Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 08/1806/261. The contractual start date was in November 2009. The final report began editorial review in August 2013 and was accepted for publication in March 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Peckham et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
It is estimated that some 15 million people in England have a long-term condition (LTC) and that this number will continue to increase. People with a LTC have, to varying degrees, a long-standing relationship with local health services. Concern about whether or not the NHS meets the needs of people with LTCs emerged in the 1990s. 1 The previous Labour government emphasised the need for better services developing a national strategy for people with LTCs, service developments, improved patient and public involvement (PPI) and supporting new service developments. 2,3 PPI was a key element of policy responses to developing services for people with LTCs, with a particular emphasis on PPI in commissioning. 4
Importantly, however, the emphasis on PPI has been continued by the current government and the NHS Mandate5 places a responsibility on the NHS to improve the co-ordination of care for people with LTCs. In particular, NHS England and Clinical Commissioning Groups (CCGs) are required to improve services and, in particular, develop commissioning strategies that address the needs of people with chronic LTCs, support strategies for self-help and engage them in decisions about the services they receive. 6 In Equity and Excellence: Liberating the NHS,7 the coalition government explicitly set a key task for the new NHS commissioning board (NHS England) to champion patient and carer involvement, and stated that the Secretary of State would hold it to account for progress. This represents a significant challenge, not only for NHS England but also for local CCGs. However, there has been an important change in language and terminology. Equity and Excellence refers to engagement as a key route for clinical commissioners to take rather than involvement, which was a term used previously in policy documents and guidance. While such a change may, in reality, be semantic, meanings are quite important; as we shall discuss later in this report, a problem exists of terms being used interchangeably while, at the same time, different stakeholders and individuals confer different meanings to the same terms. 8 Involvement and engagement were terms used interchangeably in the data. We have used the term PPI where it was clear that it related to PPI. Patient and public engagement and involvement (PPEI) has been used in this report as an overarching term to describe activities involving engagement and involvement.
In 2007, government proposals for people with LTCs suggested that user groups were to be key to increasing the devolution of decisions to practice-based commissioners (now abolished) and the development of ‘strategic commissioning’ between health and social care agencies. 9 Guidance for commissioning agencies, published in 2007, placed great importance on how commissioners could procure care that promoted the health and well-being of individuals in consultation with local people. 10 These were incorporated into the commissioning competencies, needs assessment frameworks and performance regimes across health and social care, and there was a clear emphasis on increasing the role of the third sector. 11–13 The NHS Next Stage Review14 highlighted changing public expectations related to ‘control, personalisation and connection’, and building partnerships with patients and LTC user groups.
While the policy direction for commissioning was clear, implementation was variable as primary care trusts (PCTs) coped with a complex blend of incentives and regulatory arrangements. Practice-based commissioning (PBC) was seen as integral to the success of commissioning strategies for LTCs but remained underdeveloped, had little significant effect on the redesign of services and did not sufficiently engage most general practitioners (GPs) in commissioning. 15,16 Good commissioning for people with LTCs requires not only developing a set of skills for commissioning responsive and appropriate patient pathways that provide relevant choices for service users, but also developing approaches to sustaining user engagement. Research on engaging users in the NHS and on user involvement in change management in health services has demonstrated a willingness and commitment to engagement, but few, if any, concrete examples of effective influence by users or evidence of change. 17,18
While the importance of PPI in commissioning has been recognised since the initial development of NHS purchasing in the 1990s, there has not been any significant evidence that such engagement has influenced commissioning decisions. 8,17–19 In 2007, a Picker Institute survey found that, while PCTs had a number of mechanisms and defined management responsibilities for PPI, ‘. . . there is a disconnect between these activities and the relatively low expectation that patient, public and community groups will have significant influence on commissioning decisions’ (p. 15). 18 Key barriers identified were difficulties in reaching marginalised, isolated or deprived groups, a lack of understanding among the public of ‘commissioning’ and a lack of reliable data about patients’ experiences. However, when respondents to the Picker survey were asked what approaches PCTs were considering for future engagement, there was a continued emphasis on methods such as formal consultations, patient panels, citizens’ juries and surveys.
It was in this context that our original proposal to the National Institute for Health Research (NIHR) was developed. The research brief highlighted a number of areas for research relating to the organisation and processes of commissioning, with particular reference made to commissioning for people with LTCs. Our project responded to these general issues and explicitly focused on the question in the brief related to PCTs and their PBCs to ensure that ‘voice’ and community engagement, as set out in both Our Health, Our Care, Our Say White Paper and World Class Commissioning, are achieved.
Aims and objectives
The projects initial aim was, therefore, to examine how commissioners enable voice and engagement of people with LTCs and identify what impact this has on the commissioning process and pattern of services. A key outcome of the research will be guidance on the skills and expertise needed by different commissioners, what actions are most likely to lead to responsive services and the most effective mechanisms and processes for active and engaged commissioning for people with LTCs. Our specific objectives were to:
-
critically analyse the relationship between the public/patient voice and the impact on the commissioning process
-
determine how changes in the commissioning process reshape local services
-
explore whether or not any such changes in services impact on the patient experience
-
identify if and how commissioners enable the voice and engagement of people with LTCs
-
identify how patient groups/patient representatives get their voice heard and what mechanisms and processes patients and the public use to make their voice heard.
While the specific aim of the research did not change, the specific focus on methods had to be adapted to undertaking the research within a dynamic and rapidly changing context. However, this did provide the opportunity to investigate how PPI developed at this time of transition and what specific processes and structures for PPI were being developed within the new emerging commissioning architecture of the English NHS. As such, the aims and objectives remained the same but we have adapted our research protocol to address this changing context (see Chapter 3).
The study
Over the last 10–15 years, there has been an increasing recognition that the NHS needs to improve the support and service that it provides to people with LTCs. The current context for this is within a framework where commissioners are expected to develop stronger roles in shaping and planning local services that are responsive to local needs. In relation to LTCs, policies of choice and PPI are key to how this will be achieved. The key objectives of this study were to examine processes – how people were involved in local commissioning decisions – and impact – what was the result of that involvement.
However, the study was undertaken during a period of extensive change within the English NHS. In particular, the abolition of PCTs and development of CCGs created an ever-changing local context for our case study research, but this was only part of a much wider and far-reaching reorganisation of the English NHS introduced by the coalition government and enshrined in the Health and Social Care Act 2012 (discussed further in Chapter 2). 20 This had a significant impact on the conduct of the research in terms of both the activities we initially intended undertaking and conducting the case study research which was designed to incorporate interviews with key informants on a regular basis.
In 2009, when the project commenced, PCTs were the main commissioning organisations within the NHS, with practice-based commissioners having been developed in some areas. The original study design was focused on case studies of PCTs and our case studies were selected to reflect differences between PCTs (rural, urban, strong PBC presence, etc.). At this time it was clear that increasing emphasis was being placed on the role of PBCs and, as a result of reduced management cost funding and stronger PBCs, some PCTs were already merging into larger commissioning organisations. 21 With the election of the new coalition government in 2010 and publication of Equity and Excellence: Liberating the NHS,7 the pace of change increased, with proposals for a major restructuring of the English NHS. In particular, commissioning responsibilities, which had predominantly been invested in PCTs, were now redistributed across new GP-led commissioning groups, NHS England and local authorities (see Appendix 11). The reforms led to further PCT mergers into clusters and the development of new GP commissioning groups, with a formal Pathfinder CCG programme launched at the end of 2010. 22 By April 2012, all areas of the country had emerging CCGs and PCT clusters were beginning to reform into commissioning support organisations. During 2012–13, these groups then went through an authorisation process to become statutorily responsible for NHS commissioning from April 2013.
Patient and public involvement has been a key theme in health policy in the UK since the introduction of the internal market by the Conservative government in the early 1990s and continues to be prominent in the current coalition government policy. 7 The changes introduced by the Health and Social Care Bill also involved further reorganisation of PPI structures. The government has dismantled much of the PPI infrastructure of the previous Labour government, replacing it with new developments at the primary care level and in the role of local authorities. The only aspect of previous PPI structures that has been retained is the governance of NHS foundation trusts with the emphasis on membership from staff, patients and the public. CCGs, which will be led by GPs, will be commissioning health care to meet the needs of their local population. They ‘will need to engage patients and the public on an ongoing basis as they undertake their commissioning responsibilities, and will have a duty of public and patient involvement’ (p. 7). 7 Key changes to the role of local authorities in health care aim to align PPI with the ‘democratic oversight’ role of councils.
We planned to undertake a scoping review of PCT PPI activities across England. We commenced this work to plan in late 2009, drawing data from websites and then selecting a sample of PCTs to follow up in more detail where we identified particular good practice (see Chapter 2 for details). However, with the abolition of PCTs, this information has become redundant, and it was decided, and agreed with NIHR, that we would not produce a scoping review report. We also faced problems in case study site recruitment and access, given the extent of the reorganisation. During the research, many of the NHS staff we initially interviewed left their jobs, and new staff, in new organisations, took over responsibilities. This created a number of difficulties tracking developments in case study areas. While the research was being undertaken, we had the opportunity to collaborate with research being undertaken by the Policy Research Unit in Commissioning and the Healthcare System (PRUComm). This involved surveys of all CCGs (in December 2011 and May 2012) and case study research in eight CCGs. We negotiated and discussed questions on PPI in order to enrich our data collection. We discussed this and agreed the change with NIHR.
However, the delays in case study recruitment meant that we needed further time for data collection. The team also felt that it would be most useful if we could have sufficient time to explore changes being introduced by the new CCGs. We approached NIHR to ask for an extension to July 2013. This would allow us to undertake an analysis of CCG approaches to PPI in authorisation plans and draw on the PRUComm data. This was agreed and the end date for the research was changed from November 2012 to July 2013.
As an integral element of our study, we responded to a call to apply for funding for a management fellow to work with the project team. We were successful in being awarded funding for a NHS manager from one of our case study sites to work part-time with the research team and who undertook further research training.
Thus, the study draws on data from a literature of commissioning and PPI as well as PPI related to LTCs, case study data collected as part of this research, survey and case study findings from the PRUComm research (see Chapters 4–7) and an analysis of CCG authorisation plans.
Structure of this report
This report presents the key findings of the research and sets these within the context of the recent changes to the organisation and structure of the English NHS and key conceptual frameworks relating to PPEI. Chapter 2 discusses the background to the project and a summary of the key NHS changes that occurred during the period within which the research was undertaken. In Chapter 3, we set out the methods used, and challenges faced, in the process of undertaking the research. Chapters 4–6 present the findings from our three case studies. Chapter 7 discusses the organisational changes in the NHS in more detail, focusing on the development of CCGs and the extent to which PPI has been prioritised and embedded in practice. This chapter draws on data from surveys and case study research undertaken by PRUComm (directed by Peckham) and undertaken at the same time as the research in this study, as well as an analysis of authorisation plans of a sample of CCGs. Chapter 8 discusses our findings. In Chapter 9, we summarise the main conclusions of our research in relation to the key research objectives. In order to provide some summative assessment of the impact of PPEI, we also include here the responses from an expert reference group who independently reviewed three selected exemplars drawn from our case study research. Drawing on the findings of the research, we then identify key guidance points for national and local organisations and make recommendations for future research.
Chapter 2 Background
Introduction
The treatment and management of LTCs is one of the greatest challenges facing health systems around the world today and is recognised as being of particular importance within the UK NHS. 23 The strategies used by health professionals to engage, support and empower people with LTCs have an important role in improving health outcomes. 24–26 However, there is continued recognition that the NHS has not provided sufficient support for people with LTCs or managed their care to their, or the NHS’s, benefit.
It is suggested that there are around 15 million (almost one in three) people who have one or more LTCs in England and this accounts for in excess of 70% of the total health and social care budget. 27 This relates to around 50% of all GP visits, 64% of all hospital outpatient appointments and 70% of all inpatient bed-days. 28 People with LTCs experience poor co-ordination of care, leading to adverse events and increased hospitalisations. International comparisons suggest that the UK lags behind other countries in supporting people with LTCs. 29,30 While it is difficult to identify exact numbers of people with specific conditions given the rise in multimorbidity, the numbers of people with diabetes, neurological problems or rheumatoid arthritis (RA) do differ, with the first of these three conditions comprising the largest number of patients. It is currently estimated that 2.5 million people in England are living with diabetes, and a further 850,000 people in the UK have diabetes but either are unaware or have no confirmed diagnosis. 31 The NHS spends approximately £10B per annum on treating diabetes and 80% of NHS spending on diabetes goes into managing avoidable complications. People with diabetes account for around 19% of hospital inpatients at any one time, and have a 3-day-longer stay on average than people without diabetes. Most type 2 diabetes costs are due to hospitalisation. 31
Taken together, neurological conditions are common. For example, 8 million people in the UK suffer from migraine. 32 Altogether, approximately 10 million people across the UK have a neurological condition. 33 These account for 20% of acute hospital admissions and are the third most common reason for seeing a GP. Around 17 people in a population of 100,00034 are likely to develop Parkinson’s disease and two people in a population of 100,000 experience a traumatic spinal injury every year. 32 An estimated 350,000 people across the UK need help with daily living because of a neurological condition and 850,000 people care for someone with a neurological condition. 33
Rheumatoid arthritis affects some 580,000 people in England. There are around 12,000 children under the age of 16 with the juvenile form of the disease. The total cost to the UK (including indirect costs and work-related disability) are estimated to be between £3.8B and £4.75B per year. 35 Uncontrolled RA increases mortality through an increased risk of cardiovascular disease such as heart attacks and strokes; thus, early detection and treatment and good management of the disease are important. 35
Government policy on long-term conditions
Since the NHS Plan, the government has been committed to improving support for people with LTCs and set public service agreements in 2005 to reduce emergency bed use and introduce case management for high intensive service users. 1,36–38
The Department of Health policy Your Health, Your Way39 identified five key outcomes for people with LTCs: an improved quality of life, health and well-being and more independence; better supported self-care; more choice and control, with services built around their needs; influence over the design of services that would be more integrated, proactive and responsive; and high-quality, efficient and sustainable services.
This builds on the quality requirements for people with LTCs set out in the National Service Framework for Long-Term Conditions38 that provided a framework for commissioning and service delivery.
A key policy theme has been enabling ‘person-centred’ or ‘personalised’ care. 2 Commissioning is central to this process and to the achievement of policy on LTCs. 9 Yet commissioning for health, and in particular, commissioning in the NHS has received much criticism. 40–42 Research highlights the need for substantial management investment and a range of needs assessment, clinical, contracting and relationship management skills. 40,41,43,44
Commissioning for long-term conditions
When the study commenced, it was already clear that additional investment in expanding commissioning management was unlikely, given concerns about whether or not the additional cost would produce sufficient gains in productivity. 42 In fact, in 2009, it was already identified that savings would need to be made in management costs in the NHS as part of a package of measures to address future NHS funding shortfalls. 45,46 With the introduction of changes outlined in Equity and Excellence: Liberating the NHS7 and enacted in the Health and Social Care Act 2012, the challenges facing commissioners have intensified. In particular, reductions in the overall management allowance mean that there are fewer resources available to support commissioning activities, including PPI. In addition, the proposals, which involved the largest restructuring of the NHS since its inception, created a more complex commissioning structure than that which existed prior to 2010, with responsibilities now spread between a number of local and national agencies (see Appendix 13).
Equity and Excellence set out the rationale behind the proposed changes to commissioning, arguing that the closer involvement of GPs in the commissioning of care would ensure more effective dialogue between primary and secondary care; decision-making ‘closer to the patient’; and increased efficiency. 7 The White Paper argued explicitly that ‘we will learn from the past’ (p. 28)7 and claimed that the government had built upon lessons learned from previous clinically-led commissioning initiatives, including GP Fundholding and Total Purchasing Pilots from the 1990s. 47,48 The reforms were set out in the Health and Social Care Bill which became the 2012 Act following a controversial passage through parliament with a substantial number of amendments. 22 With the Health and Social Care Act 2012 passed by parliament, additional guidance was published by the Department of Health (and subsequently by the shadow NHS Commissioning Board) (Box 1). A timetable was set out for CCGs to apply for full ‘authorisation’ as statutory bodies from July 2012, with the first CCGs taking full responsibility for commissioning from April 2013.
-
Developing Clinical Commissioning Groups: Towards Authorisation. 49
-
The Functions of GP Commissioning Consortia. A Working Document. 50
-
Commissioning Support: Clinical Commissioning Group Running Costs Tool. A ‘Ready Reckoner’. 51
-
Towards Establishment: Creating Responsive and Accountable Clinical Commissioning Groups. 52
-
Developing Commissioning Support: Towards Service Excellence. 53
-
Clinical Commissioning Group Governing Body: Roles Outlines, Attributes and Skills, in April 2012. 54
Two hundred and eleven CCGs worked towards becoming authorised by the National Commissioning Body, NHS England, by the end of March 2013 (see Chapter 7 for a discussion of the authorisation process). Since April 2013, they have been responsible for contracts with providers of health care in their communities amounting to around £65B per annum.
In relation to commissioning services for people with LTCs, commissioners need to demonstrate how they can achieve maximum benefit within existing resource levels by focusing activities on those that bring most patient benefit. This approach is central to the Quality, Innovation, Productivity and Prevention (QIPP) agenda for LTCs. 55 One approach currently under discussion is greater integration of health services along the lines of the USA’s integrated purchaser/provider models or making greater use of soft methods of persuasion. 1,42 The previous government placed an emphasis on developing choices by engaging local users and organisations for people with LTCs, rather than individual patients, to ensure an appropriate range of services that meet people’s needs. The 2007 Department of Health consultation on choices for people with LTCs focused on shifting away from a ‘one size fits all’ model to one maintaining independence and providing people with more choice and control over their care with benefits for patients and the NHS. 4 With regard to people with LTCs, the emphasis was on developing clinical pathways and care management programmes. 1,42 However, evidence of the effectiveness of such approaches in many chronic conditions is limited,56–59 and there is no evidence of significant service user input influencing the development of such pathways. 60,61 The development of pathways may also create tensions with policies on choice and it would seem critical that to develop responsive pathways that provide meaningful choices will require significant service user input as well as collaboration with health-care commissioners and providers. 4,62,63 Current policies focus more on individual management through approaches such as the Year of Care model with flexible commissioning and self-management programmes. 4,31
The current emphasis on developing integrated pathways for managing LTCs reflects the need to address issues of comorbidity and fragmented service models. Recent policy, together with the structural reforms introduced in the Health and Social Care Act 2012, have also highlighted the need for more generic, integrated pathways for LTCs, as these might prove more successful in generating cost savings. 64 However, the evidence is not conclusive and it could take a number of years to show any meaningful impact. 65,66 This changing context in which commissioners have to operate is a complex and turbulent environment presenting significant challenges for health-care commissioners. 55 Prior to April 2013, the NHS LTCs QIPP work stream managed by local PCTs promoted a holistic model for management of LTCs – and was focused not just on specific diseases but also on providing support for patients to co-manage multiple conditions. This programme of work has now been taken over by NHS England and it is not clear how they will be taking forward this work or what direction they will be headed, as they were still in the process of developing their work programme during our study. Outcomes from the QIPP work stream included risk stratification, integrated teams and co-managed care for people with LTCs. It also introduced the Year of Care model as an alternative to Payment by Results.
Despite the large consultation undertaken in 2012 to develop a cross government LTC strategy, the new government has placed the responsibility for developing a strategy around LTCs5 with the new national commissioning board, NHS England. The strategy67 will seek to see a change in the quality of life for people with LTCs (NHS outcome framework domain 2). However, the final output from this has not been published and is now part of the work of NHS England – who may, or may not, develop their own strategy for LTCs. This is interesting as there was a long consultation in 2012 with a number of user groups and organisations but at the present time it is not clear what is being done with this information. 64 Elements of the LTC model (risk stratification/integrated pathway/maximising numbers with co-managed care) are being used to develop Quality and Outcomes Framework (QOF) for general practice to place an emphasis on ‘patient-centred care’. However, there are criticisms of QOF regarding both patient-centred care and how it relates to quality of care. 68,69
Patient and public involvement: variety of organisations
While there have been numerous changes to structures and processes for PPI in the NHS, there have been no formal mechanisms for PPI established since the 1970s. 8,62,69,70 Recent changes to the English NHS have reformed many previous structures but continue to emphasise the importance of engagement and involvement. 22 At a local level, there are a wide variety of patient and user organisations. 71 Patients, users and carers with a collective illness identity have long organised themselves, often independently of government, but these organisations are diverse and hence difficult to categorise and analyse. 72 Research suggests that local organisations are often patchy in coverage,71,72 although at a national level, groups such as Carers UK, National Voices [formerly the Long Term Medical Conditions Alliance (LMCA)] and the Patients Forum [replaced by the Local Involvement Networks (LINks) and recently replaced by local Healthwatch] are closely involved in the policy process and some support local group engagement with the NHS and social services. 72,73 Specific case studies of HIV (human immunodeficiency virus)/AIDS (acquired immunodeficiency syndrome) groups, maternity, physical disability and mental health users suggest that local groups do get engaged in policy and service issues and that patient/advocacy and voluntary organisations are important in promoting PPI with the NHS. 74–77 Such investigations have, however, paid relatively little attention to the outcomes of PPI. 17
Recent policy on patient and public involvement
Recent policy (since 2001) identifies that the NHS needs to be responsible to patients and service users and more accountable to citizens who fund it. 20 This rhetoric is further played out within the recent NHS reforms of the coalition. The Health White Paper7 detailed intentions around shared decision-making – ‘nothing about me without me’ – through choice and increased voice of local people, service users and patients. Responses from consultations suggested that there needed to be a stronger voice of the public78 and recent NHS reform planning echoes this ambition. 79
The 2012 Health and Social Care Act made clear the duties of the new organisations established under the Act, such as the NHS Commissioning Board and CCGs, around implementing proposals to give patients and the public more say and greater involvement in care and treatment decisions within the new health-care system, holding the board to account for delivery through its NHS mandate. 5 However, much of the recent policy vocabulary on involvement or engagement is patient centred and individual, with a focus on empowerment in decisions about own care rather than about patients and the public having a strategic role, either collectively or individually, in helping to shape health care. 49 Examples of this approach can be seen in the emphases on embedding care planning, shared decision-making and support for people to manage their own conditions – including a pledge to care planning written into the NHS constitution, roll-out of personal health budgets and support for telehealth/telecare, as well as producing a compendium of information to support commissioning LTC care, aimed at commissioners. It appears to be more about patient engagement (in own care) rather than public involvement in commissioning health care.
Patient and public involvement/engagement in commissioning health care
The recent health reforms present a new set of issues and challenges for PPI in commissioning health care. The majority of health-care services in England will now be commissioned by CCGs led by GPs. This is not the first approach to primary care-led commissioning in the UK, with GP fundholding introduced in 1991 and followed by a number of variants of engaging GPs in health-care commissioning. 80 Research suggests that in these previous approaches to primary care-led commissioning there has been little involvement of patients and the public. 80
Patient and public: there is little evidence to suggest that practices engaged patients and public in their commissioning activities in a meaningful way. Across the different schemes since 1990, GPs believed that, by definition, they had an excellent understanding of patient needs and could act as reliable proxies for their patients; as a result, they did not think of formal PPI as a priority. 81–83 Where efforts to consult patients were made, this was often seen as a box-ticking exercise. 82 In primary care groups, where approaches to involve patients and public had been initiated, this was more at the informing rather than at the participatory level. It has been suggested that PPI is relatively underdeveloped in primary care and GPs need to be educated about its value. 84
Clinical Commissioning Groups are held accountable by a National Commissioning Board, NHS England, which formally authorises CCGs. Currently, there are 211 CCGs authorised to commission NHS services as of April 2013. Despite a number of policy levers and local incentives to develop PPI,49,67,85 it is unclear whether or not CCGs will be able to fully embrace PPI within their culture. Given the lack of evidence of effective models of PPI in commissioning, as well as a lack of reliable data on patient involvement18,86 and the fact that many CCGs are likely to buy in commissioning support services from ex-PCT personnel, this lack of a creative PPI culture looks likely to continue. Many do not have the skills, time or resources. A recent study of CCG leaders for patient and public engagement87 revealed that, although CCG leads were keen to engage with patients and public, there was some lack of understanding of what engagement was and how it might be used within the whole commissioning cycle, particularly for procurement and monitoring. Commissioning, particularly for LTCs, is resource intensive. 88 However, the new health-care landscape involves CCGs developing strategic alliances and partnerships with existing and new organisations such as the Health and Well-Being Board (HWBB) and Healthwatch, which, in the case of the HWBB, requires the development of joint strategies with their local authority, who have a culture of public/community engagement, thereby providing some direction and potential for cross-learning.
Patient and public involvement influencing commissioning decisions: is it working?
The importance of PPI in commissioning has been recognised since the initial development of NHS purchasing in the 1990s. However, there has been no significant evidence that such engagement has influenced commissioning decisions. 8,17–19 In 2007 the Picker Institute published the results of a survey of PCTs examining PPI in commissioning. They found that while PCTs had a number of mechanisms and defined management responsibilities for PPI, there was a disconnect between the emphasis on processes and structures for PPI and the relatively low expectation that patient, public and community groups would have any significant influence on commissioning decisions. 18 Key barriers identified were difficulties in reaching marginalised, isolated or deprived groups, a lack of understanding among the public of ‘commissioning’ and a lack of reliable data about patients’ experiences. However, when asked what approaches PCTs were considering for future engagement, there was a continued emphasis on methods such as formal consultations, patient panels, citizens’ juries and surveys. These approaches did not identify engagement or involvement of user and patient groups for people with LTCs, despite this approach being promoted by the government’s policy on choice for people with LTCs. 4,9 Guidance for commissioning agencies placed great importance on how care that promotes the health and well-being of individuals in consultation with local people was procured10 forming the basis for commissioning competencies, needs assessment frameworks and performance regimes across health and social care. 10,12 There was also a clear emphasis on increasing the role of the third sector. 13 The NHS Next Stage Review also highlighted changing public expectations related to ‘control, personalisation and connection’, and building partnerships with patients and LTC user groups. 14 At the start of this research project (November 2009), we undertook an extensive scoping exercise of national changes in commissioning for LTCs. The project protocol highlighted a number of key areas for investigation: Department of Health pilot sites and demonstrators, website analysis [PCTs, strategic health authorities (SHAs) and national patient organisations] and documentary analysis (associated policies, budgets, commissioning power and choice sets). Websites were traversed using key words (identified via project objectives, research questions, literature review, health policy, commissioning models) with a search for key documents associated with LTCs/PPI and/or commissioning. Key documents were identified as Joint Strategic Needs Assessment (JSNA); World Class Commissioning Panel reports; LTC strategies; commissioning strategy; communication and engagement strategies; PPI strategies; and a 5-year strategic plan.
We found that many PCTs recognised the need to improve data collection, knowledge management and address intelligence gaps in relation to needs assessment. PPI within this context was variable; methods included the use of existing PPI mechanisms, steering group membership, workshops, stakeholder events and facilitation by social enterprise organisations. LTCs were addressed in all JSNAs reviewed and was referenced, either explicitly or implicitly, in all key documents. Correlations between an ageing population and LTCs were highlighted, with such conditions often described as a disease burden. Emphasis was placed on effective management; this included care closer to home, patient education, self-care, capacity building in general practice, targeted risk assessment, the reduction of emergency admissions and exploiting new technologies. As such, we found that in general the localised strategic viewpoint mirrored Department of Health-related documentation and LTC models. Of particular relevance – especially given the changes to commissioning that occurred during the period of research – was that PBC was seen as a key vehicle for LTC commissioning; however, organisational development at this time was variable, with limited PPI evident.
Generally, PCT PPI strategy focused on well-recognised methods, with one-third of the PCTs having a panel or membership schemes in operation and otherwise an emphasis on expert patient programmes, volunteering, Patient Advocacy Liaison Service (PALS) and reader panels. However, specific involvement in relation to LTCs was more limited.
A lack of innovative approaches could explain World Class Commissioning panel report results for competency 3 (influence on local health opinions, PPI, improvement in patient experience). In 2008–9, no PCT (n = 114) had obtained the highest level 3 competency (67% operating at level 2 and 33% at level 1). In 2009, assessments of the quality of commissioning published on the NHS Choices website showed that only 2% of PCTs were coded as excellent, the majority gaining ‘good’ at 51%. PPI in specialised commissioning groups was even less well developed, with 50% having no visible ‘involvement’ section on their website. Data collection and analysis were terminated in August 2010 following changes in health policy and the planned abolition of PCTs.
A search for recent evidence of impact of PPEI within LTCs health care revealed limited literature, particularly in relation to the specific LTCs relating to this project, as well as a lack of robust evaluative data. This reflects Sullivan and Skelcher’s89 view that lay representatives may be marginalised and have less influence than senior executives and NHS decision-makers. Nevertheless, from the small number of varied qualitative studies appraised (n = 9), a number of themes emerged. Involvement initiatives led to some positive outcomes for the service users involved: increasing knowledge, self-confidence and self-esteem,90–92 with a resulting increased capacity to become involved with decision-making. 92,93 Much of involvement or engagement was limited to sharing information, through helping the development or design of patient information material or commenting on experience of a service, rather than helping to actively plan and shape services,91,93,94 and were largely professional rather than service-user led or codesigned. Service users also demonstrated broader ‘critical awareness’ but were unlikely to be involved at a strategic or active level, such as that of service development. 95 As most studies lacked robust evaluative data, it was difficult to attribute service improvements to PPEI specifically, even though many reported positive outcomes in some areas. In addition, levels of involvement varied between studies; while some showed that there was involvement at a limited, consultation level,94,96 others were more in-depth,95,97 and this made between-study comparisons meaningless.
Our findings reflected those of the Picker Survey as well as contemporary research on PBC which also highlighted its integral role for the success of commissioning strategies for LTCs, although these remained underdeveloped and ‘yet to have a significant effect on the redesign of services’ and that ‘the incentives and infrastructure to support PBC are not currently sufficient to engage most GPs in commissioning’, a finding supported by research on PBC. 15,16 While PBC provided much of the stimulus for the development of CCGs, early research on their development does not suggest significant differences in their approach to PPI – as is discussed later in this report.
The challenges for PPI in the NHS are well discussed in the wider literature. Research has identified key contextual factors that pose challenges for effective PPI such as lack of time and resources, lack of interest among professionals and the public, and lack of knowledge of how to translate PPI into changes in health services. 98 Tritter and McCallum’s99 analysis of the state of play in user involvement suggested three areas of weakness: time and expertise for developing trust, capacity to participate effectively, and a lack of consensus on agenda and goals. Commissioners may also face the problem of who exactly to involve (e.g. patient groups or the general public), how to achieve proper representation, and the difficulty of reconciling different agendas (e.g. between organisational and professional interests and the variety of interests of the public). Some researchers draw attention to the importance of clinical champions for successful PPI. 100 Past research indicates that it is unlikely that new commissioning groups will have the required skills, resources, time or inclination to develop PPI. 81
Patient and public involvement can employ a variety of mechanisms of involvement depending on the degree of actual power invested in the public. 101 Direct/indirect involvement refers to the absence or presence of mediating agents (e.g. GPs in health care are mediating agents for patients). Passive/active involvement refers to whether it is health professionals or the public who are setting the agenda or are being instrumental in actual decision-making. 72,100,102 Deliberative/non-deliberative involvement refers to the presence or absence of face-to-face interaction with the public. Examples of deliberative mechanisms are focus groups, health panels and citizens’ juries, while non-deliberative approaches include postal questionnaires and public consultations through postal or electronic voting.
Research has yielded scant evidence about concrete outcomes achieved by PPI in commissioning. The impact of PPI on services is often not clear, acting potentially as a disincentive to engage. Limited tools exist for measuring or assessing patient involvement. 103 When evaluating impact of user involvement strategies we should look at indicators of success that include both process and outcomes including economic evaluation. 104 Evaluating outcomes, however, is not easy, as it may take years before the outcomes of PPI can be measured. Equally, outcomes of PPI may be difficult to disentangle from other interventions. Some benefits are easier to prove, such as user satisfaction, opportunities of meeting others in a similar situation and increased knowledge about the availability of services related to their condition. 94 Gibson et al. 105 identify a series of key questions to be addressed in assessing the impact of PPEI:
-
Does the new system allow a plurality of public arenas where the service user voice can be heard?
-
Which areas of decision-making will be open to influence by PPI and which will not?
-
Which proposed solutions will be acceptable and unacceptable to the various stakeholders?
-
Is the host organisation prepared to change to accommodate some of these solutions?
These also link to what Barnes106 and others106–110 refer to as emotional and figurative deliberation based on experiential knowledge. They argue that patient and public experience is as important as more purposive-rational deliberations.
It is not surprising, therefore, that PPI has often remained a ‘window dressing’ exercise, with actual implementation of policy by local managers being rather lukewarm and unsuccessful. Involvement, if it happens, tends to be passive. 111,112 When it is active, it tends to relate more to existing service users than to members of the broader community. 100,113 One review concluded that ‘primary care-led commissioning organisations have struggled to engage patients and the public in a meaningful way’ (p. 3). 114 Despite some guidance available on skills development, such as in the Smart Series guide for commissioning,115 there would appear to still be a need to develop the required culture for PPI, and, until there is evidence available about what is working/effective etc., it is going to be difficult to create that culture. 86 The previous World Class Commissioning and central guidance on commissioning was not specific for GP practice which may explain why, in the past, there has not been enough work or guidance on skills development around PPI for GPs. This is gradually being developed and the Royal College of General Practitioners (RCGP) Centre of Commissioning competencies for clinically led commissioning (August 2011) include engaging the public. 116
Conclusion
Good commissioning for people with LTCs requires not only developing a set of skills for commissioning responsive and appropriate care that provides relevant choices for service users, but also developing approaches to sustaining user engagement. While previous research on engaging users in the NHS and on user involvement in change management in health services has demonstrated a willingness and commitment to engagement, there are few concrete examples of effective influence by users or evidence of change. 17
It was against this background that this study was developed. As described in the previous chapter, the study was undertaken at a time of substantial change in the NHS which commenced in 2009 with moves to reduce NHS management costs through PCT mergers,46 an increasing focus on integrated care and approaches to self-management2,14 and substantial organisational reform introduced by the coalition government in 2010 which developed from the end of 2010 and formally came into practice in April 2013.
With agreement from NIHR, the research period was extended to enable the research team to explore some of the early impacts of this changing commissioning environment during 2012 and early 2013 (reported in Chapter 7). However, the key aim of the study remained an examination of how commissioners enable voice and engagement of people with LTCs, and to identify what impact this has on the commissioning process and pattern of services. Our key research questions were:
-
What kinds of relationships existed, and were developing, between the public/patients and commissioners?
-
What impact did the public/patient voice have on the commissioning process and decisions made by commissioners?
-
To what extent did any changes in the commissioning process reshape local services?
-
Did any such changes in services impact on the patient experience?
-
How did, if at all, commissioners enable the voice and engagement of people with LTCs in the commissioning process?
-
How did patient groups/patient representatives get their voice heard and what mechanisms and processes did patients and the public use to make their voice heard?
The findings of this project will contribute to supporting the development of relevant skills and mechanisms for engagement for commissioners and service users and representatives within this new health-care landscape.
Chapter 3 Methods
Research design
The aim of this project was to develop an understanding of some of the complex issues of involving patients and the public in commissioning health care. In order to investigate this phenomenon, a case study design was adopted in order to develop an in-depth analysis of the processes, structures and context of PPI. Case study methods are a recognised and well-established approach to conducting research in a variety of ‘real life’ settings including health care. 117 Yin defines case study research as ‘an empirical study that investigates contemporary phenomena within a real-life context, when the boundaries between the phenomena and context are not clearly evident and which multiple sources of evidence are used’ (p. 18). 118 This approach allowed us to employ a range of social science research techniques and designs, mainly qualitative, to gain some in-depth understanding of the nature of engagement between service users, the public and local NHS organisations within their specific organisations. It also provided the methodological flexibility to generate some theoretical insights from our results. 119 We were thereby able to adopt an interactive approach to data collection and analysis, allowing theory development grounded in empirical evidence, a main strength of this design. 120,121
A multilayered approach was used, combining mapping of activity at national and local levels, analysis of local context and detailed case studies in three locations. Specific methods were employed including interviews, focus groups and workshops with a range of stakeholders, observation of key commissioning and PPEI meetings, and analysing documentary data, as well as using an adapted Likert Scale ‘Star Chart’ to measure perceptions of engagement and involvement over time.
Recruitment
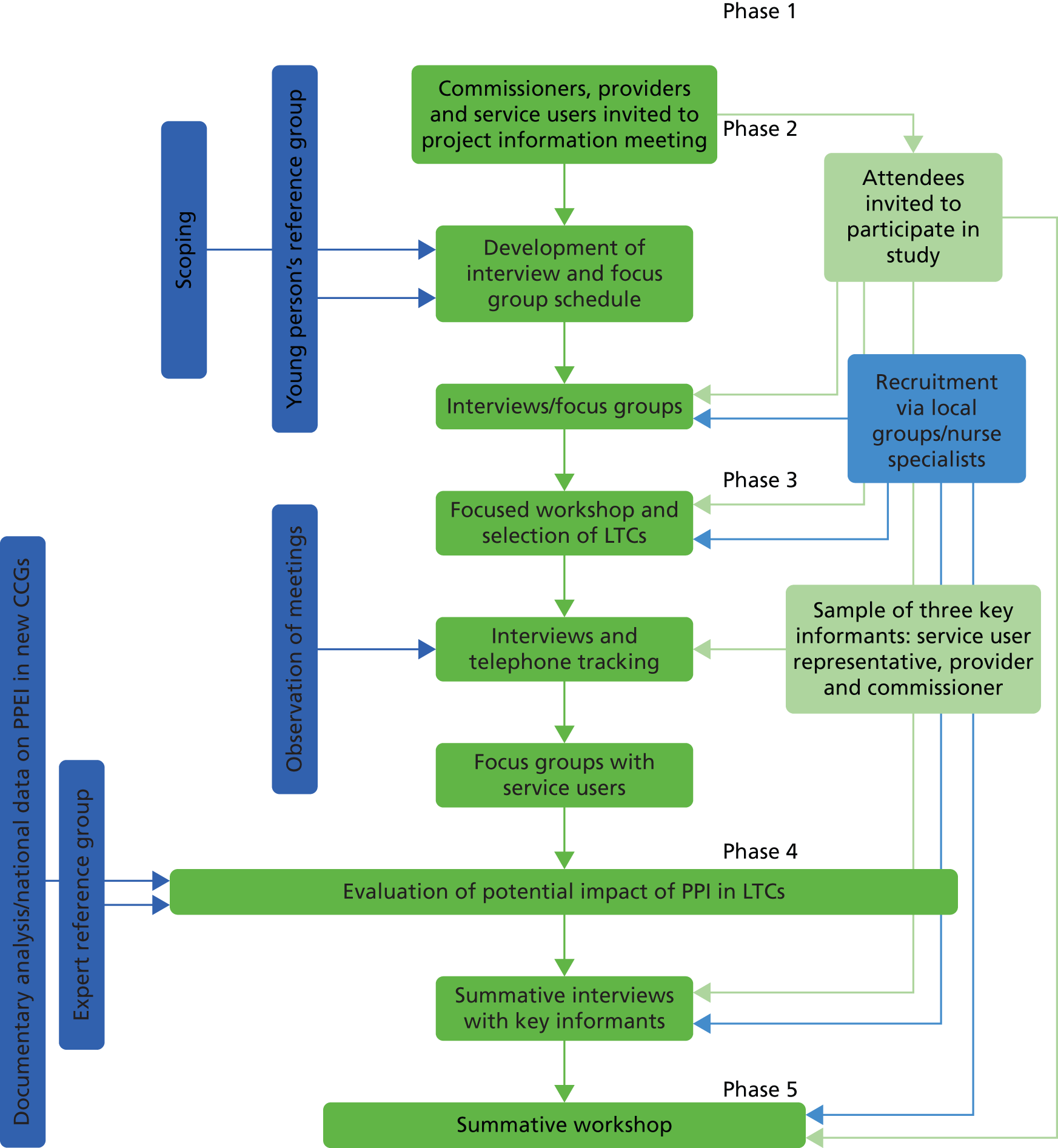
As this study was undertaken during a period of great change within the NHS, recruiting NHS personnel became a challenge. This was particularly significant during the tracking phase of the study, as respondents moved on to different organisations and roles and responsibilities were not always clearly defined during the transition to CCG stage. We therefore had to adapt our methodology during the tracking stage of the study to ensure that we collected relevant data from those who were in the appropriate posts. In some cases, this meant interviewing new personnel in the latter stages of the study, including some who had new PPEI roles and responsibilities in the new health-care structures. This is explained more fully in our findings (see Chapter 3). To support the iterative process, and enable comparisons between each site during the course of the study, the case study sites were recruited in turn (Figure 1).
