Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 09/1801/1029. The contractual start date was in October 2010. The final report began editorial review in November 2013 and was accepted for publication in April 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Richard Baker reports grants from the National Institute for Health Research during the conduct of the study.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Tarrant et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction and background
Summary of the study
Providers of primary care services do not always respond to the needs of diverse groups of patients, and certain groups of patients may be underserved and, therefore, disadvantaged. General practitioner (GP) practices are increasingly being encouraged to become more responsive to the needs of their patients in order to address these inequalities. Our aim in this study was to develop a patient-report questionnaire that could be used as a measure of patient experience in the context of efforts to improve responsiveness. We aimed to develop a questionnaire that could be used by diverse patient groups (including those with learning disabilities, and those who do not read or write English) and that was suitable for use by a range of different primary care organisations (PCOs), including GP practices and walk-in centres.
This involved, first of all, finding out what responsiveness means. To this end, we conducted a literature review, and interviews and focus groups with patients and staff in 12 PCOs in the East Midlands. We developed a questionnaire and tested it with patients from six of these PCOs. We then asked 15 PCOs across three different regions in England to distribute it to a large sample of patients. We checked the questionnaire for validity and consistency. We refined the questionnaire for different PCO settings and for specific patient groups. We investigated existing ways of population mapping which GP practices could use to increase their understanding of the needs of their populations in relation to responsiveness.
Summary of this chapter
This background chapter describes evidence for inequalities in patient experience in primary care. Within English policy, ‘responsiveness’ has been identified as a possible solution to this problem. The meaning of responsiveness in the current context of English primary care is explored. The existing measures of responsiveness and their deficiencies are summarised, and the need for a specific patient-report questionnaire on responsiveness that will allow the voice of all patients to be heard is identified.
Background
Inequalities in patient experience in primary care
One consistent finding across primary care patient experience surveys is that certain patient groups tend to report less positive experiences. 1 Patients from black and minority ethnic (BME) backgrounds, patients with poor health status, poor mental health or disabilities, less affluent patients, and younger patients tend to report poorer experiences of accessing and using primary care. 2–5 The reasons for this variation in experiences across different patient groups are not well understood. 1,5 In the case of patients from BME groups, some of this variation may be explained by the fact that these patients tend to be clustered in generally poor-performing practices, although many BME patients report less positive experiences than other patients within the same practice. 5 The variation in patients’ experiences of care between practices and across different patient groups has been described as unacceptable. 6 These inequalities are a cause for concern, as poorer experience of primary care is likely to impact on and perpetuate inequalities in health across diverse patient groups.
Responsiveness as means of addressing inequalities: an emerging concept
These concerns led to a focus in English policy from around 2008 onwards, under the Labour government, on efforts to improve access and responsiveness in primary care. Primary care providers were encouraged to work to be more ‘responsive’ – to move from a ‘one size fits all’ approach to delivering their services, towards a more flexible and responsive approach that takes into account the specific needs of their local populations. Guidance from the Department of Health (DH) underlined this aspiration, stating that, ‘there is no “one size fits all” model, it is for practices to personalise their services to meet their patients’ preferences’7 (see Chapter 3, Inequalities and the needs of diverse groups).
The concept of responsiveness was seen as closely linked with access, with the DH explicitly conceptualising practice responsiveness as a component of patient experience of access in primary care. 5 Definitions of the concept incorporate communicating and engaging with patients and carers, making efforts to identify and meet their non-clinical needs (i.e. their needs in terms of accessing and using services, rather than health needs or needs relating to the consultation or the clinician–patient relationship) and engaging in efforts to support patients from specific groups who may be vulnerable or experience particular difficulties in using primary care.
Practice responsiveness is the way in which a practice communicates and engages with its patients and their carers and responds to their non-clinical needs and preferences, reflecting the different ways in which they might prefer to access the service and an appropriate clinician, book, or indeed cancel an appointment. It includes the practice’s attitude to customer service and friendliness of staff, the environment in which patients wait to be seen and the way in which they interact and support patients from particular groups, such as those with hearing or sight loss or people from a black or minority ethnic background. 7
p. 15
The importance of supporting patients from diverse groups to access and use primary care services was underlined by a subsequent report on improving the experience of BME patients. 8 The report identified multiple reasons for the poorer access and experience of primary care of patients from BME groups; these included language and culture barriers, poorer health status, variable quality of GP services, and different expectations of BME patients. The report suggested that practices needed to work in partnership with BME patients, plan for their needs and ensure that the services were personalised to meet identified needs, and concluded that, ‘more responsive and personalised care will mean benefit for all members of the community – black and white – through the lessons learnt in service development’ (p. 3). 8
This focus on identifying and responding to the non-clinical needs of patients from diverse groups represented a shift in thinking, in that much of the work on inequalities and patient experience in primary care has tended to be concerned with clinical or health needs, and features of the consultation. This has included research into communication skills and barriers, patient-centredness and cultural competence, and issues such as patient–physician gender and race concordance. 9–11
Improving responsiveness
A review of key English policy and discussion documents highlights the key domains of service which have been identified in policy and guidance as those that GP practices should attend to in improving their responsiveness. These include engagement and communication with patients; practice opening hours; ease of contacting the practice; the ability of patients to easily make appointments that meet their needs for urgency, timing, and choice of practitioner; equity of access; alternative modes of consultation; the use of information technology (IT) to facilitate information and access; availability of premises and appropriateness of the physical environment, including accessibility; customer care; and adjustments for specific groups, including minority ethnic groups, disabled people, young people and carers. 7,12–15
Policy directives on responsiveness from 2008 onwards were accompanied by efforts to support and incentivise primary care providers to become more responsive. In 2008–9, a Primary Care Service Framework for accessible and responsive primary care13 was developed, setting out standards for care provision to improve responsiveness, and providing guidance for primary care trusts (PCTs) as to how practices might demonstrate their responsiveness. Under this framework, GP practices could claim financial reward for demonstrating their uptake of elements of responsiveness set out in the framework. Alongside this, the Practice Management Network produced extensive guidance on how to improve access and responsiveness in the form of a ‘how to’ manual,14 and a DVD to train reception staff on improving the patient experience. 15 These guides remain available, and give examples of good practice, and advice for practices in improving customer care, improving access for groups who are disadvantaged, and effectively engaging with patients. At the time that these resources were launched, they were accompanied by a training programme organised by the Royal College of General Practitioners (RCGP).
Responsiveness in the current context of primary care
Responsiveness was a highly prominent theme in English primary care policy under the Labour government (predominantly between 2003 and 2010). Despite significant political changes and NHS reorganisation, responsiveness remains a core aspiration for primary care. The DH White Paper Equity and Excellence, produced under the coalition government, calls for a ‘genuinely patient-centred approach in which services are designed around individual needs, lifestyles and aspirations’. 16 The new Clinical Commissioning Groups (CCGs) have a constitutional duty to reduce inequalities between patients in relation to their ability to access primary care services, and the outcomes achieved,17 and as such, issues of accessibility and responsiveness of local primary care providers are likely to be of concern to them. There have been some slight shifts in focus. Under the coalition government, responsiveness has become associated with the personalisation and choice agenda:16
In future, patients and carers will have far more clout and choice in the system; and as a result, the NHS will become more responsive to their needs and wishes.
p. 16
In recent years there has also been a growing emphasis on the role of patient engagement and involvement in promoting responsiveness. Interest groups such as the National Association for Patient Participation (NAPP) have taken a keen interest in responsiveness, emphasising the importance of ‘effective patient participation [in] ensuring the quality and responsiveness of services and health outcomes for patients and the wider community continuously improve’. 18
Responsiveness has also been highlighted as a key element of ‘the right culture’ post Francis, with a focus on responding to patients’ needs and preferences, encouraging a patient-centred philosophy, responding to complaints, and listening to patients. 19
A range of initiatives and programmes continue to be made available to support efforts to improve responsiveness in primary care. These include the ongoing RCGP Quality Practice Award programme; its ‘patient centred care module’20 sets standards relevant to responsiveness, and indicates evidence that practices can provide to demonstrate their performance in these areas. Initiatives such as Productive General Practice (developed by the now defunct NHS Institute for Innovation and Improvement, and still in use),21 and The King’s Fund’s experience-based codesign toolkit,22 provide guidance and support for primary care providers in involving patients in the task of identifying unmet needs within local populations, and aligning the design and delivery of services with the needs of the patients. There remains a need for research to inform approaches to addressing inequalities on health care in cost-effective ways; research into access, quality, cost and effectiveness of services for disadvantaged groups has been identified as important. 23
Measures of responsiveness
Responsiveness can best be understood as a feature of the PCO: the extent to which the organisation (1) has processes and systems in place to help them to understand the non-clinical needs of patients and how best to address them; (2) designs their services in ways that are directed at meeting these identified needs; and (3) takes a flexible and personalised approach to delivering services and helping patients gain access to the services they need.
It is evident that responsiveness of a PCO can be assessed through relatively ‘objective’ measures of these efforts, for example the extent to which the practice has clearly-defined strategies to identify the needs of their patient population, or the extent to which the practice provides different routes for patients to book appointments that are appropriate to the needs of the local population.
Alongside this, it is also important that the views of patients are sought. Responsiveness is ultimately reflected in patients’ perceptions of whether or not the service provided actually meets their non-clinical needs. Users of a service will have a range of needs and preferences, and the patterns of these will vary across services and localities; changes in service provision targeted at improving responsiveness may meet the needs of some groups of patients, but fail to address the needs of others, meaning that groups who are disadvantaged may be no better served.
While there are a number of validated and widely used patient experience questionnaires for primary care, including the annual national GP patient survey,24 there are currently no patient-report questionnaires that are designed specifically as measures of patient experience of responsiveness in primary care. Existing questionnaires include some non-clinical aspects of care (primarily issues relating to access and the behaviour of reception staff), but also include more extensive questions on the clinical aspects of care (quality and experience of the consultation).
There is extensive evidence on what matters to patients (across clinical and non-clinical domains of primary care25,26). A useful distinction has been made between relational aspects of care (e.g. dignity, empathy), and ‘functional’ aspects (e.g. access, waiting):1 non-clinical aspects of care may fall within both of these dimensions. The recent NHS Patient Experience Framework brings together evidence on patient experience and sets out the key elements of patient experience across the NHS. 27 The framework includes some ‘non-clinical’ elements, particularly access, privacy, and transition and continuity.
The framework is designed to be used flexibly, and it is acknowledged that, ‘different areas of the framework will be more significant in particular settings for different groups of patients and therefore demographics, equality, and environment will need to be considered when applying the framework’. 28 It is not clear, however, which non-clinical features of primary care are most salient for patients from different groups in judging the responsiveness of primary care services to their needs.
It is important to recognise that the boundary between clinical and non-clinical needs may be blurred, but the focus on responsiveness brings attention to the specific issues of whether or not patients find services easy to access and use, and whether or not they feel that services are aligned with their personal, cultural or lifestyle-related needs. If a questionnaire is to act as a valid measure, it is essential that it cover these issues.
A further consideration is that existing patient experience measures tend to achieve a low response rate from patients from traditionally disadvantaged groups. The term ‘seldom heard’ has been used to describe these groups, defined as those who do not have an effective voice in relation to public and voluntary service providers, and who are the most vulnerable to ill health because of social and economic disadvantage. This includes minority ethnic groups, people with disabilities or mental health problems, refugees, travellers, homeless people, ex-offenders, migrants who do not speak English and others who are socially excluded. 29,30 Accessing the views of these ‘seldom-heard’ groups is critical in assessing whether or not practices are responding fairly to the needs of all. There has been some recognition of the need to find ways of gathering more targeted and detailed information about experiences across patients from different groups. 1
In this study, we aim to develop a measure of patient experience of responsiveness that includes the non-clinical needs identified as most important for patients across diverse groups; is worded to tap into responsiveness in terms of ease of getting needs met (rather than simply measuring experience); and is designed to be appropriate for use with patients who are traditionally seen as ‘hard to reach’ and hence ‘seldom heard’.
Diversity of primary care providers
We aim to develop approaches to measuring responsiveness across a range of primary care providers. While the GP practices remain core providers of primary care, there is a diverse set of organisations that fall under the umbrella of primary care, and these organisations differ in the types and nature of services they deliver. Walk-in centres, minor injury units and urgent care centres all provide primary care services which are accessible without appointments and are open to patients outside traditional working hours. Traditional general practices have diversified, with the emergence of specialist practices providing services to vulnerable groups such as asylum seekers and homeless patients; large health and social centres enable patients to access a wide range of services under a single roof. In addition, patients consult pharmacists for advice, and pharmacies commonly offer extended health services such as health checks. There may be specific challenges to responsiveness across these different types of organisations, and patients are likely to have different expectations of the types of services they can access and the way in which these will be organised and delivered across the different providers. These differences have implications for approaches to measuring responsiveness in primary care.
Summary and discussion
Responsiveness in primary care continues, across two governments, to be seen as an important element in reducing inequalities and, thus, providing equitable quality care. Understanding how responsiveness can be measured and improved requires an understanding of the needs of the primary care population. In the absence of an existing way to measure their non-clinical needs, the requirement to develop a patient-report questionnaire is clearly identified. Existing objective measures may contribute to understanding how responsive a PCO may be, but alongside these we need to assess patients’ own perceptions of whether or not their non-clinical needs are met.
The need to hear from those who are traditionally ‘seldom heard’ is essential in any effort to measure and increase responsiveness, as it is traditionally these disadvantaged groups who provide the greatest challenge in terms of ‘access’ but who also may have the most to benefit from a responsive primary care system.
Measures of responsiveness need to take into account the specific challenges and contexts of different types of primary care provider.
Chapter 2 Methods
Summary of this chapter
The primary aim of this study was to develop a measure of patient experience of the responsiveness of primary care providers to their needs. The study involved a review of policy documents and literature, and qualitative research with patients (see Chapter 5) and primary care staff (see Chapter 4), in order to define and operationalise responsiveness. Based on this work, a questionnaire was drafted and piloted (see Chapter 6) across a range of primary care service providers before final testing, including how to optimise the use of the questionnaire to access the views of diverse patient groups (see Chapter 7).
A secondary aim was to explore the mapping of diversity in primary care. It became clear that the aim of developing guidance for practices on mapping their patient populations would not be feasible, and that there would be more value in exploring of the significant barriers and challenges to practices in undertaking this (see Chapter 8).
Summary of methods
Development and testing of the questionnaire had three main stages. The overall study design is described below and in Figures 1–4. Further details of the methods are provided for each part of the study in the corresponding chapter of this report.
Stage 1: literature review and interviews with patients and staff
This stage commenced with a literature review on the meaning and measurement of responsiveness (Figure 1). Different fields in which responsiveness has emerged as a core concept were scoped, and from this literature we identified key items and followed narrative threads.
FIGURE 1.
Stage 1: literature review and qualitative interviews. a, In 12 PCOs both staff and patient interviews were conducted, while in one PCO only staff interviews were conducted.
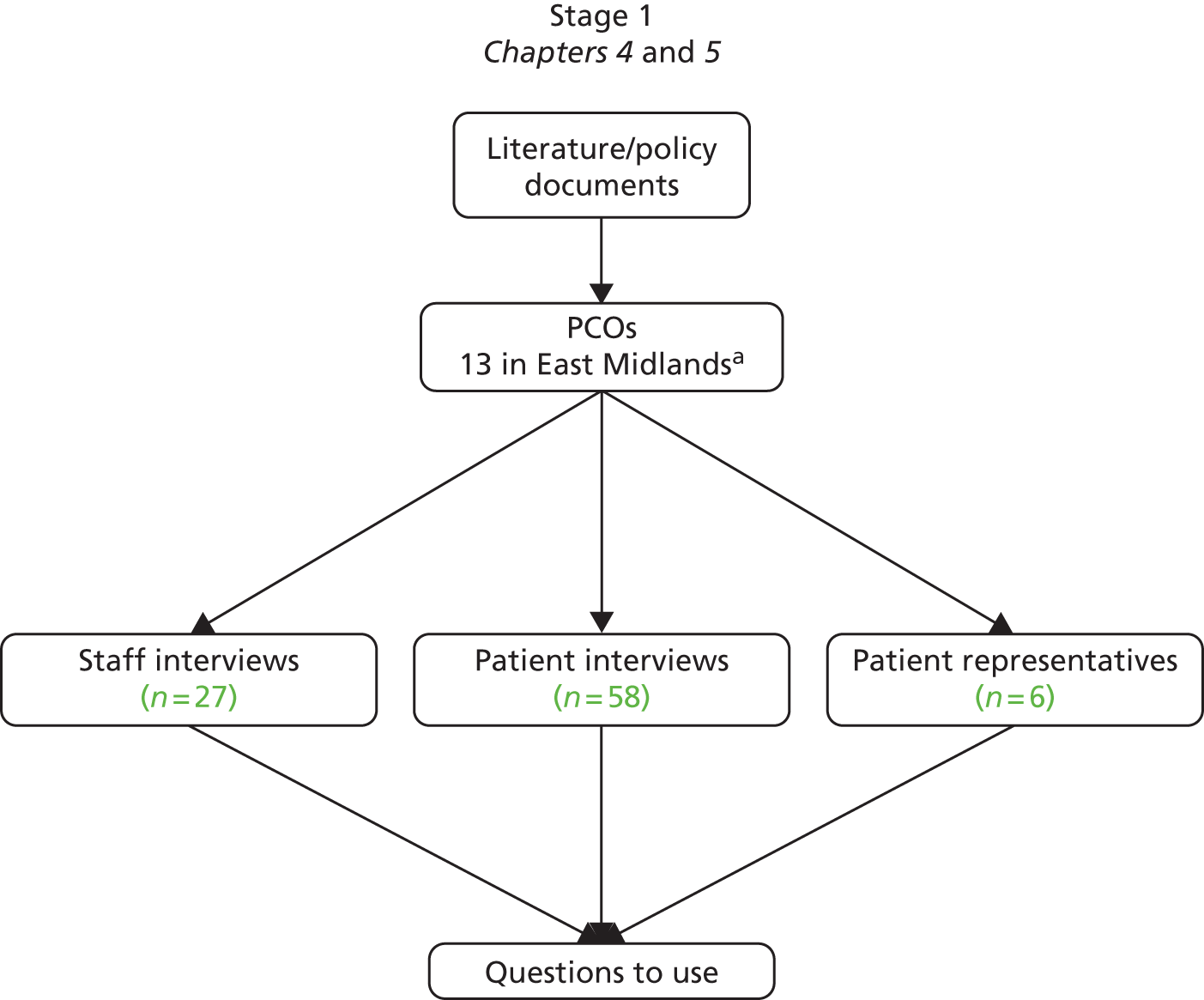
We then conducted qualitative work with patients and professionals in order to understand how patients experienced responsive primary care, the ways in which practices had attempted to deliver responsive service, and the barriers and facilitators to this. We also explored the important features of a questionnaire on responsiveness for patients and for PCOs. We conducted semistructured interviews with staff (n = 27), patient representatives (n = 6) and patients (n = 58) from 13 PCOs in the East Midlands. Recruitment was supported by the Primary Care Research Network (PCRN) for the East Midlands and South Yorkshire; practices in the South Yorkshire region were not included. Thirteen PCOs were identified through the PCRN and were selected to include mainstream GP practices of varying size, population demographics and location, as well as other types of PCO, including a walk-in centre, pharmacies and a specialist GP practice for homeless patients (Table 1).
| PCO | Type | Location | Sizea | Region | Deprivation decileb | Stage 1 | Stage 2 pilot 1 | Stage 2 pilot 2 | Stage 3 |
|---|---|---|---|---|---|---|---|---|---|
| 01 | GP surgery | Urban | Large | East Midlands | 5 | ✓c | – | – | – |
| 02 | Pharmacy | Inner-city | Large | East Midlands | 4 | ✓ | – | ✓ | ✓ |
| 03 | Pharmacy | Rural | Large | East Midlands | 10 | ✓ | – | ✓ | ✓ |
| 04 | GP surgeryd | Town centre | Large | East Midlands | 5 | ✓ | ✓ | – | – |
| 05 | GP surgery | Rural | Medium | East Midlands | 10 | ✓ | – | – | – |
| 06 | GP surgery | Inner-city | Small | East Midlands | 4 | ✓ | – | ✓ | – |
| 07 | Homeless GP surgery | Inner-city | Small | East Midlands | 2 | ✓ | – | – | ✓ |
| 08 | Health and social care centred | Inner-city | Large | East Midlands | 1 | ✓ | – | – | ✓ |
| 09 | WIC | Urban | Large | East Midlands | 4 | ✓ | – | – | ✓ |
| 10 | GP surgery | Urban | Large | East Midlands | 4 | ✓ | – | ✓ | – |
| 11 | GP surgery | Urban | Medium | East Midlands | 6 | ✓ | ✓ | – | – |
| 12 | GP surgery | Rural | Small | East Midlands | 8 | ✓ | ✓ | – | – |
| 13 | GP surgeryd | Inner-city | Small | East Midlands | 3 | ✓ | – | – | ✓ |
| 14 | Pharmacy | Inner-city | Large | Greater London | 1 | – | – | – | ✓ |
| 15 | Pharmacy | Inner-city | Large | Greater London | 2 | – | – | – | ✓ |
| 16 | GP surgerye | Inner-city | Small | Greater London | 1 | – | – | – | ✓ |
| 17 | WIC | Inner-city | Large | Greater London | 1 | – | – | – | ✓ |
| 18 | GP surgery | Urban | Medium | Greater London | 1 | – | – | – | ✓ |
| 19 | GP surgery | Recruited for stage 3 but withdrew prior to data collection | |||||||
| 20 | GP surgery | Rural | Small | Northern & Yorkshire | 10 | – | – | – | ✓ |
| 21 | GP surgery | Rural | Medium | Northern & Yorkshire | 8 | – | – | – | ✓ |
| 22 | GP surgerye | Town centre | Small | Northern & Yorkshire | 2 | – | – | – | ✓ |
| 23 | WIC | Town centre | Large | Northern & Yorkshire | 2 | – | – | – | ✓ |
| 24 | Pharmacy | Town centre | Large | Northern & Yorkshire | 3 | – | – | – | ✓ |
Based on the analysis of these interviews, we generated descriptions of the key components of responsive primary care as experienced by patients, and used these to develop a set of potential questions for the questionnaire.
Stage 2: developing the questionnaire
We conducted three patient focus groups specifically targeted at patients from ‘seldom-heard’ groups, to explore and validate understanding and acceptability of the questions. As a result of the focus groups, the questions were refined. Although we had intended to develop a short, generic questionnaire that would be applicable to all primary care providers, including GP practices, pharmacies and walk-in centres, the findings from the interviews and focus groups suggested this would not be feasible or acceptable to patients. We elected to lead with the development of a questionnaire for GP practices, which would then be adapted and modified to make it more appropriate to other specific primary care settings.
A draft questionnaire was developed including the revised questions, open questions to allow comments, and sociodemographic questions. A version was produced in paper and another online. The draft questionnaire was subject to two rounds of piloting, involving administration of the questionnaire to patients in primary care, semistructured interviews with responders to assess face validity and acceptability to patients, and cognitive interviews to assess comprehensibility. Piloting informed the refinement of questions, and provided insight into the feasibility of use of the questionnaire across different service providers (Figure 2).
FIGURE 2.
Stage 2: piloting of the questionnaires.
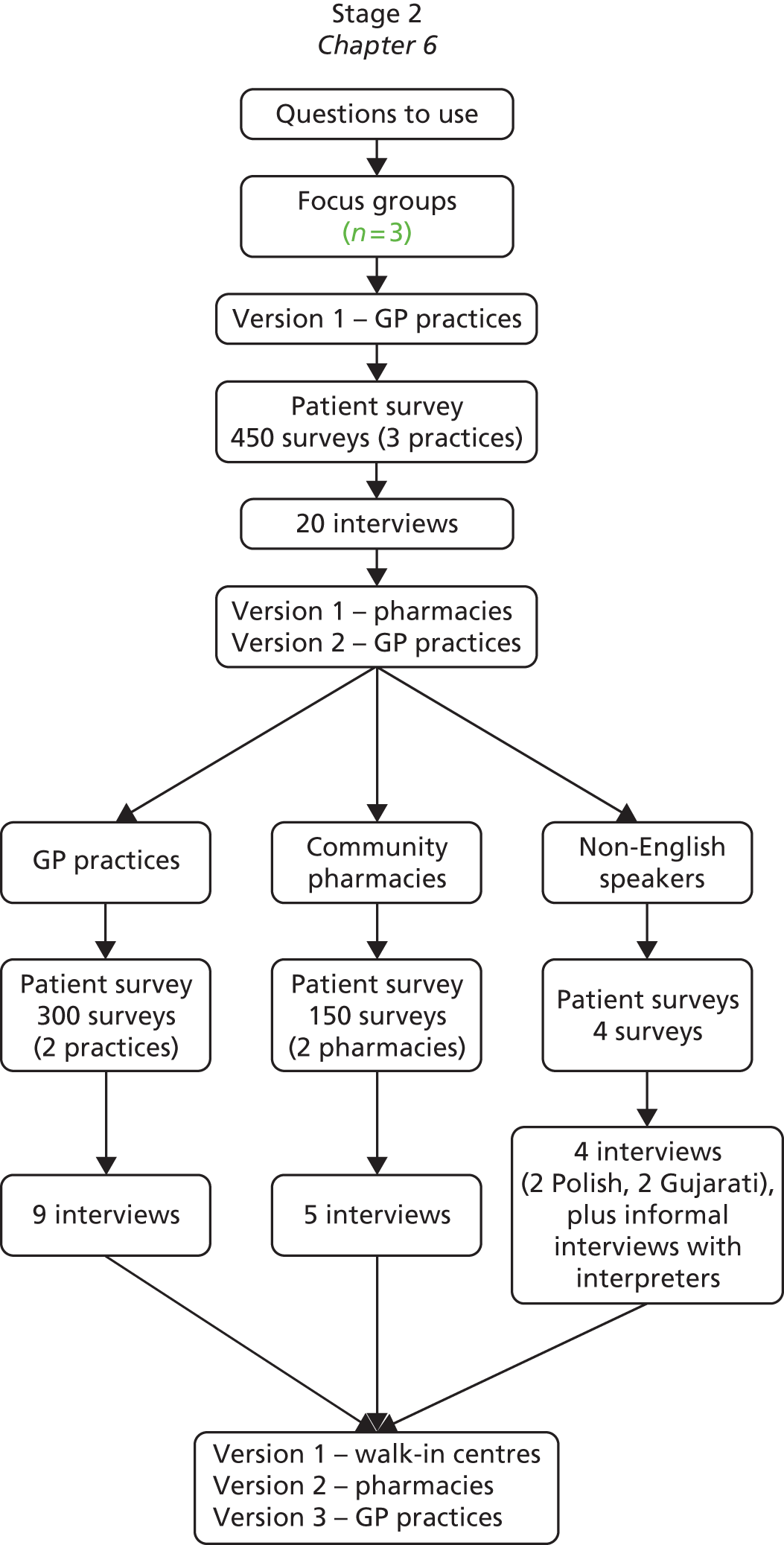
Version 1 of the questionnaire related to GP surgeries only, with the plan to adapt for other primary care providers. The first pilot was conducted in three GP practices selected from the 12 PCOs remaining after stage 1 (one practice withdrew during stage 1). A patient survey was handed out to 150 patients in each practice and a purposive sample of responders who expressed an interest were invited to take part in semistructured interviews to assess face validity and acceptability. The questions were modified and a pharmacy version was developed. The second pilot was conducted in a different set of two GP practices and in two pharmacies. In this second pilot, 450 patients received a questionnaire and cognitive interviews were conducted with a sample of responders to identify problems with question wording or questionnaire design.
We also conducted a consultation with relevant groups and individuals, using contacts through the advisory group (e.g. learning disability organisations, community organisations representing patients from ethnic minority groups, people with visual impairment) to identify preferences for a range of formats, and approaches to administering the questionnaire; members of the project team also contributed to this.
The questionnaire and the approaches to administering the questionnaire were revised iteratively in the light of the findings from the pilots. Version 1 of the GP surgery questionnaire was tested in pilot 1, and then amended to version 2 in pilot 2. Version 1 of the pharmacy questionnaire was developed for pilot 2. In stage 3 (see Figure 3), version 3 of the GP surgery questionnaire and version 2 of the pharmacy questionnaire were tested, and version 1 of the walk-in centre questionnaire was developed and tested.
Stage 3: testing the questionnaire
To assess the reliability, validity and acceptability of the questionnaire, a large-scale pilot was undertaken in 16 PCOs across three regions in England: six of the PCOs recruited for stage 1 of the study, five new PCOs from the Northern and Yorkshire/North West region, and five new PCOs from Greater London (Figure 3). PCOs were selected to ensure a diverse sample, and included eight GP surgeries, five pharmacies, three walk-in centres and one Health and Social Care centre (Table 1). The questionnaire was handed to a sample of up to 200 users attending most PCOs, except the two pharmacies and a small specialist homeless practice recruited from stage 1 that handed out 100 each. As one practice withdrew before it had handed out any patient packs, these 200 were split between four other practices; hence four GP practices were asked to hand out 250. Two practices did not manage to hand out their full quota during the time scale of the study. Responders who expressed an interest were mailed a second copy of the questionnaire, to enable test–retest reliability to be assessed. Feedback was gained from staff in participating PCOs on their experiences of administering the questionnaire, and the value of the data to them in informing changes to practice.
FIGURE 3.
Stage 3: large-scale testing of the questionnaires.
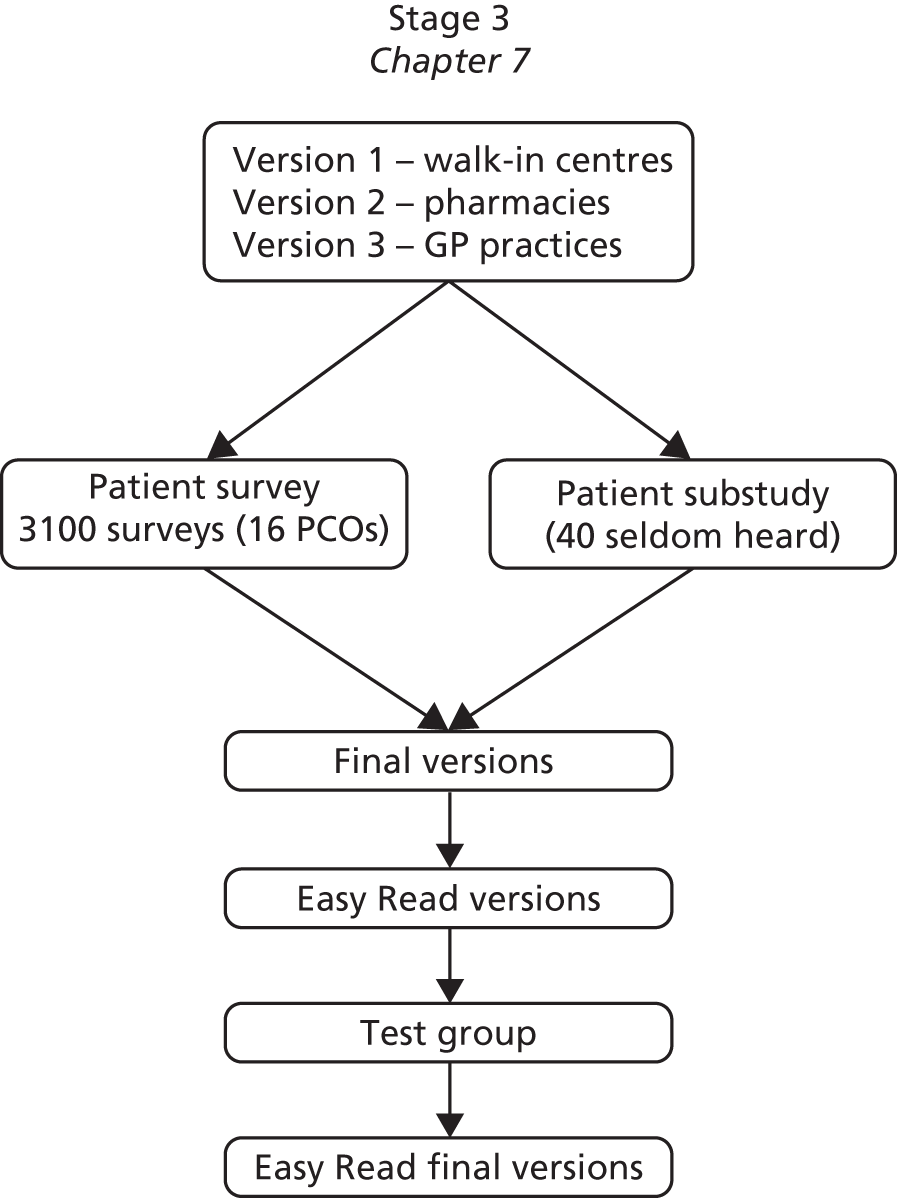
As part of stage 3, we worked with a sample of PCOs to explore ways of including patients from ‘seldom-heard’ groups in the survey process. We conducted informal interviews with staff co-ordinating the survey to identify the ‘seldom-heard’ groups within their patient population and to discuss ways of supporting these patients to become involved. The study team provided support and resources to practices to enable them to undertake additional work to include ‘seldom-heard’ groups in the survey, in ways that were tailored to the needs of specific patient groups. We also engaged a specialist in Easy Read materials to produce an Easy Read version of the questionnaire. This was subject to small-scale testing with people with learning disabilities.
The questionnaire developed as a result of this process is available in three versions: a GP surgery version, a pharmacy version and a walk-in centre version. The majority of questions are common across the three versions, but each contained some questions specific to the particular type of PCO. The questionnaire was designed as a self-completion paper questionnaire in standard and Easy Read formats, but can also be interviewer-administered (including via an interpreter) or completed online.
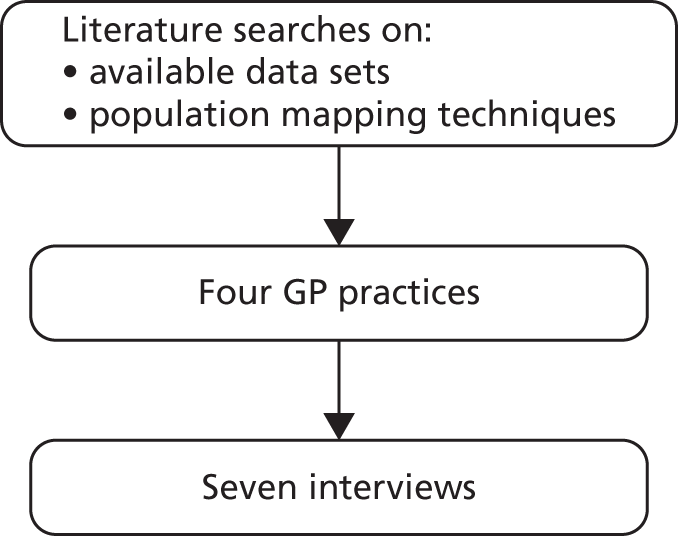
Mapping population diversity substudy
We also undertook a substantial substudy to explore approaches to and attitudes towards mapping diversity in primary care. This involved a review of available methods for population mapping and the challenges to this, and interviews with staff in four participating GP surgeries about their experiences of and attitudes to exploring the characteristics of their patient populations (Figure 4).
FIGURE 4.
Population mapping.
Data analysis
For the initial staff and patient interviews, and for narrative interviews in pilot 1, data were analysed using a combination of framework analysis and the constant comparative approach, which involved both deductive and inductive elements. An initial coding frame was generated from the research questions, which acted to guide, but not constrain, the analysis; themes and subthemes were added and iteratively revised as additional interviews were coded. The cognitive interviews were coded and charted with a focus on comprehension and response selection. NVivo 8 (QSR International, Warrington, UK) was used to organise the qualitative data.cr.
For pilots 1 and 2, we used SPSS (IBM Corporation, Armonk, NY, USA) to generate descriptive statistics for each question. In pilot 3, we carried out an exploratory factor analysis to investigate the structure of the GP questionnaire, and to identify key questions to form the basis of scores for the questionnaire which could be used as a measure of patient experience of responsiveness. We conducted analysis to provide initial evidence about reliability and validity. 32,33 We used Cronbach’s alpha coefficients to assess internal consistency for scores from identified subfactors. Pearson correlations were calculated between the scale scores from our questionnaire, and three indicators of construct validity. Kappa and intraclass correlation coefficients (ICCs) were calculated for the test–retest questionnaires to assess test–retest reliability.
Ethical considerations/governance
An advisory group was convened at the start of the project (see Appendix 1). We sought to include a variety of members with an interest in responsiveness in primary care, including academics, policy-makers and commentators, representatives from disadvantaged and traditionally ‘seldom-heard’ groups, and members of professional bodies. The remit for the group was to provide an insight into the meaning of responsiveness from their individual perspectives, and to provide feedback on our work in progress. The group’s advice and views have been invaluable throughout the project, and we are extremely grateful for their participation.
The study received a favourable opinion from the Nottingham Research Ethics Committee 2 on 28 May 2010. Research management and governance (RM&G) approval was received from all localities where the study was taking place. Seven substantial amendments were submitted throughout the course of the project, and all received a favourable ethical opinion and RM&G approval.
Assessment of the method
Strengths of the method
Our greatest success was ensuring we received the views from ‘seldom-heard’ patients. Given our focus on developing a questionnaire that reflected the needs and preferences of all patients, it was paramount that we both sought the views of these patients and tested the questionnaire with them. We achieved this using a combined approach. First, we ensured a diverse membership of the advisory group, including patient representatives from organisations that sought to promote the well-being of people with hearing and sight loss and learning difficulties, and ethnic minorities. Second, we included a specialist GP practice for homeless patients throughout the study, and recruited PCOs with diverse patient populations. Third, we devised a substantial substudy with two GP surgeries, to target two groups of ‘seldom-heard’ patients: Turkish speakers, and vulnerable (often homeless) patients attending a community group.
Another success was our sample of participants in all stages of the study, which was both large and diverse. The PCOs taking part in stage 1 were drawn from a variety of surgery locations (rural, suburban and urban; deprived and affluent; mixed ethnicities) with both large and small practice list sizes. In addition, we sought to include patients who were not well represented in the main sample. We recruited patients and patient representatives through charities supporting non-English speakers, people with learning difficulties, and people with hearing and sight loss both through the advisory group and by cold-calling organisations directly.
We also feel that exploring the meaning of the concept of responsiveness from a range of perspectives (through a literature review across different fields, from the perspective of staff across different PCOs, and from the perspectives of diverse groups of patients) has allowed us to generate a deep understanding of the complexities of the concept, and has generated valuable learning to inform work to improve responsiveness.
Methodological challenges
The greatest challenge was to provide the time and material resources to support the PCOs in their participation. As with most primary care research, there was a continuum of commitment and engagement from the participating PCOs. Some were extremely keen and contributed quickly and efficiently, with little input from the research team. At the other extreme were PCOs that needed regular reminders and prompting to ensure their continued participation. Some required material input, such as having ready-printed letters provided for use rather than printing the letters themselves on their headed paper. Unfortunately, one GP practice withdrew due to internal staffing changes during stage 1 (after the staff interviews, prior to the patient interviews). Another practice that agreed to participate in stage 3 eventually withdrew after many failed attempts on behalf of the research team to get data collection started.
Ensuring that the ‘seldom heard’ were included in stage 3 pilot was difficult. The two practices that engaged with the substudies to reach out to ‘seldom-heard’ groups were keen to participate and found the experience extremely rewarding. However, other PCOs were less interested in committing the time and resources. Administration of the substudy required additional administrative time and constant management.
Some of our methods were iterative and reactive to previous experience. During the 3-year project, we submitted seven substantial amendments to the research ethics committee and associated RM&G offices. These were time-consuming in terms of both preparation and approval processes. Although all amendments were ultimately successful, the project was held up on several occasions while we waited for approvals.
Two further methodological challenges arose. The first related to our aim of developing a measure of patient experience of responsiveness. Our initial intention was to design this to include a small number of generic, high-level and relatively abstract questions which would produce a single score. However, testing this approach with focus groups demonstrated that this was not acceptable to patients, and was unlikely to be valid. Patients wanted concrete questions that they could relate to their experiences. As a result, the questionnaire we developed was more specific and detailed than planned. However, our work in pilot 3 demonstrates that, despite this, it can be used to produce responsiveness ‘scores’.
The second methodological challenge relates to our aim of producing a measure that would be generic. For the reasons described above, this was not seen as acceptable to patients, so we instead developed a core questionnaire for GP practices and adapted this for pharmacies and walk-in centres. This means that the additional versions were not subject to the same level of development and testing as the GP questionnaire and are likely to require more work before they are ready for use.
Summary and discussion
This chapter has provided an overview of the methods we have used in the project. The qualitative interviews and focus groups, and the subsequent development of the questionnaires, are described. The methods of piloting of the questionnaires are introduced. Description of each of these methods is expanded within each of the following chapters of the report. We have also described the ethical considerations and governance arrangements employed during the study, provided a critique of our methods, and shared our main successes and challenges.
Chapter 3 Literature review: meaning and measurement of responsiveness
Introduction
We conducted a literature review on the meaning and measurement of responsiveness. The aim of this was to describe the range of work around the concept and to identify common and divergent themes. This provides a contextual background to our work to develop a measure of patient experience of responsiveness in the specific field of primary care.
A systematic search provided a starting point for scoping out the different fields in which responsiveness has emerged as a core concept; from this literature, we identified key items and followed narrative threads. We do not claim this to be a comprehensive and systematic review, and do not cite all papers identified through systematic searches. Rather, we draw on the literature to present a narrative overview of the diverse ways in which responsiveness has been conceptualised, and the implications of this.
Methods
We conducted systematic searches of MEDLINE and Web of Knowledge from January 2001 to March 2011 for papers relating to the meaning and measurement of responsiveness. This initial search was supplemented with searches of the internet and of reference lists of identified reports and papers, to identify relevant ‘grey’ literature. Identified abstracts were screened for relevance. The paper/reports were summarised into a chart which was used to generate an overview of the range and nature of work on this concept. The search strategy and methods for review and analysis are described in Appendix 2.
We present a narrative scoping review of the literature on the key fields of work relating to the meaning and measurement of responsiveness, and identify the themes that have emerged within these fields. In writing the narrative review we have referenced wider literature that was ‘signposted’ by papers identified through the core search.
Findings
Our review of the literature indicated that responsiveness is a rather fuzzy concept, with a range of meanings and definitions evident across different fields of the literature. We identified three distinct but overlapping conceptualisations of responsiveness in the literature, corresponding to domains of literature relating to service quality; inequalities and the needs of diverse groups (in health or other services); and consumerism and patient involvement.
Service quality
Responsiveness has a long history of being considered as a core element of service quality. 34 Service quality has been defined as the ability of the organisation to meet or exceed customer expectations. 35 Parasuraman and colleagues’ widely accepted model of service quality includes five key dimensions: tangibles (features of the service environment); reliability; responsiveness; assurance (the extent to which the organisation and its employees are perceived as credible and trustworthy); and empathy. Within this context, responsiveness has been defined as an organisation’s employees’ ‘willingness to help customers and provide prompt service’ (p. 23). 35
Service quality is seen as important for customer-serving organisations in marketing,36 achieving success and profitability through helping to attract and retain customers,37 and promoting customer satisfaction. Responsiveness is recognised as particularly important to the public image of customer-serving organisations; in the UK, the Institute of Customer Service38 makes a high-profile annual People’s Choice award for ‘Most Responsive Organisation’.
The notion of responsiveness as an element of service quality also features in the health literature. Several papers speak of responsiveness as part of a high-quality service, and as a feature of customer service or interactions between staff and patients. For instance, in a qualitative study of patients’ expectations and experiences of public and private providers, patients were found to expect more responsiveness and better quality of care and to be willing to pay for it. 39 A study of predictors of hospital patient satisfaction ratings in the USA found that nursing staff communication with patients had an important bearing on perceived responsiveness. 40
The field of work on service quality has generated a number of measures; the most widely used of these is the SERVQUAL scale. 35,41 This incorporates the five dimensions of service quality described above. The SERVQUAL scale includes a subscale of four questions to measure responsiveness:
-
P10: employees of XYZ tell you exactly when services will be performed
-
P11: employees of XYZ give you prompt service
-
P12: employees of XYZ are always willing to help you
-
P11: employees of XYZ are never too busy to respond to your requests.
SERVQUAL has been used extensively across a wide range of settings to measure service quality, either in its original form or adapted to the specific setting. 42,43
The SERVQUAL dimensions have been found to be applicable and stable in the measurement of service quality in health care,44–46 and specifically in primary care,47 with responsiveness remaining a core element of service quality in this context. SERVQUAL has been adapted and used in studies of service quality in a range of health-care settings48–51 but has not found wide application in the context of primary care. A version of SERVQUAL designed to assess the quality of hospital services has been developed,52 and SERVQUAL has been adapted for use in a primary care clinic in the USA. 53 The revised scale was assessed for factor structure, reliability and validity; responsiveness remained a core element of the scale. Four questions on responsiveness were included, relating to prompt service; employee willingness to help; staff never too busy to respond to requests; and convenient opening hours.
The conceptualisation of responsiveness as an element of service quality has several key implications. First, responsiveness is tied to customer service – the quality and promptness of interactions between employees and customers (or between staff and patients) – rather than other features of the organisation. Second, the notion of service quality focuses on improving customer experience, exceeding expectations, increasing satisfaction, and even ‘delighting’54 the customer. It is seen as a route to attracting and retaining customers, and increasing market share. Within this literature, responsiveness is not seen as a ‘duty’ or essential feature of an organisation, but as a ‘value adding’ feature of service. Third, the focus is not on diverse or disadvantaged groups, but on improving the experience of all customers/patients.
Inequalities and the needs of diverse groups
The concept of responsiveness is also prominent in the field of work relating to health inequalities. Seminal work undertaken by the World Health Organization (WHO) in the late 1990s and early 2000s identified responsiveness as one of the three intrinsic goals of health systems (along with good health and fair financing). 55 Responsiveness involves health systems meeting the needs of the patients they serve, and is based on the idea that there are fundamental needs, or basic human rights, that health systems should meet for all patients. These needs are seen as relating to the non-clinical domains of health service provision. Responsiveness is defined as ‘how well the health system meets the legitimate expectations of the population for the non-health enhancing aspects of the health system. It includes seven elements: dignity, confidentiality, autonomy, prompt attention, social support, basic amenities, and choice of provider’ (p. 1). 56 It is suggested that if a health system is responsive, the interactions that people have within the health system may improve their well-being, irrespective of improvements to their health. 57
The WHO argues that the measurement of responsiveness is essential to assessing the performance of health systems, and importantly, involves measuring ‘both the overall level of achievement (average over the whole population) as well as the distribution (equitable spread of this achievement to all segments of the population)’ (p. 1). 56 It is clear that this conceptualisation of responsiveness involves fairness and avoiding inequalities across the patient population.
By their definition, the WHO sought to measure responsiveness objectively by looking at how patients perceive what happens in their experience of using health care. 56 They developed a responsiveness instrument58 and tested it across 35 countries. Factor analysis revealed the seven elements used in their definition, above. 59 Levels of responsiveness were measured using a patient-report questionnaire, split into two sections: patients were asked, first, to rate their experience with the system, and second, to rate how important each element was to them. Each element comprised 3–7 questions. 56 Questions were formatted to assess the extent to which patients felt their needs for each dimension were met, for example:
-
In the last 12 months, how often did the office staff, such as receptionists or clerks there, treat you with respect?
-
always
-
usually
-
sometimes
-
never.
-
Data on inequalities in distribution of responsiveness were generated through surveys completed by key informants in each country; informants were asked about whether or not they felt that particular patient groups were discriminated against with regard to responsiveness in their country. 60
The WHO responsiveness measure has been widely used in studies to assess health system responsiveness internationally. 61,62 This has included work to identify predictors of health system responsiveness; evidence suggests that health-care expenditures per capita, and educational development, are positively associated with responsiveness, while public sector spending is negatively associated with responsiveness. 63 The WHO definition has also been used as the basis of work to identify unmet needs in disadvantaged groups, including a literature review to identify the extent to which people who access mental health services were not having their needs met. 64
The WHO work focuses on responsiveness of health systems, rather than individual providers such as GP practices. The WHO definition was adapted for primary care by Canadian researchers to produce a definition of responsiveness as the ‘ability of the primary care unit to provide care that meets the non-health expectations of users in terms of dignity, privacy, promptness, and quality of basic amenities’ (p. 341). 65 They argued that the operationalisation of responsiveness was problematic due to lack of distinctness from other concepts such as whole-person care. Their earlier work to develop national indicators suggested two core questions to ask about responsiveness: ‘Are patients satisfied that the Primary Health Care organization and providers respect their right to privacy, confidentiality and dignity? Are patients confident that PHC organizations and providers are responsive to their culture and language needs?’66
The focus in health on responsiveness as involving providing services equitably and meeting the needs of all, across diverse groups, is echoed in work on responsiveness in the field of education. Responsiveness to learners’ needs has been considered in terms of meeting individual student needs, information, support, respect and opportunities to air views; these dimensions have been included in the National Learner Satisfaction Survey. 67
As discussed earlier, arguments for the need to promote responsiveness in primary care tend to draw heavily on the inequalities agenda with a recognition that responding to specific groups’ needs might help to reduce inequalities. 68 However, needs are framed in a slightly different way from the notion of universal legitimate expectations that is central to the WHO work. Instead, the focus is on the diverse needs of different patient groups, and ensuring that individual patient needs are met through individualised and proactive care. 69,70 Alignment with the needs of different patient groups is seen to be important, and there has been particular focus on the need for cultural alignment with minority groups. Research has shown how cultural self-reflection and self-awareness on the part of staff can be helpful, and how developing a reciprocal understanding of needs can lead to a flexible responsive service. 71 However, the evaluation of a human immunodeficiency virus mental health service that actively valued cultural responsiveness (acknowledging clients’ cultural identities, taking their beliefs, norms and values into account in the interventions) struggled to separate out whether cultural responsiveness or integrated care affected observed findings independently or in combination. 72
With responsiveness defined as an approach to reducing inequalities, the onus is on providers to ensure that they understand their practice populations, and can segment them based on need. 13,73 There is also an emphasis on finding proactive ways to reach out to marginalised groups who may find it difficult to access health care. 74,75
One challenge raised within this field relates to the nature of needs, expectations and demands. A distinction has been made between needs and demands in the context of health needs assessment, and this distinction may be useful in conceptualising needs in relation to non-clinical aspects of care. Under this framework, needs have been described as areas in which there is capacity to benefit, and as ‘normative’, i.e. they should be met. 76 Demands are what patients ask for (implicit in this is the notion that it may or may not be appropriate for providers to respond to demands). One study, exploring the views of staff about needs and demands in relation to public services, concluded that responsiveness related to identifying unmet needs (with a focus on cultural needs), and finding the right balance of managing needs and demands. 77 The authors define needs as rational demands (consistent and evidence-based) as opposed to demands as ‘desires’. They argue that public services should try to meet users’ demands, but that other forms of demand management may be required to realign these demands with users’ needs. They suggest that practical demand management in needs-based public service requires knowledge of users’ demand for services; content analyses of users’ demands to identify any misinformed demands; conversion of any misinformed demands into evidence-based specifications of needs; and formulating coherent evidence-based demands on behalf of users who cannot do so themselves. They acknowledge the tension between needs assessment being professionally controlled rather than responsive to users. 77
The key implications of considering responsiveness as relating to inequalities include, first, that responsiveness relates to a broad set of non-clinical features of service organisation and delivery. Second, responsiveness is seen as a core duty of an organisation – providing a level of service that meets patients’ needs fairly across all patient groups (although there are some differences in emphasis in relation to whether this refers to basic universal needs or specific needs of different patient groups or individual patients, and a recognition that responsiveness may involve managing demands). Third, the focus is on diverse groups and ensuring that no patient groups are disadvantaged in their experiences of receiving services. Under this definition, achieving responsiveness requires more than just good customer service; it requires an understanding of population characteristics, and proactive planning to meet needs and avoid disadvantage. Finally, measures of responsiveness need to pick up on differentials between different groups, and identify whether or not certain groups are disadvantaged (e.g. BME groups, deprived groups, males, females).
Consumerism and patient involvement
The focus on responsiveness has been linked with the shift towards consumerism and consumer demand for services that are tailored to individual needs. Responsiveness is seen as a way of bringing the NHS in line with other services such as retail and banking, which are geared towards being adaptable to individual needs, and offering more convenience, choice and flexibility. Fundamental to this shift is the idea that services should be geared to the interests of users rather than the convenience of producers. 78 Increasing user participation is described as core to this; an advisory document reporting on group discussions and a citizens’ forum found that:
Overall, people think that a responsive public service is one that: provides easy and appropriate access to services; encourages the individual to use and shape services in ways that suit them; actively seeks to learn from public involvement and develop services accordingly. 70
p. 5
People’s ideas on how public services could be made more responsive included making communication simple and obvious, keeping people informed throughout, involving people as early as possible, and shared responsibilities and shared outcomes. 70 User ‘choice’ and ‘voice’ are also seen critical: exit and voice (communicating user demands) have been described as two ‘recuperation’ mechanisms for making organisations responsive. 79
In the context of public service and administration literature, responsiveness has been contrasted with collaboration. 80 The authors described responsiveness as responding to requests for action or information. They viewed responsiveness as a mostly passive, unidirectional reaction to people’s needs and demands, whereas collaboration was a more active, bidirectional act of participation, involvement and unification of forces between two or more parties. Some definitions of responsiveness in primary care and patient involvement literature are more in line with this notion of collaboration.
Responsiveness in primary care has been defined as synonymous with patient participation, engagement and involvement. 81 NAPP suggest that being responsive requires practices to engage with patients; that patient experience is a key part of a responsive practice; and that improved communication and responsiveness are needed for a successful practice and patient participation group (PPG). 81 A discussion piece summarising the meaning of responsiveness included involving patients with service planning. 74 The authors found two ways that this was enacted. First, some seek to involve patients in the planning of care. Second, others make attempts to reach out to groups who find it difficult to access health care. A Scottish study of Local Health Care Co-operatives highlighted the need to engage patients and local communities, and defined responsiveness in terms of proactively engaging patients in planning services. 82
The close link between responsiveness and patient engagement is highlighted by the inclusion in a directed enhanced service (DES) framework on responsiveness of an eligibility criteria relating to engagement with patients,13 as the report states:
Improving access and responsiveness needs to be strongly founded on engagement with patients and should be a dynamic process. Providers should be required to demonstrate active engagement with people and local communities in developing services . . . Providers should demonstrate how they respond to patient feedback and this is to be used to shape and improve services . . . Local Involvement Networks (LINks), the voluntary sector and patient advocacy organisations are all further mechanisms to seek active involvement in service planning, delivery and monitoring.
p. 6
There are limitations to the conceptualisation of responsiveness as dependent on choice, voice and patient involvement. Changing providers is not always cost-neutral for users, and exercising voice adds practical burdens with little reward, hence users who exercise voice may be few, self-selected and apparently ‘unrepresentative’. 79 Many people with common health conditions, such as mental health problems, are reluctant or unable to engage in the ‘user movement’, hence undermining the effectiveness of patient involvement. 69
The key implications of definitions of responsiveness within the consumerism/patient engagement literature are, first, responsiveness framed in this way is about patients as consumers taking responsibility for defining78 and asserting their needs. The implication of this is that less responsibility is placed upon providers to proactively plan for and support disadvantaged groups. This is in tension to some extent with the notion of responsiveness as a duty of providers and as a way of reducing inequalities (as discussed above). Reliance on patient choice and voice may result in responsiveness to those who are most eloquent and demanding, at the expense of the vulnerable and needy. There has been much focus on the need for groups who are disadvantaged to have a voice, and on providers working to involve, and hear the voices of, ‘seldom-heard’ groups. Second, a distinction can be made within this literature between the notion that responsiveness can be defined as the extent to which providers engage with patients and enable choice and voice, and the view that patient involvement and engagement is a key means of achieving or improving responsiveness (by helping providers better understand patient characteristics and needs, particularly those of groups who are disadvantaged). Third, this suggests that measures of responsiveness should assess aspects of patient choice and engagement, and the extent and quality of dialogue between providers and patients.
Summary and discussion
We have demonstrated that the literature on responsiveness falls into three broad, overlapping themes. Service quality literature speaks of responsiveness as part of a high-quality service. Responsiveness is closely linked with good customer service – providing for customer needs in a quick, efficient and polite manner. Literature on inequalities casts responsiveness as a duty of providers and as involving meeting the needs of all patients across different patient groups. A third body of literature links responsiveness to the shift towards consumerism and patient participation: being a responsive GP practice means engaging with patients, for example, through working with PPGs and involving patients in planning services.
These three distinct conceptualisations of responsiveness have different implications and connotations. With responsiveness conceptualised as service quality, it is seen as something that adds value to a service, and as a way of attracting customers and building market share. It is not seen as a ‘duty’ or essential feature of an organisation, but as a ‘value adding’ feature of service. This conceptualisation has a focus not on diverse or disadvantaged groups, but on improving the experience of all customers/patients. When responsiveness is defined as relating to inequalities, it becomes seen as a core duty of an organisation, and the focus shifts to considering the needs and experiences of disadvantaged patient groups. Conceptualising responsiveness as relating to patient involvement shifts the responsibility away from the provider and sees it as held by or shared with the patient.
In English policy, definitions of and debates about responsiveness reflect the different conceptualisations emerging from these three bodies of literature, as can be seen in the definition presented in the report Improving GP access and responsiveness:7
Practice responsiveness is the way in which a practice communicates and engages with its patients and their carers and responds to their non-clinical needs and preferences, reflecting the different ways in which they might prefer to access the service and an appropriate clinician, book, or indeed cancel an appointment. It includes the practice’s attitude to customer service and friendliness of staff, the environment in which patients wait to be seen and the way in which they interact and support patients from particular groups, such as those with hearing or sight loss or people from a black or minority ethnic background.
It is potentially problematic that the definition of responsiveness in primary care draws on all three conceptualisations of responsiveness, all with different implications about how responsiveness might be achieved and measured, meaning that responsiveness in primary care remains a fuzzy and poorly delineated concept. In subsequent qualitative work, this study sought insight into what responsiveness in primary care actually means to staff and patients, and how it can be measured and then improved.
Chapter 4 Staff interviews
Summary of this chapter
We conducted interviews with a purposive sample of clinical, management and administrative staff from GP practices, pharmacies and walk-in centres. We aimed to gain insight into the meaning of responsiveness for PCOs, the strategies and approaches to improving responsiveness to diverse patient needs in primary care, and the key barriers and challenges. We also explored what measures PCOs currently used to assess their responsiveness, and their preferences for features of a new questionnaire.
Methods
Recruitment
Semistructured interviews were conducted with members of staff recruited from 13 PCOs in the East Midlands of England (see Table 1). Purposive sampling ensured that a range of PCO staff (management, clinical and reception) were involved. Staff were approached directly by a study researcher, with permission from a senior member of staff, or were approached by our main contact at the PCO. Two members of staff were invited to be interviewed at each PCO. One PCO was a practice managed by a large national company; here, we invited a member of staff at the head office, in addition to the practice staff.
Interviews
Most of the interviews were conducted by EA or JW on PCO premises, and one was conducted over the telephone. A topic guide was developed and used flexibly to guide the conduct of the interviews. Participants were asked to give their views on what responsiveness meant to them and their PCO, how responsiveness was enacted in their PCO, and successes and difficulties they had faced in their attempts to be responsive to patients’ needs and preferences. The topic guide for the GP surgery and walk-in centre staff is included in Appendix 3; this was adapted slightly for pharmacy staff. Interviews were digitally recorded and transcribed verbatim.
