Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 09/2001/21. The contractual start date was in November 2010. The final report began editorial review in October 2012 and was accepted for publication in May 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Stephen T Green is a NHS consultant and director of QHA Trent. QHA Trent is a British company delivering accreditation and consultancy services for hospitals and clinics located internationally.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Lunt et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Section 1 Background
Chapter 1 Introduction
This study explores the role and impact of medical tourism, defined here as travel by patients to non-local providers incurring out-of-pocket and third-party payments for medical treatments but excluding state-funded cross-border care available under the European Union (EU) directive. 1 Our focus is on both inward and outward flows of medical tourists seeking treatments to and from the UK. The study examines the implications of medical tourism for the NHS across a range of specialties and services including dentistry, bariatric surgery, fertility services and cosmetic surgery. The multidisciplinary research team worked across four analytical streams of activity to examine:
-
consumerism and patient decision-making
-
quality, safety and risk (including in the clinical context)
-
economic implications
-
medical tourism provider and market development.
Beyond anecdotal reports and media speculation, relatively little is known about the implications for the NHS of inward or outward out-of-pocket medical tourism. This is despite an estimated 50,000 UK patients travelling overseas for treatment annually2 and significant numbers of overseas patients using UK NHS private and independent sector facilities. The study sought to understand these flows in greater detail and to explore the opportunities and risks. The study provides insights for NHS policy-makers, managers, regulators, commissioners, providers, clinicians and consumer interest groups. The study contributes to a better understanding of macro and local factors: costs; quality and safety; administrative and legal dimensions; decision-making; and unintended and unforeseen consequences for the NHS of inward and outward medical tourists.
Background
The impact of globalisation in health and health care has paralleled emerging trends towards increased reliance on individualised health-care provision and ‘consumer’-led access to ‘health-related’ information. Wider system developments include the growth of the cross-border supply of health-related goods and services, greater overseas investment in domestic provision and increased movement of professionals and health providers, as well as trends towards consumption of health care abroad and discounted travel incentives included as part of medical assessment and treatment packages. 3–8 One increasingly popular form of consumer expenditure is what has become commonly known as ‘medical tourism’, a type of patient or ‘consumer’ mobility in which individuals travel outside their country of residence for the consumption of health-care services abroad. 9
Medical tourism takes place when individuals opt to travel overseas with the primary intention of receiving medical (usually elective surgery) treatment. These journeys may be long distance and intercontinental, for example from Europe and North America to Asia, and cover a range of treatments including dental care, cosmetic surgery, bariatric surgery and fertility treatment. 10–12 Some speculate that medical tourism is a US$60B industry internationally. 13
A medical tourist may be defined in two ways depending on the type of health system and how it is funded. First, there are medical tourists who can be categorised as ‘consumers’ because they use purchasing power expressed through the market to access a range of dental, cosmetic and elective medical treatment. There are related questions about access to insurance, the portability of insurance and whether or not voluntary insurance systems extend to the choice of overseas services. Within the USA, for example, several domestic private insurers have looked towards purchasing services overseas. In addition, there are increasing numbers of underinsured consumers who need to pay out of pocket for treatments. 14–17
Second, at a European level, medical tourism may involve exercising citizenship rights to receive medical treatment in another EU member state (better known as cross-border care) and request their national purchaser to reimburse the cost of treatment (see European Court of Justice judgments18–20). The European Parliament and the Council of Ministers formally adopted the patients’ rights to cross-border health care directive1 in March 2011 in an attempt to codify development and clarify the situation for EU citizens (see Appendix 1).
However, although current knowledge of the demand and supply of cross-border health care is growing at European and national levels,21–24 there are no comprehensive data on inward and outward out-of-pocket and third party-funded flows (including government-sponsored) and their health and economic impact. 8 This study therefore contributes to further understanding of patient mobility and its implications for the NHS. 7,25,26 The study was particularly timely given the current global financial context and the likely implications for health expenditure and national health budgets,27,28 and also attempts to encourage NHS institutions to be more outward looking through the launch of NHS Global in 2010:29
While there are already strong examples of NHS Trusts and organisations successfully sharing their ideas and products abroad, we want to create a more systematic approach to this work, and in doing so bring benefits back to the NHS and the UK taxpayer . . . It is now more important than ever to maximise the international potential of the NHS.
NHS foundation trusts will also have more opportunity to undertake international activities should they wish to, including treating international patients (as inward medical travellers are known). Under the 2012 Health and Social Care Act30 the pre-existing cap on non-NHS income, which varied across foundation trusts, was increased. This allowed all foundation trusts to earn 49% of income from non-NHS work, including international patient activity within private activities (in force from 1 October 2012).
How the increase in private activity impacts on the NHS and its patients is not clear and is dependent on whether or not the particular foundation trust is operating close to capacity and whether additional capacity is generated to treat private patients or existing capacity is used. 31 NHS patients may receive benefits if new or enhanced facilities are shared between private and NHS patients. However, if private patients are of greater priority there will – all things unchanged – be a growth in waiting lists and waiting times for NHS patients (Section B155–B156). 31 There is currently no evidence to judge whether or not this will be the case.
A number of factors have possibly contributed towards the growth in outward medical tourism. These include improved disposable incomes, increased willingness of individuals to travel for health services, lower-cost air travel and the expansion of internet marketing – which is a major platform of information for those seeking and providing such treatments. Why do patients choose to travel overseas for treatments when evidence suggests that most patients prefer to be treated closer to home?32,33 Before this research was conducted, purported reasons to travel were said to include cost (e.g. dentistry), availability of treatment, privacy, perceived quality and for the purposes of combining treatment with an overseas vacation (especially for diaspora populations). For instance, UK patients may have to wait to meet NHS criteria on age or circumstance before being offered some treatments, or may be ineligible according to the current criteria [e.g. in vitro fertilisation (IVF), gender reassignment surgery, renal transplantation], and private treatment in the UK may be costly and not offer the range of preferred techniques and technology. Conversely, the reputation of private providers in the UK, and the perceived or actual quality of care in many countries, mean that in some areas of medical activity there is a desire for foreign nationals to seek treatment in the UK. Having completed the project, the evidence about decision-making and drivers is now on a far firmer footing.
Currently, medical tourism for the UK is limited to the private, out-of-pocket sector. However, there are important implications for a publicly funded and provided system such as the NHS. For instance, there may be a range of beneficial and detrimental consequences, such as cost savings from those voluntarily seeking care abroad, costs of follow-up care for those who have been treated overseas, and costs and benefits associated with patients travelling into the UK for paid treatments. There will also be a range of associated health impacts.
Research objectives
Media reports and speculation notwithstanding, we knew little about the historical and likely future development and impact of medical tourism for the UK NHS. The objectives of our study were to:
-
generate a comprehensive documentary review of (1) relevant policy and legislation and (2) professional guidance and legal frameworks governing inward and outward flows of medical tourists to and from the UK
-
better understand the information, marketing and advertising practices used in medical tourism, within both the UK and provider countries of Europe and beyond (and the benefits and drawbacks of them)
-
examine the magnitude and economic and direct health-related consequences of inward and outward medical tourism for the NHS
-
understand how decision-making frames, assessments of risk and associated factors shape health treatments for patients (including how prospective medical tourists assess provider reputation and risk) and to collate evidence on the role of intermediaries and brokers in facilitating medical tourism
-
better understand treatment experience, continuity of care and postoperative recovery for inward and outward flows of patients
-
elicit the views and perspectives of professionals and key stakeholder groups and organisations with a legitimate interest in medical tourism (exploring patient and professional choice, benefit, safety, harm and liability)
-
map out the medical tourism industry and chart its development within the UK and assess the likely future significance for the NHS.
Research streams
A preliminary scope of the literature and practical issues identified four streams of evidence that would inform a better understanding of medical tourism and advise policy-makers on strategies to capitalise on its benefits and minimise risks it may present:
Stream 1: consumerism and patient decision-making
We knew little about how patients made their decisions concerning treatments and destinations and what forms of hard intelligence (performance measures, quality markers, safety information) and soft intelligence (website information, friends, internet chat rooms) they use. What role do networks play in decision-making? How informed are patients when making their choices?34 Are factors that encourage cross-border exchanges (including type of care, reputation of provider, urgency of treatment, gender, age, location and socioeconomic status of patient) (e.g. reference 21) similar to those that shape out-of-pocket exchanges? What is the role of general practitioners (GPs) and web-based resources in encouraging or discouraging UK residents considering undertaking medical tourist treatments?
Stream 2: quality, safety and risk
Modern health care is an inherently risky undertaking with the potential for clinical errors and medical incompetence and malpractice, particularly in treatment areas that are not regulated by national laws and guidelines. How do patients understand the elements of risk involved in undertaking treatment overseas? There are also potential ethical, legal and insurance issues, which can influence the patient decision-making procedure. Research was needed to collect evidence on the experiences and outcomes of treatment abroad (benefits, satisfaction, unintended and dysfunctional clinical consequences). The importance of communication between professionals and aftercare, privacy and confidentiality vis-à-vis information sharing, the use of information technology (IT) information by professionals, and how patient information flows are all important areas in which data are needed. What attempts are being made to regulate the industries – by national governments or organisations themselves? What is the use of independent international health-care accreditation in European settings, such as that provided by Joint Commission International (JCI)?
Stream 3: economic implications
What are the economic implications of medical tourism for the UK NHS? There are no routinely collected data concerning inward and outward flows of medical tourists to and from the UK; however, we sought to explore what information existed [within the International Passenger Survey (IPS) and within foundation trusts themselves] and to examine the implications of such data.
Stream 4: medical tourism providers and market development
There has been a steady rise in the number of companies and consultancies offering brokerage arrangements for services and providing web-based information for prospective patients about available services and choices. This can be attributed to the transaction costs associated with medical tourism, which patients would want to reduce. Typically brokers and their websites tailor surgical packages to individual requirements: flights, treatment, hotel and recuperation. Some brokers or concierges offer medical screening. A series of inter-related questions arose with regard to the precise role of brokers and intermediaries in arranging overseas surgery. How do organisations determine their market? How do medical tourism facilitators source information, select providers and subsequently determine the most appropriate advice? Further, what are the relationships between clinical providers and such intermediaries? What are the implications of the majority of medical tourism websites being commercially driven and intermediaries relying on advertising revenues and commission?
Chapter 2 Methods and structure
Research approach and methodology
The study involved integrating policy analysis, desk-based work, economic analysis and treatment case studies. We used a mixed-method approach of qualitative and quantitative data collection and the study included both primary and secondary data collection/analysis. Activity comprised a preliminary systematic review and broad data collection to address the four research streams. In this chapter we focus on the broad methodology, outlining why a number of data sources were required to understand medical tourism, and the challenges of implementing a project of this nature (see Appendix 2 for the study protocol). The research conducted for this project has been ambitious in that it was trying to establish the level of current evidence and knowledge in an area in which robust routine data are lacking. This required innovative approaches, including in the recruitment of patients but also in obtaining data on inward medical tourism through freedom of information requests. Specific issues with regard to the research process and sample sizes are addressed in this chapter. The entire research project adopted an iterative approach, with authors regularly reviewing methods for data collection. Data collected were triangulated with other sources to ensure that findings presented are an accurate reflection of the data.
The NHS fieldwork was undertaken in the English NHS [with primary care trusts (PCTs) and foundation trusts] although the medical tourists that we interviewed were located UK-wide (including Wales, Scotland and Northern Ireland). The IPS data relate to the UK whereas our trust data for economic costs relate to England. A number of the broader issues regarding outward medical travel and patient decision-making, safety and experience are common to the wider UK population but there are differences between how the English NHS and non-English NHS are organised (e.g. with regard to foundation trust status and commissioner/provider relationships). The policy directions on potentially expanding private care and the directive on NHS Global do not extend outside of the English NHS.
Preliminary systematic review activity
The study was underpinned by a systematic overview [based on NHS Centre for Reviews and Dissemination (CRD) guidelines for systematic review35] of previously published literature on medical tourism (reported fully in Chapter 3). Although the research project overall drew on grey literature and industry surveys to triangulate findings when required (and as specified), the systematic review focused on published literature. This was to ensure the robustness of findings and to retain feasibility, given the overwhelming quantity of data published on the subject.
Secondary data analysis
Data provided by the IPS and foundation trusts’ responses to freedom of information requests were analysed to understand patient flows and their financial consequences.
Desk-based activity
Desk-based activity was undertaken to collect both primary and secondary data around patient safety and service quality – legal dimensions, education and information, external quality assessment (EQA) and quality information systems (QISs). The methods and results are reported fully in Chapters 6–8.
Interviews
We undertook in-depth interviews with a range of key stakeholders and interests involved with medical tourism (n = 134 plus 23 overseas providers) between March 2011 and August 2012. All interview schedules are provided in Appendix 3. Interviews were conducted with the following groups.
Professional associations and stakeholders
Individuals representing a range of professional associations, clinical interests and representative bodies were interviewed. This ranged from the Royal Colleges to bodies concerned with quality control and those representing nurses and doctors. Overall, we interviewed 16 individuals across this range of interests, including from legal, cosmetic, dental, fertility, primary care and travel health services. The project team drew up a list of key interests and individuals and discussed their coverage. Individuals were invited to be interviewed, either in a personal capacity or as spokespeople of their clinical specialty or organisation. There was also an element of further snowball recruitment. Interviewees were typically interviewed face to face; interviews lasted for between 30 and 60 minutes and were recorded and transcribed.
Medical tourism businesses and employees
Individuals representing the perspectives of businesses and employees within medical tourism (including facilitators, website operators, insurance providers, private fertility counsellors) were interviewed. The project team drew up a list of key interests and undertook a review of recent conference speakers, literature and websites to identify medical travel interest. The recruitment net was cast widely and we sought to understand the wider dynamics, drivers and aspirations of the individuals and companies. Overall, we interviewed 18 individuals across this range of interests, including from legal, cosmetic, dental, fertility and travel health services.
Individuals were interviewed over the telephone or using Skype™ (Skype Ltd, Rives de Clausen, Luxembourg), although a number were also interviewed at trade fairs and conventions. There was also an element of further snowball recruitment. Interviews lasted for between 20 and 60 minutes and were recorded and transcribed.
NHS managers
We sought to interview individual managers within PCTs and foundation trusts who could illuminate our understanding of the inward and outward flows of patients and the impact of such flows on the NHS. An element of snowball and convenience recruitment was used. To access individuals with commissioning insights, the study was publicised by listservs to those with commissioning knowledge and interest in overseas/cross-border patients. Individuals who had attended a cross-border health-care seminar at which the research team was present were also contacted. The NHS Confederation circulated our call for interviewees to members and, of our 23 NHS interviewees, six held commissioning roles.
For NHS providers, we identified trusts that were seen to have a longstanding interest in, or aspiration to further develop, international patient work. There is a strong network of interests (particularly around London) focused on private and international services by the NHS; individuals were approached to participate. Interviews were conducted face to face and lasted for 25–60 minutes. Interviews were usually recorded and transcribed. The NHS Confederation circulated our call for interviewees to members. We interviewed 13 NHS providers, which along with the six commissioners and four relevant practitioners, gave us a total sample of 23 NHS interviewees.
Patient interviews
A total of 46 people were categorised to our medical tourist and diaspora samples across four treatment case studies and ‘other treatment’ categories. In addition to these respondents, we also spoke to a total of 31 individuals as part of our ‘diaspora’ category (Table 1). Not all of these individuals provided interviews, instead opting to take part in a more communal discussion appropriate to the cultural dynamics of the group.
| Treatment type | Number of respondents | Procedures covered | Locations of treatment |
|---|---|---|---|
| Fertility | 9 | IVF, intracytoplasmic sperm injection, egg donation, sperm donation | Czech Republic, Ukraine, Sweden, Spain, Cyprus |
| Bariatric | 11 | Gastric band, gastric bypass, gastric wrap, gastric sleeve, duodenal switch, pancreatic diversion and duodenal bridge | Belgium, France, Czech Republic |
| Dental | 11 | Crowns, bridges, routine work and check-ups, fillings, braces, dental plates, implants | Hungary, Germany, Croatia, India, Poland, Italy, Lithuania |
| Cosmetic | 9 | Facelift, liposuction, tummy tuck, minimal access cranial suspension facelift, nose, face and eyes | Belgium, Poland, Czech Republic, Pakistan |
| Other | 6 | Nerve surgery, gynaecology, ultrasound, immunotherapy, shoulder stabilisation, needle for Dupuytren's contracture | France, Greece, Belgium, Germany, USA |
| Diaspora | 31 | Diagnostic, dental | Germany, India |
Our core sample of 46 medical tourists was sourced through a variety of means. In the first instance we posted a call for interviewees on our medical tourism project website as well as trialling an advert in a local newspaper. The advert was unsuccessful and over the 18 months of the project our online contact form yielded four responses. We came to increasingly rely on posts made to online support or information forums. This proved particularly successful, especially in terms of our bariatric and fertility samples (Appendix 7 details the range of sites and networks that we utilised for recruitment). In some cases we made contact with those whose stories had been reported elsewhere, for example in media publications or as patient testimonials. A sample of 46 is clearly not a representative sample, although the team attempted to source a wide range of travel experiences, including major and more minor procedures, a range of treatments and those who perceived themselves as having good and less successful outcomes. Attracting respondents proved extremely difficult, especially the dental sample as there appeared to be no online ‘community’.
Our diaspora sample consists of individuals from three community groups (two urban Somali groups and one Gujarati group). Access to these groups involved the support of individuals who acted as informal gatekeepers to the communities, often organising meetings with interviewees, a location in which to meet and, in some instances, interpreters.
Individuals were approached to participate and interviews were conducted face to face or, when a preference was expressed, by telephone and Skype. Interviews lasted for between 30 and 100 minutes and were recorded and transcribed. The interviews explored a range of dimensions including drivers, decision-making, treatment experience and postoperative care. They also asked about the costs that were incurred during travel abroad, including for treatment, accommodation, insurance, recuperation and aftercare.
Overseas providers
A total of 23 people were interviewed regarding overseas provision. Here, a range of recruitment and interview techniques was adopted. We undertook five full interviews by telephone and face to face, but also used opportunities at trade shows and conferences in the UK and Europe to meet and talk with overseas providers, taking field notes. These contacts and discussions went far beyond our initial expectation of 10 providers.
Interview process
As already described the recruitment of patients evolved and we revised the recruitment strategy several times. The different kinds of treatments that formed the basis for the case studies developed in the analysis were informed by findings from the initial systematic review of the literature. This identified bariatric, fertility, dental and cosmetic treatment and diaspora travel as types of procedures for which patients travel to receive treatment.
Initially, we had anticipated hip and heart patients as a further group of patients travelling for higher-risk and higher-cost procedures but, although these were targeted in our initial recruitment strategy, they proved much harder to identify. This is a likely reflection of the project’s UK focus as patients resident in the UK are unlikely to travel for high-cost and complex procedures given that these are available for free on the NHS. This is opposite to the case in the USA where patients may feel more compelled to travel for treatment for complex procedures given the high costs and much larger associated savings.
We made a conscious effort to interview similar numbers of patients across the different groups to maintain a balance within the findings across different treatment types and ensure that the findings can reflect on medical tourism overall, rather than specific conditions. Attempts to identify specificities and commonalities across treatment conditions also informed the analysis process described below.
Although the number of interviews gathered was in part determined by constraints in timing and challenges faced in recruitment, especially of patients, we stopped the interviewing process only once a saturation point was reached and no new themes were emerging from the interviews. Although the sample is not representative of all medical tourists, clear commonalities in motivation and experiences of patients emerged across the sample of interviews.
Interview analysis
Both quantitative and qualitative data analysis involves the common steps of data reduction (and data cleaning), data organisation and data interpretation. The study interview data were analysed using the ‘framework method’ of thematic analysis. 36,37 This allowed a search for conceptual definitions, typologies, classifications, form and nature (process, system, attitudes, behaviours) and explanations. 38 The study had clear research streams and specific questions that it sought to explore. We examined the data for particular ‘outliers’, searching for negative or disconfirming evidence that appeared to be inconsistent with the emerging analysis.
When consent was provided, all interviews were recorded and transcribed (see transcriber confidentiality agreement in Appendix 4). Transcripts were reviewed by four authors undertaking primary data collection and analysis (NL, DH, HK, JH). Interviews were grouped into categories defined in the study framework (e.g. professional associations or patients.). Patient interviews were further grouped into the following categories: bariatric, cosmetic, fertility, dental, diaspora and ‘other’ tourism. Authors read all transcripts and met to generate initial themes for the analysis. Themes were specific to groups of transcripts, for example themes for the analysis of fertility tourists differed from those used for professional associations. Once themes were agreed, one author took the lead on thematic analysis of the specific group of interviews and drafting of texts. These were then cross-checked by a second author to ensure accuracy and avoid bias. As a final step, completed drafts of the texts were reviewed and commented on by all authors.
Given the highly sensitive nature of the patient and provider data, we endeavoured to ensure the confidentiality and anonymity of individuals and organisations when reporting the findings.
Case study synthesis
The research design included treatment case studies that would allow the team to synthesise findings across the range of data sources (qualitative and, when possible, quantitative) and to draw together primary and secondary knowledge. Five case studies were developed: bariatric, fertility, dental, cosmetic and diaspora (see Section 3). Case study selection was informed by the review of the literature, which indicated that these areas were likely to be of value in understanding medical travel.
This method allows a better understanding of the varying specialties within medical tourism and the dynamics of patient consumer decision-making, risk-taking, and quality and safety of particular treatments. Multiple case study analysis also provides insight over and above that of individual case studies and has advantages over simply seeing the whole data set ‘in the round’. 39
Each case comprises around 10 interviews with patients to illuminate decision-making processes and treatment experiences (e.g. dentistry or bariatric). Cases included quantitative data analysis where possible, based on descriptive statistics covering aspects such as expenses incurred. Case studies also introduced analysis of relevant website and print advice (commercial and professional sources) for that particular specialism. The case studies drew on interview data from industry and clinical interests with a view to assessing current and emerging developments.
The case studies helped facilitate understanding of aspects of medical tourism that were treatment specific and those that were common across different types of treatment. This proved particularly valuable for the analysis of patient motivation and in the costing work. It also helped validate the data.
Ethics
We sought NHS ethical approval to interview representatives of NHS purchaser and provider organisations in the localities selected (managers and non-clinicians within PCT or foundation trust settings). The full ethics application ‘Implications for the NHS of inward and outward medical tourism’ was submitted to the Sheffield Research Ethics Committee for consideration and approval (11/H1308/3). Local research and development approval and appropriate letters of access were then gained for each of our final fieldwork locations (11 sites in total). Sampling for medical tourism patients did not require access to the NHS, nor patient records or materials. We sought clarification with the local National Institute for Health Research Research and Design Service and local NHS research ethics committee and ethics approval for patient recruitment was not required. We recruited ‘medical tourists’ through networks and snowball recruitment, not through the NHS.
Informed consent was a fundamental part of the study approach. Each interviewee was provided with details of the study (which they could retain) and asked to complete a consent form (see Appendices 5 and 6, respectively, for examples of these).
Fieldwork challenges
The project had a number of challenges. It included data collection in familiar health services territory (including NHS managers and professional associations and use of NHS financial information). But it also required fuller engagement with non-NHS interests and groups (non-NHS patients, commercial interests beyond the NHS). A range of data sources was required for the research team to meet its objectives and offer insight around decision-making, patient safety, economic implications and market and provider development.
Sourcing and completing interviews with medical tourists required significant effort, as well as intensive networking, patience and substantial persistence. In some areas of activity (e.g. cosmetic treatment) we recruited in a context in which media outlets would pay hefty fees for patient stories and testimonials. We were also talking about potentially sensitive issues across a range of treatment areas. Each strategy, network and site (detailed extensively in Appendix 7) contributed some part towards meeting our final sample target. The project team was supported by an advisory group (see Appendix 8 for advisory group terms of reference and membership).
For NHS managers, particularly those on the purchasing side, the impending reorganisation of PCTs provided recruitment obstacles. In two sites where we gained ethics approval, interviewees were unable or unwilling to participate in the research. Given the number of recruitment sites (up to 15), obtaining local research and development approvals and access was very time-consuming but necessary under existing governance arrangements.
Changes from protocol
There were two main departures from the envisaged study design. First, the proposal envisaged undertaking a survey in addition to the in-depth qualitative interviews. This would collect more detailed demographic and financial information from a larger number of travellers. Although we were successful in securing the qualitative interviews, recruitment numbers were not high enough to allow for a survey element. Some indicative financial information was collected in the detailed patient interviews, some of which is detailed in the treatment pathways (see Appendix 9).
Second, we anticipated recruiting 10 inward medical tourists within our overall figure of 50. However, given the typically high-end treatment focus and government-sponsored nature of these patients, this proved difficult. There were also no support forums and clear gatekeepers through which such patients could be accessed. Time constraints did not allow us to build the necessary relationships with embassies and health attachés that may have provided these recruitment opportunities. Aside from this we were able to collect data on the context within which these patients travelled to the UK. These data were collected by talking to a range of managers within the NHS foundation trusts and those working within the independent sector. Table 2 summarises our data collection process.
| Data collection method | Description | Collected by | Research objective | Report coverage |
|---|---|---|---|---|
| Interviews | ||||
| Patients (treatment groups n = 46; diaspora n = 31) | Treatment groups: cosmetic, dental, bariatric, dental, cultural, other | DH, JH, LM, HK, NL | Understand decision-making frames, assessments of risk and associated factors; better understand treatment experience, continuity of care and postoperative recovery | Chapters 9 – 14 |
| NHS (n = 23) | Purchaser and provider roles | NL | Elicit the views and perspectives of key stakeholder groups | Chapters 9 – 15 |
| Stakeholders (professional associations n = 16) | Representatives of professional associations | NL/JH | Elicit the views and perspectives of key stakeholder groups; map out the medical tourism industry and chart its development | Chapters 9 – 15 |
| Stakeholders (businesses, employees n = 18) | Individuals working within the private sector of medical tourism | LM, DH, JH | Map out the medical tourism industry and chart its development | Chapter 4 |
| Overseas providers (n = 23) | Country strategies | JH/DH/NL | Map out the medical tourism industry and chart its development | Chapter 4 |
| Desk-based work | ||||
| Review of websites | 100 sites reviewed, guideline search | DH, HK, NL, RS, JH | Better understand information, marketing and advertising practices | Chapters 6 and 8 |
| Review of quality and safety accreditation | 150 sites reviewed | NL/HK | Understand decision-making frames, assessments of risk and associated factors | Chapters 6 and 8 |
| Secondary data analysis | ||||
| IPS | 2000–11 | DH, JH, RS | Examine the magnitude of inward and outward medical tourism | Chapter 5 |
| Costing | Freedom of information requests 28 NHS trusts | JH/RS/NL | Examine the economic and direct health-related consequences of inward and outward medical tourism | Chapter 16 |
| Systematic review | ||||
| Review of medical tourism literature | JH/RS | Comprehensive documentary review | Chapters 3 and 7 | |
The impact of departure from the protocol on findings
In light of the challenges reported and the obvious further insights that could be gained by having a greater number of cases or interviews, for example of NHS managers, we have been careful not to overstate the findings and potential weaknesses resulting. We addressed challenges in data collection through innovative data collection methods, for example the freedom of information requests to fill in the limited information available on inbound UK tourists.
For the subgroups for whom data were collected, a saturation point was reached in the interviews as themes repeated themselves. The lack of interviews with inbound medical tourists to the UK means that research findings do not address motivation and limit the insights offered of their experiences of the NHS. There is also a need for further research to better understand the effects of inbound medical tourism on the NHS.
In addition, a large-scale survey (had it yielded statistically significant results) may have enabled further quantitative analysis of medical tourism. However, as the study interviewed the largest sample of UK medical tourists to date, we feel strongly that it presents the most valid insights and the most robust data on patient motivation and experience available to date. We carefully triangulated all findings and recommendations to ensure the validity of the findings stated.
Report structure
The report is structured as follows. The remainder of Section 1 provides a systematic review of the medical tourism literature (see Chapter 3), highlighting where major gaps in knowledge exist. Chapter 4 provides an introduction to the medical tourism industry. Drawing across all interview data (industry, overseas providers and professional associations, and medical tourists) it undertakes broader conceptualising to explore services involved, the ways in which information is sought, and supply/provider chains. Chapter 5 provides a critique of existing estimates and extrapolations around medical tourist flows and an analysis using IPS data provided by the Office for National Statistics (ONS).
Section 2 examines issues related to patient safety and service quality including the legal and policy context (see Chapter 6), education (see Chapter 7) and EQA and QISs (see Chapter 8), and synthesises interviews from professional associations and NHS managers.
Section 3 includes the treatment case studies. This section contains an initial synthesis (see Chapter 9) followed by five case studies of different treatments (bariatric, fertility, dental and cosmetic; see Chapters 10–13) and diaspora travel (see Chapter 14). The cases include patient interview data, wider interview data relevant to the treatment case (professional, industry, overseas) and material drawn from earlier sections.
Section 4 presents the data and discussion on inward patient flows of international patients into the NHS (policy and background, processes and perspectives) (see Chapter 15), outlines the economic considerations (see Chapter 16) and draws together the policy, management and research implications (see Chapter 17).
Chapter 3 Systematic review: what do we know about medical tourism?
Introduction
Medical tourism – people travelling abroad with the expressed purpose of accessing or receiving medical treatment – is a growing phenomenon associated with processes of globalisation. 40 This includes cheaper and more widely available air travel and cross-border communication through the internet, which allows medical providers from one country to market themselves to patients in another. At the same time, increased movement of health workers for education means greater consistency of care offered in origin and destination countries. This has been coupled with an increase in foreign direct investment in health-care providers in destination countries, including by private medical insurance companies. In some instances, US private insurers now allow patients to have treatment abroad. The increasing acceptance of health-care portability is evident in Europe where greater patient mobility led to a EU directive1 on cross-border health care. Together with a rise in out-of-pocket expenditures for health in many high-income countries at a time of economic crisis, these factors (travel, communication, consistency of care, cost and an increased acceptance of the portability of health care) conspire to form a perfect storm for medical tourism.
As a consequence, even in countries with a universal public health-care system, such as the UK NHS, patients are now travelling abroad to receive medical treatment. Data from the ONS indicate that in 2010 63,00041 people travelled abroad for medical treatment.
However, understanding of medical travel is limited. Little is known about which patients choose to travel and why. Details of the volume of patient flows and resources spent remain uncertain. This has hampered efforts to understand the economic costs to and benefits for countries experiencing inflows and outflows of patients. 8 Similarly, the medical tourism industry and the role of private providers, brokers and marketing remains a ‘black box’. 40 Although interest in the issue has grown over the past decade, the effects on patients and health systems are not fully understood. Given the emerging nature of medical travel research, the evidence base is not yet clearly mapped.
This review of the literature aims to outline the current level of knowledge on medical tourism and to better understand this phenomenon, including its impact on the UK NHS. Specific objectives are to better understand patient motivation, the medical tourism industry, the volume of medical travel and the effects of medical tourism on originating health systems. These objectives informed the search strategy and review criteria set out in Appendix 10. The results of the literature review are reported and discussed with reference to subthemes that emerged; special attention is devoted to findings directly relevant to the NHS. Conclusions are presented on current levels of knowledge, critical gaps and future research priorities on medical travel.
Methods
The review was conducted between September and December 2011, considering all papers published by this date, and adapted the strategy employed by Smith et al. 42 The strategy was reviewed and amended by a project advisory board consisting of academics, policy-makers and practitioners. The search strategy and inclusion criteria for the review are provided in Appendix 10 and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart is provided in Appendix 11. In total, 100 papers were selected for inclusion in the review. 8,10–12,17,26,40,42–134
Results
An increase in medical tourism research is evident from the prominence of the issue. In 2010 and 2011, five journals devoted special editions to medical tourism: Global Social Policy, Body and Society, Anthropology and Medicine, Tourism Review and Signs.
A rapidly expanding literature over the past 5 years (with an ‘explosion’ in 2010 and 2011) is reflected in the publication dates of papers reviewed, as evident from Appendix 12 (see Figure 9); 73 papers were published in 2010 and 2011. 40,42–45,47,50–52,54–57,59–61,64,67–78,80–95,97,99,102–104,107–121,123,125–127,129–133 This underlines the increase in medical travel and its importance as an issue in UK health-care provision.
Types of studies reviewed
Papers included in the review were classified into the following categories:
-
empirical: denoting papers based on primary research, interviews, surveys, analysis of data sets, or the calculation of revenue and tourist flows, and case studies of patients
-
reviews: literature, scoping and systematic reviews of medical tourism websites
-
analysis: papers that, although drawing on secondary sources, provide substantive new insights or conceptualise medical tourism in a new way (a number of papers presented frameworks)
-
overview articles: papers that give an introduction to the issue of medical tourism.
The results are summarised in Appendix 12 (see Figure 10). In total, 47 papers17,43,44,47–49,51,57,62,65,66,68,71,76,78,81–83,85–87,93,94,96–100,103–106,110–114,116,118–120,124,126,127,132,133 presented findings from empirical research, 25 provided an overview of issues,10,11,26,46,50,52,53,58–60,63,67,73,79,80,91,97,100,115,120,122,128,130,135,136 15 were classified as analysis8,54,56,61,69,75,84,88,108,109,119,123,125,129,131 and 11 were reviews. 40,42,55,70,72,78,89,90,92,95,133 Of the 47 empirical studies, 19 reported findings from quantitative research12,17,43,47,76,81,85,93,96,98,99,103–106,110,114,116,124 (in most cases a survey), 15 were qualitative studies,44,57,62,68,71,74,82,87,94,112,113,116,118,120,132 eight reported case studies of patients51,66,83,101,102,111,119,127 and a further five48,49,65,86,93 reported the results of an experiment, cost calculation or evaluation of an intervention. In total, 32 of the empirical findings were published between 2010 and 2011, underlying the provenance of the issue.
Geographical focus
Papers were grouped according to which region the research investigated. Papers that provided a general overview that was not focused on a specific region or country were classed as global. A total of 43 papers fell into this category. 8,10–12,17,26,45–47,52–55,58,59,63,64,67,69,70,72,73,78–81,89,90,92,93,95,107,111,119,121–123,129–133,135 Europe was the focus of 27 papers,40,42,44,48–50,57,60–62,65,66,75,76,83,84,91,94,98,100–102,104–106,114,126 with 13 explicitly focusing on the UK42,57,62,65,66,76,83,94,98,101,102,104,114 in their study design and a further 11 papers10,40,43,50,53,90,91,99,105,106,119 from across the entire sample referring to either UK patients or the NHS. The geographical distribution of papers is summarised in Appendix 12 (see Figure 11).
Evidence from studies reviewed suggests a regional dimension to medical tourism. Japanese companies send their employees to Thailand10 or to countries in the Gulf. 43,116 A study of medical tourists in Tunisia found that these were from neighbouring countries. 85 Thailand, Singapore, Malaysia109 and India8 and others have marketed themselves as medical tourism destinations. Countries are known for specific areas of medicine: Singapore for high-end procedures,86 Thailand for cardiac, orthopaedic and gender reassignment surgery,11 Eastern Europe for dental tourism108 and Spain for fertility treatment. 72
Although some destinations were recognised as being popular with UK patients, for example Budapest for dental treatment, proximity alone does not appear to explain preference for one destination over another.
Issues covered
Most papers made reference to push and pull factors determining patients’ decision to travel. These relate to cost, perceived quality, familiarity, waiting lists or delays in treatment or the lack of availability of certain treatments in the country of origin. 61 As this list demonstrates, these are often complex57 and may vary according to the treatment for which a patient travels. A patient travelling for cosmetic surgery, for example, may enjoy the anonymity of a destination far from their country of origin,53 whereas migrants may prefer to travel to their country of origin to feel more comfortable with the language or type of care provided. 87
A subset of papers reviewed focused on specific types of medical tourism.
Diaspora travel
A number of studies refer to a group of medical travellers classified as diaspora travellers. Studies describe this in relation to India, China, Korea and Mexico, with recent migrants returning to their ‘home’ country to access treatment that is either not available or perceived to be not available in their country of residence, or perceived to be more effective in their ‘home’ country. 43,71,87,94
Glinos et al. 61 developed a typology for patient motivation (availability, affordability, familiarity, perceived quality of care), cross-referenced with whether a patient has funding or not. The authors applied this typology to understand patient motivation in a range of case studies from the literature and found that diaspora patients return because of reasons of familiarity with the system, as well as affordability.
Fertility tourism
Reproductive or fertility tourism is comparatively better documented than other forms of medical tourism. 40 Sixteen papers44,47,57,59,60,72,74,79,98,100,106,113,114,129,130,132 were identified for inclusion in this review; seven59,74,79,113,129,130,132 focused on equity and ethical issues relating to fertility tourism, including the rights of women in recipient countries.
Four papers57,98,106,114 specifically examined cross-border reproductive care (CBRC) in Europe. Two106,114 of these papers presented findings of surveys monitoring patient flow and services accessed across Europe and a third paper98 presented the results of the effects of such travel on patients giving birth in a central London hospital. One57 provided a qualitative, in-depth study of UK patients and their motivations for travelling abroad.
One paper47 presented findings from an online survey of prospective and actual tourists. Four papers44,60,79,100 provided a general overview of the issues relating to fertility tourism. Hudson et al. 72 presented a review of the literature on CBRC. Results included the consistent gap in empirical research; of 54 papers reviewed only 15 were based on findings from empirical investigation. The authors note the absence of studies and knowledge about patients’ backgrounds and factors motivating their travel, and a gap in the research on the industry.
Three papers57,98,114 explicitly explore the effects on the NHS. The study by McKelvey et al. 98 of multiple births over the past 11 years found that over one-quarter of high-order pregnancies in a UK foetal medicine unit occurred in patients who had travelled abroad to access fertility treatment. The qualitative study by Culley et al. 57 showed the complex motivations for travelling abroad, but concurred with other research that cost of treatment and the greater number of gametes available abroad or more easily accessible gametes played a part in decision-making. This was echoed by the results of a survey114 in which UK respondents were most likely to name difficulty in accessing fertility treatment as motivation for travel.
Dental, bariatric and cosmetic tourism
A further area of medical tourism is dental tourism. 137 Three papers101,105,122 focused on the issue of patients travelling for dental treatment. These indicated that this is likely to be an area of increasing travel by UK residents given the high cost of dentistry in the UK private sector, limited availability in the public sector and the lower cost in Eastern Europe. 101 Some countries, such as Hungary and Poland, have marketed themselves as dental centres of excellence. 137 A survey of dental clinics in Western Hungary and Budapest105 showed the largest group of patients (20.2%) originating from the UK, with lower prices being cited as the main motivating factor.
Two papers focused in depth on issues surrounding bariatric surgery. One explored the ethical challenges117 and the other was a case study of complications experienced by a US patient. 127
Papers by Birch et al. 134 and Miyagi et al. 102 focused on complications from cosmetic tourism in UK patients. A poll conducted amongst members of the UK public found that 92% would consider travelling abroad for cosmetic surgery. 104 The possibility of a large number of UK patients seeking cosmetic surgery abroad appears to be supported by a survey conducted by the British Association of Plastic, Reconstructive and Aesthetic Surgeons (BAPRAS),76 which found that 37% of respondents had seen patients in the NHS with complications from overseas surgery.
Risks
The issue of risks to the patient in terms of health outcomes was covered in 30 papers. 11,26,40,51,53,55,63,64,66,67,70,72,76,77,79,83,91,92,99,102,104,107,111,114,115,117,119,127,128,135 Perhaps surprisingly, only seven of these51,64,83,91,99,102,111 focused exclusively on the issue; 10 studies51,55,65,98–101,117,127,132 mentioned longer-term health outcomes of patients. Four papers51,66,83,111 reported cases of infection that resulted from patients travelling to receive medical treatment. Three51,83,111 described the recent outbreak of NDM-1-producing Enterobacteriaceae following patients receiving treatment in India, which highlighted some of the dangers of medical tourism and microbial resistance. The fourth66 described an outbreak of hepatitis B in a London hospital traced to a patient recently returned from surgery in India.
Effect on recipient country health system
As summarised in Appendix 12, 36 papers8,17,42,43,48,49,51,56,65,68,71,74,78,83,85–88,92,94,97,102,103,105,106,108,109,113–116,120,124,125,128,132 focused on the effects on the recipient country health system. Issues highlighted include the potential for medical tourism to result in the retention of doctors in, or attraction of doctors to, low- and middle-income countries, thus preventing or reversing a brain drain, and to generate foreign currency. 86 Also considered is the danger of creating a two-tiered health system, resulting in increasing inequities in access and quality of health care for the local population in destination countries. 78,125 Explanations are twofold: first, a rise in price in countries that do not provide public health services free at the point of use and, second, the potentially greater concentration of doctors in the private sector. 103
A total of 34 papers8,17,42,47–49,56,57,65,66,71,76,77,81,83,87,91,94–96,98–101,104,106–108,114,117,118,127,129,132 focused on potential effects on the health system of originating countries. These referred to factors leading to travel by patients, including a rise in costs. Studies documented patients returning with complications,99 including to the NHS. 102 Research highlighted the need for regulation, the lack of quality control of overseas providers and the cost (potential or real) arising to the originating country from treating complications. Two papers94,96 calculated the potential cost savings and benefits of sending patients abroad. When papers focused on the effects on the health system of originating countries, this was mainly on perceived negative consequences.
Industry
Thirty-nine of the papers reviewed8,10,11,17,43,44,50,53,56,57,60,62,68,69,71,72,76,81,85,88–92,95,97,98,103,104,106,107,109,113,116,122,124,128,132,135 focused at least partly on providers of medical tourism. Less attention was paid to facilitators (n = 19). 47,50,56,57,59,70,77,81,89–92,104,113,117,118,132,133,135 A subset of 19 papers8,50,56,62,68,69,76,81,88–90,92,95,107,109,118,124,132,133 studied the medical tourism industry in a more focused way. This included reviews of websites,90 market analysis,82 qualitative analysis of the role of medical tourism facilitators118 and a more general review,92 as well as a model for tourism development. 69 Articles examining communication materials and websites highlighted the limited information on follow-up care and redress in case of complications. 79 They also pointed to an emphasis on testimonies from patients rather than formal accreditation or qualification of clinicians and the great focus on tourism aspects of the destination and offering services ‘as good as at home’. 80 In addition, the low cost of treatment was used as a selling point.
There were two qualitative studies of medical tourism facilitators (interview samples included nine118 and 1282 interviewees, respectively); facilitators were presented as a heterogeneous group with a range of motivations.
Studies tended to mention regulation but only two123,130 reviewed this more systematically; both pointed to a vacuum in regulation.
Many studies mentioned individual hospitals or recounted an example of a medical tourism provider at the country level to give a flavour of the industry. 53,82 However, only four studies85–88 reported findings of a more systematic assessment of the industry and its operations. One study,40 evaluating past experiences of EU cross-border care, examined contracting arrangements and their effects on health outcomes.
Trade in health services: revenue and volume
Medical travel – the consumption of health services abroad – is defined as a trade under the General Agreement on Trade in Services (GATS) mode 2 and the majority of papers included in this review implicitly or explicitly focused on this form of trade in health services. 8 A subset of seven papers75,85,94,103,116,125,128 included a detailed discussion of other forms of trade in health services, including cross-border provision of services (GATS mode 1) and movement of health workers (GATS mode 4). Many overview papers mentioned the investment by US providers in Asian hospital groups without explicitly exploring this (GATS mode 3). Four papers8,46,75,94 analysed policy processes and challenges to trade in health services.
The actual volume of trade (the flow of medical patients) was referred to in many papers but investigated in few. 74,85,105,114,116 Studies by the United Nations Economic and Social Commission for Asia and the Pacific124 and Leng88 all provided further estimates or trends. The studies by Lautier,85 Siddiqi et al. 116 and NaRanong and NaRanong103 were the only ones that calculated the total volume of trade in health services (for 13 countries), including the actual costs and effects on recipient country health systems. For example, NaRanong and NaRanong103 calculate the contribution of medical tourism to the Thai gross domestic product (GDP) (0.4%), with medical tourists with their higher purchasing power likely to increase the cost of health services and lessen access in the public sector.
Most papers cited similar figures for patient flow but often sources were not accessible or figures were based on media reports or on other academic papers, which in turn quoted inaccessible sources. When sources for patient numbers were cited these have been summarised in Appendix 12.
One of the most commonly cited sources for patient flows was other academic papers. Seven papers67,81,92,93,108,129,131 referred directly to a report by Deloitte17 and six10,40,50,58,67,68 referred to a report by McKinsey;12 the exact ways in which figures in these reports were calculated remain unclear. Even when these reports were not referenced, the figures cited suggest that these two reports were used as sources. For example, a paper by Nassab et al. 104 cites the Economist, stating that 750,000 US patients travelled abroad for treatment in 2007. This is the figure provided in the report from Deloitte17 in 2008. Eight papers85,88,103,105,106,114,116,124 had either generated or collected their own data on patient flows.
Discussion
Perhaps the most surprising finding was the increase in number of papers presenting findings from primary research – a shortfall or gap that had been noted by the earlier literature reviews. 42,55,70 The recent publication date of many papers confirms the increasing amount of research being carried out on medical travel.
Medical tourism is a phenomenon in the private health-care market, which makes it hard to monitor and regulate patient flows. 137 Despite the rapid increase in number of publications over the past 2 years, reliable calculations of the actual volume of patient flow remain rare. This confirms findings from an earlier review,42 which also noted the lack of information on how the figures in the reports by Deloitte Consultancy17 and McKinsey12 were calculated.
The body of literature focusing on medical tourism as a trade in health services indicates that further research investigating levels of such trade is needed. Data on costs and benefits of medical tourism are rare and this limits accurate assessments of its effects to inform policy decision-making. Studies are also needed to empirically observe the effects of medical tourism in practice. The definitions of trade in health services provided,8 together with the framework for measuring its level provided by Siddiqi et al. ,116 set out a methodology for such research.
Understanding of the industry is limited. None of the research-driven papers captured the entire value chain of medical tourism. It is not evident how different industry actors (e.g. referring clinician, websites, facilitators, travel agents and receiving clinicians or hospitals) link together and how their relationships may influence patient experiences and health outcomes. Three papers referred to the role of medical tourism facilitators, drawing on small samples, demonstrating the need for further research in this area, especially to enable regulation or to address the ethical dimensions discussed in the papers reviewed. 118,131,133
Types of medical tourism
The literature reviewed clearly indicates that medical tourism is no unified phenomenon. Subthemes as distinct areas covered by research were evident from the review, such as diaspora or fertility travel or travel for bariatric surgery or dental or cosmetic work. The papers on diaspora travel highlight that medical tourism and decisions by patients to travel are not simply guided by cost considerations or even clinical outcomes. Rather, the literature points to a complex matrix of perceptions of care, waiting times, cost and other factors.
The different types of medical travel allow some inferences about patient motivation, for example cost or availability in cosmetic procedures, regulation in the case of fertility and so on. However, a lack of information about patients’ characteristics limits a deeper understanding of push and pull factors.
Impact on the NHS: lack of studies focusing on long-term health outcomes
Evidence demonstrates that patients travelling abroad to receive treatment and returning to the UK may face complications or infections requiring follow-up in the public sector. Seven papers65,66,76,83,98,101,102 reported on patients who were treated in the NHS as a result of complications resulting from treatment abroad. Based on the literature reviewed, cosmetic procedures appear to be an area of growth for medical travel by UK patients and are likely to result in costs to the NHS from resulting complications. This underlines the need for further research to ascertain the potential impact and costs for the NHS arising from medical tourism.
In addition, little is known about the longer-term health outcomes of medical tourists beyond these incidental reports of complications. No literature on inward medical travel and its effects on the NHS was identified, pointing to a gap in knowledge.
Conclusions
This review provides a map of current knowledge on medical tourism and identifies a series of subthemes. The reviewed papers demonstrate the multidisciplinary nature of medical tourism research. There has been an ‘explosion’ in research on medical tourism over the past 2 years. This review clearly identifies limits to current knowledge; many papers remain hypothetical and there are many areas in which further research is needed.
There is still a lack of information on the background of patients and the numbers of patients travelling abroad for treatment. This limits insights into why some patients travel and others do not and restricts evidence about the possible costs and benefits of medical travel.
The absence of information on patients’ social, economic and demographic backgrounds hampers the ability to understand patient decision-making and determinants of travel. The studies reviewed indicate that motivation is complex. Further information is needed to fully understand this decision-making process. It is especially relevant to gain insight into why patients from countries with public health-care systems such as the UK choose to travel abroad.
Little is known about the industry beyond reviews of information materials and websites. Further research, especially qualitative and survey-based research, is needed to better understand how the sector operates and what its motives are to ultimately understand how it drives or affects trade in health services and health outcomes of medical travellers.
Although case studies of patients returning from treatment abroad with complications were reported, these did not quantify the potential cost of medical travel to the patients’ ‘home’ health systems. Given the evidence of an increase in medical travel such research is urgently needed.
There is no research examining the long-term health outcomes of UK medical tourists. Further qualitative and quantitative research, beyond immediate clinical outcomes, is needed to truly understand the effect of medical travel on patients and its cost to the health system.
Implications for the NHS
-
There is a need to collect data on the number of patients who return from treatment abroad and are treated within the NHS.
-
There is a need for additional surveys and quantitative research to understand more fully the volume of patients who travel abroad and their social and economic characteristics. This will enable a more accurate understanding of the scale of the issue and factors determining patient travel. These ‘push factors’ may in themselves hold valuable lessons that reflect on the NHS.
-
There is a need for research to assess the long-term health outcomes of medical travellers to fully understand the effects on individual and population health.
Chapter 4 The context of medical tourism
This chapter provides an introduction to medical tourism services, processes, providers and countries’ strategies. Drawing across the composite data set, including interview data (encompassing commercial interests, overseas providers, professional associations and stakeholders, and medical tourists) supported by the desk-based activity (e.g. website review), we seek to conceptualise and typologise, unravelling the bigger picture of medical tourism, as viewed through the perspective of respondents. The chapter is structured around four themes:
-
services: highlighting the range of treatment and ancillary services within medical tourism (offered by providers, marketed on the internet and purchased by patients)
-
information: conceptualising the ways in which information is made available
-
clinical provision: outlining the range of clinical providers within medical tourism and their supply chains
-
country strategies: a review of five country strategies aimed at growing medical tourism and their perspectives on UK market opportunities.
The chapter summarises the emerging implications for the NHS.
Services
Medical tourism treatment pathways involve a number of services (both clinical and ancillary) that together give an overall experience. Although not all of these services are integrated in each and every patient journey, the variety of services illustrates the full range of possibilities:
-
conferences and media activities: for example fertility trade fairs that market, inform and connect potential travellers with overseas services
-
websites: prospective travellers use the internet to find out about medical travel and to support decision-making, including clinic websites, portals (which may contain details of numerous clinics) and consumer-driven sites such as chat rooms and discussion boards
-
intermediaries: (facilitators and brokers) provide information (web-based and one-to-one) for prospective patients about treatments and services and make arrangements for treatment and services
-
preconsultation: this may take place in the UK or abroad at a preliminary clinic undertaken by the surgeon or doctor, or screening may be provided by a contractor based within the UK
-
treatment: (provided by clinics and hospitals) may involve outpatient treatment, day surgery or longer-stay hospital admission
-
forms of accreditation: (available to clinics, hospitals and facilitators) seek to offer assurance around the quality and safety of products; accreditation is itself typically a commercial activity with competing accreditation bodies offering their services
-
financial products: available to patients to fund the costs of travel and treatment
-
insurance products: developed to insure for travel and loss, and seek to cover the costs of further treatments that may be required as a result of complications and dissatisfaction following surgery abroad
-
travel, hotel and concierge: flights, accommodation (for accompanying family and companions, or for patient recuperation) and support services (e.g. translation) are purchased
-
tourism and wellness: for some medical tourist destinations and treatments, attempts are made to promote the cultural, heritage and recreational opportunities
-
aftercare: may be arranged within the treatment country or within the home country (including dressings, stitches, pharmaceutical arrangements, monitoring and follow-up).
There are particular stages in the treatment pathway during which issues arise that have a bearing on the NHS. First, can individuals obtain appropriate information to ensure that they are able to make an informed choice and ensure their safety? For example, is non-commercial advice and input available at trade fairs and on websites, for example travel guidance and checklists? Second, what advice should the Department of Health, commissioning bodies and GPs provide to individuals seeking to travel abroad? Finally, are appropriate aftercare arrangements made, given that there may be expectations of receiving NHS care and financial implications if aftercare services are required.
Information
Searching for information may be time-consuming, confusing and overwhelming. Individuals may be unclear how best to go about finding and validating trustworthy sources of information. Looking across the range of patient, commercial and stakeholder interviews, analysis identified three idealist models whereby prospective medical tourists gather information and source their destination and provider (see Appendix 13).
Model 1: facilitator-enabled provision
A range of intermediaries – known as brokers or facilitators – arrange services and phases of treatments. Such intermediaries may specialise in particular target markets or procedures or destination countries (e.g. from our own interviews these included sites focused on fertility treatment or on a particular destination for a range of treatments). Facilitators may be physically located in a home country, have a presence overseas or both. As well as e-mail and telephone communication, they may undertake chaperoning and translation functions during the travel and treatment phases. The potential for intermediaries can be attributed to the transaction costs associated with medical tourism.
Model 2: consumer-driven access to information and provision
In the consumer-driven model individuals use various forms of soft/hard intelligence to inform decision-making around medical and ancillary products, relying on marketing imagery, or evidence on quality and outcomes. They take the lead in searching and arranging. Our patient interview data suggest that individuals consult websites to compare costs and to reduce their own transaction costs when putting together a particular treatment journey (particularly related to search and information costs). As outlined in Section 3, decisions are likely to vary for different treatments (e.g. fertility treatments, for which patients are likely to be health literate about success rates and risks). Decisions to be made include selecting country, clinic and clinician and arranging travel insurance or specialist insurance, finance, travel, accommodation and concierge, and aftercare.
Model 3: networked access to information and provision
The final type of access to medical travel information relies predominantly on network dynamics. 138 Individuals source information through treatment-based, cultural-based and professional networks.
Cultural- or treatment-based networks involve patients drawing on the advice, relationships and socialisation influence of a wider group:
-
Cultural-based networks: for example, Section 3 outlines how British residents and citizens with cultural and historic ties to Indian and Somali populations travel to India and Germany, respectively, for dental treatment and diagnostics based on informal recommendations from close friends and within the wider community network.
-
Treatment-focused networks include organised discussion forums and self-help groups that cohere around treatments/conditions such as bariatric, fertility and cosmetic treatment. As Section 3 outlines, these networks may also be enmeshed in delivering treatments themselves, including offering services for support and aftercare (e.g. bariatric and fertility support groups).
Professional networks involve professional ties and connections mediating information and choice:
-
Professional networks can involve clinicians and professionals advising and linking individuals to clinicians and hospitals across national boundaries. For example, as detailed in Section 3, some private fertility clinics have links to partner clinics overseas (where perhaps wider treatment choices are available). Clinicians will also directly recommend amongst their own networks (reflecting education, training and experiences). As Chapter 15 outlines, when overseas governments are paying for NHS treatment, the choice of provider is explained by network knowledge and strong ties (e.g. where referring clinicians trained or undertook postqualifying training or where attachés have strong links).
These three network configurations sharply contrast simple market relationships of buyer and seller making trade-offs around price/quality.
To reiterate, these three idealist models (facilitators, individuals and networks) explain how information is sourced for medical tourism. These three types are clearly evidenced within our patient stories and wider interviews. As ideal types they are not mutually exclusive, and patient stories will contain one or more such sources of information, for example there is overlap between models 2 and 3 with regards to consumers’ engagement with professionals.
There are also clear advantages and disadvantages of such sources of information. In Appendix 13 we develop an analysis of the potential advantages and drawbacks of these three information sources, informed by what medical tourists and commercial interests suggested during interviews.
Clinical provision
Within medical tourism there is a diversity of participating clinics and providers [as Ackerman139 suggests, ‘cottage industries and transnational enterprises’ (p. 405)]. Providers are primarily from the private sector but are also drawn from public sectors. Relatively small clinical providers may include solo practices or dual partnerships, offering a wide range of treatments in areas such as cosmetic surgery. At the other end of the scale are extremely large medical tourism facilities in which clinical specialism is the order of the day. Hospitals may be part of large corporations or wider affiliations of general and specialist clinics. Although there are smaller independent, specialist clinics, it is these large complexes that dominate the Spanish industry.
Larger clinics and providers have moved to offer a range of services (financial products, insurance, hotel, translation, accommodation, aftercare) within a horizontally integrated supply chain. Services may be more loosely or fully integrated and emphasise upstream integration (finance, preconsultation, travel), downstream integration (recuperation, aftercare, follow-up) or both.
Country strategies
A range of national government agencies and policy initiatives (both in Europe and beyond) have sought to stimulate and promote medical tourism in their countries. Many countries see significant economic development potential in the emergent field of medical tourism. Before and during our fieldwork period we attended large international trade fairs and conferences supported by the Hungarian, Maltese, Croatian and Turkish governments, all of which sought to promote their comparative advantage as medical tourism destinations. In Appendix 14 we present a synopsis of what we assess their strategies and developments to be (drawing on provider and wider industry discussions, trade fairs and online information).
Implications for the NHS
-
The wide range of clinical, ancillary and support services involved in medical tourism complicates efforts to inform and educate medical tourists, or to regulate aspects of the industry.
-
Some European countries and beyond are seeking to explicitly market to prospective UK patients.
-
There is strong competition, as well as volatility and changeability within mainland European provision, for some treatments.
-
Medical tourists use a range of information points (intermediaries, direct and networks), which complicates practical attempts to improve information quality.
-
The European market for medical tourism is dominated by solo practices and small providers, although there are some moves to national organisation and professional affiliation in some countries. Monitoring quality and outcomes across this range of providers (and outside of the large and publicly financed institutions) is problematic.
Chapter 5 Mapping patient inward and outward flows
Problems with numbers
Authoritative data on numbers and flows of medical tourists between nations and continents are difficult to identify. Although there is consensus that the medical tourism industry has grown over the past decade, and that there are particular bilateral flows, there remains disagreement as to the current and potential size of the industry.
A key issue is that the primary source of data relating to numbers and flows is the industry stakeholders themselves. Given the possible scope of what is often a private and confidential industry in an increasingly borderless world, it is inevitable that the industry stakeholders are best placed to provide the most reliable information. The problem of course is that such information may not be reliable at all; aside from the fact that such stakeholders have a vested interest in presenting a picture of a vibrant and growing industry, those prepared to accurately record patient numbers, flows and profiles face a range of difficulties.
Whether estimates are taken from industry stakeholders, the grey literature or the academy, they are consistent in one respect: all of the numbers cited are either estimates or extrapolations. These estimates of the global numbers of medical tourists generally lie on a continuum between statistics published by the Deloitte management consultancy at one end of the spectrum and a more conservative estimate by McKinsey at the other. Deloitte placed the number of US citizens leaving the country in search of treatment at 750,000 in 2007 and this number was projected to reach somewhere between 3 and 5 million by 2010. 17,140 Given that US tourists are thought to represent roughly 10% of the global number of medical tourists,12 this would suggest that total worldwide figures would lie somewhere between 30 and 50 million medical tourists travelling for treatment each year. However, analysts at McKinsey suggest that, although the potential for such large numbers exists, a more accurate worldwide figure would be between 60,000 and 85,000 medical tourists per year,12 although these numbers do appear rather small and unrealistic.
The real problem when searching for reliable data is, as mentioned, that it is stakeholders with a vested interest who are providing the data. 141 So successful have these stakeholders been that their numbers and the numbers offered by Deloitte have transcended commercial literature, with Deloitte’s ‘750,000 Americans’ statistic being reproduced not only on commercial sites but also in grey literature as well as peer-reviewed academic literature. It could be argued that, by providing the parameters within which the industry is discussed (i.e. huge), Deloitte has managed to normalise the rather grandiose claims of organisations such as Bumrungrad International Hospital as well as countless national tourism boards.
None of this is problematic of course if Deloitte’s statistics are correct, but here we encounter a real problem. In both Deloitte’s original 2008 publication17 as well as in their 2009 updated projections,140 the numbers cited have not been generated by any scientific method. Indeed, the source of their numbers is simply an online article for India Daily,142 which simply states that 750,000 Americans will travel in 2007 and that by 2010 the number will reach 6 million. No evidence is offered; the figure is an estimate provided with no source of support and there is absolutely no suggestion that the figure has been reached as a consequence of any data collection. Approaching industry estimates with caution may seem like common sense, but it is important to note that such sources have also informed the wider grey and academic literatures, often being repeated in articles within well-respected journals.
So where should we look for data? Ideally we would look to well-designed, unbiased empirical studies from within the academy. Here, though, it is clear that there exists no credible authoritative data at the global level. The empirical work that has been published is generally small-scale and qualitative and these studies often avoid making market estimates. The reality is that no authoritative, reliable and unbiased data at the global level exist in the public domain. Although this cannot be fully addressed, the IPS can provide some illumination with regards to the flows into and out of the UK. The survey has some methodological flaws, especially in terms of how representative it is, but it is nonetheless an unbiased, quantitative source of data that allows time series analysis over the last decade.
The IPS, conducted by the ONS, collects information from passengers as they enter or leave the UK. Started in 1961, it aims to collect data on credits and debits in the UK balance of payments; provide information on visitors to the UK to inform tourism policy; provide data on migration; and collect information to help aviation and shipping authorities (IPS, J Hanefeld, London School of Hygiene and Tropical Medicine, 2012, personal communication). Passengers are randomly selected as they travel through passport control (entering or leaving) and a brief survey is administered. This includes basic questions about an individual’s age, sex, origin and destination, as well as questions about whether the travel is part of a package, with company or for business, the class of travel and the likely length of stay abroad or in the UK and likely pattern of expenditure. One of the survey questions asks passengers to define the primary purpose of their travel and ‘medical treatment’ is one of the possible answers, thus providing insight into the number of passengers travelling for this reason.
The main limitation of these data is the number of passengers sampled. In 2007, for example, 255,000 interviews were conducted, representing 0.2% of travellers to and from the UK overall. 41 However, given the absence of other reliable data on numbers of medical tourists, their characteristics and where they travel, the IPS does represent the single most comprehensive data quantifying medical travel to and from the UK. The IPS data have important limitations, which inhibit nuanced statistical analysis. As such, a more descriptive analysis is appropriate and, given the dearth of trustworthy data pertaining to medical tourism, is incredibly valuable.
Data from the International Passenger Survey
As Figure 1 shows, the number of people from the UK travelling to access medical treatment has increased steadily over the past decade. The number of patients travelling to the UK has held reasonably steady over the decade. (The IPS codes all passengers travelling from the Channel Islands and the Isle of Man as inbound medical travellers, that is, those coming to the UK to access treatment. As these patients are part of the NHS and are likely to have been referred for medical treatment to the mainland UK, these have been excluded from the sample of inbound patients to give an accurate picture of the numbers.) At the time of data analysis, figures for 2011 were available only for three quarters of the year, so are not included in the graph (see Appendix 15 for a regional breakdown).
FIGURE 1.
Line chart showing the numbers of people who travelled into or out of the UK for medical treatment during the period 2000–10.