FIGURE 1.
Plan of research.
Ethics
This project had NHS approval [Research Ethics Committee (REC) reference 10/H0713/24] obtaining favourable approval by the REC on 6 July 2010 with minor protocol changes agreed by ethics (Table 1). The project was originally funded for 3 years and the main focus was to investigate PPEI within the PCT commissioning structure. An extension of 9 months was granted to enable data collection within the transition stages of the new commissioning environment. A revised research plan to reflect the extension was written. All changes to the research protocol were also reported to, and agreed with, NIHR.
| Protocol | Detail of amendment | Date approved by REC |
|---|---|---|
| Initial protocol | 6 July 2010 | |
| Amendment 1 | To allow young persons option of being interviewed face to face or by telephone or within a focus group. Amendments to interview schedules, consent forms and information for participant forms made to reflect changes | 7 February 2011 |
| Amendment 2 | Amendment to age of consent for interview for young person to be reduced from 13 to 12 years. No changes to interview schedules/information/consent forms required | 7 February 2011 |
Methodology
The research was carried out in five distinct phases from October 2009 to July 2013. The project flowchart (see Figure 1) illustrates the phases of the research and methods employed.
Phase 1: scoping national changes in commissioning and case study selection
As referred to earlier in this report, we were unable to complete this phase of the study due to the abolition of PCTs. However, we did look at public information available from PCTs and this was used to inform case study selection and to initially draft the Star Chart tool (see Appendix 15) used in agreement with Health Services and Delivery Research (HSDR).
Phase 2: contextualisation
Aim
This phase was to establish detailed information on the three local case study sites selected for the study. The aim was to contextualise the specific range, type and actions of the three tracer condition based groups that would be examined in more depth in phase 3.
Sampling strategy: selection of case study sites
Three case study areas (PCTs) were purposefully selected to provide a range of demographic and geographical variation to include urban/rural, different cultural and ethnic populations as well as including a range of local NHS agencies (see Table 2). During the course of the research, the PCT in case study 1 (CS1) merged with other adjacent PCTs into a larger cluster. However, the emerging single CCG within CS1 covered the original PCT population. In case study 2 (CS2) and case study 3 (CS3), the PCT remained a single entity and these were replaced during 2012 by single CCGs.
Table 2 lists the main characteristics of the three sites.
| Case study | Setting | Population/ethnicity | Secondary care provider | PBC/CCGs |
|---|---|---|---|---|
| CS1 | Mixed urban/rural | Some ethnic minority groups, but mainly white | District general hospital | Single CCG |
| CS2 | City based | Average-size BME population | Teaching hospital | Well-developed PBC, single CCG |
| CS3 | Urban | High BME population | Foundation trust district general hospital | Single CCG |
Sampling strategy: selection of tracer long-term conditions
Three LTCs, reflecting varying known relationships across the health and social care divide as well as demand for services, were chosen for study in each location (Table 3). It was anticipated that by selecting diverse populations and levels of engagement and involvement we would identify a range of different levels of PPI. Previous studies suggest that people who participate in local health-care decision-making are generally older, wealthier and better educated than the general population and are less likely to be from black and minority ethnic (BME) communities or from other vulnerable communities. 122,123 These patient groups were specifically selected as they reflected a wide age range for study, including children and young people with LTCs, who are less likely to have a voice in their care than adults with LTCs. In addition, we purposively selected one case study with an ethnically diverse and large BME population (see CS3). The research design was structured to avoid only examining decision-making and service changes where the process was framed by the health service and its approach to engaging patient or user involvement. 124
| LTCs | Characteristics |
|---|---|
| Diabetes | Vocal patient groups, large population, established services |
| RA | Less established patient groups and services |
| Neurological conditions | Variety of patient groups and services with substantial local variation in services |
Sampling
Purposeful sampling was employed to target practice-based and PCT commissioners and public involvement staff, provider organisations and patient representatives for each of the tracer conditions. Interview targets were set, with each site aiming to recruit up to seven PCT, PBC and PPEI leads, one provider from each tracer condition and around five patient and public representatives, including adults as well as young people and carers, from each tracer condition. In order to address problems of recruiting only patient representatives who were already involved with local health agencies, we recruited participants via local voluntary groups and support groups as well as through advertising in clinics and practices and identifying participants who were not in formal groups. 123,124 For example, in one case study, site participants with RA were not involved in any group or health-care organisation approaches to PPI. Theoretical data saturation also guided sampling, in that sampling relevant cases would continue until no new theoretical insights emerged from the data. One case study site exceeded the target sample due to staff reorganisation as a result of the health reforms, necessitating targeting the new ‘PPEI’ staff and patient/public leads. A total of 102 participants were interviewed for the study across phases 2 and 3. Table 4 shows the total number and range of participants interviewed in each site. Table 5 shows the full range of roles.
| Case study | Service users and representatives | Commissioners (PCT, GP, CCG/LA and PPEI leads) | Providers | Total number of interviews |
|---|---|---|---|---|
| CS1 | 33 | 11 | 4 | 48 |
| CS2 | 11 | 9 | 5 | 25 |
| CS3 | 11 | 13 | 5 | 29 |
| Total interviewed in range | 55 | 33 | 14 | 102 |
| Role | CS1 | CS2 | CS3 |
|---|---|---|---|
| PCT commissioners | 2 | 1 | 2 |
| PCT PPEI leads | 1 | ||
| GP commissioners | 1 | 2 | |
| GP practice managers | 1 | 2 | |
| PCT/CCG transition PPEI project leads | 3 | 1 | 1 |
| CCG PPEI executive leads | 1 | ||
| CCG PPEI representatives | 8 | 1 | |
| CCG medical director | 1 | ||
| Local Healthwatch | 1 | ||
| HWBB | 1 | ||
| Service providers | 3 | 3 | 3 |
| Service users and representatives | 12 | 10 | 9 |
| PCT/LA diversity lead | 1 | ||
| CCG clinical lead (diabetes) | 1 | ||
| Local authority PPEI executive | 1 | 1 | |
| GP commissioning support (SHA) | 1 | ||
| PCT/LA commissioning (YP) | 1 | ||
| Provider PPEI lead | 1 |
In addition to the people interviewed, the local workshops involved other service users and their representatives, providers and commissioners. For example, initial workshops were attended by between 30 and 40 people in each case study, with service users from a wide variety of age ranges and backgrounds. In the second workshops, 76 people attended across the three case study sites and 30 people attended focus groups structured to address the tracer topics, with two of these being with people from BME communities. There was some overlap between those attending initial workshops in phase 1, the follow-up workshops in phase 2, focus groups and interviewees.
Inclusion and exclusion criteria
We set out to include as many local service users and their representatives as possible through running local workshops which were advertised to as many people and organisations in each of the three tracer groups, proactive work to recruit young people and use of snowballing techniques to reach as wide a population as possible. Overall, in the study we included:
-
service users and representatives from age 12 (no upper age limit), with diabetes or RA or a neurological LTC receiving services in the case study site (PCT)
-
informal carers
-
parents of children 0–16 years old.
We excluded:
-
younger people whose parents/guardians did not consent to their participation
-
service users and informal carers who were unable to speak or read English and for whom translation services within the research team or locally were unavailable
-
informal carers of adult patients who had not consented for the carer to be approached.
Data collection
Initial meeting and workshop
An initial set-up meeting was organised by the research team with key stakeholders from the PCT in each case study site. This was carried out with those leading on commissioning and providing services for people with LTCs. The aim of this meeting (alongside providing information about the study and an invitation to participate) was to discuss local provision for the three tracer conditions and how patients and the public are currently involved. Information gathered from this meeting, along with additional local scoping of patient and public groups, was used to identify and map the key organisations and groups, as well as the institutional structures for local commissioning of health care for the three tracer conditions. Representatives from these organisations and groups, including primary, community and secondary providers, health-care commissioners as well as patient and public representatives, were purposefully selected to represent the tracer conditions and to reach as many people with an interest in the research topic as possible; they were invited to attend an initial workshop, or information meeting, within each case study site. We specifically mapped as many relevant patient groups and organisations, voluntary groups related to people with diabetes, neurological conditions and RA in each area as possible (including support groups run by services, local groups of national organisations), as well as contacting some specific individuals identified through a snowballing technique to ensure that we reached as wider patient/user community as we could. 122–124 The aim of this meeting was to map the terrain of local PPEI to understand the contextual features impacting on each case study. It was also used to identify any key issues, projects or mechanisms for PPEI, which we aimed to follow up in more depth in the next phase.
Interviews
Following the initial workshop, a series of mainly individual in-depth semistructured interviews were carried out with a purposive selection of commissioners, providers and service users and representatives for each site (see Table 5 for total numbers interviewed in each site). Data saturation guided the sample limit. The interview aimed to elicit views on the issues, processes and current activity relating to commissioning health care for people with LTCs across the three tracer conditions. Interviews were carried out face to face, normally at the participant’s place of work or leisure, or by telephone if requested, following the researcher’s obtaining of full consent. The interview schedule, information on interview and consent forms are attached at Appendices 3–6. Following interview, the participant was asked to complete the Star Chart tool to obtain some assessment of the individual’s understanding and experience of PPEI.
Data from young people
It was planned to hold a series of focus groups with young people to obtain their perspectives on involvement during this phase of the research. The research team consulted guidelines for the operation of research with young people125–127 and these were taken into account, especially to ensure that the principles of how to conduct fieldwork with young people with age-appropriate sensitivity were adhered to. 128,129 However, the project represented an attempt to include young people within a project adopting an inclusive approach across the life course and in a new area, that of patient-led commissioning. Moreover, we encountered a number of gatekeeper issues that were unanticipated. The team had difficulty recruiting young people to a focus group (see Chapter 8, Power and control). In discussions with our young person reference group, it was agreed that individual telephone interviews might result in more success in recruitment. Following approval of this revision to the protocol by the REC and NIHR, a total of 10 young people and their carers were interviewed in this phase of the study.
Follow-up workshop
Focused, or follow-up, workshops (one in each case study site) were held at the end of phase 2 to explore local issues and approaches to commissioning people with LTCs in more depth. Examples or issues around PPEI, identified during earlier interviews and discussions with stakeholders, were used to guide some of the discussion. PCT, local authority and practice-based commissioners as well as clinical leads (commissioner, provider) and representatives from user groups and patient organisations from the three tracer conditions, plus key representatives from consumer and patient organisations, were invited to attend. In total, 76 participants attended these workshops across the three sites. These represented a mix of commissioners, service users/representatives and providers. The workshop also served to identify specific exemplars of PPEI practice suitable for follow up as ongoing in-depth analysis over time in phase 3 of the project. For CS1, this was identified as a third-sector targeted approach to support local commissioning of neurological conditions and a schools-based diabetes project, for CS2 an integrated diabetes service with PPEI input and for CS3 a proposed community diabetes service for the local BME population.
Dissemination of findings
It was originally intended that we would share results and outcomes of these workshops with participants through a shared website. We developed a project-specific website at the beginning of the project. This was a secure site in order to share documents, resources and findings within the project team, who had intended to use this as a method of dissemination with participants. However, following discussions with participants during workshops and interviews, a process of e-mailing workshop reports out to participants was considered preferable to requiring people to engage with another ‘internet site’, particularly in the current climate of change and turmoil.
Phase 3: evaluation of the impact of involvement on local health policy processes
Aim
In this phase, we aimed to identify the impact of involvement on local health policy processes such as service reconfiguration, service delivery and service development. This was through an exploration of public/patient views and perceptions of how the public voice is heard and if/how it impacts on change. Processes relating to the potential exemplars of PPEI practice identified in phase 2 were focused on, with the aim of exploring the extent to which participants felt that they were able to successfully influence local health policy processes in the past year, as well as issues that they were currently trying to place on local policy agenda or attempts to influence current commissioning policy/strategies on LTCs. Their development was tracked during this phase. (See Appendices 6–8 for exemplars.)
Methods of data collection
Interviews (phase 3 interviews and telephone tracking)
A purposive sample of three key informants (service user representative, commissioner and service provider) were selected for each case study site. They were interviewed soon after the exploratory focused workshop in phase 2. The original plan was to carry out a series of short tracking telephone calls as well as a further two interviews (one in the middle of the 18-month tracking and one at the end), with the purpose of tracking case study site activity and to explore any impact of PPEI on local health policy process. At the end of each interview, measurement of the interviewee’s perception of changes in user involvement was to be made through the Star Chart tool. However, staff changes (with key commissioning informants lost from all three of the sites at varying stages of the study) meant that tracking could not be undertaken in the manner it was intended and the Star Chart tool was of limited use. Tracking was, nevertheless, carried out with those who were still in place and further interviews were undertaken with some of the new commissioning and PPEI personnel where available. (See the case study site findings in Chapters 4–6 for further information.)
Focus groups
A number of focus groups were held with a selection of service users within this phase to complement the data collected from interviews and observation. Focus groups are group discussions that are carried out to examine a specific set of topics. 130 This was done in order to hear issues which may not readily emerge from interviews or observations alone, and to capture the shared, lived experience with the possibility, through the synergy of conversation, of developing unique data or ideas. 131 As Ivanhoff and Hultberg suggest, the strength of the focus group method is that researchers are provided with an opportunity to appreciate the way people perceive their own reality and get ‘closer to the data’ (p. 126). 132 Focus groups also provide a safe environment for some individuals or groups, such as those from similar socioeconomic or ethnic backgrounds, who might find interviews intimidating, and can serve to provide a voice from seldom-heard or marginalised groups. We had originally planned to carry out focus groups with young people in phase 2 but had to adapt our plans, as emerging data from interviews indicated that this would not be the preferred option for this group and we had to amend our protocol to include interviews as an option. No focus groups were held with young people in phase 2 or 3 of this project.
A selection of service users were recruited using convenience or snowball sampling methods to ensure adequate coverage of a range of patient groups.
Four focus groups with service users were carried out in this phase, with a total number of 30 participants (Table 6 gives a breakdown of numbers and characteristics of participants). The focus groups were facilitated by two members of the research team, with one acting as main facilitator and the other taking notes. The focus group discussions were recorded with consent and transcribed verbatim. Notes taken during the focus group were used to clarify the discussion and aid analysis.
| Case study | Number of participants and focus groups | Characteristics of focus group |
|---|---|---|
| CS1 | Six participants in one focus group | Service users (adult) with neurological LTCs |
| CS2 | Four participants in one focus group | Service users (adult) with RA |
| CS3 | Twenty participants in two focus groups | Service users (adult BME) with diabetes |
Some of the issues or findings emerging from the initial workshop and interviews were used to explore further in the focus group. As previously discussed earlier, many of the statements contained within the Star Chart tool were no longer valid as commissioning had changed so much. However, the statements that were still meaningful in the new context were used to guide some of the discussion within the focus groups. In two of the focus groups, vignettes developed from phase 2 interviews were used to trigger discussion on their involvement in LTC service commissioning. In one of the case study sites, focus groups were carried out with groups with very little or no spoken English and were therefore conducted through a translator. (See Appendices 9 and 10 for focus group topic guides and information provided to participants.)
In total, 10 key commissioning and PPEI meetings were observed across all the case study sites and relevant documents collected for analysis during phases 2 and 3. The central aim was to observe the nature of PPEI within these meetings, how and in what way the lay voice is heard and acted upon. Field notes of the meetings were recorded and used as appropriate for analysis.
In order to better understand the position of PPI within the emerging new health structures, data were obtained on PPEI processes and structures from a national survey on emergent CCGs (via PRUComm) as well as from a selection of CCGs undergoing authorisation (refer to Checkland et al. 22 for details of methods in the PRUComm study). (See Chapter 7 for further information and findings.)
Phase 4: confirmation of outcome measures
Aim
Following an initial analysis of data in phases 2 and 3, the aim of this phase was to identify outcome measures related to commissioning including direct evidence of service change, changes in investment, satisfaction with changes and processes of engagement.
Methods of data collection
An expert reference group was formed, consisting of a number of external key people with a wide variety of expertise and experience relating to patient involvement, clinical skills and knowledge and clinical practice around LTCs in general and/or specific to the tracked tracer conditions. These acted as a virtual panel to provide comments on the identified exemplars of PPEI practice tracked in phase 3. The aim was to bring some external verification of whether or not the interventions, services or processes, developed through PPEI, were likely to lead to improvements and benefits for patients. (See Appendix 9 for expert reference group list.)
We had originally planned to carry out a number of summative focus groups with a purposive sample of commissioners, providers and service users to discuss outcomes of commissioning. However, in the rapidly shifting staff turnover, focus groups were not possible and individual as well as small group interviews (as in CS1) were carried out instead. These were conducted with a purposive sample of commissioners, service users, providers and PPEI staff to discuss changes in services and process of engagement. This was also supplemented by participant and non-participant observation of specific related commissioning meetings where field notes were made about evidence of service changes, including changes in investment, processes of PPEI as well as any perceived satisfaction with any changes.
Phase 5: summative workshop
Aim
The aim of this phase was to present the findings from the study to date to a range of stakeholders, assess the current situation and discuss the way forward. The summative workshop formed part of the initial analysis and synthesis stages of the research and was used for both the presentation of findings and also to explore the validity of our preliminary analysis of the data.
Methods
A summative workshop, with patient and public representatives, commissioners, PPEI executive/lay leads and providers from all three case study sites, was held in London in April 2013. Over 40 stakeholders attended this meeting. Preliminary analysis was presented to the audience for discussion and clarification. The workshop was chaired by the chair of the Engagement and Voice in Commissioning (EVOC) advisory group and facilitated by a lay representative who had experience in supporting emerging CCGs on PPEI at the SHA level and was involved in assessing the PPEI part of the CCG authorisation process for a number of CCGs. Data obtained from this workshop was used to refine the analysis. A report from the workshop was written and circulated as a project output (see Appendix 10).
Analysis and synthesis
Comparative case study analysis was used to identify and explain patterns across and within organisations and case study sites. The strategy for analysis was to:
-
observe, describe and explain the interaction between commissioning approaches identified and the way that patients and the public are engaged in these processes
-
identify and explain patterns of commissioning LTC services in each case study
-
examine the relative influence of patient and public views on LTC commissioning processes to identify lessons for future development of policy and practice.
Extensive notes were made of workshops and workshop material collected and analysed by the research team. Interviews and focus groups were transcribed verbatim and explored to uncover main themes. Transcripts were analysed using qualitative software (NVivo, QSR International, Warrington, UK) to enable thematic coding. Documents were coded to identify key themes and decisions were made. Framework matrices were developed using coded themes to summarise and condense data sources by codes and themes. Visual Star Charts were translated into Likert scale measurements and interpreted numerically. National and local contextual information was obtained from undertaking a discourse analysis of key policy documents and data from a range of national patient and public organisations. Data from a national survey of emerging CCGs were extracted to provide further information on the direction of travel for PPEI within the new health structures, and a selection of first wave CCGs undergoing authorisation were analysed thematically in relation to the evidence supplied around PPEI.
The analysis was structured around Ritchie and Spencer’s ‘Framework’ for applied policy research. 133 An iterative approach to data collection and analysis was employed throughout the project. Initial analysis was discussed between the team and Advisory Group to inform data collection and results. Interviews and focus group transcripts were read by at least two team members, their content being organised into a priori and emergent themes. To ensure that findings were empirically grounded, pairs of transcripts were exchanged to compare inter-related reliability, any differences in interpretation discussed at team meetings and a common thematic list agreed. A comparison between and within themes, case studies and organisational type, and over time, was conducted. This was aided by the use of NVivo software via a shared server to promote consistency of analysis.
Analysis focused on identifying implications for local policy and practice as well as contributing to an understanding of the process of local policy development, highlighting inter-relationships between context, role of local organisations and the local policy agenda. By submitting our initial findings and analyses to external critique via phase 4 interviews and group discussions, expert reference group and phase 5 summative workshop, we were able to validate our analyses and ensure that they were informed by a number of stakeholder and theoretical perspectives.
Within the report discussion, we employ two explanatory frameworks to interrogate our findings further. First, we draw upon the work of Barnes106–109 on public participation and synthesise this with the theoretical framework suggested by Gibson et al. 105 in order to map our findings against the ‘ideal’ PPEI processes. Second, we use normalisation process theory to identify the work required to sustain PPEI as normal practice within the new structures. 134,135
Patient and public involvement in Engagement and Voice in Commissioning
The acronym EVOC was employed as a working title for the duration of the project. EVOC was supported by a project advisory group, the members of which are listed on the acknowledgements in this report.
The advisory group was chaired by a lay person who had a long history of PPEI and was former chair of the external reference group for the Department of Health National Service Framework for LTCs. Lay members of this group consisted of representatives from a range of national LTCs organisations as well as patient representatives drawn from the Patient Involvement in Research Group (PIRG), an established group of service users and members of the public supporting research within the Centre for Research in Primary and Community Care (CRIPACC) at the University of Hertfordshire. Adequate representation to this advisory group was informed through discussions with the PIRG during the early stages of the study. The advisory group supported the conceptual and methodological approaches utilised in the research, providing critical commentary during the development of the project. They also provided advice and guidance on the development of research tools, such as interview schedules and contributed to reviewing sections of this report, including help in the dissemination of findings.
A young persons’ group, comprising a number of young people either with or supporting people with a LTC were involved in the development of supporting information relating to children and young people.
The expert reference group, described above and also listed in Appendix 9, also included a number of patient representatives, providing critical feedback for the exemplars of PPEI practice described.
In addition to the interviews and focus groups carried out with a range of service users and patient representatives, invitations were provided to local patients, services users and representatives to the two workshops held in each case study site. The summative, or consensus workshop, held at the end of the project, included a number of service users and their representatives from a variety of LTCs including diabetes, osteoporosis, arthritis and neurological conditions (see Appendix 10 for the report from summative workshop).
Chapter 4 Research findings: case study 1
Background
Case study 1 was the first study site to be recruited, with an initial workshop held in May 2010. Amalgamated from three smaller PCTs in 2006, CS1 was, at the start of the EVOC study, a PCT with an active research agenda focused on patient involvement and engagement. Data collection in this site falls into two eras, the first during a relatively stable period with well-established PCT structures, and the second during transition to the CCG. Some respondents (including all service users and representatives) participated in EVOC during its lifetime; however, inevitably, a number of PCT staff moved on during the transition phase.
Case study setting
Case study 1 is located in the south east of England and is less ethnically diverse than the rest of England. The main population centre is a new town; other population centres are mainly rural. The average life expectancy is higher than the national average but there is a mixed picture of deprivation; one of the three local authorities in CS1 is in the bottom 30% of most deprived local authorities, whereas another is in the top 5% least deprived. CS1 commissions the majority of acute care from the local district general hospital which includes an accident and emergency department. In case study 1, there are 39 GP practices in three commissioning consortia, and compared with many areas of the country, PBC in CS1 was well established. One district in CS1 has a lower prevalence of chronic diseases, while another district has a higher prevalence for diabetes and hypertension. The third district has a higher prevalence than the national average for all chronic diseases.
Processes and supporting structures for patient and public involvement
When the study commenced, the PCT’s rhetoric suggested that PPI was an underpinning ethos within the organisation. In the World Class Commissioning report in 2010, CS1 increased its competency rating and the score for engaging with public and patients was increased to level 2. Level 3 was not attained as it was unclear how patient experience data influenced commissioning and hence improvements in quality of care. At the first workshop, an array of initiatives aimed at enhancing PPI or guided by the principles of PPI was described by the participants (Table 7).
| PPI structures | PPI activities |
|---|---|
| PPI projects | Patient Experience Blog. An interactive online blog-based tool that seeks to gain patient narratives on their experiences of local health services, and their views on local health services Marie Curie Delivering Choice project. A 2-year project assessing end-of-life care provision and gaps |
| Service user-led PPI structures | PINpoint. Recommendations from prostate cancer survivors are directly fed to commissioners Networks. Neurological, stroke and diabetes led by voluntary sector LINks Local Voluntary Action Groups |
| Organisation-led structures with PPI | Children’s Trust Board (includes younger service users) Maternity services engage with service users End-of-life preferred place of care Personal Health Plans pilot Long-term conditions Pathways PALS General practice health forums |
Early discussions and interviews suggested a strong ‘will’ for PPI. There was a close working relationship with the local LINks organisation, and a history of locally based action groups and health forums which were drawn upon by the PCT for service user representation. The PCT’s lead on patient experience reported directly to the Director of Nursing and Quality who was the board lead for public engagement. The patient experience lead used a combination of proactive view seeking (particularly via the Voluntary Action groups and LINks) and gaining feedback from the Patient Experience survey and PALS. At that time, there were some local issues around the perceived lack of interpretation services, and the lead was able to improve accessibility through the use of the Voluntary Action Group’s newsletter.
A key initiative developed jointly between the PCT and local researchers was the Patient Experience Blog project. This was a move away from reliance on the Patient Experience survey and sought to capture patients’ stories and experiences as a continuous dialogue between service user and commissioner. The blog allowed patients and the public to tell their stories anonymously via the internet. Once checked, these narratives then appeared on the website. Feedback to commissioners happened monthly as a themed summary and also as targeted feedback if, for example, the story was about a particular GP surgery. It was also possible for NHS staff to anonymously respond to the patient stories. Dissemination about the blog initially happened via established service user groups [e.g. the prostate cancer support group and local Multiple Sclerosis (MS) Society branch] and publicity material at GP surgeries. While, early on, service users met the blog with enthusiasm, this became tempered by time as service users received no feedback about any response to their postings. This was mirrored in the provider services, with staff complaining that commissioners were not passing on the summaries to them:
. . . the PEBL [Patient Experience Blog] site is obviously a commissioner tool, it’s not a provider tool but actually, and that’s I think again an issue because commissioners are collecting, we collect and whether the two match up and marry up and whether the service users really understand that who are providing feedback, because I suspect that a lot of service users who put stuff on to PEBL think that that information’s coming directly through to the provider unit.
CS1 neurological provider
When data collection commenced in 2010, the recent split between commissioner and provider of services was also reflected in the way in which PPEI was defined and understood by the different stakeholders. For providers, PPEI was about ‘fine-tuning services’ and being used as leverage on commissioners:
I think that in terms of advantages certainly in terms of sort of informing our commissioner, informing our partner organisations, to have feedback from service users is absolutely crucial in terms of service redesign, in terms of how the service is delivered.
CS1 neurological manager
Providers also felt that they were often left to deal with service user representatives who, because of their sense of ownership of a service, may not respond well to a major service redesign. Service user representatives also had to engage with a new cadre of people – the commissioners. This often resulted in well-established relationships with providers being seen as less useful at a strategic level, but for the ‘grass root’ service user the provider service was the only tangible organisation to engage with.
Involvement of service users with long-term conditions
Although targeted at the whole PCT population, the blog was particularly taken up by people with LTCs. The PCT had a number of other structures in which service users with LTCs were involved. At board level, the PCT had lay representation on its LTCs programme board and there was service user involvement in the development of the diabetes pathway. In most condition-specific development work, providers had, traditionally, been asked to suggest suitable patients to be involved. As the diabetes pathway was developed, an alternative approach to recruitment was taken:
. . . we tried to take a different approach to avoid that and we advertised in the local newspaper for representatives on our network and then interviewed them, and what we got out of that is we ended up with one retired gentleman who was a type 2, but we also ended up with the parent of a child with diabetes and our type 1 lady, who is young and who works, but obviously we‘ve at least got an input from a slightly different group of people.
CS1 PCT commissioner 1
There was also some involvement of younger people in a diabetes users group whose feedback helped to reverse a PCT decision to supply a single model of glucometer:
. . . we had a younger girl there who had type 1 diabetes and she said ‘you know, when you’re growing up, you know, you hate testing your blood glucose and if there’s a particular meter you like because it looks cool or whatever it is, where it only takes five second or whatever, then you should be giving people whatever they need which would kind of mean they’re more likely to test’ . . . and we said ‘what about if we kind of promoted that as sort of the meter for choice but again didn’t restrict if someone wanted a different one that was absolutely fine’. And she thought that would be really useful so yeah, exactly we kind of adjusted our thoughts based on kind of the feedback that we had.
CS1 PCT commissioner 2
The commissioners’ focus on diabetes resulted in the other two tracer conditions being less visible in terms of PPI. Within CS1, RA service users engaged solely with providers and framed involvement purely at the level of care (e.g. shared decision-making); this also appeared the case at a local patient group. Similarly, providers of RA services had an equally narrow view limiting their definition of PPI as patient complaints through the PALS. In contrast, service user representatives had a more strategic vision of the potential for PPI, realised their low visibility to commissioners and actively strove to get their voice heard:
. . . we are relatively powerless, don’t really have much to lever any change with, you know, it’s not, MS is not a media issue, we can’t really use that, you know, it’s not topical, it’s not sort of highlighted in the press a lot, and I think compared to all the other services that the PCT look at I think those sort of neurological conditions are pretty low down on the list . . .
CS1 service user MS 1
The MS Society, Parkinson’s UK and other smaller organisations for long-term neurological conditions had formed a strategic alliance across the region to amplify their voice to commissioners. At meetings with commissioners (e.g. neurological network, QIPP commissioning support events), these organisations presented a united voice in an attempt to raise their constituents’ profile. Although this strategy was clearly understood by the service user representatives and local service users engaged at branch level, as pointed out by a service provider, reliance on voluntary organisations as the sole voice for a condition resulted in a number of service users not being included in that voice. This was clear during the focus group with service users and carers living with MS or Parkinson’s disease. Similarly to participants with RA, these respondents viewed PPI as being limited to care level and feedback on services.
Evidence of influence
Despite this limited view, the members of the focus group all benefited from a service improvement influenced by the voluntary organisations. Both the MS Society and Parkinson’s UK had put a strong case forward for a nurse specialist role in the respective conditions, and had provided some pump-prime funding. Following focused lobbying, service user representatives were added to the appointment panel and had a sense of continued ownership over this post. Although hard data are not available, both commissioners and service user representatives reported that the appointment of these nurses had improved quality of life and reduced avoidable hospital admissions.
However, while this example of service change demonstrated a partnership approach to meeting a need, CS1 also provides another exemplar of influence and service change that was initiated by service users themselves. A group of parents had approached the local LINks in order to address issues they were having with local primary schools supporting their child with type 1 diabetes:
. . . they’re [parent] having trouble getting help for diabetic children, in their school. I took this through to the county wide group . . . the LINk and we’ve ventured on a project which will, along with the county education authority and the health group, it has resulted in a protocol being . . . how to treat people who are youngsters in schools, it really is very important because if they can’t get . . . and this is just about diabetes we’ve done this, but hopefully this will be adapted for other problems we’ve had with children in schools.
CS1 LINks chairperson
The parents, LINks and PCT worked with the CS1 local education authority and Diabetes UK (regional office), a paediatric diabetes specialist nurse from a local hospital and other interested parties to create a protocol for implementation in CS1 schools. The protocol (see Appendix 16) was a set of guidelines to ensure that school staff were supported and given the right equipment to support pupils with diabetes. The protocol outlined recommendations on how schools can provide medical care and emotional support to children who have diabetes. This included an individual care plan for each child and providing a place for a child to test their blood glucose levels or administer their insulin injection, extra training for school staff to prevent situations where children are unable to participate in day outings or residential trips, and allowing children to eat snacks to regulate their blood glucose levels.
Clinics at some hospitals are very reluctant to put a child on a better regime because it might mean an injection at lunchtime and so they don’t do it because of the issues surrounding schools. Well we’ve now recently got a protocol up and running for schools to look at, of all the information that they need regarding insurance, just the care of a child with diabetes, everything they need to know is in this document that they can refer to and we’re hoping that it will be rolled out nationally.
CS1 parent 1
Feedback from the expert reference panel suggested that the protocol was highly likely to be adopted by schools and lead to improved health outcomes of children with diabetes.
The voice of parents is strong and it is evident that involvement/representation on the working group has highlighted key issues that are important to the lives of children with diabetes. If implemented through discussion to develop tailored health plans, based on partnership working between the PDSN [paediatric diabetic specialist nurse]/parents and school, it will improve health outcomes.
Diabetes charity representative
I am of the opinion that the likelihood of the protocol leading to health improvement for children with diabetes would be greatly increased. Schools need to have expert guidance in dealing with their children with complex health needs and diabetes is one of these conditions. A robust protocol to support the children, parents, carers and school staff is essential for the children to have good experiences in school while living alongside their condition.
Specialist diabetes nurse
However, in tracking interviews, the parent above reported her disappointment in the slow uptake by local schools, and a growing resignation that, unless a mandatory requirement, the protocol was unlikely to be high on a school’s priority list. The need for a more mandatory approach was echoed by the expert panel respondents, who expressed concern that insufficient attention was given to implementation.
The wider question about this policy and its development process is how it is delivered in practice and monitoring/feedback processes. There does not appear to be a defined delivery or monitoring plan involving the schools/teachers themselves.
Diabetes charity representative
While supportive, one panel member – a head teacher – also raised some concerns.
I have had only one child who developed Diabetes towards the end of her time with us and a document like this would have been invaluable – but for non-medical people also a bit scary . . . Just as a point, some staff may well not want any responsibility for a diabetic and in a small school this could be an issue . . . I feel this is a sensible protocol which would be adopted in schools. Primary, and secondary schools are now educating children with a wide range of illnesses, some are even life limiting which cause emotional strain. We are doing it with very little support and so the protocol is a HELPFUL document which can be our guidance. I particularly liked the Notification process . . . [but] . . . Soon there will be very little LA [local authority] left to inform. FYI School Nurses are also very few and far between nowadays.
Head teacher
As an alternative strategy, this parent then attempted to use the patient reference group (PRG) as a forum to promote the protocol; this is discussed in later sections of this chapter.
Involvement of children and younger people
Despite the above parent-led initiative, it was acknowledged in CS1 that the involvement of younger people and children was challenging:
. . . once we had a meeting, a day’s meeting, under the auspices of a Children and Young People’s Strategic Partnership, and I can’t remember what we called it, it doesn’t matter what it was called, and we did have a few young people along for that and then you know, they’d be peeling off into small groups and that information would be fed back, but it is very, very difficult.
CS1 PCT lay representative and LINks member
Nevertheless, within CS1 we conducted interviews with three young people. One young person had set up a school council for students with diabetes to meet and talk about their issues. This diabetes awareness group was set up with the support of a teacher who had helped this young person through her struggles. This young person described how she found clinic sessions to be a bad experience and that she received a lot of support from her diabetes nurse outside the clinic on diet and insulin levels.
Yeah it was a big help, she answered a lot of questions that I’d had but couldn’t ask in the clinic, just from being upset so it was nice to have them answered finally . . .
CS1 young person 1
Her experience of the clinic was that no one responded to her attempts to make contact by telephone or e-mail during a period where she needed support. She felt that within the school council there were several voices who would like to be heard regarding service provision but she did not know who she could go to or talk to with ideas and suggestions. Neither did she believe that they could make an impact.
Another young person had regular online activity with ‘diabetes support’ for peer support and to share information and experiences but, again, she did not think that the group had any influence on services. Her experience of care in school was not good and she felt that no support was offered to her. Examples she gave were having to inject her insulin in the toilets rather than in the medical room, and not being given appropriate facilities to eat during examination periods.
I did see a nurse [at school] because I had to go into hospital because I wasn’t very well, and when I came out of that I went to see a nurse then, and she was like ‘is there anything we can do?’ and I, sort of, said the things but nothing become of it, they never did anything about it, so I did try.
CS1 young person 3
We also conducted interviews with five parents. Parents felt that support groups provided opportunities to talk to other families in similar situations and share their experiences of accessing support, which enabled them to question what they were being told by professionals and pinpoint where care was failing. One parent felt that the support group had power to make changes through ‘campaigning and bombarding people with e-mails’. This parent also sat on the CS1 diabetes network group as a representative for meetings with the PCT; however, she felt that she had little influence:
Whenever I try and say something and put my point across, they all say, ‘oh yes, there – there’ and take no notice.
CS1 parent 3
Another parent reported that her child’s school always responded appropriately to any care needed. The parent is involved in training school staff to support her child to use her insulin pump. This parent also felt that voluntary groups could provide examples of what has worked when writing to GPs and consultants for service provision.
I feel you’re acting as an individual but you feel as if, supported, that you have the power of them [the group] behind you even though the power doesn’t actually do anything.
CS1 parent 5
Patient and public involvement: embedded within the primary care trust?
In the early phases of the research, there was a mixed picture of PPI within CS1. There was evidence that the PCT as an organisation had ‘signed up’ to PPI, and, while acknowledging many of the challenges, was undertaking some quite innovative work. The main issue was that many of these initiatives were ad hoc and at the first workshop there was recognition of silo working and poor sharing of good practice in PPI locally. Indeed, both workshops provided the opportunity for many participants to learn about each other’s approaches.
At board level, PPI was often interpreted in terms of patient experience, with feedback and complaints used to illustrate methods of ‘PPI’. However, commissioners working at service design level were able to describe the benefits of involving patients:
. . . you sometimes perceive it’ll be more difficult than it would be, sometimes you perhaps have an anxiety that it might be a difficult meeting if you’ve got patients there. I have to say, my experience is usually that it isn’t actually, and particularly if you’ve got consultants in the room they tend to behave better actually if there are members of the public there, and they’re often more engaging . . .
CS1 PCT commissioner 1
The evidence of service change presented earlier suggests that PPI was not tokenistic on many occasions. However, there were also a number of examples of reservations from commissioners and providers about a potentially demanding public with a personal agenda. In contrast, many of the service users and their representatives were aware of this perception and sought to allay it:
. . . a commissioner who achieved a lot, you know, was like, ‘Well there is no money, It’s no good getting people coming in here and telling me all the stuff they want because I don’t want to raise expectation, because there is no money’. And when we try to get these networks set up we have to sort of reassure commissioners, . . . agree what we would like to see and then understanding that there are certain realities and what can we do working together to maximise the resources that are available.
CS1 service user representative Parkinson’s disease
The impact of changing processes
The second workshop in CS1 coincided with a PCT board extraordinary meeting to discuss how the transition to the new structures (in particular the clustering of PCTs as a first stage) would be managed. There was a general anxiety that the current PPI infrastructure would be lost and that local GPs were unlikely to have the experience or will to embrace the PPI agenda:
. . . the history of GP engagement with this sort of stuff isn’t good and it’s quite difficult really to see the patients having much influence. I mean, I’m quite concerned, as a nurse by background, how some of the other professions are represented, so I can’t imagine patients would find it easy to get their voice heard.
CS1 PCT commissioner 1
This perceived GP antipathy towards PPI appeared evident in one interview:
. . . all they say is how they have got rights and how their rights should be, that they’ve looked it up and they want it and they feel it is right for them and when they can afford to have it, despite being aware of the costs and risks and everything and they’ve paid their taxes and why shouldn’t they should have it and it all goes back to what they’re personally going to get and not get. I think they‘ve just been too empowered with this idea of informed choice and rights.
CS1 GP commissioner
However, despite these rather negative perspectives, some key mechanisms played out in CS1 resulting in a firmer embrace of the PPEI agenda than suggested above.
Mechanisms for patient and public engagement and involvement within the transitional structures
The PCT medical director was confirmed as medical director in the shadow and subsequently authorised CCG. As a strong proponent of PPEI, she had undertaken an increasingly public facing role in the former PCT, could describe how the PPEI agenda had developed in her own GP practice, and clearly articulated her vision for PPEI within the new CCG:
PPEI in the CCG is absolutely right through, I’m absolutely clear about that. So and it’s a two way process, it’s not just us hearing them, and one of the challenges is how do you create a public group who have enough knowledge of the principles of healthcare without having been subverted into an agenda that, you don’t want. You know, that’s actually the health agenda but are able to be critical friends, critical partners and contribute, and have enough knowledge of the jargon and the processes that they can feel confident as well to contribute and challenge.