Analysis
Analysis progressed alongside the interviews using NVivo to organise the data. Data were analysed using a combination of framework analysis83 and the constant comparative approach, which involved both deductive and inductive elements. An initial coding frame was generated from the research questions and focused on the meaning of responsiveness, examples of implementation, meeting the needs of different groups, and barriers and facilitators to providing a responsive service. We used this coding frame to map staff descriptions of the strategies available to them to develop responsive primary care services. The coding frame acted to guide and bound the analysis of staff interviews to ensure a focus specifically on ‘responsiveness’, not just broad experiences of primary care (e.g. ensuring that the focus remained on ‘non-clinical’ aspects of care). However, we were careful to ensure that the coding frame did not unduly constrain the analysis; themes and subthemes were added and iteratively revised as additional interviews were coded. As such, themes were tested and developed inductively to produce a description of the strategies PCOs use to be responsive, grounded in staff’s views and experiences. In interpreting the data, we drew on concepts around market orientation and customer orientation developed in the marketing literature. 84,85
In the initial part of the findings, we focus on data from the GP practices; we reflect on similarities and differences in the accounts of walk-in centre and pharmacy staff in a separate section.
Findings
Twenty-seven members of staff were interviewed, including GPs, practice and pharmacy managers, administrators, receptionists, and a nurse (Table 2). We interviewed six men and 21 women: 22 white British, four South Asians and one Filipino. Staff had worked at their respective PCOs for between 8 months and 25 years (median 4 years, mean 6 years) (see Table 2).
| Job role | Sex | Age group (years) | Total | ||||
|---|---|---|---|---|---|---|---|
| 18–24 | 25–34 | 35–44 | 45–54 | 55–64 | |||
| GP | M | – | 1 | 1 | 1 | – | 3 |
| F | – | 1 | 1 | – | – | 2 | |
| Nurse | F | – | – | 1 | – | – | 1 |
| Practice manager | M | – | – | – | 1 | 1 | 2 |
| F | 2 | 1 | 1 | 2 | 6 | ||
| Receptionist | F | 2 | 1 | 2 | 2 | 1 | 8 |
| Head office | F | – | 1 | – | – | – | 1 |
| Pharmacy manager | M | – | 1 | – | – | – | 1 |
| F | – | – | – | 1 | – | 1 | |
| Pharmacy staff | F | – | – | – | 1 | 1 | 2 |
| Total | 2 | 7 | 6 | 7 | 5 | 27 | |
General practitioner practices
Meaning of responsiveness
Responsiveness was seen by the majority of staff to be about how the practice meets the needs of their patients, particularly around gaining access to the care they need. Staff commonly talked about meeting the needs of vulnerable groups who may need additional support to access the services they need, and ensuring that patients from diverse groups were treated fairly. These groups included patients with particular characteristics (e.g. older people, people from a BME background, non-English speakers); illnesses, conditions and disabilities (such as the blind or partially sighted, deaf or hard of hearing, and those with specific conditions such as cancer, diabetes and epilepsy); and situation, location and lifestyle (busy or working people, carers, people living in deprivation or who are homeless, travellers).
Giving appointments that the patients require, they are getting the telephone access that they require, they are getting the treatment that they require. [. . .] It’s aligning with the patient’s agenda I think.
S09, GP
From my point of view, responsiveness is being there for the patients and responding to what their needs are, and making sure the surgery provides what the patient population needs. [. . .] The needs of the patients here are a lot different to [our other practice]. [. . .] Here, you have got a mixture of young Asian families and elderly white folk, at [our other practice] I would say 99.9 of the population are Muslims.
S25, practice manager
Some staff, particularly practice managers and reception staff, understood responsiveness in terms of how they dealt with individual patients’ needs at the point at which the patient used the service.
So responsiveness is dealing with the problem I think as fast and as promptly as you can.
S03, practice manager
What approaches do primary care organisations use to make their services more ‘responsive’ to the needs of patients?
Staff described various activities undertaken at their PCO to improve the extent to which they could meet the needs of their patients. From these descriptions we developed a typology of approaches to providing a responsive primary care service. We found that approaches fell into three distinct categories that varied in the extent to which they were proactive or reactive, and the extent to which they were focused at the level of the practice population or the individual patient. These categories were (1) proactive population orientated approaches (approaches that involved PCOs planning ahead to design systems and services around the anticipated needs of the different groups of patients that used their services); (2) reactive population orientated (attempts to elicit and respond to patients’ expressed needs, feedback and complaints); and (3) individual patient orientated (providing flexibility and support at the level of the individual patient), which is also primarily reactive. These themes are summarised in Figure 5.
FIGURE 5.
Strategies for responsiveness: themes.
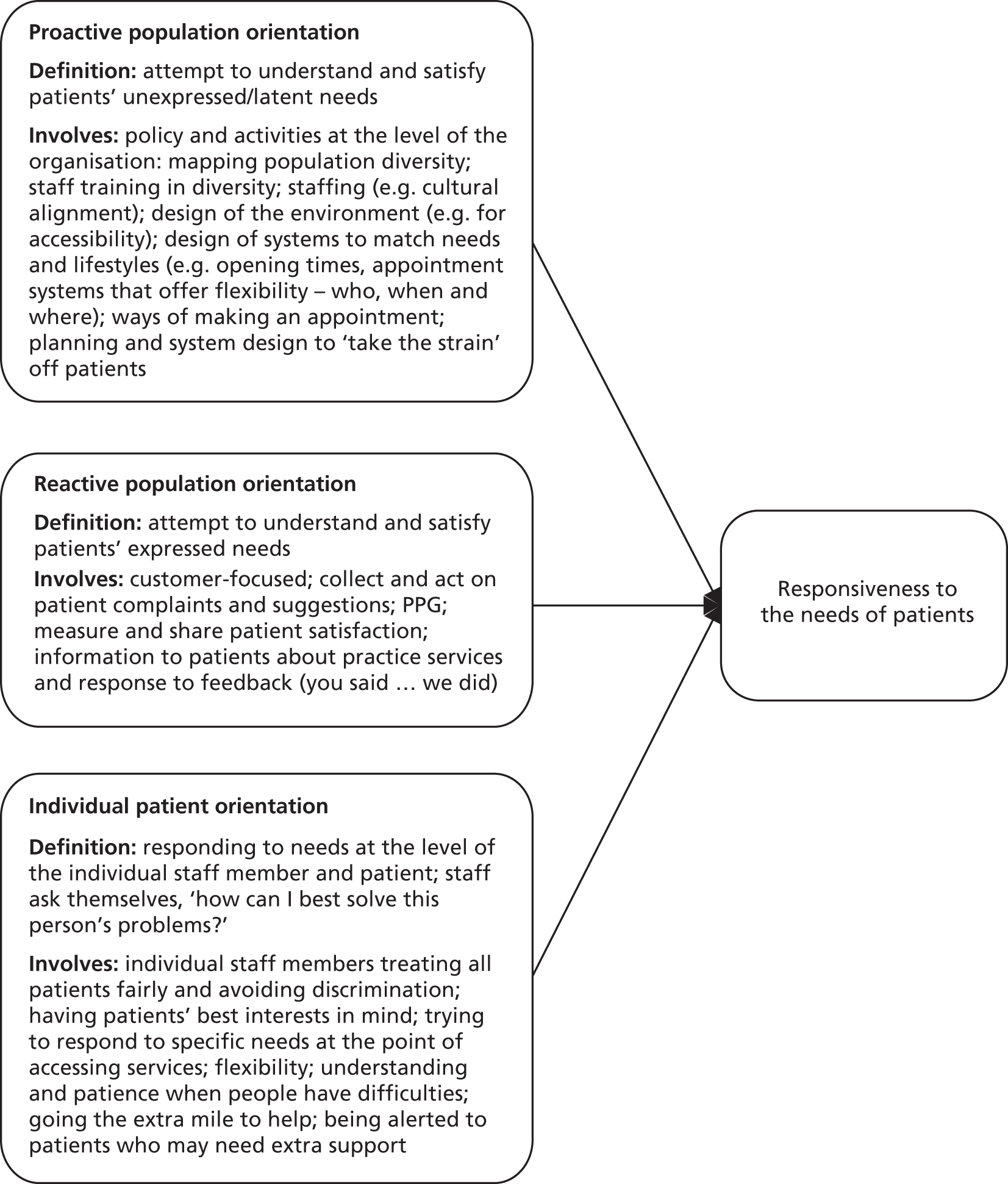
Proactive population-orientated strategies
One prominent theme in staff accounts of strategies for responsiveness reflected the attempts of practices to develop an awareness of the diverse patient groups they served and their specific needs, and to proactively design and organise their services so that they could respond to the needs of specific patient groups.
It’s looking at different groups of people and trying to work out what they want and need, and looking at ways to provide that, . . . it’s trying to find ways to firstly kind of identify the problems and then work out ways to change things.
S15, GP
A minority of practices had developed an understanding of their patient populations through formal mapping, but the majority described their understanding as based on informal staff knowledge of the local patient population. (The issue of practices’ awareness of the characteristics of their patient population is explored in more detail in Chapter 8. )
[Site 1] has a lot of Muslim patients and South Asian patients, [site 2] has some as well but less . . . a lot of Polish patients as well. I don’t know about our Afro-Caribbean population, no idea. There definitely are some but I have no idea what proportion we would have.
S02, GP
The steps that practices took to proactively plan for and support the needs of diverse groups included adapting the physical environment and technology, providing interpreters and other communication support, staff training on diversity, considering the design of appointment and booking systems, and using tailored approaches to contacting specific groups of patients and delivering services to meet their needs.
The physical environment was talked about commonly in the context of how improvements to the building had been made in ways that met the needs of diverse groups. This was particularly in relation to patients with disabilities, although staff also talked about how consideration had been given to the way the environment could be set up to better meet the needs of other groups, including teenagers and families with young children.
One of the things when we had the building refurbished was improving disabled access, because we used to have a horrible desk where . . . the receptionist [was] standing behind a chest-high hatch with a grill, whereas we have got that low desk now.
S12, practice manager
The teenage population . . . for them, . . . as you come just inside the surgery, there is a huge notice board there and we put things there, because we feel that the teenagers coming in might not want to come fully into the surgery, they can just come into that first bit the foyer, see what they need to see and if anything there, does interest them, then they can come in further.
S14, receptionist
Staff also talked about provision for communication support for specific patient groups, including non-English speakers and patients with a sensory impairment:
We have got quite a lot of patients who don’t speak English as their first language. So things like the screen that patients use to book in when they arrive at the surgery: . . . if they speak a different language then that is all written in the language that they speak.
S15, GP
Staff training in diversity issues, and in supporting the specific needs of specific patient groups, was also seen as critical to providing a responsive service.
I think probably [we need] more training and awareness for staff . . . It’s maybe that education about the range of issues that may be faced from mental disabilities, visual impairment, hearing impairment, physical disabilities . . . to make sure that we try and consider things from the perspectives of every one of our patients.
S27, head office
For some groups of patients, the key issue was seen to be planning to enable diverse patient groups to access the services, particularly groups of patients who would be disadvantaged by standard opening times and appointment systems. Staff described ways that their practice had adapted the systems for appointments around the needs of these patient groups.
We have obviously got some surgeries that support care homes, you know, you have got people that have mobility issues, so we tend to do regular GP visits, . . . we will say the GP is going to be here on a Monday afternoon and a Thursday afternoon. [. . .] So we do try to accommodate the needs that we have.
S27, head office
Many staff recognised that tailored approaches could be required to help patients from disadvantaged groups to access services and have their needs met. Being responsive often involved practices ‘doing things differently’ in the way that they communicated and engaged with patients.
We have got a few [patients] in [location] that couldn’t read or write. So we were sending out absolutely loads of letters, for all chronic diseases, for immunisations, follow-ups for smears. Our postage was extortionate, but I think we were having no results [. . .]. So then we started to actually telephone, to actually ring them up . . . and that was quite successful.
S03, practice manager
We do the learning disability health checks here . . . and they gave us literature for people with learning disabilities and told us how to set things out, for somebody with a learning disability . . . Just sending them a standard letter, they are going to think ‘oh no’, but this had pictures and things on it so that was very useful.
S25, practice manager
In some practices, initiatives that had been developed to help improve the services or support provided to specific groups within the practice population. Setting up registers of patients with specific needs could help practices to identify patients who might benefit from additional support and to direct them to appropriate services.
Initially I set up the carers register in [the practice computer system], well there was one there [already], but updated it, [I] . . . now we have a specific carer support worker, so any GP can refer to [her]. She comes in every Wednesday and she takes it from there. [She] contacts the carers, and basically they have an assessment, she lets them know what the benefits are due to them, [and] where they can go for support.
S20, practice manager
There were examples of practices going ‘one step further’ in their efforts to meet the needs of their patients: actively working with local community to engage ‘seldom-heard’ patients in using services.
We have worked very closely with the PCT and the local community to manage the Romany population. [. . .] What we agreed was that every Wednesday morning we would run a clinic where they could just walk in and they would be seen, and we would have two translators there, and then the community leaders spread that round the community so that everybody knows. So that worked so well.
S27, head office
Overall, being responsive through proactive planning was not a discrete task but a process, involving the ongoing monitoring by practice staff of the changing needs of their practice population, and the willingness to proactively seek solutions to these problems.
Recently I have noticed about the Slovakian people . . . there is language assistance problem, so [we are working towards getting] the language assistance.
S26, receptionist
Reactive population-orientated strategies
The second theme that emerged related to attempts to listen to, involve and engage with patients, and to react to their expressed priorities and needs. In contrast to the first theme, this approach to responsiveness was one which was reactive – being led by the expressed needs and priorities of patients.
Staff felt that listening to and involving patients was important in ensuring that they were aware of the needs of their patient population, and how best to address them. Many staff felt that responsiveness involved taking patient feedback seriously, and being willing to make changes, and try new things, to address the issues that were important to patients.
We are very open here, I mean we are as a practice very much for change, we don’t just say ‘well we will do it this way and that’s it’, we look at ways. And if something doesn’t work, or if we get a complaint, or we get a suggestion we do look at it and see if we can act upon it, and we discuss it. So we are very open to change and we are changing all the time really to try and improve services.
S03, practice manager
Practices used a range of processes to listen to patients. These included collecting and acting on patient survey data, suggestions and complaints, and involving patients through a PPG or engagement with the local community.
We have worked hard with the patient participation group in the practice, we run every 2 months, and they have been great in two ways – one is telling us how they have observed our practice and what other people have been saying so they are giving us feedback. [. . .] The other thing, the patient participation group just gives us ideas about how we can keep improving.
S09, GP
In a special case of a GP service for homeless patients, a GP cited how important it was to get feedback, not only from patients themselves but also from partner organisations that also worked with the same patient group.
We have learnt a lot over the last 10 years about being responsive to the needs of our patient group. So we try to listen very hard, to what their needs are. We have a multidisciplinary meeting every week with our partner agencies, with the hostel staff and the mental health team and the drug workers, so information gets shared and fed back at that point.
S10, GP
Acting on patient survey data or patient feedback was seen to be a key element of responsiveness, but not always sufficient in itself. Another feature of providing a responsive service was described in terms of ‘closing the loop’ – finding ways of communicating to patients about how changes would (or would not) be made in response to their comments or complaints. This was seen as important not only in ensuring that patients felt that the practice was listening to them, but also so that patients could get to know about changes that had been made to better meet their needs.
We have introduced [appointment] the system, it’s currently working, we need to advertise it a bit more, we need to get the patient participation groups more involved so they are advocating it. [. . .] We have got leaflets that we can hand out to [patients]. Whenever I get a complaint that says ‘can’t get through’, I immediately use [leaflets] to show them this new service.
S01, practice manager
This element of responsiveness, therefore, involved engaging in dialogue with patients about their needs and the practice’s response to these needs.
Patient-orientated strategies
While the first two themes include approaches that are oriented towards the patient population as a whole, or specific groups of patients, staff also commonly talked about their efforts to be responsive in terms of meeting the needs of individual patients at the point of delivery. For many staff, responsiveness was most evident at the point at which individual patients accessed the service.
You respond individually to that person that is in front of you . . . depending on their needs.
S21, pharmacist
Responsive service delivery was seen to be dependent on attitudes and behaviour of staff (particularly reception staff) towards patients; willingness to operate systems flexibly around the needs of patients; and the approach of the practice towards helping and supporting patients who had higher levels of need or faced particular challenges in accessing services.
Delivering a responsive service was seen to depend heavily on the extent to which a practice had a patient-oriented philosophy. This was most important in relation to the way that reception staff treated patients. Interviewees commonly emphasised the need for reception staff to be friendly, approachable and helpful towards patients, to treat patients as individuals, and to be sensitive to their needs and circumstances. They felt staff needed a willingness to help and to support patients who faced difficulties in using the service.
I think just overall it’s just a positive approach to patients . . . what we have got to remember, when these patients are ringing up, no matter how cross they are, or frustrated or confused, or even happy, we have got to remember we are here to help and we have to do everything that we can, within our capabilities, to help them.
S04, practice manager
We have a large elderly population . . . and you know we are just very aware and more helpful to the elderly.
S14, receptionist
Interviewees emphasised the role of reception staff as gatekeepers, in terms of managing demand on the service, but felt that reception staff needed to be willing to work with patients to help find the most appropriate solution for them within the constraints of the system.
We don’t ever say ‘we can’t do it’, see you have got to try and find a solution for the patient’s needs at that time. Because you know, that is what you are here for, to provide a service.
S19, receptionist
Responsiveness was reflected in a willingness to operate systems flexibly around the needs of patients, particularly patients from groups who are disadvantaged who may struggle to access the services they needed.
We don’t take prescription requests over the telephone, [but] if a patient is real sick, like say for cancer [patients] or elderly can’t get out, we do take them over the telephone, so that is quite responsive.
S06, practice manager
Staff highlighted the value of systems that alerted them to individual patients who had particular needs, so that these needs could be accounted for at the point at which the patient accessed the service.
You can put alerts on the patient home screen and you can put it in order of severity . . . On the front screen, you can have an alert. For example if someone you know is extremely unwell with mental health issues, or they are Down’s or anything like that, an alert can pop up on the screen to say ‘please accommodate where possible’.
S20, practice manager
Patient needs and expectations
Importantly, as well as recognising that there was a range of strategies that practices should consider in making their services more responsive to the needs of their patients, staff felt that responsiveness was a not simply a matter of organisational systems and service delivery. Rather, it was better seen as involving alignment between service provision and the needs of patients. Some staff recognised that this involved judgements of legitimacy of these needs, and of the extent to which services could stretch to meet expectations/demands.
Patients’ needs and demands were balanced against the realities of what practices could provide in the context of limited resources, and staff recognised that they could not always meet needs or expectations because of these limitations. In some cases, patients’ expectations were seen as unrealistic or, even if legitimate, impossible for the provider to respond to owing to practical or resource constraints.
I don’t think we are very responsive and I don’t see how we can do better. [. . .] They want too much. [. . .] Or maybe their expectations aren’t unreasonable, people pay their taxes [and] they feel they have this free service and there is no limit placed to anything, which is unrealistic.
S07, practice manager
Staff also felt that achieving alignment between service delivery and needs or expectations could involve managing patient expectations, to bring them more in line with what the practice could be expected to provide. Addressing this mismatch between patient expectations and service provision could sometimes require explanation to patients in order to change expectations and help them to use the service more effectively. Practices also highlighted the value of working to educate patients who struggled to get their needs met because of a lack of understanding about how systems worked.
There is always an element of patient education in this, and . . . training them to [understand] what we can and can’t do.
S12, practice manager
[New] Eastern European [patients] . . . don’t seem to understand, they think they can walk in and see a doctor there and then because that’s what they do in their own country. It’s just, it’s just training really and re-educating them that it doesn’t work like that.
S19, receptionist
Walk-in centres
Staff at the walk-in centre shared many of the views of staff at the GP surgeries. Responsiveness, as interpreted by walk-in centre staff, is responding to what patients want.
. . . basically providing the service that the patients want and need.
S18, nurse
It means answering or dealing with their problem as quickly as you can, and as appropriately as you can.
S19, receptionist
Because of the way walk-in centres are set up, staff felt that they contributed to the ability of primary care services across a locality to respond to patient needs, by offering patients the option of quick and easy access to an appointment. An additional benefit was seen to be that medical care could be provided to patient groups who might otherwise struggle to access mainstream general practice.
We are reacting to people who say ‘we want evening appointments.’ [. . .] If somebody rings up after 5 tonight then you know we have probably got two appointments on each doctor that we could book into. [. . .] so I think that is responding to a need of the patients . . . because people don’t work normal hours anymore.
S19, receptionist
Because of the nature of the walk-in anybody can walk in from anywhere . . . anyone can walk in. There have been a few travellers that just use the walk-in centre, because they will get treated and they will get seen.
S20, practice manager
Strategies for responsiveness described by walk-in centre staff tended to be reactive. The walk-in centre did not have policies for dealing with specific patient groups; staff felt that all patients were treated the same. They did, however, recognise the need to plan and to be prepared for patients who may have difficulties using the service, such as patients who do not speak English.
I think everybody is generally treated the same, I mean, people with disabilities have an equal access to anybody else. It’s harder sometimes, especially with the Polish population, because a lot of them really struggle with their English. To me they are making a really good effort, I take my hat off to them because I can’t speak another language, but I have an app on my iPhone that translates and I have used it a few times now and it’s cracking.
S18, nurse
There were particular challenges to providing a responsive service at the walk-in centre. Patient perceptions and expectations were seen as the main barriers (not understanding what nurse practitioners can offer, not wanting to use the touch-screen appointment system, or expecting to be able to see a particular doctor any time).
They want to see the doctor of their choice, at the time of their choice. Patients are still very uneducated about nurse practitioners, they still see a doctor [as] better than a nurse.
S20, practice manager
There were also practical considerations, such as maintaining the safety of women in refuges.
Women who live in refuge centres, that is difficult because they don’t have a postcode, it’s like a PO Box number and you have to go through a few avenues to get to them and only certain members of staff do because of the confidentiality side of things.
S20, practice manager
One member of staff spoke about the difficulties that arose at the GP surgery adjoined to the walk-in centre.
I mean ‘yes, in an ideal world you would be able to be seen now’, but where I work is not a walk-in centre. But they expect, I think, because there is a walk-in centre [next door], that everyone will perhaps work the same.
S18, nurse
Pharmacies
The pharmacy staff’s definition of responsiveness was more literal (akin to a dictionary definition) than that of staff at GP surgeries and walk-in centres. They felt that it was about the way in which and how quickly they responded to patients’ requests.
. . . a lot of it is responding immediately to phone calls or to patients wanting something or asking us something.
S21, pharmacist
Pharmacy staff enacted responsiveness in similar ways to GP surgeries. Their patient-orientated strategies included responding to the needs of customers on an individual basis: providing a speedy and efficient service at the customers’ convenience, such as delivering goods and services to homes; being open 365 days a year; stocking the products and brands that people wanted; or recognising that first-time mothers need reassurance or that visually-impaired customers may need extra help and time.
. . . we liked to think that we go that extra bit for the patients in the traditional [way], I mean we deliver if they want delivering and we do everything we can to make the patient happy.
S21, pharmacist
Well, as soon as you see them or hear [a blind person] coming through the door you speak to them across everybody else, so they know that they have been noticed and somebody will be with them, and then you help them to the counter. And then you just go through everything with whatever [medication] they want, you spend time showing them stuff and explaining how tops open and things.
S22, pharmacy staff
The business model appeared to affect staff’s views of responsiveness. While GP surgeries are also small businesses, their primary source of income is the NHS. Surgeries try to keep patient lists to a manageable size, and work towards meeting the needs of patients as they present at the surgery. Pharmacies, on the other hand, are in direct competition with other pharmacies: the key to attracting ‘customers’ (as opposed to patients) is the quality of customer service.
. . . the only way we can differentiate ourselves in this market is by customer service so we try and make sure that they always get a smile when they come in and just make them feel as if we genuinely care. It’s not just a case of, you know, bring them in and let’s show them the door as quickly as possible.
S23, pharmacy manager
Many members of GP surgery staff spoke about ‘bending over backwards’ for patients, but pharmacy staff took this even further.
So the opening hours are 9 a.m. ‘til 8.30 p.m. [. . .] but the key, the determining factor is 7 days a week, 365 days a year, so Christmas Day, Boxing Day, New Year’s Day . . . Yeah, bank holidays, never close, it never closes.
S23, pharmacy manager
Pharmacies’ reactive population-orientated strategies involved staff using customer surveys, approaching people who were obviously smokers to see if they wanted to attend the smoking cessation clinic, and looking out for patients who might need a medicines-use review. Staff were also aware of the characteristics of their potential customers, for example providing an emergency hormonal contraception service in an inner-city area with a large student population. Pharmacies wanted to know about the characteristics of their population and to gain feedback from customers, mainly to understand how to improve their customer service and to attract and retain customers.
. . . we obviously have our own annual customer survey that we do and generally, we’re always quite impressed with the results that we see so, it’s always good, I mean, you always get a few, couple of negative comments which you’ve got to take constructively and try and work on and try and improve upon the but general feedback is always well received.
S23, pharmacy manager
There were no obvious references in the pharmacy staff interviews to demonstrate proactive population strategies, such as surveying their populations to identify and quantify the various patient groups. However, there were a multiple examples where the pharmacies recognised that different groups had different needs and had proactively designed and organised their services to meet these needs, by providing cheap baby products, smoking cessation clinics, additional training to provide flu vaccines, health promotion initiatives for people with hypertension or diabetes, different processes for people with drug addiction, and additional staff.
. . . it’s all about prevention rather than cure, so we are trying to [focus] on health promotion activities and trying to get the public and the patients that we look after to a better place with any little bits of lifestyle advice that we can give, especially to the hypertensive or the diabetics. The smoke cessation clinics, that’s really done well out of this branch.
S23, pharmacy manager
Although the priority of pharmacies appeared to be speed and quality of service and providing for the customers’ wants and needs, there were limits. Staff recognised that people expected a quick service and to be able to buy whatever they want, but that there were limits to the speed at which a prescription could be filled and rules about what could be sold.
It’s not like a doctors’ system or the dentist system where it’s just inherent that there is an appointment. That’s often kind of the drawback in pharmacy, people feel that access should be immediate, they feel they shouldn’t have to wait, and sometimes they walk in with a big prescription, they want it yesterday.
S23, pharmacy manager
The challenges to pharmacies are quite different from those experienced by GP surgeries, mostly due to their business model. Smaller pharmacies have to compete with larger pharmacies, chains and supermarkets that have superior buying power and can offer cheaper products. PCT-led services can be at the mercy of budget cuts and are restricted to certain patients. Private health checks can be more flexible and responsive, but the customer has to pay.
. . . the supermarkets, the Boots, the likes of them, are able to offer things, they sometimes retail at prices that we’re buying at. It’s sheer muscle power that they have when they’re doing their procurement which, when we have a customer perhaps thinking ‘well I can get this cheaper in Asda’, it’s a frustration . . .
S23, pharmacy manager
Practical constraints for pharmacies included opening times that are not convenient for working people, lack of toilet facilities and wheelchair access, having time to do the extra things, and training required for certain jobs. Staffing could also be an issue because of the long opening hours.
Yes, sometimes you think, you know, oh perhaps there was a little bit more you could have done, but time is restricting you. You are just so busy.
S22, pharmacy staff
One of the difficulties of having a pharmacy that’s open all the hours is that you don’t always have the same staff working there. So one of the main difficulties we’ve found is . . . it always has been a challenge to try and make sure that the customer would get the same level of service whether they come on a Monday afternoon or a Sunday evening. That’s always been very difficult, you know, just trying to make sure that the staffing is right, not just in numbers but in terms of calibre.
S23, pharmacy manager
Pharmacy staff felt that they wanted to accommodate both needs and expectations as part of delivering a service that would attract and retain customers.
I suppose their day-to-day requirements, or if they have got an illness then they need something to sort that out, but the wants and needs are very, they are very close. And most of the time, would be the same, sometimes won’t.
S21, pharmacist
Barriers and challenges in delivering responsive primary care services
The majority of interviewees concurred with the view that responsiveness was an important aspiration in primary care, and felt that their PCO made at least some attempts towards responsiveness. There were few examples of staff stating explicitly that responsiveness was not important.
[Responsiveness means] responding to the, hopefully the needs not the wants of our patients, so it’s reflecting on, on their needs and then trying to see within our budgetary constraints if we can meet those.
Is that something that is important to you as a PCO?
Extremely, yes.
Translating this aspiration into practice was not straightforward. Efforts to improve responsiveness were complicated by staff and patient attitudes and expectations, lack of resources, practical constraints and tensions with other internal and external demands on service provision.
Attitudes and expectations
Being responsive requires tolerance and flexibility, and a willingness to help to support patients who were struggling to get their needs met. Notions of responsiveness became challenging when patients were perceived to be unduly demanding or aggressive.
I think they are quite demanding, certainly in the last few months the abuse that has taken place from patients to receptionists . . . is outrageous and I do think if you went to McDonalds, and you kicked off you would be asked to leave. [. . .] You get like a select few that are really quite hard to deal with.
S20, practice manager
While recognising the value of flexibility, and of staff going ‘beyond the call of duty’ to help vulnerable patients, staff were very aware of the potential negative consequences of this flexibility.
We ask people to allow 48 hours [for prescriptions] but there is always somebody who, with the best will in the world, realises that they have made a mistake and they have woken up and found they have got no tablets left, and we will do that on the day. But we actually found that that was happening so often, that we have had to clamp down . . ., try and educate people and make a note of the ones who keep on doing it, and just try and encourage them to organise their lives a bit better.
S12, practice manager
Staff were concerned that efforts to respond to patient needs could mean that excessive demands were put on staff. In one example, a member of staff felt that the PCO’s explicitly flexible attitude could have negative repercussions for her team, and needed to be brought into check.
As far as me and the little nursing team are concerned, I think we are generally [responsive] [ . . . but] you feel so put upon sometimes, you think ‘right, now I am putting my foot down’ and you just say ‘no, no, it can’t be done that way because we are not doing that, why should we miss our lunch break because of that?’
S18, nurse
Resources
Lack of funding, staffing and time due to internal and external pressures were commonly cited as barriers to a PCO’s ability to be more responsive to patients.
We will undertake looking after patients with substance misuse, we do people with alcohol, . . . not for the money but again we do it simply because it’s good patient care. [. . .] Really, sometimes it’s an awful lot of work and it can put pressure on top of you. . . . Unfortunately, the resources don’t always meet the need.
S03, practice manager
Practical constraints
The physical environment caused problems for some PCOs. Some staff felt that the building in which the PCO was hosted was unsuitable, and made it difficult for them to provide the accessibility and comfort that patients expected. Staff expressed frustration when they were unable to make improvements, such as providing extra services or additional opening hours, owing to practical constraints.
It’s an old building. So it is sometimes challenging to get around the building because we have got lots of floors and lots of sets of stairs, but there is a lift, there are little stair lifts up even just two or three stairs, and ramps and things as well. [. . .] It’s not an ideal building for disabled people but I think we hopefully try and get round that the best we can.
S15, GP
From a practical point of view . . . our waiting area is shared with another service; when they close, we can’t, at the moment, open [. . .]. That poses us with a problem.
S10, GP
Internal and external context
The ability of PCOs to be responsive to their population needs was seen to be influenced by features of the organisation and the population they served. In particular, staff felt that, in larger practices, it could be more difficult to respond to the needs of individual patients at the point of service, and to respond to patient preferences for continuity of care.
[Our patients] would probably say we are growing too much, too fast, they are not seen as patients any more, they are seen as numbers, and we are not offering the amount of routine appointments with their own GPs, this is the biggest thing – it’s the patient’s GP that they want to see.
S20, practice manager
Several barriers external to the PCO were identified by staff. Curiously, only one staff member referred to the NHS restructuring that was taking place during 2011 in the wake of the change of government. More commonly mentioned was the plethora of bureaucratic rules by which PCOs are expected to abide. These could take the form of targets or actions dictated by the (former) PCTs or the wider government through locally or centrally enforced policy objectives, some of which were felt to be inappropriate for local populations.
Time is the only [thing], I would say time and pressure of work. Deadlines . . . working to, jumping through hoops sometimes for the PCT. [. . .] When you have got all of those other pressures and things that you have to do, you can’t always do what you want to do?
S03, practice manager
In some cases, a lack of support from organisations higher up the chain of command was felt to be obstructive.
The health authority [are] a very difficult bunch to deal with. [They] are asking me to [do something that is] just highly impossible. So from that I don’t feel like I have got much support.
S20, practice manager
Views on patient experience measures
Use of data from existing patient experience surveys
Staff at the GP practices used various sources of patient feedback to learn about issues that patients considered important. The most common source was the GP patient survey. Some staff found these data useful for identifying problems common to most patients, such as not being able to get through by telephone or not being able to make an appointment with a preferred GP.
I think it’s important that we get the patient’s point of view, and what they want from the surgery, so that we can work towards doing what they want to, if it’s feasibly possible. Yes and [the survey feedback] shows us areas where we need to work on, again one thing that always comes up is the access to the phones, and we are looking into getting extra lines put in, and having a direct service so you get directed to different places for different issues or queries that you have got.
S04, practice manager
Questionnaires about specific elements of the service were also used. Staff found these useful, especially if the results showed that patients’ reactions were positive.
We did have, for the extended hours there was a questionnaire asking, you know, ‘would you use this service again?’ ‘Did you get an appointment [and] in what time scale?’ . . . ‘Were you happy with what happened, by coming to a different surgery?’ There were questionnaires about that, which seem to be quite positive, you know.
S19, receptionist
Although the national GP patient survey was used in many of the practices, most of the staff interviewees identified problems in using the data. The response rate was consistently low, and only certain patient groups returned their survey, leading to ‘biased’ results. In addition, some staff were concerned that this lack of representativeness may lead to the ‘seldom-heard’ being excluded, such as people with low literacy, non-English speakers, people with dyslexia, homeless people and older people. In some cases, these were the people from whom staff wished to hear. On the other hand, some staff were concerned that the surveys were also sent to people from whom they did not wish to hear, such as patients who have not used the services recently.
We don’t see much meaning in them because our response rate from our practice is about 15/20% and we know that patients who are more likely to complain are more likely to fill them in. So I am not sure whether that’s the representative sample that they are capturing. [. . .] I really don’t know how one could capture a representative sample because the response rates are so low.
S09, GP
I think they are given out to patients who may not have accessed the practice anyway. We know for a fact [that someone known to us] got one and he hasn’t been near a GP in several years. How is he supposed to know whether he feel the opening hours are appropriate [. . .]. Their answers will be: ‘it’s a shame they don’t offer evening appointments’ yes, we do. It will be: ‘a shame they close on Thursdays’, which we don’t . . .
S02, GP
In addition to low response rates and lack of representativeness, the questions that were asked in the national survey caused concern among staff. Some felt that the questions were difficult to understand and that the survey was too long. Others were aware that sending questionnaires by post was not necessarily the most effective way of reaching some patients.
We have got the national survey but I think that’s rubbish. [. . .] Because as I say I think the questions are hard to understand.
S02, GP
The survey, the mechanism [by] which [it] is delivered is not helpful for this population, it’s by post. I don’t know what percentage but I am guessing 50% of our patients use this building as their c/o address. So we simply receive the questionnaire, which sits in our reception waiting for us to see the patient and hand it out, so a significant reduction is made in the number of people who even receive their questionnaire. And then it’s a postal measure, and I know that our numbers for returns are very low. The quality of the information received or the positive feedback that we get seems to be very good but I know that the numbers must be a handful really.
S10, GP
Some members of staff felt that existing questionnaires were worded in a leading way and that questionnaires should be solution-based rather than problem-based.
I think specific [questions] can sometimes lead to, I guess, coercion sometimes, can’t it. Yes I would like a very open ‘how do you feel?’ Very, it’s very qualitative, there is no exact measure. [. . .] I would like to see some encouraging solutions, based on responses, as opposed to ‘this is a problem’. I guess if you get presented with a number of problems it’s actually very difficult to accommodate that, whereas if you say ‘actually that sounds like a very good solution to a problem’.
S17, GP
The delay in receiving the results was also considered a problem by staff. Staff received not the raw data but, rather, aggregated feedback, often with targets to reach in response to the issues raised. While this may be useful for incentive-based systems such as Quality and Outcomes Framework (QOF), the delayed nature of the feedback prevented staff from making changes to practice in real time.
For us the national patient survey has got a real time lag on it obviously, because it takes a long time to collate all the information, so it’s always kind of 6 months out of date, and it’s rolling averages, and it can be a bit difficult to extract very quick changes.
S27, head office
So the annual patient survey . . . you get points you know they give you a percentage. . . . I think there is a target, you know, what’s acceptable, sort of 90% of patients and you know, how you measure up. I mean I think we usually came either round about just over, or with the odd thing just slightly under, so we were obviously sort of more or less on target for that. But there hasn’t been, there is nothing that I am aware of recently to give us any sense of how we are doing, other than feedback from patients, which by its nature tends to be negative.
S12, practice manager
Other sources of feedback about patients’ experiences and views
The most common sources of patient feedback that practices reported using were informal and in real time. This included ad hoc feedback from individual patients (n = 1), through comments forms and boxes (n = 5), monitoring complaints received (n = 17) or not received (n = 2), exit questionnaires and postcards (n = 4), websites (including NHS Choices, n = 4) and the PPG (n = 17).
Patient participation groups were a popular source of feedback. Staff tended to use feedback from PPGs in a similar way to survey results, identifying issues upon which staff could act. However, staff expressed concern that membership of such groups was likely to be ‘biased’ and may not include patients who are hard to reach.
. . . having spoken to the PPG they would like to see continuity from the partners and are happy to see any doctor for the urgent stuff so we are hoping to try and move towards a model like that.
S02, GP
It’s mostly elderly that come [to the PPG meetings] I am trying to get somebody that is young with a baby but that hasn’t happened as yet.
S03, practice manager
We tend not to get a decent representation of the practice. Often these sorts of things, there tends to be a little bit of bias, I find, from the type of patient who will come to that type of group. And so in reality that tends to be unproductive.
S17, GP
Complaints were also a common source of feedback, through either not receiving them (no action required by the practice) or receiving them (action may be required by the practice or the issue may be resolved on the spot). Complaints were submitted in writing, verbally or via the NHS Choices websites.
We are not getting any complaints anymore, so [laughs] that’s good.
S25, practice manager
There is a complaint form but that obviously goes to the managers. So if a patient does want to complain we always tell them to either write, we always get them to write in, erm and it is dealt from there. [. . .] if it’s something significant, and that needs to be improved then yes it does, be informed in the [team] meetings.
S16, receptionist
Comments forms and suggestion boxes were also used by staff, as trends could be identified and acted upon.
I think the comments box in reception can sometimes not be where they would like to leave their comments. It’s not about a blame culture at all, it’s about getting some honest feedback, and you know you can see when trends start developing, that you can work with those staff to manage their performance and to give them the training that they need, but that means patients can be very honest about their feedback which is really valuable for us.
S27, head office
Ad hoc feedback from individual patients could also be a useful source of evidence that there may be an issue that needs addressing, bearing in mind the bias that this may introduce.
. . . the fairly informal feedback that you get from patients as they come into the room tends to be fairly actually quite useful, as in: ‘I have struggled to get an appointment this week’ and then if you hear that on a number of occasions, that tends to, I guess, bear some sort of interest in your mind that actually there is perhaps, perhaps more of a problem here than one person’s particular opinion. So I guess you have got, it is important to listen to individual opinions . . . but again sometimes individual opinions do have a little bit of bias and they do have different agenda.
S17, GP
Advice for our questionnaire
Most (n = 25) of the interviewees provided us with advice about our questionnaire. The most common advice was about the types of questions we should ask. Eighteen members of staff advised on the mode of delivery, and nine on the participants we should target and the formats we should use.
Question topics
Fifteen members of staff gave advice about the topics we should ask patients about. Five members of staff wanted to know how patients felt about the service they provided, whether or not they were happy, specifics about what the PCO was doing right or wrong, and whether or not patients felt they were receiving a quality and timely service. Two members of staff suggested that it would be most useful if patients could explain why they felt that the service was poor, rather than ticking yes/no boxes. Four members of staff would be interested to hear how patients might suggest how to improve the system and what changes they would make to achieve this improvement.
I would ask them what they thought of the service, how we could improve the service, why, have they got examples of what we have not done right, because you need to get their perception of things. So I would delve into more deeply I suppose, why you don’t think we achieve that, you know.
S03, practice manager
Some members of staff cited particular areas of interest that they would like to see on the questionnaire, such as the telephone system (n = 4), the appointment system (for instance how soon and far ahead you can book) (n = 6), opening times (n = 2), receptionists (n = 2), information provision (such as how easy it is to get information and advice, whether or not staff get back to patients if they do not know the answer) (n = 2), and accessibility of the building for people with physical disabilities (n = 1).
To see are they are happy, I suppose, with the practice, really the main thing is as long as they are happy we are happy as such. But, if they can get the appointments and things like that, that’s really all it is.
S05, receptionist
Three members of staff suggested that the questionnaire should include questions about the clinical consultation, perhaps due to a misunderstanding of responsiveness. Another two interviewees were keen that the clinical aspects should be separated out.
Some staff felt that it was important that the questionnaire included ‘something different’, beyond appointments and telephone systems. Suggestions included what patients thought about backroom staff and the referrals process, how well complaints are handled, how services had been improved in recent times, and how service reconfigurations such as practice mergers had affected patients.
But [I’d] like to come up with a question that is a bit more, that we can get explanation from, not ‘I can’t see my doctor in 3 days, I was on the phone for 20 minutes’. [. . .] I would like to see how they, how they felt about backroom staff, if they have ever had any dealings with, I don’t know, their referrals, how did that go, you know ‘have you ever complained?’ . . . It would be nice to ask if they feel something has improved, if they feel the service has improved . . .
S20, practice manager
One member of staff also felt that it was important to include customer-focused questions – asking the ‘awkward’ questions, the answers to which might prove challenging for the PCO to respond to.
Two interviewees, both practice managers with a background in business, felt that it was more important to measure responsiveness objectively through systems and procedures as well as seeking the patients’ views.
Question wording
Twelve members of staff provided advice about how the questions might be worded. Seven were keen to stress the importance of open-ended questions, to allow patients to express their views in their own words to create a rich source of data to inform service improvement. Four wanted the questions to be solution-focused – how can the service be changed to make it better – rather than simply asking patients what they like and don’t like.
. . . how would you change it, how would you change the appointment system, how would you change you know the phone queuing system. Yes, do that. Definitely do that, I would like to see what they say.
S20, practice manager
The ability to measure change over time was important to three members of staff.
something that can measure change, that, you know, if services are changing you could see a change, it was responsive to change, in terms of you can measure it and the measure would be valid, that there has been an improvement.
S09, GP
Answer formats
As well as the wording of the questions, 11 members of staff referred to the format of the answers that patients could give. Eight members of staff spoke about tick boxes and six about yes/no questions. Five members of staff felt that closed questions were of little value and encouraged ‘satisficing’. In contrast, four members of staff preferred closed questions as they were simple for patients to complete and less work for staff to interpret. Two members of staff had a mixed response to closed questions – they were easy to analyse and prevented difficult issues arising, such as suggestions that would not be implementable, but were limited in usefulness.
Tick boxes and yes/nos are useful, but actually there is going to need to be some space within it, for people to flesh out what their experience has been and/or what their issue has been.
S10, GP
Data analysis
Two members of staff talked about the importance of data analysis: being able to feed back to specific members of their team and being able to provide feedback to patients quickly. Staff also felt that comparative national data would be valuable.
I think the time frame of getting the responses needs to be turned around very quickly, that it’s not 3 months later you are addressing a problem, you are actually addressing it there and then, and then the patients feel like ’I have made a comment and someone has listened to me’.
S27, head office
I think some information about national averages should be provided.
S07, practice manager
Participants and format
Nine members of staff provided advice on participants and format. Seven interviewees were keen that the responsiveness questionnaire be accessible to particular patient groups, including those with dyslexia (n = 1), those with low levels of literacy (n = 2), non-English speakers (n = 4) and older people (n = 1). Four members of staff talked more generally about ensuring that a PCO targets the appropriate patients.
I think trying to get the populations involved, that you want to hear from. So trying to engage with people with learning disabilities and their carers, and people who don’t speak the language . . . trying to get those people who maybe wouldn’t put themselves forward or, maybe, you know, would have difficulties in communicating with you trying to get their views.
S15, GP
Six members of staff were concerned about the format of the questionnaire. They wanted it to be accessible (n = 3), anonymous (n = 1), short (n = 3) and tailored for different patient groups (n = 1). Two interviewees hoped that a simple format would help with analysis.
It couldn’t just be in the written form, because it would have to either, well there would have to be different options, I don’t think one size would fit all.
S15, GP
Mode of delivery
The mode of delivery was important to 18 interviewees. The modes of delivery they discussed included using technology, such as the booking-in touch-screens or hand-held tablets (n = 10), paper-based by post or in the PCO building (most of these acknowledged the difficulties with this method) (n = 6); online (n = 5); face to face (n = 5); providing help with completion (n = 4); using lay interviewers (n = 2); offering incentives (n = 2); and using patient groups to help deliver it in the PCO (n = 1).
There is no reason why you can’t have machines in the reception area where the patients can fill it in. Or a tablet you give out, they fill it in, give it to the next patient.
S09, GP
Summary and discussion
We identified three categories of strategies for achieving responsive primary care within the staff interviews in relation to GP practices: developing an awareness of the needs of the local population through proactive population-orientated strategies; adapting systems and services to better meet these needs through reactive population strategies; and ensuring that staff are willing and able to respond sensitively and flexibly when patients use the services by employing patient-orientated strategies. Staff placed most emphasis on reacting to patients’ needs at the point of accessing services and on individual patients in one-to-one interactions. In contrast, systematic efforts to understand the population and target services to reduce inequalities seemed to be less of a focus.
Responsiveness was not simply a property of an organisation, but involved the alignment of service provision with patient needs and expectations. As well as reflecting the ability of the PCO to identify and meet needs, it also reflected judgements about the legitimacy of patients’ needs or expectations. Sometimes responsiveness was seen to involve working with patients to manage expectations, to bring these into alignment with the level of service that the PCO could provide. In some cases, where needs are seen to be legitimate but beyond the scope of the PCO to meet, then specialist primary care services could be seen as a more appropriate solution.
Responsiveness was seen in slightly different ways by staff from walk-in centres: they emphasised that these organisations were part of the wider picture of responsiveness to patients’ needs across a locality, enabling patients to get quick and convenient access in ways that might not be possible in mainstream GP practices, but that they may not meet other needs for which patients may prefer to use GP surgeries. Their focus tended to be on reactive strategies – trying to be prepared and flexible to support and meet the needs of patients who walked through the door. Pharmacies differed significantly from GP practices and walk-in centres; their business model is different, with a focus on attracting and retaining customers. The pharmacy staff interviews tended to focus more strongly on customer service aspects of responsiveness.
Staff gave a range of perspectives on what they would like the questionnaire to include, its format, and what would make a questionnaire work for them. Key issues included ensuring that the questionnaire was designed to access the views of hard-to-reach patients, making it available in different formats, and the need for quick feedback of the results.
In this qualitative work, we were able to access the views of a diverse group of primary care staff, with a range of job roles and time spent at the PCO, based in a variety of different PCOs with differing responsive cultures. We have been able to identify the key non-clinical aspects of care that staff feel are important to patients across diverse groups, and the specific issues which impact on staff’s ability to implement responsiveness in the primary care setting. The understanding of responsiveness we developed through these interviews primarily reflects responsiveness in GP practices; walk-in centres and pharmacies had different underlying models and philosophies, and hence their focus in terms of what responsiveness means and the drivers for responsiveness were somewhat different to those of GP practices. Despite this, there were some commonalities, meaning that the idea of a parallel measure of responsiveness across these settings is not unreasonable.
This work helped to clarify the meaning of responsiveness in primary care, and to identify limitations and challenges arising from the way primary care staff understood and enacted strategies to promote responsiveness. This work also fed into considerations about questionnaire content, and about approaches to administering the questionnaire.
Chapter 5 Understanding patients’ experiences of responsiveness
Introduction
Some of the key aspects of delivering responsive services highlighted in staff interviews, such as efforts to assess the needs of the PCO’s patient population, or the development of systems for acting on patient feedback, may in fact not be directly experienced by patients, and may be better assessed by objective measures. There is extensive research evidence on the attributes of primary care that are particularly important to patients. 25,26 It is not clear, however, which of these features are most salient for patients in judging the responsiveness of a PCO to their needs. In order to develop a patient-report questionnaire on responsiveness, we need a clear understanding of how responsiveness is experienced by patients.
We conducted interviews with a diverse group of patients and patient representatives in order to identify the key dimensions of their experiences that reflected responsiveness. We aimed to explore (i) the attributes of the organisation and delivery of primary care that impacted on patients’ experiences of primary care as responding well (or poorly) to their needs, and (ii) whether or not experiences of these attributes differed across different patient groups, particularly for disadvantaged groups. Based on this work, we aimed to develop a framework of key attributes on which to base the development of the questionnaire.
Methods
Recruitment
A diverse group of patients and patient representatives were recruited from 12 PCOs in the East Midlands of England, comprising eight GP practices with varying characteristics, a primary care walk-in centre, two pharmacies and a specialist GP practice for homeless patients (see Table 1). Patients were recruited from only 12 of the 13 practices from which we recruited staff, as one of the practices (PCO1) withdrew owing to staffing changes and time pressure.
In mainstream GP practices, random samples of adult patients stratified by age were drawn from practice lists and contacted by post and patients who expressed an interest were purposively sampled for interview. In other PCOs, the receptionist or counter assistant introduced the study to consecutively attending patients and a study researcher approached those who expressed an interest in person. To ensure the inclusion of patients from ‘seldom-heard’ groups and ‘groups who are disadvantaged’, targeted mailings to carers and people with sensory disabilities were conducted in three PCOs; we also recruited via a BME group charity, a learning disabilities specialist and an organisation for travelling families.
Interviews
Semistructured interviews were conducted by EA or JW, in the participant’s own home (34 people) or on PCO (n = 18) or local organisation (n = 6) premises. All bar one patient contacted by letter chose to be interviewed at home and all patients recruited in the homeless GP practice, walk-in centre and pharmacies chose to be interviewed on the PCO premises. The travelling women and the BME patients requiring an interpreter chose to be interviewed in the local support organisation premises. Some interviews included more than one participant (at the participants’ request), for example a husband and wife, a mother and daughter, and a group of travelling women. All were counted as individual participants in reporting the total number of participants. Six stakeholders were recruited to represent the views of particular groups of patients, based on their knowledge, experiences and priorities of these patient groups, representing carers (n = 2), people with learning difficulties (n = 2), BME patients (n = 1) and travellers (n = 1).
A topic guide was developed and used flexibly to guide the conduct of the interviews. The topic guide included open-ended questions about participants’ recent experiences of non-clinical aspects of care from PCOs, and about ways in which services did or did not respond well to their needs. We included prompts derived from the literature and policy documents on responsiveness in primary care. The topic guide was adapted slightly for different patient groups (e.g. homeless patients) and for different PCOs. The core topic guide is included in Appendix 4. Interviews were digitally recorded and transcribed verbatim.
Analysis
Data were analysed using a modified version of framework analysis, which involved both deductive and inductive elements. 83 Themes identified from a review of English policy documents acted as an initial organising framework for the analysis. Our initial analysis focused on identifying core themes relating to responsiveness of GP practices. We used the thematic framework to code patients’ accounts relating to GP practices using NVivo. The framework acted to guide and bound the analysis of patient interviews to ensure a focus specifically on ‘responsiveness’, not just broad experiences of primary care (e.g. ensuring that the focus remained on ‘non-clinical’ aspects of care). However, we were careful to ensure that the initial framework did not unduly constrain the analysis, in line with the recognition that the elements of patients’ experience of responsive service might not mirror the elements required to deliver responsive service. Themes and subthemes were added and iteratively revised during coding. Themes were tested and developed inductively to produce a description of responsiveness of GP practices grounded in patients’ experiences. Following the initial analysis, we used the themes generated from the analysis of data relating to GP practices to code data relating to pharmacies and walk-in centres, while ensuring that we were sensitive to identifying divergent issues.
Findings
We interviewed 64 participants, comprising 58 patients and six patient representatives.
Of the 58 patients, 45 were recruited from participating PCOs [mainstream GP surgeries (n = 43), homeless GP surgery (n = 5), pharmacies (n = 6), walk-in centre (n = 4)], and 13 via other organisations (charity and community organisations). We interviewed 25 men and 33 women, aged from 18 to ≥ 85 years (Table 3). Fourteen participants identified themselves as carers. The sample was diverse and included a high proportion of patients from groups who are disadvantaged and ‘seldom heard’. Nineteen participants had physical disabilities, five had hearing impairments, four had visual impairments, and six had learning difficulties. Seven participants were from a South Asian background, three were travellers and six were homeless.
| Characteristics | n (%) of participants (N = 58) |
|---|---|
| Sex | |
| Female | 33 (57) |
| Male | 25 (43) |
| Ethnicitya | |
| Asian or Asian British | 7 (12) |
| White | 49 (84) |
| Age (years)a | |
| 18–24 | 3 (5) |
| 25–34 | 4 (7) |
| 35–44 | 7 (12) |
| 45–54 | 11 (19) |
| 55–64 | 8 (14) |
| 65–74 | 13 (22) |
| 75–84 | 8 (14) |
| 85 or over | 1 (2) |
Patient representatives were recruited from a local BME research organisation, a local parent and carers’ council, a carers’ charity, and two NHS organisations for people with learning difficulties (Table 4).
| Patient representative | Group of patients represented | Basis for representing them |
|---|---|---|
| 1 | BME patients | Research centre co-ordinator at a PCT |
| 2 | Parents and carers | Family support worker at a local charity |
| 3 | People with learning difficulties | Learning disability lead at a health-care trust |
| 4 | Carers | Manager at a local charity |
| 5 | People with learning disabilities | Health facilitator at a PCT |
| 6 | Travelling families | Travelling families lead at a health-care trust |
Attributes of responsiveness for general practitioner practices
We identified five key attributes of the organisation and delivery of primary care that patients directly experienced, and that impacted on their perceptions of how well the GP practice responded to their needs. These were ease of access to services; the alignment of the physical environment with patient needs; diversity awareness and cultural alignment; staff attitudes and behaviours; and co-ordination and support for their ongoing care. Although issues relating to keeping patients informed, and patient involvement and engagement, are prominent in recommendations for the delivery of responsive primary care, these elements featured less prominently in patients’ accounts of their experiences of responsive primary care.
These five key attributes were common across all patient groups, and across different primary care providers, but certain groups were more likely to have negative experiences of certain dimensions of care.
Ease of access to services
The most prominent non-clinical aspect that emerged in patients’ accounts of responsive and unresponsive primary care was how easy the GP practice made it for them to access appropriate services. In the case of GP surgeries, this included how easy it was for patients to initiate contact in order to arrange a visit or consultation, and how easy it was for them to negotiate an appointment that met their needs, for example for urgency, timing or choice of practitioner.
Initiating contact
In terms of ease of making contact, some patients described having to go to some inconvenience just to ‘get through’ by telephoning repeatedly, or having to turn up and wait outside before opening time. This was an example, for many patients, of a lack of responsiveness to patients’ needs.
The only way you can get an appointment is either you phone up at 8 o’clock, or you go at 7.30 in the morning and you queue up outside and because I hate hanging on the telephone and hearing recorded voices for 10 minutes or more and running up a big phone bill, I always go at 7.30 and queue up outside. In the depth of winter you have to stand there in the cold.
Interview 01, patient with mobility problems
While it was important for all patients that they could easily make contact with the GP practice to arrange an appointment or to speak to someone, this was a particular issue for certain vulnerable groups. Systems for getting in touch with GP practices in the first place could present significant barriers for patients who lacked capacity or resources (e.g. those with learning disabilities or who did not speak English), and the alignment of systems for making contact with specific patient needs was critical.
[The touch-tone phone system] gives you so many options for different things.
Sometimes then we do it again and they go through them all again, don’t they?
Because you have missed what they have said?
Yes, yes.
Yes, they do it so fast.
Interview 45, mother and daughter with learning difficulties
It’s a very poor area, some people don’t have a landline, they only have a mobile [telephone], if they have to ring from their mobile and they are put on hold, . . . they haven’t got the money to spend on that.
Interview 01, patient with mobility problems
Getting an appropriate appointment
Patients wanted to be able to easily get an appointment that suited their needs, namely one that was at the ‘right’ or convenient time for them, and with the ‘right’ health professional; this could be, for example, their usual GP, a doctor or nurse who was of the same sex as them, or someone who spoke their language.
I do think the main thing is that you can book in advance to see your own doctor if you wish to, because I think that is really important.
Interview 09, patient with mobility problems
However, patients were aware of the realities of providing primary care, and recognised that resources were not limitless: they acknowledged that responsiveness was not just about giving patients everything they wanted. Patients recognised that they might have to make trade-offs between their preferences for who they saw, when they were seen and how long they waited (e.g. having to wait a few more days to see the GP of their choice, or seeing a nurse practitioner in order to be seen sooner).
She said that the nurse could deal with that, nurse practitioner, that she can do any prescriptions or anything like that, I said ‘oh’, and so I said ‘fine’ . . . I could have seen a different doctor if I had wanted to, but I couldn’t have got an appointment that day, or the next day, so I saw the nurse.
Interview 18, patient with hearing, sight and mobility problems
Patients wanted practices to operate appointment systems that had some flexibility and offered choice in order to enable them to make trade-offs, and to make it easy for them to find an acceptable option without having to make unacceptable compromises (such as having an excessively long wait for an appointment with their preferred GP).
You can only book a routine appointment for 3 weeks’ time but if you want one before that 3 weeks they tell you to ring on the Tuesday and they’ll see if they can fit you in on the Thursday. But if they haven’t got nowt on that Tuesday for that following Thursday . . . then you’ve got to wait until the following Tuesday to go for that [next] Thursday.
That’s why a lot of travellers go to hospital.
Group interview, travellers
Patients felt that practice responsiveness to their needs for access was not only about the features of practice appointment systems, but also about how these systems were operated by reception staff. It was seen as critical that staff were willing and able to operate the appointment system flexibly at the point of access; this was a particular issue for patients who had higher levels of need or lower resources. Patients described the importance of staff being willing to ‘bend the system’ or ‘fit people in’ when they had genuine and pressing needs.
I did need an appointment and at first [the receptionist] said ‘no, there’s no appointments left’ and I said ‘well I really do need to see somebody’ because I couldn’t stand another night with what we’d had. [. . .] She went back on the computer and then she said . . . ‘I’ll book you in’.
Interview 23, carer of adult son with learning difficulties
If people have particular difficulties like waiting in waiting rooms, having that flexibility to be able to have maybe the last appointment of the day.
Interview 50, health facilitator for people with learning difficulties
It was evident that some groups of patients, particularly those who were homeless, faced such challenges in accessing primary care that it was difficult for mainstream practices to respond to their needs. These patients lacked the resources or capacity to organise their lives around the systems for accessing mainstream care, and often felt unable to negotiate with reception staff to get what they needed. For many of these patients, their needs were better served by specialist services which were able to respond to the specific needs of these groups by ensuring they were extremely permeable. 86 Some of the homeless patients we interviewed felt that they were able to access primary care only because the specialist homeless practice they used placed few demands or restrictions on their access – they were able to simply turn up when they needed to.
That is the good thing about it, you just come in . . . and you sit down and wait to be called. [. . .] I am not very good with phones.
Interview 28, homeless patient with learning difficulties, mental health and mobility problems
Alignment of physical environment with patient needs
Another key issue that impacted on patients’ experiences of GP practices as responsive (or unresponsive) to their needs was that of how well the physical environment aligned with their needs.
