Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 09/1801/1066. The contractual start date was in August 2010. The final report began editorial review in March 2013 and was accepted for publication in October 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Corrections
-
This article was corrected in March 2016. See Drennan VM, Halter M, Brearley S, Carneiro W, Gabe J, Gage H, et al. Corrigendum: Investigating the contribution of physician assistantsto primary care in England: a mixed-methods study. Health Serv Deliv Res 2016;2(16):137–138. http://dx/doi.org/10.3310/hsdr02160-c201603
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Drennan et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
This study addresses questions of the implications of the changing workforce in primary care. It is focused, in the first instance, on providing information that addresses the questions of general practitioners (GPs), managers and those involved in commissioning services and education programmes in the UK. This chapter provides the background and rationale to the study by presenting contextual information about primary care, the workforce in general practice, mid-level practitioners including physician assistants (PAs) and the evidence at the point the study was commissioned (December 2009). The aims and objectives of the study are presented, followed by brief detail of the advisory mechanisms and public involvement to the study team. The chapter concludes with an outline of the rest of the report.
Rationale
Primary health care has a pivotal role in the NHS, as in other countries. 1 In all countries of the UK, the policy direction over the past 20 years has been to increase the delivery of health care outside hospitals at the same time as addressing issues of effectiveness, accessibility, equity, patient choice and affordability in primary care. 2–8 This policy stream, together with views from within the profession of general practice itself, argues that the delivery of services will require differently skilled and different types of health professionals working in general practice. 9 The changing demands on health-care systems combined with financial pressures and/or shortages of professionals raise questions of effectiveness and efficiency in all health-care workforce structures and/or staff deployment. 10 Task-shifting from one occupational group to another, substitution of one professional for another and the growth of support workers (in direct health-care and administrative roles) are three strategies evident in primary and secondary care in many countries. 11–14 These strategies are evident in the changes in the UK general practice workforce, including the use of ‘mid-level’ providers. ‘Mid-level’ health practitioner is a term that has been used to describe a qualified health professional (non-medical and non-dental) practising at a level above that of the basic level of qualification for most health professionals in the UK and with authority to assess, investigate and commence or change treatment within the agreed scope of practice with their employer and/or clinician supervisor. 15 PAs and nurse practitioners (NPs) are two examples of mid-level practitioners among a diversity of titles and roles worldwide. 16
We outline first of all the developments in the general practice workforce before providing information on PAs in primary care and the rationale for the study.
Developments in the UK general practice workforce
There are about 10,000 general practices in the UK and, as a sector, these have been characterised by entrepreneurial developments in service delivery as well as in practice organisational forms. 17,18 Many of these developments have arisen through individual enthusiasms and values19,20 and others have developed in response to incentives and health professional labour market fluctuations. 21,22 The flexibilities created both by the new General Medical Services Contract23 and other forms of contracts for primary care24,25 created opportunities for different organisational forms and skill mixes appropriate to the needs of patient populations and to the provision of out-of-hours and extended hours services. GPs, as both health-service professionals and employers, exemplify the human resource policy stream articulated first in the human resource strategy for the NHS Improvement Plan in 2002: ‘more staff working differently‘. 26 The GP workforce has, in the last 10 years, both grown and diversified, with increased numbers of part-time and salaried, rather than partner, GPs. 27–30 However, it should be noted that shortages of GPs and their distribution are not uniform across the country. For example, the number of GPs per 10,000 population in England in 2011 ranged from 6.3 in the east of England region to 7.7 in the south-west region. 27 There have also been changes in the types and volume of consultations undertaken in general practice, with shifts of responsibilities from secondary care to primary care, for example in chronic diseases management and the development of GPs with special clinical interests. 31
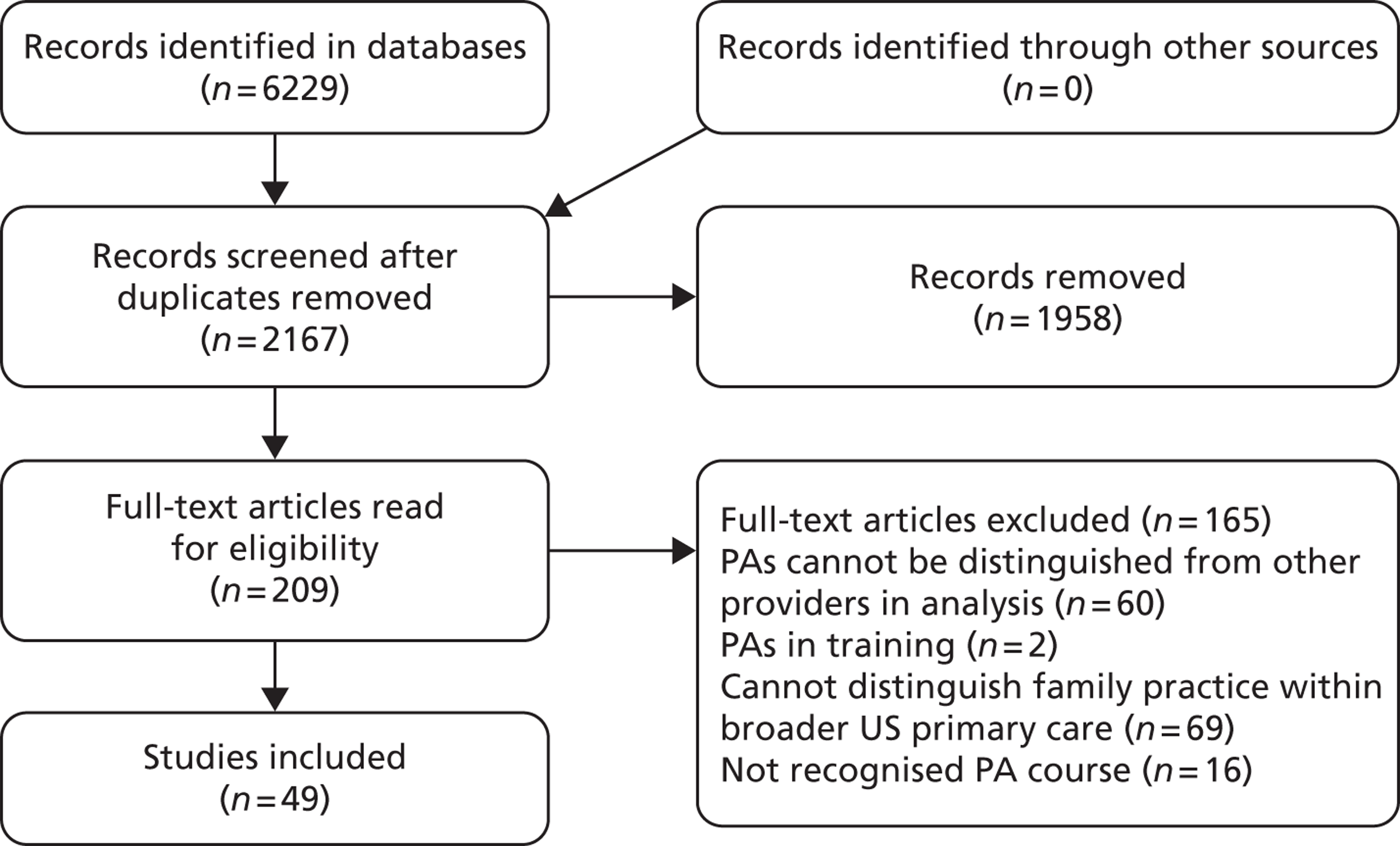
These shifts have been accompanied by GPs moving to employ a wider skill mix within general practice teams. 29 Such a development is evident in the growth over the past 25 years in numbers of administrative staff, nurses and others providing direct care. 27,28 Current statistics for general practice staff in England are illustrated in Figure 1.
FIGURE 1.
Composition of general practice workforce in England, 2011. FTE, full-time equivalent. Data source: NHS Information Centre. 32
In the UK, the solo GP with only a receptionist is an organisational model of the past. 33 However, debates continue within the profession of general practice regarding the appropriate mix of staff and skills for a general practice team. 20,34 It is evident from annual surveys in general practice in Scotland that nurses, together with direct care staff such as health-care assistants (HCAs), account for increasing volumes of patient consultations (30% in 2011). 35 Analysis indicates that these are not consultations in which patients present with undifferentiated diagnosis but are follow-up consultations for monitoring or review activities. 35 This suggests that the nursing and direct care staff are both supplementing the work of the doctor and undertaking delegated tasks. Outside general practice itself there are suggestions, such as from a HM Treasury-commissioned report, that NPs could provide a form of substitution, undertaking at least 25% of the work undertaken by GPs. 36 A Cochrane Review published in the same year37 suggested that the evidence was more nuanced. Previous systematic reviews indicated that patient health outcomes were broadly the same for NP and doctor consultations but that patient satisfaction was higher, the length of consultation was longer and the rate of investigative tests was higher for nurse consultations than for consultations with doctors. 38,39 The Cochrane Review excluded observational studies and also separated analysis between those studies in which the nurses were taking ongoing responsibility for chronic disease management and those in which they substituted for the doctor in first-contact, urgent consultations. 37 It was reported that in the studies of ongoing chronic disease management ‘there were no appreciable differences between doctors and nurses in health outcomes for patients, process of care, resource utilisation or cost’. 37 In the five included studies of first-contact, urgent consultations, broadly similar health outcomes for patients were reported for nurses and doctors. Differences reported between the two were lengthier nurse consultations, greater rates of recall by nurses, but higher satisfaction scores for nurse consultations than for doctor consultations. 37 The authors reported that the ‘impact on physician workload and direct cost of care was variable’. 37
By the turn of the twenty-first century there was a policy impetus for a redesigned workforce, particularly in primary care and first-contact services,21 an acute shortage of nurses and doctors applying to work in primary care and encouragement to develop and test new roles from a national body for service innovation known as the NHS Modernisation Agency. 40 At this point, some GPs with others who were looking for workforce solutions began to consider the contribution that another type of ‘mid-level’ practitioner, the PA, working in the USA, could make to the NHS. Before examining this occupational group in the UK, the following section provides contextual information on PAs in the USA and other countries.
Physician assistants
Physician assistants were introduced as a new professional group in the USA in the 1960s in response to medical shortages and misdistribution. 41 PAs are ‘graduates of an accredited PA educational program who are nationally certified and state licensed to practice medicine under physician supervision’. 42 The 170 educational programmes in the USA last an average of 27 months and require applicants to have qualifications in basic science and behavioural sciences and experience of health care. 42 The courses are based on medical education programmes and include 2000 hours of clinical experience practice. 42 Each qualified PA is required to undertake continuing medical education and recertification every 6 years. 42 PAs undertake physical examinations, investigations, diagnosis, treatment, and prescribing within their scope of practice as agreed with their supervising doctor. 43 They have to be registered in the state in which they want to work, and each state has separate regulations and limitations on the prescribing authority of PAs. There are similar numbers of PAs44 and NPs45 in the USA, and about one-quarter of PAs work in family medicine settings46 (Table 1).
| Role | Total number practising in the USA | Percentage practising in family medicine |
|---|---|---|
| Doctors of Medicine (2009) | 766,836144 | 1244 |
| NPs (2006) | 81,43345 | 2545 |
| PAs (2009) | 62,960144 | 2646 |
Studies have demonstrated that PAs, as an occupational group in the USA, provide equivalent and safe care to physicians for the case mix they attend and are acceptable to patients. 47,48 PAs have been shown to have the same task productivity of between 50% and 80% of a physician, dependent on practice setting and experience of the PA, with attendant cost savings to the organisation dependent on the remuneration levels of both the PAs and the physicians they are replacing. 49–51
A number of other countries have PAs in their health-care systems and have developed PA educational programmes. Hooker et al. 52 provide an overview of international developments. Canada introduced PAs in the military in 1984 and in the civilian health service in 1999. Taiwan (Province of China) converted a group of nurses to PAs in 1997 and introduced a PA programme, as did the Netherlands in 2001. The health services in Australia ran pilot projects in rural and remote areas in Queensland starting in 2009, developed the first PA education programme in 201053 and are looking to develop this workforce further. 54 New Zealand has also run a demonstration project and is about to commence a second in rural areas and in primary care. 55 The International Association of PA Educators reported that in 2012 there were 12 countries with PA education programmes: Australia, Canada, England, Germany, Ghana, India, Kenya, the Netherlands, Saudi Arabia, Scotland, South Africa and the USA. 56 Key issues in all countries have been how to achieve recognised accreditation and regulation mechanisms as well as authority for prescribing. 52 The earliest record of GPs in the UK exploring the use of PAs was in 1980. 57 We will now describe the UK experience of PAs from 2000 to 2009.
Physician assistants in the UK
In undertaking a review of the literature, it became evident that in the UK setting the term ‘physician assistant’ was being used in two ways. The first was by some hospital trusts in the UK to describe medical technicians with national vocational qualifications (NVQs) at level 2 or 3. The second was in relation to PAs either trained in the USA or trained in the UK at postgraduate level to the American model. This study is concerned with the second group.
Under the auspices of the policy for the modernisation of the workforce, many developments in new roles were encouraged in the first decade of the century. Small-scale, local pilots of training for roles such as PAs (although often under different role titles) were developed in many parts of the country. 58 The central government health department interest in exploring the utilisation of PAs was evident in two ways. The first was the support of the development of the anaesthetist practitioner programme, later PAs (Anaesthesia), with the Royal College of Anaesthetists in 2003. 59 The second was the funding of pilot projects deploying PAs in support of a wider range of medical teams. Two large-scale pilot projects were funded from central health departments in which USA-trained PAs were employed in a variety of health-care settings: primary care, emergency departments, intermediate care, orthopaedics and surgical specialties in England (2002–5)60 and Scotland (2005–8). 61 The pilot in England arose specifically out of the difficulties of recruiting GPs to deprived communities and the interest in the PA role as a potential solution from a nurse partner in a personal medical services practice, some local GPs and the local primary care trust managers. 60 The evaluations reported that they were very well received by patients, received without problems by other professionals, worked at the level of either a NP or a doctor in training and were reported to be safe in clinical practice. Caveats were noted; for example, demands on mentors were higher than anticipated and a tendency towards slightly longer consultations was reported. 60,61 The evaluation study in England reported on eight USA-trained, experienced PAs working in GP practices. 60 Mixed methods were used including interviews, electronic appointment data and PA- and supervisor-completed forms of types of patients seen and their clinical activities over specified weeks. The PAs were found to provide a similar number of consultations a day (an average of 16.5 per day) to GPs (17 per day) and see, broadly, the same types of patients, with variations between individuals according to prior experience, subspecialisation and practice organisation. 62 Issues that were reported included a period of acclimatisation to the NHS and medical practice in the UK being necessary for American PAs, and a lack of prescribing rights resulting in a greater demand on supervising GP time than would be usual in the USA. 62 It was also noted that the PAs expanded the scope of types of services offered in some practices and allowed others to increase their numbers of registered patients. 62 The Scottish pilot evaluated supernumerary PA posts, of which five were in general practice. Mixed methods were used, including interviews with staff and patients and self-completion work activity by the PAs and events diaries by the PAs and their supervisors. 61 In the primary care setting, the findings concurred with the reports of the English pilot. 63 In their conclusions, both evaluations pointed to the need for research that considered cost-effectiveness more systematically. 60,61
Concurrent with these pilots, PA educational programmes were initiated62 and then further developed by the Department of Health, involving the Royal Colleges of Physicians and General Practitioners. Together these organisations have agreed a competency and curriculum framework for PAs’ education,64 modelled closely on that of the USA. By 2009, postgraduate diploma courses for PAs had commenced in four English universities and a further three trained PAs in the specialty of anaesthesia only. 59 The first of their students had graduated by 2009. These developments were supported by national PA networks and structures. The PAs in anaesthesia established an Association of Physicians’ Assistants (Anaesthesia), which has an agreed curriculum and competency framework with the Royal College of Anaesthetists and the Association of Anaesthetists of Great Britain and Ireland, and holds a voluntary managed register of qualified PAs (Anaesthesia). 65 The UK Association of Physician Assistants was established in 2005. 66 Together with the UK and Ireland Universities Board for Physician Assistant Education (UKIUBPAE), it established the Physician Assistant Managed Voluntary Register (PA MVR) in 2010. 67 The Department of Health agreed an updated version of the competency and curriculum framework64 to reflect this last development. 68
Although both the medical and the nursing professions have in the past been hostile to the introduction of the PA role,59,69,70 there has been increasing acceptance that the addition of PAs to multidisciplinary teams, such as first-contact services, can enhance the delivery of care. 71 At the same time, the number of general practices employing PAs, although small, is growing. 72 In an interview study of 20 GPs, respondents reported that they were motivated to employ PAs in order to increase the practice capacity to manage patient demand within government targets for access, while considering value for money and broadening the skill mix in their teams. 72 The GPs reported that the PAs were primarily being used to see ‘same-day’ and ‘urgent’ appointment patients, although some had also forward-booked appointment clinics and chronic disease management clinics, and some undertook home visits. That study did not quantify or collect details on the work activity of PAs. 72
It was evident that there was growing interest from potential employers in PAs and a potential supply of UK-trained PAs. The UK evidence was limited in 2009 as to the effect of introducing PA personnel into general practice on issues of patient outcomes, service efficiency and safety. This study aimed to address the knowledge gap and provide information to inform decision-makers in health services, commissioning and higher education institution (HEI) settings.
Study aims and objectives
This study aimed to investigate the contribution of PAs to the delivery of patient care in primary care services in England. The research questions addressed were:
-
How are PAs deployed in general practice and what is the impact of including PAs in general practice teams on the patients’ experience and outcomes?
-
What is the impact of including the PAs in general practice teams on the organisation of general practice, the working practices of other professionals, relationships with these professionals and the practice costs?
-
What factors support or inhibit the inclusion of PAs as part of English general practice teams at the local and macro levels?
The full protocol has been published on the National Institute of Health Research (NIHR) Health Service and Delivery Research Programme website. The study team had the benefit of both an advisory group and a patient and public involvement group (see Appendix 1). Both of these groups met during the course of the study to help inform study tool development and research processes, and participated in the seminar in which emerging findings were presented and discussed. In between meetings, communication was electronic, using a newsletter and a website. In addition, the study team were successful in applying for a NIHR management fellow to work alongside the team, allowing synergy between the NHS management community and the research community. Further details are provided in Appendix 2.
The following chapters provide details of the study methods (see Chapter 2) and the findings reported in four chapters. The report concludes with the discussion and recommendations.
Chapter 2 Methods
This investigation employed an evaluative framework suggested by Maxwell73 to examine the contribution that PAs make to the effectiveness, appropriateness, equity, efficiency, acceptability and costs of primary health care. The study had two phases of enquiry. The first investigated the research questions at the macro and meso level of health-care systems through (a) a review of evidence, (b) a scoping survey74 of key informants at national and regional levels and (c) a survey of the current work deployment of PAs in UK general practice. The second phase used a comparative case study design75 of 12 general practices to investigate the research questions at the micro level of the health-care system. Each of these phases is described in detail below. The evidence from each of these elements was then synthesised by the research team and brought to a wider consultative group of people who had participated in the study, including the advisory group and public and patient involvement group.
Phase 1: investigating at the macro and meso levels of health systems
This phase had three elements: (1) a review of evidence, (2) a scoping survey74 of key informants at a national and regional level and (3) a survey of current work deployment of PAs in UK general practice.
The review of evidence
In this element we undertook three review activities. The first was a review of empirical evidence using a rapid review methodology76 for empirical evidence of the deployment and impact of PAs (research questions 1 and 2; see Chapter 1, Study aims and objectives). The second was a narrative review77 of published commentaries and opinions of the PA role in the UK setting. The third was a narrative review77 of national and international policy and developments on health-care workforce planning in relation to PAs and primary care. The last two activities addressed the question as to factors supporting or inhibiting the presence of PAs in the primary care workforce.
The review of empirical evidence
A review78 was conducted to investigate the evidence of the contribution of PAs to primary care as applicable to a European model. The European model of general practice/family medicine was that given by the European region of the World Organization of Family Doctors79 (WONCA Europe). Seven databases [British Nursing Index, Cumulative Index to Nursing and Allied Health Literature (CINAHL), EMBASE, MEDLINE, PsycINFO, Social Sciences Citation Index (SSCI) and Scopus] were searched from 1967 (or start date if later) to September 2010. A broad range of search terms was used singly and in combination: physician assistant, primary health care, family practice, general practice, family physician, general practitioner (see Appendix 3).
The inclusion criteria were defined as follows:
-
The PA role was one with a recognised PA qualification.
-
The setting was of general practice/family medicine (including community paediatrics in the USA) or the data were identified as pertaining to ‘family medicine’ within other findings from broader ‘primary care’.
The exclusion criteria were defined as follows:
-
Settings of secondary care, in-patient care ambulatory or outpatient care.
-
Health care provided by primary care specialists in the USA (obstetrics, gynaecology, internists or primary care physicians) that would be regarded as secondary care in the UK.
-
The personnel were student PAs or nurses/others who had received special training as medical assistants (that is, without a recognised PA course) for a particular disease condition.
-
The data presented did not distinguish either between PAs and other professionals or between the general practice/family medicine setting from ‘primary care’ overall in its presentation of results.
Retrieved abstracts were screened and full papers, where available, were obtained. Each full paper was assessed for inclusion by two researchers independently and a third (HG, SdeL, VMD, and MH) in cases of indecision or disagreement. A data extraction framework was developed which included categories of PA activities, study methods and key findings. Study outcome measures were categorised using Donabedian’s80 framework of structure, process and outcome. Owing to the wide range of methods used in the retrieved studies, a broad quality assessment of the studies was undertaken using critical appraisal tools81 appropriate to the papers’ methods (e.g. qualitative, cohort, health economic) with additional questions derived from the British Medical Journal’s guidance for peer reviewers. 82 The heterogeneity of the retrieved studies precluded any pooling of data and a narrative synthesis was undertaken using the Donabedian80 framework.
Review of commentaries
A documentary analysis83 was undertaken of published commentaries and opinion pieces about PAs in the UK health-care system or addressed to UK audiences. The published material was identified in two ways: first, through the electronic database search described in the previous section and, second, by an internet search using the Google™ (Mountain View, CA, USA) search engine. The internet search used a combination of terms: physician assistant, physician assistants, National Health Service (NHS), primary care, secondary care, England, Scotland, Wales, Northern Ireland, pilots and workforce, and was repeated at intervals by WC from April 2011 until December 2012. ‘Published’ was defined as in print and electronic formats including online forums between 1980 and 2012. The lower date was determined by our previous knowledge of the first paper published on the experience of a PA in UK primary care. 58 A data extraction framework was developed which included a categorisation of the author (journalists, doctors, nurses, health service managers, etc.), the intended audience, any catalyst for the item (e.g. another published item), inclusion of any empirical evidence and from which country, evidence of support, resistance or neutrality in the publication. The items were recorded chronologically with the data extraction in a Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) spreadsheet. A narrative synthesis was drawn from the data.
Review of workforce policy and developments
The purpose of this review was both to identify policy and developments pertaining to PAs in the primary health-care workforce in the UK and internationally in order to both help the research team contextualise the study and to identify supporting or hindering factors in the development of the PA profession in the English health-care workforce. The review drew on the methods of the documentary review. 83 Publications were identified through the searches described above. Additional searches were performed to identify polices and reports on health-care workforce planning and development relevant to, primarily, the education and employment of PAs and, secondarily, primary care. The time period covered was from the mid-1990s to the present day. The searches were conducted by:
-
visiting key websites in the UK, for example government health departments in each of the four countries, the Centre for Workforce Intelligence (CfWI) and Strategic Health Authority (SHA) websites
-
using keyword searches in the Google search engine for open source materials related to the topics of interest, for example ‘primary care workforce’, ‘physician assistant/s’ (and other titles to describe this profession, such as medical care practitioners) and ‘health care workforce’
-
snowballing techniques of references and website links.
The documents identified in this way were screened to include only those with relevance to health-care workforce in primary care. Research team alerts of new policy or reports relevant to the study were generated by one researcher (WC). A data extraction framework was developed to classify the document by country, type of author, type of document (e.g. policy, analysis of primary data, opinion and evaluative reports), any reference or absence of reference to PAs and key points from or about the document. The information was saved on an electronic database with full references, any URLs and electronic copies of the original. A narrative synthesis was undertaken addressing the questions of interest.
Scoping survey
A scoping survey74 was undertaken to address research question 3: what supports or inhibits the use and development of PAs in the primary care? (See Chapter 1, Study aims and objectives. ) The method is one element of a scoping review74 and allows for data to be gathered from those knowledgeable in the issue of interest, providing a range of perspectives to ensure breadth in the analysis. 84 It is an approach that has been widely used, most recently in exploring European perspectives on human health resource issues. 85 A purposive sample of key informants at national and regional levels in England and Wales was approached to participate. These were individuals at a senior level from central departments of health, professional organisations, regulatory organisations, patient organisations, and commissioning bodies who are concerned with the development of primary care services, workforce development and health professional regulation. At the point of the design of the study (2009) the Department of Health and Social Services (Wales), unlike the Departments of Health for England and Scotland, had not explored the use of PAs. In order to consider diversity in national environments, individuals were approached to participate in England and Wales. Individuals were identified for approach through an internet search of public domain organisational sites, suggestions of the study advisory group and members of the research team, and snowball techniques from participants. An aide-memoire was developed of topic areas, based on the issues of interest, to be used in semi-structured interviews83 which were offered either face to face or by telephone, dependent on participant preference. The aide-memoire explored knowledge of mid-level practitioners, PAs and perceptions of the factors that currently and will in the future support or inhibit their use and development in the UK settings. Notes were taken during the interview and, with permission, digitally recorded. These were transcribed, anonymised and the recordings deleted. The transcriptions and notes were analysed using the constant comparison method86 by two researchers (WC and VMD) independently, compared and further analysis confirmed with a third researcher (JG). The analysis of the early interviews assisted in identifying further stakeholder groups from whom views were sought. This element of the study was deemed service evaluation by the NHS ethics query service and as such not for research ethics review. It conformed to all university requirements.
Survey of current use of physician assistants in general practices in England
An online, anonymous, self-completion survey was developed and piloted with two PAs who had previously worked in general practice in England. It posed questions of career history, work environment, work activities and estimates of volumes of work. PAs known to working in primary care were invited to participate in 2010 through e-mails sent out by the UK Association of Physician Assistants (UKAPA), course leaders of PA courses in English universities and practices identified as employing PAs in previous research. 72 All invitation e-mails included a link to the survey website and requested forward distribution to any other PAs thought to be working in primary care. UKAPA estimated that there were about 25 of their member PAs employed in primary care. The electronic survey was open for responses for 7 weeks (7 October to 30 November 2010). It addressed three areas: the activities and role of PAs in the primary care team, their primary care setting and their qualifications. Those interested in volunteering for the second phase of the study were given an opportunity to give their contact details at the end of the survey. The survey did not require NHS ethical review and fulfilled all university requirements for the ethical conduct of research. Descriptive analysis of the data was undertaken using Statistical Product and Service Solutions (SPSS) (IBM Corporation, Armonk, NY, USA).
Phase 2: the micro level
A comparative case study design75 was used to address the three overarching research questions at the micro level of analysis through examination of 12 case studies: six general practices currently employing PAs and six matched practices not including PAs in their staffing. A mixed-methods approach87 allowed for both description and the quantification of the impact of PAs in the context of general practice. This element of the study addressed specific additional questions:
-
How are PAs deployed and supervised in general practice and how do their roles and responsibilities compare with those of the doctors, NPs and practice nurses?
-
How do PA outcomes of care differ from those of GPs, specifically with respect to prescriptions rates, referrals, investigations, reattendances for the same problem within 2 weeks, patient safety, and patient satisfaction?
-
How do patients understand the role of PAs and what is the experience of patients when consulting PAs?
-
How does employment of PAs affect practice organisation, staffing configurations and costs?
-
What are the factors that support or inhibit the employment of PAs?
The six practices employing PAs were identified either by the PAs initially volunteering through the survey (see Survey of current use of physician assistants in general practices in England) or by an expression of interest from a practice. The volunteering PA practices achieved diversity in features such as general practice size, practice population sociodemographic characteristics, rural and urban coverage, and in the country in which the PAs had qualified. The comparative that was designed required some similarity between PA and comparator GP practices. Following the agreement to participate from PA employing practices, comparison practices were sought in the same health economy and with similar characteristics and patient population size. After the adoption of the study by the UK Clinical Research Network (UKCRN) Primary Care Research Network (PCRN), officers in five local PCRNs made the initial approaches and requests for comparison general practices. Practices expressing interest were then contacted and provided with information, and an initial meeting was set up between the researchers (VMD and MH) and the GP, the practice manager and, in those employing practices, the PA. A summary description of the practices is provided at the end of Chapter 2 (see Table 5).
The general practices and staff likely to be included in the study were provided with full participant information sheets for all research activities. Written agreement and consent for the practice to participate was obtained from the senior partner GP. Procedures for obtaining individual informed consent for each of the research activities are described below.
Data were gathered through the activities detailed in the following sections in this chapter. The analysis is described in each section and the economic analysis in Economic analysis. Analyses were then combined and synthesised to address the research questions as outlined in Table 2.
| Research questions | Data |
|---|---|
| (a) How are PAs deployed and supervised in general practice and how do their roles and responsibilities compare with those of the doctors, NPs and practice nurses? | Interviews with practice staff |
| Work activity diaries | |
| Administrative data | |
| Observation of consultations/meetings | |
| (b) How do PA outcomes of care differ from those of GPs, specifically with respect to prescriptions rates, referrals, investigations, reattendances for the same problem within 2 weeks, patient safety and patient satisfaction? | Consultation record review and patient survey |
| Clinical review of reconsultations | |
| Observation of consultations | |
| (c) How do patients understand the role of PAs and what is the experience of patients when consulting PAs? | Patient interviews |
| Patient survey | |
| (d) How does employment of PAs affect practice organisation, staffing configurations and costs? | Interviews with practice staff Work activity diaries |
| Administrative data | |
| (e) What are the factors that support or inhibit the employment of PAs? | Interviews with practice staff |
Semi-structured interviews with practice staff
Semi-structured interviews83 were undertaken with PAs, GPs, practice managers, receptionists and practice nursing staff. A purposive sample in each practice was approached, provided with information and invited to participate. Aide-memoires for each professional group were developed addressing the questions (a), (b), (d) and (e), above, but allowing flexibility to explore new issues or ideas raised in the interview. GPs, PAs and nurses were also asked to describe their responsibilities and activities within the practice. In addition, practice managers and GPs were invited to provide any practice documents that would provide the research team with information about the practice, its working practices, services provided, staffing and planning. If documents on staffing were not available, the practice managers were asked to provide this information verbally. The interviews were conducted face to face or by telephone as preferred by the participant, digitally recorded with consent, transcribed and erased after analysis. Thematic analysis was undertaken88 initially by one researcher (RL), with further analysis by two other researchers (VMD and MH) and interpretative discussion with the wider research team. Documentary evidence on staffing was read and data extracted as relevant to providing contextual information for each practice.
Consultation record review and linked patient survey
The consultation record review and linked patient survey, which addressed question (b) above, was of patients presenting in urgent or same-day surgeries. This was the type of surgery that PAs were predominately working in as identified from the national survey (p. 9). Each practice identified time periods in summer and winter periods (known as reference periods) during 2011 and 2012 in which they were able to assist the research team in data gathering. The length of time periods were based on the practice’s estimation as to the number of surgeries required to reach the sample size. Each practice made staff and patients aware of the research during the reference periods in keeping with their usual practice, for example via notices at the reception desk.
The patient surveys
The validated General Practice Assessment Survey (GPAS)89 focuses on patient outcomes and consultation experience and was used with permission (Paula Metcalfe, GP Patient Survey Team, 12 October 2010, personal communication). During a meeting of the study’s public and patient participation group (see Chapter 1, Study aims and objectives) the GPAS was scrutinised and amendments suggested to improve the clarity of the wording and to specifically address the experience of a consultation with a PA. The amended, self-completion GPAS (see Appendix 4) was then to be offered to adult patients in each designated surgery during the reference periods. The method of distribution and collection varied in each practice, according to their working practices. In some practices, the GP or PA handed the patient a sticker to return to the receptionist, following the consultation, to collect a survey pack (containing a questionnaire, participant information sheet, and business reply envelope). In other practices, the survey pack was sent by post either the same day or the next. All completed questionnaires could be returned in a sealed envelope to a collection box in the practice reception or by post to the research team. The questionnaire did not include any information that could identify the person. Each questionnaire had a unique study identifier (study ID). Practice staff kept a log of the dates of survey administration (the index event) and recorded the unique practice identifier of the patient against the study ID. Practice staff were asked to send out a research team prepared reminder and duplicate survey pack to all those who had taken or been sent a questionnaire who had not responded. The practice staff did not have any access to any of the completed questionnaires, ensuring that anonymity was protected. Data were entered onto a SPSS spreadsheet and descriptively analysed. The data were then also added to the data drawn from the consultation record review as described below.
In the PA-employing practices, the survey pack included additional material inviting patients to participate in a face-to-face or telephone interview. A separate consent form and business reply envelope were provided to respond to the invitation.
Consultation record review
This review addressed the primary outcome of the study: the rate of reattendance in general practice or an urgent care facility defined for the study as GP out-of-hours care, emergency department, walk-in centre, minor injury unit or other direct entry emergency unit (e.g. early pregnancy assessment unit) within 2 weeks of the initial consultation (the index consultation) with a PA or GP, and questions of whether or not the initial consultation activity by the PA or GP was appropriate in the light of the subsequent reattendance. The consultation records also provided the data for the process measures of advice, investigations, treatments, referrals and prescriptions.
The sample
The sample size required for the primary outcome was based upon randomised controlled trial data which compared the rate of reattendance in general practice within 2 weeks and outcomes of care delivered by NPs and GPs in the UK for patients attending ‘same-day appointments’. These studies reported figures ranging from a self-reported 18.2%90 through to extracted medical records 28.4%91 and 29%92 for patients seeing GPs and 20.4%, 31% and 37.2% for NPs, respectively. Taking Venning et al. ’s91 analysis as the most robustly adjusted of these, the reattendance rate within 2 weeks of the consultation for this sample size calculation was taken as 28.4% for GPs and 37.2% for NPs. Assuming an OR of 1.5 and adjusting for slight multicollinearity as reported by Venning et al. ,91 we estimated that a sample size of 205 in each group (consultations with a PA or a GP) was needed to give 80% power at a significance level of 5% for a logistic regression using the covariates of age, gender and general practice. We estimated that anonymised clinical records data might be required for up to approximately 600 patients each attended by PAs and GPs in the 12 practices in the data collection periods in order to meet the required sample size, assuming a response rate of 30% to the patient survey. However, in conducting the study, two problems arose. The first was that a condition of the research ethics approval was that child consultations were excluded from the survey element but could be included in the review of clinical records. We therefore included all child consultations in the designated surgeries in the reference periods as our review and survey had shown that PAs were consulted by children and their parents. The second problem arose through inaccurate research team and practice staff estimates of patient survey return rates in their practice (i.e. lower than our assumptions) resulting in more surgeries being designated for survey distribution. In some practices, clinical records were passed to the research team some months after the designated surgeries and only then did it become apparent to the research team that these had much greater numbers than anticipated. In addition, in some practices, there was a lack of fidelity to the protocol in that not all eligible patients were offered the survey (in some instances only 30% were offered). This was apparent to the research team staff only when they returned to discuss the participant numbers and check that the reference periods were similar to those of the preceding weeks for the practice. As the possibility of selection bias could not be eliminated, the research team decided to include all of the clinical records sent by the practices. This resulted in a larger sample than in the study design.
The data
Data from the electronic records of those patients who consulted in the designated surgeries during the reference periods were extracted and all patient identifiers removed in the practice. These data were then passed to the research team using the unique study ID number only. The data extraction occurred at a time point more than 2 weeks after the end of the reference period. The data extracted by the practice staff for the index event included the consultation date, person consulted (PA or GP) and length of consultation; the patient’s age, gender, ethnicity and postcode; the patient’s presenting conditions; number of prescriptions from the consultation; the number and type of Quality and Outcome Framework93 chronic conditions registers the patient was entered on; the number of repeat prescriptions; and the number of times the patient had contact with the practice in the three months preceding the index event. For any consultations in the following 2-week period, the location of consultation, the professional consulted, presenting condition(s) and number of prescriptions issued were recorded. The research team used the postcode on each record to assign the Index of Multiple Deprivation (IMD)94 and then deleted the postcode. The practice records varied in the extent to which Read codes95 were used for the presenting problem or diagnosis. The research team subsequently reviewed each record and assigned Read codes95 to presenting problems that were documented but not coded by practice staff and assigned study codes for groups of diagnostic tests, referrals, procedures, certificates, medicine management and advice given (see Appendix 5). Each consultation record was coded by one member of the research team and then checked by a second. Uncertainties were discussed and resolved with a third member of the team. A categorisation of the presenting problems in the index consultation was also assigned to each patient record in order to examine the case mix of the consulting patients. This classification of acute, chronic, minor/symptoms, prevention and processes was an adaptation of that used by de Jong et al. ,96 developed by the research team in which the GP in the research team (SdeL) made the final decisions on categorisation and assignment. The method of assignment of a condition category to each patient is presented in Appendix 6.
Each index consultation that had subsequent consultations was identified. Each subsequent consultation was coded by two research team members to identify whether it was for exactly the same, a linked or a different problem to that of the index consultation. The method for designation was developed and refined with the GP research team member (SdeL).
All data were entered into a SPSS spreadsheet, to which the data from the patient survey (where available) could be matched by the study unique identifying number.
The data were then analysed descriptively, involving summary measures of location (e.g. means /medians/proportions) and dispersion [standard deviations (SDs)/percentiles] appropriate for the type and distribution of the individual variables. Differences in processes and outcome between those practices with and without PAs were assessed by generalised estimating equation models. 97 The resulting ORs or rate ratios were adjusted for the case mix and IMD variables where they were significant predictors or notably confounded the relationship between practice type and the dependent variable. The correlation matrix was set to be exchangeable, that is to say patients were assumed to have some shared characteristics within each practice, whether from demographics or organisation of the practice.
The clinical review of reconsultations records
All records in which a patient had reconsulted within 2 weeks for the same or a linked problem were assigned to clinical record review. The review of medical records, or ‘chart review’, is a longstanding method of assessing the consultation98 used in assessing overall quality99 and considered reliable in detecting prescribing errors. 100
An anonymised printout of the computerised medical record system was reviewed to assess the quality of the record and to assess the appropriateness and safety. The data on whether it had been a GP or PA who had conducted the index consultation were removed, as well as any other references that might identify the practice or its geographical area (e.g. hospital name). A clinical review process, which addressed the question as to whether or not, in the light of the subsequent consultation(s), the first consultation had been appropriate, was developed by the GP member of the research team (SdeL) in consultation with the clinical review team of four GPs. The four GPs all had experience of assessing the quality of the consultation and, to a more limited extent, of the medical record. They were all active in education: one was a trainer while the other three took medical students in their practices; two were research active; two were male, two were female. They were trained in two 2-hour training sessions led by SdeL.