CS1 CCG medical director
In contrast to the earlier data suggesting some silo working, PPEI was now envisaged as synergistic across the health, local authority and voluntary sectors. The PPEI agenda had another prominent champion within the CCG, the Director of Development and Strategy, whose portfolio included being the Public and Patient Engagement Executive Lead. She described four key aims for PPI within the CCG:
-
to be different from how PPI was enacted pre CCG
-
to be present and embedded within all CCG decision-making processes
-
to have an active influence over CCG decision-making
-
to support people to make active changes over lifestyle, particularly those with diabetes type 2.
The first aim was a recurring theme with CCG and local authority respondents in the post PCT phase of this study and will be explored further in Chapter 7. The executive lead offered the following evidence on the CCG’s commitment to PPEI:
. . . we’ve got this strong will to do things differently but we’ve not been resourced to do so. So what’s important to know is that we have just offered positions to Communication and Engagement Managers within the CCG and we’re a bit different from other CCG’s because others are just buying it from commissioning support . . . we interviewed two weeks ago and we had some exceptional candidates and we have been a bit naughty [laughs] and now recruiting two managers.
CS1 CCG PPE [patient and public engagement] lead
In addition to the two CCG champions, a small project team headed by a lead bought in as a consultant by the CCG cluster developed the PPEI strategy for the authorisation process; having a very experienced and effective project team who role-modelled engagement during the development of the strategy was an important mechanism within the CCG. The project lead highlighted the initial challenges as getting the shadow CCG board to attend engagement events, and that these events had been too large and were prone to being used as ‘an opportunity to have a moan and to complain about things’. Nevertheless, a clear and coherent set of work streams resulted in a comprehensive strategy for PPEI. While the overall PPEI structure is presented in Figure 2, this was supplemented by a number of tools. First, the close links between the CCG and Public Health based in the local authority would provide the CCG with data for the representative population and advice on what kind of engagement approach would suit this population. Second, a database of existing PPI groups and service user representatives was being created:
. . . we’ve built up all our contacts and we’ve checked with our equality colleagues within (cluster) as to the type of groups that we should be interacting with and making initial contacts with them and then once you’ve got all those people and you’ve kind of identified them in this database that we’ve created, or built up, you then can be very targeted about, approach about recruiting people in, so for example a clinical lead on a, one of their commissioning priorities, urgent care will say, ‘I actually need two or three lay reps,’ so you can then say, ‘Right, for your area what coverage do you want there to be?’ and then you write out to the people in that area and say ‘Here’s an opportunity for you, you’ve said you wanted to either get involved at this level or you’ve said specifically you’re interested in A&E [accident and emergency] issues, you know, what may be classified as urgent care, do you want to put yourself forward?
CS1 PPEI project lead
FIGURE 2.
Patient and public engagement and involvement structure in CS1. PPE, patient and public engagement.
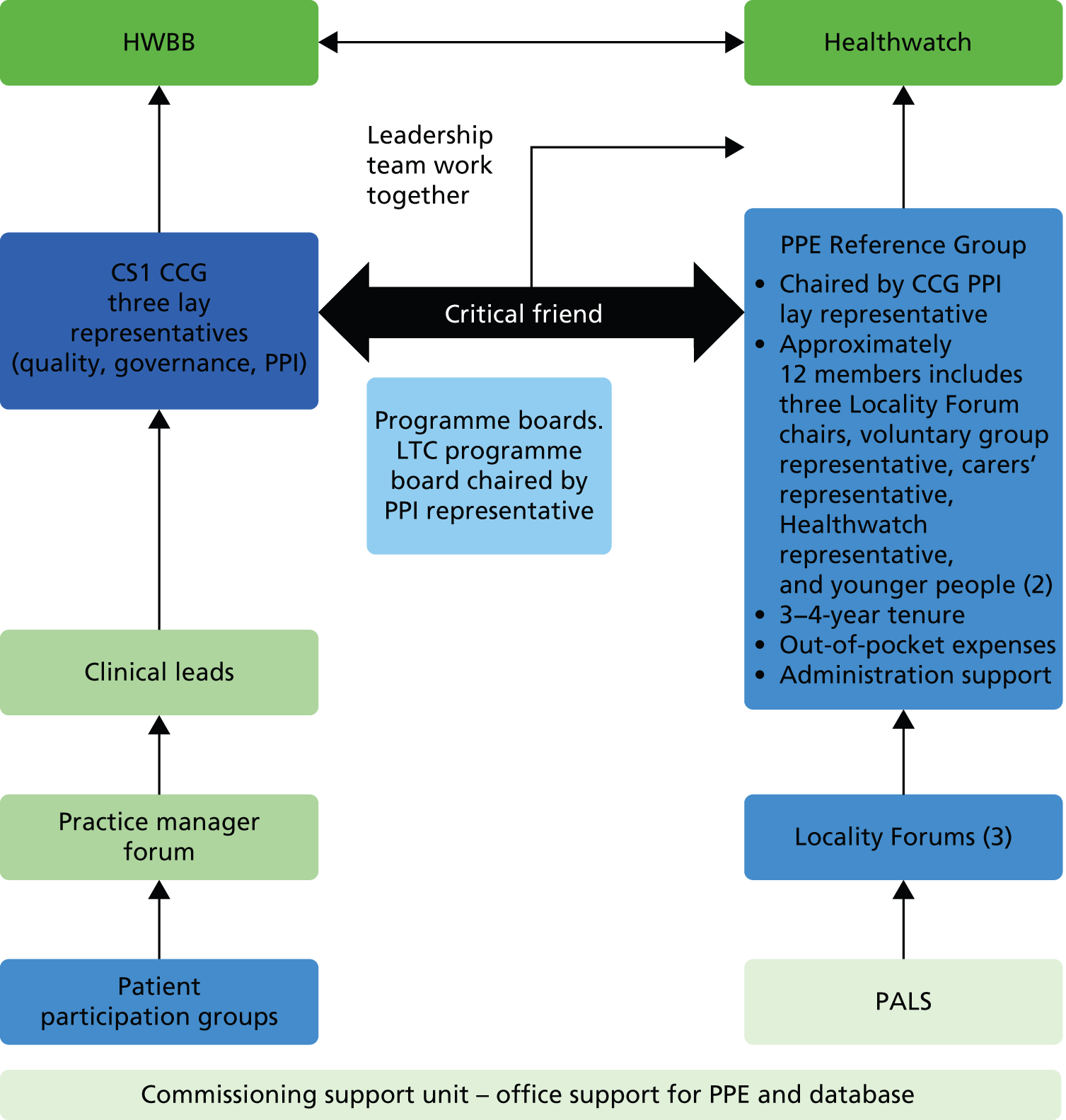
Third, the Patient Experience Blog described earlier took on a new importance in the eyes of the commissioners and was seen as a key tool for PPEI. This represented a complete turnaround from the rather ambivalent attitude of GPs to the Patient Experience Blog project in its early days. As one of the original catalysts of Patient Experience Blog, the loss of enthusiastic PCT commissioners in the NHS reorganisation had left the project floundering. Observation of a shadow CCG board meeting also suggested that the GPs initially perceived Patient Experience Blog as being a ‘twitter like tool which was just about patient’s [sic] having their say’ (field notes). However, specific championing by the PPEI project lead and a SHA PPEI consultant resulted in the Patient Experience Blog being a key pillar of the CCG PPEI strategy and, indeed, it was rolled out to other CCGs within the cluster.
The targeted approach to PPEI as articulated by the CCG PPEI project lead was mirrored by the project lead for the shadow Healthwatch. He described focusing on areas where they could potentially have the most influence: large budget holders and being the voice of the ‘ignored middle’, i.e. the everyday person who did not usually get their voice heard.
While strong links with the voluntary sector were integral to CS1 PPEI strategy, there were some reservations from respondents representing these groups:
I haven’t had any links or contact with CS1 CCG, I don’t even know whether they have a neurology lead, but I have been able to make contact with [a neighbouring CCG] and they were looking into whether there was anybody leading in this area but they haven’t got back to me yet . . . [January 2013]
CS1 service user representative MS
This represented a more general view voiced by service users, that while the CCG was creating its PPEI strategy it was a one-way ‘don’t call us, we’ll call you’ approach. However, there was some acknowledgement, too, that CCGs were so focused on the authorisation exercise that there was less capacity at that stage to operationalise PPEI in the spirit intended.
Concurrent to the PPEI development within the CCG, the Directed Enhanced Service (DES) payment was resulting in the setting-up of local patient participation groups (PPGs) attached to general practices. CS1 included some relatively affluent areas where there was some history of PPGs:
. . . at [xxx] Health Centre and that’s been going now for about 13 years, it was one of the originals . . . our Chairman is an ex-partner of the practice, retired . . . he instigated it really, you see, and so we’re very fortunate and the senior partner, you know, attends all our meetings so we‘re very lucky. What’s the role of that particular group? Simply communication between the patients and the partners . . .
CS1 service user CCG reference group
However, the DES was encouraging more practices to set up these groups:
. . . other practice managers I’ve spoken to and said, well what does your do and how does yours work and . . ? You know, and it was like well, you know, it’s very much about fundraising and they don’t quite have as much involvement maybe and things like that. And then, of course, when the discussion about the DES came out, we had a draft DES and thought well, you know, this probably gives us the impetus to say let’s now do something about it . . .
CS1 practice manager
Nevertheless, while there was enthusiasm for PPGs from some local practices, in CS1 there was little evidence on how they had been closely aligned to the overall CCG PPEI structure; as illustrated in Figure 2, they appear at the periphery. In addition, there were proportionately fewer active PPGs than in other case study sites and, of those active, there were more that were functioning as a virtual group rather than face to face (Figure 3).
FIGURE 3.
General practitioner practice patient groups for CS1.
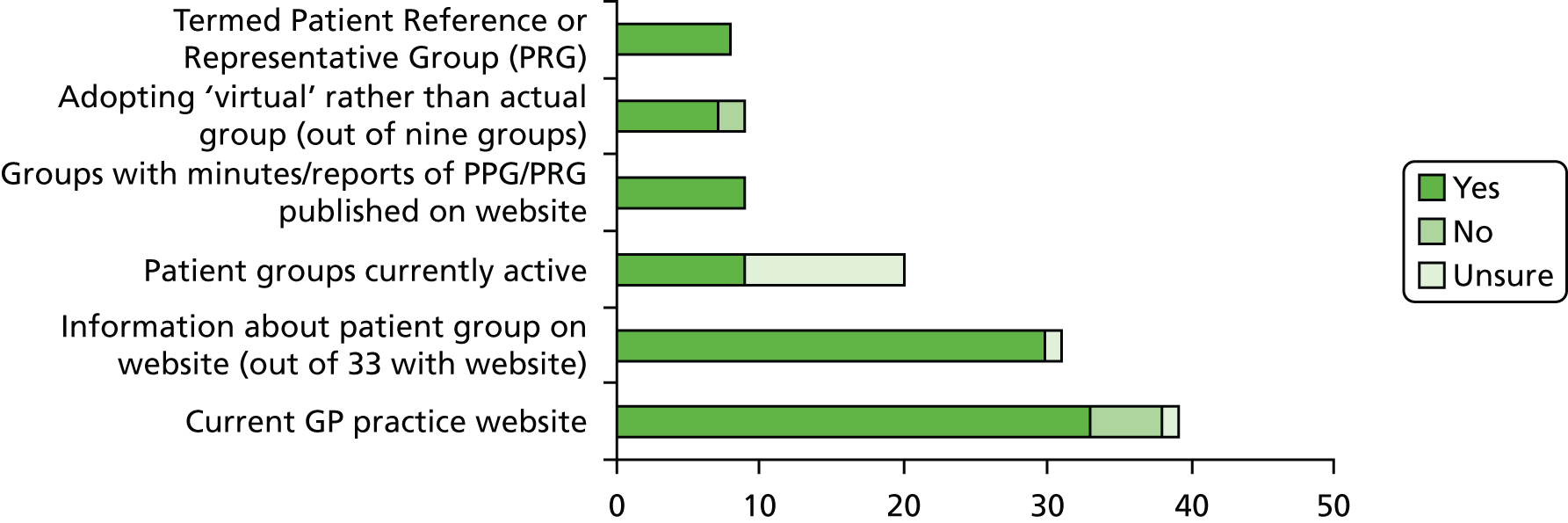
Access
Within CS1, there was a real desire from the CCG and local authority to take a new approach to PPI and recruit new people. In the earlier phase of the study, service user respondents in a PCT lay role or LINks members described a long history of PPI often stretching back to community health councils. As described by the project lead for the shadow HWBB, there was an initial assumption from LINks that there would be an automatic transition into the new PPI structure. Indeed, in the early days of the shadow HWBB, this was exactly what happened. However, the formal recruitment processes adopted by the CCG, HWBB and Healthwatch ensured that a ‘refresh’ process occurred. Key lay positions on all three bodies were via a formalised recruitment process. In the case of the HWBB, LINks had formally objected to this process and so were invited to present their approach (open invitation) to the scrutiny committee which then voted for the formalised approach. The Healthwatch project lead had also designed a recruitment process to emulate the Olympics ‘Gamesmaker’ model in order to get the ‘right people’.
While the three lay positions on the CCG board were advertised within local media, the reality was that all appointees were previously known to the CCG and were actively encouraged to apply. However, there was an acknowledgement of the need not only for ‘new blood’, but also not to alienate those who had undertaken years of lay involvement:
. . . it’s also not wanting to seem like an organisation that doesn’t value a group of the public because that defeats what you’re trying to do. But it’s how to not alienate them, get them to feel involved but allowing a wider range of comment. And you have the same thing with the lobby groups and it’s how do you harness their energy and their knowledge without it railroading everybody else?
CS1 CCG medical director
The PRG was seen as the main forum to prevent alienation and continue the involvement of these long-serving lay people. In contrast to lay appointments to the CCG board, the PRG had less of a formal recruitment process and was generally offered to lay people serving in an existing role. Within CS1, the PRG was chaired by the PPI lay non-executive CCG board member. Both she and the appointed chairperson of Healthwatch were chief executives of local charities serving marginalised groups, and had a long history of non-statutory service to the local population. The PRG chair was focused on moving the PRG agenda on from a personal one:
I threw down a challenge at our first meeting and just said ‘I hear what you’re all saying, I really do and I’ve got every sympathy’ . . . but we can all talk about that, we can all sit and nod and we can all talk about it again next time and nothing will change. So my challenge to everybody around the table is that our group will be solutions focused.
CS1 CCG board lay member 1
As data collection completed, the PRG had met only four times, and, as described by the PRG chair and the CCG PPE lead, the group were still in the ‘storming’ phase of group development. It was also acknowledged that the next steps were seen as focusing on engaging harder to reach groups, in particular younger people.
Agenda
When looking at access to the new PPEI structures in CS1, it appeared that the PRG was being used as a ‘holding area’ for patients and the public with a long history of health service involvement and lobbying activities. There was also some evidence that the PRG chair was acknowledging that it would take time to change the ‘personal agenda’ of many of the PRG members:
I had a sort of review meeting with the Chair and the Chief Accountable Officer last week and we had quite a good and frank discussion, where I said ‘Look, this is my day job, but please don’t think I’ve got a magic wand’, because to move forward there is a piece of work that we need to do with the people that are currently engaged, because if you flip them off, instead of them being your ambassadors and your advocates, they will become your enemies.
CS1 CCG board lay member 1
Interestingly, there was some evidence that service user-led initiatives, such as the schools diabetes protocol discussed earlier, were being removed from the agenda by the PRG members themselves:
. . . someone started to talk about the diabetes pathway at the last meeting, legitimate issues, things about. . . actually it boiled down to children, how people with a reliance on insulin need something during the day, and they were talking about a programme that had been established . . . nobody responded, nobody said ‘That’s really good, I can roll that out, I can take it back to my forum’, and the end result was we came back to GP access . . . You know, the person that sat there [parent presenting the protocol], what would be their incentive, what would be their ‘what’s in it for me to come back to that sort of environment?’
CS1 CCG board lay member 1
It was too early to tell what impact the PRG was having on the CCG decision-making process, and, indeed, the CCG lay board members felt that it was too early to assess their own impact on the agenda.
Agenda-setting within the new structures was understood as the role of the executive officers, with an acknowledgement that lay representatives would have the opportunity to influence discussion of the items on the agenda. For the CCG, key challenges were identified as occurring in 2014 with service restrictions, and the CCG PPE lead described PPEI as a key tool in getting difficult decisions through. For the CS1 Healthwatch, the agenda was set around its self-definition of being ‘an evidence-based market research organisation’. There was some evidence that the voluntary sector was trying to change or influence the agenda. For example, the carer of someone living with MS was encouraged and helped by the MS Society to successfully apply for Healthwatch in order to ensure that the MS population voice would be heard. However, it was clear when interviewing this member that he perceived the importance of being able to understand the health issues facing the broader population and being able to contribute more strategically.
Summary
Case study 1 had a strong pedigree of PPI initiatives; however, even with this history there were only a few notable examples of service user voice having a major impact on service delivery. The will for PPEI transferred over to the CCG board, although there was evidence that this intent did not extend to all GPs. Nevertheless, the employment of a dedicated project lead to develop the PPEI strategy demonstrated a commitment. However, when data collection completed there was a general feeling that the aims of the strategy would take longer to achieve than anticipated, and that it was too early to be able to fully evaluate whether or not the service user voice was being heard and responded to in the CCG decision-making processes.
Chapter 5 Research findings: case study 2
Background
Case study 2 was the second site to be recruited. Merged from four separate health organisations in 2006, CS2 had a long-standing tradition of patient involvement and public engagement, with a PPI strategy that focused on partnership working and active involvement.
Case study setting
Case study 2 is situated in an inner-city area in the north of England. It is culturally diverse, with a growing BME population. Life expectancy is marginally below the national average and the site reflected high levels of health inequalities, with areas and pockets of deprivation. Differences between life expectancy between the best-off and worst-off neighbourhoods was marked (around 14 years in 2008) and prevalence of chronic diseases showed a consistent and high relationship with indicators of deprivation at ward level. CS2 commissions services from a variety of providers, including acute, community services and specialist hospitals. Primary care is provided through 88 general practices, forming four locality-based, practice-based, commissioning groups.
Processes and supporting structures for patient and public involvement
Public and patient engagement and involvement appeared well established in CS2, primarily through CS2’s relationship with the local authority. The city council was an active partner in health and social care, with an established track record in community development, as well as increasing public involvement via community assemblies. The voluntary sector was highly developed, with over 150 charities and voluntary organisations operational. PPEI structures, such as a third sector assembly, brought together voluntary and community organisations, faith groups and social enterprise organisations with statutory services.
The first workshop identified various PPI initiatives that were operating within the case study site. Significantly, participants found the information exchange informative, and discussion identified that many of the initiatives were not adequately or widely communicated. Sharing information was seen as essential (Table 8).
| PPI structures | PPI activities |
|---|---|
| Organisational-led structures | Expert patient programme |
| Quality Improvement Academy – led by PCT chief executive, attended by LINk and service users, focus on care pathways | |
| Readers Panel | |
| Health Inspectors – young people (11–19 group) inspecting children services re: fit for purpose | |
| Patient Involvement in redesign of hospital car park | |
| Lay involvement in steering groups | |
| Patient stories | |
| Big Health Conversation – public consultation for JSNA | |
| Shadow Board for Coronary Heart Disease | |
| PPI projects | Experience-based design – the collection of real-time data focusing on how patients are feeling at each stage of pathway |
| Person-centred planning – patient redesigned care pathway transition from child to adult learning disabilities services, results identified reduction in hospital admissions and healthier lifestyle | |
| Service user-led PPI structures | LINks |
| Local voluntary action groups | |
| NRAS – directly approaching general practices to raise issues |
Interviews, discussions and documentary analysis showed a diversity of methods utilised within the case study site in relation to PPEI (2010–13) (Table 9). The development of PPGs was evident at practice level. Patient participation group recruitment was often via invitation, and involvement covered areas such as practice environment, patient education and self-help, advocating access to services and involvement in public events. Lay representation was identified in a number of working groups – this included areas such as Partnership for Mental Health, Health Panels, commissioning/public/multidisciplinary meetings and virtual groups. A focus group with local National Rheumatoid Arthritis Society (NRAS) members identified the use of the press as a way of making their views heard.
| Method of involvement | Used or led by | Level of involvement |
|---|---|---|
| Lobbying local press | Service users | Information exchange |
| Lay representation on health panels/forum | Commissioner Consortia |
Information exchange Feedback |
| Patients as champions | Patients | Participatory |
| Lay representation in commissioning meetings | Commissioner | Information exchange Feedback |
| Lay representation in working groups | Commissioner | Information exchange Feedback |
| Voluntary organisations facilitating public engagement events | Service user representatives | Participatory Consultative |
| PPGs | Initiated by practice personnel User led |
Participatory |
| Practice leaflets/letters | Provider | Information giving |
| Diabetes support group | User led | Participatory |
| Consortium/practice website | Provider | Information giving Feedback |
| Comment box | Provider | Feedback |
| Lay representation in public meetings | Commissioner | Information exchange |
| Involvement network | Commissioner/patients | Participatory |
| Enter and view visits | User led | Feedback |
| Press releases | Commissioner | Information giving |
| Graffiti wall | Commissioner | Feedback |
| Public consultation exercises | Commissioner | Consultative |
| Questionnaire – patient satisfaction | Commissioner/provider | Feedback |
| Lay representation in forums | Commissioner/local authority | Information exchange |
| Survey | Provider | Feedback |
Some of the examples focused on information exchange, with a strong emphasis on feedback. Data collection tools such as survey, questionnaire and comment boxes were highlighted as well as a number of public consultation events. Newsletters and practice leaflets were also identified, as well as the use of consortium websites, with strong emphasis on providing patient information but also offering ways to become involved. Discussion with LINk representatives highlighted the use of ‘enter and view’ at hospitals and GP surgeries. There was PCT involvement (PPEI team) in citywide PPEI networks and expert patient programme groups; in relation to tracer conditions, there were a number of consortia-led groups such as diabetes planning and commissioning group/long-term neurological conditions forum.
A diabetes support group had been involved in service redesign and had the ability to work independently of the practice, setting its own agenda and offering support and social networking. Patients were also acting as champions at practice level, which involved supporting other patients and helping them to access appropriate services. Patient involvement in educational programmes such as DESMOND (Diabetes Education and Self-Management for Ongoing and Newly Diagnosed) had also led to increased involvement, for example in changes made to adolescent services. In addition, there were some examples where voluntary groups had been asked to run public consultation events; for example, the Royal National Institute for Deaf People (RNID, now known as Action on Hearing Loss) was involved with hearing aid services redesign. In relation to tracer conditions, PPEI was evident in the redevelopment of musculoskeletal services, with the PCT instigating a number of service provision reviews focusing on physiotherapy, podiatry and chronic pain services. PPEI focused strongly on consultation, with the predominant use of questionnaire and survey. Although there was a Long-term Neurological Conditions forum, with patient and public representation, documentary analysis revealed no evidence in relation to the impact of the forum.
Assessment of methods and approaches of PPI reviewed within the case study site (see Table 9) highlighted a continuing focus on commissioner-led initiatives, with fewer examples of participatory involvement. This would suggest that overall control of the agenda had rested within the PCT itself.
Local policy and embedding of patient and public engagement and involvement
Consultation, partnership working and knowledge exchange had all impacted on the development of the PCT PPI strategy, with three key priorities emerging:
-
focus resources on creative engagement of the seldom heard
-
maintain effective engagement through agreed approaches
-
patient involvement in the development, purchase of appropriate services and monitor their effectiveness (ensuring that service users were part of the strategic procurement cycle).
Interview data from the evaluation suggested that creative engagement with seldom-heard groups was linked to the restructuring of the Communications and Engagement Teams within the PCT. This involved the abolition of the Engagement Team in 2010, with a social enterprise organisation contracted to run 8–10 consultations each year. The organisation had an established relation with the PCT with experience of being involved in a number of consultations relating to ‘hard-to-reach’ communities. The rationale for this significant move was explored and discussions identified a refocusing of PPI initiatives, moving consultation out into specific communities, and bypassing established community meetings.
I mean the way that the Engagement Team before worked was that they, they used sort of traditional methods like going through the voluntary sector organisations, going through established groups that support some of those communities, but we felt we were probably getting opinions from the same people through that route. Whereas using this company, they, I mean they’ll go and speak to people within those communities, they don’t just attend the meetings that get attended by the same people if you know what I mean, they’ll actually go out and speak to more people . . .
CS2 assistant director of PPI, PCT
Some informants thought that there was a broad range of representation within initiatives but also saw that seeking a wider opinion was beneficial. However, some professionals still felt that the use of proxy-users was acceptable. Furthermore, creating wider diversity was seen as problematic; one commissioner highlighted the usual type of person who becomes involved as being too enthusiastic or opinionated, and that there was a struggle to attract minority ethnic groups.
Documentary analysis revealed actual and potential examples of PPEI within the case study period (2010–13) with emphasis on the use of advisory panels/forums, joint training initiatives (professional/public), partnership working and consultation. A review of public consultations by the PCT (2008–12) reflected a variety of health-related topics; however, none specifically related to the tracer conditions of the research project. Website analysis identified a prominent place for patient stories; involvement initiatives included health education programmes, volunteering and polls as well as the provision of links to other involvement networks.
There was also evidence of PPEI as part of the strategic procurement cycle. Interviews with providers and commissioners identified the importance of PPI both as a policy directive and within the commissioning process. Discussion with commissioners highlighted the value and essential nature of PPI in ensuring that services fit local patient need and facilitated service buy-in. The concept was also seen as an opportunity to be involved in and informed about service provision.
Public involvement is trying to, for us or for me is about matching services to meet the needs of patients and having them involved in that process as best as we can.
CS2 GP commissioner
. . . effective commissioning is heavily dependent on good, constructive and meaningful patient engagement in the development and redesign of services. Without it there’s a danger that we design systems and care processes that patients, the public and service users don’t understand and don’t buy into . . .
CS2 commissioner
Interviews with service providers identified that patients needed to be involved in any changes to services and that such involvement was part of the effective shaping and development of service provision.
I think if you’re not careful a lot of well meaning people develop a service without necessarily the true input of how someone actually on the receiving end of the service is actually going to feel about it . . .
CS2 NHS provider
Service user discussions identified lay involvement should be proactive, linked to improved patient care and effective design or redesign.
Because we’re on the receiving end of all this care and so it’s important that you get the feedback on how we are finding it and what we feel the hospital is doing well and what they could do better. It just needs different peoples point of views, you know, not just the actual carers but the patients themselves.
CS2 service user representative
Respondents gave examples of where PPI was discussed in specific service redesign contexts. This highlighted that the concept of PPI was an essential element of the redesign process and that it was embedded within the PCT operations and processes.
We did completely unpick the previous service model for community physiotherapy, and we ran a series of engagement exercises, partly at practice level and partly at wider community level . . . we actually had some very good constructive points of detail which helped develop the specification to a level that was more productive, and that was as a result of, if you like, public input.
CS2 PCT commissioner
As with other the case study sites, public involvement was viewed as resource intensive; cost implications were identified in relation to large-scale engagement events. Involvement was also seen as time-consuming with the potential to slow down decision-making, with limited staff available for such work. Voluntary organisation representatives identified difficulties with funding, recruitment and workload.
There was limited documentary evidence in relation to the place of PPI within PBC and general practice as a whole, although PPGs and Patient Opinion work were operated by a number of practices.
Evidence of influence
There was some evidence of involvement leading to identifiable changes, although examples tended to focus on small gains. Initiatives relating to the diabetes service gave a number of examples:
-
patient retention of medication on admission to hospital
-
redesign of leaflets
-
development of exemptions to the standardisation of blood sugar meters
-
accurate register of patients with diabetes
-
use of patient-friendly letters
-
greater localisation of eye-screening.
The LINk was involved in the evaluation of a care home directory; following involvement, the directory was redesigned to be more user-friendly. This organisation was also involved in challenging the planned closure of two care homes; successful campaigning resulted in the care homes remaining open. Furthermore, feedback from ‘enter and view’ initiatives at local hospitals had led to the implementation of an action plan for change; however, it was unclear whether or not the suggested changes had been implemented.
Public involvement in relation to physiotherapy services had led to the rationing of such services, i.e. six treatments only before review. Public involvement in hearing-aid service redesign had led to an improvement in the quality of the specification and a service that was more cost-effective. PPGs had also made a number of successful changes such as adjustment of practice opening times, patient confidentiality at reception, changes in the waiting area layout, increased access to chiropody services and increased and quicker access to physiotherapy services (identified within contractual arrangements).
However, the main exemplar of influence and service redesign related to the development and implementation of a model of enhanced diabetes care within primary care settings in 2009. The transfer of diabetes services from a predominantly secondary care-based service to a community-based model had a number of drivers and this included disease projections, demands on secondary care, policy drives, service gaps and stakeholder feedback. Public consultation events (n = 2200) had identified three public priorities for diabetes services:
-
improved communication
-
care nearer home and at a single location
-
better engagement with diabetic patients from BME groups.
I mean the diabetes community group hasn’t come out of just practitioners thinking this is a good idea, this was from long-term listening to patients saying ‘actually, you know, why do we have to go to the hospital for this, why can’t it be done at a GP surgery? Why do we have to traipse up there when we can’t park?’
CS2 service user representative
A Clinical Commissioning Planning Group (CCPG) was activated to support the transition of this service; although PCT-led, this group had lay membership in the form of Diabetes UK representatives. Interviews with commissioner and service user representatives suggested active involvement and the valuing of lay input. The new service was evaluated by patients at each stage (e.g. scoping, piloting and post implementation). This included an additional evaluation by the social enterprise organisation (see exemplar).
With the evaluation that’s going on at the moment, what we determined was that we didn’t want it just to be fed back to the patients, but we very much wanted them to be part of that evaluation. So, we’ve looked at – we’ve got service data; we’ve got the effects on hospital spend, etc. going off; we’ve got access. But what we also did do is put a strand in and we got a PR [public relations] company doing some work for us that actually asked patients what they thought about the new service.
CS2 PCT commissioner
However, assessment of the PPI initiative by the Expert Reference Panel identified a number of problems with this exemplar. A diabetologist felt that there was insufficient attention paid to implementation and outcomes.
We have a tripartite service with poor communication between primary, community and secondary care and at least 3 different IT [information technology]/data collection systems. if not multiplicity and delays in referral confusion in clinical responsibility. Have to demonstrate good governance/quality of care.
Member of expert panel
Similar concerns were echoed by the GP:
. . . possibility that the proposed new service configuration might be difficult to implement and lead to problems during the transition phase (such as a disruption of care for patients).
Member of expert panel
In terms of the process, the representative from the national diabetes patient organisation felt that there had clearly been some engagement with service users but was critical of the outcome measures:
The outcomes that are not described are the more intermediate outcomes of patient engagement in their own individual care, confidence in the care delivered, increased capacity and confidence to self-manage their diabetes. 95% of a person with diabetes life is spent managing their own condition and only a maximum of 5% is spent in contact with the clinical system of care, therefore ability to cope, understand, knowledge and engagement outcomes are important.
Member of expert panel
There was concern among the expert panel members that the overall focus of the exemplar was on clinically defined outcomes which, while recognised as important, primarily focused on process outcomes with little attention to issues related to the predominantly self-management of diabetes and clear demonstration of a wider patient-focused engagement in process and outcome measures.
Involvement of children and younger people
Three interviews were conducted with three young people within CS2 and one interview with a parent; as with other case study sites, gaining access to such interviewees proved time-consuming with limited success.
A number of issues were highlighted within the interviews such as the importance of support. One young person with complex conditions was not involved with any support group due to risk of infection. She looked to her family and her consultant for support, and her experience was that the children’s hospital was responsive to her needs.
Two young people interviewed had set up their own support and social group for local teenage girls with type 1 diabetes. The group aims to provide a forum for social activities and for people to gain support, information and advice from each other. The children’s hospital was encouraging in helping the group to make contact with other young people and supportive to the needs of the group.
So I think they’re quite, you know, they‘re very supportive of us and I think if we did need an extra service or more help the nurses and people would help us and back us up on that.
CS2 young person 1
One young person who had been involved in starting up the group said she felt that more members would strengthen the group in terms of getting their ideas listened to.
I think it would just be a good idea to get other people but I think people do listen to us because you know, obviously this is a long-term condition so it is something that you know probably would need to be looked at if we did need another service.
CS2 young person 1
The parent interviewed had also been involved in the setting up of the young persons’ support group for local teenage girls with type 1 diabetes. She has also attempted to set up a support group for families of children who receive diabetes care at a local hospital. One of the challenges of reaching out to families who might want to participate in such a group was making contact. Advertising and word of mouth tends to be how families find out about the group.
. . . we can’t be given people’s names and addresses.
CS2 parent 1
This parent had a good understanding of the commissioning process and organisational processes taking place and she felt that young people should certainly be involved in decision-making but also that young people’s views were not sought or represented.
But at the moment I don’t know, I don’t see anybody asking them for their opinion in terms of commissioning I think there was a paper, I think it was about services for disabled people a few years ago, which was entitled, sort of, ‘nothing about us without us’, and I do think that unless you involve the people, i.e. the young people who this affects and their parents and carers who support them, you won’t actually get the best solution, I think it needs everybody.
CS2 parent 1
She was happy with the services provided for her daughter at the children’s hospital, which she described as flexible and person-centred, and she felt that she could easily approach the diabetes team to discuss any additional services, if needed. She went on to say, however, that the service was responsive rather than actively seeking user opinion.
So although the service is very good and they are responsive to you as an individual . . . I don’t recall in 7 years at . . . children’s hospital ever being asked, ‘What’s your opinion of the services?’
CS2 parent 1
The impact of changing processes
The data collection period for the study was extended until March 2013 to capture major health policy changes, which included the abolition of the local PCT and LINk and the establishment of a CCG as well as the development of the local Healthwatch and HWBB. The PCT communications team was incorporated into a patient partnership group based at the NHS Teaching Hospitals Foundation Trust. It was expected that there would be representation from Healthwatch on the Patient Partnership Committee. Some PCT personnel transferred over to the newly developed commissioning support unit (CSU) in order to perform an advisory role as well as have some responsibility for external public consultation on behalf of the CCG. Although health policy had advocated a ‘smooth transition’ between organisational responsibilities, interviews with PCT commissioners highlighted a number of issues regarding strategic development and the implementation of services.
. . . in terms of the commissioning, contracting, that pushing, shoving, making happen, managing, monitoring, implementation, managing performance, working with, you know, all that type of stuff I can’t see where that actually is in the new organisation, which makes me really worried.
CS2 PCT commissioner
Officially we transferred, supposedly transferred, in August, but then we were transferred again supposedly in October. But I don’t really know . . . I think for diabetes . . . we have made such enormous strides forward that it’s – you just think well, where’s this going to go? What’s the future? Will this progress?
CS2 PCT commissioner
Discussions with lay representatives also identified frustration about what was seen as having to start again with a new process of involvement.
And, you know, they often throw the baby out with the bath water. We had a very good system going and it’s now gone. And I’m not sure that what’s going to be there instead will be any better.
CS2 service user representative
The PALS was split, with the CCG chief nurse having responsibility for the continuing care aspect of this organisation; PALS in respect of GP-related issues remained independent of the CCG, resting within local area team structure.
Getting heard
The restructuring of local services and organisations had impacted on PPI in several ways. Firstly, interviews with service user representatives and commissioners highlighted a reduction in PPI activity. One example of this was service user representation in relation to the community diabetes service (see exemplar). A CCPG for this service, which had representation from Diabetes UK, had been disbanded following the successful implementation of the new service into one locality. This left representatives feeling that they had very little contact with the newly developing shadow CCG, affecting their ability to be heard.
Well, I can tell you that everything’s fallen apart completely . . . the commissioning group of the PCT has been disbanded and the patient group that we were involved with, we haven’t met because there’s been nothing to meet about. And they’re in a process of reorganisation into consortia, and how it’s going to work, I don’t know.
CS2 service user representative
The CCPG was seen as a key vehicle for involvement, enabling a systematic ongoing dialogue between PCT commissioners and service users. Importantly, it had acted as a feedback mechanism between clinicians, managers and lay representatives. Dissolving the group had impacted on communication; for example, the service user representative was unaware that the community service had been rolled out citywide.
. . . we had key people at the Primary Care Trust who we could contact as patients and keep the kettle boiling, kind of thing. But now we don’t; I mean, we’re waiting and waiting for the new systems to get into place. At the moment I have got the lead GP as a contact and that’s about it.
CS2 service user representative
[Re: community service] . . . I can’t tell you how it’s going really, ‘cause I don’t know . . . I know they were planning for it to go city-wide, but I didn’t know it actually had.
CS2 service user representative
Communication had become more individualised rather than maintaining an organisational systematic approach. Key members of staff had also resigned or been transferred, which had led to concerns over the loss of expertise and organisational knowledge.
So like yesterday I was bouncing e-mails backwards and forwards to one of the ones of the group. But that’s because I know this person and I keep her informed. But in terms of where’s the formal route of doing this? I can’t see anything much happening.
CS2 PCT commissioner
I think we’ve gone from having something really good and robust and we’re clinging hold of it and determined we’re going to continue with getting patient involvement in there, but it feels as if we’re doing that outside of now what is in place or what is supported by the organisation.
CS2 PCT commissioner
Discussions highlighted the importance of effective communication to increase the visibility of voluntary organisations.
. . . the main problem is telling – is patients being told about Diabetes UK meetings and about services it offers and you’re reliant on that . . . you can give people information, but they may not pass it on.
CS2 service user representative
The development of new processes had meant that voluntary groups had to be proactive to ensure that they had a voice in the new structure; this included asking the GP lead for diabetes (shadow CCG) to attend local voluntary meetings and leaving information regarding Diabetes UK at individual GP practices. There were also concerns about a new approach to diabetes as a condition; with all LTCs having been incorporated into an umbrella group (LTC committee), interviewees questioned whether or not specific conditions would remain visible within this new structure. Acting as a specific group was seen as important in relation to being heard:
I mean, some of the best engagement groups are where you’ve got people with the same condition being involved together and then that voice can come from all of them, because they have all been able to have a say.
CS2 LINk representative
The need to re-establish relationships was seen as unhelpful and time-consuming, demand for involvement had dropped, difficulties with recruitment remained and fund-raising had halved.
Well, it’s not just getting representation, it’s getting any volunteers to do anything.
CS2 service user representative
For some interviewees, there was a loss of influence; however, for other groups this had never been attained. Those with mainstream conditions, such as diabetes, cancer and heart disease, were seen as groups more likely to have a voice. Focus group data analysis showed that groups such as the local NRAS group did not feel that they were visible and it was difficult to get their voice heard – this may explain why this group would tend to use the local press to air issues.
Other public involvement initiatives had stalled to some respect; specific consultation initiatives by the social enterprise company had been operationalised but the report was delayed, perhaps suggesting loss of organisational focus by the local PCT:
. . . this has been one of the things that has fallen a bit through the gap; that actually getting through from them their end report or even a recent progress, hasn’t been there.
CS2 PCT commissioner
Access
Some stakeholders took advantage of the need to develop new structures. For example, the development of Healthwatch was described as a coproduction between local citizens and local government, and incorporated 18 months of stakeholder engagement focusing on the role and remit.
. . . we wanted to take the approach that the citizens . . . sort of co-design and lead on the development of our Healthwatch, you know, the scale of how do you get something that represents what 500,000 very different sort of people might want.
CS2 city council representative
Selection of the organisation to run Healthwatch went through a robust tendering process; however, difficulties were noted in relation to funding.
. . . I think some of the challenges for us have been that information from the Department of Health has come out very late in the process and so for example we still don’t know what level of funding settlements are that we’re going to get.
CS2 city council representative
The tendering process finished in January 2013, with the contract given to a consortium of local voluntary organisations, leaving little time for organisational and partnership development before going live in April.
Within the case study, the 88 general practices formed one single CG, with practices divided into four localities. The CCG board had two lay members, as well as a clinical executive team, with specific GPs taking on portfolio specialities such as PPI and diabetes. The HWBB was seen as a useful vehicle in supporting the development of PPI in the CCG, and there was GP membership at board level.
. . . I do also sit on the Health and Wellbeing Board for the city and that’s been very supportive, and there’s similar conversations going on there about making sure that we’re doing what the public and the patients want us to be doing to the best of our ability.
CS2 GP lead PPI CCG
There was also the development of a LTCs committee, an umbrella group for all LTCs. During the data collection phase, it was unclear whether there was any patient or public representation on this committee.