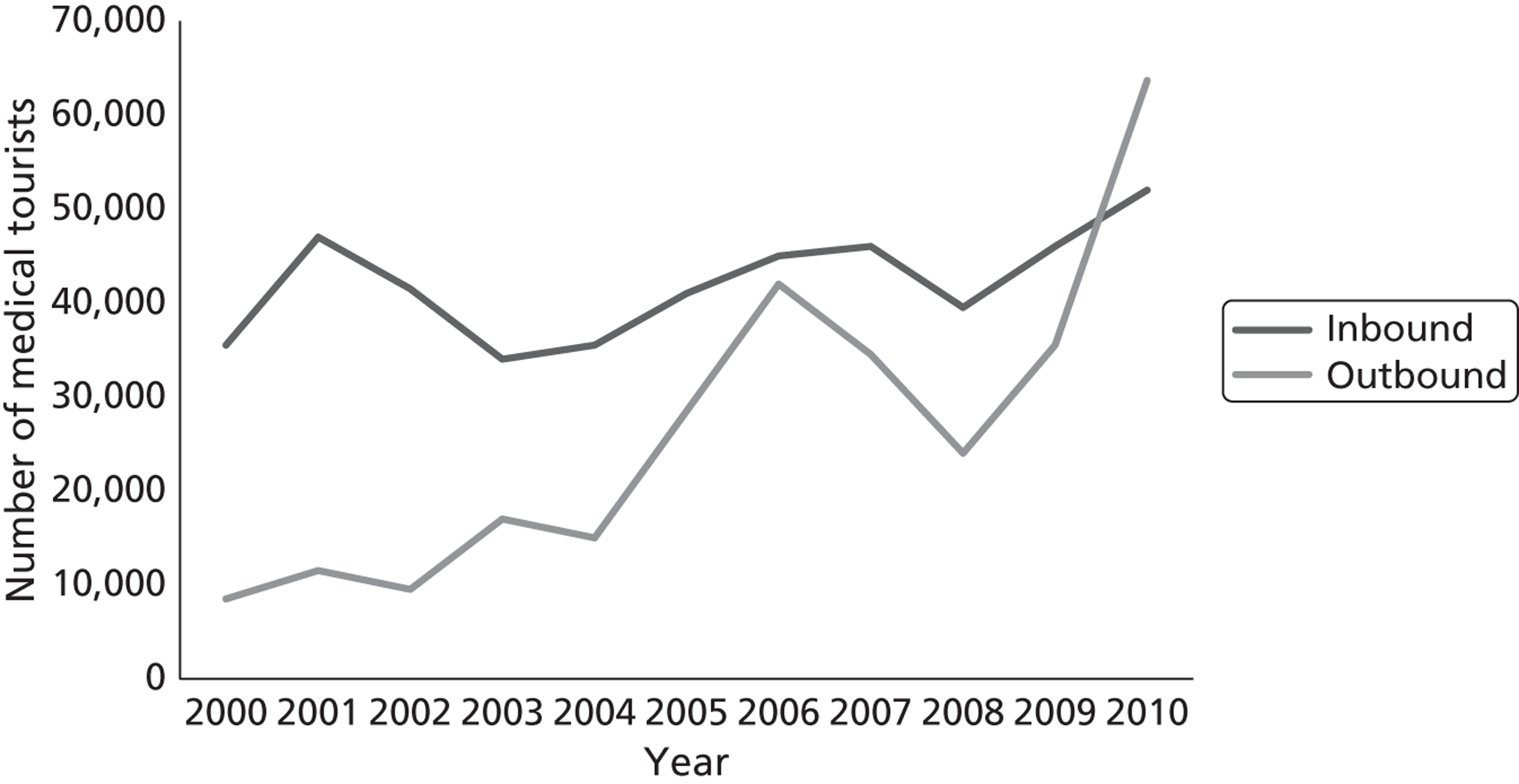
Destination of UK outbound medical travellers
For UK residents who travel abroad for medical treatment, Northern, Western and Southern Europe are the most common destination regions, as evident from Figures 2 and 3, with France being the most visited country over the decade. Appendix 15 charts these trends over time.
FIGURE 2.
Pie chart showing total outward medical travel by UK residents by destination region over the time period 2000–10.
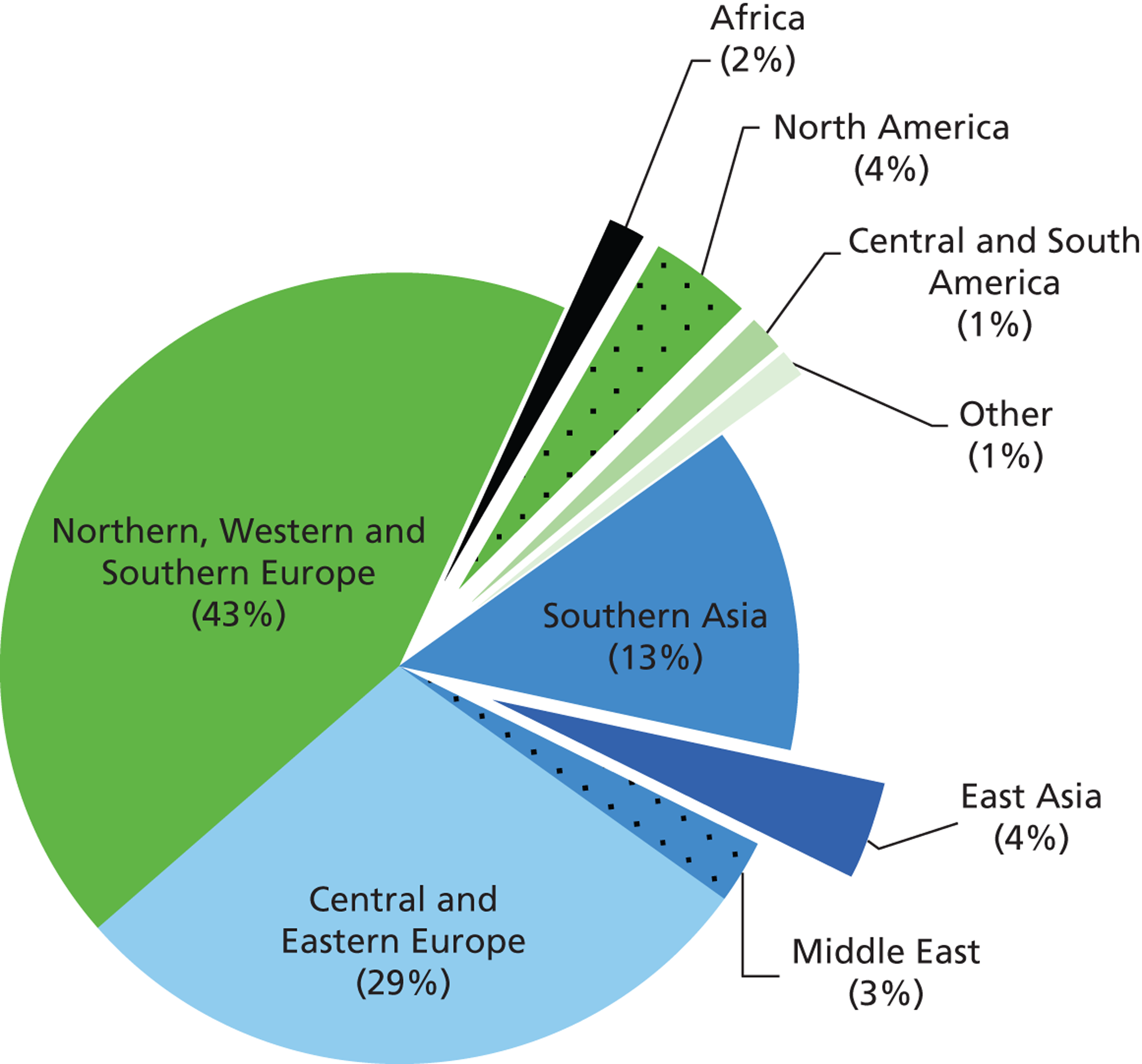
FIGURE 3.
Map depicting total numbers of medical travellers from the UK and their destinations over the period 2000–10.
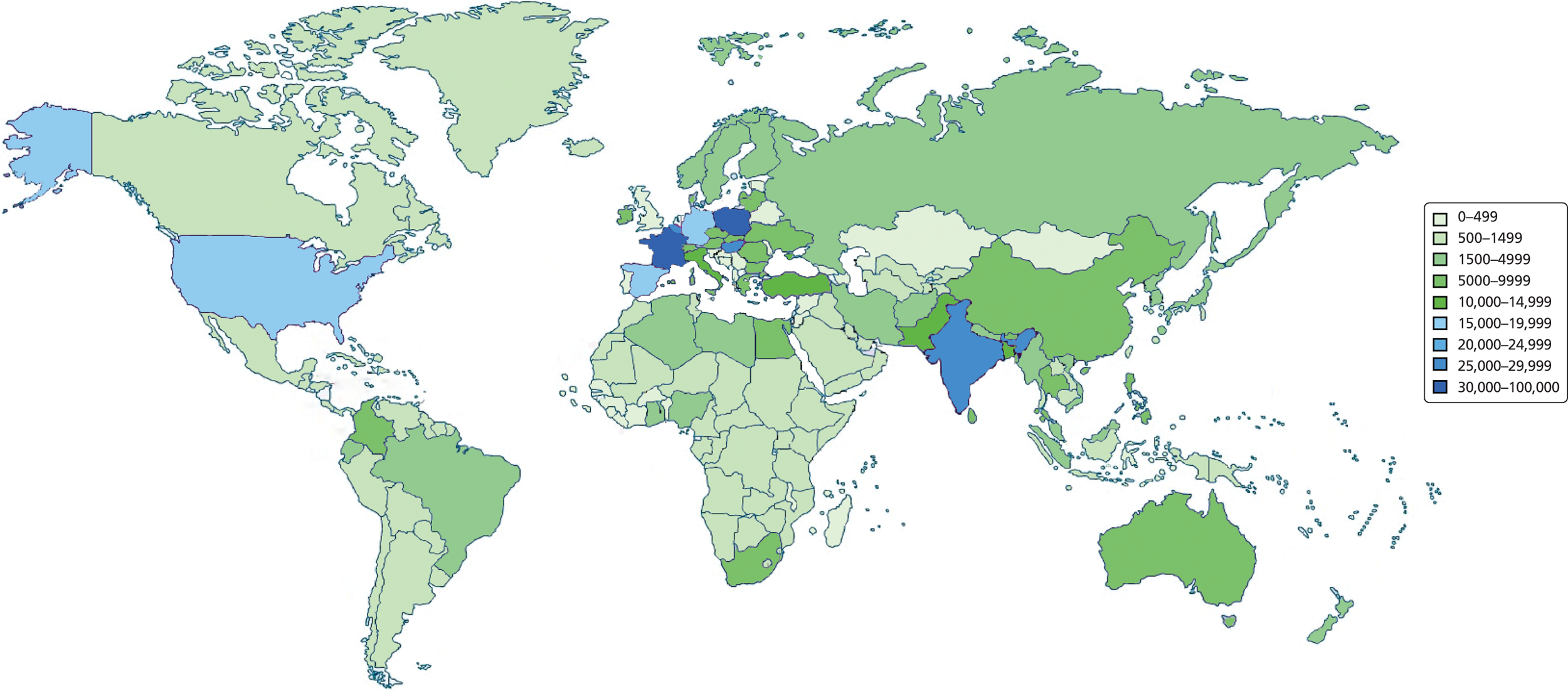
Central and Eastern Europe are the second most popular destinations. Appendix 15 (see Figure 15) clearly shows high numbers of travellers visiting Poland, the second most popular travel destination over the decade, and the most popular in recent years with approximately 11,000 and 13,500 travellers in 2009 and 2010 respectively. It also indicates the popularity of medical travel to Hungary since 2006.
South Asia (primarily India) attracts large numbers of UK patients, making it the most frequently visited non-European region (see Figure 2). The most recent data show the relatively stable pattern of travel to India, Pakistan and (in much lower numbers) Sri Lanka and Bangladesh. Medical travel to East Asia shows a different pattern to that for South Asia. No medical travellers from the UK to East Asia were recorded by the IPS before 2003, when 1500 people travelled from the UK to East Asia. In 2010 > 4000 people made the same journey, which represents an increase of 171%. By 2010, 15% of all UK medical travellers went to East Asia. North America, the Middle East, Africa and Central and Southern America account for a small percentage of those undertaking medical travel.
As Appendix 15 (see Figure 15) illustrates, France, Poland and India are the most popular destinations for UK medical tourists, with France holding relatively steady, India demonstrating a gradual increase and Poland experiencing a rapid increase as of 2007. The French case may be explained as a historical and geographical option, with its proximity to the UK proving convenient alongside a familiarity of British holidaymakers with France. Similarly, both Belgium and Spain can be found in the top 10 destinations across the decade (fifth and eighth, respectively), perhaps for similar reasons.
Poland has demonstrated the largest surge in popularity and by 2009 was the most visited destination for medical travellers from the UK. This may reflect the fact that the UK is home to a large population of people with historic and familial ties to Poland, a population that has burgeoned considerably during the second half of the last decade. Although this is likely to be the case, the proximity to and accessibility of Central and Eastern Europe and the emergence of a reputation for high-quality cosmetic care (whether this is accurate or not) are also undoubtedly factors. Hungary, with a reputation as a leader in dental care, is, like Poland, easily accessible by low-cost airlines operating from the UK and is the fourth most visited destination by UK travellers. Similarly, the Czech Republic is the 12th most visited destination and, like both Hungary and Poland, has developed a reputation for particular types of treatment and is well served by budget airlines.
India has proven to be a popular and increasingly visited destination during the time period analysed, which, as with Poland, might reflect the fact that the UK has a large population with historic ties to India and that travel to this region has become much more accessible in recent years. Indeed, it may even be that those travelling retain Indian citizenship. Similarly, Pakistan was the 10th most popular destination for UK medical travellers, once again possibly a reflection of a large population of people in the UK with historic ties to Pakistan.
Inward medical travel
The largest numbers of inbound medical travellers are from Northern, Western and Southern Europe (Figure 4). Looking at individual countries, the greatest numbers of patients travelling into the UK for treatment are from Ireland and Spain and these two countries also show a growing trend of patients coming to the UK. In the case of Spanish (and perhaps French) residents, it is highly likely that a substantial number will be UK expatriates and it is unclear whether these engage in out-of-pocket medical treatment or whether they use NHS services. The numbers of Greeks and Cypriots travelling into the UK to access treatment rose rapidly in 2009 and 2010. This increase may be the result of the economic crisis, which in turn has meant severe public sector cuts including in health. 143
FIGURE 4.
Map depicting total numbers of medical travellers to the UK and their countries of origin over the period 2000–10.
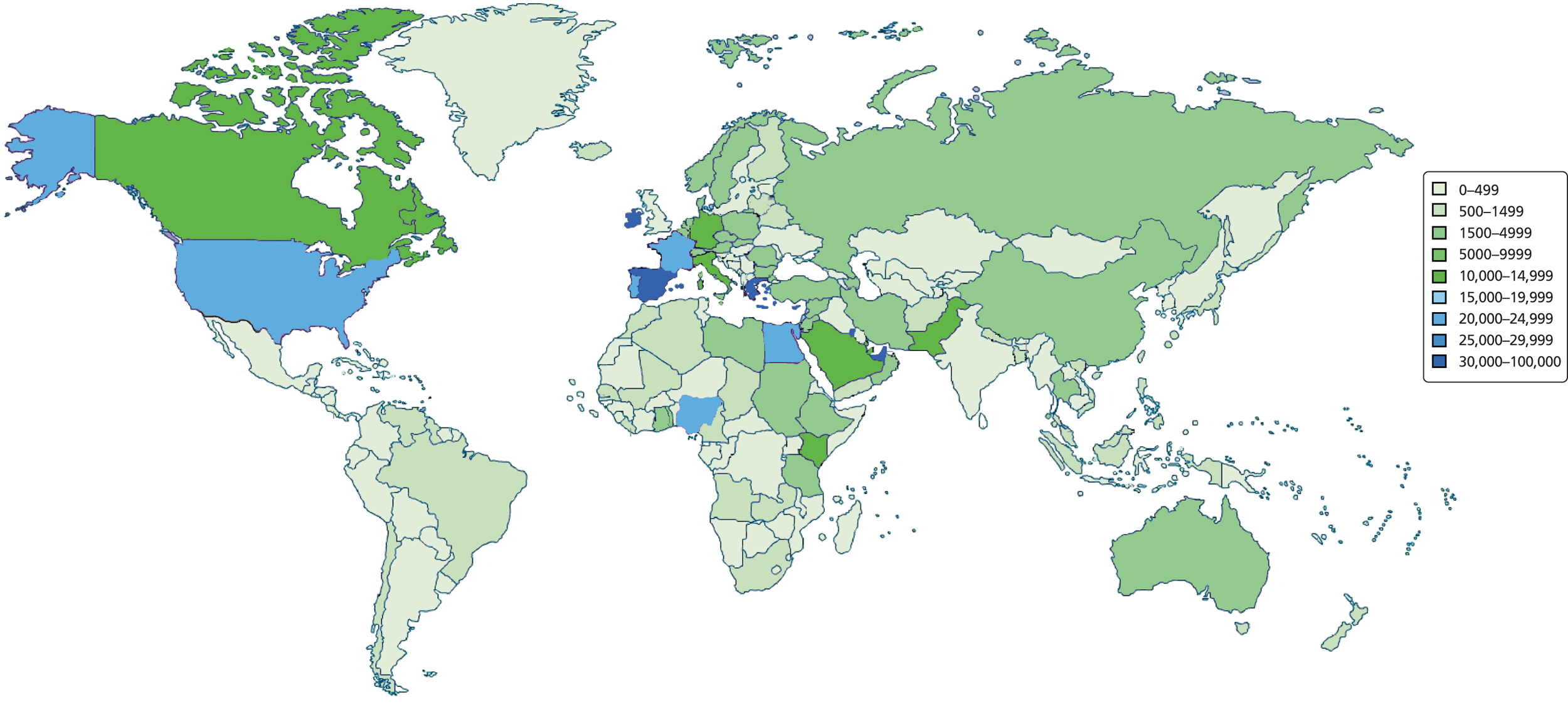
A significant number of patients also travel from countries in the Middle East (specifically from the United Arab Emirates and Kuwait, although visitor numbers dropped sharply in 2008 and 2009 respectively).
Despite some variation over the years, a stable inward flow of medical travellers from Nigeria is also evident over the past decade.
Comparing numbers of inbound and outbound medical travellers from 2000 to 2010 (see Appendix 15), a trend in increasing outbound medical travel is visible. Despite a temporary drop in patients from the UK travelling to access treatment in 2008, the data show that the number of outbound travellers in 2010 exceeded the number of inbound travellers for the first time.
Characteristics
Most inbound medical tourists are in the age group 35–44 years (22%), with 18% of medical tourists between the ages of 45 and 54 years and 19% between the ages of 55 and 64 years; 16% were aged ≥ 65 years. A much smaller number of children and young adults were inbound medical travellers.
Interestingly, this differs from the demographic profile of those travelling from the UK to seek treatment abroad. Almost one-third (30%) of all UK patients travelling abroad are aged between 25 and 34 years, 20% are aged between 35 and 44 years and 16% are aged between 45 and 54 years. Overall, Figure 5 shows outbound medical travellers to be comparatively younger than those who travel into the UK to access medical treatment.
FIGURE 5.
Medical travellers by age.
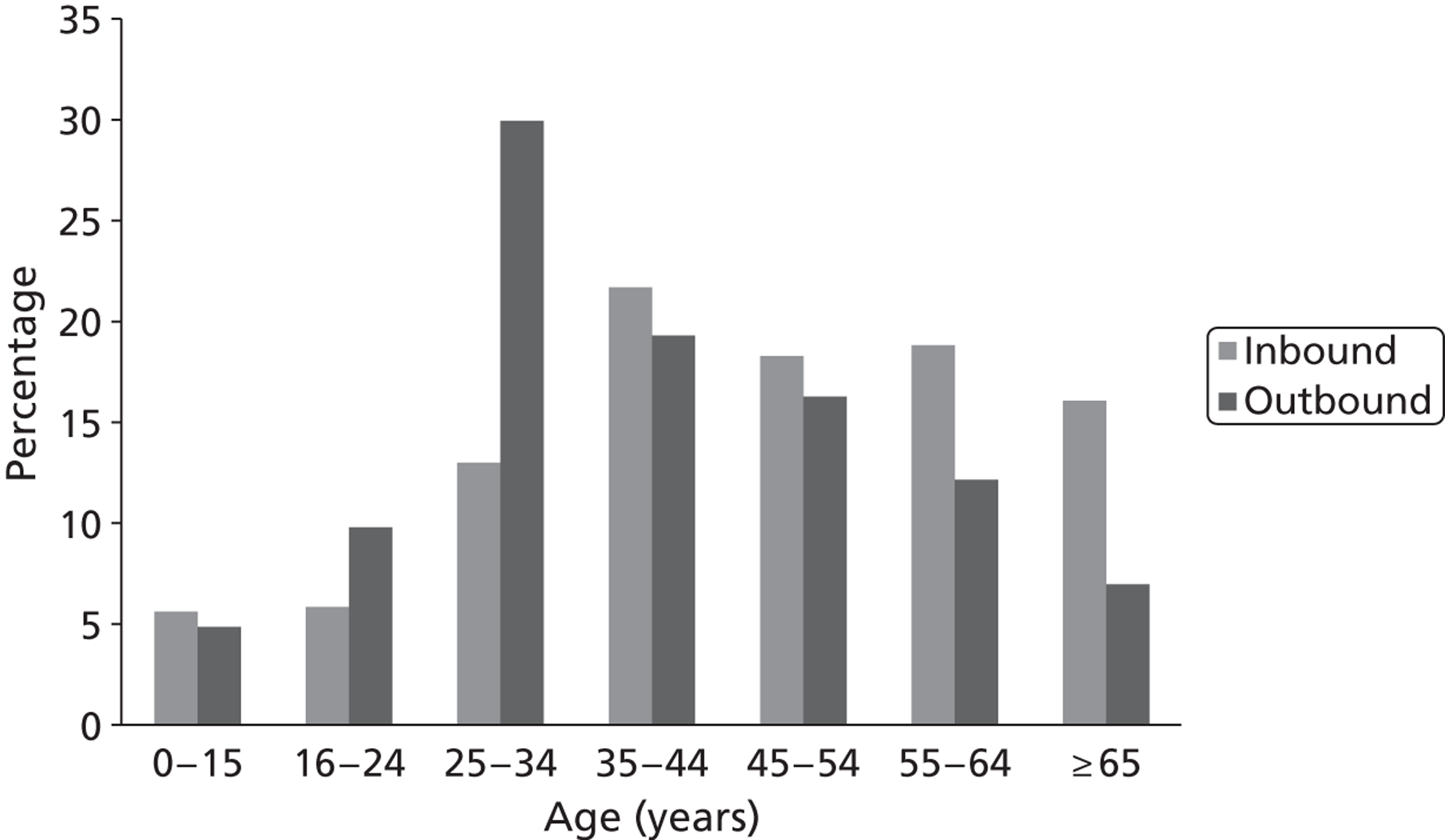
There is also a difference in gender split between inbound and outbound medical tourists. More women than men travel out of the UK to access medical treatment, whereas a greater number of inbound medical tourists are male. This appears stable across the decade when looking at the average across 2000–10 and considering the last couple of years individually.
Discussion
Data analysis highlights the characteristics of inbound and outbound UK medical travel. The largest number of patients travelling into the UK are from Ireland and more than half of all UK patients travel to Europe (both Northern, Western and Southern Europe and Eastern and Central Europe) to access treatment, with France being the most popular destination country for UK patients when looking across the decade (see Appendix 15, Figure 15). This seems to confirm the importance of proximity for patient choice of destination observed in other empirical work. 85,116
It is also worth highlighting the fact that many of those who have travelled into the UK for treatment may be expatriates, especially those travelling from countries such as France and Spain. It is possible that this group of people may be using – knowingly or otherwise – NHS services when they are not entitled to do so. Given that such high numbers of inward travellers are from regions with high concentrations of UK expatriates, this issue deserves further study.
Travel to South Asia on the other hand has remained relatively stable over the past years. Studies that demonstrate the importance of diaspora linkages for medical travel87,94 may offer a likely explanation for this. Diaspora linkages could also be an explanation in the past for the large number of inbound medical travellers from Ireland.
Data confirm that the UK is a destination for medical travellers, including from the Gulf States in the Middle East (see Appendix 15, Figure 16). Taken together with the information available on age groups of inbound medical travellers, it may be likely that patients from the Middle East are accessing specialist care in the UK private sector.
Demographic factors such as age and sex of outbound medical travellers from the UK – comparatively younger and more women – could potentially indicate that cosmetic and fertility treatments are key areas of medicine for which patients travel, as has been shown in incidental reports102 and recent survey results. 104
Trends
Analysis over time confirms recent media reports of a growing number of medical travellers to Poland and Hungary. This is likely to include patients travelling for cosmetic, dental and fertility treatment. These were confirmed in our research as areas of medicine for which both countries are marketing themselves.
Examining time trends also shows how medical travel is changing. Notable in this respect is the growth in medical travel to East Asia. No patients travelled to this region before 2003 yet in 2010 17% of all UK medical travellers visited the region. At the same time, although the overall volume of patients from the UK seeking treatment abroad grew, a comparatively smaller percentage of these were travelling to Europe. For example, in 2009 70% of all UK patients seeking treatment abroad travelled to Europe, whereas in 2010 this had reduced to 58%. This may indicate a changing trend in medical travel from Europe towards long-haul destinations, although it should be noted that Europe remains the most popular destination for medical travel and Central and Eastern Europe have seen a steady increase across the decade.
The rapid increase in the number of travellers from Ireland to the UK over the past 3 years could be an effect of the economic crisis, which has resulted in greater limitations on services available within the public sector in Ireland. This would then infer that these patients are likely to access care in the public sector. Similarly, the growing number of inbound medical travellers from Greece over the past 2 years may be associated with the effects of the economic crisis there. This is particularly likely given the documented impact that this has had on health. 143 The ‘dip’ in both inbound and outbound medical travel evident in Figure 1 in 2008 may be attributable to the onset of the crisis. Examining the number of travellers by quarter there was a much lower number of inward and outward medical travellers in quarter 3 of 2008 during the onset of the crisis than during the rest of 2008 or in quarter 3 of 2009.
Data confirm an overall rising trend in the number of patients traveling from the UK to access treatment but a stabilisation and decline in numbers of patients traveling into the UK to access medical services. The year 2010, the last year for which data were analysed, represented a tipping point at which the UK became a net importer of health-care services with a greater number of patients traveling out of the UK to access treatment and care than patients seeking services in the UK. Given the age of outbound medical travellers – the largest percentage of whom are 25–34 years old – this trend seems likely to continue.
This study offers the most extensive analysis of the most robust data set on inward and outward UK medical travel to date. This data set is not without its limitations. First, the data are useful only if passengers have answered the survey questions honestly; as we have encountered throughout this project, many do not wish to discuss health matters. Second, the sampling strategy employed by the ONS is not without flaws. Third, upscaling raw data regarding destination countries and countries of origin on the basis of an estimate of the proportion of passengers sampled is risky. That said, some of the results of this analysis add credence to some of the hypotheses and trends described in the recent academic literature and show that medical travel is complex and not a uniform phenomenon. Given that the IPS data indicate that 63,000 UK citizens or 0.1% of a population of 65 million travel per annum from a country with a NHS, it may be that the often-touted figure of 500,000–750,000 or 0.2% of Americans travelling abroad is realistic, although this will include large numbers of diaspora travellers, especially to Mexico. We can probably suggest that the debate should be firmly moved on from the estimates provided by McKinsey. 12
A growing number of patients from the UK are travelling abroad to access treatment. The majority of patients travel within Europe but an increasing number are seeking treatment further afield. Findings show a growing trend in UK patients travelling specifically to Poland and Hungary in Central and Eastern Europe, and a growth in travel to East Asia. Findings also confirm a slight overall decline in inbound medical travel, but a growth in numbers of travellers from Ireland, Greece and Nigeria.
Furthermore, the data support some of the characteristics of medical travel described in the literature. This includes the importance of proximity in determining where patients travel to seek medical treatment and the importance of diaspora linkages for patients traveling abroad. Some of the findings appear unexpected, such as the recent increase in inbound travel from Nigeria, which could be an indication of economic growth in the country.
At the same time the findings still provide only limited demographic information on patients who travel and their conditions and expenditure. Specific further research is required to investigate some of the observations that our analysis allows. This includes the decline in numbers of travellers from the Middle East, the effects of the economic crisis on inbound medical travel and the increase in outbound medical travel to East Asia. Further information on these would allow an even better understanding of why patients travel and the impact of this trade in health services on the NHS and other health systems.
Based on this data analysis, including the relative youth of patients from the UK, outbound medical tourism looks set to grow with the UK becoming an importer of health care. The impact of medical travel on the UK public, including patients returning with complications or ongoing care needs in the absence of clear and reliable guidance, looks set to offer increasing challenges to policy-makers in the UK and globally.
More broadly, our analysis highlights health services as a tradable commodity that behaves just as financial markets do – sensitive to external events. The increase in the number of patients visiting the UK from Greece and Ireland shows the effects of the economic crisis on medical travel. Similarly, the ‘drop’ in travel observed from some countries and the growth of travel from Nigeria all reflect wider developments in the global economy, showing how medical travel acts as an indicator of globalisation and its effects on health.
Section 2 Patient safety and service quality
Section 2 focuses on patient safety and service quality. It draws on two sets of data. The first includes desk-based material that was collected to understand the context and practice of patient safety and service quality in the context of medical tourism. The second includes interviews with NHS managers (primarily those with commissioning and public health roles) and a range of interested stakeholders representing professional societies and those with expertise regarding issues such as malpractice and indemnity, health policy and travel health. This part is organised around four themes, reflecting the key factors that we perceive as enabling quality, safety and choice:
-
legal: a review of the legal context and background (see Chapter 6)
-
education: issues relating to informing and educating medical tourists (e.g. regarding website resources and guidelines) (see Chapter 7)
-
quality and safety: explores the role of EQA (see Chapter 8)
-
performance and outcomes: details the relevant dimensions of QISs (see Chapter 8).
For explanatory purposes these four points can be viewed as a patient safety and service quality diamond for medical tourism (Figure 6).
FIGURE 6.
Medical tourism patient safety and service quality diamond.
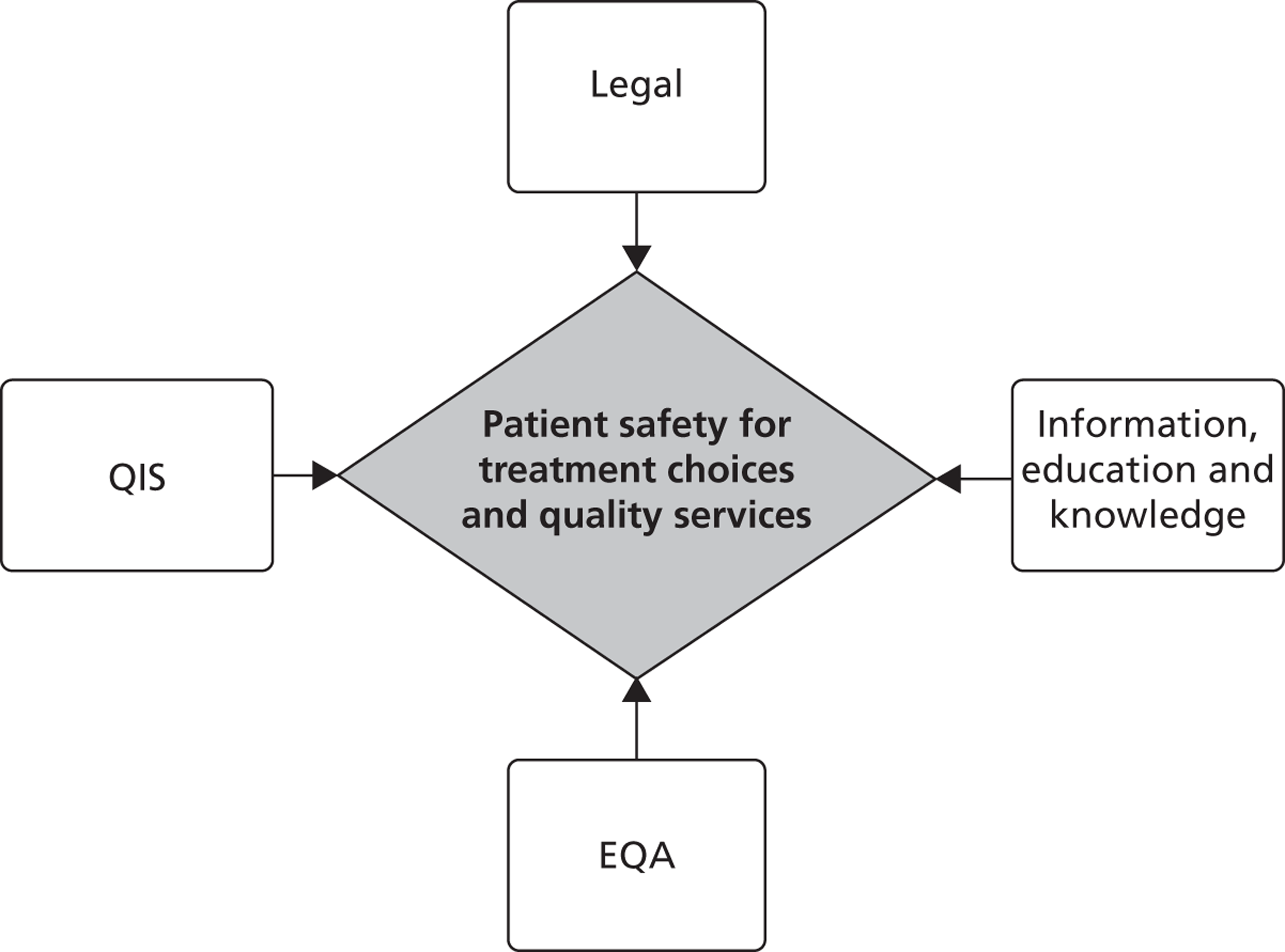
Chapter 6 Legal dimensions of outward medical travel
The medical tourist faces uncertain legal difficulties at each point in the treatment process (Figure 7). Health-care consumers face particular challenges in making choices given the often episodic nature of health care, information asymmetries with providers and problems of measuring and assessing quality both before and following treatment. Particular problems include:
-
Initial advertising and search for information. Prospective medical travellers require information and opportunities to identify clinicians and clinics, sometimes using companies that act as intermediaries to facilitate this search. Such information searches, and the associated promotion and advertising of treatments and facilities, present difficulties.
-
Purchasing treatment and ancillary services. There are decisions to make about what treatments to ‘purchase’, whether or not to use a broker, whether or not to take out travel insurance and opportunities for pretreatment consultation. A combination of services may contribute towards the medical tourist experience at different stages of the process, including product advertising, initial internet consultation, brokerage services, the treatment itself and various combinations of the above. There are a number of uncertainties, including who is liable when there is a deficiency in the quality of treatment (health-care professional, clinic or broker) and the precise coverage of insurance. Sellers of insurance products in the UK may themselves be subject to regulation by the Financial Services Authority (FSA). Questions include who has responsibility for meeting the additional costs of complications that arise during, or as a result of, surgery and how is redress best pursued.
-
Longer-term aftercare. Beyond the immediate treatment, there are questions about a surgeon’s and a clinic’s legal duty to provide follow-up if the procedure results in adverse outcomes for the patient, both immediately following the procedure as well as in the future.
FIGURE 7.
The patient journey.
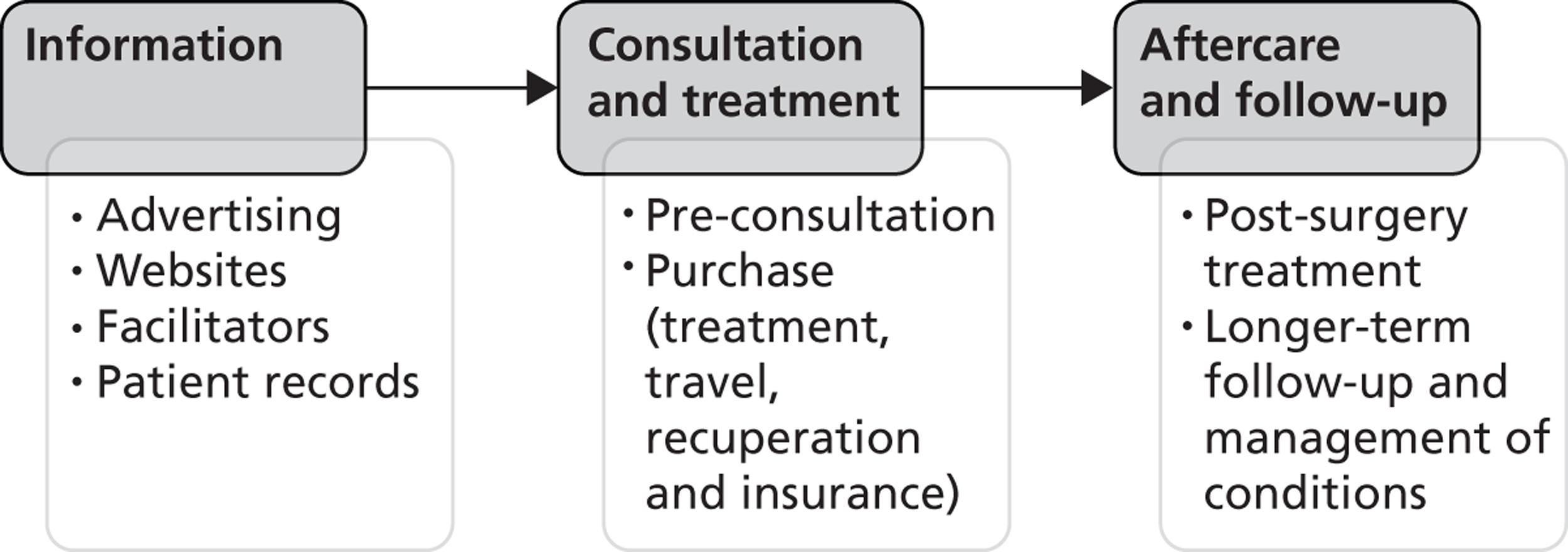
Obtaining personal and provider information
To begin their treatment journeys, patients (at some point in their decision-making) may seek to obtain their own personal medical (or dental) records and attempt to ensure that they have adequate information about medical treatments available overseas. Individuals in the UK are entitled (under the Data Protection Act 1998144) to have access to their personal health information, including NHS and private health records held by a GP, optician or dentist or by a hospital (e.g. dental records and radiographs). An administration fee may be charged depending on whether records are held electronically or in paper format. Under the Data Protection Act, requests for access to records are required to be met within 40 days. However, government guidance for health-care organisations states that they should aim to respond within 21 days. A request may be refused if it is believed that releasing the information may cause serious harm to an individual’s physical or mental health or that of another person.
With regards to provider information, medical tourism services are marketed and advertised vigorously and a key driver for such promotion is the high-profile technological platform afforded by the internet for consumers to access health-care information and advertising from anywhere in the world. Within the UK, the advertising of medicines for human use is tightly legislated and is regulated by a unit within the Medicines and Healthcare products Regulatory Agency (MHRA). The advertising of treatment services, including medical travel abroad, is outside the MHRA’s remit of responsibility for medicines and devices.
Within the UK, health care has not traditionally been viewed as simply another product to be advertised. However, the marketing of domestic cosmetic surgery is increasingly commonplace in the UK (including billboards) and the Committee of Advertising Practice has released guidance on the interpretation of rules in the British Code of Advertising. 145 The Advertising Standards Authority (ASA), which is independent of the government and the advertising industry, is the main body responsible for dealing with complaints in the UK. The ASA investigates complaints and proactively monitors and takes action against ‘misleading, harmful or offensive advertisements, sales promotions and direct marketing’. 146 If a complaint is upheld, the advertiser must withdraw or amend the advertisement and not use the advertising approach again. The remit of the ASA includes online advertising for paid advertisements, marketing messages on a provider’s own website and marketing communications in spaces that include Twitter™ and Facebook™. ASA’s coverage is limited, however, to UK websites.
The ASA has on occasions ruled on domestic advertising of treatment services. For example, it ruled against advertising that promoted invasive cosmetic surgery as being without risk and ‘safe’. It stated that such content was irresponsible and misleading and breached clauses relating to social responsibility and truthfulness. 147 The body has also criticised a billboard advertising campaign that emphasised the speed and costs of cosmetic treatment because, in its judgement, this trivialised cosmetic surgery and conflicts with advice elsewhere in the advertisement about the need for consultation before surgery. 148
From the standpoint of professional standards, a major function of the General Medical Council (GMC)149 is to foster good medical practice. Its good medical practice guidelines150 contain a number of implications for treatment promotion and marketing, noting:
If you publish information about your medical services, you must make sure the information is factual and verifiable.
You must not make unjustifiable claims about the quality or outcomes of your services in any information you provide to patients. It must not offer guarantees of cures, nor exploit patients’ vulnerability or lack of medical knowledge.
You must not put pressure on people to use a service, for example by arousing ill-founded fears for their future health.
Reproduced with permission from GMC. Good medical practice 2006. URL: www.gmc-uk.org/Good_Medical_Practice_Archived.pdf_51772200.pdf (accessed 9 September 2013). © GMC.
It should be noted that the 2006 guidelines, quoted here, were withdrawn on 22 April 2013 and replaced with an updated set of guidelines (see www.gmc-uk.org/gmp for the latest edition). The GMC also has responsibility for keeping an up-to-date register of qualified doctors and seeks to deal firmly and fairly with doctors whose fitness to practise is in doubt.
The EU E-Commerce Directive (2000/31/EC)151 has implications for website quality and requires all companies to display ways in which the website can be contacted. The European Court of Justice has ruled that this may include a telephone number and a contact form that is answered within an hour. The ruling impacts on e-businesses operating within the EU and requires that the name of the service provider, the geographical address of the service provider and service provider details including the e-mail address where it may be contacted at short notice must be provided before a contract can be entered into through the website. As our own review of websites found, many European sites (but not all) adhere to these requirements and the vast majority carry clear privacy statements on how personal data are protected.
Potential medical tourists face the dilemma that there is no guarantee of the veracity or legitimacy of claims made on websites. Treatment outside of jurisdiction poses problems for the effective regulation of advertising and promotion. Although the ASA will refer complaints about advertising that originate from outside the UK to the European Advertising Standards Alliance (covering 24 European countries) and to some countries outside of Europe (including India), the reach of these is unlikely to prevent companies breaking regulations through their internet-based advertisements. The sheer number of websites operating in the medical tourism field further complicates the issue. Similarly, cross-border complaints against GMC-registered clinicians operating outside of the UK are less likely to result in charges than if such individuals were practicing within the UK.
In summary, the rise of medical tourism has been a largely online phenomenon and it is the internet that provides the arena in which all key stakeholders (from the patients, through the facilitators, to the providers) can interact. In the offline world where such decisions are taken in doctors’ surgeries and hospitals, there is at least a sense that information is authoritative, impartial and trustworthy. There is a general appreciation of the existing and potential problems related to health information on the internet, especially given the increasing quantity of health-related websites. Issues of accuracy have long been a concern, although perhaps compounded by the burgeoning number of sites whose primary purpose is to market products rather than inform. What is less clear is how (if at all) the quality of information provided to medical tourists should be regulated, with suggestions beyond legislative control ranging from codes of conduct to self-taken quality labels, user guidance tools and third-party quality and accreditation labels.
Legal redress
The lack of an internationally agreed framework to regulate medical tourism or offer legal redress begs a number of difficult questions concerning:
-
the grounds for seeking legal redress
-
who is responsible – the clinic, surgeon or broker?
-
in which jurisdiction to seek redress
-
the time frame to seek legal redress.
It is common practice in many countries for a patient to sue for negligence if he or she has suffered avoidable harm as a result of poor-quality medical treatment. Under the law of ‘tort’, a patient may seek compensation if he or she can provide proof of fault. He or she can also claim under a breach of contract. The grounds for seeking redress vary from country to country. For example, in the case of an Australian citizen,152 domestic legislation would provide an additional third potential route for redress in the form of action under the misrepresentation of Trade Practices (contracts) Act 1974,153 which in January 2011 was replaced by the Competition and Consumer Act 2010. 154
In the UK, treatment is considered negligent if the court accepts that a patient has suffered injury and loss as a result of the negligence, or that the doctor or surgeon is in breach of his or her duty of care to the patient and has failed to act in accordance with the accepted standards of a competent practitioner in his or her area of expertise. 155 However, some foreign companies may insist that medical tourists sign a legal disclaimer before their treatment. These may include clauses that seek to limit where a case can be held, the law that governs the claim and liability limitation, which can reduce potential options for redress. (An emergent area of specialist legal services provides clients with the opportunity to seek legal redress for adverse outcomes of medical tourism. Some legal practitioners specialise in particular treatments, for example fertility treatment abroad.) In the UK, exemption clauses that exclude a doctor or clinic from liability for negligence are not enforceable and disclaimers are subject to legislation governing the fairness and legality of their contract terms.
When attempting to sue for medical malpractice abroad, there are decisions to be made about who the patient should sue (clinic, surgeon or facilitator) and the particular jurisdiction where any legal case would be heard and the laws and legislation that would be used. Ordinarily, when both the patient and the clinician are within the EU, the clinician has to be sued in his or her home country. However, as patients are likely to be considered as consumers, under EU consumer contract rules they can opt to sue in their home country. 155 Clinics outside of the EU would be subject to the same issues discussed above, for example if they advertise in the EU they can be sued in the EU.
The case for seeking legal redress in the UK is strengthened if any initial consultations, written consent or the signing of contracts or payment have taken place within the UK. 155 A clinic that consulted in London and treated in Belgium was recently successfully pursued using grounds of negligence and breach of contract. 155 The initial consultation was in English, the contract was signed and agreed in England and payment was made in sterling. For litigation purposes it can work in a patient’s favour if an overseas clinic has advertised within the UK. Clinics that specifically target UK citizens, for example by advertising in the UK, having an office based in the UK or having a ‘.co.uk’ website address, may become subject to the jurisdiction and laws of the UK, which has implications for litigation. Overseas clinics with a UK base or a UK-targeted advertising campaign may not be fully aware of the implications. Payment for treatment using a credit card could allow a case to be brought in the UK against the consumer credit card company under Section 75 of the 1974 Consumer Credit Act. 156 This route has been pursued for the cost of replacing Poly Implant Prosthèse (PIP) implants in cases in which the surgery was undertaken in the UK.
Beyond the liability of brokers, surgeons and clinics, questions arise with regard to potential liability issues for UK-based health professionals (e.g. within the fertility field). For example, when the initial consultation and advice are delivered privately in the UK but treatment is subsequently obtained overseas, albeit recommended through the UK facility, who is liable? Under such circumstances, should UK facilities be expected to accredit physicians within their overseas treatment network (and, if so, how would they do this)? Are such UK health professionals likely to be subject to vicarious liability if complications arise from treatment, or is this avoidable through their clear statement of disclaimers?
Medical clinics are normally liable for the failings of their employees, including surgeons. A clinic is usually responsible for advertising and arranging a patient’s treatment and the patient’s contract will be with the clinic. It is therefore the responsibility of the clinic to pursue litigation against a surgeon if it so wishes. As Vick155 states: ‘despite offering the package of care to the patient clinics may seek to divert blame to surgeons with whom the patient had no contract’ (p. 108). Even if the surgeon is registered with the GMC in the UK, his or her indemnity cover [with the Medical Defence Union (MDU) or Medical Protection Society (MPS) in the UK] is unlikely to cover treatment undertaken outside the UK. 157 Conversely, the surgeon’s insurance may not cover the clinic and thus clinics must also ensure that they have adequate insurance in place. If a clinic is not insured for a case brought in the UK, it may not be possible to enforce a judgement in a UK court and turn the award into financial payment. Once liability is established, it may be necessary for the patient’s legal representative to apply to the court in the clinic’s home country for recognition of the UK judgement and permission to enforce it in that jurisdiction. 157 Finally, in some cases the jurisdictions of both the patient and the clinic may be applied.
A patient may have to pursue legal action in the country where the operation took place. This could result in the patient having to return to that country and having to instruct a specialist lawyer in that country, all at extra personal expense. If a patient seeks legal action abroad he or she must be prepared to deal with complications related to language, local culture and unfamiliar law and legal traditions. Some argue that there is a particularly high risk of foreign patients not being adequately protected from malpractice in developing countries. 26 Patients should be made aware that other countries might have different malpractice laws and legal traditions and that these will impact on the size of malpractice payouts. For example, Malaysian standards for proving medical negligence are said to defer to physicians to determine whether the standard of care has been breached, rendering it extremely difficult for foreign patients to successfully prosecute. 26 In India a civil case could be brought using the Fatal Accidents Act158 and Section 357 of the Code of Criminal Procedure159 (or via a consumer route under consumer protection legislation); however, 95% of cases are said to be dismissed because there is not a culture of professional critique. 160 Favourable judgements handed down in an overseas jurisdiction may therefore be very difficult to enforce. Some countries may have a damages cap on the amount of compensation or may not allow compensation, for example for loss of earnings or the cost of care. For example, in India the level of compensation is likely to be extremely modest compared with Western standards. 26 In the UK and many other jurisdictions, for example, when a patient is awarded compensation this usually includes general damages for the psychological and physical consequences of the negligence and special damages for past and future financial losses incurred from the negligence. 157
A further issue concerns the time frame within which legal redress may be sought, which varies from country to country. Adverse after-effects arising from a particular treatment may not occur for several years, for example as has been the case in the recent PIP implant debate. 161 As illustrated by the PIP events, surgeons may be difficult to trace and clinics may no longer be in business. 162 In the UK the deadline for filing a personal injury claim is 3 years from the treatment or the patient’s date of knowledge of complications, but other countries may have shorter time frames for seeking legal redress. Even within the EU the time limit varies, for example from 1 year for claims in Spain to 3 years for claims in the UK. 155
In summary, we are entering relatively uncharted and rapidly changing territory with regards to the legal dimensions of outward medical travel, and the increased use of the internet further complicates this legal uncertainty (see Appendix 16 for a discussion of this in relation to fertility treatment). There is no clear legislative picture or developed body of case law to guide practice in this area. There are clear limitations in the current legal framework that blunt one point of the medical tourism safety and quality diamond. Although cases have been successfully argued (see Appendix 17 for an example), patients looking to rely on the existing UK framework in the event of adverse outcomes should be warned: caveat emptor – buyer beware.
Implications for the NHS
-
Prospective patients may not be aware of the lack of clear avenues for redress should treatment abroad give rise to unexpected complications.
-
Legal uncertainty and complexity bedevils all phases of treatment abroad: access to information, preconsultation, treatment itself, aftercare and follow-up.
-
Longstanding safeguards for UK health care (e.g. GMC registration) may have little relevance if treatment is received out of jurisdiction.
-
The need to seek redress and the subsequent legal implications may become apparent many years following treatment, when complications have emerged.
Chapter 7 Education and information
The second point of the safety and quality diamond focuses on educating and informing prospective medical travellers and, potentially, doctors and allied health professionals in the UK with whom they may consult. To explore education and information, we undertook two empirical reviews: first, we looked in detail at websites that promote and market treatment services abroad and, second, we reviewed the range of travel guidance and checklist documents around medical tourism that are available.
Website analysis of outward medical travel
A key driver of medical tourism is the platform provided by the internet for consumers to access health-care information and for advertising. The aim of the following discussion is to provide a systematic review of medical tourism websites, describe their range and content and begin to examine their quality and the implications of this in relation to decision-making.
We first present an overview of medical tourism websites and a conceptual framework to understand these. This is followed by a detailed review of 100 commercial medical tourism websites for dental tourism using checklists adapted from proposed questions that consumers should ask, according to a number of national-level bodies. Finally, we present a consideration of the broader implications of these findings.
There has been a burgeoning of websites dedicated to providing information for medical tourists in recent years. Although restricting its coverage to English-language websites, one scoping study suggests that a useful typology of websites can be drawn: (1) commercial portals (to aid the search for treatments and information about them); (2) media sites (e.g. carrying weekly features and updates); (3) consumer-driven sites (including discussion boards and blogs); (4) commerce-related sites (advertising ancillary products such as finance or accommodation); and (5) professional contributions (from professional associations, policy-makers and regulators). 90
Medical tourism websites perform a range of functions. First and foremost the scope of the websites is to introduce and promote services to the consumer. The main functions of the websites can be separated into five main processes: as a gateway to medical and surgical information; to provide connectivity to related health services; for the assessment and/or promotion of services; commerciality; and an opportunity for communication. 90
The range of medical tourism websites and related content raises familiar concerns associated with unregulated online health information. 163–165 The sites are relatively cheap to set up and run and contributors may post information without being subject to clear quality controls. A contextual deficit means that selective information may be presented, or information may be presented in a vacuum, ignoring issues such as the need for and availability of postoperative care and support. There is also the possibility of unreliable products being marketed via the internet: poor-quality surgery or inadvisable treatments or unnecessary and even dangerous medical care.
Clear evidence from other studies suggests that the quality of health information online is variable and should be used with caution. There have been some suggestions that the quality of information has been improving as a consequence of the increasing use of peer reviewing of information on increasingly interactive websites;166 however, it is still best characterised as being of variable and suspect quality. 167–169 In one study concerned with the quality of information on the internet pertaining to inflammatory bowel disease, researchers found that only 14% of websites offered high-quality information. 170
A review171 of patient-oriented methotrexate information on the internet found many of the same issues identified by Bernard et al. ,170 especially that the level of technical language was restrictively high and so not easily understandable by prospective consumers. However, this study did note that there were some examples of extremely high-quality information that were not only available but also presented on the first page of the Google™ search engine returns. One of the issues that they identified was not that information supplied by websites was erroneous but rather that some of the information that experts would expect to be provided was simply missing. 165
It is of course possible that missing information simply reflects the specific focus of a website or perhaps is even a reflection of frequently asked questions (FAQs) posed of a site. However, there is also the scope to provide misinformation simply through the omission of important information. Mason and Wright95 suggest that this is a very real concern where medical tourism websites are concerned. Their review of 66 medical tourism websites noted a distinct overselling of the positive aspects of medical tourism and a significant downplaying of the risks.
Systematic review: sites promoting commercial dental and weight loss surgery
Two samples of commercial websites, the first offering treatment services abroad in the field of dental surgery and the second offering weight loss surgery abroad, were identified in the first instance (Table 3). Building on published methodologies,163,165,169–171 50 sites were selected by interrogation of the Google search engine with lay terms for both treatment types. Although there is variation in the precise methodology adopted, the literature is replete with examples of studies adopting this broad approach. We believe that our samples are an accurate reflection of the type of sites that consumers are presented with when searching the internet. The major assessment of the sites then involved the utilisation of two similar, although not identical, clinical checklists (see Appendix 18 for methods and protocols). A detailed analysis of the websites is provided in Appendix 19.
| Country location of dentist/clinic | Number of sites in dental sample | Number of sites in weight loss sample | Total number of sites |
|---|---|---|---|
| Hungary (mostly Budapest) | 25 | 1 | 26 |
| Multiple locations | 10 | 7 | 17 |
| Belgium | 0 | 13 | 13 |
| Czech Republic | 1 | 9 | 10 |
| Spain/Tenerife | 2 | 3 | 5 |
| Poland | 3 | 1 | 4 |
| Turkey | 2 | 1 | 3 |
| Mexico | 0 | 3 | 3 |
| India | 0 | 3 | 3 |
| Ukraine | 2 | 0 | 2 |
| Lithuania | 0 | 2 | 2 |
| USA | 0 | 2 | 2 |
| Italy | 0 | 1 | 1 |
| Tunisia | 0 | 1 | 1 |
| France | 1 | 0 | 1 |
| Slovenia | 1 | 0 | 1 |
| Switzerland | 1 | 0 | 1 |
| Germany | 1 | 0 | 1 |
| Total | 49 (plus 1 with broken link) | 47 (plus 3 with broken link) | 100 (including 4 with broken link) |
Discussion
The rise of medical tourism has been a largely online phenomenon and it is the internet that provides the arena in which all of the key stakeholders (from the patients through to the facilitators to the providers) are connecting. But it is not necessarily a safe arena; in the offline world where such decisions are taken in doctors’ surgeries and hospitals there is at least a sense that information is authoritative, impartial and trustworthy. The internet does not offer this and it is hard not to see the marketing interests behind even the most reassuring information found on the internet. With regard to the websites that we reviewed, there were many affirmations of integrity, quality and caring services. There was an abundance of guarantees of professionalism, safety and a continuation of care. However, there can be no assurance that such guarantees are anything but empty promises. How we reconcile the potential of the internet, its endowment of individuals with ever-increasing levels of choice, with the risks inherent with an unregulated and uncontrollable content in a way that empowers patients is unclear and undoubtedly not straightforward.
Evidence shows that health-care consumers increasingly use the internet to access both information and health-care products and that an even greater proportion of people would consider doing so. 172 This includes people who are using, or would consider using, the internet to organise treatment abroad. 173 It is evident that information is often confusing, overwhelming and even contradictory – a fact that is acknowledged by many health-care regulatory bodies. 137
Medical tourism is a consumer industry primarily marketed online and as such there are serious potential issues facing those considering travelling abroad for treatment. Issues of accuracy are longstanding, although perhaps compounded by the burgeoning number of websites whose primary purpose is marketing products, as is the case with websites that promote medical tourism. It is common to identify misinformation, unsubstantiated scientific claims, fear-provoking threats and a lack of information on the uncertainties and the risks of particular services. On the whole, websites do not mention long-term risks or problems, limiting themselves to acknowledging that further treatment may be necessary as a consequence of hitherto unknown circumstance. 95,174
Whether or not it is possible to guarantee a universal minimum standard for the quality of medical tourism information is unclear. To this end, suggestions range from the development of codes of conduct, user guidance tools and third-party quality and accreditation labels,166 to educating users and assisting those wishing to search for information. 164,165,169 However, a large and ever-increasing number of quality measurement tools (many of which represent commercial ventures) exist, which makes selecting an authoritative tool impractical. Moreover, many of these systems are not accessible to a lay audience. 175,176
Some studies also recommend that prospective e-patients or e-health consumers should be educated by their ‘offline’ medical professional. Lawrentschuck et al. 169 go as far as to suggest that professionals should take the time to provide a steer to ethical, accurate, readable and accessible websites. This is echoed by Scullard et al. 165 and both studies make the recommendation that, if health-care professionals can direct patients to government websites or other such reputable sources of information, patients will be able to minimise risk. There are of course several problems with this approach. First, patients are motivated on the basis of what they find on the internet, rather than from having visited a health-care professional offline. Second, even when potential e-patients/consumers have visited health-care professionals it is not necessarily the case that these professionals will be aware of reputable sites beyond perhaps the broad and often general sites such as NHS Direct. Third, some of the sites assumed to conform to quality-based expectations do indeed fall short.
Others argue that debates over the quality of information should simply ‘move on’. 166 The new features of many websites brought about by the advent of Web 2.0 have, they insist, inspired a ‘health 2.0’ to emerge. They argue that the increased interactivity through the use of blogs, wikis and podcasts, often provided by not just health-care professionals but also researchers and the general public, has helped formulate a new e-health era that is tailored to the needs of those who access it. Crucially, this ‘bottom-up’ approach involves a process that is analogous to peer reviewing, drawing on real-life experiences, but always ensuring that an expert source is nearby. However, the findings of our study, alongside with other findings mentioned in this discussion, suggest that, at least for those new to searching the internet for health information, there is a lot of poor-quality information that is likely to be found, and discerning what is useful and what is not is no easy task.
It is perhaps easy, albeit misleading, to think of the relationship between patients and health-care providers having fundamentally and irrevocably changed as a consequence of the internet. Even now there is a feeling that word of mouth is still the main driver behind new patients registering with dental practices177 and that this relationship of trust between professional and patient may hold the key to how the internet can be best harnessed for patients, with trusted professionals playing a larger role in providing health-care information online.
Analysis of medical tourism travel information, advice and guidance
Given that web-based resources have clear commercial interests, prospective medical tourists may seek to look towards more objective impartial advice. Travel for medical treatment combines both the potential uncertainty of travel arrangements (travel delays and cancellations, risks to personal safety) and the risks inherent in receiving medical treatment. We sought to understand the range and nature of travel advice that prospective medical tourists could access to assist them in making informed decisions about overseas travel for treatments.
An internet-based search was conducted to determine where potential medical tourists are able to find information, advice and guidance and what that may include. The research team identified and discussed the potential professional, regulatory and policy organisations in which there were clear implications of medical tourism or that had commented, published or spoken about medical tourism. These sites, alongside those suggested by a broader search of keyword combinations (‘guidance’, ‘guidelines’, ‘advice’, ‘checklists’, ‘travel’, ‘treatment’, ‘surgery abroad’, ‘medical tourism’), contributed towards the corpus. We also explored the sites of consumer/advocacy organisations and during our website review (see Appendix 20) recorded sites on which guidance and advice was offered by commercial providers and entities. When repetition was evident within these searches, and leads did not provide additional sites to investigate, we took this to signal that data saturation had been achieved.
A total of 30 websites were identified as potential sources of information, advice and guidance; these were reviewed for their content about medical travel. The sites can be grouped into four different types: professional, regulatory, consumer and commercial. Table 4 details a small, non-exhaustive selection of organisations that offer information, advice and guidance regarding medical tourism. These are grouped based on the primary role of the organisation, although there is likely to be some overlap, especially between professional and regulatory organisations.
| Primary role of organisation | Examples |
|---|---|
| Professional | British Association of Aesthetic Plastic Surgeons, BAPRAS, Foreign & Commonwealth Office, National Travel Health Network and Centre (NaTHNaC), NHS Choices, Department of Health |
| Regulatory | Human Fertilisation and Embryology Authority, General Dental Council, GMC |
| Consumer or advocacy | Which?, Infertility Network UK, British Obesity Surgery Patient Association |
| Commercial | Medical Tourism Association, International Medical Travel Journal, JCI |
Half of the professional sites did not contain information, advice or guidance about medical treatment, medical travel or medical tourism. Regarding the information, advice and guidance that was available to medical tourists (in particular from professional and regulatory bodies), such material was often difficult to find, requiring specific searches within organisation websites, and was rarely signposted from industry sites. Information, advice and guidance were in a number of formats and the depth and quality of advice varied considerably. Information and checklists are the most common formats across all types of sites, but a few sites from across the types include guidelines or FAQs sections. A total of 14 sites provided detailed information, advice and guidance specifically related to travelling abroad for treatment.
The FAQs across the websites vary from focusing on practical questions that prospective patients are likely to ask, such as ‘how do I know if the clinic is clean and safe?’,178 to more generic ones about the industry, such as ‘what types of treatment do people travel for?’179 Guidelines often take the form of information provision, such as the British Association of Aesthetic Plastic Surgeons consumer safety guidelines. 180 Checklists and ‘questions to ask’ are tick box exercises that attempt to ensure that patients have all of the information, advice and guidance that they need. A more detailed analysis of the advice, information and guidance can be found in Appendix 20.
Implications for the NHS
-
There remain doubts about whether or not website information facilitates treatment choice which ensures that care is ‘effective, personal and safe’.
-
The risks of treatments are not fully detailed; unsurprisingly, there exists an imbalance of information and marketing material.
-
A range of UK advice exists for prospective travellers; typically, this focuses on treatment decisions and does not clearly identity the lack of a clear framework for redress and that patients may be personally liable for treatment costs that do not fall within NHS entitlements.
-
The onus is on prospective medical tourists to locate guidance and advice.