Based on the problem-orientated medical record format,101 the experienced GP reviewers were asked to judge each element of the consultation, the overall appropriateness and whether a GP or a PA had been consulted. Weed’s taxonomy,101,102 for the elements of a problem-orientated medical record, was used as an measure of quality of the record, and the opinion of experienced GPs about appropriateness of the content of each part was used for the problem presented. The GP raters also gave an overall assessment. Weed’s101,102 approach was to suggest that there were four key elements of the record, described by the acronym SOAP:
-
Subjective: what the patient complains of, the problem from the patient’s perspective.
-
Objective findings from the consultation (e.g. blood pressure measurement).
-
Analysis by the clinician of the problem.
-
Plan for future action, including follow-up.
We modified this by making it explicit that the plan could have different elements: investigations, prescriptions and other aspects of the plan, such as referral or follow-up (Table 3).
| Weed’s SOAP | Modified SOAP | Includes | Explanation | |
|---|---|---|---|---|
| 1 | Subjective | Subjective | History | Patients’ complaint(s) |
| 2 | Objective | Objective | Exam | Objective findings (e.g. blood pressure recording) |
| 3 | Analysis | Analysis | Problem | May include diagnosis, recorded as the problem or reason for encounter |
| 4 | Plan | Investigation | Tests | Laboratory tests, X-rays, other tests initiated in primary care |
| 5 | Prescription | Acute, repeat or recommendation for over the counter | ||
| 6 | Other aspects of the plan | Referral |
Each record was assessed by a GP and 20% by two GPs independently using a study-designed form (see Appendix 7). Data were entered into a SPSS spreadsheet, analysed descriptively and inter-rater reliability was assessed. Inter-rater reliability is a measure of the extent to which the reviewers agreed with each other in their responses. Fleiss’s kappa103 is a simple measure of this inter-rater reliability. A kappa score of 0 indicates no more agreement than one would expect to occur simply by chance, and a score of 1 indicates complete agreement on all the data that were rated. Negative scores indicate agreement that is worse than chance. It is often said that a kappa score of 0.0–0.2 is ‘poor’, one of 0.21–0.4 is ‘fair’, 0.41–0.6 is ‘moderate’, 0.61–0.8 is ‘good’, and 0.81–1.0 is ‘very good’. 104 The raters assessed one case/medical record as a group. Next, they analysed three cases on their own and checked back afterwards. They then did a further 10 cases, which were assessed for inter-rater reliability.
Patient interviews
Patients who had consulted PAs and received a survey were also invited to participate in telephone or face-to-face interviews. This was designed to address question (c): how do patients understand the role of PAs and what is the experience of patients when consulting PAs? An aide-memoire was developed to explore issues not captured by the patient survey such as patient choice, understanding of the role of the PA, perceptions of the consultation with regard to communication and perceived expertise. A researcher (WC) contacted those who responded to the invitation as soon after the index consultation as possible. With consent, the interviews were digitally recorded, transcribed and analysed thematically88 by three researchers (LJ, MH, WC) using the NVivo software programme (QSR International Pty Ltd, Doncaster, Australia) (LJ, MH).
Observation of physician assistants and general practitioners
Patient consultations were video recorded, with consent of the practitioner and the patients, during one surgery per PA and GP. This element addressed questions (a), (b) and (e). We recorded GPs and PAs using two video channels, and assessed competence at consulting using the validated Leicester Assessment Package (LAP) rating scale. 105 Video recording is an established method of assessing the consultation106 and the use of two channels was a compromise between the multichannel recording we planned106 and what we could gain the NHS REC permission for.
Patients in the designated surgeries were provided with information and consent was sought in writing by a researcher in the waiting room before recording commenced. Recording was stopped at the end of each consultation. Patients were then asked whether they continued to give consent or would prefer that it was withdrawn and the recording deleted. Practitioners also reconsented to the inclusion of each recording or could ask for a recording to be withdrawn at the end of the surgery. The recordings were made using ALFA: a computer-mediated consultation observation technique developed to provide an analysable overview of the consultation. 107 Each consultation was assessed by two GPs independently using the LAP105 for assessing competence in general practice on dimensions of interviewing and history taking, patient management, problem solving and behaviour and relationship with patients.
The LAP for video consultation is a tool for measuring competence by direct observation. It was initially developed in the 1990s and demonstrated to have validity108–110 and reliability across levels of clinical competence. 107 Testing of reliability found a range of mean scores between 51.3% and 70.2% in one study, depending on levels of experience,110 and between 45% and 75% in another looking at the effect of interruption. 109 Although it has been criticised, no better package has been developed. 111,112 The LAP has also been used in a range of clinical contexts – assessment of cancer patients,112 the needs of caregivers113 and in the assessment of psychosexual problems. 114 This package has also been used in an international setting, where a 50% pass mark was included,115 for assessing practice nurses116 and medical students. 117
Grades were given by the four raters, using the seven main categories of the assessment package, and the results were then analysed. The seventh element of the package, the record, could not be rated as it could not be properly observed from the two-camera set-up used. Record keeping referred to how the health-care professional (HCP) interacted with the computer. It was not possible to view the detail of the individual record being collected by the HCP owing to the fact that only two channels of video were being recorded, and an additional channel is required for recording video directly from the HCP’s computer screen. Three of the seven categories – interview/history taking, patient management and problem solving – are given a double weighting, and count for 20% of overall marks (Table 4). When combined, this means that the LAP scale total is 100, allowing final results to be expressed as a mean score (out of 5 for each category) or be expressed as a total percentage score.
| LAP105 component | Weighting (%) |
|---|---|
| Interview/history taking | 20 |
| Physical examination | 10 |
| Patient management | 20 |
| Problem solving | 20 |
| Behaviour/relationship with patients | 10 |
| Anticipatory care | 10 |
| Record keeping | 10 |
A workshop was held to discuss the findings with the raters (unblinded) which was video recorded and transcribed.
Observation was also undertaken in a sample of practice clinical meetings in which PAs and GPs were both present to understand more broadly how the PAs interact with the GPs in clinical decision-making in the practice. Permission and invitations was sought from the practice manager, the GPs and the PA. Permission and consent to observe was sought at each meeting that the research team was invited to. Field notes were made of only the activity and interaction of the team members. Analysis of these notes was used to complement data from the staff interviews (see Semistructured interviews with practice staff) and consultation video observations.
Work activities of physician assistants and general practitioners
Work activity diaries, using the 2006–7 general practice workload survey,118 were offered to PAs to complete for 1 week in the summer and winter. This addressed question (a), above. Early discussions with GPs made it evident that these diaries were unlikely to be completed by practice professionals other than the PAs and the data were therefore sought through interviews (see Semi-structured interviews with practice staff) and administrative systems. Data were entered onto a SPSS spreadsheet and analysed descriptively.
Economic analysis
The economic analysis was conducted at two levels:
-
The resource implications and costs of different team configurations were explored using practice-level data on staffing. Skill mixes, and the relative contribution of different practitioners, were compared within and between practices that do and do not employ PAs, after consideration of case mix differences. Nationally validated scales119 were used to calculate total human resource costs and costs per patient.
-
The impact of PAs, compared with GPs, on consultation processes (e.g. prescribing, referral and investigations), consultation outcomes (e.g. reattending, consultation satisfaction) and length, at individual patient level, as analysed in the clinical record element were incorporated in a high-level analysis of costs and effectiveness.
Practice level
Data
Each of the 12 practices (six with and six without a PA) was asked in November 2012 to provide information about their staffing configurations – headcounts and whole-time equivalents (WTEs) of:
-
clinical personnel
-
– GPs (partners and salaried/other)
-
– mid-level professionals – PAs and NPs
-
– nursing and other staff engaged in direct patient care – practice nurses (PNs), HCAs, phlebotomists
-
-
support staff
-
– managers and professionals [e.g. for information technology (IT), finance]
-
– secretarial, reception, clerical.
-
The number of patients on the list of each practice and the proportions aged > 65 years and < 15 years were obtained from the Department of Health NHS Commissioning Board. 120 IMD 2010 for each practice was obtained from the NHS Information Centre. 121
Costs
Unit costs of clinical personnel were obtained from validated national sources. 119 These unit costs provide a value, per annum, that covers remuneration, on-costs, qualifications (where relevant), training, capital and other overheads associated with each role (see Appendix 8). PAs were costed as Band 7 nurses (secretary of UK Association of PAs, 2012, personal correspondence). The same costs were applied to GP partners and salaried GPs because evidence on this was contradictory. One study suggested that partners cost less than salaried GPs122 and others argued partners cost slightly more123 or the same. 124
The remuneration levels of management and other support staff were obtained by looking at several job vacancies within the NHS for each role (outside London rates) in January 2013, and inferring an average salary. The on-costs and overheads associated with each role were assumed to be equivalent to those of clinical NHS staff working in general practice with the same remuneration. For example, the salary of a NP was £38,800 and job advertisements for practice managers were around the same level, so the on-costs and overheads of the NP were used to estimate the costs of a practice manager.
Analysis
The numbers of WTE staff in each category, and numbers of patients per GP, were calculated and compared within and between practices with and without a PA. Reported vacancies were included in the calculations.
Staffing costs were calculated for each category in each practice on an annual basis by multiplying the WTE by the unit cost. Total staff costs for each practice per annum were obtained by summing across all staff categories. An average cost per patient per practice was calculated, and compared within and between practices with and without a PA.
The sample of practices included in the study in both the PA and no-PA groups were compared with national staff headcount data from the NHS Information Centre 2012125 with respect to the proportions of GPs who were salaried (vs. partners), and the numbers of administrative/clerical staff and nurses/direct patient care staff per GP.
Patient level
Analysis
The patient-level analysis used findings from the analysis of consultation records and the patient survey to compare the costs and effectiveness of consultations by PAs and GPs. The mean length of consultations in minutes for PAs and GPs was calculated from available data recorded by the ‘time enter’ and ‘time leave’ functions on practice management systems. Nationally validated unit costs119 were applied to mean consultation lengths to explore differences between PA and GP practices in the cost of consultations. Other ways in which the use of PAs may affect practice costs were also considered, such as GP time spent in supervision and training, but could not be quantified as data were not available. The relative effectiveness of PAs and GPs was judged by rates of reconsultation (primary outcome), patient satisfaction, and rates of referring, prescribing, testing, fitness to work certification, procedures and advice giving (process outcomes). Adjusted values of variables were used, after controlling for covariates.
Ethics and research governance
Phase 2 of the study required a number of types of reviews and agreements. The research ethical review was undertaken by NHS Research Ethics Committee (REC) South East Coast – Surrey who gave approval but required that child patients were not included in some elements (REC reference number: 10/H1109/28). Local NHS primary care research governance approvals were obtained using different local processes from five different bodies. The procedures for local agreement of the UKCRN NHS service support costs to research in general practice varied in each area. Agreements were obtained for each participating general practice.
The case study settings
Twelve practices participated in the study in the south-west, east and south-east of England. They were diverse in the sociodemographic features of their locale, the number of practice partners and the size of their registered patient population. These data are presented within ranges, to ensure anonymity for the practices, in Table 5.
| Practice study ID | Type of locationa | IMD | Practice partners (WTE) | Patient list size | Employing a PA |
|---|---|---|---|---|---|
| 1 | Rural-50 | 11–15 | 1–3 | 5001–10,000 | Yes |
| 2 | Rural-50 | 6–10 | 4–6 | > 10,000 | No |
| 3 | Rural-80 | 6–10 | 4–6 | > 10,000 | No |
| 4 | Rural-50 | 11–15 | 4–6 | 5001–10,000 | No |
| 5 | Rural-50 | 16–20 | 1–3 | 5001–10,000 | Yes |
| 6 | Significant rural | 16–20 | 4–6 | > 10,000 | Yes |
| 7 | Significant rural | 11–15 | 4–6 | > 10,000 | No |
| 8 | Major urban | 31–35 | 1–3 | < 5000 | No |
| 9 | Major urban | 31–35 | 1–3 | 5001–10,000 | No |
| 10 | Major urban | 31–35 | 4–6 | < 5000 | Yes |
| 11 | Other urban | 11–15 | 1–3 | > 10,000 | Yes |
| 12 | Major urban | 46–50 | 1–3 | 5001–10,000 | Yes |
The report now turns to presenting the findings.
Chapter 3 Findings: evidence at the macro and meso levels
In this chapter we report on the findings from the first phase of the study: (a) the review of evidence, (b) the scoping survey74 of key informants at a national and regional level and (c) the survey of current work deployment of PAs in UK general practice.
The review of evidence
In this section we report on our rapid review76 of different types of documentary evidence. This includes a systematic review of empirical evidence, a review of commentaries and a review of workforce policies (see Chapter 2, The review of evidence for the method).
The systematic review of empirical evidence
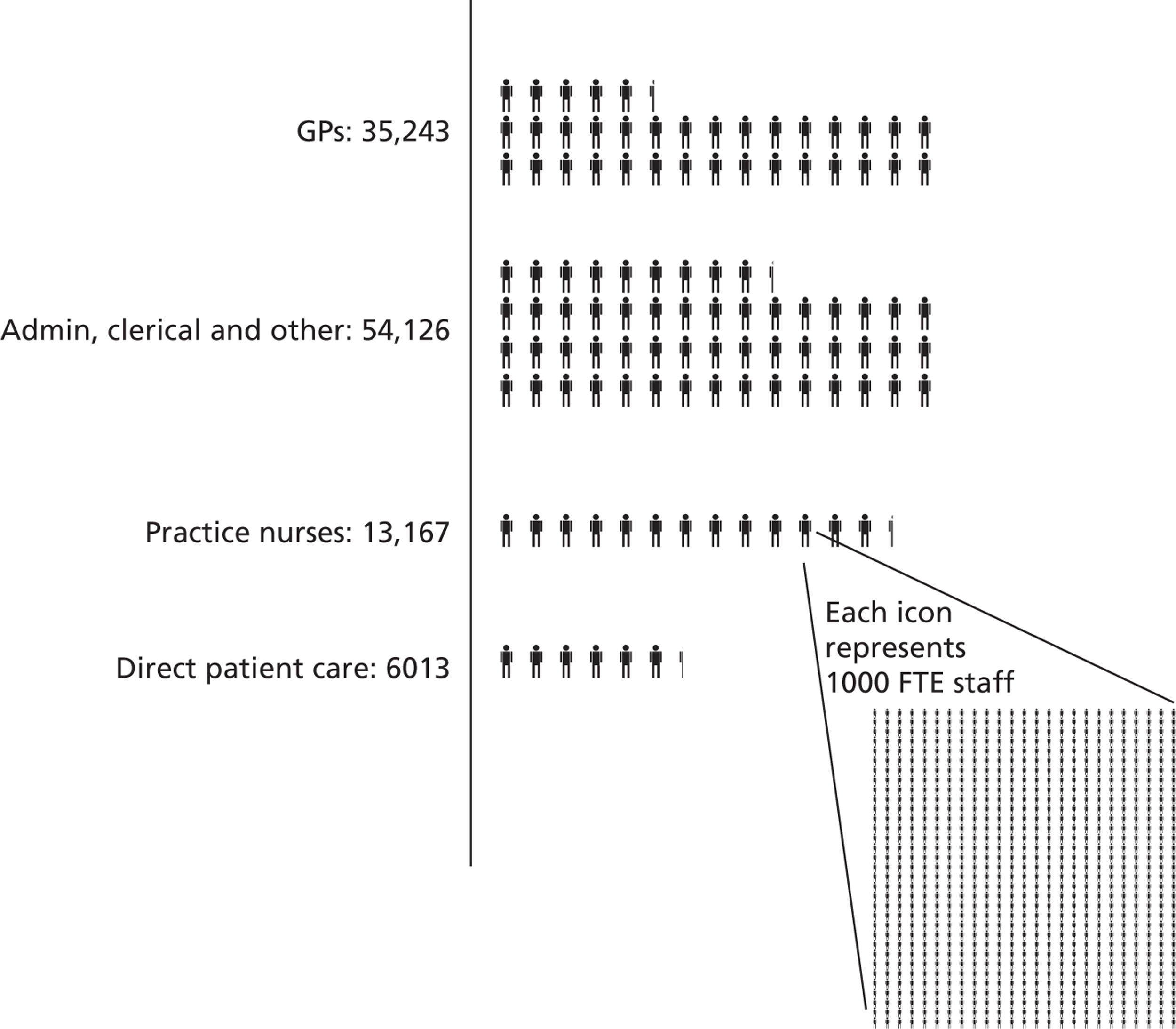
Of the 2167 publications identified and screened, 49 met the inclusion criteria49,62,127–161 as presented in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)162 diagram in Figure 2.
Of these included studies, 46 were from the USA, and one each was from the UK,62 Australia,163 and the Netherlands. 164 The heterogeneity of the types of studies (Table 6) and their outcome measures mean that any meta-analysis was not possible and a narrative review is presented. The overall judgement of the quality of the research was that it was weak to moderate with few studies providing comparative data about other occupational groups.
| Method and data source | Number of studies |
|---|---|
| Quantitative surveys | 27 (five are secondary analyses) |
| Medical record review | 5 |
| Structured/quantitative observations of practice | 3 |
| Individual or focus group interviews | 4 (three qualitative analysis) |
| Administrative cost data analysis | 1 |
| Mixed methods | 9 |
Evidence regarding structural aspects of PAs in primary care was found in 24 studies62,127–149 ranging in date from the late 1970s to 2007. These studies focused predominantly on PAs as a human resource in primary care, investigating questions as to the numbers employed in primary care, the willingness of physicians and managers to employ PAs, perceptions of barriers to employment and issues in retention rates. In the USA, the numbers of PAs are seen to have grown over time. Although studies vary in their findings, several suggest that approximately half of those with PA qualifications work in primary care. 128–132,139 Support for the concept is mostly reported to be high among family doctors,62,142–148 with the potential for releasing the doctors’ time to allow them to focus on more complex patients (and thereby increase practice productivity)143–146 being one of the most prominent reasons, alongside perceptions of patient satisfaction. 146,147 Retention is not considered problematic. 140,141
Aspects of the process of care were reported in 24 studies49,62,134,137,140,144,147,151–161,164–168 ranging from the late 1970s to 2009. The majority of these studies describe the work activities of the PA and the patient groups who consult them. The greater part of the PA work is reported to be in consultations with patients with acute presentations. 140,150,151,153–155,158,160 Two studies suggest that doctors who are in the same primary care facility as PAs attend more patients with chronic conditions49,153 and one suggests that the doctors attend more patients with more serious problems. 140 The evidence indicates that, while PAs can be consulted by patients of all types, primary care facilities have systems which direct particular groups of patients to the PA. 156 The activity level of PAs’ work is reported in a number of studies but without conclusive evidence. Varying levels of PAs’ productivity in patient throughput have been reported compared with those of family physicians, suggesting that there is near equivalency62 and up to 60% physician whole-time equivalence. 164 PAs are consistently reported to require supervision from physicians, although this is low in actual patient care episodes154,165,166 apart from when PAs are not afforded prescribing rights. 62 Some evidence suggests that the employment of PAs provides greater capacity and efficiency in the provision of primary care. 62,149,153,164 Seven papers49,154,155,157,158,167,168 report on investigations in the USA about the issue of cost and the impact on practice finances. Only one provides data after the year 2000. 49 Again, no conclusive evidence is provided, with four suggesting that the employment is not financially advantageous for the practice49,155,156,168 and four suggesting otherwise. 38,154,158,167
Evidence about the outcomes of care was found in 14 papers. 140,141,144,154,155,160,163,168–173 Overall, PAs were reported as acceptable to patients,141,155,160,168–171 although this decreased in a rural setting in which patients were not offered the choice to see a doctor. 141 One study involving hypothetical scenarios suggested that patients were less willing to consult a PA in primary care if they had more complex conditions. 173 The evidence on technically appropriate care provided by PAs was weak and mainly from the 1970s. 140,144,154,155,168,169,174 While evidence was mainly positive regarding the appropriateness of care, some less favourable comparisons with other providers were also reported. 155,175 It is noteworthy that most of these studies were concerned with care for people with chronic conditions, for example diabetes; however, the evidence suggests that this patient group are in the minority in the PA workload.
Despite 40 years of studies, the evidence pertaining to PAs in family practice remains descriptive and weak, accentuated by poor reporting. While the review provides some evidence of the consequences of changing from physicians to PAs, it also makes it clear that research questions remain which would benefit from country-specific, good-quality investigation.
The findings of this systematic review are reported in full elsewhere. 176
Review of commentaries
This section reports on the findings of the review of commentaries and published opinions. This was one element of the study that contributed to investigating the question as to what supports or inhibits the development of PAs in primary care in the UK. The review was undertaken as reported earlier (see Chapter 2, The review of evidence). One hundred and seventeen published (print and electronic) commentaries and opinions were found that met the criteria for the review and these are listed in Appendix 9. They were found in sources with public, medical and nursing audiences (Table 7).
| Source type | Number |
|---|---|
| Journals and magazines targeted primarily to medical audiences (print and electronic) | 65 |
| Journals and magazines targeted primarily to nursing audiences (print and electronic) | 28 |
| Journals and magazines targeted to health-service managers | 9 |
| National newspapers | 7 |
| Other types of journals | 8 |
| Total | 117 |
The commentaries ranged in date from 1980 to 2012, with the greatest number published between 2004 and 2006 (Table 8). This was the period in which a Department of Health-funded pilot project was being conducted in England. 60
| Time period | ||||
|---|---|---|---|---|
| Pre 2000 | 2000–3 | 2004–6 | 2007–12 | |
| Published commentaries (n) | 6 | 28 | 58 | 25 |
Journalists were the most frequent type of author (n = 28), followed by medical staff (n = 24), including those with clinical backgrounds and senior medical practitioners, and by academics (n = 20). A notable absence was a patient or public perspective. Only one member of the public177,178 pointed out that the public were not asked for their views and questioned the need for new roles in the NHS. Many of the commentaries were unclear as to the competencies of a PA. In some, the author confused a PA trained in the USA model with a similarly named role in the UK in which individuals are trained to undertake only technical tasks such as taking bloods under the direction of a doctor.
Fifty-one of the commentaries gave a positive view of PAs, 24 gave negative opinions and the remainder were neutral, often suggesting that more information was required to help inform opinion. The positive opinions were authored for the most part by senior medical practitioners and academics. The doctors were mainly from the acute setting and, either from direct experience or from consideration of their current staffing issues, could envisage a place for PAs in their teams. Some of the more recent opinions relate to the potential for PAs to provide solutions to contemporary health policy requirements such as those found in the Quality, Innovation, Productivity and Prevention programme174,179 and as support to GPs in the new commissioning structure. 180 The majority of the negative opinions were authored by GPs and nurses. None of these had direct experience of PAs. Issues raised included the transferability of a US model to a UK setting; confusion for the public when faced with multiple roles; concern that PAs were not cost-effective in general practice when compared with GPs; and a viewpoint that nurses and NPs fulfilled this role in the UK health-care workforce and offered greater value to patients than another professional trained in the medical model. Conflicting views were authored from junior doctors; some reported that PAs made their working lives better as they could delegate routine tasks, while others questioned whether or not they would be in competition for jobs for which PAs would be seen as preferable by managers because they were cheaper.
There was little citation of empirical publications to support opinions in the commentaries, with most referring to other opinion pieces. It is possible to detect a trend over time to more positive, or at least neutral, opinions as more direct experiences of PAs in the UK were reported.
We turn now to the findings from reviewing the workforce policy documents and associated material.
Review of workforce policies and developments
One hundred and thirty-three documents were identified. Those concerned with international developments regarding PAs in primary care informed the context for the study (reported in Chapter 1). Twenty documents were published after 2010 (the year of the election of the Coalition government) by central government departments or regional bodies responsible for NHS workforce and education planning. There was a lack of reference to PAs in all of the English policy documents and, similarly, in the House of Commons Health Committee Report into the workforce and education. 181 At a local level we did identify a few NHS trusts in England with plans to employ PAs (e.g. see University Hospitals of Leicester NHS Trust Annual Operational Plan 2011–12182). The only mention of PAs in Welsh documents was in reference to the health workforce in rural areas, but no commitment to develop or support the role of PAs in this context was made. 183 In contrast, there was more evidence of recognition for PAs in Scotland where they were cited in central government policy documents both as an example of workforce efficiency184 and as a potential addition to the remote and rural health-care workforce. 185 To this end, NHS Grampian, as the lead NHS organisation for workforce development, was working actively with the University of Aberdeen to establish and recruit to a PA education programme. 185 There was little reference to PAs in other types of workforce review documents which were intended to inform decision-making bodies.
Support for PAs was, however, evident in the medical colleges. The support of the Royal College of Anaesthetists for PAs (A) was noted earlier in Chapter 1, as was the support of the Royal College of General Practitioners and the Royal College of Physicians (RCP) in establishing competency and curriculum frameworks. More recently, the Royal College of General Practitioners referred to PAs in their review of general practice34 and also included PAs in their membership via their General Practice Foundation. The Royal College of Physicians of Edinburgh also offered foundation membership to PAs. 186 PAs were also cited by the Director of the Medical Workforce Unit at the RCP187 as one of the solutions to the problems facing medical workforce planning, medical training and complying with the European Working Time Directive. 188
Against this backdrop of limited recognition in policy, we go on to report the findings from the scoping survey.
The scoping survey
This section reports on the findings of the scoping survey, which addressed the question of what supports or inhibits the use and development of PAs in primary care. Fifty people were identified and approached as described earlier (see Chapter 2, The scoping survey). Thirty people agreed to the invitation and 25 participated in an interview. While not necessarily representing their organisation’s views, they provided perspectives as individuals active in the work of a range of organisations at national and regional levels (Table 9). It should be noted that most of them were in very senior positions and that they often held multiple positions and roles. For example, one GP participant was a senior partner in a general practice, a role that involved caring for patients, leading the practice and also employing staff. In addition, this participant had involvement in a Clinical Commissioning Group (CCG), the emerging local education and training board (LETB) and Department of Health national working groups as a member of the Royal College of General Practice. A participant from an organisation representing patients was the leader of this organisation, was involved in consultative processes with both the Department of Health and professional regulatory bodies and was a member of a steering group for research into hospital workforce changes. All of the participants had had some involvement in aspects of health workforce development: planning, redesign, review or research, provision and/or quality assurance of education and training programmes or regulation. Some were authors of reports on aspects of health-care workforce that were used in national- and regional-level policy and planning decisions.
| Types of organisations | Number of individuals interviewed |
|---|---|
| Regional and national level of the NHS in England and Wales | 5 |
| Organisations representing patients | 2 |
| Organisations involved in workforce analysis, planning and development within and without the NHS | 3 |
| Organisations providing primary care general medical services and clinical commissioning | 4 |
| Organisations providing medical education and advice at regional and national level on medical workforce planning | 3 |
| Organisations representing doctors | 2 |
| Organisations representing nurses and nurses working in primary care | 4 |
| Organisations representing PAs | 2 |
| Total | 25 |
The interviews were undertaken in 2011 and early 2012. The backdrop to which all the participants referred was the major debates on the reorganisation to the NHS as described in the 2010 White Paper,6 consulted on through the NHS Future Forum work189 and enacted in the Health and Social Care Act 2012. 190
Health-care workforce changes
Health-care workforce redesigns and changes were seen as ongoing and inevitable by all respondents. They identified the current and future drivers which included the demographic and epidemiological changes in the population; the need to contain health-care costs and the impact of the general economic environment; the technological changes in medical treatments and communications; public and patient expectations in health-care delivery; and employment legislation and changes to professional education and regulatory requirements, specifically with regard to medicine and also the implementation of the European Working Time Directive. 188
Most informants had either observed or been involved in some way in shifts in work roles between occupational groups and envisaged this movement continuing. For example, the participants from patient organisations described the growth in employment of HCAs in NHS hospitals, who were undertaking what had been previously registered nurses’ activities. Some described the shift in terms of ‘the blurring of boundaries’ between occupational roles, while others described planning for some groups to gain competencies (assessed in some way) to take over roles or tasks of other occupational groups, as in this exemplar:
So we take the approach of developing registered professionals into, you know, roles that will support medics or even, you know, replace some of the work of the junior doctors because with less junior doctors being around, you know, we’ve got a real capacity issue so registered professionals are currently filling that gap.
Participant 17: regional workforce development organisation
Workforce changes in primary care
In considering additional factors that impacted on workforce developments in primary care, participants noted the policy drive to deliver more care in primary care settings, reduce unplanned hospital admissions and increase the availability and accessibility of primary care. In addition, one GP predicted changes in the actual GP workforce, for example increased part-time working, and their possible impact:
I think in general practice there’s going to be a much greater feminisation of the workforce, so I mean that’s going to cause a tension because of people, you know, working out of normal working hours and kind of family and caring commitments making that very difficult, so you might almost get two types of workforces, those who work evenings and nights and those who work, you know, main work days.
Participant 5: GP and primary care organisation
There seemed to be general agreement as to the direction of travel of developments in the workforce in primary care. These included (1) greater numbers of staff (medical, nursing, allied health professions, support staff and administrative staff) to provide the range of services moving from hospital to primary care settings and accessible for longer hours, 7 days a week, (2) increased availability in primary care of medical specialists in ambulatory sensitive conditions, (3) increased subspecialism by GPs, and (4) increased stratification in some occupational groups, for example more clinical nurse specialists and advanced NPs, fewer registered nurses and more HCAs.
Experience and knowledge of physician assistants
Aside from those involved in organisations concerned with PAs, about half of the participants had no direct experience of an aspect of the PAs movement in the UK. Those without prior knowledge, such as participants from patient organisations, could easily translate the concept and sought additional information to check their understanding. Of those who had direct experience, this ranged from involvement in early pilot projects of PAs or staff like them to consultations of professional bodies on the Department of Health-agreed national competencies for the PA programme,64 to engagement with provider organisations on the commissioning of places on PA programmes. This did not necessarily translate to knowledge of any current developments in the PA movement in the UK.
And you have to look back, not so long ago, but we had this thing called the ‘NHS Plan Modernisation Agency’ and with it, there were all these calls for workforce development. And one of the calls was for England to develop the role of physician assistant to increase capacity and capability within both secondary and primary care. Now, as a response to that, a working party was set up looking at the education programme that SHAs would commission from HEIs for the physician assistant, and I was on that working party . . . but I had assumed that we had very few out there now.
Participant 9: nursing profession organisation
Participants also commented that they thought there was little awareness or knowledge of PAs among the public or, indeed, professionals.
So you know if you talk about physician assistants I actually don’t think many people in this country really understand what they are.
Participant 15: GP and medical profession organisation
Factors influencing demand for and employment of physician assistants
Around half of the participants saw potential for the PA role in primary care, although there were caveats expressed, as outlined below. Other participants were more neutral in their opinions, requiring more information and evidence. None expressed a completely negative view of the potential for PAs to be employed in primary care settings.
For those who could envisage a role for PAs in primary care, that role tended to be one of triage or dealing with patients with minor, self-limiting illnesses in general practices and other first-contact settings such as walk-in centres. The explanations for this were that this was the area of patient pressure on the practices, but also that the role could free up the doctors’ time to deal with patients’ more complex problems or with other types of activities such as commissioning. Some participants reported that PAs were increasingly being employed in secondary care settings.
Something like seven out of ten of the PAs working in the UK now are in secondary care . . . something like 19 trusts are now employing PA’s across the UK. There are none in Wales that I know of and none in Northern Ireland but the vast majority are in England.
Participant 16: PA organisation
This echoed views reported to one of the research team members when interviewing senior staff involved in the New Zealand pilots of PAs (see Chapter 1).
The factors that participants considered were particularly likely to create demand for PAs were lack of medical applicants to work in particular areas or types of primary care services; the need to have continuity in medical team personnel; and the need to free medical personnel from the more routine aspects of patient care to either undertake their medical training or undertake other types of work. Some participants debated whether it was nurses at advanced level or clinical nurse specialists that were required or whether or not it was PAs. Most considered that they needed further information before taking a view, although one participant from a professional nursing organisation considered that the nurse added value in ways the PA would not.
Having had a long conversation with one of the PAs [at professional meeting] to actually do a direct comparison of what were the pros and cons of an ANP [advanced nurse practitioner], because they couldn’t understand what an ANP was and say ‘Well, why would you need ANPs, you’ve got physician’s assistants’ so we were like diametrically opposed and I’m going ‘Well, why do you want physician assistants because we can get that and more from an advanced nurse practitioner’.
Participant 11: nursing professional organisation
Participants from medical education and medical professional organisations could see particular problems for consultant teams created by the changes in postgraduate medical training, which roles such as PAs could address. One participant noted that in a LETB, representatives of trusts that had experience of training and employing PAs were voicing requirements for a greater supply of PAs.
. . . the consultants there who’ve hired now four physician assistants, they were losing training roles because their trainees couldn’t get in, because they were having to do the ward work and couldn’t get into surgery. With physician assistants in place they have the ward covered, they’re not hiring locums, they’re now getting more training posts because they can actually train those people.
Participant 24: medical education organisation
In contrast, in a different region of England, a participant from a workforce planning organisation reported a lack of interest by trusts in PAs specialising in anaesthesia.
Yeah, I mean we constantly look at the potential around PAs in the region and have had little uptake really locally. We’ve had a few events where we’ve explored what physician assistants are but none of the trusts have wanted to go forward with them.
Participant 17: regional workforce development organisation
Participants also raised questions and offered views as to why PAs might not be employed in primary care settings. Foremost were questions (not in any order) as to the cost and value for money compared with other staff groups, the lack of legislated authority for PAs to be an independent prescriber and the lack of oversight by a statutory regulatory body. Opinions seemed to vary as to whether or not there was a shortage of doctors applying to general practice to which PAs might offer an alternative but that may have reflected regional variations in settings. Participants had different views as to whether or not PAs represented value for money when compared with doctors. Most used the evidence from studies of NPs, reporting that compared with doctors (particularly in general practice) their consultations with patients were longer, resulting in no financial gain to the service. They considered that the evidence about PAs would be similar.
Practices have tried nurse practitioners and generally they take twice as long to see the patients and don’t come to the conclusion or the management as quickly. So you actually often end up when you look at the, and there’s been published papers to show it, when you look at the cost actually the nurse practitioner doesn’t become any cheaper.
Participant 15: GP and medical professional organisation
The participant from the patients’ organisation also raised issues of opportunity costs to patients in consulting a PA who could not prescribe.
It seems to me that if the physician assistant can’t actually prescribe then, you know, you’re duplicating . . . you’re repeating what has happened with, you know, some of the walk-in centres experience, where people have gone, you know, thinking I won't need to bother with the GP. They see a nurse at the end of which the nurse says, ‘Well I think you'd better go and see your own GP service.’ . . . So actually how much, how effective is delegation if people just bounce back through again because the GP’s the only one who can make a particular decision?
Participant 12: patient organisation
Issues of acceptance and patient preference were mentioned by a range of participants. A number cited experience and research that demonstrated patient preference for consulting with a doctor rather than a nurse, although some also pointed out that many patients, particularly those with long-term conditions, were also discerning as to the expertise level they required and found acceptable.
Concerns were also expressed that the PAs were not a professional group regulated by legislation, although, as one participant from a patients’ organisation pointed out, the existence of a regulatory body would not necessarily result in regular checks of individual competence. The absence of such a body was considered by some, but not all GPs, as a barrier to employment:
No, I didn’t realise that [there was no regulatory body for PAs], not in a million years would I employ someone.
Participant 5: GP and primary care organisation
Participants from the PA organisations reported the existence of a voluntary register for UK PAs which recorded individual PAs’ credentials. In addition, it was reported that UKAPA had tried to be included in the remit of the Health Professions Council but, following the government’s announcement not to regulate any further groups,191 this was not currently possible.
Finally, a number of participants made comment as to the risk-averse, essentially conservative attitudes of many NHS managers and employers towards innovation. In comparison, one GP participant noted how ‘nimble’ general practices were like small independent businesses in the speed at which making decisions and testing innovations could occur, particularly when compared with large NHS trusts. Others observed the need for evidence and information so that employers and commissioners could make decisions. Some participants considered more widely the factors in diffusion in innovation and offered a broader analysis that included a NHS cultural aversion to the importation of ideas from other countries such as the USA.
So, I think this is an opportunity to try and move some of these ideas. You know, they may not be right of course. So, ‘Do they feel right?’ but I don’t think physician assistants have ever had enough scope to run a NICE [National Institute for Health and Care Excellence] trial on their VFM [Value for Money] and impact. Which is probably part of the thing that drags you back down. It’s almost like you’d need to reach that tipping point even in terms of evidence or just acceptability to get it done. And the weird thing is that ‘and not invented here, culture’, [you] can’t point to 175,000 American physician assistants and say, ‘Oh yeah, it does work’ you know, cos it’s not here.
Participant 20: workforce development organisation and national and regional level
The scoping survey suggested that there was awareness of potential benefits of the role but also recognition of the current drawbacks and a desire for more information.
This section has reported on the findings of the scoping survey as to perceived factors influencing the use and development of PAs in primary care at the macro and meso levels. We now turn to the evidence as to the employment of PAs in England in primary care.
The national physician assistant survey
The online electronic survey was completed by 16 PAs working in primary care in 2010. Using the UKAPA estimate at that point of time of 25 PAs employed in primary care, this gave an estimated response rate of 64%. Four surveys had missing responses. Fifteen respondents were female, eight were aged between 30 and 39 years and five were aged over 50 years. Half of the respondents (n = 8) were graduates of PA courses in the UK, the others of US courses. Two respondents omitted the question about their employment setting. The remainder were all employed in general practice, with three reporting additional employment in walk-in-centres, urgent care and primary care out-of-hours services. Most had worked in their current practice for over 1 year, with two PAs reporting working for over 5 years in the same practice. Two worked in settings described as rural, two in urban non-deprived settings and eight in settings described as urban and deprived. The patient list size of the employing practices ranged from under 3000 to over 20,000. Three PAs worked in practices that had only partner GPs. Nine PAs reported working in practices that employed salaried doctors and eight in practices that also employed NPs. The most frequently reported clinical activity was seeing patients (classified as same day/urgent and non-urgent) in booked surgery appointments. In addition, this was reported as the greatest number of hours of their working week engaged in this activity. The next most frequent activity was reported as reviewing test results. Only seven undertook booked appointments with patients for chronic disease management activities. A range of other activities were reported by individual respondents including home visits, cryotherapy, teaching, clinical audit and supervision of other staff such as HCAs. This is an adapted version of findings reported in detail in Drennan et al. 192 Some respondents also volunteered to be potential participants in the second phase of the study.
