample of studies that they had retrieved from a systematic search and, as analysis developed, they used theoretical sampling of further papers to challenge their developing theory. However, the difficulty remains of how to determine which are the most useful papers without reading them. As the sheer volume of available knowledge increases, other methods for identifying relevant data are developing. For example, the Economic and Social Research Council is exploring the use of ‘text mining’ in knowledge reviews. 434 Text mining identifies specific phrases or combinations of relevant words to target specific areas of knowledge amidst large volumes of data.
Another way to limit the number of studies is to include only those that we think are very good or ‘key papers’. A common approach in quantitative research synthesis, recently adopted in qualitative synthesis, is to use sensitivity analysis to allow the reviewer to assess the impact of including ‘lower-quality’ studies on the conclusions of a synthesis. Carroll and colleagues435 used sensitivity analysis to show the possible benefits of quality appraisal for qualitative research synthesis. The difficult question is how to determine what is good. It is a challenge to determine the impact of including studies of diverse quality if we do not agree on what good quality is. In short, it is difficult to decide what should and what should not be included. We therefore made the decision to systematically search for, and include, all papers that we felt were ‘good enough’.
Methodological and conceptual quality: two sides of the same coin?
We need to consider why we are spending a lot of time appraising studies: do we intend to exclude studies on the basis of our appraisal; does our appraisal have an impact on our interpretation? Qualitative researchers cannot ignore the debate about quality, and their intuitive certainty about what is ‘good’ should not remain sacrosanct;436 in other words, it is not good enough to say that we ‘know’ quality when we see it. Some researchers have begun to consider the impact of ‘quality’ on qualitative research syntheses and a growing number of researchers are appraising studies for the purpose of qualitative systematic reviews. Hannes and Macaitis32 report that the percentage of qualitative syntheses including quality appraisal increased from 40% in 1988–2004 to 72% in 2005–8. Although some argue that appraisal is not compatible with qualitative research, there is little doubt that we do make judgements about the quality of research. A central issue for quality appraisal, which is transferable to quantitative research synthesis, is that quality comprises both method and concept. 436
What is the value of methodological quality?
First, we need to consider whether or not we exclude methodologically weak studies and, if so, how do we decide what is inadequate. Although Campbell and colleagues28 argue that the ‘inclusion of poorer quality qualitative research . . . is unlikely to be as damaging’ (p. 45), should we include studies that are not methodologically sound, even if they show conceptual insight? Although they suggest that analysis needs to be rigorous enough to meet the research aim, they do not move from here to exclude papers on grounds of quality. 28 In contrast, Dixon Woods and colleagues29 exclude studies that they judge to be ‘fatally flawed’, and give some guidelines for determining this. Our team and advisory group agreed that methods had to be good enough.
We agreed that several areas were integral to methodological quality. Fundamentally, does the study present a reflexive account of the research process, which allows the reader to make a sensible judgement about the authors’ interpretation? In short, can I judge how the context of the research affects the interpretation? Do the authors show how the findings are supported by the data? Do the researchers show how they have challenged their interpretation? For example, readers need a clear description of the research context to allow them to judge whether or not the final interpretation has come from the data. Reader also need to be able to judge for themselves whether or not the interpretation has been cherry picked to support a priori views. Although interpretations are inevitably influenced by a priori concepts, an important facet of ‘methodological integrity’ is whether or not the concept is grounded in the data (inductive) or is imposed on the data (deductive). This is supported by both Campbell and colleagues23 and Dixon-Woods and colleagues:29 ‘an interpretive synthesis does not float free of any empirical anchor: an interpretive synthesis of primary studies must be grounded in the data reported in those studies’ (p. 46). 29
The research report should show how the interpretation is supported by the data and how the authors have challenged their interpretation. This supports the guidelines for determining fatally flawed papers suggested by Dixon-Woods and colleagues. 29 The tension between inductive and deductive approaches is not new437 and it may be more useful to interpret these approaches as two poles on a continuum. For the purposes of meta-ethnography, we agreed that studies should gravitate towards the inductive pole and that studies reporting deductive methods (e.g. studies that developed a framework for analysis from a literature review) or studies that imposed a priori structures on the data would not be included. As methodological reporting is the only means that we have of judging ‘inductiveness’, methods need to be reported well enough to allow readers to judge this. Although we intuitively felt that some studies would be ‘good enough’ (e.g. references 309 and 379), the brevity of the reports meant that we did not have enough information to make this decision and, thus, these studies were excluded. Although some might say that we have spent a disproportionate amount of time appraising studies, we argue that method is an important facet of quality that cannot be ignored (even if difficult to define). In particular, if there are aspects of method that might have a significant impact on the authors’ interpretation, and thus the integrity of the synthesis, we would consider this ‘fatally flawed’ and not include it in the analysis.
What is the value of conceptual quality?
Researchers, readers and journal editors should consider the value that they place on ‘methodological integrity’ vis-à-vis conceptual insight. 28 Conceptual insight is integral to meta-ethnography and concepts are the data of meta-ethnography. However, methodological flaws can be easier to ‘pin down’436 and therefore tend to be picked up in quality appraisal. Some therefore argue that excluding studies from qualitative research syntheses on the basis of quality appraisal criteria may mean that insightful studies are excluded. 28 Campbell and colleagues28 chose to include conceptually rich studies with a poor report of method, arguing that meta-ethnography is concerned primarily with conceptual development. Some authors argue that there may be a positive relationship between sound methodological reporting and a positive contribution to the synthesis,435 although others suggest that there may be a negative relationship. 28 Campbell and colleagues28 chose to include ‘classic’ studies in their meta-ethnography, assuming ‘methodological integrity’ in the absence of fully reported methods. Emphasising the importance of conceptual insight they state that: ‘There appears almost to be an inverse correlation between methodological quality and the quality of insight and theory-building displayed in many papers’ (p. 44). 28
We did not find data to support this statement and did find insightful studies that clearly described their methods, notably those by Osborn and Smith66,342–344 and Snelgrove and Liossi. 358 Although we agree that conceptual insight is fundamental to meta-ethnography, deciphering concepts from descriptive studies is not always straightforward. In other words, it is not always easy to see ‘the wood through the trees’. If a concept is an idea that develops by comparing particular instances, this will depend on the personal experience and background of the reader. Thus, it is not surprising that different readers fail to agree about which papers are conceptually rich or ‘key papers’. Agreement may mean only that we are exploring something from the same, arguably limited, perspective. It does not necessarily mean that we have been able to determine the truly ‘key papers’. Although the emphasis placed on the quality of concepts has its roots in qualitative research,67 it is not foreign to quantitative researchers, who also consider conceptual decision-making in their assessment of quality. For example, they might ask whether a study is measuring useful constructs (internal validity), or whether the study conclusions are relevant and transferable beyond this study (external validity). The difficulty remains, for both qualitative and quantitative methodologies, that the quality of conceptualisation is a matter of judgement, which is likely to remain elusive.
It might be more useful to see method and concept as two sides of the same coin. Therefore, studies should be methodologically good enough or ‘satisfactory’ to allow us to judge the interpretation made. However, studies that include useful concepts or challenging ideas may be ‘key’. We also need to consider that the concept of quality is constructed and dynamic. The criteria by which we judge quality are not fixed but shift and change over time and in relation to context. 438
Is it useful to use appraisal tools for qualitative synthesis?
Although appraisal tools are often used in qualitative synthesis,32 the majority of qualitative syntheses (27 out of 41) identified by Campbell and colleagues28 did not use appraisal criteria to determine inclusion. When tools are used to appraise the quality of qualitative research, there tends to be low agreement between researchers. 57 Although we also found that agreement was low, the CASP appraisal tool was useful in framing our discussions and encouraging us to ‘read the papers carefully and systematically’ (p. 44). 28 Although we did not intend to use a cut-off score, it was striking that we generally considered studies scoring < 20 to be ‘fatally flawed’. This may illustrate that appraisal tools help us to determine methodological weakness. Although we remain convinced that checklists will continue to produce inconsistent judgements regarding quality, analysis of potential reasons for variation is lacking, and this would be an extremely interesting area of research.
We found it more difficult to distinguish a ‘key’ or conceptually rich paper from a ‘satisfactory’ paper. Studies that we ranked as ‘key’ were not given a particularly higher CASP score (score 18–27) than those that we ranked as ‘satisfactory’ (score 20–28), and the range in scores was similar for both. This may reflect the emphasis on methods in the CASP score and may show that the CASP score does not necessarily reflect conceptual insight. Although we considered exploring the possibility of carrying out ‘sensitivity analysis’ by ranking papers, this would have been impossible as we did not agree on either score or ranking. (In quantitative syntheses, sensitivity analyses involve comparing the results of two or more analyses using different assumptions. For example, you might perform the analysis on higher- or lower-ranking studies to see whether the results are affected.)
In summary, if we see method and concept as two sides of the same coin, appraisal tools may help us to determine what is good enough or ‘satisfactory’ and to exclude studies with methodologically ‘fatal flaws’. We did not find any benefit from using any particular method of appraising studies. The tools did not help us to determine the quality of conceptual insight and, thus, the possible impact on our interpretation. In short, we did not always agree on what was conceptually rich or ‘key’ to the analysis. However, our innovative method of collaborative interpretation to define second-order constructs ensured that areas that were conceptually weak were not incorporated in the analysis, even if they were ‘good enough’ methodologically.
Is it possible to include 77 papers in a conceptual synthesis?
We knew at the outset that this synthesis was likely to include a large number of studies. Some authors (including Noblit and Hare20) argue that it is not possible to maintain familiarity with this number of primary studies28 and that we should find ways of limiting the number of studies included. Some suggest that meta-ethnography is more suited to smaller syntheses. However, we have discussed the inherent issues involved with making decisions about what to include when there is a large number of studies meeting inclusion criteria. Our unique innovations allowed us to analyse 77 studies within the time and budget allowed and to produce a conceptual model that is grounded in a large body of knowledge. Central to our method was our collaborative approach to interpreting second-order constructs. This allowed us to produce a glossary of concepts that we successfully synthesised into a line of argument model. Although this was time-consuming, incorporating the interpretations of three team members made us confident that we remained true to the original studies. NVivo 9 allowed us to link the full original studies to all stages of the developing analysis, including team notes about the team members’ ideas and descriptions of concepts.
Limitations
The findings of qualitative research will inevitably be only one possible interpretation of the data. As qualitative analysis is iterative, it can be difficult to present exactly how you have reached your conclusions, or where your conclusions specifically come from. Researchers will always bring existing ideas and points of view into the analysis. We made great efforts to work collaboratively to challenge our individual interpretations at each stage of the analysis. The strength of our team was that members felt free to agree, disagree or change their mind within the safety of the group. This facilitated a dialectic process in which our ideas were challenged and modified. To illustrate the stages of this process we have included a full glossary of second-order concepts along with tables showing which of these concepts supported our categories (see Appendices 3 and 4). It is also important to consider that the strength of qualitative research is its focus on interpretation. Meta-ethnography is an interpretive form of knowledge synthesis that aims to develop new conceptual understandings. This process is iterative and utilises an ongoing form of knowledge production (thesis–antithesis–synthesis). Therefore, bringing ideas into a study is not necessarily a limitation, as long as these a priori ideas are challenged. In this way, Blumer439 distinguishes between definitive concepts, which precisely define the object of enquiry, and sensitising concepts, which give ‘a general sense of reference and guidance in approaching empirical instances’ (p. 7). Although we propose a model that ‘explains’ the conceptual categories, this model is our interpretation based on a rigorous process carried out over 2 years. We do not claim that this is the only way that these concepts could be explained and invite readers to consider their own interpretations in the light of ours, with the ultimate aim of improving patient care.
Clinical application
Our line of argument supports a model of health care in which the health-care professional sits alongside the person in pain. Affirming a person’s experience and allowing an empathetic interpretation of their story is not an adjunct, but integral to health care. In this way our model supports an embodied, non-dualistic approach that may be transferable to other chronic conditions.
Our model also suggests possibilities that might help patients to move forward alongside their pain:
-
an integrated relationship with the painful body
-
redefining a positive sense of self now and in the future
-
communicating to, rather than hiding from, others the experience of pain
-
knowing that I am not the only one with pain (but I am still valued)
-
regaining a sense of reciprocity and social participation
-
recognising the limitations of the medical model
-
being empowered to experiment and change the way that I do things without the sanction of the health-care professional.
Chapter 6 Conclusion
This meta-ethnography provides a synthesis of concepts and suggests a model for pulling these concepts together. We focus on the constant daily struggle facing people with chronic MSK pain, which may distinguish it from other kinds of pain. For example, someone with cancer pain might not feel the need to prove that they are in pain. This suggests a very different starting point for people with chronic MSK pain. In spite of this struggle, our model suggests how a person can move forward alongside pain by listening to their body rather than fighting it; letting go of the old self and finding a new self; becoming part of a community and not feeling like the only one; telling others about pain and redefining relationships; realising that pain is here to stay rather than focusing on diagnosis and cure; and becoming the expert and making choices.
Our findings challenge some of the cultural notions about illness, in particular the expectation that the doctor will find a diagnosis and offer an effective treatment. These cultural expectations are deep-rooted and can affect the experience of pain. For example, not having a diagnosis can produce powerful feelings, such as worthlessness, fear, shame and guilt. Our model also shows that not feeling believed can have an impact on a person’s participation in everyday life. Qualitative research has consistently shown that people with chronic MSK pain do not think that doctors believe them, and this finding has not changed in more recent studies. This has clear implications for clinical practice and education. Our model suggests that central to the relationship between patient and practitioner is the recognition of the patient as a person whose life has been deeply changed by pain. Our model suggests that feeling valued is not simply an adjunct to the therapy or an optional extra, but central to it.
In the context of recent developments in pain management, it would be useful for qualitative research to focus on the following experiences:
-
how a person in pain experiences their own body
-
the meaning of acceptance for both patients and clinicians
-
reconciling hope with acceptance that pain is here to stay
-
other specific MSK pain conditions, for example shoulder pain
-
other chronic pain conditions, for example chronic visceral pain.
Additional syntheses would also help us to understand the experience of chronic pain. For example, there is already a growing body of qualitative research exploring the experience of osteoarthritis. Efforts to synthesise qualitative research will help to make sure that qualitative research is accessible to a wider relevant audience.
Our research shows that meta-ethnography can be used to elicit concepts that increase our understanding of patients’ experience and enable us to explain the context in which people make decisions about health care. Conceptual models developed from meta-ethnography can have an impact on quality of care. Our model opens up possibilities for therapies that aim to help a person to move forward alongside pain. Although developed from studies of people with MSK pain, our model may also be transferable to other long-term conditions. Further research is needed that compares our model with the experiences of people with other chronic conditions.
Acknowledgements
We would like to thank all authors and research participants involved in the qualitative research studies included in this meta-ethnography.
Thanks to Sue Robertson, Ambrose Phillips and Dor Wilson for their valuable support with the systematic search.
We would also like to thank the advisory group for their valuable contribution throughout this project.
Contributions of authors
Francine Toye (Researcher, Qualitative Research) contributed to the conceptual design, interpretation and analysis, wrote the first draft of the final report, made important intellectual contributions to the study and approved the final draft.
Kate Seers (Professor, Health Research) contributed to the conceptual design, interpretation and analysis, made important intellectual contributions to the study and approved the final draft.
Nick Allcock (Associate Professor, Nursing) contributed to the interpretation and analysis, made important intellectual contributions to the study and approved the final draft.
Michelle Briggs (Professor, Nursing) contributed to the interpretation and analysis, made important intellectual contributions to the study and approved the final draft.
Eloise Carr (Professor, Nursing) contributed to the interpretation and analysis, made important intellectual contributions to the study and approved the final draft.
JoyAnn Andrews (Researcher, Qualitative Research) contributed to the interpretation and analysis, made important intellectual contributions to the study and approved the final draft.
Karen Barker (Clinical Director, Musculoskeletal Services, and Senior Research Fellow) contributed to the interpretation and analysis, made important intellectual contributions to the study and approved the final draft.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Croft P, Blyth FM, van der Windt D, Croft P, Blyth FM, van der Windt D. Chronic pain epidemiology. From aetiology to public health. Oxford: Oxford University Press; 2010.
- Price C, Ellis B, Taylor A. members of the Pain Summit Steering Group . Putting Pain on the Agenda: The 2012. www.painsummit.org.uk/sites/painsummit/files/page/7376/downloads/puttingpainontheagendafullreport.pdf (accessed 12 July 2013).
- Croft P, Peat G, van-der-Windt D. Primary care research and musculoskeletal medicine. Prim Health Care Res Dev 2010;11:4-16. http://dx.doi.org/10.1017/S1463423609990272.
- Merskey H, Bogduk N. Classification of chronic pain. Definitions of chronic pain syndromes and definition of pain terms. Seattle, WA: IASP Press; 1994.
- Tracey I, Bushnell C. How neuroimaging studies have challenged us to rethink: is chronic pain a disease?. J Pain 2009;10:1113-20. http://dx.doi.org/10.1016/j.jpain.2009.09.001.
- Pain: breaking through the barrier. London: Department of Health; 2008.
- Breivika H, Collettb B, Ventafriddac V, Cohend R, Gallacherd D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006;10:287-333. http://dx.doi.org/10.1016/j.ejpain.2005.06.009.
- Elliott AM, Smith BH, Penny KI, Smith WC, Chambers WA. The epidemiology of chronic pain in the community. Lancet 1999;354:1248-52. http://dx.doi.org/10.1016/S0140-6736(99)03057-3.
- König HH, Bernert S, Angermeyer MC, Matschinger H, Martinez M, Vilagut G, et al. Comparison of population health status in six European countries: results of a representative survey using the EQ-5D questionnaire. Med Care 2009;47:255-61. http://dx.doi.org/10.1097/MLR.0b013e318184759e.
- Covinsky KE, Lindquist K, Dunlop DD, Yelin E. Pain, functional limitations, and aging. J Am Geriatr Soc 2009;57:1556-61. http://dx.doi.org/10.1111/j.1532-5415.2009.02388.x.
- Smith B, Elliott A, Chambers W, Carins-Smith W, Hannaford P. The impact of chronic pain in the community. Fam Pract 2001;18:292-9. http://dx.doi.org/10.1093/fampra/18.3.292.
- Phillips C, Main C, Buck R, Aylward M, Wynne-Jones G, Farr A. Prioritising pain in policy making: the need for a whole systems perspective. Health Policy 2008;88:166-75. http://dx.doi.org/10.1016/j.healthpol.2008.03.008.
- Gibson SJ. Older people’s pain. Pain Clin Updates 2006;15:1-4.
- McBeth J, Jones K. Epidemiology of chronic musculoskeletal pain. Best Pract Res Clin Rheumatol 2007;21:403-25. http://dx.doi.org/10.1016/j.berh.2007.03.003.
- NHS Quality Improvement Scotland . Getting to GRIPS With Chronic Pain in Scotland 2008. www.nationalpainaudit.org/media/files/GRIPS_booklet.pdf (accessed 12 July 2013).
- Welsh Assembly Government . Chronic Non-Malignant Pain. Services Development and Commissioning Directives n.d. http://education.wales.gov.uk/dhss/publications/health/strategies/chronicpain/chronicpaine.pdf?lang=en&ts=1 (accessed 12 July 2013).
- Price B. Illness careers: the chronic illness experience. J Adv Nurs 1996;24:275-9. http://dx.doi.org/10.1046/j.1365-2648.1996.02047.x.
- Royal College of General Practitioners . Chronic Pain n.d. www.rcgp.org.uk/clinical-and-research/clinical-resources/chronic-pain.aspx (accessed 2 July 2013).
- Roehr B. US needs new strategy to help 116 million patients in chronic pain. BMJ 2011;343. http://dx.doi.org/10.1136/bmj.d4206.
- Noblit G, Hare R. Meta-ethnography: synthesising qualitative studies. Newbury Park, CA: Sage Publications; 1988.
- Noyes J, Popay J, Pearson A, Hannes K, Booth A, Higgins J, et al. Cochrane handbook for systematic reviews. Chichester: John Wiley; 2008.
- Britten N, Campbell R, Pope C, Donnovan J, Morgan M, Pill R. Using meta ethnography to synthesise qualitative research: a worked example. J Health Serv Res Policy 2002;7:209-15. http://dx.doi.org/10.1258/135581902320432732.
- Campbell R, Pound P, Pope C, Britten N, Pill R, Morgan M, et al. Evaluating meta-ethnography: a synthesis of qualitative research on lay experience of diabetes and diabetes care. Soc Sci Med 2003;56:671-84. http://dx.doi.org/10.1016/S0277-9536(02)00064-3.
- Malpass A, Shaw A, Sharp D, Walter F, Feder G, Ridd M, et al. ‘Medication career’ or ‘moral career’? The two sides of managing anti-dperessants: a meta-ethnography of patients’ experience of antidepressants. Soc Sci Med 2009;68:154-68. http://dx.doi.org/10.1016/j.socscimed.2008.09.068.
- Dixon-Woods M, Booth A, Sutton A. Synthesizing qualitative research: a review of published reports. Qual Res 2007;7:375-422. http://dx.doi.org/10.1177/1468794107078517.
- Sandelowski M, Barrosso J. Writing the proposal for a qualitative research methodology project. Qual Health Res 2003;13:781-814. http://dx.doi.org/10.1177/1049732303013006003.
- Sandelowski M, Barroso J. Handbook for synthesising qualitative research. New York, NY: Springer; 2007.
- Campbell R, Pound P, Morgan M, Daker-White G, Britten N, Pill R, et al. Evaluating meta-ethnography: systematic analysis and synthesis of qualitative research. Health Technol Assess 2011;15.
- Dixon-Woods M, Agarwal S, Jones D, Young B, Sutton A. Synthesising qualitative and quantitative research evidence: a review of possible methods. J Health Serv Res Policy 2005;10:45-53.
- Barnett-Page E, Thomas J. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol 2009;9. http://dx.doi.org/10.1186/1471-2288-9-59.
- Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy making in the field. J Health Serv Res Policy 2005;10:6-20. http://dx.doi.org/10.1258/1355819054308576.
- Hannes K, Macaitis K. A move to more systematic and transparent approaches in qualitative evidence synthesis: update on a review of published papers. Qual Res 2012;12:402-42. http://dx.doi.org/10.1177/1468794111432992.
- Garrett R, Gask L, Hays R, Cherrington A, Bundy C, Dickens C, et al. Accessing primary health care: a meta-ethnography of the experiences of British South Asian patients with diabetes, coronary heart disease or a mental health problem. Chronic Illn 2012;8. http://dx.doi.org/10.1177/1742395312441631.
- Monforte-Royo C, Villavicencio-Chavez C, Tomas-Sabado J, Mahtani-Chugani V, Balaguer A. What lies behind the wish to hasten death? A systematic review and meta-ethnography from the perspective of patients. PLoS One 2012;7. http://dx.doi.org/10.1371/journal.pone.0037117.
- Seitz D, Prorok J, Horgan S. Health care experiences of persons with dementia and their caregivers: a meta-ethnography of qualitative studies. Alzheimers Dement 2012;8. http://dx.doi.org/10.1016/j.jalz.2012.05.1515.
- Hubbard G, McLachlan K, Forbat L, Munday D. Recognition by family members that relatives with neurodegenerative disease are likely to die within a year: a meta-ethnography. Palliat Med 2012;26:108-22. http://dx.doi.org/10.1177/0269216311402712.
- Hilber AM, Kenter E, Redmond S, Merten S, Bagnol B, Low N, et al. Vaginal practices as women’s agency in sub-Saharan Africa: a synthesis of meaning and motivation through meta-ethnography. Soc Sci Med 2012;74:1311-23.
- Franzel B, Heusser P, Lauche R, Schwiegershausen M, Berger B. Meta-ethnography: the perspective of patients choosing alternative and complementary medicine regarding individualized medicine and integrative care. BMC Complement Altern Med 2012;12. http://dx.doi.org/10.1186/1472-6882-12-S1-P403.
- Heinze E, Nolan T. Parental decision making for children with cancer at the end of life: a meta-ethnography. J Pediatr Oncol Nurs 2012;29:337-46. http://dx.doi.org/10.1177/1043454212456905.
- Malpass A, Carel H, Ridd M, Shaw A, Kessler D, Sharp D, et al. Transforming the perceptual situation: a meta-ethnography of qualitative work reporting patients’ experiences of mindfulness-based approaches. Mindfulness 2012;3:60-75. http://dx.doi.org/10.1007/s12671-011-0081-2.
- Beck C. A metaethnography of traumatic childbirth and its aftermath: amplifying causal looping. Qual Health Res 2011;21.
- Adams E, McCann L, Armes J, Richardson A, Stark D, Watson E, et al. The experiences, needs and concerns of younger women with breast cancer: a meta-ethnography. Psychooncology 2011;20:851-62. http://dx.doi.org/10.1002/pon.1792.
- McInnes E, Seers K, Tutton L. Older people’s views in relation to risk of falling and need for intervention: a meta-ethnography. J Adv Nurs 2011;67:2525-36. http://dx.doi.org/10.1111/j.1365-2648.2011.05707.x.
- Tonkin-Crine S, Yardley L, Little P. Antibiotic prescribing for acute respiratory tract infections in primary care: a systematic review and meta-ethnography. J Antimicrob Chemother 2011;66:2215-23. http://dx.doi.org/10.1093/jac/dkr279.
- Banning M. Employment and breast cancer: a meta-ethnography. Eur J Cancer Care 2011;20:708-19. http://dx.doi.org/10.1111/j.1365-2354.2011.01291.x.
- Purc-Stephenson RJ, Thrasher C. Nurses’ experiences with telephone triage and advice: a meta-ethnography. J Adv Nurs 2010;66:482-95. http://dx.doi.org/10.1111/j.1365-2648.2010.05275.x.
- Chang YT, Hayter M, Wu SC. A systematic review and meta-ethnography of the qualitative literature: experiences of the menarche. J Clin Nurs 2010;19:447-60. http://dx.doi.org/10.1111/j.1365-2702.2009.03019.x.
- Elmir R, Schmied V, Wilkes L. Women’s perceptions and experiences of a traumatic birth: a meta-ethnography. J Adv Nurs 2010;66:2142-53. http://dx.doi.org/10.1111/j.1365-2648.2010.05391.x.
- Schumm K, Skea Z, McKee L, N’Dow J. ‘They’re doing surgery on two people’: a meta-ethnography of the influences on couples’ treatment decision making for prostate cancer. Health Expect 2010;13:335-49. http://dx.doi.org/10.1111/j.1369-7625.2010.00624.x.
- Greenwood N, Mackenzie A. Informal caring for stroke survivors: meta-ethnographic review of qualitative literature. Maturitas 2010;66:268-76. http://dx.doi.org/10.1016/j.maturitas.2010.03.017.
- Shaw R, Booth A, Sutton A, Miller T, Smith J, Young B, et al. Finding qualitative research: an evaluation of search strategies. BMC Med Res Methodol 2004;4.
- McKibbon K, Wilczynski N, Haynes R. Developing optimal search strategies for retrieving qualitative studies in PsycINFO. Eval Health Prof 2006;29:440-54. http://dx.doi.org/10.1177/0163278706293400.
- Hopewell S, Clarke M, Lefebvre C, Scherer R. Handsearching versus electronic searching to identify reports of randomized trials. Cochrane Database Syst Rev 2007;2. http://dx.doi.org/10.1002/14651858.MR000001.pub2.
- Eakin J, Mykhalovskiy E. Reframing the evaluation of qualitative health: reflections on a review of appraisal guidelines in the health sciences. J Eval Clin Pract 2003;9:187-94. http://dx.doi.org/10.1046/j.1365-2753.2003.00392.x.
- Barbour R. Checklists for improving rigour in qualitative research: a case of the tail wagging the dog?. BMJ 2001;322:1115-17. http://dx.doi.org/10.1136/bmj.322.7294.1115.
- Systematic reviews – CRD’s guidance for undertaking reviews in healthcare. York: Centre for Reviews and Dissemination, University of York; 2009.
- Dixon-Woods M, Sutton A, Shaw R, Miller T, Smith J, Young B, et al. Appraising qualitative research for inclusion in systematic reviews: a quantitative and qualitative comparison of three methods. J Health Serv Res Policy 2007;12:42-7. http://dx.doi.org/10.1258/135581907779497486.
- Dixon-Woods M, Shaw R, Agarwal S, Smith J. The problem of appraising qualitative research. Qual Saf Health Care 2004;13:223-5. http://dx.doi.org/10.1136/qhc.13.3.223.
- Critical Appraisal Skills Programme . Critical Appraisal Skills Programme: Making 2010. www.casp-uk.net/wp-content/uploads/2011/11/CASP_Qualitative_Appraisal_Checklist_14oct10.pdf (accessed 12 July 2013).
- Atkins S, Lewin S, Smith H, Engel M, Fretheim A, Volmink J. Conducting a meta-ethnography of qualitative literature: lessons learnt. BMC Med Res Methodol 2008;8. http://dx.doi.org/10.1186/1471-2288-8-21.
- Pound P, Britten N, Morgan M, Yardley L, Pope C, Daker-White G, et al. Resisting medicines: a synthesis of qualitative studies of medicine taking. Soc Sci Med 2005;61:133-55. http://dx.doi.org/10.1016/j.socscimed.2004.11.063.
- Joanna Briggs Institute Qualitative Assessment and Review Instrument . QARI Critical Appraisal Instrument. The Joanna Briggs Institute Reviewers Manual 2011. http://joannabriggs.org/Documents/sumari/Reviewers%20Manual-2011.pdf (accessed 12 July 2013).
- Seale C. The quality of qualitative research. London: Sage Publications; 1999.
- Schütz A. Collected papers 1. The Hague, Netherlands: Martinus Nijhoff; 1962.
- Paterson BL, Dubouloz C-J, Chevrier J, Ashe B, King J, Moldoveanu M. Conducting qualitative metasynthesis research: insights from a metasynthesis project. Int J Qual Methods 2009;8:22-33.
- Smith JA, Osborn M. Pain as an assault on the self: an interpretative phenomenological analysis of the psychological impact of chronic benign low back pain. Psychol Health 2007;22:517-35. http://dx.doi.org/10.1080/14768320600941756.
- Charmaz K. Constructing grounded theory. Thousand Oaks, CA: Sage Publications; 2006.
- Pope C, Mays N, Popay J. Synthesizing qualitative and quantitative health research: a guide to methods. Maidenhead: Open University Press; 2007.
- Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P. Qualitative research methods in health technology assessment: a review of the literature. Health Technol Assess 1998;2.
- Benjaminsson O, Biguet G, Arvidsson I, Nilsson-Wikmar L. Recurrent low back pain: relapse from a patients perspective. J Rehabil Med 2007;39:640-5. http://dx.doi.org/10.2340/16501977-0104.
- Carter B, Lambrenos K, Thursfield J. A pain workshop: an approach to eliciting the views of young people with chronic pain. J Clin Nurs 2002;11:753-62. http://dx.doi.org/10.1046/j.1365-2702.2002.00642.x.
- Dewar A, White M, Posade ST, Dillon W. Using nominal group technique to assess chronic pain, patients’ perceived challenges and needs in a community health region. Health Expect 2003;6:44-52. http://dx.doi.org/10.1046/j.1369-6513.2003.00208.x.
- Henriksson CM. Living with continuous muscular pain – patient perspectives. Part II: strategies for daily life. Scand J Caring Sci 1995;9:77-86. http://dx.doi.org/10.1111/j.1471-6712.1995.tb00391.x.
- Henriksson CM. Living with continuous muscular pain – patient perspectives. Part I: encounters and consequences. Scand J Caring Sci 1995;9:67-76. http://dx.doi.org/10.1111/j.1471-6712.1995.tb00390.x.
- Reid M. An assessment of health needs of chronic low back pain patients from general practice. J Health Psychol 2004;9:451-62. http://dx.doi.org/10.1177/1359105304042353.
- Collen M. Life of pain, life of pleasure: pain from the patients’ perspective – the evolution of the PAIN exhibit. J Pain Palliat Care Pharmacother 2005;19:45-52. http://dx.doi.org/10.1080/J354v19n04_08.
- Becker B. Narratives of pain in later life and conventions of storytelling. J Aging Stud 1999;13:73-87. http://dx.doi.org/10.1016/S0890-4065(99)80007-3.
- Dekkers W. Hermeneutics and experiences of the body. The case of low back pain. Theor Med Bioeth 1998;19:277-93.
- Dubin RE, King C, Vlack V. Stop this ride I want to get off! The chronic pain roller-coaster: fueled by stress and conflict. Pain Res Manag 2010;15:100-1.
- Steihaug S, Malterud K. Stories about bodies: a narrative study on self-understanding and chronic pain. Scand J Prim Health Care 2008;26:188-92. http://dx.doi.org/10.1080/02813430802177305.
- Williams G. Hope for the humblest? The role of self-help in chronic illness: the case of ankylosing spondylitis. Sociol Health Illn 1989;11:135-59. http://dx.doi.org/10.1111/1467-9566.ep10844329.
- Ashby S, Richards K, James C. The effect of fear of movement on the lives of people with chronic low back pain. Int J Ther Rehabil 2010;17:232-9.
- Bowman JM. The meaning of chronic low back pain. AAOHN J 1991;39:381-4.
- Bowman JM. Reactions to chronic low back pain. Issues Ment Health Nurs 1994;15:445-53. http://dx.doi.org/10.3109/01612849409006920.
- Bowman JM. Experiencing the chronic pain phenomenon: a study. Rehabil Nurs 1994;19:91-5. http://dx.doi.org/10.1002/j.2048-7940.1994.tb01316.x.
- Brown M, Dean S, Hay-Smith EJ, Taylor W, Baxter GD. Musculoskeletal pain and treatment choice: an exploration of illness perceptions and choices of conventional or complementary therapies. Disabil Rehabil 2010;32:1645-57. http://dx.doi.org/10.3109/09638281003649896.
- Bury M. Chronic illness as biographical disruption. Sociol Health Illn 1982;4:167-82. http://dx.doi.org/10.1111/1467-9566.ep11339939.
- Carnes D, Anwer Y, Underwood M, Harding G, Parson S. Influences on older people’s decision making regarding choice of topical or oral NSAIDs for knee pain: qualitative study. BMJ 2008;336:142-5. http://dx.doi.org/10.1136/bmj.39401.699063.BE.
- Dean SG, Smith JA, Payne S, Weinman J. Managing time: an interpretative phenomenological analysis of patients’ and physiotherapists’ perceptions of adherence to therapeutic exercise for low back pain. Disabil Rehabil 2005;27:625-36. http://dx.doi.org/10.1080/0963820500030449.
- Ewan C, Lowy E, Reid J. ‘Falling out of culture’: the effects of repetition strain injury on sufferers’ roles and identity. Sociol Health Illn 1991;13:168-92. http://dx.doi.org/10.1111/1467-9566.ep11340787.
- Gannik D, Jespersen M. Lay concepts and strategies for handling symptoms of disease. A sample of adult men and women experiencing back pain symptoms. Scand J Prim Health Care 1984;2:67-76. http://dx.doi.org/10.3109/02813438409017707.
- Hawtin H, Sullivan C. Experiences of mindfulness training in living with rheumatic disease: an interpretative phenomenological analysis. Br J Occup Ther 2011;74:137-43. http://dx.doi.org/10.4276/030802211X12996065859283.
- Howden S, Jones D, Martin D, Nicol M. Employment and chronic non-cancer pain: insights into work retention. Work 2003;20:199-204.
- Hush JM, Refshauge K, Sullivan G, De Souza L, Maher CG, McAuley JH. Recovery: what does this mean to patients with low back pain?. Arthritis Rheum 2009;61:124-31. http://dx.doi.org/10.1002/art.24162.
- Hwang EJ, Kim YH, Jun SS. Lived experience of Korean women suffering from rheumatoid arthritis: a phenomenological approach. Int J Nurs Stud 2004;41:239-47. http://dx.doi.org/10.1016/S0020-7489(03)00132-9.
- Krohne K, Ihlebaek C. Maintaining a balance: a focus group study on living and coping with chronic whiplash-associated disorder. BMC Musculoskelet Disord 2010;11. http://dx.doi.org/10.1186/1471-2474-11-158.
- Kugelmann R, Tolman CW, Cherry F, van Hezewijk R, Lubek I. A phenomenological analysis of mental and physical pain. Problems of Theoretical Psychology 1996:342-50.
- Lillrank A. Back pain and the resolution of diagnostic uncertainty in illness narratives. Soc Sci Med 2003;57:1045-54. http://dx.doi.org/10.1016/S0277-9536(02)00479-3.
- Magnussen L, Nilsen S, Raheim M. Barriers against returning to work – as perceived by disability pensioners with back pain: a focus group based qualitative study. Disabil Rehabil 2007;29:191-7. http://dx.doi.org/10.1080/09638280600747793.
- McPhillips-Tangum CA, Cherkin DC, Rhodes LA, Markham C. Reasons for repeated medical visits among patients with chronic back pain. J Gen Intern Med 1998;13:289-95. http://dx.doi.org/10.1046/j.1525-1497.1998.00093.x.
- Medina-Mirapeix F, Escolar-Reina P, Gascon-Canovas JJ, Montilla-Herrador J, Collins SM. Personal characteristics influencing patients’ adherence to home exercise during chronic pain: a qualitative study. J Rehabil Med 2009;41:347-52. http://dx.doi.org/10.2340/16501977-0338.
- Ong BN, Hooper H, Dunn K, Croft P. Establishing self meaning in low back pain narratives. Sociol Rev 2004;52:532-49. http://dx.doi.org/10.1111/j.1467-954X.2004.00494.x.
- Ostlund G, Cedersund E, Alexanderson K, Hensing G. Developing a typology of the ‘duty to work’, as experienced by lay persons with musculoskeletal disorders. Int J Soc Welf 2002;11:150-8. http://dx.doi.org/10.1111/1468-2397.00209.
- Rogers A, Allison T. What if my back breaks? Making sense of musculoskeletal pain among South Asian and African-Caribbean people in the North West of England. J Psychosom Res 2004;57:79-87. http://dx.doi.org/10.1016/S0022-3999(03)00570-1.
- Ross MM, Carswell A, Hing M, Hollingworth G, Dalziel WB. Seniors’ decision making about pain management. J Adv Nurs 2001;35:442-51. http://dx.doi.org/10.1046/j.1365-2648.2001.01859.x.
- Sale JE, Gignac M, Hawker G. How ‘bad’ does the pain have to be? A qualitative study examining adherence to pain medication in older adults with osteoarthritis. Arthritis Rheum 2006;55:272-8. http://dx.doi.org/10.1002/art.21853.
- Shaw WS, Huang YH. Concerns and expectations about returning to work with low back pain: identifying themes from focus groups and semi-structured interviews. Disabil Rehabil 2005;27:1269-81. http://dx.doi.org/10.1080/09638280500076269.
