Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 08/1809/255. The contractual start date was in December 2009. The final report began editorial review in July 2013 and was accepted for publication in February 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Paula Whitty has been employed as Director of Research, Innovation and Clinical Effectiveness at one of the research study’s mental health trust study sites since April 2011 (and by the trust’s predecessors as Consultant in Medical Care Epidemiology since 1998). David Hunter is an appointed governor of one of the acute foundation trust hospital study sites involved in this research project and was a member of the commissioning board for the National Institute for Health Research (NIHR) Service Delivery and Organisation programme between 2009 and 2012, and the NIHR Health Services and Delivery Research programme between 2012 and 2014. Jonathan Erskine was a non-executive director of one of the primary care trust study sites until October 2011. Martin Eccles received a salary one day a month as a senior mentor for the National Institute for Health and Care Excellence Fellows and Scholars programme.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Hunter et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Policy context and background
The North East Transformation System (NETS) was a unique experiment in the adoption of transformational change in a complex system, namely the NHS in North East England. If the initiative had been allowed to evolve and mature, it might have become a blueprint for other regions to copy. However, it was unexpectedly interrupted and required to take a different direction following the UK coalition government’s proposals to reorganise the NHS, announced in July 2010. 1 In this scene-setting introductory chapter, we locate the NETS in its broader policy context.
Launched in 2007, the NETS was both pioneering and novel in terms of its purpose and scope. However, it did not exist in isolation from other quality initiatives that also sought to improve service delivery and quality of care, while also reducing waste and variation. Government policy during this period was influenced by several factors. First was the election of a Labour government that sought to distance itself from its predecessor’s health-care reforms, which emphasised internal markets and competition as a mechanism to stimulate health service improvements. In addition, the appointment in 1999 of Liam Donaldson as Chief Medical Officer for England proved both timely and significant. Donaldson had been a major proponent of patient safety in his previous role as Regional General Manager of the former Northern and Yorkshire Regional Health Authority. He was also a principal architect of clinical governance arrangements. Clinical governance has been defined as ‘a framework through which NHS organisations are accountable for continuously improving the quality of their services and safeguarding high standards of care by creating an environment in which excellence in clinical care will flourish’. 2 Many of the concerns and concepts embraced by clinical governance were encompassed in the NETS.
The NETS therefore evolved and took root within a policy context that was sympathetic and receptive to its overall aims, purpose and approach. This introductory chapter sets out the key elements of the government’s focus on quality improvement (QI) which formed the broad policy context for, and background to, the NETS. Chapter 3 provides a brief history of the origins and evolution of the NETS, which formed the backdrop to the evaluation of its evolution and its impact over the period of the study.
A focus on quality and QI has been a central feature of NHS policy since 1997, although the interest in quality goes much further back. The Labour government, elected in May 1997, invested heavily in a range of initiatives intended to improve quality. In a White Paper published in 1997 (The New NHS: Modern, Dependable), it stated: ‘The new NHS will have quality at its heart . . . Every part of the NHS, and everyone who works in it, should take responsibility for working to improve quality’3 [© Crown copyright 1997, contains public sector information licensed under the Open Government Licence v2.0 (www.nationalarchives.gov.uk/doc/open-government-licence/version/2)].
The government expressed concern about the unacceptable variations in performance and practice. It sought to address the problem by putting quality at the top of the NHS agenda. The objective was to align local clinical judgements with clear national standards that incorporated best practice. This was described in detail in an important consultation document published by the Department of Health in 1998, A First Class Service: Quality in the new NHS. 4 The plan was for national standards to be set through national service frameworks and through the establishment of a new body, the National Institute for Clinical Excellence (NICE) (in April 2013 this became the National Institute for Health and Care Excellence).
At local level, standards were to be delivered by a clinical governance system that was informed by the latest evidence and guidance on what worked best for patients. The approach was also supported by lifelong learning for staff and modernised professional self-regulation. Clinical governance is the process by which each part of the NHS assures its quality and ensures that clinical decisions are aligned with its principles. The intention was to introduce a system of continuous improvement into the operations of the whole NHS. Quality was to be everybody’s business and was based upon partnerships within health-care teams comprising health professionals and managers. The new emphasis on quality was to be established at all levels of the NHS. It was stressed that the drive to place quality uppermost on the NHS agenda was concerned with changing thinking, rather than merely ticking checklists.
Central to the government’s focus on quality was the clinical governance framework which included a comprehensive programme of QI activity and processes for monitoring clinical care. Developing a structured and coherent approach to clinical quality was central to the whole endeavour. This included an emphasis on attracting, developing, motivating and retaining high-calibre health-care professionals, managers and staff. Continuing professional development was viewed as central to continuous QI, which was termed ‘action for quality’. The 10-year strategy acknowledged that the issues were complex and could not be tackled overnight. The vision for quality aimed to create a NHS culture that encouraged innovation and success, and one that fostered a learning culture which made good use of best practice exemplars. This was seen as the bedrock of continuous improvement, as well as a focus on partnership working rather than competiton. 4
The drive to improve quality was considered to involve major cultural change for all. Part of supporting such a change in culture entails developing organisations to deliver change. 4 The crucial elements to achieve success were excellent leadership and the involvement of staff. These were important because, in some QI work, there has tended to be a separate focus on either clinically led improvement or improvement led from a management perspective. The result was discrete, parallel activities within organisations with misaligned objectives, duplication of effort and a lack of focus. 5 The challenge for health-care organisations is to improve both clinical and managerial quality, as in practice they interact – or should do. The government acknowledged this in 1998. When the NETS was conceived nearly 10 years later, it was similarly informed by such an approach.
Many of the ideas set out in the government’s 1998 consultation document were lost in the subsequent series of NHS reforms that started with the NHS Plan in 2000. 6 Further waves of structural and other changes to various NHS organisations proved both disruptive and distracting. Quality and patient safety only came back into vogue as a result of two particular developments. First, the period of increased investment in the NHS came to an end in 2007 owing to the global economic slowdown and the subsequent collapse of the banking system. Attention therefore focused on using resources more efficiently and effectively. The Quality Innovation Productivity and Prevention (QIPP) initiative was introduced specifically with this aim in mind. It was intended to avoid a retrenchment response to spending pressures through adopting a more intelligent approach to commissioning decisions that avoided putting quality at risk. Initiatives like the NETS were seen by some NHS leaders at the Department of Health as being especially important for the whole NHS, and were being looked to as pioneers providing lessons for the rest of the system. This was because they offered the potential to improve services without sacrificing staff or losing any of the gains resulting from previous additional investment stemming from the Wanless report. 7 The second factor which reinstated QI as a central objective of government policy was Lord Darzi’s next stage review of the NHS. 8 Commissioned by the then prime minister, QI was given particular prominence by Darzi, an eminent cardiac surgeon. In his view, one of the ‘core elements’ of leadership was a focus on continuous improvement. Aligning clinical and managerial approaches to quality was seen as critical.
A review of QI in health care published in 2008 concluded that having an improvement method is important to achieve outcomes, but the particular method adopted is not important. 9 Failures are usually due to intractable problems in relationships or leadership rather than in the tools or methods adopted. These conclusions are supported by our research. The architects of the NETS approach saw it as a transformational change initiative that sought to achieve a change in overall culture. It specifically addressed the issues of leadership and relationships through the Vision and Compact. The evidence demonstrates that it is important for leaders to adopt and commit to whichever tool or method is chosen ‘for as long as it takes to deliver the results for patients’8 (Our NHS Our Future: NHS Next Stage Review – Leading Local Change, © Crown copyright 2008). Øvretveit provided evidence that leadership is associated with, and influences, successful improvement and is a factor contributing to slow, partial or failed improvement. 10 However, the highly contextual nature of change makes generalisation difficult.
The early development of the NETS initiative was informed by these findings, although how far this was explicit or implicit is unclear. The origins of the NETS are described in Chapter 3, drawing on a scoping review conducted in 2008 which formed the basis for the main study. 11 Before doing so, however, we set out why the NETS was important, its particular features which set it apart from other QI initiatives, and our research aims and objectives.
The generalisation of results is an important, if often contested, issue in research that investigates complex adaptive systems of the type to be found in the NHS. 12 Walshe13 commented that with QI research
the aim is not to find out ‘whether it works’, as the answer to that question is almost always ‘yes, sometimes’. The purpose is to establish when, how and why the intervention works and to unpick the complex relationship between context, content, application and outcomes.
Having undertaken these tasks, the issue remains one of how far it is reasonable to offer generalisable findings, as the precise combination of factors making for success may be particular to that setting and not possible to replicate elsewhere. On the other hand, it is likely that the presence of some features will serve as generic drivers of change which can be usefully highlighted and disseminated more widely. Of course, how they are then applied in practice in varying settings will determine their precise configuration and impact. The Health Foundation’s work on spreading improvement demonstrates that with the right learning and support systems, the NHS has the potential to spread good practice across the system to the universal benefit of staff and patients. However, realising this potential is far from straightforward. 14
The North East Transformation System: key features, research aims and objectives
The NETS is of national and international importance because NHS North East (NHS NE), until its demise in March 2013, was the first Strategic Health Authority (SHA) to adopt a region-wide strategy that aimed to transform an entire health-care system. The initiative was bold and ambitious because the SHA served a population of 2.4 million people and the NHS in the region employed 77,000 staff. Up until that time, the implementation of lean and similar tools and methods in the NHS had involved relatively small-scale interventions confined to particular hospital departments and support services. 15 However, NHS NE was committed to addressing more complex system-wide issues, including addressing transformational change, culture and the relationship between clinicians and managers. Many aspects of the NETS were aligned with Darzi’s NHS next stage review conclusions about how best to ensure service redesign. 16
The NETS started with seven pathfinders that represented a wide range of NHS organisations, including the SHA, primary care trusts (PCTs), acute trusts and mental health trusts. These pathfinders constituted wave 1 of the NETS initiative. Subsequent waves included other NHS NE organisations that were programmed to undertake NETS training at regular intervals of around 12 months. The NETS took much of its inspiration and guidance from the Virginia Mason Production System (VMPS) whose lean method was derived from the Toyota Production System (TPS).
Although NHS NE was committed to supporting a full evaluation of the NETS, it was anxious to capture the learning from its early experiences. To this end, a 6-month scoping study of the background and initial steps was commissioned from Durham and Newcastle Universities. 11 The scoping study took place between January and July 2008 and investigated the NETS, its aims and objectives and the initial developments that had occurred in the seven first-wave pathfinder organisations. It prepared the ground for the main study, whose aims and objectives are described below.
Research aims and objectives
This research has:
-
Produced a literature review that focused upon change management in health systems; the adoption of TPS/lean in health-care organisations; and learning from lean in manufacturing. This builds on the literature review undertaken for the scoping study. 11
-
Evaluated the impact of the NETS (comprising Vision, Compact, Method) and its evolution over time, including the impact on NHS organisational and clinical cultures (including staff engagement and empowerment); the quality and efficiency of health care in respect of technical quality, safety, patient experience, access and equity; reduced waiting times and waste; and reduced variation across specialties, departments and hospitals.
-
Identified the factors facilitating (or acting as barriers to) successful change, including an evaluation of rapid process improvement workshops (RPIWs).
-
Evaluated the role of the NETS project team in co-ordinating progress and supporting the transfer of learning, including the mechanisms used for identifying and disseminating best practice.
-
Investigated the extent to which the changes introduced through the NETS (and through other means in the case of non-NETS study sites) have become embedded and sustained.
-
Assessed the impact of the NETS on service users, for example patients or carers and/or family and friends.
Conducting the North East Transformation System study
The NETS research team was drawn from Durham and Newcastle Universities. Members of the team included health professionals, and academics who were specialists in health policy, human resource management, operations management, strategy and statistics. Project management was provided by one of the co-investigators (Erskine) who was located with the principal investigator (PI) at Durham University. Part of this important role was to organise and support team meetings. These occurred frequently and rotated between Durham’s Queen’s Campus on Teesside and Newcastle University Business School. In addition, and apart from regular e-mails and telephone calls, the team set up a password-protected virtual research environment on a secure server for sharing key documents and managing communications. Second, an external advisory group (EAG) was established to guide and support the study throughout its duration. Membership of the group and its terms of reference are provided in Appendix 1. Between them, EAG members possessed a wealth of experience of managing and researching health-care services and of improvement science methods. The EAG met approximately every 6 months and members provided useful guidance and advice on various aspects of the study during its data gathering and writing-up stages.
The third feature to note was that the study was allocated a Management Fellowship. The Management Fellowship scheme was established by the former Service Delivery and Organisation (SDO) programme to address concerns about translating research into practice. A part-time management fellow (MF) was seconded from the NHS and commenced work in April 2010. A report on her activities, and the way the role evolved during the course of the study, is included in Appendix 2.
Chapter 2 Literature review
A literature review was undertaken for the scoping study. This involved searching a wide body of published work that included professional and managerial tribalism in health systems, organisational culture, leadership styles and the evolution of lean thinking in manufacturing, public services and the NHS. 11
The review of literature on professional–managerial relations, organisational culture, leadership styles and complex adaptive systems is only briefly reported here. The review focuses on the evolution of lean and its application to the NHS and how this can relate to the NETS. The section Lean in health care has been updated to reflect how this particular area has developed since the original scoping study was produced.
Management–profession interface
The tension between managerial and professional values is well documented in the literature and underpins the rationale for a Compact. A BMJ editorial in 2001 posed the question: why are doctors unhappy?17 It suggested that the causes were multiple, although one in particular was highlighted: ‘the mismatch between what doctors were trained for and what they are required to do’. 17 Trained in some specialty or field of medicine, ‘doctors find themselves spending more time thinking about issues like management, improvement, finance, law, ethics, and communication’. 17 In an article in the BMJ the following year, Edwards et al. suggested that the cause of doctors’ unhappiness ‘is a breakdown in the implicit compact between doctors and society: the individual orientation that doctors were trained for does not fit with the demands of current healthcare systems’. 18 They described the old compact and why it is no longer regarded as legitimate, and outlined what a new compact might look like. The old compact comprised two aspects: what doctors give and what they get in return (see lists below). The mismatch between these has been the cause of dissonance over what doctors might have reasonably expected the job to be and how it now is. Some commentators have suggested that the psychological contract – or compact – is a useful concept to explain this problem. 18–20
What doctors give:
-
sacrifice early earnings and study hard
-
see patients
-
provide ‘good’ care as the doctor defines it.
What doctors get in return:
-
reasonable remuneration
-
reasonable work/life balance later
-
autonomy
-
job security
-
deference and respect.
A new and more sustainable Compact is required because the old promise to doctors is either no longer valid or can act as a barrier to modernisation. Among the new imperatives to be addressed in a revised Compact are the following:18
-
greater accountability (e.g. guidelines)
-
patient-centred care
-
becoming more available to patients, providing a personalised service
-
working collectively with other doctors and staff to improve quality
-
evaluation by non-technical criteria and patients’ perceptions
-
a growing blame culture.
Edwards et al. asserted that it was not possible to return to the old compact and that clinical leaders and managers must create ‘a new compact that improves care for patients, improves the effectiveness of the healthcare organisation, and helps create a happier workforce’. 18 The following year, once again in the BMJ, Davies and Harrison returned to the theme of the discontented doctor and argued that a principal reason for the dissatisfaction doctors experienced was their relationship with managers. 21 This manifests itself in a perceived sense of diminished autonomy and reduced dominance. The authors argued for ‘better alignment between doctors and the organisations in which they provide services’ while noting that the extent of ‘cultural divergence between managers, doctors, and other professional groups suggests that such a realignment will be far from easy’. 21 They concluded by insisting that there is no practicable alternative to doctors engaging with management. Yet, despite such calls, the unease felt by many doctors and their lack of being valued has persisted. 22 This was a major reason for inviting a surgeon, Ari Darzi, to lead the next stage review of the NHS, which had clinicians and other front-line staff at the heart of the change process – change that is ‘locally-led, patient-centred and clinically driven’16 (High Quality Care For All: NHS Next Stage Review Final Report, © Crown copyright 2008).
For their part, managers are also unhappy with their lot. They can appear beleaguered functionaries in a system that is more politicised than ever and whose political heads regard themselves as its leaders. 23 A major exponent of lean in the UK, Seddon, considered that distortions in the health system ensure that the patient is not put first. 24 The result is an elaborate set of managerial ploys which are, in effect, forms of cheating or gaming to arrive at the results desired by their political masters. But it is a further contributor to the unhappiness felt on both sides of the management–medicine divide.
The awkward and often dysfunctional relationship between managers and professions is far from being a new phenomenon. In their study of hospital organisation in 1973, Rowbottom et al. 25 noted that
the position of doctors . . . presents a fascinating, and possibly unique, situation to any student of organisation. Never have so many highly influential figures been found in such an equivocal position – neither wholly of, nor wholly divorced from, the organisation which they effectively dominate.
The work of Degeling et al. 26,27 demonstrated the importance of getting professionals and managers to:
-
recognise interconnections between the clinical and financial dimensions of care
-
participate in processes that will increase the systematisation and integration of clinical work and bring it within the ambit of work process control
-
accept the multidisciplinary and team-based nature of clinical service provision and accept the need to establish structures and practices capable of supporting this
-
adopt a perspective which balances clinical autonomy with transparent accountability. 27,28
The findings from Degeling’s work pointed to significant profession-based differences on each of the four elements of the reform agenda. 26–28 They also demonstrated the barriers that face those seeking to introduce changes in the delivery of health care. For those changes to happen there needs to be a common sense of purpose and a set of core values shared by the key stakeholders. These prior conditions do not exist. Degeling’s work showed that all attempts to impose managerial controls on clinical work are doomed to failure unless a different approach to managing change and engaging with clinicians and other health-care staff is adopted. 26,27
Organisational culture and leadership styles in health care
Culture is something of a weasel word that may simply be empty rhetoric. It is often invoked too readily and simplistically in a health-care context, the belief being that if culture change can occur then issues of organisational performance will be resolved. Despite this, culture does matter. Many commentators such as Schein29 and Mannion et al. 28 have emphasised the importance of culture in shaping organisational behaviour and hence achieving improved performance. However, change can be stifled by culture. As Mannion et al. stated, culture constitutes the informal social aspects of an organisation that influence how people think, what they regard as important, and how they behave and interact at work. 28 Organisational culture has been defined by Schein29 as:
the pattern of shared basic assumptions – invented, discovered or developed by a given group as it learns to cope with its problems of external adaptation and internal integration – that has worked well enough to be considered valid and, therefore, to be taught to new members as the correct way to perceive, think, and feel in relation to those problems.
Culture is therefore not merely that which is observable in social life but also the shared cognitive and symbolic context within which a society or institution can be understood. 28 But Mannion et al. 28 resisted the temptation of searching for a ‘magic bullet or simple cultural prescription for the ills of the NHS’ (pp. 214–15). In their view, ‘what works’ is contingent upon context ‘and on how and by whom efforts targeted at culture reform are evaluated and assessed’ (pp. 214–15). They counselled against the adoption of a ‘one size fits all’ approach to culture management in the NHS and ‘encourage[d] the adoption of more nuanced strategies which seek to deploy a judicious mix of instruments and supporting tactics depending on setting and application’ (pp. 214–15). One of the principal components of effective culture management relates to leadership styles. 30 Much has been written about leadership and hundreds of definitions offered but, as Goodwin observed, ‘it is principally local context that largely determines the leadership approach to be adopted, meaning local challenges, the history and relative strength of local relationships, local resource issues and local ways of doing things’ (p. 330). 31
Some writers on leadership subscribe to a trait or competency approach, i.e. one size fits all, which ignores context. The NHS competency framework is an example of this. Competencies have been criticised for being overly reductionist, overly universalistic or generic, focusing on past or current performance, focusing on measurable behaviours and outcomes, and resulting in a limited and mechanistic approach to development. 32 Critics also believe that ‘such frameworks reinforce the underlying assumption that leadership resides in the individual’ (pp. 32–3). 33 They are regarded as too generic and ignore ‘the context of a situation and the complexity of running very challenging and diverse workplaces’ (pp. 32–3). As Western argued, ‘the experience on the ground may be that there is little room for seizing the future and empowering others when the context feels disempowering due to a production-line atmosphere where success is measured against meeting targets and deadlines’ (pp. 32–3). 33 Situational leadership is therefore regarded as more appropriate in the context of complex adaptive systems.
In their study of the impact of leadership on successful change in the NHS, Alban-Metcalfe and Alimo-Metcalfe found that competencies did not predict effectiveness but that ‘engaging’ leadership styles significantly predicted motivation, satisfaction, commitment, reduced stress and emotional exhaustion, and team effectiveness/productivity. 34 For them, leadership was viewed as a shared or distributed process and one that was embedded in the culture.
Like other writers on leadership, Goodwin30,31 also noted that leadership is not a characteristic of one person but rather is a process ‘played out between leaders and followers, without whom leadership cannot exist’ (p. 330). 31 Not all commentators believe that leadership and management are entirely separate entities, but those who do consider that leaders are different from managers because they view people from an emotional perspective, seeing them as individuals. 33 But managers can demonstrate leadership and a leader can have managerial skills. Bennis defined leaders as those who ‘master the context’ whereas managers ‘surrender to it’ (p. 45). 35 Leadership is about passion, vision, inspiration, creativity and co-operation, rather than control, which is the hallmark of management. 33 A variant on this view is that a leader creates change whereas a manager creates stability. Running through all these definitions is the derogatory assumption that management is the ‘other’ to leadership; a view of the manager as an outdated mechanistic functionalist. Leadership is very clearly in vogue and ‘sexy’; whereas managers are regarded as transactional in their approach, leaders are seen as transformational.
In keeping with this view of leadership as being about emotions and meaning rather than control, Goodwin claimed that leadership is a dynamic, relationship-based process that uses a twofold approach:
-
creating an agenda for change using a strong vision; and
-
building a strong implementation network to get things done through other people. 30
In their Leadership for Health Improvement framework, Hannaway et al. 36 applied improvement science thinking, which borrowed many of its ideas and principles from lean. The approach has been applied in the NHS as a result of the work of the former NHS Modernisation Agency and its successor, the NHS Institute for Innovation and Improvement, which has been superseded by the NHS Leadership Academy. The 10 High Impact Changes for Service Improvement Delivery includes the optimisation of flow and the reduction of bottlenecks, the application of systematic approaches, improved access and role redesign. 37
Complexity and health
It is generally accepted that leading and managing a health system is a complex business where there are few certainties and where ambiguity and paradox are often present. These need to be managed rather than denied or obscured by an inappropriate managerial model. Failure in public policy and public services occurs, according to Chapman, because ‘assumptions of separability, linearity, simple causation and predictability are no longer valid’ (p. 65). 38 Under such conditions of growing complexity, it is essential that those responsible for managing and governing take on a wider, more holistic perspective, ‘one that includes complexity, uncertainty and ambiguity’ (p. 65). 38 Systems thinking marks a shift away from regarding the entities being managed as if they were linear, mechanical systems. As Plsek (Paul E. Plsek & Associates, Inc., 2003) commented in materials distributed at a Leadership for Health Improvement workshop held in York in 2006, ‘existing principles of management and leadership are based on old metaphors that fail to describe adequately or accurately complex situations’ (© 2003 Paul E. Plsek & Associates, Inc.; reproduced with permission from Plsek P. An Organisation is not a Machine! Principles for Managing Complex Adaptive Systems. Materials prepared for Leadership for Health Improvement programme. York: Unpublished; 2006). In a complex system, the complex adaptive manager and/or leader:
-
manages context and relationships
-
creates conditions that favour emergence and self-organisation
-
lets go of ‘figuring it all out’
-
relies on ‘good enough’ analysis of the problem and its solution
-
requires minimum specifications to act rather than prescribing actions in advance.
Plsek, in the workshop materials referred to above, defined a complex adaptive system as ‘[a] collection of individual agents with freedom to act in ways that are not always totally predictable, and whose actions are interconnected so that one agent’s actions changes the context for other agents’ (© 2003 Paul E. Plsek & Associates, Inc.; reproduced with permission from Plsek P. An Organisation is not a Machine! Principles for Managing Complex Adaptive Systems. Materials prepared for Leadership for Health Improvement programme. York: Unpublished; 2006).
The remainder of the literature review presented below focuses on lean thinking and tools, as these have been central to the NETS initiative and, in particular, in demonstrating that successful change is possible and motivational for staff. The sections The evolution of lean, Fordism and Toyota Production System focus on the origins and evolution of lean in the manufacturing sector, including its impact in the North East region of England. Lean in the UK examines the recent take-up of lean thinking in the UK NHS as well as the public services sector more widely.
The evolution of lean
Lean production evolved from established production management approaches. These include the concept of interchangeable parts devised by Eli Whitney, scientific management developed by Taylor, Henry Ford’s mass production and the TPS. 39–41
Taylor found that in craft systems, skills and knowledge were transferred through the apprentice model. 39 Braverman considered that management was buying knowledge which was the workers’ capital. 42 There were variations in the volume and quality of work performed by different individuals as they had different ways of performing tasks. Taylor used the term ‘soldiering’ to describe workers who deliberately did work slowly. 40 He noted that there was conflict between management and workers fighting over the control of work and pay. There was a lack of standardised working methods and training. The end result was that there was waste, which was to the detriment of both the workforce and management. 43
The scientific management movement was very influential in the development of modern institutions which carry out labour processes. 42 Taylor stated that: ‘the principal object of management should be to secure the maximum prosperity for the employer, coupled with the maximum prosperity for each employee’ (p. 9). 39 Taylor believed that this required each individual to maximise efficiency by producing the greatest possible daily output.
Taylorism is based upon four principles:
-
It is necessary to systematically analyse work through time and motion studies to develop standardised methods.
-
Organisations should train employees in best practice approaches rather than leaving them to train themselves.
-
Workers should be provided with detailed instructions that prescribe how to undertake standardised tasks.
-
There should be a separation between ‘planning’, undertaken by managers using scientific management principles, and ‘doing’, performed by workers. 44,45
The core elements of Taylorism are (1) that operations should be standardised and optimised scientifically using time and motion studies and (2) the division of labour between managers and workers. 46 Taylor highlighted the importance of training as a mechanism for ensuring that individuals were able to work at maximum efficiency. 39
Taylorism has several limitations. 45 It creates non-value-adding supervisors and other indirect workers, which increases costs. Flexibility is reduced by the reliance on semiskilled workers and high levels of demarcation. However, new workers can be integrated quickly into the production process, which increases numerical flexibility. It becomes unattractive to work on the shop floor. Taylorism is widely considered to be anti-worker. 42
Fordism
Ford developed mass production at the Highland Park plant in 1913. His approach incorporated many aspects of Taylorism. He automated the production of standard parts using repetitive processes and introduced a continuously moving assembly line. 40 The pace of work and the volume of production were determined by the line speed. The combination of Taylorist approaches and assembly lines, together with a rigorously controlled and well-paid workforce, became known as ‘Fordism’,43 which achieved economies of scale through the division of labour. The objective was to minimise the unit cost through high-volume manufacturing. Production workers were not responsible for quality; there were specialist inspectors and repair staff. There was also a strict separation between the planning and execution of work, and a high division of labour. 46
Toyota Production System
The TPS was developed by Taiichi Ohno. 41 He identified several barriers to implementing mass production approaches in Japan. After the Second World War there was limited domestic demand. Furthermore, customers required a large variety of vehicles, so there was a requirement for low volume and high variety. Workers were reluctant to work in a system that considered them to be a variable cost, owing to legislation that strengthened workers’ rights during the period of American occupation. Japanese companies were starved of capital and foreign exchange; therefore, companies were unable to purchase expensive Western equipment. There was intense competition from overseas manufacturers that were keen to enter the Japanese market while defending their established markets. 47 Toyota could not afford to fund the working capital required to maintain the buffers that would be needed to maintain the high utilisation of production lines that were subject to line imbalances, quality problems and other sources of variability. Toyota therefore developed an alternative solution, which was to operate with minimum inventory while simultaneously maintaining high resource utilization. 48 The TPS is based upon two concepts. First, costs are reduced through the elimination of all forms of waste (those things that do not add value to the product). Second, there is a need to fully utilise workers’ capabilities. 49
The TPS may be viewed as a set of tools for reducing waste or as the set of principles that led to the development of the tools. 50 Liker51 identified 14 principles associated with four themes: (1) long-term philosophy; (2) the right process will produce the right results; (3) add value to the organisation by developing people; and (4) continuously solving route problems drives organisational learning.
Lean in the UK
In the 1980s and 90s inward investment by Japanese automotive companies exposed the uncompetitiveness of many UK automotive components suppliers. 52,53 The Society of Motor Manufacturers and Traders collaborated with the Department of Trade and Industry to form the Industry Forum in 1996. 54,55 This initiative was supported by major automotive companies. They seconded staff with expertise in improving manufacturing processes, who became ‘master engineers’. 56,57 Their role was to train UK engineers in the use of ‘best practice’ manufacturing tools and techniques in order to increase the competitiveness of the UK suppliers. The Industry Forum developed training programmes that used a ‘Common Approach Toolkit’. The ‘building blocks’ included clear out, configure, clean and check, conformity, custom and practice (5C)/sorting, set in order, systematic cleaning, standardising and sustaining (5S),58 the seven wastes,59 standardised work and visual management. The workshops also included training in data analysis, problem solving, set-up improvement and line balance. 56 Skills, knowledge and delivery techniques were disseminated through ‘Master Classes’,60,61 which included training and practical, shop floor-based process improvement activities. The aim of the Master Class is to introduce staff to best practice approaches and to improve performance in terms of quality, cost and delivery. 56
The superior performance of Japanese exemplars encouraged the dissemination of lean principles and tools to other contexts, including service industries and health care. However, Western organisations have often been able to adopt specific lean tools but have found it difficult to change the organisational culture and mindset. The impact of lean interventions is often localised. Organisations often fail to achieve the desired improvements to the overall system. 62
Lean philosophy and strategies
The TPS was developed in Japan by Ohno and Shingo and forms the basis of lean manufacturing. 63 Vollmann et al. 64 considered the goal of lean to be zero inventories, zero defects, zero disturbances, zero set-up time, zero lead time, zero transactions and routine operations that operate consistently day to day. Transactions consist of (1) logistical transactions (ordering, execution and confirmation of material movement); (2) balancing transactions, associated with planning that generates logistical transactions (production control, purchasing, scheduling); (3) quality transactions (specification and certification); and (4) change transactions (engineering changes, etc.).
In lean manufacturing, waste may be viewed as any activity that creates cost without producing value. 65,66 Ohno outlined seven forms of waste:67
-
Overproduction, i.e. making too many items or making items before they are required. The result is extended lead times and increased inventory, which incurs carrying costs.
-
The waste of waiting, i.e. time when materials or components are not having value added to them.
-
The waste of transportation, i.e. the movement of materials within the factory, which adds cost but not value.
-
The waste of inappropriate processing describes the use of a large, expensive machine instead of several small ones leads to pressure to run the machine as much as possible rather than only when needed.
-
The waste of unnecessary inventory, which increases lead times, reduces flexibility and makes it difficult to identify problems. This form of waste increases carrying costs and may cause waste through obsolescence.
-
The waste of unnecessary motions relates to ergonomics. If operators become physically tired it is likely to lead to quality and productivity problems.
-
The cost of defects is caused by internal failures within the factory, including scrap, rework and delay, as well as external failures that occur outside the manufacturing system (repairs, warranty cost and lost custom).
Bicheno59 identified additional ‘new’ wastes: untapped human potential; inappropriate systems that add cost without adding value; wasted energy and water; wasted materials; wasted customer time; and the waste of defecting customers – it may cost many more times to acquire a customer than it does to retain one.
Lean comprises a philosophy, a way of thinking that focuses upon value. Often this is considered in terms of cost reduction:62
This migration from a mere waste reduction focus to a customer value focus opens essentially a second avenue of value creation . . . Value is created if internal waste is reduced, as the wasteful activities and the associated costs are reduced, increasing the overall value proposition for the customer . . .
The other main emphasis is on continuous improvement that is usually based upon teamwork undertaken by empowered employees.
Lean initiatives in the North East of England
In 2000, the level of productivity (measured in terms of gross value added, i.e. the value of outputs minus the value of inputs) in the North East was 25% lower than the national average. 68 This situation had made the support of manufacturing companies a major policy objective of One North East (ONE), the regional development agency (RDA) (RDAs were abolished in 2012 as part of the government’s deficit reduction programme). In 2002, ONE funded the North East Productivity Alliance (NEPA), which aimed to improve the productivity of regional companies by training employees in lean tools using the Master Class approach.
The NEPA Master Classes selectively trained employees in the following tools: (1) 5S/5C; (2) standard operations; (3) skill control; (4) Kaizen; (5) visual management; (6) process flow; (7) problem solving; (8) Single-Minute Exchange of Dies (SMED); (9) production-led maintenance; (10) work measurement; (11) failure mode effect analysis; (12) poka-yoke (mistake-proofing); (13) value stream mapping (VSM); and (14) advanced problem solving. 69
The NEPA approach was further developed in 2008 through the European Regions for Innovative Productivity (ERIP) project. Research led by Newcastle University developed an improved lean implementation approach for small business that aimed to standardise processes and reduce costs while improving quality and delivery performance. 70 This approach was applied in 25 small- and medium-sized enterprises (SMEs) across the North Sea Region of Europe. Policies for improving the productivity and efficiency of SMEs had not been fully resolved by any of the European member states. Therefore, a transnational approach was advocated to develop a transferable solution. Building on the research highlighted above, a grant was awarded by the European Regional Development Fund (Interreg funding) to support the transfer of lean into SMEs across the North Sea Region. The objective of the ERIP project was to develop a methodology, using the knowledge developed in the North East of England (building on the NEPA work), which could be used by SMEs across the North Sea Region of Europe to implement lean to become more competitive. A key challenge identified through the research was that SMEs found it difficult to allocate the necessary time and resource to undertake the improvement activities. To address this, a new approach was developed through the research, called bite-sized lean. 70 This demonstrated that while lean could be applied in various contexts, it needed to be tailored. The next sections review research relating to lean in the public and health-care sectors respectively.
Lean in the public sector
McNulty and Ferlie71 argued that the UK’s new public management (NPM) reforms, which began in the early 1980s, eventually evolved, by the mid-1990s, into what they termed ‘NPM 4’. NPM 4 is characterised by a melange of private and public sector management ideas, emphasising a value-driven approach, concerned with the quality of service, and a continuing commitment to a distinctive public sector ethos of collective provision. Although McNulty and Ferlie had reservations about the application of private sector models such as business process re-engineering (BPR) to public sector settings (within the context of NPM 4), they concluded that the shift to a NPM model has made the public sector more receptive to ideas of process redesign. Lean is focused on process rather than product, and to this extent McNulty and Ferlie’s observations are highly relevant. For example, they found that a number of public sector organisations experience a problem over organising their work with regards to process and functional principles. 71 This is precisely the tension described by Seddon72 when he criticised local government for setting up ‘front office/back office’ call centres to process the various requests and demands from local citizens.
Although BPR and total quality management (TQM) have certainly attracted considerable attention in the public sector – including health care – there is evidence from recent literature that lean management and the TPS are currently more in vogue in a variety of public service settings. 73 For example, Hines and Lethbridge74 reviewed a project that implemented a lean value system in a university. The authors found a number of case studies relating to lean initiatives in academic settings, and they engaged in a 3-year initiative to embed lean methods and thinking in a client university. 74 Radnor and Bucci75 investigated the use of lean in UK business schools and universities. They found that the application of lean in UK universities was still relatively new and primarily applied in support and administrative functions.
Hines et al. 76 explored the use of lean in the Portuguese and Welsh legal public sectors, particularly in court services. McQuade77 discussed the organisational transformation brought about by lean thinking in a UK social housing group. Erridge and Murray78 reported on the application of lean principles to local government procurement processes, using the example of procurement contracts drawn up by Belfast City Council. The authors concluded that ‘lean supply’ was compatible with the best value approach to procurement, as long as characteristics of lean that are most closely aligned to manufacturing are adapted to fit the culture of local government. Scorsone79 considered the implementation of lean by the city government of Grand Rapids, MI, USA, in the face of fiscal restrictions and a dwindling workforce. Radnor and Bucci80 evaluated a lean programme undertaken in Her Majesty’s Court Services. The programme sought to focus on administrative functions as part of the operational aspects of court services. The underlying challenge of the project was to improve the delivery of service through a waste elimination programme, as well as simplify processes and free up capacity to be able to do more work. The outcome of the evaluation found that the programme had created impact within the court services. Leadership played a key role along with the dedicated project team. Other findings identified the understanding of why there is a need to change, changing and updating practices which had not been revisited, and engaging with the workforce in a manner that promotes a desire to change. Radnor and Bucci provided a framework to support the implementation of lean in public services. This framework requires an understanding of an organisation’s processes, customer requirements and types of demand. These factors are identified as key to ensuring that any lean programme can be successful. 80
One of the most wide-ranging evaluations of lean in the public sector – in terms of the scope of the research undertaken – is the report titled Evaluation of the Lean Approach to Business Management and Its Use in the Public Sector. 81 This document aimed to provide a comprehensive assessment of the success of the lean philosophy and tools in transforming a number of public sector organisations in Scotland. The report, commissioned by the Scottish Executive, covered eight case studies and three pilot sites, including local authorities, health agencies and a government (Royal Air Force) agency. It described a range of levels of engagement with lean, from full implementation (acceptance of lean thinking across all levels of an organisation, and use of lean tools and techniques, together with some likelihood of sustainable transformation) to light-touch lean [adoption of a ‘quick win’, toolkit approach, usually based on rapid improvement events (RIEs)]. These case studies collectively warn against a lean implementation approach that relies too heavily on the lean/TPS ‘toolbox’ without a complementary commitment to lean thinking at all levels of the organisation. The implication is that the tools of lean/TPS (RIEs, 5S, Kaizen blitz, etc.) are less likely to become embedded and have sustainable value unless they are part of a wider package of organisational reform. Furthermore, Radnor and Walley82 suggested that many public sector organisations lack an understanding of process management. Organisations that only gain quick wins, usually via RIEs [or rapid process improvement workshops (RPIWs) in VMPS parlance], find it difficult to sustain improvement in the long term. In a number of cases, the authors found a lack of alignment between the lean/TPS implementation and the organisations’ strategic objectives.
An over-reliance on the lean/TPS toolbox can make it difficult to embed process-oriented thinking. Radnor et al. 81 found that a common public sector response has been to avoid specific, transformational, quick win tools, believing these to be unwelcome imports from a manufacturing environment and inappropriate for use in public service. The message here is that balance is required. The case studies showed that the success of lean/TPS implementation was context dependent, and relied to a large degree on a number of organisational and cultural factors. When lean is not fully aligned with the strategy of a public sector organisation, there is a risk that it will not be sustainable in the long term. Having a critical mass of people who are trained in lean and accepting of it as a transformational agent is also essential.
As a brief summary, Radnor et al. 81 identified the following critical success factors for implementing lean in public service organisations:
-
organisational culture and development
-
organisational readiness
-
management commitment and capability
-
external support from consultants (at least initially)
-
having a strategic approach to service improvement
-
teamwork and whole-systems thinking
-
timing – setting realistic timescales and making effective use of staff commitment and enthusiasm
-
effective communication channels across the whole organisation.
These points were reinforced by a range of papers in a special issue of Public Money & Management (February 2008). These considered the relevance of lean in improving public sector services; aspects of lean thinking that ‘fit’ public service organisations; the transfer of lean experience from other sectors; and the extent to which lean is a distraction or a panacea.
Lean in health care
Most of the research on lean in health care has focused on hospitals. Spear83 highlighted a series of avoidable medical errors and patient safety issues in the US hospital sector. He advocated the use of the TPS to remove ambiguities in processes and to empower health-care workers to solve problems as they arise, rather than opting for work-around solutions. Spear pointed out that ‘No organisation has fully institutionalised to Toyota’s level the ability to design work as experiments, improve work through experiments, share the resulting knowledge through collaborative experimentation, and develop people as experimentalists’. 83
Radnor et al. 84 investigated the introduction of lean in four UK NHS hospital trusts. They found a widespread use of lean tools that led to small-scale and localised productivity gains and highlighted significant contextual differences between health care and manufacturing that made it difficult to move towards a more system-wide approach. In particular, some of the principles proposed by Womack et al. 47 do not apply. ‘Customer value’ in health care is different to manufacturing because the patient is normally a recipient of treatment and does not commission or pay for the service. The provision of health care is often subject to budgetary constraints that make it capacity led; there is limited ability to influence demand or reallocate resources saved by improvement measures.
Fillingham15 described the use of the TPS for improving patient care at the Royal Bolton Hospital in the UK, which has been widely considered to be an exemplar case. He reported a 42% reduction in paperwork, better multidisciplinary teamworking, a reduction in length of stay by 33% and a 36% reduction in mortality. Ballé and Régnier85 reported on the use of lean to reduce medication distribution errors, nosocomial infection rates and catheter infections in a French hospital. Although the initiative was deemed successful, the authors identified resistance to the standardisation of clinical and nursing practices. Gowen et al. 86 investigated the application of continuous QI, Six Sigma and lean in US hospitals. They concluded that lean was significant in reducing the sources of errors, but that it did not improve organisational effectiveness. Chiarini87 researched an improvement project utilising lean and Six Sigma tools to reduce safety and health risks to nurses and physicians who managed cancer drugs in an Italian hospital. The author identified that the tools helped improve health and safety and reduced pharmaceutical inventory. Yeh et al. 88 looked at the application of lean thinking and Six Sigma and how they could be used to improve processes in treating an acute myocardial infarction. The outcome was that the medical quality improved, as did market competitiveness. Esain and Rich89 focused on improving patient flow through hospitals to reduce waiting times.
Outside the hospital sector, Boaden and Zolkiewski90 conducted a process study of the non-clinical aspects of a UK general practice, with particular attention to the relationship between the patient and the managerial and administrative aspects of the organisation. Endsley et al. 91 considered process and flow issues in family medical practice in the USA. They focused upon understanding patient needs and administrative procedures, which led to reduced waste. Endsley et al. made a good case that, from the patient’s perspective, many of the frustrations involved in accessing general practitioner (GP) services arise not from direct contact with the physician, but from missing paperwork, unacceptably long waiting times, and poorly managed hand-offs between doctor, practice nurse and receptionist. 91
One of the most frequently cited exemplars of lean in health care is the Virginia Mason Medical Center (VMMC). It adopted the TPS to create the VMPS. The research on VMMC has included work by Weber,92 who investigated how improved logistics and productivity reduced costs and defects; Furman and Caplan,93 who outlined the patient safety alert system; Nelson-Peterson and Leppa,94 who described the elimination of waste in nursing procedures; McCarthy95 on the application of the TPS; Bush96 on eliminating waste; Kowalski et al. 97 on nurse retention and leadership development; and Pham et al. 98 on the redesign of care processes.
The next chapter considers the origins and evolution of the NETS, which was supported by consultancy from VMMC and Amicus.
Chapter 3 The origins and evolution of the North East Transformation System
In this chapter, the key influences and factors that led to the introduction of the NETS and the pivotal role of NHS NE are considered. The NETS comprised three principal components: Vision, Compact and Method. It drew heavily on the seminal influence of the VMPS which was derived from the TPS and from Amicus.
Why the North East Transformation System?
In the North East of England the NHS performs well in terms of meeting targets and performance measures, but the population has poor health due to the region’s industrial heritage and socioeconomic factors. 99 Although this might seem to be a paradox at first glance, it is not really, as good health is determined by factors that lie outside the health-care system. 100 The social and economic circumstances in which people live and work can have a significant impact on their state of health, as Marmot’s work on the social determinants of health and the life course amply demonstrates. 101,102 Nevertheless, while in existence, NHS NE believed that the NHS could do much better by focusing on quality and patient safety and adopting a whole-systems approach to an individual’s and community’s health state. 11
The NETS was instigated as a result of the SHA board’s conviction that a new approach to the way in which it conducted its business was both required and essential. At a meeting held to share information about lean activities across trusts in the North East of England in February 2011, the SHA’s medical director, one of the chief champions of the NETS, commented that the solution was no longer simply doing ‘the same thing but harder’, but doing it smarter. Merely doing what had always been done would deliver exactly the same result. To shift the paradigm or do something genuinely different required changing the rules of the game and transforming the culture of the system. This is something Don Berwick and his colleagues at the Boston-based Institute for Healthcare Improvement in the USA had known for a long time. 103 It was a central theme in his report to the coalition government on the lessons to be learned from the failures at Mid Staffordshire hospitals. 104 NHS NE sought to achieve system-wide rather than localised transformation through a major change programme that would engage all parts of the health system in the North East, including commissioners as well as providers of services. There was an early intention to encourage GPs to undertake training in the principles of the NETS, but it was recognised that GP practices were unlikely to form part of the vanguard, as they lacked the required resources to do so.
Throughout the NHS there was considerable interest in organisational change and the tools available to embed and sustain it. These were reviewed in a National Institute for Health Research (NIHR)-funded study by Isles and Sutherland,105 intended for health-care managers, professionals and researchers. The study concluded that change in the NHS will not be straightforward. The NHS was an example of a ‘complex adaptive system’, which Plsek and Greenhalgh defined as ‘a collection of individual agents with freedom to act in ways that are not always predictable, and whose actions are interconnected so that one agent’s actions changes [sic] the context for other agents’. 12 Complex adaptive systems invariably have fuzzy boundaries, with changing membership and members who simultaneously belong to several other systems or subsystems. In such contexts, tension, paradox, uncertainty and ambiguity are natural phenomena and cannot necessarily or always be resolved or avoided. Instead, they need to be embraced by the various stakeholders and harnessed in such a way that they result in sustainable solutions to complex problems. Arising from such concerns, the term ‘whole-systems thinking’ is now routinely used by managers and clinicians to capture the particular features of a complex health-care system and reflect the following features:
-
an awareness of the multifactorial nature of health care and an acknowledgement that complex health problems – often termed ‘wicked problems’ because they have no simple or easy solutions – lie beyond the ability or capacity of any one practitioner, team or agency to fix106
-
an interest in designing and managing organisations as dynamic interdependent systems committed to providing safe, integrated care for patients. 105
The NETS and its evaluation was informed by systems thinking. A system cannot be considered in isolation from its context and overall environment,107 nor do systems constitute neat chains of linear cause-and-effect relationships which can be isolated and understood in their own terms. In health-care systems, complex networks of inter-relationships are the norm. 108
Isles and Sutherland’s 2001 review noted that the problems and situations that occur cannot be resolved through the use of a single tool or strategy. 105 Consequently, NHS managers had to acquire the ability to diagnose different situations, as well as the skill to find the right tool to use in the particular circumstances that they face. NHS NE’s choice of the NETS and its three main components was certainly informed by such a diagnosis as well as exposure to the VMMC’s adoption of a change programme. The VMPS was derived from TPS principles and methods that were subsequently adapted to suit the North East context.
The NETS comprises three components, familiarly known as the ‘three-legged stool’: Vision, Compact and Method. These components are not individually pioneering. It is the combination that constitutes the NETS approach to transformational change and lends it particular novelty as far as the NHS is concerned.
Vision
The Vision adopted by NHS NE was for it to be a leader in excellence in health improvement and health-care services. To achieve this, the SHA adopted a zero tolerance approach and proceeded to articulate a powerful, uncompromising vision for health-care services in the North East, underpinned by the ‘seven no’s’:99
-
no barriers to health and well being
-
no avoidable deaths, injury or illness
-
no avoidable suffering or pain
-
no helplessness
-
no unnecessary waiting or delays
-
no waste
-
no inequality.
The sheer bravura of such a list had an immediate impact which made staff in the NHS take stock. The NETS was seen as one of the pillars for implementing the Vision set out in NHS NE’s strategy, Our Vision, Our Future. 99 Of course, achieving the Vision was to prove immensely challenging, but the SHA board, led by its chairman, wanted to set the bar high. The Vision set out the fundamental objectives and direction of the NHS in the region and it was intended to be a living document with which all staff could engage. It was shared with other public bodies, embedded in a suite of local strategy documents, promoted by local managers and cascaded down to front-line staff. The architects of the NETS intended each NHS trust in the North East to draw on the regional Vision for inspiration, but also to create their own Vision, relevant to their organisation’s purpose and values and ‘owned’ by their staff. Otherwise, the Vision risked being imposed from on high, which could have resulted in resistance from front-line staff.
Compact
The Compact arose from the enduring tension between managerial and professional values and the attempt to find some accommodation between the two groups with their differing cultures. It was influenced by the Physician Compact introduced by the VMMC at an early stage of its change journey. The concept of a compact was simple enough: an explicit deal between two parties which, in the case of the VMMC, comprised the clinicians and the VMMC organisation. 109 The intention was to move from an implicit compact to a new explicit one which reflected changes in health care and its management.
Such tensions were not confined to the VMMC or even the USA. In the UK, successive governments have sought to change the way the NHS operates and is managed. Central to these efforts has been shifting the frontier between medicine and management in favour of the latter. It was a development that began in earnest with the first major reorganisation of the NHS in 1974 and has been an enduring theme ever since. However, the effect of a growing managerial encroachment into medicine was not unanimously welcomed by clinicians. Many were suspicious of such developments and opposed to what they perceived to be an erosion of their clinical freedom. An editorial in the BMJ in 2001 posed the question: why are doctors unhappy?17 It suggested the causes were multiple, but highlighted one in particular, which concerned the training doctors received and the nature of the work they were subsequently required to perform. Despite their medical training in a particular specialty, the reality of life on the front line required doctors to think about other matters, including management, finance, ethics and communication. 17 Edwards et al. 18 suggested that the cause of doctors’ unhappiness lay in a breakdown between them and society at large. Doctors were trained to function as individuals with a fair degree of autonomy, but the demands of modern health-care systems required them to be accountable for their actions and to operate as members of a team. They described the old compact which underpinned the NHS and why it was no longer regarded as legitimate, and outlined what a new compact might look like. The old compact comprised two aspects: what doctors gave and what they got in return (Table 1). The mismatch between these was the cause of the dissonance over what doctors might have reasonably expected the job to be and what it now was. Some commentators have suggested that the psychological contract – or compact – is a useful concept to explain this problem. 18–20 Jack Silversin from Amicus, an international consultancy specialising in health-care system improvement, was an influential figure during this period on both sides of the Atlantic. His contribution to the debate was significant because he had worked on the Physician Compact at VMMC and subsequently provided an input into the NETS and its development of the Compact.
| What doctors give | What doctors get in return |
|---|---|
| Sacrifice early evenings and study hard | Reasonable remuneration |
| See patients | Reasonable work/life balance later |
| Provide ‘good’ care as the doctor defines it | Autonomy |
| Job security | |
| Deference and respect |
A new and more sustainable compact was required because the old promise to doctors was either no longer valid or could act as a barrier to modernisation. Among the new imperatives to be addressed in a new compact were those listed in Box 1.
-
Greater accountability (e.g. guidelines).
-
Patient-centred care.
-
More available to patients, providing a personalised service.
-
Work collectively with other doctors and staff to improve quality.
-
Evaluation by non-technical criteria and patients’ perceptions.
-
A growing blame culture.
Edwards et al. 18 were of a view that returning to the old compact was not possible and that doctors and managers should work together to devise a new compact that: was fit for modern health-care systems, sought to improve patient care and the effectiveness in which they worked, and would result in a happier workforce. Apart from the issues with patients and their care, a principal reason for the discontent among doctors was the dissatisfaction they experienced in their relationship with managers. It manifested itself in a perceived sense of diminished autonomy and reduced dominance. To address these concerns, Davies and Harrison21 argued in favour of a better alignment between doctors and the organisations in which they worked. However, given the tensions and cultural differences that existed between doctors, managers and their professional groups, they were under no illusions that such a task would be easy or straightforward. They concluded by insisting that there was no practicable alternative to doctors engaging with management. Despite such calls, there was still unease felt by many doctors who perceived that they were not valued. 22 This was a major reason for Ari Darzi being invited by the government to lead the next stage review of the NHS. As noted in Chapter 1, this was an attempt to re-engage clinicians in the reform effort together with other front-line staff so that they were at the heart of the change process – change that was ‘locally-led, patient-centred and clinically driven’. 16
However, the unhappiness felt was, and is, not confined to clinicians. Managers are also unhappy with their lot, a situation that has arguably, and for many, deteriorated further in recent years as a result of being subjected to continuous organisational change whose precise purpose is often unclear and whose impact often falls short of expectations. Combined with a culture of fear and ‘terror by targets’,110 the outcome is an environment which, as the Berwick report put it, ‘is toxic to both safety and improvement’. 104 The ‘harvest of fear’ evident at Mid Staffordshire resulted in
a vicious cycle of over-riding goals, misallocation of resources, distracted attention, consequent failures and hazards, reproach for goals not met . . . A symptom of this cycle is the gaming of data and goals; if the system is unable to be better, because its people lack the capacity or capability to improve, the aim becomes above all to look better, even when truth is the casualty.
Berwick 2013104 [A Promise to Learn – A Commitment to Act: Improving the Safety of Patients in England, © Crown copyright 2013, contains public sector information licensed under the Open Government Licence v2.0 (www.nationalarchives.gov.uk/doc/open-government-licence/version/2/)]
Managers in such a dysfunctional environment can appear beleaguered functionaries in a system that seems more politicised than ever and whose political heads regard themselves as its true leaders. 23 Indeed, critics of the waves of reform under the Labour government between 1997 and 2010 hold that the ‘terror by targets’ regime was largely responsible for distortions in the health system which, unintentionally, ensured that the patient was not put first. 110 The result, as Berwick noted, is an elaborate set of managerial ploys, often labelled ‘gaming’, to arrive at the results desired by their political masters and mistresses.
The term ‘culture’ is often invoked too readily and simplistically in a health-care context, especially in the aftermath of the Francis report into the events at Mid Staffordshire Hospital between 2005 and 2009. 111 It is assumed that culture change will address issues of organisational performance. Culture is important in terms of shaping organisational behaviour and improving performance. 28 Change can also be stifled by culture. Mannion et al. 28 commented that culture comprises the informal social aspects of an organisation that influence how people think, what they regard as important, and how they behave and interact at work. Organisational culture has been defined as29
the pattern of shared basic assumptions – invented, discovered or developed by a given group as it learns to cope with its problems of external adaptation and internal integration – that has worked well enough to be considered valid and, therefore, to be taught to new members as the correct way to perceive, think, and feel in relation to those problems.
Culture is therefore not merely that which is observable but also the shared cognitive and symbolic context within which a society or institution can be understood. 28 But Mannion et al. counselled against the adoption of a ‘one size fits all’ approach to culture management in the NHS and encouraged ‘the adoption of more nuanced strategies which seek to deploy a judicious mix of instruments and supporting tactics depending on setting and application’ (pp. 214–15). 28 These issues were very much at the heart of the NETS and how it sought to win ‘hearts and minds’ across the North East region. Those leading the initiative recognised the importance of establishing shared goals, cultural change and collaborative working.
As the literature review in Chapter 2 revealed, a principal component of effective culture management is leadership style. 30 Perhaps the key factor to note is that leadership entails much more than the actions or behaviour of an individual, as such a focus ignores the importance of both context and complexity. Situational leadership is therefore regarded as more appropriate in the context of complex adaptive systems. Alban-Metcalfe and Alimo-Metcalfe,34 in their study of leadership and successful change in the NHS, found that a culture of ‘engaging’ leadership significantly predicted motivation, satisfaction, commitment, reduced stress and emotional exhaustion, and team effectiveness/productivity. Leadership, then, is not about control but about co-operation and creating an agenda for change using a strong vision.
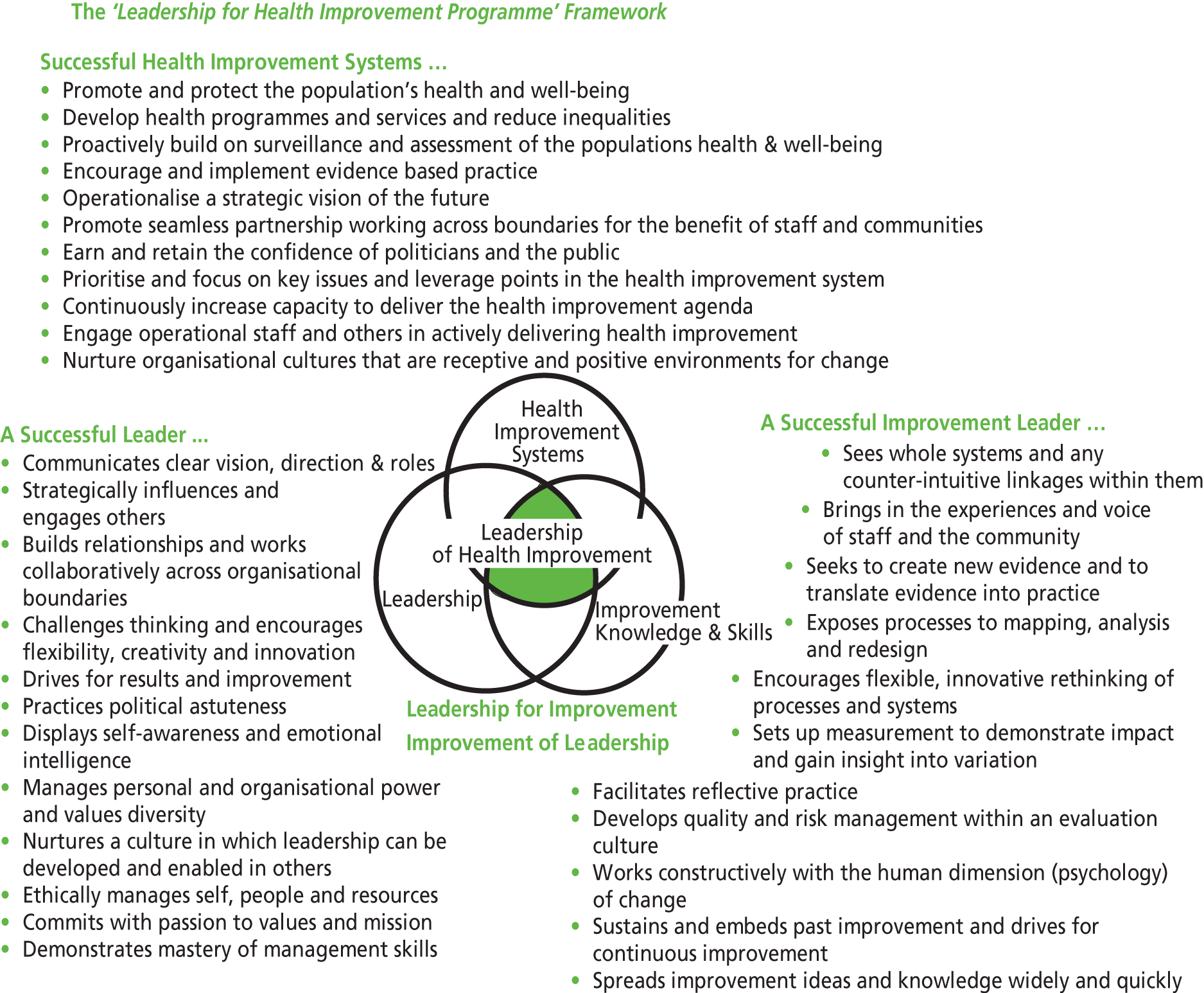
In their Leadership for Health Improvement framework (Figure 1), Hannaway et al. 36 employed a mix of improvement science concepts together with softer notions of emotional intelligence and political astuteness.
FIGURE 1.
The ‘Leadership for Health Improvement’ framework (reproduced with permission from Figure 7.2 in Hunter DJ, editor. Managing for Health. London: Routledge; 2007. p. 158). 36
Method
We now turn to the third leg of the stool – the Method. The particular method used within the NETS approach was considered less important than the commitment to QI. It is important to adopt a contingency approach to achieve fit between the local context, the needs of the organisation and the Method. However, the VMPS was by far the preferred approach and was strongly supported by the SHA, which invested resources in it to encourage wider engagement and commitment.
The NHS NE’s desire was to develop and roll out across the region a NE Production System modelled on the VMPS. The SHA anticipated that the VMPS would enhance patient safety and increase capacity through making better use of existing resources. The objective was to increase patient and staff satisfaction, shorten the patient pathway, stimulate continuous improvement and encourage a new culture of clinical care. 11 This was to be achieved by making full use of the potential skills and strengths of all team members.
The implementation of the NETS began in mid-2007 and was led by a small project team based at the SHA. This team of enthusiasts actively promoted the approach and provided a link with the consultants engaged in delivering elements of the initiative, notably Amicus (Compact work in its early stages) and VMMC (lean method training). The SHA also hosted meetings, acted as a repository of information about lean and other aspects of the NETS, and maintained communication channels with NETS organisations that were not employing VMPS as their method of choice.
Conclusions
In later chapters, we describe and assess the journey taken by the NETS from its inception to the present time. Large-scale transformational change is challenging and often problematic in any complex adaptive system. This is especially so when considering a large region’s entire health-care system. 71 There are multiple reasons for this. Constituent organisations have conflicting aims, different cultures and varying skill mix. These issues were evident in the NHS organisations participating directly in, or more loosely associated with, the NETS. External forces, often unforeseen and unexpected, can also have a decisive impact on what happens regionally and locally. This occurred to the NETS in mid-2010, when the coalition government elected in May 2010 announced a major restructuring of the NHS in England. The research reports on the impact of the NETS within the North East region and how it adapted to a changing environment.
Chapter 4 Study design and methods
The research comprised a longitudinal evaluation of the NETS conducted over 3.5 years, from 1 December 2009 to 31 May 2013. The NETS comprises three principal components: Vision,99 Compact18 and Method,51 the ‘three-legged stool’ with patients at the centre. 18,51,99 The study design aimed to answer the research questions set out in the proposal, which are of significance to practitioners, policy-makers and researchers studying transformational change in health systems. The research questions were as follows:
-
How have the various manifestations of the NETS and non-NETS approaches evolved over time?
-
How receptive have NHS organisations in the North East been to transformational change, including the adoption of either VMPS, TPS or other lean tools?
-
What has the impact of the different NETS approaches been on the quality and efficiency of health care in respect of technical quality, safety, patient experience, access and equity?
-
How far has variation been reduced across specialties, departments and hospitals?
-
How far has work-related stress been reduced?
-
How far has the ‘Compact’ with clinicians, to secure their commitment to the NETS approaches, been made a reality?
-
How far have staff been empowered to take control of their work?
-
What are the factors facilitating, and/or acting as barriers to, successful change?
The research team drew on their multidisciplinary skills and expertise in the areas of health policy and management, engineering, operations management, strategy, human resource management and statistics. Team members had first-hand and extensive experience of working, and researching, in an NHS environment. According to Eisenhardt:112
Multiple investigators . . . enhance the creative potential of the study. Team members often have complementary insights which add to the richness of the data, and their different perspectives increase the likelihood of capitalizing on any novel insights which may be in the data.
The research environment was complex in terms of scale (the NHS in the North East employed approximately 77,000 people and served a population of 2.4 million); scope (geographically dispersed, primary and secondary care, commissioning, delivery and management); and orientation [policy, organisation, leadership, human resources (HR) and operations]. Towards the end of the study, the research had unexpectedly to contend with a major reorganisation of the NHS. It followed the UK general election in May 2010 which ushered in the coalition government, which published proposals for an extensive restructuring of the NHS within months of entering office.
The study sites, which are referred to in this report in the form ‘site xx’, where ‘xx’ is the internal project code, comprised two clusters of PCTs, two mental health and learning disability trusts, three hospital trusts, an ambulance trust and a community services trust. Furthermore, there were many actors at different levels in the organisations including managers, clinicians, nurses, ancillary staff and administrative and operational areas.