It was important to all patients that the building and facilities were appropriate and easy to use. They wanted to be able to wait in comfort, and for the practice to help make waiting less stressful, for example through providing toys for children. There was little discussion of the time patients had to wait at the surgery: for patients using GP surgeries, it was much more important to be able to get a suitable appointment in the first place. Patients wanted an environment that protected their privacy – they wanted to be able to speak to the reception staff without being overheard, and to be able to easily book in when they arrived and know when it was their turn to be seen.
It’s all open and [reception staff] are all sort of in a line. [. . .] You know, somebody wants to ask something personal at the, perhaps a test result or something, I mean all and sundry can hear and I just don’t think that is right [. . .]. All right it may not be, not top secret but it’s just a little bit lack of confidentiality I think.
Interview 10, no health problems
Alignment of the practice environment with physical accessibility needs was seen as a critical aspect of responsiveness by patients with disabilities. Patients with physical disabilities generally found GP practices’ premises accessible, as most practices had adapted or built their surgeries to suit the needs of patients with physical disabilities. However, facilities were not always seen as suitable and there were some problems with disabled parking systems. Many patients with sensory and learning disabilities found primary care environments poorly aligned with their needs and, consequently, difficult to use.
Most people with visual issues have some residual vision and they need high contrast, so you walk in and I can’t think of any sort of obvious high contrast pathway that kind of leads you in from the door way to the reception areas. So you could be left high and dry.
Interview 51, advocacy manager for carer organisation
Diversity awareness and cultural alignment
For certain groups of patients, including patients from BME groups and travellers, the service provider’s understanding of and efforts to align services with their language, culture and lifestyle was an important element of responsiveness.
If you knew about the culture [you would understand] that suddenly there will be a lot of demand for appointments just before Ramadan starts.
Interview 54, BME patient
Practices that served areas with a large population of patients from particular ethnic groups were often, by default, well aligned with the cultural and language needs of these patients; for example, they tended to employ reception staff from the local community who were able to communicate with non-English speakers in their own language. This level of alignment meant that patients could easily access and use services.
All the receptionists either speak Gujarati or Urdu which they can communicate with [. . .]. No language problem.
Interview 49, non-English speaker with mobility and other health problems
Even in practices where a patient group was in a minority, it was possible for patients to experience services that were delivered in ways that aligned with their needs, and so experienced as responsive. This tended to be the case when practices had actively planned for supporting patients with specific language or cultural needs, in terms of both the services they provided and the attitudes and awareness of staff.
Things like knowing that [traveller women] might not have transport [. . .]. So the receptionist now will say ‘have you got any transport today?’ or ‘what time are you expecting your husband home? Shall we make it later on this afternoon?’
Group interview, traveller representative
Staff attitudes and behaviours
The attitudes and behaviour of non-clinical staff, particularly reception staff, was an important issue for all patients. Patients felt that a responsive practice was one in which staff were friendly, treated all patients with respect and understanding, and were willing to be flexible, helpful, and supportive towards patients at the point at which they accessed the service.
I feel in a way they are always quite flexible. I feel they are approachable. If I felt that if I needed something or if I was asking a question about something they would listen.
Interview 12, no health problems
Staff attitudes and behaviour was an issue of particular importance for patients from certain groups who feared discrimination or disadvantage – this included some older people, homeless people, travellers and people with disabilities.
Quite often there is this sharpness still there towards older people, almost like, because they are maybe being a little seemingly awkward or difficult they are being treated like a naughty child.
Interview 43, patient with a physical disability and other health problems
Nine times out of 10, you are a homeless person, you go into a doctor’s, respect is the last thing you are going to get. [. . .] But the receptionists at the [practice are] friendly, welcoming, courteous, respectful.
Interview 30, homeless patient with mental health problems
Patients wanted staff to be patient-centred and willing to help them to access and use services. Patients with disabilities wanted to feel confident that staff would help them to use and navigate the environment; patients who had difficulty communicating wanted staff to be sensitive in their approach and willing to take extra time to help them communicate.
If you are incapable of walking, bad hips, bad knees, they have a little stair-lift for you to ride up, and it is there for your use, and somebody will help you, you will not be left alone.
Interview 48, patient with a hearing impairment
Co-ordination and support for ongoing care
A further feature of practices that were seen as responsive or unresponsive to patients’ needs related to the extent to which patients felt supported by the practice in keeping up to date with their care. Patients described positive experiences when administrative systems ran smoothly and efficiently to co-ordinate their care both within the GP practices and with other providers; this included systems for arranging repeat prescriptions and for co-ordinating their care with hospitals. They valued reception staff who were ‘on the ball’, supported by practice systems that ensured that patient information was up to date and accessible. Correspondingly, they reported negative experiences when systems did not seem joined up or did not operate smoothly, resulting in patients having to chase things up themselves.
Recently I went to pick up my prescription and had a note with my tablets saying the doctor wants to see you about your thyroid, so that was quite good – saying you are due for another blood test. Otherwise you just forget, won’t you, that it’s been 6 months since you last had it checked, so they are quite good.
Interview 19, patient with health problems
This aspect of care was most important for patients with complex long-term conditions and patients who found it difficult to take responsibility for their own ongoing care – these included elderly patients, patients with learning disabilities, and patients with difficult lives such as those who were homeless. Where practices took responsibility for proactively identifying these patients, and worked in partnership with patients to organise and co-ordinate their care, patients were more likely to be able to easily access and use the services that they needed.
For the annual health checks, the practice manager went out of his way to actually do the Easy Read letters, follow people up, ring people if necessary [. . .]. [He] went out of his way to actually make sure people were booked and follow [up] people that hadn’t turned up as well.
Interview 50, health facilitator for people with learning difficulties
Information and engagement
Although informing and engaging with patients is seen by practice staff, and in policy, as a key element of delivering responsive primary care, information and engagement did not feature prominently as an important element of patients’ experiences of responsive primary care.
Few patients felt that their practice made efforts to keep them informed about the services it provided or its opening times, but for most patients this did not matter. Some even felt that efforts to keep patients informed would be a waste of resources.
Well I don’t think there is a great flow of information from the surgery, let’s put it like that. And you do learn what is going on, while you are there, by reading notices and just looking at the screen you know because they have got one of these computer screens. [But] they are not forthcoming with the information. But I don’t know whether that presents us with a problem or not really. It doesn’t present me with a problem because I am quite adaptable.
Interview 42, patient with physical disabilities
The issue of engaging and listening to patients was not commented on by many, although those who did raise this issue felt that it was important that practices made it easy for patients to make complaints and suggestions, and showed evidence of responding to this feedback.
It was actually because I belong to that meeting thing [PPG], it was us that asked for [the touch screen]. And they put it in, so they are actually listening to patients.
Interview 21, patient with mobility problems and other health issues
Attributes of responsiveness for other primary care organisations (walk-in centres and pharmacies)
The key attributes of responsiveness identified from the analysis of data relating to GP practices mapped well onto the findings on patients’ experiences of responsiveness from the walk-in centre and from pharmacies. In Tables 5 and 6, we summarise similarities and differences across the PCO types organised by theme, and provide illustrative quotes.
| Attribute | Description | Illustrative quotes |
|---|---|---|
| Ease of access to services | Patients valued the lack of barriers to access to care in WICs (there was no need to make an appointment, the patient could simply turn up and wait), and the ability to access the service out of hours. They recognised that having this level of access involved trade-offs with other priorities including waiting time, and choice of professional |
|
| Alignment of physical environment with patient needs | The issues that arose corresponded with those that arose for GP practices |
|
| Diversity awareness and cultural alignment | Owing to the small sample of WIC users, this theme was not explored | |
| Staff attitudes and behaviours | The issues that arose corresponded with those that arose for GP practices |
|
| Co-ordination and support for ongoing care | This theme was not prominent in accounts of patients from WIC, as they generally used the centres for one-off acute conditions | |
| Information and engagement | This theme was not prominent in accounts of patients from WICs |
|
| Attribute | Description | Illustrative quotes |
|---|---|---|
| Ease of access to appropriate services | Patients described ease of access relating to the times pharmacies were open, the ability to drop in at a time that was convenient to them, who they could see (particularly if they could see someone of their own sex), how long they had to wait to be served, ease of collecting prescriptions, and whether or not they were offered advice |
|
| Alignment of physical environment with patient needs | The issues that arose corresponded with those that arose for GP practices, but also included the cleanliness and orderliness of the shop, and ease of finding required items |
|
| Diversity awareness and cultural alignment | Owing to the small sample of pharmacy users, this theme was not explored | |
| Staff attitudes and behaviours | The issues that arose corresponded with those that arose for GP practices |
|
| Co-ordination and support for ongoing care | This theme was not prominent in accounts of patients from pharmacies | |
| Information and engagement | This theme was not prominent in accounts of patients from pharmacies |
|
Generation of questions
We used the framework developed from the analysis of patient interviews to generate a set of initial questions for the questionnaire. We phrased the questions in relation to GP practices, but our intention was to generate a set of high-level, generic questions that would link with the core attributes of responsive primary care, and which could be adapted through slight changes in wording to be equally applicable to other primary care providers, including pharmacies and walk-in centres. The initial set of questions is shown in Table 7 organised by the key attributes of responsiveness identified from the patient interviews.
| Attribute | Wording of questions | Response options |
|---|---|---|
| Ease of access to appropriate services | 1. Does the practice make it easy for you to contact them to arrange to see a doctor or nurse? | Yes, it’s very easy; it’s quite easy; no, it’s difficult |
| 2. Does the practice make it easy for you to get an appointment that suits you? | Yes, it’s very easy; it’s quite easy; no, it’s difficult | |
| Alignment of physical environment with patient needs | 3. Does the practice make it easy for you to get into the building and use the facilities? | Yes, it’s very easy; it’s quite easy; no, it’s difficult |
| Diversity awareness and cultural alignment | 4. Does the practice try to support your individual needs? | Yes; to some extent; no |
| Staff attitudes and behaviours | 5. Do receptionists try to be helpful? | Yes, they always try to be helpful; they sometimes try to be helpful; no, they don’t try to be helpful |
| 6. Do practice staff treat you with respect? | Yes, they always treat me with respect; they sometimes treat me with respect; no, they don’t treat me with respect | |
| Co-ordination and support for ongoing care | 7. Does the practice make it easy for you to keep up to date with your care and treatment? | Yes, it’s very easy; it’s quite easy; no, it’s difficult |
| 8. Does the practice make it easy for you to access other health care services that you need? | Yes, it’s very easy; it’s quite easy; no, it’s difficult | |
| Information and engagement | No questions included |
Summary and discussion
We identified five key attributes of responsive general practice that arose consistently in the accounts of patients across diverse groups. These were easy access to an appropriate appointment or services; an accessible and patient-centred environment; a provider that understood specific cultural or language needs; friendly, non-discriminatory and supportive non-clinical staff; and support in the co-ordination of patient care. Information and engagement featured less prominently as an aspect of responsiveness in patients’ accounts.
The importance of each attribute to patients from diverse groups varied, and within each element of care, certain patients groups were more likely to describe negative experiences.
Importance for ease of access was the perceived ease of initiating contact and then negotiating an appropriate appointment. Patients were aware of the realities of limited resources and were willing to make trade-offs when necessary. Patients wanted staff to use the appointment system flexibly when there was a pressing need but this may challenge the staff member in knowing how far to ‘bend the system’ while maintaining equality of access. Thus, reactive individual orientated responsiveness should balance reactive population responsiveness.
Accessing appropriate care could be problematic for patients whose lifestyles made it difficult for them to fit in with rigid systems. This was particularly evident for some homeless patients and travellers who could struggle to access care if appointment systems were inflexible and staff were not accommodating. Services designed to respond to their needs, such as homeless GP practices where pre-booked appointments are not required, fit the needs of this group who are disadvantaged. Walk-in centres and pharmacies may offer similar advantages here.
Patients with physical disabilities described difficulties with parking, getting around practice buildings and using facilities. They appreciated efforts to make buildings and facilities more accessible, and valued staff who were aware of their particular needs and were willing to support them. Some patients, including older people, homeless people, travellers and people with disabilities, felt that they were not always treated equitably, taking into account their greater needs or disadvantaged position. For these patients, any indications that a GP practice had considered the issues for patients like them, and that staff had been trained in diversity and had positive attitudes, were greatly welcomed. Patients with complex long-term conditions, and those who found it difficult to take responsibility for their own ongoing care, had a particular need for their GP practice to efficiently and proactively co-ordinate their care. Interestingly, although patient involvement, choice and voice is seen in policy as a key way of ensuring responsiveness, most patients were not interested in being, or did not feel able to be, engaged or involved with their PCO.
These themes were also reflected in patients’ descriptions of their experiences of walk-in centres and pharmacies, although the issues discussed in relation to the key themes differed somewhat for the different providers. Diversity awareness and cultural alignment, and co-ordination of care, did not feature in accounts of these providers, but this may be partly due to the small numbers of patients interviewed.
These findings suggest that patient experience of responsiveness reflects the extent to which PCOs have systems that are well designed to meet the needs of their main practice population groups, particularly those who are often disadvantaged in using primary care services, and staff who have the knowledge, concern and interpersonal skills to implement these systems flexibly, in a way that is sensitive to both the needs of patients and the demands on clinical staff. Interviewees commonly described examples of lack of responsiveness, indicating that there remains a significant need to improve responsiveness, in particular for patients from the ‘seldom-heard’ groups.
We were able to interview a relatively large sample of patients across a range of PCOs within diverse settings. We were successful in hearing the views and experiences of patients from ‘seldom-heard’ or hard-to-reach groups, including homeless patients, patients with a range of disabilities, patients from the travelling community, and patients for whom English was not a first language. The main limitations of this work were that we had fewer patients from walk-in centres and pharmacies, and so the findings from these settings are somewhat tentative.
The findings of the patient interview study provided a framework of five key attributes of responsiveness to form the basis of a questionnaire. This was used to generate an initial set of questions for testing with focus group participants to assess wording and comprehension, and to check whether or not the questions captured the key issues for patients in their experience of responsive primary care, prior to piloting.
Chapter 6 Developing and piloting the questionnaires (pilots 1 and 2)
Summary of this chapter
Having developed an initial set of candidate questions for inclusion in the questionnaire, we then went on test the acceptability of the questions through three focus groups with diverse patient groups. This informed the development of version 1 of the questionnaire, which was about GP practices. This was subject to two rounds of piloting, the revisions to the questionnaire being made based on the results of each pilot. The first involved 450 patients in three GP practices and the second involved 300 patients in two GP practices. In both rounds of piloting, completion rates and distribution of responses to questions were assessed to help refine the questions. Each pilot also included interviews with a sample of up to 20 responders; the first set of interviews aimed to test the face validity of the questionnaire, and the second set were cognitive interviews to help refine the wording and layout of the questionnaire. Informed by the results of pilot 1, we developed version 2 of the GP surgery questionnaire and version 1 of the pharmacy questionnaire. The pharmacy version was piloted with 150 patients in two pharmacies and was subject to a small number of cognitive interviews.
During this phase, we conducted a consultation with our advisory group members about their priorities for the provision of a number of different formats for the questionnaire. Following piloting, version 3 of the GP questionnaire was prepared (along with version 2 of the pharmacy version and version 1 of the walk-in centre version) to go on to be tested for reliability and acceptability in a large-scale pilot (see Chapter 7).
Developing version 1 of the questionnaire: focus groups
Methods
We conducted three focus groups with patients from diverse groups to test the initial set of questions. We wanted to access the views of patients from diverse groups to ensure that the questions were relevant to their specific needs and experiences, and to enable us to test the questions with patients who are traditionally ‘seldom heard’,87 to ensure that our questionnaire included issues that were important for these patient groups. We chose to hold one group with patients who were members of a PPG at a large inner-city practice in a deprived locality (seven participants), one with individuals from a BME background with few or no English-speaking skills (Gujarati-speakers) (10 participants) and one with people with physical disabilities (eight participants). PPG members were recruited by a postal invitation issued by the GP practice, accompanied by a visit by the researcher to a PPG meeting to introduce the study and answer questions. Patients who did not speak English, or had limited English, were recruited through information leaflets (translated into Gujarati) distributed to learners at a community IT education project. The focus group involving patients with physical disabilities was held at a social group set up by a local charity.
Focus groups were facilitated by JW, with EA in attendance to take notes and act as scribe, using a flipchart to display the main points. The focus group with Gujarati speakers was jointly facilitated by JW and an interpreter from the community IT project. The topic guide is given in Appendix 5. Groups lasted between 1 hour 10 minutes and 2 hours 8 minutes, and were held at locations convenient for the participants. With participants’ permission, the discussions by each group were digitally recorded and transcribed verbatim. A framework approach83 was used for the analysis of the data. A coding framework was developed in NVivo by EA, based on notes taken during the focus groups. The framework described each question in terms of issues that participants talked about when answering the questions, and misunderstandings and suggestions for improvement to wording. Verbatim transcripts were imported and coded to the framework. The coded data were summarised into a chart.
Results
Findings from the focus groups
Appendix 6 shows the resulting summary framework of the issues arising from the initial draft questions in the focus groups. This was used to inform revisions to the initial draft questions, to produce a set of questions for version 1 of the GP questionnaire. Key issues are summarised in Table 8.
| Question | Focus group comments | Action (questions for pilot 1) |
|---|---|---|
| Q1 and 2: contacting practice and getting a suitable appointment | Participants found it difficult to differentiate between questions 1 and 2, and talked about arranging an appropriate appointment in relation to both questions | Version 1 of the GP questionnaire was formatted so that questions about ability to get an appointment that met patient’s needs came first, followed by a separate question on how easy it was to arrange the appointment |
| Q2: getting a suitable appointment | Participants felt that their answer to this question would differ depending on what it was they wanted; it was generally harder to get an appointment if they wanted a specific GP | This question was split into separate questions about what the patient wanted when they arranged their appointment (e.g. an urgent appointment, to see their preferred GP), and whether or not they could get this |
| Q3 accessing the building and facilities | This question worked well, although participants suggested splitting into getting to the practice and accessing the building. They felt that more subquestions would be helpful | We split this question and added subquestions on using the facilities |
| Q4&5: reception staff helpful, practice staff treat with respect | These questions worked well, but participants were not always clear about whether or not question 5 referred to clinical staff. Focus group participants highlighted important aspects about the way they were treated by reception staff | These questions were revised to produce a set of questions about reception staff, covering welcome, respect, listening to patients, communicating well, understanding patient circumstances and helpfulness |
| Q6: support your individual needs | This was generally interpreted as relating to clinical needs, but also raised a lot of issues around support and co-ordination of ongoing care | Questions on co-ordination of ongoing care were developed |
| Q7: help keep up to date with care | This was generally interpreted as relating to clinical aspects of care, but also highlighted the importance of the practice being proactive | This issue was covered by including questions on organisation and co-ordination of care |
| Q8: access other services | This question was seen as important but participants felt that examples of other services would be helpful | Question retained and examples added |
| General issues | (i) Participants preferred ‘GP surgery’ to ‘GP practice’; (ii) clarify that the questionnaire relates to non-clinical issues; (iii) include ‘do not know’/’no opinion’ response options | These issues addressed in producing pilot 1 |
Revisions to the questions
Key decisions made at this stage included (1) the decision to include a larger number of more detailed questions in the questionnaire – a common theme across focus groups was that patients felt that some of the high-level questions were too abstract, and it was clear from inspection of the topics discussed during the focus group that the question wording for some questions was not cueing patients effectively to consider the issues that we expected; and (2) the decision to frame questions by asking patients about the ‘last time’ they visited the GP, to overcome the problem of patients struggling to answer a general question relating to making an appointment (they felt that their experiences depended on what they wanted on a particular occasion, such as to see their usual GP or to be seen quickly).
We consulted widely used and validated primary care patient experience/satisfaction questionnaires to identify relevant questions and question wording to inform development of questions for the first draft of the responsiveness questionnaire. 88–91 During the process of drafting the initial version of the questionnaire, the advisory group were consulted for feedback on the wording and ease of use, and to gain insight into the appropriateness of the pilot version for different patient groups. Feedback was collated and version 1 of the questionnaire was developed for testing in the first pilot.
Questions on demographics were developed, drawing on other validated measures where possible, including the national GP patient survey (questions on sex, age, occupation, parent/carer status, sign language, sexuality), the General Practice Assessment Questionnaire (question on ethnicity), and the Scottish Patient Experience Survey (question on disability).
Version 1 related to GP surgeries only, consistent with our approach, which was to develop a GP version of the questionnaire which could then be adapted for other primary care providers. Version 1 of the questionnaire is included in Appendix 7. Version 1 was produced in paper and online (using SurveyMonkey: www.surveymonkey.com) formats.
Pilot 1: general practitioner questionnaire version 1 – survey and narrative interviews
Methods
The first pilot took place over 3 months (June–August 2012). Three mainstream GP practices were chosen for the first pilot (one in a central area of a large town, another in a deprived suburban area of a town, and the third in a small village in rural surroundings). Practices were asked to hand out 150 patient packs to consecutively attending patients coming into the surgeries during a 2-week period. Patients could return their questionnaire to a box on the reception desk, or directly to the research team using a freepost envelope. The questionnaire included a website address for patients to complete the survey online, if they preferred.
Patients were asked to return a reply slip with the questionnaire if they were willing to be interviewed. On receipt of the reply slip (or e-mail for the online version), participants were contacted by telephone by the interviewer and a date was arranged with patients who were agreeable: patients were offered the choice to be interviewed either in their own home or at their GP premises. A topic guide was used in interviews (see Appendix 8) to elicit patients’ accounts of their recent encounters with their GP practice. It included direct questions about the content of the questionnaire: whether or not patients felt that the questions allowed them to articulate their views; whether any questions were missing or redundant; and how easy it was to complete. Interviews were recorded on a digital recorder and transcribed verbatim.
Interview transcripts were uploaded into NVivo software and coded according to a predefined coding framework which included the broad themes of the questionnaire. Additional codes were generated for issues that did not fit this framework, and for issues relating to problems and suggestions for improvement. A validation exercise was conducted in which the coded text from the nine randomly selected interviews was compared against the list of questions in the questionnaire by EA and CT. An approach based on content analysis was used to identify whether or not each theme was discussed by each individual patient, and to identify any additional themes. We collated examples of the issues people discussed within these themes, and the terms that were commonly used to describe these issues, to inform refinements to the wording of the questionnaire. The additional transcripts were read to ensure that no further issues arose. Across the whole sample, we also explored participants’ expressed views on the wording, content and format of the questionnaire.
This analysis from the interviews was used in conjunction with analysis of descriptive statistics from the pilot survey to develop the next iteration of the questionnaire. The draft was circulated to members of the team for feedback, and the content and format of version 2 was agreed.
Results
Survey
Across the three GP practices, 450 questionnaires were handed out. An overall response rate of 52% was achieved, ranging from 43% in PCO04 to 59% in PCO11. A total of 232 completed questionnaires were returned (Table 9). This response rate was higher than anticipated.
| PCO | Number returned | Response rate (% of 150) |
|---|---|---|
| 04 | 65 | 43% |
| 11 | 89 | 59% |
| 12 | 78 | 52% |
| Total | 232 | 52% (of 450) |
Responders included 124 women, 92 men and one transgender person (data were missing for 15), aged from < 18 years to ≥ 85 years. Thirty-two patients had physical disabilities or mobility problems, 20 had hearing impairments, none had visual impairments, and two had learning difficulties. Only 7% were from BME groups. The majority of patients were either working (full- or part-time) or retired/out of work, with a small number in full-time education (Table 10).
| Characteristics | n (%) of participants (N = 232) |
|---|---|
| Sex | |
| Female | 124 (53) |
| Male | 92 (40) |
| Transgender | 1 (< 1) |
| Missing data | 15 (6) |
| Age (years) | |
| Under 18 | 3 (1) |
| 18–24 | 21 (9) |
| 25–34 | 41 (18) |
| 35–44 | 24 (10) |
| 45–54 | 42 (18) |
| 55–64 | 34 (15) |
| 65–74 | 38 (16) |
| 75–84 | 18 (8) |
| 85 or over | 2 (1) |
| Missing data | 9 (4) |
| Ethnicity | |
| White British | 207 (89) |
| Black or Black British | 5 (2) |
| Asian or Asian British | 7 (3) |
| Mixed British | 1 (< 1) |
| Chinese | 1 (< 1) |
| Other ethnic group | 2 (1) |
| Missing data | 9 (4) |
| Health conditionsa | |
| Deafness or severe hearing impairment | 20 (9) |
| Blindness or severe visual impairment | 0 (0) |
| A condition that substantially limits ability to carry out basic activities, e.g. walking, climbing stairs, lifting or carrying | 32 (14) |
| A learning disability | 2 (1) |
| A long-standing mental health problem | 11 (5) |
| Any other long-standing illness | 56 (24) |
| Working statusa | |
| Full-time paid work (30 hours or more each week) | 75 (32) |
| Part-time paid work (under 30 hours each week) | 31 (13) |
| Full-time education at school, college or university | 6 (3) |
| Not in paid work/retired | 99 (43) |
| English as first language | |
| Yes | 209 (90) |
| No | 6 (3) |
| Bilingual/multilingual | 3 (1) |
| Missing data | 14 (6) |
SPSS was used to generate descriptive statistics for each question (see Appendix 9). There were very few missing data or incorrect responses. The distribution of responses for most questions was skewed towards positive responses, with a greater distribution for some of the individual questions.
Narrative interviews
Of the 232 patients who returned a questionnaire across the three GP practices, 28 expressed an interest in being interviewed (12%). Of these, 20 were purposively selected based on sex, age and health problems/disability. We interviewed 10 women, nine men and one transgender person. Most (n = 19) were White British. Nearly half (n = 8) of the interviewees were aged 55–64 years, with a fairly even distribution through the other age groups. Two had a learning difficulty, four had mobility problems, two a mental health problem, and nine had other illnesses. Three were carers (Table 11).
| Characteristics | n of interviewees (N = 20) |
|---|---|
| Sex | |
| Female | 10 |
| Male | 9 |
| Transgender | 1 |
| Ethnicity | |
| Asian or Asian British | 1 |
| White | 19 |
| Age (years) | |
| 18–24 | 1 |
| 25–34 | 1 |
| 35–44 | 3 |
| 45–54 | 4 |
| 55–64 | 2 |
| 65–74 | 8 |
| 75–84 | 2 |
| 85 or over | 0 |
Validation exercise
The results of the validation exercise suggested that the themes included in the questionnaire reflected the issues that were important to patients (Table 12). The interviews highlighted the value of including a question on getting in contact with the surgery, and the importance to some patients of the surgery being proactive and helping to organise their care.
| Theme | Number of patients who referenced the themea | Additional issues raised (positive experiences) | Additional issues raised (negative experiences) |
|---|---|---|---|
| Ease of access to appropriate services (arranging an appointment) | 9 | The usefulness of telephone consultations; being able to see other doctors if preferred GP is unavailable; doctors arranging further appointments on patient’s behalf; getting appointments sooner than expected; ‘Dr First’ system; ease of telephoning surgery (any time of day); GP recommending colleague | Long waits on the telephone; having to wait a long time to see preferred doctor; issues of GPs vs. nurse-led care; continuity of care; receptionists answering phones and manning the front desks: long waits to make appointment; long waits in surgery, patient had to leave; difficulties in getting same-day appointments or at suitable time; having to telephone as specified times; patient does not want to give symptoms over the telephone |
| Staff attitudes and behaviours (how well the reception staff treat you) | 8 | Staff being caring, efficient, pleasant, friendly, polite, good-humoured and sympathetic; staff doing what they are supposed to do (i.e. not giving medical advice); staff being professional, well organised and not pushy; staff proactively communicating when clinics are running late | Receptionists not answering telephones; staff being abrupt |
| Alignment of physical environment with patient needs (how easy it for you to visit the surgery) | 9 | Availability of parking spaces; pharmacy on GP premises or nearby; availability of services (e.g. X-ray); nice atmosphere in the waiting room, and not crowded; preference for GP calling patients rather than a screen | Availability of parking spaces; preferences for receptionists over a touch screen to book in; difficulties arranging for volunteer care to bring patient to the surgery |
| Co-ordination and support for ongoing care (how good the surgery is at organising your care) | 9 | Reminders about flu jabs and appointments; flexibility of the 48-hour rule for prescriptions when needed; online prescription orders; proactive follow-up of patient; professional service; services closer to home (minor surgery, X-ray) rather than at hospital | Slow communication from hospital (not the fault of the GP surgery); patient wants GP to chase hospital |
| Information and engagement (how good the surgery is at listening and communicating with patients) | 4 | Ways in which information is communicated, e.g. plasma screen, leaflets if you want them | One patient explicitly stated that they did not wish to hear from the surgery |
| Diversity awareness and cultural alignment (how good the surgery is at meeting your needs) | 2 | Patients mainly talked in general terms, although specific items included efficiency, caring attitudes of staff, and continuity of care for ongoing illness |
Patients’ views on the questionnaire
When patients were directly asked in interviews if they felt that there were any problems with the questionnaire, none raised any problems. Patients felt that the time to complete the questionnaire was acceptable, and times ranged between ‘2 or 3 minutes’ and 20 minutes, with most taking between 5 and 10 minutes. Patients felt that the questionnaire was fully comprehensive, and none felt that there were any irrelevant questions. Three patients had felt that something might have been missed, but subsequently found the sections in the questionnaire where their concerns were put to rest.
I feel it was quite good. Yes. I think so, I remember at the time thinking it was quite thorough and I couldn’t think of anything which could be added.
P101
I think the terminology. It’s very layman’s terminology isn’t it, it’s easy to read, it’s not, ‘what does that mean?’, or ‘how do you interpret that?’ the questions are to the point.
P102
No, I think, like I say, I think everything in there covered everything that, you know, I would have thought about when I, when I go there, do you know what I mean?
P103
But elsewhere in the interviews, patients expressed some minor concerns: that the questionnaire was not geared towards infrequent users (n = 1); that some of the language was not understandable (this related to the use of the term ‘straight’ relating to sexuality in the demographic section) (n = 1); that it was too long (n = 1); that the patient’s last visit was not like previous visits and so his or her answers were not representative of the practice as a whole (n = 1); and that the question about age may cause patients to feel that they had been put in a box (n = 1). There were several specific suggestions to improve the questionnaire, which were considered when designing the next iteration of the questionnaire (Table 13).
| Suggestion | Quote |
|---|---|
| Would prefer to be asked about the general experiences rather than being focused on last visit |
|
| More room to elaborate |
|
| Room to talk about planned changes at the surgery |
|
| Parking |
|
| Should have a ‘not applicable’ option |
|
| KISS test |
|
Revisions to questions: changes from the first to the second pilot
The changes suggested by patients were considered along with the distribution of responses from the survey, tables of correlations between questions, and the extent to which questions discriminated between practices. The following changes were made.
Some questions removed that were found to duplicate other questions or add no new information
Four questions were removed from the section about reception staff (making you feel welcome, taking time to listen, making efforts to communicate, and understanding circumstances) because the questionnaire data suggested that they were non-discriminating questions (if a patient answered ‘yes’ to treating with respect, or being helpful, then they were likely to answer ‘yes’ to all the others). In addition, these specific issues were not commonly raised in the interviews.
In the section about how easy it is to visit the GP surgery, just one question was removed: about travel to the surgery. This was after lengthy discussion within the research team. Although this topic was mentioned often in the interviews and appeared to be an issue for patients according to the questionnaire data, we decided that we should include only questions about which the PCO could take action in response. As parking arrangements are so often beyond the control of the PCO, this question was removed.
The final section, about how well the GP surgery meets patients’ needs, was significantly reduced: three questions were removed (flexibility, help and support, and organisation of care) as a relatively high number of respondents chose ‘no opinion’, and it was felt that they did not add new information over and above the more specific questions.
New questions added where the first pilot failed to address an important issue
Two new questions were added to the first section about arranging appointments. The first asked how easy it was for patients to get in touch with the surgery. The second provided patients with a list of potential problems and asked them to indicate whether or not they had experienced any of them. These were designed to include the issues that were raised during the interviews that did not easily fit within the previous questions, such as difficulties getting through on the telephone and waiting too long for an appointment.
The revised section, about how well patients were treated by reception staff, included a new ‘overall’ question. We hoped that this would capture any other aspects of receptionists’ behaviour that were not covered by the reduced list of questions in this section. A similar question was also added to the section about how easy it was to visit the surgery, and how good the surgery was at helping to co-ordinate care.
A new question was added to the end of the questionnaire, allowing patients to write about their positive experiences of responsive care at their GP surgery. The previous version did not include such a question, and patients were often keen to include positive stories as well as suggestions for improvement. This was also a key feature of the interviews – patients often tempered their negative experiences with narratives of when things went well.
Amended wording to make it clearer and prevent misunderstanding
The preamble at the start of the questionnaire was completely rewritten to encourage participation. The previous version was mainly descriptive and explained the purpose of the questionnaire, and possibly ‘assumed’ that the patient would complete the questionnaire. The revised version accentuated the importance of individuals’ responses, and what would happen if they did not respond. We included an estimation of how long the questionnaire might take to complete, as the interviews suggested that it looked quite daunting.
A few questions in the first section (appointments) were amended slightly to make the meaning clearer, for instance adding ‘no opinion’ to the response options, adding more options to the preferences for who the appointment was with, and adding ‘overall’ to the question about being able to arrange a suitable appointment.
The second and third sections (reception staff and visiting the surgery) were revised from the present to the past tense, focusing on the patient’s last visit rather than their experiences in general, to bring these in line with the first section.
The section about co-ordinating care was amended to provide more examples, as the meaning of ‘keeping up to date’ and ‘organising your health care with hospitals’ was not clear to patients. We also changed the ‘no opinion’ response option to ‘not applicable’, as patients sometimes hand-wrote ‘N/A’ if the question did not apply to their situation. The free-text question inviting patients to provide additional comments was also amended to make it clear that we wanted to hear about problems and solutions rather than just suggestions for improvement.
In the final section about meeting patients’ needs, the section title was amended to ‘overall, how do you feel about this GP practice?’, as this more closely reflected the reduced list of questions. We also changed the wording of the question about circumstances to make it personal to the patient rather than ‘for people in your circumstances’.
Formatting improved for ease of completion
The overall format of the questionnaire remained unchanged. Just one revision was made: reordering the questions in the appointments section (to more closely reflect the patient journey from initial contact to getting a suitable appointment).
Changes to the ‘about you’ section
These included:
-
bolding to the statement telling patients that if they did not want to answer a question, they could leave it blank
-
a new response option for ‘transgender’ (as one patient added this option to the previous version)
-
a new response option for ‘Gypsy or traveller’, as this was omitted from the first version
-
examples of ‘other long-standing illness’, as patients often wrote down their ailments if they felt that the list was inadequate
-
changing ‘tick as many as you need to’ to ‘please tick only one’ for the question about working status
-
removal of ‘if you are working’ from the question about taking time away from work to see the doctor
-
adding a response option of ‘I would prefer not to say’ to the question about sexuality, as some interviewees did not wish to answer this question
-
changing ‘what language(s) do you speak?’ to ‘what is your first language?’ as a list of languages did not add information and potentially caused a burden on the patient.
The revised questionnaire – GP questionnaire version 2 – is shown in Appendix 10.
Developing version 1 of the pharmacy questionnaire
A first version of a parallel questionnaire for use by pharmacies was developed for testing in pilot 2. This mirrored the GP questionnaire, but was adapted to make it appropriate for use in pharmacies, informed by the findings of the interviews in stage 1. The key differences between the pharmacy version 1 and the parallel version 2 GP questionnaire are summarised in Table 14.
| Theme | Comparison of pharmacy and GP questionnaire |
|---|---|
| Ease of access to appropriate services | Making appointments is not relevant to most pharmacy visits; pharmacy questionnaire instead included questions about how easy it was to get the advice or medication they needed, and to get to see their preferred member of staff. It also asked about speed of service. These issues of levels of stock and speed of service emerged as important during patient interviews |
| Staff attitudes and behaviours | Mirrored GP questions about whether or not staff were friendly, respectful, helpful |
| Alignment of physical environment with patient needs | Mirrored GP questions about getting around the building, talking to staff without being overheard, and knowing what it is your turn to be seen. Included some different questions, relating to getting supplies needed, finding what wanted on shelves |
| Co-ordination and support for ongoing care | Pharmacies have less input into co-ordination of care than GP, so questions in this section differed from GP questionnaire, and covered providing advice, co-ordinating with GP (e.g. about repeat prescriptions), fitting patients circumstances (e.g. home delivery of prescriptions), informing patients about other useful services |
| Diversity awareness and cultural alignment | Mirrored overall question from GP questionnaire on whether or not service meets needs |
| Information and engagement | Mirrored overall questions from GP questionnaire |
Version 1 of the pharmacy questionnaire is also shown in Appendix 10.
Administering the questionnaire: feedback from practices and consultation about alternative formats
Feedback from participating practices
Feedback was gained from participating practices about their experiences of administering the questionnaire. The feedback highlighted some of the challenges for practices in handing out the questionnaire to patients attending the surgery. These mainly included patient resistance to taking a questionnaire; receptionist reluctance to bother patients by asking them to take a questionnaire; and lack of time to explain to patients why they were being given a questionnaire. Practices felt that they were able to overcome these challenges by persistent reminders and support to receptionists from the practice manager, conveying enthusiasm, and concentrating their efforts to hand out the questionnaire into discrete periods (although there is the potential for this to bias the sample).
We have handed quite a few out, they are being handed out to patients as they arrive, we have not had any challenges. [. . .] Some patients who are offered them don’t want to do them so I think that’s why it’s taking a while to do them.
PCO11, by e-mail
I think reception staff are hard to motivate to do this and find it difficult to do, they perhaps think in terms of accosting strangers with something unwelcome.
PCO12, by e-mail
Although administration of the questionnaire in person to patients attending the practices generated a reasonable response rate, there is little control over the quality of the patient sample, and patients who do not regularly attend their GP practice are less likely to be included in the sample. There were suggestions that this approach could be onerous. In pilot 2, we included postal administration, and the use of lay people to support administration of the questionnaire and help patients to complete it if needed.
Consultation about alternative formats
We proposed to develop a questionnaire that would be accessible across different patient groups, and in pilot 1 we began to consider possibilities for different formats for the questionnaire. Advisory group and team members were sent a list of six possible format options and were asked to rank their preferences regardless of cost. These format options were collated from various patient experience questionnaires; for example, the national GP patient survey is available in many formats – pencil and paper, online, British Sign Language, large print and Braille, a telephone helpline to help people complete the questionnaire, and information and a telephone service in 13 languages other than English.
Seven responses were received from four research team members, an expert member of the advisory group, a representative from a learning disabilities charity, and a representative from a network for patients and staff in primary care.
The questionnaire from pilot 1 was already available in a standard paper and an online version. The ranks allocated to each proposed alternative format are shown in Table 15.
| Format | Rank (1–6) | Mean (min., max.) |
|---|---|---|
| Easy Read/pictorial version | 3, 1, 3, 1, 1, 2, 4 | 2.14 (1, 4) |
|
||
|
||
|
||
| Translated into other languages (on paper, online and/or audio) | 4, 4, 5, 4, 5, 3, 1 | 3.71 (1, 5) |
|
||
| Spoken audio (online or DVD) | 5, 4, 4, 3, 5, 6, 2 | 4.14 (2, 6) |
|
||
|
||
|
||
| Braille | 6, 6, 6, 6, 5, 4, 5 | 5.43 (4, 6) |
|
||
| Administered by lay people or community ambassadors | 1, 2, 1, 2, 1, 1, 3 | 1.57 (1, 3) |
|
||
|
||
|
||
| Administered by telephone | 2, 3, 2, 5, 1, 5, 6 | 3.43 (1, 6) |
|
||
|
||
|
Easy Read92 and lay-administered emerged as the preferred options for alternative formats for the questionnaire. This was reinforced by open comments that accompanied the ranking forms:
People with a learning disability will often need support to complete questionnaires, this is not always available. It may also take them longer to complete the forms and will need an explanation of what is required. Use easy words with not too many options to choose from and use a size 14 font. Many of them do not have access to the internet, so online is not an option.
I think you have covered most formats. I have marked high those that I think will be acceptable for a wide and diverse group of patients. I do think that the use of lay interviewers appropriately briefed can be very good. I cannot think of alternative options.
Pilot 2 provided an opportunity to test the feasibility of involving suitably briefed lay people in administering the questionnaire. The development of an Easy Read version was delayed until an initial analysis of pilot 3 data had been conducted to ensure that the Easy Read version was comparable with the final standard version.
Summary of pilot 1
Pilot 1 allowed initial testing of the GP version of the questionnaire. From inspection of responses to the survey, and checking content validity based on patient interviews, we identified changes required to improve the questionnaire. Based on feedback from the team and members of the advisory group about formats to improve accessibility of the questionnaire, we chose to focus on lay and interpreter administration, and developing an Easy Read version. We also developed a pharmacy version. We went on to test these further in pilot 2.
Pilot 2: general practitioner questionnaire version 2 and pharmacy questionnaire version 1 – survey and cognitive interviews
Methods
The second pilot took place over 3 months (October–December 2012). For the second pilot, two GP practices were chosen (one small practice in a non-English speaking inner-city area, and one very large practice in a deprived town). In addition, two pharmacies (one inner-city and one rural) were invited to pilot the pharmacy version.
While the first pilot exclusively employed face-to-face methods to distribute the patient packs, the second pilot included postal methods in one GP practice. Based on evidence on improving response rates,93,94 the process entailed:
-
Sending patients a prenotification letter informing them that they would soon receive a questionnaire through the post.
-
Sending patients the patient pack (containing an invitation letter, information sheet, questionnaire and reply-paid envelope) 1–2 weeks later.
-
Sending patients a follow-up letter 1–2 weeks later. This letter thanked patients who had returned the questionnaire, and reminded those who had not to complete and return the questionnaire. It included some frequently answered questions about concerns that patients may have about completing questionnaires.
The questionnaire was posted out to 150 patients in one practice, selected randomly from the patient list for patients who had visited the surgery in the previous 6 months. An online version was made available.
The other GP practice (PCO10) asked members of their PPG to distribute the patient packs in the waiting rooms; this enabled us to assess the feasibility and effectiveness of involving lay people in administering the questionnaire, which was identified in the consultation in pilot 1 as a potentially important way of improving accessibility and uptake. PPG members handed waiting patients a patient pack, briefly explained the study, and offered to help patients to complete the questionnaire if they wished. It was hoped that this offer of help might increase the response rate from those who may have literacy or sight problems, and those for whom English is not their first language.
In the pharmacies, 75 packs were handed out to adult patients attending for medical advice or prescriptions. Customers were excluded if they were simply using the pharmacy as a shop, for example to buy toiletries, or if staff felt that it would be inappropriate to include them, for example due to a recent bereavement.
Patients completing the questionnaire were invited to return their contact details to express an interest in being interviewed. The aim was to interview up to 20 patients. Cognitive interview techniques,95 drawing on the ‘verbal probing’ method,96 were used to identify problems with questions and misinterpretation: specifically, how participants understood each question on the questionnaire; how they answered it; and how the question might be improved. The topic guide for the interviews is shown in Appendix 11. Interviews were conducted by JW, mostly in participants’ homes (two chose to be interviewed on university premises). We aimed to involve non-English speakers in the cognitive interview process; we recruited Polish speakers in the waiting room of one of the participating GP practices (PCO06), and Gujarati speakers from the community organisation involved in recruitment to the focus groups. An interpreter assisted patients in completing the questionnaire and participating in interviews. The interpreters were interviewed by JW about the experience and difficulties of translating the questionnaire for responders.
Transcripts were uploaded into NVivo for analysis, and coded and charted to identify key issues relating to comprehension, response options and interviewer difficulties97,98 (for the interpreted questionnaires). We identified suggestions for improvements.
The findings from the cognitive interviews were used in conjunction with data from the survey to refine the questionnaire to develop a near-final version. Version 3 of the GP questionnaire and version 2 of the pharmacy questionnaire were then tested for reliability and validity in pilot 3, along with version 1 of the walk-in centre questionnaire.
Results
Survey
Across the two practices and the two pharmacies that took part in the second pilot, a response rate of 36% was achieved, ranging from 19% in PCO02 to 76% in PCO03 (both pharmacies). A total of 163 completed questionnaires were returned (Table 16).
| PCO | Number returned | Response rate |
|---|---|---|
| PCO type: GP practice | ||
| 06 | 54 | 36% (of 150) |
| 10 | 38 | 25% (of 150) |
| GP practice total | 92 | 31% (of 300) |
| PCO type: pharmacy | ||
| 02 | 14 | 19% (of 75) |
| 03 | 57 | 76% (of 75) |
| Pharmacy total | 71 | 47% (of 150) |
| Total | 163 | 36% (of 450) |
Responders included 92 women, 62 men and one transgender person, aged from under 18 to over 85 years. Twenty-eight patients had physical disabilities or mobility problems, nine had hearing impairments, two had a visual impairment, and two had learning difficulties. Three patients were black, 12 were from a South Asian background, two were mixed and 12 classified themselves as ‘other’ ethnic group. The majority of patients were either working (full- or part-time) or retired/out of work, with a small number in full-time education (Table 17).
| Characteristics | Number (%) of participants for GP surgeries (N = 92) | Number (%) of participants for pharmacies (N = 71) | Number (%) of participants for all (N = 163) |
|---|---|---|---|
| Sex | |||
| Female | 47 (43) | 45 (63) | 92 (56) |
| Male | 40 (51) | 22 (31) | 62 (38) |
| Transgender | 1 (1) | 0 (0) | 1 (< 1) |
| Missing data | 4 (4) | 4 (6) | 8 (5) |
| Age (years) | |||
| Under 18 | 0 (0) | 1 (1) | 1 (< 1) |
| 18–24 | 9 (10) | 1 (1) | 10 (6) |
| 25–34 | 14 (15) | 4 (6) | 18 (11) |
| 35–44 | 9 (10) | 7 (10) | 16 (10) |
| 45–54 | 16 (17) | 16 (23) | 32 (20) |
| 55–64 | 21 (23) | 16 (23) | 37 (23) |
| 65–74 | 14 (15) | 16 (23) | 30 (18) |
| 75–84 | 6 (7) | 4 (6) | 10 (6) |
| 85 or over | 0 (0) | 1 (1) | 1 (< 1) |
| Missing data | 3 (3) | 5 (7) | 8 (5) |
| Ethnicity | |||
| White British | 66 (72) | 59 (83) | 125 (77) |
| Black or Black British | 3 (3) | 0 (0) | 3 (2) |
| Asian or Asian British | 7 (8) | 5 (7) | 12 (7) |
| Mixed British | 2 (2) | 0 (0) | 2 (1) |
| Chinese | 0 (0) | 0 (0) | 0 (0) |
| Other ethnic group | 10 (11) | 2 (3) | 12 (7) |
| Missing data | 4 (4) | 5 (7) | 9 (6) |
| Health conditions | |||
| Deafness or severe hearing impairment | 7 (8) | 2 (3) | 9 (6) |
| Blindness or severe visual impairment | 1 (1) | 1 (1) | 2 (1) |
| A condition that substantially limits your ability to carry out basic activities, e.g. walking, climbing stairs, lifting or carrying | 19 (21) | 9 (13) | 28 (17) |
| A learning disability | 1 (1) | 1 (1) | 2 (1) |
| A long-standing mental health problem | 5 (5) | 5 (7) | 10 (6) |
| Any other long-standing illness | 32 (35) | 24 (34) | 56 (34) |
| Missing data | 2 (2) | 4 (6) | 6 (4) |
| Working status | |||
| Full-time paid work (30 hours or more each week) | 33 (36) | 16 (23) | 49 (30) |
| Part-time paid work (under 30 hours each week) | 13 (14) | 16 (23) | 29 (18) |
| Full-time education at school, college or university | 2 (2) | 0 (0) | 2 (1) |
| Not in paid work/retired | 40 (44) | 36 (51) | 76 (47) |
| Missing data | 3 (3) | 3 (4) | 6 (4) |
| English as first language | |||
| Yes | 73 (79) | 58 (82) | 131 (80) |
| No | 12 (13) | 5 (7) | 17 (10) |
| Bilingual/multilingual | 5 (5) | 3 (4) | 8 (5) |
| Missing data | 2 (2) | 5 (7) | 7 (4) |
Cognitive interviews
Of the 163 patients who returned a questionnaire, 28 expressed an interest in being interviewed (17%). Interviews were conducted with a purposive sample of 14 patients. Five had completed a pharmacy questionnaire and nine a GP questionnaire.
We interviewed eight women and six men. Eleven were white British. There was a fairly even distribution of age groups, although no patient was under 25 years. Four had mobility problems, three had a mental health problem and nine had other illnesses. One was also a carer (Table 18).
| Characteristics | Number of interviewees (N = 14) |
|---|---|
| Sex | |
| Female | 8 |
| Male | 6 |
| Ethnicity | |
| Black or Black British | 1 |
| White | 11 |
| White non-British | 1 |
| Unknown | 1 |
| Age (years) | |
| 18–24 | 0 |
| 25–34 | 2 |
| 35–44 | 1 |
| 45–54 | 2 |
| 55–64 | 4 |
| 65–74 | 1 |
| 75–84 | 2 |
| 85 or over | 1 |
| Unknown | 1 |
In addition, two Polish speakers and two Gujarati speakers completed the questionnaire and took part in cognitive interviews conducted by researchers who spoke their language. Both researchers reported back the key issues arising from the cognitive interviews and from their experiences of interpreting the questionnaire for non-English speakers.
Key issues arising in the cognitive interviews are summarised in Table 19.
| Questionnaire | Theme | Key issues |
|---|---|---|
| GP | Ease of access to appropriate services (arranging an appointment) | Section is complex and difficult to complete Not exhaustive (e.g. want GP who speaks own language) ‘Last visit’ may not be representative |
| Alignment of physical environment with patient needs (how easy it for you to visit the surgery) | Travelling to the surgery and parking are important Need to give examples of other facilities, not just toilets The term ‘booking in’ caused confusion The word ‘comfort’ could be misunderstood; ‘feel at ease’ would be better |
|
| Co-ordination and support for ongoing care (how good the surgery is at organising your care) | The term ‘community services’ is not well understood; need more examples | |
| Diversity awareness and cultural alignment (how good the surgery is at meeting your needs) | The term ‘people like you’ caused problems; ‘for you’ would be better The term ‘feel comfortable’ is confusing |
|
| Pharmacy | Overall | Not being overheard/being able to have a private consultation with staff was important Whether or not the pharmacy had what they needed in stock was also important Question about getting the medication, supplies or advice they needed was seen as covering too many issues Could be difficult to remember the specifics of the last visit Some confusion about the terms ‘comfort’, ‘comfortable’, ‘signpost’ and ‘other services’ |
| Generic comments | Easier if questions were more uniform; use stem ‘how easy’ Concern that ‘last visit’ may not be representative of general experiences ‘Overall’ questions caused confusion/seen as repetitive and unnecessary |
Revisions to questions: changes from the second to third pilot
Based on inspection of the pilot data, and informed by the findings of the cognitive interviews, we made the following changes to the GP and pharmacy questionnaires:
Some questions were removed as they were considered to duplicate other questions or did not add new information
The ‘overall’ question at the end of each section and the corresponding free-text box asking for further comments were removed. This was mainly for the purposes of shortening the questionnaire. Question 25 provided an overall question about how well the surgery met patients’ needs, and this was felt to be sufficient.
The list of potential problems when making an appointment was removed from the GP surgery version. Cognitive interviews suggested that the first section included too many questions and was rather complex. We reflected on the findings of the cognitive interviews, and held team discussions around how best to frame questions in a way that matched our conceptualisation of responsiveness as relating to the extent to which patients were able to easily access and use services in ways that met their needs. This resulted in the decision to rephrase questions throughout the questionnaire using the stem ‘how easy’ and ‘how good’. For the section on access, this enabled us to return to asking about general experiences (rather than the patient’s last visit), which fitted with our original intentions, while allowing the questionnaire to account for the fact that patients’ experiences differ depending on what their specific needs are when they try to make an appointment.
The question about whether or not the PCO staff were respectful was removed as it did not add any new information to the section about staff.
The question about whether or not the patient could get the medicines, supplies or advice that they needed was removed from the pharmacy version, as these issues were covered in other questions. Several questions were removed from the section about organising and providing services in the pharmacy version because the survey data suggested that these questions did not perform well.
New questions were added where the second pilot failed to address an issue considered to be of importance
Four new questions were added to the section about making an appointment in the GP surgery version of the questionnaire: interpreters, home visits, telephone consultations and finding out about opening hours. The question about opening hours was previously part of a question about the provision of information, but was moved to this section as it closely relates to how easy it is for patients to get in touch with the PCO. Similarly, a new question about the provision of translated or Easy Read information was added to the section about visiting the surgery. This ensured that we covered the key issues that arose consistently from patient interviews across different patient groups, as well as issues that were highly important for specific patient groups.
The question about travelling to the PCO was reinstated because it was mentioned by so many patients.
A question about politeness was added to the section about PCO staff, replacing the question about respect. Many patients spoke in the interviews of the importance of staff being polite, and we felt that this concept was sufficiently distinct from other questions in this section (friendliness, helpfulness) to warrant inclusion.
A new question about getting repeat prescriptions was added to the GP surgery questionnaire, as interviewees mentioned this frequently.
Wording was amended to make it clearer and to prevent misunderstanding
The titles of both questionnaires were amended to simplify them, and section headers were amended to make them more succinct, to ensure that they accurately described the questions that followed; for instance, ‘About how good this GP surgery is at helping to co-ordinate your care’ was amended to ‘Helping to organise your ongoing care’.
More examples were added to some questions to ensure that patients understood the question; for instance, the question about facilities in the surgery gave the example of toilets in the previous version, and we added ‘the waiting area, baby changing room’.
The question about ‘waiting in comfort’ was amended to ‘helping you feel at ease’ as ‘comfort’ caused problems in understanding, especially for those who did not speak English. Similarly, the question about booking in on arrival was amended to ‘let staff know that you have arrived’, as ‘booking in’ caused confusion for some of the interviewed patients. The question about knowing when it was your turn to be seen was amended to make it clear that this was about being seen by the doctor or nurse rather than by the receptionist. In the pharmacy questionnaire, the term ‘signpost’ was replaced by ‘letting you know’.
The overall question on how well the PCO met patients’ needs was reworded to make it clear that this was about whether or not the service suited the patient well.
The wording of the questions about listening and communicating were amended. The revised versions ask separate questions about making suggestions, listening to complaints and acting on feedback.
The free-text box at the end of the main questionnaire was revised to include an invitation for patients to use the box to explain any of their other answers, as well as to suggest improvements.
Both versions were professionally designed by a designer in the Audio-Visual Services department at the University of Leicester, and formatting was improved to make it easier to complete
The designer developed a full-colour front cover using appropriate picture banks. She suggested a new title for the questionnaires, and advised on format and colour throughout.
Interviews indicated that although patients were able to complete the questionnaire in a short time, the length of the questionnaire was initially off-putting. For the amended versions, we introduced a double-column format, essentially halving the number of pages. This had the dual benefit of reducing the length and aligning the branding of the questionnaires with other NHS questionnaires, such as the national GP patient survey.
The header reminding patients to think about their own circumstances when answering the questions was removed, as it was felt to be unnecessary.
The order of questions in the pharmacy version was improved, and a new question was added about the home delivery of prescriptions (as this was considered important by interviewees). Wording was amended to aid understanding.
A few minor changes were made to the ‘About you’ section.
In addition to the changes from pilot 2 to pilot 3, we added a new section to the back of the questions. This page included nine questions from the SERVQUAL questionnaire (comprising the SERVQUAL scales ‘responsiveness’ and ‘empathy’)35 for validation purposes, and we included an invitation for patients to provide their contact details if they would be willing to complete the questionnaire for a second time (for test–retest validity) (see Chapter 7).
The revised questionnaires – GP version 3 and pharmacy version 2 – are shown in Appendix 13.
Developing version 1 of the walk-in centre questionnaire
A first version of a parallel questionnaire for use by walk-in centres was developed for testing in pilot 3. This mirrored the GP questionnaire, but was adapted to make it appropriate for use in walk-in centres, informed by the findings of interviews in stage 1. The key differences between the walk-in centre version 1 and the parallel version 3 GP questionnaire are summarised in Table 20.
| Theme | Comparison WIC and GP questionnaire |
|---|---|
| Ease of access to appropriate services | Making appointments is not relevant to WICs; WIC questionnaire instead included similar questions to the pharmacy questionnaire, about how easy it was to get what you wanted without a long wait, and how easy it was to get to see their a member of staff of their own sex/same language |
| Staff attitudes and behaviours | Mirrored GP questions about whether or not staff were friendly, helpful, polite |
| Alignment of physical environment with patient needs | Mirrored GP questions about: getting around the building, using facilities, talking to staff without being overheard, knowing what it’s your turn to be seen, feeling at ease, and provision of appropriate information |
| Co-ordination and support for ongoing care | WICs have less input into co-ordination of care than GP. A single question on ‘letting you know about health or community services available elsewhere’ was included |
| Diversity awareness and cultural alignment | Mirrored overall question from GP questionnaire on whether or not service meets needs |
| Information and engagement | Mirrored overall questions from GP questionnaire |
Version 1 of the walk-in centre questionnaire is also shown in Appendix 13.
Summary of pilot 2
Pilot 2 allowed additional testing and refinement of the GP version of the questionnaire based on inspection of responses to the survey and findings from cognitive interviews. The pharmacy questionnaire was also subject to testing, and a parallel walk-in centre version was developed for testing in phase 3. The involvement of PPG members in handing out the questionnaire and helping patients complete it was welcomed by PPG members and patients, although it did require commitment of time from PPG members and did not generate a high response rate. Postal administration was used in only one practice, but they found it burdensome and were concerned about a low response rate from ‘seldom-heard’ groups, particularly non-English speakers.
Discussion
We conducted two rounds of piloting involving administering the questionnaires to 450 patients in GP surgeries and pharmacies, narrative interviews to check content validity and cognitive interviews to explore problems with wording and layout. At the end of this stage, we had a relatively final version of the questionnaire, available in three parallel forms: GP practice, pharmacy and walk-in centre.
We found that handing out questionnaires to consecutively attending patients in GP surgeries and pharmacies was acceptable and generated a reasonable response rate in most participating PCOs. The exception to this was one pharmacy in which only a 19% response was achieved. This was attributed by pharmacy staff to a lack of interest from staff and patients, as well as to language problems because a significant number of their patients did not speak English. The large majority of responders overall were white British, and it is likely that ‘seldom-heard’ groups will be under-represented in this sample as they are less likely to respond to this recruitment method. We used additional recruitment strategies to include patients from one specific hard-to-reach group in the cognitive interviews: non-English speakers. This involved recruiting in person in the waiting room of one of the GP practices and through contact with a community organisation.
While the nature of the sample is relatively unproblematic in terms of piloting and refining the questionnaire, it is important that when the questionnaire is used in practice, the views of hard-to-reach groups are sought: PCOs can get a valid picture of their responsiveness only if they hear the views of patients across from diverse and disadvantaged groups within their practice population. In pilot 3, we conducted a substudy in two GP practices to explore feasible ways of identifying and accessing the views of patients from hard-to-reach groups as part of conducting a survey using the questionnaire.
We found the involvement of a designer to be important at this stage; the designer brought additional expertise in formatting the questionnaire in ways that would improve its appeal to diverse patient groups and make it easier to use.
Following pilot 2, the revised questionnaires were subject to large-scale testing to assess reliability and validity.
Chapter 7 Testing the questionnaires (pilot 3) and accessing the views of diverse groups substudy
Summary of this chapter
Version 3 of the GP questionnaire, version 2 of the pharmacy questionnaire and version 1 of the walk-in centre questionnaire were subject to large-scale testing to assess reliability, validity and acceptability. The questionnaires were distributed to more than 3000 patients across 16 PCOs in three regions of England. Patients were offered the opportunity to complete the questionnaire for a second time, to assess the test–retest validity of the instruments.