Mechanisms for patient and public engagement and involvement within the transitional structures
The PPI strategy for the CCG was at the stage of a draft plan by the end of data collection. Three main involvement vehicles were advocated: CCG-wide membership scheme (open to all practice patients), a patient engagement panel (PEP) and PPGs.
Both the membership scheme and the PEP were only at the stage of potential vehicles in March 2013. The membership scheme, if implemented, would certainly have increased access to participation. The remit of the PEP was unresolved at the end of data collection; however, there was some discussion that its membership could potentially come from Healthwatch. One of the lay members on the CCG board was also a member of an organisation within the consortium which had won the tender for Healthwatch, and therefore had established links.
However, the development of PPGs was visible within the case study area. By March 2013, 65 out of 88 practices (74%) had established a PPG in some form; this included virtual and actual groups, with Patient Opinion, again, increasing access to participation, with 81% of practices offering a publicly accessible website.
The draft CCG PPEI plan (see Figure 4) did not clearly elaborate on how each element of the structure would function, communicate or relate to each other; this could potentially lead to compartmentalisation, with each operating as separate entities. This concern was also highlighted in discussion:
My worry is that information doesn’t find its way up and concerns don’t find their way up from the shop floor, as it were.
CS2 GP PPI lead CCG
FIGURE 4.
Patient and public involvement structure in CS2. CET, clinical executive team.
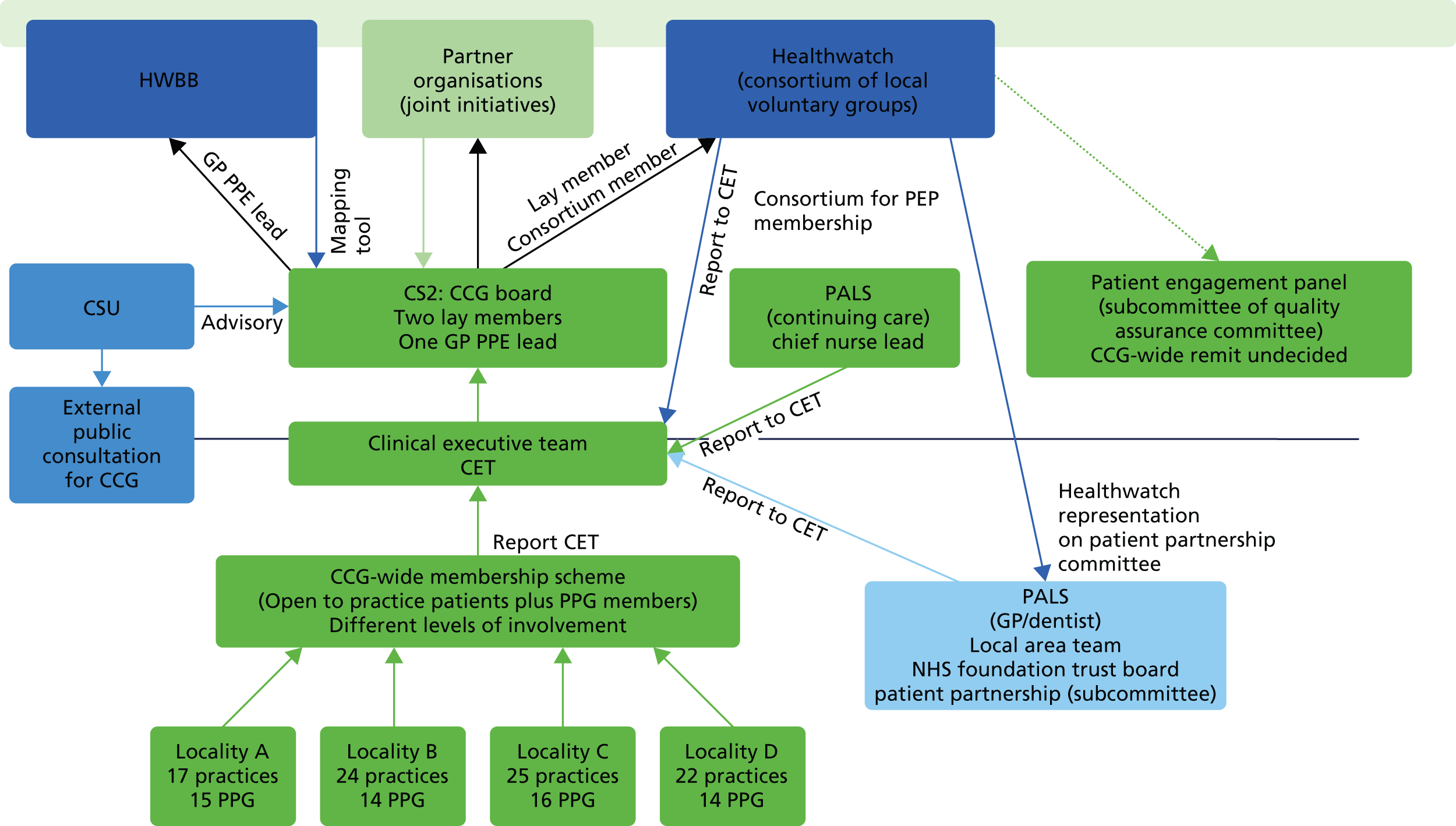
Agenda setting
A review of early CCG initiatives showed that initiatives such as the membership scheme and PEP had been generated by CCG staff rather than through consultation with the local population. Discussion identified the importance of the authorisation process, rather than a vision and strategy for PPI.
The CCG had taken a portfolio approach in relation to some of its roles and functions; such portfolios were held by GPs, for example diabetes and PPI. The GP lead for PPI had developed the draft proposals, in conjunction with other GPs and a lay board member, again suggesting that CCG personnel were setting the agenda at this point in time.
When discussing the proposed PEP, the CCG PPI lead stated that ‘. . . I’ve got a meeting about that this afternoon, where we’re going to decide about the terms of reference and the attendance of that panel . . .’
Summary
Case study 2 had a long-standing tradition of PPEI initiatives, with a strong emphasis on partnership working. As can be seen from the findings, there were a number of examples of service user voice influencing service development and delivery. However, there was limited documentation in relation to impact of such involvement. The development and expansion of PPGs was evident in general practice during the research period. During the data collection period, the CCG had only formulated a PPEI draft plan, rather than a strategy, with a GP lead in this area rather than a stand-alone appointment. Discussions and documentation identified a number of potential PPEI vehicles within the new organisation such as a membership scheme and PEP; however, it was unclear, during this period of time, how these structures would function within the organisation or how the service user voice would feed into service development and, overall, decision-making.
Chapter 6 Research findings: case study 3
Background
Case study 3 was the last of the three case study sites to be recruited to the project (April 2011). CS3 was, at the time of recruitment, in the process of a major restructure, which included divesting its community provider services. For the past 2 years, the PCT, in addition to its role of commissioning health care for its locality, has been working to support its emerging CCG, which received authority to function as a commissioning organisation in April 2013. Hence much of the data collection for this site has taken place in a climate of major organisational change with its resultant confusion and uncertainty over futures and services.
Case study setting
Case study 3 was located within a large urban town situated in the south of England, close to the capital, London. It is an ethnically diverse town with a large BME population (over 40%) and a higher than average birth rate and population of young people, as well as a rising rate of people within the older age group. Health, in general, was poorer for the population of CS3 than the average for the people in England. Life expectancy and infant mortality was considerably lower than national rates (in the bottom quartile) and, like CS1, there was a mixed picture of deprivation, with a large proportion of CS3’s population living within the top 10% most deprived areas of England. CS3 currently commissions most of its acute services from one local acute trust, mental health services from its local mental health trust and community services from its recently divested community provider, now located within a neighbouring NHS community trust. CS3 comprises 32 GP practices with below-national density of GP to patient (around 2000 patients to each GP). There were, until recently, two PBC consortia in CS3 which merged into one in July 2011 and were functioning as a shadow CCG for the majority of this research project. CS3, as a whole, had a higher than national average prevalence of diabetes and a higher than national average mortality rate for cardiovascular disease.
Processes and supporting structures for patient and public involvement
Approaches and methods for patient and public involvement
During the time of data collection for this study, CS3 did not have a dedicated lead for PPI. Despite this, CS3 had performed relatively well within the World Class Commissioning competencies for PPI in 2010, having made some significant improvements for competencies 2 and 3 (working with community partners and engaging with public and patients). However, it was not clear how CS3 had involved patients, including those with LTCs, in developing choices of services, and the organisation was focused on improving this this through a variety of PPEI initiatives and activities (Table 10).
| PPI structures | PPI activities |
|---|---|
| Service user-led PPEI structures | LINks |
| Network/user forums: neurological, diabetes, stroke, COPD, HIV. Led by voluntary sector | |
| Organisation-led structures with PPEI | Diabetes service redesign |
| PALS | |
| Children’s joint commissioning: You’re Welcome programme, young carers’ network | |
| Equality Deliver System | |
| Neighbourhood Governance Programme (community engagement strategy, LA ward level) | |
| GP practice groups | |
| Expert patient programme |
From data collected during workshops and interviews, it was evident that there was strong agreement about the value of including service users in the process of commissioning.
Participants at the first workshop spoke about service users bringing local knowledge and expertise at community, service and clinical level and of the importance this had in ensuring effective commissioning of services. A list of PPEI structures and activities were described by the participants (see Table 10).
However, it was also acknowledged that PPEI was not always effectively managed within the system, and that they (the health service) were ‘not very good at it’. Evidence of good PPEI was particularly lacking for LTCs as well as within GP practice in this site. There was no one leading PPEI at the helm and no organisational strategy in place for user engagement.
Tensions around the proposed changes in health services certainly played a part in some of the comments expressed at this workshop. Commissioners spoke about the current uncertainty on funding services and how this impacted on their communication with service users and providers; ‘information can’t be passed on because the commissioners don’t know whether the funding will be there one day to the next’ was one comment expressed by a commissioner at the workshop. Service users and representatives spoke about the need to build trust and relationships with those planning and organising health services and that they were unsure at the time of what commissioners had planned for them. GPs were also generally concerned or unsure about their new responsibilities, including those around PPEI, arising from the recent White Paper.
Despite this climate of ambiguity and chaos, there was evidence that service users were actively involved or engaged at some level, either individually or collectively, in health care. These approaches and methods of engagement and involvement are summarised in Table 11.
| Method of involvement | Used or led by | Reason(s) |
|---|---|---|
| Complaints systems (PALS) | Service user groups Individual service users Commissioners (NHS) |
To complain about local services To inform services |
| Lobbying MP | Service users | To change services |
| Patient/user surveys | Commissioners (NHS) Providers |
To inform/improve service provision/strategies |
| Patient representative on health committee (LIG) | Service user(s) | To provide information on experience |
| Public representative on health/public committee(s) | LINk member | To provide public perspective |
| Informal discussions with service users | GP practice group manager | To gain insight into quality of services |
| One to one with patients | Clinical providers | To get feedback on personal experience |
| Patient participant groups | Practice manager | To inform development/improve service provision |
| Website | Service users | To gain knowledge on condition/local services |
| Responding to consultations | LINks representative | To provide patient/public perspective to those organising services |
| Meetings with commissioners | Patient group representative | To provide information to commissioners to help improve services for patient group |
| Attending clinical network meetings | Patient group representative | To provide patient perspective to providers of services |
| Attend local disease-related support group | Service users/carers | Knowledge/understanding of condition/gain support from others/raise public awareness/fundraise |
| Targeting and meeting local community groups | Commissioners/providers | To reach hard to reach communities/specific disease related/to help commission/provide/improve services |
| Education groups | Providers | To provide information and guidance on services and self-management |
| Workshops on services | Commissioners (NHS) | To consult and plan/feedback on services |
However, much of this was through informal or ad hoc approaches and, prior to the formation of the new CCG, there was a distinct lack of a strategic approach for PPEI within the organisation. There was also a lack of evidence of PPEI within all stages of the commissioning cycle, particularly within the planning and evaluating stages.
Despite this lack of evidence, there was a strong sense of commitment for PPEI in general across the site and a determination, among those participating, to make improvements. This was expressed in interviews, workshops and observation of meetings throughout the timeframe of the study.
Some viewed the recent NHS changes including the ‘Pause’ as an opportunity to make new inroads for PPEI. Motivating factors varied from personal interest or altruism (service users) to viewing it as a necessary part of their job role (commissioners, providers). Involving patients and public was seen as important not only for effective service provision and improving staff morale but also for avoiding service user criticism (commissioners, providers). As one NHS commissioner put it, ‘people are more likely to be critical if not involved’. However, financial incentives such as the DES for PPEI were also viewed as a prime motivating factor within primary care practice. As one practice manager said, ‘I’d say that the PPG DES has probably had more of an influence and raised, you know, sort of, the profile of patient participation more than any of the commissioning documents, . . . in my opinion’. This is further illustrated in that GP practice PPGs grew from only four prior to the introduction of DES, to 26 (out of a total of 31 practices) at the end of data collection in the study.
For NHS commissioners, the focus of PPEI was more about obtaining patient feedback using patient surveys or for providing information through community consultation events as well as through links with a number of local patient groups, such as Diabetes UK or the LINk. However, not everyone agreed that this was the best approach, as it was recognised that some groups might be missed and more of a targeted approach was needed. One of the common themes emerging from the data at this site throughout the project was whether or not there was adequate representation for PPEI. Patients and the public had representation at both local and strategic levels of commissioning. At the local specific service organisation and delivery level, patient representatives normally came through organisations such as the LINks, the local voluntary organisations or representation through a local charity (often condition specific). Here, commissioners felt that they were not always reaching the right groups and some (often minority ethnic) groups were perceived as not having their voice heard. There was a reliance on the ‘same old faces’ for patient and public representation, the ‘usual suspects’ who volunteer their services as patient or public representatives. They were often from the ‘white middle-class male population’. Getting the ‘hard-to-reach, minority’ audience was seen as important for take up of services, particularly for redesigning or reorganising clinical services. As one PCT commissioner commented, ‘It’s pointless having a service if only half the population is actually accessing it because they don’t understand it’. But it was also important to have the ‘right’ representative, not only for representing the group but also in having knowledge and experience of the specific condition and service. Most of those commissioning and providing services felt that involving genuine local patients or carers, those who have ‘walked the journey’, rather than patient representatives from an organisation such as LINks or a local charity, was an important factor for commissioning services. One NHS commissioner spoke about her recent tactic of going out into the community to reach minority or so called local ‘hard-to-reach’ groups in order to ensure that she would have a representative voice to commission local diabetes services. There was also some discussion within the shadow CCG about developing some guidance to GP practices on ensuring adequate representation within the newly formed practice PPGs. However, in such a diverse population it was recognised that it would be difficult to get good representation and that people might be missed if only vulnerable groups were targeted.
From a service user perspective, apart from engaging with the health authority through the local LINk or a patient group, normally organised through a voluntary organisation with a ‘disease’ focus, there were limited opportunities to engage in commissioning local health care. However, where these were observed, they often involved, at some level, the local authority, either singularly or through joint commissioning with health. This was demonstrated in a consultation on reablement services, where patient and public stakeholders were invited to provide their ideas, thoughts and feedback on the development of pathways from hospital discharge into reablement. The outcomes from these workshops fed back directly into the pathways. One (joint) commissioner pointed out ‘we’re already implementing some of their patient experience and feeding that into development of pathways now, so we are utilising their feedback directly into how we’re trying to improve the quality of pathways.’ Children’s health services, jointly commissioned, also demonstrated some level of engagement. Young people were involved in designing and testing an asthma log for the asthma pathway and there were plans to do a similar exercise for the child epilepsy pathway. Another group of young people were involved in assessing a range of health services for being ‘young-person friendly’ through the ‘You’re Welcome’ local authority programme. The ‘You’re Welcome’ programme helps PCT and children’s trusts commissioners to transform the health services (NHS and non-NHS providers) they commission by improving the acceptability, accessibility, quality and choice of services for young people. The local authority had recently developed its community engagement programme to consult with its local community on key priorities which include health, but these were generally around public health with a focus on individual lifestyle. Within the provider arena, process and methods of engagement and involvement existed primarily through feeding back experience through PALS.
Involvement of service users with long-term conditions
Although there was some discussion at PCT level about forming a LTC patient user group, there were limited opportunities within the organisation for services users with LTCs to be involved in commissioning services for LTCs. At the strategic level, patient representation was through patient representative (single) on an area-health-level LTC clinical working group. At a local service level, there was service user involvement in service redesign through membership of a committee set up for this purpose or through taking part in a focus group, workshop or consultation exercise organised by one of the providers or commissioner. Other opportunities existed outside the organisation, through membership of a local charity or community group.
Within the three tracer conditions, there was limited evidence of local PPEI activity for commissioning, even within diabetes, which was, at the time, undergoing a redesign. The diabetes service redesign committee included a patient representative with diabetes type 2 as a member. As previously mentioned, the commissioning lead for LTCs was keen to engage with real patients who receive local services and to reach out to ‘hard-to-reach’ service users who represented poor uptake of services. She was reluctant to adopt an ‘in-house’ workshop approach, often used by other commissioners, to help to inform decisions.
Because to get the numbers of people to come in for a, sort of, workshop, which is the old way that we’ve been doing it, again, you don’t necessarily get the right people, but if you take it out where there are large numbers of patients that meet socially and support groups, then you’re going to get much more honest answers about what is going on and what you’re proposing and how they think that would work.
CS3 PCT commissioner 2
She was also reluctant to consult with focus groups of ‘patient representatives’, often organised through the LINk, who she felt were not representative of local patients.
. . . LINk is a bit of a worry for me because it’s not the real people.
CS3 PCT commissioner 2
Involvement of children and younger people
As described in other chapters of this report, access to children and young people with LTCs was a challenge and only one young person with epilepsy was recruited for interview for this site. This person appeared quite informed about her own condition and of local support services, including engagement forums for young people such as Epilepsy Action. However, motivating factors for engagement were limited to personal needs for information, rather than wanting to become involved in supporting or helping others:
I think I’ve got past all of that. I mean, I know it’d probably be good to go on there and help other people, but I don’t, I don’t go on there, I don’t feel like I need to ask questions on there.
CS3 young person 1
Interviews with commissioners also revealed the existence of a specific young person’s group organised through the paediatric department of the local acute services trust. The provider trust’s paediatric clinical lead reported that this group met regularly and provided feedback to the trust on the quality of services provided for young people with a variety of LTCs. However, despite a number of meetings, telephone and e-mail correspondence with clinical and management personnel over a number of months, we were unable to access this group for our research.
Evidence of influence
There was some feeling, specifically among some service users and representatives, that the balance of service user power in commissioning rested with the voices of the larger, national charities as well as those representing the conditions the commissioners are prioritising, for example those conditions perceived as preventable and with a high cost to the NHS, such as diabetes. One exception was RA, which appeared to have quite effective local patient support groups and a (self-)perception of some influence and autonomy.
Although examples were provided of PPI, it was not clear if very much of this was meaningful. In effect, many of those interviewed (commissioners, providers and PPI leads) suggested that service users did not have much power, that there was some engagement but only up to a certain level and they were not having much influence on ‘real’ health decisions, including changing services. This is further illustrated by a comment provided by the lay representative on the diabetes reconfiguration local implementation group (LIG), suggesting that agendas were set by the organisation and professionals.
I really came into that too late to say very much, because the pattern of what they were wanting to do was really set, and I don’t think there was really very much likelihood that a layperson could affect the pattern that they had laid down . . .
CS3 service user 2
In the case of primary care, a key area for people with LTCs, some patients involved in practice groups felt that they had very little clout, as the group often lacked a clinical presence to take forward any issues or concerns. Some saw this to be more of a tick-box exercise with service users or representatives not taken seriously and a ‘done to’ rather than ‘done with’ approach to service delivery.
This was despite some innovative approaches to involvement, such as one patient representative organisation targeting commissioners to present a business case for service development for people with MS. Linked to a lack of power was a feeling of inequity which was mentioned by many of the service users and representatives within the case study site. One service user said that he found it difficult to understand the medical jargon at health meetings (diabetes) and felt reluctant to speak up.
. . . I think that’s very difficult for me to say they do listen, yes . . . absolutely no idea why. You know, I think because there’s so many other people could be listened to and my opinion sometimes might not matter to them, you know?
CS3 service user 3
This is further illustrated in this following dialogue at the same interview.
. . . when they talk about medical things, you know, me as a patient as a non-medical person it’s very difficult to sometimes understand . . . I mean, when they talk about long-term conditions and long-term patients’ problems; as a patient, you know, the medical jargon, it’s sometimes very difficult to understand. [Interviewer: And do you tell them this?] If I don’t understand, I don’t speak there and then. I probably will ask somebody in a little corner. Yeah, I would. I sometimes do it. [Interviewer: Have they changed anything as a result of you saying something . . .?] No, not really.
CS3 service user 3
However, there were some exceptions. A large and well-attended patient group organised through the NRAS argued for the appointment of two physiotherapists for RA, which was set up by the provider following a meeting with clinicians. The service user felt empowered by the strength of the group voice.
. . . it was something the rheumatology consultants and nurses were pushing for, but I think, when he was, sort of, confronted by . . . 50 people, 60 people and we were all saying ‘well, you know, we really could do with this’, I think it was just all firmed up.
CS3 service user 4
In addition, within children’s services, the implementation of the ‘You’re Welcome’ initiative allowed young people some say in local health services for children and young people. One PCT commissioner did feel that things were changing, that it had been lip service in the past but now it was more meaningful as commissioners and others involved in planning services were becoming much more aware of how useful educated and well informed service users could be.
. . . I think the Health Service was guilty of just giving lip service to them [service users] and saw them more as irritants. I think when they are powerful is if they can lobby MPs and what have you.
CS3 commissioner, joint PCT/local authority
Despite the level of commitment to PPEI, there were few examples provided of PPEI initiating or effecting change in health-care services for LTCs in the site. In fact, when asking for recent evidence of where PPI initiated change, it was very difficult to get local current case site examples, many providing examples of previous roles or roles in other organisations, suggesting that this might be more of a case site specific or historical phenomena. Where examples were given, they usually centred around using PPEI for developing service specs or for providing feedback on services already in place. These included examples of meaningful public engagement for reablement and some children’s services and, through patient-led organisations, services relating to RA and Parkinson’s disease. There were very few examples of having service user input at every stage of the commissioning cycle.
This did have consequences in some areas. For instance, one example was provided where service users were involved in the specs for new musculoskeletal services in the community and patients were involved in choosing the specs and recruitment of the service provider but not in the procurement of the premises. The premises ended up being situated on a busy roundabout with limited access for those the services were aimed at. Had service users been involved in the discussions on location and access, this might well have been avoided.
Negative outcomes from PPEI were also observed. As part of the diabetes redesign, local health-care commissioners and providers have been consulting with the BME community about how it could best meet its needs. A number of meetings and focus groups (facilitated by the EVOC research team) had been undertaken with diabetic service users from the Bangladeshi community within their local community centre, situated in one of the high prevalence of diabetes wards. Representatives from this community have indicated, through a series of focus groups, interviews and surveys, that they would welcome diabetic services, including advice and guidance on self-management, within their community, rather than through their GP or general NHS community health centre (see Appendix 6 for a full account of this example). PPEI in commissioning diabetes services for this community was tracked as part of the project for a period of 18 months. The project (plan to set up an integrated community-based diabetic and other LTCs service clinic for this specific BME group situated ideally within their own community centre) was subject to a series of delays due, in part, to NHS staff capacity and organisational restructure, including the loss of the lead commissioner in December 2012. The new commissioner is currently in the process of reviewing the business plan and it is not clear if this development will be on the agenda as initially envisaged as service specs had not been defined and funding had not yet been agreed. One of the community providers is now thinking of providing a community ‘drop-in service’ in the future where health promoting advice and guidance would be offered, rather than the provision of integrated health and social care services as originally considered.
Frustrated by the slow pace and delays/turnaround by the local NHS in developing the service, the director of the BME community centre is now pursuing alternative funding (BIG Lottery) to help develop the community centre as a diabetes advice and information centre.
Some of the feedback from the expert reference panel indicated that the failure was probably down to poor PPEI planning and practice. Much of the PPEI was around needs assessment. As members of the expert reference panel commented:
. . . This in itself is not ‘engaging’. Patients and communities will only see themselves as being ‘engaged’ if needs assessment is followed by continuing communication and further tangible action such as involvement in planning and/or redesigning services. Neither appears to have been carried out effectively here.
Policy officer for PPE national patient organisation
I have some criticisms of the process of PPE and some doubts about how they could know whether the intervention will be successful or not. . . . The PPE is very basic and seems to me to be flawed in at least 2 ways. It appears ad hoc and lacking in clear structure, without any clear sense of representation at any of the decision points.
Representative from diabetes patient organisation
The expert panel also made specific reference to the way in which health agencies need to work with BME communities.
With minority communities where information and communication may present significant barriers to the success of such patient involvement (literacy in English, health literacy, culturally appropriate information and information support, etc.) these interventions need to be located within the right context of appropriately designed services and consultation. In my view this would be much more likely within a genuine partnership between the statutory services and the community ‘hubs’ (community centre and mosque, for example), and probably requiring the training of a cohort of Bengali health trainers or assistants who would then be capable of providing support to people’s self care and self management. It would be much less likely with the ‘drop in’ health promotion service that is now inferred.
Policy officer for PPE national patient organisation
This experience of having needs surveyed and then engagement which results in no action is not untypical of the experience of minority communities with the NHS. Alternative models of involvement such as experiential or coproduction might have proved more successful in this instance.
Other negative aspects of involvement, again in diabetes services, have resulted from the experience of the service representative on the LIG, who felt ineffective as a result of being invited to the meeting at a late stage, ‘once things had already been decided’, and did not feel able to contribute much due to the technical nature of the meeting:
But at this moment, I am seriously wondering whether I can actually make much of a contribution to what they’re going to be discussing. As I see it, and I haven’t seen any agenda yet for 2012, they’re likely to be quite technical issues, medical issues which, really, I don’t have any impact.
CS3 service user 2
Attributing specific service-level outcomes to user input is always a challenge, as service users are only part of the commissioning jigsaw. Much of the evidence provided within this study site was of the process and actions of involvement rather than what impact this had on patient experience or service design. However, there was one example provided of where positive outcomes (for both provider and user) were directly attributed to service user input. A GP practice used feedback from people with LTCs (the PPG advised on GP rota systems) to change booking appointment systems, which led to a true cost saving for the practice and reduction in the did-not-attend rates for people with LTCs.
The impact of changing processes
As stated earlier, while there was a stated commitment or will for PPEI within the organisation, there was a fragmented approach to its operation, little supportive infrastructure with no real strategy in place and no one championing or leading it within the PCT (as stated earlier, the PPEI lead had left the organisation a number of years earlier and was not replaced, and PPEI was thereafter taken up by the communications team). In addition, despite a local authority with evidence of innovative community engagement activities, evidence of a strong collective public voice for local health services was not apparent.
This project commenced shortly after the new health reforms were announced and captured some of the initial tensions and anxieties of a major change and restructure. It was acknowledged that GPs did not have a history of good PPEI in the area, and there were issues of communication and trust between service users, commissioners and providers. Uncertainty around budgets and resources, including staff capacity, added to the unease. All of those interviewed within the NHS said that PPI was resource intensive and that there was a lack of resources for this within the new commissioning arrangements. There was the suggestion that by having PPEI you inevitably put up costs as patient suggestions often involve added costs and PPI does ‘slow things down’. As the health service was engaged in making cost/efficiency savings, with increasingly scarce resources, this presented its own challenge. The recent restructure placed an extra strain on this agenda, specifically within the children’s services, who had recently lost their key member of staff for PPEI, a health participation manager who acted as the local authority’s link with the NHS for young people. Yet there was realisation that good engagement would lead to a cost saving in the long run, particularly from the providers who viewed patient involvement as ‘becoming more aware of own condition and taking more responsible for one’s own health, as well as family and friends’, thereby reducing the NHS disease burden.
However, some saw this as a real opportunity to change things: to create an organisational strategy for more effective and meaningful PPEI, and to create a CCG where PPEI is firmly embedded at every level of CCG decision-making.
The new CCG structure, in theory, provides increased opportunities for patients and the public to be engaged and involved in commissioning local health services, at both the strategic and the grass roots level. Figure 5 shows a draft structure of PPEI governance within the CCG as described by the current communications and engagement lead and local authority community engagement lead (note: a steering group was established to develop new governance arrangements and was due to report in the summer of 2013 after the end of the research).
FIGURE 5.
Clinical Commissioning Group PPEI structure for CS3. a, PPG n = 15–20. Each PPG nominates one or two members to sit on PRG. LA, local authority; LBC, local borough council; FRS, fire and rescue services; R&I, research and information; VCS, voluntary and community sector; YP, young persons.
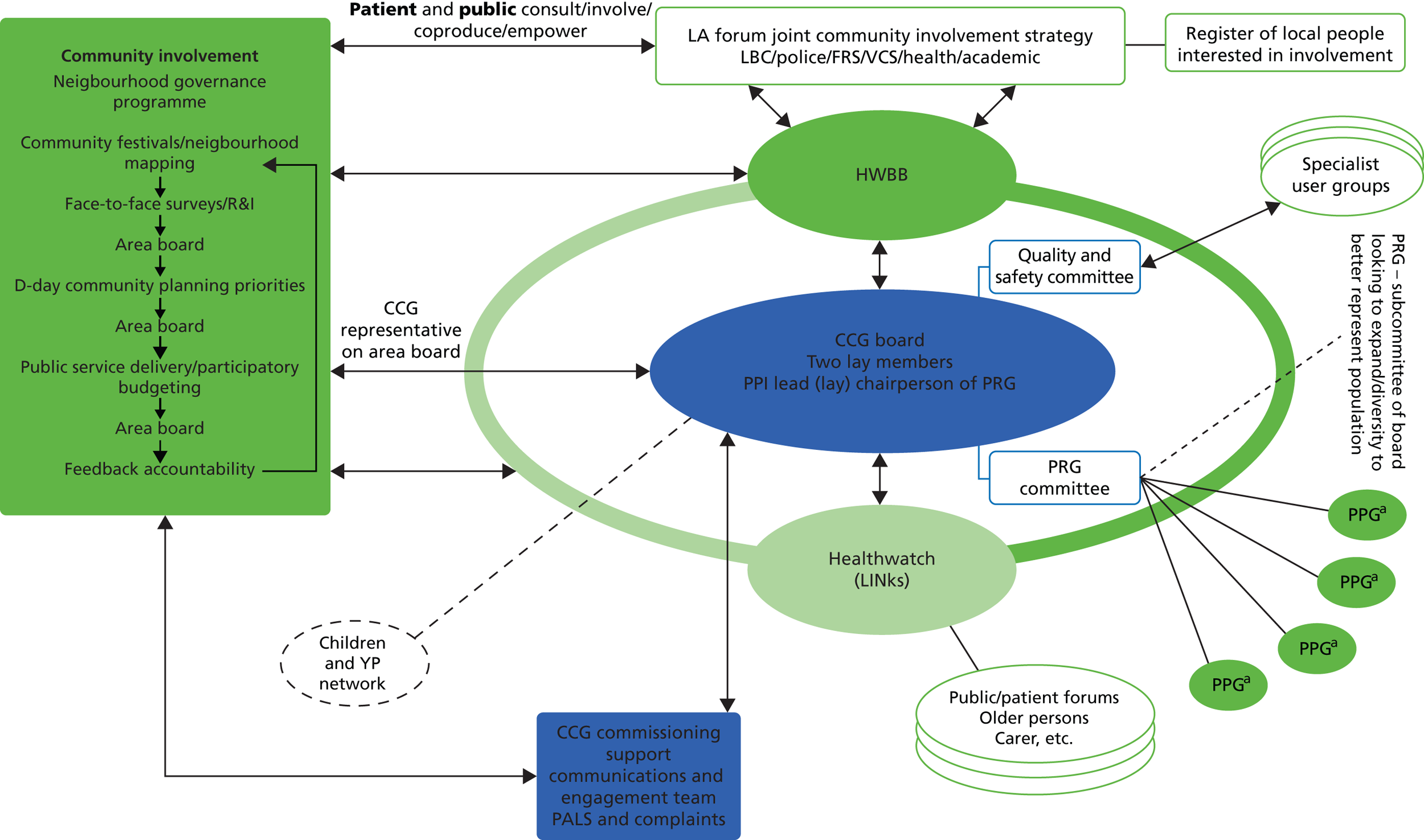
A new accountability officer has been appointed with a record of leading pioneering and award-winning PPEI within a neighbouring urban multicultural PCT. The new mechanism for PPEI describes a partnership approach between the local authority (the stronger partner for PPEI) and the health service within the newly formed HWBB.
The CCG board currently comprises three lay representatives (only two were in place at the time of data collection), with one leading on PPEI. Input from service users of primary care is direct to the board through the PRG (one of six subcommittees of the board) where each GP practice is represented by up to two service user representatives. Communication and Engagement is being contracted by the CCG. There is also user representation through the HWBB, which has Healthwatch representation, and direct links with the local forum’s community involvement strategy (the forum is a joint working forum of community stakeholders including the PCT, local authority, fire and police services as well as academic and local businesses) and neighbourhood governance programme (a CCG member sits on the local area boards) as well through the equality and diversity strategy. There were also talks about having a Children and Young People’s network feeding into the CCG board. At the time of writing the new Healthwatch had yet to be officially launched, and the community and engagement strategy, submitted in draft form as part of the CCG authorisation process, was still in discussion.
As the data collection for the study completed at the same time the new CCG was established, it was not possible to follow up on how PPEI governance arrangements are working and how users are actively influencing commissioning decisions. Perhaps the key distinction of this approach to PPEI is having primary care strategically placed in the governance system through the PRG. This group is chaired by the lay board member and membership comprises representatives of up to two members of local practice groups (practice participation groups) as well as members from the communications and engagement team. This did raise some questions about how representative this might be. One communication team member observed that the meeting comprised mostly white men over 60 years. Further research revealed that these early meetings (only three had taken place during the data collection part of the study) included representation from only nine of the 31 primary care practices, despite at least 26 having established practice participation groups through the DES initiative. Plans were afoot to enlarge this group to include other patient and public representatives, such as local patient and voluntary organisations.
Access
Some restrictions to being a lay representative in the new structures were observed in CS3. At the primary care level, service users spoke about difficulties in accessing information from their GP, particularly about how to become more involved outside their own health and care. Some were not aware that their local GP either had or was recruiting for a practice participation group. Clarity and standardisation about what these groups were and how they would be used was lacking from a number of practices. From a brief desktop scoping of GP practice websites in CS3 (Figure 6), following the introduction of the DES payment for PPEI, only 17 out of the current active GP websites provided information about their PPGs and there was often varying information about the aims and objectives as well as how to become involved. Many were indicating that these were for providing feedback for the surgery for specific areas of practice. Some were asking for a virtual group only, and only a few were indicating that these groups fed into the CCG’s strategy. Only a small number published minutes of meetings and terms of references. However, some, probably four or five, were implementing more meaningful/strategic PPI where patients had input into decision-making about local health services. It was interesting to note that one of these four had a GP on the CCG board. Incentives often drive practice and perhaps the reason for the variation in PPG practice was that much of this was not required as a condition for payment for year 1. The DES has been extended for another year with more clear outputs for quality which might have the effect of driving up standards as well as access.
FIGURE 6.
General practitioner practice patients groups in CS3.
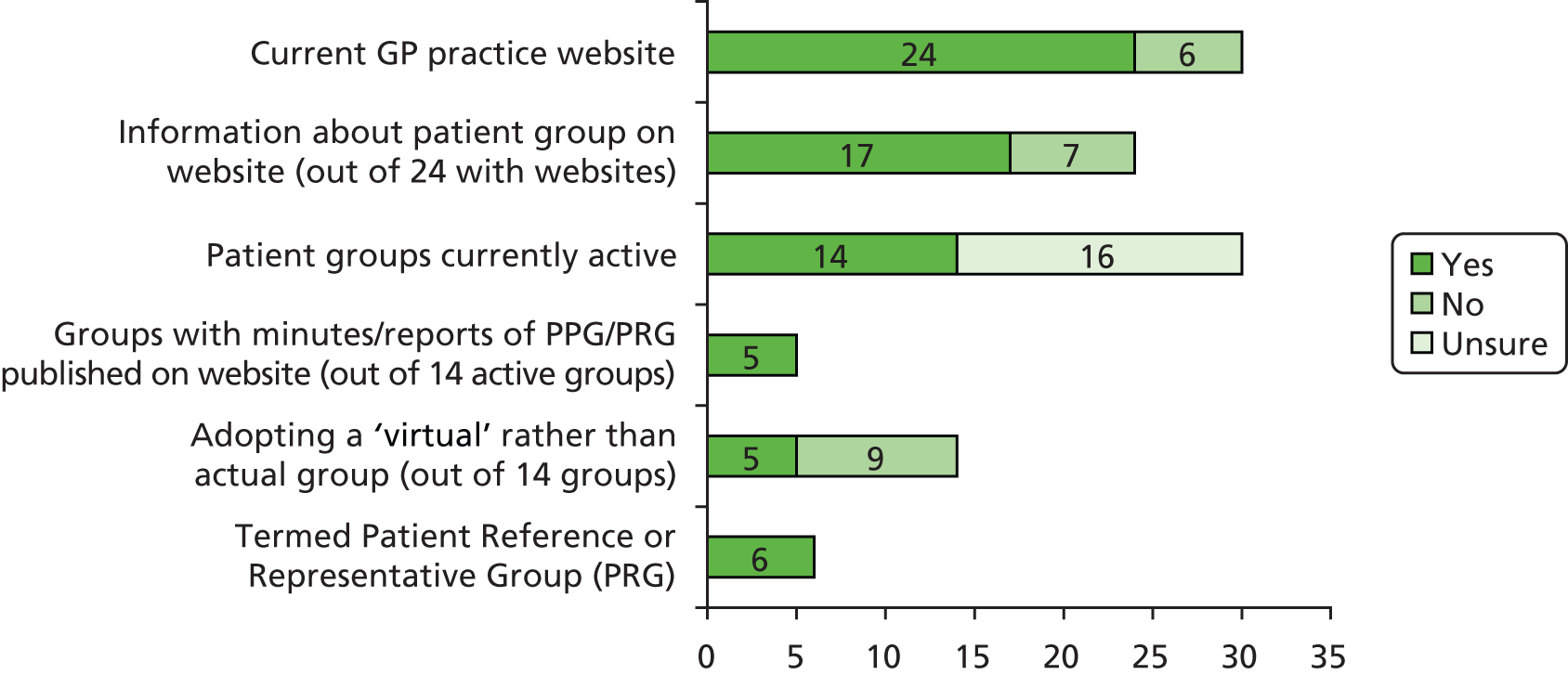
Summary
Case study 3 did not have a marked history of PPEI within the PCT; nevertheless, they employed a variety of different methods to involve and engage with their community. There was, however, little evidence of much meaningful engagement particularly within primary care, an area of increasing significance for people with LTCs. Some efforts were made to ensure that services were planned to meet the needs of particular sections of the community but failed due, in part, to poor PPEI planning and execution. As a consequence of the health reforms, the CCG is better placed to ensure that PPEI is firmly embedded in all areas of commissioning decisions in the future and new staff and structures are planned to enable this to happen. There is a strong commitment and will to make a difference but time will tell if this is successful.
Chapter 7 Clinical Commissioning Groups and patient and public engagement and involvement
Introduction
As discussed earlier in this report, this project was undertaken at a time of substantial change in the English NHS following the election of the coalition government in 2010. Despite an initial promise that there would be ‘no more top-down reorganisations of the National Health Service’,136 one of the first actions of the coalition government was to propose a substantial reorganisation of the English NHS – so large it is ‘visible from space’. 137 In July 2010, the coalition government published a White Paper, Equity and Excellence: Liberating the NHS,7 which had significant implications for arrangements within the NHS for PPEI as well as for this research project. Box 2 sets out the main proposals contained in the White Paper, Equity and Excellence. 7
-
PCTs to be abolished, with responsibility for commissioning (purchasing) services handed over to groups of GPs.
-
The abolition of regional SHAs.
-
The creation of a new ‘arm’s length’ body to oversee the NHS called the NHS Commissioning Board (NHSCB).
-
The transfer of responsibility for public health to local authorities and the creation of a new national body, Public Health England.
-
The establishment of local authority-based Health and Wellbeing Boards, responsible for the development of strategic assessment of local health and well-being needs.
