Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 09/1001/52. The contractual start date was in February 2011. The final report began editorial review in January 2013 and was accepted for publication in July 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Peckham et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Since the 1970s there has been a growing policy and practice interest in the public health role of primary care. The 1978 World Health Organization Alma Ata declaration1 set the context for exploring the relationship between primary care and its role in prevention and population health. In the UK, the government highlighted the importance of health promotion in general practice in its 1987 White Paper Promoting Better Health2 and the introduction of health promotion payments in the 1990 general practitioner (GP) contract. This introduced, for the first time, specific payments for health promotion activities and provided the first key national policy interest in the public health role of general practice. Despite this, very little formal attention was paid to the public health role of general practice in the UK until the turn of the century. The introduction of the new General Medical Services (GMS) contract and the Quality and Outcomes Framework (QOF) in 2004, and recommendations in the Wanless Review3 on public health, provided a new impetus and focus on the role of general primary care and, more specifically, general practice.
Alongside an interest in how services were to be delivered, there was also an increasing focus on the effectiveness of interventions delivered in public health. However, much of the research on effectiveness has produced equivocal outcomes and, on the whole, has not addressed the contextual issues that might affect the final outcome of such interventions. Understanding how public health services are delivered and organised has been highlighted as an important area for public health research. 4 Concern about the public health role of primary care has been identified as an area of concern in the UK since the mid-1990s, with professional bodies exploring the extent to which the professional practice of GPs and nurses should include prevention. 5–7 A number of commentators have also specifically addressed the extent to which prevention and health improvement should be an integral part of general practice. 8–15
In order to explore the role of general practice and primary care in health improvement activities, this project was developed with an explicit focus on the delivery and organisation of such activities. The project was designed to examine who delivers these interventions, where they are located, what approaches are developed in practices, how individual practices organise such public health activities within general practice and how these contribute to health improvement. Our focus was on health promotion and prevention activities. However, these are contested concepts and their meanings are often confused and unclear,16 and they are frequently used as a synonyms for ‘public health’, which also lacks clarity and certainty as a descriptor of activity. 4,17 It is important, in carrying out a review of health-promoting and health improvement activities, to be as clear as possible about what is understood by such terms.
The need for this scoping study has been identified based on previous and existing research being undertaken by the research team members and discussions with practitioners in primary care. The need to develop public health in primary care was highlighted by Derek Wanless3 in his report on public health. Current research on the QOF has also shown that there are important changes in the activities and roles of practice-based staff in relation to health-promoting activities. The recent King’s Fund review of GP quality highlighted the need to examine the wider role of the primary health-care team in general practice and their contribution to health improvement. 18 In a recent review of health promotion opportunities for general practice, Watson15 noted that ‘there has been a dearth of information about the effectiveness of health promotion in the primary care setting’ (p. 180). In advocating a health-promoting general practice model, he concludes that there is a need for further research to demonstrate ‘health benefits for local communities . . . and also a need to identify potential practical and organisational difficulties’. Finally, Health England has identified that ‘there are significant gaps in the evidence base for primary prevention interventions in primary medical care’. 19
The aim of this scoping exercise was to identify the current extent of knowledge about the health improvement activities in general practice and the wider primary health-care team. The key objectives were to provide an overview of the range and type of health improvement activities, and to identify gaps in knowledge and areas for further empirical research.
Our specific research objectives were:
-
to map the range and type of health improvement activity undertaken in general practice and primary care
-
to scope the literature on health improvement in general practice and identify gaps in the evidence base
-
to synthesise the literature and identify effective approaches to the delivery and organisation of health improvement interventions in a general practice setting
-
to identify the priority areas for research as defined by those working in general practice.
The focus of this scoping review and evidence synthesis was to identify where further research on the provision of public health in general practice is needed. To this extent the review seeks to identify areas of practice where there is evidence to support health improvement, and areas of practice that lack research evidence or where the current evidence base is incomplete. Our aim was not to provide a systematic review of the evidence base or provide a comprehensive and detailed account of all areas of public health practice in primary care.
The purpose of this research was, therefore, to identify areas where there is good evidence of effective approaches to the delivery of interventions in general practice and areas where there is an insufficient evidence base to support practice and where further research will support the development of practice. In particular, we focused on identifying:
-
the range and type of activities that are best suited to the general practice context
-
the roles and responsibilities of practice-based staff in relation to what they should be doing
-
community-focused (rather than individual-focused) health improvement activities
-
the efficacy of incentivised and non-incentivised health improvement activities and how these affect health improvement activity in the practice
-
other interventions that primary care staff can undertake that contribute to health improvement that are currently not universally undertaken.
So that the review findings provide a substantive evidence base for the implementation of effective health improvement programmes, we adopted two approaches to the review. The first focused on assessing the quality and strength of the research evidence while the second examined the extent and nature of the literature to identify where additional research is required. Given that our focus was on service delivery and organisation, we have drawn on a broader assessment of study quality than is used in systematic reviews and also incorporated papers where there was some description of services. While more weight has been given to studies and papers with some evaluative component, we also felt it important to include more descriptive studies to provide an overview of the delivery and organisation of health improvement activities in general practice. However, it became clear from very early on in the study that providing a comprehensive overview and identifying approaches supported by evidence of effectiveness would be complex. An initial review of Cochrane studies relevant to this review suggested that we would not find significant numbers of studies that included assessments of the way that interventions were delivered and organised. In addition, the range and nature of the studies was enormous as was the breadth of topics.
Rather than make a systematic assessment of the evidence, we have attempted to draw together an assessment of quality, relevance, theory, integrity of interventions, context and sustainability of interventions and outcomes. While randomised controlled trials (RCTs) are considered a gold standard of quality of evidence, we have also examined, and included where relevant, non-RCTs, such as controlled before-and-after studies, interrupted time series and comparisons with historical controls or national trends. These may not always represent the best available evidence. Relevant qualitative research has also been included in order to help identify the factors that enable or impede the implementation of an intervention, describe the experience of the participants receiving it and their subjective evaluations of outcomes, and understand the diversity of effects across studies, settings and groups. 20
It was recognised from the beginning that the task of assembling information and evidence on the delivery and organisation of health improvement activities in general practice would create a number of challenges in terms of developing the search strategy and identifying papers that provided details of service and delivery of health improvement activities. Substantial investment was made in trying to refine a search that would provide a wide range of information that when synthesised would contribute to improving knowledge and understanding of current practice. This involved refining our research protocol and approach. We narrowed our searches to review UK papers only. This was partly driven by the volume of studies identified in our literature searches but was also to ensure relevance, taking into account the different context of UK general practice from the delivery and organisation of primary care in other countries. Following early discussions with practitioners in practices and public health agencies, we also changed our approach to consultations with practitioners. Originally we planned to hold stakeholder events but, because of the unprecedented upheavals in the NHS during the period of the research, arranging meetings was extremely difficult. In addition, the substantial task of dealing with the extensive literature meant that we had to allocate more staff resources to this element of the study, further limiting our ability to undertake an extensive practitioner scoping study as outlined in our original application. It was, therefore, agreed with the National Institute for Health Research (NIHR) Service Delivery and Organisation (SDO) programme that we would instead draw on discussions with individual practitioners in practices and public health agencies and in group discussions with GPs when these could be arranged.
Structure of this report
The main elements of the report provide details of the literature review. The review was developed from a reading of all selected papers, but not all these are referred to in the report because of the substantial amount of material. Chapter 3 provides details of how we approached the literature and dealt with the complexities of conducting the review. Chapters 4–6 provide details of the literature. Chapter 4 describes the main aspects of the literature including the quality, topic areas and extent of the literature found. The chapter also includes a brief outline of some of the key themes emerging from discussions with practitioners. Chapter 5 provides details of the range of activities identified in the literature. Chapter 6 provides details of the evidence about effective ways to organise and deliver health improvement interventions in general practice or by the primary health care team. Given the changes currently being introduced in the English NHS, in Chapter 7 we examine how these changes impact on the public health role of general practice. The aim of this chapter is to set the findings of the scoping review within the context of the recent changes to the organisation of public health and health-care services in England resulting from the Health and Social Care Act 2012. 21 Finally, in Chapter 8 we identify some of the key messages arising from the review and set out the implications for practice and further research.
Chapter 2 Background
Since the 1970s there has been a growing interest in the role of primary care, and general practice in particular, in public health activities. The main focus of attention has been the important health promotion role of general practice. General practice has traditionally been the first point of contact with the NHS and there are 300 million patient consultations in England every year. 22 The role of general practice is to act as the gatekeeper to the NHS, managing the health care for the practice population and referring relevant cases to secondary care services. This places general practice in a unique position not just to provide medical care but also to promote the health and well-being of the practice population.
This chapter provides a brief overview of the key themes and discusses a number of concepts relating to the public health role of general practice health improvement activities associated with the practice and primary health-care team. It is not intended to be a detailed review of the issues, as there have been a number of previous studies that have explored the relationship between general practice and public health18 and the broader relationship between public health and primary care. 23,24 The aim of this review is to examine how health improvement activities are organised and delivered within general practice, and this chapter provides a discussion of those issues which focused the proposal on this aspect of general practice activity.
Organisationally, the history of UK public health is complex, involving a number of changes in the responsibility, structure and roles of different professionals engaged in public health practice. 25–27 Over the past 20 years there has been a shift towards highlighting the role of primary care in public health alongside a renewed focus on partnerships, and the development of a multidisciplinary workforce and the introduction of public health targets such as those for reducing health inequalities, improving detection rates for cancer and smoking cessation. However, despite a policy focus on reducing health inequalities, the infant mortality gap has widened and, while life expectancy is increasing overall, it is increasing more slowly in socially and economically deprived areas. 28 The Wanless Report3 on improving the public health function in England argued that public health activities at a local level needed to be prioritised and adequately resourced in order to develop long-term sustainable action to improve population health and that there is a need to evaluate existing activities against a common framework (including their cost-effectiveness). The report identified the need to develop incentives, shared local targets and performance management in primary care trusts (PCTs) to enable them both to prioritise public health issues and to work in partnership with local authorities (LAs) on public health. In response, policy-makers began to focus on specific public health measures, such as doubling the capacity of smoking cessation interventions, targeting prevention of cardiovascular disease (CVD) by increasing coverage of antihypertensives and statins, and improving the detection of cancer. These more clinical interventions are delivered at a primary care level, making the role of GPs and practice nurses in particular crucial to the delivery of public health improvements and reductions in health inequalities. This expansion of activities has been supported in a number of ways through contractual mechanisms and by wider debate about public health roles of practice staff.
The public health role of primary care was also highlighted by the Marmot Review29 on health inequalities. There is good evidence to suggest that people from lower socioeconomic groups have their cancer diagnosed at a later stage and are less likely to participate in cardiovascular screening affecting treatment options and outcomes – areas where the general practice role is critical. 30,31 In examining how to reduce inequalities, the Marmot Review29 focused attention on the role of general practice and reiterated the important leadership function of GPs and the NHS in tackling health inequalities. 32 The task-group report on priority conditions highlighted a number of key areas relevant to general practice including CVD, obesity, alcohol and drug misuse, mental health, and the health and well-being of older people. 33 In addition, the delivery systems and mechanisms task group32 highlighted the key role of primary care and the use of incentive systems such as the QOF. The Marmot Review29 paid specific attention to the impact of the QOF and its role as a mechanism for contributing towards reductions in health inequalities. It was recognised, however, that the QOF had limitations, and Exworthy et al. in the Task Group 7 report cautioned that the QOF is mainly concerned with secondary prevention for existing chronic disease (Exworthy M, Marmot Review. Task Group 7: Delivery systems and mechanisms Topic 3: Structural reorganisations and their impact on the ability of the health system to focus on population health. Unpublished; 2009). There are therefore few indicators which relate to primary prevention (10 of the 146 indicators). There is therefore a risk that primary preventative activities will be overlooked. It is significant that Marmot29 therefore made a specific recommendation about extending the use of the QOF to include more primary prevention activities, while recognising that the QOF should not be viewed as the only vehicle for promoting primary prevention within general practice.
Introduced at the same time as the QOF, the Local Enhanced Service (LES) element of the 2004 GMS contract has made a significant contribution to supporting public health in general practice. LESs have been particularly effective in involving GPs in locally driven public health efforts supporting a wide range of evidence-based public health activities, such as identifying CVD risk and providing long-acting contraceptives, and in 2009/10 they accounted for some £370M. 34 Having the option of LESs in the contract has provided a way for GPs to reduce preventable morbidity, and it could continue to do so in the future. This option would be especially helpful in the context of a more diverse provider landscape.
With the election of the new government in 2010, there have been a number of key developments that have an impact on the public health role of general practice. The 2010–15 coalition government’s programme published in May 2010 made explicit reference to proposals to restructure the NHS and specifically to incentivise GPs to tackle public health problems. 35 These proposals were further developed with the publication of two White Papers, Equity and Excellence: Liberating the NHS36 and Healthy Lives, Healthy People: Our Strategy for Public Health in England,37 which signalled substantial organisational changes in the NHS and a shift in public health policy. With the Health and Social Care Act 2012,21 PCTs and strategic health authorities have been abolished. Clinical Commissioning Groups (CCGs) and the new NHS Commissioning Board (NHS England) took on responsibility for health-care commissioning from April 2013. Of particular significance are the role of NHS England as the contractor for general practice and the transfer of public health responsibilities to LAs. Many of the activities previously funded through LES, including sexual health, smoking cessation, prevention and treatment of alcohol misuse, falls prevention and mental health promotion, are now commissioned through the public health budget of LAs, while the GP contract is currently the responsibility of NHS England. These shifts are likely to affect the role of general practice in public health and are discussed later in this report (see Chapter 7).
Other developments include an expanded role for the National Institute for Health and Care Excellence (NICE) with an increasing emphasis on the development of public health guidance and its new responsibility for developing QOF indicators. To date, NICE has published 39 potentially relevant guidance documents covering topics such as accidents and injuries, alcohol, behaviour change, CVD, child health, diabetes, maternal health, obesity and diet, physical activity, sexual health, smoking and tobacco, vaccine-preventable diseases, and working with and involving communities (see list at www.nice.org.uk/guidance/published?type=ph). However, reference to general practice and the wider primary health-care team is limited in this guidance. For example, NICE Public Health Guidance number 21, Reducing Differences in the Uptake of Immunisations38 identifies the practice and its staff as key practitioners as well as other key primary care settings within the community and also, for young people, the important role of schools, nurseries and social care settings involving health-care, social care and education staff. This guidance draws on international evidence, which may limit applicability to a UK general practice context.
Of particular relevance to this review is the fact that such evidence rarely takes into account the different international or local contexts of evidence. For example, a systematic review of RCTs on lifestyle interventions in primary care39 included seven studies: three from the UK as a whole, one from England, one Finnish, one Australian and one from New Zealand. No account is taken of different payment, organisational or system contexts. The only key delivery variable referred to is whether it was undertaken by a nurse or a physician, although these are stated without any further detail. Similarly, a systematic review of brief alcohol interventions40 included 24 studies across north America, Europe, Africa and Australia; and a systematic review of interventions in routine clinical practice on nutrition and physical activity for reduction of diabetes risk41 included 12 studies, with three from the UK, one Japanese, one Italian, two Swedish, three from the USA, one Finnish and one Australian. Routine clinical practice locations varied and, while they were predominantly delivered by physicians, this was not always clear. The aim of this review is to examine the delivery and organisation of health improvement activities in UK general practice or by the primary health-care team from the practice. The context of the practice or location and the way the activity is organised, who delivers it, etc. are critical to providing an overview of such activity. One key problem in examining the public health role of primary care is the lack of single, stable and bounded definitions of both health improvement and primary care.
Defining public health and primary care
There is some ambiguity about whether the term ‘public health’ is primarily about NHS activity or something wider. This ambiguity reflects a longstanding debate about the nature of public health itself. The most widely used definition of public health is that provided in 1988 by Acheson,42 who defined public health as ‘the science and art of preventing disease, prolonging life, and promoting health through the organised efforts of society’ (p. 1). The UK Faculty of Public Health endorses this definition; it suggests that public health is population based; it suggests that there is a collective responsibility for health, protection and disease prevention; it accepts the key role of the state; and it suggests that tackling public health problems involves a concern for the underlying socioeconomic and wider determinants of health as well as disease, and involves partnerships between all those who contribute to the health of the population. The faculty identifies three key domains of public health practice:
-
health improvement
-
inequalities
-
education
-
housing
-
employment
-
family/community
-
lifestyles
-
surveillance and monitoring of specific diseases and risk factors
-
-
improving services
-
clinical effectiveness
-
efficiency
-
service planning
-
audit and evaluation
-
clinical governance
-
equity
-
-
health protection
-
infectious diseases
-
chemicals and poisons
-
radiation
-
emergency response
-
environmental health hazard.
-
In the 2010 Public Health White Paper,37 the government set out five domains of public health which were to be covered by a public health outcomes framework:
-
domain 1 – health protection and resilience: protecting people from major health emergencies and serious harm to health
-
domain 2 – tackling the wider determinants of ill health: addressing factors that affect health and well-being
-
domain 3 – health improvement: positively promoting the adoption of ‘healthy’ lifestyles
-
domain 4 – prevention of ill health: reducing the number of people living with preventable ill health
-
domain 5 – healthy life expectancy and preventable mortality: preventing people from dying prematurely.
The scope of this review falls mainly in the area of health improvement and domains 3 and 4 outlined in Healthy Lives, Healthy People. 37 However, identifying clear-cut public health activities or responsibilities is complex, and many activities overlap the domains defined by the Faculty of Public Health and those in the public health outcomes framework. For this review, the definition of health improvement draws on that used by the World Health Organization, first outlined by Leavell and Clark in 1958. 43
Primary prevention: activities designed to reduce the incidence of an illness in a population and thus to reduce, as far as possible, the risk of new cases appearing and to reduce their duration. Primary prevention can be defined as the action taken prior to the onset of disease, which removes the possibility that the disease will ever occur. It signifies intervention in the pre-pathogenic phase of a disease or health problem. It includes the concept of ‘positive health’, a concept that encourages achievement and maintenance of an acceptable level of health that will enable every individual to lead a socially and economically productive life. Primary prevention may be accomplished by measures designed to promote general health and well-being, and quality of life of people, or by specific protective measures.
While not all of these areas of activity relate to primary care or even specifically general practice, key activities such as lifestyle advice, nutrition and health are as much part of practice as immunisation, safe use of drugs, etc.
Secondary prevention: activities aimed at detecting and treating pre-symptomatic disease. It is defined as an action which halts the progress of a disease at its incipient stage and prevents complications. Secondary prevention attempts to arrest the disease process, restore health by seeking out unrecognised disease and treating it before irreversible pathological changes take place, and reverse communicability of infectious diseases.
There is an obvious and clear link between the role of general practice and primary medical care, and secondary protection. The individual focus of general practice, especially in the UK, places the primary care practitioner in a key position to identify areas for secondary prevention and, where relevant, undertake action.
Tertiary prevention: activities aimed at reducing the incidence of chronic incapacity or recurrences in a population, and thus to reduce the functional consequences of an illness; including therapy, various rehabilitation techniques and interventions designed to assist the patient to return to educational, family, professional, social and cultural life. This level involves the treatment and monitoring of people with disease, and general practice plays a key role in this in the UK. For the purposes of this review we have categorised this as treatment and outside our review.
However, strict demarcation between levels is not always possible, as some activities cut across these levels. For example, protecting others in the community from acquiring an infection can involve providing secondary or even tertiary prevention for the infected and primary prevention for their potential contacts. Some activities do not differentiate between levels so promoting smoking cessation is directed at those without any health problems as well as those already identified as having a specific disease. Froon and Benbassat44 have argued that, given the inconsistencies in the way the different definitions of levels of prevention are used in practice, this approach should be abandoned. They argued that interventions should be defined by their objective, target population and type of intervention.
This refocusing of health promotion frameworks has already been promoted in government public health policy. In Choosing Health: Making Healthy Choices Easier,45 the government set out proposals for more integrated approaches to prevention and health promotion for children through Children’s Trusts and Children and Family Centres, and using schools as settings for health promotion working with children and their families. Primary care was also seen as an integral part of a community-based approach to health promotion. It is not clear, however, how far the shift has permeated current policy thinking in relation to primary care and public health activities of general practice. Current policy appears to have demarcated general practice with a stronger emphasis on the GP role and using consultation opportunities to address individual lifestyle issues. The 2010–15 coalition agreement The Coalition: Our Programme for Government35 announced that the Department of Health (DH) would strengthen the role and incentives for GPs and GP practices on preventative services, both as primary care professionals and as commissioners. As primary care professionals, GPs and GP practices play a critical role in both primary and secondary care prevention. They have huge opportunities to provide advice, brief interventions and referral to targeted services through the millions of contacts they have with patients each year. It is clear that current government policy continues to emphasise the important role of general practice and primary care that cut across the different levels of intervention and domains of practice.
Similarly, there is a longstanding debate about the nature of primary care. 46–49 In the UK, ‘primary care’ generally refers to services provided by general practice, dental practice, pharmacists and opticians. There is little discussion about the range of services that this encompasses. In 1994 the US Institute of Medicine defined primary care as the provision of ’integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs, developing a sustained partnership with patients, and practicing in the context of family and community’ (p. 15). 50 Starfield47 has discussed the parameters of primary care, focusing on the role of primary care in dealing with the whole person in a holistic way over the long term and providing co-ordination of care for individuals. Starfield47 identified four unique features of a primary care service: first contact access, person-focused care over time, comprehensiveness and co-ordination. Hogg et al. 51 suggest that other important aspects of primary care include patient–provider relationships as defined by communication, holistic care and an awareness of the patient’s family and culture. They also argue that primary care performance needs to be set within a broader structural environment that recognises the wider health-care system, the practice context and the organisation of the practice. This reflects an increasing acceptance of the role of the health-care delivery system, including issues of governance and accountability, resources, inter-relationships between primary care and other health and social care services, and person-centred care. 52,53 Kringos et al. 53 undertook a systematic review to identify the core dimensions of primary care, identifying 10 core dimensions. The review identified preventative and health promotion activities as elements of primary care and, in particular, how such activities are underpinned by dimensions such as co-ordination of care and equity. However, they concluded that a primary care system can be defined and approached as a multidimensional system contributing to overall health system performance and health. The broad nature of primary care and the difficulty of providing a clear definition were highlighted by Peckham and Exworthy. 48 In the UK, primary care is variously equated with general practice, the primary health-care team and a broader view of a wide variety of community-based services. For the purposes of this review we identified our focus as those health improvement activities that are undertaken in general practice or by staff located in practices but which are delivered outside the practice. This definition was not without its problems, and relating definitions to search terms was complex (see Chapter 3). There are, however, specific aspects of policy and practice that directly relate to the organisation and delivery of health improvement within general practice and primary care settings and are directly relevant to this review, including contractual issues in general practice, pay for performance, its organisation and staffing, and relationship to professional public health practice.
The general practitioner contract
Historically, GPs’ status as independent contractors to the NHS has meant general practice has been relatively free of direct management and monitoring compared with other parts of the NHS and has predominantly provided a demand-led sickness service. Thus, any focus on public health has tended to be more focused on a secondary level of prevention, although GPs have always provided general lifestyle advice, vaccination, etc., as a normal part of good practice. 48,54 GPs’ income was based on allowances, capitation and fees for a limited set of services, and the nature and quality of care was undefined and left to professional discretion. 54 There is a range of general incentives for GPs and the wider primary health-care team to engage in public health activities. Capitation payment systems (such as that for UK GPs) provide a general incentive for health promotion and managing long-term care problems to minimise inappropriate use of primary care services – particularly when compared with fee-for-service payment systems. 55,56 However, practice in the UK falls short of this aspiration. 57,58 In addition, wider influences such as national policy frameworks, guidelines, professional competencies, and practice guidelines and educational programmes seem to influence physician practice and encourage more preventative health interventions and practice, but the evidence is limited. 59
Before the introduction of the latest GMS contract in 2004, practices were given financial incentives to provide health promotion. For example, cervical cancer screening is undertaken predominantly within general practice by GPs and practice nurses. Target payments (for achieving 50% and 80% coverage rates) were introduced in 1990 as part of the revised GP contract and, while provision of this financial incentive increased coverage from 53% to 83% of GPs achieving the 80% target, these improvements bore no relation to local need. 60,61 However, for GPs and practices which found it difficult to achieve even 50% coverage, there was no real incentive to try and maximise the uptake of screening. 60
The new GMS contract of 2004 continued the trend of increasing regulation of clinical practice to improve quality of clinical care, with a pay-for-performance system rewarding practices for the quality of their services. 62 The main principles of the new contract were:
-
a shift from individual-GP to practice-based contracts
-
contracts based on workload management, with core and enhanced service levels
-
a reward structure based on the new QOF and annual assessments
-
an expansion of primary care services
-
modernisation of practice infrastructure (especially information technology systems).
The contract is not universal, as there are alternative contract types alongside the GMS contract, including Personal Medical Services, which cover about 30% of practices and were developed in the 1990s; Alternative Provider Medical Services aimed at contracting private sector companies to run GP practices; and Specialist Provider Medical Services contracts for specific GP services such as those for homeless people. The core contract includes general patient care, with prevention seen as an integral part of the provision of such care. Over the years, specific aspects of prevention have been identified beyond clinical care, such as health checks for new patients. LESs also provided a way for PCTs to contract for specific areas of health promotion such as drug and alcohol services, extending stop-smoking services, breastfeeding initiatives and dealing with other locally identified public health problems. By 2009, LES expenditure represented a significant investment in locally defined services. 63
The QOF has also been used to target some preventative activities, although to date their extent has been limited. There were recommendations in the Marmot Review29 for greater use to be made of the QOF for reducing health inequalities. Currently, despite the inclusion of key clinical areas and an increasing emphasis on prevention, there is little evidence to support any substantial beneficial impact of the QOF on either preventative activities or reducing health inequalities. 64,65 However, there is some evidence to show that the QOF has contributed to a reduction in the delivery of clinical care related to area deprivation,66 and a systematic review of the impact of pay-for-performance schemes on health inequalities concluded that inequalities have largely persisted since the introduction of schemes. 67 The Healthcare Commission report68 noted that the QOF is unlikely to encourage practices to try and include the most ‘hard to reach’, since no further points are received once 90% coverage has been achieved. Typically, QOF points are awarded to reflect workload and consist of both a minimum performance threshold (payments beginning once 40% of eligible practice population have been treated) and a maximum threshold (e.g. 90% of those eligible) with graduated payments in between.
Few QOF indicators directly address health outcomes and primary prevention. The evidence suggests that the QOF has improved health outcomes for some conditions, but has had a limited impact on others, including adverse effects for population subgroups and non-incentivised activities. Current research also highlights the limitations of the QOF scores awarded in improving health outcomes, due to the indicators’ ceiling thresholds and the suboptimal clinical targets set compared with national clinical guidelines. 69,70 One key exception has been the inclusion of smoking targets. These were included in early versions of the scheme and was associated with the universal uptake by GPs for recording the smoking status and providing smoking cessation advice for patients with various comorbid factors [coronary heart disease (CHD), stroke or transient ischaemic attack, hypertension, diabetes, chronic obstructive pulmonary disease (COPD) or asthma and, from 2008, chronic kidney disease, schizophrenia, bipolar disorder or other psychoses]. Notably, the original QOF threshold for intervening with smokers without comorbidity factors was simply that status was recorded at any time. This was changed in 2006, when recording smoking status in non-morbid patients was required periodically (every 27 months), rather than ‘ever’, to attract payment. However, only one indicator is solely focused on the achievement of an actual health outcome (i.e. the number of epilepsy patients who have been seizure free in the last 15 months), whereas the remaining intermediate outcomes relate to targets which are an indirect measure of one’s health (e.g. cholesterol < 5 mmol/l). The QOF points available are also weighted towards particular conditions such as diabetes (88 points) and CHD secondary prevention (69 points), compared with scores available for COPD (30 points), depression (31 points) and other mental health conditions (40 points).
The QOF also allows GPs to ‘exception report’ to ensure that they are not penalised by patients who do not attend reviews of their medication or where patients are unable to tolerate medication, possibly because of side effects. Exception reporting is supposed to ensure that GP performance is measured only against a viable practice population. However, it is possible for reporting to be ‘gamed’ to exclude high-risk patients or those for whom GPs have missed targets, thereby decreasing the patient pool and maximising QOF scoring. 71
The organisation of preventative activities in primary care settings
A Cochrane review72 on the secondary prevention of ischaemic heart disease stated it succinctly: while the benefits of individual medical and lifestyle interventions are established, the effectiveness of interventions which seek to improve the way secondary preventative care is delivered in primary care or community settings is less so. A review by The King’s Fund18 examining the quality of general practice identified that a key challenge to improving the quality of public health and ill-health prevention is that there is a lack of evidence about the effectiveness of interventions carried out by primary care practitioners. The authors concluded that:
Evidence about the effectiveness and cost-effectiveness of public health interventions is growing . . . However, more needs to be done to help understand how general practice can effectively tackle ill-health prevention. General practice, public health practitioners and academics all have the responsibility to work together to improve this evidence base.
p. 3118
While it is clear that there is a substantial commitment, in terms of both policy and practice, for general practice to be engaged in public health activities, the literature tends to discuss this in one of three ways. The first way is in the focus at a conceptual level examining the links between primary care and public health. The second is the focus on the public health role of primary care professionals. Finally, the literature has examined the role of the practice as a location for public health activity. We examine each of these areas in turn.
Primary health care as public health
There has been a longstanding debate within general practice about the extent to which ‘primary health care’ has both a community and an individual orientation. 47,48 There is good evidence to demonstrate that primary care can effectively contribute to individual health. Health promotion activities can be categorised as individual, practice and community based, and these may be primary or secondary prevention activities.
The development of public health policy and practice in the second half of the twentieth century was marked by two major inter-related tensions: whether public health is a largely medical domain or a multidisciplinary one, especially given the wider determinants of health, and whether public health is a specialist or generalist activity. 27 These two tensions are central to discussions about the role of general practice in public health. Primary care has been seen as a logical location for local public health action, and its role was specifically identified in the Alma Ata declaration. 1 However, in many Western industrial countries this link has not been so clearly identified and a more individualistic, medicalised system of primary medical care has developed. This is particularly true in the UK. 48,73 Since the late 1970s there has been an increasing recognition that primary care should encompass a population health perspective and that prevention and health improvement are key constituents of high-quality primary health care. 1,47,53
Experience suggests that, while the public health activity of practices is located in the community, primary care professionals do not necessarily engage with the community about public health issues and about the relevance of their activity to the community’s health priorities. 12 Generally, the structures and cultures of primary care organisations reflect the dominant medical model, which inhibits the development of community perspectives on health. 12,74 Many professionals, then, confine their public health activity to a strictly clinical agenda. Those who do engage with the community on wider public health issues go beyond their formal role,8,10,12,75 although there is a tradition of public health within UK general practice, and of activist doctors addressing health inequalities in deprived communities. 13,14 Direct policy support for public health came with the 1990 GP contract, which introduced the first payments for reaching cervical screening and immunisation targets, and for running ‘health promotion’ clinics. The development of primary care organisations in the 1990s shifted the focus towards population approaches, seemingly building on incentives for health promotion and education, as well as secondary prevention, that already existed in UK general practice. 48,76,77 However, none of these incentives succeeded in drawing GPs ‘beyond the surgery door’, and they still focused on what were essentially clinical activities. 10,78 Generally, GPs focus prevention interventions on patients at high risk rather than taking a population approach or maximising opportunities for health promotion advice to all patients who might benefit. 79 Nevertheless, prevention is seen as an important element of the role of primary care practitioners. 80,81
Professional public health practice in general practice and primary care
The range of professionals engaged in general practice and primary care include all staff who work within the practice, are based or located at the practice or are part of the primary health-care team linked to the practice. There has been discussion about the public health role of such professionals for many years. Policy tends to focus on the role of the practitioner, with the main emphasis on the GP, although there has been an increasing recognition of the roles of other practitioners based in general practice or providing primary care services. However, the main funding mechanism for general practice remains the GMS contract, which is negotiated with the GP principals in the practice, and most payment mechanisms are historically associated with GP activities. For example, while the QOF is essentially a reward system for GPs to undertake specific activities with patients, it is practice nurses who actually undertake much of the work. 82
Tannahill83 has argued that public health in primary care incorporates clinical and non-clinical dimensions and that it challenges GPs to more proactively address their patient population’s needs. This view was supported by the coalition government of 2010–15, which identified the need to extend the public health role of GPs and further incentivise public health activity through the QOF. 37 The Royal College of General Practitioners also supports a stronger, proactive role for GPs in carrying out public health activities and interventions, with health promotion representing a core element of the general practice curriculum (Box 1). 7
-
A wide knowledge of the public’s health and prevalence of disease.
-
The ability to judge the point at which a patient will be receptive to the concept and the responsibilities of self-care.
-
Knowledge of patient’s expectations and the community, social and cultural dimensions of their lives.
-
Understanding the importance of ethical tensions between the needs of the individual and the community, and to act appropriately.
-
Working with other members of the primary health-care team to promote health and well-being by applying health promotion and disease prevention strategies appropriately.
-
The ability to work as an effective team member over a prolonged period of time and understand the importance of teamwork in primary care.
-
Understanding the role of the GP and the wider primary health-care team in health promotion activities in the community.
-
Understanding approaches to behavioural change and their relevance to health promotion and self-care.
-
Changing patients’ behaviour in health promotion and disease prevention.
-
Helping the patient to understand work–life balance and, where appropriate, help patients achieve a good work–life balance.
-
Describing the effects of smoking, alcohol and drugs on the patient and his or her family.
-
Promoting health on an individual basis as part of the consultation.
-
Negotiating a shared understanding of problems and their management (including self-management) with the patient, so that the patient is empowered to look after his or her own health and has a commitment to health promotion and self-care.
-
Giving information on acute and chronic health problems, on prevention and lifestyle, and on self-care.
Source: Royal College of General Practitioners. Healthy People: Promoting Health and Preventing Disease. 2007. URL: www.rcgp-curriculum.org.uk/pdf/curr_5_Healthy_people.pdf (accessed 10 June 2010). 7
At the heart of the relationship between general practice and public health is an ethical balance between individual and collective freedom. For primary care practitioners, the roles of patient’s advocate and population planner may conflict with one another. 84 Many practitioners are ambivalent about the place of health promotion alongside their more central clinical caring role. Some GPs question the idea that they should be vested with responsibilities for social engineering that are really the proper role of government. 85 General practitioners are also often untrained as health educators, and may have a narrow view of health promotion and limited experience of community development activities. The potential for primary care practitioners to influence public health is also shaped by the role of local health purchasers, which redistribute resources between geographical areas, clinical disciplines and practices to support a public health agenda. However, the GP contract has for nearly 20 years included a number of aspects of health promotion, and more recently the Marmot Commission on health inequalities29 has focused some attention on developing the performance elements of the contract, within the QOF.
There has also been a longstanding debate about the public health role of nurses and allied health professionals. 86 In particular, the health promotion role of nurses has long been recognised by professional and regulatory bodies that have advocated a stronger public health role in nursing. 87 Following the publication of Making a Difference: Strengthening the Nursing, Midwifery and Health Visiting Contribution to Health and Healthcare,88 there has been an increasing policy emphasis on developing the public health role of nurses. However, there has been an increasing trend towards more clinical specialisms, and concerns have also been raised about supporting the public health roles of key groups such as health visitors and school nurses. 89–91 There has been less discussion about the public health role of district and other specialist nurses. 86 However, over the last 20 years, practice nurses have experienced a substantial change in their involvement in public health activities. The introduction of health promotion banding payments in the 1990s, the focus on screening and the introduction of the QOF in 2004 have had a significant impact on the role and workload of practice nurses and also led to the introduction of more health-care assistants working in general practice. 92,93 Practice nurses are undertaking a substantial amount of the screening and monitoring activities in general practice for blood pressure, diabetes, asthma, etc., creating a stronger health promotion role with symptomatic patients. There has also been an increase in practice nurses undertaking smoking cessation work. 94,95
Changes in the role of health visitors in the past 20 years have involved a more targeted focus on disadvantaged groups and families. This has involved closer working with developments such as Sure Start and family/children centres. 96 While the specific role of the public health nurse (as in Scotland) has not been developed in England, health visitors remain the most public-health-focused nursing role. 97 However, the coalition government of 2010–15 was committed to increasing the health visiting workforce by 4200 health visitors by 2015. This commitment was supported by the Health Visiting Implementation Plan,98 which uniquely set out the government’s determination for health visitors to be the key drivers for child and family public health through the vehicle of the Healthy Child Programme. 99 This is on target to be achieved, although the evidence base for health-visiting interventions remains relatively weak. 100
More broadly, however, there has been a clear shift in thinking about practitioner roles that increasingly highlights a health promoting role and one that also emphasises the practitioner’s role as a facilitator as well as medical or health professional expert. The growing emphasis on self-care, coproduction and supporting self-management has influenced approaches to health promotion. However, in general practice the emphasis appears to have been an increasing focus on individual lifestyle and clinical interventions with patients identified with specific risk factors or with existing morbidities. The shift has been reflected in the definition of core professional values and the incorporation of population health as a core professional value80,81 but does not appear to incorporate core public health skills such as those identified in the public health skills framework. 101 This has been developed by Public Health England (PHE) to provide a clear structure for public health practice and professional development in public health.
There has also been a growing interest in the roles of non-nursing, non-practice-based community staff such as community pharmacists. 102,103 Agomo undertook a scoping study exploring the range of roles that community pharmacists were providing in public health. 104 Dominant activities were smoking cessation, healthy eating and lifestyle advice, provision of emergency hormonal contraception, infection control and prevention, promoting cardiovascular health and blood pressure control, and prevention and management of drug abuse, misuse and addiction. However, the study identified gaps in the UK evidence base and in knowledge of what activities were being undertaken in some geographical areas (e.g. London).
General practice as a location for public health activity
General practice has been seen as an ideal location for health promotion activities, as it is the location of most individual contacts with the health service in the UK. In 2008/9 there were just over 300 million GP consultations in England. The average number of patient consultations each year has been gradually increasing from 3.9 in 1995/6 to 5.5 in 2008/9. Since 2004 in particular, there has been a change in the proportion of patients seen by nurses in primary care, with the proportion of nurse consultations increasing from 21% to 34%, and consultations with GPs reducing from 75% to 62%, reflecting changing workload patterns. This shift may reflect a change in recording of nurse consultations as well as an increase in the numbers of patients seen. This represents a high degree of contact with practice populations. While recent changes in out-of-hours care, increased advice roles for pharmacists and the development of telephone advice lines and walk-in centres have provided alternative points of contact, general practice remains the main first point of contact and ideally placed to develop and support health improvement activities.
However, in many ways the boundaries of the practice have changed, as many community activities are linked to general practice through the activities of community nurses and there is a recognition that some activities traditionally associated with general practice may be better provided in other community locations including people’s homes, schools and community pharmacies. In addition, there is a greater expectation that the role of general practice is to refer people to preventative activities such as specialist stop-smoking services, weight loss services and exercise activities. Developing closer links with schools – for sexual health and other health support services for young people – has led to not just school nurses but other health professionals working in schools. With changes to the structure and delivery of health services, some activities traditionally seen as part of general practice can now be delivered by a range of agencies such as community organisations delivering the NHS Health Check.
Watson15 has suggested that, rather than focus attention on general practice as a location for health promotion, the development of the concept of a health-promoting practice should be employed. Drawing on ideas in the World Health Organization Ottawa Charter for Health Promotion,105 Watson argues that it is possible to conceptualise the practice as a setting. While the focus of ‘settings’ has been on the community or schools and workplaces, the principles of the ‘settings’ concept can be applied to primary care. ‘Settings’ literature has emphasised key central concepts that involve the desire to act on policies, reshape environments, build partnerships and develop empowerment and ownership as well as developing personal competencies for public health. 106,107 There is also a shift from medical expert to change facilitator for health promotion. This broadens the perspective of activities and who undertakes them, where they are undertaken and how they are delivered. It shifts attention away from specific interventions for individuals and places health promotion practice in general practice within a broader social and environmental context. In undertaking this review we have drawn on this concept to structure our data collection and analysis.
Conclusion
The discussion of current issues raises a number of concerns about examining the public health role of general practice and primary care. These relate to two broad themes. The first is methodological. While there has been a substantial number of research papers and reviews on health promotion in general practice, the focus has been on the intervention. Very little attention appears to have been paid to the way interventions are delivered or organised. Reviews, in particular, have not addressed this organisational context. The second is that many reviews draw on international evidence and this raises important questions about their relevance to UK general practice. While not unique in terms of its structure and organisation, UK general practice has a particular organisational form, tradition and funding structure which are different from most other countries. Such differences – the QOF being a good example – are likely to create different incentives and contexts within which health promotion takes place.
It is also clear that much of the literature and research on health promotion focuses on the relationship between the practitioner and the individual patient. UK general practice operates within an individualised medical model. 48 Developments in recent years have tended to strengthen this focus, with an emphasis on individual, clinical (predominantly pharmaceutical) preventative interventions. Broader, more community-based approaches – such as those advocated by Julian Tudor-Hart,14 for example – tend not to be supported by policy or professional and regulatory guidelines. Following the Marmot Review29 there has been more policy interest in developing the public health role of general practice, and new QOF criteria to promote preventative activities are being developed by NICE. However, there remains a degree of uncertainty within general practice itself about its public health role and how preventative interventions are best delivered.
Chapter 3 Methods
Introduction
Our methodological approach was based on the standard methodology for scoping reviews. 108,109 It consisted of two components: (1) literature review and (2) consultation with key stakeholders. The findings from these components were integrated to establish how well current knowledge mapped onto priorities and issues identified by stakeholders, to identify gaps in knowledge and future priorities.
The aim was to conduct a synthesis of the research evidence and wider literature on public health and primary care. Reviews of health improvement interventions pose numerous challenges due to multicomponent interventions, diverse study populations, multiple outcomes measured, the wide range of approaches and study designs used, and the effect of context on intervention design, implementation and effectiveness. 110 An initial scoping of the literature identified in excess of 20,000 papers that may be relevant to the topic area, and we developed strategies designed to manage paper selection and data extraction. The aim was to undertake a review of the extant literature on health improvement and primary care, focusing on the contribution of activities undertaken in or associated with general practice, wider practice and the primary health care team. However, following changes to the NHS and developments in public health service provision in England, the scope of the review was extended to include non-practice-based health improvement activity. This included exploring the roles of primary health care team members in the community and schools, and community pharmacists. However, the focus remained primarily on those activities associated with general practice, and our search strategies were based upon this central premise.
The review focused on examining the health improvement role of general practice in England, Scotland, Wales and Northern Ireland. We initially intended including English-language papers on health improvement roles in health systems with similar general practice organisational arrangements (e.g. Holland, Sweden, Canada, New Zealand), however, the initial literature searches identified a substantial number of papers and, given the specific nature of UK general practice and the need to produce findings relevant to the delivery and organisation of public health activities in UK general practice, it was decided to restrict the searches to UK studies only.
This study was not a systematic review of the literature but, in order to provide a comprehensive synthesis of the evidence, the team approached the review drawing on systematic methods. The conceptual complexity of both public health and primary care raised a number of initial problems in identifying key words for the literature search. In addition, the team also recognised that a focus on service delivery and organisation would create difficulties in identifying relevant literature. It was decided to approach the review in a number of stages including a hand search of selected primary care/public health journals and NHS public health reports. This was to be followed by an initial search of key databases and then broadened to cover all relevant databases. Dependent on the number of papers found, we would then develop a strategy for paper selection.
Ethics
Formal NHS ethical approval was not required, as the study sought information only on current service delivery. The study was classified as service evaluation as defined by current National Research Ethics Committee guidelines: Defining Research, published by the NHS Health Research Authority. 111 The research was conducted in line with ethical standards relevant to applied research and had approval from the London School of Hygiene and Tropical Medicine ethical committee.
Preliminary hand searches
To facilitate the development of search terms for the literature search, preliminary hand searches of key journals and PCT public health reports were undertaken. The purpose of this preliminary work was to create a more useful list of keywords for our search. We selected two recent director of public health reports from each strategic health authority: one from a rural PCT and one from an urban PCT (based on calculated population density). The reports were reviewed for references to ‘GP’, ‘general practice’, ‘primary care’ and ‘primary health care’. Each report was also skimmed to make sure relevant references were identified. We recorded any discussion of health problems in relation to general practice and any mention of general practice interventions as well as noting the common words or phrases used.
Journals included in the hand search were the British Journal of General Practice, Health Promotion International, the Journal of Public Health and Primary Health Care Research and Development. Tables of contents from 1990 to the present were skimmed for titles relating to health promotion or disease prevention services delivered in general practice or by general practice staff. Broad selection criteria were used, and all study types were considered. Full-text papers were downloaded and skimmed and, if the paper still fitted our topic, three pieces of data were recorded for each paper: relevant keywords used, health problem discussed and type of intervention discussed.
In addition to these hand searches, the research team met with public health experts, local public health managers and staff in general practices. The aim of these discussions was to help focus the review and provide a rationale for paper selection. As a result it was decided that we would categorise papers that were selected for review into one of four categories:
-
include for evidence synthesis of approaches to delivery/organisation of health improvement
-
include because tells us about health improvement activities undertaken in primary care
-
mark as a paper ‘of interest’
-
reject paper.
While the evidence synthesis focused on the first category, we also decided to include papers in the second category in the review, as they provided useful information about the range of activities being undertaken in general practice.
Preliminary results
There was a wide variation in the amount that GPs were mentioned in PCT public health reports. Several reports did not mention general practice at all while others listed innovative measures that general practices were implementing to tackle public health problems.
Four journals were searched for papers on general practice provision of public health services between 1990 and 2010. Numbers of relevant papers from each journal were 75 from the British Journal of General Practice, six from Health Promotion International, 15 from the Journal of Public Health and six from Primary Health Care Research and Development.
Based on this list of terms, we undertook a MEDLINE search, which yielded over 100,000 hits. A rapid review of a small selection of abstracts showed that few papers were likely to be relevant. This result suggested that our search strategy was too wide. However, we also found that a number of the papers that we uncovered in our hand search had not been detected by this broad search strategy. Our next step was the practical one of narrowing our search finding to a manageable number of papers. We developed a second search strategy that identified specific keywords that appeared to generate substantial relevant hits from within our original list of terms. We also restricted our search to the UK to try to identify a manageable pool of references. See Appendix 1 for the literature search strategy.
Initial literature search
Thus, an initial search of Ovid MEDLINE, informed by the keywords obtained from the hand searches, was conducted by combining synonyms for primary care, public health and the UK. The search strategy is listed in Appendix 1. Results were limited to academic papers published in the English language between 1990 and 2010. The search yielded 14,948 references. Bearing in mind that the final literature search was planned to be conducted on four databases, this high number of papers from one database was deemed to be unmanageable for paper selection. Steps were therefore taken to further refine this search.
Refinement of literature search
The initial search was refined by replacing the public health search terms with synonyms for three areas of public health highlighted in the Healthy Lives, Healthy People White Paper. 37 These were ‘prevention’, ‘health improvement’ and ‘health promotion’. Thus the search was a combination of synonyms for these three areas of public health, primary care and the UK. The search was run on four databases, namely MEDLINE, EMBASE, Global Health and CINAHL Plus, using strategies designed specifically for each database, described in Appendix 2. Results were limited to academic papers published in the English language between 1990 and 2010. This search yielded 7209 results in total after duplicate references were removed using EndNote X4 software (Thomson Reuters, CA, USA).
The discrepancy between 7209 results from four databases in the refined search and 14,948 results from one database in the initial search led to concerns that the refined search may have missed relevant papers. In order to investigate this, a sample of references published in June of each year from 1990 to 2010 which were retrieved by the initial search but not by the refined search were examined. From this, eight additional areas to supplement the refined search were identified. These were alcohol and drug addiction, brief interventions, exercise therapy, immunisation, lifestyle, risk reduction, screening and smoking cessation. Synonyms for the eight areas were combined with search terms for primary care and the UK, and limited to academic papers published in English between 1990 and 2010, as before. The search strategies for each of the four databases are shown in Appendix 2.
The final literature search results consisted of references retrieved by combining the search strategies used in our refined search (see Appendices 1 and 2). Duplicate references were removed using EndNote X4 software. The process was repeated on 12 May 2012 to identify papers published in 2011 and early 2012. The total number of references retrieved for the years 1990–2012 was 16,791.
Paper selection
Paper selection was conducted in three sequential stages: by title, by abstract and by full text. At each stage, the following inclusion criteria were used:
-
Is it focused on primary care?
-
Is it health improvement (defined as primordial, primary, secondary or tertiary prevention, and also encompassing health promotion)?
-
Is it, or could it be, related to service delivery or organisation?
-
Does it report research findings or, alternatively, does it contain a description of health improvement activities undertaken in practice?
If the answers to all four questions were yes, the paper was progressed to the next stage. Where abstracts were unavailable or did not provide sufficient information to assess the paper’s relevance, the full text was obtained in order to assess relevance.
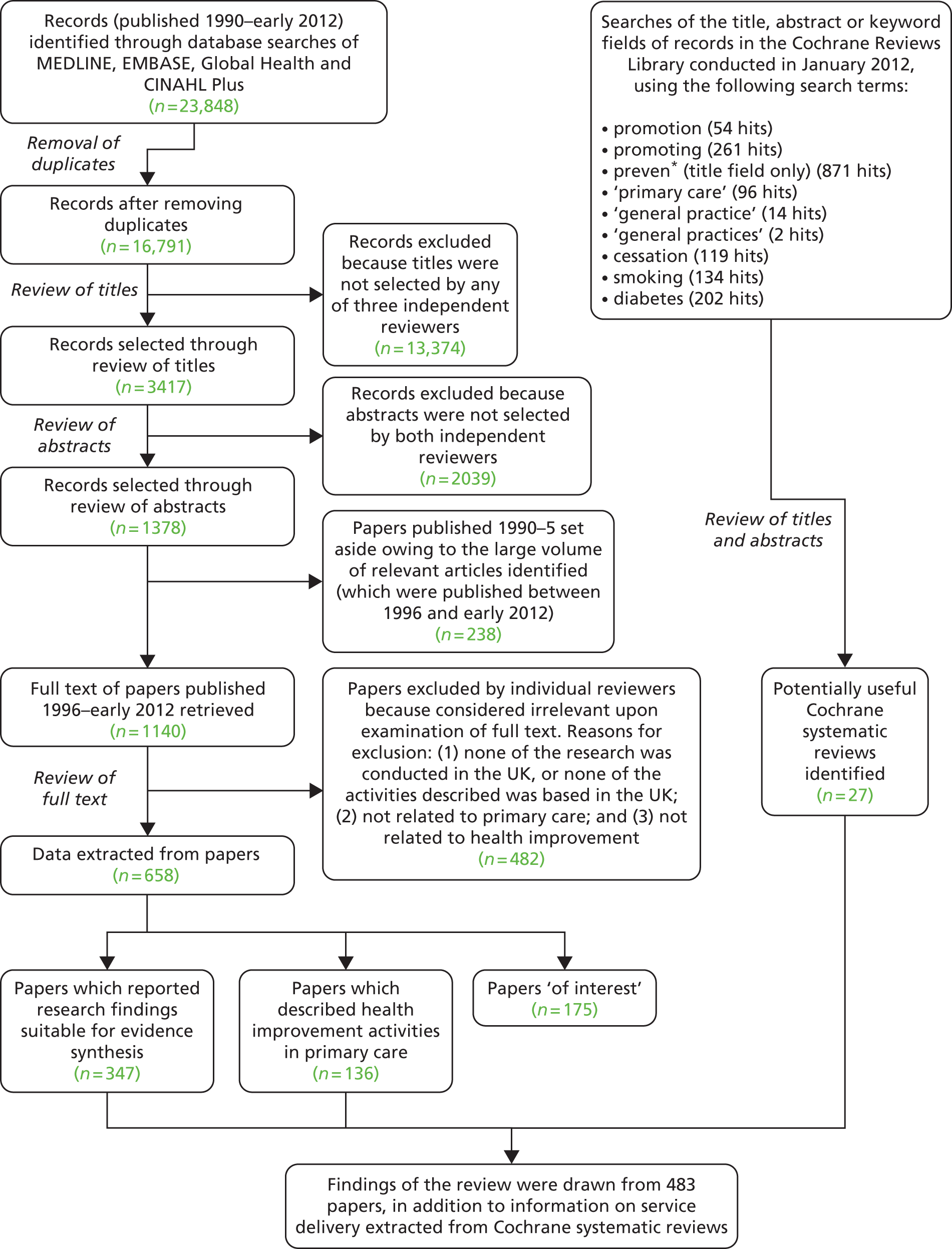
The 16,791 references were divided so that, in the title selection stage, the title of each paper was reviewed separately by three reviewers. If any one reviewer considered a paper to be relevant, it was progressed to the abstract selection stage. In the abstract stage, references were divided so that each abstract was reviewed separately by two reviewers. If both reviewers considered a paper to be relevant, it was progressed to the full-text stage. In the full-text stage, data from each paper were extracted by individual reviewers. There was also an opportunity to discard papers at this stage, if considered to be irrelevant upon examination of the full text. The overall search and paper selection process is shown in Figure 1.
FIGURE 1.
Flow diagram of review process.
Supplementary searches
In addition to our database searches we undertook a search of The Cochrane Library to identify potential reviews that might have relevance to our review. Searches of the title, abstract or keywords of reviews in The Cochrane Library were performed in January 2012 using the search terms listed below:
-
promotion – 54 results
-
promoting – 261 results
-
preven* (search restricted to title field only) – 871 results
-
‘primary care’ – 96 results
-
‘general practice’ – 14 results
-
‘general practices’ – 2 results
-
cessation – 119 results
-
smoking – 134 results
-
diabetes – 202 results.
The results were manually reviewed to identify potentially relevant reviews.
We then examined each of the final results for any information relating to public health service delivery and organisation in primary care. We identified 27 potentially useful reviews (see Appendix 3). In addition there were three reviews in progress that were possibly relevant and we also identified a review on Interventions to implement prevention in primary care that was registered in 2001 but then withdrawn in 2005 owing to a lack of resources available to undertake the review.