A substudy was conducted, involving two practices, to explore feasible ways of identifying and accessing the views of hard-to-reach groups within the patient population.
Following data analysis, the questionnaires were subject to minor revisions to produce the final versions. These final versions were used to develop Easy Read versions for people with learning difficulties. The Easy Read versions were tested with a group of people with learning difficulties, and amendments were made in response to the issues they raised.
Methods
This phase of the study subjected the questionnaires to piloting on a large scale to enable testing of reliability and validity. Although we administered all three versions in pilot 3, we conducted validity and reliability analysis only on the GP version of the questionnaire. This was partly due to sample size restrictions, and partly because the GP version can be seen as providing a template for the other questionnaires. The results of this pilot can be taken as a good indicator of the reliability and validity of the GP measure, but the pharmacy and walk-in centre measures will require further work to develop and validate them.
We aimed to assess the factor structure of the questionnaire, and whether or not a subset of questions could be used to generate responsiveness ‘scores’ that could act as measures of patient experience of responsiveness across different practices or different patient groups. We aimed to check validity by administering two validated measures alongside the responsiveness questionnaire; these were two subscales from the SERVQUAL questionnaire,35,41 ‘responsiveness’ and ‘empathy’. The SERVQUAL subscales were chosen as they are validated measures of relevant constructs, and we would expect our measure to show moderate, negative correlation with these scales (due to the direction of scoring of the questions). The SERVQUAL responsiveness scale focuses on customer service, while the empathy scale looks at the extent to which the GP practice understands patients’ needs and has patients’ best interests at heart. We elected not to use the WHO responsiveness questionnaire;58 this is a valid measure, but because it measures responsiveness of health systems rather than individual providers it was not considered appropriate for this purpose. We also asked a subsample of responders to complete the questionnaire again after a period of around 2 weeks, to check test–retest reliability.
This final testing phase took place over 6 months (March to August 2013). Prior to this, additional PCOs were recruited in London and the north-west of England. The corresponding PCRNs helped with recruitment in identifying appropriate GP surgeries (n = 8), walk-in centres (n = 3) and pharmacies (n = 5) (characteristics of the PCOs are shown in Chapter 2).
Our original protocol specified 3000 questionnaires, with an expected response rate of 40%, in order to attain 1200 completed questionnaires. The original sample size stated that if 493 responders were sent the second mail-out, allowing for a 60% response rate (n = 296), this would allow an ICC of 0.75 from the test–retest reliability to be estimated with 95% confidence limits extending in either direction (two-tailed) of no further than 0.05.
This was revisited in the context of testing the three parallel questionnaires. We elected to administer 1700 questionnaires in GPs practices, 800 in pharmacies and 600 in walk-in centres. Allowing for a conservative response rate, this would provide 680, 320 and 240, respectively, for test–retest analysis. For the smallest figure of n = 240, this would allow an ICC of 0.75 to be estimated with 95% confidence limits of 0.055, and therefore only minimally increasing the confidence limits from the original sample size. This sample size was calculated in nQuery (Statistical Solutions, Saugus, MA, USA).
For factor analysis, there have been multiple publications on recommendations regarding the minimum sample size necessary to obtain factor solutions that are adequately stable. These recommendations vary widely from as little as a minimum of 100 up to 500. 99 Comrey and Lee100 offered a rough rating scale for adequate sample sizes in factor analysis: 100 = poor, 200 = fair, 300 = good, 500 = very good, 1000 or more = excellent. The anticipated sample size for the GP questionnaire of 680 is within the upper range for recommendations for factor analysis, while the smallest sample size available for this study (n = 240) is at the lower end of these recommendations.
We aimed to ask PCOs to hand out 200 patient packs to patients attending for appointments or medical advice. One specialist practice for homeless patients handed out 100 patient packs as this was a more realistic number for their small patient list. Two pharmacies both had two branches, and so 100 were handed out in each. Two other pharmacies also had a sample size of 100, as they participated in pilot 2 as well as pilot 3. During this phase, one GP surgery withdrew from the study, so four other surgeries were asked to distribute a further 50 patient packs each to make up the numbers. Two GP surgeries were asked to take part in a substudy to encourage seldom-heard patients to complete the questionnaire (see Substudy: accessing the views of diverse groups). An additional 20 questionnaires were handed out by these practices (Table 21).
| PCO | Region | Number of forms (N = 3140) |
|---|---|---|
| GP surgery | ||
| 07 | East Midlands | 100 |
| 08 | East Midlands | 250 |
| 13 | East Midlands | 200 |
| 16 | London | 250 |
| 18 | London | 220 |
| 20 | North West | 250 |
| 21 | North West | 250 |
| 22 | North West | 220 |
| GP surgery total | 1740 | |
| Pharmacy | ||
| 02 | East Midlands | 100 |
| 03 | East Midlands | 100 |
| 14 | London | 200 |
| 15 | London | 200 |
| 24 | North West | 200 |
| Pharmacy total | 800 | |
| WIC | ||
| 09 | East Midlands | 200 |
| 17 | London | 200 |
| 23 | North West | 200 |
| WIC total | 600 | |
We chose the in-PCO distribution method as the postal method was problematic during stage 2 – the workload associated with a prenotification letter, the patient packs and a follow-up letter was prohibitive and the response rate was low – and we wanted to ensure that we chose a method that was practical for PCOs, both during the research project and when in general use post project. Patients were invited to return their completed questionnaire to the PCO or to return it directly to the research team using a freepost envelope. A website address was provided for patients wishing to complete the questionnaire online.
Based on the analysis of the data, we made further minor amendments to the questionnaires. PCOs received feedback on their results from the questionnaire.
Results
Across the eight GP practices, 1529 questionnaires were handed out. In the five pharmacies, 800 were handed out. In the three walk-in centres, 600 were handed out. An overall response rate of 39% was achieved, ranging from 22% in PCO7 (a GP practice for homeless patients) to 79% in PCO03 (a pharmacy). A total of 1139 questionnaires were returned (Table 22). Only the GP results are reported in the remainder of this section.
| PCO | Number returned | Response rate |
|---|---|---|
| GP practice | ||
| 07 | 22 | 22% (of 100) |
| 08 | 98 | 39% (of 250) |
| 13 | 19 | 17% (of 104a) |
| 16 | 69 | 34% (of 205b) |
| 18 | 114 | 52% (of 220) |
| 20 | 136 | 54% (of 250) |
| 21 | 139 | 56% (of 250) |
| 22 | 33 | 22% (of 150c) |
| GP practice total | 630 | 41% (of 1529) |
| Pharmacy | ||
| 02 | 24 | 24% (of 100) |
| 03 | 79 | 79% (of 100) |
| 14 | 49 | 25% (of 200) |
| 15 | 43 | 22% (of 200) |
| 24 | 51 | 26% (of 200) |
| Pharmacy total | 246 | 31% (of 800) |
| WIC | ||
| 09 | 65 | 33% (of 200) |
| 17 | 123 | 62% (of 200) |
| 23 | 75 | 38% (of 200) |
| WIC total | 263 | 44% (of 600) |
| Total | 1139 | 39% (of 2929) |
Responders included 363 women and 243 men, aged from under 18 to over 85 years old, with the largest age group being the newly retired. One hundred and twenty-eight patients had physical disabilities or mobility problems, 64 had hearing impairments, 20 had visual impairments, and 19 had learning difficulties. Fourteen per cent were from BME groups. The majority of patients were either working (full- or part-time) or retired/out of work, with a small number in full-time education (Table 23).
| Characteristics | Number (%) of participants for GP surgeries (of 630 responses) |
|---|---|
| Sex | |
| Female | 363 (58) |
| Male | 243 (39) |
| Incorrectly answered | 2 (< 1) |
| Missing data | 24 (4) |
| Age (years) | |
| Under 18 | 5 (1) |
| 18–24 | 25 (4) |
| 25–34 | 72 (11) |
| 35–44 | 87 (14) |
| 45–54 | 94 (15) |
| 55–64 | 114 (18) |
| 65–74 | 136 (22) |
| 75–84 | 67 (11) |
| 85 or over | 8 (1) |
| Incorrectly answered | 3 (< 1) |
| Missing data | 19 (3) |
| Ethnicity | |
| White British or European background | 508 (81) |
| Mixed/multiple ethnic background | 5 (1) |
| Asian background | 48 (8) |
| Black/African/Caribbean background | 28 (4) |
| Other ethnic group | 4 (1) |
| Incorrectly answered | 17 (3) |
| Missing data | 20 (3) |
| Health conditionsa | |
| Deafness or severe hearing impairment | 64 (10) |
| Blindness or severe visual impairment | 20 (3) |
| A condition that substantially limits your ability to carry out basic activities, e.g. walking, climbing stairs, lifting or carrying | 128 (20) |
| A learning disability | 19 (3) |
| A long-standing mental health problem | 79 (13) |
| Any other long-standing illness | 140 (22) |
| Working statusa | |
| Full-time paid work (30 hours or more each week) | 116 (18) |
| Part-time paid work (under 30 hours each week) | 80 (13) |
| Full-time education at school, college or university | 11 (2) |
| Unemployed | 65 (10) |
| Fully retired from work | 212 (34) |
| Long-term sick or disabled | 57 (9) |
| Not in work/other | 112 (18) |
| English as first languagea | |
| Yes | 515 (82) |
| No | 71 (11) |
| Bilingual/multilingual | 30 (5) |
| Missing | 23 (4) |
Data entry and cleaning
Data were entered onto SPSS v20. Descriptive summaries (frequency tables and charts) were used to check for any incorrect data (see Appendix 14). If a responder had ticked more than one option, then the higher (more negative) number was taken. For the SERVQUAL scale, where a respondent had circled two adjacent numbers, the lower (more negative) number was taken. Where a respondent had circled two numbers within two points of each other, the middle value was taken (e.g. if 3 and 5 circled, 4 was entered). Where a respondent circled two non-adjacent numbers more than two points apart, this was counted as missing data. We calculated scores for the two dimensions of the SERVQUAL scale: responsiveness (four questions: A–D) and empathy (five questions: E–I), by calculating the mean score on each dimension for each respondent. SERVQUAL scores were calculated for individuals with up to one missing data point.
Questionnaire structure: factor analysis
We carried out an exploratory factor analysis to investigate the structure of the GP questionnaire, and to identify key questions to form the basis of scores for the questionnaire which could be used as measures of elements of responsiveness. Questions were excluded from the factor analysis on the basis of initial results, and based on consideration of the content of questions in the questionnaire. We aimed to include generic questions (relating to universal needs and relevant to the majority of patients, regardless of which group they belonged to), and remove questions specific to certain groups (where there were a high proportion of ‘don’t know’ answers, indicating that these questions were only relevant to certain patients, e.g. the questions about getting a home visit and getting to see a doctor or nurse who spoke the patient’s language).
The final round of factor analysis included 15 generic questions. The analytic approach involved varimax rotation, with factors generated based on the criteria of MINEIGEN = 1. Missing data were handled using ‘pairwise deletion’.
Factor analysis generated a three-factor solution. Together, the three factors explained 57.7% of the variance. The factors do not correspond exactly with the sections of the questionnaire, but can be described as:
-
factor 1 (five questions): ease of access to a suitable appointment
-
factor 2 (seven questions): welcome, help, and support for ongoing care
-
factor 3 (four questions): ease of using the building and facilities, and information.
In Table 24, coefficients below 0.3 are suppressed.
| Questions | Component | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| 3. How easy is it for you to book an appointment in advance, for a time that suits you? | 0.748 | – | – |
| 2. How easy is it for you to get an urgent appointment on the same day? | 0.729 | – | – |
| 4. How easy is it for you to get to see your preferred doctor? | 0.715 | – | – |
| 8. How easy is it for you to get a telephone consultation, when you want one? | 0.696 | – | – |
| 1. How easy is it for you to get in touch with the surgery to make an appointment? | 0.695 | – | – |
| 11. Are the reception staff willing to try their best to help? | 0.393 | 0.708 | – |
| 10. Are the reception staff friendly? | 0.359 | 0.703 | – |
| 17. How easy is it for you to talk to receptionists without being overheard? | – | 0.689 | – |
| 19. How good it this surgery at helping you to feel at ease while you are waiting? | – | 0.585 | 0.448 |
| 23. How good it this surgery at helping to organise your health care with hospitals (e.g. letting you test results, chasing hospital letters)? | 0.430 | 0.582 | – |
| 21. How good it this surgery at helping you keep up-to-date with your health care (e.g. sending you reminders about appointments, letting you know what to do next)? | 0.434 | 0.569 | – |
| 15. How easy is it for you to use the facilities at the surgery (e.g. the waiting area, toilets, baby changing room)? | – | – | 0.835 |
| 14. How easy is it for you to get around the building? | – | – | 0.775 |
| 20. How good is this surgery at providing information in a form that you can understand (e.g. translated or Easy Read information leaflets)? | 0.370 | – | 0.583 |
| 18. How easy is it for you to know when it is your turn to be seen by the doctor or nurse? | – | 0.394 | 0.487 |
Internal consistency of scales: Cronbach’s alpha
Cronbach’s alpha coefficients were calculated to assess internal consistency of three subscales identified through factor analysis. High alpha scores suggest that scales are measuring the same underlying construct (Table 25). Missing data were deleted list-wise.
| Questions | n | Cronbach’s alpha | Cronbach’s alpha based on standardised items | No. of Items |
|---|---|---|---|---|
| Factor 1 (ease of access to an appropriate appointment) | 351 | 0.848 | 0.848 | 5 |
| Factor 2 (welcome, help and support) | 428 | 0.834 | 0.843 | 7 |
| Factor 3 (using the facilities and information) | 432 | 0.661 | 0.684 | 4 |
Factors 1 and 2 showed ‘good to excellent’ internal consistency (0.7–0.9), while factor 3 was ‘acceptable to good’ (0.6–0.7). The lower scores for factor 3 may partly reflect the smaller number of items in factor 3, but there would be value in testing the measure again with another data set to confirm the factor structure. This suggests that it would be appropriate to compute scores for each of the three factors.
Calculating scores for the questionnaire
We calculated scores from the questionnaire: we calculated an average score for each of the three factors for each patient, by averaging the scores across the questions included in the factor. For each factor, we calculated scores for individuals who had answered all questions or omitted no more than one question. Table 26 shows mean scores and standard deviations for each of these scores. Lower scores indicate more positive experiences.
| Questions | n | Minimum | Maximum | Mean | Standard deviation |
|---|---|---|---|---|---|
| Factor 1 (ease of access to an appropriate appointment) | 561 | 1.00 | 4.00 | 2.07 | 0.695 |
| Factor 2 (welcome, help and support) | 566 | 1.00 | 3.83 | 1.79 | 0.584 |
| Factor 3 (using the facilities and information) | 603 | 1.00 | 3.50 | 1.37 | 0.433 |
External validity: correlations between the responsiveness scores and SERVQUAL dimensions
Pearson correlations were calculated between the scale scores from our questionnaire, and scores on the ‘responsiveness’ and ‘empathy’ subscales of SERVQUAL. We expected a modest negative correlation, as the content of the SERVQUAL scales differs somewhat from the content of the responsiveness questionnaire, and SERVQUAL is scored in the reverse direction to the questions on our questionnaire, i.e. higher scores are more positive. Correlations are shown in Table 27.
| Questions | SERVQUAL responsiveness score | SERVQUAL empathy score |
|---|---|---|
| Factor 1 (ease of access to a suitable appointment) | ||
| Pearson correlation | –0.538a | –0.564a |
| Sig. (two-tailed) | 0.000 | 0.000 |
| n | 542 | 536 |
| Factor 2 (welcome, help, and support for ongoing care) | ||
| Pearson correlation | –0.673a | –0.648a |
| Sig. (two-tailed) | 0.000 | 0.000 |
| n | 547 | 543 |
| Factor 3 (ease of using the building, facilities, and information) | ||
| Pearson correlation | –0.396a | –0.405a |
| Sig. (two-tailed) | 0.000 | 0.000 |
| n | 579 | 572 |
The correlations between the factors and the SERQUAL scores were all in the expected direction. All correlations were significant at p < 0.001. The correlations between factor 3 and the SERVQUAL scales were relatively low. This is to be expected, as the issues to which this factor relates (buildings and facilities, and supporting communication) are not covered directly in the SERVQUAL scales.
Test–retest reliability
The consistency of individual responses between the original and retest questionnaire were assessed using Kappa for individual questions and ICCs for scores.
Kappa scores: consistency of responses for individual questions
Kappa scores were calculated for each of the 15 questions to compare the extent to which individuals responded consistently to the original questionnaire and the retest questionnaire. Kappa tests produce a score between 0.00 and 0.99, with higher scores indicting overall higher agreement. It is generally accepted that a kappa value of 0.01–0.20 indicates slight agreement; 0.21–0.40 fair agreement; 0.41–0.60 moderate agreement; 0.61–0.80 substantial agreement; and 0.81–0.99 almost perfect agreement. 101
Kappa values across the 15 questions ranged from 0.37 to 0.73. Five of the questions had kappa scores between 0.21 and 0.40 (fair agreement); eight had kappa scores between 0.41 and 0.60 (moderate agreement); and two had kappa scores between 0.61 and 0.80 (substantial agreement). All were significant at p < 0.001.
Inspection of cross-tab tables indicated that in the majority of cases where there was a mismatch between responses to the first and retest questionnaires, this was due to a shift of one point on the response scale (usually between ‘very easy’ and ‘quite easy’).
Intraclass correlation coefficients: consistency of factor and overall scores
The consistency of factor scores was calculated to assess the extent to which the score for each factor was consistent for individual patients between the original questionnaire and the retest questionnaire. ICCs (average measures) were computed for each of factor scores across all patients (e.g. comparing factor 1 score on the original questionnaire and factor 1 score on the retest questionnaire), using type C ICCs and a two-way mixed effects model (Table 28).
| Questions | ICC (average measures) | 95% CI | F-test with true value 0 | |||
|---|---|---|---|---|---|---|
| Value | df1 | df2 | Sig. | |||
| Factor 1 (ease of access to an appropriate appointment) | 0.901 | 0.861 to 0.930 | 10.122 | 132 | 132 | 0.000 |
| Factor 2 (welcome, help and support) | 0.895 | 0.853 to 0.926 | 9.553 | 133 | 133 | 0.000 |
| Factor 3 (using the facilities and information) | 0.735 | 0.630 to 0.810 | 3.774 | 138 | 138 | 0.000 |
All correlations are high and significant at p < 0.001, suggesting that scores on each factor are stable across the original and retest questionnaire. The caveat is that individuals might score the same mean score on the first and second questionnaires, while answering slightly differently on individual questions. However, as described above, the kappa scores suggest reasonable levels of consistency for individual questions.
Data display: data from the questionnaire for individual practices
Practices may wish to look at the frequency of positive responses for each individual question in comparison with other practices, in order to identify areas in which their patients report less positive experiences. An example for practice 16 factor 1 is given below (Figure 6). This reports the percentage selecting ‘very easy’ on each question within the practice, compared with the percentage selecting this option in the overall sample across all practices. The graph suggests that this practice performs better than average on making it easy for patient to get an urgent appointment on the same day, to see a doctor or nurse of their own sex, and to get a home visit if they need one, but worse than average on seeing their preferred doctor, making it easy for patients to see someone who speaks their language, and getting a telephone consultation.
FIGURE 6.
Percentage responding ‘very easy’ to the questions ‘How easy is it for you to . . .’: overall sample vs. practice 16.
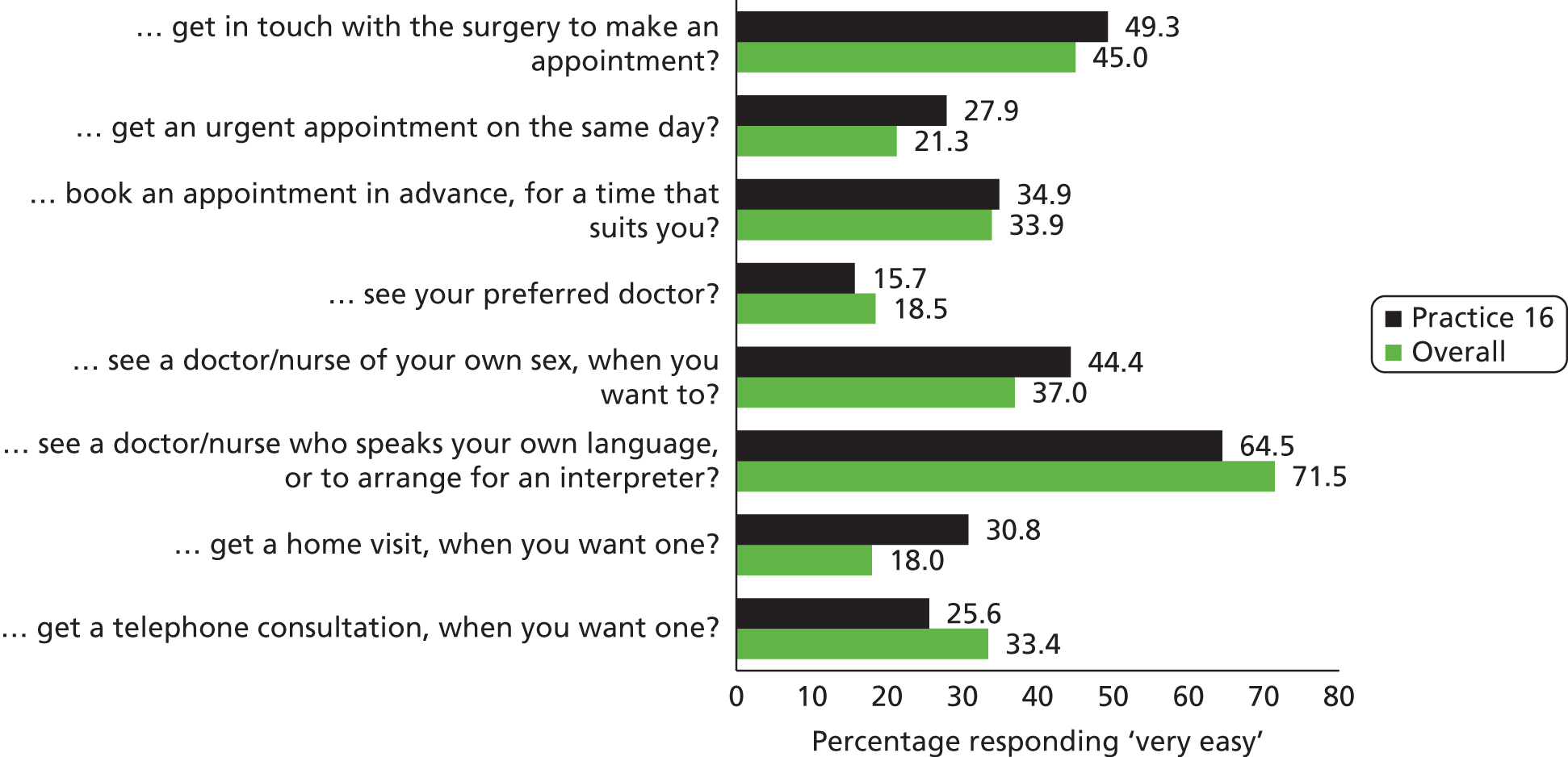
It is important to note, however, that responsiveness relates to the extent to which different patient groups are supported in accessing and using services. In order to assess responsiveness in a valid way, the data produced must be based on a sample that is representative of the patient population; achieving this may require a range of strategies, as discussed later in this chapter.
Data display: comparative data across practices
The questionnaire could be potentially be used to compare practices to provide feedback on how their level of responsiveness differs from other similar practices. This may be useful at a local level, for example to help identify where quality improvement efforts or where additional funding may be needed, to help practices improve their responsiveness.
The scores for each practice are shown in Figures 7–9. A higher score indicates a less positive overall experience.
FIGURE 7.
Means and confidence intervals (CIs) for factor 1 scores (error bars 95% CI).
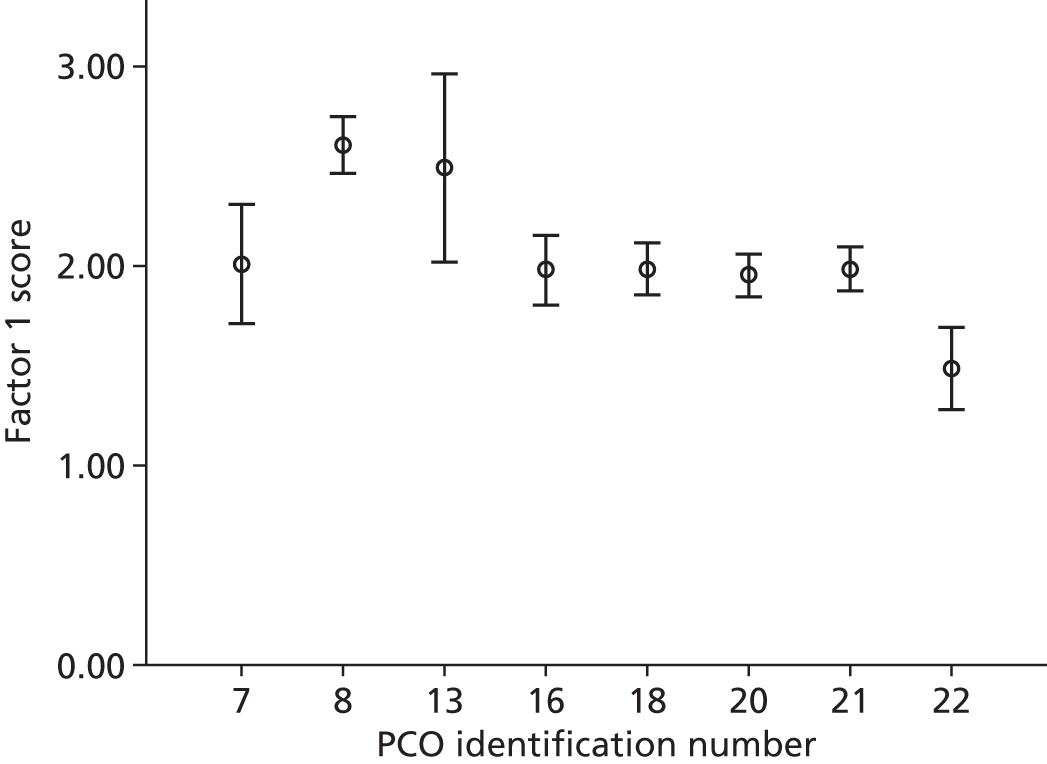
FIGURE 8.
Means and confidence intervals (CIs) for factor 2 scores (error bars 95% CI).
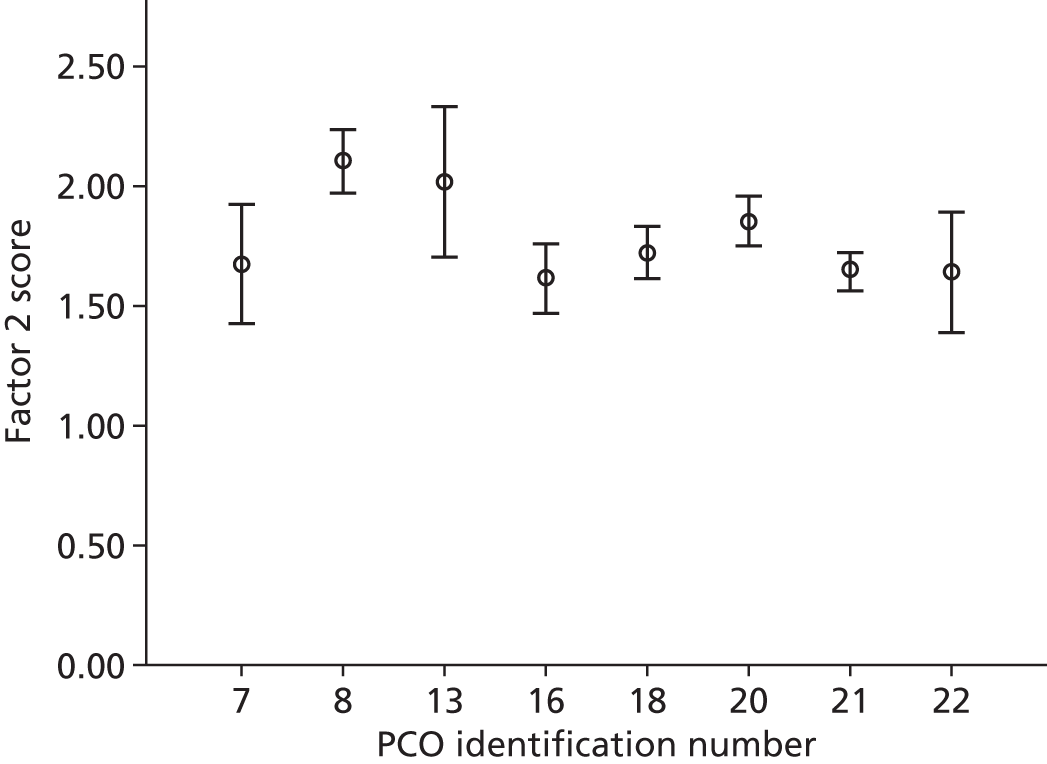
FIGURE 9.
Means and confidence intervals (CIs) for factor 3 scores (error bars 95% CI).
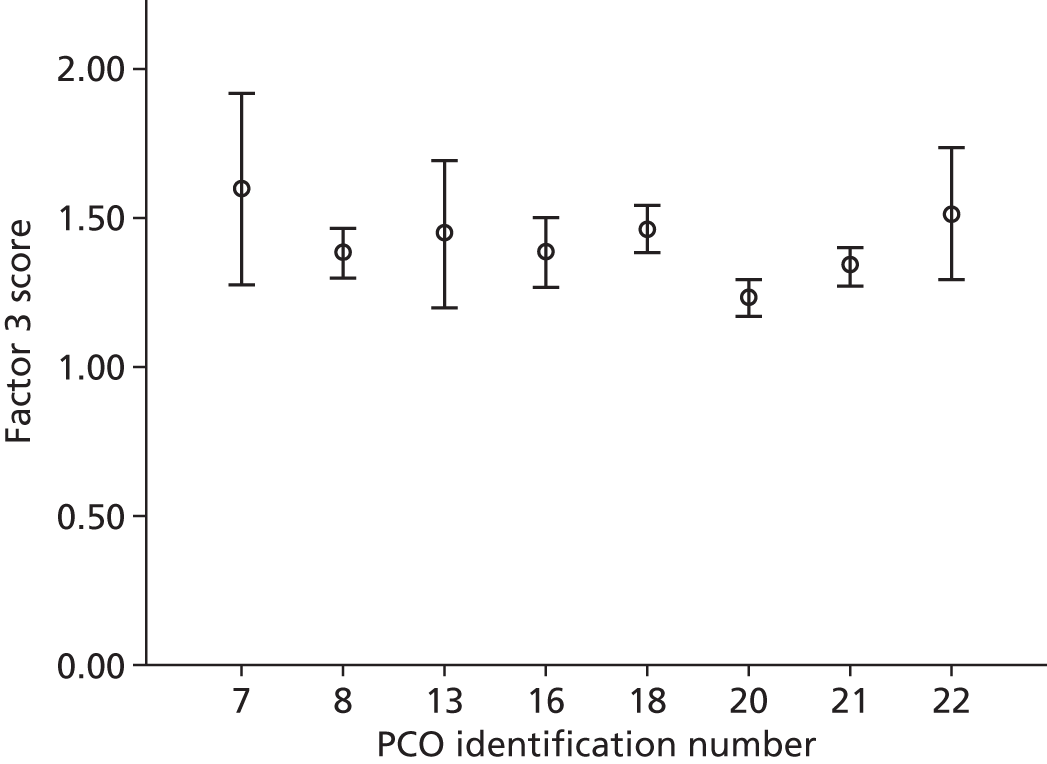
Caution should be exercised in drawing conclusions from these comparative data, as scores are likely to be highly influenced by local contextual factors (such as practice 22 sharing its premises with a walk-in centre), and characteristics of the local population (such as practice 8 serving a population with a high level of deprivation; this population might be expected to find it more difficult to use services).
However, this type of comparative data is likely to be of value in identifying areas where efforts are required to improve the alignment of services with patient need. This potential would be strengthened by further research to test the discriminant validity of the measure.
Revisions of the questionnaires to produce final versions
Decisions about which questions we would remove were based on inspection of the descriptive data, and checks against the findings from the set of patient interviews conducted in stage 1. We were also informed by the exploratory factor analysis. We aimed to reduce the number of questions to make the questionnaire more manageable. In summary, revisions included:
-
Removing some redundant or poorly performing questions to reduce the length of the questionnaire. These included questions on finding out about the PCO’s opening hours and services; whether or not the reception staff are polite; how easy it is to let staff know that you have arrived for your appointment; and how good the PCO is at acting on patients’ suggestions and complaints.
-
Removing the question on travel to the surgery: this had been the source of some dispute as it is an issue important to patients. It was decided to remove this as it is outside the control of PCOs. The question on home delivery of prescriptions was removed as this could be assessed objectively.
-
Minor rewording to improve clarity.
Final versions of the questionnaire are included in Appendix 15.
Summary of analysis
Testing suggests that the questions are reliable and valid, and can be used to produce scale scores. We suggest that the results would be easier to interpret if scoring were reversed, i.e. so that high scores indicate better performance.
More research is required before these are put into use to develop guidance for sampling and for administering the questionnaire, and for interpreting scores. There needs to be consideration of how this measure can be integrated into a more holistic assessment of responsiveness, which may include ‘objective’ measures of practices’ responsive activities, and systematic sampling and surveying of diverse patient groups.
Practices may also like to explore the data from different patient groups to identify whether or not certain groups have less positive experiences, and why. This would provide a starting point for identifying how to address these problems. The questionnaire could be used to compare the experiences of patients within certain groups, for example patients with disabilities, within and between practices. We have provided some examples in this section of how data from the questionnaire could be displayed for use by providers. Sophisticated approaches to making data accessible, and displaying them in ways that are intuitive and easy to interpret, have been developed for existing patient-experience and other quality measures,31,102,103 and there would be value in learning from these approaches to optimise the display of data on responsiveness.
Overview of evolution of questionnaires
Tables 29–31 provide a summary of the evolution of questions in the GP, pharmacy and walk-in centre versions of the questionnaire, from pilot 1 through to the final version. Comments on the reasons for changes are also included.
| Theme | Stage 1: focus group questions | Stage 2: pilot 1 questionnaire, GP V1 | Stage 2: pilot 2 questionnaire, GP V2 | Stage 3: pilot 3 questionnaire, GP V3 | Final version: GP V4 |
|---|---|---|---|---|---|
| Ease of access to appropriate services | Does the practice make it easy for you to contact them to arrange to see a doctor or nurse? Does the practice make it easy for you to get an appointment that suits you? |
|
|
|
|
| Staff attitudes and behaviours | Do receptionists try to be helpful? Do practice staff treat you with respect? |
|
|
|
|
| Alignment of physical environment with patient needs | Does the practice make it easy for you to get into the building and use the facilities? |
|
|
|
|
| Co-ordination and support for ongoing care | Does the practice make it easy for you to keep up to date with your care and treatment? Does the practice make it easy for you to access other health-care services that you need? |
|
|
|
|
| Diversity awareness and cultural alignment | Does the practice try to support your individual needs? |
|
|
|
|
| Information and engagement | No questions included |
|
|
|
|
| Key changes (for GP questionnaire – mirrored in changes to pharmacy and walk-in questionnaires) |
|
|
|
|
| Theme | Stage 2: pilot 2 questionnaire, pharmacy V1 | Stage 3: pilot 3 questionnaire, pharmacy V2 | Final version: pharmacy V3 |
|---|---|---|---|
| Ease of access to appropriate services |
|
|
|
| Staff attitudes and behaviours |
|
|
|
| Alignment of physical environment with patient needs |
|
|
|
| Co-ordination and support for ongoing care |
|
|
|
| Diversity awareness and cultural alignment |
|
|
|
| Information and engagement |
|
|
|
| Theme | Stage 3 : pilot 3 questionnaire, WIC V1 | Final version: WIC V2 |
|---|---|---|
| Ease of access to appropriate services |
|
|
| Staff attitudes and behaviours |
|
|
| Alignment of physical environment with patient needs |
|
|
| Co-ordination and support for ongoing care |
|
|
| Diversity awareness and cultural alignment |
|
|
| Information and engagement |
|
|
Substudy: accessing the views of diverse groups
A substudy was conducted to investigate ways in which ‘seldom-heard’ patients might be encouraged to participate.
We invited two GP surgeries to take part. The sample was pragmatic and based on the high level of engagement between the research team and the practice staff; the speed with which they handed out the questionnaires (and hence how realistic it would be to ask them to conduct extra work in a short time scale); and the interim data analysis (which indicated less diversity in responders than might be expected given the characteristics of the practice population). Practice managers at the two GP surgeries were approached to ask if they would be interested in the substudy, and both agreed. A researcher undertook informal interviews with the practice managers to discuss which groups of patients they would like to involve, and possible ways in which these groups might be successfully engaged.
A general practitioner practice with a large non-English-speaking Turkish population
The area in which PCO18 is based has a low literacy rate. The practice manager identified three ‘seldom-heard’ groups: Somali women; males, in particular Caribbean males; and Turkish patients. Turkish patients make up 15% of the practice list. Those who can speak some English still find it difficult to communicate with non-Turkish staff members. The practice manager noted that Turkish patients highly frequent the practice: ‘40 times a year as opposed to the 3–4 times a year on average from other patients. Each time they demand the Turkish doctor and refuse to see another’.
At the time of the interview, the practice employed a Turkish doctor and two part-time Turkish receptionists but there were days when no Turkish speakers were present at the surgery. When the Turkish doctor is away on leave, the vast majority of the Turkish patient population cancel any pre-booked appointments. The interim data analysis indicated a lack of questionnaires returned by patients self-ascribing as Turkish or Kurdish.
For previous patient surveys, staff sat in the waiting room with as many Turkish patients as possible, going through each question and noting their answers. They had not had the resources or the time to do this with the stage 3 responsiveness questionnaires. This approach also has disadvantages in that patients may not feel able to be totally honest about their experiences when a staff member is acting as a translator.
Engagement strategy
With agreement from the practice manager, the researcher secured an independent interpreter fluent in Kurdish and Turkish and arranged for him to visit the surgery over three mornings to fill in the questionnaires with Turkish- and Kurdish-speaking patients who were willing to participate. The patients were approached in the waiting room prior to their appointments and were asked to fill in the questionnaire after their consultation.
Twenty questionnaires were successfully completed within three mornings (12 hours).
Feedback from the interpreter
The interpreter provided feedback over the telephone about the success of this engagement strategy:
-
Patients were really happy to fill in the forms and to see another Turkish person in reception ready to help them.
-
No one who was approached refused the questionnaire.
-
Most respondents were female.
-
Most patients started to complete the forms before their consultation, as they had arrived early. All were keen to give their views and they patiently waited in line after their appointment to complete the questionnaire that they had started pre consultation. The interpreter was surprised that the patients were willing to wait.
-
When answering questions, some patients indicated to the interpreter which box to tick, while others explained their answers.
-
Most informal comments made after each question were comparisons with other GP surgeries, praising the fact that PCO18 had a Turkish-speaking doctor. Some had moved out of the area but still wished to remain registered with the Turkish-speaking GP.
-
More than 15 patients spoke no English. They did not like to use interpreters during their clinical consultations, citing the great difference between telling the doctor directly and telling their problem through a third person. They also felt ashamed to speak about their ailments and conditions through a third party. Basic communication at reception included stating their name and the time of appointment.
-
Patients said that there used to be a Turkish-speaking receptionist but he or she had left.
-
Some patients said that they disliked the reception area, as it was too open and lacked privacy. In addition, the waiting room was big but empty: no magazines or toys for children, or no water machine.
-
For Q7, ‘How easy is it to get a home visit, when you want one?’, many were not aware that this was available.
A general practitioner practice providing enhanced services
PCO22 is a GP surgery providing enhanced services (substance misuse, homeless, sexual health and mental health). Enhanced service workers proactively search for ‘seldom-heard’ groups and groups who are disadvantaged rather than relying on them attending the practice. This includes visiting their homes, shelters, bed and breakfast hotels, a local community group (which is very well attended), and a centre for substance misuse (also very well attended).
The practice had previously attempted to engage with these groups by organising a PPG but there was always a low turnout at scheduled meetings. The few who attended regularly complained about their treatment and the speed of the services delivered to them as individuals. None commented on practice processes. The practice never receives suggestions for improvement or feedback from patients.
Engagement strategy
The practice manager agreed to assign two staff members (who were not core members of practice staff) to assist with the completion of the questionnaires while out on their routine visits to a community-based service frequented by ‘seldom-heard’ patients and disadvantaged groups. The centre has a breakfast club once a week at which health professionals provide health checks. Attendees were reported to feel more comfortable with staff with whom they were familiar, and would not tend to engage with other unknown staff members. Following patients’ check-ups with the nurse, two staff members sat with the patients, explained what the questionnaire was about and then helped them to complete it, if they were willing.
Staff completed the substudy over a period of approximately 4 weeks, due to the weekly schedule. No attendees refused to complete the questionnaire.
Feedback from practice staff
A member of reception staff provided feedback over the telephone about the success of the strategy:
-
A receptionist and nurse conducted the substudy at the breakfast club.
-
The receptionist described the experience as ‘very interesting’.
-
Staff tried to have a one-to-one with all service users and encouraged honesty in all answers.
-
Nobody refused to complete the questionnaire.
-
Most breakfast club attendees were male.
-
The substudy took a few weeks, as the same faces had been attending the breakfast club and it was difficult to find new people.
Discussion
We worked with practices to find methods that were practical for PCOs during the research project but these would be equally feasible for use as part of routine surveys in order to include ‘seldom-heard’ groups. PCOs need to understand their practice populations and which groups will be ‘seldom heard’ using traditional approaches, and to invest time and resources in accessing these ‘seldom-heard’ groups. We found very good acceptance of questionnaire by ‘seldom-heard’ groups when they were offered the questionnaire in a tailored way.
Substudy: developing an Easy Read version of the questionnaires
The final versions of the questionnaire were used as a basis for developing Easy Read versions, developed by Easy Read specialists (The Clear Communications People Ltd: www.communicationpeople.co.uk/). The specialists met with their advisory group (comprising people with learning difficulties who advise them on their work) to get a sense for the difficulties that the questions presented and how the questionnaires might translate best into Easy Read. The Easy Read versions were developed iteratively through discussion between the specialists and the study researcher.
The Easy Read questionnaire for GP practices was piloted with 14 people with learning difficulties. The pilot was undertaken by the staff team and two volunteers who support the visitors to the day centre where the pilot took place. Of the 14 who completed the questionnaire, 12 people were users of the day service and two were volunteers at the centre.
People had a variety of needs: one was deaf, one person had dyslexia, three had autism, 12 had a learning disability, three had a physical disability, four had additional health needs such as diabetes and epilepsy, and one person had a language other than English as their first language.
The team also tried to administer the questionnaire with a further nine people with learning disabilities. These people had a more profound disability and the team felt that they did not have the capacity to understand the concepts in a meaningful way. The day centre supports a wide range of people with learning disabilities, some of whom need additional support. It was felt that these nine people’s family carers or home staff should complete the questionnaires on their behalf.
Of the nine with profound disabilities, nine needed help to understand the questions, and five people needed help to write. The five people who needed help to write also needed help to understand the questions.
The staff team and volunteers felt that the introduction to the questions helped them to explain the ideas to the people filling in the questionnaires and that the pictures were useful to illustrate the ideas.
Other comments included:
-
‘Some questions are tricky because people’s carers make appointments on their behalf.’
-
‘The “please tell us about the help you had” question should be at the back not the front of the questionnaire as you’re not sure what help someone will need until you’ve done it.’
-
‘It’s very awkward asking people about their sexuality – as a supporter, it feels intrusive.’
-
‘There should be a box to say you have autism.’
-
‘I liked doing it.’
-
‘Well-spaced out.’
-
‘Nice big words make it easy to read.’
-
‘The “tell us about yourself” section is very clear and easy to follow.’
Suggested changes included rewording questions to make them clearer, deleting unnecessary words, and replacing ‘don’t know’ with ‘doesn’t apply’. In addition, we were advised to move the ‘tell us about the help you had’ question to the back page, to add an autism option in the demographics section and to take out the sexuality question.
The team also commented that people selected the range of response options (i.e. from ‘very’ to ‘not at all easy’), which suggests that questions have been explained and understood. In most questionnaires, people ticked yes to friendly staff and helpful staff, but either ‘hard’ or ‘don’t know’ to speaking to a receptionist without other people hearing, which suggests that people have understood the issues in the reception staff section.
The final versions are shown in Appendix 16.
Summary and discussion
We conducted a large-scale pilot to test the reliability and validity of the GP questionnaire. The results indicated that the questionnaire was reasonably well received – response rates varied, but this is likely to reflect the level of enthusiasm and engagement of the PCO in handing out and encouraging patients to complete the questionnaire, and the willingness of patients to complete it. Qualitative data (cognitive interviews) from pilot 2 do indicate that the questionnaire is acceptable to patients.
While PCOs may find it useful to inspect results from individual questions, results from factor analysis indicated that a subset of questions could be used to create scores across three factors (ease of access to a suitable appointment; welcome, help and support for ongoing care; and ease of using the building and facilities, and information). These scales had good internal consistency, and construct validity based on correlations with SERVQUAL subscales. Test–retest reliability analysis showed fair to excellent stability for individual questions, and very good stability for the scores. The scores were shown to discriminate between practices.
We identified the need for caution in interpreting these findings as responsiveness is influenced not only by the way a practice organises and delivers its services, but also by the features of the practice population and the extent to which they may have needs which are more difficult than average to meet. The questionnaire measures patient experience of responsiveness on each of three factors and overall, and these scores can be used in identifying areas where alignment between patient need and service delivery is low, to inform further work to identify how best to improve that alignment. In a similar way, it could be used to identify whether or not there are particular patient groups across a locality who are less likely to experience primary care as responsive to their needs.
We did further work in this stage to explore ways of accessing the views of hard-to-reach groups, and found that it was possible to do this without an excessive amount of time or resource, but that achieving it required a level of motivation and commitment on the part of the PCO. The two practices that did engage in this work found it illuminating and valuable.
As part of ensuring that the questionnaire would be accessible across diverse groups, we also worked with a specialist organisation to develop an Easy Read version.
The limitations of this work primarily relate to the fact that we were unable to fully test the pharmacy and walk-in centre questionnaires; these will need further development and testing work before they are ready for use.
Chapter 8 Collecting and using diversity data in primary care
Introduction
Health-care services provided by PCOs are an integral part of the NHS health-care system in England. Quality and access to care are intertwined with socioeconomic status and patient demographics. 104 Assessing these aspects within general practice populations is important for providing an accessible and adequate practice service for every patient. Mapping GP practice populations using good-quality data would be a step closer to providing high-quality care, both for those who present themselves frequently at practices and for those on the practice list who do not actively seek help. 104 Without knowing the complete details about these patients’ non-clinical characteristics, it is difficult for primary care providers to provide them with a tailored service.
This section of the report is in four parts and focuses on GP practices. The first part aims to investigate the different sources of information that are currently available and publicly accessible about GP practice populations, at an individual practice level. The second part will look at methods of mapping primary care patient data in order to display a set of results that are ‘meaningful’ to the practice, i.e. to accurately display practice population details in a way that can be acted upon to improve service delivery at a local level. The third will discuss the concerns and arguments identified in the literature around collecting and recording diversity data, and will describe some examples of good practice in overcoming these challenges. Part 4 reports a qualitative study of the views of clinical and non-clinical practice staff on collecting and mapping local patient population data.
Part 1: availability of data about practice populations
For a practice to be responsive, comprehensive data on population characteristics at an individual practice level are necessary. We conducted an informal literature search to describe the data sources available to practices containing information about the characteristics of their patient population.
Methods
Systematic and non-systematic literature searches were conducted of published materials, ‘grey’ literature and websites, to identify data sets containing information about practice populations, and publicly available information about practice patient profiles. Initial searches yielded results from local PCT websites, the DH and other informational NHS-related pages. A search was conducted of the databases MEDLINE, Scopus, The King’s Fund Library, Web of Science and Science Direct from January 2001 to March 2011. Search terms included terms such as ‘PATIENT DATA’, ‘DEMOGRAPHICS’ and ‘PROFILING’ combined with terms such as ‘PRIMARY CARE’ and ‘GENERAL PRACTICE’. Articles from the year 2000 onward were included in the primary search. When search combinations produced results of 2500 or more, the searches were refined using subject headings. Articles were then read to identify instances where practice population data from a particular general practices (or a group of known general practices) had been stated, included, referenced or displayed. Over one-third of the search results were duplicated throughout all the databases. Reference snowballing was also conducted on articles, and papers of relevance were added. Secondary searches of the literature were conducted using the titles of the local primary care toolkits and the names of general practice resources found within the initial ‘grey’ searches, coupled with primary care-related terms.
Results
Data sets
Primary care electronic patient records systems
Electronic patient records systems hold the most comprehensive data on local practice populations. Practices currently use their systems for many practice processes in addition to recording non-clinical patient details and patient medical histories. Uses include appointments, integration of NHS Choose and Book facilities, and integrated collation of functions for QOF targets among many others. Electronic patient records systems such as EMIS (EMIS Web, Egton Medical Information Systems Limited, Leeds, UK) and SystmOne (TPP, Horsforth, UK)105 use the Read Code hierarchy to record patient data. 106 Within both systems, tools are available to conduct some ‘population reporting’, including facilities to perform real-time searches and to create reports on data by selecting the fields of interest. The value of electronic records for mapping patient populations depends on the completeness and quality of data on population characteristics. Diversity data tend to be poorly recorded in primary care,107 and the challenges involved in collecting and recording such data are described in the subsections below (see Part 3: challenges to collecting and recording diversity data in primary care and Part 4: interviews with general practice staff). In addition, extracting data from electronic records to map population characteristics may be complex and time-consuming for individual practices.
Hospital Episode Statistics
Linkage of primary care records to other data sets including hospital data108 has the potential to improve data completeness. 109 Hospital Episode Statistics (HES) can be used to improve the completeness of patient data in primary care. When a patient is admitted to hospital, the patient details are taken and they are recorded as a hospital episode. Each hospital episode is then linked to the GP practice at which the patient is registered, using the unique practice code. The main, non-clinical, patient-related data sets recorded by the HES are age group, gender, ethnicity or ethnic category and deprivation score. 110,111
Hospital Episode Statistics data can be easily linked to general practice data in one of the national anonymised patient databases, and strong correlations were reported between the HES data and the General Practice Research Database (GPRD). 112 In a study within general practices in London where self-ascribed ethnicity recording at practice level was above 75%, HES data for ethnicity proved to be a closer, more accurate match to the practice-collected data than the census data. 113 HES data are, however, recorded only for those who have been admitted for treatment in hospitals.
National databases
A number of studies106,114–123 on general practice used three national databases – the Doctors’ Independent Network (DIN), the GPRD and The Health Improvement Network (THIN) database. 124
Doctors’ Independent Network
The DIN, developed in the late 1990s, sourced data from anonymised patient records from over 300 general practices across the UK. 125 Data sourced from the practices include medical diagnoses, symptoms and prescriptions, as well as patient registration information. 125 The DIN was able to work with the privately owned ACORN classification tool to link socioeconomic postcode data to individual patient data sourced from the general practices. 116,125
The General Practice Research Database
The GRPD, now part of the Clinical Practice Research Datalink, is a primary care database126 which holds anonymised general practice patient records at a national level. 127–130 It is a collection of around 8% of the UK population’s patient records, including demographic details, diagnoses and symptoms. 127,131,132
The Health Improvement Network database
The Health Improvement Network also provides anonymised general practice data sets to medical researchers, and there are many studies that used the data to research primary care. 133–137 The CSD Medical Research group aided in the development of the database, which now holds an estimated 6% of the UK population’s health records. 131,138 As the collection method is attached to a live electronic record system, the anonymous bank of patient records is continually updated. Over 500 general practices are currently connected to the system. THIN data are organised into nine categories, covering patient demographics, socioeconomic data attached to patient records, additional non-clinical aspects of a patient’s lifestyle, and medical diagnoses, symptoms and prescriptions. 131,138
Another, less well known database, the IMS Disease Analyser,139,140 was also found to contain anonymous patient data from general practice records extracted on a national level.
Publicly available practice profiles
Further investigation aimed to characterise information sources which use available data to profile the clinical care and characteristics of patient populations for individual practices. These sources display information about practice populations at an individual practice level. Such profiles have the potential to enable practices to easily glean information about their patient population without the need to extract data themselves from their electronic records systems.
Public health observatories
There are currently 12 public health observatories (PHOs) regionally situated within the UK and Ireland. The PHOs aim to organise raw, pre-existing data sets in ways that are beneficial and meaningful to health-care providers, managers and policy-makers and can inform improvements to public health services. 141,142 Researchers have also used the PHO resources to source data. 143
Public health observatories combine data sets from QOF scores, data sets from needs assessment indicators based on Middle Super Output Area, patient age and gender, Indices of Multiple Deprivation (IMDs), patient experience data from the national GP patient survey, ethnicity and disease prevalence estimates. The information is displayed in the form of easy-to-understand tables, charts and graphs.
A tool available on the Network of Public Health Observatories (formerly the Association of Public Health Observatories) website is the National General Practice Profiles (NGPPs), allowing the user to view the data for a specified general practice. 127,144 It is an online resource that has been and is being used in a variety of ways. The NGPPs have been used to provide information to map the prevalence of disease within a practice population145 and to chart current and future trends of clinical conditions within a practice. 146
NHS iView
The NHS iView is an online tool provided by the NHS Information Centre. 147 It allows access to practice-level data for each general practice in the UK. 148 The tool sources its data from the Centre’s Indicator’s Portal, which lists 280 patient data indicators (a mix of clinical and sociodemographic-related indicators). Indicators include gender, age group, number of patients in nursing homes, estimated number of disability allowance claimants, data sets from QOF scores, expected prevalence of four chronic conditions, IMD, practice infrastructure (staff and IT) and patient experience data from the national GP patient survey. 147,149 NHS iView allows users to modify the display format, switching between grid and graphical form.
General Practice Profiles for Cancer
The General Practice Profiles for cancer were created by the National Cancer Intelligence Network to help GP practice staff to think about the cancer-related services they provide for their patients. 150,151 Information for over 95% of registered general practices is displayed on one spreadsheet. Indicators include cancer screening waiting times, the number of new cancer cases and the number of cancer referrals for each practice. Demographic data include the total patient population figure for each practice, the number of patients over the age of 65 (from the yearly practice-based commissioning guidance) and socioeconomic deprivation quintiles (from IMD data). 152
Quality and Outcomes Framework data
The QOF database houses QOF figures assessing the performance of every GP practice in the UK and Ireland. 153–155 Results for each practice can be viewed on the NHS Information Centre website under the practice’s unique code. Within the ‘organisational indicator’ group, there is an indicator for ‘practice management’. Here, GP practices are assessed to see whether or not they have gained points ‘for the identification of carers and a mechanism for the referral of carers for social services assessment’.
Discussion
Electronic patient records have the potential to be used for mapping population characteristics, but this is dependent on the quality and completeness of the data recorded, and it may be complicated and time-consuming for individual practices to extract and display these data. Tools and approaches for practices or CCGs to map the features of individual practices’ patient population, based on electronic records and other information, are described in Part 2: existing population mapping techniques, below.
A number of large searchable databases of primary care patient data exist, but these are not primarily designed to provide detailed, practice-level information about the characteristics of the patient population. The national databases (DIN, GPRD and THIN) are primarily designed to be used for research purposes based on anonymised individual patient data. It would not be possible to identify and single out the data for one GP practice.
There are a number of sources of practice profiles that are easy for practices to access but the information they contain is often incomplete. The PHO NGPPs are easily accessible and provide very basic categories of practice data. It is possible for practices to see an overview of the practice in clinical and non-clinical terms, but the profiles do not provide defined patient population characteristics. In addition, the depth of information displayed is not adequate for viewing detailed information on a particular patient population: the QOF scores display the performance of the practice under the various indicator categories, but further details about the practice population characteristics are not available. The NHS iView displays a greater number of non-clinical categories that could potentially be used to improve practice responsiveness, but the total number remains low. The tool is focused on displaying figures on clinical information. QOF data are also of limited value in assessing practice patient characteristics.
Part 2: existing population mapping techniques
Methods
Informal literature searches were performed to draw out existing mapping techniques in use or proposed to generate information about population characteristics at the level of individual practices. A literature search was conducted with the terms ‘MAPPING’, ‘PROFILING’, ‘NON-CLINICAL DATA’, ‘PRIMARY CARE’, ‘GENERAL PRACTICE’ and their variants, from 2000 onwards. These terms were used to search online databases including Science Direct, MEDLINE and Web of Science, and searches refined using subject headings. Identified articles were screened for relevance by reviewing titles. A ‘grey’ literature search was conducted using similar terms, and key websites/reports identified in the formal literature were retrieved.
Results
Methods of mapping populations: generic/national
Productive General Practice
The Productive General Practice156 programme was developed by the now-defunct NHS Institute for Innovation and Improvement and continues to be promoted by NHS Improving Quality and delivered by accredited partners. The module ‘Knowing how we are doing’ provides guidance on mapping the characteristics of a practice’s patient population, and uses a range of approaches to gain a better understanding of their needs.
Health Needs Assessment
Individual practices can undertake a Health Needs Assessment (HNA) of their practice. 157 The process comprises a description of the practice, an investigation, a write-up and, finally, an action plan. Within the investigation section is a quantitative study of the general practice population including a demographic profile, socioeconomic status, morbidity data, health-related behaviour data, immunisation and prescription data. NHS Mid Hampshire PCT has a step-by-step HNA toolkit for general practices that wish to conduct an assessment of their practice population. 158
The Joint Strategy Needs Assessment
The Joint Strategy Needs Assessment (JSNA) employs both quantitative and qualitative data collection methods to paint a picture of the target area’s health needs. The JSNA has been used by some NHS authorities to produce population-level data for general practices. The JSNA has an inventory of data collection areas that may be of interest to those wishing to carry out an assessment, with one of the five sections focusing solely on population characteristics.
Taxonomy of general practices
The DH Health Inequalities National Support Team (HINST) produced many ‘how to’ guides to help care providers, including primary care services, reduce the inequalities in their populations. HINST have produced a step-by-step guide to creating taxonomy of general practices for each PCT area. Individual general practice data can be easily extrapolated.
The taxonomy sources data from many large databases, such as the census. As the census is carried out every 10 years, the information collated will not be dynamic enough to reflect more short-term changes in patient demographics, for example Eastern European migration to the UK. The usefulness of these data for responsiveness is, therefore, questionable.
NHS Strategic Health Asset Planning and Evaluation application
Strategic Health Asset Planning and Evaluation (SHAPE, Public Health England, London, UK) is mapping software for the analysis of general practice data, and offers a highly promising approach to mapping local population needs. Primary care patient populations can be mapped by both clinical activity and demographic indicators. These include age, ethnicity and socioeconomic status as well as other primary care factors. The software is based on geographical mapping, and can map patient characteristics and accessibility of health services in particular localities. It focuses on geographical localities rather than on a practice’s registered population.
Johns Hopkins Adjusted Clinical Groups system
Johns Hopkins Adjusted Clinical Groups (ACG®) system (Johns Hopkins University, Baltimore, MD, USA) is a method of mapping that measures the morbidity burden of a given population, and so can be adjusted to focus on individuals in a set area. Using data from a variety of clinical and non-clinical sources such as medical records and insurance claims, the measure is able to identify and distinguish between high-risk, high-dependency patients and lower-risk, lower-dependency patients. Organisations licensed to use the system can then begin to map the variation in morbidity burden of the patients using their particular health service.