- Skelton AM, Murphy EA, Murphy RJL, O’Dowd T. Patient’s views of low back pain. Br J Gen Pract 1996;46:153-6.
- Steihaug S, Ahlsen B, Malterud K. ‘I am allowed to be myself’: women with chronic muscular pain being recognized. Scand J Public Health 2002;30:281-7. http://dx.doi.org/10.1080/14034940210133960.
- Strunin L, Boden LI. Family consequences of chronic back pain. Soc Sci Med 2004;58:1385-94. http://dx.doi.org/10.1016/S0277-9536(03)00333-2.
- Tveito TH, Shaw WS, Huang YH, Nicholas M, Wagner G. Managing pain in the workplace: a focus group study of challenges, strategies and what matters most to workers with low back pain. Disabil Rehabil 2010;32:2035-45. http://dx.doi.org/10.3109/09638281003797398.
- Wrapson W, Mewse AJ. Does the doctor or the patient control sick leave certification? A qualitative study interpreting patients’ interview dialogue. Fam Pract 2011;28:202-9. http://dx.doi.org/10.1093/fampra/cmq088.
- Young AE, Wasiak R, Phillips L, Gross DP. Workers’ perspectives on low back pain recurrence: ‘it comes and goes and comes and goes, but it’s always there’. Pain 2011;152:204-11. http://dx.doi.org/10.1016/j.pain.2010.10.033.
- Arvidsson SB, Petersson A, Nilsson I, Andersson B, Arvidsson BI, Petersson IF, et al. A nurse-led rheumatology clinic’s impact on empowering patients with rheumatoid arthritis: a qualitative study. Nurs Health Sci 2006;8:133-9. http://dx.doi.org/10.1111/j.1442-2018.2006.00269.x.
- Baird CL. Living with hurting and difficulty doing: older women with osteoarthritis. Clin Excell Nurse Pract 2000;4:231-7.
- Brown S, Williams A. Women’s experiences of rheumatoid arthritis. J Adv Nurs 1995;21:695-701. http://dx.doi.org/10.1046/j.1365-2648.1995.21040695.x.
- Davis GC, Hiemenz ML, White TL. Barriers to managing chronic pain of older adults with arthritis. J Nurs Scholarsh 2002;34:121-6. http://dx.doi.org/10.1111/j.1547-5069.2002.00121.x.
- Hughes JG. ‘When I first started going I was going in on my knees, but I came out and I was skipping’: exploring rheumatoid arthritis patients’ perceptions of receiving treatment with acupuncture. Complementary Ther Med 2009;17:269-73. http://dx.doi.org/10.1016/j.ctim.2009.06.002.
- Kee CC. Living with osteoarthritis: insiders’ views. Appl Nurs Res 1998;11:19-26. http://dx.doi.org/10.1016/S0897-1897(98)80041-4.
- Keysor JJ, Sparling JW, Riegger-Krugh C. The experience of knee arthritis in athletic young and middle-aged adults: an heuristic study. Arthritis Care Res 1998;11:261-70. http://dx.doi.org/10.1002/art.1790110407.
- Maly MR, Krupa T. Personal experience of living with knee osteoarthritis among older adults. Disabil Rehabil 2007;29:1423-33. http://dx.doi.org/10.1080/09638280601029985.
- Seomun GA, Chang SO, Lee PS, Lee SJ, Shin HJ. Concept analysis of coping with arthritic pain by South Korean older adults: development of a hybrid model. Nurs Health Sci 2006;8:10-9. http://dx.doi.org/10.1111/j.1442-2018.2006.00262.x.
- Good BJ. Medicine rationality and experience. Cambridge: Cambridge University Press; 1994.
- Asbring P, Narvanen AL. Women’s experiences of stigma in relation to chronic fatigue syndrome and fibromyalgia. Qual Health Res 2002;12:148-60. http://dx.doi.org/10.1177/104973230201200202.
- Soderlund A, Skoge AM, Malterud K. ‘I could not lift my arm holding the fork . . .’. Living with chronic fatigue syndrome. Scand J Prim Health Care 2000;18:165-9.
- Howell SL. A theoretical model for caring for women with chronic nonmalignant pain. Qual Health Res 1994;4:94-123. http://dx.doi.org/10.1177/104973239400400107.
- Howell SL. Natural/alternative health care practices used by women with chronic pain: findings from a grounded theory research study. Nurse Pract Forum 1994;5:98-106.
- Dudgeon BJ, Tyler EJ, Rhodes LA, Jensen MP. Managing usual and unexpected pain with physical disability: a qualitative analysis. Am J Occup Ther 2006;60:92-103. http://dx.doi.org/10.5014/ajot.60.1.92.
- Warms CA, Marshall HM, Hoffman AJ, Tyler EJ. There are a few things you did not ask about my pain: writing on the margins of a survey questionnaire. Rehabil Nurs 2005;30:248-56. http://dx.doi.org/10.1002/j.2048-7940.2005.tb00120.x.
- Hansson KS, Fridlund B, Brunt D, Hansson B, Rask M. The meaning of the experiences of persons with chronic pain in their encounters with the health service. Scand J Caring Sci 2011;25:444-50. http://dx.doi.org/10.1111/j.1471-6712.2010.00847.x.
- Schlesinger L. Chronic pain, intimacy, and sexuality: a qualitative study of women who live with pain. J Sex Res 1996;33:249-56. http://dx.doi.org/10.1080/00224499609551841.
- Clarke KA, Iphofen R. Accepting pain management or seeking pain cure: an exploration of patients’ attitudes to chronic pain. Pain Manag Nurs 2007;8:102-10. http://dx.doi.org/10.1016/j.pmn.2007.03.006.
- Carson MG, Mitchell GJ. The experience of living with persistent pain. J Adv Nurs 1998;28:1242-8. http://dx.doi.org/10.1046/j.1365-2648.1998.00843.x.
- Keponen R, Kielhofner G. Occupation and meaning in the lives of women with chronic pain. Scand J Occup Ther 2006;13:211-20. http://dx.doi.org/10.1080/11038120600672975.
- Lansbury G. Chronic pain management: a qualitative study of elderly people’s preferred coping strategies and barriers to management. Disabil Rehabil 2000;22:2-14. http://dx.doi.org/10.1080/096382800297079-1.
- Bustin BM, Hughes OG. Residential pain management programmes: participants’ hopes and expectations. Int J Ther Rehabil 2009;16:139-45.
- Cartwright T. ‘Getting on with life’: the experiences of older people using complementary health care. Soc Sci Med 2007;64:1692-703. http://dx.doi.org/10.1016/j.socscimed.2006.11.034.
- Hall-Lord ML, Larsson G, Steen B. Chronic pain and distress among elderly in the community: comparison of patients’ experiences with enrolled nurses’ assessments. J Nurs Manag 1999;7:45-54. http://dx.doi.org/10.1046/j.1365-2834.1999.00991.x.
- Miles A, Curran HV, Pearce S, Allan L. Managing constraint: the experience of people with chronic pain. Soc Sci Med 2005;61:431-41. http://dx.doi.org/10.1016/j.socscimed.2004.11.065.
- Evans S, de Souza L. Dealing with chronic pain: giving voice to the experiences of mothers with chronic pain and their children. Qual Health Res 2008;18:489-500. http://dx.doi.org/10.1177/1049732308315433.
- Allcock N, Elkan R, Williams J. Patients referred to a pain management clinic: beliefs, expectations and priorities. J Adv Nurs 2007;60:248-56. http://dx.doi.org/10.1111/j.1365-2648.2007.04400.x.
- Silverman M, Nutini J, Musa D, Schoenberg NE, Albert SM. ‘Is it half full or half empty?’ Affective responses to chronic illness. J Cross Cult Gerontol 2009;24:291-306. http://dx.doi.org/10.1007/s10823-009-9097-7.
- Dewar AL, Gregg K, White MI, Lander J. Navigating the health care system: perceptions of patients with chronic pain. Chronic Dis Can 2009;29:162-8.
- Bates S, Rankin-Hill L, Sanchez-Ayendez M. The effects of the cultural context of health care on treatment of and response to chronic pain and illness. Soc Sci Med 1997;45:1433-47. http://dx.doi.org/10.1016/S0277-9536(97)00068-3.
- Honkasalo ML. Chronic pain as a posture towards the world. Scand J Psychol 2000;41:197-208. http://dx.doi.org/10.1111/1467-9450.00188.
- Honkasalo ML. Vicissitudes of pain and suffering: chronic pain and liminality. Med Anthropol 2001;19:319-53. http://dx.doi.org/10.1080/01459740.2001.9966181.
- Van Huet H, Innes E, Whiteford G. Living and doing with chronic pain: narratives of pain program participants. Disabil Rehabil 2009;31:2031-40. http://dx.doi.org/10.1080/09638280902887784.
- Clarke KA, Iphofen R. A phenomenological hermeneutic study into unseen chronic pain. Br J Nurs 2008;17:658-63.
- Higgins I. The experience of chronic pain in elderly nursing home residents. J Res Nurs 2005;10:369-82. http://dx.doi.org/10.1177/174498710501000402.
- Gudmannsdottir GD, Halldorsdottir S. Primacy of existential pain and suffering in residents in chronic pain in nursing homes: a phenomenological study. Scand J Caring Sci 2009;23:317-27. http://dx.doi.org/10.1111/j.1471-6712.2008.00625.x.
- Hall-Lord ML, Larsson G, Steen B. Chronic pain and distress in older people: a cluster analysis. Int J Nurs Pract 1999;5:78-85. http://dx.doi.org/10.1046/j.1440-172x.1999.00157.x.
- Casarett D, Karlawish J, Sankar P, Hirschman K, Asch DA. Designing pain research from the patient’s perspective: what trial end points are important to patients with chronic pain?. Pain Med 2001;2:309-16. http://dx.doi.org/10.1046/j.1526-4637.2001.01041.x.
- Wessely S. Women experienced chronic fatigue syndrome and fibromyalgia as stigmatising. Evid Based Ment Health 2002;5:127-8. http://dx.doi.org/10.1136/ebmh.5.4.127.
- Asbring P. Chronic illness – a disruption in life: identity-transformation among women with chronic fatigue syndrome and fibromyalgia. J Adv Nurs 2001;34:312-19. http://dx.doi.org/10.1046/j.1365-2648.2001.01767.x.
- Schoofs N, Bambini D, Ronning P, Bielak E, Woehl J. Death of a lifestyle: the effects of social support and healthcare support on the quality of life of persons with fibromyalgia and/or chronic fatigue syndrome. Orthop Nurs 2004;23:364-74. http://dx.doi.org/10.1097/00006416-200411000-00005.
- Van-Houdenhove B, Neerinckx E, Onghena P, Vingerhoets A, Lysens R, Vertommen H. Daily hassles reported by chronic fatigue syndrome and fibromyalgia patients in tertiary care: a controlled quantitative and qualitative study. Psychother Psychosom 2002;71:207-13. http://dx.doi.org/10.1159/000063646.
- Dudgeon BJ, Gerrard BC, Jensen MP, Rhodes LA, Tyler EJ. Physical disability and the experience of chronic pain. Arch Phys Med Rehabil 2002;83:229-35. http://dx.doi.org/10.1053/apmr.2002.28009.
- Upshur CC, Bacigalupe G, Luckmann R. ‘They don’t want anything to do with you’: patient views of primary care management of chronic pain. Pain Med 2010;11:1791-8. http://dx.doi.org/10.1111/j.1526-4637.2010.00960.x.
- Roberto KA, Reynolds SG. Older women’s experiences with chronic pain: daily challenges and self-care practices. J Women Aging 2002;14:5-23. http://dx.doi.org/10.1300/J074v14n03_02.
- Roberto KA, Ermann LS, Savla J. Older women’s assessment and management of chronic pain in their daily lives. J Pain Manag 2009;1:345-56.
- Martensson L, Dahlin-Ivanoff S. Experiences of a primary health care rehabilitation programme. A focus group study of persons with chronic pain. Disabil Rehabil 2006;28:985-95. http://dx.doi.org/10.1080/09638280500476246.
- Tollefson J, Usher K, Foster K. Relationships in pain: the experience of relationships to people living with chronic pain in rural areas. Int J Nurs Pract 2011;17:478-85. http://dx.doi.org/10.1111/j.1440-172X.2011.01963.x.
- Fisher GS, Emerson L, Firpo C, Ptak J, Wonn J, Bartolacci G. Chronic pain and occupation: an exploration of the lived experience. Am J Occup Ther 2007;61:290-302. http://dx.doi.org/10.5014/ajot.61.3.290.
- Sofaer B, Moore AP, Holloway I, Lamberty JM, Thorp TA, O’Dwyer J. Chronic pain as perceived by older people: a qualitative study. Age Ageing 2005;34:462-6. http://dx.doi.org/10.1093/ageing/afi139.
- Sofaer-Bennett B, Holloway I, Moore A, Lamberty J, Thorp T, O’Dwyer J. Perseverance by older people in their management of chronic pain: a qualitative study. Pain Med 2007;8:271-80. http://dx.doi.org/10.1111/j.1526-4637.2007.00297.x.
- Smith AA. Intimacy and family relationships of women with chronic pain. Pain Manag Nurs 2003;4:134-43. http://dx.doi.org/10.1016/S1524-9042(03)00030-4.
- Grime J, Richardson JC, Ong BN. Perceptions of joint pain and feeling well in older people who reported being healthy: a qualitative study. Br J Gen Pract 2010;60:597-603. http://dx.doi.org/10.3399/bjgp10X515106.
- Damsgard E, Dewar A, Roe C, Hamran T. Staying active despite pain: pain beliefs and experiences with activity-related pain in patients with chronic musculoskeletal pain. Scand J Caring Sci 2011;25:108-16. http://dx.doi.org/10.1111/j.1471-6712.2010.00798.x.
- Douglas C, Windsor C, Wollin J. Understanding chronic pain complicating disability: finding meaning through focus group methodology. J Neurosci Nurs 2008;40:158-68. http://dx.doi.org/10.1097/01376517-200806000-00006.
- Scherer M, Schaefer H, Blozik E, Chenot JF, Himmel W. The experience and management of neck pain in general practice: the patients’ perspective. Eur Spine J 2010;19:963-71. http://dx.doi.org/10.1007/s00586-010-1297-x.
- Sjostrom R, Melin-Johansson C, Asplund R, Alricsson M. Barriers to and possibilities of returning to work after a multidisciplinary rehabilitation programme. A qualitative interview study. Work 2011;39:243-50.
- McPherson KM, Brander P, Taylor WJ, McNaughton HK. Consequences of stroke, arthritis and chronic pain – are there important similarities?. Disabil Rehabil 2004;26:988-1000. http://dx.doi.org/10.1080/09638280410001702414.
- Baker TA, Wang CC. Photovoice: use of a participatory action research method to explore the chronic pain experience in older adults. Qual Health Res 2006;16:1405-13. http://dx.doi.org/10.1177/1049732306294118.
- Bates MS, Rankin-Hill L. Control, culture and chronic pain. Soc Sci Med 1994;39:629-45. http://dx.doi.org/10.1016/0277-9536(94)90020-5.
- Bendelow G. Pain perceptions, emotions and gender. Sociol Health Illn 1993;15:273-94. http://dx.doi.org/10.1111/1467-9566.ep10490526.
- Bendelow GA, Williams SJ. The end of the road? Lay views on a pain-relief clinic. Soc Sci Med 1996;43:1127-36. http://dx.doi.org/10.1016/0277-9536(96)00033-0.
- Blomqvist K, Edberg A. Living with persistent pain: experiences of older people receiving home care. J Adv Nurs 2002;40:297-30. http://dx.doi.org/10.1046/j.1365-2648.2002.02371.x.
- Blomqvist K, Hallberg IR. Managing pain in older persons who receive home-help for their daily living. Perceptions by older persons and care providers. Scand J Caring Sci 2002;16:319-29. http://dx.doi.org/10.1046/j.1471-6712.2002.00087.x.
- Borell L, Asaba E, Rosenberg L, Schult ML, Townsend E. Exploring experiences of ‘participation’ among individuals living with chronic pain. Scand J Occup Ther 2006;13:76-85. http://dx.doi.org/10.1080/11038120600673023.
- Bremander A, Bergman S, Arvidsson B. Perception of multimodal cognitive treatment for people with chronic widespread pain – changing one’s life plan. Disabil Rehabil 2009;31:1996-2004. http://dx.doi.org/10.3109/09638280902874139.
- Cairncross L, Magee H, Askham J. Pain in older people: a hidden problem: a qualitative study 2007. www.pickereurope.org/assets/content/pdf/Project_Reports/Paincarehomes_final.pdf (accessed 11 September 2013).
- Clarke K, Iphofen R. Issues in phenomenological nursing research: the combined use of pain diaries and interviewing. Nurse Res 2006;13:62-74.
- Gran SV, Festvag LS, Landmark BT. ‘Alone with my pain – it can’t be explained, it has to be experienced’. A Norwegian in-depth interview study of pain in nursing home residents. Int J Older People Nurs 2010;5:25-33. http://dx.doi.org/10.1111/j.1748-3743.2009.00195.x.
- Hellström C. Temporal dimensions of the self-concept: entrapped and possible selves in chronic pain. Psychol Health 2001;16:111-25. http://dx.doi.org/10.1080/08870440108405493.
- Higgins I, Madjar I, Walton JA. Chronic pain in elderly nursing home residents: the need for nursing leadership. J Nurs Manag 2004;12:167-73. http://dx.doi.org/10.1046/j.1365-2834.2003.00437.x.
- Kodiath MF, Kodiath A. A comparative study of patients with chronic pain in India and the United States. Clin Nurs Res 1992;1:278-91. http://dx.doi.org/10.1177/105477389200100307.
- Lofvander M. Attitudes towards pain and return to work in young immigrants on long-term sick leave. Scand J Prim Health Care 1999;17:164-9. http://dx.doi.org/10.1080/028134399750002584.
- Lofvander M, Lindstrom MA, Masich V. Pain drawings and concepts of pain among patients with ‘half-body’ complaints. Patient Educ Counsel 2007;66:353-60. http://dx.doi.org/10.1016/j.pec.2007.01.011.
- McParland JL, Eccleston C, Osborn M, Hezseltine L. It’s not fair: an interpretative phenomenological analysis of discourses of justice and fairness in chronic pain. Health 2011;15:459-74. http://dx.doi.org/10.1177/1363459310383593.
- McParland JL, Whyte A. A thematic analysis of attributions to others for the origins and ongoing nature of pain in community pain sufferers. Psychol Health Med 2008;13:610-20. http://dx.doi.org/10.1080/13548500701842966.
- Nilsen G, Elstad I. Temporal experiences of persistent pain. Patients’ narratives from meetings with health care providers. Int J Qual Stud Health Well-Being 2009;4:51-6. http://dx.doi.org/10.1080/17482620802416129.
- Ohman M, Soderberg S, Lundman B. Hovering between suffering and enduring: the meaning of living with serious chronic illness. Qual Health Res 2003;13:528-42.
- Peolsson M, Hyden LC, Larsson US. Living with chronic pain: a dynamic learning process. Scand J Occup Ther 2000;7:114-25.
- Peolsson M, Saljo R, Satterlund U. Experiencing and knowing pain – patients’ perspectives. Adv Physiother 2000;2:146-55.
- Persson D, Andersson I, Eklund M. Defying aches and revaluating daily doing: occupational perspectives on adjusting to chronic pain. Scand J Occup Ther 2011;18:188-97. http://dx.doi.org/10.3109/11038128.2010.509810.
- Richardson JC. Establishing the (extra)ordinary in chronic widespread pain. Health 2005;9:31-49. http://dx.doi.org/10.1177/1363459305048096.
- Richardson JC, Ong BN, Sim J. Remaking the future: contemplating a life with chronic widespread pain. Chronic Illn 2006;2:209-18. http://dx.doi.org/10.1177/17423953060020030201.
- Richardson JC, Ong BN, Sim J. Is chronic widespread pain biographically disruptive?. Soc Sci Med 2006;63:1573-85. http://dx.doi.org/10.1016/j.socscimed.2006.03.040.
- Richardson JC, Ong BN, Sim J. Experiencing chronic widespread pain in a family context: giving and receiving practical and emotional support. Sociol Health Illn 2007;29:347-65. http://dx.doi.org/10.1111/j.1467-9566.2007.00496.x.
- Richardson JC, Ong BN, Sim J. Experiencing and controlling time in everyday life with chronic widespread pain: a qualitative study. BMC Musculoskelet Disord 2008;9. http://dx.doi.org/10.1186/1471-2474-9-3.
- Seers K. The patients’ experiences of their chronic non-malignant pain. J Adv Nurs 1996;24:1160-8. http://dx.doi.org/10.1111/j.1365-2648.1996.tb01021.x.
- Shariff F, Carter J, Dow C, Polley M, Salinas M, Ridge D. Mind and body management strategies for chronic pain and rheumatoid arthritis. Qual Health Res 2009;19:1037-49. http://dx.doi.org/10.1177/1049732309341189.
- Smith AA, Friedemann ML. Perceived family dynamics of persons with chronic pain. J Adv Nurs 1999;30:543-51. http://dx.doi.org/10.1046/j.1365-2648.1999.01123.x.
- Soeker MS, Wegner L, Pretorius B. I’m going back to work: back injured clients’ perceptions and experiences of their worker roles. Work 2008;30:161-70.
- Soklaridis S, Cartmill C, Cassidy D. Biographical disruption of injured workers in chronic pain. Disabil Rehabil 2011;33:2372-81. http://dx.doi.org/10.3109/09638288.2011.573056.
- Sorajjakool S, Thompson KM, Aveling L, Earl A. Chronic pain, meaning, and spirituality: a qualitative study of the healing process in relation to the role of meaning and spirituality. J Pastoral Care Counsel 2006;60:369-78.
- Tveiten S, Knutsen IR. Empowering dialogues – the patients’ perspective. Scand J Caring Sci 2011;25:333-40. http://dx.doi.org/10.1111/j.1471-6712.2010.00831.x.
- Werner A, Malterud K. ‘The pain isn’t as disabling as it used to be’: how can the patient experience empowerment instead of vulnerability in the consultation?. Scand J Public Health Suppl 2005;66:41-6. http://dx.doi.org/10.1080/14034950510033363.
- Wrapson W, Mewse AJ. Supervisors’ responses to sickness certification for an episode of low back pain: employees’ personal experiences. Disabil Rehabil 2011;33:1728-36. http://dx.doi.org/10.3109/09638288.2010.544836.
- Miller WL, Yanoshik MK, Crabtree BF, Reymond WK. Patients, family physicians, and pain: visions from interview narratives. Fam Med 1994;26:179-84.
- Rodham K, Rance N, Blake D. A qualitative exploration of carers’ and ‘patients’ experiences of fibromyalgia: one illness, different perspectives. Musculoskelet Care 2010;8:68-77. http://dx.doi.org/10.1002/msc.167.
- Snelling J. The effect of chronic pain on the family unit. J Adv Nurs 1994;19:543-51. http://dx.doi.org/10.1111/j.1365-2648.1994.tb01119.x.
- Fox P, Solomon P, Raina P, Jadad A. Barriers and facilitators in pain management in long-term care institutions: a qualitative study. Can J Aging 2004;23:269-80. http://dx.doi.org/10.1353/cja.2004.0032.
- Baszanger I. Deciphering chronic pain. Sociol Health Illn 1992;14:181-215. http://dx.doi.org/10.1111/1467-9566.ep11343694.
- Breen A, Austin H, Campion-Smith C, Carr E, Mann E. ‘You feel so hopeless’: a qualitative study of GP management of acute back pain. Eur J Pain 2007;11:21-9. http://dx.doi.org/10.1016/j.ejpain.2005.12.006.
- Davies C, Howell D. A qualitative study: clinical decision making in low back pain. Physiother Theory Pract 2012;28:95-108. http://dx.doi.org/10.3109/09593985.2011.571752.
- Daykin AR, Richardson B. Physiotherapists’ pain beliefs and their influence on the management of patients with low back pain. Spine 2004;29:783-95. http://dx.doi.org/10.1097/01.BRS.0000115135.19082.97.
- Lovering S. Cultural attitudes and beliefs about pain. J Transcult Nurs 2006;17:389-96. http://dx.doi.org/10.1177/1043659606291546.
- Ryan S, Hassell A, Thwaites C, Manley K, Home D. Developing a new model of care for patients with chronic musculoskeletal pain. J Nurs Manag 2007;15:825-30. http://dx.doi.org/10.1111/j.1365-2934.2007.00761.x.
- Lee EO, Park YS, Song M, Lee IS, Park Y, Kim HS. Family functioning in the context of chronic illness in women: a Korean study. Int J Nurs Stud 2002;39:705-11. http://dx.doi.org/10.1016/S0020-7489(02)00009-3.
- Lemmens G, Verdegem S, Heireman M, Lietaer G, Van Houdenhove B, Sabbe B, et al. Helpful events in family discussion groups with chronic-pain patients: a qualitative study of differences in perception between therapists/observers and patients/family members. Fam Syst Health 2003;21:37-52. http://dx.doi.org/10.1037/h0089500.
- Lindenmeyer A, Griffiths F, Hodson J. ‘The family is part of the treatment really’: a qualitative exploration of collective health narratives in families. Health 2011;15:401-16. http://dx.doi.org/10.1177/1363459310384493.
- Sherwood G, Adams-McNeill J, Starck PL, Nieto B, Thompson CJ. Qualitative assessment of hospitalized patients’ satisfaction with pain management. Res Nurs Health 2000;23:486-95. http://dx.doi.org/10.1002/1098-240X(200012)23:6<486::AID-NUR7>3.0.CO;2-5.
- Guy L, Short D. Rehabilitation of workers with musculoskeletal injury and chronic pain. Health Sociol Rev 2005;14:77-83. http://dx.doi.org/10.5172/hesr.14.1.77.
- Laerum E, Indahl A, Sture J. What is ‘the good back-consultation’? A combined qualitative and quantitative study of chronic low back pain patients’ interaction with and perceptions of consultations with specialists. J Rehabil Med 2006;38:255-62. http://dx.doi.org/10.1080/16501970600613461.
- Oien AM, Iversen S, Stensland P. Narratives of embodied experiences – therapy processes in Norwegian psychomotor physiotherapy. Adv Physiother 2007;9:31-9.
- Oien AM, Råheim M, Iversen S, Steihaug S. Self-perception as embodied knowledge – changing processes for patients with chronic pain. Adv Physiother 2009;11:121-30.
- Hansson M, Bostrom C, Harms-Ringdahl K. Living with spine-related pain in a changing society – a qualitative study. Disabil Rehabil 2001;23:286-95.
- Hooper H, Ong BN. When Harry met Barry, and other stories: a partner’s influence on relationships in back pain care. Anthropol Med 2005;12:47-60. http://dx.doi.org/10.1080/13648470500049842.
- Kralik D, Kotch T, Price K, Howard N. Taking action to create order. Chronic illness self-managment. J Clin Nurs 2004;13:259-67. http://dx.doi.org/10.1046/j.1365-2702.2003.00826.x.
- Subramaniam V, Stewart MW, Smith JF. The development and impact of a chronic pain support group: a qualitative and quantitative study. J Pain Symptom Manage 1999;17:376-83.
- Martin R, Williams J, Hadjistavropoulos T, Hadjistavropoulos D, MacLean M. A qualitative investigation of seniors’ and caregivers’ views on pain assessment and management. Can J Nurs Res 2005;37:142-64.
- Buijs PC, Lambeek LC, Koppenrade V, Hooftman WE, Anema JR. Can workers with chronic back pain shift from pain elimination to function restore at work?. J Back Musculoskelet Rehabil 2009;22:65-73.
- Morris AL. Patients’ perspectives on self-management following a back rehabilitation programme. Musculoskelet Care 2004;2:165-79. http://dx.doi.org/10.1002/msc.68.
- Muhli UH. Accounts of pain experience in an elderly care context. Commun Med 2010;7:55-64.
- Steihaug S, Ahlsen B, Malterud K. From exercise and education to movement and interaction. Treatment groups in primary care for women with chronic muscular pain. Scand J Prim Health Care 2001;19:249-55.
- Spiers J. Expressing and responding to pain and stoicism in home-care nurse–patient interactions. Scand J Caring Sci 2006;20:293-302. http://dx.doi.org/10.1111/j.1471-6712.2006.00407.x.
- McCluskey S, Brooks J, King N, Burton K. The influence of ‘significant others’ on persistent back pain and work participation: a qualitative exploration of illness perceptions. BMC Musculoskelet Disord 2011;12. http://dx.doi.org/10.1186/1471-2474-12-236.
- Blomqvist K, Hallberg IR. Pain in older adults living in sheltered accommodation – agreement between assessments by older adults and staff. J Clin Nurs 1999;8:159-69. http://dx.doi.org/10.1046/j.1365-2702.1999.00241.x.
- Blomqvist K, Hallberg IR. Recognising pain in older adults living in sheltered accommodation: the views of nurses and older adults. Int J Nurs Stud 2001;38:305-18.
- Blomqvist K. Older people in persistent pain: nursing and paramedical staff perceptions and pain management. J Adv Nurs 2003;41:575-85. http://dx.doi.org/10.1046/j.1365-2648.2003.02569.x.
- Undeland M, Malterud K. Diagnostic interaction: the patient as a source of knowledge?. Scand J Prim Health Care 2008;26:222-7. http://dx.doi.org/10.1080/02813430802325086.
- Miller J, Timson D. Exploring the experiences of partners who live with a chronic low back pain sufferer. Health Soc Care Community 2004;12:34-42. http://dx.doi.org/10.1111/j.1365-2524.2004.00466.x.
- Jinks C, Ong BN, O’Neill T. ‘Well, it’s nobody’s responsibility but my own’. A qualitative study to explore views about the determinants of health and prevention of knee pain in older adults. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-148.
- Beaton DE, Tarasuk V, Katz JN, Wright JG, Bombardier C. ‘Are you better?’ A qualitative study of the meaning of recovery. Arthritis Rheum 2001;45:270-80. http://dx.doi.org/10.1002/1529-0131(200106)45:3<270::AID-ART260>3.0.CO;2-T.
- Borkan J, Reis S, Hermoni D, Biderman A. Talking about the pain: a patient-centered study of low back pain in primary care. Soc Sci Med 1995;40:977-88. http://dx.doi.org/10.1016/0277-9536(94)00156-N.
- Calnan M, Wainwright D, O’Neill C, Winterbottom A, Watkins C. Making sense of aches and pains. Fam Pract 2006;23:91-105. http://dx.doi.org/10.1093/fampra/cmi077.
- Calnan M, Wainwright D, O’Neill C, Winterbottom A, Watkins C. Illness action rediscovered: a case study of upper limb pain. Sociol Health Illn 2007;29:321-46. http://dx.doi.org/10.1111/j.1467-9566.2007.00543.x.
- France NEM, Farrell K, Kearney B, Myatt S. Women living with fibromyalgia: ‘do no harm’. Int J Hum Caring 2008;12:21-6.
- Glenton C. Chronic back pain sufferers – striving for the sick role. Soc Sci Med 2003;57:2243-52. http://dx.doi.org/10.1016/S0277-9536(03)00130-8.
- Hansson M, Boström C, Harms-Ringdahl K. Sickness absence and sickness attendance – what people with neck or back pain think. Soc Sci Med 2006;62:2183-95. http://dx.doi.org/10.1016/j.socscimed.2005.10.002.
- Hilbert RA. Acultural dimensions of chronic pain. Soc Probl 1984;31:365-78. http://dx.doi.org/10.1525/sp.1984.31.4.03a00010.
- Larsson ME, Nordholm LA, Ohrn I. Patients’ views on responsibility for the management of musculoskeletal disorders – a qualitative study. BMC Musculoskelet Disord 2009;10. http://dx.doi.org/10.1186/1471-2474-10-103.
- May S. Patients’ attitudes and beliefs about back pain and its management after physiotherapy for low back pain. Physiother Res Int 2007;12:126-35. http://dx.doi.org/10.1002/pri.367.
- McIntosh A, Shaw CF. Barriers to patient information provision in primary care: patients’ and general practitioners’ experiences and expectations of information for low back pain. Health Expect 2003;6:19-2. http://dx.doi.org/10.1046/j.1369-6513.2003.00197.x.
- Miller JS, Pinnington MA, Stanley IM. The early stages of low back pain: a pilot study of patient diaries as a source of data. Fam Pract 1999;16:395-401. http://dx.doi.org/10.1093/fampra/16.4.395.
- Ong BN, Jinks C. ‘Walking like John Wayne’: open-format diaries of people with knee pain and disability. Chronic Illn 2006;2:21-6. http://dx.doi.org/10.1179/174592006X93842.
- Ong BN, Hooper H. Comparing clinical and lay accounts of the diagnosis and treatment of back pain. Sociol Health Illn 2006;28:203-22. http://dx.doi.org/10.1111/j.1467-9566.2006.00488.x.
- Sheppard J, Kumar K, Buckley CD, Shaw KL, Raza K. ‘I just thought it was normal aches and pains’: a qualitative study of decision-making processes in patients with early rheumatoid arthritis. Rheumatology 2008;47:1577-82. http://dx.doi.org/10.1093/rheumatology/ken304.
- Tang NK, Salkovskis PM, Hodges A, Soong E, Hanna MH, Hester J. Chronic pain syndrome associated with health anxiety: a qualitative thematic comparison between pain patients with high and low health anxiety. Br J Clin Psychol 2009;48:1-20. http://dx.doi.org/10.1348/014466508X336167.
- Vroman K, Warner R, Chamberlain K. Now let me tell you in my own words: narratives of acute and chronic low back pain. Disabil Rehabil 2009;31:976-87. http://dx.doi.org/10.1080/09638280802378017.
- Walker JM. Caring for elderly people with persistent pain in the community: a qualitative perspective on the attitudes of patients and nurses. Health Soc Care Community 1994;2:221-29. http://dx.doi.org/10.1111/j.1365-2524.1994.tb00168.x.
- Wiitavaara B, Barnekow-Bergkvist M, Brulin C. Striving for balance: a grounded theory study of health experiences of nurses with musculoskeletal problems. Int J Nurs Stud 2007;44:1379-90. http://dx.doi.org/10.1016/j.ijnurstu.2006.07.009.
- Wiitavaara B, Brulin C, Barnekow-Bergkvist M. When the body makes itself heard – the experience of bodily illness among people with neck-shoulder problems. Adv Physiother 2008;10:85-9. http://dx.doi.org/10.1080/14038190701760627.
- Wiitavaara B, Lundman B, Barnekow-Bergkvist M, Brulin C. Striking a balance--health experiences of male ambulance personnel with musculoskeletal symptoms: a grounded theory. Int J Nurs Stud 2007;44:770-9. http://dx.doi.org/10.1016/j.ijnurstu.2006.02.007.
- Liedberg G. Time use and activity patterns in women with long term pain. Scand J Occup Ther 2004;11:26-53. http://dx.doi.org/10.1080/11038120410019081.
- Kenny DT. Constructions of chronic pain in doctor–patient relationships: bridging the communication chasm. Patient Educ Couns 2004;52:297-306. http://dx.doi.org/10.1016/S0738-3991(03)00105-8.
- Keen S, Dowell AC, Hurst K, Klaber JAJ, Tovey P, Williams R. Individuals with low back pain: how do they view physical activity?. Fam Pract 1999;16:39-45. http://dx.doi.org/10.1093/fampra/16.1.39.
- Meijer EM, Hugenholtz NIR, Sluiter JK, Frings-Dresen MHW. What do referred patients with upper extremity musculoskeletal disorders expect of a multidisciplinary treatment and what is the perceived value?. Disabil Rehabil 2008;30:541-51. http://dx.doi.org/10.1080/09638280701355744.
- Mannerkorpi K, Gard G. Physiotherapy group treatment for patients with fibromyalgia--an embodied learning process. Disabil Rehabil 2003;25:1372-80. http://dx.doi.org/10.1080/09638280310001616367.
- Steihaug S. Women’s strategies for handling chronic muscle pain: a qualitative study. Scand J Prim Health Care 2007;25:44-8. http://dx.doi.org/10.1080/02813430601016944.
- Glenton C. Developing patient-centred information for back pain sufferers. Health Expect 2002;5:319-29. http://dx.doi.org/10.1046/j.1369-6513.2002.00196.x.
- Jinks C, Ong BN, Richardson J. A mixed methods study to investigate needs assessment for knee pain and disability: population and individual perspectives. BMC Musculoskelet Disord 2007;8. http://dx.doi.org/10.1186/1471-2474-8-59.
- Woolhead G, Gooberman-Hill R, Dieppe P, Hawker G. Night pain in hip and knee osteoarthritis: a focus group study. Arthritis Care Res 2010;62:944-9. http://dx.doi.org/10.1002/acr.20164.
- Coutu MF, Baril R, Durand MJ, Cote D, Rouleau A, Cadieux G. Transforming the meaning of pain: an important step for the return to work. Work 2010;35:209-19.
- Glenton C, Nilsen ES, Carlsen B. Lay perceptions of evidence-based information – a qualitative evaluation of a website for back pain sufferers. BMC Health Serv Res 2006;6.
- Wootton IM, Wood V, Cook F. Who wants expert patient programmes for chronic mechanical spinal pain? An investigation into the value of, and recruitment to, an expert patient programme as part of the physiotherapy management of chronic spinal pain. Physiotherapy 2008;94:78-85. http://dx.doi.org/10.1016/j.physio.2006.12.012.
- Crooks VA. Exploring the altered daily geographies and lifeworlds of women living with fibromyalgia syndrome: a mixed-method approach. Soc Sci Med 2007;64:577-88. http://dx.doi.org/10.1016/j.socscimed.2006.09.025.
- Henriksson CM. Factors of importance for work disability in women with fibroymyalgia. J Rheumatol 2000;27:1271-76.
- Svajger A, Winding K. Perceptions of possibilities of returning to work with chronic musculoskeletal disorders. Work 2009;32:443-55.
- Alsaker S, Josephsson S. Occupation and meaning: narrative in everyday activities of women with chronic rheumatic conditions. OTJR 2010;30:58-67. http://dx.doi.org/10.3928/15394492-20100312-01.
- Charmaz K. Identity dilemmas of chronically ill men. Sociol Q 1994;35:269-88. http://dx.doi.org/10.1111/j.1533-8525.1994.tb00410.x.
- Koch T, Kralik D. Chronic illness: reflections on a community-based action research programme. J Adv Nurs 2001;36:23-31. http://dx.doi.org/10.1046/j.1365-2648.2001.01939.x.
- Östlund G, Cedersund E, Alexanderson K, Hensing G. ‘It was really nice to have someone’ – lay people with musculoskeletal disorders request supportive relationships in rehabilitation. Scand J Public Health 2001;29:285-92. http://dx.doi.org/10.1177/14034948010290041401.