The results of these reviews were incorporated into the findings from our literature search. While there is inevitably some overlap of papers, we conducted a brief cross-check. Given the differences in search strategies, review focus and quality assessment, this was limited.
We also examined NICE guidance on public health and primary care but this was more limited. NICE started undertaking public health reviews only recently. However, where relevant, the guidance is referred to in this review.
Finally, we searched for other reviews that focus on public health and primary care. Two key reviews were identified. The first was undertaken in Canada23 and the other was by the Committee on Integrating Primary Care and Public Health Board on Population Health and Public Health Practice, US Institute of Medicine. 24 Both these reviews examined the relationship between primary care and public health. The first of these had a very broad focus and had little direct relevance to general practice or actual health improvement activities. The US review was very specific on the US context and the potential for developing public health in primary care. Neither review added anything substantial to our own searches but they are referred to where relevant.
Data extraction
Given the large volume of relevant papers identified, a decision was made to perform data extraction on a subset of papers published from 1996 to early 2012. We identified that older papers tended to be selected less and decided that we would therefore restrict full data extraction to after 1995. We retained the selected references for 1990–5 and, where relevant, examined and included papers in the review where they added additional information. The topic ranges for these papers focused on a small number of themes including health checks for older people, smoking cessation, health promotion payments (under the 1990 GMS contract) and CVD. There was a large number of papers describing activities in general practice and the community. There has been a substantial number of changes to the funding and organisation of primary care since the mid-1990s, and therefore we focused mainly on the more recent papers. Details of selected papers are given in Chapter 4.
Data were extracted from each relevant paper into an Access 2010 (Microsoft Corporation, Redmond, WA, USA) database using a standardised form, which is included in Appendix 4. The form had been designed by the research team and contained fields to capture information on the type of study, outcomes, population targeted, service provider and main results. For intervention studies there were fields for describing the intervention and how it related to service delivery or organisation. Designing a single data extraction form for use across all types of studies was complex and the final format did not provide a single structured way to extract data from qualitative studies. The limitations of the data extraction form were:
-
The depth and nuances of the information extracted from qualitative studies may have been limited by all researchers extracting data not having a ‘rule’ about which findings to extract from qualitative papers, other than ‘a summary of the results and conclusions’.
-
It relied on researchers using individual judgement to interpret the ‘outcome assessment (risk of measurement bias)’ criterion of the quality assessment section about how appropriately and reliably data were collected in the qualitative studies to address their aims.
To counter this we undertook extraction on a group of papers and compared results between researchers to obtain some cross-researcher consistency. In addition, when drafting results sections authors returned to a number of key full texts to ensure correct data interpretation. During data extraction, papers were grouped in terms of whether they simply described health improvement activities in primary care, or they reported research findings which could be included for evidence synthesis. Quality assessment was conducted on the latter group of studies.
Quality assessment
Several tools exist for determining the quality of studies for reviews. However, given the large volume of papers included in this review, and the diversity of study designs which were both quantitative and qualitative, it was not possible to find one tool that would be sufficient for the task. Instead, a general assessment of the quality of each study was formed by critiquing five areas:
-
quality of the sampling process (including the sample size)
-
appropriateness of the analysis
-
comparability of the intervention and comparison groups
-
quality of the intervention delivery (including whether consistency of the intervention was measured or there was risk of contamination)
-
outcome assessment.
For each area, reviewers stated in the data extraction form whether or not the approaches taken in the study on these five criteria were applicable to the study design. The reviewers indicated, under each area, whether they had no concerns, minor concerns or major concerns. Studies were graded as:
-
A, high quality, if there were no concerns across the applicable areas
-
B, good quality, if there were one or two minor concerns
-
C, lower quality, if there were major concerns or multiple minor concerns
-
D, poor quality or not assessable, if there were major concerns or insufficient detail.
The goal of our search strategy was to identify a body of literature on the delivery and organisation of health promotion and disease prevention undertaken in general practice. We expected problems in identifying relevant papers, but the main problem was that we found many unrelated results while missing out some relevant ones. Several challenges were identified that make it difficult to (1) define the topic of general practice and public health and (2) identify the literature on this topic. These challenges can be categorised as ‘practical challenges’ and ‘conceptual challenges’ as follows.
Practical challenges
In our search strategy, papers needed to have a GP or primary care-related term in the title or abstract in order to be picked up. This was clearly necessary to keep findings relevant to our topic, but this strategy misses the body of research on clinical interventions that are delivered in a different setting rather than in general practice. For example, some studies on smoking cessation or exercise on prescription were not done in general practice, so these papers did not have a ‘GP term’ in the keyword list, title or abstract. However, these interventions are in reality often delivered by GPs, so these studies were relevant to our scoping study. This problem was discovered when investigating papers from the hand search that did not appear in the literature search results, and accounts for some of the papers we ‘missed’ in our database search.
Conversely, many of the studies that do involve general practice are surveys of GP knowledge and attitudes, audits of GP patient lists, or surveys of patient reactions to GP-provided services. These qualitative studies are useful for defining a problem or gaining patient perspective, but seldom provide evidence on outcomes of interventions. The abundance of this type of study became clear after a quick scan of the results from our database search, and it partially explains the large number of studies we recovered with our search terms that were not relevant to service delivery.
There are several types of interventions and diseases that are particularly common in the literature of GPs and health promotion, for example behaviour modification and CVD. It would be useful to do broad searches that include these terms to ensure that we have covered these topics, as they relate to our questions, in their entirety. However, the terminology used for these and many other topics is not straightforward. For example, behavioural interventions use a variety of phrases such as ‘health behaviour’, ‘lifestyle management’ and ‘behaviour modification’. Relevant studies on CVD use the terms ‘cardiovascular disease,’ ‘coronary heart disease’ and ‘coronary risk factors’ among others. This use of different keywords to describe the same disease or same type of health interventions makes it difficult to be sure of the completeness of a search. This is a problem for those trying to do review studies, but it also makes it difficult for practitioners at every level (from GPs to PCT public health officials) to find information quickly on a given topic.
As in many fields, the hand search showed that research priorities in general practice and public health have changed over time. These changes in research reflect changes in disease prevalence (as in the case of the rapid increase in obesity-related studies) as well as changes in policies and GP contracts. For example, studies on health checks for over-75-year-olds that were introduced in the 1990 GP contract have been largely replaced by studies of health checks for over-40-year-olds. These changing priorities over time raise questions for our research focus and whether to focus more on the more ‘current’ issues or to give equal weight to all topics that have been researched since 1990.
Finally, a key challenge was to identify papers that specifically addressed service delivery and organisational aspects of health improvement in general practice. It was not possible to use organisational criteria in the search so it was necessary to examine each paper for any reference to delivery and organisational issues. Most papers focused on the intervention and its efficacy or describing the intervention but provided less detail on how it was delivered.
Conceptual challenges
Public health is, by definition, about the health of populations. A good example of what this means for research is displayed on the Cochrane Public Health Group website, which states that: ‘The CPHG [Cochrane Public Health Group] facilitates the production of systematic reviews of the effects of public health interventions to improve health and other outcomes at the population level, not those targeted at individuals’ (their emphasis). 112 But GPs usually deal with health by treating one individual at a time, which seems to conflict with the concept of ‘public health’. However, the collective action of primary care and some individual interventions – such as immunisation – can be seen as having a population effect. Because our research is focused on delivery methods and organisational factors, it attempts to look beyond the individual patient interaction, but research on interventions delivered in general practice ultimately comes down to a one-on-one interaction. This definitional conflict raises questions for our inclusion criteria and how to determine whether or not a study truly qualifies as being about ‘public health’.
The prevalence of chronic diseases and the new focus on their prevention has complicated notions of primary, secondary and tertiary prevention. For example, in the case of a person who has a poor diet and is physically inactive, then goes on to become overweight, and then develops high blood pressure and abnormal cholesterol levels, where does the disease process start? Is primary prevention the prevention of becoming overweight, developing hypertension or developing CVD? Similarly, many titles retrieved in our search focus on self-care for chronic diseases such as diabetes or asthma. Technically, these are about managing an ongoing condition, but the goal of self-care is to prevent progression of disease or hospitalisation, so they could also be thought of as prevention. With topics in the ‘prevention’ literature ranging from recommending healthy diets to managing patients after a heart attack, it becomes difficult to assemble the evidence or even decide what to include in a review of prevention interventions.
Two related questions that have revealed themselves both in the hand search and in a quick review of our search results are (1) where, physically, does general practice end and (2) who constitute the general practice team? Considering the physical space of the general practice gives a different answer from considering the staff of a general practice, as health visitors work with a GP surgery but by definition practise outside the surgery door. And if we extend our focus to all primary care staff the picture becomes even more clouded. Who exactly constitutes a primary health-care provider? Our literature review brought up a large number of results about dentists, school nurses and community pharmacists. While we can easily draw our own boundaries and eliminate certain types of providers or locations of service from our review, the results of our searches caused us to reconsider our initial definitions of general practice, as it brought up types of providers that we had not previously considered.
Consultations with stakeholders
Our original plan was to hold regional stakeholder events and invite practitioners to these to discuss public health issues. However, the period during which the research was undertaken was one of substantial upheaval in the NHS. Following discussion with key stakeholders and with NIHR Evaluation, Trials and Studies Coordinating Centre SDO Programme staff, this approach was amended to one whereby we would undertake more individual discussions with practitioners in general practice and with other key informants. In addition, we were able to draw on interviews conducted for a study on early developments in CCGs and some group discussions with GPs.
The research team undertook a number of discussions with key general practice stakeholders. Initial discussions were held in 2011 with NHS public health, general practice and health promotion staff in England and Wales:
-
two primary care health promotion advisors in Wales
-
a director of public health (London)
-
two practice visits in Wales involving interviews with four GPs, two practice nurses and one practice manager
-
two practice visits in England involving interviews with three GPs, three practice nurses, one community nurse and two practice managers.
These visits and interviews were exploratory and helped shape the initial scoping of the literature. The researchers explored key issues as identified by the staff members. Key issues and themes were noted by the researchers. We were also able to capitalise on research being undertaken on emerging CCGs by the Policy Research Unit in Commissioning and the Healthcare System, which is directed by Professor Stephen Peckham. This involved interviews with staff in PCTs, emerging CCGs and practices in eight areas in England and were conducted in 2012. These interviews explored public health roles and responsibilities and the potential impact of organisational changes currently under way in England. Research team members were also involved in concurrent research on primary care, and the opportunity was taken to ask GPs and practice staff in a number of practices in London, the Midlands and the North West to discuss health improvement activities in their practices. In total we drew data from 45 interviews undertaken with practitioners. These included 11 GPs and 11 practice nurses interviewed within the context of their practice, 16 CCG board members (15 GPs and one nurse), three lay members and four public health specialists/consultants.
In addition to individual interviews, two group sessions were held with GPs in two locations to discuss public health roles. One group consisted of 38 GPs in a 3-hour session on public health and general practice. GPs in this group included GP principals, salaried GPs and some trainees. In addition, research team members held a group meeting of eight GP principals, including one GP trainer. Finally, during the research one researcher was involved in the King’s Fund review of quality in general practice,18 which included two discussions with a wide range of stakeholders (GPs, public health specialists, nurses and patient organisations) on health promotion in general practice. Given that the aim of this element of the research was to inform the scoping review and our analysis, interviews and discussions were not recorded and we relied on researcher notes.
The data from these discussions and interviews were in the form of interview extracts (from the research on CCGs), field notes and observations from group meetings, and notes from individual discussions with practitioners. Researchers discussed the notes and interview extracts, and used these to develop key themes. These were used in refining search terms (described earlier in this chapter) and in interpreting literature findings. The discussions and interviews also highlighted the significant impact of the changes in the English NHS that occurred during the period of the research. These data have informed the discussion of this report and the key themes arising from the interviews and discussions are reported in Chapter 4.
Evidence synthesis
For this review a key challenge was to identify evidence on the delivery and organisation of health improvement interventions rather than the effectiveness of a specific intervention irrespective of the context within which it is delivered. As Rychetnik et al. 113 have argued (p. 119):
Public health interventions tend to be complex, programmatic, and context dependent. . . . The evaluation of evidence must distinguish between the fidelity of the evaluation process in detecting the success or failure of an intervention, and the relative success or failure of the intervention itself.
In particular they argued that, where an intervention is unsuccessful, it is important that the evidence should help to determine it was inherently faulty as a result of the failure of intervention concept or theory, or simply badly delivered. It is also important that there be sufficient descriptive information on the intervention and its context to allow for the proper interpretation of the evidence.
In our review we were reliant not only on whether or not contextual issues had been included in the study but also on whether or not these details were reported in the published papers – which was not always the case. Given the breadth and diversity of the topics and papers, and the limited amount of data on service delivery and organisation, the research team agreed that a narrative synthesis would be the most appropriate approach. 114,115 All the papers were allocated topic tags and a member of the research team then examined groups of papers (e.g. on smoking, screening, CVD, child health) and key findings were reviewed to identify any common themes and if there was any evidence to support particular approaches to the delivery and organisation of health improvement activities. Given the range of material, we adopted a textual narrative synthesis, trying to group studies and data into more homogeneous groups. 116 Our approach was to develop an interpretive synthesis of the literature. 117,118 We developed the synthesis along two broad themes:
-
what kinds of activities were described in the papers
-
what evidence there was for effective approaches to service delivery and organisation.
Drawing on these data we then explored themes around the ways interventions were organised, who delivered them and where they were delivered to identify common issues.
Limitations of the review
This was a complex review to undertake because of problems about definition of terms and also because of the diversity of the topic. The research team made substantial efforts to identify appropriate search terms and develop inclusion and exclusion criteria. We had to take an approach that required only brief scanning of our original search results to reduce the numbers of potential papers. We adopted a checking system for papers initially discarded to ensure completeness. However, we recognise that our eventual strategy produced a particular set of results and that it is possible that other search strategies could have produced a fuller set of results in some areas of public health activity. However, without some initial scoping research in practices and across the literature, identifying these specific areas would have been difficult. For example, with emphasis on primary care/general practice we are aware that a number of more community-based health initiatives that might be usefully classified as primary care were not picked up in our search.
The rejection of papers identified as treatment or tertiary prevention may also have limited the final paper selection. Having completed the searches, we are aware that some topics may be better reviewed as a single group incorporating all activities relating to prevention, including all levels of prevention and treatment. Based on the experience of this review it is possible that in undertaking such a review there would still be very few data on the delivery and organisation of health improvement activities. It is probable that further primary research would be required to identify these aspects of how such interventions are undertaken in practice.
Our conclusions about the delivery and organisation of health improvement activities are also limited by the information provided in the published papers. Generally this was very limited, with the main focus placed on the intervention. There were papers that examined different interventions by different practitioners; for example, screening by nurses or GPs, pharmacists undertaking health checks, smoking advice given by GPs, nurses or health promotion specialists. There were also papers that discussed the provision of activities in different specific locations such as the practice, schools or pharmacies. However, very few papers made any comparison between different practitioners or locations. Most comparisons examined different interventions; for example, offering screening or screening and advice, or comparing verbal and written information but often without details of who did what.
While the selection of papers was undertaken by multiple researchers, the final selected papers were read by only one researcher and data extracted using the standard form. While we adopted a checking process comparing how all researchers read a selected set of papers to ensure consistency of approach and use of the data extraction form, it is possible that there were still differences in interpretation of papers between researchers – especially given the broad range of material reviewed. However, it is unlikely that such differences would have had a significant impact on the eventual conclusions in this review, as all researchers faced similar problems about the lack of detail and data irrespective of topic.
Presentation of findings
The results of the analysis of the literature are presented in three sections. In order to provide an overview of the range and type of literature and research, we have provided a descriptive analysis of the papers in the next chapter (see Chapter 4). Here the aim is to examine what topics and issues research has addressed, when it was published, and key characteristics in terms of quality and focus. We then present our analyses of the data in the papers on what kinds of activities are undertaken (see Chapter 5) and then what evidence there is of effectiveness (see Chapter 6).
Chapter 4 Description of papers and overview of findings
Introduction
This chapter provides an overview of the results of the literature search. The aim of this chapter is to provide some detail of the literature review results. It does not examine the evidence itself but rather provides an indication of the areas in which academic and research activity has been focused. The chapter also includes a brief resume of the key points arising from discussions with public health/health promotion staff in PCTs and local health boards, and primary care practitioners in general practice.
In the process of undertaking the review it was clear that there were important trends and features of the literature that are important. The first section of this chapter provides an overview of the search results by publication year and then the extracted papers are examined in relation to their assessed quality, type of prevention activity and details of the type of intervention, where it was provided and by whom. While 658 papers from our initial pool of 12 papers were extracted for more detailed examination, a number of these provided insufficient detail of interventions or were general discussion papers. Initially it was hoped to include data from these in general discussion sections, but generally these papers were not of specific use for describing either interventions or how they are organised. The number of references retrieved by the final literature search by year of publication is shown in Figure 2.
FIGURE 2.
Number of hits from literature search by publication year.
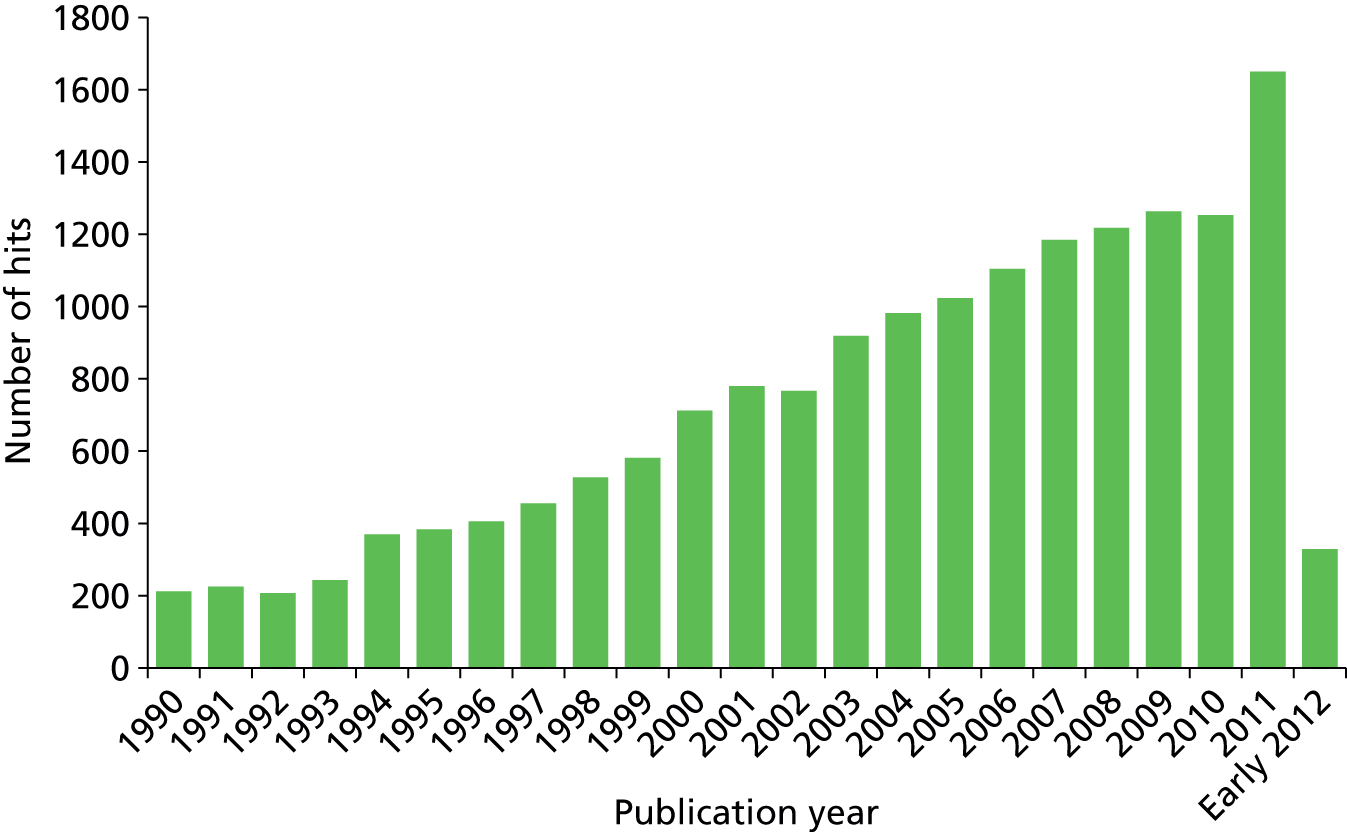
Figure 3 provides details of the numbers of papers extracted for review. What is interesting is the leap in numbers of papers extracted after 2006. We also looked at papers published between 1990 and 1996. Of the 1639 search hits, only 365 were selected for further review and of these 262 were considered for full-text review and inclusion in the study, but only a small proportion – approximately 20% – were research studies that provided evidence relevant to the review. However, examination of these papers revealed that many dealt with issues that were relevant only to the circumstances at that particular time. For example, a number of papers examined the development of health promotion interventions developed in response to the introduction of health promotion banding payments in the 1990 GMS contract. Others specifically examined the impact of the payments on activity. It was not clear, therefore, that these papers would provide relevant data for inclusion in a discussion about current practice. It was decided, therefore, to exclude papers from before 1996 unless they had directly relevant findings that could add to the general body of knowledge.
FIGURE 3.
Number of papers selected for data extraction by publication year.
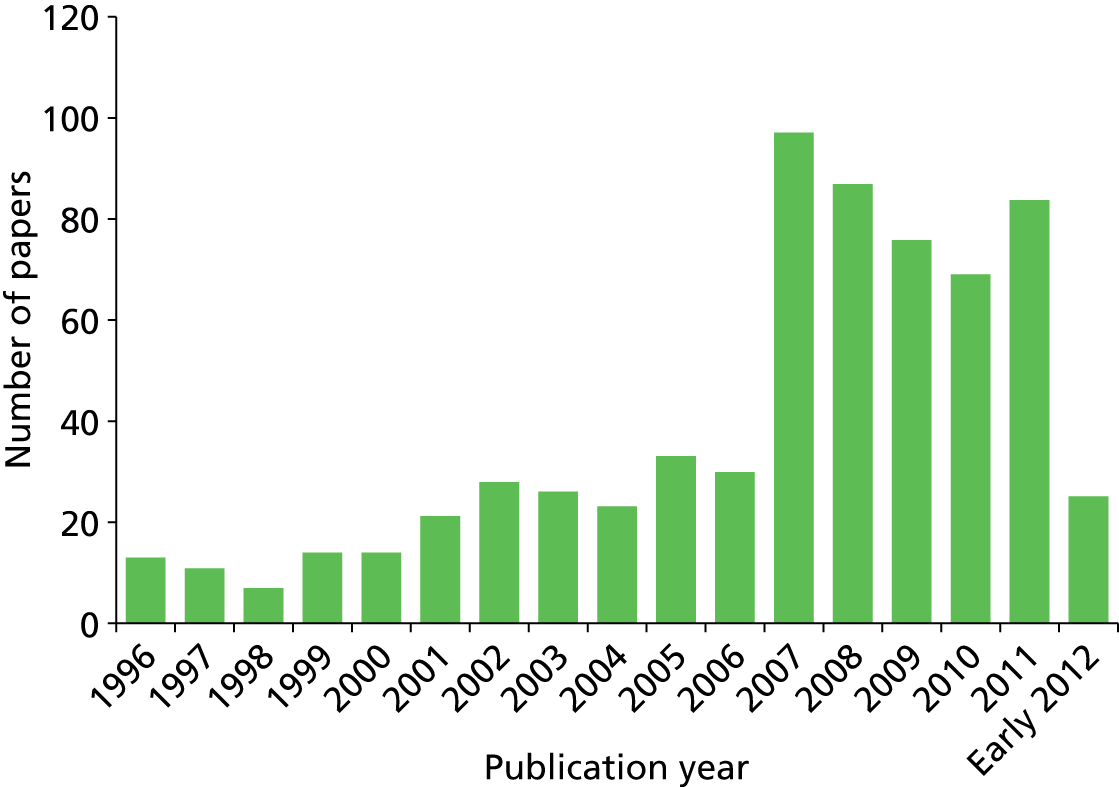
It was clear from the search that there were key journals in which papers were published. Figure 4 shows the top 20 journals in terms of the number of hits from the final literature search, and Figure 5 shows the numbers of papers in key journals selected for extraction. These demonstrate an enormous leap in the number of papers selected for review after 2006. This may indicate an increase in papers that address issues of delivery and organisation aspects of health improvement. One driver may be papers examining issues related to the QOF or a growing interest in health promotion research more generally.
FIGURE 4.
Top 20 journals in terms of the number of hits from the literature search. BMC, British Medical Council; BMJ, British Medical Journal.
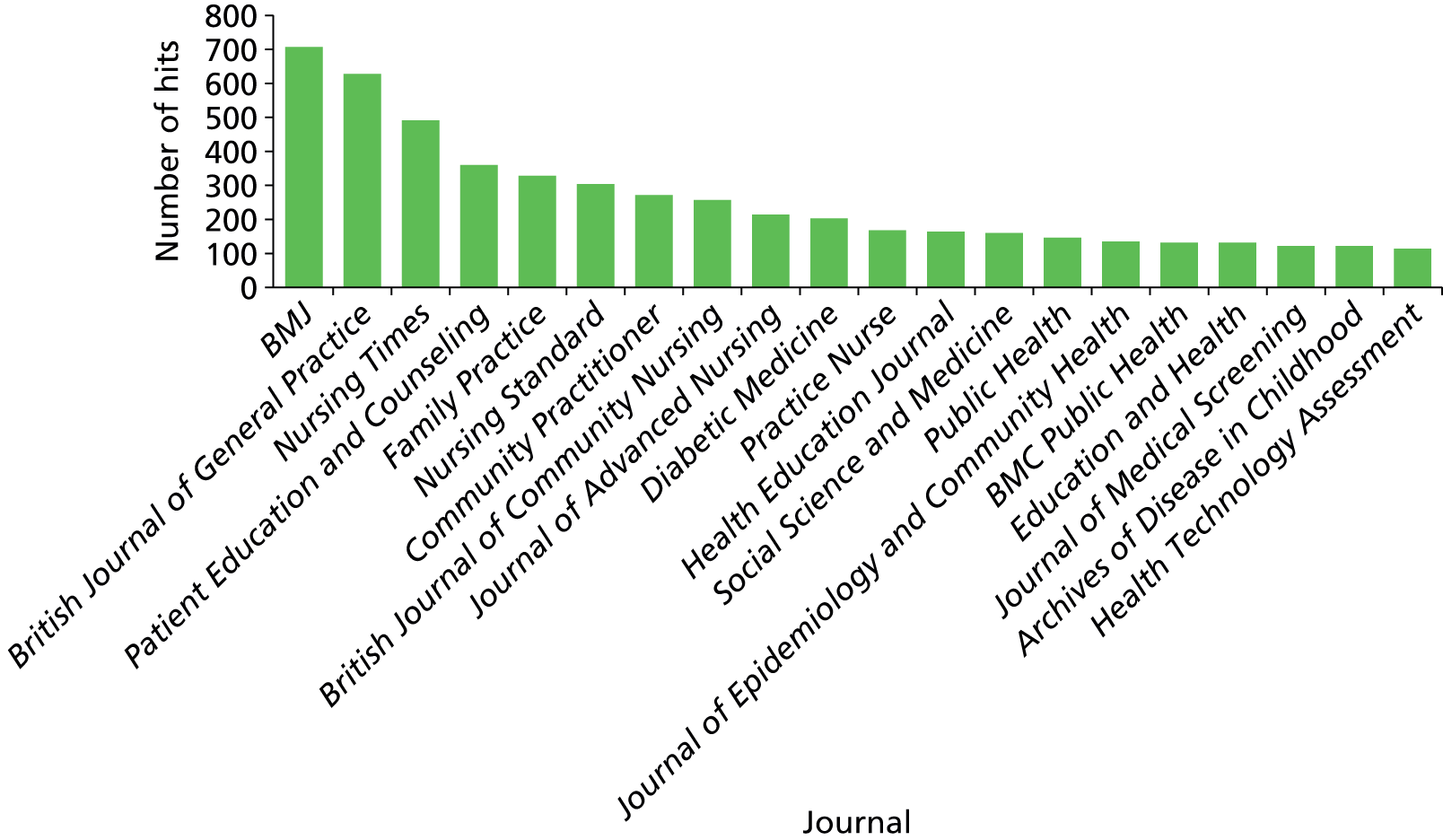
FIGURE 5.
Top 20 journals in terms of the number of papers selected for data extraction. BMC, British Medical Council; BMJ, British Medical Journal.
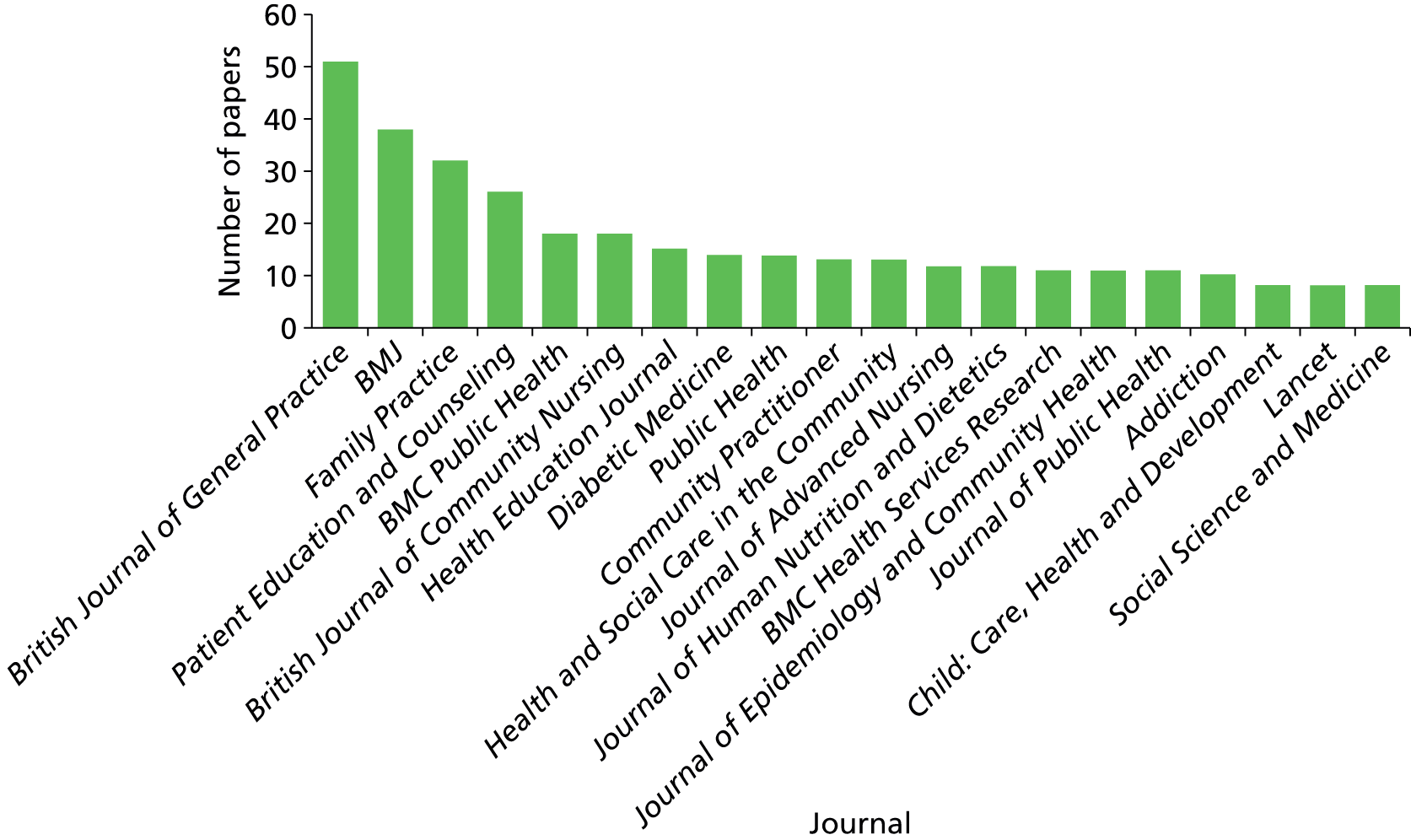
We then analysed the papers by topic. Each paper was allocated a topic tag based on assessment of the paper. These were categorised into primary topic and subtopics. A number of studies did not fit into topic categories and these were labelled ‘No specific topic’ or ‘Other specific topics’. Papers categorised as no specific topic were health improvement interventions that were either broad in scope or not aimed at a specific health problem. Examples of these types of interventions were community interventions and welfare advice. In addition, some papers focused on a practitioner role in relation to health promotion, such as school nurses or community nurses. Papers in the ‘Other specific health topics’ category were topic areas where only one or two papers were identified in our search. For example, these included papers examining hepatitis B screening, skin cancer, kidney disease, glaucoma and haemoglobin disorders screening. The main areas where papers were located were for CVD (15%), obesity (10%), diet and exercise (10%) and smoking (10%). This provides a broad indication of where the focus of activities, and to a certain extent research, is in relation to health improvement activities in general practice. However, following a review of the papers only 137 were selected for the evidence synthesis. The distribution of topics in these papers is shown in Figure 6. We then examined the numbers of papers selected for the evidence synthesis by topic area as shown in Figure 7.
FIGURE 6.
Distribution of topics of papers selected for the review.
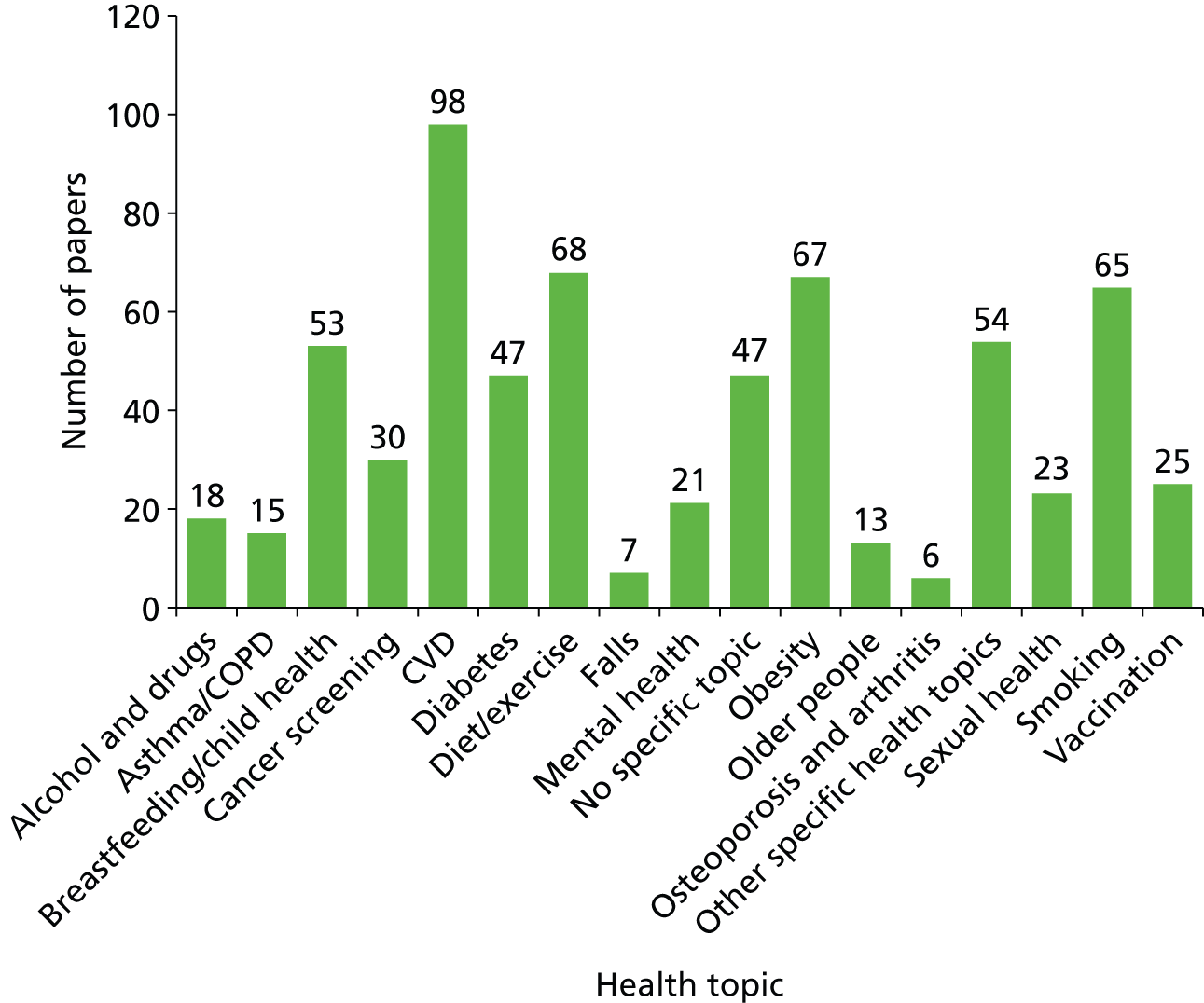
FIGURE 7.
Distribution of topic of papers included in evidence synthesis.
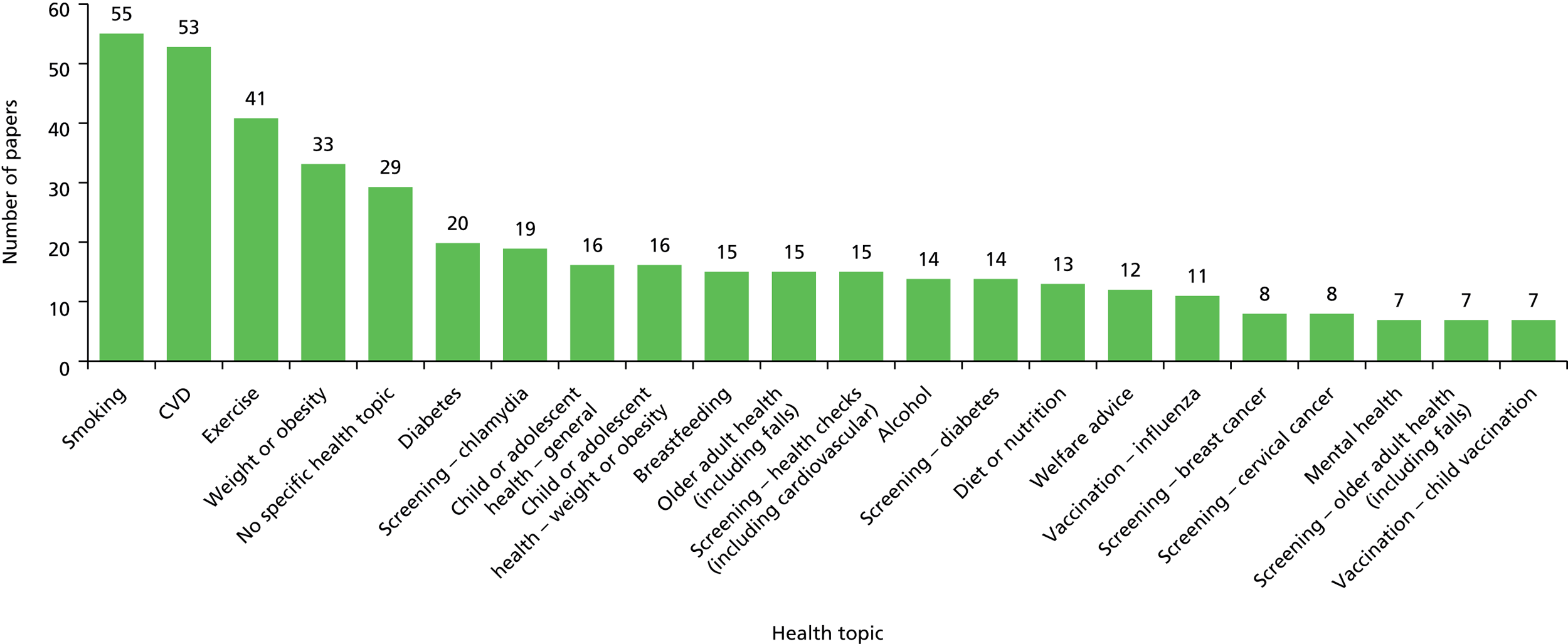
Comparing Figures 6 and 7 shows how the range of activities discussed in the literature does differ from what topics tend to be most commonly studied. Of the 347 papers selected for evidence synthesis, we graded them on the basis of an assessment of the quality of the research methods (see Chapter 3):
-
A, high quality (no concerns): 153
-
B, good quality (one or two minor concerns): 132
-
C, low quality (multiple minor concerns or major concern): 50
-
D, poor quality or not assessable (major concerns or lacked sufficient detail): 12.
The proportion of papers within each assessment grade is shown in Figure 8.
FIGURE 8.
Quality assessment of papers included for evidence synthesis.
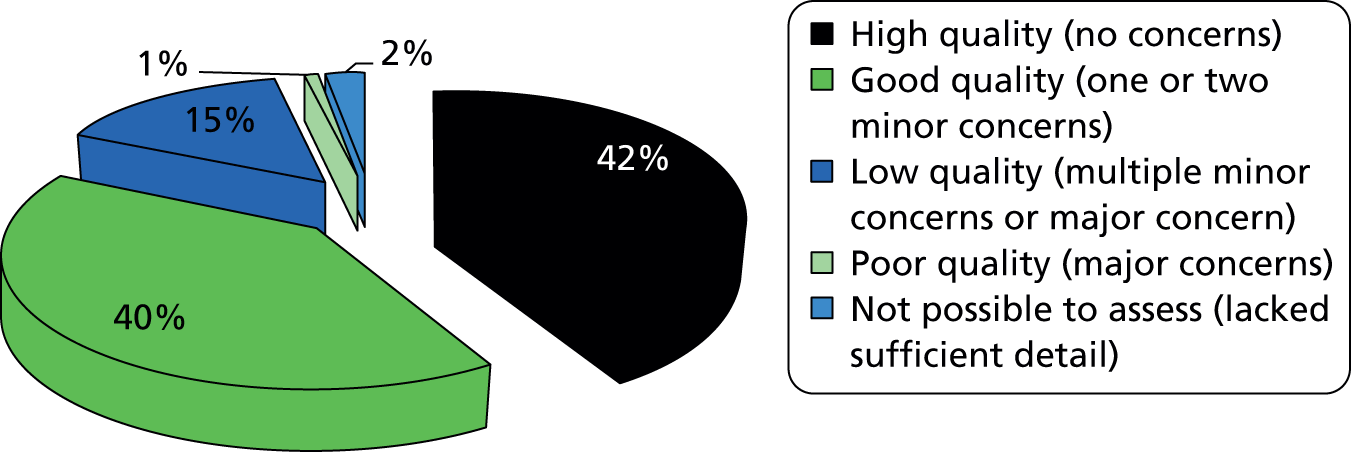
The selected papers encompassed a wide variety of research designs. Where details were provided we indicated the research design in the data extraction form. However, we did not rank study quality on a hierarchal basis as used in systematic reviews or meta-analysis. We assessed each paper as far as possible for rigour in the design used and whether or not the methods supported confidence in the reported outcome. The range of study designs is shown in Figure 9. It is important to note that the study design and quality assessment relate to the paper as a whole and they do not indicate whether or not we were able to make confident statements about the effectiveness of any particular approach to service delivery or organisation reported in the paper unless this was the specific subject of the research being reported on.
FIGURE 9.
Distribution of study designs.
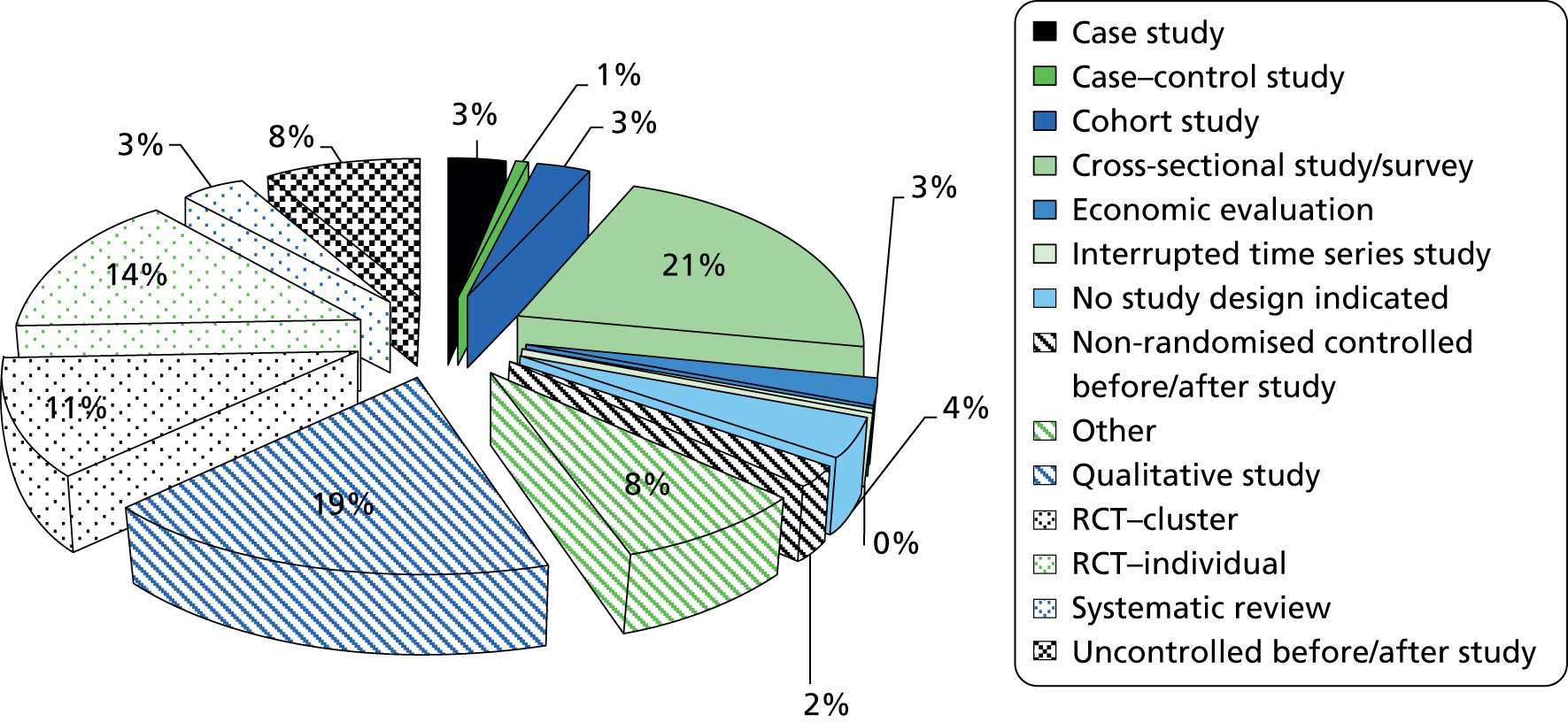
The biggest groups of papers were for qualitative methods studies and cross-sectional studies or surveys. Cross-sectional studies and surveys were primarily used to examine patient or practitioner knowledge or behaviour about, or as a result of, a health improvement intervention. The majority of these were in specific topic areas such as screening, smoking, and weight or exercise interventions (Figure 10). These tended to focus on the views or perceptions of patients/users and practitioners. None specifically compared groups and few provided before-and-after data related to an intervention.
FIGURE 10.
Distribution of topics of cross-sectional and qualitative studies. Note that total may be greater than 100% due to rounding.
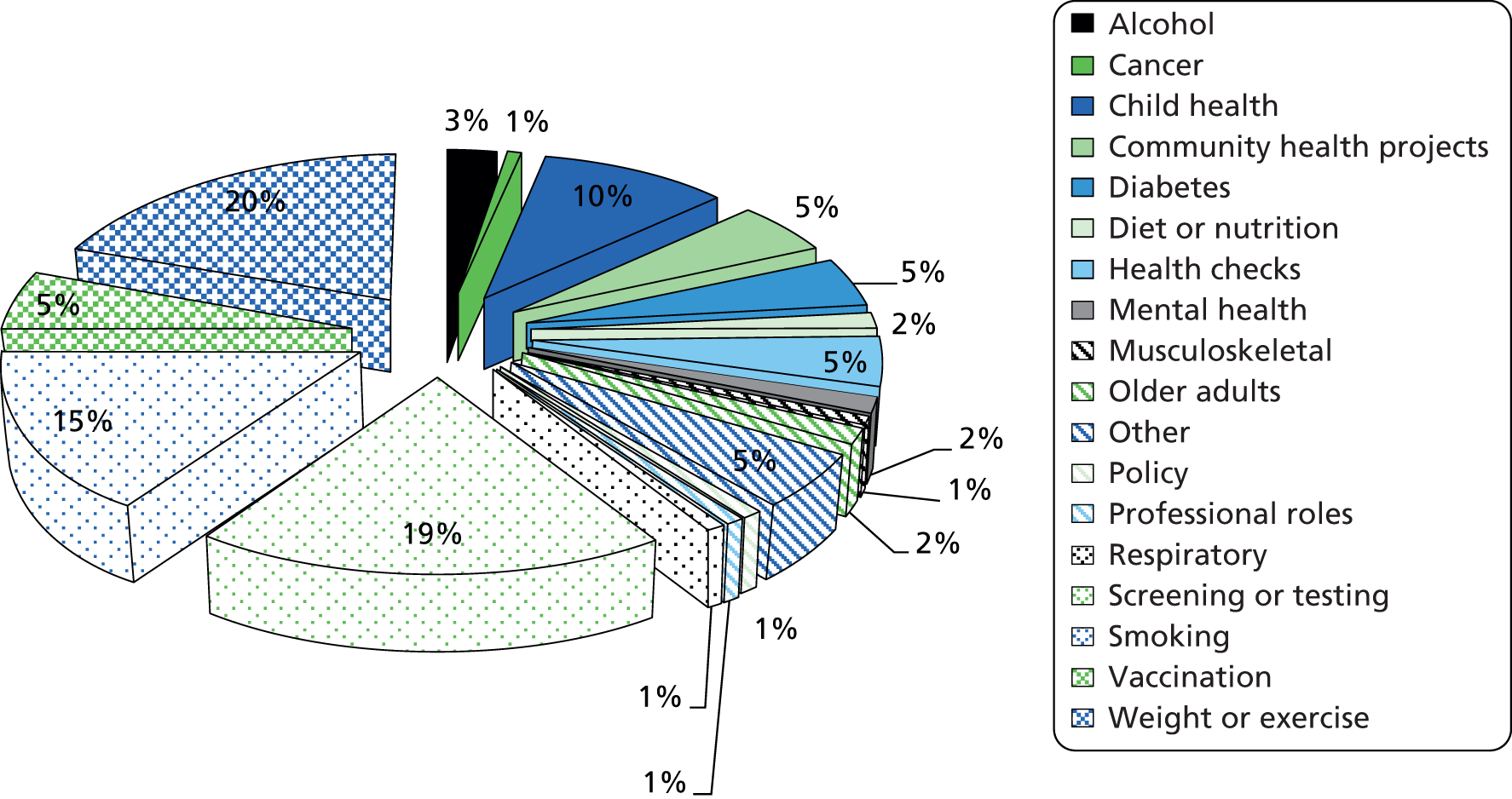
We were particularly interested in those papers classified as evaluating an intervention or evaluating a service delivery. The majority of papers identified as evaluating an intervention had little information on the context or organisation of the way in which the intervention was delivered. For example, interventions included a 10-week physical activity course delivered in schools but with no details of the actual programme or who ran the programme. Similarly, many educational interventions lacked details of who delivered it, where, in what way, etc. Generally papers contained few specific data on the content and context of interventions. There were 89 papers that evaluated the service delivery and organisation of interventions or aspects of practice. There was a mix of research designs, with many studies merely examining patient or practitioner views. Some studies – for stop-smoking interventions and weight/exercise – did look at outcomes but often the descriptions of the delivery of the intervention were limited in the published paper. Lack of detail or of focus on service delivery and organisation aspects of interventions was a general feature of the papers included for review.
We initially attempted to distinguish between three broad areas of health improvement activity: screening, primary prevention and secondary prevention. We excluded tertiary prevention from the study, as we classified this as treatment and outside the scope of the study. Defining papers and categorising them was not without problems. The distribution of papers selected for review and then for the evidence synthesis is shown in Figure 11.
FIGURE 11.
Distribution of topics in selected papers for review and for synthesis. Note that some papers cover more than one area.
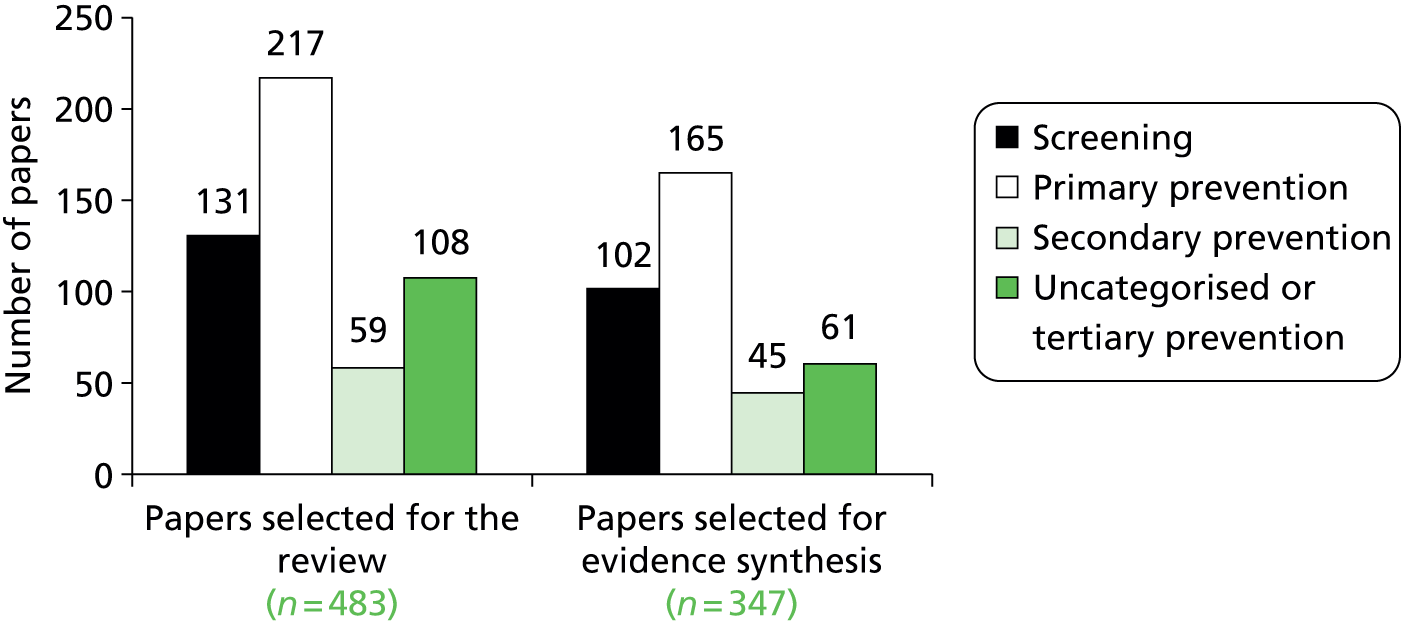
Description of papers on screening activities
Overall, 148 papers provided details of some aspects of screening, although only 84 papers specifically examined research relating to a screening programme. Other mentions of screening were included in papers examining other interventions. Of the papers that were specifically examining aspects of screening, the topics covered are shown in Figure 12.