Chapter 8 External quality assessment and quality information systems
There are many definitions of quality in health care, with the US Institute of Medicine’s being probably the most influential, with health-care quality defined as the extent to which health services provided to individuals and patient populations improve desired health outcomes. In this sense care should be based on the most robust clinical evidence and provided in a technically and culturally competent manner with good communication and shared decision-making. Important dimensions of quality commonly associated with health care include effectiveness, efficiency, safety, equity, appropriateness, timeliness, acceptability, patient responsiveness, satisfaction, health improvement and continuity of care.
The measurement and assessment of health-care quality is beset by confusion, with different regulatory bodies promoting different processes and no way to reconcile common standards across borders [Charles Shaw and Paul Stennett, independent accreditation expert and Chief Executive, United Kingdom Accreditation Service (UKAS), 2012, personal communication]. Some have suggested that the lack of transparency with regard to quality prevents the medical tourism market from flourishing. 12 Indeed, the lack of robust clinical governance arrangements and quality assurance procedures in provider organisations has led to concerns over the quality and safety of some overseas providers. 181 EQA has the capacity for improving clinical effectiveness, quality and safety and ensuring public accountability,182 although such processes themselves face calls for greater transparency in the evidence base on which they are reliant. 183
The most common EQA models are statutory inspection, public sector education programmes for training and testing private providers, industry-based assessments such as International Organization for Standardization (ISO) certification, and health care-based assessment through peer review. 182 A more detailed discussion of EQA is provided in Appendix 21.
The importance of external quality assessment for medical tourism
There is a diverse range of different types of EQA and regulation employed by organisations (for a full review see Appendix 22) and consumers are therefore likely to feel confused and anxious when trying to assess which clinic to access.
When making a decision about which clinic and surgeon to select, medical tourists are likely to expect safe treatment as a minimum and are also likely to be motivated by considerations including quality and cost. How best to judge quality and safety is one of the most difficult issues for a prospective medical tourist to address in their decision-making process. In searching for providers, there is a plethora of labels and symbols (on website and marketing materials) professing some form of accreditation, certification or professional registration. However, few would understand the bewildering array of EQA and badges used by different companies and countries. With a lack of international regulation or legislation governing this field, providers and patients alike may look to accreditation and certification to prove their standards and inform their decisions respectively.
As part of our investigation into this area, empirical research was undertaken to examine the role of accreditation and certification used by providers. A systematic review of websites for dental, bariatric and cosmetic surgery was undertaken to understand how they reported their EQA and registration status.
Dental surgery external quality assessment: an empirical review
Following our review of 50 websites advertising dental treatment abroad, the same sample was used to further investigate the forms of (1) accreditation, (2) certification and (3) professional registration that they lay claim to. Of the 49 websites with working links, 24 displayed a range of different forms of accreditation and professional registration. However, none provided details on precisely what these meant or an explanation of whether they were a form of accreditation or professional registration.
Bariatric surgery external quality assessment: an empirical review
Using the bariatric surgery website data set, 50 sites were further systematically investigated for forms of accreditation, certification and national regulation. Of the 49 sites that were accessible, 25 sites displayed some form of EQA, although the amount of detail varied considerably.
Cosmetic surgery external quality assessment: an empirical review
Finally, 50 sites used by Lunt and Carrera184 in their discussion of patient advice and sources of information for decision-making were revisited and analysed for EQA. Similar to the bariatric surgery review, a large range of bodies was cited, 46 in total. However, only 18 websites provided any details of accreditation, certification or regulation. Further details of these three sets of findings may be found in Appendix 22.
Quality information systems
The public release of information on the absolute and relative performances of health-care providers may improve the quality of care and promote transparency and accountability among health-care consumers and payers. 185,186 There is a range of information systems reporting on the quality or performance of providers of health care (‘quality information systems’) that could, plausibly, be of value to prospective medical travellers.
Quality information systems may have multiple aims and objectives including facilitating patient choice, improving quality by changing provider behaviour and systems, and providing greater clarity and accountability for provider–commissioner relationships. However, development of such systems is patchy, particularly among those countries that are lower-cost destinations. 185 Aside from the availability of such information, evidence suggests that there is a low uptake of published information, it does not sufficiently meet patients’ information needs and it is not easily understood. 187–189
With regard to the UK context, for example, there are a range of dimensions for the publicly funded system (Table 5). However, it would appear that relatively few systems exist that are publicly available and accessible for the prospective medical tourist and facilitators seeking to arrange travel to other EU and non-EU countries. For example:
-
Thailand. There are no clear information portals or sources that gather/compare health-care providers for purposes of statutory reporting requirements. Beyond a site provided by the Tourism Authority of Thailand that lists hospitals and other providers of medical services, there is little available information. There are numerous privately owned websites, but information is descriptive with regard to the services, treatments and facilities that are available. Information is not routinely collected/published for key indicators by national or regional agencies and so meaningful comparison across facilities is difficult (e.g. infection, outcomes, adverse effects).
-
Spain. There are numerous commercial sites providing details of hospitals and facilities, which may include statements about the quality standards that are held by institutions. The Ministry of Health website provides information on the Spanish NHS system; however, there does not appear to be a solid information system on quality. There are extensive reports on accreditation and quality in terms of patient safety but there are no comparisons between providers.
-
India. Although it is possible to identify > 5500 hospitals by region, there are no clear quality assessment results. There are commercial search engines but no QIS data that would facilitate an informed choice. The Ministry of Health and Family Welfare, the governmental body that looks after quality control in hospitals and clinics, is said to be establishing minimum quality standards to reassure patients seeking treatment abroad.
-
Cyprus. Most large health-care providers are owned by the public sector and there are no clear comparisons between them. On the Ministry of Health website there is a section that is supposed to provide statistical information on hospitals but it does not work in either English or Greek. Again, most of the websites that list providers are international ones for promotional purposes.
-
Poland. Nothing was identified that details information on quality or allows comparison between providers.
| Organisation | Source of quality information |
|---|---|
| NHS Choices | Trust quality accounts provide information on quality of care, specific clinics, treatments and staff information. Key performance indicators are examined; results are colour coded and graded 1–10. Patient feedback is available including patient survey scores. Includes indicators that stress underachievers and low quality |
| Dr Foster Intelligencea | Provides information on NHS mortality rates, patients discharged within 56 days and waiting times |
| Care Quality Commissionb | Reports whether or not trusts meet standards set by the Commission. Examples include treating patients with respect, providing care that meets people's needs, patient safety, staffing and quality, and the suitability of management. Summary of assessment provided. Latest inspection reports available for review |
| Patient-reported outcome measure (PROM)c | PROMs calculate health gain after surgical treatment using pre- and postoperative surveys for four procedures: hip replacement, knee replacement, hernia and varicose veins |
| Monitord | Information mainly on financial and risk indicators |
Implications for the NHS
-
There is a plethora of EQA and registration details displayed on websites.
-
There are no clear patterns in take-up of different EQA forms, perhaps reflecting that European clinics within the medical tourism market are relatively small.
-
How EQA and registration details are presented assumes significant health literacy by website users.
-
EQA does not fulfil the function of providing relevant signposting to patients.
As part of the research, 16 representatives of professional associations and agencies (including Royal College and Clinicians’ Associations representatives) were selected in a purposeful sample based on their knowledge and experience of the possible impact or consequences of medical travel to and from the UK and were interviewed. We also interviewed individuals within NHS commissioning organisations to explore issues and implications for the NHS arising from UK populations travelling abroad for treatment. These included six NHS managers based in PCTs and strategic health authorities (roles included director of public health, head of commissioning and community partnerships). Further, we spoke to a small number of NHS clinicians who wished to share their insights on specific issues arising from medical tourism (in bariatric surgery, hepatology). Overall, the aim was to better understand the impact of medical travel on the UK NHS including considerations around the patient safety and service quality diamond: legal, education, EQA and QIS dimensions. The detailed data are provided in Appendix 23. In summary:
-
Specialists (often in the private sector), dentists and cosmetic clinics are likely to see a greater number of complications and follow-up cases after treatment abroad, whereas GPs or NHS clinicians are likely to interact with a comparatively smaller number of patients.
-
The recent PIP breast implant scandal is an example of how there can be a significant delay in complications, making it harder for patients and doctors to contact the original treating physician.
-
Adequate mechanisms to collect information about the ongoing costs of medical tourism are required to sample GPs, private clinics, dentists, accident and emergency (A&E) departments, NHS surgical facilities and infectious disease facilities.
-
There is a need to clarify the role of the new strategic NHS Commissioning Board and clinical commissioning groups in providing information, advice and support with regard to medical tourism.
-
There is a need to clarify the role of the Care Quality Commission (CQC) with regard to upholding the quality and safety of care provided to outward medical tourists.
Section 3 Treatment group case studies
Chapter 9 Common themes within experiences of medical tourism
In this section we draw on in-depth interview data to provide a discussion of the general experience of being a medical tourist, before outlining the peculiarities of different forms of medical tourism. In both the general overview and our treatment case studies, the interview data collected from our medical tourist respondents play a key role in shaping the discussion. However, a wider context is provided by interviews with NHS staff, professional associations and other related stakeholders, and respondents from the wider industry, which includes those with a commercial interest in medical tourism. Further depth is provided by engagement with the wider academic literature.
This chapter seeks to detail what can tentatively be referred to as a typical medical tourism journey. In reality there is no typical process, even among those who travel to the same place for the same procedure. However, we have found that certain issues are common to many of our medical tourist respondents, even if the relative importance of such issues differs between individual patients or various forms of medical tourism. This chapter draws on some literature and interviews with professional or industry respondents, but is primarily shaped by the responses of our medical tourist sample. Table 6 gives an overview of this sample and further details of the individual respondents and their treatment pathways can be found in Appendix 9.
| Treatment type | Number of respondents | Procedures covered | Locations |
|---|---|---|---|
| Fertility | 9 | IVF, intracytoplasmic sperm injection, egg donation, sperm donation | Czech Republic, Ukraine, Sweden, Spain, Cyprus |
| Bariatric | 11 | Gastric band, gastric bypass, gastric wrap, gastric sleeve, duodenal switch, pancreatic diversion and duodenal bridge | Belgium, France, Czech Republic |
| Dental | 11 | Crowns, bridges, routine work and check-ups, fillings, braces, dental plates, implants | Hungary, Germany, Croatia, India, Poland, Italy, Lithuania |
| Cosmetic | 9 | Facelift, liposuction, tummy tuck, minimal access cranial suspension facelift, nose, face and eyes | Belgium, Poland, Czech Republic, Pakistan |
| Other | 6 | Nerve surgery, gynaecology, ultrasound, immunotherapy, shoulder stabilisation, needle for Dupuytren's contracture | France, Greece, Belgium, Germany, USA |
| Cultural | 31 | Diagnostic, dental | Germany, India |
Chapters 10–14 provide a series of case studies focusing on different types of medical tourism. In these case studies we present a more focused account of dental, bariatric, cosmetic and fertility surgery tourism, as well as a discussion around those who travel for familial or cultural reasons or reasons linked to diaspora. Again, we draw on medical tourists’ interview data, especially when highlighting the peculiarities of each case study; however, greater emphasis is placed on professional interviews and the wider literature. These case studies will also reflect on issues such as quality, safety, risk, legal uncertainties and regulation, as identified earlier in this report.
Combining the general discussion of common traits with more focused case studies will enable us to highlight some of the broad implications of medical travel that are perhaps easy to conceptualise, with more complex implications related to the types of treatment for which people travel.
Although there were most certainly different stories being told by our respondents, all discussed their experience of the NHS, motivations for travelling for treatment, the process of travelling and their experiences of care abroad. Within these four themes there were also many common issues addressed and these are discussed within the broader themes.
The NHS
Across each treatment type our respondents all had something to say about the NHS. Their responses (whether positive or not) usually reflected whether or not they had ‘got what they wanted’ out of the NHS. Of course, given that we have sampled only those who have travelled abroad for treatment, opinions will be skewed towards those who did not get what they wanted. Despite this, discussion around the NHS was not wholly negative. Indeed, there are many examples of people praising the support of NHS staff throughout their treatment journey, even if they had been initially disappointed to learn that their treatment could not be provided on the NHS:
I have an extremely, extremely lovely doctor and she gave me all my medication for free. I’ve been able to consult with her all the way through from the very beginning. She’s the best doctor that I’ve ever had.
FT3
When I came back I told him I’d had the surgery and what had taken place and he has been very supportive since that.
BT6
Yeah, I’ve spoken to my GP about it. I do get a lot of help from my GP and he does give me tablets to try and counter my weight problems.
CT6
Discussion of the NHS loosely fell into three subthemes: availability, distrust or dissatisfaction, and aftercare. We will discuss in more detail the issue of availability in the section on motivations but, in brief, the overwhelming majority of our sample travelled abroad mainly because they could not access their desired treatment in the UK. However, even within this common theme there exists much variance: for some, treatment was simply not practised or not commonly practised within the NHS (most notably with bariatric surgery) whereas, for others, the treatment was available but they were not eligible. In many cases issues of eligibility and whether the procedures were regularly performed within the NHS were less prominent than the waiting times to access treatment. Here, we encounter yet more variance, with some suggesting that the long waiting times had been conveyed by professionals, others hearing from friends, some reaching this conclusion having read published figures and others appearing to have simply assumed long waiting times:
With regard to the egg donation I was told [by a friend] there’s a five year waiting list at that time for eggs.
FT4
I then had to wait a long time on the waiting list. I would phone up the secretary and see where I was on the waiting list to be pretty much told there are people with cancer out there and you’re not a priority [. . .] I’d been told that I was going to be done in the January and then in January I was told June and I thought I don’t think I can hang on till June.
BT8
The second subtheme that emerges clearly from our interview data related to the NHS is that of distrust or dissatisfaction with previous treatment. Interestingly, those who held such views were often those who had cultural or familial ties to other health systems (e.g. OT2). This was also linked with treatments for which there is no NHS eligibility/provision, such as cosmetic surgery or cosmetic dental treatment, rather than fertility or bariatric surgery. Indeed, this distrust was not confined to the NHS, with many of those who talked of distrust or dissatisfaction extending that feeling to private provision in the UK as well: ‘So I actually went to see a private dentist and I always thought I’d get better and prompter treatment and that is just an illusion’ (DT3).
The issue of aftercare in the NHS was also discussed, sometimes at length, by a range of respondents. Again, those who had travelled for procedures that they may have hoped or even expected to have been provided on the NHS, such as bariatric or fertility services, generally had some form of interaction with the NHS on their return as part of some ongoing care. In many cases this was care that would not have been needed (although other care may have been needed at some stage) and can be described as a pressure on NHS resources entirely as a consequence of medical travel. How NHS staff were described as responding to this desire for post-travel care seems to differ depending on what type of treatment our respondents accessed abroad. Those who travelled for cosmetic or dental work were less likely to seek NHS aftercare, but those who did were less likely to be provided with aftercare than those who had travelled for bariatric or fertility treatment. The response to bariatric travellers was much more varied than the response to those who had travelled for fertility treatment. In their entirety, our fertility sample all accessed NHS antenatal care and in many cases neonatal care. In each case, irrespective of any previous frustrations with NHS ‘rationing’, respondents were wholly positive of the antenatal and, when relevant, neonatal care that they received. There was a sense from both cosmetic and bariatric travellers that there was unwillingness on the part of individual GPs to engage with them after they had travelled for treatment. Whether this was genuinely the case or simply perceived is hard to ascertain; however, as the literature suggests, some GPs may be mindful of assuming responsibility, and perhaps even clouding issues of liability, by providing aftercare. 190 On the other hand, some of our respondents simply never visited their GPs on their return.
I went to a private doctor at a skin clinic and got antibiotics and just paid £20 for them rather than go to the NHS. Mainly because of my pride really. I don’t want a GP waving his finger and going you shouldn’t have done it and I told you so.
CT4
Interestingly, no respondents who travelled for fertility treatment mentioned any examples of unwillingness on the part of the NHS to provide continuation of care that had, in essence, begun overseas.
Motivations for travelling
Availability
As alluded to above, a lack of availability on the NHS is a key motivator for those who travel abroad. Only a couple of our medical tourists had no engagement with the NHS before their decision to seek treatment outside the UK. Although the reasons for traveling abroad varied (from required procedures not being covered to patients being ineligible, or from a perceived lack of quality or expertise in the NHS to long waiting times), the inability or unwillingness to access NHS care can be seen in most cases as a primary motivator for seeking private treatment, which with our sample saw them leave the UK. In the literature there is reference to this being best termed a form of ‘medical exiling’ rather than tourism. 191 However, that term may not be wholly appropriate in the UK because in many cases care was available and our respondents travelled to avoid waiting times or for what they perceived as better care. That said, among our sample, statements such as the following were not uncommon:
Well, the NHS wouldn’t even consider us. It was just a non-starter.
FT5
No [there was no chance of treatment on the NHS], because of my age.
FT1
But basically she said I just wouldn’t get funded to have it done on the NHS.
BT9
If the inability or unwillingness to access NHS care provided the primary motivation for our sample to seek private treatment, it was a combination of secondary motivations that saw these private treatment journeys travel overseas. In particular, issues of cost, the experience of overseas practitioners, the distance that people would need to travel, tourism, and cultural or familial links to destinations were prominent within our interview data.
Cost
Cost was discussed by all of our respondents and in almost all cases was an important motivator for travel abroad. Commercial literature clearly cites cost as the key selling point of medical tourism, and this sentiment is shared by a range of the professional interviewees who spoke to us (e.g. NHS15). Indeed, cost is important, with many speaking of considerable savings available abroad. Cost played a particularly strong role among our cosmetic tourists and dental tourists who had no cultural or familial ties to the destinations to which they travelled. Although cost was important to our bariatric respondents, it did not take precedence to the same extent, rather being a contributing factor, albeit an important one, alongside others. The story was much more mixed among our fertility and cultural samples. Similarly, cost was discussed only fleetingly by those who travelled for treatment not covered by our case studies (OT1–6), such as our respondent who travelled to the USA for pioneering nerve surgery. Indeed, although some who travelled for fertility treatment cite cost savings as having played some role, many were aware that cost savings were unlikely. Similarly, many of our ‘cultural’ respondents actually spent a considerable amount to simply access diagnostic treatment abroad and one of our other respondents who sought experimental, ‘high-end’ treatment abroad has incurred considerable expense.
What is unclear is the degree to which cost in the UK was prohibitive to our sample. It clearly was in some cases, but on the whole there was a sense that people were simply driven by a perception of better value for money overseas.
Expertise
Our respondents often used terms such as ‘experience’ and ‘success rates’ as well as ‘expertise’. Here, perhaps more than with any other motivator, we see a clear distinction between those who have travelled for fertility treatment and those who have undertaken different forms of treatment. For those who sought cosmetic, bariatric and, to a lesser degree, dental treatment, expertise seemed bound to the desire to obtain value for money; if our respondents were not going to access NHS treatment, why spend more money in the UK, especially when the surgeons abroad were seen to have more experience of carrying out the surgery? Indeed, both bariatric and cosmetic tourists mentioned that they had travelled to specific locations and clinics either as the procedure that they desired had been pioneered there or the clinician was acclaimed. Of particular interest is the fact that perceived expertise binds our bariatric, cosmetic and dental tourists to many of the ‘cultural’ medical tourists as well as those who travelled for procedures not captured in our case studies. As with the pioneering cosmetic and bariatric surgery, our respondents who travelled for ‘other’ procedures were motivated first by a lack of NHS provision and second by a pull towards areas of expertise. In one case our respondent has maintained his connection to a French clinic even though the treatment that he requires is now available on the NHS, as he sees his French surgeon as best qualified.
With the diaspora group there is again a sense that expertise plays an important role in motivating travel, although in many cases this may be more a reflection of a lack of confidence in the services that they receive from UK health care. One of our professional respondents (PA5) answered this charge by stating that there was often a tendency to link perceived action with expertise, when often action is not required.
Despite the clear discussion of expertise, respondents were often vague as to how they had assessed such expertise and by what criteria they had judged their clinicians or the facilities to which they decided to travel. When success rates were mentioned, they were not critically assessed in comparison with UK data. As one professional noted (PA12), irrespective of their discussion of expertise, a nicely branded website was as likely to shape the choice of clinic as hard data on success rates. Although this appears to be sound analysis in the main, some of our bariatric sample had noted the number of procedures that a surgeon had performed.
Cultural/familial
We interviewed members of the Somali and Gujarati communities regarding their experiences of travelling for medical treatment; here, the issue of diaspora was prominent, but these were not the only interviews to touch on this subject. An ability to speak a certain language, the existence of family members in the vicinity of the health-care facility or, in the case of some of those who travelled for fertility treatment, phenotypical similarities with likely donors were all important motivators for travel and, most importantly, for determining where to travel. Such considerations were not confined to a particular treatment type and undoubtedly reflected the sample who we recruited.
Figure 8 provides a graphical representation of the various motivations cited by our sample and the relative importance of each within our bariatric, fertility, cosmetic and dental samples. This underscores the point raised that many of the motivations were common to all treatment types; however, the relative importance varied between our treatment case studies. The graphic represents the importance of the motivations on a 0–5 scale with 0 (at the centre) indicative of a motivation that was not of import within our sample. Some motivations register scores of 0 in each of our case studies but have been included as they have been highlighted as important in other studies. Individual motivation wheels for each treatment case study can be found in Appendix 24.
FIGURE 8.
Motivation wheel depicting the relative importance of various motivations in the four treatment case studies.
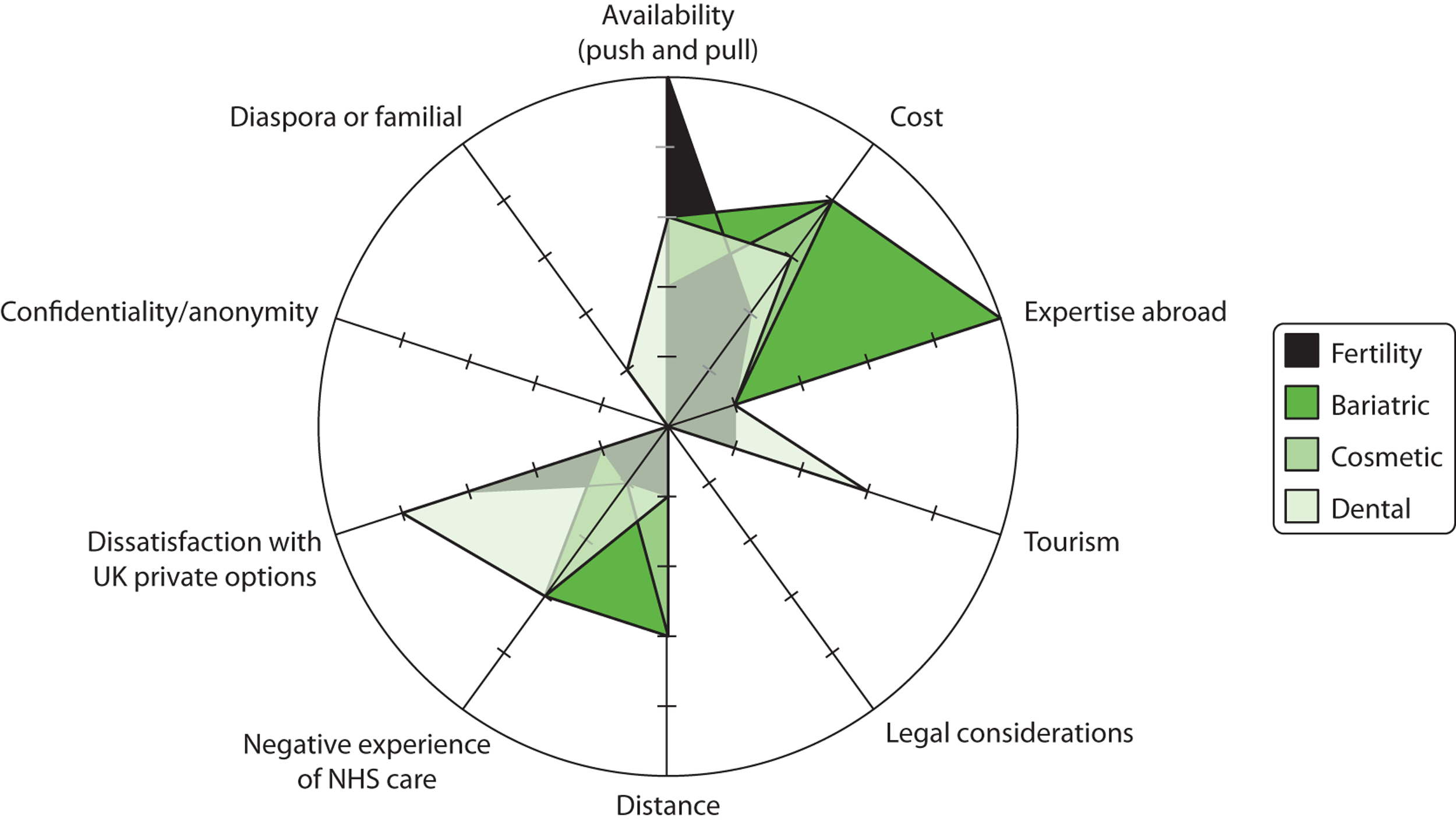
The medical tourism process
In this section we look at how people found their information regarding the facilities that they eventually visited, how they then organised their care and the process of travelling for care.
Information gathering
We have noted in this report that the internet plays a pivotal role within the medical tourism industry. This suggests that, with the exception of entrenched trade patterns, medical tourism is very much an online phenomenon. With that comes a series of issues relating to the quality of information online, the regulation of services online and, in turn, risk online. With only a very small number of exceptions, our sample had made some use of the internet to gather information regarding medical tourism abroad. For some, internet searching played a role in determining what treatment they wanted as well as where they would travel for that treatment. Indeed, in some cases it was through this informational search for the treatment sought that our respondents became aware of medical tourism as a possibility. Very few of our respondents mentioned, let alone appeared to have assessed, issues of risk, liability or even aftercare. Many of our respondents seem to conform to the expectations of the professional interviewee mentioned earlier: a well-presented and clear website and, more importantly, a feeling that people were receiving a personalised service were deemed much more important than hard information such as success rates. Some respondents did suggest that they found it reassuring to see that their chosen clinician was a member of a body such as the GMC or the General Dental Council (GDC). However, none of our respondents mentioned checking whether or not such memberships were still valid. Neither had any of our interviewees explored the qualifications and overseas memberships of the clinicians to whom they entrusted their care. It is worth noting that there is very little to stop a person who has been suspended or banned from practising in the UK from setting up in another country and, although they should not display suspended or deleted credentials, there is little oversight.
Although clinics that boast GDC- or GMC-registered staff, or profess to meet Human Fertilisation and Embryology Authority (HFEA) guidelines, are required to do very little to justify such claims, our respondents were either unaware of this or were simply less interested in this ‘hard’ information. One respondent neatly underlines the lack of knowledge that some – we would argue many – medical tourists possess with regard to quality, safety and risk in their discussion of accreditation. This respondent was one of the only interviewees we spoke to who seemed to have lent the issue much thought:
The firm we went to are called [company name] and I looked at their website and it gives the CVs of the two dentists. I looked at their accreditations on there and I then went to the university they said they were accredited with. I followed those through as far as I could and they looked bona fide. You don’t know if they’ve got that accreditation but they had an honest look about them and I then also got on to other people who had been with them who said it was a comfortable experience. That was what I was mainly concerned about.
DT1
Interestingly, a website having a ‘seal of approval’ from a commercial organisation seemed to provide an equal level of reassurance as being able to view curriculum vitaes (CVs) and professional memberships:
When you get something like the [medical tourism] website thing they would tend to give you the established practitioners. If you’re just looking at somebody’s website, I could set you up a website that made you look the most fantastic dentist in York. You’ve got no idea what you’re going to get and from that point of view having an organisation like [medical tourism website] gives a little bit of credence to it.
DT1
In clinical terms, being accredited by a commercial organisation, especially one with a commercial interest in encouraging growth within the medical tourism market, is worth nothing. Yet we have seen from a range of medical tourists as well as professional respondents that a neat and tidy website, which presents information that comforts readers irrespective of the level of protection it affords them, is extremely powerful. When people have already completed offline a large degree of research into the type of treatment that they are seeking, perhaps with support from health-care professionals in the UK, the online risk is confined to the choice that is made regarding location. This can still be extremely significant; however, the potential for greater misinformation is increased for those who combine the online gathering of information about a procedure with online information gathering with regard to the location and clinic. Here, one of the major problems is that, as our website review highlighted, even the most professional-looking websites are clearly playing down the risks associated with treatment. Our interviews underscore just how risky this can be with some suggesting that they had carried out very little research and others believing themselves well informed as a consequence of the research that they had carried out online before their treatment.
The respondents who seemed most informed and aware of the issues of risk were those who had spent time engaging with NHS care. Primarily we are referring here to our fertility travellers and, to a lesser extent, our bariatric sample. As our fertility sample had nearly all engaged with NHS care related to their fertility problems, many were aware of exactly what treatment they desired and the associated chances of success and risks. Indeed, for this group the internet played a still significant but perhaps relatively smaller role in information gathering. Here, a wider network of information, from health-care professionals to support forums and online sources, was utilised. It has been reported that in some countries, especially Italy, this represents the most common form of information gathering. 114 That is not to say that our fertility travellers represent a group of super-informed ‘risk minimisers’; it was clear that some of this sample had engaged only partially with information that alluded to risk, perhaps because of the level of determination and optimism that these respondents had about their ‘last chance’. In particular, issues around donation were addressed with only minimal discussion and seemingly little critical appraisal. Wider issues such as how donors are treated were discussed at length by professional interviewees but only fleetingly by those who travelled for fertility treatment.
Booking
The wider networks mentioned above were also evident in discussions around the procedure that our sample engaged with when organising their treatment. Some visited clinics on the recommendation of others, including friends or relatives, people in online support forums or health-care professionals. Generally, booking fell into one of two categories with people either booking direct with the provider or using some form of intermediary such as a broker or facilitator. In the vast majority of cases, our sample organised their treatment with the provider. In some instances, accommodation and flights were also organised in this fashion. Some respondents had used a facilitator or broker, either to make the process easier or because the broker represented a gatekeeper to services as in the case of one of our fertility travellers who required egg donation. In a small selection of cases our respondents had dealt directly with a private clinic in the UK that then organised treatment with a partner clinic overseas. In such cases it was unclear where our respondents would seek recourse should any complications arise.
The literature is replete with suggestions that facilitators and brokers play an important role in the global medical tourism industry;118,192 however, our sample made rather mixed use of such services. This perhaps reflects a sense of agency and responsibility that emerged from the interviews with many of our respondents. One respondent stated: ‘Maybe some people need some hand-holding and for that hand-holding a couple of hundred quid and you might have swallowed it’ (FT8). This came through most in the interviews with bariatric travellers, many of whom spoke at length about taking control of their health care, to a certain extent by engaging in medical treatment.
Whether respondents dealt with their provider directly or through an intermediary, what exactly the service covered ranged from treatment alone at one end of the spectrum to pretreatment tests, treatment, drugs, flights and accommodation at the other end. Most respondents sorted at least some part of their journey in isolation from their treatment provider.
Travelling abroad
In nearly every case our respondents travelled with a companion. When they had travelled as part of a package, the companion was an extra cost rather than included in the price. Those who elaborated explained that the ability to travel with a companion was extremely important, suggesting that without a companion the journey would have been too daunting. It is unclear whether this was not the case for those who did not discuss their companions at length or whether they simply took for granted that they would travel with their partner or friend. In more than one case a respondent discussed the conflict between their desire to keep their treatment plans secret and their need for companionship and support.
With regard to how long people travelled abroad for, this largely depended on whether or not they were travelling for particularly invasive procedures and whether or not they had family in or near their destination country. For most of our sample, treatment dictated that they would stay for at least 2 days but could, should they wish, travel home soon after. None of our sample talked of getting off the plane, having treatment and then returning on the same day. The most common approach was to travel to the country, have pretreatment checks and perhaps treatment on day 1, either recover on day 2 or have treatment followed by a day of recovery and then journey home.
Tourism
The popular conception within the medical tourism promotional literature, which echoes the views of some of those we have interviewed from a commercial background, is that the holiday plays an important role in medical tourism. Many have criticised the label ‘medical tourism’ as underplaying the process of travelling abroad to access health care, most notably when discussing fertility tourism or potentially life-saving treatment. 57,72 The notion of tourism is increasingly being applied to dental and cosmetic treatment; however, this is perhaps not an accurate reflection of the process. Within our sample it was clear that tourism played a peripheral role in the decision-making process. With the exception of those who travelled to see family and decided to ‘fit in’ a trip to the GP or dentist, decisions were taken first and foremost for health-care reasons. Even in cases in which our respondents stayed and enjoyed their destination country for a couple of weeks after treatment, travelling abroad was motivated by the need for treatment not the desire for tourism. This is not to say that some of our sample did not engage in tourist pursuits, of course; a reasonable number did.
The popular notion of sun, sea, sand and surgery10 was not, however, one that many of our respondents shared. This may of course be a reflection of our sample and it is important to note that we sampled the same number of cosmetic tourists as bariatric tourists. In reality, cosmetic tourism is likely to account for much more of the medical tourism market than fertility and bariatric treatment combined. It should also be acknowledged that recruiting samples proved extremely complex, in particular those undergoing forms of treatment that are seen as less invasive. We did not, for example, manage to recruit those who are often referred to as ‘tweakenders’, who do pop abroad for the weekend to have minor cosmetic work, or rather fit such minor treatments into a luxury holiday. We did not interview anybody who had travelled for breast augmentation or related surgery – apparently a common medical tourism procedure. It may very well be that we have oversampled the medical and undersampled the tourists, but in our sample tourism was clearly not a priority.
The medical tourism experience
In this section we discuss how our respondents found their experience, their satisfaction levels with regard to the process and, to a certain extent, the clinical outcomes (although this is rather limited as it was not the focus of our study), their feelings about the level of aftercare that they received and the ongoing support that they were given.
Satisfaction and dissatisfaction
It is easy to regard the patient testimonies on commercial websites with much scepticism, and addressing this potential imbalance in our knowledge of the medical tourism process is crucial. However, it would be possible to use the transcripts of nearly all of our interviews across all treatment types to produce the kinds of quotes that furnish these very websites. The overwhelming message that we received was one of satisfaction, even if the respondents had not achieved the clinical outcome that they desired. Typical statements were:
This is the best thing I’ve ever done.
FT9
It was amazing. It’s not a country I’d ever been to. It’s very European cosmopolitan, lovely cafes. It was beautiful weather because it was the summertime.
FT4
Very helpful, very friendly it’s just unfortunate it’s so far away that you can’t have the treatments you could have if you lived there. It was a very positive experience it’s just unfortunately it didn’t turn out good for me.
BT3
It was commonly observed that the facilities were clean, often being compared favourably to NHS facilities, and that language barriers were very rarely an issue. In only a small number of cases did any of our respondents suggest that their experience was negative and nearly all insisted that they would recommend the process to others. However, the implications of this finding are not straightforward. First, once again the sample we have recruited is undoubtedly skewed for a number of reasons. For example, recruitment of a sample is difficult as it is unclear where best to target communicational literature. Much success came from contacting online forums and it is likely that many of these hosted a number of people wishing to share their experiences. It is perhaps the case that it is easier to share positive experiences than negative and as such it may be that we had easier access to success stories. This was definitely apparent in a couple of cases in which prospective medical tourists agreed to take part in our study only to change their mind after not achieving a successful outcome. Of course, there is the possibility that people who have received particularly poor treatment would be motivated to share their story; however, we encountered only one example of this. It may also be that those using online forums are part of a supportive and possibly well-informed network and as such our respondents had been able to avoid many of the potential risks associated with medical tourism. In our fertility sample all had conceived, either as a result of their treatment or subsequent to it. It would have been useful to hear from those who had not, although this would undoubtedly be a very difficult experience to share.
Another issue is that we may have to question some of the positivity that our sample shared. In particular, our bariatric sample consisted of many people for whom treatment had not worked particularly well. In some cases our respondents were in a rather serious state of ill health, requiring constant care. And yet these very respondents were extremely positive about their experience, being very quick to defend both their decision to seek treatment and the surgeons who conducted the treatment. It may be that this reflects a clear sense of agency that emerged from our bariatric sample. Our bariatric surgery respondents seemed to use their organising and travelling for treatment as a form of exerting control over a hitherto uncontrollable part of their lives. Indeed, as researchers it was often quite difficult to reconcile the clear divide between the lack of clinical success and the levels of positivity with which our respondents regarded their treatment. As our purpose was to understand how our respondents felt and still feel about their treatment rather than report clinical outcomes, we must restate that the overwhelming sense was one of satisfaction. However, it is important to note that there was clearly a vested interest among our respondents in presenting a positive experience. Even with our fertility sample, all of whom it can be argued had experienced a successful procedure, there were clearly less positive issues that were pushed to the periphery of our conversations. Respondents discussed not feeling wholly prepared and feeling uneasy about the donation process, and at times unsupported, yet all of this was clearly deemed insignificant in the wider context of a successful pregnancy.
Support
In particular, it was unclear from many interviews what support our respondents had received, especially from their treatment providers. Often our respondents were keen to stress that their ‘friendly’ clinician had reassured them that they could pop back should any issues arise. Whether a return journey would have been physically or financially possible is not clear. As highlighted, a large proportion of our bariatric and fertility surgery samples were critical of the NHS support that they had received before and after organising treatment. But it is difficult to identify any obvious support being offered by the overseas treatment providers. It would appear in many cases that the NHS was seen as unsupportive because the respondents were unable to access NHS care, whereas the overseas providers, by giving the desired care, were viewed as supportive. The fact that this care had been bought rather than provided free of charge as it would have been on the NHS seems lost in many interviewees’ discussions. Some did mention a degree of support being forthcoming throughout their journey, with some providers or facilitators providing practical advice in a patient and warm manner. This ranged from providing advice regarding pretreatment drugs to practical support with regard to the organisation of travel and accommodation.
What can be thought of as more clinical support, especially psychological support, is largely missing from our respondents’ stories. When it is discussed it is seen as a deficiency in the process, with two respondents directly highlighting a lack of, or inappropriate, psychological support as particularly upsetting. The issue of psychological support is picked up by three professional interviewees (NHS17, NHS18, IND18) who note that the lack of psychological support, especially beyond ‘implicational counselling’, is a key concern regarding overseas treatment. Most patients relied on online or face-to-face support groups for this, although the high number of patients reporting membership in a support group may be the result of a sample bias. Similarly, family and friends, especially the companions who accompanied our respondents on their journeys, were clearly an invaluable form of support, even when our respondents wished to keep their treatment a secret from most.
Aftercare
Support extends beyond the conclusion of treatment and, as noted, support forums are clearly an important source of such support. However, it is important to highlight that, as well as support, care also continues after treatment. This can vary from check-ups and minor adjustments to corrective or further treatment. Even with dentistry, perhaps seen as the least invasive and traumatic treatment accessed by our sample, care is ongoing. At the most obvious, implants often need readjusting as swelling settles and the mouth changes shape. In addition, pain relief may be an issue for some and, most importantly, teeth, veneers and implants all have to be maintained; a trip abroad does not represent the end of treatment. However, returning to the place of treatment is not always possible, no matter how welcoming the clinician is and how prepared the clinician is to offer aftercare free of charge.
What is clear from our interviews is that the continuation of care occurred primarily in the UK, often within the NHS. The immediate aftercare while our respondents were still in their destination country was usually provided by the clinician or clinic and often the medication or tools required for aftercare were provided. However, when the overseas clinic provided drugs or required blood samples, our respondents were responsible for ensuring that medication was taken or that blood samples were provided. In some cases respondents would use syringes provided by the clinic and then post them from the UK. When aftercare for dentistry or cosmetic treatment was needed, most sought private care or reported being refused NHS care. One respondent even claimed to have removed his own stitches rather than ask his GP to remove them. It is clear that, had any of our bariatric or cosmetic surgery travellers required emergency treatment, the NHS would have been their chosen provider and it is likely that the burden would have fallen there. Indeed, as our bariatric case study outlines, the NHS is likely to play a key role in providing aftercare for bariatric patients, many of whom were clearly not fully aware that there would indeed be a continuation of care required.
Even with our fertility sample, for whom traditional conceptions of aftercare were not required, the resulting pregnancies, which have a higher likelihood of multiple births and premature births,98,193 were supported through the NHS. With both antenatal care and neonatal care (much more likely to be required as a consequence of IVF pregnancies) being extremely expensive, this is sure to be of concern.
Implications for the NHS
We have seen that medical tourism, irrespective of the treatment that is being sought, involves much that is similar across all patients. It is clear that accessing the required treatment in the desired time frame is the primary motivator for travel, but that issues of cost, culture and even to a lesser degree tourism all play a role. We have also seen that the internet, as well as networks both online and offline, play an important role in informing prospective medical tourists, but that on the whole it does not appear that those who travel are truly informed, especially with regard to the risks involved. Despite this, our respondents have nearly all registered satisfaction with their experience and would travel again, or recommend the process to others.
The positives must be set in a wider context that is at least cautious. Our sample is undoubtedly skewed towards those who are satisfied with their experience and yet even here we can see quite profound examples of ill health, poor clinical outcomes and what are likely to be long and expensive requirements for ongoing care. Clearly, with some of our respondents this must be offset against the ill health and need for care that was already being experienced, but it important to note that treatment abroad represents no panacea, either for those who travel or for the NHS.
Subsequent chapters detail the nuances of particular forms of medical tourism and their implications. At the broader level we can say that medical tourism presents the following potential implications for the NHS:
-
Medical tourists are unlikely to be fully informed or understanding of all associated clinical risks.
-
Medical tourists pay more heed to soft information than hard clinical information.
-
There is little effective regulation of information, hard or soft, online or overseas.
-
Patients travelling overseas leave the regulatory safety of the UK and the NHS. Although patients may not ever be fully informed or understanding, if they access care within the NHS then health-care professionals will have played an important role in ensuring that appropriate treatment is being administered. This cannot be guaranteed abroad. There is clearly scope for health-care professionals within the NHS to become part of the networks of information and support that can be accessed, even by those who in the end do still seek treatment abroad.
-
Even when medical tourists travel to professional, reputable clinics, returning for aftercare or continued support is not usually viable.
-
Aftercare in some form is usually required.
-
Aftercare or ongoing care can be extremely intensive.
-
The NHS will play some role in providing ongoing care for many of those who travel for treatment. This can be expensive and can continue through the life course. It may be that the treatment that has been accessed overseas was risky or inappropriate and alternatives in the UK could have been offered.
-
Interviews with professional stakeholders clearly identify the need for guidance and information for patients and staff working within the NHS. Our analysis points to a vacuum in policy guidance. It highlights the need for information and guidance about quality and safety issues that patients may wish to consider before travelling.
-
Clarification is needed in relation to the roles and responsibilities of the NHS in pre and post care and this should be communicated effectively to those who may engage in medical tourism.
-
Further Department of Health guidance for NHS providers and patients on what to request from foreign providers may go some way to address the challenges in continuity of care described.
Chapter 10 Bariatric surgery case study
An area that has seen rapid growth in the numbers of patients travelling abroad, as well as patients in the UK undergoing surgery, is bariatric or weight loss surgery. 194 The UK, like many other countries globally, has seen a rapid increase in the numbers of overweight and obese patients, with the Department of Health estimating that one-quarter of the UK population is now clinically obese, that is, with a body mass index (BMI) of ≥ 30 kg/m2. 195 Obesity has several long-term health effects including an increased incidence of diabetes and cardiovascular disease. In addition to behavioural interventions such as exercise, counselling and pharmacological interventions (appetite suppressants), several surgical procedures are available to assist weight loss.
The two most common procedures are a gastric band and a gastric bypass. A ‘band’ is the less invasive procedure. It limits food intake by placing a restrictive string around the top end of the stomach. This band has to be regularly adjusted to allow patients to consume food while maintaining weight loss. When a band is too tight it can prevent patients from eating, whereas a loose band means that patients can eat as much as they wish. The bypass is a much more invasive procedure in which part of the patient’s stomach is partitioned and his or her capacity to absorb food is limited. As a result of a bypass, patients need to monitor their food intake carefully to ensure that they receive the nutrition that they require. Given the body’s reduced capacity to absorb nutrients and specific vitamins and minerals, supplements have to be taken by patients for the rest of their lives to ensure adequate nutrition. 196
In the UK, bariatric surgery is a relatively new field of surgery. It is available as treatment on the NHS and National Institute for Health and Care Excellence (NICE) guidelines197 recommend or make available bariatric surgery in individuals with a BMI > 40 kg/m2. However, the implementation and interpretation of the guidelines depend on the PCT and on the assessment by a GP. Research has indicated a reluctance by GPs to prescribe such surgery. 195
In this research, 13 in-depth interviews were conducted with patients who travelled abroad for bariatric surgery. These discussed the themes explored in the patient interviews described in Chapter 9, for example patients’ experiences of the NHS before and after treatment, and how they identified the treatment provider abroad. In addition, three professionals from organisations working in bariatric surgery in the UK were interviewed to gain further understanding.
Findings from bariatric surgery patients
Although many issues identified across our sample of patients were common to bariatric patients’ motivation to travel (such as issues relating to distance and eligibility), there were also clear differences within each subtheme identified that were specific to bariatric tourism. These hold important lessons when trying to understand and address the specific factors determining bariatric patients’ travel and follow-up needs.
Motivation for travelling abroad for bariatric surgery: an emerging field of expertise in the UK
As with many other medical tourists, bariatric surgery patients were keen to stress that cost had not been the only factor in them choosing to travel for surgery, and only 2 of the 13 patients interviewed cited this as their sole motivation. More than for any other group interviewed, expertise (in bariatric surgery) was the biggest pull factor. In total, 11 out of the 13 had travelled to Belgium, which was perceived to be more advanced in the field of bariatric surgery at the time that the patients interviewed had undertaken treatment (between 2004 and 2009). In several cases patients specifically described how the surgery that they had opted for had not been available to them within the NHS, or that surgeons in the UK had conducted only a small number of procedures, or that there was only limited expertise in these areas.
Of the 13 patients interviewed, half reported that the surgeon having conducted the procedure many times before was a key factor in their decision-making. The experience of the surgeon was contrasted in some cases with a general distrust of the NHS:
[My motivation for travel was] mainly the cost but also because the surgeon was very highly recommended. Also in general all-round the whole experience. I mean, there’s quite a big issue with MRSA [methicillin-resistant Staphylococcus aureus] which they didn’t have at all abroad.
BT4
Availability
Several issues relating to the availability of treatment were factors in the decision of where to seek treatment. This relates to bariatric surgery specifically, as it is a comparatively new field in the UK (see also p. 69). For example, two patients from Northern Ireland reported that, at the time of their surgery, it was not available in the province and surgery would have required them to travel (to mainland Britain) in any case. Similarly, a patient from Scotland reported that she would have had to travel to England to receive the procedure under the NHS.
Patients also mentioned that they had seen a NHS doctor and had been judged eligible but that the waiting time for the operation had put them off having it done on the NHS. In some cases this appeared to be the actual reported waiting times; in others it was unclear if the patient had just anticipated the long wait.
Eligibility on the NHS: a ‘postcode lottery’?
As in other cases, such as fertility surgery, several patients reported that they had been found to be ineligible for treatment on the NHS. Although NICE guidelines exist that recommend or make available bariatric surgery for individuals with a BMI > 40 kg/m2,197 the implementation and interpretation of these guidelines depends on the PCT and on assessment by the GP. Several patients interviewed referred to the resulting inequities and the sense of a ‘postcode lottery’. In some cases this was because people were deemed to have a BMI considered too low to qualify for surgery, or patients were considered healthy despite having a very high BMI and fearing for their long-term health. This may in part be the result of GPs looking at bariatric surgery as a ‘last resort’ and an expense rather than a cost-saving treatment. A recent survey of GPs conducted by the Office of Health Economics195 found that the vast majority try to avoid prescribing surgery for obesity, regardless of BMI.
Distance: Belgium, a perceived centre of expertise
As with other patients, distance played a key role in decision-making. Specific to bariatric patients was that Belgium, as a centre of expertise in bariatric surgery at the time that interviewees had travelled (between 2004 and 2009), was easily accessible via Eurostar. Ten of the 13 people interviewed had travelled to Belgium: several mentioned its proximity, including specifically the ease of access by Eurostar. This has particular relevance for weight loss surgery, as some patients are cautioned against flying following the procedure.
Based on this analysis, the decision by patients to travel for weight loss surgery was rarely the result of a single motivating factor; rather, it was a combination of cost, expertise, availability and distance, with different patients giving different weight to each of these. Unique to this group was the specific emphasis given to the experience of the surgeon. This was a direct result of bariatric surgery being a newer field of investigation in the UK; as expertise grows in the UK it is likely that these differences will disappear or become less pronounced. A representative of a Royal College working on these issues highlighted that bariatric surgery had been a very new field in the UK in 2004, but that the field was rapidly growing now with increasing expertise in the UK.
Treatment pathway and experience: high rate of complications
The treatment pathway for bariatric patients did not vary greatly from the general model set out in Chapter 9, with most patients describing the use of the internet to identify and research providers.
What did set the experience of bariatric patients somewhat apart from the general experience was the level of complications and aftercare required for most procedures. Of the 13 patients interviewed, four experienced complications directly relating to the surgery and had to be resubmitted to hospital for additional surgery while still abroad. Many of the patients interviewed experienced long-term health problems relating to the surgery undertaken or the longer-term care needs resulting from these. However, what resonated across accounts of immediate complications and longer-term issues was the responsibility that patients took for the health outcomes of their procedures. This again seemed to be specific to bariatric patients in the study sample.
Follow-up and aftercare
The most common procedures for which patients travelled abroad, gastric banding and gastric bypass, both require lifelong follow-up care and maintenance. In the case of a gastric band, this has to be adjusted to ensure that patients continue to lose weight while being able to consume enough food to obtain the nutrition that they require to survive. The gastric band is an elastic band filled with fluid that can be adjusted to tighten or loosen it. People with a gastric band are required to have the band adjusted at regular intervals.
In the case of a gastric bypass, although the procedures may vary, a part of a person’s gut is removed and his or her capacity to absorb minerals and vitamins is limited. Therefore, patients who have undergone a gastric bypass have to rely on supplements to avoid malnutrition and patients have to undergo regular blood tests to monitor this. A professional interviewed for this research referred to the ‘maintenance’ that patients require following bariatric surgery and how this is a lifelong condition.
Aftercare and follow-up from bariatric surgery can be divided into the needs immediately following surgery and the ongoing maintenance of the results achieved from the procedure.
Several patients reported complications with their bands. One patient had a ‘faulty’ band emptied and removed because of the problems that she experienced with it; this interviewee reported that the replacement was also problematic.
Two patients reported more severe long-term health consequences. One (who had had a gastric bypass) reported having been hospitalised for 2 years following a life-threatening complication and was still unable to work. Although the patient had returned to the original surgeon abroad to have the complication dealt with, she was now unable to afford further follow-up visits to him. Despite the complication arising from the original surgery, the patient retained a greater trust in the original surgeon’s abilities than in the NHS as he had been able to resolve the issue whereas the NHS had been unable to:
Now, unfortunately two years down the line and I’m still not 100 per cent. I’m still on morphine every day and I’m still underweight. So I still have long-term problems so I don’t know if that will ever be sorted out.
BT6
The other described how the long-term consequences of a bypass had led to severe health issues, including tears and fistulas.
Continuity of care emerged as a clear challenge for all patients. However, in bariatric surgery this differed between the complications resulting from the surgery and the long-term care needs resulting from the surgery. Some of the complications experienced were severely debilitating, while the need for aftercare and ‘maintenance’ of a gastric band make continuity of care more important than for some of the other areas of surgery for which people travelled and which are reviewed here.
The specific clinical requirements of aftercare for bariatric treatment also led to specificities in the industry models. Many of the Belgian providers offered aftercare services to English patients (such as the filling of bands) in London or other UK locations at an additional cost. This was specific to providers of bariatric services.
National Health Service
Unlike other groups of patients, all patients interviewed had been in contact with the NHS (specifically their GP) in relation to their weight before and after the surgery. Six patients specifically recounted the refusal by their GP to refer them for surgery; two of these explicitly mentioned that they were eligible for the surgery according to NICE guidelines but that their GP had told them that no funding was available.
Overall, the vast majority of patients reported limited support from GPs. This was more common than in other groups of patients interviewed. In many cases patients reported that this may be based on limited knowledge. One interviewee summed it up as follows:
The GP that was here just used to look at me blank if I mentioned my obesity. They didn’t offer anything at all, no support whatsoever [. . .] It’s not that they’re not supportive they just don’t know what to do. They don’t know anything about them.
BT7
Interviewees also reported a difference in attitude between surgeons and GPs, which they felt was mainly due to surgeons’ greater knowledge of bariatric surgery.
Moreover, all patients interviewed reported that insufficient services were provided within the remit of the NHS for overweight and obese patients. There was a clear sense that the approach by NHS staff had been cautious in relation to surgery and that as a result the patients interviewed for the research felt that the treatment that they required was unavailable to them.
Compared with the overall sample of medical tourists, there were several distinct aspects to bariatric tourism. Three key factors were uncommon compared with other patients’ experiences. First, all bariatric patients interviewed had been in contact with the NHS before making their decision to travel for treatment. Second, the lack of expertise within the NHS was a greater factor for motivating bariatric patients than for motivating other medical tourists. Third, the need for aftercare and the high level of complications experienced by bariatric surgery patients set this group apart. It underlines the need for better information and a full understanding of risk amongst this group of medical tourists before they travel. This has also led to specific industry developments by providers, with follow-up consultations in London, and equally specific requirements of the NHS when maintenance is not provided by the original clinic.
Bariatric surgery outcomes have long-term consequences; as this is a comparatively ‘young field’ some of these and the effects of treatment abroad will likely emerge only in the future. The SurgiCal Obesity Treatment Study (SCOTS) at the University of Glasgow (a longitudinal study of bariatric surgery patients)198 will in the future provide important results in this respect.
Across the interviews there was a sense that patients felt that they lacked the entitlement for surgery on the NHS as their weight was a result of their own ‘behaviour’. Some of the patients addressed this explicitly and described how their interactions with the NHS had left them feeling this way; most patients had had some contact with the NHS about weight loss and felt abandoned, with the NHS not recognising the value of weight loss surgery. Even when patients described this negative experience as an example of policy that had to change, they were equally keen to convey a sense of responsibility that they had taken on through their actions, that is, choosing to travel and have surgery to address a health issue, which all of them felt would have become worse otherwise. In addition, even in cases in which weight loss surgery may be inadvisable from a medical perspective, the fact that patients felt compelled to travel indicated that current approaches to overweight and obesity by the NHS are not working. Many patients reported a sense of frustration as they felt that they had saved the NHS substantive future health-care expenditure related to being overweight and obese. Patients had a sense of being judged for being overweight or obese.
Implications for the NHS
-
The need for clearer guidance on bariatric surgery or for patients considering bariatric surgery is evident. Patients lacked consistent information on possible complications, but also on the long-term consequences of surgery and the maintenance requirements, whether they were travelling abroad or seeking treatment in the UK.
-
Equally, greater information for and education of GPs is needed to enable them to educate patients and to deal with the possible consequences of weight loss surgery. Our data suggest that, even when patients travel abroad to access treatment for obesity, they are likely to consult their GP. This presents the opportunity to provide guidance and information either on procedures or on medical travel or both.
Chapter 11 Fertility surgery case study
The rationale for adopting the phrase ‘medical tourism’ throughout this report has already been discussed. The limitations of the term are perhaps most stark when discussing fertility tourism. Indeed, the term ‘fertility tourism’ is not common among the academic literature with the exception of noting its lack of suitability. Instead, a rather extensive and diverse range of terms, from ‘cross-border fertility treatment’ to ‘transnational reproduction’, is adopted. 47,72,114 The most frequently used and seemingly acceptable term appears to be ‘cross-border reproductive care’, which is adopted widely and most notably in the works of Hudson et al. ,72 Culley et al. 57 and Shenfield et al. 114 However it is labelled, fertility tourism or CBRC appears to be on the rise (PA7, PA11, NHS15, Hudson et al. 72). With this comes a range of potential issues. Many of these, such as patient safety and risk, legal uncertainties and long-term care, are similar (although not identical) to those that arise from all forms of medical tourism. However, there are often additional moral and ethical debates surrounding CBRC. 199–201
Distinctive features of fertility tourism
Although there are many similarities between travelling for fertility treatment and travelling for other forms of medical treatment, there is much that sets fertility tourism apart. Discussion here is informed by interviews with NHS professionals, representatives of professional associations and those who play a role (be it commercial or otherwise) in overseas treatment, as well as those who have travelled for some form of what can be termed ‘fertility treatment abroad’. The purpose here is to highlight the differences between fertility treatment abroad and other forms of medical tourism, and attempt to explain such differences.
As with the findings of other studies, the availability of treatment in the UK was the single biggest motivator to travel abroad for fertility treatment. All respondents discussed their ineligibility for publicly funded treatment, which again was the consequence of a range of factors: some were outwith the age criterion, others were deemed as having an extremely low chance of success, one had exhausted her publicly funded opportunities and one, although eligible, could not access the treatment in a time scale that she felt was reasonable. Typical comments were:
Well, the NHS wouldn’t even consider us. It was just a non-starter.
FT5
No [there was no chance of treatment on the NHS], because of my age.
FT1
Despite this, all respondents reported positive experiences of the NHS. For some, frustration or disappointment regarding a lack of eligibility was balanced by high levels of support from their GP or other NHS staff throughout their treatment journey, in terms of both help received with organising tests and accessing required fertility drugs before treatment and the antenatal care accessed after pregnancy was successfully achieved. When respondents were less positive regarding the support that they had received pretreatment abroad, they were unanimous in their satisfaction with subsequent NHS antenatal care. Perhaps surprisingly, not all were frustrated with their ineligibility for publicly funded fertility treatment, with one respondent remarking:
It’s my choice in a way that I’m this age wanting to have a family [. . .] so in a way I think it was my lifestyle choice and I knew that that could be a potential issue in the future so I’m not sure health-care systems should have to pay for my lifestyle choice.
FT1
An interesting finding from our interviews was that support from NHS staff for those who had undertaken private treatment varied. In some instances NHS staff aided patients in accessing necessary pretreatment scans and tests free through the NHS, whereas others would provide no such access to drugs and scans:
She looked at the list and she said I can make an excuse to have that one done for you and that one and that one and that one. So she did absolutely as many as she could on the NHS, which was fantastic of her.
FT5
I tried to go to my GP to get the blood tests done but he wouldn’t do it. It depends on your GP. He told me to go to my local GUM [genitourinary medicine] clinic and pretend I’d slept with a waiter on holiday to get a test for HIV [human immunodeficiency virus] and Hep and stuff.
FT8
Here, it is likely that a complex range of considerations has informed a GP’s decision whether or not to provide NHS resources, from a desire to help at the most human level perhaps to a fear of vicarious liability at the other end of the spectrum. As one NHS respondent noted (NHS18), some NHS staff may worry about playing a role in facilitating the overseas journey of a patient to a country with different ethical and legal principles of medicine.
The main reason cited by our respondents for travelling abroad for fertility treatment was waiting times; even privately in the UK, the wait for egg donors in particular can feel prohibitive for those seeking fertility treatment:
With regard to the egg donation I was told there’s a five year waiting list at that time for eggs. This would have been in about 2002/03. So I thought about it and I thought well I’m 40 so if I wait five years I’m going to be 45, my son is going to be eight, I don’t think I can wait that long.
FT4
Although there is the hope that recent legislative changes allowing greater remuneration for sperm and egg donors will increase supply, numbers are still low (PA7). In total, five of our respondents required egg donation (sometimes alongside other procedures) and for all the lack of availability both publicly and privately in the UK precipitated their decision to travel. Other studies suggest that a high proportion of those travelling globally for fertility treatment are receiving some form of egg donation. Shenfield et al. 114 suggest figures of roughly 45% Europe-wide and Culley et al. 57 report figures of 59% in a small study of UK fertility travellers. The figure is even higher for patients from Germany where there is a shortage of donors. 202 It was not only the availability of donor eggs that motivated our respondents to travel; in one case concerns were raised regarding the quality of UK-sourced eggs (FT8).
A review of the literature suggests three other common motivations for seeking CBRC: success rates, legal restrictions and issues of anonymity. 72 In our sample, as with other UK-focused studies,57 there was no discussion of legal restrictions. With regards to anonymity, only one respondent (FT2) suggested that this had played a role in travelling abroad and even here it was a minor consideration. On the contrary, other respondents who did mention anonymity professed to find the anonymity offered to donors abroad to be a concern (FT1). This was clearly the case for one respondent (FT9) who struggled to access vital information when her offspring was being tested for certain genetic conditions. This is perhaps surprising in the context of the interviews we conducted with professionals and stakeholders, as well as the wider literature. Here the suggestion seems to be that anonymity is a key motivator for those who seek fertility treatment abroad (NHS17, NHS56). Perhaps equally surprising was the fact that only two respondents (FT6, FT8) directly addressed the issue of success rates and in only one case (FT6) did this seem to be a key (although still not the sole) motivator. One NHS professional (NHS15) did remark that it was unlikely that overseas clinics could actually offer better success rates than are available in the UK, or innovative procedures that are unavailable in the UK.
Unlike other forms of medical tourism, information gathering on the internet was limited to searching for clinics, rather than information about procedures. GPs and other NHS staff represented the main source of information regarding the procedures that our sample travelled for. The internet was simply a location in which the clinics offering the required treatment could be identified.
The websites of clinics were not the only source of information that respondents engaged with. Most had some contact with an online fertility support group or forum, which proved useful in terms of both gaining information about the experiences of others and obtaining specific clinician reviews:
I went to [support forum] website and through there I started looking at clinics. And I saw similar problems to mine so I contacted the [clinic] and went for a consultation.
FT2
So I had heard from people on [support forum] website about the clinic in the Czech Republic and they had been successful there and they just said it’s a wonderful clinic.
FT2
The role played by support forums is clearly substantial here, with one respondent from a support organisation presenting extremely large membership figures (IND2). Moreover, they acknowledge the power that a post on such trusted sites can have, with visitors to sites happy to take the recommendations of others based on a clinic or clinician being ‘nice’ over ‘hard’ evidence regarding success rates (PA12).
Although the internet played an extremely important role in identifying and selecting overseas clinics, it would appear that it played a much more minor role, if any, in gathering information regarding the conditions that people suffer from and possible treatment options. Rather, all had engaged with the NHS (or the French national health system in one case) and diagnosis had occurred here. Further diagnosis may have occurred at private clinics, but regardless of the public or private setting much of the information gathering regarding the procedures that our sample travelled for was undertaken as part of the diagnosis procedure. As such, it can be argued that the fertility patients in our sample could have been considered as having expertise beyond that of lay persons when searching the internet for foreign clinics. As one professional association respondent noted (PA12), all had a clear idea of what procedure was needed and the questions they would need answering.
With regards to how fertility travellers organise their treatment, the picture was mixed. At one end of the spectrum we heard from somebody who paid a flat fee to a private UK clinic, which then organised all pretreatment tests, flights, accommodation, treatment and follow-ups:
It’s all included. They basically arrange it on different budgets. So there’s an expensive hotel in [city], there’s a cheaper hotel in [city]. I think you get all your meals. It’s very, very well organised. They tell you what flights you can have. You’re quite limited on your flights [. . .] I took my son with me because we didn’t have a babysitter really and he was about eight at the time. So they arranged everything.