-
Changes to the role of Monitor (previously the body responsible for regulating foundation trusts) and its establishment as an ‘economic regulator’.
-
All NHS trusts to become foundation trusts.
These changes represented a significant redistribution of responsibilities within the English NHS and, ultimately, for the structures and processes developed for PPEI. For GPs, membership of what came to be called CCG is compulsory via their practices, with some kind of quality payment available for those who fulfil their commissioning responsibilities successfully. While initially the policy was deliberately permissive, with, for example, the size and composition of CCGs not centrally specified, over time many aspects of the development process became increasingly proscribed, leading to a formal authorisation process in 2012–13. In a letter to GPs in September 2010, Sir David Nicholson stated that:
We would want to enable new organisations, and particularly [CCGs], to have the maximum possible choice of how they operate and who works for them. It is important that GP practices be given time and space to develop their plans to form commissioning consortia. PCTs should provide support for this process and empower consortia to take on new responsibilities quickly when they are ready to do so, but it is important that solutions develop from the bottom up and are not imposed from above.
p. 5138
In October 2010, groups of GPs wishing to move ahead with setting up their local CCG were invited to come forward to join a ‘Pathfinder programme’. The objective of this was to allow aspiring CCGs to begin to work out the best way to organise themselves, facilitated by their local SHAs. The process gained momentum quickly, and by June 2011, more than 90% of England was covered by a Pathfinder CCG. In the summer of 2012, a formal authorisation process commenced in four waves to establish fully-fledged CCGs from April 2013. The data presented in this chapter draw on an analysis of a sample of CCG authorisation submissions and the findings from case study and survey research undertaken by the Department of Health PRUComm. 22
Background and context
Equity and Excellence set out the rationale behind the proposed changes, arguing that the closer involvement of GPs in the commissioning of care would ensure more effective dialogue between primary and secondary care; decision-making ‘closer to the patient’; and increased efficiency. 7 It was argued explicitly that ‘we will learn from the past’ (p. 28),7 claiming to have built upon lessons learned from previous clinically-led commissioning initiatives including GP Fundholding and Total Purchasing Pilots from the 1990s. 47,139 As discussed in Chapters 1 and 2, the reforms were set out in the Health and Social Care Bill which became the 2012 Act following a controversial passage through Parliament with a substantial number of amendments. 48 With the Health and Social Care Act 201220 passed by Parliament, additional guidance was published by the Department of Health (and subsequently by the shadow NHS Commissioning Board) (see Chapter 2). A timetable was set out for CCGs to apply for full ‘authorisation’ as statutory bodies from July 2012, with the first CCGs taking full responsibility for commissioning from April 2013. The authorisation process was based on a number of key principles:
-
A process ‘fit for purpose’ – sufficiently robust to enable a thorough and cost-effective assessment of the CCG’s capacity and capability to carry out its functions.
-
A process viewed by both the NHS Commissioning Board and CCGs as developmental and as adding value and helping improve quality and overall patient experience and outcomes.
-
Setting the tone for the future positive relationship between CCGs and the NHS commissioning board.
-
Minimising administrative demands for both emerging CCGs and the review team(s), and delivering a process which is both rigorous and efficient.
-
Evidence required should be a by-product of core business, as far as is possible.
-
Recognising that this is a unique process – as ‘start-up’ bodies, CCGs will be building a track record of performance; therefore, authorisation will focus on confidence in their potential to deliver, drawing on their participation in, for example, improving LTC care, clinical care in general and other aspects of QIPP, but will also draw on their track record to date as subcommittees of PCTs to whom certain commissioning responsibilities have been delegated.
-
A nationally consistent approach – so that all emerging CCGs can have confidence that the same standards are being applied.
Authorisation was undertaken in four waves. The aim of the process was to enable the NHS commissioning board (NHS England) to determine the level of commissioning responsibility and agree with each emerging CCG the nature of the development support needed, or conditions to be placed upon the CCG, in becoming established.
Two hundred and eleven CCGs worked towards becoming authorised by the National Commissioning Body, NHS England, by the end of March 2013. From April 2013, they have been responsible for contracts with providers of health care in their communities amounting to around £65B per annum. The first wave of 34 CCGs were authorised in December 2012, having submitted evidence of their competence against 119 authorisation criteria across six domains. 140 These required competence to be evidenced in clinical focus, engagement, clear and credible plans, proper constitutional and governance arrangements, collaborative arrangements, and leadership (Figure 7). Domain 2 was headed ‘Meaningful engagement with patients, carers and their communities’.
FIGURE 7.
Clinical Commissioning Group authorisation: the six domains.
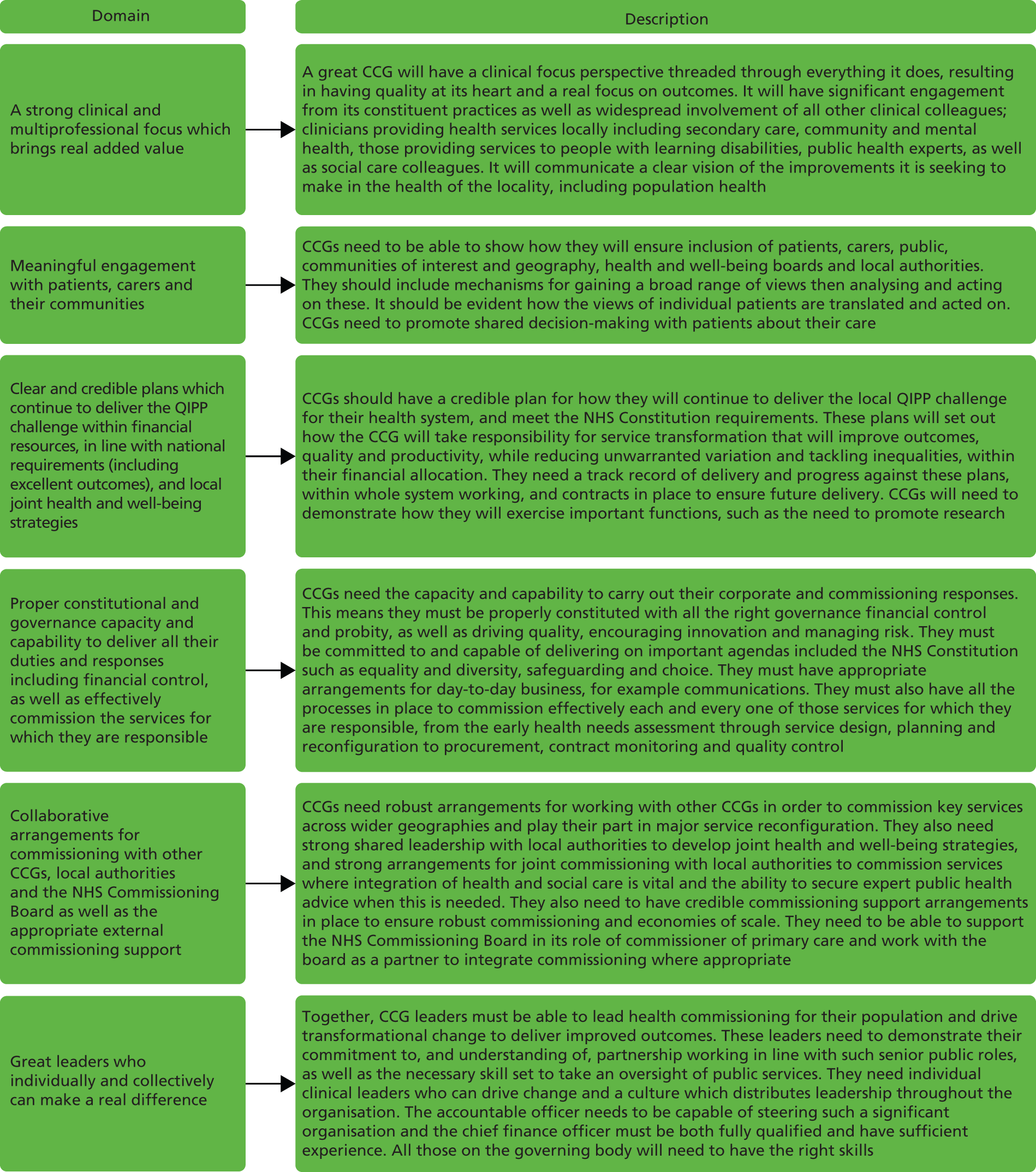
The challenge for CCGs is illustrated by the speed of the change in the expectations of government of primary care health services to involve the public and patients in their decisions. In April 2011, a Patient Participation DES scheme was introduced which provided GP practices with financial incentives ‘to ensure that patients are involved in decisions about the range and quality of services provided’ by setting up and supporting PPGs. 141 There was no compulsion to participate. By contrast, domain 2 of the authorisation process requires the CCG to ensure that ‘Arrangements are in place to ensure appropriate ongoing patient and public involvement in CCG decision making’. While the requirement for CCGs is at a different level, the shift from voluntary engagement/involvement to mandatory engagement/involvement demonstrates a shift in policy focus. PPEI has become a clear requirement rather than an option.
In the first phase of research leading up to authorisation, the research demonstrated that PPE was not a key priority for most CCGs. However, PPE did figure as an issue for discussion among CCGs although not always with any priority:
I presented the proposed plan to the CCG in September which they noted, and I would stress the word noted.
Manager, London CCG
However, there was a clear recognition that PPE was important and that it needed to be developed to ensure real engagement. For example, in one CCG there had been discussion about strategy development, with the board member lead arguing that:
What we have is we have a 1-year strategy, which is a strategy from now until next March, for the CCG which is going to the next CCG board, um, this month, um, so it kind of sets the groundwork. But my thoughts, what I want to do is over the next 6 months is as we go out and engage with people on a range of CCG issues, strategy, and vision, and values, that actually we gather information from that as well to prepare a three year engagement strategy ready for April 2013, which is informed by the people that we’re engaging with. Because otherwise, you know, it’s a bit . . . it would be ironic to produce an engagement strategy that we didn’t engage people in the development of. It’s kind of not very good practice I think.
GP board member, south-west England CCG
In May 2012, a second survey of 211 (reduced from 253 following mergers) CCGs was undertaken. The PRUComm survey asked CCGs about the membership of the main decision-making committee. Figure 8 shows the type of membership by profession or background. When the survey was undertaken (May 2012) there had been little guidance on membership. At that time, three broad groups of lay members were identified: members of the public, LINk members and councillors.
FIGURE 8.
Clinical Commissioning Group governing body membership. GB, governing body.
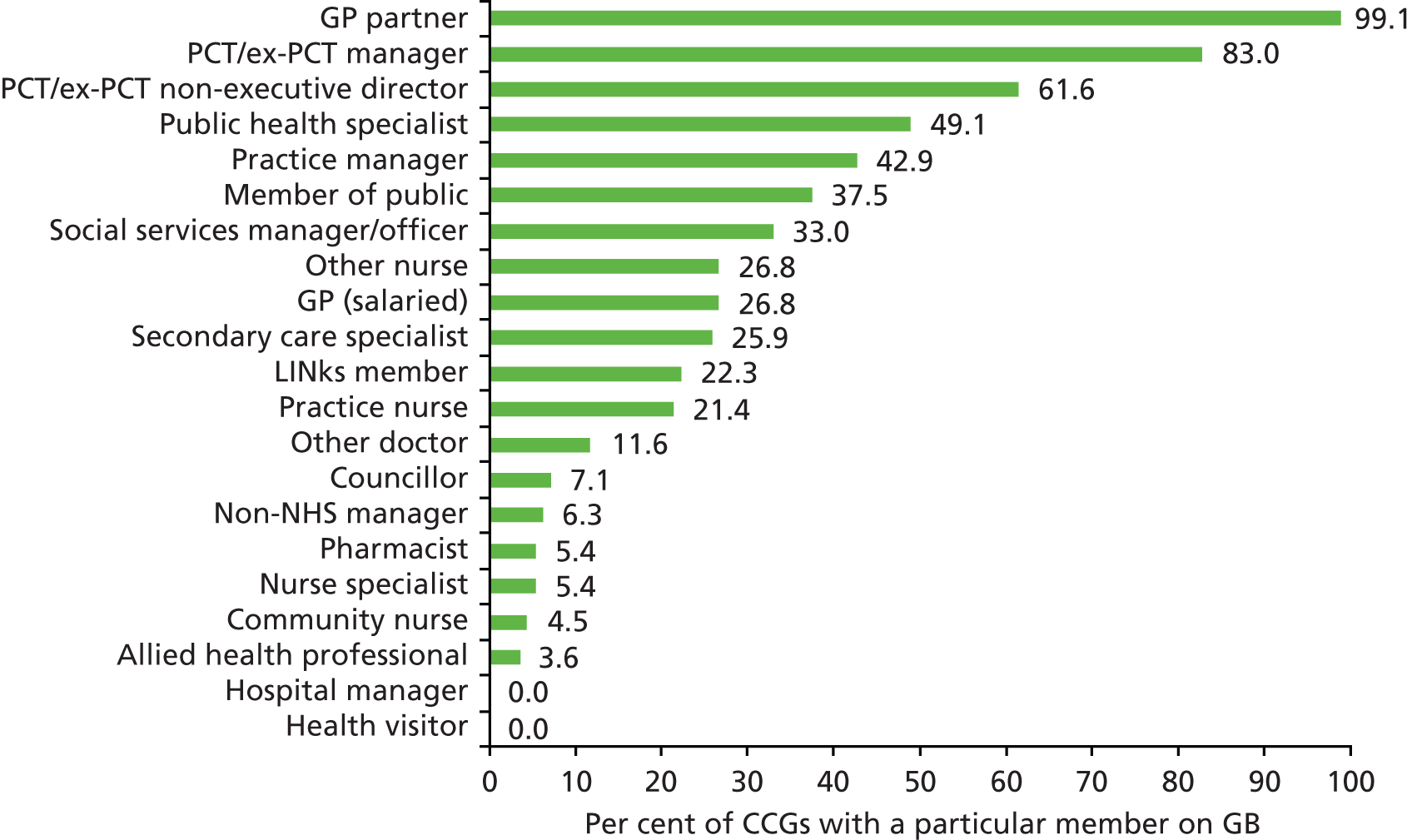
All of the case study sites in the PRUComm research expressed a commitment to genuine involvement of patients and the public in their work. Many included such a commitment in their statement of their ‘vision’ or ‘mission’, and were keen to demonstrate a new approach:
No, absolutely. I mean, the other thing, probably, just the stress, because, it’s been a bit of a journey for us, you know, us thinking that if we really want patients, at the heart of what we do, then, people leading on, how do we reach out to the communities, the individuals, both, through the practices, through any, you know, having that patient and public engagement, we felt that, in the PCT, it was, almost, over here, as a, kind of, tick box part of the organisation, whereas, us, trying to bring that into mainstream and whatever piece of work we do, putting it through the lens of, well, from your perspective, how do we reach the customers we need to, has been really important.
Ex-PCT manager, central England
Engaging with patients and the public was seen as a ‘good’ in and of itself, but many respondents also gave clear explanations of the value added by true public engagement. This manager had spent some time considering the issue, and explained it thus:
Well, I think there’s four reasons you do public engagement, and that’s what I worked out in this study. One is, you need to know whether things are happening, right. Secondly, you’ve got to be aware of public needs, public feelings for the commissioning process that you decide what you’re going to do. . . . Then you’ve got to . . . you’ve then got to, to some extent, have a two-way liaison because you . . . sometimes if you’re trying to pursue policies that need people to change their behaviour, you’ve got to take people with you . . . And the fourth one I think is long term caring, long-term conditions. You’ve got to involve people much more in that, you know, supporting people who have long-term conditions. So that’s four reasons, that’s it.
Manager, north-east England CCG
However, this suggests engaging through communication but not necessarily engaging in discussions about decisions or involvement in decision-making. The importance placed on developing PPE is reflected in one CCG’s approach to embed PPE in its founding principles (these draft principles were intended to guide the shadow CCG through the delegation process and help it on the path to authorisation, in advance of a communications and engagement strategy being developed):
-
Partnership approach to decision-making. The principle is for the CCG Communications and PPG to have two-way communications. The CCG acknowledges that it is a membership organisation in which practices are the members – not just board but also practices and population. Use this (membership structure) as a core mechanism. The CCG will work with constituent practices to utilise the knowledge and experiences of local stakeholders to assess needs, review existing service provision, decide priorities, design services and develop its annual plan. Where this approach does not give a fully representative view, additional mechanisms will be used to support disengaged communities.
-
Cross-boundary working – not only about diversity of population but also about common needs. The CCG recognises that people living in different localities may often have different needs and require different approaches. However, wherever possible, the CCG will adopt a cross-boundary approach to its business while recognising the specific needs of localities.
-
Integrated engagement – between health and social care. The CCG recognises that working closely with local stakeholders can add value to its work, but that fragmented engagement can result in duplication. The CCG’s over-riding approach will be one of integrated engagement working through, and within, existing structures.
Concerns about PPE were also linked to questions about accountability and all CCGs in the PRUComm case studies had spent time discussing the meaning, dimensions and importance of this. 22 As one GP reflected:
I think what we haven’t done yet and what we’re trying to organise now in this locality is go one step further and recognise that we are after all accountable to the public, we’re there to serve them, we are paid by them, we’re there to provide their health needs. So actually it only makes sense to actually be in discussion and contact with them and this has been a long sought after chalice to have, you get public engagement made meaningful in the Health Service and no-one’s ever done it successfully in my view.
GP, central England CCG
Similarly, in a CCG in the north-west the board were keen to embed PPE within the accountability framework of the CCG:
We need to let the public know that their voice is valued. As time goes on the patient voice and experience will be put more prominently into contracts with providers – quality measures. Also could be linked to CQINS [Commissioning for Quality and Innovation]. This should be seen as ground breaking and very positive.
GP
In the PRUComm research, CCGs identified a wide range of different approaches and initiatives to engage with both patients and the public, some planned and some already established, with many sites planning to use more than one approach. These included:
-
Local patient forums – either generic or for specific patient groups.
-
Patient participation groups at individual practice level. Many case study CCGs were looking at ways to bring these groups together to provide wider intelligence about local services.
-
Community involvement groups – bringing together representatives from carers’ organisations, voluntary sector groups and patients. In some areas, these types of groups were constituted as a subgroup of the CCG.
-
Steering group – one CCG had set up a ‘steering group’ which brought together PCT Cluster representatives with LINks members, carers’ representatives, voluntary groups, local clinical networks etc. This group met periodically and offered advice and comment to the CCG governing body.
-
Clinical reference groups – these are usually set up jointly with local acute trusts, and generally focus upon particular service areas such as diabetes, etc.
-
Stakeholder group – this is a group of local patients and the public who are asked to comment on proposed major service changes.
-
Public events – for example, one of our case study sites was planning a series of ‘road shows’ in supermarket car parks which would offer health checks as well as providing information about the development of the CCG.
-
Citizens panel – this is a group of interested individuals specifically convened to discuss in depth a proposed service development.
-
Patient experience network – this is a network which focuses upon the collation of patient experiences of different types of health care, including both primary and secondary care.
-
Newsletter – at least one site was planning a public-facing newsletter.
-
CCG board open public meeting – after authorisation, all CCGs will be required to hold some of their governing body meetings in public. Many are starting to do this already, reasoning that it would be good practice to begin to get used to this. Some were holding alternate monthly meetings in public, using the other internal meetings to work on organisational development.
Many of these approaches were already in place as part of the local PCT’s work or the PBC group which was in existence before. However, many CCGs reported that they were keen to develop more effective public/patient engagement than had been achieved by PCTs in the past, but at the time of the PRUComm research (2011–12, i.e. pre authorisation), there were not any active initiatives that were significantly different from those which had gone before. The issues identified in the PRUComm study reflect the findings of the case study research undertaken within the EVOC study (see Chapters 4–6).
The authorisation process
Leading up to authorisation, CCGs adopted both structured and piecemeal approaches to PPE. The most structured involve incorporating engagement into governance structures. For example, some CCGs have established a patient committee reporting directly to the board. A more usual approach has been to establish a PRG for the CCG, often drawn from the membership of PPGs within individual practices. Sometimes this is very structured, including examples where every practice in the CCG has a PPG and has a representative on the CCG PRG, such as identified in CS3 of the EVOC study (see Chapter 6). It is usual for this to report to a board committee, often the Quality Committee, and for this to be reflected in the terms of reference of the Quality Committee.
Another structured approach identified in authorisation plans was to provide an engagement and involvement strategy together with evidence that it is being rigorously implemented. Some of these were first class. One case was over 100 pages and demonstrated detailed understanding of the needs of its patients, clear and substantial action plans to achieve engagement and demonstrable progress and achievements against the plan. One of the strongest structures was a CCG for whom improving services for those patients with LTCs was one of three strategic objectives. Their governance structure included a Communications and Engagement Committee which sat alongside the Quality and Performance Committee and reported directly to the board. There was also a Patient and Public Advisory Group and a Practice Manager Forum, which informed the work of the Communications and Engagement Committee.
However, not all CCGs demonstrated such a structured approach. Part of the authorisation process included a requirement to submit brief summaries of case study examples to illustrate their work. Many CCGs used their response as an opportunity to demonstrate examples of engaging patients and the public. In many cases, that supplemented an engagement strategy which was more a statement of intent than a report of achievements to date. They included examples of proactive involvement in the redesign of services as well as consultation about proposed service changes. This was reflected in the 10 case study examples the NHS Commissioning Board supplied from the work of the first wave of CCGs when they announced their authorisation. For example, NHS Warrington CCG described their transformation of the service for LTC patients with lung conditions who are now looked after in the community wherever possible and have a central contact point where they can request support without visiting hospital. The chief clinical officer of the CCG is quoted as confirming the commitment to PPEI.
We’re keen to build on this success in other areas in the future and are working closely with partners and engaging with the public to make sure health services are joined up and meet people’s needs.
p. 8142
However, there was also evidence in the PRUComm study of PPEI being managed in order to present the right information for the authorisation process:
[A GP] said that she didn’t think the public were very concerned about the way that they run the CCG – but that they should go public – it is good practice and we are ready. She felt that they should do it sooner rather than later. She said that the press do not usually come, they use public minutes and then phone up and ask questions. There was various discussion about this – someone said that it will look good for authorisation.
Field notes from observation of CCG board, emphasis in original
It might be expected that strategies for engagement would draw on acknowledged best practice to inform them. For example, the authorisation criteria required CCGs to demonstrate how it would achieve shared decision-making between health professional and patients and translate those views into commissioning decisions. Applications as part of their strategies could have drawn on the evidence of what works, including research from The King’s Fund. 143 None of the applications for authorisation reviewed for this study did so. Similarly, there was no reference to the leading research into the quality of the engagement work in primary care, including notable practice. 86
The impact of involvement
In their authorisation documents, some CCGs quoted case study examples of commissioning decisions that have been influenced by individual patients and by public consultation.
These included the redesign of services for people with LTCs. Initiatives to deliver care across sectors and disciplines in an integrated way featured largely in these examples. Fewer demonstrated how patient feedback systematically informs their work and helped them achieve improved patient experience. A minority did not provide any evidence but reported having a strategy for the future. In one case, the minutes of a meeting held in July 2012 as part of an application submitted in October 2012 included the statement ‘the detail around exactly how the CCG was going to engage with its communities was still being worked on’. This reflects the findings of the PRUComm research, although some CCGs were more engaged in thinking about both PPE and how this would be delivered post authorisation:
There’s two GPs leading for that, and myself as like the PCT cluster lead. Um, what we’ve done is we‘ve set up a steering group made up of people within the PCT cluster and people from outside, LINks and some of our voluntary sector organisations. Um, and we’re going to get some patients and members of our public networks on there to help steer us through. So we have a work plan from the authorisation, and we’re working through that to make sure that we’re delivering that. So we have other people that are involved in that to help us and steer us.
GP, south-west CCG
The case study examples included in the NHS Commissioning Board’s announcement of the first wave of authorised CCGs included examples relating to commissioning decisions including North Staffordshire where the redesign took account of both the clinical perception and user experience to shape a new and improved service – this is surely what clinical commissioning is all about. 144
While there are many similar examples, not one of the 16 submissions assessed for this study was explicit about the impact of the involvement of patients, i.e. how the outcome was different from what it would have been if the involvement had not occurred. For example, in one case a CCG submitted a schedule which described, in tabular form, the issue, who was involved, what feedback was forthcoming, what decision was made and how the engagement influenced the decision. The content of the table, however, comprised issues for which, in the main, evidence already exists about the views of patients. These included issues relating to diabetes services where patients were asked about their views about self-care programmes and what they would want included, when there is already no shortage of knowledge about what diabetes patients want to support their self-management of their condition. It was, therefore, not surprising that it was unclear how different decisions were taken as a result of the engagement.
There was a similar lack of compelling evidence that patient experience is informing other types of decisions. For example, the role of the Quality Committee as part of the governance structure of a CCG and its use of patient experience and feedback to establish indications of a failing service was often contained in the CCGs Constitution, but it was rare to find examples of that working in practice. To some extent, the lack of evidence of engagement in decision-making in practice was a reflection of the early stage of development of a CCG. It was not unusual for a Quality Committee to have been formed only shortly before the CCG applied for authorisation.
Achieving impact is dependent in large part on the CCG leadership making it a priority in practice. Again, the evidence is very varied. At one extreme were the organisations that had a long track record of leadership championing engagement at practice level. For example, CCGs in Lincolnshire are building on the excellent foundations of GP leadership in NHS Lincolnshire. This is illustrated by the handbook they published in March 2011 ‘setting out 10 principles for GPs leading programmes of commissioning change by working with their local population’. 145 At the other extreme are those who seemed not to grasp the distinction between communication, engagement and involvement. In one example, the chairperson of a CCG referred in the foreword to their integrated plan to their commitment to keeping the public informed about the decisions made by the CCG and made no reference to active involvement in the work of the CCG. Similar differences were found in our three case study sites (see Chapters 4–6).
Proposals for voices to be heard after authorisation
It is pertinent to recognise that engagement has been regarded as an important but not urgent part of the work of CCGs to date. The result is that delivering on engagement plans in the future is more significant for the cause of engagement than the work to date.
It has been fundamental to the authorisation process to ensure that £65B of public money is safe in the hands of the authorised CCGs. Governance, leadership, clinical competence and patient safety are fundamental to this. The view that engagement, at least in the short term, is not a prerequisite is reflected in the Draft Applicants Guide issued by the NHS Commissioning Board and the results of the first wave of authorisation. The applicants guide states that the thresholds for authorisation reflect ‘coherence with ongoing assurance and thresholds for early intervention in relation to failure. The criteria in relation to risk on quality, safety and financial management and related governance, planning and capacity and capability therefore have relatively high thresholds’. 146 Note that engagement is not included in that list. This is also suggested by the results of the first two waves of authorisations.
Of the 34 CCGs who were authorised, eight had no conditions attached to the approval. Twenty-six were given ‘minor’ conditions because they did not meet fully the thresholds of one or more of the 119 criteria in the six domains. A total of 96 conditions were listed, of which just eight related to domain 2. Only six CCGs had conditions relating to domain 2. Fifteen of the 67 CCGs authorised in the second wave were given conditions relating to domain 2, 11 of the 62 CCGs authorised in wave three and 13 of the 38 authorised in wave four. In all waves, the main areas of conditions were in respect of domain 3 and 4, which address finance, governance and effective commissioning.
The process from the outset has emphasised that authorisation is the first stage of a process leading to first-class commissioning groups. The Draft Applicants’ Guide includes a section for each domain on ‘potential beyond authorisation’. For domain 2, it includes a series of inspiring objectives including ‘CCGs will recognise that communication and engagement drives transparency, accountability and ultimately better services and outcomes . . . CCGs enable patients to make choices and shared decisions about their care and treatment. They have clear plans to extend the potential for patients to exercise choice about their care and treatment’ (p. 15). 146
What is not yet clear, and what is crucial for delivering this vision, is how NHS England will ensure that authorisation is the first part of a long-term process. A mechanism is needed for CCGs to be held to account for the delivery of the engagement strategy they supplied as part of their application for authorisation. A commitment is needed from NHS England to a methodology for giving assurance about delivery post authorisation. Active dialogue with CCGs about progress in implementing strategies and plans is a practical step that would help to ensure an appropriate focus remains on engagement activity. Other sectors demonstrate that service user engagement takes time to embed and can flourish.
One further key component for ensuring that intentions become reality will be that the work is adequately resourced. Many CCGs believe that the management allowance is not adequate. There is a danger that management and support services in practice become focused on issues which have short-term impact on quality and safety as opposed to the longer-term development of engagement. Many CCGs are resourcing at least some of management of their engagement work from CSUs, organisations which are being established to provide management services to groups of CCGs. The challenge about securing appropriate support specifically for engagement in these arrangements was illustrated by one application for authorisation which stated that they were ‘insisting that a Communication and Engagement Manager is based within the Clinical Commissioning Group for the majority of the time’.
Conclusion
Some CCGs have already delivered excellent examples of engagement which have impacted on decisions about commissioning. Others can point to future plans. More can quote some case study examples which demonstrate some good work but which fall short of a strategy being systematically implemented. Some have put in place governance structures which facilitate engagement. Many of those are only now being put into practice.
It is widely acknowledged that effective PPE is difficult to achieve. The findings from our case study sites, the PRUComm research and our analysis of authorisation submissions suggest that CCGs are wrestling with many of the issues that research into PPE have identified in the past. Firstly, while there is widespread recognition that individual patient voices are important, it is also important that those appointed to forums or engagement groups see themselves as representing the wider community as well as feeding in their own experiences. Where wider engagement activities are attempted, it remains difficult to access those whose voices are not usually heard. Some CCGs have tried to tackle this by engaging with existing patient and voluntary groups. However, this can also be difficult, as there are a myriad of such groups, many of which have diverging agendas. Secondly, in some sites we found some concern as to which different aspects of the CCG’s work could most usefully seek engagement. While many remained committed to engaging the public in all aspects of the CCGs work, others argued that commissioning and the strategic aspects of service change were actually not of interest to the public.
Key to ensuring that voices are heard and acted upon will be the success of CCGs in delivering their plans for engagement that they have all submitted as part of the authorisation process. Delivery will be partly dependent on there being leadership from the CCG and also from service users in engagement so that the work is championed, prioritised and resourced. There must be decision-making structures within the CCG which enable patients and the public to engage, influence and, in the future, scrutinise. The NHS commissioning board can also facilitate delivery through their future work. The potential beyond authorisation that the commissioning board itself has articulated can become reality.
Chapter 8 Discussion
Introduction
Commissioners are required to procure care that promotes the health and well-being of individuals. Since 2007, consultation of local populations has been seen as key to this process,10 and this is particularly important in LTCs where service users have extensive experience of local services and specific issues of living with their condition. The EVOC study was focused on investigating PPEI in commissioning for LTCs. However, the study was conducted during a time of unparalleled change for the NHS, and while this led to challenges in conducting research in organisations undergoing the turmoil of transformation, it also provided a unique opportunity to investigate how the policy imperative for PPI evolved within the transitional structures. The need to adapt our protocol to the new structures enabled us to specifically focus on how, in terms of PPEI, transition processes were managed, how the new patterns and structures for PPEI varied from pre-organisation change and what evidence there was of the new structures being embedded within the infrastructure. In order to illuminate this within the discussion, we draw on normalisation process theory as an explanatory framework. During the transition processes we also sought evidence on whether the patient and public voice was, or could potentially be, more easily heard and responded to. To explore this further, we map our findings against the theoretical frameworks developed by Gibson et al. and Barnes. 105–109
Involvement or engagement?
When the project commenced in 2009, policy documents and local operational plans used the term ‘involvement’ to indicate that patients and the public should be part of the decision-making processes in commissioning, service planning and care provision. 2,7 However, Equity and Excellence7 highlighted engagement as a key route for clinical commissioners to take. This change in language characterises the move in emphasis from PPI at all levels of care from individual to strategic planning, to the bounding of involvement just at care level as exemplified by the third edition of the LTC compendium. 147
Our data, which were also supported by previous research,148,149 suggested that PPI was understood in different ways by the main stakeholders. For commissioners, PPI was identified as being integral to a rational approach to decision-making and a potentially useful tool for difficult decisions framed by the need to ration resources. While providers identified PPI as being part of ‘fine-tuning’ services, they also recognised that there was the potential for PPI to act as leverage on commissioners. Reflecting the variety of roles they had at the time (e.g. LINks member, service user group member), service users and representatives defined PPI in a number of different ways. These ranged from involvement in care to the strategic long-term planning of services for a population. While variation in understanding PPI was expected, the introduction of the term ‘engagement’ further compounded tensions in the different understandings between stakeholders. 150 Our data indicated that engagement and involvement were being used as interchangeable terms, but were represented by markedly different levels of patient and public participation. Engagement was limited to information giving (e.g. public engagement events) and obtaining feedback on services (e.g. through a survey or public consultation meeting). Engagement was not described in terms of active involvement in decision-making.
Mapping the boundaries between engagement and involvement from our data, and supported by definitions from National Voices151,152 and the Department of Health,79 involvement was the active response to a combination of patient and public experience of living with the LTC and health and social care services, and engagement which we define as a commitment to respond or interact (Figure 9). The implications for CCGs and other organisations with a PPEI mandate is significant, for if patients and the public are engaged but have no meaningful mechanism for involvement, this will inevitably lead to frustration and a disengaged public. Our findings suggested that this particularly occurred with service user groups who felt that their voice was not heard and that they were not being involved in decision-making. For example, a service user group of people with RA in CS2 were clearly engaged with the health system but, because they lacked any active involvement in decision-making processes, used complaints to the press and MP as the first course of action in getting their voice heard. Equally, in CS3, engagement of a service user group of people with diabetes and a BME background led to a breakdown in relationship when this was not followed by involvement.
FIGURE 9.
Engagement and involvement.
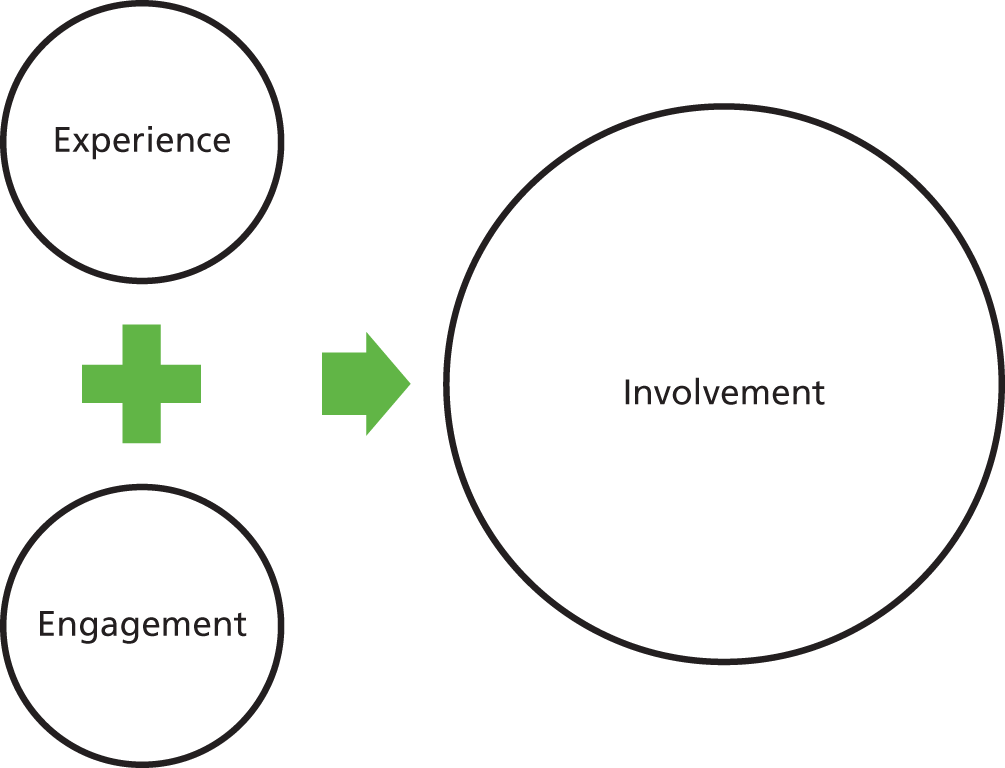
Although we have marked out the boundaries between engagement and involvement, guidance for CCGs on engagement (e.g. InHealth Associates Engagement for commissioning success Smart Guides87) quite clearly use the term to indicate the nature of the relationship between commissioner, service user and the public. 150 As discussed in Chapter 7, CCGs were required to state within the authorisation process how they would ensure meaningful engagement with patients, carers and their communities. The PRUComm survey, CCG authorisation review and the EVOC case studies suggests a continuum of strategies from operationalising PPEI at a purely information-giving and feedback level, to participatory involvement of a broad range of public and patients at all levels of commissioning. However, our findings also suggest that engagement and involvement is not a linear process; rather, it is a circular process which is fragile and can be broken – if involvement becomes tokenistic or ends then the service user becomes disengaged, and as a prerequisite involvement cannot occur without engagement. During the transition period between PCT and CCG, there was evidence that this cycle was often broken, sometimes as a deliberate cutting of ties but also because of the turmoil of change.
Patient and public engagement and involvement: the transition from primary care trust to Clinical Commissioning Group
Responses to plans for PPEI within the transition period can be characterised by anxiety from PCT commissioners and service user representatives about loss of relationships and GPs’ lack of experience in PPEI, counterbalanced by some respondents (particularly CCG shadow board members and local authorities) seeing it as an opportunity for a more strategic approach and starting anew. However, our findings indicate that PPEI processes and impact were being affected in the case studies by varying degrees of organisational amnesia. 153 As described in CS2 (see Chapter 5), an initiative underpinned by PPEI to transfer diabetes care from the acute to primary care sector was seen by PCT commissioners as likely to flounder during the transition phase. This was confirmed by service user representatives who felt that the focus on this initiative had been lost and communication from commissioners had ceased, a situation echoed in CS3 with the planned reconfiguration of diabetes services for the BME population.
In all our case studies, there was evidence that the speed of implementing the reforms153 and the sharp focus on the CCG authorisation process resulted in a number of projects with PPEI being lost from the radar. This was further compounded by the accompanying downsizing and loss of PCT staff who had been leading these projects. In all case studies, our original PCT commissioners had moved onto other organisations, indicative of the career-jumping that is suggested as one of the characteristics of a reformed public sector organisation. 154 Those staff who were still in post were working in great uncertainty about their future position, and were negotiating continually changing short-term roles. 154 In two of the three case studies, there was outsourcing of Communication and Engagement, with only one of our case studies retaining this in-house. This use of outside agencies may contribute to organisational amnesia by removing PPEI from the central radar. Observation of meetings indicated that major decisions were being made within a very short time frame (often as quickly as 24 hours), and supporting documentation was solely electronic. This ‘time compression’ and change in mode of record-keeping154 inevitably made PPEI in the decision-making process more challenging. There was evidence that there was insufficient time for lay members of the shadow CCG boards to keep abreast and informed of changes, and, therefore, meaningful involvement was lost.
However, the move to the CCG structure was seen as an opportunity to be innovative and move away from the former PPEI models. The relative freedom allowed by Equity and Excellence7 to determine local CCG structures resulted in a variety of structures, again indicative of recent reforms of public sector organisations. 154 While the PRUComm survey and EVOC case studies indicated the varied positioning of PPEI in these structures, our case studies also suggested that there was an ongoing tension between representatives of the previous PPEI structures and of the new. 153 The innovators saw the previous model of LINks as failing to be a conduit to harder-to-reach groups, and for perpetuating a very narrow representation. In CS1, this tension was openly acknowledged and addressed and there was evidence of a concerted effort to maintain a balance between change and continuity. 155 However, in all case studies, continuity in terms of service user representation appeared to be outweighing change. Although more recently housed in different structures such as PRGs, the majority of our service user respondents remained unchanged during the EVOC project. At the start of the project, many had been LINks or service user group members, and all were committed to maintaining their local PPEI role. In many ways, they became the organisational memory and were able to refer back to PPEI initiatives that had been successful in the past. However, it was more of a challenge for them to have this memory acknowledged and listened to during the frenetic period of reorganisation. The resourced project lead in CS1 enabled some organisational memory to be retained through the development of an extensive database of service user groups and public involvement representatives. Nevertheless, this project lead was an outsider on a fixed contract and there was some evidence towards the end of the data collection period that the achievability of the PPEI strategy was being questioned. Within the other two case studies, the development of the PPEI strategy was part of a shadow CCG board member’s workload, with an inevitable lack of focus demonstrated by the comparatively late production of the PPEI strategy. It was also significant that both leads were relatively inexperienced in PPEI, and much of this work was done alongside outsourced PPEI resources (CS2) and complementary projects such as the Equality and Diversity Strategy (CS3). Having a key project running in tandem both informed and shaped the PPEI strategy, and affected the way PPEI was understood in this case study. 153 The transition phase resulted in significant rehousing, with communication and engagement teams and PALS being outsourced or moved to provider trusts or CSUs. Containing PPEI within the overarching Communication and Engagement strategy made it vulnerable to being overshadowed by the CCG’s organisational priorities around communication with staff and provider services. Only one of the EVOC case studies had retained Communications and Engagement within the CCG (CS1). There are questions of sustainability for the other case study sites – external organisations and CSUs may be transitory.