- Pilkington FB, Kilpatrick D. The lived experience of suffering: a parse research method study. Nurs Sci Q 2008;21:228-37. http://dx.doi.org/10.1177/0894318408319274.
- Stamm T, Lovelock L, Stew G, Nell V, Smolen J, Jonsson H, et al. I have mastered the challenge of living with a chronic disease: life stories of people with rheumatoid arthritis. Qual Health Res 2008;18:658-69. http://dx.doi.org/10.1177/1049732308316348.
- Mengshoel AM. Living with a fluctuating illness of ankylosing spondylitis: a qualitative study. Arthritis Rheum 2008;59:1439-44. http://dx.doi.org/10.1002/art.24103.
- Gronning K, Lomundal B, Koksvik HS, Steinsbekk A. Coping with arthritis is experienced as a dynamic balancing process. A qualitative study. Clin Rheumatol 2011;30:1425-32. http://dx.doi.org/10.1007/s10067-011-1836-9.
- Maly MR, Cott CA. Being careful: a grounded theory of emergent chronic knee problems. Arthritis Rheum 2009;61:937-43. http://dx.doi.org/10.1002/art.24611.
- Lempp H, Scott D, Kingsley G. The personal impact of rheumatoid arthritis on patients’ identity: a qualitative study. Chronic Illn 2006;2:109-20. http://dx.doi.org/10.1177/17423953060020020601.
- Stamm T, Lovelock L, Stew G, Nell V, Smolen J, Machold K, et al. I have a disease but I am not ill: a narrative study of occupational balance in people with rheumatoid arthritis. OTJR 2009;29:32-9. http://dx.doi.org/10.3928/15394492-20090101-05.
- Iaquinta ML, Larrabee JH. Phenomenological lived experience of patients with rheumatoid arthritis. J Nurs Care Qual 2004;19:280-9. http://dx.doi.org/10.1097/00001786-200407000-00016.
- Ryan S. Living with rheumatoid arthritis: a phenomenological exploration. Nurs Stand 1996;10:45-8.
- Sanderson T, Morris M, Calnan M, Richards P, Hewlett S. ‘It’s this whole picture, this well-being’: patients’ understanding of ‘feeling well’ with rheumatoid arthritis. Chronic Illn 2010;6:228-40. http://dx.doi.org/10.1177/1742395310377672.
- Donovan JL, Blake DR. Qualitative study of interpretation of reassurance among patients attending rheumatology clinics: ‘just a touch of arthritis, doctor?’. BMJ 2000;320:541-4. http://dx.doi.org/10.1136/bmj.320.7234.541.
- Busch H. Appraisal and coping processes among chronic low back pain patients. Scand J Caring Sci 2005;19:396-402. http://dx.doi.org/10.1111/j.1471-6712.2005.00348.x.
- Chew CA, May CR. The benefits of back pain. Fam Pract 1997;14:461-5. http://dx.doi.org/10.1093/fampra/14.6.461.
- Cudney SA, Butler MR, Weinert C, Sullivan T. Ten rural women living with fibromyalgia tell it like it is. Holist Nurs Pract 2002;16:35-4.
- De Souza LHL, Frank AO. Experiences of living with chronic back pain: the physical disabilities. Disabil Rehabil 2007;29:587-96. http://dx.doi.org/10.1080/09638280600925852.
- Liedberg GM, Burckhardt CS, Henriksson CM. Young women with fibromyalgia in the United States and Sweden: perceived difficulties during the first year after diagnosis. Disabil Rehabil 2006;28:1177-84. http://dx.doi.org/10.1080/09638280600551534.
- Morone NE, Lynch CS, Greco CM, Tindle HA, Weiner DK. ‘I felt like a new person’: the effects of mindfulness meditation on older adults with chronic pain: qualitative narrative analysis of diary entries. J Pain 2008;9:841-8. http://dx.doi.org/10.1016/j.jpain.2008.04.003.
- Raak R, Wahren LK. Health experiences and employment status in subjects with chronic back pain: a long-term perspective. Pain Manag Nurs 2006;7:64-70. http://dx.doi.org/10.1016/j.pmn.2006.02.001.
- Reid J, Ewan C, Lowy E. Pigrimage of pain: the illness experiences of women with repetition strain injury and the search for credibility. Soc Sci Med 1991;32:601-12. http://dx.doi.org/10.1016/0277-9536(91)90295-N.
- Schaefer KM. Struggling to maintain balance: a study of women living with fibromyalgia. J Adv Nurs 1995;21:95-102. http://dx.doi.org/10.1046/j.1365-2648.1995.21010095.x.
- Silva FC, Sampaio RF, Mancini MC, Luz MT, Alcantara MA. A qualitative study of workers with chronic pain in Brazil and its social consequences. Occup Ther Int 2011;18:85-9. http://dx.doi.org/10.1002/oti.302.
- Sokunbi O, Cross V, Watt P, Moore A. Experiences of individuals with chronic low back pain during and after their participation in a spinal stabilisation exercise programme – a pilot qualitative study. Man Ther 2010;15:179-85. http://dx.doi.org/10.1016/j.math.2009.10.006.
- Tavafian SS, Gregory D, Montazeri A. The experience of low back pain in Iranian women: a focus group study. Health Care Women Int 2008;29:339-48. http://dx.doi.org/10.1080/07399330701876356.
- Wade BL, Shantall HM. The meaning of chronic pain: a phenomenological analysis. S Afr J Physiother 2003;59:10-9.
- May CR, Rose MJ, Johnstone FC. Dealing with doubt. How patients account for non-specific chronic low back pain. J Psychosom Res 2000;49:223-5.
- Holloway I, Sofaer B, Walker J. The transition from well person to ‘pain afflicted’ patient: the career of people with chronic back pain. Illn Crisis Loss 2000;8:373-87.
- Schaefer KM. Health patterns of women with fibromyalgia. J Adv Nurs 1997;26:565-72. http://dx.doi.org/10.1046/j.1365-2648.1997.t01-17-00999.x.
- Aegler B, Satink T. Performing occupations under pain: the experience of persons with chronic pain. Scand J Occup Ther 2009;16:49-56. http://dx.doi.org/10.1080/11038120802512425.
- Allegretti A, Borkan J, Reis S, Griffiths F. Paired interviews of shared experiences around chronic low back pain: classic mismatch between patients and their doctors. Fam Pract 2010;27:676-83. http://dx.doi.org/10.1093/fampra/cmq063.
- Bair MJ, Matthias MS, Nyland KA, Huffman MA, Stubbs DL, Kroenke K, et al. Barriers and facilitators to chronic pain self-management: a qualitative study of primary care patients with comorbid musculoskeletal pain and depression. Pain Med 2009;10:1280-90. http://dx.doi.org/10.1111/j.1526-4637.2009.00707.x.
- Campbell C, Guy A. ‘Why can’t they do anything for a simple back problem?’ A qualitative examination of expectations for low back pain treatment and outcome. J Health Psychol 2007;12:641-52. http://dx.doi.org/10.1177/1359105307078171.
- Campbell C, Cramb G. ‘Nobody likes a back bore’ – exploring lay perspectives of chronic pain: revealing the hidden voices of nonservice users. Scand J Caring Sci 2008;22:383-90. http://dx.doi.org/10.1111/j.1471-6712.2007.00541.x.
- Cook FM, Hassenkamp AM. Active rehabilitation for chronic low back pain: the patients’ perspective. Physiotherapy (London) 2000;86:61-8.
- Coole C, Watson PJ, Drummond A. Staying at work with back pain: patients’ experiences of work-related help received from GPs and other clinicians. A qualitative study. BMC Musculoskelet Disord 2010;11. http://dx.doi.org/10.1186/1471-2474-11-190.
- Coole C, Drummond A, Watson PJ, Radford K. What concerns workers with low back pain? Findings of a qualitative study of patients referred for rehabilitation. J Occup Rehabil 2010;20:472-80. http://dx.doi.org/10.1007/s10926-010-9237-5.
- Coole C, Watson PJ, Drummond A. Low back pain patients’ experiences of work modifications; a qualitative study. BMC Musculoskelet Disord 2010;11. http://dx.doi.org/10.1186/1471-2474-11-277.
- Cooper K, Smith BH, Hancock E. Patients’ perceptions of self-management of chronic low back pain: evidence for enhancing patient education and support. Physiotherapy 2009;95:43-50. http://dx.doi.org/10.1016/j.physio.2008.08.005.
- Cooper K, Smith BH, Hancock E. Patient-centredness in physiotherapy from the perspective of the chronic low back pain patient. Physiotherapy 2008;94:244-52. http://dx.doi.org/10.1016/j.physio.2007.10.006.
- Crowe M, Whitehead L, Gagan MJ, Baxter GD, Pankhurst A, Valledor V. Listening to the body and talking to myself – the impact of chronic lower back pain: a qualitative study. Int J Nurs Stud 2010;47:586-92. http://dx.doi.org/10.1016/j.ijnurstu.2009.09.012.
- de Vries H, Brouwer S, Groothoff JW, Geertzen JH, Reneman MF. Staying at work with chronic nonspecific musculoskeletal pain: a qualitative study of workers’ experiences. BMC Musculoskelet Disord 2011;12. http://dx.doi.org/10.1186/1471-2474-12-126.
- Dickson GL, Kim JI. Reconstructing a meaning of pain: older Korean American women’s experiences with the pain of osteoarthritis. Qual Health Res 2003;13:675-88. http://dx.doi.org/10.1177/1049732303013005006.
- Dragesund T, Råheim M. Norwegian psychomotor physiotherapy and patients with chronic pain: patients’ perspective on body awareness. Physiother Theory Pract 2008;24:243-55. http://dx.doi.org/10.1080/09593980701738400.
- Gustafsson M, Ekholm J, Ohman A. From shame to respect: musculoskeletal pain patients’ experience of a rehabilitation programme, a qualitative study. J Rehabil Med 2004;36:97-103. http://dx.doi.org/10.1080/16501970310018314.
- Hallberg LR, Carlsson SG. Psychosocial vulnerability and maintaining forces related to fibromyalgia: in-depth interviews with twenty-two female patients. Scand J Caring Sci 1998;12:95-104. http://dx.doi.org/10.1111/j.1471-6712.1998.tb00482.x.
- Hallberg LR, Carlsson SG. Coping with fibromyalgia. A qualitative study. Scand J Caring Sci 2000;14:29-36. http://dx.doi.org/10.1111/j.1471-6712.2000.tb00558.x.
- Harding G, Parsons S, Rahman A, Underwood M. ‘It struck me that they didn’t understand pain’: the specialist pain clinic experience of patients with chronic musculoskeletal pain. Arthritis Rheum 2005;53:691-6. http://dx.doi.org/10.1002/art.21451.
- Hunhammar C, Nilsson-Wikmar L, Lofgren M. Striving to master variable pain: an interview study in primary care patients with non-specific long-term neck/shoulder pain. J Rehabil Med 2009;41:768-74. http://dx.doi.org/10.2340/16501977-0421.
- Johansson E, Hamberg K, Lindgren G, Westman G. ‘I’ve been crying my way’ – qualitative analysis of a group of female patients’ consultation experiences. Fam Pract 1996;13:498-503. http://dx.doi.org/10.1093/fampra/13.6.498.
- Johansson EE, Hamberg K, Lindgren G, Westman G. ‘How could I even think of a job?’ – ambiguities in working life in a group of female patients with undefined musculoskeletal pain. Scand J Prim Health Care 1997;15:169-74. http://dx.doi.org/10.3109/02813439709035022.
- Johansson EE, Hamberg K, Westman G, Lindgren G. The meanings of pain: an exploration of women’s descriptions of symptoms. Soc Sci Med 1999;48:1791-802. http://dx.doi.org/10.1016/S0277-9536(99)00080-5.
- Lachapelle DL, Lavoie S, Boudreau A. The meaning and process of pain acceptance. Perceptions of women living with arthritis and fibromyalgia. Pain Res Manag 2008;13:201-10.
- Liddle SD, Baxter GD, Gracey JH. Chronic low back pain: patients’ experiences, opinions and expectations for clinical management. Disabil Rehabil 2007;29:1899-909. http://dx.doi.org/10.1080/09638280701189895.
- Lofgren M, Ekholm J, Ohman A. ‘A constant struggle’: successful strategies of women in work despite fibromyalgia. Disabil Rehabil 2006;28:447-55. http://dx.doi.org/10.1080/09638280500197891.
- Lundberg M, Styf J, Bullington J. Experiences of moving with persistent pain – a qualitative study from a patient perspective. Physiother Theory Pract 2007;23:199-20. http://dx.doi.org/10.1080/09593980701209311.
- Madden S, Sim J. Creating meaning in fibromyalgia syndrome. Soc Sci Med 2006;63:2962-73. http://dx.doi.org/10.1016/j.socscimed.2006.06.020.
- Mannerkorpi K, Kroksmark T, Ekdahl C. How patients with fibromyalgia experience their symptoms in everyday life. Physiother Res Int 1999;4:110-22. http://dx.doi.org/10.1002/pri.157.
- Mengshoel AM, Heggen K. Recovery from fibromyalgia – previous patients’ own experiences. Disabil Rehabil 2004;26:46-53. http://dx.doi.org/10.1080/09638280410001645085.
- Osborn M, Smith A. The personal experience of chronic benign lower back pain: an interpretative phenomenological analysis. Br J Health Psychol 1998;3:65-83. http://dx.doi.org/10.1111/j.2044-8287.1998.tb00556.x.
- Osborn M, Smith JA. Living with a body separate from the self. The experience of the body in chronic benign low back pain: an interpretative phenomenological analysis. Scand J Caring Sci 2006;20:216-22. http://dx.doi.org/10.1111/j.1471-6712.2006.00399.x.
- Osborn M, Smith A. The fearfulness of chronic pain and the centrality of the therapeutic relationship in containing it: an interpretative phenomenological analysis. Qual Res Psychol 2008;5:276-88. http://dx.doi.org/10.1080/14780880701826143.
- Patel S, Greasley K, Watson PJ. Barriers to rehabilitation and return to work for unemployed chronic pain patients: a qualitative study. Eur J Pain 2007;11:831-40. http://dx.doi.org/10.1016/j.ejpain.2006.12.011.
- Paulson M, Danielson E, Soderberg S. Struggling for a tolerable existence: the meaning of men’s lived experiences of living with pain of fibromyalgia type. Qual Health Res 2002;12:238-49. http://dx.doi.org/10.1177/104973202129119865.
- Paulson M, Norberg A, Danielson E. Men living with fibromyalgia-type pain: experiences as patients in the Swedish health care system. J Adv Nurs 2002;40:87-95. http://dx.doi.org/10.1046/j.1365-2648.2002.02343.x.
- Raheim M, Haland W. Lived experience of chronic pain and fibromyalgia: women’s stories from daily life. Qual Health Res 2006;16:741-61. http://dx.doi.org/10.1177/1049732306288521.
- Raymond MC, Brown JB. Experience of fibromyalgia. Qualitative study. Can Fam Phys 2000;46:1100-6.
- Rhodes LA, McPhillips-Tangum CA, Markham C, Klenk R. The power of the visible: the meaning of diagnostic tests in chronic back pain. Soc Sci Med 1999;48:1189-203. http://dx.doi.org/10.1016/S0277-9536(98)00418-3.
- Sallinen M, Kukkurainen ML, Peltokallio L, Mikkelsson M. Women’s narratives on experiences of work ability and functioning in fibromyalgia. Musculoskelet Care 2010;8:18-26. http://dx.doi.org/10.1002/msc.162.
- Sallinen M, Kukkurainen ML, Peltokallio L. Finally heard, believed and accepted – peer support in the narratives of women with fibromyalgia. Patient Educ Counsel 2011;85. http://dx.doi.org/10.1016/j.pec.2011.02.011.
- Sanders C, Donovan J, Dieppe P. The significance and consequences of having painful and disabled joints in older age: co-existing accounts of normal and disrupted biographies. Sociol Health Illn 2002;24:227-54. http://dx.doi.org/10.1111/1467-9566.00292.
- Satink T, Winding K, Jonsson H. Daily occupations with or without pain: dilemmas in occupational performance. OTJR 2004;24:144-50.
- Skuladottir H, Halldorsdottir S. The quest for well-being: self-identified needs of women in chronic pain. Scand J Caring Sci 2011;25:81-9. http://dx.doi.org/10.1111/j.1471-6712.2010.00793.x.
- Slade SC, Molloy E, Keating JL. ‘Listen to me, tell me’: a qualitative study of partnership in care for people with non-specific chronic low back pain. Clin Rehabil 2009;23:270-80. http://dx.doi.org/10.1177/0269215508100468.
- Slade SC, Molloy E, Keating JL. Stigma experienced by people with nonspecific chronic low back pain: a qualitative study. Pain Med 2009;10:143-54. http://dx.doi.org/10.1111/j.1526-4637.2008.00540.x.
- Snelgrove S, Liossi C. An interpretative phenomenological analysis of living with chronic low back pain. Br J Health Psychol 2009;14:735-49. http://dx.doi.org/10.1348/135910709X402612.
- Soderberg S, Lundman B, Norberg A. Struggling for dignity: the meaning of women’s experiences of living with fibromyalgia. Qual Health Res 1999;9:575-87. http://dx.doi.org/10.1177/104973299129122090.
- Soderberg S, Lundman B. Transitions experienced by women with fibromyalgia. Health Care Women Int 2001;22:617-31. http://dx.doi.org/10.1080/073993301753235389.
- Sturge-Jacobs M. The experience of living with fibromyalgia: confronting an invisible disability. Res Theory Nurs Pract 2002;16:19-31. http://dx.doi.org/10.1891/rtnp.16.1.19.52994.
- Teh CF, Karp JF, Kleinman A, Reynolds CFC, Weiner DK, Cleary PD. Older people’s experiences of patient-centered treatment for chronic pain: a qualitative study. Pain Med 2009;10:521-30. http://dx.doi.org/10.1111/j.1526-4637.2008.00556.x.
- Toye F, Barker K. ‘Could I be imagining this?’ – the dialectic struggles of people with persistent unexplained back pain. Disabil Rehabil 2010;32:1722-32. http://dx.doi.org/10.3109/09638281003657857.
- Toye F, Barker K. Persistent non-specific low back pain and patients’ experience of general practice: a qualitative study. Prim Health Care Res Dev 2012;13:72-84. http://dx.doi.org/10.1017/S1463423611000387.
- Toye F, Barker K. ‘I can’t see any reason for stopping doing anything, but I might have to do it differently’ – restoring hope to patients with persistent non-specific low back pain – a qualitative study. Disabil Rehabil 2012;34:894-903. http://dx.doi.org/10.3109/09638288.2011.626483.
- Undeland M, Malterud K. The fibromyalgia diagnosis: hardly helpful for the patients? A qualitative focus group study. Scand J Prim Health Care 2007;25:250-5. http://dx.doi.org/10.1080/02813430701706568.
- Walker J, Holloway I, Sofaer B. In the system: the lived experience of chronic back pain from the perspectives of those seeking help from pain clinics. Pain 1999;80:621-8. http://dx.doi.org/10.1016/S0304-3959(98)00254-1.
- Walker J, Sofaer B, Holloway I. The experience of chronic back pain: accounts of loss in those seeking help from pain clinics. Eur J Pain 2006;10:199-207. http://dx.doi.org/10.1016/j.ejpain.2005.03.007.
- Werner A, Steihaug S, Malterud K. Encountering the continuing challenges for women with chronic pain: recovery through recognition. Qual Health Res 2003;13:491-509. http://dx.doi.org/10.1177/1049732302250755.
- Werner A, Malterud K. It is hard work behaving as a credible patient: encounters between women with chronic pain and their doctors. Soc Sci Med 2003;57:1409-19. http://dx.doi.org/10.1016/S0277-9536(02)00520-8.
- Werner A, Isaksen LW, Malterud K. ‘I am not the kind of woman who complains of everything’: illness stories on self and shame in women with chronic pain. Soc Sci Med 2004;59:1035-45. http://dx.doi.org/10.1016/j.socscimed.2003.12.001.
- Afrell M, Biguet G, Rudebeck CE. Living with a body in pain – between acceptance and denial. Scand J Caring Sci 2007;21:291-6. http://dx.doi.org/10.1111/j.1471-6712.2007.00475.x.
- Arnold LM, Crofford LJ, Mease PJ, Burgess SM, Palmer SC, Abetz L, et al. Patient perspectives on the impact of fibromyalgia. Patient Educ Counsel 2008;73:114-20. http://dx.doi.org/10.1016/j.pec.2008.06.005.
- Crowe M, Whitehead L, Jo M, Baxter D, Panckhurst A. Self-management and chronic low back pain: a qualitative study. J Adv Nurs 2010;66:1478-86. http://dx.doi.org/10.1111/j.1365-2648.2010.05316.x.
- Cunningham MM, Jillings C. Individuals’ descriptions of living with fibromyalgia. Clin Nurs Res 2006;15:258-73. http://dx.doi.org/10.1177/1054773806291853.
- De Souza L, Frank AO. Patients’ experiences of the impact of chronic back pain on family life and work. Disabil Rehabil 2011;33:310-18. http://dx.doi.org/10.3109/09638288.2010.490865.
- Gullacksen AC, Lidbeck J. The life adjustment process in chronic pain: psychosocial assessment and clinical implications. Pain Res Manag 2004;9:145-53.
- Hellström O, Bullington J, Karlsson G, Lindqvist P, Mattsson B. A phenomenological study of fibromyalgia. Patient perspectives. Scand J Prim Health Care 1999;17:11-6.
- Holloway I, Sofaer-Bennett B, Walker J. The stigmatisation of people with chronic back pain. Disabil Rehabil 2007;29:1456-64. http://dx.doi.org/10.1080/09638280601107260.
- Kelley P, Clifford P. Coping with chronic pain: assessing narrative approaches. Soc Work 1997;42:266-77. http://dx.doi.org/10.1093/sw/42.3.266.
- Lempp HK, Hatch SL, Carville SF, Choy EH. Patients’ experiences of living with and receiving treatment for fibromyalgia syndrome: a qualitative study. BMC Musculoskelet Disord 2009;10. http://dx.doi.org/10.1186/1471-2474-10-124.
- Liedberg GM, Henriksson CM. Factors of importance for work disability in women with fibromyalgia: an interview study. Arthritis Rheum 2002;47:266-75. http://dx.doi.org/10.1002/art.10454.
- Paulson M, Danielson E, Larsson K, Norberg A. Men’s descriptions of their experience of nonmalignant pain of fibromyalgia type. Scand J Caring Sci 2001;15:54-9. http://dx.doi.org/10.1046/j.1471-6712.2001.1510054.x.
- Schaefer KM. The lived experience of fibromyalgia in African American women. Holist Nurs Pract 2005;19:17-25.
- Steen E, Haugli L. From pain to self-awareness – a qualitative analysis of the significance of group participation for persons with chronic musculoskeletal pain. Patient Educ Counsel 2001;42:35-46. http://dx.doi.org/10.1016/S0738-3991(00)00088-4.
- Strong J, Ashton R, Chant D, Cramond T. An investigation of the dimensions of chronic low back pain: the patients’ perspectives. Br J Occup Ther 1994;57:204-9.
- Strong J, Large RG. Coping with chronic low back pain: an idiographic exploration through focus groups. Int J Psychiatry Med 1995;25:371-87. http://dx.doi.org/10.2190/H4P9-U5NB-2KJU-4TBN.
- Leder D. The absent body. Chicago, IL: University of Chicago Press; 1990.
- Frank A. The wounded storyteller. Body illness and ethics. Chicago, IL: University of Chicago Press; 1995.
- Engel G. The need for a new medical model: a challenge for biomedicine. Science 1977;196:129-36. http://dx.doi.org/10.1126/science.847460.
- Turner V. The forest of symbols. Ithaca, NY: Cornell University Press; 1967.
- Illich I. Limits to medicine; medical nemesis: the expropriation of health. London: Marion Boyars Publishers; 1976.
- Bury MR. Sociol Health Illn 2001;23:263-85. http://dx.doi.org/10.1111/1467-9566.00252.
- Merleau-Ponty M. Phenomenology of perception. London: Routledge; 1962.
- Kleinman A. The illness narratives. Suffering, healing and the human condition. New York, NY: Basic Books; 1988.
- Canguilhem G. Normal and the pathological. New York, NY: Zone Books; 1989.
- Frank A. Bringing bodies back in: a decade review. Theory Cult Soc 1990;7:131-62. http://dx.doi.org/10.1177/026327690007001007.
- Turner B. Missing bodies – towards a sociology of embodiment. Sociol Health Illn 1991;13:265-73. http://dx.doi.org/10.1111/1467-9566.ep11340829.
- Wall P. Pain: the science of suffering. London: Phoenix; 1999.
- Chiesa A, Serretti A. Mindfulness-based interventions for chronic pain: a systematic review of the evidence. J Altern Complement Med 2011;17:83-9. http://dx.doi.org/10.1089/acm.2009.0546.
- Morley S. Possible selves in chronic pain: self-pain enmeshment, adjustement and acceptance. Pain 2005;115:84-9. http://dx.doi.org/10.1016/j.pain.2005.02.021.
- McCracken L, Velleman S. Psychological flexibility in adults with chronic pain: a study of acceptance, mindfulness, and values-based action in primary care. Pain 2009;148:141-7. http://dx.doi.org/10.1016/j.pain.2009.10.034.
- Vowles KE, McCracken LM. Comparing the role of psychological flexibility and traditional pain managment coping strategies in chronic pain treatment outcomes. Behav Res Ther 2010;48:141-6. http://dx.doi.org/10.1016/j.brat.2009.09.011.
- Thompson T, McCracken L. Acceptance and related processes in adjustment to chronic pain. Curr Pain Headache Rep 2011;15:144-51. http://dx.doi.org/10.1007/s11916-010-0170-2.
- McCracken LM, Carson JW, Eccleston C, Keefe F. Acceptance and change in the context of chronic pain. Pain 2004;109:4-7. http://dx.doi.org/10.1016/j.pain.2004.02.006.
- Pincus T, Morley S. Cognitive-processing bias in chronic pain: a review and integration. Psychol Bull 2001;127:599-617. http://dx.doi.org/10.1037//0033-2909.127.5.599.
- Higgins ET. Self-discrepancy: a theory relating self and affect. Psychol Bull 1987;94:319-40. http://dx.doi.org/10.1037//0033-295X.94.3.319.
- Leder D. Toward a phenomenology of pain. Rev Existential Psychol Psychiatry 19:255-66.
- World Health Organization . Towards a Common Language for Functioning, Disability and Health. The International Classification of Functioning, Disability and Health 2002. www.who.int/classifications/icf/training/icfbeginnersguide.pdf (accessed 12 July 2013).
- Towards a common language for functioning, disability and health. The international classification of functioning, disability and health. Geneva: World Health Organization; 2002.
- Morris DB. The culture of pain. Berkeley, CA: University of California Press; 1993.
- Foucault M. The birth of the clinic. Abingdon: Routledge Classics; 2003.
- Mead N, Bower P. Patient-centredness: a conceptual framework and review of empirical literature. Soc Sci Med 2000;51:1087-110. http://dx.doi.org/10.1016/S0277-9536(00)00098-8.
- Brett-MacLean P. Use of the arts in medical and health professional education. Univ Alta Health Sci J 2007;4:26-9.
- Helman C. Culture, health and illness. London: Hodder Arnold; 2007.
- Lupton D. Medicine as culture. London: Sage Publications; 1994.
- Annandale E. The sociology of health medicine. A critical introduction. Cambridge: Polity Press; 1998.
- Grace V. Embodiment and meaning. J Conscious Stud 2003;10:41-60.
- Csordas TJ, Good B, Fischer MMJ, Willen SW, Delvecchio-Good M-J. A reader in medical anthropology. Theoretical trajectories, emergent realities. Chichester: Wiley-Blackwell; 2010.
- Kleinman A. Concepts and a model for the comparison of medical systems as cultural systems. Soc Sci Med 1978;12:85-9. http://dx.doi.org/10.1016/0160-7987(78)90014-5.
- Grace V. Mind/body dualism in medicine: the case of chronic pelvic pain without organic pathology. A critical review of the literature. Int J Health Serv 1998;28:127-51. http://dx.doi.org/10.2190/M38P-QMDT-5EKD-NBMA.
- Grace V. Pitfalls of the medical paradigm in chronic pelvic pain. Ballieres Best Pract Res Clin Obstet Gynaecol 2000;14:525-39. http://dx.doi.org/10.1053/beog.1999.0089.
- Sontag S. Illness as metaphor. New York, NY: Farrar, Straus & Giroux; 1978.
- Sontag S. AIDS and its metaphors. New York, NY: Farrar, Straus & Giroux; 1989.
- Goffman E. Presentation of self in everyday life. Carden City, NY: Doubleday Anchor Books; 1959.
- Turner V. The anthropology of performance. New York, NY: PAJ Publications; 1987.
- Honkasalo M-L. Vicissitudes of pain and suffering: chronic pain and liminality. Med Anthropol 2001;19:319-53. http://dx.doi.org/10.1080/01459740.2001.9966181.
- Williams G, Radley A. Worlds of illness: biographical and cultural perspectives on health and disease. New York, NY: Routledge; 1993.
- Sim J, Madden S. Illness experience in fibromyalgia syndrome: a metasynthesis of qualitative studies. Soc Sci Med 2008;67:57-6. http://dx.doi.org/10.1016/j.socscimed.2008.03.003.
- Parsons S, Harding G, Breen A, Foster N, Pincus T, Vogel S, et al. The influence of patients’ and primary care practitioners’ beliefs and expectations about chronic musculoskeletal pain on the process of care. Clin J Pain 2007;23:91-8. http://dx.doi.org/10.1097/01.ajp.0000210947.34676.34.
- Smith JA, Flowers P, Larkin M. Interpretative phenomenological analysis. Theory, method and research. London: Sage Publications; 2009.
- Baszanger I. Pain: its experience and treatments. Soc Sci Med 1989;29:425-34. http://dx.doi.org/10.1016/0277-9536(89)90291-8.
- Jackson E. Stigma, liminality, and chronic pain: mind–body borderlands. Am Ethnol 2005;32:332-53. http://dx.doi.org/10.1525/ae.2005.32.3.332.
- n.d. www.ncrm.ac.uk/RMF2012/programme.php?id=F7.
- Carroll C, Booth A, Lloyd-Jones M. Should we exclude inadequately reported studies from qualitative systematic reviews? An evaluation of sensitivity analyses in two case study reviews. Qual Health Res 2012;22:1425-34. http://dx.doi.org/10.1177/1049732312452937.
- Toye F, Seers K, Allcock N, Briggs M, Carr E, Andrews J. ‘Trying to pin down jelly’ – exploring intuitive processes in quality assessment for meta-ethnography. BMC Med Res Meth 2013;13.
- Boychuk-Duchscher JE, Morgan D. Grounded theory: reflections on the emergence vs forcing debate. J Adv Nurs 2004;48:605-12. http://dx.doi.org/10.1111/j.1365-2648.2004.03249.x.
- Smith J, Hodkinson P, Denzin N, Lincoln Y. The Sage handbook of qualitative research. London: Sage; 2005.
- Blumer H. ‘What is wrong with social theory’. Am Sociol Rev 1954;18:3-10. http://dx.doi.org/10.2307/2088165.
- High quality care for all: NHS Next Stage Review final report. London: Department of Health; 2008.
- Helme R, Gibson S. The epidemiology of pain in elderly people. Clin Geriatr Med 2001;17:417-23. http://dx.doi.org/10.1016/S0749-0690(05)70078-1.
- Bevan S, Quadrello T, McGee R, Mahdon M, Vavrovsky A, Barham L. Fit for work? Musculoskeletal disorders in the European workforce. London: The Work Foundation; 2009.
- Werner A, Isaksen LW, Materud K. I am not the kind of woman who complains of everything: illness stories on self and shame in women with chronic pain. Soc Sci Med 2004;59:1035-45. http://dx.doi.org/10.1016/j.socscimed.2003.12.001.
- Bendelow G, Williams S. Transcending the dualism: towards a sociology of pain. Sociol Health Illn 1995;17:139-65. http://dx.doi.org/10.1111/1467-9566.ep10933376.
- Corbett M, Foster NE, Ong BN. Living with low back pain – stories of hope and despair. Soc Sci Med 2007;65:1584-94. http://dx.doi.org/10.1016/j.socscimed.2007.06.008.
- Good BJ, Good M-JD, Brodwin PE, Good BJ, Kleinman A. Pain as human experience. Berkeley, CA: University of California Press; 1992.
- Jackson JE, Good M-JD, Brodwin PE, Good BJ, Kleinman A. Pain as human experience. Berkeley, CA: University of California Press; 1992.
- Lillrank A. Back pain and resolution of diagnostic uncertainty in illness narratives. Soc Sci Med 2003;57:1045-54. http://dx.doi.org/10.1016/S0277-9536(02)00479-3.
- May C, Rose M, Johnstone F. Dealing with doubt. How patients account for non-specific chronic low back pain. J Psychosom Res 2000;49:223-5.
- Miles A, Curran H, Pearce S, Allan L. Managing constraint: the experiences of people with chronic pain. Soc Sci Med 2005;61:131-41. http://dx.doi.org/10.1016/j.socscimed.2004.11.065.
- Nettleton S. I just want permission to be ill: towards a sociology of medically unexplained symptoms. Soc Sci Med 2006;62:1167-78. http://dx.doi.org/10.1016/j.socscimed.2005.07.030.
- Paulson M, Danielson E, Norberg A. Nurses’ and physicians’ narratives about long-term non-malignant pain among men. J Adv Nurs 1999;30:1097-105. http://dx.doi.org/10.1046/j.1365-2648.1999.01162.x.
- Rhodes L, McPhillips-Tangum A, Markham C, Klenk R. The power of the visible: the meaning of diagnostic tests in chronic back pain. Soc Sci Med 1999;48:1189-203. http://dx.doi.org/10.1016/S0277-9536(98)00418-3.
- Skuladottir H, Halldorsdottir S. Women in chronic pain: sense of control and encounters with health professionals. Qual Health Res 2008;18:891-90. http://dx.doi.org/10.1177/1049732308318036.
- Thomas S. A phenomenological study of chronic pain. West J Nurs Res 2000;22:683-705. http://dx.doi.org/10.1177/019394590002200604.
- Van Huet H, Innes E, Whiteford G. Living and doing with chronic pain: narratives of pain program participants. Disabil Rehabil 2009;31:2031-40. http://dx.doi.org/10.1080/09638280902887784.
- Walker J, Holloway I, Sofaer B. In the system: the lived experience of chronic back pain from the perspective of those seeking help from pain clinics. Pain 1999;80:621-8. http://dx.doi.org/10.1016/S0304-3959(98)00254-1.
- Walker J, Sofaer B, Holloway I. The experience of chronic pain: accounts of loss in those seeking help from pain clinics. Eur J Pain 2006;10:199-207. http://dx.doi.org/10.1016/j.ejpain.2005.03.007.
- Werner A, Malterud K. Its hard work behaving as a credible patient: encounters between women with chronic pain and their doctors. Soc Sci Med 2003;57:1409-19.
- Werner A, Steihaug S, Malterud K. Encountering the continuing challenges for women with chronic pain: recovery through recognition. Qual Health Res 2003;13:491-50. http://dx.doi.org/10.1177/1049732302250755.
- Morley S, Eccleston C, Williams A. Systematic review and meta-analysis of randomised controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache. Pain 1999;80:1-13.
- Guzmán J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C. Multidisciplinary rehabilitation for chronic low back pain: systematic review. BMJ 2001;322:1511-16. http://dx.doi.org/10.1136/bmj.322.7301.1511.
- Williams S. Chronic illness as biographical disruption or biographical disruption as chronic illness? Reflections on a core concept. Sociol Health Illn 2000;22:40-67. http://dx.doi.org/10.1111/1467-9566.00191.
- Eccleston C, McCracken L. Coping or acceptance: what do we do about chronic pain. Pain 2003;105:197-204.
- Parsons T. The social system. New York, NY: New York Free Press; 1951.
- Wong S, Wilczynski N, Haynes R. Developing optimal search strategies for detecting clinically relevant qualitative studies in MEDLINE. Stud Health Technol Inform 2004;107:311-16.
- Briggs M, Nelson E. Topical agents or dressings for pain in venous leg ulcers. Cochrane Database Syst Rev 2006;1. http://dx.doi.org/10.1002/14651858.CD001177.
- Briggs M, Flemming K. Living with leg ulceration: a synthesis of qualitative research. J Adv Nurs 2007;59:319-28. http://dx.doi.org/10.1111/j.1365-2648.2007.04348.x.
- Gorecki C, Brown J, Lamping D, Nelson E, Briggs M, Schoonhoven L, et al. On behalf of the European Quality of Life Pressure Ulcer Project (EQUIP) group. A systematic review of quality of life issues in pressure ulcers. J Am Geriatr Soc 2009;57:1175-83.
Appendix 1 Protocol
A META-ETHNOGRAPHY OF PATIENTS’ EXPERIENCE OF CHRONIC NON-MALIGNANT PAIN – REVISED FOLLOWING RECOMMENDATIONS BY BOARD
Aims and objectives
The aim of this study is to:
-
Increase our understanding of patients’ experiences of chronic non-malignant pain and therefore have an impact on quality of care.
-
Utilise existing research knowledge to improve understanding and thus best practice in patient care.
-
Contribute to the development of methods for qualitative research synthesis.
These aims meet the HSR programme objectives.
Objectives
-
To produce a conceptual synthesis of qualitative findings related to chronic non-malignant pain using the methods of meta-ethnography proposed by Noblit and Hare,20 and developed for use in health research. 22,23,61
-
To contribute to the development of methods for qualitative research synthesis and produce a qualitative synthesis that is rigorous, accessible and relevant to academics, practitioners, patients and policy makers.
This research will increase understanding and knowledge of chronic non-malignant pain, and thus directly inform best clinical practice by providing new understandings regarding patient experience and their treatment. We will contribute to a more patient focused research agenda. A qualitative synthesis would enable policy makers to determine whether or not the treatment for chronic non-malignant pain is meeting the needs of quality improvement as defined by the Department of Health’s report – ‘High quality care for all’440 where patient experience is seen as fundamental to quality of care. A greater understanding of patient experience of care has potential to provide new opportunities to deliver services differently and directly influence patient redesign of health services.