FT4
At the other end of the spectrum respondents had contacted clinics directly, had organised their own flights and accommodation and had responsibility for organising any pretreatment scans and drugs. In the most extreme case there was no guidance offered as to which drugs, tests and scans were needed and when they were needed:
That was the only thing about having treatment abroad is that they don’t tell you that you have to have anything prior to going out there. I was using my own eggs so therefore I had to take all these drugs prior to going out to [destination]. But having done four cycles in the UK I knew the procedure [. . .] so I organised those scans privately in a private hospital in [UK city].
FT3
As with other types of treatment most plotted a journey in between these two extremes, with parts of the process packaged with the treatment. What is hard to tell is whether our respondents opted for a more or less comprehensive package as a reflection of a desire to relinquish or take control. Even in cases in which our respondents have an increased level of responsibility, say for organising tests, scans and drugs, they are following an extremely prescriptive and strict plan. Other studies have highlighted the importance of agency and the feeling that fertility travellers were their own ‘project manager’ (p. 577). 203 We have certainly witnessed this with other treatment types, notably bariatric treatment; however, the tone of our interviews does not seem to suggest that the process has been engaged with as a form of exerting control over a part of life that is out of the respondents’ control. Although the fertility issues are clearly out of the respondents’ control, there appears in our interviews to be a sense of this being a last chance rather than a means to assert control. Indeed, when the issue of control is addressed it is an admission that the process does not endow the person seeking treatment with any control: ‘If people wanted complete and utter control over it then that’s fatal. You don’t have control over the process’ (FT7).
What is particularly interesting is that, even with regard to the organising of tests, scans and drugs, for which respondents have responsibility if only a little control, most had at least attempted to source these through the NHS.
Overall, the experiences of our travellers mirror those that our professional interviewees have come across and those that have been discussed in published studies inasmuch as they are largely positive. 72 There is undoubtedly a sampling issue here as all of our interviewees had been successful in achieving pregnancy. Indeed, potential respondents have withdrawn their participation as a consequence of treatment being unsuccessful.
All mentioned that clinical staff were proficient in the English language although quite often nurses had little command of English. Communication was not seen as an issue by any of the respondents, although it had been a concern in advance of travelling for some. Interestingly, almost all of the respondents seemed at pains to highlight how clean the overseas clinics were, with some contrasting the clean, clear and ‘un-hospital-like’ nature of the overseas clinics with conditions in UK clinics and hospitals (FT1, FT4).
In contrast to other treatment types, such as bariatric or cosmetic surgery, there was little to probe with regard to aftercare and complications. As alluded to earlier, for all the majority of aftercare was dealt with on the NHS as with any ‘traditional’ pregnancy. All respondents mentioned that they received follow-up communications from their private clinic and some attended a first scan and blood test post implantation at their private clinic, although this was usually for those who had travelled abroad through a UK clinic. However, there was no detailed or continuous care or communication. None of the respondents seemed to expect this and seemed happy to engage with NHS antenatal services. In only one case did a respondent discuss a complication from the treatment that she had received, expressing frustration that the apparently well-known risk of such a complication was not communicated to her (FT4). Here, the intracytoplasmic sperm injection (ICSI) procedure precipitated a twin pregnancy that resulted in a premature birth at 29 weeks and subsequent intensive treatment.
Multiple births
Although others do not speak directly of complications, a number of respondents had multiple births as a consequence of their fertility treatment abroad. In all cases, whether we consider multiple births as a complication or not, these outcomes of fertility treatment abroad were addressed in the UK within the NHS. One professional respondent (NHS15) suggests that complications are extremely rare, with the outcome simply being pregnancy or non-pregnancy. Others were keen to stress the seriousness of multiple births, with regard to not only the chance that a pregnancy would last until term, but also complications such as disabilities that might not manifest or present themselves until months after the birth (PA7, PA12). Multiple births have long been seen as more likely after assisted reproductive technology (ART) than after spontaneous conception,98,193 but evidence also suggests that the likelihood is even higher when patients undergo ART abroad. 98 This is almost certainly a consequence of higher numbers of embryo transfers being permitted in some countries than in the UK (PA7). In our sample, one respondent even speaks of having four embryos transferred (FT3). This is particularly worrying if we consider the implications of fertility tourism or CBRC for the NHS. As both professional association and NHS respondents are keen to stress, the cost of care during and after multiple pregnancies is considerably higher than that for singleton pregnancies (NHS15, NHS17, PA7, PA11). Neonatal care is itself an expensive process, which, within the NHS, is subsidised in part by private income generated from other procedures. Simply increasing the number of births is a problem but, given that the average length of pregnancy for a carrier of triplets is only 35 weeks and that premature birth is extremely common with multiples, the cost of neonatal treatment is a major burden for the NHS (NHS15, PA7).
Fertility tourism or CBRC clearly shares some similarities with other forms of medical travel while at the same time standing apart in many ways. Our respondents have shared motivations and experiences that are common with those in other studies, while never engaging with the legal and ethical dimensions that mark much of the academic debate. Our respondents are satisfied on the whole yet some of their stories allude to quite substantial risks faced by those who travel for fertility treatment and the implications of these risks for the NHS. Ultimately, as our professional respondents noted, when a patient travels abroad certain best practices cannot be guaranteed, from the way that donors are treated to the number of embryos that are transferred (NHS17, PA7). Until a degree of global regulation can be guaranteed, which does not seem viable, or provision within the UK meets demand, UK citizens will travel abroad and the associated risks cannot be easily controlled.
Implications for the NHS
We have discussed the broad implications common to all forms of medical tourism but fertility tourism often exacerbates some of the issues common to medical tourism more generally, as well as presenting others:
-
Aftercare or the continuation of care is not required in the same sense as with bariatric treatment or even cosmetic treatment; however, the NHS bears the cost of antenatal care, which is expensive, in nearly all cases.
-
Furthermore, IVF treatment is, ceteris paribus, more likely than non-assisted fertilisation to result in a multiple pregnancy, which in turn increases the likelihood of premature birth or miscarriage. Neonatal costs are extremely high.
-
In addition, not all countries have strict legislation governing the number of embryos that can be transferred. With every additional transfer beyond the UK limit of two, the likelihood of multiple pregnancies/births increases, along with the risk of premature birth and the need for neonatal care.
-
Unclear regulatory frameworks overseas mean that patient data may not always be held in the detail expected within the NHS and it is not always possible to retrieve data. When countries have anonymous donor laws this is exacerbated.
Chapter 12 Dental surgery case study
Although commercial sources have undoubtedly talked up the numbers travelling for all forms of medical tourism, it is clear that dental tourists represent a large proportion of whatever the global figure is for medical tourists. One commercial survey suggests that dental tourism represents 32% of all medical tourism204 and this is echoed by the consumer watchdog Which?’s survey,179 which finds that dental treatment is the most popular form of medical tourism among its sample of UK-based medical tourists. In addition, media sources both in the UK and beyond have reported the dental tourism phenomenon for over a decade, and in the UK dental tourists have often been tied to commentary on a perceived crisis within NHS provision. Countless newspapers articles and BBC news reports have highlighted the difficulties of registering with a NHS dental practice. Once British patients have accepted this they will rationally seek cheaper treatment offered abroad. 205,206
This case study centres on interviews with 11 people who have travelled for some form of dental care, with responses from NHS professionals, professional associations and other stakeholders in the dental tourism industry (alongside a rather scant literature base) providing a wider context. There are many differences between dental tourism and other forms of treatment abroad. Not least is the fact that the very term ‘dental tourism’ appears much more palatable than other treatment tourisms such as fertility tourism. Indeed, as we discuss, many of our respondents place their treatment journey within a tourism context, reflecting the portrayal of dental treatment abroad that is commonly found online.
The distinctiveness of dental tourism
As with other treatment types, lack of NHS availability can be seen as a primary motivator for seeking overseas dental treatment. However, this was not the case for five of our respondents: unlike for fertility or bariatric treatment, for example, not all of our dental respondents had sought NHS treatment (DT6, DT8, DT10) and, even when they had, it was not necessarily a lack of availability that had prompted overseas treatment (DT2, DT3). Other core reasons cited were a distrust of or scepticism about NHS dentists (DT3, DT8, DT10), a perceived lack of availability (rather than experienced) (DT8), dissatisfaction with NHS dental care received previously (DT3) and cultural reasons (DT5, DT6, DT8, DT10). Similar to studies of other treatment types, the decision to travel abroad for dental treatment was in no case motivated by a single factor but rather a combination of factors.
For some a distrust of the NHS played a key role in looking for private treatment:
I’ve never heard any good stories about UK dentists so I thought if I have to pay here I might just go home and pay there as well.
DT10
I wouldn’t dream of it [using an NHS dentist]. I’ve just seen a colleague, funnily enough a couple of hours ago, who was just about to go to an NHS dentist. She had a provisional crown in one of her front rows of teeth for a proper replacement and it looked so amateurish. No I just wouldn’t dream of it. I’d rather jump on a flight and bear the cost for that.
DT3
Even among those who would at some stage have sought NHS treatment had it been available there was a sense that the standard of care was not as high as they would hope, often drawing on personal experience:
The NHS did the cheapest job they could and for two or three years I’d had problems and the infection spread to my gums and affected other teeth. So in the end I lost more teeth than I should have done. If the NHS had been up to snuff I would never have needed to go.
DT1
Whether our respondents had decided to seek private treatment as a consequence of issues with NHS dental care or because of other factors, the decision to seek this private care abroad was shaped by four issues: a wider distrust of UK dentistry, cost, culture and the opportunity for a holiday.
The distrust of or dissatisfaction with UK private health care was a common theme for those who had been born or who had spent a considerable amount of time outside the UK (DT3, DT6, DT8, DT10). Here, the sense is that British dentistry, private or otherwise, is of a low standard (DT10). One respondent reflected on her experience of private UK treatment: ‘So I actually went to see a private dentist and I always thought I’d get better and prompter treatment and that is just an illusion’ (DT3).
Cultural and familial reasons to travel were not limited to those who returned home; one respondent (DT5) travelled to her partner’s country of origin after a poor personal experience of NHS dental care. As with others who travelled home (as well as five British citizens who travelled to destinations to which they had no previous connections), this respondent located her dental treatment within a holiday. It is perhaps one of the major differences between the motivations of dental tourists and the motivations of other medical travellers; whereas some who travelled for bariatric or fertility treatment may have built a holiday or some sightseeing around the planned treatment, with some dental respondents the holiday was as central as the treatment. In this respect dental and cosmetic tourism perhaps best fit the label of medical tourism. One respondent has even returned to her dental destination for a holiday whereas another scheduled his treatment to coincide with a ‘stag party’:
The places we went were fantastic and it was a good holiday. I think we went back three or four times.
DT1
I’d been wanting to go for ages so when my mate said he was going to do Hungary for the stag I just thought, done.
DT11
Perhaps the most surprising finding from the interviews was that cost was not seen as a key driver by most. Cost was likely to be more important to those with no cultural ties beyond the UK. In our sample only six mentioned cost and in only four cases was cost the most important factor for choosing overseas treatment rather than UK private treatment. In each of these cases, however, the cost savings were felt to be significant by the interviewees and in two cases (DT1, DT7) the perceived savings were > £20,000. Given the media attention that has focused on the cost of dental treatment abroad, it is perhaps surprising that cost was not a factor for more of our respondents. Indeed, when asked what they thought the key motivations for travelling were, our professional association respondents ranked cost as being the only real reason to travel (PA9, PA16).
With regard to the experience of travelling for dental treatment, the organisation of the journey was rather mixed. In some cases our respondents had pretreatment consultations in the UK. Although ‘package’ treatment and holiday offers are readily available on the internet, none of our respondents had travelled on such a deal (although two did have their accommodation organised by the treatment provider). In addition, none of our respondents had used brokers or facilitators. Instead, all organised their journeys direct with the clinic and organised their own flights.
In terms of the experience, for 10 of our 11 respondents it was overwhelmingly positive:
Yeah, the experience we had there was excellent.
DT1
Yeah, wonderful. They said that these were guaranteed for 10 years.
DT2
She [the dentist] was brilliant. I can’t praise her high enough. I’m not being emotional about it. She was very, very good. She listened first and foremost. She didn’t rip me off and she charged very reasonable and at the same time she didn’t cut herself short.
DT9
However, as one of our professional association respondents (PA9) and the wider literature caution,207 problems may not reveal themselves until months or even years down the line.
An unregulated industry
One respondent (DT4) did not have a positive experience. Having travelled for what she called a full restoration of her smile, numerous implants were provided. In fact, the implants were initially placed in the UK before the respondent travelled to Hungary for the subsequent stages of treatment:
Some of my existing teeth which had been filed back too far and therefore caused a lot of pain because the nerves, the pulp was exposed . . . There was no trial of whether they were the right size or the correct whatever. The final work, it ended up that they were all far, far too big for the size of my mouth. They weren’t in the right place of my original teeth. They completely cramped my tongue. I couldn’t speak. I had no room to speak because they were too high. I couldn’t close my mouth. And I was in a considerable amount of pain, which wasn’t taken any notice of at all.
The respondent has subsequently had all of the work redone bringing the total cost to in excess of £40,000 and has suffered for a number of years while the problem was being addressed. This is only one case in our sample but it underscores the potential negative outcomes of dental surgery. Indeed, our professional association respondents (PA9, PA16) suggest that corrective work is commonly requested by those who have travelled abroad. A survey by the Irish Dental Association in 2010208 even suggested that 75% of those who had travelled abroad for dental surgery and then subsequently re-engaged with the Irish dental system required corrective work. Even if these figures are incorrect, the success rate for non-complicated implants ranges between 93% and 98%,207 which means that even when best practice is observed complications will arise. When these have occurred within a different legal and regulatory framework the problems faced by the patient can be difficult to address. One professional association respondent (PA8) stated that he would never feel comfortable referring a patient for treatment overseas as there is too much that cannot be controlled.
A clear issue is the lack of regulation governing dental practice overseas, especially when procedures are considered cosmetic in nature. Not unlike cosmetic tourism, dental tourism is marketed very much as a commodity rather than as a health service. This, as we have seen, has a profound impact on the quality of information that exists and in turn on how well protected potential dental tourists are from issues of risk. That many of the dentists who operate abroad have trained in the UK or been registered with the GDC is clearly of great comfort to many of those who travel for dental treatment. But how reassuring is such registration? Dental tourists are unlikely to look beyond whether a practitioner is registered with the GDC, perhaps to explore clinical memberships beyond the UK and the comprehensiveness of their safeguards. Moreover, it is unrealistic to expect prospective dental tourists to assess the veracity of any claims made regarding memberships. In the UK it is relatively straightforward to ascertain whether or not a dentist is deemed as being in good standing with the GDC. It is extremely unlikely that any professional who has been suspended or deleted from the GDC’s register could practise for long without being dealt with by the GDC. However, this may not be the case abroad. Indeed, one of our professional association interviewees (PA9) points to the case of a celebrated dentist in one country who had actually been suspended from the GDC’s list in the UK. The dentist in question continued to actively market himself to UK customers, even maintaining that he was registered with the GDC when in fact he was suspended.
It is possible to think of dental treatment abroad as reflecting more closely the consumer-driven ideal of choice in medical services and perhaps best befitting the label ‘medical tourism’. But as one respondent noted (DT4), although dental tourism does not necessarily involve life-threatening medical treatment, it most definitely can involve life-changing medical treatment. As in this case, this change will not always be positive.
Implications for the NHS
Although many in the UK undergo private dental treatment, it is clearly possible that people who have had dental work abroad may seek NHS care on their return. As the NHS are unlikely to offer anything beyond the most basic corrective work (if patients are in great pain), dental tourism does still present some implications for the NHS:
-
The lack of comprehensive regulation of dentistry outside the UK means that there is a genuine risk of wholly inadequate care being received abroad. Although the NHS is likely to perform emergency treatment only, often with the purpose of relieving pain, there is the potential for a large number of such cases to occur as a consequence of dental tourism.
-
Many clinics offering dental treatment, especially in selected locations, also offer what is marketed as minor cosmetic treatment. In many cases it is unclear whether or not they are qualified to do so.
-
The key issue relates to the lack of clarity regarding patient records. In particular, when a patient has travelled for treatment, the apparent linguistic ability of clinicians may not be reflected in records. It is entirely possible that continuation of care will take place within the NHS, sometimes in circumstances in which the precise treatment undertaken abroad is unknown.
Chapter 13 Cosmetic surgery case study
Distinctive features of cosmetic tourism
Unlike all other forms of treatment, it is unlikely that those who require cosmetic surgery will have had much contact related to their treatment with the NHS. As one NHS commissioner remarked:
We have a very, very tight cosmetic approval process which we’ve had for a number of years. Every GP is aware of it so the numbers of people who actually get referred – we call it IFR, Individual Funding Request – is quite small.
NHS6
As our interviews confirmed, people are generally aware that cosmetic procedures are rarely provided on the NHS and as such there is an understanding from the outset that treatment will be privately funded and provided. There are notable exceptions, for example following bariatric surgery some may hope to have loose skin removed. Likewise, those who use the NHS dental service may assume that cosmetic dentistry can be provided through the NHS. In both of these examples people who seek cosmetic surgery may engage with the NHS in the hope that treatment will be provided, although as the quote above implies such treatment is unlikely to be approved.
The mindset that surrounds cosmetic treatment is perhaps then different to that which surrounds other forms of treatment. It is generally understood that to seek cosmetic treatment is to seek private treatment. Even when it comes to aftercare, our respondents either were turned away by their GP or opted to utilise private facilities from the outset. In one case a respondent discussed visiting their GP for the removal of stitches: ‘I had to go and get my stitches out 15 days later. The doctor that took them out was very unimpressed, very angry, that I’d gone to get four stitches taken out that had been for private treatment’ (CT2).
The consequence of this is that, for those seeking cosmetic surgery, value for money and overall costs appear extremely important. Although one study found that 66% of its respondents would never consider cosmetic surgery abroad and only 4% would consider it for reduced costs,209 a consensus of commercial, professional and academic sources, as well as our sample of medical tourists, suggest that cost is the key driver behind those who travel for cosmetic treatment. ‘The cost generally does seduce you . . . I thought to myself if I’m going to pay £5000 and not get any result at all and be back to stage one why not go to Cyprus and pay £800 and get the same thing’ (CT4).
Patients felt that it was important and useful that prices were upfront and made readily available on websites of foreign providers, in comparison to UK providers at which an enquiry and consultation would first be necessary. Almost half (four out of nine) of the sample opted for multiple procedures as part of a package; this was particularly cost-effective. For example, CT3 explained how the surgeon offered to ‘throw in some extras’ to make it a more attractive package: ‘It was £5000 for my arms alone. In Belgium I paid £6000 for my arms, my tummy and he said because you’re having all that done we’ll do some liposuction and reshape you. So he did that as well’ (CT3).
The cosmetic tourism industry
The value-for-money nature of cosmetic tourism reflects a wider approach from within the industry and combined with intensive marketing, there is a potential for risks to be not only heightened but also misunderstood by those who travel. All of our interviewees, whether they had travelled for treatment, worked in the NHS, represented a professional association or had a commercial interest in cosmetic tourism, presented a picture of a process that is very much marketed as tourism. This is not to say that our medical tourists agreed with the notion of cosmetic treatment being reconcilable with a holiday:
I don’t understand this image that you’re going to have an operation and then go and lie on the beach for a week and have cocktails. Because you’re big swollen and painful – whatever you’ve had done [. . .] so I think it’s naughty for companies to advertise as sort of holiday surgery breaks because it’s not like that.
CT4
Contrasting this point with the image presented by many online sources and verbalised by one interviewee with commercial interests is particularly stark:
It’s not just about going for medical treatment. [Location] is an absolutely stunningly beautiful city so don’t just think about it as going for a quick nip or tuck. Actually take an extra few days out of your diary and actually spend some time doing sightseeing.
IND14
There is clearly an issue with how cosmetic treatment is marketed in general, with the role of television, from reality TV shows to adverts, linked to an increasing prevalence of people deciding to undergo procedures. 210 Although our professional respondents were all keen to underscore the fact that cosmetic surgery is still surgery and as such should be considered as a medical procedure (PA8, PA17), cosmetic surgery, especially abroad, is marketed more as a commodity than a procedure. This has clear consequences for the quality of information that is presented, especially online.
We saw in Chapter 7 that the quality of information that can be found on cosmetic tourism websites is poor. This is perhaps even more problematic given that it is unlikely that potential cosmetic tourists will have discussed their treatment plans with a health-care professional. This lack of quality is exacerbated by the broader consumer rather than medical focus of the cosmetic tourism industry. Interviews with industry professionals demonstrated a level of concern for patients opting to travel abroad for financial reasons, as this can result in patients overlooking more important factors such as qualifications and aftercare.
Even those who engage with an online community find themselves under- or ill-informed. Indeed, there appears much less balance to the online community that surrounds cosmetic tourism than can be found in bariatric or fertility surgery forums. As one respondent noted (CT8), forums on cosmetic surgery provider sites are heavily monitored to remove any negative comments about the treatment received.
Risk
The picture that is painted by those with commercial interests in the cosmetic tourism industry is one that plays up the tourism dimension, attempts to normalise the notion that one would travel to have cosmetic surgery and seriously underplays the risks involved. This has a profound impact on how people view the risks involved and, in turn, through being under- or ill-informed, how they experience risks. The poor quality and lack of regulation of information online is found across all forms of medical tourism; however, a wider lack of regulation surrounds cosmetic tourism, even within the UK. One professional respondent suggested that, within the UK, cosmetic treatment is being offered by people without the necessary qualifications and that this is certainly the case overseas as well (PA8). Turning to overseas cosmetic surgery the same interviewee explained that, as things stand, there was no good clinical reason to travel for treatment:
By and large nobody encourages the principle of people going into a foreign land, not knowing the culture, often not knowing the language and also not knowing how to check on who the surgeon is, what qualifications they have and where they have the surgery whether they have similar standards to those imposed by the Care Quality Commission here in the UK.
PA8
Regulation is quite simply missing. 211 Despite our interviewees from the commercial sector playing down the risks of cosmetic treatment, both in general and abroad, evidence from academic and professional sources suggests that there are numerous clinical risks and examples of quite serious complications arising from cosmetic tourism abroad. 76,102,134,212,213 We can draw examples of quite severe complications even from our cosmetic tourists:
I’d got a pocket full of fluid inside of my face. I’d got infection all round my neck and I’d got this pocket full of fluid.
CT5
I’m left with a hole in my stomach because they just couldn’t be bothered to sort it out properly.
CT8
We should probably note that none of our sample had travelled for cosmetic surgery involving their breasts. A survey of clinicians by BAPRAS212 recorded a higher rate of complications related to such cosmetic surgery than for any other type of surgery.
The reality is that many of the health implications are likely to present after the period that a cosmetic tourist spends abroad (PA8, PA17). It is unlikely that people will be willing or able to travel, perhaps in great pain, to the country in which they underwent treatment and, even if they did, there are no guarantees that the original provider would offer treatment. The recent PIP breast implant scandal underscores the unclear legal and regulatory frameworks that exist around cosmetic tourism as well as the clinical risks faced by those who undergo cosmetic treatment abroad.
An additional issue that is addressed in the literature,213,214 and which was discussed by our professional association interviewees but not by our cosmetic tourists, is that of psychological support. One representative of a professional association stressed that psychological support is woefully lacking in general and even more so abroad. Moreover, in her opinion:
Cosmetic surgery patients are amongst the most vulnerable patients in this society and they can be taken advantage of. Many patients, the vast majority of them, who think about cosmetic surgery, they feel embarrassed to talk about it. They don’t even go and discuss it with their GP.
PA8
This sentiment is echoed by both Bradbury213 and McGrath,214 who discuss the psychological impact of cosmetic surgery and breast implant surgery respectively. Indeed, it is worth reflecting on the fact that cosmetic surgery abroad may often involve vulnerable people who may have little interaction with health-care professionals, who have been exposed to poor-quality information, who travel for possibly life-changing procedures and who do so with no professional psychological support.
Implications for the NHS
Cosmetic tourism involves people leaving a rather weak regulatory framework in the UK to have what can be serious and complex procedures in countries that may offer even fewer safeguards than the UK. This has a number of consequences and presents the following possible implications for the NHS:
-
Complications from cosmetic surgery often do not occur immediately. Once patients have returned to the UK it is likely that any serious complications will be addressed by the NHS.
-
Perhaps even more than for those who travel for any other form of medical treatment abroad, cosmetic tourists are likely to be exposed to poor-quality information that is not balanced through interaction with health-care professionals.
-
The lack of psychological support offered by private providers, especially overseas, leaves many at risk of undergoing inappropriate procedures or procedures that are unlikely to offer outcomes that meet what may be unrealistic expectations. The consequences of this are once again likely to fall on the NHS.
Chapter 14 Diaspora case study
Of particular interest to this project is the experience of diaspora patients who choose to travel abroad, to their countries of origin or to a third country, for medical treatment. There are a number of reasons why these patients choose to travel, in particular the desire to access primary care, which is freely available in the UK. Research demonstrates that black and minority ethnic (BME) and migrant communities often encounter difficulties when accessing health care in the UK, and this is also often the case in other countries. 215
Three individuals were interviewed regarding their experiences of travelling abroad to a country that they had a familial connection with for medical treatment. In addition, focus groups were conducted with members of the Somali communities in Manchester and Camden and the Gujarati community in Leicester. Here it has been necessary to deviate from the hitherto-used method of interviewee identification, in which individual identifiers have been attached to verbatim quotes. Given that the diaspora groups were often interviewed within a group setting, sometimes with the facilitation of a cultural gatekeeper, it was not possible to give individuals unique identifier labels. Although patients travelled for a range of treatments, diagnostics was the predominant reason. Despite representing different ethnic communities, there were a number of commonalities across all patients that marked this as a distinct group within our patient sample, with specific characteristics differing from those of the general medical tourism experience. This included patients’ motivation for travel and their use of information and awareness.
Destination
Within the diaspora category there were several different strands to the diaspora element of patients travelling abroad. The three individuals travelled to familial countries within Europe (France and Germany); two travelled to their country of origin and the third travelled to his wife’s country of origin. They had strong links with family and friends and previous experience of the health-care system. Industry professionals explained that members of specific ethnic communities within their catchment areas would often travel ‘home’ for various treatments and combine this with visiting family and friends.
The Gujarati community travelled to a specific area of Gujarat in India. However, none of the individuals had direct familial links to this city. All of the members had been born or grown up in East Africa and moved to the UK in the 1970s. Although their families originated from Gujarat, there was a specific religious element to their choice of destination. All of the community members follow a certain branch of Hinduism and they have become followers and travel to Gujarat as part of an annual religious pilgrimage. The choice of destination by this group was not primarily determined by any of the considerations evident for other medical tourists interviewed for this research.
Members of the Somali community predominantly travelled to Germany and occasionally to Italy. Research from both Sweden216 and Holland217 demonstrates that members of the Somali communities in these countries also travel to Germany for medical treatment, in particular diagnosis, for similar reasons. German doctors have advertised on Somali television for many years and this has developed as the main medical tourism route for the Somali communities that we spoke with. A minority of the groups have travelled to other European destinations, including Italy and Holland. Community members stay with members of the Somali communities in both of those countries. Holland was a prominent destination for Somali refugees during the 1990s and Italy has a colonial connection with Somalia. Industry professionals also considered this a reason for Somali community travel. Members of the community were keen to highlight that it is commonplace within their nomadic culture to travel, including for health purposes, and therefore this may be specific to Somali diaspora.
Motivation
Motivation for travel differed vastly amongst diaspora travellers in contrast to the motivation for travel for all other outbound medical tourists.
Expertise
The overwhelming motivating factor for the mixed and Somali diaspora groups was their desire to seek a quick and thorough diagnosis. This was paired with a willingness to travel and pay out of pocket for services normally available on the NHS. Although the Gujarati community also displayed such willingness, cost took precedence for these patients. The willingness to travel and seek a quick diagnosis is combined with a lack of confidence in the UK system and in some cases not having a full awareness of all services offered. Tiilikainen and Koehn218 found that a key motivation for Somali patients to travel is a negative perception of the host nation’s health-care system, including a lack of understanding of the system and a lack of trust in the diagnosis given. However, for both the Somali and the Gujarati communities, cost was also an influencing factor as they were able to access diagnostics more cheaply abroad than in the UK.
Across the board, patients were generally unhappy with the diagnostics that they receive from their GPs. For example, OT6 explained:
I don’t like to go to doctors and have the feeling that right from the get go the examination or even the way the diagnosis is being formulated, I don’t like to have the impression that I’m going to have to come back or see another doctor.
Patients expressed the belief that a GP should undertake a thorough diagnostics process, including any necessary testing (e.g. blood tests), during the first visit and be able to prescribe treatment or medication as appropriate. They often felt that their GPs went through a process of vague questioning and prescribing of either paracetamol or antibiotics with the proviso that if their complaint did not improve they should return in a month or so. This led members of the Somali communities to refer to their local GPs as ‘Dr Paracetamol’, demonstrating their dissatisfaction. This has been corroborated by other studies. 219
The Somali focus groups revealed that Somali patients tell their GP their problems and expect tests and a diagnosis immediately, rather than having to return for tests or results at a later date. One individual said: ‘Somalis feel that their GPs don’t care about people – they provide no diagnosis, no results and no evidence and so, people travel’.
Research has found this to be the case in America as well, where Somali patients expect to receive immediate results and a diagnosis, in some cases causing tension for patients and physicians. 220 The expectation to be diagnosed immediately has also been reported in other Somali diaspora communities. 216 Warfa et al. 221 found that some Somali patients seek treatment in A&E departments to bypass their GP, which was corroborated by our focus group discussion. A report for the Department of Health into BME experiences of health care in the UK found that there is a ‘mismatch between the health needs and requirements of BME and the services on offer, leading to dissatisfaction and unmet need’ (p. 5). 215
Many patients reported a lack of faith in GPs. Having had an unsatisfactory experience a number of years ago and rectified the situation through private treatment in her country of origin, one interviewee continues to travel for check-ups and any necessary diagnoses or treatment with the same provider abroad:
I don’t know why but for some reason when I go to UK doctors I just don’t feel – I don’t have a lot of confidence in their diagnostics. I don’t know why they don’t make me feel like I can trust what they’re telling me. And often if I don’t go for a check-up but go for a specific problem the medicine they give me doesn’t work and end up having to go and see another doctor.
OT6
For two individuals, access to treatment in the UK was further complicated by a lack of availability of their chosen treatment on the NHS. Although the treatment for his rare condition is now available in the UK, one individual prefers to continue to travel to France because of the expertise there and because he can combine this with visiting his in-laws. The other interviewee travels ‘home’ for ultrasound, which although available through the NHS is not available for her condition. In Germany, this is freely available without a referral and is cheap compared with the cost in the UK.
Cost
As for all medical tourists interviewed, cost is a factor in deciding to be treated abroad. All patients were able to receive a diagnosis and treatment abroad for significantly less than in the UK. Members of the Gujarati community seek dental treatment in particular during their trips to India. For example, patients were quoted £3000–5000 for dental implants in the UK compared with £110 in India. The price of dental treatment in the UK is prohibitively high for them. This is also the case for the Somali community. In addition, both diaspora communities perceived private health care in the UK to be out of their means. Patients interviewed described that they are not wealthy but that a person’s health is considered paramount and that therefore the community will ‘chip in’ to ensure that they are able to travel for diagnostics in serious cases. One Somali said:
Culturally and religiously we’re close-knit so what generally tends to happen is we help each other. So if people know that somebody is in a really bad way and they need treatment or they need money to be collected to get them something then that’s what we do. It’s like an obligation as a community to do it. Even people when they have nothing will find a way to help. And that’s kind of how people survive. So it’s not that people have this disposable income it’s just they find a way if it’s really serious. If people are so sick that people are worried then they’ll do something.
What is distinct to diaspora patients is that the choice of destination is not determined by cost but rather by cultural or personal affinity or a perception that members of their community are likely to receive a better service abroad. In many cases, such as in the Gujarati community, treatment is not the primary motivation for travel but rather travel provides an opportunity for treatment.
Information and marketing
Contrary to other medical tourism patients, diaspora tourists do not rely heavily on the internet for information. Community and family relationships play a key role in decision-making. Two of the patients travelled to countries that they had a familial relationship with and relied on personal recommendations from their family or friends in that country when seeking treatment.
When patients travel with the primary purpose of treatment this is often combined with a familial visit:
I do go to see my mom from time to time but otherwise I know that there are times where I’m just going specifically. I make phone calls to make appointments and I leave for my checks up. Maybe I take a week where I can just go to all of my doctors in that week and I just go to France.
OT6
Personal recommendations also form the basis of decision-making within the Gujarati community. Interviewees requested recommendations through the religious organisation that they are members of and these are shared within the community. This contrasts with the Somali community, which relies heavily on oral information and mainstream sources, such as the internet. Media and papers are not consulted, leading them to be described as ‘oral communities’. 219 In Manchester community leaders were key in distributing information to the community. Some community members may not be able to access written information, available in different languages, such as leaflets about local NHS services, because of illiteracy. The oral dimension has a significant impact on community members’ decision-making processes and how they view services available for them. For example, all negative experiences of the NHS and GPs are shared within the community, which increases mistrust. 219
Another key source of information is Somali television channels, available by satellite. This helped develop the connection with German clinics and doctors. German clinics are the only ones to advertise on Somali television in Somali and these adverts are usually at peak viewing times, for example before the early evening news. Once one patient has been to visit a doctor this then rapidly spreads through the community through word of mouth. For example, one Somali explained:
We’re a close-knit oral community so if someone comes around and says I’m not well then they might say there’s this doctor I’ve been to. So lots of advice from word of mouth but they’ve got Somali channels now and they do adverts on them. So they’ll have advertisements for hospitals abroad. The doctors out there I think have clued on and they advertise. So people get that if they have satellite TV.
These examples highlight how health information, including information about medical providers abroad, is spread within specific diaspora communities. It is also clear that specific clinics, such as German clinics, market themselves to specific segments of diaspora markets. This was echoed by the Gujarati community interviewed who reported that in Gujarat there are now a number of clinics targeting returning non-resident Indians, who have greater resources than domestic patients.
Language barriers: a key motivation for diaspora travel
The issue of language is a key area of divergence in experience within this diaspora category. For members of the Gujarati community and other diaspora patients, language was not a barrier to accessing or receiving health care in the UK. However, language barriers exist for members of the Somali community in the UK and these are key to their experience of, and interaction with, the NHS. This can prove problematic on a practical level and lead to misunderstandings. For example, one Somali explained:
Sometimes if you’re not feeling well and you go to the GP and sometimes you don’t know the words. They cannot find a way for an interpreter. So it can be a bit difficult and so you have to point to it. Sometimes there’s a misunderstanding.
This frustration expressed by Somali women at language and cultural barriers, including brief and rushed appointments, results in further mistrust, which is also the case for Somali women in other countries. 220
This can also affect the services that patients receive: ‘Sometimes if they know your English is not good they just brush you away’. However, the language barriers between members of the Somali community and their GPs can be seen as one aspect of poor health literacy within the community. 222
In one of our focus group areas, additional funding had been sourced to employ a Somali nurse at the local surgery who acted as the first point of contact for Somali patients. This was extremely well received and successfully ensured that language and cultural differences could be both understood and interpreted in partnership with the GP. However, the majority of patients said that translators were rarely available. This was a key determining factor in their seeking treatment with private Somali doctors in the UK or their choosing to travel abroad. Across the two Somali communities interviewed, accessing a Somali doctor in the UK was their first choice.
The reason they go is because he speaks the same language and you don’t have to look for a translator. You don’t feel like he doesn’t understand you. Sometimes when you go to a GP you feel like they don’t understand you so you always have doubt. But he 100 per cent understands and we understand him as well.
However, this option was significantly more expensive than travelling abroad and therefore was rarely used. Notably, doctors accessed abroad are not necessarily always of Somali origin. For example, some of the most popular German doctors do not speak Somali but provide translators as standard. In contrast, when patients return to a country with familial ties, language does not pose a barrier.
Treatment experience
Patients’ experiences of treatment and care in the clinics abroad were overwhelmingly positive and some compared their experience to their experience of care in the UK. For example, one patient described her experience of diagnosis and tests abroad:
If you see a specialist you usually see them in their private office. It’s a nicer environment. Here you go to the hospital and you’re in a big waiting room, unless you see someone privately. It’s a lot more busy. It feels a lot more like you’re on a conveyor belt.
OT2
Despite this, she went on to say that, ‘With my experience it’s very difficult to compare because it’s not like for like really. I wouldn’t say that care is necessarily better. You get things much quicker in Germany’.
Throughout the Somali and Gujarati communities, members discussed how happy they were with the treatment received abroad. In particular, the sense of value for money compared with private care in the UK is important in this process.
The reasons why diaspora patients travel differ from the motivations observed in other medical tourists. Mainly they lie in cultural ties and connections to the place of treatment, or in opportunistically making use of a ‘holiday’ or a return ‘home’, which could be in part for treatment but may be motivated by other reasons. At the same time the high numbers of patients from specific ethnic groups (in our case the Somali community) who travel to receive treatment in a third country could be indicative of a lack of communication or outreach by the NHS to specific sections of the population, rather than a more general phenomenon of medical tourism.
Regardless of cause, providers have clearly developed to capture this niche, as is evident from German clinics and from the medical industry in India catering for non-resident Indians who return ‘home’ for their medical treatment.
Implications for the NHS
Diaspora patients, especially those of the diaspora Somali community, described cultural and specifically language barriers to accessing the NHS, including local GPs. When services are accessed, the treatment and care received may in some cases not meet patient needs. More needs to be done to address these needs, which act as the main determinant for travel. This includes communication in diaspora languages not limited to print materials and the use of health mediators from diaspora communities in local GP surgeries. It could include health information on diaspora radio and television stations, as well as greater engagement of community leaders to disseminate health information, including information on services provided by the NHS.
Section 4 Inward travel, costings and conclusions
Chapter 15 International patients and associated activities within the NHS
Background
The discussion below presents analysis of inward international patient flows to the NHS. Discussion is based on data gathered from seven foundation trusts, based on semistructured interviews with a range of NHS providers (n = 13), and three key stakeholder discussions with individuals who have significant experience of international patients flows, including a Department of Health official and a business consultant with significant experience of the NHS and private activity. Except for one, all foundation trusts were based within London. The roles of interviewees within trusts included the commercial and strategic oversight of activity, contract and business development and managing private and international patient activity.
The focus on inward flows is around the booked and planned admission of international patients treated as private patients within NHS facilities. This could include outpatient admission and day surgery as well as overnight stays. Possible payers for these patients include government-sponsored patients, private/employer insurance, and those funding treatment out of pocket.
The emphasis was on booked and planned admissions for which the foundation trusts could reasonably expect reimbursement (prepaid or through an embassy or insurer ‘letter of guarantee’). Individuals travelling from outside the UK for booked and planned treatment should be distinguished from categories of ‘overseas’ and ‘eligible’ or ‘non-eligible’ patients. For example:
-
Individuals might travel to the UK and receive NHS services (as a result of initial admission to A&E or through GP referral) but not be eligible for these services (which could include maternity, dialysis, cancer or human immunodeficiency virus treatments). This links to a pejorative meaning of health tourism,223 in which there is no booked and planned admission with a clear reimbursement pathway.
-
Overseas nationals could be admitted to A&E and could then be transferred to private patient facilities if their costs were covered by insurance or self- or embassy guarantee.
-
EU nationals who access A&E or planned treatments using their rights as clarified under the EU directive (Directive 2011/24/EU of the European Parliament and of the Council). 1
The background and policy context to international patient activity is detailed in Appendix 25.
Size and scope of international patient activity
Data from the IPS suggest that, overall, international patient flows were in the region of 62,000 in 2010. Within this overall figure, major source countries include Ireland, Spain, Greece, Cyprus and the Middle East.
From the freedom of information requests we submitted it was clear that trusts could not always clearly identify international patients within their pool of private patients because nationality was not recorded: ‘With [international private] patients, a lot of them have an address in England and so that’s the address that will go on the systems. So we may never have a record of where they come from’ (NHS20).
Those whose treatment was funded by foreign embassies were more easily identified, but foreign nationals based/living in the UK may undergo treatment as private NHS patients in the UK, the costs of which are paid by their overseas employer or insurer or are funded out of pocket.
The NHS foundation trusts participating in the study were purposely sampled as we sought to understand the experiences of and ambitions for treating international patients. The London-based foundation trusts had longstanding international patient flows (including single-specialty hospitals as well as those offering a broader range of specialties). Countries identified as sending patients were primarily those from the Middle East (including Kuwait, the United Arab Emirates, Oman and Qatar, with smaller numbers from Saudi Arabia), and there were also strong flows from Cyprus and Greece. Types of treatment centred on complex tertiary procedures (including paediatrics and heart surgery).
Trusts that had delivered care to international patients over a number of years were keen to maintain and consolidate such activity. A number sought to explore opportunities to develop further international patient flows. The one trust based outside London had some limited experience but a growing interest in developing its international activity.
As we note in Chapter 16, the size of international private patient flows across trusts and foundation trusts varies. Similarly, across the seven trusts within our sample, activity ranged from being relatively marginal to being one-third of their total private work. The great majority of international patient treatment and payment pathways were organised by embassies and national institutional links. Very few patients within the NHS private system were reported to be out-of-pocket payers.
Respondents suggested that sender countries’ governments valued the NHS brand:
Overseas, it’s a great brand.
NHS16
A lot of those countries feel it’s quite politically supportive to actually send their patients through to NHS facilities rather than to direct private facilities.
NHS3
As we note below, these views regarding brand perception and reputation were also associated with individual NHS providers.
Strategic and commercial considerations
Respondents emphasised strongly that international patient flows must be seen within a wider picture of pressure on NHS resources, broader international activities and linkages and the lifting of the cap on private income earned by foundation trusts.
First, broader commercial imperatives facing the NHS were highlighted by interviewees, and treating international patients was seen as a means to an end (improving services for NHS patients and developing NHS facilities). The current financial climate for the NHS was viewed as a major challenge, and commercial income, private patient income and international income were seen as possible routes to ameliorating pressure on stretched NHS resources: ‘I think going forward all NHS organisations are financially challenged in some way or other . . . . Our best chance is actually by growing income from the private sector which will be used to subsidise the NHS’ (NHS15).
However, any commercial imperatives were balanced with strong statements regarding the core NHS role, centred on NHS services and prioritising NHS patient care:
Why else would we be having a commercial operation if it wasn’t to deliver a surplus that we can then reinvest on the NHS side?
NHS19
You have to balance. You cannot compromise our NHS responsibility. That is number one responsibility of the hospital. What we’re trying to do in these difficult times is manage the whole element of trying to achieve the overheads and costs that we have and manage that in a way that we at least generate some additional monies.
NHS3
We’re in the business of making a profit after we have done our core job which is making people better.
NHS5
It helps us launch services or buy kit that we couldn’t buy otherwise and employ people that we may not be able to employ.
NHS16
International patients were seen as an opportunity, as was domestic private activity. Both domestic and international activities provided opportunities to utilise spare capacity, particularly operating theatre time that was available out of hours. The NHS was viewed as having excellent back-up facilities, particularly in intensive care units. A common view was that, if not carried out at NHS sites, private work would be undertaken elsewhere and that there was an advantage in retaining clinicians on-site because they could be accessed by NHS patients.
There was little interest in actively accessing other patient flows (e.g. EU cross-border flows) given that tariff rates were not perceived as particularly attractive. One trust, for which one-third of its private work is international, directly commented on the advantage of international patients (funded by governments) being on higher tariffs than patients from domestic insurance companies: ‘So to be honest they [embassies] were paying more than insurance companies in this country, we had limited capacity, so why not for the NHS gain as much as we can and put back into the NHS?’ (NHS16).
For one commercial director, the board’s interest in and enthusiasm for exploring commercial opportunities required expectation management with regard to international patient opportunities: ‘What is really uncertain is what are the procedures people will travel for and what countries are they in’ (NHS5).
Such issues of non-NHS activity were invariably contentious. As the Department of Health policy manager stated: ‘It’s a very sensitive issue to the public about how much of the NHS is retained in its original format or how much of it change to opening up a more commercial approach’ (PA15).
Local and national political sensitivities of engaging in private patient and international activity were recognised. Indeed, one commercial manager spoke of the importance of being able to ‘Demonstrate that you’re doing it with additional capacity and it’s not making NHS patients wait and you’re doing it in a way that generates additional income which then goes to benefit patients’ (NHS1).
Second, established traditions and practices of having wider international clinical linkages and exchange were correlated with international patient activity. Institutions had longstanding international consultancy arrangements, collaborations and linkages and harboured ambitions to see these develop and flourish. Some were organisationally driven whereas some lay outside the hands of individual trusts:
So lots of our consultants go overseas to do lots of things. Some of it is charitable, some if it is rather more formal than that but that’s not the same as the organisation doing it . . . It gets quite complicated that in the NHS you’ve got an organisation that may or may not choose to do something but that organisation is made up of a load of clinical staff who will go off and do their own thing anyway.
NHS19
As discussed below, these activities raised the profile of consultants and hospitals and contributed significantly towards international patient referrals.
Third, closely linked to private patients (and thereby international private flows) was the cap limiting earnings from private activity. Fieldwork interviews were conducted during the passage of the Health and Social Care Act 2012. 30 The lifting of the cap was broadly welcomed within the trusts, although differing views were expressed regarding how, and whether, it would make an immediate difference. An interviewee from one trust stated that:
It’s a really very important constraint for us given our location and given the low level of the cap at the moment relative to other organisations . . . an expected policy move to lift the cap will be very important for the future of this organisation.
NHS15
This particular trust pointed to major difficulties with the measurement of the private cap contribution whereby billing counted towards private income (even if unpaid) and treatments that were not necessarily planned and booked were included in the count. One example provided was a treatment bill of £200,000 that was unlikely to be collected but which was nevertheless set against the cap of this particular trust. For some trusts the impact of the cap was dependent on location and also capacity:
I think for some hospitals it’s just a non-starter because of the area they’re in but for us in an area like this . . . it’s very international and affluent. You stand a far better chance of being run over by a Bentley or a Porsche than you do by a normal car out here.
NHS15
Thus, this trust intended to explore opportunities with embassies from a range of countries (e.g. getting on embassy ‘lists’ of preferred providers) once the cap was lifted. Another trust identified how the changes were absolutely vital to its future growth and development; this particular trust had developed two business models for the upcoming year, premised on the cap being lifted at different points in time. For another trust, however, although its earnings were close to the cap, when it was raised capacity issues would continue to constrain any growth of private/international income.
Referral and treatment pathways
There are distinct processes of referral and patient management for international patients. Two central considerations are organisational reputation and ongoing relationships.
First, beyond a broad view of ‘the NHS’, the reputations of individual trusts and hospitals were identified as crucial:
We’ve got a certain brand, particularly around the Middle East.
NHS2
Patients just want to come here . . . to be honest, the trouble we have is the capacity to fit international patients in.
NHS1
We’re actually very protective of that brand so we tend not to formally partner with people overseas.
NHS19
The international patient activity that was referred to NHS facilities was viewed as specialist and typically not possible to treat locally because of relatively small volumes and the complex nature of the treatment required.
Second, relationships, primarily clinical ones, were paramount in maintaining flows of international patients. Patient flows were perceived to develop from clinical relationships, including training links resulting from overseas referring doctors training within the UK or spending time alongside receiving consultants. One individual spoke of their trust’s experience of treating international patients as ‘a clinically convenient relationship presented a commercial opportunity to make a profit’ (NHS5). Another individual suggested that ‘we shouldn’t forget that we have lots of doctors who have come from overseas to train here who then go back to their own countries’ (NHS20).
Some trusts continuously developed and consolidated such links by offering clinical training to overseas consultants and staff exchange and educational programmes. ‘Show and tell days’, either locally or in locations where individual clinicians travelled overseas, were also identified:
The number one factor is the super-specialised doctors we have in London Teaching Hospitals having these links with the referring doctors in Kuwait, or the Emirates or Saudi Arabia.
NHS1
A lot of the international work we do now comes from a variety of sources but a lot of it is to do with our own consultants who have an international reputation.
NHS20
Having clinicians at the centre of relationship building was not without its problems, given that such activity was time-consuming:
I guess the key way of doing it is around getting clinician out there actually and spending a bit of time on the ground with the local clinicians to build up their links . . . providing education, assistance with research, maybe going over and doing some operating lists . . . the problem is really around getting access to these clinicians’ time in a busy NHS hospital.
NHS2
Alongside clinician links there were also cultural preferences that favoured specific London hospitals. For example, Middle East nationals were said to prefer particular London localities for treatment; similarly, a strong connection was identified between some parts of London and Greek and Cypriot populations. ‘I think the patients feel at home in London. Their relatives will come over and get a flat on [name of road] and go buy cuisine they’re familiar with in that area’ (NHS1).
Embassies and health attachés of sender countries were seen to occupy central roles in the market for international patients. A referral typically began with doctors at the local hospital board identifying a patient for overseas treatment and suggesting a particular country and doctor. This recommendation moves forward to an overseas treatment board with responsibility for all hospitals for approval. The decision would be passed to an overseas health department where locally based health attachés may have their own recommendation on choice of consultant/institution. The local health attaché takes responsibility for ongoing clinical liaison.
Embassies generate ‘letters of guarantee’ to provide reimbursement assurance for a trust for what may be a very expensive programme of treatment. Detailed patient records may not always accompany the travelling patient and so detailed checks and diagnostics are undertaken on arrival. Complex cases and lengthy stays will necessarily generate very large bills and sometimes payment is a drawn-out process. Line-by-line billing was the norm, with each item being detailed, rather than packages (self-funders are expected to pay upfront for treatments and are seen as financially riskier propositions given that they lack institutional surety). Staff who we interviewed from NHS trusts offered various forms of patient liaison (which may be 24/7), but not hotel-type concierge services. Translation services were either provided through individual patient liaison (e.g. fluent Arabic speakers) or sourced through NHS lists. There was no door-to-door service; return travel arrangements, for example, were typically made by embassies.
Personal relations and trust were perceived as key in fostering embassy and government institutional links (including military and health departments). One trust identified having 15 different embassy-type relationships and thus potential referral points for international government-sponsored patients. A great deal of institutional marketing centred on embassies and there were fairly regular visits to embassies and discussions to better understand their needs.
There were downsides of such activity, however. Income was not subject to contracts, unlike more continuous PCT income. Business could be volatile – ‘lucrative and transient’ suggested one patient manager (NHS12) – and referrals could dry up relatively quickly from embassy sources without a clear rationale. The role of attachés was central: ‘If they change you might get different favourites [places for referral]. It depends on where they trained, who they trained with, who they think is good. You can get a sudden change in referral patterns if that happens’ (NHS1).
Some interviewees perceived that there was greater competition among London teaching hospitals for referrals and that embassies were likely to explore options and be price sensitive: ‘I think there’s more competition between trusts now to attract international patients. And I don’t think that the pool has grown particularly’ (NHS2).
Some referral sources were said to be shrinking. One trust, for example, outlined that Cyprus was sending only very complex cases for treatment, and as countries developed expertise in particular procedures these were performed locally.
There were instances of facilitators and intermediaries approaching trusts offering to broker work between trusts and embassies. Such offers were often declined by trusts, and individuals involved in embassy liaison and patient support were trust employees (i.e. we did not identify instances of commission-type incentives for individuals bringing business). Specialty had a bearing on the overall pattern of referrals. When opportunities existed for patient self-referral, it meant that embassy referral was only one of a number of sources and website presence could be more significant for trusts.
Market development
All staff interviewed in the trusts perceived their international work as significant and were intending to maintain – or expand – such activity (unsurprising given our purposive sample). There was a distinction between those undertaking some (albeit limited) marketing outside of the UK activities, including attendance at large international trade shows and the use of brochures, and those not undertaking any marketing. Some viewpoints suggested that although such trade shows did not lead directly to additional business they were important for profile raising. There had been some attempts to share the costs of publicity, for example joint marketing of seven of the London specialist hospitals, including a brochure and a hotline. NHS private providers also meet regularly within London.
There was a view that to leverage greater opportunities would require fuller attention to marketing and customer care, and these were challenges in the current NHS environment. Two main points emerged.
First, the private health sector was perceived to have certain advantages, including marketing expertise derived from longstanding involvement. Some arguments were made that large international private health-care organisations were able to undertake general surgical marketing far more effectively given their experience of negotiating with insurance companies and were able to offer a dedicated marketing approach (and a greater customer care focus). One commercial manager perceived opportunities presented by possible private NHS activity being partnered with private health care: ‘If you travel first class your safety risk is the same but you just get a nicer experience. And we do the safe thing well, we don’t do the nice experience that well’ (NHS1).
Foundation trusts were seen as being particularly hampered by not having a commercial team, alongside having limited marketing budgets and also potential internal perceptions about private work:
I think to really leverage that sort of thing the organisation would need to become much better at managing [arrangements]. Because at the high end you are dealing with the sort of people who will want a number of other things.
NHS15
Like anything we’ve got limited budgets so we want to make sure we also use it for the biggest bang for our buck.
NHS16
We’re an NHS facility and the monies that we make through private patient activity feed into the trust so there isn’t a lot of that to enable us to go and do the sort of things that perhaps would generate additional monies.
NHS3
One interviewee argued that customer-focused processes required further attention within the NHS: ‘London has rested on its laurels a bit and sort of got away with it because people want to come and because the clinical standards are good’ (NHS1).
Traditionally, the NHS orientation was a passive one whereas private and international activity may involve more marketing and proactivity engaging overseas markets.
The second point to emerge was the need to manage both internal and local stakeholder views of such NHS commercial developments. One trust was explicitly developing an internal communications strategy that emphasised the contribution of private income to its NHS facilities. ‘The whole point of being a Foundation Trust Hospital is you make choices about how you’re going to generate your money and where you’re going to spend it’ (NHS5).
There were image issues (both internal and external) and a number of managers identified public misunderstanding around the role of NHS private patient activity. Sometimes these perceptions were linked to the pejorative notion of ‘health tourists’.
A number spoke of the benefits of ‘collaboration’. However, balancing the promotion of a NHS ‘brand’ against the interests of individual institutions presented a dilemma:
We should be trying to do it [collaborate] and share the costs. But then obviously I want the business to come to me. That’s what the trust employs me for. But getting the NHS brand out there is certainly going to help me and if we can share it great and if people want to ride on the back of that it’s up to them.
NHS16
A senior Department of Health policy manager commented (speaking some months before the launch of Healthcare UK): ‘So there are related functions across government that sometimes work together and sometimes don’t necessarily work effectively but [are] in the same sort of territory’ (PA15).
A number of trusts were keen for UK Trade and Investment (T&I) and NHS Global to help gain access to markets and foster activity overseas. Some expressed a lack of clarity of roles between T&I and NHS Global at the current time. They were unclear how an organisation that aimed to broker NHS international activities will be structured and located, for example whether it would be a closed subscription body or would be for all NHS trusts: ‘I’m not sure what NHS Global has actually managed to achieve’ (NHS19).
Market competition was seen as both national (including public and private) and international: ‘There’s a lot of competition within the NHS, within the private and that’s before you even start looking at Belgium, Germany, Paris’ (NHS16). For example, hospital consultants may receive a referral and have a choice where to undertake the work (privately or in the NHS), or be invited to operate overseas. ‘We have a number of competitors in London. Largely private hospitals . . . They are competitors but a lot of our own consultants also work in those hospitals’ (NHS20).
Germany was seen as competing for Middle Eastern activity, as well as a number of international developments within the Gulf region itself (although some Gulf developments were said to face challenges of consultant and nurse recruitment and volumes of activity).
Implications for the NHS
-
International patient income was identified as significant within a number of trusts, particularly within the London area. Other parts of the country may hardly benefit from international patients.
-
The lifting of the private income cap has stimulated further activity in search of international patients.
-
Foundation trusts do not always fully distinguish between domestic and international private income. New reporting requirements (under the Health and Social Care Act 201230) and a wish to further promote activities abroad may sharpen this distinction (for trust boards and Monitor).
-
Foundation trusts vary in their ability to compete for further international activity and in what is the appropriate role of health care.
-
Our study did not focus on accounting systems and how tariffs are determined for international patients who receive treatment within the NHS, or controls to limit costs of private treatment being cross-subsidised by the NHS; research activity is required on these topics.
-
Given the ongoing global financial instability, are there greater risks to trusts from international bad debts?
-
Trusts were cautious in balancing their NHS responsibilities with the opportunities presented for income generation from international patients.
-
Given the importance of referral networks, will changes to UK education and training opportunities facing non-EU medics (because of an EU focus and visas restrictions) impact on referrals over the medium term?
Chapter 16 The financial value associated with medical tourism
Many estimates of the potential value of the medical tourism industry are reported in the media, although these are mostly based on industry reports in which there is often an incentive to exaggerate the possible income streams coming from medical tourism. For example, the value of the Indian medical tourism sector is often cited as being worth some US$1B by 2012, which originates, as does much in the literature, from the McKinsey report12 (see discussion in Chapter 5). A report by the industry research company Tourism Research & Marketing (TRAM)224 puts the overall value of the medical tourism industry in 2006 at US$20B, predicting this to double by 2010. However, it is not clear how either of these figures were calculated or whether current estimates validate these predictions.
One of the few empirical studies reported in the academic literature investigating the revenue generated by medical tourism was carried out in Thailand. 103 Drawing on survey data, the Thai market was estimated to be worth between 59 and 110 billion baht (between £1.1B and £2B) in 2012, contributing a total of 0.4% of the Thai GDP. In another empirical study, Johnson and Garman225 estimated the number of inbound and outbound medical travellers to and from the USA to calculate the volume of trade in health services. They estimated that the value of inbound travel for medical care was between US$491M and US$1.2B, whereas the loss to the US economy from medical fees paid to foreign providers ranged from US$87M to US$209M, leading them to conclude a surplus of between US$404M and US$1B for the US economy. Both of these studies are based on extensive data sets of inbound and outbound medical tourists obtained from their national Ministries of Health.
However, there are no such studies concerned with the value of medical tourism for the UK. We therefore set out to estimate the financial value that may be associated with medical tourism from the UK perspective, considering the income generated by inbound medical travellers, the savings to the NHS resulting from people travelling abroad to receive treatment that they may be eligible for on the NHS and the costs arising to the NHS from possible complications and follow-up care.
Within the scope of this research project we focused on the available data and the analysis and insights that these allowed. There is limited availability of reliable data and further primary research emerged as a key recommendation from this work. The analysis in this chapter presents a first picture of some of the economic implications on the basis of the data currently available. Despite this caveat it represents the clearest indication to date of the economic impact of medical tourism on the UK (NHS, general economy and social services).
Although the overall focus is on costs incurred or averted by the NHS, when direct costs relating to social services were clearly avoided, as in the case of bariatric patients, social services expenditure was considered. The costings included here consider scenarios in which there is an additional cost to the NHS from returning medical tourists who require follow-up treatment as a result of procedures that would not have been covered by the NHS. When patients opt to receive treatment abroad that they would have been entitled to under the NHS, this represents a saving to the NHS (but not a source of revenue), unless these patients experience complications. In addition to the actual costs of the treatment incurred, future health and social security spending averted are considered in one case for which reliable models for costing were available. We focused specifically on three areas of treatment (fertility, cosmetic and bariatric), included among the case studies for this research and in which we interviewed a number of patients.
Income generated by inbound medical travellers
Tourism revenue from inbound medical travellers
We calculated the economic contribution from medical travellers to the UK per annum based on available data from the IPS, based on the most recent data set for inbound medical tourists (2010), excluding the Channel Islands and the Isle of Man (as explained in Chapter 3) (J Hanefeld, London School of Hygiene and Tropical Medicine, 2012, personal communication). As respondents in the IPS survey specifically state that they are visiting for health care, we have assumed that this is their main purpose and that they would not have otherwise been visiting the UK and thus are an addition to visitor/tourist numbers to the UK. Hence, any spending would be seen to be a net benefit not otherwise coming to the UK.
Based on hospital data for the ‘average patient’ (both medical tourists and UK patients) treated within NHS hospitals, we assumed that 20% of inbound medical travellers receive treatment as inpatients and the remainder undergo day-case procedures.
We calculated the expenditure of patients staying in the UK for a number of different scenarios, ranging from those who stay for 4 days to receive outpatient treatment to those who receive inpatient treatment for 10 days and stay a further 2 weeks for follow-up (Table 7). These assumptions were based on data that we collected and on an average hospital stay for inpatients (not only medical tourists) in 2010–11 from the NHS Hospital Episode Statistics. 226 We assumed that patients would likely arrive some days before treatment and remain for additional days to fully recuperate or to take the opportunity for additional tourism activities.
| Inbound medical travellers | Number | Nights in hotel | Cost of hotel (£) | Expenditure (£) | Total expenditure (£) |
|---|---|---|---|---|---|
| Total | 52,000 | ||||
| Inpatients | 10,400 | ||||
| Hospital for 10 days (75%) (75% from Middle East) | 7800 | 14 | 8,736,000 | 10,920,000 | 19,656,000 |
| Hospital for 5 days (25%) (5% from Middle East) | 2600 | 7 | 1,456,000 | 1,820,000 | 3,276,000 |
| Subtotal inpatients | 10,192,000 | 12,740,000 | 22,932,000 | ||
| Accompanying persons inpatients | 16,380 | ||||
| Hospital for 10 days (75%) (75% from Middle East) | 13,650 | 24 | 26,208,000 | 32,760,000 | 58,968,000 |
| Hospital for 5 days (25%) (5% from Middle East) | 2730 | 12 | 2,620,800 | 3,276,000 | 5,896,800 |
| Subtotal accompanying persons | 28,828,800 | 36,036,000 | 64,864,800 | ||
| Total inpatient and accompanying | 39,020,800 | 48,776,000 | 87,796,800 | ||
| Outpatients | 41,600 | ||||
| 4-day stay (25%) | 10,400 | 4 | 3,328,000 | 4,160,000 | 7,488,000 |
| 7-day stay (40%) (2.75% from Middle East) | 16,640 | 7 | 9,318,400 | 11,648,000 | 20,966,400 |
| 14-day stay (35%) (2% from Middle East) | 14,560 | 14 | 16,307,200 | 20,384,000 | 36,691,200 |
| Subtotal outpatients | 28,953,600 | 36,192,000 | 65,145,600 | ||
| Accompanying persons outpatients | 41,600 | ||||
| 4-day stay (25%) | 10,400 | 4 | 3,328,000 | 4,160,000 | 7,488,000 |
| 7-day stay (40%) (2.75% from Middle East) | 17,098 | 7 | 9,574,880 | 11,968,600 | 21,543,480 |
| 14-day stay (35%) (2% from Middle East) | 14,809 | 14 | 16,586,080 | 20,732,600 | 37,318,680 |
| Subtotal accompanying persons outpatients | 42,307 | 29,488,960 | 36,861,200 | 66,350,160 | |
| Total outpatient and accompanying | 131,495,760 | ||||
| Total | 219,292,560 |
Based on our research findings reported in Chapter 15 (corroborated by an earlier survey by Which? magazine179), we assumed that people travel with one companion, apart from those travellers from the Middle East who we assumed to travel with two companions. Data obtained from interviews indicated that patients themselves are in many cases reluctant to report that they travel for treatment. We therefore assume that accompanying travellers do not identify themselves as travelling for treatment, that is, figures for inbound travellers captured by the IPS are solely those for patients (not their companions). According to the IPS, 21% of inbound medical patients were from the Middle East. Moreover, we assumed that the majority of these patients travelled to the UK for more complex inpatient procedures, given the cost and the initial length of travel.