Organisational memory is also stored through the norms and values of the organisational culture. In each of our case studies, the data suggested that PPEI could be mapped onto an intersecting continuum (Figure 10). The findings suggested a continuum of motivation for lay people to become involved ranging from an individualistic perspective to collective. 156 Our respondents included service users whose involvement had been triggered by a personal health agenda, but more commonly were motivated to undertake PPEI from a volunteerism perspective. Narratives from commissioners and providers also indicated that organisations were undertaking PPEI because it underpinned the organisational ethos, and (rather than a simple alternative view) because it was a statutory requirement or externally incentivised. During the transition period, there was evidence of some shift, albeit relatively subtle, on the continuum. This shift was influenced by the new structures, relationships within these structures and changes in key stakeholders in each case study. Interestingly, we could find evidence in only one of the case studies (CS1) of a shift towards an embedded ethos of PPEI. In the other two case studies, the sheer pressure of change was evoking PPEI strategies and responses more attuned to the top-down requirement of the reorganisation (see Figure 10).
FIGURE 10.
Continuum of PPEI.
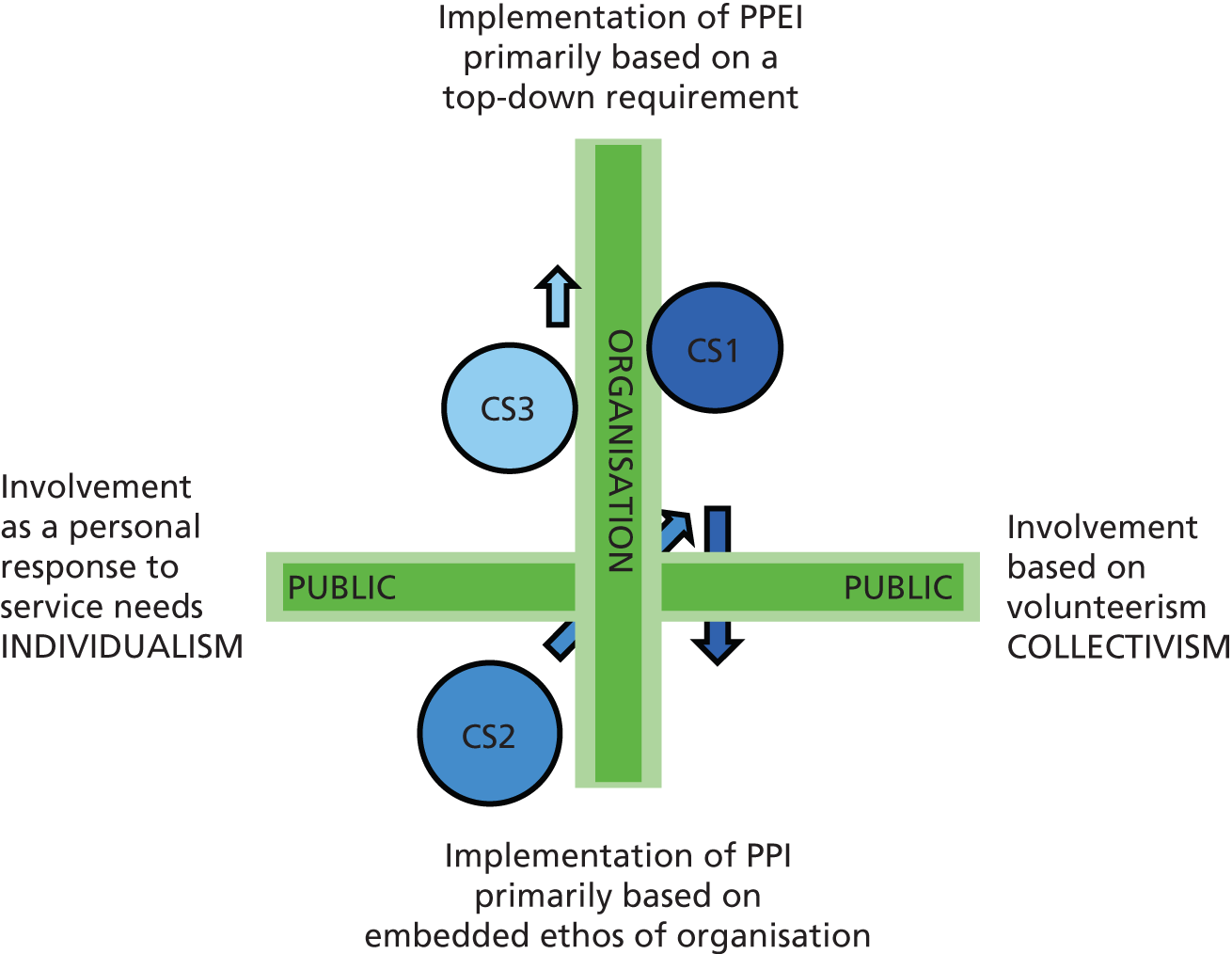
Changing patterns and structures of patient and public engagement and involvement
When data collection commenced, there were different histories and leaders of PPEI in each case study site. While all case study sites contained a local authority with strong pedigrees of PPEI activity, the PCTs varied considerably in terms of PPEI history. Furthermore, even in the case studies with significant PPEI activity, this tended to be fragmented with no overall joined-up strategy. Before the reorganisation, PPEI had been housed within the PCT, service user groups, PALS, local authorities and LINks, and tended to be focused within condition-specific pathway work, with an emphasis on service user feedback to proposed developments. Tritter157 categorises gathering feedback from service user groups as indirect collective involvement. Our findings also indicated that there were attempts, particularly by voluntary groups, towards direct, collective and proactive involvement. We found examples in each case study site where Diabetes UK, MS Society, Parkinson’s UK and the NRAS had actively influenced decision-making. In many ways, having a pathway-focused structure was an enabling feature for these organisations to have influence, and the shift away from this pattern resulted in a loss of relationships and concern over the move towards a more generic landscape.
The CCG PPEI structures in the EVOC case studies (see Chapters 4–6) and the reflections from the CCG authorisation review (see Chapter 7) indicated a significant movement towards integrated PPEI between the CCG and social care. During the transition process, it was evident from our data that clinical commissioners and local authorities were working more closely together to engage with their local populations, not least because of the move of Public Health from the NHS to local authorities. Models for involvement from the local authorities expanded the horizon of PPEI in the eyes of the clinical commissioners. Our discussions with local authority informants suggested a real enthusiasm for this closer joined-up working on PPEI. However, there was a significant difference between each case study site in the relationship between local community involvement structures and the CCG board. In CS3, community involvement was enacted through the Neighbourhood Governance Programme (see Figure 5) and reflected the local authority’s rich tradition of engaging with a very diverse population. However, in the other two case studies, community involvement appeared defined by the remit of the local Healthwatch and HWBBs [see Figure 2 (CS1) and Figure 4 (CS2)] and evidence of community engagement programmes within these two case study sites often had a public health focus.
While the closer linkage with local authorities and local populations significantly changed the landscape of PPEI in each case study site, conversely the pull towards local authorities was mirrored by less linkage with provider service PPEI groups. With the exception of the community diabetes service in CS2, we experienced increasing difficulty in engaging provider services with the EVOC project, and found access to any established provider service user group difficult. For example, in CS3 commissioners had alerted us to an active young person user group at the local provider hospital, but despite research governance approval we were prevented from making contact by the gatekeeper.
Although there appeared to be continued levels of silo working in PPEI, particularly between CCGs and provider services, many of our service user respondents were acting as a bridge. It was unusual for a service user or representative to be a member of just one committee or group. In reality, many of our respondents were concurrent members of different PPEI forums including provider service user groups, CCG-affiliated structures such as PRGs, and their local GP PPG. While the observation of different meetings with varying health professionals and managers but the same service user representative may suggest a range of arenas where the public voice can be heard,105 but a limited range of service user perspective, it also suggests that these service users were acting as boundary spanners between the different constituent parts of the whole structure. What is perhaps more important is whether or not they were enabled to perform in this role, and particularly whether or not they were seen as credible and hence listened to in this role (we will discuss this further in the following section).
As mentioned above, many of our service user respondents were members of existing or developing PPGs based at general practices. There was a marked difference between case study sites on where PPGs sat in the overall PPEI structure and how important they were seen to be within the PPEI strategy. This positioning alongside the relationship with local community involvement can be demonstrated in a matrix illustrating the key differences in the emerging structures of PPEI during the transition period (Figure 11).
FIGURE 11.
Matrix of emerging structures of PPEI.

The mapping of the case studies onto this matrix contrasts with the direction of travel, as illustrated in Figure 11. While the data on CS1 indicate that there was a subtle shift towards an embedded ethos of PPEI, this may not be sustained in view of the more marked separation between the CCG board and the voice of the ground roots patient and community. Equally, in CS3, which showed a direction of PPEI travel directed by a top-down requirement, it will be interesting to explore whether or not the flatter, networked structure creates a reversal of direction. As the positioning of PPGs within the new structures appears emblematic of this paradox, they will be explored more in-depth.
Patient participation groups
General practitioner patient groups are not a new initiative. Historically, PPGs have existed in the UK since 1972, and have grown in number through support from a national member association [the National Association for Patient Participation (NAPP)] and a joint campaign by NAPP, RCGP, the British Medical Association (BMA) and NHS Alliance to establish PPGs in around 40% of all English GP practices in 2009, and estimates of around 75% in 2012. However, research revealed that these groups exhibited a number of concerns, including equity of access, unrepresentative membership, diversity of purpose, variation and difficulties around assessing cost and benefit. 158 A recent review86 found most of these groups demonstrated little influence on practice management or service development, functioning primarily as a provider of feedback on services with a subservient role within the practice. Nevertheless, within Equity and Excellence,7 PPGs were seen as a potentially important tool for ensuring the patient voice was heard within the proposed structures. 159
To incentivise GP practices, a 2-year Patient Participation DES was implemented in 2011. 141,160 There was evidence from all our case studies that this had had a significant impact on developing these groups, and was seen by some as the most important PPEI initiative at that time. Information on PPGs in each case study is presented in Chapters 4–6. However, there are some interesting comparisons and points to be made. Firstly, as with the confusions of terminology between PPE and PPI highlighted earlier, GP practice-based PPGs also went through a blurring of titles. The DES required qualifying practices to establish a ‘Patient Reference Group (PRG). This may be a formal Patient Participation Group (PPG) or a similar group that is representative of the practice population . . .’ (p. 4). 160 However, we found no standard terminology in our case study sites, with around a half-and-half split in CS1 and CS3 of PPGs versus PRGs, and in CS2 nearly all were termed PPGs. This confusion is further compounded as many CCGs have a main PRG directly reporting or linking with the CCG and distinct from GP practice PRGs (for clarity, we will continue to use PPG to denote GP practice PRG or PPG).
When we compared GP websites in each case study site, only 27% of CS1 websites had any mention of an active PPG, in contrast to 58% in CS3 and 93% in CS2. This marked difference is reflected in each case study site’s PPEI structure. In CS2, PPGs reported directly to the clinical executive team; in CS3, PPGs fed into the CCG PRG committee which then reported to the CCG board. However, in CS1 where there was the least evidence of active PPGs, these were remote from the CCG board and any viewpoint would need to navigate the practice manager’s forum and then the clinical leads before reaching the CCG board. Furthermore, CS1 had a much larger percentage of virtual rather than actual groups. While it was too early to explore fully the consequences of these differences, our findings from the qualitative data and analysis of documents such as PPG terms of reference do suggest a tentative typology that would merit further exploration. The differences between PPGs could, to a certain extent, be differentiated in terms of who led the group, and whether it was virtual or face to face (Figure 12).
FIGURE 12.
Typology of PPGs in CCG structures.
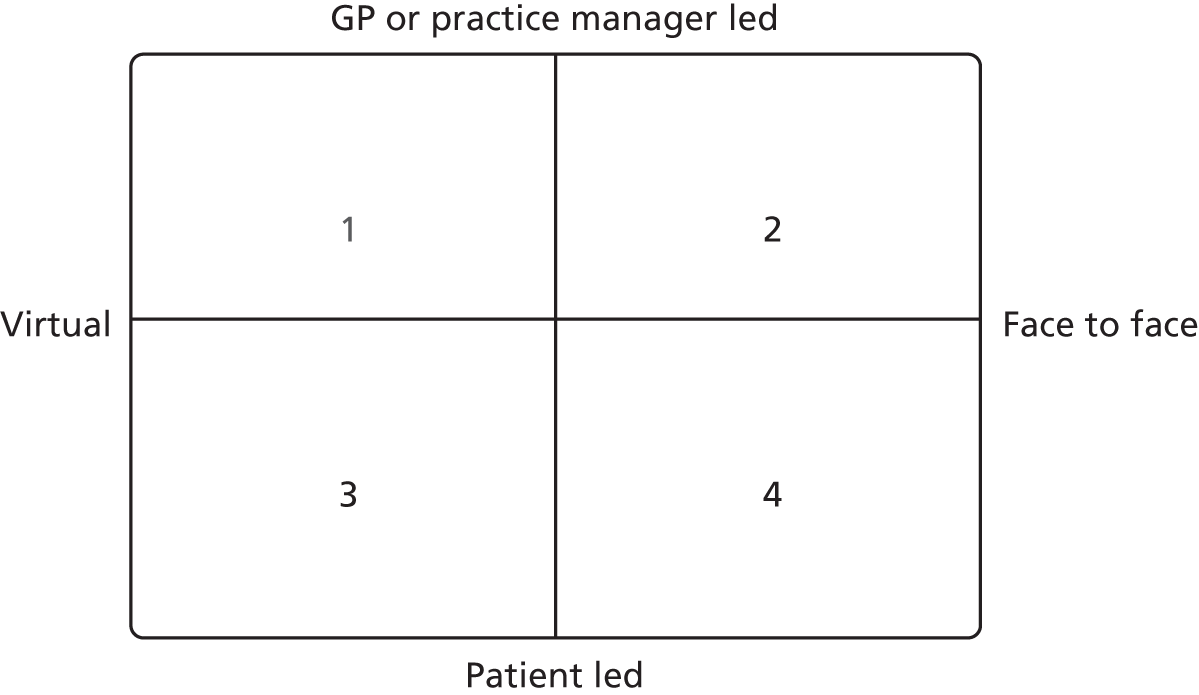
There is evidence to suggest some implications from each quadrant. In quadrant 1, there may be a selected customer feedback output, but it is questionable how representative this is, and how meaningful this form of PPEI is. Quadrant 2 will ensure that the agenda is set by the GP practice, but this may not include those issues most relevant for patients. Quadrant 3 may enable personal narratives (e.g. the Patient Experience Blog project in CS1), but there is also the risk that these narratives will end up in a void. Finally, quadrant 4 allows the agenda to be set by local patients, but may be at risk of focusing on personalised single agendas.
As a number of respondents in case studies 2 and 3 quite clearly felt that PPGs were a key tool in ensuring that the ‘grass roots’ voice was heard, and being a mechanism to engaging GPs with the reforms, their operationalisation and route to the CCG board is important. Equally, PPGs’ ability to be an effective voice for patient’s views and experiences is also important, as they are seen as a key source of information for the Care Quality Commission to draw upon when regulating GP practices. 161
While PPGs’ impact and future is uncertain, the DES payment was, quite clearly, a major incentive in the establishment of PPGs. The financial incentives associated with PPGs were, however, not replicated within the overall PPEI structure.
Resources for patient and public engagement and involvement
Although it was generally agreed that PPEI was resource intensive and had cost implications, resource implications, interestingly, were rarely highlighted as a major barrier to PPEI during the interviews. However, using resources on PPEI in the current financial climate was also highlighted by respondents to indicate their level of commitment to PPEI. At our final stakeholder workshop, participants raised concerns that CCG resources were unlikely to be adequate for PPEI and were currently targeted at communication rather than at engagement and involvement. In acknowledging the potential for the CCG agenda to be dominated by budgetary issues, many attendees suggested that PPEI work needed to show its impact on highlighting potential cost savings. This fitted with our data from service user representatives, particularly those from the condition-specific voluntary groups, who acknowledged the need to present potential cost savings alongside PPEI initiatives and suggested development of new services. This balanced approach was linked to being seen as rational and credible, a key criteria for shadow CCGs selection of lay representatives.
Power and control
Inevitably, PPEI brings with it questions of power and control. Earlier in this report, we mapped out the policy direction in PPEI which aimed to change the relationship between service users, the public and the NHS. 157 Equity and Excellence7 sought to further challenge this relationship, and the EVOC study has been in a position to watch any unfolding of a different dynamic during the transition process.
Specifications for lay representation: who did Clinical Commissioning Groups want?
As the reforms began to be implemented, the emerging CCGs were reminded that they were not working with a clean PPEI sheet and were encouraged to work on developing established relationships. 78,162 The PRUComm survey also suggested that PPEI initiatives in the pre-authorisation CCGs tended to be a continuation of work commenced by the PCT, and this was also reflected in some of the EVOC case studies. However, there was also evidence that the shadow CCGs in our case studies had an agenda to ‘refresh’ PPEI and move away from a reliance on LINks members as the PPEI representatives. There was a general concern that these members were of a particular background (white, middle class and retired), and were not representative of those sections of the public the CCGs were most keen to have a conversation with: the ‘harder-to-reach’ or seldom-heard groups. Prior to and during the transition process, our case studies had tried to address this by outsourcing PPEI to a social enterprise organisation which worked with these groups (CS2), by the appointment as CCG lay member of a chief executive officer running a local charity working with vulnerable groups (CS1), and through commissioners going out into the community to reach these seldom-heard groups in their own settings (CS3).
While there was some evidence of successful engagement within public health initiatives led jointly with local authorities, if we take children and younger people as an example of a harder-to-reach group then there was little evidence of successful engagement during the data collection period. Although we contacted national voluntary organisations and local groups in each case study site, very few young people were identified for interview. Despite following up potential contacts from organisations, in many instances telephone calls and e-mails were not returned. In CS1, a meeting with community nurses for young people with diabetes and juvenile arthritis resulted in only one interview, despite the enthusiastic efforts of the nurses to make personal contact with and recruit each eligible young person. In contrast, direct contact via LINks with a key member of a national advocacy group for children with diabetes resulted in several interviews with parents and young people in CS1. However, despite a parent in CS2, who ran a young person and family group for young people with arthritis, acting as an intermediary, we failed to recruit any young people through that route. In CS2, we had mixed success via local support groups and in CS3 we interviewed only one young person recruited via a diabetes nurse specialist.
A lack of engagement with young people was evident in the interviews with parents and young people. Parents said that there was little in the way of support groups for young people, and those parents who had been involved in trying to set up groups come across many obstacles particularly in gaining access to the young people themselves. This seemed to mirror the difficulties that we encountered with recruiting and gate-keeping. Young people who used support forums tended to use them to look up information rather than for contact with similar others sharing their condition.
As well as the difficulties in accessing young people, it was evident from those who were interviewed that many did not want to talk about their condition. For some, this was because they found it intrusive or did not want to be identified by their condition. Some young people declined an interview and their interviewed parents reported that this was due to ‘overload’. For example, one young person had recently taken part in clinical trials, been involved in the CS1 schools protocol launch and had given a diabetes presentation at his school. Hence, once a young person had become engaged, there was a process of disengagement because of involvement overload. This is in contrast to Figure 10 and suggests that a different model of engagement and involvement is required for young people.
While there was a desire for ‘new faces and fresh blood’ and engagement with harder-to-reach groups, there was also an acknowledgement that long-established relationships should not simply be cut. Although local LINks members were not seen as being an effective conduit to the harder-to-reach groups, they were acknowledged as having a long history of involvement in the local health service and as understanding how the system worked. Hence a balancing act was evident during the transition phase between developing new PPEI strategies and retaining and valuing established PPEI relationships. One mechanism employed for this balancing was to limit157 the LINks PPEI representatives to certain areas and use selective access criteria for the new PPEI roles.
Barnes et al. 107 describe the discursive practices of an organisation that helps define who is seen as a ‘legitimate public’. Legitimacy appeared to be normatively defined by commissioners in terms of what experience the lay person bought with them, and how they should behave (Figure 13). This definition was framed by an understanding of PPEI as a facet of consumerism, a binary division between ‘usual suspects’ and ‘hard-to-reach groups’, and an assumption that the public could be neatly packaged into distinct groups. 108
FIGURE 13.
Clinical Commissioning Groups’ ideal PPEI representative.
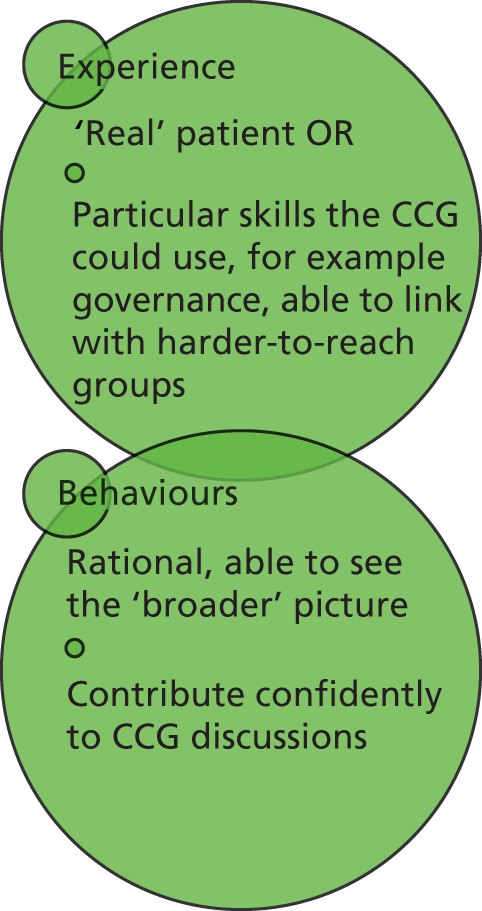
While commissioners in our case study sites were able to articulate the ‘ideal’ PPEI representative, it was clear that the members of the public, service users and their representatives identified their capacity to represent in similar terms, through their personal experience (e.g. living with a LTC), personal characteristics (e.g. able to function effectively within a committee), and through merit of their links via informal networks. Legitimacy, therefore, seemed to rely more on who the shadow CCG felt that they could work with, and the more formalised approach to recruitment ensured that this was focused on.
Patient and public engagement and involvement: who was leading the agenda?
As PCT commissioners faced increasing uncertainty in terms of their future and current service developments, there was evidence in our case studies of decreasing PPEI and the creation of a void. Service user groups felt the impact of this void; conversations with commissioners ceased and the service user voice hit a vacuum. The early transition phase was characterised by service user representatives desperately searching for the new agenda leaders in the embryonic organisations. Voluntary organisations that were used to playing an active role in decision-making with commissioners (e.g. Diabetes UK) were suddenly outside any communication loop and had little knowledge of how service initiatives were developing.
Voluntary groups played a major role in each of our case studies prior to the reorganisation and some were particularly effective in lobbying. Our case studies had examples of where the MS Society and NRAS had influenced local service commissioning. However, these groups were also in competition with each other108 and were very aware that diabetes was commissioners’ key priority. Furthermore, where smaller groups representing people with long-term neurological conditions had strategically merged, there was evidence that they were actively keeping out other long-term neurological condition organisations representing larger populations to ensure that their own voice was not drowned out. The PRUComm research also suggested that commissioners were grappling with such groups having a very condition-specific focus rather than being the voice of the wider community. Nevertheless, these groups and their alliances are likely to continue trying to influence commissioners’ agendas through increasingly sophisticated ways. For example, the Neuronavigator was a web-based tool developed by Neurological Commissioning Support and promised to be a user-friendly tool designed to help to deliver QIPP for neurology. This is an example of service user representatives responding to the broad NHS agenda (QIPP), and trying to ensure representation at the local NHS table by offering a clear ‘added value’ that was of immediate use to local commissioners. The tension between having to respond to an agenda set by someone else and then shaping it any way possible to serve the needs of the service users represented was often evident within all three case studies.
Nevertheless, at shadow CCG board level there was little evidence of the service user voice influencing the agenda. While this probably reflected the frenetic focus on the authorisation process, it is interesting that PPEI representatives in both the EVOC research and another external evaluation163 were periphery to decisions being made during authorisation. It was too early to tell whether or not this reflected earlier findings from some of our case studies, where PPEI representatives were invited only once key decisions had been made. Our shadow CCG board lay representatives suggested that they were listened to by the CCG, but were less certain about the amount of influence they would have on the agenda, reflecting Sullivan and Skelcher’s89 suggestion that lay representatives may be marginalised and have less influence than senior organisational members on a board. The EVOC summative workshop was attended by CCG board members outside the EVOC case study sites; there was a minority who reported a sense of marginalisation, which was exemplified by their being the only board members without voting rights.
Mapping the case studies against the ‘ideal’
In addition to highlighting tensions in the rules and norms of public participation, specifically access, agenda and deliberation, the work of Barnes et al. 106–109 also reveals the importance of emotional and figurative deliberation based on experiential knowledge. Enabling forms of exchange designed to offer recognition of the patient and public experience is seen as an essential feature of deliberation alongside purposive-rational discussion. This not only enables commissioners to understand the service user perspective but also demonstrates ‘deliberation with care’. 106 This embrace of emotional and expressive narratives is characterised by four moral principles of care: attentiveness to others, responsibility for action, competence in deliberative care and responsiveness to the service user and carer perspective. 110 These moral principles underpin one of the evaluative questions posed by Gibson et al. 105 as new PPEI structures are developed. These questions interrogate the notions of legitimacy through asking whether or not the new structures relate to the public solely in purposive-rational terms or whether or not they also fully attend to the emotional and expressive narratives. As can be seen from Figure 13, while ‘real’ patients were sought, their expected behaviour was bounded by rationality and a business-like confidence in meetings. Gibson et al. go on to ask four further questions of proposed structures:
-
Does the new system allow a plurality of public arenas where the service user voice can be heard?
-
Which areas of decision-making will be open to influence by PPI and which will not?
-
Which proposed solutions will be acceptable and unacceptable to the various stakeholders?
-
Is the host organisation prepared to change to accommodate some of these solutions?
While we can map the case studies to these questions to a certain extent (Table 12), our data collection ceased at the time of CCG authorisation and hence it was too early to judge the impact and responses to PPEI-initiated solutions.
| Structures relate to public in purposive-rational terms | CS1 had developed a Patient Experience Blog to capture patient narratives illustrating, albeit in virtual form, some attentiveness to service user perspectives. However, the response to these narratives was questioned, and a clear line of responsibility for action was unclear. None of the case studies engaged directly with patients with an explicit intention of listening to their narratives | Structures also relate to public in terms of expressive-narrative terms |
| Few arenas where public voice is heard | CS1 and CS3 had developed a number of arenas for the public voice to be heard. In CS2, it was less clear how the arena was being multiplied other than a process of outsourcing | Plurality of public arenas |
| Decision-making not influenced by PPEI | There was minimal evidence of PPEI influencing decision-making during data collection in the transitional phase to CCG | Decision-making influenced by PPEI |
| Solutions suggested by PPEI unacceptable to CCG | There was minimal evidence of PPEI initiated solutions during the transition phase to CCG | Solutions suggested by PPEI acceptable to CCG |
| CCG not prepared to change to accommodate proposed solutions | Too early to judge whether or not the established CCG in each of the EVOC case study sites would be prepared to change in response to PPEI-initiated solutions | CCG prepared to change to accommodate some of these solutions |
In addition, while Gibson’s framework provides a set of idealistic evaluative criteria, it needs to be framed in terms of resource and other constraints. Therefore, if PPEI-initiated solutions would be impossible to operationalise, then they are unlikely to be acceptable to the CCG. However, the EVOC evidence suggests that the majority of service user representatives were cognisant of these constraints and were willing to work within them. What appeared clearer within our data is that the new structures were enabling a plurality of arenas in at least two of our case studies, but that it was not clear how the expressive-narrative service user voice was being captured and listened to by the shadow CCGs.
In addition to it being too early to evaluate our case studies on all of Gibson et al. ’s criteria,105 the complexity of the new structures may be further compounded as new processes become embedded. In particular, the housing of PPEI across the local authority–health service interface will inevitably lead to some tensions in terms of existing institutional frameworks, professional, political and organisational norms. 108 Hence the journey has only just begun and these new relationships need to be navigated.
The future of patient and public engagement and involvement: what work needs to be done to embed it?
While incentives clearly trigger increased operationalisation of PPEI such as in research164 and general practice,141,160 this does not necessarily lead to a scenario where PPEI is normalised. As data collection completed, structures for PPEI had yet to embed within the new infrastructure; however, some case studies provided more evidence of work around this embedding than others. Normalisation process theory134,135 provides a useful explanatory framework to explore the differences further, and to usefully tease out the work needed to be done in order to make PPEI an integral part of a CCGs work. The theory was originally developed to assist in explaining why complex interventions often failed to be incorporated into routine practice134,135 and was developed from secondary analyses of qualitative data from a broad range of studies investigating complex interventions. Normalisation process theory focuses on how legitimate space is created for the work of the intervention to become a routine part of the landscape. 165 It is increasingly being used as a retrospective explanatory framework whereby thematic findings from qualitative data can be mapped against the key constructs,166,167 and has recently been used as a theoretical underpinning for PPI in research. 168
Patient and public engagement and involvement: issues of sustainability
Normalisation process theory suggests that, in order to sustain PPEI as normal practice, four areas of work must be achieved. First, PPEI in the new structures must be understood individually and collectively as something different from that previously known (coherence). Second, there needs to be an individual and shared understanding of what PPEI requires of each stakeholder, and that it is seen as potentially valuable by all (cognitive participation). Third, the actual tasks and resources required to sustain PPEI (collective action), and, finally, individual and communal appraisal of PPEI and adjustments to structures and processes if assessed as necessary (reflexive monitoring). 135
Coherence and cognitive participation
The respondents in our case studies could clearly identify the potential value of PPEI for their work; however, this was not without caveats around potential barriers. It was also clear that commissioners and service users and the public offered slightly different interpretations of the role requirement. 149 At the time of data collection, we did not find any clear role specification for the PPEI representatives, and participants at the summative workshop identified this as an essential tool for sustainability.
As already discussed, there was a palpable tension between continuity and bringing in new approaches and PPEI representatives. Our service user respondents remained largely unchanged and, equally, their narratives on PPEI demonstrated little shift. However, the new cadre of commissioners did speak of PPEI in different terms, particularly in describing PPEI at the strategic level. For future sustainability, the individual and communal specification of what PPEI is will need closer alignment.
Embedding PPEI also requires a key individual to drive it forward and that stakeholders continue to support it. We found clear evidence in one of the EVOC case studies that having an external project lead had led to the working up of a more developed strategy. Conversely, relying on an external source for this leadership may have future consequences in terms of continued support. It was too early to explore the consequences of having an internal or external PPEI project lead on continued buy-in.
Collective action
Perhaps the most obvious area of PPEI sustainability within the normalisation process theory framework is the performance and appropriate allocation of tasks required by PPEI, the relationships between stakeholders and the organisational support for PPEI. The reliance on just a few service user or lay representatives could lead to overwork and disillusion,169 with participants at the summative workshop highlighting the need for co-option and time-limited appointments. However, this was balanced with the need for time to develop relationships and trust, a key component for successful PPEI. There was evidence that PPEI representatives for the CCG board were being selected because this relationship had already been developed; potential candidates already known to CCG board members were being actively approached as they had been ‘good to work with’ in the past.
Perhaps the largest gap identified in the sustainability of PPEI was the lack of training for these new roles, for both the lay representative and the professional. In two of our case study sites, CCG board members did have access to a training programme run by the SHA. However, as can be seen by the structures presented in each case study, they were a very small, albeit central, part of the overall PPEI structure. During interviews, discussions and workshops, the need for training and preparation for PPEI was a repeated theme. While we did observe some training workshops that had a combined lay and professional audience, in view of the different interpretations of PPEI highlighted above a more extensive joint programme would be merited.
Reflexive monitoring
The final area of work within normalisation process theory is around systematically evaluating PPEI and reconfiguring PPEI strategies and processes in the light of this appraisal. There was little evidence of how this was to be approached within our case study sites. However, participants at the summative workshop suggested a number of approaches to monitoring PPEI (Box 3).
-
Record changes made as a result of PPI (as routine).
-
Evaluate outcomes – having measurable outputs agreed by patients and public.
-
Performance dashboard at CCG board.
-
Equality analysis (legal requirement).
-
Through provider contract with ‘consequences’.
-
National Commissioning Board to overview.
-
Annual PPEI report.
-
Research – how CCG services look from different perspectives – 360 degree (national GP survey, hospital survey, LINks – compare and contrast).
-
Disseminate research outcomes.
-
JSNA and use of LA – powerful monitoring tool.
-
Healthwatch as monitor.
-
Use of website – results of feedback – actions taken (you said – we did).
-
CQC inspection of GP practices.
-
Benchmarking: throughout patient pathway and against ‘most similar family’ (comparable CCGs).
-
Capturing patient experience over time/throughout service changes.
CQC, Care Quality Commission; LA, local authority.
While PPEI during the transition phase from PCT to CCG had evolved from pathway focused to a strategic level, issues around sustainability still need to be explored. Equally, if the health service is to fit the needs of the service user rather than vice versa,170 then PPEI needs not only to be sustained but also to be developed further.
Some future models of patient and public engagement and involvement
When the EVOC project commenced, our remit was focused on exploring PPEI within the LTC pathways and set against the choice agenda. This landscape changed significantly, with PPEI functioning at a more strategic level and within an environment increasingly framed by limited resources. Within some of the case studies, we found perceptions from some commissioners that the public would be unwilling to engage in decision sharing over limited resources. However, our findings suggest that the service user and public respondents were often only too aware of the challenges facing the health service and were willing to enter dialogue on these issues, a finding mirrored elsewhere. 171 This desire for active involvement in decision-making is in contrast to an alternative model of patient-focused commissioning which draws on virtual patient narratives. Experience-led commissioning is a model developed by a private consultancy in association with the Health Experiences Research Group at the University of Oxford. They suggest that using the Healthtalkonline (www.healthtalkonline.org) national data set of qualitative interviews of over 2000 patients living with 55 different conditions provides equivalent narratives when compared with the local patient population, and can be used when supplemented by a local needs analysis to commission services. However, it is not clear how this virtual form of patient experience will help the commissioners in making difficult decisions, or how it fits with the drive to localism which was expressed by a number of the EVOC respondents.
Perhaps more congruent with our findings from EVOC are the suggestions offered around the concept of patient leaders. Gilbert169 suggests that PPEI involves a twofold role: first, to be a community channel and provide a conduit to local communities and wider perspectives, and second, to be a critical friend ‘offering strategic advice from a non-institutional perspective’. These roles were clearly reflected in the EVOC data. With the appropriate learning and training, Gilbert also suggests the emergence of two types of patient leader: those who want to improve health and social care by being involved in the transformation of systems, and those who want to actively improve health and well-being within their local communities. However, robust support and development will be key to these leadership roles, an area lacking to date. 170,172 Resources to provide appropriate training for all concerned are scarce and will continue to be so. However, within the EVOC study, we saw the continuation of forms of PPEI silo work. While the CCG PPEI plans took a more strategic approach and built linkages with the local authorities, at the same time other links were being loosened or lost, for example with provider PPEI groups and some voluntary groups. The potential for sharing resources for PPEI training and development is significant, particularly in the new landscape and burgeoning of PPEI within new structures such as the Academic Health Science Networks and second wave of Collaborations for Leadership in Applied Health Research and Care (CLAHRCs). This may be the way forward for developing a more synergistic and effective PPEI.
Chapter 9 Conclusions and recommendations
Introduction
The project’s initial aim was to examine how commissioners enable voice and engagement of people with LTCs and to identify what impact this has on the commissioning process and pattern of services. A key outcome of the research was to provide guidance for commissioners on the skills and expertise needed by different commissioners, what actions are most likely to lead to responsive services and the most effective mechanisms and processes for active and engaged commissioning for people with LTCs. Our specific objectives were to:
-
critically analyse the relationship between the public/patient voice and the impact on the commissioning process
-
determine how changes in the commissioning process reshape local services
-
explore whether or not any such changes in services impact on the patient experience
-
identify if and how commissioners enable the voice and engagement of people with LTCs
-
identify how patient groups/patient representatives get their voice heard and what mechanisms and processes patients and the public use to make their voice heard.
In addition to our key objectives, we were also able to observe how the NHS reforms in England impacted on approaches to PPEI. These reforms commenced before the start of our research with the merger of PCTs into clusters during 2009–10. However, following the election of the coalition government in 2010 and publication of the White Paper Equity and Excellence: Liberating the NHS,7 the path of reform shifted to include a complete restructuring of commissioning arrangements in the English NHS. From January 2011, new ‘Pathfinder’ GP-led commissioning groups began to develop, leading eventually to the establishment during 2012 of new CCGs. These CCGs took over statutory responsibility for some 60% of the NHS budget from April 2013 to commission local community and hospital services. At the same time, PCT clusters evolved into CSUs and NHS England was established with responsibility for 40% of the NHS budget with a specific emphasis on specialist services, national GP, ophthalmic, pharmaceutical and dental contracts, prison health, armed forces and a number of national public health programmes (see Appendix 11). In addition, public health, including the commissioning of public health services, moved from PCTs to local authorities.
While all three new commissioners – CCGs, NHS England and local authorities – have responsibility for commissioning services for people with LTCs, our study specifically focused on local relationships and, therefore, did not examine what developments have occurred in relation to NHS England on PPEI except where this organisation established the authorisation process for CCGs. The commissioning activities of local authorities of public health interventions that affect people with LTCs did not commence until the very end of our study (from April 2013), and so it was not possible to explore the impact of this. Thus, the findings from this study relate specifically to the developing role of CCGs and PPEI and, in particular, the relationships between local commissioners, local providers and patients and the public.
In this chapter, we summarise our main findings for each of our key research questions. We then go on to discuss some reflections on the research process and limitations of our research. Finally, drawing on the key findings discussed in the case studies, analysis and discussion, we provide guidance for national organisations, local health-care commissioners and providers, and patient and third-sector organisations, identify key local and national policy issues and make recommendations for further research.
What kinds of relationships existed, and were developing, between the public/patients and commissioners?
In common with previous research on PPEI,149,150 we found that there were different understandings of involvement in terms of how it was understood and what is was for. Our findings demonstrate some clear distinctions between commissioners, providers, patients and the public about what the purpose of PPEI is (Box 4).
Commissioners: view involvement as a rational process, part of the activities that are undertaken within the commissioning cycle. The emphasis is on getting the structures and processes that feed into the commissioning process right.
Providers: view involvement as a ‘fine-tuning’ process to get their services right or a way of exerting leverage on commissioners. PPEI is, therefore, predominantly a self-interested activity.
Patients and the public: view involvement as a wide spectrum of activities ranging from involvement in care to more strategic purposes. Identify a need for a variety of occasions and places in which they can be engaged and involved.
We also identified that there are distinct different meanings associated with, or attached to, ‘involvement’ and ‘engagement’. We suggest that engagement is a pre-determinant of involvement and that involvement is seen as ‘active’; engagement is a passive activity but forms part of a commitment to involve. As discussed in Chapter 8, these different understandings and perceptions are important in terms of what PPEI takes place locally and how it is supported.
We found that the factors that drove PPEI in commissioning organisations were broadly threefold:
-
In some organisations there was a clear organisational ethos for PPEI. It was seen as central to the activity of the organisation. This view was reflected in our case studies 1 and 2.