There are methodological issues that need to be addressed if qualitative synthesis is to be effectively used to enhance best practice:21,22 A systematic search of the qualitative literature is not straightforward. 22,51 There is a lack of consensus regarding the most appropriate way to judge what should be included in a qualitative synthesis. 56,57
Background
Chronic pain has been acknowledged as a condition in its own right,5 and has become the focus of recent government policy in the UK. 6,15,16 Each year over five million people develop chronic pain. 6 As many as 19% of adults in Europe suffer with moderate to severe chronic pain,7 and 7% have chronic pain that is severe and disabling. 11 Persistent pain may affect more than 50% of older persons living in the community. 441 Pain has a high impact on the individual’s physical, psychological and social wellbeing. 12 For example, 49% of patients with persistent pain experience depression, 25% lose their jobs and 16% feel their chronic pain is so bad that they sometimes want to die. 6 In terms of cost, musculoskeletal pain may account for 2% of the Gross Domestic Product of Europe. 442
Rationale – Qualitative research addresses a central concern of the NHS – patient experience. 440 Patient experience is one of the dimensions of quality integral to the NHS. In 2008, Darzi’s report ‘High Quality Care for All’ stated that the patient’s experience of the NHS is fundamental to the quality of care and is of central concern. ‘Quality of care means quality of caring’ which can only be improved by understanding patients experience. 440 Qualitative research aims to understand the experience of illness, and make sense of the complex processes involved. It aims to enrich human discourse and help to generate concepts that allow us to understand behaviour. 20 It can thus lead to substantial improvements in health care and policy decisions by enabling clinicians and policy makers to understand the appropriateness, and meaningfulness of interventions. In particular, by understanding the experience of those with chronic pain clinicians, policy makers and patients can be empowered to make more informed decisions about care. Insights from several meta-ethnographies in health care have contributed to a greater understanding of complex processes such as medicine taking,22 adherence to treatments for diabetes23 and use of antidepressants. 24 Excluding qualitative research from evidence based practice may mean that we neglect vital information from decisions related to policy and practice. 25 Syntheses of qualitative research should thus be used alongside those of quantitative research, to underpin policy decisions. Concepts generated from qualitative research synthesis will help researchers, policy makers, clinicians and patients to ask questions that will enhance the validity of subsequent research.
Qualitative findings can help to formulate relevant research questions, identify the components of interventions, understand the outcome of interventions and conflicting results, and to identify barriers to treatment. However, the proliferation of studies exploring the experience of chronic non-malignant pain97,140,206,214,250,261,296,327,342,343,348,363,379,385,427,433,443–460 makes it difficult for clinicians and policy makes to use this knowledge to inform practice and policy, and increases the danger that these findings are ‘doomed never to be visited’. 27 Research findings need to be accessible if they are to have an effect on care and policy. The Cochrane Qualitative Research Methods Group acknowledges the importance of including qualitative findings within evidence based healthcare, and stress that ‘evidence from qualitative studies can play an important role in adding value to systematic reviews for policy, practice and consumer decision-making’21 571. Syntheses of the existing body of qualitative research can also help to identify gaps in knowledge and to target these gaps. To date, there has been no synthesis of qualitative research related to chronic non-malignant pain, and thus the proposed research is timely. 25
A qualitative synthesis would aim to offer conceptual insights into health experience that could have a direct effect on care. For example, there may be a place for a conceptual theory regarding disability from chronic pain based on the concepts derived from qualitative synthesis. Such a theory could be used to inform the development of ‘risk’ tools for assessment of patients with chronic pain. We know that psychosocial factors seem to predict the outcome of treatment but we do not fully understand why some are disabled by their pain and others are not. 461,462 Some patients with chronic pain are able to accept their limitations and successfully revise their sense of self and others are not. 427,463 Although there has been some research exploring adaptation to pain,450 the role of acceptance has not been fully explored. 464
There is large body of qualitative research exploring patients’ experience of chronic pain, and although certain themes seem to be consistent, there has been no attempt to systematically search the qualitative literature with an aim to increase our conceptual understanding. Qualitative studies show that patients with persistent unexplained back pain remain committed to the medical model of pain even though this model does not fit their experience. 327,344,451 The medical model takes disease to be an objective biomedical category that can be accounted for by a specific etiology. This model also implies an illness trajectory whereby, following diagnosis and treatment, a person’s health is restored. 465 Studies also report that patients feel that they are not believed,97,250,427,443,447,448,452,460 and may even start to doubt their own experience of pain. 327,433,447,448,451,457 These findings are supported by a meta-synthesis of patient experiences of Fibromyalgia. 429 Patients with chronic pain also present a certain moral narrative393 in order to legitimize their condition,443,449,452,459 and use social comparison to rank themselves in relation to others. 342,443,450,453,458 Qualitative studies have also shown the importance of self-identity, yet at the same time, an acceptance of changes to identity. 427,454,460
The aim of qualitative synthesis is to systematically review and integrate the findings of qualitative research in order to increase conceptual understanding. The aim is to make ‘a whole into something more than the parts imply’ [48:28]. This synthesis would be accessible to health professionals, researchers, policy makers and patients, thus having a far-reaching impact on the processes of health care. Policy makers and clinicians need to draw on various sources of evidence in order to improve the quality of patient care. 31 Qualitative synthesis can thus add value to evidence on the effectiveness of interventions. 21 Synthesis of qualitative research aims to move beyond narrative description and generate ‘theories that can inform the development of interventions’,31 thus informing the implementation of more appropriate and effective patient focused interventions. 21,60
Need
This research meets the classifications of research need outlined by the NIHR Health Services Research Programme. In particular, a meta-ethnography aims to build on exiting work and generate new knowledge.
-
Building on existing work. One of the specific aims of this study is to utilise existing research knowledge to improve understanding and thus best practice. Specific to meta-ethnography is the aim of making a whole that is greater than the sum of its parts,20 in order to generate a new conceptual understanding based on the comparison of multiple accounts. A meta-ethnography of chronic non-malignant pain will therefore enhance and add value to the body of existing knowledge in the field of pain.
-
Capacity to generate new knowledge. A qualitative synthesis would offer a greater conceptual understanding of patients’ experiences and offer insights into effective care. This meta-ethnography would help us to identify gaps in the knowledge that are not addressed by existing research and therefore add to the validity of further research in this area. For example, we have said that certain patients are able to successfully revise their sense of self and others are not. 427,463 This study is likely to offer conceptual insights into this process. 464
-
Health need. Chronic pain has a huge impact on the quality of life of adults in the UK,6,7,11,12,441 and this is recognised in recent UK policy documents. 6,15,16 The research may be used to inform the development of quality of life tools to be used in chronic pain. This research may also contribute to the dialogue with patients about their chronic pain and how policy makers and clinicians can meet their needs. It could thus have a direct impact on quality of care as outlined in ‘High Quality Care for all’. 440
-
Expressed need. A greater conceptual understanding of chronic pain is highly relevant and has been highlighted as important in recent policy documents in the UK. The Chief Medical Officers report in 2009, ‘Pain breaking through the Barrier’6 identifies chronic pain as important to NHS policy. In addition to this, an NHS report on ‘getting to GRIPS with chronic pain in Scotland’15 identified a need to improve knowledge about chronic pain. Chronic non-malignant pain is also recognised as one of the key areas for improvement by the Welsh Assembly Government. 16 Specifically, the Chief Medical Officer recommended that training in chronic pain should be included in the curricula of all healthcare professionals. 6 This meta-ethnography may be used to inform education initiatives related to chronic pain.
-
Sustained interest and intent. Chronic pain has been highlighted as a future priority for NHS policy. 6 If patients with pain are managed more effectively this may reduce unnecessary interventions such as emergency department visits, hospital admissions, secondary and tertiary referrals and inappropriate diagnostic testing. Conceptual understanding may contribute to the development of care pathways for chronic non-malignant pain. Poor quality pain management in the elderly and in care home residents has been highlighted by the Patients Association. 181 This finding is of particular social importance in view of the ageing population in the UK and the potential effect on demand for pain services. Demand for the treatment of chronic pain is likely to increase with increasing age.
-
Organisational focus consistent with HSR mission. This study will inform the organisation of appropriate services for chronic pain. There is currently no synthesis of qualitative evidence available to understand patients’ views of the feasibility and acceptability of interventions for chronic pain. This is fundamental as qualitative research has been highlighted as important in informing health care policy and best practice. 21,56
-
Generalisable findings and prospects for change. Whilst qualitative research is contextual and therefore can be complex to apply to decision making processes, qualitative synthesis can be used to generate findings that can more clearly inform practice. We have given the example of how findings could be used to inform the development of ‘risk’ tools for assessment of patients with chronic pain. Similarly, we have suggested the findings could be used to inform the development of chronic pain care pathways within the NHS, thus having a direct effect on decision-making regarding treatment.
Method
A figure outlining the research process is shown below.
Flow chart of research process.
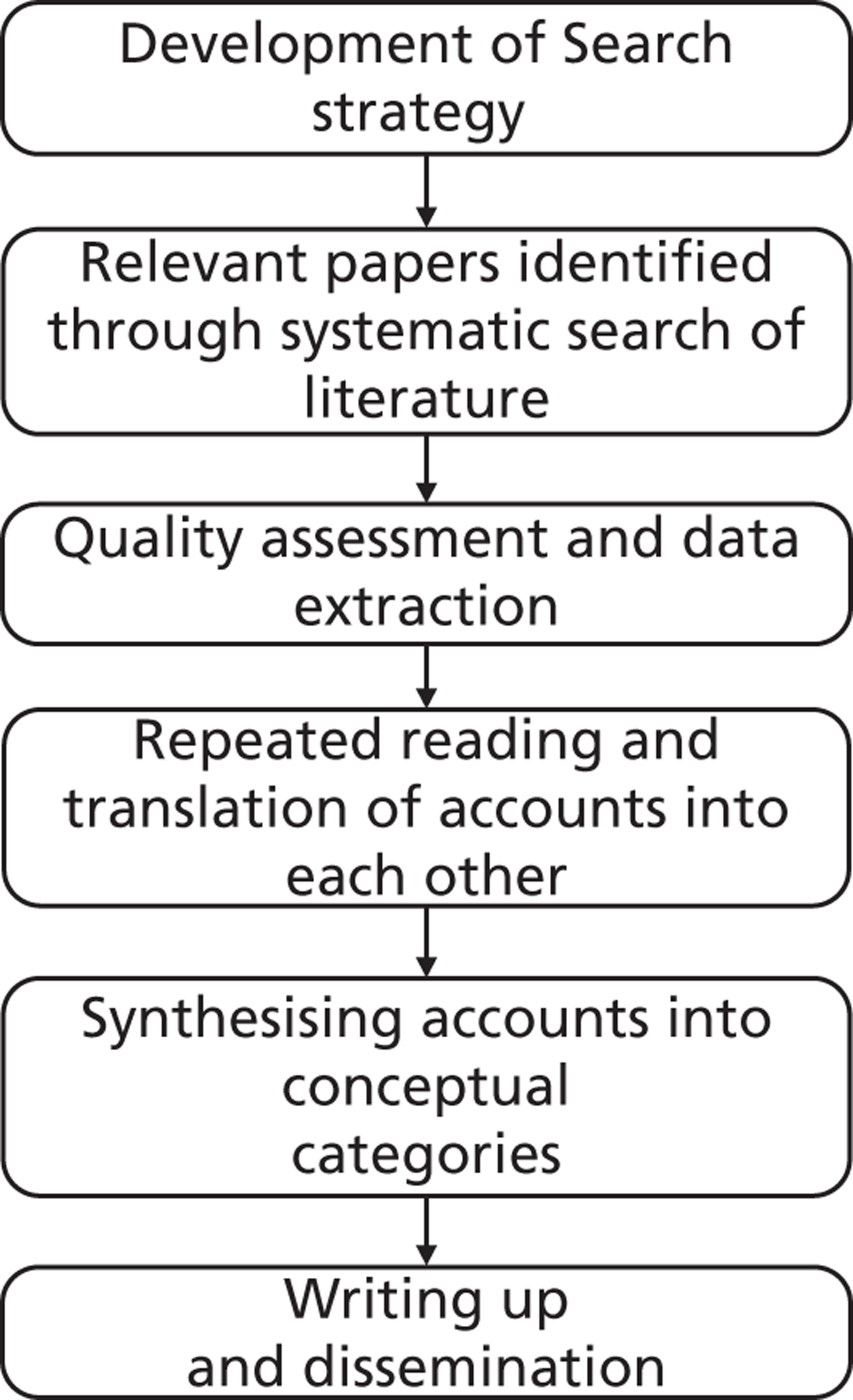
Search strategy
Initial scope of literature – We undertook an initial search of the published literature in order to determine the scope of the meta-ethnography and to refine the research question. Using MEDLINE from 1950 to the present, we used the ‘Clinical Query’ limit to search for articles filtered as using qualitative research methods. We used the widest scope available in this option. Using ‘pain’ as our key word within title or abstract, we identified 1200 articles in English. One of the research team (FT) read through the titles and identified 206 as qualitative studies pertinent to chronic non-malignant pain. A further 31 were excluded after reading through the abstracts, leaving 175. The number of studies for each condition is shown in Table 1. Searching for qualitative studies can be problematic,51 and we did not expect to identify all available studies by conducting this search only in MEDLINE. Interestingly, the results for Fibromyalgia (FM) were comparable to a recent meta-synthesis of qualitative findings in FM. 429 However, we know that the search did not identify all studies related to back pain. The search demonstrated that there is a body of knowledge available for a meta-ethnography of patient experience of chronic non-malignant pain.
| Condition | Number of studies identified |
|---|---|
| Chronic non-malignant/chronic widespread (mainly musculoskeletal) | 39 |
| Back and neck pain | 36 |
| Hip and knee osteoarthritis (OA) | 27 |
| Fibromyalgia | 20 |
| Cross cultural studies | 12 |
| Rheumatoid arthritis | 9 |
| Other* | 1–3 |
We will conduct a systematic search of the qualitative literature on patient experiences of chronic non-malignant pain, using the guidelines provided by the Centre for Reviews and Dissemination (www.york.ac.uk/inst/crd/intertasc/). Final decisions on scope will be made after the searching is complete.
The research team will include a full time information scientist for 6 months to help develop the search strategy in consultation with the research team. The information scientist will be responsible for performing the search and retrieving the literature with guidance from the research team. The progress of the search will be discussed amongst the team at regular project team meetings. Using several search strategies can facilitate optimal retrieval of relevant articles,51,466 and the search strategy will include the following:
-
(a) A systematic search of relevant databases in order to identify all qualitative studies exploring patients’ experiences of chronic non-malignant pain. Databases will include CINAHL, EMBASE, MEDLINE, OVID, PsychINFO, as indicated by CRD guidelines. The search aims to include all patients aged 18 and over, and all available dates.
-
(b) We will follow up references from identified papers.
-
(c) We will search the indexes of specific journals identified by the research team as known to report the findings of qualitative studies in depth (e.g. Social Science and Medicine, Qualitative Health Research, Journal of Advanced Nursing) for the previous 10 years. Hand-searching journals is an important strategy for comprehensively identifying relevant qualitative studies. 51,52 A Cochrane Methodology Review found that hand-searching is necessary in order to identify relevant studies. 53 A list of journals will be developed at an early research team meeting and refined as the search strategy is developed. We will also search for work by authors identified as having done research in this area.
-
(d) Personal Communication. Each member of the team is familiar with the literature on chronic pain and will use contacts to further widen the search.
-
(e) Grey literature
Once relevant articles have been identified, the process as outlined by Sandelowski and Barroso will be used to exclude articles that do not meet the inclusion criteria. 27 This is shown in Figure 1. A detailed description of the search strategy and reasons for excluding studies will be kept.
Strategy for determining inclusion of studies
Although methods for determining the quality of qualitative research have been suggested, there is currently no consensus and the use of quality criteria is widely debated. 54–56 Although structured checklists may not produce consistent judgements about quality in qualitative research,57 they may be useful in providing a focus for consensus discussions. Some argue that quality appraisal should not be used to exclude studies from qualitative synthesis. 31 It could be argued that the determination of quality for inclusion in a meta-ethnography is determined by its ability to be translated and to enhance the development of conceptual categories. To be utilised within a meta-ethnography, studies must therefore provide sufficient description of concepts to allow translation. 20
To assist with appraisal for inclusion, the team will use questions developed by the critical appraisal skills programme (CASP)59 that have been adapted and used for appraising quality of studies for meta-ethnography. 23,60,61 We will use the initial screening questions used in these studies:
-
Does this paper report on findings from qualitative research in people aged 18 and over and did that work involve both qualitative methods of data collection and analysis?
-
Is this research relevant to the synthesis?
This process will be carried out independently by two people, any disagreement will be discussed, and where required will be reviewed by a third person. All members of the team have experience of appraising and conducting qualitative research. If no consensus is reached, the paper will be included. Following quality assessment, data will be extracted and included on a data extraction form developed by the research team.
Each team member will also categorise papers as suggested by Dixon-Woods. 57 Is this paper:
-
A ‘key paper’(KP) – ‘conceptually rich and could potentially make an important contribution to the synthesis’
-
A ‘satisfactory paper’ (SAT)
-
A paper that is irrelevant to the synthesis (IRR)
-
A paper that is methodologically fatally flawed (FF)
This method of determining inclusion has been used in a recent meta-ethnography,24 and will allow us to compare two methods of appraisal for inclusion into meta-ethnography.
Design and theoretical/conceptual framework
This study will use the methods of meta-ethnography as proposed by Noblit and Hare. 20 Various methods for synthesizing the results of qualitative research have been suggested. 27,29,30 Meta-ethnography is an interpretive form of knowledge synthesis, as opposed to the aggregate form more commonly used in the meta-synthesis of quantitative research. 29 It thus aims to develop new conceptual understandings. Meta-ethnography20 is currently the most frequently used method of qualitative synthesis used in health care research,25 and provides one of the most explicit methods of synthesising qualitative studies. 30 It has been suggested that we need to interpret the findings of meta-ethnography for policy makers;30 the research team will provide an accessible interpretation and make suggestions for policy and practice, and policy makers will be part of the steering group to assist with this process. Meta-Ethnography has been used to synthesis qualitative findings in several areas of health care. 23–25,61 For example, Malpass et al. 24 conducted a meta-ethnography which aimed to more fully understand patients non-adherence to anti-depressants. This study shows how meta-ethnography can have a direct effect on clinical practice by suggesting ways in which general practitioners can facilitate concordant relationships with patients. In a similar way, Pound et al. 61 use meta-ethnography to synthesise qualitative studies of medicine taking, and suggest that research should focus on developing ways of making medicine-taking safe.
Analysis involves translating the concepts of qualitative research findings, and exploring how these translations are related to each other, thus ‘translating qualitative studies into one another’. 20 The process of translation involves reading and re-reading accounts and constantly comparing the concepts of the original texts in order to ensure that the translations are grounded in the original studies. This is comparable to the constant comparative method of Grounded Theory. 67 Constant comparison allows us to see the similarities and differences and thus generate new concepts. Through comparing and translation, the synthesis aims to provide further conceptual understanding of a particular phenomenon. Once formulated, translations can be, reciprocal (in agreement), refutational (disagree), or brought together to form a line of argument. 20 Translations are integrated into a conceptual interpretation that deepens understanding of the phenomenon. It may be more useful to think of translation and integration as ongoing and simultaneous processes, rather than sequential acts. As in other qualitative research methods, data collection does not precede analysis but informs it. 67 The process of meta-ethnography involves continually returning to the ‘data’ in order to ensure that the translations are recognisable and convey the meaning of the source research.
Contribution to collective research effort and research utilisation
Outputs
We anticipate the following outputs from this research:
-
Publication in high impact journals related to:
-
(a) Chronic pain
-
(b) Research methodology.
-
-
A conceptual framework for chronic non-malignant pain. This would help ensure that domains important to the patients are addressed in the complex management of chronic non-malignant pain.
-
A summary of the research for practitioners, policy makers and patients.
-
Identification of research questions not currently addressed by body of qualitative knowledge.
-
Dissemination of research utilising technology such as Podcasts.
Methods of dissemination
The Steering Group will include members with access to practice, policy and patient arenas to advise on appropriate dissemination. The research team have wide experience of research dissemination and are active in the field of chronic pain.
We would expect research findings to be disseminated through
-
PODCAST/DVD production. The Centre for Qualitative Research at Bournemouth University has a strand of ‘Performative Science’ which works with qualitative researchers to produce visual outputs. (www.bournemouth.ac.uk/cqr/rescqrpss.html.) It is powerful in the ‘promotion of knowledge’ beyond traditional outputs.
-
Key high impact journals.
-
International conferences e.g. International Association for the Study of Pain (IASP), European Federation of IASP Chapters (EFIC).
-
Patient groups, including the British Pain Society Patient Liaison.
-
Special interest groups (British Pain Society and IASP).
-
NHS Evidence.
-
Electronic open source publication via BioMed Central.
-
Linking a summary of report into key patient websites.
Plan of investigation and timetable
A plan of the study with monthly schedule has been drawn up and is shown below.
| Metaethnography Chronic Pain: Project Time Plan with key phases, meetings, progress reports to HSR and key milestones | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Date | 10 Nov | 10 Dec | 11 Jan | 11 Feb | 11 Mar | 11 Apr | 11 May | 11 Jun | 11 Jul | 11 Aug | 11 Sep | 11 Oct | 11 Nov | 11 Dec | 12 Jan | 12 Feb | 12 Mar | 12 Apr | 12 May | 12 Jun | 12 Jul | 12 Aug | 12 Sep | 12 Oct |
| Key Phases | Develop search strategy and systematic search | |||||||||||||||||||||||
| Critical appraisal and data extraction ongoing | ||||||||||||||||||||||||
| Translating accounts and developing themes ongoing | ||||||||||||||||||||||||
| Synthesis of translations and development of lines of argument | ||||||||||||||||||||||||
| Writing up and preparation of final report | ||||||||||||||||||||||||
| Project team meetings** | SG* | SG PP* | PP | SG | PP | |||||||||||||||||||
| PT* | PT | PT | PT | PT | PT | PT | PT | PT | PT | PT | PT | PT | PT | PT | PT | PT | PT | PT | PT | PT | PT | PT | PT | |
| HSR progress report (6/12) | HSR | HSR | HSR | HSR | ||||||||||||||||||||
| Milestones | Initial search completed and set up to rerun | Complete initial translation of accounts | Line of argument developed and prepared for write up | Rerun search & integrate findings | DVD production | |||||||||||||||||||
Ethics
This meta-ethnography would not involve patient participants and does not require ethical approval.
Project management
There will be a clear project documentation system, with careful version control. This will be developed by the PI and agreed by the project team at their first meeting. It will include a detailed Gantt chart; roles and responsibilities of each project team member; a risk register; a brief communication strategy setting out principles for communication, updating and discussion within the project team; a dissemination strategy and reference management plan using Endnote. The PI will be responsible for the day-to-day running of the study, and the project team will meet monthly using a combination of face-to-face meetings, teleconferencing and Skype. Progress against agreed objectives and budget monitoring will be part of each meeting. A steering group will be established and meet three times during this study to offer advice to the project team.
Service users
Steering group membership
-
A member of the Nuffield Orthopaedic Centre, Patient Research Engagement Forum (PREF) who has recent experience of treatment for non-malignant pain.
-
A patient with an interest in research will be recruited from UNTRAP based at Warwick University (www2.warwick.ac.uk/fac/cross_fac/healthatwarwick/untrap/). UNTRAP is a partnership between users of health and social care services and carers, the University of Warwick and the NHS. UNTRAP aims to support the involvement of service users and carers in teaching and research.
-
Beverly Collett [past Pain Society President], Assistant Medical Director, Consultant in Pain Management & Anaesthesia, Leicester Royal Infirmary NHS Trust, who has been actively involved in policy decisions for chronic pain, has agreed to be part of the steering group.
-
Department of Health representative with an interest in patient and public involvement.
-
Two members of NHS staff working in chronic non-malignant pain.
The steering group will meet a minimum of 3 times spread throughout the study (see study timetable) and aims to provide advice from a broad perspective.
2. Involvement in Analysis – The UNTRAP user will also be active in the synthesis stage of the research (see study timetable). This person will attend 3 key analysis meeting and contribute to the conceptual development of this study. This person will paid at the agreed UNTRAP rate.
Expertise and justification of support required
The main costs for this proposal will be to support the research team. Full details of costing are given in the application form. We realise the likely number of papers will be challenging and so have constructed this team taking this into account. We will allocate each paper to two members of the research team in a rotational system, so that each researcher has the opportunity to work with every member of the team. This will allow a broader perspective on appraisal and interpretation of each paper. We know that meta-ethnography is feasible for studies incorporating smaller numbers of studies. 22,23,61 A meta-synthesis incorporating a large number of studies will contribute to the understanding of the feasibility of meta-ethnography for use in areas of healthcare where a large body of qualitative knowledge exists.
Research team
Dr Francine Toye (FT) – FT will be responsible for overall project management and coordination of the team. She will work closely with the research fellow and information scientist to develop the search strategy and data collection methods. She will be financed to work on the project 1.5 days per week (0.3FTE) for the duration of the study, and will support the research fellow during this time. She will work jointly with the other team members to translate and synthesise the studies and to disseminate findings. FT is familiar with the literature in this field and has experience of qualitative analysis. She has a social science degree (2.1) in Anthropology, awarded by Cambridge University, and has a continued interest in medical anthropology. For her PhD, FT used interpretative phenomenological analysis (IPA) to explore patient’s perceptions of health care need (total knee replacement). During her doctoral and post-doctoral qualitative research FT has developed the skills needed to identify and analyse qualitative data. She uses IPA and grounded theory in her own research and has attended courses in IPA analysis and qualitative synthesis and meta-ethnography. She has a recent qualitative publication related to patients’ experience of pain [80] which used grounded theory to explore how patients with persistent unexplained pain interpret and utilise the biopsychosocial model. She also teaches qualitative research methods to research colleagues within her NHS Trust. Her current role also involves consulting with and supervising clinicians involved in qualitative research. FT is currently involved as a qualitative research consultant at the clinical trials unit (University of Warwick).
Professor Kate Seers (KS) – KS has extensive qualitative research experience, is supervising seven qualitative PhDs and has supervised eight qualitative PhDs to completion. One of these was a complex meta-ethnography, a publication from which is currently under review. KS’s topic expertise is within pain management where she has a detailed knowledge and has published widely. She has also undertaken and published two quantitative systematic reviews in pain management, and is feedback editor of the Cochrane Pain, Palliative and Supportive Care Group, so is used to extracting data and assimilating large amounts of data. KS also has extensive experience in leading large research teams and working collaboratively. KS will be responsible for contributing to the development of the meta-ethnography, and working with the team to extract themes and translate concepts across studies.
Dr Eloise Carr (EC) – EC is an experienced pain and mixed methods researcher spanning over twenty years. All her research studies have involved a qualitative element and she would have access to the international ‘Centre for Qualitative Research’ in the School of Health & Social Care at Bournemouth University. She has supervised doctoral students to successful completion (3 in qualitative methods) and currently supervises six students in pain research. Her most recent grant (Health Foundation £456K) has focused on the management of chronic low back pain in primary care and she has considerable subject knowledge of the topic area. EC is experienced in leading complex projects and working collaboratively. EC will work with other team members to translate and synthesise the studies and contribute to dissemination of the outputs.
Dr Nick Allcock (NA) is director of the Nottingham Centre for Evidence Based Practice Nursing, Midwifery and Physiotherapy a collaborating centre of the Joanna Briggs collaboration and has been trained in the process of qualitative research synthesis. Clinically involved in the management of chronic pain, he has planned and completed qualitative studies into patient experiences of chronic pain. 141 NA works in the School of Nursing, Midwifery and Physiotherapy, and is director of the MSc in research methods. He has successfully supervised PhD and Masters Dissertations.
Michelle Briggs (MB) MB has broad experience in systematic reviews. She is an author of a Cochrane systematic review467 and has served as a Cochrane Wounds Group editor from 2003–2008 and is currently a reviewer for The Cochrane Pain, Palliative Care and Supportive Care Collaborative Review Group. She has completed syntheses of qualitative research during her NIHR post doctoral training using Joanna Briggs QARI methodology. The Cochrane Qualitative Methods group recently asked permission to use the publication of this synthesis468 as an exemplar of qualitative synthesis in a qualitative workshop at the Singapore Cochrane Colloquium Oct 2009. She also has supervised others in mixed methods reviews of quality of life issues in pressure ulcers using a combined synthesis of qualitative and quantitative research based on Bayesian synthesis methods involving the generation of a prior distribution of likely factors and their relative importance and using content analysis to generate common categories and themes from findings. 469
Dr Karen Barker (KB) is the Clinical Director and research lead for the rehabilitation arm of the NIHR supported Musculoskeletal Biomedical Research Unit a collaboration between the Nuffield Orthopaedic Centre NHS Trust and Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Science at University of Oxford. She has experience in conducting research trials with patients with chronic back pain and has participated in a number of systematic reviews. She has supervised PhD and MPhil students to completion and is currently supervising PhD and MPhil students.
Collaborators
Information Scientist (IS) – Full time for 6 months. This will allow time to develop and refine the search strategy within the team. The role of the IS would be to work with the team to develop and refine the search strategy, to identify and retrieve all relevant articles. The quality of this type of synthesis relies on optimising retrieval, and this role is important to the quality of output.
Research Fellow (RF) – 0.5 FTE post (2.5 days) over the 24 months. The research fellow would work with the team in all stages of the project (quality appraisal, data extraction, analysis).
Other costs
Include travel for team and servicer users to attend meetings, NVivo to assist analysis and dissemination costs. These are broken down in detail within the application form.
Building research capacity
This project will provide FT the opportunity to develop her post doctoral experience to undertake a large synthesis of qualitative research within an experienced team of qualitative researchers. With the proliferation of qualitative research findings, the ability to synthesise findings is likely to become an increasingly important facet informing best clinical practice.
Planned or active research grants
We have not planned, nor are in receipt of any other research grants for this project.
History of past or existing NIHR programme research
Current
KS Principal investigator on NIHR Research for Patient Benefit Grant: PB-PG-0407-12243 – Research for Patient Benefit (Diabetes Urgent Care) September 2008-November 2010. £230,963
MB Co-Investigator on NIHR Research for Patient Benefit Grant: October 2009–October 2012 PI SJ Closs. Towards culturally competent pain management for older people £239,000
MB Co-Investigator on NIHR Programme Grant for Applied Research. PURPOSE Pressure UlceR Programme of ReSEarch. Feb 2008–Feb 2013 PI J Nixon £1,995,549
MB Principal Investigator NIHR Post Doctoral Award Jan 2006–June 2010. Self-management for people with painful leg ulcers: the development of a complex intervention using qualitative synthesis of research, realistic synthesis and grounded theory. £231,000
Completed
KS Co-investigator Service Delivery and Organisation (SDO) Grant August 2005. PI Rycroft-Malone. Clinical decision making (protocol based care). £93,000
KB Principal investigator on NIHR Research for Patient Benefit Grant: PB-PG-0407-13216 Rehab after RHA. Evaluation of a specific physiotherapy programme following resurfacing arthroplasty – is it more effective at improving function and muscle strength than standard rehabilitation? November 2008–October 2011 £232,046.
Appendix 2 Search syntax for meta-ethnography of pain
MEDLINE
-
RESEARCH, QUALITATIVE/
-
ATTITUDE TO HEALTH/
-
INTERVIEWS AS TOPIC/
-
FOCUS GROUPS/
-
NURSING METHODOLOGY RESEARCH/
-
LIFE EXPERIENCES/
-
(qualitative OR ethno$ OR emic OR etic OR phenomenolog).mp
-
(hermeneutic$ OR heidegger$ OR husserl$ OR colaizzi$ OR giorgi$ OR glaser OR strauss).mp
-
(van AND kaam$ OR van AND manen OR constant AND compar$).mp
-
(focus AND group$ OR grounded AND theory OR narrative AND analysis OR lived AND Experience$ OR life).mp
-
(theoretical AND sampl$ OR purposive AND sampl$ OR ricoeur OR spiegelberg$ OR merleau).mp
-
(field AND note$ OR field AND record$ OR fieldnote$ OR field AND stud$).mp;
-
(participant$ adj3 observ$).mp
-
(unstructured AND categor$ OR structured AND categor$).mp
-
(maximum AND variation OR snowball).mp
-
(metasynthes$ OR meta-synthes$ OR metasummar$ OR meta-summar$ OR metastud$ OR meta-stud$).mp
-
“action research”.mp
-
(audiorecord$ OR taperecord$ OR videorecord$ OR videotap$).mp
-
exp PAIN/
-
exp ARTHRITIS, RHEUMATOID/
-
exp FIBROMYALGIA/
-
exp OSTEOARTHRITIS/
-
MUSCULOSKELETAL DISEASES/
-
exp ARTHRITIS/
-
1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18
-
19 OR 20 OR 21 OR 22 OR 23 OR 24
-
25 AND 26
-
cancer.mp
-
27 NOT 28
-
29 [Limit to: English Language and Humans and (Age Groups All Adult 19 plus years)];
Allied and Complementary Medicine Database
-
exp MUSCULOSKELETAL DISEASE
-
exp LOW BACK PAIN/ OR exp BACK PAIN/ OR exp MUSCULOSKELETAL PAIN/
-
exp ARTHRITIS/
-
exp ARTHRITIS RHEUMATOID/
-
exp FIBROMYALGIA/
-
exp PAIN/
-
EXPERIENCE.ti,ab
-
ATTITUDE.ti,ab
-
QUALITATIVE.ti,ab
-
(qualitative OR ethno$ OR emic OR etic OR phenomenolog).mp
-
(hermeneutic$ OR heidegger$ OR husserl$ OR colaizzi$ OR giorgi$ OR glaser OR strauss).mp
-
(van AND kaam$ OR van AND manen OR constant AND compar$)
-
(focus AND group$ OR grounded AND theory OR narrative AND analysis OR lived AND experience$
-
OR life).mp
-
(theoretical AND sampl$ OR purposive AND sampl$ OR ricoeur OR spiegelberg$ OR merleau).mp
-
results.
-
(field AND note$ OR field AND record$ OR fieldnote$ OR field AND stud$).mp
-
(participant$ adj3 observ$).mp; 397 results.
-
(unstructured AND categor$ OR structured AND categor$).mp
-
(maximum AND variation OR snowball).mp
-
(metasynthes$ OR meta-synthes$ OR metasummar$ OR meta-summar$ OR metastud$ OR meta-stud$).mp
-
“action research”.
-
PATIENT ACCEPTANCE OF HEALTH CARE/
-
INTERVIEWS/ OR interview$.af
-
1 OR 2 OR 3 OR 5 OR 6 OR 8
-
9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 34
-
25 AND 26
-
child$.af
-
27 not 30
-
cancer.ti,ab
-
31 NOT 32 [Limit to: (Languages English)]
Cumulative Index to Nursing and Allied Health Literature
-
qualitative OR ethno$ OR emic OR etic OR phenomenology$
-
hermeneutic$ OR heidegger$ OR husserl$ OR colaizzi$ OR giorgi$ OR glaser OR strauss.mp
-
van AND kaam$ OR van AND manen OR constant AND compar$.mp
-
focus AND group$ OR grounded AND theory OR narrative AND analysis OR lived AND experience$
-
OR life AND experience$.mp
-
theoretical AND sampl$ OR purposive AND sampl$ OR ricoeur OR spiegelberg$ OR merleau.mp
-
field AND note$ OR field AND record$ OR fieldnote$ OR field AND stud$.mp
-
participant$ adj3 observ$.mp
-
nonparticipant$ adj3 observ$.mp
-
unstructured AND categor$ OR structured AND categor$.mp
-
maximum AND variation OR snowball.mp
-
exp QUALITATIVE STUDIES/
-
exp PHENOMENOLOGY/ OR exp ETHNOGRAPHY/
-
exp OBSERVATIONAL METHODS/
-
exp LIFE EXPERIENCES/
-
exp ETHNOLOGICAL RESEARCH/
-
exp ETHNONURSING RESEARCH/ OR exp FOCUS GROUPS/
-
exp GROUNDED THEORY/ OR exp PHENOMENOLOGICAL RESEARCH/
-
exp QUALITATIVE VALIDITY/ OR exp PURPOSIVE SAMPLE/ OR exp theoretical sample/
-
exp FIELD STUDIES/ OR exp FIELD NOTES/
-
exp CONTENT ANALYSIS/ OR exp THEMATIC ANALYSIS/
-
metasynthes$ OR meta-synthes$ OR metasummar$ OR meta-summar$ OR metastud$ OR
-
meta-stud$.mp
-
exp OSTEOARTHRITIS/
-
exp ARTHRITIS/
-
exp FIBROMYALGIA/
-
exp DIAGNOSIS, MUSCULOSKELETAL/ OR exp MUSCULOSKELETAL DISEASES/ OR exp MUSCULOSKELETAL SYSTEM/
-
exp ARTHRITIS, RHEUMATOID/
-
cancer.ti,ab
-
1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18
-
OR 19 OR 20 OR 21
-
exp CHRONIC PAIN/ OR exp PAIN CLINICS/ OR exp BACK PAIN/
-
25 OR 26 OR 27 OR 29 OR 31 OR 34
-
34 AND 35
-
36 NOT 32[Limit to: (Language English) and (Age Groups All Adult)
PsycINFO
-
(“semi-structured” OR semistructured OR unstructured OR informal OR “in-depth” OR indepth OR
-
“face-to-face” OR structured OR guide OR guides) adj3 (interview* OR discussion* OR questionnaire*).mp
-
(focus AND group* OR qualitative OR ethnograph* OR fieldwork OR “field work” OR “key
-
informant”).mp
-
exp QUALITATIVE RESEARCH/ OR exp INTERVIEWS/ OR exp GROUP DISCUSSION/ OR
-
qualitative study.mp
-
exp CONTENT ANALYSIS/
-
exp LIFE EXPERIENCES/
-
exp PHENOMENOLOGY/
-
exp ETHNOGRAPHY/.