This chapter has provided the findings from the macro and meso levels of the study. The report now turns to the findings at the micro level through the comparative case studies.
Chapter 4 Case studies: evidence from the practice as an organisation
This chapter reports on findings from the comparative case studies, using data from the GP and practice staff interviews, the work diaries and the observations in the practice clinical meetings. The first section considers the data from PA employing practices in addressing, first of all, questions of deployment, the place of the PA in the work of the practice team, supervision, professional relationships, and views on the perceptions of patients. It then moves to consider the data from the GPs and practice managers in both PA-employing and non-PA-employing practices as to their views on the factors that shape staffing decisions in general practice, including the employment of PAs. Interviews were conducted with the GP, the practice manager, the PA, a nurse or NP and a receptionist in all of the PA-employing practices (except one practice where we were unable to interview a receptionist). A lead GP and the practice manager were interviewed in five of the six non-PA-employing practices (the sixth declined to participate in this element).
The deployment and role of physician assistants in practices
The PAs were all employed in practices that also employed other professionally qualified staff, including salaried GPs, NPs and practice nurses (Table 10). The PAs in the study had a variety of work experience and training backgrounds, including some who were UK and some US trained.
| Practice study ID | Patient list size | Practice partners (WTE) | Employing salaried GP(s) | Employing NP(s) | Employing nurse(s) | Employing PA(s) |
|---|---|---|---|---|---|---|
| 1 | 5001–10,000 | 1–3 | Yes | No | Yes | Yes |
| 5 | 5001–10,000 | 1–3 | Yes | No | Yes | Yes |
| 6 | > 10,000 | 4–6 | No | Yes | Yes | Yes |
| 10 | < 5000 plus walk-ins | 4–6 | Yes | Yes | Yes | Yes |
| 11 | > 10,001 | 1–3 | Yes | No | Yes | Yes |
| 12 | 5001–10,000 | 1–3 | Yes | Yes | Yes | Yes |
Physician assistant activities: an overview from the work diaries
The work diaries (confirmed in interviews with PAs) indicated that the majority of the PAs’ working hours were spent in providing clinical consultations (direct patient contact in face-to-face or telephone appointments), although the proportion of the time they reported on this ranged from 58% to 92% (Table 11). The majority of these hours were in same-day appointment sessions but PAs also undertook booked appointment sessions. These were mostly for the follow-up of patients with long-term conditions.
| PA | Time reported | ||||
|---|---|---|---|---|---|
| Total hours reported on | Clinical activities | Non-clinical activities | |||
| Hours | Per cent of reported time | Hours | Per cent of reported time | ||
| 1a | 125 | 111 | 88.8 | 14 | 11.2 |
| 5b | 37.75 | 21.75 | 57.6 | 16 | 42.4 |
| 6 | No diaries received | ||||
| 10a | 11.75 | 74.5 | 62.7 | 44.25 | 37.3 |
| 11c | 8.75 | 7.75 | 88.6 | 1 | 11.4 |
| 12d | 36.25 | 33.5 | 92.4 | 2.75 | 7.6 |
The non-clinical activities could be related to either patient consultations, such as arranging referrals or processing laboratory results, or other professional activities such as attending practice meetings or training days. The most frequently reported non-clinical activities by PAs were dealing with test results and referrals to other professionals. Some PAs also reported attending training and carrying out clinical governance activities and condition/case-specific duties (such as child protection work). It was evident that the wider the range of non-clinical activities, reported by individual PAs, the greater the proportion of time spent on these activities compared with clinical activities (as with PA 10) (see Table 11).
From the staff interviews, it was evident that each practice deployed the PAs according to a number of parameters. These included deployment that fitted with the practice organisational requirements, for example to telephone triage in a practice that used that system, or by clinical competence as judged by the senior or lead GP, as in this exemplar:
[The PAs] don’t usually see under-1s but depends on [their] experience.
GP 11–5
This is further explored in the following sections, where the variety in the scope of practice reported to be undertaken by the individual PAs is clear.
Same-day appointment clinical consultations
The deployment of PAs in the practices was primarily to provide clinician time for same-day/urgent appointments. The range of scope of practice was evident in the manner in which same-day appointment patients were assigned to a PA or to a GP. In some practices, it was evident that the receptionists treated PAs as the doctors assigned to that type of surgery, as noted here:
He [the PA] sees a surgery of patients morning and afternoon every day, which are almost entirely unselected. We have selected out under ones because he is not trained for those, but other than that he sees the full range of problems that present.
GP 1–2
In other practices, more nuanced systems had been developed so that the GPs and PA were seeing different types of patients, with the GP more likely to see either the more complex patients or those with more chronic conditions, as in this exemplar:
So the doctors and the physician assistant, the nurses between them have developed a, like a list, a triage type list. So if someone rings up and says ‘I’ve got this, that or the other’, they [the reception staff] can look on the list and decide whether it should see a doctor or a physician assistant or a nurse practitioners, depending on who’s on. So they’re a sort of triage but not in-depth triage, just pointed in the right direction.
Practice manager 6–4
The practices varied in the length of the appointment slots they assigned to PAs. Most – but not all – assigned longer slots (15 minutes) to PAs than to GPs (10 minutes), but often shorter appointment times than those allocated for nurses.
Chronic disease management consultations
The extent to which PAs were involved in the ongoing management of patients with chronic diseases also varied among practices. For example, in one practice the PA undertook the diabetic review clinic, among other chronic condition review clinics. Another PA estimated that about 50% of the patients he saw were ‘regular routine follow-up of chronic patients’ (PA 5–3).
Some of the practices had nuanced ways of separating the work the PA undertook in chronic disease management from that of the nurses in the practice. For example, in most practices the nurses were described as not seeing patients with depression or other mental health problems or with musculoskeletal problems, whereas the PAs would attend to those types of patients. In general, the division of labour appeared to be based on clinical expertise and confidence, as in this example:
When the physician assistant that we have here, when she started a lot of my chronic disease patients [were] then allocated to [the PA], especially COPD, she does spirometry, which she’s been trained for . . .
Practice nurse 10–3
It was observed by a number of participants that the difference between nurses and PAs in their chronic disease management was often recognisable through the point at which the patient was referred back to the doctor. PAs were described as often managing more problems and transition points, whereas the nurses referred back for any problem or change. The differences in activity between the PA and the NP were exemplified in this description:
She [the PA] does all the things the nurse practitioner will do on the day but she also does a couple of other things because she’s covered the training. So she is happy to see straightforward depressions, which the nurses, none of our nurse are prepared to at present . . . And she is happy to see back pains also which the nurses haven’t covered so they don’t do that. Another difference is the PA will do some of her own referrals [to secondary care] whereas the nurse practitioner would refer the patient to the doctor who would be responsible for doing the referral.
GP 6–2
More evident in the descriptions were situations in which PAs and nurses flexibly covered the work required in the practice as the demands of each day unfolded. These were reported by PAs, nurses and practice managers; for example, PAs might cover the work of nurses absent through sickness, while one nurse described assisting with booked chronic disease management review patients in the absence of a PA.
Income-generating work
In addition, some practices were also developing their PA to undertake work that contributed specifically to the practice income as part of either Quality and Outcomes Framework (QOF)93 indicators, such as maintaining the register of people with learning disabilities, or clinical activities that attracted specific payments under local or nationally agreed enhanced service elements of the General Medical Services (GMS) or Personal Medical Services (PMS) contract,23 for example initiation of insulin in primary care. Each of the activities referred to by the PA in this exemplar is an activity associated with specific payments:
What else do I do? I’m responsible for the warfarin patients, I do all the bridging for surgery [changing the warfarin pre-surgery to another drug and restarting post a surgical operation]. I do contraceptive implants and there’s only one or two in the practice who do that so that’s quite a big role . . . and I do a lot of paperwork, so I run the palliative care meetings 3-monthly . . . the GP would normally do that but I’ve taken that off their hands. And I’m now starting to do initiation of insulin in primary care. We had one GP that was doing that but he retired.
PA 6–3
Authority and lack of authority to order tests, refer and prescribe
There was a reported difference between PAs in different practices and between PAs and nurses as to the recognised authority to order pathology and radiological tests and also to make referrals to secondary care. In general, the PAs were described as having been given more authority to order tests and make referrals to secondary care (although some needed countersigning in some areas by the GP) than the nurses, who mainly described usual practice as referral back to the GP, as described in this exemplar:
Can you authorise an X-ray referral?
No that goes on our prescription board [a way of leaving items such as prescriptions for the doctor to sign] and the doctor will sign it. Obviously it is a trust thing, they know what I can do and trust me.
And if they needed investigations of any other kind, would there be something you authorise or . . .?
Bloods. I would obviously do that myself and authorise myself. I think X-rays, most other things, scans and things would be the doctor or PA.
And if they need a hospital referral?
Yeah doctor or PA because they wouldn’t take any notice of me at the hospital.
Physician assistants are not authorised to prescribe medicines in the UK. The lack of ability to prescribe was reported to cause frustration and additional time to the PAs, the GPs and the patients. Each practice had developed systems to try to minimise the delay caused by getting the GP to sign prescriptions. This varied from a system of knocking on the GPs’ consulting room door, messaging by computer, hovering in corridors to speak to the next available GP, and leaving the prescription in a designated place for the next available doctor to review the notes and sign, to offering to send the signed prescription to the local pharmacist later for collection. It was evident that the GPs developed trust in the clinical competency of the PAs over time, which had the effect of reducing the amount of time they spent reviewing consultations before signing prescriptions, as illustrated in this exemplar:
When I first qualified and also when any new doctor starts there’ll be a period where when they are signing my prescription you would tend to give them a lot more information about what you are doing . . . explain a bit more what it’s about, because they have got to learn to trust you and understand it, because ultimately they are signing the prescription, . . . so it’s just about building up a trust and an understanding of your competencies which is fair enough.
PA 10–2
In the PA-employing practices, the nurses with the qualifications to prescribe medications were in the minority. Consequently, most of the nurses, whether with a title of nurse practitioner, senior practice nurse or practice nurse, were using the same systems as the PA to obtain GP signatures on patient prescriptions.
Supervision of physician assistants’ clinical practice
The GPs, practice managers and PAs all described an induction process of establishing the PAs’ competency in clinical work, confidence in working in the practice team and with practice systems through additional training and supervision sessions offered by the GP.
When they [PA] first start they sit in with all the doctors, they sit in with the nurses, sit in reception, go out with the district nurses . . . and they meet quite regularly with the mentor [GP] and so they will watch the mentor deal with patients. Then they will do consultations with the mentor observing and then . . . and then they’ll pick cases, [the PA] will then bring cases for discussion.
Practice manager 12–3
There was agreement from most participants, across all professional roles, as to the importance of ongoing supervision and mentorship. The PAs tended to report a mixture of informal advice as and when needed in clinical sessions together with regular more formal supervision sessions, as illustrated in these exemplars:
There’ll always be somebody who is instructed as my mentor for the day . . . and it tends to be the person’s on call. So if I have any problems during the day I go and see them and if I want them to see a patient with me then they will.
PA 6–3
Dr [name] routinely and regularly looks at my work and patient care notes to see if there is anything he needs to reassess or talk to me about.
PA 5–3
It was evident from the GPs that they valued what they described as the PAs knowing their own limitations in clinical practice, and that this added to the GPs’ confidence that the PA was a safe clinician.
A number of practice managers described how the appointment slots for the supervising GP were tailored to ensure that there were free slots to compensate for interruptions and discussions. One noted that in the event that all of the GPs were absent from the premises, for example doing home visits, the PA would not see patients during that time period.
Relationships with other practice staff
Knowledge of PAs among other practice staff, prior to the employment of the first PA, was reported to be negligible. Some practice managers were more involved than others in decisions to seek a PA to employ. It was reported by some GPs and practice managers that a few previously employed nurses, usually named as NPs, saw the PAs as a threat to their role and were less than enthusiastic about the employment of the PA. The PAs themselves noted that very occasionally they had felt that a NP was hostile to them. The nurses and NPs interviewed for the study did not raise any negative views about PAs. Most were positive about the role as an asset in managing the workload of the practice, in being complimentary in skills or knowledge to themselves and as a source of information on some things, as illustrated in the following exemplar:
So I think the advantage of having a PA is that she’s on the wavelength of the doctor . . . I feel I am better placed dealing with the chronics [patients] and she’s better placed dealing with she’s doing with the others, the non-urgent referrals, with the follow ups and things like that.
NP 12–4
On the other hand, many of the practice staff and nurses observed that the PA could sometimes be seen to be aligned with the nursing staff, or sometimes as a bridge between nursing and medical staff.
Participants described a range of working relationships with the medical staff, dependent in part on the configuration of the practice, the experience of the PA and the turnover of medical staff such as GP registrars, salaried doctors, and locums. In some practices, there were close working relationships between the named mentor and the PA. In the observed clinical meetings it was evident that the PAs were considered integral to the practice team. They contributed information, opinions, and potential solutions and took proactive roles in administration and patient management.
Patients and the physician assistant role
Most of the practices described the ways in which they assisted their patients in understanding this new type of clinical professional. There was a range of ways in which practices informed patients of the PAs within the practice team. This included posters in waiting rooms, leaflets, and information on their practice leaflet and website. Some of the PAs reported that they ensured that each patient understood that they were a PA, not a doctor, with a ‘script’ introducing themselves on starting the consultation. Others reported that they did not have time to do that with each patient. The reception staff in some practices reported how they described the role to patients and the responses, as in this exemplar:
We always say he [the PA] is qualified and he’s covered by a GP, if he is not sure about anything he will call the GP who is supervising him. So it’s ‘yeah ok’ or ‘well no I’d rather see a doctor’ and then I would say ‘well he is covered by a doctor, he is qualified, he can generate prescriptions though he can’t sign them and he will always call a doctor in’. And some of them are happy and some of them aren’t. We don’t push it.
Receptionist 1–3
Some practice staff stated that they were not sure if the patients quite understood about PAs, particularly if the PA was American, with the patient assuming that it was a US medical role. Others suggested that there were always some patients who did not receive or retain the information as to who they were consulting.
Most patients were reported to be content to see the PA, although some were reported to prefer to see the GP; this was also described as occurring with NPs. A number of the participants described the GPs as educating patients as to the consulting competency of PAs and NPs. Participants also reported groups of patients requesting to see individual PAs, as in this exemplar:
We’ve had people really want to see the PA. They’re high-quality clinicians as well and effective communicators . . . they are clinically sound and people want that continuity.
GP 12–1
The report now turns to the staff resource evidence from the study.
Comparative staff resources
Key comparisons of staff resources between practices with and without a PA are shown in Table 12. Owing to the small number of practices, and to preserve anonymity, results are not presented at the individual practice level. There is variation within both groups of practices (those with and without PAs) with respect to list sizes, proportions of older patients, IMD, and numbers (WTE) of GPs, nursing, management and other support staff, reflecting the practice matching that occurred when the sample of practices was selected for inclusion in the study.
| Variables | Practices employing PAs (n = 6) | Practices without PAs (n = 6) | ||
|---|---|---|---|---|
| Range | Mean | Range | Mean | |
| List size (number of patients) | 4316–15,000 | 9357 | 4385–13,635 | 9637 |
| Percentage of patients > 65 years | 8.5–22% | 13.7% | 4.9–22.3% | 16.0% |
| IMD (high is more deprivation) | 11.05–48.2 | 23.7 | 6.4–33.39 | 17.2 |
| Number of GPs (partners and salaried) | 3–9.3 | 5.3 | 2.4–7.1 | 4.9 |
| Patients per GP | 1233–2304 | 1818 | 719–4292 | 2339 |
| PAs | 1 (n = 5); 2 (n = 1) | 0 | ||
| NPs | 0 (n = 3); 1.4 (n = 1); 1.0 (n = 2) | 0 (n = 4); 1 (n = 2) | ||
| Nurses, others in patient care (PN, HCA, phlebotomists) | 1.2–6.5 (n = 6) | 3.4 (median) | 1.5–4.6 | 2.6 |
| Management, other professional | 1.35–2.75 (n = 6) | 2.2 (median) | 1.1–4.5 | 2.3 |
| Secretarial, reception, clerical | 4.6–11.6 (n = 6) | 7.8 (median) | 4.6–10.1 | 7.6 |
| Total annual staff cost (£M) | 0.96–14.15 | 1.57 | 0.8–2.07 | 1.39 |
| Average cost per patient (£) | 146–273 | 176 | 68–405 | 170 |
There is large variation in the number of patients per GP, particularly in the group of practices without PAs. Data on staffing were provided by practices and could not be verified by other means. Two practices without PAs had one NP each. Two practices with PAs employed two NPs each. Average costs per patient per annum varied between practices; those with the lowest number of patients per GP tended to have the highest average costs.
Comparisons between national headcount data125 and the practices included in the study are shown in Table 13. While the staffing ratios of practices without PAs are similar to national averages, the practices with PAs have higher proportions of salaried GPs. However, there was substantial variability in ratios within groups and the findings need to be treated with caution. Large proportions of staff (in all roles) were reported to be working part-time and headcounts are likely to provide an inaccurate picture in a small sample.
| Ratio | National average | Practices without PAs (n = 6) | Practices with PAs (n = 6) | |
|---|---|---|---|---|
| PAs counted as GP | PAs counted as nurses | |||
| Proportion of all GPs who are salaried (%) | 24 | 28 | 49 | 56 |
| Nurses and direct care staff per GP | 0.95 | 0.91 | 0.73 | 1.04 |
| Administrative/clericala staff per GP | 2.3 | 2.5 | 1.9 | 2.2 |
Decisions about medical and practice staffing
This section uses data from both practices employing PAs and those not employing PAs. Those in non-PA-employing practices often had little knowledge of PAs but most had experience and knowledge of NPs as other mid-level practitioners.
Those GP partners interviewed who had been in general practice since the 1980s commented on the change in the work of practices and the increased need for other types of staff, noting in particular the rise in numbers of nurses, HCAs and administrative staff in different guises. All commented that they could see future changes to the primary care workforce as a result of shifts in demography, pressures on finance for health care, new medical and communication technologies and consequent reductions for hospital inpatient stays but possible increases in local care facilities.
It was evident that GP partners considered multiple factors when making decisions about both new partners in the practice and employed staff. The practice managers echoed these factors, although involvement in decision-making in some aspects, for example on partnerships, was described as mainly the domain of the partners. The factors included (in no order of priority) practice income levels, clinical expertise required to meet patient profile, quality of life of GP partners, GP partners’ own previous experiences in working with different types of staff, efficiency (including cost) in meeting patient demand and/or contract requirements, availability or shortage of GPs and experienced practice nurses to work in their area, other interests beyond the GMS/PMS contract activities (such as training), innovation and research, and the ‘fit’ of individuals within relatively small practice partnerships and staff teams.
All participants reported trying to use staff most efficiently to cover the work required, as in this exemplar:
There is an active attempt to feed work down to the person most appropriate to do it if you see what I mean, I mean it’s pointless paying your mostly highly paid and qualified staff to do tasks that can be done by others.
GP 7–2
While there appeared to be a consensus that the workforce would change, there was no consensus on the likely replacement of doctors by NPs or PAs in substantial numbers. GPs and practice managers drew on both personal experience and published evidence in their arguments. Some suggested that GPs were required to appropriately identify the very small percentage of urgent and complex problems presented which NPs or PA were not trained to identify. Others argued that using the GP as the first contact, particularly in triage systems, was more effective and cost-efficient owing to their expertise levels and ability to take risk.
A further argument was made that the lower productivity levels of nurses and PAs compared with GPs made them more costly. This productivity issue was not just about the appointment times, as illustrated here:
Does [cost] come into it, yes it certainly does. I mean if you could have an experienced PA performing a largely similar role to a salaried doctor then clearly the practice is able to employ more staff to achieve, to provide consultations to patients because the money goes further. However, you have to set against that the fact that there’s supervision time, there’s education time that’s required for PAs, there’s the fact that they aren’t fully registered here.
GP 11–2
One GP noted that making these types of judgements was based on the individual capabilities of PAs and the requirements of a practice and, consequently, it was hard to generalise to an occupational group. Others pointed to the wider considerations to be made in decisions about practice staffing, as in this exemplar:
I think probably it’s the cost actually, more than anything else, to be honest. We used to have one [NP], but we just can’t afford it anymore so the idea with having partners is that they all sort of carry the can more and work more for less really, that’s the bottom line at the moment, to be honest.
Practice manager 8–2
Those who commented that there was a place for replacing doctors with PAs also commented that there were problems to be overcome. Chief among these was the lack of regulation for PAs combined with the consequent lack of authority to prescribe (as described in the exemplar above). A second issue was the lack of a ‘supply’ or ‘pool’ of UK PAs to recruit from, combined with reported problems in attracting US PAs (including visas and higher salaries in the USA). The participants were not convinced that NPs would be a viable group to employ in general practice, in terms of both shortage of supply and their training, as illustrated in this exemplar:
The last time we advertised for a nurse practitioner, it took us about four or five months to recruit. It took ages to recruit because a lot of people will call themselves nurse practitioners, but when you actually look into their qualifications and skills they haven’t got what you need in practice . . . Here, they have to make their own decision and that makes it a different ball game.
Practice manager 7–1
Chapter summary
This chapter has considered the deployment and role of PAs and their relationships within the practices. It then considered the comparative staff resources and the factors that influence the decisions by GPs in staffing their practices. Differences of staffing configurations between PA- and non-PA-employing practices appear to reflect the divided opinions among GPs, primarily, as to the place, viability and/or cost consequences of PAs or other mid-level practitioners in the general practice team.
Chapter 5 Case studies: evidence from the consultation records and linked patient surveys
Patient consultation records were collected for all patients attending a same-day appointment (the index event) in the allocated study periods in each of the participating general practices (see Chapter 2,Consultation record review and linked patient survey). These records were analysed to describe and compare PA and GP activity in the following ways: the work activity of PAs and GPs, the consultation process outcomes and the primary study outcome of reconsultation for the same problem within 14 days of the index event. A subset of these patients received a patient satisfaction survey, any responses to which could be linked to the patient’s consultation records and, therefore, to the study outcome. Cost-effectiveness analyses have also been applied using the process, outcome and satisfaction results.
This chapter addresses each of these components in turn: the consultation records overall (sample numbers, demographics and health characteristics, consultation process outcomes and rate of reconsultation); the patient satisfaction survey (sample numbers, representativeness of the survey subsample and of respondents and satisfaction measures); and analysis of cost-effectiveness.
Consultation records
The consultation records overall are described in terms of the sample numbers, demographics and health characteristics, consultation process outcomes and rate of reconsultation.
Consultation records sample numbers
The sample initially identified for inclusion in the study consisted of 2260 patients, reduced to 2086 after exclusions, for analysis. Figure 3 presents a flow chart of the inclusion and exclusion of the patient consultations forming the study sample.
FIGURE 3.
Flow chart of inclusion and exclusion to the consultation records and patient survey.
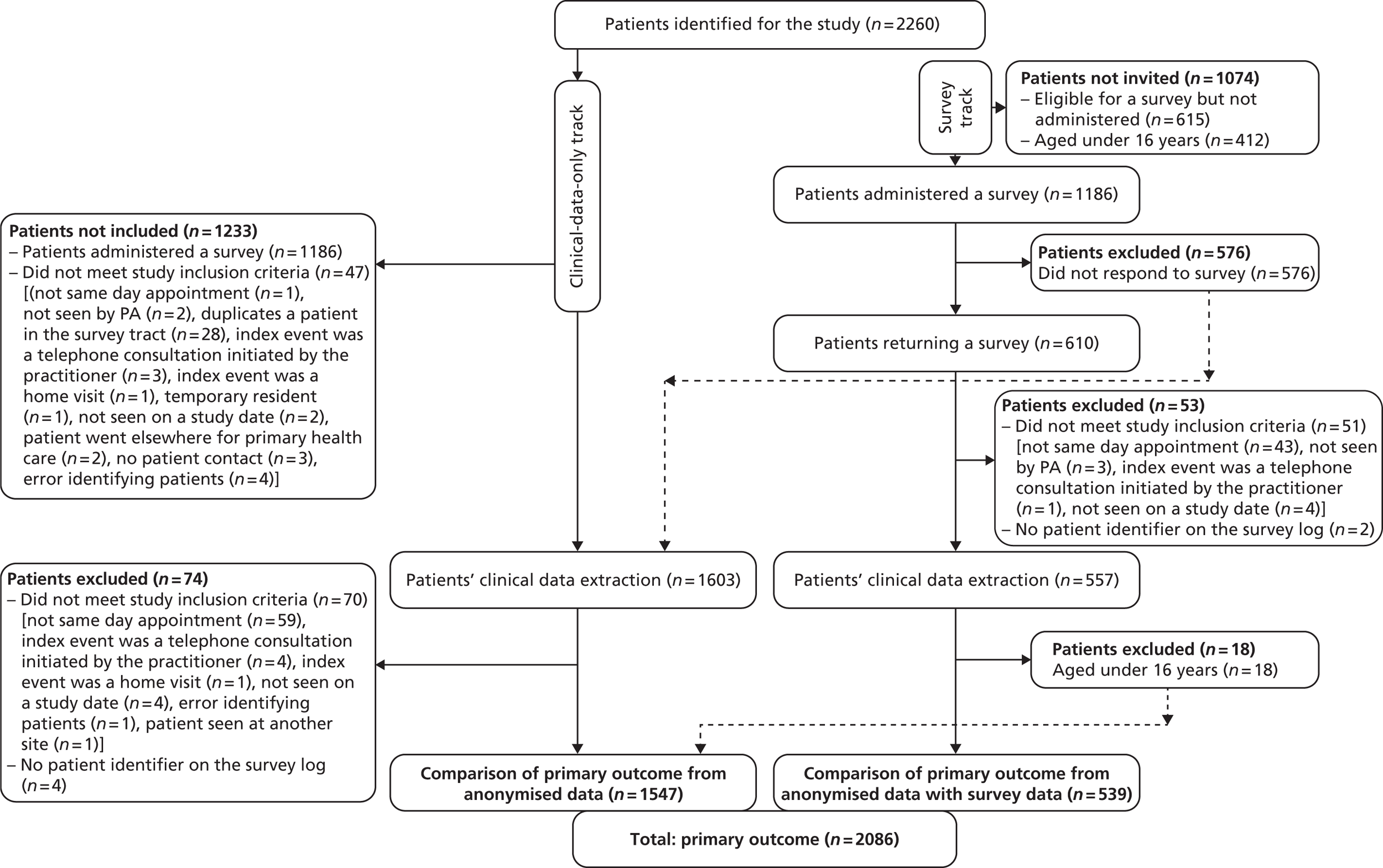
In total, 932 consultations with PAs and 1154 with GPs were included for analysis. The number of patient consultations per practice ranged from 90 to 255 among the PA practices and from 136 to 304 among the GP practices.
These differences reflect the amount of time the practice could commit to the study, the proportion of patients seen who were under the age of 16 years and the proportion of eligible patients to whom a survey was offered.
Work activity of physician assistants and general practitioners in the consultation record sample
The work activity of PAs and GPs in the sample for the index events is described in this section through the demography of the consulting patients and a characterisation of the health problems of the sample.
The demography of the consulting patients
The sample is described in terms of the patients’ age, sex, ethnicity and IMD,94 constructed from the domains of income deprivation, employment deprivation, health deprivation and disability, education, skills and training, barriers to housing and services and the living environment of their home postcode.
The patients consulting both PAs and GPs show a wide range and a fair spread across the age range and in IMD (Table 14). PAs see significantly younger patients than the GPs in this sample [t = −7.971; 95% CI −10.567 to −6.394; degrees of freedom (df) 2081; p < 0.001] but see patients with higher deprivation (t = 9.496; 95% CI 4.902 to 7.454; df 2075; p < 0.001).
| Descriptive statistics | Age at index event | IMD | ||||
|---|---|---|---|---|---|---|
| All | PA consultation | GP consultation | All | PA consultation | GP consultation | |
| n | 2083 | 929 | 1154 | 2077 | 929 | 1148 |
| Missing | 3 | 3 | 0 | 9 | 3 | 6 |
| Mean | 39.15 | 34.35 | 42.93 | 18.57 | 21.99 | 15.81 |
| SD | 24.50 | 23.20 | 24.87 | 15.06 | 16.61 | 13.04 |
| Minimum | 0 | 0 | 0 | 1.04 | 2.04 | 1.04 |
| Maximum | 97 | 91 | 97 | 64.68 | 64.68 | 60.61 |
| Percentiles | ||||||
| 25 | 19 | 15 | 23 | 7.31 | 8.19 | 5.62 |
| 50 | 40 | 35 | 44 | 12.39 | 15.23 | 10.16 |
| 75 | 58 | 51 | 64 | 29.50 | 35.87 | 24.53 |
Female patients are over-represented in the whole sample but no difference is seen in the pattern of male and female patients consulting PAs or GPs (Table 15) (Fisher’s exact test 0.823).
| Sex | All, n (%) | PA consultation, n (%) | GP consultation, n (%) |
|---|---|---|---|
| Female | 1234 (59.2) | 548 (58.8) | 686 (59.4) |
| Male | 850 (40.7) | 382 (41.0) | 468 (40.6) |
| Total | 2084 (99.9) | 930 (99.8) | 1154 (100.0) |
| Missing | 2 (0.1) | 2 (0.2) | 0 (0) |
| Total | 2086 (100.0) | 932 (100.0) | 1154 (100.0) |
The ethnicity of patients is spread across the census categories, although the majority of the sample are classified as white British (Table 16). A large minority of the patients in the sample had no ethnicity recorded by their practice. Comparison of those in the white British ethnicity category with any other ethnicity groups (where this is known) suggests that PAs see slightly more patients in the white British category than do GPs, although this does not reach statistical significance (Fisher’s exact test 0.049).
| Ethnicity (2011 census categories) | Consultation type | ||
|---|---|---|---|
| All, n (%) | PA, n (%) | GP, n (%) | |
| White-British | 948 (45.4) | 420 (45.1) | 528 (45.8) |
| White-Irish | 22 (1.1) | 10 (1.1) | 12 (1.0) |
| Any other white background | 101 (4.8) | 44 (4.7) | 57 (4.9) |
| Mixed-white and black Caribbean | 6 (0.3) | 5 (0.5) | 1 (0.1) |
| Mixed-white and black African | 17 (0.8) | 11 (1.2) | 6 (0.5) |
| Mixed-white and Asian | 3 (0.1) | 1 (0.1) | 2 (0.2) |
| Any other mixed background | 16 (0.8) | 5 (0.5) | 11 (1.0) |
| Asian or Asian British-Indian | 14 (0.7) | 8 (0.9) | 6 (0.5) |
| Asian or Asian British-Pakistani | 10 (0.5) | 7 (0.8) | 3 (0.3) |
| Asian or Asian British-Bangladeshi | 3 (0.1) | 3 (0.3) | 0 (0) |
| Any other Asian background | 57 (2.7) | 15 (1.6) | 42 (3.6) |
| Black or black British-Caribbean | 50 (2.4) | 25 (2.7) | 25 (2.2) |
| Black or black British-African | 95 (4.6) | 52 (5.6) | 43 (3.7) |
| Any other black background | 10 (0.5) | 4 (0.4) | 6 (0.5) |
| Chinese or other ethnic group-Chinese | 5 (0.2) | 3 (0.3) | 2 (0.2) |
| Any other ethnic group | 27 (1.3) | 25 (2.7) | 2 (0.2) |
| Subtotal | 1384 (66.3) | 638 (68.5) | 746 (64.6) |
| Missing | 702 (33.7) | 294 (31.5) | 408 (35.4) |
| Total | 2086 (100.0) | 932 (100.0) | 1154 (100.0) |
Characterisation of the health problems of the consultation record sample
The sample’s health problems are characterised through the number of problems the patient presented with at the index event, the patient being registered on one or more QOF93 disease registers, the number of repeat prescriptions issued to the patient in the year preceding the index event, the number of attendances at the general practice in the 3 months preceding the index event, and a classification of the severity and acuity of the presenting patient as a whole through a combination of their presenting problems (building on de Jong et al. 96) and their presence on QOF registers. This is referred to as the ‘PA study condition classification’.
The number of problems the patient presented with and which were recorded in the index event ranged from one to eight in both PA and GP patient consultations, though 73.9% of the sample presented with just one problem and another 17.9% with two problems. The remainder of the patients, in steadily diminishing numbers (each with less than 5% of the sample), had from three to eight different problems recorded in the index consultation (Table 17). No difference is observed between the PA and GP consultations.
| Descriptive statistics | Number of problems patient presented with at the index event | Number of QOF registers the patients were recorded on | Number of repeat prescriptions recorded in year preceding the index event | Number of visits to practice in the 3 months before the index consultation | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | PA | GP | All | PA | GP | All | PA | GP | All | PA | GP | |
| n | 2086 | 932 | 1154 | 2084 | 932 | 1152 | 2085 | 931 | 1154 | 2085 | 931 | 1154 |
| Missing | 0 | 0 | 0 | 2 | 0 | 2 | 1 | 1 | 0 | 1 | 1 | 0 |
| Mean | 1.39 | 1.40 | 1.38 | 0.73 | 0.55 | 0.87 | 2.24 | 1.81 | 2.60 | 2.44 | 2.12 | 2.70 |
| SD | 0.81 | 0.85 | 0.78 | 1.16 | 0.99 | 1.26 | 3.39 | 3.02 | 3.63 | 2.93 | 2.83 | 2.99 |
| Minimum | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Maximum | 8 | 8 | 8 | 7 | 6 | 7 | 27 | 17 | 27 | 30 | 30 | 25 |
| Percentiles | ||||||||||||
| 25 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 50 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 2 | 1 | 2 |
| 75 | 2 | 2 | 2 | 1 | 1 | 1 | 2 | 2 | 3 | 3 | 2.4 | 3 |
Patients in the sample presented with being on up to seven QOF registers, though 60.8% were on no registers, another 20.5% were registered on just one, and the remainder, in much smaller numbers (each with less than 10% of the sample), were on between two and seven QOF registers (see Table 17).
The majority of the patients in the sample had between zero (27.1%) and three (11.2%) visits to the practice in the previous 3 months (see Table 17). The remaining upper quartile of patients was spread, in steadily decreasing numbers, between 4 and 30 previous visits to the practice.
The number of repeat prescriptions patients were recorded as having been prescribed in the year preceding the index event ranged from none for 45.9% of the sample, one for 14.2% and two for 10.0% up to 26 and 27 repeat prescriptions for one person each in the sample (see Table 17).
Descriptively, GPs appear to be consulted by patients whose average number of QOF registers is higher, who have attended the practice more often in the 3 months preceding the index event and who have had a higher number of repeat prescriptions in the year preceding the index event than those patients consulting PAs.
The ‘PA study condition classification’ sought to address severity, acuity (medical immediacy) and complexity of the presenting complaint(s) in the context of other health characteristic information about the patient, and placed some patients in each classification of acute, chronic, minor/symptoms, prevention and processes for both PAs and GPs. One thousand, one hundred and forty-seven Read code descriptors existed for the presenting problems of the 2086 patients at their index events. Nineteen per cent (n = 213) of these were listed by de Jong et al. 96 in their classification of acute or minor problems. The largest grouping was the minor/symptoms category (Table 18). Significant differences were found between patients consulting PAs and GPs, with PAs tending to see more patients with problems classified as ‘minor/symptoms’ than GPs, while the GPs saw more patients classified as ‘chronic’ or ‘acute’ (χ2 = 34.51; df 4; p < 0.001).
| Consultation type | PA study condition classification | All | ||||
|---|---|---|---|---|---|---|
| Acute | Chronic | Minor/symptoms | Prevention | Process | ||
| PA, n (%) | 34 (3.6) | 305 (32.7) | 586 (62.9) | 1 (0.1) | 6 (0.6) | 932 (100.0) |
| GP, n (%) | 61 (5.3) | 504 (43.7) | 579 (50.20) | 3 (0.3) | 7 (0.6) | 1154 (100.0) |
| All, n (%) | 95 (4.6) | 809 (38.8) | 1165 (55.8) | 4 (0.2) | 13 (0.6) | 2086 (100.0) |
The ‘PA study condition classification’ appears to be correlated with patient age. The patients classified as having a ‘chronic’, ‘acute’ or ‘process’ presentation have a higher mean age than those classified as having a ‘minor/symptoms’ or ‘prevention’ presentation (Table 19).
| Descriptive statistics | Age at index event | ||||
|---|---|---|---|---|---|
| Acute | Chronic | Minor/symptoms | Prevention | Process | |
| n | 95 | 809 | 1162 | 4 | 13 |
| Missing | 0 | 0 | 3 | 0 | 0 |
| Mean | 47.42 | 54.05 | 28.13 | 21.25 | 41.31 |
| SD | 20.272 | 20.087 | 21.804 | 10.372 | 17.918 |
| Minimum | 4 | 2 | 0 | 6 | 1 |
| Maximum | 86 | 95 | 97 | 29 | 67 |
| Percentiles | |||||
| 25 | 32 | 40 | 7 | 10.5 | 31 |
| 50 | 44 | 56 | 26 | 25 | 44 |
| 75 | 67 | 70 | 44 | 28.25 | 56.5 |
These findings suggested that all analyses of process and outcome would benefit from statistical adjustment for the ‘PA study condition classification’ and for the patient’s age as a baseline.
Consultation process outcomes
The process outcomes within the consultation have been measured as follows: the number of procedures carried out in the consultation; number of investigations or tests carried out or ordered; number of prescriptions from the index event; number of referrals made to other services; general advice given; advice on the management of medicines; advice on the use of over the counter medicines; and the issue of Fitness to Work certificates.