-
Other organisations engaged in PPEI because it was a statutory requirement – something they had to do. Responses to the CCG authorisation process are an example of this.
-
The third group of organisations responded mainly to external incentives to undertake PPEI, such as the provision of resources and funding. The development of practice-based PPGs following the introduction of the DES supplement to the General Medical Services contract is a good example of this.
It was clear from our research that commissioners continue to define who has a legitimate lay voice. As Barnes et al. 107 have described, PPEI is framed by an understanding that there are two distinct legitimate voices based on (1) experience where CCGs identify useful skills and (2) behaviour where the lay voice is viewed as rational and can, therefore, contribute with confidence. The corollary of this is that there is a group of ‘non-legitimate’ lay voices to be kept out of processes. This distinction has been observed over many years8 but still seems to be a key factor in current practice.
While incorporating the experiences of young people proved a challenge in this project, we were able to identify some key issues relating to PPEI and young people. Our research also demonstrates that young people and adults have different experiences and perceptions. We found that, for adults, engagement and experience provide the key underpinning for developing involvement in decision processes (see Chapter 8, Figure 10). However, for young people the combination of experience and engagement tends to lead to a withdrawal of interest. From our research it is not clear why this should be so, although there was a general reluctance by young people to discuss their experiences of the process of PPEI. It is critical that further research is undertaken with young people to understand the reasons for this and how young people’s involvement can be supported and sustained.
The structural changes to the English NHS affected both the organisation and roles of commissioners, and the more formal structures and processes for PPEI. In commissioning organisations, people changed roles and organisations or left the NHS. This severed existing relationships, requiring new ones to be formed. In addition, the shift from the previous LINks structures to the new PPEI structures was also disruptive and created tension and a lack of sign-up to the new processes. More needs to be done to keep individuals ‘on board’ during periods of transition. We found that PPEI at a grassroots level became removed from the core CCG through the creation of various hierarchies – both within the CCG and in newly established structures for developing PPEI. Investing in a designated lead and getting whole-CCG sign-up and investment helped, but involved a substantial resource and energy investment into building relationships. Incentivising and having a budget for PPEI would be useful to support this type of work.
What impact did the public/patient voice have on the commissioning process and decisions made by commissioners?
As research on CCGs has shown,22 the reforms led to a lack of clear focus on commissioning developments. For CCGs, the key focus through 2012 was on the authorisation process. Given the substantial changes occurring in local commissioning structures and the impact that this had on PPEI activities, it is not surprising that we did not identify many examples of public and patient voice impact on commissioning decisions. Not only was organisational change a key focus of local organisations, but we found a lack of continuity of staff within the evolving organisations, meaning that initiatives and activities such as PPEI were disjointed or, as in our CS3, started from the beginning again. It is perhaps instructive, however, that we found little evidence of any PPI in this process at CCG level. This peripheralisation of PPEI representatives was also found in another study. 163
Successful approaches by patients to influencing commissioning agendas were generally evidenced where voluntary and larger patient organisations were involved. These groups played a significant role in trying to influence commissioners. The importance of collectivity was also observed where small groups of patients collaborated to influence agendas and to ensure that their voice was heard as well as, or in cases, instead of that of larger patient organisations. Larger user groups appear to be well placed to provide tools for commissioners, although generally this was observed as responding to NHS agendas (such as QIPP) but trying to shape that agenda to meet the needs of service users. We did not, however, find any strong evidence of PPEI influence on commissioning discussions at board level; in particular, lay board members were unsure about their level of influence, even if they were listened to.
To what extent did any such changes in the commissioning process reshape local services?
Given the difficulties described in this report about continuity and the limited evidence of impact that resulted from the impact of reform, we found few examples of how PPEI impacted on service changes. However, we found some evidence that PPEI in commissioning did lead to the reshaping of local services for people with LTCs. This was perhaps strongest where national third-sector organisations were involved, such as in the example provided for MS and Parkinson’s disease services. Service user representatives lobbied for support in the form of dedicated nurse specialists for their respective conditions and these were eventually commissioned (supported by pump-prime funding from the respective third-sector national organisations) in CS1 and CS3. At a more local level, service users also managed to influence the development of a protocol for supporting children with diabetes in schools in CS1 as well as others having a major role in reshaping local diabetes services in CS2. For RA there was less evidence of direct influence, but one local group in CS3 did push for the provision of a dedicated ‘rheumatoid arthritis’ physiotherapy service within their local trust.
Our findings relating to identifying changes were significantly limited by the rapidly changing organisational and commissioning environment. This led to interrupted developments as those responsible for service developments left organisations. For example, in CS3, the work on developing a commissioning strategy for people with LTCs was restarted when responsibility moved from the old PCT to the CCG. The exception was the development of the protocol for children with diabetes (in CS1). Here, there was continuity, as the protocol was developed outside of the NHS. However, implementation was a problem because there was no mandatory application of the protocol in schools. Our findings highlight the importance of organisational stability and the need for continuity and for processes that ensure responsibility and accountability for implementation. In CS3, the service that was identified in the exemplar case of diabetes services for people in BME communities was noted by the expert reference group as a service that was based on good clinical practice – and therefore likely to be of benefit – but was not influenced by the engagement activity with BME groups.
Did any such changes in services impact on the patient experience?
Given the time frame of the research, it was anticipated that most of the data we would collect would examine process aspects of PPEI and identify whether changes had been made in services or new initiatives commenced as a result of PPEI. Given the lack of research evidence on impact, a key objective of this research was to identify outcomes that were beneficial to patients. As described in the methods chapter, we established an expert reference group to review a selected number of exemplar initiatives. We selected exemplars that were sent to a virtual expert reference group consisting of a number of external key people with a wide variety of expertise and experience relating to patient involvement, clinical skills and knowledge and clinical practice around LTCs in general and/or specific to the tracked tracer conditions. We asked the ‘experts’ to provide comments on the identified exemplars of PPEI practice tracked in phase 3. The aim was to bring some external verification of whether or not the interventions, services of processes, developed through PPEI, were likely to lead to improvements and benefits for patients, given that within the time frame of the research this was not possible. This stage of the research was undertaken after we had analysed our data and identified our key findings (as outlined in the previous chapter). The purpose of this external assessment was, therefore, to identify whether or not our conclusions were valid and, thus, this information is presented here rather than as part of the general discussion of our findings.
The examples provided in our case studies demonstrated that impact on patient experience was more of a challenge as there were limited ‘hard’ service evaluative data to make an overall assessment. Some of the changes were too recent and had not yet been evaluated (RA, physiotherapy) and others had not yet been implemented (schools protocol for diabetes). Data obtained from qualitative interviews suggest that the specialist support nurses for MS and Parkinson’s disease had improved patients’ quality of life, which is supported by previous research. 173 The case has also been made by the MS Trust and Parkinson’s UK that these nurse specialists reduce unplanned hospital admissions and are cost-effective. 174,175 Evaluative data from the diabetes service reconfiguration in CS2 revealed that the service was popular with the public as well as meeting other quality and efficiency targets (see Chapter 5 and Appendix 5).
We selected three examples of practice, or exemplars, reflecting developments initiated by patients and/or the public. The selection of case study exemplars was based on data from each case study and in each case a diabetes service development was selected. Summaries of these were sent to expert reference group members (see Appendices 5–7 for details). We asked members of the expert reference group to comment on both the process of involvement and whether or not the initiative identified sufficiently demonstrated a high degree of patient/public involvement, and what the potential benefit of the development would be to patients. In this sense, we were asking about more than just clinical or health benefit.
For the exemplar in CS1, we selected a protocol developed by parents for supporting children with diabetes in school. Interestingly, as discussed elsewhere in this report, this initiative was developed by parents who engaged with schools and only later was supported by the local LINk. In a sense this was undertaken outside the health system, yet of the three initiatives – all relating to diabetes – this one was rated as having the potential for the most patient benefit. The reference group members’ assessment of the exemplars from CS2 and CS3 was critical both of clinical benefit and of the process of engagement; this was particularly true for the exemplar from CS3, which involved a development that was intended to address the needs of people in BME communities with diabetes. The assessment of these exemplars demonstrates some of the key findings of this study relating to the fragility of PPEI where it occurs, poor PPEI processes and the lack of support by health agencies, issues of short-termism and impact of constant health service reorganisation. Yet they also suggest that PPEI can have positive impacts and that, where initiatives are driven by strong lay perceptions built on experience, there is the potential to develop approaches of real benefit to patients. Getting formal support from health-care agencies can, however, be difficult and, in the case of the school protocol, the lack of a mandatory system for ensuring that it was implemented in schools limited the potential of the protocol and the work put in by parents and others.
The expert reference group also identified a number of key weaknesses in process, such as the focus on a single group in CS3 or relying on communication (in CS2) as a means of engagement without considering how the patient/public voice is heard or taken into consideration. These themes emerged across our case studies and are reflected in the wider PPEI literature.
How did commissioners enable the voice and engagement of people with long-term conditions in the commissioning process?
Our study found that commissioners use a range of approaches to PPEI. However, while we identified an extensive range, the move to CCGs suggests some broad common themes emerging. Our study was able to observe how the organisational changes in commissioning impacted on PPEI during January 2011 to May 2013. It was clear from our case study research and also from the findings of the PRUComm research and analysis of CCG authorisation documents that CCGs saw themselves as wanting to be more innovative in their PPEI strategies and activity. In some cases CCGs were critical of previous approaches to PPEI, such as the role of LINks perpetuating a limited approach to representation – especially from harder-to-reach groups. However, it was clear from our study that the organisational changes to the NHS led to fragility in PPEI initiatives and some – such as in our CS3 – were lost completely. At the same time, while commissioning organisations suffered substantial changes in organisation and staff, there was a degree of continuity in the patients and public involved in lay structures – moving from the old to the new PPEI structures. In addition, despite the commitment to innovation, we observed that PPEI was, in many cases, brought under the umbrella of communication and engagement strategies within CCGs, with the activity then outsourced to CSUs or other external agencies. Such moves may make PPEI vulnerable to CCG organisational priorities. Two of our exemplars (CS1 and CS2) show how NHS and/or clinical priorities are prioritised over lay perspectives.
One of the key findings from our research is the fact that PPEI is a fragile activity that is subject to pressure from organisational change and pressure from policy directives. Only one of our case studies (CS1) had sought to embed PPEI within its organisational ethos, while activity in the other two case studies was driven mainly by top-down policy and guidance. NHS reform adds another dimension of fragility and contributes to short-termism in approaches to PPEI. These factors are reflected in the assessment of the exemplars discussed above. In particular, the CS3 exemplar demonstrates how changes in the organisational structure of the NHS have a detrimental impact on PPEI. It is also clear from our data that engagement and involvement is not a linear process. There is a circular process and this is, in itself, extremely fragile. This circular process can be ‘virtuous’, in that good engagement can lead to improved involvement if it is not tokenistic and does not lack sustainability. However, where involvement is tokenistic or ends, patients and the public become disengaged and less involved, and this can be described as a ‘vicious circle’.
Drawing on the data from our case studies, we identified a number of different ways in which local structures for PPEI were developing. The organisational structures for PPEI identified in each of the case studies show how these structures are developing differently in each of. In CS1 and CS2, the PPEI structures are hierarchal in one sense, but with separate pathways developing between PPEI driven from PPGs and broader representation from community and voluntary sector groups. In contrast, in CS3 PPEI appears to be developing a more complex system, with a number of distinct elements feeding into the CCG mediated through Healthwatch and the HWBB as well as through specialist groups. One result of this formalisation of PPEI structures and processes is to remove PPEI from the core work of CCGs as commissioning organisations. In addition, these do not represent model structures, but demonstrate how distinct structures can emerge which do not, in themselves, pre-determine the nature or quality of PPEI. It is instructive that the service initiative found, in this study, to represent the most potential beneficial impact for patients (assessed by the external reference group as most beneficial) was the school diabetes protocol (CS1), which was developed outside the health-care system and whose implementation relied predominantly outside the health system.
In Chapter 8, we mapped the case study activity against an ideal model. 105 Key to supporting PPEI is the requirement for a plurality of arenas where the patient and public voice can be heard. These were found more in CS1 and CS3. These were, from our data, the only elements of what might constitute an ‘ideal’ that were observed. While this may be a reflection of the early stage of CCG development and more general impact of the very recent reorganisation of the NHS, it does highlight how such structural change can impact on PPEI which is already a fragile area of activity. As shown in CS3, the preceding work developing PPEI with BME groups simply disappeared with the change and a whole new process is to be started. Our findings also suggest that there is a lack of reflexive monitoring to learn from experience. While organisational changes and restructuring had a part to play in our study, there was also evidence that organisations constantly restart PPEI processes.
Consultation events where patients and carers are invited were characteristic of approaches used in our case studies. This reflects the findings of other research on PPEI18,104 and also on commissioning for LTCs. 55 Interestingly, the study by Smith et al. 55 also highlights the involvement of providers, often in the same forums as patients and carers. Our study supports the view that for people with LTCs, greater collaboration between commissioners and providers is important for service development – particularly to support stronger PPEI building on existing, and often, extensive contact between providers and patients and their carers as well as groups representing patient and carer interests. Recent research in Scotland has highlighted that building on existing ‘volunteerism’ in participation provides a useful way of engaging and involving patients and the public in local decision-making and this needs to be done by identifying whether particular groups are marginalised or excluded rather than being classed as unrepresentative. 176
None of our case studies had developed ways of measuring or systematically identifying the benefits or otherwise of PPEI. There was no attempt to build in processes for monitoring the impact or costs of PPEI. This is an issue that has been identified in the existing literature on PPI. 103 The findings of this study reflect discussions in the literature on PPEI regarding the accepted view that PPEI is a good thing in its own right – that its benefit is self-evident. 177,178 Current evidence focuses mainly on the impact of involvement on those participating, with less emphasis on the benefits to decision-making in health care. As a recent review by RAND concluded:
We find evidence for the developmental role of public involvement – such as enhancing awareness, understanding and competencies among lay participants of healthcare decision-making – while the evidence for instrumental benefits of public involvement initiatives, that is whether public involvement improves decision-making and policy in terms of processes and/or outcomes, is less well documented. Yet overly focusing on outcomes of public involvement risks missing the normative argument that involving the public in the process may be seen to be of intrinsic value in itself.
p. ix178
Commissioners, and providers, in our study tended to focus more on the idea that patients and the public should be involved, without determining how the benefit, or otherwise, of that involvement would be measured.
How did patient groups/patient representatives get their voice heard and what mechanisms and processes did patients and the public use to make their voice heard?
Our study found that patient groups and representatives employed a number of mechanisms and processes to make their voice heard. While patient group involvement may be viewed as ‘meliorist’179,180 in trying to support health-care agencies (commissioners and providers) to make improvements to the way they do things the strategies used varied. These could be broadly mapped upon a continuum between benefit and threat. For the latter, there was evidence of patient groups actively following the ‘threat route’ by initiating complaints and using the press and local parliamentarian to coerce commissioners into change. The demarcation between this approach and those employing an asset-based strategy was often marked particularly at the EVOC workshops. Patient groups following the ‘benefit route’ ensured a strategic message to commissioners that highlighted the benefit, generally in terms of cost, of their suggestions for service development. In common with other studies, our findings suggest that measures of success for patients and the public are often different and more incremental than for health agencies, and that networking resources, such as funded support workers or support from larger voluntary groups, is a crucial support factor for PPEI. 181
During the transition period to CCG, the lack of certainty about who the actual commissioners were resulted in less of a coercive response and more of a focused effort to ensure that the patient and public voice remained audible by proactively highlighting the benefits of adopting the patient/public representatives’ suggested PPEI processes. In some of our case studies, LINks were particularly active in this through endeavouring to shape recruitment processes for PPEI, and attempting to take on a consultancy-type role in advising shadow CCGs on PPEI. The ensuing negotiation between established PPEI representatives and new emerging forums such as the local Healthwatch involved establishing structures which provided an arena for previous PPEI groups such as LINks and neighbourhood forums, but also developed new arenas where the ‘new PPEI’ representatives would sit. The funnelling of ‘new’ and ‘old’ PPEI into various components of the overall PPEI structure was enabled by CCG outsourcing or targeted recruitment. There were also proactive attempts to ensure a seat within the new components of the structure, such as in CS1 where the local MS Society branch had encouraged one of their members to be recruited onto Healthwatch. It was also clear, however, how fragile even well-developed approaches to engaging service users were at this time of change. In CS3, considerable community and health service resources had been involved in working with BME communities to input into service development. Despite this, the new commissioners decided to disengage from the process and start their own new approach to service development, demonstrating the fragility of even well-developed processes.
Key conclusions from study findings
The finding that there were different understandings of involvement was not surprising. However, the different understandings between commissioners, providers and patients and the public are of particular importance. These understandings lead to different to important differences in not only the perceived purpose of PPEI but also how it is undertaken. Our findings suggest that getting a shared understanding of the purposes and form of PPEI is key to developing effective PPEI processes. It is also clear that getting processes for implementation is essential to success. To develop circles of PPEI that inform the development of services, it is important that there is demonstration of actual influence. We also found that providers are of particular importance in PPEI processes. In our case studies, the structures for PPEI tended to formalise PPEI within structures that were not central to commissioning activity within CCGs. Commissioners need to work with providers on developing more integrated approaches to working in partnership with patients and the public. The need for more close working between commissioners and providers has also been highlighted in a study of commissioning for people with LTCs. 55
In considering PPEI in commissioning, we identify three areas that frame approaches to PPEI and provide an analytical framework for evaluating PPEI. These draw on the theoretical concepts developed by Barnes et al. and Gibson et al. 105–109 and the three main paradigmatic stances towards PPEI. 168 When explored through NPT concepts,134,135 viewing PPEI by asking whether or not it is moral, whether or not it is approached methodologically and how the policy imperative is enacted begins to help to shape a potential evaluative frame for PPEI. Table 13 shows how this framework sets the context and analytical framework for considering PPEI, and provides possible applications in practice. Implementing these practice applications across all three PPEI stances enables a more holistic approach to PPEI, recognising and bringing together the differing viewpoints we found in our study in order to move towards a more congruent approach.
| NPT concept | Sense making | Evaluation frame | Application in practice |
|---|---|---|---|
| Moral | PPEI as a right for the tax-paying citizen in a democracy, and the moral argument of ‘nothing about me without me’ | Does everyone have a voice? Is there deliberation with care? Is involvement seen as a moral right? Is there more transparency? | Ensuring PPEI processes and structures enable the voice of the public who are the most vulnerable such as people with long-term health conditions (mental health problems; dementia; learning disabilities), long-term socioeconomic conditions (homeless people, traveller groups, sex workers, refugees, asylum seekers, prisoners/ex-offenders, people living with persistent poverty/lower levels of education), and those from BME communities Enabling deliberation with care through having a highly visible and accessible main point of contact for the public and focusing on relational integration such as the fostering of relationships and trust. Consistently providing timely and informative feedback Provision of clear and accessible information regarding service users and the public’s rights in involvement with local health and care services |
| Methodological | PPEI as a tool for quality improvement, improved patient safety and increased efficiency | Has quality improved in terms of patient experience and safety? Are there economic benefits? |
Developing an evaluative framework to measure how PPEI has led to improved patient experience and safety Using patient experience and collaborative work with the public to commission and develop experience-based services Measuring the potential economic costs benefit of more effective PPEI |
| Policy | PPEI undertaken as a policy imperative | Is PPEI being implemented as per policy? | Conducting policy evaluations to understand the mechanisms associated with embedding PPEI as a policy initiative Collecting indicative data to understand the local contextual enablers and barriers to implementing PPEI Sharing and learning from best practice in PPEI |
However, congruence is difficult to maintain during times of significant change, and a key theme that emerges from our data is the need for stability in order for relationships to develop. As Barnes has argued, enabling forms of exchange designed to offer recognition of the patient and public experience is seen as an essential feature of deliberation alongside purposive-rational discussion. 108,109 Our findings have clearly demonstrated that more needs to be done to maintain PPEI processes and activities during periods of transition. Of concern is our finding that PPEI at a grassroots level became removed from the core activities and functions of the CCG through the creation of various hierarchies within the CCG. Of more concern, though, was the removal of grassroots-level PPEI from the newly established structures for developing PPEI.
Reflections on and limitations of the research
Researching PPEI is complex and the changing organisational context of the English NHS occurring during the undertaking of this research, while offering a unique opportunity to observe change, also created methodological problems and a need to make revisions to our research protocol. We were also faced with a number of key challenges in undertaking this project which have had an impact on our research findings. These included:
-
the changing organisational context in our case study sites
-
gaining access to case study sites
-
staff changes in commissioning organisations
-
undertaking research with young people.
The changing organisational context in our case study sites
We have discussed elsewhere in this report the substantial changes to the organisational context in which we were undertaking research. The lack of commissioner continuity and the uncertainties created by both the reforms themselves and the uncertainties that emerged until the Health and Social Care Act was given Royal Assent led to a number of problems in applying our original methodology. Access and staff turnover were two key problems and these are discussed separately. However, organisational turbulence, fragmentation and uncertainty led to significant challenges. Changes led to substantial loss of organisational and institutional memory. 154 In many cases, there were periods where organisational structures were transitory and it was not clear which organisation was responsible for what. Negotiating and maintaining relationships with key stakeholders was both time-consuming and very complex. It also involved having to restate the purposes of the research over and over again. Changing organisations also raised problems for research governance, as we had to constantly gain permission and access to staff members and patients.
Gaining access to case study sites
While access to CS1 was facilitated by good existing relationships and keenness of the PCT to engage with the research and support a management fellow, access to the two other sites was more complex. In CS2, the existence of a strong PBC was identified via the local CLAHRC. While a positive focus, the PBC was at that time in a state of reform responding to changes in 2010 as a result of the new plans for NHS commissioning outlined in Equity and Excellence. 7,163 This led to a period of disengagement, given the organisational change priorities. However, the team was supported by key local stakeholders, enabling the research to develop around a key priority area (diabetes) that had been identified by the PBC. However, recruiting a third site was frustrated by the rapid organisational changes, and while a number of potential sites were approached, there was uncertainty about who the lead commissioner organisation was or it was the case that the organisations were too involved in changes to want to be involved in the research project. Thus, it was some time before a third case study site was recruited, leading to a delay in the phasing of the research. In the end, we treated each case study site separately, undertaking the phases of research as set out in the research protocol but concurrently across sites. This had the effect of lengthening the overall time frame for the research project.
Given this, we also felt that this provided an opportunity to examine some of the changing context in more detail and follow developments up to the point at which the new CCGs became statutorily responsible for commissioning in April 2013. As a result, we suggested to NIHR that the research should be extended by 9 months. This would enable this project to draw on data from the case study research and surveys on CCGs being undertaken by the PRUComm being undertaken in 2011–12 (which involved the principal investigator of this research project). In addition, we were able to undertake an analysis of PPEI plans in CCG authorisation documentation. This involved an analysis of the process and criteria and detailed documentary analysis of a sample of CCG authorisation submissions.
Staff changes in commissioning organisations
One of the key impacts of the NHS reforms was on staff. As Pollitt150 has previously described, organisational reform can lead to career jumping and staff continually negotiating changing short-term roles. These were distinct features observed in our research. Our original protocol involved longitudinal data collection in phase 3. Our original research method was to track some specified developments in each case study with a purposive sample of stakeholders. This involved repeated interviews and the completion of ‘Star Charts’ (see Chapter 3 for further details). However, we found that commissioning staff, in particular, changed very rapidly and it was not possible to follow staff members over time. This led to a lack of longitudinal and comparative information over time. We were able to collect sufficient data in order to provide a rich picture. It is perhaps ironic that the main continuity over the period that we undertook our research was in the patient/public representatives and this represents a key lesson for organisations and perhaps an important factor for underpinning why PPEI is crucial.
Implications for research with young people
The inclusion of young people in projects relating to LTCs is important to consider, as young people have distinctive service needs and experiences of their conditions from adults.
The difficulties encountered in this project of recruiting young people and even gaining access to ask them if they wanted to participate, however, illustrate some of the key challenges for researchers in obtaining a young person’s perspective. The project team adhered to the recommendations in relation to research with young people and our approach was in line with existing work in the field. 122–126 We wish to highlight the importance of such strategies in the context of research that spans new and emerging domains of work, but we identify the following lessons from this project that highlight the need for future research to consider the following:
-
The challenge of involving young people needs to be anticipated from the outset and sufficient dedicated resources allocated to this aspect.
-
Young people are likely to require specialised and specific information that needs to be developed in partnership with young people.
-
Young people may require specific approaches to the conduct of the research that impacts on the project organisation and methodology of the research; for example, they may not be in, or wish to join, condition-specific groups. Including charities that work with children and young people in the proposal development stage may be one way to address this issue and improve recruitment. This may also help to allay the concerns of gatekeepers about the participation of young people in research.
The involvement of a management fellow
The research team were extremely positive about the inclusion of a management fellow, and Joanne Reay’s role was key in the early stages of the research. We were fortunate to get support from the PCT in CS1 and the PCT was particularly keen to nominate a management fellow. Having the fellow played a key role in supporting access to the case study in terms of both the contacts of the management fellow and the support received for the fellow which made the PCT more aware of the research. The management fellow’s insights to commissioning processes and NHS structure were also extremely helpful. In the later stages of the research, the role of the management fellow became more uncertain. There were two reasons for this. The first was the NHS reorganisation, which resulted in the management fellow’s NHS job being placed at risk. Her NHS role was reorganised a number of times and also included a period of potential redundancy and uncertainty about her future. This impacted on the contribution she could make to the research project. It also meant that the original support structure within the PCT also disappeared. Thus, the original intention of the management fellow acting as a bridge between research and practice was severely curtailed. The other reason for uncertainty was due to the changes within NIHR and the seeming withdrawal of the management fellow programme and support structures within NIHR. This left the fellow and the research team uncertain about how the management fellow concept was to be incorporated into research activities.
Reflecting on our experience, we would definitely support the idea of involving NHS managers and practising clinicians in research projects. This would require stability and continuity from NHS organisations to facilitate the maximum benefit from a fellow. The selection of fellows is extremely important and both the research team and the employing organisation need to be clear about joint objectives. It would help if fellows have some research training – probably through postgraduate education programmes – prior to being involved in research projects, but additional training should be a key element of the management fellowship. It is important that NIHR supports management fellows across research projects.
Guidelines for practice and recommendations for future research
The findings set out in this report identify some key areas where improvements to practice in relation to PPEI can be made. In particular, these findings point to two broad areas of action. The first relates to the framework or infrastructure arrangements for PPEI and how PPEI can be supported in the NHS and other organisations. The second area of action relates to the process for PPEI and how it should be undertaken. These action areas are relevant to national organisations (and the new regional structures and organisations developing within the reformed English NHS) and to local commissioners (the CCGs) and service providers. In addition, the research has identified a number of key research issues about methodology and areas for further research that should be considered by research funders and researchers.
Implications for national organisations
-
National agencies should ensure that training and development programmes on PPEI for commissioners, providers and patients and the public are implemented: these can be delivered nationally or support local training and development initiatives.
-
National organisations such as NHS England and National Healthwatch need to develop monitoring criteria for PPEI.
-
There needs to be clarity about terminology, with agencies being specific about the meaning of terms such as engagement and involvement. These terms carry different meanings to different people.
-
National and regional agencies need to develop and support a sustainable environment for PPEI in which local relationships can develop and flourish.
-
At a regional level, organisations need to ensure that resources and structures for PPEI are shared, for example supporting networks, sharing resources, jointly supporting infrastructures.
Implications for health-care commissioners and providers
-
Commissioners need to embed PPEI throughout the commissioning cycle.
-
Commissioners need to understand that strategies for engagement, while important, do not substitute for involvement – this is a contributing stage but does not constitute active participation.
-
Commissioners and providers need to agree measurable outcomes of PPEI with patients and public, and evaluate these annually.
-
Commissioners and providers need to work together on PPEI as providers have more opportunities for engaging with patients and carers.
-
Commissioners, providers, patients and the public should work together to develop a shared vision of PPEI.
-
Agencies should participate in existing networks and forums – such as participation in a neurological network.
-
Agencies should co-operate on the mapping of local PPEI.
-
While PPEI requires an organisation-wide approach, organisations require dedicated resources (staff, funding) for PPEI.
-
Commissioners and providers should develop a shared framework for evaluating PPEI and its outcomes – for example, in relation to improved patient experience and safety.
-
Indicative data should be collected to understand the local contextual enablers and barriers to implementing PPEI.
-
PPEI processes and structures should enable the voice of the public who are the most vulnerable, such as people with long-term health conditions (mental health problems, dementia, learning disabilities) or long-term socioeconomic conditions (homeless people, traveller groups, sex workers, refugees, asylum seekers, prisoners/ex-offenders, people living with persistent poverty/lower levels of education) and those from BME communities.
-
A highly visible and accessible main point of contact for the public should be provided, focusing on relational integration such as the fostering of relationships and trust and consistently providing timely and informative feedback.
Recommendations for future research
-
Our research suggests that further research is urgently required to examine how PPEI is being developed within the reformed English NHS. Our research has demonstrated the fragility of PPEI and how reorganisation can impact negatively of PPEI processes and developments.
-
Research on PPEI among young people and children requires dedicated research projects where all resources and activity are focused on accessing, involving and supporting young people.
-
This project has demonstrated the value of linking research between similar research projects – in this case linking with the PRUComm research on CCGs – allowing the pooling of data.
-
This project has demonstrated the value of participative and iterative methods for investigating PPEI and researchers should be encouraged to utilise similar methods in future studies.
-
There is still a need for research to measure the potential economic costs/benefits of PPEI.
Acknowledgements
We would like to extend our thanks to all the service users, patient representatives and members of staff who participated in the study. We would also like to thank the advisory group, especially Diana Whitworth (chair), Vina Mayor, Diane Munday, Vicki Matthews, Alice Hamilton, Lynda Dent, Helena Wythe, Paul Wike and Ann Nugent, as well as members of our expert reference group, who are listed in Appendix 9, and also our young person reference group.
Contributions of authors
Professor Stephen Peckham (Professor of Heath Policy and Director of the Centre for Health Services Studies, University of Kent; Professor of Health Policy, Department of Health Services Research and Policy: London School of Hygience & Tropical Medicine; Director of the Policy Research Unit in Commissioning and the Healthcare System): principal investigator, designed the study, provided overall direction, analysed data and drafted sections of the report.
Dr Patricia Wilson (Reader in Patient Experience, Centre for Research in Primary and Community Care): co-applicant, designed the study, research lead for one of the case studies, collected and analysed data, and drafted sections of the report.
Lorraine Williams (Research Fellow, Department of Health Services Research and Policy): co-ordinated the project, research lead for one of the case studies, collected and analysed data, and drafted sections of the report.
Dr Jane Smiddy (Research Fellow, Centre for Research in Primary and Community Care): research lead for one of the case studies, collected and analysed data, and drafted sections of the report.
Professor Sally Kendall (Professor of Nursing and Director of Centre for Research in Primary and Community Care): co-applicant, advised on study and reviewed chapters of the report.
Professor Fiona Brooks (Professor of Adolescent and Child Health, Centre for Research in Primary and Community Care): co-applicant, advised on young person section of the study and drafted section on recommendations for children and young persons.
Joanne Reay (management fellow): collected and analysed data.
Douglas Smallwood (Patient and Public Engagement and Involvement Consultant): contributed to the section on CCG authorisation and contributed to phase 5 of the study.
Linda Bloomfield (Research Fellow, Centre for Research in Primary and Community Care): collected and analysed data for the young person section of the report, drafted section of the report on children and young persons.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Ham C. Chronic care in the English National Health Service: progress and challenges. Health Aff 2009;28:190-201. http://dx.doi.org/10.1377/hlthaff.28.1.190.
- Our Health, Our Care, Our Say. London: The Stationery Office; 2006.
- Next Steps Review: Interim Report. London: The Stationery Office; 2007.
- Generic Choice Model for Long-Term Conditions. London: The Stationery Office; 2007.
- NHS Mandate. London: Department of Health; 2012.
- The CCG Outcomes Indicator Set (2013/14). London: NHS Commissioning Board; 2012.
- Equity and Excellence: Liberating the NHS. London: The Stationery Office; 2010.
- Lupton C, Peckham S, Taylor P. Managing Public Involvement in Healthcare Purchasing. Milton Keynes: Open University Press; 2008.
- Commissioning Framework for Health and Well-Being. London: Department of Health; 2007.
- Guidance on Joint Strategic Needs Assessment. London: Department of Health; 2007.
- World Class Commissioning: Vision. London: Department of Health; 2007.
- Commissioning Assurance Handbook. London: Department of Health; 2008.
- NHS Next Stage Review: What it Means for the Third Sector. London: Department of Health; 2008.
- High Quality Care for All: the NHS Next Steps Review Final Report. London: The Stationery Office; 2008.
- Is the Treatment Working? Progress with the NHS System Reform Programme. London: Audit Commission; 2008.
- Checkland K, Coleman A, Harrison S, Hiroeh U. Practice Based Commissioning in the National Health Service: Interim Report of a Qualitative Study. Manchester: National Primary Care Research and Development Centre; 2008.
- Harrison S, Milewa T, Dowswell G. Public and user ‘involvement’ in the National Health Service. Health Soc Care Community 2002;10:1-4. http://dx.doi.org/10.1046/j.1365-2524.2002.00342.x.
- Chisholm A, Redding D, Cross P, Coulter A. Patient and Public Involvement in PCT Commissioning: A Survey of Primary Care Trusts. Oxford: Picker Institute Europe; 2007.
- PCT Surveys. Manchester: National Primary Care Research & Development Centre; 2004.
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
- ‘Commissioning.’ Fourth report of session 2009–2010. London: The Stationery Office; 2010.
- Checkland K, Coleman A, Segar J, McDermott I, Miller R, Wallace A, et al. Exploring the Early Workings of Emerging Clinical Commissioning Groups: Final Report. London: Policy Research Unit in Commissioning and the Healthcare System (PRUComm); 2012.
- Wanless D. Securing Our Future Health: Taking a Long Term View. London: HM Treasury; 2002.
- Realising the Potential of Patient Empowerment for Tackling Chronic Disease. London: BUPA; 2011.
- Wilson T, Buck D, Ham C. Rising to the challenge: will the NHS support people with long-term conditions?. BMJ 2005;330. http://dx.doi.org/10.1136/bmj.330.7492.657.
- UN Secretary General . Prevention and Control of Non-Communicable Diseases 2011. www.ghd-net.org/sites/default/files/UN%20Secretary-General’s%20Report%20on%20NCDs.pdf (accessed 8 February 2013).
- Quality and Outcomes Framework 2010–11. London: Health and Social Care Information Centre; 2011.
- Long Term Conditions Compendium of Information. London: Department of Health; 2012.
- Rosen R, Asaria P, Dixon A. Improving Chronic Disease Management. London: The King’s Fund; 2007.
- Schoen C, Osborn R, Doty MM, Bishop M, Peugh J, Murukutla N. Toward higher performance health systems: adults’ health care experiences in seven countries. Health Aff 2007;26:w717-34. http://dx.doi.org/10.1377/hlthaff.26.6.w717.
- State of the Nation 2012 England. London: Diabetes UK; 2012.
- Supporting People with Long-Term Conditions. An NHS and Social Care Model to Support Local Innovation and Integration. London: Department of Health; 2005.
- Neuro Numbers: a Brief Review of the Numbers of People in the UK with a Neurological Condition. London: Neurological Alliance; 2003.
- Ford HL, Gerry E, Johnson M, Williams, R. A prospective study of the incidence, prevalence and mortality of multiple sclerosis in Leeds. J Neurol 2002;249:260-5. http://dx.doi.org/10.1007/s004150200002.
- Panayi G. What is RA?. Maidenhead: National Rheumatoid Arthritis Society; 2003.
- The NHS Plan. London: The Stationery Office; 2000.
- Choosing Health. London: Department of Health; 2004.
- The National Service Framework for Long-Term Conditions. London: Department of Health; 2005.
- Your Health, Your Way – a Guide to Long-Term Conditions and Self Care. Information for Healthcare Professionals. London: Department of Health; 2009.
- Weiner J, Lewis R, Gillam S. US Managed Care and PCTs: Lessons to a Small Island from a Lost Continent. London: The King’s Fund; 2001.
- Mays N, Hand K. A Review of Options for Health and Disability Support in New Zealand. Wellington: New Zealand Treasury; 2000.
- Ham C. World class commissioning: a health policy chimera?. J Health Serv Res Policy 2008;13:116-21. http://dx.doi.org/10.1258/jhsrp.2008.007177.
- LeGrand J, Mays N, Mulligan J. Learning from the NHS Internal Market. London: The King’s Fund; 1998.
- Figueras J, Robinson R, Jakubowski E. Purchasing to Improve Health System Performance. Maidenhead: Open University Press; 2005.
- Dixon J. Making Progress on Efficiency in the NHS in England: Options for System Reform. London: Nuffield Trust; 2010.
- Lamb-White J. New challenges set for the NHS (UK). Leadership Health Serv 2010;23.
- Mays N, Goodwin N, Killoran A, Malbon G. Total Purchasing: A Step Towards Primary Care Groups: National Evaluation of Total Purchasing Pilot Projects. London: The King’s Fund; 1998.
- Field S. NHS Future Forum. Summary Report on Proposed Changes to the NHS. London: Department of Health; 2011.
- Developing Clinical Commissioning Groups: Towards Authorisation. London: Department of Health; 2012.
- The Functions of GP Commissioning Consortia. A Working Document. London: Department of Health; 2011.
- Commissioning Support: Clinical Commissioning Group Running Costs Tool. A ‘Ready Reckoner’. London: Department of Health; 2011.
- Towards Establishment: Creating Responsive and Accountable Clinical Commissioning Groups. NHS Commissioning Board; 2012.
- Developing Commissioning Support: Towards Service Excellence. NHS Commissioning Board; 2012.
- Clinical Commissioning Group Governing Body: Roles Outlines, Attributes and Skills, in April 2012. NHS Commissioning Board; 2012.
- Smith J, Shaw S, Porter A, Rosen R, Blunt I, Davies A, et al. Commissioning High Quality Care for People with Long-Term Conditions. Southampton: National Institute for Health Research Service Delivery and Organisation Programme; 2013.
- Ofmann JJ, Badamgarav E, Henning JM, Knight K, Gano A, Levan RK, et al. Does disease management improve clinical and economic outcomes in patients with chronic diseases? A systematic review. Am J Med 2004;117:182-92. http://dx.doi.org/10.1016/j.amjmed.2004.03.018.
- Taylor S, Bestall J, Cotter S, Falshaw M, Hood S, Parsons S, et al. Clinical service organisation for heart failure. Cochrane Database Syst Rev 2005;2.
- Sulch D, Evans A, Melbourn A, Kalra L. Does an integrated care pathway improve processes of care in stroke rehabilitation? A randomised controlled trial. Age Ageing 2002;31:175-9. http://dx.doi.org/10.1093/ageing/31.3.175.
- Weingarten SR, Henning JM, Badamgarav E, Knight K, Hasselbad V, Gano A, et al. Interventions used for patients with chronic illness – which ones work? Meta-analysis of published reports. BMJ 2002;325:925-33. http://dx.doi.org/10.1136/bmj.325.7370.925.
- McDonald PS, Whittle CL, Dunn L, de Luc K. Shortfalls in integrated care pathways. Part 1: what don’t they contain?. J Integr Care Pathw 2006;10:17-2. http://dx.doi.org/10.1258/j.jicp.2006.126.
- McDonald PS, Whittle CL, Dunn L, de Luc K. Shortfalls in integrated care pathways. Part 2: how well are we doing?. J Integr Care Pathw 2006;10:23-7. http://dx.doi.org/10.1258/j.jicp.2006.127.
- Stronger Voice, Better Care. London: Department of Health; 2008.
- Wilson PM, Bunn F, Morgan J. A mapping of the evidence on integrated long term condition services. Br J Community Nurs 2009;14:202-6. http://dx.doi.org/10.12968/bjcn.2009.14.5.42078.
- QUIPP National Workstream Updated. London: Department of Health; 2013.
- National Evaluation of the Department of Health’s Integrated Care Pilots: Final Report. Prepared for the Department of Health. RAND Europe, Ernst & Young LLP; 2012.
- Bardsley M, Smith J, Car J. Evaluation of the First Year of the Inner North West London Integrated Care Pilot. London: Nuffield Trust; 2013.