We assumed an average cost of £80 per night for accommodation and £100 per day as spending for patients and their travel companions when they were not in hospital.
Based on these assumptions, our calculations, summarised in Table 7, suggest that, even without taking the cost of the actual medical treatment into account, medical travellers for fertility, dental and cosmetic procedures contribute around £219M in additional ‘tourism spending’ to the UK economy per year.
Health-care revenue from inbound medical travellers
To estimate as accurately as possible the spend on medical procedures in NHS facilities by inbound medical tourists we submitted freedom of information requests for data on income from private patients in NHS hospitals, including UK and non-UK patients, to 28 NHS foundation hospitals (see list in Appendix 26). These 28 hospitals reported a combined income from private patients of around £195M. Of these hospitals, 18 were able to provide data on the percentage of income that resulted from non-UK resident patients. The remainder were unable to differentiate between private UK and non-UK resident patients.
Those who were able to provide differentiated data indicated that £42M of the total income was from non-UK resident patients; looking across these 18 hospitals, close to 25% of the income was from incoming medical tourists. Although our sample of hospitals was weighted towards large London-based facilities that may experience a higher number of medical tourists, income ranged vastly between the hospitals surveyed: from > £20M to just £2466, with a mean of £2.47M.
Those hospitals that were able to provide numbers of patients reported a total of 6722 patients from abroad out of a total of 88,775 private patients counted, that is, 7% of private patients were inbound medical tourists. It might therefore appear that medical tourists are especially profitable, yielding almost a quarter of revenue from only 7% of volume.
However, it is likely that these figures are an underestimate as, for example, one of the hospitals was able to supply a figure only for private patients reimbursed by foreign embassies and this alone was responsible for 7% of its private patients. There was also great variation between hospitals with regard to numbers of patients treated, ranging from one non-UK resident patient to > 1880 patients, with the median being 147 patients per hospital. Unsurprisingly, the largest numbers of inbound medical tourists were treated in the large hospitals that are internationally known for their specialism; foremost among these was Great Ormond Street Hospital, which reported income of > £20M from 656 patients. We excluded Moorfields Eye Hospital as a review of the data across different hospitals indicated that this was an outlier. Given the focus on eye medicine, it has a very large number of patients visiting for outpatient procedures at a very low cost. These data also demonstrate the range of procedures carried out and the average income per patient. Whereas Great Ormond Street Hospital has a high average cost of treatment per patient (approximately £31,600), University College London Hospitals NHS Foundation Trust (UCLH), despite seeing more than double the number of private non-UK resident patients (n = 1881), has an income of only £1.53M from these patients (a very low average treatment cost of £813), indicating the differences in the cost of procedures as well as the challenges in estimating the total market value given these variations. The low treatment cost per patient at UCLH was somewhat of an outlier but we chose to include this to highlight the range of costs paid by inbound medical travellers and because UCLH covers a broader spectrum of treatment than Moorfields Eye Hospital. Data summarised in Appendix 26 also highlight the variation in the percentage of income that non-UK resident patients represent for hospitals; to some, especially the large hospitals in London, it marks a significant part or even the majority of the private patient income whereas for others it contributes a very small percentage of funding.
Despite the variations in numbers of patients visiting different hospitals and income per patient, the number of medical tourists was comparatively smaller than the percentage of income generated by them (7% of patients generating close to 25% of private income). This indicates that spending by private non-UK residents per procedure was much higher than spending by private UK residents. These figures suggest that non-UK residents travelling to the UK for medical treatment seek high-end specialist and expensive procedures.
Drawing on our data to gain a picture of inbound medical tourists more generally, we calculated that the average income per non-UK patient across the 18 hospitals was £6252. If we scale up the average cost per incoming patient using data from the IPS, medical tourists coming to the UK spend a total of £325M per annum on health services. To further triangulate this figure we used the median earned per patient across the hospitals sampled (a lower figure of £3402 per patient) and scaled this up to the total number of inbound medical tourists to give a total spend of £178M per annum. We conclude that expenditure by inbound medical tourists on health services is in the range of £178–325M per annum. Although we recognise that our sample of hospitals is biased towards London and other locations that attract inbound medical tourists, it is likely that the majority of inbound medical travellers will visit these centres.
The UK private health-care sector as a destination
From the available data it is not known what percentage of the total number of incoming medical tourists estimated by the IPS access treatment in the NHS and what percentage access treatment in the private medical sector. Given the international reputation and prolific nature of ‘Harley Street’ medicine, it is fair to assume that a significant number of inbound medical tourists will access treatment in the private sector. Because the cost per procedure in the private sector may be higher, it is probable that patients undertaking serious and more complex procedures will be more likely to have these carried out within the NHS (as highlighted in the previous chapter).
A 2012 report by the Office for Fair Trading investigating the private health-care sector in the UK227 concluded that in 2009 the market was worth £5B in total and that 2.4% of this was income generated by foreign patients (i.e. £120M was generated by medical tourists).
Based on the available data and the assumptions made and set out earlier, total spending by incoming medical tourists (i.e. taking together spending on medical treatment and additional ‘tourism spend’) ranges from £397M to £544M per annum. Although this does represent a sizable market and one that obviously could grow, this represents < 0.5% of the projected government spend on the NHS of £130B in 2012–13. However, as reflected in our sampling of NHS hospitals, we consider it likely that the majority of inbound medical travellers will visit London and select other urban medical centres in the UK. Considering the tourism and health expenditure by medical tourists as concentrated more in these locations, this may represent a very significant stream of income in specific areas.
Given the revenue estimated earlier it is likely that medical tourists may represent a useful stream of income to some large trusts but at present not a significant market segment. Of course, as the caps on private patients are raised there is the potential for expansion of this market, although it is hard to imagine (given the greater level of competition with the private sector) that this it become anything other than a niche area, although with possibly lucrative margins.
An additional benefit from having a greater number of inward medical tourists undergoing specialist treatments within NHS hospitals may lie in the ability of doctors to further develop a specialism, for example in relation to surgical learning curves.
Costs to the UK NHS resulting from outbound medical travel
Based on the case studies of different types of medical travel identified by this research and further described in Chapter 7, we sought to identify the likely costs to and savings for the UK NHS from medical travel. In one case there also appeared to be additional savings for wider social services as a result of overseas travel.
Fertility tourism
Multiple pregnancy is associated with increased risks for the mother and babies. The mother is at increased risk of hypertensive disorders, anaemia, gestational diabetes, haemorrhage, preterm labour and operative delivery (including caesarean section).
Risks to babies include low birth weight and immaturity needing admission to a neonatal intensive care unit, congenital malformations, cerebral palsy, and impaired physical and cognitive development.
Reproduced with permission from NICE. Fertility: assessment and management (update). London: NICE; 2012 (p. 1). 228 For updated documentation see www.nice.org.uk/nicemedia/live/14078/62770/62770.pdf
Although it is clear that multiple births can present complications for the mother and the child, in the analysis presented in this report we are concerned with the costs arising to the NHS associated with the medical tourist. In this case, once the child is born (and of course obtains its own unique NHS patient identifier) then it is a NHS patient who is not a medical tourist. Therefore, in our analysis we have not been concerned with possible implications for the child but only the mother, in the same way that we are concerned with effects for the patient undergoing bariatric surgery or cosmetic surgery. If we undertake to cost the implications for those other than the medical tourist then this generates discussion of the breadth of effects to cover. This also moves us, for instance, to consider ethical issues such as those associated with organ donation and transplantation (e.g. when the organ donor is not a medical tourist but the recipient is, it is not clear whether the costs of complications in the donor are incorporated in the cost exercise or not). We accept that in many ways this means that the ‘cost’ of fertility treatment may be underestimated compared with if these costs for the child were taken into account. We have pointed to the literature that discusses the costs incurred through complications related to the child,229,230 but this issue needs further discussion. For instance, even when the child is totally healthy there are arguably still costs stemming from them simply existing. Therefore, should this perfectly healthy child be seen as a ‘cost’ of infertility treatment? Or is their productive future a benefit? Is a child itself a ‘complication’ of the treatment? These profound ethical issues cannot be addressed here and hence we have simply restricted ourselves to issues surrounding the health and care of the mother. Here we focus on costs to the NHS of multiple pregnancies and births rather than longer-term health outcomes of the child, but note that the model on which these calculations are based considers child health for up to 1 year in its costings.
As indicated, multiple births can present severe complications. Infertility treatment, including IVF, has been shown to increase the chances of multiple births. To calculate the likely number of multiple births and costs to the NHS resulting from fertility travel we draw on a longitudinal study by consultants in obstetrics and gynaecology at University College London who observed that multiple births submitted to their ward were often the result of women having received fertility treatment overseas (including IVF and intrauterine insemination). 98 The authors studied all multiple births over a period of 10 years and found that more than one-quarter were as a result of patients having travelled overseas to receive fertility treatment.
All patients interviewed by us travelled abroad for IVF and none of these was eligible for further treatment on the NHS (some had exhausted their free rounds on the NHS). We triangulated findings from our interviews by drawing on the literature relating to CBRC, including the findings by Shenfield et al. 114 reporting on a six-country study of cross-border fertility care and in-depth qualitative work conducted by Culley et al. ,57 in which a large sample of fertility tourists was interviewed. We assumed that patients seeking CBRC would not be eligible for fertility treatment on the NHS and thus did not represent a saving for the NHS.
We drew on ONS data231 on multiple births in the UK for the latest available year. In 2010, 11,053 women gave birth to twins, 169 to triplets and six to quads and above in England and Wales, giving a total of 11,228 multiple births.
We further assumed that the cohort studied by McKelvey et al. 98 was slightly swayed towards medical tourists as it was based in an urban population in central London. Therefore, we assumed that 20% of multiple births (a total of 2246 women giving birth to multiples) were as a result of fertility treatment received abroad. This is supported by our analysis of data from the IPS in which a comparatively larger number of women between the ages of 24 and 45 years travel abroad to access fertility treatment.
Women with multiple pregnancies require increased and more complex monitoring, which is sometimes not available in the routine NHS setting. Women with multiple pregnancies also require a greater number of antenatal visits. However, their exact needs are highly variable. We therefore drew on an earlier study by the Cost of Multiple Births Study Group,193 which calculated the expense of multiple births compared with singleton pregnancies in 2006 and reported costs of £3313 for the birth of a singleton, £9122 for twins and £32,354 for triplets. We estimated that these costs had increased by 3% per year between 2006 and 2010 and then calculated the additional cost of a twin or triplet pregnancy over that of a singleton birth (Table 8). This gave an estimate of £15.5M for the cost of multiple births resulting from fertility travel in 2010.
| Type of multiple birth | Number of births | Resulting from fertility treatment abroad | Additional cost (£) | Cost resulting from fertility treatment abroad (£) |
|---|---|---|---|---|
| Twins | 11,053 | 2210.6 | 6506 | 14,382,164 |
| Triplets | 169 | 33.8 | 32,526 | 1,099,379 |
| Total | 15,481,542 |
The long-term costs resulting from assisted reproductive technologies, including cases of multiple pregnancies, will not differ between medical tourists and fertility patients who received care in the UK. However, our research indicates that patients will travel in search of reproductive care to countries with regulations that will allow fertility treatment likely to result in a higher number of multiple births. Any effort to address the rise in multiple births in the UK therefore needs to take account of medical travel and involve specific targeted information to be effective.
Cosmetic tourism
A comparatively greater focus in relation to the costs and complications of medical tourism falling on the UK NHS has been on cosmetic tourism. As observed in the review of the literature in Chapter 3, there are reports highlighting complications arising from cosmetic treatment received abroad,134 including survey results indicating the percentage of doctors who have treated complications within the NHS (37%) as a result of cosmetic tourism. 76 In addition, a recent study by Miyagi et al. 102 described a cohort of patients seen in a tertiary facility who reported with problems arising from cosmetic surgery abroad over a period of 3 years. The authors calculated the cost of treatment provided within the NHS for complications, highlighted the reimbursement received by the hospital from the PCT (which was less than the expenditure of the hospital) and provided a mean cost per patient (this included patients who were seen but who did not receive follow-up treatment) of £6360. However, as can be expected, costs varied widely, ranging from £114 to £57,968.
Based on IPS data on age and gender of outbound travellers we estimated that 30% (18,300) of patients who travelled abroad for medical treatment travelled for cosmetic surgery. We triangulated this with the survey conducted by Which? magazine,179 which found that 28% of medical tourists travelled for cosmetic procedures, recent survey findings that 95% of all people considering cosmetic surgery would travel abroad for this104 and the survey results of medical doctors reported above. 76 This makes it likely that the estimate of 30% of patients travelling for cosmetic surgery is at the lower end of the spectrum.
Based on our interview findings and the survey results reported by Jeevan et al. ,76 we estimated that 10% of those who travel abroad for cosmetic treatment will require some form of aftercare, even if this is limited to dealing with an infection or removing stitching. However, drawing on Miyagi et al. 102 we assumed a great variation in the level of aftercare required, with some complications (such as infections or the removal of stitches) being resolved at the GP surgery level, for example through one consultation and a course of antibiotics. Based on our interview sample and cases reported in the literature, we assumed that 20% of complications in those travelling for cosmetic surgery would require a visit to a tertiary facility, either as an emergency or through referral. For this we used the average cost of the four higher-cost cases described by Miyagi et al. 102 We assumed that other complications would be resolved at a much lower cost (for this we used the average cost of the two lowest-cost cases described in Miyagi et al. ’s study) and would likely require only one GP visit to remove stitches with more complex cases dealt with at primary care level.
Based on these assumptions and drawing on the mean costs provided by Miyagi et al. 102 we calculated that, in 2010, 1890 patients would seek follow-up care (some major, some minor) from the NHS, at a cost of £8.2M (Table 9).
| Total | Severe complications | Minor complications | |
|---|---|---|---|
| Number of cosmetic tourists | 18,900 | ||
| Number with complications | 1890 | 378 | 1512 |
| Cost (£) | 8,251,740 | 7,867,692 | 384,048 |
The cost incurred by the NHS for patients who have travelled abroad for cosmetic procedures may give an indication of the level of complications that occur in the cosmetic surgery sector in the UK. Although there are no reliable figures for the size of the sector in the UK, the recent PIP breast implant scandal gave an indication of just how sizeable this market is. The UK NHS estimated that 45,000 women had been fitted with the implant, with only 900 of these as NHS patients and the rest in the private medical sector. 232 Given the size of this market in the UK and the complications experienced by returning medical travellers, it appears opportune to address this gap in regulation. The government launched a consultation process to this effect in August 2012 and findings from our research underline the need for this.
Savings (or not) from outbound medical tourism
Bariatric surgery
With 25% of the UK population classified as clinically obese, there has been some focus on the costs of obesity and how to tackling obesity in a cost-effective way. The financial impact on the NHS of obesity is calculated by the Department of Health to be £4.3B. 195
The National Institute for Health and Care Excellence has developed a cost guide197 alongside its 2009 obesity guidelines. 195 This modelled a reduction in cost to the NHS of £16M per year through prescription of medications and surgery. This saving was primarily based on saved GP contacts as a result of these prescriptions. Moreover, a study by the National Audit Office in 2001233 estimated that 18 million working days were lost as a result of obesity. A study by Hawkins et al. 234 in 2007 demonstrated that in a cohort of 59 bariatric patients there was a 32% increase in the number of patients in paid work after surgery.
Given the global rise in obesity a number of cost-effectiveness studies and systematic reviews summarising the evidence concerning bariatric surgery have been published (e.g. see Picot et al. 196). A study in Health Technology Assessment from 2009196 found that, for morbid obesity, incremental cost-effectiveness ratios (base case) ranged between £2000 and £4000 per quality-adjusted life-year (QALY) gained. The authors reported that this was both at a lower cost per QALY than non-surgical interventions and within the cost range deemed efficient by NICE.
Taking this as a starting point, a recent study by the Office of Health Economics195 focused specifically on the cost-effectiveness of bariatric surgery in the UK. The author estimated that between 11,000 and 140,000 people would have qualified for bariatric surgery in 2009/10 but only 3607 were given surgery on the NHS. The range of 11,000–140,000 patients is based on the assumption that between 1% and 25% of patients eligible for bariatric surgery will choose to undergo this. The authors then calculate savings to the UK economy by deducting the cost of the surgical intervention from workdays gained and savings in social benefits, including unemployment, disability and housing benefits. Based on this range, additional income is estimated at £46–578M per year and the savings in benefit payments are estimated in the range of £10–151M per year. These calculations explicitly exclude any costs of complications or follow-up care. Further research is currently under way to examine the long-term effects of obesity surgery, specifically the SurgiCal Obesity Treatment Study (SCOTS) at the University of Glasgow. 198
For our sample we used the national tariff costs for a gastric band and gastric bypass obtained through a freedom of information request to calculate the cost savings for patients who we interviewed who had opted to travel abroad to have bariatric surgery. The cost of procedures saved by the NHS was a total of £58,816 for the 13 patients interviewed. If we use the model employed by the Office of Health Economics – both savings in health and social services and additional income (including through taxation on additional days worked) – the total savings and additional income would rise to £112,506.
Even if this was a high estimate, the key point remains that patients travelling abroad to receive bariatric surgery are likely to represent a sizeable saving to the NHS and social services. At the same time the limited knowledge of long-term costs and effectiveness of bariatric surgery beyond the immediate clinical outcomes remains a major limitation of the research.
To fully understand the costs of and savings from bariatric surgery for both health and social services, further research is required including into the long-term medical and social outcomes of such surgery, including a comparison of outcomes in medical tourists and patients who have received this treatment in the UK.
Based on the patient histories collected for this research, the literature on bariatric surgery seems highly optimistic. Only one of the bariatric tourists had not experienced any complications and all 13 required ongoing treatment and care. This echoes the findings from a systematic review of the cost-effectiveness of bariatric surgery conducted in 2009. 196 This research found that all studies reviewed reported bariatric surgery to be cost-effective but equally found flaws in all of the models and studies. Picot et al. 196 use the methodological insights from studies reviewed to further develop a model for economic evaluation and also find bariatric surgery to be cost-effective. The review of the cost-effectiveness literature stresses the need to consider a longer (minimum of 5 years) time frame to understand morbidity and complications associated with weight-loss surgery. This seems to be corroborated by our research findings.
In relation to medical tourism, our findings highlight that, first, the complications likely to occur as a result of bariatric surgery received abroad will happen at a time when the patient may be unable to return abroad or claim compensation from a clinician or clinic abroad. Second, the cost of the surgery incurred by patients when they travel abroad is negligible compared with the potential future savings in health and social services to the state or in health-care costs (to either the patient or the health-care worker) that may result from the procedure. Our research indicates that, when complications occur, these may be catastrophic in the long term with no savings and high costs to the individual and a publicly funded health-care system.
Implications for the NHS
-
Both inbound and outbound medical tourism have the potential for cost savings and, in the case of inbound tourism, for additional income to be generated for the NHS.
-
Given the level of complications experienced in the three areas of medical travel explored in this research, guidance to the public is urgently needed to ensure that patients travelling abroad pay greater attention to issues of patient safety. This will minimise costs to the NHS and patients resulting from outbound medical tourism.
-
For bariatric and fertility treatment, the long-term costs (and potential savings) for health and social services associated with the procedures and outcomes far outweigh those in the short term. To fully assess the cost of medical tourism to health and social services it is therefore important to understand the differences between the long-term health and social effects resulting from treatment received abroad and those resulting from treatment received in the UK. For bariatric surgery this is currently not known. Research examining long-term outcomes between UK patients and medical tourists to enable a full understanding of the costs and savings of bariatric surgery is required.
-
For fertility treatment there is a strong rationale to address the determinants (including regulation) of people travelling and provide greater information and sensitisation on this issue. Studies suggest that the incidence of multiple births is significantly higher (we estimated 20%, as set out earlier) as a result of people having sought and received treatment abroad. This is not a result of ‘different’ treatment but rather of differences in regulation, with other countries allowing different numbers of embryos to be transferred. Thus, any cost to the NHS as a result of multiples born in the UK will increase as a result of medical tourism (because of the increase in incidence of multiples born to couples who have travelled abroad to receive fertility treatment).
-
Greater guidance and regulation of the cosmetic surgery sector is needed. The rate of complications for cosmetic surgery observed by others102 may also give an indication of the level and cost of complications in the largely private cosmetic sector in the UK. In many cases complications may not be reported as patients simply return to the original clinic. Our research further indicates that patients are likely to significantly under-report cosmetic procedures and complications. Therefore, the true level of complications resulting from cosmetic surgery is not known. Although the cost of cosmetic tourism to the NHS overall may seem low, all estimates presented here would increase substantively should outbound medical tourism further expand in the absence of clearer regulation and guidelines.
-
Unified data collection among NHS hospital trusts with regard to private patients, including whether or not these are from the UK, is needed. This will enable the NHS nationally and individual trusts to plan for and assess this market. This seems to be a particular oversight in light of the changing patient caps within the NHS (Health and Social Care Act 201230).
-
The current level of income from inbound medical tourists highlights the potential of this market, in particular for specialist hospitals that have a particular ‘brand’ to market.
-
Finally, in terms of bariatric surgery, the balance of costs and savings for health and social services suggests that the NHS might ‘encourage’ people to go abroad for this procedure, but also provide guidelines on what to look for, as it represents a net saving to the NHS and the social security system. This is especially important as complications resulting from bariatric procedures appear to be particularly severe.
Chapter 17 Conclusions and research recommendations
The premise for undertaking this study was that little was known about the inward and outward flows of patients and the implications for the NHS of these flows were not well understood. Our study focused on combining a wide range of evidence about the nature and scale of international patient flows, including:
-
an understanding of legislation, policy and practice with regard to medical tourism
-
sources of information and marketing and advertising practices with regard to medical tourism
-
the influences on and shapers of medical tourism decision-making
-
treatment processes and experiences of using medical tourism services
-
professionals’ and key stakeholder group perspectives on medical tourism
-
the magnitude of flows of inward and outward medical tourism and the economic and direct health-related consequences of this for the NHS.
In this chapter we interpret our findings, highlight the key implications for policy and practice in the NHS and look forward at the emerging research agenda in this area. The practical implications for the NHS are detailed in a series of text boxes.
Patient decision-making
Eligibility for access to domestic health-care services is a strong influence on the decision to seek medical care overseas. Patients are prepared to travel abroad when a treatment is not available within the NHS, when they do not meet strict eligibility requirements or when they have exhausted their entitlement (e.g. for IVF treatment). Individuals choose to pay for treatment abroad rather than domestically primarily for reasons of cost but also because of the perceived expertise of clinicians overseas; family or cultural connections with overseas destinations are also contributing factors.
Outward medical tourism involves a range of medical and ancillary services and typically a range of small-scale providers and clinics. We identify an emerging trend for patients to travel beyond Europe for treatment, but also the key role of diaspora networks and relations in shaping the favoured travel destinations of medical tourists.
Information, guidance and risk
Decision-making around outward medical travel involves a range of information sources; the internet plays a key role in addition to information from informal networks of friends and peers. It would appear that medical tourists often pay more attention to soft information than hard clinical information and there is little effective regulation of information (be it hard or soft) online or overseas. Because prospective travellers source information from intermediaries, direct from websites and internet marketing, and among networks, it complicates practical attempts to improve the quality of information provided to medical tourists.
A broad range of advice, information and guidance exists for prospective travellers, including the NHS Choices website235 and information developed by the National Travel Health Network and Centre (NaTHNaC) (see www.nathnac.org/travel/misc/medicaltourism_010911.htm). 236 Although potentially valuable, the onus is on prospective medical tourists to seek out such information; presently there is little evidence that they routinely do this. There is clearly scope for health-care professionals within the NHS to become part of the networks of information and support that can be accessed by potential medical tourists.
Information and advice available to potential medical tourists should highlight the lack of a clear framework for redress in many countries should complications arise from treatment abroad. Potential travellers should be made fully aware of current NHS eligibility and commissioning rules, and costs for which patients may be personally liable, including non-emergency care, to rectify any poor outcomes of treatments received overseas.
Our review of the legal framework attests that individuals are willing to travel for treatment to locations that are not regulated by national laws and guidelines. It is apparent that patients do not fully understand the scale and nature of the risk associated with seeking treatment overseas, including the difficulties relating to redress when something goes wrong. This uncertainty bedevils all phases of treatment decision-making, including access to information, preconsultation, treatment itself, aftercare and follow-up.
The wide range of clinical, ancillary and support services involved in medical tourism complicates efforts to inform and educate medical tourists, or to regulate aspects of the industry. It is clear that across many websites of facilitators, clinics and hospitals, treatment risks are underplayed, and there exists an imbalance of objective information and promotion and advertising used for marketing purposes.
Although there has been a recent proliferation of systems of EQA and audit, these, along with the registration details displayed on websites, do not always make for better-informed patients.
Information for potential medical tourists needs to be packaged and disseminated in such a way that it will reach them, some of whom may not consult their GP or indeed a specialist website before travelling.
It is clear that safeguards for UK health care (e.g. GMC registration) have little relevance if treatment is received out of the national jurisdiction. The need to seek redress and subsequent legal implications may occur many years after treatment and once complications have emerged. Although advice, information and guidance do exist for travellers, it must have appropriate coverage and be widely accessed. To provide sufficient safeguards from risk, guidance needs to be proactively available. Currently, the onus is on prospective medical tourists to locate this information.
Beyond generic travel advice for medical tourists, the need for clearer guidance on bariatric surgery, or for patients considering bariatric surgery, is evident. Patients lacked consistent information on possible complications and also on the long-term consequences of surgery and the ongoing aftercare. Equally, greater information for and training of GPs is needed to enable them to advise patients and to deal with the possible negative consequences associated with weight-loss surgery.
GPs need support and training to enable them to advise patients not only on the broad consequences of medical tourism but also on the implications of specific forms of treatment that may present particular concerns.
For fertility the situation is particularly complex. IVF treatment is, ceteris paribus, more likely than non-assisted fertilisation to result in multiple births, which are in turn associated with higher risks than single births. UK legislation is geared towards reducing the likelihood of multiple births, in particular governing the number of embryos that can be transferred. However, such legislation varies cross-nationally. Furthermore, unclear regulatory frameworks overseas mean that patient data may not always be held in the detail expected within the NHS and it is not always possible to retrieve data; these issues are exacerbated when countries have anonymous donor laws. With diaspora travel, we have seen that many of the issues outlined here can be further compounded and complicated by wider misunderstandings and often unrealistic culturally rooted expectations about a wide range of issues related to NHS care.
Specific attention is needed to ensure that information is provided in a manner that is accessible to all; this includes tailored information for ethnic or linguistic minorities. It is important that all feel that they can trust the information that is provided.
The size and economic impact of the medical tourism market
Individuals travelling for medical treatment are often ill-informed or under-informed and this heightens the risks associated with medical travel. The most robust data available clearly show that this affects many UK residents. Although the limitations of the IPS mean that we cannot banish all uncertainty that surrounds market estimates, the data show that, in 2010, at least 63,000 UK residents travelled abroad for medical treatment and at least 52,000 residents of foreign countries travelled to the UK for treatment. These are likely to be conservative estimates but even these numbers underscore that medical tourism is a very real phenomenon.
To better understand the collective risk faced by medical travellers it is imperative that robust, reliable data are collected that not only map the size of the medical tourism market but also provide useful information about who travels when and for what purpose.
It is also important to better understand the similarities and differences between inward and outward medical travel. We have seen that inward medical travel to the UK occurs across a range of clinics and providers, including to private facilities within the NHS and the independent sector. These inward referrals and flows of international patients are shaped by clinical networks and longstanding relationships that are fostered between clinicians within sender countries and their NHS counterparts; in this sense they may be different to outward flows. Those travelling to the UK for treatment as NHS international patients are more likely to receive complex and expensive treatment underwritten by their national governments, in sharp contrast to outward medical travel from the UK.
Despite important caveats, our calculations show that there are costs and benefits to the UK economy and the NHS resulting from inward and outward medical travel. Our estimates show that inward medical travellers and their companions contribute in the region of £219M per annum to the UK economy in additional tourism spends. We also found spending on medical treatment in the range of £178–325M. Together this amounts to a contribution of between £397M and £544M per annum to the UK economy.
In addition, our research revealed costs and savings resulting from UK residents travelling abroad to seek treatment. When complications occur and these are dealt with by the NHS, or when surgery undertaken will require lifelong maintenance, this represents additional expenditure for the NHS. Although the costs of such complications can be comparatively small (e.g. an infection following cosmetic surgery that requires a GP visit and a course of antibiotics), they can also be very high (e.g. in the case of failed bariatric surgery patients may need full-time care and may be, or continue to be, unable to work). The costs of corrective surgery and ongoing care can be extremely high.
Our research demonstrates equally that, when people opt to travel abroad to access treatment and this is successful and they return to work, savings may be substantial for domestic health and social services. Most importantly, if medical travel increases, so will these costs and savings.
The industry: providers and market development
We are now better able to understand the nature of medical travel providers and ancillary services, including the role of intermediaries. Our research demonstrated a range of different models marketed by providers and by which patients travel to receive treatment. There are clearly legal uncertainties at the interface of these and clinical provision.
Our research reveals a picture of a complex market; surprisingly few of the patients interviewed were using brokerage or facilitator arrangements unless these were built in by the clinic itself. Models also differed by type of medical tourism and clinical procedure for which travel occurred. For example, bariatric patients may have had consultations before and after overseas treatment with a representative of the clinic in London, whereas fertility patients appeared to undertake pretreatment tests privately in the UK in advance of travel, but at the request of the overseas provider.
Findings, including interviews with patients and providers, also highlight recent industry development. Patients are now travelling to further or ‘new’ markets in medical tourism, highlighting development and diversification within the market, with higher-end and lower-end destinations emerging.
International patient income generated for NHS trust hospitals, particularly in London, is significant. Although the analysis of data on patient flows shows a change in origin of travellers from the Middle East towards a greater number of Europeans, this market appears stable. Many NHS trusts do not always fully distinguish between domestic and international private income earned. This has some bearing on the ability to identify and further target particular overseas market segments. It is therefore not possible at the moment to gain a full picture of the types of procedures that incoming patients access, nor the specific hospitals that they target. Nonetheless, our research findings clearly underline the power of the brand that large NHS hospitals have, the extent to which this attracts foreign capital and the potential for generating further income. In light of the lifting of the cap on private income, some specialist providers may wish to market themselves more aggressively.
Separately recorded private income from domestic and international sources will enable trusts to have a more accurate picture of their income. It will also provide a more accurate picture of inward medical flows and allow for better planning and decision-making in this area.
New reporting requirements under the Health and Social Care Act 2012,30 and a wish to further promote activities abroad, may focus greater attention on the distinction between private domestic and international income, both within trust boards and by regulators. A more accurate national picture of the inbound patient flow could allow targeted marketing of NHS facilities.
Given the importance of clinician networks in attracting referrals of international patients, there are uncertainties about how changes to UK education and training opportunities for non-EU health-care professionals (because of an EU focus and visa restrictions) will change the shape and dynamics of international networks and linkages, thereby impacting on referrals over the medium to long term.
The missing link: patients’ health
A key limitation across the areas of medical tourism information, activity, income and industry is the current lack of evidence on medium- and long-term health outcomes of patients travelling to receive treatment abroad. This includes how these may differ from the outcomes of those patients receiving treatment in the NHS.
A review of the literature reveals that there is currently no long-term comparative evidence of clinical outcomes in medical travellers and clinical outcomes in those who have been treated at home. This restricts the ability to estimate long-term costs and to fully understand the effects of medical travel, as well as its potential for savings and better patient care.
Our sample of patients highlights that medical travel is rarely without complications or costs to the individual. Although some people have minor or no problems following treatment abroad, others face severe health problems that in some cases are exacerbated by an inability to ensure continuity of care or obtain patient records to address their needs. This research did not set out to assess long-term clinical outcomes of medical tourists. However, our findings did reveal that, although the scale of the issue may (arguably) not as yet be overwhelming, the effect on individual patients can in some cases be catastrophic. This raises a number of related ethical questions and issues. These aside it poses a limitation on the ability to fully weigh up the benefits and costs of treatment abroad compared with domestic treatment.
Research agenda
This study has addressed many of the key questions relating to recent developments in medical tourism and the implications of these for the NHS. To obtain an even more complete understanding of the costs and benefits of medical tourism and to move the debate beyond discussing its potential to a stage at which we can understand its impact better, further research needs to be undertaken.
Future research should:
-
Seek to better understand the medium- and long-term health and social outcomes of treatment for those who travel from the UK for medical treatment. Specifically, comparative research is needed with patients undergoing similar treatment within the UK. This will enable a direct comparison between the costs and benefits of domestic treatment and those of treatment abroad. There are likely to be not only costs and benefits to the NHS but also costs and benefits to social services. Such research is of particular value as our findings demonstrate that medical treatment has medium- and long-term outcomes that may be evident only in later stages as complications or unintended consequences of medical tourism arise. Routinely recording and analysing the ongoing care needs of those who have travelled abroad for treatment will also enable professionals to provide guidance to patients who are considering treatment abroad. Furthermore, a greater understanding of the clinical outcomes of medical travellers that extends beyond the short term will enable a more robust and nuanced understanding of the costs to the NHS of outward medical tourism.
-
Generate more robust data that better capture the amount of activity and the flows of medical travel. This is needed to provide a deeper understanding of why UK residents seek treatment abroad. It will also enable further work on costs and savings to the NHS, to other social services and to the UK economy as a whole that may result from inward and outward medical tourism. Such data should also include sociodemographic data as well as information about what procedures patients are travelling for to better understand patient motivation for travel.
-
Aim to better understand inward flows of medical travellers. This includes data on where patients travel to, the procedures they undergo, the price of these and their sources of funding. Data show that the UK’s immediate neighbours are the source of many medical travellers to the UK, but so are many Middle Eastern nations. Do these represent very different medical tourists? Are we correct in assuming that many of the travellers from the Middle East are those requiring ‘high-end’, complex and expensive treatment? Is this conducted within the NHS and without? Are those residents of France and Spain actually expats? If so, how are they funding their treatment?
-
Gather a greater level of information on patients, including their origins, procedures undertaken and outcomes, to allow for the development of better economic costings. This could include costs and revenue experienced by the NHS as well as the wider economic and social costs and benefits, which may be both public and private.
-
Explore further the issues of clinical relationships and networks. Our research suggests that clinical relationships and networks explain the dynamics and patterns of international patient referrals into the NHS. Linkages are generated through education, training, consultancy and research collaborations. However, further studies are required to understand the precise shape and nature of these networks, including how they may be fostered and the impact of policy and broader social developments on their expansion. For example, visa requirements, increased costs of studying and the emergence of alternative training destinations may weaken established networks in the medium and longer term.
-
Consider the importance of the NHS brand. Recent policy initiatives are promoting the notion of a NHS brand. Research to explore this brand perception internationally would allow better communication and targeting of activities. It would also identify where potential opportunities, if any, exist for promoting the UK as a destination for medical tourists.
Chapter 18 Synopsis
This project set out to increase our understanding of medical tourism, both as a process undertaken by patients and as a broader commercial activity and industry. Given the private nature of treatment as well as the range of commercially focused treatment providers and ancillary services, it would be unrealistic to expect to capture the ‘whole’ picture. However, using an innovative application of a mixture of methods, our understanding of both the overseas treatment process and the wider supply-side effects has been enriched. We have produced the first, high-quality study of the phenomenon of patients paying out of pocket for treatment abroad. In short, we can say with confidence that medical tourism involving travellers to and from the UK is on the increase, that the motivations behind such travel are varied and complex, that the economic implications of medical tourism are diverse and that there are opportunities for savings for the NHS as well as costs, that these depend largely on future developments and that there are wide-ranging risks and uncertainties for patients with regard to a number of aspects of medical tourism. We are now well positioned to develop the wider theoretical and conceptual debate that is clearly of importance.
As with any project of this size, there are a number of limitations. Largely these stem from unexpected barriers, which created difficulties accessing information that we had reasonably felt would be forthcoming. In particular, one major deviation from the protocol involved the abandonment of a survey of medical tourists. It was felt that, although the survey would have been useful, we would not have been confident of achieving a sufficient sample size and a high-quality survey without better access to potential sampling frames held by a range of commercial organisations. We sought to avoid an extremely small n survey, which offers no real insights. Instead, we redirected our resources to a deeper analysis of the qualitative interviews, which proved remarkably fruitful. A clear finding regarding inward medical travel that may assist future planning of such a survey is that many of those travelling to the UK are either expatriates or those who utilise existing networks of support, such as embassies, to access treatment in the UK.
In a similar vein, the economic analysis proved more difficult and time-consuming than anticipated. Given that many foundation trusts employed an ‘international patient manager’ (or similar), it was anticipated that hospitals would routinely collect data pertaining to inward medical travellers who booked and planned treatment in the UK. This proved not to be the case – there are difficulties in distinguishing amongst the broader private patient group for whom clear data were available. Data were incomplete and this inhibited the modelling of some important elements. However, there was sufficient evidence to support a tentative estimate – likely to be an underestimate – of the economic implications for the NHS and the wider UK economy of inward medical travellers. Given the frailties of the data, we have adopted a precautionary principle and present estimates when we are confident that these describe an accurate trend. We envisage this as a basis for future research.
Given that the scope of the study was largely limited to an exploration of out-of-pocket payments for treatment, we chose not to focus explicitly on the EU directive on cross-border health care. 1 Although we acknowledge that such patients are likely to represent a different type of medical traveller and merit further study, they are distinct from the type of private medical travel researched as part of this project.
It is important to note that, despite including a large sample of medical tourism interviewees, this was not a representative sample. Not all questions have been fully answered (we would wish to understand more about the costs and the ongoing health implications of treatment abroad), even some of those that had appeared to be straightforward at the outset.
Despite these limitations the study has generated new evidence and insights into several aspects of medical tourism; contrary to the public image presented in the media, medical tourism is still a sensitive issue. Those who have travelled or who are considering travelling are reluctant to discuss their experiences. This presented challenges in terms of our recruitment of medical tourists. Equally, the industry is largely suspicious of academic interest and those within the NHS do not seem to have a consistent strategy for dealing with medical tourism, whether inward or outward. Indeed, it is clear that in many areas within the NHS this is a rather unknown and not widely understood phenomenon. By utilising a mixed-methods approach, which was often innovative, we uncovered the processes of referral of international patients travelling into the UK. Similarly, we identified a confusing array of accreditation, registration and licensing that exists internationally. This is important if, as our study demonstrates, medical tourism is a process that carries inherent and often serious risks and is on the increase.
In spite of the limitations of our study, we have advanced the evidence base on medical tourism, as well as confirming insights from other studies. Results from this research demonstrate reliably for the first time that a growing number of patients travel for treatment. Although many of the numbers presented by commercial sources are indeed overestimates, large numbers of UK residents are engaging in medical tourism and an equally sizeable number of overseas residents are travelling to the UK for treatment as international patients within the NHS and the independent sector. The implications of this depend on several factors, including where patients travel to or from and what types of procedures they travel for, as well as a range of demographic and socioeconomic factors. Contrary to previous assumptions, outward medical travel appears to involve lower-cost procedures within Europe, with fewer tourists travelling further afield or accessing more complex procedures abroad.
This study has identified two streams within inward medical tourism: the first involves expatriates and the second is driven by nationals of countries with which the UK has longstanding ties. Both groups merit further study. It may also be that the previously muted impact of the EU directive1 will yield a very different type of medical tourist and that further study will be required as the directive becomes more frequently utilised.
Our evidence demonstrates that medical tourism represents potential income for some trusts. The estimates presented in this report are based on the available evidence but equally the limited data suggest that these figures may be underestimates and may be set to grow. There may be potential savings in future health and social services spending averted when patients travel abroad for treatment. This is closely linked to specific procedures and of course relies on quality control. Without a detailed study of the direct and wider costs associated with procedures such as bariatric surgery it is unclear what level such cost savings could conceivably reach and as such further study is essential.
Our study provides clearer evidence on how prospective medical tourists gather information about destinations and treatment. This includes greater information on individual internet searches, the role of facilitators and the place of networks based around treatments and culture, and also influenced by the knowledge and preferences of referring clinicians. Providers are primarily from the private sector but public sectors are also constituents of these emerging treatment relationships. Private activity may include small clinical partnerships offering a wide range of treatments and extremely large medical tourism facilities where clinical specialism is the order of the day. Larger clinics and providers overseas have moved to offer a range of ancillary products and services. The precise requirements of domestic regulation and the role of accreditation schemes are typically confusing and unclear to medical travellers. Much treatment activity does not have clear regulation in place.
Our findings also allow us to question some of the assumptions within the medical tourism field. This includes making realistic estimates of how much medical tourism activity countries may expect to attract. Pre-existing networks, history and relationships may provide insights into medical tourist flows and the success of particular destinations in attracting patients.
Confirming that medical tourism is indeed a real phenomenon affecting a cross-section of society, a phenomenon that occurs in a diverse industry without regulation or even a clear sense of direction, requires consideration of how patients can be safeguarded. We interviewed individuals with serious and complex health needs. Whether these can genuinely not be met within the NHS or, rather, these individuals simply perceive that their needs would be better met elsewhere, we can say with confidence that > 60,000 UK residents each year make the decision to travel abroad for treatment. In so doing they leave behind the regulatory framework and relative safety of the NHS. Patients often have information that is at best incomplete and at worst incorrect. They often travel for inappropriate procedures, delivered with lower standards of care than are guaranteed in the NHS, and do not consider continuity of care. Quite simply they are often at risk and are rarely fully aware of such risks. Perhaps the most important finding of this report is that in some instances relatively minor changes to practice can severely minimise these risks.
Acknowledgements
The project team acknowledges the support and advice of the advisory group; individually and collectively they made a huge contribution during the life of the project. Thank you.
We thank our many interviewees. We are very grateful for their time, their willingness to take part and their honesty.
Particular thanks go to Nina Lakhani, Martin Rathfelder, Ubah Egal and Ken Clare for their assistance with recruitment.
A number of individuals provided research support during the project: Gavriil Tsolos, Lauren Hutchinson and Chris Clarke.
Thanks go to Dr Charles Shaw, Elizabeth Boultbee and Lila Skountridaki for providing context and materials.
Alicia Wooding and Atholynne Lonsdale assisted in the final preparation of the manuscript.
Many professionals and clinicians provided background context and clarification during the project: Evangelos Efthimiou, Dimitrios Pournaras, Ashley Brown, Aneez Esmail, Simon Kay, Alex Milosevic, Jacqueline Joyce, Alaana Woods and Suzanne Wynne-Jones.
The views and conclusions outlined in this report remain the sole responsibility of the authors.
Contribution of authors
Dr Neil Lunt was Principal Investigator and had overall responsibility for the design, data collection, analysis, research governance and preparation of the final document. He undertook data collection (including interviews and website analysis) and contributed towards the policy context and background. He gave final approval of the report to be published.
Professor Richard D Smith was a co-applicant. He conducted the analysis of costings, oversaw the systematic review and was involved in the overall planning and preparation of the final document. He gave final approval of the report to be published.
Professor Russell Mannion was a co-applicant. He contributed towards the background context and analysis of patient safety and service quality and advised on the final write-up. He gave final approval of the report to be published.
Professor Stephen T Green was a co-applicant. He contributed towards the background context and analysis of patient safety and service quality. He gave final approval of the report to be published.
Professor Mark Exworthy was a co-applicant. He contributed towards the background context and analysis of NHS policy and advised on the final write-up. He gave final approval of the report to be published.
Dr Johanna Hanefeld conducted the interviews and analysis and the analysis of the costing work and the IPS. She was responsible for the preparation of the final document. She gave final approval of the report to be published.
Dr Daniel Horsfall was responsible for the day-to-day planning and administration of the project. He conducted the interviews and analysis and the analysis of the IPS. He was responsible for the preparation of the final document. He gave final approval of the report to be published.
Dr Laura Machin was responsible for the project start-up, led on the initial ethics applications and governance and conducted the interviews. She gave final approval of the report to be published.
Dr Hannah King conducted the interviews and analysis and provided background context on patient safety. She gave final approval of the report to be published.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
Publication
Lunt N, Machin L, Mannion R, Green S. Are there implications for quality of care for patients who participate in international medical tourism? Expert Rev Pharmacoecon Outcomes Res 2011;11:133–6.
References
- Official Journal of the European Union . Directive 2011 24 EU of the European Parliament and of the Council of 9 March 2011 on the Application of patients' Rights in Cross-Border Healthcare 2011.
- Youngman I. Medical tourism statistics: why McKinsey has got it wrong. Int Med Travel J 2009. www.imtjonline.com/articles/2009/mckinsey-wrong-medical-travel/ (accessed 9 September 2013).
- Smith RD. Foreign direct investment and trade in health services: a review of the literature. Soc Sci Med 2004;59:2313-23. http://dx.doi.org/10.1016/j.socscimed.2004.03.021.
- Blouin C, Drager N, Smith RD. International trade in health services: debates on the GATS. Washington, DC: World Bank; 2005.
- Holden C. The internationalization of corporate healthcare: extent and emerging Trends. Compet Change 2005;9:201-19. http://dx.doi.org/10.1179/102452905X45409.
- Smith RD. Trade and Health – the Role and Impact of the Private Sector n.d.
- Smith RD, Lee K. Trade and health: an agenda for action. Lancet 2009;373:768-73. http://dx.doi.org/10.1016/S0140-6736(08)61780-8.
- Smith RD, Chanda R, Tangcharoensathien V. Trade in health-related services. Lancet 2009;373:593-601. http://dx.doi.org/10.1016/S0140-6736(08)61778-X.
- Bridge M. Medical tourism; the pros and cons. The Times 2007. www.thetimes.co.uk/tto/money/consumeraffairs/article2206101.ece (accessed 9 September 2013).
- Connell J. Medical tourism: sea, sun, sand and … surgery. Tourism Manag 2006;27:1093-100. http://dx.doi.org/10.1016/j.tourman.2005.11.005.
- Horowitz MD, Rosensweig JA, Jones CA. Medical tourism: globalization of the healthcare marketplace. MedGenMed 2007;9.
- Ehrbeck T, Guevara C, Mango PD. Mapping the Market for Medical Travel 2008. http://cureandcareindia.com/writereaddata/McKinsey-9547270771.pdf (accessed 9 September 2013).
- Crone RK. Flat medicine? Exploring trends in the globalization of health care. Acad Med 2008;83:117-21. http://dx.doi.org/10.1097/ACM.0b013e318160965c.
- Milstein A, Smith M. America's new refugees – seeking affordable surgery offshore. N Engl J Med 2006;355:1637-40. http://dx.doi.org/10.1056/NEJMp068190.
- Repasky M. A cut below: Americans look abroad for health care. ABC News 2006. http://abcnews.go.com/Business/IndustryInfo/story?id=2320839&page=1 (accessed 13 August 2013).
- Herrick DM. Medical tourism: global competition in health care. Dallas, TX: National Center for Policy Analysis; 2007.
- Keckley PH, Underwood HR. Medical tourism: consumers in search of value. Washington, DC: Deloitte Center for Health Solutions; 2008.
- Judgement of the European Court of Justice: Case C-372/04 (the Watt case). Luxembourg: EUCJ; 2005.
- Judgement of the European Court of Justice: Case C-158/96 (the Kohll case). Luxembourg: EUCJ; 1998.
- Judgement of the European Court of Justice: Case C-120/95 (the Decker case). Luxembourg: EUCJ; 1998.
- Exworthy M, Kanavos P. Cross-border patient flows for health care in Europe: a feasibility study. London: Department of Health; 2001.
- Lowson K, West P, Chaplin S, O’Reilly J. Evaluation of patients travelling overseas: final report. York: York Health Economics Consortium; 2002.
- Burge P, Devlin N, Appleby J, Rohr C, Grant J. Do patients always prefer quicker treatment?: a discrete choice analysis of patients' stated preferences in the London Patient Choice Project. Appl Health Econ Health Policy 2004;3:183-94. http://dx.doi.org/10.2165/00148365-200403040-00002.
- Bertinato L, Busse R, Fahy N, Legido-Quigley H, McKee M, Palm W, et al. Cross-border health care in Europe. Denmark: World Health Organization; 2005.
- Rosenmöller M, McKee M, Baeten R. Patient mobility in the European Union: learning from experience. Copenhagen: World Health Organization; 2006.
- Cortez N. Patients without borders: the emerging global market for patients and the evolution of modern health care. Indiana Law J 2008;83:71-131.
- Smith RD. The Crisis in Global Finance and Trade: What Are the Implications for Health? n.d.
- Ham C. Health in a cold climate: developing an intelligent response to the financial challenges facing the NHS Nuffield Trust. London: Nuffield Trust; 2009.
- Nicholson D. NHS Global 2010. http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/en/Publicationsandstatistics/Lettersandcirculars/Dearcolleagueletters/DH_114587 (accessed 9 September 2013).
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
- Health and Social Care Bill 2011. Coordinating document for the impact assessments and equality impact assessments. London: Her Majesty's Stationery Office; 2011.
- Fotaki M, Boyd M, Smith L, McDonald R, Roland M, Sheaff R, et al. Patient choice and the organisation and delivery of health services: scoping review. Manchester: Manchester Business School, University of Manchester; 2005.
- Exworthy M, Peckham S. Access, choice and travel: implications for health policy. Soc Policy Admin 2006;40:267-87. http://dx.doi.org/10.1111/j.1467-9515.2006.00489.x.
- Carter H. Nip, tuck, hard sell: don't let ads seduce you, plastic surgeons warn. The Guardian 2008. www.theguardian.com/society/2008/sep/19/cosmeticsurgery.advertising (accessed 9 September 2013).
- Systematic Reviews: CRD's Guidance for Undertaking Systematic Reviews in Health Care. York: Centre for Reviews and Dissemination; 2009.
- Ritchie J, Spencer L, Bryman A, Burgess R. Analysing qualitative data. London: Sage; 1993.
- Ritchie J, Lewis J. Qualitative research practice: a guide for social science students and researchers. London: Sage; 2003.
- Miles M, Huberman MB. Qualitative data analysis. Beverly Hills, CA: Sage; 1984.
- Stake RE, Denzin N, Lincoln Y. The Sage handbook of qualitative research. Thousand Oaks, CA: Sage; 2005.
- Lunt N, Carrera P. Medical tourism: assessing the evidence on treatment abroad. Maturitas 2010;66:27-32. http://dx.doi.org/10.1016/j.maturitas.2010.01.017.
- International passenger survey. Newport: ONS; 2012.
- Smith R, Martínez Álvarez M, Chanda R. Medical tourism: a review of the literature and analysis of a role for bi-lateral trade. Health Policy 2011;103:276-82. http://dx.doi.org/10.1016/j.healthpol.2011.06.009.
- Alsharif MJ, Labonte R, Lu Z. Patients beyond borders: a study of medical tourists in four countries. Global Social Policy 2010;10:315-35. http://dx.doi.org/10.1177/1468018110380003.
- Bergmann S. Fertility tourism: circumventive routes that enable access to reproductive technologies and substances. Signs 2011;36:280-9. http://dx.doi.org/10.1086/655978.
- Birch DW, Vu L, Karmali S, Stoklossa CJ, Sharma AM. Medical tourism in bariatric surgery. Am J Surg 2010;199:604-8. http://dx.doi.org/10.1016/j.amjsurg.2010.01.002.
- Blouin C. Trade policy and health: from conflicting interests to policy coherence. (Special Theme: Health and Foreign Policy.). Bull World Health Organ 2007;85:169-73. http://dx.doi.org/10.2471/BLT.06.037413.
- Blyth E. Fertility patients' experiences of cross-border reproductive care. Fertil Steril 2010;94:E11-15. http://dx.doi.org/10.1016/j.fertnstert.2010.01.046.
- Botten G, Grepperud S, Nerland SM. Trading patients. Lessons from Scandinavia. Health Policy 2004;69:317-27.
- Brouwer W, van Exel J, Hermans B, Stoop A. Should I stay or should I go? Waiting lists and cross-border care in the Netherlands. Health Policy 2003;63:289-98.
- Carrera P, Lunt N. A European perspective on medical tourism: the need for a knowledge base. Int J Health Serv 2010;40:469-84. http://dx.doi.org/10.2190/HS.40.3.e.
- Chan HL, Poon LM, Chan SG, Teo JW. The perils of medical tourism: NDM-1-positive Escherichia coli causing febrile neutropenia in a medical tourist. Singapore Med J 2011;52:299-302.
- Cohen E. Medical travel – a critical assessment. Tourism Recreation Res 2010;35:225-37.
- Connell J, Woodside AG, Martin D. Tummy tucks and the Taj Mahal? Medical tourism and the globalization of health care. Tourism Management: Analysis, Behavior and Strategy 2008:232-44. http://dx.doi.org/10.1079/9781845933234.0232.
- Cook PS. Constructions and experiences of authenticity in medical tourism: the performances of places, spaces, practices, objects and bodies. Tourist Stud 2010;10:135-53. http://dx.doi.org/10.1177/1468797611403048.
- Crooks VA, Kingsbury P, Snyder J, Johnston R. What is known about the patient's experience of medical tourism? A scoping review. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-266.
- Crooks VA, Turner L, Snyder J, Johnston R, Kingsbury P. Promoting medical tourism to India: Messages, images, and the marketing of international patient travel. Soc Sci Med 2011;72:726-32. http://dx.doi.org/10.1016/j.socscimed.2010.12.022.
- Culley L, Hudson N, Rapport F, Blyth E, Norton W, Pacey AA. Crossing borders for fertility treatment: motivations, destinations and outcomes of UK fertility travellers. Hum Reprod 2011;26:2373-81. http://dx.doi.org/10.1093/humrep/der191.
- de Arellano ABR. Patients without borders: the emergence of medical tourism. Int J Health Serv 2007;37:193-8. http://dx.doi.org/10.2190/4857-468G-2325-47UU.
- Donchin A. Reproductive tourism and the quest for global gender justice. Bioethics 2010;24:323-32. http://dx.doi.org/10.1111/j.1467-8519.2010.01833.x.
- Ferraretti AP, Pennings G, Gianaroli L, Natali F, Magli MC. Cross-border reproductive care: a phenomenon expressing the controversial aspects of reproductive technologies. Reprod Biomed Online 2010;20:261-6. http://dx.doi.org/10.1016/j.rbmo.2009.11.009.
- Glinos IA, Baeten R, Helble M, Maarse H. A typology of cross-border patient mobility. Health Place 2010;16:1145-55. http://dx.doi.org/10.1016/j.healthplace.2010.08.001.
- Glinos IA, Baeten R, Maarse H. Purchasing health services abroad: practices of cross-border contracting and patient mobility in six European countries. Health Policy 2010;95:103-12.
- Gray HH, Poland SC. Medical tourism: crossing borders to access health care. Kennedy Inst Ethics J 2008;18:193-201. http://dx.doi.org/10.1353/ken.0.0006.
- Hall CM, James M. Medical tourism: emerging biosecurity and nosocomial issues. (Special Issue: Health and Medical Tourism.). Tourism Rev 2011;66:118-26. http://dx.doi.org/10.1108/16605371111127288.
- Hanna SA, Saksena J, Legge S, Ware HE. Sending NHS patients for operations abroad: is the holiday over?. Ann R Coll Surg Engl 2009;91:128-30. http://dx.doi.org/10.1308/003588409X359411.
- Harling R, Turbitt D, Millar M, Ushiro-Lumb I, Lacey S, Xavier G, et al. Passage from India: an outbreak of hepatitis B linked to a patient who acquired infection from health care overseas. Public Health 2007;121:734-41.
- Helble M. The movement of patients across borders: challenges and opportunities for public health. Bull World Health Organ 2011;89:68-72. http://dx.doi.org/10.2471/BLT.10.076612.
- Heung VCS, Kucukusta D, Song H. Medical tourism development in Hong Kong: an assessment of the barriers. Tourism Manag 2011;32:995-1005. http://dx.doi.org/10.1016/j.tourman.2010.08.012.
- Heung VCS, Kucukusta D, Song HY. A conceptual model of medical tourism: implications for future research. J Travel Tourism Mark 2010;27:236-51. http://dx.doi.org/10.1080/10548401003744677.
- Hopkins L, Labonte R, Runnels V, Packer C. Medical tourism today: what is the state of existing knowledge?. J Public Health Policy 2010;31:185-98. http://dx.doi.org/10.1057/jphp.2010.10.
- Horton S, Cole S. Medical returns: seeking health care in Mexico. Soc Sci Med 2011;72:1846-52. http://dx.doi.org/10.1016/j.socscimed.2011.03.035.
- Hudson N, Culley L, Blyth E, Norton W, Rapport F, Pacey A. Cross-border reproductive care: a review of the literature. Reprod Biomed Online 2011;22:673-85. http://dx.doi.org/10.1016/j.rbmo.2011.03.010.
- Hunter D, Oultram S. The ethical and policy implications of rogue medical tourism. Global Soc Policy 2010;10:297-9. http://dx.doi.org/10.1177/14680181100100030204.
- Inhorn MC. Globalization and gametes: reproductive ‘tourism’, Islamic bioethics and Middle Eastern modernity. Anthropol Med 2011;18:87-103. http://dx.doi.org/10.1080/13648470.2010.525876.
- Jarman H, Greer S. Crossborder trade in health services: lessons from the European laboratory. Health Policy 2010;94:158-63.
- Jeevan R, Birch J, Armstrong AP. Travelling abroad for aesthetic surgery: informing healthcare practitioners and providers while improving patient safety. J Plast Reconstruct Aesthet Surg 2011;64:143-7. http://dx.doi.org/10.1016/j.bjps.2010.04.022.
- Johnston R, Crooks VA, Adams K, Snyder J, Kingsbury P. An industry perspective on Canadian patients' involvement in medical tourism: implications for public health. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-416.
- Johnston R, Crooks VA, Snyder J, Kingsbury P. What is known about the effects of medical tourism in destination and departure countries? A scoping review. Int J Equity Health 2010;9. http://dx.doi.org/10.1186/1475-9276-9-24.
- Jones CA, Keith LG. Medical tourism and reproductive outsourcing: the dawning of a new paradigm for healthcare. Int J Fertil Womens Med 2006;51:251-5.
- Karuppan CM. Healthcare tourism: accelerating diffusion through a more effective use of communication channels. J Commun Healthc 2010;3:24-36.
- Karuppan CM, Karuppan M. Changing trends in health care tourism. Health Care Manag 2010;29:349-58.
- Karuppan CM, Karuppan M. Who are the medical travelers and what do they want?: A qualitative study. Health Market Q 2011;28:116-32. http://dx.doi.org/10.1080/07359683.2011.545339.
- Kumarasamy KK, Toleman MA, Walsh TR, Bagaria J, Butt F, Balakrishnan R, et al. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: a molecular, biological, and epidemiological study. Lancet Infect Dis 2010;10:597-602. http://dx.doi.org/10.1016/S1473-3099(10)70143-2.
- Laugesen MJ, Vargas-Bustamante A. A patient mobility framework that travels: European and United States-Mexican comparisons. Health Policy 2010;97:225-31. http://dx.doi.org/10.1016/j.healthpol.2010.05.006.
- Lautier M. Export of health services from developing countries: the case of Tunisia. Soc Sci Med 2008;67:101-10. http://dx.doi.org/10.1016/j.socscimed.2008.01.057.
- Lee CG, Hung WT. Tourism, health and income in Singapore. Int J Tourism Res 2010;12:355-9. http://dx.doi.org/10.1002/jtr.755.
- Lee JY, Kearns RA, Friesen W. Seeking affective health care: Korean immigrants' use of homeland medical services. Health Place 2010;16:108-15. http://dx.doi.org/10.1016/j.healthplace.2009.09.003.
- Leng CH. Medical tourism and the state in Malaysia and Singapore. Global Soc Policy 2010;10:336-57.
- Lunt N, Carrera P. Systematic review of web sites for prospective medical tourists. (Special Issue: Health and Medical Tourism.). Tourism Rev 2011;66:57-6. http://dx.doi.org/10.1108/16605371111127224.
- Lunt N, Hardey M, Mannion R. Nip, tuck and click: medical tourism and the emergence of web-based health information. Open Med Inform J 2010;4:1-11. http://dx.doi.org/10.2174/1874431101004010001.
- Lunt N, Machin L, Green S, Mannion R. Are there implications for quality of care for patients who participate in international medical tourism?. Expert Rev Pharmacoeconom Outcomes Res 2011;11:133-6. http://dx.doi.org/10.1586/erp.11.4.
- Lunt N, Smith R, Exworthy M, Green S, Horsfall D, Mannion R. Medical Tourism: Treatments, Markets and Health System Implications: A scoping review. Paris: OECD; 2011.
- Martin DS, Ramamonjiarivelo Z, Martin WS. MEDTOUR: a scale for measuring medical tourism intentions. (Special Issue: Health and Medical Tourism.). Tourism Rev 2011;66:45-56. http://dx.doi.org/10.1108/16605371111127233.
- Martinez Alvarez M, Chanda R, Smith RD. The potential for bi-lateral agreements in medical tourism: A qualitative study of stakeholder perspectives from the UK and India. Globalization Health 2011;7. http://dx.doi.org/10.1186/1744-8603-7-11.
- Mason A, Wright KB. Framing medical tourism: an examination of appeal, risk, convalescence, accreditation, and interactivity in medical tourism web sites. J Health Commun 2011;16:163-77. http://dx.doi.org/10.1080/10810730.2010.535105.
- Mattoo A, Rathindran R. How health insurance inhibits trade in health care. Health Aff (Millwood) 2006;25:358-68.
- Mazzaschi A. Surgeon and safari: producing valuable bodies in Johannesburg. Signs 2011;36:303-12. http://dx.doi.org/10.1086/655941.
- McKelvey A, David AL, Shenfield F, Jauniaux ER. The impact of cross-border reproductive care or ‘fertility tourism’ on NHS maternity services. BJOG 2009;116:1520-3. http://dx.doi.org/10.1111/j.1471-0528.2009.02294.x.
- Melendez MM, Alizadeh K. Complications from international surgery tourism. Aesthetic Surg J 2011;31:694-7. http://dx.doi.org/10.1177/1090820X11415977.
- Michelmann HW, Himmel W. Considering the possible and choosing the justifiable – The problem of “tourism” in infertility treatment. Journal Fur Reproduktionsmedizin Und Endokrinologie 2007;4:118-23.
- Milosevic A. Dental tourism – A global issue?: Perspectives. J Esthetic Restorative Dent 2009;21:289-91. http://dx.doi.org/10.1111/j.1708-8240.2009.00277.x.
- Miyagi K, Auberson D, Patel AJ, Malata CM. The unwritten price of cosmetic tourism: an observational study and cost analysis. J Plast Reconstr Aesthet Surg 2012;65:22-8. http://dx.doi.org/10.1016/j.bjps.2011.07.027.
- NaRanong A, NaRanong V. The effects of medical tourism: Thailand's experience. Bull World Health Organ 2011;89:336-44. http://dx.doi.org/10.2471/BLT.09.072249.
- Nassab R, Hamnett N, Nelson K, Kaur S, Greensill B, Dhital S, et al. Cosmetic tourism: public opinion and analysis of information and content available on the Internet. Aesthetic Surg J 2010;30:465-9. http://dx.doi.org/10.1177/1090820X10374104.
- Osterle A, Balazs P, Delgado J. Travelling for teeth: characteristics and perspectives of dental care tourism in Hungary. Br Dent J 2009;206:425-8. http://dx.doi.org/10.1038/sj.bdj.2009.308.