-
exp BACK PAIN/ OR exp CHRONIC PAIN/ OR exp PAIN/ OR exp PAIN MANAGEMENT/
-
exp MUSCULOSKELETAL DISORDERS/ OR exp MUSCULOSKELETAL SYSTEM/
-
exp ARTHRITIS/ OR exp RHEUMATOID ARTHRITIS/
-
exp ARTHRITIS/ OR exp KNEE/ OR exp PAIN/ OR exp HIPS/ OR exp CHRONIC PAIN/ OR exp
-
PAIN MANAGEMENT/ OR exp RHEUMATOID ARTHRITIS/
-
exp FIBROMYALGIA/
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10
-
11 or 12 or 13 or 14 or 15
-
cancer.mp
-
16 AND17
-
19 AND18
-
20 [Limit to: English Language and (Age Groups 300 Adulthood age 18 yrs and older)]
EMBASE
-
(hermeneutic$ OR heidegger$ OR husserl$ OR colaizzi$ OR giorgi$ OR glaser OR strauss).mp
-
(van AND kaam$ OR van AND manen OR constant AND compar$).mp
-
(focus AND group$ OR grounded AND theory OR narrative AND analysis OR lived AND experience$ OR life).mp
-
(theoretical AND sampl$ OR purposive AND sampl$ OR ricoeur OR spiegelberg$ OR merleau).mp
-
(participant$ adj3 observ$).mp
-
(unstructured AND categor$ OR structured AND categor$).mp
-
(maximum AND variation OR snowball).mp
-
(metasynthes$ OR meta-synthes$ OR metasummar$ OR meta-summar$ OR metastud$ OR meta-stud$).mp
-
(metasynthes$ OR meta-synthes$ OR metasummar$ OR meta-summar$ OR metastud$ OR meta-stud$).mp
-
“action research”.mp
-
(audiorecord$ OR taperecord$ OR videorecord$ OR videotap$).mp
-
(field AND note$ OR field AND record$ OR fieldnote$ OR field AND stud$).mp
-
(qualitative OR ethno$ OR emic OR etic OR phenomenolog).mp
-
exp QUALITATIVE ANALYSIS/ OR exp QUALITATIVE RESEARCH/
-
exp PHENOMENOLOGY/
-
exp GROUNDED THEORY/ OR exp NURSING METHODOLOGY RESEARCH/
-
exp EXPERIENCE/
-
1 or 2 or 3 or 4 or 11 or 5 or 6 or 7 or 8 or 9 or 10 or 13 or 14 or 15 or 16 OR 17
-
exp CHRONIC PAIN/ OR exp HIP PAIN/ OR exp KNEE PAIN/ OR exp LOW BACK PAIN/ OR exp 20. MUSCULOSKELETAL PAIN/ OR exp PAIN CLINIC/
-
exp OSTEOARTHRITIS/
-
exp RHEUMATOID ARTHRITIS/
-
exp FIBROMYALGIA/
-
19 or 20 or 21 OR 22
-
18 AND 23
-
cancer.mp
-
24 NOT 25
-
25 [Limit to: English Language and (Human Age Groups Adult 18 to 64 years or Aged 65+ years)]
Health Management Information Consortium
-
exp QUALITATIVE ANALYSIS/ OR exp QUALITATIVE RESEARCH/ OR exp QUALITATIVE TECHNIQUES/
-
exp NURSING RESEARCH/
-
exp INTERVIEWS/ OR interview$.mp
-
phenomenol$.mp
-
exp BACK PAIN/ OR exp LOW BACK PAIN/ OR exp PAIN/ OR exp PAIN CLINICS/ OR exp PAIN MANAGEMENT/
-
Chronic ADJ pain.mp
-
exp ARTHRITIS/ OR exp RHEUMATOID ARTHRITIS/
-
exp OSTEOARTHRITIS/
-
exp FIBROMYALGIA/
-
exp MUSCULOSKELETAL SYSTEM DISEASES/
-
1 or 2 or 3 or 4
-
5 or 6 or 7 or 8 or 9 or 10
-
11 AND 12
-
cancer.mp
-
13 NOT 14
-
child$.mp
-
15 not 16 [Limit to: (Language Type English)]
Appendix 3 Second-order constructs
Musculoskeletal second-order constructs
Aegler 2009:312 challenge to finish performance
Frequently not able to finish a performance and needed strong intent. However, occupations completed even if body racked by pain as this brought a sense of satisfaction. Sometimes completed task in spite of potential consequences and increased pain (e.g. because of social pressure, reminded of old self, sick of interruptions).
Aegler 2009:312 performing as an ongoing attraction
Describes how keeping occupied is important; organise and adapt occupations to remain active. Participants engaged in joyful occupations when they felt low levels of pain to be able to be attracted by their doing and not go off the things they loved to do. However enjoying an occupation did not have an impact on the pain.
Aegler 2009:312 taking breaks not easy
Interruption became a pattern of behaviour. Difficult to switch off emotionally and cognitively during breaks. Organised performance around breaks. Three strategies to manage interruptions:
a. constant awareness of body in order to know when to take a break. This reduced concentration on the activity itself (I am not really present) and therefore difficult to attain quality of activity
b. fixed day schedule; planned activities and breaks. This could be frustrating if couldn’t comply with it
c. split goals into sub goals so could still enjoy a result.
Afrell 2007:372 acceptance typologies – active process of change
Pro-active decision to make adaptations. ‘a change from an earlier, more or less, total lack of body awareness to a relation where the body is looked upon as a speaking partner and a teacher. In this interplay, the subjects have grown as individuals and have begun to look at their future with optimism, although they know it will require great effort’ (p. 295).
Afrell 2007:372 acceptance typologies – hope and resignation
Self; the profound change of life conditions imposed by constant pain, puts the subject into a state of ambivalence. Oscillate between accepting and refusing the aching body: hope/despair. Ambiguous relationship with body; listen to body/shut it off. Acceptance is a process punctuated with bouts of fighting against pain and giving-up of hope. Balance returns as one realises that acceptance of pain is the only way forward.
Afrell 2007:372 acceptance typologies – rejecting the body
‘Integrating the aching body is totally impossible. The ache is neither possible to comprehend, nor accept, and it is unfair. The body is an enemy . . . there is a tiny little hope of recovery’ (p. 294). Rejection of body makes it disconnected from the self and self-esteem diminished.
Afrell 2007:372 acceptance typologies – surrendering to fate
‘Listening to the signals of the body comes quite naturally in everyday life. There is a sensitive cooperation between self and body’ (p. 293). Come to accept pain and the unpredictability of the body as part of life. Acceptance of aching body. Imagery of the body being broken into pieces by pain but brought together as a whole by sheer acceptance of, and adaptation to, the unpredictability of pain.
Allegretti 2010:313 goal to reduce pain
Patients described primary goal to reduce pain (versus physician which was to improve function). Patients described their frustration at the lack of pain relief and questioned their doctors’ understanding that their pain was ‘real’. Felt that physicians were unable to effectively treat pain and physician blocked prescription of pain medication for fear of addiction [this differs from other studies? USA].
Allegretti 2010:313 importance of diagnosis
Patients continued to seek a biomedical test for their pain (versus physician). Discouraged by negative test results.
Allegretti 2010:313 biomedical versus biopsychosocial
Patients adhered to biomedical explanatory model and emphasised the concrete physical explanations [versus physician who used bio-psychosocial model].
Bair 2009:314 barriers to self-management – fear of hurt
Fear of increased pain – acute fear of aggravated pain if one exercises.
Bair 2009:314 barriers to self-management – GP just describes painkillers
No instruction given in pain self-management strategies from primary care physicians, instead physicians almost exclusively relied on analgesics to treat pain.
Bair 2009:314 barriers to self-management – lack of social support
Lack of understanding and encouragement at home and at work is a barrier to self-management.
Bair 2009:314 barriers to self-management – pain
Though desire for activity may be strong, pain imposes limitations to exercising.
Bair 2009:314 facilitators – relieve depression
Relief of depression – improved mood, ‘mental focus’, motivation, and a more positive outlook that all contributed to patients being able to better manage their pain.
Bair 2009:314 facilitators – social comparison
Comparing oneself with others – others patients perceived as worse off (in greater pain) than themselves bolstered ability to not dwell on one’s own pain so much and put their pain in perspective.
Bair 2009:314 barriers to self-management – strategies do not work
Difficulty in doing the exercises and experiencing exercises as ineffective also a barrier. Why do it if it does not work?
Bair 2009:314 barriers to self-management – stress and depression
Depression and stress contribute to lack of motivation to undertake self-management.
Bair 2009:314 facilitators – support of others
Support of others; empathy, encouragement, understanding and cheer from family, friends, programme care workers and pets buttressed patients against the effects of their pain, while enabling and sustaining participation.
Campbell 2007:315 back to square one
Feel entrapped in a medical system where GP is gatekeeper to other treatments. Reticent to re-engage with a system that previously had little to offer, but things may have moved on now. Feel that a cure (for something so simple) is now possible and should be made available. Tenacity rather than acquiescence evident (versus Illich391).
Campbell 2007:315 future and past
Sense of hopelessness for future. Feelings of uselessness attributed to the dependency that participants felt would naturally ensue as their pain became increasingly intractable.
Campbell 2007:315 getting something done
The reason sufferers pursue treatments or interventions with such a short-lived effect, often at great expense to themselves, is the belief that at least something is being done to alleviate the pain. Something has to be done; having ‘something done’ seen as an ACTIVE endeavour inherent in medical model (even if results short lived). Inability of health-care professionals to find cure is seen as inactivity on their part. There is a responsibility to ‘do something’ to get rid of pain. Metaphors of body as machine used which reinforce dualism of mind and body.
Campbell 2007:315 health professionals (allied)
All sought help from alternative or complementary practitioners and were optimistic about the outcome. Felt that other these knew more about pain than the medical profession and that failure of treatment was due to it not working ‘for them’ rather than limitation of the treatment itself. Practitioner seen as ACTIVE rather than PASSIVE (medics).
Campbell 2007:315 importance of self
Don’t let it beat you; persevere despite pain. Here expectations were focused towards individual ability to persevere despite the pain and what they could do themselves. However pain has negative impact on important relationships which leads them to direct energies further towards pursuit of treatment and cure.
Campbell 2007:315 unmet expectations
Patients expect an explanation, diagnosis, treatment and cure but this is not forthcoming. Leads to frustration and anger at impotence of medical system. Feel that they are not believed because of invisibility of pain; seek to make invisible visible in order to legitimise pain. They have failed a medical test. Anger and frustration at the perceived ineptitude of the medical profession was evident. Leads to engendering personal remedies.
Campbell 2008:316 dependence and social withdrawal
Feelings of dependence dominated this theme with the result that participants chose to withdraw from their social circles rather than to be perceived as a complaining ‘back bore’ or ‘wet weekend’. Image here of growing dependence but a desire not make it noticeable or to complain. Felt accepting help was demeaning and made them feel alienated from former lives.
Campbell 2008:316 normal compared with others
Described how sufferers struggled for normalcy despite their constant pain. ‘There was an almost constant comparison with others being made as they made every effort to not be perceived as malingering’ (p. 386). Patients made ‘an effort to look “normal”; however, paradoxically this often made others think that there was nothing wrong with them’ (p. 386).
Campbell 2008:316 striving for self-management
‘Participants actively sought to empower themselves and to be empowered’ (pp. 387–8). Concerns over side effects and dependency of medication; some preferred to take generic pain medicines to avoid this. Reluctant to discuss with GP who did not condone complementary medications. Some used drugs or alcohol to block out pain. ‘ “Coming to terms” with pain and the related changes in sufferers’ life situations was recognized as a major part of the process of learning to live with chronic pain’ (p. 387). ‘Instead of trying to rid themselves of “it” and embarking on what is often a fruitless search for a cure, they had undertaken to co-exist with “it” ’ (p. 388).
Cook 2000:317 relationship with health-care professional
Overwhelming faith and dependence on health-care professionals.
Coole 2010:318 no employment help from GP – clinicians increase concerns
Advice from health-care practitioners often negative. Warnings linked harm to duties at work and increased concerns about staying in work; ‘be careful’; ‘take is steady’. Did not contact employers or advise on temporary modifications.
Coole 2010:318 no employment help from GP – doubt what GP can offer
Did not expect their GP to give advice regarding work, but only to prescribe medication or issue sickness certificates.
Coole 2010:318 no employment help from GP – GPs write sick notes
GPs wrote sick notes rather than suggesting modifications to work duties. Most of the advice about returning to work did not follow the occupational guidelines and many either did not return to work or had to request additional information on their certificates to permit them adjusted work duties. Some patients felt they simply had to comply with what the GP said. Others signed off work while awaiting tests and results.
Coole 2010:318 no employment help from GP – lack of dialogue between GPs, health-care professionals and employers
Any joined up dialogue and action missing. This need is therefore undertaken by the patient who then worries whether his explanations will be accepted as valid by the employer.
Coole 2010:318 no employment help from GP – no effective advice from GPs
GPs advised them to stay at work but did not understand the difficulties of this or make any helpful suggestions. Information about return to work from GPs inadequate.
Coole 2010:319 concern about sickness record
Concerns that sick leave perceived negatively and had an impact on employment record and job security. Use holiday leave rather than sick leave. Paradox – only seen as legitimate if they have a sick note, not self-certified – so damned if I do and damned if I don’t! i.e. need sick record to be legitimate but don’t want a sick record.
Coole 2010:319 concerns about future at work
Perceived condition as progressive and had concerns about maintaining work or life quality after work. May be unable to enjoy leisure retirement. Also considered effect of ageing on on-going pain.
Coole 2010:319 difficulty coping with flare-ups
Uncertainty at the unpredictable nature of their pain which made them unable to work at times. Effect on consistency of ability to work. Loss of confidence. Concerned that employer would not tolerate this unpredictability.
Coole 2010:319 justifying back pain
Cautious about disclosing pain for fear of appearing as either a fraud or as unreliable due to disability. Wanted to legitimise illness by diagnosis or specific cause. Needed to attribute some cause. Some used their own explanations based on physical origin e.g. wear and tear, heavy lifting.
Coole 2010:319 reluctance to use meds
Although saw medication as main role of GP: sceptical of effectiveness of medication; worried about side effects.
Coole 2010:320 occupational health – advice overcautious
Graded return to duties usually replaced by advice to avoid task altogether (against occupational guidelines). Some remained on light duties long after sick leave.
Coole 2010:320 occupational health – dependent on causation
Employers take up of occupational health advice varied. Employers more likely to listen to advice from occupational health if injury occurs at work. Also influenced by other factors e.g. litigation.
Coole 2010:320 patient control
Easier to modify work and stay at work if had the freedom to make their own modifications to working practise. Small changes could make a lot of difference. Could rely on colleagues but there were limits to this. Flexibility of working for self, enabled them to stay in work. However, if worked alone had no one to share work with and would be committed to finish.
Coole 2010:320 employers – help depends on managers
Some received help from managers and colleagues to adjust their work so they could maintain reciprocal working. Short term flexibility allowed them to feel valued at work. If work was reduced indefinitely then they felt a burden that they were not part of team and that colleagues would not support them indefinitely. Exacerbated by lack of belief and cuts to workforce.
Coole 2010:320 employers – managers with back pain
Perceived managers who had had back pain were more supportive.
Coole 2010:320 occupational health – modifications left to manager
Both manager and physician expected patient to be conduit between occupational health, employer and GP. Lack of a clear and effective communication strategy. No opportunity for consultation or discussion.
Coole 2010:320 occupational health – service for employees
Referral to occupational health left to the manager or employer, with non-systematic procedure in place. Often perceived as employer-led (way of managing absence rather than helping them remain at work). Agreement to attend seen as compulsory and there were concerns over confidentiality or future employability. Decision-making/assessments seemed to be based on discussions rather than an actual visit to the place of work.
Coole 2010:320 employers – overcautious support
Some managers could be overcautious as worried about their responsibility for back pain.
Cooper 2008:322 communication
Communication was important to the individual and an important facet of patient care; ‘good communication involved: taking time over explanations; using appropriate terminology; listening, understanding and getting to know the patient; and encouraging the patient’s participation in the communication process’ (p. 247).
Cooper 2008:322 decision-making
Happy for physiotherapist to make treatment decisions as long as they explained options and aims (good communication), it was based on their expertise and it was tailored to individual needs.
Cooper 2008:322 individual care
Valued being able to ask questions and have their opinions taken on board in deciding course of treatment. Felt physiotherapist should take their lifestyles into account. Wanted care to suit individual needs. Felt a thorough assessment important to facilitating effective individual care. Good communication central to individualised care.
Cooper 2008:322 information sharing
Wanted physiotherapist to explain what was wrong with their back (diagnosis); this need not always met. Peer information sharing generally found to be extremely helpful.
Cooper 2008:322 organisation
This was around access and timelines for treatment. Wanted shorter waits, easy access during flare-up and longer and more frequent sessions.
Cooper 2008:322 the physiotherapist
Patient-centred care a complex combination of factors. Caring important but not integral to patient centred care. Competence (as experts) and personality (pleasant and not abrupt, caring) most valued. Did not blame physiotherapist if rehabilitation did not work.
Cooper 2009:321 typology – non-self-managing looking for cure
Hoping that new treatment would come out that could cure and often seeking alternative treatments. Generally felt that physiotherapy did not meet their goals.
Cooper 2009:321 typology – self-managing but want future access
Self-managing pain but wanted access in future, in particular for flare-ups; saw physiotherapist as expert and felt they needed a continued relationship with them in order to motivate, check or provide reassurance. Some felt telephone checks were adequate; others wanted predetermined checks and others happy with ad hoc arrangement.
Cooper 2009:321 typology – self-managing and do not want future access
A small group felt no need for future contact with physiotherapist as confident in knowledge of appropriate exercises. Many in this group felt physiotherapy not meeting their needs but appreciate being able to make some form of long term contact (e.g. by telephone).
Crowe 2010:374 direct heat (heading doesn’t match concept)
The approach to living with chronic low back pain of ‘putting up with it’ and ‘getting on with it’ pervaded the interviews. Used self-learned strategies (e.g. pacing, diversion). Direct heat was effective in the form of showers, baths, electric blankets or wheat packs.
Crowe 2010:374 taking medication
Preferred over-the-counter medication as opposed to prescribed. Reluctant to use, and when done usually because it was the only way to be able to get on with what they wanted/needed to do.
Crowe 2010:323 alteration to self
Pain had altered the self-image. I am not what I used to be (capable and productive). Tension between what I want to be and how I see myself now. Giving up careers had a particular impact.
Crowe 2010:323 externalisation of the body
Process of ‘objectifying’ body often referred to as ‘listening’ and ‘talking’ to the body. Talked about body as if it was external to the self. Dualism between body and mind. Body external to self.
Crowe 2010:323 need for vigilance
Because it is unpredictable you need to be constantly vigilant about what you were doing and how you move. People became cautious to attempt things they had always taken for granted. Related to body differently; loss of spontaneity even for previously routine activities.
Crowe 2010:323 unpredictability
Pain unpredictable and not related to any trigger. This evoked a sense of one being unable to control the body. A sense of tension it seems, as one waits for pain to ‘appear’ at any time; expecting it without warning.
De Souza 2011:376 children and parents
Physical and emotional burden placed on wider family including grandchildren. Influence of chronic pain spreads up and down the generations. Influence on children age related.
De Souza 2011:376 spouses and partners
Help and support from spouse/partner valued but also caused feelings distress and helplessness. Strain on marital relationships due to both stress and reluctance to have a sexual relationship due to pain. Additional stress of chronic pain can be tipping point for weak relationship, but in other relationships there was closeness and support to deal with the pain together.
De Souza 2011:376 work-related problems
Impacts on ability to work and how a person is viewed in workplace.
Dickson 2003:325 reconstructing meaning of pain – managing and tolerating
Continued to seek out traditional means to manage their symptoms, alongside search for cure. Shift from pain being symptom of disease to being part of ageing [positive view of aging in Korean culture]. Women gained control over their pain and began to interpret their experience as part of growing older.
Dickson 2003:325 reconstructing meaning of pain – striving to reduce pain
Striving to reduce pain using eastern alternative methods, and restore self-esteem by focusing away from one’s pain. They stopped complaining of pain to others and pain became theirs alone.
Dickson 2003:325 reconstructing meaning of pain – struggling to remove pain
Disappointment in western medicine – search (complicated by the language barriers) for cure not met by western or Korean American health-care professionals. Socially shared experiences with similar others lessens sense of isolation in suffering.
Dickson 2003:325 reconstructing meaning of pain – stumbling along with pain
Stumbled along failing to relieve their pain when treated as a disease symptom and realised that western medicine had little to offer. Instead they exchanged experiences with others in pain and realised the benefits of social support and self-care and seeing pain is a sign of ageing.
Dickson 2003:325 reconstructing meaning of pain – suffering with pain
At first women ignored pain but when pain limited activity they sought cause and treatment from western medicine. At this point the pain became a symptom of a disease that could be treated.
Dragesund 2008:326 associations about the body
Body a limitation AND a possibility for some; unpredictable body limits opportunities – body has an existence of its own. Become MORE PRESENT IN THE BODY. New opportunities for participation connected to an increased ability to prevent pain from dominating. Not about controlling body but listening to it. No longer at mercy of the body.
Dragesund 2008:326 aware of body
Greater sensitivity to body and symptoms; different to previous pain free experience of detachment from one’s body. Physical exercise and knowledge of bodily symptoms gave a sense of control over pain and tiredness. Need to respect limits on body (and life) imposed by pain.
Harding 2005:330 living with and planning for the future
With time there came a sense of resignation to the pain and accepting it as a part of life for the foreseeable future. Acceptance of pain and whether it would ever eventually end dominated this theme. Some reported the notion of an increased pain threshold to accommodate the pain. This acceptance marked a significant point of the patients’ pain career and was characterised by a sense of active adaptation.
Harding 2005:330 unmet expectations
A person needs their doctors to bear witness to their pain experience. This has a profound effect on their functioning as individuals. Expectations of medical system are not met. Loss of faith in medical system due to GPs’ inability to diagnose and treat; their lack of time to listen and understand patient condition; disbelief of patient descriptions and lack of concern; not being taken seriously. Could receive a range of different sometimes contradictory opinions from medical professionals as to the cause pain and way to treat it. Search for an alternative remedy is taken up.
Harding 2005:330 making sense of pain
Tried to make sense of the cause of pain by locating it in the context of their lives (e.g. cancer, bereavement, diabetes etc.). Used diverse explanations to explain their pain. Doctors were perceived as not helping them make sense of their pain but only providing a medical interpretation for it. For most, there was a consistent tendency to not wholly subscribe to the medical interpretation.
Harding 2005:330 spoiled identity
The reductions required by chronic pain have an impact on sense of identity and cause people to perceive themselves as different from others. There is a tension between outward appearance remaining ‘normal’ and internal changed identities. Some felt that they had ‘given in’ to pain; other grudgingly accommodated the changes and lowered expectations.
Holloway 2007:379 stigma at work
All described struggle to stay at work and stories of unsympathetic encounters with colleagues who could be hostile. This created an environment of mistrust. Media reports of back pain being ‘real’ reason to be off sick do not help.
Holloway 2007:379 stigma by significant others
Lack of diagnosis and invisibility of pain raised suspicion that pain is not real. Spouses faced isolation, role tension, marital conflict reduced sexual activity. Could lead to divorce. Patients tried to meet the expectations of others, and this could not only aggravate pain but make others feel that they were putting it on.
Holloway 2007:379 stigma in everyday life
Patients felt stigmatised socially for having an invisible illness; people don’t believe that there is anything wrong at all. Provoked by media reports of benefit fraud.
Holloway 2007:379 stigmatisation in health-care systems
Often disbelieved by health professionals and told pain was ‘all in the head’. This has an impact on benefits and compensation as patients perceived as malingerers.
Hunhammar 2009:331 striving to master variable pain – disruptions to daily life
The multidimensional nature of pain and how this impacted on a range of activities associated with living (physical and psychological).
Hunhammar 2009:331 striving to master variable pain – space for health
The experience of chronic non-specific pain added an additional burden to life which required a space to meet these demands such as physiotherapists’ appointments or time to keep fit. Gender differences emerged with childcare a main consideration for women.
Hunhammar 2009:331 striving to master variable pain – strategies for pain control
Balance and concealment of pain were two important approaches to handling pain. Balancing incorporated physical adaptations as well as utilisation or primary care resources. Pain was often concealed from others to avoid feeling negative about experiencing the pain.
Hunhammar 2009:331 striving to master variable pain
This core category describes the variability and unpredictable nature of pain. Thoughts of the future were hopeful but did not include an expectation that there would be a full recovery. Concerns about work emphasised the need to keep on working and not take sick leave. This category included an attitudinal approach to pain which encompassed a ‘getting on with life in spite of the pain’.
Johansson 1996:332 strategies to get doctor’s attention – claiming under cover
Diverse strategies of obtaining information about the illness from the doctor through ‘naive’ questioning.
Johansson 1996:332 strategies to gain self-respect – condemning
Sceptical of usefulness of encounters with the doctor, their willingness to help and their knowledge of the illness.
Johansson 1996:332 experience of distrust
All patients felt distrusted in the consultation by the doctors, and wanted a diagnosis for reasons of credibility. They described a vulnerable position. As patients they were subject to the doctor’s ability to define the illness and decisions over treatment. Concern doctor might turn hostile; felt ignored, disregarded and rejected.
Johansson 1996:332 expectations of a ‘creditable’ consultation
Unfulfilled expectations of the ‘diagnosis’ (i.e. a ‘creditable consultation’) emerged: to be taken seriously, to get time for an informative dialogue, and to achieve an ongoing relationship to the doctor.
Johansson 1996:332 strategies to get self-respect – martyrising
Although they described constant pain, and ‘pilgrimages’ for help to different doctors, they also, conveyed the image of ‘silent sufferer’, never complaining, ‘working beyond’ their power.
Johansson 1996:332 strategies to gain self-respect – mystifying
One way to accept the absence of a creditable diagnosis was to adopt a self-image of being an incomprehensible case. Therefore the doctor was not to be blamed.
Johansson 1996:332 strategies to get doctor’s attention
Dramatic weeping or begging in order to elicit information from the doctor.
Johansson 1996:332 strategies to get doctor’s attention – somatising
All about trying to be seen as a credible (and illness not imaginary) patient by doctor through very physical bodily descriptions to the doctor.
Johansson 1996:332 I am under the doctor now
Image of the doctor as a sort of manager who can be useful in helping patient on the road to recovery, but can limit the patient’s initiative in their recovery process.
Johansson 1997:333 family considerations
Managing job and family responsibilities (such as child care) a balancing act premised on complex choices (fewer hours, working unsociable hours, etc.) in order to make more time for home and the family.
Johansson 1997:333 to get along moneywise
Saw having a job as vital to getting on with life, but stuck with low income jobs, and difficult to get back into education to improve job prospects.
Johansson 1997:333 getting out to be stimulated
A job holds potential for stimulating activity if flexible and not onerous. Described social tensions at their workplace, involving workplace reorganization, threat of redundancy, and some even bullying.
Johansson 1997:333 sick role process
Work capacity constrained by illness. Tensions surrounding inability to work, having to be at home and the desire for financial benefit compounded by a revaluing of more ‘traditional’ family roles (and the woman’s place in the home) – ‘how could I even think of getting a job’. For older participants a feeling of shame at being sick listed along with a sense of entitlement.
Johansson 1997:333 to be somebody
A job could play a part (as one of other factors) in improving one’s self-esteem as individuals felt needed, but many frustrated with lack of recognition. ‘If you don’t have a job you are nobody’.
Johansson 1999:334 consequences for activity
Pain impacted capacity to undertake everyday tasks. Some patients even felt these limitations made them incompetent workers or made them appear to be whiners to family members. The pain limited pleasure in undertaking hobbies.
Johansson 1999:334 bodily presentations
Pain a threat of something going wrong in the body. Pain unpredictable and uncontrollable. Started in a distinct location and then dispersed. Pain a constant invisible alien enemy. Patient feels detached from the painful body part and unable to connect with it as a familiar part of their own body; an uncontrollable intruder; and can be triggered with one small body part being affected, then pain spreading throughout body.
Johansson 1999:334 explanations
Focus here on the patient’s search for the cause of their condition with reasons ranging from physical injuries to emotional tension and even spiritual retribution and genetic predisposition.
Johansson 1999:334 self-perception
Invisibility of symptoms damaging to ones reputation as it evoked disbelief on the part of others. Being at home could increase expectations about household duties. At the same time, if she managed this, then neighbours were suspicious – why can’t she work! Can affect a woman’s very sense of being a capable woman (wife, mother, sexual partner). Uncertain about how to deal with limitations imposed by illness on work capacity, especially as many patients felt that going out to work improved their image socially despite their perpetual struggle with the physical pain.
Liddle 2007:336 expectations from treatment
As individuals took more responsibility for their recovery the need for individual exercise and advice was increasingly important. Supervision was considered important to make individual corrections. There was a need for follow-up and support as this was reassurance that the exercises were being performed correctly.
Liddle 2007:336 treatment received
Disappointment at unmet expectations of treatment. Frustration at inability of medical system to relieve pain, and diversity of attempts to resolve the problem. GPs over-emphasised use of medication. Participants were concerned that this was treating the symptom without addressing the source of their condition.
Lundberg 2007:338 failed adaptation
Did not accept the radical change to lives caused by pain. Frustration, low mood, sleep deprivation, abuse of meds. Avoided movement which aggravated and adopted ‘passive’ strategies; lying down etc.
A strong, well-functioning body was an important source of identity, so this limitation in their ability to use their bodies led to identity loss. The lost identity was expressed as low self-esteem, bitterness, and shame. Exacerbated by negative encounters with health-care professionals and socially. Mourned previous life without pain.
Lundberg 2007:338 finding the way out
Found time to accept body in pain. Positive encounters with others helped this. They had previously taken their bodies for granted and paid no attention to it. The experience of pain forced them to think about their body and in so doing, their existence and identity came into focus. Thoughts about body and mind were more clearly expressed in this than in the other typologies. I have learnt to separate my body from my self; learned new things about themselves. They developed their empathetic abilities and gained patience both with themselves and others. The informants experienced the vibrancy of and the good in life despite difficulties and persistent pain.
Lundberg 2007:338 identity restoration
At first experienced low self-esteem, shame, loss of self, social isolation. Time of chaos and abandonment. Went through a process of reconsidering their existence and identity. A new identity was created based on the reality they had to face. With guidance from physical therapists, the informants achieved increased awareness of their bodies, which helped them to transform their way of being in the world of pain. This gave an increased confidence in the future (with some doubt). Reorientation was described in terms of how their previous life had been re-evaluated and having reconsidered their definition of quality of life.
Osborn 1999:342 comparing this self with other selves
Compare self with others and past/future self.
a. I am not like the old me who was fit and able to work hard. Some defined themselves as bereaved. Grieved for the old self. I am not my happy previous self – look back nostalgically. Painful reminder of loss. Past self considered to represent the real self replaced by new false persona. Pain denies me my right to be me.
b. Fear what future will bring. Feelings of uncertainty.
c. Constantly comparing to others and put emphasis on disability. Took refuge in thinking of those who were worse off, but this could make them think of a possibly worse future (also this does not compensate for my loss).
Osborn 1999:342 not being believed
No visible sign of suffering. Uncertainty about pain made them vulnerable to judgements of those around them. Continual need to justify self. It is real; I am not mad or bad. Faced threat of rejection even by nearest and dearest. Pain has caused a shift in familial reciprocal roles. I am a burden but also people don’t believe me. Lack of credible evidence made them feel guilty of the burden they were placing on their families. Uncomfortable about not being able to reciprocate but becoming the one that is cared for. Appearing too healthy or mobile threatened credibility. Forced to appear ill but this meant bearing burden of not being seen as self by others (‘I’m not a cripple’). Denied opportunity to relate to others in a world free of the influence of pain.
Osborn 1999:342 searching for an explanation
Strong motivation to know why they had pain. Couldn’t believe nothing could be done. Pain felt to have its own volition. Sense of bewilderment of why I am suffering. There must be something wrong. Reality can’t be explained in a meaningful way. Uncertainty and ambiguity pervades.
Osborn 1999:342 withdrawing from others
Rather than meet demands of managing appearance of pain, withdrew from public view. Easier to conceal their condition than rely on the understanding of others. Avoided social events at risk of appearing unsociable. Avoided potential for embarrassment and rejection. Tension with not wanting to become isolated. Relationships at risk. Hide distress to avoid rejection. Dilemma: can’t appear healthy but don’t want to go on about pain and risk rejection. Social world now threatening. Retreated to private world. ‘Social world could not accommodate people who had chronic pain’.
Osborn 2006:343 living with body separate from self
Pain has made me aware of my body now. Separation of painful body from self. Self and body opposing entities. Painful part NOT ME. Unpleasant and relentless presence of a body that is ‘not me’. Living with pain affects who I am [self]. New body alien. I feel powerless against this alien body. Dysfunctional part of body NOT ME. There was a distinction made between the original self and that self which had emerged due to pain.
Osborn 2008:344 fearfulness of pain
Powerful affective element. Describes how pain is sucking the life out of me. Violent imagery of pain. Pain a hostile presence; an aggressor. I am powerless. Pain is a malevolent force intent on damaging me. Pain is malevolent like the ‘devil’ as it harasses and disables. Pain is a parasite. Pain is vindictive. [Anthropomorphising pain – it has a will]. Humiliating and punishing assault from another [person] Pain threatens my body and me. Pain undermines and isolates me socially. Pain is punishing. Pain makes me a monster. Pain makes me not me and intrudes on others. Imagery of isolation. The malice and cruelty they ascribed to their pain interfered with their relationships by making them both intolerant and hostile.
Osborn 2008:344 containing fear through social connection (post-hypnotic intervention)
Pain remained unchanged as an object of thought but they felt better able to manage the fear it evoked. Their pain possessed the same meanings and was no different in its threatening potential and unpleasantness: each participant felt more able to manage his or her pain, they reported an increase in the degree of self-confidence they felt in the face of their on-going pain and a reduction in the level of fear and worry. Therapeutic alliance eased sense of isolation, vulnerability, and fear. Someone else is part of the experience.
Patel 2007:345 personal obstacles – age
Older patients felt double disadvantage of age and disability. Older persons resistant to retraining (as close to retirement) and feared rejection from employers because of their disability.
Patel 2007:345 uncertainty – benefits
Patients not only perceive leaving benefits as risky but also returning back to benefits as time consuming and bureaucratic. Feared leaving benefits but saw employment as making them better off. Return to benefits within a year of coping unsuccessfully with work (government initiative) perceived as daunting and as not offering financial stability.
Patel 2007:345 benefits organisation – (limited)
Limited support on advice from benefits officer about return to work. Felt jobs offered were inappropriate to their condition.
Patel 2007:345 perceptions at work – employers’ limited understanding
Employer support and understanding limited due to a lack of awareness, negative perceptions (that the ill person will frequently be off work) and, perhaps, lack of personal experience. Patients feel that use of walking aids may make their case appear more plausible to employers; However, employers may also see such persons as more ‘risky’ to employ.
Patel 2007:345 perceptions at work – fear of letting employer down
Letting people down was expressed in terms of a threat to the patient’s own self-image as a worker: Some left work voluntarily for fear of letting employers down or not being seen as a good worker.
Patel 2007:345 health-care barriers
Trapped in a cycle of repeated consultations that stopped return to work. Long waits and not being taken seriously by health-care professionals exacerbated this. Some had been classified unsuitable to work by benefits medical officers. This assessment for work eligibility became a deterrent to taking on rehab to return to work.
Patel 2007:345 perceptions at work – job availability
‘Patients held the perception that healthy individuals would be more appealing from an employer’s perspective therefore; there is little point in attempting to return to work’ (p. 837). Reported negative attitude and discrimination from employers exacerbated in competitive work market.
Patel 2007:345 uncertainty – pain and health
The unpredictability of the severity of pain and limitation, and the duration of a flare-up made it very difficult for patients to foresee how they would cope with returning to and remaining in work: inability to cope with fluctuating nature of pain makes return to work less possible (as flexible working patterns not very common). Disadvantage in competitive working market.
Patel 2007:345 benefits organisation – permitted work
Government initiatives to ease patients back into work are perceived by patients as limiting their capacity to earn, while placing them in the additional dilemma of having to choose to remain in work or cease working once permitted work period ends.
Patel 2007:345 psychological barriers
Sense of being unable to control/manage pain leads to feelings of low mood, depression, fear, loss of confidence and frustration, heightened by limited positive treatment outcomes and disappointing results of high expectations from health care. The search for other medical treatments results in a cycle of consultation that can be frustrating.
Patel 2007:345 personal obstacles – qualifications and experience
High-level skills could be a barrier for return to work as applicants did not want to be trapped in a job that was not commensurate with their level of training. Those with low level skills thought lack of training was also a barrier to return to work.
Patel 2007:345 perceptions at work – resistance to change
Anxious about prospect of having to change job or field.
Patel 2007:345 benefits organisation – staff skills
Benefits officers lacked skills to help return to work for patients with chronic pain. Focus on unemployment rather than returning to work with chronic pain. Most dreaded attending for an assessment.
Patel 2007:345 uncertainty – future
Pessimistic about future and avoided thinking about it. Unable to plan a return to work because of unpredictable nature of pain. Lived day by day rather than making plans they could not realise.
Patel 2007:345 uncertainty – working capacity
Did not feel that they had received advice on what type of work they could return to and that benefits officers lacked skills to do this. Some reported being advised not to return to work by their GPs.
Rhodes 1999:350 aligned or alienated
Aligned – tests fit the anatomical model. For some patients diagnostic tests produce ‘results’ (‘black and white’ X-rays, tests) for which the visual image corresponds exactly with their experience of pain. Tests seem so positively transparent and simplistic; they give proof. Deviation should show up and be susceptible to repair.
Alienated – don’t fit anatomical model; feel guilty and disillusioned. Some experienced a discrepancy between their own ‘inner’ experience of pain and the diagnosis and needed to legitimise what they felt. This can lead to feelings of guilt, disillusionment with medicine, doubts about the tests and frustration. (I am certain but I have no proof).
Rhodes 1999:350 anatomical body
Anatomical understanding corresponds to visual images of the inside of the body. We perceive that variations can be measured based on what is typical and what is deviant. While in pain awareness of the body increases, becoming an ‘alien presence’ or ‘foreign thing’. Pain patients may see ‘images’ of their pain specific to their own cultural model.
Sanders 2002:353 cultural connotations of ageing
Change in expectations came with older adulthood BUT at the same time the desire to distance themselves from the negative stereotypes of old age; e.g. embarrassed about walking sticks. Want to present an image of ‘ageing well’ i.e. not conforming to stereotypes. Striving to appear ‘normal and without arthritis’. Ambiguity – old age made disability become invisible ‘you cannot be considered old and disabled’; i.e. they were not viewed as being legitimately disabled because they were old. ‘operating simultaneously in creating an experience of symptoms which is both biographically normal and abnormal’.
Sanders 2002:353 disrupted biographies
Although ‘normal’, pain also disruptive; effect on relationships, isolation, depression, and fear of dependence in future. Varying degrees of social or relational disruption due to illness. However this ‘talk’ of disruptive biography balanced with playing down the significance of osteoarthritis and ‘putting on a brave face’. There was a degree of stoicism in their accounts. Family relationships paradoxical: a source of both support and conflict. Participants experienced fear of possible future dependency affecting relationship with extended family, but seemed more positive about relations with a disabled spouse with whom there was mutual support.
Sanders 2002:353 normal aspect of biography
Pain is a normal inevitable part of ageing; normal and integral to biography; an ‘expression of their history’; Onset often tied up with biography e.g. varying hardship; bound up with self. Reluctant to seek treatment, ‘there is nothing they can do’. Those with rapid onset and deterioration and younger adults did see this as disruptive to self and ‘not normal’ (e.g. hereditary, trauma).
Satink 2004:354 aiming to collaborate with pain
Found ways to build relationship with their pain and to accept it [up to a point].
Pain become part of me; learnt to listen and accept it as part of me. Became focused on the present moment. became more aware of need to participate and care for others.