FIGURE 12.
Range of topics within papers examining screening. HIV, human immunodeficiency virus.
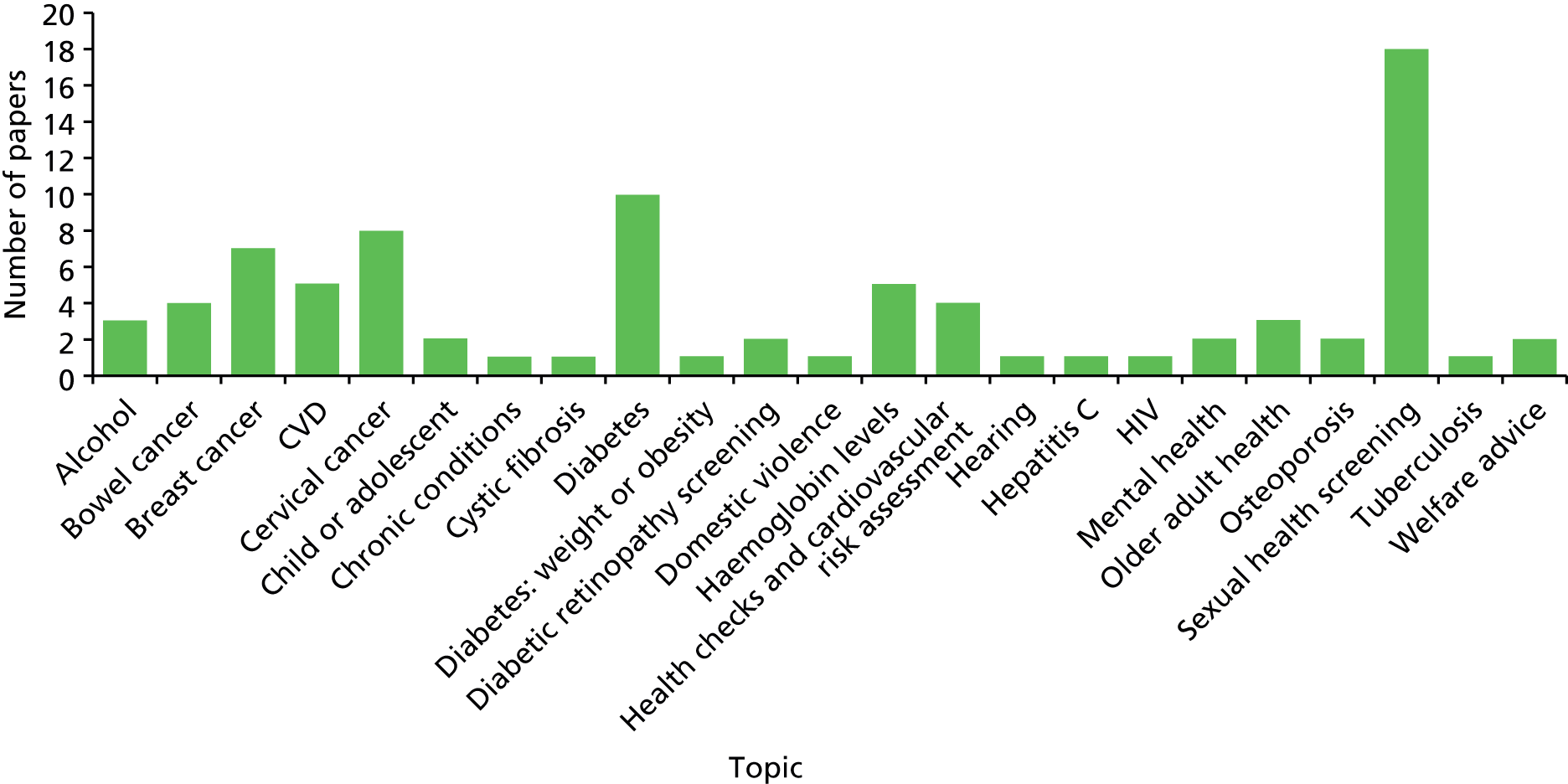
Description of primary prevention papers
Based on the original concept of levels of prevention,119 primary prevention is the action taken prior to the onset of disease, which removes the possibility that the disease will ever occur. Two approaches to primary prevention fall under the broad approaches of health promotion and specific protection. In the review of papers it was often difficult to identify whether or not the activities being described were primary prevention. While appearing to be primary prevention in nature, they could have been applied in practice to patients with an existing health issue, for example CVD. There was often insufficient detail to allocate papers between primary and secondary prevention. Unless specifically stated, papers that addressed primary prevention activities but did not refer to patients with existing disease were classified as primary prevention and are considered here. The data presented here reflect the papers selected for this review and may not provide an exhaustive description of all primary prevention activities undertaken in general practice or primary care more generally. The aim is to present what literature we found where there is evidence relating to the effectiveness of interventions.
In total we extracted 326 papers to include in the review of primary prevention activities. Of these, 164 were included in the evidence synthesis. Of these 164, the majority related to child health (50 papers), smoking (49 papers), exercise and weight (40 papers) and vaccination (22 papers). In addition there were a number of papers that related specifically to CVD (8 papers). The remainder deal with falls, diabetes and mental health. Some of the categories overlapped, providing higher numbers of papers for some topics such as child health and smoking where, for example smoking related to young people or where diet, nutrition and exercise were specifically related to young people. In addition, we included 18 papers on community participation and a further 11 papers on welfare advice services in general practice. The distribution of the primary topics is shown in Figure 13.
FIGURE 13.
Distribution of topics of papers classified as primary prevention.
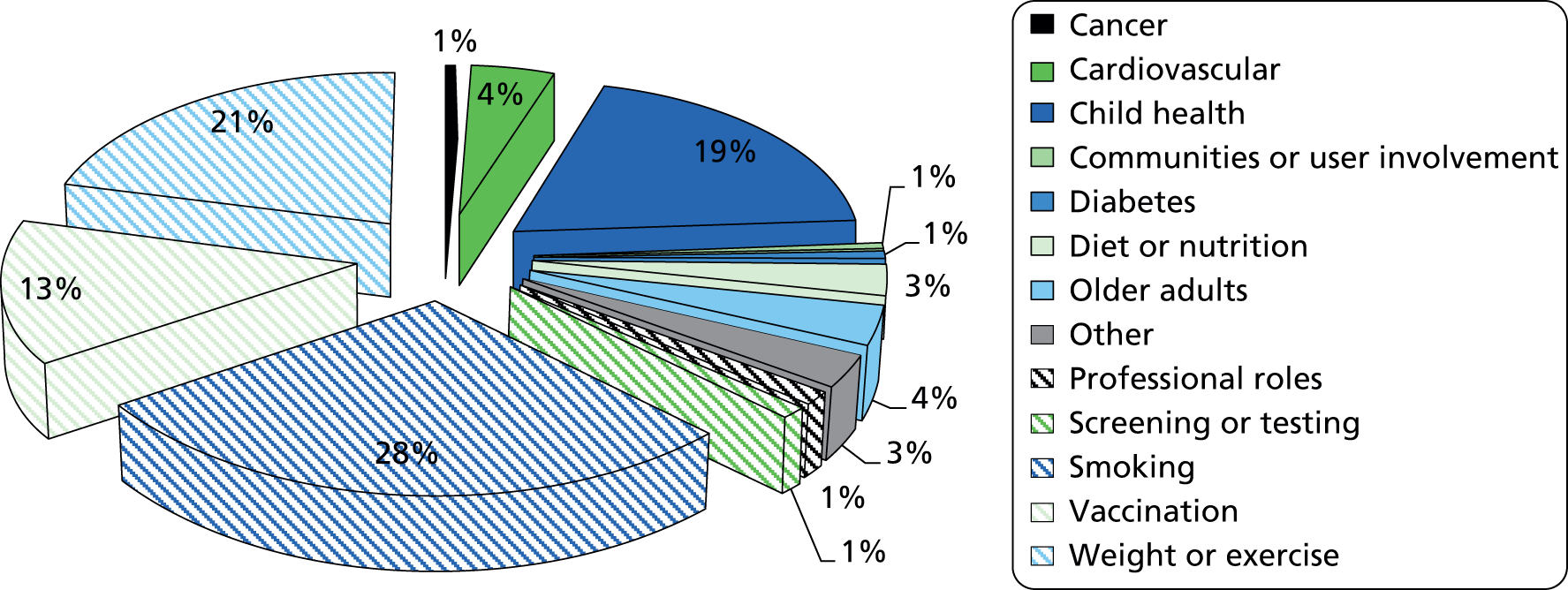
We also examined the 64 papers that were unclassified by the level of prevention (which included welfare advice and community initiatives) but were mainly interventions that addressed particular population groups without clearly defined problems; see Figure 14.
FIGURE 14.
Unclassified papers by population focus.
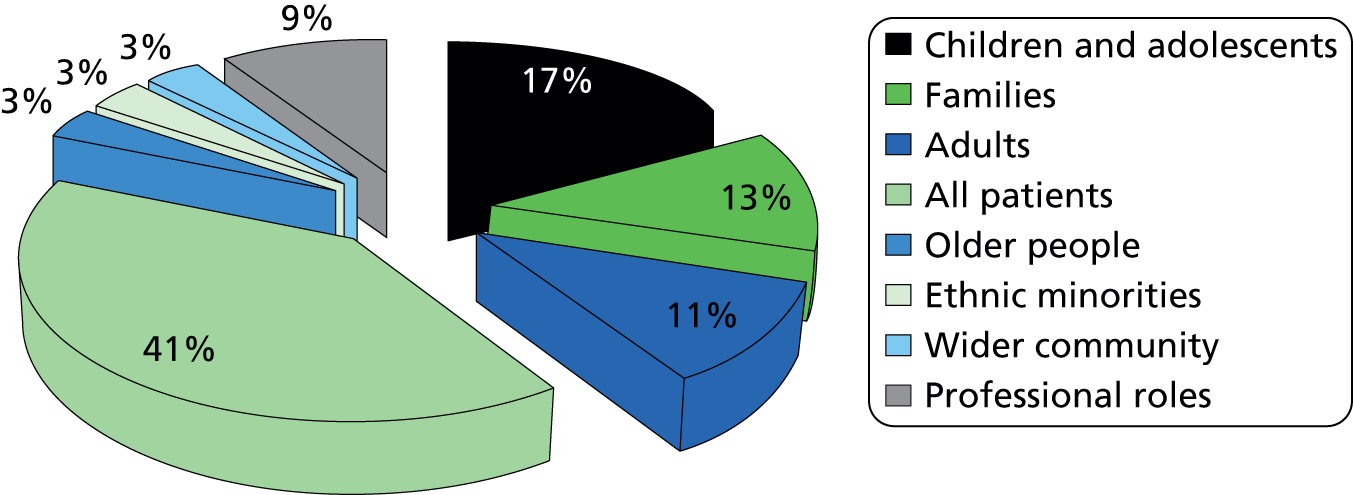
There were also 176 papers that provided additional and relevant information about public health activities undertaken in general practice. The majority referred to aspects of primary prevention or screening although some were not clear about their target population. Of these, 162 were reviewed in relation to primary prevention but did not provide significant detail of interventions or their impact.
Few papers addressed issues such as cancer or alcohol misuse. Many papers that discussed exercise and weight loss were in relation to people with an existing health problem; they were defined as secondary prevention and are included in the description of secondary prevention activities below. Similarly, stop-smoking interventions are both primary and secondary, and potentially tertiary. Primary prevention focuses on smoking prevention and smoking cessation programmes before any disease, secondary prevention limits the sequelae of a disease and would fall within smoking cessation programmes, and tertiary prevention keeps those who are disabled from experiencing more severe effects, such as in pulmonary rehabilitation programmes.
Within this group of papers we also identified those that examined community-based activities related to general practice and services, such as welfare and employment advice where undertaken, in general practice. Whereas these may be seen as primordial prevention activities, the rationale here is that they are provided within the general practice context as a primary intervention, such as stopping smoking, and many of the papers are concerned with the health impact or at least direct impact on the patient or health services. It is also true that some of the patients referred to such services have pre-existing conditions and thus such services could also be classified as secondary prevention interventions.
Description of secondary prevention papers
We identified 126 papers within the evidence synthesis that were secondary prevention interventions. The most frequent area researched was CVD, with 43 papers addressing this area specifically (including health checks), but there were also 25 papers addressing weight and exercise for people with symptomatic disease. Figure 15 provides an overview of secondary prevention topics.
FIGURE 15.
Overview of secondary prevention paper topics.
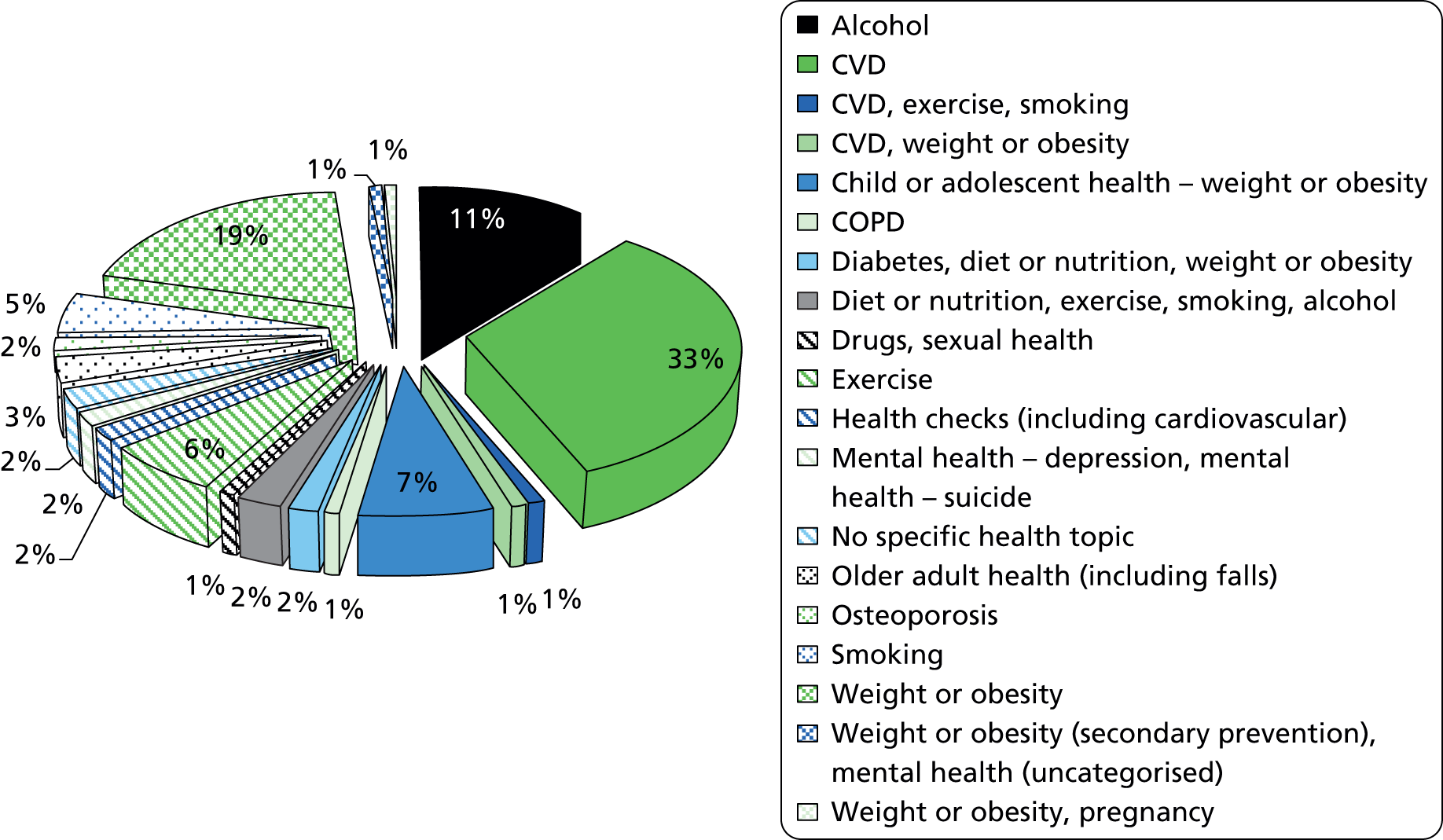
It is not clear how far these should all be classified as secondary prevention, as information about patient/population groups and whether they were symptomatic or asymptomatic was not clear. Many of these were therefore seen as primary prevention activities whether they included symptomatic patients or not. Most remaining papers were then related to CVD and pharmaceutical interventions although there were some lifestyle interventions.
Given that much of general practice prevention activity – such as that supported in the QOF – relates to clinical interventions, it is surprising that there were not more papers included in the evidence synthesis. Reviewing the topics of papers identified in the search and selected for review, but not included in the evidence synthesis, does show a high proportion of papers examining clinical prevention interventions. However, many of these had no information or did not address delivery and organisation aspects of interventions, but were merely clinical trial data or evaluations of the clinical intervention. For example, a number of papers examined the use of statins to reduce cholesterol levels without any discussion of the process. Similarly, papers about the effectiveness of clinical measures to reduce blood pressure were identified but examined only the pharmaceutical effectiveness of the drug, not how it was provided or by whom. Descriptions of secondary prevention activities or how these are related to broader health improvement activities were significantly under-represented in our final paper selection. These were more likely to be categorised as chronic disease management or tertiary prevention and outside of our inclusion criteria.
Description of interventions
The papers selected for review encompassed not only a wide range of topics but also the type of intervention, where it took place and who delivered it. This type of data was not available in all papers and, given that some papers examined patient or practitioner views, it was not possible to identify the organisation and delivery of many types of interventions. For example, a number of papers examined brief interventions. However, these papers included those delivered by GPs,120,121 pharmacists and nurses, and covered smoking, alcohol, exercise, weight management and sexual health. Some papers examined the brief intervention itself, others reported on studies that combined brief interventions with screening and other forms of advice or treatment, and others examined training and support for professionals to deliver brief interventions and advice and support. 121–124 While the majority of brief interventions appeared to be delivered in practices by GPs and nurses, some were delivered in the community or pharmacies. 121,122 Taking just one topic area – brief interventions for alcohol – there were papers that combined interventions,122,123 examined the link between screening and a brief intervention,124 studied training for practitioners giving advice122 and investigated a pharmacy-based intervention. 121 It was not possible, therefore, to draw substantive synthesised findings about these intervention types. However, more information about where and who delivered interventions was identifiable from the studies.
Description of papers by location of health improvement activity
We examined the location of the delivery of the health improvement activity in the 483 papers that were selected for the review process. The main location of intervention delivery was general practice (Figure 16). While this may have been affected by the search strategy, the fact that we specifically looked for studies in pharmacies and activities by primary care professionals in the community, the distribution of papers suggests that the main focus of research interest is in relation to interventions delivered in general practice locations (Figure 17). The papers selected for the evidence synthesis show a similar distribution, although proportionally more papers that examined community, the home and pharmacy-based interventions were excluded from the synthesis.
FIGURE 16.
Where the interventions in papers selected for the review were delivered.
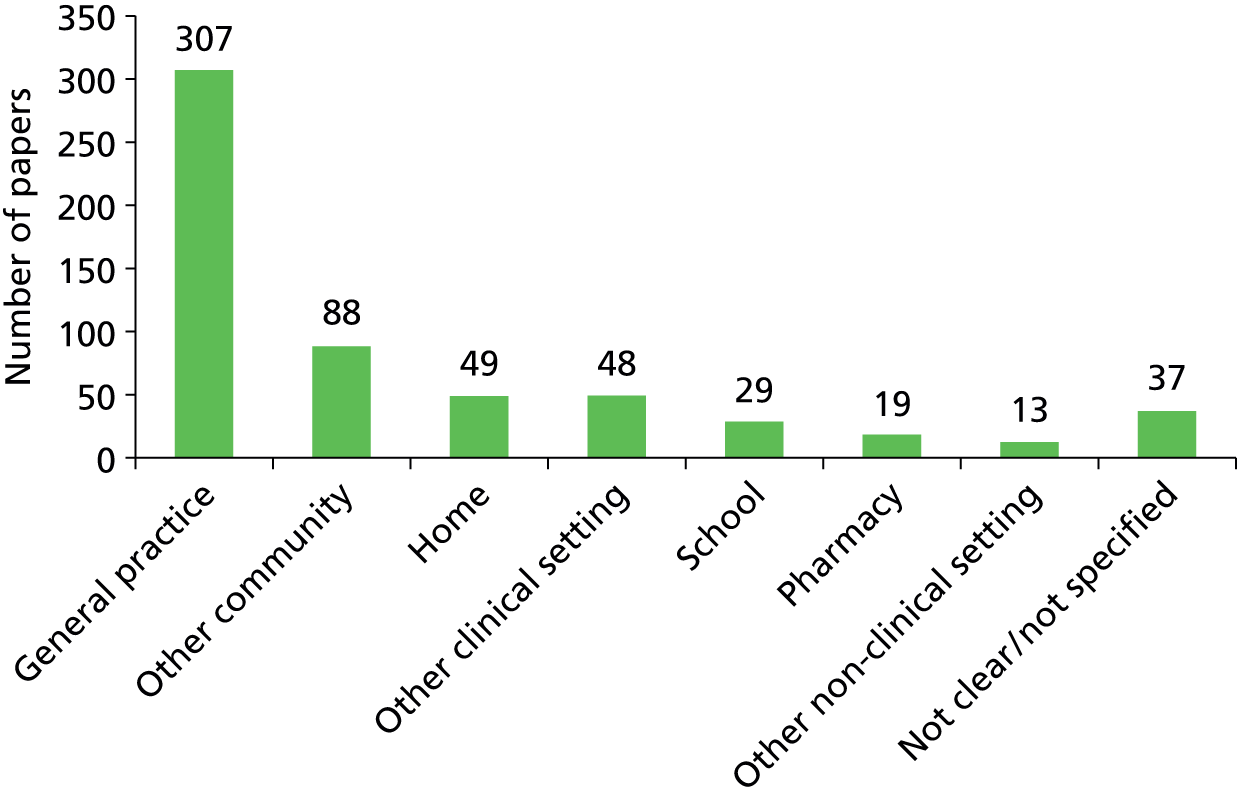
FIGURE 17.
Where the interventions in papers selected for evidence synthesis were delivered.
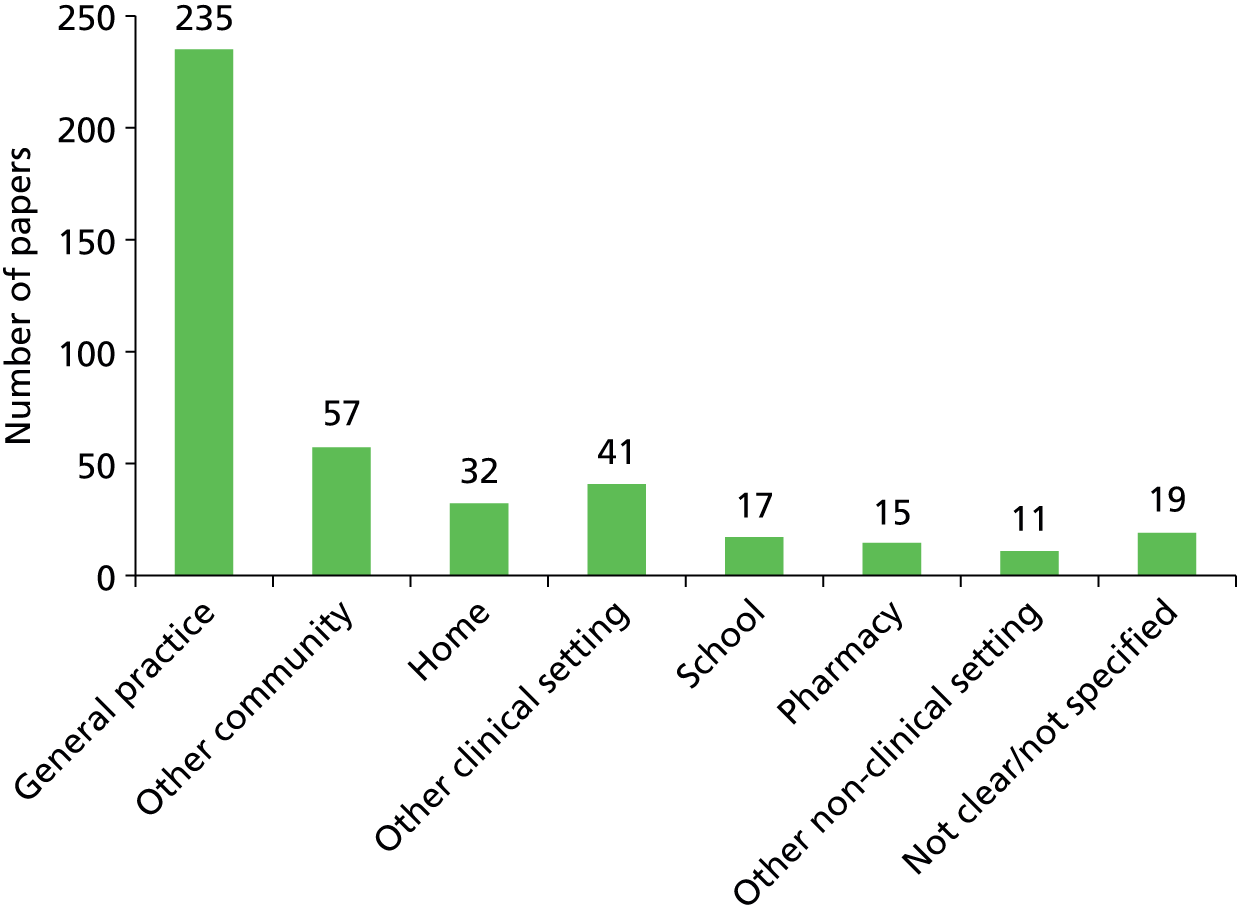
One key problem was a lack of detail in papers clearly defining where activities were performed. For example, papers identifying general practice as the location of the intervention do not necessarily distinguish between whether the activity was in the consultation with a GP or nurse, part of a group or clinic, or some other part of the practice. Similarly, the designation of community is very broad and in most cases did not include a specific venue. Often a number of venues were referred to without any reference to whether or not location was an important element of the delivery and organisation of interventions.
Description of papers by who undertook the intervention
We also examined who delivered the interventions. The majority were delivered by a GP or nurse, and this was reflected in papers selected both for review and for the evidence synthesis (Figures 18 and 19). There is a substantial other category which includes specialist health promotion practitioners, smoke-stop counsellors, other community staff, welfare advisers, etc. However, the findings do underline the key roles of GPs and practice nurses in delivering health improvement activities, but also show that many other professionals contribute to the prevention and health promotion activities related to primary health care and general practice itself.
FIGURE 18.
Who delivered the interventions in papers selected for review.
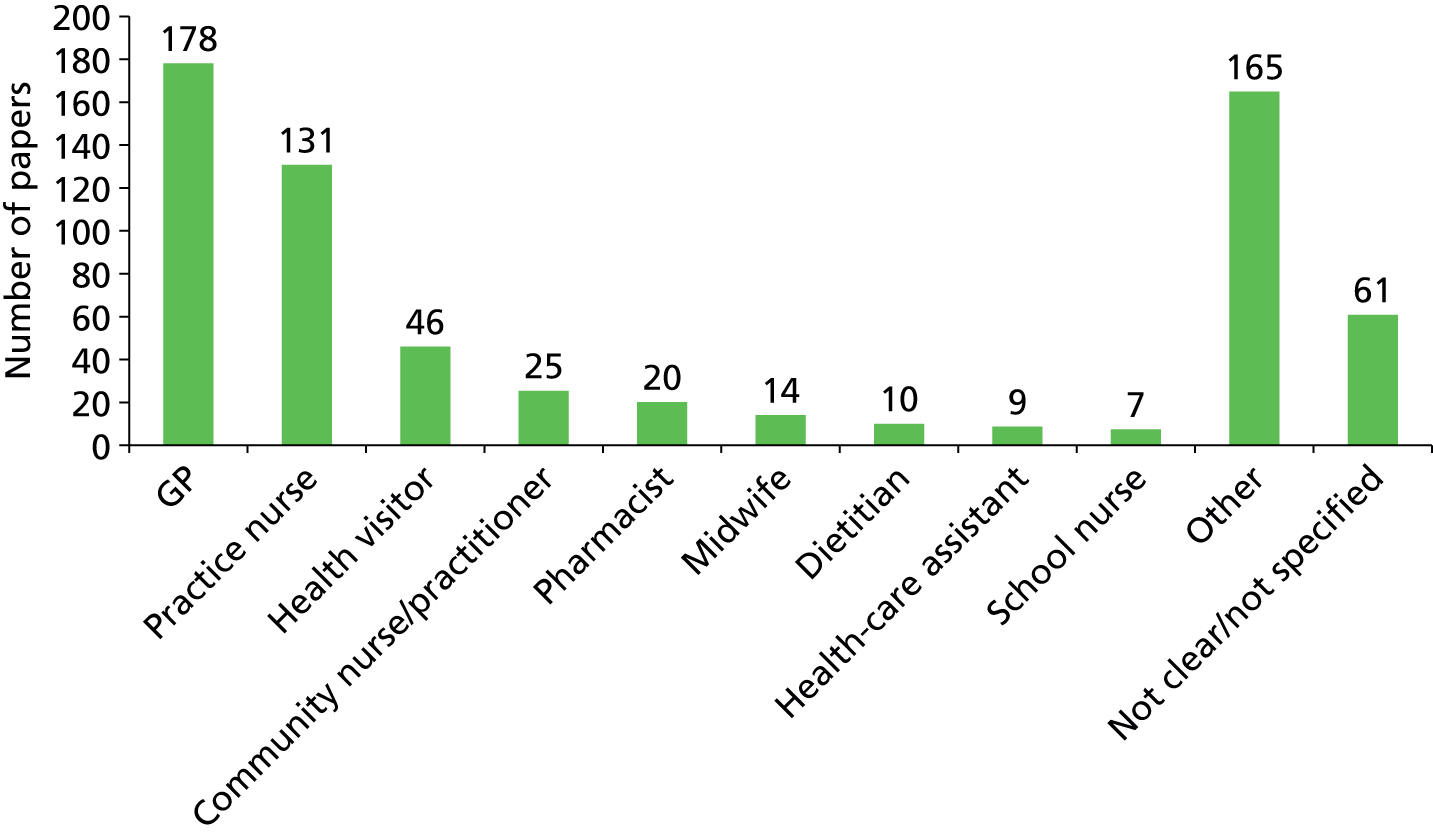
FIGURE 19.
Who delivered the interventions in papers selected for evidence synthesis.
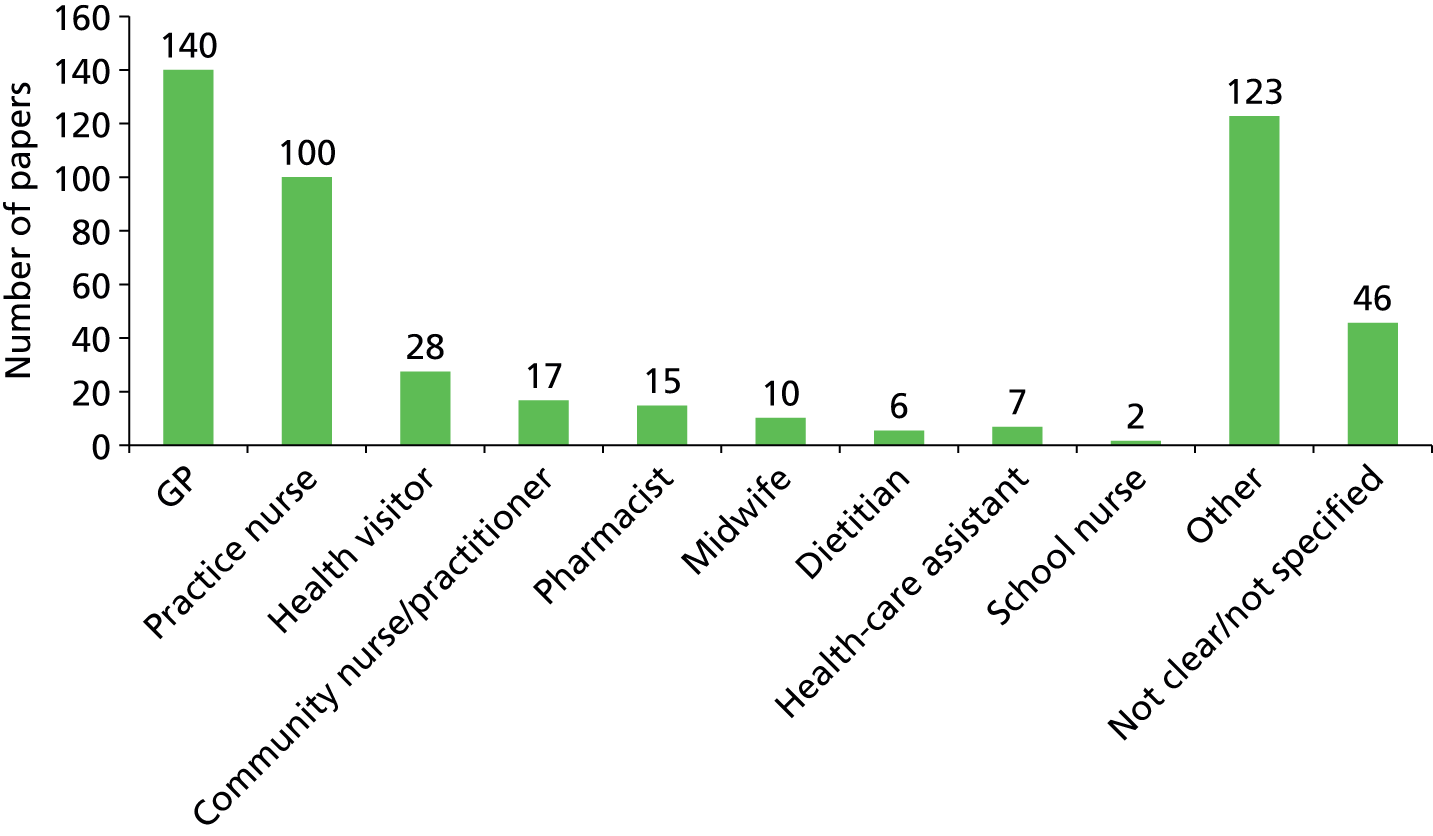
Key themes arising from discussions with practitioners
As described in the previous chapter, during the study we interviewed a number of primary care and public health practitioners in practices, PCTs and local health boards in London, the Midlands, North West of England and in South Wales. We also held two group discussions with GPs in the south of England to discuss their views about public health. The purpose of these interviews and group discussions was to identify issues; they were not designed or intended to provide specific data on activities undertaken in practices. Early interviews were used to help shape the literature review and raise issues to inform the data synthesis and analysis. Interviews and group meetings were not recorded but researchers took notes and wrote up filed observation notes. In addition, we were able to obtain data from a concurrent study looking at the development of CCGs, which, thanks to the involvement of researchers from this study in the research team, included questions about public health issues. Researcher notes were shared between researchers and thematically analysed by two researchers to derive a list of key themes.
Key themes that arose from the interviews and group discussions were:
-
There appears to be a dichotomy between practitioners about whether the focus of general practice should be on more clinical interventions for individuals, and thus prioritising secondary prevention, or general practice should have a more holistic perspective within which health improvement and prevention is a key focus.
-
There were mixed views regarding the QOF and its impact and potential for supporting health promotion in general practice. Some GPs did not see that they should ‘interfere’ directly with some areas of lifestyle advice for patients, although most recognised that a general level of advice was appropriate.
-
Views varied about the usefulness of screening activities, but many GPs felt that current policies were placing more and more responsibilities on them to screen and advise patients, which was difficult in normal patient consultations.
-
GP interviewees generally appeared keen to take on health improvement roles but acknowledged that there is a wide variation in activity and motivation between practices and between practitioners. GPs and other practice staff reported a wide range of health promotion activity ranging from information to proactive approaches.
-
Key areas of concern remain, however, specific clinical conditions such as diabetes and CVD, although smoking and obesity were also highlighted by respondents. GPs tend to identify themselves as proactive in their approach to prevention but focus mainly on individual contacts. Some practices have adopted a range of health promotion activities for their patients. This appears unrelated to recent initiatives and incentives in the QOF but is part of how these practitioners view their practice and the services they offer.
-
More common activities are in clinical areas such as cancer screening, CHD and diabetes in response to key national priority areas and also responding to local issues.
-
There were concerns about what contact practices will have with public health in the future.
-
Practices were receiving specific health promotion support from their PCTs or local health boards, including education and training, additional resources and involvement in wider community-based projects. This was undertaken by dedicated staff in local health boards and PCTs and there was a concern that this support and help would not be there in the future.
-
GPs involved in CCGs were particularly concerned about the future relationship with public health specialists in terms of getting public health advice and also advice specifically for commissioning. There were concerns that good links developed through PCTs will be lost with the move of public health departments to LAs.
-
GPs did not express much interest in or awareness of non-financial incentives. One or two said they would value extra ring-fenced funding to employ extra staff or to invest in their premises. GPs in group discussions generally viewed the additional income from the QOF as a way of investing in new, often nurse-led, activities. However, capacity was clearly an issue regarding whether practices can run health promotion clinics or prevention activities are undertaken during individual consultations.
-
There was a recognition and an acceptance that the QOF had been important, not specifically because it was paid but because it had created a standardised system. However, it was clear that how this standardised system was implemented in practices varied considerably.
-
Practice nurses generally welcomed the additional responsibilities regarding risk assessment, screening and monitoring patients. However, while some practices have a lot of nurse-led clinics, other practices still embed this activity in individual patient consultations.
-
There was a lack of knowledge about wider health improvement issues and services that were not practice-based. GPs had variable knowledge about other services in the local community that provide or support health improvement, such as smoke-stop service, community groups, activities in local schools, etc.
-
Discussions with GPs and public health practitioners – particularly as part of the research undertaken with the Policy Research Unit in Commissioning and Primary Care – identified key concerns about arrangements after April 2013. There was concern about the future relationship of public health departments and CCGs with general practice more generally when public health departments move to LAs.
Conclusion
In this chapter we have provided a brief analysis of the papers identified in the review and those selected for inclusion in the review and evidence synthesis. The process of reviewing papers reduced the initial 1143 papers to 483 that provided some information or evidence on the delivery and organisation of health improvement interventions in general practice or by primary care practitioners. In the end only 347 papers were included in the evidence synthesis and many of these had few details about the type, process and location or who provided the intervention. Generally, our review has demonstrated that little attention is paid in the literature to examining the impact of the organisational context on the way services are delivered or how this affects the effectiveness of health improvement interventions in general practice. Often even those papers describing activities had little detail about the implementation and delivery of interventions.
Key themes arising from discussions with practitioners demonstrated that in practice there are a wide variety of views and concerns about health improvement. There are also substantial variations in the way that health improvement activities are undertaken in the practice, with differences in who does them and how they are organised. This reflects the findings from the literature.
Chapter 5 Health improvement activities undertaken in general practice and primary care
Introduction
The aim of this chapter is to describe the types of health improvement activities undertaken in general practice or by practice staff in other locations. This includes activities undertaken in community pharmacies and in schools by primary health-care staff. The information in this chapter is drawn from all papers selected for the review including those that were marked only as ‘of interest’.
Variation in practice and activity was evident in the literature. As discussed earlier in this report, we identified a substantial number of papers that described specific activities or interventions undertaken in general practice. However, closer examination of papers provided less information about how activities were organised. The data presented here provide a general overview of health improvement approaches and are grouped broadly into specific topic areas. The selected papers included a wide range of prevention activities and intervention types. As discussed earlier in this report, it was difficult to distinguish between levels of prevention, with many papers not distinguishing between interventions with asymptomatic and symptomatic individuals. In addition, examining the papers for details of the organisation of the delivery of these interventions was not straightforward but primarily related to who delivered the service, where it was delivered or some other aspect of its organisation. For ease of presentation the findings have been summarised around key areas of activity:
-
screening
-
child health
-
exercise promotion and weight reduction (including interventions aimed at the prevention of specific diseases)
-
smoking cessation
-
CVD
-
community activities
-
welfare benefits advice.
Types of screening activities undertaken in general practice
We identified 148 papers that examined the delivery and organisation of screening services. Most of these papers addressed specific screening programmes undertaken in general practice or examined the involvement of practice and primary care staff in national screening programmes. Others focused on screening as part of child health programmes, cardiovascular prevention or treatment, or addressed health checks for people with learning disabilities or the new NHS Health Check programme.
Systematic screening
Several activities aimed at identifying health conditions, or risk factors which predict ill health, are delivered systematically to a target population. The role of general practice in systematic screening programmes includes performing cervical smears, child health surveillance and providing health checks as part of the NHS Health Check programme.
Cervical screening
The national cervical screening programme is delivered by primary care in conjunction with regional screening centres, which manage the call and recall system for inviting eligible women who are due for screening. General practice is the major location of sample taking for cytology, the first stage in cervical screening. Around 90% of all samples that were examined by pathology laboratories in 2010/11 and 2011/12 originated from general practices. 125 Although both GPs and practice nurses are involved in sample taking, it has been reported that practice nurses take the majority of smears, and when GPs perform smears it is often on an opportunistic basis. 126 General practices also have an important role in checking the lists of women registered with them who are due to be invited for screening, in order to identify cases where invitations for screening should be postponed or ceased. 127
The national cervical screening programme has been operational for over two decades and has been credited with considerable reductions in cervical cancer mortality. 128 The literature identified by our review tended to focus on screening coverage and women’s experiences of the process, including the extent to which informed consent was promoted. A few studies explored patient views on non-attendance for cervical screening, including qualitative research conducted in deprived areas and the Somali community. 129–131 One study examined women’s views on communication of cytology results, highlighting the importance of co-ordination between general practice teams and screening centres to ensure the provision of consistent messages. 132
Health checks and cardiovascular risk assessment
The NHS Health Check programme was introduced in England in 2009 and aims to screen people aged 40–74 years old for risk of heart disease, stroke, diabetes and kidney disease. Papers reporting on this specific programme described screening occurring in a variety of settings including general practice, community pharmacy, workplaces and even a mobile screening bus. 133–136 The NHS Health Check can be delivered in different ways in general practice. For example, three broad approaches have been employed simultaneously at two general practices in the West Midlands region of England, and reported in a descriptive study. 137 These were invitations to people to make booked appointments, a drop-in clinic and an opportunistic approach utilising electronic flags in patient notes. The authors considered a combination of the approaches to be beneficial.
Prior to the introduction of the NHS Health Check, similar initiatives geared to identifying cardiovascular risk and related risk factors, such as diabetes, were also delivered in a range of locations. These were general practice,138 community pharmacy,139,140 general practice and community pharmacy,141 and community settings including workplaces, pubs, leisure centres and religious buildings. 142–145 Three cardiovascular screening and health promotion studies in the early 1990s, including the Oxford and Collaborators Health CHECK (OXCHECK) and British Family Heart Study RCTs, were general practice based. 146–148 In these three studies, practice nurses were tasked with screening and provision of health promotion advice.
Where health-check screening occurred in general practice, it was carried out by nurses in the majority of cases, although health-care assistants and PCT employed staff were also mentioned. 133,134,138,148–150 However, in one programme in inner-city Birmingham, some of the participating GPs were paid to provide health checks, which included taking blood samples. 141
With regard to health-check projects delivered in community locations, screening was conducted by a wide range of personnel including practice nurses,145 health visitors,142 staff from an independent sector organisation144 and district nurses working in conjunction with lay health workers. 143 Onward referral of screening participants to smoking cessation clinics or to general practice, for example in cases of raised blood sugar level, was noted in two papers. 142,143
Screening specifically for diabetes
Although the objectives of many health-check programmes have included identifying undetected diabetes or risk of developing diabetes, studies have also been conducted to examine systematic screening focused specifically on diabetes. The 2003–5 national pilot diabetes-screening programme and the Anglo-Danish-Dutch Study of Intensive Treatment In People with Screen Detected Diabetes in Primary Care (ADDITION)-Cambridge cluster RCT occurred in 24 general practices in relatively deprived areas of England and 49 general practices in the east of England, respectively. 151,152 The ADDITION-Cambridge study formed part of a larger multinational study with sites in Denmark and the Netherlands, termed ADDITION-Europe. It is noteworthy that recently published results from ADDITION-Cambridge have shown that screening for type 2 diabetes was not associated with reductions in mortality over a 10-year period. 153 ADDITION-Europe found that screening followed by intensive management of patients diagnosed with type 2 diabetes was associated with a small, but non-statistically significant, reduction in cardiovascular events and death. 154
Notwithstanding the generally negative results of the ADDITION research with respect to the UK context, publications arising from ADDITION-Cambridge and the national pilot diabetes-screening programme have provided some useful information for this review with respect to how the screening was delivered. This has relevance in light of the inclusion of diabetes risk assessment in the more recently introduced NHS Health Check programme. A study examining the implementation of screening activities at six general practice sites in ADDITION-Cambridge highlighted the involvement of a range of practice staff in screening, including practice nurses, health-care assistants, GPs, practice managers/administrators and reception managers. 155 Practice nurses seemed to have significant involvement in delivering the screening, the involvement of GPs seemed to be limited and information on the specific contributions of health-care assistants, practice managers/administrators and reception managers was patchy. One paper reporting on the delivery of the national pilot diabetes screening programme at five of the 24 general practice sites described the employment of health-care assistants to perform screening at four practices, with the remaining practice employing a practice nurse. 156 In the same paper the screening was described as generally being led by practice managers and practice nurses, with one practice manager stating that ‘the GP doesn’t get involved because GPs are busy seeing patients’ (p. 80). 156 Interestingly, several practice nurses had taken it upon themselves to conduct the screening at the start of the programme, but had subsequently delegated an increasing amount of the work to health-care assistants because of time constraints. The consensus that emerged over time was that the most appropriate staff member to carry out the screening was a health-care assistant, and care was taken to ensure that health-care assistants would refer patients to practice nurses when uncertain of their needs. 156
In both the national pilot diabetes-screening programme and the ADDITION-Cambridge study, inconsistency between participating practices in how screening activities were delivered was encountered, despite attempts by programme designers to standardise it. 151,155 Practice teams ‘adapted the work according to the size of the practice, the numbers to be screened, the way that they made decisions in the team and their particular interests’ (p. 391). 155 Recent research on the implementation of the NHS Health Check suggests that there is considerable diversity in general practices’ implementation of the NHS Health Check. 157
Health checks for people with learning disabilities
Several research studies on health checks for people with learning disabilities were found among our selected papers. There seemed to be wide variation in service delivery. For example, checks were carried out in different locations including GP surgeries and people’s homes,158,159 and different practitioners carried out the checks, including GPs, practice nurses and community nurses. 159–161 Despite the inconsistency in service delivery, a systematic review of the impact of health checks for people with intellectual disabilities found that they had consistently led to the detection of unmet health needs, and actions to address those needs. 159
Assessment of the health needs of older people
Policies such as the inclusion of health checks for people over 75 years in the 1990 GP contract and the 2001 National Service Framework for Older People have emphasised preventing ill health and promoting health among those in older age. Examples of different strategies for targeting the older population for health needs assessment were found. Some approaches involved offering a health check to all people on general practice lists aged over 75, to be carried out either at their home162,163 or in the general practice with the offer of home visits for those unable to attend. 164
Alternatively, people ‘at risk’ were identified by asking them to complete posted questionnaires. 165,166 Of these, ‘Health Risk Appraisal for Older people’ was notable in its use of a computer expert system to analyse questionnaire responses and provide tailored information for both patients and their GPs. 166 A project also examined the feasibility of a team made up of community nurses and social welfare officers from a voluntary sector organisation in assessing the health and social care needs of people over 75 years deemed to be potentially ‘at risk’, through not having contacted their GP in the last year or not responding to a call for a routine health check. 167 The team referred people defined as having unmet needs to a wide variety of services including those concerned with health care, social care, housing, leisure and transport. The highest percentage of referrals was to GPs.
Opportunistic screening
Opportunistic screening can be said to occur when people attend a service provider for a matter related or unrelated to the condition being screened for. The distinction between systematic and opportunistic screening is not absolute, as opportunistic approaches may be used in general practices to increase the screening uptake of systematic programmes. 126,137 While identifying smoking status is a key role for practices and has been included in the QOF, a discussion of smoking is included later in this chapter alongside interventions on smoking.
Screening activities driven by the Quality and Outcomes Framework
A general survey on screening sent to GPs in Essex and north-east London in 1996 asked, among numerous other questions, whether they offered screening for hypertension, cholesterol and diabetes to all adults, on an opportunistic basis or for other reasons. 168 A major limitation to this section of the survey was a lack of clarity in terms of how and when screening was offered and what was meant specifically by offering screening ‘to all adults’. However, the results are perhaps of note in that variation in reported practice was found, and a high proportion of GPs reported offering some form of ‘screening’ for each of hypertension, cholesterol and diabetes. With regard to hypertension, 51% of GPs offered screening ‘opportunistically or for a combination of reasons’, 42% of GPs offered screening ‘to all adults’, 2% of GPs did not offer screening, 2% of GPs offered a test for medical reasons only, 1% of GPs offered a test on patient request only and 2% of GPs did not specify whether or how they offered it. A relevant question to current research into service delivery is how the QOF, introduced into the GP contract in 2004, has affected screening activity in general practice. The QOF adjusts target payments of specified conditions, including CHD, hypertension and diabetes, for the prevalence of the condition in the practice population, and thus in theory provides a financial incentive to find and register cases.
Although several studies have examined the impact of the QOF on the quality of care delivered in general practice, few have specifically examined its effect on the identification of new cases of disease. Two studies that have touched on this issue suggest that the effect of the QOF on uncovering undiagnosed disease has been modest and geographically variable. 65,169 The epidemiological analysis conducted by Soljak et al. 169 suggested that a large proportion of undiagnosed CHD and hypertension remained in many areas of England in 2007, 3 years after the introduction of the QOF. Through qualitative research with GPs in deprived areas, Dixon et al. 65 found that ‘for the most part, practices were engaged in opportunistic case finding, screening patients with family members with particular conditions, or patients who looked overweight; but the exact causal relationship between the QOF and case finding was difficult to discern in most cases, as most practices that did extensive screening said they did it pre-QOF’ (p. 106). The method employed to adjust QOF payments for achievement of targets for particular diseases, which involved using the square root of the prevalence of the disease, potentially dampened the incentive to identify new cases of disease. 65 In 2009 the square-rooting arrangement in the calculation of QOF payments was discontinued and now actual prevalence rates are used to calculate QOF payments.
The QOF may have had a greater impact on screening rates for complications of existing disease. 65,170 Taking diabetes as an example, a study using QOF data in Northern Ireland reported that the increase in the prevalence of diabetic nephropathy recorded on general practice registers from 2004/5 to 2006/7 was proportionally greater than the increase in the prevalence of diabetes recorded on practice registers in the same period. 170 However, this study also found considerable variation among general practices with regard to the proportion of diabetic patients recorded on their registers as having diabetic nephropathy.
Chlamydia screening
In 2008–9, the two locations in which the highest proportion of chlamydia screening in England occurred were community contraception/sexual health services and general practice, with 25.0% and 16.1% of chlamydia screening activity, respectively. 171 Both GPs and practice nurses offer chlamydia tests in general practice. 172–174 Furthermore, three papers identified in this review reported the involvement of receptionists in distributing leaflets or discussing screening with patients. 175–177 Treatment of chlamydia infection and partner notification can be provided by programme area screening team offices. 176 Alternatively, a study conducted in one practice described patients with a positive result being invited to discuss their results and receive treatment, and being offered referral to a local genitourinary medicine clinic for contact tracing. 178
Screening and brief intervention for alcohol misuse
Patients are often asked in general practice about their alcohol consumption, although it is not routine for all patients on practice lists to be asked on a regular basis. 179,180 GPs may be unaware of potentially problematic drinking behaviour in many of their patients whose alcohol consumption is only moderately above recommended levels. 179 Between 1999 and 2009 there was a trend towards patients being asked more about drinking, with 40% of GPs reporting in a closed survey question in 2009 that they asked about alcohol ‘all of the time’ or ‘most of the time’, in situations where the patient does not ask them first. 180
Several types of professionals have been involved in delivering screening and brief intervention for alcohol misuse in primary care including GPs, practice nurses, psychologists, counsellors and community pharmacists. 124,181,182 However, nurse involvement in alcohol intervention was reported as being low in a paper published in 2003,183 and community pharmacists in Scotland were found to provide little advice on alcohol use in a paper published in 2011. 182
Within general practice, asking about alcohol consumption tends to occur when patients are not specifically seeking help for alcohol problems, usually in the context of new patient registration forms, during health checks or during consultations. 179,181 Within consultations, GPs report asking patients in a wide range of scenarios including those presenting with psychological conditions such as depression and anxiety, social problems, as well as physical conditions. 180 GPs have described some awkwardness in enquiring about drinking and seem to have responded with strategies such as either embedding the question about alcohol consumption within a list of questions about lifestyle or reassuring the patient that they ‘ask everyone’. 179
The term ‘brief intervention’ has been used broadly with respect to alcohol to refer to interventions which last between 5 and 60 minutes, usually consisting of no more than a few sessions, and focusing on providing counselling and education. 184 Because of a complex combination of factors, having ascertained a patient’s drinking status as risky does not necessarily mean that GPs will follow this with a brief intervention aimed at changing their behaviour. 185 A paper reporting on the ‘real world’ implementation of screening and brief alcohol intervention in a primary care setting in three countries described the development of two levels of brief intervention as part of an action research approach taken in England. 124 This allowed a simple brief intervention (structured advice needing only a few minutes to deliver) or an extended brief intervention (behavioural counselling taking 20–30 minutes, plus repeat consultations where thought to be beneficial) to be employed by practitioners depending on the patient’s level of drinking and level of interest in discussing alcohol consumption. The research in England involved GPs and practice nurses, and to a lesser extent practice managers, receptionists and voluntary sector counsellors. However, it did not delineate the roles of these staff members in delivering the simple and extended brief interventions.