The Johns Hopkins ACG does not seek to access data sets aside from those that will provide information about the physical and mental health of individuals, established through medical diagnosis. This is because the measure’s primary function is to provide a clinical health map of a group of individuals. The measure does not take into account non-clinical aspects of health, although it does provide an example of a methodology for mapping characteristics of a patient population.
Methods of mapping populations: local example
EMIS Web Tower Hamlets
The ability to search through the data of registered patients in the locality has previously been granted to Tower Hamlets PCT for the monitoring of health inequalities in primary care, with the aid of EMIS Web. 159 There is potential for a general practice to apply to view such data for their own practice. With EMIS Web, practices can extract large numbers of data and have them displayed as graphs and other visual methods.
Discussion
There are a number of tools and methodologies for mapping and displaying data on population characteristics in primary care, but their usefulness depends heavily on the quality and completeness of existing diversity data.
Part 3: challenges to collecting and recording diversity data in primary care
Numerous NHS organisations, both local and regional, have been known for their lack of adequate, reliable data collection on diversity, especially for people who fall into the protected groups as defined by the Equality Act 2010. 160 Effective diversity monitoring is necessary to chart any potential inequalities in access and experience across different patient groups. The collection of diversity data provides an evidence base for addressing non-clinical needs. 161
The quality of clinical data in computerised records within general practices is frequently studied106 but non-clinical data have received less attention. Segments of data have been put under the spotlight, the most notable being ethnicity. Data collection and recording of other characteristics (disabilities, gender and religion, among others) has not received equal attention. Below, we use ethnicity data as an example to illustrate the challenges in collecting and recording diversity data. It is likely that the collection of other types of diversity data, particularly around disability, sexuality and religion, will be subject to the same challenges.
Concerns and challenges: ethnicity data
Ethnicity data in primary care are not collected systematically or recorded to a high standard. 162 Missing ethnicity data within routine data sets in primary care have hindered comprehensive assessments of health inequalities experienced by ethnic minority groups. Any drive to reduce inequalities for these groups has tended to lack focus and measurable elements for evaluating successful initiatives. 163 Without a comprehensive data set, the NHS and other public services cannot say whether they have or have not delivered race equality outcomes. 164 There has been a growing interest in filling in the gaps in ethnicity data to enable effective equality monitoring. 165
The DH recommends the collection of ethnicity data ‘as indicated by the national minimum ethnicity dataset’ (p. 7), covering both ethnicity and first language. 166 There has been a drive to improve race equality in relation to mental health patients in both primary and secondary care, prompting the launch of the Mental Health Minimum Data Set (2003–8) to include new collections of data (including ethnicity) and the National Mental Health and Ethnicity Census in 2005. 167
The NHS Practice Management Network suggests that general practices begin to understand their communities. It forms the first step of the five-step plan to ‘improve access for patients from black and minority ethnic groups’ (p. 95). They encourage the practice managers to put measures in place to monitor ‘ethnicity and preferred language plus all other diversity pointers’, seeing this as vital to providing a responsive service to patients. 14
Studies have explored the practicalities surrounding ethnicity data collection within general practices. 165,168,169
One of the main barriers to systematic collection of ethnicity data is the lack of understanding within primary care teams (and the NHS as a whole)170 as to the potential added benefits to service delivery from collecting and analysing these data. It is thought that the unsuccessful attempts to relay the benefits around the mass collection of ethnicity data, coupled with the lack of incentives for ethnicity data collection at PCO level, has led to low recording rates overall. 171,172 The collection of ethnic monitoring data is incentivised in QOF, attracting one QOF point, providing some financial incentive for practices to engage in this data collection. Systematically collecting ethnicity data within PCOs requires significant time and resources. 81,173 The financial value of the QOF incentive is fairly minimal in terms of the effort and resources necessary.
Staff resistance to asking patients for ethnicity and other personal data, and patient resistance to providing such data, are key challenges. Staff resistance emerged an a significant barrier to the collection of ethnicity data in a Liverpool initiative;174 staff could not envisage the added benefits in the collection of ethnicity data, and felt that the additional value of the collection was less than the additional workload demand it would cause. A study of primary care patients’ perspectives on the collection of ethnicity data found that patients had reservations about data collection and the possibility of abuse of information they deemed sensitive. 170
Another key challenge to collecting and recording ethnicity data relates to the level of detail to be recorded. Collecting and storing data under multiple self-ascribed classifications would enable a detailed overview of the practice population. However, general practices that have attempted to record ethnicity data about their patients have generally done so in order to monitor and target treatment for chronic diseases more prevalent in certain ethnic groups. 175 For this purpose, using less descriptive categories is often preferred;176 this makes for easier data analysis when studying disease prevalence and management at a practice level. The problem with this approach is that, when considering tailoring service delivery to practice populations, the broader categories may systematically suppress the subgroups that are potentially more useful. Broader categories are less useful to tailoring to non-clinical aspects of care that are concerned with improving patient access to and their experience of care. If practices already record less ‘fine-grained’ ethnicity data, they may be unwilling to collect more detailed data concurrently.
A recent review by the Race Equality Foundation162 summarised the challenges in routinely collecting ethnicity data:
-
difficulties in obtaining an accurate classification
-
reluctance to request data for fear of giving offence
-
no meaningful incentive to collect or provide data
-
reluctance on the part of service users to supply data
-
inability to supply data owing to language barriers
-
lack of understanding as to how data can or will be used.
The report argued that ‘successful ethnic monitoring requires a strong regulatory framework complemented by proactive, committed leadership’ (p. 1), and emphasised the need to increase the extent and quality of ethnic data collection and to ensure that data are used to inform and improve practice.
Examples of projects to improve the collecting and recording of diversity data at practice level
Individual Patient Registration Profile (Lambeth area)
A pilot study was conducted with 12 practices in south London to improve the recording of ethnicity and other patient characteristics as part of the Individual Patient Registration Profile project. The project included the provision of templates for data collection, staff training on diversity and on asking patients for information, funding for data entry, and financial incentives for data collection. Practices started with newly registered patients, and then sent questionnaires to existing patients. Although successful, and now spread to more practices, the project has faced practical challenges, particularly around producing templates, coding data and engaging staff. 177,178
Liverpool Primary Care Trust
Patient profiling in Liverpool first began in 1997 in one Liverpool health care centre,179 and now takes place for all 98 registered GP practices in Liverpool. This work has been highly commended by the DH. 179 Patient profiling data are recorded using ethnicity Read codes and are stored on GP systems so that they remain dynamic in nature, constantly being updated. Data are shared to enable work, such an assessment of the prevalence of coronary heart disease (CHD), diabetes and obesity, in 20 GP practices by gender and ethnicity. Data collection has been incentivised by a DES and the QOF, and heavily promoted and supported by the (former) PCT. Practices are supported through the provision of a toolkit including a data collection form and protocols for data entry, and training so that staff understand why profiling is important. Key challenges have included overcoming staff resistance, and avoiding data collection being seen as a ‘tick-box’ exercise. 180
Princes Park Health Centre, Liverpool: ethnic profiling
Princes Park Health Centre Service Development Initiative174 was established to assess the health needs of patient groups self-ascribing to particular ethnicities and countries of origin, and aimed to collect data on patient characteristics from all registered patients within a single practice. The project involved a mailing of questionnaires to all registered patients and a set of strategies for overcoming non-response; the questionnaire and mailing strategy was designed in consultation with local community leaders. Although the focus was on the adequate recording of ethnicity, the form allowed for data to be collected on a wider variety of issues relating to the patient, resulting in the creation of a ‘patient profile’ rather than an exclusive ethnic profile within a non-clinical data set.
The response rate to the questionnaire was 75%. The data were used to develop a strategy to reduce the mortality and morbidity rates from CHD in BME communities, but also for tailoring other parts of the PCO’s service delivery. The data were useful not only in guiding the ways in which clinical care delivery could be improved, but also in determining the health centre’s service provision which tended to the non-clinical aspects of patient care. Data also informed staff recruitment, inviting staff with particular language skills to apply for future vacancies.
The team emphasised the importance of systematic, rather than opportunistic, data collection; involving community leaders; getting staff ‘on board’; paying special attention to the data collection form; and ensuring that data are used in meaningful ways to change practice so that ‘tokenistic’ data collection is avoided.
Patient profiling pilot project: Dr Pugh and Partners Surgery, Kilmarnock
NHS Ayrshire and Arran, in partnership with Information Services Division Scotland, carried out a pilot project to highlight the potential staff and patient benefits of collecting more personal information from registered patients. 181 The processes involved a range of strategies including adjusting the patient registration form to include more detailed patient information and to improve readability; adjusting the touchscreens that patients interact with on arrival in order to include ethnicity, disability and impairment sections; and assigning Read codes for all the additional information recorded for future retrieval. Staff training was also provided. The project recommendations stated a need for the collection of additional patient information to become mandatory in order for any significant patient profiling to take place. The team suggested that practices might require financial incentives to encourage them to invest in this activity.
Toolkits to support diversity data collection
A number of toolkits have been developed to support work to improve data collection on ethnicity and other demographic data. These include the Practical Guide to Ethnic Monitoring in the NHS,182,183 the Health Research and Educational Trust Disparities Toolkit (developed in the USA), and NHS Scotland’s ‘Happy to ask, happy to tell’ programme,184 which focuses on overcoming staff and patient resistance to collecting diversity data, and includes guidance and training materials. This is accessible in the form of a DVD or a printed manual. The effectiveness of these toolkits requires further evaluation.
Part 4: interviews with general practice staff
We conducted interviews with practice staff to explore their views and experiences of collecting diversity data, the availability and quality of non-clinical information they have about their patient populations, and the use they make of these data.
Methods
Semistructured interviews were conducted with practice managers and GPs at four practices with diverse demographics (multicultural city centre; high-deprivation city fringe; suburban, largely elderly population and less deprived; and inner-city, high minority ethnic population). Three practices were chosen from those already involved in the main study. One GP worked for the head office of a large private company (of which PCO13 is a part) and spoke about the local GP practice where he also worked. Inclusion criteria were largely pragmatic and included practices with diverse patient populations and that were willing to be involved. The topic guide included questions about types of data collected by the practices and about staff views on mapping practice population characteristics and on using these data (see Appendix 17). Data were analysed using a combination of framework analysis and the constant comparative approach. 83 A stage of familiarisation involved reading the transcripts and making notes. An initial coding frame was generated based on themes of interest, relating to what data were collected within the practices; the extent to which practices used the data, and the barriers to collecting and using diversity data. Data were entered into the coding frame using NVivo, and care was taken to add new codes for data that did not fit the existing coding frame. Data summaries were produced for each theme.
Results
Seven interviews were conducted, with four GPs and three practice managers. Quotations are labelled GP for general practitioners and PM for practice managers.
We describe variation between practices in the extent of non-clinical data they recorded for each patient, and how they went about capturing, recording and using these data. We also explore staff views on the value of such data, and of the barriers and challenges to both collection and use of non-clinical diversity data.
Approaches to collecting and using non-clinical data
Non-clinical information in electronic patient records
All practices routinely collected some non-clinical data for each patient and recorded them within their patient records. Recorded data categories included personal details (name, address and contact details), age, sex, ethnicity, language, visual impairments, hearing impediments, employment status, housebound status, disabilities, learning difficulties and carer status, but the comprehensiveness of data collection was variable between practices (Table 32).
| Practice | Visual impairments | Hearing Impediments | Sex | Age | Carer status | Learning difficulties | Ethnicity | Language | Housebound status | Employment status | Disabilities |
|---|---|---|---|---|---|---|---|---|---|---|---|
| PRAC1 | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ | ✗ | ✓ |
| PRAC2 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| PRAC3 | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✗ | ✗ | ✓ |
| PRAC4 | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✗ | ✗ | ✓ |
Practices primarily collected these data from patients at the time of first registration, either in person or by asking the patient to complete a paper or online registration form. The data were then transferred to the patient’s electronic patient record.
We record it when new patients register with us, so we have to record their ethnicity, their language that they use, and then that gets put on their records.
GP01
Although this data collection was focused on new patients, three practices also described efforts to improve the data by recording information about existing patients when they consulted. One practice said that they were not actively trying to collect data from those patients who had registered previously.
[Data collection is] mainly at the point of registration, but we are back-dating when patients come in if we notice that it’s not been recorded, we shall ask them.
PM03
[In the system] there used to be a warning that ethnicity data [were] missing.
GP04
Staff recognised that their data collection at registration was not always consistent and comprehensive. Staff also recognised that relying on the front desk and ad hoc data collection methods risked missing out on collecting details from patients and carers who are less frequent visitors to the practice, and those whose status changed after registration.
We just ask them on an ad hoc basis when they come in. For patients that never come in, they unfortunately [do] not get [recorded].
PM03
If they came to see us to say ‘I’m blind’ or something [it might be recorded but], it wouldn’t automatically get asked for when they were to register.
GP01
Staff at all four practices felt that the non-clinical data they held about their patient population was very incomplete.
Non-clinical information from other sources
Practices described drawing on other sources of information about their patient population. One practice described gaining insights from its PPG about the characteristics and needs of its patients, while another used the demographics of responders from its annual patient survey as a source of information about its patient demographics.
So there is also a section on [the annual patient survey] about ethnicity, male/female, age, do you work, don’t you work, retired etc. [. . .] I analyse all that out, so we’ve got the results and I can tell you how many white British answered it, and how few non-white British answered it.
PM01
There are obvious drawbacks to these approaches: PPGs are small and unlikely to be fully representative of the views of the patient population; similarly, the annual survey captures the diversity details of only a small (and not necessarily representative) proportion of the practice population.
As described earlier, data displays such as the NGPPs and NHS iView are publicly available. Only one GP was familiar with both data sources. Two practice managers were aware of the NGPPs, and the remaining interviewees had not heard of either.
I think it’s probably appropriate to look at what is going on and I wasn’t aware of this NHS iView or the National General Practice profile, not that I have time to go through any of these websites.
GP04
Most commonly, staff felt that their awareness of their population characteristics and needs came not from systematic collection and analysis of data, but from informal knowledge gained from daily interactions with patients.
Rather than practically looking at data and doing this, of course these things come to light in normal surgery, so I have been here for 5 years . . . you get enough experience to know what sort of things you need, what services you need and roughly how much percentage.
GP04
Understanding diversity: the use of non-clinical data from the electronic patient record
There were few examples of practices actively using non-clinical data in electronic patient records to help them understand the characteristics of their population. Only one GP described drawing on population data to plan services; and this GP was an exception in having the enthusiasm and the skills to make use of other data sets, including the Personal Demographics Service, alongside practice electronic records.
Do I want to hire one of my GPs, or more than one of my GPs who speak any of the Asian languages, so they can see our patients, or do I want to go to the expense of actually not getting multiple-language-speaking staff and relying on Language Line call centre? . . . So in order for me to decide one way or the other obviously have to rely on my data.
GP03
Other members of staff felt that, although they did not use data in this way, in principle there would be value in doing so if they had easier access to good-quality data.
Obviously languages, we need to make sure we’re providing our information in the right languages and that we’ve got correct interpretive services in place. Ethnicity, there are certain diseases that are obviously more prevalent in certain ethnic groups, so we need to understand that a bit better. The other things we need to understand [is] the deprivation. [. . .] So it’s those sorts of things. Understanding all of that so you can actually target things to your patient groups.
PM02
It was more common for staff to describe non-clinical data as useful on an individual patient level. Staff gave examples of how they used non-clinical information in patients’ records to ‘flag up’ individual patients who had specific needs.
We try to encourage the receptionists to look to see if a person is a carer when booking appointments so that we can be as flexible with them as possible.
PM02
Most staff said that although they collected and recorded non-clinical information about their patients, they made little use of these data.
The last 6 or 7 years we’ve, when they register we’ve been collecting ethnicity data, age, sex. [. . .] What we do with it I would say is nothing, with that particular data set.
PM01
Challenges to systematically collecting and using non-clinical data
We identified a number of barriers and challenges to the systematic collection of non-clinical patient data, and to the use of data from electronic records systems to map the features of the patient population.
Barriers and challenges to collecting non-clinical data
A significant barrier to systematic collection of data on patients’ non-clinical characteristics was perceived lack of utility of such data sets. Some staff saw the value of comprehensive data sets for understanding their patient population and planning services. In contrast, other staff were unsure of what they would do with the data and felt that the investment of time and resources in collecting the data would not be worthwhile.
We don’t do anything with the 7000, 8000 [patients with full data] that we’ve got so why would we want to waste the postage or the time of the patients collecting data we’re going to do nothing with, and I’d have to enter it and that, that would take me a long time. [. . .] I don’t know how useful it would be to have definite figures.
PM01
A lack of resources and time were cited as key barriers to undertaking systematic collection of non-clinical data from the patient population, even by staff who felt that, in principle, such data would be useful.
I think the time and money involved in doing that would be maybe prohibitive in collecting the whole, you know, or enough to make it meaningful of the data.
PM02
Some members of staff felt that staff reluctance to ask patients for personal information, and patient reluctance to provide such information, was problematic. One staff member felt very strongly against collecting employment status data and saw it as an encroachment on patient privacy. Another perceived the patient’s electronic record itself as personal to the patient and their doctor, and thought it improper for non-clinical data to be stored within it. The changing nature of an individual’s employment status over time was also a potential drawback because, unlike ethnicity, it is less stable and may require regular updating.
It’s always a bit of a tricky one, isn’t it? Because you’re asking people for personal information that they may not be happy to give and I think that’s part of why we don’t have robust information. People don’t like to ask it.
PM02
Some patients aren’t prepared to answer. So no, I don’t think there is ease of doing it.
PM03
Staff highlighted practical difficulties in obtaining a comprehensive data set. Collecting and updating data about long-standing patients and from individuals who do not frequent the practice was seen as challenging. All practices felt that their data about long-standing patients were patchy and incomplete.
I would suspect that part of why we haven’t got a lot of this recorded is historical. We would have some patients here with us for, you know, 70 years and it’s just never been properly recorded because it wasn’t when they first registered with us.
PM02
Mundane problems in ensuring completeness of data also arose from patients failing to complete forms correctly, difficulties in ensuring that information on paper forms was transferred to electronic records system, and the risk of transcription errors.
Some people will complete it when they’re doing registrations and some won’t. [. . .] So it’s whether it’s been put on the computer. [. . .] Some of it I think is about making sure that patients have completed the forms correctly, and about [reception staff] then recording it correctly when they register the patients.
PM02
Barriers and challenges to using non-clinical data to understand practice populations
As discussed earlier, although all practices collected data, these were not used in any way. Various barriers to using non-clinical data to map the characteristics and needs of their patients were identified.
Staff attitudes about the value of profiling their patient population could be a barrier. Some staff felt that systematically mapping diversity data would add little to their current, informal knowledge of the practice population.
So do you think mapping . . . would benefit you?
Probably not. Because I do [know] most of them are, in fact all my patients are Asian, 85% are Muslim and then the rest are Hindus.
Other staff were more positive about the idea of profiling their patient population, but described barriers and challenges to making more use of patient record data to do this. Workload, time and resources were significant barriers.
I would say that time is a big limiting factor, especially if clinicians have to go through . . . data because there really is very little time, there is meetings and all sorts of quality stuff and stuff going on in the practice.
GP04
In one practice, both interviewees felt that, owing to high levels of demand in their practice, they did not have the capacity to do anything more than react to demand. They felt that finding the time and resources to map their population would be difficult. They were unsure as to how a practice population profile would be useful to them, and felt concerned that any efforts to understand their population would only mean identifying unmet needs that they would be unable to address.
I mean if you tried it, you might find that there were things you didn’t do, things you maybe should be doing, but at the moment I’m not sure how useful it would be. [. . .] There’s probably a whole load of people who don’t walk through the door that have got significant health needs that we don’t know about, but then it would be how we target those people if we did have that information, and at the moment we’re so over-run with everything we haven’t got much capacity to be looking for more work for us to do really.
GP01
This practice was experiencing a number of pressures, including high levels of missed appointments. Staff did not consider whether or not collecting, mapping and analysing their diversity data may identify patterns that could point to reasons for these levels of demand, and help to find solutions.
Practical challenges in making use of non-clinical data held on patients’ records included issues relating to the quality and completeness of data, and lack of training and support in using these data effectively.
All interviewees felt that a lack of completeness in the non-clinical data they held diminished their value for use in generating a profile of their patients, or informing the design or delivery of services.
I did actually do a quick search this morning on our computer system . . . And for a large number of our patients, the majority of patients we don’t actually have recorded their ethnicity or their language or, you know, any of those key things that you need to start looking at. So, very little information.
PM02
Running simple searches and analysing the data was seen to be relatively straightforward, but required a level of skill and knowledge, meaning that staff training and support might be needed – or that experienced staff had to find the time to provide this training. Some aspects of preparing and extracting the data could be complex and time-consuming, requiring higher levels of expertise.
It wasn’t easy [to check for missing language data]. You would have to put every single language in and do a recode for every single language that is worldwide. I did it once and it was very hard [laughs].
PM03
The two electronic patient record systems used across the four practices were both capable of displaying data as graphs. However, these features required the practices to make additional software purchases to upgrade the minimal search facilities to more user-friendly functions.
External influences on the collection and use of non-clinical data
External incentives for data collection provided a motivating force for practices to engage in recording non-clinical patient data. Ethnicity data in particular tended to be routinely recorded, as this was necessary as evidence for the fulfilment of a QOF target up until 2011. However, other non-clinical data were reported as being at a relatively lower standard. This resulted in variations in the quality of different sets of non-clinical data.
Things that are necessary for the, for example for the quality outcomes framework . . . like ethnicity and stuff, and those are quite well recorded but all the other information things like occupation, the family structure and stuff like that, I think it’s probably going to be quite poor.
GP03
Quality and Outcomes Framework targets specified recording for new registrants, including one non-clinical data set for the ethnicity data. Practices were still routinely collecting these data following their removal as a QOF indicator. The collection of these data for existing patients has not been incentivised via QOF. This meant that practices’ efforts were directed towards collecting complete data for new registrants but not for current patients, resulting in an incomplete data set which was of little value to practices.
The structure of external incentives for data collection risked data collection that was driven by incentive value, rather than the intrinsic value of the data. There was evidence, to some extent, of collection for collection’s sake, to meet government targets or for a financial benefit. This meant that practices were investing in collecting data without fully considering how they could optimise data collection for their own purposes, or utilise the data to make improvements to their own service.
And why do you collect the non-clinical data, for example ethnicity, language, etc.?
The basic answer is that, 3 years ago, the PCT made it part of the contract to record this information. It was integrated into the QOF GP surgeries adhere to. We have collected it ever since.
We don’t do anything, we don’t do any searches on it, we don’t produce it for anybody, we started to collect it because it was a government initiative to collect it.
This suggests external incentives for data collection can drive this data collection, but may not result in data being put to effective use.
External incentives could, however, have a positive impact, when their requirements were aligned with clinical practice and involved collection of data in ways that enhanced the value of such data to practices. One practice agreed to register a large group of elderly patients who required relocating to a new practice. The patient transfer was conducted under a local enhanced service (LES), generating extra income for the practice. The LES required that data on non-clinical needs such as mobility and visual impairments should be recorded. The need to collect these data for the LES prompted the practice to develop an electronic template, to ensure the collection of such data for all new patients.
Part of the local enhancement service [sic] is to be able to fulfil certain criteria, otherwise you will not be paid for that service. [. . .] All those patients, we have to capture certain data about them, part of that data is visual impairment, hearing impairment, incontinence, mobility and so on and so on. [. . .] Sometimes it may seem irrelevant to start with, but . . . as we capture more data we discover more and more uses for them.
GP03
Although the practice had not initially been intrinsically motivated to collect these data, the fulfilment of the LES brought other potential uses of such data to the fore. Once the data were available, it became evident to the practice that the data could be useful to them clinically, and in planning services. Information that had not previously been regarded as useful was now seen as valuable.
One GP suggested that, while the ability to collect and use data on population characteristics might be useful for individual GP practices, they were likely to be critical for CCGs as commissioners.
With the advent of . . . clinical commissioning groups, any of that data becomes absolutely necessary for us to make decisions about the clinical services we’re trying to commission, . . . because ultimately if I’m going to go out and, as a commissioning group, and let’s say commission an optician for their services, . . . without me having an idea how many of my population are actually partially sighted, or how many of them have difficulty mobilising and so on and so on, I cannot effectively commission that service. I might be overpaying for it, underbudgeting for it, either way it’s no good. So however much data I can capture, or the more data I can capture the better.
GP03
Discussion
All four practices collected some non-clinical data, usually when a patient first registered with the practice. Subsequent changes to patient information were less likely to be recorded.
Some staff understood that non-clinical data could improve clinical outcomes for patients and could be used for tailoring services, for example recruiting multilingual staff or restructuring the appointment system. Financial incentives and government policies provided motivation to collect some types of data, such as ethnicity, but not other types of non-clinical data. Practices did little with the data they collected.
Discussion and conclusions
There are a number of national and publicly available databases containing non-clinical information on the patient population and examples of where the data have been used to inform improvements to services. All of the databases considered in this substudy had limitations and/or drawbacks. Being able to understand the characteristics of the patient population within a practice is highly dependent on the completeness and quality of data collected by practices. The four practices varied in their knowledge of existing databases (some were not aware of the better known databases such as NGPP and NHS iView) and there were differences in the types of data collected, when and how they were collected and how they were (or could be) used.
All practices recorded some non-clinical data for each patient within their patient records but the views of staff about the value of such data varied within and between practices. Data were collected either at the front desk or by ad hoc means – neither method was systematic and data were less likely to be captured for less frequent attenders. Post-registration data collection was limited in all four practices. Not all practices had systems in place to alert them to missing data. Data collection was not seen as a priority. Practices did very little with the data they held, and collection of such data was mostly motivated by government policy and financial incentives, rather than by the desire to reduce inequalities or tailor services to patients.
Barriers and challenges were identified to both collection and use of non-clinical diversity data, including a lack of awareness of the value of such data, staff reluctance to request information from patients and patient resistance to providing personal information.
This substudy is limited by the fact that the interviews were conducted with a small number of staff in four practices, three of which were located within a single region. The findings do, however, suggest some important implications.
For PCOs to be motivated to collect diversity data they need an appreciation of the value of such data in terms of the practical benefits to service provision and improving practice efficiency (such as monetary savings due to more effective resource allocation). This will help to motivate staff to record and use data, and to monitor and improve data collection processes. Staff may also need training and support in collecting these data, and practices may not be aware that resources are available. 184
Recording non-clinical data and mapping population needs should be central to service planning and not seen as an additional priority,185 especially when add-on priorities tend to be the first to be to sidelined in difficult times. Monetary incentives to collect data may not translate into their effective use, although intelligent use of incentives in ways that integrate with information for clinical care and for improving efficiency may be effective.
Knowing about and making efforts to access ‘seldom-heard’ groups in the patient population is critical for responsiveness, in terms of both understanding the characteristics of the patient population to plan for their needs and gaining an accurate measure of their experiences. The questionnaire we have developed should be used in conjunction with intelligence about which groups within the practice population may be disadvantaged and hard to reach, and efforts to use appropriate strategies to reach these patients. Both of these strategies are dependent on practices having a valid picture of the demographics of their patient population.
Chapter 9 Study discussion and conclusions
Definition of responsiveness
In Chapter 3, we reported that the literature review highlighted three overlapping but qualitatively different ways of conceptualising responsiveness: that of service quality, inequalities and patient participation. That these are all reflected in the DH definition makes responsiveness a potentially fluid or ‘fuzzy’ concept; our aim was to add structure and firm up the concept in order to inform measurement and improvement in everyday practice.
We have explored what responsiveness means to staff and patients in primary care settings. Perhaps unsurprisingly, staff mentioned all three concepts but there was most emphasis on inequalities in terms of helping groups who are disadvantaged. Staff interviews highlighted components of service organisation and delivery that were important for responsiveness: proactive population orientation, reactive population orientation and individual patient orientation (Figure 10). All of these components were important in ensuring that a PCO was aware of the diverse needs within its patient population and was delivering its services in ways that were designed to meet these diverse needs.
FIGURE 10.
Strategies for increasing responsiveness in primary care.
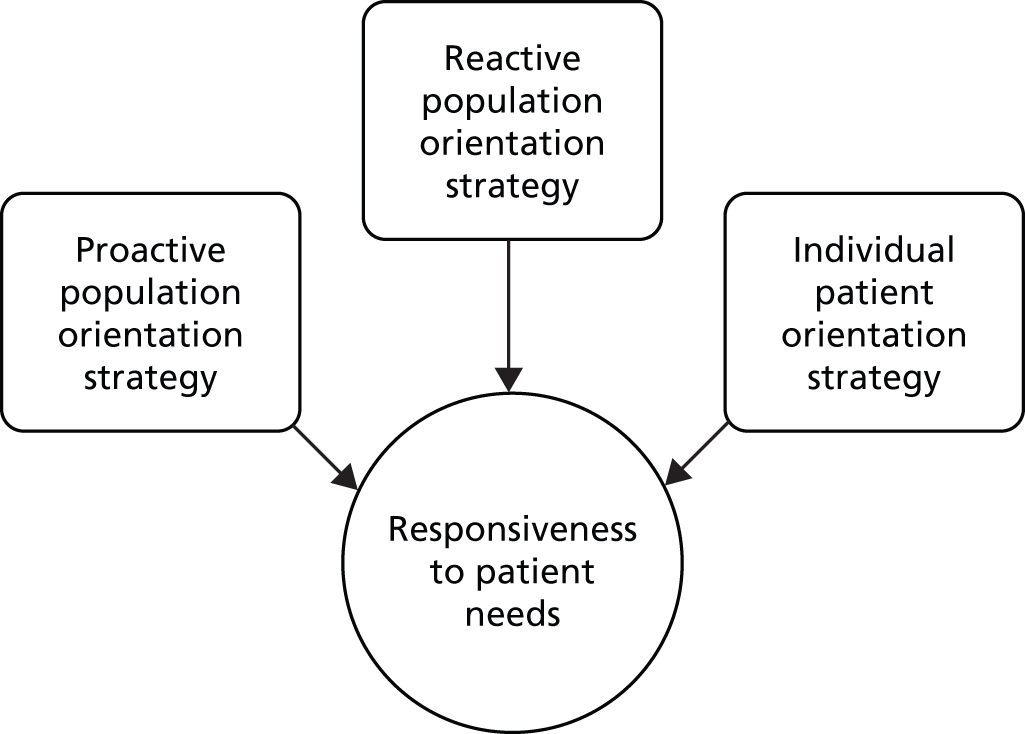
So what does being responsive mean in daily work? Proactive population-oriented strategies involve systematically identifying the different patient groups within the practice population, and being aware of their (sometime latent) needs and the implications of this for the way services are delivered. One example might be recognising that the practice has a responsibility towards the learning disabled people within their practice population, and making appropriate patient information material available. Matching appointment slots to practice population lifestyles is another instance of a population-based strategy, for example planning for requests for appointments during Ramadan. Reactive population-oriented strategies are those that enable a practice to hear patients’ expressed needs, for example through working with the PPG and inviting patient suggestions and complaints, but, importantly, this should involve dialogue, so that patients get feedback about what changes have been made to better meet their needs. Individual patient orientation relates to the extent to which staff are able to be flexible and accommodating to needs when patients try to access and use the service. It can mean, for example, that a receptionist feels able to be flexible in reacting to an anxious and stressed mother who rings up for a same-day appointment for her son with a learning disability, fitting her in even if no appointments are available.
Alongside this, staff and patients highlighted the problem of distinguishing between patient needs and ‘wants’, and recognised that responsiveness involved judgements of legitimacy of expressed needs, and the feasibility of responding to needs in the context of capacity and resource limitations in primary care.
We argue that responsiveness is best understood as an interplay between the needs and expectations of patients across diverse patient groups (both latent and expressed needs and expectations), and the way that primary care services are organised and delivered, and is reflected in successfully achieving alignment between patient needs and service delivery across diverse patient groups. Inherent in this definition is that responsiveness will require primary care services to use the multiple strategies described above to try to align services with patient needs, but may also require work to help manage patients’ expectations to bring them in line with the limits of primary care provision. Although responsiveness can be seen as a responsibility of individual primary care providers, it is important to recognise that the limitations of providing generalist care may make it impossible for providers to achieve a high degree of alignment for certain patients or patient groups with particularly high levels of need (examples in this study included patients with complex social and personal circumstances, such as individuals who were homeless, substance misusers and asylum seekers). In these cases, specialist primary care services which were able to plan for the specific needs of these patient groups, and deliver services in flexible and tailored ways, were needed to ensure responsive care.
Although the concept of responsiveness is complex, we have drawn limits around it, aiming for a meaningful working definition for use within primary care.
Developing the measure
In terms of developing the questionnaire which would act as a measure of patient experience of responsiveness, the study identified key non-clinical features of primary care; these were aspects of non-clinical care for which patients across different groups consistently expressed needs, and for which patients felt that alignment between their needs and the provision of services by PCOs was most important. Key aspects of good care were access to a suitable appointment; staff attitudes and behaviours; alignment of the physical environment with patient needs; co-ordination and support for ongoing care; and diversity awareness and alignment. We included questions on listening to patients; although this was not a theme that emerged as particularly important to patients, it could act as a useful indicator of PCO success within the second component of responsiveness – reactive patient orientation. Themes were identified through the patient interviews, and questions addressing these issues were developed and refined through focus groups and subsequent piloting and iterative development of the questionnaire. These features form the basis for the final questionnaires and a means of measuring patient perceptions of responsiveness.
We had initially planned to develop a generic measure which could be applied across primary care providers. It became clear, however, that the context of primary care providers, such as walk-in centres and particularly pharmacies, was very different from that of a GP practice. The pharmacy setting is characterised by a significantly different underlying business model. GP practices and walk-in centres are tied to the CCG structure, whereas pharmacies will either be part of a wider commercial organisation or be totally independent. Although pharmacies and GP practices are businesses, key issues for GP practices and walk-in centres are managing, and possibly reducing, demand, whereas pharmacies have a business model which favours attracting and retaining customers and encouraging more visits. The issues relevant for GP practice (particularly around access) are quite different from those for pharmacies and walk-in centres. We developed and tested parallel measures for pharmacies and walk-in centres, although these are likely to require further testing and development to ensure that they fully represent the different issues within each of these contexts.
The final versions of the GP, pharmacy, and walk-in centre questionnaires (in standard and Easy Read format) are available for use free of charge with the written permission of the University of Leicester.
The themes identified in this research are in line with what is already known about what matters to patients. 25,26 Our questionnaire includes these specific themes as they emerged as those that were consistently important across different patient groups. Responses to individual questions can be inspected to give a comprehensive picture of patient experiences of the extent to which the PCO responds to their needs. We have demonstrated that a subset of the questions can be used to produce scores (for three factors: accessing an appropriate appointment; using the building, facilities and information; and staff attitudes and support for ongoing care).
Our questionnaire differs from currently available measures of primary care patient experience in a number of ways. First, it is focused specifically on the non-clinical aspects of service delivery that matter to patients. This is important in terms of how we envisage the measure being used. Practices may wish to focus on improving the way that they organise and deliver their services to meet the needs of diverse patient groups. While improving the quality of clinical aspects of care rests with the clinicians who provide it, efforts to improve service organisation and delivery may involve work by practice managers and administrative staff in collaboration with patients, and, in this context, a specific measure of the ‘non-clinical’ aspects of care is likely to be of most value in highlighting the issues that are amenable to change by those involved.
Second, the questions are framed not as reports of experiences (did this happen, and how did you feel about this?), or of satisfaction (‘how satisfied were you with . . .’), but, where possible, in terms of ‘how easy . . .’ it was for the patient to get their needs meet for each of the included questions. This reflects our understanding of responsiveness as relating to the extent to which PCOs facilitate and support patients in getting their needs met.
Third, the questionnaire asks for general perceptions, rather than reports of the patients’ last visit; this was seen as important to patients, as sometimes their last visit was not representative or they wanted to report on their experiences when they wanted different things, such as to book an urgent appointment versus an appointment to see their preferred GP. After some difficulties in working out what was the best approach to this, we arrived at a solution which allowed patients to report on their general experiences but to differentiate between what happened when they had different needs.
Fourth, we designed the questionnaire to be acceptable and easy to use by patients from different groups, and have provided evidence that it can be used to access the views of ‘seldom-heard’ groups as long as investment is made in approaching these groups in appropriate ways. We made the questionnaire available online, but uptake of the online questionnaire was low. We also developed a version in ‘Easy Read’ format and this has been well received by patients with learning disabilities.
Although GP practices have access to readily available patient experience data from national patient surveys, we identified that GP practices tend to make little use of these data. Key reasons included the low response rate and lack of representativeness in national surveys, the types of questions included in the questionnaire and the delay in return of results. Staff tended to see the annual GP patient survey as a relatively isolated activity they were ‘required’ to do, rather than as something that was purposeful and integrated into an active process of quality improvement. The approaches to gaining feedback that practices tended to actively use and rely upon were ad hoc, reactive and ‘real-time’, including responding to complaints, using suggestion boxes, and reacting to feedback from their PPG. The limitations of these approaches, however, are that they are not systematic, and they can still fail to include the views of diverse and hard to reach groups. We suggest that there is a need to find ways of collecting high-quality data systematically, in a manner that meets the needs of practices for gaining quick, locally relevant feedback from diverse patient groups. While questionnaires such as those used in the national GP patient survey could be used for this purpose, our measure has been designed explicitly to be acceptable to diverse patient groups, and to explore the key issues identified as important across these groups. We have generated recommendations about how practices can use the measure to access hard-to-reach populations, and we suggest that the measure could be actively used as part of a process of improvement to generate quick and locally relevant data on the views of patients across the practice population.
It is important to note that the questionnaire produces a measure of patient experience of responsiveness: we would expect PCOs in which there is better alignment between patients’ needs and the way services are organised and delivered to be experienced as more responsive by patients, and hence receive better scores on the questionnaire. The existence and extent of the three responsiveness strategies (see Figure 10) could be measured using a variety of means, through looking at aspects of service organisation and delivery, for example whether a practice has an active PPG or a suggestions/complaints box or a means of regularly updating non-clinical patient information. Some aspects cannot be measured from the patients’ point of view, particularly the extent to which a practice uses proactive population-level strategies. Our questionnaire provides a measure of the patient perspective, and might be usefully employed in conjunction with more ‘objective’ measures of practice organisation and delivery.
Hearing the seldom heard
Responsiveness is about making sure that primary care services can meet the needs of all patients, even the ‘hard to reach’ or ‘seldom heard’. 29,30 This has implications both for efforts to improve responsiveness and for the use of the questionnaire. We reflect on how successful we were in involving ‘seldom-heard’ groups in the research process, and identify lessons for future research.
Efforts to improve responsiveness
This study found that PCO staff do not necessarily think about responsiveness in the complex way outlined in this report; PCOs tend to think of responsiveness in terms of being reactive: responding to individual patients as they access the service, and responding to patient complaints or suggestions, or patient survey data. There was less evidence of PCOs thinking about responsiveness proactively. Few had attempted to systematically map their patient population or plan actively for their patients’ needs. This restricted approach has significant limitations in that PCOs might respond only to those who make themselves heard and who take an active role. The patient interviews indicated that most patients were not interested in or able to engage or be involved and that this is this is particularly likely to be the case for patients from disadvantaged and vulnerable groups.
To be responsive to all, PCOs need to invest in finding out more about the disadvantaged groups in their patient population, particularly those who may not access services because they face significant barriers in doing so. This may mean PCOs (or CCGs) having to give extra support or make extra effort for some patient groups, and there are implications of this in terms of time and resources.
It is important to recognise that, while the questionnaire assesses how easy it is for patients to get their needs met (such as their need to easily access an appropriate appointment), what this means to an individual might vary tremendously. For example, ‘a convenient time’ will vary, with daytime appointments perhaps preferred by the elderly and early or late appointments by those at work. Being responsive involves identifying gaps in meeting needs, and understanding how best to meet those needs for underserved patients.
This reinforces the need for each practice to identify their particular ‘seldom-heard’ (and underserved) patients. Practice populations differ considerably, and patients’ needs and wants will vary accordingly. For example, a practice with high numbers of retired British-born nationals may need to focus on physical aspects of the practice to maximise accessibility, whereas an inner-city multiethnic practice will need to give special attention to responding to multilanguage challenges. There is a potentially large number of different and overlapping groups. The complexity of differing patient populations and their needs and wants means that there is not a ‘one-size-fits-all’ solution to increasing responsiveness. The challenge of being inclusive and responsive is significant.
Interestingly, although patient involvement, choice and voice are seen in policy as key ways of ensuring responsiveness, we found that notions of involvement, choice and voice did not feature in patients’ accounts of responsiveness. Instead, we found that, while many patients want to be involved in decisions on an individual level186 – in terms of their individual treatment and care – on the whole this desire for involvement did not seem to extend to collective decisions at the organisational level. Most patients were not interested in being or did not feel able to be engaged or involved in shaping the design or delivery of services. For most patients, particularly those from vulnerable groups, responsiveness was reflected in the extent to which practices ‘took the strain’, i.e. did the work of identifying needs, planning service delivery and providing support to patients to use services and to help organise their care. Patients from disadvantaged groups may struggle to act as active and involved partners in the design and delivery of health care. They need primary care providers to take responsibility for enabling them to overcome barriers to using services.
This study suggests that pluralisation of primary care providers can have a positive impact on responsiveness, but that this is unlikely to be due the effects of choice and competition driving up responsiveness. Rather, this is due to the emergence of specialist providers that are better able to accommodate to and meet diverse needs. Examples include the introduction of walk-in centres that enable patients to access services without the need to wait or make appointments, and the emergence of specialist providers such as specialist practices for homeless patients and asylum seekers.
Models of health-care provision that focus on empowering patients to drive improvement through choice and involvement may, in fact, disadvantage the most vulnerable. Instead, there is a need to ensure that primary care providers are better placed to support the least empowered.
Use of the questionnaire
Reaching diverse groups with the questionnaire was a challenge for this study, and will remain a challenge for those who want to use the questionnaire in practice. The questionnaire has been designed to maximise its acceptability to a range of diverse patient groups: patients with disabilities, homeless patients, travellers and non-English speakers were closely involved in its design, and it was piloted with different ‘seldom-heard’ groups. This included conducting cognitive interviews with non-English speakers to check for problems in translation if the questionnaire is used with an interpreter. It also included targeting homeless patients, vulnerable patients and non-English speakers in pilot 3. We worked with a specialist organisation to develop an Easy Read version.
It is critical that future users of the questionnaire recognise the need to use appropriate strategies to access the views of diverse groups. Simply handing out questionnaires to a consecutively attending sample of patients or mailing to a random patient sample will not ensure that the views of diverse patient groups are heard. The validity of the measure is dependent on steps being taken to include the ‘seldom-heard’. There are multiple barriers to be overcome, ranging from a lack of willingness to engage with surveys, to language barriers, to barriers to completing questionnaires caused by limitations arising from physical, sensory or cognitive impairment. Gaining a genuine picture of responsiveness to the needs of diverse groups requires (i) information on the characteristics of the population to be surveyed; and (ii) the time, resources and motivation to invest in efforts to access the views of these groups.
There is guidance available on accessing the views of hard-to-reach groups. 187 This is not as challenging as it may be assumed to be. In pilot 3, we conducted a substudy specifically aimed at accessing hard-to-reach groups in two PCOs. Neither PCO had reliable data on the characteristics of their patient population, but both were able to identify vulnerable patient groups whom they served, who were unlikely to be reached through traditional survey methods. The first practice identified that they had a significant number of patients who spoke only Turkish or Kurdish. We arranged for an interpreter to be available in the practice for three mornings (12 hours), and were able to get 20 completed questionnaires. This involved a small cost, but generated data from a hard-to-reach group. The second practice provided a substantial enhanced service to patients with complex needs (substance misuse, homeless, sexual health and mental health). They had struggled to hear from and involve this patient group, but were able to gain 20 completed questionnaires and huge insight into the experiences of these patients by assigning two staff members (not core practice staff) to spend a small amount of time over a 4-week period on their routine visits to a breakfast club for vulnerable people, encouraging and assisting patients to complete the questionnaire.
Our experience suggests that with a small commitment of resources, and careful consideration of appropriate strategies, the views of ‘seldom-heard’ people can be accessed. Such efforts are also likely to be valuable in opening up lines of communication with hard-to-reach groups.
It is a key consideration as to how much effort practices will be willing to put in to get the participation of people who find it particularly difficult to participate. It is unknown what practices need to see, in terms of benefits for them, to engage in such a labour intensive process which requires commitment and investment of resources.
Involving the ‘seldom heard’ in research
We were very keen to involve patients from hard-to-reach, or ‘seldom-heard’, groups in our study, as we felt that this would be critical in designing a measure that was accessible and appropriate for all. We had considerable success in this, using the following approaches:
-
making links with experts, specialist practices, and community organisations
-
having a study advisory group which included representatives of diverse and hard-to-reach patient groups; advisory group members helped with snowball sampling, and reviewing the measure
-
working with local community groups and voluntary organisations to recruit patients and get feedback on the questionnaire
-
working with specialist providers (e.g. a GP practice serving homeless patients
-
attending local events (e.g. a ‘Big Health Day’ for people with learning disabilities)
-
working with a specialist organisation to develop Easy Read version.
-
-
seeking to involve diverse groups actively in the study
-
providing interpreters and involving carers/advocates in focus groups and interviews
-
flexibility in research methods (e.g. face-to-face recruitment with homeless patients).
-
Using these approaches, we were able to access the views of diverse patient groups, including travellers, non-English speakers and patients with learning disabilities.
We found that ‘seldom-heard’ groups were not so hard to involve in the research process. Our success was dependent on the advice we received from our advisory group; efforts to build relationships with key individuals, local community groups and voluntary organisations; and having a flexible and adaptive approach to conducting the research, such as going out from the PCOs and into the community setting for the purposes of administering the questionnaire, and working with interpreters and carers. We found that working with diverse patient groups was extremely valuable for questionnaire design, helping to improve the validity and acceptability of the final product, and understanding how to access the views of diverse groups. The support we received from the specialist organisation in developing and testing the Easy Read version was particularly important.
Implications for practice
Use of the measure for service planning
Primary care in England is facing several related challenges. 188 The demand for care is increasing as the population ages and the numbers of people with several comorbidities rise. The supply of GPs is insufficient to meet the demand,189,190 funding is constrained,191 action to reduce the burden on hospital services is needed,192 and at the same time general practice has taken on lead responsibility for commissioning many services, a role that requires the acquisition of new attributes, including a community perspective. 193 Responses to these challenges have included proposals for the creation of federations of practices that are able to share policies and resources to improve efficiency and effectiveness,6 greater integration of care with general practice playing a key role,194 whole-person care,195 and the greater adoption of a public health perspective in primary care. 195 Although a detailed and national plan for the reform of general practice and primary care to meet the current challenges has not yet been set out or implemented, all of the pressures and suggested responses indicate that primary care will need to improve the planning of services (both those delivered in primary care and those commissioned from other health and social care sectors), a process that will rest on an improved understanding of the needs of populations and communities, and better monitoring of the extent to which those people with potential to benefit from health care do have access to the appropriate care. Responsiveness to the needs of populations is, therefore, fundamental to the delivery of primary care in the coming years.
The instrument we have developed has several potential roles in assisting primary care meet the new need for responsiveness. Providers (practices, CCGs, primary care federations) will be able to use the measure to monitor whether or not care is responsive, i.e. whether or not care is reaching those sections of the population in need to care, and therefore reducing the need for the secondary care of complications or late-stage disease or reducing the need for social care. A key influence in acceptance of the questionnaire will be the local PPG. The questionnaire could even be ‘owned’ by the PPG and form a focal part of the PPG–practice relationship (or, more widely at a local level, the public–CCG relationship). PPG guidance would be beneficial in leading efforts to reach the ‘seldom heard’. Perhaps the ideal approach at practice level may be a ‘ground-up’ push led by the local PPG, with a top-down push and support from the CCG.
Population mapping
Mapping the population to understand the characteristics of the populations is important for several reasons: first, to gain greater insight to the characteristics/demographics of the practice population; second, to help identify specific groups who may be ‘seldom heard’ via traditional survey method; third, to interpret the results in an informed way; and, finally, to identify areas for improvement.
Population mapping aids the federation, CCG or practice to plan their population (reactive and proactive)-orientated strategies by informing the practice of the characteristics of their population. Once ‘seldom-heard’ groups are identified, then a plan can be developed to ensure these groups are heard when the questionnaire is used. Learning gained from this study can illuminate approaches to successfully reaching the ‘seldom heard’ and can be utilised by PCOs.
Improving responsiveness
The definition of responsiveness developed in this study has several implications for efforts to measure and improve responsiveness. The first is that PCOs may wish to target the questionnaire at specific patient groups as part of a process of improving the experiences of these groups. The second relates to the potential for the measure to be used more widely across a CCG, a region, or nationally. This could involve, for example, using the measure comparatively to identify specific GP practices where patients report lower levels of responsiveness. In doing this, it would be important to recognise that the measure would not, in itself, be an objective measure of ‘quality’ of the provider. Instead, the measure would be better viewed as a tool to be used in the early stages of service delivery planning, as a means of identifying problems and gaps, and for the purposes of issue stimulation.
The scores can be seen as reflecting the level of alignment between the way the PCO organises and delivers its services, and the needs of the local population. Clearly, responsiveness not only depends on the way a PCO delivers its services, but is also highly dependent on the level and type of need of local patients, and the challenges they may face in accessing and using services. Addressing this lack of alignment may require the PCO to (1) improve the way in which they organise and deliver services by attending to the three key components of responsiveness; and (2) work with local patients to manage needs and expectations (e.g. in our study one practice worked with local patients who were recent immigrants, and who had little understanding of how English primary care worked, to educate them about how to use services and hence bring their expectations in line with what the PCO could provide). However, it may require attention to the range and nature of services available locally in order to identify if there are gaps in meeting patients’ needs that would be better met by specialist primary care services or by working closely with other services (such as social care or charities). This level of consideration implies a need for strategic involvement and planning, possibly at a CCG level.
This study raises an important question about the most appropriate ways of improving responsiveness across different care providers. Our findings are most pertinent for GP practices. Identifying the features of the business model, or model of operation, that underpins the work of particular organisations, and considering the implications of this for what responsiveness means in terms of patient benefit, and how best to encourage and support it, is likely to be important.
Responsiveness at primary care organisation and locality level
Our work on responsiveness raises the question of what the roles and responsibilities of an individual GP practice or PCO, and of the CCG, might be in measuring and increasing responsiveness. Through this study, we have developed a measure of patient experience of responsiveness at a PCO level. PCOs have responsibility for their own services and how they are delivered, and so are responsible for their own level of responsiveness. As the definition above suggests, however, a possible way forward in improving the responsiveness of primary care services might be to consider the role of CCGs in assessing and improving responsiveness across their locality.
Our study found that GP practices may lack the skills and incentives to make use of data on the characteristics of their patient population, and CCGs may have a role to play in supporting and incentivising activities around population mapping, either at the level of individual PCOs or across a locality – making the task more cost-efficient due to the larger scale.
We found that the provision of specialist services within a locality could have an important impact on responsiveness to the needs of certain vulnerable groups, such as homeless patients, asylum seekers and patients with substance misuse problems. This points to the value of service planning at a locality level, not just at the level of the individual PCO, in order to meet the needs of diverse groups. A particular driver for considering responsiveness at the locality level is that this is inclusive of all patients, not just those who are currently registered with a GP practice. Those individuals who are not registered, or who do not access primary care services, may have the greatest needs and be repeat users of acute care, especially accident and emergency (A&E) services; increasing the responsiveness of primary care services across a locality could potentially help alleviate the pressure on other parts of the health system, notably A&E departments.
What are the drivers and incentives for responsive primary care?
There are differing and overlapping drivers and incentives for patients, PCOs and the wider NHS system to embrace the concept of responsiveness. For patients, increased responsiveness in primary care should mean better and more equitable care with resulting increased satisfaction. Many GP practices and staff also wish to decrease inequalities in care and may see the benefits in targeting efforts to high-needs/high-wants patients, taking a proactive rather than reactive approach to increase efficiency and avoid acute presentations.
Responsiveness requires PCOs to engage in work to commit time and resources to mapping the population and collecting and analysing patient views. The concept of responsiveness may require a significant change in mindset in primary care, in that it requires a change from being almost entirely reactive and dealing with patients who present, to being responsible for the population, which means having an obligation to seek out what the population need and want. For this to happen may require a cultural and professional change in attitudes and behaviour.
Since the study started, the economy has worsened and the economic pressures on health care have increased. A reasonable question to pose, therefore, is that in a time of austerity, with a growing population and increasing comorbidities, together with a static resource, can we afford responsiveness? There may be little incentive for PCOs in identifying the unmet needs of groups in their practice population if they do not have the resources to meet these needs. Use of the questionnaire and extra effort to reach the ‘seldom heard’ and ‘underserved’ may be seen as a lot of effort for minimal data return even if they are important data to have. It is likely that unless responsiveness is seen as part of the solution196 – with a recognition that improving the alignment between service provision and need will improve efficiency, and that addressing inequalities may reduce the burden on the system – then it risks ‘being put on the shelf’.
We have identified that there is a range of barriers for PCOs in becoming more responsive to the needs of their patients, in terms of mapping their patient populations (see Part 3: challenges to collecting and recording diversity data in primary care), gathering and using patient feedback (see Chapter 4, Views on patient experience measures), and making changes to their services to better meet patient needs (see Chapter 4, Barriers and challenges in delivering responsive primary care services). Some of these barriers are, to a large extent, outside the control of the individual PCO: resources; internal pressures such as workload and demand; and external priorities and pressures. Efforts to improve responsiveness are likely to require more than goodwill on the part of individual PCOs: there may be a need for a clearer strategic direction, support for activities to improve responsiveness at a local (CCG) level, and incentives for improvement.
Strengths and limitations
The greatest strength of the study was our success in involving hard-to-reach and ‘seldom-heard’ patients in the research process as advisors and partners in the development of the questionnaire and as participants in its testing. Overall, we feel that our study methods provide a model for others who wish to involve ‘seldom-heard’ groups in the research process. These successes combined to ensure that our patient-report questionnaire was valid and reliable across all patient groups.
We were able to generate a deep understanding of the concept of responsiveness through exploring the meaning of the concept from a range of perspectives. This has produced valuable learning to inform work to improve responsiveness.
Our questionnaire piloting achieved a reasonable response rate, but this varied across PCOs. One important issue is that using the questionnaire as a measure of patient experience of responsiveness requires PCOs to hear from groups who may be underserved or disadvantaged. These groups are also often hard to reach. We have demonstrated that PCOs can access the views of such groups if they are motivated to do so, and this involves a small but not insignificant investment of time and resources. It is likely that PCOs that are less responsive will be less interested in putting in this work to access hard-to-reach groups, and this undermines the validity of the measure. This study has not addressed this issue of how best to encourage or support PCOs to access hard-to-reach groups when they use the questionnaire, but this may need to be considered.
Our testing of the final versions of the measure for reliability, validity and acceptability were limited, and this is discussed in the following section. We generated scores for the GP questionnaire and have provided initial evidence of reliability and internal consistency for these scores. This suggests that it would be acceptable to use composite scores from the questionnaire as measures of responsiveness. However, further consideration of scoring rules, and guidance to users on scoring, are required.
We were not able to develop an approach for PCOs to use to describe the characteristics of users of different PCOs, but we reviewed available sources of data and explored the challenges inherent in collecting and using data about patient populations to inform improvement.
Our study has highlighted the different requirements of different primary care agencies, and the lack of a proactive culture towards non-clinical data. We have identified some promising strategies for reaching elusive and disadvantaged patient groups. However, the study was developmental and exploratory in nature, and only included practices from three regions in England, and as such these findings should be considered preliminary in terms of their generalisability.
Lessons learned
We reflect on decisions made during the questionnaire development process, and highlight the implications of these decisions in terms of the content and format of the questionnaire, the need for further development and testing, and for the potential future use of the measure.
Generation of content
The generation of items for our questionnaire was driven by the conceptual model developed from interviews; the first draft of questions included eight items which reflected key themes that had emerged from the qualitative data. This decision was taken in line with our aims to develop a short, generic, high-level questionnaire. Findings from focus groups held to explore their experience of completing the questionnaire indicated that patients found generic questions difficult to answer. Based on these data and a review of the qualitative coding of subthemes, we generated a longer set of more specific questions organised by higher-level theme, which were closely linked to the most important concepts identified in the qualitative data. Although we explored content validity extensively, it is possible that using the alternative approach of generating a large pool of items to be reduced through iterative testing may have optimised content validity and questionnaire performance. Further research may be of value to assess and refine item selection.
The final versions of the measures do not include a recall period: patients are asked to report on their overall experiences of a PCO. Decisions about whether to ask patients about their last visit or about ‘overall experiences’ were carefully considered during questionnaire development, and the decisions to frame the questionnaires in terms of overall experiences was seen to be most acceptable to patients. If the measure is to be used to evaluate change or improvement in ‘responsiveness’, then an appropriate recall period (‘over the last 3 months’) could be included in the questionnaire. The choice of an appropriate recall period will require further research.
The process of development and piloting
Questionnaire development was iterative throughout stage 2, and the process involved integration of the conceptual framework, the quantitative analysis, and qualitative assessment. Significant changes were made in stage 2, including changes to response options as a result of cognitive interviews. More time and intensive work at the development stage, involving smaller-scale pilot evaluations and more in-depth cognitive interviews, might have facilitated more thorough testing and development of the measures (including the walk-in centre and pharmacy versions) prior to large-scale piloting. The decisions to develop three separate questionnaires along with Easy Read versions led to compromises in terms of how far we could successfully assure reliability and validity. On reflection, we feel that there may have been value in undertaking the qualitative work as a separate, preliminary study, to inform a proposal for work to develop the measure; this would have enabled us to better take into account the evidence from the qualitative data on the ideal features of the ‘end product’ in our design for the process of questionnaire development.
Reliability and validity
As a result of our findings in the qualitative phase of the study, we recognised that the development of a single short measure of responsiveness that would be applicable across different primary care settings would not be feasible or acceptable to patients. We retained a strong focus on acceptability and content validity. We used qualitative methods to identify the key issues to include in the questionnaire, and narrative and cognitive interviews to assess face validity, content validity and acceptability to patients. Our approach meant that our understanding of what should be included in the questionnaire, how it should be worded and formatted, and how it might best be used was grounded in the qualitative data and emergent throughout the study. We explored ways of optimising the use of the measure to access the views of diverse groups. We produced some preliminary findings that suggest that the GP measure is sound in terms of reliability and validity, and conducted exploratory factor analysis to assess the feasibility and appropriateness of generating scores from the GP measure. We were not able to test the parallel version for pharmacies and walk-in centres as extensively as the GP version.
We acknowledge that ‘gold-standard’ methodological approaches and structured frameworks exist for developing rigorous patient-reported outcome measures (known as PROMs or, sometimes, PROs). 197,198 Although we drew on accepted recommendations for good practice in questionnaire design,32,33,93,199 we recognise that our approach did not follow that now required in the development of PROMs and does not meet the rigorous methodological requirements for design and assessment of reliability and validity that may have been achieved through adhering to such frameworks. We also acknowledge that the decision to pursue the development of three separate measures for different PCOs, along with Easy Read versions, compromised the extent to which we were able to test and assure the quality of each. Nonetheless, we believe that we were extremely successful in developing measures that meet criteria of content validity and acceptability to patients. A key next step for research is to rigorously test our measures to higher standards. Until this information is available, the measure should be used with caution.