Research on transformational change benefits from a sociotechnical perspective that takes account of both the behavioural and cultural context, described in Chapter 3, as well as the technical challenges involved in bringing about change. This is because ‘organisational objectives are best met not by the optimisation of the technical system and the adoption of a social system to it, but by the joint optimisation of the technical and social system’ (p. 62). 113 Alternative aspects of reality and different research questions require appropriate methods of enquiry. 114 It has been argued that the complexities of human phenomena require mixed-methods approaches to capture deep insights. 115 Furthermore, the purposes of using mixed-methods include triangulation, to ensure the corroboration of data or convergent validation; complementarity to clarify, explain or elaborate the results of analyses; and guiding additional sampling data collection and analysis. 116
Research design
Transformational change may be viewed in terms of content, context, process and outcomes. 117 Furthermore, there is a distinction between episodic and continuous change. 118 This led to different types of research questions that needed to be addressed through qualitative and/or quantitative methods. 119 Various typologies of mixed-methods research have been proposed that consider sequence, priority, purpose, etc. 120 The research methods included semistructured interviews, observation, documentary analysis, focus groups, attendance at meetings and presentations and interrupted time series (ITS) analysis.
The research approach is shown in Table 2, which identifies the sources of qualitative and quantitative data that were used to evaluate processes and outcomes. The priority and sequence of the data collection and methods varied according to the quadrant and also the research question being addressed. Initially, a deductive approach was adopted and employed to aid the analysis of qualitative data at the end of the first year of the study, and to assist in identifying key issues associated with transformational change. As the study progressed, emerging themes were analysed inductively to complement the deductive approach. 121,122 The research methods also took into account multiple levels of analysis; for example, at the level of specific interventions the stakeholders included a sponsor, a process owner, a workshop leader, a team leader, a subteam leader, an advisory group and participants. 123 The NETS included formal evaluations of the impact of the interventions after 30, 60 and 90 days.
| Data type | Qualitative | Quantitative |
|---|---|---|
| Process | Interviews | Documentary data |
| Observation | Target progress sheet | |
| Focus groups | Value stream map | |
| Attended Coalition meetings | Takt/cycle time | |
| Seven wastes categorisation | ||
| Spider diagrams | ||
| Outcome | Interviews | Documentary data (including self-reported routinely collected data) |
| Focus groups | Routinely collected data for five RPIWs (ITS analysis) | |
| Attended report-outs |
Study sites
Stratified purposive sampling is an approach where certain cases are selected to ensure that they vary according to preselected parameters. 115 This approach was adopted so that the sample of cases included organisations that were representative of the scale, scope and geographic location of the participating trusts. A similar strategy was adopted within each case to ensure that the respondents selected for interview were representative of the various professional groups, skill mix and band level.
The plan outlined in the initial proposal was to conduct research in five pathfinders that had implemented the VMPS and two non-pathfinders as controls. The pathfinders were subdivided into two waves: the first wave started in 2008 and the second in 2009. This was intended to reflect organisations at different stages of the NETS journey. The actual design was modified to reflect the range of methods used to achieve transformational change (including study sites not using the VMPS as their Method), as well as the changes to NHS organisations across the North East that occurred following the 2010 general election and came to be enshrined in the Health and Social Care Act 2012. 124
The research design (see Figure 2) included 14 study sites (Table 3) which formed the basis of nine case studies (as some organisations operated on multiple sites). Four cases were wave 1 pathfinders, one was a wave 2 pathfinder and four were non-pathfinders. All stages of the research involved multiple investigators to allow for triangulation and to enable different perspectives to be obtained from multiple observers. 112
| Site | Context and background | NETS information | Staff (approximate number) | Annual budget (£M) |
|---|---|---|---|---|
| 01 | University teaching hospital NHS FT. Operates across two acute hospital sites, one large and one smaller. Granted FT status in May 2009. Took over running local community health services in April 2011, including a number of smaller primary care and community hospitals | A non-VMPS NETS organisation, using a mix of different improvement methodologies | 9000 | 523 in 2012 |
| 02–05 | This cluster of four PCTs is treated as a single entity for the purposes of the NETS evaluation. The PCT cluster operated under a single CEO, but with four separate boards, during the evaluation period | A non-VMPS NETS organisation | Numbers varied over the period of the study, from many thousands in 2009 (including community health service staff) to fewer than 300 in 2012/13. This decrease in staff numbers reflected the major changes in the structure and governance of commissioning organisations in the NHS from 2010 onwards | 1100 (2011/12 data) |
| 06 | This organisation provided NHS community services from its original creation in 2007 to April 2011, when it became part of a NHS hospital FT. Its functions and services are now provided through one of the clinical divisions of site 01. The data below refer to the study site pre 2011 | A non-VMPS NETS organisation, which made use of a variety of improvement methodologies | 1000 (2010 figure) | 44 (2010 data) |
| 07 | This NHS ambulance trust was formed around July 2006 following the merger of the previous service and part of three other transportation services | A VMPS NETS organisation, which joined the NETS training programme during its second wave | 2000 | 106 |
| 08 | This NHS acute mental health and learning disability trust was formed in 2006, and became a FT in December 2009 | A VMPS NETS organisation, which joined the first wave of NETS training | 6000 | 300 |
| 09 | Established as a NHS hospital FT in 2005 | A VMPS NETS organisation, which joined the first wave of NETS training | 3000 | 190 |
| 10 | This NHS mental health and learning disability trust was created in April 2006, following the merger of two other mental health and learning disability trusts. FT status granted in mid-2008 | A VMPS NETS organisation, which joined the first wave of NETS training | 5700 | 270 |
| 11–13 | This cluster of three PCTs is treated as a single entity for the purposes of the NETS evaluation. A single management team operated the day-to-day PCT activities during the evaluation period | A VMPS NETS organisation, which joined the first wave of NETS training | 4000 | 1323 (2011/12 data) |
| 14 | This trust, which manages hospital, community and adult social care services, became a FT in 2006 | A non-VMPS NETS organisation, which uses a mix of different improvement methods. Involvement in structured QI activities predates the NETS programme by several years | 6000 | 420 |
Longitudinal research design, including timetable
A representation of the research project is shown in Figure 2, which contains an overview of the work conducted during each year of the 3-year research study. Figure 2 is a schematic diagram intended to provide a visual reminder of the elements of the design; details are explained in the remainder of this section.
FIGURE 2.
Research design. KPO, Kaizen Promotion Office; OD, organisational devolvement.
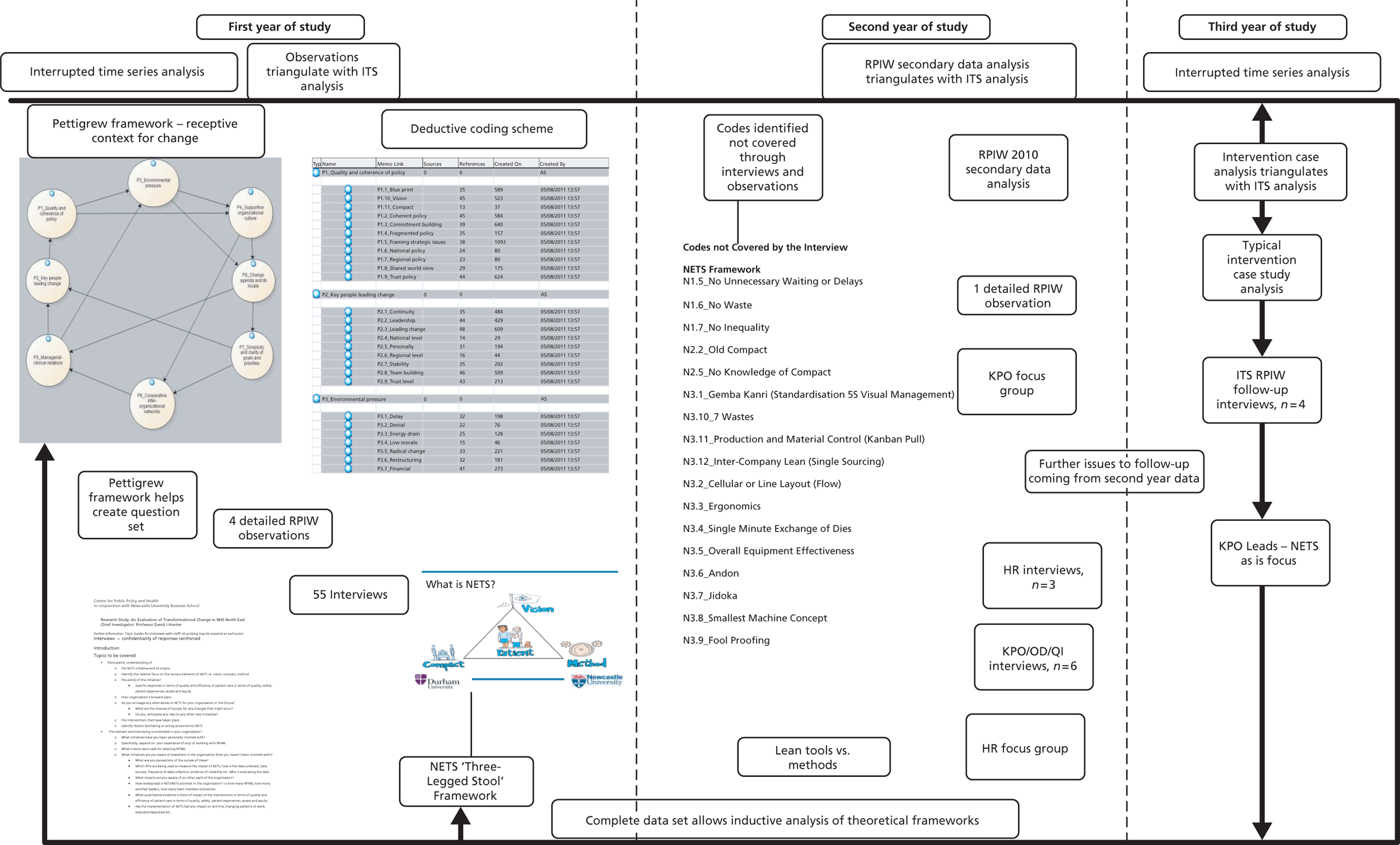
Year 1
The research used two frameworks to evaluate the process of transformational change: the Pettigrew et al. 125 framework of ‘receptive contexts for change’ which was developed in a study of strategic change in the NHS in the 1980s; and the ‘three-legged stool’ (Vision, Compact and Method) that was adopted as the basis of the NETS.
The research aims and objectives the study set out to address were derived from the scoping study and influenced by the Pettigrew et al. framework. 125 In year 1, interviews were conducted with 55 key respondents at different levels throughout the study site organisations. The interviews were coded deductively against the Pettigrew et al. framework and the ‘three-legged stool’. Detailed observations were made during four RPIWs that sought to improve processes in two important pathways. Each RPIW was of a week’s duration. Three of the RPIWs were part of the same clinical pathway (a ‘superflow’ RPIW), which demonstrated a value stream approach. Secondary data, including standard NETS RPIW documents and training materials, fieldwork notes and photographs were collected and analysed.
The team regularly attended quarterly meetings of the NETS Coalition Board which co-ordinated the NETS activities, and ‘report-outs’ where the RPIW participants presented the results of their interventions. In addition, a pilot ITS study was conducted in a mental health trust. Once the deductive analysis was completed, an inductive analysis was undertaken, thereby allowing other themes and issues to emerge. Through a combination of deductive/inductive analysis a list of topics and issues were captured which were explored further and added to during years 2 and 3 of the study.
Year 2
In the second year, follow-up in-depth interviews were undertaken with nine participants. Focus groups were conducted with HR managers (two participants) and Kaizen Promotion Office (KPO) certified leaders (three participants). Secondary data from all training RPIWs conducted in 2010 were analysed. These data were coded deductively against the two frameworks as well as against the inductive codes that emerged from the analysis of data at the end of year 1 of the study. A further inductive analysis was undertaken to see if any further issues and themes emerged from the data collected in year 2. The team continued to collect and analyse secondary data, and to attend Coalition meetings and report-outs.
Year 3
The focus in the third year of the study was to identify and analyse typical interventions in a range of settings. These were selected using a purposive sampling technique115 that drew on seven of the case studies. Within this sample, three of the case studies were selected as they were also being analysed through the ITS method. One was included as it was a commissioning organisation; two were chosen as non-VMPS organisations using alternative methods; and the final one was included as it was a wave 2 organisation. A further four interviews were conducted with key NHS staff associated with the RPIWs that were being analysed using ITS. Finally, the third-year data collection concluded with a small number of further interviews being conducted with KPO leaders and the NETS Coalition managers to ascertain how NETS was evolving as a mechanism of transformational change across NHS NE. These data were again coded against the two frameworks developed in year 1 of the study as well as any codes that emerged inductively from years 1 and 2. Finally, the data from year 3 were analysed to identify any further codes and themes.
Methods
This section outlines the key methods used to obtain, manage and analyse the data that resulted from our research work.
Literature review
A literature review was undertaken throughout the duration of the project and the main themes from this were presented in Chapter 2 and highlighted in Chapter 3. It provided the theoretical background and helped to focus the data collection methods. This built on and extended the review undertaken during the scoping study commissioned by the SHA as a prelude to the main evaluation study. 11
Interviews
In total, 55 semistructured interviews were conducted in year 1. The interviewees were selected through a snowball sampling approach to represent a wide range of stakeholders and functional roles, and included clinicians, managers, administrators and board members. 119 The aim of the first-year interviews was to understand the transformational change process, and the context, content, scope, organisation and outcomes of the NETS. Those responsible for leading and delivering change were interviewed as well as participants at all levels of the organisations. Some of the respondents who had visited the VMMC in Seattle, WA, and the Toyota Museum in Japan were able to compare local practices with global exemplars. Many participants had multiple roles including learning and applying best practice and how to translate it to their local context; leading and managing change; and diffusing knowledge throughout their organisations.
The interviewers used a question schedule (see Appendix 3), designed to ensure that similar ground was covered in each interview but also to allow for questioning to reflect the particular interests and expertise of the interviewees. The interviews were conducted by at least two team members to provide complementary insights, check for consistency and ensure accuracy. The interviews were digitally recorded and participant consent forms were signed and collected from all interviewees. The recordings were transcribed and checked for accuracy by at least two team members. Clarification was sought from participants when necessary.
NVivo 9 (QSR International, Warrington, UK) was used to manage and analyse the data that were collected at all stages of the project. The transcripts were added to a NVivo database. A hierarchical, two-level coding framework was developed deductively based upon the ‘receptive contexts of change’ framework described by Pettigrew et al. 125 Each transcript was independently coded by two members of the research team. The codes were then compared for consistency and any differences were discussed and resolved. Another team member also independently checked and compared the coding of the transcripts to ensure reliability. A second two-level coding framework was also developed deductively based upon the NETS ‘three-legged stool’. Finally, the data were coded inductively to identify emergent issues that were not addressed by the deductive frameworks.
Observations
To examine the NETS method in more detail, four RPIWs were observed, three of which took place concurrently during a single week. These cases were selected to complement the ITS analysis described in Chapter 7, Summary of findings for the rapid process improvement workshops included in the interrupted time series. 126,127 The selection criteria were related to the availability of sufficient pre- and post-intervention data to provide sufficient power for the ITS analysis. At least two team members were present throughout the workshops to provide complementary insights, check for consistency and ensure accuracy. The observations provided rich data on the process, whereas the ITS aimed to provide a systematic quantitative evaluation of outcomes in terms of specified performance indicators. The observations included data on how the facilities were configured, the structure of the intervention, training materials, the configuration of the team (sponsor, process owner, workshop leader, team leader, subteam leader, advisory group and participants), how the team interacted and used the lean tools, how the team progressed and how it proposed to implement the outcomes. Observations provided a mechanism for revealing softer aspects that a purely quantitative approach could not detect. Detailed notes were taken and evaluated to understand the context of the proposed improvements and how they related to transformational change. These data were triangulated with the interview, focus group and documentary data.
Focus groups
Focus groups were conducted among HR managers (two participants) and KPO leaders (three participants) in year 2. They were facilitated by two researchers and discussions were recorded and detailed notes taken. A research protocol was prepared in advance of the meetings, which provided sufficient flexibility to allow the participants to raise and discuss matters that they felt were relevant and important. The purpose of conducting a focus group with HR managers was to discover how the Compact was developed and how it was being used in their respective organisations; in the case of the KPO leaders, the aim was to obtain data on their role in leading transformational change within their trusts.
Dissemination of early research findings
An interactive dissemination event was held at the midpoint of the project with 30 participants attending. This provided an opportunity to feed back interim findings from the first year of the study to key stakeholders and to obtain further data in respect of verifying the authenticity of our emerging findings. There were six round tables (two each for Vision, Compact and Method), each of which had a team member as facilitator. The table discussions were recorded and notes of key points written up.
Documentary materials
The complexity of the project (14 study sites; multiple research objectives; hundreds of potential QI activities over 3.5 years; an unstable policy context) meant that the research team was faced from the outset with an avalanche of possible sources of documentary materials. To manage this volume of data and to render subsequent analyses viable, decisions about which materials to request and collect were based first on their relevance to the key research objectives, and subsequently on their contribution to themes that emerged in the first 2 years of the project.
Documentary materials collected in phase 1 of the project concentrated on:
-
reports and presentations from the study sites, NHS NE and the NETS Coalition Board that concerned the origins of the NETS and its start-up period with wave 1 and 2 pathfinder organisations
-
training materials used by the study sites to promote their QI programmes, particularly those relating to the VMMC and TPS, the Unipart Way, the Institute for Innovation and Improvement and the Lean Academy
-
evidence linked to knowledge sharing and learning (KSL) activities (share-and-spread events, report-outs, documentation shared across the NETS organisations)
-
NETS Coalition Board meeting papers
-
documents offered by interviewees in support of their views on NETS development.
During phase 2, the researchers continued to collect documents in a variety of formats that were linked to the core elements of the NETS (Vision, Compact and Method; KSL activities). The research team also obtained DVD films of typical region-wide report-outs, documents that reported on awards won by NETS organisations in recognition of successful improvement projects and further NETS Coalition Board papers.
In phase 3, the research team mainly focused on collecting documentation in support of case studies:
-
internal trust documents that self-reported the benefits resulting from RPIWs (including the RPIWs chosen for ITS analysis)
-
photographs of 5S activities
-
further evidence of the processes followed during QI activities [e.g. project forms, target sheets, value stream maps, 30/60/90 newspapers (formal, structured progress reports at 30-, 60- and 90-day intervals after the improvement activity) and report-out information, visual management boards].
North East Transformation System Coalition Board papers were accessed via the NETS Coalition website, particularly those which contained data on the changing shape of the NETS post 2010. Documentary materials in electronic format were stored on a secure, password-protected server; paper documents and DVDs were placed in a secure, locked filing cabinet. All documentary materials were anonymised.
Qualitative data analysis
The Pettigrew et al. 125 framework of the ‘receptive contexts for change’ (Figure 3) was adopted as a theoretical construct to investigate and understand transformational change in NHS NE. It comprises eight factors: (1) quality and coherence of policy; (2) availability of key people leading change; (3) long-term environmental pressure to trigger change; (4) supportive organisational culture; (5) effective managerial–clinical relations; (6) co-operative interorganisational networks; (7) simplicity and clarity of goals and priorities; and (8) fit between the change agenda and its locale.
FIGURE 3.
The ‘receptive contexts for change’ framework [reprinted with permission of SAGE Publications, London, Los Angeles, New Delhi and Singapore, from Pettigrew AM, Ferlie E, McKee L. Shaping Strategic Change: Making Change in Large Organizations: The Case of the National Health Service. London: SAGE; 1992 (© SAGE, 1992)]. 125
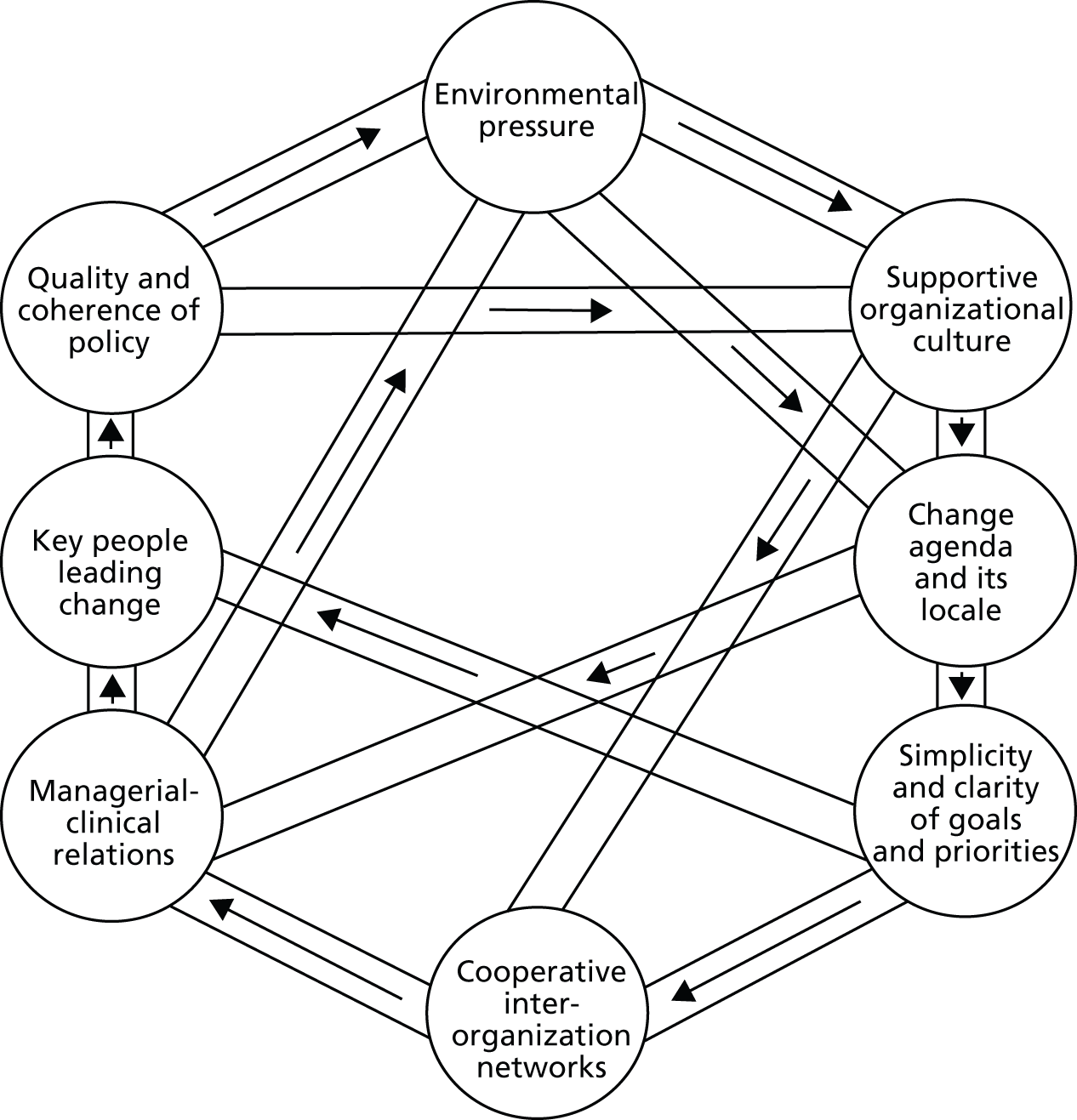
From these eight factors a series of subcodes were derived through a detailed exploration of the explanation of the interaction of these factors offered by Pettigrew et al. 125 The coding framework is set out in Table 4.
| Code | Subcode |
|---|---|
| Quality and coherence of policy | Blueprint |
| Vision | |
| Coherent policy | |
| Fragmented policy | |
| Framing strategic issues | |
| National policy | |
| Regional policy | |
| Shared world view | |
| Trust policy | |
| Commitment building | |
| Key people leading change | Continuity |
| Leadership | |
| Leading change | |
| National level | |
| Personality | |
| Regional level | |
| Stability | |
| Team building | |
| Trust level | |
| Environmental pressure | Delay |
| Denial | |
| Energy drain | |
| Low morale | |
| Radical change | |
| Restructuring | |
| Financial | |
| Supportive organisational culture | Achievement |
| Challenging and changing beliefs | |
| Deep-seated assumptions | |
| Flexibility | |
| Hierarchies | |
| Openness | |
| Risk taking | |
| Role models | |
| Value base | |
| Managerial–clinical relations | Blocking change |
| Common ground | |
| Communication | |
| Honesty | |
| Identifying needs | |
| Trust | |
| Relationship building | |
| Co-operative interorganisational networks | Boundary spanners |
| Communication points | |
| Informal links | |
| Purposeful | |
| Sharing and learning activities | |
| Bargaining | |
| Simplicity and clarity of goals and priorities | Conflict resolution |
| Key priorities | |
| Organisational framework | |
| Patience | |
| Persistence | |
| Managing complexity | |
| Change agenda and its locale | Pace of change |
| Change in power balance | |
| Trust-level culture | |
| Regional-level culture | |
| National-level culture | |
| Workforce changes | |
| Opportunities |
The researchers engaged in three iterations to arrive at the final deductive framework. The approach considered a pattern of association rather than direct causation between the independent and dependent variables. 128 The framework considers receptive conditions for change which are dynamic and reversible through changes in personnel or management action. The approach identifies patterns in processes and recognises emergence, possibility, precariousness and iteration. The framework is based on the following principles (1) change is studied over time in the context of interconnected levels of analysis; (2) change is considered in terms of the past, present and future; (3) the relationship between context and action is explored; and (4) change is considered to be neither linear nor singular. All qualitative data (e.g. interview data, focus group data, etc.) were coded against this framework.
During the next step of the analysis, the data were coded deductively against the NETS ‘three-legged stool’ (Vision, Compact, Method) to provide the NETS organisations with analysis that would correspond more directly to their transformational change ambitions. The framework was developed through an analysis of the SHA’s policy documents on NETS. The codes associated with the Vision were coded against the ‘seven no’s’ which were central to NHS NE’s approach to QI. The Compact codes were developed by looking at the policy documents that set out the mutual expectations between staff and the organisation. The psychological contract aimed to ensure that all staff and managers were clear about the expected approach and behaviours that should be demonstrated in the workplace. The codes developed for the Method focused on the lean tools that were adopted in the workplace and used in the RPIWs or equivalent improvement events for non-VMPS sites. An identical approach to developing the NETS ‘three-legged stool’ framework and the coding process as outlined above was adopted to ensure consistency and reliability. Again, all qualitative data (e.g. interview data, focus group data, etc.) were coded against this framework. The coding framework is shown in Table 5.
| Code | Subcode |
|---|---|
| NETS Vision | No barriers to health and well-being |
| No avoidable deaths, injury or illness | |
| No avoidable suffering or pain | |
| No helplessness | |
| No unnecessary waiting or delays | |
| No waste | |
| No inequality | |
| General NETS Vision | |
| NETS Compact | Unhappiness |
| Old Compact | |
| New imperatives | |
| New Compact | |
| No knowledge of Compact | |
| NETS Method | Gemba Kanri (standardisation, 5S and visual management) |
| Seven wastes | |
| Production and material control (Kanban Pull) | |
| Intercompany lean (single sourcing) | |
| Organisation for change (teamworking, continuous improvement and QC) | |
| TQM (focus on the customer) | |
| Cellular or line layout (flow) | |
| Ergonomics | |
| SMED | |
| OEE | |
| Andon | |
| Jidoka | |
| Smallest machine concept | |
| Fool proofing |
Qualitative data analysis faces the challenge that other researchers may interpret the data in a different way, and this issue had to be addressed as part of the study. Miller and Crabtree129–131 argued that five iterative phases needed to be undertaken, namely describing, organising, connecting, corroborating/legitimating and representing the account. By following this approach, the crystallising, corroborating and legitimating aspects of the data analysis process were achieved.
In summary, the deductive frameworks were developed to initiate the investigation of transformational change in NHS NE. The first stage of analysis was to deductively code all qualitative data to these frameworks. Secondly, all qualitative data were then coded inductively, allowing themes and issues that the two deductive frameworks did not detect to be identified. This was an iterative process that occurred continuously throughout the 3 years of the study period.
Interrupted time series
Increasingly, ITS analyses are being used to evaluate the impact of health-care interventions, including the effects of health service and policy interventions. ITS analysis is most effective in detecting the impact of the intervention when the intervention takes place over a short period of time, as opposed to being spread over time. 126 ITS analysis is the strongest observational design for evaluating the impact of interventions and takes into account the trend in outcome measures as well as the pre-intervention level. 127
At the micro level, the impact of selected RPIWs was evaluated using a controlled ITS design. The ITS approach was adopted owing to the strength of the design and the short period over which RPIW interventions took place. The ITS design utilises multiple observations over time that are ‘interrupted’, usually by an intervention or treatment,132 and allows for the statistical investigation of potential biases in the estimate of the effect of the intervention. 133,134 Short time series need to have at least three observation points in each of the pre- and post-intervention phases. 135 Therefore, data in this study were collected for at least three time points pre intervention, and for at least three time points post intervention (and the ability to obtain these data was a key inclusion criterion for RPIWs that could be subjected to this form of evaluation). The ITS design can be further strengthened by the inclusion of one or more control groups, and therefore the research aimed to identify control units where possible. 132
Data and data sources
The initial intention was to evaluate at least one RPIW within five pathfinders using ITS analysis. However, appropriate RPIWs with suitable historic data were not available in each pathfinder. The result was that one RPIW was analysed from site 09, and four RPIWs were analysed from site 10. The five RPIWs evaluated were:
-
purposeful inpatient admission (PIPA) (site 10)
-
community psychosis, referral (site 10)
-
community psychosis, treatment (site 10)
-
community psychosis, discharge (site 10)
-
acute surgical admissions (abdominal pain) (site 09).
Internal controls were available for three RPIWs (community psychosis referral, treatment and discharge). However, no external controls were available for these RPIWs owing to the different service structures in the comparator trust (which, during the time period under study, did not have separate psychosis and non-psychosis community teams). External controls were explored for the other RPIWs but difficulties in obtaining data for the intervention RPIWs indicated that there would not be sufficient time within the study to obtain the external control data.
The RPIW studies consisted of multiple observations over time that were ‘interrupted’ by the RPIW intervention, with the time point specified as the RPIW week. Outcome measures include clinical measures, such as the percentage compliance with a standard, and efficiency measures, such as the length of stay in hospital. These were intended to measure (1) the outcome of the targeted change; and, where possible, (2) ‘halo effect’ indicators (indicators of change that could be hypothesised to also occur if the targeted change is successful) and (3) indicators of unintended consequences.
The performance of RPIWs should be measured and recorded on a target sheet at the baseline and after 30, 60 and 90 days as specified by the RPIW process (with one of these data sets incomplete for the selected RPIWs). However, these data were not available for the period before the intervention. Therefore, it was necessary to select RPIWs for which there was routinely collected data for a sufficient period prior to the RPIW to provide a minimum of three pre-intervention data points. Data could be obtained from electronic record systems (where these existed) or via extracts from other ‘in-house’ systems such as radiology and theatre information systems. Using these systems, data were available for at least a year prior to the RPIW. In one case, concerning the PIPA RPIW in site 10, it was possible to construct a data set covering several years before and after the intervention from two hospital information systems, following males and females through three ward changes, including a move to a new hospital, linked by a unique anonymised patient identifier (see Chapter 7, Site 10 purposeful inpatient admission rapid process improvement workshop).
An alternative approach would have been for the research team to collect bespoke data prior to a planned RPIW. However, despite reviewing RPIW forward programmes in all of the study sites, it became clear that there were no RPIWs planned for which such prospective data collection was possible for a sufficient time period in advance of a RPIW. This was usually because the RPIW leaders had not identified their outcome metrics sufficiently far in advance, or the organisation’s forward RPIW programmes were uncertain.
The shortcoming of using routine data was that the range of measures available was limited and it was necessary in some cases to use proxy measures rather than directly measuring the desired outcomes. However, where this was necessary, the staff responsible for planning and conducting the RPIWs agreed that the proxy measures had a clear relationship with the outcome data they were collecting within the RPIW process. The available routine data were also too limited to be able to identify ‘halo effect’ or ‘unintended consequences’ indicators. However, an advantage of using retrospective data was the opportunity to include RPIWs that had commenced before the research (historic RPIWs).
The researchers engaged with the leaders of the selected RPIWs to identify the appropriate data that related most closely to the targeted outcomes of the RPIW. The data identified to evaluate the outcomes of each of the selected RPIWs are provided (see Table 6), as are some of the issues encountered in finalising these choices (see Table 7).
Data collection
The researchers liaised with the trusts’ information staff to identify and obtain extracts of the appropriate anonymous data. The next section gives more details on the data sets provided (see Table 6), and defines the measures and shows the data used to calculate them (see Table 7). For one RPIW (site 10, PIPA RPIW), a review of the first draft of the analysis report with the trust’s information staff revealed that the data set provided was missing some key variables, and a new data set was provided for analysis.
Quantitative data analysis: interrupted time series
Although some of the time series comprised an extended set of observations, the data were analysed using the repeated measures approach recommended for short time series. This approach comprised the following steps. First, for each dependent variable an appropriate error structure was selected; second, for continuous variables a normal error structure was adopted; third, for binary variables a binomial error structure was assumed and finally, for variables in the form of a count, either a Poisson or negative binomial error structure was chosen. When there were data from a number of units, variation between the units was included as a random effect to allow for the correlation of repeated responses from the same unit. In each case, the appropriateness of the choice of error structure was evaluated, and where this procedure indicated a problem an appropriate transformation of the variable of interest was considered. In general, variables in the form of time to event were transformed using a suitable log transformation.
Once an appropriate baseline model had been identified (generally a constant term with the appropriate error terms), a number of nested models were then considered. For evaluations with no control units these models included:
-
a general trend over time
-
a simple difference pre–post introduction of the RPIW
-
a model with both these terms to allow us to estimate the impact of the RPIW, controlling for an underlying trend
-
a model with different trends pre–post the introduction of the RPIW.
When there were data from control units, the difference between control and intervention units was considered as a fixed effect and the estimate of the impact of the RPIW was based on an interaction between the types of unit (control or intervention) and time (pre–post introduction of the RPIW).
For some variables there were clearly seasonal effects. For example, operations undertaken in accident and emergency (A&E) on a weekend clearly differed from those carried out during the week. In such cases, the impact of the RPIW was re-estimated, taking into account the difference between appropriate units (day of the week and/or month of the year). Prior to modelling, the dependent variables were explored extensively using graphical plots to identify obvious trends and any unexpected features.
Where possible, draft analysis reports were ‘sense checked’ with the clinical leaders of the RPIWs who had originally assisted with identifying the appropriate data for the evaluation. The outcome measures and data sources can be seen in Table 6. The outcome measures and the data definitions and issues encountered can be seen in Table 7.
| RPIW | Outcome measures for ITSa | Data sources and data sets |
|---|---|---|
| PIPA | Length of stay (in hospital) Length of stay on ward Time from admission to ward to discharge from hospital |
For individual anonymised records, extracted from two information systems (patient administration system for 1 April 2005 to 31 December 2008, and patient record information system for 1 April 2008 to 31 December 2012): Date of admission to hospital Date of admission to or transfer to ward Date of discharge from or transfer out of ward Date of discharge from hospital Gender Anonymised unique patient identifier A linked data set for males and females was created across the full period from April 2005 to October 2012, covering the following wards: Male/female wings in single ward (2005–06) Male ward, old hospital (2006–11) Female ward, old hospital (2006–11) Male ward, new hospital (2010–12) Female ward, new hospital (2010–12) |
| Community psychosis (referral) | Duration from referral received to first allocation Duration from referral received to first successful face-to-face contact % DNAs at first appointment |
For individual anonymised records extracted from the electronic patient record information system, for the period 1 January 2009b to 31 July 2012 for all referrals to eight adult community psychosis teams (3 × intervention sites; 5 × control sites): Anonymised unique patient identifier Team name Team locality Gender Referral received date First allocation date First successful face-to-face contact date Second successful face-to-face contact date Referral close date First cluster of referral score Latest cluster score First assessment date First assessment type Latest care plan assessment date Latest care plan type Community contact date(s) Community contact task Community contact outcome |
| Community psychosis (treatment) | Duration from referral received to first assessment Duration from referral received to formulation Percentage of patients with a care plan after formulation meeting |
|
| Community psychosis (discharge) | Discharge rates Duration from referral received to discharge Rejected: ‘treatment complete’ rates Rejected: percentage of discharged patients with a cluster allocated Rejected: cluster score at discharge Rejected: latest cluster score |
|
| Acute surgical admissions for abdominal pain | Percentage of patients attending A&E with abdominal pain receiving an abdominal X-ray For those who receive an X-ray, mean time from arrival in A&E to X-ray Percentage of A&E attendances with abdominal pain admitted to hospital Percentage of admissions who get a surgical procedure during their stay For those who receive a surgical procedure, mean time from arrival in A&E to procedure Percentage of admissions who get a US during their stay For those who receive a US, mean time from arrival in A&E to US Percentage of days when emergency theatres started before 10.00; percentage of days when they finished before 20.00 |
For individual anonymised records extracted from a linked data set created from the trust’s A&E, radiology and patient administration systems, linked by hospital number, for the period 1 September 2009 to 30 September 2012 for all attendees at A&E presenting with abdominal pain: Anonymised unique patient identifier Date of attendance at A&E Arrival time at A&E Abdominal X-ray in A&E (yes/no) A&E abdominal X-ray date A&E abdominal X-ray time A&E abdominal US (yes/no) A&E abdominal US date A&E abdominal US time Admitted (yes/no) Admission date Time of admission Inpatient surgical procedure (yes/no) Surgical procedure date Procedure time Inpatient US (yes/no) Inpatient US date Inpatient US time Inpatient US type Inpatient abdominal X-ray (yes/no) Inpatient abdominal X-ray date Inpatient abdominal X-ray time Emergency theatre start and finish times for individual anonymised records for emergency theatres extracted from the trust theatre system, ‘Ormis’, for the period 1 September 2009–30 September 2012: Anonymised unique patient identifier Surgery date Specialty (not requested/used) Anaesthetic start time Leave theatre time |
| RPIW | Outcome metrics for ITS | Relevant data fields for each measure | Comments |
|---|---|---|---|
| PIPA | Length of stay (in hospital) (A) | (A) Admission date, discharge date | The objective of the RPIW was not focused on reducing length of stay (see Chapter 6, Case study 1: purposeful inpatient admission rapid process improvement workshop for objectives), but this was one of the key metrics used to track impact of the RPIW internally. Other metrics used by the trust (e.g. incidents of violence and aggression, staff sickness rates) were either not available from the two information systems or not for the period required for the ITS Ward staff had maximal control over measure (B) but measure (C) was also included to avoid missing perverse impacts |
| Length of stay on ward (B) | (B) Date of admission to or transfer to ward, date of discharge from or transfer out of ward | ||
| Time from admission to ward to discharge from hospital (C) | (C) Admission date, date of discharge from hospital | ||
| Community psychosis (referral) | Duration from referral received to first allocation | Referral received date First allocation date |
Referrals of interest were all new episodes (patients may well have been seen by services in the past but had been discharged previously) |
| Duration from referral received to first successful face-to-face contact | Referral received date First successful face-to-face contact date |
||
| Percentage DNAs at first appointment | ‘Outcome’ field = ‘DNA/failed to attend’ where ‘community contact date’ is the first date recorded for that patient ID | ||
| Community psychosis (treatment) | Duration from referral received to first assessment | Referral received date Date of first assessment Where ‘assessment’ is defined as ‘task’, field is not equal to ‘practical, care coordination, or interventions’ |
From discussion with the clinicians, every contact usually involves some sort of assessment but the aim of this measure is to focus on those encounters where the primary aim is assessment. Therefore, the clinicians advised defining this by a process of exclusion |
| Duration from referral received to formulation Proportion of referrals with diagnosis/formulation recorded |
Referral received date Date of ‘task’ field = diagnosing/formulation Date of ‘task’ field = diagnosing/formulation or = ‘assessment’ ‘Task’ field = diagnosing/formulation, or ‘task’ field = diagnosing/formulation or = ‘assessment’ |
The clinicians advised that only doctors would use ‘diagnosing/formulation’ as the task for this. Nurses and others might often use ‘assessment’ as the task instead The clinicians therefore suggested two measures: ‘time to diagnosing/formulation’ and ‘time to diagnosing/formulation and/or assessment’ (They were confident that no other tasks would be used) Production of this additional measure was a necessary precursor to the measure above, so was added to the analysis plan |
|
| Not done (see Comments): percentage of patients with a care plan after formulation meeting | Latest care plan date any team Where ‘latest care plan type’ = ‘CARE PLAN (20??)’; ‘CARE PLAN REVIEW (AD09)’ Date of formulation meeting (identified as above – both options) If ‘latest care plan date any team’ (as defined) is after date of formulation, this variable is ‘yes’ |
From discussion with the clinicians, there were two descriptors which could be focused on: ‘care plan (20??)’ and ‘care plan review’, so we proposed to use only these types. However, on examination of the fields provided in the data set, there were other possible fields for ‘care plan’, so the variable definition was inconclusive. On this basis, this measure was omitted during the analysis | |
| Community psychosis (discharge) | Discharge rates | ‘Ref close date’ means discharge date Percentage of patients where ‘ref close date’ contains a date |
|
| Duration from referral received to discharge | Referral received date Ref close date |
||
| Rejected: ‘treatment complete’ rates | ‘Outcome’ = ‘TREATMENT COMPLETE’ | The clinicians advised that this only applies to a single treatment/therapist – does not mean discharged/treatment overall complete. Therefore the measure was rejected | |
| Rejected: percentage of discharged patients with a cluster allocated | This was rejected after determining that almost 100% of records had a cluster allocated | ||
| Rejected: cluster score at discharge | Where ‘ref close date’ contains a date Latest cluster score |
‘Cluster scores’ (reference the definitions, methodology) are intended to reflect patient need rather than outcome. Although within the psychosis clusters (10–17) reduction of cluster score after a period of treatment would usually be expected as needs for intervention reduce, the consultant psychiatrist who we consulted did not think it was appropriate to use as an outcome measure (although using cluster score as a casemix variable could have been explored) Measures rejected for the ITS on this basis |
|
| Rejected: latest cluster score | Latest cluster score | ||
| Acute surgical admissions for abdominal pain | Percentage of patients attending A&E with abdominal pain receiving an abdominal X-ray | Abdominal X-ray in A&E (yes/no) | |
| For those who receive an X-ray, mean time from arrival in A&E to X-ray | Abdominal X-ray in A&E (yes/no) Arrival time at A&E A&E abdominal X-ray date A&E abdominal X-ray time |
An initial review of the data set suggested some outliers with implausible times. A discussion with the lead clinician for the RPIW on plausible times produced the following: Time from attendance to X-ray in A&E: minimum plausible time is 15 minutes Time from attendance to admission: minimum plausible time is 1.5 hours (90 minutes) |
|
| Percentage of A&E attendances with abdominal pain admitted to hospital | Admitted (yes/no) | While the A&E information system was only able to select attendances for inclusion on the basis of a category of generic ‘abdominal pain’ as a presenting complaint, the clinicians would ideally have wanted to exclude ‘gynaecological pain’ from the data set extracted. A more selective data set would be predicted to be more sensitive to the impact of the RPIW (which aimed to influence the general surgical pathway) | |
| Percentage of admissions who get a surgical procedure during their stay | Admitted (yes/no) Inpatient surgical procedure (yes/no) |
||
| For those who receive a surgical procedure, mean time from arrival in A&E to procedure | Inpatient surgical procedure (yes/no) Arrival time at A&E Procedure time |
||
| Percentage of admissions who get a US during their stay | Admitted (yes/no) Inpatient US (yes/no) |
||
| For those who receive a US, mean time from arrival in A&E to US | Inpatient US (yes/no) Arrival time at A&E Inpatient US time |
An initial review of the data set suggested some outliers with implausible times. A discussion with the lead clinician for the RPIW on plausible times produced the following: Time from admission to inpatient X-ray: minimum plausible time is 30 minutes Time from admission to inpatient US scan: minimum plausible time is 30 minutes |
|
| Percentage of days when emergency theatres started before 10.00 Percentage of days when they finished before 20.00 |
Surgery date Anaesthetic start time Surgery date Leave theatre time |
Further discussion was required with the RPIW clinical lead to determine how to deal with the timings of what would appropriately be considered as urgent (‘life or limb’) surgery which must happen outside these hours. As a result, the metrics were more tightly defined as: Proportion of days when a procedure was started between 08.00 and 10.00 Proportion of days when all procedures that were started before 20.30 were also finished before 20.30 |
Chapter 5 Perspectives on the North East Transformation System
The NETS initiative involved thousands of NHS staff in the North East of England. Hundreds were certified to train others in formal methods of QI and transformational change – whether using the VMPS, Productive Series modules, the Unipart Way, or other tools and/or programmes borrowed and adapted from health-care organisations elsewhere. Many more received NETS-related training, took part in the improvement activities (in site 10 the number reached 50% of the total workforce by mid-2011), and were either involved in or exposed to the creation of new organisational Visions and Compacts. Links were established with further education providers in the region to deliver NETS-related qualifications.
Although the NETS initially focused principally on NHS provider and commissioning trusts, it was intended to include the general practice community and go beyond the confines of NHS organisations. This was because care pathways include the primary, community and social care sectors. It was recognised that adopting the NETS approach would be difficult for GPs. This was because human and financial resource limitations could make lengthy periods of non-clinical training problematic. Primary care organisations were not included in this study as they had been addressed by previous research. 136
This chapter explores perceptions of the evolution of the NETS, particularly in relation to its three fundamental elements: Vision, Compact and Method. It draws on transcripts of interviews and focus groups, field observations, notes of a research team dissemination meeting with the NETS study sites, NETS Coalition Board papers and internal trust documents.
The development of the Vision
The initiators of the NETS emphasised the development of a Vision to create a shared value system. It was an essential means to ensure that improvements were driven from the bottom up, as well as from the top down. In January 2011, one of the SHA’s most senior staff members made the point that although the NHS was adept at publishing and formally adopting standards for improved patient care, sound finances and better patient safety, it seemed to struggle to apply these effectively at the point of delivery. The Vision (regional and local) was seen as a central, enabling link between aspiration and action on the ground:
. . . it is crucial that the vision is shared, truly believed and firmly embedded in the minds of people and the very fabric of organisation thinking. Without this the purpose and goals to which people are striving become less clear and potentially misaligned.
NHS NE99
A 2010 NETS Coalition Board briefing on the history of the VMPS stressed the importance of the regional Vision (the ‘seven no’s’) as a psychological tool to strongly encourage a shift from a mindset that is tolerant of, and expects, errors and defects, to one that believes the perfect patient experience is possible. The Compact sought to shape the psychological contract between staff and the organisation in which they worked. Thus, both the Vision and Compact were mutually reinforcing and aimed to bring about transformational change through aligning stakeholders’ values in order to achieve a patient-centred organisation. The Method, the most visible component of the NETS though not the most important, provided a toolkit that facilitated the improvement of operations to achieve the Vision.
An organisation cannot usually adopt a complex management practice without shaping the Method to meet its specific context and requirements. Therefore, the way the NETS was adapted by trusts varied. Views varied concerning the study sites’ success in creating, sharing and embedding a vision that was more than just rhetoric or well-meaning words. However, nearly all of the sites had produced a written statement of the Vision. A number of sites incorporated these into highly visible graphics that were used on official documents and websites, displayed as posters in public areas, and even produced as staff badges.
Senior SHA leaders were convinced about the purpose of a clearly stated Vision as a unifying rallying point. However, there was variation between the study sites in terms of the widespread understanding of the Vision. Some interviewees said that, on becoming part of the NETS, their organisation made use of an existing Vision statement to avoid repeating an exercise that was considered to be already complete. In one case, this was a contributing factor in deciding not to adopt the VMPS version of the NETS, as explained by a senior director of a hospital trust: ‘. . . our plea was . . . we have just gone through a 3-year . . . assessment process and we have a vision . . . What we want to do is focus on implementing that . . . as opposed to we start again . . .’ (site 14, senior director).
However, some interviewees from the VMPS study sites commented that the development of the Vision, Compact and Method had to be considered as a holistic package. In VMPS study site 10, the alignment of the Vision with the Compact and Method was reinforced through the distribution of a prompt card that reminded staff of the Vision and its surrounding values, the behaviours linked to those values and a summary of key lean tools. A senior member of the KPO team saw the prompt cards as a way for junior staff to challenge upwards, to hold leaders to account: ‘If we’re working with junior staff I often challenge them to challenge their leaders, because if leaders are not following our trust Vision and Compact then I think staff have every right to question it’ (site 10, KPO team member).
Not all VMPS sites – even wave 1 pathfinders – made significant progress in embedding their NETS-inspired Vision throughout the organisation. The medical director of one site, which had focused on its drive to attain foundation trust (FT) status, commented that the Vision was understood by senior staff, but had not been shared sufficiently at all levels. This was because operational problems facing middle managers took priority over the dissemination of the Vision. In general, board members and senior managers appreciated the importance of linking the Vision and Compact and disseminating these throughout their organisations. This was the case even in a study site (02–05) that had decided not to pursue the VMPS version of the NETS after some initial interest. This was one of the NHS organisations disbanded at the end of March 2013. The acting chief executive officer (CEO) expressed the view that implementing the Vision and Compact was still important irrespective of the impending reorganisation.
The utility of the organisation-wide Vision, as well as the regional Vision, was recognised by many interviewees as a means to unite staff behind a ‘flag’. It acted as a memorable shorthand for a number of strategic objectives and communicated the organisation’s values to patients, public and other, external agencies. Some interviewees saw significant value in adapting the process of creating and communicating a Vision to organisational units or initiatives. This approach supported the development of business units within FTs with their own leadership teams, budgets and targets.
Compact development
It was recognised by NHS NE that a step change in its approach to change management was required to achieve transformational change. The Compact focused upon aligning people and organisations to the Vision. To quote NHS NE’s 2008 strategy Our Vision, Our Future, Our North East NHS: A Strategic Vision for Transforming Health and Healthcare Services Within the North East of England:99
Whilst necessary, developing vision is clearly not sufficient and the NETS approach insists upon the vision being complemented in equal measure with a compact that aligns culture and behaviour as well as consistent method for continuous improvement.
[The Compact] describes the unwritten rules, the behaviours and the signals that are sent by managers.
It explicitly sets out the ‘unwritten rules’ making them written and transparent, it sets out the expectations and behaviours that are required to be more effective in delivering change and it is mutually binding and enforced.
It is a reciprocal contract for the ‘give and the get’.
In defining the Compact in these terms, NHS NE explicitly recognised the critical nature of this particular leg of the ‘three-legged stool’, and therefore the role of people in delivering transformational change.
The following subsection examines interviewees’ perceptions of the role of the Compact within the NETS, how Compacts were developed and implemented, and how trusts sought to integrate the Compact with existing managerial practices, including the management of change.
Perceptions of the role of the Compact
The role of the Compact in the NETS was accepted by the majority of interviewees who felt that Vision and Method had to be accompanied by a clear set of expectations, the ‘gives and the gets’, in order for transformational change to occur.
. . . we could give you all the tools in the world but it won’t make a jot of difference unless you’ve got people’s hearts and minds in the right place.
Site 02–05, senior director
. . . the issue for me was if you don’t genuinely talk to people about the behaviours that you expect, the fact that this is going to feel different for individuals and it’ll be quite challenging for them, if you don’t do that, then you can spend as much time as you like agreeing what the vision might be, agreeing how you measure stuff, but when push comes to shove you will not enact the change. And we learnt that and we saw it in Japan, we saw it in Seattle. So from my perspective I think the Compact is the bit that we neglect at our peril.
Site 11–12, senior director
There’s a lot of little empires and a lot of this is how we’ve always done it, and there’s a lot of resistance to change in any shape or form. And I think telling people that we’re going to be able to do change in a week when for some of them it’s 20 years is a short time.
Site 07, senior manager
The Compact is about changing cultures, having a formal agreement between managers and clinicians and administrators so that everyone knows what behaviours are expected, the gives and the gets.
Site 14, matron
. . . it’s not just about doing the bit of work, you have to behave in a particular way, you have to have that Compact, managers have to behave in a particular way, people have to understand that by being involved in the change process they aren’t going to be disadvantaged in any sort of way.
Site 10, senior director
The tensions between managerial and professional staff in the NHS have been well documented, as noted in Chapter 2. A number of interviewees commented on the need for changes in behaviour, particularly among doctors. They recognised that doctors occupy a more powerful and pivotal position than other staff and, as a result, a Compact was regarded as beneficial for supporting change.
. . . so we’re trying to get more and more medics through different development which would improve behaviours and make it more likely that they work in teams . . . so if you have to force the issue you can force it in the end more with nurses than you can with doctors.
Site 01, board member
This trust included a new section in the contract of employment on values. It also changed the process for interviewing consultants to emphasise expected values and behaviour: ‘. . . new consultants coming in, sign up to these behaviours’ (site 01, nurse manager).
There was very little overt scepticism of the need for, and value of, a Compact, although occasionally such views were expressed. One example follows:
. . . maybe I should come out at this particular point and not declare myself a sceptic but declare myself to be overall completely content and supportive of the intentions, as I understand them to be, which is to make things more efficient and to reduce waste in the organisation and to continually look at the way you do things and see if you can do them better. If the cynical side of me came out I would say that I remember going through a fairly similar process myself . . . only we called it ‘total quality’. So therefore all this terminology about compacts and this kind of stuff leaves me a little cold. It doesn’t mean I don’t support the process itself, but I just find it somewhat amusing I suppose that these days we have to badge all of the things that we do in the name of sensible sound management techniques into something which has a sort of glitzy attachment to it in terminology.
Site 07, board member
How the Compact was developed
The development and dissemination of the Compact varied between trusts. Staff consultation was a common theme in trusts where the Compact was well developed and widely recognised. Consultation often took place over a long period of time, and involved road shows; focused interviews with professional groups; meetings that cut across functional groups; departmental meetings; and the distribution of copies of the Compact.
In one trust the Compact was developed over a relatively short period of time, but it was acknowledged that further development was needed:
. . . we’ve got a Compact, I think we spent about 3 months doing it, and in the end it turns out it’s a piece of paper that sits in the corner because you don’t live and breathe it . . . let’s just stand back from it all now, let’s do things and then we’ll test what people think our Compact is and then we’ll refine it, then we’ll refine it again and then we’ll refine it again.
Site 14, business unit director
Some trusts made little progress on their Compacts. In response to the question, ‘Does your trust have a Compact?’ focus group members working in HR responded as follows:
I don’t think we do.
We don’t, we’ve debated it . . . we haven’t picked up that Compact issue yet [reflecting the fact that in this trust the focus had been on vision and process].
No, I don’t think you’d find many people that have heard a lot about it to be honest. It might be one of those headquarters things that they know about that we don’t.
Not all trusts gave equal weight to the Compact element of the ‘three-legged stool’. One trust deliberately avoided using the word ‘Compact’ because managers felt it ‘was not really helpful’. Instead, the trust employed what it called ‘250 events’ where groups of senior staff brought together groups of approximately 250 staff to examine particular issues and to ‘get a staff consensus and get an agreed way forward’ (site 10, senior clinician). Compacts typically occupy one side of A4 paper and comprise a series of ‘gives and gets’. Box 2 shows an example of some of the expectations included in the staff Compact of one trust; these were clearly focused on providing a receptive context for change.
Staff will be ‘involved in and supported through the process of change and managing the process of change’; there will be ‘no compulsory redundancies should job numbers reduce as a consequence of quality improvement activities’.
StaffStaff are expected ‘To respond to the changing needs of patients and the people who use our services, as well as changes to the requirements of other “customers” and changes in demand for services’; be willing to ‘support, co-operate with and contribute to quality improvement activities and especially with the testing of new ideas and innovations’; ‘be flexible with regard to the breadth of work undertaken and the location of their work.’
Both VMPS and non-VMPS trusts recognised the key role of clinicians and made efforts to ensure that they were involved in the development of Compacts:
Clinicians came on board really, really rapidly, but I made sure that, I was very careful in the early days to make sure that the medical director, clinical directors and associate clinical directors were on board, kept up to speed.
Site 10, senior director
. . . it isn’t a Compact as such. When we listen to what they talked about it was largely geared towards consultants and the fact that in effect consultant medical staff are aligned more to their profession than they are to the organisation, and this Compact was something that sort of acted as a bridge across the two. You know, we’ll do this for you and therefore you can do this for us.
Site 06, business development manager
So you’ve got to get, in my opinion, the key movers and shakers in your organisation committed, on board and tooled up.
Site 11–13, senior director
All interviewees considered that the Compact should apply to all staff and this was reflected in their approach to the development of Compacts.
How trusts are integrating the concept of the Compact with existing managerial practices
Compacts were made visible to staff by being posted on notice boards known as ‘visibility walls’; one trust sent a copy of the Compact to all staff with their payslips. This was followed up with staff meetings when awareness was judged to be between ‘5% and 10%’ (senior director, site 10). A staff member commented:
I can probably honestly say that the admin staff wouldn’t have any idea whatsoever what you’re talking about . . . I have a basic idea so I would have to go back and have another read of that to be able to answer your question in a bit more depth.
Site 10, medical secretary
At some sites the expectations of the Compacts were incorporated into other aspects of management/staff relationships. For example, it was included as part of the recruitment and selection process; induction; leadership and development activities; appraisal; and, in one case, the disciplinary procedure (applied when standards of behaviour did not match those set out in the Compact).
. . . we wrap it around everything we do. So if there is a service reconfiguration and you get the normal tensions you do, this gets wrapped around it. And it’s just part of our parlance now that nobody raises an eyebrow when we go, our managers get you know, what does the code tell us about this? How does that help shouting at each other and the code says we shouldn’t be doing that, why are we shouting? And it just gives us a different language to manage. It’s put like the emotional life of the organisation in a place that’s acceptable.
Focus group participant
The value of the Compact was summed up by one interviewee in the following terms: ‘. . . when we ever felt that a wheel had come off and we analyse why, it’s always because we haven’t done enough of the Compact stuff’ (site 01, senior director).
The adoption and use of the Method
Although the SHA initiators of the NETS encouraged use of the VMPS as the Method of choice, it is noteworthy that early official documents often make mention of generic improvement methods:
What we require is change at every level, a focus on behaviours, culture and proven improvement methods and a wider recognition through the systematic use of the quality equation of the links between appropriateness, outcomes/effectiveness, quality of service/personalisation and elimination of unnecessary waste when assessing overall quality.
NHS NE99
This was reflected in the different QI tools adopted by the NETS organisations. These included the TPS-based VMPS, the Unipart Way, the NHS Institute for Innovation and Improvement’s ‘Productive Series’ and a variety of borrowings and adaptations from lean programmes as practised by a range of health-care organisations in the UK, Europe and further afield. All of these approaches were intended to promote and improve quality by
focusing on value-added activity, systematically removing waste (or non-value adding activity) and eliminating defects. It considers quality through the eyes of people and patients . . . to demonstrate the relationship between different features that impact on the value of care as experienced by our patients and people.
NHS NE99
A number of interviewees thought that, despite the promotion of all three elements of the NETS, the Method was generally overemphasised:
. . . I think we draw that NETS triangle as Vision, Compact, Method and Vision’s at the top. But we behave in a way that almost the Method is at the top and maybe that’s where we’ve got it slightly wrong . . . if your Vision and Compact’s in place you’ll find a Method.
Site 08, KPO
I think we’re very much focused on, you know . . . Method – I think we know a lot about the Method, we know about the tools and, you know, the RPIW’s not the be all and end all.
Site 11–13, service improvement manager
The reasons given for this varied. One phase 3 interviewee complained that the very success of one VMPS RPIW in reorganising and streamlining an important and highly visible care pathway had led to a rush of enthusiastic interest in repeating the process in related areas of the organisation. However, this meant that the staff who were involved in the original RPIW were unavailable to run the standard 30-, 60- and 90-day report-outs, and the share-and-spread activity was conducted piecemeal. This was borne out to some extent by the difficulty the research team encountered in many of the VMPS study sites in obtaining the 30-, 60- and 90-day documentation that was supposed to follow each RPIW.
A few interviewees, including some from non-VMPS sites, said that it was tempting to achieve ‘quick wins’ by using the range of available lean tools. This was not seen as necessarily bad practice – indeed, the VMMC recognised that this was a powerful way to achieve early acceptance of the value of lean thinking among staff – except in so far that it could divert attention away from the need also to pursue development of the Vision and the Compact.
Finally, the Method was clearly associated with recognition and reward. During the period of our study, several NETS organisations were nominated for, and won, Health Service Journal and Lean Academy awards. The SHA and the central NETS team regularly organised large-scale report-out sessions at which up to 100 or more staff were present to showcase process improvement. Research team members attended several of these events, and observed that Compact or Vision development appeared to play a peripheral role. The trust’s Vision might be a visible element, but it was not celebrated per se. Changes in staff behaviour and trust culture that had an impact on patients were sometimes highlighted, but the emphasis was mostly on process improvements and changes to the physical environment.
The value of visual management
According to the Lean Management Institute, visualisation is a valuable tool commonly used in lean practice. Among the benefits of visualisation we should include improved clarity over the pace and quality of work, which leads to easier problem solving and sustainable gains. 137
A number of participants interviewed supported this view. For example, as a senior director in one trust explained:
Oh yeah, and I think we have, we have translated a lot of that. Generally a lot of the work that we’ve done, I mean we’ve got our, we keep the . . . report-out wall . . . that we corporately use using visual controls . . . to make sure we’re aware of what we’re working on. We do use a lot of simulation in our change projects. They are, we have been doing the Kaizen work, 3P [Production Preparation Process] work that we’ve been doing around the organisation.
Site 10, senior director
Another interviewee from a non-VMPS site agreed that visual management helped improve the quality of services:
So the type of information that we have on the board is generally non-sensitive, so this is about has the doctor seen the patient, has the discharge prescription been written, has the ambulance been booked for the patient to go home? Anything that you would expect in a patient’s pathway of care that is about that flow happening, so obviously utilising the lean stuff that we want it to flow, has that, can we see it visually? So it’s about that visual management.
Site 01, nurse manager
With increased visual management comes the pressure to sustain any improvements through quickly identifying any deterioration. This allows all individuals to focus on the same key issues and maintain the improvements implemented:
We took this approach, did it with a team, rolled it out across the whole organisation, and we actually went not just to the top quartile, we ended up as the best trust nationally against that. And that was massively around the use of visual control was one of the key things in that, having very clear standard work in place. And we’re just reauditing that, and I’m told that the audit so far – forgot what they’re called now, anyway it’s the National [unclear] Audit process, it’s coming out we’ve maintained that improvement around that one.
Site 10, senior director
Another participant highlighted how visual management provides information and also promotes communication that supports continuous improvement:
Well we’ve got our tier 4 boards, tier 4 visibility boards in all of our teams. They’re all again at various degrees of kind of success, on the shop floor visibility boards as we call it. So they’re currently in place to encourage our staff to continuously talk about what it is that they’re doing and look at their performance and then strive to make improvements.
Site 11–13, senior nurse business manager
It is clear that increased visibility has been achieved by adopting visual management principles.
Lean tools
Lean tools provided the means to achieve continuous improvement. They are complementary and synergistic. However, if lean training introduces too many tools there is a risk of shallow learning, whereas if too few are covered it is not possible to achieve holistic improvement.
The VMPS study sites adopted the VMPS as the ‘Method’, which used 5-day RPIWs. These are based upon a standard framework that includes (1) an overview (introducing team members and assessing the current situation; analysing process flow, Takt time,138 targets and boundaries); (2) an analysis of standard work; and (3) a progress report that measures prior performance and targets (for space, inventory, staff walking distance, parts travel distance, lead time, quality, productivity, 5S and set-up reduction).