- NHS England . Putting Patients First: The NHS England Business Plan for 2013 14–2015 16 2013. www.england.nhs.uk/pp-1314–1516/ (accessed 30 April 2013).
- Peckham S, Wallace A. Pay for performance schemes in primary care: what have we learnt?. Qual Prim Care 2010;18:111-16.
- Chew-Graham CA, Hunter C, Langer S, Stenhoff A, Drinkwater J, Guthrie EA, et al. How QOF is shaping primary care review consultations: a longitudinal qualitative study. BMC Fam Pract 2013;14. http://dx.doi.org/10.1186/1471-2296-14-103.
- Making Partnership Work for Patients, Carers and Service Users. London: Department of Health; 2003.
- Wood B. Patient Associations in Britain and America. Buckingham: Open University Press; 2000.
- Baggott R, Allsop J, Jones K. Speaking for Patients and Carers: the Role of Health Consumer Groups in the Policy Process. Basingstoke: Palgrave; 2005.
- NAVCA/NCVO . Regional Voices Briefing Paper, Briefing on Changes to Local Commissioning 2011 n.d. www.navca.org.uk/commissioning-policy-briefings (accessed 24 April 2014).
- Tyler S. Comparing the profile of maternity user groups in Europe – can we learn anything useful?. Health Expect 2002;5:136-47. http://dx.doi.org/10.1046/j.1369-6513.2002.00172.x.
- Weekes J, Aggleton P, McKevitt C, Parkinson K, Taylor-Laybourn A. Community and contracts: tensions and dilemmas in the voluntary sector responses to HIV and AIDs. Policy Stud 1996;17:107-22. http://dx.doi.org/10.1080/01442879608423699.
- Bond M, Irving L, Cooper C. Public Involvement in Decision Making in Primary Care Groups. Sheffield: University of Sheffield School of Health and Related Research; 2001.
- Milewa T, Harrison S, Ahmad W, Tovey P. ‘Citizens’ participation in primary health care planning: innovative citizenship practice in empirical perspective. Crit Public Health 2002;12:39-53. http://dx.doi.org/10.1080/09581590110113295.
- Liberating the NHS: Greater Choice and Control – a Consultation on Proposals. London: Department of Health; 2010.
- Better Health, Better Experience, Better Engagement. London: Department of Health; 2011.
- Miller R, Peckham S, Checkland K, Coleman A, McDermott I, Harrison S, et al. Clinical Engagement in Primary Care-Led Commissioning: a Review of the Evidence. London: Policy Research Unit in Commissioning and the Healthcare System (PRUComm); 2012.
- Coleman A, Checkland K, Harrison S. Still puzzling: patient and public involvement in commissioning. J Integr Care 2009;17:23-30. http://dx.doi.org/10.1108/14769018200900043.
- Dixon J, Goodwin N, Mays N. Accountability and Total Purchasing Pilots. London: National Evaluation of Total Purchasing Pilot Projects Working Paper; 1998.
- Wyke S, Mays N, Street A, Bevan G, McLeod H, Goodwin N. Should general practitioners purchase health care for their patients? The total purchasing experiment in Britain. Health Policy 2003;65:243-59. http://dx.doi.org/10.1016/S0168-8510(03)00040-X.
- Elbers M, Regen E. Public and User Involvement in Primary Care Groups and Trusts: Alien or Ally? A Study that is Part of HSMC’s National Evaluation of Primary Care Groups and Trusts. Birmingham: University of Birmingham, Health Services Management Centre; 2001.
- NHS Improvement . QIPP Domain 2 n.d. www.improvement.nhs.uk/Default.aspx?alias=www.improvement.nhs.uk/qipp (accessed 8 February 2013).
- Parsons S, Winderbottom A, Cross P, Redding D. The Quality of Patient Engagement and Involvement in Primary Care: an Inquiry into the Quality of General Practice in England. London: The King’s Fund; 2010.
- InHealth Associates . Embedding PPE 2013. www.networks.nhs.uk/nhsnetworks/documents/documents/ppe/FINAL%20Embedding%20patient%20and%20public%20engagement.pdf (accessed 24 April 2013).
- Smith J, Mays N. GP led commissioning, a time for cool appraisal. BMJ 2012;344. http://dx.doi.org/10.1136/bmj.e980.
- Sullivan H, Skelcher C. Working Across Boundaries: Collaboration in Public Services. London: Palgrave; 2002.
- Rhodes P, Nocon A, Booth M, Chowdrey MY, Fabian A, Lambert N. A service users’ research advisory group from the perspectives of both service users and researchers. Health Soc Care Community 2002;10:402-9. http://dx.doi.org/10.1046/j.1365-2524.2002.00376.x.
- Coad J, Flay J, Aspinall M, Bilverstone B, Coxhead E, Hones B. Evaluating the impact of involving young people in developing children’s services in an acute hospital trust. J Clin Nurs 2008;17:3115-22. http://dx.doi.org/10.1111/j.1365-2702.2008.02634.x.
- Evaluation of the User Involvement in Local Diabetes Care Project. London: Diabetes UK; 2011.
- Matthews R. Involving patients in service improvements. Nurs Manag 2010;16:16-9. http://dx.doi.org/10.7748/nm2010.03.16.10.16.c7608.
- Fudge N, Wolfe D, McKevitt C. Assessing the promise of user involvement in health service development: ethnographic study. BMJ 2007;336. http://dx.doi.org/10.1136/bmj.39456.552257.BE.
- Kielmann T, Huby G, Powell A, Sheikh A, Price D, Williams S, et al. From awareness to involvement? A qualitative study of respiratory patients’ awareness of health service change. Health Expect 2011;14:321-33. http://dx.doi.org/10.1111/j.1369-7625.2010.00631.x.
- Poulton B. User involvement in identifying health needs and shaping and evaluating services: is it being realised?. J Adv Nurs 1999;30:1289-96. http://dx.doi.org/10.1046/j.1365-2648.1999.01224.x.
- Curry R. Vision to reality: using patients’ voices to develop and improve services. Br J Community Nurs 2006;11:438-45. http://dx.doi.org/10.12968/bjcn.2006.11.10.21966.
- Florin D, Dixon J. Public involvement in health care. BMJ 2004;328:159-61. http://dx.doi.org/10.1136/bmj.328.7432.159.
- Tritter JQ, McCallum A. The snakes and ladders of user involvement: moving beyond Arnstein. Health Policy 2006;76:156-68. http://dx.doi.org/10.1016/j.healthpol.2005.05.008.
- Anderson E, Shepherd M, Salisbury C. ‘Taking off the suit’: engaging the community in primary health care decision-making. Health Expect 2006;9:70-8. http://dx.doi.org/10.1111/j.1369-7625.2006.00364.x.
- Arnstein S. A ladder of citizen participation. Am Instit Planners J 1969;35:216-24. http://dx.doi.org/10.1080/01944366908977225.
- Oliver SR, Rees RW, Clarke-Jones L, Milne R, Oakley AR, Gabbay J, et al. A multidimensional conceptual framework for analysing public involvement in health services research. Health Expect 2008;11:72-84. http://dx.doi.org/10.1111/j.1369-7625.2007.00476.x.
- Staniszewska S, Herron-Marx S, Mockford, C. Measuring the impact of patient and public involvement: the need for an evidence base. Int J Qual Health Care 2008;20:373-4. http://dx.doi.org/10.1093/intqhc/mzn044.
- Richardson A, Sitzia J, Cotterell P. ‘Working the system’. Achieving change through partnership working: an evaluation of cancer partnership groups. Health Expect 2005;8:210-20. http://dx.doi.org/10.1111/j.1369-7625.2005.00332.x.
- Gibson A, Britten N, Lynch J. Theoretical directions for an emancipatory concept of patient and public involvement. Health 2012;16:531-47. http://dx.doi.org/10.1177/1363459312438563.
- Barnes M. Passionate participation: emotional experiences and expressions in deliberative forums. Crit Soc Polit 2008;28:461-81. http://dx.doi.org/10.1177/0261018308095280.
- Barnes M, Newman J, Knops A, Sullivan H. Constituting ‘the public’ in public participation. Public Admin 2003;81:379-99. http://dx.doi.org/10.1111/1467-9299.00352.
- Barnes M, Newman J, Sullivan H. Power, participation, and political renewal: theoretical perspectives on public participation under New Labour in Britain. Soc Polit 2004;11:267-79. http://dx.doi.org/10.1093/sp/jxh034.
- Barnes M. The same old process? Older people, participation and deliberation. Ageing Soc 2005;25:245-59. http://dx.doi.org/10.1017/S0144686X04002508.
- Tronto CJ. Moral Boundaries: a Political Argument for an Ethic of Care. New York, NY: Routledge; 1993.
- Kirk S, Bailey J, Glendinning C, Burkey Y. Involving communities in health service planning in primary care. Health Soc Care Community 1997;5:398-407. http://dx.doi.org/10.1111/j.1365-2524.1997.tb00137.x.
- Martin D, Abelson J, Singer P. Participation in health care priority-setting through the eyes of the participants. J Health Serv Res Policy 2002;7:222-9. http://dx.doi.org/10.1258/135581902320432750.
- Crawford M, Rutter D, Manley C, Weaver T, Bhui K, Fulop N, et al. Systematic review of involving patients in the planning and development of health care. BMJ 2002;325:1263-7. http://dx.doi.org/10.1136/bmj.325.7375.1263.
- Smith J, Mays N, Dixon J, Goodwin N, Lewis R, McClelland S, et al. A Review of the Effectiveness of Primary Care-Led Commissioning and its Place in the NHS. London: The Health Foundation; 2004.
- Craig A. Engagement for Commissioning Success. Smart Guides to Engagement 2012. www.networks.nhs.uk/nhs-networks/smart-guides (accessed 30 April 2012).
- Effective Patient and Public Involvement: Briefing Guide. London: Royal College of General Practitioners Centre for Commissioning; 2011.
- Exworthy M, Peckham S, Powell M, Hann A. Shaping Health Policy: Case Study Methods and Analysis. Bristol: The Policy Press; 2012.
- Yin RK. Case Study Research, Design and Method. London: Sage Publications; 2009.
- Marinetto M, Exworthy M, Peckham S, Powell M, Hann A. Shaping Health Policy: Case Study Methods and Analysis. Bristol: The Policy Press; 2012.
- Hartley J, Cassell C, Symon G. Qualitative Methods in Organisational Research, a Practical Guide. London: Sage; 1994.
- Hartley J, Cassell C, Symon G. Essential Guide to Qualitative Methods in Organisational Research. London: Sage; 2004.
- Public and Patient Involvement in the NHS: Third Report of Session 2006–7. London: The Stationery Office; 2007.
- Martin GP. Representativeness, legitimacy and power in public involvement in health service management. Soc Sci Med 2008;67:1757-65. http://dx.doi.org/10.1016/j.socscimed.2008.09.024.
- Armstrong N, Herbert G, Aveling EL, Dixon-Woods M, Martin G. Optimizing patient involvement in quality improvement. Health Expect 2013;16:e36-47. http://dx.doi.org/10.1111/hex.12039.
- Tales K. The Evaluator’s Cookbook: Participatory Evaluation Exercises, a Resource for Work with Children and Young People. Birmingham: National Evaluation of the Children’s Fund; 2005.
- Young People in Research: How to Involve us. London: National Children’s Bureau; 2010.
- Shaw C, Brady CM, Davey C. Guidelines for Research with Children and Young People. London: National Children’s Bureau; 2011.
- Hill M. Children’s voices on ways of having a voice: children’s and young people’s perspectives on methods used in research and consultation. Childhood 2006;13:68-89. http://dx.doi.org/10.1177/0907568206059972.
- Ireland L, Holloway I. Qualitative health research with children. Child Soc 1996;10:155-64. http://dx.doi.org/10.1002/(SICI)1099-0860(199606)10:2<155::AID-CHI15>3.0.CO;2-Q.
- Kitzinger J, Holloway I. Qualitative Research In Health Care. Maidenhead: Open University Press; 2005.
- Steward DW, Shamdasani PN. Focus Groups: Theory and Practice. Newbury Park, CA: Sage; 1990.
- Ivanhoff SD, Hultberg J. Understanding the multiple realities of everyday life: basic assumptions in focus group methodology. Scan J Occup Ther 2006;13:125-32. http://dx.doi.org/10.1080/11038120600691082.
- Ritchie J, Spencer L, Bryman A, Burgess R. Analysing Qualitative Data. London: Routledge; 1994.
- May C, Finch T. Implementing, embedding and integrating practices: an outline of normalization process theory. Sociology 2009;43:535-54. http://dx.doi.org/10.1177/0038038509103208.
- May C, Finch T, Mair F, Ballini L, Dowrick C, Eccles M, et al. Understanding the implementation of complex interventions in health care: the normalization process model. BMC Health Serv Res 2007;7. http://dx.doi.org/10.1186/1472-6963-7-148.
- The Coalition: our Programme for Government. Freedom, Fairness, Responsibility. London: HM Government, Cabinet Office; 2010.
- Timmins N. Never Again? The Story of the Health and Social Care Act 2012: A Study in Coalition Government and Policy Making. London: The King’s Fund; 2012.
- Nicholson D. Letter to All Chief Executives and Arm’s Length Bodies: Equity and Excellence: Liberating the NHS – Managing the Transition. London: Department of Health; 2010.
- Glennerster H, Matsaganis M, Owens P, Hancock S. Implementing GP Fundholding. Wild Card or Winning Hand?. Buckingham: Open University Press; 1994.
- Clinical Commissioning Group Authorisation Outcomes: Wave 1. NHS Commissioning Board; 2012.
- Patient Participation Directed Enhanced Service (DES) for GMS Contract – Guidance and Audit Requirements for 2011/12–2012/13. London: NHS Employers; 2011.
- Case Studies from Around England. NHS Commissioning Board; 2012.
- Coulter A, Collins A. Making Shared Decision-Making a Reality. London: The King’s Fund; 2011.
- Clinical Commissioning Groups Authorised in Wave 1. NHS Commissioning Board; 2013.
- McShane M. Publically Engaged GP Leadership. A Handbook Setting Out 10 Principles for GPs Leading Programmes of Commissioning Change by Working with their Local Population. NHS Lincolnshire; 2011.
- Clinical Commissioning Group Authorisation: Draft Guidance for Applicants. NHS Commissioning Board; 2012.
- Long Term Conditions: Compendium of Information. London: Department of Health; 2012.
- Forbat L, Hubbard G, Kearney N. Patient and public involvement: models and muddles. J Clin Nurs 2009;18:2547-54. http://dx.doi.org/10.1111/j.1365-2702.2008.02519.x.
- Rise MB, Solbjør M, Lara MC, Westerlund H, Grimstad H, Steinsbekk A. Same description, different values. How service users and providers define patient and public involvement in health care. Health Expect 2013;16:266-76. http://dx.doi.org/10.1111/j.1369-7625.2011.00713.x.
- Keep J. PPE – A synthesis of Perspectives for CCGs Towards and Beyond Authorisation. Leicester: Healthskills; 2012.
- INVOLVE . What Is Public Involvement in Research? 2012. www.invo.org.uk/find-out-more/what-is-public-involvement-in-research-2/ (accessed 12 November 2012).
- National Voices . Patient Involvement n.d. www.nationalvoices.org.uk/patient-involvement (accessed 25 April 2014).
- Wettenhall R. Organisational amnesia: a serious public sector reform issue. Int J Public Sector Manag 2011;24:80-96. http://dx.doi.org/10.1108/09513551111099235.
- Pollitt C. Bureaucracies remember, post-bureaucratic organizations forget?. Public Admin 2009;87:198-21. http://dx.doi.org/10.1111/j.1467-9299.2008.01738.x.
- Macfarlane F, Exworthy M, Wilmott M, Greenhalgh T. Plus ca change, plus c’est la meme chose: senior NHS managers’ narratives of restructuring. Soc Health Illn 2011;33:914-29. http://dx.doi.org/10.1111/j.1467-9566.2011.01338.x.
- Kreindler SA. Patient involvement and the politics of methodology. Can Public Admin 2009;52:113-24. http://dx.doi.org/10.1111/j.1754-7121.2009.00062.x.
- Tritter JQ. Revolution or evolution: the challenges of conceptualising patient and public involvement in a consumerist world. Health Expect 2009;12:275-87. http://dx.doi.org/10.1111/j.1369-7625.2009.00564.x.
- Brown I. Patient participation groups in general practice in the NHS. Health Expect 1999;2:169-78. http://dx.doi.org/10.1046/j.1369-6513.1999.00057.x.
- Nagraj S, Gillam S. Patient participation groups. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d2333.
- Patient Participation Directed Enhanced Service (DES) for GMS Contract. London: British Medical Association & NHS Employers; 2011.
- A Guide for Working Together: the Care Quality Commission and Patient Participation Groups. Newcastle upon Tyne: Care Quality Commission; 2013.
- Liberating the NHS: Commissioning for Patients. London: Department of Health; 2010.
- Craig A, Gilbert D. Embedding Patient and Public Engagement. A Report On Learning From Interviews With CCG Leaders. London: InHealth Associates and Moore Adamson Craig Partnership; 2013.
- McKevitt C. Experience, knowledge and evidence: a comparison of research relations in health and anthropology. Evid Policy 2013;9:113-30. http://dx.doi.org/10.1332/174426413X663751.
- Willis K, Small R, Brown S. Using documents to investigate links between implementation and sustainability in a complex community intervention: the PRISM study. Soc Sci Med 2012;75:1222-9. http://dx.doi.org/10.1016/j.socscimed.2012.05.025.
- Bamford C, Heaven B, May C, Moynihan P. Implementing nutrition guidelines for older people in residential care homes: a qualitative study using Normalization Process Theory. Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-106.
- Gallacher K, May CR, Montori VM, Mair FS. Understanding patients’ experiences of treatment burden in chronic heart failure using normalization process theory. Ann Fam Med 2011;9:235-43. http://dx.doi.org/10.1370/afm.1249.
- Mathie E, Wilson P, Poland F, McNeilly E, Howe A, Staniszewska S, et al. Consumer involvement in health research: a UK scoping and survey. Int J Consum Stud 2014;38:35-44. http://dx.doi.org/10.1111/ijcs.12072.
- Gilbert D. The rise of the patient leader. Health Serv J 2012. http://m.hsj.co.uk/5040463.article (accessed 2 July 2012).
- Crisp N. Patient power needs to be built on strong intellectual foundations: an essay. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e6177.
- Broqvist M, Garpenby P. To accept, or not to accept, that is the question: citizen reactions to rationing. Health Expect 2014;17:82-9. http://dx.doi.org/10.1111/j.1369-7625.2011.00734.x.
- Millar R, Snelling I, Brown H. Liberating the NHS: Orders of Change?. Birmingham: University of Birmingham Health Services Management Centre; 2011.
- Forbes A, While A, Dyson L, Grocott T, Griffiths P. Impact of clinical nurse specialists in multiple sclerosis – synthesis of the evidence. J Adv Nurs 2003;42:442-62. http://dx.doi.org/10.1046/j.1365-2648.2003.02644.x.
- Mynors G, Perman S, Morse M, Mynors G, Perman S, Morse M. Defining the Value of MS Specialist Nurses. Letchworth: Multiple Sclerosis Trust; 2012.
- Parkinson’s Nurses – Affordable, Local, Accessible and Expert Care: A Guide for Commissioners in England. London: Parkinson’s UK; 2011.
- Greer SL, Stewart EA, Wilson I, Donnelly P. Victory for volunteerism? Scottish health board elections and participation in the welfare state. Soc Sci Med 2014;106:221-8. http://dx.doi.org/10.1016/j.socscimed.2014.01.053.
- Stewart E. What is the point of citizen participation in health care?. J Health Serv Res Policy 2013;18:124-36. http://dx.doi.org/10.1177/1355819613485670.
- Conklin A, Morris ZS, Nolte E. Involving the Public in Healthcare Policy. Cambridge: RAND Corporation; 2010.
- Naylor C, Mundle C, Weaks L, Buck D. Volunteering in Health and Care Services: Securing a Sustainable Future. London: The King’s Fund; 2013.
- South J, White J, Gamsu M. People-Centred Public Health. Bristol: Policy Press; 2013.
- Nathan S, Stephenson N, Braithwaite J. Sidestepping questions of legitimacy: how community representatives manoeuvre to effect change in a health service. Health 2014;18:23-40. http://dx.doi.org/10.1177/1363459312473617.
Appendix 1 Interview guide
Interview guide: commissioners/providers/patient and public involvement and service users’ representatives
-
General role and experience of PPI:
-
Can you tell me a bit about your role?
-
What is your general understanding of what PPI means?
-
What is your personal experience of PPI?
-
-
General understanding of PPI and commissioning:
-
Do you think PPI is necessary in the commissioning process? Why or why not?
-
What is the reasoning behind PPI forums?
-
What do you think are the advantages and disadvantages of PPI in commissioning?
-
One of the themes that has come up in workshops is that service users can identify gaps in services. What is your experience of this?
-
Can you give me a specific example of PPI in commissioning?
-
-
Impact of PPI on decision-making in commissioning:
-
Thinking more about the example you have given me can you tell me how and in what way service users’ views were listened to?
-
What lines of communication were there between the commissioners and the public? Who talked to whom and who didn’t?
-
Were there any disagreements or challenges and what happened?
-
Did PPI actually change services and in what way? If not what were the barriers?
-
-
Representativeness:
-
Is PPI the best way to represent the views of a particular population?
-
Does representativeness actually matter?
-
What about under-represented groups?
-
Are there over-represented groups – what impact do they have?
-
Who are PPI accountable to? What is their accountability?
-
-
Power:
-
Do you feel the service representatives have any power or is it just a ‘tick-box’ exercise?
-
-
Future:
-
What do you think should happen to PPI in commissioning? How realistic would this be?
-
Appendix 2 Information about interview
Appendix 3 Consent form
Appendix 4 Case study 1 exemplar
Appendix 5 Case study 2 exemplar
Appendix 6 Case study 3 exemplar
Appendix 7 Focus group topic guide
Appendix 8 Information for participants of focus group
Appendix 9 Expert reference panel
| Exemplar | Name of expert | Role | Perspective |
|---|---|---|---|
| Schools protocol | Vivienne Marsh | Paediatric Asthma Nurse Specialist at NHS Dudley | Clinical/children |
| Bridget Turner | Head of Policy, Diabetes UK | PPI/diabetes | |
| Lynda Edwards | Specialist Community Practitioner (School Nursing) | Clinical/school nursing | |
| Pat Boyer | Ex-head teacher of primary school | Teacher in primary education | |
| Sandra Ashby | Head teacher of primary school | Teacher in primary education | |
| Diabetes service reorganisation | Dr Colin Johnston | Director of Patient Safety, West Hertfordshire Hospitals NHS Trust (Diabetologist) | Clinical (diabetes) |
| Bridget Turner | Head of Policy, Diabetes UK | PPI (diabetes) | |
| Professor Azim Majeed | Professor of Primary Care and Head of Primary Care and Public Health, Imperial College, London | Clinical (diabetes) | |
| Diabetes service for BME population | David Jones | Head of Involvement and Improvement Diabetes UK |
PPI (diabetes) |
| Don Redding | Policy Director, National Voices | PPI (general) |
Appendix 10 Report from summative workshop
Appendix 11 NHS fact sheet
Commissioning fact sheet for Clinical Commissioning Groups July 2012
This fact sheet sets out the services to be commissioned by Clinical Commissioning Groups (CCGs) from April 2013. It also sets out the complementary services to be commissioned by the NHS Commissioning Board (NHS CB), local authorities and Public Health England (PHE). A number of previous documents have described commissioning responsibilities, but this fact sheet is intended to be a helpful summary, with further clarity on certain aspects. It is not a substitute for legislation or guidance or your own legal advice.
In general, you as CCGs will be responsible for commissioning health services to meet all the reasonable requirements of your patients, with the exception of: certain services commissioned directly by the NHS CB; health improvement services commissioned by local authorities; and health protection and promotion services provided by PHE.
You will play a key role in promoting integrated care and, as a member of your local health and wellbeing board(s), in assessing local needs and strategic priorities. This will mean working collaboratively with local authorities and the NHSCB. You may decide to pool budgets or have collaborative commissioning arrangements.
Your commissioning responsibilities (for the areas set out in part 1) will include: planning services, based on assessing the needs of your local population; securing services that meet those needs; and monitoring the quality of care provided.
In most cases, you will also be responsible for meeting the cost of the services provided. There will be some services that you commission for your geographic area (e.g. A&E services) where the costs for an individual patient may be charged to another CCG (i.e. in an area where the patient is registered or, if unregistered, where they live). There will be guidance on this in due course, which it is expected will follow the current ‘responsible commissioner’ arrangements.
Local authorities will take the lead for improving health and coordinating local efforts to protect the public’s health and wellbeing. They will also provide advice and expertise on how to ensure that the health services you commission best improve population health and reduce health inequalities. For health improvement activities transferring to local authorities, such as smoking cessation, sexual health and drug/alcohol services, you may wish to agree joint commissioning arrangements. You should also consider how best to work with local authorities to ensure that health improvement activities are an integral part of the healthcare services that you commission (more detail on local authorities’ commissioning responsibilities can be found at: www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_131901.pdf).
A new executive agency, PHE, will take the lead for public health at a national level. It will deliver a number of national health services and support the development of the public health workforce. The NHS CB will also commission some public health services nationally as agreed with the Secretary of State.
This fact sheet includes information that is subject to secondary legislation. For example, the list of specialised and highly specialised services that the Board will be required to commission has not been finalised; the final list will be included in regulations, which are expected to be laid before Parliament in the Autumn.
Services to be commissioned by CCGs
Unless otherwise indicated (such as for urgent and emergency care), your commissioning responsibility will be for your local population. Your local population includes registered patients (some of whom may live in a different area) and unregistered patients usually resident in your area. It does not include members of the armed forces, or their families if they are registered with Defence Medical Services (DMS) rather than a NHS GP practice, nor does it include those detained in prison and other custodial settings.
Local authorities will provide public health advice to CCGs on the commissioning of these services.
| CCG commissioning | Related NHS CB commissioning |
|---|---|
| Urgent and emergency care (including 111, A&E and ambulance services) for anyone present in your geographic area | |
| Out-of-hours primary medical services (for everyone present in your area), except where this responsibility has been retained by practices under the GP contract | Urgent care provided under GP contracts Urgent dental care |
| Elective hospital care | Specialised and highly specialised services Hospital and community dental services Public health services for children from pregnancy to aged 5 (Healthy Child Programme 0–5) including health visiting and family nursing partnership (commissioned on behalf of Secretary of State) Antenatal and newborn screening aspects of maternity services Health services (excluding emergency care) and public health services for people in prisons and other custodial settings Health services (excluding emergency care services) for members of the armed forces and their families (those registered with DMS) |
| Community health services (such as rehabilitation services, speech and language therapy, continence services, wheelchair services, and home oxygen services, but not public health services such as health visiting and family nursing) | |
| Other community-based services, including (where appropriate) services provided by GP practices that go beyond the scope of the GP contract | |
| Rehabilitation services | |
| Maternity and newborn services (excluding neonatal intensive care) | |
| Children’s healthcare services (mental and physical health) | |
| Services for people with learning disabilities | |
| Mental health services (including psychological therapies) | Mental health interventions provided under GP contract Some specialised mental health services Secure psychiatric services |
| NHS continuing health care | Operation of Independent Review Panels |
| Infertility services | Infertility services for the armed forces and some infertility services for veterans in receipt of compensation under the Armed Forces Compensation Scheme on grounds of infertility |
Services to be commissioned by the NHS CB
| NHS CB commissioning | Related CCG commissioning |
|---|---|
| Essential and additional primary medical services through GP contract and nationally commissioned enhanced services Out-of-hours primary medical services (where practices have retained the responsibility for providing OOH services) |
Out-of-hours primary medical services (where practices have opted out of providing OOH services under the GP contract) Community-based services that go beyond scope of GP contract (akin to current Local Enhanced Services) Resources attached to current Local Enhanced Services (LES) (except for public health LES) are proposed to be included in CCG funding |
| Pharmaceutical services provided by community pharmacy services, dispensing doctors and appliance contractors | Meeting the costs of prescriptions written by member practices (but not the associated dispensing costs) |
| Primary ophthalmic services, NHS sight tests and optical vouchers | Any other community-based eye care services and secondary ophthalmic services |
| All dental services, including primary, community and hospital services and including urgent and emergency dental care | |
| Health services (excluding emergency care) and public health services for people in prisons and other custodial settings (adult prisons, young offender institutions, juvenile prisons, secure children’s homes, secure training centres, immigration removal centres, police custody suites) | Emergency care, including 111, A&E and ambulance services, for prisoners and detainees present in your geographic area Health services for adults and young offenders serving community sentences and those on probation Health services for initial accommodation for asylum seekers |
| Health services for members of the armed forces and their families (those registered with DMS) Prosthetics services for veterans (Primary care for members of the armed forces will be commissioned by the Ministry of Defence) |
Health services for veterans or reservists (when not mobilised), for whom normal commissioning responsibilities apply Emergency care, including A&E and ambulance services, for serving armed forces and families registered with DMS practices present in your geographic area |
| Specialised and highly specialised services | Related services along patient pathways |
Public health services to be commissioned by the NHS CB
| Public health services for children from pregnancy to age 5 (Healthy Child Programme 0–5), including health visiting, family nurse partnership, responsibility for Child Health Information Systems (Responsibility for children’s public health 0–5 due to transfer to local authorities in 2015) |
| Immunisation programmes |
| National screening programmes |
| Public health care for people in prison and other places of detention |
| Sexual assault referral services |
Further detail on the arrangements for commissioning these services will be confirmed in Autumn 2012.
Public health services to be provided or commissioned by local authorities
In addition to the functions set out below, local authorities will be responsible for providing population health advice, information and expertise to CCGs to support them in commissioning health services that improve population health and reduce inequalities.
Local authorities will also need to ensure plans are in place to protect the health of their population and will have a supporting role in infectious disease surveillance and control and in emergency preparedness and response.
| Local authority commissioning | Related CCG commissioning | Related NHS CB commissioning | |
|---|---|---|---|
| Children’s public health 5–19 | Healthy Child Programme for school-age children, including school nursing | Treatment services for children, including Child and Adolescent Mental Health Services (CAMHS) | Healthy Child programme (pregnancy to five years old), including health visiting and family nurse partnership Immunisation programmes |
| Sexual health | Contraception over and above GP contract Testing and treatment of sexually transmitted infections (excluding HIV treatment) Sexual health advice, prevention and promotion |
Promotion of opportunistic testing and treatment Termination of pregnancy services (with consultation on longer-term arrangements) Sterilisation and vasectomy services |
Contraceptive services commissioned through GP contract Sexual assault referral centres HIV treatment |
| Public mental health | Mental health promotion, mental illness prevention and suicide prevention | Treatment for mental ill health | Mental health interventions under GP contract Some specialised mental health services |
| Physical activity | Local programmes to address inactivity and other interventions to promote physical activity | Advice as part of other health-care contacts | Brief interventions in primary care |
| Obesity programmes | Local programmes to prevent and address obesity, e.g. National Child Measurement Programme and weight management services | Advice as part of other health-care contacts NHS treatment of overweight and obese patients |
Brief interventions in primary care Some specialist morbid obesity services |
| Drug misuse | Drug misuse services, prevention and treatment | Advice as part of other health-care contacts | Brief interventions in primary care |
| Alcohol misuse | Alcohol misuse services, prevention and treatment | Alcohol health workers in a variety of health-care settings | Brief interventions in primary care |
| Tobacco control | Local activity, including stop smoking services, prevention activity, enforcement and communications | Brief interventions in secondary care and maternity care | Brief interventions in primary care |
| Nutrition | Any locally-led initiatives | Nutrition as part of treatment services, dietary advice in health-care settings | Brief interventions in primary care |
| NHS Health Check Programme | Assessment and lifestyle interventions | NHS treatment following NHS Health Check assessments and ongoing risk management |
Support in primary care for people with long term conditions identified through NHS Health Checks |
| Reducing and preventing birth defects | Population level interventions to reduce and prevent birth defects (with PHE) | Maternity services | Interventions in primary care such as pre-pregnancy counselling or smoking cessation programmes Some specialist genetic services Antenatal and newborn screening aspects of maternity services |
| Health at work | Any local initiatives on workplace health | NHS occupational health services | |
| Dental public health | Epidemiology, dental screening and oral health improvement, including water fluoridation (subject to consultation) | Oral health as part of dental contracts | |
| Accidental injury prevention | Local initiatives such as falls prevention services | ||
| Seasonal mortality | Local initiatives to reduce excess deaths | Flu and pneumococcal vaccination programmes |
Some of the above services will be mandated for local authorities and the commissioning of other services will be discretionary. More information is available at: www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_ 131901.pdf.
Public health services to be provided or commissioned by PHE and related NHS CB/CCG commissioning
| PHE | Related CCG commissioning | Related NHSCB commissioning | |
|---|---|---|---|
| Prevention and early presentation | Health improvement support for local authorities and NHS CB Social marketing and behaviour change campaigns including campaigns to prompt early diagnosis via awareness of symptoms |
Promoting early diagnosis as part of community health services and outpatient services | Promoting early diagnosis as part of primary care |
| Infectious disease | Current functions of the Health Protection Agency (HPA) in this area Public oversight of prevention and control, including co-ordination of outbreak management (with supporting role for local authorities) |
Treatment of infectious disease Co-operation with PHE and local authorities on outbreak control and related activity |
Co-operation with PHE and local authorities on outbreak control and related activity Some specialist infectious disease services |
| Emergency preparedness and response | Current functions of HPA Emergency preparedness including pandemic influenza preparedness (supported by local authorities) |
Emergency planning and resilience remains part of the core business for the NHS | Mobilising the NHS in the event of an emergency |
| Health intelligence and information | Intelligence and information on health improvement and health protection (with local authorities), including many existing functions of Public Health Observatories, Cancer Registries, National Cancer Intelligence Network, HPA and National Treatment Agency for Substance Misuse’s National Drug Treatment Monitoring System | NHS data collection and information reporting systems (for example, Secondary Uses Service) | NHS data collection and information reporting systems |
Appendix 12 Star Chart tool
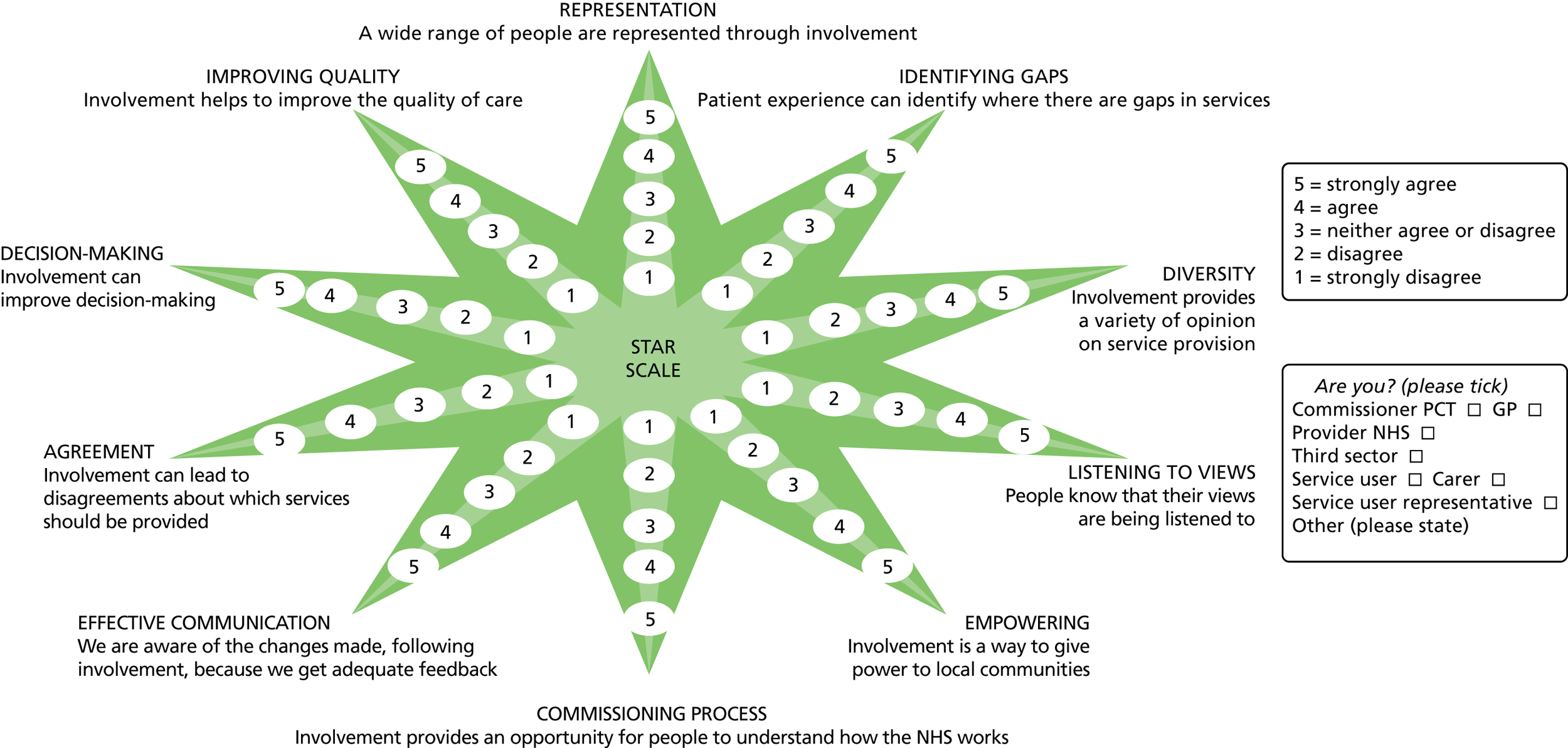
Appendix 13 Documentary analysis
| Documents | Sites | ||
|---|---|---|---|
| CS3 | CS2 | CS1 | |
| NHS Trust documents |
|
||
| CCG related (PPI/PPE focus) |
|
|
|
| Local Demographics (Health) |
|
|
|
| Equality Delivery System |
|
||
| General PPI |
|
|
|
| GP/primary care |
|
|
|
| LA |
|
|
|
| Community services |
|
|
|
| LTCs general |
|
|
|
| LTCs specific |
Diabetes
|
Diabetes
|
Diabetes
|
| Local Pathfinder PPI |
|
||
| PCT/cluster |
|
|
|
| Focus of documents | Documents |
|---|---|
| CCG |
|
| Children’s |
|
| Commissioning for LTCs |
|
| Engagement strategies | |
| HWBB |
|
| Health service research |
|
| Healthwatch |
|
| Integrated care |
|
| National Voices |
|
| CCG PPI/PPE Pathfinder |
|
| Patient representative role |
|
| PPI/PPE |
|
| QIPP LTC |
|
List of abbreviations
- BME
- black and minority ethnic
- CCG
- Clinical Commissioning Group
- CCPG
- Clinical Commissioning Planning Group
- CLAHRC
- Collaboration for Leadership in Applied Health Research and Care
- CS1
- case study 1
- CS2
- case study 2
- CS3
- case study 3
- CSU
- commissioning support unit
- DES
- Directed Enhanced Service
- EVOC
- Engagement and Voice in Commissioning
- GP
- general practitioner
- HWBB
- Health and Well-Being Board
- JSNA
- Joint Strategic Needs Assessment
- LIG
- local implementation group
- LINk
- Local Involvement Network
- LTC
- long-term condition
- MS
- multiple sclerosis
- NAPP
- National Association for Patient Participation
- NHSCB
- NHS Commissioning Board
- NIHR
- National Institute for Health Research
- NRAS
- National Rheumatoid Arthritis Society
- PALS
- Patient Advocacy Liaison Service
- PBC
- practice-based commissioning
- PCT
- primary care trust
- PEBL
- Patient Experience Blog
- PEP
- patient engagement panel
- PPE
- patient and public engagement
- PPEI
- patient and public engagement and involvement
- PPG
- patient participation group
- PPI
- patient and public involvement
- PRG
- patient reference group
- PRUComm
- Policy Research Unit in Commissioning and the Healthcare System
- QIPP
- Quality, Innovation, Productivity and Prevention
- QOF
- Quality and Outcomes Framework
- RA
- rheumatoid arthritis
- RCGP
- Royal College of General Practitioners
- REC
- Research Ethics Committee
- SHA
- strategic health authority