Application and acceptability to primary care organisations
Our questionnaire development focused primarily on acceptability to patients. We did engage, to some extent, in efforts to work with practice staff to explore how to optimise the measure, and approaches to administering it, to try to ensure that it would be appropriate and meet the needs of practices. We achieved this by exploring in practice staff interviews (in phase 1) the limitations of measures that were currently available to them, and the features that they would like to see in a new measure. We requested feedback from practice staff at all stages of piloting measure about their experiences of administering the measure, barriers to achieving a high response rate, and approaches to accessing hard-to-reach groups. Owing to time constraints arising from the longer-than-expected time needed to complete pilot 3, we were subsequently unable to collect feedback systematically from PCO staff on their experiences of running the survey, or the value of the results. It is possible that more extensive involvement of practice staff as ‘end users’ of the tool, both in the design of the questionnaire and in the approach to using it, would have enhanced the process.
Conclusions and recommendations for further research
Conclusions
Responsiveness is a complex concept, involving alignment of service delivery and the needs of diverse patient groups. Achieving responsive primary care requires PCOs to use reactive and proactive strategies at individual and population level. In practice, responsiveness tends to be understood and enacted in a limited way; PCOs focus on reacting to patients’ requests and being accommodating when patients access the service, and/or on reacting to patient feedback and complaints. There is less evidence of proactive planning for diverse patient needs across primary care, or of understanding how to best manage and meet the needs of diverse patient groups.
We found that responsiveness is important to patients, and patients from vulnerable groups often experience primary care as failing to be responsive to their needs. This reinforces the emphasis in policy on improving responsiveness, and suggests that there is still much work to be done in this area. Being responsive means providing good care equally to all, and some groups may require extra support. What this extra support is will differ reflecting the different patient populations, and so knowledge of the practice population is essential to be responsive. However, practices do not systematically collect or use diversity data, and lack of understanding of the value of such activities, as well as lack of resources, is a significant barrier.
We developed parallel versions of a patient-report measure of responsiveness for GP practices, walk-in centres and pharmacies. We provided preliminary evidence of reliability and validity for the GP measure, but additional testing is required. Our questionnaire has the potential to be used as a measure within PCOs, between PCOs, and across different patient groups. It will have most value when used as a part of a process of mapping local populations, surveying patients across diverse groups to identify where there is lack of alignment between needs and service provision, and developing efforts to address this gap. The validity of the measure depends on PCOs’ efforts to involve hard-to-reach groups; a challenge exists in that PCOs that are less responsive are less likely to invest in the time and effort required to hear from these groups. An understanding of how to incentivise and support PCOs to engage in this is required.
Future research
The following research requirements emerge from this study.
Further testing of reliability, validity and acceptability of the measures
A research priority is to assure the quality, reliability and validity of the measures (GP, pharmacy, walk-in centre and Easy Read versions) to the current standards required for outcome measures,200 and to meet the standards of reliability and validity required for national measures for use in commissioning, service development and quality improvement. 201–203 There is a need for further testing of item inclusion, reliability and validity of the measures on a larger scale, and across different populations, for example non-English speakers.
While the current study provides some evidence of reliability, validity and acceptability, further testing should systematically explore these issues, building on the current study to generate further evidence of (1) measurement properties including data quality and precision (missing values); reliability; content and face validity; construct validity; longitudinal validity/responsiveness to important change; the ability of the measure to discriminate between poor performing and well-performing practices; and interpretation of scores; and (2) practical properties including acceptability, respondent burden and feasibility. Further consideration of the approach to scoring the questionnaires is also required.
Optimising response rates for diverse groups
Response rates to primary care surveys tend to be low, and this was the case for several practices that took part in the piloting of the measure. We were able to demonstrate that practices can access the views of hard-to-reach groups using tailored approaches. There would be value in additional work testing different approaches to administering the measure, to inform future users about ways of optimising response rates.
Facilitating the use of patient experience data in primary care
We found that staff in PCOs tend to make little use of data from national patient experience surveys. There is evidence that use of patient feedback data is dependent on staff attitudes and a supportive culture, and that staff commonly report having little training in collecting or using patient feedback. 204 We identified some key barriers to investing in collecting good-quality patient experience data, and in using the data effectively to inform improvements to practice. There would be value in further, focused qualitative research into the barriers to using patient feedback to inform improvements in primary care, and how these barriers could be overcome.
The needs of CCGs and federations for monitoring levels of responsiveness require investigation if primary care is to maintain the health of as many people as possible efficiently.
Implementing responsiveness
Our study has highlighted the strategies that PCOs can use to become more responsive to the diverse needs of their patient population. The framework of strategies includes proactive patient orientation (population mapping and planning); reactive population orientation (listening to patients); and individual patient orientation (flexibility at the point of service delivery). The study also highlights the need to manage patient expectations alongside improving services.
There is a need for further research into how this knowledge can be put into practice to improve responsiveness. This will require attention to the issue of ways of incentivising/supporting activities to improve responsiveness; identifying how to implement these strategies ‘on the ground’, in particular, attending to the question of whether such activities should be focused on individual practices or at CCG level; and how to involve patients in a meaningful and appropriate way in the process of improving responsiveness.
There are a number of tools available that could support PCOs to improve their responsiveness, including the toolkit developed by the Practice Management Network,14,15 and elements of the Productive General Practice programme (module: ‘knowing how we are doing’). 156 These have not been implemented systematically across English PCOs, and have not been systematically evaluated. Patient involvement is likely to play an important role, but despite incentives for practices to engage patients through PPGs and patient surveys, patient and public involvement is not yet mainstream. Evidence-based models of involvement are lacking and it is not clear how patients can be involved in meaningful and appropriate ways. 205
There is a need for responsiveness interventions to be designed (or adapted) to reflect the definition of responsiveness and the framework of strategies for responsiveness developed in our study. Interventions should be piloted and evaluated for feasibility and impact.
Population mapping
In terms of population mapping, there is very little information on what practices currently know about the populations they serve. How do practices, and also CCGs and federations, understand their populations, and what do they do, if anything, to gain insight? Identifying what is already happening and what approaches and systems appear helpful would facilitate the sharing of best practice.
Understanding the motivators and facilitators for responsiveness
In those practices that take a proactive view of responsiveness, key questions are around understanding the incentives and motivations for why they are proactive and their view on what the benefits are of this. This insight will be important as it appears that the concept of responsiveness is at risk of being disregarded because it requires investment of time and other resources for uncertain benefit. So, what motivates a practice to be proactive, what the benefits gained are and if staff feel it is worthwhile would all be areas for exploration. It is also unclear how interested primary care staff are in the concept of responsiveness and in having comparative data available. Exploration of these topics would help to inform future national initiatives.
Investigation of the current and potential role of practice managers in responsiveness would be valuable. Practice managers appear to be a heterogeneous group, and so characterisation of their roles, responsibilities and experience, alongside how they influence the approach taken to responsiveness in the practice, could be enlightening. Responsiveness, focusing on non-clinical aspects, fits well with the role of the practice manager.
Testing hypotheses about the predictors and outcomes of responsiveness
Once the measure has been tested and assured to a high standard, it will have extensive potential for use in research testing hypotheses about the predictors of, and outcomes associated with, responsiveness. We would hypothesise that practices which are more responsive to patient needs have greater equality in outcomes across sociodemographic groups for selected conditions than those which are less responsive; the measure could be used to test this hypothesis and provide evidence to support efforts to improve responsiveness. It would be worthwhile to make an international comparison and look at countries with low inequalities and see how responsive their primary care systems are. If we postulate that responsiveness reduces health inequalities, we would expect primary care providers in countries that have low inequalities to be more responsive than providers in countries with greater inequalities.
Acknowledgements
Janet Willars for conducting interviews and focus groups; Clare Gillies for expert statistical advice; Janette Camosso-Stefinovic for conducting the literature searches; Lisa Hallam for administrative support and data entry; Jessica Wright for data entry; Jessica Tarrant for help with coding; Liz Shaw for help with writing and formatting the report; Angela Chorley for designing the final versions of the questionnaires; The Communications People (especially Mike Leat) for designing and testing the Easy Read versions of the questionnaires; the patient organisations that helped with recruitment and testing of the questionnaire (eCooke Learning, Mosaic, Leicestershire Partnership Trust, NHS Northamptonshire, The Big Health Day); individuals from patient support organisations and elsewhere who agreed to be part of the advisory group; practices, pharmacies and walk-in centres for participating; and SAPPHIRE (Social Science Applied to Healthcare Improvement Research) researchers for feedback on the questionnaire.
Contributions of authors
Dr Carolyn Tarrant (Senior Lecturer in Health Psychology) led the study, including research design, critical thinking, data analysis and report writing.
Emma Angell (research associate) managed the project on a day-to-day basis, conducted the data analysis and contributed to the report.
Professor Richard Baker (Professor of Quality in Health Care), Professor Peter Jackson (Professor of Economics and Strategy), Professor George Freeman (Emeritus Professor of General Practice), Professor Mary Boulton (Professor of Health Sociology) and Dr Patricia Wilkie (Honorary President and Chairman of NAPP) contributed to the research design, critical thinking, data analysis and the report.
Fatimah Wobi (research intern) managed the patient mapping substudy, conducted the data analysis and contributed to the report.
Diane Ketley contributed to critical thinking and to writing the report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Robert G, Cornwell J, Brearley S, Goodrich J, Joule N, Levenson R, et al. What Matters to Patients? Developing the Evidence Base for Measuring and Improving Patient Experience. Coventry: NHS Institute for Innovation and Improvement; 2011.
- Campbell J, Ramsay J, Green J. Age, gender, socioeconomic, and ethnic differences in patients’ assessments of primary health care. Qual Health Care 2001;10:90-5. http://dx.doi.org/10.1136/qhc.10.2.90.
- Kontopantelis E, Roland M, Reeves D. Patient experience of access to primary care: identification of predictors in a national patient survey. BMC Fam Pract 2010;11. http://dx.doi.org/10.1186/1471-2296-11-61.
- Mead N, Roland M. Understanding why some ethnic minority patients evaluate medical care more negatively than white patients: a cross sectional analysis of a routine patient survey in English general practices. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b3450.
- Lyratzopoulos G, Elliott M, Barbiere J, Henderson A, Staetsky L, Paddison C, et al. Understanding ethnic and other socio-demographic differences in patient experience of primary care: evidence from the English General Practice Patient Survey. BMJ Qual Saf 2012;21:21-9. http://dx.doi.org/10.1136/bmjqs-2011-000088.
- Improving the Quality of Care in General Practice. London: The King’s Fund; 2011.
- World Class Commissioning for GP services: Improving GP Access and Responsiveness. London: Department of Health; 2009.
- Lakhani M. No Patient Left Behind: How Can We Ensure World Class Primary Care for Black and Minority Ethnic People?. London: Department of Health; 2008.
- Perloff RM, Bonder B, Ray GB, Ray EB, Siminoff LA. Doctor-patient communication, cultural competence, and minority health. Am Behav Sci 2006;49:835-52. http://dx.doi.org/10.1177/0002764205283804.
- Fernandez A, Schillinger D, Grumbach K, Rosenthal A, Stewart AL, Wang F, et al. Physician language ability and cultural competence. J Gen Int Med 2004;19:167-74. http://dx.doi.org/10.1111/j.1525-1497.2004.30266.x.
- Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, et al. Race, gender, and partnership in the patient–physician relationship. JAMA 1999;282:583-9. http://dx.doi.org/10.1001/jama.282.6.583.
- Developing General Practice: Listening to Patients. London: BMA; 2009.
- Primary Care Service Framework: Accessible and Responsive General Practice. London: NHS Primary Care Contracting; 2008.
- Improving Access, Responding to Patients. A ‘How To’ Guide for GP Practices. London: NHS Practice Management Network; 2009.
- Improving the Patient Experience. A Training DVD Resource for GP Practices. London: NHS Practice Management Network; 2010.
- Public Health White Paper. Equity and Excellence: Liberating the NHS. London: HMSO; 2010.
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
- National Association for Patient Participation . Vision and Values 2012. www.napp.org.uk/vision.html (accessed 23 November 2013).
- The King’s Fund . Highly Responsive to Patients’ Needs and Preferences 2012. www.kingsfund.org.uk/projects/francis-inquiry-creating-right-culture-care/highly-responsive-patients-needs-and-preferences (accessed 23 November 2013).
- Royal College of General Practitioners . Quality Practice Award n.d. www.rcgp.org.uk/professional_development/team_quality/qpa.aspx (accessed July 2011).
- NHS Improving Quality . Productive General Practice n.d. www.nhsiq.nhs.uk/capacity-capability/productive-gp.aspx (accessed 21 November 2013).
- The King’s Fund . Experience-Based Co-Design Toolkit: Working With Patients to Improve Care n.d. www.kingsfund.org.uk/projects/ebcd (accessed 20 November 2013).
- Malmivaara A. On decreasing inequality in health care in a cost-effective way. BMC Health Serv Res 2014;14. http://dx.doi.org/10.1186/1472-6963-14-79.
- The GP Patient Survey 2008–09 Summary Report. London: Ipsos MORI; 2009.
- Cheraghi-Sohi S, Bower P, Mead N, McDonald R, Whalley D, Roland M. What are the key attributes of primary care for patients? Building a conceptual ‘map’ of patient preferences. Health Expect 2006;9:275-84. http://dx.doi.org/10.1111/j.1369-7625.2006.00395.x.
- Entwistle V, Firnigl D, Ryan M, Francis J, Kinghorn P. Which experiences of health care delivery matter to service users and why? A critical interpretive synthesis and conceptual map. J Health Serv Res Policy 2012;17:70-8. http://dx.doi.org/10.1258/jhsrp.2011.011029.
- NHS Patient Experience Framework. London: Department of Health; 2011.
- Department of Health . A Framework For NHS Patient Experience n.d. www.gov.uk/government/news/a-framework-for-nhs-patient-experience (accessed 18 October 2013).
- Coote A, Andersson E, Tritter J, Wilson R. Healthy Democracy: The Future of Involvement in Health and Social Care. London: Involve and NHS National Centre for Involvement; 2006.
- Andersson E, Tritter J, Wilson R. Healthy Democracy: The Future of Involvement in Health and Social Care. London: Involve and NHS National Centre for Involvement; 2006.
- Public Health England . National General Practice Profiles n.d. http://fingertips.phe.org.uk/profile/general-practice/data (accessed 24 February 2014).
- Streiner DL, Norman GR. Health Measurement Scales: a Practical Guide to their Development and Use. Oxford: Oxford University Press; 2008.
- Oppenheim AN. Questionnaire Design, Interviewing and Attitude Measurement. London: Continuum; 1992.
- Parasuraman A, Zeithaml VA, Berry LL. A conceptual model of service quality and its implications for future research. J Market 1985;49:41-50. http://dx.doi.org/10.2307/1251430.
- Parasuraman A, Zeithaml VA, Berry LL. SERVQUAL: a multiple item scale for measuring customer perceptions of service quality. J Retail 1988;64:12-40.
- Brand RR, Cronin JJ, Routledge JB. Marketing to older patients: perceptions of service quality. Health Mark Q 1998;15:1-31. http://dx.doi.org/10.1300/J026v15n02_01.
- Zeithaml VA, Berry LL, Parasuraman A. The behavioral consequences of service quality. J Market 1996;60:31-46. http://dx.doi.org/10.2307/1251929.
- Institute of Customer Service . UK Customer Satisfaction Awards n.d. www.instituteofcustomerservice.com/11,167/UK-Customer-Satisfaction-Awards.html (accessed 22 November 2012).
- Pongsupap Y, Lerberghe WV. Choosing between public and private or between hospital and primary care: responsiveness, patient-centredness and prescribing patterns in outpatient consultations in Bangkok. Trop Med Int Health 2006;11:81-9. http://dx.doi.org/10.1111/j.1365-3156.2005.01532.x.
- Elliott MN, Kanouse DE, Edwards CA, Hilborne LH. Components of care vary in importance for overall patient-reported experience by type of hospitalization. Med Care 2009;47:842-9. http://dx.doi.org/10.1097/MLR.0b013e318197b22a.
- Parasuraman A, Zeithaml V, Berry L. Refinement and reassessment of the SERVQUAL scale. J Retail 2004;67.
- Yang Z, Jun M, Peterson RT. Measuring customer perceived online service quality: scale development and managerial implications. Int J of Operations Product Manage 2004;24:1149-74. http://dx.doi.org/10.1108/01443570410563278.
- Ye N, Jianmin J. Proceedings of ICSSSM ’05: International Conference on Services Systems and Services Management, 13–15 June 2005. IEEE; 2005.
- Kilbourne WE, Duffy JA, Duffy M, Giarchi G. The applicability of SERVQUAL in cross-national measurements of health-care quality. J Serv Market 2004;18:524-33. http://dx.doi.org/10.1108/08876040410561857.
- Dean AM. The applicability of SERVQUAL in different health care environments. Health Mark Q 1999;16:1-21. http://dx.doi.org/10.1300/J026v16n03_01.
- Clemes MD, Ozanne LK, Laurensen WL. Patients’ perceptions of service quality dimensions: an empirical examination of health care in New Zealand. Health Mark Q 2001;19:3-22. http://dx.doi.org/10.1300/J026v19n01_02.
- Papanikolaou V, Zygiaris S. Service quality perceptions in primary health care centres in Greece. Health Expect 2012;17:197-20. http://dx.doi.org/10.1111/j.1369-7625.2011.00747.x.
- Andaleeb SS. Service quality perceptions and patient satisfaction: a study of hospitals in a developing country. Soc Sci Med 2001;52:1359-70. http://dx.doi.org/10.1016/S0277-9536(00)00235-5.
- Lam SS. SERVQUAL: a tool for measuring patients’ opinions of hospital service quality in Hong Kong. Total Qual Manage 1997;8:145-52. http://dx.doi.org/10.1080/0954412979587.
- De Man S, Gemmel P, Vlerick P, Van Rijk P, Dierckx R. Patients’ and personnel’s perceptions of service quality and patient satisfaction in nuclear medicine. Eur J Nucl Med Mol Imaging 2002;29:1109-17. http://dx.doi.org/10.1007/s00259-002-0869-3.
- Scardina SA. SERVQUAL: a tool for evaluating patient satisfaction with nursing care. J Nurs Care Qual 1994;8:38-46. http://dx.doi.org/10.1097/00001786-199401000-00008.
- Babakus E, Mangold WG. Adapting the SERVQUAL scale to hospital services: an empirical investigation. Health Serv Res 1992;26.
- Headley DE, Miller SJ. Measuring service quality and its relationship to future consumer behavior. J Health Care Mark 1993;13:32-41.
- Oliver RL, Rust RT, Varki S. Customer delight: foundations, findings, and managerial insight. J Retail 1997;73:311-36. http://dx.doi.org/10.1016/S0022-4359(97)90021-X.
- The World Health Report 2000. Health Systems: Improving Performance. Geneva: World Health Organization; 2000.
- Darby C, Valentine N, Murray CJL, de Silva A. World Health Organization (WHO): Strategy on Measuring Responsiveness. Geneva: World Health Organization; 2000.
- Gostin L, Hodge JG, Valentine N, Nygren-Krug H. The Domains of Health Responsiveness – a Human Rights Analysis. Geneva: World Health Organization; 2003.
- World Health Organization . Health System Responsiveness: Responsiveness Questionnaires n.d. www.who.int/responsiveness/surveys/en/ (accessed 20 August 2014).
- de Silva A, Valentine N. Measuring Responsiveness: Results of a Key Informants Survey in 35 Countries. Geneva: World Health Organization; 2000.
- Valentine NB, de Silva A, Murray CJL. Estimating Responsiveness Level and Distribution for 191 Countries: Methods and Results. Geneva: World Health Organization; 2000.
- Coulter A, Jenkinson C. European patients’ views on the responsiveness of health systems and healthcare providers. Eur J Public Health 2005;15:355-60. http://dx.doi.org/10.1093/eurpub/cki004.
- Schoen C, Osborn R, Huynh PT, Doty M, Davis K, Zapert K, et al. Primary care and health system performance: adults’ experiences in five countries. Health Aff (Milllwood) 2004;W4:487-503.
- Robone S, Rice N, Smith PC. Health systems’ responsiveness and its characteristics: a cross-country comparative analysis. Health Serv Res 2011;46:2079-100. http://dx.doi.org/10.1111/j.1475-6773.2011.01291.x.
- Hopkins J, Loeb S, Fick D. Beyond satisfaction, what service users expect of inpatient mental health care: a literature review. J Psychiatr Ment Health Nurs 2009;16:927-37. http://dx.doi.org/10.1111/j.1365-2850.2009.01501.x.
- Haggerty J, Burge F, Lévesque JF, Gass D, Pineault R, Beaulieu MD. Operational definitions of attributes of primary health care: consensus among Canadian experts. Ann Fam Med 2007;5:336-44. http://dx.doi.org/10.1370/afm.682.
- Haggerty J, Martin C. Evaluating Primary Health Care in Canada: the Right Questions to Ask. Ottawa, ON: Health Canada; 2005.
- Framework for Excellence: Survey Questions under Consideration for Inclusion within the Responsiveness to Learners’ Key Performance Indicator. London: Learning and Skills Council; 2007.
- Box G. Access and Responsiveness: What Matters to Patients?. Walton-on-Thames: NAPP; 2008.
- Campbell SM, Gately C, Gask L. Identifying the patient perspective of the quality of mental healthcare for common chronic problems: a qualitative study. Chronic Illn 2007;3:46-65. http://dx.doi.org/10.1177/1742395307079193.
- Future Services: a Consumer Blueprint for Responsive Public Services. London: NCC/CBI; 2005.
- Cross V, Shah P, Bativala R, Spurgeon P. ReGAE 2: glaucoma awareness and the primary eye-care service: some perceptions among African Caribbeans in Birmingham UK. Eye 2006;21:912-20. http://dx.doi.org/10.1038/sj.eye.6702461.
- Winiarski M, Beckett E, Salcedo J. Outcomes of an inner-city HIV mental health programme integrated with primary care and emphasizing cultural responsiveness. AIDS Care 2005;17:747-56. http://dx.doi.org/10.1080/09540120412331336733.
- Report of the National Improvement Team for Primary Care Access and Responsiveness. London: Department of Health; 2008.
- Smith T. Towards a more responsive health system?. Qual Saf Health Care 2003;12:156-8. http://dx.doi.org/10.1136/qhc.12.2.156.
- Building on the Best. Choice, Responsiveness and Equity in the NHS. London: Department of Health; 2003.
- Wright J, Williams R, Wilkinson JR. Health needs assessment: development and importance of health needs assessment. BMJ 1998;316. http://dx.doi.org/10.1136/bmj.316.7140.1310.
- Sheaff R, Pickard S, Smith K. Public service responsiveness to users’ demands and needs: theory, practice and primary healthcare in England. Public Admin 2002;80:435-52. http://dx.doi.org/10.1111/1467-9299.00312.
- Clarke JH, Clarke J, Newman J, Vidler E, Westmarland L, Smith N, et al. Creating Citizen-Consumers: Changing Publics and Changing Public Services. Thousand Oaks, CA: Pine Forge Press; 2007.
- Pickard S, Sheaff R, Dowling B. Exit, voice, governance and user-responsiveness: the case of English primary care trusts. Soc Sci Med 2006;63:373-83. http://dx.doi.org/10.1016/j.socscimed.2005.12.016.
- Vigoda E. From responsiveness to collaboration: governance, citizens, and the next generation of public administration. Public Adm Rev 2002;62:527-40. http://dx.doi.org/10.1111/1540-6210.00235.
- Growing Patient Participation – Promoting Quality and Responsiveness in General Practice. Walton-on-Thames: National Association for Patient Participation; 2009.
- Simoens S, Scott A. How are Scottish integrated primary care organisations managed?. J Health Organ Manag 2003;17:25-36. http://dx.doi.org/10.1108/14777260310469292.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analyzing Qualitative Data. London: Routledge; 1994.
- Narver JC, Slater SF, MacLachlan DL. Responsive and proactive market orientation and new-product success. J Prod Innovation Manage 2004;21:334-47. http://dx.doi.org/10.1111/j.0737-6782.2004.00086.x.
- Saxe R, Barton A. Weitz. The SOCO scale: a measure of the customer orientation of salespeople. J Market Res 1982;19:343-51. http://dx.doi.org/10.2307/3151568.
- Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol 2006;6. http://dx.doi.org/10.1186/1471-2288-6-35.
- Faugier J, Sargeant M. Sampling hard to reach populations. J Adv Nurs 1997;26:790-7. http://dx.doi.org/10.1046/j.1365-2648.1997.00371.x.
- Baker R. The reliability and criterion validity of a measure of patients’ satisfaction with their general practice. Fam Pract 1991;8:171-7. http://dx.doi.org/10.1093/fampra/8.2.171.
- Mead N, Bower P, Roland M. The general practice assessment questionnaire (GPAQ) – development and psychometric characteristics. BMC Fam Pract 2008;9. http://dx.doi.org/10.1186/1471-2296-9-13.
- Greco M, Powell R, Sweeney K. The Improving Practice Questionnaire (IPQ): a practical tool for general practices seeking patient views. Educ Prim Care 2003;14:440-8.
- The GP Patient Survey . GP Patient Survey Results – National Reports and Data 2012. www.gp-patient.co.uk/results/ (accessed 12 November 2012).
- Office for Disability Issues . Easy Read and Makaton n.d. http://odi.dwp.gov.uk/inclusive-communications/alternative-formats/easy-read-and-makaton.php (accessed 22 November 2012).
- Dillman DA, Smyth JD, Christian LM. Internet, Mail, and Mixed-mode Surveys: The Tailored Design Method. Hoboken, NJ: John Wiley & Sons; 2008.
- Edwards P, Roberts I, Clarke M, DiGuiseppi C, Pratap S, Wentz R, et al. Increasing response rates to postal questionnaires: systematic review. BMJ 2002;324. http://dx.doi.org/10.1136/bmj.324.7347.1183.
- Beatty PC, Willis GB. Research synthesis: the practice of cognitive interviewing. Public Opin Q 2007;71:287-311. http://dx.doi.org/10.1093/poq/nfm006.
- Priede C, Farrall S. Comparing results from different styles of cognitive interviewing: ‘verbal probing’ vs. ‘thinking aloud’. Int J Soc Res Methodol 2011;14:271-87. http://dx.doi.org/10.1080/13645579.2010.523187.
- DeMaio TJ, Landreth A, Presser S, Rothgeb JM, Couper MP, Lessier JT, et al. Methods for Testing and Evaluating Survey Questionnaires. Hoboken, NJ: John Wiley & Sons; 2004.
- Presser S, Couper MP, Lessler JT, Martin E, Martin J, Rothgeb JM, et al. Methods for testing and evaluating survey questions. Public Opin Q 2004;68:109-30. http://dx.doi.org/10.1093/poq/nfh008.
- MacCallum RC, Widaman KF, Zhang S, Hong S. Sample size in factor analysis. Psychol Methods 1999;4. http://dx.doi.org/10.1037/1082-989X.4.1.84.
- Comrey AL, Lee HB. A First Course in Factor Analysis. Abingdon: Psychology Press; 2013.
- Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med 2005;37:360-3.
- NHS England . The GP Patient Survey Analysis Tool n.d. http://results.gp-patient.co.uk/report/10/result.aspx (accessed 24 February 2014).
- Health and Social Care Information Centre . Quality and Outcomes Framework: GP Practice Results n.d. http://qof.hscic.gov.uk/search/ (accessed 24 February 2014).
- Goodwin N, Dixon A, Poole T, Raleigh V. Improving the Quality of Care in General Practice: Report of an Independent Inquiry Commissioned by The King’s Fund. London: The King’s Fund; 2011.
- NHS Connecting for Health . GPSoC Supplier Systems n.d. www.connectingforhealth.nhs.uk/systemsandservices/gpsupport/gpsoc/systems/suppliers.
- Jordan K, Porcheret M, Croft P. Quality of morbidity coding in general practice computerized medical records: a systematic review. Fam Pract 2004;21:396-412. http://dx.doi.org/10.1093/fampra/cmh409.
- Tarrant C, Wobi F, Angell E. Tackling health inequalities: socio-demographic data could play a bigger role. Fam Pract 2013;30:613-14. http://dx.doi.org/10.1093/fampra/cmt071.
- Payne RA, Abel GA, Simpson CR. A retrospective cohort study assessing patient characteristics and the incidence of cardiovascular disease using linked routine primary and secondary care data. BMJ Open 2012;2. http://dx.doi.org/10.1136/bmjopen-2011-000723.
- Aspinall PJ, Jacobson B. Why poor quality of ethnicity data should not preclude its use for identifying disparities in health and healthcare. Qual Saf Health Care 2007;16:176-80. http://dx.doi.org/10.1136/qshc.2006.019059.
- HES Online . Data Dictionary: Inpatients 2010. www.hscic.gov.uk/media/1358/HES-Hospital-Episode-Statistics-HES-Admitted-Patient-Data-Dictionary/pdf/HES_Inpatients_DD_Sept10.pdf (accessed 20 August 2014).
- HES Online . Data Dictionary: Outpatients 2010. www.hscic.gov.uk/media/1359/HES-Hospital-Episode-Statistics-HES-Outpatient-Data-Dictionary/pdf/HES_Outpatient_DD_Dec10.pdf (accessed 20 August 2014).
- Eaton SC, Williams TJ, Puri S, Van-Staa T. The feasibility of linking the English Hospital Episode Statistics to the GPRD. Pharmacoepidemiol Drug Saf 2008;17.
- Hull SA, Rivas C, Bobby J, Boomla K, Robson J. Hospital data may be more accurate than census data in estimating the ethnic composition of general practice populations. Informatics in Primary Care 2009;17:67-78.
- Dregan A, Moller H, Murray-Thomas T, Gulliford MC. Validity of cancer diagnosis in a primary care database compared with linked cancer registrations in England. Population-based cohort study. Cancer Epidemiol 2012;36:425-9. http://dx.doi.org/10.1016/j.canep.2012.05.013.
- Bremner SA, Carey IM, DeWilde S, Richards N, Maier WC, Hilton SR, et al. Early-life exposure to antibacterials and the subsequent development of hayfever in childhood in the UK: case–control studies using the General Practice Research Database and the Doctors’ Independent Network. Clin Exp Allergy 2003;33:1518-25. http://dx.doi.org/10.1046/j.1365-2222.2003.01794.x.
- Calvert M, Shankar A, McManus RJ, Lester H, Freemantle N. Effect of the quality and outcomes framework on diabetes care in the United Kingdom: retrospective cohort study. BMJ 2009;338. http://dx.doi.org/10.1046/10.1136/bmj.b1870.
- DeWilde S, Carey IM, Richards N, Whincup PH, Cook DG. Trends in secondary prevention of ischaemic heart disease in the UK 1994–2005: use of individual and combination treatment. Heart 2008;94:83-8. http://dx.doi.org/10.1136/hrt.2006.111757.
- Shafe ACE, Lee S, Dalrymple JSO, Whorwell PJ. The LUCK study: Laxative Usage in patients with GP-diagnosed Constipation in the UK, within the general population and in pregnancy. An epidemiological study using the General Practice Research Database (GPRD). Therap Adv Gastroenterol 2011;4:343-63. http://dx.doi.org/10.1177/1756283X11417483.
- Calvert MJ, Shankar A, McManus RJ, Ryan R, Freemantle N. Evaluation of the management of heart failure in primary care. Fam Pracy 2009;26:145-53. http://dx.doi.org/10.1093/fampra/cmn105.
- Jordan K, Clarke AM, Symmons DPM, Fleming D, Porcheret M, Kadam UT, et al. Measuring disease prevalence: a comparison of musculoskeletal disease using four general practice consultation databases. Br J Gen Pract 2007;57:7-14.
- Kapur N, Hunt I, Lunt M, McBeth J, Creed F, Macfarlane G. Primary care consultation predictors in men and women: a cohort study. Br J Gen Pract 2005;55:108-13.
- Myles PR, Hubbard RB, Gibson JE, Pogson Z, Smith CJP, McKeever TM. Pneumonia mortality in a UK general practice population cohort. Eur J Public Health 2009;19:521-6. http://dx.doi.org/10.1093/eurpub/ckp081.
- Sammon CJ, McGrogan A, Snowball J, de Vries CS. Factors associated with uptake of seasonal and pandemic influenza vaccine among clinical risk groups in the UK: an analysis using the General Practice Research Database. Vaccine 2012;30:2483-9. http://dx.doi.org/10.1016/j.vaccine.2011.11.077.
- Mathur R, Grundy E, Smeeth L. Availability and Use of UK Based Ethnicity Data for Health Research. Southampton: National Centre for Research Methods; 2013.
- Carey IM, Cook DG, De Wilde S, Bremner SA, Richards N, Caine S, et al. Developing a large electronic primary care database (Doctors’ Independent Network) for research. Int J Med Inf 2004;73:443-53. http://dx.doi.org/10.1016/j.ijmedinf.2004.02.002.
- Herrett E, Thomas SL, Schoonen WM, Smeeth L, Hall AJ. Validation and validity of diagnoses in the General Practice Research Database: a systematic review. Br J Clin Pharmacol 2010;69:4-14. http://dx.doi.org/10.1111/j.1365-2125.2009.03537.x.
- Simkiss DE, Spencer NJ, Stallard N, Thorogood M. Health service use in families where children enter public care: a nested case control study using the General Practice Research Database. BMC Health Serv Res 2012;12. http://dx.doi.org/10.1186/1472-6963-12-65.
- Hawkins NM, Scholes S, Bajekal M, Love H, O’Flaherty M, Raine R, et al. Community care in England: reducing socioeconomic inequalities in heart failure. Circulation 2012;126:1050-7. http://dx.doi.org/10.1161/CIRCULATIONAHA.111.088047.
- Huerta C, Rivero E, Rodriguez LAG. Incidence and risk factors for psoriasis in the general population. Arch Dermatol 2007;143:1559-65. http://dx.doi.org/10.1001/archderm.143.12.1559.
- Tsang C, Majeed A, Aylin P. Routinely recorded patient safety events in primary care: a literature review. Fam Pract 2012;29:8-15. http://dx.doi.org/10.1093/fampra/cmr050.
- Martín-Merino E, Fortuny J, Rivero E, García-Rodríguez LA. Validation of diabetic retinopathy and maculopathy diagnoses recorded in a UK primary care database. Diabetes Care 2012;35:762-7. http://dx.doi.org/10.2337/dc11-2069.
- Hansell A, Hollowell J, Nichols T, McNiece R, Strachan D. Use of the General Practice Research Database (GPRD) for respiratory epidemiology: a comparison with the 4th Morbidity Survey in General Practice (MSGP4). Thorax 1999;54:413-19. http://dx.doi.org/10.1136/thx.54.5.413.
- Cai B, Xu W, Bortnichak E, Watson DJ. An algorithm to identify medical practices common to both the General Practice Research Database and The Health Improvement Network database. Pharmacoepidemiol Drug Saf 2012;21:770-4. http://dx.doi.org/10.1002/pds.3277.
- Taggar JS, Coleman T, Lewis S, Szatkowski L. The impact of the Quality and Outcomes Framework (QOF) on the recording of smoking targets in primary care medical records: cross-sectional analyses from The Health Improvement Network (THIN) database. BMC Public Health 2012;12. http://dx.doi.org/10.1186/1471-2458-12-329.
- Langley T, Szatkowski L, Wythe S, Lewis S. Can primary care data be used to monitor regional smoking prevalence? An analysis of The Health Improvement Network primary care data. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-773.
- Hall G, Carroll D, McQuay H. Primary care incidence and treatment of four neuropathic pain conditions: a descriptive study, 2002–2005. BMC Fam Pract 2008;9. http://dx.doi.org/10.1186/1471-2296-9-26.
- Blak BT, Smith HT, Hards M, Maguire A, Gimeno V. A retrospective database study of insulin initiation in patients with Type 2 diabetes in UK primary care. Diabetic Med 2012;29:e191-8. http://dx.doi.org/10.1111/j.1464-5491.2012.03694.x.
- CSR Medical Research n.d. http://csdmruk.cegedim.com/about-us/about-us.shtml (accessed 20 August 2014).
- Young AH, Rigney U, Shaw S, Emmas C, Thompson JM. Annual cost of managing bipolar disorder to the UK healthcare system. J Affect Disord 2011;133:450-56. http://dx.doi.org/10.1016/j.jad.2011.06.016.
- McColl BW, Allan SM, Rothwell NJ. Systemic infection, inflammation and acute ischemic stroke. Neuroscience 2009;158:1049-61. http://dx.doi.org/10.1016/j.neuroscience.2008.08.019.
- Hill A, Cooke H, Jenner D, Somervaille L. Mini-symposium – Public Health Observatories: building public health skills and capacity in the English regions. Public Health 2005;119:235-8. http://dx.doi.org/10.1016/j.puhe.2005.01.002.
- Wilkinson J, Coyle E. Mini-symposium – Public Health Observatories: development of public health observatories in the UK, Ireland and Europe. Public Health 2005;119:227-34. http://dx.doi.org/10.1016/j.puhe.2005.01.006.
- Bellis MA, Hughes K, Tocque K, Hennell T, Humphrey G, Wyke S. Mini-symposium – Public Health Observatories: assessing and communicating the health and judicial impact of alcohol use. Public Health 2005;119:253-61. http://dx.doi.org/10.1016/j.puhe.2005.01.005.
- Battersby J. Using practice-level data to improve health. Pract Nurs 2012;23:207-10. http://dx.doi.org/10.12968/pnur.2012.23.4.207.
- Hayes L, Hawthorne G, Unwin N. Undiagnosed diabetes in the over-60s: performance of the Association of Public Health Observatories (APHO) Diabetes Prevalence Model in a general practice. Diabet Med 2011;29:115-20. http://dx.doi.org/10.1111/j.1464-5491.2011.03389.x.
- Holman N, Forouhi NG, Goyder E, Wild SH. The Association of Public Health Observatories (APHO) Diabetes Prevalence Model: estimates of total diabetes prevalence for England, 2010–2030. Diabet Med 2011;28:575-82. http://dx.doi.org/10.1111/j.1464-5491.2010.03216.x.
- HSCIC Indicator Panel . NHS Information Centre for Health and Social Care 2012. https://indicators.ic.nhs.uk/webview (accessed 20 August 2014).
- Purdy S, Griffin T, Salisbury C, Sharp D. Emergency admissions for coronary heart disease: a cross-sectional study of general practice, population and hospital factors in England. Public Health 2011;125:46-54. http://dx.doi.org/10.1016/j.puhe.2010.07.006.
- Griffin T, Peters TJ, Sharp D, Salisbury C, Purdy S. Validation of an improved area-based method of calculating general practice–level deprivation. J Clin Epidemiol 2010;63:746-51. http://dx.doi.org/10.1016/j.jclinepi.2009.07.019.
- Bottle A, Tsang C, Parsons C, Majeed A, Soljak M, Aylin P. Association between patient and general practice characteristics and unplanned first-time admissions for cancer: observational study. Br J Cancer 2012;107:1213-19. http://dx.doi.org/10.1038/bjc.2012.320.
- National Cancer Intelligence Network . General Practice Profiles for Cancer 2010. www.ncin.org.uk/cancer_information_tools/profiles/gp_profiles.aspx (accessed 11 October 2012).
- National Cancer Intelligence Network . General Practice Profiles for Cancer: Meta-Data for Profile Indicators 2010. www.ncin.org.uk/cancer_information_tools/profiles/gp_profiles (accessed 20 August 2014).
- Saxena S, Car J, Eldred D, Soljak M, Majeed A. Practice size, caseload, deprivation and quality of care of patients with coronary heart disease, hypertension and stroke in primary care: national cross-sectional study. BMC Health Serv Res 2007;7. http://dx.doi.org/10.1186/1472-6963-7-96.
- Ashworth M, Seed P, Armstrong D, Durbaba S, Jones R. The relationship between social deprivation and the quality of primary care: a national survey using indicators from the UK Quality and Outcomes Framework. Br J Gen Pract 2007;57:441-8.
- Dixon A, Khachatryan A, Tian Y. Socioeconomic differences in case finding among general practices in England: analysis of secondary data. J Health Serv Res Policy 2012;17:18-22. http://dx.doi.org/10.1258/jhsrp.2012.011112.
- A Guide to Productive General Practice. Coventry: NHS Institute for Innovation and Improvement; 2012.
- National Institute for health and Clinical Excellence . Health Needs Assessment 2005. http://admin.nice.org.uk/nicemedia/documents/Health_Needs_Assessment_A_Practical_Guide.pdf (accessed 20 August 2014).
- Mid Hampshire PCT . Health Needs Assessment Toolkit 2002. http://courses.essex.ac.uk/hs/hs915/Mid%20Hampshire%20PCT%20HNA%20Toolkit.pdf (accessed 24 November 2013).
- Hutt P, Gilmour S. Tackling inequalities in general practice. London: The King’s Fund; 2010.
- Ali S, Burns C, Grant L. Equality and diversity in the health service: an evidence-led culture change. J Psycholo Issues Organ Culture 2012;3:41-60. http://dx.doi.org/10.1002/jpoc.20095.
- Lodge KM, Milnes D, Gilbody SM. Compiling a register of patients with moderate or severe learning disabilities: experience at one United Kingdom general practice. Ment Health Fam Med 2011;8:29-37.
- Fulton R. Ethnic Monitoring: Is Health Equality Possible Without It?. London: Race Equality Foundation; 2010.
- Thorlby R, Curry N. PCTs and Race Equality Schemes. London: The King’s Fund; 2007.
- Widger T, Prosser TS, Rogers S, Hutton C. The Performance of the Health Sector in Meeting Public Sector Equality Duties: Moving towards Effective Quality Outcomes. London: Equality and Human Rights Commission; 2011.
- Raleigh VS. Collection of data on ethnic origin in England. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a1107.
- Lakhani M. No Patient Left Behind: How Can We Ensure World Class Primary Care for Black and Ethnic Minority People?. London: Department of Health; 2008.
- Aspinall PJ. Informing progress towards race equality in mental healthcare: is routine data collection adequate?. Adv Psychiatr Treat 2006;12:141-51. http://dx.doi.org/10.1192/apt.12.2.141.
- Jones M, Kai J. Capturing ethnicity data in primary care: challenges and feasibility in a diverse metropolitan population. Divers Health Soc Care 2007;4:211-20.
- Siva N. Race relations in the UK’s National Health Service. Lancet 2009;373:1935-6. http://dx.doi.org/10.1016/S0140-6736(09)61050-3.
- Iqbal G, Johnson MRD, Szczepura A, Wilson S, Gumber A, Dunn JA. UK ethnicity data collection for healthcare statistics: the South Asian perspective. BMC Public Health 2012;12. http://dx.doi.org/10.1186/1471-2458-12-243.
- Ipsos MORI. The GP Patient Survey 2011. www.gp-patient.co.uk/info/ (accessed February 2011).
- Perry G, Van Cleemput P, Peters J, Moore J, Walters S, Thomas K, et al. The Health Status of Gypsies and Travellers in England. Sheffield: School of Health and Related Research, University of Sheffield; 2004.
- Pringle M, Rothera I. Practicality of recording patient ethnicity in general practice: descriptive intervention study and attitude survey. BMJ 1996;312:1080-2. http://dx.doi.org/10.1136/bmj.312.7038.1080.
- Lee B, Gardner KK, Jones B, Qassim TA. Ethnicity Profiling in Primary Care – the Princes Park Health Centre Model. Liverpool: Public Health Sector, Liverpool John Moores University; 2000.
- Mathur R, Hull SA, Badrick E, Robson J. Cardiovascular multimorbidity: the effect of ethnicity on prevalence and risk factor management. Br J Gen Pract 2011;61. http://dx.doi.org/10.3399/bjgp11X572454.
- Kumarapeli P, Stepaniuk R, De Lusignan S, Williams R, Rowlands G. Ethnicity recording in general practice computer systems. J Public Health 2006;28:283-7. http://dx.doi.org/10.1093/pubmed/fdl044.
- Iqbal G, Johnson MR, Szczepura A, Gumber A, Wilson S, Dunn JA. Ethnicity data collection in the UK: the healthcare professional’s perspective. Divers Equal Health Care 2012;9:281-90.
- Race for Health . Lambeth PCT Peer Review 2006. www.raceforhealth.org/storage/files/Lambeth_Outcome.pdf (accessed 20 August 2014).
- Mitchell P. Patient Profiling Report Update. Liverpool: Liverpool Primary Care Trust; 2010.
- Race for Health . Liverpool PCT . . . Know Your Patients Better, Save More Lives n.d. www.raceforhealth.org/resources/case_studies/liverpool (accessed 21 November 2013).
- Savory E, Jamieson J. Patient Profiling Pilot Project n.d. www.isdscotland.org/Health-Topics/Equality-and-Diversity/Publications/Final_pugh-patient-profiling-pilot-project%20(3).pdf (accessed 20 August 2014).
- Practical Guide to Ethnic Monitoring in the NHS and Social Care. London: Department of Health; 2012.
- Health Research and Educational Trust . HRET Disparities Toolkit n.d. www.hretdisparities.org/ (accessed 22 November 2013).
- Happy to Ask, Happy to Tell: Handbook for Trainees. Edinburgh: NHS Health Scotland; 2012.
- Caton S, Starling S, Burton M, Azmi S, Chapman M. Responsive services for people with learning disabilities from minority ethnic communities. Br J Learn Disabil 2007;35:229-35. http://dx.doi.org/10.1111/j.1468-3156.2007.00454.x.
- Say R, Murtagh M, Thomson R. Patients’ preference for involvement in medical decision making: a narrative review. Patient Educ Couns 2006;60:102-14. http://dx.doi.org/10.1016/j.pec.2005.02.003.
- Wilkinson S, Stöckl A, Taggart D, Franks W. Surveying Hard to Reach Groups – Final Report. NHS Great Yarmouth and Waveney; 2009.
- NHS England London . Transforming Primary Care in London: General Practice – A Call to Action 2013.
- 2022 GP: a Vision for General Practice in the Future NHS. London: Royal College of General Practitioners; 2013.
- Atherton H, Dalton A, Fleming S, Hirst J, Nunan D, Selwood M, et al. Are there enough GPs in England to detect hypertension and maintain access?. Br J Gen Pract 2013;63:346-7. http://dx.doi.org/10.3399/bjgp13X669103.
- Investment in General Practice 2008/09 to 2012/13 England, Wales, Northern Ireland and Scotland. Leeds: Health & Social Care Information Centre; 2013.
- Baker R, Bankart MJ, Rashid A, Banerjee J, Conroy S, Habiba M, et al. Characteristics of general practices associated with emergency-department attendance rates: a cross-sectional study. BMJ Qual Saf 2011;20:953-8. http://dx.doi.org/10.1136/bmjqs.2010.050864.
- Working with Communities, Developing Communities. Guidance for Primary Care. London: Royal College of General Practitioners; 2013.
- General Practice and the Integration of Care. An RCGP Policy Report. London: Royal College of General Practitioners; 2013.
- Bickerstaffe S. Towards Whole Person Care. London: IPPR; 2013.
- Richards T. European health systems must adapt to austerity, conference hears. BMJ 2013;347. http://dx.doi.org/10.1136/bmj.f6073.
- Gorecki C, Brown JM, Cano S, Lamping DL, Briggs M, Coleman S, et al. Development and validation of a new patient-reported outcome measure for patients with pressure ulcers: the PU-QOL instrument. Health Qual Life Outcomes 2013;11. http://dx.doi.org/10.1186/1477-7525-11-95.
- U.S . Food and Drug Administration. Wheel and Spokes Diagram: Clinical Outcome Assessments 2013.
- McColl E, Jacoby A, Thomas L, Soutter J, Bamford C, Steen N, et al. Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients. Health Technol Assess 2001;5.
- Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res 2010;19:539-49. http://dx.doi.org/10.1007/s11136-010-9606-8.
- The NHS Outcomes Framework 2014/15. London: Department of Health; 2013.
- Commissioning Outcomes Framework – Engagement Document. Redditch: NHS England; 2011.
- CCG Outcomes Indicator Set 2014/15: Technical Guidance. Redditch: NHS England; 2013.
- de Silva D. Measuring Patient Experience. London: Health Foundation; 2013.
- Fudge N, Wolfe CD, McKevitt C. Assessing the promise of user involvement in health service development: ethnographic study. BMJ 2008;336:313-17. http://dx.doi.org/10.1136/bmj.39456.552257.BE.
Appendix 1 Advisory group membership
| Name | Organisation |
|---|---|
| Anuila Ahmad | Volunteer Family Support Worker, Parent and Carer Council |
| Asma Sader | Leicester Centre for Ethnic Health Research |
| Beth McCarron-Nash | Chair, BMA General Practitioners’ Committee |
| Brian Fisher | Chair, NHS Alliance PPI steering group |
| Charles Huddleston | Manager, CLASP – The Carers Centre |
| Geoff Gaisford | Force4Change |
| Iona Heath | President, RCGP |
| Jane Hall | Family Support Worker, Parents and Carers Council |
| Janet Butterworth | Deputy Director, Service Experience Directorate, NHS North West |
| Jeannie Haggerty | Associate Professor, McGill University, Department of Family Medicine |
| Leicester City LD partnership board | Leicester City Learning Disabilities Partnership Board (to provide help with making the questionnaire accessible) |
| Leon Charikar | Programme Manager, Pacesetters |
| Mark Shrimpton | Deputy Chief Executive, The Royal Association for Disability Rights |
| Mike Warburton | National Director for Dental and GP Access, Department of Health |
| Paul McQuone | Force4Change |
| Paula Wray | Northamptonshire LINk and PPI lead for LNR CLAHRC |
| Russell Vine | Steering Group member, Practice Management Network |
| Sue Brookes | Community Development Officer, Mencap |
| Sue Freeman | Nurse Consultant, Learning Disabilities, Berrywood Hospital |
| Sue Mason | Board member, Leicester LINk |
| Sue Williams | Age Concern Leicestershire and Rutland |
| Wendy Collett | Business and Finance Manager, Tiptree Medical Centre (winner of NHS Alliance responsiveness prize) |
Appendix 2 Search strategy for literature review
Outline of systematic search strategy
MEDLINE and Web of Knowledge were searched on 15 March 2011, using terms such as ‘responsiveness’, ‘customer-focused’, combining these with terms for ‘patient experience’, ‘user needs’, etc. In both databases, a set of terms relating to ‘primary care’ was used to limit results to literature of specific relevance to general practice. A separate search strategy was designed for use in Web of Knowledge to identify literature on responsiveness of services in the public sector. Finally, a simple, one-line search was carried out in Web of Knowledge for literature mentioning the term ‘SERVQUAL’ (a multi-item quality scale developed to assess customer perceptions of service quality in service and retail businesses).
In developing the search strategies, relevant indexing terms were used, where available (such as general practice/, Quality Indicators, Health Care/), in combination with free-text terms (such as family physician$). Publication date filtering was applied, so as to limit results to articles published during the past 10 years (from 2001 until March 2011). In Web of Knowledge, results were restricted to the two general categories: ‘SOCIAL SCIENCES’ OR ‘SCIENCE & TECHNOLOGY’.
Due to the significant volume of literature identified in MEDLINE (in excess of 1600 results), a pragmatic decision was made to further limit search results in this database to literature of particular relevance to the UK by using an unvalidated search filter (lines 57 to 67 in the MEDLINE search strategy).
The database search generated 980 references. These were reviewed for duplicates, and 25 duplicate references were removed, resulting in a set of 955 references.
This initial search was supplemented with searches of the internet, and of reference lists of identified reports and papers, to identify relevant grey literature. This included searches of the websites of key UK commercial and charity organisations for papers on responsiveness of primary care and measures of responsiveness or patient experience of primary care; searches of DH websites for key policy documents on responsiveness; and Google searches (using terms responsiveness/respond/responsive in combination with patient/customer/student; measure/survey/questionnaire).
The search for grey literature generated 207 papers and reports. This meant that a total of 1162 references were identified.
As the parameters of our search were relatively wide and unfocused (in order to try to collect a wide range of work relevant to the meaning and measurement of responsiveness), the initial search generated many irrelevant articles. In order to reduce the number of articles with low relevance, we conducted a search of identified articles to include only those with the terms ‘responsiveness’ or ‘responsive’ in the title or abstract.
This generated 119 references: 85 originating from the database searches and 34 from the grey literature.
These were screened by reading the abstract (by CT and EA), with reference to the inclusion and exclusion criteria described below. As we were interested in gaining an overview of the body of work on this concept, we did not assess quality of included literature, and did not use quality assessments as exclusion criteria.
Inclusion criteria
-
Empirical, review or discussion paper.
-
Concerns responsiveness of organisations to customer/patient/client needs.
-
Relates to the meaning or measurement of responsiveness.
Exclusion criteria
-
Duplicate reference.
-
Papers focusing on clinical aspects of care only, decision-making, interpersonal care in the consultation, physician responsiveness to patients (staff patient relationships, staff–patient communication, shared decision-making, patient-centred consultations, consultation skills, etc.).
-
Papers reporting ‘responsiveness’ as a psychometric attribute of a questionnaire.
-
Papers focusing on responsiveness within organisations (e.g. employer–employee, or organisational responsiveness to the business climate).
-
Papers focusing on responsiveness of technology or environments.
-
Papers focusing on research methodology.
-
Mention of responsiveness only, no discussion of meaning or measurement.
As a result of this process, 87 references were excluded, leaving 32 papers and reports (13 from the database searches and 19 from the search for grey literature).
The full papers/reports were obtained. The paper/reports were summarised into a chart, to give an indication of the disciplinary area and an overview of the features of responsiveness as described in the paper. If the paper reported a survey or questionnaire, information about this was also recorded. The chart was used to generate an overview of the range and nature of work on this concept.
We present a narrative scoping review of the literature on the key fields of work relating to the meaning and measurement of responsiveness, and identify the themes that have emerged within these fields. In writing the narrative review, we have referenced wider literature that was ‘signposted’ by papers identified through the core search.
Formal search strategy
MEDLINE and Web of Knowledge were searched on 15 March 2011, using terms such as ‘responsiveness’, ‘inverse care’, combining these with terms for ‘patient experience’, ‘user needs’, etc. In both databases, a set of terms relating to ‘primary care’ was used to limit results to literature of specific relevance to general practice. A separate search strategy was designed for use in Web of Knowledge to identify literature on responsiveness of services in the public sector. Finally, a simple, one-line search was carried out in Web of Knowledge for literature mentioning the term ‘SERVQUAL’ (a multi-item quality scale developed to assess customer perceptions of service quality in service and retail businesses). RATER, the ‘successor’ to SERVQUAL, was not included.
In developing the search strategies, relevant indexing terms were used, where available (such as general practice/, Quality Indicators, Health Care/), in combination with free-text terms (such as family physician$, inverse care.ti,ab.). Publication date filtering was applied, so as to limit results to articles published during the past 10 years (from 2001 until March 2011). In Web of Knowledge, results were restricted to the two general categories: ‘SOCIAL SCIENCES’ OR ‘SCIENCE & TECHNOLOGY’.
Owing to the significant volume of literature identified in MEDLINE (in excess of 1600 results), a pragmatic decision was made to further limit search results in this database to literature of particular relevance to the UK by using an unvalidated search filter (lines 57 to 67 in the MEDLINE search strategy below).
In addition to the database searches, the NatCen, MORI, Picker Institute and Joseph Rowntree Foundation websites were searched, using the terms ‘responsiveness’ and ‘patient involvement’.
MEDLINE strategy (primary care), revised
21 January 2011 plus rough UK filter
-
exp primary health care/
-
exp family practice/
-
exp general practice/
-
exp physicians, family/
-
exp nurse/
-
(gp$ or general practi$ or family physician$ or family doctor$ or primary health care or primary care or nurse$ or health visitor$).ti,ab.
-
(gp$ or general practi$ or family physician$ or family doctor$ or primary health care or primary care or nurse$ or health visitor$).tw.
-
or/1-7
-
responsiveness.ti,ab.
-
inverse care.ti,ab.
-
((inequit$ or equit$) adj2 access).tw.
-
(equit$ adj2 quality adj2 care).tw.
-
(access$ adj2 quality adj2 care).tw.
-
(coordinat$ adj2 primary adj2 care$).ti,ab.
-
(fairness adj2 treatment).tw.
-
(fairness adj2 access).tw.
-
(Differentials adj2 quality adj2 management).tw.
-
(Differentials adj2 quality adj2 prevention).tw.
-
flexible health care.tw.
-
operational agreement$.ti,ab.
-
flexible booking.tw.
-
(customer-focused adj2 approach$).tw.
-
(engage$ adj2 (patient$ or user$)).ti,ab.
-
(involv$ adj2 (patient$ or user$)).ti,ab.
-
active listening.tw.
-
interpersonal continuity.ti.
-
(continuity adj2 care).ti.
-
Continuity of Patient Care/
-
cultural sensitivity.ti,ab.
-
Health Services Accessibility/
-
Cultural Diversity/
-
Quality Indicators, Health Care/
-
Physician-Patient Relations/
-
practice feature$.ti.
-
Ethnic Groups/
-
(ethnic adj2 group$).ti.
-
(ethnic adj2 minorit$).ti.
-
or/9-37
-
((patient$ or user$) adj2 need$).ti,ab.
-
((patient$ or user$) adj2 participat$).ti,ab.
-
((patient$ or user$) adj2 consult$).ti,ab.
-
((patient$ or user$) adj2 expectation$).ti,ab.
-
((patient$ or user$) adj2 experience$).ti,ab.
-
((patient$ or user$) adj2 prefer$).ti,ab.
-
((patient$ or user$) adj2 view$).ti,ab.
-
patient report$.ti,ab.
-
(non-health adj2 expectation$).ti,ab.
-
(non-clinical adj2 (preference$ or factor$ or need$)).tw.
-
(non-health adj2 benefit$).tw.
-
or/39-49
-
8 and 38 and 50
-
Primary Health Care/og [Organization & Administration]
-
responsive$.ti,ab.
-
52 and 53
-
51 or 54
-
limit 55 to yr="2001 -Current"
-
exp Great Britain/
-
UK.in.
-
welsh.ti,ab.
-
(England or wales or Ireland or Scotland).tw.
-
united kingdom.ti,ab.
-
"uk".ti,ab.
-
"gb".ti,ab.
-
english.ti,ab.
-
scottish.ti,ab.
-
Britain.ti,ab.