Screening for other conditions
Our literature review also identified papers on a wide range of other screening activities that can be conducted in general practice. These included antenatal screening for haemoglobin disorders,91,186,187 screening for dementia,188,189 falls,190–192 osteoporosis,193,194 atrial fibrillation,195 depression,196 domestic violence,197 adult hearing,198 hepatitis C,199 human immunodeficiency virus,200 oral cancer,201 syphilis202 and tuberculosis. 203
Support of screening programmes delivered outside general practice
Aside from performing screening activities, general practice also has an information provision and advocacy role with respect to screening programmes delivered outside practice sites. This applied to breast screening, which is usually provided at units run by hospital staff, and bowel screening using home testing kits, which is organised centrally and conducted by post. General practice involvement included GPs verbally recommending screening,204–207 practices sending GP-endorsed screening invitation letters or information leaflets,208–212 and interventions to promote opportunistic reminders for people to attend screening. 210,211 One RCT investigated the effectiveness of nurse visits to women who had not attended breast screening. 213
Child health
There were a large number of papers (50) addressing issues in primary prevention among the child population. These spanned a range of topics relating to breastfeeding, accident prevention, weight management and exercise. Many of the studies focused on the activities of community nurses, school nurses and health visitors with activities taking place outside the practice: in the home, community or schools. The majority of the studies were rated as of good methodological quality, although some were qualitative and descriptive rather than studies of effectiveness. There are gaps in both knowledge of activities actually undertaken and evidence to support interventions. For example, a review on the effectiveness of school nurse interventions89 found little research of acceptable quality and little could be said about its effectiveness.
Most research papers examined changes in patient behaviour as a result of the intervention but few examined clinical outcomes. Studies fell into three broad categories. The first group examined interventions within practices or by primary health-care team staff to identify children at risk of health problems, accidents, etc. In this area of activity, interventions were often targeted at specific groups of children. The second group were interventions aimed at intermediary organisations such as changing school policies or practices. This included training and educational interventions for teachers. 214,215 The third group examined interventions or activities in the community or in schools. 216–219 With respect to childhood and adolescent obesity, some studies suggest that GPs are less inclined to blame their young obese patients for their condition and to hold less negative and stigmatised views towards them, but, as with their obese adult patients, there is a sense of futility and lack of confidence evident in GPs’ approaches to treatment. 220 Generally, however, GPs are less involved in addressing obesity in childhood than other primary health-care staff and teachers. There is some potential for GPs to adopt a more population approach to childhood obesity and play a more active role.
Breastfeeding promotion is largely conducted by health visitors and community-based midwives. One of the few papers that addressed the context of a breastfeeding intervention policy221 discusses the variance in outcomes of a RCT of a community based breastfeeding support group. Through ethnographic enquiry of the complex intervention, they found there was variation in the way that services were organised, which could be explained through a Hierarchy of Service Attributes Model. In the study sites where breastfeeding rates increased, the model was underpinned by good personnel resources and organisational stability, and demonstrated reflective action cycles at its apex. In localities where breastfeeding declined, the authors found that managers focused on solving the problems within the model, such as staff shortages, rather than ways to deliver the policy. The model provides a useful approach to understanding and explaining delivery of public health interventions in primary care and could be usefully applied to other scenarios.
Provision of childhood vaccinations is a key component of public health for children and adolescents. Proactive campaigns by general practices do seem to increase uptake of vaccinations. 222–226 GP recommendation appears to improve uptake compared with non-primary care and other primary care staff. 223
Exercise, weight reduction and diet
Most of the papers on exercise targeted the general patient population although one referred to people with mental health problems and another three to older people. The majority of papers on weight loss were focused on people who already had risk factors or a health issue, primarily CVD. There were few very good-quality studies; most were of medium quality with some mainly minor concerns about sampling, analysis and outcome assessment. Previous reviews227,228 have also found few good-quality studies and described research as suboptimal. Interventions ranged from lifestyle advice to specific interventions such as exercise or weight loss classes. There was a mixture of interventions delivered by practice and community nurses, GPs, specialists (e.g. nutritionists, dieticians), community workers and health promotion specialists.
In 2009, the QOF included physical activity for the first time under a ‘cardiovascular risk assessment and management’ indicator. 229 The indicator set a target that between 40% and 70% of newly diagnosed hypertensive patients should be ‘given lifestyle advice in the last 15 months for: increasing physical activity, smoking cessation, safe alcohol consumption and healthy diet’. The QOF has been a major driver in the development of more systematic approaches to public health interventions. 65,230 While this appears to have stimulated such advice, with practices introducing clinics and ‘lifestyle reviews’, the evidence on its effectiveness is limited. This area of activity is also being driven by the introduction of the NHS Health Check.
The prevalence of overweight and obesity is rapidly increasing in both the developed and the developing worlds, while tobacco use is largely declining or has levelled off in the developed world. A 2007 study of 168,000 patients in 63 countries showed that 64% of men and 57% of women were overweight or obese. 231 In England in 2007, 24% of all adults were classified as obese, an increase of 37.5% since 1993, along with 16.5% of children aged 2–15 years, an increase of 11.5% since 1995. 232 We found 16 papers that examined primary care interventions that addressed weight loss and obesity. Much of the research is of poor quality, with only one study rated as high quality.
Overweight people rarely turn first to their GP or the formal health-care system for help in losing weight. They try various self-help approaches first, despite consistently citing their GP as the most trusted source of advice on matters regarding diet and nutrition. 233 GPs regard obesity, both its treatment and its genesis, as largely the responsibility of the patient, and believe that their capacity to effect positive change in their obese patients’ weight status is seriously limited,234–238 despite having higher than average frequency of contact with their obese patients. 239 Clearly this attitude stands in stark contrast with the move by public health and obesity experts to treat obesity as a chronic disease. The biggest obstacle is health professionals’ inability to recruit patients. This may relate to their limited knowledge of potential benefits. 240 There is also likely to be a resulting underutilisation of pharmacotherapy and weight loss services, as fewer than 40% of GPs view these options as effective, despite their evidence-based inclusion in practice guidelines for both adults and young people. 234 GPs (and practice nurses) make relatively few referrals in a rather haphazard way owing to lack of time, lack of feedback, medicolegal concerns or their view that patients are unlikely to go/respond, and because exercise is not a priority during consultations. They are uncertain about their own influence. 241 As with offering a smoking cessation intervention, and for similar reasons relating to lack of faith in efficacy, GPs are hesitant to raise the issue of weight loss with obese patients if they feel it will negatively impact on their relationship with the patient. 235 Many GPs believe that obesity does not belong within the medical domain. 234
Smoking cessation
There is a vast body of literature on issues related to smoking cessation, ranging from the effectiveness of various pharmacotherapy and behavioural interventions to the role of public policy and government. This review focuses on what GPs are currently known to do when promoting smoking cessation and what the literature says about the effectiveness of various smoking cessation approaches. It was not always possible to distinguish between stopping-smoking services that targeted all smokers and those focusing on smokers with an existing health problem. Services were often provided generically.
General practitioners in England have access to much smoking cessation guidance and numerous best practice documents, including those produced by NICE and the Health Education Authority. 242,243 There is also an emphasis on GPs and other primary care professionals raising smoking in consultations and visits, with brief interventions highlighted as particularly important. 244 Brief interventions are generally defined as lasting between 5 and 10 minutes and include one or more of the following: asking the patient to stop smoking; assessing the patient’s willingness to stop; offering pharmacotherapy and/or other behavioural support; providing self-help materials; and referring the patient to specialist counselling.
There is good evidence that services for helping people quit smoking are cost-effective and the evidence suggests that a belief in clinical effectiveness and cost-effectiveness is an important influence over whether or not GPs offer smoking cessation advice or interventions. 245–247 Smoking is a major contributor to health inequalities, and cessation services do help reduce these. 248–250 However, few studies examined specific population groups although one study suggests a lack of services for ethnic minority groups despite some evidence of the benefit of community outreach services. 251,252 Identifying strategies to find and support smokers from disadvantaged groups is, therefore, of key importance. 253 This systematic review identified 48 papers. Some papers were of poor quality, most were observational studies and many did not report findings for disadvantaged smokers. Nevertheless, several methods of recruiting smokers, including proactively targeting patients on GP registers, routine screening or other hospital appointments, were identified. Barriers to service use for disadvantaged groups were identified, and providing cessation services in different settings appeared to improve access. Overall, the evidence on the effectiveness of some interventions in increasing quitting behaviour and access in disadvantaged groups is limited. While many studies collected socioeconomic data, very few analysed their contribution to the results. 253
Many studies demonstrated that there was poor recording of smoking status in practice patient records and more can be done to identify patients who smoke. 254,255 While recording improved following the introduction of the new GMS contract in 2004 (for patients with various comorbid factors: CHD, stroke or transient ischaemic attack, hypertension, diabetes, COPD or asthma254,256), a 2008 study showed that levels of recording were still low in some practices. This study of practices in Nottingham found a range of recorded smoking status between 39% and 100%. 255 However, of key importance was the fact that, while in many practices the ascertainment of smoking status was incomplete and/or inaccurate, it was the failure to intervene appropriately on known status that remained the biggest challenge. 255
A GP’s query regarding a patient’s smoking status and subsequent recording of this status are the first steps in an effective smoking cessation intervention, as indicated by NICE, the Health Education Authority/Thorax and the US Department of Health and Human Services guidelines. 242 Virtually all English GPs (98%) report following these steps. 257 It is clear that in the UK the universal uptake by GPs of the QOF process258 and its reimbursement for recording smoking status and providing smoking cessation advice have had an impact on levels of recording smoking status, although rates of recording do vary. 254–256 Smoking cessation is a good example of the QOF changing the way in which practices work, by providing prompts and reminders which have helped to ensure practices try and reach people. In group discussions GPs also referred to systems and prompts, but there was some disagreement among GPs about whether these were helpful or not.
However, knowing a patient smokes does not routinely trigger a smoking cessation intervention by the GP. Fewer than half of all GPs consistently advise patients to stop smoking. 257,259–261 The reasons for this are complex. In addition to not believing that the patient is motivated enough to quit smoking, many GPs report concern about harming the doctor–patient relationship by broaching the topic of smoking cessation with a potentially unreceptive patient, deciding, on balance, that protecting this relationship is more important than providing a smoking cessation intervention with questionable odds of succeeding. 262–267 Pilnick and Coleman267 argue that smoking cessation is complex and that offering help on how to quit is difficult. They also suggest that the benefits of nicotine replacement therapy may be due not simply to the clinical effects but also to the legitimisation of the view that stopping smoking is an appropriate problem for medical intervention.
A randomised controlled study of 74 GPs in England has shown some success in overcoming GPs’ concerns about harming the doctor–patient relationship by providing GPs with a simple desktop resource which triggers a smoking cessation intervention. 263 Furthermore, English GPs are more likely to initiate discussion regarding smoking when the patient presents in the surgery with a smoking-related problem. 268,269 Training GPs and nurses in effective delivery of stop-smoking interventions results in better outcomes. 94 Other research supports or encourages such action, including evidence from a Cochrane review. 259,270–272 A lack of knowledge among GPs about how to affect behaviour change when working with addiction, even among GPs who regularly initiate smoking cessation interventions, presents evidence of the need for further specialised training for GPs. 273
Overall, few papers examined the delivery and organisation of smoking cessation services and only two compared different service approaches. There is a mix of activity in general practice and communities more widely but there appears to be little evidence on how best to organise services despite an increase in the recording of smoking status and incentives to promote smoking cessation. 255,256,274–277 In practices, GPs and nurses provide smoking cessation interventions and, while more nurses may be involved, they have restricted prescribing rights. 278 Lack of time in consultations remains a key barrier to services, as do concerns about how to raise smoking issues within the consultation. 279 However, increasing awareness of smoking status, targeting smokers and provision of training to health-care professionals increase cessation interventions in primary care. 261,280–283 There is some evidence to suggest that patients prefer specialist smoking cessation services but that not all GPs make appropriate referrals for these services. 284
Cardiovascular disease
Papers discussing prevention activities related to CVD were one of the most common groups found in our initial literature search and were the largest group of papers included in the evidence synthesis. Within these, by far the most common activity taking place in primary care with regard to the prevention of CVD is the attempt to modify lifestyle risk factors in symptomatic and asymptomatic patients who are deemed to be in the ‘at risk’ category. The risk factors that are commonly targeted are obesity, poor diet, lack of exercise, alcohol use and smoking. Other key areas were the monitoring of, and strategies to control, blood pressure in symptomatic patients, especially those patients with peripheral arterial disease, patient compliance with medications (especially statins), strategies to improve patient outcomes for people with angina and the cost-effectiveness of nurse-led clinics for those with existing CVD. In addition there were a number of studies looking at GP and practice nurse knowledge and behaviour with regard to guidelines for CVD.
Ten papers directly addressed lifestyle risk factor improvement in asymptomatic patients. 285–294 Five papers285–289 looked specifically at trying to alter patients’ behaviour regarding the amount of exercise they took, their diet and other risk factors (e.g. smoking). This was delivered through short interventions which employed a wide range of activities, such as tai chi, exercise classes, guided walks, counselling sessions and, in one case, a home exercise kit. Two papers looked specifically at the effect of risk factor awareness on asymptomatic patients’ behaviour. 290,291 The first of these studies looked specifically at the level of awareness of risk factors for cancer and CVD. 290 It found that there was a good level of understanding for the lifestyle risk factors for CVD but that risk factors for cancer were less well understood. One study focused on lifestyle risk factors with particular reference to patients with high blood pressure where patients were given information and advice about diet and weight loss to help lower blood pressure. 292
Some of the papers provided details about who delivered the interventions. The role of the GP in giving advice concerning lifestyle risks was considered specifically in two papers. 293,294 The first of these examined the use of ‘pop-up’ reminders on practice computers to improve GPs’ awareness of patients with CVD risk factors. The ‘nudge’ screen would prompt the GP to offer advice and give information about lifestyle risk factors for the patient. The second study examined tailored practice care plans which included ‘motivational interviewing’ and target setting for lifestyle change delivered in a primary care setting.
There were five studies on the effectiveness of nurse-led clinics for secondary CVD prevention in a primary care setting. 295–299 All of the studies looked at clinics where practice nurses monitored lipid levels, blood pressure, medication use and other risk factors such as diet, exercise and smoking. Three studies300–302 looked at the effect of nurse-led interventions in primary care on patient compliance with drug regimens for high blood pressure.
Three studies looked specifically at the management of patients with peripheral arterial disease. One study303 looked specifically at the patterns of management of patients with CVD and peripheral arterial disease. It found that, while most patients were given advice concerning smoking cessation and blood pressure, fewer than half were given advice about weight loss or exercise. The second study304 looked specifically at the treatment received by patients who presented with either peripheral arterial disease alone or peripheral arterial disease and CVD. It found that those patients who had peripheral arterial disease alone were given suboptimal care. The third was a simple description of prescribing practices for peripheral arterial disease patients in Ireland. It found that prescribing patterns varied widely and that patient compliance was less likely when they were required to take a number of different medications. It was also found that prescribing patterns for this group of patients was influenced strongly by budgetary concerns, as some of the medications were expensive.
Two papers looked specifically at ethnicity and CVD. 305,306 Murray et al. 305 looked at a strategy to reduce health inequalities between the white ethnic majority and ethnic minorities in Wandsworth, London. It was a 10-year study using blood pressure and cholesterol measurements as proxy markers for CVD. It was difficult to assess whether or not a significant narrowing of inequalities between ethnic groups had been achieved and there were also insufficient data in the paper to assess the approach. An additional problem was that small numbers of some ethnic minorities and South Asians from different countries were pooled. Previous studies have found that CVD risk is not necessarily uniform among the South Asians population, and there are important differences between Indians, Pakistanis and Bangladeshis. The second study306 looked at the feasibility of using screening services to reach ethic minority groups in Sandwell. It was a series of community-based screening events for CVD and diabetes. The screening events were very popular with the ethnic minorities who attended them, but it unclear if the strategy actually resulted in any lifestyle risk factor change, as this does not appear to have been assessed.
Two papers looked at sex and CVD. 307,308 One study used computerised data from primary care practices to investigate how CVD is treated. 308 The results showed that considerable variation existed between practices, though women were consistently given suboptimal care with regard to prescribing and diagnostic tests. Also, doctors did not always follow the guidelines and procedures. The second study307 looked at the clinical management of patients with stable chronic angina pectoris. Women received a lower level of risk factor assessment, secondary prevention therapy, cardiac investigation and coronary revascularisation.
There was just one paper that looked specifically at deafness and screening for cardiovascular risk. 309 The study was carried out in Sandwell and was part of a community-based programme to provide health promotion advice in a deaf community. The approach in the study did not reduce estimates of CVD risk after 6 months among deaf people determined to be at ‘high risk’, despite the high-risk group of deaf people being given advice and being referred to their GP. A speculative link with language barriers was identified (e.g. a lower reading ability preventing access to information on health promotion, and the discovery that there was no sign for cholesterol in British Sign Language).
Community participation
Community participation in general practice and the role of primary health-care teams in tackling population health beyond the surgery door have long been championed. However, the research literature betrays a focus in favour of a biomedical and technical approach to public health. Most papers concern what might be called ‘preventative medicine’ rather than more complex community-based interventions. Regarding this subset, three immediate observations can be made.
Firstly, there was a paucity of papers – only 18 papers in this category – reflecting the focused nature of our original search strategy. Secondly, few studies focus on outcomes: most papers described case studies and used interviews with key stakeholders to illustrate the potential benefit of participatory approaches. Few studies attempted to measure health processes or outcomes. Thirdly, methodological quality was poor. The evaluation of complex community interventions is a study in itself. Unfortunately, beyond rather woolly references to ‘action research’ and the complexity involved, few studies were of the quality required to ground firm conclusions. In many instances, the initiative had apparently progressed without the necessary resources to undertake detailed evaluation.
Six papers examined health promotion initiatives from the vantage of different groups involved. 310–315 For example, Daykin and Naidoo310 explored the views of health professionals on promoting health in areas of poverty with low-income clients. They questioned the assumption that primary health care is the best setting for health promotion; several constraints are identified as limiting its effectiveness. Firstly, the emphasis on individual lifestyle change that often informs government strategy for health promotion causes frustration among health professionals. Characteristics of primary health care limited its scope in addressing socioeconomic inequalities and engaging in multiagency initiatives. Their interviews indicate that, despite these constraints, workers in primary care demonstrate high levels of awareness and commitment to a social model of health promotion. On the other hand, Abbott and Riga311 exposed limited understanding of the links between deprivation and ill health among health-care professionals in east London. Better professional education on equality, diversity and public health approaches, and improved patient education to overcome knowledge barriers were proposed solutions but their views seemed to be anecdotal rather than evidence-based. Both studies suggested a need for resources and training.
Conceptual uncertainties are mirrored in the views of deprived residents. Parry et al. 312 found that they conceptualised health in both physical and non-physical (e.g. being happy, peace of mind) terms. Sense of place affected health through three key levers: physical structures (e.g. quality of housing), social structures (e.g. friendliness of neighbours) and provision of services (e.g. transport). The interplay between these factors was complex and fear was a common node in many of the pathways residents described linking place with health.
A survey of faith groups in Dundee313 found they were already involved to different degrees in health promotion and ready to engage in more. They constitute an untapped resource whose potential has been evidenced in the USA. Kennedy and colleagues314,315 have explored the benefits arising from lay involvement in community-based nutrition programmes in poor neighbourhoods. These include increased service coverage and the ability to reach populations, personal development and enhanced social support.
A similar gulf in expectations characterised health professional views on health visiting in an orthodox Jewish community. 316 The community only partially understood or valued the health visitors’ role, while health visitors’ awareness of aspects of Jewish culture was limited. Closer partnership is required to develop a service that the community finds valuable.
Participatory approaches to health-needs assessment have gained credence as an effective substitute for traditional, epidemiological approaches. A comprehensive literature review found that research on African and Afro-Caribbean populations was limited and uneven, focusing on specific particular diseases. Okereke et al. 317 used a triangulation approach to identify the community’s perspectives on local priorities.
A narrative review of published research on community capacity to manage hypertension among black groups identified 27 relevant studies. 318 However, collaborative methods yielded insufficient evidence of effectiveness in terms of quantifiable outcomes. Intrinsic assumptions about the homogeneity of communities and how they are represented were challenged.
The Community Health Educator is a model developed through a series of participatory action research projects in UK cancer screening during the 1990s. However, little is known about its effectiveness, or how researchers/practitioners engage with communities. 319 Researchers and practitioners need to be flexible in accommodating the ambiguity implicit in the concepts of ‘community’ and ‘ethnicity’. The efficacy of social networks has similarly been questioned. 320 The prevailing assumption that the community health educators’ personal networks are ethnically and neighbourhood-bounded has influenced intervention design but may not reflect the complexity of urban communities. Concepts such as ‘social capital’ and ‘embeddedness’ are notoriously difficult to operationalise.
Welfare advice services
We evaluated eight papers that described or reported research findings on welfare advice services in general practice. These papers constituted a focused assessment of the organisation, role and impact of advice services for practice populations. The general conclusion of these papers was that welfare advice services are an excellent strategy by which primary care organisations address the social, economic and environmental influences on the health of their population. 321,322 In addition, studies show that services are valued by patients and practice staff323,324 and lead to positive social and health outcomes for patients. 325–328
While a number of the studies were small, the quality of the research was mainly rated as A or B (see Chapter 3 for definitions) and the cumulative findings suggest that there are measurable health benefits for those patients who achieve additional income and high levels of patient satisfaction. There were no cost-effectiveness studies of these services. However, most services were delivered by existing welfare services, with practices merely providing premises.
Organisational issues
The focus of most studies we examined in the review was on general practice, although a number of papers described or evaluated activities linked to the primary health care team but delivered in community settings, people’s homes or schools. Generally those activities outside the practice seldom involved GPs and were predominantly delivered by community nurses or other professionals (e.g. health promotion specialists, pharmacists). The papers reviewed identified a number of important issues related to the location of health improvement activities. For example, there is evidence to support the use of community and school-based locations for health improvement activities with people from ethnic minorities. Evidence shows that schools are more likely to be the most appropriate setting for family-based interventions for ethnic minority groups because of easier access and availability, and the relationship between healthy lifestyle and curriculum. Places of worship are more likely to engage in a dialogue around traditional food practices. Places of worship also provide access to the wider family, including grandparents, and offer opportunity for culturally and family-specific support. 329
In group discussions with GPs, the variation in approach and how services were organised and delivered was very evident. Some practices had invested in training and developing their practice nurses and employing health-care assistants to undertake routine screening and monitoring. In some cases this activity was undertaken by running clinic sessions or group sessions while in others it was based on individual patient recall systems. Younger GPs tended to focus more on the impact of the QOF on these sorts of activities. There was much debate about the impact of the QOF not only on preventative interventions but on the way the practices organised activities and patient care. There are some new issues that have been forged by the QOF such as a more embedded emphasis on systematised models of care through the use of disease registers, computerised working methods and greater use of clinical templates. 93 The literature on the impact of the QOF also suggests that it has focused on individual interventions with patients and more depersonalised care. 93,330
While there has been a particular focus on GPs, it is clear that primary care approaches to public health involve all workers in the practice, as well as the wider primary health-care team. There has been an increasing involvement of practice nurses in patient care, particularly for routine screening and review activities, although the majority of consultations are still with the GP. The introduction of the QOF has been important in opening up new opportunities for practice nurses, although these are a continuation of pre-QOF trends (increasing employment of health-care assistants, delegation of clinical work from GPs to nursing staff). 331 These approaches are also reflected in general practice approaches to prevention and health promotion. 65
While this review describes a wide range of activity, there does not appear to be any consistency in how services are organised between practices. From the papers examined in this review it does seem that many of the interventions have been successful in improving record keeping in practice. In areas such as CVD, diabetes, etc., there is an emphasis on identifying risk factors and on education, most of which seems to have limited benefit. Interventions aimed at changing lifestyle (e.g. for weight management, exercise and CVD) of patients who are asymptomatic seems to be limited in terms of any long-lasting impact. Studies tend to be short in duration and rely on self-reported behaviour change. Studies suggest that there are huge variations in prescribing practices, and the amount of information and advice given by GPs. A number of papers report that GPs feel ill-equipped to give that sort of advice. Practice nurses are used more often to provide information and monitoring of patients, both those ‘at risk’ and symptomatic patients. Generally speaking, patients seem to like this, but with disappointing outcomes with regard to patient benefit. However, it is also not clear how far lifestyle advice is either delivered or remembered by patients. In a study of patient views on health promotion and lifestyle advice in general practice, only 6% of patients recalled receiving advice on diet, 4% on exercise and smoking and only 2% on alcohol. 332 Few papers examined services for specific groups of people or reducing health inequalities between groups.
More attention needs to be paid to skill mix in general practice, although the nature of general practice varies. In this sense, although the systematisation of activity provided by QOF has been seen as restrictive for many practices, it has also been helpful. 65,93,331,333
General practitioners also referred to other financial support for public health activity in practices. Some GPs recognised that the principle of capitation funding should provide some incentive to explore prevention activities but felt that limited time in consultations and the demands of clinical practice made this difficult. Some PCTs have been using other elements of the GMS contract such as LES to support health promotion activity based on financial incentives. However, some respondents questioned if such activity being incentivised was already covered either within the core contract or through the QOF. 63 In a more recent study on the early development of CCGs, the researchers identify a number of uncertainties in this area and report mixed views among CCGs and public health staff about the relationships between GP practices and public health. 334 Data from this study also suggest that there is considerable uncertainty and concern about how public health will work in the new system.
Conclusion
The focus of attention is mainly on individual prevention approaches, with practices engaging in both primary and secondary prevention. The focus is on medical conditions related to prevention of specific diseases such as diabetes or CHD. GP activity appears to be driven by specific contractual incentives and conditions. However, the wider literature also suggests that general practice is also affected by other factors such as peer pressure, relationships with public health departments, education and training. While direct incentives such as contracted standards or the QOF do influence practice, there is some debate about whether or not GPs simply react to maximise their income and do not prioritise activities towards those most in need. The use of thresholds can provide perverse incentives and there is some evidence that GPs use exception reporting to maximise their points score and income. However, there is some evidence that the wider primary care team, such as health visitors, are engaged in health improvement interventions such as breastfeeding support where variance in outcomes have been explained from a service delivery perspective. 221
There appears to have been little shifting from the position described by Lawlor et al. ,79 who argued that GPs do not adopt a population approach as they focus on high-risk patients and adopt a predominantly medical approach. They also argued that GPs felt that giving lifestyle advice interfered with the doctor–patient relationship. However, it is clear that many GPs see health promotion as an integral part of practice, whether as individual approaches to primary or secondary health improvement or as a practice approach to improving the health of their patients.
There is little evidence to show that GPs undertake wider public health roles in terms of population surveillance beyond contractually defined screening and monitoring. These do not target major areas of health concern (such as mental health, eye problems and oral health), which receive less attention despite the potential of general practice to play a leading preventative role. While there is good evidence, for example, that GPs address eye health for people with diabetes, less is known about their wider role in screening for eye problems. It is important that GPs link mental and physical health issues, as people with mental health problems, particularly severe mental illness, are at increased risk of a number of physical health problems. 335
Chapter 6 Evidence on effectiveness of health improvement activities undertaken in general practice and primary care
Introduction
The evidence on the impact and overall effectiveness of prevention activities was limited in both scope and quality. We included 347 papers in the evidence synthesis. A list of reviewed papers is included as Appendix 5. The extent to which selected papers discussed the organisation and delivery of health improvement activities, or the interaction of general practice and primary health-care team staff with services such as screening that are offered through national programmes, varied considerably. Therefore, not all papers are directly referred to in this discussion; references are given where specific or detailed comments have been made, or where papers support general statements. It is important to note that the focus of the discussion is not necessarily on the effectiveness of the intervention per se. Our aim was to examine whether or not there was evidence of effectiveness of different ways of organising and delivering intervention programmes, for example differences in who delivered an intervention, where it was located or how something was provided. Very few studies provided comparisons of approaches and many studies lacked sufficient detail in the papers to make judgements about effectiveness.
Where they are of value we have referred to relevant Cochrane reviews. We found few data on service delivery and organisation in the reviews but where relevant this is incorporated in the discussion. The chapter is split into sections by area of activity. Key points relating to the organisation and delivery of activities are summarised at the end of the chapter in relation to evidence on:
-
cost-effectiveness
-
interventions with patients
-
interventions with practitioners
-
location of the intervention.
Child health
With regard to targeted interventions to identify children at risk of ill health and provide support to them, the evidence suggests that the most effective approach involves consistent and ongoing engagement with families and parents. 218,336,337 Approaches to identifying children at risk of ill health did not lead to significant improvements or changes in behaviour, and the provision of advice by nurses or GPs did not have any impact on behaviour change. 338,339 The evidence on the effectiveness of interventions aimed at intermediary organisations and interventions undertaken in the community and schools suggests that these generally have a positive outcome, although such impacts were small. For interventions with children and their parents, location of activity is important. For the promotion of breastfeeding, delivery needs to be in premises seen by mothers as suitable. 221 Interventions also need to engage a range of professionals and the community. 340–342
While schools were found to be good locations for conducting health promotion, there is little evidence of any substantial change to children’s diet, exercise levels and weight loss. With regard to pre-school children, a systematic review of weight loss initiatives in children aged under 5 years found little robust evidence, and no significant evidence of effect was found. 217
The evidence on the benefit of interventions to promote and support safety advice to reduce accidents suggests that such schemes do not reduce overall numbers of childhood accidents. 337–339,343 One key area of current concern relates to the prevention of obesity in children. Evidence from a recent Cochrane review344 which examined studies from a range of countries in a variety of settings (including schools, home-based and community settings) concluded that child obesity prevention interventions can be effective, especially when assessed using body mass index as an outcome measure. However, the finding should be interpreted cautiously because of ‘unexplained heterogeneity and the likelihood of small study bias’ (p. 2). 344 It was also difficult to know if the outcomes of short-term interventions can be sustained over the longer term (studies were included if they evaluated interventions that were in place for a minimum of 12 weeks). Delivery of effective interventions tended to focus on schools and home settings with input from primary care professionals such as school nurses, health visitors or community support workers rather than within GP practices.
Delivery and organisation of screening services
Despite the importance of general practice as a location of service delivery for a range of screening activities, only a small number of studies systematically compared or explored alternative approaches to performing these activities. While 83 papers were identified for inclusion in the evidence synthesis, 36 were graded as A and 34 as B, with a substantial number of cross-sectional surveys and few trials or evaluations.
Nurse-led cardiovascular screening was one of the few areas in which quantitative evidence on service organisation and delivery could be drawn together, albeit from a few studies with evidence of limited effectiveness of the interventions overall. This has relevance to the NHS Health Check programme, for which little evaluative research has been published yet, owing to its relatively recent introduction. For most other screening services delivered in primary care, our review did not find literature on the effectiveness of different modes of organisation. Instead, the papers addressing particular screening services often focused on different issues. For example, in the case of cervical screening, three studies explored women’s views on non-attendance,129–131 two studies investigated informed consent,126,345 one study examined women’s views on result communication,132 one study assessed the effect of an intervention to improve screening uptake346 and one study examined general practice factors associated with uptake. 347 For some areas, including promoting the uptake of cervical and chlamydia screening, papers provided indications of important considerations for effective service delivery and organisation when considered collectively. In other areas, namely nurse-led systematic screening for atrial fibrillation, alcohol screening and health risk appraisal for older people, evidence was limited to the results of single studies.
One central debate about the delivery of screening relates to targeted, opportunistic and universal screening for diabetes and CVD. These are particularly pertinent in relation to the introduction of the NHS Health Check. 151,348–350 At the time of this review, no substantive evaluations of the NHS Health Check had been completed. However, Dalton et al. 133 found that uptake was only 45% and that uptake was variable between different population subgroups. While many South Asian and younger men in their study had higher than average uptake, many people at higher risk were not screened, which may unintentionally lead to increasing health inequalities. Internationally, it has been shown that screening in other health-care environments can be an effective way of reaching a wider population. 351–354 However, such approaches are not without problems in determining cost-effectiveness, identifying appropriate screening tests and integrating screening into business practices such as pharmacies. 136,352 One pilot project that used opportunistic screening in a supermarket did succeed in reaching specific at-risk groups, although again the ability to do a full range of screening tests limited the overall success of the project. 355 However, extending accessibility to screening may not be a sufficiently effective approach to reducing CVD risk, and studies suggest that multiple risk factor interventions in primary prevention, comprising counselling, education and drug treatments, are more likely to be effective in high-risk groups than in the general population. 356
Nurse-led approaches to cardiovascular risk assessment and health promotion
A few studies of good quality, including the OXCHECK and British Family Heart Study RCTs, have demonstrated small reductions in risk factors for CVD, such as high cholesterol, through a nurse-led health checks approach. 138,146,147 Patient care was organised in these studies so that health checks were followed by nurse-delivered lifestyle intervention146,147 or, in one approach, health promotion advice from the nurse or GP referral to receive medication (e.g. to control hypertension or high cholesterol), depending on the results of the check. 138 Comparison of the results from the British Family Heart Study and the OXCHECK study suggested that the nurse-led approach of the former, which targeted whole families and offered intensive follow-up, was more effective in terms of increasing life expectancy, but less cost-effective than the less intensive approach of the OXCHECK study, where follow-up was negotiated between nurses and participants. 357 However, as neither of the studies was designed to collect empirical data to assess long-term sustainability of changes over more than 10 years, the results of this comparison of the cost-effectiveness of approaches differing in intensity of follow-up should be interpreted with caution. Furthermore, observation of routine practice of nurse-led health checks at 18 general practices, which had relatively low rates of intensive follow-up, concluded there was no beneficial effect over a 2-year period. 148
Cervical screening uptake
Although cervical screening is a national programme, in the late 1980s, when it was clear the programme was not working, there was substantial interest in determining how to improve uptake among marginalised groups. Improvements to the actual delivery and quality control borrowed much from the national breast cancer screening programme but it was the introduction of financial incentives for hitting targets in GP contracts that substantially increased coverage. 358
An important issue for the national cervical screening programme is its population coverage. 130 Two qualitative studies assessed to be of high quality suggest a few considerations likely to be important for increasing screening uptake among specific groups of women. Focus groups with Somali women highlighted the importance of a female sample-taker being available, and the influence that GPs have on screening attendance through giving advice. 129 In a similar study undertaken in a deprived area, the personal skills of the practitioner taking the sample were mentioned as potentially influencing future attendance. 131 Both studies found that practical factors such as lack of child-care provision and inconvenient appointment times were likely to discourage women from participating in screening. 129,131 The importance of addressing practical barriers, including appointments that fit in with work and child-care commitments, was supported by a survey of good methodological quality, which involved face-to-face interviews with 580 randomly selected women in England. 130
Only one intervention study based in the UK and specifically focused on cervical screening uptake was identified. It used an uncontrolled before-and-after design to examine the effect of sending a letter to women who had repeatedly not responded to cervical screening invitations. 346 The letter offered a home visit by a health visitor to discuss screening. Twenty-six of the 70 women who agreed to a visit subsequently attended for cervical screening within 3 months. Interestingly, 16 of the 67 women who declined a visit also subsequently attended for screening, although the authors did not provide an interpretation of this particular finding.
Screening and brief intervention for alcohol misuse
The effectiveness of brief intervention for reducing risky drinking in primary care populations has been established by a Cochrane systematic review, with a caveat that the benefit was not clear for women. 181 The results are likely to be relevant to the UK general practice setting, as 66% of the included trials were based in English-speaking countries (the USA, the UK, Canada, Australia) and the remainder were based in Europe. Moreover, 83% of included trials were conducted in a general practice setting. However, aside from providing general evidence on brief intervention as an effective service delivery strategy, the review did not assess the effectiveness of other aspects of service organisation and delivery, for example in terms of the type of professional delivering the intervention and precisely how it was delivered. Our review of the literature found evidence in these areas to be limited.
With regard to how brief alcohol intervention should be delivered, researchers collaborating with five general practices in the Tyne and Wear area in England in an action research study found it useful to operationalise screening and brief alcohol intervention in routine practice by developing two different levels of brief intervention. 124 However, the study was primarily aimed at examining the process of implementation and describing how the intervention was implemented rather than evaluating the approach adopted. Furthermore, the representativeness of the five general practices selected could not be judged, as details were not provided on their characteristics or why they were chosen from the 12 general practices that applied to participate (apart from perhaps to provide a geographical spread across the Tyne and Wear area).
With regard to the type of health professional delivering brief alcohol intervention, RCTs have been conducted to examine the promotion of alcohol screening and brief intervention among GPs and practice nurses. However, by design they focused on changing practitioner rather than patient behaviour and did not directly compare service delivery by GPs and practice nurses within the same study. 122,183 The trial with nurses found that nurses were more likely to mismanage patients (by administering brief intervention to non-risky drinkers, or failing to intervene with risky drinkers) when provided with training than when sent written guidance only. 183 The earlier trial with GPs did not explore this issue of practitioner error, and was assessed as of lower quality because of concerns with the sampling process. 122 A pilot study to inform the development of a large-scale randomised trial on screening and brief intervention for alcohol misuse in community pharmacies has been recently conducted, so high-quality evidence regarding effectiveness in this setting may become available in future years. 121
Chlamydia screening uptake
Young people, screening co-ordinators and health professionals feel that chlamydia screening should be offered in general practice, particularly to increase population coverage. 175,176,359,360 The barriers to achieving the chlamydia screening uptake required to impact on the infection’s prevalence are fairly well researched. From the health professional point of view, the major barrier seems to be time. 359,361,362 Since chlamydia screening is generally provided opportunistically, GPs and practice nurses have to allocate time within routine consultations to raise the topic of sexual health, offer the test and discuss its implications. Studies have also found that raising the topic of sexual health in unrelated consultations can be challenging in general practice. 176,362 From the service user perspective, qualitative research with young women and men supports the suggestion that the time constraint within routine consultations is a major barrier to increasing testing rates. 360,363 Furthermore, stigma associated with chlamydia is an important issue, and young people do not want to feel they have been ‘singled out as “needing” a Chlamydia screen’ (p. 7). 360
Opportunities may exist to tackle the time constraint by involving reception staff in the screening process. 176,359 For example, one study reported receptionists identifying 16- to 24-year-old women attending the practice and making initial contact with a leaflet about chlamydia for them to read before their consultation. 175 This also led to receptionists being asked questions about chlamydia screening, which, although handled in different ways, had the potential to save further time during consultations. However, concerns about the appropriateness of receptionist involvement, including problems with privacy, have been expressed by both general practice staff and patients. 177,360,364 Additional factors that may be important for effective organisation and delivery of chlamydia screening in general practice were identified in a qualitative study by McNulty et al. 176
Chlamydia screening has been found to be feasible in the community pharmacy setting, and the provision of emergency contraception by pharmacies provides an opportunity to provide chlamydia screening kits simultaneously. 365,366 However, there is a lack of evidence comparing the effectiveness of chlamydia screening in community pharmacy with general practice. Nevertheless, the available evidence suggests pharmacists have experienced some challenges similar to those of general practices, such as lack of privacy and the difficulty of raising the subject of chlamydia in consultations. 366,367
Nurse-led systematic screening for atrial fibrillation
One RCT compared nurse-led systematic screening for atrial fibrillation, where invitations were sent to people’s homes, with opportunistic screening, where a reminder flag was placed in people’s medical records. 195 The results suggested that nurse-led systematic screening was the more effective approach in terms of the proportion of patients screened and the proportion of patients detected as having atrial fibrillation. However, a need for electrocardiogram confirmation of diagnosis and ongoing monitoring of anticoagulation were highlighted as important resource implications.
Assessment of the health needs of older people
A RCT compared standard care with a health risk appraisal health risk appraisal approach to health promotion of adults 65 years of age or older. 166 The health risk appraisal approach involved collecting data from individuals by self-completed mailed questionnaires, which were fed into decision support software to provide individualised written feedback, concerning health promotion, to both patients and their GPs. This allowed issues to be addressed either directly or opportunistically according to patient or professional discretion. No significant differences in self-reported health behaviours or uptake of preventative care measures (except pneumococcal vaccination) were found after 1 year. The authors suggested that a more systematic approach to engaging patients with the feedback from the software may be required to obtain positive results, such as through face-to-face consultations outside routine encounters. In a related cohort study, health risk appraisal for older people was shown to be feasible for repeated use. 368 However, the people who did not respond to the mailed questionnaire repeatedly over time were found to be more likely to have a lower income or to smoke.
Currently, the over-75-year-old health check includes vision screening. However, all evidence to date suggests that such universal approaches bring limited benefit. 369 A Cochrane review specifically examining the screening of older adults for visual impairment found no evidence of impact on vision of screening services which had a vision component to the assessment. 370 The six RCTs in the review were located in community settings including general practice, four were based in the UK and screening was delivered by either a nurse or health visitor. However, such tests do not screen for glaucoma, and intraocular pressure testing may provide an important targeted preventative screening intervention for vision impairment. 371 The converse is true for auditory screening, where a universal programme – especially for people aged over 75 years – would lead to substantial benefits, although it would place additional strains on NHS hearing services. 372
Support for screening programmes delivered outside general practice
Besides providing screening, general practice also has an important (public health) role in providing information to patients about bowel and breast cancer screening, and recommending participation in these programmes. A few studies of variable quality, including one well-conducted RCT, suggest general practices can improve uptake of screening in their area, even with relatively superficial actions such as posting endorsement letters to patients. 209,210,212 A qualitative study exploring factors affecting screening uptake among men and women invited to participate in bowel screening noted the influence of GPs in encouraging screening participation. 205 This finding resonated with the views of many Somali women, who reported that they had taken up cervical screening following advice from their GP. 129
Among other studies related to the role of general practice with regard to the breast and bowel screening programmes, an interesting initiative focused on increasing the coverage of breast screening in a PCT area using a ‘whole-systems approach’. 211 This included the following interventions targeted at primary care: financial incentives to GPs, training on screening provided to general practices by public health teams, endorsement of invitation letters by general practices and establishment of an alert system in practices to provide opportunistic reminders for women to attend breast screening. 211 Although it was not possible to disaggregate the effect of the interventions in primary care from the other components, the initiative showed promising results overall.
Work is currently under way to design a definitive RCT to assess the effectiveness of GP endorsement on participation in the national bowel cancer screening programme. 373 GPs have stressed their need for high-quality information to support them in helping patients make an informed choice to undergo bowel screening, and this issue may be of increasing importance if general practice is called on to be more proactive in encouraging participation in off-site screening programmes. 374
The organisation and delivery of weight management, diet and exercise interventions
There is some evidence to support strategies which have shown promise for incorporation into GP weight management practices, including referral to commercial slimming services375 – supported by evidence that such services may have better long-term outcomes than commonly reported376 – and partnering with other health-care providers such as dieticians. 236,238,377 However, there is no evidence that the effectiveness of weight management in general practice is long lasting. A review217 on weight management programmes for children found no good-quality evidence of a beneficial effect.
Similarly, in relation to exercise referral schemes (ERSs), the evidence suggests that there may be limited initial benefit but no strong evidence for long-term effects. 228,378–380 There are problems with non-attendance; younger people in particular are less likely to attend. Practice nurses and health educators get better responses than GPs. 380–382 The evidence suggests that there is some benefit in discussing exercise in general practice and that systematic approaches to identifying individuals and to providing sustained advice and support – especially by nurses and health educators – may have some beneficial impact. Lawton et al. 383 have shown in a RCT that physical activity promotion can improve behaviours in general practice care when co-ordinated with exercise on referral, which is widely accessible in the UK. However, the impact appears to be short-term and limited, although one RCT384 suggested that differences can be sustained for 12 months. A systematic review found that lifestyle counselling interventions delivered by primary care providers in primary care settings to patients at low risk (primary prevention) appeared to be of marginal benefit. 39 Resources and time in primary care might be better spent on patients at higher risk of CVD, such as those with existing heart disease or diabetes.
There was very limited evidence to support the use of brief interventions for exercise. 228 Brief interventions (3–10 minutes) or simple pedometer-based programmes delivered through health professionals can lead to substantial increases in patients’ activity levels (by ≈ 30%). 385 Marginal improvements may, however, be cost-effective. 386 Most studies were based in general practice but one study in a breast-screening clinic found that women were interested in obtaining advice and information on weight loss. 387 While evidence on the effect of brief interventions for exercise and physical activities in primary care appears mixed, they have been recommended as an effective intervention in the USA. 385 Current NICE guidance also supports brief interventions and recommends that primary care practitioners ‘should take the opportunity, whenever possible, to identify inactive adults and advise them to aim for 30 minutes of moderate activity on 5 days of the week (or more)’ (p. 4). 388
Weiler and Stamatakis389 have argued that regular intervention built on existing, longstanding primary care relationships may have a significant impact on patients. There is, however, only limited support for this approach. 390 In addition, there is little strong evidence to support the benefits, especially in the long term, of ERSs. A Health Technology Assessment review in 2011391 concluded that ‘there remains very limited support for the potential role of ERS for impacting on PA [physical activity] and, consequently, public health . . . Although ERS programmes in our review aimed to increase medium to long-term PA, they were typically based on only a 10- to 12-week leisure centre based period intervention’ (p. xi). The cost-effectiveness of such schemes is also questionable. 386
There have been three relevant Cochrane reviews392–394 that directly examined evidence for general exercise and weight loss interventions. In addition, there were a number of reviews that specifically addressed diet, exercise and weight loss for the prevention of specific conditions including diabetes395–397 and CVD. 398 All the reviews drew on the findings of international literature and therefore their direct relevance to UK general practice cannot be assumed. The reviews concluded that it is not possible to draw any firm conclusions about the effectiveness of interventions aimed at changing the behaviour of health professionals or the organisation of care to promote weight reduction in overweight and obese adults. 393 Neither is there any consistent evidence to support the hypothesis that multicomponent community-wide interventions are effective at increasing levels of physical activity. 394 The third review found that professional advice with ongoing support has only a moderate effect on increasing self-reported physical activity in the short to mid-term. 392 However, in the studies for this review most participants were volunteers, limiting its applicability to a general practice population. Generally, however, the evidence supports systematic approaches working through disease registers and targeting patients most in need. Systematic programmes of support/advice241,399 are more likely to be effective than opportunistic approaches. 400
The success of smoking cessation interventions is generally supported by good evidence and they are seen as cost-effective. 401–404 There is some variation in reported success rates of smoking cessation interventions. 405 Quit rates in the range of 10–20% of smokers exposed to a smoking cessation intervention are commonly cited. 405–410 It should be noted that there is no universally accepted definition of ‘quit rate’, although most studies use a minimum period of 6 months of abstinence from tobacco use – with the definition of ‘abstinence’ itself being the subject of some disagreement. Brief smoking cessation interventions within general practice settings with patients who smoke are marginally effective. 403 Unassisted 12-month quit rates in the general population are in the range of 2–3%. While brief interventions by GPs may increase this level by an additional 1–3%,411,412 this could lead to a further 75,000–92,000 patients per year in England who could quit smoking if GPs increased the number of smoking cessation intervention initiatives by 50% and accompanied them with nicotine replacement therapy or other pharmacotherapy. 242,413,414 Motivational interviewing by GPs over a number of multiple sessions may be more effective but there is no evidence to identify the optimal number of sessions required. 404 Brief interventions by nurses were not found to be as effective as those by primary care physicians. 402 Community pharmacists who provide support to patients to quit smoking may, when trained, have a positive impact but the evidence is limited. 401 The evidence on community-based interventions lacked sufficient quality and detail to provide guidance on who should deliver interventions or how they should be delivered.
There is also debate within the literature regarding the optimal degree of brevity versus intensity of these interventions. 410,411 Research shows that the move towards guidance favouring ‘intensive’ brief interventions is misguided,415 but no apparent disagreement exists regarding their utility and cost-effectiveness, regardless of intensity. 242 The use of pharmacotherapy, such as nicotine replacement therapy, varenicline or bupropion, with or without a brief GP intervention, increases quit rates considerably, by upwards of 1.5 to 3 times. 407,409,411,413,416–419 Following a brief GP-led smoking cessation intervention, referral of patients to specialist programmes, such as those offering behavioural support, or even guidance to telephone help lines, has also been shown to enhance rates of smoking cessation. 257,415
Overall, the evidence suggests that smoking cessation advice provided by trained, specialist advisors delivered over a number of sessions with follow-up support provides the most effective interventions. Brief interventions by GPs supported by pharmacological support may also have an important impact on smoking rates in absolute terms.
Cardiovascular disease
Of the 10 papers that provided evidence on interventions aimed at lifestyle risk factor improvement in asymptomatic patients, five285–289 examined altering patients’ behaviour regarding the amount of exercise they took, their diet and other risk factors (e.g. smoking). All these papers reported improved behaviour after the study period was complete, and one288 reported a significant improvement in waist circumference at the end of the study. Three of the papers suggested that the intervention programmes were worthwhile and cost-effective (see Evidence on cost-effectiveness). However, there were concerns about the quality of some of the evidence. For example, one of the studies288 was conducted over a very short period (12 weeks), limiting its claim of significant improvement, one was a pilot study285 and one relied on self-reported levels of behaviour change. 289 One study289 pointed out that the programme had ‘failed to engage’ with the ‘hard to reach’ population, especially people from deprived areas and men. In relation to lifestyle risk, some papers described providing information to patients but the effect of risk factor awareness on asymptomatic patients’ behaviour was shown in only one study. 291 This concluded that, even when patients are fully informed of their personalised disease risk factors such as lack of exercise, this knowledge is in itself unlikely to change their behaviour. In another study, where patients with high blood pressure were given information about diet and weight loss to help lower blood pressure, it was found that after 6 months there was no improvement in the study group, either in their risk factors or their blood pressure readings. 292 As discussed earlier in this chapter, in the OXCHECK study the nurse-led approach, which targeted whole families and offered intensive follow-up, was more effective in terms of increasing life expectancy, but less cost-effective, than the less intensive approach of the OXCHECK study, highlighting the need for more intensive and consistent intervention programmes. 357
The use of information technology systems to prompt practitioners to offer advice had no impact on whether or not physicians offered such advice to patients, but it did improve practice record keeping. 294 Another trial, examining motivational interviewing and care plans provided by practitioners, found that they did not lead to benefits in terms of blood pressure, cholesterol or health-related quality of life, although it found that there was a reduction in the number of hospital admissions. 293 Studies that examined the effectiveness of clinics where practice nurses monitored lipid levels, blood pressure, medication use and other risk factors such as diet, exercise and smoking suggest that these led to improvements in some aspects of secondary prevention except for smoking cessation and exercise levels. However, what small improvements there were may be misleading, as they relied on patients self-reporting. 295–299 In a study that looked at the effect of nurse-led interventions in primary care on patient compliance with drug regimens for high blood pressure, Schroeder et al. 300 found that there was no effect on patient compliance, while another study302 found that there was some improvement. Bane et al. 301 concluded that compliance was more likely if patients felt that they had been ‘listened to’ by their GP in the initial consultation.
Murray et al. 305 looked at a strategy to reduce health inequalities between the white ethnic majority and ethnic minorities in Wandsworth, London. It was a 10-year study using blood pressure and cholesterol measurements as proxy markers for CVD. Although the intervention had resulted in a lowering of the risk factors across the board, there were methodological problems such as the small numbers of some ethnic minorities and the pooling of South Asians from different countries, which limit an assessment of effectiveness. Two papers looked at the effect of educational programmes on outcomes for patients with angina. 420,421 The first examined the cost-effectiveness of a personalised health education programme for people with angina in Belfast. Those in the intervention group had three visits per year from a health visitor, whose brief was to discuss ways of living more easily with their disease and ways in which risks of further events might be reduced. The results showed significant improvements in survival and self-assessed quality of life in the study group. The second looked at a similar programme of education for angina patients. The intervention group received personalised health promotional advice from a practice nurse four times a year for two years. The results showed that the study group had improved quality of life and physical mobility, and there were significantly fewer deaths in the study group than in the control group. It also showed that it was important that GPs gave advice to patients concerning physical mobility but that GPs were reluctant to do this because they felt ill-equipped to give it, and that they lacked the training.
Community-based approaches
Despite growing recognition of the potential of community-based efforts to improve public health, the costs and ‘added value’ of such approaches remain unclear. The most substantial systematic review sought studies that included controls of suitable comparative groups and measured both outcome and costs. 422 Of 4405 references screened, 152 records were potentially relevant, but just eight studies met the inclusion criteria. Seven of these reported positive findings, but none was designed to evaluate impact or cost-effectiveness. The review found tentative evidence that community engagement is part of a multifaceted approach to health promotion, may have positive effects and could be cost-effective. As discussed earlier in this chapter, Cochrane reviews of community interventions for exercise and weight loss, and for smoking found little robust evidence of positive effect on smoking prevalence or sustained weight loss. 394,414 The studies also either said little about who delivered the interventions or found little difference in who delivered interventions or how they were organised.