Numbers of patient consultations recording process outcomes
The number of patient consultations with each these process measures recorded is shown in Table 20.
| Consultation process measure | Consultation type | ||
|---|---|---|---|
| PA, n (%) | GP, n (%) | All, n (%) | |
| Number of diagnostic tests ordered at index consultation | |||
| 0 | 686 (73.6) | 863 (74.8) | 1549 (74.3) |
| 1 | 174 (18.7) | 210 (18.2) | 384 (18.4) |
| 2 | 59 (6.3) | 64 (5.6) | 123 (5.9) |
| 3 | 13 (1.4) | 11 (1.0) | 24 (1.2) |
| 4 | 0 (0) | 5 (0.4) | 5 (0.2) |
| Number of procedures carried out during the index consultation | |||
| 0 | 924 (99.1) | 1140 (98.9) | 2064 (99) |
| 1 | 8 (0.9) | 13 (1.1) | 21 (1.0) |
| Number of prescriptions from index event | |||
| 0 | 349 (37.5) | 513 (44.5) | 862 (41.3) |
| 1 | 396 (42.5) | 464 (40.2) | 860 (41.2) |
| 2 | 139 (14.9) | 121 (10.5) | 260 (12.5) |
| 3 | 35 (3.8) | 36 (3.1) | 71 (3.4) |
| 4 | 10 (1.1) | 15 (1.3) | 25 (1.2) |
| 5 | 2 (0.2) | 5 (0.4) | 7 (0.3) |
| Number of referrals made from index consultation | |||
| 0 | 849 (91.1) | 1023 (88.7) | 1872 (89.8) |
| 1 | 78 (8.4) | 129 (11.2) | 207 (9.9) |
| 2 | 5 (0.5) | 1 (0.1) | 6 (0.3) |
| General advice given at the index consultation | |||
| Yes | 479 (51.4) | 264 (22.9) | 743 (35.6) |
| No | 453 (48.6) | 889 (77.1) | 1342 (64.4) |
| Advice on medication management given at the index consultation | |||
| Yes | 159 (17.1) | 145 (12.6) | 304 (14.6) |
| No | 773 (82.9) | 1008 (87.4) | 1781 (85.4) |
| Advice given about over-the-counter medications at the index consultation | |||
| Yes | 191 (20.5) | 109 (9.5) | 300 (14.4) |
| No | 741 (79.5) | 1044 (90.5) | 1785 (85.6) |
| Fitness to Work certificate issued at index consultation | |||
| Yes | 29 (3.1) | 45 (3.9) | 74 (3.6) |
| No | 902 (96.9) | 1108 (96.1) | 2010 (96.4) |
The data show that:
-
Very few procedures were carried out at the index consultation by either PAs or GPs (mean 0.1, median 0 for PAs; mean 0.1, median 0 for GPs). The types of procedure reported in the data are described in Table 21.
-
Investigations and tests are much more common than procedures for both PAs and GPs, although the largest single group remains those patients for whom no investigation or test was recorded (mean 0.36, median 0 for PAs; mean 0.34, median 0 for GPs). The types of investigation or test reported in the data are described in Table 22.
-
The number of prescriptions from the index event was most commonly none or one for both groups (mean 0.89, median 1.00 for PAs; mean 0.78, median 1.00 for GPs).
-
For referrals, a large majority of patients had no onward referral made at the index event (mean 0.9, median 0 for PAs; mean 0.11, median 0 for GPs) and the commonest type of referral was to secondary medical care. The types of referral reported in the data are described in Table 23.
-
General advice is the most commonly recorded activity of the processes measured in this study, being reported for approximately half of the patient consultations, followed by advice on medication management and the use of over-the-counter medicines in a large minority (see Table 20).
| Procedure conducted at index consultation | Consultation type | ||
|---|---|---|---|
| PA, n (%) | GP, n (%) | All, n (%) | |
| No procedure | 924 (99.1) | 1140 (98.9) | 2064 (99.0) |
| Injection/vaccination | 3 (0.3) | 0 (0) | 3 (0.1) |
| Wound care | 2 (0.2) | 5 (0.4) | 7 (0.3) |
| Removal of sutures | 0 (0) | 1 (0.1) | 1 (0) |
| Cryotherapy | 0 (0) | 1 (0.1) | 1 (0) |
| Electrocautery | 0 (0) | 1 (0.1) | 1 (0) |
| Therapeutic injections | 0 (0) | 1 (0.1) | 1 (0) |
| Ear irrigation (syringe/clean) | 2 (0.2) | 1 (0.1) | 3 (0.1) |
| Nebuliser | 1 (0.1) | 3 (0.3) | 4 (0.2) |
| Total | 932 (100.0) | 1153 (100.0) | 2085 (100.0) |
| Investigation or testa | Consultation type | ||
|---|---|---|---|
| PA (n) | GP (n) | All (n) | |
| No diagnostic test | 686 | 857 | 1543 |
| Blood test ordered | 68 | 117 | 185 |
| Blood test taken | 10 | 13 | 23 |
| Urine test – dipstick | 61 | 33 | 94 |
| Urine test – sent to lab | 42 | 32 | 74 |
| Cervical smear/LBC | 2 | 2 | 4 |
| ECG | 16 | 14 | 30 |
| 24-hour ECG | 1 | 5 | 6 |
| Echocardiogram | 0 | 4 | 4 |
| Helicobacter pylori test | 1 | 4 | 5 |
| Spirometry/peak flow | 18 | 23 | 41 |
| Stool sample | 14 | 7 | 21 |
| Swab | 28 | 20 | 48 |
| Ultrasound | 9 | 25 | 34 |
| Radiography | 5 | 8 | 13 |
| Screening tool or questionnaire | 41 | 62 | 103 |
| CT scan | 0 | 4 | 4 |
| MRI | 1 | 2 | 3 |
| Pregnancy test | 3 | 2 | 5 |
| Nail, hair or skin sample | 4 | 0 | 4 |
| Other test | 0 | 5 | 5 |
| Total | 1010 | 1239 | 2249 |
| Referrala | Consultation type | ||
|---|---|---|---|
| PA (n) | GP (n) | All (n) | |
| No referral | 849 | 1023 | 1872 |
| Secondary medical care or treatment | 38 | 69 | 107 |
| Allied health professionals and dental | 10 | 28 | 38 |
| Health promotion/public health services | 0 | 2 | 2 |
| Psychological therapies | 5 | 7 | 12 |
| GP within the same practice | 23 | 4 | 27 |
| For a procedure within the same practice | 11 | 15 | 26 |
| Community nursing services | 0 | 1 | 1 |
| Other | 1 | 2 | 3 |
| GP with special interest | 0 | 3 | 3 |
| Total | 937 | 1154 | 2091 |
Comparison of physician assistant and general practitioner consultations in recording process outcomes
The above descriptive accounts of the processes recorded in the consultations give some indication of where there may be similarity or difference between the actions of PAs and GPs.
Unadjusted analyses suggest no difference in the number of procedures carried out, the number of investigations or tests ordered or undertaken, or the issuing of Fitness to Work certificates, but suggest that patients consulting a PA are more likely to receive a prescription for medicine; PAs are more likely to make a referral to another service; and PAs are more likely to record giving general advice, advice on medication management and advice about over-the-counter medications (Table 24).
| Consultation process measure | Unadjusted | Adjusted | |||
|---|---|---|---|---|---|
| χ2 | p-value | Rate ratio | 95% CI | p-value | |
| Number of procedures carried out during the index consultationa,b | 0.37 | 0.66 | 0.85 | 0.34 to 2.15 | 0.734 |
| Number of diagnostic tests ordered at index consultationc | 5.61 | 0.23 | 1.08 | 0.89 to 1.30 | 0.439 |
| Number of prescriptions from index eventd | 16.46 | 0.006 | 1.16 | 0.87 to 1.53 | 0.309 |
| Number of referrals made from index consultationb,e | 8.07 | 0.018 | 0.95 | 0.63 to 1.43 | 0.797 |
| Consultation process measure | χ2 | p-value | OR | 95% CI | p-value |
| General advice given at the index consultationf | 182.49 | < 0.001 | 3.30 | 1.689 to 6.4532 | < 0.001 |
| Advice on medication management given at the index consultationf | 8.32 | 0.004 | 1.72 | 1.0831 to 2.73 | 0.022 |
| Advice given about over-the-counter medications at the index consultationf,b | 50.99 | < 0.001 | 1.74 | 0.62 to 4.88 | 0.295 |
| Fitness to Work certificate issued at index consultationg | 0.93 | 0.34 | – | – | – |
Once adjusted for covariates of relevance to each of the process outcome measures (detailed in Table 24 footnotes) and for clustering in the data at practice level, the unadjusted differences in the number of prescriptions, number of referrals and the giving of advice about over-the-counter medications diminish and are no longer statistically significant (see Table 24). Key in the adjustment of difference is the ‘PA study condition classification’ of the case as acute, chronic, minor/symptom, prevention or process. After statistical adjustment, PAs remain more likely to document giving general and medication management advice to patients (see Table 24).
Consultation process: length of consultation and advice taking
Length of consultation
The length of consultation recorded by the ‘patient enter’ and ‘patient leave’ functions of the practices’ electronic databases were available for 1812 (86.9%) consultations. Missing data were predominantly from three practices and for specific reasons: in one GP practice the surgery session management data (i.e. functional data other than the patient’s clinical record) had already been removed from the database before study data collection took place; in one GP practice the ‘patient enter’ time for telephone consultations was the time the patient telephoned to request an appointment, not the time they spoke with the GP; and in one PA practice the ‘patient enter’ time was infrequently used.
For the 1812 consultations with a time available, PA consultations were seen to have a significantly longer mean consultation time, 5.5 minutes in excess of the GP consultations (95% CI 4.8 to 6.2 minutes; p < 0.001 by t-test), in unadjusted comparisons (Table 25).
| Descriptive statistics | Consultation type | |
|---|---|---|
| PA consultations | GP consultations | |
| n | 896 | 916 |
| Missing | 36 | 238 |
| Mean | 16.79 | 11.28 |
| Percentiles | ||
| 25 | 11.00 | 7.00 |
| 50 | 15.00 | 10.00 |
| 75 | 21.00 | 14.00 |
Differences are seen by practice (Figure 4), although the lack of obvious pattern by newly qualified or experienced PAs, missing data about the length of experience in primary care of all the GPs and the variety of practice organisation of appointment times and type of work make adjustment for potentially confounding factors untenable.
FIGURE 4.
Box plot of length of consultation by practice.
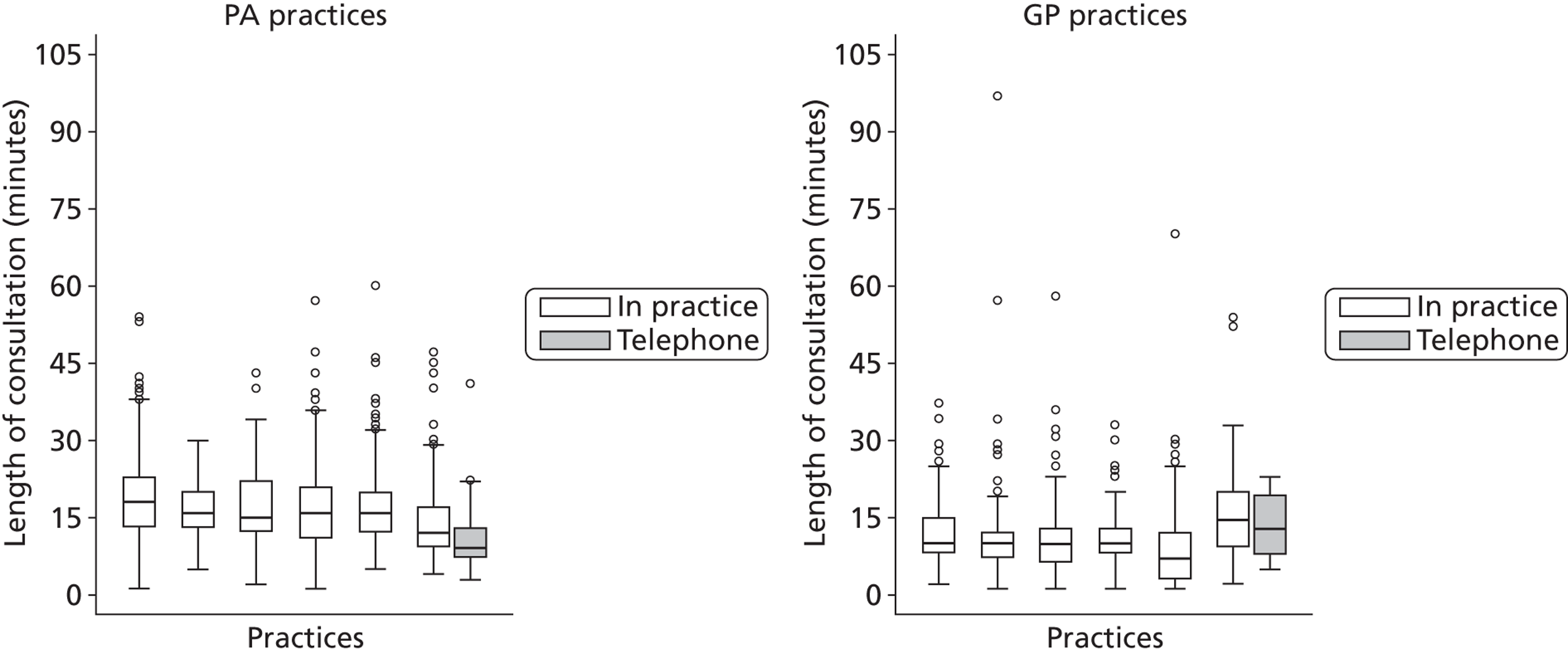
In practice 11 (the furthest right in the box plot for PA practices), the mean length of consultation is obviously shorter than that in the remainder of the PA practices. Here, the PA undertakes both telephone and in-person consultations. Telephone consultations have a mean of 10.4 minutes (SD 8.9 minutes; range 3–41 minutes) and in-person consultations have a mean of 14.5 minutes (SD 5.7 minutes; range 4–47 minutes), being closer to (but still shorter than) the remaining PA practices. Similarly, in practice 8 (the furthest right in the box plot for GP practices), telephone consultations are also routinely carried out for same-day appointments, and the mean length of consultation for these is lower than that for in-practice consultations (although length of consultation data were available for only three such cases).
After adjustment for the ‘PA study condition classification’, age, age squared and the number of problems, the mean difference remained statistically significantly different for practice type (PA or GP) and for the interaction of practice type with age. This difference in length of consultation between PAs and GPs, however, varies by patient age, increasing with age before tailing off at the older ages. The marginal effects at different ages are shown in Table 26.
| Patient age (years) | Difference in length (minutes) of consultation between GPs and PAs (marginal effects) |
|---|---|
| 20 | 5.33 |
| 30 | 5.58 |
| 40 | 5.84 |
| 50 | 6.09 |
| 60 | 6.34 |
| 70 | 6.59 |
| 80 | 6.85 |
The average participant in this study has an age of 38.7 years, where there is a marginal (averaged over all covariates) effect of 5.8 minutes (95% CI –3.54 minutes to –8.06 minutes). All of these are significant differences.
Advice taking
Physician assistants recorded that advice was taken from a supervising doctor in 53 (35.3%) of their index consultations, whether this was at the time of the consultation or later routine quality assurance by the doctor. This was highly significantly different from the GPs, where there was just one case of taking advice documented (χ2 = 68.581, df 1, p < 0.001).
Consultation outcome: reconsultation within 2 weeks
The study’s primary outcome is considered in terms of the numbers of patients reconsulting and the rate of reconsultation, a comparison of rates between PAs and GPs, the type of professional seen at the reconsultation and the planning of reconsultations.
Rate of reconsultation for the same problem
Reconsultation within 2 weeks of the index event was found following 664 (31.8%) of the 2086 index consultations. For 22.6% (n = 150) of those reconsulting, the return visit was for a different/unrelated problem and these cases are not further analysed. For the remaining 514 consultations, the reconsultation was judged, from Read codes95 and free-text consultation record data, to have been for the same (85.0%, n = 437) or a closely related (linked) (14.8%, n = 76) problem, while one case had insufficient data to allow a decision to be made. Those who did reconsult did so between 1 and 20 times in the 2 weeks following the index event. In the majority of cases at least one of the patient’s reconsultations for the same or a linked problem was at the practice (n = 417, 81.1%), the remaining 97 patients reconsulting only at local urgent care facilities.
The following sections describe the unadjusted and adjusted rates of reconsultation for PAs and GPs for the data split into three groupings (not mutually exclusive): reconsultation anywhere for a condition classified as the same or linked to the index consultation, reconsultation anywhere for a condition classified only as the same as the index consultation, and reconsultation only at the practice for a condition classified as the same as the index consultation. The latter is the primary outcome measure for the study (see Chapter 2).
The rate of reconsultation at the practice for the same problem is 0.22 (1 in every 4.5 patients) for those consulting a PA and 0.20 (1 in every 5 patients) for those consulting a GP per fortnight (Table 27).
| Index consultation type | Rate of reconsultations for a linked or the same condition per fortnight | Rate of reconsultations for a linked or the same condition at the practice per fortnight | Rate of reconsultations for exactly the same condition per fortnight | Rate of reconsultations for exactly the same condition at the practice per fortnight |
|---|---|---|---|---|
| PA | ||||
| Mean | 0.373 | 0.277 | 0.317 | 0.236 |
| Percentiles | ||||
| 25 | 0 | 0 | 0 | 0 |
| 50 | 0 | 0 | 0 | 0 |
| 75 | 0 | 0 | 0 | 0 |
| GP | ||||
| Mean | 0.354 | 0.244 | 0.286 | 0.198 |
| Percentiles | ||||
| 25 | 0 | 0 | 0 | 0 |
| 50 | 0 | 0 | 0 | 0 |
| 75 | 0 | 0 | 0 | 0 |
Comparisons of the rates of reconsultation between PAs and GPs
Comparison of the mean number of reconsultations for the same or linked, same or same at practice problems for PA or GP index consultations shows equivalence against the study’s primary outcome for PAs and GPs, with no difference found in the rates of reconsultation for the two groups, unadjusted or adjusted for potential confounding factors (Table 28).
| Consultation process measure | Adjusteda | ||
|---|---|---|---|
| Rate ratio | 95% CI | p-value | |
| Reconsultation for a condition the same or linked to the index consultation at the practice or an urgent care facility | 1.240 | 0.861 to 1.789 | 0.247 |
| Reconsultation for a condition the same or linked to the index consultation at the practice only | 1.328 | 0.926 to 3.968 | 0.123 |
| Reconsultation for a condition the same as the index consultation at the practice or an urgent care facility | 1.314 | 0.843 to 2.049 | 0.228 |
| Reconsultation for a condition the same as the index consultation at the practice only | 1.385 | 0.928 to 2.066 | 0.111 |
Type of professional seeing patients at their first or only reconsultation
For those patients who did reconsult with the same problem (at the practice or an urgent care facility), the largest group consulted a GP at their only or first reconsultation, although PAs are also found to see 35% of their reconsulting patients again themselves (Table 29).
| Reconsultation | Index consultation | |
|---|---|---|
| PA, n (%) | GP, n (%) | |
| GP | 96 (49.5) | 210 (92.1) |
| PA | 67 (34.5) | 0 (0) |
| Nurse | 9 (4.6) | 8 (3.5) |
| NP | 6 (3.1) | 3 (1.3) |
| ED doctor | 2 (1.0) | 7 (3.1) |
| Foundation doctor | 5 (2.6) | 0 (0) |
| Practice nurse | 4 (2.1) | 0 (0) |
| GP trainee | 3 (1.5) | 0 (0) |
| GP locum | 1 (0.5) | 0 (0) |
| Midwife | 1 (0.5) | 0 (0) |
Planning of reconsultations
Some of the PAs and GPs documented that the reconsultation was planned, that is to say it was intended that the patient would return in a specified time period. This documented planning differed between PAs and GPs, with PAs documenting planning more follow-up in the practice than GPs, with Table 30 detailing this for reconsultations for the same problem at the practice or urgent care facility (χ2 = 5.779, df 1, p = 0.019) and for reconsultations for the same problem at the practice only (χ2 = 2.315, df 1, p = 0.080).
| Consultation type | Reconsultation for the same condition at the practice or urgent care facility | Reconsultation for the same condition at the practice only | ||
|---|---|---|---|---|
| Unplanned | Planned | Unplanned | Planned | |
| PA, n (%) | 85 (57.0) | 64 (43.0) | 83 (56.8) | 63 (43.2) |
| GP, n (%) | 119 (70.0) | 51 (30.0) | 102 (65.4) | 54 (34.6) |
| Total, n (%) | 204 (63.9) | 115 (36.1) | 185 (61.3) | 117 (38.7) |
When comparison of the rate of reconsultation for the same problem at the practice or urgent care facility between PAs and GPs is further adjusted for whether or not the reconsultation was documented as planned, the previous finding of no difference in reconsultation rate remains true (rate ratio 1.183; 95% CI 0.914 to 1.531; p = 0.202).
Patient survey
Evidence from the patients’ perspectives was collected from patients whose same-day appointment consultation was entered into the case studies, as described in Consultation records, above. All adult patients recruited were able to offer their perspective through the completion of a survey.
In this section, we describe first of all the sample, then the response rate, and then turn to the responses.
The patient survey sample
The sample identified for inclusion in this element of the study consisted of 1020 adult (aged 16 years or over) patients (n = 490 PA consultations, n = 590 GP consultations). Figure 3 (see Chapter 4) details the identification of cases for inclusion/exclusion in the study, including the patient survey route of entry into the study. The survey sample differed from the overall sample of patients’ consultation records primarily by the exclusion of children aged under 16 years. Table 31 presents descriptive data of the survey sample against the overall consultation record sample for age, Table 32 for IMD, Table 33 for sex and Table 34 for ethnicity.
| Descriptive statistics | Age at index event | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Survey sample | Consultation record sample | Respondents | |||||||
| All | PA | GP | All | PA | GP | All | PA | GP | |
| n | 1017 | 427 | 590 | 2083 | 929 | 1154 | 538 | 219 | 319 |
| Missing | 3 | 3 | 0 | 3 | 3 | 0 | 1 | 1 | 0 |
| Mean | 48.86 | 45.25 | 51.47 | 39.15 | 34.35 | 42.93 | 52.99 | 48.78 | 55.89 |
| SD | 18.311 | 16.808 | 18.914 | 24.50 | 23.20 | 24.87 | 17.956 | 16.945 | 18.082 |
| Minimum | 16 | 16 | 16 | 0 | 0 | 0 | 16 | 18 | 16 |
| Maximum | 97 | 90 | 97 | 97 | 91 | 97 | 94 | 90 | 94 |
| Percentiles | |||||||||
| 25 | 35 | 32 | 36.75 | 19 | 15 | 23 | 39.00 | 36.00 | 42.00 |
| 50 | 47 | 44 | 51.00 | 40 | 35 | 44 | 53.00 | 48.00 | 58.00 |
| 75 | 64 | 57 | 68.00 | 58 | 51 | 64 | 67.00 | 63.00 | 70.00 |
| Descriptive statistics | IMD | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Survey sample | Consultation record sample | Respondents | |||||||
| All | PA | GP | All | PA | GP | All | PA | GP | |
| n | 1015 | 427 | 588 | 2077 | 929 | 1148 | 537 | 219 | 318 |
| Missing | 5 | 3 | 2 | 9 | 3 | 6 | 2 | 1 | 1 |
| Mean | 20.123 | 21.666 | 19.002 | 18.57 | 21.99 | 15.84 | 16.28 | 17.582 | 15.377 |
| SD | 15.044 | 15.787 | 14.392 | 15.06 | 16.61 | 13.04 | 13.44 | 14.033 | 12.96 |
| Minimum | 1.04 | 2.04 | 1.04 | 1.04 | 2.04 | 1.04 | 1.04 | 2.04 | 1.04 |
| Maximum | 64.68 | 64.68 | 60.61 | 34.68 | 64.68 | 60.61 | 56.55 | 56.55 | 56.55 |
| Percentiles | |||||||||
| 25 | 8.18 | 8.63 | 7.47 | 7.31 | 8.19 | 5.62 | 7.10 | 8.19 | 5.55 |
| 50 | 13.82 | 15.23 | 13.47 | 12.39 | 15.23 | 10.16 | 11.45 | 12.32 | 10.16 |
| 75 | 31.05 | 34.97 | 29.50 | 29.50 | 35.87 | 24.53 | 21.64 | 20.46 | 22.10 |
| Sex | Consultation record sample | Survey sample | Respondents | ||||||
|---|---|---|---|---|---|---|---|---|---|
| All, n (%) | PA, n (%) | GP, n (%) | All, n (%) | PA, n (%) | GP, n (%) | All, n (%) | PA, n (%) | GP, n (%) | |
| Female | 1234 (59.2) | 548 (58.8) | 686 (59.4) | 621 (60.9) | 268 (62.3) | 353 (59.8) | 322 (59.7) | 128 (58.2) | 194 (60.8) |
| Male | 850 (40.7) | 382 (41.0) | 468 (40.6) | 397 (38.9) | 160 (37.2) | 237 (40.2) | 217 (40.3) | 92 (41.8) | 125 (39.2) |
| Total | 2084 (99.9) | 930 (99.8) | 1154 (100.0) | 1018 (99.8) | 428 (99.5) | 590 (100.0) | 539 (0) | 220 (100.0) | 319 (100.0) |
| Missing | 2 (0.1) | 2 (0.2) | 0 (0) | 2 (0.2) | 2 (0.5) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Total | 2086 (100.0) | 932 (100.0) | 1154 (100.0) | 1020 (100.0) | 430 (100.0) | 590 (100.0) | 539 (100.0) | 220 (100.0) | 319 (100.0) |
| Ethnicity | Consultation record sample | Survey sample | Respondents | ||||||
|---|---|---|---|---|---|---|---|---|---|
| All, n (%) | PA, n (%) | GP, n (%) | All, n (%) | PA, n (%) | GP, n (%) | All, n (%) | PA, n (%) | GP, n (%) | |
| White British | 948 (45.4) | 420 (45.1) | 528 (45.8) | 605 (59.3) | 279 (64.9) | 326 (55.3) | 432 (80.1) | 181 (82.3) | 251 (78.7) |
| Any other ethnicity | 436 (20.9) | 218 (23.4) | 218 (18.8) | 243 (23.8) | 89 (20.7) | 154 (26.1) | 102 (18.9) | 35 (15.9) | 67 (21.0) |
| Missing | 702 (33.7) | 294 (31.5) | 408 (35.4) | 172 (16.9) | 62 (14.4) | 110 (18.6) | 5 (0.9) | 4 (1.8) | 1 (0.3) |
| Total | 2068 (100.0) | 932 (100.0) | 1154 (100.0) | 1020 (100.0) | 430 (100.0) | 590 (100.0) | 539 (100.0) | 220 (100.0) | 319 (100.0) |
Response rate and respondents
Of the 1020 eligible patients given a survey, 52.8% (n = 539) responded with a completed survey, with 51.2% (n = 220) of those surveyed and consulting a PA responding and 54.1% (n = 319) of those surveyed and consulting a GP responding.
Tables 31 to 34 present descriptive data of the survey respondents against the survey sample for age, IMD, sex and ethnicity. These data suggest that survey recipients are older than the overall sample (explained by the exclusion of those aged under 16 from the sample) and that respondents are an older group still; that the IMD of survey recipients is higher than that of the overall sample but that of respondents is lower (indicating less deprivation among respondents); that sex is consistent across the consultation, survey and respondent samples; and that ethnicity appears to show the biggest difference between groups with survey recipients and survey respondents showing an increasing proportion of participants classifying their ethnicity as white British (although the reduction in missing data for these groups is dramatic and may have influenced the proportions).
The survey responses
The survey measured the patients’ experiences against a number of measures as follows: how good the PA or GP was at giving enough time, asking about symptoms, explaining tests and treatments, involving the patient in decisions about their care, treating the patient with care and concern, and taking problems seriously; confidence and trust in the PA or GP seen; satisfaction with the care received from the PA or GP at the index consultation; satisfaction with the general care at the general practice; willingness to recommend the general practice; and willingness to see a PA rather than a GP.
Table 35 describes the responses in total and by consulting with PA and GP groups and the unadjusted and adjusted comparison between PA and GP groups.
| Consultation process measure | Response option | Crude | Adjusted | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Very good, n (%) | Good, n (%) | Neither good nor poor, n (%) | Poor, n (%) | Very poor, n (%) | Doesn’t apply, n (%) | p-value | OR (95% CI) | p-value | |
| Judgement of practitioner for | |||||||||
| Giving time | |||||||||
| PA | 161 (74.5) | 49 (22.7) | 6 (2.8) | 0 (0) | 0 (0) | 0 (0) | 0.97 | 0.97 (0.48 to 1.94) | 0.93 |
| GP | 232 (74.4) | 68 (21.8) | 8 (2.6) | 3 (1.0) | 0 (0) | 1 (0.3) | |||
| Asking regarding symptoms | |||||||||
| PA | 153 (71.5) | 52 (24.3) | 8 (3.7) | 0 (0) | 1 (0.5) | 0 (0) | 0.39 | 1.19 (0.62 to 2.29) | 0.60 |
| GP | 231 (74.0) | 61 (19.6) | 13 (4.2) | 1 (0.3) | 1 (0.3) | 5 (1.6) | |||
| Listening | |||||||||
| PA | 157 (73.0) | 49 (22.8) | 9 (4.2) | 0 (0) | 0 (0) | 0 (0) | 0.20 | 1.30 (0.63 to 2.68) | 0.47 |
| GP | 242 (77.3) | 60 (19.2) | 7 (2.2) | 2 (0.6) | 0 (0) | 2 (0.6) | |||
| Explaining tests, etc. | |||||||||
| PA | 135 (63.1) | 48 (22.4) | 14 (6.5) | 1 (0.5) | 0 (0) | 16 (7.5) | 0.63 | 1.07 (0.84 to 2.08) | 0.84 |
| GP | 197 (64.2) | 66 (21.5) | 15 (4.9) | 2 (0.7) | 1 (0.3) | 26 (8.5) | |||
| Taking seriously | |||||||||
| PA | 156 (72.6) | 46 (21.4) | 11 (5.1) | 0 (0) | 1 (0.5) | 1 (0.5) | 0.57 | 1.12 (0.66 to 1.93) | 0.67 |
| GP | 229 (73.4) | 58 (18.6) | 13 (4.2) | 3 (1.0) | 1 (0.3) | 8 (2.6) | |||
| Involving in decisions | |||||||||
| PA | 120 (56.1) | 53 (24.8) | 12 (5.6) | 4 (1.9) | 0 (0) | 25 (11.7) | 0.53 | 1.10 (0.73 to 1.67) | 0.65 |
| GP | 185 (59.7) | 64 (20.6) | 24 (737) | 2 (0.6) | 1 (0.3) | 34 (11.0) | |||
| Treating with care | |||||||||
| PA | 156 (72.9) | 48 (22.4) | 10 (4.7) | 0 (0) | 0 (0) | 0 (0) | 0.67 | 1.09 (0.59 to 2.01) | 0.79 |
| GP | 226 (72.9) | 64 (20.6) | 10 (3.2) | 3 (1.0) | 0 (0) | 7 (2.3) | |||
| Consultation process measure | Response option | Unadjusted | Adjusted | ||||||
| Yes, definitely, n (%) | Yes to some extent, n (%) | No, not at all, n (%) | Don’t know/can’t say, n (%) | Mann–Whitney p | OR (95% CI) | p-value | |||
| Confidence and trust in the PA/GP | |||||||||
| PA | 175 (80.6) | 39 (18.0) | 2 (0.9) | 0 (0) | 0.05 | 1.55 (0.61 to 3.96) | 0.36 | ||
| GP | 271 (87.1) | 36 (11.6) | 3 (1.0) | 0 (0) | |||||
| Very satisfied, n (%) | Satisfied, n (%) | Neither satisfied nor dissatisfied, n (%) | Dissatisfied, n (%) | Very dissatisfied, n (%) | Mann–Whitney p | OR (95% CI) | p-value | ||
| General satisfaction with the care | |||||||||
| PA | 164 (75.9) | 40 (18.5) | 11 | 0 | 0.82 | 1.00 (0.42 to 2.36) | 0.99 | ||
| GP | 241 (76.5) | 61 (19.4) | 10 (3.2) | 2 (0.6) | 1 (0.3) | ||||
| Very satisfied to see PA again, n (%) | Satisfied to see the PA again, n (%) | Neither satisfied nor dissatisfied, n (%) | Dissatisfied and prefer to see a GP, n (%) | Very dissatisfied/prefer to see a GP, n (%) | |||||
| Satisfied with seeing the PA again? | |||||||||
| 136 (62) | 62 (28.3) | 8 (3.7) | 7 (3.2) | 2 (0.9) | N/A | ||||
| Very willing to see the PA, n (%) | Willing to see the PA, n (%) | Neither willing nor unwilling, n (%) | Unwilling to see the PA, n (%) | Very unwilling to see PA, n (%) | |||||
| Willing to see a PA instead of the GP? | |||||||||
| 15 (4.7) | 69 (21.6) | 60 (18.8) | 87 (27.2) | 74 (23.1) | N/A | ||||
The majority of respondents were satisfied or very satisfied with their consultation with both PAs and GPs. The measures for which lower percentages of respondents reported themselves to be very satisfied were ‘explaining about tests and procedures’ and ‘involving you in decision-making’. There was no difference between PAs and GPs.
Positive correlation, significant at p < 0.01, was found between general satisfaction with the index event consultation and all other measures of satisfaction collected in the survey: giving enough time, asking about symptoms, listening, explaining tests and treatments, taking problems seriously, involving the patient in decision-making, treating the patient with care and concern, confidence and trust and willingness to see a PA. The majority of these measures were also correlated.
No statistically significant correlation was found between any measures of satisfaction and the study’s primary outcome, that is, the rate of reconsultation with the same problem.
Economic analysis
The mean consultation time was higher for PAs than for GPs (16.79 minutes vs. 11.23 minutes), an unadjusted difference of 5.5 minutes. This reflects the appointment times set in the study practices, which were 10 minutes for GPs and 15 minutes for PAs (20 minutes in one practice). Controlling for other covariates (set at their mean values), the difference in consultation times for the average patient (age 38.7 years) increased to 5.8 minutes (17.03 minutes vs. 11.23 minutes) minutes. This increase reflects, in part, the fact that, compared with GPs, a higher proportion of PA consultations are for minor symptoms (mean consultation time 13.5 minutes) and a lower proportion are for chronic and for acute conditions which require longer consultation times (14.35 minutes and 17.3 minutes respectively).
Although GPs see more patients per hour (three patients for every two seen by PAs), their salary and related costs are more than twice those of PAs (see Appendix 8), and so PA consultations are still less costly. Using national figures,119 GP and PA consultations cost £3.08 and £1.67 per minute (based on consultations of 11.7 minutes at £36 and 15 minutes at £25), giving consultation costs within this study (for the adjusted consultation lengths of 17.03 minutes and 11.23 minutes) of £34.36 and £28.14, respectively, a saving of £6.22.
In adjusted analyses that controlled for variations in the case mix of GPs and PAs, no significant differences between the professionals were found in rates of reconsultation, referring, prescribing, ordering investigations or undertaking procedures, and so no attempt was made to cost these activities.
Physician assistants provided significantly more general and medicines management advice than GPs, and this may have contributed to the longer mean length of PA consultations. Providing advice may be valued by patients and contribute to self-management, but this was not reflected in feedback from patients, which suggested no differences between the skills of GPs and PAs regarding explanations of tests and treatments.
Physician assistants thus appear to deliver similar outcomes from same-day consultations as GPs, at lower cost. However, the apparent cost advantage of PAs is eroded when broader factors are taken into consideration. GPs spend time on training and supervising PAs; in addition, GP consultations are interrupted for signing PA prescriptions and when PAs seek advice about patients (23 occasions in this study vs. 1 by GPs). No data were available to enable an assessment of the extent to which such factors affect comparative consultation costs.
Summary of key findings from the consultation records
The analyses of the workload activities, consultation processes and consultation outcomes of the PAs’ and GPs’ consultations and the subsequent economic analyses have suggested that:
-
PAs and GPs in the sample attend patients with differing demographic and health characteristics, with GPs being consulted by an older patient group with a higher incidence of measures of comorbidity.
-
From the clinical record of the consultation, PAs and GPs conduct many processes within the consultation similarly but PAs record that their patients receive more general and medication management advice.
-
PAs’ consultations are significantly longer than those conducted by GPs in the study.
-
PAs take and document advice from supervising doctors in just over one-third of consultations.
-
The outcomes of consultations as measured by reconsultation rates do not differ between the PAs and the GPs in the sample.
-
Patient satisfaction with both PAs and GPs is high, with no difference in responses in the two groups.
-
PA consultations are less costly than those of GPs, taking salary, caseload and length of consultation/productivity into account.
-
PAs appear to deliver similar outcomes from same-day consultations as GPs, at this lower cost.
-
Any apparent cost advantage of PAs is eroded when the training and supervision of PAs by GPs and interruptions to GP consultations by advice-seeking PAs are considered.
Chapter 6 Case studies: evidence from the clinical review of consultation records and video observations
This chapter reports on how effective the PAs were at delivering the core business of primary care: the clinical consultation. In the previous chapter, analysis of the study’s primary outcome – the rate of reconsultation for the same problem – was seen not to differ between PAs and GPS. Against this background, clinical review was carried out of the medical records of the index consultation where there was a repeat consultation for the same problem to assess the quality of medical records made at the index consultation and appropriateness in light of any subsequent attendance. Clinical review was also carried out with direct (video) observation of the consultation to assess competence at consulting. The methods for each of these were reported in Chapter 2. This chapter addresses each of these aspects of clinical review in turn.
Quality of consultation records and appropriateness of the index consultation
The quality of the medical records made at the index consultation and the appropriateness of any subsequent attendance are reported.
Sample numbers
Selection of cases with a reconsultation for the same or a linked problem (at the practice or any urgent care facility) identified 511 cases for review. After exclusions, 475 cases (93%) were used to explore the quality of the medical record as a surrogate for consultation quality and appropriateness (Table 36).
| Clinical review process | Reconsultation for the same or a linked problem, n (%) |
|---|---|
| Eligible for review | 511 (100) |
| Used in training the review raters | 12 (2.3) |
| Missed by researchers | 2 (0.4) |
| Review not completed (in full) | 22 (4.7) |
| Review completed | 475 (93) |
Review of reconsultations for the same condition at the practice or urgent care facility
The assessment of the quality of computerised medical record entries for the key consultation components (using Weed’s SOAP classification101,102 as described in Chapter 2, The clinical review of reconsultations records), for cases with a reconsultation for the same problem (n = 388) at the practice or urgent care facility within 14 days, is presented in Table 37.
| Consultation type | Judgement of appropriateness, n (%) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Subjective information | Examination | Investigation | Prescription | Problem | Overall | |||||||
| Inappropriate | Appropriate | Inappropriate | Appropriate | Inappropriate | Appropriate | Inappropriate | Appropriate | Inappropriate | Appropriate | Inappropriate | Appropriate | |
| PA | 37 (20.2) | 146 (79.8) | 48 (26.2) | 135 (73.8) | 29 (15.8) | 154 (84.2) | 48 (26.2) | 135 (73.8) | 32 (17.5) | 151 (82.5) | 38 (20.8) | 145 (79.2) |
| GP | 132 (64.7) | 72 (35.3) | 138 (67.3) | 67 (32.7) | 90 (43.9) | 115 (56.1) | 104 (50.7) | 101 (49.3) | 84 (41.0) | 121 (59.0) | 106 (51.7) | 99 (48.3) |
| Total | 169 (43.7) | 218 (56.3) | 186 (47.9) | 202 (52.1) | 119 (30.7) | 269 (69.3) | 152 (39.2) | 236 (60.8) | 116 (29.9) | 272 (37.1) | 144 (62.9) | 244 (70.1) |
| Unadjusted difference | χ2 = 77.611, df 1, p < 0.001 | χ2 = 65.402, df 1, p < 0.001 | χ2 = 35.791, df 1, p < 0.001 | χ2 = 24.361, df 1, p < 0.001 | χ2 = 25.454, df 1, p < 0.001 | χ2 = 39.663, df 1, p < 0.001 | ||||||
The PAs were judged to record the key consultation components more frequently in the computerised medical record, with each element reaching statistical significance for the difference. The PAs recorded appropriate index consultation records nearly 80% of the time (145 out of 183), whereas GPs made appropriate records in just under 50% of the time (99 out of 205; p < 0.001) (see Table 37).