Satink 2004:354 aiming to be normal
Image of struggle to not accept pain of its limitations, but be as active as previously/normally was. Recognise pain has ‘won’ and overpowered them. A losing battle and growing realisation of need to change behaviour due to pain.
Satink 2004:354 aiming to control and reduce
Hope that less social/occupations participation would mean less pain. This way of controlling pain results in emotional pain due to the effects of this withdrawal; imprisoned in a very small world of limited daily activity. Further, despite this sacrificial adaptation the physical pain remained.
Skuladottir 2011:355 quest for normalcy – avoid sick role and maintain dignity
Took trouble to maintain appearance which meant that some did not realise or understand how they felt. Some tried to hide pain or conceal that there was anything wrong. Wanted to appear normal and maintain a sense of dignity. Felt this was respectable and made them more like ‘normal’ people’. If you look too good it doesn’t look like you are suffering.
Skuladottir 2011:355 quest for normalcy – need to participate
Need to participate in family activities even if it makes me worse for a while. Being an observer increases isolation. Having a job, being involved, being active and participating important. ‘Give up and be depressed or to try to live a good life with this’.
Skuladottir 2011:355 quest for normalcy
Retain optimism hope positive thinking goals at same time be realistic. Although pain has changed me I am still a strong person. Gaining a sense of achievement from the things I CAN do. More of a focus here on positive thinking and seeking meaningful activities to occupy time and focus in order to maintain good mood and optimism.
Skuladottir 2011:355 quest for normalcy – involved in decision-making
Women felt they were the experts in their own pain and valued participation in decision-making surrounding pain. Realised the limitations of health-care professionals and that I am the expert of my pain. I am in charge.
Skuladottir 2011:355 quest to learn to live with pain – need diagnosis
Diagnosis – the women ambivalent about getting a diagnosis: not having one increased probability of stigma and label of its all being in ‘the mind’. Receiving a diagnosis made some patients feel they may be ill for life.
Skuladottir 2011:355 quest to learn to live with pain – need for effective treatment
Effective treatment – pain alleviation/coping strategies ranged from exercise and reflexology, to diet, distraction and medication. Some made unilateral decision to stop taking medication.
Skuladottir 2011:355 quest to learn to live with pain – need for help, advice and information
Most had experienced a lack of information and felt they were left to fend for themselves and find out information about their illness. Sought advice from health-care professionals but communication itself important. ‘An approachable health professional not only gave information and advice but allowed expression on their part as well’ (p. 85).
Skuladottir 2011:355 quest to learn to live with pain – need to take care of self and find a new pace
Slow process; need to learn to protect self from unfair demands. Found a new pace and pattern of life through organising and preparing self.
Skuladottir 2011:355 quest for support, caring and connection – need for health-care professional
Professional support from health-care professionals valued for the encouragement provided during early stages of pain. Health-care professional care through listening and concern also valued, with patients not receiving this frequently experiencing dejection and misery.
Skuladottir 2011:355 quest for support, caring and connection – need for practical support
Torn between wanted to keep role and do household tasks themselves but needing help. Some obliged to do it because nobody else did it.
Skuladottir 2011:355 quest for support, caring and connection – need someone who cares
All felt a need to share their experience with someone (family) close who cared about them, and not to feel as though they were bearing the burden alone.
Skuladottir 2011:355 quest for support, caring and connection – need to be connected and care for someone
Caring for children increase pain but was satisfying and fulfilling. They were needed and had a role. Someone relies on me and this drives me on.
Slade 2009:356 engagement with health care – ask me
All participants reported that engagement with their health-care provider improved if they were explicitly asked for their opinions and goals.
Slade 2009:356 engagement with health care – assertiveness
They acquired an ability to assert their needs through a process of trial and error.
Slade 2009:356 engagement with health care – continuity and connectedness
Poor continuity of care and abandonment by care providers was perceived by all participants. Follow-up contact valued.
Slade 2009:356 listen to me – explain it so I can understand (title doesn’t match concept)
Need a ‘competent and empathetic listener’. Health-care professional needs to listen and be empathetic; I am not taken seriously; I have to keep telling my story; listen to what I am saying.
Slade 2009:356 listen to me – I know my body
Learned about responses of body and limitations imposed on it by pain over time. This knowledge empowers.
Slade 2009:356 engagement with health care – partnership
‘All participants expressed the need for mutual enquiry, problem-solving, negotiation and renegotiation between care-provider and care-seeker to establish mutual therapeutic goals’ (p. 273). Patients wanting to feel that their opinions are sought and considered through every part of their care pathway.
Slade 2009:356 engagement with health care – understand me
Desire for care providers to view them holistically and consider their life circumstances, personal preferences and their perceptions in order to develop individualised exercise programmes.
Slade 2009:357 stigma – community, friends and family
Judgement extended to family, friends and community. People see back pain as an excuse for non-participation and poor performance. The invisibility of pain is a barrier to legitimacy.
Slade 2009:357 stigma – pathology-driven validation
Medical validation valued as it bestows credibility. Absence of validation is a significant barrier to participation; it is physiologically, psychologically and socially disabling. Patients felt validity of illness in question as imaging tests revealed no cause/evidence of pain. Expressed relief when an X-ray or MRI demonstrated pathology. Compounded by misdiagnosis or change in imaging findings. Feel need to legitimise self as not ‘mad’ or ‘bad’.
Slade 2009:357 stigma – sickness versus wellness model
Participants’ feelings ranged from anger to frustration in their search for understanding, legitimacy, validation, and knowledge, and this highlights the dominance and essential weakness of the biomedical model to their situation. The medical model makes it difficult to engage in treatment and regain control of their lives. Current societal attitudes reinforce these obstacles. Preferred incorporation of ‘normalcy’ rather than ‘sickness’ in rehabilitation.
Slade 2009:357 stigma – relative positioning
Comparing themselves with other patients helped some patients gauge severity of their own condition. Some were judgemental of others with back pain.
Slade 2009:357 stigma – health-care professionals
A long patient journey reported, in their search for knowledge of illness, and appropriate and empathetic care. Majority unsatisfied with encounters with health-care professionals. They felt blamed, guilty, perceived as having an ulterior motive (such as seeking gain through their illness), or that were imagining it. Perception that practitioners did not position them as capable of understanding pathology or management approaches. They wanted to feel valued, believed and connected with practitioner. Felt practitioners emphasised medication and did not give advice; they lacked empathy and understanding and did not seem to take them seriously.
Slade 2009:357 tell me
Strong motivation to understand their pain. Patients wanted lots of information in a clear jargon-free way that they can understand.
Slade 2009:357 stigma – workplace
Many felt responsible for back injuries despite poor workplace policies. This guilt compounded by judgements by colleagues. Culture of judgement exacerbated by compensable bodies. Reputation for being ‘workshy’ despite attempts to stay in work.
Smith 2007:66 continuum or trajectory
Paradox:
a. Use strategies to try and prevent erosion of ‘good’ self.
b. At the same time a resignation that pain has irreparably altered self.
This represents as a process along a continuum. Cannot tell if this necessarily a process from one to the other or could go in either direction. Over time ability to wrestle self back from the pain. Initially fight to be same as always, realise it is not possible and therefore adapt into new person with chronic pain as part of who they are.
Smith 2007:66 directing it at others
Negativity contaminates relationships. Patients felt that their internal negative emotions brought on by chronic pain are directed outwardly to others in the form of malevolence and spite in taking pleasure in the suffering of others. Narrative – My pain is so bad that I am a terrible person now; it is so bad it has changed who I am. An expression of lasting change; this is how bad the pain is.
Smith 2007:66 negative impact on self
Pain significantly impacts on one’s identity and perception of self, resulting in denigrative mental inner conflict between the ‘two selves’: the ‘mean me’ and the ‘nice me’. There is a battle to ‘retain a good self’ and this struggle can be more distressing than even the pain itself.
Smith 2007:66 public arena makes it worse
Social isolation appealing as less pressure to hide ‘miserable self’. Patients felt reduced to ‘a bit of a person’ as unable to fulfil (familial) roles to their ideal standards; felt vulnerable to ridicule or punishment from others; and felt perceived as a ‘burden’ and without ‘value’ by society. Sense of SHAME.
Smith 2007:66 the sting in the tail
Concealed pain for fear of social judgement and consequences. Feared retribution for ‘mean’ behaviour premised on a ‘moral’ sense that ‘what goes around comes around’. Sense of justice – I will be punished for becoming so bad. Linked to a sense of SHAME and retribution.
Snelgrove 2009:358 maintaining integrity – cause of pain
Explanation for pain physical not psychological; often described as caused when doing something virtuous. Patients’ explanations couched in a previously virtuous life (moral narrative) and they are therefore blameless.
Snelgrove 2009:358 crucial nature of pain – emotional response
Low mood and anger impact negatively on relationships with others including health-care professionals and inwardly to self.
Snelgrove 2009:358 crucial nature of pain – loss of social role
Discrepancy between present and past self. Loss of independence and family role compared to the past.
Snelgrove 2009:358 crucial nature of pain – loss of spontaneity
Loss of ability to do even most mundane and taken for granted activities of daily living. Loss of spontaneity; need to plan everything I do.
Snelgrove 2009:358 managing the pain – medication dependency
Ambivalent relationship to medications as even though medication needed to relieve pain, it can be ineffective and lend to one becoming medication-dependent.
Snelgrove 2009:358 maintaining integrity – not being believed
Difficult to maintain credibility due to invisibility of pain and disbelief.
Snelgrove 2009:358 crucial nature of pain – body/self/pain as a threat
Body separate from real self. IT (pain) versus ME (body). Pain threatens to take over self by taking ownership of body.
Snelgrove 2009:358 crucial nature of pain – physicality
Emphasised physicality of pain: unpredictable, hopeless, intrusive, overwhelming, unbearable.
Snelgrove 2009:358 managing the pain – relationship with health-care professionals
Loss of faith in medication and the health professionals but continued to adhere to a medical model and continued to have faith in medical technology.
Steen 2001:385 awareness of self
Now more aware of self and body in everyday life and did things differently.
Steen 2001:385 community
Being in within the walls of ‘the room’ brought a sense of relief, sharing and community, validation and safety to many.
Steen 2001:385 accepting self and others
Acceptance – of self and others increased as group discussions allowed for comparisons and validation. Being able to express innermost thoughts and feelings (and to cry) valued by patients and appeared to impact positively on their self-esteem.
Steen 2001:385 change of focus
Increased consciousness of bodily signals and of how one needs to respond to these (rather than ‘fighting the pain’) in order to effectively manage pain. This may require a change in one’s way of thinking.
Steen 2001:385 drop-outs
Some patients not comfortable with psychological inference, physical proximity and embarrassment of exercising.
Steen 2001:385 experimenting
Narrative of discovery [learning to trust own opinions]. This seemed to capture how the group and leaders gave them permission to explore, be curious and be creative. The feelings generated to be celebrated and not hidden. A respect for patient opinions about illness and exercise choices although they may have limited experience of these processes. Also seems to be about patients valuing freedom to try things out, such as different methodological approaches (and make mistakes), rather than only following the instructions from health professionals.
Steen 2001:385 gender
While some felt that discussions would have been ‘different’ if men participated in their group, some males were glad to have been able to be a part of a group.
Steen 2001:385 group leaders
The humankind of believing the patient – different from usual health-care professionals. Behaved like human beings and treated patients like one. This did not impact on professionalism in a negative way (rather positively). Valued if they joined in not just issued instructions.
Strong 1995:387 how are you coping?
Most patients perceived themselves as ‘copers’ being able to get on with life, despite pain. This perception appears to be characterised by an attitude of acceptance of pain over time. Where such acceptance was absent (usually for a patient still relatively new to the pain), it was usually characterised by attempts to ignore pain as an approach to managing it.
Strong 1995:387 what helped you to cope?
Distinct changes over time for the majority of patients as they realised that pain might be there to stay. However they remained open to any new advancement. This realisation was usually accompanied by accepting responsibility for managing pain, and appreciating the roles of planning, compromising and prioritising in undertaking tasks. Get the maximum you can out of life because life goes on – the pain is always going to be there regardless of what you do, so get out and do it. A general sense that inactivity was not a viable option as it only made the pain worse. Movement here from high patient expectations of an omniscient health professional, to greater self-reliance in addressing the symptoms of their illness.
Teh 2009:362 participation in pain treatment – don’t want to be harmed
Some patients wanted to maintain a compliant [traditional] relationship with their doctor and be seen as a ‘good patient’; for some this was because of fear of harm if you didn’t do as the doctor told you – the doctor knows best.
Teh 2009:362 importance of relationship with health-care professional
Relationship with health-care professional valued: being understood, seeing them as a person, being remembered and continuity of care means that you feel known, safe and legitimate. Being unknown, not heard or understood means isolation and de-legitimacy.
Teh 2009:362 participation in pain treatment – involved in decisions
Patients were involved in decisions by rejecting or withdrawing from suggested treatments, or by asking for specific treatments. Those who had a good relationship with the health-care professional were more successful self-advocates. Power to take control of treatments may lead to withdrawal from treatment and subsequent suffering. Mixed view about speaking up and being assertive about health-care needs and options.
Teh 2009:362 participation in pain treatment – working outside health-care professional relationship
Patients sometimes changed pain medications without consulting health-care professional, due to dislike of pain medications and fear of reliance on these. Working on own to manage pain: change own medication, taking supplements or exploring alternative remedies. Patients resourceful in accessing alternative health strategies.
Toye 2010:363 loss of credibility
Most described situations where they had not been believed by healthcare professionals, friends, family or colleagues. Difficult to appear credible when you have back pain because; it is very common, symptoms continually vary, it is medically invisible; a person looks well. It also is stigmatised and carries various stereotypes.
Toye 2010:363 could I be imagining this
Paradox:
a. I need a diagnosis to be legitimate (even though this is counterintuitive because I don’t want to be ill).
b. However, I know that psychosocial factors contribute to my pain (mind over matter metaphor).
Toye 2010:363 I am not like the others
Paradox:
a. Meeting others with pain confirmed legitimacy.
b. BUT I am not like the others. Patients were ambivalent in their relationships with other patients, and also stressed how they were ‘not like them’. Social comparison and moral narrative used to rank self and confirm legitimacy.
Toye 2010:363 I am still me but not me
Paradox:
a. You have to learn to live with it [use of cultural rhetoric].
b. I am still me and I will fight to be [use of cultural rhetoric].
These are not mutually exclusive; can accept defeat but still fight on [lose battle; win war].
Toye 2010:363 mustn’t look too ill
Paradox:
a. Consistency or persistence of pain behaviour an important dimension of judging whether or not someone was genuine.
b. But don’t look too ill all the time or people won’t believe you. There is a ‘right way to be in pain’.
Patients had to negotiate a balance between not looking ‘too ill’ and yet looking ill enough. Often resolved this by hiding their illness even from those close to them.
Toye 2012:364 being fobbed off
This describes how patients felt that they were not being listened to or understood as a person whose life had been changed by back pain.
Toye 2012:364 being fobbed off – I see buckets of people like you
GPs make light of something that is very serious to the person (I see loads like you, there is nothing much wrong with you), and this also makes them feel guilty for wasting doctors time.
Toye 2012:364 being fobbed off – just take the tablets
Saw GPs as keen to dish out drugs and this was not a cure. Medication was described as part of the process of being ‘fobbed off’. Particularly annoyed if given anti-depressants as not seen as dealing with real pain.
Toye 2012:364 being fobbed off – I just want to be heard
Patients described how it was important to know that the GP understood them as an individual and the impact the pain was having on their lives.
Toye 2012:364 being fobbed off – I didn’t get a thorough examination
Did not accept that a doctor could diagnose a problem without performing a thorough examination, including physical and diagnostic tests such as palpation, X-rays, scans or blood tests. Patients interpreted this as a) not being believed or b) not being taken seriously.
Toye 2012:364 you are just a GP – not leaving until I see a specialist
Patients described the GP’s reluctance to refer to the specialist. They felt they had to make a strong case for their referral or the GP would not ‘sign that piece of paper’. This was described as a battle and some described feeling guilty for putting pressure on the doctor.
Toye 2012:364 being fobbed off – nothing else we can do
Patients described how the doctor told them to accept their pain and to get on with life, perhaps even to expect things to become worse. This left them feeling that they had not been heard or taken seriously. There was a nagging doubt that for some that maybe there really is nothing that can be done (but this leaves me with no hope).
Toye 2012:364 who is the back expert
Over time patients began to doubt the existence of a ‘back expert’. Having accessed the specialist, patients had expected a definitive diagnosis on the basis of thorough examination and expert opinion, but often got conflicting advice.
Toye 2012:364 you are just a GP – you are not a back expert
Patients described how GPs lacked specialist knowledge that would allow them to effectively treat back pain, and this is why they ‘fobbed you off’.
Toye 2012:365 restoring hope – constructing an acceptable explanatory model
Successful patients had accepted a link between mind and body and embraced psychological interventions. However, physical explanations were still important, and they constructed a new model, which described the body as out of balance rather than broken, thus being able to retain legitimacy in spite of having no medical diagnosis. Unsuccessful patients held onto medical model.
Toye 2012:365 restoring hope – constructing acceptable self-identity
Successful patients felt that they were ‘still me’. They had made some ‘acceptable changes’ to themselves. For example; I need to be strict with myself now, I don’t need to be a perfectionist. They described pacing as a way of gradually increasing activity levels over time, rather than being used to limit activities. Unsuccessful patients described overwhelming loss of self and saw pacing activities as restricting their activities and therefore their lives.
Toye 2012:365 restoring hope – deconstructing fear of specific movements
Described how prior to pain management, fear of moving had made them avoid specific movements. Several factors helped to deconstruct fear: learning that hurt does not mean harm, seeing other patients in the group perform feared movements, performing feared movements themselves, working through flare-ups under supervision of physiotherapist.
Walker 1999:367 being in the system – all in the mind
Absence of proper diagnosis contributed to patients feeling that medical professionals felt that the pain was ‘made-up’. They were often referred onto different physicians.
Walker 1999:367 being in the system – battling for benefits
Forced to stay in benefit system; no perceived advantage of coming out of it, even though they did want to work. This concept underscores the challenges generated by the state.
Walker 1999:367 being in the system – compensation claims
Some patients felt others were at least partly responsible for their back pain problem and that they should be compensated.
Walker 1999:367 being in the system – damned if you do and damned if you don’t
Compensation claims could alienate you from colleagues at work OR force you to seek medical diagnosis and treatment. Negative consequences of applying for compensation and apportioning blame. This describes being alienated because of legal process BUT if you don’t then you won’t get compensation [team note; link to Karl Marx: system covertly suppresses claims for what you deserve].
Walker 1999:367 being in the system – establishing a legitimate claim
Participants describe a struggle to be seen as ‘genuine’ benefit applicants. Living with back pain and living with disability benefit reflects the battles to prove disability
Walker 1999:367 being in the system – feeling insignificant
Communication with health-care professionals not based on relationship between two equals. Professional language often alienated the patient and inhibited good communication. Feel like you have not been understood as a person. Failure of medical professionals to ‘believe’ them, this being compounded by nothing appearing on X-rays, and patients being seen by different professionals in ‘parts’ and never holistically.
Walker 1999:367 being in the system – getting nowhere
Attempts to understand, diagnose and treat pain unfulfilled – feel thwarted.
Walker 1999:367 being in the system – losing faith
Felt health-care professionals had given up on finding a diagnosis and cure, and blamed the patient for their own condition. Patients lost faith in doctors who did not understand their world.
Walker 1999:367 being in the system – passing the medical test
Need to prove that there is significant disability to enable the claim to be processed. Physician bias and ‘malingerophobia’, compounded by the patient’s own determination to lead a ‘normal’ life. This can contribute to patients failing their physical examination and impact their being unable to receive compensation and benefits. [test – powerful of language TEST]
Walker 1999:367 being in the system – the medical process
Medical system consuming their lives but is failing them.
Walker 1999:367 being in the system – waiting
Feeling like a ‘shuttlecock’ long periods of waiting and being sent back and forth for non-productive treatments. All patients felt too much time wasted waiting in vain for ‘productive’ assistance in the medical system.
Walker 1999:367 being in the system – your life is not your own
Deservingness of benefits payment out of the hands of patients, resting solely on the opinion of medical professionals/benefits officers.
Walker 2006:368 loss – employment
Sense of loss related to work exacerbated by lack of understanding from employers, particularly if employment had been longstanding. Felt a sense of betrayal by employer as pressure felt to leave work. Feel like they are treated ‘just like a number’ even when work had been valued prior to pain. Patients went to great lengths to find employment and often hid back pain from their employers (e.g. by taking holiday instead of sick leave). Guilt and resentment at losing/not finding suitable employment.
Walker 2006:368 loss – financial
‘Descent into poverty and social dislocation’; Changes in accustomed lifestyle as a result of financial loss. Inability to support family led to feeling guilty. Difficulty accessing statutory financial support related to invisibility of pain. Lack of economic dissatisfaction appeared linked to age (pension aged people did not necessarily feel the loss).
Walker 2006:368 loss – ability and role
Physical and mental effects of pain (e.g. lack of concentration) prevented patients from performing every day and valued activities. Unable to maintain employment or valued family activities. Interfere with valued life plans. Came to rely on important others (loss of reciprocity). Become ‘socially and environmentally restricted’. Acceptance or rejection of these limitations appears linked to age related expectations.
Walker 2006:368 loss – hope
Turmoil, chaos, turbulence. Patient wrestles powerful emotions of uncertainty about the future, fears of potential worsening of illness, and feelings of vulnerability and helplessness. Inability to make plans; need to live each day as it comes; not knowing what the future holds; fear of getting worse. Like Arthur Frank’s389 CHAOS narrative – ‘being shipwrecked by the storm of disease’ (p. 54). Describe life as imprisoned by pain with no knowledge of release.
Walker 2006:368 loss – identity
Patients distinguished private and public self. Agonised over what people thought and feared being seen as a ‘faker’. I am no longer who I was and I don’t like what I have become. At the same time, I am still the same person but others can no longer see it. This is exacerbated by reactions of others (e.g. why isn’t he giving up his seat?!) [Paradox: I am no longer the same person – I am still the same person]: private/public; old me/new me; fake/real. Gender expectations of behaviour exacerbate this dilemma.
Walker 2006:368 loss – relationships
Irritability, need to be alone, loss of trust and disbelief, lead to breakdown of physical and emotional relationship with partners. Also became isolated from friends and work. Came to know who to trust and who true friends were. For older people, dependence could sometimes increase contact with the family [doesn’t talk about the quality of this contact]
Werner 2003:369 applying the competence – encountering others
With renewed self-esteem following the programme patients were less reactive to and concerned about what others felt about their chronic pain, and less preoccupied with gaining approval.
Werner 2003:369 why can’t she just do it? – family
Negative reactions from husbands or others who could become annoyed or angry. They still expected them to be in charge of household tasks/usual roles. This made it more difficult for the participants to make use of the competence acquired from the treatment programme.
Werner 2003:369 applying the competence – focusing on resources (not pain)
Learnt to be less focused on pain and more on personal resources and enhancement i.e. what can I actually DO rather than how do I FEEL; simply to ‘treat’ oneself or enjoy a pleasurable activity and mobility; making adjustments to amount of tasks to be undertaken in relation to bodily capacity and letting others know about this work capacity.
Werner 2003:369 why can’t she just do it? – friends
Well-intended advice from friends could also make it more difficult to apply the treatment benefit. The women often felt they were given advice as an accusation for not having been clever enough or working sufficiently hard to become healthy. Friendships could break down.
Werner 2003:369 why can’t she just do it? – health-care professionals
Health-care providers were mentioned as a cause of obstruction, by obstructing women’s desired treatment/not referring to specialist.
Werner 2003:369 applying the competence – informing others
Women now let others know of their limitations and capabilities. Being outspoken about personal needs and desires was said to be a constantly on-going internal and external process of work.
Werner 2003:369 for better or worse – awareness of needs
Responding to bodies fluctuating needs. Become more aware of signals of bodies needs and able to act upon them. More competent to allocate capacity in response to limitations. Yet within this dynamic is the constancy of pain that forces the patient to accept (however reluctantly) and readjust to bodily limitations.
Werner 2003:369 applying the competence – knowing my body
I now know the capacity and limitations of my body and am prepared to respect it; I now have permission to adapt to capacity.
Werner 2003:369 for better or worse – recognition gives strength
Recognition and respect demonstrated within groups strengthened participants’ self-confidence and self-esteem while diminishing feelings of guilt for not being restored to full health. The participants described the strength, confidence, and awareness gained from the treatment programme as being useful bodily and emotionally, and gave social competence outside the group context.
Werner 2003:369 for better or worse – sorrow at loss
a. Negative effects due to the increased level of awareness which leads to sorrow at loss of aspects of self. An increased feeling of despair is caused by having to realise that you might never be restored to your former healthy state. Sorrow and bitterness at having to revise the picture of self.
b. Feelings of loss at the cessation of the group treatment therapy and its emotional support and reinforcement that they had experienced.
Werner 2003:369 applying the competence – thinking of me
Learnt to think about myself and the things I can do for me.
Werner 2003:370 I don’t give up unless I have to
Women encountered significant difficulty in being accepted as credible patients by the benefits and medical systems, partners and friends. They dealt with these barriers mainly by persevering, being assertive, and not giving up. Felt ‘tested’ for mental disorder. Worked hard to ‘past test’.
Werner 2003:370 I feel I should look groggy
Have to negotiate their appearance (healthy, pretty, and smartly dressed) in encounters with health-care professionals as this impacted on whether or not these professionals would believe their stories of pain. Have to strike a balance between appearing too healthy/not too healthy. If you look too good or bad people won’t believe you.
Werner 2003:370 you have to tread rather softly
Women reported simply ‘accepting’ in silence the negative treatment meted out by social services and health-care professionals. They either chose to terminate the relationship or to allow someone else to present their arguments so that these professionals were not antagonised.
Werner 2004:371 I have always been so strong
I have always been physically strong but pain has made me physically weak. I have always been emotionally strong but there are times that pain is so bad that it has made me emotionally weak. Paradox – I am still a strong person. I have not chosen this. It is not my fault.
Werner 2004:371 some people pour out their troubles
Narrative of strength. Important to be strong and fighter not weak and complaining. On the one hand I am like those other women (because I have pain) but I am different (not one of those whiners). I am strong, I have a positive attitude, I don’t whine, I am never sick; I don’t go to the doctors. Women work to appear credible and distance themselves from ‘the others’. I am not to blame.
Fibromyalgia second-order constructs
Arnold 2008:373 cognitive impairment
Cognitive processes affected by fibromyalgia: forgetfulness, inability to drive, lack of motivation to undertake tasks and ‘fibro fog’; difficult to articulate thoughts; difficult to plan things; difficult to focus or keep attention.
Arnold 2008:373 function and quality of life – education
Could miss out on higher education because of inability to sit in class or concentrate for long periods.
Arnold 2008:373 emotional impact
Emotional disturbances – included depression and anxiety. Also embarrassed by having to explain illness or inability to undertake ‘simple’ tasks; frustrated by lack of medical and social understanding and at their own lost capabilities. Guilt over putting their needs first. Felt isolated and a burden on family.
Arnold 2008:373 function and quality of life – family
Described as ‘time spent with families was often reduced, and families frequently had to compensate for the participant’s absence by taking on more chores. Those who were mothers could not assist their children with homework or other school-related activities. Participants also mentioned not being able to go on family trips. Alternatively, fibromyalgia allowed the women to legitimise taking more time for themselves when they would otherwise have focused their energies on others’.
Arnold 2008:373 fatigue
Fatigue could be worse than pain; it was a constant presence in the lives of participants, who often had to limit activities to ensure that the tasks set for the day could be accomplished. They frequently cited the need to take naps and mentioned their tendency to fall asleep during the day.
Arnold 2008:373 pain
Pain constant and difficult to pinpoint.
Arnold 2008:373 function and quality of life – partners
Burden on family members and partners increased as they take on more chores and responsibilities. Sexual libido is affected leading to loss of intimate relationships.
Arnold 2008:373 sleep
Fatigue and pain interfered with sleep, making mornings especially difficult for most; bodies were racked with pain.
Arnold 2008:373 function and quality of life – social life
Unpredictability of fibromyalgia and fear of being judged unreliable prevented them becoming involved in social events. Some people were sceptical about pain and this could lead to loss of friendships.
Arnold 2008:373 function and quality of life – work
Frequently had to stop or change work due to inability to do competitive tasks or lack of concentration. This could have a financial impact, particularly in view of medical costs. Also impact on loss of identity; no longer ‘respected in my field’.
Cunningham 2006:375 living with the symptoms of fibromyalgia
Symptoms constant yet varying and unpredictable. Unable to engage in everyday life; need to give up former roles and activities and employment. Interferes with social life. Participants felt a burden to their families due to their disability. Invisibility of symptoms made it more difficult to manage psychologically.
de Vries 2011:324 success factors (work) – adjustment latitude
Involves a range of crucial adaptation strategies around prioritising work, being flexible in execution of tasks (e.g. using a mobile phone that allowed one to not be confined to a desk), adapting ways of working with colleagues (delegation of tasks and accepting assistance) and working in partnership with families (i.e. accepting support as may be necessary). Not everyone at work experiences this latitude at work
de Vries 2011:324 success factors (work) – coping with pain
Ambivalence about medication: for some it enabled them to stay in work, others did not want to take medication for fear it would mask symptoms or make them drowsy at work. Some wanted to stop medications and take control of the pain themselves. Others avoided provocative movements or were attentive to body signals. Many felt that acceptance was important to continuing at work and needed to stay active.
de Vries 2011:324 success factors (work) – pain beliefs
Pain threshold of all participants reported by them as being above average, allowing them to work despite pain. Sometimes this threshold diminished over time.
de Vries 2011:324 success factors (work) – personal characteristics
Moral narratives (character traits described as crucial to stay in work): perseverance, ambition, positive outlook, communicative, assertive, self-confident.
de Vries 2011:324 success factors (work) – use of health-care services
Some patients satisfied with advice and treatment options that allowed them to stay in work, while others were disappointed with the health-care services.
de Vries 2011:324 consequences of staying at work
Patients generally felt staying in work had many benefits. Dis-benefits included reduced opportunities for a social life and to pursue hobbies. Diminished capacity for leisure and pleasurable activities; increased pain and fatigue.
de Vries 2011:324 motivators for staying at work – work as income
A strong motivator, especially if one owned the company.
de Vries 2011:324 motivators for staying at work – work as responsibility
A few perceived their work role as indispensable and that others relied on them. Therefore felt their absence impacted on work productivity as they could not be substituted, therefore worked through pain to meet work responsibilities and to not place a burden on their colleagues.
de Vries 2011:324 motivators for staying at work – work as therapy
Work is place for healing and recovery. Work distracts me from my pain. Work gives me energy to go on. Work gives my life structure and gives control over pain. Work gives social contact which further distracts from pain. Gives me self-respect and self-worth.
de Vries 2011:324 motivators for staying at work – work as value
Work gave recognition, approval, self-realisation and self-respect. Work gives status and offers opportunity to be valued by peers. Work provides a mission to life. Gave link to society and value to life. Work is the ‘normal’ thing to do.
Gullacksen 2004:377 stage 1 – prelude
Slow to change as pain often regarded as temporary at first. As sick periods got longer and effected life – reached a critical point.
Gullacksen 2004:377 stage 1 – self-deception
Continued to hide pain and maintain ‘normality’. Various coping strategies adopted to hide illness, precluding social support for social survival, even though pain only worsens. Isolated in pain and in worry about future. Difficulty to explain situation to others and felt isolated and inadequate.
Gullacksen 2004:377 stage 1 – struggling to restore life
Hoping for recovery and restored self. Person aimed to restore previous life and hold onto former identity. Maintaining ‘normal life’ outwardly and coping with pain an immense strain which they tried to keep hidden.
Gullacksen 2004:377 stage 1 – acknowledgement
Acknowledging that pain was not temporary was crucial to adjustment. Necessary to give up the aspiration to return to life as ‘normal’. This grew as an ‘inner certainty’. No longer possible to hide situation. Now turned toward the future, although this did create anxiety about what future holds. Stopped waiting for a cure to be found and turned to own resources. Hope for recovery maintained BUT NO LONGER AN OBSTACLE to alternative possibilities. Change begun.
Gullacksen 2004:377 stage 1 – confirmation by health-care professional
This helped to explain to others and increased understanding. Health-care professional diagnosis and attitude important in adjustment. Women had to ‘prove’ to others that they were ill and this could be construed as being ‘obsessive’. Disbelief by health-care professionals described as insulting and a threat to patients ‘reason’. All pervading doubt a drain on personal resources.
Gullacksen 2004:377 stage 2 – losing oneself
Difficult to automatically perform usual tasks. Uncertain about what body was capable of and this disrupted self-esteem and self-confidence. This a major threat to self-image. What have I become? Inability to rely on the body damages self-image and confidence.
Gullacksen 2004:377 stage 2 – sorrow and loss
Admission that pain not temporary often succeeded by an emotional crisis. Sorrow and loss strong (sometimes voiced and others hidden). They missed life as it used to be.
Gullacksen 2004:377 stage 2 – working through
Admission that pain was not temporary the beginning of adjustment. Cognitive and emotional acceptance that pain may be permanent and exploring new ways of dealing with limitations imposed by pain.
Gullacksen 2004:377 stage 2 – defining problems
Medical explanations important to removal of focus from body and self to other things in life (family, etc.) and finding a new sense of personal completeness.
Gullacksen 2004:377 stage 2 – finding solutions
Focus on repairing existence and relearning to live with pain.
Gullacksen 2004:377 stage 2 – leaving the sick role
As pain not temporary, taking on sick role (rest, withdrawal, and support from others) becomes problematic. Expectation of return to normal life entailed by sick role not fulfilled. Sick role behaviour becomes less desirable and did not want to be dependent on others. Tried to create new patterns and routines to achieve independence and ‘normality’. Sometimes difficult for others to accept need for independence in certain tasks. Patient rejection of support often confusing for others. Patients generally preferred emotional empathetic support.
Gullacksen 2004:377 stage 3 – maintenance (a new attitude)
Strength had to be rationed to prioritise activities. Had to come to terms with uncertainty of fluctuating symptoms. Had to balance desire versus capability. Sometimes chose to worsen pain to perform certain valued acts.
Gullacksen 2004:377 stage 3 – a new course of life
A challenging process of adopting new coping strategies in search to re-establish self and a sense of control. Difficult to sustain: constantly changing.
Gullacksen 2004:377 stage 3 – maintenance (handling future changes)
Normalising life in spite of pain demands skilful strategies of coping. Increased self-knowledge gained through this (hidden) struggle.
Gullacksen 2004:377 stage 3 – maintenance (regular self-care)
Although self-discipline and regularity were required for the successful undertaking of tasks, there was some pleasure and astonishment at being able to learn to live with pain despite all initial doubts.
Gustaffson 2004:327 developing body awareness
Theoretical and practical knowledge on course used a year later to improve energy, concentration, relaxation, confidence. Transformed from ignorance to knowledgeable.
Gustaffson 2004:327 changing self-image – handling the pain
Moved from trying to ignore pain to finding new ways (self-reflection and rest) of handling pain. No longer shame and self-doubt of pain; learnt to self-reflect, respect pain and limit demands.
Gustaffson 2004:327 changing self-image – housekeeper identity
New housekeeping strategies to reduce demands from self to others, listening to body and leave time for self. This category captured the day to day management of households and how their approach changed from being the slave to normality before the programme, to using the knowledge to manage the household chores differently.
Gustaffson 2004:327 changing self-image – self-confidence
Programme made them more willing to talk about pain. Pain now legitimate. Less doubt. More confidence.
Gustaffson 2004:327 setting limits – adjust workload
Change priorities, ask for help; leave time for myself. Decrease unpredictability of pain.
Gustaffson 2004:327 setting limits – adjusting self-demands
Through understanding and listening to their bodies and the boundaries they were able to set limits on their activity.
Gustaffson 2004:327 shame to respect
Started rehabilitation with feelings of shame and self-doubt. Felt disbelieved by health professionals and misunderstood by family. The group interaction realised a change from these negative emotions to a greater sense of respect and self-worth with more positive relations with others.
Gustaffson 2004:327 changing self-image – boundaries imposed
Boundaries imposed and curtailing life were seen as more flexible and could be determined by the person with chronic pain. Pacing activities and resting became ways to manage the pain.
Gustaffson 2004:327 shame to respect – negative factors
This captures the hopelessness often felt by not being able to enjoy activities which normally gave pleasure. A struggle with constant pain impacts on employment. Not being able to work as one wanted or had done previously, nor being able to undertake desired tasks and hobbies evoked a sense of despair and frustration.
Gustaffson 2004:327 shame to respect
Started rehabilitation with feelings of shame and self-doubt. Felt disbelieved by health professionals and misunderstood by family. The group interaction realised a change from these negative emotions to a greater sense of respect and self-worth with more positive relations with others.
Gustaffson 2004:327 shame to respect
Started rehabilitation with feelings of shame and self-doubt. Felt disbelieved by health professionals and misunderstood by family. The group interaction realised a change from these negative emotions to a greater sense of respect and self-worth with more positive relations with others.
Gustaffson 2004:327 setting limits – telling others
Programme has taught them to tell others about their condition and thus reduce demands on themselves [learn to say NO].
Hallberg 1998:328 maintaining forces – family support
Pain changes the roles within the family; husband takes on caring duties; children get less attention from mum; wife becomes dependent on husband; no longer viewed as sexual. Social and leisure activities outside of home decreased.
Hallberg 1998:328 psychosocial vulnerability – overcompensatory perseverance
Perseverance – over-compensating for illness by working harder than the norm at meeting the demands of life. Despite this over-compensation the women still felt inadequate and as though they did not measure up.
Hallberg 1998:328 maintaining forces – pain benefits
This category describes any advantages, implicitly or explicitly expressed in the interviews, of having chronic pain. When on sick-list, the women seemed to be relatively satisfied with their lives, partly due to a perceived balance between the external demands and their own resources.
Hallberg 1998:328 psychosocial vulnerability – pessimistic life view
Pain described bio-medically and dissatisfied that doctors had taken a long time to identify the problem. Uncertain about what they could now manage. Pain demanding much of the patient’s time and attention and made them less confident about managing things in the future. Life less meaningful.
Hallberg 1998:328 maintaining forces – professional care
Disbelieved by health-care professionals therefore hesitant about seeking their help, but also exaggerated condition when they did speak to them. Felt health-care professionals had no faith in their own capacity to help people with chronic pain. Diagnosis brought sense of relief as offered a form of validation, making it easier to tell others about illness, including employers.
Hallberg 1998:328 psychosocial vulnerability – traumatic life history
Emotional wear and tear over time: specific negative (e.g. alcoholism of a parent) and even traumatic past life events (such as death of a loved one or divorce) that escalate with the onset of illness and evoke a sense of hopelessness, helplessness, powerlessness and despair.