A further uncontrolled study looked at the impact of a training programme in community-oriented primary care on 11 practices. This detailed benefits to staff, for example learning new skills, and to patients in terms of intermediate health outcomes. Costings suggested the projects undertaken were likely to be cost-effective. 423 Overall, the dearth of evidence suggests the desirability of community engagement at all stages of project development to capture the community’s priorities and perspectives, and assess appropriately the costs and benefits of engagement.
A large literature described case studies located in different parts of the country. These predominantly involved urban, deprived populations but rural communities were also covered. These provided testimony to the impact of the programmes under consideration, for example through interviews and focus groups, often supplemented by process data (e.g. attendance rates). However, other measures of impact were seldom forthcoming. The aim was to share good practice and provide learning for others.
Taket and Edmans,424 for example, listed key elements in a framework for community involvement in health and regeneration:
-
work at the most local level
-
involve community in decision-making at all stages
-
local recruitment to paid posts involved, wherever possible
-
ensure that work involved supports local economy in all sectors
-
build capacity
-
train
-
give specific attention to planning and management of change
-
specific attention to building partnership between organisations
-
work towards building trust and openness
-
adopt innovative and multiple ways/processes of working
-
recognise the importance of facilitation
-
adopt a participatory action research approach
-
adopt a holistic approach
-
keep a high profile
-
recognise the need to work creatively on constraints/challenges imposed by funding conditions
-
see regeneration as intimately involved with changing, where necessary, the way that mainstream services operate
-
recognise, respect and work with diversity, in an empowering fashion
-
recognise that it takes time
-
build in external evaluation.
Such learning may also identify barriers. 425,426 Inadequate resource allocation and poor continuity of structures/personnel are frequently barriers to community-based partnership programmes. Ritchie et al. 425 made recommendations to address them (e.g. the need for contingency plans and funding to deal with indeterminate aspects). Studying a social exclusion partnership in Scotland, Carlisle426 identified rival relationships between key partners and the sometimes conflicting priorities of health promotion versus community development as potential barriers.
The literature on community participation identified some important methodological issues and highlighted the inconclusive nature of much of the research. The specific role of primary health-care professionals was seldom described and the contribution of GPs was notably absent. Given our search terms, it is likely that this absence of a GP contribution accurately reflects the literature in this area. Previous reviews of public health and primary care have also noted the limited engagement of general practice and GPs in community-based public health activities, although community nurses have been more engaged in such activity. 73
Summary of the evidence on health improvement in general practice
The evidence synthesis reported here is not designed to provide a comprehensive assessment of the effectiveness of health improvement interventions undertaken in general practice or by primary health team practitioners. Our interest was rather to explore the nature of the evidence, its scope and limitations and to specifically identify what evidence there is on the way health improvement interventions are organised and delivered.
Evidence on cost-effectiveness
Cost-effectiveness evidence for health promotion interventions included in this study was very limited. Only 13 of the 347 papers retrieved for the evidence synthesis had a cost-effectiveness outcome measure. Four papers examined exercise and weight loss,386,400,427,428 and there were two papers in each of the following topic areas: CVD,298,429 NHS Health Checks,149,150 and health checks for people with learning disabilities. 158,161 The other three papers examined sickle cell screening,430 breast screening210 and smoking cessation. 380 Generally there was little substantial evidence to make general conclusions about the cost-effectiveness of health improvement interventions in general practice. The evidence is often poor and very mixed.
Effectiveness of interventions aimed at patients
Interventions that directly focus on the patient include those aimed at changing behaviour through the provision of information, brief interventions, lifestyle counselling, non-medical interventions such as welfare advice or ERSs, and medication, or some combination of these. The evidence supporting interventions with patients was generally poor, and few discussed how interventions were delivered. Interventions aimed at changing lifestyle factors in patients who are asymptomatic have little success, as the impact is short-term. One problem is that studies tend to be short in duration and rely on self-reported behaviour change. In symptomatic patients there is a similar obsession with changing lifestyle but the evidence suggests that outcomes are slightly more positive, especially in angina patients, although these are still fairly limited. Very few papers examined impacts on health inequalities; for example, in relation to CVD we identified only one paper on the experience of deaf people,309 two on race305,306 and two on gender,307,308 all of which showed a real problem that was not really being addressed. There is some evidence to support opportunistic brief interventions for stopping smoking by physicians. While the evidence is weak, the potential for population health gain is high.
Effectiveness of interventions aimed at practitioners
Our review of primary prevention papers supports the findings of NICE in its Prevention of Cardiovascular Disease. 431 In consultations with practitioners it found that the role of primary care was complicated and sometimes contradictory. In group and practice-based interviews, some GPs and public health specialists highlighted the fact that GPs may be more comfortable with a secondary, rather than primary, prevention role, which may explain why some health promotion and public health staff find it difficult to engage GPs in CVD prevention programmes. Conversely, other interviewees viewed primary care staff as crucial partners in CVD prevention. This reflects evidence from other studies, which have found that many GPs state they lack the skills needed to delivery effective health promotion and that the lack of skill may also affect their attitude to giving advice. 228,268,269,432 Many GPs are concerned that giving lifestyle advice may be detrimental to the doctor–patient relationship,79,85 and are also unconvinced that their efforts to counsel patients on lifestyle issues are effective in changing behaviours.
Yet, while practitioners often to do not feel qualified or experienced in preventative work, a survey of GPs undertaken for the King’s Fund Quality Review found that GPs tended to rate the quality of their own health promotion and ill-health prevention activities as better than that of general practice as a whole. 433 Advocacy among other local organisations may be a key role, as is referral of patients to relevant services. However, practitioners are often unaware of the range of local services, or relevant services do not exist. Engaging primary care and keeping practitioners appropriately informed requires tailored approaches. In addition, lack of time has been cited as a key problem. For example, where primary care is involved in CVD prevention programmes, practices need to receive appropriate resources to free up staff time.
The role of nurses within the practice has become increasingly important. There is some weak evidence to show that nurse interventions for a number of screening and advisory interventions is effective. For example, studies involving nurses providing smoke-stop advice were rated as effective although there were no direct comparisons with physicians or others offering similar advice. However, the limited prescribing rights of nurses meant that more effective advice and clinical interventions were more difficult. In addition, studies consistently show that specialist services with specialist staff were most effective at stopping people smoking; this may include specially trained nurses. Where there were comparisons,183 the outcome was unclear, as nurses were more cost-effective in terms of the number of patients they counselled, but were more likely to misdirect patients, whereas GPs were less like to misdirect patients and gave better advice. In a study on hypertension the researchers concluded that to improve nurse effectiveness an algorithm to assess and steer care more effectively needed to be developed – similar to the one already used by GPs. 302
In relation to primary care provision, the introduction of the QOF has provided a key activity incentive for general practice. While limited in terms of supporting preventative activities, a number of QOF criteria relate to intermediate outcomes. The evidence from studies examining the impact of the QOF suggests that it has led to an improvement in intermediate health outcomes for some conditions (such as diabetes), although the results are mixed for others (such as CHD). 330 While some studies state that the management of blood pressure and cholesterol has improved for CHD since the introduction of the QOF,434 others claim that the improvement is not significantly higher than the underlying trend which existed before the QOF was introduced, as is the case for hypertension and asthma. 435,436 However, as the methodological quality of the latter studies is higher thanks to the inclusion of additional time points before and after the QOF, combined with stronger statistical results, the evidence supporting the hypothesis of no improvement above the underlying pre-QOF trend seems more convincing.
The results also demonstrate that despite a surge of improvement during its introductory period for some conditions, levels of achievement have reached a plateau in later years. As mentioned by Calvert et al. ,70 this may be a result of a ceiling effect caused by the maximum threshold levels set for each indicator. Achievement thresholds for the clinical domain indicators are mostly between 50% and 90%. This specifies the minimum and maximum percentages of patients that are required to achieve the target before the minimum and maximum scores are rewarded for that indicator (not to be confused with the different clinical targets referred to in the QOF, for example blood pressure < 140/80 mmHg). Studies that examined the impact of the QOF on non-incentivised activities of care and associated health outcomes suggest that non-incentivised areas were neglected and had declining performance. 437,438
Effectiveness of interventions related to location
While few studies specifically examined the differing effectiveness of locations, our review suggests that location is important for health improvement. For example, there is good evidence to support the use of schools as a setting for health improvement activities. For some weight loss and exercise activities, non-general-practice locations are preferable. On the other hand, general practice provides an ideal location for opportunistic interventions, such as on smoking, because of the numbers of patient contacts. While many lifestyle and brief interventions are not well supported in terms of effectiveness, where low-cost interventions can be delivered there may still be significant health gains across the population. In a study examining the control of hypertension, it was found that what seemed to work best was nurse-led interventions within primary care, and that interventions in the community or by telephone were less effective. 302
Conclusion
Our review of the literature suggests that there is little robust evidence to demonstrate positive behaviour change or clinical outcomes for preventative activities in primary care. Most papers examining primary prevention were either descriptions of services, commentary about primary prevention or research studies that were rated as of low quality. Few high-quality studies were identified in all key areas of primary prevention. The main exception was in relation to smoke-stop services, where services to support quitting are viewed as cost-effective and approaches that provide ongoing support for smokers wanting to stop, or those who have quit, delivered in a targeted way, are more likely to be effective. 252,439–442 In addition, there is still potential for better identification of smokers and raising smoking awareness by a range of health and other care professionals. The evidence to support interventions for increasing exercise or reducing weight was limited and suggested that such approaches in primary care or in schools have little impact and that any benefit is generally only short-term. In particular, the cost-effectiveness of primary preventative lifestyle interventions is difficult to determine because of the diverse nature of the interventions (type and organisation, different target groups) and research methodology. 442,443 There is good qualitative evidence from a large study of breastfeeding support to demonstrate the health services attributes that might be necessary to deliver interventions effectively. 221
Clearly advice from the GP is still rated highly by patients and may be acted upon. In terms of secondary prevention, there is evidence that more is being done but it is not clear how effective this is. For example, in relation to CHD, general practice has been identified as an ideal setting for delivering secondary prevention. However, the evidence indicates that provision is not as effective as it could be and, while the provision of secondary prevention can be improved by using specific disease management programmes, the optimal mix of their components remains uncertain. 444,445 There is insufficient evidence to make clear decisions about the balance between universal, opportunistic and targeted health promotion interventions. A key point, however, is that multiple risk factor interventions in primary prevention comprising counselling, education and drug treatments were more likely to be effective in high-risk groups than in the general population. 356
Finally, the current interest in incentivising health improvement practice through performance payment systems such as the QOF has had an important impact on both the areas of activity that are prioritised and how services are organised. There is good evidence that practices have responded in different ways to these incentives in terms of how they organise practice. What is clear from the evidence and discussions with practitioners is that there has been a shift to employ nurses and health-care assistants to do much routine prevention work including screening. The QOF has also led to improved recording of the health status of patients in their practice. Interestingly, a Europe-wide survey of GPs in other countries highlighted the lack of reimbursement as a key reason for not engaging in health promotion activities. 446 As the discussion on CVD demonstrates, the use of financial incentives is more likely to lead to GPs following guideline advice. However, the focus on single disease risk factors has been widely criticised and can lead to a number of problems or skew practice to the neglect of non-incentivised areas of practice. 437,438,447,448
Chapter 7 Impact of changes in the Health and Social Care Act 2012 and Public Health White Paper
Introduction
The coalition government (2010–15) policies since 2010 highlighted the potential for greater GP involvement in public health. The changes to the structure of the NHS and to public health oversight introduced in April 2013 were designed to strengthen local public health, although the extent to which this will support and increase GP involvement is not clear. The combined implications of the government’s proposals for public health in England set out in Healthy Lives, Healthy People37 (and subsequent consultation papers) and the changes contained in the Health and Social Care Act 201221 on the structure and delivery of public health in England have been enormous. In this chapter we discuss those implications which have a direct impact on the public health role of general practice. In the White Paper and other public statements, the government outlined an increased role for GPs and general practices in public health. GPs and their practice teams have a crucial role in promoting health and preventing disease. Each year there are over 300 million consultations with primary care professionals – the majority with GPs but increasingly with practice nurses and other practice-based healthcare staff – with every consultation an opportunity to detect early warning signs that prevent illness and disease. 18 This was recognised by the coalition government of 2010–15 in its White Paper on public health arguing that GPs ‘have huge opportunities to provide advice, brief interventions and referral to targeted services through the millions of contacts they have with patients each year’ (p. 61). 35 In addition, since January 2012 there has been a call to NHS professionals to ‘Make every contact count’449 in a campaign to improve public health via every contact between a NHS professional and the public. As well as all aspects of primary and secondary prevention, there has also been an effort to incorporate the guidance into wider aspects of public health such as homelessness. 450 Furthermore, in 2011 the DH published the Health Visiting Implementation Plan,98 which proposed an increase in the health visitor workforce by 4500 new health visitors by 2015, with the concomitant emphasis on public health outcomes for children and families at all levels.
However, how these roles are developed, supported and sustained within the new public health and commissioning structures of the NHS in England is still not clear. The development of CCGs, new public health commissioning and delivery roles for LAs, and an expanded national public health role through PHE as well as a public health commissioning role for NHS England create a new and potentially more complex commissioning and service delivery environment for many public health activities in primary care. 36,98,451 There are particular concerns about the fragmentation of public health functions and service delivery agencies, the distribution of resources between responsible agencies and how proposals for commissioning and organising public health will provide a cohesive and co-ordinated public health system with a clear general practice role. The aim of this chapter is to set the context of this review within the recent changes to commissioning and public health introduced in April 2013. The chapter provides a critical analysis of the organisational changes and policy implications of the Health and Social Care Act 201221 as they relate to the organisation and delivery of public health within general practice.
The changes
Until April 2013 public health was delivered through a number of different mechanisms:
-
DH – setting policy and funding a number of health intelligence programmes including the observatories and cancer registries
-
government offices
-
National Treatment Agency for Substance Misuse – drug treatment monitoring
-
strategic health authorities – strategic oversight and performance of each region
-
PCTs – commissioning of programmes to deliver health service outcomes/joint commissioning with LAs
-
provider trusts – delivery of public health programmes, for example community services
-
LAs – a number of different services provided by local government that have an impact on the public’s health such as environmental health, leisure, planning, housing
-
Health Protection Agency – health protection services.
Following the Health and Social Care Act 2012,21 most of these organisations either were abolished or have taken on significantly different responsibilities. In addition, new commissioning and public health organisations have been established. The key strategic changes are as follows:
-
Strategic health authorities were abolished at the end of March 2013.
-
PCTs were abolished at the end of March 2013.
-
PHE was established in April 2013, encompassing the National Treatment Agency and Health Protection Agency, and is responsible for a number of health intelligence functions including the cancer registries and regional observatories, and former government office functions.
-
Ring-fenced budgets for public health have been allocated to LAs: unitary authorities and upper-tier authorities (i.e. county councils, not district councils). Directors of public health are employed within these authorities and are joint appointments between PHE and the appointing LA.
-
CCGs are now responsible for the commissioning of secondary and community-based health care.
-
NHS England (a national commissioning organisation) is accountable for CCGs and oversees the commissioning of specialised services and primary care services (GMS contract).
-
A range of provider organisations (‘any qualified provider’) including foundation trusts, charities, independent sector and social enterprise.
In Healthy Lives, Healthy People,37 the government proposed key changes to the provision of public health. The two key changes involved the establishment of PHE in April 2013 and the transfer of local NHS public health responsibilities to LAs. PHE is responsible for funding and ensuring the provision of a wide range of services such as health protection, emergency preparedness, recovery from drug dependency, sexual health, immunisation programmes, alcohol prevention, obesity, smoking cessation, nutrition, health checks, screening, child health promotion (including those led by health visiting, school nursing and general practice), some elements of the GP contract (including parts of the QOF such as those relating to immunisation), contraception and dental public health. It does not have direct commissioning responsibility but will grant funding to LAs and it will need to work through NHS England to commission services, such as screening services, and the relevant elements of the GP contract.
The 2010–15 coalition government announced its intention in The Coalition: Our Programme for Government35 that the DH would strengthen the role and incentives for GPs and GP practices on preventative services, both as primary care professionals and as commissioners. There was a recognition that primary care professionals, GPs and GP practices play a critical role in both primary and secondary care prevention. Key areas highlighted by the government were practitioners’ opportunities to provide advice, brief interventions and referral to targeted services through the millions of contacts they have with patients each year. 37
Healthy Lives, Healthy People37 (para. 451) sets out specific ways by which the DH intends to strengthen the public health role of GPs. These involve a mix of support and incentives:
-
PHE and the NHS Commissioning Board will work together to support and encourage CCGs to maximise their impact on improving population health and reducing health inequalities. This includes looking specifically at equitable access to services and outcomes.
-
Information on achievement by practices will be available publicly, supporting people to choose their GP practice based on performance. By increasing transparency about how effective different GP practices are in giving public health advice, PHE will enable local communities to challenge GPs to enhance their performance.
-
Incentives and drivers for GP-led activity will be designed with public health concerns in mind, for example in terms of prevention-related measures in the QOF. To increase the incentives for GP practices to improve the health of their patients, the DH has proposed that a sum at least equivalent to 15% of the current value of the QOF should be devoted to evidence-based public health and primary prevention indicators from 2013. The funding for this element of the QOF will be within the PHE budget. However, in 2013/14 this has not translated into many additional or different indicators.
-
PHE will strengthen the focus on public health issues in the education and training of GPs, nurses and health visitors as part of the DH’s development of a workforce strategy.
These changes have had a significant impact on general practice and its public health role. In particular, five changes potentially increased both GPs’ needs for public health knowledge and practices’ need to increase their provision of health promotion and disease prevention services. The changes also provide significant challenges.
-
The now abolished PCTs were responsible for the GMS contract and supporting local practices. The PCT also provided public health support to local practices and delivered some health promotion services such as specialist smoke-stop and sexual health services for young people. In many areas, PCTs developed additional prevention services in collaboration with practices funded through LES within the GMS contract. It is not clear how the new system will continue such support.
-
With the abolition of PCTs, newly created LA Health and Wellbeing Boards (HWBs) now have to make decisions about public health priorities for their geographical area. GP representatives from CCGs sit on these boards, and they will probably be expected to contribute to the understanding of what the local health demands are, as well as the ways that general practice and other primary care services can improve health outcomes in these areas.
-
General practitioner-led CCGs have taken over the commissioning role of PCTs. This could include some public health commissioning, although the details of which will depend on what NHS England chooses to ‘pass down’ to them. Commissioning public health services will require knowledge of how and where these services are best delivered.
There is a new Commissioning Outcomes Framework which will be used by NHS England to assess CCG performance. The aim of the framework is to allow NHS England to identify the contribution of CCGs to achieving the priorities for health improvement in the NHS Outcomes.
-
The QOF will be adjusted so that 15% is made up of evidence-based public health and primary prevention indicators by 2013. 36 While the substance of these changes remains unclear and no change has yet occurred, GPs should be preparing for a shift towards payments for prevention.
-
Although funding for public health will be ‘ring-fenced’, overall budget cuts may increase the focus on prevention rather than expensive treatments, a shift which is likely to extend to general practice. Whereas in the past such pressures within PCTs have tended to squeeze out public health expenditure, the protected LA budget will not be at risk of being shifted towards clinical services.
General practice and the new commissioning arrangements
The emphasis on CCGs being responsible for the well-being of their whole community and the stronger role of the HWBs was recommended in the NHS Future Forum report449 and ensured that public health became a shared responsibility across local commissioning organisations. However, the splitting of public health resources across general practice, CCGs, LAs and PHE/NHS England presents new challenges for the organisation and delivery of public health in England. For example, drug, alcohol and mental health services will all be commissioned via LAs. From 2015, LAs will also commission the health visiting services, which may have the effect of separating health visiting from the general practice population. These important public health challenges often overlap and are best dealt with by joint services, which may include GPs and community health professionals in shared-care arrangements if locally appropriate. These services are a good example of how, by commissioning similar public health services by one body (in this case, LAs), there can be streamlining of service delivery and inclusion of GPs where beneficial, but this grouping together will be effective only if there is enough funding to support these joint endeavours.
Commissioning has been split between local and national commissioners. While NHS England has local offices, co-ordination between commissioners is important. It is also be important to ensure that CCGs and GPs more generally are linked to broader public health commissioning arrangements. For example, public health services for children aged under 5 years, which include pre-established programmes and services that fall outside the NHS, are contracted centrally by NHS England, but GPs play a huge role in the care of under-5s and work collaboratively with local health visiting teams and other community staff, who also work closely with LA and third sector organisations – all of which are commissioned by different bodies. It is not clear how the necessary linkages are being made between GPs and community services (and local council services) when it comes to the local organisation and delivery of care and prevention programmes to under-5s.
Some degree of co-ordination will possibly be achieved through CCG representation on HWBs. The boards are seen as key to co-ordinating the local health system:
The joint local leadership of CCGs and local authorities through the health and wellbeing board will be at the heart of this new health and social care system . . . [and] enable greater local democratic legitimacy of commissioning decisions, and provide an opportunity for challenge, discussion, and the involvement of local representatives.
p. 115451
Clinical Commissioning Groups have an avenue, therefore, to be involved in local decisions about public health resource allocation – an important way of maintaining GP involvement in public health. Concerns about CCG access to public health support were raised in discussions with GPs and CCG staff, and also identified in research on the early development of CCGs. 334
However, the most dominant role of the CCG is in commissioning secondary care services, which provides a new set of challenges as well as opportunities for improvement in public health and ill-health prevention. Research on practice-based commissioning found that GPs focused more on preventing ‘unnecessary’ hospital admissions than on primary prevention. 452 Analyses of previous primary care commissioning similarly found GPs used traditional models of general practice and did not address key public health problems. 57,76,258,453 However, this is not a reason to take public health out of GP commissioning responsibilities. In fact, researchers have suggested that GP budgets for commissioning health services be aligned with budgets for commissioning public health. 454 On a more positive note, it is possible that, by giving CCGs responsibility for standard health service commissioning as well as some public health services, they may be forced to think more broadly about their communities. CCGs should have responsibility for, or at least be directly involved in, commissioning those public health activities that most closely relate to the ones they provide themselves via the GP contract (such as contraception services and cervical cancer screening). Aligning these responsibilities puts GPs’ existing knowledge of service provision to work, and helps to ensure that patients have access to the most streamlined pathways for these services (as well as the best-quality ones).
One key area of public health activity is the support for commissioners. Systems developed within PCTs for supporting GPs with epidemiological analyses are likely to have been substantially disrupted with changes to public health departments. New relationships, systems and processes need to be developed to provide what is critical support for the new commissioning bodies. Additionally, this is being done at a time when new organisational structures for public health are being established in LAs, placing further strains on developing relationships.
There is continuing tension around the relationship between general practice commissioning and public health. The evidence from previous approaches to primary care-led commissioning suggests that public health has not been a priority for GP commissioners. 453 The development of primary care groups and, more specifically, PCTs did start to embed a more public health perspective in commissioning, but current changes to both public health and health-care commissioning may simply exacerbate what has often been a troublesome relationship between GP commissioners and public health. 77,453
The General Medical Services contract and public health
Currently many public health activities in primary care are supported by the GMS contract. There are three funding strands:
-
core standard tasks – expected in normal practice (advice, information, etc.)
-
aspects of the QOF
-
Local Enhanced Service elements of the contract.
Where clinical services are closely linked to public health activities such as screening, immunisation, obesity and sexual health services, part of the service is being provided by GPs as part of the GP contract (cervical cancer screening, childhood and elderly vaccinations, and contraception services), but other, similar services are being commissioned by LAs or NHS England (i.e. additional cancer screening, booster vaccinations, sexually transmitted infection screening and treatment, and general screening such as the NHS Health Check). This could lead to a situation where similar services that can be most effectively provided side by side (most obviously, contraception and sexually transmitted infection services) may be available from different providers because they are commissioned by different groups. Greater co-ordination of commissioning and service delivery will be essential. Thought needs to be given to arrangements for lead commissioning with the flexibility such as that available between the NHS and LAs under the 1999 Health Act455 for partnership funding for the commissioning of all aspects of key prevention services by one commissioner.
Local Enhanced Services have been particularly effective in involving GPs in locally driven public health efforts supporting a wide range of evidence-based public health activities, such as identifying CVD risk and providing long-acting contraceptives, and in 2009/10 they accounted for some £370M. 34 Having the option of LESs in the contract has provided a way for GPs to reduce preventable morbidity, and it could continue to do so in the future. This option would be especially helpful in the context of a more diverse provider landscape. However, many of the activities currently funded through LESs, including sexual health, smoking cessation, prevention and treatment of alcohol misuse, falls prevention and mental health promotion, are now commissioned by LAs, with the GP contract the responsibility of NHS England. LESs are commissioned by the local area teams of NHS England, yet the teams do not have any real levers or necessarily the knowledge needed to do this. This appears to be a key weakness in the new system.
One key element of the contract where it is proposed to incentivise more primary prevention in general practice is through the QOF. In the White Paper the government proposed that NICE adjust QOF to ensure that 15% is devoted to ‘evidence-based public health and primary prevention indicators’ (p. 62). 35 Currently, QOF continues to have only two indicators that it designates as ‘primary prevention’; otherwise it focuses mainly on secondary prevention and uses proxy or process outcomes. QOF has had a major impact on how practices undertake public health and other activities leading to more systemisation of public health activity – particularly through use of protocols and special clinics, but mainly with a secondary and medical focus. 65,456 While having some impact on primary and secondary prevention by stimulating GPs to run ill-health prevention clinics for screening and monitoring blood pressure etc., QOF has mainly supported secondary prevention activities. 32,65,93 To date, the evidence that the QOF has improved health outcomes or promoted a public health approach is very limited. 18,65,330 However, financial incentives that are effective in changing practice and more outcomes-based contracts, rather than activity-related incentives, could encourage a more proactive approach. 32 The impact of proposed changes by NICE will, to a large extent, dictate how much GPs are involved in improving the health of their patient population, which will, in turn, be affected by the future organisation of public health commissioning and service delivery.
There are, however, concerns about the extent to which NICE’s rigidly evidence-based approach is relevant for the development of many public health interventions and also whether or not such approaches are relevant to primary care itself. 457–460 In particular, there are concerns about what the contract encourages in the way of public health activity in general practice. There is an important trade-off here: RCT-based ‘certainties’ around expensive technical interventions versus ‘riskier’ but potentially more impactful interventions such as, for example, brief interventions for smoking, which have low impact but are very low cost and, while having a small impact, affect a large number of people. 460 Similarly, many areas of activity such as community-oriented activities or even welfare advice are not currently rewarded.
The implications of the fragmentation of public health services
Not only is the commissioning of similar services undertaken by different bodies, but there is also a more general likelihood of fragmentation of delivery of public health services due to the ‘any qualified provider’ model. The idea behind this approach to commissioning is to increase quality of care via a wider field of competition, on the presumption that increased competition will drive out poor providers and reduce the total number of providers. However, there is a risk that the overall effect of this policy will be that public health-related care is divided over a larger number of providers. The effect on GPs may be twofold. The first is simply that services that were once provided by GPs will be provided elsewhere, such as NHS Health Checks. The second effect, which is likely to be the more common one, is that patients will have to seek out many geographically separated providers for services such as sexually transmitted disease treatment, cancer screening and nutrition advice. This may be confusing and frustrating to patients as well as GPs, requiring good communication between different agencies to minimise this confusion. GPs must be kept aware of which providers are providing which services so they can properly advise their patients on where to seek care. Additionally, GPs must be able to keep track of what care their patients have received from other providers. Co-ordinating with other providers and keeping detailed records of their patients’ care, particularly when it comes to routine screening and immunisation, are key roles of the GP. It will be crucial to build in a way for all commissioners and providers of public health services to share their knowledge and records with GPs so that GPs can continue to do their jobs effectively. For example, there has been a long tradition of health visitors being ‘GP attached’, and parents and children within GP practices will lose this direct relationship with their GP services when health visitors are commissioned by the LA to provide a community-based service.
Ultimately, this will lead to postcode variation in provision or a variant of the ‘inverse prevention’ law if commissioning is more effectively supported and undertaken in healthier, wealthier areas (as, historically, has tended to be the case).
The opening up of public health delivery and practice to a more diverse range of providers calls into question the future role of entire categories of providers already working in public health, including health visitors, midwives and school nurses. Investment in health visiting is discussed in the White Paper37 and is welcome, but other key members of the local primary health care team who deliver public health are not mentioned. For example, the crucial role of school nurses is not mentioned in the documents and it is not clear where this service will need to focus its attention or how it will be integrated into the rest of public health delivery.
One mechanism for prioritising the general practice role in public health is via the Public Health Outcomes Framework. 37 As it currently stands, the Public Health Outcomes Framework indicates the few places where responsibility for achieving indicators is shared with the NHS. Just eight indicators in the entire list refer to the NHS, and most of them are around reducing premature death in people with chronic diseases rather than disease prevention or health promotion. It is not clear what this shared responsibility refers to: provision of funding or delivery/planning of services. Looking at the entire list of public health indicators it is clear that GPs, and therefore the NHS, can be instrumental in delivering many services beyond the ones singled out – in services relating to sexual health or smoking cessation, to name just two areas. When LAs and local HWBs are considering how to best respond to these indicators (which they are driven to do by the ‘health premium’ payments), they should keep GP services in mind for many indicators beyond those with designated NHS involvement. Additionally, the boards may find that GPs are particularly well primed to the idea of indicators, having now been working with the QOF for over 6 years. While these two sets of indicators are very different in character, GPs may be comfortable with the idea of indicators and may have ideas for how to incorporate this new set into their practices.
While HWBs have been given a key co-ordinating role, it is questionable how far they will be able to fulfil all the expectations placed upon them. At the current time there remains considerable ‘fuzziness’ around the exact role of HWBs. The lack of statutory powers given to the boards means that it is only by developing good local relationships that they will be able to fulfil their potential. In recent research on the development of CCGs, the development of a strong ‘co-ownership’ model, where CCGs, LAs and HWBs saw themselves as joint owners of the developing strategy, with all partners being actively involved, was noted in some areas. However, in others, CCGs were developing quite separately from their HWBs, with CCG representatives attending meetings but contributing little. 63,334 Marks et al. 63 have highlighted the difficulty of aligning priorities across large geographical areas and where organisations were not coterminous. This may prove a problem again, as many of the 211 CCGs cover smaller populations than their HWB, and the ability to respond to local concerns and problems will be important as HWBs develop. Ultimately, despite HWBs having ‘strategic influence over commissioning decisions across health, public health and social care’ as one of their main roles,461 there is a danger that, as new local public health systems develop, they may become more fragmented in terms of the relationships between LAs, CCGs and HWBs as well as having to cope with a new national context with PHE and NHS England. This may create additional complexities for local co-ordination by the HWBs and raises important questions about how public health activities in general practice will be incentivised, managed and supported in the future. This uncertainty was of concern to many of the GPs we talked to during the research.
Current developments
In line with the government’s coalition agreement (of 2010–15) policy focused on the health improvement role of general practice. 35 In addition to proposals to revise the QOF to include more primary prevention criteria, the recent Mandate for the NHS Commissioning Board highlights prevention within the concept of making ‘every contact count’, ‘in focusing the NHS on preventing illness, with staff using every contact they have with people as an opportunity to help people stay in good health – by not smoking, eating healthily, drinking less alcohol, and exercising more’ (p. 8). 462 This approach is now reflected in NICE Public Health Guidance with the publication of the draft revision of physical exercise guidelines (currently out for consultation). The proposed revised guidelines specifically target primary care practitioners proposing that they:
Assess the physical activity levels of all adults in contact with primary care services and identify those who are not currently meeting the UK physical activity guidelines. This could be done:
opportunistically during a consultation with a GP or practice nurse (or while people are waiting)
as part of a planned session on management of long-term conditions run by a practice nurse
as part of a consultation with a pharmacist.
p. 8463
With this guidance, primary care practitioners are being encouraged to identify inactive patients, assess their level of activity and deliver a brief intervention to encourage them to increase levels of activity. Concerns have been raised about whether or not it is appropriate for more and more elements to be placed on GPs and nurses given the limited consultation time in practice. These questions have also been raised in connection with a pilot study that examined adding cancer-screening questions into the NHS Health Check. The pilot study involved a screening survey of 4250 patients with high cardiovascular risk undergoing NHS Health Checks. The study, reported at the October 2012 Society of Academic Primary Care conference in Glasgow, found that the process involved substantial nurse and GP time but led to only four cases being identified. 464
Conclusion
The Royal College of General Practitioners argues that GPs should be proactive in carrying out public health activities and interventions, and it is expected that GPs should possess a wide range of skills related to ill-health prevention and public health. 7 Since 1990, GPs in particular, have been encouraged to carry out more public health activities through changes to their contract and the potential of the primary care public health role was highlighted in the Wanless Report on public health. 3,48 However, research continues to find that the relationship between public health and general practice in England focuses primarily on secondary prevention, and many GPs state they lack the skills needed to deliver effective health promotion. 432 The King’s Fund Inquiry on quality in general practice concluded that there is enormous potential for general practice to take a more proactive role in ill-health prevention and public health. 18,465 In fact, a key criticism of much of general practice (when it comes to public health) is that it focuses on either secondary prevention or just information and advice. While both of these activities are useful, other interventions can be more effective. All of these considerations and criticisms are of particular importance when it comes to the QOF, which is a key driver of GP practice.
The Public Health White Paper37 outlines a number of key changes to the organisation and delivery of public health in England. However, while the public health role of general practice has been the subject of much debate over the past few decades, the government does not appear to have grasped how this role can be integrated, developed and supported within the proposed changes. Relying on changes to the QOF is both short-sighted and overly narrow. The fragmentation of the commissioning and delivery of public health is likely to lead to problems of co-ordination. It is not clear how HWBs – responsible for local public health co-ordination – will build integrated approaches with both CCGs and PHE as well as the wide range of local delivery organisations, including general practices. Previous approaches to primary care-led commissioning have not demonstrated that GPs can work closely with LAs or other agencies. 453 A further problem may be the attitude of many GPs themselves, as studies suggest that they are more comfortable managing illness than promoting health. How effective the new proposals will be at engaging GPs and other primary care staff in public health activities is still open to question, as for many GPs there is still a significant amount of distrust. 334
In this chapter we have identified a number of potential problems that may result from current policy developments and organisational changes. While an emphasis on health improvement is welcome, there are a number of potential threats to the ability of primary care, and general practice more specifically, to deliver public health. First, commissioning approaches need to be aligned across the different agencies that will be responsible for aspects of public health. In particular, commissioning agencies need to urgently identify how services from existing groups of primary care-based public health providers (midwives, school nurses, etc.) are commissioned and supported within the new structures. Thought also needs to be given to how health improvement activities that have formerly been funded through GMS, PMS and other local contractual arrangements can be continued, and how local variations in funding and service delivery can be incorporated into the new systems and structures. Developments in health improvement in general practice have benefited from local negotiation and relationships with the public health department in the PCT. Concerns have been raised about the ongoing links between public health and general practice now that LAs have taken on public health responsibilities. While policy is increasingly emphasising public health roles being embedded in primary care practice, many of the current organisational changes are creating potential problems for the commissioning and delivery of many important health improvement activities.
Chapter 8 Discussion and conclusion
Introduction
The aim of this study was to identify the current extent of knowledge about health improvement activities in general practice and the wider primary health-care team. The primary focus of the review was on activities that were specifically related to activities undertaken in the practice and by primary health-care staff linked to the practice. With the publication of the White Paper on public health,37 this focus was extended to include the role of pharmacies and prevention activities undertaken by primary health-care teams in settings outside the practice such as schools and in the community. Thus activities by school nurses and health visitors were included, but wider public health and health education activities in schools – by the schools themselves – were excluded.
The original focus of the research was to undertake a scoping review of health improvement activities undertaken in general practice or by the primary health-care team to determine the nature and extent of research evidence about these. Through discussions with practitioners we sought to identify how such activities were organised and delivered. An overall aim was to define areas of practice that needed further research. We were also requested by the NIHR SDO programme to focus the research on producing an evidence synthesis rather than merely scoping the research. The key objectives of the review were, therefore, revised in order to provide an overview of the range and type of health improvement activities being undertaken, assess the strength of evidence for such activities where possible and identify gaps in knowledge and areas for further empirical research. As a result, the stakeholder consultations were more limited than originally envisaged and were primarily used to inform the literature review and interpretation of findings.
Key questions for the review team were:
-
What was the range and type of health improvement activity undertaken in general practice?
-
What evidence was there on effective approaches to the delivery and organisation of health improvement interventions in general practice settings?
-
What gaps were there in the evidence base?
-
What are the priority areas for future research?
Essentially our focus was twofold, involving:
-
an assessment of the efficacy of approaches to the delivery and organisation of health improvement interventions to identify areas of public health that can be delivered in a general practice setting (including identifying the roles of general practice and the staff working in general practice and methods of delivery and organisation)
-
identifying research gaps and priorities for further research.
This chapter draws on the findings of the review and discusses them in the context of current developments in the NHS. The chapter summarises our key findings and sets this within a framework that structures the relationship between public health and primary care, and how health improvement activities are delivered and organised.
General practitioners and their practice teams have a crucial role in promoting health and preventing disease. Every consultation is an opportunity to detect early warning signs that prevent illness and disease. GPs and the wider primary health-care professionals are, therefore, ideally placed to ‘make every contact count’. 449 While this rhetoric pervades the NHS and public health discourse, the evidence that primary care consultations can effectively deliver this is less clear from our review. The Royal College of General Practitioners agrees that GPs should be proactive in carrying out public health activities and interventions, and it expects GPs to possess a wide range of skills related to ill-health prevention and public health, as reflected in the Member of the Royal College of General Practitioners curriculum. 466 However, research continues to find that the relationship between public health and general practice in England focuses primarily on secondary prevention,18 and many GPs state they lack the skills needed to deliver effective health promotion. For example, currently GPs respond to requests for support in smoking cessation more often than they proactively engage their patients. Therefore, there is enormous potential for general practice to take a more proactive role in ill-health prevention and public health. NICE public health guidance advises primary care professionals, such as GPs, to opportunistically carry out activities such as brief interventions. 244,388 The White Paper on public health acknowledges this role, stating that GPs have huge opportunities to provide advice, brief interventions and referrals to targeted services. 35
The evidence
The evidence synthesis and review of activities undertaken in primary care focused on how health improvement interventions and activities have been, and are, organised and delivered. We undertook a broad search for relevant literature with the aim of identifying both the extent and the quality of evidence supporting approaches to organising and delivering health improvement interventions. Given the breadth and huge number of potential papers identified in our original searches, we refined our search criteria to focus specifically on papers describing or evaluating UK practice.
While we identified 1140 papers from our original literature search, when they were examined for relevance and then for quality we found that only 347 (30%) met our inclusion criteria for the evidence review. We assessed the quality of each paper in terms of whether or not the research methods supported the outcomes in the paper. We used a grading system based on critiquing five areas:
-
quality of the sampling process (including the sample size)
-
appropriateness of the analysis
-
comparability of the intervention and comparison groups
-
quality of the intervention delivery (including whether consistency of the intervention was measured or whether there was risk of contamination)
-
outcome assessment.
For each paper we identified whether there were no concerns about the methods or data presented, minor concerns or major concerns. Studies were described as of high quality (A) if there were no concerns across the applicable areas, good quality (B) if there were one or two minor concerns and lower quality (C or D) if there were major concerns or multiple minor concerns.
As detailed in Chapters 4–6, the range and diversity of papers was substantial. In order to examine selected papers we grouped them into broad topic areas. However, even within these there was significant variation between papers. For example, papers classified as child health covered childhood screening, breastfeeding, accidents, diet, sexual health, weight and exercise, etc. Assessing papers presented a number of key difficulties for reviewers. We foresaw that identifying data on service delivery and organisation would be difficult and we expected to exclude many papers because they did not address these issues at all. However, even amongst selected papers in the review it was difficult to summarise the evidence or draw any substantial conclusions from the evidence.
In addition, there is a widely recognised problem about the relevance of much research to general practice. The increasing importance being placed on the role of primary care within health systems raises questions about how an appropriate evidence base for practice can be supported, developed and applied. A simple view of knowledge production and use would see this as a linear process, whereby scientists find out new things about the world that are published in academic journals. Then people who want that knowledge search for it and put it into use. In this classic knowledge-driven model, research generates knowledge, which impels action; thus, where knowledge is generated and by whom is less relevant than ensuring the production of high-quality research findings. 467 This is an oversimplified view of a complex process. 468,469 An interactive, social model of knowledge is more useful. Gibbons et al. 470 make the case for two ‘modes’ of knowledge production. As Sweeney et al. 457 have argued, not only does research needs to be statistically and clinically relevant but there should also be recognition of personal significance and the importance of applying research evidence to the individual within the social context.
Producing evidence on health improvement interventions in general practice raises important questions about the type of evidence required and how it is produced. As Rychetnik et al. 113 argue, evidence needs to be clear not only about whether the intervention is successful or has failed, but also about how it is delivered – especially if failure of an intervention is a result of bad delivery. Furthermore, De Maeseneer et al. 458 have argued that ‘[c]ontextual evidence is necessary to assist doctors to address the challenge of how to treat a particular patient in a given situation’ (p. 1316). Where service delivery needs to be supported by research that is both appropriate and context-relevant – as is the case for much health improvement activity – it is best conducted within primary care. The study by Hoddinott et al. 221 has cast important light on how analysis of the context of service delivery can be explanatory regarding success and failure of interventions. Hospital-based clinical research is not always relevant to the primary care context, and the findings of clinical trials based in secondary care cannot easily be translated into primary care practice. In addition, primary care practice involves an interest in the appropriateness of care and low-technology interventions such as many health improvement activities that require being responsive to individual patient circumstances. In an analysis of NICE guidelines for GPs the researchers concluded that as few as 2% were directly relevant for general practice. 471 The need for a different approach to primary care research is set out in the recent Society for Academic Primary Care Paper Blue Sky Research for Primary Care: A Discussion Paper. 472 Watt concludes that:
The contribution of generalist clinical practice to health improvement is achieved via the sum of care provided for all patients. . . . Such activity is an important determinant of population health, although it is often excluded from public health discourse and from consideration of public health research needs.
p. 11472
From the analyses in our review we conclude that more relevant research needs to be developed that adequately reflects both the context of primary care and other settings where health improvement interventions are undertaken as well as ensuring that service delivery and organisational issues are researched as well. In addition, research needs to compare different methods of delivery and organisation; for example, comparing the role of different professionals and different locations as well as different delivery methods in order to determine the effectiveness of not just the specific intervention but also how it is delivered.
What is done, by whom and where
The selected papers encompassed a wide variety of research designs across a broad range of topic areas. Generally papers had little information on the context or organisation of the way in which the intervention was delivered. There were a substantial number of papers that examined individual interventions without any comparison or were simply studies of patient or practitioner views and perceptions. Much prevention activity in general practice relates to clinical interventions and it was surprising that more such papers were not included in the evidence synthesis. However, we found that a high proportion of papers examined clinical prevention interventions yet had no information about, or did not address, delivery and organisation aspects of interventions but were merely clinical trial data or evaluations of the clinical intervention. There were some data on the type of practitioner and location of the intervention delivery but there were few data that allowed statements to be made about the comparative effectiveness of different locations, or person, delivering the intervention.
The problem of identifying service issues is a common problem in this area of research. For example, a recent cost-effectiveness analysis for brief interventions in general practice for physical exercise argued that the main reason for a lack of evidence was that
it was not possible to disentangle the effectiveness (and hence efficiency) of brief advice interventions from either more intensive counselling, exercise delivery programmes (n = 7) or from other lifestyle advice (n = 10). The problem of disentangling was a function of study design as well as choice of outcome measures.
p. 31473
It is understandable, therefore, that we found little robust evidence to demonstrate positive behaviour change or clinical outcomes for preventative activities in primary care. The evidence on the effectiveness of different approaches by different practitioners and in different locations was very limited. For example, most papers examining primary prevention were either descriptions of services or commentary about primary prevention or research studies that were rated as of low quality. The main exception was in relation to smoking cessation services, where services to support quitting are viewed as cost-effective and approaches that provide ongoing support for smokers wanting to stop, or for those who have quit, when delivered in a targeted way, are more likely to be effective. In addition, there is still potential for better identification of smokers and raising the subject of smoking with patients by a range of health and other care professionals. We found little similar evidence for other areas of prevention activity. The evidence to support interventions for increasing exercise or reducing weight was limited and suggests that such approaches in primary care or in schools have little impact and that any benefit is generally only short-term. In particular, the cost-effectiveness of primary preventative lifestyle interventions is difficult to determine because of the diverse nature of the interventions (type and organisation, different target groups) and research methodology.
The papers examined in this review also appear to show that GPs often feel ill equipped to give prevention and health promotion advice to patients. There is clear evidence that practice nurses are increasingly being used to provide prevention and health promotion and also to monitor symptomatic and asymptomatic (but deemed at risk) patients. While patients seem to like this, there is little evidence of positive outcomes or other patient benefit. There is little evidence to suggest that any lifestyle advice is recalled by patients, let alone acted upon, which may contribute to lower levels of effectiveness. 332 In addition, patients may prefer alternative sources of information for such advice, such as magazines and television. 332 Generally, the evidence is only from short studies, with methodological problems, and benefits demonstrated were only marginal. However, a recent international review of the literature on the role of primary care in improving health literacy among patients suggests that there are effective measures that may help improve people’s knowledge about health and contribute to improved health outcomes. Its authors conclude that:
group and individual interventions . . . in both primary health care and community settings may all be useful in supporting sustained change in health literacy for change in behavioural risk factors. There may be scope for some tailoring of the site and type of interventions depending [on the] risk factor.
p. 10474
The authors conclude that less-intense interventions may be as effective as more intensive ones but caution that more research is needed on the specific intervention type. They note that different interventions produced different results and that similar interventions produced different results depending on the health issue being targeted. Similarly, different locations produced different results as did different degrees of intensity of the intervention.
There is some evidence to suggest that short interventions are effective in general practice, particularly where the GP has done these (e.g. smoking, alcohol, older people), although effects are very small. However, concerns have also been raised about adding more and more advice interventions into the limited consultation time. Making sufficient time available for health promotion and prevention remains a crucial issue. Limited consultation time is seen as a key problem restricting how health issues – such as smoking and lifestyles – can be raised. In a review of the relationship between the GP consultation length, process and outcomes, Wilson and Childs475 concluded that a consistent finding from studies was that GPs with ‘longer than average consultation lengths prescribed less and were more likely to include lifestyle advice and preventive activities’ (p. 1018).
Evidence on effectiveness of different approaches to service delivery and organisation
We were able to identify a wide range of intervention processes that were of interest in terms of how health improvement services are delivered and organised. However, the evidence is disparate and covers a number of different topics. For example, brief interventions by GPs are effective in helping people stop smoking. However, there are numerous concerns about the way smoking is raised in consultations by GPs and it is not clear whether similar interventions by other practitioners are equally effective. Brief interventions by GPs for other health issues have also been examined – such as with people with alcohol problems – but there is less definitive evidence of their effectiveness. There is good evidence as well that specialist stop smoking services are effective, but the evidence suggests that GPs are poor at making referrals to such services.
Since the 1990s there has been a growth in the number of screening intervention programmes undertaken in general practice. Since the introduction of the QOF there has been an increase in more systematic approaches to screening for health risks for blood pressure, cholesterol, etc. 65,93,330 Increasingly, emphasis appears to be focused on these types of interventions with population screening by primary care practitioners seen as important health improvement activities. The introduction of NHS health checks, chlamydia screening, recent proposals for exercise screening, and extending health checks to include other screening questions appear to be promoting more systematised approaches to care. Such moves are not without controversy464,476 both in terms of whether or not the evidence supports the benefits of these interventions but also in terms of changing the way primary care practitioners practice. 477,478
The focus of attention is mainly on individual prevention approaches, with practices engaging in both primary and secondary prevention. Health improvement activity in general practice also tends to be focused on medical conditions related to specific disease prevention such as diabetes or CHD. There is substantial evidence to suggest that GP activity is driven by specific contractual incentives and conditions. However, the wider literature also suggests that general practice is also affected by other factors such as peer pressure, relationships with public health departments, education and training. 18 While direct incentives such as contracted standards or the QOF do influence practice, there is some debate about whether or not GPs simply react to maximise their income and do not prioritise activities on those most in need. The evidence from studies examining the impact of the QOF suggests that the QOF has led to an improvement in intermediate health outcomes for some conditions (such as diabetes), although the results are mixed for others such as CHD, and improvements may be more reflective of general improvement trends rather than a result of the introduction of financial incentives.
The evidence supporting interventions with patients was generally poor and few discussed how interventions were delivered. Interventions aimed at changing lifestyle factors in patients who are asymptomatic have little success, as the impact is short-term. One problem is that studies tend to be short in duration and rely on self-reported behaviour change. There also appears to have been little shift from the position described by Lawlor et al. ,79 who argued that GPs do not adopt a population approach, as they focus on high-risk patients and adopt a predominantly medical approach. They also argued that GPs felt that giving lifestyle advice interfered with the doctor–patient relationship. However, it is clear that many GPs see health promotion as an integral part of practice, whether as individual approaches to primary or secondary health improvement or as a practice approach to improving the health of their patients. Attention needs to be paid to the context and approaches to health improvement in general practice to improve both the delivery and uptake of interventions. 221
There is little evidence to show that GPs undertake wider public health roles in terms of population surveillance beyond contractually defined screening and monitoring. Given that these do not target major areas of health concern (such as mental health and oral health), these are areas which receive less attention despite the enormous potential of general practice to play a leading preventative role in these areas. While there is good evidence, for example, that GPs address eye health for people with diabetes, less is known about their wider role in screening for eye problems. It is important that GPs link mental and physical health issues, as people with mental health problems, particularly severe mental illness, are at increased risk of a number of physical health problems. 335
Generally there was little substantial evidence to make general conclusions about the cost-effectiveness of health improvement interventions in general practice. The evidence is often poor and very mixed. More research is needed on the economic effectiveness of primary care interventions for health improvement.
The role of primary health care in public health
There is no doubt that general practice and the wider primary care team play an important role in the delivery of health improvement interventions with local populations. Reviews that have examined the relationship between primary care and public health support a clear, common core of shared principles. 1,23,24 Our review has demonstrated that general practice and those that work in, or with, general practice undertake many key public health functions. While the relationship between primary health care and public health has long been recognised, systems of primary care in different countries do not necessarily fulfil all the elements of primary health care as reflected in the Alma Ata declaration. 46 Concerns about the nature of UK general practice have been identified for some years. 46,48
General practice fulfils many of the key elements of primary health care. However, this review has identified that much prevention activity is undertaken in general practice itself by primary care practitioners. Other activities that are clearly associated with the principles of primary care are delivered by other professionals or workers either in general practice or in other locations, including homes, the community, pharmacies and schools. This suggests that, in developing public health practice and policy in this area, consideration needs to be given to a wider concept of primary care. Policies in the Public Health White Paper37 and also in many guidance documents tend to focus on the role of the general practice. We would argue that this is too narrow a focus.
This review supports the role of primary care professionals as having an important public health function. GPs have always viewed prevention and health promotion as a core part of their role. In a survey of GPs in one English region in 1990, a large majority of respondents claimed to discuss health-related topics with their patients when indicated. However, fewer made specific efforts to discuss smoking habits (64%), alcohol intake (26%), diet (12%) or exercise (11%) as a matter of routine with all their adult patients. 479 Most GPs said they usually offered simple advice, leaflets or other aids when they had identified a problem, but few said they would refer these patients to the practice nurse. However, at that time few GPs undertook systematic screening for risk factors and lifestyle advice for all patients. The introduction of the 1990 contract with specific health promotion banding payments and the introduction of guidelines on screening, the QOF and now Public Health Guidance from NICE has pushed practices towards more systematic prevention and health promotion interventions.
With 30 million patient contacts a year and registered practice populations, it is clear that general practice provides an important location for health improvement initiatives. More importantly, as services such as welfare advice demonstrate, practices provide a location for other services that can also have an impact on health. Conversely, there is good evidence to show that some interventions are best delivered outside the practice. Yet general practice does, along with many other locations, provide opportunities to promote health. There has been criticism of the increasing individual and specific disease focus that is driven by measures such as the QOF and clinical guidelines. In particular, there is concern that practices serving more deprived communities are disadvantaged by such systems but also that many of the primary focuses of policy and practice guidelines – such as smoking, weight loss and cholesterol measurement – do not address wider underlying problems faced by patients, whether health problems, such as alcoholism, or wider socioeconomic issues. 480 Reporting on the experiences of the Scottish Deep End project, Norbury et al. argue that:
practices in severely deprived areas can improve patient’s health and narrow health inequalities [only] by increasing the volume and quality of the care . . . but . . . lack time in consultations to address the multiple morbidity, social complexity and reduced expectations that are typical of patients living in severe socio-economic deprivation.
p. 3481
The way public health is conceptualised in general practice currently tends to focus on specific interventions by specific professionals. Changes in the way that general practice and its relationship with patients is conceptualised has important implications for much health improvement activity. Marteau and Kinmonth482 have questioned the top-down public health approach to issues such as screening and lifestyle advice, arguing for a more nuanced approach to working with patients, and Getz et al. 483 have questioned the ethical basis of opportunistic prevention in practice. Drawing on these kinds of criticisms of health improvement has led to the development of different ways of conceptualising the role of general practice in public health. Watson15 has argued that the practice should not be seen as just a location for public health, and develops proposals for a health-promoting practice. We suggest that this concept be taken one step further, with the practice being seen as a setting for public health. To view general practice as a setting requires a focus on key central concepts that involve the desire to act on policies, reshape environments, build partnerships, and develop empowerment and ownership as well as developing personal competencies. 106,107 In public health the concept of settings has been used successfully in relation to schools and work places, for example. In developing the practice as a setting, the focus is not on what practitioners can provide as interventions but examines what kinds of interactions can be undertaken with those who work in, work with and use the practice. Attention would then be paid to what should be delivered in the practice (and by whom) and if there are circumstances where the practice may simply direct people to other services.