- Pennings G, Autin C, Decleer W, Delbaere A, Delbeke L, Delvigne A, et al. Cross-border reproductive care in Belgium. Hum Reprod 2009;24:3108-18. http://dx.doi.org/10.1093/humrep/dep300.
- Perfetto R, Dholakia N. Exploring the cultural contradictions of medical tourism. Consumption Markets Cult 2010;13:399-417. http://dx.doi.org/10.1080/10253866.2010.502417.
- Piazolo M, Zanca NA. Medical tourism – a case study for the USA and India, Germany and Hungary. Acta Polytechnica Hungarica 2011;8:137-60.
- Pocock NS, Phua KH. Medical tourism and policy implications for health systems: a conceptual framework from a comparative study of Thailand, Singapore and Malaysia. Globalization Health 2011;7. http://dx.doi.org/10.1186/1744-8603-7-12.
- Reddy SG, York VK, Brannon LA. Travel for treatment: students' perspective on medical tourism. Int J Tourism Res 2010;12:510-22. http://dx.doi.org/10.1002/jtr.769.
- Rogers BA, Aminzadeh Z, Hayashi Y, Paterson DL. Country-to-country transfer of patients and the risk of multi-resistant bacterial infection. Clin Infect Dis 2011;53:49-56. http://dx.doi.org/10.1093/cid/cir273.
- Sarkar SK, Sarkar PK, Gretzel U, Law R, Fuchs M. Information and Communication Technologies in Tourism 2010. Vienna: Springer; 2010.
- Sarojini N, Vrinda M, Anjali S. Globalisation of birth markets: a case study of assisted reproductive technologies in India. Globalization Health 2011;7. http://dx.doi.org/10.1186/1744-8603-7-27.
- Shenfield F, de Mouzon J, Pennings G, Ferraretti AP, Andersen AN, de Wert G, et al. Cross border reproductive care in six European countries. Hum Reprod 2010;25:1361-8. http://dx.doi.org/10.1093/humrep/deq057.
- Shetty P. Medical tourism booms in India, but at what cost?. Lancet 2010;376:671-2. http://dx.doi.org/10.1016/S0140-6736(10)61320-7.
- Siddiqi S, Shennawy A, Mirza Z, Drager N, Sabri B. Assessing trade in health services in countries of the Eastern Mediterranean from a public health perspective. Int J Health Plan Manag 2010;25:231-50. http://dx.doi.org/10.1002/hpm.989.
- Snyder J, Crooks VA. Medical Tourism and Bariatric Surgery: More Moral Challenges. Am J Bioethics 2010;10:28-30. http://dx.doi.org/10.1080/15265161.2010.528510.
- Snyder J, Crooks VA, Adams K, Kingsbury P, Johnston R. The ‘patient's physician one-step removed’: the evolving roles of medical tourism facilitators. J Med Ethics 2011;37:530-4. http://dx.doi.org/10.1136/jme.2011.042374.
- Snyder J, Dharamsi S, Crooks VA. Fly-By medical care: Conceptualizing the global and local social responsibilities of medical tourists and physician voluntourists. Globalization Health 2011;7. http://dx.doi.org/10.1186/1744-8603-7-6.
- Solomon H. Affective journeys: the emotional structuring of medical tourism in India. Anthropol Med 2011;18:105-18. http://dx.doi.org/10.1080/13648470.2010.525878.
- Tresidder R, Robinson P, Heitmann S, Dieke P. Research Themes for Tourism. Wallingford: CABI Publishing; 2011.
- Turner L. Cross-border dental care: ‘dental tourism’ and patient mobility. Br Dent J 2008;204:553-4. http://dx.doi.org/10.1038/sj.bdj.2008.403.
- Turner LG. Quality in health care and globalization of health services: accreditation and regulatory oversight of medical tourism companies. Int J Qual Health Care 2011;23:1-7. http://dx.doi.org/10.1093/intqhc/mzq078.
- Medical Travel in Asia and the Pacific. Challenges and Opportunities. Thailand: UN ESCAP; 2007.
- Vijaya RM. Medical tourism: revenue generation or international transfer of healthcare problems?. J Econ Issues 2010;44:53-69. http://dx.doi.org/10.2753/JEI0021-3624440103.
- Wagner C, Linder R. The demand for EU cross-border care: an empirical analysis. J Manag Health Care 2010;2:176-87.
- Whiteman RG. Medical tourism and bariatric surgery. Surg Obes Relat Dis 2011;7:652-5. http://dx.doi.org/10.1016/j.soard.2011.05.016.
- Whittaker A. Pleasure and pain: medical travel in Asia. Global Public Health 2008;3:271-90. http://dx.doi.org/10.1080/17441690701463936.
- Whittaker A. Challenges of medical travel to global regulation: a case study of reproductive travel in Asia. Global Soc Policy 2010;10:396-415. http://dx.doi.org/10.1177/1468018110379981.
- Whittaker A. Cross-border assisted reproduction care in Asia: implications for access, equity and regulations. Reprod Health Matters 2011;19:107-16. http://dx.doi.org/10.1016/S0968-8080(11)37575-1.
- Whittaker A, Manderson L, Cartwright E. Patients without borders: understanding medical travel. Med Anthropol 2010;29:336-43. http://dx.doi.org/10.1080/01459740.2010.501318.
- Whittaker A, Speier A. “Cycling overseas”: care, commodification, and stratification in cross-border reproductive travel. Med Anthropol 2010;29:363-83. http://dx.doi.org/10.1080/01459740.2010.501313.
- Cormany D, Baloglu S. Medical travel facilitator websites: an exploratory study of web page contents and services offered to the prospective medical tourist. Tourism Manag 2011;32:709-16. http://dx.doi.org/10.1016/j.tourman.2010.02.008.
- Birch J, Caulfield R, Ramakrishnan V. The complications of ‘cosmetic tourism’ – an avoidable burden on the NHS. J Plast Reconstr Aesthet Surg 2007;60:1075-7.
- Connell J, Connell J. Medical Tourism. Wallingford: CABI Publishing; 2011.
- Conrady R, Buck ME. Trends and Issues in Global Tourism. Berlin and Heidelberg: Springer; 2008.
- Connell J. A new inequality? Privatisation, urban bias, migration and medical tourism. Asia Pac Viewp 2011;52:260-71.
- Smith KP, Christakis NA. Social networks and health. Ann Rev Sociol 2008;34:405-29.
- Ackerman SL. Plastic paradise: transforming bodies and selves in Costa Rica’s cosmetic surgery tourism industry. Med Anthropol 2010;29:403-23.
- Keckley PH, Eselius LL. Survey of health care consumers: key findings, strategic implications. Washington DC: Deloitte Center for Health Solutions; 2009.
- Connell J. Contemporary medical tourism: conceptualisation, culture and commodification. Tourism Manag 2013;34:1-13.
- Baliga H. Medical tourism is the new wave of outsourcing from India. India Daily n.d. www.indiadaily.com/editorial/14858.asp (accessed 9 September 2013).
- Kentikelenis A, Karanikolos M, Papanicolas I, Basu S, McKee M, Stuckler D. Health effects of financial crisis: omens of a Greek tragedy. Lancet 2011;378:1457-8.
- Data Protection Act 1998. London: The Stationery Office; 1998.
- Committee of Advertising Practice . Advertising Codes n.d. www.cap.org.uk/Advertising-Codes.aspx (accessed 9 September 2013).
- Advertising Standards Authority . About Regulation n.d. www.asa.org.uk/About-ASA/About-regulation.aspx (accessed 9 September 2013).
- Complaint reference 71102. London: Advertising Standards Authority; 2008.
- Complaint reference A11–170051. London: Advertising Standards Authority; 2011.
- Medical Act 1983. London: HMSO; 1983.
- General Medical Council . Good Medical Practice 2006 n.d. www.gmc-uk.org/Good_Medical_Practice_Archived.pdf_51772200.pdf (accessed 9 September 2013).
- Official Journal of the European Communities . Directive 2000 31 EC of the European Parliament and of the Council of 8 June 2000 on Certain Legal Aspects of Information Society Services, in Particular Electronic Commerce, in the Internal Market (Directive on Electronic Commerce) 2000.
- Svantesson DJB. From the airport to the surgery to the courtroom – private international law and medical tourism. Commonwealth Law Bull 2008;34:265-76.
- Commonwealth of Australia . Trade Practices (contracts) Act 1974 1974. www.austlii.edu.au/au/legis/cth/num_act/tpa1974149/ (accessed September 2013).
- Commonwealth of Australia . Competition and Consumer Act 2010 n.d. www.austlii.edu.au/au/legis/cth/consol_act/caca2010265/ (accessed September 2013).
- Vick L. The perils of cosmetic surgery/medical tourism. AvMA Med Legal J 2012;18:106-9.
- Consumer Credit Act 1974. London: The Stationery Office; 1974.
- Vick L. Medical Toursim: Legal Issues n.d.
- Central Government Act . Fatal Accidents Act n.d. http://indiankanoon.org/doc/594667/ (accessed September 2013).
- Central Government Act . Code of Criminal Procedure 1973 n.d. http://indiankanoon.org/doc/445276/ (accessed September 2013).
- Howze KS. Medical tourism: symptom or cure?. Georgia Law Rev 2007.
- Sixteenth report – PIP breast implants and regulation of cosmetic interventions. London: The Stationery Office; 2012.
- Smith R, Lunt N, Hanefeld J. The implications of PIP are more than just cosmetic. Lancet 2012;379:1180-1.
- Eysenbach G. What is e-health?. J Med Internet Res 2001;3.
- Lichtenfeld LJ. Can the beast be tamed? The woeful tale of accurate health information on the internet. Ann Surg Oncol 2012;19:701-2.
- Scullard P, Peacock C, Davies P. Googling children’s health: reliability of medical advice on the internet. Arch Dis Child 2010;95:580-2.
- Deshpande A, Jadad AR. Trying to measure the quality of health information on the internet: is it time to move on?. J Rheumatol 2009;36:1-3.
- Honekamp W, Ostermann H. Evaluation of a prototype health information system using the FITT framework. Inform Prim Care 2011;19:47-9.
- Langille M, Bernard A, Rodgers C, Hughes S, Leddin D, van Zanten SV. Systematic review of the quality of patient information on the internet regarding inflammatory bowel disease treatments. Clin Gastroenterol Hepatol 2010;8:322-8.
- Lawrentschuk N, Sasges D, Tasevski R, Abouassaly R, Scott A, Davis I. Oncology health information quality on the internet: a multilingual evaluation. Ann Surg Oncol 2012;19:706-13.
- Bernard A, Langille M, Hughes S, Rose C, Leddin D, Veldhuyzen van Zanten S. A systematic review of patient inflammatory bowel disease information resources on the World Wide Web. Am J Gastroenterol 2007;102:2070-7.
- Thompson AE, Graydon SL. Patient-oriented methotrexate information sites on the internet: a review of completeness, accuracy, format, reliability, credibility, and readability. J Rheumatol 2009;36:41-9.
- Ni Riordain R, McCreary C. Dental patients’ use of the internet. Br Dent J 2009;207:583-6.
- Harris CE, Chestnutt IG. The use of the internet to access oral health-related information by patients attending dental hygiene clinics. Int J Dent Hyg 2005;3:70-3.
- Illes J, Kann D, Karetsky K, Letourneau P, Raffin TA, Schraedley-Desmond P, et al. Advertising, patient decision making, and self-referral for computed tomographic and magnetic resonance imaging. Arch Intern Med 2004;164:2415-19.
- Bernstam EV, Sagaram S, Walji M, Johnson CW, Meric-Bernstam F. Usability of quality measures for online health information: can commonly used technical quality criteria be reliably assessed?. Int J Med Inform 2005;74:675-83.
- Bernstam EV, Shelton DM, Walji M, Meric-Bernstam F. Instruments to assess the quality of health information on the World Wide Web: what can our patients actually use?. Int J Med Inform 2005;74:13-9.
- Hancocks S. Dentist 50533 does dentistry. Br Dent J 2010;209.
- British Association of Plastic, Reconstructive and Aesthetic Surgeons . Cosmetic Surgery Tourism – Patient Information 2011. www.bapras.org.uk/guide.asp?id=353 (accessed 15 August 2013).
- We Expose Medical Tourism Pitfalls: Do Your Homework before You Go, Urges Which? 2008. www.which.co.uk/news/2008/03/we-expose-medical-tourism-pitfalls-135137/ (accessed 1 November 2011).
- British Association of Aesthetic Plastic Surgeons . BAAPS Issue Consumer Safety Guidelines 2004. www.baaps.org.uk/about-us/press-releases/132-baaps-issue-consumer-safety-guidelines (accessed 9 September 2013).
- Zahir K. Clinical governance in the UK NHS. London: Department for International Development Health Resource Centre; 2001.
- Green ST. The movement of patients across borders – emerging challenges and opportunities for health care systems: quality control and accreditation of health service providers and facilities. Kobe: World Health Organization; 2009.
- Greenfield D, Braithwaite J. Developing the evidence base for accreditation of healthcare organisations: a call for transparency and innovation. Qual Saf Health Care 2009;18:162-3.
- Lunt N, Carrera P. Advice for prospective medical tourists: systematic review of consumer sites. Tourism Rev 2011;66:57-6.
- Cacace M, Ettelt S, Brereton L, Pedersen J, Nolte E. How health systems make available information on service providers: experience in seven countries. Santa Monica, CA: RAND Corporation; 2011.
- Exworthy M, Smith G, Gabe J, Jones IR. Disclosing clinical performance: the case of cardiac surgery. J Health Organ Manag 2010;24:571-83.
- Mannion R, Goddard M. Impact of published clinical outcomes data: case study in NHS hospital trusts. BMJ 2001;323:260-3.
- Mannion R, Goddard M. Public disclosure of comparative clinical performance data: lessons from the Scottish experience. J Eval Clin Pract 2003;9:277-86.
- Mannion R, Goddard M. Performance measurement and improvement in health care. Appl Health Econ Health Policy 2002;1:13-2.
- Asai RG, Jones KD. Am I obligated to treat a patient whose need for emergency care stems from dental tourism?. J Am Dent Assoc 2007;138:1018-19.
- Inhorn MC, Shrivastav P, Patrizio P. Assisted reproductive technologies and fertility ‘tourism’: examples from global Dubai and the Ivy League. Med Anthropol 2011;31:249-65.
- Gan LL, Frederick JR. Medical tourism in Singapore: a structure–conduct–performance analysis. J Asia Pac Bus 2011;12:141-70.
- Ledger WL, Anumba D, Marlow N, Thomas CM, Wilson ECF. the Cost of Multiple Births Study Group . Fertility and assisted reproduction: the costs to the NHS of multiple births after IVF treatment in the UK. Br J Obstet Gynaecol 2005;113:21-5.
- Snyder B, Wilson T, Mehta S, Bajwa K, Robinson E, Worley T, et al. Past, present, and future: critical analysis of use of gastric bands in obese patients. Diabetes Metab Syndrome Obes 2010;3:55-6.
- O’Neil P. Shedding the pounds: obesity management, NICE guidance and bariatric surgery in England. London: Office of Health Economics; 2010.
- Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess 2009;13.
- National Institute for Health and Care Excellence (NICE) . Costing report. Obesity: Guidance on the Prevention, Identification, Assessment and Management of Overweight and Obesity in Adults and Children n.d. www.nice.org.uk/nicemedia/live/11000/48323/48323.pdf (accessed 10 October 2013).
- Logue J, Sattar N, Bruce J, Bruce D, Lindsay R, Ford I, et al. SurgiCal Obesity Treatment Study: A Prospective Cohort Study n.d. www.controlled-trials.com/ISRCTN47072588/ (accessed 23 September 2013).
- Storrow RF. The pluralism problem in cross-border reproductive care. Hum Reprod 2010;25:2939-43.
- Storrow RF. Assisted reproduction on treacherous terrain: the legal hazards of cross-border reproductive travel. Reprod Biomed Online 2011;23:538-45.
- Van Hoof W, Pennings G. Extraterritoriality for cross-border reproductive care: should states act against citizens travelling abroad for illegal infertility treatment?. Reprod Biomed Online 2011;23:546-54.
- Pennings G, Ombelet W, Tournaye H. Facts, views and vision in obstetrics and gynaecology. Genk: ESHRE; 2010.
- Hudson N, Culley L. Assisted reproductive travel: UK patient trajectories. Reprod Biomed Online 2011;23:573-81.
- Treatment Abroad . Medical Tourism Research: The Treatment Abroad Medical Tourism Survey 2012 n.d. www.treatmentabroad.com/medical-tourism/medical-tourist-research-2012/ (accessed 9 September 2013).
- Leidig M. Tooth tourism transforms town as dental patients flock to Hungary. The Telegraph n.d. www.telegraph.co.uk/news/worldnews/europe/hungary/1409328/Tooth-tourism-transforms-town-as-dental-patients-flock-to-Hungary.html (accessed 9 September 2013).
- O’Neill T. UK’s Dental Tourists Drive Boom n.d. http://news.bbc.co.uk/1/hi/uk/4872884.stm (accessed 15 August 2013).
- Barrowman RA, Grubor D, Chandu A. Dental implant tourism. Aust Dent J 2010;55:441-5.
- Irish Dental Association . New Survey Shows 6,000 Patients Per Annum Receive Corrective Treatment Following Dental Work Abroad n.d. http://idamembers.hostireland.com/resources/news/showarticle.jsp?id=959 (accessed 7 May 2012).
- Molina A, Baker R, Nduka C. ‘What women want’ – the UK’s largest cosmetic surgery survey. Eur J Plast Surg 2012;35:607-12.
- Crockett RJ, Pruzinsky T, Persing JA. The influence of plastic surgery ‘reality TV’ on cosmetic surgery patient expectations and decision making. Plast Reconstr Surg 2007;120:316-24.
- Latham M. A poor prognosis for autonomy: self-regulated cosmetic surgery in the United Kingdom. Reprod Health Matters 2010;18:47-55.
- British Association of Plastic, Reconstructive and Aesthetic Surgeons . Cosmetic Surgery Tourism Facts and Figures 2011. www.bapras.org.uk/guide.asp?id=61 (accessed 15 August 2013).
- Bradbury E. Clinical risk in cosmetic surgery. Clin Risk 2009;15:227-31.
- McGrath MH. The psychological safety of breast implant surgery. Plast Reconstr Surg 2007;120:103-9.
- No patient left behind. London: HMSO; 2008.
- Svenberg K, Skott C, Lepp M. Ambiguous expectations and reduced confidence: experience of Somali refugees encountering Swedish health care. J Refug Stud 2011;24:690-705.
- Gerritsen A, Bramsen I, Devillé W, van Willigen L, Hovens J, van der Ploeg H. Physical and mental health of Afghan, Iranian and Somali asylum seekers and refugees living in the Netherlands. Soc Psychiatry Psychiatr Epidemiol 2006;41:18-26.
- Tiilikainen M, Koehn PH. Transforming the boundaries of health care: insights from Somali migrants. Med Anthropol 2011;30:518-44.
- Feldmann CT, Bensing JM, de Ruijter A. Worries are the mother of many diseases: general practitioners and refugees in the Netherlands on stress, being ill and prejudice. Patient Educ Couns 2007;65:369-80.
- Pavlish CL, Noor S, Brandt J. Somali immigrant women and the American health care system: discordant beliefs, divergent expectations, and silent worries. Soc Sci Med 2010;71:353-61.
- Warfa N, Bhui K, Craig T, Curtis S, Mohamud S, Stansfeld S, et al. Post-migration geographical mobility, mental health and health service utilisation among Somali refugees in the UK: a qualitative study. Health Place 2006;12:503-15.
- Safeer RS, Keenan J. Health literacy: the gap between physicians and patients. Am Fam Physician 2005;72:463-8.
- Borman E. Health tourism. BMJ 2004;328:60-1.
- Medical tourism: a global analysis. Tilburg, the Netherlands: Association for Tourism and Leisure Education (ATLAS); 2006.
- Johnson TJ, Garman AN. Impact of medical travel on imports and exports of medical services. Health Policy 2010;98:171-7.
- Health & Social Care Information Centre . Hospital Episode Statistics n.d. www.hscic.gov.uk/hes (accessed 9 September 2013).
- Private healthcare market study. Report on the market study and final decision to make a market investigation reference. London: Office for Fair Trading; 2012.
- Fertility: assessment and management (update). London: NICE; 2012.
- Connolly MP, Hoorens S, Chambers GM. The costs and consequences of assisted reproductive technology: an economic perspective. Hum Reprod Update 2010;16:603-13.
- Koivurova S, Hartikainen A-L, Gissler M, Hemminki E, Järvelin M-R. Post-neonatal hospitalization and health care costs among IVF children: a 7-year follow-up study. Hum Reprod 2007;22:2136-41.
- Office for National Statistics . Statistical bulletin. Live Births in England and Wales by Characteristics of Birth, 2010 n.d. www.ons.gov.uk/ons/dcp171778_241936.pdf (accessed 10 October 2013).
- Meikle J. PIP breast implants pose no long-term health threat, say experts. The Guardian n.d. www.theguardian.com/world/2012/jun/18/pip-breast-implants (accessed 9 September 2013).
- Tackling obesity in England. London: The Stationery Office; 2001.
- Hawkins SC, Osborne A, Finlay IG, Alagaratnam S, Edmond JR, Welbourn R. Paid work increases and state benefit claims decrease after bariatric surgery. Obes Surg 2007;17:434-7.
- NHS Choices . Cosmetic Surgery Abroad n.d. www.nhs.uk/Livewell/Treatmentabroad/Pages/Cosmeticsurgeryabroad.aspx (accessed 9 September 2013).
- National Travel Health Network and Centre . Travellers. Travel Health Information Sheets n.d. www.nathnac.org/travel/misc/medicaltourism_010911.htm (accessed 9 September 2013).
- Legido-Quigley H, Passarani I, Knai C, Busse R, Palm W, Wismar M, et al. Cross-border healthcare in the European Union: clarifying patients' rights. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d296.
- Human Fertilisation and Embryology Act 1990. London: HMSO; 1990.
- Consultation on proposals to transfer functions from the Human Fertilisation and Embryology Authority and the Human Tissue Authority. London: HFEA; 2012.
- McDonagh C. Quangoing, going, gone: what should happen to the HFEA?. BioNews 2012.
- Cook JL, Collins J, Buckett W, Racowsky C, Hughes E, Jarvi K. Assisted reproductive technology-related multiple births: Canada in an international context. J Obstet Gynaecol Can 2011;33:159-67.
- Laurent MR, Vickers TJ. Seeking health information online: does Wikipedia matter?. J Am Med Inform Assoc 2009;16:471-9.
- General Dental Council . Going Abroad for Your Dental Treatment. What You Need to Know before You Go n.d. www.gdc-uk.org/newsandpublications/publications/publications/going%20abroad%20for%20your%20dental%20care.pdf (accessed 9 September 2013).
- Health on the Net Foundation . The HON Code of Conduct for Medical and Health Websites (HONCode) n.d. www.hon.ch/HONcode/Conduct.html (accessed 9 September 2013).
- Meric F, Bernstam EV, Mirza NQ, Hunt KK, Ames FC, Ross MI, et al. Breast cancer on the world wide web: cross sectional survey of quality of information and popularity of websites. BMJ 2002;324:577-81.
- Khazaal Y, Fernandez S, Cochand S, Reboh I, Zullino D. Quality of web-based information on social phobia: a cross-sectional study. Depress Anxiety 2008;25:461-5.
- Shaw C, Groene O, Mora N, Sunol R. Accreditation and ISO certification: do they explain differences in quality management in European hospitals?. Int J Qual Health Care 2010;22:445-51.
- Nicklin W, Dickson S. The value and impact of accreditation in health care: a review of the literature. Toronto: Accreditation Canada; 2009.
- Shaw C, Bruneau C, Kutryba B, de Jongh G, Suñol R. Towards hospital standardization in Europe. Oxford: Oxford University Press; 2010.
- Shaw C, Braithwaite J, Moldovan M, Nicklin W, Grgic I, Fortune T, et al. Profiling healthcare accreditation organisations: an international survey. Int J Qual Health Care 2013;25:222-31.
- Shaw C. Quality and accreditation in health services: a global review. Geneva: World Health Organization and International Society for Quality in Health Care; 2003.
- Braithwaite J, Westbrook J, Pawsey M, Greenfield D, Naylor J, Iedema R, et al. A prospective, multi-method, multi-disciplinary, multi-level, collaborative, social-organisational design for researching health sector accreditation. BMC Health Serv Res 2006;6:1-10.
- Greenfield D, Braithwaite J. Health sector accreditation research: a systematic review. Int J Qual Health Care 2008;20:172-83.
- Mihalik GJ, Scherer MR, Schreter RK. The high price of quality: a cost analysis of NCQA accreditation. J Health Care Finance 2003;29:38-47.
- Joint Commission International . JCI Accredited Organizations 2011. www.jointcommissioninternational.org/JCI-Accredited-Organizations/ (accessed 15 August 2013).
- Woodhead A. Scoping medical tourism and international hospital accreditation growth. Int J Health Care Qual Assur 2013;26:688-702.
- Hospital Corporation of America . NHS Ventures 2012. www.hcahospitals.co.uk/about-hca-partnering.asp (accessed 3 October 2012).
- Timmins N. NHS trusts set up deals to avoid private income caps. Financial Times 2007.
- Great Ormond Street Hospital . Gulf Office 2012. www.gosh.com.kw/about-us/gulf-office/ (accessed 15 August 2013).
- Moorfields . Moorfields Eye Hospital Dubai 2012. http://moorfields.ae (accessed 3 October 2012).
- AMEinfo.com . Moorfields Turns Its Sights on Enhancing Patient and Customer Services 2011. www.ameinfo.com/269582.html (accessed 15 August 2013).
- AMEinfo.com . Moorfields Eye Hospital Dubai, Now Health International Sign Medical Services Provider Agreement 2011. www.ameinfo.com/272363.html (accessed 15 August 2013).
- Clover B. FT plans 20 per cent growth in private patient income. Health Serv J n.d. www.hsj.co.uk/ft-plans-20-per-cent-growth-in-private-patient-income/5034288.article (accessed 15 August 2013).
- Health and Social Care Act 2003. London: The Stationery Office; 2003.
- Birtwistle M. Guy'S Breaching Private Patient Cap After Twins Procedure n.d. www.hsj.co.uk/hsj-local/acute-trusts/guys-and-st-thomas-nhs-foundation-trust/guys-breaching-private-patient-cap-after-twins-procedure/5036152.article (accessed 9 September 2013).
- White Paper. Equity and excellence: liberating the NHS. London: Department of Health; 2010.
- Great Ormond Street Hospital . NHS Work at Great Ormond Street Hospital 2012. www.gosh.nhs.uk/news/press-releases/2012-press-release-archive/nhs-work-at-great-ormond-street-hospital/ (accessed 15 August 2013).
- Exworthy M, Frosini F, Jones L. Are NHS foundation trusts able and willing to exercise autonomy? ‘You can take a horse to water . . .’. J Health Serv Res Policy 2011;16:232-7.
- The plan for growth. London: The Stationery Office; 2011.
Appendix 1 The implementation of the EU directive on cross-border health care: potential relevance for medical tourism
Introduction and background
European Union directives outline end results to be achieved by every member state. National authorities must adapt their laws to meet these goals but have the freedom to decide how this is done. In 2006 the European Parliament voted for the exclusion of health services from the scope of the Services Directive 2006/123/EC, designed to increase internal service trade within the European zone. The directive relevant to cross-border health care was proposed, which treats health with these specificities. Under this directive, which came into force in 2013, EU patients are able to access health care across borders as a right – under certain conditions.
Health care that falls outside of the directive includes:
-
long-term care
-
organ transplants
-
vaccination programmes.
This summary assesses the implementation of the directive and comments on/highlights potential points of relevance for medical tourism within the UK context. The points of focus are:
-
entitlements and authorisation
-
care while abroad and continuity of care
-
patient information
-
regulation of advertising.
Throughout this discussion the ‘state of affiliation’ refers to the state that is competent to offer the patient authorisation to travel under the directive. The ‘state of treatment’ refers to the member state on whose territory health care is provided to the patient. Cross-border health care refers to health care provided or prescribed in a member state other than the member state of affiliation (under the directive).
Entitlements and authorisation
What treatments are patients entitled to cross borders for under the directive?
Patients may receive treatment in another EU country under the directive for treatments to which they are entitled in their state/country of affiliation. 1,237 In addition, the treatment must be unavailable within a reasonable time frame in the country of affiliation, that is, the directive explicitly aims to address undue delay for treatment found to be offered elsewhere in the EU in a shorter time period. The state of affiliation (not state of treatment) determines whether at a local or national level the patient is entitled to the health care (Chapter III, Article 7.3). Under the clarified rights there are only certain circumstances under which health care can be refused.
Do patients need to obtain authorisation?
There are certain circumstances under which patients must acquire prior authorisation before choosing to cross a border for health care. These include when the treatment involves overnight hospital accommodation for at least one night; requires the use of highly specialised cost-intensive medical infrastructure or equipment; involves treatment that has the potential to pose a particular risk to the patient (or population); or when there could be serious concerns about quality and safety of care (Article 8, Part 2). The state of affiliation may object if the health care offered by a provider raises serious and specific concerns relating to quality of care and patient safety. Authorisation can also be rejected if the health care can be provided on the member state’s own territory within a time limit that is medically justifiable, taking into account the current state of health and the probable course of illness of each patient concerned [Article 8, Section 6(d)].
Under the directive, member states organise their own method of administrative formalities for reimbursement of health care. For example, a member state may require that patients receive a referral from a GP before receiving hospital care. If a member state does introduce prior authorisation, then this must be identified and made publicly available (Article 42). The directive also advises that this must be carried out in a transparent manner and ‘should not impose any additional burden on patients seeking healthcare in another member state in comparison to patients being treated in their State of affiliation, and that decisions should be made as quickly as possible’ (Article 37).
States of treatment may object to treating foreign patients in certain circumstances, the main reason being if a patient’s request for treatment would interfere with planned national health systems, for example if the treatment centre did not have the capacity to treat non-domestic patients. The directive outlines that foreign patients must not be favoured over domestic patients.
How are patients reimbursed?
Under the directive, reimbursement for treatment is based on the rate of the treatment state and reimbursement to the patient is determined by the rate of the state of affiliation. The treatment providers are not allowed to charge incoming patients at a different rate from their domestic patients. Patients will be reimbursed only up to the amount that it would cost in their state of affiliation.
Member states are required to reimburse specifically for the health care received as a minimum. In addition to this, the state of affiliation may decide to reimburse other costs such as accommodation and travel, ‘or extra costs which persons with disabilities might incur due to one or more disabilities when receiving cross-border healthcare’. This will be in accordance with national legislation and there must be sufficient documentation setting out these costs (Chapter III, Article 7.4).
Relevance for medical tourism
In the UK context of cross-border care, patients are typically reimbursed specifically for the health care received. However, if NHS patient eligibility for domestic travel benefits were expanded to include cross-border travel this would have implications (see www.nhs.uk/NHSEngland/Healthcosts/Pages/Travelcosts.aspx). Any expansion to the NHS Low Income Scheme would remove potential cost barriers for lower-income groups to access care under the directive. Those that fall outside the scheme would still need to meet their costs of travel (for further information on the travel costs scheme see http://www.nhs.uk/NHSEngland/Healthcosts/Pages/Travelcosts.aspx).
Under the directive patients’ needs must be considered on a case-by-case basis, which includes medical need and the ability to carry out professional activity. This requirement will complicate the possibility of issuing clear statements of eligibility for both GPs and patients.
If GPs become the route to prior authorisation, this may impact on those travellers who are seeking a service abroad that they could be expected to receive within the primary care setting. This will therefore require GPs to be educated and sensitised should they become gatekeepers for cross-border travel.
Care while abroad and continuity of care
In the UK, when patients make the choice to travel abroad (for both out-of-pocket and cross-border care) it is up to them to make sure that they are insured and that they are aware of what NHS entitlements will cover. The directive stipulates that:
Member states should ensure that mechanisms for the protection of patients and for seeking remedies in the event of harm are in place for healthcare provided on their territory and that they are appropriate to the nature and extent of the risk. However, it should be for the Member State to determine the nature and modalities of such a mechanism.
Article 24
Medical travellers who pay out of pocket may benefit from clarification being developed around cross-border care. A reinstatement of NHS eligibility and responsibility may allow the opportunity to clarify a range of patient circumstances, including what aftercare will be given and aspects of care that are the patient’s own responsibility and when the NHS will not assume liability.
Continuity of care is another aspect for which there may be spillover effects for medical tourism that result from clarifying cross-border rights. The directive outlines that patients who have received care in another state are entitled to a written or electronic medical record of such treatment [Article 4(f)]. In addition, when a patient has received cross-border health care and medical follow-up proves necessary, the same medical follow-up is available as would have been if that health care had been provided on the patient’s territory [Article 5(c)].
However, matters are complicated concerning redress. Under the directive, the NHS is required to treat the patient only in relation to medical need. Outside of this, redress would need to be followed up in the state of treatment, which may incur further travel and accommodation costs to the patient.
Patient information
The means of carrying out the objectives of the directive are largely left to the individual member states. Under the directive, member states will be required to have national contact points that aim to facilitate the exchange of information. A certain amount of information must be provided by these contact points and is likely to be put forward voluntarily. All information made available through national contact points must be easily accessible and shall be made available by electronic means and in formats accessible to people with disabilities, as appropriate (Chapter 2, Article 6.5). Member states will also be able to decide on the number of national contact points and these can be designed to be built into pre-existing information centres (Article 49). Medical tourism may receive some spillover benefits from the provision of information by contact points.
The contact points will play differing roles when acting as treatment states or states of affiliation. When acting as the treatment state, the contact point must make available information on quality and safety standards and guidelines, patient rights, redress mechanisms and complaints procedures. States of treatment are required to provide, on request, relevant information on standards and guidelines. This includes information on the provisions for supervision and assessment of health-care providers; which health-care providers are subject to these standards and guidelines; and the accessibility of hospitals for persons with disabilities [Chapter 2, Article 4(a)]. The contact points must also provide information on the legal and administrative options available to help patients settle disputes, including in the event of harm arising from cross-border health care (Chapter 2, Article 6.3). Medical tourists may use such information to inform their own out-of-pocket treatment decisions.
A state of affiliation must make available on request information on patient rights and entitlements in that member state relating to receiving cross-border health care, in particular regarding the terms and conditions for reimbursement of costs, and procedures for accessing and determining those entitlements and for appeal and redress if patients consider that their rights have not been respected [Article 5(b)].
In addition to the national contact points, health-care providers will also need to provide relevant information for a patient to make an informed choice about treatment and the availability, quality and safety of the health care provided in the state of treatment. They must also provide clear invoices and clear information on prices [Chapter 2, Article 4(b)]. This should already be provided to domestic patients. These requirements may again have spillover effects for medical travellers who seek treatment outside of the directive. Greater transparency around quality and safety and invoicing may inform the treatment decisions of outward medical travellers. The requirement for NHS facilities to provide further information on tariffs may have implications for international patients’ decision-making as they look across NHS providers and make comparisons with the private sector and facilities elsewhere in Europe and further afield.
Although the directive outlines that member states must make information available, there is likely to be great variation in the way in which this information is received.
Irrespective of how much information about rights is provided by countries under the directive, the decision to travel will remain that for the individual to make. Patients are to be informed about what is available to them, yet this should be without the intention of promoting the services abroad. Accurate and transparent reporting on use of the directive and its implementation, including when complications may arise, will require some form of oversight body.
Regulation of advertising
In addition to the directive, treatment providers must adhere to general provider guidelines in European directives designed to increase internal service trade within the European zone. These include making information available with regard to informed choice, treatment options and risks. Health-care providers will need to provide relevant information, including on the availability, quality and safety of the health care that they provide in the state of treatment, so that patients can make an informed choice about treatment options. They must also provide clear invoices and clear information on prices [Chapter 2, Article 4(b)]. Such requirements will have a bearing on advertising practices. Given that information may be sourced through a number of ways (internet, by word of mouth, community television), marketing is more complex to regulate.
Appendix 2 Protocol
Appendix 3 Example interview questions
Example interview questions for medical tourists
-
What treatment/s have you gone overseas for? Where did you go?
-
Why did you not have the treatment in the UK?
-
How did you first find out that it was possible to have treatment overseas? From whom?
-
Did you ask anyone or look for advice on how to go about having treatment overseas?
-
How did you choose which agency/hospitals/clinician to have your treatment with? What factors were a priority when choosing?
-
What additional services were you made aware of by the agency/hospital when planning your treatment?
-
Did you take out any travel insurance for your trip/treatment?
-
Did you require any pretreatment checks? Who carried these out and where?
-
Did anyone travel/stay with you when going overseas for treatment?
-
How was your experience of accessing treatment overseas? How could it have been improved? Would you say you are satisfied with the outcome of your treatment abroad?
-
Was the language barrier between you and the hospital staff a concern for you?
-
How were you made aware of any risks associated with the treatment before it began?
-
Did you have any postoperative care requirements? How were these met? By whom?
-
What responsibility does the NHS have to those people who travel overseas for treatment?
-
How do you feel about people travelling to the UK to have treatment on the NHS?
-
Would you recommend going overseas for treatment to others?
Costs
-
Travel/accommodation/transfers.
-
Self/accompanied.
-
How long stay.
-
Aftercare/after-service:
-
which/what
-
hotel/recuperation
-
pharmacy
-
bandages/dressings, etc.
-
removal of sutures, etc.
-
follow-up appointments/consultations.
-
-
Tourism/visiting, etc.
-
Other costs (visa, insurance).
Example interview questions for industry
-
Tell me about the work you do here/your role.
-
How did you get into this business?
-
What services does your business offer? Insurance? Sightseeing, transfer of medical records, transport?
-
Can you identify your closest competition?
-
How do you attract customers to use your services that don’t rely on/use/have access to the internet?
-
Can you explain the process after someone contacts your agency/views your website and wishes to go overseas for treatment (telephone, e-mail, face to face?)
-
Is your advice sought after by potential medical tourists? Do you see that as part of your role – to draw on your experience?
-
How do you and medical tourists overcome the language barriers that arise from accessing treatment overseas?
-
How do you choose which hospitals/clinics to work with? Are they chosen by the customer already or do you advertise particular venues/experts?
-
Have you any insights into how your customers handle the postop care arrangements? Does your business deal with the recovery needs of the customers?
-
How do you deal with customers reporting bad experiences to you? What are the ramifications for your company? The hospital and surgeon?
-
Are there aspects of the medical tourism industry that you don’t yet provide or conduct that you wish to in the future? Particular groups of customers that you wish to attract?
-
What is needed for the medical tourism industry to grow? What could hinder the future growth of the medical tourism industry?
Example interview questions for NHS commercial/international/private patient managers
Background
-
Numbers of international tourists (type of treatment, country, age/gender, etc.).
-
Where is funding from? Out of pocket, central government, third-party insurers?
-
Reasons for patient travelling – cost, quality, etc.
-
Trends – which areas in above are growing/declining?
-
How services are marketed to different groups.
-
Which patients generate most revenue/profit?
-
Price elasticity of treatment – how sensitive are different patient groups/treatments to increasing/lower prices?
Development
-
Implications of lifting private patient cap on recruiting international patient groups above.
-
Marketing strategies (including websites) used for different potential patient groups – branding, etc.
-
Problems with entry (e.g. visas) and suggestions for overcoming barriers to entry.
-
Competitors for specific treatments/patient groups:
-
national
-
international.
-
Wider policy considerations
-
Complications and unintended consequences of international patients. Any knock-on costs for the UK?
-
Central government support and enterprise support for developing services – trade missions, etc.
-
Plans for the future.
Example interview questions for NHS managers (commissioning)
-
Tell me about the work you do here/your role.
-
How did you get into this role?
-
Why do you believe that people pay for medical treatment overseas?
-
Do you view people accessing treatment overseas as patients, customers or consumers? Does your perception vary according to which treatment is being sought after?
-
Do you foresee any risks with opting to pay for treatment overseas?
-
How can we make accessing treatment overseas safer?
-
In your opinion, are there aspects of the medial tourism process that bring up ethical or legal dilemmas?
-
Are there particular treatments that you believe should not be available through medical tourism agencies?
-
What impact does medical tourism have on the NHS? Its staff? Budget? Its public perception? In the long and short term?
-
Can medical tourism provide opportunities for the NHS?
-
Are you aware of people travelling to the UK to access treatment through the NHS or private clinics? What do you believe are the issues that arise from this travel and care?
-
Have you any insight into how medical tourists handle the postop care arrangements? Are you aware of hospitals that have dealt with the recovery needs of medical tourists?
-
Whose responsibility is it to deal with any complications that arise after medical treatment paid for overseas?
-
In the current economic climate, what does the future hold for the medical tourism industry?
Example interview questions for professional associations
-
Tell me about your role within the association.
-
What role does the association provide to its members?
-
Does the association have a role within wider society? Within government?
-
Is it the role and responsibility of the association to provide advice or guidelines to potential medical tourists? Those working within the medical field?
-
Why do you believe that people pay for medical treatment overseas?
-
Is there enough regulation around the medical tourism industry?
-
Do you foresee any risks with opting to pay for treatment overseas?
-
How can we make accessing treatment overseas safer?
-
In your opinion, are there aspects of the medial tourism process that bring up ethical or legal dilemmas?
-
Are there particular treatments that you believe should not be available through medical tourism agencies?
-
Do you see/hear about medical tourism having implications for your members? Your profession?
-
Have you any insight into how medical tourists handle the postop care arrangements? Are you aware of hospitals that have dealt with the recovery needs of medical tourists?
-
Whose responsibility is it to deal with any complications that arise after medical treatment paid for overseas?
-
Are you aware of people travelling to the UK to access treatment through the NHS or private clinics? What do you believe are the issues that arise from this travel and care?
-
In the current economic climate, what does the future hold for the medical tourism industry?
Example interview questions for overseas providers
-
Numbers of international tourists (type of treatment, country, age/gender, etc.) and types of services offered/utilised.
-
Trends – which areas above are growing/declining? Where are they seeking to develop?
-
How services are marketed to different groups:
-
marketing strategies (including websites), word of mouth, clinician referral, brokers.
-
-
Treatment pathways:
-
preconsultations
-
use of brokers.
-
-
Competitors for specific treatments/patient groups:
-
national
-
international.
-
-
Observations on quality of care.
-
Do you foresee any risks with opting to pay for treatment overseas?
-
How can we make accessing treatment overseas safer?
-
role of accreditation
-
role of national/international guidance/legislation.
-
-
Aftercare and follow-up – whose responsibility is it to deal with any complications that arise after medical treatment paid for overseas?
-
Ethics and legal – in your opinion, are there aspects of the medial tourism process that bring up ethical or legal dilemmas?
-
Plans for the future – any possible problems/barriers with regard to developing services?
Appendix 4 Confidentiality agreement for transcriber
Appendix 5 Research participation information sheet
Appendix 6 Consent form
Appendix 7 Recruitment networks and calls for information
Online channels through which recruitment was attempted
Beauty in Prague Forum.
Big Matters.
Cosmedia.
Cosmetic Compare.
Cosmetic Surgery Forums.
Donor Conception Network.
eHealth Forum.
Fertility Friends.
Gay Family Web.
Infertility Network UK.
Linda Briggs forum.
Look Your Best.
Michelmores.
MoneySave Supermarket.
National Gamete Donation Trust.
Patient Opinion.
PlacidWay.
RealSelf.
Secret Surgery.
So feminine.
Surgery Overseas Forum.
Treatment Abroad.
Weight Loss Surgery Information and Support [site and Facebook (Facebook, Inc., Menlo Park, CA, USA)].
Journals which carried article about the study and recruitment
International Medical Travel Journal (IMTJ) and The Probe Magazine.
Network gatekeepers assisting with sample recruitment
Martin Rathfelder, Somali Adult Social Services, Nina Lakhani and Ubah Egal.
Project website
Appendix 8 Advisory group terms of reference and membership
Advisory group terms of reference and membership (PDF download)
Appendix 9 Treatment pathways for medical tourists interviewed as part of the study
Bariatric surgery
| Patient | Procedure | Destination | Motivation | Treatment pathwaya | Cost savings (£)b |
|---|---|---|---|---|---|
| BT1 | Gastric band | Belgium | Experience, distance, cost | Model 5, internet, online patient forum | 7000 |
| BT2 | Gastric band | France | Recommendations, NHS waiting list, mortality rate | Media, personal contact | 3500 |
| Gastric bypass | Poland | ||||
| BT3 | Gastric wrap | Prague, Czech Republic | Cost | Online patient forum, booked through facilitator | 1000 |
| BT4 | Gastric band | Bruges, Belgium | Cost, surgeon experience | Internet | 4000 |
| BT5 | Gastric band | Belgium | NHS criteria not met, distance, cost | Online patient forum, internet | 7000 |
| BT6 | Gastric bypass | Bruges, Belgium | Treatment not available, experience, cost | Web forum | 5000 |
| BT7 | Gastric band, tummy tuck | Belgium | NHS criteria, cost, no wait | Internet, facilitator, preconsultation in London | 8000 |
| BT8 | Duodenal switch | Belgium | Waiting list, experience, treatment not available at the time | Online patient forum | 7000 |
| BT9 | Gastric band | Brussels, Belgium | NHS said no, agency, cost | Online patient forum | 5400 |
| BT11 | Pancreatic diversion and duodenal bridge | Belgium | NHS criteria, experience | Personal recommendation | 5000 |
| BT12 | Gastric band | Belgium | Cost | Internet, London contact | 10,000 for both patients |
| BT13 | Abdominoplasty and liposuction | Poland | Cost | Internet | 2300 |
Fertility surgery
| Patient | Procedure | Destination | Motivation | Outcomes/complication | Cost (and savings) |
|---|---|---|---|---|---|
| FT1 | IVF/egg donation | Brno, Czech Republic | Needed donor eggs/time, not eligible on NHS (age) | Pregnancy/multiple births | None, cost £10,000–14,000 |
| FT2 | IVF | Czech Republic | Low likelihood of success meant not available free on NHS, cost and experience of UK private treatment | No pregnancy – followed up with egg donation in Dublin | Cost £2400 compared with £7500 in the UK |
| FT3 | IVF/ICSI | Cyprus (North) | Exhausted free NHS cycles, cost of private treatment | Pregnancy | Cost £3650 excluding flights and premedication, but inclusive of all other treatment and accommodation. Meds cost £800 (although this was not paid). This is compared with £6000 in Edinburgh |
| FT4 | IVF/egg donation/ICSI | Kiev, Ukraine | Early menopause, no provision on the NHS, donor needed | Pregnancy/twins, early pregnancy | Cost £20,000 |
| FT5 | IVF/egg donation | Kiev, Ukraine | No provision on the NHS, multiple miscarriages and extremely high risk of Down syndrome, donor | Pregnancy (third cycle) | Cost £22,000 |
| FT6 | IVF | Sweden | NHS waiting time –exacerbated by long diagnosis time of endometriosis, didn’t like private UK treatment | Pregnancy (three children from two cycles) | Cost roughly £8000 (reading between lines). Represented a £2000 saving (ish) but this was offset by travel and taking time off work |
| FT7 | IVF | Czech Republic | NHS waiting time, private costs and desire for ignorance | No pregnancy despite four cycles | £1000 for treatment compared with £3500 in the UK. Medication £500 (sourced in the Czech Republic) compared with £1000 in the UK. With flights and accommodation total cost £3000, so roughly a £1500 saving |
| FT8 | IVF/egg donation (prospective) | Madrid | Not eligible on NHS, waiting times, private costs | Prospective | Hard to tell, all in it appears to be £12,000, which FT8 seems to believe is a major saving |
| FT9 | IVF/sperm donation/egg donation | Alicante, Spain | Not eligible on NHS or French SS | Two failed cycles in the UK and one successful in Alicante, pregnancy to term | £7000 for treatment in Alicante but a total of > £21,000 for all treatment |
Dental surgery
| Patient | Procedure | Destination | Motivation | Outcomes/complication | Cost (and savings) |
|---|---|---|---|---|---|
| DT1 | Crowns and bridges for multiples | Croatia | No NHS treatment and then cost. Cost the motivator for overseas treatment rather than UK private treatment | Satisfied | Cost £4000 – saving of £36,000? |
| DT2 | Implants | Hungary | Cost, experience of dentist | Satisfied | Saving |
| DT3 | Emergency and cosmetic | Germany | Bad UK private experience | Satisfied | Minimal |
| DT4 | Restoration? 11 implants | Hungary | Word of mouth | Work had to be redone | Cost £40,000 to have rectified |
| DT5 | Brace to bottom jaw | Poland | Lack of NHS treatment – waiting times and cost, boyfriend speaks Polish, word of mouth, holiday | Satisfied | Even including the cost of flights, the total cost was less than half |
| DT6 | Routine | India | Cultural | Satisfied | No saving |
| DT7 | Bridge and plate | Croatia | No NHS treatment and then cost. Cost the motivator for overseas treatment rather than UK private treatment | Satisfied | Estimated anywhere between £15,000 and £35,000 |
| DT8 | Routine | Italy | Cultural | Satisfied | No costs incurred |
| DT9 | Crowns and fillings | Lithuania | Cost | Satisfied | Cost £5200 including flights compared with £18,000 |
| DT10 | Routine | Germany | Distrust of NHS and cultural reasons | Satisfied | No cost saving |
| DT11 | Implant | Hungary | Cost and holiday | Satisfied | Cost £400 plus flights; perceived all-in saving of £200 (cost for treatment in UK £1200) |
Cosmetic surgery
| Patient | Procedure | Destination | Motivation | Outcomes/complication | Cost (£) |
|---|---|---|---|---|---|
| CT1 | Facelift | Prague | Price, previous experience | Satisfied | 3300 |
| CT2 | Thigh liposuction | Prague | Price, expertise | 1200 + | |
| CT3 | Tummy tuck, liposuction, arm lift | Belgium | Price | 6600 | |
| CT4 | Minimal access cranial suspension lift | Brussels, Belgium | Price, expertise | Satisfied | 2000 |
| CT5 | Facelift | Prague, Czech Republic | Price | 4000 | |
| CT6 | Abdominoplasty, liposuction | Poland | Price | Satisfied | 3500 |
| CT7 | Face and neck lift | Lahore, Pakistan | Price | Satisfied | 3800 |
| CT8 | Caesarean section tummy tuck | Prague | Price | Major infection | 2600 |
| CT9 | Nose, face, eyes | Poland | Price | Complication | 5000 |
Other medical tourists
| Patient | Procedure | Destination | Motivation | Outcomes/complication | Cost (£) |
|---|---|---|---|---|---|
| OT1 | Buttock/nerve surgery | Los Angeles, California | Pain, expertise, lack of NHS availability | Needed second operation but hasn’t worked | 78,000 |
| OT2 | Ultrasound | Germany | Lack of NHS availability | Ongoing visits | 0–150 |
| OT3 | Shoulder stabilisation | Belgium | Poor NHS response, pain/lack of faith | Some restriction of movement | 2500 |
| OT4 | Needle for Dupuytren’s contracture | France | Lack of NHS availability | Ongoing treatment | 30 |
| OT5 | Immunotherapy for breast cancer | Athens, Greece | Lack of NHS availability | In remission but ongoing treatment | Free treatment (travel) |
| OT6 | Check-ups (GP/gynaecology/eyes/dermatology) | Paris, France | Lack of faith in NHS | Ongoing visits | Free treatment (travel) |
Appendix 10 Search strategy for systematic review
The systematic review of the literature followed a number of strategies. Key papers in journals and other researchers working on the issue of medical tourism were identified, including through the interviews. Follow-up with several academics was conducted to ensure that additional research and emerging publications would be considered as part of the review.
A review of key literature databases was conducted in October and December 2011 using the terms ‘medical tourism’, ‘health tourism’, ‘tourism AND medicine’ and ‘tourism AND health’. No restrictions in terms of publication dates were made.
The following table lists the databases searched, the search terms used and the exact number of hits achieved for each database.
| Database | No. of hits | Search terms |
|---|---|---|
| MEDLINE | 360 | ‘health tourism’, ‘medical tourism’, ‘medicine, tourism AND health’, ‘tourism AND medicine’ |
| ISI Web of Science | 878 | ‘medical tourism’, ‘health tourism’, tourism AND medicine’, ‘tourism AND health’ |
| EMBASE | 546 | ‘health tourism’, ‘medical tourism’, ‘medicine, tourism AND health’, ‘tourism AND medicine’ |
| Global Health | 514 | ‘medical tourism’, ‘health tourism’, tourism AND medicine, and tourism AND health’ |
| Health Management Information Consortium (HMIC) | 77 | ‘health tourism’, ‘overseas treatment’, ‘overseas patients’, ‘health tourism’ |
| EconLit | 280 | ‘medical tourism’, ‘health tourism’, ‘tourism AND medicine’, ‘tourism AND health’ |
In total, 2295 papers (including duplicates) were identified through the database searching. Two papers were also included based on recommendations from people interviewed as part of the research project. 91,102
Review criteria
The initial selection of papers was undertaken following a review of titles that had a general focus on medical tourism. The following were excluded: papers on well-being or travel for assisted suicide, news items, commentaries, laws or directives and conference proceedings. One exception was made in the case of a news report published in the Lancet. Only articles published in English and German were included.
Following a review of titles and abstracts, 425 papers remained. Out of this sample a further 21 papers focusing on stem cell tourism and 29 papers focusing on transplant tourism were excluded as these are distinct areas of tourism with specific ethical issues. In addition, one guideline from the American Medical Association was excluded, leaving 374 papers.
Of the 374 remaining papers, the abstract or entire paper for each was reviewed to determine whether or not to include it in the review. In addition, references of the papers identified through the review of the literature were further examined to ensure that all relevant papers were included.
In line with the overall research objectives, papers were selected to see how much they could contribute to understanding medical tourism as an industry, as a trade in health services and from a patient perspective.
Emphasis was on papers published in peer-reviewed journals that had a global focus on medical tourism or a focus specific to the UK (i.e. the review excluded papers that focused exclusively on medical tourism to one country or the effects of medical tourism on one country, for example the USA, unless there was a specific UK link) or to dental, fertility, cosmetic, bariatric or diaspora tourism, which form specific case studies within the overall research project. Articles were included when primary research had been conducted in one country but the framework, conclusions and discussion demonstrated that findings were transferable.
The research project is also undertaking a review of websites to better understand the industry and providers. Given this emphasis, papers focusing on medical tourism provider websites were included. Papers that focused from an industry perspective on the management or organisational issues (e.g. on how to lead virtual teams working within the medical tourism industry) were excluded when these did not draw wider conclusions on the issue of medical tourism as a whole.
There is a body of literature examining issues relating to medical tourism, including issues of transplant, stem cell and surrogacy tourism, from an ethical and philosophical perspective. This literature has not been considered here.
A number of studies explored the impact of medical tourism on the health-care system and professionals within a specific country; these have not been included in this review of the literature unless their findings shed light on the wider phenomenon of medical tourism. Papers focusing exclusively on the implementation of the EC directive on cross-border patient care (e.g. Hawkins et al. 234) were also excluded.
On the basis of these criteria 276 papers were excluded. Following the review of the papers, four additional studies were included that had not emerged from the initial literature searches. Two papers were not accessible and were therefore excluded. Based on these criteria 100 papers8,10–12,17,26,40,42–134 were included in this review.
Review process
Two authors independently reviewed the papers and then met to compare results. A third author tested a sample of papers. The initial results of the review were presented to the study advisory board and following input a further search term of ‘cross-border care’ was run. However, this did not yield any additional papers that had not already been included in the original search.
Appendix 11 Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram for literature review of medical tourism
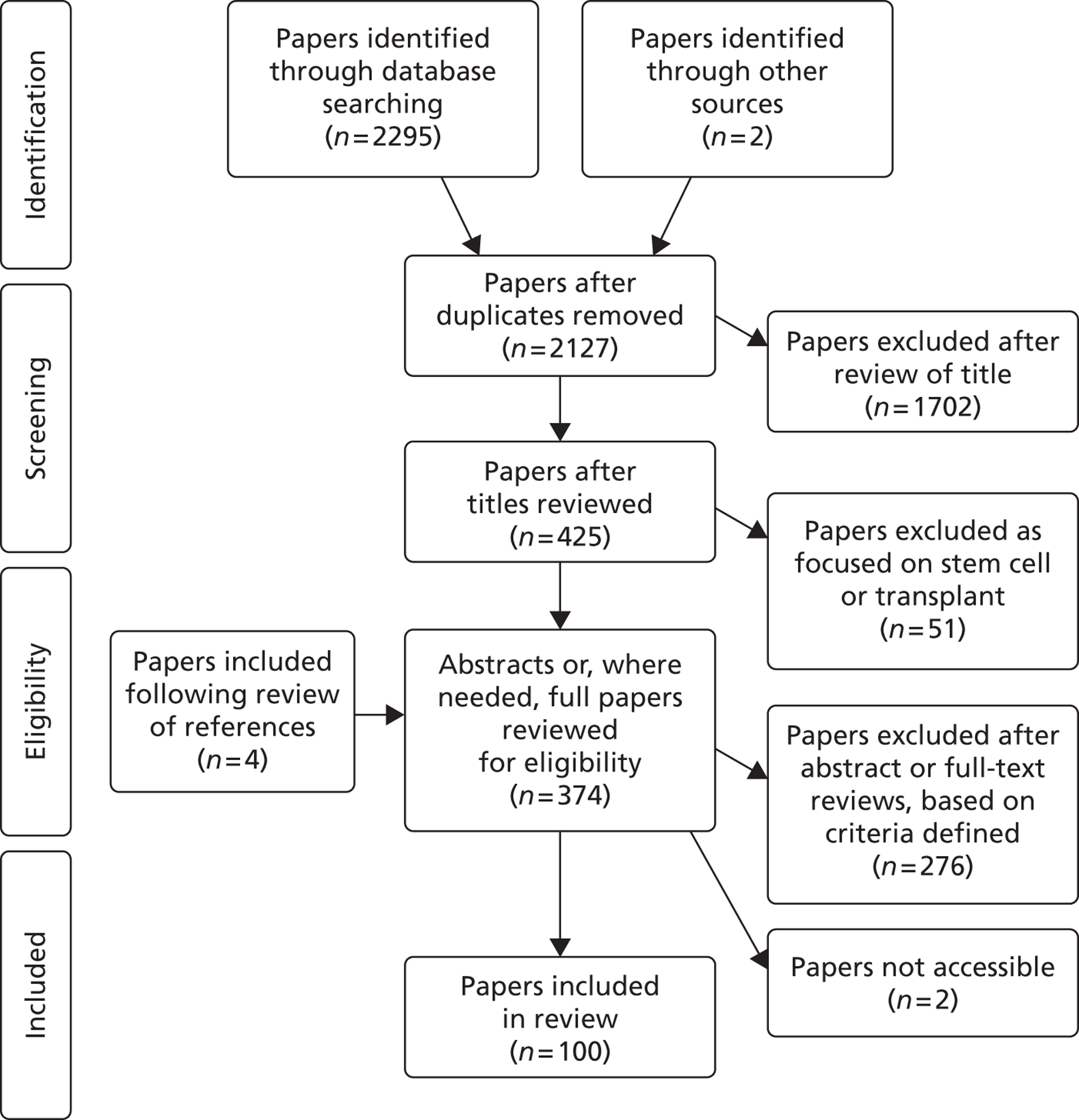
Appendix 12 Results of the literature search
What do we know about medical tourism? A review of the literature
| Database searched | No. of hits |
|---|---|
| MEDLINE | 360 |
| ISI Web of Science | 878 |
| EMBASE | 546 |
| Global Health | 514 |
| Health Management Information Consortium (HMIC) | 77 |
| EconLit | 280 |
| Issue | No. of papersa |
|---|---|
| Fertility | 16 |
| Cosmetic | 5 |
| Dental | 3 |
| Diaspora | 5 |
| Bariatric | 2 |
| Risks in health outcomes | 29 |
| Focus on recipient country health system | 37 |
| Focus on originating country health system | 34 |
| Industry category | No. of papersa |
|---|---|
| Providers | 41 |
| Tourism facilitators | 19 |
| Focused on industrya | 22 |
| Website review | 5 |
| Market review | 4 |
| Communication | 4 |
| Model | 1 |
| Facilitators | 3 |
| Regulation | 2 |
| At country level | 4 |
| Contracts | 1 |
FIGURE 9.
Number of publications by year of publication.
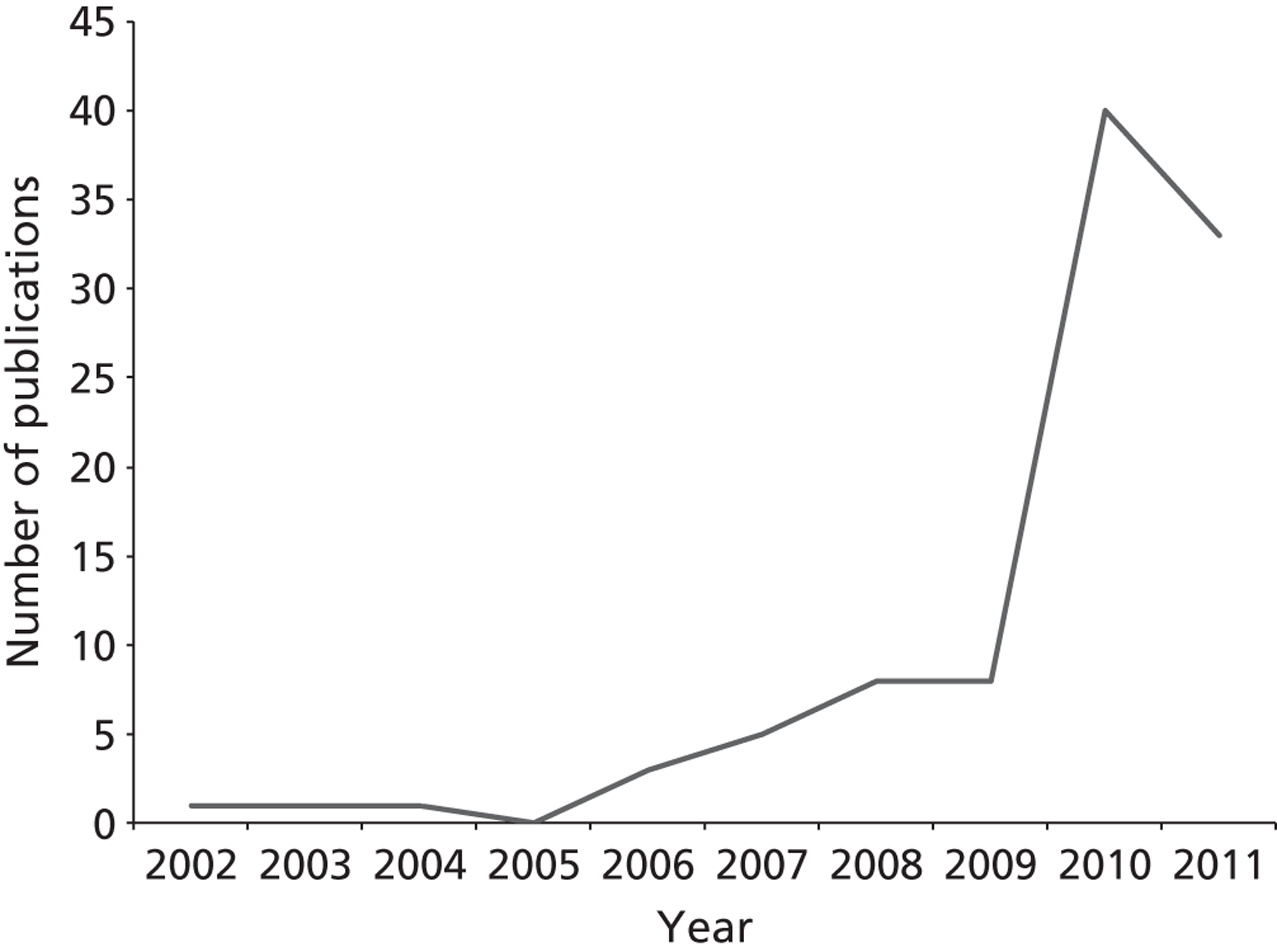
FIGURE 10.