This difference remained the same across all of the elements of the medical record that were observed. GPs had an excess of appropriate over inappropriate records only for investigations. The risk ratio of a PA making an appropriate record compared with a GP was 1.64 (95% CI 1.40 to 1.93; p < 0.001; see Table 37 for raw data), that is to say those consulting a PA are 64% more likely to get an appropriate medical record, as judged by the reviewers.
Review of reconsultations for a linked condition at the practice or urgent care facility
The assessment of the quality of computerised medical record entries as above for cases with a reconsultation for a linked condition (n = 75) at the practice or urgent care facility within 14 days is presented in Table 38.
| Consultation type | Judgement of appropriateness, n (%) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Subjective information | Examination | Investigation | Prescription | Problem | Overall | |||||||
| Inappropriate | Appropriate | Inappropriate | Appropriate | Inappropriate | Appropriate | Inappropriate | Appropriate | Inappropriate | Appropriate | Inappropriate | Appropriate | |
| PA | 12 (37.5) | 20 (62.5) | 6 (18.8) | 26 (81.3) | 7 (21.9) | 25 (78.1) | 8 (25.0) | 24 (75.0) | 5 (15.6) | 27 (84.4) | 3 (9.4) | 29 (90.6) |
| GP | 24 (55.8) | 19 (44.2) | 20 (46.5) | 23 (53.5) | 17 (39.5) | 26 (60.5) | 22 (51.2) | 21 (48.8) | 18 (41.9) | 25 (58.1) | 18 (41.9) | 25 (58.1) |
| Total | 36 (48.0) | 39 (52.0) | 26 (34.7) | 49 (65.3) | 24 (32.0) | 51 (68.0) | 30 (40.0) | 45 (60.0) | 23 (30.7) | 52 (69.3) | 21 (28.0) | 54 (72.0) |
| Unadjusted difference | χ2 = 2.465, df 1, p = 0.161 | χ2 = 6.243, df 1, p = 0.015 | χ2 = 2.630, df 1, p = 0.136 | χ2 = 5.233, df 1, p = 0.032 | χ2 = 5.939, df 1, p = 0.022 | χ2 = 9.604, df 1, p = 0.002 | ||||||
The same judgement of the difference between the medical record entries of PAs and GPs for a linked problem as for the same problem was made: just over 90% of PA records (90.06%, 29 out of 32) and just under 60% of GP records (58.1%, 25 out of 43) were thought appropriate. Again, PAs were much more likely to make appropriate records, in all domains. The numbers are smaller, which may reflect in fewer significant differences between professions. The risk ratio of a PA making an appropriate record for these ‘linked’ consultations compared with a GP was 1.56 (95% CI 1.18 to 2.06; p < 0.001, see Table 38 for raw data), that is to say those consulting a PA are 56% more likely to get an appropriate medical record, as judged by the reviewers.
Review of all repeat consultations
The PAs made better records of their consultations, and the reviewers felt that they indicated safe practice. They did not feel that any of the consultation records represented unsafe practice.
Effectiveness of blinding/reviewers’ judgement of who conducted the consultation
The blinding of records to remove any indication of whether the consultation was with a PA or a GP was considered to be successful. Reviewers were unable to judge whether the index event had been consulted by a PA or GP in both the review of cases for the same condition and those for a linked condition.
For cases with a reconsultation for the same problem, reviewers gave an opinion in nearly all cases (98.2%, 381 out of 388); in the remainder of the consultations the reviewers stated that they were unable to decide. Where they could decide, there was low sensitivity and specificity; they judged 57% of PA consultations reviewed for the same problem to have been those of a GP (к = 0.196; Table 39).
| Consultation type | Reviewers’ judgement whether the index consultation conducted by a PA or a GP? | |
|---|---|---|
| PA, n (%) | GP, n (%) | |
| PA | 77 (43.0) | 102 (57.0) |
| GP | 48 (23.8) | 154 (76.2) |
| Total | 125 (32.8) | 256 (67.2) |
For cases with a reconsultation for a linked condition, reviewers were similarly unable to judge whether the index event for these linked reconsultations had been carried out by a PA or GP, though they gave an opinion for all 75 cases. In the case of linked consultation, the reviewers judged 66% of PA consultations for a linked problem to have been those of a GP (к = 0.141; Table 40).
| Consultation type | Reviewers’ judgement whether the index consultation conducted by a PA or a GP? | |
|---|---|---|
| PA, n (%) | GP, n (%) | |
| PA | 11 (34.4) | 21 (65.6) |
| GP | 9 (20.9) | 34 (79.1) |
| Total | 20 (26.7) | 55 (73.3) |
Overall, 58.3% (123 out of 211) of the consultations actually with a PA were thought on the basis of the records to have been with a GP. Thirty-nine per cent (57 out of 145) of the consultations that the reviewers thought were by a PA were actually by a GP. The raters were neither sensitive nor specific: diagnostic OR 2.36 (95% CI 1.58 to 3.53; Pearson chi-squared p < 0.001), sensitivity 42% (95% CI 35.1% to 48.3%) and specificity 77% (95% CI 71.4% to 82%).
Inter-rater reliability
Ten clinical review cases were rated by all four reviewers independently immediately following the review raters’ training exercise. The assessment of inter-rater reliability using Fleiss’s kappa103 for the assessment of the quality of computerised medical record entries for the key consultation components is presented in Table 41.
| Key consultation component | к | 95% CIs |
|---|---|---|
| Subjective information | 0.76 | 0.51 to 1.00 |
| Examination | 0.69 | 0.43 to 0.94 |
| Investigation | 0.90 | 0.65 to 1.00 |
| Prescription | 1.00 | 0.75 to 1.00 |
| Problem | 1.00 | 0.75 to 1.00 |
| Appropriateness | 1.00 | 0.75 to 1.00 |
| PA or GP | 0.12 | –0.15 to 0.39 |
Taken against the consideration that a kappa score of 0.0–0.2 is ‘poor’, of 0.21–0.4 is ‘fair’, of 0.41–0.6 is ‘moderate’, of 0.61–0.8 is ‘good’ and of 0.81–1.0 is ‘very good’,104 the inter-rater reliability of the reviewers here was very good when assessing the quality of the computerised medical records, but very poor agreement on the type of practitioner (reviewers blinded to this) carrying out the consultation.
Comparison of reconsultation rates with judgements of appropriateness
The rate of reconsultation for PAs and GPs was presented in Chapter 5 (see Rate of reconsultion for the same problem), indicating that there were no differences in the rate of repeat consultations within the 2 weeks following the index consultation by type of professional seen at the index consultation.
After adjustment for the judgement of appropriateness (and practice clustering), the rate of reconsultation for the same problem at the practice or urgent care facility, or at the practice only, does not suggest any statistically significant difference between the rates for PAs or GPs:
-
same problem at the practice or urgent care facility: rate ratio 1.124, 95% CI 0.918 to 1.374, p = 0.257 (see raw data in Table 42)
-
same problem at the practice only: rate ratio 1.217, 95% CI 0.981 to 1.506, p = 0.074 (see raw data in Table 43).
| Practice type | Number of reconsultations for exactly the same condition | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 18 | ||
| PA practice | ||||||||
| Was the index consultation appropriate? | ||||||||
| Inappropriate, n (%) | 3 (7.3) | 26 (63.4) | 11 (26.8) | 1 (2.4) | 0 (0) | 0 (0) | 0 (0) | 41 (100.0) |
| Appropriate, n (%) | 24 (13.2) | 119 (65.4) | 26 (14.3) | 6 (3.3) | 4 (2.2) | 2 (1.1) | 1 (0.5) | 182 (100.0) |
| Total, n (%) | 27 (12.1) | 145 (65.0) | 37 (16.6) | 7 (3.1) | 4 (1.8) | 2 (0.9) | 1 (0.4) | 223 (100.0) |
| Non-PA practice | ||||||||
| Was the index consultation appropriate? | ||||||||
| Inappropriate, n (%) | 17 (13.7) | 79 (63.7) | 21 (16.9) | 5 (4.0) | 1 (0.8) | 1 (0.8) | 124 (100.0) | |
| Appropriate, n (%) | 25 (19.5) | 76 (59.4) | 15 (11.7) | 10 (7.8) | 2 (1.6) | 0 (0) | 128 (100.0) | |
| Total, n (%) | 42 (16.7) | 155 (61.5) | 36 (14.3) | 15 (6.0) | 3 (1.2) | 1 (0.4) | 252 (100.0) | |
| Total | ||||||||
| Was the index consultation appropriate? | ||||||||
| Inappropriate, n (%) | 20 (12.1) | 105 (63.6) | 32 (19.4) | 6 (3.6) | 1 (0.6) | 1 (0.6) | 0 (0) | 165 (100.0) |
| Appropriate, n (%) | 49 (15.8) | 195 (62.9) | 41 (13.2) | 16 (5.2) | 6 (1.9) | 2 (0.6) | 1 (0.3) | 310 (100.0) |
| Total, n (%) | 69 (14.5) | 300 (63.2) | 73 (15.4) | 22 (4.6) | 7 (1.5) | 3 (0.6) | 1 (0.2) | 475 (100.0) |
| Practice type | Number of practice reconsultations for exactly the same condition | Total | |||||
|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 9 | ||
| PA practice | |||||||
| Was the index consultation appropriate? | |||||||
| Inappropriate | 7 (17.1) | 30 (73.2) | 4 (9.8) | 0 (0) | 0 (0) | 0 (0) | 41 (100.0) |
| Appropriate | 46 (25.3) | 113 (62.1) | 17 (9.3) | 4 (2.2) | 1 (0.5) | 1 (0.5) | 182 (100.0) |
| Total | 53 (23.8) | 143 (64.1) | 21 (9.4) | 4 (1.8) | 1 (0.4) | 1 (0.4) | 223 (100.0) |
| Non-PA practice | |||||||
| Was the index consultation appropriate? | |||||||
| Inappropriate | 47 (37.9) | 64 (51.6) | 11 (8.9) | 1 (0.8) | 1 (0.8) | 124 (100.0) | |
| Appropriate | 42 (32.8) | 73 (57.0) | 10 (7.8) | 3 (2.3) | 0 (0) | 128 (100.0) | |
| Total | 89 (35.3) | 137 (54.4) | 21 (8.3) | 4 (1.6) | 1 (0.4) | 252 (100.0) | |
| Total | |||||||
| Was the index consultation appropriate? | |||||||
| Inappropriate | 54 (32.7) | 94 (57.0) | 15 (9.1) | 1 (0.6) | 1 (0.6) | 0 (0) | 165 (100.0) |
| Appropriate | 88 (28.4) | 186 (60.0) | 27 (8.7) | 7 (2.3) | 1 (0.3) | 1 (0.3) | 310 (100.0) |
| Total | 142 (29.9) | 280 (58.9) | 42 (8.8) | 8 (1.7) | 2 (0.4) | 1 (0.2) | 475 (100.0) |
Post-analysis observations of reviewers
At the post-review workshop, the GP raters, no longer blinded, felt that they had clearly mistaken the more thorough medical records made by the PAs for those of GPs. They wondered the extent to which this might reflect training: PAs might have more emphasis on systematic data recording; GPs might tend to make a more global assessment of the patient. Finally, they also speculated on the extent to which time to write records might be an issue (i.e. PA 15-minute consultation vs. GP 10-minute consultation).
Assessment of competence from video observation
Here, an assessment of competence at consulting is made from an analysis, based on real videotaped consultations, using a validated rating scale.
Sample numbers: physician assistants and general practitioners who volunteered to be video recorded
A further 62 consultations were video recorded: 21 (33.9%) with four PAs and 41 with five GPs. The number of consultations varied between 3 and 13 for the GPs and their patients who consented to be video recorded, and between two and seven for PAs (Table 44). These consultations were then reviewed by at least two reviewers.
| HCP | PA | GP | Total |
|---|---|---|---|
| GP1 | 0 | 8 | 8 |
| GP2 | 0 | 12 | 12 |
| GP3 | 0 | 3 | 3 |
| GP4 | 0 | 5 | 5 |
| GP5 | 0 | 13 | 13 |
| PA1 | 6 | 0 | 6 |
| PA2 | 7 | 0 | 7 |
| PA3 | 2 | 0 | 2 |
| PA4 | 6 | 0 | 6 |
| Total | 21 | 41 | 62 |
Leicester Assessment Package scores: how the physician assistant consultations compared with the general practitioner consultations
Grades were given by four raters using six of the seven main categories of the assessment package. These data were not normally distributed: median, interquartile range (IQR) and Mann–Whitney U-test to compare GPs and PAs are presented in Table 45. Higher median scores were found for GPs than for PAs across all the dimensions of competence in the LAP. GPs were generally rated above 50% for each element of the LAP; PAs’ median scores were mainly 60%, with some at 40%, although the lower range score was the same for GPs and PAs on all competence dimensions bar problem solving. It was noted by the assessors that the PAs gave the computer more attention and may be writing better medical records.
| Competence | Weight | PAs, median (IQR) (n = 45) | GPs, median (IQR) (n = 85) | p-value, Mann–Whitney U-test |
|---|---|---|---|---|
| Interview/history taking | 20% | 3.0 (2.0–3.5) | 3.5 (2.0–4.0) | 0.011 |
| Physical examination | 10% | 3.0 (2.0–3.0) | 3.5 (3.0–4.0) | 0.003 |
| Patient management | 20% | 2.0 (2.0–3.0) | 3.0 (2.0–3.5) | < 0.001 |
| Problem solving | 20% | 3.0 (1.5–3.5) | 3.5 (3.0–4.0) | < 0.001 |
| Behaviour/relationship with patients | 10% | 3.0 (2.0–4.0) | 3.5 (2.0–4.0) | 0.009 |
| Anticipatory care | 10% | 2.0 (2.0–3.0) | 3.0 (2.0–3.0) | 0.024 |
| Record keeping | 10% | Not assessed | Not assessed | Not assessed |
The weighted scores showed similar differences; GPs scored higher across all competencies (Figure 5). The median overall percentage for the practising GPs was 58.6% (25th centile 50.7%; 75th centile 69.7%). For PAs, the median percentage was 47% (25th centile 30.6%; 75th centile 60.0%). These data were not normally distributed; the differences were statistically significant [Mann–Whitney U-test (two-tailed) p = 0.012].
FIGURE 5.
Range of results with the LAP: a box plot comparing PAs and GPs.
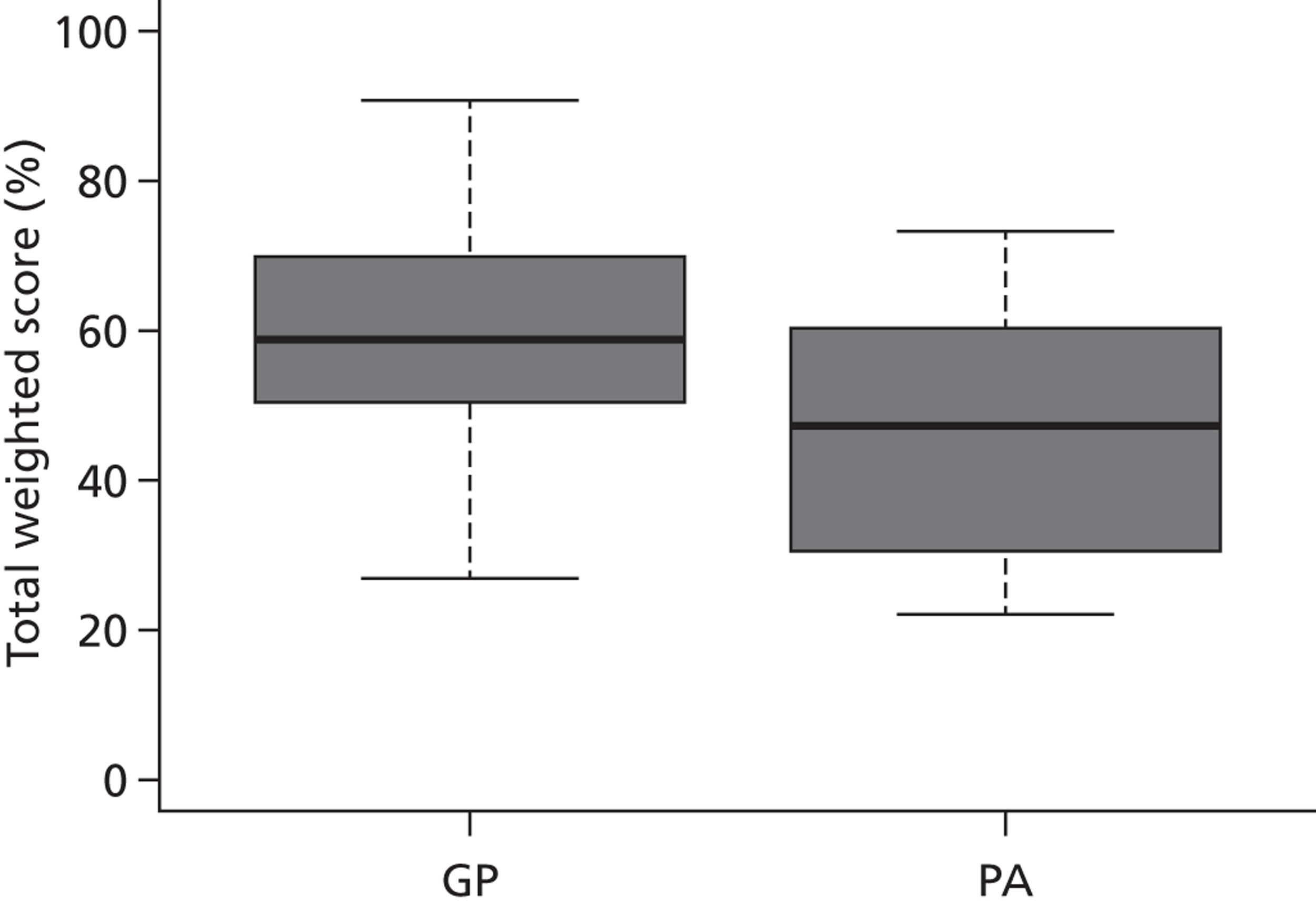
The raters did not consider any of the health-care professionals to be unsafe to practise.
Inter-rater reliability
The Cohen and Fleiss kappa,103 also referred to as ‘Cohen’s kappa’, was used to measure inter-rater reliability. Across all the ratings, kappa just fell into the poor agreement category104 (к = 0.193); there was fair agreement104 for the GP assessments (к = 0.225), but poor agreement104 for the PA assessments (к = 0.121).
Workshop with raters
At the workshop, the GP raters, no longer blinded, felt that the following themes should be taken into account when comparing records:
-
PAs were much more systematic in their approach to record writing, and GPs were much more likely to make global assessments in their records. Possibly there were differences in training with regard to records and what to record when assessing patients.
-
Raters felt that there was a difference in caseload between GPs and PAs, with the GPs having a more complex caseload. However, the PAs were effective in managing a core part of the primary care caseload, and the nature of emergent histories was such that many of the cases were complex.
-
Raters felt that the longer PA consultations may allow the creation of better medical records.
-
The only aspect of PA consultations that raters would criticise was that some PAs did not correct the patient calling them doctor. Clearly, the patient was comfortable with this misapprehension; however, this appeared undesirable and reminiscent of when medical students were introduced as ‘young doctors’.
-
The need to get prescriptions signed appeared to fit into the workflow in the consultation, much as in the way that GPs support nurse prescribing.
-
Raters reiterated their view that they did not identify any patient safety problems, and that PAs demonstrated expertise across a range of consultations.
Chapter summary
This chapter has described findings of the clinical review of, first of all, medical records where there was a repeat consultation for the same problem within 2 weeks and, secondly, direct (video) observation of the consultation to assess competence at consulting. In summary, this chapter has reported that:
-
The PAs were judged competent at consulting across a wide range of presentations, and appeared to fit well into the primary health-care team.
-
PAs produced more appropriate and systematic medical records than GPs in this sample (80% vs. 50% appropriate).
-
Raters did not correctly identify PA records.
-
GPs scored higher on the LAP for consultation competence; the raters did not consider any of the health-care professionals to be unsafe to practise.
Chapter 7 Case studies: evidence from interviews with patients consulting a physician assistant
The patient experience with PAs and GPs was explored through the patient surveys (reported in Chapter 5). The patient experience and understanding of the PA, a role which was new to the UK, was also explored through semi-structured interviews by telephone with a sample of those consulting PAs, as described in Chapter 5 (see The patient survey). This chapter reports on the findings from the interviews.
Participants
All of those invited to participate in a survey and consulting a PA (n = 430) were invited to participate in an interview. The response to the invitation to participate in an interview is shown in Figure 6, resulting in 34 interviews with patients (described in this chapter as participants) who had consulted a PA. Participants were purposively recruited from each of the six PA employing practices. One interview was face to face in a practice setting and 33 were conducted by telephone, lasting between 10 and 20 minutes. Four interviews were subsequently excluded from the analysis.
FIGURE 6.
Flow chart of invitation and response to participate in an interview.
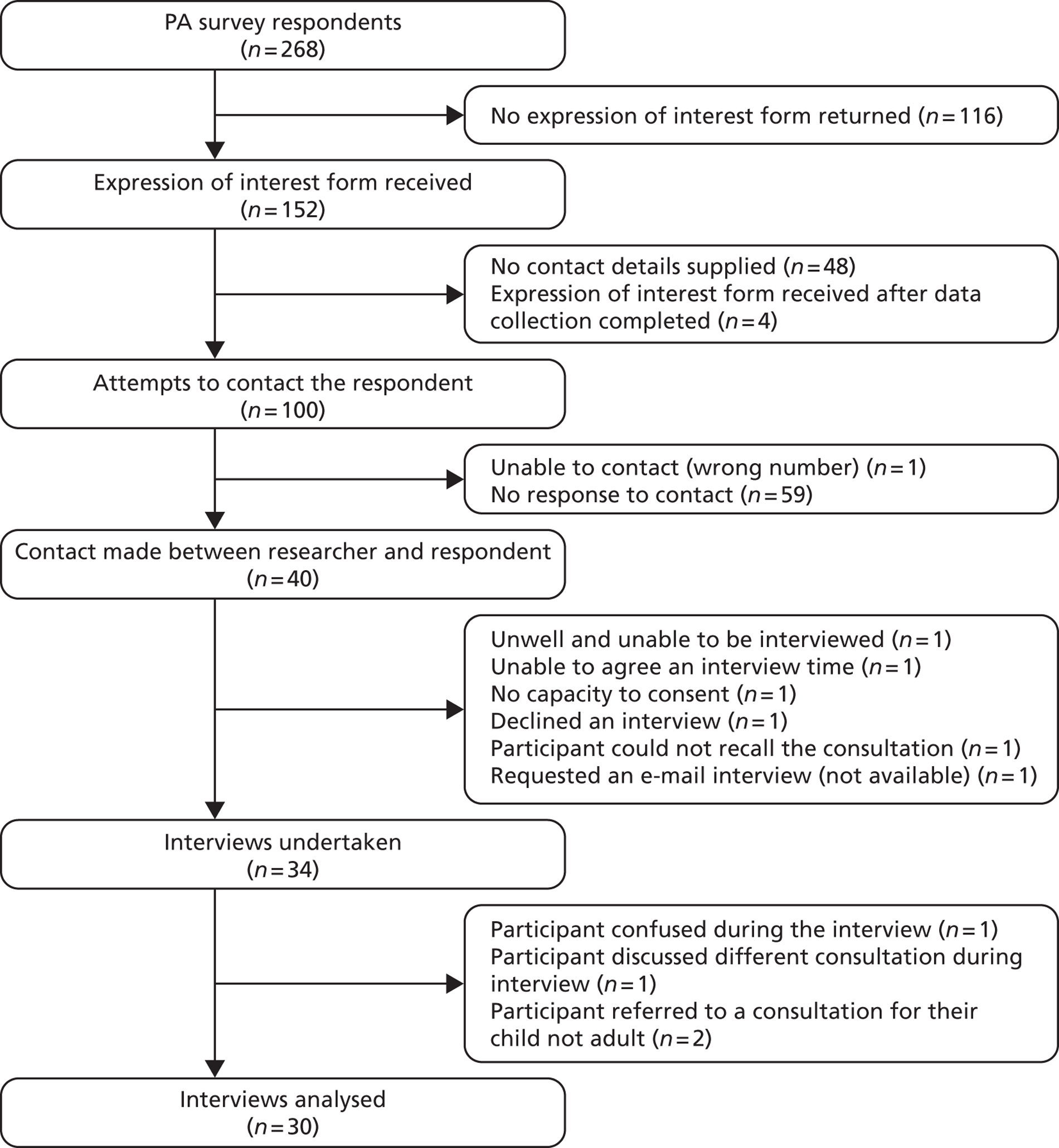
Eighteen (60%) participants were male and 12 (40%) were female. Participants' age spanned 63 years (from 27 to 90 years) with a mean age of 58 years. The majority of participants were of white British ethnicity (Table 46).
| Ethnic group | Number of participants | Per cent |
|---|---|---|
| White–British | 24 | 82.8 |
| White–Irish | 1 | 3.4 |
| Any other Asian background | 1 | 3.4 |
| Black or black British–Caribbean | 2 | 6.9 |
| Black or black British–African | 1 | 3.4 |
| Total | 29 | 100.0 |
The experience of consulting a physician assistant
Overall, the majority of participants described their experience of consulting a PA as positive, finding them praiseworthy and ‘doing a good job’. Some reported less satisfactory experiences and understanding of the role. Explanations for the positive and less positive views were identified and are reported here in three interlinked themes: (a) understanding and conceptualising the role of the PA, (b) trust and confidence in the PA role and (c) the impact of the PAs’ lack of authority to prescribe. Each of these themes also features in explanations of the contingent willingness of participants to consult a PA in the future, which was found in the interviews. The themes are described separately and then drawn together in a summary, with further discussion and interpretation undertaken in Chapter 8.
Understanding and conceptualising the role of the physician assistant
The participants’ accounts of consultations with PAs revealed diversity in terms of being familiar with the PA who they consulted in this study. A small number of participants confirmed that this had been their first contact, while others had had varying levels of previous contact; for example:
I’ve actually seen [PA name] in the past, I had earache sort of, I don’t know, some time last year and I’ve actually seen him before.
Participant 15
Some participants also described prior interaction owing to the PA’s previous treatment of a spouse or child. Three participants described an ongoing relationship with the PA as their clinician in the treatment of a long-term condition.
It was in these descriptions of the relationship with the PA that some of the participants revealed how they understood and conceptualised the role of the PA, with many using the word ‘doctor’ to refer to the PA, as in this example:
Mr X, do you remember is this the first time that you’ve seen this particular health professional?
By health professional you mean my GP or hospital visits?
The medical, no, the medical care practitioner at your GP surgery.
Err, Dr X [the PA]?
It was evident that there were accurate and inaccurate conceptualisations of the PA role.
Those with an accurate conceptualisation of the role appeared to derive this from previous personal or family experience and/or because the practice routinely informed its registered population about the PA role with leaflets, posters and explanations. These participants conceptualised the PA role in relation to doctors, a ‘GP with a difference’ (Participant 22), or, as in this more detailed illustration:
They’re just like doctors . . . I asked them about physician assistants and they gave me a leaflet and then I had a chat with the person . . . and he explained about his education, and his background . . . and you know I realised then that they’re almost doctors, they just can’t do everything here that they can, that a doctor could do.
Participant 17
The inaccurate conceptualisations reported included believing that the PA was a professional in training, a nurse, a qualified doctor from another country who could not prescribe in the UK or a qualified medical doctor. Unfortunately, some in this group had not known that the person they had seen was not a doctor until this information emerged during the research interview, and were puzzled as to why they were not given more information, as in this exemplar:
I called him doctor because I thought he was a doctor . . . I don’t know why they didn’t tell me, I’m not sure whether they didn’t want me to think he wasn’t a doctor and to think that he wasn’t going to do such a good job, but I was very open to whatever he was going to say to me anyway so I wasn’t judging him because he wasn’t.
Participant 03
These participants reported a varying level of both being informed and being able to recall the information about this new role. There were also those who described receiving information from the practice or the PA but then not understanding the implications of that information, described as in this exemplar:
She did explain, she said I’m from America.
Participant 31
Several participants described a deductive process whereby they had picked up on clues that the PA was not a doctor, and ‘worked that out myself’ (Participant 29), most obviously with the issue of prescription signing, as in the next example:
Then when I went to her to write out a prescription, she said, ‘No, I must get the doctor to sign it.’ Then I realised. So, I think that’s the right way to go about it because it’s better because then if the patients are, ‘Oh no, she’s not a doctor . . .’
Participant 32
Despite the inaccuracies in conceptualisation and the lack of information for some, most of these participants then turned to describing positive qualities or a desirable outcome from seeing the PA. This mirrored the positive views expressed by those who had an accurate conceptualisation of the role and links to the next theme of trust and confidence in the PA.
Trust and confidence in the physician assistant
The issue of trust and confidence in the PA was raised in most of the interviews, in response either to general questions about the consultation or direct questioning by the interviewer. Where the response was to a direct question, participants generally used unambiguously positive words such as ‘certainly’ or ‘absolutely’ or gave a percentage score, for example:
Did you feel trust and confidence in that episode of care?
Definitely. Yeah, 95–99%.
The reasons for the levels of trust and confidence can be grouped into subthemes: the personal attributes of the PA, demonstration of clinical competence and positive outcomes of the consultation, similarity of the consultation with that with a GP, and trust in their GPs and the wider NHS to provide appropriate, safe and effective care. Each of these is discussed in turn. The section ends by considering explanatory factors given by patients who did not express high levels of trust or confidence.
Attributes of the physician assistant
Evidence of trust in the PA was expressed in a number of different descriptions of their positive qualities or personal attributes, closely related to their communication skills. Their capacity to listen and to respond with clear explanations was commonly reported by participants, as were characteristics such as being ‘likeable’, ‘friendly’ ‘caring’ or like ‘doctors used to be’. Furthermore, attributes such as the PA seeming confident or knowing what they were talking about, checking with the patient, and knowing their own boundaries were cited by participants as those that gave them confidence in consulting the PA, as in this exemplar:
I had no hesitation in going to an appointment with him because I’d seen him before, so I was quite happy that he was confident and knew where his boundaries laid and yeah I was more than happy.
Participant 34
Demonstration of clinical competence of the physician assistant
Participants reported trust and confidence in the PA because the PA demonstrated clinical competence and qualities such as those described as being ‘professional’, ‘thorough’, ‘efficient’ and ‘confident’. This was very closely linked to judgements made by participants on the basis of the outcome of the consultation. Participants gave examples, such the PA offering appropriate advice, ordering or initiating investigations, treating conditions or making appropriate referrals to other services as a range of positive outcomes of the consultation. Some participants cited examples of PAs identifying additional health issues that needed medical attention as evidence of their clinical competence, as exemplified here:
She pointed something out my dad wasn’t aware of. He went with a certain complaint and then when she was examining his body she saw like a sort of a lump in his neck and she was saying, ‘Mr X, what’s this?’ And he was saying, ‘Oh, no, this is because of old age,’ and she was saying, ‘I don’t think so, I think I need to refer you because maybe this is linked to what you’re complaining about’.
Participant 02
In particular, trust appeared to have grown for participants who reported that the PA had provided advice or treatment that either had already resolved the problem by the time they were interviewed or was anticipated to be an appropriate potential solution.
Well they’ve never given a diagnosis that I didn’t think was a good diagnosis, they’ve always given the right medicine in my opinion, it’s always worked. So I’ve never, ever had a problem, that’s why I feel confident with them. It’s as if you’re seeing a doctor.
Participant 17
Most participants perceived that their consultation with a PA was either no different from or very similar to a consultation with a GP. This similarity was given as an explanation for trust and confidence in the PA. Participants described being asked the same questions and given the same types of examination and investigations that they would have received from a GP, as in this exemplar:
Yeah, I had no idea that he wasn’t a fully qualified GP, and there was nothing in his, the way he spoke to me, the questions he asked, he did an examination, the examination that he did for me was all really professional and exactly as I would expect him to do, which is why, when I walked out of the door I said ‘thank you Doctor’, because for me he did everything that I was expecting, he gave me the right advice, answered my questions, so I was completely happy with it.
Participant 03
Many participants understood that the PA was in a hierarchical relationship with the GP and their judgement of clinical competence derived from the knowledge that the PA would check with or refer to the GP if it was necessary, as in this exemplar:
I didn’t necessarily think that he wasn’t a GP if you see what I mean. I know that he isn’t because I knew the difference and that the help was next door if he needed it, so I was more than happy with seeing him and that would make me confident to see him again.
Participant 34
Trust in their general practitioners and the wider NHS
Participants also expressed trust in the PA derived from their trust and confidence in their general practice, particularly the senior partners, and also in the wider system of the NHS. Participants trusted their GPs to employ appropriate and competent staff. Examples of their evidence for competence based on trust of the wider NHS system were the direct referral by a PA to a hospital specialist without checking with the GP and the fact PA had had appropriate training and was employed in this way within the NHS.
Limited trust and confidence in physician assistants
Despite a high level of trust and confidence being expressed by many participants, this was not universal. Trust and confidence among participants could be limited or even lost where the participant felt rushed or like an inconvenience, if they were not able to gain an answer about a presenting problem or if the outcome was considered unsatisfactory or contrary to their expectations, as shown here:
I felt it was very much on the surface and I came away, and they gave me this form and I thought at that time, I wasn’t happy with that, it didn’t work for me . . . I was disappointed with the non-outcome of that visit.
Participant 08
In contrast to those who had trusted the PA because they could check with a doctor, some participants reported having lost confidence when the PA’s inability to deal with the medical complaint subsequently led to delays in receiving an appropriate consultation from a doctor, as illustrated by the following participant:
I went in there and I really was nearly in tears with the pain. He [PA] listened to me in fairness, went out of the room because he has to then run it by a doctor. I waited 20 minutes and it came back and his words to me were ‘she said you’ll have to come back tomorrow’. And I had to walk out of that surgery in agony. Now that isn’t satisfactory . . . As I say, he went to a doctor and he done what he probably had to do, he wasn’t qualified to do . . .
Participant 14
Some of the reasons given for the presence or lack of trust and confidence in the PA were articulated in terms of comparison with consultations with GPs. One aspect of this was the PAs’ lack of authority to prescribe, which is considered next.
The impact of physician assistants’ lack of authority to prescribe medications
Participants reported having become aware that PAs were unable to prescribe either through the explanations given to them prior to the appointment or during their consultation. For those participants who described having required a prescription, different methods to organise this had been experienced. Most reported the PA leaving the consulting room to discuss the case with a GP and then return with the signed prescription while the patient waited either in the consulting room or in the waiting room. Some patients also reported collecting the signed prescription from reception then or later, or having it faxed to the pharmacy.
The need for prescriptions to be verified and signed by a GP was reported by most participants to cause no apparent or significant delay. A small number of participants reported delays of 5–10 minutes, with a minority reporting longer waiting times ranging from 15 to 30 minutes. Short delays appeared generally to cause no particular problem to participants and were considered reasonable or understandable. A minority, however, felt that any delay caused by the PAs’ lack of prescribing authority was problematic, as exemplified here:
It’s quite annoying, actually, because, I mean, I feel that if people can prescribe it they should be able to sign it.
Interview 23
Participants, however, were mostly understanding of this potential limitation and it appeared that a consultation experience that was in other ways a positive one was not viewed negatively because of the need to wait for a prescription.
Each of the above themes features in responses to the final issue explored, which was participants’ willingness to consult a PA again.
Willingness to see a physician assistant again
A small number of participants had actively sought an appointment with a PA and gave the following types of reasons: a shorter waiting time to see a PA than a GP, dissatisfaction from prior appointments with GPs and trust in the PA based on previous contact. Most of participants reported that they had not been offered a choice of whether they saw a PA or GP when they booked their same-day appointment. Those who had been offered a choice chose the PA, as this option provided them with an earlier appointment.
Most of the participants stated a willingness to see a PA again for any condition, while one participant stated that they would not wish to consult a PA again as it had resulted in delays in a consultation with a GP.
The willingness of other participants to consult was expressed as contingent on a number of factors. Some participants who were interviewed at a point very close to the time of their consultation with the PA described their willingness to consult as contingent upon the success of their current course of treatment. Others described themselves as willing but differentiated which professional was appropriate to consult according to how serious or complex the problem(s) were that they wished to consult about. Broadly speaking, participants with complex medical conditions or more complex prescribing needs considered it more appropriate and preferred to consult a GP rather than a PA. Minor conditions or complaints were seen as appropriate for consultation with a PA, as in this example:
I think if it was just a general complaint he [relative] wouldn’t mind seeing [the PA] but regarding his prescription, he’s a bit fussy about his medicine, he would prefer to see a doctor.
Participant 02
Willingness to return to see a PA again also appeared to be influenced by the participants’ beliefs about pressures faced by the GP and recognition that not all medical problems required the attention of a doctor, as in this example:
I am very aware that I don’t want to take up appointments when it isn’t really that necessary. So the thought that there is a role within the surgery where I could go and see somebody who isn’t as pressurised as the doctor, to see, to understand, to and go and see them for something that’s like not trivial particularly, but I don’t necessarily need to see a doctor for then I feel that that role is a really good thing to have in the surgery and I feel that I would be happy to utilise that again, definitely.