In the international nursing field the concept of ‘positive practice environments’484,485 has been developed to enable nursing, frequently undertaken in under-resourced communities internationally, to be delivered in settings that support good human resource practice and empower the staff to develop positive attitudes and change their own behaviour. The concept could be considered and applied to primary care settings in England. Key to developing such an approach will be to strengthen relationships within the primary health-care team – especially with health visitors and other public health-oriented staff. Whether or not the development of public health within LAs can support such developments is not yet clear and this is an area that HWBs are unlikely to prioritise. Similarly, the new CCGs are not focused on health improvement issues in the short term given the scale of other commissioning priorities that need to be addressed. 334
It is important that GPs and the wider primary health-care team stay involved in public health, and to encourage an even greater level of participation. However, as discussed in Chapter 7, we are concerned by several aspects of the government’s proposals and the impact this could have on the public health role of general practice and the wider primary health-care team’s involvement in health improvement activities. These include the breaking down of relationships between public health and general practice, which are already fairly tenuous in many places, and the need to support improved education and training for staff – especially for newly developing roles such as health-care practitioners, who undertake a substantial amount of routine screening and monitoring work in practices.
The new NHS organisation and structure in England presents a number of challenges to the provision of public health by general practice and the broader primary health-care team. Up until April 2013, PCTs held contracts with primary and community care services and provided public health services and advice. From April 2013, commissioning responsibilities that affect public health services are split between CCGs, the NHS Commissioning Board and LAs.
The issue of clarifying who is a primary care provider and who is responsible for providing public health services, needs to be established as the new commissioning structure for public health is established. For example, school nurses and pharmacists appear in the ‘primary care and public health’ literature and carry out vital public health services, but they did not feature in the public health White Paper37 at all. Traditional services may also have to compete with other public-health service providers, in line with the ‘any willing provider’ policy, to continue to provide public health services. For example, currently NHS Health Checks are provided mainly by general practice but also by pharmacists in community pharmacies. Since April 2013, LAs can commission other organisations to undertake health checks, raising issues of continuity of care. This issue is further complicated by the fact that much of the public health commissioning is at the local level, by LAs and GP consortia. The lack of any consensus on who should be providing services may mean local variation in the future roles of school nurses, community pharmacists and other practitioners who have been providing public health services.
The proposed changes to the QOF to increase the public health focus will affect almost all GPs. The White Paper on Public Health37 states that by 2013 15% of the QOF will be dedicated to evidence-based public health and primary prevention indicators. There are currently just two indicators in the QOF that are categorised as ‘primary prevention’, both related to patients who have been diagnosed with hypertension, and there are six recommended indicators that are categorised as ‘public health’, which are related to obesity and exercise promotion. It is not clear how the increase in primary care and public health indicators will happen and the extent to which primary care practitioners will be involved in developing the indicators. If new indicators are developed, where along the spectrum of a chronic disease will they target their effect?
Another consideration for the QOF public health indicator development is how the indicators will take into account the way public health research priorities have changed over time. Obviously the evidence base should be as current as possible, but, if the indicators just reflect the most recent research trends, they will probably encompass a different set of diseases and types of interventions from if they took a more long-term approach to the evidence. This question applies not just to the QOF, but also to the new proposed public health outcomes framework, which will reward LAs for meeting local public health targets. 37
In Healthy Lives, Healthy People,37 the government acknowledged the need for more research on public health practice. One key development has been the establishment of a new NIHR School for Public Health Research. This new school needs to invest in research that examines the question of the role of public health research in relation to general practice. As we saw in our research, there are some health intervention studies that could apply to general practice and are not carried out in a general practice setting, and there are many general practice studies that are not focused on actual intervention delivery. We found very little research that addressed the context of delivery and organisation in general practice. However, it is often very difficult to actually set research in general practice, when GPs and practice nurses have limited time for treating patients. Infrastructure and research support needs to be given to general practice, and public health research needs to be prioritised to ensure any guidance is context relevant and likely to produce real health gains. It is also necessary to develop a system that allows GPs, practice nurses and other primary care practitioners to be involved in more research in their natural setting, which may help to improve the quality of research on public health interventions in general practice. The concept of positive practice environments may be worth considering as a way of promoting settings for public health interventions, although the evidence for this is largely based on international health-care systems. 485
Conclusion
This review provides a broad overview of the literature on UK health improvement practices in general practice and by the broader primary health-care team associated with the practice. We also included some aspects of school- and pharmacy-based interventions. The aim of the review was not to systematically review all the evidence on health improvement interventions but rather to identify the nature and extent of the evidence on the delivery and organisation of the health interventions. As expected in our original research proposal, we found that the evidence was mixed in terms of detail and methodological quality, and that identifying sufficient information about the context and organisation of the delivery of health improvement interventions was very limited. Given this, undertaking any systematic approach to even a narrative evidence synthesis was not possible.
In the review we have therefore highlighted some key areas where there are evidence strengths and specific shortcomings in the evidence. While it was foreseen at the start of this process, it is clear that further scoping work and specific research is required to fully understand the health improvement role of general practice and identify effective approaches to the delivery and organisation of health improvement in general practice/primary care settings and by primary care practitioners.
Our key conclusion is that there is currently insufficient evidence to strongly support many of the health improvement interventions undertaken in general practice and primary care more widely. This is not to conclude that there are no interventions that provide population health improvements; brief interventions for stopping smoking are a good example. There is, however, some evidence to support specific interventions being undertaken with some patient groups and in some locations. Further research is needed to strengthen these areas to provide more supportive and clear evidence.
What was the range and type of health improvement activity undertaken in general practice?
The range and type of activities undertaken in general practice or by primary health-care practitioners is diverse. However, there are areas where, because of national policies and incentives for practice, more activity takes place. Areas incentivised by the QOF have become increasingly researched in the last few years, stimulating a growth in the number of studies but increasingly focused on clinical, individual risk factors or diseases. The studies also tend to examine only a single parameter such as the QOF incentive rather than the broader context of the delivery of interventions such as who undertakes the work. The review also suggests that research is focused on a limited number of health behaviours and conditions seen as clinically important.
While our approach to searching the literature limited the range and type of evidence, we are confident that our eventual pool of papers provided a good reflection of the wider literature. Although we did not specifically look for literature that examined community-based initiatives and interventions, there is a clear indication from the literature that health improvement undertaken in or by general practice is focused on the individual rather than involving local communities. Finally, the recent reorganisation of public health services in England creates a number of key challenges for supporting and delivering health improvement in general practice.
What evidence was there on effective approaches to the delivery and organisation of health improvement interventions in general practice settings?
Overall, we found that the evidence base is very limited. There is insufficient good-quality evidence to draw clear conclusions about many areas of health improvement practice in general practice. There is an urgent need to develop this further and to undertake better-quality and more relevant research studies that examine the way interventions are delivered and organised to support continuing developments in health promotion and prevention that are being prioritised in policy and practice.
Implications for policy and practice
Policy
-
If more emphasis is to be placed on the role of general practice in public health, more consideration will need to be given to how to provide support for research within primary care and by primary care practitioners.
-
National policy tends to focus on key clinical issues, and interventions supported by incentives have tended to focus on individuals (e.g. the QOF). This can result in a skewing of activity, and consideration needs to be given to supporting alternative incentive structures.
-
Policy tends to focus on the narrow clinical role of general practice. This may result in a narrow range of activity, and local public health organisations and LAs more generally should consider how they support a wider concept of primary care.
-
Current changes in commissioning and the delivery of public health services may lead to less engagement with general practice on public health issues. Without clear guidelines and processes, gaps in communication and action may develop between LAs and general practice. Local authority public health staff need to be aware of the importance of maintaining close contact with GPs and other primary care staff.
-
Educational providers and commissioners need to consider professional development frameworks for primary care practitioners and consider what aspects of the public health skills framework should be incorporated in core curricula.
Practice
-
Local agencies responsible for public health need to be aware of the risks posed to service provision in primary care-based public health providers (midwives, school nurses, health visitors, etc.) by the new commissioning arrangement. Attention needs to be given to developing appropriate support structures.
-
NHS England, LAs and CCGs may need to consider how existing health improvement activities that have been funded through GMS, Personal Medical Services and other local contractual arrangements can be continued and how local variations in funding and service delivery can be incorporated into the new systems and structures.
-
In the past, developments in health improvement in general practice have benefited from local negotiation and relationships with the public health department in the PCT. Concerns have been raised about the ongoing links between public health and general practice following the transfer of public health professionals to LAs, and maintaining and developing these links must be a key priority for public health services and CCGs.
What gaps were there in the evidence base?
The findings of this review suggest that there is not just a lack of evidence for effectiveness (e.g. obesity/exercise promotion) from existing research, or even just a lack of research. There is also a problem in that much literature has a medicocentric focus. While there is a lot of research on the views of professionals, few studies examine lack of evidence within the existing literature about issues such as professional roles and, where this is examined, the research tends to focus on their clinical role.
Even in the best-researched areas relating to secondary prevention (e.g. CVD, diabetes) there are very few studies of economic effectiveness. There is also a lack of research that examines the costs/benefits in terms of health outcomes of primary preventative interventions tackling anything other than unhealthy behaviours, for example the impact of welfare benefits advice in general practice. Similarly, there is little research on the effectiveness of different approaches to shared decision-making or costs/benefits in different clinical domains. There is insufficient evidence that compares different ways of organising and delivering health improvement in general practice and primary care. Research needs to explore whether different models of interventions, different professionals or different locations are more or less effective than others.
There needs to be more research that examines contextual issues relating to the patient and to local context. The impact of wider socioeconomic and cultural factors may be of particular importance in determining effective interventions with some patients and populations. There is a clear gap in the research related to some neglected population groups including, for example, teenagers, young/middle-aged men and black and ethnic minority groups.
What are the priority areas for future research?
Research on health improvement in primary care needs to move beyond clinical research to include delivery systems, and here there is an overriding imperative for such research to be conducted in a primary care context to ensure that research is relevant and hence more likely to be transferred to practice. One important driver for primary care physician involvement in research is the need to improve quality of care. 486 More needs to be done to support the development of research within and by primary care.
Currently the major areas of research tend to be driven by clinical interest and be associated with specific disease groups. There needs to be more discussion about the type and range of disease burdens in primary care – perhaps moving away from areas such as CVD, where rates are declining, to other areas. Attention needs to shift to examining areas such as other chronic disease burdens: mental health of young people, cancer, dementia and other disabilities of old age.
The type of research needs to change. We found substantial numbers of cross-sectional studies examining patient and professional views but less research that examined what was being done and how. Currently there is little substantive research that examines whole areas of health improvement. Studies tend to be grouped around specific aspects of diseases such as identifying risk factors or provision of information. Further reviews could be commissioned that examine the whole prevention pathway for health problems that are managed within primary care drawing together research from general practice, pharmacy, community engagement, etc., to provide a rich, in-depth picture and analysis of the role of primary care in prevention. In some areas this would involve primary research informed by initial reviews. For example, while for stopping smoking it is possible to provide good evidence about the relative roles of general practice and specialist interventions and also about the intensity and delivery of services – including cost-effectiveness – there are few other areas where this is possible. Thus studies would examine interventions in a specific condition (e.g. cancer), for a population group (e.g. older people) or an intervention type (e.g. welfare advice).
Key recommendations for future research
-
More research needs to be developed that adequately reflects both the context of primary care and other settings where health improvement interventions are undertaken.
-
Research is needed that compares different methods of delivery and organisation, for example comparing different locations as well as different delivery methods in order to determine the effectiveness of not just the specific intervention, but also how it is delivered.
-
More research is required about the specific roles of professionals in primary care. Current studies tend to focus on the views of practitioners rather than their actions.
-
There is an urgent need for cost-effectiveness studies and research on the wider costs and benefits of health improvement activities in general practice and primary care.
-
More comparative research is required that explores whether different models of interventions, different professionals, or different locations are more or less effective than others.
-
Research is needed that examines ‘neglected population groups’ including, for example, teenagers, young/middle-aged men, and black and ethnic minority groups.
-
Further reviews should be commissioned that examine the whole prevention pathway for health problems that are managed within primary care, drawing together research from general practice, pharmacy, community engagement, etc.
-
Where relevant, consideration should be given to commissioning primary research (informed by these initial reviews).
Acknowledgements
The research team thanks Anna Peckham Dip. Lib. for checking and formatting of the references.
Contribution of authors
Professor Stephen Peckham: project lead and corresponding author; involved in all aspects of the research and responsible for the drafting of the final report.
Ms Jane Falconer: librarian; conducted literature searches and retrieval of full-text papers.
Professor Steve Gillam: coinvestigator; refined methods, reviewed papers and commented on the report.
Dr Alison Hann: coinvestigator; refined methods, reviewed papers, drafted report sections and commented on the final report.
Professor Sally Kendall: coinvestigator; refined methods, reviewed papers and commented on the report.
Dr Kiran Nanchahal: coinvestigator; refined methods, reviewed papers.
Mr Benjamin Ritchie: researcher from October 2011; worked with the librarian on searches, managed the data extraction process, reviewed papers, drafted report sections.
Dr Rebecca Rogers: intern researcher until June 2011; worked with the librarian on searches, managed the data extraction process.
Dr Andrew Wallace: researcher until July 2011; worked with the librarian on searches.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- World Health Organization. Declaration of Alma Ata n.d.
- Promoting Better Health. London: HMSO; 1987.
- Wanless D. Securing Good Health for the Whole Population. London: HM Treasury; 2004.
- Peckham S, Hunter DJ, Hann A. The delivery and organization of public health in England: setting the research agenda. Public Health 2008;122:99-104. http://dx.doi.org/10.1016/j.puhe.2007.05.003.
- Lindsay J, Craig P. Nursing for Public Health: Population-Based Care. Edinburgh: Churchill Livingstone; 2000.
- Nurses as Partners in Delivering Public Health. London: Royal College of Nursing; 2007.
- Royal College of General Practitioners . Healthy People: Promoting Health and Preventing Disease 2007. www.rcgp-curriculum.org.uk/pdf/curr_5_Healthy_people.pdf (accessed 10 June 2010).
- Abbott S, Florin D, Fulop N, Gillam S. Primary Care Groups and Trusts: Improving Health. London: The King’s Fund; 2001.
- Anderson W, Florin D, Gillam S, Mountford M. Every Voice Counts: Primary Care Organisations and Public Involvement. London: The King’s Fund; 2002.
- Gillam S, Abbott S, Banks-Smith J. Can primary care groups and trusts improve health?. BMJ 2001;323:89-92. http://dx.doi.org/10.1136/bmj.323.7304.89.
- Peckham S, Hann A, Boyce T. Health promotion and ill-health prevention: the role of general practice. Qual Prim Care 2011;19:317-23.
- Taylor SM, Elliott S, Robinson K, Taylor S. Community-based heart health promotion: perceptions of facilitators and barriers. Can J Public Health 1998;89:406-9.
- Toon PD. What is good general practice? A philosophical study of the concept of high quality medical care. Occas Pap R Coll Gen Pract 1994;65:1-55.
- Tudor-Hart J. A New Kind of Doctor: The General Practitioner’s Part in the Health of the Community. London: Merlin Press; 1988.
- Watson M. Going for gold: the health promoting general practice. Qual Prim Care 2008;16:177-85.
- Seedhouse D. Health Promotion: Philosophy, Prejudice and Practice. Chichester: Wiley; 2004.
- Baggott R. Health and Health Care in Britain. Basingstoke: Palgrave Macmillan; n.d.
- Boyce T, Peckham S, Hann A, Trenholm S. A Pro-active Approach: Health Promotion and Ill-Health Prevention. London: The King’s Fund; 2010.
- Le Grand J, Srivastava D. Economic Incentives for Long-Term Health Gain: A Report for Health England. London: Health England; 2008.
- Undertaking Systematic Reviews of Research on Effectiveness: CRD’s Guidance for Carrying Out or Commissioning Reviews. York: NHS Centre for Reviews and Dissemination, University of York; 2001.
- The Health and Social Care Act 2012. London: The Stationery Office; 2012.
- Hippisley-Cox J, Fenty H, Heaps M. Trends in Consultation Rates in General Practice 1995 to 2006: Analysis of the QRESEARCH Database. London: QResearch and The Information Centre for Health and Social Care; 2007.
- Martin-Misener R, Valaitis R. A Scoping Literature Review of Collaboration between Primary Care and Public Health: A Report to the Canadian Health Services Research Foundation. Ottawa: Canadian Health Services Research Foundation; 2008.
- Primary Care and Public Health: Exploring Integration to Improve Population Health. Washington, DC: Institute of Medicine of the National Academies; 2012.
- Lewis J. What Price Community Medicine? The Philosophy, Practice and Politics of Public Health since 1919. Brighton: Wheatsheaf Books; 1986.
- Baggott R. Public Health: Policy and Politics. Basingstoke: Palgrave Macmillan; 2000.
- Hunter DJ, Marks L, Smith K. The Public Health System in England: A Scoping Study. Part 1: An Interim Report Commissioned by the NHS SDO R&D Programme. Durham: School for Health, Durham University; 2007.
- Tackling Health Inequalities: 2003–05 Data Update for the National 2010 PSA Target. London: Department of Health; 2006.
- Marmot M. Fair Society, Healthy Lives: Strategic Review of Health Inequalities in England post 2010. London: Marmot Review; 2010.
- Adams J, White M, Forman D. Are there socioeconomic gradients in stage and grade of breast cancer at diagnosis? Cross sectional analysis of UK cancer registry data. BMJ 2004;329. http://dx.doi.org/10.1136/bmj.38114.679387.AE.
- Soljak M, Browne J, Lewsey J, Black N. Is there an association between deprivation and pre-operative disease severity? A cross-sectional study of patient-reported health status. Int J Qual Health Care 2009;21:311-15. http://dx.doi.org/10.1093/intqhc/mzp033.
- Whitehead M, Doran T, Exworthy M, Richards S, Matheson D. Delivery Systems and Mechanism for Reducing Inequalities in Both Social Determinants and Health Outcome: Marmot Review Task Group Report 7. London: Department of Health; 2010.
- Maryon-Davis A, Bambra C, Bellis M, Hughes S, Greatley A, Greengross S, et al. Priority Public Health Conditions: Marmot Review Task Group Report 8. London: Department of Health; 2010.
- Marks L, Cave S, Wallace A, Mason A, Hunter DJ, Mason JM, et al. Incentivising preventative services in primary care: perspectives on Local Enhanced Services. J Public Health 2011;33:556-64. http://dx.doi.org/10.1093/pubmed/fdr016.
- The Coalition: Our Programme for Government. London: Cabinet Office; 2010.
- Equity and Excellence: Liberating the NHS. London: The Stationery Office; 2010.
- Healthy Lives, Healthy People: Our Strategy for Public Health in England. London: The Stationery Office; 2010.
- Reducing Differences in the Uptake of Immunisations. London: National Institute for Health and Clinical Excellence; 2009.
- Fleming P, Goodwin M. Lifestyle interventions in primary care: a systematic review of randomized controlled trials. Can Fam Physician 2008;54:1706-13.
- Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med 2005;165:986-95. http://dx.doi.org/10.1001/archinte.165.9.986.
- Cardona-Morrell M, Rychetnik L, Morrell SL, Espinel PT, Bauman A. Reduction of diabetes risk in routine clinical practice: are physical activity and nutrition feasible and are the outcomes from reference trials replicable? A systematic review and meta-analysis. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-653.
- Acheson D. Public Health in England: The Report of the Committee of Inquiry into the Future Development of the Public Health Function. London: HMSO; 1988.
- Leavell HR, Clark EG. Preventive Medicine for the Doctor in His Community. New York, NY: McGraw-Hill; 1958.
- Froon P, Benbassat J. Inconsistencies in the classification of preventive interventions. Prev Med 2000;31:153-8. http://dx.doi.org/10.1006/pmed.2000.0689.
- Choosing Health: Making Healthy Choices Easier. London: The Stationery Office; 2004.
- Macdonald JJ. Primary Health Care: Medicine in its Place. Abingdon: Earthscan; 1993.
- Starfield B. Primary Care: Balancing Health Needs, Services and Technology. New York, NY: Oxford University Press; 1998.
- Peckham S, Exworthy M. Primary Care in the UK: Policy, Organisation and Management. Basingstoke: Palgrave; 2003.
- Van Lerberghe W. The World Health Report 2008: Primary Health Care – Now More than Ever. Geneva: World Health Organization; 2008.
- Defining Primary Care: An Interim Report. Washington, DC: National Academy Press; 1994.
- Hogg W, Rowan M, Russell G, Geneau R, Muldoon L. Framework for primary care organizations: the importance of a structural domain. Int J Qual Health Care 2008;20:308-13. http://dx.doi.org/10.1093/intqhc/mzm054.
- Starfield B, Shi L, Macinko J. Contribution to health systems and health. Milbank Q 2005;83:457-502. http://dx.doi.org/10.1111/j.1468-0009.2005.00409.x.
- Kringos DS, Boerma WG, Hutchinson A, van der Zee J, Groenewegen PP. The breadth of primary care: a systematic literature review of its core dimensions. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-65.
- Moon G, North M. Policy and Place: General Medical Practice in the UK. Basingstoke: Macmillan; 2000.
- Barnum H, Kutzin J, Saxenian H. Incentives and provider payment methods. Int J Health Plan M 1995;10:23-45. http://dx.doi.org/10.1002/hpm.4740100104.
- Zuvekas SH, Hill SC. Does capitation matter? Impacts on access, use, and quality. Inquiry 2004;41:316-35. http://dx.doi.org/10.5034/inquiryjrnl_41.3.316.
- Coulter A. Engaging Patients in their Healthcare. Oxford: Picker Institute Europe; 2006.
- Ellins J, Coulter A. How Engaged Are People in Their Health Care? Findings of a National Telephone Survey. London: Health Foundation; 2005.
- Rice N, Smith PC, Mossialos E, Dixon A, Figueras J, Kutzin J. Funding Health Care: Options for Europe. Buckingham: Open University Press; 2002.
- Austoker J. Cancer prevention in primary care: screening for ovarian, prostatic and testicular cancers. BMJ 1994;309:315-20. http://dx.doi.org/10.1136/bmj.309.6950.315.
- Langham S, Gillam S, Thorogood M. The carrot, the stick and the general practitioner: how have changes in financial incentives affected health promotion activity in general practice?. Br J Gen Pract 1995;45:665-8.
- Smith PC, York N. Quality incentives: the case of UK general practitioners. Health Aff 2004;23:112-18. http://dx.doi.org/10.1377/hlthaff.23.3.112.
- Marks L, Cave S, Hunter D, Mason J, Peckham S, Wallace A. Governance for health and wellbeing in the English NHS. J Health Serv Res Policy 2011;16:14-21. http://dx.doi.org/10.1258/jhsrp.2010.010082.
- McLean G, Guthrie B, Sutton M. Differences in the quality of primary medical care for CVD and diabetes across the NHS: evidence from the Quality and Outcomes Framework. BMC Health Serv Res 2007;7. http://dx.doi.org/10.1186/1472-6963-7-74.
- Dixon A, Khachatryan A, Wallace A, Peckham S, Boyce T, Gillam S. The Quality and Outcomes Framework: Does It Reduce Health Inequalities? Final Report. Southampton: NIHR Service Delivery and Organisation programme; 2011.
- Doran T, Fullwood C, Kontopantelis E, Reeves D. Effect of financial incentives on inequalities in the delivery of primary clinical care in England: analysis of clinical activity indicators for the quality and outcomes framework. Lancet 2008;372:728-36. http://dx.doi.org/10.1016/S0140-6736(08)61123-X.
- Alshamsan R, Majeed A, Ashworth M, Car J, Millett C. Impact of pay for performance on inequalities in health care: systematic review. J Health Serv Res Policy 2010;15:178-84. http://dx.doi.org/10.1258/jhsrp.2010.009113.
- State of Healthcare. London: The Stationery Office; 2008.
- Fleetcroft R, Steel N, Cookson R, Howe A. Mind the gap! Evaluation of the performance gap attributable to exception reporting and target thresholds in the new GMS contract: national database analysis. BMC Health Serv Res 2008;8. http://dx.doi.org/10.1186/1472-6963-8-131.
- Calvert M, Shankar A, McManus RJ, Lester H, Freemantle N. Effect of the Quality and Outcomes Framework on diabetes care in the United Kingdom: retrospective cohort study. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b1870.
- Gravelle H, Sutton M, Ma A. Doctor Behaviour under a Pay-for-Performance Contract: Further Evidence for the Quality and Outcomes Framework. York: Centre for Health Economics, University of York; 2008.
- Buckley BS, Byrne MC, Smith SM. Service organisation for the secondary prevention of ischaemic heart disease in primary care. Cochrane Database Syst Rev 2010;3. http://dx.doi.org/10.1002/14651858.CD006772.pub2.
- Turton P, Peckham S, Taylor P, Lindsay J, Craig P. Nursing for Public Health: Population-Based Care. Edinburgh: Churchill Livingstone; 2000.
- Peckham S, Taylor P, Orme J, Powell J, Taylor P, Harrison T, et al. Public Health for the 21st Century: New Perspectives on Policy, Participation and Practice. Maidenhead: Open University Press; 2003.
- Anderson W, Florin D. Consulting the public about the NHS. BMJ 2000;320:1553-4. http://dx.doi.org/10.1136/bmj.320.7249.1553.
- Kai J, Drinkwater C. Primary Care in Urban Disadvantaged Communities. Oxford: Radcliffe Medical Press; 2004.
- Peckham S, Dowling B, Glendinning C. The New Primary Care: Modern, Dependable, Successful?. Maidenhead: Open University Press; 2003.
- Gillam S. Provision of health promotion clinics in relation to population need: another example of the inverse care law?. Br J Gen Pract 1992;42:54-6.
- Lawlor DA, Keen S, Neal RD. Can general practitioners influence the nation’s health through a population approach to provision of lifestyle advice?. Br J Gen Pract 2000;50:455-9.
- Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N, Evans T, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet 2010;376:1923-58. http://dx.doi.org/10.1016/S0140-6736(10)61854-5.
- Plochg T, Klazinga NS, Schoenstein M, Starfield B. Health Reform: Meeting the Challenge of Ageing and Multiple Morbidities. Paris: OECD Publishing; 2011.
- McDonald R, Campbell S, Lester H. Practice nurses and the effects of the new general practitioner contract in the English National Health Service: the extension of a professional project?. Soc Sci Med 2009;68:1206-12. http://dx.doi.org/10.1016/j.socscimed.2009.01.039.
- Tannahill A. Health promotion: the Tannahill model revisited. Public Health 2009;123:396-9. http://dx.doi.org/10.1016/j.puhe.2008.05.021.
- Pratt J. Practitioners and Practices: A Conflict of Values?. Oxford: Radcliffe Medical Press; 1995.
- Fitzpatrick M. The Tyranny of Health: Doctors and the Regulation of Lifestyle. London: Routledge; 2001.
- Scriven A. Health Promoting Practice: The Contribution of Nurses and Allied Health Professionals. Basingstoke: Palgrave; 2005.
- Whitehead D. Health promoting hospitals: the role and function of nursing. J Clin Nurs 2005;14:20-7. http://dx.doi.org/10.1111/j.1365-2702.2004.01012.x.
- Making a Difference: Strengthening the Nursing, Midwifery and Health Visiting Contribution to Health and Healthcare. London: Department of Health; 1999.
- Wainwright P, Thomas J, Jones M. Health promotion and the role of the school nurse: a systematic review. J Adv Nurs 2000;32:1083-91. http://dx.doi.org/10.1046/j.1365-2648.2000.01579.x.
- Jinks A, Smith M, Ashdown-Lambert J. The public health roles of health visitors and school nurses: a survey. Br J Community Nurs 2003;8:496-501. http://dx.doi.org/10.12968/bjcn.2003.8.11.11819.
- Thomas P, Oni L, Alli M, St Hilaire J, Smith A, Leavey C, et al. Antenatal screening for haemoglobinopathies in primary care: a whole system participatory action research project. Br J Gen Pract 2005;55:424-8.
- McDonald R, Checkland K, Harrison S, Coleman A. Rethinking collegiality: restratification in English general medical practice 2004–2008. Soc Sci Med 2009;68:1109-205. http://dx.doi.org/10.1016/j.socscimed.2009.01.042.
- Peckham S, Wallace A. Pay for performance schemes in primary care: what have we learnt?. Qual Prim Care 2010;18:111-16.
- Hall S, Vogt F, Marteau TM. A short report: survey of practice nurses’ attitudes towards giving smoking cessation advice. Fam Pract 2005;22:614-16. http://dx.doi.org/10.1093/fampra/cmi082.
- Hall S, Marteau TM. Practice nurses’ self-reported opportunistic smoking cessation advice in three contexts. Nicotine Tob Res 2007;9:941-5. http://dx.doi.org/10.1080/14622200701488434.
- Bryans A, Cornish F, McIntosh J. The potential of ecological theory for building an integrated framework to develop the public health contribution of health visiting. Health Soc Care Comm 2009;17:564-72. http://dx.doi.org/10.1111/j.1365-2524.2009.00856.x.
- Peckham S, Wirrmann E, Davies C. The Future Health Workforce. Cambridge: Cambridge University Press; 2003.
- Health Visiting Implementation Plan. London: Department of Health; 2011.
- The Healthy Child Programme: Pregnancy and the First Five Years of Life. London: Department of Health; 2009.
- Bunn F, Kendall S. Does nursing research impact on policy? A case study of health visiting research and UK health policy. J Res Nurs 2011;16:169-91. http://dx.doi.org/10.1177/1744987110392627.
- Public Health Online Resource for Careers, Skills and Training (PHORCAST) n.d. www.phorcast.org.uk/page.php?page_id=44 (accessed 4 March 2014).
- Blenkinsopp A, Anderson C, Armstrong M. Systematic review of the effectiveness of community pharmacy-based interventions to reduce risk behaviours and risk factors for coronary heart disease. J Public Health 2003;25:144-53. http://dx.doi.org/10.1093/pubmed/fdg030.
- Holden M. Weight management is likely to become a priority for community pharmacists. Pharm Pract 2008;18:277-80.
- Agomo C. The role of community pharmacists in public health: a scoping review of the literature. J Pharm Health Serv Res 2012;3:25-33. http://dx.doi.org/10.1111/j.1759-8893.2011.00074.x.
- Ottawa Charter for Health Promotion. Geneva: World Health Organization; 1986.
- Baric L. Health Promotion and Health Education in Practice. Module 2: The Organisational Model. Altrincham: Barns Publications; 1994.
- Grossman R, Scala K. Health Promotion and Organisational Development: Developing Settings for Health. Geneva: World Health Organization Europe; 1993.
- Anderson S, Allen P, Peckham S, Goodwin N. Asking the right questions: scoping studies in the commissioning of research in the organisation and delivery of health services. Health Res Policy Syst 2008;6. http://dx.doi.org/10.1186/1478-4505-6-7.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Res Methods 2005;8:19-32. http://dx.doi.org/10.1080/1364557032000119616.
- Jackson N, Waters E. Guidelines for systematic reviews of health promotion and public health interventions taskforce: the challenges of systematically reviewing public health interventions. J Public Health 2004;26:303-7. http://dx.doi.org/10.1093/pubmed/fdh164.
- Defining Research. London: NHS Health Research Authority; 2009.
- Cochrane Public Health Group . About the Cochrane Public Health Group (CPHG) n.d. http://ph.cochrane.org/about-cochrane-public-health-group-cphg (accessed 4 March 2014).
- Rychetnik L, Frommer M, Hawe P, Shiell A. Criteria for evaluating evidence on public health interventions. J Epidemiol Community Health 2002;56:119-27. http://dx.doi.org/10.1136/jech.56.2.119.
- Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Policy 2005;10:6-20. http://dx.doi.org/10.1258/1355819054308576.
- Pope C, Mays N, Popay J. Informing policy making and management in healthcare: the place for synthesis. Healthc Policy 2006;1:43-8. http://dx.doi.org/10.12927/hcpol.2006.17874.
- Barnett-Page E, Thomas J. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol 2009;9:1-11. http://dx.doi.org/10.1186/1471-2288-9-59.
- Dixon-Woods M, Agarwal S, Jones D, Young B, Sutton A. Synthesising qualitative and quantitative evidence: a review of possible methods. J Health Serv Res Pol 2005;10:45-53. http://dx.doi.org/10.1258/1355819052801804.
- Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol 2006;6. http://dx.doi.org/10.1186/1471-2288-6-35.
- Leavell HR, Clark EG. Textbook of Preventive Medicine. New York, NY: McGraw-Hill; 1953.
- Little P, Kelly J, Barnett J, Dorward M, Margetts B, Warm D. Randomised controlled factorial trial of dietary advice for patients with a single high blood pressure reading in primary care. BMJ 2004;328. http://dx.doi.org/10.1136/bmj.38037.435972.EE.
- Watson MC, Inch J, Jaffray M, Stewart D. Screening and brief interventions for alcohol misuse delivered in the community pharmacy setting: a pilot study. Int J Pharm Pract 2011;19.
- Kaner EF, Lock CA, McAvoy BR, Heather N, Gilvarry E. A RCT of three training and support strategies to encourage implementation of screening and brief alcohol intervention by general practitioners. Br J Gen Pract 1999;49:699-703.
- Copello A, Templeton L, Orford J, Velleman R. The relative efficacy of two levels of a primary care intervention for family members affected by the addiction problem of a close relative: a randomized trial. Addiction 2009;104:49-58. http://dx.doi.org/10.1111/j.1360-0443.2008.02417.x.
- McCormick R, Docherty B, Segura L, Colom J, Gual A, Cassidy P, et al. The research translation problem: alcohol screening and brief intervention in primary care – real world evidence supports theory. Drugs Educ Prev Policy 2010;17:732-48. http://dx.doi.org/10.3109/09687630903286800.
- Cervical Screening Programme, England 2011–12. Leeds: Health and Social Care Information Centre; 2012.
- Chew-Graham C, Mole E, Evans LJ, Rogers A. Informed consent? How do primary care professionals prepare women for cervical smears: a qualitative study. Patient Educ Couns 2006;61:381-8. http://dx.doi.org/10.1016/j.pec.2005.04.017.
- Campbell C, Anandan C, Appleton S, Elton R, Patnick J, Weller D. Avoiding inappropriate invitations to cancer screening programmes: the role of primary care. J Med Screen 2011;18:12-7. http://dx.doi.org/10.1258/jms.2011.009122.
- Peto J, Gilham C, Fletcher O, Matthews FE. The cervical cancer epidemic that screening has prevented in the UK. Lancet 2004;364:249-56. http://dx.doi.org/10.1016/S0140-6736(04)16674-9.
- Abdullahi A, Copping J, Kessel A, Luck M, Bonell C. Cervical screening: perceptions and barriers to uptake among Somali women in Camden. Public Health 2009;123:680-5. http://dx.doi.org/10.1016/j.puhe.2009.09.011.
- Waller J, Bartoszek M, Marlow L, Wardle J. Barriers to cervical cancer screening attendance in England: a population-based survey. J Med Screen 2009;16:199-204. http://dx.doi.org/10.1258/jms.2009.009073.
- Logan L, McIlfatrick S. Exploring women’s knowledge, experiences and perceptions of cervical cancer screening in an area of social deprivation. Eur J Cancer Care 2011;20:720-7. http://dx.doi.org/10.1111/j.1365-2354.2011.01254.x.
- Goldsmith M, Austoker J, Marsh G, Kehoe S, Bankhead C. Cervical screening result communication: a focus-group investigation of English women’s experiences and needs. Qual Saf Health Care 2008;17:334-8. http://dx.doi.org/10.1136/qshc.2007.023275.
- Dalton AR, Bottle A, Okoro C, Majeed A, Millett C. Uptake of the NHS Health Checks programme in a deprived, culturally diverse setting: cross-sectional study. J Public Health 2011;33:422-9. http://dx.doi.org/10.1093/pubmed/fdr034.
- Khunti K, Walker N, Sattar N, Davies M. Unanswered questions over NHS health checks. BMJ 2010;342. http://dx.doi.org/10.1136/bmj.c6312.
- Martin H. Delivering NHS health checks to all. Br J Health Care Manage 2011;17:250-5. http://dx.doi.org/10.12968/bjhc.2011.17.6.250.
- McNaughton RJ, Oswald NT, Shucksmith JS, Heywood PJ, Watson PS. Making a success of providing NHS Health Checks in community pharmacies across the Tees Valley: a qualitative study. BMC Health Serv Res 2011;11. http://dx.doi.org/10.1186/1472-6963-11-222.
- Kumar J, Mawby Y, Chambers R, Leese C, Iqbal Z. Implementing the NHS health check in general practice. Nurs Pract 2011;59:10-2.
- McCluskey S, Baker D, Percy D, Lewis P, Middleton E. Reductions in cardiovascular risk in association with population screening: a 10-year longitudinal study. J Public Health 2007;29:379-87. http://dx.doi.org/10.1093/pubmed/fdm045.
- Donyai P. Coronary heart disease risk screening: the community pharmacy Healthy Heart Assessment Service. Pharm World Sci 2009;31:643-7. http://dx.doi.org/10.1007/s11096-009-9338-4.
- Horgan JM, Blenkinsopp A, McManus RJ. Evaluation of a cardiovascular disease opportunistic risk assessment pilot (‘Heart MOT’ service) in community pharmacies. J Public Health 2010;32:110-16. http://dx.doi.org/10.1093/pubmed/fdp092.
- Lambert AM, Burden AC, Chambers J, Marshall T. Cardiovascular screening for men at high risk in Heart of Birmingham Teaching Primary Care Trust: the ‘Deadly Trio’ programme. J Public Health 2012;34:73-82. http://dx.doi.org/10.1093/pubmed/fdr052.
- Mathews G, Alexander J, Rahemtulla T, Raj B. Impact of a cardiovascular risk control project for South Asians (Khush Dil) on motivation, behaviour, obesity, blood pressure and lipids. J Public Health 2007;29:388-97. http://dx.doi.org/10.1093/pubmed/fdm044.
- Kane K. Case-finding in the community: the results 2. Br J Community Nurs 2008;13:265-9. http://dx.doi.org/10.12968/bjcn.2008.13.6.29458.
- Kirkcaldy AJ, Robinson JE, Perkins ES, Forrest D. Older men’s experiences of community-based health checks in Knowsley, UK. Glob Public Health 2011;6:15-27. http://dx.doi.org/10.1080/17441691003720247.
- White J, South J. Health trainers can help people manage long-term conditions. Prim Health Care 2012;22:26-31. http://dx.doi.org/10.7748/phc2012.03.22.2.26.c8963.
- Wood DA, Kinmonth A-L, Pyke SD, Thompson SG. Randomised controlled trial evaluating cardiovascular screening and intervention in general practice: principal results of British family heart study. BMJ 1994;308:313-20. http://dx.doi.org/10.1136/bmj.308.6924.313.
- Muir J, Lancaster T, Jones L, Yudkin P. Effectiveness of health checks conducted by nurses in primary care: final results of the OXCHECK study. BMJ 1995;310:1099-104. http://dx.doi.org/10.1136/bmj.310.6987.1099.
- Dowell AC, Ochera JJ, Hilton SR, Bland JM, Harris T, Jones DR, et al. Prevention in practice: results of a 2-year follow-up of routine health promotion interventions in general practice. Fam Pract 1996;13:357-62. http://dx.doi.org/10.1093/fampra/13.4.357.
- Langham S, Thorogood M, Normand C, Muir J, Jones L, Fowler G. Costs and cost effectiveness of health checks conducted by nurses in primary care: the OXCHECK study. BMJ 1996;312:1265-8. http://dx.doi.org/10.1136/bmj.312.7041.1265.
- Kumar J, Chambers R, Mawby Y, Leese C, Iqbal Z, Picariello L, et al. Delivering more with less? Making the NHS Health Check work in financially hard times: real time learning from Stoke-on-Trent. Qual Prim Care 2011;19:193-9.
- Goyder E, Wild S, Fischbacher C, Carlisle J, Peters J. Evaluating the impact of a national pilot screening programme for type 2 diabetes in deprived areas of England. Fam Pract 2008;25:370-5. http://dx.doi.org/10.1093/fampra/cmn054.
- Sargeant LA, Simmons RK, Barling RS, Butler R, Williams KM, Prevost AT, et al. Who attends a UK diabetes screening programme? Findings from the ADDITION-Cambridge study. Diabet Med 2010;27:995-1003. http://dx.doi.org/10.1111/j.1464-5491.2010.03056.x.
- Simmons RK, Echouffo-Tcheugui JB, Sharp SJ, Sargeant LA, Williams KM, Prevost AT, et al. Screening for type 2 diabetes and population mortality over 10 years (ADDITION-Cambridge): a cluster-randomised controlled trial. Lancet 2012;380:1741-8. http://dx.doi.org/10.1016/S0140-6736(12)61422-6.
- Griffin SJ, Borch-Johnsen K, Davies MJ, Khunti K, Rutten GE, Sandbæk A, et al. Effect of early intensive multifactorial therapy on 5-year cardiovascular outcomes in individuals with type 2 diabetes detected by screening (ADDITION-Europe): a cluster-randomised trial. Lancet 2011;378:156-67. http://dx.doi.org/10.1016/S0140-6736(11)60698-3.
- Graffy J, Grant J, Williams K, Cohn S, Macbay S, Griffin S, et al. More than measurement: practice team experiences of screening for type 2 diabetes. Fam Pract 2010;27:386-94. http://dx.doi.org/10.1093/fampra/cmq022.
- Carlisle J, Lawton J, Goyder E, Peters J, Lacey EA. The role of healthcare assistants in screening for diabetes: a qualitative study. Qual Prim Care 2007;15:77-83.
- Nicholas JM, Burgess C, Dodhia H, Miller J, Fuller F, Cajeat E, et al. Variations in the organization and delivery of the ‘NHS health check’ in primary care. J Public Health 2013;35:85-91. http://dx.doi.org/10.1093/pubmed/fds062.
- Romeo R, Knapp M, Morrison J, Melville C, Allan L, Finlayson J, et al. Cost estimation of a health-check intervention for adults with intellectual disabilities in the UK. J Intellect Disabil Res 2009;53:426-39. http://dx.doi.org/10.1111/j.1365-2788.2009.01159.x.
- Robertson J, Roberts H, Emerson E, Turner S, Greig R. The impact of health checks for people with intellectual disabilities: a systematic review of evidence. J Intellect Disabil Res 2011;55:1009-19. http://dx.doi.org/10.1111/j.1365-2788.2011.01436.x.
- Felce D, Baxter H, Lowe K, Dunstan F, Houston H, Jones G, et al. The impact of repeated health checks for adults with intellectual disabilities. J Appl Res Intellect Dis 2008;21:585-96. http://dx.doi.org/10.1111/j.1468-3148.2008.00441.x.
- Chauhan U, Kontopantelis E, Campbell S, Jarrett H, Lester H. Health checks in primary care for adults with intellectual disabilities: how extensive should they be?. J Intellect Disabil Res 2010;54:479-86. http://dx.doi.org/10.1111/j.1365-2788.2010.01263.x.
- Drennan V, Iliffe S, Tai SS, Lenihan P, Deave T. Can primary care identify an ‘at risk’ group in the older population. Br J Community Nurs 2007;12:142-8. http://dx.doi.org/10.12968/bjcn.2007.12.4.23248.
- Jenkins P, Baker E, White B. Promoting good health in people aged over 75 in the community. Nurs Older People 2009;21:34-9. http://dx.doi.org/10.7748/nop2009.03.21.2.34.c6872.
- Lloyd K, Wise K, Wyllie E. Implementing health checks for the over-75s. Nurs Times 2002;98:34-5.
- Walker L, Jamrozik K. Effectiveness of screening for risk of medical emergencies in the elderly. Age Ageing 2005;34:238-42. http://dx.doi.org/10.1093/ageing/afi055.
- Harari D, Iliffe S, Kharicha K, Egger M, Gillmann G, von Renteln-Kruse W. Promotion of health in older people: a randomised controlled trial of health risk appraisal in British general practice. Age Ageing 2008;37:565-71. http://dx.doi.org/10.1093/ageing/afn150.
- Drennan V, Iliffe S, Haworth D, Tai SS, Lenihan P, Deave T. The feasibility and acceptability of a specialist health and social care team for the promotion of health and independence in ‘at risk’ older adults. Health Soc Care Community 2005;13:136-44. http://dx.doi.org/10.1111/j.1365-2524.2005.00541.x.
- Li PL, Logan S. The current state of screening in general practice. J Public Health Med 1996;18:350-6. http://dx.doi.org/10.1093/oxfordjournals.pubmed.a024517.
- Soljak M, Samarasundera E, Indulkar T, Walford H, Majeed A. Variations in cardiovascular disease under-diagnosis in England: national cross-sectional spatial analysis. BMC Cardiovasc Disord 2011;11. http://dx.doi.org/10.1186/1471-2261-11-12.
- Magee GM, Hunter SJ, Cardwell CR, Savage G, Kee F, Murphy MC, et al. Identifying additional patients with diabetic nephropathy using the UK primary care initiative. Diabet Med 2010;27:1372-8. http://dx.doi.org/10.1111/j.1464-5491.2010.03105.x.
- The Bigger Picture: The National Chlamydia Screening Programme 2008/09 Annual Report. London: National Chlamydia Screening Programme; 2009.
- Joshi UY, Dixon W. General practitioners’ views on the screening for genital Chlamydia trachomatis infection and partner notification. Int J STD AIDS 2000;11:588-91. http://dx.doi.org/10.1258/0956462001916579.
- Griffiths C, Cuddigan A. Clinical management of chlamydia in general practice: a survey of reported practice. J Fam Plann Reprod Health Care 2002;28:149-52. http://dx.doi.org/10.1783/147118902101196315.
- Senok A, Wilson P, Reid M, Scoular A, Craig N, McConnachie A, et al. Can we evaluate population screening strategies in UK general practice? A pilot randomised controlled trial comparing postal and opportunistic screening for genital chlamydial infection. J Epidemiol Community Health 2005;59:198-204. http://dx.doi.org/10.1136/jech.2004.021584.
- Perkins E, Carlisle C, Jackson N. Opportunistic screening for Chlamydia in general practice: the experience of health professionals. Health Soc Care Community 2003;11:314-20. http://dx.doi.org/10.1046/j.1365-2524.2003.00437.x.
- McNulty CA, Freeman E, Oliver I, Ford-Young W, Randall S. Strategies used to increase chlamydia screening in general practice: a qualitative study. Public Health 2008;122:845-56. http://dx.doi.org/10.1016/j.puhe.2007.10.009.
- Freeman E, Howell-Jones R, Oliver I, Randall S, Ford-Young W, Beckwith P, et al. Promoting chlamydia screening with posters and leaflets in general practice: a qualitative study. BMC Public Health 2009;9. http://dx.doi.org/10.1186/1471-2458-9-383.
- Harris DI. Implementation of chlamydia screening in a general practice setting: a 6-month pilot study. J Fam Plann Reprod Health Care 2005;31:109-12. http://dx.doi.org/10.1783/1471189053629590.
- Rapley T, May C, Kaner EF. Still a difficult business? Negotiating alcohol-related problems in general practice consultations. Soc Sci Med 2006;63:2418-28. http://dx.doi.org/10.1016/j.socscimed.2006.05.025.
- Wilson GB, Lock CA, Heather N, Cassidy P, Christie MM, Kaner EF. Intervention against excessive alcohol consumption in primary health care: a survey of GPs attitudes and practices in England 10 years on. Alcohol Alcohol 2011;46:570-7. http://dx.doi.org/10.1093/alcalc/agr067.
- Kaner EF, Beyer F, Dickinson HO, Pienaar E, Campbell F, Schlesinger C, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev 2007;2. http://dx.doi.org/10.1002/14651858.cd004148.pub3.
- McCaig D, Fitzgerald N, Stewart D. Provision of advice on alcohol use in community pharmacy: a cross-sectional survey of pharmacists’ practice, knowledge, views and confidence. Int J Pharm Pract 2011;19:171-8. http://dx.doi.org/10.1111/j.2042-7174.2011.00111.x.
- Kaner E, Lock C, Heather N, McNamee P, Bond S. Promoting brief alcohol intervention by nurses in primary care: a cluster randomised controlled trial. Patient Educ Couns 2003;51:277-84. http://dx.doi.org/10.1016/S0738-3991(02)00242-2.
- Boland B, Drummond C, Kaner E. Brief alcohol interventions: everybody’s business. Adv Psychiatr Treat 2008;14:469-76. http://dx.doi.org/10.1192/apt.bp.105.002063.
- Kaner EF, Heather N, Brodie J, Lock CA, McAvoy BR. Patient and practitioner characteristics predict brief alcohol intervention in primary care. Br J Gen Pract 2001;51:822-7.
- Tsianakas V, Calnan M, Atkin K, Dormandy E, Marteau TM. Offering antenatal sickle cell and thalassaemia screening to pregnant women in primary care: a qualitative study of GPs’ experiences. Br J Gen Pract 2010;60:822-8. http://dx.doi.org/10.3399/bjgp10X532602.
- Brown K, Dormandy E, Reid E, Gulliford M, Marteau T. Impact on informed choice of offering antenatal sickle cell and thalassaemia screening in primary care: a randomized trial. J Med Screen 2011;18:65-7. http://dx.doi.org/10.1258/jms.2011.010132.
- Milne A, Culverwell A, Guss R, Tuppen J, Whelton R. Screening for dementia in primary care: a review of the use, efficacy and quality of measures. Int Psychogeriatr 2008;20:911-26. http://dx.doi.org/10.1017/S1041610208007394.
- Bond J, Graham N, Padovani A, Mackell J, Knox S, Atkinson J. Screening for cognitive impairment, Alzheimer’s disease and other dementias: opinions of European caregivers, payors, physicians and the general public. J Nutr Health Aging 2010;14:558-62. http://dx.doi.org/10.1007/s12603-010-0268-6.
- Barr RJ, Stewart A, Torgerson DJ, Seymour DG, Reid DM. Screening elderly women for risk of future fractures: participation rates and impact on incidence of falls and fractures. Calcif Tissue Int 2005;76:243-8. http://dx.doi.org/10.1007/s00223-004-0101-5.
- Spice CL, Morotti W, George S, Dent TH, Rose J, Harris S, et al. The Winchester falls project: a randomised controlled trial of secondary prevention of falls in older people. Age Ageing 2009;38:33-40. http://dx.doi.org/10.1093/ageing/afn192.
- Dickinson A, Horton K, Machen I, Bunn F, Cove J, Deepak J, et al. The role of health professionals in promoting the uptake of fall prevention interventions: a qualitative study of older people’s views. Age Ageing 2011;40:724-30. http://dx.doi.org/10.1093/ageing/afr111.
- Brankin E, Mitchell C, Munro R. Closing the osteoporosis management gap in primary care: a secondary prevention of fracture programme. Curr Med Res Opin 2005;21:475-82. http://dx.doi.org/10.1185/030079905X38150.
- Emmett CL, Redmond NM, Peters TJ, Clarke S, Shepstone L, Lenaghan E, et al. Acceptability of screening to prevent osteoporotic fractures: a qualitative study with older women. Fam Pract 2012;29:235-42. http://dx.doi.org/10.1093/fampra/cmr069.
- Morgan S, Mant D. Randomised trial of two approaches to screening for atrial fibrillation in UK general practice. Br J Gen Pract 2002;52.
- Subramanian DN, Hopayian K. An audit of the first year of screening for depression in patients with diabetes and ischaemic heart disease under the Quality and Outcomes Framework. Qual Prim Care 2008;16:341-4.
- Feder G, Davies RA, Baird K, Dunne D, Eldridge S, Griffiths C, et al. Identification and Referral to Improve Safety (IRIS) of women experiencing domestic violence with a primary care training and support programme: a cluster randomised controlled trial. Lancet 2011;378:1788-95. http://dx.doi.org/10.1016/S0140-6736(11)61179-3.
- Koopman J, Davey E, Thomas N, Wittkop T, Verschuure H. How should hearing screening tests be offered?. Int J Audiol 2008;47:230-7. http://dx.doi.org/10.1080/14992020801908236.
- Anderson EM, Mandeville RP, Hutchinson SJ, Cameron SO, Mills PR, Fox R, et al. Evaluation of a general practice based hepatitis C virus screening intervention. Scott Med J 2009;54:3-7. http://dx.doi.org/10.1258/rsmsmj.54.3.3.
- Prost A, Griffiths CJ, Anderson J, Wight D, Hart GJ. Feasibility and acceptability of offering rapid HIV tests to patients registering with primary care in London (UK): a pilot study. Sex Transm Infect 2009;85:326-9. http://dx.doi.org/10.1136/sti.2008.033233.
- Macpherson LM, McCann MF, Gibson J, Binnie VI, Stephen KW. The role of primary healthcare professionals in oral cancer prevention and detection. Br Dental J 2003;195:277-81. http://dx.doi.org/10.1038/sj.bdj.4810481.
- Knussen C, Bingham D, Flowers P. The acceptability of health service and community-based venues for syphilis testing amongst men who have sex with men: the views of potential service users in Scotland. Public Health 2008;122:959-61. http://dx.doi.org/10.1016/j.puhe.2007.12.006.
- Griffiths C, Sturdy P, Brewin P, Bothamley G, Eldridge S, Martineau A, et al. Educational outreach to promote screening for tuberculosis in primary care: a cluster randomised controlled trial. Lancet 2007;369:1528-34. http://dx.doi.org/10.1016/S0140-6736(07)60707-7.
- Barter-Godfrey S, Taket A. Understanding women’s breast screening behaviour: a study carried out in South East London, with women aged 50–64 years. Health Educ J 2007;66:335-46. http://dx.doi.org/10.1177/0017896907083155.
- Chapple A, Ziebland S, Hewitson P, McPherson A. What affects the uptake of screening for bowel cancer using a faecal occult blood test (FOBt): a qualitative study. Soc Sci Med 2008;66:2425-35. http://dx.doi.org/10.1016/j.socscimed.2008.02.009.
- Damery S, Clifford S, Wilson S. Colorectal cancer screening using the faecal occult blood test (FOBt): a survey of GP attitudes and practices in the UK. BMC Family Practice 2010;11. http://dx.doi.org/10.1186/1471-2296-11-20.