Types of studies included in the review.
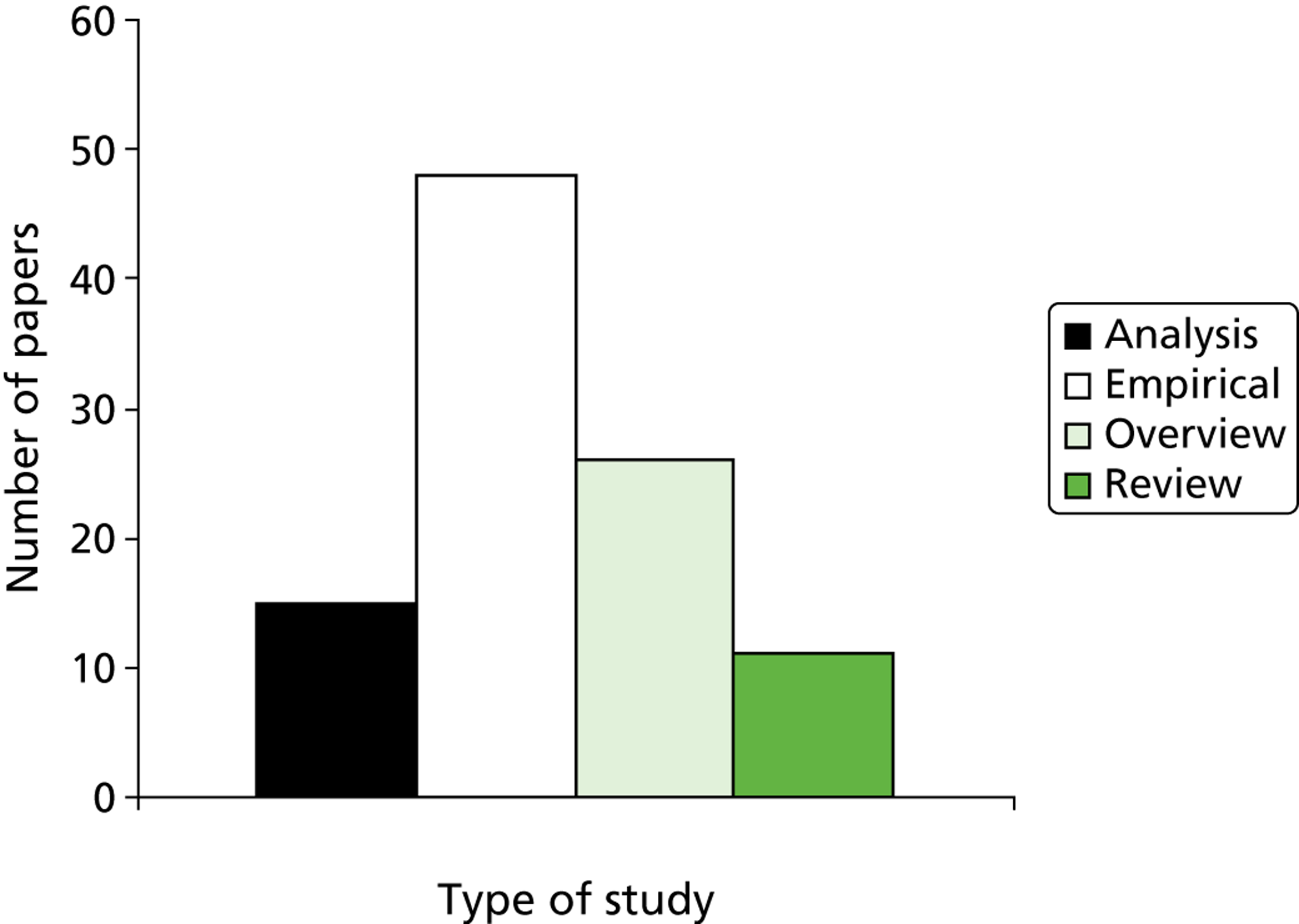
FIGURE 11.
Geographic focus of studies included in the review. Numbers denote the number of papers investigating each region. Papers could fall into more than one category, and some comparative papers focused on two regions or countries from within two regions.
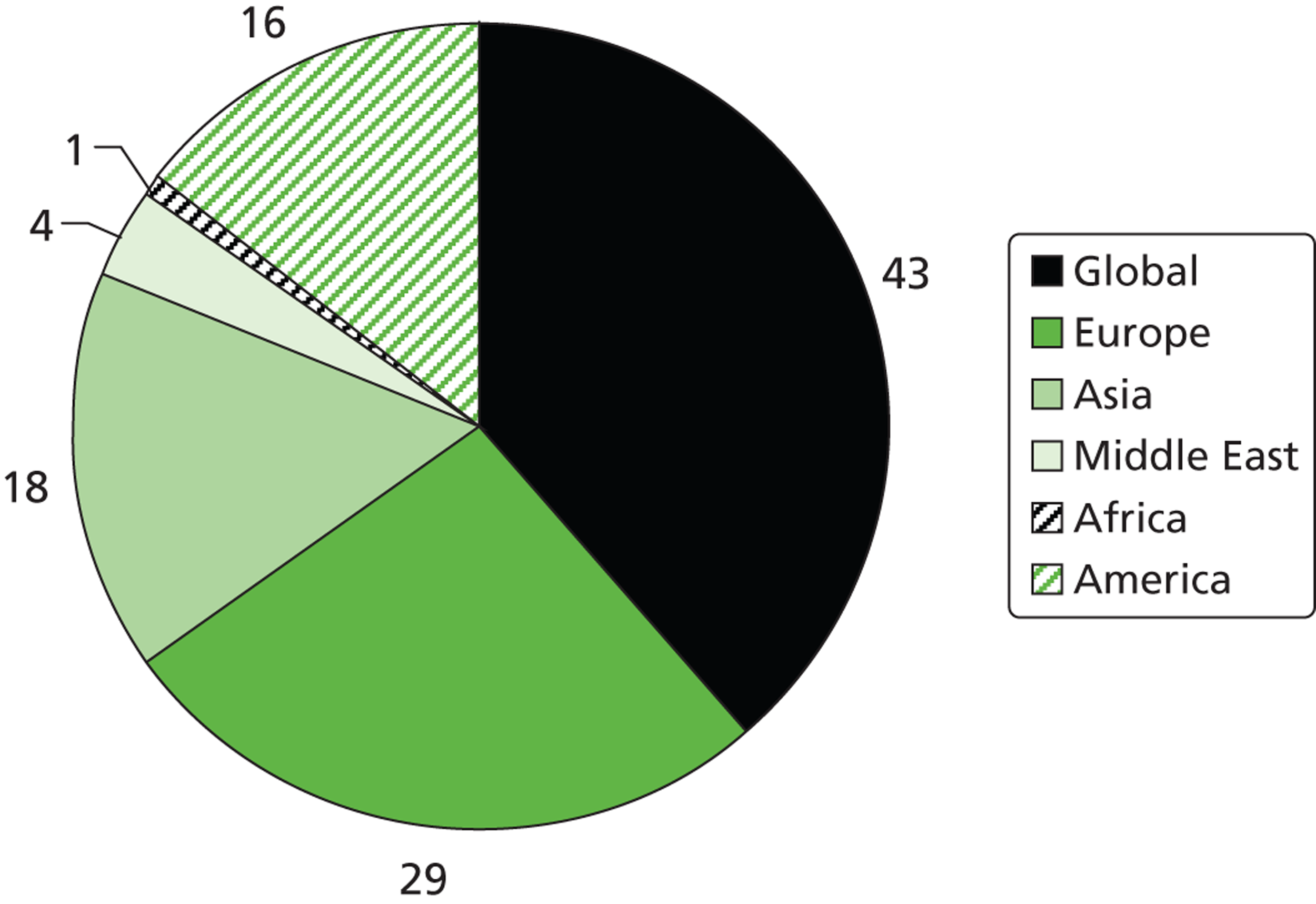
FIGURE 12.
Data sources for patient numbers quoted in studies included in the review.
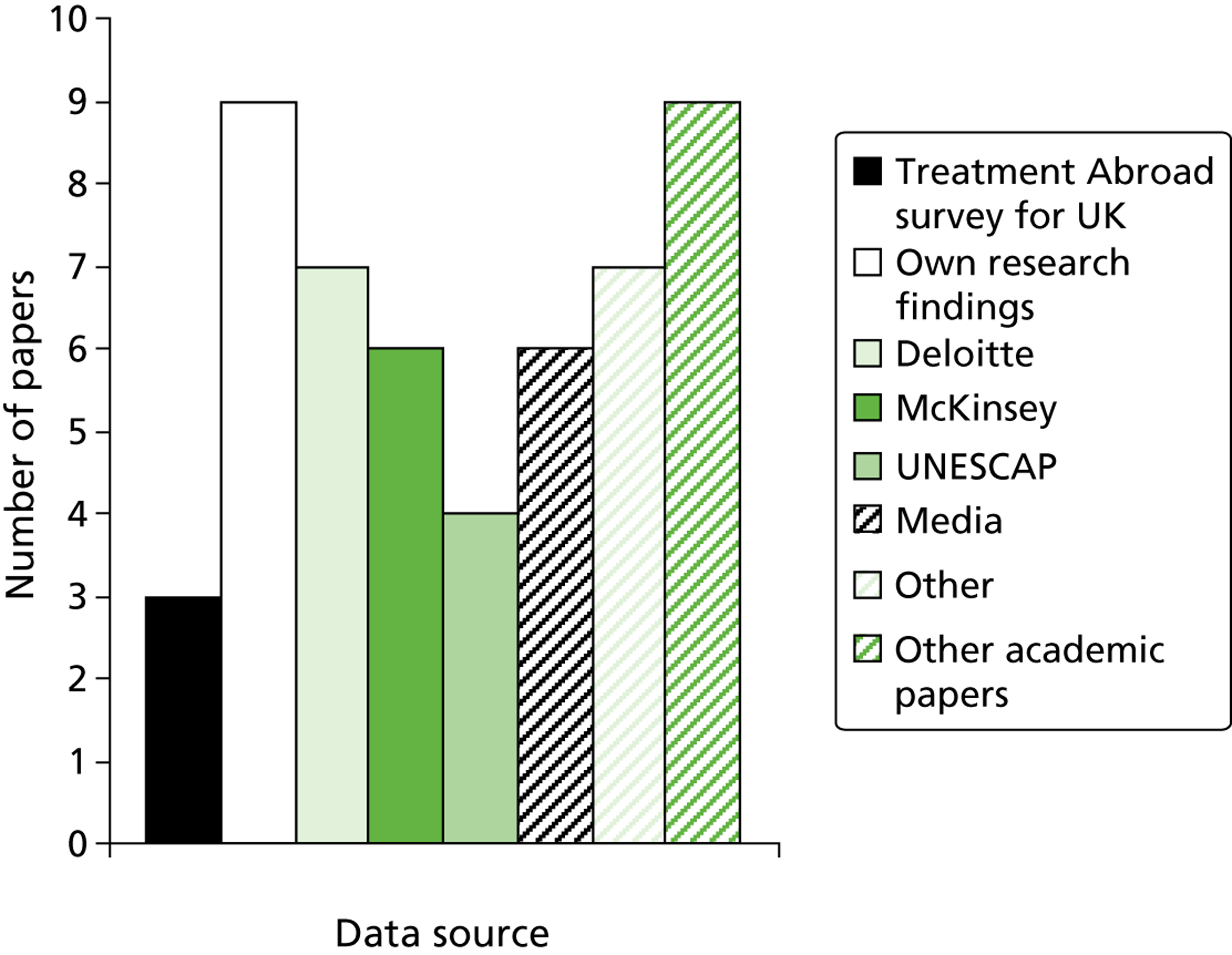
Appendix 13 Models of information and their advantages and disadvantages
| Key features | Advantages | Disadvantages |
|---|---|---|
| Facilitator-enabled provision | ||
|
|
|
| Consumer-driven model | ||
|
|
|
| Network provision | ||
|
|
|
Appendix 14 Country strategies: case examples
Belgium
Medical tourism in Belgium is dominated by small independent clinics often specialising in one broad treatment area, the most common being bariatric surgery, cosmetic surgery and fertility surgery. These smaller clinics do market themselves to European, including UK, trade; however, word-of-mouth recommendations are increasingly important in capturing UK tourists. Although cheaper costs available in Belgium are a draw for citizens of other European countries, many clinics are also able to boast pioneering or field-leading surgeons, especially in terms of cosmetic and bariatric surgery. UK citizens who have travelled to Belgium have noted that the cost of travel to and accommodation within Belgium is often cheaper than for London, where the UK alternatives are usually located.
Spain
The Spanish medical tourism industry has a long history built on low costs and an active wider tourism industry. For Britons it has historically not been uncommon to combine low-level medical treatment such as dentistry with conventional tourism to Spain; however, Spain’s medical tourism industry primarily serves continental Europe rather than the UK. Indeed, a senior consultant at one of Spain’s large health-care institutions suggested that UK medical tourists made up only an insignificant proportion of medical tourists to the organisation. The only exception to this is fertility tourism, which brings a large number of UK citizens to Spain.
Medical tourism in Spain is primarily hosted within large multipurpose clinics or hospitals that often deal with a range of treatments. For example, an organisation such as the Barcelona Medical Centre actually represents an affiliation of a number of general and specialist clinics. Much private treatment also occurs within public hospitals. Although there are smaller independent, specialist clinics, it is these large complexes that dominate the industry. The main exception to this is the case of fertility clinics, with a number of smaller clinics attracting medical tourists alongside the larger clinics.
Turkey
The Turkish medical tourism industry is an increasingly national project with small and large clinics soliciting business alongside governmental and quasi-governmental bodies. Although small clinics offering a narrow range of treatments are common, it is larger clinics that are driving the Turkish medical tourism industry. These clinics are usually ‘hotel like’ in their front-of-house appearance, whilst marketing state-of-the-art medical facilities. Such clinics are frequently ‘one-stop’ clinics where a wide range of procedures are performed. Although Turkish providers are happy to court the UK market, UK travellers to Turkey have historically travelled for less complex and lower-cost treatment (often cosmetic). As one provider noted, although this is useful, it does not represent a stable foundation for a viable business model. Clinics are actively courting ‘en masse’ those requiring higher-end procedures. To this end, Turkish clinics are actively seeking partnerships with medical insurance companies, both in Europe and in the Middle East. Although individual clinics are in competition, there is a degree of unity behind what appears to be a national programme aimed at establishing Turkey as medical tourism hotspot ‘where East meets West’. Organisations such as Health in Turkey (an association of the Foreign Economic Relations Board and the Health Tourism Business Council) and the Turkish Healthcare Development Council represent a loose alliance of Turkish medical tourism providers who agree to support certain ventures with the aim of benefitting the wider medical tourism industry in Turkey. These organisations are linked at arm’s length to the Turkish government’s Ministry of Tourism and Culture.
Hungary
The Hungarian Ministry of Health is actively pursuing a medical tourism strategy and is keen to market the country as a destination for patients from abroad. The UK is clearly considered a market for this strategy as the Ministry of Health recently financed its first medical tourism symposium in London. The country is recognised for its expertise in dentistry and has excess capacity in dentistry. Within Hungary, specific regions attract patients from different countries based on proximity and accessibility. Many of the Hungarian dentists catering to UK clients appear to have facilitators in the UK who are the first point of call for patients.
Cosmetic surgery and non-surgical cosmetic procedures are areas targeted at patients abroad with providers from Hungary marketing themselves to UK patients and patients of neighbouring countries. Fertility tourism appears to be an area of growth in Hungary. Cost aside, regulations governing IVF in Hungary (which allow for four embryos to be implanted) were cited as a pull factor for patients. Hungary has the highest European concentration of spas and thermal waters and the Hungarian Ministry of Health and the country’s tourist association are keen to attract a greater number of UK tourists to its spas for medical purposes.
The Hungarian Minister of Health clearly outlined that the government sees the connection between the good reputation of the country’s medical education and the growth in its medical tourism industry. In 2009, concern among the more established larger clinics that medical tourism might risk the reputation of Hungarian dentistry internationally led to the formation of the Association of Leading Hungarian Dental Clinics. This includes a number of clinics that commit themselves to follow a code of practice on professional ethics and quality assurance.
Thailand
Thailand is one of the main medical tourism destinations in Asia and the country has invested in its infrastructure to market itself as a medical tourism centre. Thailand has provided medical services for foreign patients including medical tourists and foreigners working in the country. The country has also targeted regional medical tourists with expatriates from neighbouring countries visiting Thailand for treatment. Thai consuls provide information on treatment and prices and the country provides a specific visa for medical tourism. Most patients, originating mainly from the USA, the UK and Japan, are treated in three hospitals in Bangkok. Thai hospitals generally have also attracted foreign investment, with 24 hospitals part privately owned in 2001.
Appendix 15 Line charts illustrating inward and outward medical travel trends from the International Passenger Survey 2000–10
FIGURE 13.
Line charts illustrating the numbers of UK residents who travelled for medical treatment in 2000–10 by destination region. (a) Africa, Southern Asia and East Asia; (b) the Middle East, Central and Eastern Europe and Northern, Western and Southern Europe; and (c) North America, Central and South America and other regions.
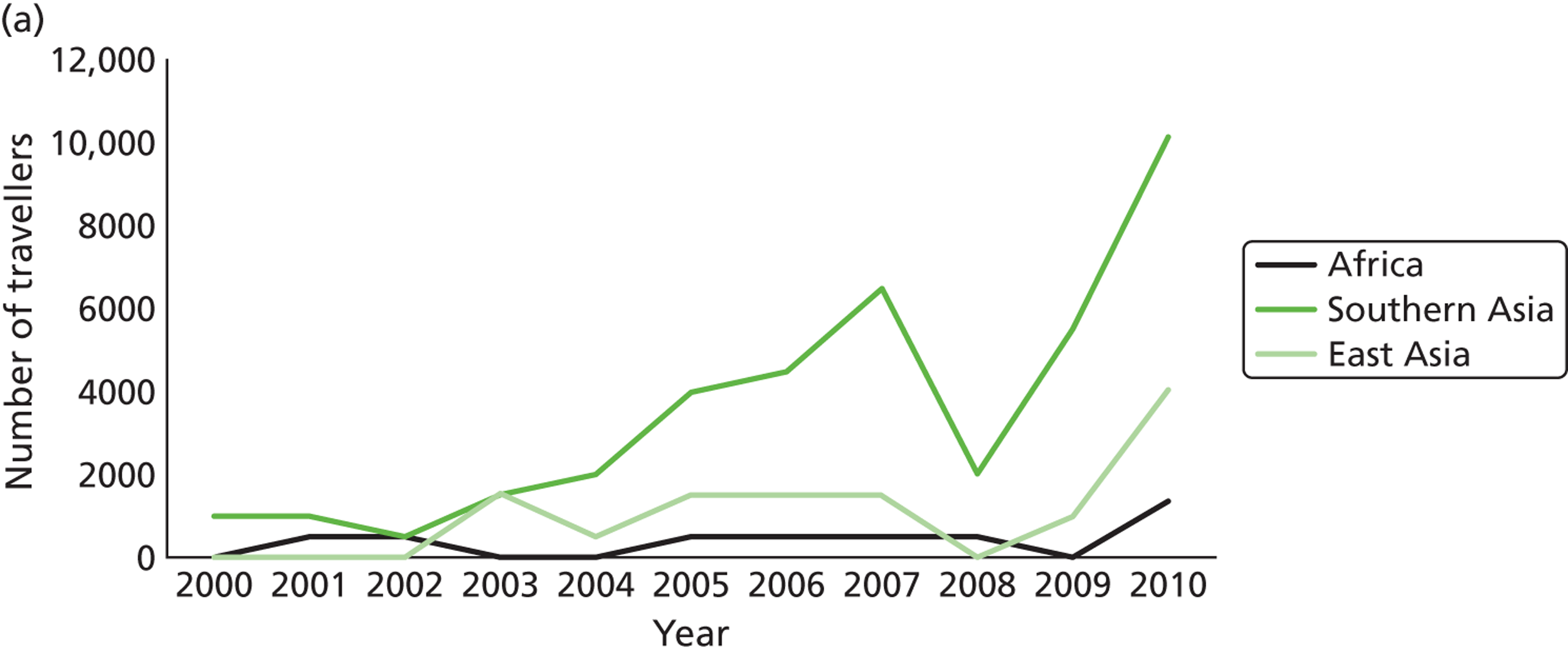
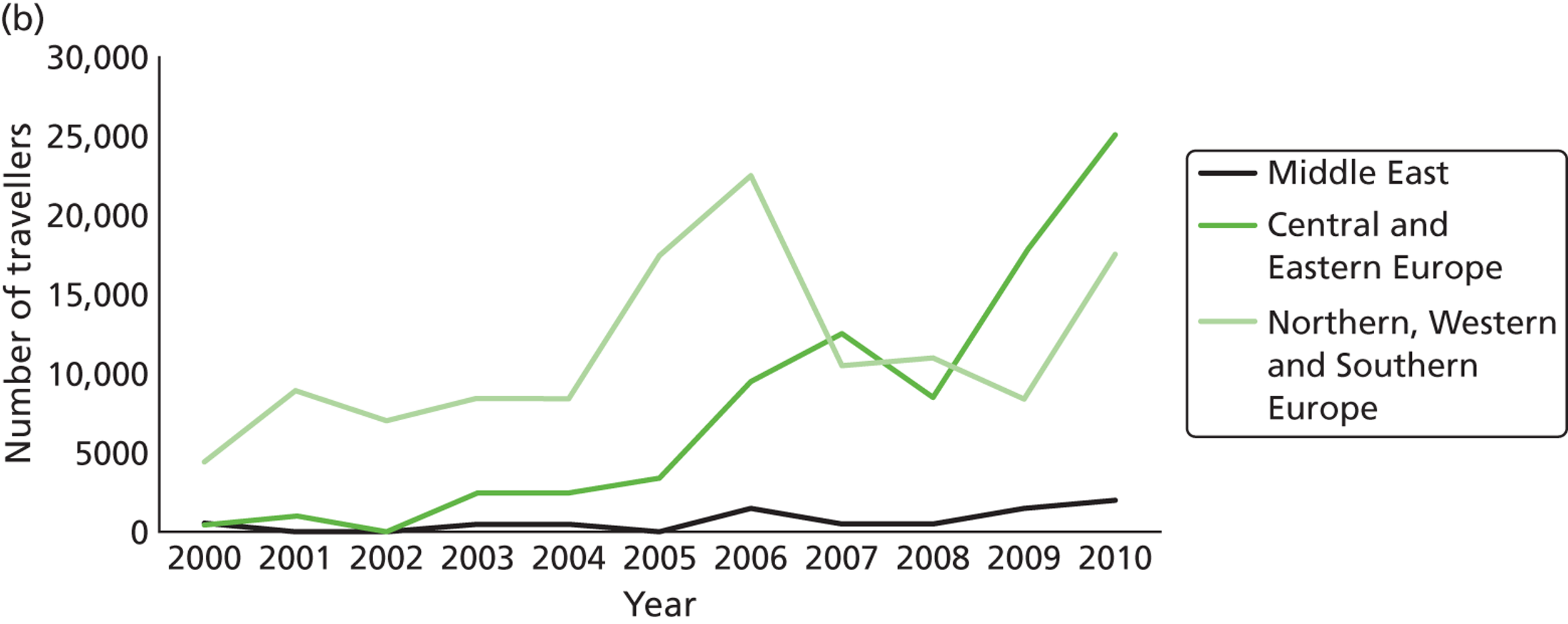
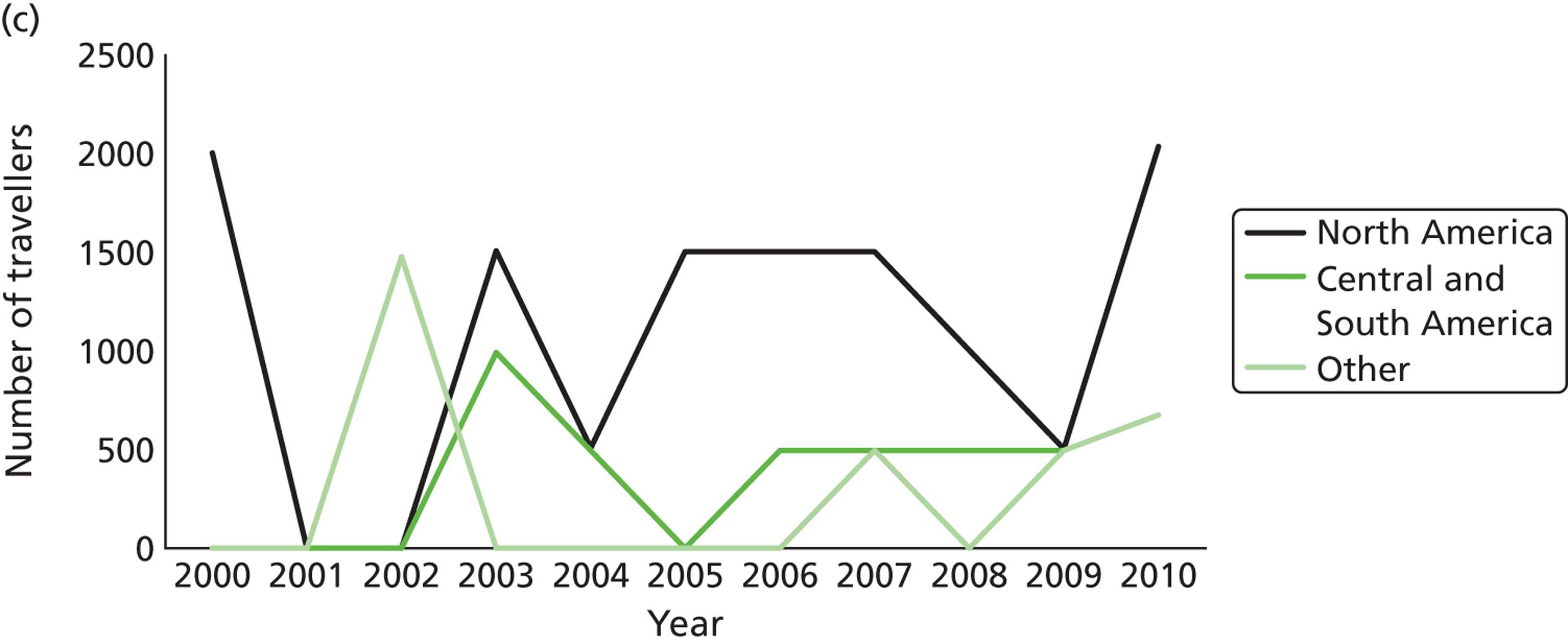
FIGURE 14.
Line charts illustrating the numbers of people who are resident outside the UK and who travelled to the UK for medical treatment in 2000–10 by region of origin. (a) Africa, Southern Asia and East Asia; (b) the Middle East, Northern, Western and Southern Europe and Central and Eastern Europe; and (c) North America, Central and South America and other regions.
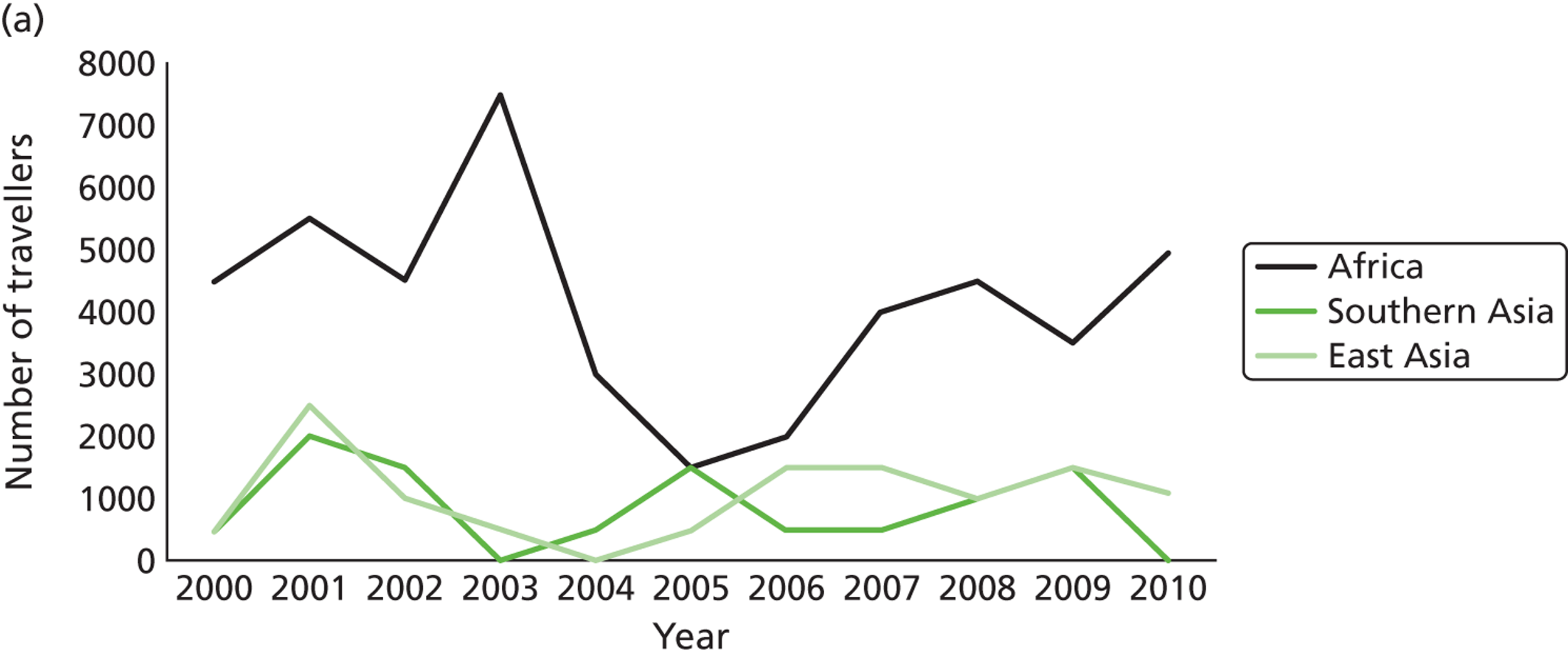
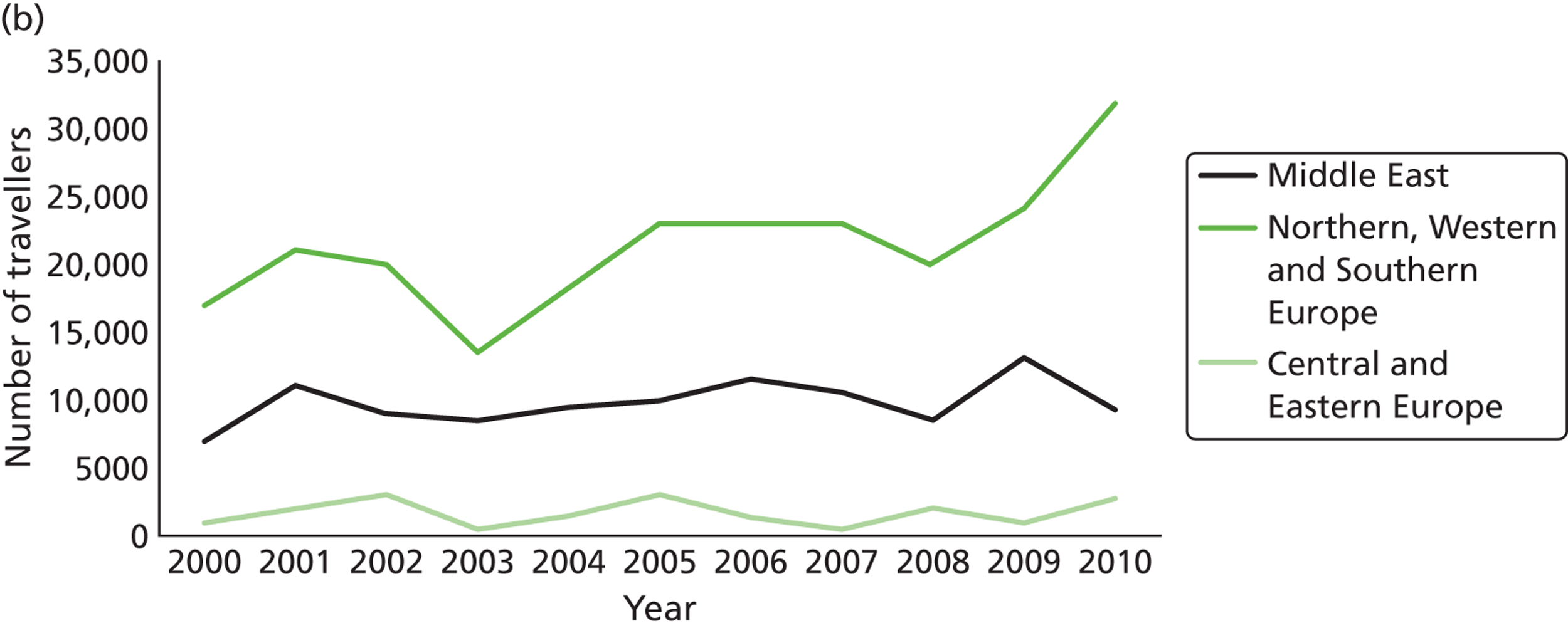
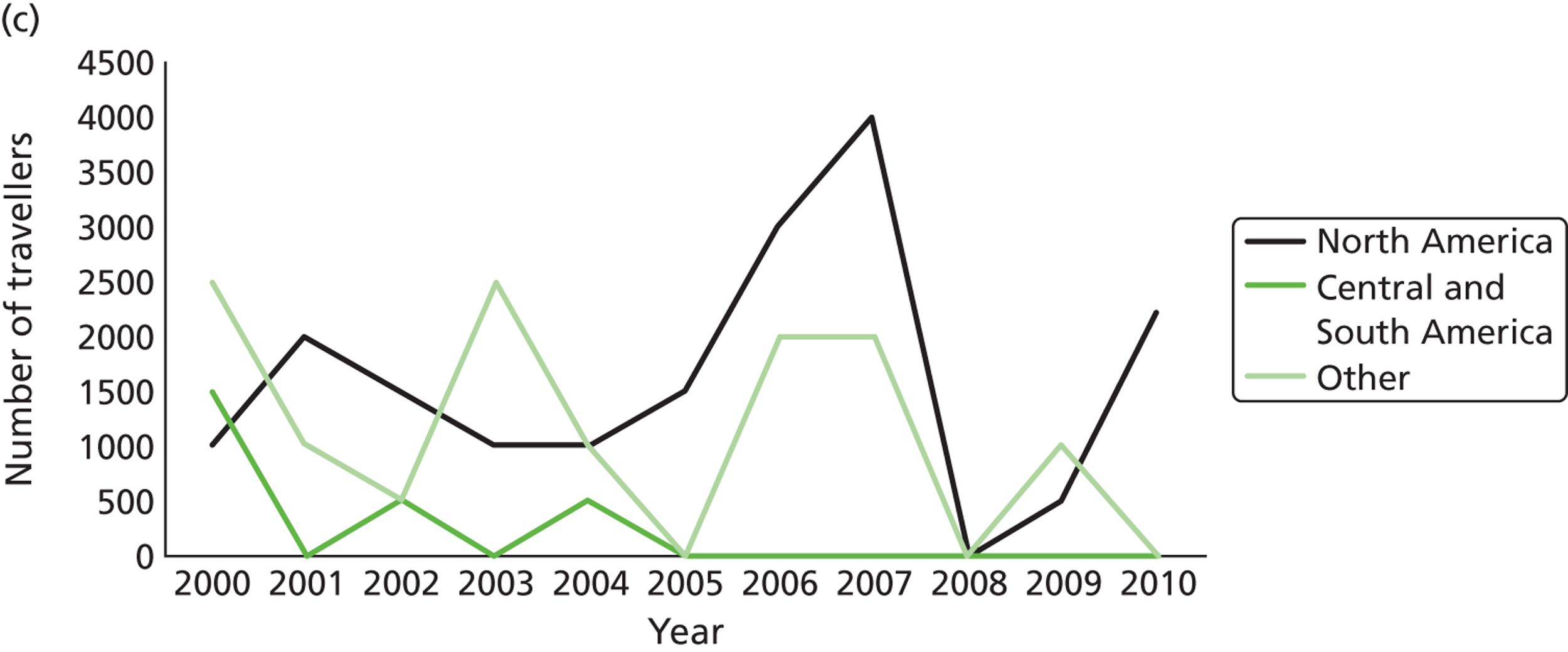
FIGURE 15.
Line charts illustrating the nine most popular destinations of UK residents who travelled for medical treatment in 2000–10. (a) France, Poland and India; (b) Hungary, Belgium and Germany; and (c) USA, Spain and Turkey.
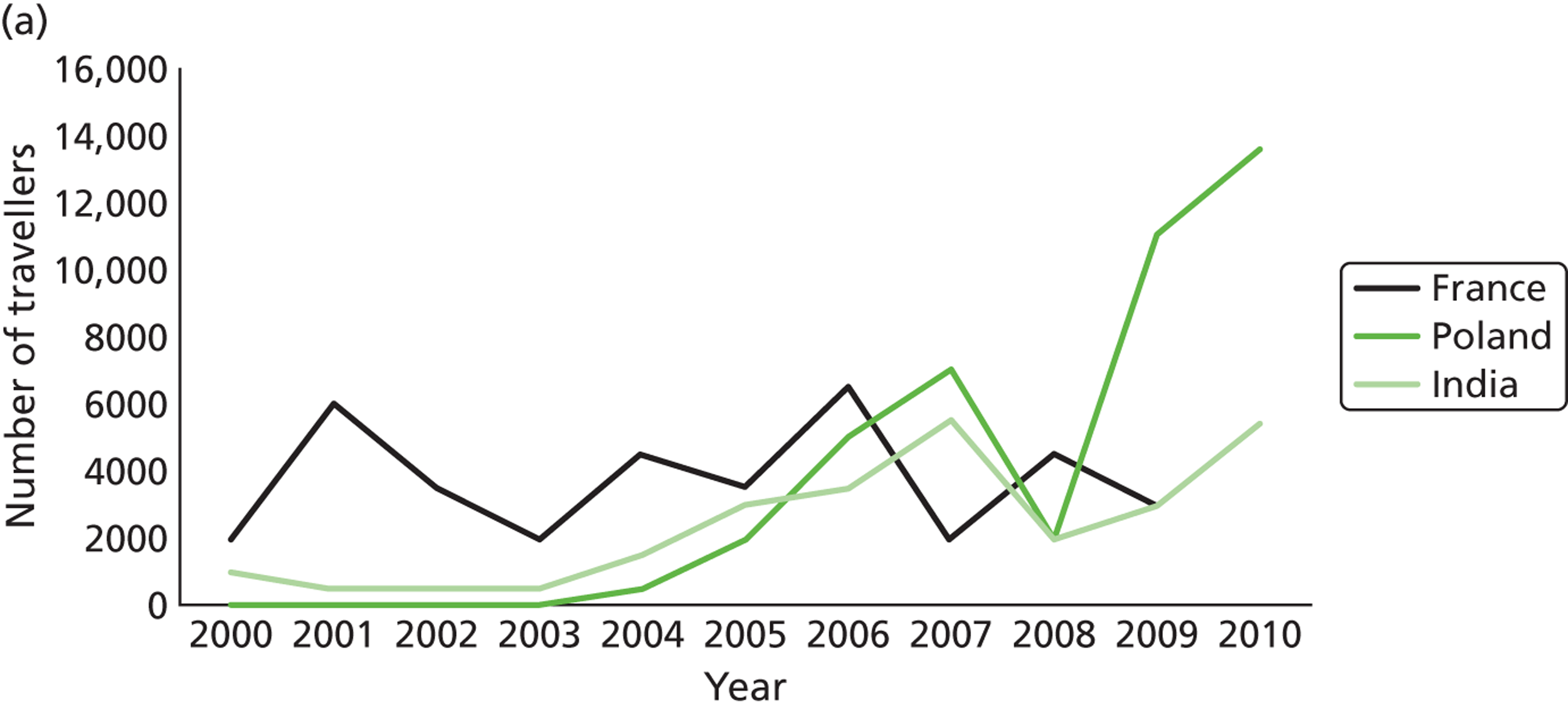
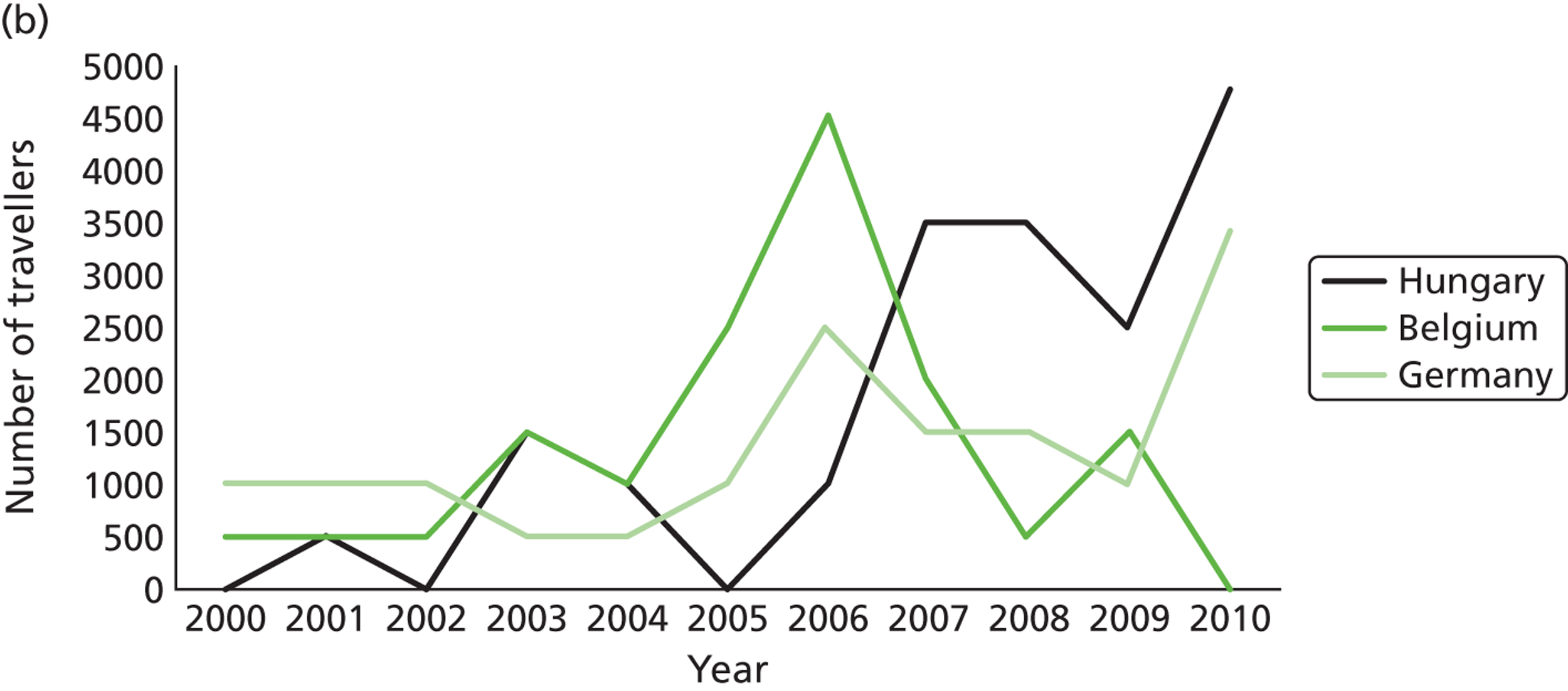
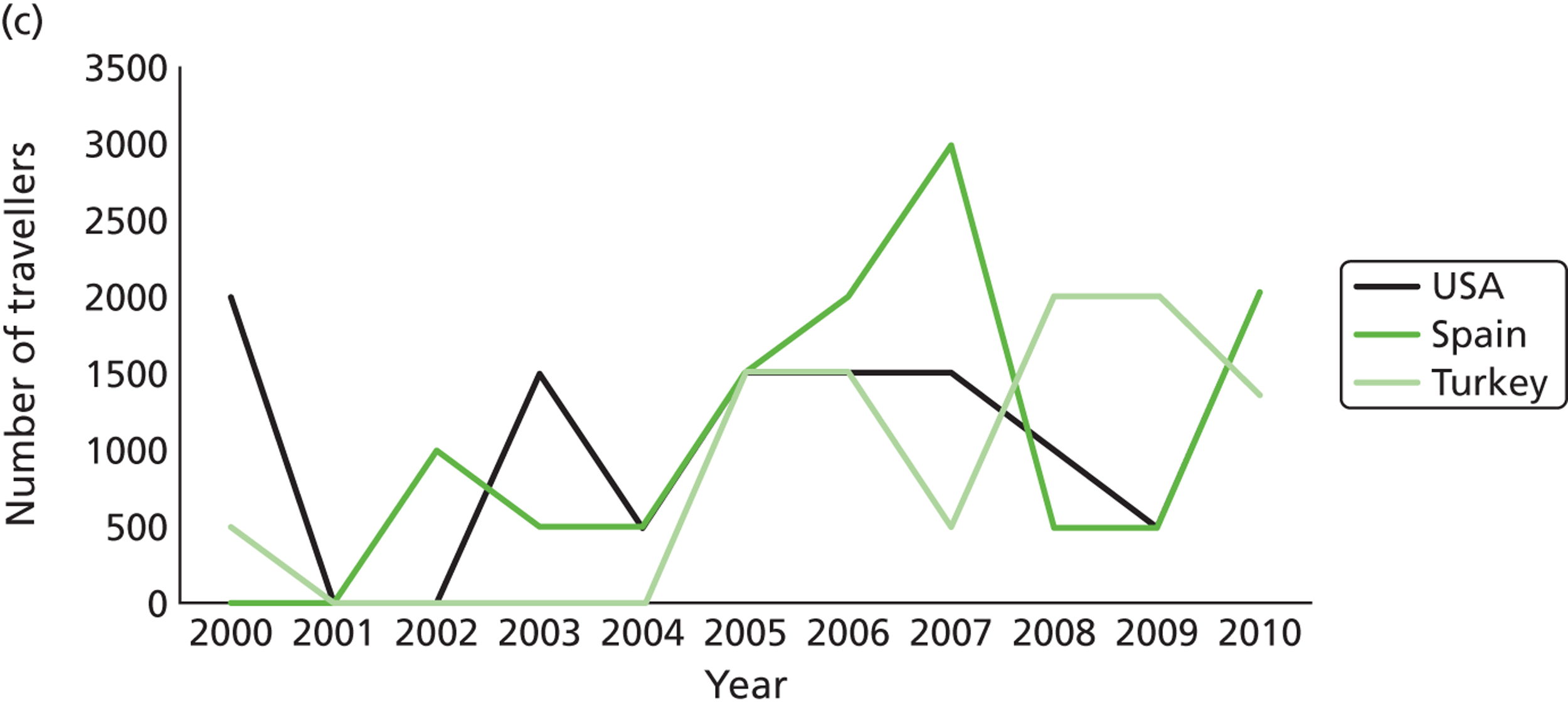
FIGURE 16.
Line charts illustrating the nine most common countries of origin for those who travelled to the UK for medical treatment in 2000–10. (a) Ireland, Spain and the United Arab Emirates; (b) Kuwait, Nigeria and Greece; and (c) France, Cyprus and Portugal.
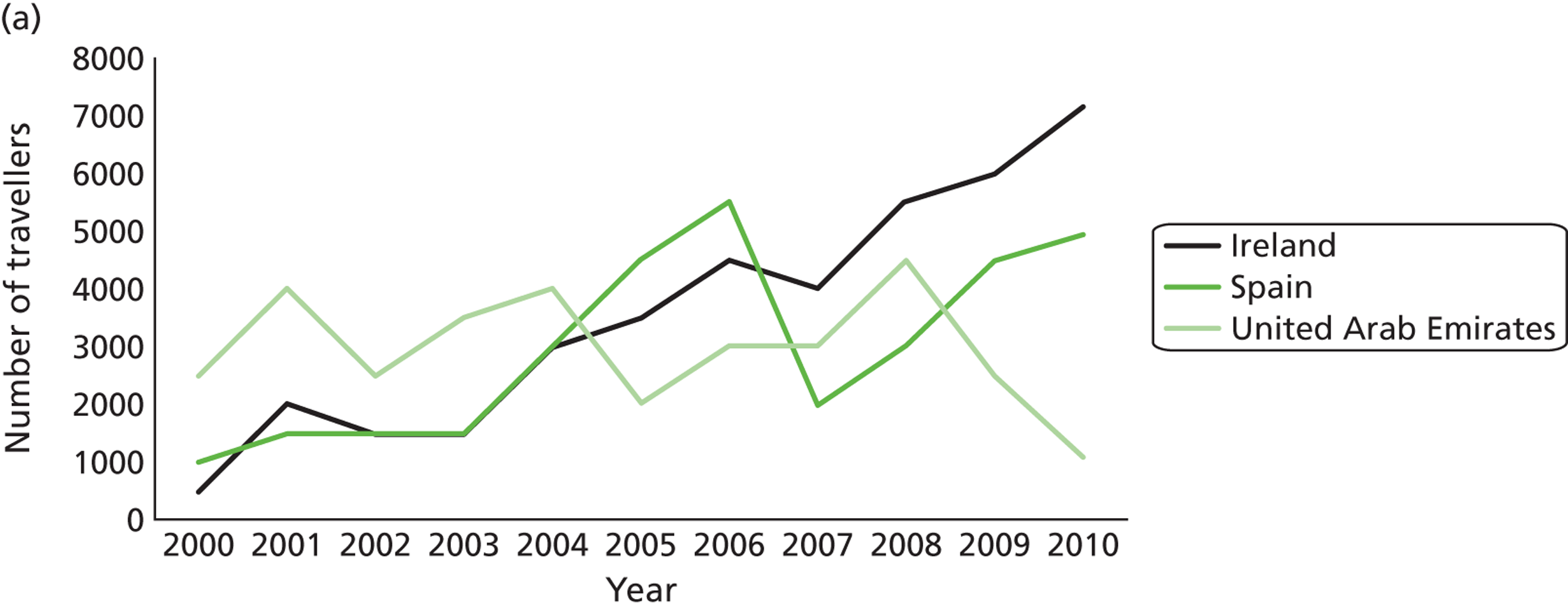
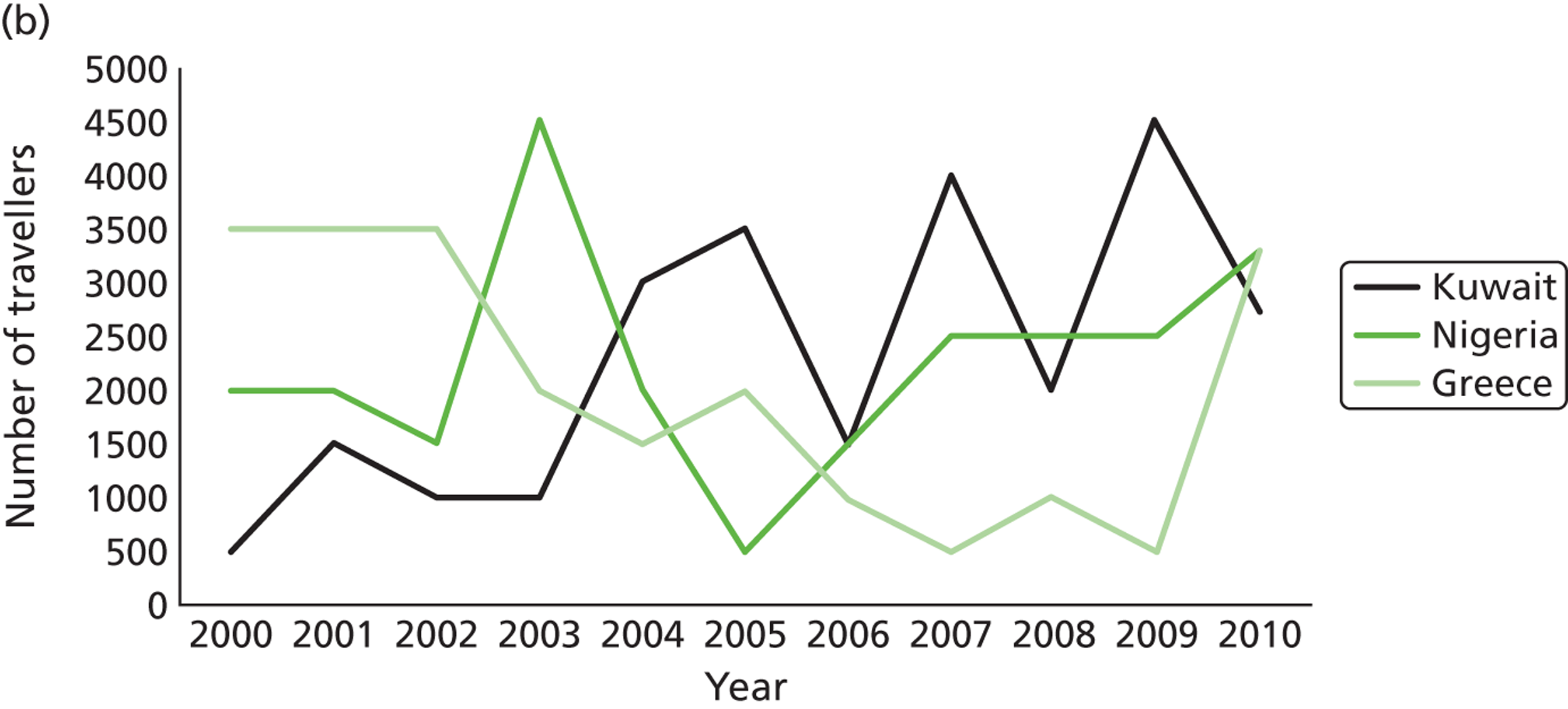
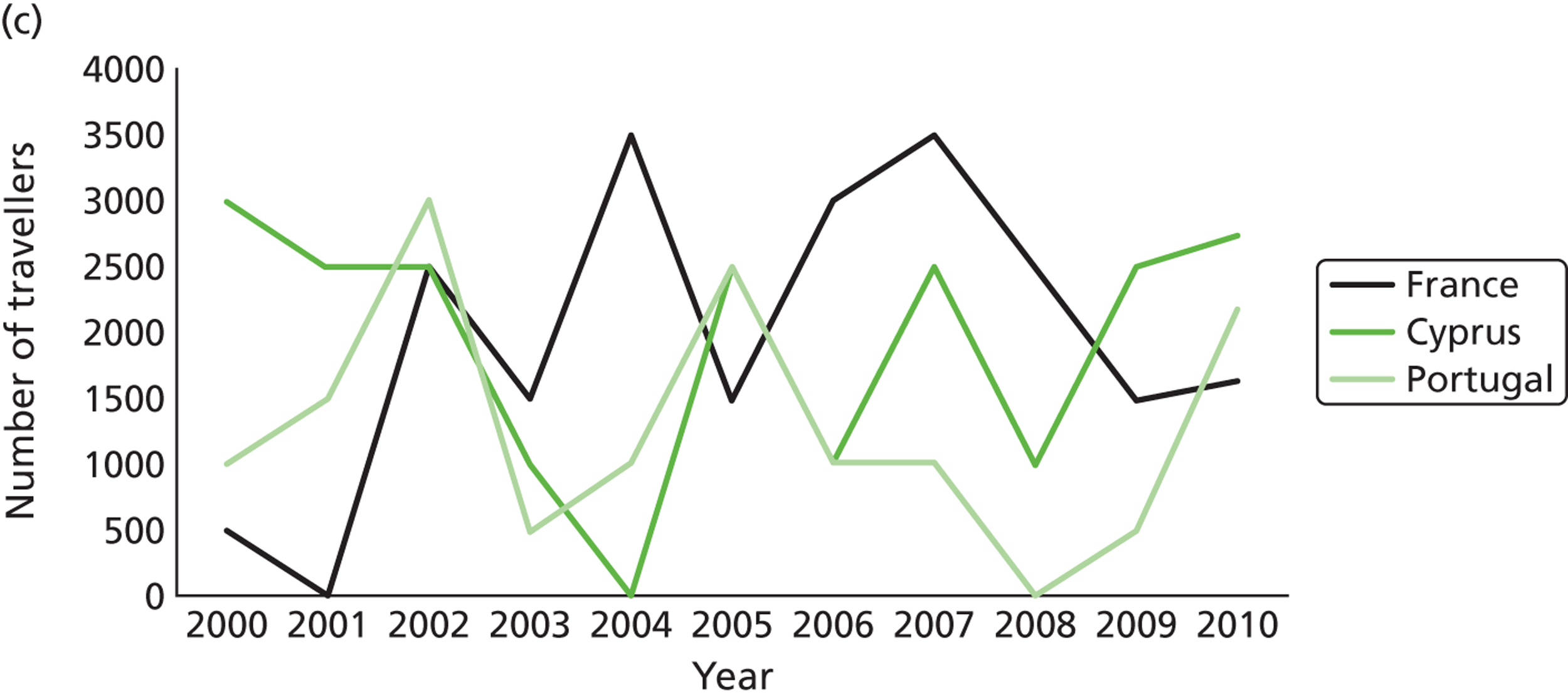
Appendix 16 Fertility treatment abroad and the wider legal and regulatory complexities
Alongside the pioneering techniques and continued innovation in fertility treatment, the UK has advanced regulatory and legal frameworks overseen by the HFEA, which governs assisted reproduction standards.
The Human Fertilisation and Embryology Act238 established the HFEA and since 1990 it has licensed and monitored UK fertility clinics, regulated research and fertility procedures, maintained a register of donors, treatments and any resulting births, published a code of practice, provided advice to clinics and patients and advised the appropriate Secretaries of State on issues related to fertility. Although it is unclear whether the HFEA will continue in its current form or whether some or all of its functions will be transferred to bodies such as the CQC,239,240 the HFEA currently ensures that:
-
All fertility clinics in the UK receive a license through the HFEA for which they are periodically inspected. Details of their services, facilities and success rates are available through the HFEA and in that sense are transparent and independently validated.
-
Fertility clinics transfer a maximum of two embryos (only increased in exceptional circumstances), thus reducing the risk of multiple births.
-
Counselling is provided to all those who seek fertility treatment.
-
Donors receive a set payment and their health and well-being is considered throughout.
-
Facilities do not breach legal or ethical codes in advertising donor services or recruiting donors.
-
A register is maintained of all procedures carried out by registered UK clinics.
-
Sperm and egg donors are identifiable to a child once they reach the age of 18 years.
-
A maximum of 10 families are created per donor.
-
Research on embryos is strictly controlled.
By travelling abroad for fertility treatment, patients remove themselves from a system with the above guarantees and safeguards. In many countries there are frameworks covering ART; however, there is a large degree of variance with regard to what is addressed by such frameworks. Moreover, the principles enshrined in one may run contrary to those guaranteed by others. 114
It is difficult to state that patients travelling abroad for fertility treatment present clear legal difficulties. However, there is much to be considered simply by removing the guarantees listed above. The interviews conducted in this study alone have highlighted instances in which the guarantees above were absent or may have been absent and in each case it has been detrimental to the immediate and future well-being of the patient and offspring. Of particular concern is that the transfer of embryos is not regulated in some countries or higher limits are set. 241 Higher transfer levels are directly related to an increased risk of multiple births and with that comes a raft of related risks and costs, which as we have seen are being borne by the NHS irrespective of where fertility treatment occurs. 98,193
Legislation and, perhaps more importantly, record keeping surrounding donation abroad are clearly variable. Beyond the wider ethical implications of lower or a lack of standards regarding the commercialisation of donation abroad, the anonymity of donors presents two major points for consideration. First, especially if combined with an inconsistent or not particularly thorough record-keeping system, the information that patients receive about donors is at best unreliable. Second, when unexplained or suspected genetic conditions present in offspring, information can be difficult to retrieve.
Appendix 17 The perils of cosmetic surgery/medical tourism by Laurence Vick
This article has been reproduced with permission from AvMA Medical & Legal Journal 2012;18:106–9. 155
The perils of cosmetic surgery/medical tourism by Laurence Vick (PDF download)
Appendix 18 Detailed methods for website review and checklists for dental and bariatric surgery websites
Drawing on previous studies we used (on 20 January 2012) the most popular search engine, Google165,242 to search for both dental and weight loss surgery offered abroad. Evidence suggests that interested searchers are unlikely to travel beyond the first page of a search engine. 165,170,242 As such, we limited the search to the first three pages of returns for what we identified as our major search terms; additional terms were searched to the first page only. We also followed the ‘sponsored’ advertisements that appear at the top of a Google search page as well as any advertisement banners that appear on the right-hand-side of the search return page. In addition, we followed a sample of links from any portal website that appeared in the first page of returns.
Our search of dental websites consisted of the following major search terms: ‘dental surgery’, ‘dental surgery abroad’ and ‘dentist abroad’. These returned a high number of relevant sites although there was much overlap. We supplemented these terms with further lay searches such as ‘dental implant’, ‘dental implant abroad’, ‘crowns abroad’ and ‘teeth whitening’ as well as perhaps more technical searches such as ‘veneers’, ‘cosmetic dentistry’ and ‘cosmetic dentistry prices’. With regard to weight loss websites we searched using the following major lay search terms: ‘weight loss surgery’, obesity surgery’ and ‘bariatric surgery’. These lay terms produced a high number of returns and these, alongside our informed understanding of the online community surrounding weight loss treatment, led us to supplement these lay terms with a small number of more technical searches. These were ‘gastric bypass’, ‘lap band’, ‘gastric band’, ‘VSG’ (vertical sleeve gastrectomy) and ‘gastric balloon’. For both topics search terms were entered as listed here and then subsequently with the terms ‘abroad’, ‘Asia’ and ‘Europe’ after each term. This approach mirrored previous studies that focused on the quality of information on the web pertaining to cosmetic surgery89 and oncology information. 169
Sites that were returned were included in our two 50-site samples if they satisfied the criteria of being ‘active’ (had been updated recently), offering surgery abroad directly through the website and not being an extension of a website that had already been included. This means that we have used portals to access other websites but that the portals have not formed part of our sample. As a final check regarding the robustness of our sampling strategy the major search terms were entered into the search engines Bing™, Yahoo™ and Alta Vista™; we found that the majority of our sites, including all those that appeared on page 1 in Google, were found in the first three pages of these alternative search engines’ returns.
Overall, our dental sample consisted of four sites that were accessed through portals returned by the Google search, eight that were not returned in the Google search but which were followed through the banners on the right-hand side of the page and three that were similarly accessed through adverts at the top of the Google return. The remaining 35 sites were listed in the Google returns although there were a small number of these that also appeared either in a portal or as a banner. Of the 50 websites searched, only one did not work, displaying a home page with broken links. For the 49 remaining websites, four were found to provide answers to two or less of the questions used to interrogate the sites.