The report-outs included a value stream map, Takt time calculations and work flow diagrams that showed the status before and after the intervention, as well as 30-, 60- and 90-day follow-ups (part of the RPIW process). The lean tools covered by the VMPS are 5S/workplace organisation;139 visual control; Kanban; flow of materials; standard operations; Jidoka; the VMPS house; VSM; autonomous maintenance; production levelling; fool proofing; and set-up time reduction. Measuring the impact of improvement activities is necessary for determining the usefulness of the event and whether or not the desired benefits have been achieved. 123 The Method was the key difference between the VMPS and non-VMPS sites. Interviewees from VMPS sites talk about the process in the following terms:
I think [of] the toolset as the number of processes, such as value stream mapping, 5S, Kaizen, 3P that we use, RPIWs, the strategies . . . around patient safety . . . so just in time, the levelling. So when I say we’re using the Virginia Mason’s toolset it’s the tools and strategies and you get that within the Virginia Mason toolset and strategy map.
Site 10, improvement manager
Although the RPIWs were deemed useful, they were also considered to be resource intensive.
And I think it is the priorities of the Trust plus literally the amount of capacity we have anyway in terms of to support RPIWs that shapes those RPIWs . . . so you get your specialist support, the team leader role, the person who does lots of the preparation before, the observation, helps with producing value stream maps and target sheets ahead of the RPIW.
Site 08, senior HR manager
The RPIWs were highly standardised, whereas non-VMPS sites were more flexible in tailoring the implementation to suit their context. The particular Method adopted was less important than the clarity of purpose, i.e. moving towards achieving the Vision. The following subsections assess the adoption of the various lean principles and tools.
Waste
One of the key principles of lean is the identification and elimination of waste to increase effectiveness and efficiency. This is achieved by a value stream map that identifies waste that can be eliminated by using 5S. One interviewee demonstrates this:
Yeah, because that’s what you’re observing. Like you’ve agreed the steps in your process map, your timings on your form will be what you can identify, what’s value-added and not, and using the tools that we use, we put those on the process maps, then identify which step you can perhaps have the biggest impact in terms of reducing the waste. And occasionally we’ll just take that step out altogether, sometimes you can do that.
Site 09, medical services manager
Once people see the benefits and are able to contextualise how removing waste and applying lean tools can help, the Method can become a focal point:
Yeah, well I never found Compact very revolutionary I suppose. For me Compact was, Compact for other people seemed to be very revolutionary but to me what was revolutionary was continuous flow. It was removal of waste. It was thinking about product, it was redesigning a process, visual control, those things were revolutionary.
Site 10, senior clinician
Another interviewee noted that lean tools helped individuals to identify wasteful activities and challenged the way work was undertaken and whether or not better approaches could be adopted:
I mean I think there’s those people who have that personality of kind of 5S, that’s giving them permission to go back and to sort things out in a way that’s kind of acceptable to others now as well because it’s not just about what they want. It’s about this is a philosophy, this is some methodology that we can implement and has meaning behind it, so that’s been well embraced, so 5S in principle goes down really well. The waste, looking at aspects of waste and how we can address that . . . has been again greatly appreciated I think because lots of people have been able to identify that, this aspect of what they do, that is wasteful that nobody’s ever challenged before.
Site 11–13, senior nurse manager
Standardisation
The concept of standardisation in a health context is contested on the grounds that every patient is different, as this interviewee suggests:
So whereas I understand the concept of lean and process and so on, and if you look at the context of, let’s say, I don’t know, a coronary artery bypass graft or if you’re doing a hernia operation or if you’re doing cataracts or so forth, then I can really see that for a lot of that kind of stuff, you’re going to have pretty predictable outcomes. You can look and compare unit by unit. But if you’re looking at something like pneumonia or even stroke or diabetes even, my area of specialist interest, and if you look at all the patients I see with type 1 diabetes, all of them are so different with so many different personal impacts on the chronic disease that it’s hard to know how, on the individual patient-level basis, you can really apply a lot of the lean and other production processes because they very much depend on you having the same kind of system operating all the time. Do you see what I’m getting at?
Site 01, member of management group
Although every patient is different, there are clinical best practices with prescribed processes that may be varied according to the clinical need. The administration is also standardised, for example forms to be completed and data entry requirements. Lean seeks to minimise waste (muda), variation (mura) and work overload (muri). The adoption of standard work allows variation to be reduced by adopting clinical best practice.
Yes. I think somewhere along the way because standard work is such a fundamental bit of what Toyota did I think there’s been a misconception that you mustn’t change anything which seems almost overly paradoxical in a system that’s very much about change and if you change anything you’re breaking the fidelity and it won’t work. I think that’s been part of the problem for some people and why it’s been perceived to be or thought as you do it this way because that’s the standard work but to me the standard work only exists in the Toyota production to reduce variation in the outputs. So it has a particular purpose so the concepts underneath that were trying to reduce variation and outputs and because we’re in the service context how we tackle things in some service contexts might have to be different to how they’re tackled in production contexts.
NETS Coalition manager
Another interviewee provided an example of where standardisation worked well:
Again this is back to, you know, standard forms where . . . it was things like where are the forms going to when they’ve signed these forms, you know, we’re finding them in cupboards and things like that. Well no, now we know the standard work is you’ve booked, and you do the training. Fred the trainer gives it to this person, this person, this person, which goes back into the file which wasn’t there. And I think it would have happened without the RPIW, but I think it would have taken a lot longer to do it.
Site 07, senior manager
But the issue of resistance to standardisation needed to be managed, according to a nurse business manager:
We do try to promote the standard work quite a lot. We try to get people to understand that people should always [have] been able to have that same kind of repeatable aspect of work delivered in that same way, and I think that’s a difficult concept for people in health to get their head around. So we often have quite a debate around, you know, I’m different to that practitioner there and my clients are very different to that one and you can’t just bog standard say that assessment’s going to be an hour or whatever. But I think when we talk through what the actual principles are and how we’re trying to look at the benefits for patients around what they should be gaining from the health visits and the contacts and things then I think sometimes the penny drops and people don’t see it as threatening but I think maybe the term standard work at first was a bit threatening to them.
Site 11-13, senior nurse business manager
Another interviewee highlighted how the tools used as part of the Method link together. For example, being able to see what equipment is available in treatment rooms (visualisation) allows staff to order the right quantities of supplies (waste removal):
All the trolleys have got what should be in the drawers and everything, and they’re labelled as well, and there’s pictures, and where treatment rooms and everything, the sluices and that have all got labels and things. Then we have stock levels and things so that we don’t go over a certain amount of anything and in more clinical rooms, we’ve got the plastic sleeve in so when you’ve used so many, you just top it up to the amount instead of having millions in.
Site 08, dystonia team member
Training
There are two training elements associated with RPIWs. First, workshop and team leaders are required to run a specified number of RPIW events to become certified team leaders. Second, the participants involved in the RPIWs need to be trained in the application of lean tools. Under this model, the number of RPIWs was constrained by the number of certified leaders available. Thus, it was necessary to have a programme of RPIWs which took into account the development of certified leaders as well as identifying areas that would benefit from performance improvement. As one member of the KPO focus group put it:
I mean we call it the scattergun approach to improvement in years 1 and 2 was something which we did because we tried to scatter improvement across a wide variety of clinical directorates and corporate teams. I think year 3 onwards we became more focused towards delivering against the Trust strategic goals. So I’d probably agree there is a need for both types of approach, probably early on in your lean journey a scattergun approach so you get buy in and champions across a number of divisions and corporate service areas, and then as you get more and more buy in, start then to focus on specific goals.
Focus group participant
One of the first stages of planning a RPIW was to identify the staff who would be involved. There was a potential problem of staff feeling demotivated if they were not invited to take part. The formation of ‘in’ and ‘out’ groups was potentially divisive. It was therefore important for the trusts to have an inclusive approach. The point is well made by one of our interviewees:
It has been selective, but I think its involvement is part of the training as well, so we try to involve as many of the staff in RPIWs in the Kaizen events as we possibly can . . . We’ve moved away from having sort of smaller groups of very defined people and handpicked people to well let’s try and have a much broader church in terms of the people who are attending these events. And obviously then there’s some training elements in there, but the, you know, we have a team of modernisation facilitators as well that are linked to all of our services, and they have all been trained in doing the RPIWs and the Virginia Mason tools etc., and it’s about they’re on a rolling programme [and] are going out to staff meetings . . .
Site 11–13, intermediate care business manager
In the early years of the NETS, some RPIWs were focused on the training of certified leaders as opposed to focusing solely on the improvements. A KPO lead reflected on the nature of the training:
Well I think from our point of view, I mean we’ve had over 2500 employees have been part of improvement activity on a workforce of over 5600, so that’s a significant number of the workforce have been directly involved in improvement activity. It is a 10-year journey and we’re still growing with new staff. The end of last month was the first two RPIWs in [location], and we were still back to engaging home teams, rapid change with the shock and how do they link to compact, the values and the behaviours to improving activity. And war wall this morning there were still some negative comments from the home teams about 5S activity, despite the fact that we’ve put in a lot of effort. So we still learn, it’s still an ongoing process. We did those two RPIWs during sensei week, we’ve got the sensei report yesterday, and sensei has given us more recommendations around engaging home teams and training, tailored training for new process owners and sponsors.
Focus group participant
Another interviewee reinforced the point relating to the capacity and reach of training activities and the time taken to filter down through the organisation:
I think as an organisation, I mean we’ve ran a tremendous amount of events now. We’ve got somewhere in the region of 50 certified leads. You know, some of those have been . . . trained as such, some of them have been through the VMPS model, but at the end of this year I think we’ll have about 50 certified leads who can do training. We’re doing events on a regular basis. So when you look at it like that it has started to go down into the organisation. We always take the opportunity to do some 5S with teams when we do it, so most people now, I’d say probably a good 50, 60% of people have been involved in some sort of RPIW or some improvement event or whatever.
Site 10, service development manager
Rapid process improvement workshop leaders require accreditation and periodic reaccreditation in order to be qualified to run events. The selection and planning of RPIWs therefore needs to accommodate initial training and reaccreditation requirements. Participation in training events is an additional activity outside the normal work of staff. This needs to be accommodated in the plan for RPIWs:
I actually sort of ask people up front when I can expect to get their time, so the presumption is always that they will be able to support in some way, shape or form and, obviously, to keep up registration, well the qualification. We always say that’s the agreement, it’s two RPIWs or a number of Kaizen events anyway, so that’s the premise on which I’ve sort of worked, but linked it in with the cost improvement programme. And obviously then the commitment from the board to say that people have to be free to actually attend events and stuff, so as long as your parameters are set up in the first place.
Focus group participant
The training element is a key component in the VMPS owing to the role RPIWs play in bringing about change. In the early years of NETS, the VMPS sites focused more on running improvement events and training workshops for team leaders. The planned improvements were a by-product of these activities. As the NETS initiative matured a more strategic approach was adopted due to the availability of suitably qualified and experienced leaders.
Undertaking improvements and sustainability
An interviewee commented that sustaining improvements was just as, if not more, important than the RPIW. Therefore, it was better to have embedded change rather than maximise the number of interventions:
The short-term bit is you get the spike and everybody kind of does it and has a focus on it. And then how do you sustain that going forward and don’t revert back to type or whatever else, and that is really the crux of doing it. That’s why I think you go back to the culture and the management group to try and get them clear about their understanding and trying to make sure that . . . they’re responsible because we can’t be everywhere. And it is about having the right thinking and the right kind of mentality in the organisation.
Site 07, senior HR manager
Rapid process improvement workshops are standardised and have produced good results. However, some individuals saw them as a panacea to solve all problems and did not appreciate their limitations. This was highlighted by a service improvement head:
As kind of issues and problem areas arise on part of that work, and then you need to have a discussion about, is a RPIW, is that a good use, like is that a good tool for that, because I do think there is, well there was, initially it was almost like a RPIW that’ll solve everything. So it was almost like if we’ve got a problem let’s do a RPIW on it. And actually, really, we needed to stand back and say well actually that might not be appropriate, it’s too big, it’s too small, it’s only a tool. You know, well it’s a tool with tools with it, do you know what I mean? It’s only one way of doing things.
Site 11–13, senior service improvement manager
Summary
The initiators of the NETS emphasised the development of a Vision to create a shared value system. It was an essential means to ensure that improvements were driven from the bottom up, as well as from the top down. An organisation cannot usually adopt a complex management practice without shaping the method to meet its specific context and requirements. The way the NETS was adapted by trusts varied. Senior SHA leaders were clear about the purpose of an explicit Vision as a unifying rallying point. However, there was variation between the study sites in terms of the widespread understanding of the Vision. It was acknowledged, primarily by the VMPS study sites, that the development of the Vision, Compact and Method had to be considered as a holistic package. It was also acknowledged that a number of the study sites had made significant progress in embedding their NETS-inspired Vision throughout the organisation.
In some trusts there were large numbers of staff involved in developing Compacts. In these cases there was a low level of cynicism and little resistance to their development and dissemination. However, in most trusts the Compact was not given equal weight compared with the Vision and Method. This was despite widespread recognition of the significance of the Compact among senior staff. This research found that trusts see value in addressing the behavioural aspects of the employment relationship through the use of ‘gives and gets’ and explicit statements on standards of behaviour. Some trusts have taken a strategic decision to integrate work on the Compact with other aspects of the way they manage staff. The Compact has been used to develop a supportive organizational culture including managerial–clinical relations in order to facilitate transformational change that is at the heart of the NETS. 123
Despite the promotion of all three elements of the NETS in some sort of equilibrium, the Method was generally overemphasised. It was noted that it was tempting to achieve ‘quick wins’ by using the range of available lean tools which could inadvertently divert attention away from the need to also pursue development of the Vision and the Compact. The Method also became associated with recognition and reward. The VMPS RPIW method was highly standardised, whereas non-VMPS sites were more flexible in tailoring the implementation of their QI programme to suit their context. It was found that the Method adopted was less important than the clarity of purpose, i.e. moving towards achieving the Vision. In the early years of NETS, the VMPS sites focused more on running improvement events and training workshops for team leaders. It was clear that sustaining improvements was more important than the actual Method adopted. Some individuals saw the Method as a panacea to solve all problems and did not always appreciate its limitations.
Chapter 6 Case studies
This chapter presents four case studies that were chosen to illustrate the use of the NETS as a programme for QI activities (VMPS RPIWs plus other approaches) (Table 8). Case studies 1–3 were selected as typical RPIWs for which quantitative and qualitative data were available. It is important to consider both quantitative and qualitative data, as the perceived benefits of the RPIW events go far beyond the RPIW outcomes measured by a limited set of metrics. Case study 4 brings together some higher-level observations concerning a number of different types of NETS organisations:
-
A wave 2 VMPS pathfinder, which, by its own judgement, made steady progress in implementing NETS training.
-
NETS in a health-care commissioning environment. Lean methods in health care have usually been applied to provider organisations, so it was important to include the experiences of this PCT cluster.
-
NETS in a hospital trust that initially used the ‘productive series’ improvement tools, and carried out a lot of ward-based activities.
-
NETS in a hospital trust that made use of an eclectic suite of methodologies for improvement and culture change.
Case studies 1–3 include summaries of the ITS analysis of the RPIWs. Full details of these analyses are provided in Chapter 7 [see sections Summary of findings for the rapid process improvement workshops included in the interrupted time series, Site 09 surgical pathway (abdominal pain), Site 10 purposeful inpatient admission rapid process improvement workshop and Site 10 community psychosis rapid process improvement workshops (referral, treatment, discharge)].
| Case study | Study site code | Type of organisation | NETS characteristics | Notes |
|---|---|---|---|---|
| 1 | 10 | Mental health trust | VMPS | Early RPIW case study (2008) |
| Wave 1 | ||||
| 2 | 10 | Mental health trust | VMPS | Complex, large-scale RPIW activity (a ‘superflow’ of three linked RPIWs) |
| Wave 1 | ||||
| 3 | 09 | Acute hospital trust | VMPS | RPIW activity linked to a changing model of care |
| Wave 1 | ||||
| 4 | 07 | Ambulance trust | VMPS | Development of Method, Compact and Vision |
| Wave 2 | ||||
| 4 | 11–13 | PCT cluster | VMPS | NETS in a commissioning organisation |
| Wave 1 | ||||
| 4 | 01 | Acute hospital trust | Non-VMPS | NETS on the ward |
| 4 | 14 | Acute hospital trust | Non-VMPS | NETS and clinical leadership |
Case study 1: purposeful inpatient admission rapid process improvement workshop
This case study concerned an early NETS RPIW undertaken by one of the wave 1 NETS pathfinder organisations. It took place in early 2008 – prior to the start of the research study – and thus provided a baseline comparison with later RPIW case studies. The RPIW was an attempt to apply the NETS VMPS methods to problems associated with inpatient wards throughout the trust; these are summarised in data obtained from the RPIW project form (Table 9).
| RPIW element | Information provided by RPIW team |
|---|---|
| Problems identified |
|
| Targets |
|
| Resources | Sponsor: trust clinical director Workshop leader: not defined on project form Team leader: assistant clinical director Team members:
|
Study site 10 was one of the first organisations in NHS NE that agreed to become a wave 1 pathfinder and train staff in VMPS methods of quality management. Senior leaders were therefore concerned to apply the NETS version of the VMPS to areas of the trust’s work that were likely to result in successful, demonstrable improvements to quality, patient safety and staff satisfaction. The process for inpatient admission and subsequent treatment was recognised to be in need of overhaul and improvement. Furthermore, it was acknowledged that several previous improvement attempts had failed, reportedly because previous projects had been under-resourced or not sufficiently supported by key staff; a successful RPIW with sustained evidence of a better service would therefore achieve significant recognition and have an impact throughout the organisation. As a senior clinician commented:
But I suppose the pressing issues for our area and why we got involved is there’d been a number of issues for a number of years, that there’d been several improvement events and techniques already tried and had failed . . . much slower processes to a certain degree, ones that just dragged on over months with no changes being made . . . that again just fizzled out so the changes weren’t made.
Site 10, clinical psychologist
Another main driver for tackling inpatient admissions was the 2-year timetable for moving some wards to new accommodation. This was seen as an opportunity to introduce changes to processes and to relationships between staff, patients and families, in advance of moving to a different environment. As the same interviewee noted:
We wanted for the first time to be able to look ahead and say right we’re moving into a new unit in 2 years’ time, do we want to move in doing the same old thing we’ve been doing here that’s not working or do we actually seriously want to plan ahead and be able to move into this. But there was also that awareness of what the future environment’s going to look like, there’s going to be a reduction in beds that we’re going to have to face. If we could improve something, maybe that wouldn’t be as painful, and that’s how it turned out to be. We could reduce the number of beds pretty painlessly compared to other places . . .
Site 10, clinical psychologist
Patient and staff safety was also a major concern, particularly the number of incidents of violence and aggression, and the consequent use of control and restraint techniques. Unsurprisingly in these circumstances, the trust received a number of complaints directly from patients and families, and via the Patient Advice and Liaison Service, in the months leading up to this RPIW. Staff sickness rates were felt to be unacceptably high over the year preceding the RPIW – on occasions reaching 10–15% of staff working time – which in turn caused a high number of overtime hours to be worked.
In general, it was clear to senior leaders and to staff working on the wards that the processes involved in inpatient admission, treatment and discharge were inefficient, contributed to a chaotic environment, caused a considerable waste of resources, left staff dissatisfied and were not focused on the best outcomes for patients.
Rapid process improvement workshop support
Study site 10 was fully committed to the key elements of the NETS – developing the organisation’s Vision and Compact, adopting the VMPS Method, and using trainers from VMMC and Amicus – from the outset. The RPIW had high-level support from the chief operating officer, the trust’s clinical director and the KPO lead as workshop leaders, and a consultant psychologist as the process owner. The trust’s most senior leaders were early adopters of the NETS principles and enthusiastic ‘converts’. As one of them commented during an interview:
[The NETS has] . . . been transformational in terms of the way I think about health care – probably the most interesting thing since going into mental health actually.
Site 10, senior clinician
Pre-rapid process improvement workshop work
The evidence from analysis of documentary materials and interview transcripts shows that the process owner and workshop leaders had prepared the ground carefully for this RPIW. A number of pre-RPIW meetings were held to define and review the problems to be tackled and the overarching aims (‘what we want’). The KPO staff had observed the existing inpatient admission process on a number of occasions (n = 27) and had recorded some baseline data on the time taken for initial assessment and decision to admit, the quality of the physical environment (judged through 5S) and the distance that staff covered during each patient assessment.
A trust presentation produced after the RPIW, in support of its submission to a national health-care award, made it clear that the key internal drivers were patient and carer views (via a service user questionnaire and a ward round audit); serious untoward incident (SUI) recommendations; the constraints of managing a multidisciplinary team; the impending move to a new hospital environment; and a staff desire to make changes. The same presentation noted some central flaws in the pre-RPIW processes, including wide variations in the experience of care, practice that did not reflect policies and a culture that allowed defects to continue while being intolerant of mistakes.
It is not clear from the analysis of the available documents, however, to what extent some of these issues were quantified or supported by data. Staff at all levels appeared to have been fully aware of the shortcomings in the care for patients attending for assessment, admission and treatment. However, this did not equate to having accurate metrics available in all areas. In fact, the process of carrying out the RPIW seems to have acted as a catalyst for a reassessment of what should be measured. As a clinical psychologist noted:
. . . the data collection before and what we collected data on afterwards were different things really in a way. So they had to be retrospective to get some of the baseline stuff, because we didn’t know what was going to come out and the changes that were going to happen.
Site 10, clinical psychologist
Outputs and outcomes
The list below provides an overview of some of the outputs from this RPIW. It is not exhaustive, as the large volume of available material obliged the research team to make a selection. However, the list provides a comprehensive perspective on the range of changes that were made as a result of the RPIW. Some of these outputs relied on data that were routinely collected by the trust (e.g. bed occupancy rates) but the format and purpose of the documents below was specifically related to the RPIW outcomes:
-
30-, 60- and 90-day report-out documents (progress updates)
-
standard process/standard operations documents for:
-
specialist nurse practitioners
-
formulation meetings at different stages of the patient’s treatment
-
admissions by different routes: community mental health team, crisis team, consultant referral
-
transfer of patients to acute hospital
-
care co-ordinators
-
nursing staff
-
clinical psychologists
-
reception
-
pharmacy
-
review meetings
-
senior house officers
-
consultants
-
-
spreadsheet data on admissions and readmissions
-
data on bed occupancy rates
-
data on admissions through crisis requests
-
standard information for patients and family/carers, including discharge planning
-
comparative data on numerous metrics compiled for all adult mental health assessment treatment wards in the trust, for the period of time considered by this RPIW
-
comprehensive evidence of this RPIW being repeated in other wards across the trust and supported by share-and-spread activities
-
inclusion in trust internal communications documents and board papers
-
RPIW submitted to, and a runner-up in, a NHS award for ‘transforming services’.
The trust made considerable efforts to record the views of service users and staff on the effects of the changes brought about by the RPIW. These were incorporated into a report that brought together clinical and performance data, with impressionistic evidence and visual images. These illustrated improvements to the ward environment, to co-operative working between managers and clinicians and to the information provided to service users. The report was illustrative of how the trust reflected on its processes for making judgments about improvements. Charts showing reduced rates of incidents of violence and aggression were juxtaposed with graphs that represented fewer complaints from service users; a significant reduction in the number of beds was set against the picture of improving staff-to-patient ratios; the flow diagram that documented the new care pathway was followed by quotations from staff, patients and carers that were chosen to highlight the improvements made to different steps in the process. The overall effect was to present a holistic account of the RPIW that encompassed its rationale, the available data and evidence, outcomes and effects on staff and patients.
The original intention of this RPIW was to trial a number of changes to inpatient admissions with a view to implementing them (if successful) in every ward in the trust. RPIW report-out information in the form of RPIW ‘newspapers’, from many different wards over the ensuing 4 years, showed that this objective was implemented. Note that the spread of this new way of working was not achieved by ‘telling’ or ‘commanding’. Each ward carried out its own RPIW, led by VMPS-qualified trust staff. Teams were encouraged to take the core learning from the original RPIW and adapt it to their local circumstances, with standard process documents updated as necessary where an innovation warranted this.
This RPIW was frequently mentioned by interviewees as an exemplar that demonstrated the positive benefits of the NETS programme. It received national recognition through the Health Service Journal awards and was cited by senior staff as evidence that lean thinking should apply to issues of quality and safety first and foremost. Financial savings were a likely but secondary consideration. A senior clinician commented that many of the successful outcomes were (self-)reported by the trust, including an unforeseen consequence for levels of patient violence and aggression:
. . . things we didn’t expect to get out were things like violence and aggression . . . it was never an aim to improve violence and aggression . . . if you walked on the wards then compared to now the difference would be striking . . . when you look at what we did, you can see why those things changed because . . . the ward staff, the patients, the families and carers weren’t as frustrated as they had been previously.
Site 10, clinical psychologist
The same member of staff claimed that by taking a classic TPS approach to focusing on customer (patient) needs and removing waste from the processes associated with care and management of inpatients, doctors, nursing staff and pharmacists were freed from many hours of non-value-added work. This was to the benefit of patients and their families. However, the most important change brought about by the RPIW was said to be conceptual: a re-examination of the purpose of inpatient admission. As indicated by the lengthy list of problems to be tackled by the RPIW, staff were essentially ‘firefighting’, carrying out a great deal of rework caused by inefficient procedures and following a pathway that had developed piecemeal over many years. The RPIW empowered staff to stop focusing on the reason for admission (e.g. overdose) and concentrate on the aim: to assess and stabilise the patient, and then to treat prior to discharge for further therapy and support. This re-evaluation of the service, coupled with practical process changes, was widely claimed to have led to a reduction in length of stay on the ward, better clinical outcomes for patients and improved staff satisfaction and sickness rates.
Interrupted time series analysis
Before commenting on the ITS analysis of a number of metrics associated with this RPIW, it is worth recalling the nature of the problems identified and the targets set. The problems were expressed in terms of a lack of standardisation in many parts of the PIPA process; a high level of variation within and between different wards; a lack of clarity over roles and responsibilities of staff; and a need to make significant improvements to staff communication. The targets concerned service user and staff ‘experience’; the creation of standard work; the flow of patients through the pathway; and better decision-making processes. In other words, the problems identified and the targets set were not associated with routinely collected data such as the length of time that patients spent on wards. Some of the problems and targets identified could be associated with metrics either post hoc or as proxies for a more efficient inpatient pathway; the reported reduction in incidents of violence; the apparent improvement in staff sickness rates; or the recorded decrease in bed numbers apparently associated with the trust’s analyses showing reduced length of stay on the targeted wards. However, only one of these (length of stay) corresponds with the metrics chosen for the ITS analysis, for reasons explained in Chapter 4, Data and data sources.
It is important to emphasise, in this case study and those studies described in Chapter 7 [see Site 09 surgical pathway (abdominal pain), Site 10 purposeful inpatient admission rapid process improvement workshop and Site 10 community psychosis rapid process improvement workshops (referral, treatment, discharge)] that, as a quantitative analysis, the ITS must use metrics. Although these were clearly of significant interest, they were associated with only a small element of the overall impact of the RPIW, as the organisations were generally not able to measure a wider range of important outcomes using routinely available data. Owing to the limitations of routinely available data, the ITS metrics tended to fall into the category of effects on efficiency and performance that resulted from work to achieve higher-order targets. This was in line with the expectation that better-quality care should be the main driver behind many of the NETS-inspired improvement initiatives, with other benefits such as cost savings, shorter length of stay or faster flow of patients resulting as a consequence of that focus.
The PIPA ITS analysis examined several length-of-stay variables for male and female patients (see Chapter 7, Site 10 purposeful inpatient admission rapid process improvement workshop for further details), with the results for ‘time spent on the ward’ being easier to understand more immediately. As a result of the RPIW intervention, the ITS analysis showed that:
-
the length of time that female patients spent on the ward decreased
-
the length of time that male patients spent on the ward is ambiguous.
Several issues with the findings are noted in Chapter 8, Reflections on the interrupted time series, which may partly explain the finding that a greater proportion of patients were transferred into the ward (from other wards) after the RPIW. This was particularly true for men; after the RPIW, the proportion of male patients who had been admitted elsewhere rose to 18% from 1% prior to the RPIW. When this factor was taken into account in the analysis, the reduction in length of stay for men also became statistically significant. However, it was not possible to determine whether or not the changes in admission pattern were also due to the RPIW, which makes it difficult to interpret these results.
Case study 2: community psychosis ‘superflow’ rapid process improvement workshop
This case study concerned a ‘superflow’ RPIW event in study site 10 that took place in early 2011, almost 3 years after case study 1. The term ‘superflow’ indicates that, in effect, a number of interlinked RPIWs were carried out concurrently; in this case, three RPIWs, corresponding to distinct elements (referral, assessment and discharge) of the patient pathway for psychosis in the adult mental health service.
The scope of the superflow RPIW was ambitious (Table 10). The week-long event required considerable organisational and logistical planning, together with the active involvement of a large number of staff. In itself, this demonstrates emerging confidence and trust in using the study site’s quality improvement system (QIS). The key problems addressed were multifactorial: a lack of standard work across the whole pathway; variation in practice in different geographical locations; poor communication with patients, carers, family members and other NHS staff; and a lack of reliable and useable data on quality and performance.
| RPIW element | Information provided by RPIW team |
|---|---|
| Problems identified |
|
| Targets | The documents associated with this highly complex ‘superflow’ RPIW reveal a very large number of individual targets, corresponding with many steps in the patient pathway, from referral to assessment and eventual discharge. The targets fall into areas such as creating standardised processes for handovers between different staff groupings within the trust, and between trust staff and external agencies; improvements to communication; greater patient choice; effecting reductions in the time taken to carry out several elements of the patient pathway, as well as the number of appointments required; improvements to the quality of data held on patients; overall productivity of the process The high-level aims and targets, as set out on day 1 of the RPIW by the sponsor, were:
|
| Resources | This RPIW involved MDTs from three different geographical locations, with approximately 30–35 people present at any time during the week The sponsor and the team leaders were senior trust clinicians; workshop leads were trained KPO staff. Participants included clinical and administrative staff, GPs, a service user representative and care assistants |
Rapid process improvement workshop support
This ‘superflow’ event consisted of three interlinked RPIWs that collectively addressed the assessment, treatment and discharge of patients on the psychosis care pathway. Fieldwork notes revealed that this was recognised as ambitious and innovative. It was predicated on the successful outcomes of previous RPIWs and other QIS activities, as well as the availability of a well-resourced KPO and a suitable number of VMPS-trained staff. Despite thorough preparation, a straw poll of the staff taking part in the RPIW on day 1 revealed some concern about the complexity and level of ambition, as well as a perceived lack of consistency in the commitment shown by the different geographical teams.
Senior trust leaders were present during the planning phase and the superflow RPIW itself, and others were available remotely via telephone and e-mail to lend support and to enable some critical decisions to be made. The KPO leads had arranged for the event to take place outside trust premises. The location allowed for the large number of participants to gather in one space and the group could be divided into three when necessary. Supporting documentation and data were available on a laptop, or on request via telephone and e-mail.
Pre-rapid process improvement workshop work
This RPIW was carefully planned for months prior to the RPIW week. Documentary materials showed that at least four meetings were held at intervals of several weeks. These mapped the existing processes and drew up a high-level overview of the activities associated with each of the three main elements of the care pathway: referral, assessment and discharge. The overview document provided clear descriptions of work that were classified as waste; opportunities to reconsider processes from the customer’s point of view (where the customer may be a patient, a member of a different trust team, or an external agent such as a GP or social worker); inconsistencies in practice; and variations in inputs, outputs and outcomes. The conclusions reached during these meetings were data driven; for example, concerns were raised over significant variations in the length of time that patients spent in the care pathway, when comparing different teams based in different locations with similar demographic and clinical characteristics. The location and setting of the RPIW was also given thorough consideration. Aside from a considerable effort to ensure a high-quality environment for the RPIW week, much thought was given to the composition of the three teams (organised by the role of individual participants in the referral, assessment and discharge phases) and to later interaction with the RPIW ‘home’ teams.
Rapid process improvement workshop outputs and outcomes
The scale and scope of the superflow RPIW were reflected in a long list of outputs, initially in the form of standard process description (SPD) and patient management documentation (Table 11).
| Referral | Assessment | Discharge |
|---|---|---|
| DNA letters × 2 | 12-week formulation letter | Absence recording sheet |
| SPD first contact | 5 P’s formulation guidelinesa | Case note recording for activity (template and example) |
| SPD DNA management | 5 P stress vulnerability diagram | CPA GP letter |
| SPD initial referral | Initial formulation flow chart | CPA review standard format |
| SPD referral allocation | Intervention plan template | Discharge checklist |
| SPD visual control board | Letter to GP after initial appointment | Pre-discharge letter to GP |
| SPD transfer of care | Pictorial team formulation | SPD CPA review |
| SPD transfer | Psychosis assessment and discharge | SPD formulation meeting 6-month review |
| Visual control board | Psychosis superflow formulation documentation | SPD loss of contact or disengagement |
| SPD assessment appointment 1 | SPD medication review appointments | |
| SPD assessment appointment 2 | SPD planned discharge | |
| SPD formulation initial meeting | SPD service user declines service | |
| SPD formulation meeting (care co-ordinator) | SPD staff absence | |
| SPD formulation meeting (medical staff) | SPD treatment activity recording | |
| SPD psychological assessment | ||
| Standard care plan template |
All of the outputs listed in Table 11 were produced in support of a standardised care pathway, as shown in Figure 4.
FIGURE 4.
Psychosis superflow overview: the standardised post-RPIW care pathway (adapted with permission from a study site diagram). CPA, Care Programme Approach; DNA, did not attend. Information supplied and permission granted by a senior member of staff in study site 10’s QI team, 2011, personal communication.
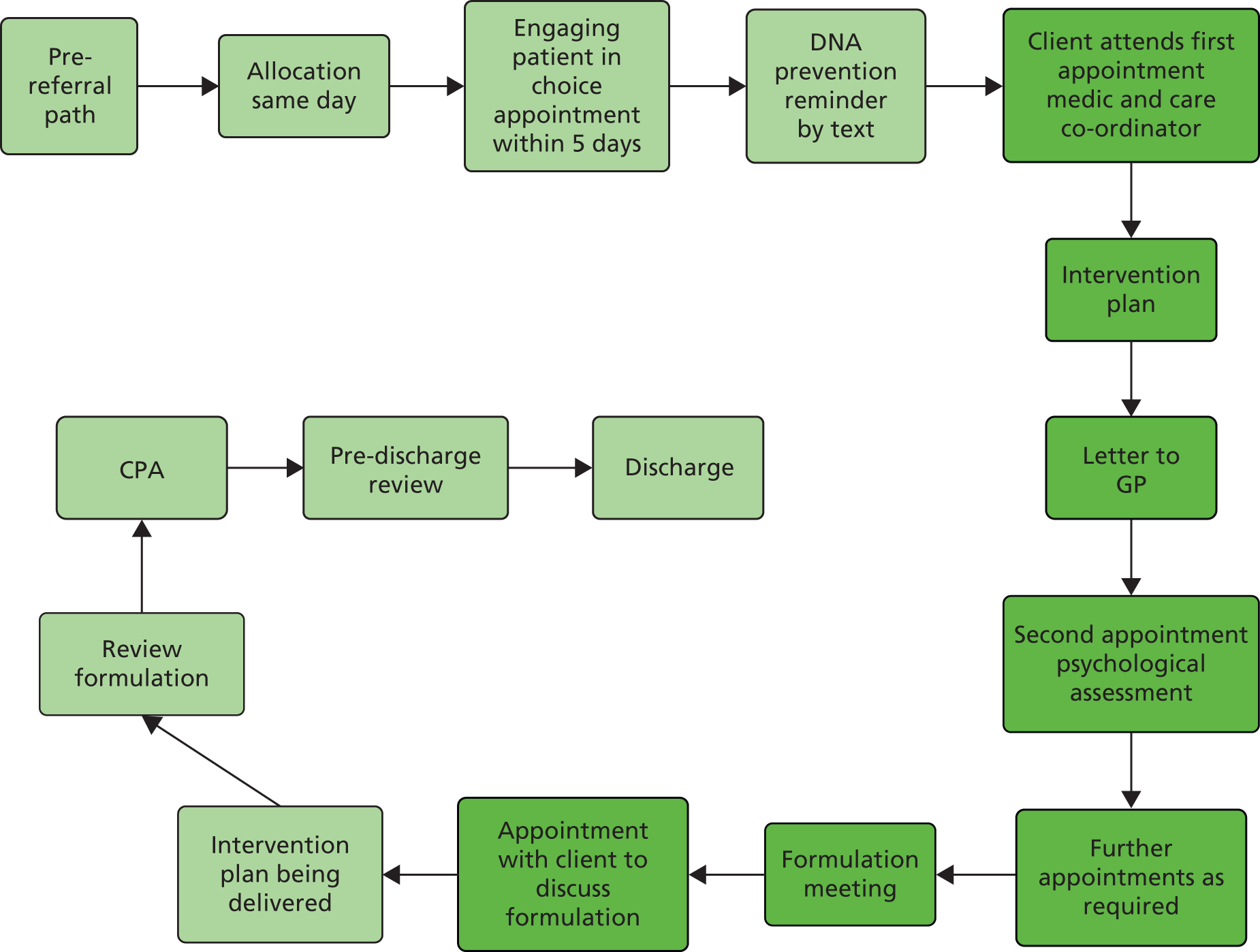
The longer-term outcomes of the superflow RPIW were almost as varied as the immediate outputs summarised in Table 11. Four months after the superflow event had taken place, those staff closely associated with the implementation of the RPIW reported a number of positive changes that were directly attributable to having standardised processes supported by common documentation:
-
Psychosis team care co-ordinators were better equipped to deal with their workload and staff sickness absence had reduced. An initial concern that staff would find the new and unfamiliar ways of working stressful proved unfounded.
-
Acceptance of standard work had highlighted gaps in the structures of the multidisciplinary teams in different locations, but had also empowered staff to make requests for – and obtain – team members with the professional skills to fill those gaps.
-
The superflow RPIW had demonstrated the need to make changes to the study site’s electronic record-keeping system, which had proved occasionally unwieldy and ill-suited to the new ways of working. In particular, the system had been shown to be poorly equipped to provide historical evidence of a patient’s clinical history and previous treatments, and this was being addressed as a priority.
-
Staff were now often able to move from one team to another without having to learn new protocols.
-
Patients and staff had a much clearer understanding of the purpose of admission and treatment within the psychosis pathway.
-
There was positive feedback from GPs, who were reported to be pleased with the new forms of communication with patients.
-
Patients assessed as needing treatment elsewhere, either in primary care or in mental health secondary care, were transferred in a timely way, with no waiting for handovers between different agencies.
Not every outcome of the superflow RPIW was reported as positive. Staff noted, for example, considerable variation in the implementation of the standard work across different locations. This was attributed to a combination of factors, including a historical lack of commitment to change in some of the psychosis teams and some failings in team leadership. The formulation of standard work had also highlighted gaps in the study site’s existing metrics and data, and some staff expressed doubts that these problems would be overcome quickly.
Interrupted time series analysis
The referral, assessment and discharge subpathways were each subject to their own RPIW, and ‘problems identified’ were therefore set out separately for each. The problems identified fell into two broad categories: a lack of standard work practices across different localities, and within the processes themselves; and a high degree of variation in caseload due to poorly understood and controlled flow of patients.
The high-level targets were mainly concerned with achieving a redesign of the pathway, addressing patient and carer needs, improving quality of care, and value for money indices. However, they included reduction in waiting time for ‘customers’. Some of the detailed targets, such as those that directly concerned the length of time taken to undertake some elements of the pathway, were strongly associated with the RPIW metrics.
As set out in Chapter 7, Site 10 community psychosis rapid process improvement workshops (referral, treatment, discharge), the ITS metrics concerned the time that patients spent on the Adult Mental Health Psychosis pathway, from referral to first allocation; first successful face-to-face contact; first assessment; formulation; and discharge. ITS metrics were also used to analyse the number of ‘did not attends’ (DNAs) at the first appointment and recorded discharge rates. The results are shown in Table 12.
| Metric | Result of ITS analysis |
|---|---|
| Duration from referral received to first allocation | Time to allocation fell more in control sites but mainly because time to allocation had already fallen considerably in intervention sites 6 months prior to the intervention |
| Duration from referral received to first successful face-to-face contact | No evidence of significant impact on time to first contact (though a non-significant reduction was observed) compared with control sites |
| Duration from referral received to first assessment | No evidence of a significant impact (though a non-significant reduction was observed) compared with control sites |
| Duration from referral received to formulation | No evidence of a significant impact (though a non-significant reduction was observed) compared with control sites |
| Duration from referral received to discharge | Analysis suggests that mean time to discharge fell in control localities but increased in the intervention localities |
| DNAs at first appointment | No evidence of a significant impact (though a non-significant reduction was observed) compared with control sites |
| Recording of discharge rates | No change |
These results represented a mixed picture, and a consistent feature of these analyses was that large changes in most of the key variables were also observed in the control localities. In some cases there were counter-intuitive outcomes, even when the metrics available for ITS analysis corresponded directly, one to one, with the targets chosen for the RPIW. In fact, the majority of targets, and nearly all of the problems identified, focused on reducing variation in practice across the trust’s locality teams, and improving the quality of the service offered to patients and their families. Improving the quality of service was partly related to reducing the length of time patients spent in certain areas of the pathway. Many of the targets addressed other quality issues, and this was reflected in some enthusiastic claims for improvements that addressed variation and the patient and staff experience. This was highlighted in staff interviews and RPIW ‘newspapers’. Key individuals were realistic about the ability of the trust to share and spread the new ways of working. They admitted that RPIW outcomes were variable across the trust localities. This was even when RPIWs had been repeated. The complexity of the pathway meant that even successful changes could take a considerable time to bed in.
Case study 3: surgical pathways assessment area (abdominal pain) rapid process improvement workshop in an acute hospital
This case study was based on a RPIW event that took place in an acute hospital study site in October 2011 (Table 13). The study site was a wave 1 NETS pathfinder that had contributed to the NETS programme from its inception.
| RPIW element | Information provided by RPIW team |
|---|---|
| Problems identified |
|
| Targets |
|
| Resources | The RPIW sponsor was a senior executive officer in the trust. The workshop and team leaders, and the process owner, were senior clinicians. Participants (n = 13) included nursing staff, a bed manager, ward managers, surgical staff at various levels, senior house officers, A&E staff, an emergency care practitioner and representatives of the medical assessment area. Days 1 and 2 of the RPIW took place in a trust training room; subsequent activity took place in a ward environment |
Rapid process improvement workshop support
This RPIW was viewed as a key element in the process leading up to the occupation of a new-build surgical block on the trust’s main hospital site. The layout and arrangement of existing facilities were thought to reinforce some of the traditional boundaries between medical and surgical departments. The design of the new building was intended to help overcome these barriers and to provide a more patient-centred service. The RPIW was thus an attempt to both standardise and improve the processes of assessment and admission of patients on the abdominal pain part of the surgical pathway. It was a means to embed new working practices that would be used after the move to a new building.
The RPIW sponsor (a senior trust director) came to visit the RPIW team on day 3 and spent time asking questions and offering support to the RPIW participants. Some of the participants had taken part in previous RPIWs or other QI activities, but others joined the RPIW as novices.
The bulk of the improvement activity was carried out in situ in a ward environment, with ‘real’ patients, where a number of bed bays had been reorganised to reflect the likely layout in the new building. Time was set aside at the end of each day to reflect on what had worked well and which problems could be addressed. The ward environment featured prominent displays of the trust’s Vision statement, as well as reference information on a variety of lean tools.
Pre-rapid process improvement workshop work
This trust was one of the original ‘pathfinder’ NETS sites. By October 2011 many staff had been trained in the NETS and VMPS and had taken part in formal QI activities. These spanned a wide range of clinical areas, as well as problems linked to logistics, administration, estates and diagnostics. This RPIW was clearly aligned to one of the study site’s strategic objectives: a successful move to new facilities and a more patient-centred environment. Most of the participants were at least aware of previous improvement activities.
The original intention for this RPIW was to increase the amount of time staff had in contact with patients in the adapted ward environment. The workshop leads had organised a training session 2 weeks prior to the RPIW week, at which participants were introduced to the use of lean tools and other NETS concepts. However, attendance at that session was poor, and day 1 of the RPIW was therefore used to recap some of the basic introductory material.
Outputs and outcomes
This was a ‘hands-on’, highly practical approach to a RPIW, where staff were immediately putting into practice the new procedures and processes that had been agreed during the first 2 days of the week. Reception and A&E staff were instructed that patients presenting with appropriate symptoms should be sent immediately to the assessment unit (after an initial telephone call to the bed manager). The ward bays had been set up to reflect the future environment in the new building. A visual control board was in place to manage the patients through assessment and their onward referral or discharge. Mobile trolleys were arranged with a standardised complement of equipment and recording material. Some staff were asked to collect ‘patient stories’, to be used later in share-and-spread NETS activities.
A mini report-out was arranged during day 3 of the RPIW. During this, staff commented that:
-
a single point of access to the assessment unit had improved the ‘grip’ of bed managers on demand and capacity
-
staff on the inpatient wards were pleased with patient flow and the accompanying quality of information
-
A&E reported a major improvement in waiting times (and hence better-quality patient experience)
-
inefficiencies had been unearthed in patient transport and use of emergency theatre time.
According to key RPIW participants, no 30-, 60- or 90-day report-outs were carried out, and there was therefore a lack of documentary material on later outcomes. However, interview data showed that the improvements associated with the assessment of patients with abdominal pain were swiftly replicated for other types of surgical pathways (abscess, gynaecology, vascular and general surgery). GPs were reported to be pleased with the improvements to the patient length of stay:
. . . [patients] come to us, they go to theatre and they’re discharged by dinner time whereas at one time they used to take beds up for 2 or 3 days at a time . . . the GPs think that’s really good . . .
Site 09, ward sister
The same data also indicated better co-ordination of tasks:
. . . [people] would probably be shipped up to the ward . . . the nurse would see them, obviously take a few minor details and that would be it whereas obviously they come up here [the assessment unit] now and we do everything straightaway.
Site 09, ward sister
The above improvements to processes were recognised by RPIW participants. However, in general they were unable to quantify the improvements in terms of the number of patients seen, reduced waiting times or other performance indicators. The lack of data was recognised, and attributed to the speed at which changes were implemented, and the introduction of a new electronic patient management system that did not provide historical data.
Interrupted time series analysis
The ITS metrics analysed for this RPIW fell into two categories: (1) changes in the percentage of patients who received certain procedures; and (2) changes to the time taken to carry out activities within the pathway. The problems identified and the targets set on the RPIW project form were largely concerned with trialling a new system for potential candidates for surgical procedures, reducing variation in existing procedures and introducing standard assessment tools. However, one of the problems identified was that of long waiting times between assessments and decision-making, which could potentially cause delays in treatment. It is therefore of interest to examine the results of ITS analysis in relation to improvements to this area. These are summarised in Table 14.
| Metric | Result |
|---|---|
| Time from arrival in A&E to being X-rayed | Waiting time reduced significantly (around 11.5 minutes) |
| For those receiving a surgical procedure, times from arrival in A&E to procedure | No evidence of any effect |
| For those receiving an inpatient US, times from admission to US | No evidence of any effect |
A simple reading of the results of the ITS analysis would suggest that the RPIW was effective at the ‘front end’ of the process (from a patient arriving at A&E to being X-rayed). Evidence of effectiveness in the parts of the pathway that concern inpatients is inconclusive. To some extent, it can be concluded that the RPIW made an impact on one of the original problems, as set out in the RPIW project form. On balance, however, this had a relatively minor effect, compared with the reported improvements to co-ordination of tasks, bed management, staff and patient satisfaction, and approval of the changes from GPs.
The surgical pathway RPIW was conducted against a background of a significant rising trend in overall attendances at A&E (thought to be due to the closure of a local ‘walk-in’ centre in October 2010), which was also likely to have resulted in a change in the casemix of those attending, so that the proportion of attendees with abdominal pain that required admission was probably falling. This background would have made it more difficult to detect any significant impacts of the RPIW, as ITS analysis controls for background trends.
Case study 4: other North East Transformation System environments
Case studies 1, 2 and 3 concentrated on specific RPIW events in two wave 1 provider organisations that used the VMPS as their method for change and QI. This case study brings together a number of considerations that derive from a study of the NETS in a different set of environments: a wave 2 VMPS pathfinder; a commissioning organisation; and two provider trusts that employed a range of different, non-VMPS lean tools as their preferred method.
The North East Transformation System in a wave 2 organisation
Study site 07 joined the NETS programme as a ‘wave 2’ organisation in mid-2009. It followed the path, established by the wave 1 organisations, of sending a small group of senior trust staff to undergo training in Seattle, WA (with VMMC), and Japan. Initial NETS/VMPS training was facilitated by staff from VMMC and Amicus. Formal QI events (RPIWs, 5S, 3P, etc.) began in early 2010, focusing on internal processes (stores, logistics, training and inspections), apparently at the expense of a more patient-centred approach. However, as indicated by interviewees who took part in these events, the efficiency and effectiveness of front-line services depended to a large degree on having supplies and equipment in working order, in the right place at the right time. Even those RPIWs that were only concerned with internal processes and value-for-money considerations (such as a road traffic accidents RPIW) had an immediate impact on the trust’s finances, which in turn helped improve the quality of service. One example of such an intervention was the RPIW on the storage and supply of stores items throughout the trust (Table 15), which took place in October 2010.
| RPIW element | Information provided by RPIW team |
|---|---|
| Problems identified |
|
| Targets |
|
| Resources | Two senior sponsors were assigned to this RPIW, plus a workshop leader, two team leaders, a VMPS coach and a process owner. In addition, team members included an estates professional, a paramedic, a team leader, an equipment specialist, an IT specialist and representatives from finance and stores |
| The RPIW took place in a single site |
Rapid process improvement workshop support
Although the central Kaizen team for this study site was small relative to those of some of the wave 1 NETS organisations, it was well prepared for undertaking training in the NETS and VMPS. Two of the key staff had extensive experience of business change management methods, Six Sigma principles, process control and the principles of lean, which they gained prior to working in the NHS.
It was not possible to obtain evidence of pre-RPIW activities directly linked to this RPIW. However, general NETS training documents from 2010 showed that presentation materials had been developed that explained the key elements of the TPS and the VMPS in detail. These materials explained the way in which the study site intended to use the NETS to further the strategic aims of the organisation. The Vision, Compact and Method were given comparable attention in these presentations. This was perhaps an indication that early lessons about the appropriate balance between the three elements of the NETS had been learned from the wave 1 organisations. The purpose and nature of service improvement was made clear to staff, as shown by a presentation slide used in the NETS training, which indicated that the main thrust of service improvement activities was to support the trust’s Vision by using VMPS to bring about positive changes to quality, costs and service delivery.
The Kaizen team carried out a number of observations of the central stores area prior to the RPIW, recording metrics such as space used for storage, the value of inventory items, staff walking distance, lead time, parts travel distance and quality defects (availability of audit data, missing items from orders and number of reported health and safety breaches). As recorded on the RPIW target sheet, much of the focus of the RPIW was on environmental, health and safety factors, which were judged on a scale of 1 to 5 (1 being the lowest score).
Outputs and outcomes
The target sheet contained data on the progress towards targets over the 5 days of the RPIW, as well as the sustained improvements at 30 and 60 days after the event. No data were available for the 90-day follow-up.
From day 3 of the RPIW onwards, the improvements in the environmental, health and safety standards were recorded as significant, moving from a score of 1 to 4 by day 5, and remaining at that level over the 30- and 60-day follow-ups. This improvement was achieved through the application of 5S principles. The target of reducing staff walking distance by 50% was reported to have been achieved and sustained. The value of the inventory showed a small decrease, but not at the 5–10% target level; however, this was not the primary focus of the RPIW.
The reason for staff health and safety being such an important element in this RPIW was revealed in the comments from trust staff during interviews:
The space was restricted for various reasons . . . the ways they were working created concern for everybody . . . I mean one member of staff said to me, do you know, it was so bad that I actually considered not coming into work . . .
Site 07, service improvement manager
Such concerns were clearly voiced during the preparatory pre-RPIW phase. A service improvement update document recorded a request to stores staff to identify the work streams for the RPIW. These resulted in top priority being given to the cluttered, potentially dangerous state of the environment. This was an almost ‘textbook’ case of improvement by a RPIW. It was driven by communication with the people who did the work, backed up by evidence and data recorded on the ‘current state’ value stream map, and sustained by follow-up events and further refinements. The service improvement update reports that staff ideas are of the greatest importance in improving the process.
Additional findings
In addition to the case study material summarised in The North East Transformation System in a wave 2 organisation, interview data and documentary materials also revealed other significant findings in relation to study site 07 and the NETS:
-
Site 07 joined the NETS as a wave 2 VMPS pathfinder in part because of a perceived need to gain a competitive edge over other potential providers, and because the site could see that the NETS initiative had achieved significant momentum by 2010.
-
Senior staff were highly impressed by the VMPS/TPS approach of using incremental changes to drive a larger, system-wide transformation.
-
Opportunities to train with other NHS NE organisations, to jointly redesign pathways and to speak the same language of improvement, were highly valued.
-
Compact development had not proceeded as quickly as originally planned during the first 18 months of the NETS activity, in part because the site had a geographically dispersed staff.
-
The NETS programme within the site was not resourced as generously as some of the other VMPS NETS sites, in terms of numbers of full-time staff devoted to training and running improvement activities.
-
A number of the key VMPS certified leaders had previous experience of lean and other QI programmes outside the NHS environment (e.g. Nissan, IKEA and local authorities); one of these was instrumental in gaining board approval for the NETS programme within the site.
-
The long-term goal was widely understood to be that of embedding a different culture in the organisation.
-
The NETS was seen as a means to achieve QIPP targets, cost savings and FT status.
-
The NETS impact on health and safety targets was also seen as very important to the organisation.
The North East Transformation System in a commissioning organisation
Site 11–13 was a cluster of PCTs that, prior to 2010, provided both health-care commissioning and provider functions, the latter in the form of a community health service. During the course of this study the community health service was transferred to the control of local hospital trusts, and the remaining commissioning function prepared for transfer to the emerging Clinical Commissioning Groups (CCGs). The site therefore had to operate in a rapidly changing environment which saw many staff change role or leave to join other organisations. The site had joined the NETS as a wave 1 pathfinder. It maintained an active involvement in the programme until its demise in March 2013.
A senior director in study site 02–05 – also a commissioning organisation, but much less committed to the NETS – summed up a view that gained ground among some senior staff when his PCT cluster was first introduced to the NETS concepts, which he contrasted with his previous experience in another trust:
On the PCT commissioning side, I think it’s fair to say that people were perhaps struggling to see what the application was of quality improvement systems in commissioning . . . I think what they were struggling to see is how we could introduce that into a commissioning function, other than to champion it in our providers . . .
Site 02–05, senior director
In fact, study site 11–13’s senior leaders did see how a QIS could be directly applied in a commissioning environment, by concentrating efforts on those aspects of the health and care system that cross many boundaries, between hospital environments, general practice, community services and social services. A range of such improvement events were identified, including:
-
breast feeding
-
local enhanced services (LESs)
-
bringing drug users into effective treatment
-
Tier 2 smoking cessation
-
hospital discharge
-
mental health services
-
access to contraception services
-
safeguarding children and adults.
The above were all areas which required multiagency, multiprofessional collaboration, which would benefit from leadership from a commissioning organisation to bring together the appropriate and relevant actors. This is not to underestimate the difficulties faced by the study site in carrying out such complex improvement activities. The interested parties were dispersed across a wide region, had different arrangements for cover and some might have required payment to attend. Most importantly, the parties had different expectations and were accustomed to different organisation cultures. There would have been no single, unifying Vision, unless it was effectively and actively promoted by the commissioning organisation.
Despite these potential difficulties, the above improvement activities did take place during 2010, and we have chosen one of them – the multi-agency hospital discharge RPIW – to compare with RPIWs run by other, provider study sites (Table 16).
| RPIW element | Information provided by RPIW team |
|---|---|
| Problems identified |
|
| Targets |
|
|
|
|
|
|
|
|
|
|
|
|
|
| Resources | Sponsors × 4 |
| Workshop leaders × 2 | |
| Team leader × 1 | |
| Process owners × 4 | |
| KPO specialist × 1 | |
| Team manager, hospital discharge team | |
| Social worker, hospital discharge team | |
| Team manager, older person’s team | |
| Social worker, older person’s team | |
| Social worker, adults duty team | |
| Administrator, older person’s team | |
| Home care manager | |
| Community equipment | |
| Ward manager, ward X | |
| Senior nurse, ward X | |
| Ward manager, ward Y | |
| Ward manager, ward Z | |
| Ward manager, ward W | |
| Discharge liaison nurse, PCT provider services | |
| Occupational therapist, PCT provider services | |
| Team lead, PCT provider services | |
| Lead occupational therapist, hospital | |
| Mental health liaison nurse, PCT provider services | |
| Lead occupational therapist, hospital | |
| Administrator, adults duty team | |
| PPI lead, commissioning organisation | |
| The total number of people involved in this RPIW was 33. We list the individual job roles to illustrate the complexity of the task and the highly heterogeneous nature of the RPIW team |
Rapid process improvement workshop support
This RPIW was carefully planned for many weeks before it took place, not least because of the logistical difficulties involved in arranging for a large number of staff, from four different NHS organisations, to be able to attend during the same time frame. The four organisations were an acute hospital trust, a commissioning organisation (study site 11–13), a metropolitan borough council and a mental health trust. Participants came from every level of the hierarchies in these organisations, from senior directors and managers to student nurses and occupational therapists.
Pre-rapid process improvement workshop work
A background briefing document set out the reasons for the RPIW:
-
Hospital discharge was seen as complex and often contentious.
-
Although goodwill and determination had resulted in occasional improvements to discharge processes and procedures, fundamental system faults persisted.
-
The faults were largely linked to difficulties in spanning organisational boundaries.
-
The study site’s hospital discharge policy (2009) made it clear that each transfer of care should be well planned and dealt with sensitively. It was important to maintain good interagency communications that involved patients, relatives, carers and professionals.
-
A Care Quality Commission (CQC) inspection from 2009 had noted frequent reports of untimely referrals and avoidable residential care admissions, as well as failures to engage with Independent Mental Capacity Act advocates.
-
The CQC post-inspection action plan recommended a multi-agency RPIW to address the issues highlighted in the CQC report, with its scope identified as being the overall discharge process for patients referred to social care from a total of three wards at two different hospitals.
In light of the above challenges, the RPIW sponsors asked for a 50% reduction in the baseline calculation for inventory (bed-day costs and the costs of readmissions within 7 and 28 days); a 50% reduction in lead time; a 100% reduction in inappropriate and incomplete referrals to social care; transfers to long-term care direct from the acute ward; and readmissions within 7 and 28 days. The sponsors also requested a 100% improvement in the patient experience of the discharge process, as measured by a patient survey.
Rapid process improvement workshop outputs and outcomes
The current and future state value stream maps for this RPIW showed that by the end of the RPIW week there was
-
no reduction in lead time (maintained at 33 days)
-
a small reduction in processing time to 26 hours, from a baseline of 28 hours
-
no change to value-added time (26 hours) and almost no change in non-value-added time (774 hours, from a baseline of 776 hours).
However, the same documents showed a significant change to the steps involved in processing patients from admission to discharge, in terms of the ordering of elements in the patient pathway. The post-RPIW process, for example, introduced multidisciplinary team meetings early in the pathway – described as ‘pull’ systems – which were explicitly tasked with preventing inappropriate and incomplete referrals. The overall lead time hardly reduced at this point, but there had been a major change to the way in which that time was used by staff.
The RPIW 5-day newspaper reported that, of the targets specified by the workshop sponsors, there was an expectation that inappropriate and incomplete referrals would be reduced to zero over time, and that patient dissatisfaction with the discharge process would also be reduced to zero. The same document anticipated significant progress towards the other targets, over time.
After the RPIW was completed, the study site RPIW team and KPO lead produced a ‘feedback pack’ for the use of all those who had participated in the event. This was a substantial document, which recorded in detail the context of the improvement event, the targets and progress made against them, the full range of ideas generated during the RPIW, feedback comments from each of the RPIW subteams, a series of RPIW newspapers and a complete contact listing for all of the participants. This pack also contained a summary message from the sponsors, which stated their assessment of progress made and necessary further work. It was clear from this summary that the sponsors were genuinely surprised by the poor quality of existing discharge information available for patients and carers, and would prioritise this area for urgent development.
Additional findings
In addition to the case study material summarised in Pre-rapid process improvement workshop work, interview data and documentary materials also revealed other significant findings in relation to the study site 11–13 and the NETS:
-
The site joined the NETS programme at a time when senior managers had been looking for a way for their PCT cluster to go ‘further, faster’, and had already examined a number of possible ways of achieving whole-system reform.
-
The VMPS approach was favoured because it emphasised having a long-term vision that sought to stabilise the existing system and then build on that to effect change in the desired direction.
-
The NETS’s region-wide approach fitted well with the links that this organisation already had with local authorities, provider organisations, and public health and community services.
-
Compact development was seen as a useful lever to change relationships with other organisations, particularly the FTs.
-
Service improvement staff recognised the fragility of the NETS in the face of mounting pressures within the system, and felt that ultimately it would be owned and run by the quasi-independent provider organisations.
-
The NETS programme was seen as key to initiating and sustaining some large-scale reforms in the management of certain chronic diseases in the community and paediatric services.
-
The initial NETS-sponsored visits to VMMC had a deep and lasting impact on key staff:Site 11–13, Senior Director
. . . when you go to Seattle you’ll see . . . people just talk the talk, walk the walk, and you can see that these people are focused in a different way to probably anywhere else I have seen, on improving quality, eliminating waste, and it [is] just the way they do business . . . And there are just some absolutely stunning examples of how they have changed, you know, clinical services, physical buildings, and you know that this just works and it is stunning.
-
KPO leads felt that the ‘territoriality’ of many NHS organisations was a potential barrier to sustaining the NETS, particularly in the face of flatlining budgets.
Non-Virginia Mason Production System North East Transformation System: study site 01
Site 01 was not a VMPS pathfinder organisation, but it was an early adopter of the NETS philosophy of applying the ‘three-legged stool’ of Vision, Compact and Method to QI and organisational development. In the first 2 years of the study, this site made use of a version of the NHS Institute for Innovation and Improvement’s ‘Productive Series’ tools as the method of choice. At a later stage, the study site came to adopt a more eclectic approach, introducing some VMPS elements such as RPIWs, and joining the NETS Coalition Board as an active partner.
This site had made a determined and sustained effort to communicate its Vision, which emphasised excellence in patient safety, quality and continuous improvement, to all staff, and to deepen this by setting out ‘core values’ and the means to realise them. The core values focused on two main areas: being patient centred and seeking continuous improvements to services. Patient-centred values included expectations that staff would treat patients honestly and directly; encouragement of partnership working; protecting the patient’s rights to dignity, privacy and their spiritual and cultural needs; and zero tolerance of pain, suffering, delays and waste. The values linked to continuous improvement included commitments to efficient and effective teamworking; partnership across health and social care; ensuring a clean, safe environment that promotes patient comfort and well-being; using standards and outcome measurements; following best practice; accepting an environment of mutual challenge; and celebrating excellence in service delivery.
The nature of the QI activities undertaken in this study site meant that it is not possible to provide case study material that is equivalent to those study sites that conducted RPIWs. However, an analysis of interview data and documentary evidence revealed the following findings:
-
The site took a ward-by-ward, department-by-department approach to training staff in the Method. This ensured that nursing staff were engaged from the outset and were less likely to see the programme as imposed by management.
-
The emphasis on ward-level improvement activities – many of them highly visible and involving patients – ensured that much of the drive for standardisation and redesign of processes came from nursing staff and health-care assistants.
-
The trust had absorbed staff from the local community services organisations (site 06). It was aware that many community services staff had been trained in their own version of a lean-inspired QI programme, but felt strongly that they should adapt to the new environment, rather than the other way around.
-
Some senior managers were sceptical about the lean aspect of the NETS. They felt that the variability of cases in a hospital would make it difficult to apply. There was also some evidence from interview data of resistance to the Productive Series approach from doctors.