Hallberg 1998:328 psychosocial vulnerability – unsatisfying work situation
‘This category is comprised of four substantive codes, “low-valued job”, “strenuous job”, “controlled work tasks”, and “personal dissatisfaction”, and describes the women’s view of their work situation’ (p. 99).
Hallberg 2000:329 preoccupied with pain – pain communication
Pain made patients irritable which in turn affected the way in which they behaved towards others, although there were rigid attempts to conceal emotions (low mood, tears etc.), even from closest friends. This made them appear perfectly cheerful and healthy externally while racked with pain internally.
Hellström 1999:378 avoiding thoughts of future
Focused on limitations of illness and held onto safe and familiar routines to avoid thinking of the future.
Hellström 1999:378 demands on self
Unable to manage the high demands they placed on themselves and undertake previous activities. For some fibromyalgia gave a chance to slow down. Patients struggled to balance the deficit between ideal and achievable self.
Hellström 1999:378 managing threatened failure
Irresistible fatigue given as a reason to delay decision-making and deal with the incapacitating effects of illness (I really want to do it but I can’t). The texts seemed to demonstrate the patients’ attempts to connect a feared inability and the existence of an incapacitating illness.
Hellström 1999:378 onset
Onset temporal well defined and linked to significant unpredictable life event e.g. car crash.
Hellström 1999:378 search for a cause
Looked for meaning and cause of illness within their lives. FELT disbelieved as many felt the women were experiencing pain that was all in the head. Rejected psych explanations but felt illness led to mental problems.
Hellström 1999:378 search for confirmations as ill
Search for diagnosis validates; diagnosis gave relief as ‘not serious’ disease but diagnosis of fibromyalgia made it difficult for them to convince doctors that they had any other illness. Only others who are ill understand me.
Hellström 1999:378 unpredictable, invisible, incapacitating
Illness unpredictable, invisible incapacitating.
Kelley 1997:380 changes over time
Less focus on losses over time, and greater acceptance; new sense of empowerment. Fears of ongoing need of advocacy and support groups for the future.
Kelley 1997:380 feeling understood
Feeling understood important for overall sense of wellbeing. All discussed loss of validation (family, friends, and some health-care professionals). Diagnosis validating. Grateful for validation. As group progressed they became more accepting of partial understanding and that total understanding.
Kelley 1997:380 group approach
Appreciation of emphasis on whole person and coping strategies, that aided controlling life irrespective of pain and ‘refocusing’ to pain as a part of a process of acceptance, adopted from group sessions.
Kelley 1997:380 loss
Overwhelming loss (work, leisure, home, relationships, independence).
Kelley 1997:380 resources
Participants became more resourceful in pacing and substituting activities to cope with illness.
Kelley 1997:380 self-esteem
Not feeling validated, not able to help others, not wanting to ask for help ‘feel like a burden or failure’. As they learned to externalise the condition as not intrinsic to themselves, fighting the effects of their illness made them feel stronger.
Kelley 1997:380 support and empowerment
Learned to ask for help from friends and family; linked to most positive self-esteem.
Lachapelle 2008:335 barriers to acceptance – support and belief of others
Lack of support and belief from others is a barrier to acceptance. It was important to have a concrete diagnosis to feel legitimate and get support from others. Friends, colleagues and families began to treat them the same as the health-care professionals did. Delays in diagnosis damaging to fibromyalgia women’s social (support) networks.
Lachapelle 2008:335 barriers to acceptance – unrelenting pain and fatigue
Unrelenting pain and fatigue – women drained of physical and emotional resources.
Lachapelle 2008:335 barriers to acceptance – fight to be normal
Mounting losses and fight to be normal; struggle to maintain pre-pain identity. Felt they had let the pain ‘win’. Struggled to maintain normalcy; ‘put on a play’ ‘cover it up’. Acceptance meant you had to take on changes and accept changed identity (sometimes felt guilty for this e.g. gender roles).
Lachapelle 2008:335 facilitators to acceptance – self-management education
Having a diagnosis was a key turning point for them to seek out information about their condition. Effective self-management linked to the undertaking of non-medical strategies that improved ability to perform activities desired despite pain, empowering patients to take control of their lives. Women with fibromyalgia more self-reliant in educating themselves about illness compared to women with arthritis who received greater access to information for health and specialist organisational sources.
Lachapelle 2008:335 facilitators to acceptance – perceived social support
Emotional support from friends and balanced counterbalanced by a concern over not overburdening. Limited by a lack of understanding on the part of supporters and fears the possible onset of supporter fatigue. Support groups ambiguous; some offered a safe haven whilst others perceived as discouraging and designed to force on participants a particular agenda. Professional counselling could help to mourn loss of old self and redefine new identity.
Lachapelle 2008:335 meaning of acceptance
Meaning of acceptance ambiguous; implies giving in/resignation. Patients ‘preferred expressions such as “embracing”, “dealing” or “coming to terms” with their pain’ (p. 203). Means pursuing life activities in spite of pain. I am willing to engage rather than avoid. Hope for improvement in pain and symptoms not incompatible with acceptance of current state. Retained hope for reduced pain at the same time as accepting chronicity of pain, and that there was no cure for pain. Acceptance begins with giving up hope of cure.
Lachapelle 2008:335 process of acceptance – ongoing process
Acceptance was not an all or nothing process. Repeated moments of reflection. You made decisions on a daily basis and setbacks occurred on bad days. Easier to accept pain on a cognitive than an emotional level.
Lachapelle 2008:335 process of acceptance – realising need for help, getting diagnosis, realising no cure, it could be worse
Four stages of acceptance:
realisation that this is not normal and I need medical help;
receiving a diagnosis (and thus legitimacy as ‘real’);
realisation there is no cure and had to get on with it (this stage often repeated time and time again when hope of a cure are raised (by medicines or surgery);
realisation things could be worse (comforted by identification of people who are worse off).
Lachapelle 2008:335 process of acceptance – redefining normal
Letting go of pre-pain self-expectations and shifting their focus to what they could accomplish now, despite the pain, was an important next step. The knowledge that no return to pain-free status possible. Followed by a grieving of losses and a redefinition of goals, although conscious of having the power to also choose a path of giving in to negative emotions.
Lempp 2009:381 change in health identity
Illness became increasingly intrusive in life and began to undermine their confidence and sense of self. Self-esteem undermined. Fear of not being able to rely on body and the unpredictability of the illness.
Lempp 2009:381 quality of care – ethnicity
Black and ethnic minority patients were uneasy about prescription medicines and mistrusted health-care professionals
Lempp 2009:381 quality of care – GPs
GPs sympathetic but don’t spend enough time, unresponsive to needs and limited to prescribing medication.
Lempp 2009:381 quality of care – hospital specialists
Hospital outpatient departments were criticised for poor organisation (e.g. cancelled appointments) and professional attitudes.
Lempp 2009:381 change in health identity – impact on social life
Patients became less able to go out, particularly spontaneously (physical difficulties or embarrassment) and became socially isolated. Those who left work became isolated from colleagues; those who remained at work also became isolated because of lack of understanding. In public patients felt misunderstood and stigmatised. Viewed as ‘invalids’ by people around them. Some tried to hide their disability. Had to find a balance between wanting/needing support but retaining independence. Illness took its toll on relationships. Patients worried about the future, becoming dependent on others and how to fill their own caring roles.
Lempp 2009:381 quality of care – interventions
Ambivalence to medication; concern over dependence and that it might mask symptoms but not ‘cure’ the disease. Drugs ineffective for pain relief and most ‘followed their own intuition rather than medical advice’. Physiotherapy whilst positive for some, on the whole brought up negative memories. Many tried alternative medicine/therapy, again with little relief apart from use of heat.
Lempp 2009:381 change in health identity – mental distress
Depression, anxiety, cognitive problems and lack of co-ordination were all reported. People described feeling suicidal and spiralling down. The inability to remember things was referred to as ‘fibro fog or foggy brained’ and this was distressing.
Lempp 2009:381 change in health identity – physical problems
Virtually constant overwhelming total body pain has physical and mental toll, as well as having an effect on their usual behaviour. Some could not remember a pain free day. Many unable to function ‘normally’ due to chronic sleeplessness resulting in debilitating fatigue. Co-morbidities and abdominal symptoms exacerbated their condition. Also discussed difficulty with mobility and resulting isolation.
Liedberg 2002:382 structural social factors – commuting
An additional strain in terms of getting to work and many of the respondents were dependent on others helping them with transportation.
Liedberg 2002:382 structural social factors – finances
Finances not always the motivator to stay in work. Some had spousal support in terms of finances, single mothers found that finances dominated their decision to remain in work, and other patients preferred to decrease hours of work to maintain a work role.
Liedberg 2002:382 values and norms – fulfilment in work
Conflict between accepting new limitations imposed by illness and desire to be responsible workers. Participants describe themselves as dutiful, responsible and loyal and gain fulfilment from their work. They find it hard to relinquish roles.
Liedberg 2002:382 values and norms – meaning of work
Work valued by respondents as it made them feel useful members of society, appreciated by others and able to socialise. Many mourned over their lost professional identity [you are what you do at work]. Experience loss of work role and social contacts that go with it.
Liedberg 2002:382 values and norms – organised time structure
Work role important perceived as integral to time structure for daily routine in personal pain management. Disliked sick leave as disrupted this time pattern. They endeavour to maintain some kind of time structure and routine even if professional role lost, and new ‘work’ is simply that of helping others.
Liedberg 2002:382 working conditions – physical work
Tasks that allow varied work posture preferred. Sleep disturbances made many of the women tired, and this impacted on their undertaking and maintaining the requirements of work/employment.
Liedberg 2002:382 working conditions – psychosocial environment
Work relations important for motivation to return to work and for job satisfaction. Employment related changes often disruptive to these relationships. Understanding from colleagues and employer confidence in their ability to accomplish their work roles valued. Opportunities to influence work schedule and hours to facilitate return to work also valued.
Liedberg 2002:382 other commitments – social relations
Cut off from social contacts made when previously employed and family relations are affected for those who remain in work and wrestle with fatigue and other symptoms of their illness at the end of the work day.
Liedberg 2002:382 other commitments – unpaid work
Home maintenance, raising children and looking after elderly relatives were all commitments these women had. Other aspects were commitments due to their spouses’ career, e.g. receiving guest at home. Women highlighted the difficulty of having enough energy for family and work. Spousal support valued as this allowed for sharing of household responsibilities. A need to prioritise responsibilities, with leisure activities often being neglected and the time used to rest instead.
Liedberg 2002:382 structural social factors – work restructuring
Restructuring in the labour market has meant changing roles and in some instances increased workload and hours of work. This creates instability, uncertainty about the future and increased pain as fibromyalgia patients struggle to cope with these pressures. Unable to rely on colleagues to help as they too are stretched. The attitude experienced at work is that if someone can’t manage the tasks or the environment has to be changed they shouldn’t be at work.
Lofgren 2006:337 social support
Described as: ‘To know that family members knew, supported and understood, gave strength and helped the informants keep the self-confidence to go on struggling’ (p. 452).
Lofgren 2006:337 constant struggle – being knowledgeable
Described this as ‘learning everything there is to know about fibromyalgia. They read the journals and the Internet and/or discussed with others. The knowledge gave them both self-esteem and respect for others similarly placed. It helped them find new ways to cope and encouraged them in thinking about their pain as not dangerous’ (p. 452).
Lofgren 2006:337 constant struggle
Every aspect of life changed and there would be no release.
Lofgren 2006:337 constant struggle – creative solutions
This concept was about ways in which sufferers managed everyday tasks and activities in a way which enabled them to complete them; in their own time. Planning and adapting activities assists in dealing with effects of illness. Found creative solutions to adapt day to make it more manageable.
Lofgren 2006:337 constant struggle – enjoying life
Making time for pleasures of every day. Conscious strategy to enjoy the small things in life (like putting a candle on the table).
Lofgren 2006:337 grieving
The sense of loss of a previous life but also the time when the process of grieving allows a turning point and new opportunities. Entailed working through loss of former self and body to reach a point of finding new ways to live life. Work through feelings of disappointment, self-blame, sadness, despair, regret. Grieving process important to rehabilitation.
Lofgren 2006:337 constant struggle – positive thinking
Making the best of life. Trying to be content and seeing the advantages of fibromyalgia for a more positive outlook on illness and its effects. Adapting one’s lifestyle as one gains improved understanding of the limits of the illness.
Lofgren 2006:337 constant struggle – setting limits
Described this as ‘It was important to set limits by prioritising and lowering one’s demands; it was also a matter of adapting life and oneself to one’s limitations. It was difficult to learn how to keep a slow pace and divide up strenuous activities; and how to stop in time. The informants used trial and error to learn their limits’ (p. 451).
Lofgren 2006:337 constant struggle – taking care of yourself
Striving for bodily balance; taking care of the balance of rest and exercise to reduce stressing the body.
Lofgren 2006:337 constant struggle – using pain as a guide
Become experts in body awareness. Increased awareness of body used to avoid worsening of pain when they were able. At other times they chose to accept an increase in pain. Explored pain without fear and chose to stop or ignore it. Responsiveness to pain signals enhanced by avoiding medication. Medication more useful if one was unable to stop activity at the point of pain.
Lofgren 2006:337 constant struggle – walking a tight-rope
Everything in life had to be planned with regard to their bodies; e.g. rest at weekend to be able to work. Describes the precariousness of being able to work and ways to balance/manage life to ensure they could work.
Madden 2006:339 seeking answers – biomedical ambiguity
Fibromyalgia symptoms wide-ranging and ambiguous; difficulty of locating specific symptoms with the illness. This led to confusion over definition of diagnosis; feeling that no one really knows what it is. ‘the diagnosis is seemingly adapted to suit the presentation of the illness, rather than the illness fitting within a predefined diagnostic framework’ (p. 2971).
Madden 2006:339 discovering a disease – fibromyalgia empty diagnosis
Participants felt that they had received an empty diagnosis: difficult to explain to others as not really understood by patient – ‘uncertainty based hitherto on a lack of knowledge was replaced by a new type of uncertainty, stemming from a diagnosis that conveyed no meaning, inspired little confidence, and created no real basis for understanding or coping with the illness experience’ (p. 2967).
Madden 2006:339 discovering a disease – identifying an organic being
Diagnosis perceived by patients as validation of suspicions of illness – ‘the diagnosis is the product of an interaction between the doctor and the individual’s body, and the person’s self is effectively excluded. The diagnosis also legitimates the person’s claim that the illness exists, thereby validating it to the wider social world’ (p. 2966).
Madden 2006:339 seeking answers – invisibility of fibromyalgia
Invisibility makes it difficult to explain to others – ‘informants interpreted information given to them as trivializing the illness, as it failed to acknowledge the nature and authenticity of the illness experience. Although such language may be intended to reassure the patient, in effect it is interpreted as invalidating the diagnosis’ (p. 2970).
Madden 2006:339 seeking answers – patterns of acceptance
Acceptance ranged from complete (did not acknowledge uncertainty of diagnosis); partial (continued to search for meaning in face of uncertainty. Clinical uncertainty allowed them to retain hope that uncertainty would be resolved); reject (fibromyalgia and an umbrella term with no meaning as an illness).
Madden 2006:339 seeking answers – resolving uncertainty
Health-care professionals seem to avoid discussion on meaning of the diagnosis. All new symptoms not investigated but put down to fibromyalgia – fibromyalgia gains master status. Expected to accept and move forward. ‘Informants assume a diagnosis to operate within a biomedical framework, where a diagnosis has a uniform meaning. However, FMS appears to have a continually changing definition, which is adapted by health professionals and support group literature to suit the presentation of the illness’ (p. 2968).
Madden 2006:339 seeking answers – why me?
Participants searched for reason or cause for their fibromyalgia, often looking for physical triggers e.g. a car accident. They need to make sense of their illness within their own lives. Many questions remained unanswered for patients.
Mannerkorpi 1999:340 giving up
Symptoms dominated every aspect of their lives which was now very limited. Could not plan or participate in life. Symptoms frightening and unmanageable. This despondency made some give up activities previously enjoyed and submit to the inevitable dominance of pain.
Mannerkorpi 1999:340 despair
Could not cope and found life task unmanageable. Lack of clinical findings increased despair. Felt changed in an incomprehensible and negative way. Sense of dejection and anguish.
Mannerkorpi 1999:340 adapting
Understanding of limitations imposed by pain and operating within these seemed to convey some sense of control over life despite presence of pain. Shared resources between work and social. Wanted to continue working as it brought fulfilment, but at some time ambivalent due to strain it brought. Expectations of others that they could not fulfil was a source of tension although this made them feel tougher (a sense of the SURVIVOR here).
Mannerkorpi 1999:340 struggling
Struggled to mobilise resources to manage pain and fatigue. Leisure activities reduced but work given higher priority and improved self-esteem. Many chose to be active even if they could not manage as felt activity was beneficial. For mothers, looking after children took priority (‘that’s what mums do’).
Mengshoel 2004:341 a new interpretation
Come to understand that diagnosis fibromyalgia had its limits and only a label for pain in muscles. No longer preoccupied with seeking biomedical explanation. They talked about strategies to end the pain which involved listening to their body and take things slowly when needed. Realise there is a close link with pain and life events. Cause of symptoms sought in everyday life. They described living life on a knife edge and they need to take precautions to stay healthy. Learned to slow down and assess situation to avoid relapse. New strategy of analysing life events.
Mengshoel 2004:341 ambivalence about diagnosis
Patients still want a biomedical diagnosis and are unhappy to have a diagnosis based on subjective criteria. Diagnosis of fibromyalgia a relief (as not a fatal disease) as well as a burden (as not rooted in fully treatable biological signs and viewed with much scepticism).
Mengshoel 2004:341 redefining obligations and goals
The women were very aware and determined women who could reflect on their experience and formulate a plan for recovery. They understood what they could change and what they couldn’t. Therefore they were able to achieve their goals in life by giving themselves more time to do things and giving more priority to their own needs. This developed their self-esteem and self-awareness.
Mengshoel 2004:341 resisting a sick role
Adapting to fibromyalgia can mean adopting a passive sick role. This conflicted with their view of themselves as active subjects with demanding social roles. There was a discrepancy between how they saw themselves and how others saw them. They felt there were conscientious with work whereas as others accused them, directly or indirectly, of being work shy and classed their health problem as fictitious. Recovery is about avoiding perceptions of ‘being sick’ and at the same time redefine what is essential goals and meaning for their lives. This ability to come OUT of sick role empowered recovery.
Mengshoel 2004:341 uncertainty of treatment
This study includes women who have recovered – restoration narratives. Viewed fibromyalgia as temporary and curable. Dissatisfaction over lack of effective treatment. Many treatments tried to find a cure. Explained disease and recovery through medicalised explanations e.g. pregnancy, penicillin. (Confirms Frank’s389 medical plot.)
Mengshoel 2004:341 unwilling to celebrate illness
The women actively resisted the sick role through participation in the fibromyalgia patients’ association and non-disclosure to employers, for example; did not want to ‘celebrate illness’ with other sufferers. Described it as a fellowship designed to endure a hopeless fate. Keep it quiet.
Paulson 2001:383 calm and difficult phases
The pain went in waves. In the calm phase, the men imagined a healthy future. They began to work harder and risked overstepping their capacity. In the difficult phase life turned darker when the rebound comes. This phase was when the pain was at its worst and most frightening. The difficult phases appear to get longer and longer over time. Although they become specialists in their own pain they cannot describe it to others to make them understand. Men earnestly affirm that pain is in their body; they use a metaphor to describe pain.
Paulson 2001:383 local to spread-out pain
Localised pain can spread out over all of body. Exercise helped only in early stages, and then it became too painful to use this strategy to relieve pain. Frustrating.
Paulson 2001:383 worrying and not worrying pain (concept not developed)
Single areas of the body that ached but were mobile were less worrying than a situation where multiple areas experienced intense pain.
Paulson 2002:346 striving to endure – living as normally as possible
Tried to maintain contact with family and friends during less painful periods and valued these moments. Tried not to express how they were feeling as did not wish to appear to be whiners. Role models of older men in family of being stoical; I can do it too. Sad for loss of family life but comforted themselves with the thought that things might have been worse.
Paulson 2002:346 body as obstruction – living day by day
Fluctuations in pain mean you have to live by the moment, not plan for future. Need to live life at your own speed so you can maintain participation.
Paulson 2002:346 being a different man – not being the same
No longer a whole man. Had lived life at high tempo, cheerful, kind, offered help. Not the same – could no longer manage multiple activities due to failing strength and inability to concentrate (compounded by feelings of sorrow for lost abilities; isolation when not treated like others at work; irritability that affected relationships; and suicidal thoughts due to these). Anger, often directed towards family. Over time came to accept and worry less what people felt.
Paulson 2002:346 being a different man – not understood
People might believe me but do not understand. I used to think that people with back pain were exaggerating. Realised why others found it difficult to understand. Sad that children could not understand why they couldn’t be a ‘normal’ dad.
Paulson 2002:346 striving to endure – nurturing hope
The men had come to terms with a future that may not be pain free. This seemed to help them to be hopeful for the future. Keep courage.
Paulson 2002:346 body as obstruction – reluctant body
Reluctant body – body in constant pain (whether active or still) that pervaded all over. Image of it as unresponsive to person’s desire for activity. Loss of capacity to play and work as before. Work capacity diminished, making men anxious about the financial implications.
Paulson 2002:346 striving to endure – search for alleviation
Felt lives could be different if pain went. Searched for ways to lessen pain and improve quality of life. May include medication, or trying to work through pain or even periods alone. Peace of mind found from gaining access to disability pensions as no longer had to explain invisible symptoms.
Paulson 2002:347 feeling hopeful
Still hopeful of a cure even after years of trying various medical and non-medical treatments. Relieved when other bodily discomforts diagnosed as symptom of illness.
Paulson 2002:347 feeling neglected
This seemed to encapsulate the feelings of not being believed by health professionals and treated disrespectfully. Men felt that over time doctors lost interest in them as not a high profile condition (and no cure found). Felt doctors thought they were exaggerating their condition. Aware or stigma of being ‘lazy’ associated with non-specific pain. Also too many different professionals, so difficult to establish a relationship or sustain quality of care.
Paulson 2002:347 feeling no recovery
Specialist clinic gave strategies to relieve pain along with awareness that there was no cure.
Paulson 2002:347 guinea pig
About wanting thorough examination but not wishing so many different ‘trial and error’ treatments. Men felt that they were being subjected to a range of treatments with no benefits. Also dissatisfied with physicians prescribing medication without discussing other treatment options.
Paulson 2002:347 not being a whiner
Most of the men seemed to have remained with pain until a point of (near) collapse before seeking medical help (often persuaded by their partner) as they did not wish to appear as whiners. Even when sick leave was recommended by physician and allowed by employer the men insisted on getting back to work as soon as possible. Were aware of lack of credibility of fibromyalgia and were reluctant to divulge all symptoms or anxiety there were causing.
Raheim 2006:348 typologies – ambivalence
Ambivalence – not quite managing to keep control through day; mechanisms breaking down; unable to ask for the help needed. A constant balance between taking and losing control. Finding ways to gain control gives hope but this is taken away by a body which lets one down. Asking for help and explaining pain is difficult.
Raheim 2006:348 typologies – coping
A dialogue between the body and self creates a caring relationship despite its treachery. Dialogue with partner and family about pain and resulting needs integral to adjustment and gaining the support of others. Working with the body and not against.
Raheim 2006:348 theoretical interpretation – lived time and space
This captures both the trapped dimensions of being caught in the rhythms of a life with no structure (an endless here and now) and one of reaching beyond this enclosure to an outside world (establishing a structure or routine to deal with unwilling body).
Raheim 2006:348 theoretical interpretation – lived body
There now exists a dialogue between self and body which is either positive or negative.
impossible enemy – antagonistic (parasitic) dualism; homeless in body
friendly dialogue – symbiotic dualism; at home in my body.
Participants describe dualism in body in pain with a distinction between self and body. No longer unconscious of the body but more aware of it, while paradoxically feeling ‘homeless in one’s own body’ and wanting to escape from it. Other patients do not report feelings of disintegration, but rather view the body in pain as a ‘problematic friend’ with which they can cope.
Raheim 2006:348 theoretical interpretation – lived relations
Chronic pain alters the relationships we have and can either destroy (detached/dissociated relationship/destroy) or allow us to build new relationships (mutuality/reciprocal relationship/build up) as we redefine who we are.
Raheim 2006:348 typologies – powerlessness
At will of the painful body: feeling powerless to control body and carry through daily routines or plans. Feels misunderstood and unsupported by husband, with additional feelings of guilt in being unable to meet needs of family or work. Feels hopeless at inability to prevent growing distance between self and family.
Raymond 2000:349 establishing coping strategies
Understanding illness enabled accommodation. Gathering information was an important step. Patients also reported a perceived need to be allowed to mourn loss of previous capabilities. Came to recognise the individual nature of coping strategies (what works for you). Person also has to learn their own limits by trial and error. Accepting and acknowledging limitations enabled coping strategies (e.g. establishing routines) BUT felt loss/grief over former self. Useful to meet others with fibromyalgia at first (I am not the only one) but over time this lost its value.
Raymond 2000:349 experiencing symptoms
Women felt some specific event (and mostly stress) precipitated illness.
Raymond 2000:349 seeking a diagnosis
Achieving a diagnosis challenging – everyone says I am in perfect health. Disbelieved by health-care professionals. Lack of understanding and acknowledgement of symptoms by those close to them. It is an invisible illness. This results in social isolation for fear of rejection. Relief at getting a diagnosis was a springboard to gathering information yet short lived due to concern over future.
Sallinen 2010:351 confusion
This describes a search for diagnosis and the challenge of validity in dealing with health-care professional disbelief. Tension: knowing something is wrong but not what it is. Dr keeps saying nothing wrong. Invisibility an obstacle for being seen as ‘real’ patient.
Sallinen 2010:351 coping with fluctuating symptoms
Process of learning to live with fluctuating symptoms but adopting strategies of prioritising, pacing and work adjustments. Others experienced release from work an amnesty, as it allowed them to break down tasks and listen to their body. Able to maintain role with some compromises. Coping was expressed as an acceptable goal of recovery, thus recognizing that full remission might not be possible.
Sallinen 2010:351 being over the edge
Work saps resources until no reserve. Forced out of work by sheer exhaustion of struggling to work. Negative events in personal life (divorce, death of relative, etc.) can sap remaining strength and force decision to leave work. Resources run dry.
Sallinen 2010:351 being in-between
Refers to the process of moving back and forth between full work ability and work disability.
a. working in poor health and exceeding capacity
b. forced out of work into long term sick yet access to benefits denied = stress and financial difficulties.
Sallinen 2011:352 experiential knowledge
Fibromyalgia experienced as an ‘unreal disease’. This theme captures the thirst for knowledge about their condition as experienced by others but also the scientific knowledge made available through a specialist centre. Learning from the practical experience of others with fibromyalgia was an important part of changing this perception. Helped them to see fibromyalgia as something ‘real’ that was experienced on a daily basis by others who could provide practical knowledge.
Sallinen 2011:352 permission to talk
Peer encounters often a turning point after wrestling with disbelief for a long time. Had kept feelings to themselves so as not to jeopardise existing relationships. Now had ‘permission to talk’ with genuinely interested peers. It captures the relief and joy of feeling free to unburden the experiences of pain with those who did not judge.
Sallinen 2011:352 reciprocity
Describes the strong felt need to give back the comfort and support derived from others but at the same time recognising that for some sufferers their lives demanded too much and they were not able to provide this. Receiving and giving support, comfort and understanding important. The feeling of being an outsider replaced by feeling part of a group and not alone. Able to share with peers with a similar illness trajectory and life events. Sharing of experiences often based on desire for this to help others. Value of group reciprocity diminished over time as many too ill or too well to benefit from this.
Sallinen 2011:352 self-evaluation through comparison
Group interaction allows for comparisons that can change one’s perspective of one’s life as one is able to walk in another person’s shoes albeit for just a little while (there is always folk worse than you). Compared themselves favourably to those with diseases (e.g. rheumatoid arthritis or depression). Saw themselves as ‘mentally strong’ compared to others. Seeing those with worse condition motivated them to take care of themselves.
Schaefer 2005:384 secrecy makes it easier
A certain amount of secrecy makes it easier to live with the illness. Intolerance of society toward people with illness and disability, and in particular fibromyalgia which is difficult to explain. Secrecy from family was more about not wanting to be a burden.
Schaefer 2005:384 support from self and spiritual connections
This emphasis how many women found inner strength through reflection and their own personal approaches to help themselves. It often appeared to follow on from a period of anger or hopeless about their condition.
Schaefer 2005:384 accused of taking a free ride
Being accused of ‘taking a free ride’ angers them. The illness often led to disbelief in others.
Schaefer 2005:384 camouflaging with medications
Medication camouflaged pain and made women overdo things. Weighing the effect of the medicines and the degree of symptom reduction, several of the women decided they might feel better off the medicines, so they stopped taking them. Sought out alternatives.
Schaefer 2005:384 becoming a self-advocate
Being disbelieved or not given a diagnosis was commonly described. Once they had a diagnosis they sought out information from the internet, other sufferers and gained strength from the information gleaned.
Soderberg 1999:359 loss of freedom – body in pain
Pain pervades the entire body. Difficult to describe (patients often alluding to metaphors for assistance).
Soderberg 1999:359 loss of freedom – changed everyday life
Life more regulated; difficult to plan ahead or be spontaneous. Often dependant on others. Missed their old lives. Social life restricted.
Soderberg 1999:359 threat to integrity – credibility and invisibility
Lack of belief from others; not taken seriously; others felt it imaginary or psychological. Naming the illness meant that it existed. If you don’t look sick you are not sick. Diagnosis and participation in research increased credibility. Felt lucky to be believed. Lack of belief a threat to their human dignity, thus depriving opportunity to be a whole human being. Engagement implies ‘fraternity’ i.e. treat someone like your brother.
Soderberg 1999:359 loss of freedom – economic restrictions
Economic loss due to inability to work; limited possibilities for alternate therapies.
Soderberg 1999:359 loss of freedom – fatigue
Absolute and overwhelming fatigue and loss of energy. Impacts on ability to undertake daily tasks.
Soderberg 1999:359 threat to integrity – lack of knowledge and negative attitude
Participants felt that dissemination of knowledge is important for social awareness of condition, and dissolution of negative social attitudes. Negative attitudes violated patients’ sense of respect as human beings. Threatened their integrity.
Soderberg 1999:359 struggle for understanding – seeking explanations
To be stricken with illness without understanding why is the classic dilemma of Job. An explanation does more than identify biological process. Explanation and understanding give relief. Diagnosis positive because you know the illness is not grave. Also makes unbelievable acceptable. Also makes it easier to accept and know you are not alone. Understanding through experience gives relief. ‘An explanation can contribute to living a life of dignity’ (p. 581).
Soderberg 1999:359 struggle for understanding – seeking relief and planning life
Tried many treatments in struggle to adapt to manage life. Reliant on a process of trial and error linked to medical and alternative treatments, but important to managing of everyday life.
Soderberg 2001:360 learning to live with fibromyalgia
Learnt to live with restrictions and take your time. Changes that the women struggle to make go mostly unnoticed and unappreciated by others.
Soderberg 2001:360 transitions – social life
No longer had energy to meet socially. Big impact on social life. Friends don’t necessarily understand. A sense of sharing with others who are also ill. Illness had made them more tolerant of others. Socially people commented on how good they looked.
Soderberg 2001:360 transitions – family life
Relationship with husband and children altered. Women’s family lives become more passive. Forced to ask for help. Some family did not understand the invisible alteration. Children have to help more in the home. Guilt about now helping older relatives. Change in intimate relationships.
Soderberg 2001:360 transitions – working life
Unable to sustain work. Lack of understanding form colleagues led to feeling of alienation. (One example of boss who’ tailor made’ job to suit). Leaving work had impact on self-value. A sense of sorrow about having to make these changes. Some changed jobs or did job retraining.
Soderberg 2001:360 transitions – daily life
Daily life disrupted as ‘the spirit is willing but the flesh is weak’ and there is diminished strength to undertake previous activities. Monotonous lifestyle. Life more passive. Unable to plan day or future. Most getting used to this new way of living but also angry and bitter, though generally hopeful for a cure in the future.
Sturge-Jacobs 2002:361 dealing with flare-ups
Flare-ups are fluctuating, unpredictable and uncontrollable. Characterised by worsening of physical and cognitive impairments of fibromyalgia.
Sturge-Jacobs 2002:361 fatigue invisible foe
Fatigue engulfing, insurmountable and overwhelming, insidious, unseen and uncontrollable. Affects all aspects of life. Activities had to be avoided or prioritised. Fear of becoming a burden on friends and family (i.e. non-reciprocal relationships). Always receiving help and not giving.
Sturge-Jacobs 2002:361 living within boundaries
Seeking some measure of control over limitations imposed by illness through acceptance that there are limitations, and diverting energies into positive activities rather than complaining. This acknowledgment was vital to their being in control of the condition, rather than the condition controlling them.
Sturge-Jacobs 2002:361 longing for a normal life
Conflict between the ‘normal’ exterior versus inner pain. Took great efforts to retain normalcy of life. Participants make a conscious effort to convey to others that their lives and that of their families are no different than other families not dealing with a chronic illness. Need to be seen as a person not just ‘a disease’; don’t want others to think of them as different to their normal self [am still the same person]. This linked to self-worth and self-value.
Sturge-Jacobs 2002:361 pain constant presence
Constant agonizing nature of pain. Pain continually present and limited ability to do things. However as not visible was not understood/believed by others. Lacked validity by health-care professional and significant others as no pathology. Pain difficult to control and left women feeling powerless. Resulted in social isolation as well as loss of intimate relationships. Pain limits intimacy and, hence, evokes a sense of withdrawal and social disruption. Also affected ‘normal’ gendered social roles (mother, wife, grandmother, friend). Undermines self-worth.
Sturge-Jacobs 2002:361 power of diagnosis
Fruitless visits to medics in constant quest for diagnosis. Dismissed as psychological illness but women continued to seek diagnosis. Often endures inappropriate treatment and labels of their pain being ‘all in the head’.
Sturge-Jacobs 2002:361 thinking in a fog
Brain ‘in a fog’; unable to concentrate or think clearly. Difficulties with problem solving, abstract thinking, and the inability to make appropriate judgement calls or on-the-spot decisions were areas of concern for all participants. Mind and body ‘constantly at odds’. Sense of being in a dark place. Could affect ability to continue meaningful employment.
Undeland 2007:366 diagnostic uncertainty
Patients search for a diagnosis impeded by GPs reluctance to use a diagnosis of fibromyalgia. Patients saw doctors hoping for relief and explanations but had difficulty explaining their symptoms. Several participants described doctors who were hesitant or dismissive, claiming fibromyalgia was a fashion tag.
Undeland 2007:366 relief of name but diagnosis becomes a burden
Relief at diagnosis (not terminal and I have GOT something) followed by conflict (what is the cause, no cure, fear of stigma, meant inevitable disability, disbelief by others, or not taken seriously ‘just a bit of fibromyalgia’). Diagnosis brought no understanding or appreciation. Despair and sorrow when they realised the impact of fibromyalgia on their lives. This process was lonely. Some people expected improvement after diagnosis and it was difficult for the women to explain the lack of progress. Some women remarked that their doctors felt that fibromyalgia was just a word associated with hysterical women. This turmoil leads some to continue to search for a different diagnosis.