Our bariatric sample consisted of 28 sites returned by the Google search, 13 sites solely from portals that were returned by Google, six sites that were accessed solely by following right-hand banners and three sites that were advertised at the top of the Google returns pages. A small number of the 28 sites could also be found as adverts, banners or through portals. Three sites were no longer working when they came to be reviewed.
In our combined sample a wide range of destinations was covered, although Hungary was easily the most frequently advertised dental destination and Belgium was advertised by the largest number of weight loss tourism sites. The overall visual impact and content of sites varied widely. Most were professional, attractive and well designed with alluring images of beauty, health and vitality; a small number, however, were extremely basic and did not reflect advanced web design and marketing techniques and practices.
The major assessment involved the utilisation of two similar, although not identical, clinical checklists. The checklists were adapted from a series of similar checklists aimed at assessing the quality of information pertaining to other clinical areas such as cosmetic surgery (NaTHNaC,236 NHS Choices,235 GDC243) before being finalised with the help of dental and bariatric experts. We also supplemented these clinical checklists with a qualitative assessment of the non-clinical quality of the websites. Here, the HONcode [Health on the Net (HON) Code of Conduct for Medical and Health Web sites]244 was extremely useful, providing us with a platform to assess how accessible, accurate and authoritative the websites are (see Meric et al. ,245 Lunt and Carrera89 and Khazaal et al. 246).
Although the checklists differed slightly for our two treatment types, both sought to establish the quality of information pertaining to four main categories: the clinicians, the clinic, regulation and aftercare.
Having developed the respective lists of criteria against which to judge our samples of sites, roles were divided within the five-person research team. Two members of the team performed the initial assessment of the dental websites against our checklist while at the same time noting any interesting features of the websites according to the HONcode and broader qualitative reflections. This process was also undertaken for our weight loss sites by two other members of the research team. After completion, the two research teams swapped samples and as part of a moderation exercise any variations were explored. As a final check, a fifth member of the research team assessed a random sample of the sites and, again, any disparities were discussed and addressed. Such procedures extend those adopted in similar methodologies165,171 in an attempt to avoid many of the limitations acknowledged by Meric et al. 245
Dental tourism websites
Clinicians
-
I. Is the dental practitioner named?
-
II. Are dental qualifications listed?
-
III. Is the dental practitioner a specialist?
Clinic
-
IV. Does the practitioner speak English/have translation?
-
V. Is the clinic equipped for medical emergencies?
-
VI. Are there any side effects or risks associated with the procedure?
-
VII. Who will be responsible for any clinical failures and their costs?
Regulation
-
VIII. Who is the practitioner’s regulatory body?
-
IX. Does both the practitioner and the clinic have professional indemnity cover?
-
X. Does the clinic have a complaints procedure?
Aftercare
-
XI. Will I be given a copy of my dental records on completion?
-
XII. What continuing care will be required?
-
XIII. What is the overall cost of the procedure?
Bariatric tourism websites
Clinicians
-
I. How many years practising?
-
II. Experience of performing procedure (number given)?
-
III. Opportunity of preoperative consultation (UK)?
-
IV. Qualifications/organisations listed?
Clinic
-
V. English-speaking surgeon/clinic (medical notes)?
-
VI. Facilities and back-up (e.g. how would the clinic deal with an emergency if serious complications were to arise during the procedure)?
-
VII. Are there any side effects or risks associated with the procedure?
-
VIII. What are the rates of success, complications and infection?
-
IX. Who will sort out complications (and pay, etc.)?
Regulation
-
X. Is there a body that regulates the clinic or practice?
-
XI. Does the clinic/operator have the correct medical indemnity in place should anything go wrong with the procedure?
Aftercare
-
XII. What type of care will I need after the treatment? Who will provide check-ups in the UK?
-
XIII. Who can I contact for advice once I’m back in the UK?
-
XIV. Overall cost of the treatment?
Appendix 19 Detailed analysis of website review data
Clinician details
Websites were interrogated whether or not they provided details regarding the experience, qualifications and professional memberships of clinicians. The bariatric surgery websites were also investigated to assess whether a preoperative consultation was possible. Of the dental sites, 35 (70%) provided varying degrees of information about the clinicians employed within surgeries. Of these, all named the dental practitioners and 31 gave details of the dentists’ qualifications, often a full curriculum vitae of qualifications and experience. These numbers were lower in the bariatric surgery sample, with 25 (50%) sites giving some clinician information, mostly pertaining to how long a clinician had been practising and his or her qualifications. However, in both samples the provision of information was not uniform. Some sites simply stated the institution and year of qualification; in comparison, other sites provide extensive details on clinicians’ credentials, including certification and current membership of professional bodies. Many websites (31 in total) enabled potential clients to ascertain whether a dentist is a specialist and, if so, in what area, whereas only 12 weight loss sites allowed viewers to establish how many and what type of procedures clinicians had undertaken and only one site reported the treatment success rate of an individual clinician. In addition, only nine sites displayed any information pertaining to the possibility of preoperative consultation for bariatric treatment. As Exworthy et al. 186 note, for public health care the named clinician is not always the person who does the procedure; however, it should signify that he or she supervises junior staff performing much of the routine work.
Clinics
The majority of websites include photographs of the staff and the clinic, along with videos and even virtual tours of the facilities available. However, a number of the photographs appeared somewhat random and unrelated to dentistry or bariatric surgery and many were duplicated in different sections of the site or even on different websites (perhaps reflecting the interests of website builders). There were few sites giving exact details on the number of dentists employed or the number of treatment rooms. For some, UK media coverage that they had received was seen as a major asset. The most sophisticated websites belonged to large ‘one-stop’ clinics that provided dental, cosmetic and weight loss treatments amongst others. Most dental websites were aesthetically strong; however, many websites for small weight loss clinics in Western Europe were little more than an electronic flyer hosted on the internet.
Assessing whether English was spoken at the clinics, either by the clinicians or by the support staff, was not straightforward. Of our dental sample, 29 (58%) stated that their clinicians speak English and often other languages (mostly German and French), whereas only 16 (32%) weight loss sites made the same claim. However, all of the websites accessed were written in English and there was an implicit suggestion that, when information was presented in English, clients could assume that communication would not be a problem. That said, the grammar and spelling were poor on a number of sites, which is unlikely to reassure potential patients of the clinic that clinicians have the ability to communicate proficiently in English. Roughly half of all sites quoted prices, although these ranged from a sample ‘offer’ price to a full breakdown of prices for all services. However, all sites did carry a caveat that the final price would depend on personal circumstances and treatment plan.
Very few websites acknowledge the possibility of something going wrong during treatment and it is therefore unsurprising that only two of the 50 dental websites explicitly said that their clinic was equipped for medical emergencies. Although weight loss sites were generally better at discussing possible side effects and risks, only 21 of the 47 working sites addressed the issue of risk and only four sites had any statistics pertaining to success rates. When risk was addressed it was often downplayed and, despite many forms of bariatric surgery involving complicated, risk-laden procedures, only three weight loss sites provided details of what would happen should anything go wrong. Although it may be unsurprising that only two dental clinics advertised their access or proximity to emergency facilities, only four weight loss clinics advertised such facilities, which seems remarkably low. It can also be extremely difficult for a prospective client to work out who would be held responsible if something does go wrong, with only three weight loss sites discussing who would be responsible for any clinical failures and their costs.
The issue of responsibility and guarantees highlights a major difference between the dental sites and the bariatric sites. Although none of the websites explicitly state that they will be responsible for clinical failures and any associated costs, 31 dental sites provide some form of guarantee for the dental treatment that their clinic or dentist provides. These guarantees vary for different types of treatment and are often tied to the marketing of a particular ‘brand’. Although all guarantees are replete with an extensive list of conditions and exemption clauses, the existence of such guarantees is a potential source of comfort to prospective dental tourists that is not offered by any weight loss site.
Regulation and quality
There are also substantial differences between the two samples with regard to the issue of regulation. In total, 17 dental sites mentioned a regulatory body either that their practitioners are registered with or whose standards they adhere to; however, no weight loss sites provided such details. Similarly, no weight loss sites provided information regarding medical indemnity to cover cases in which complications arise. Although dental sites did have more information regarding regulation, it is undoubtedly difficult for a lay audience to assess what the varied forms of regulation mean and how rigorous the standards are. Interestingly, even when a number of clinics operate in the same country, they cite different regulatory bodies and authorities. Dental sites frequently make statements pertaining to being regulated but do not clarify the precise details. For example, one website states that it is a ‘fully accredited British Dental Practice Abroad’, whereas another claims to ‘conform to and often exceed all the most stringent of EU regulations and requirements’. There were also 10 websites which declared that they comply with ISO standards and two mention adhering to a commercial provider’s Code of Practice.
Aftercare and follow-up
On the whole, websites provide very little detail about any aftercare services that may be required following the initial treatment. Twelve dental websites made some form of reference to aftercare; for eight of these it is simply to state that check-ups are available in their London clinic at extra cost. Only six weight loss websites directly address issues of aftercare and continuation of advice and care, although when advice was offered it was often detailed. One website even offered an ‘aftercare only’ package in the UK for those who had travelled for weight loss surgery abroad.
The lack of discussion regarding aftercare is perhaps unsurprising given the rather meagre discussion of risks, side effects and complications. Overall, sites sought to convey a sense of ‘popping overseas’ for a treatment holiday, something one site referred to as ‘tweakending’.
Appendix 20 Analysis of guidance available for medical tourism
Professional and consumer
A number of different professional and consumer organisations provide information, advice and guidance for prospective medical tourists. For both of these types of organisations there were overlaps concerning advice about choosing a private provider in the UK and generic travel advice. The Royal Colleges did not appear to provide any form of information, advice and guidance on aspects of medical tourism. How thorough the websites were in covering the core issues varied considerably. Common across all types of organisation and information, advice and guidance was the need to inform patients about the normal risks associated with treatment, especially surgery, and the potential heightened risks if travelling abroad, including issues such as complications arising from the actual travel. There was also an emphasis on standards abroad differing from those in the UK and the potential risks from infection and transmission of disease. Patients are also consistently advised to find out certain information from the medical tourism provider before travelling, such as the qualifications and experience of staff; success, infection and mortality rates; and aftercare arrangements.
However, beyond this the information, advice and guidance varies and there are a number of issues that are covered by only a few websites. For example, only one website specifically addresses the legal situation in terms of redress if things go wrong (Which?). Consequently, unless a potential medical tourist has consulted this site, they may be unlikely to have considered, or be aware of, the inherent challenges in seeking redress. The Which? site also advises of the need to exercise caution over money transactions, who you arrange your treatment with and their liability to you (the clinic or broker). Furthermore, only three websites advise about the difficulties of securing travel and medical insurance covering treatment abroad. Communication problems, especially language differences, are also mentioned rarely.
One of the most dependable sources of information, advice and guidance is the NHS Choices website, which has distinct sections for different types of treatment and a very useful ‘Questions to ask the Surgeon or Dentist’ section. Along with a number of other agencies, such as the NaTHNaC, the website emphasises the importance of consulting with your local GP or dentist first. The importance of researching your chosen treatment, clinic and surgeon and having a consultation before deciding on treatment are stressed across the sectors. A number of websites point out that, although outlay costs for treatment abroad may be cheaper than those for treatment in the UK, the patient is responsible for covering costs if things go wrong, which could be substantially more. Generally, warnings about regulatory differences are not easy to find, with only vague inferences on sites that ‘things may be different abroad’. Related to this, it appears that only NaTHNaC mentions EQA in a list provided of international accreditation schemes.
Sector-specific information, advice and guidance
As well as generic information, advice and guidance for medical travel overseas, there is also more specialist treatment provision advice. This is particularly the case for fertility treatment with the regulatory body in the UK (the HFEA) providing very thorough information, advice and guidance and a checklist for prospective fertility tourists, along with the guidelines that they adhere to. The HFEA covers a number of issues, including multiple birth rates; legislation and legal, social and ethical implications; donor and surrogacy issues; counselling and support; and the management of patient data. As a result, those travellers who consult the website are more likely to be better informed and to ask the right questions of the provider. However, this is not the case for other forms of treatment, including cosmetic and dental treatment. These other sectors provide generic information, advice and guidance that is pertinent to all medical tourists. Professional bodies specialising in cosmetic surgery do emphasise consumer safety, in particular warning against the holiday sell and ‘tweakender’ rhetoric, highlighting that all surgery carries risks, is likely to be painful afterwards and requires some form of aftercare.
Appendix 21 Background context for external quality assessment
Terminology
There is a great deal of complexity when exploring EQA, including terminology. For example, the term ‘accreditation’ has a number of different meanings. Historically, the original use of the term ‘accreditation’ in health care related to training programmes. More recently, it has come to be accepted as meaning the recognition of competent assessors, such as the ISO and the EU. 247 However, in the vocabulary of the ISO, hospital accreditation is actually called certification. This in turn would mean that a hospital had met defined requirements, verified by an independent auditor (Charles Shaw and Paul Stennett, 2012;personal communication).
Lack of standardisation
A second complication arises with the lack of standardisation across accreditors. 248 Although standards are reasonably considered to be a level of achievement, a benchmark for comparison or a requirement of regulation, they vary both across and within countries. An American organisation, ISO is also regulated in Europe and provides standards for organisations to be measured against for accreditation or certification purposes. Originally focusing on quality management systems for manufacturing, the ISO 9000 series of standards has been extended to assess hospitals and other medical providers. Standards that materialise at a national level can be incorporated at regional levels, but unless adopted by government they carry no legal weight. For example, the British Standard (BS) 5750 on quality systems was adopted as European Norm (EN) 29000 and then internationally as ISO 9000 (Charles Shaw and Paul Stennett, 2012; personal communication). Although ISO 9001:2000 is considered to be an excellent health-care quality management tool, it differs from hospital accreditation, which tends to have a strong clinical dimension. 182
The International Society for Quality in Healthcare (ISQua) also plays a key role in this area, assessing external health-care organisations against published standards. In addition, it promotes and benchmarks health-care standards and organisations. Here, health-care accreditation of a provider organisation (termed ‘certification’ by the ISO) includes peer review assessment against these standards, which have been specifically designed. 249 In 2010 there were 46 national health-care accreditation organisations operating around the world. 250 EQA thus varies across and within countries, with a range of badges being used and no consistency in terms of standards, assessment or regulation.
Selective coverage
A third complication is that hospital accreditation is by no means universal across Europe (or more globally) and there is a very unequal distribution of take-up across countries. For example, 100% of eligible hospitals in France (780 hospitals) participate in nationally available programmes in comparison to < 15% in Spain (four hospitals). There are also questions about the motivations of institutions for pursuing accreditation. Shaw et al. 250 found that, although ‘quality improvement’ was identified by schemes as the key motivator for hospitals to seek accreditation, there were also a number of other incentives. Medical tourism was an incentive for > 27% of accrediting organisations, along with marketing for 50% and as a legal requirement for 34%. The question thus arises as to what and whose interests do forms of EQA serve.
Value of forms of external quality assessment
There are debates about the precise value of accreditation/certification. 183,251 In their investigation of accreditation and ISO certification in Europe, Shaw et al. 247 found that, of the participating hospitals, those with either accreditation or certification were safer and better than those with neither. However, they also found that accredited hospitals consistently appeared to score higher on measures of hospital management, patient safety and clinical organisation and practice than hospitals with ISO certification. Despite this, there is some debate over the value of accreditation and the evidence to support claims of its importance as an EQA method. As Braithwaite et al. 252 have highlighted, ‘empirical evidence to sustain many claims about the benefits of accreditation is currently lacking’ (p. 8). Indeed, in a later systematic review of health sector accreditation research, Greenfield and Braithwaite253 concluded that accreditation was consistently having a positive impact in only 2 of 10 categories (promoting change and professional development).
Cost and affordability
A further challenge facing accreditation is how internationally accessible and affordable it is. Accreditation schemes often come with an expensive price tag, often prohibitively so for providers in developing countries, especially smaller ones. In addition, the commercial aims of the scheme may overshadow the purpose of the process. Very few accreditation schemes openly publish information about their charges and associated expenses on their websites. The 2003 study by Mihalik et al. ,254 which analysed the costs of the National Committee for Quality Assurance accreditation process, estimated an annual cost of around £400,000 a year for participation in the accreditation process for a typical, medium-sized US-based organisation.
The USA’s JCI publishes an average accreditation survey cost of £29,700, and an explanation of additional costs, including onsite costs for the team (travel, accommodation, food), preparation and other consultations. 255 With members in over 70 countries, the JCI is one organisation accredited by ISQua. 253 Research undertaken in July 2011 found that the JCI had conducted 90% of all international accreditations, with the total number of JCI hospitals reaching 329. 256
Non-enforceable standards and guidance
A number of other organisations internationally issue standards and guidance, although without clear methods of enforcement. For example, the World Health Organization issues both general guidance on health care and also documents on specific issues such as safe surgery. 252 Within Europe there are a number of examples of attempts to harmonise standards in the medical field by the EU, including for professional training and clinical practice. Despite there being no standardised system for quality and safety, efforts have been made to share best practice, such as through the European network for Health Technology Assessment (EUnetHTA) and the European Network for Patient Safety (EUNetPaS) project. 249
Voluntary and commercial initiatives
Outside of formal EQA and accreditation, voluntary and commercial schemes exist in which providers sign up to ‘codes of practice’ or become ‘partners’ of other organisations. Many medical tourism facilities and facilitators state that they adhere to commercial ‘codes of practice’. Claiming to be a partner of another organisation is also common, although this is also a grey area in terms of how this ‘partnership’ helps ensure the quality and safety of the actual provider.
Statutory regulation
In addition to accreditation and certification, all countries have some form of inspectorate for health services that provides a minimum level of regulation for both public and private sector providers. In the UK, the CQC regulates facilities whereas the GMC regulates standards for the practice of medicine. In addition, there are a number of bodies that provide and promote standards and training within specialist areas, such as the Royal Colleges (Surgeons, Psychiatrists, GPs). A RAND185 study found that the structure, remit and values of medical regulation vary significantly between different countries. For example, some countries have a unitary state-authorised regulator (such as the UK in medicine and dentistry), whereas others have decentralised polycentric systems, such as Spain, where different bodies and processes exist depending on the region.
The Health & Care Professions Council (the UK body responsible for keeping a register of health and care professionals) hosts a searchable online database of health regulators and professional bodies for health professionals (see www.hpc-uk.org/). A wide range of countries and specialisms are included with links referring individuals to (typically non-English) websites.
Appendix 22 Analysis of external quality assessment statements on websites
Dental clinics external quality assessment
The different credentials can be categorised into:
-
ISO standards, e.g. ISO 9001
-
national regulations, e.g. GDC (UK)
-
domestic professional associations, e.g. British Academy of Cosmetic Dentistry
-
accreditation organisations/companies, e.g. Technical Inspection Association (TÜV)
-
voluntary associations and codes of practice
-
those remaining, as other.
Ten websites identified some form of ISO certification, usually ISO 9001, although not all displayed details. Only one other accrediting body was mentioned, TÜV, with two sites claiming accreditation.
The majority of websites detailed some form of national regulation. Unsurprisingly, given the proliferation of Hungarian dental providers, the most commonly cited were the Hungarian Chamber of Dentists and the Hungarian Medical Chamber, which incidentally oversees the former. The UK GDC was also mentioned by two websites in recognition of the need to be registered (with the GDC) to hold consultations in the UK. However, no explanation is given to highlight that its regulation extends only to those practising on British soil. Other national regulatory bodies included the Romanian Dental Council and the Ministry of Health of the Czech Republic.
Websites also claimed some form of affiliation to a domestic professional association within the home country, usually some form of Hungarian Dental Academy (although these claims are typically inaccessible for consumers who search in English). Four websites claimed some form of British registration, although this ranged from credible (GDC) to unverifiable through online English searches (‘British Dental Practice Abroad’). Further non-verifiable claims included being a member of the ‘Cosmetic Dentistry Guide’. Two further European voluntary associations were also mentioned by single websites: the European Dental Association and the European Association of Cosmetic Dentistry. A further two displayed ‘Treatment Abroad Code of Practice’ labels but with no detail as to what this involved (see full list in table below).
The lack of explanation for prospective tourists about the differences between accreditation, certification and national regulation, and the failure to provide any details of what any of these mean, render assessment of a dental clinic’s credentials particularly difficult.
| ISO standards | Domestic professional associations | Voluntary associations (Europe and other) | National regulation | Accreditation organisation/company | Other |
|---|---|---|---|---|---|
| ISO 9001 ISO 9001:2000 |
Academy of Leading Hungarian Dental Clinics British Academy of Cosmetic Dentistry Hungarian Academy of Aesthetic Dentistry |
Treatment Abroad Code of Practice European Association of Cosmetic Dentistry European Dental Association |
Romanian Dental Council Ministry of Health of the Czech Republic Hungarian Chamber of Dentists Hungarian Medical Chamber UK GDC |
TÜV – German, also certificates ISO | British Dental Practice Abroad – not found online General Medical Office – not found online GDC of Hungary – not found online |
Bariatric clinics external quality assessment
Overall, 23 different types of credentials were mentioned. However, seven of those were US specific and were on one American website. Here, extensive details of the seven credentials were provided with a brief explanation and some links to the source of the accreditation [e.g. the American College of Surgeons: Level 1A Accredited Bariatric Center, Adult and Pediatric (15 years and above)].
Once again, ISO certification was strongly evident, with nine providers claiming to meet one of their standards, including ISO 9001, ISO 15189, ISO 14001 and ISO 13001. Five websites claimed either certification or partnership with Treatment Abroad or the Medical Tourism Association. Two websites claimed HON certification; however, HON no longer offers certification for medical tourism sites. A further two displayed a Better Business Bureau rating.
Five clinics displayed a connection with domestic professional associations, including the Czech Obesity Society and the Indian Association of Gastrointestinal Endosurgeons. Three websites claimed professional registration with the GMC, the national regulating body in the UK, but again failed to highlight that the GMC’s regulation extends only as far as the British borders.
A large number of clinics claimed some form of professional allegiance to or partnerships with institutions including Apollo Hospitals, Harvard Medical School and Worldwide Medical Partners. It was rare for precise details of the arrangements to be provided beyond a symbol demonstrating the affiliation.
Other individually cited memberships included the ‘GLC’ and the ‘FEQH’ (Forum for Enhancement of Quality in Healthcare) quality certificates, neither of which are traceable through English-based internet searches. Further unverifiable statements found on some bariatric sites included ‘licensed health care hospital’ and ‘Our company is British and so we adhere to the regulations of the British Government’, with no further detail on what these regulations may be (for full list see table).
| ISO standards | Domestic professional associations | Voluntary associations (Europe and other) | National regulation | Accreditation organisation/company | Other |
|---|---|---|---|---|---|
| ISO 9001 ISO 13001 ISO 14001 ISO 15189 |
Czech Obesity Society Czech Bariatric Chapter Association of Gastrointestinal Endosurgeons American Society for Bariatric Surgery: Center of Excellence American College of Surgeons [Level 1A Accredited Bariatric Center, Adult and Pediatric (15 years and above)] |
International Federation for the Surgery of Obesity Anthem Blue Cross and Blue Shield: Blue Distinction Program, Center of Excellence for Bariatric Services Aetna: Aetna Preferred Bariatric Center Network Medical Mutual of Ohio: Medical Mutual of Ohio Center of Excellence for Bariatric Surgery Cigna: Center of Excellence Program for Bariatric Surgery |
UK GMC | Occupational Health and Safety Advisory Services (OHSAS 18001) HON code certified 2009/10 |
Better Business Bureau rating Medical Tourism Association membership Online Medical Tourism Partner Medical tourism certificate issued by the State of Baja California ‘FEQH’ quality certificate Treatment Abroad member/partner ‘GLC’ quality certificate |
Cosmetic clinics external quality assessment
Finally, 50 sites analysed by Lunt and Carrera89 in their discussion of patient advice and sources of information for decision-making were revisited and analysed for EQA. Similar to the bariatric review, a large range of bodies was cited (46 in total); however, only 18 websites provided any details of accreditation, certification or regulation.
As with both the dental and bariatric reviews, ISO certification was identified, with five provider websites citing ISO 9001:2000 and two citing ISO 14001. Membership of domestic professional associations was most frequently cited, although rarely were links provided to these associations’ websites. Twenty-one different domestic professional associations were highlighted by the websites, with the Polish Society of Plastic and Reconstructive Surgery the most frequently cited (by four sites), along with the American Society for Aesthetic Plastic Surgery (three sites) and the Spanish Society of Plastic, Reconstructive and Aesthetic Surgery (two sites).
Membership of international voluntary associations was also evident, with four websites claiming membership of the International Society of Aesthetic Plastic Surgery and three claiming allegiance with the International Confederation for Plastic, Reconstructive and Aesthetic Surgery. National regulation through domestic medical councils or chambers was cited infrequently, with two mentioning the UK GMC.
As with both other reviews, a number of other forms of accreditation or certification were claimed with no explanation as to their meaning or why they had been awarded. For example, one website claimed that it had received a ‘Slovak Gold Exclusive’ award and displayed a gold medal symbol. However, it proved impossible to verify through English-language internet searches what this was (for full list see table).
| ISO standards | Domestic professional associations | Voluntary associations (Europe and other) | National regulation | Accreditation organisation/company |
|---|---|---|---|---|
| ISO 9001:2000 ISO 14001 PN-N-18001:2004 Occupational Health and Safety Management Certificate |
ÁNTSZ – Hungarian National Public Health and Medical Officer Service MPHEST – Hungarian Society for Plastic, Reconstructive and Aesthetic Surgery Polish Society of Plastic and Reconstructive Surgery SSPES – Slovak Society of Plastic and Aesthetic Surgery Belgian Society for Plastic Surgery Netherlands Society for Aesthetic Plastic Surgery French Society for Lipoplasty SOF-CPRE – French Society of Plastic Reconstructive and Aesthetic Society SETGRA – Spanish Society of Fat Transfer Applications SECPRE – Spanish Society of Plastic, Reconstructive and Aesthetic Surgeons SEMAL – Spanish Society of Anti-aging Medicine AECEP – Spanish Association of Aesthetic Plastic Surgery Croatian Society for Plastic, Reconstructive and Aesthetic Surgery Society of German Otorhinolaryngologists Society of Croatian Otorhinolaryngologists Royal College of Surgeons of Thailand (Plastic Surgeons) Society of Aesthetic Plastic Surgeons of Thailand Society of Plastic and Reconstructive Surgeons of Thailand Thai Society of Cosmetic Dermatology and Surgery International member of American Society of Plastic Surgeons |
International Confederation for Plastic, Reconstructive and Aesthetic Surgery International society of Aesthetic Plastic Surgery European Academy of Cosmetic Surgery International Federation for Adipose Therapeutics And Science World Society of Anti-Ageing Medicine American Society for Aesthetic Plastic Surgery European Society of Plastic, Reconstructive and Aesthetic Surgery European Academy of Facial Plastic Surgery International College of Surgeons (Plastic Surgeons) |
Czech Republic Medical Chamber UK GMC Slovak Medical Chamber French Society for Cosmetic Surgery |
HON code PN-N-18001:2004 Occupational Health and Safety Management Certificate Health Care Surveillance Authority |
Appendix 23 Interviewee perspectives on patient safety and service quality
Background
Stakeholders interviewed differed markedly in their areas of expertise and in their roles with regard to medical travellers. They ranged from GPs who had dealt with returning patients’ medical problems in their surgery to policy-makers developing guidance on patient safety. Despite these differences, a set of key themes and perspectives emerged clearly from the interviews.
A number of interviewees based in PCTs identified drivers that encouraged individuals to travel to overseas destinations. These included the tightening of eligibility for services (e.g. the general unavailability of cosmetic breast surgery paid for by PCTs), a broader consumer orientation and the influence of advertising: ‘They are seeing what’s available on the shelves and deciding that there’s actually more available on the shelves of different country’ (NHS13).
Primary care trusts reported receiving a number of treatment requests that were outside their eligibility criteria and which may prompt private (including overseas) treatment as a result: ‘[We receive] a lot of requests for what we would consider cosmetic or plastic procedures. Endless requests for breast augmentation or reductions or nips and tucks and abdominal plastics and so forth’ (NHS9).
Across the different groups of actors interviewed, the absence of reliable data on the scale of outbound medical tourism and on the costs and any problems was highlighted.
You really come up against a lot of industry based information but very limited and fast facts about the numbers of people trying to access healthcare abroad. And obviously there are discrepancies between industry sources and figures for the UK, for instance, when you look at the international passenger survey data. [. . .] frustrated not being able to find good information or reliable information.
PA11
At the same time there was a sense that medical travel and any resulting complications posed potentially serious issues and were worthy of further attention but that this was not an overwhelming challenge either for the organisations that the interviewees were representing or for the NHS as a whole. A representative from one of the Royal Colleges summarised:
[It] doesn’t happen too much I think in the UK. Not that much because actually most people don’t speak languages. Most people don’t want to go abroad to have treatment, to be honest. [. . .] They want to be treated at their local hospital.
PA5
The experience of the NHS in the early 2000s, which provided patients on waiting lists with the option of travelling under a NHS contract to another European country, was also cited as relevant to understanding the level of outbound medical travel and the motivation for it.
Primary care trust interviewees reported examples of complications that had occurred after medical tourists returned back to the UK:
So we’re not infrequently getting requests from people to go abroad for surgery or other things. Not infrequently getting people coming back from having gone abroad with problems.
NHS7
People have gone and had a gastric band fitted in Holland and then come back and had problems and expect the NHS to either pay for that care or to pick up the follow-up care which they’re not entitled to do
NHS6
There were also said to be subsequent requests for cosmetic surgery to remove excess skin following overseas bariatric surgery. However, although examples were given (a couple of bariatric cases in one PCT, a bariatric case and gender reassignment in another), the scale was not overwhelming when viewed in the context of PCT activity. A director of public health suggested: ‘The totality of all this, at least in terms of the stuff that comes back in our direction, is very small’ (NHS7).
Medical tourists returning with diagnostics was also mentioned in the case of some minority ethnic cultural groups:
I’ve heard of lots of people that are turning up with files an inch or two thick with ridiculously over detailed packs of diagnostics for essentially a dermatology condition. Or something which would be an endoscopy and you’ve had full body scan.
NHS6
Many people travel for treatments that are not available on the NHS. This was the case for many of the patients interviewed for this research (see Section 3) and also helps explain the seemingly greater number of providers of elective procedures (especially dental treatment and cosmetic surgery) and fertility treatment. A difference in perception of the scale of the issue between professionals working in different medical sectors was clearly evident from the interviews. However, although complications were not identified as significant (albeit within the small number of PCTs that we spoke to), what was also clear was the absence of a clear mechanism for recording such complications (e.g. to identify patterns): ‘Nobody would come back [to the PCT] because that would be taken care of in primary care generally or even if it need[ed] secondary care, they wouldn’t really have a way to feed that back to us’ (NHS9).
Education and information
Many professionals pointed to the absence of clear guidance (and related regulation), both for patients travelling abroad and for those returning with complications. Interviewees highlighted the need for greater guidance for patients travelling abroad for medical treatment including what the minimum standards for providers and overseas treatment should be. This relates closely to how information is packaged, how it is provided and by whom. Many of the interviewees offered ideas on how information could be better provided, either through GPs or the Royal Colleges, but also through greater public awareness of these issues.
Providing reliable independent information on medical travel was seen as a key challenge and an important step in addressing issues of patient safety, to limit some of the likely negative consequences of medical tourism (including complications and insufficient aftercare). One of the main problems with the current provision of information is that it is often provided by agents:
At the moment if you look at the information sources out there they appear to be so swayed towards internet sites that have a vested interest in getting people on planes and abroad and having treatment we really need to have a thing that is free from commercial interest.
PA5
Interviewees referred to information in the media being sensationalist, with individual stories of complications being reported or stories generally having negative undertones. This leads to medical tourism overall having negative connotations, which in turn limits open discussion and accurate debate of the issues involved. Actors highlighted the need to get reliable institutions involved in providing information but also the need to make this easily accessible to patients.
Representatives of the Department of Health interviewed for the research pointed to the need for greater patient information and highlighted that such advice and guidance would be developed as part of the implementation of the EU directive on cross-border care. 1 PCTs did identify NHS Choices and the Department of Health as portal points where prospective medical tourists could be directed.
Those professionals working on issues relating to cosmetic treatments highlighted that patients often did not speak to a doctor or their GP in the UK before seeking treatment abroad: ‘Cosmetic surgery patients are amongst the most vulnerable. The vast majority of them who think about cosmetic surgery feel embarrassed to talk about it. They do not even go and discuss it with their GP. They quietly go away’ (PA8).
Doctors working within the NHS, especially GPs, were seen as central to the provision of information and in guiding medical patients as they contemplate travelling abroad for medical treatment. In this respect, several professionals interviewed highlighted the importance of GPs being open to patients discussing their plans for medical travel with them and providing a safe space for advice.
External quality assessment and quality information systems
All interviewees commented on the vast variety of standards of treatment and procedures undertaken abroad. There was a general recognition that this depended entirely on the provider and that people travelling abroad may receive excellent health care but equally may receive very poor treatment. One of the clinicians working for a professional organisation observed: ‘Some of the work I see from oversees is excellent and some of the work I see from my peers in the UK is not always great. So I think it depends on who you see’ (PA16).
However, given the very large variation in providers and quality, patient safety was mentioned as a key concern by all professional actors interviewed. The absence of reliable universal benchmarking or quality control mechanisms was described as a key limitation for patient safety and a critical issue to address. One of the actors interviewed highlighted that in the absence of the CQC or its equivalent many patients travel into the unknown:
The vast majority of people who go on holiday would not dream of going to a hairdresser abroad [. . .]. Yet they go abroad and they trust their body, their health, their wellbeing to somebody they have no idea who he or she is and in circumstances where you do not know whether they meet the necessary requirements of safety.
PA8
Producing guidance or guidelines would not be a straightforward task. An interviewee from a professional association suggested: ‘In order to have guidelines you need to have evidence and facts . . . what are the outcomes not only of operations abroad but of operations in this country. I’m afraid they’re sadly lacking at the moment ‘ (PA2).
Fertility travel, in which many patients travel to have access to treatment not allowed by UK regulations, poses specific threats to patient safety. Professionals working in reproductive care repeatedly mentioned the resulting increase in risk of complications including multiple births. A representative from an organisation working in reproductive care (PA12) commented that ‘the desire for a child is so all-consuming, it takes over rationality on occasions’.
Interviewees also referred to accreditation as a way of ensuring greater patient safety. International accreditation schemes, such as JCI, offer greater credibility but come at a higher cost. This will be reflected in the price of the treatment as these costs have to be passed on to the patient. It is therefore more likely that patients who search for the cheapest possible treatment will have inadvertently compromised on safety standards. Professionals noted that cosmetic surgery is referred to as the ‘Wild West’ as no quality standards exist.
Continuity of care was seen as a particular concern. All of the professionals interviewed referred to follow-up care and complications as an issue. Although the scale of medical tourism did not seem overwhelming, all interviewees were aware of (or had treated) complications arising from treatment abroad. The greatest challenges experienced were due to a lack of continuity of care provided to the patient, including challenges faced by doctors in the UK providing aftercare. Several issues were highlighted in this respect.
Professionals also reported that it was not uncommon to see patients who had been to one or more providers, having already seen a number of different clinicians, often adding to the confusion over the treatments carried out. Contributing to the lack in continuity of care was that complications and the need for aftercare often arise much later than the original treatment. In many cases patients would experience problems years after the surgical procedures had been carried out.
Of the medical professionals interviewed, several referred to the lack of reliable patient records as a key challenge to providing follow-up care to patients who may experience complications. Either records do not exist or they may be in a different language. A senior representative of the professional dental community described several negative experiences in terms of record keeping. He described a long delay in receiving patient records from the overseas provider, which in many cases are in a different language and therefore need to be translated to be of any value, but also how these are often meaningless.
Legal considerations and NHS entitlement
Medical insurance providers and quality control agencies highlighted different levels of indemnity cover across countries. Many providers do not offer this and this was noted as a concern for patients if things go wrong. Specific industry models were also reported as being particularly limiting to patients’ ability to assure quality. Patients who pay up front for treatment, especially when they pay a broker without having seen the clinician or doctor, raised concerns with professionals about the consent to medical treatment and safeguarding this principle. Certainly, amongst the sample of patients interviewed for this research were some who had not fully understood the procedure that they were receiving and consenting to.
Representatives from the Department of Health were very clear on NHS responsibility for dealing with complications and follow-up care resulting from medical travel:
It comes back to the fact that the NHS is a universal healthcare service therefore if you live in this country those services are available to you. Whether you’ve been dealt with badly in another country and if you’re living here you have the right to access the NHS and that extends to putting right treatments.
PA14
This ‘no fault’ treatment issue was captured by another provider viewpoint that those trusts with A&E facilities face key issues that PCTs must deal with:
We take everybody in and then only get to decide whether you pay or not and if you don’t wish to pay well there’s only so much we can do about it. So I think from an acute side its very much all routes lead into us from whether it’s a private hospital to us when it goes wrong, whether it’s done overseas that treatment has gone wrong, or whether it’s GPs saying I didn’t check the status because it’s not my problem.
NHS10
Interviewees conveyed that, although complications would be dealt with, this may not necessarily involve longer-term management of patients’ follow-up care and needs.
Professional associations of NHS doctors described patients’ requests for pretreatment tests and investigations as a dilemma, especially at a time of limited resources. One GP described how prospective medical tourists were dealt with using the same principle as for those seeking treatment in the private sector in the UK and consulting their GP in advance. However, when the tests required by patients would be part of a NHS treatment plan, the surgery would provide these for patients seeking to travel abroad or receive treatment in the private sector. When these are different from or are additional to what the NHS prescribes they are not provided.
A number suggested that outward medical travel should simply be seen within the wider context of private care: ‘We have received cases of patients who have had a private operation and then want to come back within the NHS’ (NHS8).
The NHS as a treatment facility was viewed as the eventual recipient of all patients with complications that could not be rectified in the private sector:
If you were an overseas provider you would just give people the advice that our private sector providers down the road give their patients. If you’ve got any problems go to your local NHS hospital, which is what they do. The private sector doesn’t take a particularly pastoral approach to the management of some of the complications.
NHS15
Overall, among the different professional stakeholders there appeared to be a lack of clarity on NHS responsibility to provide information, deal with complications and provide follow-up care. Given the overall remit of the NHS there was a sense that in all likelihood all complications would be dealt with in the NHS. Those interviewed pointed to the government’s responsibility, specifically the Department of Health, to provide clear information and guidance on the responsibility of the NHS both to NHS doctors and to patients.
Appendix 24 Motivation wheels: bariatric, fertility, dental and cosmetic treatment
Bariatric treatment
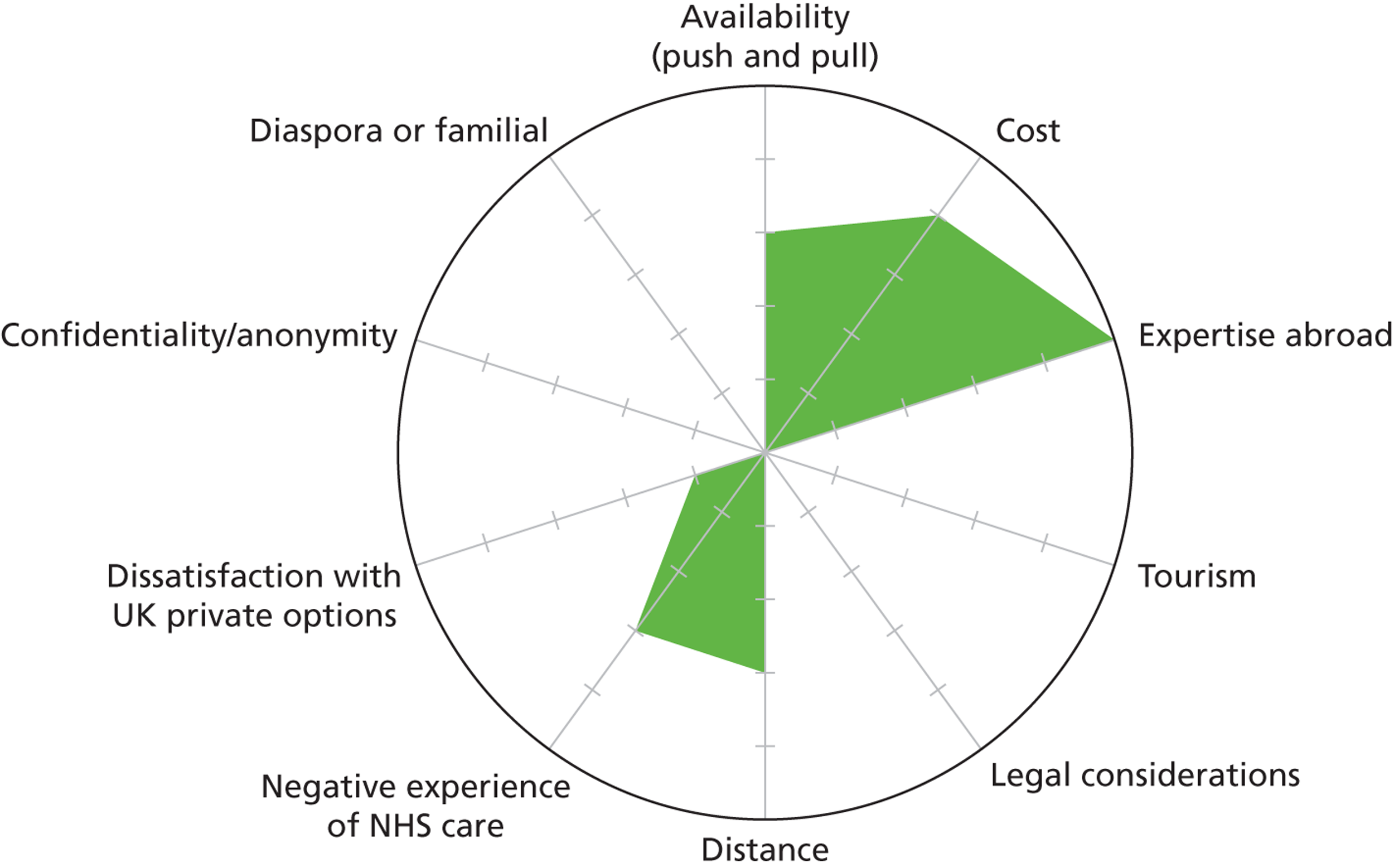
Fertility treatment
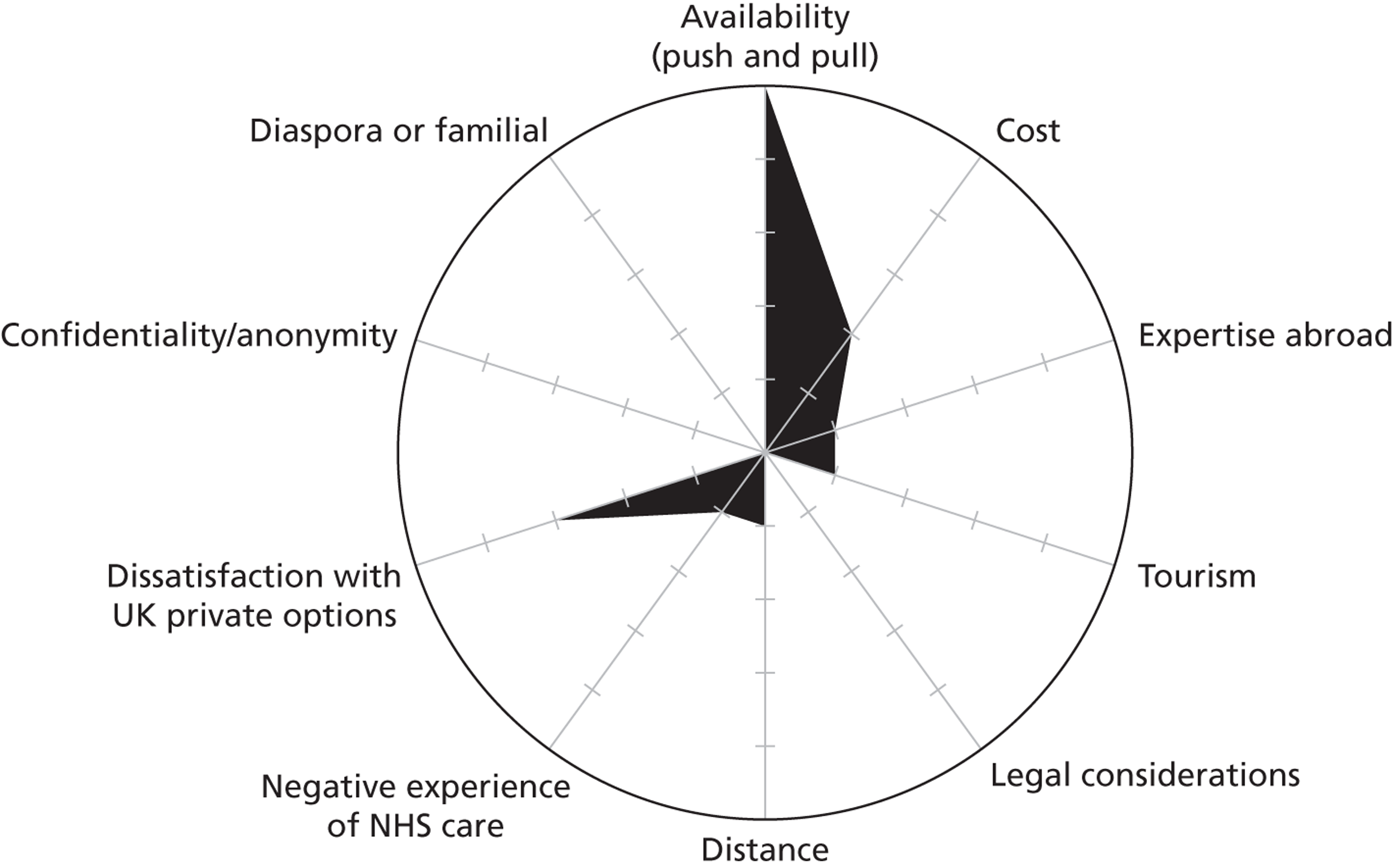
Dental treatment
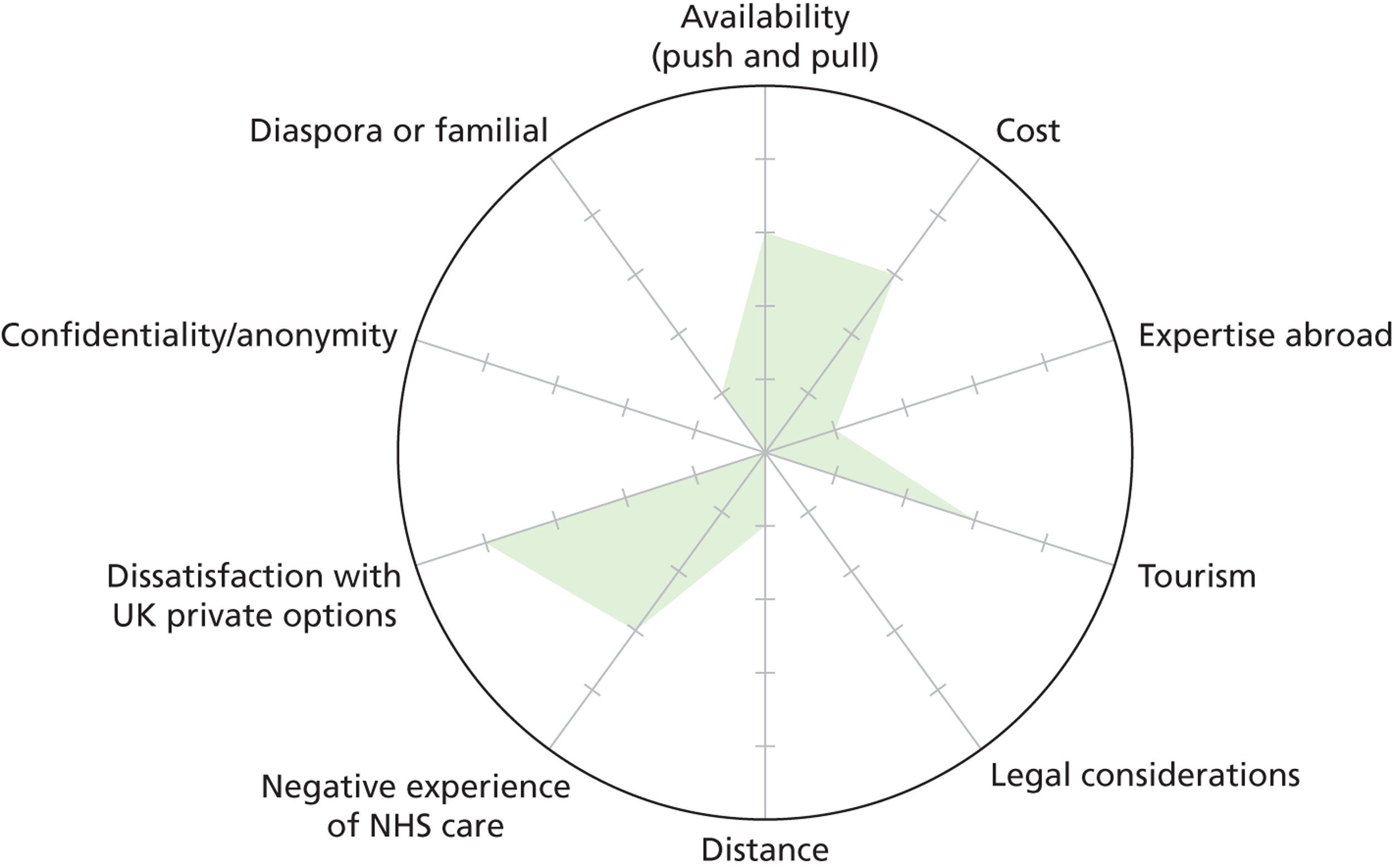
Cosmetic treatment
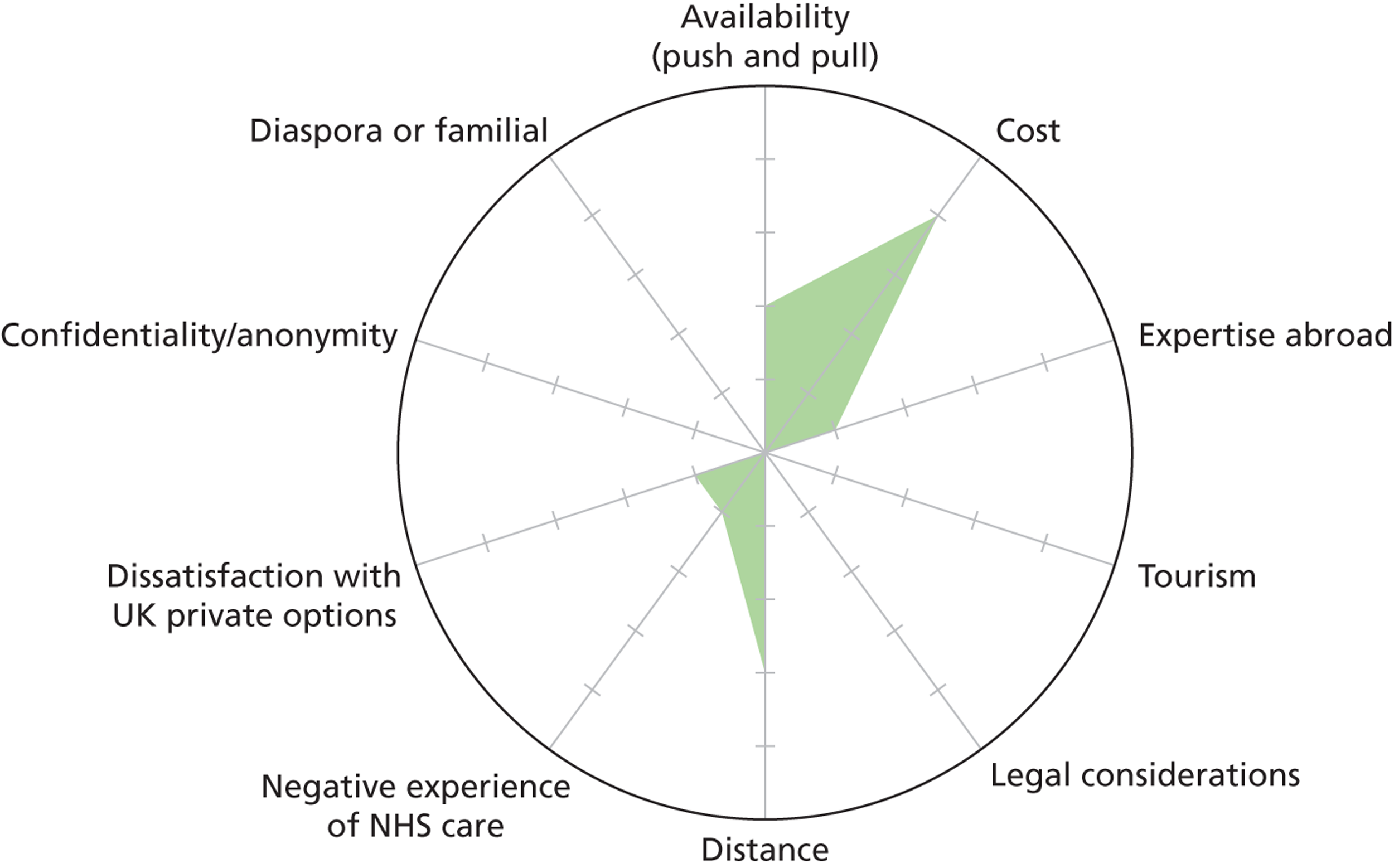
Appendix 25 International patients and associated activities: background and policy context
Specialist NHS facilities have a long tradition of treating international patients; there are also established collaborative clinician networks and programmes with regard to training, education and consultancy. NHS trusts adopt a range of commercial models and approaches to the organisation of services and their delivery to international patients. First, some foundation trusts partner private commercial interests. For example, Hospital Corporation of America (HCA) NHS Ventures has a number of partnership arrangements with NHS trusts whereby patients are treated exclusively in private settings. 257 HCA’s first such venture was the 2006 partnership arrangement with UCLH. This was to develop Harley Street at UCLH (a complex cancer centre facility). This has resulted in HCA taking over the hospital’s private patient wing, leasing space and paying for services and sharing profits from private patients with the hospital. 258 A 2010 partnership with Christie NHS Foundation Trust in Manchester led to the Christie Clinic, a new trust/HCA joint venture.
Second, some specialist London hospitals have opened branches in the Middle East or partnered with commercial interests and health-care developments in the region. Imperial College London Diabetes Centre opened its Abu Dhabi facility in 2006, specialising in diabetes treatments, research and training. The Gulf region in particular has a significant British and Western expatriate population.
Great Ormond Street Hospital opened a regional office at Dubai Healthcare City in 2006 aiming to:
-
improve the quality of services provided to children and families referred to Great Ormond Street Hospital from the Gulf region
-
develop the international business of the hospital through service improvement and development
-
maintain and develop the profile of Great Ormond Street Hospital as a provider of health care for children.
Great Ormond Street Hospital’s Gulf office averages 300 patient contacts annually. It offers support to patients and families travelling from the region to London that parallels support undertaken by facilitators within the wider medical travel industry: advice on investigations and pretreatment; information and assistance with accommodation and transport to the hospital and information on services and London; and assistance obtaining visas. On return to the Gulf, the office claims to provide medical records and adequate information for the referring hospital/doctor, continuity of care with regard to equipment or medication, and ongoing contact with families and communication with clinicians at Great Ormond Street Hospital. 259
In 2007 Moorfields Eye Hospital opened a facility in Dubai Healthcare City that operates as an overseas arm of the hospital. Its doctors have typically undergone training at Moorfields and are based in Dubai permanently rather than rotating between London and Dubai. 260 The hospital treats around 11,000 patients per year at its purpose-built campus, with around 70% coming from the Emirati and expat Arab communities. 261 The hospital has established 18 insurance affiliations and many of the patients are covered by insurance, the number of insured patients rising strongly as a proportion of the total patient base. 262 In March 2011, Moorfields Eye Hospital NHS Foundation Trust took the decision not to expand its Dubai facilities. 263 There is also emerging international competition within the region, with the US-owned and run Cleveland Clinic scheduled to open in Abu Dhabi in 2013. A number of the specialist teaching hospitals have close clinical relationships with hospitals in Middle Eastern countries and offer clinical training, education and ongoing support, which may be more or less formalised (at hospital or national level). Great Ormond Street Hospital activity, for example, is undertaken through partnerships with the Dubai Health Authority. This provides a visiting consultant programme to the main government hospitals. 259 Similarly, a programme of education and training for paediatric services is run in partnership with the Kuwaiti Ministry of Health to enhance delivery of its government hospitals.
Third, within the NHS, private services are offered to patients (including private patients from abroad) within both integrated and standalone facilities. Integrated facilities involve the use of shared theatres and treatments; activities are co-located because of the need for intensive care units and specialist support (e.g. shared theatres with private wards for private maternity patients). For some treatments there may be dedicated facilities with private operating theatre space and ward facilities.
Private patient income cap
A limit on the amount of income that hospitals can raise from private activities was introduced by the Labour government in 2003 as part of the legislation to establish NHS foundation trusts (Health and Social Care Act 2003264). The cap for foundation trusts was fixed at that existing in the 2002–3 base financial year and so varied from hospital to hospital. As well as private patient income, the percentage could include income from external business ventures such as commercialisation of research and development, training and consultancy. Although typically the cap on hospital income from private activity was around 2%, for a small number of specialist facilities it was much higher. The Royal Marsden, for example, had a 30% cap on income from private activity The cap limited hospitals from increasing the amount of private work and income beyond their base-year proportion and foundation trusts were monitored to ensure compliance. There were reported cases of single expensive treatments taking foundation trusts over their cap. The Health Service Journal (6 October 2011)265 reported Guy’s Hospital breaching its private patient cap by £700,000 because of treatment relating to one set of overseas twins. Non-NHS trusts were not subject to the cap and a number had private patient income far in excess of that of many foundation trusts. Since the cap was introduced, several NHS foundation trusts have established charity, joint venture or other arrangements with private sector interests to raise additional income or protect existing sources of income raised from private patients.
There ensued considerable discussion about the cap and the merits or otherwise of its removal. The White Paper Equity and Excellence: Liberating the NHS266 argued for ‘Abolishing the arbitrary cap on the amount of income foundation trusts may earn from other sources to reinvest in their services and allowing a broader scope, for example to provide health and care services’ (Section 4.22).
The NHS Confederation and the Foundation Trust Network both backed the lifting of the cap. Additional private sector income was explicitly identified in the Health and Social Care Bill31 in the form of ‘additional non-EEA overseas private patients’ who under previous arrangements could not be treated in the NHS if trusts were close to their cap. The chief executive of Great Ormond Street Hospital suggested that ‘The lifting of the “private patient cap” would allow us, as a Foundation Trust, to treat more private patients but also, through reinvestment, to help more NHS patients as well’. 267 Advocates of legislation foresaw opportunities to secure greater numbers of patients travelling from overseas for treatment as part of wider commercial developments. Critics pointed to the further privatisation of the NHS. These non-UK patients will potentially be sponsored by governments, funded by insurers or paying out of pocket. Under the Health and Social Care Act 201230 the cap for foundation trusts was increased and now 49% of income can be earned from non-NHS work (in force since 1 October 2012). However, the core legal duty of foundation trusts remains unchanged (that of caring for NHS patients and delivering authorised services).
How the increase in private activity will impact on the NHS and its patients is not clear and is dependent on whether a particular foundation trust is operating close to capacity and whether additional capacity is generated to treat private patients or existing capacity is used. 31 NHS patients may receive benefits if new or enhanced facilities are shared between private and NHS patients. However, if private patients have greater priority there will – all things unchanged – be a growth in waiting lists and waiting times for NHS patients (Section B155–B156). 31 There is no evidence to judge this.
The final legislation passed in March 2012 made key provisos with respect to the impact of private income on NHS services:
Each annual report prepared by an NHS foundation trust must give information on the impact that income received by the trust otherwise than from the provision of goods and services for the purposes of the health service in England has had on the provision by the trust of goods and services for those purposes.
Any major increases in private sector income require governance approval at board level:
An NHS foundation trust which proposes to increase by 5% or more the proportion of its total income in any financial year attributable to activities other than the provision of goods and services for the purposes of the health service in England may implement the proposal only if more than half of the members of the council of governors of the trust voting approve its implementation.
The NHS ‘brand’
Since 2010 there have been clear attempts to support international activities of NHS trusts and organisations. NHS Global was launched in 2010 by the chief executive of the NHS:29
While there are already strong examples of NHS Trusts and organisations successfully sharing their ideas and products abroad, we want to create a more systematic approach to this work, and in doing so bring benefits back to the NHS and the UK taxpayer . . . It is now more important than ever to maximise the international potential of the NHS.
The 2010 White Paper266 also highlighted the potential of the NHS to exploit the power of its international reputation and financially gain from the NHS ‘brand’ when marketing NHS services to overseas patients. 31 To date, however foundation trusts have often been unwilling or unable to take full advantage of all of their ‘apparent freedoms’. 268
NHS Global is hosted outside the Department of Health by the NHS Institute for Innovation and Improvement. Its stated aims include identifying commercial opportunities, generating demand, brokering partnerships and advising on legalities and risks. The Treasury has an expressed interest in these developments. As the Plan for Growth269 outlined: ‘The Government will work with the NHS and industry to design and establish a proactive entrepreneurial NHS Global to make the most of the brand internationally and to offer support and advice to NHS Trusts’.
In early August 2012 the Healthcare UK scheme was launched, supported by the Department of Health and T&I. The aim is to further promote and encourage overseas investment and activities from within the NHS with the aim of providing profit streams for reinvestment in core NHS services.
Appendix 26 Results of freedom of information requests to NHS trusts 2012
Results of freedom of information requests to NHS trusts 2012 (PDF download)
List of abbreviations
- A&E
- accident and emergency
- ART
- assisted reproductive technology
- ASA
- Advertising Standards Authority
- BAPRAS
- British Association of Plastic, Reconstructive and Aesthetic Surgeons
- BME
- black and minority ethnic
- BMI
- body mass index
- CBRC
- cross-border reproductive care
- CQC
- Care Quality Commission
- EQA
- external quality assessment
- EU
- European Union
- FAQ
- frequently asked question
- GATS
- General Agreement on Trade in Services
- GDC
- General Dental Council
- GDP
- gross domestic product
- GMC
- General Medical Council
- GP
- general practitioner
- HCA
- Hospital Corporation of America
- HFEA
- Human Fertilisation and Embryology Authority
- HON
- Health on the Net
- ICSI
- intracytoplasmic sperm injection
- IPS
- International Passenger Survey
- ISO
- International Organization for Standardization
- ISQau
- International Society for Quality in Healthcare
- IVF
- in vitro fertilisation
- JCI
- Joint Commission International
- MHRA
- Medicines and Healthcare products Regulatory Agency
- NaTHNaC
- National Travel Health Network and Centre
- NICE
- National Institute for Health and Care Excellence
- ONS
- Office for National Statistics
- PCT
- primary care trust
- PIP
- Poly Implant Prosthèse
- PROM
- patient-reported outcome measure
- QALY
- quality-adjusted life-year
- QIS
- quality information system
- T&I
- UK Trade and Investment
- TÜV
- Technical Inspection Association
- UCLH
- University College London Hospitals NHS Foundation Trust