-
Service improvement managers had ensured that Compact development and attention to the behavioural and cultural aspects of the transformation programme were given a high profile at an early stage: ‘. . . there’s no point applying a methodology if really we need to sort the behaviours first . . .’ (site 01, organisation development manager). Compact development was promoted across the whole organisation, whereas the implementation of the Method appeared to be carried out on a ward-by-ward basis.
-
Some senior clinicians and managers felt that the pressures on FT hospitals – increases in rate of admissions, A&E attendance, compliance with patient safety standards – were undermining the trust’s transformational change programme by changing priorities for the use of resources and staff time.
Non-Virginia Mason Production System North East Transformation System: study site 14
Site 14 had been involved in exploring and applying improvement methodologies for some years before the NETS was conceived. This was initially through involvement in the Kaiser Club (NHS organisations that were learning from the approach of the USA’s Kaiser Permanente to integrated health-care management). In part, this was why the site did not join the NETS as a pathfinder. The need for a strong, shared Vision was acknowledged, and senior managers understood the potential advantages of the Compact. There was a consensus view that the organisation had already made progress in these areas and that a change of direction would be disruptive. There was also some resistance to the idea that NHS NE would set the agenda for transformational change.
The site made use of a number of different improvement methodologies, including the Lean Academy tools, the Productive Series and ideas borrowed from other health-care organisations in the UK and overseas. A senior director summarised this eclectic approach:
So what we wanted to try to do was to build a system where we had our own visions, strategy, values, and we had a set of tools in the box, and one day they’d be lean and another . . . they’d be something else . . . and we’d use them appropriately.
Site 14, senior director
-
The QI activities undertaken in this study site during the research study were not documented in a comparable way with the VMPS site RPIWs. However, analysis of interview data and documentary evidence revealed the following findings. Senior managers at site 14 had a clear understanding that the Vision and Compact should focus on value for the public. It was noteworthy that pre-2007 trust documents used the word ‘public’ in this context, rather than ‘patient’. Interviews with senior directors showed that the Vision was seen as providing a service to the wider community, beyond the ‘traditional’ confines of the hospital environment. This was reflected in the organisational and physical structure of the trust, which converted to FT status at an early stage. It managed both acute and community hospitals, as well as adult social care services towards the end of our study period.
-
Senior management recognised that achieving far-reaching changes in culture and behaviour would take many years to accomplish, and that this process should include the public as well as staff.
-
The study site’s transformational change programme relied heavily on clinicians rather than managers – at all levels – to provide the impetus for new ways of working.
-
Many of the interviewees felt that if it was important to learn from the experience of Japanese companies, suitable examples could be found in the UK, and there was probably no need to travel to Japan and the USA.
-
Senior nursing staff had a clear view of the links between the quality of the patient experience, financial resources and prioritisation of improvement activities. They employed a scoring system to help in deciding which activities to pursue.
-
Leadership development was highly valued, but not at the expense of team development. This reflected a strongly held view that progress in transformational change would be achieved by enabling networking and communication between health-care professionals working in the same area.
-
Compact development was seen as a long-term, dynamic project, which should not be rushed.
-
There was some evidence that this site genuinely saw wrong turns and mistakes in changing processes as opportunities for staff to learn, rather than reasons to apportion blame.
Summary
This chapter has presented four case studies chosen to illustrate the application of the NETS as a programme for QI activities. Case studies 1 to 3 were chosen to provide some background and context against which to view the results of the ITS analysis of five RPIWs. Case study 4 brought together some higher-level observations about a number of different types of NETS organisations, including a wave 2 VMPS pathfinder, NETS in a health-care commissioning environment, NETS in a hospital trust that initially used the ‘Productive Series’ and NETS in a hospital trust which made use of an eclectic suite of methodologies. From this analysis it was identified that the Method seemed to be less important than the ability to bring about improvements. These had to be driven by the people who had a key understanding of the challenges faced, namely the staff, who needed training in lean tools and the support of colleagues and senior managers. It appeared that the non-VMPS sites were able to pick and choose which improvement methods to adopt and when, implying a freer application to enable more flexible working in comparison with the structured RPIW format which the other sites were required to follow.
A key outcome of the case studies reviewed was an emphasis on removing inefficient processes and practices, standardisation, identifying if the ‘system’ was operating as planned (visibility) once any improvement had been made, and monitoring the outcomes. The QI activities often resulted in an improved understanding that measurement was an important part of any Method adopted. In addition, staff often also realised that suitable metrics were not available, or that the data were of poor quality.
Chapter 7 The impact of the North East Transformation System
This chapter evaluates the impact of the NETS on individual NHS organisations in the North East of England, and on the region’s health-care system as a whole. The findings cover:
-
the performance of NHS organisations in the North East region, measured in terms of improvements to patient safety, quality of care and the patient experience
-
the role and development of the central NETS Coalition Board
-
communication through visual management in the NETS organisations
-
the impact of the NETS on patients and the public
-
the outcomes of the ITS analysis of a number of selected RPIW events
-
factors that facilitate, or act as barriers to, the adoption of the NETS.
Our analysis of these issues is based on the mixed deductive and inductive approach adopted for the study and applied to the qualitative data collected (see Chapter 4, Qualitative data analysis). For the deductive analysis we used the receptive contexts for change framework by Pettigrew et al. 125 comprising eight factors, and the NETS ‘three-legged stool’ of Vision, Compact and Method. These factors are explicitly drawn out in some of the analysis (see, for example, Managerial–clinical relations). However, to ease the narrative flow and avoid a rigidly structured and potentially repetitive presentation of findings, this report more often allows these factors to permeate and underpin as appropriate the discussion of leadership, organisational culture, environmental pressures, intra- and interorganisational communications, goal and priority setting, and the coherence of policy in regard to QI programmes.
Impact on performance
The range, scope, volume and complexity of the multiple NETS activities carried out in the study sites from 2009 to 2012 made it necessary to adopt a sampling approach. Interviews, focus groups, documentary materials and observational fieldwork were used to evaluate the impact of the NETS on patient safety; the quality of care; the patient experience; the efficiency of processes; productivity; and staff satisfaction. The interviewees in phases 1, 2 and 3, whether individual or in focus groups, were remarkably congruent in their assessments of the effects of the NETS on the performance of their respective organisations and on the NHS region as a whole. Most NHS staff had experienced many reorganisations (locally, regionally and nationally) and had been introduced to a variety of change programmes; they were therefore disinclined to be overly optimistic about the likely impact of the latest initiative.
Patient safety
Patient safety is implicit in several of the ‘seven no’s’ that provide the basis of the Vision of NHS NE (particularly, and most obviously, in ‘no avoidable deaths, injury or illness’ and ‘no avoidable suffering or pain’). The development of the NETS focused on achieving existing and future patient safety targets. Emphasising safety was deliberate. Senior SHA and trust leaders were aware that the lean component of the NETS could be interpreted as a prelude to cost-cutting and staffing reductions. It was thought essential to direct the NETS towards safety and quality of care, which were of prime concern to clinicians, nurses and managers. As noted in the 2008 scoping study, patient safety was seen as the main ‘selling point’ for staff involved in the NETS initiative.
It is difficult to disentangle the direct contribution of the NETS to improvements in patient safety from the many other factors that influence the safety culture of the NHS. These include, but are not confined to, medical/clinical education and training, conformity with national standards, guidelines and best practice, recruitment procedures, professional performance assessment and procurement practice. The influence of the NETS on safety programmes in the study sites was evaluated.
Safety culture
The development of the Compact in the NETS organisations – ‘the gives and the gets’ – was intended to empower staff to challenge behaviours and processes that acted as barriers to patient-centred, high-quality care. As discussed in Chapter 5, the focus and attention given to Compact development varied among the study sites. However, in some cases there was clear evidence from interviews that the Compact was having the intended effect. This was true for small-scale, everyday interactions between staff, as one interviewee claimed:
. . . about 6 months after I started was the first case of where a nurse having said nicely to a senior consultant ‘we have a bare below the elbow so you must leave your jacket here and roll up your sleeves’, finally when he refused a third time [she] did report it up to the Director of Nursing and the man was disciplined. And to me that was a big turnover point of where a nurse could actually report a senior consultant and say this is, you know, we impose it.
Site 01, senior board member
The Compact was also having an impact on larger-scale, strategic relationships that affected safety in a broader sense. The following comment from a HR director makes the point:
Well what typically comes up is in the kind of commissioning/providing type of discussion . . . the fact that there should be no surprises, that people should act with integrity and honesty, and that if things are going wrong there’s a mechanism to flag that they’re going wrong and a route so that people can air those concerns and address them.
Site 11–13, HR director
Interviews with HR directors showed that the introduction of a Compact had been influential (in some cases, at least) in shifting the emphasis of work on patient safety from a rule-based, process-oriented approach to one that addressed issues of organisation culture:
And what’s been intriguing, I was with a member of staff yesterday, a manager who was doing an investigatory hearing, and it’s all behavioural issues so she came for some advice on how the case should be framed. So . . . years ago the one yesterday would have been a drug administration error, so it would have been a competency issue. It’s not, and she’s right it’s not, it’s a behavioural issue between the team.
Site 01, HR manager
Safety communication: from ward to board
In two of the five RPIW events observed, members of staff commented that the NETS had given them a method and a reason to make improvements to procedures. They knew that previous ways of working were flawed, but they had become ingrained and seemingly intractable over time. This was the case for front-line staff as well as managers and senior directors. Some of the NETS study sites opted to implement their QI programme vertically – department by department, or ward by ward – rather than horizontally across the whole organisation. In these cases (sites 01 and 14), staff at different levels of the organisations were well informed about the specifics of particular improvement activities. Improvements were reported up from the ward or department to board level. For example, the chair of a hospital trust was informed about the use of visual management techniques to prevent accidents and errors:
I mean for example one of the things that we do is we have patient information boards and reporting boards on every ward which has to be visible. And so they have targets, for example, I mean it’s the numbers of infections, the number of falls, the number of pressure sores all have to be visible to everybody coming through the ward, and they have targets for those that come through . . . We have reports every month on all the patient safety issues, and yes down to a very, a considerable degree of detail. I mean we spend about a third of our time I think of each board meeting on patient safety issues.
Site 01, senior board member
A senior member of the nursing staff in another, non-VMPS trust emphasised the use of specific ward-level data for making decisions about how to make improvements to the trust’s patient safety record:
We run patient safety days where we would take more teams away, so there’s a consultant manager, nurses, domestics . . . you know, a whole team, and I don’t organise them, [name] does . . . but I go and teach on them . . . They’re then provided with a load of data about their ward areas, then they’re sat down to start developing a PDSA [Plan, Do, Study, Act] plan of what improvement they’re going to go back into.
Site 14, matron
The VMPS NETS study sites communicated patient safety improvements through internal and regional report-outs (attended by staff at all levels and senior sponsors); formal KSL events; and, in the case of RPIW events, discussions with the ‘home teams’ (those not involved in RPIWs) which were expected to support putting the redesigned processes into practice.
Embedded patient safety
Many of the interviewees felt that training and involvement in the NETS had helped them to make a strong case for making patient safety the highest priority for all staff. This included those who were not in direct contact with patients. The emphasis on patient safety became embedded in all processes and activities. A number of interviewees in study site 07, a wave 2 ambulance trust, made these points repeatedly in relation to the choice of improvement activities in their organisation. The trust’s training RPIWs, listed in Appendix 4, included a large number of improvement activities that were not directly focused on patient safety, the patient experience or quality of care. The list includes, for example, RPIWs that tackled vehicle inspections, recording of staff sickness, processes in the stores and warehouses and the database used for keeping staff training records up to date. However, our interviewees believed strongly that improved service department or back office functions contributed directly to achieving the key priorities of the trust. This was summed up in its Vision statement, which focused on improving quality through integration of care and transport in order to ensure equity and excellence for patients. In the case of vehicle inspections, for instance, a service improvement manager commented:
As a statutory requirement, we inspect our vehicles before we get in them and drive them, right? It’s a legal requirement and everybody has to do it but we only have 8 minutes to respond to a Category A call. So if people are inspecting the tyres and the lights . . . then that takes 2 or 3 minutes or even longer, how do you respond to a call before you get in the vehicle and go?
Site 07, service improvement manager
Some staff in the same organisation, with a background outside the NHS, saw parallels between the focus on the customer in well-run private companies, and the approach the NETS was intended to encourage:
I worked for [company name] for about . . . 20 years managing a production line. I have extreme difficulty coming to terms with the fact that in industry you produce because if you don’t produce you don’t make money. The service departments were there to make sure that you could do what you wanted and I often feel that this runs the other way around [in the NHS].
Site 07, operations manager
North East Transformation System and the quality of care
From its inception, the NETS focused on making measurable improvements to clinical care. A number of interviewees said that this emphasis was adopted in large part because of a need to convince initiative-weary doctors and nurses of the value of the principles of the NETS, and to gain their commitment to the programme. One study site exemplifies this view particularly well:
I was particularly keen that in the early days of this we didn’t attach anything to do with efficiency or cost savings or anything like that because I think that it’s not going to hook clinicians in at all. They’re interested in improving the quality, and to be honest I think we should be as well.
Site 06, business development manager
. . . we tried to make it very clear it was about changing hearts and minds, and it was about quality, increasing quality for patients, which is obviously very important for our clinicians.
Study site 06, QI manager
Most interviewees saw quality and safety as very closely linked. Therefore, the views expressed above in respect of patient safety (see Embedded patient safety) were often echoed when staff reflected on the NETS and improvements to the quality of care. The lean programmes (VMPS, Unipart Way or the Productive Ward) taught staff that QI would arise from removing and reducing waste, focusing on adding value and concentrating on seeing processes from the patient’s point of view.
The NETS was effective in reinforcing and encouraging a whole-system view of quality. For example, back office staff could understand how their work could contribute to QIs on the front line. An administrator in study site 07, for example, explained that his first experience of NETS training had resulted in the establishment of a better process for managing insurance claims. He estimated that potential savings of several hundred thousand pounds could be achieved across the whole organisation. He explicitly linked this cost saving to an improved service for patients.
The message about the primacy of QI was not universally accepted. During one observation of a series of linked VMPS improvement activities, an attempt to make use of 5S techniques to create a better working environment was rebuffed by a number of staff. They were unwilling to accept the suggestions and pleas from their colleagues. QI staff were aware that the department had an embedded culture of resisting change. However, they regarded the failure of this project as a positive reason to review how they implemented the organisation-wide Compact.
Some interviewees expressed the view that the NETS insistence on QI, rather than, say, cost saving or raw productivity, acted as a useful means to ‘flush out’ colleagues who were not pulling their weight, or who were overly concerned with their place in the organisation’s hierarchy. Two staff gave the example of a reorganisation of practices in their department which was designed to more effectively meet the needs of a particular cohort of vulnerable patients. The reorganisation required more and better communications between different professional roles. This was difficult for two senior team members to accept, who were subsequently moved to a different part of the organisation. The planned reorganisation was then successfully implemented and team morale improved considerably. In effect, the focus on quality of care had positive consequences for both patients and staff.
The role and development of the North East Transformation System Coalition
The ‘NETS Coalition’ was the term used to describe the collective of NHS organisations that were involved in the NETS programme. It included organisations committed to involvement in wave 1, VMPS pathfinders and those likely to take part in waves 2 and 3, as well as non-VMPS organisations that had agreed to follow the Vision/Compact/Method approach to QI.
In practice, early NETS Coalition activities were directed largely by the representatives of the pathfinders (wave 1, and later wave 2) who were committed to VMPS training. These representatives attended meetings as the NETS Coalition Board, chaired by senior SHA staff. The name of this group – the co-ordinating committee of the NETS, in effect – changed over time, from the ‘North East Transformation Coalition Board’ to the ‘VMPS Coalition Board’, and eventually the ‘NETS Coalition Board’, to reflect the changing activities and interests of its membership. For simplicity, we have used the terms ‘NETS Coalition’ and ‘NETS Coalition Board’ throughout.
Administrative support for the NETS Coalition Board, as well as practical resources (funding, desk space, meeting rooms, and so on), were provided by the SHA from 2007 to 2010. The SHA also provided some resources for managing contract negotiations with VMMC and Amicus; co-ordinating VMMC training; arranging training visits to Seattle, WA, and Japan; and KSL activities. Funds were made available to support the region-wide report-out sessions that were an important feature of the first years of the NETS. They provided the opportunity for large numbers of NHS staff to see the outcomes of improvement activities carried out by many different organisations. Staff gained direct experience of speaking at a region-wide event, using a common language of improvement.
The NETS was a complex and large-scale transformational change initiative. Agendas and minutes of the NETS Coalition Board provided a high-level view of the impact of the NETS across the region and documented variations in the number of NETS Coalition members over time. There were significant changes following the announcement of the NHS restructuring in July 2010. The key points from these documents are summarised in Tables 17 and 18 (presented separately to assist legibility).
| 2007 | 2008 | 2009 |
|---|---|---|
| First meetings of the Coalition Board, comprising wave 1 pathfinders and the SHA; Regional Director of Public Health to chair the board | Further Kaizen trips to Japan planned | Wave 2 starts |
| First visits to Japan and Seattle, WA, arranged and attended | First pathfinder compacts drafted | Links established with other regional agencies (NEPA, Teesside University, Gateshead College) and with national organisations (NHS Institute for Improvement and Innovation) |
| First training RPIWs undertaken | A standard ‘NETS script’ developed (to represent the NETS to organisations outside the Coalition) | VMMC contracts for 2009 and 2010 approved |
| Initial certified leader training organised (with VMMC); objective of 90 pathfinder certified leaders within 18 months established | North East NETS workshop organised | KSL training programme starts |
| Initial work on the Compact (with Amicus) | Increased emphasis on Compact development | Discussions around the differences between the ‘Coalition’ and ‘NETS’ |
| Standard communications plan initiated | Contract established with VMMC to allow use of Virginia Mason training materials | Japan and Seattle, WA, visits and feedback continue |
| First visits from VMMC CEO and other VMMC staff | First discussions of NETS branding | Plans made for wave 3 |
| Agreement on central support and funding from SHA resources | Discussions about evaluation of the NETS | Seattle, WA, visits made optional |
| TPS made central to the Coalition’s programme | Exploration of running ‘see/feel’ experience in the North East and Japan visits to be shortened, or ‘boot camp’ to be established in the North East | |
| Region-wide KSL programme implemented | Discussions over the name of the Coalition Board: ‘VMPS Coalition’ or ‘NETS Coalition’? ‘NETS Coalition’ preferred as being more inclusive | |
| Patient safety themes given prominence | ||
| Resources released to employ a NETS programme manager |
| 2010 | 2011 | 2012 |
|---|---|---|
| Japan and Seattle, WA, visits continue through to the middle of the year | Interest in FTs joining the Coalition, reflecting their acquisition of community service organisations | Trials of new NETS training materials |
| More emphasis on leadership development | Initial discussions about ending the contractual arrangements with VMMC. Debate over acquisition of IP rights to NETS training materials, and use of VMMC materials | Negotiations with VMMC over IP |
| Reviews of VMPS tools and standard work | New model for the NETS discussed, offering products and services to a wider audience | Bid for Health Foundation funding |
| New members join the Coalition Board (which now has 14 members) | Consideration of making changes to the training schedules, to better fit with the needs of local organisations | Certified leaders and coaches now trained via NETS staff |
| Standard process descriptions developed for VMPS certification, with the option of visiting Seattle, WA, or organisations in the North East | More emphasis on Compact development, and tying this to staff contracts, job descriptions and performance management processes | Initial consideration of how to include CCGs |
| Development of a regional VMPS KPO | NETS case studies produced and distributed | Formal work started on registering IP for the NETS |
| Foundation degree under development with the University of Sunderland | First steps in creating NETS (as opposed to VMMC) certified leaders | Emphasis on the NETS becoming self-sufficient and sustainable, through offering training and services to a wider range of NHS organisations |
| NETS Coalition function transfers to acute hospital trust (study site 09) | NETS IP to be jointly hosted in the Coalition Board | Debate over the need for a NETS Coalition Board, or whether or not the region’s KPO leads meetings have come to fulfil the same function |
Communication via visual management in the North East Transformation System organisations
Visual management was an important component of interventions. One of the key outcomes was increased visibility of processes and performance. This was the case for a range of situations: front office or back office; ward or full pathway; and whether using RPIWs or other methods. Increased visibility allowed staff to be more informed, which helped them to fulfil their role effectively. For example, one interviewee highlights the visibility of a patient’s status in the following terms:
We have yeah, we do have actually the big wall thing that as I say we put all of the referrals on to, and it was decided that . . . the way we did it previously we didn’t, but this is just as you say a visual way of sort of being able to see straightaway how many patients there are, who they’ve been allocated to, how long it’s been since they were referred, and how long it took to get them through the system and things like that. So yes, we have a big wall board in our office, in the admin office, because we’re like all admin and it’s all in there.
Site 10, medical secretary
Another interviewee identified the advantage of communicating the plan of activities using visual management:
And so for example you can very clearly as you walk round the hospital, you can see the wards that have done it, because what you’ll see as before and after is just de-cluttering and the store cupboard is better and so on. And in some of them, for example the staff will decide to put the prices of things on the store cupboard shelves so that you’re making an instant choice knowing the price of it.
Site 01, senior board member
Visual management allowed staff to identify the key information that they required and needed to communicate to others. This in turn allowed staff to compare their performance (internally and externally):
Yes, we have, like I say I think we’ve got tiers of information that we collect. I mean obviously . . . internally each service has its own sort of barometer in terms of service requirements, and we use things like visibility walls et cetera to share that with the staff. And it can vary, I mean for example it can be things around uptake of the flu, you know, immunisation, sickness levels, we vary it as required. But again we’re very immature I think in terms of where we’re at with that, compared to maybe our colleagues in the foundation trust who have reams of information they can pull out at the press of a button.
Site 11–13, business manager
Improving the visibility of information and data has also helped improve the quality and accuracy of reports:
We didn’t know because unfortunately prior to doing the RPIW we didn’t have a fantastic reporting regime. The culture of the trust was quite poor where staff felt that we hadn’t got time to fill in a large A3 piece of paper for nothing to happen, for the feedback to be negative or non-existent. So the reporting culture was very poor. So as a result staff feel more empowered, just hearts and minds really. Reporting as I say has gone up approximately 75% now. So it means our workload has gone up 75% because we are, even though the forms are shorter, we’re getting 75% more reports, but we now reply to everyone, give feedback, acknowledge receipt of the incident report.
Site 07, finance administrator
At the opposite end of the continuum, visibility can highlight where data and information can take time to filter through to the people who need it. The following comment makes the point:
Trying to think of another example where we might have had to, I think that it’s, again it’s not a symptom of specifically health but it’s probably a reflection of community services in the NHS is that we find it difficult to provide performance information in as timely a way as we would like.
Site 02–05, senior board member
The sheer volume of reporting and associated data made the collation and management of information important:
Well it doesn’t always happen, but what should happen is in each organisation they should basically have the high-level, the very high-level value stream maps. Basically they should know what’s happening in the organisation, but we know that no it doesn’t happen, so you’ve got your high-level maps, and in terms of strategic goals for the organisations, it could be for yearly goals for example, they should be looking at their vision and what are they looking to achieve in the near future. And as a result of that in terms of scoping and planning you will get your topics so to speak from that. And in working with and if you do have a kaizen promotion office and you do have champions in various departments across the organisations, it’s a way of tapping in and then saying right we’re going to look at a particular process.
Site 09, NETS co-ordinator
Visual management helped to identify key performance indicators and the costs of providing a high-quality service:
Your performance element is very much around, why we did this was because we’ve got staff working in some of our services and some of the staff sort of higher up in those services as such might know all about the business side of that service, what the key performance indicators are, all that sort of thing, but actually sometimes in some services quite a few of those staff weren’t aware of what the key performance indicators were, how much things were costing. Things cost an awful lot of money in the NHS, and actually making that very visible and very visual kind of highlights to every member of staff what they’re striving to achieve with the view that if everybody understands that, then people are focused on what you need to do to meet the vision mission and aims of the organisation.
Site 06, QI manager
Standardisation of products and services is a core component of lean. It reduces variation so that a product or service is delivered exactly the same way every time. The use of visual management highlighted variations in the approaches developed by different RPIW teams. This suggests that a standardised approach would be beneficial:
There were some other areas like cardiothoracic ward and orthopaedic wards and surgical wards that also put their own patient status at-a-glance boards in. And then what we realised was actually we were creating a risk across the organisation because all of the symbols were different. They were all producing their own system which if you worked across the trust was just going to cause all sorts of problems. So we knew we needed to do something about that.
Site 01, nurse manager
This section has looked at how the Method applied visual management techniques. Through increasing visibility, staff were able to obtain information that helped them perform their roles more effectively. Both VMPS and non-VMPS sites achieved similar benefits.
The North East Transformation System and patient involvement
Baggott141 noted that patient and public involvement (PPI) had received considerable attention in the NHS since the late 1990s. PPI should inform decisions concerning the allocation of health and health-care resources, health policy (at local, regional and national levels) and system planning. However, despite the ambitions of successive administrations, meaningful and effective PPI has often proved elusive. Baggott identified five barriers to successful PPI:
-
poor understanding of the multidimensional nature of PPI
-
a confusing and complex mixture of different initiatives to encourage PPI
-
PPI structures that lack ‘independence and integrity’
-
a lack of evidence-based analysis of the weaknesses of patients and the public in the face of powerful forces within the health-care system
-
‘. . . institutional changes may be insufficient to promote genuine empowerment of citizens . . . cultural change is probably more important . . . Small-scale institutional changes may achieve more than completely new structures, particularly if existing institutions can be modified to involve and engage with patients, users and carers more effectively’.
The fifth point is highly relevant to the findings in relation to the NETS and PPI. The NETS was conceived to encourage staff to see the world through the eyes of patients, their families and carers, and to focus on making changes to processes only where they were of direct benefit to these ‘customers’. It was a ‘bottom-up’ approach, with senior leadership commitment and resourcing supplied ‘top down’, and it was promoted as achieving transformational change through small-scale but continuous improvements to processes.
The NHS staff who had visited the VMMC in Seattle, WA, or who had had exposure to VMMC trainers, were generally impressed by the benefits accruing from active patient involvement in improvement activities. One interviewee summed up his experience of seeing PPI in action in Seattle thus:
[There was] a great emphasis on getting patient feedback in very simplistic ways. It could just be how did we do today, and it [could] just be putting a counter in a box saying very good, good, poor . . .
Site 10, service development manager
The same interviewee remarked that, over time, the NETS emphasised using metrics to inform and sustain change. It also encouraged the involvement of patients and the use of patient feedback to make judgements about clinical outcomes following the redesign of care pathways.
A VMPS KPO manager (site 08) also stated that the NETS had been a spur to take PPI seriously, to build networks and to include service users on project boards. Within the organisation, the profile of staff charged with promoting PPI had risen considerably: ‘But I work quite closely with our . . . patient involvement lead, whereas perhaps 18 months ago I knew her name but now we’re regularly in contact’ (site 08, KPO manager).
Some of the non-VMPS study sites also had strong messages about the importance and value of involving patients in the redesign of processes and working practices. However, in these cases the PPI appeared to focus more on ward-level activity, rather than policy setting or influencing strategic objectives. The emphasis here was on promoting a safety culture:
. . . we’re using these information centres now for each, each ward [shows visual control board to interviewer] . . . And this bit here is the real change, because that’s about patient and relative involvement and what patients and relatives can do to actually make [trust name] a better place to be in and a safer place to be in.
Site 01, nurse manager
The same interviewee saw the mobilisation of patients, carers and family members as a way to augment staffing levels and provide another perspective on safety concerns. A senior nursing director from another study site (site 14), which made use of an eclectic array of improvement methodologies, felt that PPI had been integrated into QI initiatives for ‘some time’, and gave an example of involving children in decisions about their health care:
In child health, we decided 18 months ago one of our priorities was doing something more locally with children, and that’s a raging success . . . [A child] got involved in this group . . . and as a result of that he’s coming to clinic, he’s talking about what they want in the clinic appointment and their own handling of their illness.
Site 14, senior nurse manager
These accounts of PPI seem to offer some evidence of the barriers identified by Baggott141 being overcome, at least partially. In some cases, the NETS appeared to have encouraged staff to think harder about PPI as a multidimensional activity. A single, patient-centred QI programme instead of a complex mix of initiatives may have helped to create a coherent focus that gave it the independence status and credibility that would otherwise have been missing. In relation to Baggott’s fifth barrier, the NETS concentrated on cultural change and small-scale, incremental improvements.
It was not possible to conduct interviews directly with patients. The evaluation of the impact of the NETS in terms of PPI was therefore based upon staff interviews. Some proxy measures found in documentary materials such as board reports and supporting documents for awards were also used. These secondary sources do not, on the whole, present as positive a picture as the interview data. In part, this may be because the learning curve involved in setting up PPI was steep. The study sites may not have felt confident in claiming success in the early years of the NETS. In addition, many early improvement activities were concerned with internal processes, where it would have been difficult (or impossible) to put PPI into practice. Patient stories feature frequently in annual reports and proposals for awards. However, without comprehensive and consistent reporting of how patients and the public were engaged in improving processes and pathways, it remains difficult to judge the effectiveness of the NETS in this regard.
Interrupted time series analysis of selected rapid process improvement workshops
As described in Chapter 4, Data and data sources, the data obtained for the ITS analysis were analysed using the repeated measures approach recommended for short time series. The detailed findings from each analysis are provided below [see Site 09 surgical pathway (abdominal pain), Site 10 purposeful inpatient admission rapid process improvement workshop and Site 10 community psychosis rapid process improvement workshops (referral, treatment, discharge)]. A summary of the key findings for each RPIW included in the ITS is provided in the next section.
Summary of findings for the rapid process improvement workshops included in the interrupted time series
The analysis of 19 variables is shown in Table 19. There was a prespecified expected direction of effect for 15 of these variables. In practice, the ITS analyses provided indicative evidence of a change that was consistent with the hypothesised impacts of the RPIWs in only seven variables. For three other variables, there was indicative evidence that there was a change over time, but it was in the opposite direction to that hypothesised. For the other variables, the results were ambiguous with no clear evidence of a positive or negative impact of the RPIWs.
| RPIW | Variable | Hypothesised effect | Result |
|---|---|---|---|
| Abdominal pain | Proportion of patients X-rayed in A&E | Not specified | Reductiona |
| Time from arrival in A&E to being X-rayed | Reduction | Reductionb | |
| Proportion of A&E attendances with abdominal pain admitted to hospital | Reduction | Increasea | |
| Proportion of admissions who get a surgical procedure during their stay | Increase | Reductionc | |
| Time from arrival in A&E to having a surgical procedure | Reduction | No change/reductionb | |
| Proportion of admissions who have a US scan during their stay | Not specified | Reductiona | |
| For those who receive an inpatient US, times from admission to US | Reduction | No changea | |
| Emergency theatre start (between 08.00 and 10.00) and finish (before 20.30) times | Increase | No changea | |
| Purposeful inpatient admission | Number of patients admitted or transferred on to the wards per month | Not specified | Increase for men; no change for womena |
| Proportion of patients admitted directly on to ward | Not specified | Reductiona | |
| Length of spell on ward | Reduction | No change for men; reduction for womenb | |
| Time between admission to ward and discharge from hospital | Reduction | Increase for men; no change/reduction for womena | |
| Community psychosis | Duration from referral received to first allocation | Reduction | No change/increasec |
| Duration from referral received to first successful face-to-face contact | Reduction | No change/reductionb | |
| Proportion of DNAs at first appointment | Reduction | No change/reductionb | |
| Duration from referral received to first assessment | Reduction | No change/reductionb | |
| Duration from referral received to diagnostic formulation | Reduction | No change/reductionb | |
| Proportion of patients for whom a discharge date is specified | Increase | No changea | |
| Duration from referral received to discharge | Reduction | No change/increasec |
Site 09 surgical pathway (abdominal pain)
The main data set examined for this analysis was for all attendees at A&E presenting with abdominal pain, for the period 1 September 2009 to 30 September 2012. The analysis of emergency surgery theatre start and finish times used a different data set from the theatre system and included all patients (see Table 6 for more details of data sets and data definitions). The RPIW week was in September 2011. Attendance at A&E by patients with abdominal pain increased over the period of follow-up (Figure 5). There was a corresponding increase in the number of patients admitted but this was not reflected in the number of patients being X-rayed.
FIGURE 5.
Attendees at A&E presenting with abdominal pain from 2009 to 2012. Dashed line indicates the date of the RPIW intervention.
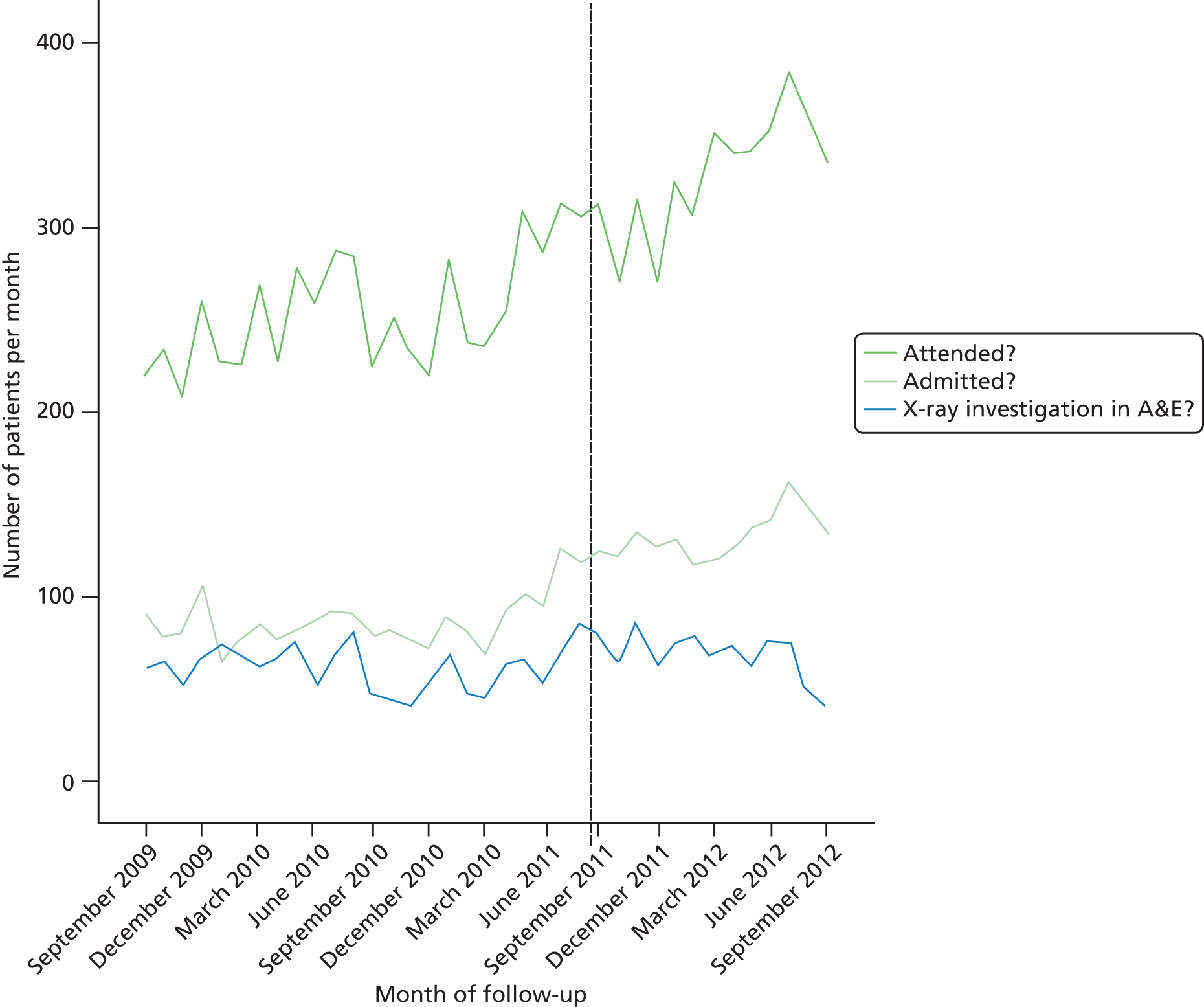
Proportion of patients X-rayed in accident and emergency
The proportion of patients X-rayed in A&E was investigated using logistic regression analysis. The first stage of the analysis was to ascertain whether or not there was any trend in the proportion of patients X-rayed over the entire period of follow-up. This baseline model suggested a significant downwards trend over time. The reduction in odds of an X-ray corresponding to a change of 1 year was 0.85 [95% confidence interval (CI) 0.81 to 0.89]. The second step was to determine whether or not there was a shift in the general level of X-ray requests following the RPIW in September 2011. The estimated change in the odds of requesting an X-ray was 1.18 (95% CI 0.99 to 1.40), which was of borderline significance (p = 0.06). The final step was to investigate whether or not there was a different trend after the RPIW compared with before. This produced a significantly better model. Prior to the RPIW, the reduction in odds of requesting an X-ray corresponding to an increase in time of 1 year was 0.85 (95% CI 0.77 to 0.94); following the RPIW the corresponding reduction in odds was 0.47 (95% CI 0.37 to 0.61). The difference in slopes was highly significant (p < 0.001).
Time from arrival in accident and emergency to being X-rayed
The time taken for patients to be X-rayed was analysed using linear regression. On average patients spent about 2 hours in A&E before being X-rayed. Fitting a linear trend at step 1 suggested an annual increase in time to being X-rayed of 10.0 minutes (95% CI 7.0 to 13.0 minutes) over the period from September 2009 to September 2012. Adding a difference in mean corresponding to the introduction of the RPIW at step 2 suggested that the RPIW had the immediate impact of reducing the time to being X-rayed by 11.5 minutes (95% CI 2.0 to 21.1 minutes). The third step in the analysis was to fit different slopes before and after the RPIW. The difference in the gradients was significant (difference = 17.3 minutes per year, with 95% CI 1.1 to 31.6 minutes per year). This final model suggested that after an initial impact of the RPIW the change was not sustained; the rate of increase in time to being X-rayed after the RPIW was greater than that before.
Checking the fit of the regression model, it was noted that there were a number of suspiciously short and long times recorded in the data. To investigate the impact of these outliers, the analysis was repeated using a plausible range of times defined as being between 15 and 600 minutes of arrival in A&E. The difference in slopes before and after the intervention was no longer statistically significant. The revised model suggested that the impact of the intervention was a reduction of 10.3 minutes in the time spent before being X-rayed (95% CI 2.7 to 17.9 minutes).
Proportion of accident and emergency attendances with abdominal pain admitted to hospital
Whether or not a patient was admitted was investigated using logistic regression analysis. Fitting a linear trend (step 1) suggested that over time (September 2009 to September 2012) the proportion of patients admitted increased; each year the odds of a patient being admitted increased by a factor of 1.13 (95% CI 1.08 to 1.18). Fitting an impact of RPIW at step 2 suggested that the trend observed in step 1 could be attributed to a general increase in the likelihood of admission following the RPIW. The odds of admission increased by a factor of 1.30 (95% CI 1.12 to 1.51). Fitting a more complex model with a different trend before and after the intervention (step 3) did not generate a significant improvement in fit. The most parsimonious model is one that only includes an impact of the RPIW. This estimated impact of the RPIW based on this final model is an increase in the odds of admission by a factor of 1.26 (95% CI 1.16 to 1.36). In practice this corresponds to a change in the proportion of patients being admitted from 34.9% to 45.2%.
Proportion of admissions who receive a surgical procedure
Approximately 14% of patients who were admitted went on to have a surgical procedure during their stay (Figure 6).
FIGURE 6.
Proportion of patients admitted who went on to have a surgical procedure.
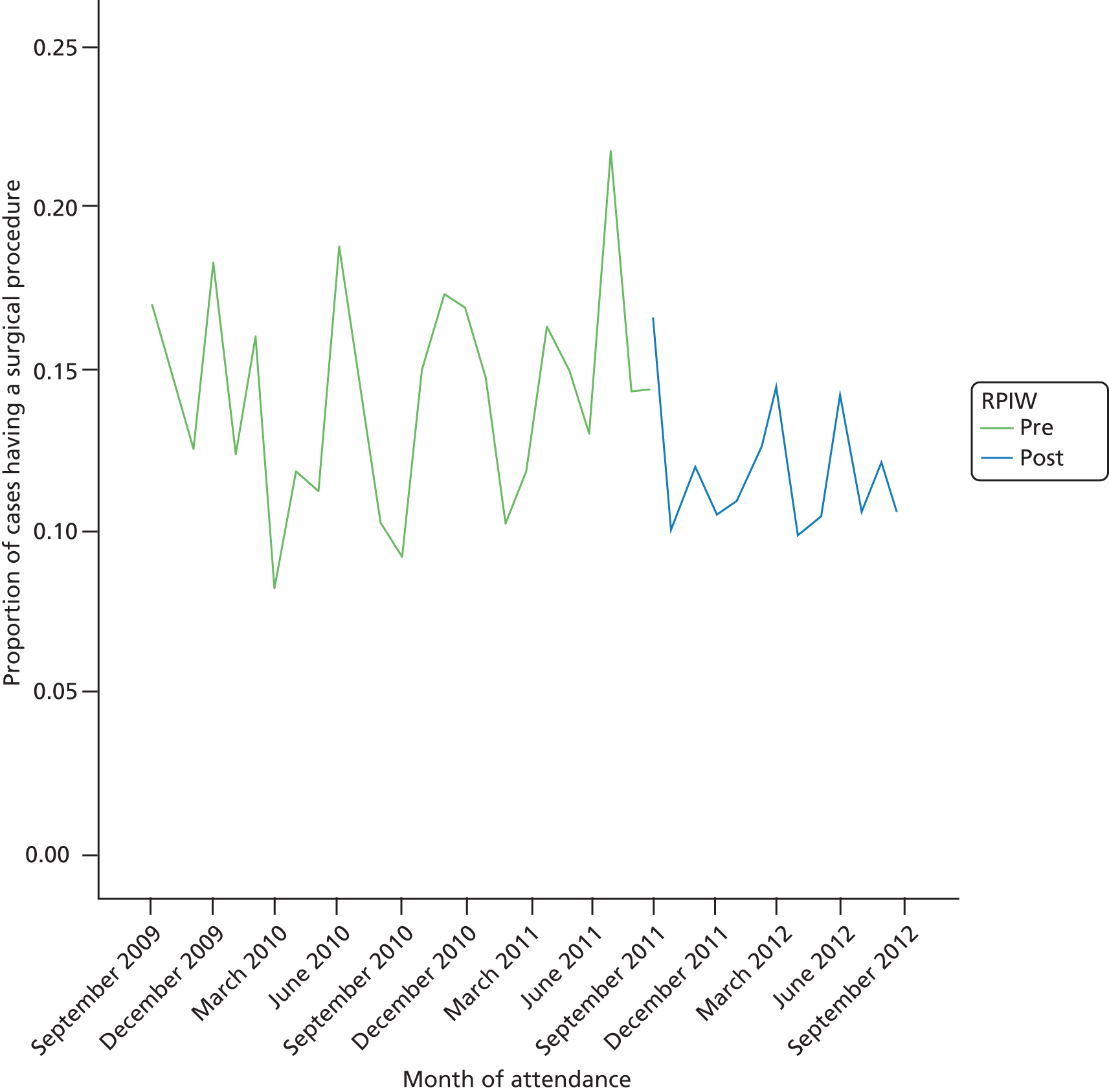
Whether or not a patient underwent a surgical procedure was analysed using logistic regression. Fitting a linear trend (step 1) provided some evidence of a downwards trend over time, with the odds of a patient having surgery changing annually by a factor of 0.91 (95% CI 0.82 to 1.00; p = 0.06). Adding an impact of the RPIW (step 2) suggested that the odds of surgery following the RPIW changed by a factor of 0.74 (95% CI 0.53 to 1.03; p = 0.08). Fitting a different trend before and after the RPIW (step 3) did not improve the fit of the model.
It was noted that, at step 2, fitting an impact of the RPIW appeared to explain the trend observed in step 1. With a term corresponding to the RPIW included in the model, the estimated background trend was no longer significant (p = 0.69). This suggested fitting a more parsimonious model with just a reduction in the likelihood of a surgical procedure following the RPIW. Removing the trend suggested that the impact of the RPIW was to reduce the odds of patients having surgery by a factor of 0.78 (95% CI 0.64 to 0.95).
Time from arrival in accident and emergency to having a surgical procedure
Time from arrival in A&E to having a surgical procedure was heavily skewed (Figure 7).
FIGURE 7.
Distribution of time to surgical procedure (n = 518). Mean 2413.07 minutes, standard deviation 3607.403 minutes.
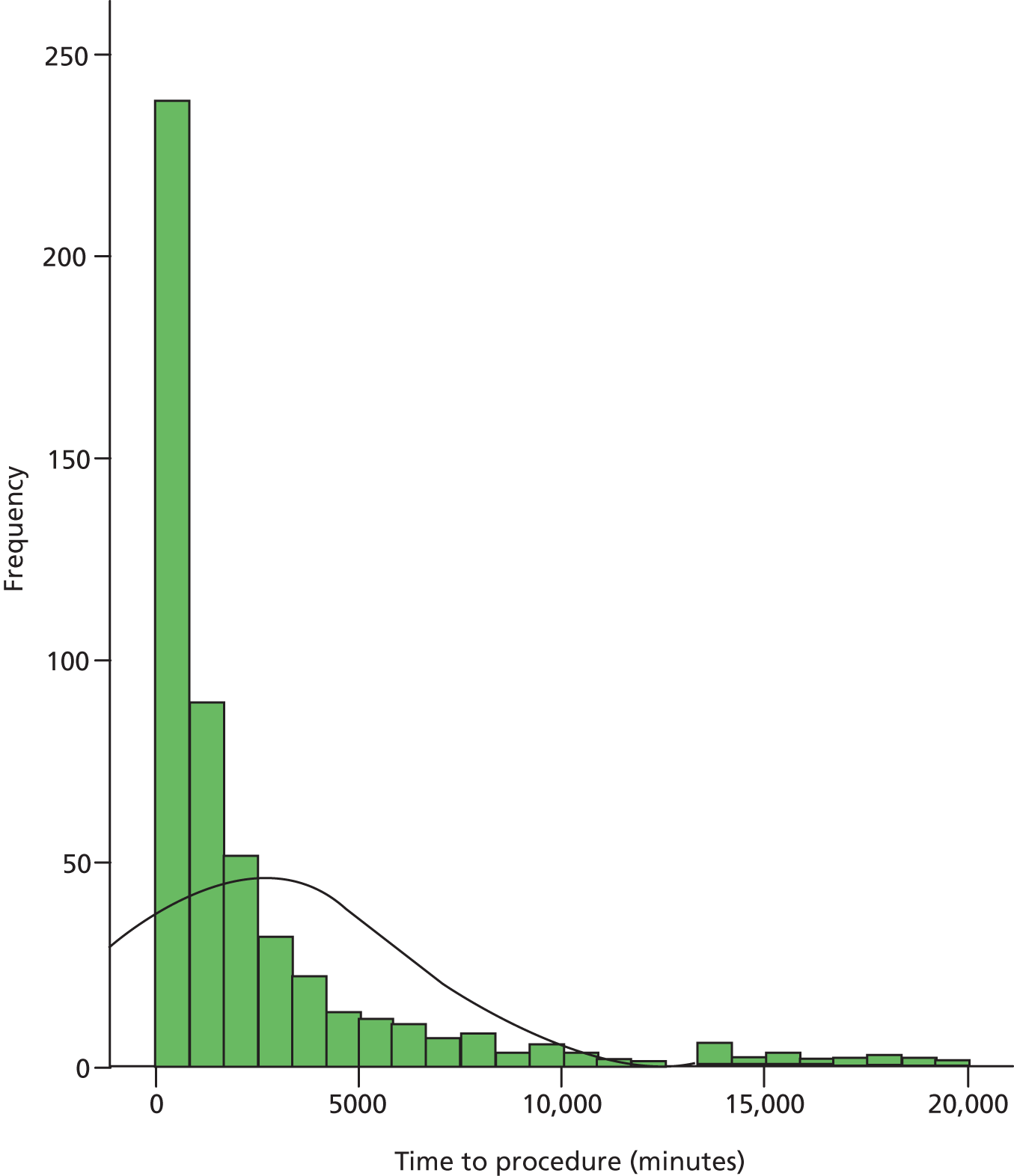
Removing cases where time to surgery was more than 2 weeks and taking a log transformation provided a variable that had a more symmetric distribution (Figure 8). The monthly means of the log-transformed variable are plotted in Figure 9.
FIGURE 8.
Distribution of time to surgical procedure (n = 524). Mean 6.93 minutes, standard deviation 1.491 minutes.
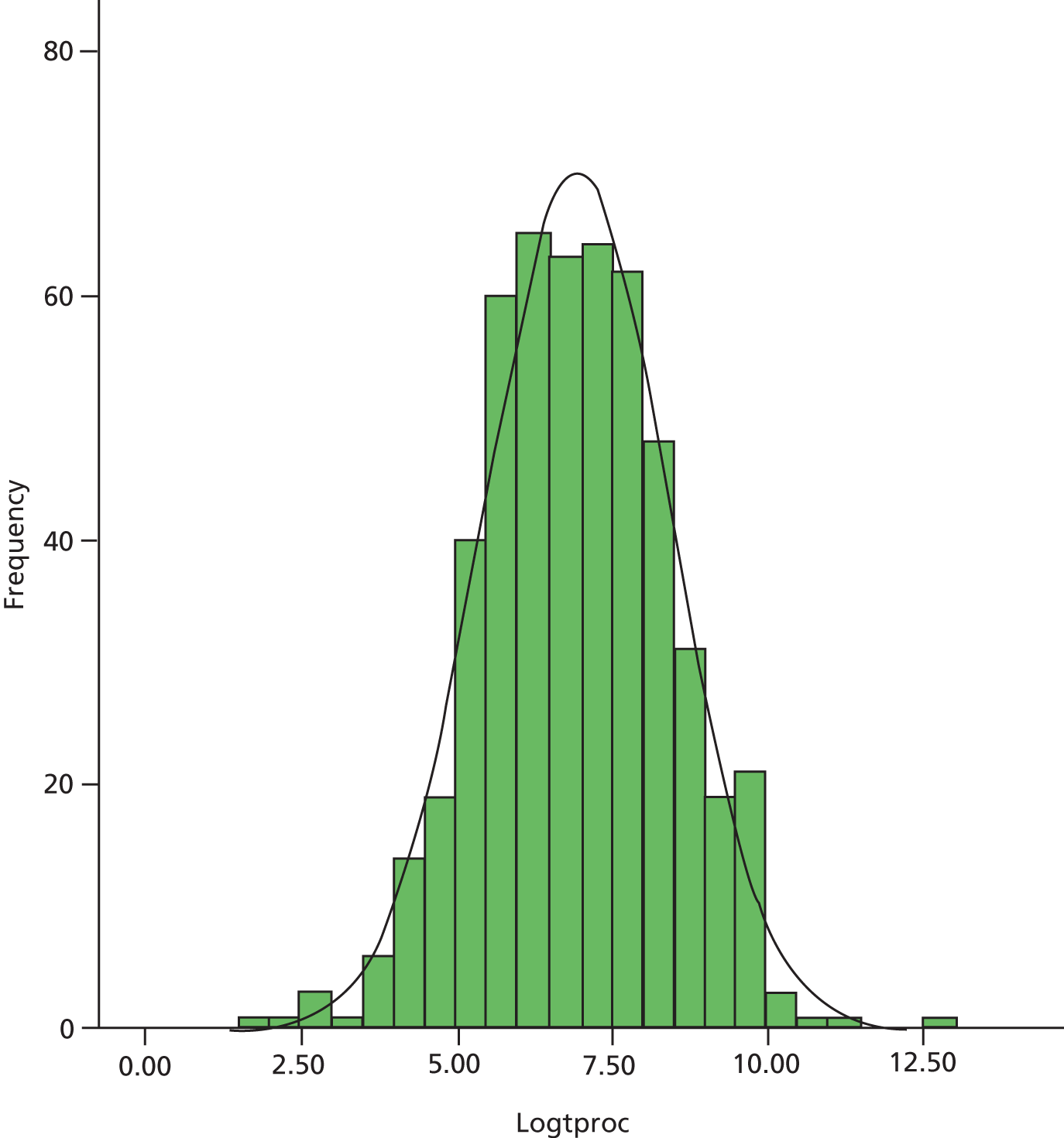
FIGURE 9.
Log-time to procedure by month of follow-up.
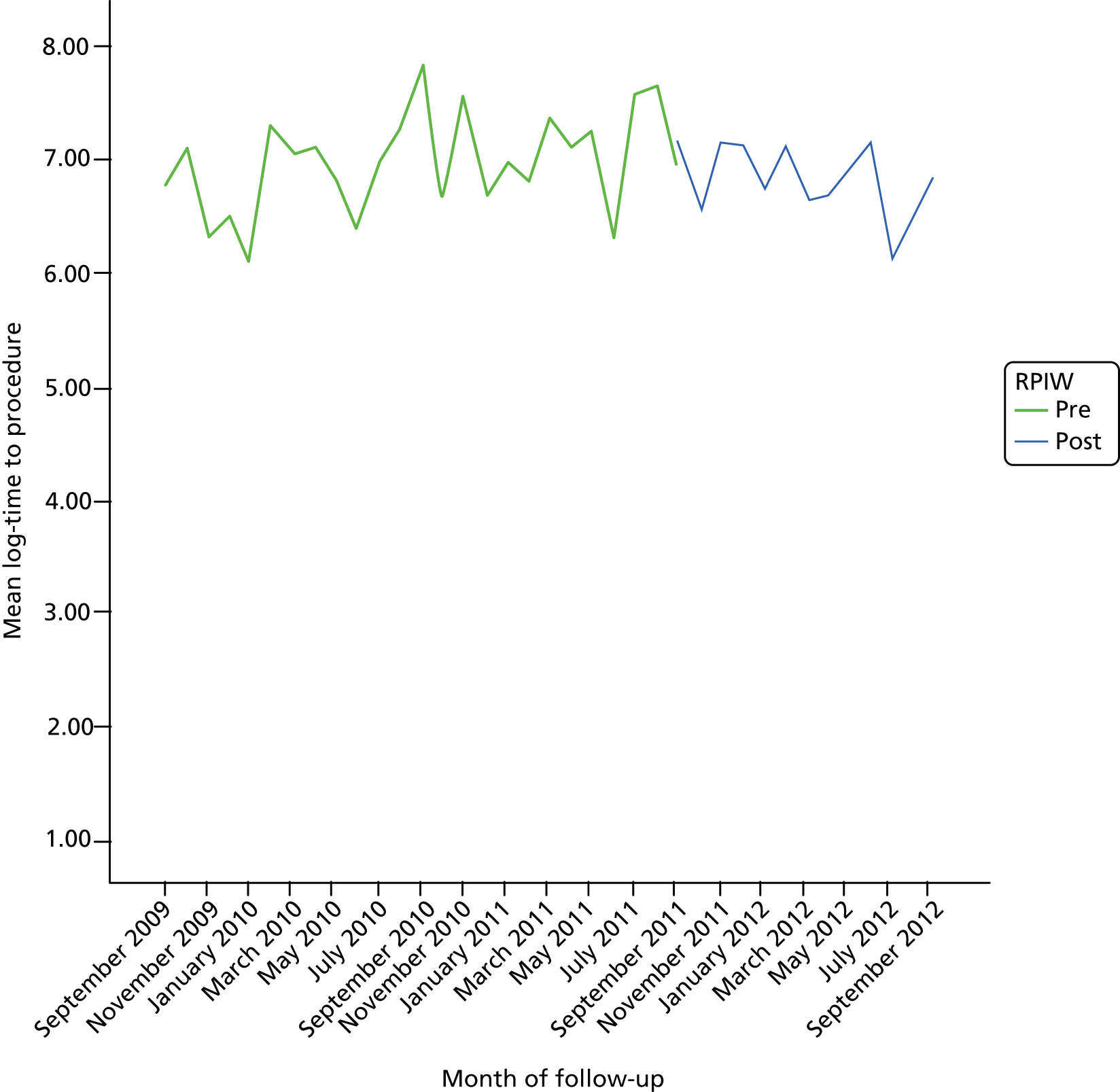
The log-time to procedure was analysed using linear regression. At step 1 there was no suggestion of a linear trend; the annual change in log-time to procedure was 0.01, with 95% CI –0.14 to 0.15. Adding an impact of the RPIW (step 2) suggested that it may have produced a very slight change in log-time to procedure (change = –0.53, 95% CI –0.99 to –0.07). However, by fitting a model with an impact of the RPIW with no annual trend the estimated impact fell to –0.18 (95% CI –0.45 to 0.10). Finally, a more complex model with a different trend before and after the RPIW suggested that the slope after the RPIW (–0.48, 95% CI –1.17 to 0.21) was less than the slope before the RPIW (0.35, 95% CI 0.08 to 0.62) (difference in slopes = –0.83, 95% CI –1.57 to –0.84). There was very little difference in terms of goodness of fit between the alternative models. Any impact of the RPIW was fairly modest when considered alongside the natural variability in this variable.
Proportion of admissions who have an ultrasound scan
Thirty-one per cent of patients admitted had an ultrasound scan. The monthly data varied considerably over the period of follow-up (Figure 10).
FIGURE 10.
Proportion of admissions who had an ultrasound scan by calendar month.
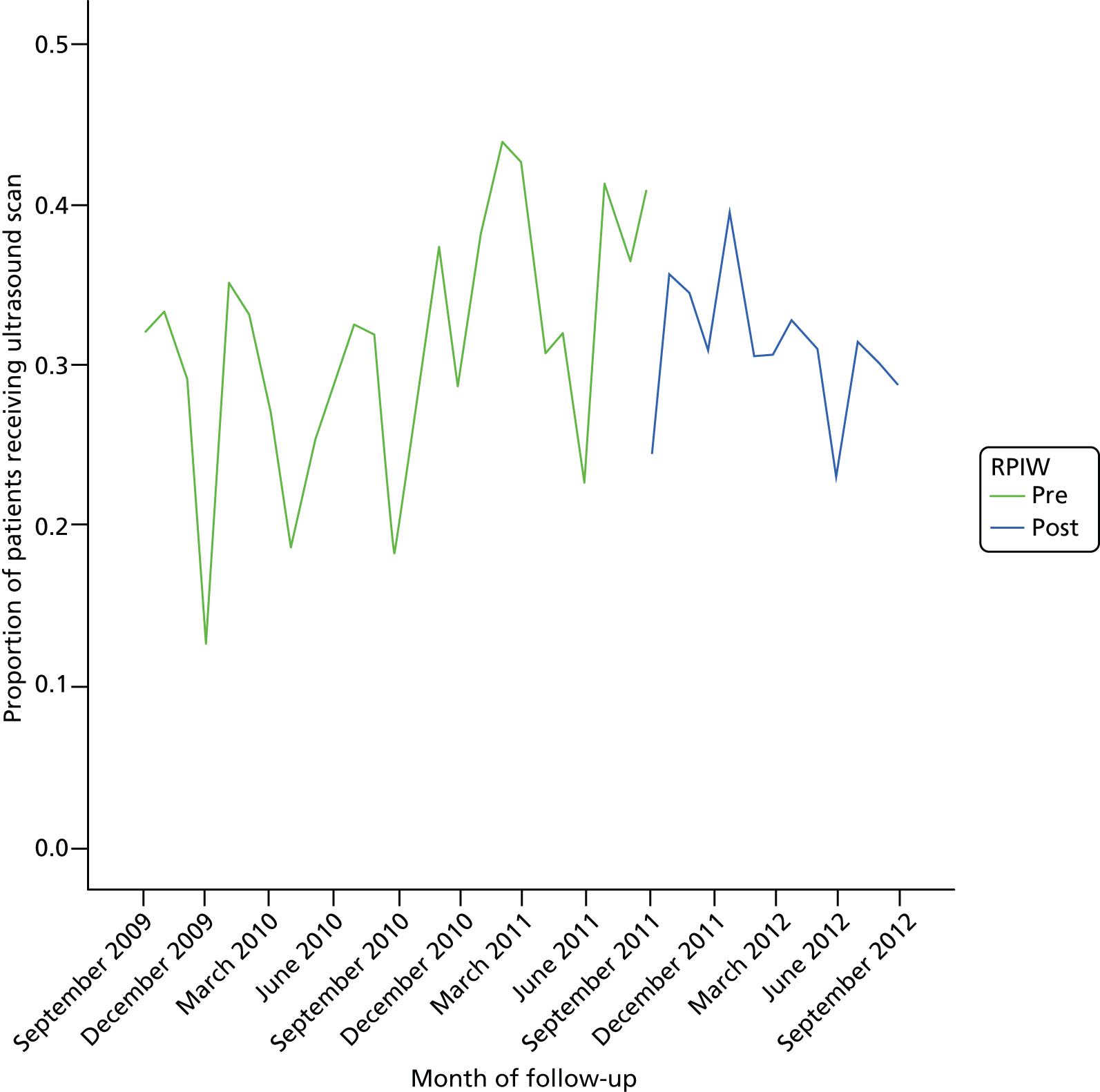
The likelihood of a patient having an ultrasound scan was investigated using logistic regression. Fitting a linear trend (step 1) suggested that, annually, the odds of a patient having a scan increased by a factor of 1.06 (95% CI 0.98 to 1.15; p = 0.13). Adding an impact of the RPIW (step 2) suggested that after the RPIW the odds of a patient having a scan changed by a factor of 0.77 (95% CI 0.60 to 0.99; p = 0.04). Fitting a different trend before and after the intervention (step 3) suggested that the RPIW had an impact on the proportion of patients receiving an ultrasound scan. Prior to the RPIW, there was an increasing trend in the proportion of patients who had an ultrasound scan. After the RPIW the trend was reversed, and over time fewer patients had an ultrasound scan (the difference in slopes on the logistic scale was –0.508 with 95% CI –0.884 to –0.132; p = 0.008).
Inpatient ultrasound: times from admission to ultrasound
The time to ultrasound was skewed and typically between 1 hour and 1 week. A plot of the geometric means by calendar month is shown in Figure 11.
FIGURE 11.
Geometric mean time to ultrasound by calendar month.