- McIlfatrick S, Taggart L, Truesdale-Kennedy M. Supporting women with intellectual disabilities to access breast cancer screening: a healthcare professional perspective. Eur J Cancer Care 2011;20:412-20. http://dx.doi.org/10.1111/j.1365-2354.2010.01221.x.
- Hart AR, Barone TL, Gay SP, Inglis A, Griffin L, Tallon CA, et al. The effect on compliance of a health education leaflet in colorectal cancer screening in general practice in central England. J Epidemiol Community Health 1997;51:187-91. http://dx.doi.org/10.1136/jech.51.2.187.
- Bell TS, Branston LK, Newcombe RG, Barton GR. Interventions to improve uptake of breast screening in inner city Cardiff general practices with ethnic minority lists. Ethn Health 1999;4:277-84. http://dx.doi.org/10.1080/13557859998056.
- Richards SH, Bankhead C, Peters TJ, Austoker J, Hobbs FD, Brown J, et al. Cluster randomised controlled trial comparing the effectiveness and cost-effectiveness of two primary care interventions aimed at improving attendance for breast screening. J Med Screen 2001;8:91-8. http://dx.doi.org/10.1136/jms.8.2.91.
- Eilbert KW, Carroll K, Peach J, Khatoon S, Basnett I, McCulloch N. Approaches to improving breast screening uptake: evidence and experience from Tower Hamlets. Br J Cancer 2009;101:S64-7. http://dx.doi.org/10.1038/sj.bjc.6605393.
- Hewitson P, Ward AM, Heneghan C, Halloran SP, Mant D. Primary care endorsement letter and a patient leaflet to improve participation in colorectal cancer screening: results of a factorial randomised trial. Br J Cancer 2011;105:475-80. http://dx.doi.org/10.1038/bjc.2011.255.
- Sharp DJ, Peters TJ, Bartholomew J, Shaw A. Breast screening: a randomised controlled trial in UK general practice of three interventions designed to increase uptake. J Epidemiol Community Health 1996;50:72-6. http://dx.doi.org/10.1136/jech.50.1.72.
- Sahota P, Rudolf MC, Dixey R, Hill AJ, Barth JH, Cade J. Evaluation of implementation and effect of primary school based intervention to reduce risk factors for obesity. BMJ 2001;323:1027-9. http://dx.doi.org/10.1136/bmj.323.7320.1027.
- Syson-Nibbs L, Peters J, Saul C. Can health visitor intervention change sun safety policies and practice in preschool establishments? A randomised controlled study. Health Educ J 2005;64:129-41. http://dx.doi.org/10.1177/001789690506400205.
- Warren JM, Henry CJ, Lightowler HJ, Bradshaw SM, Perwaiz S. Evaluation of a pilot school programme aimed at the prevention of obesity in children. Health Promot Int 2003;18:287-96. http://dx.doi.org/10.1093/heapro/dag402.
- Bond M, Wyatt K, Lloyd J, Welch K, Taylor R. Systematic review of the effectiveness and cost-effectiveness of weight management schemes for the under fives: a short report. Health Technol Assess 2009;13. http://dx.doi.org/10.3310/hta13610.
- Barlow J, Whitlock S, Hanson S, Davis H, Hunt C, Kirkpatrick S, et al. Preventing obesity at weaning: parental views about the EMPOWER programme. Child Care Health Dev 2010;36:843-9. http://dx.doi.org/10.1111/j.1365-2214.2010.01107.x.
- Banks J, Shield JP, Sharp D. Barriers engaging families and GPs in childhood weight management strategies. Br J Gen Pract 2011;61:e492-7. http://dx.doi.org/10.3399/bjgp11X588466.
- van Gerwen M, Franc C, Rosman S, Le Vaillant M, Pelletier-Fleury N. Primary care physicians’ knowledge, attitudes, beliefs and practices regarding childhood obesity: a systematic review. Obes Rev 2008;10:227-36. http://dx.doi.org/10.1111/j.1467-789X.2008.00532.x.
- Hoddinott P, Britten J, Pill R. Why do interventions work in some places and not others: a breastfeeding support group trial. Soc Sci Med 2010;70:769-78. http://dx.doi.org/10.1016/j.socscimed.2009.10.067.
- McDonald P, Friedman EH, Banks A, Anderson R, Carman V. Pneumococcal vaccine campaign based in general practice. BMJ 1997;314:1094-8. http://dx.doi.org/10.1136/bmj.314.7087.1094.
- Kyaw MH, Nguyen-Van-Tam JS, Pearson JC. Family doctor advice is the main determinant of pneumococcal vaccine uptake. J Epidemiol Community Health 1999;53:589-90. http://dx.doi.org/10.1136/jech.53.9.589.
- Lamden KH, Gemmell I. General practice factors and MMR vaccine uptake: structure, process and demography. J Public Health 2008;30:251-7. http://dx.doi.org/10.1093/pubmed/fdn036.
- Cockman P, Dawson L, Mathur R, Hull S. Improving MMR vaccination rates: herd immunity is a realistic goal. BMJ 2011;343. http://dx.doi.org/10.1136/bmj.d5703.
- Jackson C, Cheater FM, Harrison W, Peacock R, Bekker H, West R. Randomised cluster trial to support informed parental decision-making for the MMR vaccine. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-475.
- Ashenden R, Silagy C, Weller D. A systematic review of the effectiveness of promoting lifestyle change in general practice. Family Practice 1997;14:160-76. http://dx.doi.org/10.1093/fampra/14.2.160.
- Lawlor DA, Hanratty B. The effect of physical activity advice given in routine primary care consultations: a systematic review. J Public Health Med 2001;23:219-26. http://dx.doi.org/10.1093/pubmed/23.3.219.
- GOV.UK . Summary of QOF Indicators n.d. www.gov.uk/government/uploads/system/uploads/attachment_data/file/213226/Summary-of-QOF-indicators.pdf (accessed 4 March 2014).
- Peckham S, Wallace A, Gillam S, Siriwardena AN. The Quality and Outcomes Framework: QOF – Transforming General Practice. Abingdon: Radcliffe Publishing; 2011.
- Balkau B, Deanfield JE, Després JP, Bassand JP, Fox KA, Smith SC, et al. International Day for the Evaluation of Abdominal Obesity (IDEA): a study of waist circumference, cardiovascular disease, and diabetes mellitus in 168 000 primary care patients in 63 countries. Circulation 2007;116:1942-51. http://dx.doi.org/10.1161/CIRCULATIONAHA.106.676379.
- National Health Service Information Centre for Health and Social Care . Statistics on Obesity, Physical Activity and Diet: England, February 2009 2009. www.hscic.gov.uk/catalogue/PUB00188/obes-phys-acti-diet-eng-2009-rep.pdf (accessed 4 March 2014).
- Obesity: The Prevention, Identification, Assessment and Management of Overweight and Obesity in Adults and Children. London: National Institute for Health and Clinical Excellence; 2006.
- Ogden J, Flanagan Z. Beliefs about the causes and solutions to obesity: a comparison of GPs to lay people. Patient Educ Couns 2008;71:72-8. http://dx.doi.org/10.1016/j.pec.2007.11.022.
- Epstein L, Ogden J. A qualitative study of GPs’ views of treating obesity. Br J Gen Pract 2005;55:750-4.
- Hankey CR, Eley S, Leslie WS, Hunter CM, Lean ME. Eating habits, beliefs, attitudes and knowledge among health professionals regarding the links between obesity, nutrition and health. Public Health Nutr 2003;7:337-43.
- Ogden J, Bandara I, Cohen H, Farmer D, Hardie J, Minas H, et al. General practitioners’ and patients’ models of obesity: whose problem is it?. Patient Educ Couns 2001;44:227-33. http://dx.doi.org/10.1016/S0738-3991(00)00192-0.
- Morris SE, Lean ME, Hankey CR, Hunter C. Who gets what treatment for obesity? A survey of GPs in Scotland. Eur J Clin Nutr 1999;53:S44-8. http://dx.doi.org/10.1038/sj.ejcn.1600801.
- Counterweight Project Team . Obesity impacts on general practice appointments. Obes Res 2005;13:1442-9. http://dx.doi.org/10.1038/oby.2005.174.
- Hillsdon M. Promoting physical activity: issues in primary health care. Int J Obes Relat Metab Disord 1998;22:S52-4.
- Graham R, Dugdill L, Cable N. Health professionals’ perspectives in exercise referral: implications for the referral process. Ergonomics 2005;48:1411-22. http://dx.doi.org/10.1080/00140130500101064.
- West R, McNeill A, Raw M. Smoking cessation guidelines for health professionals: an update. Thorax 2000;55:987-99. http://dx.doi.org/10.1136/thorax.55.12.987.
- Smoking Cessation Services in Primary Care, Pharmacies, Local Authorities and Workplaces, Particularly for Manual Working Groups, Pregnant Women and Hard to Reach Communities. London: National Institute for Health and Clinical Excellence; 2008.
- Brief Interventions and Referral for Smoking Cessation in Primary Care and Other Settings. London: National Institute for Health and Clinical Excellence; 2006.
- Herbert R, Coleman T, Britton J. U.K. general practitioners’ beliefs, attitudes, and reported prescribing of nicotine replacement therapy in pregnancy. Nicotine Tob Res 2005;7:541-6. http://dx.doi.org/10.1080/14622200500186015.
- Vogt F, Hall S, Marteau TM. General practitioners’ beliefs about effectiveness and intentions to prescribe smoking cessation medications: qualitative and quantitative studies. BMC Public Health 2006;6. http://dx.doi.org/10.1186/1471-2458-6-277.
- Vogt F, Hall S, Marteau TM. General practitioners’ beliefs about effectiveness and intentions to recommend smoking cessation services: qualitative and quantitative studies. BMC Fam Pract 2007;8. http://dx.doi.org/10.1186/1471-2296-8-39.
- Bauld L, Judge K, Platt S. Assessing the impact of smoking cessation services on reducing health inequalities in England: observational study. Tob Control 2007;16:400-4. http://dx.doi.org/10.1136/tc.2007.021626.
- Gray J, Eden G, Williams M. Developing the public health role of a front line clinical service: integrating stop smoking advice into routine podiatry services. J Public Health 2007;29:118-22. http://dx.doi.org/10.1093/pubmed/fdm011.
- Twigg L, Moon G, Szatkowski L, Iggulden P. Smoking cessation in England: intentionality, anticipated ease of quitting and advice provision. Soc Sci Med 2009;68:610-19. http://dx.doi.org/10.1016/j.socscimed.2008.11.032.
- White M, Bush J, Kai J, Bhopal R, Rankin J. Quitting smoking and experience of smoking cessation interventions among UK Bangladeshi and Pakistani adults: the views of community members and health professionals. J Epidemiol Community Health 2006;60:405-11. http://dx.doi.org/10.1136/jech.2005.040345.
- Begh RA, Aveyard P, Upton P, Bhopal RS, White M, Amos A, et al. Promoting smoking cessation in Pakistani and Bangladeshi men in the UK: pilot cluster randomised controlled trial of trained community outreach workers. Trials 2011;12. http://dx.doi.org/10.1186/1745-6215-12-197.
- Murray RL, Bauld L, Hackshaw LE, McNeill A. Improving access to smoking cessation services for disadvantaged groups: a systematic review. J Public Health 2009;31:258-77. http://dx.doi.org/10.1093/pubmed/fdp008.
- Coleman T, Lewis S, Hubbard R, Smith C. Impact of contractual financial incentives on the ascertainment and management of smoking in primary care. Addiction 2007;102:803-8. http://dx.doi.org/10.1111/j.1360-0443.2007.01766.x.
- Murray RL, Coleman T, Antoniak M, Fergus A, Britton J, Lewis SA. The potential to improve ascertainment and intervention to reduce smoking in primary care: a cross sectional survey. BMC Health Serv Res 2008;8. http://dx.doi.org/10.1186/1472-6963-8-6.
- Coleman T. Do financial incentives for delivering health promotion counselling work? Analysis of smoking cessation activities stimulated by the Quality and Outcomes Framework. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-167.
- McEwen A, West R, Owen L, Raw M. General practitioners’ views on and referral to NHS smoking cessation services. Public Health 2005;119:262-8. http://dx.doi.org/10.1016/j.puhe.2004.05.016.
- Peckham S. The new general practice contract and reform of primary care in the United Kingdom. Healthc Policy 2007;2:34-48. http://dx.doi.org/10.12927/hcpol.2007.18873.
- Twardella D, Brenner H. Lack of training as a central barrier to the promotion of smoking cessation: a survey among general practitioners in Germany. Eur J Public Health 2005;15:140-5. http://dx.doi.org/10.1093/eurpub/cki123.
- Young JM, Ward JE. Implementing guidelines for smoking cessation advice in Australian general practice: opinions, current practices, readiness to change and perceived barriers. Fam Pract 2001;18:14-20. http://dx.doi.org/10.1093/fampra/18.1.14.
- McEwen A, West R. Smoking cessation activities by general practitioners and practice nurses. Tobacco Control 2001;10:27-32. http://dx.doi.org/10.1136/tc.10.1.27.
- Guassora AD, Gannik D. Developing and maintaining patients’ trust during general practice consultations: the case of smoking cessation advice. Patient Educ Couns 2009;78:46-52. http://dx.doi.org/10.1016/j.pec.2009.05.003.
- McEwen A, West R, Preston A. Triggering anti-smoking advice by GPs: mode of action of an intervention stimulating smoking cessation advice by GPs. Patient Educ Couns 2006;62:89-94. http://dx.doi.org/10.1016/j.pec.2005.06.008.
- Cleland J, Thomas M, Pinnock H. The views and attitudes of general practitioners and smokers toward provision of smoking cessation advice: a qualitative study. Prim Care Respir J 2004;13:144-8. http://dx.doi.org/10.1016/j.pcrj.2004.05.003.
- Coleman T, Wilson A. Anti-smoking advice from general practitioners: is a population-based approach to advice-giving feasible?. Br J Gen Pract 2000;50:1001-4.
- Pilnick A, Coleman T. Death, depression and ‘defensive expansion’: closing down smoking as an issue for discussion in GP consultations. Soc Sci Med 2006;62:2500-12. http://dx.doi.org/10.1016/j.socscimed.2005.10.031.
- Pilnick A, Coleman T. Do your best for me: the difficulties of finding a clinically effective endpoint in smoking cessation consultations in primary care. Health (London) 2010;14:57-74. http://dx.doi.org/10.1177/1363459309347489.
- Wynn A, Coleman T, Barrett S, Wilson A. Factors associated with the provision of anti-smoking advice in general practice consultations. Br J Gen Pract 2002;52:997-9.
- Coleman T, Wilson A. Factors associated with provision of anti-smoking advice by general practitioners. Br J Gen Pract 1999;49:557-8.
- Zwar NA, Richmond RL. Role of the general practitioner in smoking cessation. Drug Alcohol Rev 2006;25:21-6. http://dx.doi.org/10.1080/09595230500459487.
- Anderson P, Jane-Llopis E. How can we increase the involvement of primary health care in the treatment of tobacco dependence? A meta-analysis. Addiction 2004;99:299-312. http://dx.doi.org/10.1111/j.1360-0443.2003.00672.x.
- Lancaster T, Silagy C, Fowler G. Training health professionals in smoking cessation. Cochrane Database Syst Rev 2000;3. http://dx.doi.org/10.1002/14651858.cd000214.
- Coleman T, Cheater F, Murphy E. Qualitative study investigating the process of giving anti-smoking advice in general practice. Patient Educ Couns 2004;52:159-63. http://dx.doi.org/10.1016/S0738-3991(03)00020-X.
- Coleman T, Wynn AT, Barrett S, Wilson A, Adams S. Intervention study to evaluate pilot health promotion payment aimed at increasing general practitioners’ antismoking advice to smokers. BMJ 2001;323:435-6. http://dx.doi.org/10.1136/bmj.323.7310.435.
- Coleman T, Wynn AT, Stevenson K, Cheater F. Qualitative study of pilot payment aimed at increasing general practitioners’ antismoking advice to smokers. BMJ 2001;323:432-5. http://dx.doi.org/10.1136/bmj.323.7310.432.
- McEwen A, Akotia N, West R. General practitioners’ views on the English national smoking cessation guidelines. Addiction 2001;96:997-1000. http://dx.doi.org/10.1046/j.1360-0443.2001.9679978.x.
- Millett C, Gray J, Saxena S, Netuveli G, Majeed A. Impact of a pay-for-performance incentive on support for smoking cessation and on smoking prevalence among people with diabetes. Can Med Assoc J 2007;176:1705-10. http://dx.doi.org/10.1503/cmaj.061556.
- Wilkes S, Evans A, Henderson M, Gibson J. Pragmatic, observational study of bupropion treatment for smoking cessation in general practice. Postgrad Med J 2005;81:719-22. http://dx.doi.org/10.1136/pgmj.2005.032433.
- Ulbricht S, Meyer C, Schumann A, Rumpf HJ, Hapke U, John U. Provision of smoking cessation counseling by general practitioners assisted by training and screening procedure. Patient Educ Couns 2006;63:232-38. http://dx.doi.org/10.1016/j.pec.2005.11.005.
- Lennox AS, Osman LM, Reiter E, Robertson R, Friend J, McCann I, et al. Cost effectiveness of computer tailored and non-tailored smoking cessation letters in general practice: randomised controlled trial. BMJ 2001;322:1396-400. http://dx.doi.org/10.1136/bmj.322.7299.1396.
- Coleman T, Wilson A, Barrett S, Wynne A, Lewis S. Distributing questionnaires about smoking to patients: impact on general practitioners’ recording of smoking advice. BMC Health Serv Res 2007;7. http://dx.doi.org/10.1186/1472-6963-7-153.
- Gilbert H, Nazareth I, Sutton S. Assessing the feasibility of proactive recruitment of smokers to an intervention in general practice for smoking cessation using computer-tailored feedback reports. Fam Pract 2007;24:395-400. http://dx.doi.org/10.1093/fampra/cmm028.
- McRobbie H, Hajek P, Feder G, Eldridge S. A cluster-randomised controlled trial of a brief training session to facilitate general practitioner referral to smoking cessation treatment. Tob Control 2008;17:173-6. http://dx.doi.org/10.1136/tc.2008.024802.
- Springett J, Owens C, Callaghan J. The challenge of combining ‘lay’ knowledge with ‘evidence-based’ practice in health promotion: Fag Ends Smoking Cessation Service. Crit Public Health 2007;17:243-56. http://dx.doi.org/10.1080/09581590701225854.
- Davey R, Cochrane T, Iqbal Z, Rajaratnam G, Chambers R, Mawby Y, et al. Randomised controlled trial of additional lifestyle support for the reduction of cardiovascular disease risk through primary care in Stoke-on-Trent, UK. Contemp Clin Trials 2010;31:345-54. http://dx.doi.org/10.1016/j.cct.2010.04.002.
- Joyce KE, Smith KE, Henderson G, Greig G, Bambra C. Patient perspectives of Condition Management Programmes as a route to better health, well-being and employability. Fam Pract 2010;27:101-9. http://dx.doi.org/10.1093/fampra/cmp083.
- Ward M, Phillips CJ, Farr A. Heartlinks: a real world approach to effective exercise referral. Int J Health Promot Educ 2010;48:20-7. http://dx.doi.org/10.1080/14635240.2010.10708176.
- Craigie AM, Barton KL, Macleod M, Williams B, van Teijlingen E, Belch JJ, et al. A feasibility study of a personalised lifestyle programme (HealthForce) for individuals who have participated in cardiovascular risk screening. Prev Med 2011;52:387-9. http://dx.doi.org/10.1016/j.ypmed.2011.03.010.
- Watt G, O’Donnell C, Sridharan S. Building on Julian Tudor Hart’s example of anticipatory care. Prim Health Care Res Dev 2011;12:3-10. http://dx.doi.org/10.1017/S1463423610000216.
- Sanderson SC, Waller J, Jarvis MJ, Humphries SE, Wardle J. Awareness of lifestyle risk factors for cancer and heart disease among adults in the UK. Patient Educ Couns 2009;74:221-7. http://dx.doi.org/10.1016/j.pec.2008.08.003.
- Price HC, Griffin SJ, Holman RR. Impact of personalized cardiovascular disease risk estimates on physical activity: a randomized controlled trial. Diabet Med 2011;28:363-72. http://dx.doi.org/10.1111/j.1464-5491.2010.03212.x.
- Bazian Ltd . Advice about diet and lifestyle does not reduce blood pressure in people with hypertension. Evid Based Healthc Public Health 2004;8:348-9.
- Gillespie P, O’Shea E, Murphy AW, Byrne MC, Byrne M, Smith SM, et al. The cost-effectiveness of the SPHERE intervention for the secondary prevention of coronary heart disease. Int J Tech Assess Health Care 2010;26:263-71. http://dx.doi.org/10.1017/S0266462310000358.
- Holt TA, Thorogood M, Griffiths F, Munday S, Friede T, Stables D. Automated electronic reminders to facilitate primary cardiovascular disease prevention: randomised controlled trial. Br J Gen Pract 2010;60:e137-43. http://dx.doi.org/10.3399/bjgp10X483904.
- Campbell NC, Ritchie LD, Thain J, Deans HG, Rawles JM, Squair JL. Secondary prevention in coronary heart disease: a randomised trial of nurse led clinics in primary care. Heart 1998;80:447-52. http://dx.doi.org/10.1136/hrt.80.5.447.
- Mant J. Secondary prevention of coronary heart disease in primary care: the evidence. Br J Cardiol 2002;9:S6-10. http://dx.doi.org/10.1370/afm.1620.
- Reilly V, Cavanagh M. The clinical and economic impact of a secondary heart disease prevention clinic jointly implemented by a practice nurse and pharmacist. Pharm World Sci 2003;25:294-8. http://dx.doi.org/10.1023/B:PHAR.0000006526.55922.8d.
- Raftery JP, Yao GL, Murchie P, Campbell NC, Ritchie LD. Cost effectiveness of nurse led secondary prevention clinics for coronary heart disease in primary care: follow up of a randomised controlled trial. BMJ 2005;330. http://dx.doi.org/10.1136/bmj.38342.665417.8F.
- Connolly S, Holden A, Turner E, Fiumicelli G, Stevenson J, Hunjan M, et al. MyAction: an innovative approach to the prevention of cardiovascular disease in the community. Br J Cardiol 2011;18:171-6.
- Schroeder K, Fahey T, Hollinghurst S, Peters TJ. Nurse-led adherence support in hypertension: a randomized controlled trial. Fam Pract 2005;22:144-51. http://dx.doi.org/10.1093/fampra/cmh717.
- Bane C, Hughes CM, Cupples ME, McElnay JC. The journey to concordance for patients with hypertension: a qualitative study in primary care. Pharm World Sci 2007;29:534-40. http://dx.doi.org/10.1007/s11096-007-9099-x.
- Clark CE, Smith LFP, Taylor RS, Campbell JL. Nurse led interventions to improve control of blood pressure in people with hypertension: systematic review and meta-analysis. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c3995.
- Dunkley A, Stone M, Sayers R, Farooqi A, Khunti K. A cross sectional survey of secondary prevention measures in patients with peripheral arterial disease in primary care. Postgrad Med J 2007;83:602-5. http://dx.doi.org/10.1136/pgmj.2007.060806.
- D’Souza J, Patel NN, Rocker M, Townsend E, Morris-Stiff G, Magee TR, et al. Management of cardiovascular risk factors by primary care physicians in patients with peripheral arterial disease. Surg J R Coll Surg E 2008;6:144-7. http://dx.doi.org/10.1016/s1479-666x(08)80109-6.
- Murray J, Saxena S, Millett C, Curcin V, de Lusignan S, Majeed A. Reductions in risk factors for secondary prevention of coronary heart disease by ethnic group in south-west London: 10-year longitudinal study (1998–2007). Fam Pract 2010;27:430-8. http://dx.doi.org/10.1093/fampra/cmq030.
- Patel JV, Gunarathne A, Lane D, Lim HS, Tracey I, Panja NC, et al. Widening access to cardiovascular healthcare: community screening among ethnic minorities in inner-city Britain – the Healthy Hearts Project. BMC Health Serv Res 2007;7. http://dx.doi.org/10.1186/1472-6963-7-192.
- Crilly M, Bundred P, Hu X, Leckey L, Johnstone F. Gender differences in the clinical management of patients with angina pectoris: a cross-sectional survey in primary care. BMC Health Services Research 2007;7. http://dx.doi.org/10.1186/1472-6963-7-142.
- de Lusignan S. An educational intervention, involving feedback of routinely collected computer data, to improve cardiovascular disease management in UK primary care. Methods Inform Med 2007;46:57-62.
- Patel JV, Gill PS, Chackathayil J, Ojukwu H, Stemman P. Short-term effects of screening for cardiovascular risk in the deaf community: a pilot study. Cardiol Res Pract 2011;2011. http://dx.doi.org/10.4061/2011/493546.
- Daykin N, Naidoo J. Poverty and health promotion in primary health care: professionals’ perspectives. Health Soc Care Comm 1997;5:309-17. http://dx.doi.org/10.1111/j.1365-2524.1997.tb00127.x.
- Abbott S, Riga M. Delivering services to the Bangladeshi community: the views of healthcare professionals in East London. Public Health 2007;121:935-41. http://dx.doi.org/10.1016/j.puhe.2007.04.014.
- Parry J, Mathers J, Laburn-Peart C, Orford J, Dalton S. Improving health in deprived communities: what can residents teach us?. Crit Public Health 2007;17:123-36. http://dx.doi.org/10.1080/09581590601045253.
- Fagan DM, Kiger A, van Teijlingen E. A survey of faith leaders concerning health promotion and the level of healthy living activities occurring in faith communities in Scotland. Glob Health Promot 2010;17:15-23. http://dx.doi.org/10.1177/1757975910383927.
- Kennedy LA, Milton B, Bundred P. Lay food and health worker involvement in community nutrition and dietetics in England: roles, responsibilities and relationship with professionals. J Hum Nutr Diet 2008;21:210-24. http://dx.doi.org/10.1111/j.1365-277X.2008.00876.x.
- Kennedy L. Benefits arising from lay involvement in community-based public health initiatives: the experience from community nutrition. Perspect Public Health 2010;130:165-72. http://dx.doi.org/10.1177/1757913910369090.
- Abbott S. Lay and professional views on health visiting in an orthodox Jewish community. Br J Community Nurs 2004;9:80-6. http://dx.doi.org/10.12968/bjcn.2004.9.2.12424.
- Okereke E, Archibong U, Chiemeka M, Baxter CE, Davis S. Participatory approaches to assessing the health needs of African and African-Caribbean communities. Diversity Health Soc Care 2007;4:287-301.
- Connell P, Wolfe C, McKevitt C. Preventing stroke: a narrative review of community interventions for improving hypertension control in black adults. Health Soc Care Community 2008;16:165-87. http://dx.doi.org/10.1111/j.1365-2524.2007.00737.x.
- Chiu L. Engaging communities in health intervention research/practice. Critical Public Health 2008;18:151-9. http://dx.doi.org/10.1080/09581590701771725.
- Chiu LF, West RM. Health intervention in social context: understanding social networks and neighbourhood. Soc Sci Med 2007;65:1915-27. http://dx.doi.org/10.1016/j.socscimed.2007.05.035.
- Greasley P, Small N. Providing welfare advice in general practice: referrals, issues and outcomes. Health Soc Care Community 2005;13:249-58. http://dx.doi.org/10.1111/j.1365-2524.2005.00557.x.
- Burrows J, Baxter S, Baird W, Hirst J, Goyder E. Citizens advice in primary care: a qualitative study of the views and experiences of service users and staff. Public Health 2011;125:704-10. http://dx.doi.org/10.1016/j.puhe.2011.07.002.
- Harding R, Sherr L, Singh S, Sherr A, Moorhead R. Evaluation of welfare rights advice in primary care: the general practice perspective. Health Soc Care Community 2002;10:417-22. http://dx.doi.org/10.1046/j.1365-2524.2002.00393.x.
- Hoskins RA, Smith LN. Nurse-led welfare benefits screening in a general practice located in a deprived area. Public Health 2002;116:214-20. http://dx.doi.org/10.1038/sj.ph.1900848.
- Abbott S, Hobby L. Impact on individual health of the provision of welfare advice in primary health care settings. Men Health Learn Disabil Care 2000;3:260-2.
- Abbott S, Hobby L. Welfare benefits advice in primary care: evidence of improvements in health. Public Health 2000;114:324-7. http://dx.doi.org/10.1016/s0033-3506(00)00356-5.
- Harding R, Sherr L, Sherr A, Moorhead R, Singh S. Welfare rights advice in primary care: prevalence, processes and specialist provision. Fam Pract 2003;20:48-53. http://dx.doi.org/10.1093/fampra/20.1.48.
- Abbott S, Hobby L, Cotter S. What is the impact on individual health of services in general practice settings which offer welfare benefits advice?. Health Soc Care Community 2006;14:1-8. http://dx.doi.org/10.1111/j.1365-2524.2005.00582.x.
- Maynard MJ, Baker G, Rawlins E, Anderson A, Harding S. Developing obesity prevention interventions among minority ethnic children in schools and places of worship: the DEAL (DiEt and Active Living) study. BMC Public Health 2009;9. http://dx.doi.org/10.1186/1471-2458-9-480.
- Gillam S, Siriwardena A, Steel N. Pay-for-Performance in the United Kingdom: impact of the Quality and Outcomes Framework – a systematic review. Ann Fam Med 2012;10:461-8. http://dx.doi.org/10.1370/afm.1377.
- McDonald R, Harrison S, Checkland K, Campbell SM, Roland M. Impact of financial incentives on clinical autonomy and internal motivation in primary care: ethnographic study. BMJ 2007;334. http://dx.doi.org/10.1136/bmj.39238.890810.BE.
- Duaso M, Cheung P. Health promotion and lifestyle advice in a general practice: what do patients think?. J Adv Nurs 2002;39:472-9. http://dx.doi.org/10.1046/j.1365-2648.2002.02312.x.
- Checkland K, Harrison S. The impact of the Quality and Outcomes Framework on practice organisation and service delivery: summary of evidence from two qualitative studies. Qual Prim Care 2010;18:139-46.
- Checkland K, Coleman A, McDermott I, Segar J, Miller R, Pestoulas C, et al. Exploring the Early Workings of Emerging Clinical Commissioning Groups: Final Report. London: Policy Research Unit in Commissioning and the HealthCare System; 2012.
- Robson D, Gray R. Serious mental illness and physical health problems: a discussion paper. Int J Nurs Stud 2007;44:457-66. http://dx.doi.org/10.1016/j.ijnurstu.2006.07.013.
- Emond A, Pollock J, Deave T, Bonnell S, Peters TJ, Harvey I. An evaluation of the First Parent Health Visitor Scheme. Arch Dis Child 2002;86:150-7. http://dx.doi.org/10.1136/adc.86.3.150.
- Watson M, Kendrick D, Coupland C, Woods A, Futers D, Robinson J. Providing child safety equipment to prevent injuries: randomised controlled trial. BMJ 2005;330. http://dx.doi.org/10.1136/bmj.38309.664444.8F.
- Clamp M, Kendrick D. A randomised controlled trial of general practitioner safety advice for families with children under 5 years. BMJ 1998;316:1576-9. http://dx.doi.org/10.1136/bmj.316.7144.1576.
- Kendrick D, Marsh P, Fielding K, Miller P. Preventing injuries in children: cluster randomised controlled trial in primary care. BMJ 1999;318:980-3. http://dx.doi.org/10.1136/bmj.318.7189.980.
- McInnes RJ, Stone DH. The process of implementing a community-based peer breast-feeding support programme: the Glasgow experience. Midwifery 2001;17:65-73. http://dx.doi.org/10.1054/midw.2000.0236.
- Graffy J, Taylor J, Williams A, Eldridge S. Randomised controlled trial of support from volunteer counsellors for mothers considering breast feeding. BMJ 2004;328. http://dx.doi.org/10.1136/bmj.328.7430.26.
- Hoddinott P, Pill R, Chalmers M. Health professionals, implementation and outcomes: reflections on a complex intervention to improve breastfeeding rates in primary care. Fam Pract 2007;24:84-91. http://dx.doi.org/10.1093/fampra/cml061.
- Kendrick D, Marsh P. Injury prevention programmes in primary care: a high risk group or a whole population approach?. Inj Prev 1997;3:170-5. http://dx.doi.org/10.1136/ip.3.3.170.
- Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2011;12. http://dx.doi.org/10.1002/14651858.cd001871.pub3.
- Adab P, Marshall T, Rouse A, Randhawa B, Sangha H, Bhangoo N. Randomised controlled trial of the effect of evidence based information on women’s willingness to participate in cervical cancer screening. J Epidemiol Community Health 2003;57:589-93. http://dx.doi.org/10.1136/jech.57.8.589.
- Campbell H, MacDonald S, McKiernan M. Promotion of cervical screening uptake by health visitor follow-up of women who repeatedly failed to attend. J Public Health Med 1996;18:94-7. http://dx.doi.org/10.1093/oxfordjournals.pubmed.a024468.
- Ibbotson T, Wyke S, McEwen J, Macintyre S, Kelly M. Uptake of cervical screening in general practice: effect of practice organisation, structure, and deprivation. J Med Screen 1996;3:35-9.
- Janssen P, Gorter K, Stolk R, Rutten G. Low yield of population-based screening for type 2 diabetes in the Netherlands: the ADDITION Netherlands study. Fam Pract 2007;24:555-61. http://dx.doi.org/10.1093/fampra/cmm052.
- Woolthuis EPK, de Grauw WJ, van Gerwen HE, van den Hoogen HJ, van de Lisdonk EH, Metsemakers JF, et al. Yield of opportunistic targeted screening for type 2 diabetes in primary care: the Diabscreen Study. Ann Fam Med 2009;7:422-30. http://dx.doi.org/10.1370/afm.997.
- Robson J, Boomla K, Hart B, Feder G. Estimating cardiovascular risk for primary prevention: outstanding questions for primary care. BMJ 2000;320:702-4. http://dx.doi.org/10.1136/bmj.320.7236.702.
- Gill B, Meltzer H, Hinds K, Pettigrew M. Psychiatric Morbidity among Homeless People. London: HMSO; 1996.
- Howse JH, Jones S, Hungin AP. Screening and identifying diabetes in optometric practice: a prospective study. Br J Gen Pract 2011;61:436-42. http://dx.doi.org/10.3399/bjgp11X583227.
- Krass I, Mitchell B, Clarke P, Brillant M, Dienaar R, Hughes J, et al. Pharmacy diabetes care program: analysis of two screening methods for undiagnosed type 2 diabetes in Australian community pharmacy. Diabetes Res Clin Pract 2007;75:339-47. http://dx.doi.org/10.1016/j.diabres.2006.06.022.
- Lawal AG, Patel MG, Wong IC, Chrystyn H. Opportunistic screening for type 2 diabetes within inner city community pharmacies. Int J Pharm Pract 2003;11.
- Dachsel M, Lee E. Opportunistic health checks in a retail environment. Lond J Prim Care 2011;4:5-10.
- Ebrahim S, Smith GD. Systematic review of randomised controlled trials of multiple risk factor interventions for preventing coronary heart disease. BMJ 1997;314:1666-74. http://dx.doi.org/10.1136/bmj.314.7095.1666.
- Wonderling D, Langham S, Buxton M, Normand C, McDermott C. What can be concluded from the OXCHECK and British family heart studies: commentary on cost effectiveness analyses. BMJ 1996;312:1274-78. http://dx.doi.org/10.1136/bmj.312.7041.1274.
- Summers A, Fullard B. Improving the coverage and quality of cervical screening: women’s views. J Public Health Med 1995;17:277-81.
- Ma R, Clark A. Chlamydia screening in general practice: views of professionals on the key elements of a successful programme. J Fam Plann Reprod Health Care 2005;31:302-6. http://dx.doi.org/10.1783/147118905774480806.
- Hogan AH, Howell-Jones RS, Pottinger E, Wallace LM, McNulty CA. ‘. . . They should be offering it’: a qualitative study to investigate young people’s attitudes towards chlamydia screening in GP surgeries. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-616.
- Santer M, Warner P, Wyke S, Sutherland S. Opportunistic screening for chlamydia infection in general practice: can we reach young women?. J Med Screen 2000;7:175-6. http://dx.doi.org/10.1136/jms.7.4.175.
- McNulty CA, Freeman E, Bowen J, Shefras J, Fenton KA. Barriers to opportunistic chlamydia testing in primary care. Br J Gen Pract 2004;54:508-14.
- Santer M, Wyke S, Warner P. Women’s experiences of chlamydia screening: qualitative interviews with women in primary care. Eur J Gen Pract 2003;9:56-61. http://dx.doi.org/10.3109/13814780309160403.
- Pimenta JM, Catchpole M, Rogers PA, Perkins E, Jackson N, Carlisle C, et al. Opportunistic screening for genital chlamydial infection. I: acceptability of urine testing in primary and secondary healthcare settings. Sex Transm Infect 2003;79:16-21. http://dx.doi.org/10.1136/sti.79.1.16.
- Baraitser P, Pearce V, Holmes J, Horne N, Boynton PM. Chlamydia testing in community pharmacies: evaluation of a feasibility pilot in south east London. Qual Saf Health Care 2007;16:303-7. http://dx.doi.org/10.1136/qshc.2006.020883.
- Brabin L, Thomas G, Hopkins M, O’Brien K, Roberts S. Delivery of chlamydia screening to young women requesting emergency hormonal contraception at pharmacies in Manchester, UK: a prospective study. BMC Women’s Health 2009;9. http://dx.doi.org/10.1186/1472-6874-9-7.
- Dabrera G, Pinson D, Whiteman S. Chlamydia screening by community pharmacists: a qualitative study. J Fam Plann Reprod Health Care 2011;37:17-21. http://dx.doi.org/10.1136/jfprhc.2010.0003.
- Kharicha K, Iliffe S, Harari D, Swift CG, Goodman C, Manthorpe J, et al. Feasibility of repeated use of the Health Risk Appraisal for Older people system as a health promotion tool in community-dwelling older people: retrospective cohort study 2001–05. Age Ageing 2012;41:128-31. http://dx.doi.org/10.1093/ageing/afr126.
- Smeeth L, Fletcher AE, Hanciles S, Evans J, Wormald R. Screening older people for impaired vision in primary care: cluster randomised trial. BMJ 2003;327. http://dx.doi.org/10.1136/bmj.327.7422.1027.
- Smeeth L, Iliffe S. Community screening for visual impairment in the elderly. Cochrane Database Syst Rev 2006;3.
- Cioffe GA, Mansberger S, Spry P, Johnson C, Van Buskirk EM. Frequency doubling perimetry and the detection of eye disease in the community. Trans Am Ophthalmol Soc 2000;98:195-202.
- Smeeth L, Fletcher AE, Ng ES, Stirling S, Nunes M, Breeze E, et al. Reduced hearing, ownership, and use of hearing aids in elderly people in the UK: the MRC Trial of the Assessment and Management of Older People in the Community – a cross-sectional survey. Lancet 2002;359:1466-70. http://dx.doi.org/10.1016/S0140-6736(02)08433-7.
- Damery S, Smith S, Clements A, Holder R, Nichols L, Draper H, et al. Evaluating the effectiveness of GP endorsement on increasing participation in the NHS Bowel Cancer Screening Programme in England: study protocol for a randomized controlled trial. Trials 2012;13. http://dx.doi.org/10.1186/1745-6215-13-18.
- Woodrow C, Rozmovits L, Hewitson P, Rose P, Austoker J, Watson E. Bowel cancer screening in England: a qualitative study of GPs’ attitudes and information needs. BMC Fam Pract 2006;7. http://dx.doi.org/10.1186/1471-2296-7-53.
- Lavin JH, Avery A, Whitehead SM, Rees R, Parsons J, Bagnall T, et al. Feasibility and benefits of implementing a Slimming on Referral service in primary care using a commercial weight management partner. Public Health 2006;120:872-81. http://dx.doi.org/10.1016/j.puhe.2006.05.008.
- Lowe MR, Miller-Kovach K, Phelan S. Weight-loss maintenance in overweight individuals one to five years following successful completion of a commercial weight loss program. Int J Obes Relat Metab Disord 2001;25:325-31. http://dx.doi.org/10.1038/sj.ijo.0801521.
- Pritchard DA, Hyndman J, Taba F. Nutritional counselling in general practice: a cost effectiveness analysis. J Epidemiol Community Health 1999;53:311-16. http://dx.doi.org/10.1136/jech.53.5.311.
- Lamb SE, Bartlett HP, Ashley A, Bird W. Can lay-led walking programmes increase physical activity in middle aged adults? A randomised controlled trial. J Epidemiol Community Health 2002;56:246-52. http://dx.doi.org/10.1136/jech.56.4.246.
- Lowther M, Mutrie N, Scott EM. Promoting physical activity in a socially and economically deprived community: a 12 month randomized control trial of fitness assessment and exercise consultation. J Sports Sci 2002;20:577-88. http://dx.doi.org/10.1080/026404102760000071.
- Greaves CJ, Middlebrooke A, O’Loughlin L, Holland S, Piper J, Steele A, et al. Motivational interviewing for modifying diabetes risk: a randomised controlled trial. Br J Gen Pract 2008;58:535-40. http://dx.doi.org/10.3399/bjgp08X319648.
- Dugdill L, Graham RC, McNair F. Exercise referral: the public health panacea for physical activity promotion? A critical perspective of exercise referral schemes; their development and evaluation. Ergonomics 2005;48:1390-410. http://dx.doi.org/10.1080/00140130500101544.
- Tulloch H, Fortier M, Hogg W. Physical activity counseling in primary care: who has and who should be counseling?. Patient Educ Couns 2006;64:6-20. http://dx.doi.org/10.1016/j.pec.2005.10.010.
- Lawton BA, Rose SB, Elley R, Dowell AC, Fenton A, Moyes S. Exercise on prescription for women aged 40–74 recruited through primary care: two year randomised controlled trial. Br J Sports Med 2009;43:120-3.
- Elley CR, Kerse N, Arroll B, Robinson E. Effectiveness of counselling patients on physical activity in general practice: cluster randomised controlled trial. BMJ 2003;326:793-6. http://dx.doi.org/10.1136/bmj.326.7393.793.
- Marcus BH, Williams DM, Dubbert PM, Sallis JF, King AC, Yancey AK, et al. Physical activity intervention studies: what we know and what we need to know: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity); Council on Cardiovascular Disease in the Young; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research. Circulation 2006;114:2739-52. http://dx.doi.org/10.1161/CIRCULATIONAHA.106.179683.
- Anokye NK, Trueman P, Green C, Pavey TG, Hillsdon M, Taylor RS. The cost-effectiveness of exercise referral schemes. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-954.
- Fisher B, Dowding D, Pickett KE, Fylan F. Health promotion at NHS breast cancer screening clinics in the UK. Health Promot Int 2007;22:137-45. http://dx.doi.org/10.1093/heapro/dal043.
- Four Commonly Used Methods to Increase Physical Activity: Brief Interventions in Primary Care, Exercise Referral Schemes, Pedometers and Community-Based Exercise Programmes for Walking and Cycling. London: National Institute for Health and Clinical Excellence; 2006.
- Weiler R, Stamatakis E. Physical activity in the UK: a unique crossroad?. Br J Sports Med 2010;44:912-4. http://dx.doi.org/10.1136/bjsm.2010.073726.
- Laws R. Counterweight Project Team . A new evidence-based model for weight management in primary care: the Counterweight Programme. J Hum Nutr Diet 2004;17:191-208. http://dx.doi.org/10.1111/j.1365-277X.2004.00517.x.
- Pavey TG, Anokye N, Taylor AH, Trueman P, Moxham T, Fox KR, et al. The clinical effectiveness and cost-effectiveness of exercise referral schemes: a systematic review and economic evaluation. Health Technol Assess 2011;15. http://dx.doi.org/10.3310/hta15440.
- Hillsdon M, Foster C, Thorogood M. Interventions for promoting physical activity. Cochrane Database Syst Rev 2005;1.
- Flodgren G, Deane K, Dickinson HO, Kirk S, Alberti H, Beyer FR, et al. Interventions to change the behaviour of health professionals and the organisation of care to promote weight reduction in overweight and obese people. Cochrane Database Syst Rev 2010;3. http://dx.doi.org/10.1002/14651858.cd000984.pub2.
- Baker PR, Francis DP, Soares J, Weightman AL, Foster C. Community wide interventions for increasing physical activity. Cochrane Database Syst Rev 2011;4. http://dx.doi.org/10.1002/14651858.cd008366.pub2.
- Norris SL, Zhang X, Avenell A, Gregg E, Schmid CH, Lau J. Long-term non-pharmacological weight loss interventions for adults with prediabetes. Cochrane Database Syst Rev 2005;2. http://dx.doi.org/10.1002/14651858.cd005270.
- Nield L, Summerbell CD, Hooper L, Whittaker V, Moore H. Dietary advice for the prevention of type 2 diabetes mellitus in adults. Cochrane Database Syst Rev 2008;3. http://dx.doi.org/10.1002/14651858.cd005102.pub2.
- Orozco LJ, Buchleitner AM, Gimenez-Perez G, Roque IFM, Richter B, Mauricio D. Exercise or exercise and diet for preventing type 2 diabetes mellitus. Cochrane Database Syst Rev 2008;3. http://dx.doi.org/10.1002/14651858.cd003054.pub3.
- Hooper L, Bartlett C, Davey SG, Ebrahim S. Advice to reduce dietary salt for prevention of cardiovascular disease. Cochrane Database Syst Rev 2004;1. http://dx.doi.org/10.1002/14651858.cd003656.pub2.
- McKenna J, Vernon M. How general practitioners promote ‘lifestyle’ physical activity. Patient Educ Couns 2004;54:101-6. http://dx.doi.org/10.1016/S0738-3991(03)00192-7.
- Boehler CE, Milton KE, Bull FC, Fox-Rushby JA. The cost of changing physical activity behaviour: evidence from a ‘physical activity pathway’ in the primary care setting. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-370.
- Sinclair HK, Bond CM, Stead LF. Community pharmacy personnel interventions for smoking cessation. Cochrane Database Syst Rev 2004;1. http://dx.doi.org/10.1002/14651858.cd003698.pub2.
- Rice VH, Stead LF. Nursing interventions for smoking cessation. Cochrane Database Syst Rev 2008;1. http://dx.doi.org/10.1002/14651858.cd001188.pub3.
- Stead LF, Bergson G, Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst Rev 2008;2. http://dx.doi.org/10.1002/14651858.cd000165.pub3.
- Lai DT, Cahill K, Qin Y, Tang JL. Motivational interviewing for smoking cessation. Cochrane Database Syst Rev 2010;1. http://dx.doi.org/10.1002/14651858.cd006936.pub2.
- Buffels J, Degryse J, Decramer M, Heyrman J. Spirometry and smoking cessation advice in general practice: a randomised clinical trial. Respir Med 2006;100:2012-17. http://dx.doi.org/10.1016/j.rmed.2006.02.014.
- Rennard SI, Daughton DM. Smoking cessation. Chest 2000;117:360S-4S. http://dx.doi.org/10.1378/chest.117.5_suppl_2.360S.
- Sutherland G. Current approaches to the management of smoking cessation. Drugs 2002;62:53-61. http://dx.doi.org/10.2165/00003495-200262002-00006.
- Pieterse ME, Seydel ER, DeVries H, Mudde AN, Kok GJ. Effectiveness of a minimal contact smoking cessation program for Dutch general practitioners: a randomized controlled trial. Prev Med 2001;32:182-90. http://dx.doi.org/10.1006/pmed.2000.0791.
- Sippel JM, Osborne ML, Bjornson W, Goldberg B, Buist S. Smoking cessation in primary care clinics. J Gen Intern Med 1999;14:670-6. http://dx.doi.org/10.1046/j.1525-1497.1999.11088.x.
- Aveyard P, Brown K, Saunders C, Alexander A, Johnstone E, Munafo MR, et al. Weekly versus basic smoking cessation support in primary care: a randomised controlled trial. Thorax 2007;62:898-903. http://dx.doi.org/10.1136/thx.2006.071837.
- Stead LF, Perera R, Bullen C, Mant D, Lancaster T. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev 2009;1.
- Pomerleau J, McKee M. Issues in Public Health. London: Open University Press; 2005.
- Raw M, McNeill A, West R. Smoking cessation: evidence based recommendations for the healthcare system. BMJ 1999;318:182-5. http://dx.doi.org/10.1136/bmj.318.7177.182.
- Secker-Walker RH, Gnich W, Platt S, Lancaster T. Community interventions for reducing smoking among adults. Cochrane Database Syst Rev 2002;3. http://dx.doi.org/10.1002/14651858.cd001745.
- Aveyard P, Foulds J. The 2008 US Clinical Practice Guideline: The Key Recommendations and a Commentary 2009. www.treatobacco.net (accessed 1 March 2012).
- Cahill K, Stead LF, Lancaster T. Nicotine receptor partial agonists for smoking cessation. Cochrane Database Syst Rev 2012;1. http://dx.doi.org/10.1002/14651858.cd006103.pub6.
- Hughes JR, Stead LF, Lancaster T. Antidepressants for smoking cessation. Cochrane Database Syst Rev 2007;1. http://dx.doi.org/10.1002/14651858.cd000031.pub3.
- The Clinical Effectiveness and Cost Effectiveness of Bupropion (Zyban) and Nicotine Replacement Therapy for Smoking Cessation. London: National Institute for Health and Clinical Excellence; 2002.
- Silagy CA, Stead LF, Lancaster T. Use of systematic reviews in clinical practice guidelines: case study of smoking cessation. BMJ 2001;323:833-6. http://dx.doi.org/10.1136/bmj.323.7317.833.
- O’Neill C, Normand C, Cupples M, McKnight A. Cost effectiveness of personal health education in primary care for people with angina in the greater Belfast area of Northern Ireland. J Epidemiol Community Health 1996;50:538-40. http://dx.doi.org/10.1136/jech.50.5.538.
- Cupples ME, McKnight A, O’Neill C, Normand C. The effect of personal health education on the quality of life of patients with angina in general practice. Health Educ J 1996;55:175-83. http://dx.doi.org/10.1177/001789699605500107.
- Mason AR, Hill RC, Myers LA, Street AD. Establishing the economics of engaging communities in health promotion: what is desirable, what is feasible?. Crit Public Health 2008;18:285-97. http://dx.doi.org/10.1080/09581590802277366.
- Gillam S, Joffe M, Miller R, Gray A, Epstein L, Plamping D. Community-oriented primary care: old wine in new bottles. J Interprof Care 1998;12:53-61. http://dx.doi.org/10.3109/13561829809014087.
- Taket A, Edmans T. Community led regeneration: experiences from London. Int J Healthc Tech Manag 2003;5:81-95. http://dx.doi.org/10.1504/IJHTM.2003.003334.
- Ritchie D, Gnich W, Parry O, Platt S. ‘People pull the rug from under your feet’: barriers to successful public health programmes. BMC Public Health 2008;8. http://dx.doi.org/10.1186/1471-2458-8-173.
- Carlisle S. Tackling health inequalities and social exclusion through partnership and community engagement? A reality check for policy and practice aspirations from a Social Inclusion Partnership in Scotland. Crit Pub Health 2010;20:117-27. http://dx.doi.org/10.1080/09581590802277341.
- Munro JF, Nicholl JP, Brazier JE, Davey R, Cochrane T. Cost effectiveness of a community based exercise programme in over 65 year olds: cluster randomised trial. J Epidemiol Community Health 2004;58:1004-10. http://dx.doi.org/10.1136/jech.2003.014225.
- Trueman P, Haynes SM, Lyons GF, McCombie EL, McQuigg MS, Mongia S, et al. Long-term cost-effectiveness of weight management in primary care. Int J Clin Pract 2010;64:775-83. http://dx.doi.org/10.1111/j.1742-1241.2010.02349.x.
- Marshall T, Rouse A. Resource implications and health benefits of primary prevention strategies for cardiovascular disease in people aged 30 to 74: mathematical modelling study. BMJ 2002;325. http://dx.doi.org/10.1136/bmj.325.7357.197.
- Bryan S, Dormandy E, Roberts T, Ades A, Barton P, Juarez-Garcia A, et al. Screening for sickle cell and thalassaemia in primary care: a cost-effectiveness study. Br J Gen Pract 2011;61:e620-7. http://dx.doi.org/10.3399/bjgp11X601325.
- Prevention of Cardiovascular Disease. London: National Institute for Health and Clinical Excellence; 2010.
- Laws R, Kirby S, Powell Davies G, Williams AM, Jayasinghe UW, Amoroso CL, et al. ‘Should I and can I?’ A mixed methods study of clinician beliefs and attitudes in the management of lifestyle risk factors in primary health care. BMC Health Serv Res 2008;8. http://dx.doi.org/10.1186/1472-6963-8-44.
- Goodwin N, Ross S, Smith A. The Quality of Care in General Practice: Capturing Opinions from the Front Line. London: The King’s Fund; 2010.
- Millett C, Gray J, Wall M, Majeed A. Ethnic disparities in coronary heart disease management and pay for performance in the UK. J Gen Intern Med 2009;24:8-13. http://dx.doi.org/10.1007/s11606-008-0832-5.
- Campbell SM, Reeves D, Kontopantelis E, Sibbald B, Roland M. Effects of pay for performance on the quality of primary care in England. N Engl J Med 2009;361:368-78. http://dx.doi.org/10.1056/NEJMsa0807651.
- Simpson CR, Hannaford PC, Ritchie LD, Sheikh A, Williams D. Impact of the pay-for-performance contract and the management of hypertension in Scottish primary care: a 6-year population-based repeated cross-sectional study. Br J Gen Pract 2011;61:e443-51. http://dx.doi.org/10.3399/bjgp11X583407.
- Doran T, Kontopantelis E, Valderas J, Campbell S, Roland M, Salisbury C, et al. Effect of financial incentives on incentivised and non-incentivised clinical activities: longitudinal analysis of data from the UK Quality and Outcomes Framework. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d3590.
- Campbell SM, McDonald R, Lester H. The experience of pay for performance in English family practice: a qualitative study. Ann Fam Med 2008;6:228-34. http://dx.doi.org/10.1370/afm.844.