-
57 or 58 or 59 or 60 or 61 or 62 or 63 or 64 or 65 or 66
-
56 and 67
Web of Science: strategy 1 (primary care)
-
#24 #21 AND #20 Refined by: Publication Years=(2006 OR 2010 OR 2008 OR 2007 OR 2009 OR 2001 OR 2003 OR 2002 OR 2004 OR 2005 OR 2011) AND General Categories=(SCIENCE & TECHNOLOGY OR SOCIAL SCIENCES)
-
#23 #21 AND #20 Refined by: Publication Years=(2006 OR 2010 OR 2008 OR 2007 OR 2009 OR 2001 OR 2003 OR 2002 OR 2004 OR 2005 OR 2011)
-
#22 #21 AND #20
-
#21 #19 OR #18 OR #17 OR #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1
-
#20 Title=(primary same care or "general practi*" or "family practice" or "family doctor*" or "family physician*" or "primary care same nurs*" or "health visitor*")
-
#19 Title=(consumer* same preference*)
-
#18 Title=(consumer* same experience*)
-
#17 Title=(consumer* same perspective*)
-
#16 Title=("non-health benefit")
-
#15 Title=("patient expectation*")
-
#14 Title=(responsive*)
-
#13 Title=(respond*)
-
#12 Topic=("inverse care")
-
#11 Title=("service delivery")
-
#10 Title=("service quality")
-
#9 Title=("patient participation")
-
#8 Title=("patient preference*")
-
#7 Title=("patient need*")
-
#6 Title=("patient consultation*")
-
#5 Title=("patient experience")
-
#4 Title=("patient report*")
-
#3 Topic=("non-health expectation*")
-
#2 Topic=(divers* same workforce)
-
#1 Topic=(segmentation same population)
Web of Science: strategy 2 (public services), revised
#30 #27 AND #20
Refined by: Publication Years=(2009 OR 2001 OR 2010 OR 2005 OR 2000 OR 2008 OR 2007 OR 2004 OR 2002 OR 2006 OR 2003 OR 2011) AND General Categories=(SOCIAL SCIENCES OR SCIENCE & TECHNOLOGY)
#29 #27 AND #20
Refined by: Publication Years=(2009 OR 2001 OR 2010 OR 2005 OR 2000 OR 2008 OR 2007 OR 2004 OR 2002 OR 2006 OR 2003 OR 2011)
-
#28 #27 AND #20
-
#27 #26 OR #25 OR #24 OR #19
-
#26 Title=(user* same experience*)
-
#25 Title=((user* same preference*))
-
#24 Title=((user* same need*))
-
#23 #20 AND #19
-
Refined by: General Categories=(SOCIAL SCIENCES OR SCIENCE & TECHNOLOGY) AND Publication Years=(2009 OR 2005 OR 2010 OR 2006 OR 2008 OR 2007 OR 2004 OR 2002 OR 2003 OR 2001)
-
#22 #20 AND #19
-
Refined by: General Categories=(SOCIAL SCIENCES OR SCIENCE & TECHNOLOGY)
-
#21 #20 AND #19
-
#20 #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1
-
#19 #18 OR #17 OR #16 OR #15 OR #14 OR #13 OR #12 OR #11
-
#18 Title=(consumer* same service*)
-
#17 Title=(consumer* same need*)
-
#16 Title=(consumer* same preference*)
-
#15 Title=(consumer* same experience*)
-
#14 Title=(customer* same experience*)
-
#13 Title=(customer* same preference*)
-
#12 Title=(customer* same need*)
-
#11 Title=(customer* same service*)
-
#10 Title=(performance same index)
-
#9 Title=(cross-cultural same approach)
-
#8 Title=(market segmentation)
-
#7 Title=(measuring same quality)
-
#6 Title=(measuring same service)
-
#5 Title=(measure same quality)
-
#4 Title=(measure same service)
-
#3 Title=(service same quality)
-
#2 Title=(respond)
-
#1 Title=(responsive*)
Web of Science: strategy 3 (public services: SERVQUAL)
#1 Title=(SERVQUAL) Refined by: Publication Years=(2009 OR 2004 OR 2005 OR 2008 OR 2006 OR 2010 OR 2007 OR 2001 OR 2003 OR 2002)
Appendix 3 Staff interviews topic guides (stage 1)
Interview topic guide for staff at GP surgeries and walk-in centres.
Introduction
Thank you for seeing me today. Have you had a chance to read the information sheet?
The study
If I could just explain very briefly what our study is about . . . we are hoping to develop a patient-report measure of primary care responsiveness that can be completed a diverse group of patients (so for instance, we would like to include those with sensory or learning disability or who may not read or write English or who are from a BME background). It may take the form of a paper questionnaire but we will look at other formats, so as to ensure that it is accessible to all patients. It is hoped that the questionnaire will be suitable to be used by a range of different primary care organisations (PCOs) including GP practices, walk-in centres and pharmacies. So what I’m hoping to discuss with you today and get your views and feelings on is what do you feel is important when we talk about responsiveness.
What is responsiveness? So just to explain what we mean by responsiveness, we are not talking about what happens in the consultation with the doctor or nurse, or about how good the medical treatment is at this GP practice. But we are interested in everything else that goes around this, like: how easy or hard it is to make an appointment, or to get into the practice, the welcome and the customer service. There may be other issues that you feel are important to patients and we are interested in these too.
So I’ll be asking you questions around what responsiveness means to you, what are the things that you are currently doing, how you might be measuring this, what things would you like to do and possibly what are the barriers or facilitators to being as responsive as you would like to be.
Does that sound okay to you?
Recording and data
So before we take each of these points individually, I just want to make sure that you are okay with me digitally recording the interview. As I mentioned in the information sheet, we transcribe each interview verbatim and then anonymise the data prior to analysis. This ensures that everything that you say is confidential and nothing can be traced back to you. Is this okay? Also just to re-emphasise that this is voluntary and we are very grateful that you are willing to take part, but if you wish to withdraw at any time then that is fine. Do you have any questions at all about the study that you would like me to answer?
Please could you can sign the consent form to confirm this [check that they have signed and dated the consent form].
[Switch on the digital recorder]
[Get verbal consent for the recording again.]
General
[Only if the About The Practice questionnaire hasn’t been completed] So maybe to start with I wonder if you could give me a picture of what your practice is like?
[Probe specifically types of services they provide, patient population.]
Could you tell me what responsiveness means to you?
Would you say that responsiveness is something that is important to you as a PCO?
Responsiveness in their own experience
Could you give me a picture of what your practice is like in terms of responsiveness?
Can you tell me about any specific examples of ways in which you feel that your PCO is successful at being responsive to patients?
You mentioned [xxx] as an area that you have been successful in. Why do you believe that you have been successful in this area? Has anything been particularly helpful in bringing about these changes?
Did you face any difficulties in trying to implement these changes?
Do you have any other examples of you being successful in terms of improving the responsiveness of your practice?
[When interviewee gives ‘reactive’ examples, ask when you ask them about responsiveness.] Have you done anything or are you doing anything proactively to help meet the needs of your patients, such as thinking about your appointment systems, flagging up carers, redesigning their waiting room for people with a disability?
On the flip side, can you think of any examples of ways in which you feel your PCO is not particularly responsive to your patients? [Probe specifically if they feel that they may not be particularly responsive to a particular group of patients.]
What do you think are the reasons for this? [Probe actions of staff, systems, policies of the service, etc.]
What do you think would need to happen to improve in this area?
Are you doing anything currently to improve your responsiveness? Why?
If we were to ask the patients who visit this practice, what do you think they would say at this moment in time if we asked them how responsive the practice is?
Bearing in mind the characteristics of your patient population, are there any particular needs or wants that you are aware of, for example, in particular subgroups of the population (e.g. mothers want urgent appointments)?
Some groups of patients find it harder to use primary care services, e.g. disabled people, people who don’t speak English, people from other minority groups like LGBT, travellers. Is there anything you do as a practice to try to make it easier for potentially disadvantaged groups of people?
What are the difficulties?
What would you say makes it easier for you to be responsive to the needs of your specific patient population (i.e. what are the facilitators)?
On the other hand what would you say are the barriers to being responsive to your specific patient population?
Development of a measure
As I mentioned we are trying to develop a measure that practices are can use to measure responsiveness.
Do you have any measurements or indicators to let you know how responsive you are as a practice? [Probe survey data, actions of staff, systems, policies of the service, etc.]
What do you think of these indicators/measurements? [Probe are they useful or not.]
What do you think a measure should look like? What would it be like to work for you? Or maybe not be like?
Conclusion
Thank you for your time is there anything else that you would like to add that you feel is possibly important but hasn’t been covered in today’s discussion?
Any questions that you would like to ask?
Thanks again, would you be interested in a copy of the results?
Appendix 4 Patient interviews topic guide (stage 1)
Interview topic guide for patients at mainstream GP practices.
Introduction
We are trying to develop a questionnaire about how well GP practices and other primary care organisations (e.g. pharmacies, walk-in centres) respond to the needs of their patients.
We contacted you because you’re a patient at [practice].
And I would like to ask you about how well you feel this practice responds to your needs, and why you think that.
We want to talk to patients so we can make sure our questionnaire includes the issues most important to patients.
When we talk about responding to needs, we are not asking about what happens in the consultation with the doctor or nurse, or about how good your medical treatment was. We are interested in things like: how easy or hard it is to make an appointment that suits you, and to get into the practice, as well as the welcome and the customer service you get. You may have other needs from the practice so we are interested in these too.
Give information about anonymity, withdrawal from the study, etc.
Any questions?
Check and gain consent.
Background
The interview is split into three parts – the first is about your most recent visit, the second is about your experience of the practice over the past year or two, and the third contains some more general questions.
But to start with, can you tell me often have you visited this GP practice in the past year?
And when was the last time you visited or contacted this practice?
Thinking about this most recent experience of visiting or contacting this practice . . .
Can you talk me through what happened the last time you visited or contacted this practice? [Probe for the following, and for each, ask whether this was easy/hard OR good/not so good, and why.]
-
Making an appointment
Getting in to the practice
-
How the receptionists treated you/feeling welcome and treated like an individual.
-
Booking in and being called to the appointment.
-
Getting around the surgery, the facilities in the practice.
-
Getting information/keeping up to date with the practice, e.g. new appointment systems/clinics.
-
Having your particular needs supported (e.g. disabled access).
Did you have anything you particularly wanted or needed on your last visit (e.g. an appointment at a particular time, a telephone consultation, an interpreter)?
Did you feel that you got what you wanted/needed on this last visit? Was this easy or hard? Why – what happened?
What would have made this visit better for you?
Thinking more generally about your experience of this practice (e.g. over the past year or two)
Have you ever had an experience where you felt the practice was particularly flexible or went out of their way to help you and meet your needs? What happened, and why?
Have you ever had an experience where you felt the practice was particularly inflexible, unhelpful, or didn’t try hard to meet your individual needs? What happened, and why?
Generally, would you say that this practice is good at meeting the needs of patients like yourself (with a disability/who don’t speak English/older patients/young mothers, etc. [also refer to ‘about you’ form])? In what areas is it good, and in what areas could it be better? Can you give examples?
Generally, would you say that this practice is good at listening to and communicating with its patients? In what areas is it good, and in what areas could it be better? Can you give examples?
What could this GP practice do to make them more responsive to patients’ needs?
[Notes: (1) If the patient has only used the service once, which may be the case for walk-in centres, ask about their experience of primary care more generally. (2) For patients using the walk-in centre and the pharmacy, also ask ‘why did you decide to use this service rather than going to your GP?’ – probing for what needs they had and why this service meets them better than the GP practice.]
Responsiveness more generally
Imagine in an ‘ideal’ world you had a GP practice that was really responsive. Can you describe this organisation, what would it be like?
Imagine you had a GP practice that was really unresponsive. Can you describe this organisation, what would it be like?
Some people would say that responsiveness is about giving patients exactly what they want from a service. What do you think?
Anything else you would like to add?
Ask for feedback on the interviews (how could we make it better)
Any other questions?
Thank and ask if would like a copy of results.
Appendix 5 Patient focus groups topic guide (stage 1)
Introduction
We are trying to develop a questionnaire about how well GP practices and other primary care organisations (e.g. pharmacies, walk in centres) respond to the needs of their patients.
When we talk about responding to needs, we are not thinking about what happens in the consultation with the doctor or nurse, or about how good the medical treatment was. We are interested in how easy it is for people to use the service – to make an appointment that suits them, and to get into the practice building, and as well as things like how helpful receptionists are.
This is important because we know that some groups of people struggle to have these needs met, and if we develop a questionnaire then practices can find out what their own patients think, and try to improve.
We want to be sure that the questionnaire includes the issues that are most important to patients. We have come up with some questions and we want to find out how people would answer them, and whether we could make them better. This is what we’ll be asking you about over the next hour and a half.
Questions
I’m going to ask you some questions. I would like you to think about your own GP practice and try to answer them. There are no right or wrong answers, we just want to know what you think.
A. For each of the questions I ask, please think about your own GP practice and tick the box on the questionnaire which best represents your views. I will then ask you to say how you have answered the question and the sorts of things you thought about in coming to that answer.
Put each question up in turn on an OHP or flipchart, and read out.
-
Does the practice make it easy for you to contact them, to arrange to see a doctor or nurse?
-
How did you answer this question about your own GP practice? Why? What sort of things did you think about in deciding whether or not your practice makes it easy for you to contact them to arrange to see a GP or nurse?
-
PROMPT IF NEEDED: Thinking about the last time you used the practice, was it easy or hard to arrange to see a GP/nurse (e.g. did you have to ring up at a particular time of day, and the phone was engaged)? What would have made it easier for you?
-
-
Can you tell me in your own words what you think this question is asking about?
-
PROMPT if people are struggling to understand the question – these are the types of things we are interested in when we ask this question (see description of themes).
-
-
Was it difficult for you to answer this question, and why?
-
How do you think we could make this question better/what words should we use to make it easier for people to understand the question?
-
-
Does the practice make it easy for you to get an appointment that suits you?
-
How did you answer this question about your own GP practice? Why? What sort of things did you think about in deciding whether or not your practice makes it easy for you to get an appointment that suits you?
-
PROMPT IF NEEDED: Thinking about the last time you used the practice was it easy to get an appointment that suited you? What did you want, e.g. did you want to be seen quickly, or to see a particular doctor? What would have made it easier for you?
-
Can you tell me in your own words what you think this question is asking about?
-
PROMPT if people are struggling to understand the question – these are the types of things we are interested in when we ask this question (see description of themes).
-
Was it difficult for you to answer this question, and why?
-
How do you think we could make this question better/what words should we use to make it easier for people to understand the question?
-
-
Does the practice make it easy for you to get into the building and use the facilities?
-
How did you answer this question about your own GP practice? Why? What sort of things did you think about in deciding whether or not your practice makes it easy for you to get into the building and use the facilities?
-
PROMPT IF NEEDED: Thinking about the last time you used the practice, was it easy to get into the building and use the facilities. Did you have any problems? What facilities did you use? What facilities were you unable to use? Were there any other facilities that you needed that were not available?? What would have made it easier for you?
-
PROMPT if people are struggling to understand the question – these are the types of things we are interested in when we ask this question (see description of themes)
-
Can you tell me in your own words what you think this question is asking about?
-
PROMPT if people are struggling to understand the question – these are the types of things we are interested in when we ask this question (see description of themes).
-
-
Was it difficult for you to answer this question, and why?
-
How do you think we could make this question better/what words should we use to make it easier for people to understand the question?
-
-
-
Do receptionists always try to be helpful?
-
How did you answer this question about your own GP practice? Why? What sort of things did you think about in deciding whether or not receptionists always try to be helpful to you?
-
PROMPT IF NEEDED: Thinking about the last time you used the practice, did you feel the receptionists tried to be helpful? Did you have any problems? Did the receptionists make it awkward for you in any way? What would have made it better for you?
-
Can you tell me in your own words what you think this question is asking about?
-
PROMPT if people are struggling to understand the question – these are the types of things we are interested in when we ask this question (see description of themes).
-
-
Was it difficult for you to answer this question, and why?
-
How do you think we could make this question better/what words should we use to make it easier for people to understand the question?
-
-
Do practice staff treat you with respect?
-
How did you answer this question about your own GP practice? Why? What sort of things did you think about in deciding whether or not staff treat you with respect?
-
PROMPT IF NEEDED: Thinking about the last time you used the practice did you feel practice staff treated you with respect? Did you have any problems? What would have made it better for you?
-
Can you tell me in your own words what you think this question is asking about?
-
PROMPT if people are struggling to understand the question – these are the types of things we are interested in when we ask this question (see description of themes).
-
-
Was it difficult for you to answer this question, and why?
-
How do you think we could make this question better/what words should we use to make it easier for people to understand the question?
-
-
Does the practice try to support your individual needs?
-
How did you answer this question about your own GP practice? Why? What sort of things did you think about in deciding whether or not the practice tries to support your individual needs?
-
PROMPT IF NEEDED: Thinking about the last time you used the practice did you feel the practice supported your individual needs? How would you describe your individual needs? Did you have any problems in conveying these to the staff? In getting help appropriate to these needs? What would have made it better for you?
-
Can you tell me in your own words what you think this question is asking about?
-
PROMPT if people are struggling to understand the question – these are the types of things we are interested in when we ask this question (see description of themes).
-
-
Was it difficult for you to answer this question, and why?
-
How do you think we could make this question better/what words should we use to make it easier for people to understand the question?
-
-
Does you practice make it easy for you to keep up to date with your care and treatment?
-
How did you answer this question about your own GP practice? Why? What sort of things did you think about in deciding whether or not the practice makes it easy for you to keep up to date with your care and treatment?
-
Can you tell me in your own words what you think this question is asking about?
-
PROMPT if people are struggling to understand the question – these are the types of things we are interested in when we ask this question (see description of themes).
-
-
Was it difficult for you to answer this question, and why?
-
How do you think we could make this question better/what words should we use to make it easier for people to understand the question?
-
-
Does your practice make it easy for you to access other health care services you need?
-
How did you answer this question about your own GP practice? Why? What sort of things did you think about in deciding whether or not the practice makes it easy for you to access the other health-care services you need?
-
Can you tell me in your own words what you think this question is asking about?
-
PROMPT if people are struggling to understand the question – these are the types of things we are interested in when we ask this question (see description of themes).
-
-
Was it difficult for you to answer this question, and why?
-
How do you think we could make this question better/what words should we use to make it easier for people to understand the question?
-
-
B. Is there anything else that’s important for you when you use your GP practice, that we haven’t included in our questions?
Thank, travel claims/gift token. Ask if would like feedback.
Appendix 6 Summary framework from patient focus groups (stage 1)
| Question | People with disabilities | Members of a PPG at a practice in a deprived area (some disabilities and chronic conditions) | Non-English speaking |
|---|---|---|---|
| Q1: Does the practice make it easy for you to contact them to arrange to see a doctor or nurse? | Phone is engaged (have to phone again, cost); phone stacking (no indication of where you are in the queue); holding on (cost); competition with others who are physically at the practice – all the appointments are gone; different receptionists: ask personal questions; confidentiality in a crowded waiting room; walk-in clinics are good; booking online might be helpful; parking charges, so make appointment on phone not in person, or don’t live near enough; can’t see GP of choice. Question wording: ‘. . . to see any doctor . . .’ | Some answered Q2 within Q1, i.e. can be a long wait to see your own GP, easier to see any GP (but they can’t always handle complex cases); hanging on the phone then no appointments left; costly (repeated) phone calls (is this why people don’t bother to cancel appointments and there are so many DNAs?); can come in to make appointment but sometimes too ill; administrative errors (duplicate appointments); practice are bound to a telephone contract (0845 number); repeated phone calls then not enough appointments; season and day dependent. Question wording: some answers encompassed Q2, need to separate these more obviously. Suggestion: do the communication systems enable you to get through? | Long time to answer phone; costly (0845); easier to get an appointment in person (Q2?); appointments too far in advance (Q2); one problem per appointment (Q2); no triage, all appointments are 15–20 days in advance (Q2); difficult for working people; fully booked, even for emergencies (Q2); hard to see own doctor – continuity of care. Question wording: surgery not practice; can be interpreted as clinical; need to make it more obvious that it’s not about making the appointment but just getting in contact; suggestion: remove the latter part of the question so it ends at ‘. . . contact them?’ |
| Q2: Does the practice make it easy for you to get an appointment that suits you? | Once you get through, it’s moderately easy; receptionist-dependent; GP might be on annual leave; depends if you have a preference for a particular GP (which depends on the ailment: continuity vs. emergency). Question wording: ‘. . . that suits your needs’. Need extra option of ‘moderately easy’ | See Q1 above. There were no additional points to be made by the time we got onto Q2 | Can sometimes get appointments, it’s a lottery; receptionists don’t explain why there are no appointments; telephone consultations not face to face, just give prescriptions; one appointment, one problem, so have to make another appointment; sometimes told to ring back in case a cancellation becomes available; have to keep phoning back; fully booked, 2–4 week wait, ‘it’s not my fault’; refused an emergency appointment; daytime appointments not good for children at school; no problems for some people, especially in single-handed practices; continuity of care is a problem; so many new doctors, don’t know their names; if not urgent, some patients happy to wait; trial and error medication (clinical). Question wording: surgery not practice, otherwise worked well apart from the odd clinical need creeping in |
| Q3: Does the practice make it easy for you to get into the building and use the facilities? | Automatic doors; slopes for wheelchairs; disabled toilets; car parking (need one, need a bigger one, need more disabled spaces, if can’t get a spot then have to park on street which can mean a long walk in the rain, or the snow, which is tricky for people with mobility issues); need wider doors inside the surgery (auto door to get in, but not wide enough inside for large scooter or wheelchair). Question wording: separate into external and internal | Welcoming; slope up to door is too steep and no handrail; facilities inside are clearly visible; good signage; pharmacy on site; comfortable seating (but not for everyone, some get backache); lighting not good for people with sight problems and the call screen is too small – could use a verbal call from the receptionist for people whose notes are flagged; car park is quite a long walk from the front door; there can be long queues at reception (back problems); disabled parking spaces are misused (want blue badge spaces). Question wording: ‘your personal needs’ instead of ‘for you’; make it clear it’s for your personal situation rather than generic; most didn’t think about parking; most thought of inside the building | No bus, difficult to walk with mobility problems; doctors are upstairs, no lift; difficult to park at busy times; automatic doors; parking too far from surgery; seating, cleanliness, toilets, disabled access, lift. Question wording: need two questions, one for getting to the building and one for inside the building |
| Q4: Do receptionists try to be helpful? | Receptionist-dependent; depends on how busy they are; helps to be recognised and have a good relationship (more helpful); sometimes feel rushed – tricky when you need time to think; can feel like a number. Question wording: fine as is, three options are fine | Depends on the receptionist – some are very helpful, others are very rude; depends on how busy they are; they can assume too much knowledge (don’t explain); [appointment systems, continuity of care]; you need to be assertive to get what you want; rule-driven, lack of flexibility and communication; perhaps lack of training?; don’t smile enough. Question wording: ‘. . . helpful to you?’ | Sometimes busy in morning so have to phone again the afternoon (Q1); they do sometimes try to give you an appointment (Q2?); don’t answer phone if busy (Q1); face to face is more helpful than over the phone; if fully booked then have to phone again tomorrow, can’t help, no reassurance; don’t try to understand; depends on receptionist/their mood/the surgery; face to face is easier as you have body language to help; respect (Q5), listen, give you what you want; good customer service, polite; Gujariti-speaking (Q7?); no interpreters available, tried to help but was not satisfactory (Q7?); depends on expectation. Question wording: what kinds of things do people need help with, give examples, e.g. appointments, hospital reports, prescriptions, medical advice; perhaps two questions: one for face to face and one for over the phone |
| Q5: Do practice staff treat you with respect? | Staff try to use first names; it helps to be known; can feel hurried and rushed (it can be a waste of time if you have to come back for another appointment, and this is expensive – taxi fares). Question wording: what does ‘practice staff’ mean? Everyone, everyone except the doctors, everyone except the receptionists? Could say ‘. . . everyone at the practice, e.g . . .’ | Once you get an appointment, respect is fine (appointment system is the hurdle; continuity of care); lack of dignity in care (clinical); depends on what you want, e.g. follow-up appointments are difficult to book, staff (reception and GPs) can be rushed at the end of the day and try to push you out. Question wording: who are the practice staff: receptionists, everybody, GPs, physios, nurses, district nurses – list who we mean | How they talk to you has improved (used to be bad but more polite now); good systems for prescriptions (Q4); receptionists informing patients that there will be delay in patient’s appointment time (Q4); respectful face to face but not over the phone – they don’t try to understand; polite, always get a good answer (full answer, well explained); smile. Question wording: surgery not practice; do we mean receptionists or everybody; perhaps two questions, one for clinical and one for non-clinical |
| Q6: Does the practice try to support your individual needs? | This was interpreted as a clinical question initially; depends on expectations; depends on the type of need; have to ask/not proactive; had to tell them carer status and disabled status many times (now computerised in notes); communication/continuity/having to start again each visit; plain English; GP-dependent/continuity of care. Question wording: ‘. . . practice staff, e.g. . . .’ | Lack of or conflicting information between primary and secondary care; not working with parents to make (clinical) decisions; GPs don’t admit lack of (clinical) knowledge; patients are prescribed generic medication that can have side-effects (e.g. castor oil) so should be informed of changes (clinical); lack of privacy in pharmacy; [lack of continuity of care]. Question wording: this question was generally interpreted as clinical | Reminders (Q7); make blood test appointments automatically and just phone back to confirm (Q7/8); one GP refused to write a letter to confirm mobility problems prevented a patient from getting a discount on a piece of equipment; supports clinical needs (clinical); one problem, one appointment, not enough time in appointment; provides support (appointments) but not at patient’s convenience (Q2); support with prescriptions (Q7); refused a home visit for an elderly (96 years) parent; no after-clinic appointments (Q2). Question wording: surgery not practice; interpreted as clinical (doctor), or just receptionists, or everybody (need clarity). Answers didn’t really reflect what we were trying to get at. Needs work |
| Q7: Does the practice make it easy for you to keep up to date with your care and treatment? | Have to ask/not proactive (this sums it up); would be helpful to receive a letter that an appointment is due; don’t tell you that checks are necessary, they just give you a repeat prescription and then use ad hoc opportunities to do checks, e.g. when you go in for something else; underuse of IT (e.g. e-mails); text reminders would be helpful. Question wording: more options needed | Some interpreted as clinical (GP answers questions); reminders; fast track urgent test results; automatic checks for 70+ years; younger people must instigate any contact; repeat prescriptions are fine, they can provide in < 48 hours if urgent; can deliver medicines. Question wording: need to make it clear it’s non-clinical | Good proactive communication from doctor (clinical); can be interpreted as clinical; doctor saying (and sometimes phoning to say) need a blood test (clinical); have to ask and be proactive; reminders for blood tests and text reminders for appointments; expectations: been here longer, know how the system works and know what you need, if been here only a short time, tend to be more satisfied; referral to optician (Q8); one practice used to have reminders but not any more – ‘it’s your responsibility to remember’ with no explanation as to why the change happened. Question wording: surgery not practice; hard to answer if haven’t been registered for long or if don’t visit the surgery often; include a not applicable option? |
| Q8: Does the practice make it easy for you to access other health-care services that you need? | What’s available? How do you access it? Word of mouth; fragmentation; need a ‘care officer’ to manage pathways; too many forms to complete (duplication, hard work); isolation/abandonment/vulnerability/voice not heard (even if you had a voice, which you don’t at that time of shock); lack of knowledge about benefits; have to ask/not proactive. Question wording: fine as is | Access is okay but the communication from secondary care back to primary care is not good (takes ages); some GPs are not referring to specialists; lack of knowledge about what services are available. Question wording: should we include a list of possible services? | Can get referral letter for hospital; there is a diabetes nurse at the surgery; it’s easier nowadays; the surgery arranges everything; there are now more facilities on site, e.g. for blood tests, previously had to make appointment elsewhere for 3 weeks’ time; GPs repeat previous prescriptions without examining or listening to you (clinical). Question wording: surgery rather than practice; what does ‘access’ mean; give examples of other health-care services; this question is hard to answer if you don’t need other services; include a not applicable option |
| Other: Is there anything else that’s important for you when you use your GP practice that we haven’t included in our questions? | Length of appointment (one appointment, one problem); length of wait after appointment time – not knowing where you are in the queue or how many people are in front of you | The practice provides a good service, especially the nurses; one patient said that respect wasn’t covered (even though it was), so it couldn’t have registered with her | No indication of when the GP will phone back – tied to the phone; if there were phone queuing systems, people would hang up of they were 15th in the queue; busy phone lines 8–9:30 a.m., have to phone later; when visiting walk-in centre or hospital, need medical card or passport; information provision, e.g. leaflets put forward by interpreter but not an issue for the participants |
Appendix 7 General practitioner questionnaire, version 1 (stage 2, pilot 1)
Reproduced with permission from the University of Leicester.
General practitioner questionnaire, version 1 (stage 2, pilot 1) (PDF download)
Copyright © 2013 University of Leicester. All rights reserved.
Appendix 8 Patient interviews topic guide (stage 2, pilot 1)
Introduction
Give background to study
This stage of the study involves trying to find out how well the questionnaire works, and whether it allows people to report on the things that are most important to them.
Definitions
-
primary care
-
responsiveness (we are interested in NON-CLINICAL aspects of care).
Give information about anonymity, withdrawal from the study, etc.
Any questions? Check and gain verbal consent
Face validity
Recent experiences of consulting: Can you tell me just very briefly about the visit to your practice when you were given this questionnaire – when was this, and generally, what were you going for (don’t need medical details, just generally, e.g. was it to see the doctor with a new or ongoing medical problem, to get more medication, etc.).
I’d like to talk you through the things that were covered in the questionnaire, and ask you about how these were for you, this last time you used the practice. Also as we go through them you can tell me more generally how good you think your practice is in each of the areas.
-
Tell me about how it went arranging an appointment
-
PROMPTS: What did you need, and how easy or hard was it to get an appointment that suited you? Was there anything particularly good about your experience of arranging an appointment? Was there anything you were unhappy about?
-
-
Tell me about how the reception staff treated you
-
PROMPTS: Was there anything particularly good about how reception staff treated you? Was there anything you were unhappy about?
-
-
Tell me about how easy it was for you get to the GP surgery and what it’s like to wait at the surgery and to use their facilities
-
PROMPTS: Was there anything that was particularly difficult for you around travelling to the practice, waiting to be seen, and using the facilities in the practice? Was there anything that made this particularly easy or good for you?
-
-
Tell me, more generally, about how good you feel this GP surgery is at organising your care (Things like organising repeat prescriptions, sending you reminders, and coordinating your care with other services)
-
PROMPTS: Is there anything your practice is particularly good at, and anything you have been unhappy about around organising your care?
-
-
Tell me about how good you think this GP surgery is at listening and communicating with patients
-
Overall, how good would you say that this surgery is at meeting your needs, and the needs of patients like you? Why do you think this?
Feedback on the questionnaire
Was there anything important about your recent experience(s) of using primary care services that wasn’t on the questionnaire? REMIND – it’s not about the consultation or clinical care.
Was there anything on the questionnaire that you thought shouldn’t be there – that didn’t really matter to you?
About how long did it take you to fill in the questionnaire?
What did you think about the instructions on filling in the questionnaire?
Did you find it easy or difficult to complete?
Was there anything you didn’t really understand?
Overall, what are your views on the questionnaire?
Is there anything you would change to make it better?
Anything else you would like to add?
Any other questions? Thank and ask if would like a copy of results.
Appendix 9 Data analysis: descriptive statistics (stage 2, pilot 1)
Patient characteristics
Are you male or female?
| Response | n (%) |
|---|---|
| Male | 92 (39.7) |
| Female | 124 (53.4) |
| Transgender | 1 (0.4) |
| Total | 217 (93.5) |
| Missing | 15 (6.5) |
| Total | 232 (100.0) |
How old are you?
| Response | n (%) |
|---|---|
| Under 18 years | 3 (1.3) |
| 18–24 years | 21 (9.1) |
| 25–34 years | 41 (17.7) |
| 35–44 years | 24 (10.3) |
| 45–54 years | 42 (18.1) |
| 55–64 years | 34 (14.7) |
| 65–74 years | 38 (16.4) |
| 75–84 years | 18 (7.8) |
| 85 years or over | 2 (0.9) |
| Total | 223 (96.1) |
| Missing | 9 (3.9) |
| Total | 232 (100.0) |
What is your ethnic group?
| Response | n (%) |
|---|---|
| White British | 207 (89.2) |
| Black or black British | 5 (2.2) |
| Asian or Asian British | 7 (3.0) |
| Mixed British | 1 (0.4) |
| Chinese | 1 (0.4) |
| Other ethnic group | 2 (0.9) |
| Total | 223 (96.1) |
| Missing | 9 (3.9) |
| Total | 232 (100.0) |
Do you have any of the following conditions? Please tick any that apply.
Deafness or severe hearing impairment?
| Response | n (%) |
|---|---|
| No (not ticked) | 207 (89.2) |
| Yes (ticked) | 20 (8.6) |
| Total | 227 (97.8) |
| Missing | 5 (2.2) |
| Total | 232 (100.0) |
Blindness or severe visual impairment?
| Response | n (%) |
|---|---|
| No (not ticked) | 227 (97.8) |
| Missing | 5 (2.2) |
| Total | 232 (100.0) |
A condition that substantially limits your ability to carry out basic activities (e.g. walking, climbing stairs, lifting or carrying)?
| Response | n (%) |
|---|---|
| No (not ticked) | 195 (84.1) |
| Yes (ticked) | 32 (13.8) |
| Total | 227 (97.8) |
| Missing | 5 (2.2) |
| Total | 232 (100.0) |
A learning disability?
| Response | n (%) |
|---|---|
| No (not ticked) | 225 (97.0) |
| Yes (ticked) | 2 (0.9) |
| Total | 227 (97.8) |
| Missing | 5 (2.2) |
| Total | 232 (100.0) |
A long-standing mental health problem?
| Response | n (%) |
|---|---|
| No (not ticked) | 216 (93.1) |
| Yes (ticked) | 11 (4.7) |
| Total | 227 (97.8) |
| Missing | 5 (2.2) |
| Total | 232 (100.0) |
Any other long-standing illness?
| Response | n (%) |
|---|---|
| No (not ticked) | 171 (73.7) |
| Yes (ticked) | 56 (24.1) |
| Total | 227 (97.8) |
| Missing | 5 (2.2) |
| Total | 232 (100.0) |
Which of these describes what you are doing at present? (Tick as many as you need to.)
Full-time paid work (30 hours or more each week)
| Response | n (%) |
|---|---|
| No (not ticked) | 141 (60.8) |
| Yes (ticked) | 75 (32.3) |
| Incorrectly answered | 1 (0.4) |
| Total | 217 (93.5) |
| Missing | 15 (6.5) |
| Total | 232 (100.0) |
Part-time paid work (under 30 hours each week)
| Response | n (%) |
|---|---|
| No (not ticked) | 186 (80.2) |
| Yes (ticked) | 31 (13.4) |
| Total | 217 (93.5) |
| Missing | 15 (6.5) |
| Total | 232 (100.0) |
Full-time education at school, college or university
| Response | n (%) |
|---|---|
| No (not ticked) | 211 (90.9) |
| Yes (ticked) | 6 (2.6) |
| Total | 217 (93.5) |
| Missing | 15 (6.5) |
| Total | 232 (100.0) |
Not in paid work/retired
| Response | n (%) |
|---|---|
| No (not ticked) | 118 (50.9) |
| Yes (ticked) | 99 (42.7) |
| Total | 217 (93.5) |
| Missing | 15 (6.5) |
| Total | 232 (100.0) |
If you are working, is it easy for you to take time away from your work to see a doctor?
| Response | n (%) |
|---|---|
| Yes | 61 (26.3) |
| No | 47 (20.3) |
| Incorrectly answered | 2 (0.9) |
| Not applicable | 78 (33.6) |
| Total | 188 (81.0) |
| Missing (legitimately) | 1 (0.4) |
| Missing | 43 (18.5) |
| Total | 44 (19.0) |
| Total | 232 (100.0) |
Are you registered at this GP surgery?
| Response | n (%) |
|---|---|
| Yes | 213 (91.8) |
| No | 7 (3.0) |
| Not applicable | 1 (0.4) |
| Total | 221 (95.3) |
| Missing | 11 (4.7) |
| Total | 232 (100.0) |
Are you a parent or a legal guardian for any children aged under 16 living in your home?
| Response | n (%) |
|---|---|
| Yes | 60 (25.9) |
| No | 152 (65.5) |
| Total | 212 (91.4) |
| Missing | 20 (8.6) |
| Total | 232 (100.0) |
Are you a carer for anyone with an ongoing health problem or disability?
| Response | n (%) |
|---|---|
| Yes | 35 (15.1) |
| No | 178 (76.7) |
| Total | 213 (91.8) |
| Missing | 19 (8.2) |
| Total | 232 (100.0) |
Which of the following best describes how you think of yourself?
| Response | n (%) |
|---|---|
| Heterosexual/straight | 199 (85.8) |
| Gay/lesbian | 2 (0.9) |
| Bisexual | 4 (1.7) |
| Other | 2 (0.9) |
| I would prefer not to say | 7 (3.0) |
| Total | 214 (92.2) |
| Missing | 18 (7.8) |
| Total | 232 (100.0) |
Would you say that English is your first language?
| Response | n (%) |
|---|---|
| Yes | 209 (90.1) |
| No | 6 (2.6) |
| Bilingual/multilingual | 3 (1.3) |
| Total | 218 (94.0) |
| Missing | 14 (6.0) |
| Total | 232 (100.0) |
Patients expressing an interest in being interviewed
| Response | n (%) |
|---|---|
| Yes | 49 (21.1) |
Distribution of responses, missing and incorrect responses
About arranging an appointment . . .
Q1. The last time you used the GP surgery, what did you want?
| Response | n (%) |
|---|---|
| To see a doctor or nurse at the surgery | 188 (81.0) |
| To speak to doctor or nurse on the phone | 14 (6.0) |
| To arrange a home visit | 5 (2.2) |
| I wanted something else | 8 (3.4) |
| I didn’t mind/wasn’t sure what I wanted | 3 (1.3) |
| Incorrectly answered | 5 (2.2) |
| Total | 223 (96.1) |
| Missing | 9 (3.9) |
| Total | 232 (100.0) |
Were you able to get what you wanted?
| Response | n (%) |
|---|---|
| Yes | 179 (77.2) |
| No | 15 (6.5) |
| Total | 194 (83.6) |
| Missing (legitimately) | 1 (0.4) |
| Missing | 37 (15.9) |
| Total | 38 (16.4) |
| Total | 232 (100.0) |
Q2. The last time you used the GP surgery, did you have any preferences about who the appointment was with?
| Response | n (%) |
|---|---|
| Yes, I wanted a particular doctor | 102 (44.0) |
| Yes, I wanted a particular nurse | 7 (3.0) |
| Yes, I wanted someone of my own sex | 7 (3.0) |
| No, I didn’t mind who I saw | 107 (46.1) |
| Incorrectly answered | 4 (1.7) |
| Total | 227 (97.8) |
| Missing | 5 (2.2) |
| Total | 232 (100.0) |
If yes: were you able to get an appointment with right person for you?
| Response | n (%) |
|---|---|
| Yes | 91 (39.2) |
| No | 28 (12.1) |
| Answered incorrectly | 20 (8.6) |
| Total | 139 (59.9) |
| Missing (legitimately) | 80 (34.5) |
| Missing | 13 (5.6) |
| Total | 93 (40.1) |
| Total | 232 (100.0) |
Q3. The last time you used the GP surgery, did you have any preferences about when the appointment was?
| Response | n (%) |
|---|---|
| Yes, I wanted it as soon as possible | 107 (46.1) |
| Yes, I wanted to make an advance appointment for a particular time | 56 (24.1) |
| No, I didn’t mind when it was | 57 (24.6) |
| Incorrectly answered | 1 (0.4) |
| Total | 221 (95.3) |
| Missing | 11 (4.7) |
| Total | 232 (100.0) |
If yes: were you able to arrange an appointment at a time that was right for you?
| Response | n (%) |
|---|---|
| Yes | 134 (57.8) |
| No | 35 (15.1) |
| Answered incorrectly | 11 (4.7) |
| Total | 180 (77.6) |
| Missing (legitimately) | 36 (15.5) |
| Missing | 16 (6.9) |
| Total | 52 (22.4) |
| Total | 232 (100.0) |
Q4. Did the GP surgery make it easy for you to arrange this appointment?
| Response | n (%) |
|---|---|
| Very easy | 108 (46.6) |
| Quite easy | 85 (36.6) |
| Quite difficult | 20 (8.6) |
| Very difficult | 7 (3.0) |
| No opinion | 7 (3.0) |
| Total | 227 (97.8) |
| Missing | 5 (2.2) |
| Total | 232 (100.0) |
About how well reception staff treat you . . .
Q5. At this GP surgery, do reception staff . . .
Make you feel welcome?
| Response | n (%) |
|---|---|
| Yes | 181 (78.0) |
| To some extent | 33 (14.2) |
| No | 5 (2.2) |
| Incorrectly answered | 1 (0.4) |
| No opinion | 10 (4.3) |
| Total | 230 (99.1) |
| Missing | 2 (0.9) |
| Total | 232 (100.0) |
Treat you with respect?
| Response | n (%) |
|---|---|
| Yes | 191 (82.3) |
| To some extent | 24 (10.3) |
| No | 5 (2.2) |
| Incorrectly answered | 1 (0.4) |
| No opinion | 9 (3.9) |
| Total | 230 (99.1) |
| Missing | 2 (0.9) |
| Total | 232 (100.0) |
Take time to listen to you?
| Response | n (%) |
|---|---|
| Yes | 173 (74.6) |
| To some extent | 40 (17.2) |
| No | 5 (2.2) |
| Incorrectly answered | 1 (0.4) |
| No opinion | 10 (4.3) |
| Total | 229 (98.7) |
| Missing | 3 (1.3) |
| Total | 232 (100.0) |
Make efforts to communicate well with you (e.g. using language you can understand)?
| Response | n (%) |
|---|---|
| Yes | 189 (81.5) |
| To some extent | 25 (10.8) |
| No | 3 (1.3) |
| No opinion | 9 (3.9) |
| Total | 226 (97.4) |
| Missing | 6 (2.6) |
| Total | 232 (100.0) |
Understand your circumstances?
| Response | n (%) |
|---|---|
| Yes | 147 (63.4) |
| To some extent | 58 (25.0) |
| No | 8 (3.4) |
| No opinion | 16 (6.9) |
| Total | 229 (98.7) |
| Missing | 3 (1.3) |
| Total | 232 (100.0) |
Seem willing to try their best to help you?
| Response | n (%) |
|---|---|
| Yes | 179 (77.2) |
| To some extent | 35 (15.1) |
| No | 9 (3.9) |
| No opinion | 7 (3.0) |
| Total | 230 (99.1) |
| Missing | 2 (0.9) |
| Total | 232 (100.0) |
About how easy it is for you to visit the GP surgery . . .
Q6. How easy is it for you to . . .
Travel to the surgery?
| Response | n (%) |
|---|---|
| Very easy | 128 (55.2) |
| Quite easy | 67 (28.9) |
| Quite difficult | 14 (6.0) |
| Very difficult | 7 (3.0) |
| Incorrectly answered | 1 (0.4) |
| No opinion | 10 (4.3) |
| Total | 227 (97.8) |
| Missing | 5 (2.2) |
| Total | 232 (100.0) |
Get into the building?
| Response | n (%) |
|---|---|
| Very easy | 175 (75.4) |
| Quite easy | 36 (15.5) |
| Quite difficult | 4 (1.7) |
| Very difficult | 3 (1.3) |
| No opinion | 9 (3.9) |
| Total | 227 (97.8) |
| Missing | 5 (2.2) |
| Total | 232 (100.0) |
Get around, once you are inside the building?
| Response | n (%) |
|---|---|
| Very easy | 160 (69.0) |
| Quite easy | 51 (22.0) |
| Quite difficult | 5 (2.2) |
| Very difficult | 1 (0.4) |
| No opinion | 10 (4.3) |
| Total | 227 (97.8) |
| Missing | 5 (2.2) |
| Total | 232 (100.0) |
Use the facilities at the surgery (e.g. toilets)?
| Response | n (%) |
|---|---|
| Very easy | 143 (61.6) |
| Quite easy | 52 (22.4) |
| Quite difficult | 10 (4.3) |
| Very difficult | 2 (0.9) |
| No opinion | 20 (8.6) |
| Total | 227 (97.8) |
| Missing | 5 (2.2) |
| Total | 232 (100.0) |
Book in when you arrive?
| Response | n (%) |
|---|---|
| Very easy | 172 (76.1) |
| Quite easy | 42 (18.1) |
| Quite difficult | 1 (0.4) |
| Very difficult | 2 (0.9) |
| No opinion | 9 (3.9) |
| Total | 226 (97.4) |
| Missing | 6 (2.6) |
| Total | 232 (100.0) |
Talk to receptionists without being overheard?
| Response | n (%) |
|---|---|
| Very easy | 55 (23.7) |
| Quite easy | 53 (22.8) |
| Quite difficult | 67 (28.9) |
| Very difficult | 37 (15.9) |
| No opinion | 13 (5.6) |
| Total | 225 (97.0) |
| Missing | 7 (3.0) |
| Total | 232 (100.0) |
Know when it is your turn to be seen?
| Response | n (%) |
|---|---|
| Very easy | 126 (54.3) |
| Quite easy | 74 (31.9) |
| Quite difficult | 13 (5.6) |
| Very difficult | 3 (1.3) |
| No opinion | 10 (4.3) |
| Total | 226 (97.4) |
| Missing | 6 (2.6) |
| Total | 232 (100.0) |
Can you wait in comfort?
| Response | n (%) |
|---|---|
| Yes | 153 (65.9) |
| To some extent | 53 (22.8) |
| No | 10 (4.3) |
| No opinion | 7 (3.0) |
| Total | 223 (96.1) |
| Missing | 9 (3.9) |
| Total | 232 (100.0) |
About how good this GP surgery is at organising your care . . .
Q8. Is this GP surgery good at . . .
Helping you keep up to date with your health care (e.g. letting you know about test results, making it easy to get repeat prescriptions)?
| Response | n (%) |
|---|---|
| Very good | 88 (37.9) |
| Quite good | 92 (39.7) |
| Not very good | 15 (6.5) |
| Not at all good | 7 (3.0) |
| No opinion | 25 (10.8) |
| Total | 227 (97.8) |
| Missing | 5 (2.2) |
| Total | 232 (100.0) |
Organising your health care with hospitals?
| Response | n (%) |
|---|---|
| Very good | 77 (33.2) |
| Quite good | 70 (30.2) |
| Not very good | 9 (3.9) |
| Not at all good | 4 (1.7) |
| Incorrectly answered | 1 (0.4) |
| No opinion | 62 (26.7) |
| Total | 223 (96.1) |
| Missing | 9 (3.9) |
| Total | 232 (100.0) |
Helping you to get other community care services you need (e.g. family planning, counselling, social care)?
| Response | n (%) |
|---|---|
| Very good | 39 (16.8) |
| Quite good | 58 (25.0) |
| Not very good | 7 (3.0) |
| Not at all good | 2 (0.9) |
| Incorrectly answered | 1 (0.4) |
| No opinion | 112 (48.3) |
| Total | 219 (94.4) |
| Missing | 13 (5.6) |
| Total | 232 (100.0) |
About how good this GP surgery is at listening and communicating with patients . . .
Q9. Is this GP surgery good at . . .
Keeping you informed about their services?
| Response | n (%) |
|---|---|
| Very good | 54 (23.3) |
| Quite good | 90 (38.8) |
| Not very good | 23 (9.9) |
| Not at all good | 5 (2.2) |
| Incorrectly answered | 1 (0.4) |
| No opinion | 51 (22.0) |
| Total | 224 (96.6) |
| Missing | 8 (3.4) |
| Total | 232 (100.0) |
Listening to patients’ complaints and suggestions?
| Response | n (%) |
|---|---|
| Very good | 57 (24.6) |
| Quite good | 61 (26.3) |
| Not very good | 13 (5.6) |
| Not at all good | 4 (1.7) |
| Incorrectly answered | 2 (0.9) |
| No opinion | 84 (36.2) |
| Total | 221 (95.3) |
| Missing | 11 (4.7) |
| Total | 232 (100.0) |
About how good the GP surgery is at meeting your needs . . .
Q10. Is this GP surgery willing to be flexible to fit you in when it really matters to you?
| Response | n (%) |
|---|---|
| Very willing | 65 (28.0) |
| Quite willing | 110 (47.4) |
| Not very willing | 22 (9.5) |
| Not at all willing | 6 (2.6) |
| No opinion | 22 (9.5) |
| Missing | 7 (3.0) |
| Total | 232 (100.0) |
Q11. Is this GP surgery willing to do all they can to help and support you?
| Response | n (%) |
|---|---|
| Very willing | 84 (36.2) |
| Quite willing | 97 (41.8) |
| Not very willing | 12 (5.2) |
| Not at all willing | 3 (1.3) |
| No opinion | 28 (12.1) |
| Total | 224 (96.6) |
| Missing | 8 (3.4) |
| Total | 232 (100.0) |
Q12. Does this GP surgery take steps to organise your care?
| Response | n (%) |
|---|---|
| Yes, completely | 72 (31.0) |
| Yes, to some extent | 64 (27.6) |
| No, not really | 11 (4.7) |
| No, not at all | 4 (1.7) |
| No opinion | 72 (31.0) |
| Total | 223 (96.1) |
| Missing | 9 (3.9) |
| Total | 232 (100.0) |
Q13. Does this GP surgery provide good services and support for people in your circumstances?
| Response | n (%) |
|---|---|
| Yes, completely | 86 (37.1) |
| Yes, to some extent | 65 (28.0) |
| No, not really | 9 (3.9) |
| No, not at all | 2 (0.9) |
| No opinion | 61 (26.3) |
| Total | 223 (96.1) |
| Missing | 9 (3.9) |
| Total | 232 (100.0) |
Q14. Overall, do you feel comfortable using this GP surgery?
| Response | n (%) |
|---|---|
| Very comfortable | 137 (59.1) |
| Quite comfortable | 64 (27.6) |
| Not very comfortable | 8 (3.4) |
| Not at all comfortable | 4 (1.7) |
| Incorrectly answered | 1 (0.4) |
| No opinion | 11 (4.7) |
| Total | 225 (97.0) |
| Missing | 7 (3.0) |
| Total | 232 (100.0) |
Discrimination between practices
| Question | Valuea | Significance (two-sided) |
|---|---|---|
| Q1. The last time you used the GP surgery, what did you want? | N/A | |
| Were you able to get what you wanted? | 1.959 | 0.376 |
| Q2. The last time you used the GP surgery, did you have an preferences about who the appointment was with? | N/A | |
| If yes: were you able to get an appointment with right person for you? | 2.277 | 0.685 |
| Q3. The last time you used the GP surgery, did you have any preferences about when the appointment was? | N/A | |
| If yes: were you able to arrange an appointment at a time that was right for you? | 10.344 | 0.035 |
| Q4. Did the GP surgery make it easy for you to arrange this appointment? | 28.918 | 0.000 |
| Q5. At this GP surgery, do reception staff make you feel welcome? | 30.736 | 0.000 |
| At this GP surgery, do reception staff treat you with respect? | 35.171 | 0.000 |
| At this GP surgery, do reception staff take time to listen to you? | 24.932 | 0.002 |
| At this GP surgery, do reception staff make efforts to communicate well with you (e.g. using language you can understand)? | 37.155 | 0.000 |
| At this GP surgery, do reception staff understand your circumstances? | 7.179 | 0.305 |
| At this GP surgery, do reception staff seem willing to try their best to help you? | 30.812 | 0.000 |
| Q6. How easy is it for you to travel to the surgery? | 35.791 | 0.000 |
| How easy is it for you to get into the building? | 36.916 | 0.000 |
| How easy is it for you to get around, once you are inside the building? | 39.937 | 0.000 |
| How easy is it for you to use the facilities at the surgery (e.g. toilets)? | 39.415 | 0.000 |
| How easy is it for you to book in when you arrive? | 25.964 | 0.001 |
| How easy is it for you to talk to receptionists without being overheard? | 33.456 | 0.000 |
| How easy is it for you to know when it is your turn to be seen? | 22.421 | 0.004 |
| Q7. Can you wait in comfort? | 46.430 | 0.000 |
| Q8. Is this GP surgery good at helping you keep up to date with your health care (e.g. letting you know about test results, making it easy to get repeat prescriptions)? | 56.426 | 0.000 |
| Is this GP surgery good at organising your health care with hospitals? | 47.068 | 0.000 |
| Is this GP surgery good at helping you to get other community care services you need (e.g. family planning, counselling, social care)? | 15.390 | 0.118 |
| Is this GP surgery good at keeping you informed about their services? | 50.846 | 0.000 |
| Q9. Is this GP surgery good at listening to patients’ complaints and suggestions? | 16.548 | 0.085 |
| Q10. Is this GP surgery willing to be flexible, to fit you in when it really matters to you? | 21.022 | 0.021 |
| Q11. Is this GP surgery willing to do all they can to help and support you? | 23.722 | 0.003 |
| Q12. Does this GP surgery take steps to organise your care? | 11.214 | 0.190 |
| Q13. Does this GP surgery provide good services and support for people in your circumstances? | 19.832 | 0.011 |
| Q14. Overall, do you feel comfortable using this GP surgery? | 37.867 | 0.000 |
Appendix 10 General practitioner questionnaire, version 2; pharmacy questionnaire, version 1 (stage 2, pilot 2)
General practitioner questionnaire, version 2
Reproduced with permission from the University of Leicester.
General practitioner questionnaire, version 2 (PDF download)
Pharmacy questionnaire, version 1 (stage 2, pilot 2)
Reproduced with permission from the University of Leicester.
Pharmacy questionnaire, version 1 (stage 2, pilot 2) (PDF download)
Appendix 11 Cognitive interviews topic guides (stage 2, pilot 2)
Patient topic guide
Introduction
Give background to study.
This stage of the study involves trying to find out how well the questionnaire works and whether any of the wording might be confusing to people.
Make it clear that if people struggled to answer any question(s) then we want to know, so we can make the questionnaire better.
Give information about anonymity, withdrawal from the study, etc.
Any questions? Check and gain verbal consent.
Cognitive interview to explore responses
[N.B. This involves assessing what people are thinking, and how they interpret questions, when they complete the questionnaire. This will help identify sources of difficulty or misunderstandings.]
Why did you decide to fill in the questionnaire?
How long did it take to fill in?
For each question, the researcher will ask a series of general and specific probes (examples given below)
Were there any particular questions that you found difficult to answer?
[Researcher to start with these questions suggested by the interviewee]
Can you repeat this question in your own words?
Can you tell me what [e.g. ‘an urgent appointment’] means to you?
What sorts of things were you thinking about when you answered that question?
How did you arrive at that answer? Why not [higher or lower score]?
Was it easy or hard to answer?
If question was not completed – why?
Particular questions of interest to the research team
General practitioner questionnaire
Q6 (list of problems arranging an appointment)
Q8 (the meaning of ‘treated you well’, and the heading for this section)
Q10 (the meaning of ‘comfort’)
Q12 (what do they think about when they read ‘organising your health care with hospitals’? Can you rephrase ‘helping to coordinate your care ‘? What might that involve?)
Q15 and Q16 (the meaning of these questions)
Any issues with ‘About You’
Pharmacy questionnaire
Q1a (the list of what they want)
Q6 (the meaning of ‘treated you well’, and the heading for this section)
Q8 (the meaning of ‘comfort’)
Q10 (how they felt about the list of services)
Q12 and Q13 (the meaning of these questions)
Any issues with ‘About You’
Feedback on the questionnaire
Overall, what are your views on the questionnaire?
Is there anything you would change to make it better?
Anything else you would like to add?
Any other questions? Thank and ask if would like a copy of results.
Interpreter topic guide
Go through the questionnaire page by page and ask Q1 and Q2.
-
Were there any questions that were difficult to translate?
-
–Particular concepts that don’t translate?
-
–Particular words that are difficult to put into your language?
-
-
Where there any questions that you noticed people found difficult to answer? Why?
Feedback on the interpreting experience
-
How might we improve the interpreting experience?
-
–Reword the questions in English?
-
–Produce some guidance alongside the questionnaire to explain the meaning of the questions in more detail?
-
Appendix 12 Data analysis: descriptive statistics (stage 2, pilot 2)
Patient characteristics (general practitioner surgeries)
What is your gender?
| Response | n (%) |
|---|---|
| Male | 40 (43.5) |
| Female | 47 (51.1) |
| Transgender | 1 (1.1) |
| Total | 88 (95.7) |
| Missing | 4 (4.3) |
| Total | 92 (100.0) |
How old are you?
| Response | n (%) |
|---|---|
| 18 to 24 years | 9 (9.8) |
| 25 to 34 years | 14 (15.2) |
| 35 to 44 years | 9 (9.8) |
| 45 to 54 years | 16 (17.4) |
| 55 to 64 years | 21 (22.8) |
| 65 to 74 years | 14 (15.2) |
| 75 to 84 years | 6 (6.5) |
| Total | 89 (96.7) |
| Missing | 3 (3.3) |
| Total | 92 (100.0) |
What is your ethnic group?
| Response | n (%) |
|---|---|
| White British | 66 (71.7) |
| Black or black British | 3 (3.3) |
| Asian or Asian British | 7 (7.6) |
| Mixed British | 2 (2.2) |
| Other ethnic group | 10 (10.9) |
| Total | 88 (95.7) |
| Missing | 4 (4.3) |
| Total | 92 (100.0) |
Do you have any of the following conditions? Please tick any that apply.
Deafness or severe hearing impairment?
| Response | n (%) |
|---|---|
| No (not ticked) | 83 (90.2) |
| Yes (ticked) | 7 (7.6) |
| Total | 90 (97.8) |
| Missing | 2 (2.2) |
| Total | 92 (100.0) |
Blindness or severe visual impairment?
| Response | n (%) |
|---|---|
| No (not ticked) | 89 (96.7) |
| Yes (ticked) | 1 (1.1) |
| Total | 90 (97.8) |
| Missing | 2 (2.2) |
| Total | 92 (100.0) |
A condition that substantially limits your ability to carry out basic activities (e.g. walking, climbing stairs, lifting or carrying)?
| Response | n (%) |
|---|---|
| No (not ticked) | 71 (77.2) |
| Yes (ticked) | 19 (20.7) |
| Total | 90 (97.8) |
| Missing | 2 (2.2) |
| Total | 92 (100.0) |
A learning disability?
| Response | n (%) |
|---|---|
| No (not ticked) | 89 (96.7) |
| Yes (ticked) | 1 (1.1) |
| Total | 90 (97.8) |
| Missing | 2 (2.2) |
| Total | 92 (100.0) |
A long-standing mental health problem?
| Response | n (%) |
|---|---|
| No (not ticked) | 85 (92.4) |
| Yes (ticked) | 5 (5.4) |
| Total | 90 (97.8) |
| Missing | 2 (2.2) |
| Total | 92 (100.0) |
Any other long-standing illness (e.g. asthma, diabetes)?
| Response | n (%) |
|---|---|
| No (not ticked) | 58 (63.0) |
| Yes (ticked) | 32 (34.8) |
| Total | 90 (97.8) |
| Missing | 2 (2.2) |
| Total | 92 (100.0) |
Which of these describes what you are doing at present?
| Response | n (%) |
|---|---|
| Full-time paid work (30 hours or more each week) | 33 (35.9) |
| Part-time work (under 30 hours each week) | 13 (14.1) |
| Full-time education at school, college or university | 2 (2.2) |
| Not in paid work/retired | 40 (43.5) |
| Incorrectly answered | 1 (1.1) |
| Total | 89 (96.7) |
| Missing | 3 (3.3) |
| Total | 92 (100.0) |
Is it easy for you to take time away from your work to see a doctor?
| Response | n (%) |
|---|---|
| Yes | 34 (37.0) |
| No | 20 (21.7) |
| Not applicable | 35 (38.0) |
| Total | 89 (96.7) |
| Missing | 3 (3.3) |
| Total | 92 (100.0) |
Are you registered at this GP surgery?
| Response | n (%) |
|---|---|
| Yes | 89 (96.7) |
| No | 1 (1.1) |
| Total | 90 (97.8) |
| Missing | 2 (2.2) |
| Total | 92 (100.0) |
Are you a parent or a legal guardian for any children aged under 16 living in your home?
| Response | n (%) |
|---|---|
| Yes | 17 (18.5) |
| No | 70 (76.1) |
| Total | 87 (94.6) |
| Missing | 5 (5.4) |
| Total | 92 (100.0) |
Are you a carer for anyone with an ongoing health problem or disability?
| Response | n (%) |
|---|---|
| Yes | 6 (6.5) |
| No | 83 (90.2) |
| Total | 89 (96.7) |
| Missing | 3 (3.3) |
| Total | 92 (100.0) |
Which of the following best describes how you think of yourself?
| Response | n (%) |
|---|---|
| Heterosexual/straight | 83 (90.2) |
| Gay/lesbian | 1 (1.1) |
| Bisexual | 3 (3.3) |
| Incorrectly answered | 2 (2.2) |
| Total | 89 (96.7) |
| Missing | 3 (3.3) |
| Total | 92 (100.0) |
Would you say that English is your first language?
| Response | n (%) |
|---|---|
| Yes | 73 (79.3) |
| No | 12 (13.0) |
| Bilingual/multilingual | 5 (5.4) |
| Total | 90 (97.8) |
| Missing | 2 (2.2) |
| Total | 92 (100.0) |
Patients expressing an interest in being interviewed
| Response | n (%) |
|---|---|
| Yes | 19 (20.7) |
Patient characteristics (pharmacies)
What is your gender?
| Response | n (%) |
|---|---|
| Male | 22 (31.0) |
| Female | 45 (63.4) |
| Total | 67 (94.4) |
| Missing | 4 (5.6) |
| Total | 71 (100.0) |
How old are you?
| Response | n (%) |
|---|---|
| Under 18 years | 1 (1.4) |
| 18 to 24 years | 1 (1.4) |
| 25 to 34 years | 4 (5.6) |
| 35 to 44 years | 7 (9.9) |
| 45 to 54 years | 16 (22.5) |
| 55 to 64 years | 16 (22.5) |
| 65 to 74 years | 16 (22.5) |
| 75 to 84 years | 4 (5.6) |
| 85 years or over | 1 (1.4) |
| Total | 66 (93.0) |
| Missing | 5 (7.0) |
| Total | 71 (100.0) |
What is your ethnic group?
| Response | n (%) |
|---|---|
| White British | 59 (83.1) |
| Asian or Asian British | 5 (7.0) |
| Other ethnic group | 2 (2.8) |
| Total | 66 (93.0) |
| Missing | 5 (7.0) |
| Total | 71 (100.0) |
Do you have any of the following conditions? Please tick any that apply.