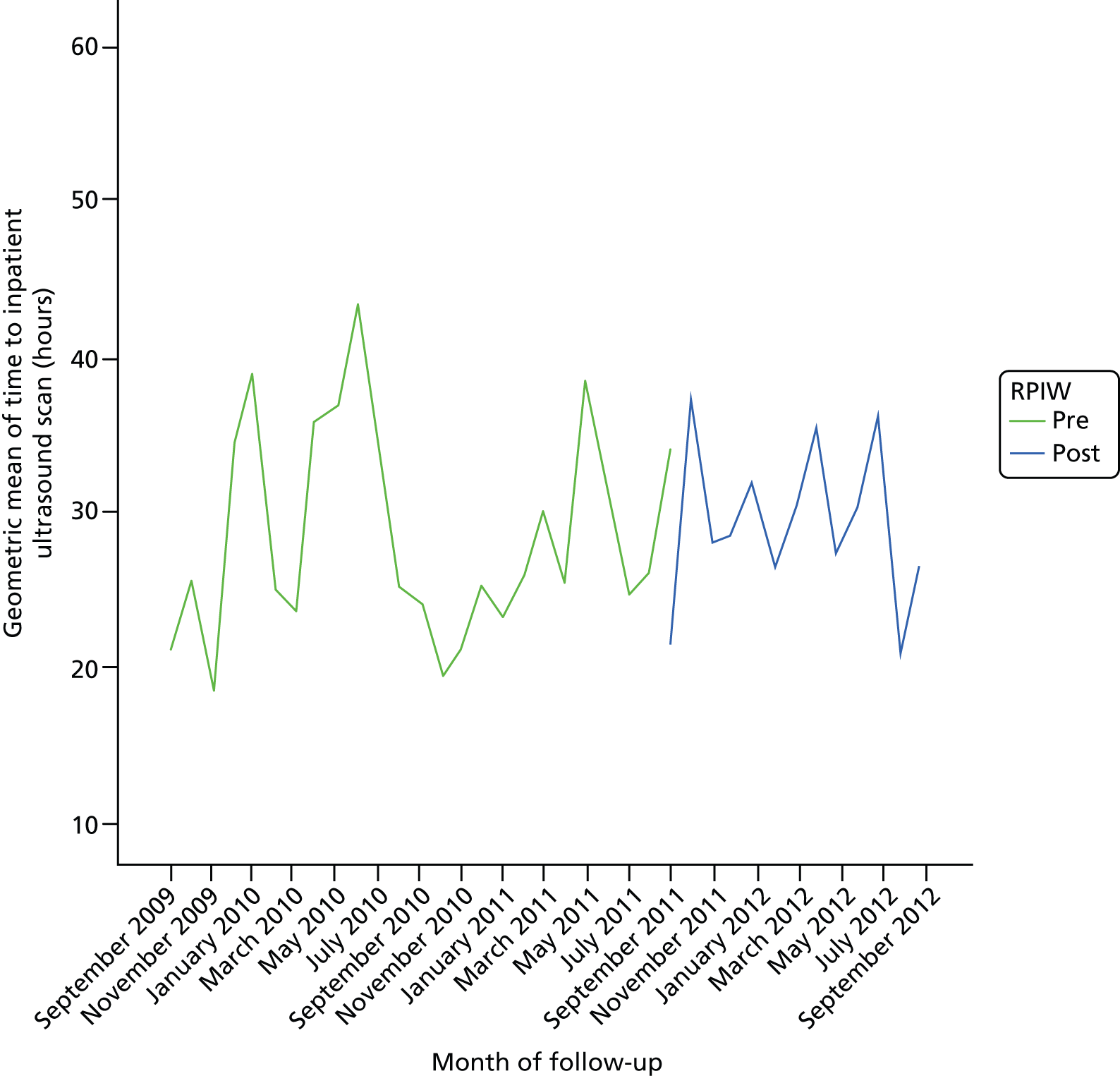
The time to inpatient ultrasound was analysed using normal regression after undertaking a log transformation. The distribution of log-transformed data is shown in Figure 12.
FIGURE 12.
Distribution of log-transformed time to ultrasound scan (n = 1201). Mean 7.42 minutes, standard deviation 1.025 minutes.
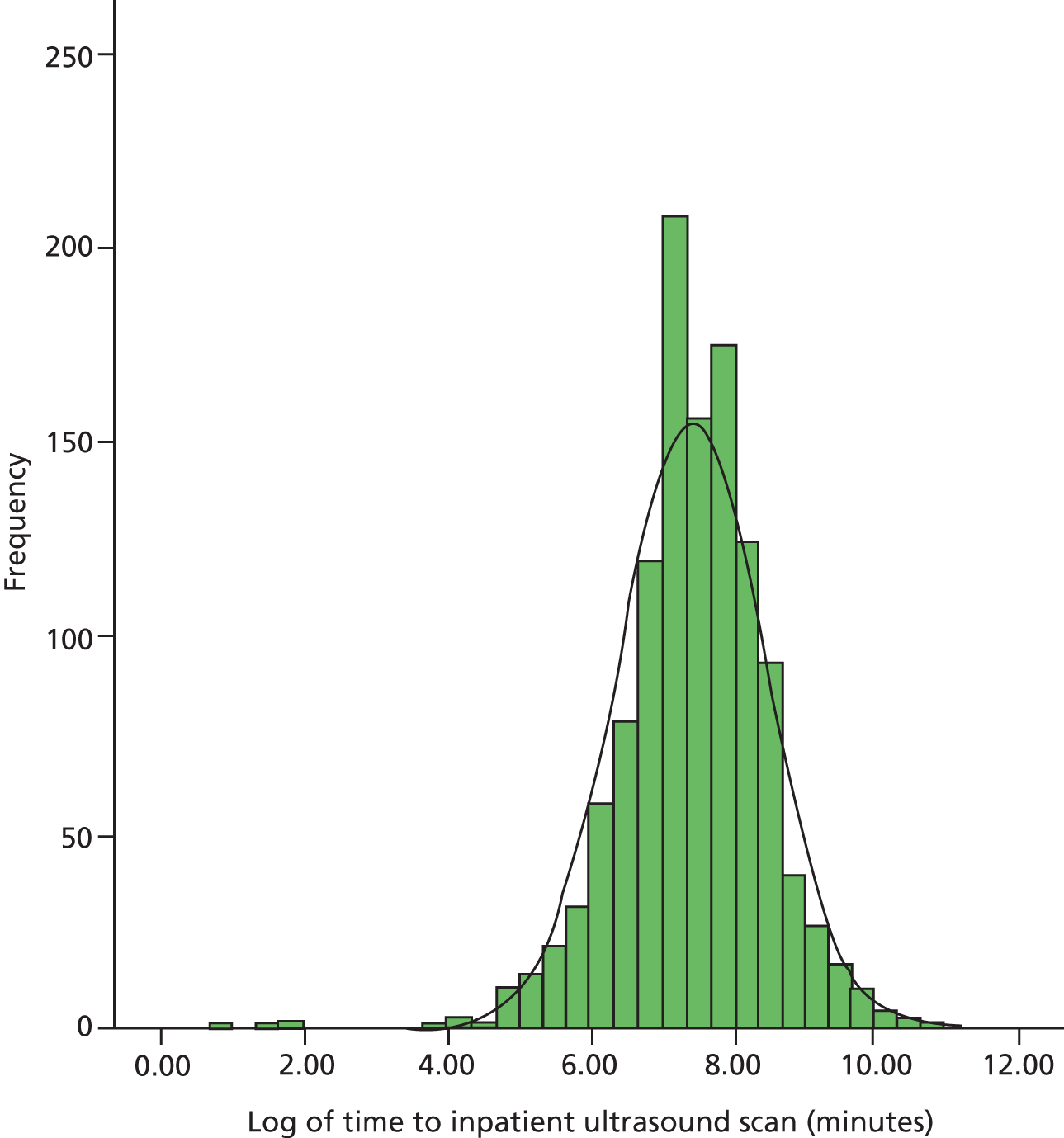
Fitting a linear trend (step 1) across the entire period of interest suggested a slight annual increase in log-time to ultrasound of 0.06, with 95% CI 0.01 to 0.13 (p = 0.07). In step 2, when an impact of the RPIW was added, the estimated change in log-time to ultrasound was 0.05 with 95% CI –0.15 to 0.26 (p = 0.62). Finally, fitting a different slope before and after the intervention (step 3) did not produce a significant improvement in fit. There was no evidence that the RPIW had a clinically significant impact on time to ultrasound.
Emergency theatre start (between 08.00 and 10.00) and finish (before 20.30) times
One of the aims of the RPIW was that the period when routine procedures (non-‘life or limb’) in the emergency theatre are undertaken should commence prior to 10.00 and finish before 20.30. The data set included the start and finish times of all procedures but there was no variable to indicate which procedures were ‘routine’ and which were ‘life or limb’. A pragmatic solution to this problem was to regard any procedure that commenced either prior to 8.00 or after 20.30 as ‘life or limb’. These procedures were then excluded from the analysis. For each day, it was determined whether or not the first ‘routine’ procedure started before 10.00 and the last finished before 20.30.
The target of starting before 10.00 and finishing before 20.30 was achieved on 47.5% of the 1119 days considered. There was considerable variation between days of the week, as shown in Table 20. Differences between days were statistically significant (χ62 = 32.6, p < 0.001).
| Day | Start before 10.00 and finish before 20.30? | Total | |
|---|---|---|---|
| No, n (%) | Yes, n (%) | ||
| Sunday | 58 (36.5) | 101 (63.5) | 159 |
| Monday | 100 (63.3) | 58 (36.7) | 158 |
| Tuesday | 86 (53.8) | 74 (46.3) | 160 |
| Wednesday | 89 (55.3) | 72 (44.7) | 161 |
| Thursday | 70 (43.8) | 90 (56.3) | 160 |
| Friday | 89 (55.6) | 71 (44.4) | 160 |
| Saturday | 95 (59.0) | 66 (41.0) | 161 |
| Total | 587 (52.5) | 532 (47.5) | 1119 |
The target was achieved most often on Sundays and least often on Mondays.
In contrast, the differences between calendar months were not significant (χ112 = 15.7, p = 0.15). Plotting the monthly figures (Figure 13) suggests an upwards trend over the 3-year period commencing in September 2009.
FIGURE 13.
Proportion of days with procedures starting before 10.00 and finishing before 20.30, by month.
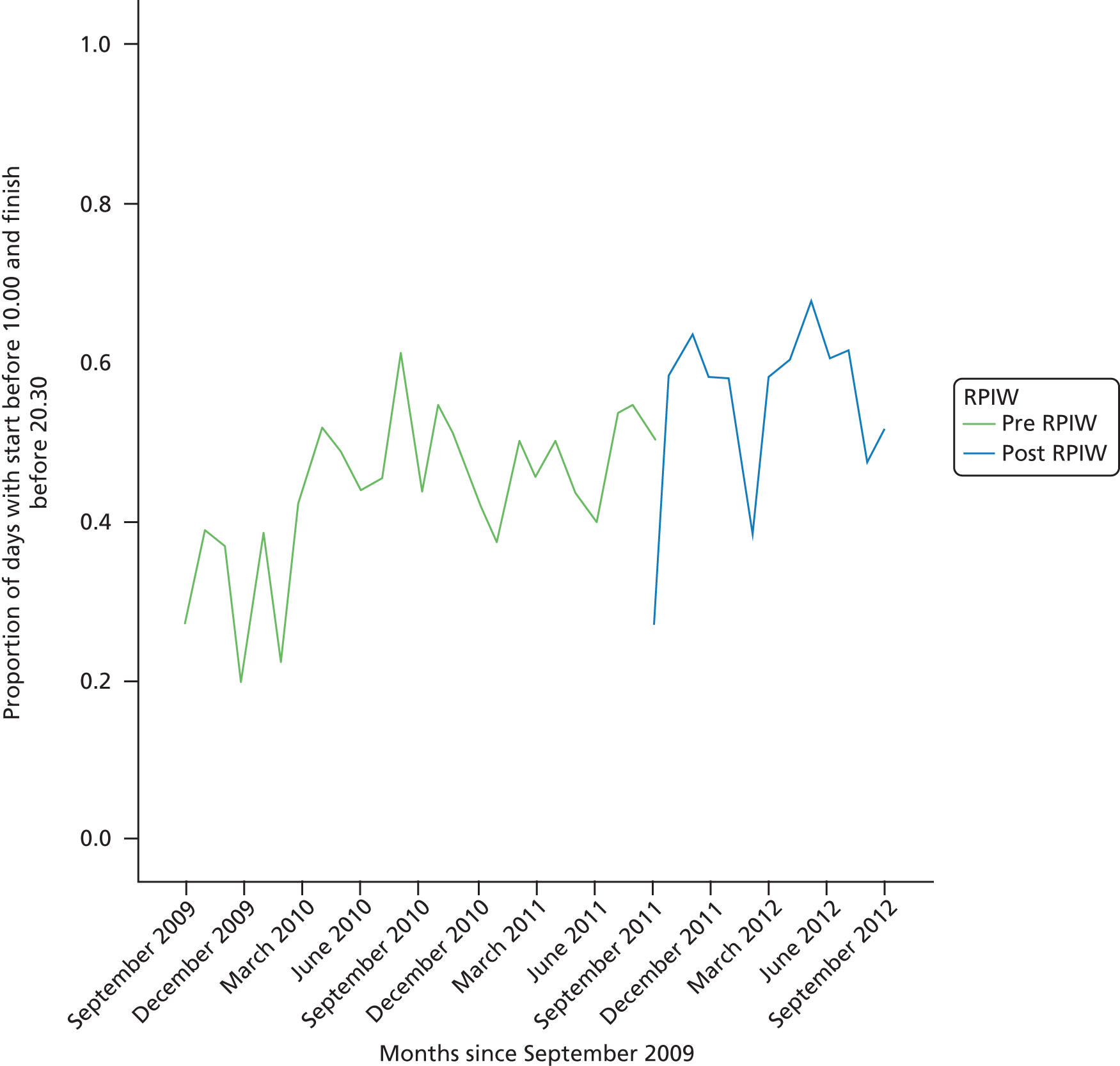
The data were analysed using logistic regression. Given the difference between days of the week, this categorical variable was included as the baseline model. At the next step a linear trend was included. This was highly significant. Each year the odds of achieving the target increased by a factor of 1.40 (95% CI 1.22 to 1.61, p < 0.001). The next step was to fit an impact of the RPIW. There was almost no change in the odds of achieving the target following the RPIW (odds ratio 0.98, 95% CI 0.62 to 1.49). Finally, fitting an interaction between the effect of the RPIW and the linear trend indicated that the RPIW had no impact on the rate of change. The difference in trends on the logistic scale before and after the RPIW was –0.30 with 95% CI –1.03 to 0.44. Prior to the RPIW, the target was achieved on only 43% of occasions; after the RPIW this figure rose to 55.7%. However, the above analysis suggests that it is likely that this increase would have occurred anyway, given the underlying trend in the 2 years from September 2009.
Site 10 purposeful inpatient admission rapid process improvement workshop
The data set used for this analysis was linked across several ward changes for males and females across the period from April 2005 to October 2012 (see Chapter 4, Table 6 for details). For the purposes of the analysis, the RPIW was assumed to be April 2008 for males and October 2008 (‘share and spread’) for females.
The key variables for this analysis related to the length of time the patient spent receiving care in hospital and, specifically, on the intervention wards. There were a number of potential dependent variables (see Chapter 4, Tables 6 and 7). Note that in the analysis, ‘length of stay in hospital’ is equal to the time between admission to hospital and admission to the ward, plus the length of spell on the ward and the time from discharge from the ward to discharge from hospital.
However, as can be seen in Figure 14, a number of the variables were highly correlated. Generally, the length of stay on the ward was highly correlated with the length of stay in the hospital. However, patients may have been admitted to the hospital some time before being transferred to the ward. Although most patients were discharged from the hospital when they left the ward, there were some patients who were transferred elsewhere within the hospital prior to being discharged. It was decided that the two most important variables to analyse were the time that the patient spent on the ward (which could be most influenced by staff behaviour) and the time from admission to the ward to discharge from hospital (to allow for apparently shortened stays which were actually due to transfers to other wards). Other variables of interest were the time between admission to hospital and start date on the ward, and the time between discharge from the ward and discharge from hospital. Before considering the impact of the RPIW on the time spent on the ward, a number of processes of care variables were examined so as to understand the concomitant changes that were happening during the period of interest.
FIGURE 14.
Length of stay in days in hospital and on the ward. (a) Total length of stay by time spent on ward; (b) time between admission to ward and discharge from hospital by time spent on ward; (c) time between admission to ward and discharge from hospital: frequency distribution (n = 4195; mean 13.01 days, standard deviation 81.338 days); and (d) total length of stay by time between admission to ward and discharge from hospital.
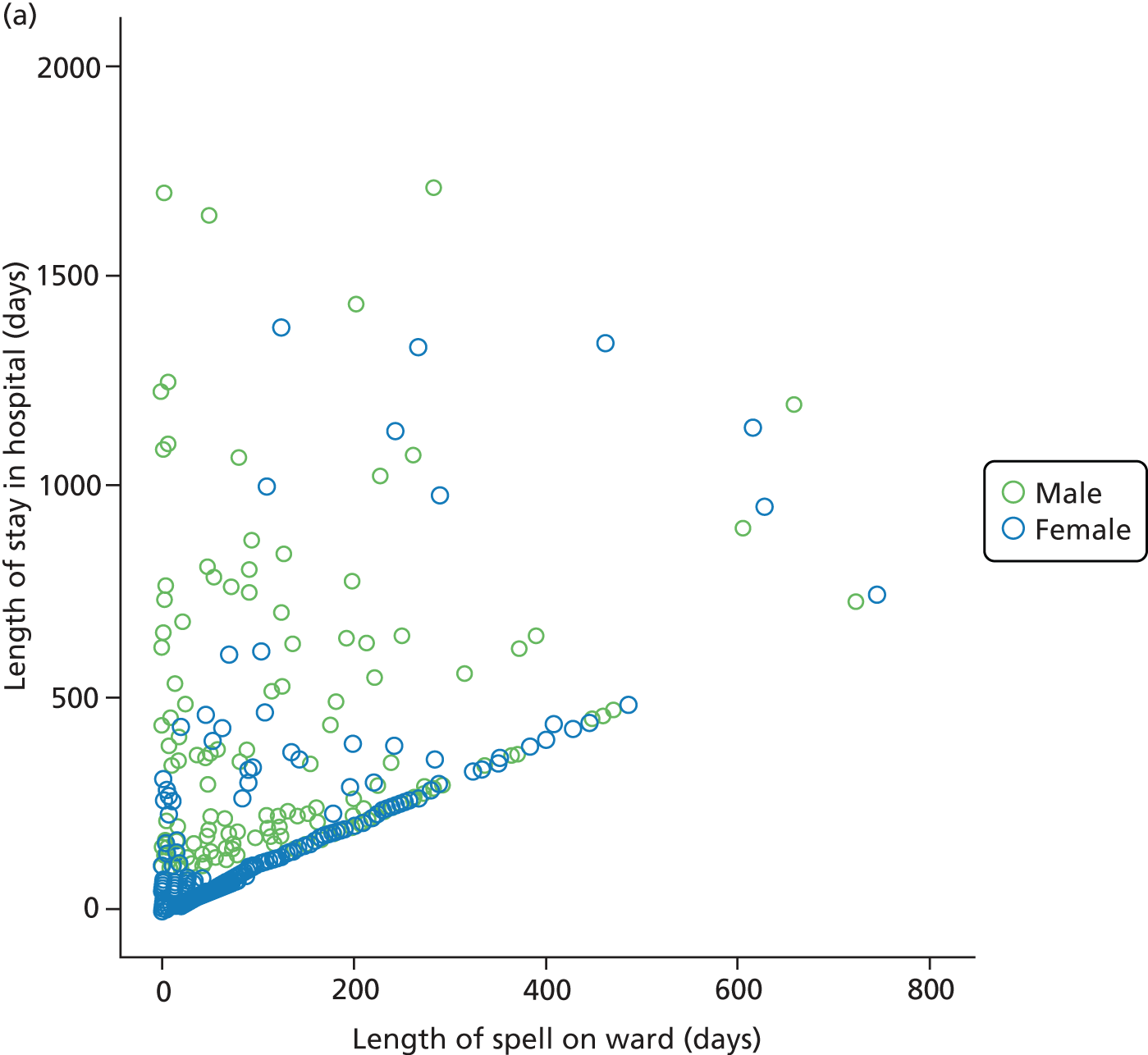
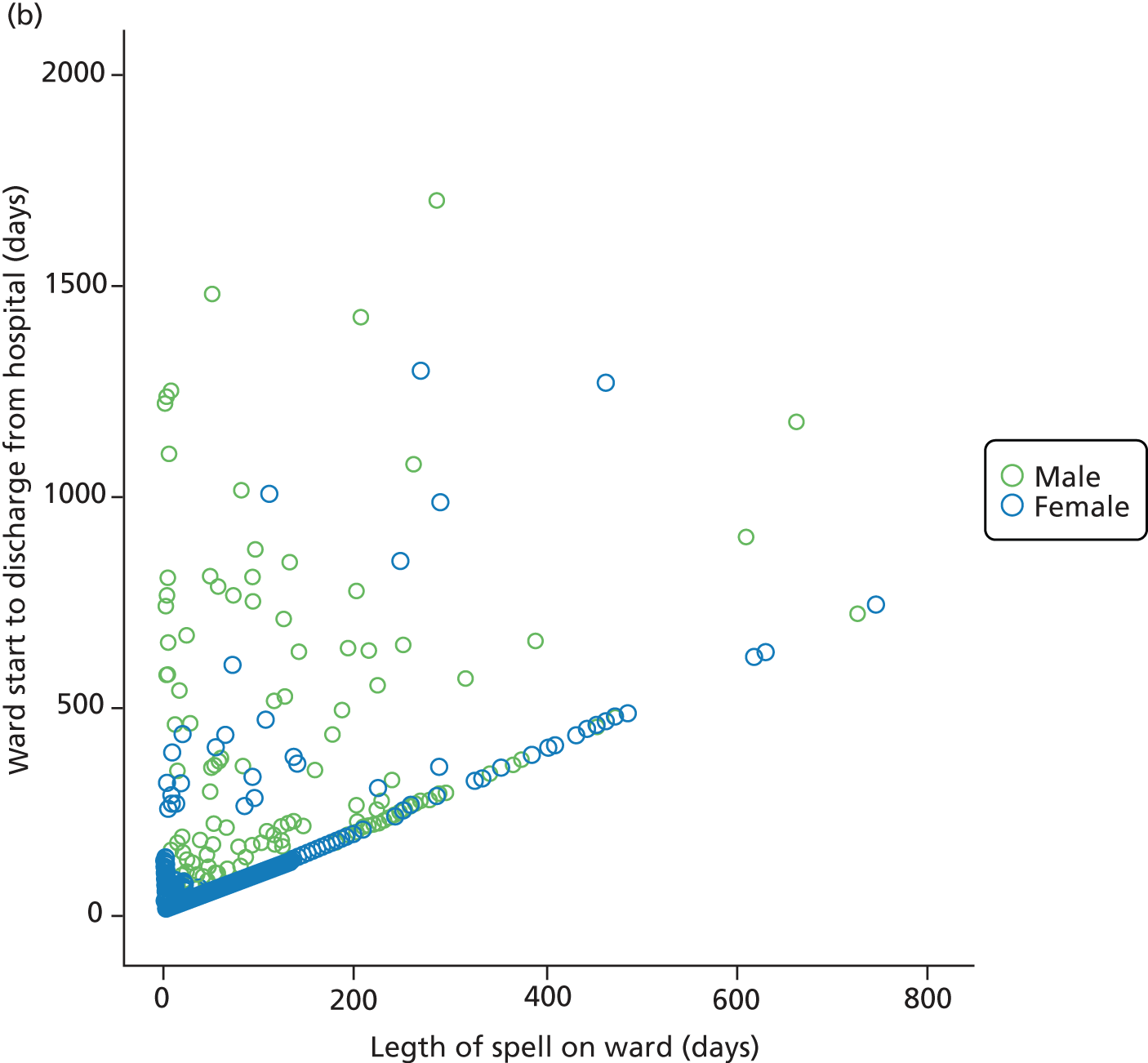
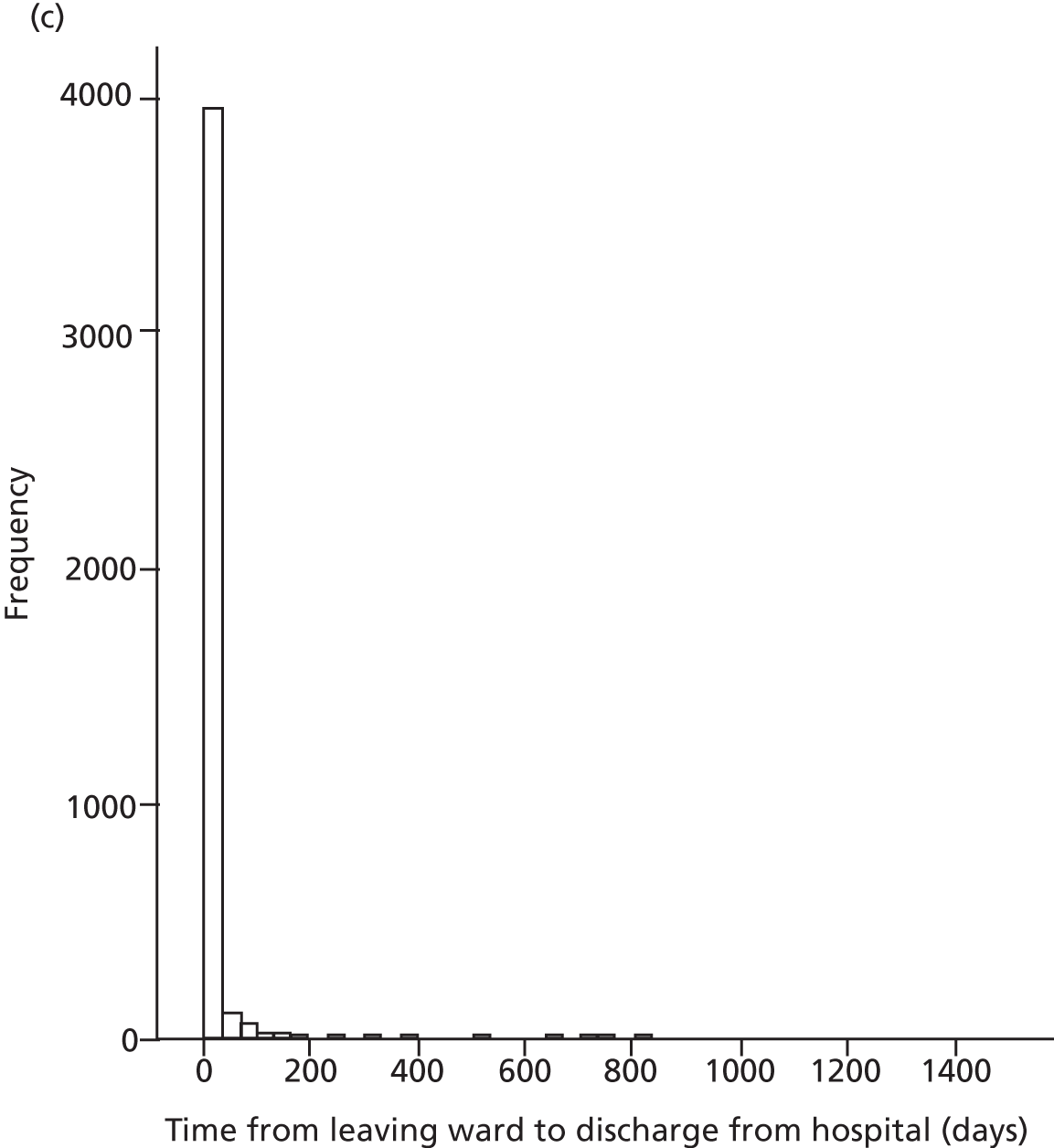
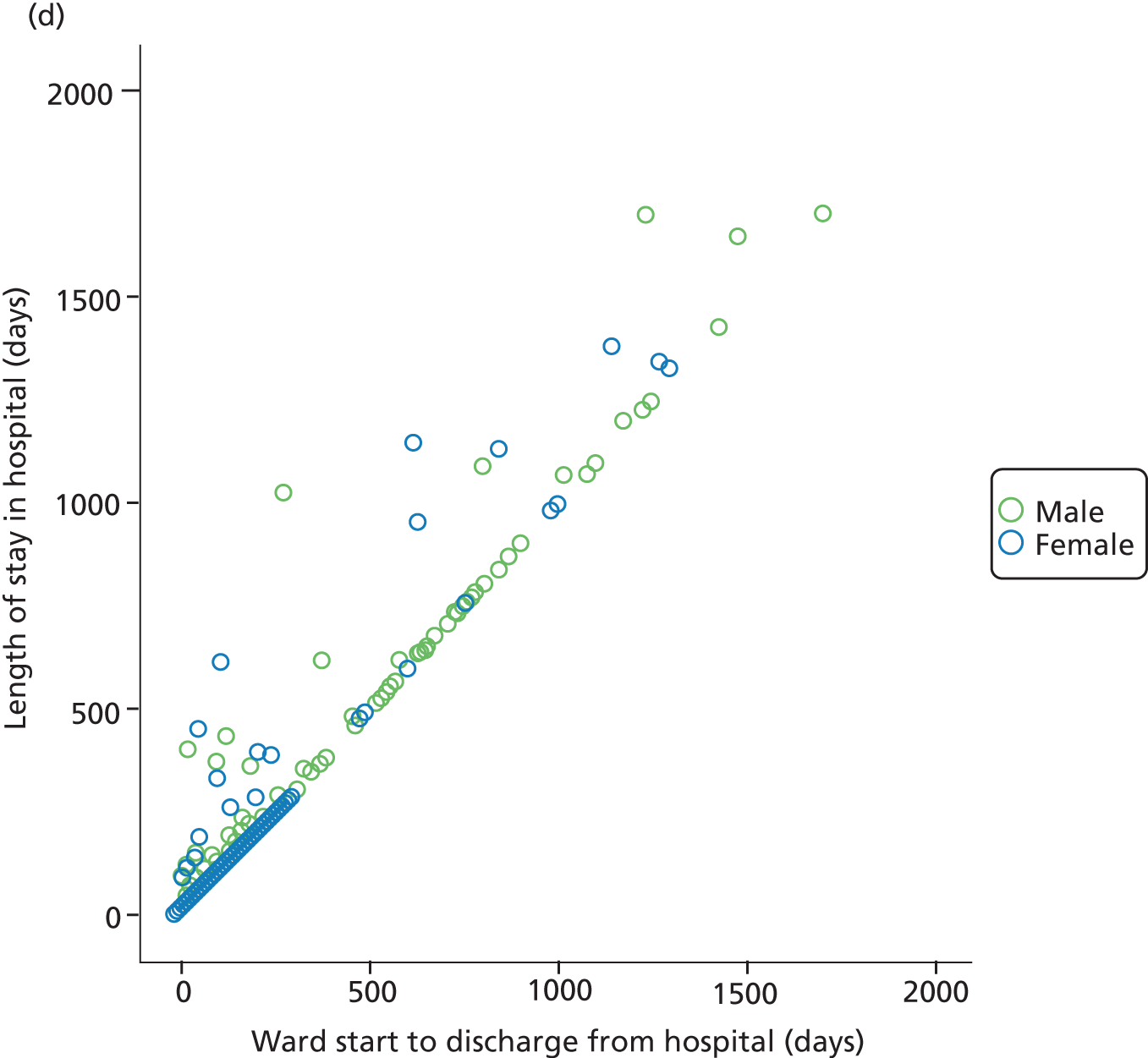
Number of patients admitted or transferred on to the wards per month
The number of patients admitted or transferred on to the wards is shown in Figure 15. The number of male patients admitted or transferred on to the ward fell from a mean of 27.6 per month prior to the RPIW to 22.2 after the RPIW (difference in means = –5.4, 95% CI –7.8 to –3.0). In contrast, the number of female patients admitted or transferred increased slightly from 18.0 per month to 20.9 per month, although this change was not statistically significant (difference in means = 2.9, 95% CI –0.6 to 5.3).
FIGURE 15.
Admissions and transfers to hospital wards by calendar month.
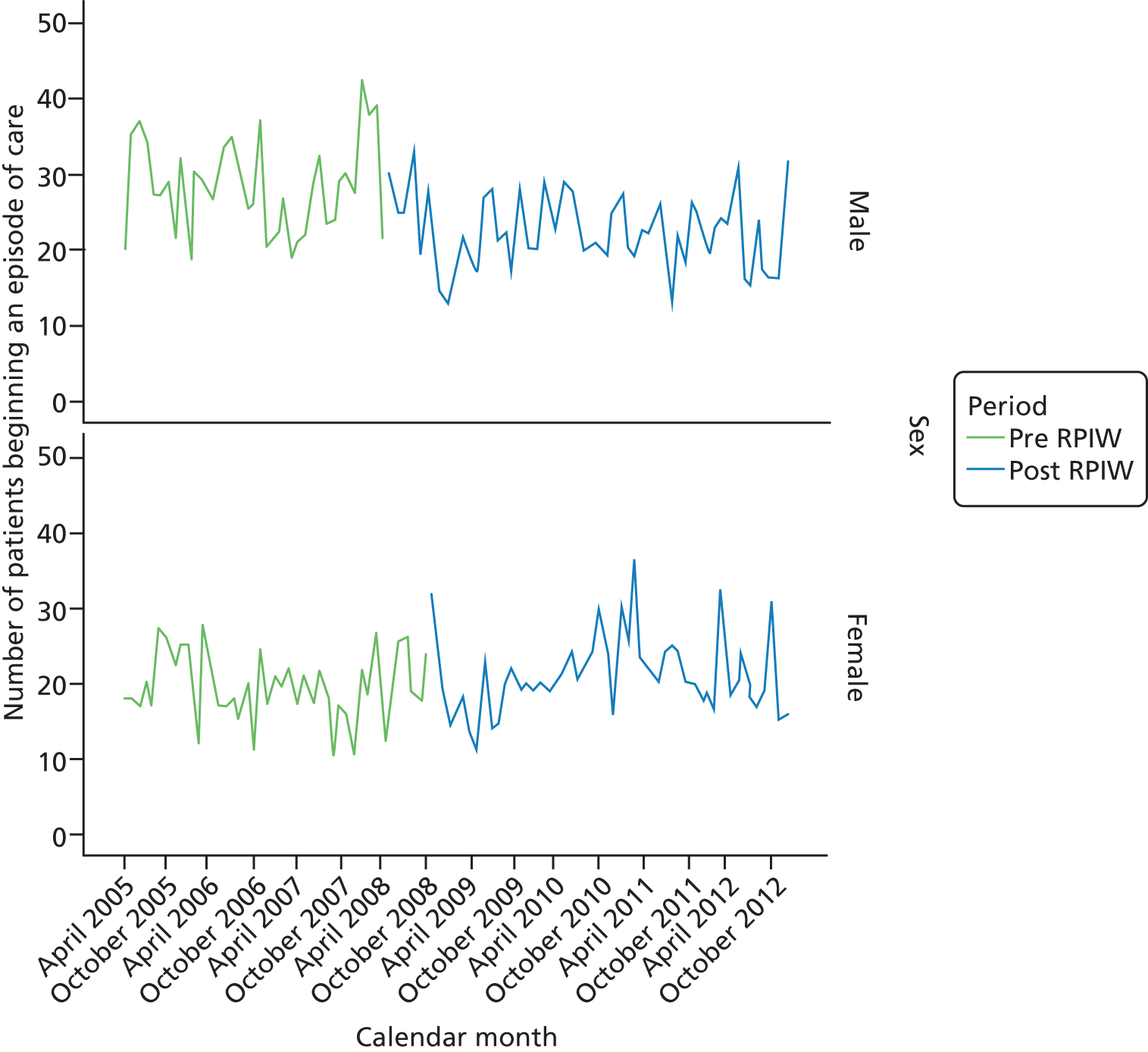
Proportion of patients admitted directly on to the ward
The proportion of patients admitted directly on to the ward was smaller after the RPIW (Table 21); a greater proportion of patients were being transferred to the ward. This was particularly true for men, with 18.3% of male patients after the RPIW having been admitted elsewhere.
| Sex | RPIW | Patient admitted directly to ward? | Total | |
|---|---|---|---|---|
| No, n (%) | Yes, n (%) | |||
| Male | Pre RPIW | 11 (1.1) | 1031 (98.9) | 1042 |
| Post RPIW | 228 (18.3) | 1016 (81.7) | 1244 | |
| Total | 239 (10.5) | 2047 (89.5) | 2286 | |
| Female | Pre RPIW | 6 (0.7) | 828 (99.3) | 834 |
| Post RPIW | 95 (9.1) | 952 (91.9) | 1047 | |
| Total | 101 (5.4) | 1780 (94.6) | 1881 | |
| Total | Pre RPIW | 17 (0.9) | 1859 (99.1) | 1876 |
| Post RPIW | 323 (14.1) | 1968 (85.9) | 2291 | |
| Total | 340 (8.2) | 3827 (91.8) | 4167 | |
Time between admission to hospital and admission to the ward
Most patients were admitted directly on to the ward. For those patients who were not directly admitted to the ward, the mean time between admittance to hospital and transfer to the ward was 38.1 (95% CI 11.4 to 65.0) days for men and 51.6 (95% CI 10.3 to 92.8) days for women.
Length of spell on the ward
For each patient, the time between admission or referral to the ward and leaving the ward was calculated. The data were normalised by taking a log transformation (Figure 16).
FIGURE 16.
Distribution of log-transformed length of stay with superimposed normal curve (n = 186). Mean 2.55 days, standard deviation 0.362 days.
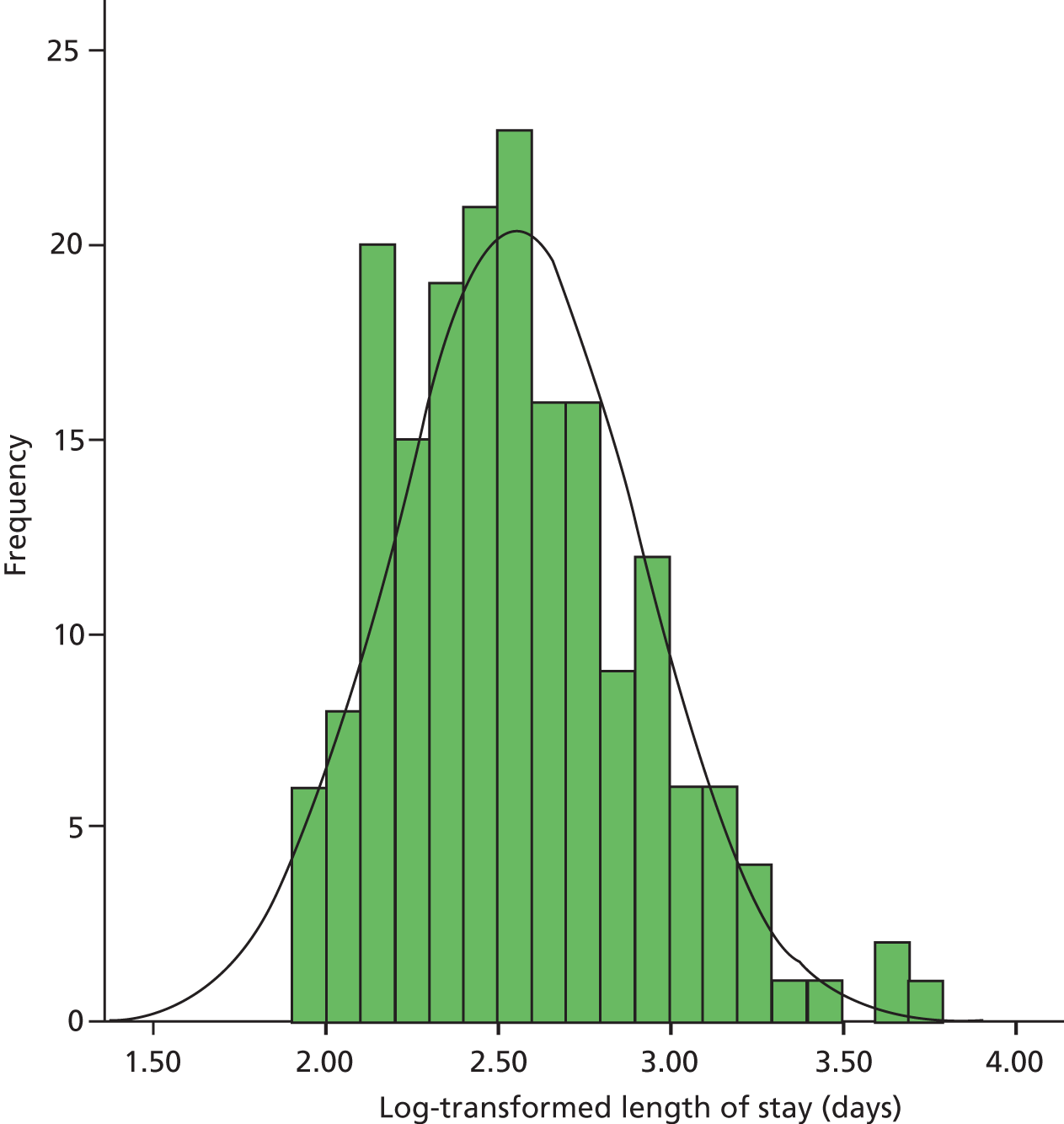
For each calendar month the mean of the log-transformed length of stay was calculated and the antilog taken to give the geometric mean (Figure 17).
FIGURE 17.
Geometric mean length of spell on ward, in days, by month of admission by sex.
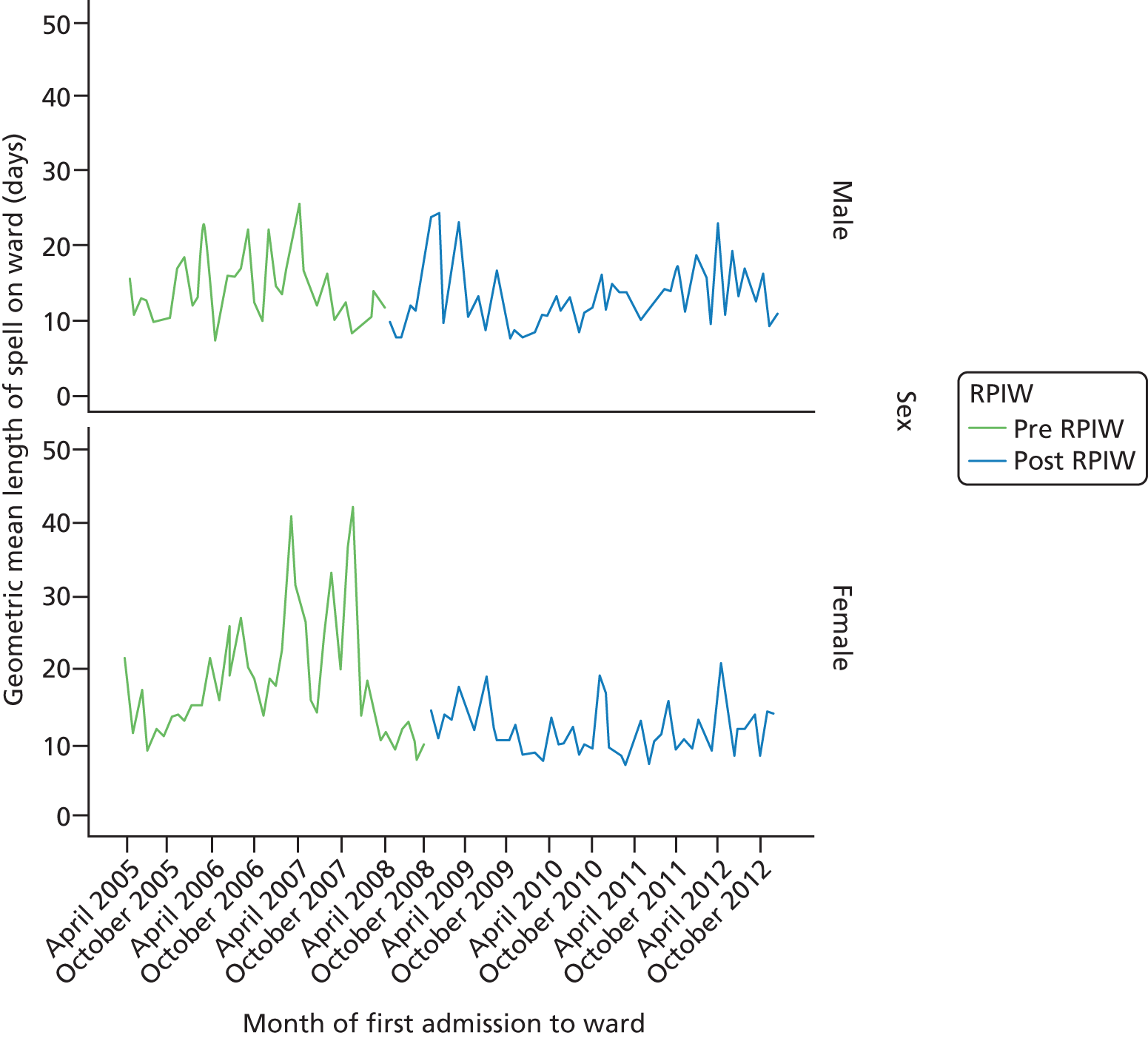
There appears to be a considerable variability in the length of stay, with some particularly large geometric mean values for women during 2007. The log-transformed length of stay was analysed using linear regression.
At step 1 a linear trend was fitted across the period April 2005 to November 2012. The length of stay on the ward fell by 3.9% (95% CI 2.3% to 5.6%).
Adding an impact of the RPIW at step 2 suggested that the RPIW led to a reduction in the length of time spent on the ward; the time spent on the ward following the RPIW fell by 18.0% (95% CI 4.3% to 29.7%). With a difference from pre to post RPIW, the effect of a linear trend was no longer significant and this term was removed from the model.
Given the systematic differences between wards, a difference in the impact of the RPIW was fitted for male and female patients. There was a significant interaction effect. There was a significant impact of the RPIW for female patients but not for male patients; length of spell on the ward was reduced post RPIW to
-
68.4% (95% CI 60.8% to 80.0%) of pre-RPIW values for women
-
93.4% (95% CI 83.9% to 103.9%) of pre-RPIW values for men.
A concern with these results was that they primarily reflected the spikes in length-of-stay times for women admitted in 2007. It is possible that length of stay was already falling for female patients by the beginning of 2008. The above results may reflect a regression to the mean. The other issue with this analysis was that admissions were categorised by whether they occurred before or after the RPIW. Some patients who were admitted prior to the RPIW were discharged following it. This issue was addressed by the following analysis.
Time between admission to the ward and discharge from hospital
The time to discharge from hospital (starting from the first admission to the ward) was analysed using a Cox proportional hazards model with time-varying covariates. All patients who were admitted to the ward after 1 April 2005 were included in the regression analysis.
In this analysis the intervention variable was a time-varying covariate. The length of spell for those patients who were on the ward at the time of the RPIW was split into two periods; in the first their management was undertaken pre RPIW and in the second it was undertaken post RPIW. The results from the modelling were calculated as hazard ratios. A higher hazard indicated a faster rate of discharge of patients from the ward (one of the aims of the RPIW).
Fitting a trend at step 1 indicated that there was an annual increase in the rate of discharge (hazard ratio 1.015, 95% CI 1.001 to 1.030). Adding an impact of the RPIW at step 2 suggested that if allowing for an annual increase in the rate at which patients were discharged the RPIW was to decrease the rate of discharge (hazard ratio 0.80, 95% CI 0.72 to 0.90).
The next steps were to investigate separate effects for men and women. Allowing for an annual trend, the estimated impacts of the RPIW were
-
a reduction in the rate of discharge for men; hazard ratio 0.70 (95% CI 0.60 to 0.81)
-
very little change in the rate of discharge for women; hazard ratio 0.93 (95% CI 0.77 to 1.11).
For comparison purposes, assuming no annual trend, the corresponding unadjusted estimates were
-
a reduction in the rate of discharge for men; hazard ratio 0.89 (95% CI 0.82 to 0.97)
-
an increase in the rate of discharge for women; hazard ratio 1.12 (95% CI 1.02 to 1.23).
The true impact of the RPIW was likely to be between the adjusted and unadjusted estimates. Any trend in discharge rates was in the hypothesised direction for women admitted to the study wards, but the analysis suggested that male patients were waiting longer to be discharged.
Summary
The number of men admitted to the ward each month fell after the RPIW. The proportion of patients admitted directly on to the ward (date of admission = ward start date) fell after the RPIW. This was true for both male and female patients but was particularly noticeable for men, with the proportion of male patients being transferred in from elsewhere increasing from 1% to 18%. The length of time that women spent on the ward decreased following the RPIW, whereas the impact on the length of time that men spent on the ward was ambiguous. When considering the total length of time between arrival on the ward and discharge from hospital, there was some evidence that men may have been discharged more slowly. There may have been a slight increase in the rate of discharge for women. Both of these results suggest that some patients were being transferred to other wards for extended treatment following the RPIW.
Site 10 community psychosis rapid process improvement workshops (referral, treatment, discharge)
The data set analysed for these RPIWs consisted of all referrals to eight adult community psychosis teams (three interventions, five controls) for the period 1 January 2010 to 31 July 2012 (see Table 5 for more details). There were 3036 episodes of care included in the analysis. The RPIW week was in January 2011.
Duration from referral received to first allocation
Time from ‘referral received’ to ‘first allocation’ was highly skewed (Figure 18).
FIGURE 18.
Time in days from referral received to first allocation.
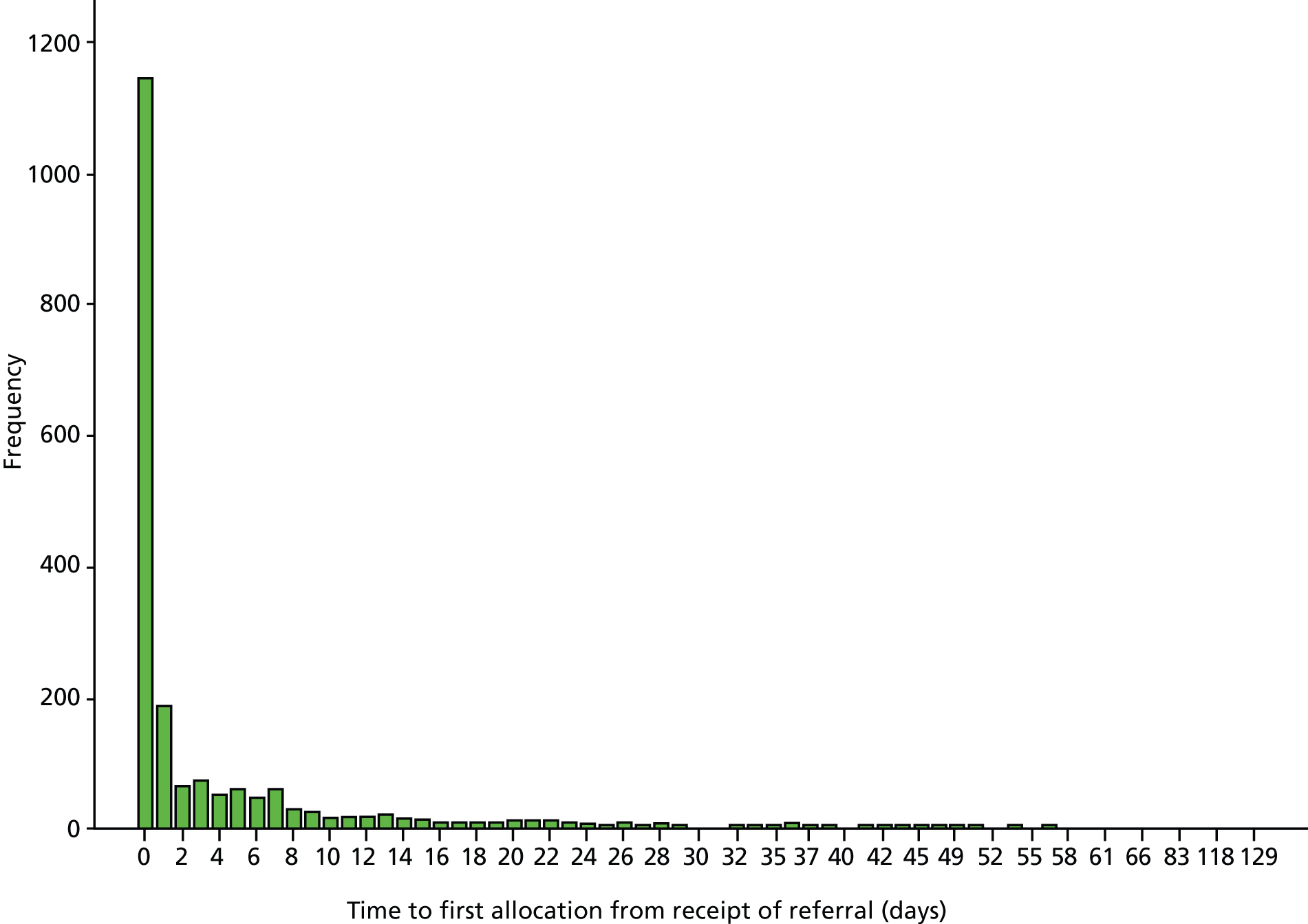
The mean was 4.1 days and the standard deviation was 10.3 days. For 59% of patients (95% CI 56% to 61%) the date of first allocation was the same as the date that the referral was received. Initial exploration suggested that the most appropriate way to model the data was to fit a zero inflated negative binomial regression model. Using this procedure the likelihood of being allocated on the date that the referral was received, and for other patients, the length of time spent waiting (that is, those for whom the date of allocation was not the same as the date of referral) were modelled simultaneously. Summary data corresponding to these variables were plotted by calendar month as shown in Figures 19 and 20.
FIGURE 19.
Proportion of patients allocated on the day that the referral was received.

FIGURE 20.
Mean time to allocation for those patients who did not receive an allocation on the day that the referral was received.
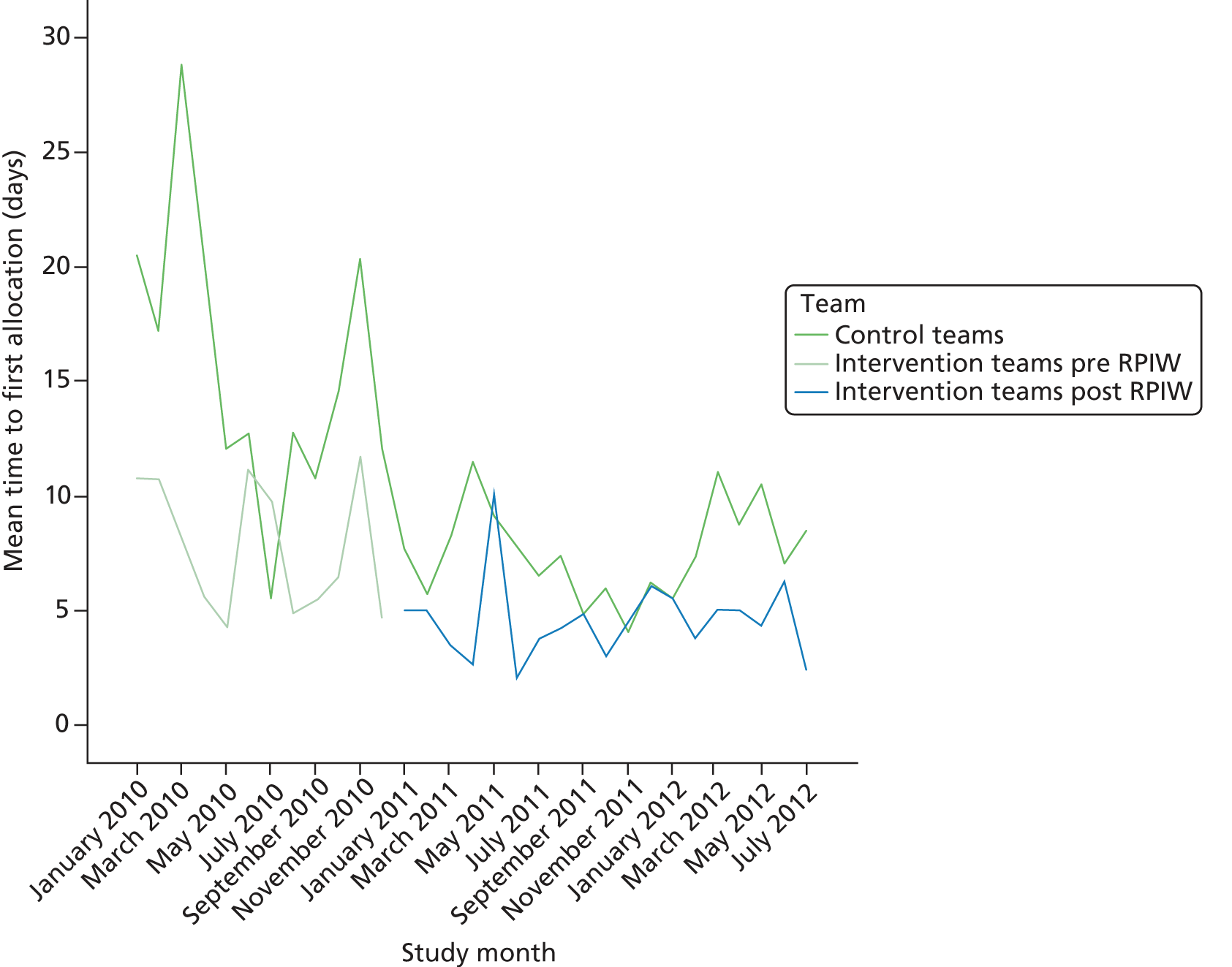
Any effect of the RPIW appeared to be in the hypothesised direction. There appeared to be a higher proportion of patients allocated on the day that the referral was received in intervention sites following the RPIW. The mean time to allocation for the remaining patients appeared to be lower than in the control sites following the intervention. Of note is the apparent fall in the mean time to first allocation in the control sites in 2011–12 compared with 2010.
Using a zero inflated negative binomial regression model we simultaneously modelled the probability that a patient was allocated on the day that the referral was received and time to allocation for the remaining patients. The dependent variable was time in days to first allocation. The first step was to include a trend over time in each part of the model. Both trends were significant:
-
annual trend in the proportion on a logistic scale = –0.29 (95% CI –0.56 to –0.02)
-
annual trend in time to allocation on a log scale = –0.45 (95% CI –0.57 to –0.32).
The negative coefficients indicated an overall reduction in the proportion of patients allocated on the day of referral (which would be in the opposite direction to the hypothesised impact of the RPIW) and a reduction in the time to allocation for other patients (which would be consistent with the hypothesised impact of the RPIW).
The second step was to adjust for differences between mental health teams. There were eight teams. Adding differences between teams in both halves of the model improved the fit significantly (change in –2 log likelihood = 296.3 for the loss of 14 degrees of freedom). The adjusted estimates of trend were
-
annual trend in the proportion on a logistic scale = –0.12 (95% CI –0.32 to 0.08)
-
annual trend in time to allocation on a log scale = –0.45 (95% CI –0.58 to –0.32).
There was almost no change in the trend in time to allocation, but the estimated trend in the proportion of patients allocated on the day of referral was reduced substantially. The third step was to add a step change in all sites (both intervention and control) following the introduction of the RPIW. There were four parameters of interest:
-
annual trend in the proportion on a logistic scale = –0.25 (95% CI –0.64 to 0.14)
-
estimated step change in the proportion on a logistic scale = 0.22 (95% CI –0.36 to 0.81)
-
annual trend in time to allocation on a log scale = –0.14 (95% CI –0.40 to 0.12)
-
estimated step change in the time to allocation on a log scale = –0.58 (95% CI –0.98 to 0.18).
None of these coefficients differed significantly from zero but the CIs were fairly wide. The fourth step was to fit an impact of the RPIW by adding a binary indicator variable to the model that contrasted intervention sites after the RPIW with intervention sites pre intervention and control sites for the entire period from 2010 to 2012. The parameter estimates were
-
annual trend in the proportion on a logistic scale = –0.25 (95% CI –0.63 to 0.13)
-
estimated step change in the proportion on a logistic scale = 0.08 (95% CI –0.52 to 0.69)
-
estimated impact of the RPIW on the proportion on a logistic scale = 0.45 (95% CI –0.16 to 1.06)
-
annual trend in the time to allocation on a log scale = –0.15 (95% CI –0.40 to 0.11)
-
estimated step change in the time to allocation on a log scale = –0.72 (95% CI –1.13 to –0.30)
-
estimated impact of the RPIW on the time to allocation on a log scale = 0.54 (95% CI 0.08 to 1.00).
This model suggested that the impact of the RPIW was to increase the proportion of patients who were allocated on the day that the referral was received, but that the time to allocation for other patients increased (although neither effect was statistically significant).
Given that neither of the two trend terms differed statistically from zero, they were removed and the model re-estimated as follows:
-
estimated step change in the proportion on a logistic scale = –0.24 (95% CI –0.61 to 0.12)
-
estimated impact of the RPIW on the proportion on a logistic scale = 0.45 (95% CI –0.17 to 1.07)
-
estimated step change in the time to allocation on a log scale = –0.91 (95% CI –1.16 to –0.67)
-
estimated impact of the RPIW on the time to allocation on a log scale = 0.53 (95% CI 0.07 to 0.99).
The estimated impacts of the RPIW generated by this model were almost identical to those obtained from the previous model, but the model itself enabled a much clearer interpretation of the results. The estimated step changes in the model corresponded to the estimated change for control teams following the introduction of the RPIW. Considering the proportion of patients allocated on the day of referral, this fell for control teams (change = –0.24 with 95% CI –0.61 to 0.12) and was therefore not statistically significant. The corresponding change for intervention teams was an increase of 0.21 with 95% CI –0.29 to 0.70. The difference between these figures was the estimated impact of the RPIW, which was 0.45 (95% CI –0.17 to 1.07). These figures were consistent with the data shown in Figure 18. The estimated impact of the RPIW corresponded to an odds ratio of 1.57 (95% CI 0.84 to 2.90). None of these effects were statistically significant. Considering the time to allocation for the remaining patients, the estimated change for control teams on the log scale was –0.91 (95% CI –1.16 to –0.67). There was also a reduction in the time to allocation in intervention sites; the estimated change on the log scale was –0.38 (95% CI –0.77 to 0.01) (although this was smaller and only of borderline significance; p = 0.06). The difference between these changes did, however, differ significantly from zero and was the estimated impact of the RPIW (0.53, 95% CI 0.07 to 0.99). These figures were consistent with the data shown in Figure 20. The time to allocation fell more in control sites, but this was primarily attributed to the fact that the time to allocation had already fallen considerably in the intervention sites 6 months prior to the intervention. There was much less room for improvement in the intervention sites, which may explain the modest reduction in time to allocation observed in those sites. It was very difficult to explain the very large reduction observed in the control sites (and this was not explored as part of the study).
Duration from referral received to first successful face-to-face contact
Time to first contact was highly skewed (Figure 21).
FIGURE 21.
Frequency distribution of time in days to first contact.
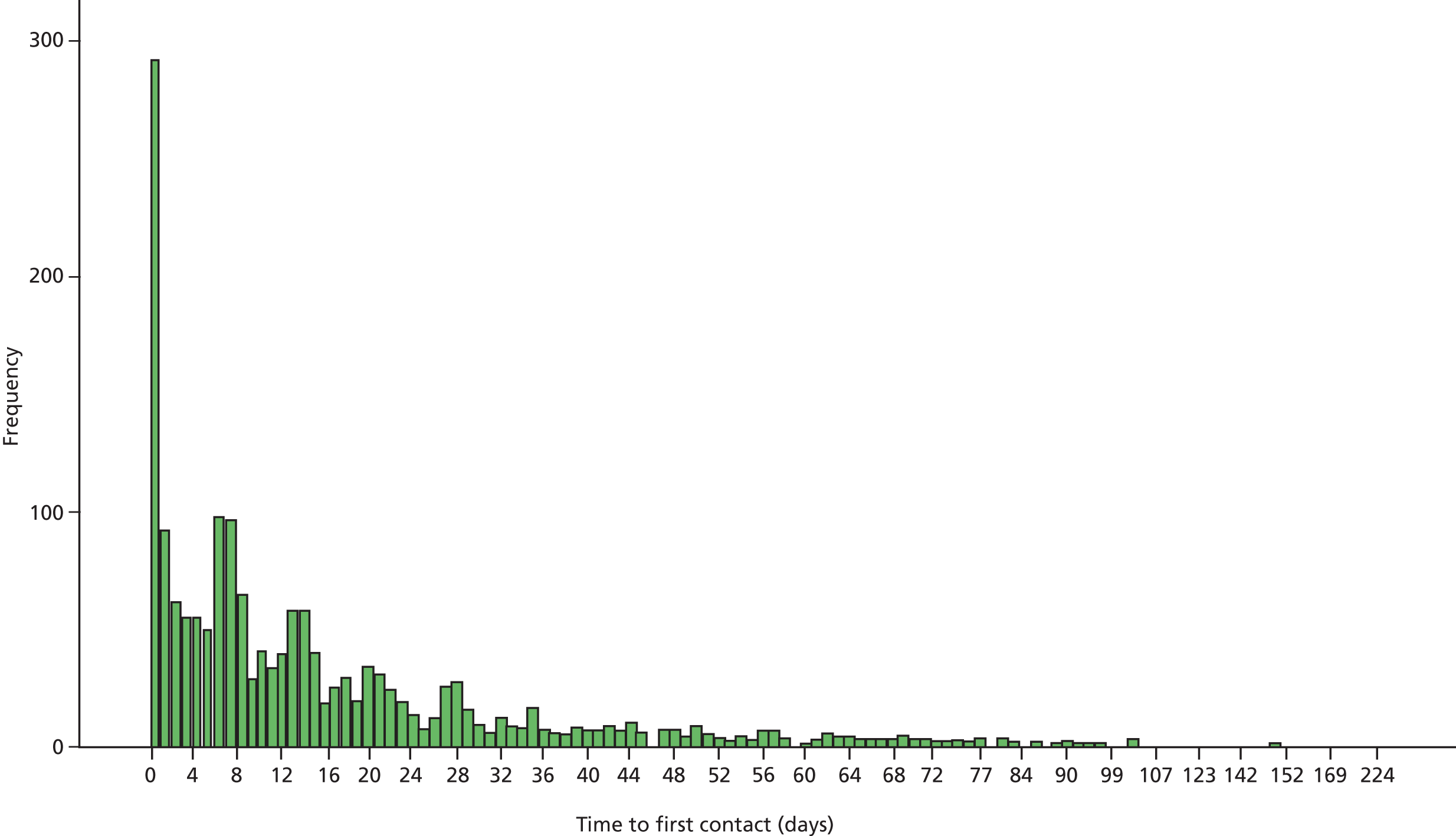
The mean time to first face-to-face contact was 18 days, with a standard deviation of 25 days. Sixteen per cent (95% CI 14% to 18%) of patients had their first face-to-face contact the day that the referral was received (Figure 22).