Participant 03
For some participants, regardless of how satisfied they were with the PA (or the GP) in a single consultation, maintaining continuity of their care with one professional was considered equally as important as, if not more important than, having a preferred type of practitioner. Consequently, participants who had already consulted a GP or a PA about a particular problem preferred to consult the same practitioner again, to achieve continuity of care:
I’m trying to make her my regular, I say doctor, but my regular person I see at the surgery . . . she seems to understand my needs. I get on really well with her. She listens to me; she makes me feel very comfortable. She seems to, you know, she gives good advice as well. She understands my situation very well, and she’s the only one, she’s actually the only one at the doctors at the moment that seems to be able to give me that response. As I said, because it’s a [type of practice], you’re sort of shuttled around from doctor to doctor. You don’t really get to make a relationship with anybody.
Participant 21
Other participants also referred to the benefits of their longer-term relationships with the PA and cited this as a reason for willingness to reconsult with a PA. Some gave positive accounts of the PA’s ability to recall personal details such as a medical history, the names of extended family members, or work and social circumstances, as well as seeing the PA as part of the community.
Chapter summary: the patient experience
This chapter reports on the exploration of patients’ experience in consulting a PA in same-day appointments in general practice, a professional role new to the UK. As in the results of the patient survey (see Chapter 5, The patient survey), mainly positive experiences and outcomes were reported. However, the accurate conceptualisation and understanding of this novel role was not universal. Participants were most accurate in their conceptualisation in practice settings where multiple mechanisms had been used to routinely inform patients. One explanation for the positive experiences (and the less positive experiences) lay in the level of trust and confidence the participants had in the PAs. This trust and confidence were not given automatically and derived from multiple, interacting factors. These included the PA’s personal attributes (particularly communication skills), their clinical competence as demonstrated by successful treatment or appropriate actions, the similarity of their consultation to that of the GPs and the wider trust participants placed in their GPs and the NHS to provide appropriate care. A willingness, or otherwise, to consult a PA in the future demonstrated a sophisticated decision-making process by participants. This involved not just previous experiences but also judgements about the seriousness of the problem, the rapidity with which it needed medical attention, the medical skill level appropriate to deal with it and the benefits of long-term conditions being dealt with by the same rather than different professionals. This latter factor, continuity of health professional, often appeared to outweigh others. Further interpretation of these findings in the context of the other findings is undertaken in the concluding chapter.
Chapter 8 Discussion and conclusion
This chapter summarises the findings and presents a synthesis of the study. It draws on the discussions in the emerging findings seminar which was held with participants of the study, patient and public representatives and advisory group members in February 2013. We address, first of all, our three study questions:
-
How are PAs deployed in general practice and what is the impact of including PAs in general practice teams on the patients’ experiences and outcomes?
-
What is the impact of including the PAs in general practice teams on the organisation of general practice, the working practices of other professionals, relationships with these professionals and the practice costs?
-
What factors support or inhibit the inclusion of PAs as part of English general practice teams at the local and macro levels?
We present a synthesis against a framework of dimensions to judge the quality of health services. 73 We then discuss the limitations of the study before turning to our conclusions and summary of recommendations.
The deployment of physician assistants in general practice
Evidence from the national survey (see Chapter 3, The national physician assistant survey) and the case studies (see Chapters 4 and 5) demonstrated that the PAs provide clinician time for patient consultations in the practice. The majority of these consultations were in same-day appointment surgeries, and the employing GPs expected the PAs to hold their own consultations and, within their competency, as agreed by their supervising doctor, to assess, diagnose and treat the patients they saw. In most practices, the PAs also had forward-booked appointments for follow-up with individual patients and/or review and management of those with chronic diseases. The deployment of PAs in UK primary care to patients attending mainly same-day appointment surgeries has been reported qualitatively before72 and confirmed here, similar to the international literature. 176,193
The lack of legal authority to prescribe in the UK deterred the GPs and practice managers from deploying PAs to home visits. This concurs with evidence from previous studies in the UK. 60,61,72 PAs in the USA have prescriptive authority in all states, although the scope may vary in different federal jurisdictions. 194
Most of the PAs spent the majority of their time in direct patient contact, with the non-clinical activities usually being linked to direct patient management (see Chapter 3, The national physician assistant survey and Chapter 4). Those undertaking other activities in the practice reported spending a greater percentage of their time on non-clinical activities (defined as any non-patient-facing activity). 118 This resonates with the findings in the National General Practice Work Load Survey181 in which NPs, salaried GPs and GP partners were found to spend, on average, 8.2 hours, 7.0 hours and 13.6 hours per week, respectively,195 on non-clinical activities.
All of the practices gave the PAs longer appointment time slots than GPs (and in one instance double the time) or the same length of appointment slots but with some free slots to allow for consultation or prescription signing with a GP (see Chapter 4). Appointment time slots were not reported in either of the previous UK studies. 60,61 Contextual information as to the length of appointment slots is also missing from previous UK studies of NPs91,92 offering same-day appointments in general practice. Of two studies of practice nurses, trained specifically to offer minor illness appointments, one reported that with experience built up over time (unspecified) the nurse worked to 10-minute appointment slots196 and the other reported that the nurses and doctors were both given 10-minutes appointment slots. 90
There was evidence from the PA and practice staff interviews (see Chapter 4) that some practices had decided to deploy their PAs in ways which increased the practice income. Examples included giving the PAs responsibility for ensuring that the activities required under QOF for certain patient registers had been completed and the provision of clinical activities that were promoted and incentivised by local and national commissioners. These were clinical activities that were preventative in nature (e.g. provision of intradermal, long-acting contraceptives) or reduced activity in hospital settings (e.g. initiation of insulin in type 2 diabetes). This has not been described before in the UK setting. Our review of evidence did not identify this in literature from other countries, although the previous restrictions in the USA on claiming reimbursement from federal funds for clinical activities carried out by PAs rather than doctors had been noted as a deterrent to their employment in the past. 149
The impact of including physician assistants in general practice teams on the patients’ experiences and outcomes
The patients’ experiences
The majority of patients who responded to the survey in this study reported that they were satisfied or very satisfied with their consultation with the PA (see Chapter 5, Patient survey). These findings mirror the national results of general practice patient surveys. 197 A high level of patient satisfaction with general practice consultations is not an unusual finding; however, this is the first time that patient satisfaction concerning PAs in the UK has been reported from such a large sample drawn from a variety of general practice settings. This mirrors the findings in medium- and large-scale surveys of primary care patients consulting PAs in the USA. 155,160,168–171
Patients consulting a PA described factors such as continuity of clinician and perceived complexity of their illness as important in their willingness to consult the PA again or their preference for consultation with a GP. These types of factors have been evident in other studies regarding patient views on consultations in primary care. 198,199 A small number of patients indicated their preference to always consult a GP in future consultations (see Chapter 5, Patient survey). This is important in that studies investigating patient preferences following consultation with another type of clinical professional (nurse or pharmacist) in UK primary care have reported one-third or more expressing a preference for future consultations with a GP despite high levels of satisfaction with the initial consultation. 90,92,200,201
It is noteworthy that, of the patients who were surveyed in practices not employing PAs, 28% were willing or very willing to consult a PA and 20% were neither willing nor unwilling (see Chapter 5, The survey responses). This is a lower percentage than in studies carried out in three other countries where PAs are relatively unknown. Those studies, however, were more in-depth, hypothetical studies posing scenarios of different lengths of waiting time to see the PA or a physician in ambulatory care settings. 173,202,203 One explanation in the UK setting may be that a common feature of general practice since the 1990s has been the employment of other types of staff such as nurses,20 which is not as common in many other countries.
The average length of consultation for same-day appointments with a PA (16.79 minutes) was significantly longer than the average consultation time with a GP (11.28 minutes). The national workload survey has reported 11.7 minutes, 12.1 minutes, 16.4 minutes and 15.5 minutes as the mean consultation lengths with a GP partner, salaried GP, GP registrar and NP, respectively,204 suggesting that the study’s data for GPs, at least, are representative. Previous UK studies of PAs do not report length of consultation. 60–63 Past UK studies of nurses providing this mid-level practitioner activity with same-day-appointment patients also report longer consultation times for GPs. Kinnersley et al. 92 reported a median of 6 minutes (range 4–8 minutes) for GPs and a median of 10 minutes (range 7–14 minutes) for NPs, reducing to 8 minutes (range 6–11 minutes) when the time for obtaining a signature on a prescription was removed. Venning et al. 91 reported a mean consultation duration of 11.57 minutes for NPs (SD 5.79 minutes) and 7.28 minutes (SD 4.80 minutes) for GPs. Shum et al. ,90 in a study of practice nurses with additional minor illness training providing same-day appointments compared with GPs, reported that both were given 10-minute appointment slots and that the nurses had a mean consultation time of 10.2 minutes (SD 5.7 minutes) compared with a GP consultation time mean of 8.3 minutes (SD 6.4 minutes). Further investigation is required as to the variation in consultation lengths by differently skilled and experienced clinicians adjusted for patient case mix and when using surgery systems such as telephone triage.
Patients reported varying levels of understanding and conceptualisation of this new professional role in UK primary care. Similar findings were reported in studies investigating understandings of general householders in the early introduction of PAs in the USA. 172 The practices in the current study had a range of strategies to inform their patients about the role, some more evident than others. Our interviews suggest that those practices using multiple methods, including a script for receptionists and explanation by the PA, were more successful in achieving understanding. This suggests implications for operational practice in general practice and a role for the national PA organisations in sharing best practice.
The patients’ outcomes
All of the patients in this sample were attending ‘same-day appointments’, that is having a problem or symptom that required consultation that day as decided by the patient or the practice using telephone triage. GPs were consulted by an older patient group with a higher incidence of measures of comorbidity than those patients consulting the PA (see Chapter 5, Consultation records). PAs tended to be consulted by more patients with problems classified by the study as ‘minor/symptoms’, while GPs were consulted by patients whose problems were more likely to be classified in this study as ‘acute’ or ‘chronic’, that is to say having greater medical acuity or complexity in terms of comorbidity (see Chapter 5, Characterisation of the health problems of the consultation record sample). Previous UK and international studies of PAs in primary care have not included a measure of severity or acuity of presenting medical problems. One recent US study also has evidence that PAs see patients who are less medically complex than those seen by doctors,193 using the patients’ diagnostic care group (DCG) score as the measure of complexity. DCG is a predictor of future health-care expenditure based on age, sex and comorbidities. 205
After adjusting the data for covariates and clustering, it was found that consultations with PAs resulted in the same rate of reconsultation for the same problem in the 2 weeks after the index event as with GPs: our primary outcome measure. They also resulted in the same rate of process outcomes: procedures, investigations or tests ordered or undertaken, prescriptions, referrals and advice on over-the-counter medicines (see Chapter 5, Consultation records). This is the first time that these process and outcome measures have been reported for PAs in the UK primary care setting. One US study from the 1970s showed that two PAs in comparison with nine family practice physicians had higher medication costs, although they also had higher laboratory costs (not found in the present study) and higher rates of good outcomes for patients. 167 A more recent study of a single PA in the Netherlands showed no difference in referral rates to secondary care from the PA compared with those of the GPs. 164 The only other UK evidence of mid-level practitioners, from studies comparing NPs with GPs in same-day consultations in the UK, provides more mixed evidence. Similar to our findings for PAs, Kinnersley et al. 92 reported no difference between NPs and GPs in the issuing of prescriptions and making referrals. Shum et al. 90 also reported that nurses and doctors issued prescriptions for similar proportions of patients. In contrast, Venning et al. 91 reported that NPs undertook significantly more procedures, ordered more tests and investigations and were significantly more likely to ask the patient to return within 2 weeks.
The adjusted figures also showed that PAs were more likely than GPs to have documented that the patient had been given general and medicine management advice (see Chapter 5, Comparison of physician assistant and general practitioner consultations in recording process outcomes). It could be argued that this may be an artefact of differences in record-keeping styles between doctors and PAs. It could equally be associated with the longer consultation time of PAs. The variation in electronic record keeping in general practice has been noted before206 and the more detailed completion of records by NPs has been observed in comparison with GPs in the UK. 207 In the current study, however, differences between professional groups were not apparent to the independent GP assessors, who were blinded to whether the author of records was a GP or PA (see Chapter 6). This finding has not been reported before in the UK or international settings. For another mid-level practitioner group, NPs, a UK study also found that they delivered more advice in longer consultations. 92 The analysis of the audiotaped consultations with NPs and GPs reported that nurses talked significantly more about treatments, including how to carry out or apply a treatment. 208
Clinical assessment of the consultations
The clinical judgement as to the appropriateness of the initial consultation in the light of the patient reconsulting for the same problem within 2 weeks found that the PAs had documented appropriate clinical activities in the majority of consultations (80%) compared with half of the cases by the GPs (see Chapter 6). This finding may be an artefact of the documentation as noted in the section above but, again, the blinded reviewers were not able to correctly identify GP records from PA records. This is the first published report establishing the higher rate of documented appropriateness in initial consultations by PAs than by GPs for reconsulting patients. A previous study from the USA reported poor documentation from PAs. 155 The finding of high rates of reconsultation with GPs following an initial consultation in which not all elements of appropriate clinical activity have been documented requires further investigation.
The clinical judgement as to the consulting activities of the PAs compared with GPs, as video-recorded, found the PAs competent and safe at consulting across a wide range of patient presentations. Although GPs achieved higher scores in their upper range, the comparative scores for PAs and GPs were similar in their lower ranges. The structured comparative analysis of consulting styles is the first to be reported in the UK or internationally.
The PAs were competent at consulting across a wide range of presentations, and appeared to fit well into the primary health-care team.
The impact of including the physician assistants in general practice teams on the organisation of general practice, the working practices of other professionals, relationships with these professionals and the practice costs
We address each of the sections of this study question in turn.
Impact on the organisation of the practice
From the scoping survey (see Chapter 3, The scoping survey), it was evident that those closely associated with general practice could see a potential role for PAs within general practice teams but were looking for more evidence with regard to impact. From the case study element (see Chapter 4), the PA and practice staff interviews revealed that PAs were employed to fit into the organisation of the practice and the aim was for minimal impact per se, as with any other member of staff. The newness of both the occupational group and, in some instances, the individual’s qualification had some effect. For those practices new to employing PAs, one effect was the need to ensure that other staff understood this new-to-the-UK role. The next effect was a need to assign a supervising doctor and ensure time for that supervision (whether about an individual patient consultation or as a regular supervision session), and for newly qualified PAs to arrange ongoing professional development. The extent to which the role of the PA developed within each practice appeared to depend both on the interests and knowledge of the PA and on the opportunities presented within the organisation of the practice. This is captured in the discussion of deployment, earlier in this chapter (see The deployment of physician assistants in general practice).
Impact on the working practices and relationships with other professionals
In the case studies, it was evident that the PAs had an impact on the working practices of some of the GPs. In some practices, they were employed specifically to release GP time for attending to more complex patients or other aspects of the GP workload. GPs described how more of their work was with patients with more complex needs and patients outside the scope of practice of the PA (see Chapter 4). This was confirmed in the clinical consultations entered into the case study, where it was evident that PAs were consulted by younger patients with a lower incidence of measures of comorbidity compared with those consulting GPs (see Chapter 5, Consultation records). A previous UK study of a smaller sample of PAs suggested that PAs saw older patients than GPs but concurred that the PAs saw a similar but less complex case mix to GPs. 62 This was also evident in the observation of clinical meetings (see Chapter 4), in which the GP partners were focused on the care of patients with multiple physical, mental health and social problems and also on ensuring that salaried GPs, GP registrars and nurses were supported in the management of such patients.
The extent to which PAs impacted on the work in each surgery of the supervising doctor varied depending on the experience of the PA and the systems in place to signal the PA’s need for consultation about a patient and/or prescription signing. While PAs’ lack of authority to sign a prescription was an issue in all of the practices, it should be set in the context that, firstly, in most of the practices the nurses did not have prescribing qualifications and were also dependent on efficient systems (see Chapter 4) and, secondly, that most consultations (with either a GP or a PA) did not result in the issuing of a prescription (see Chapter 5). The types of actions to minimise the consequences from lack of authority to sign prescriptions have been noted before in the UK context61–63,72 and in other countries developing the PA role. 164,209
The boundaries between the work of the PA and that of the nurses in the practices were described as delineated and agreed without overlap (see Chapter 4), a point also noted in the primary care pilots of PAs in Scotland. 61 The PAs were reported to be flexible in their skills, and so were often able to cover nurse absences, a feature again noted in the earlier study of PAs in England. 60 It was evident from the interviews with the practice managers and GPs (see Chapter 4) that the priority was to deploy available staff most efficiently against the practice service delivery needs and the demands of each day. While some GPs noted that there had been disquiet from some NPs when PAs were first employed, we were able to find evidence of only positive relationships and working practices between PAs and nurses in the case studies. This has been noted before in the UK60,61 and in other settings where PAs have been introduced in primary care more recently. 209
The impact of including the physician assistants on practice costs
This study has shown that, after controlling for case-mix differences, GP and PA consultations resulted in similar levels of prescribing, referral, tests, procedures, reconsultations and patient satisfaction. The observed difference in consultation times between PAs and GPs (16.8 minutes vs. 11.3 minutes) is very similar to the national data for NPs and GPs (15 minutes vs. 11.7 minutes). 119 After adjusting for covariates, a PA consultation for the ‘average’ patient is 5.8 minutes longer than a GP consultation for the same patient, at a marginal cost of £6.22. Although PAs’ consultations are longer than GPs’, they document giving more advice to their patients, and the lower costs associated with their consultations mean that they still deliver care more cheaply. This analysis does not, however, take account of extra costs associated with the use of PAs, including GP time in supervising, training and signing prescriptions, which was not quantified in this study.
In the absence of other studies of the relative costs and effectiveness of PAs and GPs in the UK setting, comparative evidence can be drawn from research that has compared GPs with NPs, another mid-level practitioner group. The findings of one randomised controlled trial in English general practice over a decade ago were similar to those in the current study of PAs; the NPs had similar rates of prescribing, referring, testing and reattending as GPs, and they delivered more advice in longer consultations. 92 Another UK-based comparison of GPs and NPs at about the same time concluded that the clinical care and costs of GPs and NPs were similar; a higher propensity of NPs to order tests and for patients to return for follow-up appointments offset lower consultation costs. 91 A systematic review showed that patients were more satisfied with NPs than with doctors, and while there were no differences in prescribing, referrals and reconsultations, NPs had a higher propensity to order investigations. 39 A modelling study based on the review calculated that there was no significant difference in costs from the NHS or practice perspective because the GP time that goes into the supervision and reconsultations arising from the use of NPs offsets the lower consultation cost per minute of NPs, although sensitivity analysis showed that if the supervisory time input of GPs was halved, NP consultations were cheaper. 210 In a recent study in the Netherlands, NPs provided equivalent outcomes to doctors for a lower cost; the mean saving per consultation was € 8.21,211,212 which is similar to the saving recorded for PAs in this study of £6.22.
Factors supporting or inhibiting the inclusion of physician assistants as part of English general practice teams at the micro, meso and macro levels
The introduction, adoption and diffusion of innovation in health-care services is known to be influenced by determinants in the sociopolitical environment, the characteristics of the organisation, the characteristics of the person and the surrounding team or peers adopting the innovation, and the characteristics of the innovation such as the complexity, the risk and the relative advantage. 212,213
At the meso and micro levels, that is to say the organisational and personal levels, the GP partner(s) made the decisions to employ PAs as an innovation in their practice teams (see Chapter 4, Decisions about medical and practice staffing). Comparisons between national headcount data and the practices included in the study showed that while the staffing ratios of practices without PAs were similar to national averages, the practices with PAs had higher proportions of salaried GPs, suggesting that there may be differences in approach to staffing decisions. Internal and external organisational factors as well as characteristics of the innovation were considered in making the decision. These included factors such as practice income, costs, productivity of PAs, local availability of GPs and experienced practice nurses; in addition, beliefs about the value of differently skilled professionals in their general practice were evident. General practice in the UK has long employed staff with different skill sets and professional qualifications,20 in contrast to other countries where solo medical practice is the norm. 214 The effect of the 2004 GMS contract23 in shifting some work roles between doctors and nurses has been demonstrated in a longitudinal survey. 215 The changing nature of general practice, primary care, GPs themselves and their views of their roles has been well evidenced. 216–218 There were divided views among the GPs as clinician managers in our study as to whether a Taylorist approach,219 involving the delegation of certain types of patients in unscheduled appointments to mid-level practitioners (PA or NP), achieved greater efficiency or whether greater efficiency and less risk was achieved by the forward deployment of an experienced GP to see all unscheduled patients, with the GP then delegating tasks to others. This difference of views as to the most effective organisation of general practice services is echoed in the GP literature, in which the need for evidence is highlighted. 20,34 In this study, the difference in opinion about the value of other types of professional seemed to apply irrespective of whether the mid-level professional was a PA or a NP, and opinions on both were compared with opinions about the employment of salaried GPs. The views of GPs and practice managers as to the relative advantage of each type of health professional was set in the local, external context of their availability, both now and in the future. The desire for information and evidence on the value and productivity of PAs to inform GPs decision-making about this innovation in their workforce was evident from those practices that volunteered to participate and did not currently employ a PA.
At the macro level, which encompasses the sociopolitical environment and the organisation of the NHS beyond the individual practice, this study examined both policy influencers’ views and policy documents to investigate factors influencing the adoption of this workforce innovation. The scoping survey participants described the wider factors influencing change in the profile of the health-care workforce including primary care (see Chapter 3, The scoping survey), as did those working in general practice. These factors included demographic changes, an ageing primary care workforce and restricted public finances for the NHS. These forces have been underlined in subsequent reports pointing to a shortfall in GPs against the increased likely demands for services in primary care settings. 220,221 All participants could see the place of, and make the argument for, increased numbers of staff working at the mid level, such as PAs and NPs, in primary care settings. Positive opinions and advocacy for PAs as one innovatory solution were evident from those who had had contact in some way with PAs, while others were more neutral in their opinions. Most participants, including those representing patients, considered that further evidence was required as to the effectiveness and efficiency of PAs to influence the decision for further development and use of them as an innovation in the UK setting. Most participants noted that, for PAs to be further introduced in the NHS, a key macro-level factor was their inclusion in the state regulatory mechanisms, which would both address issues of public safety and open the way for their inclusion in the legislation for authority to prescribe.
The history of health professional groups is one of a dynamic system of shifting role boundaries that are sometimes challenged not only because of cautious responses to innovation but also because each shift has the potential to affect another group’s access to resources, rewards and status. 222 The introduction of a completely new health professional group, the PA, has that potential within the UK system. In the main, the nurses interviewed in the scoping survey did not view PAs as a challenge to the nursing profession, although one offered the perspective of NPs, arguing that PAs could be competitors not for jobs but for investment via NHS-funded education and training. The group more likely to see PAs as competitors for jobs were junior doctors, as suggested in our analysis of published commentaries (see Chapter 3, Review of commentaries). In this, our study provides evidence that there is stratification within both the medical and the nursing professions,223 resulting in different opinions in support of or in opposition to PAs as a new health professional group in the NHS.
At the macro and meso levels, the NHS is a publicly funded system which includes the planning of future national and local health-care workforce and the funding of health professionals’ education and training. 6 A review of workforce planning and policy documents was undertaken to gauge the support for innovation of PAs at this level. In the planning and policy documents in England and Wales, PAs were noticeably absent; this is in contrast to those in Scotland, where high-level policy decisions had been made to support the development of PAs as part of the health-care workforce (see Chapter 3).
Evidence synthesis
This study is framed by the dimensions proposed by Maxwell73 for judging health-care services and is applied here to the innovation of PAs in primary care. The dimensions are acceptability, effectiveness (including safety), equity (fairness), and efficiency (including costs of primary health care).
Physician assistants were found to be an acceptable group of health professionals to contribute to primary care teams at the macro, meso and micro levels. They were found to be acceptable and appropriate to professionals, managers, commissioners and patients, although many in these roles sought more information. Caveats included that any employer and PA needed to ensure that patients, the public, administrative staff and the professionals understood the PAs’ competency levels and that the PAs’ role was dependent on a supervising doctor. Inclusion of PAs in the state regulatory processes for health professions was viewed as important in terms of both their acceptability and the perceived effectiveness. This factor requires support at the macro, sociopolitical level.
Within the universal provision of primary care in the UK, PAs provided clinical care mainly to patients seeking same-day (unscheduled) appointments whose presenting condition was of less medical severity and who were of less medical complexity than those consulting GPs. There was no indication that this was inequitable (unfair) to any group of patients or that patients were not given appointments with preferred GPs (and preferred PAs) if requested. The PAs were working in complementary ways to the activities of the GPs rather than as substitutes. 14
The case study elements demonstrated PAs’ effectiveness in providing appropriate and safe care at the same time as not increasing costs to the wider health-care system. The analysis of cost demonstrated that they deliver care more cheaply to the patient case mix they work with than GPs. However, this analysis was unable to account for all opportunity costs to the GP(s) through consultation interruptions and supervision, although the extent of this was dependent on the expertise level of the PA and the preferred working practices of the GP.
While acceptable, effective, equitable and efficient, PAs do not feature at the macro level in the planning for a primary care workforce or in the regulatory framework for health professionals. The introduction of a new health-care professional is influenced by support at sociopolitical levels as well as at the organisation and individual levels. 213,224 The policies supporting greater delivery of health care in primary care settings suggest that more mid-level staff will be required irrespective of the type of provider organisation. 190 PAs are drawn from a different labour pool from nurses, being mainly science graduates, and as such are likely to be an additional solution in addressing the future perceived shortages for primary care. 34,220 They potentially offer more flexibility to a primary care workforce in that they have a shorter education programme than that for GPs. The PA benchmarked and nationally agreed curriculum offers consistency and uniformity among those graduating from courses, unlike NPs in the UK. For there to be a supply of PAs available for recruitment into primary care, there has to be demonstrable NHS workforce planning support, at the very least at the local level in order to allocate opportunities for clinical placements in their educational programmes.
Limitations
This was a mixed-methods study incorporating comparative case studies of a small number of general practices and, as such, has both strengths and limitations. Although two practices reported list sizes per GP that were approximately double the national average of around 2000 per GP, they are not inconsistent with other evidence that shows a rising trend. 225 General practices are very busy, as small organisations, and the study was shaped by the extent to which the practice staff were able to participate in the anticipated way, in the face of competing demands and priorities. The variation in the completion of workload diary sheets was an example of this. There are limitations in the data collection tools. Using the anonymised clinical records reduced the reliance on clinical staff having to undertake additional work and ensured that we collected data that were representative of usual practice. However, this could be open to the challenge that there was a lack of study-prescribed uniformity in data collected. Data collection covered relevant case-mix factors that might confound the analysis of outcomes, and information from a large sample of consultations, that included summer and winter periods for all practices, were gathered. There were limitations to the health economic analysis; for example, data were not available on the time taken for seeking advice or prescriptions from GPs, as described in more detail in Chapter 5 (see Economic analysis). Uncertainties surround the costs of GPs, but use of validated national rates provided a sound estimate of the likely average situation. The costing analysis takes no account of practice income and budgets, which are sensitive issues and for which information was not available.
While the patient satisfaction survey was based on a widely used and validated tool, it is recognised that such surveys tend to produce positive results. The patient interviews went some way towards providing more nuanced data.
The case study element was not a trial which randomised patients to PA or GP, but rather was a pragmatic approach that was adopted based on usual systems in place in the participating practices. The sample size was relatively small, although well powered for the analyses undertaken. Ethical constraints meant that children seen by PAs were not included in the patient satisfaction survey or the observed consultation, and children are a large patient group in primary care. Similarly, the proportion of each record that we were allowed to use was limited. The PAs had no experience of being videoed before, unlike GPs, in whose vocational training it is commonplace, and this factor may have stilted the PAs’ behaviours.
The use of Read codes in patient records was limited and variable between professionals and practices. We were not able to find any UK-published general practice patient classification system for medical acuity of presenting complaint and complexity of the person (including both medical and social aspects). We built on a published patient condition severity classification system developed in the records28 but our additions were novel and require further validation.
Conclusions
Physician assistants were found to be acceptable, effective and efficient in complementing the work of GPs. PAs could provide a flexible addition to the primary care workforce. They offer another labour pool, with a shorter training period than that for GPs or NPs, to consider in workforce planning at local, regional and national levels. However, in order to maximise the contribution of PAs in primary care settings, consideration needs to be given to the appropriate level of regulation and the potential for giving PAs authority to prescribe medicines.
Recommendations
-
Physician assistants have the potential to be a competent and flexible addition to current and future primary care staffing teams. Patients, the public and primary care professionals need more information to understand both the role and its potential contribution to the NHS. There may be a role for professional organisations, general practices and local primary care organisations in doing this.
-
General practitioners and managers of primary care services should consider the inclusion of PAs within their staffing configurations, and CCGs (and their equivalents outside England) should consider their potential in future service and innovation planning.
-
The efficiency of PAs in primary care is likely to be enhanced by the legal authority to prescribe, which can be achieved only by including PAs in the regulatory framework for health-care professionals. This has implications for policy with regard to regulatory frameworks for health professionals in the UK.
-
In order for there to be a supply of PAs, there needs to be cognisance of this group in health profession education commissioning at a local and national levels (Health Education for England and its equivalent in other UK countries). Educational commissioners at local and national levels should consider the contribution PAs could make to a future flexible primary care workforce.
Further investigation
This study has highlighted a number of questions that require further investigation. These include:
-
the contribution of PAs in other first-contact services as well as secondary services
-
the contribution and impact of all mid-level practitioners, PAs and NPs in first-contact services
-
the extent and impact of supervision and conferring on patients for mid-level practitioners, PAs and NPs in different types of primary care settings, for example GP practices or urgent care facilities
-
the influence of sociodemographic and geographic factors, such as inner-city, remote and rural settings, on the demand for PAs and other mid-level practitioners, in a flexible primary care workforce
-
the reliability and validity of classification systems for both primary care patients and their presenting condition and their consequences for health-resource utilisation
-
the factors and influences in GP partner and manager decision-making as to staffing and skill mix in general practice, with particular reference to beliefs, preference, evidence and use of financial data.
Acknowledgements
Our thanks go to all the PAs and GPs who volunteered to participate, and to all the practice staff and patients who participated and generously helped the study staff. In the busy world of general practice we appreciated all the support of the study.
This report presents independent research commissioned by the NIHR. The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, Health Service and Delivery Research (HSDR) or the Department of Health.
Contributions of authors
Dr Vari M Drennan (Professor of Health Care and Policy Research) led the study, contributed to all elements of the study, led the overall synthesis of findings and drafted the final report.
Dr Mary Halter (Senior Research Fellow, Health Service Research) project managed the study, and contributed to all elements of the study, leading on the data collection and analysis within practices and with patients and prepared the results for publication. She also contributed important intellectual content to the revisions of the final report.
Sally Brearley (patient and public involvement) contributed to all elements of the study, led on the patient and public involvement including chairing of the emerging findings seminar. She contributed important intellectual content to the revisions of the final report.
Wilfred Carneiro (NIHR Research Management Fellow) contributed to all elements of the study, provided expert health service management knowledge as applied to workforce development, undertook scoping interviews, policy review and prepared results for publication, as well as patient interviews. He contributed important intellectual content to the revisions of the final report.
Dr Jon Gabe (Professor of Sociology) contributed to all elements of the study, provided expert knowledge in sociology applied to health care and qualitative methods, undertook scoping interviews and analysis of qualitative data. He contributed important intellectual content to the revisions of the final report.
Dr Heather Gage (Professor of Health Economics) contributed to all elements of the study, provided expert knowledge in health economics, led on the economic analysis and prepared results for publication. She contributed important intellectual content to the revisions of the final report.
Robert Grant (Senior Research Fellow in Quantitative Methods) contributed to all elements of the study, provided expert advice and undertook the statistical analysis. He contributed important intellectual content to the revisions of the final report.
Dr Louise Joly (Research Associate, Health Care Research) contributed to all elements of the study from February 2012, organised and undertook data collection within the practices, led on preparation of data for analysis, and undertook data analysis. She contributed important intellectual content to the revisions of the final report.
Dr Simon de Lusignan (General Practitioner and Professor of Primary Care and Clinical Informatics) contributed to all elements of the study, provided expert general practitioner and primary care knowledge in clinical record data extraction, and led on the clinical record review and analysis of video observations and prepared results for publication. He contributed important intellectual content to the revisions of the final report.
Acknowledgements of the contributions of others to the study
Kaushik Chattophadhay (August 2010–July 2011) and Jennifer Yiallouros (January 2011–September 2012) were research associates assisting in the rapid review, liaison with the practices, administration of surveys and data extraction.
Ros Levenson, independent researcher, undertook interviews with all practice staff in 2012 and prepared internal study reports to inform analysis.
Caragh Flannery, researcher, assisted Professor Gage in the health economics analysis.
Ayoub Ali, researcher, assisted Professor de Lusignan in the analysis of clinical reviews and video observations.
Alexander Courtney-Hatcher, Phillip Crisp, Nicholas Duncan and Dr Julia Wood assisted in data management and coding.
Hugh Claridge, Lucy Drennan, Sian Jones and James Norton provided administrative support at different time points.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
Publications
Drennan V, Halter M, Brearley S, Carneiro W, Gabe J, Gage H, et al. Physician assistants in English primary care teams: a survey. J Interprof Care 2012;5:416–18.
Drennan V, Halter M, Brearley S, Carneiro W, Gabe J, Gage H, et al. The contribution of physician assistants in primary care: a systematic review. BMC Health Serv Res 2013;13:233.
References
- World Health Report 2008: Primary Health Care - Now More than Ever. Geneva: World Health Organization; 2008.
- White Paper. Promoting Better Health Care: The Government’s Programme for Improving Primary Health Care. London: HMSO; 1987.
- White Paper. Choice and Opportunity. Primary Care: The future. London: HMSO; 1996.
- Caring for People Beyond Tomorrow: A Strategic Framework for the Development of Primary Health and Social Care. Belfast: DHSSPSNI; 2005.
- White Paper. Our Health, Our Care, Our Say: A New Direction for Community Services. London: The Stationery Office; 2006.
- White Paper. Equity and Excellence: Liberating the NHS. London: The Stationery Office; 2010.
- Delivering Quality in Primary Care National Action Plan. Edinburgh: The Scottish Government; 2010.
- Setting the Direction: Primary and Community Services Strategic Delivery Plan. Cardiff: The Welsh Assembly Government; 2010.
- The Future Direction of General Practice: A Road Map. London: RCGP; 2007.
- The World Health Report 2006: Working Together for Health. Geneva: World Health Organization; 2006.
- Task Shifting: Rational Redistribution of Tasks Among Health Workforce Teams – Global Recommendations and Guidelines. Geneva: World Health Organization; 2008.
- Buchan J, Dal Poz MR. Skill mix in the health care workforce: reviewing the evidence. Bull World Health Organ 2002;80:575-80.
- Dubois CA, Singh D. From staff-mix to skill-mix and beyond: towards a systemic approach to health workforce management. Human Res Health 2009;7. http://dx.doi.org/10.1186/1478-4491-7-87.
- Laurant M, Harmsen M, Faber M, Wollersheim H, Sibbald B, Grol R. Revision of Professional Roles and Quality Improvement: A Review of the Evidence. London: The Health Foundation; 2010.
- Watson P, Hendey N, Dingwall R, Spencer E, Wilson P. The Mid-level Practitioner: A Review of the Literature on Nurse Practitioner and Physician Assistant Programmes. Sheffield: Sheffield University, Trent Institute Discussion Papers; 1996.
- Chong YS, Tan EK. Midlevel health-care providers key to MDG 5. Lancet 2011;377:1127-8. http://dx.doi.org/10.1016/S0140-6736(11)60166-9.
- Huntingdon J, Meads G. Future Options for General Practice. Oxford: Radcliffe Medical Press; 1996.
- Meads G, Riley AJ, Harding G, Carter YH. Personal medical services: local organizational developments. Prim Health Care Res Dev 2004;5:193-201. http://dx.doi.org/10.1191/1463423604pc213oa.
- Jones R, Rosen R, Tomlin Z, Cavanagh MR, Oxley D. General practitioners with special interests: evolution and evaluation. J Health Serv Res Policy 2006;11:106-9. http://dx.doi.org/10.1258/135581906776318929.
- Iliffe S. From General Practice to Primary Care: The Industrialization of Family Medicine. Oxford: Oxford University Press; 2008.
- Investing in Primary Care Scheme. London: Department of Health; 2002.
- Exworthy M, Wilkinson EK, McColl A, Moore M, Roderick P, Smith H, et al. The role of performance indicators in changing the autonomy of the general practice profession in the UK. Soc Sci Med 2003;56:1493-504. http://dx.doi.org/10.1016/S0277-9536(02)00151-X.
- Investing in General Practice: The New General Medical Services Contract. London: Department of Health; 2003.
- The National Health Service (Primary Medical Services) (Miscellaneous Amendments) Regulations 2004. London: The Stationery Office; 2004.
- National Health Service Act 1977 Alternative Provider Medical Services (No.2) Directions. London: The Stationery Office; 2005.
- HR in the NHS Plan: More Staff Working Differently. London: Department of Health; 2002.
- General and Personal Medical Services England 2001–2011. London: The NHS Health and Social Care Information Centre; 2012.
- A Profile of UK General Practitioners. RCGP Information Sheet. London: Royal College of General Practitioners; 2006.
- General Practice – GP Workforce and Practice Population Statistics to 2012. Edinburgh: Information Services Division Scotland; 2012.
- StatsWales . General Practitioners Workforce Headcounts and Whole Time Equivalents by Local Health Board, Gender and Year 2006–2012 n.d. https://statswales.wales.gov.uk/Catalogue/Health-and-Social-Care/General-Medical-Services (accessed 31 January 2013).
- General Practitioners with Special Interests. RCGP Information Sheet. London: Royal College of General Practitioners; 2006.
- NHS Information Centre . NHS Staff, General Practice 2001–2011 Tables 2012. www.hscic.gov.uk/catalogue/PUB05214 (accessed 30 April 2014).
- Loudon I, Horder J, Webster C. General Practice Under the National Health Service 1948–1997. Oxford: Oxford University Press; 1998.
- Gerada C, Mathers N, Thomas M. Patients, Doctors and the NHS in 2022: A Compendium of Evidence. London: Royal College of General Practitioners; 2012.
- Practice Team Information Annual Update 2011/12. Edinburgh: Information Services Division cotland; 2012.
- Wanless D. Securing Good Health for the Whole Population: Final Report – February 2004. London: HM Treasury; 2004.
- Laurant M, Reeves D, Hermens R, Braspenning J, Grol R, Sibbald B. Substitution of doctors by nurses in primary care. Cochrane Database Syst Rev 2004;4. http://dx.doi.org/10.1002/14651858.CD001271.