Deafness or severe hearing impairment?
| Response | n (%) |
|---|---|
| No (not ticked) | 65 (91.5) |
| Yes (ticked) | 2 (2.8) |
| Total | 67 (94.4) |
| Missing | 4 (5.6) |
| Total | 71 (100.0) |
Blindness or severe visual impairment?
| Response | n (%) |
|---|---|
| No (not ticked) | 66 (93.0) |
| Yes (ticked) | 1 (1.4) |
| Total | 67 (94.4) |
| Missing | 4 (5.6) |
| Total | 71 (100.0) |
A condition that substantially limits your ability to carry out basic activities (e.g. walking, climbing stairs, lifting or carrying)?
| Response | n (%) |
|---|---|
| No (not ticked) | 58 (81.7) |
| Yes (ticked) | 9 (12.7) |
| Total | 67 (94.4) |
| Missing | 4 (5.6) |
| Total | 71 (100.0) |
A learning disability?
| Response | n (%) |
|---|---|
| No (not ticked) | 66 (93.0) |
| Yes (ticked) | 1 (1.4) |
| Total | 67 (94.4) |
| Missing | 4 (5.6) |
| Total | 71 (100.0) |
A long-standing mental health problem?
| Response | n (%) |
|---|---|
| No (not ticked) | 62 (87.3) |
| Yes (ticked) | 5 (7.0) |
| Total | 67 (94.4) |
| Missing | 4 (5.6) |
| Total | 71 (100.0) |
Any other long-standing illness (e.g. asthma, diabetes)?
| Response | n (%) |
|---|---|
| No (not ticked) | 43 (60.6) |
| Yes (ticked) | 24 (33.8) |
| Total | 67 (94.4) |
| Missing | 4 (5.6) |
| Total | 71 (100.0) |
Which of these describes what you are doing at present?
| Response | n (%) |
|---|---|
| Full-time paid work (30 hours or more each week) | 16 (22.5) |
| Part-time work (under 30 hours each week) | 16 (22.5) |
| Not in paid work/retired | 36 (50.7) |
| Total | 68 (95.8) |
| Missing | 3 (4.2) |
| Total | 71 (100.0) |
Is it easy for you to take time away from your work to visit the pharmacy?
| Response | n (%) |
|---|---|
| Yes | 17 (23.9) |
| No | 11 (15.5) |
| Not applicable | 34 (47.9) |
| Total | 62 (87.3) |
| Missing | 9 (12.7) |
| Total | 71 (100.0) |
Why did you choose to use this particular pharmacy?
| Response | n (%) |
|---|---|
| This is the pharmacy I usually use | 58 (81.7) |
| This pharmacy was convenient for me today | 4 (5.6) |
| None of the above | 1 (1.4) |
| Incorrectly answered | 2 (2.8) |
| Total | 65 (91.5) |
| Missing | 6 (8.5) |
| Total | 71 (100.0) |
Are you a parent or a legal guardian for any children aged under 16 living in your home?
| Response | n (%) |
|---|---|
| Yes | 14 (19.7) |
| No | 51 (71.8) |
| Total | 65 (91.5) |
| Missing | 6 (8.5) |
| Total | 71 (100.0) |
Are you a carer for anyone with an ongoing health problem or disability?
| Response | n (%) |
|---|---|
| Yes | 9 (12.7) |
| No | 57 (80.3) |
| Total | 66 (93.0) |
| Missing | 5 (7.0) |
| Total | 71 (100.0) |
Which of the following best describes how you think of yourself?
| Response | n (%) |
|---|---|
| Heterosexual/straight | 63 (88.7) |
| Missing | 8 (11.3) |
| Total | 71 (100.0) |
Would you say that English is your first language?
| Response | n (%) |
|---|---|
| Yes | 58 (81.7) |
| No | 5 (7.0) |
| Bilingual/multilingual | 3 (4.2) |
| Total | 66 (93.0) |
| Missing | 5 (7.0) |
| Total | 71 (100.0) |
Patients expressing an interest in being interviewed
| Response | n (%) |
|---|---|
| Yes | 15 (21.1) |
Distribution of responses, missing and incorrect responses (general practitioner surgeries)
Distribution across PCOs
| PCO | n (%) |
|---|---|
| PCO06 | 54 (58.7) |
| PCO10 | 38 (41.3) |
| Total | 92 (100.0) |
About arranging an appointment . . .
Q1. The last time you used the GP surgery, how easy was it for you to get in touch with them to make the appointment?
| Response | n (%) |
|---|---|
| Very easy | 54 (58.7) |
| Quite easy | 30 (32.6) |
| Not very easy | 7 (7.6) |
| Not at all easy | 1 (1.1) |
| Total | 92 (100.0) |
Q2a. The last time you used the GP surgery, what type of appointment did you want?
| Response | n (%) |
|---|---|
| An appointment at the surgery | 84 (91.3) |
| To speak to doctor or nurse on the phone | 5 (5.4) |
| I didn’t mind/wasn’t sure what I wanted | 1 (1.1) |
| Something not listed above | 2 (2.2) |
| Total | 92 (100.0) |
Q2b. Were you able to get the type of appointment you wanted?
| Response | n (%) |
|---|---|
| Yes | 87 (94.6) |
| No | 3 (3.3) |
| No opinion | 1 (1.1) |
| Total | 91 (98.9) |
| Missing | 1 (1.1) |
| Total | 92 (100.0) |
Q3a. The last time you used the GP surgery, did you have any preferences about when the appointment was?
| Response | n (%) |
|---|---|
| Yes, I wanted it as soon as possible | 38 (41.3) |
| Yes, I wanted to make an appointment for a particular day/time | 22 (23.9) |
| No, I didn’t mind when it was | 31 (33.7) |
| Total | 91 (98.9) |
| Missing | 1 (1.1) |
| Total | 92 (100.0) |
Q3b. Were you able to get an appointment at a time that was right for you?
| Response | n (%) |
|---|---|
| Yes | 74 (80.4) |
| No | 12 (13.0) |
| No opinion | 3 (3.3) |
| Total | 89 (96.7) |
| Missing | 3 (3.3) |
| Total | 92 (100.0) |
Q4a. The last time you used the GP surgery, did you have any preferences about who the appointment was with?
| Response | n (%) |
|---|---|
| Yes, I wanted a particular doctor | 29 (31.5) |
| Yes, I wanted a particular nurse | 4 (4.3) |
| Yes, there was a particular doctor/nurse I wanted to avoid | 2 (2.2) |
| Yes, I wanted someone of my own sex | 2 (2.2) |
| No, I didn’t mind who I saw | 55 (59.8) |
| Total | 92 (100.0) |
Q4b. Were you able to get an appointment with the person you wanted?
| Response | n (%) |
|---|---|
| Yes | 54 (58.7) |
| No | 8 (8.7) |
| No opinion | 28 (30.4) |
| Total | 90 (97.8) |
| Missing | 2 (2.2) |
| Total | 92 (100.0) |
Q5. Overall, did the GP surgery make it easy for you to arrange an appointment that suited you?
| Response | n (%) |
|---|---|
| Very easy | 37 (40.2) |
| Quite easy | 42 (45.7) |
| Not very easy | 12 (13.0) |
| Not at all easy | 1 (1.1) |
| Total | 92 (100.0) |
Q6. Did you have any of the following problems in arranging an appointment? (Please tick any that apply)
It was difficult to get through on the phone
| Response | n (%) |
|---|---|
| No (not ticked) | 77 (83.7) |
| Yes (ticked) | 15 (16.3) |
| Total | 92 (100.0) |
I had to keep phoning back to get an appointment
| Response | n (%) |
|---|---|
| No (not ticked) | 85 (92.4) |
| Yes (ticked) | 7 (7.6) |
| Total | 92 (100.0) |
There were no appointments available on the day/at the time I wanted
| Response | n (%) |
|---|---|
| No (not ticked) | 73 (79.3) |
| Yes (ticked) | 19 (20.7) |
| Total | 92 (100.0) |
The wait for a non-urgent appointment was too long
| Response | n (%) |
|---|---|
| No (not ticked) | 81 (88.0) |
| Yes (ticked) | 11 (12.0) |
| Total | 92 (100.0) |
The wait for an appointment with my preferred GP or nurse was too long
| Response | n (%) |
|---|---|
| No (not ticked) | 80 (87.0) |
| Yes (ticked) | 12 (13.0) |
| Total | 92 (100.0) |
I wasn’t able to book in advance for the time I wanted
| Response | n (%) |
|---|---|
| No (not ticked) | 86 (93.5) |
| Yes (ticked) | 6 (6.5) |
| Total | 92 (100.0) |
About how well reception staff treated you . . .
Q7. Did you feel that the reception staff . . .
Were friendly towards you?
| Response | n (%) |
|---|---|
| Yes | 76 (82.6) |
| Yes, to some extent | 14 (15.2) |
| No | 2 (2.2) |
| Total | 92 (100.0) |
Treated you with respect?
| Response | n (%) |
|---|---|
| Yes | 77 (83.7) |
| Yes, to some extent | 13 (14.1) |
| No | 2 (2.2) |
| Total | 92 (100.0) |
Tried their best to help you?
| Response | n (%) |
|---|---|
| Yes | 76 (82.6) |
| Yes, to some extent | 14 (15.2) |
| No | 2 (2.2) |
| Total | 92 (100.0) |
Q8. Overall, did you feel that the reception staff treated you well?
| Response | n (%) |
|---|---|
| Very well | 61 (66.3) |
| Quite well | 28 (30.4) |
| Not very well | 3 (3.3) |
| Total | 92 (100.0) |
About how easy it was for you to visit the GP surgery . . .
Q9. How easy was it for you . . .
To get around the building?
| Response | n (%) |
|---|---|
| Very easy | 77 (83.7) |
| Quite easy | 15 (16.3) |
| Total | 92 (100.0) |
Use the facilities at the surgery (e.g. toilets)?
| Response | n (%) |
|---|---|
| Very easy | 66 (71.7) |
| Quite easy | 13 (14.1) |
| No opinion | 12 (13.0) |
| Total | 91 (98.9) |
| Missing | 1 (1.1) |
| Total | 92 (100.0) |
Book in when you arrived?
| Response | n (%) |
|---|---|
| Very easy | 68 (73.9) |
| Quite easy | 21 (22.8) |
| Quite difficult | 2 (2.2) |
| No opinion | 1 (1.1) |
| Total | 92 (100.0) |
Talk to receptionists without being overheard?
| Response | n (%) |
|---|---|
| Very easy | 19 (20.7) |
| Quite easy | 24 (26.1) |
| Quite difficult | 35 (38.0) |
| Very difficult | 11 (12.0) |
| No opinion | 3 (3.3) |
| Total | 92 (100.0) |
Know when it is your turn to be seen?
| Response | n (%) |
|---|---|
| Very easy | 63 (68.5) |
| Quite easy | 24 (26.1) |
| Quite difficult | 4 (4.3) |
| Very difficult | 1 (1.1) |
| Total | 92 (100.0) |
Q10. Could you wait in comfort?
| Response | n (%) |
|---|---|
| Yes | 60 (65.2) |
| Yes, to some extent | 31 (33.7) |
| No | 1 (1.1) |
| Total | 92 (100.0) |
Q11. Overall, how easy was it for you to use the GP surgery building and its facilities?
| Response | n (%) |
|---|---|
| Very easy | 61 (66.3) |
| Quite easy | 29 (31.5) |
| Incorrectly answered | 1 (1.1) |
| No opinion | 1 (1.1) |
| Total | 92 (100.0) |
About how good this GP surgery is at helping to co-ordinate your care . . .
Q12. Is this GP surgery good at . . .
Helping you keep up to date with your health care (e.g. sending you reminders about upcoming appointments, making it easy to get repeat prescriptions)?
| Response | n (%) |
|---|---|
| Very good | 43 (46.7) |
| Quite good | 32 (34.8) |
| Not very good | 8 (8.7) |
| Not at all good | 3 (3.3) |
| Not applicable | 6 (6.5) |
| Total | 92 (100.0) |
Organising your health care with hospitals (e.g. letting you know hospital test results, chasing the hospital when letters go missing)?
| Response | n (%) |
|---|---|
| Very good | 30 (32.6) |
| Quite good | 35 (38.0) |
| Not very good | 9 (9.8) |
| Not at all good | 3 (3.3) |
| Incorrectly answered | 2 (2.2) |
| Not applicable | 13 (14.1) |
| Total | 92 (100.0) |
Helping you to get other health and community care services you need (e.g. family planning, counselling, social services)?
| Response | n (%) |
|---|---|
| Very good | 13 (14.1) |
| Quite good | 24 (26.1) |
| Not very good | 5 (5.4) |
| Not applicable | 47 (51.1) |
| Total | 89 (96.7) |
| Missing | 3 (3.3) |
| Total | 92 (100.0) |
Q13. Overall, how good is this GP surgery at helping to co-ordinate your care?
| Response | n (%) |
|---|---|
| Very good | 31 (33.7) |
| Quite good | 41 (44.6) |
| Not very good | 5 (5.4) |
| Not at all good | 2 (2.2) |
| No opinion | 11 (12.0) |
| Total | 90 (1.0) |
| Missing | 2 (2.2) |
| Total | 92 (100.0) |
About how good this GP surgery is at listening and communicating with patients . . .
Q14. Is this GP surgery good at . . .
Keeping you informed about their services?
| Response | n (%) |
|---|---|
| Very good | 23 (25.0) |
| Quite good | 36 (39.1) |
| Not very good | 14 (15.2) |
| Not at all good | 2 (2.2) |
| No opinion | 16 (17.4) |
| Total | 91 (98.9) |
| Missing | 1 (1.1) |
| Total | 92 (100.0) |
Listening to patients’ complaints and suggestions?
| Response | n (%) |
|---|---|
| Very good | 24 (26.1) |
| Quite good | 21 (22.8) |
| Not very good | 6 (6.5) |
| Not at all good | 2 (2.2) |
| Incorrectly answered | 1 (1.1) |
| No opinion | 37 (40.2) |
| Total | 91 (98.9) |
| Missing | 1 (1.1) |
| Total | 92 (100.0) |
Overall, how do you feel about this GP practice?
Q15. Thinking about your own lifestyle and personal circumstances, does this GP surgery provide a good service for people like you?
| Response | n (%) |
|---|---|
| Yes, completely | 53 (57.6) |
| Yes, to some extent | 32 (34.8) |
| No, not really | 5 (5.4) |
| Total | 90 (97.8) |
| Missing | 2 (2.2) |
| Total | 92 (100.0) |
Q16. Do you feel comfortable using this GP surgery?
| Response | n (%) |
|---|---|
| Very comfortable | 60 (65.2) |
| Quite comfortable | 26 (28.3) |
| Not very comfortable | 4 (4.3) |
| Not at all comfortable | 1 (1.1) |
| Total | 91 (98.9) |
| Missing | 1 (1.1) |
| Total | 92 (100.0) |
Distribution of responses, missing and incorrect responses (pharmacies)
Distribution across PCOs
| PCOs | n (%) |
|---|---|
| PCO02 | 14 (19.7) |
| PCO03 | 57 (80.3) |
| Total | 71 (100.0) |
About your visit to the pharmacy . . .
Q1a. The last time you used the pharmacy, what did you want?
| Response | n (%) |
|---|---|
| To collect a prescription | 55 (77.5) |
| I wasn’t sure what I wanted | 1 (1.4) |
| Something not listed above | 6 (8.5) |
| Incorrectly answered | 8 (11.3) |
| Total | 70 (98.6) |
| Missing | 1 (1.4) |
| Total | 71 (100.0) |
Q1b. Were you able to get what you wanted?
| Response | n (%) |
|---|---|
| Yes | 65 (91.5) |
| No | 2 (2.8) |
| Total | 67 (94.4) |
| Missing | 4 (5.6) |
| Total | 71 (100.0) |
Q2. Were you happy with the speed of service?
| Response | n (%) |
|---|---|
| Yes | 68 (95.8) |
| No | 2 (2.8) |
| Total | 70 (98.6) |
| Missing | 1 (1.4) |
| Total | 71 (100.0) |
Q3a. If you wanted to speak with someone, did you have any preferences about who spoke with?
| Response | n (%) |
|---|---|
| Yes, I wanted a particular pharmacist | 1 (1.4) |
| Yes, I wanted a particular member of the pharmacy staff | 8 (11.3) |
| No, I didn’t mind who I saw | 36 (50.7) |
| I didn’t want to speak with anyone | 21 (29.6) |
| Incorrectly answered | 2 (2.8) |
| Total | 68 (95.8) |
| Missing | 3 (4.2) |
| Total | 71 (100.0) |
Q3b. Were you able to speak with the person you wanted?
| Response | n (%) |
|---|---|
| Yes | 37 (52.1) |
| No | 1 (1.4) |
| Answered incorrectly | 1 (1.4) |
| No opinion | 11 (15.5) |
| Total | 50 (70.4) |
| Missing | 21 (29.6) |
| Total | 71 (100.0) |
Q4. Overall, did the pharmacy make it easy for you to get what you wanted?
| Response | n (%) |
|---|---|
| Very easy | 58 (81.7) |
| Quite easy | 8 (11.3) |
| Not at all easy | 1 (1.4) |
| Total | 67 (94.4) |
| Missing | 4 (5.6) |
| Total | 71 (100.0) |
About how well pharmacy staff treated you . . .
Q5. The last time you used the pharmacy, did you feel that the staff . . .
Were friendly towards you?
| Response | n (%) |
|---|---|
| Yes | 67 (94.4) |
| To some extent | 2 (2.8) |
| No | 1 (1.4) |
| Total | 70 (98.6) |
| Missing | 1 (1.4) |
| Total | 71 (100.0) |
Treated you with respect?
| Response | n (%) |
|---|---|
| Yes | 67 (94.4) |
| To some extent | 1 (1.4) |
| No | 1 (1.4) |
| Total | 69 (97.2) |
| Missing | 2 (2.8) |
| Total | 71 (100.0) |
That the staff tried their best to help you?
| Response | n (%) |
|---|---|
| Yes | 67 (94.4) |
| To some extent | 1 (1.4) |
| No | 1 (1.4) |
| Total | 69 (97.2) |
| Missing | 2 (2.8) |
| Total | 71 (100.0) |
Q6. Overall, did you feel that the staff treated you well?
| Response | n (%) |
|---|---|
| Very well | 64 (90.1) |
| Quite well | 5 (7.0) |
| Not at all well | 1 (1.4) |
| Total | 70 (98.6) |
| Missing | 1 (1.4) |
| Total | 71 (100.0) |
About how easy it was for you to visit the pharmacy . . .
Q7. How easy was it for you to . . .
Get around the building?
| Response | n (%) |
|---|---|
| Very easy | 48 (67.6) |
| Quite easy | 19 (26.8) |
| Very difficult | 1 (1.4) |
| Total | 68 (95.8) |
| Missing | 3 (4.2) |
| Total | 71 (100.0) |
Find what you wanted on the shelves?
| Response | n (%) |
|---|---|
| Very easy | 33 (46.5) |
| Quite easy | 29 (40.8) |
| Quite difficult | 3 (4.2) |
| No opinion | 3 (4.2) |
| Total | 68 (95.8) |
| Missing | 3 (4.2) |
| Total | 71 (100.0) |
Talk pharmacy staff without being overheard?
| Response | n (%) |
|---|---|
| Very easy | 15 (21.1) |
| Quite easy | 32 (45.1) |
| Quite difficult | 15 (21.1) |
| Very difficult | 2 (2.8) |
| No opinion | 4 (5.6) |
| Total | 68 (95.8) |
| Missing | 3 (4.2) |
| Total | 71 (100.0) |
Know when it is your turn to be served?
| Response | n (%) |
|---|---|
| Very easy | 39 (54.9) |
| Quite easy | 28 (39.4) |
| Quite difficult | 1 (1.4) |
| Very difficult | 1 (1.4) |
| Total | 69 (97.2) |
| Missing | 2 (2.8) |
| Total | 71 (100.0) |
Q8. Could you wait in comfort?
| Response | n (%) |
|---|---|
| Yes | 34 (47.9) |
| Yes, to some extent | 27 (38.0) |
| No | 6 (8.5) |
| No opinion | 3 (4.2) |
| Total | 70 (98.6) |
| Missing | 1 (1.4) |
| Total | 71 (100.0) |
Q9. Overall, how easy was it for you to use the pharmacy building and its facilities?
| Response | n (%) |
|---|---|
| Very easy | 50 (70.4) |
| Quite easy | 20 (28.2) |
| Quite difficult | 1 (1.4) |
| Total | 71 (100.0) |
About how good this pharmacy is at providing and signposting services . . .
Q10. Is this pharmacy good at . . .
Providing advice on your health problem(s)?
| Response | n (%) |
|---|---|
| Very good | 45 (63.4) |
| Quite good | 18 (25.4) |
| Not very good | 2 (2.8) |
| Not applicable | 6 (8.5) |
| Total | 71 (100.0) |
Providing advice on how to have a healthier lifestyle?
| Response | n (%) |
|---|---|
| Very good | 24 (33.8) |
| Quite good | 22 (31.0) |
| Not very good | 2 (2.8) |
| Not at all good | 1 (1.4) |
| Not applicable | 20 (28.2) |
| Total | 69 (97.2) |
| Missing | 2 (2.8) |
| Total | 71 (100.0) |
Disposing of medicines you no longer need?
| Response | n (%) |
|---|---|
| Very good | 45 (63.4) |
| Quite good | 3 (4.2) |
| Not at all good | 1 (1.4) |
| Not applicable | 19 (26.8) |
| Total | 68 (95.8) |
| Missing | 3 (4.2) |
| Total | 71 (100.0) |
Coordinating with the GP (e.g. ensuring that repeat prescriptions are ready for you, checking your prescriptions are correct)?
| Response | n (%) |
|---|---|
| Very good | 53 (74.6) |
| Quite good | 11 (15.5) |
| Not very good | 3 (4.2) |
| Not applicable | 4 (5.6) |
| Total | 71 (100.0) |
Fitting in with your life circumstances (e.g. offering home delivery of prescriptions)?
| Response | n (%) |
|---|---|
| Very good | 21 (29.6) |
| Quite good | 14 (19.7) |
| Not very good | 1 (1.4) |
| Not at all good | 1 (1.4) |
| Not applicable | 29 (40.8) |
| Total | 66 (93.0) |
| Missing | 5 (7.0) |
| Total | 71 (100.0) |
Helping patients get the best out of the service (e.g. offering advice such as how to save money on a prescription)?
| Response | n (%) |
|---|---|
| Very good | 27 (38.0) |
| Quite good | 13 (18.3) |
| Not very good | 2 (2.8) |
| Not applicable | 26 (36.6) |
| Total | 68 (95.8) |
| Missing | 3 (4.2) |
| Total | 71 (100.0) |
Providing advice about relevant health services or information available elsewhere?
| Response | n (%) |
|---|---|
| Very good | 19 (26.8) |
| Quite good | 14 (19.7) |
| Not very good | 2 (2.8) |
| Not applicable | 28 (39.4) |
| Total | 63 (88.7) |
| Missing | 8 (11.3) |
| Total | 71 (100.0) |
About how good this pharmacy is at listening and communicating with patients . . .
Q11. Is this pharmacy good at . . .
Keeping you informed about their opening hours?
| Response | n (%) |
|---|---|
| Very good | 41 (57.7) |
| Quite good | 25 (35.2) |
| No opinion | 4 (5.6) |
| Total | 70 (98.6) |
| Missing | 1 (1.4) |
| Total | 71 (100.0) |
Keeping you informed about their services?
| Response | n (%) |
|---|---|
| Very good | 35 (49.3) |
| Quite good | 29 (40.8) |
| No opinion | 6 (8.5) |
| Total | 70 (98.6) |
| Missing | 1 (1.4) |
| Total | 71 (100.0) |
Listening to patients’ complaints and suggestions?
| Response | n (%) |
|---|---|
| Very good | 38 (53.5) |
| Quite good | 9 (12.7) |
| Not at all good | 1 (1.4) |
| No opinion | 20 (28.2) |
| Total | 68 (95.8) |
| Missing | 3 (4.2) |
| Total | 71 (100.0) |
Overall, how do you feel about this pharmacy?
Q12. Thinking about your own lifestyle and personal circumstances, does this pharmacy provide a good service for people like you?
| Response | n (%) |
|---|---|
| Yes, completely | 59 (83.1) |
| Yes, to some extent | 10 (14.1) |
| Total | 69 (97.2) |
| Missing | 2 (2.8) |
| Total | 71 (100.0) |
Q13. Do you feel comfortable using this pharmacy?
| Response | n (%) |
|---|---|
| Very comfortable | 62 (87.3) |
| Quite comfortable | 6 (8.5) |
| Not very comfortable | 1 (1.4) |
| Total | 69 (97.2) |
| Missing | 2 (2.8) |
| Total | 71 (100.0) |
Discrimination between practices
| Question | Valuea | Significance (two-sided) |
|---|---|---|
| About arranging an appointment . . . | ||
| Q1. The last time you used the GP surgery, how easy was it for you to get in touch with them to make the appointment? | 0.769 | 0.857 |
| Q2a. The last time you used the GP surgery, what type of appointment did you want? | 3.848 | 0.278 |
| Q2b. Were you able to get the type of appointment you wanted? | 0.771 | 0.680 |
| Q3a. The last time you used the GP surgery, did you have any preferences about when the appointment was? | 2.156 | 0.340 |
| Q3b. Were you able to get an appointment at a time that was right for you? | 3.680 | 0.159 |
| Q4a. The last time you used the GP surgery, did you have any preferences about who the appointment was with? | 14.182 | 0.007 |
| Q4b. Were you able to get an appointment with the person you wanted? | 1.930 | 0.381 |
| Q5. Overall, did the GP surgery make it easy for you to arrange an appointment that suited you? | 2.970 | 0.396 |
| Q6. Did you have any of the following problems in arranging an appointment? (Please tick any that apply) | ||
| It was difficult to get through on the phone | 0.013 | 0.911 |
| I had to keep phoning back to get an appointment | 0.008 | 0.931 |
| There were no appointments available on the day/at the time I wanted | 7.263 | 0.007 |
| The wait for a non-urgent appointment was too long | 5.088 | 0.024 |
| The wait for an appointment with my preferred GP or nurse was too long | 10.055 | 0.002 |
| I wasn’t able to book in advance for the time I wanted | 1.607 | 0.205 |
| About how well reception staff treated you . . . | ||
| Q7. Did you feel that the reception staff . . . | ||
| Were friendly towards you? | 9.854 | 0.007 |
| Treated you with respect? | 3.736 | 0.154 |
| Tried their best to help you? | 6.776 | 0.034 |
| Q8. Overall, did you feel that the reception staff treated you well? | 5.544 | 0.063 |
| About how easy it was for you to visit the GP surgery . . . | ||
| Q9. How easy was it for you . . . | ||
| To get around the building? | 0.013 | 0.911 |
| Use the facilities at the surgery (e.g. toilets)? | 1.540 | 0.463 |
| Book in when you arrived? | 9.210 | 0.027 |
| Talk to receptionists without being overheard? | 12.204 | 0.016 |
| Know when it is your turn to be seen? | 4.496 | 0.213 |
| Q10. Could you wait in comfort? | 10.445 | 0.005 |
| Q11. Overall, how easy was it for you to use the GP surgery building and its facilities? | 3.648 | 0.302 |
| About how good this GP surgery is at helping to co-ordinate your care . . . | ||
| Q12. Is this GP surgery good at . . . | ||
| Helping you keep up to date with your health care (e.g. sending you reminders about upcoming appointments, making it easy to get repeat prescriptions)? | 1.600 | 0.809 |
| Organising your health care with hospitals (e.g. letting you know hospital test results, chasing the hospital when letters go missing)? | 0.277 | 0.998 |
| Helping you to get other health and community care services you need (e.g. family planning, counselling, social services)? | 0.966 | 0.809 |
| Q13. Overall, how good is this GP surgery at helping to co-ordinate your care? | 5.839 | 0.322 |
| About how good this GP surgery is at listening and communicating with patients . . . | ||
| Q14. Is this GP surgery good at . . . | ||
| Keeping you informed about their services? | 2.016 | 0.733 |
| Listening to patients’ complaints and suggestions? | 3.807 | 0.578 |
| Overall, how do you feel about this GP practice? | ||
| Q15. Thinking about your own lifestyle and personal circumstances, does this GP surgery provide a good service for people like you? | 1.350 | 0.509 |
| Q16. Do you feel comfortable using this GP surgery? | 2.319 | 0.509 |
Discrimination between pharmacies
| Question | Valuea | Significance (two-sided) |
|---|---|---|
| About your visit to the pharmacy . . . | ||
| Q1a. The last time you used the pharmacy, what did you want? | 1.417 | 0.841 |
| Q1b. Were you able to get what you wanted? | 1.056 | 0.304 |
| Q2. Were you happy with the speed of service? | 8.235 | 0.004 |
| Q3a. If you wanted to speak with someone, did you have any preferences about who spoke with? | 7.236 | 0.124 |
| Q3b. Were you able to speak with the person you wanted? | 4.928 | 0.177 |
| Q4. Overall, did the pharmacy make it easy for you to get what you wanted? | 20.687 | 0.000 |
| About how well pharmacy staff treated you . . . | ||
| Q5. The last time you used the pharmacy, did you feel that the staff . . . | ||
| Were friendly towards you? | 12.537 | 0.002 |
| Treated you with respect? | 8.092 | 0.017 |
| That the staff tried their best to help you? | 8.092 | 0.017 |
| Q6. Overall, did you feel that the staff treated you well? | 16.660 | 0.000 |
| About how easy it was for you to visit the pharmacy . . . | ||
| Q7. How easy was it for you to . . . | ||
| Get around the building? | 5.193 | 0.075 |
| Get the medicines, supplies or advice that you needed? | 7.312 | 0.007 |
| Find what you wanted on the shelves? | 4.791 | 0.188 |
| Talk to pharmacy staff without being overheard? | 12.124 | 0.016 |
| Know when it is your turn to be served? | 9.587 | 0.022 |
| Q8. Could you wait in comfort? | 0.882 | 0.830 |
| Q9. Overall, how easy was it for you to use the pharmacy building and its facilities? | 4.166 | 0.125 |
| About how good this pharmacy is at providing and signposting services . . . | ||
| Q10. Is this pharmacy good at . . . | ||
| Providing advice on your health problem(s)? | 2.425 | 0.489 |
| Providing advice on how to have a healthier lifestyle? | 5.923 | 0.205 |
| Disposing of medicines you no longer need? | 20.695 | 0.000 |
| Co-ordinating with the GP (e.g. ensuring that repeat prescriptions are ready for you, checking your prescriptions are correct)? | 12.360 | 0.006 |
| Fitting in with your life circumstances (e.g. offering home delivery of prescriptions)? | 6.622 | 0.157 |
| Helping patients get the best out of the service (e.g. offering advice such as how to save money on a prescription)? | 12.447 | 0.006 |
| Providing advice about relevant health services or information available elsewhere? | 3.959 | 0.266 |
| About how good this pharmacy is at listening and communicating with patients . . . | ||
| Q11. Is this pharmacy good at . . . | ||
| Keeping you informed about their opening hours? | 3.988 | 0.136 |
| Keeping you informed about their services? | 2.722 | 0.256 |
| Listening to patients’ complaints and suggestions? | 6.290 | 0.098 |
| Overall, how do you feel about this pharmacy? | ||
| Q12. Thinking about your own lifestyle and personal circumstances, does this pharmacy provide a good service for people like you? | 6.383 | 0.012 |
| Q13. Do you feel comfortable using this pharmacy? | 4.809 | 0.090 |
Appendix 13 General practitioner questionnaire, version 3; pharmacy questionnaire, version 2; walk-in centre questionnaire, version 1 (stage 3)
General practitioner questionnaire, version 3
Reproduced with permission from the University of Leicester.
General practitioner questionnaire, version 3 (PDF download)
Pharmacy questionnaire, version 2
Reproduced with permission from the University of Leicester.
Walk-in centre questionnaire, version 1 (stage 3)
Reproduced with permission from the University of Leicester.
Walk-in centre questionnaire, version 1 (stage 3) (PDF download)
Appendix 14 Data analysis: descriptive statistics (stage 3)
Distribution of responses, missing and incorrect responses (general practitioner surgeries)
| Questions | Responses, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Very easy | Quite easy | Not very easy | Not at all easy | Don’t know/not applicable | Incorrectly answered | Total | Missing | Total | |
| Q1. How easy is it for you to get in touch with the surgery to make an appointment? | 280 (44.4) | 234 (37.1) | 80 (12.7) | 27 (4.3) | 3 (0.5) | 2 (0.3) | 626 (99.4) | 4 (0.6) | 630 (100) |
| Q2. How easy is it for you to get an urgent appointment on the same day? | 122 (19.4) | 256 (40.6) | 136 (21.6) | 57 (9.0) | 51 (8.1) | 3 (0.5) | 625 (99.2) | 5 (0.8) | 630 (100) |
| Q3. How easy is it for you to book an appointment in advance, for a time that suits you? | 203 (32.2) | 221 (35.1) | 122 (19.4) | 52 (8.3) | 26 (4.1) | 2 (0.3) | 626 (99.4) | 4 (0.6) | 630 (100) |
| Q5. How easy is it for you to get to see a doctor or nurse of your own sex, when you want to? | 106 (16.8) | 246 (39.0) | 155 (24.6) | 66 (10.5) | 50 (7.9) | 2 (0.3) | 625 (99.2) | 5 (0.8) | 630 (100) |
| Q6. How easy is it for you to get to see a doctor or nurse who speaks your own language, or to arrange for an interpreter? | 233 (37.0) | 66 (10.5) | 14 (2.2) | 13 (2.1) | 289 (45.9) | 2 (0.3) | 617 (97.9) | 13 (2.1) | 630 (100) |
| Q7. How easy is it for you to get a home visit, when you want one? | 34 (5.4) | 48 (7.6) | 46 (7.3) | 60 (9.5) | 424 (67.3) | 1 (0.2) | 613 (97.3) | 17 (2.7) | 630 (100) |
| Q8. How easy is it for you to get a telephone consultation, when you want one? | 134 (21.3) | 171 (27.1) | 64 (10.2) | 32 (5.1) | 219 (34.8) | 2 (0.3) | 622 (98.7) | 8 (1.3) | 630 (100) |
| Q9. How easy is it for you to find out about the surgery’s opening hours and services? | 431 (68.4) | 150 (23.8) | 13 (2.1) | 29 (4.6) | 0 (0.0) | 1 (0.2) | 624 (99.0) | 6 (1.0) | 630 (100) |
| Questions | Responses, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes, very | Yes, to some extent | No, not very | No, not at all | No opinion | Incorrectly answered | Total | Missing | Total | |
| Q10. Are the reception staff friendly? | 401 (63.7) | 176 (27.9) | 30 (4.8) | 9 (1.4) | 7 (1.1) | 4 (0.6) | 627 (99.5) | 3 (0.5) | 630 (100) |
| Q11. Are the reception staff willing to try their best to help? | 402 (63.8) | 177 (28.1) | 30 (4.8) | 7 (1.1) | 6 (1.0) | 3 (0.5) | 625 (99.2) | 5 (0.8) | 630 (100) |
| Q12. Are the reception staff polite? | 426 (67.6) | 167 (26.5) | 19 (3.0) | 5 (0.8) | 5 (0.8) | 3 (0.5) | 625 (99.2) | 5 (0.8) | 630 (100) |
| Questions | Responses, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Very easy | Quite easy | Not very easy | Not at all easy | No opinion | Incorrectly answered | Total | Missing | Total | |
| Q13. How easy is it for you to travel to the surgery? | 394 (62.5) | 176 (27.9) | 43 (6.8) | 8 (1.3) | 5 (0.8) | 1 (0.2) | 627 (99.5) | 3 (0.5) | 630 (100) |
| Q14. How easy is it for you to get around the building? | 471 (74.8) | 129 (20.5) | 14 (2.2) | 2 (0.3) | 8 (1.3) | 2 (0.3) | 626 (99.4) | 4 (0.6) | 630 (100) |
| Q15. How easy is it for you to use the facilities at the surgery (e.g. the waiting area, toilets, baby changing room)? | 470 (74.6) | 115 (18.3) | 6 (1.0) | 3 (0.5) | 28 (4.4) | 1 (0.2) | 623 (98.9) | 7 (1.1) | 630 (100) |
| Q16. How easy is it for you to let staff know that you have arrived for your appointment? | 509 (80.8) | 104 (16.5) | 10 (1.6) | 1 (0.2) | 2 (0.3) | 1 (0.2) | 627 (99.5) | 3 (0.5) | 630 (100) |
| Q17. How easy is it for you to talk to receptionists without being overheard? | 136 (21.6) | 168 (26.7) | 205 (32.5) | 102 (16.2) | 13 (2.1) | 3 (0.5) | 627 (99.5) | 3 (0.5) | 630 (100) |
| Q18. How easy is it for you to know when it is your turn to be seen by the doctor or nurse? | 395 (62.7) | 176 (27.9) | 41 (6.5) | 7 (1.1) | 6 (1.0) | 2 (0.3) | 627 (99.5) | 3 (0.5) | 630 (100) |
| Questions | Responses, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Very good | Quite good | Not very good | Not at all good | No opinion/not applicable/don’t know | Incorrectly answered | Total | Missing | Total | |
| Q19. How good it this surgery at helping you to feel at ease while you are waiting? | 213 (33.8) | 275 (43.7) | 70 (11.1) | 11 (1.7) | 56 (8.9) | 1 (0.2) | 626 (99.4) | 4 (0.6) | 630 (100) |
| Q20. How good is this surgery at providing information in a form that you can understand (e.g. translated or Easy Read information leaflets)? | 249 (39.5) | 169 (26.8) | 23 (3.7) | 14 (2.2) | 168 (26.7) | 1 (0.2) | 624 (99.0) | 6 (1.0) | 630 (100) |
| Q21. How good is this surgery at helping you keep up-to-date with your health care (e.g. sending you reminders about appointments, letting you know what to do next)? | 242 (38.4) | 197 (31.3) | 85 (13.5) | 25 (4.0) | 68 (10.8) | 3 (0.5) | 620 (98.4) | 10 (1.6) | 630 (100) |
| Q22. How good it this surgery at making it easy for you to get repeat prescriptions? | 354 (56.2) | 174 (27.6) | 36 (5.7) | 6 (1.0) | 56 (8.9) | 1 (0.2) | 627 (99.5) | 3 (0.5) | 630 (100) |
| Q23. How good it this surgery at helping to organise your health care with hospitals (e.g. letting you test results, chasing hospital letters)? | 206 (32.7) | 211 (33.5) | 81 (12.9) | 21 (3.3) | 104 (16.5) | 3 (0.5) | 626 (99.4) | 4 (0.6) | 630 (100) |
| Q24. How good it this surgery at helping to get any other health or community services that you need (e.g. family planning, counselling, physiotherapy, social services, support for housing applications)? | 133 (21.1) | 133 (21.1) | 37 (5.9) | 17 (2.7) | 298 (47.3) | 2 (0.3) | 620 (98.4) | 10 (1.6) | 630 (100) |
| Question | Responses, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes, completely | Yes, to some extent | No, not really | No, not at all | No opinion | Incorrectly answered | Total | Missing | Total | |
| Q25. Thinking about your own needs and personal circumstances, do you feel that this surgery provides a service that suits you well? | 327 (51.9) | 226 (35.9) | 34 (5.4) | 16 (2.5) | 20 (3.2) | 4 (0.6) | 627 (99.5) | 3 (0.5) | 630 (100) |
| Questions | Responses, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Very good | Quite good | Not very good | Not at all good | Don’t know | Incorrectly answered | Total | Missing | Total | |
| Q26. How good it this surgery at encouraging patients to make suggestions about the surgery could do better (e.g. a suggestion box, website feedback form)? | 140 (22.2) | 171 (27.1) | 75 (11.9) | 27 (4.3) | 208 (33) | 2 (0.3) | 623 (98.9) | 7 (1.1) | 630 (100) |
| Q27. How good it this surgery at listening to patients’ complaints? | 112 (17.8) | 117 (18.6) | 48 (7.6) | 27 (4.3) | 313 (49.7) | 1 (0.2) | 618 (98.1) | 12 (1.9) | 630 (100) |
| Q28. How good it this surgery at acting on patients’ suggestions and complaints? | 75 (11.9) | 102 (16.2) | 40 (6.3) | 19 (3.0) | 382 (60.6) | 1 (0.2) | 619 (98.3) | 11 (1.7) | 630 (100) |
Distribution of responses, missing and incorrect responses (pharmacies)
| Questions | Responses, n (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Very easy | Quite easy | Not very easy | Not at all easy | Don’t know/not applicable | Total | Missing | Total | |
| Q1. How easy is it for you to collect a prescription? | 203 (82.5) | 32 (13.0) | 4 (1.6) | 0 (0.0) | 2 (0.8) | 241 (98.0) | 5 (2.0) | 246 (100) |
| Q2. How easy is it for you to get health-care advice? | 160 (65.0) | 66 (26.8) | 5 (2.0) | 1 (0.4) | 9 (3.7) | 241 (98.0) | 5 (2.0) | 246 (100) |
| Q3. How easy is it for you to get what you want without a long wait? | 131 (53.3) | 96 (39.0) | 10 (4.1) | 2 (0.8) | 2 (0.8) | 241 (98.0) | 5 (2.0) | 246 (100) |
| Q4. How easy is it for you to speak with a particular member of the pharmacy staff, when you want to? | 143 (58.1) | 80 (32.5) | 4 (1.6) | 0 (0.0) | 13 (5.3) | 240 (97.6) | 6 (2.4) | 246 (100) |
| Q5. How easy is it for you to get to speak with someone of your own sex, when you want to? | 134 (54.5) | 49 (19.9) | 16 (6.5) | 4 (1.6) | 38 (15.4) | 241 (98.0) | 5 (2.0) | 246 (100) |
| Q6. How easy is it for you to get to speak with someone who speaks your own language, or to arrange for an interpreter? | 118 (48.0) | 13 (5.3) | 4 (1.6) | 5 (2.0) | 100 (40.7) | 240 (97.6) | 6 (2.4) | 246 (100) |
| Q7. How easy is it for you to find out about the pharmacy’s opening hours and services? | 198 (80.5) | 32 (13.0) | 5 (2.0) | 0 (0.0) | 6 (2.4) | 241 (98.0) | 5 (2.0) | 246 (100) |
| Questions | Responses, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes, very | Yes, to some extent | No, not very | No, not at all | No opinion | Incorrectly answered | Total | Missing | Total | |
| Q8. Are the pharmacy staff friendly? | 228 (92.7) | 14 (5.7) | 1 (0.4) | 0 (0.0) | 0 (0.0) | 1 (0.4) | 244 (99.2) | 2 (0.8) | 246 (100) |
| Q9. Are the pharmacy staff willing to try their best to help? | 220 (89.4) | 19 (7.7) | 3 (1.2) | 1 (0.4) | 0 (0.0) | 0 (9.0) | 243 (98.8) | 3 (1.2) | 246 (100) |
| Q10. Are the pharmacy staff polite? | 222 (90.2) | 16 (6.5) | 2 (0.8) | 1 (0.4) | 1 (0.4) | 0 (0.0) | 242 (98.4) | 4 (1.6) | 246 (100) |
| Questions | Responses, n (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Very easy | Quite easy | Not very easy | Not at all easy | No opinion | Total | Missing | Total | |
| Q11. How easy is it for you to travel to the pharmacy? | 188 (76.4) | 46 (18.7) | 8 (3.3) | 0 (0.0) | 0 (0.0) | 242 (98.4) | 4 (1.6) | 246 (100) |
| Q12. How easy is it for you to get around the building? | 194 (78.9) | 41 (16.7) | 4 (1.6) | 0 (0) | 3 (1.2) | 242 (98.4) | 4 (1.6) | 246 (100) |
| Q13. How easy is it for you to find what you want on the shelves? | 131 (53.3) | 90 (36.6) | 12 (4.9) | 1 (0.4) | 9 (3.7) | 243 (98.8) | 3 (1.2) | 246 (100) |
| Q14. How easy is it for you to talk to pharmacy staff without being overheard? | 113 (45.9) | 70 (28.5) | 36 (14.6) | 7 (2.8) | 17 (6.9) | 243 (98.8) | 3 (1.2) | 246 (100) |
| Q15. How easy is it for you to know when it is your turn to be served? | 156 (63.4) | 72 (29.3) | 11 (4.5) | 3 (1.2) | 1 (0.4) | 243 (98.8) | 3 (1.2) | 246 (100) |
| Questions | Responses, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Very good | Quite good | Not very good | Not at all good | No opinion/not applicable | Incorrectly answered | Total | Missing | Total | |
| Q16. How good it this pharmacy at helping you to feel at ease while you are waiting? | 154 (62.6) | 67 (27.2) | 12 (4.9) | 1 (0.4) | 9 (3.7) | 0 (0.0) | 243 (98.8) | 3 (1.2) | 246 (100) |
| Q17. How good is this pharmacy at providing information in a form that you can understand (e.g. translated or Easy Read information leaflets)? | 138 (56.1) | 43 (17.5) | 8 (3.3) | 0 (0.0) | 52 (21.1) | 1 (0.4) | 242 (98.4) | 4 (1.6) | 246 (100) |
| Questions | Responses, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Very good | Quite good | Not very good | Not at all good | No opinion/not applicable/don’t know | Incorrectly answered | Total | Missing | Total | |
| Q18. How good is this pharmacy at working with the doctors’ surgery (e.g. making sure that repeat prescriptions are ready for you, checking that your prescriptions are correct)? | 165 (67.1) | 40 (16.3) | 6 (2.4) | 1 (0.4) | 30 (12.2) | 0 (0.0) | 242 (98.4) | 4 (1.6) | 246 (100) |
| Q19. How good is this pharmacy at offering home delivery of prescriptions, if you need it? | 114 (46.3) | 23 (9.3) | 1 (0.4) | 1 (0.4) | 103 (41.9) | 0 (0.0) | 242 (98.4) | 4 (1.6) | 246 (100) |
| Q20. How good it this pharmacy at letting you know about health or community services available elsewhere that might be helpful for you? | 88 (35.8) | 49 (19.9) | 10 (4.1) | 1 (0.4) | 93 (37.8) | 1 (0.4) | 242 (98.4) | 4 (1.6) | 246 (100) |
| Q21. How good is this pharmacy at disposing of medicine you no longer need? | 137 (55.7) | 21 (8.5) | 4 (1.6) | 1 (0.4) | 79 (32.1) | 0 (0.0) | 242 (98.4) | 4 (1.6) | 246 (100) |
| Question | Responses, n (%) | ||||||
|---|---|---|---|---|---|---|---|
| Yes, completely | Yes, to some extent | No, not really | No opinion | Total | Missing | Total | |
| Q22. Thinking about your own needs and personal circumstances, do you feel that this pharmacy provides a service that suits you well? | 206 (83.7) | 32 (13) | 1 (0.4) | 4 (1.6) | 243 (98.8) | 3 (1.2) | 246 (100) |
| Questions | Responses, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Very good | Quite good | Not very good | Not at all good | Don’t know | Incorrectly answered | Total | Missing | Total | |
| Q23. How good is this pharmacy at encouraging patients to make suggestions about the pharmacy could do better (e.g. a suggestion box, website feedback form)? | 73 (29.7) | 54 (22.0) | 10 (4.1) | 2 (0.8) | 104 (42.3) | 0 (0.0) | 243 (98.8) | 3 (1.2) | 263 (100) |
| Q24. How good it this pharmacy at listening to patients’ complaints? | 93 (37.8) | 35 (14.2) | 6 (2.4) | 2 (0.8) | 105 (42.7) | 1 (0.4) | 242 (98.4) | 4 (1.6) | 263 (100) |
| Q25. How good it this pharmacy at acting on patients’ suggestions and complaints? | 71 (28.9) | 25 (10.2) | 4 (1.6) | 2 (0.8) | 140 (56.9) | 0 (0.0) | 242 (98.4) | 4 (1.6) | 263 (100) |
Distribution of responses, missing and incorrect responses (walk-in centres)
| Questions | Responses, n (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Very easy | Quite easy | Not very easy | Not at all easy | Don’t know/not applicable | Total | Missing | Total | |
| Q1. How easy is it for you to get what you want without a long wait? | 107 (40.8) | 107 (40.7) | 25 (9.5) | 8 (3.0) | 11 (4.2) | 258 (98.1) | 5 (1.9) | 263 (100) |
| Q2. How easy is it for you to get to see a doctor or nurse of your own sex, when you want to? | 39 (14.8) | 50 (19.0) | 22 (8.4) | 6 (2.3) | 139 (52.9) | 256 (97.3) | 7 (2.7) | 263 (100) |
| Q3. How easy is it for you to get to see a doctor or nurse who speaks your own language, or to arrange for an interpreter? | 102 (38.8) | 19 (7.2) | 9 (3.4) | 7 (2.7) | 118 (44.9) | 255 (97.0) | 8 (3.0) | 263 (100) |
| Q4. How easy is it for you to find out about the walk-in centre’s opening hours and services? | 188 (71.5) | 54 (20.5) | 7 (2.7) | 2 (0.8) | 9 (3.4) | 260 (98.9) | 3 (1.1) | 263 (100) |
| Questions | Responses, n (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Yes, very | Yes, to some extent | No, not very | No, not at all | No opinion | Total | Missing | Total | |
| Q5. Are the reception staff friendly? | 210 (80.8) | 39 (14.8) | 9 (3.4) | 1 (0.4) | 1 (0.4) | 260 (98.9) | 3 (1.1) | 263 (100) |
| Q6. Are the reception staff willing to try their best to help? | 202 (76.8) | 44 (16.7) | 5 (1.9) | 1 (0.4) | 8 (3.0) | 260 (98.9) | 3 (1.1) | 263 (100) |
| Q7. Are the reception staff polite? | 209 (79.5) | 41 (15.6) | 8 (3.0) | 1 (0.4) | 0 (0.0) | 259 (98.5) | 4 (1.5) | 263 (100) |
| Questions | Responses, n (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Very easy | Quite easy | Not very easy | Not at all easy | No opinion | Total | Missing | Total | |
| Q8. How easy is it for you to travel to the walk-in centre? | 149 (57.1) | 90 (34.5) | 18 (6.9) | 4 (1.5) | 0 (0.0) | 261 (99.2) | 2 (0.8) | 263 (100) |
| Q9. How easy is it for you to get around the building? | 175 (66.5) | 64 (24.3) | 10 (3.8) | 13 (5.0) | 0 (0.0) | 261 (99.6) | 1 (0.4) | 263 (100) |
| Q10. How easy is it for you to use the facilities at the walk-in centre (e.g. the waiting area, toilets, baby changing room)? | 187 (71.1) | 42 (16.0) | 3 (1.1) | 1 (0.4) | 28 (10.7) | 261 (99.2) | 2 (0.8) | 263 (100) |
| Q11. How easy is it for you to talk to receptionists without being overheard? | 50 (19.0) | 94 (35.7) | 73 (27.8) | 32 (12.2) | 10 (3.8) | 259 (98.5) | 4 (1.5) | 263 (100) |
| Q12. How easy is it for you to know when it is your turn to be seen by the doctor or nurse? | 146 (55.5) | 67 (25.5) | 25 (9.5) | 10 (3.8) | 11 (4.2) | 259 (98.5) | 4 (1.5) | 263 (100) |
| Questions | Responses, n (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Very good | Quite good | Not very good | Not at all good | No opinion/not applicable | Total | Missing | Total | |
| Q13. How good it this walk-in centre at helping you to feel at ease while you are waiting? | 106 (40.3) | 108 (41.1) | 16 (6.1) | 7 (2.7) | 24 (9.1) | 261 (99.2) | 2 (0.8) | 263 (100) |
| Q14. How good is this walk-in centre at providing information in a form that you can understand (e.g. translated or Easy Read information leaflets)? | 103 (39.2) | 63 (24.0) | 8 (3) | 2 (0.8) | 84 (31.9) | 260 (98.9) | 3 (1.1) | 263 (100) |
| Q15. How good it this walk-in centre at letting you know about health or community services available elsewhere that might be helpful for you? | 63 (24.0) | 71 (27.0) | 18 (6.8) | 5 (1.9) | 102 (38.8) | 259 (98.5) | 4 (1.5) | 263 (100) |
| Question | Responses, n (%) | ||||||
|---|---|---|---|---|---|---|---|
| Yes, completely | Yes, to some extent | No, not really | No opinion | Total | Missing | Total | |
| Q16. Thinking about your own needs and personal circumstances, do you feel that this walk-in centre provides a service that suits you well? | 151 (57.4) | 91 (34.6) | 9 (3.4) | 7 (2.7) | 258 (98.1) | 5 (1.9) | 263 (100) |
| Questions | Responses, n (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Very good | Quite good | Not very good | Not at all good | Don’t know | Total | Missing | Total | |
| Q17. How good it this walk-in centre at encouraging patients to make suggestions about the walk-in centre could do better (e.g. a suggestion box, website feedback form)? | 66 (25.1) | 59 (22.4) | 16 (6.1) | 9 (3.4) | 107 (40.7) | 257 (97.7) | 6 (2.3) | 263 (100) |
| Q18. How good it this walk-in centre at listening to patients’ complaints? | 55 (20.9) | 45 (17.1) | 5 (1.9) | 4 (1.5) | 142 (54.0) | 251 (95.4) | 12 (4.6) | 263 (100) |
| Q19. How good it this walk-in centre at acting on patients’ suggestions and complaints? | 41 (15.6) | 31 (11.8) | 4 (1.5) | 1 (0.4) | 168 (63.9) | 245 (93.2) | 18 (6.8) | 263 (100) |
Appendix 15 Final versions of the questionnaires (general practitioner, pharmacy, walk-in centre)
General practitioner questionnaire, final version
Reproduced with permission from the University of Leicester.
General practitioner questionnaire, final version (PDF download)
Pharmacy questionnaire, final version
Reproduced with permission from the University of Leicester.
Walk-in centre questionnaire, final version
Reproduced with permission from the University of Leicester.
Appendix 16 Final versions of the Easy Read questionnaires (general practitioner, pharmacy, walk-in centre)
Easy read general practitioner questionnaire, final version
Reproduced with permission from the University of Leicester.
Easy read general practitioner questionnaire, final version (PDF download)
Easy read pharmacy questionnaire, final version
Reproduced with permission from the University of Leicester.
Easy read pharmacy questionnaire, final version (PDF download)
Easy read walk-in centre questionnaire, final version
Reproduced with permission from the University of Leicester.
Easy read walk-in centre questionnaire, final version (PDF download)
Appendix 17 Staff interviews topic guide on mapping populations
-
Can you tell me about what your role is here?
-
How long have you been here?
-
We are interested in how practices know about the different patient groups within their population. What information do you currently have about the diversity of your practice population? (e.g. age, ethnicity, deaf, visually impaired, learning difficulties, employment status or whether they are a commuter)
-
How do you collect this information?
-
How do you use this information?
-
How would you describe the successes of your method?
-
What methods do you use to map the needs of your practice population?
-
Are you aware of online resources like APHO and NHSiView? (Explanation if necessary)
-
[If yes] What is your opinion about their usefulness?
-
Do you think you could use them to help improve the service provided by your practice?
Patient data/patient-related data held by practices
-
Aside from the explicitly medical aspects, what other data do you currently have about your patients, like the different categories, i.e. sex?
-
At what point(s) is these data collected for each user? (Probe any non-clinical data they might have/more about the non-clinical they do have)
-
Currently, do you have a way of checking patient records that have one or more of the above elements missing?
-
How might you use the information already in your electronic patient records to map the diversity of your practice population?
-
[Direct to non-clinical staff]: Judging from visiting patients, are there any groups of patients who could be helped more? By this I mean can the practice improve the patient’s experience of using the practice in any way? And from any angle?
-
What are the barriers to the collection of information from patients? (Probe whether it is it too late to ask for info. Is it a poor data recording tool when patients register, that does not include easy questions that can help them in being more responsive? etc.)
-
If you had a stronger data set of these non-clinical characteristics, what would you like to do with it?
-
What are your views on mapping the diversity of your population?
-
What are you views on collecting more non-clinical data?
-
What do you think would work for you in identifying diversity in your practice population, i.e. knowing the different sets of people who use you practice?
-
How would it help you to do things differently?
-
How would it benefit the practice? (Probe money savings, time savings, etc.)
-
Would you like a mapping system in place? If yes, why?
Practice-specific questions
Not included here to protect the PCOs’ anonymity. They focus on particular aspects of the practices’ processes.
Explanation of NHS iView and Association of Public Health Observatories
NHS iView and the Association of Public Health Observatories feature publicly accessible online tools that display information about general practices nationwide. You simply enter your surgery’s code (or search for your practice’s name) and the information will be displayed in graphical and tabular forms. Currently, they display your practice’s QOF data, sociodemographic information of the patients at your practice, so age, gender, ethnicity, deprivation scores and additional results obtained from the GP survey.
List of abbreviations
- A&E
- accident and emergency
- ACG
- Adjusted Clinical Groups
- BME
- black and minority ethnic
- CCG
- Clinical Commissioning Group
- CHD
- coronary heart disease
- DES
- directed enhanced service
- DH
- Department of Health
- DIN
- Doctors’ Independent Network
- GP
- general practitioner
- GPRD
- General Practice Research Database
- HES
- Hospital Episode Statistics
- HINST
- Health Inequalities National Support Team
- HNA
- Health Needs Assessment
- ICC
- intraclass correlation coefficient
- IMD
- Index of Multiple Deprivation
- IT
- information technology
- JSNA
- Joint Strategy Needs Assessment
- LES
- local enhanced service
- NAPP
- National Association for Patient Participation
- NGPP
- National General Practice Profile
- PCO
- primary care organisation
- PCRN
- Primary Care Research Network
- PCT
- primary care trust
- PHO
- public health observatory
- PPG
- patient participation group
- PROM
- patient-reported outcome measure
- QOF
- Quality and Outcomes Framework
- RCGP
- Royal College of General Practitioners
- RM&G
- research management and governance
- THIN
- The Health Improvement Network
- WHO
- World Health Organization