FIGURE 22.
Proportion of patients with face-to-face contact on day of receipt of the referral, by calendar month.
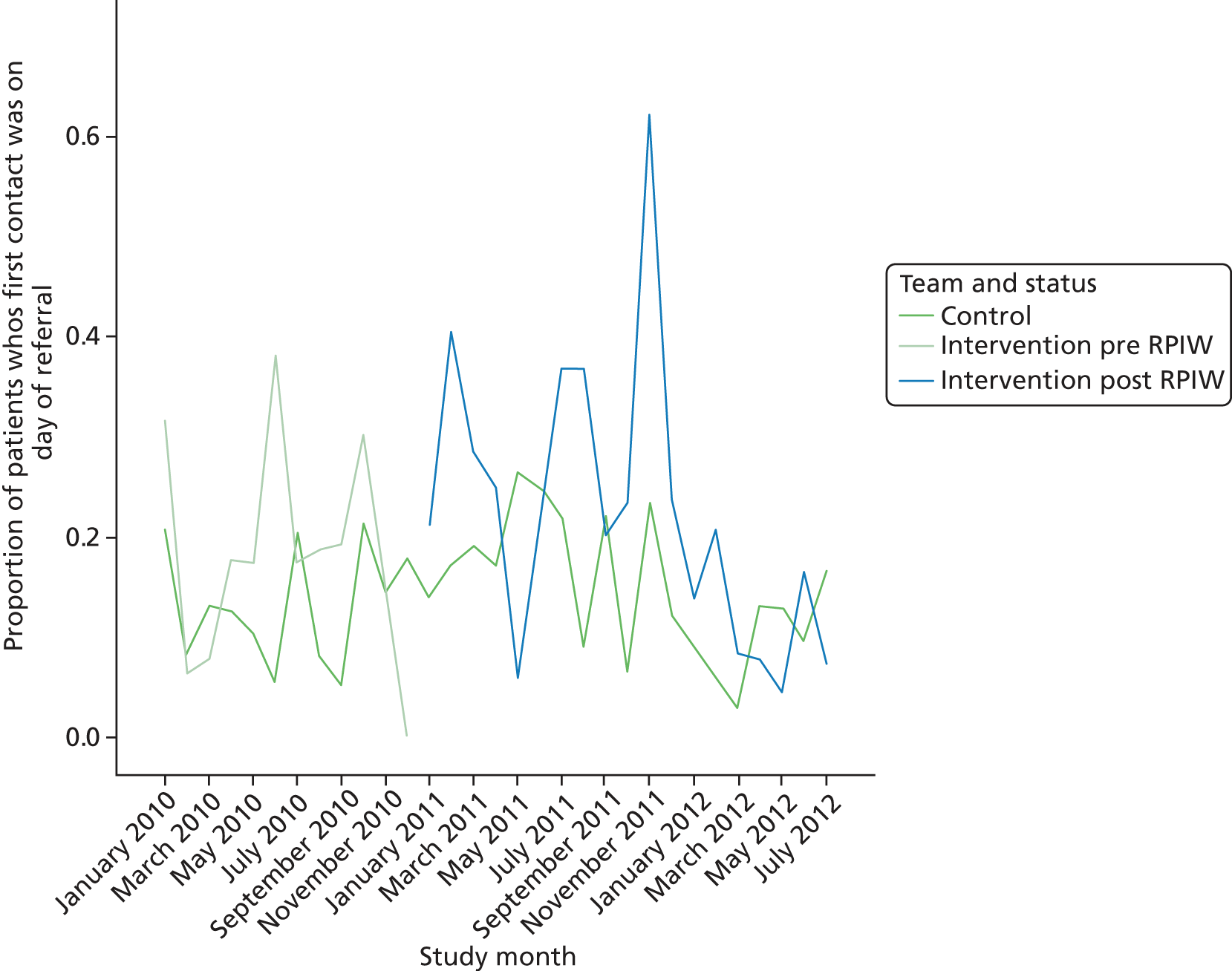
There appeared to be very little difference between control and intervention sites over the period 2010–12.
The mean time to first face-to-face contact for other patients is shown in Figure 23.
FIGURE 23.
Mean time to first face-to-face contact for patients whose contact was not on the day that the referral was received, by calendar month.
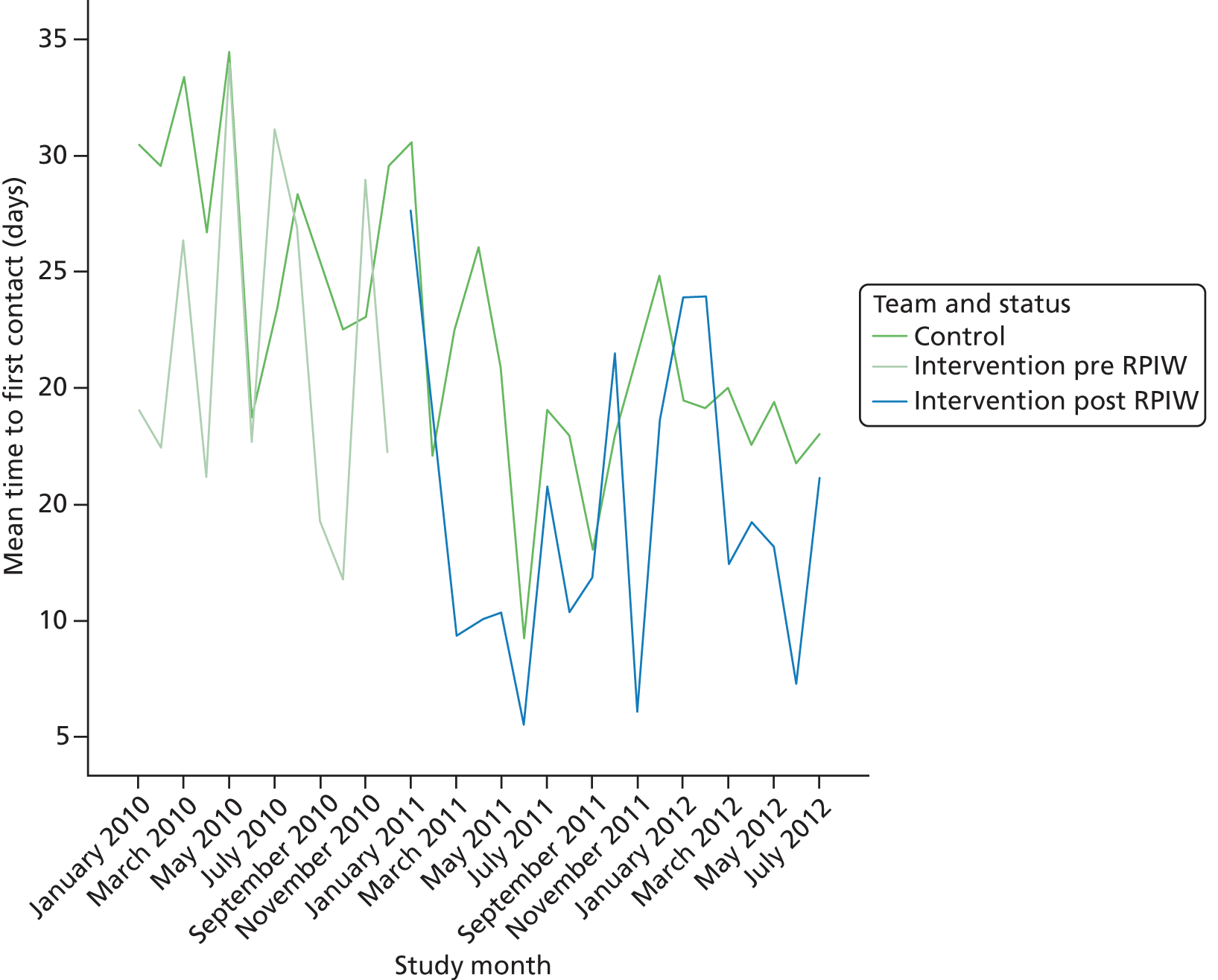
The time to the first face-to-face contact for other patients appeared to decrease steadily over the period 2010–12 but there was considerable monthly variability. The time in days to first contact was analysed using a zero inflated negative binomial regression model. A trend over time was fitted for both parts of the model and was adjusted for differences between teams (fitted as fixed effects). The estimated annual trends were
-
annual trend in the proportion of patients with face-to-face contact on the day that the referral was received (on a logistic scale) = –0.12 (95% CI –0.40 to 0.16)
-
annual trend in the time to face-to-face contact for other patients (on a log scale) = –0.29 (95% CI –0.37 to –0.21).
Consistent with Figures 21 and 22, there was a downwards trend in the time to first face-to-face contact for other patients, but the trend in the proportion of patients seen on the day of receipt of referral did not differ significantly from zero. The trend was removed from the inflation part of the model and a step change that corresponded to the introduction of the RPIW was included in both parts.
-
Step change in the proportion of patients with a face-to-face contact on the day that the referral was received (on a logistic scale) = 0.18 (95% CI –0.26 to 0.63).
-
Annual trend in the time to face-to-face contact for other patients (on a log scale) = –0.17 (95% CI –0.30 to –0.03).
-
Step change in the time to face-to-face contact for other patients (on a log scale) following the RPIW = –0.22 (95% CI –0.43 to –0.00).
The step change in the proportion of patients with a time to contact of zero did not differ significantly from zero. For other patients, both the trend over time and a step change coincident with the RPIW were statistically significant. Modelling the impact of the intervention in both halves of the model:
-
step change in the proportion of patients with a face-to-face contact on the day that the referral was received (on a logistic scale) = 0.40 (95% CI –0.28 to 1.07)
-
impact of the RPIW on the proportion of patients with a face-to-face contact on the day that the referral was received (on a logistic scale) = –0.46 (95% CI –1.41 to 0.50)
-
annual trend in the time to face-to-face contact for other patients (on a log scale) = –0.16 (95% CI –0.30 to –0.03)
-
step change in the time to face-to-face contact for other patients (on a log scale) following the RPIW = –0.16 (95% CI –0.39 to 0.06)
-
impact of the RPIW on the time to face-to-face contact for other patients (on a log scale) = –0.19 (95% CI –0.44 to 0.07).
There was no evidence that the RPIW had a marked impact on the time to first contact. However, the time to first contact decreased steadily over the period of follow-up for all sites. Again, the improvement in the control group militated against being able to conclude a positive effect of the intervention.
‘Did not attends’ at first appointment
One hundred and eleven patients out of 1924 did not attend the first scheduled face-to-face contact (proportion = 5.8%, 95% CI 4.7% to 6.9%). There was considerable variability in this figure from month to month (Figure 24).
FIGURE 24.
Proportion of DNAs at first contact by calendar month.
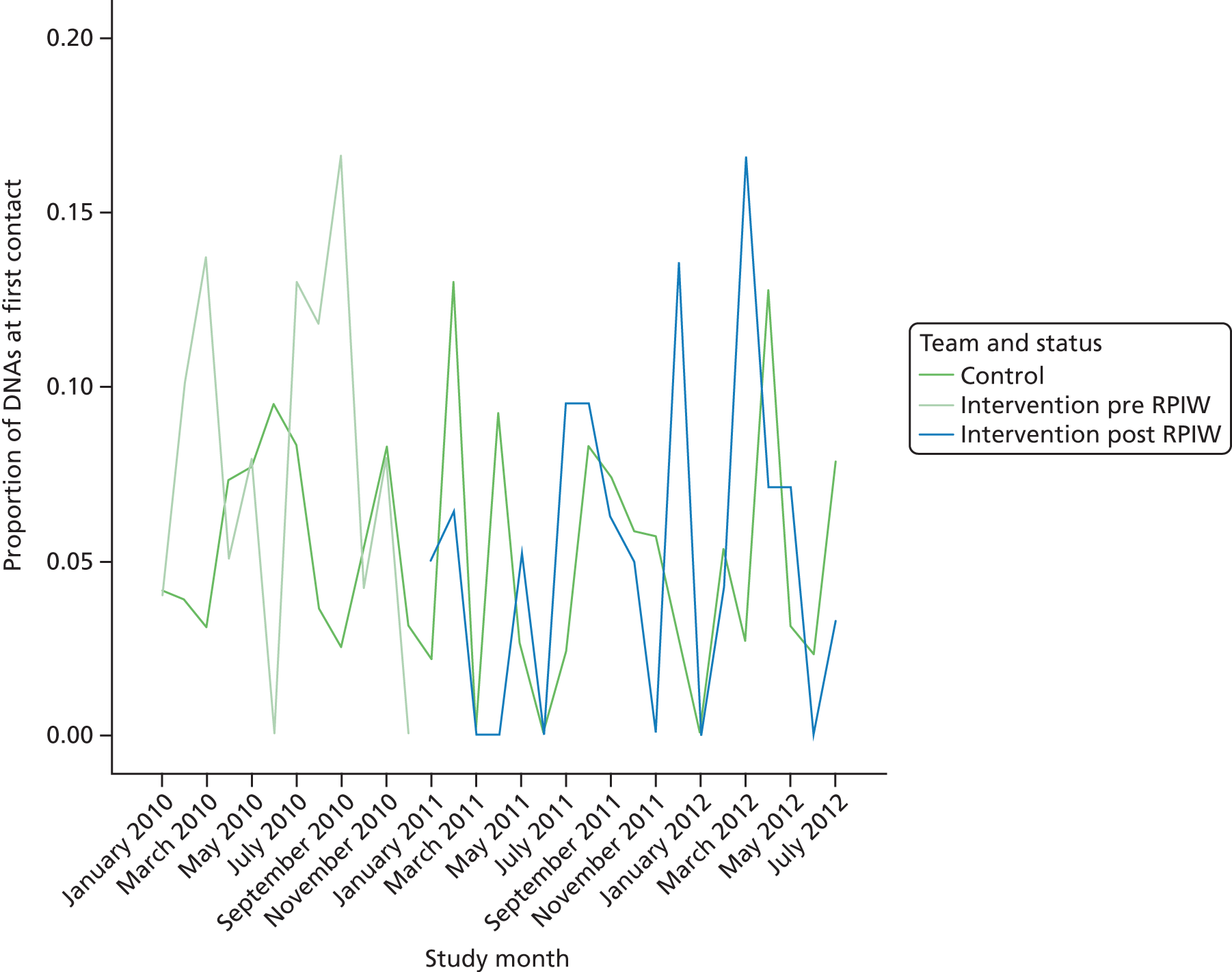
Whether or not a first contact resulted in a DNA was analysed using logistic regression. At step 1, after including differences between community teams as fixed effects, a linear trend was fitted. Each year the odds of a DNA changed by a factor of 0.82 (95% CI 0.62 to 1.06), which does not differ significantly from 1 (corresponding to no change). At step 2 the trend was removed and separate changes following the intervention were fitted for control and intervention sites:
-
change in likelihood of a DNA on a logistic scale in the control sites = –0.19 (95% CI –0.69 to 0.32)
-
change in likelihood of a DNA on a logistic scale in the intervention sites = –0.62 (95% CI –1.50 to 0.00).
There was a slight reduction in the likelihood of a DNA in both control and intervention sites (although in neither case was the reduction statistically significant). The estimated impact of the RPIW was the difference between these two figures (–0.43, 95% CI –1.24 to 0.37), which corresponded to an odds ratio of 0.65 with 95% CI 0.29 to 1.45. Although the CI spanned 1 (corresponding to no impact of the intervention), it was very wide. This suggested that there was insufficient power to detect an impact of the intervention against such very large background variation.
Duration from referral received to first assessment
The time to assessment was highly skewed (Figure 25) with a mean of 24.1 days and standard deviation of 54.8 days.
FIGURE 25.
Distribution of time in days from referral received to assessment.
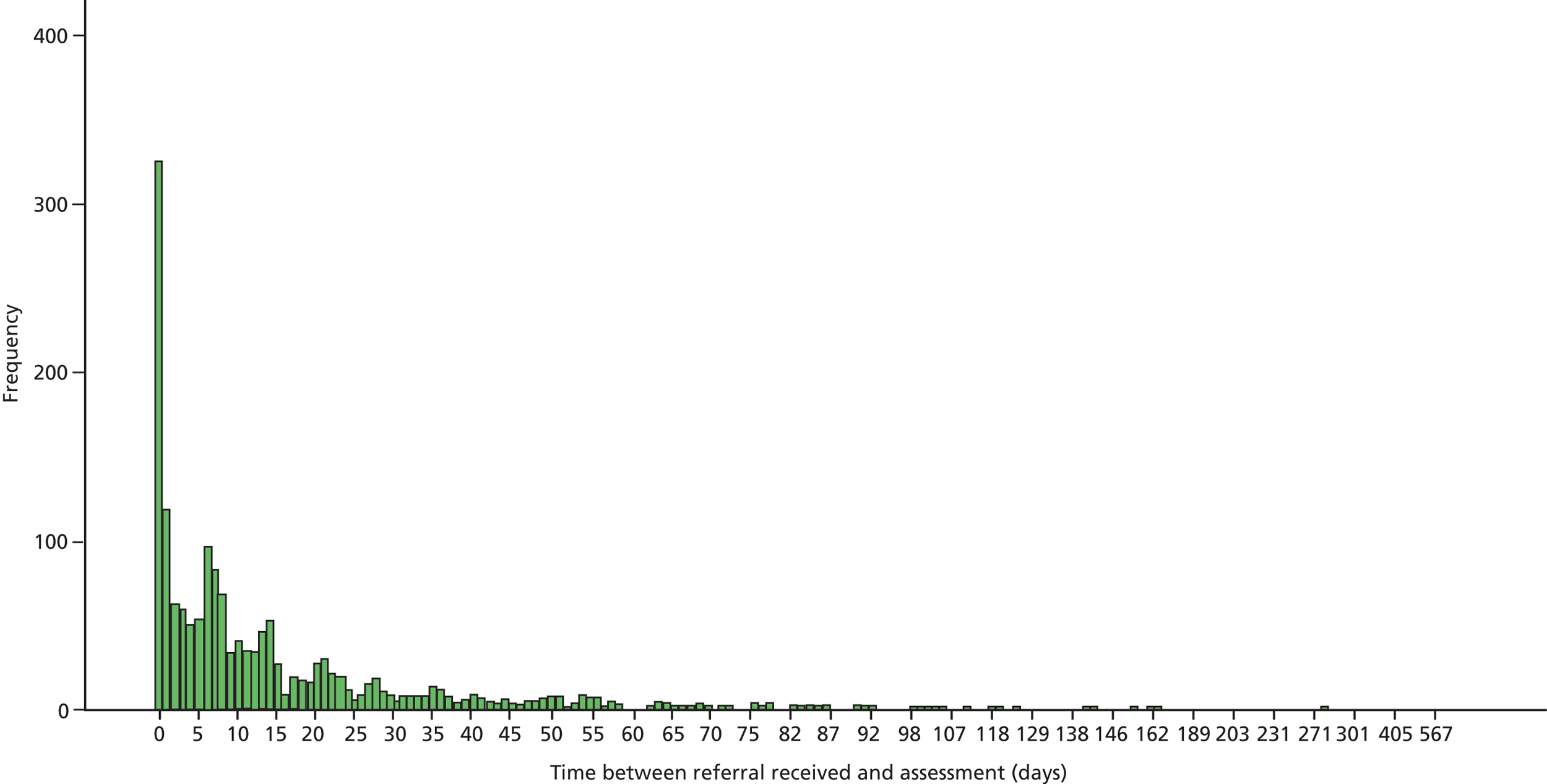
An assessment was recorded the day that the referral was received in 18.3% of cases (95% CI 16.5% to 20.2%). This proportion was similar for control and intervention localities (Figure 26), although there appears to be a spike corresponding to November 2011.
FIGURE 26.
Proportion of cases where assessment was recorded on day of receipt of referral by calendar month.
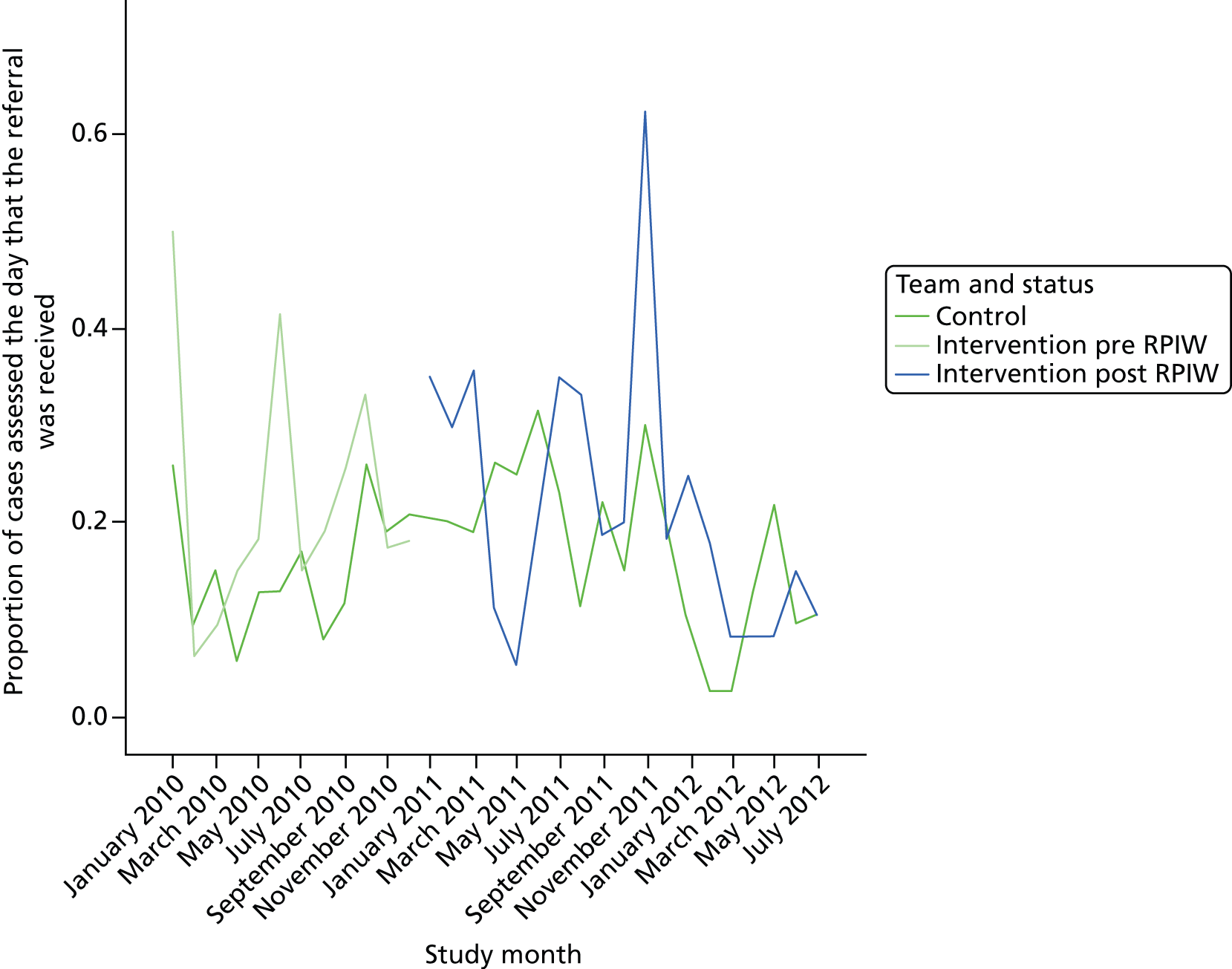
The distribution of mean time to assessment for the other cases is shown in Figure 27. A notable feature of this graph is the downwards trend in time to assessment in control sites.
FIGURE 27.
Mean time in days to assessment for patients not assessed on day referral was received by calendar month.
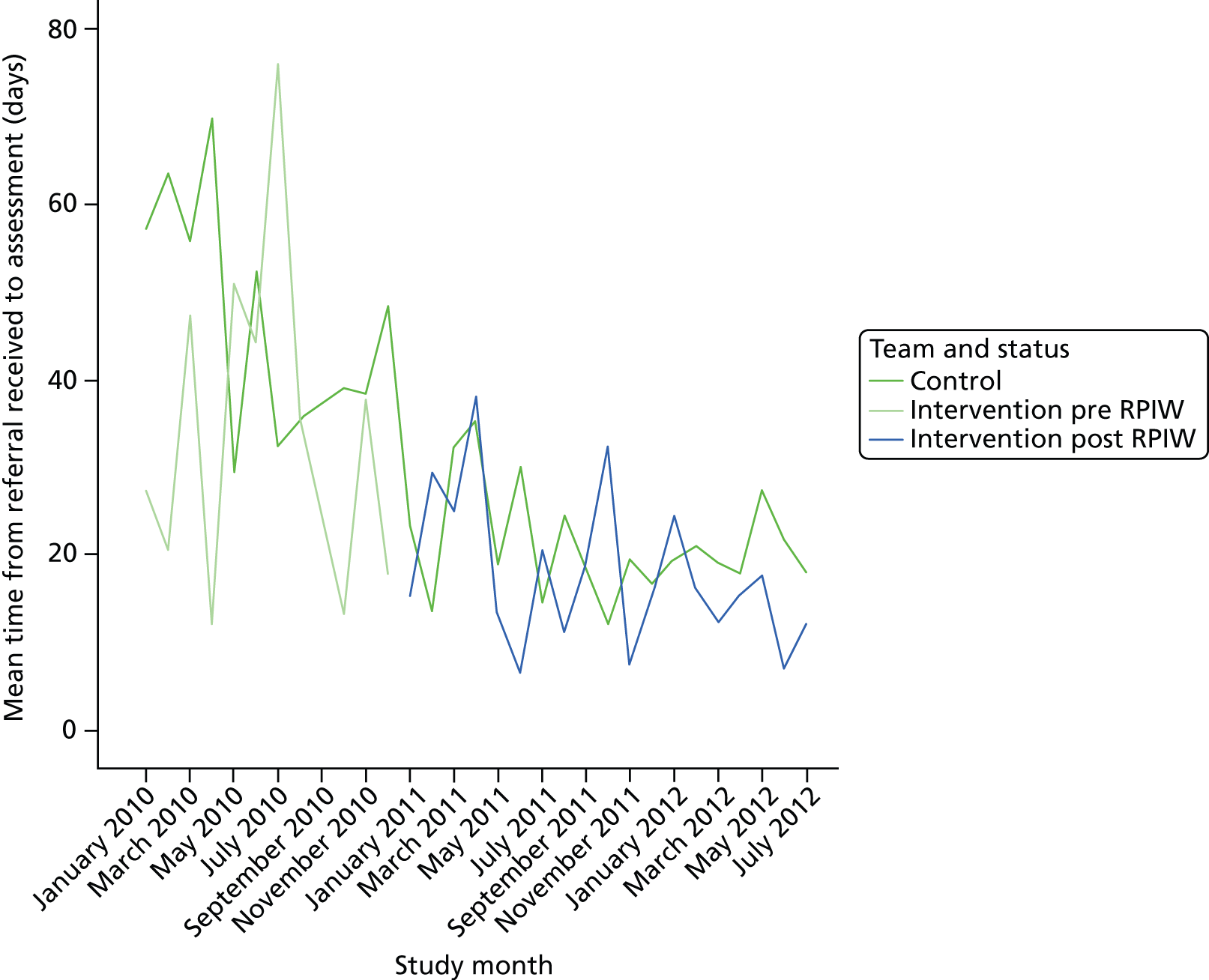
Logistic regression indicated no impact of the intervention on the proportion of patients assessed on the day of referral (odds ratio 0.96, 95% CI 0.59 to 1.56). Time to assessment was analysed using a negative binomial regression model. Fitting a trend over time yielded the following estimate:
-
annual trend in time to assessment (on a log scale) = –0.10 (95% CI –0.17 to –0.03).
Adding a difference pre/post January 2011 yielded the following estimates:
-
annual trend in time to assessment (on a log scale) = 0.10 (95% CI –0.01 to 0.22)
-
change post January 2011 in time to assessment (on a log scale) = –0.37 (95% CI –0.55 to –0.19).
This suggests that most of the change over time can be explained by a drop after January 2011. Removing the trend over time gives
-
change post January 2011 in time to assessment (on a log scale) = –0.24 (95% CI –0.34 to –0.14).
Fitting different changes for intervention and control localities:
-
change post January 2011 in time to assessment in control localities (on a log scale) = –0.20 (95% CI –0.31 to –0.09)
-
change post January 2011 in time to assessment in intervention localities (on a log scale) = –0.31 (95% CI –0.45 to –0.17).
There was a larger reduction in intervention localities. The estimated impact of the intervention (the difference between these figures on a log scale) was –0.11 (95% CI –0.26 to 0.04). The direction of effect was as predicted but the effect did not differ significantly from zero. This estimate on the log scale corresponded to a reduction in time to assessment of 10% (with the 95% CI indicating a change that was between a reduction of 23% and an increase of 4%).
Duration from referral received to diagnostic formulation
For each referral there were multiple records corresponding to different tasks undertaken by the community team. For each referral the first task with the descriptor ‘diagnosing/formulation’ or ‘assessment’ was identified and the duration between referral and this task was calculated. The mean time to diagnostic formulation across all referrals received in a calendar month is shown in Figure 28.
FIGURE 28.
Mean time to diagnostic formulation by calendar month.
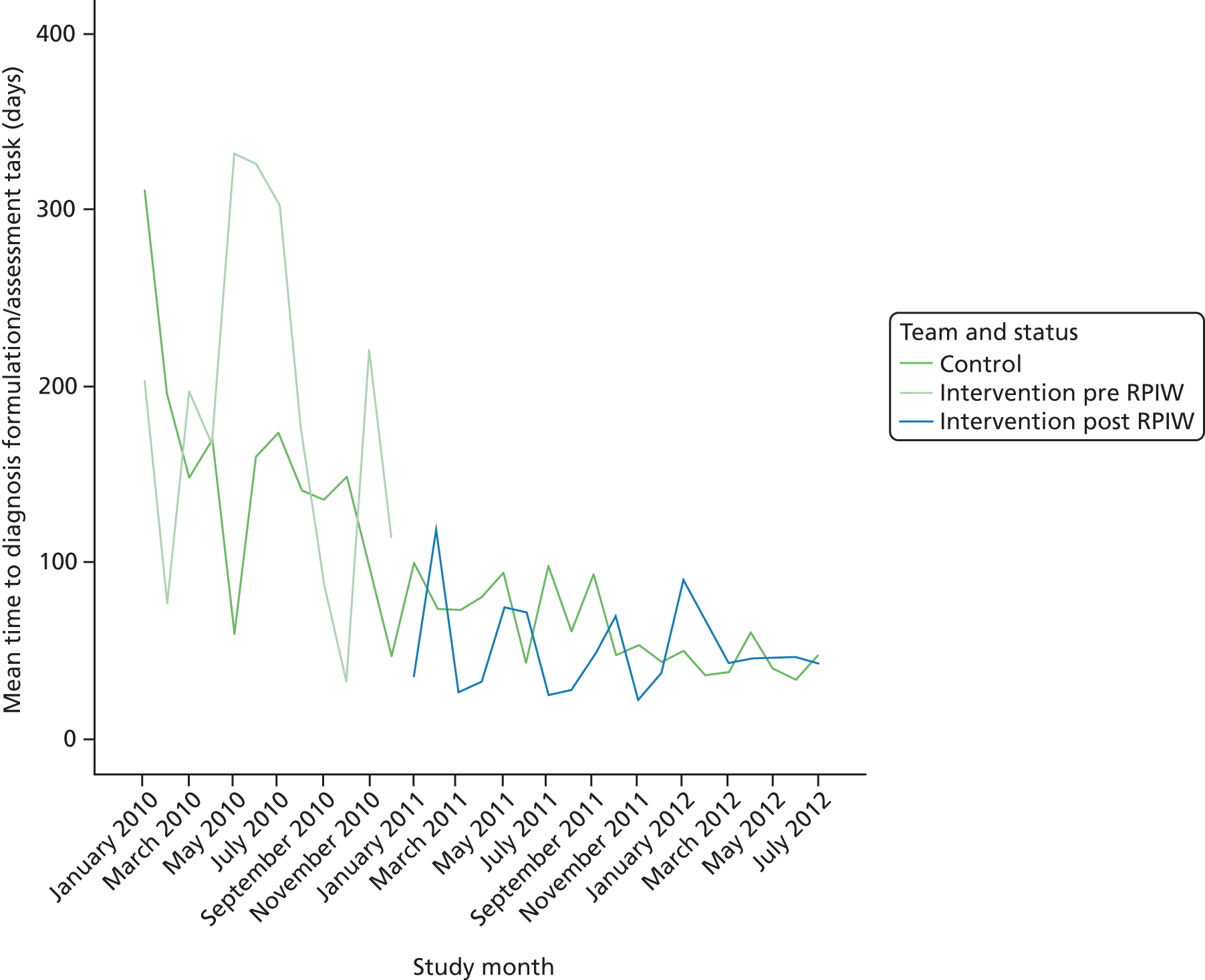
The time between the referral being received and the diagnostic formulation was then log transformed and analysed using a multilevel normal regression model. At step 1 a trend over time was included in the model. There was a significant annual decrease in the time to diagnostic formulation:
-
annual change in log (time to diagnostic formulation) = –0.46 (95% CI –0.60 to –0.32).
At step 2, a step change post January 2010, corresponding to the implementation of the RPIW, was introduced to the model:
-
annual change in log (time to diagnostic formulation) = –0.17 (95% CI –0.41 to 0.08)
-
estimated step change in log (time to diagnostic formulation) = –0.52 (95% CI –0.88 to –0.16).
Separate changes were fitted for the control and intervention teams:
-
annual change in the log (time to diagnostic formulation) = –0.16 (95% CI –0.40 to 0.09)
-
estimated step change in the log (time to diagnostic formulation) in the control sites = –0.47 (95% CI –0.85 to –0.09)
-
estimated step change in log (time to diagnostic formulation) in the intervention sites = –0.64 (95% CI –1.08 to –0.19).
There was a reduction in the time to diagnostic formulation in both control and intervention sites. The estimated impact of the intervention was the difference between these two figures (–0.16, 95% CI –0.40 to 0.09) which, back transformed, corresponds to a reduction in time to diagnostic formulation of 15%, although this was not statistically significant (95% CI corresponds to between a reduction of 41% and an increase of 23%).
In practice, there was a reduction in the time to diagnosis formulation in the intervention localities which may or may not have been a result of the RPIW. However, there was a similar change in non-intervention (control) localities. Pooling this information suggested that the effect of the RPIW was not statistically significant. It is difficult to explain the large reduction in time to diagnostic formulation in the control sites (and, as noted earlier, what was happening in the control sites was not explored as part of this study). Additionally, the very wide CI reflects the inherent variability in the data and suggests that we may not have had sufficient power to detect clinically important differences.
Discharge rates
One of the aims of the RPIW was to reduce the time from referral to discharge. Not all referrals had a recorded date of discharge. The first investigation was to look at the impact of the RPIW on the likelihood of a date of discharge being recorded. The number of referrals with a recorded date of discharge decreased over time (Figure 29).
FIGURE 29.
Proportion of referrals with a recorded date of discharge by calendar month.
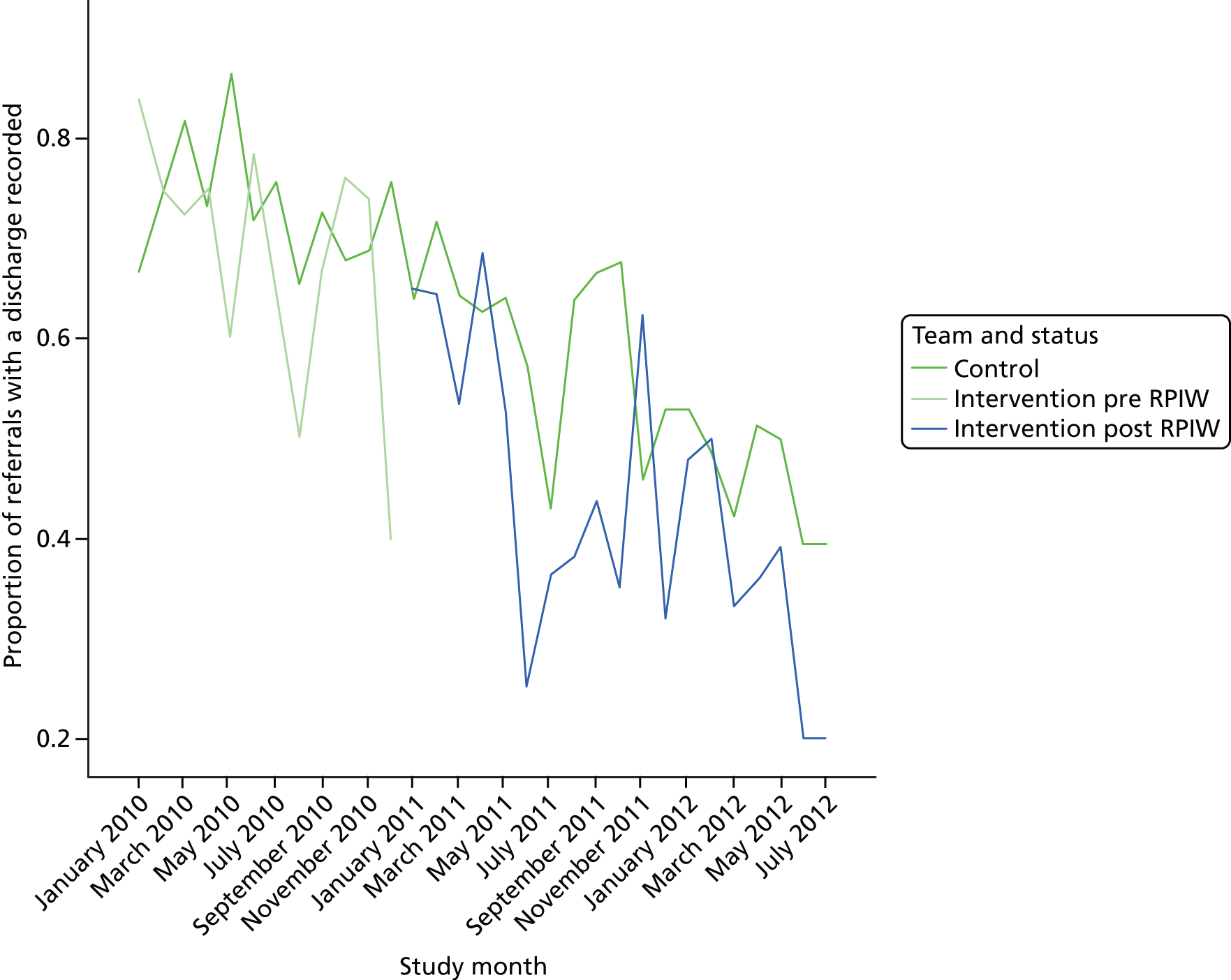
This was true for both groups. Fitting a logistic regression model with a common trend over time but a different change in each group following the introduction of the RPIW yielded the following estimates:
-
overall annual trend on a logistic scale = –0.90 (95% CI –1.16 to –0.64)
-
change after January 2011 in the control group = 0.06 (95% CI –0.36 to 0.48)
-
change after January 2011 in the intervention group = 0.03 (95% CI –0.43 to 0.49).
This model suggests that the variability in the data can be explained by a trend over time that is the same for both groups.
The estimated impact of the RPIW was the difference between the step changes (–0.03, 95% CI –0.46 to 0.40). This suggested that the RPIW had very little impact on the proportion of patients who had a recorded date of discharge. Taking the exponent, this impact corresponded to an odds ratio of 0.97 with 95% CI 0.63 to 1.50.
Duration from referral received to discharge
There were 1169 referrals in the database with a recorded time to discharge. The summary statistics are shown in Table 22.
| Locality/time | Mean (days) | n | Standard deviation (days) |
|---|---|---|---|
| Control 2010 | 279.8 | 418 | 286.9 |
| Control 2011–12 | 193.7 | 389 | 162.5 |
| Intervention 2010 | 241.0 | 187 | 241.5 |
| Intervention post RPIW | 184.6 | 175 | 156.7 |
| Total | 230.7 | 1169 | 229.7 |
The time to discharge in days was highly skewed, as can be seen in the box plots in Figure 30. The horizontal line within the box corresponds to the median time to discharge. This appears to have fallen in the control localities but increased in the intervention localities post January 2011. The times were log transformed, loge(1 + time in days) (Figures 31 and 32).
FIGURE 30.
Time to discharge in days.
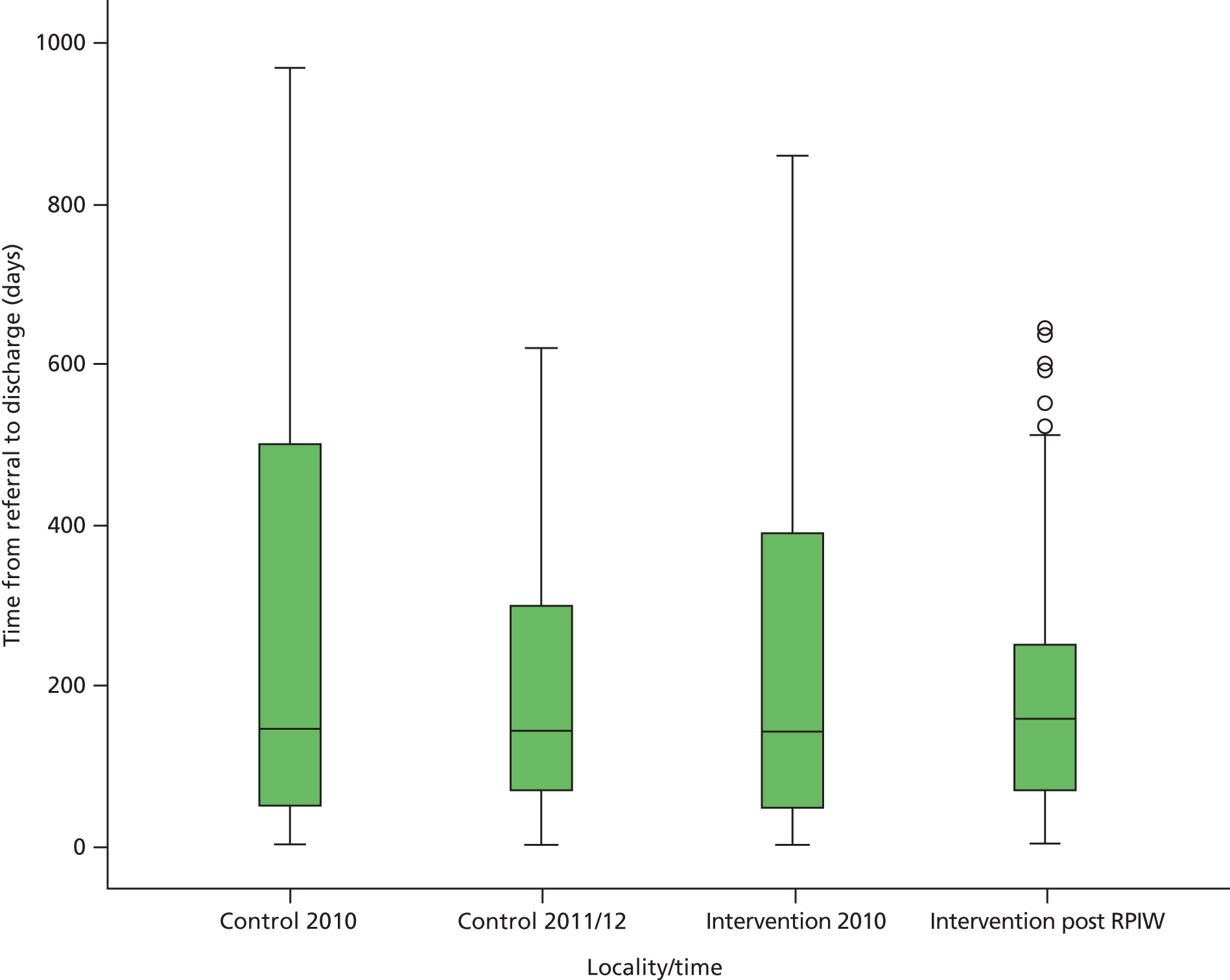
FIGURE 31.
Frequency distribution of log-transformed time to discharge (n = 1169). Mean 4.79, standard deviation 1.395.
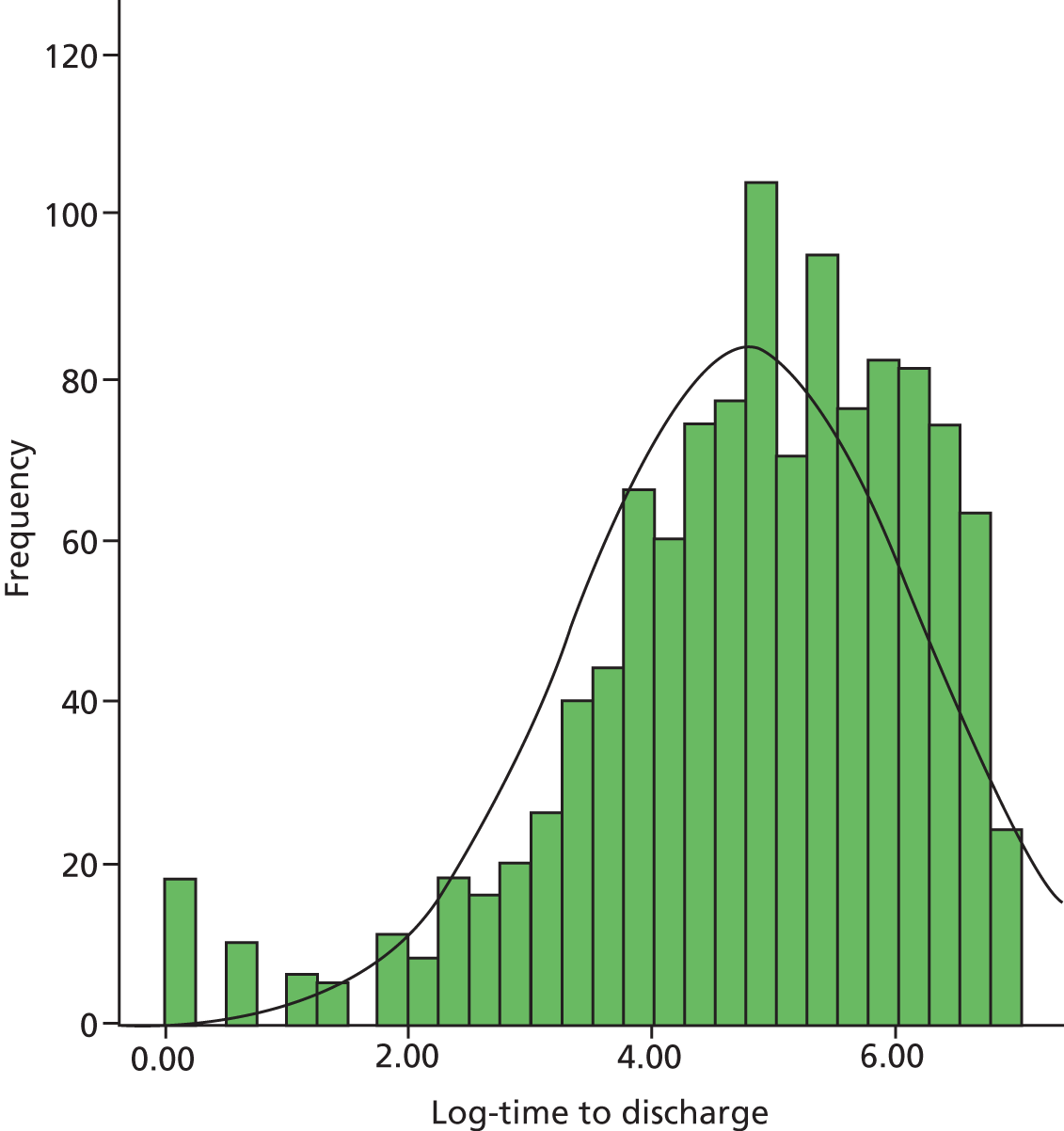
FIGURE 32.
Log-transformed time to discharge by calendar month.
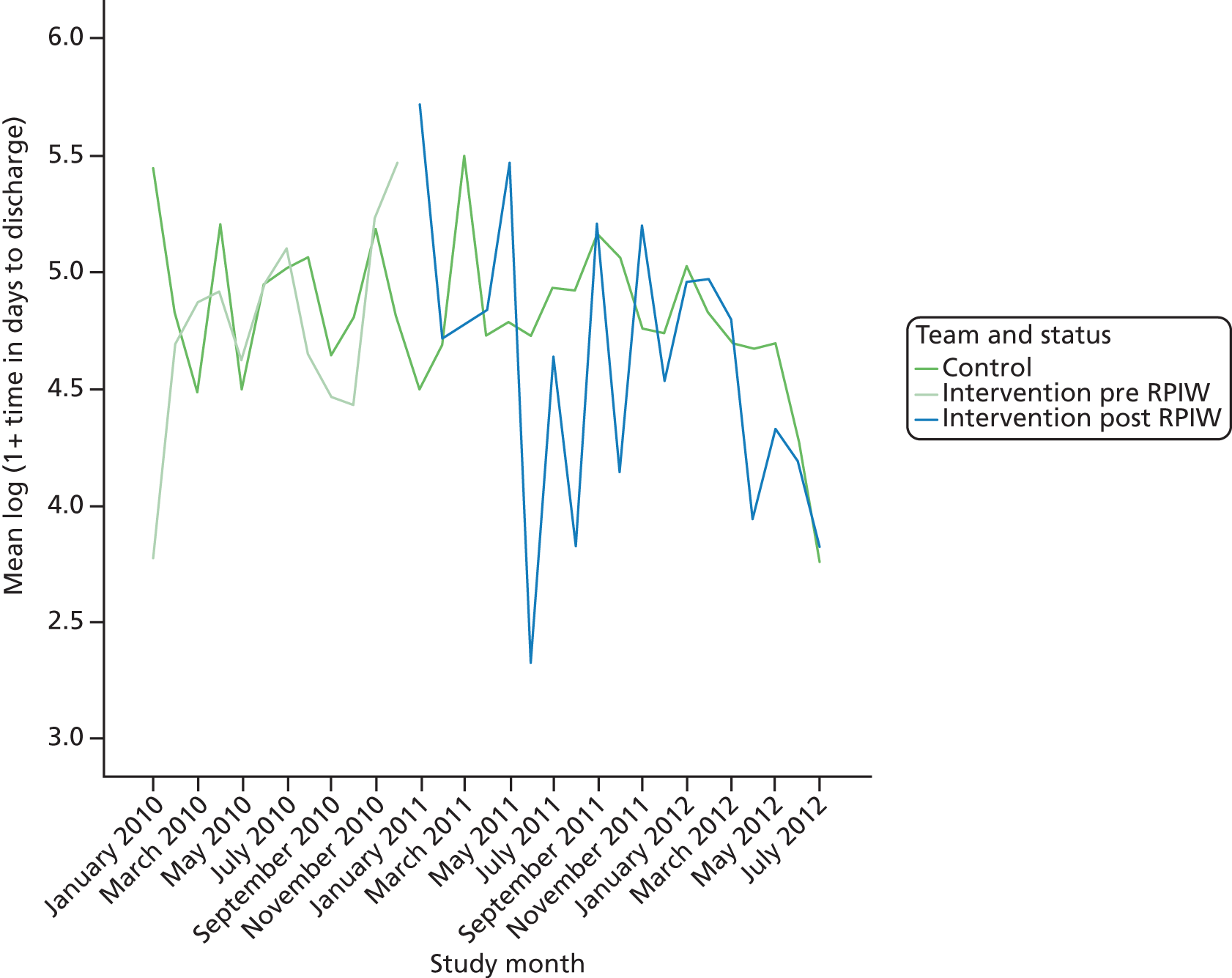
The times to discharge appeared to be broadly similar in the two groups.
A trend was fitted over time:
-
annual change in log (time to discharge) = –0.19 (95% CI –0.30 to –0.07).
Adding a step change in January 2011 across all sites:
-
annual change in log (time to discharge) = –0.26 (95% CI –0.46 to –0.05)
-
step change post January 2011 = 0.11 (95% CI –0.18 to 0.40).
Fitting different changes in the intervention and control localities:
-
annual change in log (time to discharge) = –0.26 (95% CI –0.47 to –0.06)
-
step change post January 2011 in the control localities = –0.00 (95% CI –0.30 to 0.30)
-
step change post January 2011 in the intervention localities = 0.33 (95% CI –0.03 to 0.69).
The estimated impact of the RPIW was given by the difference between the changes in the control and intervention practices (0.33, 95% CI 0.01 to 0.65). This would suggest that the impact of the RPIW was to increase time to discharge in intervention localities. In reality, time to discharge was actually getting smaller in intervention localities (we were looking at changes in both control and intervention localities while allowing for a downwards trend over time). However, the rate of decline in intervention localities was much lower than the rate of decline in time to discharge in control localities. Thus the apparent impact of the RPIW was to increase time to discharge.
Summary
A consistent feature of these analyses was that large changes in most of the key variables were observed in the control localities. Further, the direction of these changes tended to be the same as that of the effects hypothesised in the intervention groups as a result of the RPIWs. Consequently, when compared against the control group, none of the changes in the intervention group was significant in a positive direction. Indeed, this comparison led to an estimated negative impact of the RPIWs on a number of variables. Had the analysis been undertaken without the control groups, in a number of cases it would have been concluded that there had been no impact (instead of a negative impact) or a positive impact (instead of no impact) of the RPIW.
It was very difficult to explain the observed improvements in the control groups (and, as noted earlier, what was happening in the control sites was not explored as part of this study). This was a non-randomised comparison and thus systematic differences between groups were to be expected.
Factors that promoted or inhibited the adoption, implementation and sustainability of the North East Transformation System
Transformational change programmes are usually characterised by four distinct phases: (1) acceptance of the need for change; (2) adoption of the means by which change will be enacted; (3) initial implementation of the change programme; and (4) embedding sustainable practices, such that the programme continues in the medium to long term. In the case of the NETS, the first phase was successfully completed; nearly all North East NHS organisations agreed that there was an urgent case for continuous, region-wide, large-scale QI. This section presents findings in relation to the factors that promoted or inhibited the NETS through early adoption, implementation of the programme and its subsequent sustainability. These factors can be conveniently clustered within five of the areas in the Pettigrew et al. ‘receptive contexts for change’ model125 and the rest of this section is structured around these five areas.
Key people leading change
Many of our interviewees felt strongly that the successful adoption and implementation of the NETS was closely associated with committed and stable leadership at the highest level in trusts and the SHA: ‘. . . the most important thing is to have that organisational commitment and leadership and the constancy of purpose really just to keep going at it and be prepared for it to take time’ (site 10, medical director).
In one VMPS study site (site 10), the initial work on the NETS was interrupted by a need to recruit a new CEO. Board members were concerned that the new incumbent would feel a need to take QI in a different direction, and insisted that the candidates should be fully committed to the NETS and to the VMPS method. On appointment, the new CEO was fast-tracked to visit the VMMC in Seattle, WA, and returned convinced that the trust had chosen well; indeed, he subsequently described his first encounter with the VMPS as a ‘light bulb moment’, and has since proved to be one of the most committed and engaged NETS leaders, championing the provision of substantial resources to his organisation’s NETS programme.
The same interviewees were also clear that senior leaders, whether managers or clinicians, had to take a hands-on approach to driving forward NETS activities and development, and should take part in practical, day-to-day improvement events. In sum, leaders should ‘walk the walk’, not just ‘talk the talk’. A number of interviewees, particularly in the VMPS organisations, pointed out that many directors and board members had been through the process of becoming ‘certified leaders’, and continued to sponsor and take part in RPIWs and attend organisation and region-wide report-outs: ‘. . . we have so many of the senior team involved, I mean all of the directors are certified leaders, the chief exec’s a certified leader. All of the divisional managers, if they’re not they’re being trained currently’ (site 09, senior nurse manager).
Clinician leadership was seen as vital to encouraging confidence in the NETS in all of the study sites, VMPS and non-VMPS. It was clear that a key NETS message – that leadership should not be applied solely in a top-down fashion – had made an impression: ‘. . . we’ve done a lot of work . . . to try and involve all levels of staff . . . it’s about having a sort of champion . . . one of our consultants . . . leads on lean and he participates in the lean project group’ (site 09, divisional manager).
A focus group involving KPO leads echoed the above views. It was noteworthy that the KPO leads representing the organisations that we judge to have made the most progress in implementing the VMPS were clear that their role had changed over time. Initially they promoted and led the roll-out of the VMPS and NETS programme. Later, they acted as facilitators for leadership development among a range of staff. In a sense, the baton had passed, from the QI programme being done to staff, to being led and done by those same people. One KPO lead, interviewed in late 2011, commented that the KPO functions in his trust had become more distributed, as a sufficient number of clinical and managerial staff at different levels of the organisation had qualified as certified VMPS leaders. The number of staff who had been exposed to the trust’s version of the NETS had reached a critical mass.
Quality and coherence of policy
The national NHS policy environment in which the NETS operates was described in Chapter 1. This subsection concentrates on policy factors at trust and regional levels. The term ‘policy’ is used in its wider sense, to indicate a generally accepted direction of travel and a common set of principles, which may or may not be embodied in official documents. At regional level, the early enthusiasm for and commitment to a region-wide NETS programme was evident from SHA annual reports, as summarised in Table 23. As the programme expanded from the original cohort of wave 1 pathfinders, the annual reports for 2009–10 and 2010–11 covered the NETS activities and principles in some detail.
| Year of annual report | NETS description |
|---|---|
| 2008–09 |
|
| 2009–10 |
|
| 2010–11 |
|
| 2011–12 |
|
However, as the demise of the SHA loomed in 2011–12, the emphasis shifted to handover arrangements, collaboration with other QI and innovation agencies, and the role of the NETS in contributing to the productivity and financial challenges faced by the NHS.
Early SHA policy towards adoption of the NETS and its subsequent implementation was certainly coherent: senior SHA leaders chaired Coalition Board meetings, attended region-wide report-out sessions and visited individual organisations to discuss progress and offer encouragement on a regular basis. The SHA provided some central resources to negotiate contractual arrangements with VMMC and Amicus and to organise training programmes and ‘share-and-spread’ activities. No evidence was found that the original proponents of the NETS at SHA level underwent a change of heart in relation to the necessity for, and the principles of, the NETS. Rather, the weakening of support for the NETS from 2010 onwards was in part a result of force majeure: the post-2010 general election upheaval in the structures of the NHS and the imminent demise of the SHA itself. Both of these factors, which had not been expected or foreseen, necessitated a loosening of the SHA’s central role in guiding the NETS programme.
It is interesting to contrast the regional NETS policy with the variation apparent through an analysis of the annual reports published by some of the study sites. Table 24 summarises the frequency with which words or phrases linked to lean, formal QI programmes or reference to the NETS occurred, as reported in a selection of VMPS study site annual reports in 2008–12.
| Study site | 2008–09 | 2009–10 | 2010–11 | 2011–12 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lean | QI | NETS | Lean | QI | NETS | Lean | QI | NETS | Lean | QI | NETS | |
| 07a | – | – | – | – | – | – | 1 | 2 | 2 | – | – | – |
| 08 | – | – | – | 1 | 10 | 1 | 1 | 14 | – | 1 | 3 | – |
| 09 | NA | NA | NA | 3 | 10 | 3 | 5 | 6 | – | 1 | 7 | – |
| 10 | – | 21 | 1 | 4 | 32 | – | – | 26 | – | – | 37 | – |
Table 24 suggests a number of patterns. First, study site 10 had a well-developed policy of promoting and supporting the NETS from the outset. Its QI programme was given more prominence in the public documents available to Monitor (the regulator for health services in England), the CQC and the public than was the case for the other study sites in this sample. Second, although study site 10 mentioned lean specifically four times in the 2009–10 report, all references in later years were to the trust-specific QI programme; the term ‘lean’ had disappeared from the text. Third, in later years, there was little or no mention of the NETS as a region-wide programme. That is not to say that the reports did not emphasise co-operative and collaborative working with other NHS organisations; however, it is noteworthy that trust policy did not appear to be aligned with the original NETS intention to create a region-wide, common approach to QI. This may have reflected the disappearance of the term ‘region’ from the vocabulary of health reform during the initial phase of change following the July 2010 NHS White Paper. 1 Even when the term was reinstated, the North East region was subsumed within a larger geographical area known as NHS North, and became known as a ‘centre’.
Environmental pressure
The interviews and focus group discussions spanned a period in which the English NHS came under sustained pressures from a number of different directions. Significant year-on-year increases in NHS funding ended in 2008–09. A number of crises in governance and care quality were in the public domain. The Health and Social Care Bill of 2010, which later became the Health and Social Care Act 2012,124 triggered a major and controversial, not to say prolonged, upheaval in the majority of NHS organisations. 142 All of these issues resulted in significant public, political and media scrutiny. It is therefore no surprise that interviewees reflected on how they had an impact on the NETS programme and how the programme had to adapt and respond accordingly.
Efficiency and productivity versus quality and safety?
Despite general awareness of the financial constraints facing the NHS, many of the phase 1 interviewees expressed a consensus view that the NETS’s primary focus on quality and safety was both appealing to staff and correct in principle. Cost savings or increased efficiency were helpful by-products. For example, two interviewees expressed the issue in the following terms:
. . . the driver of pretty much all the transformational work that we’ve done up until very recently has been on improving quality. And the fallout from it, where the fallout has been financial, that’s almost been incidental.
Site 01, board member
Cost improvement and improvements go hand in hand, but sometimes it’s about quality and not just about cost.
Site 07, senior director
Those staff who had visited the VMMC headquarters in the USA, or who had heard the VMMC story by other means, often commented approvingly on the origins of the VMPS. It was a health-care organisation facing bankruptcy, which adopted the TPS as a means to address problems of quality, safety and the patient experience through a continuous process of removing waste from its systems and processes, and became solvent again as a result.
On a number of occasions, interviewees expressed the view that the financial crisis was in itself an urgent and compelling reason to invest in the NETS concepts and practices. This was on the basis that a whole-system approach to QI would lead to greater staff productivity and reductions in bed numbers and length of stay, and hence overall costs. However, this view was typical of the trusts involved in payment-by-results financing, either as commissioners or providers; those trusts that were subject to block contracts sometimes took a different view: ‘We have a block contract . . . so actually all you do is get paid the same and do fantastic things in terms of productivity’ (site 11–13, head of finance).