Appendix 4 Tables showing team memos and second-order constructs supporting each conceptual category
Team memos and second-order constructs for ‘alienated versus integrated body’
| Team memos describing
category: Pain external to me; self and body opposing; pain not me; still me but not me; body external to me; self vs. body; pain threatens me; pain taking ownership of body In some cases a new self with pain emerges; body alien Pain brings an awareness of the body as a foreign alien (like Leder’s dys-appearance396) |
|
| Collaborative translations supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Osborn 2008:344 fearfulness of pain Rhodes 1999:350 anatomical body Johansson 1999:334 bodily presentations Crowe 2010:323 externalisation of the body Lundberg 2007:338 failed adaptation Osborn 2006:343 living with body separate from self Snelgrove 2009:358 crucial nature of pain – body/self/pain as a threat Afrell 2007:372 acceptance typologies – rejecting the body |
Raheim 2006:348 theoretical interpretation – lived
body Raheim 2006:348 typologies – powerlessness Paulson 2002:346 body as obstruction – reluctant body Sturge-Jacobs 2002:361 thinking in a fog Raheim 2006:348 typologies – coping |
Team memos and second-order constructs for ‘negotiating an unrelenting body’
| Team memos describing
category: Unrelenting pain a constant struggle; pain constant, overwhelming, all pervading; drains my resources Described overwhelming sense of loss/sorrow and emotional impact of this (depression, anxiety, despair, hopeless, helpless, powerless) |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Hunhammar 2009:331 striving to master variable pain –
disruptions to daily life Walker 2006:368 loss – ability and role Walker 2006:368 loss – hope Snelgrove 2009:358 crucial nature of pain – physicality Bair 2009:314 barriers to self-management – stress and depression |
Lachapelle 2008:335 barriers to acceptance – unrelenting
pain and fatigue Soderberg 1999:359 loss of freedom – body in pain Lofgren 2006:337 constant struggle Gustaffson 2004:327 shame to respect – negative factors Arnold 2008:373 pain Sturge-Jacobs 2002:361 pain constant presence Lempp 2009:381 change in health identity – physical problems Paulson 2002:346 body as obstruction – reluctant body |
| Emotional impact | |
| Arnold 2008:373 emotional impact Kelley 1997:380 loss Lempp 2009:381 change in health identity – mental distress Gustaffson 2004:327 shame to respect – negative factors Hallberg 2000:329 preoccupied with pain – pain communication Gullacksen 2004:377 stage 2 – sorrow and loss Hallberg 1998:328 psychosocial vulnerability – traumatic life history Mannerkorpi 1999:340 despair Soderberg 2001:360 transitions – daily life |
|
| Fatigue | |
| Lachapelle 2008:335 barriers to acceptance – unrelenting
pain and fatigue Soderberg 1999:359 loss of freedom – fatigue Arnold 2008:373 fatigue Sturge-Jacobs 2002:361 fatigue invisible foe Hellström 1999:378 managing threatened failure Lempp 2009:381 change in health identity – physical problems Liedberg 2002:382 working conditions – physical work Arnold 2008:373 sleep |
|
| Fibrofog | |
| Arnold 2008:373 cognitive impairment Lempp 2009:381 change in health identity – mental distress Lempp 2009:381 change in health identity – physical problems Sturge-Jacobs 2002:361 thinking in a fog |
|
Team memos and second-order constructs for ‘new me not the real me’
| Team memos describing
category: Describes loss of self-identity and impact on self-esteem, self-image and confidence Struggle for old self to win; no longer whole self [old self is the real one] Grief/loss over old self; grief important to moving on? Internal conflict; good vs. bad; before vs. now Pain has altered the essence of me; good/bad me; old/new me; past to present self Paradox – need to prevent erosion of self but am irreparably altered Paradox – fight but also learn to live with (gracefully) = powerful rhetoric; strong language – will not beat me Paradox – if I am not altered am I ill (important in adversarial system where have to keep showing how I am altered) |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Satink 2004:354 aiming to be normal Crowe 2010:323 alteration to self Osborn 1999:342 comparing this self with other selves Toye 2012:365 restoring hope – constructing acceptable self-identity Smith 2007:66 continuum or trajectory Smith 2007:66 directing it at others Snelgrove 2009:358 crucial nature of pain – emotional response Lundberg 2007:338 failed adaptation Skuladottir 2011:355 quest for normalcy Toye 2010:363 I am still me but not me Lundberg 2007:338 identity restoration Campbell 2007:315 importance of self Werner 2004:371 I have always been so strong Osborn 2006:343 living with body separate from self Walker 2006:368 loss – identity Smith 2007:66 negative impact on self Werner 2003:369 for better or worse – sorrow at loss Harding 2005:330 spoiled identity |
Gullacksen 2004:377 stage 3 – a new course of
life Lachapelle 2008:335 barriers to acceptance – fight to be normal Soderberg 1999:359 loss of freedom – changed everyday life Hellström 1999:378 demands on self Raymond 2000:349 establishing coping strategies Lofgren 2006:337 grieving Gullacksen 2004:377 stage 2 – losing oneself Liedberg 2002:382 values and norms – meaning of work Paulson 2002:346 being a different man – not being the same Lachapelle 2008:335 barriers to acceptance – fight to be normal Mengshoel 2004:341 resisting a sick role Gullacksen 2004:377 stage 2 – sorrow and loss Gullacksen 2004:377 stage 1 – struggling to restore life Arnold 2008:373 function and quality of life – work |
Team memos and second-order constructs for ‘isolated not connected’
| Team memos describing
category: Loss of reciprocal roles; negativity/low mood/anger contaminated relationships I no longer am a nice person – lasting change. Changing social roles and status; lost social roles Cut off from work; the ‘normal thing’ to do Exacerbated by invisibility/lack of belief, ambiguous diagnosis; fluctuating symptoms A lonely process; exacerbated for need to hide illness or appear normal (living a lie?) |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Bair 2009:314
facilitators – support of others Satink 2004:354 aiming to control and reduce Slade 2009:357 stigma – community friends family Campbell 2008:316 dependence and social withdrawal Smith 2007:66 directing it at others Snelgrove 2009:358 crucial nature of pain – emotional response Werner 2003:369 why can’t she just do it? – friends De Souza 2011:376 children and parents Johansson 1999:334 consequences for activity Campbell 2008:316 dependence and social withdrawal Sanders 2002:353 disrupted biographies Skuladottir 2011:355 quest for normalcy – need to participate Werner 2003:369 why can’t she just do it? – family Johansson 1997:333 family considerations Campbell 2007:315 importance of self Walker 2006:368 loss – ability and role Snelgrove 2009:358 crucial nature of pain – loss of social role Skuladottir 2011:355 quest for support caring and connection – need for practical support Skuladottir 2011:355 quest for support caring and connection – need someone who cares Skuladottir 2011:355 quest for support caring and connection – need to be connected and care for someone Osborn 1999:342 not being believed Walker 2006:368 loss – relationships De Souza 2011:376 spouses and partners Holloway 2007:379 stigma by significant others Walker 2006:368 loss – financial Bair 2009:314 barriers to self-management – lack of social support |
Lachapelle 2008:335 barriers to acceptance – support and
belief of others Soderberg 1999:359 loss of freedom – changed everyday life Liedberg 2002:382 structural social factors – commuting de Vries 2011:324 consequences of staying at work Arnold 2008:373 emotional impact Lachapelle 2008:335 facilitators to acceptance – perceived social support Arnold 2008:373 function and quality of life – family Hallberg 1998:328 maintaining forces – family support Sturge-Jacobs 2002:361 fatigue invisible foe Lempp 2009:381 change in health identity – impact on social life Gullacksen 2004:377 stage 2 – leaving the sick role Raheim 2006:348 theoretical interpretation – lived relations Cunningham 2006:375 living with the symptoms of fibromyalgia Paulson 2002:346 being a different man – not being the same Paulson 2002:346 being a different man – not understood Hallberg 2000:329 preoccupied with pain – pain communication Sturge-Jacobs 2002:361 pain constant presence Arnold 2008:373 function and quality of life – partners Raheim 2006:348 typologies – powerlessness Raymond 2000:349 seeking a diagnosis Gullacksen 2004:377 stage 1 – self-deception Kelley 1997:380 self-esteem Liedberg 2002:382 other commitments – social relations Lofgren 2006:337 social support Mannerkorpi 1999:340 struggling Soderberg 2001:360 transitions – family life Soderberg 2001:360 transitions – social life Liedberg 2002:382 other commitments – unpaid work de Vries 2011:324 motivators for staying at work – work as therapy de Vries 2011:324 motivators for staying at work – work as value |
Team memos and second-order constructs for ‘unpredictable now’
| Team memos describing
category: Live with uncertainly of fluctuating symptoms; living life on a knife edge; constant need to take precautions Good and bad days cause uncertainty about future; body is unpredictable; can’t rely on it; inability to rely on the body damages self-image Difficult to plan ahead or be spontaneous; leads to isolation; have to live by the moment Pain shrinks lived time and space; hold onto safe routines and don’t think of future Don’t plan ahead; never ending here and now; routines gone; structure of life broken down; living here and now New rhythm of daily life – space of action increased; rhythm of life has changed and is related to state of the body; routines and rituals now required |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Osborn 1999:342 comparing this self with other
selves Coole 2010:319 difficulty coping with flare-ups Snelgrove 2009:358 crucial nature of pain – loss of spontaneity Crowe 2010:323 need for vigilance Patel 2007:345 uncertainty – pain and health Snelgrove 2009:358 crucial nature of pain – physicality Hunhammar 2009:331 striving to master variable pain Patel 2007:345 uncertainty – (future) Crowe 2010:323 unpredictability |
Gullacksen 2004:377 stage 3 – maintenance (a new
attitude) Mengshoel 2004:341 a new interpretation Hellström 1999:378 avoiding thoughts of future Paulson 2001:383 calm and difficult phases Lempp 2009:381 change in health identity Soderberg 1999:359 loss of freedom – changed everyday life Sturge-Jacobs 2002:361 dealing with flare-ups Lempp 2009:381 change in health identity – impact on social life Raheim 2006:348 theoretical interpretation – lived time and space Paulson 2002:346 body as obstruction – living day by day Cunningham 2006:375 living with the symptoms of fibromyalgia Gullacksen 2004:377 stage 2 – losing oneself Hallberg 1998:328 psychosocial vulnerability – pessimistic life view Raheim 2006:348 typologies – powerlessness Arnold 2008:373 function and quality of life – social life Soderberg 2001:360 transitions – daily life Hellström 1999:378 unpredictable, invisible, incapacitating Lofgren 2006:337 constant struggle – walking a tightrope |
Team memos and second-order constructs for ‘unpredictable future’
| Team memos describing
category: On balance a negative outlook for future; future unpredictable Unable to plan for future (dys-appearance of future, i.e. foregrounding – bleak to dwell on what is to come; life’s great paradox) Turning towards future can cause anxiety; can have hope for cure at same time as not being driven by finding one Clinical uncertainty allows a degree of hope?339 Hope for improvement in pain and symptoms not incompatible with acceptance of current state |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Coole 2010:319 concerns about future at
work Skuladottir 2011:355 quest for normalcy Campbell 2007:315 future and past Afrell 2007:372 acceptance typologies – hope and resignation Walker 2006:368 loss – hope Toye 2012:364 being fobbed off – nothing else we can do Snelgrove 2009:358 crucial nature of pain – physicality Afrell 2007:372 acceptance typologies – rejecting the body Osborn 1999:342 comparing this self with other selves |
Paulson 2002:347 feeling hopeful Lachapelle 2008:335 meaning of acceptance Paulson 2002:346 striving to endure – nurturing hope Madden 2006:339 seeking answers – patterns of acceptance Soderberg 2001:360 transitions – daily life Hallberg 1998:328 psychosocial vulnerability – pessimistic life view |
Team memos and second-order constructs for ‘alienated from the dominant medical model’
| Team memos describing
category: Need to find a cause; medical model doesn’t fit – failed the test; need a diagnosis – don’t want one/don’t have one It is in not in my body – so it is in my mind. I need to do something – there is nothing I can do because I haven’t ‘got anything’ wrong with me I have failed the medical test; diagnosis and medical test give credibility; seek fix/cure Medical model has implication that something should be done; need medical cause to be credible Can’t see pain so not believed; aligned/alienated – fail or pass medical test – powerful language Paradox – need a diagnosis although don’t want to be ill Paradox – common sense shows me that psychosocial has an impact on how I feel Fibromyalgia Fibromyalgia experienced as ‘unreal’; uncertainty replaced by a different uncertainty Diagnosis uncertain and often not believed. Some saw fibromyalgia as a limited diagnosis (pain in muscles) For some a key turning point (a springboard to knowledge) Problem that diagnosis of fibromyalgia gains master status; delays in diagnosis damaging as required for credibility |
|
| Second-order constructs supporting category | |
|---|---|
| MSK – alienated from medical model | Fibromyalgia – ambivalent medical diagnosis |
| Walker 1999:367 being in the system – all in the
mind Rhodes 1999:350 anatomical body Allegretti 2010:313 biomedical vs. biopsychosocial Snelgrove 2009:358 maintaining integrity – cause of pain Walker 1999:367 being in the system – feeling insignificant Campbell 2007:315 getting something done Allegretti 2010:313 importance of diagnosis Skuladottir 2011:355 quest to learn to live with pain – need diagnosis Toye 2012:364 being fobbed off – I didn’t get a thorough examination Snelgrove 2009:358 maintaining integrity – not being believed Walker 1999:367 being in the system – passing the medical test Slade 2009:357 stigma – pathology-driven validation Slade 2009:357 stigma – sickness vs. wellness model Dickson 2003:325 reconstructing meaning of pain – suffering with pain Campbell 2007:315 unmet expectations |
Undeland 2007:366 relief of name but diagnosis becomes a
burden Mengshoel 2004:341 a new interpretation Mengshoel 2004:341 ambivalence about diagnosis Lachapelle 2008:335 barriers to acceptance – support and belief of others Madden 2006:339 seeking answers – biomedical ambiguity Gullacksen 2004:377 stage 1 – confirmation by health-care professional Sallinen 2010:351 confusion Soderberg 1999:359 threat to integrity – credibility and invisibility Gullacksen 2004:377 stage 2 – defining problems Undeland 2007:366 diagnostic uncertainty Madden 2006:339 discovering a disease – fibromyalgia empty diagnosis Sallinen 2011:352 experiential knowledge Lachapelle 2008:335 facilitators to acceptance – self-management education Paulson 2002:347 feeling hopeful Kelley 1997:380 feeling understood Madden 2006:339 discovering a disease – identifying an organic being Madden 2006:339 seeking answers – invisibility of fibromyalgia Madden 2006:339 seeking answers – patterns of acceptance Hallberg 1998:328 maintaining forces – professional care Lachapelle 2008:335 process of acceptance – realising need for help, getting diagnosis, realising no cure, it could be worse Madden 2006:339 seeking answers – resolving uncertainty Soderberg 1999:359 struggle for understanding – seeking explanations Hellström 1999:378 search for confirmations as ill Raymond 2000:349 seeking a diagnosis |
Team memos and second-order constructs for ‘nobody believes me’
| Team memos describing
category: Perceived as malinger or ‘all in my head’; social stigma – seen as an excuse for non-participation and inadequacy Being fobbed off interpreted as not being believed. You look so well! Can’t be ill Variability of conditions threatens credibility; trying to meet expectations of social role [and being successful!] threatens credibility; exacerbated by media reports of fraud; self-doubt |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Family and friends don’t believe me | |
| Slade 2009:357 stigma – community friends
family Werner 2003:369 why can’t she just do it? –friends Werner 2003:370 I don’t give up unless I have to Toye 2010:363 loss of credibility Snelgrove 2009:358 maintaining integrity – not being believed Osborn 1999:342 not being believed Johansson 1999:334 self-perception Holloway 2007:379 stigma by significant others Holloway 2007:379 stigma in everyday life |
Lachapelle 2008:335 barriers to acceptance – support and
belief of others Soderberg 1999:359 threat to integrity – credibility and invisibility Kelley 1997:380 feeling understood Soderberg 1999:359 threat to integrity – lack of knowledge and negative attitude Sturge-Jacobs 2002:361 pain constant presence Hellström 1999:378 search for a cause Raymond 2000:349 seeking a diagnosis |
| Health-care professionals don’t believe me | |
| Walker 1999:367 being in the system – all in the
mind Johansson 1996:332 experience of distrust Walker 1999:367 being in the system – feeling insignificant Werner 2003:370 I don’t give up unless I have to Toye 2010:363 loss of credibility Toye 2012:364 being fobbed off – I didn’t get a thorough examination Holloway 2007:379 stigmatisation in health-care systems Campbell 2007:315 unmet expectations |
Gullacksen 2004:377 stage 1 – confirmation by
health-care professional Sallinen 2010:351 confusion Paulson 2002:347 feeling neglected Sturge-Jacobs 2002:361 power of diagnosis Hallberg 1998:328 maintaining forces – professional care Raymond 2000:349 seeking a diagnosis Gustaffson 2004:327 shame to respect Holloway 2007:379 stigmatisation in health-care systems |
Team memos and second-order constructs for ‘striving for an alternative explanation’
| Team memos describing
category: Realise link between pain and life events; seek cause in everyday life; affirmed pain in body not mind Looked for specific events as trigger; looked for meaning and cause in life Used medicalised explanations (pregnancy, penicillin) Need to make sense of illness in own life |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Toye 2012:365
restoring hope – constructing an acceptable
explanatory model Snelgrove 2009:358 maintaining integrity – cause of pain Toye 2010:363 could I be imagining this Johansson 1999:334 explanations Coole 2010:319 justifying back pain Harding 2005:330 making sense of pain Dickson 2003:325 deconstructing meaning of pain – managing and tolerating Sanders 2002:353 normal aspect of biography Osborn 1999:342 searching for an explanation Dickson 2003:325 reconstructing meaning of pain – stumbling along with pain |
Mengshoel 2004:341 a new interpretation Raymond 2000:349 experiencing symptoms Hellström 1999:378 onset Soderberg 1999:359 struggle for understanding – seeking explanations Hellström 1999:378 search for a cause Mengshoel 2004:341 uncertainty of treatment Madden 2006:339 seeking answers – why me? |
Team memos and second-order constructs for ‘ambivalent relationship with health care’
| Team memos describing
category: Don’t trust system; conspiracy – lack of faith Conflicts, expectations; lack of fit with system Conflicts with treatment; tension faith/no faith. In them or their medicines; loss of faith but still have hope If I don’t get better I am blamed, getting nowhere; trapped in the medical system Like a shuttlecock; at the mercy of it. Failing me but I am compelled to be in it (gives hope) Consumes my life but is failing me; but continue to value it Paradox; faith in it/no faith in it; expectation to be active/self-manage but trapped Reticent but compelled to engage; continuous battle Battle; conflict; struggle; doctor knows best but GP not a specialist You know best but you don’t know best; who does know best; perhaps no cure at all Fibromyalgia GP dismissive of fibromyalgia label or reluctant to give it; not believed; dismissed as psychological Used as a guinea pig – feel doctor doesn’t know what it is or what to do |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Walker 1999:367 being in the system – all in the
mind Campbell 2007:315 back to square one Johansson 1996:332 strategies to gain self-respect – condemning Slade 2009:356 engagement with health care – continuity and connectedness Teh 2009:362 participation in pain treatment – don’t want to be harmed Walker 1999:367 being in the system – feeling insignificant Walker 1999:367 being in the system – getting nowhere Werner 2003:369 why can’t she just do it? – health-care professionals Patel 2007:345 health-care barriers Teh 2009:362 participation in pain treatment – involved in decisions Walker 1999:367 being in the system – losing faith Johansson 1996:332 strategies to gain self-respect – mystifying Toye 2012:364 you are just a GP – not leaving until I see a specialist Toye 2012:364 being fobbed off – nothing else we can do Cooper 2008:322 organisation Walker 1999:367 being in the system – passing the medical test Johansson 1996:332 strategies to get doctor’s attention Patel 2007:345 psychological barriers Cook 2000:317 relationship with health-care professional Snelgrove 2009:358 managing the pain – relationship with health-care professionals Liddle 2007:336 treatment received Johansson 1996:332 strategies to get doctor’s attention – somatising Walker 1999:367 being in the system – the medical process Campbell 2007:315 unmet expectations Harding 2005:330 unmet expectations Walker 1999:367 being in the system – waiting Toye 2012:364 who is the back expert Toye 2012:364 you are just a GP – you are not a back expert Werner 2003:370 you have to tread rather softly Walker 1999:367 being in the system – your life is not your own |
Undeland 2007:366 diagnostic uncertainty Paulson 2002:347 guinea pig Lempp 2009:381 quality of care – hospital specialists Hallberg 1998:328 psychosocial vulnerability – pessimistic life view Sturge-Jacobs 2002:361 power of diagnosis Hallberg 1998:328 maintaining forces – professional care de Vries 2011:324 success factors (work) – use of health-care services |
Team memos and second-order constructs for ‘medication’
| Team memos describing
category: Medication demonstrates ambivalence to health-care system |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Allegretti 2010:313 goal to reduce pain Bair 2009:314 barriers to self-management – GP just describes painkillers Toye 2012:364 being fobbed off – just take the tablets Snelgrove 2009:358 managing the pain – medication dependency Skuladottir 2011:355 quest to learn to live with pain – need for effective treatment Snelgrove 2009:358 managing the pain – relationship with health-care professionals Coole 2010:319 reluctance to use meds Liddle 2007:336 treatment received Campbell 2008:316 striving for self-management Crowe 2010:374 taking medication Teh 2009:362 participation in pain treatment – working outside health-care professional relationship |
de Vries 2011:324 success factors (work) – coping with
pain Lempp 2009:381 quality of care – ethnicity Lempp 2009:381 quality of care – GPs Paulson 2002:347 guinea pig Lempp 2009:381 quality of care – interventions Schaefer 2005:384 camouflaging with medications |
Team memos and second-order constructs for ‘value me as a person, don’t just treat my body’
| Team memos describing
category: Understand the impact that pain has on me and my life: believe that it is not my fault Humankind of believing valued as a person had an impact on experience Doctor needs to bear witness to pain; experience of not being believed, listened to, given time, taken seriously Let me know what you are doing |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Osborn 2008:344 containing fear through social
connection Toye 2012:364 being fobbed off Cooper 2008:322 communication Johansson 1996:332 experience of distrust Johansson 1996:332 expectations of a ‘creditable’ consultation Slade 2009:356 listen to me – explain it so I can understand Walker 1999:367 being in the system – feeling insignificant Steen 2001:385 group leaders Patel 2007:345 health-care barriers Toye 2012:364 being fobbed off – I see buckets of people like you Teh 2009:362 importance of relationship with health-care professional Toye 2012:364 being fobbed off – I just want to be heard Walker 1999:367 being in the system – losing faith Skuladottir 2011:355 quest for support caring and connection – need for health-care professional Skuladottir 2011:355 quest to learn to live with pain – need for help advice and information Toye 2012:364 being fobbed off – I didn’t get a thorough examination Slade 2009:357 stigma – health-care professionals Harding 2005:330 unmet expectations Slade 2009:356 engagement with health care – ask me Johansson 1996:332 strategies to get doctor’s attention – claiming under cover Cooper 2008:322 decision-making Cooper 2008:322 individual care Slade 2009:356 engagement with health care – understand me Slade 2009:356 engagement with health care – partnership Slade 2009:357 tell me |
Gullacksen 2004:377 stage 1 – confirmation by
health-care professionals Paulson 2002:347 feeling neglected Kelley 1997:380 feeling understood Sturge-Jacobs 2002:361 power of diagnosis de Vries 2011:324 success factors (work) – use of health-care services |
Team memos and second-order constructs for ‘struggling to find the right balance’
| Team memos describing
category: Invisibility damages credibility; making invisible visible is hard work; difficulty being accepted. Worked hard to pass the test by not giving up and being assertive Try to get on with normal role – increases disbelief; difficult to know how to deal with showing limitations. Maintaining normal life an immense strain to keep hidden Have to negotiate appearance and behaviour to be believed; shame stigma; cautious about disclosure (shame, being believed, etc.) Need to enact pain in the right way; can’t look too ill or too well or people won’t believe you. There is a right balance. Some find it easier to just hide it (maybe linked to rhetoric of being brave, stiff upper lip, not whinging, etc.). Cautious about disclosure for fear of shame (weak, fraud, etc.). Want to just hide my new self from others Sense of shame at not being what I once was. Am I sick or well; normal/not normal; me/not me; dependent/dependant; recovered/still ill; ill vs. normal; conceal vs. express; control vs. not; good vs. bad day; balance support or dependence (link to negotiating reciprocity) Link to sick role – am I sick or not (can apply to all chronic illness); social recognition/belief; link to shame stigma/legitimacy Managing external projection of pain; health care in law court. Language of witnesses/advocate. Start in dock; burden of proof; not equal in eyes of society (or health care). Guilty unless proven innocent. Adversarial of pain; moral narratives a defence of self Credibility; not my fault; diagnosis, X-ray, social recognition, benefits, work. Captures inner struggle to maintain who they were and at the same time hide their symptoms Putting on a brave face. Trying to look normal and not be a ‘whiner’ (men/stoical); conceal emotions and appear cheerful Effort to look normal – I am still what I was. Resist sick role and keep it hidden. Exacerbated by need to balance need for support/not; need to be ill/not (Canguilhem’s396 discussion on normality linked) |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Skuladottir 2011:355 quest for normalcy – avoid sick role
and maintain dignity Campbell 2008:316 dependence and social withdrawal Werner 2003:370 I feel I should look groggy Coole 2010:319 justifying back pain Toye 2010:363 mustn’t look too ill Campbell 2008:316 normal compared with others Smith 2007:66 public arena makes it worse Johansson 1999:334 self-perception Harding 2005:320 spoiled identity Hunhammar 2009:331 striving to master variable pain – strategies for pain control Dickson 2003:325 reconstructing meaning of pain – striving to reduce pain Smith 2007:66 the sting in the tail Osborn 1999:342 withdrawing from others |
Lachapelle 2008:335 barriers to acceptance – fight to be
normal Lempp 2009:381 change in health identity – impact on social life Gullacksen 2004:377 stage 2 – leaving the sick role Paulson 2002:346 striving to endure – living as normally as possible Sturge-Jacobs 2002:361 longing for a normal life Paulson 2002:347 not being a whiner Hallberg 1998:328 psychosocial vulnerability – overcompensatory perseverance Hallberg 2000:329 preoccupied with pain – pain communication Sallinen 2011:352 permission to talk Lachapelle 2008:335 barriers to acceptance – fight to be normal Mengshoel 2004:341 resisting a sick role Schaefer 2005:384 secrecy makes it easier Raymond 2000:349 seeking a diagnosis Gullacksen 2004:377 stage 1 – self-deception Gullacksen 2004:377 stage 1 – struggling to restore life Mengshoel 2004:341 uncertainty of treatment Mengshoel 2004:341 unwilling to celebrate illness |
Team memos and second-order constructs for ‘struggling to show that I am a good and valuable person’
| Team memos describing
category: Not so evident in fibromyalgia Moral narratives used to support credibility; not my fault. I am not a person to be blamed for this. I have done nothing I am no longer good me but still use moral narratives to support self; narratives of previous life emphasis good me Need positive self-view; narratives of previous virtuous life emphasis I am not to blame Need to hold onto an acceptable and positive view of self Constant comparison to others to negotiate reality of their pain Tensions in social comparison (neither upward comparison or downward comparison satisfactory) |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Snelgrove 2009:358 maintaining integrity – cause of
pain Toye 2010:363 I am not like the others Werner 2004:371 I have always been so strong Johansson 1996:332 strategies to get self-respect – martyrising Slade 2009:357 stigma – relative positioning Werner 2004:371 some people pour out their troubles |
de Vries 2011:324 success factors (work) – personal
characteristics Sallinen 2011:352 self-evaluation through comparison |
Team memos and second-order constructs for ‘struggle to affirm myself as a good worker’
| Team memos describing
category: Feel treated like a number; don’t want to be seen as a ‘bad worker’; work has effect on identity; ‘if you don’t have a job you are nobody’; feeling that work adds value to self; feel respected and valued |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Walker 2006:368 loss – employment Patel 2007:345 perceptions at work – fear of letting employer down Johansson 1999:334 self-perception Johansson 1997:333 to be somebody Patel 2007:345 personal obstacles – age Patel 2007:345 perceptions at work – job availability Patel 2007:345 perceptions at work – employers’ limited understanding |
Mannerkorpi 1999:340 adapting Liedberg 2002:382 values and norms – fulfilment in work Liedberg 2002:382 values and norms – meaning of work Liedberg 2002:382 values and norms – organised time structure Mannerkorpi 1999:340 struggling Soderberg 2001:360 transitions – working life Arnold 2008:373 function and quality of life – work de Vries 2011:324 motivators for staying at work – work as responsibility de Vries 2011:324 motivators for staying at work – work as therapy de Vries 2011:324 motivators for staying at work – work as value Arnold 2008:373 function and quality of life |
Team memos and second-order constructs for ‘hostility at work isolating’
| Team memos describing
category: Changing and lost relationships of work colleagues; became isolated at work; seen as work-shy; sense of loss at work status |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Johansson 1997:333 getting out to be stimulated Coole 2010:320 employers – help depends on managers Holloway 2007:379 stigma at work Slade 2009:357 stigma – workplace |
Liedberg 2002:382 structural social factors –
commuting Lempp 2009:381 change in health identity – impact on social life Liedberg 2002:382 values and norms – meaning of work Liedberg 2002:382 working conditions – psychosocial environment Mengshoel 2004:341 resisting a sick role Liedberg 2002:382 other commitments – social relations Soderberg 2001:360 transitions – working life de Vries 2011:324 motivators for staying at work – work as responsibility |
Team memos and second-order constructs for ‘unpredictability of symptoms and the need for flexible work’
| Team memos describing
category: Unpredictability of symptoms and fear of progression; faced fear of not working Feared that no-one would employ them; need to balance other commitments at home Limit to reliance on colleagues. Exacerbated by financial climate; could continue if there was some flexibility in working arrangements |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Coole 2010:319 concerns about future at work Coole 2010:319 difficulty coping with flare-ups Coole 2010:320 patient control Johansson 1997:333 getting out to be stimulated Coole 2010:320 employers – help depends on managers Patel 2007:345 uncertainty – pain and health Johansson 1997:333 sick role process |
de Vries 2011:324 success factors (work) – adjustment
latitude Sallinen 2010:351 being in-between Sallinen 2010:351 being over the edge de Vries 2011:324 consequences of staying at work Liedberg 2002:382 structural social factors – finances Liedberg 2002:382 working conditions – physical work Liedberg 2002:382 working conditions – psychosocial environment Soderberg 2001:360 transitions – working life Lofgren 2006:337 constant struggle – walking a tightrope Liedberg 2002:382 structural social factors – work restructuring |
Team memos and second-order constructs for ‘battling the system to stay in work’
| Team memos describing
category: Negotiating benefits; no incentive to get off benefits; struggling to get benefits Deservingness out of your hands. Participants struggle to be seen as ‘genuine’ benefit applicants Disadvantages of getting better financially Damned if you do or don’t; if you don’t get benefits you lose credibility; if you do get benefits there are other losses Sense of shame of claiming benefits |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Walker 1999:367 being in the system – battling for
benefits Holloway 2007:379 stigmatisation in health-care systems Patel 2007:345 benefits organisation – permitted work Walker 1999:367 being in the system – your life is not your own Patel 2007:345 benefits organisation – (limited) Patel 2007:345 uncertainty – working capacity Coole 2010:319 concern about sickness record Walker 2006:368 loss – financial Walker 1999:367 being in the system – damned if you do and damned if you don’t Walker 1999:367 being in the system – compensation claims Johansson 1997:333 to get along moneywise Patel 2007:345 personal obstacles – qualifications and experience Patel 2007:345 perceptions at work – resistance to change |
|
Team memos and second-order constructs for ‘health-care system does not facilitate return to work’
| Team memos describing
category: No communication between health-care service and employer to facilitate return to work or access to benefits; advice to ‘be careful’ does not help graded return to work; being trapped in health-care system delays return to work; exacerbated by loss of legitimacy |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Coole 2010:320 occupational health – advice
overcautious Coole 2010:320 employers – overcautious support Coole 2010:318 no employment help from GP – clinicians increase concerns Coole 2010:320 occupational health – dependent on causation Coole 2010:318 no employment help from GP – doubt what GP can offer Coole 2010:318 no employment help from GP – GPs write sick notes Patel 2007:345 health-care barriers Coole 2010:320 occupational health – modifications left to manager Coole 2010:318 no employment help from GP – lack of dialogue between GPs, health-care professionals and employers Coole 2010:318 no employment help from GP – no effective advice from GPs Coole 2010:320 occupational health – service for employees |
|
Team memos and second-order constructs for ‘listening to and integrating my painful body’
| Team memos describing
category: Have become more present in the body (either a limitation or benefit); no longer at mercy of body but listen to it and co-operate, respect limits Respond to fluctuating needs. ‘Sensitive co-operation’; growing acceptance of, and permission for, limitations imposed by the body But – constant awareness of body can distract from being present in occupation Ambiguity (Afrell 2007372), do I listen to it or shut it off? Fight – give up hope – accept and move on? Listen to body/analyse life; working with body/knowing body; dialogue with body. Analyse life events and listen to body; become expert in body awareness Awareness that changes have to be made; live life at own speed to maintain participation’. Slow down, balance resources, set priorities, pace, rest, balance demands; balance external demands and own personal resources |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Afrell 2007:372 acceptance typologies – active
process of change Satink 2004:354 aiming to collaborate with pain Dragesund 2008:326 associations about the body Dragesund 2008:326 aware of body Werner 2003:369 for better or worse – awareness of needs Steen 2001:385 awareness of self Steen 2001:385 change of focus Lundberg 2007:338 finding the way out Slade 2009:356 listen to me – I know my body Lundberg 2007:338 identity restoration Werner 2003:369 applying the competence – knowing my body Skuladottir 2011:355 quest to learn to live with pain – need to take care of self and find a new pace Afrell 2007:372 acceptance typologies – surrendering to fate Aegler 2009:312 taking breaks not easy Werner 2003:369 applying the competence – thinking of me |
Gullacksen 2004:377 stage 3 – maintenance (a new
attitude) Mengshoel 2004:341 a new interpretation Mannerkorpi 1999:340 adapting Gustaffson 2004:327 setting limits – adjusting self-demands Gustaffson 2004:327 changing self-image – boundaries imposed Raheim 2006:348 typologies – coping Sallinen 2010:351 coping with fluctuating symptoms Lofgren 2006:337 constant struggle – creative solutions Hellström 1999:378 demands on self Gustaffson 2004:327 changing self-image – handling the pain Gustaffson 2004:327 changing self-image – housekeeper identity Soderberg 2001:360 learning to live with fibromyalgia Raheim 2006:348 theoretical interpretation – lived body Paulson 2002:346 body as obstruction – living day by day Hallberg 1998:328 maintaining forces – pain benefits Mengshoel 2004:341 redefining obligations and goals Kelley 1997:380 resources Lofgren 2006:337 constant struggle – setting limits Schaefer 2005:384 support from self and spiritual connections Lofgren 2006:337 constant struggle – taking care of yourself Liedberg 2002:382 other commitments – unpaid work Lofgren 2006:337 constant struggle – using pain as a guide |
Team memos and second-order constructs for ‘redefining normal and less focus on loss’
| Team memos describing
category: Give up aspiration of being ‘old self’ = challenging; idea of repairing existence Sense that realisation of loss and grief is important in process = redefine goals; have to do things ‘not normally’; create new patterns and routines Acceptance was not an all or nothing process; repeated moments of reflection You made decisions on a daily basis and setbacks occurred on bad days Easier to accept pain on a cognitive than an emotional level Less focus on loss and energy diverted to positive activities rather than complaining Making the best of things, realising that thinks ‘could be worse’ Letting go of pre-pain self-expectations and shifting their focus to what they could accomplish now, despite the pain Conscious of having the power to choose a path of giving in to negative emotions Can lead to pleasure at coping in spite of pain |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Skuladottir 2011:355 quest for normalcy – need to
participate Lundberg 2007:338 finding the way out Skuladottir 2011:355 quest for normalcy Werner 2003:369 applying the competence – focusing on resources (not pain) Lundberg 2007:338 identity restoration Aegler 2009:312 performing as an ongoing attraction Bair 2009:314 facilitators – social comparison Dickson 2003:325 reconstructing meaning of pain – striving to reduce pain |
Gullacksen 2004:377 stage 1 –
acknowledgement Lachapelle 2008:335 barriers to acceptance – fight to be normal Kelley 1997:380 changes over time Lofgren 2006:337 constant struggle – enjoying life Gullacksen 2004:377 stage 2 – finding solutions Lofgren 2006:337 grieving Gullacksen 2004:377 stage 3 – maintenance (handling future changes) Gullacksen 2004:377 stage 2 – leaving the sick role Lachapelle 2008:335 meaning of acceptance Sturge-Jacobs 2002:361 living within boundaries Lofgren 2006:337 constant struggle – positive thinking Lachapelle 2008:335 process of acceptance – redefining normal Lachapelle 2008:335 barriers to acceptance – fight to be normal Mengshoel 2004:341 redefining obligations and goals |
Team memos and second-order constructs for ‘being part of a community of others with pain’
| Team memos describing
category: Free to talk and unburden self without judgement; able to express self with others Positive impact on self-esteem; sense of community. Recognition, respect; feel understood; feeling of reciprocity met Group helpful for gathering info; helped them to see pain as something ‘real’ that was experienced on a daily basis by others who could provide practical knowledge; focus on coping strategies; recognition, respect self-esteem. Removed sense of isolation. But some ambiguity (I am not quite like them) |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Steen 2001:385 accepting self and others Steen 2001:385 community Steen 2001:385 gender Cooper 2008:322 information sharing Werner 2003:369 for better or worse – recognition give strength Werner 2003:369 for better or worse – sorrow at loss Dickson 2003:325 reconstructing meaning of pain – struggling to remove pain Dickson 2003:325 reconstructing meaning of pain – stumbling along with pain |
Gustaffson 2004:327 shame to respect Kelley 1997:380 feeling understood Sallinen 2011:352 permission to talk Sallinen 2011:352 experiential knowledge Hellström 1999:378 search for confirmations as ill Gustaffson 2004:327 changing self-image – self-confidence |
| But . . . I am not like others | |
| Toye 2010:363 I am not like the others | Raymond 2000:349 establishing coping
strategies Lachapelle 2008:335 facilitators to acceptance – perceived social support Sallinen 2011:352 reciprocity Mengshoel 2004:341 unwilling to celebrate illness |
Team memos and second-order constructs for ‘telling others about my pain’
| Team memos describing
category: Come out and tell others; don’t keep secret; don’t need approval of others |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Werner 2003:369 applying the competence –
encountering others Werner 2003:369 applying the competence – focusing on resources (not pain) Werner 2003:369 applying the competence – informing others Skuladottir 2011:355 quest to learn to live with pain – need to take care of self and find a new pace |
Gustaffson 2004:327 setting limits – adjust
workload Raheim 2006:348 typologies – ambivalence Raheim 2006:348 typologies – coping Kelley 1997:380 support and empowerment Gustaffson 2004:327 setting limits – telling others |
Team memos and second-order constructs for ‘realising there is no cure for my pain’
| Team memos describing
category: Acknowledging pain here to stay critical to adjustment – have to get on with it Cannot maintain ‘normal’ old self; stopped waiting for a cure; hope for cure no longer an obstacle to other possibilities Ironically this made them more hopeful |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Strong 1995:387 how are you coping? Harding 2005:330 living with and planning for the future Campbell 2008:316 striving for self-management Strong 1995:387 what helped you to cope? |
Gullacksen 2004:377 stage 1 –
acknowledgement Sallinen 2010:351 coping with fluctuating symptoms Paulson 2002:347 feeling no recovery Paulson 2002:346 striving to endure – nurturing hope Lachapelle 2008:335 process of acceptance – realising need for help, getting diagnosis, realising no cure, it could be worse Gullacksen 2004:377 stage 2 – sorrow and loss Gullacksen 2004:377 stage 2 – working through |
Team memos and second-order constructs for ‘becoming expert’
| Team memos describing
category: This is about becoming more of an expert and taking control of situation. System not working so need to become self-reliant in order to move forward Becoming flexible. Learning to think differently and change From ignorance to knowledge. Diagnosis a turning point to becoming more knowledgeable about fibromyalgia Helped self-esteem and respect |
|
| Second-order constructs supporting category | |
|---|---|
| MSK | Fibromyalgia |
| Slade 2009:356 engagement with health care –
assertiveness Crowe 2010:374 direct heat (poor title for concept) Steen 2001:385 experimenting Skuladottir 2011:355 quest for normalcy – involved in decision-making Teh 2009:362 participation in pain treatment – involved in decisions Strong 1995:387 what helped you to cope? Teh 2009:362 participation in pain treatment – working outside health-care professional relationship |
Schaefer 2005:384 becoming a self-advocate Lofgren 2006:337 constant struggle – being knowledgeable Gustaffson 2004:327 developing body awareness Raymond 2000:349 establishing coping strategies Sallinen 2011:352 experiential knowledge Lachapelle 2008:335 facilitators to acceptance – self-management education Kelley 1997:380 group approach Lachapelle 2008:335 process of acceptance – ongoing process Soderberg 1999:359 struggle for understanding – seeking relief and planning life |
List of abbreviations
- ACT
- acceptance and commitment therapies
- AMED
- Allied and Complementary Medicine Database
- CASP
- Critical Appraisal Skills Programme
- CBP
- chronic back pain
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CRD
- Centre for Reviews and Dissemination
- GP
- general practitioner
- HMIC
- Health Management Information Consortium
- HTA
- Health Technology Assessment
- IPA
- interpretive phenomenological analysis
- ISSG
- Information Specialists’ Sub-Group
- JBI-QARI
- Joanna Briggs Institute Qualitative Assessment and Review Instrument
- MSK
- musculoskeletal
- UNTRAP
- University/User Teaching and Research Action Partnership