- Brown SA, Grimes DE. A meta-analysis of nurse practitioners and nurse midwives in primary care. Nurs Res 1995;44:332-9. http://dx.doi.org/10.1097/00006199-199511000-00003.
- Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ 2002;324:819-23. http://dx.doi.org/10.1136/bmj.324.7341.819.
- Annual Report 2002. London: Department of Health; 2002.
- Hooker R, Cawley J. Physician Assistants in American Medicine. St Louis, MO: Churchill Livingstone; 2003.
- American Academy of Physician Assistants . What Is a PA? n.d. www.aapa.org/the_pa_profession/what_is_a_pa.aspx (accessed 31 January 2013).
- Mittman DE, Cawley JF, Fenn WH. Physician assistants in the United States. BMJ 2002;325:485-7. http://dx.doi.org/10.1136/bmj.325.7362.485.
- Health, United States 2008. Washington, DC: Department of Health and Human Sciences; 2009.
- American Academy of Physician Assistants . 2008 AAPA Physician Assistant Census Report 2009. www.aapa.org (accessed 25 February 2013).
- The Registered Nurse Population: Findings from the 2004 National Sample Survey of Registered Nurses. Washington, DC: US Department of Health and Human Services; 2006.
- Ruby EB, Davidson LJ, Daly B, Clochesy JM, Sereika S, Baldisseri M, et al. Care activities and outcomes of patients cared for by acute care nurse practitioners, physician assistants, and resident physicians: a comparison. Am J Crit Care 1998;7:267-81.
- Cawley JF, Rohrs FC, Hooker RS. Physician assistants and malpractice risk: findings from the national practitioner data bank. Fed Bull 1999;85:242-6.
- Gryzbicki DM, Sullivan PJ, Oppy JM, Bethke A-M, Raab SS. The economic benefit for family/general medicine practices employing physician assistants. Am J Manag Care 2002;8:613-20.
- Larson E, Hart LG, Ballweg R. National estimates of physician assistant productivity. J Allied Health 2001;30:146-52.
- Roblin DW, Howard DH, Becker ER, Adams EK, Roberts MH. Use of midlevel practitioners to achieve labor cost savings in the primary care practice of an MCO. Health Serv Res 2004;39:607-25. http://dx.doi.org/10.1111/j.1475-6773.2004.00247.x.
- Hooker RS, Hogan K, Leeker E. The globalization of the physician assistant profession. J Physician Assist Educ 2007;18:76-85.
- Miller M, Siggins I, Fowler G. The Potential Role of Physician Assistants in the Australian Context Volume 2: Literature Review. Adelaide, SA: Health Workforce Australia; 2011.
- The Potential Role of Physician Assistants in the Australian Context – Final Report. Adelaide, SA: Health Workforce Australia; 2011.
- Health Workforce New Zealand . Physician Assistant Role in New Zealand n.d. www.healthworkforce.govt.nz/new-roles-and-scopes/physician-assistant-role-in-new-zealand (accessed 31 January 2013).
- The International Association of Physician Associate Educators . PA Programs Around the World n.d. www.iapae.org/pa_programs (accessed 31 January 2013).
- Reedy BL, Stewart TI, Quick JB. Attachment of a physician’s assistant to an English general practice. Br Med J 1980;281:664-6. http://dx.doi.org/10.1136/bmj.281.6241.664.
- Abbott S, Stubbs K, Forbes-Burford J. Local pilot, new profession: developing medical care practitioners in primary care. Primary Care Res Dev 2006;7:188-93.
- The Association of Anaesthetists of Great Britain and Ireland . Physicians’ Assistants (Anaesthesia) Review 2011 n.d. www.rcoa.ac.uk/document-store/physicians-assistant-anaesthesia-review-2011 (accessed 31 January 2013).
- Woodin J, McLeod H, McManus R, Jelphs K. Evaluation of US-trained Physician Assistants Working in the NHS in England. Final Report. Birmingham: University of Birmingham; 2005.
- Farmer J, Currie M, West C, Hyman J, Arnott N. Evaluation of the Physician Assistant Pilot Study in Scotland: Final Report. Inverness: University of the Highlands and Islands Millennium Institute; 2009.
- Parle JV, Ross NM, Doe WF. The medical care practitioner: developing a physician assistant equivalent for the United Kingdom. Med J Aust 2006;185:13-7.
- Farmer J, Currie M, Hyman J, West C, Arnott N. Evaluation of physician assistants in National Health Service Scotland. Scott Med J 2011;56:130-4. http://dx.doi.org/10.1258/smj.2011.011109.
- The Competence and Curriculum Framework for the Physician Assistant. London: Department of Health; 2006.
- Association of Physicians’ Assistants (Anaesthesia) . General Information n.d. http://anaesthesiateam.com/index.php/general-information (accessed 31 January 2013).
- UK Association of Physicians‘ Assistants . About UKAPA n.d. www.ukapa.co.uk (accessed 31 January 2013).
- UK Association of Physician Assistants . The Physician Assistant Managed Voluntary Register (PA MVR) n.d. www.paregister.sgul.ac.uk (accessed 31 January 2013).
- The Revised Competence and Curriculum Framework for the Physician Assistant Register. London: Physician Assistant Managed Register; 2012.
- Castledine G. Do we need physician assistants in the UK?. Br J Nurs 1996;5.
- Hutchinson L, Marks T, Pittilo M. The physician assistant: would the US model meet the needs of the NHS?. BMJ 2001;323:1244-7. http://dx.doi.org/10.1136/bmj.323.7323.1244.
- Gavin M. Physician assistants. Many general practitioners would welcome having physician assistants. BMJ 2002;324:735-6.
- Drennan V, Halter M, Levenson R, Tye C. Physician assistants in English general practice: a qualitative study of the employers’ viewpoint. J Health Serv Res Policy 2011;16:75-80. http://dx.doi.org/10.1258/jhsrp.2010.010061.
- Maxwell R. Dimensions of quality revisited: from thought to action. Qual Health Care 1992;1:171-7. http://dx.doi.org/10.1136/qshc.1.3.171.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19-32. http://dx.doi.org/10.1080/1364557032000119616.
- Yin RK. Case Study Research. Thousand Oaks, CA: Sage Publications Inc.; 1994.
- Royal P, Milne R. Literature searching for randomized controlled trials used in Cochrane reviews: rapid versus exhaustive searches. Int J Technol Assess Health Care 2003;19:591-603.
- Dixon-Woods M, Bonas S, Booth A, Jones DR, Miller T, Sutton AJ, et al. How can systematic reviews incorporate qualitative research? A critical perspective. Qual Res 2006;6:27-44. http://dx.doi.org/10.1177/1468794106058867.
- Systematic Reviews: CRDs Guidance for Undertaking Reviews in Healthcare. York: Centre for Reviews and Dissemination, University of York; 2009.
- WONCA Europe . European Definition of General Practice Family Medicine Short Version n.d. www.woncaeurope.org/gp-definitions (accessed 25 February 2013).
- Donabedian A. The quality of care. How can it be assessed?. JAMA 1988;260:1743-8. http://dx.doi.org/10.1001/jama.1988.03410120089033.
- Critical Appraisal Skills Programme (CASP) . Critical Appraisal Checklists n.d. www.casp-uk.net/find-appraise-act/appraising-the-evidence (accessed 25 February 2013).
- British Medical Journal . Guidance for Peer Reviewers 2011. www.bmj.com/about-bmj/resources-reviewers/guidance-peer-reviewers (accessed 25 February 2013).
- Silverman D. Interpreting Qualitative Data. London: Sage Publications; 2011.
- Anderson S, Allen P, Peckham S, Goodwin N. Asking the right questions: scoping studies in the commissioning of research on the organisation and delivery of health services. Health Res Policy Syst 2008;6. http://dx.doi.org/10.1186/1478-4505-6-7.
- Kuhlmann E, Batenburg R, Groenewegen PP, Larsen C. Bringing a European perspective to the health human resources debate: a scoping study. Health Policy 2013;110:6-13. http://dx.doi.org/10.1016/j.healthpol.2012.11.002.
- Strauss A, Corbin J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Thousand Oaks, CA: Sage Publications Ltd; 1998.
- Creswell JW, Clark VL. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA: Sage Publications Ltd; 2007.
- Boyatzis RE. Transforming Qualitative Information: Thematic Analysis and Code Development. London: Sage Publications Ltd; 1998.
- Bower P, Mead N, Roland M. What dimensions underlie patient responses to the General Practice Assessment Survey? A factor analytic study. Fam Pract 2002;19:489-95. http://dx.doi.org/10.1093/fampra/19.5.489.
- Shum C, Humphreys A, Wheeler D, Cochrane MA, Skoda S, Clement S. Nurse management of patients with minor illnesses in general practice: multicentre randomised controlled trial. BMJ 2000;320:1038-43. http://dx.doi.org/10.1136/bmj.320.7241.1038.
- Venning P, Durie A, Roland M, Roberts C, Leese B. Randomised controlled trial comparing cost effectiveness of general practitioners and nurse practitioners in primary care. BMJ 2000;320:1048-53. http://dx.doi.org/10.1136/bmj.320.7241.1048.
- Kinnersley P, Anderson E, Parry K, Clement J, Archard L, Turton P, et al. Randomised controlled trial of nurse practitioner versus general practitioner care for patients requesting ‘same day’ consultations in primary care. BMJ 2000;320:1043-8. http://dx.doi.org/10.1136/bmj.320.7241.1043.
- NHS Employers . Quality and Outcomes Framework for 2012 13 n.d. www.nhsemployers.org/Aboutus/Publications/Documents/QOF_2012-13.pdf (accessed 3 January 2013).
- Noble M, McLennan D, Wilkinson K, Whitworth A, Barnes H, Dibben C. The English Indices of Deprivation 2007. London: Communities and Local Government; 2008.
- UK Terminology Centre . Read Codes n.d. www.connectingforhealth.nhs.uk/systemsandservices/data/uktc/readcodes (accessed January 10 2013).
- De Jong J, Visser MR, Wieringa-de Waard M. Exploring differences in patient mix in a cohort of GP trainees and their trainers. BMJ Open 2011;1. http://dx.doi.org/10.1136/bmjopen-2011-000318.
- Snijders TAB, Bosker RA. Multilevel Analysis. London: Sage Publications Ltd; 2011.
- Curtis P, Skinner B, Bentz E, Purvis A. Inside the chart review. J Med Educ 1982;57:841-7. http://dx.doi.org/10.1097/00001888-198211000-00004.
- Goulet F, Jacques A, Gagnon R, Bourbeau D, Laberge D, Melanson J, et al. Performance assessment. Family physicians in Montreal meet the mark!. Can Fam Physician 2002;48:1337-44.
- Tam KW, Kwok KH, Fan YM, Tsui KB, Ng KK, Ho KY, et al. Detection and prevention of medication misadventures in general practice. Int J Qual Health Care 2008;3:192-9. http://dx.doi.org/10.1093/intqhc/mzn002.
- Weed LL. Medical records that guide and teach. N Engl J Med 1968;278:593-600. http://dx.doi.org/10.1056/NEJM196803142781105.
- Weed LL. Medical records that guide and teach. N Engl J Med 1968;278:652-7. http://dx.doi.org/10.1056/NEJM196803212781204.
- Fleiss JL. Measuring nominal scale agreement among many raters. Psychol Bull 1971;5:378-82. http://dx.doi.org/10.1037/h0031619.
- Altman D. Practical Statistics for Medical Research. London: Chapman & Hall; 1991.
- Fraser RC, McKinley RK, Mulholland H. Consultation competence in general practice: testing the reliability of the Leicester assessment package. Br J Gen Pract 1994;44:293-6.
- Coleman T. Using video-recorded consultations for research in primary care: advantages and limitations. Fam Pract 2000;17:422-7. http://dx.doi.org/10.1093/fampra/17.5.422.
- de Lusignan S, Kumarapeli P, Chan T, Pflug B, van Vlymen J, Jones B, et al. The ALFA (Activity Log Files Aggregation) toolkit: a method for precise observation of the consultation. J Med Internet Res 2008;10. http://dx.doi.org/10.2196/jmir.1080.
- Fraser RC, McKinley RK, Mulholland H. Consultation competence in general practice: establishing the face validity of prioritized criteria in the Leicester assessment package. Br J Gen Pract 1994;44:109-13.
- Allen J, Rashid A. What determines competence within a general practice consultation? Assessment of consultation skills using simulated surgeries. Br J Gen Pract 1998;48:1259-62.
- Jiwa M, McKinley R, O’Shea C, Arnet H, Spilsbury K, Smith M. Investigating the impact of extraneous distractions on consultations in general practice: lessons learned. BMC Med Res Methodol 2009;9. http://dx.doi.org/10.1186/1471-2288-9-8.
- Braunholtz D. Leicester assessment package. Br J Gen Pract 1995;45:51-2.
- Halkett GK, Jiwa M, O’Shea C, Smith M, Leong E, Jackson M, et al. Management of cases that might benefit from radiotherapy: a standardised patient study in primary care. Eur J Cancer Care 2012;21:259-65. http://dx.doi.org/10.1111/j.1365-2354.2011.01314.x.
- Jiwa M, Mitchell G, Sibbrit D, Girgis A, Burridge L. Addressing the needs of caregivers of cancer patients in general practice: a complex intervention. Qual Prim Care 2010;18:9-16.
- Jiwa M, O’Shea C, Merriman G, Halkett G, Spilsbury K. Psychosexual problems in general practice: measuring consultation competence using two different measures. Qual Prim Care 2010;18:243-50.
- Fraser RC, Sarkhou ME, McKinley RK, Van der Vleuten C. Regulatory end-point assessment of the consultation competence of family practice trainees in Kuwait. Eur J Gen Pract 2006;12:100-7. http://dx.doi.org/10.1080/13814780600898353.
- Redsell SA, Hastings AM, Cheater FM, Fraser RC. Devising and establishing the face and content validity of explicit criteria of consultation competence in UK primary care nurses. Nurse Educ Today 2003;23:299-306. http://dx.doi.org/10.1016/S0260-6917(03)00013-3.
- McKinley RK, Fraser RC, van der Vleuten C, Hastings AM. Formative assessment of the consultation performance of medical students in the setting of general practice using a modified version of the Leicester assessment package. Med Educ 2000;34:573-9. http://dx.doi.org/10.1046/j.1365-2923.2000.00490.x.
- The NHS Information Centre . GP Workload Survey Results 2007. www.ic.nhs.uk/pubs/gpworkload (accessed 3 January 2013).
- Curtis L. Unit Costs of Health and Social Care 2011. Canterbury: PSSRU, University of Kent; 2011.
- Department of Health . NHS Commissioning Board n.d. www.wp.dh.gov.uk/commissioningboard/files/. ccg-practice-list.xls (accessed 13 December 2012).
- Health and Social Care Information Centre . GP Practice Indicators: Deprivation n.d. https://indicators.ic.nhs.uk/webview/ (accessed 5 March 2013).
- Ramsay Brown and Partners . Real Cost of Salaried GPs Vs Partner 2009. www.ramsaybrown.co.uk/RealcostofsalariedGPvsPartner.htm (accessed 2 March 2013).
- Torjesen I. Salaried GPs Versus Partners 2010. http://careers.bmj.com/careers/advice/view-article.html?id=20001005 (accessed 9 March 2013).
- Jacques H. GP Partners Could Be More Cost-Effective Than Salaried GPs 2011. http://careers.bmj.com/careers/advice/view-article.html?id=20002602 (accessed 10 March 2013).
- NHS Information Centre . General Practice 2002–2012 n.d. www.dh.gov.uk/health/tag/nhs-information-centre (accessed 5 March 2013).
- Office for National Statistics . Rural/Urban/Local/Authority/(LA)/Classification/(England)/(2009) n.d. www.ons.gov.uk/ons/guide-method/geography/products/area-classifications/rural-urban-definition-and-la/rural-urban-local-authority--la--classification--england-/index.html (accessed 25 January 2013).
- Scheffler RM, Gillings DB. Survey approach to estimating demand for physician assistants. Soc Sci Med 1982;16:1039-47. http://dx.doi.org/10.1016/0277-9536(82)90176-9.
- Oliver DR, Laube DW, Gerstbrein JJ, Wombacher N. Distribution of primary care physicians assistants in state of Iowa. J Iowa Med Soc 1977;67:320-3.
- Larson EH, Hart LG, Hummell J. Rural physician assistants: a survey of graduates of MEDEX Northwest. Public Health Rep 1994;109:266-74.
- Hooker RS, Freeborn DK. Use of physician assistants in a managed health care system. Public Health Rep 1991;106:90-4.
- Perry HB. Physician assistants: an overview of an emerging health profession. Med Care 1977;15:982-90. http://dx.doi.org/10.1097/00005650-197712000-00002.
- Perry HB, Fisher DW. The physician’s assistant profession: results of a 1978 survey of graduates. J Med Educ 1981;56:839-45. http://dx.doi.org/10.1097/00001888-198110000-00006.
- Muus KJ, Geller JM, Ludtke RL, Pan S, Kassab C, Luloff AE, et al. Implications for recruitment: comparing urban and rural primary care PAs. JAAPA 1996;9.
- Pan S, Geller JM, Gullicks JN, Muus KJ, Larson AC. A comparative analysis of primary care nurse practitioners and physician assistants. Nurse Pract 1997;22:14-7.
- Duryea WR, Hooker RS. ‘Elder’ physician assistants and their practices. JAAPA 2000;13:67-71.
- Larson EH, Hart LG, Ballweg R. National estimates of physician assistant productivity. J Allied Health 2001;30:146-52.
- Hooker RS, Berlin LE. Trends in the supply of physician assistants and nurse practitioners in the United States. Health Aff 2002;21:174-81. http://dx.doi.org/10.1377/hlthaff.21.5.174.
- Oliveria SA, Altman JF, Christos PJ, Halpern AC. Use of nonphysician health care providers for skin cancer screening in the primary care setting. Prev Med 2002;34:374-9. http://dx.doi.org/10.1006/pmed.2001.0995.
- Larson EH, Hart L. Growth and change in the physician assistant workforce in the United States, 1967–2000. J Allied Health 2007;36:121-30.
- Duttera MJ, Harlan WR. Evaluation of physician assistants in rural primary care. Arch Intern Med 1978;138:224-8. http://dx.doi.org/10.1001/archinte.138.2.224.
- Henry LR, Hooker RS. Retention of physician assistants in rural health clinics. J Rural Health 2007;23:207-14. http://dx.doi.org/10.1111/j.1748-0361.2007.00092.x.
- Joiner CL. Attitudes of primary care physicians in the state of Alabama toward physician assistants: a preliminary report. Ala J Med Sci 1974;11:363-5.
- Oliver D, Preston D. What Iowa family physicians, residents and medical students think about physician’s assistants. J Iowa Med Soc 1980;70:466-70.
- Ford VH, Kish CP. What’s happening. Family physician perceptions of nurse practitioners and physician assistants in a family practice setting. J Am Acad Nurse Pract 1998;10:167-71.
- Engel GV, Roy A, Martin LR, Matheny SC. Projections for the viability of the physician assistant occupation based on the intended hiring practices of family medicine physicians. Fam Pract Res J 1984;4:122-4.
- Isberner FR, Lloyd L, Simon B, Craven JM. Utilization of physician assistants: incentives and constraints for rural physicians. Perspective Physician Assist Educ 2003;14:69-73.
- Sells CJ, Herdener RS. Medex: a time motion study. Pediatrics 1975;56:255-61.
- Drass KA. Discourse and occupational perspective – a comparison of nurse practitioners and physician assistants. Discourse Process 1988;11:163-81. http://dx.doi.org/10.1080/01638538809544697.
- Dehn RW, Asprey DP. A study of PA perceptions: impediments to the practice of medicine in Iowa. JAAPA 1995;8:49-58.
- Golladay FL, Miller M, Smith KR. Allied health manpower strategies: estimates of the potential gains from efficient task delegation. Med Care 1973;B:457-69.
- Miles DL, Rushing WA. A study of physicians’ assistants in a rural setting. Med Care 1976;B:987-95. http://dx.doi.org/10.1097/00005650-197612000-00002.
- Rushing WA, Miles DL. Physicians, physicians’ assistants, and the social characteristics of patients in Southern Appalachia. Med Care 1977;B:1004-13. http://dx.doi.org/10.1097/00005650-197712000-00004.
- Nelson EC, Johnson KG, Jacobs AR. Impact of Medex on physician activities: redistribution of physician time after incorporating a Medex into the practice. J Fam Pract 1977;5:607-12.
- Frame PS, Wetterau NW, Parey B. A model for the use of physician’s assistants in primary care. J Fam Pract 1978;7:1195-201.
- Hill RF, Greenwood JG, Wert FS. An evaluation of a remote, rural clinic manned by a physician’s assistant. Public Health Rep 1979;94:60-6.
- Fethke C, Ekwo E, Daniels M. Management practices: task allocation between physicians and physician assistants. J Ambul Care Manag 1979;2:31-45. http://dx.doi.org/10.1097/00004479-197905000-00006.
- Larsen KM, Kirkwood CR. Procedures performed by family physicians, internists, and a Medex in a small group practice. J Fam Pract 1982;15:285-92.
- Martin E, Sophocles AM. Analysis of a rural family-practice-based evening clinic staffed by a PA. Physician Assist 1984;8:16-9.
- Willis JB, Cyr B, Schafft G, Steinbrueck SP. 1985 physician assistant role delineation study: ten years later. Physician Assist 1986;10:33-8.
- Mainous IAG, Bertolino JG, Harrell PL. Physician extenders: who is using them?. Fam Med 1992;24:201-4.
- Dehn RW, Hooker RS. Implications for practice and education. Clinical activities of Iowa family practice PAs. JAAPA 1999;12:63-77.
- Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 2009;6.
- Hooker RS, Harrison K, Pashen D. Are Australians willing to be treated by a physician assistant?. AMJ 2010;3:407-13. http://dx.doi.org/10.4066/AMJ.2010.325.
- Simkens ABM, van Baar ME, van Balen FAM, Verheij RA, van den Hoogen HJM, Schrijvers AJP. The physician assistant in general practice in the Netherlands. J Physician Assist Educ 2009;20:30-8.
- Ekwo EE, Dusdieker LB, Bean JA, Daniels MA. How lengths of office visits vary when primary care practices employ physician assistants. Inquiry 1980;17:145-54.
- Henry RA. Use of physician’s assistants in Gilchrist County, Florida. Health Serv Rep 1972;87:687-92. http://dx.doi.org/10.2307/4594632.
- Wright DD, Kane RL, Snell GF, Woolley FR. Costs and outcomes for different primary care providers. JAMA 1977;238:46-50. http://dx.doi.org/10.1001/jama.238.1.46.
- Kane RL, Gardner J, Wright DD, Woolley FR, Snell GF, Sundwall DN, et al. Differences in the outcomes of acute episodes of care provided by various types of family practitioners. J Fam Pract 1978;6:133-8.
- Henry RA. Evaluation of physician’s assistants in Gilchrist County, Florida. Public Health Rep 1974;89:429-32.
- Hooker RS, Cipher DJ, Sekscenski E. Patient satisfaction with physician assistant, nurse practitioner, and physician care: a national survey of Medicare beneficiaries. J Clin Outcomes Manag 2005;12:88-92.
- Cipher DJ, Hooker RS, Sekscenski E. Are older patients satisfied with physician assistants and nurse practitioners?. JAAPA 2006;19:36-9. http://dx.doi.org/10.1097/01720610-200601000-00007.
- Litman TJ. Public perceptions of the physicians’ assistant – a survey of the attitudes and opinions of rural Iowa and Minnesota residents. Am J Public Health 1972;62:343-6. http://dx.doi.org/10.2105/AJPH.62.3.343.
- Smith CW. Patient attitudes toward physicians’ assistants. J Fam Pract 1981;13:201-4.
- The NHS Quality, Innovation, Productivity and Prevention Challenge: An Introduction for Clinicians. London: Department of Health; 2010.
- Ohman-Strickland PA, Orzano AJ, Hudson SV, Solberg LI, DiCiccio-Bloom B, O’Malley D, et al. Quality of diabetes care in family medicine practices: influence of nurse-practitioners and physician’s assistants. Ann Fam Med 2008;6:14-22. http://dx.doi.org/10.1370/afm.758.
- Halter M, Drennan V, Chattopadhyay K, Carneiro W, Yiallouros J, de Lusignan S, et al. The contribution of physician assistants in primary care: a systematic review. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-223.
- Teasdale C. We Have Deeper Issues Than the US to Consider. BMJ Rapid Response 2001. www.bmj.com/rapid-response/2011/10/28/we-have-deeper-issues-us-consider (accessed 23 January 2013).
- Teasdale C. True Equality Means Dropping All the Barriers. BMJ Rapid Response 2002. www.bmj.com/rapid-response/2011/10/29/true-equality-means-dropping-all-barriers (accessed 23 January 2013).
- Moghal N. Exploring the US Physician Assistant Model: A Contribution to QIPP. HSJ 2011. www.hsj.co.uk/resource-centre/best-practice/exploring-the-us-physician-assistant-workforce-model-a-contribution-to-qipp/5026533.article (accessed 23 January 2013).
- Elegbe O. GP commissioning consortia: is there a role for physician assistants in routine care?. Br J Gen Prac 2010;60:704-5. http://dx.doi.org/10.3399/bjgp10X515601 (accessed 23 January 2013).
- Education, Training and Workforce Planning: First Report of Session 2012–13. London: The Stationery Office; 2012.
- Annual Operational Plan 2011–2012. Leicester: University Hospitals of Leicester NHS Trust; 2011.
- Delivering Rural Health Care Services. Cardiff: Welsh Government; 2011.
- Progress Report – 2009/10. Appendix 3: Potential Areas for Efficiency Savings. Edinburgh: NHS Scotland; 2010.
- Nicoll P, MacVicar R. NES Supporting Scottish Remote and Rural Healthcare. Edinburgh: NHS Education for Scotland; 2012.
- Royal College of Physicians of Edinburgh . Student and Foundation Membership n.d. www.rcpe.ac.uk/about/join/safm.php (accessed 28 February 2013).
- Goddard A. EWTD: RCP Addresses NHS Employers Annual Conference n.d. www.rcplondon.ac.uk/update/ewtd-rcp-addresses-nhs-employers-annual-conference (accessed 31 January 2013).
- European Parliament and the Council of the European Union . Directive 2003 88 EC of the European Parliament and of the Council of 4 November 2003 Concerning Certain Aspects of the Organisation of Working Time n.d. http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=CELEX:32003L0088:EN:HTML (accessed 31 January 2013).
- Proposed Change to the NHS Summary Report from NHS Future Forum (Chairman Professor Field). London: Department of Health; 2011.
- The Health and Social Care Act 2012. London: The Stationery Office; 2012.
- Enabling Excellence: Autonomy and Accountability for Health and Social Care Staff. London: The Stationery Office; 2011.
- Drennan VM, Chattopadhyay K, Halter M, Brearley S, de Lusignan S, Gabe J, et al. Physician assistants in English primary care teams: a survey. J Interprof Care 2012;26:416-18. http://dx.doi.org/10.3109/13561820.2012.686538.
- Morgan PA, Abbott DH, McNeil RB, Fisher DA. Characteristics of primary care office visits to nurse practitioners, physician assistants and physicians in United States Veterans Health Administration facilities, 2005 to 2010: a retrospective cross-sectional analysis. Hum Resour Health 2012;10. http://dx.doi.org/10.1186/1478-4491-10-42.
- Hooker RS, Cawley JF, Asprey DP. Physician Assistants Policy and Practice. Philadelphia, PA: F.A. Davis Company; 2009.
- Health and Social Care Information Centre . GP Workload Survey Results (Appendix A Table 6) 2007. http://www.ic.nhs.uk/pubs/gpworkload (accessed 23 February 2013).
- Marsh GN, Dawes ML. Establishing a minor illness nurse in a busy general practice. BMJ 1995;310:778-80. http://dx.doi.org/10.1136/bmj.310.6982.778.
- Department of Health . The GP Patients Survey Results 2012 n.d. www.gp-patient.co.uk/results (accessed 14 February 2014).
- Gerard K, Salisbury C, Street D, Pope C, Baxter H. Is fast access to general practice all that should matter? A discrete choice experiment of patients' preferences. J Health Serv Res Policy 2008;13:3-10. http://dx.doi.org/10.1258/jhsrp.2007.007087.
- Freeman GK. Progress with relationship continuity 2012, a British perspective. Int J Integr Care 2012;12.
- Redsell S, Stokes T, Jackson C, Hastings A, Baker R. Patients’ accounts of the differences in nurses’ and general practitioners’ roles in primary care. J Adv Nurs 2007;57:172-80.
- Cooper RJ, Bissell P, Ward P, Murphy E, Anderson C, Avery T, et al. Further challenges to medical dominance? The case of nurse and pharmacist supplementary prescribing. Health 2012;16:115-33. http://dx.doi.org/10.1177/1363459310364159.
- Doan Q, Hooker RS, Wong H, Singer J, Sheps S, Kissoon N, et al. Canadians’ willingness to receive care from physician assistants. Can Fam Physician 2012;58:e459-64.
- Kuilman L, Nieweg RM, van der Schans CP, Strijbos JH, Hooker RS. Are Dutch patients willing to be seen by a physician assistant instead of a medical doctor?. Hum Resour Health 2012;10. http://dx.doi.org/10.1186/1478-4491-10-28.
- Health and Social Care Information Centre . GP Workload Survey Results (Appendix A Table 5b) 2007. http://www.ic.nhs.uk/pubs/gpworkload (accessed 23 February 2013).
- Ellis RP, Ash A. Refinements to the diagnostic cost group (DCG) model. Inquiry 32:418-29.
- Thiru K, Hassey A, Sullivan F. Systematic review of scope and quality of electronic patient record data in primary care. BMJ 2003;326:1070-2. http://dx.doi.org/10.1136/bmj.326.7398.1070.
- Price A, Clark J. A quantitative study of the management of acute urinary symptoms by nurse practitioners and general practitioners in a general practice setting. Prim Health Care Res Dev 2002;3:194-20.
- Seale C, Anderson E, Kinnersley P. Comparison of GP and nurse practitioner consultations: an observational study. Br J Gen Pract 2005;55:938-43.
- Evaluation of the Queensland Physician’s Assistant Pilot: Final Report. Brisbane, QLD: Urbis Pty Ltd; 2010.
- Hollinghurst S, Horrocks S, Anderson E, Salisbury C. Comparing the cost of nurse practitioners and GPs in primary care. Br J Gen Prac 2006;56:530-5.
- Dierick-van Daele ATM, Metsemakers JFM, Derckx EW, Spreeuwenberg C, Vrijhoef HJM. Nurse practitioners substituting for General Practitioners in the care of patients with common complaints: a randomised controlled trial. J Adv Nurs 2009;65:391-40.
- Dierick-van Daele ATM, Steuten LMG, Metsemakers JFM, Derckx EWCC, Spreeuwenberg C, Vrijhoef HJM. Economic evaluation of nurse practitioners versus GPs in treating common conditions. Br J Gen Prac 2010;60:e28-35. http://dx.doi.org/10.3399/bjgp10X482077.
- Fleuren M, Wiefferink K, Paulussen T. Determinants of innovation within health care organizations: literature review and Delphi study. Int J Qual Health Care 2004;16:107-23. http://dx.doi.org/10.1093/intqhc/mzh030.
- Boerma WGW, Dubois CA, Saltman RB, Rico A, Boerma WGW. Primary Care in the Driver’s Seat? Organisational Reform in European Primary Care. Maidenhead: Open University Press; 2006.
- Gemmell I, Campbell S, Hann M, Sibbald B. Assessing workload in general practice in England before and after the introduction of the pay-for performance contract. J Adv Nurs 2009;65:509-15. http://dx.doi.org/10.1111/j.1365-2648.2008.04902.x.
- Charles-Jones C, Latimer J, May C. Transforming general practice: the redistribution of medical work in primary care. Sociol Health Illness 2003;25:71-92. http://dx.doi.org/10.1111/1467-9566.t01-1-00325.
- Jones L, Green J. Shifting discourses of professionalism: a case study of general practitioners in the United Kingdom. Sociol Health Illness 2006;28:927-50.
- Checkland K, Harrison S, McDonald R, Grant S, Campbell S, Guthrie B. Biomedicine, holism and general medical practice: responses to the 2004 general practitioner contract. Sociol Health Illness 2008;30:788-803. http://dx.doi.org/10.1111/j.1467-9566.2008.01081.x.
- Taylor F. Scientific Management. New York, NY: Prism Key Press; 2011.
- Centre for Workforce Intelligence . GP In-Depth Review Interim Report 2013. www.cfwi.org.uk/publications (accessed 3 March 2013).
- Deloitte UK Centre for Health Solutions . Primary Care: Today and Tomorrow – Improving General Practice by Working Differently 2012. www.deloitte.com/view/en_GB/uk/research-and-intelligence/deloitte-research-uk/deloitte-uk-centre-for-health-solutions/bb6e38f609817310VgnVCM3000001c56f00aRCRD.htm (accessed 3 March 2013).
- Abbott A. The System of Professions: An Essay on the Division of Expert Labor. Chicago, IL: University of Chicago Press; 1988.
- Calnan M, Gabe J, Gabe J, Calnan M. The New Sociology of the Health Service. Oxon: Routledge; 2009.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. http://dx.doi.org/10.1111/j.0887-378X.2004.00325.x.
- Rimmer A. GP Shortages Increase List Sizes As Too Many Specialists Are Trained 2012. www.gponline.com/News/article/1110536/GP-shortages-increase-list-sizes-specialists-trained (accessed 3 March 2013).
- Bullock A, Morris Z, Atwell C. A Formative Evaluation of the Service Delivery and Organisation (SDO) Management Fellowships 2012 n.d. www.netscc.ac.uk/hsdr/projdetails.php?ref=09-1003-01 (accessed February 2013).
- Stoll L, Foster-Turner J, Glenn M. Mind Shift. An Evaluation of the NHS London ‘Darzi’ Fellowships in Clinical Leadership Programme 2010. www.ioe.ac.uk/IoE_fellowship_evaluation_report_final_July_2010_Executive_Summary_final.pdf (accessed February 2013).
Appendix 1 Advisory group membership
Name Representing
Dr Phil Begg Wolverhampton University.
Joel Grey St George’s University of London.
David Kuhns Birmingham University.
Prof Jim Parle Birmingham University.
Rob Smith NHS London.
Kathy Tyler Skills for Health.
Jeannie Watkins UKAPA.
Lori Williams UKAPA.
Patient and Public Involvement Group membership
Lawrie Baker.
Joy Mills.
Simon Gardner.
Richard Omari.
Vishy Harihara.
Patricia Page.
Gwen Hunter.
Pauline Stanley.
Elizabeth Lloyd-Dehler.
Josephine Udine.
James Lindsay.
Edna White.
Tom McGill.
Appendix 2 National Institute for Health Research health research management fellow report
Introduction
This report is a reflection of my personal and subjective experience as a National Institute for Health Research – Service Delivery and Organisation (NIHR SDO) management fellow, attached to a multimethods evaluation of a new innovation for the health-care workforce. I was an integral member of the core research team for most of the duration of the research study on a part-time basis.
Background
The management fellow scheme was an innovation undertaken in 2009 by the NIHR SDO with the principal aim of encouraging utilisation of research in NHS health-care management. The wider NIHR SDO programme and the Management Fellow programme were replaced in 2012 by the Health Services and Delivery Research programme. The SDO Management Fellow programme was evaluated in 2012. 226 The aims of the Management Fellow programme were to:
-
improve the quality and relevance of the research projects through manager involvement
-
develop capacity in the NHS manager community for accessing, appraising and utilising research evidence and
-
encourage greater engagement, linkage and exchange between research and practice communities in health-care management.
The specific aims of my fellowship were to:
-
utilise my NHS expertise and experience in shaping, undertaking and interpreting stakeholder analysis to ensure there is a NHS management perspective throughout
-
enhance my personal and my NHS employer trust’s capacity and capability to undertake and utilise service delivery and organisational research.
There was a formal process of being recruited to a Management Fellowship. In the autumn of 2010, I saw an open call for expressions of interest to this management fellowship on an internal e-mail to staff in my NHS trust. I replied to the open call for expressions of interest in the Management Fellowship, and subsequently met with the principal investigator and the project manager for the study. I had a series of meetings with my NHS trust to discuss the aims and objectives of the Management Fellowship. A formal application by the principal investigator, supported by my NHS trust, was submitted to the NIHR SDO programme board. Due diligence was followed through a decision being made to award a management fellowship to this project. The process from an expression of interest to the formal start of the Management Fellowship took over 6 months to complete. As I had agreed to work on a part-time basis on the Management Fellowship over 20 months in order to gain a better experience of the research process and project, it was necessary to revise my duties with the trust and maintain a high degree of flexibility in these duties through the life of the Management Fellowship. At the time of starting and through the span of this Management Fellowship, there have been significant policy reforms190 and subsequent changes in the landscape to the NHS and within all NHS organisations. The wider study and the Management Fellowship were extended by an additional 4 months owing to unforeseen circumstances. The period of this Management Fellowship was from February 2011 to February 2013.
Work undertaken by the Management Fellow
I undertook and contributed to a wide variety of research and other activities through the duration of the project. My principal research activities included taking a key role and working closely with Professors Gabe and Drennan in shaping the national stakeholder analysis, including identifying, contacting, and undertaking semistructured interviews, and also undertaking analysis of the interviews. I took a lead role in undertaking the commentary review and health workforce and policy analysis. I drafted early versions of discussion papers for these activities, which have informed the content of these sections in the final report. Additionally, I took the lead role in contacting and interviewing patients, and in developing the coding framework for these interviews with other members of the research team.
I worked with other members of the core research team in a range of other elements on this study, including the rapid review of the literature, and in various activities undertaken with patients and staff in the visits to the case study sites. I contributed to ongoing communication with participants of the study through newsletters, and in a seminar to discuss the preliminary research findings in February 2013. Finally, I assisted in the drafting of the final report as a joint author with other members of the research team.
Knowledge mobilisation and transfer activities
During the period of the fellowship, I ensured that relevant information about health policy and operational change within the NHS was communicated to the research team as it applied to the study. I met with visiting national and international health staff to improve their understanding of the NHS, and contacted other professionals to help inform their visit to the UK. I have continued to build relationships with academic and teaching staff in the university and this has resulted in presentations by medical students, development of joint bids for small-scale research projects and sharing of my specific knowledge in the NHS and local community with academic staff to inform their current and future research. Additionally, during the period of this management fellowship, I have been actively engaged in a series of Centre for Workforce Intelligence (CfWI) workshops, sharing my experience as an NHS manager and research fellow, and disseminating relevant CfWI materials with the research team.