In the phase 2 interviews and focus group discussions conducted in mid-2011, it was found that little had changed from the positions expressed during the earlier phase 1 interviews. Most interviewees who commented on the relationship between the NETS and financial pressures acknowledged that cost control had become more urgent, but still felt that this could be addressed by concentrating on improvements to the quality of the service on offer:
. . . this is about improvement in its widest sense, some of it’s going to be cash release . . . but some of it’s also about quality and just making sure you do it as right as you should, which should generate cash savings at the end of the day . . . And it’s just taking waste out of the system.
Site 07, VMPS certified leader
One interviewee, a KPO lead in a study site that had tracked the savings associated with NETS activities, was very clear that the efficiency gains accrued over 3 years (estimated at £20M) more than compensated for the expenditure on the costs of the resources necessary to undertake the NETS programme.
Reputation and public scrutiny
From its inception, the VMPS NETS programme was predicated on an expectation that senior leaders (CEOs, medical, nursing, finance and HR directors, QI and organisation development leads) would spend time at the VMMC headquarters in Seattle, WA, and, if possible, also attend a joint tour to Japan with VMMC staff. Such activities are expensive and, particularly during a period of flatlining NHS income, carry a significant risk of being perceived as an unwise or improper use of public funds. One of the first, SHA-sponsored tours to the VMMC and Japan was subject to criticism in the region’s press, including strongly worded commentary from members of the public and local GPs who objected to financial restrictions on specialist treatment, at a time when NHS staff were being flown to Seattle and Japan. 143 The NIHR SDO MF, who was closely involved with the development of the NETS across the region, noted that similar criticisms were occasionally voiced by commissioning organisations, local authority health scrutiny committees and some NHS staff. Some felt that training in lean methods could be sourced closer to home and that the ‘see–feel’ experience could be arranged by visiting manufacturing plants in the North East or health-care organisations in England that already had experience of the lean redesign of processes and systems.
There is no doubt that public criticism of a training programme involving regular overseas travel caused some NHS organisations to have concerns about joining the VMPS version of the NETS. It may even have affected the degree of acceptance of the NETS programme in its wider context. Indeed, the NETS Coalition Board made some changes to the expectations of those staff undergoing VMPS certification. The trips to Seattle and Japan became optional and they explored how they might create the ‘see–feel’ experience closer to home. However, in the main more pragmatic views prevailed, and other barriers to adopting or continuing with the NETS programme came to the fore. These are discussed below.
Changing priorities
As noted earlier, the period of the evaluation of the NETS coincided with a number of major challenges faced by NHS organisations. The principal one of these – the redesign of the governance and organisation of the NHS as a consequence of the Health and Social Care Act 2012124 – was a background theme throughout this report. This section concentrates on two other challenges that received specific and frequent comment from interviewees at all stages of the study: the NHS QIPP programme and the requirement that NHS provider organisations should achieve self-governing FT status. In both cases, NHS organisations were assessed and judged by external agencies, which obliged boards to make difficult prioritisation decisions relating to the deployment of the skills of their senior staff and the resources at their disposal.
Two of the study sites (09 and 14) were granted FT status prior to the start of the NETS. The other provider organisations (01, 07, 08 and 10) became FTs during the NETS programme or, in the case of study site 06, merged with another FT study site.
There were mixed views on whether the NETS helped or hindered the process of achieving FT status. Some interviewees felt that the NETS’s early focus on quality, safety and eliminating waste provided a useful focus that could underpin an application to become a FT:
. . . the reason I came in when I did was because the trust had failed to get foundation trust status . . . And the reason . . . was because of infection control . . . transformation models were starting to be concentrated on in that particular way . . .
Site 01, senior board member
Other organisations experienced a pause in the NETS implementation while they chose other means to tackle the range of financial, quality and governance issues involved in meeting the requirements of FT status. This was particularly the case in site 08:
. . . the [NETS] work that we were doing around engagement of clinical staff et cetera, that’s obviously positive and helpful in every respect, and so from that point of view the work that we’ve done for NETS has helped with the foundation trust application. But . . . a lot of the work that was done . . . was . . . developing a sort of wider business, integrated business plan and going through . . . sort of financial planning scenarios of a number of kinds. Didn’t really have very much to do with NETS to be honest . . . we’ve kind of been on pause for a while as far as developing all of this is concerned because of the whole FT application.
Site 08, senior clinician
Sometimes the consequences of a shift of attention away from the NETS programme were very specific, as in the case of this RPIW: ‘Unfortunately that’s where it all fell to bits. Because we were going through foundation trust and when it came to our 30 days no one turned up’ (site 08, care pathway team member).
The North East was the first English region where all provider organisations achieved FT status. In one way, this had a direct impact on the NETS as a region-wide programme, in that the non-FT NHS organisations and networks became aware that their FT colleagues had acquired a certain degree of freedom to invest in training and to follow their own QI path. As one KPO lead explained, the FTs enjoyed autonomy of decision-making, but were able to maintain a consistent approach to the NETS through strong communication links. The strength of the FT group within the NETS, however, also ran the risk of alienating non-FT organisations: ‘. . . we have the same thing at the Coalition Board where the PCT leads are saying right it’s not an FT club, we don’t want to join an FT club’ (KPO focus group participant).
The importance of the national QIPP programme grew considerably during the period of the study, in large part as a response to the so-called ‘Nicholson challenge’144 to find savings of £20B from the NHS budget by 2014. QIPP and the NETS shared a fundamental belief that improvements to quality and a willingness to innovate will have a positive impact on health-care productivity and thereby bring about cost reductions. In theory, therefore, NETS activities should have contributed directly to QIPP targets. Fifteen of the interviewees made explicit reference to QIPP, and their responses revealed a wide range of views, as summarised in Table 25.
| Study site views of the role of the NETS in achieving QIPP targets | Hospital (VMPS) | Hospital (non-VMPS) | PCT (VMPS) | Ambulance trust (VMPS) | Mental health trust (VMPS) |
|---|---|---|---|---|---|
| NETS as a vitally important means of achieving the intra- and interorganisational process improvements that will enable QIPP targets to be met | 11–13 | 10 | |||
| NETS as one of the means to deliver QIPP targets, widely understood as such by staff | 09 | 07 | |||
| NETS as one of the means to deliver QIPP targets, but with less confidence that most staff see the link between the two | 09 | ||||
| QIPP and the NETS as occasionally complementary and mutually supporting programmes | 01 14 |
||||
| The NETS as supportive of QIPP targets, but with some adaptation required | 07 | ||||
| QIPP as potentially destabilising, with NETS as the ‘back up’ system | 11–13 |
From the interview data there was an indication that the more mature and committed NETS organisations, such as study sites 09 and 10, were more likely to see the NETS as being an essential mechanism in achieving QIPP targets. It is also noteworthy that the two non-VMPS hospital study sites (01 and 14) appeared less inclined to see the NETS as closely linked to QIPP success, whereas the VMPS commissioning organisation (study site 11–13) appeared to be strongly convinced of this connection. However, the small numbers and nature of the interviewees mean that caution should be exercised in placing too much reliance on these conclusions.
Change agenda and its locale
Pettigrew et al. 125 included ‘change agenda and its locale’ as one of the eight factors in their receptive contexts for change model. The ‘locale’ of change (the political, social and relational context wherein change takes place) may have a strong influence on facilitating or inhibiting the process of transformational change. They noted that many elements of the locale may be ‘beyond management control’ but that ‘awareness of their influence could nevertheless be important in anticipation of potential obstacles to change.’
Many of the interviewees were senior members of staff who might reasonably have been expected to possess such awareness. The interview data showed considerable appreciation of the political and policy environment in which the NETS was being developed. It was explained in Chapter 3 that the NETS was originally conceived to overcome the conundrum of the North East region having a high-performing health-care service but also high levels of poor population health and considerable levels of health inequality. These factors were well understood by most – perhaps all – of our interviewees.
Managerial–clinical relations
As mentioned in Chapter 2, Management–profession interface, Degeling et al. 26,27 showed that successful changes to the delivery of health care – whether to improve quality, ensure safety or cut costs – are strongly associated with clinician and manager acceptance that health service provision is necessarily team-based and multidisciplinary. This research found evidence that the NETS, when supported by adequate resources and senior-level commitment, contributed significantly to improved communication across these traditional professional boundaries. The VMPS-inspired report-outs (time-limited, team-based progress reports on improvement activities), or their equivalents in the non-VMPS NETS organisations, stand out as exemplars of this principle in action. Regional report-out events frequently brought together 10 or more teams from the whole spectrum of NHS organisations in the North East. Each team comprised 10–12 members, representing junior, mid-level and senior staff with a broad range of clinical, administrative and managerial roles. It was clear from the observation of these events, and from DVD recordings, that the report-outs were generally valued as an opportunity to demonstrate the successes achieved during a week of hard work. Furthermore, participants often commented on the lasting benefit they had gained – individually and collectively – through having an opportunity to tackle a poorly designed process, remove waste from the system or redesign work around patient benefit without the constraints and frustrations of day-to-day professional boundaries and hierarchies.
The NETS developed during a time of considerable financial and organisational pressure on the NHS, and against this background it is difficult – if not impossible – to form a definitive view on whether or not the principles of the initiative would enable deep and lasting changes to managerial–clinical relations. However, the buoyant enthusiasm that was evident in regional report-out sessions did appear to reflect a short- to medium-term shift in the perceptions and behaviours of those staff who took part.
Share-and-spread activities
It is important that lessons can be learned from any activities that have been undertaken, regardless of whether they are positive or not. Sharing such experiences allows other individuals to see what improvements were made and whether or not they could be adopted elsewhere in the organisation. However, this ‘sharing’ or transfer of best practice was not without its difficulties, as this interviewee explained:
I think the more difficult point is often if you then try and translate those changes to other areas where staff haven’t been directly involved in improvement events there, that is certainly much more difficult. Even if to be frank there aren’t those sort of negative consequences, because you’re just trying to get people engaged in making changes when they can’t always see for themselves why they should bother is a problem, regardless of whether there are job losses or job changes, just there is still some resistance. So we usually sort of share and spread events to try and overcome that.
Site 10, HR manager
Another interviewee linked the share-and-spread and replication stages back to the issue of standardisation and standard operations of work:
Even if you’re doing something similar oh well we’ve refined it very slightly, we’ve done it slightly differently. As soon as you put it into, like you say in the information here, as soon as you put it into an organisation of 9000 people it’s never going to be replicated. It doesn’t matter what you do, it doesn’t matter how rigid you are, it will never, ever be replicated like for like. So that ability then to reflect and to learn from that implementation is really key.
Site 07, organisation development manager
In other cases, the share-and-spread events worked quite well. A service development lead explained:
We’ve done spread and share events so an example of that would be we did antipsychotic monitoring, an event in Stockton with a psychosis team. And we then rolled it out to every psychosis team within the trust. So we did, rather than do a 5-day event, we did a reduced 4-day event, and spread out the learning. So we looked at the standard work we’d produced, we looked at the visual control boards we’d produced, we allowed some local variation but they had to have the same outcomes. So we’ve actually started doing share-and-spread events.
Site 10, service development lead
A particular challenge was how a share-and-spread event should be conducted. One interviewee provided an example of the approach used in her organisation:
Well, as an organisation the organisation develop half-day awareness sessions so that staff at every level could have an awareness just about what does the VMPS actually mean, what does NETS mean and to give them an idea about some of the basic concepts of 5S and the waste wheel. That was a half day and then they also put on full days which included how to use different tools and then there’s a week course which is the 5 days looking at how to actually put those tools in place. Now the 5 days would be what we kind of envisage our senior staff getting involved in and our modernisation facility; it’s people who take a lead in trying to, you know, have continuous improvement in things.
Site 11–13, senior nurse business manager
Share-and-spread activities had not been limited to activity within the trusts. They were undertaken with other trusts as well as with external partners, as this interviewee described:
I think there’s the Leadership Awards and the Bright Ideas Awards are coming up as well. And the thing is there’ll be people in different departments, it’s about filtering it down, because someone’s going to have an idea, but they won’t know how to share it. And I know you get your payslips and you get the Bright Ideas application and stuff like that, but I think the more people involved in that the better. We’re very good at talking about sharing, very good at oh I’ll share what we did with this RPIW. We’ve produced a case study template that was last year and getting organisations, and we’ve had a workshop as well with someone external, well she used to work in the NHS, someone [name] knew, came in, delivered a morning session, but basically it was a pilot workshop to test it out, and that went quite well, went very well actually.
Site 09, NETS Coalition co-ordinator
Cost-effectiveness
Although the cost-effectiveness of the NETS programme did not form part of the research objectives, the issue arose frequently and spontaneously in interviews and focus group discussions, and was therefore included as part of our inductive analysis of transcripts. Around one-third of the transcripts (n = 19) provided commentary on this topic.
The question of whether or not the NETS programme was cost-effective has two components: the cost-effectiveness of the NETS training, as compared with training in other methodologies for improving quality and reducing waste, and the cost-effectiveness of the NETS activities in the study sites (RPIWs, 5S and 3P events, compact development, share-and-spread workshops) compared with other ways of achieving the same, or similar, results.
It proved impossible to make a definitive comparison between the cost-effectiveness of NETS training and that of other available QI programmes, mainly because data were either unavailable to the research team or ambiguous. Some of the study sites (01 and 14, for example) were using a mix of different improvement methods, and such data as were available on the costs of training did not provide sufficient detail to understand how much of the total was devoted to NETS-specific or VMPS-specific training. A search of the documentary materials, however, revealed some data on the costs of providing VMMC training for ‘wave 3’ of the NETS in 2010, as brokered by the central NETS support team at NHS NE. This showed that, if all of the proposed VMMC-supported training, plus staff visits to Seattle, WA, and Japan, had taken place in that year, the total costs borne by NHS NE and the relevant trusts would have been comfortably in six figures. This sum only included the direct costs of payments to VMMC, and did not include the costs to the trusts of staff time to organise and administer the training, the costs of providing cover for staff engaged on the training programmes or the costs of materials and travel in the region. It is clear from just this limited set of data that the VMMC training, as part of the overall NETS programme, was not a cheap option or insignificant budget item; but this tells little about whether or not it was cost-effective and value for money. To make this judgement the following evidence would be required:
-
whether or not the NETS organisations would have organised other types of training, if not engaged in VMMC activities
-
the success of VMMC training compared with other training programmes, in terms of delivering and sustaining training objectives
-
the congruence of VMMC training with the overall aims of the NETS, again compared with other possible programmes.
The above information was not available, except in anecdotal and subjective form, so a proper assessment of the cost-effectiveness of the NETS training (and, in particular, the VMMC element of this) cannot be made.
A similar picture emerged when the cost-effectiveness of the NETS activities was considered. Many of those staff who commented on the cost-effectiveness of carrying out NETS activities spoke of the need to perform cost–benefit analyses, to understand the value-for-money aspect of the NETS programme, or simply to develop better metrics that would allow such comparative study. Sometimes the cost-effectiveness of the NETS programme was unequivocal:
Now we’re able to point to things like I’ve told you . . . I’ve got an empty surgical ward following RPIWs that have happened there . . . So the board now . . . sees the financial payback, as well as the fact that in the last set of annual health-check ratings we were double excellent, so it clearly did something in terms of quality and safety as well.
Study site 09, senior director
However, the link between NETS activities and the bottom line was often not so clear-cut. A senior director at a commissioning organisation was asked about the impact of RPIWs financially, and considered that this was not well understood:
. . . that’s one of the areas which I think we . . . do not focus sufficiently on . . . and I think . . . that’s one of the key things that we need given the economic circumstances . . . there’s not a great deal of focus I would say on the pure financial.
Study site 11–13, senior director
Perhaps this is not surprising; the driving force behind the NETS was improvements to patient safety and the quality of care, and although financial benefits were expected to flow from this focus, they were deliberately not positioned as the central driver of the programme.
The data revealed very little about the cost-effectiveness of the NETS compared with other QI initiatives. Even where interviewees and focus group members had extensive experience of other lean-based programmes, or had previously taken part in NHS experiments with Six Sigma, total quality management or quality circles, they did not comment on the comparative cost-effectiveness of the NETS programme. In truth, it would be very difficult to do so. First, the recipients of training programmes (of all kinds) often have little or no idea of the cost of providing the training. Second, those who do know the costs are often unable to put an accurate value on the outcomes of the training, especially if the focus is not directly on cost-saving. Finally, as noted in Chapter 1 of this report, the NETS was a unique, region-wide programme, with expected benefits that were intended to span organisational boundaries. In these circumstances, the cost-effectiveness of the programme would always be difficult to assess directly.
With these caveats in mind, it is worth noting that some of the more senior staff interviewed were passionately convinced that the NETS stood an excellent chance of delivering on its promises and was highly cost-effective, but that this promise was imperilled by the upheaval in NHS structures following the election in 2010. As one medical director commented:
. . . we’ve done a massive own goal getting rid of the SHAs. If I was in the Department of Health I’d be saying oh look what’s happened in the North East, the SHA has managed to galvanise not the whole health-care community but a substantial amount of it, let’s go with that, let’s build on it, let’s spin that fly wheel even more. Let’s get them talking to some of the other SHAs and say look, if you have an SHA-wide service improvement model you can deliver vast amounts of savings. Because I absolutely think that the North East would have continued to deliver more and more savings if we were allowed to carry on. And you can see it in the people’s faces the devastation that we were just on the verge of something really special.
Focus group, medical director
Summary
Patient safety and putting the patient at the centre of all activities is a key message of the NETS. Patient safety was implicit in several of the ‘seven no’s’ that provide the basis of the Vision of NHS NE, especially No avoidable deaths, injury or illness and No avoidable suffering or pain. Emphasising safety was deliberate as patient safety was perceived as the main ‘selling point’ for staff involved in the NETS initiative. The introduction of a Compact was also identified as influential in shifting the emphasis of work on patient safety from a rule-based, process-oriented approach to one that addressed issues of organisation culture. This enabled improvements to be made to procedures that were known to be flawed. It was acknowledged that the planned implementation of improvement programmes was not a key issue. Some of the NETS study sites opted to implement their QI programme vertically (i.e. department by department, or ward by ward) rather than horizontally across the whole organisation.
The NETS focused on making measurable improvements to clinical care as a way to convince initiative-weary doctors and nurses of the value of the principles of the NETS, and to gain their commitment to the programme. Quality and safety were identified as being very closely linked. The lean programmes (e.g. VMPS, Unipart Way or the Productive Ward) taught staff that QI would arise from removing and reducing waste, focusing on adding value and concentrating on seeing processes from the patient’s point of view. The NETS was effective in reinforcing and encouraging a whole-system view of quality.
The NETS encouraged staff to see the world through the eyes of patients, their families and carers, and to focus on making changes to processes only where they were of direct benefit to these ‘customers’. It was a ‘bottom-up’ approach, with senior leadership commitment and resourcing supplied ‘top down’, and it was promoted as achieving transformational change through small-scale but continuous improvements to processes. Some of the non-VMPS study sites also had strong messages about the importance and value of involving patients in the redesign of processes and working practices. However, in these cases the PPI appeared to focus more on ward-level activity, rather than policy setting or influencing strategic objectives.
Successful adoption and implementation of the NETS were found to be closely associated with committed and stable leadership at the highest level in trusts and the SHA. Senior leaders, whether managers or clinicians, were required to take a hands-on approach to driving forward the NETS activities. They were expected to take part in practical, day-to-day improvement events. Evidence of public criticism of a training programme that involved regular overseas travel caused some NHS organisations to have concerns about joining the VMPS version of the NETS. The upheaval in NHS structures that began in 2010 had a significant effect on the NETS as a regional programme, and negatively affected its progress in some of the study sites.
Chapter 8 Discussion and key themes
In this chapter we consider the key issues to emerge from the study for further analysis and comment. The research study sought to evaluate a large-scale, region-wide initiative that aimed to transform an entire health-care system. It was an ambitious and complex project that included a large number of local interventions and many co-ordinating activities. The research yielded a considerable volume of information and a rich array of insights and issues. It is not possible to do justice to them all in the confines of a single chapter. However, a number of core themes have recurred at various points throughout the study and stand out as being of particular significance. We have therefore chosen to focus on them in our discussion. This chapter draws together the key issues relating to
-
the implementation and sustainability of transformational change in a complex and changing policy and organisational context
-
the importance of leadership and its effectiveness
-
differences between lean in the manufacturing and health sectors and the nature of complexity in the two sectors
-
differences between study sites in terms of their receptiveness to the NETS and lean thinking, as well as their relative success in implementing the NETS’s founding principles
-
reflections on the ITS.
We consider each of these in turn. Thereafter, in a final section we reflect briefly on some general messages to emerge from the overall evaluation study.
The implementation and sustainability of transformational change in a complex and changing policy and organisational context
The factors that enabled or hindered transformational change were evaluated. Bringing about transformational change in health systems is regarded as particularly challenging even in the most propitious of circumstances, given the multiple complexities involved and the diverse range of stakeholders to be engaged. Health systems are complex in terms of both the challenges facing them and how these can best be addressed. Command and control approaches, though often superficially appealing, rarely succeed and risk oversimplifying the complexity of the problems facing managers and practitioners. In the NHS, complexity arises from numerous sources and factors including the political and regulatory environments, powerful groups operating nationally and locally, and the multiple groups involved in commissioning and providing health and health care.
Kotter145 argued that large-scale change can take years to bring about and goes through a series of eight distinct steps. These are establishing a sense of urgency; forming a powerful guiding coalition; creating a vision; communicating the vision; empowering others to act on the vision; planning for and creating short-term wins; consolidating improvements and producing still more change; and institutionalising new approaches. Virtually all eight steps can be discerned in respect of how the NETS was conceived and progressed. They also complement the eight factors making up the ‘receptive contexts for change’ framework. 125 However, Kotter’s schema does not include the impact of the external environment and, in particular, the political context (although it is included in the Pettigrew et al. framework125), which are among the major reasons why transformation efforts often fail in the NHS. The two factors can have a decisive effect on the direction of transformational change at all levels of the system. It is often the final two steps in Kotter’s list – consolidating improvements and institutionalising new approaches – that fall victim to changing political circumstances and fads and fashions. There was evidence from our study that such factors were at play in determining the NETS’s fate following the announcement of the NHS changes in mid-2010.
As a general point, though it may seem paradoxical, in order to effect successful transformational change there is a need for organisational stability, or a freezing of the organisation, before it can unfreeze and change. Public sector bodies, especially high-profile ones like the NHS, have over the years been subjected to increasingly frequent policy and structural changes which, while giving the semblance of change, tend to leave them remarkably unchanged – what Schön146 terms a case of ‘dynamics without change’. The consequence is that the same problems and challenges tend to recur.
The NHS changes announced unexpectedly in July 2010 were perhaps a good example of this phenomenon. Regardless of whether or not the changes were required or desirable, their impact on the NETS as originally conceived was profound. In particular, it seriously disrupted the approach adopted by NHS NE and necessitated a rethink of how the NETS’s future could be assured in a very different world. The reason for this was because the NETS aimed to achieve transformational change rather than merely apply lean thinking or a set of mechanistic tools. It was an ambitious attempt to change NHS organisations throughout an entire health-care system. To this end, the Vision, Compact and Method were, in combination, a holistic mechanism that aimed to achieve transformational change in a complex setting. This was because these three elements focused on the need for change management in the way that the NHS across the North East conducted its business; the focus was not on particular tools or methods. Overemphasis on the methods could have led to point improvements and a lack of sustainability. They were important, but only after the commitment to the Vision and Compact was in place. Those organisations which achieved this were better placed to weather the disruption unleashed by the 2010 changes. Indeed, as noted on a number of occasions, two organisations in particular stood out in terms of displaying a critical mass of activity which enabled them to achieve a degree of sustainability not found elsewhere in the study sites. That is not to say that a similar degree of embeddedness would not have developed or been possible elsewhere had the NETS been able to continue on its course. However, the immediate impact of the changes announced in mid-2010 did mean a setback in terms of achieving those hopes and aspirations. Consequently, those organisations which were less secure or developed in each of the three domains – Vision, Compact and Method – were more vulnerable to the impact of the changes which served to test the limits of the managerial and clinical commitment to the NETS.
Even so, across most of the study sites, the commitment to deep cultural change sought by the NETS remained fragile and had yet to attain the degree of embeddedness achieved in the VMMC. In particular, the Compact appeared to have received much more attention and investment there than in NHS NE. Indeed, the VMMC implemented the Compact before it became aware of the TPS. It was believed that only when the Compact was in place should the introduction of lean tools begin. In NHS NE, the three elements tended to advance simultaneously. There was a tendency in some quarters to invest more in lean thinking and tools than in the more difficult work arising from the Compact and, possibly to a lesser degree, the Vision.
In particular, the 2010 proposals for major NHS changes, which many commentators regarded as amounting to the biggest bang in the history of the NHS’s many reorganisations, disrupted the combined top-down and bottom-up approach to change which did seem to be working within the NETS study sites. 142,147 Strong and visionary leadership from the SHA was not to everyone’s taste in the region but, where it worked, it provided the momentum required to improve and embed the NETS approach. But this top-down approach could only work in those cases where there was also strong buy-in from those working at or close to the front line in the various NHS organisations. The 2010 changes put paid to the top-down dimension because the SHA’s position could not be sustained when faced with abolition in March 2013.
There were mixed views on the consequences for the NETS of the major upheaval in the NHS announced in July 2010 in the coalition government’s White Paper. 1 Some of those interviewed expressed concerns that the impending demise of familiar structures, notably the SHAs and the PCTs, and the resultant loss of organisational memory from parts of the NHS in the region, would limit progress of the NETS and would divert attention and resources from it. It was acknowledged that organisations could individually pursue the NETS if they wished to. However, the significance of what was happening in the North East as a whole in terms of a collaborative approach would be put in jeopardy without any guarantees that it would survive. But not all staff were persuaded by this view. Some of those interviewed felt that the SHA’s role had been negligible and would not be missed as long as there remained sufficient local commitment. Importantly, this view came more typically from provider organisations in the vanguard of implementing the NETS, who were more confident of their ability to continue to train staff without support from the SHA or elsewhere. In practice, some of these provider organisations did continue to support a small central NETS team to co-ordinate training and support activities, further development of the initiative and promotion of the NETS as a brand that could be offered to other NHS organisations.
The importance of leadership and its effectiveness
The important role of leaders and leadership in enabling transformational change in health-care organisations has been well established in the literature. It was certainly a key factor throughout the NETS at all levels and across all organisations in our case study sites. 148 The Pettigrew et al. 125 ‘receptive contexts for change’ framework includes as one of the eight factors ‘key people leading change’. The words were deliberately chosen to avoid connotations of heroic and individualistic ‘macho managers’. Instead, the model of leadership that is articulated refers to pluralist, distributed leadership styles that encourage team-building, group accountability and diversity of skills. The Vision and Compact were central to the leadership approach adopted; they represented the ends of the NETS project while the Method represented the means of getting there. The Vision, framed around the ‘seven no’s’, proved powerful in motivating staff to think differently about how to improve services.
A number of common themes concerning leadership emerged. First, many of the respondents were strongly of the view that embedding the principles underpinning the NETS required committed, stable, long-term leadership at the highest level. Continuity of key personnel was cited as critical to the success of change projects. Unplanned staff movements were associated with loss of purpose and commitment. In the North East there tended to be less senior staff churn than was evident in other regions, which helps embed learning and sustainability.
Second, it was important for senior leaders to have a hands-on presence. The NETS attracted both scepticism and cynicism that it was just another passing fad – one of the many fashions to sweep through the NHS without achieving much by way of impact or sustainable change. Staff therefore felt that rhetoric and exhortation were insufficient to win commitment and support from the workforce. Senior managers were required to take part in practical, day-to-day improvement activities if they were to be taken seriously. In short, they had to ‘walk the walk’, not merely ‘talk the talk’.
Third, continuity and consistency of purpose were highly valued outcomes of the NETS programme. They provided a framework and created a sense of purpose that enabled organisational change and the building of relations through the Compact, participative workshops and other knowledge-sharing activities. Clinicians were accustomed to working in a largely individualistic, competitive manner rather than in a more collegiate, team-based style, especially when it came to relationships with managers; this could act as a barrier to transformational change, which was addressed by the Compact.
Fourth, the importance of leadership skills was recognised at all levels. However, there was a tension between the type of skills that were considered to be desirable and the requirements of the top-down, target-driven culture of the NHS. The dilemma was captured by Currie and Lockett’s149 reference to ‘a managerialist form of transformational leadership’ that had been ‘promoted through government policy’ and had little connection with its academic conception. Maintaining or improving levels of quality and safety, meeting financial challenges and embedding a culture of continuous improvement were all seen to require different leadership styles from that which was commonly found throughout the NHS. In important respects, these concerns have been reinforced and confirmed by the findings from the Francis Inquiry into the failings at the Mid Staffordshire Hospitals Trust. 111 In contrast to what happened there, those closely involved in the NETS programme viewed leadership as a distributed attribute within their organisation. Leadership was characterised as an ability to empower a team, communicate a vision and be able to effectively delegate responsibility to the staff.
The research confirmed the findings of previous research which had stressed the importance of leadership in effecting successful transformational change in health-care organisations. It was recognised that shaping organisational culture and promoting teamworking were more important in achieving transformational change than the mechanics of implementing lean tools.
Differences between lean in the manufacturing and health sectors respectively, and the nature of complexity in the two sectors
From their origins in the Toyota Motor Corporation, lean production programmes spread through other manufacturing sectors, then into service industries, and more recently to a wide range of public sector organisations, including health care. Within the UK, lean in health care has been focused on single organisations, such as hospitals or smaller units. For example, Radnor et al. 84 looked at four case studies in the UK NHS and reported a number of successes across these cases, including
-
reduced waiting times
-
improved patient service
-
increased direct patient care time
-
clearer understanding of care pathways
-
removal of duplicated processes
-
exposing areas to 5S
-
enhanced staff motivation
-
removing unnecessary data fields from multiple forms.
This research has also identified similar outcomes. The NETS, however, tried to bring about transformational change in the health-care organisations across a whole region. Pettersen150 categorised four approaches that form the basis of a lean journey:
-
toolbox lean: practical and operational
-
becoming lean: practical and strategic
-
leanness: philosophical and operational
-
lean thinking: philosophical and strategic.
In order to achieve the full benefits of lean, an organisation needs to achieve ‘lean thinking’. For a manufactured commodity like a car, the customer is the commissioner, owner and user of the product. Radnor et al. 84 identified that in health care it is not clear who the customer is. The patient is the recipient of the service; the payment is made by the commissioning organisation. In a NHS context, the patient has no knowledge or interest in the price of the service or the cost of its delivery. The notion of value, central to lean thinking, is therefore ambiguous. A further issue is the number of stakeholders involved in a health-care ‘system’ (e.g. government, professional bodies, the local community, friends and family of the patient) who will have different views on what constitutes ‘value’ in this context.
Lean tools can help eliminate waste; make the product flow; standardise best practice; synchronise processes; and introduce a ‘pull’ approach. In manufacturing, it is easier to apply the tools and see the outcomes of the ‘product’ moving through the manufacturing process. In health care, it is likely to be the patient who moves through the ‘production line’, so a different approach and mindset is required for this form of ‘service’ model. Focus needs to be placed on the ‘social’ and ‘organisational’ system, not just the technical system (and the lean tools). The NETS identified these issues, which is why the Vision and Compact were so important. They provided a mechanism for aligning stakeholders’ interests and encouraging teamworking.
Patient characteristics and medical conditions may be highly variable, leading to a requirement for a high level of personalisation of care; this is in sharp contrast to the standardisation of products and processes found in many areas of manufacturing. The health-care ‘servicescape’151 provides the environment in which health professionals work, patients receive treatment and family and friends visit. The servicescape has environmental dimensions (ambient conditions, space/functions and signs, symbols and artefacts). It influences psychological moderators (cognitive, emotional and psychological) which effect stakeholder responses and behaviours (e.g. social interactions). 151 These factors make health services a more complex environment than manufacturing, which make it necessary to adopt a holistic sociotechnical approach. 113
The structure, development and implementation of the NETS has gone some way in trying to tackle these issues through the development of the Vision and Compact. This can be seen as a key difference in approach between manufacturing and health care.
Differences between study sites in terms of their receptiveness to the North East Transformation System and lean thinking, as well as their relative success in implementing the North East Transformation System’s founding principles
The study sites comprised NHS organisations that provided a range of services including acute hospital, mental health and learning disability, community, ambulance and commissioning services. The sites’ complexity varied across different dimensions: the mix of professions; the geographical spread of activities; the scope of interactions with other NHS and non-NHS organisations; and the range and type of internal processes. Apart from the inherently heterogeneous nature of the study sites, they also differed considerably in the type and extent of the external challenges and pressures they faced. Study site 06, for example, had been affected by a national policy of absorbing community service trusts within acute hospital trusts. Its staff transferred into study site 01 in April 2011. Study site 06 no longer existed, and the change also had an effect on the NETS programme within site 01. Former site 06 staff had to ‘buy into’ a different organisational Vision and an alternative Compact, and become familiar with a different set of improvement tools employed as the Method. These difficulties interrupted the rollout of site 01’s improvement programme.
Despite variations in operational priorities and internal structures, the study sites initially displayed a consistently high degree of receptiveness to the principles of the NETS. This was immediately apparent in the observation that most of the NHS organisations in the North East quickly agreed to follow the Vision/Compact/Method route to QI. Of the NHS organisations that were approached to take part in the first round of meetings in late 2007 that set the course for the NETS, only one refused to take part, and one (site 02–05) appeared to reject NETS training at an early stage.
The main reasons for the early ‘buy-in’ to the NETS were as follows.
-
NHS NE had identified, through extensive consultation with NHS leaders, a consensus view that a step change in QI required collective as well as individual action. This required changes in culture as well as the application of lean tools.
-
The boards and senior executives of NHS organisations were acutely aware that real-terms increases to NHS budgets were due to end after 2008. This was seen as both a pressing reason to find ways to remove waste from the health-care system’s processes, and an opportunity to set a new course for improvements to care quality and safety; in other words, a way to ‘keep ahead of the game’.
-
The early pilot visits to VMMC and Japan had enthused senior clinicians and managers. This positive reaction had been well communicated using existing channels across the North East. There was therefore extensive (although not universal) managerial and clinical agreement that the NETS approach should be given an opportunity to flourish.
As the NETS programme was implemented in the wave 1, and then the wave 2 pathfinder organisations, the degree of receptiveness to the Vision, Compact and Method elements began to differ among the study sites. Some appeared to be more interested in the Method component, seeing lean as a means to make an immediate impact on waste, rework and progress towards external targets such as QIPP. Others took a longer-term view that placed Compact development firmly at the centre of the NETS programme. A small number (sites 07 and 10, and possibly site 09) seemed able to make simultaneous progress with all three elements of the NETS, although, even in those sites, there was a general view that the development of the Vision component had lagged behind the others.
It is not possible to establish a strict causal relationship between receptiveness to the principles underlying the NETS (and success in implementing them) and the managerial and clinical circumstances prevailing in the various study sites. There were simply too many confounding factors to establish cause and effect with any certainty. However, we note some of the broader impressions that were formed while conducting the research (Table 26).
| Study site | Notes on receptiveness to the NETS |
|---|---|
| 01 | This site had been introducing the NHS Institute’s Productive Ward Series ‘Time to Care’ programme to a number of selected wards, prior to the start of the NETS. It initially continued to use the Productive Ward Series as the NETS Method, later introducing VMPS interventions in conjunction with other tools |
| 02–05 | After initial interest, this site decided not to take an active role in the NETS; expressed concern over the use of public monies to fund overseas training |
| 06 | This site used involvement in the NETS to develop an in-house QI programme, closely tailored to the particular needs of community service staff. However, the organisation ceased to exist in April 2011; staff transferred to study site 01 |
| 07 | For this site, operating across a very large geographical area, the NETS was an important means to share and spread QI initiatives among widely dispersed groups of staff with different organisational subcultures. The NETS was supported by a small core team whose members were well versed in the wider field of improvement science |
| 08 | After initial involvement with the NETS as a wave 1 pathfinder, this site appeared to experience an interval of approximately 1 year with less NETS activity while senior leaders focused attention on other priorities. The NETS programme did not cease, but some key staff changes also contributed to a slower pace of progress in undertaking NETS training and spreading the NETS’s message |
| 09 | This wave 1 pathfinder site made rapid early progress in implementing NETS training for a central team, which has continued to make the NETS a key component of the organisation’s QI strategy. The site has experienced some difficulties in consistently following the strict VMPS Method, but on the other hand, it has shown itself able to adapt the NETS to a wide variety of operational areas |
| 10 | This site was an early and enthusiastic adopter of the NETS. The NETS programme was seen as a vital, long-term linking mechanism between the organisation’s strategic aims and the developments necessary to improve and standardise processes, focus on value for patients and staff and achieve greater efficiencies. The principles of the NETS were widely disseminated among staff |
| 11–13 | This site saw the VMPS as key to leading cross-boundary, multidisciplinary improvements that would improve the quality and cost-effectiveness of care pathways that encompassed primary, community, hospital and social care. Took on the leadership role of bringing together the actors in these sectors |
| 14 | This site accepted the NETS’s principles as being consistent with an existing and well-established programme of quality and safety improvement; incorporated the NETS as part of an eclectic armoury of strategies to redesign work processes and change clinical culture |
At least four, and possibly five of the 14 study sites remained committed to the NETS approach throughout the study. Other sites that had adopted some of the NETS approach had not bought into the whole package (e.g. not using the VMPS Method). They also remained committed but did not consider that the precise Method chosen was of great importance. For them, demonstrating commitment and being clear about the purpose of the NETS approach were the most important factors. This issue is a manifestation of the loose–tight tension which, for many of those working in the NHS in the North East, characterised the NETS and their feelings towards it. Being permissive about means may be perfectly legitimate as long as the purposes and goals are tight, in terms of their clarity and measurability, in order to demonstrate improvement.
Reflections on the interrupted time series
The findings from the ITS analysis of the five RPIWs were mixed, with a small number of statistically significant improvements observed, some ambiguous results, several where no evidence of an impact of the RPIW could be detected and some counter-expectation findings. Clear improvements included a reduction in time from arrival of patients with abdominal pain in A&E to being X-rayed (surgical pathway RPIW) and a reduction in the length of stay on the ward for women (PIPA RPIW). Counter-expectation findings included an increase in the time to discharge (community psychosis – discharge RPIW). Overall, for 9 out of 19 variables the results tended to be ambiguous, without clear evidence of a positive or negative impact of the RPIWs. However, the ITS findings need to be placed in the context of both the limitations of any quantitative method (including the ITS method) for pragmatic evaluations and the findings of the rest of this study, as illustrated notably in the case studies.
As explained in Chapter 4, Interrupted time series, ITS is the strongest quantitative observational study design for examining the impact over time of short-term interventions, but it is acknowledged that the data requirements of multiple time points (12 for a long series) can be onerous. Nevertheless, the NETS evaluation would have presented a challenge to any prospective study as prior or baseline data are a feature of any pre–post prospective design. The ITS analysis presented within this report could be regarded as a ‘methodological experiment’ in determining whether or not this method is feasible for service evaluations of this kind within the NHS. A key problem was the requirement for multiple data points pre and post intervention, and the trade-off between the desire to measure the clinical outcomes targeted by the RPIW (which would have had to be specially collected prospectively for up to a year before the RPIW, whereas the standard method for doing RPIWs requires only baseline data collection) and the data available retrospectively pre RPIW, which could only be derived from routine information systems and was therefore limited to more administrative variables.
Other constraints included the lack of control by the research team over the construction of the variables to be used in the analysis and the consequent inability to predict data collection requirements and feasibility. Major data processing was also required on receipt of the extracted data sets, with some assumptions having to be made by the research team. It was not always feasible to verify the assumptions with hospital information staff or RPIW clinicians. There were particular challenges for the hospital information staff in constructing the linked data set for the PIPA RPIW, involving linkages over two information systems and through three ward name and/or location changes.
As noted in Chapter 4, Interrupted time series, ITS designs are strengthened by the inclusion of controls. Control data were obtained for five control localities for the community psychosis analysis but, for the reasons explained in Chapter 4, Data and data sources, it was not possible within the time frame of the study to identify controls for the other two RPIWs. It should be noted that obtaining control data is an issue for any controlled design.
A number of factors need to be considered in interpreting the findings observed from the ITS analysis, and more detail on these is found in the case studies. Of particular note for the ITS are the following:
-
The surgical pathway RPIW was conducted against a background of a significant rising trend in overall attendances at A&E (thought to be due to the closure of a local ‘walk-in’ centre in October 2010), which was also likely to have resulted in a change in the casemix of those attending, so that the proportion of attendees with abdominal pain who required admission was probably falling. This background would have made it more difficult to detect any significant impacts of the RPIW, as ITS analysis controls for background trends.
-
For the PIPA RPIW, we found that a greater proportion of patients were being transferred into the ward (from other wards) after the RPIW. This was particularly true for men, with the proportion of male patients who had been admitted elsewhere rising from 1% prior to the RPIW to 18% after the RPIW. When this factor was taken into account in the analysis, the reduction in length of stay for men also became statistically significant. However, it was not possible to determine whether or not the changes in admission pattern were also due to the RPIW, which makes it difficult to interpret these results.
-
The community psychosis RPIWs’ variables were particularly difficult to construct from the data set provided; the process required several phases of discussion with clinicians. Assumptions needed to be made in some cases that may have led to data quality issues for the more complex variables. Several variables also had to be abandoned as they could not be reliably constructed, limiting the range of impacts that could be evaluated using ITS.
In summary, although the findings from the ITS analysis are mixed, with the data acquisition problems identified, it would be possible to draw conclusions in either direction regarding evidence for the effectiveness of the RPIW interventions based on the ITS alone. The inability to obtain data on the range of clinical outcomes targeted by the RPIWs (which have, by necessity, used mainly administrative variables) may mean that the ITS missed significant impacts in the other key outcomes. The findings from the ITS should therefore be placed in the context of the remainder of the study. In the context of wishing to use quantitative analyses to make causal inferences within this study, it should also be noted that, although undertaking an ITS was problematic in the context of this study, failing to use this more robust quantitative design would leave researchers using designs considered to be at greater risk of bias (such as uncontrolled after designs). The ITS analysis has, however, provided sufficient findings of interest that it would be worth considering the development of a well-designed prospective study to evaluate the effectiveness of RPIW-type interventions.
General messages from the study
Given the complexities and ever-shifting nature of some aspects of the NETS, it is difficult to come to any firm or final conclusions about its success (or otherwise) or its impact on either services or the public’s health status in the North East. Even where there may be evidence of change and improvement, attributing these either wholly or partially to the NETS, rather than to other factors or policy drivers operating at the time, is virtually impossible. A mixed-methods approach can help to try and cover all the bases but, even then, establishing causal links as distinct from strong correlations and associations from the data and their subsequent analysis is risky, and has to be approached with considerable caution and some humility. Indeed, adopting such a stance may mean rethinking what we understand by complexity and how we seek to research it, a topic considered in the final chapter.
From the interviews, observations and documentary analysis, a range of specific issues were identified:
-
The choice of RPIWs was based upon the receptiveness to change rather than maximising return.
-
The RPIWs were possibly too standardised and not tailored to the local context.
-
The quality of follow up after 30, 60 and 90 days following a RPIW was variable, and on at least one occasion was not evident at all.
-
Share-and-spread events and report-outs served as an effective means of dissemination and creating a regional community of practice.
-
The NETS served as an enabling, ‘challenging up’ factor which gave staff permission to question and challenge existing practice and to come up with workable solutions.
-
The NETS ethos changed over time following the NHS changes announced in 2010. From having been seen as a QIS, it came to be seen by the Coalition Board as a potential source of revenue. The original region-wide focus based upon the notion of ‘we are all in it together’ was undermined to a degree by the changing context which potentially sanctioned fragmentation and competition in place of collaboration and integration.
The real challenge facing us as researchers has been what to make of such findings in the totality of what constituted the NETS and its impact. We reflect on such matters in the next and concluding chapter.
Chapter 9 Conclusions and implications
This final chapter reflects on the research and its potential benefits to the wider NHS. It considers the particular challenges of conducting research in complex systems, especially, but not only, during a time of significant shifts in the landscape and architecture of the NHS. Key recommendations derived from the research provide useful lessons and insights for others embarking on similar complex change initiatives. Finally, suggestions for future research are offered.
The original research protocol listed eight key questions which were to be investigated by the study, as follows:
-
How have the various manifestations of the NETS and non-NETS approaches evolved over time?
-
How receptive have NHS organisations in the North East been to transformational change, including the adoption of VMPS, TPS and other lean tools?
-
What has the impact of the different NETS approaches been on the quality and efficiency of health care in respect of technical quality, safety, patient experience, access, equity?
-
How far has variation been reduced across specialties, departments and hospitals?
-
How far has work-related stress been reduced?
-
How far has the ‘compact’ with clinicians, to secure their commitment to the NETS approaches, been made a reality?
-
How far have staff been empowered to take control of their work?
-
What are the factors facilitating, and/or acting as barriers to, successful change?
Inevitably, in the course of conducting any evaluation of a complex dynamic system the questions may require to be reviewed and some may be subject to change or prove impossible to pursue for various reasons. Although the evaluation has been able to address the majority of the eight questions posed, for three in particular (numbers 4, 5 and 7) there has been less success in being able to provide either conclusive or convincing evidence, although some insights into these have been provided. In response to question 4, the study has not been able to say definitively how far variation has been reduced across specialties, departments and hospitals. Nor, in regard to question 5, is the study able to state how far work-related stress has been reduced. Question 7 was concerned with how far staff had been empowered to take control of their work, and while the study has provided insights into this issue through the case studies, it has not been able to come up with a general or conclusive statement to the effect that staff have been empowered.
Potential benefits of the research for the wider NHS
Berwick103 argued that complex, ever-changing systems such as health care should be learning organisations. They need to adapt and change direction as evidence becomes available which demonstrates what is working well and what may be defective and require modification or reform. Berwick makes the point in his report on the failings at Mid Staffordshire: ‘The NHS should become a learning organisation. Its leaders should create and support the capability for learning, and therefore change, at scale within the NHS’ [© Crown copyright 2013, contains public sector information licensed under the Open Government Licence v2.0 (www.nationalarchives.gov.uk/doc/open-government-licence/version/2)]. 104 At the same time, it is also claimed that organisations like the NHS are not good at spreading and sharing learning. 14 This is even the case when examples of good practice have been documented and published. Organisations tend to be slow to adapt and hang on to outmoded procedures or ways of operating. This is because they are regarded as familiar and/or they are defended by powerful vested interests, protective of what they regard as valuable and worth preserving.
The NETS was an example of a transformational change initiative that affected an entire health region comprising numerous organisations engaged in the commissioning and provision of health and health services. Within the confines of this community that served a population of 2.4 million people, the NETS was itself an example of spreading and sharing at work. The SHA saw part of its role as ensuring that internal learning was effective throughout the region. Indeed, it was keen to commission research into the impact of the NETS as part of this process. The manner in which the study was conceived was a good example of a NHS organisation working with the NIHR Health Services and Delivery Research (formerly SDO) programme to produce the research brief which resulted in the study reported here being established.
The NETS attracted much interest from other parts of the NHS, with site visits from groups of managers and practitioners a regular feature at some of the study sites. Just as the NETS was informed by developments at the VMMC, adopting and subsequently adapting the VMPS, so the early leaders of what was to have become the North East Production System felt compelled to spread the word beyond NHS NE.
Challenges of conducting research in complex systems
The NETS is an example par excellence of a complex intervention occurring within a complex system. This poses particular challenges for research and researchers, especially with regard to the generalisability and reproducibility of findings. Arguably, the richer the appreciation of complexity, the more difficult it becomes to generalise the findings and apply them elsewhere.
It is simplistic to assume that researchers can isolate the system (in this case the NETS) from its environment, as would be usual in simple randomised controlled trials (RCTs) as a route to understanding causality. More complex, pragmatic RCTs with embedded process analyses are potentially capable of addressing these concerns and are used to do so in the areas of education, policing and the criminal justice system. However, such trials are complex and logistically complicated, but in principle they can be designed and run. Built on sound observational methods to identify a priori hypothesised covariates and important dimensions of a process analysis, they can have important advantages including the identification of causal links that can be applied elsewhere. However, the number of covariates and dimensions of process analyses will always be limited. Moreover, not everyone is convinced that it is possible to use RCTs in this way to fully comprehend complex systems and to apply the lessons elsewhere. It is the context that shapes the intervention and can even determine whether it succeeds or not. In this view, reducing phenomena to their constituent variables is not especially productive, even if it were possible to do so. Thus, key properties of the interactions are emergent rather than determined and contingent upon one another, while significant elements remain uncertain and unknown. Research can aid understanding of how such systems operate while acknowledging that it may never be possible to completely comprehend how that system functions or what the precise mix of factors might be.
The adoption of an ecological approach to complexity views it as an open system that is both dynamic and gives rise to a series of interacting processes, the outcome of which informs and shapes that complexity. 152
The research team shares the view that engaging with complexity is not simply a case of developing more carefully contructed efforts to capture additional data. Nor is it a case of developing more sophisticated models to establish causation or those factors which might account for complexity. 152 The research team has wrestled with these issues. It is not enough to acknowledge the existence of complexity in health care, but it is necessary to find ways of engaging with its dynamic variability and constantly changing context. Such issues were thrown into sharp relief when the current NHS changes were announced in mid-2010, as these had the effect of instantly shifting the ground beneath the NETS. Life was simply not the same after the NHS White Paper appeared in July 2010. 1 In short, as Cohn et al. 152 put it, ‘the challenge is how to go about studying complexity without fully unravelling it’.
Complex health interventions like the NETS will always be highly variable because of the inherent dynamic character of their constituent parts, and as a result of the inevitable adaptations that emerge from their implementation in particular contexts. These are influenced and shaped by numerous local and national factors which cannot always be foreseen or predicted. Health-care systems will therefore remain complicated to study, especially when unpredictable events occur. Moreover, evaluation methods all have their limitations.
Key implications
Given the conclusions in the previous section, it would be both presumptuous and inappropriate to list a set of firm recommendations which, if adopted, would allow the NETS to be replicated and to succeed elsewhere. The study did not follow a linear journey from the identification of a problem, through the adoption of an intervention, to final impact on quality of care. The journey itself is still ongoing, as was recognised from the outset by one of the NETS’s architects, because striving for continuous improvement, by definition, never ends. The best we can do, therefore, is to offer a set of key implications arising from the research, identifying those influences and factors that were encountered on the journey that seemed to be especially critical in bringing about sustainable change. Of course, these influences and factors may not work in quite the same way in any given situation or context. Furthermore, a recognition and acknowledgement from the outset that they cannot be applied in a simplistic ‘lift and shift’ manner ought to go some way to reducing any sense of disappointment should failure occur. The architects of the NETS, as well as the NHS organisations engaged in its implementation, also struggled with this dilemma.
The key implications arising from the research are in no particular order and are all, to a degree, inter-related.
Importance of leadership and leadership style
The research identified the importance of leadership in providing the drive for transformational change and articulating and communicating the narrative supporting it. In the two sites where the NETS achieved the greatest impact, clear, committed and consistent leadership was in place and visible. Leadership style was also critical. It was observed that leadership was not invested in charismatic or ‘heroic’ individuals but was shared or distributed across the organisations. Leadership was developed at many levels in these organisations, spanning both clinical and managerial staff. It was also evident that leadership had to be flexible and attentive to changing contexts. Therefore, a form of what has been termed ‘contingent leadership’ is desirable, which will vary and be aligned with changing organisational circumstances and the specific challenges facing leaders at a moment in time. 149
Importance of the Compact
Whether the specific term ‘Compact’ is used or not, what it represents is the development of a mutually respectful relationship between managers and clinicians (doctors, nurses and others), which is critically important. The process of reaching that agreement or concordat between stakeholders goes to the heart of the cultural challenge facing the NHS (and other health systems). The issues are difficult and cannot be addressed quickly but there needs to be a recognition of their importance. There needs to be a system in place to allow the discourse to take place, with a commitment to delivering a different way of working. Using the language of patient safety is a way of playing to the clinicians’ professional priorities and interests.
Importance of training and development
At a time of budget cuts and retrenchment, training and development is especially vulnerable and the budgets for this are often the first to suffer. The research suggests that this would be short-sighted and a serious error. Much of the success of the NETS and the commitment to it from staff at all levels can be traced back to the significant investment in training and development and the invaluable exposure certain staff members had to the VMMC and the TPS.
Avoid becoming fixated on the Method
The third leg of the NETS stool – the Method – was always regarded by the architects of the initiative as the least important. What accounted for the NETS’s appeal and central difference from other change approaches was its focus on culture change, as manifested by the attention accorded the other two legs of the stool – the Vision and Compact. Only with these in place was it likely that change could become both embedded and sustained. The Method alone cannot achieve this. It was therefore perhaps not surprising that ensuring the Vision and Compact were sufficiently embedded caused the greatest challenge for some of the study sites. They remain unfinished business for many. In contrast to applying the Method, which was relatively straightforward and had real and immediate appeal to practical managers keen to see visible results of their efforts, changing the culture was altogether a more nebulous and intangible business whose results were long term and not so easy to detect. There was some evidence that the Method absorbed rather more attention than the Vision and Compact. A lesson from the research was that this priority was misplaced, with a risk that the Method was regarded as an end in itself rather than a means to an end. The Vision and Compact were concerned with ends.
A long haul, not a quick fix
Transformational change takes time; it is a journey without end. It is not a quick fix and is therefore potentially at odds with electoral cycles and other short-term political factors that can, and do, interfere with the management of the NHS. Balancing these conflicting pressures is tricky and will often result in unexpected shifts and changes in direction, as occurred in respect of the NETS as its journey progressed. The need to be ever alert to such environmental or contextual factors is paramount and demands a degree of flexibility if what is deemed to be important is to survive. The fact that the NETS had to shift direction quite sharply following the announcement of the NHS changes in mid-2010, which led to the abolition of the SHA, was a good example of how continuity in respect of the NETS’s core values and approach was assured. In noting that the NETS was a long haul, this is not to say that quick wins along the way are not possible or desirable. They are, and in what we observed in our study many examples can be identified, ranging from successful RPIWs to ‘show and tell’ occasions where examples of innovative work were described with enthusiasm and pride.
Importance of localism
Although the ambition of the NETS was to effect region-wide transformational change, this dimension was viewed with some suspicion and wariness on the part of some local trusts within the region, whose starting point was their own organisation and bringing about change within it. They did not believe that sustainable change could be driven from either central government or from the SHA at regional level. In some respects, this scepticism was well-founded given what happened to the NETS once the SHA’s demise was announced. At the end of the day, the NETS succeeded in those local organisations which seized the opportunities provided when the initiative was conceived and announced. To this end, the SHA played an important enabling and facilitating role in terms of pointing the way forward and providing inspiration and practical support. Had this support not been terminated, it might have continued to be available, albeit on a more modest scale, but the legacy of NETS is what has been achieved, and remains in place, at a local level.
The nature and role of data
A number of the NHS staff interviewed during the study had previously worked in other organisations (such as IKEA and Nissan) that had long experience of the application of process control and lean thinking. Most of these interviewees said that their trust was at the beginning of a long journey in learning how to choose, collect, organise and analyse NHS data. They contrasted their experience in the NHS with the real-time, outcome-oriented data systems that are used in the private sector (and in some public sector organisations) to support QIs. Some interviewees commented that, although the NHS did collect some routine data that were useful to show high-level trends, this was usually aligned to answering questions about externally determined targets. The consensus view was that this approach was unlikely to help in delivering a truly patient-centred health-care system, and that improvement-oriented data collection and analysis would become a major area for investment in coming years.
Implications for future research
In the course of our evaluation, a number of further areas for research have come to light.
First, in light of the nature of complex systems and the challenges these pose for research, there is a need for adopting new and different methods to understand how change occurs, or fails to occur, in the NHS. A mixed-methods approach was adopted and it seems that the ITS component raised as many questions as it sought to address. The ITS may be a useful analytical tool under certain circumstances and when the appropriate data exist. In this context of assessing the quality of care, the requisite data were not always available, which is a comment on the (non-)availability of data that are regarded as important and the utility (for this purpose) of the data that are routinely collected. As things stand, qualitative methods would appear to offer greater potential by way of offering illuminating insights into how change occurs and with what impact. Evaluative frameworks are needed which are able to establish how causal relationships emerge.
Second, the research was wide-ranging in its sweep across a number of organisations involved in the NETS. This was intentional and there was merit in attempting to capture the totality of what the NETS sought to achieve, as the integrated approach it sought to pursue was intrinsic to its purpose and design. But although breadth was important, it inevitably meant some sacrifice in terms of depth. There is a case for exploring each of the organisations engaged in the NETS in greater depth, employing a range of methods including observational studies. Limited observational work was undertaken but this could usefully be expanded to include all levels of the organisation.
Third, the importance of leadership has been highlighted. Further exploration of its nature, and those particular features that are especially critical in driving and sustaining transformational change in complex settings, is required.
Fourth, as noted in Chapter 8, Reflections on the interrupted time series, there were limitations arising from the ITS part of the study, particularly with regard to getting access to data retrospectively. There might therefore be merit in considering a well-designed prospective study to evaluate the effectiveness of RPIW-type interventions.
Conclusion
At one level, it will never be known if the NETS would have succeeded in its ambition as it was not allowed to run its course as originally conceived. Given that the NETS embarked on a journey that had no specific end point, it is difficult to know what would have been an optimum length of time to be able to say with reasonable confidence whether it had succeeded or not. Moreover, the venture was arguably high risk in a context such as the NHS where continuous, and often disruptive, organisational change seemed to be a feature of life. Assuming that the NETS could survive intact within such a context was arguably naive. Therefore, given the numerous changes that have occurred in an already complex environment, evaluating the impact of the NETS has not been straightforward, nor has it given rise to clear outcomes which can be tracked back to the role played by the Vision, Compact and Method. The research has been able to document much of the story of the NETS as well as identify ways in which it was perceived to have had an impact on staff and services.
After 2010 the NETS continued, although in a very different form from that envisaged at the outset. However, the research captured many examples of transformational change at a local level that led to improved patient safety, increased quality of care, improved service delivery and efficiency savings. In these ways, the NETS has undoubtedly been a success, despite the fact that it did not achieve the system-wide transformational change that was its central mission and the desire of its founders. In two of the sites the NETS continues to be influential. This might not have occurred without NHS NE’s drive and enthusiasm for a new approach to transformational change inspired by VMMC and TPS. These organisations have many best practices which can be disseminated. Perhaps, in such a complex system, securing that legacy in itself is no mean feat. Moreover, it is hoped that the evaluation of the NETS has revealed a number of lessons and insights which will have a continuing resonance and value when it comes to future transformational change initiatives in the NHS. If there is one certainty, it is that such initiatives will continue to be necessary.
Acknowledgements
The research team wishes to acknowledge the contribution of the former NHS NE SHA, all the NHS trusts who agreed to take part as case studies in this research, and anyone involved in the NETS who gave so freely of their time and experience during the fieldwork conducted for the study. Without their commitment and support, this study would not have been possible.
Two members of the research team whom we would like to thank for their valuable contributions are Dr Eileen Scott, who retired in October 2011, and Allison Welsh, MF, who left the study in June 2012. Allison made a major contribution to many aspects of the study until her departure. Her knowledge and understanding of the NETS from the inside, as she had been closely associated with it as a NHS manager, proved invaluable. Her role and contribution are described in more detail in Appendix 2. Mike Cox, statistician at Newcastle University Business School, provided useful advice and support concerning the ITS component of the study.
We are also indebted to our external advisory group, who provided us with useful criticism, stimulation, wise counsel and support at all stages of the study.
Valuable secretarial and administrative support was provided initially by Christine Jawad and more recently by Gill McGowan.
Contribution of authors
David J Hunter was the principal investigator and was involved in the study design, collection of data and data analysis, and contributed to the writing of the final report.
Jonathan Erskine was project manager for the study, and was involved in the study design, collection of data and data analysis, and contributed to the writing of the final report.
Chris Hicks was involved in the study design, collection of data and data analysis, and contributed to the writing of the final report.
Tom McGovern was involved in the study design, collection of data and data analysis, and contributed to the writing of the final report.
Adrian Small was involved in the collection of data and data analysis, and contributed to the writing of the final report.
Ed Lugsden was involved in the collection of data and data analysis, and contributed to the writing of the final report.
Paula Whitty was involved in the study design, collection of ITS data and data analysis, and contributed to the writing of the final report.
Ian Nick Steen was involved in the collection of ITS data and data analysis, and contributed to the writing of the final report.
Martin Eccles acted as advisor to the study throughout its duration, commenting on data analysis and draft reports.
Publication
Erskine J, Hunter DJ, Small A, Hicks C, McGovern T, Lugsden E, et al. Leadership and transformational change in healthcare organisations: a qualitative analysis of the North East Transformation System. Health Serv Manage Res 2013;26:29–37.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Equity and Excellence: Liberating the NHS. London: Department of Health; 2010.
- Scally G, Donaldson LJ. Clinical governance and the drive for quality improvement in the new NHS in England. BMJ 1998;317:61-5. http://dx.doi.org/10.1136/bmj.317.7150.61.
- The New NHS: Modern, Dependable. London: The Stationery Office; 1997.
- A First Class Service: Quality in the New NHS. London: Department of Health; 1998.
- Berwick DM. The science of improvement. JAMA 2008;299:1182-4. http://dx.doi.org/10.1001/jama.299.10.1182.
- The NHS Plan: A Plan For Investment, A Plan For Reform. London: Department of Health; 2000.
- Wanless D. Securing Our Future Health: Taking a Long-term View. London: HM Treasury; 2002.
- Our NHS Our Future: NHS Next Stage Review – Leading Local Change. London: Department of Health; 2008.
- Boaden R, Harvey G, Moxham C, Poudlove N. Quality Improvement: Theory and Practice in Healthcare. Coventry: NHS Institute for Innovation and Improvement; 2008.
- Øvretveit J. Leading Improvement Effectively. Review of Research. London: The Health Foundation; 2009.
- Erskine J, Hicks C, Hunter DJ, Lugsden E, McGovern T, Scott E, et al. The North East Transformation System: A Scoping Study of the Background and Initial Steps. Durham: Durham and Newcastle Universities; 2008.
- Plsek PE, Greenhalgh T. The challenge of complexity in health care. BMJ 2001;323:625-8. http://dx.doi.org/10.1136/bmj.323.7313.625.
- Walshe K. Understanding what works – and why – in quality improvement: the need for theory-driven evaluation. Int J Qual Health Care 2007;19:57-9. http://dx.doi.org/10.1093/intqhc/mzm004.
- Lining Up: How Do Improvement Programmes Work?. London: Health Foundation; 2013.
- Fillingham D. Can lean save lives?. Leadersh Health Serv 2007;20:231-41. http://dx.doi.org/10.1108/17511870710829346.
- High Quality Care For All: NHS Next Stage Review Final Report. London: Department of Health; 2008.
- Smith R. Why are doctors so unhappy?. BMJ 2001;322:1073-4. http://dx.doi.org/10.1136/bmj.322.7294.1073.
- Edwards N, Kornacki MJ, Silversin J. Unhappy doctors: what are the causes and what can be done?. BMJ 2002;324:835-8. http://dx.doi.org/10.1136/bmj.324.7341.835.
- Silversin J, Kornacki MJ. Creating a physician compact that drives group success. Med Group Manage J 2000;47:54-62.
- Silversin JB, Kornacki MJ. Leading Physicians Through Change: How to Achieve and Sustain Results. Tampa, FL: American College of Physician Executives; 2000.
- Davies HT, Harrison S. Trends in doctor–manager relationships. BMJ 2003;326:646-9. http://dx.doi.org/10.1136/bmj.326.7390.646.
- A Clinical Vision for a Reformed NHS. London: NHS Confederation; 2007.
- Blackler F. Chief executives and the modernization of the English National Health Service. Leadership 2006;2:5-30. http://dx.doi.org/10.1177/1742715006060651.
- Seddon J. Freedom from Command and Control: A Better Way to Make the Work, Work. Buckingham: Vanguard Education; 2003.
- Rowbottom RW, Balle J, Cang S, Dixon M, Jaques E, Packwood T, et al. Hospital Organization: A Progress Report on the Brunel Health Services Organization Project. London: Heinemann; 1973.
- Degeling P, Hunter DJ, Dowdeswell B. Changing health care systems. J Integr Pathw 2001;5:64-9.
- Degeling P, Kennedy J, Hill M. Do professional subcultures set the limits of hospital reform?. Clinician Manag 1998;7:89-98.
- Mannion R, Davies HTO, Marshall M. Cultures for Performance in Health Care. Maidenhead: Open University Press; 2005.
- Schein EH. Organizational Culture and Leadership. San Francisco, CA: Jossey-Bass; 1985.
- Goodwin N. Leadership in Health Care: A European Perspective. Abingdon and New York, NY: Routledge; 2006.
- Goodwin N, Griffiths S, Hunter DJ. New Perspectives in Public Health. Abingdon: Radcliffe; 2007.
- Bolden R, Gosling J. Leadership competencies: time to change the tune?. Leadership 2006;2:147-63. http://dx.doi.org/10.1177/1742715006062932.
- Western S. Leadership: A Critical Text. London: Sage; 2008.
- Alban-Metcalfe J, Alimo-Metcalfe B. Leadership Culture and Its Impact on Job Satisfaction, Motivation, Commitment and Well-Being at Work n.d.
- Bennis WG. Leaders: The Strategies for Taking Charge. New York, NY: Harper & Row; 1986.
- Hannaway C, Plsek P, Hunter DJ, Hunter DJ. Managing for Health. London: Routledge; 2007.
- NHS Leadership Qualities. London: NHS Modernisation Agency; 2004.
- Chapman J. System Failure: Why Governments Must Learn to Think Differently. London: Demos; 2004.
- Taylor FW. The Principles of Scientific Management. New York, NY: Harper & Brothers; 1911.
- Hounshell DA. From the American System to Mass Production 1800–1932: The Development of Manufacturing Technology in the United States. Baltimore, MD: Johns Hopkins University Press; 1984.
- Ohno T. How the Toyota Production System was created. Jpn Econ Stud 1982;10:83-101.
- Braverman H. Labor and Monopoly Capital: The Degradation of Work in the Twentieth Century. New York, NY: Monthly Review Press; 1998.
- Eldridge JET, MacInnes J, Cressey P. Industrial Sociology and Economic Crisis. Hemel Hempstead: Harvester Wheatsheaf; 1991.
- Littler CR. Understanding Taylorism. Br J Sociol 1978;29:185-202. http://dx.doi.org/10.2307/589888.
- Pruijt H. Repainting, modifying, smashing Taylorism. J Organ Change Manag 2000;13:439-51. http://dx.doi.org/10.1108/09534810010377417.
- Dankbaar B. Lean production: Denial, confirmation or extension of sociotechnical systems design?. Hum Relat 1997;50:567-83. http://dx.doi.org/10.1177/001872679705000505.
- Womack JP, Jones DT, Roos D. The Machine That Changed the World. New York, NY: Maxwell Macmillan International; 1990.
- de Treville S, Antonakis J. Could lean production job design be intrinsically motivating? Contextual, configurational, and levels-of-analysis issues. J Oper Manag 2006;24:99-123. http://dx.doi.org/10.1016/j.jom.2005.04.001.
- Sugimori Y, Kusunoki K, Cho F, Uchikawa S. Toyota production system and Kanban system Materialization of just-in-time and respect-for-human system. Int J Prod Res 1977;15:553-64. http://dx.doi.org/10.1080/00207547708943149.
- Lander E, Liker JK. The Toyota Production System and art: making highly customized and creative products the Toyota way. Int J Prod Res 2007;45:3681-98. http://dx.doi.org/10.1080/00207540701223519.
- Liker JK. The Toyota Way: 14 Management Principles from the World’s Greatest Manufacturer. New York, NY: McGraw Hill; 2004.
- Ward M, Cheese P, Thayer B. The Lean Enterprise Benchmarking Project: Report. London: Andersen Consulting; 1993.
- Womack JP, Jones DT, Roos D. The Machine That Changed the World: How Japan’s Secret Weapon in the Global Auto Wars Will Revolutionize Western Industry. New York, NY: Harper Perennial; 1991.
- The Society of Motor Manufacturers and Traders 2006. www.smmt.co.uk/reports-publications/#uk-automotive (accessed September 2013).
- Broome G. Head to head with Graham Broome, Chief Executive, SMMT Industry Forum. Automotive Engineer 1996;21:12-3.
- Industry Forum 2006. www.industryforum.co.uk (accessed September 2013).
- Rich N, Bateman N. Companies’ perceptions of inhibitors and enablers for process improvement activities. Int J Oper Prod Manag 2003;23:185-99. http://dx.doi.org/10.1108/01443570310458447.
- Waller DL. Operations Management: A Supply Chain Approach. London: Thompson; 2003.
- Bicheno J. The Lean Toolbox. Buckingham: PICSIE Books; 2000.
- Bateman N, David A. Process improvement programmes: a model for assessing sustainability. Int J Oper Prod Manag 2002;22:515-26. http://dx.doi.org/10.1108/01443570210425156.
- Pullin J. Master class. Automotive Engineer 1998;23.
- Hines P, Holweg M, Rich N. Learning to evolve: a review of contemporary lean thinking. Int J Oper Prod Manag 2004;24:994-1011. http://dx.doi.org/10.1108/01443570410558049.
- Spear S, Bowen HK. Decoding the DNA of the Toyota Production System. Harv Bus Rev 1999;77:97-106.
- Vollmann TE, Berry WL, Whybark DC. Manufacturing Planning and Control Systems. Chicago, IL: Irwin; 1992.
- Porter ME, Michael E. Porter on Competition and Strategy. Boston, MA: Harvard Business School Press; 1991.
- Porter ME, van der Linde C. Green and competitive: ending the stalemate. Harv Bus Rev 1995;73:120-37.
- Ohno T. Toyota Production System: Beyond Large-Scale Production. Cambridge, MA: Productivity Press; 1988.
- Office for National Statistics . Annual Business Inquiry (ABI) 2005. www.ons.gov.uk/ons/index.html (accessed October 2013).
- Herron C, Braiden PM. A Method to Predict a company’s Responsiveness to Structured Productivity Interventions n.d.
- Powell D, Hicks C, McGovern T, Small A. A bitesize Lean change methodology for small and medium-sized enterprises. Lean Manag J 2013;3:7-11.
- McNulty T, Ferlie E. Reengineering Health Care: The Complexities of Organizational Transformation. Oxford: Oxford University Press; 2002.
- Seddon J. Systems Thinking in the Public Sector: The Failure of the Reform Regime – and the Manifesto for a Better Way. Axminster: Triarchy; 2008.
- Patwardhan A, Patwardhan D. Business process re-engineering – saviour or just another fad? One UK health care perspective. Int J Health Care Qual Assur 2008;21:289-96. http://dx.doi.org/10.1108/09526860810868229.
- Hines P, Lethbridge S. New development: creating a Lean university. Public Money Manag 2008;28:53-6.
- Radnor Z, Bucci G. Analysis of Lean Implementation in UK Business Schools and Universities. London: Association of Business Schools; 2011.
- Hines P, Martins AL, Beale J. Testing the boundaries of Lean thinking: observations from the legal public sector. Public Money Manag 2008;28:35-40.
- McQuade D. New development: Leading Lean action to transform housing services. Public Money Manag 2008;28:57-60.
- Erridge A, Murray JG. Lean supply: a strategy for best value in local government procurement?. Public Policy Adm 1998;13:70-85.
- Scorsone EA. New development: what are the challenges in transferring Lean thinking to government?. Public Money Manag 2008;28:61-4.
- Radnor Z, Bucci G. Evaluation of the Lean Programme in HMCS. London: AtoZ Business Consultancy; 2010.
- Radnor Z, Walley P, Stephens A, Bucci G. Evaluation of the Lean Approach to Business Management and Its Use in the Public Sector. Edinburgh: Scottish Executive Social Research; 2006.
- Radnor Z, Walley P. Learning to walk before we try to run: adapting lean for the public sector. Public Money Manag 2008;28:13-20.
- Spear SJ. Fixing health care from the inside, today. Harv Bus Rev 2005;83:78-91.
- Radnor ZJ, Holweg M, Waring J. Lean in healthcare: the unfilled promise?. Soc Sci Med 2012;74:364-71. http://dx.doi.org/10.1016/j.socscimed.2011.02.011.
- Ballé M, Régnier A. Lean as a learning system in a hospital ward. Leadersh Health Serv 2007;20:33-41. http://dx.doi.org/10.1108/17511870710721471.
- Gowen CR, McFadden KL, Settaluri S. Contrasting continuous quality improvement, Six Sigma, and lean management for enhanced outcomes in US hospitals. Am J Bus 2012;27:133-53. http://dx.doi.org/10.1108/19355181211274442.
- Chiarini A. Risk management and cost reduction of cancer drugs using Lean Six Sigma tools. Leadersh Health Serv 2012;25:318-30. http://dx.doi.org/10.1108/17511871211268982.
- Yeh H-L, Lin C-S, Su C-T, Wang P-C. Applying lean six sigma to improve healthcare: an empirical study. Afr J Bus Manag 2011;5:12356-70.
- Esain A, Rich N. Patient Streaming and Patient Flow in Acute Healthcare. Cardiff: Cardiff Business School; 2006.
- Boaden RJ, Zolkiewski JM. Process analysis in general practice – a new perspective?. Int J Health Care Qual Assur 1998;11:117-22. http://dx.doi.org/10.1108/09526869810216034.
- Endsley S, Magill MK, Godfrey MM. Creating a lean practice. Fam Pract Manag 2006;13:34-8.
- Weber DO. Toyota-style management drives Virginia Mason. Physician Exec 2006;32:12-7.
- Furman C, Caplan R. Applying the Toyota Production System: using a patient safety alert system to reduce error. Jt Comm J Qual Patient Saf 2007;33:376-86.
- Nelson-Peterson DL, Leppa CJ. Creating an environment for caring using lean principles of the Virginia Mason Production System. J Nurs Adm 2007;37:287-94. http://dx.doi.org/10.1097/01.NNA.0000277717.34134.a9.
- McCarthy M. Can car manufacturing techniques reform health care?. Lancet 2006;367:290-1. http://dx.doi.org/10.1016/S0140-6736(06)68053-7.
- Bush RW. Reducing waste in US health care systems. JAMA 2007;297:871-4. http://dx.doi.org/10.1001/jama.297.8.871.
- Kowalski K, Bradley K, Pappas S. Nurse retention, leadership, and the Toyota System Model: building leaders and problem solvers for better patient care. Nurse Leader 2006;4:46-51. http://dx.doi.org/10.1016/j.mnl.2006.09.005.
- Pham HH, Ginsburg PB, McKenzie K, Milstein A. Redesigning care delivery in response to a high-performance network: The Virginia Mason Medical Center. Health Aff 2007;26:w532-44. http://dx.doi.org/10.1377/hlthaff.26.4.w532.
- Our Vision, Our Future, Our North East NHS: A Strategic Vision for Transforming Health and Healthcare Services Within the North East of England. Newcastle upon Tyne: NHS North East; 2008.
- Graham H. Health inequalities, social determinants and public health policy. Policy Polit 2009;37:463-79. http://dx.doi.org/10.1332/030557309X445618.
- Marmot M, Allen J, Goldblatt P, Boyce T, McNeish D, Grady M, et al. Fair Society, Healthy Lives: Strategic Review of Health Inequalities in England Post-2010. London: The Marmot Review; 2010.
- Marmot M. Report on Social Determinants of Health and the Health Divide in the WHO European Region. Copenhagen: World Health Organization; 2012.
- Berwick DM. A primer on leading the improvement of systems. BMJ 1996;312:619-22. http://dx.doi.org/10.1136/bmj.312.7031.619.
- Berwick D. A Promise to Learn – A Commitment to Act: Improving the Safety of Patients in England. London: Department of Health; 2013.
- Isles V, Sutherland K. Organisational Change: A Review for Health Care Managers, Professionals and Researchers. London: National Co-ordinating Centre for NHS Service Delivery and Organisation; 2001.
- Rittel HWJ, Webber MM. Dilemmas in a general theory of planning. Policy Sci 1973;4:155-69. http://dx.doi.org/10.1007/BF01405730.
- Checkland P. Systems Thinking, Systems Practice. Chichester: Wiley; 1981.
- Senge PM. The Fifth Discipline: The Art and Practice of the Learning Organization. New York, NY: Doubleday; 1990.
- Bohmer RM, Ferlins EM. Virginia Mason Medical Center. Boston, MA: Harvard Business School; 2006.
- Bevan G, Hood C. What’s measured is what matters: targets and gaming in the English public health care system. Public Adm 2006;84:517-38. http://dx.doi.org/10.1111/j.1467-9299.2006.00600.x.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office; 2013.
- Eisenhardt KM. Building theories from case study research. Acad Manag Rev 1989;14:532-50.
- Cherns A, Pasmore W, Sherwood J. Sociotechnical System: A Source Book. La Jolla, CA: University Associates; 1978.
- Wolfer J. Aspects of ‘reality’ and ways of knowing in nursing: in search of an integrating paradigm. Image J Nurs Sch 1993;25:141-6. http://dx.doi.org/10.1111/j.1547-5069.1993.tb00770.x.
- Sandelowski M. Focus on research methods: Combining qualitative and quantitative sampling, data collection, and analysis techniques in mixed-method studies. Res Nurs Health 2000;23:246-55. http://dx.doi.org/10.1002/1098-240X(200006)23:3<246::AID-NUR9>3.0.CO;2-H.
- Greene JC, Caracelli VJ, Graham WF. Toward a conceptual framework for mixed-method evaluation designs. Educ Eval Policy Anal 1989;11:255-74. http://dx.doi.org/10.3102/01623737011003255.
- Armenakis AA, Bedeian AG. Organizational change: a review of theory and research in the 1990s. J Manag 1999;25:293-315. http://dx.doi.org/10.1177/014920639902500303.
- Weick KE, Quinn RE. Organizational change and development. Ann Rev Psychol 1999;50:361-86. http://dx.doi.org/10.1146/annurev.psych.50.1.361.
- Bryman A, Bell E. Business Research Methods. New York, NY: Oxford University Press; 2007.
- Bryman A. Integrating quantitative and qualitative research: How is it done?. Qual Res 2006;6:97-113. http://dx.doi.org/10.1177/1468794106058877.
- Pratt MG. For the lack of boilerplate: tips on writing up (and reviewing) qualitative research. Acad Manag J 2009;52:856-62. http://dx.doi.org/10.5465/AMJ.2009.44632557.
- Saunders M, Lewis P, Thornhill A. Research Methods for Business Students. Harlow: Pearson; 2012.
- Hicks C, Lugsden E, McGovern T, Small A, Eccles M, Steen N, et al. The Evaluation of Lean in Healthcare Using Quantitative and Qualitative Methods n.d.
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
- Pettigrew AM, Ferlie E, McKee L. Shaping Strategic Change: Making Change in Large Organizations: The Case of the National Health Service. London: Sage; 1992.
- Gillings D, Makuc D, Siegel E. Analysis of interrupted time series mortality trends: an example to evaluate regionalized perinatal care. Am J Public Health 1981;71:38-46. http://dx.doi.org/10.2105/AJPH.71.1.38.
- Zhang F, Wagner AK, Soumerai SB, Ross-Degnan D. Methods for estimating confidence intervals in interrupted time series analyses of health interventions. J Clin Epidemiol 2009;62:143-8. http://dx.doi.org/10.1016/j.jclinepi.2008.08.007.
- Pettigrew AM, Wilson DC, Rosenfeld RH. Managing Organizations: Text, Readings and Cases. London: McGraw-Hill; 1990.
- Miller WL, Crabtree BF, Crabtree BF, Miller WL. Doing Qualitative Research. London: Sage; 1999.
- Miller WL, Crabtree BF, Crabtree BF, Miller WL. Doing Qualitative Research. 2nd edn. London: Sage; 1999.
- Miller WL, Crabtree BF, Crabtree BF, Miller WL. Doing Qualitative Research. London: Sage; 1999.
- Cook TD, Campbell DT. Quasi-experimentation: Design and Analysis for Field Settings. Boston, MA: Howton Mifflin Company; 1979.
- Box EP, Jenkins GM. Time Series Analysis. London: Holden-Day; 1976.
- Draper NR, Smith H. Applied Regression Analysis. New York, NY: Wiley; 1996.
- Crosbie J, Gottman JM. The Analysis of Change. Mahwah, NJ: Laurance Earlbaum Associates; 1995.
- Hodges D, Rubin G, Crossland A. The Use of Lean Methods for Service Improvement in the Early Diagnosis of Lung Cancer, A Realistic Evaluation. Durham: Durham University; 2010.
- Shook J. Visual Management – The Good, the Bad, and the Ugly 2012. www.lean.org/shook/DisplayObject.cfm?o=2095 (accessed October 2013).
- Miltenburg J. One-piece flow manufacturing on U-shaped production lines: a tutorial. IIE Trans 2001;33:303-21. http://dx.doi.org/10.1080/07408170108936831.
- Gapp R, Fisher R, Kobayashi K. Implementing 5S within a Japanese context: an integrated management system. Manag Decis 2008;46:565-79. http://dx.doi.org/10.1108/00251740810865067.
- Mental Health Act 1983. London: The Stationery Office; 1983.
- Baggott R. A funny thing happened on the way to the forum? Reforming patient and public involvement in the NHS in England. Public Adm 2005;83:533-51. http://dx.doi.org/10.1111/j.0033-3298.2005.00461.x.
- Hunter DJ. Change of Government: one more big bang health care reform in England’s National Health Service. Int J Health Serv 2011;41:159-74. http://dx.doi.org/10.2190/HS.41.1.k.
- Nelson B. Fury over £84,000 NHS trip to Japan. The Northern Echo 2007. www.thenorthernecho.co.uk/news/1545818.Fury_over___84_000_NHS_trip_to_Japan/ (accessed September 2014).
- Nicholson D. The Year: NHS Chief Executive’s Annual Report 2008/09. London: Department of Health; 2009.
- Kotter JP. Leading change: why transformation efforts fail. Harv Bus Rev 1995;73:59-67.
- Schön DA. Beyond the Stable State. Public and Private Learning in a Changing Society. Harmondsworth: Penguin; 1973.
- Walshe K. Reorganisation of the NHS in England. BMJ 2010;341:160-1. http://dx.doi.org/10.1136/bmj.c3843.
- Erskine J, Hunter DJ, Small A, Hicks C, McGovern T, Lugsden E, et al. Leadership and transformational change in healthcare organisations: a qualitative analysis of the North East Transformation System. Health Serv Manage Res 2013;26:29-37. http://dx.doi.org/10.1177/0951484813481589.
- Currie G, Lockett A. A critique of transformational leadership: moral, professional and contingent dimensions of leadership within public services organizations. Hum Relat 2007;60:341-70. http://dx.doi.org/10.1177/0018726707075884.
- Pettersen J. Defining lean production: some conceptual and practical issues. TQM J 2009;21:127-42. http://dx.doi.org/10.1108/17542730910938137.
- Bitner MJ. Servicescapes: the impact of physical surroundings on customers and employees. J Mark 1992;56:57-71. http://dx.doi.org/10.2307/1252042.
- Cohn S, Clinch M, Bunn C, Stronge P. Entangled complexity: why complex interventions are just not complicated enough. J Health Serv Res Policy 2013;18:40-3. http://dx.doi.org/10.1258/jhsrp.2012.012036.
- Bullock A, Morris ZS, Atwell C. A Formative Evaluation of the Service Delivery and Organisation (SDO) Management Fellowships. Final Report. Southampton: NIHR Service Delivery and Organisation programme; 2012.
Appendix 1 Membership of the external advisory group and terms of reference
The original members of the study’s EAG were:
-
Ken Jarrold CBE (Chair), Dearden Consulting, Bishop Sutton, Somerset
-
Professor Graeme Currie, Professor of Public Services Management, Nottingham University Business School
-
Dr Zoe Radnor, Associate Professor (Reader), Warwick University Business School
-
Dr Keith Copeland MBE, Senior Engineer, Nissan Motor Manufacturing, Sunderland
-
Tony Jones, Service User Research Lead, Tees, Esk and Wear Valley NHS Foundation Trust.
At an early stage of the project Dr Copeland stood down from the EAG owing to other commitments; the other members, however, continued to attend meetings and provide guidance until the end of the project.
The terms of reference of the EAG were agreed as follows.
Aim
The NETS EAG will, as required by the research team and as set out in the original proposal submitted to the NIHR SDO programme, review and provide independent comment on, and support in regard to, the progress of the evaluation of the NETS at all stages.
Objectives
The EAG will draw on its members’ expertise to
-
offer advice on the progress of the research throughout its duration
-
review and comment on working papers as they emerge and perhaps, on occasion, and where deemed desirable or helpful, on papers in preparation for publication
-
suggest ways in which the products from the research might be disseminated throughout the NHS and other organisations to maximise their value and impact.
Method of working
The research started on 1 December 2009 and will end on 30 November 2012. The EAG will meet twice each year for the duration of the research study. These face-to-face meetings will be supplemented as necessary, and by prior agreement, by e-mail contact with some or all members of the EAG in order to seek opinion and/or advice on particular issues.
Every effort will be made to ensure that the demands made of the members of the EAG are kept to a minimum given that they are giving freely of their time and have other commitments.
All reasonable travel and associated subsistence expenses will be reimbursed to EAG members.
The contribution made by EAG members will be appropriately acknowledged in any outputs from the study.
Appendix 2 Management fellow
Having been invited to apply, and following a quite rigorous and demanding process, our application for a Management Fellowship was successful. We were able to recruit someone with senior management experience working in the NETS team at the SHA. The Fellowships had three key objectives:
-
to improve the quality and relevance of the research itself through greater managerial involvement
-
to develop capacity in the managerial community for accessing, appraising and using research evidence
-
to encourage greater engagement, linkage and exchange between the research and practice communities in health-care management.
Our proposal for a Fellowship touched on each of these objectives and the MF appointed was able to address each of them. In our submission we had noted that although ‘the research team already comprised members with considerable experience of working in both managerial and/or research capacities within or alongside the NHS, it would be considerably strengthened by having someone of the candidate’s experience and skills’. She brought to the research team ‘an intimate knowledge of the workings of the NHS, especially in respect of patient safety issues which lie at the heart of the NETS approach and in its aim of improving quality and service design through tackling waste and variation’. We also argued that the MF’s experience of being seconded to the NETS team would bring a wealth of knowledge to the research about the origins and evolution of the approach prior to the research evaluation. Together with the contacts and networks at her disposal, her input would considerably enrich the research and strengthen its potential value and impact. Any potential conflict of interest arising from her close involvement with the NETS Coalition at the SHA was avoided when the MF was seconded to the NHS Institute for Innovation and Improvement. In any event, it proved that the MF’s ‘insider’ status brought with it more benefits than risks.
The MF was appointed on 1 April 2010 and remained with the project until 31 May 2012, by which time her circumstances had significantly changed as a consequence of the NHS changes announced by the UK coalition government in May 2010. Ideally, the MF would have remained with the project until its completion in order to assist with its dissemination, both in the North East region and more widely in the NHS.
Despite the MF’s early departure from the study, while attached to the research team she made an important and significant contribution which would have been difficult to replicate through other means. She was engaged in many aspects of the study, including its overall design, collection of documentary data from various NHS sources, reading through interview transcripts for sense-making and authenticity, progress-chasing in our field sites (where she often knew the relevant people) and assisting at the interface between the research team and local policy and practice partners. She assisted with the design and organisation of a dissemination event halfway through the study. The five principal components of the MF role were:
-
active involvement in aspects of the quantitative data collection and analysis; contributing to the analysis of qualitative data, and the writing of reports and publications arising from the research
-
providing a useful check on the reliability and validity of the data being collected through the research, drawing on her close and recent ‘insider’ knowledge of the workings of the NHS and the NETS initiative from its beginnings
-
serving as an important conduit for the research, its translation and subsequent take-up and impact on practice
-
strengthening the links between research, evaluation and service improvement on the ground, working with and through relevant networks, notably the Chief Knowledge Officer role
-
contributing to increasing capacity and capability in evidence-based practice, improving the theoretical basis for NETS, and subsequently improving thinking around the NETS and how the various improvement methodologies can be synthesised into an integrated approach and sustained over time.
Although she contributed to all of these components to some degree, the MF’s focus was on the first three. The only area of activity in which we did not actively employ her was primary data gathering through interviews and focus groups. The MF kept a blog during her time with the project and posted regular blogs on the project website. She took an active part in the evaluation of the MF scheme commissioned by the NIHR SDO programme and carried out by Bullock et al. 153 from Cardiff University, and she attended national meetings of the Health Service Network attended by other MFs. She would feed back her attendance at these meetings to the research team.
Had the MF remained with the project through to its conclusion, as had been her intention, the research team would have benefited further from her counsel and experience in the data analysis stage and the presentation of findings.
On reflection, and on balance, having the MF attached to the project was a worthwhile and welcome addition to the team. However, securing the post and completing what proved to be quite a lengthy and detailed application process did take up a considerable amount of time on the part of the PI at a point when the main study was taking off. It became something of a distraction which had not been foreseen. In addition, given the MF’s own changing circumstances arising from the NHS changes commencing in 2010, there were further administrative tasks which had to be completed to retain her services, as well as other circumstances which meant that tasks she had been given were either delayed or not completed. Had the NHS reforms not got under way, it is likely the candidate would have remained on secondment from the NHS and would have remained attached to the study.
Appendix 3 Interview question schedule
Centre for Public Policy and Health in conjunction with Newcastle University Business School.
Research study: An evaluation of transformational change in NHS North East
Chief investigator: Professor David J Hunter
Further information: topic guides for interviews with staff
Interviews – confidentiality of responses reinforced
Introduction
Topics to be covered
-
Participants’ understanding of
-
The NETS initiative and its origins.
-
Identify the relative focus on the various elements of NETS, i.e. Vision, Compact, Method.
-
The aim(s) of the initiative?
-
Specific objectives in terms of quality and efficiency of patient care in terms of quality, safety, patient experiences, access and equity.
-
-
Their organisation’s forward plans.
-
Do you envisage any alternatives to NETS for your organisation in the future?
-
What are the chances of success for any changes that might occur?
-
Do you anticipate any risks to any other new initiatives?
-
-
The interventions that have taken place.
-
Identify factors facilitating or acting as barriers to NETS.
-
-
The relevant activities being co-ordinated in your organisation?
-
What initiatives have you been personally involved with?
-
Specifically, expand on your experience (if any) of working with RPIWs.
-
What criteria were used for selecting RPIWs?
-
What initiatives are you aware of elsewhere in the organisation (that you haven’t been involved with)?
-
What are your perceptions of the success of these?
-
Which KPIs (key performance indicators) are being used to measure the impact of NETS, how is the data collected, data sources, frequency of data collection, evidence of reliability, etc. Who is evaluating the data?
-
What impacts are you aware of on other parts of the organisation?
-
How widespread is NETS/NETS activities in the organisation? i.e. how many RPIWs, how many certified leaders, how many team members trained, etc.?
-
What quantitative evidence is there of impact of the interventions in terms of quality and efficiency of patient care in terms of quality, safety, patient experiences, access and equity?
-
Has the implementation of NETS had any impact on skill mix, changing patterns of work, evaluation/appraisal, etc.?
-
-
-
How much progress has your organisation made so far?
-
Can you give any specific examples of progress in relation to their definitions of success?
-
Can you give any examples of your organisation’s commitment (budgets, number of people, external support, support from NETS, what has been done internally)?
-
What mechanisms are there for capturing information and sharing knowledge and best practice within the team and more generally within NETS?
-
-
What are your organisation’s criteria for success following changes in the systems?
-
What does the success of NETS/NETS initiatives mean for you?
-
-
Have any possible inhibitors or barriers to success been identified?
-
What training and development initiatives are on offer?
-
What motivations/feelings/attitudes have you experienced or become aware of? For the RPIWs need a description of the processes, inputs [e.g. arrival patterns of patients, where patients come from (relationship to other processes), resources (including working patterns – need to look at the match between demand and supply of services – lean is all about making sure they are matched)].
How does the interviewee see the future of NETS? Note here any issues that we should be aware of which have been brought up by interviewee.
Topic guide: version 1 10 August 2009; expanded version for research team February 2010.
Appendix 4 North East Transformation System Coalition-reported training rapid process improvement workshops, November 2007 to June 2011
| RPIW date | Study site or other NHS organisation | RPIW title/topic | Aim of RPIW |
|---|---|---|---|
| 26–30 November 2007 | 11–13 | GP knee referral | Reduce unnecessary referrals and develop referral process |
| 26–30 November 2007 | PCT | HELS | Improve the physical HELS facility (in the administrative, decontamination, maintenance and general storage areas) and the internal decontamination and testing processes (from point of return to placement in the storage area) |
| 26–30 November 2007 | Acute hospital trust | Pre-assessment | To assess the number of patients receiving full pre-assessment as opposed to fitness to list. To redesign service to assess patients and determine the number whose pathway could be completed at discussion with health-care assistant regarding health-care questionnaire. To implement flexible working hours to accommodate patients from late outpatient department clinics |
| 26–30 November 2007 | 08 | Hot meal serving process | To improve the mealtime experience of patients (to serve meals to patients more quickly; to reduce the amount of waste; to improve the dining environment) |
| 26–30 November 2007 | 09 | Receipt of dirty trays, to the dispatch of sterile trays | Smoother and more effective/efficient flow. Use of supplementaries. Understanding the wastage. Loan trays |
| 26–30 November 2007 | 10 | Patient flow: MHSOP | Reduce length of stay and time in engaging other professionals/improve carer user experience in planning care/assessing needs including discharge |
| 21–25 April 2008 | PCT | HR recruitment process part 1 (vacancy identified to interview pack out) | To make it as quick and easy as possible for the PCT to recruit staff into identified and funded posts, and to reduce the burden placed on HR by their current workload and the environment they work in |
| 21–25 April 2008 | 09 | Production of discharge letters | To improve the process of the production of discharge letters in the orthopaedics department |
| 21–25 April 2008 | 11–13 | Staff induction | Reducing waste and improving quality for participants |
| 21–25 April 2008 | 08 | Medication rounds | Patient safety: medicine dispensing and administration |
| 21–25 April 2008 | 10 | Improve the patient flow through XX unit | Improve the experience for service users, their families/carers and staff. Improve the flow of the inpatient pathway |
| 21–25 April 2008 | SHA | Travel booking and payment | Significant demand for travel within the SHA. All documents currently booked through a single supplier. Does this represent best value to SHA? (NB – issues over reducing travel via better use of technology) |
| 21–25 April 2008 | Acute hospital trust | Elective pathway – bookings | To assess the number of patients receiving dates for surgery on the day of outpatient department review and pre-assessment To redesign the centralised booking process, ensuring compliance from all users in line with waiting list policy |
| 19–23 May 2008 | 08 | XX ward medication round | Patient safety: medicine dispensing and administration |
| 19–23 May 2008 | PCT | HR recruitment process part 2 (interview close to job file close, and start date to induction) | To make it as quick and easy as possible for the PCT to recruit staff into identified and funded posts and to reduce the burden placed on HR by their current workload and the environment they work in |
| 19–23 May 2008 | 09 | Redesign of the patient pathway through pre-assessment | A simplified process which will ensure all patients are fully assessed and ready for surgery whether they are day cases/day of surgery admissions/inpatients |
| 19–23 May 2008 | 11–13 | Carpal Tunnel Syndrome Primary Care Pathway | Scope = patient with suspected carpal tunnel syndrome requesting an appointment to be seen by a GP, to being seen by a specialist for treatment |
| 19–23 May 2008 | 10 | RIDDOR from incident to HSE reporting | Reduce time from incidents to final reporting; improve quality of report/quality of RIDDOR information |
| 19–23 May 2008 | Acute hospital trust | Booking of gynaecology patients/consent clinics | To assess the value of ‘consent clinics’ from a patient perspective To ensure all specialisms utilise the booking process in line with waiting list policy To improve the flow of information across different hospital sites (notes) |
| 4–8 August 2008 | PCT | Blood taking and results, and reissue/repeat prescriptions | Process for managing patients having bloods taken and documenting and actioning their results. In addition, process for initiating a prescription and the reissue/repeat of a patient prescription |
| 4–8 August 2008 | 09 | Laboratory services: blood sample processing | Will focus on the registration and specimen handling process, from receipt of specimens to placing on to analytical platforms |
| 4–8 August 2008 | 11–13 | XX hospice: patients admitted to patients having full multidisciplinary care plan | Scope: from patient being admitted to hospice to having a multidisciplinary care plan agreed |
| 4–8 August 2008 | SHA | Induction of new staff | Review and improve the process by which new staff are equipped to do their job on arrival in the organisation |
| 4–8 August 2008 | Acute hospital trust | Breast screening unit | To review processes within the breast screening unit, ensuring maximum efficiency for patients and staff |
| 4–8 August 2008 | 08 | Outpatients | Booking an outpatient appointment Running an outpatient clinic Booking follow-on appointments |
| 4–8 August 2008 | 10 | Fault reporting and repair | Improvement of communication and job completion time for the repair processes |
| 22–26 September 2008 | PCT | Chlamydia screening programme | The administrative process which supports patients being notified of their test results and arrangement for the necessary action |
| 22–26 September 2008 | 09 | Theatre (sterile instruments) | Single instruments in theatre. To consider the storage, labelling and identification of single instruments so that they can be retrieved promptly in the event of an emergency situation. To consider the processes for transporting used instruments to sterile services, to improve the flow of work and reduce turnaround times |
| 22–26 September 2008 | 11–13 | Distal fractures | The patient pathway from presenting at either MIU or A&E with a distal fracture to arrival at trauma clinic for definitive treatment |
| 22–26 September 2008 | SHA | SUI process | To review and improve the way in which SUIs are reported and managed |
| 22–26 September 2008 | Acute hospital trust | Breast assessment process Group 1: radiography/radiology; group 2: histopathology; group 3: breast care nurses/surgery |
Improving the breast assessment process from the patient’s perspective by reducing the lead time in each of the three focus areas (results conveyed to patient in shortest time possible). Aiming for zero defects throughout the value stream |
| 22–26 September 2008 | 08 | Dystonia outpatient clinic | To improve the quality of service given to patients attending the dystonia outpatient clinic, particularly with regard to waiting times |
| 22–26 September 2008 | 10 | Pre-employment recruitment checks | Further streamline systems and processes in order to reduce the time it takes to complete pre-employment recruitment checks |
| 18–22 May 2009 | PCT | Chlamydia screening programme | The process involved from notification of positive results from laboratory through to treatment being given and patient being discharged following successful compliance check |
| 18–22 May 2009 | 09 | Radiology | The aim was to improve flow through the department for patients requiring a plain film X-ray and to inform other pathways within the department. A second CT scanner was coming and nuclear medicine was being relocated to upgraded facilities within the department, adding to the congestion and number of patients passing through. Thus, the aim was to improve the flow to reduce this anticipated problem. Prior to the RPIW, patients waited at various stages through the process, typically prior to and following their X-ray, leading to congestion and subsequent privacy and dignity issues for frail, unwell and vulnerable inpatients on trolleys and in nightwear |
| 18–22 May 2009 | 08 | Triage, allocation, appointment-making | Improve the patient experience – being more responsive to provide mental health services to people when they need them. Particularly, ensuring the patient is allocated to the right service and the right clinician at the right time. To reduce the burden of work for the community treatment team |
| 18–22 May 2009 | 11–13 | IR1 process: reporting, recording and investigation of incidents across NHS XX | Scope: from when incident occurs, anywhere across the organisation, until IR1 form is filed following investigation and completion. Aim to reduce waste and improve quality of the process, data recorded and outcomes |
| 18–22 May 2009 | 10 | Recording short-term sickness | |
| 1–5 June 2009 | SHA | Incident reporting and management | To review and improve the way in which all incidents are investigated and managed |
| 1–5 June 2009 | 08 | CTT risk assessment | To reduce the lead time from undertaking the initial assessment with the patient to this being fully written up within the health-care records and letters forwarded on to the relevant parties. To improve the systems for ensuring that risk assessments are completed in a timely way and kept up to date |
| 1–5 June 2009 | 11–13 | Antiviral centres: set up and distribution of antivirals to patients | Scope: set up of one antiviral centre within 24 hours, mobilise resources, simulate and test the distribution of antivirals and have a plan in place to move from one to 26 centres |
| 1–5 June 2009 | PCT | Reporting and management of significant events including SUIs | Report incident into PCT where PCT taking a lead in investigation, and look at immediate to remedial actions. From information received to commencement of investigation |
| 1–5 June 2009 | 10 | Mandatory training | To improve the process of completion and recording of mandatory training from the point when an individual need is identified through to reporting attendance at various levels in the organisation, i.e. from individual through to board. The scope is restricted to a clinical inpatient ward, in a corporate area represented by Estates and the HR department who manage the overall process |
| 1–5 June 2009 | 09 | Majors stream A&E | Clinical processing of patients through the majors stream in A&E |
| 13–17 July 2009 | 08 | Appointment-making in 10 and 20 care teams | This was the second RPIW improving the pathway for patients referred to adult planned care services in this study site. The RPIW considered the process from point of allocation to a key worker, through the appointment-making process, to the point at which the patient attends (or is discharged owing to non-attendance) for their initial assessment appointment Aims: To increase the number of patients referred to the service who attend their appointment. To improve the timeliness of the appointment-making process with patients and improve information available to patients before their appointment. To reduce the burden of repetitive, non-value-adding work undertaken by the administrative team |
| 13–17 July 2009 | 11–13 | Speech and language | To increase the amount of direct patient contact time and further develop standard work From initial assessment to discharge |
| 13–17 July 2009 | 10 | CAMHS referral to treatment | To look at the processes involved from the receipt of the referral to the first treatment appointment within CAMHS |
| 13–17 July 2009 | PCT | GPwSI accreditation process | The RPIW addressed the GPwSI accreditation process but did not address the deanery process. The RPIW looked at reducing lead time, and addressed rework and defects to improve quality and remove non-added-value work. The RPIW looked at data flows and aimed to develop standard work. It addressed environmental and health and safety elements, and set-up reduction for panel preparation and staff walking time to reduce waste. The RPIW did not address the commissioning of a GPwSI service or anything outside the RPIW boundaries |
| 13–17 July 2009 | 09 | Stroke rehabilitation | To look at ways to improve communication within the MDT, and between the team and the patients. To free up time for clinical care currently spent in excessive walking and clerical tasks |
| 10–14 August 2009 | SHA | Regional advisory groups | The RPIW focused on the internal processes for setting up and managing regional advisory group meetings |
| 10–14 August 2009 | SHA | Initial stage of trainee recruitment process | The RPIW focused primarily on the internal process whereby authority to advertise for and recruit to any vacancies which are identified by programme directors, heads of school and appropriate consultants is granted. This covers the in-year ad hoc vacancies |
| 10–14 August 2009 | 11–13 | NHS health checks | To ensure maximum service uptake is achieved and there is a standard efficient process with standard documentation for performing a health check |
| 10–14 August 2009 | 09 | Planning for ongoing care | To agree the most rapid and clinically effective process for applying to local authority decision-making panels for 24-hour care placement. Additionally, to ensure the most effective planning process that facilitates timely discharge of service users admitted for assessment of future care needs |
| 10–14 August 2009 | PCT | Contract overperformance | From a contract overperformance red flag to a clear, auditable and communicable decision Boundaries: the event focused on a case study of S23 contracts, specifically acupuncture; however, the results can be rolled out to other areas Targets: reduce process lead time to 7 days or under |
| 14–18 September 2009 | 09 | MAU and SSU | The scope of the RPIW was the process of assessing patients, including administrative, nursing and medical staff assessment. The aim was to smooth flow and reduce overprocessing/waiting and other wastes |
| 14–18 September 2009 | SHA | Meeting rooms | To improve the method of booking and using rooms, to eliminate waste and drive down cost for the benefit of public and patients |
| 14–18 September 2009 | SHA | Catering | To improve the efficiency and process of arranging catering for staff, meetings, workshops and conferences. The aim was that the catering process in future should operate with the minimum amount of resources to provide appropriate high-quality food and drink in the correct amount, just when and where it is required, which in turn would eliminate waste through improved processes and awareness and provide good value for money for the ‘customer’ |
| 14–18 September 2009 | 09 | Community treatment orders (Mental Health Act) | To develop standard work and a locality value process supporting the management of community treatment orders To ensure a single-piece flow from the decision to place someone on a community treatment order to the second opinion |
| 14–18 September 2009 | PCT | Home visits and triage | The management of a request from a patient for a home visit, to the end point of the request A safe service that gives patients what they need, when they need it. Differentiating the service that is offered, i.e. telephone triage. Exploring a GP being on call but not having booked surgeries, using a GP-on-call model. Eliminating stress associated with urgent visits for secretarial and administrative staff and GPs |
| 14–18 September 2009 | 08 | Daily review meeting | Develop the daily review meetings with the aim of standardising process, reducing waste and improving outcomes and experience for patients and their carers (safety, clinical effectiveness and quality) |
| 14–18 September 2009 | 11–13 | Community matron | Scope: to increase the capacity of community matrons to respond to referrals in a standard way and while balancing the planned care and unplanned work The RPIW was to focus on the initial part of the patient pathway and to develop, where appropriate, a consistent approach to the attendance and streaming of patients and the packages of care offered. This would refocus how the community matron team interfaced with the available intermediate nursing teams |
| 26–30 October 2009 | 10 | Medical staff emergency experience/new deal | To develop new working patterns for emergency psychiatric teams to ensure that core registrars are able to gain the necessary experience in emergency assessment and management. The sponsor and process owners indicated a locality where the RPIW would be tested out |
| 26–30 October 2009 | PCT | CVD process – XX medical centre | The scope of the RPIW included the process from when the patients were reported as being a potential risk through to when the risk was validated, interventions were in place and the patient was registered to enable follow-up appointments to be made |
| 26–30 October 2009 | 09 | Discharge process – ward XX | Improving ward XX discharge processes, from medical decision to discharge to the patient leaving the ward |
| 26–30 October 2009 | 08 | Screening appointment – 10 care team | To create standard work for screening appointments and entry of clinical information on to the electronic patient record system. To improve utility of the screening instruments. To reduce time from screening appointment to information being entered on to the electronic patient record system. To improve the patient experience |
| 26–30 October 2009 | 11–13 | Invoice processing | To reduce the lead time of invoices, which, prior to the RPIW, took more than 30 days. To develop standard work across the three PCTs in relation to the processing of invoices |
| 9–13 November 2009 | PCT | Hospital correspondence couriered from a GP practice | To standardise the approach across all GPs, reduce the length of time taken to scan and file letters and ensure a process with no defects, specifically no missing correspondence |
| 9–13 November 2009 | 09 | Emergency surgical pathway | Process of assessment/diagnosis/treatment of patients referred to surgery via A&E with abdominal pain |
| 9–13 November 2009 | 08 | HR recruitment: shortlisting to start letter | To reduce the time it takes to recruit staff To reduce the number of defects occurring in the existing process |
| 9–13 November 2009 | SHA | Form ‘R’ | To review and improve the process of the Form ‘R’ and Educational Agreement to improve the experience of trainees by creating standard work and reducing waste relating to overproduction, defects and time. It is a national requirement that on appointment trainees complete a Form ‘R’ and Educational Agreement |
| 9–13 November 2009 | North East agency | Performers list applications | To review and improve the process for performers list applications. The agency is required, under the terms of its service-level agreement with primary care .organisations, to undertake all operational duties for the inclusion of primary care performers in performers lists |
| 7–11 December 2009 | 10 | Flow in affective disorder community teams | To agree a standard process for the initial assessment of problems and formulation of treatment plans following referral, through confirmation of appointment, completion of first contact, patient record information system entry of assessment data and decisions made about ongoing case management. To develop standard work for the preparation and content of appointments that avoids any avoidable batching, rework, waste or waiting during the process and is adopted across both geographical areas by the affective team |
| 7–11 December 2009 | 09 | HR | To reduce a number of quality defects in the existing system and to reduce the lead time for getting a member of staff into post. A pathway from vacancy control to confirmation letter |
| 7–11 December 2009 | SHA | Managing temporary staff | To improve recruitment and retention of temporary staff |
| 7–11 December 2009 | 08 | Crisis team | To streamline the action/administrative process by clinicians from return to base following assessment, to completion of assessment documentation/data recording |
| 7–11 December 2009 | 11–13 | Sexual health service | To reduce the overall lead time for patients from first attendance until final diagnosis, treatment and discharge. To focus on the initial assessment and treatment plan to treatment and discharge, to have a standard pathway for patients and reduce a range of quality defects that the patient previously experienced |
| 8–12 February 2010 | PCT | Improving patient access to GPs and nurse practitioners | To improve access for patients requesting a GP/nurse practitioner appointment and ensure that patients access the most appropriate professional/outcome |
| 8–12 February 2010 | 09 | Invoice received to payment of invoice | To improve the process from receiving an invoice into finance, to the payment of the invoice |
| 8–12 February 2010 | North England network | The network meeting process | To create standard work and reduce external set up for the network meeting process |
| 8–12 February 2010 | North England network | CHD performance report | To improve the process and content of the network’s CHD performance report so that it meets the needs of the commissioners and service |
| 8–12 February 2010 | North East agency | Manually input payment data from variations | To review and improve the process to manually input payment data from variations |
| 8–12 February 2010 | 07 | Vehicle daily inspections | Review and improve the vehicle daily inspection process in order to reduce downtime created by vehicle defects. Engage participants to improve their own processes working towards total quality. Develop learning and experience which can be applied to other improvement events |
| 8–12 February 2010 | 10 | Reduction of food waste (cook/freeze) | Identify main causes of food waste and recommendations for improving processes to reduce waste. Establish targets for the reduction of food waste. Reduce food waste in respect of patient meals to a minimum. The objective was to reduce patient food waste levels to a minimum on all trust sites operating a ‘cook/freeze’ production method. A target maximum food waste level was to be agreed following the RPIW workshop |
| 15–19 March 2010 | 09 | Paediatric outpatients services | Scope: from patient referral being received into COPD to attendance at appointment and decision to discharge or follow up. To improve the overall process by reducing lead time, introducing standard work and increasing value-added activity |
| 15–19 March 2010 | 11–13 | Breastfeeding | Increase the percentage of babies still breastfeeding at 6–8 weeks through the removal of any quality defects and maximising value-added time |
| 15–19 March 2010 | 08 | Step-down process | To identify and develop standard work across the process |
| 15–19 March 2010 | 07 | Professional standards panel | The workshop focused on improving the means by which public and patient concerns were addressed, and on learning lessons to improve the service |
| 15–19 March 2010 | PCT | Reducing cancer deaths | To develop a standardised lean pathway across primary care. Ensure safety-netting is in place. Give patients an appointment for review, and decide when it is appropriate to tell them to return ‘if it doesn’t get better’. Ensure patients attend for X-ray in a timely manner and are followed up if they do not attend. Ensure results are received and acted on in a timely manner. Ensure patients are informed of results. Improve read-coding for chest X-ray |
| 19–23 April 2010 | 10 | Disciplinary process | VSM to be completed, improve existing process by removing non-value-added stages and implement standard work |
| 19–23 April 2010 | 10 | On call out of hours | Review the existing on-call process through use of data analysis. Through the RPIW process, improve, standardise and develop clear guidance and standard work for all staff involved in triggering on call, and staff delivering non-medical managerial on call. Recognise links to business continuity plan |
| 19–23 April 2010 | 08 | Supplies delivery and top-up process | To ensure items are available when required at point of use. To improve the environment at XX clinic by improving the supplies delivery and removal processes |
| 19–23 April 2010 | North England network | Storage: capacity vs. demand | To understand and control the demand for storage and to maximise capacity through standardising processes |
| 19–23 April 2010 | 11–13 | LES development and implementation | To review the implementation of an enhanced contract, from the process that encompasses how the decision to commission a LES is taken, through initial agreement to develop such a contract, to the contract being awarded |
| 19–23 April 2010 | SHA | QA visit process | Review and improve the existing process of the QA visit by improving standard work and reducing waste in the process in terms of overproduction, defects and time. The QA visitor model is used in breast, cervical and bowel screening programmes and standard work implemented via this RPIW could be implemented across existing and any future programmes |
| 10–14 May 2010 | 08 | Referral/admission into hospital | Point of access to the service for patients who require inpatient care and treatment |
| 10–14 May 2010 | 08 | Discharge process in regional disability team | To identify and develop standard work across the process |
| 10–14 May 2010 | SHA | Independent investigations | The independent investigations process is carried out by the patient safety team of the SHA. The RPIW was to review and improve the existing process using Virginia Mason tools and training to improve the experience of the customers by creating standard work and reducing waste |
| 21–25 June 2010 | 11–13 | Bringing drug users into effective treatment from the point of arrest and test to commencement of treatment | To review process from the point of arrest/test to the point of an individual accessing structured treatment, and remaining in treatment for 12 weeks or more |
| 21–25 June 2010 | North England network | Communication – capacity vs. demand | To decrease turnaround time from receipt of request to response. To 5S the virtual workspace. To improve communication |
| 12–16 July 2010 | 08 | Laundry | The purpose of the RPIW was to redesign the laundry to ensure it could meet existing demand by focusing on the resources required to do this, reducing rework and ensuring that the workplace offered a healthy and safe environment for its staff |
| 12–16 July 2010 | 07 | Road traffic accidents | To report accidents in a timely way, so as to achieve better cost control. To improve the flow of information through implementation of standard work |
| 12–16 July 2010 | PCT | Room bookings at XX house | Streamline room booking process and eliminate wasted slots in the diary. Cut existing costs incurred by unavailability of rooms resulting in externally booked rooms |
| 12–16 July 2010 | PCT | Occupational health management referral | To reduce the overall lead time for the process of management referrals within the occupational health and hygiene service |
| 12–16 July 2010 | North England network | Heart failure programme | To improve the process by which heart failure patients experience the pathway of heart failure management |
| 12–16 July 2010 | 11–13 | Tier 2 smoking cessation: establishing new tier 2 providers – from request through training to first payment | To create standard work and reduce the lead time for the establishment of new tier 2 providers. To create a defect-free process that enables the new process to successfully deliver a high-quality service |
| 12–16 July 2010 | 09 | Shortness of breath | To reduce variation and improve the quality of shortness of breath assessment, immediate available treatment and the pathway for managing the condition |
| 16–20 August 2010 | North England network | GP palliative care registers | Ensure development and effective use of the PCR in general practice. Ensure that clinical information is up to date on the PCR. Ensure comprehensiveness of PCR. Clinical information should be accessible 24/7 to health and social care providers. Providers should have adequate IT infrastructure |
| 16–20 August 2010 | 14 | Corporate stock control of paper | To improve the process of restocking all corporate printers/copiers so corporate head office staff may see, feel and can demonstrably measure efficiency gains as a result of the trust’s first RPIW |
| 16–20 August 2010 | 07 | Recording of sickness absence | To improve the accuracy and quality of sickness absence reporting. To ensure that managers have relevant, accurate and timely information on staff absence occurrence |
| 16–20 August 2010 | PCT | Exceptional treatments procedures | To streamline the exceptional treatments procedure internal process, reduce waits in the process and eliminate waste within it |
| 16–20 August 2010 | 07 | Mandatory training process | To deliver the right training to the right people at the right time to ensure compliance with legislation and strategic objectives in a value-for-money way |
| 13–17 September 2010 | 07 | Stores order/delivery process | Review and improve the process by which stores are ordered from all ambulance stations across the trust. Review and improve the existing lead time from the order being printed off to availability of parts at station and then from delivery at station to stock on vehicles. Establish appropriate stock levels to reduce waste and inventory using 5s and other Virginia Mason tools. Engage participants to improve their own processes working towards total quality. Develop learning and experience which can be applied to other improvement events |
| 13–17 September 2010 | 11–13 | Mental health service | Scope: improve the timeliness of delivery of therapeutic interventions within a virtually integrated service from referral through therapeutic intervention to discharge |
| 13–17 September 2010 | PCT | Availability of activity information to GP commissioners | The intention is to significantly improve the process for creating and distributing information and reports to PBC/GP commissioners. Owing to the drive to reduce management costs, processes need more than ever to be efficient and lean |
| 13–17 September 2010 | 09 | Estates | To standardise and streamline the requests for category D works, reducing waste in time, overproduction and defects, while at the same time improving the user and provider experience by ensuring that the appropriate work is costed and proceeds in a timely manner |
| 11–15 October 2010 | North East community trust | Medical records processing | To review and improve the process for medical records processing |
| 11–15 October 2010 | 10 | Long-term sickness absence management | |
| 11–15 October 2010 | PCT | Availability of finance information to GP commissioners | The intention was to significantly improve the process for creating and distributing financial information and reports to PBC/GP commissioners. Owing to the drive to reduce management costs, processes need more than ever to be efficient and lean |
| 11–15 October 2010 | PCT | Room booking and cancellation process | To reduce the overall lead time for the process of booking a room at XX. Court and identify a standard process for cancellations |
| 11–15 October 2010 | 07 | Main stores processes | Review and improve the process by which central stores processes happen. Review and improve the existing lead times of different processes by focussing on 5S principles. Establish appropriate stock levels to reduce waste and inventory. Engage participants to improve their own processes working towards total quality. Develop learning and experience which can be applied to other improvement events. This event focused on applying 5S, proper layout, proper stock levels, Kanban |
| 11–15 October 2010 | North England network | Cardiac rehabilitation pathway | Cardiac rehabilitation pathway [i.e. from the point when a patient who has had PPCI is identified for cardiac rehabilitation to when the patient attends for a structured cardiac rehabilitation programme (phase 3)] |
| 11–15 October 2010 | 09 | Information management and technology | To provide a seamless, slicker and standardised approach to accessing and managing IT services |
| 8–12 November 2010 | 07 | Spa call-taking – 111 call handling | To review and improve the process, reduce the length of call and therefore increase capacity within the system. To improve the standard work around call-taking process and eliminate waste |
| 8–12 November 2010 | PCT | Informatics service desk | The intention was to significantly improve communications into the service desk from customers, between the service desk and the rest of the informatics team, and out from the service desk to customers. Owing to the drive to reduce management costs, processes need more than ever to be efficient and lean |
| 8–12 November 2010 | PCT | Taxi bookings | To reduce the overall lead time for the process of booking taxis and consider the expenditure and need in line with QIPP |
| 8–12 November 2010 | SHA | Change of circumstance form | To undertake a review of the existing use and appropriateness of change of circumstance information and resulting forms that are produced through the HR team within the LET. There is a need for improvement as to how the information is recorded, stored and retrieved and there is a requirement to sort and simplify the process and links between the HR department and the payroll team within the LET |
| 8–12 November 2010 | 09 | ENT/audiology secretaries processes | Existing processes had non-value-added elements and defects that lengthened the lead time. The aim of the RPIW was to reduce defects and introduce mistake proofing and standard work, to reduce non-value-added activities and thereby improve lead time |
| 6–10 December 2010 | PCT | Healthy Living Centre adult weight management process | To facilitate a streamlined, efficient and effective adult weight management referral process which has minimal waits, waste and quality defects. This RPIW had an overall aim to increase the available practitioner time to spend face-to-face time with patients, which would therefore improve the overall patient experience. To improve the physical environment for staff and meet health and safety regulations |
| 6–10 December 2010 | 11–13 | Access to contraception services following termination of pregnancy | Scope: teenager access to the termination-of-pregnancy service, to the point when they are discharged from hospital following the completion of the procedure. To ensure all women have access to the full range of contraception services available following a termination, with a focus on long-acting reversible contraception |
| 6–10 December 2010 | 11–13 | Safeguarding | Scope: to standardise and reduce the length of the safeguarding process with clear, appropriate role involvement leading to timely outcomes |
| 6–10 December 2010 | 09 | Portering | Reduce overall cycle time of porter job, improve patient journeys |
| 7–11 February 2011 | PCT | Stop Smoking Service | To reduce the overall lead time for the process of 4-week monthly monitoring returns and associated LES payments for pharmacies and GPs |
| 7–11 February 2011 | PCT | Psychological therapies referral process | To create a streamlined, efficient, effective referral process for use in psychological therapies services. Plan, study, test, define standard work for implementation of process. This RPIW had an overall aim to increase the available practitioner time to spend face-to-face time with patients, which would therefore improve the overall patient experience |
| 7–11 February 2011 | 11–13 | Facilities customer care | Scope: improve customer care for unplanned tasks by ensuring their request is directed to the right resource through an improved intake and dispatching process |
| 7–11 February 2011 | 07 | Dialysis transport service | To improve the performance of the trust from the customer perspective in relation to dialysis transport and to develop a quality service for responsible patients |
| 7–11 February 2011 | 07 | PTS call-taking | To review and improve the process, address issues, increase capacity for future flexibility within the system. To improve the standard work where appropriate and eliminate waste |
| 7–11 February 2011 | 14 | Wound care products | Reduction of waste associated with the process of ordering of wound care products, and waste of inventory |
| 7–11 February 2011 | PCT | IT training booking systems | To reduce delays and eliminate duplication and waste. To standardise work where possible. To streamline customer experience |
| 7–11 February 2011 | 09 | Maternity services: patient flow in outpatient clinic area | To improve the patient experience and the staff working environment. To eliminate waste in the process and reduce stresses in the clinic |
| 14–18 March 2011 | PCT 2 | Community dental autoclave community dentistry – decontamination | To develop a process flow which meets the activity demands of the department and supplies the correct instruments ‘just in time’ for the delivery of dental care |
| 14–18 March 2011 | PCT 2 | Funded nursing care and continuing health-care referral and administrative process | To reduce the overall lead time for the process from receipt of referral and associated administrative processes to reporting outcomes to stakeholders |
| 14–18 March 2011 | 07 | 999 call-taking | To review and improve the process, reduce the length of call and therefore increase capacity within the system. To improve the standard work around call-taking process and eliminate waste |
| 14–18 March 2011 | PCT 2 | Processing of primary care data | The intention was to significantly improve the support given by the primary care data quality team to the general practice/customer, with the aim of achieving high-quality, defect-free primary care data, by reducing the lead time and non-value-added processes in the processing of data by the information department |
| 14–18 March 2011 | 14 | One-to-one referrals to health training service | Removal of waste and reduction of non-value-added activities within the one-to-one referral process |
| 14–18 March 2011 | SHA | Improving efficiency and reducing risk in the ARCP process | To minimise risk and improve efficiency of the ARCP process, by ensuring appropriate communications and timely evidence in support of ARCP panels and their outcomes. Plan, test, study and define standard work for the gathering and collation of evidence for the ARCP panel. Apply mistake-proofing principles to the process; detect errors before they become defects |
| 14–18 March 2011 | 09 | Symptomatic breast clinic | To identify and eliminate non-value-added time in the patient pathways and increase value-added time. To reduce waste from unnecessary staff and patient movement. To improve quality by removing defects in the process |
| 4–8 April 2011 | 07 | Workshop stores (fleet) | Review and improve the process by which workshop stores processes happen. Review and improve the existing lead times of different processes by focusing on 5s principles. Establish appropriate stock levels to reduce waste and inventory. Engage participants to improve their own processes working towards total quality. Develop learning and experience which can be applied to other improvement events. This event focused on applying 5S, looking at layout, stock levels, Kanban |
| 4–8 April 2011 | 11–13 | Increase the uptake of repeat dispensing to reduce the waste of medicines | To streamline the patient pathway for patients in receipt of repeat prescriptions, reducing the time and effort spent both by general practice staff and patients during repeat prescribing processes, also reducing medicines waste |
| 4–8 April 2011 | PCT 2 | Continuing health care – packages of care | Receipt of continuing health care case for panel, the panel meeting and receipt of costing for packages of care |
| 4–8 April 2011 | 14 | Referrals to GUM drop-in clinic | Removal of waste and reduction of non-value-added activities within the referrals to the GUM drop-in clinic |
| 4–8 April 2011 | 09 | Radiology reporting | Reporting of plain films |
| 23–27 May 2011 | 11–13 | Initial health assessments for looked-after children | Scope: the initial health assessment process for looked-after children from the date a child becomes subject to a care order to the date the health assessment is completed. This includes the development of a care plan for the individual. To ensure all initial health assessments for looked-after children are completed within the recommended 28-day time scale |
| 23–27 May 2011 | 11–13 | Hospital breast diagnostic service | To provide a one-stop diagnostic service to all patients who are referred with suspicion of breast cancer. To ensure the patient flow within the system reflects demand |
| 23–27 May 2011 | PCT 2 | Continuing health-care service user records systems | Creating, updating and maintaining service user records. To reduce delays and eliminate duplication and waste. To standardise work where possible. To meet standards in relation to record-keeping |
| 23–27 May 2011 | North England network | Cancer peer review | Streamline the peer review process by standard operations |
| 23–27 May 2011 | 09 | Older persons’ mental health | To reduce variation, waste, defects and lead time, and to establish a standardised referral pathway |
| 20–24 June 2011 | North England Network | JIF | To standardise and simplify the completion and processing of ILR at the point of receipt of letters into the ‘holding tank’ at the SHA and upload to the SFA without errors. To plan, test, study and define standards for the verification and upload of learner records to the SFA. To apply mistake-proofing principles to each step of the process and detect errors before they become defects |
Glossary
- Jidoka
- A Japanese word meaning ‘autonomation’; may be described as ‘intelligent automation‘ or automation with a ‘human touch’.
- Kaizen
- Japanese word for ‘improvement’, or ‘change for the better’.
- Kanban
- Japanese word for ‘visual board’, used to indicate a means of visual scheduling of a production system.
- Takt time
- Derived from German; translates as ‘cycle time’.
List of abbreviations
- 3P
- Production Preparation Process
- 5C
- clear out, configure, clean and check, conformity, custom and practice
- 5S
- sorting, set in order, systematic cleaning, standardising and sustaining
- A&E
- accident and emergency
- BPR
- business process re-engineering
- CCG
- Clinical Commissioning Group
- CEO
- chief executive officer
- CI
- confidence interval
- CQC
- Care Quality Commission
- DNA
- did not attend
- EAG
- external advisory group
- ERIP
- European Regions for Innovative Productivity
- FT
- foundation trust
- GP
- general practitioner
- HR
- human resources
- ITS
- interrupted time series
- KPO
- Kaizen Promotion Office
- KSL
- knowledge sharing and learning
- LES
- local enhanced service
- MF
- management fellow
- NEPA
- North East Productivity Alliance
- NETS
- North East Transformation System
- NHS NE
- NHS North East
- NIHR
- National Institute for Health Research
- NPM
- new public management
- ONE
- One North East
- PCT
- primary care trust
- PI
- principal investigator
- PIPA
- purposeful inpatient admission
- PPI
- patient and public involvement
- QI
- quality improvement
- QIPP
- Quality, Innovation, Productivity and Prevention
- QIS
- quality improvement system
- RDA
- regional development agency
- RIE
- rapid improvement event
- RPIW
- rapid process improvement workshop
- SDO
- Service Delivery and Organisation
- SHA
- Strategic Health Authority
- SME
- small- and medium-sized enterprise
- SMED
- Single-Minute Exchange of Dies
- SPD
- standard process description
- SUI
- serious untoward incident
- TPS
- Toyota Production System
- TQM
- total quality management
- VMMC
- Virginia Mason Medical Center
- VMPS
- Virginia Mason Production System
- VSM
- value stream mapping