I was a member of the advisory group to the formal evaluation of the SDO Management Fellow programme, and participated in a series of meetings to exchange mutual experience and knowledge with other Management Fellows facilitated by the SDO network. I attended the NIHR SDO annual conferences in 2011 and 2012 and participated in knowledge-sharing discussions with other researchers at these events. As I was working in the trust on a part-time basis through the span of this Management Fellowship, I have maintained strong contact with my NHS and other colleagues and have led or been involved in active programmes of work with other staff and researchers related to my specialist field of equalities.
What was learnt from this experience?
The learning from this Management Fellowship has been in several different areas and at different levels. It has been an active and reflective process, with tangible outcomes. New skills learned included the process involved in undertaking interviews, and the coding and analysis of these interviews. The electronic skills involved in identifying various documents through several sections of this study provided additional learning, as did the extraction of information from these documents. New learning was undertaken in the use of NVivo software, with the workforce planning tools in development by the CfWI, and also through participation in a scenario generating activity by CfWI. The use of innovative cloud-based data warehouses and other electronic systems provided a new experience in sharing information with other researchers, as did the use of technical audio and video recording equipment for various elements of the study.
Additional learning was developed by reading documents critically, through formal and informal discussions and correspondence with other members of the research team and faculty staff, attending workshops and seminars on research practices, and by refining my existing communication and analysis skills. I developed an improved understanding of research methods processes, and in the ability to identify source material, assess and appraise peer-reviewed and other materials. As this was my first experience as an early researcher in a major study, I was able to both observe and reflect on the leadership and skills expressed by the principal investigator and other members of the research team. I experienced a more explicit, inclusive and collaborative style of working in the research team, alongside developing an understanding to the unpredictability of circumstances in research, and learning about the adaptability of the research team through the timescale of the project.
Plans going forward
As the Fellowship ends, I plan, where appropriate, to contribute to dissemination activities related to the study and its findings. I will seek to maintain and develop the research relationships with the research team and wider academia, specifically outside of the clinical sciences. In the last 6 months of this project, I have been actively involved in a significant staff innovation related to service improvement in a specific area. I have been able to use my increased knowledge of research to help inform the evaluation of the multiple elements in this innovation. I have facilitated discussions with other researchers to help transfer research knowledge and skills to staff within the service. The learning from this project could have a significant impact upon the patient and staff experience with NHS organisations, and we plan to use appropriate research methods to support the project and share any findings.
As my employing trust prepares for its transition to foundation trust status, it has committed to improving its capacity in research and innovation, and to developing research skills among its staff. The trust is actively engaged in research collaborations in the sector with other organisations. I plan to co-ordinate the content after the establishment of a web-based research portal for patients, the public and staff, where information and participation opportunities related to research activities in the trust and the university will be made available. I also plan, where possible, to continue discussions with other managers with research interests within the trust, explore the development of an informal network with these managers, and support initiatives to other managers in the trust in developing research capacity in service delivery and operational research. Finally, I will maintain contact with the research team and other academics and professionals I met through the span of this fellowship and participate in further dissemination activities related to the research project where appropriate.
As has been described in an evaluation of NHS London ‘Darzi’ fellowships,227 the impact of such fellowships can be far reaching on the individual, to the organisations and the wider system. The experience gained through my Management Fellowship will have an impact on my employing trust, which will be expressed in many ways. The opportunities to use the range of my newly acquired skills will need to be discussed with several senior managers and operational leads. The requirements for large sections of the NHS workforce to be adaptable and responsive in these times of change could support the development of my newly acquired abilities and skills over time. My interest in developing my research knowledge and skills further, and adapting these constructively to my workplace will require me to be politically aware, sensitive and work with my trust to make the best use of my abilities in meeting our duties as an organisation and in our public service commitments to the founding principles of the NHS.
Wilfred Carneiro, February 2013.
Appendix 3 Search strategy for PsycINFO
| Search ID# | Search terms | Search options |
|---|---|---|
| S9 | S6 and S7 | Limiters – English Language Search modes – Boolean/phrase |
| S8 | S6 and S7 | Search modes – Boolean/phrase |
| S7 | S3 or S4 | Search modes – Boolean/phrase |
| S6 | S1 or S2 or S5 | Search modes – Boolean/phrase |
| S5 | (MH “Family Practice”) | Search modes – Boolean/phrase |
| S4 | Physician* assistant* | Search modes – Boolean/phrase |
| S3 | (MH “Physician Assistants”) | Search modes – Boolean/phrase |
| S2 | General practi* | Search modes – Boolean/phrase |
| S1 | (MH “Primary Health Care) OR (MH “Physicians, Family”) | Search modes – Boolean/phrase |
Appendix 4 Patient survey
Appendix 5 Coding for clinical records
Diagnostic tests
| Code | Descriptor |
|---|---|
| 0 | None |
| 1 | Blood test ordered – includes
|
| 2 | Blood test taken includes as code 1 |
| 3 | Urine test – dipstick during consultation. Would be used to test for blood, protein, glucose, leucocytes, ketones, urobilinogen and nitrite |
| 4 | Urine – sent to laboratory, e.g. microscopy, culture and sensitivity (M, C & S) (sent to laboratory) blood, or glucose, or protein, leucocytes, ketones, urobiligen and nitrite (sent to laboratory) |
| 5 | Cervical smear/liquid-based cytology (LBC) |
| 6 | ECG |
| 7 | ECG 24-hour |
| 8 | Echocardiogram |
| 9 | Fundoscopy |
| 10 | Helicobacter pylori test |
| 11 | Intravenous urogram |
| 12 | Spirometry and/or peak flow |
| 13 | Sputum sample |
| 14 | Stool – microscopy, culture and sensitivity (MCS), ova, cysts and parasites (OCP), occult blood |
| 15 | Swab – e.g. genital, cervical, urethral, high vaginal (HVS), ear, non-specific |
| 16 | Ultrasound (specific or non-specific) |
| 17 | X-ray (specific and non-specific) |
| 18 | Screening test or questionnaire tool, e.g. alcohol-use disorder identification test, alcohol consumption questionnaire, fast alcohol screening test, PHQ-9; pre-immunisation questionnaire; Qrisk cardiovascular disease score; use of web-based tools to aid diagnosis, e.g. DermaNet |
| 19 | Other – any other test that does not fit into the previous categories. [Items coded here allocated 20 to 24] |
| 20 | CT scan |
| 21 | MRI scan |
| 22 | Pregnancy test |
| 23 | Nail, hair or skin sample |
| 24 | BM stick |
Procedures
| Code | Descriptor |
|---|---|
| 0 | None |
| 1 | Injection or vaccination |
| 2 | Wound care (renewal of dressings, removal of steristrips, wound checks) |
| 3 | Removal of sutures |
| 4 | Cryotherapy |
| 5 | Electrocautery |
| 6 | Curettage |
| 7 | Therapeutic injections used in a variety of conditions |
| 8 | Excisions |
| 9 | Incisions |
| 10 | Other procedures, which the practice is deemed competent to carry out (items coded here were later allocated codes 11 and 12) |
| 11 | Ear irrigation (syringe/clean) |
| 12 | Administration of nebuliser |
Advice (general)
| Code | Descriptor |
|---|---|
| Yes | Advice and information given (not specified) includes leaflets could be on any aspects, e.g. smoking cessation, travel health, self-referral to other services, offers of other health promotion services such as Chlamydia screening |
| No | Advised to return/call if symptoms persist |
Advice (medication management)
| Code | Descriptor |
|---|---|
| Yes | Advice on self-management of prescribed medication here, e.g. advised to use inhalers, ‘use of medication discussed’ |
| No | No advice on medication OR advice is to take medication prescribed at the index consultation |
Advice OTC (over-the-counter medicines)
| Code | Descriptor |
|---|---|
| Yes | Advice given to buy OTC medications at local pharmacist |
| No | No OTC advice given |
Fitness to Work certificate/MED3 (previously known as sickness certificate)
| Code | Descriptor |
|---|---|
| Yes | Fitness to work/MED3 (sickness certificate) given |
| No | No Fitness to work/MED3 (sickness certificate) given |
Referrals
| Code | Descriptor |
|---|---|
| 0 | None OR referral for a diagnostic test only, e.g. X-ray (covered in diagnostic test coding) |
| 1 | Secondary medical care or treatment: referral to medical consultant, service in hospital, trust or independent sector (NHS funded) includes midwives, sexual health clinic, and palliative care. NB this includes urgent referrals via A&E |
| 2 | Allied health professionals and dental, e.g. occupational therapy, physiotherapy, dietician, pulmonary rehabilitation, referral to independent medical services, private referral not NHS funded |
| 3 | Health promotion/public health services, e.g. smoking cessation clinic, exercise on prescription |
| 4 | Psychological therapies, e.g. cognitive–behavioural therapy, counselling |
| 5 | GP within the same practice |
| 6 | For a procedure within the practice, e.g. to practice nurse for immunisations, dressing, ECG, COPD review |
| 7 | Community nursing services (district nurse or health visitor) |
| 8 | Social services |
| 9 | Other |
| 10 | GPWSI (GP with special interest) |
Appendix 6 Research team classification of the presenting problems for the individual patient
| Research team classification for the individual patient | Description of the classification for each patient and presenting problem |
|---|---|
| ACUTE | At least one problem the patient presents with is classified as acute, i.e. listed by de Jong et al.96 or by GP in research team |
| CHRONIC | Patient has no acute problems AND patient has a record on one or more QOF registers (with any presenting problem/Read code) OR at least one problem the patient presents with is classified as chronic by the GP in the research team |
| SYMPTOMS | Patient has no acute problems, no record on a QOF register or no chronic problems AND at least one problem the patient presents with is classified as symptoms, i.e. the Read code95 is in chapter R or 195 or the Read code is in chapter 295 and does not diagnose the problem |
| MINOR | Patient has no acute problems, no record on a QOF register, no chronic problems or no symptoms AND the problem is classified as acute by de Jong et al.96 or by GP in research team |
| PREVENTION | Patient has no acute problems, no record on a QOF register, no chronic problems or no symptoms or no minor problems AND has presented for a health promotion or screening activity (e.g. cervical smear test as categorised) by the GP in the research team |
| ADMINSTRATIVE PROCEDURE | Patient has no acute problems, no record on a QOF register, no chronic problems or no symptoms or no minor problems AND has presented for an administrative procedure (e.g. insurance forms that require medical information) as categorised by the GP in the research team |
Appendix 7 Appropriateness of the consultation review
Clinical Review ID……………………Reviewer initials……………………….
| Patient information | |
|---|---|
| Year of birth: | Data provided by research team |
| Gender: | Data provided by research team |
| Ethnicity: | Data provided by research team |
| Number of QOF disease registers: | Data provided by research team |
| QOF disease registers name: | Data provided by research team |
| Number of repeat prescriptions: | Data provided by research team |
| No of consultations in previous 3 months: | Data provided by research team |
Was the first consultation process conducted appropriately – taking into account that one or more subsequent consultation took place in the following two weeks. i.e. With the benefit of hindsight was the first consultation as good as could reasonably be expected of an NHS GP in UK practice
Please tick either appropriate or inappropriate for each aspect of the consultation in the table. The first consultation is labelled ‘index’ or ‘initial’ with the subsequent labelled ‘Other 1, Other 2, Other X….)
Please write any comments you have regarding ‘important missing information’ or ‘issues’ in the appropriate boxes
| Weed’s SOAP | Appropriate | Inappropriate | Rationale for rating/Important missing information | Comments/Issues | |
|---|---|---|---|---|---|
| S | Subjective information | ||||
| O | Examination | ||||
| A | Investigation | ||||
| P | Prescription | ||||
| P | Problem |
Clinical Review ID…………………
Was the first consultation (the index consultation) conducted appropriately overall according to the available documentation and in the light of the subsequent consultations?
Please tick appropriate, inappropriate or unable to decide
Appropriate □
Inappropriate □
Unable to decide □
If unable, please give reasons (e.g. poor or limited documentation, the way in which problems are conceptualised)
____________________________________________________________________
____________________________________________________________________
Do you think the index clinician was a Physician Assistant or a General Practitioner?
Please tick one box
Physician Assistant □
General Practitioner □
Unable to decide □
Appendix 8 Unit costs used in calculation of practice-level costs
| Staff category | Staff role | Unit costs (per year) | Notes |
|---|---|---|---|
| Medical | GP | £172,223 | Unit costs include wages/salaries, on-costs, qualifications (except HCA and phlebotomist), training (GP only), capital and non-staff overheads, from Curtis119 |
| PA | £81,453 | ||
| NP | £81,453 | ||
| Practice nurse | £49,860 | ||
| HCA | £33,534 | ||
| Phlebotomists | £27,889 | ||
| Administrative and clerical | Practice and surgery managers | £72,097 | Remuneration levels were generated from job vacancy advertisements for appropriate NHS posts (outside of London). On-costs and overheads were added using rates from NHS clinical staff with equivalent salaries119 |
| Specialist advice (IT, finance) | £72,097 | ||
| Deputy practice managers | £40,504 | ||
| Secretaries and receptionists | £33,534 | ||
| Clerical | £27,889 |
Appendix 9 List of commentary papers reviewed, by year
1975
Hull FM. New roles for nurses in general practice – lessons from America. J Roy Coll Gen Pract 1975;25:151–3.
1980
Hambly K. Physician’s assistants in general practice. Br Med J 1980;281:284.
Reedy BLEC, Stewart TI, Quick JB. Attachment of a physician assistant to an English general practice. Br Med J 1980;281:664–6.
1996
Bayley H. Replacing doctors. Nurs Stand 1996;10:19.
Castledine G. Do we need physician assistants in the UK? Br J Nurs 1996;5:124.
Castledine G. Does the NHS need more physician assistants? Brit J Nurs 1996;115:239. URL: www.internurse.com/cgi-bin/go.pl/library/article.cgi?uid=20550;article=BJN_15_4_239_0 (accessed 30 January 2013).
Peysner J. Physician assistants: legal implications of the extended role. Br J Nurs 1996;5:592.
2000
Anon. Physicians’ assistants may attract men into health care. Br J Nurs 2000;9:535. URL: www.internurse.com/cgi-bin/go.pl/library/abstract.html?uid=6285 (accessed 30 January 2013).
Carlisle D. Past masters. HSJ, 20 April 2000. URL: www.hsj.co.uk/news/past-masters/26688.article (accessed 31 January 2013).
Davies J. The devil is in the detail. HSJ, 1 June 2000. URL: www.hsj.co.uk/news/the-devil-is-in-the-detail/27038.article (accessed 30 January 2013).
2001
Allen M. Physician assistants. BMJ Rapid Response, 25 November 2001. URL: www.bmj.com/rapid-response/2011/10/28/physician-assistants (accessed 30 January 2013).
Fenn W. Reflections on the core of the US PA model and its relation to the UK. BMJ Rapid Response, 3 December 2001. URL: www.bmj.com/rapid-response/2011/10/28/reflections-core-us-pa-model-and-its-relation-uk (accessed 30 January 2013).
Gavin M. PAs Can Help Solve the Recruitment Crisis in General Practice. BMJ Rapid Response, 29 November 2001. URL: www.bmj.com/rapid-response/2011/10/28/pas-can-help-solve-recruitment-crisis-general-practice (accessed 30 January 2013).
Hutchinson L, Marks T, Pittilo M. The physician assistant: would the US model meet the needs of the NHS? BMJ 2001;323:1244–7. URL: www.ncbi.nlm.nih.gov/pmc/articles/PMC1121704 (accessed 30 January 2013).
Law H, Sloan J. The physician assistant: an example of established practice. BMJ Rapid Response, 19 December 2001. URL: www.bmj.com/rapid-response/2011/10/28/physician-assiastant-example-established-practice-practise (accessed 30 January 2013).
Loveridge BN. The Boston experience. Accid Emerg Nurs 2001;9:86–91.
Mishra KM. Helper doc. BMJ Rapid Response, 24 November 2001. URL: www.bmj.com/rapid-response/2011/10/28/helper-doc (accessed 30 January 2013).
Morris A. Enough Doctors? BMJ Rapid Response, 1 December 2001. URL: www.bmj.com/rapid-response/2011/10/28/enough-doctors (accessed 30 January 2013).
Neary J. The Physician Assistant. BMJ Rapid Response, 23 November 2001. URL: www.bmj.com/rapid-response/2011/10/28/physician-assistant (accessed 30 January 2013).
Sivakumar R. NICE should look into its cost-effectiveness. BMJ Rapid Response, 30 November 2001. URL: www.bmj.com/rapid-response/2011/10/28/nice-should-its-costeffectiveness (accessed 30 January 2013).
Stephenson J. Deja vu. B MJ Rapid Response, 25 November 2001. URL: www.bmj.com/rapid-response/2011/10/28/deja-vu-1 (accessed 30 January 2013).
Sultan Z. Best use of a Physician’s Assistant. BMJ Rapid Response, 27 November 2001. URL: www.bmj.com/rapid-response/2011/10/28/best-use-physicians-assistant (accessed 30 January 2013).
Teasdale C. We Have Deeper Issues Than the US to Consider. BMJ Rapid Response, 25 November 2001. URL: www.bmj.com/rapid-response/2011/10/28/we-have-deeper-issues-us-consider (accessed 30 January 2013).
Fox J. The role of the PA. BMJ Rapid Response, 25 December 2001. URL: www.bmj.com/rapid-response/2011/10/28/role-pa (accessed 30 January 2013).
2002
Allen M. Physician Assistants – a unique profile for the NHS. BMJ Rapid Response, 4 September 2002. URL: www.bmj.com/rapid-response/2011/10/29/physician-assistants-%E2%80%93-unique-profile-nhs (accessed 30 January 2013).
Baines E. The next big thing – physician assistants. GP, 21 April 2003. URL: www.accessmylibrary.com/article-1G1-100726407/gp-business-next-big.html (accessed 30 January 2013).
Cawley JF, Hooker RS. Physician assistants: does the US experience have anything to offer other countries? J Health Serv Res Policy 2003;8:65–7.
Clews G. Skill-mix beats the city blues: regional focus – London. HSJ 2004;114:36-7. URL: www.hsj.co.uk/news/skill-mix-beats-the-big-city-blues/18966.article (accessed 30 January 2013).
Cohen S. Physician assistant as an export ... At the start. BMJ Rapid Response, 18 May 2002. URL: www.bmj.com/rapid-response/2011/10/29/physician-assistant-exportat-start (accessed 30 January 2013).
Editorial. The way we work now. BMJ 2002;325:8. URL: www.bmj.com/content/325/7362/0.8 (accessed 30 January 2013).
Fenn W. American idea of PAs can be anglicised. BMJ 2002;324:735. URL: www.ncbi.nlm.nih.gov/pmc/articles/PMC1122653 (accessed 30 January 2013).
Gatrad AR. The introduction of Asst. Physicians will help improve workforce problems in the UK. BMJ Rapid Response, 18 January 2002. URL: www.bmj.com/rapid-response/2011/10/28/introduction-asst-physicains-will-help-improve-workforce-problems-uk (accessed 30 January 2013).
Gavin M. Physician assistants. Many general practitioners would welcome having physician assistants. BMJ 2002;324:735. URL: www.ncbi.nlm.nih.gov/pmc/articles/PMC1122653 (accessed 30 January 2013).
Mittman D, Cawley F, Fenn W. Physician assistants in the United States. BMJ 2002;325:485–7. URL: www.ncbi.nlm.nih.gov/pmc/articles/PMC1124003 (accessed 30 January 2013).
2003
Raynsford J. Directive action. HSJ 2003;113:34–5.
2004
Anon. College aims to expand. Hosp Doct, 23 September 2004, p. 8.
Brown G. Not a quick enough solution. Nurs Stand 2004;18:23.
Cantazaro R. Physician assistants. Br J Diabetes Vascul Dis 2004;4:343.
Clarkson D. Downsides to the idea. Nurs Stand 2004;18:22.
Davies E. RCGP rejects physician practitioners scheme. GP, 19 November 2004, p. 10. URL: http://connection.ebscohost.com/c/articles/15165251/rcgp-rejects-physician-practitioners-scheme (accessed 30 January 2013).
Dix A. Assistants required. HSJ 2004;114:28–9. URL: www.hsj.co.uk/news/assistants-required/17568.article (accessed 30 January 2013).
Duffin C. New kid in town. Nurs Stand 2004;19:12–13.
Editorial. Educating with evidence. Lancet 2004;363:1485. URL: www.thelancet.com/journals/lancet/article/PIIS0140-6736(04)16181-3/fulltext (accessed 30 January 2013).
Health I. The medical care practitioner: newspeak and the duping of the public. Br J Gen Pract 2004;55:229. URL: www.ncbi.nlm.nih.gov/pmc/articles/PMC1463096 (accessed 30 January 2013).
Henry J. Medical degrees lasting two years created to fill shortage of GPs. The Telegraph, 1 February 2004. URL: www.telegraph.co.uk/news/uknews/1453156/Medical-degrees-lasting-two-years-created-to-fill-shortage-of-GPs.html (accessed 30 January 2013).
Holyoake D-D. History should allay our fears. Nurs Stand 2004;18:23.
Hutchinson L. Lets help PAs into medicine. HSJ 2004;114:24. URL: www.hsj.co.uk/news/lets-help-pas-into-medicine/17788.article (accessed 30 January 2013).
Kelly PE. Across the pond: learning from the UK National Health Service. JAAPA 2004;17:52–4.
Lamb L. Physician assistant – management perspective. Br J Diabetes Vasc Dis 2004;4:347–8.
Malik N. Physician assistants are a quick fix. Student BMJ 2004;12:133–76.
Tyke J. Re-inventing the wheel. Prac Nurse 2004;27:74.
Walton I. Why have a physician assistant? Br J Diabetes Vasc Dis 2004;4:345–6.
Wheatley M. Nurses can deliver. Nurs Stand 2004;18:23.
2005
Anon. Physician assistants: opportunity or duplication? Independent Nurse, 1 October 2005. URL: www.internurse.com/cgi-bin/go.pl/library/article.cgi?uid=73793;article=indnurse_2005_10%2000_;format=html (accessed 30 January 2013).
Anon. Detail of training and regulation for medical care practitioners revealed. Independent Nurse, 1 November 2005. URL: www.internurse.com/cgi-bin/go.pl/library/article.cgi?uid=73224;article=indnurse_2005_11%2000_;format=html (accessed 30 January 2013).
Anon. RCP lays down law on physician assistants. Hospital Doctor, 18 August 2005, p. 2.
Anon. Concern at rise in use of US-style physician assistants. Independent Nurse, 1 September 2005. URL: www.internurse.com/cgi-bin/go.pl/library/article.cgi?uid=73156;article=indnurse_2005_9%2000_;format=html (accessed 30 January 2013).
Anon. Scotland considers physician assistants. Independent Nurse, 1 September 2005. URL: www.internurse.com/cgi-bin/go.pl/library/article.cgi?uid=72312;article=indnurse_2005_9%2000_;format=html (accessed 30 January 2013).
Anon. Doctors’ fears over NHS ‘assistants’. Daily Mail, 4 November 2005. URL: www.dailymail.co.uk/health/article-367601?doctors-fears-NHS-assistnts.html (accessed 30 January 2013).
Anon. New breed of medics ‘will cut waiting times’. The Guardian 4 November 2005. URL: www.guardian.co.uk/society/2005/nov/04/health.politics (accessed 30 January 2013).
Anon. DoH defends controversial physicians assistants. Independent Nurse, 1 October 2005. URL: www.internurse.com/cgi-bin/go.pl/library/article.cgi?uid=72364;article=indnurse_2005_10%2000_;format=html (accessed 30 January 2013).
Armitage M, Shepherd S. A new professional in the healthcare workforce: role, training, assessment and regulation. Clinical Medicine 2005;5:311–14. URL: www.clinmed.rcpjournal.org/content/5/4/311.full.pdf+html (accessed 30 January 2013).
Asthana A. Doctors’ safety fears over plans for assistants. The Observer, 30 October 2005. URL: www.guardian.co.uk/news/2005/oct/30/medicineandhealth (accessed 30 January 2013).
Dayani A. City Drafts in American Medics. icBirmingham.co.uk; 2005. URL: http://icbirmingham.icnetwork.co.uk/0100news/0100localnews/2005/09/19/city-drafts-in-american-medics-50002-16148722 (accessed 30 January 2013).
Hedges JR. Physician extenders in the emergency department. Emerg Med J 2005;22:314–15. URL: http://emj.bmj.com/content/22/5/314.full (accessed 30 January 2013).
O’Dowd A. Move over, Rover: regional focus – Midlands. HSJ 2005;111:42–3. URL: www.hsj.co.uk/news/move-over-rover/15671.article (accessed 30 January 2013).
Paniagua H, Callwood I. Creating a new health-care practitioner. Practice Nursing 2005;16:540–1.
Paniagua H, Stewart A. Medical care practitioners: introducing a new profession into the UK. Br J Nursing 2005;14:405–8.
Robinson F. Are US style physician assistants needed? Hospital Doctor, 6 October 2005, p. 22. URL: www.accessmylibrary.com/article-1G1-138857012/physician-assistants-worthwhile.html (accessed 30 January 2013).
Snow T. Are physician assistants worthwhile? GP, 18 November 2005, pp. 16–17. www.accessmylibrary.com/article-1G1-138857012/physician-assistants-worthwhile.html (accessed 30 January 2013).
Robinson F. Medical care practitioners. Practice Nurse 2005;30.
Snow T. News Focus: New role criticised by nurses. Independent Nurse, 1 November 2005. URL: www.internurse.com/cgi-bin/go.pl/library/abstract.html?uid=73246 (accessed 30 January 2013).
Snow T. News Focus: Will new role help or hinder nurses? Independent Nurse, 1 September 2005. URL: www.internurse.com/cgi-bin/go.pl/library/article.cgi?uid=73149;article=indnurse_2005_9%2000_;format=html (accessed 30 January 2013).
Stewart A, Catanzaro R. Can physician assistants be effective in the UK? Clin Med 2005;5:344–8. URL: http://centrallobby.politicshome.com/Resources/epolitix/Forum%20Microsites/Royal%20College%20of%20Physicians/ClinMed2.54.344to348.pdf (accessed 30 January 2013).
Smith JS, Tevis B, Murali K. Commentary from the front lines: American physician assistants working in a United Kingdom emergency department. Emerg Med J 2005;22:322–4. URL: http://emj.bmj.com/content/22/5/322.abstract (accessed 30 January 2013).
Sparrow N, Lakhani M. Improving support for doctors in the UK: The developed of a modified physician assistant model in primary care and internal medicine. Malta Med J 2006;18:10–11. URL: www.um.edu.mt/umms/mmj/PDF/126.pdf (accessed 30 January 2013).
Tyrer L. A day in the life. How PAs live and work. JAAPA 2005;18:17–18.
2006
Anon. Prescribing key for new PA role. Independent Nurse, 1 October 2006. URL: www.internurse.com/cgi-bin/go.pl/library/article.cgi?uid=74368;article=indnurse_2006_10%2000_;format=html (accessed 30 January 2013).
Anon. Scotland PA numbers lower than hoped. Independent Nurse, 1 September 2006. URL: www.internurse.com/cgi-bin/go.pl/library/article.cgi?uid=74262;article=indnurse_2006_9%2000_;format=html (accessed 30 January 2013).
Anon. Scotland to recruit physician assistants on salaries of 40k. Independent Nurse, 1 June 2006. URL: www.internurse.com/cgi-bin/go.pl/library/article.cgi?uid=72713;article=indnurse_2006_6%2000_;format=html (accessed 30 January 2013).
Armitage M. Advanced care practitioners – friend or foe? Lancet 2006;367:375.
Davies E. Physician assistants set to replace retiring GPs. GP 2006;11. URL: http://web3.local.www.gponline.com/News/article/604916/Physician-assistants-set-replace-retiring-GPs (accessed 30 January 2013).
Dimond B. IV therapy: nurses must be competent to perform new duties. Brit J Nurs 2006;15:952–3. URL: www.internurse.com/cgi-bin/go.pl/library/article.cgi?uid=21913;article=BJN_15_17_952_953;format=pdf (accessed 30 January 2013).
Green D, Sebel PS. Anaesthesia practitioners in the UK: the high road, not yet taken. Eur J Anaesthesiol 2006;23:899–901. URL: http://journals.cambridge.org/action/displayAbstract?fromPage=online&aid=507484 (accessed 30 January 2013).
Hammond P. The transatlantic saviours of Weston-super-Mare. Guidelines in Practice 2005;9. URL: www.eguidelines.co.uk/eguidelinesmain/gip/out_of_hours/hammond_apr06.htm (accessed 30 January 2013).
Langlands E. NHS hires £43,000-a-year ‘super-nurses’. Sunday Times, 26 November 2006. URL: www.timesonline.co.uk/tol/news/uk/scotland/article650577.ece (accessed 30 January 2013).
Limb M. Medical care practitioners: an emergency response? Charted Soc Physiother 2006;11. URL: www.csp.org.uk/frontline/article/medical-care-practitioners-emergency-response (accessed 30 January 2013).
Lopes JE. General practice in the UK’s National Health Service. JAAPA 2006;19:24,26,29–30.
Parle JV, Ross NM, Doe WF. The medical care practitioner: developing a physician assistant equivalent for the United Kingdom. Med J Aust 2006;185:13–17. URL: www.mja.com.au/journal/2006/185/1/medical-care-practitioner-developing-physician-assistant-equivalent-united (accessed 30 January 2013).
Reynolds T. Medical care practitioners: a necessary import? Student BMJ 2006;14:309.
Weller DP. Workforce substitution and primary care. Med J Aust 2006;185:8–9.
2007
Anon. DoH retreats from physician assistants. Independent Nurse, 1 March 2007. URL: www.internurse.com/cgi-bin/go.pl/library/article.cgi?uid=74685;article=indnurse_2007_3%2000_;format=html (accessed 30 January 2013).
Anon. Wales funds two-year pilot to recruit US physician assistants. Independent Nurse, 1 January 2007. URL: www.internurse.com/cgi-bin/go.pl/library/article.cgi?uid=74527;article=indnurse_2007_1%2000_;format=html (accessed 30 January 2013).
Anon. Physician assistant. Pulse Today, 26 September 2008.
Begg P, Ross N, Parle J. Physician assistant education in the United Kingdom: the first five years. J Physician Assistant Educ 2008;19:47–50. URL: www.paeaonline.org/index.php?ht=a/GetDocumentAction/i/60859 (accessed 30 January 2013).
Legler CF, Cawley JF, Fenn WH. Physician assistants: education, practice and global interest. Med Teach 2007;29:e22–5. URL: http://informahealthcare.com/doi/pdf/10.1080/01421590601034696 (accessed 30 January 2013).
Saleem A. Dumbing down Doctors. Hospital Doctor 2007;33.
2008
Ross N, Parle J. Physician Assistants: a UK perspective on clinical need, education and regulation. Clin Teach 2008;5:28–32. URL: http://onlinelibrary.wiley.com/doi/10.1111/j.1743-498X.2007.00181.x/abstract (accessed 30 January 2013).
Shepherd S. New roles in the health sector. HSJ, 17 June 2008. URL: www.hsj.co.uk/resource-centre/new-roles-in-the-health-sector/1339846.article (accessed 30 January 2013).
2009
Allen M. Our Practice Needs Help – But is a Physician Assistant the Answer? Wessex Faculty e-bulletin, December 2009. URL: www.rcgp.org.uk/college_locations/english_faculties_home/southern_england_faculties/wesses_faculty_archive/ebulletin_dec_2009.aspx (accessed 7 July 2011).
Gainsbury S. Nurses accused of professional protectionism. Nursing Times, 3 November 2009. URL: www.nursingtimes.net/whats-new-in-nursing/primary-care/nurses-accused-of-professional-protectionism/5008012.article (accessed 30 January 2013).
Kharay G. The physician assistant. LSJM 2009;1:194–5. URL: http://issuu.com/lsjm/docs/thelsj (accessed 30 January 2013).
Kmietowicz, Z. Margaret Allen: A force in humanising the American healthcare system. BMJ 2009;339:b3938. URL: www.bmj.com/content/339/bmj.b3938 (accessed 30 January 2013).
Parle J, Begg P. Physician assistants: UK universities are on the case. BMJ Rapid Response, 22 October 2009. URL: www.bmj.com/rapid-response/2011/11/02/physician-assistants-uk-universities-are-case (accessed 30 January 2013).
Robinson F. The new role of physician assistant. Prac Nurse 2009;38:9–10.
Westwood O. Physician Assistant role for the UK. BMJ Rapid Response, 27 October 2009. URL: www.bmj.com/rapid-response/2011/11/02/physician-assistant-role-uk (accessed 30 January 2013).
2010
Anon. Extended roles. BMJ Careers, 22 May 2010. URL: http://careers.bmj.com/careers/advice/view-rapid-responses.html?id=20001023 (accessed 30 January 2013).
Elegbe O. GP commissioning consortia: is there a role for physician assistants in routine care? Br J Gen Prac 2010;60:704–5. URL: www.ncbi.nlm.nih.gov/pmc/articles/PMC2930240 (accessed 30 January 2013).
Goudie S. The physician assistant. BMJ Careers, 19 May 2010. URL: http://careers.bmj.com/careers/advice/view-article.html?id=20001023 (accessed January 30 2013).
Kelly P. PAs in the UK. 2010. BMJ Careers, 20 May 2010. URL: http://careers.bmj.com/careers/advice/view-rapid-responses.html?id=20001023 (accessed January 30 2013).
Sajayan A. Take it with a pinch of salt. BMJ Careers, 24 May 2010. URL: http://careers.bmj.com/careers/advice/view-rapid-responses.html?id=20001023 (accessed 30 January 2013).
Vas S. The physician assistant. Br J Gen Prac 2010;60:855. URL: www.ncbi.nlm.nih.gov/pmc/articles/PMC2965977 (accessed 30 January 2013).
2011
Dowsing T. Interface Geriatrics: A Physician Assistant’s Perspective. BGS Newsletter, October 2011, pp. 19–20. URL: www.ukapa.co.uk/files/interface-geriatrics.pdf (accessed 30 January 2013).
Moghal N. Exploring the US physician assistant model: a contribution to QIPP. HSJ, 24 March 2011. URL: www.hsj.co.uk/resource-centre/best-practice/exploring-the-us-physician-assistant-workforce-model-a-contribution-to-qipp/5026533.article (accessed 30 January 2013).
Tims A. Graduate careers: EU paves way for new healthcare roles. The Guardian, 18 June 2011. URL: www.guardian.co.uk/money/2011/jun/18/graduate-careers-healthcare-roles-physicians-assistants/print (accessed 30 January 2013).
2012
Ostler J, Vaddilas C, Parle J. Physician assistants: friends or foes to doctors? BMJ Careers, 18 July 2012. URL: http://careers.bmj.com/careers/advice/view-article.html?id=20008022 (accessed 30 January 2013).
Glossary
- Clinical Commissioning Group (CCG)
- A group including GPs, at least one registered nurse and a secondary care doctor that, since April 2013, has had responsibility for commissioning local health services in England.
- Confidence interval (CI)
- A measure of the uncertainty of statistical estimates arising from the fact that studies include only a sample and not the entire population of patients of interest. A 95% CI has a 95% probability of containing the corresponding value in the entire population.
- Family medicine
- Used in countries outside the UK, particularly the USA, to refer to the medical specialty known in the UK as general practice.
- Local education and training board (LETB)
- A local health care employer-led organisation in England that, since April 2013, has been able to plan and commission the supply of all health professionals and also allocate monies for continuing professional development training requirements.
- Logistic regression
- A statistical procedure to find the factors that predict an outcome that is either present or absent, such as whether or not advice on medication was given. The effect of each predictor is measured in terms of an odds ratio.
- Mid-level practitioner
- A term used to describe a qualified health professional (non-medical and non-dental) who is practising at a level with authority to assess, investigate and commence or change treatment within the agreed scope of practice with his or her employer and/or clinician supervisor.
- Odds ratio (OR)
- A measure of how big an effect a predictor (such as whether a PA or a GP saw the patient) has on an outcome that is either present or absent (such as whether or not advice on medication was given). If one-third of patients seeing a GP received such advice, the odds are 1/2 = 0.5 (the number with the outcome divided by the number without). An OR of 1.4 then suggests that the odds among people who saw PAs will be 1.4 × 0.5 = 0.7.
- p -value
- A statistical measure of how convincing the evidence is for a difference or effect seen in the sample also being true in the whole population of patients attending general practices. It is the probability that the observed difference (or an even greater one) could have occurred by chance if there really is no difference in the population.
- Physician assistant (PA)
- A medical professional who works as part of a team with a doctor following a 2-year postgraduate qualification. PAs perform physical examinations, diagnose and treat illnesses, request and interpret laboratory tests, and make referrals. They can work in all health-care settings.
- Primary care
- A term used in the UK setting to refer to first contact care and entry into the health-care system, continuous and ongoing patient-focused care for a defined population, co-ordination of care and comprehensiveness of services.
- Quality Outcomes Framework (QOF)
- The QOF is a voluntary annual incentive programme against nationally agreed clinical and management criteria for all GP surgeries in England.
- Rate ratio
- A measure of how big an effect a predictor (such as whether a PA or a GP saw the patient) has on an outcome that is measured as a count (such as how many reconsultations took place). If patients seeing a GP had 1.5 reconsultations per fortnight on average, then this is the rate. A rate ratio of 1.1 then suggests that the rate among people who saw PAs will be 1.1 × 1.5 = 1.65.
- Same-day appointments
- Appointments that are requested and booked on the same day (sometimes known as unscheduled, in contrast to those pre-booked in advance), which indicates a patient-perceived need for an immediate consultation.
List of abbreviations
- CCG
- Clinical Commissioning Group
- CfWI
- Centre for Workforce Intelligence
- CI
- confidence interval
- DCG
- diagnostic care group
- df
- degree of freedom
- GMS
- General Medical Services
- GP
- general practitioner
- GPAS
- General Practice Assessment Survey
- HCA
- health-care assistant
- HCP
- health-care professional
- HEI
- higher education institution
- IMD
- Index of Multiple Deprivation
- IQR
- interquartile range
- IT
- information technology
- LAP
- Leicester Assessment Package
- LETB
- local education and training board
- NIHR
- National Institute for Health Research
- NP
- nurse practitioner
- OR
- odds ratio
- PA
- physician assistant
- PCRN
- Primary Care Research Network
- PMS
- Personal Medical Services
- PN
- practice nurse
- QOF
- Quality and Outcomes Framework
- RCP
- Royal College of Physicians
- REC
- research ethics committee
- SD
- standard deviation
- SHA
- Strategic Health Authority
- study ID
- study identifier
- UKAPA
- UK Association of Physician Assistants
- UKCRN
- UK Clinical Research Network
- WTE
- whole-time equivalent