- Boyd KA, Briggs AH. Cost-effectiveness of pharmacy and group behavioural support smoking cessation services in Glasgow. Addiction 2009;104:317-25. http://dx.doi.org/10.1111/j.1360-0443.2008.02449.x.
- Bauld L, Boyd KA, Briggs AH, Chesterman J, Ferguson J, Judge K, et al. One-year outcomes and a cost-effectiveness analysis for smokers accessing group-based and pharmacy-led cessation services. Nicotine Tob Res 2011;13:135-45. http://dx.doi.org/10.1093/ntr/ntq222.
- Ronckers ET, Groot W, Ament AJ. Systematic review of economic evaluations of smoking cessation: standardizing the cost-effectiveness. Med Decis Making 2005;25:437-48. http://dx.doi.org/10.1177/0272989X05278431.
- Gordon L, Graves N, Hawkes A, Eakin E. A review of the cost-effectiveness of face-to-face behavioural interventions for smoking, physical activity, diet and alcohol. Chronic Ill 2007;3:101-29. http://dx.doi.org/10.1177/1742395307081732.
- Saha S, Gerdtham UG, Johansson P. Economic evaluation of lifestyle interventions for preventing diabetes and cardiovascular diseases. Int J Environ Res Public Health 2010;7:3150-95. http://dx.doi.org/10.3390/ijerph7083150.
- Cupples ME, Smith SM, Murphy AW. How effective is prevention in coronary heart disease?. Heart 2008;94:1370-1. http://dx.doi.org/10.1136/hrt.2007.133777.
- McAlister FA, Lawson FM, Teo KK, Armstrong PW. Randomised trials of secondary prevention programmes in coronary heart disease: systematic review. BMJ 2001;323:957-62. http://dx.doi.org/10.1136/bmj.323.7319.957.
- Brotons C, Bjorkelund C, Bulc M, Ciurana R, Godycki-Cwirko M, Jurgova E, et al. Prevention and health promotion in clinical practice: the views of general practitioners in Europe. Prev Med 2005;40:595-601. http://dx.doi.org/10.1016/j.ypmed.2004.07.020.
- Nissen SE, Tardif JC, Nicholls SJ, Revkin JH, Shear CL, Duggan WT, et al. Effect of torcetrapib on the progression of coronary atherosclerosis. N Engl J Med 2007;356:1304-16. http://dx.doi.org/10.1056/NEJMoa070635.
- Krumholz HM, Lee TH. Redefining quality: implications of recent clinical trials. N Engl J Med 2008;358:2537-9. http://dx.doi.org/10.1056/NEJMp0803740.
- Summary Report: Second Phase. London: Department of Health; 2012.
- Making Every Contact Count: A Joint Approach to Preventing Homelessness. London: Department of Communities and Local Government; 2012.
- Joint Strategic Needs Assessment and Joint Health and Wellbeing Strategies Explained: Commissioning for Populations. London: Department of Health; 2011.
- Thorlby R, Curry N. Practice-Based Commissioning. London: The King’s Fund; 2007.
- Miller R, Peckham S, Checkland K, Coleman A, McDermott I, Harrison S. Clinical Engagement in Primary Care-Led Commissioning: A Review of the Evidence. London: Policy Research Unit in Commissioning and the Healthcare System; 2012.
- Smith J, Thorlby R. Giving GPs Budgets for Commissioning: What Needs To Be Done?. London: The Nuffield Trust; 2010.
- Health Act 1999. London: HMSO; 1999.
- O’Donnell CA, Ring A, McClean G, Grant S, Guthrie B, Gabbay M, et al. The New GMS Contract in Primary Care: The Impact of Governance and Incentives on Care. London: National Institute of Health Research Service Delivery & Organisation Programme; 2010.
- Sweeney KG, MacAuley D, Gray DP. Personal significance: the third dimension. Lancet 1998;351:134-6. http://dx.doi.org/10.1016/S0140-6736(97)06316-2.
- De Maeseneer JM, van Driel ML, Green LA, van Weel C. The need for research in primary care. Lancet 2003;362:1313-19. http://dx.doi.org/10.1016/S0140-6736(03)14576-X.
- Scullard P, Abelhamid A, Steel N, Qureshi N. Does the evidence referenced in NICE guidelines reflect a primary care population?. Br J Gen Pract 2011;61:e112-17. http://dx.doi.org/10.3399/bjgp11X561177.
- Fischer A, Threfall A, Cookson R, Meah S, Rutter H, Kelly M. The Appraisal of Public Health Interventions n.d. http://dx.doi.org/10.1016/s0140-6736(13)60373-6.
- A Short Guide to Health and Wellbeing Boards. London: Department of Health; 2012.
- The Mandate: A Mandate from the Government to the NHS Commissioning Board: April 2013 to March 2015. London: Department of Health; 2012.
- Physical Activity: Brief Advice for Adults in Primary Care. London: National Institute for Health and Clinical Excellence; 2013.
- Swan D. NHS Health Checks cancer awareness pilot picks up only four patients. Pulse 2012. www.pulsetoday.co.uk/clinical/cancer/nhs-health-checks-cancer-awareness-pilot-picks-up-only-four-patients/20000605.article#.VUI_TM5U2ag (accessed 4 March 2014).
- Goodwin N, Dixon A, Poole T, Raleigh V. Improving the Quality of Care in General Practice: Report of an Independent Inquiry Commissioned by The King’s Fund. London: The King’s Fund; 2011.
- Royal College of General Practitioners . MRCGP Curriculum n.d. www.rcgp-curriculum.org.uk/trainer_support.aspx (accessed 4 March 2014).
- Hanney SR, González-Block M, Buxton MJ, Kogan M. The utilisation of health research in policy-making: concepts, examples and methods of assessment. Health Res Policy Syst 2003;1. http://dx.doi.org/10.1186/1478-4505-1-2.
- Weiss C. The many meanings of research utilization. Public Admin Rev 1979;39:426-31. http://dx.doi.org/10.2307/3109916.
- Thomas P. The Aims and Outcomes of Social Policy Research. London: Croom Helm; 1985.
- Gibbons M, Limoges C, Nowotny H, Schwartzman S, Scott P, Trow M. The New Production of Knowledge: Dynamics of Science and Research in Contemporary Societies. London: Sage; 1994.
- Abdelhamid A, Edwards H, Fleetcroft R, Howe A, Qureshi N, Song F, et al. Are NICE Recommendations for Primary Care Based on Research Conducted In, or Generalisable To, a Primary Care Setting? n.d.
- Watt G. Blue Sky Research for Primary Care: A Discussion Paper. Society for Academic Primary Care; 2011.
- Anokye N, Jones T, Fox-Rushby J. National Institute for Health and Clinical Excellence Public Health Intervention Guidance: Physical Activity – Brief Advice for Adults in Primary Care: Economic Analysis: Review of Economic Evidence. London: Brunel University; 2012.
- Taggart J, Williams A, Dennis S, Newall A, Shortus T, Zwar N, et al. A systematic review of interventions in primary care to improve health literacy for chronic disease behavioral risk factors. BMC Fam Pract 2012;13. http://dx.doi.org/10.1186/1471-2296-13-49.
- Wilson A, Childs S. The relationship between consultation length, process and outcomes in general practice: a systematic review. Br J Gen Pract 2002;52:1012-20.
- Wilkinson E. Health checks are ‘unlikely to be beneficial’. Pulse 2012. www.pulsetoday.co.uk/news/clinical-news/health-checks-are-unlikely-to-be-beneficial/20000682.article#.VUI_485U2ag (accessed 4 March 2014).
- Krogsbøll LT, Jørgensen KJ, Grønhøj Larsen C, Gøtzsche PC. General health checks in adults for reducing morbidity and mortality from disease: Cochrane systematic review and meta-analysis. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e7191.
- MacAuley D. The value of conducting periodic health checks. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e7775.
- Coulter A, Schofield T. Prevention in general practice: the views of doctors in the Oxford region. Br J Gen Pract 1991;41:140-3.
- Watt G. GPs at the deep end. Br J Gen Pract 2011;61:66-7. http://dx.doi.org/10.3399/bjgp11X549090.
- Norbury M, Mercer SW, Gillies J, Furler J, Watt GC. Time to care: tackling health inequalities through primary care. Fam Pract 2011;28:1-3. http://dx.doi.org/10.1093/fampra/cmq118.
- Marteau TM, Kinmonth AL. Screening for cardiovascular risk: public health imperative or matter for individual informed choice?. BMJ 2002;325:78-80. http://dx.doi.org/10.1136/bmj.325.7355.78.
- Getz L, Sigurdsson JA, Hetlevik I. Is opportunistic disease prevention in the consultation ethically justifiable?. BMJ 2003;327. http://dx.doi.org/10.1136/bmj.327.7413.498.
- Baumann A. Positive Practice Environments: Quality Workplaces = Quality Patient Care. Geneva: International Council of Nurses; 2007.
- Bryar R, Kendall S, Mogotlane S. Reforming Primary Health Care: A Nursing Perspective. Contributing to Health Care Reform, Issues and Challenges. Geneva: International Council of Nurses; 2012.
- Mold JW, Peterson KA. Primary care practice-based research networks: working at the interface between research and quality improvement. Ann Fam Med 2005;3:S12-20. http://dx.doi.org/10.1370/afm.303.
- Amato L, Davoli M, Ali R, Faggiano F, Farrell M, Foxcroft D, et al. Drugs and Alcohol Group. About The Cochrane Collaboration (Cochrane Review Groups (CRGs)) 2007.
- National Institute for Health and Care Excellence . NICE Guideline PH1: Brief Interventions and Referral for Smoking Cessation n.d. http://guidance.nice.org.uk/PH1 (accessed February 2010).
- National Institute for Health and Care Excellence . NICE Guideline PH17: Promoting Physical Activity for Children and Young People n.d. http://guidance.nice.org.uk/PH17 (accessed February 2010).
- National Institute for Health and Care Excellence . NICE Guidance PH21: Reducing Differences in the Uptake of Immunizations n.d. http://guidance.nice.org.uk/PH21 (accessed February 2010).
Appendix 1 Literature search
Ovid MEDLINE
Date range searched: 1990–2013.
Date of search: June 2013.
Search strategy
-
family practice/ (58,510)
-
primary health care/ (46,024)
-
physicians, family/ (14,183)
-
physicians, primary care/ (336)
-
nursing staff/ (15,236)
-
community health aides/ (2652)
-
primary care nursing/ (21)
-
community health nursing/ (17,648)
-
((primary or community) adj1 (care or health*)).ti,ab. (80,838)
-
((general or family) adj1 (practice* or practitioner*)).ti,ab. (59,896)
-
(gp adj1 (service* or practice* or clinic or clinics)).ti,ab. (751)
-
((practice or communit*) adj2 nurs*).ti,ab. (21,784)
-
health visitor*.ti,ab. (2059)
-
family practice.jw. (13,511)
-
(primary adj1 (care or health*)).jw. (5642)
-
(general adj1 (practice or practitioner*)).jw. (10,182)
-
or/1-16 (236,313)
-
exp Public Health/ (4,819,124)
-
social medicine/ (3577)
-
public health administration/ (13,831)
-
exp Health education/ (124,022)
-
health educators/ (154)
-
exp Preventive health services/ (378,490)
-
Preventive Medicine/ (10,288)
-
exp Health promotion/ (44,345)
-
public health*.ti,ab. (98,434)
-
((primary or secondary or tertiary or primordial) adj1 prevent*).ti,ab. (19,980)
-
((disease* or ill*) adj3 (reduc* or prevent*)).ti,ab. (52,929)
-
((health* or intervention*) adj2 (promot* or improve* or educat* or protect* or program*)).ti,ab. (103,386)
-
(prevent* adj2 (medicine or activi* or program*)).ti,ab. (25,787)
-
(determin* adj2 (health* or disease*)).ti,ab. (11,074)
-
education.jw. (52,717)
-
public health.jw. (81,262)
-
social.jw. (50,276)
-
prevent*.jw. (37,674)
-
community.jw. (27,019)
-
or/18-36 (5,111,715)
-
exp Great Britain/ (269,793)
-
(uk or united kingdom or britain or gb or gbr or british isles).ti,ab. (85,033)
-
(england or scotland or wales or ireland).ti,ab. (66,339)
-
(national health service or nhs).ti,ab. (18,799)
-
or/38-41 (353,245)
-
(addresses or autobiography or bibliography or biography or dictionary or directory or editorial or government publications or interactive tutorial or interview or lectures or legal cases or legislation or letter or news or newspaper article or patient education handout or periodical index or portraits or video audio media or webcasts).pt. (1,381,680)
-
17 and 37 and 42 (20,031)
-
44 not 43 (18,756)
-
limit 45 to (english language and yr=“1990 - 2010”) (14,819)
Ovid MEDLINE
Date range searched: 1990–2013.
Date of search: June 2013.
Search strategy
-
family practice/ (58,510)
-
primary health care/ (46,024)
-
physicians, family/ (14,183)
-
physicians, primary care/ (336)
-
nursing staff/ (15,236)
-
community health aides/ (2652)
-
primary care nursing/ (21)
-
community health nursing/ (17,648)
-
((primary or community) adj1 (care or health*)).ti,ab. (80,838)
-
((general or family) adj1 (practice* or practitioner*)).ti,ab. (59,896)
-
(gp adj1 (service* or practice* or clinic or clinics)).ti,ab. (751)
-
((practice or communit*) adj2 nurs*).ti,ab. (21,784)
-
health visitor*.ti,ab. (2059)
-
family practice.jw. (13,511)
-
(primary adj1 (care or health*)).jw. (5642)
-
(general adj1 (practice or practitioner*)).jw. (10,182)
-
or/1-16 (236,313)
-
exp Great Britain/ (269,793)
-
(uk or united kingdom or britain or gb or gbr or british isles).ti,ab. (85,033)
-
(england or scotland or wales or ireland).ti,ab. (66,339)
-
(national health service or nhs).ti,ab. (18,799)
-
or/18-21 (353,245)
-
Preventive Medicine/ (10,288)
-
exp immunization programs/ (7578)
-
exp primary prevention/ (101,686)
-
((disease* or ill*) adj3 (reduc* or prevent*)).ti,ab. (52,929)
-
(prevent* adj2 (medicine or activi* or program*)).ti,ab. (25,787)
-
(immuni?at* or vaccin*).mp. (293,373)
-
((primary or secondary) adj1 prevent*).ti,ab. (19,558)
-
prevent*.jw. (37,674)
-
or/23-30 (426,949)
-
(health* adj3 improve*).ti,ab. (22,492)
-
(better health or positive health).mp. (3805)
-
32 or 33 (25,980)
-
exp Health Promotion/ (44,345)
-
health education/ or exp consumer health information/ or patient education as topic/ or sex education/ (118,647)
-
health educators/ (154)
-
((health* or intervention*) adj2 (promot* or educat* or program*)).ti,ab. (78,946)
-
or/35-38 (206,242)
-
(addresses or autobiography or bibliography or biography or dictionary or directory or editorial or government publications or interactive tutorial or interview or lectures or legal cases or legislation or letter or news or newspaper article or patient education handout or periodical index or portraits or video audio media or webcasts).pt. (1,381,680)
-
17 and 22 and 31 (1403)
-
17 and 22 and 34 (497)
-
17 and 22 and 39 (2539)
-
41 not 40 (1309)
-
42 not 40 (489)
-
43 not 40 (2376)
-
limit 44 to (english language and yr=“1990 - 2010”) (961)
-
limit 45 to (english language and yr=“1990 - 2010”) (424)
-
limit 46 to (english language and yr=“1990 - 2010”) (1937)
-
or 48 or 49 (2966)
Ovid EMBASE
Date range searched: 1990–2013.
Date of search: June 2013.
Search strategy
-
((primary or community) adj1 (care or health*)).ti,ab. (95,085)
-
((general or family) adj1 (practice* or practitioner*)).ti,ab. (71,206)
-
(gp adj1 (service* or practice* or clinic or clinics)).ti,ab. (1118)
-
((practice or communit*) adj2 nurs*).ti,ab. (22,387)
-
health visitor*.ti,ab. (2100)
-
exp primary health care/ (83,783)
-
general practice/ (60,846)
-
general practitioner/ (45,161)
-
family medicine/ (5750)
-
community health nursing/ (24,379)
-
health auxiliary/ (2090)
-
community care/ or community based rehabilitation/ (42,397)
-
family nurse practitioner/ (24)
-
family nursing/ (700)
-
family practice.jx. (16,273)
-
(primary adj1 (care or health*)).jx. (10,666)
-
(general adj1 (practice or practitioner*)).jx. (11,719)
-
or/1-17 (318,809)
-
(uk or united kingdom or britain or gb or gbr or british isles).ti,ab. (139,643)
-
(england or scotland or wales or ireland).ti,ab. (158,606)
-
(national health service or nhs).ti,ab. (23,656)
-
United Kingdom/ (269,248)
-
or/19-22 (478,485)
-
(health* adj3 improve*).ti,ab. (26,276)
-
(better health or positive health).mp. (4383)
-
24 or 25 (30,304)
-
((health* or intervention*) adj2 (promot* or educat* or program*)).ti,ab. (88,594)
-
exp health education/ (193,925)
-
exp health educator/ (626)
-
or/27-29 (245,887)
-
((disease* or ill*) adj3 (reduc* or prevent*)).ti,ab. (62,343)
-
(prevent* adj2 (medicine or activi* or program*)).ti,ab. (30,546)
-
(immuni?at* or vaccin*).mp. (339,927)
-
((primary or secondary) adj1 prevent*).ti,ab. (26,470)
-
prevent*.jw. (46,037)
-
preventive medicine/ (18,969)
-
preventive health service/ (17,788)
-
primary prevention/ (20,472)
-
or/31-38 (517,885)
-
(book or editorial or erratum or letter or note or patent or press or release).pt. (1,696,203)
-
18 and 23 and 26 (683)
-
18 and 23 and 30 (3377)
-
18 and 23 and 39 (2032)
-
41 not 40 (668)
-
42 not 40 (2978)
-
43 not 40 (1815)
-
limit 44 to (english language and yr=“1990 - 2010”) (596)
-
limit 45 to (english language and yr=“1990 - 2010”) (2537)
-
limit 46 to (english language and yr=“1990 - 2010”) (1384)
-
47 or 48 or 49 (4049)
Ovid Global Health
Date range searched: 1990–2013.
Date of search: June 2013.
Search strategy
-
(uk or united kingdom or britain or gb or gbr or british isles).ti,ab. (38,414)
-
(england or scotland or wales or ireland).ti,ab. (26,826)
-
(national health service or nhs).ti,ab. (2363)
-
british isles/ or exp uk/ (69,092)
-
or/1-4 (84,298)
-
(health* adj3 improve*).ti,ab. (7936)
-
(better health or positive health).mp. [mp=abstract, title, original title, broad terms, heading words] (1339)
-
6 or 7 (9153)
-
((health* or intervention*) adj2 (promot* or educat* or program*)).ti,ab. (28,920)
-
health promotion/ (9305)
-
health education/ (9826)
-
patient education/ (102)
-
sex education/ (390)
-
nutrition education.sh. (5191)
-
or/9-14 (42,134)
-
((disease* or ill*) adj3 (reduc* or prevent*)).ti,ab. (19,963)
-
(prevent* adj2 (medicine or activi* or program*)).ti,ab. (8225)
-
(immuni?at* or vaccin*).mp. [mp=abstract, title, original title, broad terms, heading words] (108,948)
-
((primary or secondary) adj1 prevent*).ti,ab. (3531)
-
prevent*.jw. (16,556)
-
preventive medicine/ (1504)
-
prevention/ or disease prevention/ (56,750)
-
immunization programmes/ (2314)
-
or/16-23 (187,194)
-
((primary or community) adj1 (care or health*)).ti,ab. (15,546)
-
((general or family) adj1 (practice* or practitioner*)).ti,ab. (8057)
-
(gp adj1 (service* or practice* or clinic or clinics)).ti,ab. (176)
-
((practice or communit*) adj2 nurs*).ti,ab. (659)
-
health visitor*.ti,ab. (1022)
-
family practice.jw. (650)
-
(primary adj1 (care or health*)).jw. (300)
-
(general adj1 (practice or practitioner*)).jw. (317)
-
general practitioners/ (3689)
-
primary health care/ (4167)
-
community health services/ or community health/ (3954)
-
or/25-35 (26,626)
-
(annual report or annual report section or book or book chapter or bulletin or bulletin article or correspondence or editorial or patent or standard).pt. (119,097)
-
5 and 8 and 36 (170)
-
5 and 15 and 36 (572)
-
5 and 24 and 36 (994)
-
38 not 37 (133)
-
39 not 37 (466)
-
40 not 37 (800)
-
limit 41 to (english language and yr=“1990 - 2010”) (81)
-
limit 42 to (english language and yr=“1990 - 2010”) (268)
-
limit 43 to (english language and yr=“1990 - 2010”) (424)
-
44 or 45 or 46 (677)
EBSCOhost Cumulative Index to Nursing and Allied Health Literature Plus
Date range searched: 1990–2013.
Date of search: June 2013.
URL: https://www.ebscohost.com/
Search strategy
S1 (MH “United Kingdom+”) (204,333)
S2 (TI uk) or (TI united kingdom) or (TI britain) or (TI gb) or (TI gbr) or (TI british isles) (10,823)
S3 (AB uk) or (AB united kingdom) or (AB britain) or (AB gb) or (AB gbr) or (AB british isles) (20,559)
S4 (TI england) or (TI scotland) or (TI wales) or (TI ireland) (8810)
S5 (AB england) or (AB scotland) or (AB wales) or (AB ireland) (13,884)
S6 (TI nhs) or (AB nhs) or (TI national health service) or (AB national health service) (16,215)
S7 S1 or S2 or S3 or S4 or S5 or S6 (222,806)
S8 health* N3 improve* (11,982)
S9 better health or positive health (2071)
S10 S8 or S9 (13,888)
S11 (MH “Preventive Health Care+”) (138,501)
S12 (disease* N3 reduc*) or (disease* N3 prevent*) or (ill* N3 reduc*) or (ill* N3 prevent*) (52,686)
S13 (prevent* N2 medicine) or (prevent* N2 activi*) or (prevent* N2 program*) (9007)
S14 immuni?at* or vaccin* (33,410)
S15 (primary N1 prevent*) or (secondary N1 prevent*) (5486)
S16 SO prevent* (11,849)
S17 S11 or S12 or S13 or S14 or S15 or S16 (217,356)
S18 (MH “Health Promotion+”) (28,038)
S19 (MH “Health Education+”) (75,766)
S20 (MH “Health Educators+”) (2258)
S21 (health* N2 promot*) or (health* N2 educat*) or (health* N2 program*) or (intervention* N2 promot*) or (intervention* N2 educat*) or (intervention* N2 program*) (120,081)
S22 S18 or S19 or S20 or S21 (173,310)
S23 (MH “Family Practice”) (13,315)
S24 (MH “Primary Health Care”) (27,954)
S25 (MH “Physicians, Family”) (8543)
S26 (MH “Community Health Nursing”) OR (MH “Family Nursing”) (22,009)
S27 (MH “Community Health Services+”) (23,1870)
S28 (MH “Community Health Workers”) (712)
S29 (primary N1 care) or (primary N1 health*) or (community N1 care) or (community N1 health*) (91,150)
S30 (general n1 practice*) or (general N1 practitioner*) or (family N1 practice*) or (family N1 practitioner*) (24,448)
S31 (gp N1 service*) or (gp N1 practice*) or (gp N1 clinic) or (gp N1 clinics) (568)
S32 (practice N2 nurs*) or (communit* N2 nurs*) (78,933)
S33 health visitor* (2867)
S34 SO “family practice” (3309)
S35 (SO primary N1 care) or (SO primary N1 health*) (15,809)
S36 (SO general N1 practice) or (SO general N1 practitioner*) (5684)
S37 S23 or S24 or S25 or S26 or S27 or S28 or S29 or S30 or S31 or S32 or S33 or S34 or S35 or S36 (353,441)
S38 Limiters - Publication Type: Accration, Advice and Referral Website, Algorithm, Anecdote, Audiovisual, Biography, Book, Book Chapter, Book Review, Care Plan, Cartoon, Chat Groups, Classification Term, Commentary, Commercial Website, Computer Program, Consumer/Patient Teaching Materials, Critical Path, Diagnostic Images, Directories, orial, Equations & Formulas, Exam Questions, Forms, Games, Glossary, Individual Testimonial Website, Information Website, Interview, Legal Cases, Letter, Listservs, Nurse Practice Acts, Obituary, Pamphlet, Pamphlet Chapter, Pictorial, Poetry, Questionnaire/Scale, Questions and Answers, Quick Lesson, Software, Standards, Teaching Materials, Tracings, Website (1,063,759)
S39 S7 and S17 and S37 (11,000)
S40 S7 and S10 and S37 (651)
S41 S7 and S22 and S37 (12,935)
S42 S39 not S38 (7988)
S43 S40 not S38 (551)
S44 S41 not S38 (9200)
S45 S42 Limiters - Published Date from: 19900101-20101231; Language: English (7169)
S46 S43 Limiters - Published Date from: 19900101-20101231; Language: English (515)
S47 S44 Limiters - Published Date from: 19900101-20101231; Language: English (8278)
S48 S45 or S46 or S47 (12,037)
Appendix 2 Search results by database
Notes on derivation of search strategies
-
Alcohol and drug addiction strategy derived from the Cochrane Drugs & Alcohol Review Group strategy. 487
-
Brief intervention strategy derived from NICE Guideline PH1: Brief Interventions and Referral for Smoking Cessation. 488
-
Exercise therapy strategy derived from NICE Guideline PH17: Promoting Physical Activity for Children and Young People. 489
-
Immunisation strategy derived from NICE Guidance PH21: Reducing Differences in the Uptake of Immunizations. 490
-
Tobacco cessation strategy derived from NICE Guideline PH1: Brief Interventions and Referral for Smoking Cessation. 488
Ovid MEDLINE
Date range searched: 1990–2013.
Date of search: June 2013.
Search strategy
-
family practice/ (58,098)
-
primary health care/ (45,828)
-
physicians, family/ (14,165)
-
physicians, primary care/ (314)
-
nursing staff/ (15,203)
-
community health aides/ (2645)
-
primary care nursing/ (19)
-
community health nursing/ (17,628)
-
((primary or community) adj1 (care or health*)).ti,ab. (80,350)
-
((general or family) adj1 (practice* or practitioner*)).ti,ab. (59,496)
-
(gp adj1 (service* or practice* or clinic or clinics)).ti,ab. (750)
-
((practice or communit*) adj2 nurs*).ti,ab. (21,712)
-
health visitor*.ti,ab. (2046)
-
family practice.jw. (13,507)
-
(primary adj1 (care or health*)).jw. (5628)
-
(general adj1 (practice or practitioner*)).jw. (10,075)
-
or/1-16 (235,033)
-
exp Great Britain/ (266,950)
-
(uk or united kingdom or britain or gb or gbr or british isles).ti,ab. (84,527)
-
(england or scotland or wales or ireland).ti,ab. (65,572)
-
(national health service or nhs).ti,ab. (18,692)
-
or/18-21 (349,558)
-
chewing tobacco.mp. (363)
-
(pipe adj2 smok*).mp. (293)
-
(cigar* or bidi* or kretek or paan or gutka or snuff or snus or betel).mp. (57,271)
-
“Tobacco Use Disorder”/ (6764)
-
exp Tobacco/ (22,296)
-
Smoking/pc, th [Prevention & Control, Therapy] (14,103)
-
(quit* or stop* or giv* or ceas* or cessation or withdrawal).mp. (956,662)
-
or/23-28 (89,104)
-
30 and 29 (18,258)
-
smoking cessation.mp. (20,679)
-
exp “Tobacco Use Cessation”/ (17,199)
-
or/31-33 (28,451)
-
exp Substance-Related Disorders/ (329,817)
-
exp Drinking Behavior/ (50,178)
-
Psychoses, Substance-Induced/ (4149)
-
(overdos* or over-dos*).ti,ab. (12,763)
-
((drug* or substance or alcohol*) adj3 (addict* or dependen* or abuse* or misuse or withdraw* or intoxicat* or abstinen* or abstain*)).ti,ab. (83,050)
-
(alcohol* adj3 (consumption or drink*)).ti,ab. (31,550)
-
exp Amphetamines/ (30,917)
-
exp Anabolic Agents/ (11,388)
-
exp Anti-anxiety agents/ (54,092)
-
exp Antidepressive agents/ (111,358)
-
exp Barbiturates/ (48,896)
-
exp Benzodiazepines/ (55,262)
-
Cannabis/ (6240)
-
exp Cocaine/ (21,060)
-
Designer drugs/ (580)
-
exp Hallucinogens/ (20,116)
-
Heroin/ (4563)
-
Ketamine/ (8290)
-
exp Lysergic acid/ (4390)
-
exp Methadone/ (9513)
-
Opium/ (1712)
-
exp Street drugs/ (7689)
-
(alcohol or amphetamine* or angel dust or barbiturate* or cannabis or cocaine).ti,ab. (193,203)
-
(designer drug* or dexedrine or diet pill* or dissociative drug* or doping or dxm).ti,ab. (4177)
-
(ephedra or ephedrine or ecstasy or hallucinogen* or hash oil* or hashish or heroin).ti,ab. (16,983)
-
(illicit drug* or inhalant* or ketamine or lsd or lysergic-acid* or mescaline or Marihuana or marijuana).ti,ab. (29,587)
-
(mda or mdma or methadone or methcathinone or methamphetamine* or Narcotics).ti,ab. (41,670)
-
(opioid* or opiate* or opium or oxycontin or oxycodone or percocet or phencyclidine).ti,ab. (67,355)
-
(poppers or pseudophedrine or psychotomimetic* or roofies or salvia divinorum or solvent*).ti,ab. (72,729)
-
(stimulant* or steroid abuse or street-drug* or tranquili?er* or valium or vicodin).ti,ab. (20,813)
-
or/35-64 (885,117)
-
Motor Activity/ (65,534)
-
exp Exercise/ (57,752)
-
exp Exercise Therapy/ (24,179)
-
((physical$ or motor$) adj2 (activit$ or exerc$ or fitness)).ti,ab. (65,520)
-
exercis$.ti,ab. (163,000)
-
(physical$ adj5 (fit$4 or activ$3 or endur$4)).ti,ab. (47,664)
-
(exercis$3 adj5 (fit$4 or activ$3 or endur$4)).ti,ab. (11,338)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$) adj5 physical$ activit$).ti,ab. (7391)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$) adj5 exercis$).ti,ab. (25,260)
-
((self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$ or body image$) adj5 (physical activit$ or exercise$ or sport$)).ti,ab. (3633)
-
((decreas$ or reduc$ or discourag$) adj5 sedentary).ti,ab. (535)
-
(pedomet* or step counter* or walk*).ti,ab. (53,593)
-
(bicycl* or bike* or cycling or riding or rides).ti,ab. (44,518)
-
((active or activity) adj5 (transport$1 or transportation or journey$)).ti,ab. (18,426)
-
((active or activity) adj5 travel$).ti,ab. (357)
-
(travel$ adj5 (bike$ or walk$ or biking or cycle or cycling or bicycl$ or mode$1 or route$ or pattern$1 or plan$1 or planning or rollerblad$ or skateboard$ or scooter$ or rollerskat$)).ti,ab. (1097)
-
((transport$1 or transportation) adj5 (bike$ or walk$ or biking or cycle or cycling or bicycl$ or mode$1 or route$ or pattern$1 or plan$1 or planning or rollerblad$ or skateboard$ or scooter$ or rollerskat$)).ti,ab. (9416)
-
(journey$ adj5 (bike$ or walk$ or biking or cycle or cycling or bicycl$ or mode$1 or rollerblad$ or skateboard$ or scooter$ or rollerskat$ or route$ or pattern$1 or plan$1 or planning)).ti,ab. (97)
-
(commut$ adj5 (bike$ or walk$ or biking or cycle or cycling or bicycl$ or mode$1 or route$ or pattern$1 or plan$1 or planning rollerblad$ or skateboard$ or scooter$ or rollerskat$)).ti,ab. (177)
-
(school$ adj5 (bike$ or walk$ or biking or cycle or cycling or bicycl$ or route$ or rollerblad$ or skateboard$ or scooter$ or rollerskat$)).ti,ab. (439)
-
((biking or cycle or cycling or bicycl$ or walk or walking or walks) adj1 route$).ti,ab. (55)
-
((travel$ or transport or transports or transportation or commut$ or journey$) and physical$ activ$).ti,ab. (944)
-
health club$1.ti,ab. (137)
-
(leisure adj5 (centre$1 or center$1 or facilit$)).ti,ab. (125)
-
(fitness adj5 (centre$1 or center$1 or facilit$)).ti,ab. (353)
-
parks.ti,ab. (1697)
-
(fitness club$1 or wellness centre$ or wellness center$).ti,ab. (164)
-
gym$1.ti,ab. (446)
-
(pitch or pitches).ti,ab. (8061)
-
swimming pool$.ti,ab. (1441)
-
gymnasia$1.ti,ab. (24)
-
health spa$1.ti,ab. (122)
-
Public Facilities/ (623)
-
swimming pools/ (1366)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (swim$ or walk$ or running or biking or bicycl$ or bike$ or cycling)).ti,ab. (13,630)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (dance$1 or dancing or aerobics)).ti,ab. (133)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain) adj5 (sport$ or horse riding)).ti,ab. (1348)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (football or rugby or netball or cricket or hockey or rounders or athletic*)).ti,ab. (870)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (rollerblading or rollerskating or skating or skateboard$)).ti,ab. (86)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (jump$1 or jumping)).ti,ab. (1040)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (play$1 or playing or playfulness)).ti,ab. (17,244)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (games or tennis or badminton or racquet sport$)).ti,ab. (440)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (pilates or spinning or step$ class$)).ti,ab. (62)
-
physical education.ti,ab. (2248)
-
exp “Physical Education and Training”/ (12,385)
-
Dancing/ (1512)
-
exp Sports/ (93,804)
-
Recreation/ (4287)
-
“Play and Playthings”/ (6098)
-
or/66-114 (482,920)
-
exp Immunization/ (122,517)
-
exp Immunization Programs/ (7563)
-
(immuni$ not innate immunity).ti,ab. (178,208)
-
(vaccin$ not vaccinia).ti,ab. (166,796)
-
((dtp or dtap or dpt) adj3 (vaccin$ or immuni$ or jab)).ti,ab. (1324)
-
((diphtheria or tetanus or whooping cough or pertussis or polio* or hib) adj3 (vaccin$ or immuni$ or jab)).ti,ab. (13,535)
-
exp Vaccines/ (152,174)
-
(mmr vaccin$ or pluserix or priorix or trimovax or triviraten berna or virivac).ti,ab. (868)
-
(hpv vaccin$ or papillomavirus).ti,ab. (19,380)
-
(anti-HBsAg or Engerix-B or Recombivax HB).ti,ab. (633)
-
((bcg or (bacillus and calmette and guerin)) and vaccine).ti,ab. (3382)
-
or/116-126 (382,000)
-
exp Mass Screening/ (88,587)
-
(screening or screen).ti,ab. (300,285)
-
128 or 129 (333,153)
-
(brief adj3 intervention*).ti,ab. (2621)
-
counsel?ing.ti,ab. (47,595)
-
((minimal or minimum or low) adj5 (intervention* or intensity)).ti,ab. (17,234)
-
low-intensity.ti,ab. (7642)
-
advice.ti,ab. (25,098)
-
motivational.ti,ab. (9197)
-
opportunistic.ti,ab. (19,937)
-
(self-help or self help).ti,ab. (3824)
-
or/131-138 (120,933)
-
risk reduction behavior/ (5013)
-
Harm Reduction/ (1149)
-
((risk* or harm*) adj3 reduc*).ti,ab. (67,235)
-
(safe* adj2 behavi*).ti,ab. (1245)
-
or/140-143 (72,079)
-
exp LIFESTYLE/ (54,934)
-
lifestyle$.ti,ab. (36,629)
-
(inactivit$ or sedentary).ti,ab. (19,205)
-
exp Health Behavior/ (80,447)
-
health behavior.ti,ab. (3105)
-
health behaviour.ti,ab. (1390)
-
exp OBESITY/ (114,045)
-
Weight Gain/ (19,061)
-
Weight Loss/ (19,276)
-
(weight adj3 (gain or loss or change*)).ti,ab. (84,730)
-
(overweight or over weight or overeat$ or over eat$).ti,ab. (26,771)
-
((bmi or body mass index) adj2 (gain or loss or change)).ti,ab. (1591)
-
obes*.ti,ab. (126,829)
-
food habit$.ti,ab. (1246)
-
poor diet.ti,ab. (680)
-
healthy eating.ti,ab. (1649)
-
(fruit or vegetable$).ti,ab. (41,190)
-
exp *Leisure Activities/ (78,376)
-
(leisure or relax* or holiday* or vacation* or recreation* or hobbies or hobby or play*).ti,ab. (713,512)
-
or/145-163 (1,176,435)
-
(addresses or autobiography or bibliography or biography or dictionary or directory or orial or government publications or interactive tutorial or interview or lectures or legal cases or legislation or letter or news or newspaper article or patient education handout or periodical index or portraits or video audio media or webcasts).pt. (1,376,979)
-
17 and 22 and 34 (294)
-
166 not 165 (282)
-
limit 167 to (english language and yr=“1990 - 2010”) (246)
-
17 and 22 and 65 (1331)
-
169 not 165 (1249)
-
limit 170 to (english language and yr=“1990 - 2010”) (977)
-
17 and 22 and 115 (960)
-
172 not 165 (920)
-
limit 173 to (english language and yr=“1990 - 2010”) (804)
-
17 and 22 and 127 (684)
-
175 not 165 (627)
-
limit 176 to (english language and yr=“1990 - 2010”) (481)
-
17 and 22 and 130 (1791)
-
178 not 165 (1698)
-
limit 179 to (english language and yr=“1990 - 2010”) (1360)
-
17 and 22 and 139 (1790)
-
181 not 165 (1752)
-
limit 182 to (english language and yr=“1990 - 2010”) (1465)
-
17 and 22 and 144 (377)
-
184 not 165 (373)
-
limit 185 to (english language and yr=“1990 - 2010”) (349)
-
17 and 22 and 164 (2248)
-
187 not 165 (2174)
-
limit 188 to (english language and yr=“1990 - 2010”) (1870)
-
168 or 171 or 174 or 177 or 180 or 183 or 186 or 189 (5685)
Ovid EMBASE
Date range searched: 1990–2013.
Date of search: June 2013.
Search strategy
-
((primary or community) adj1 (care or health*)).ti,ab. (95,085)
-
((general or family) adj1 (practice* or practitioner*)).ti,ab. (71,206)
-
(gp adj1 (service* or practice* or clinic or clinics)).ti,ab. (1118)
-
((practice or communit*) adj2 nurs*).ti,ab. (22,387)
-
health visitor*.ti,ab. (2100)
-
exp primary health care/ (83,783)
-
general practice/ (60,846)
-
general practitioner/ (45,161)
-
family medicine/ (5750)
-
community health nursing/ (24,379)
-
health auxiliary/ (2090)
-
community care/ or community based rehabilitation/ (42,397)
-
family nurse practitioner/ (24)
-
family nursing/ (700)
-
family practice.jx. (16,273)
-
(primary adj1 (care or health*)).jx. (10,666)
-
(general adj1 (practice or practitioner*)).jx. (11,719)
-
or/1-17 (318,809)
-
(uk or united kingdom or britain or gb or gbr or british isles).ti,ab. (139,643)
-
(england or scotland or wales or ireland).ti,ab. (158,606)
-
(national health service or nhs).ti,ab. (23,656)
-
United Kingdom/ (269,248)
-
or/19-22 (478,485)
-
chewing tobacco.mp. (400)
-
(pipe adj2 smok*).mp. (300)
-
(cigar* or bidi* or kretek or paan or gutka or snuff or snus or betel).mp. (88,249)
-
tobacco/ (24,691)
-
tobacco dependence/ (9540)
-
exp smoking/pc, th [Prevention, Therapy] (6854)
-
(quit* or stop* or giv* or ceas* or cessation or withdrawal).mp. (1,216,507)
-
or/24-29 (119,253)
-
30 and 31 (24,461)
-
smoking cessation.mp. (31,866)
-
smoking cessation/ or smoking cessation program/ (29,449)
-
or/32-34 (41,216)
-
exp addiction/ (177,736)
-
drinking behavior/ (28,095)
-
alcohol consumption/ (54,246)
-
exp alcohol psychosis/ (3228)
-
(overdos* or over-dos*).ti,ab. (15,592)
-
((drug* or substance or alcohol*) adj3 (addict* or dependen* or abuse* or misuse or withdraw* or intoxicat* or abstinen* or abstain*)).ti,ab. (101,199)
-
(alcohol* adj3 (consumption or drink*)).ti,ab. (37,049)
-
exp amphetamine derivative/ (61,945)
-
exp anabolic agent/ (18,404)
-
exp tranquilizer/ (286,637)
-
exp barbituric acid derivative/ (103,845)
-
exp benzodiazepine derivative/ (125,089)
-
cannabis/ (17,546)
-
cocaine derivative/ (518)
-
designer drug/ (526)
-
exp psychedelic agent/ (44,878)
-
exp diamorphine/ (14,964)
-
exp ketamine/ (20,344)
-
exp “drugs used in the treatment of addiction”/ (88,196)
-
exp opiate/ (39,704)
-
street drug/ (2206)
-
drug withdrawal/ (82,494)
-
(alcohol or amphetamine* or angel dust or barbiturate* or cannabis or cocaine).ti,ab. (230,448)
-
(designer drug* or dexedrine or diet pill* or dissociative drug* or doping or dxm).ti,ab. (6166)
-
(ephedra or ephedrine or ecstasy or hallucinogen* or hash oil* or hashish or heroin).ti,ab. (20,234)
-
(illicit drug* or inhalant* or ketamine or lsd or lysergic-acid* or mescaline or Marihuana or marijuana).ti,ab. (33,676)
-
(mda or mdma or methadone or methcathinone or methamphetamine* or Narcotics).ti,ab. (50,802)
-
(opioid* or opiate* or opium or oxycontin or oxycodone or percocet or phencyclidine).ti,ab. (82,022)
-
(poppers or pseudophedrine or psychotomimetic* or roofies or salvia divinorum or solvent*).ti,ab. (104,755)
-
(stimulant* or steroid abuse or street-drug* or tranquili?er* or valium or vicodin).ti,ab. (22,681)
-
or/36-65 (1,140,515)
-
((physical$ or motor$) adj2 (activit$ or exerc$ or fitness)).ti,ab. (78,385)
-
exercis$.ti,ab. (193,435)
-
(physical$ adj5 (fit$4 or activ$3 or endur$4)).ti,ab. (57,906)
-
(exercis$3 adj5 (fit$4 or activ$3 or endur$4)).ti,ab. (13,420)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$) adj5 physical$ activit$).ti,ab. (9009)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$) adj5 exercis$).ti,ab. (29,110)
-
((self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$ or body image$) adj5 (physical activit$ or exercise$ or sport$)).ti,ab. (4451)
-
((decreas$ or reduc$ or discourag$) adj5 sedentary).ti,ab. (640)
-
(pedomet* or step counter* or walk*).ti,ab. (63,806)
-
(bicycl* or bike* or cycling or riding or rides).ti,ab. (54,186)
-
((active or activity) adj5 (transport$1 or transportation or journey$)).ti,ab. (18,314)
-
((active or activity) adj5 travel$).ti,ab. (446)
-
(travel$ adj5 (bike$ or walk$ or biking or cycle or cycling or bicycl$ or mode$1 or route$ or pattern$1 or plan$1 or planning or rollerblad$ or skateboard$ or scooter$ or rollerskat$)).ti,ab. (1323)
-
((transport$1 or transportation) adj5 (bike$ or walk$ or biking or cycle or cycling or bicycl$ or mode$1 or route$ or pattern$1 or plan$1 or planning or rollerblad$ or skateboard$ or scooter$ or rollerskat$)).ti,ab. (11,825)
-
(journey$ adj5 (bike$ or walk$ or biking or cycle or cycling or bicycl$ or mode$1 or rollerblad$ or skateboard$ or scooter$ or rollerskat$ or route$ or pattern$1 or plan$1 or planning)).ti,ab. (136)
-
(commut$ adj5 (bike$ or walk$ or biking or cycle or cycling or bicycl$ or mode$1 or route$ or pattern$1 or plan$1 or planning rollerblad$ or skateboard$ or scooter$ or rollerskat$)).ti,ab. (222)
-
(school$ adj5 (bike$ or walk$ or biking or cycle or cycling or bicycl$ or route$ or rollerblad$ or skateboard$ or scooter$ or rollerskat$)).ti,ab. (505)
-
((biking or cycle or cycling or bicycl$ or walk or walking or walks) adj1 route$).ti,ab. (68)
-
((travel$ or transport or transports or transportation or commut$ or journey$) and physical$ activ$).ti,ab. (1155)
-
health club$1.ti,ab. (160)
-
(leisure adj5 (centre$1 or center$1 or facilit$)).ti,ab. (166)
-
(fitness adj5 (centre$1 or center$1 or facilit$)).ti,ab. (451)
-
parks.ti,ab. (2114)
-
(fitness club$1 or wellness centre$ or wellness center$).ti,ab. (199)
-
gym$1.ti,ab. (1022)
-
(pitch or pitches).ti,ab. (8940)
-
swimming pool$.ti,ab. (1738)
-
gymnasia$1.ti,ab. (27)
-
health spa$1.ti,ab. (142)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (swim$ or walk$ or running or biking or bicycl$ or bike$ or cycling)).ti,ab. (15,826)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (dance$1 or dancing or aerobics)).ti,ab. (180)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain) adj5 (sport$ or horse riding)).ti,ab. (1786)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (football or rugby or netball or cricket or hockey or rounders or athletic*)).ti,ab. (1038)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (rollerblading or rollerskating or skating or skateboard$)).ti,ab. (92)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (jump$1 or jumping)).ti,ab. (1141)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (play$1 or playing or playfulness)).ti,ab. (20,196)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (games or tennis or badminton or racquet sport$)).ti,ab. (546)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (pilates or spinning or step$ class$)).ti,ab. (87)
-
physical education.ti,ab. (3059)
-
motor activity/ (30,313)
-
exp exercise/ (158,508)
-
exp kinesiotherapy/ (36,748)
-
exp “sports and sport related phenomena”/ or exp disabled sport/ or exp sport/ or swimming pool/ or team sport/ (100,427)
-
physical education/ (8467)
-
recreation/ or dancing/ (12,940)
-
or/67-111 (576,376)
-
(immuni$ not innate immunity).ti,ab. (187,792)
-
(vaccin$ not vaccinia).ti,ab. (188,791)
-
((dtp or dtap or dpt) adj3 (vaccin$ or immuni$ or jab)).ti,ab. (1459)
-
((diphtheria or tetanus or whooping cough or pertussis or polio* or hib) adj3 (vaccin$ or immuni$ or jab)).ti,ab. (14,397)
-
(mmr vaccin$ or pluserix or priorix or trimovax or triviraten berna or virivac).ti,ab. (1030)
-
(hpv vaccin$ or papillomavirus).ti,ab. (21,971)
-
(anti-HBsAg or Engerix-B or Recombivax HB).ti,ab. (729)
-
((bcg or (bacillus and calmette and guerin)) and vaccine).ti,ab. (3711)
-
exp immunization/ (172,171)
-
or/113-121 (387,007)
-
(screening or screen).ti,ab. (361,889)
-
exp screening/ (332,187)
-
123 or 124 (532,113)
-
(brief adj3 intervention*).ti,ab. (3223)
-
counsel?ing.ti,ab. (57,403)
-
((minimal or minimum or low) adj5 (intervention* or intensity)).ti,ab. (20,166)
-
low-intensity.ti,ab. (8623)
-
advice.ti,ab. (32,036)
-
motivational.ti,ab. (10,591)
-
opportunistic.ti,ab. (23,202)
-
(self-help or self help).ti,ab. (4809)
-
or/126-133 (145,961)
-
((risk* or harm*) adj3 reduc*).ti,ab. (84,019)
-
(safe* adj2 behavi*).ti,ab. (1427)
-
risk reduction/ (41,705)
-
harm reduction/ (1682)
-
or/135-138 (112,901)
-
lifestyle/ or lifestyle modification/ or sedentary lifestyle/ (66,362)
-
lifestyle$.ti,ab. (46,011)
-
(inactivit$ or sedentary).ti,ab. (22,406)
-
exp health behavior/ (196,458)
-
health behavior.ti,ab. (3311)
-
health behaviour.ti,ab. (1708)
-
exp obesity/ (196,733)
-
body weight/ or weight change/ or weight control/ or weight fluctuation/ or weight gain/ or weight reduction/ (239,199)
-
(weight adj3 (gain or loss or change*)).ti,ab. (101,205)
-
(overweight or over weight or overeat$ or over eat$).ti,ab. (34,036)
-
((bmi or body mass index) adj2 (gain or loss or change)).ti,ab. (2041)
-
obes*.ti,ab. (156,975)
-
food habit$.ti,ab. (1520)
-
poor diet.ti,ab. (760)
-
healthy eating.ti,ab. (2052)
-
(fruit or vegetable$).ti,ab. (51,341)
-
exp recreation/ (30,428)
-
(leisure or relax* or holiday* or vacation* or recreation* or hobbies or hobby or play*).ti,ab. (826,805)
-
or/140-157 (1,546,296)
-
(book or orial or erratum or letter or note or patent or press or release).pt. (1,696,203)
-
18 and 23 and 35 (506)
-
18 and 23 and 66 (2139)
-
18 and 23 and 112 (1303)
-
18 and 23 and 122 (779)
-
18 and 23 and 125 (2188)
-
18 and 23 and 134 (2113)
-
18 and 23 and 139 (657)
-
18 and 23 and 158 (4179)
-
160 not 159 (428)
-
161 not 159 (1915)
-
162 not 159 (1213)
-
163 not 159 (693)
-
164 not 159 (2004)
-
165 not 159 (2067)
-
166 not 159 (594)
-
167 not 159 (3832)
-
limit 168 to (english language and yr=“1990 - 2010”) (384)
-
limit 169 to (english language and yr=“1990 - 2010”) (1621)
-
limit 170 to (english language and yr=“1990 - 2010”) (1070)
-
limit 171 to (english language and yr=“1990 - 2010”) (557)
-
limit 172 to (english language and yr=“1990 - 2010”) (1705)
-
limit 173 to (english language and yr=“1990 - 2010”) (1847)
-
limit 174 to (english language and yr=“1990 - 2010”) (551)
-
limit 175 to (english language and yr=“1990 - 2010”) (3388)
-
176 or 177 or 178 or 179 or 180 or 181 or 182 or 183 (7948)
Global Health
Date range searched: 1990–2013.
Date of search: June 2013.
Search strategy
-
(uk or united kingdom or britain or gb or gbr or british isles).ti,ab. (38,414)
-
(england or scotland or wales or ireland).ti,ab. (26,826)
-
(national health service or nhs).ti,ab. (2363)
-
british isles/ or exp uk/ (69,092)
-
or/1-4 (84,298)
-
((primary or community) adj1 (care or health*)).ti,ab. (15,546)
-
((general or family) adj1 (practice* or practitioner*)).ti,ab. (8057)
-
(gp adj1 (service* or practice* or clinic or clinics)).ti,ab. (176)
-
((practice or communit*) adj2 nurs*).ti,ab. (659)
-
health visitor*.ti,ab. (1022)
-
family practice.jw. (650)
-
(primary adj1 (care or health*)).jw. (300)
-
(general adj1 (practice or practitioner*)).jw. (317)
-
general practitioners/ (3689)
-
primary health care/ (4167)
-
community health services/ or community health/ (3954)
-
or/6-16 (26,626)
-
chewing tobacco.mp. [mp=abstract, title, original title, broad terms, heading words] (178)
-
(pipe adj2 smok*).mp. [mp=abstract, title, original title, broad terms, heading words] (192)
-
(cigar* or bidi* or kretek or paan or gutka or snuff or snus or betel).mp. [mp=abstract, title, original title, broad terms, heading words] (13,783)
-
exp tobacco/ (8665)
-
tobacco smoking/ (22,143)
-
tobacco chewing/ (120)
-
(quit* or stop* or giv* or ceas* or cessation or withdrawal).mp. [mp=abstract, title, original title, broad terms, heading words] (402,110)
-
or/18-23 (28,053)
-
25 and 24 (6651)
-
smoking cessation.mp. [mp=abstract, title, original title, broad terms, heading words] (2874)
-
smoking cessation/ (572)
-
or/26-28 (6912)
-
exp substance abuse/ (9778)
-
exp addiction/ (2489)
-
alcoholism/ (6484)
-
exp poisoning/ (33,406)
-
drinking/ (2069)
-
(overdos* or over-dos*).ti,ab. (1644)
-
((drug* or substance or alcohol*) adj3 (addict* or dependen* or abuse* or misuse or withdraw* or intoxicat* or abstinen* or abstain*)).ti,ab. (10,689)
-
(alcohol* adj3 (consumption or drink*)).ti,ab. (10,559)
-
exp amphetamines/ (899)
-
exp anabolics/ (610)
-
exp neuroleptics/ (795)
-
exp antidepressants/ (1002)
-
exp barbiturates/ (811)
-
exp benzodiazepines/ (628)
-
exp cannabis/ (1568)
-
exp controlled substances/ (3772)
-
exp psychotropic drugs/ (2334)
-
ketamine/ (207)
-
methadone/ (431)
-
exp drug users/ (7774)
-
(alcohol or amphetamine* or angel dust or barbiturate* or cannabis or cocaine).ti,ab. (42,588)
-
(designer drug* or dexedrine or diet pill* or dissociative drug* or doping or dxm).ti,ab. (478)
-
(ephedra or ephedrine or ecstasy or hallucinogen* or hash oil* or hashish or heroin).ti,ab. (2948)
-
(illicit drug* or inhalant* or ketamine or lsd or lysergic-acid* or mescaline or Marihuana or marijuana).ti,ab. (3914)
-
(mda or mdma or methadone or methcathinone or methamphetamine* or Narcotics).ti,ab. (6930)
-
(opioid* or opiate* or opium or oxycontin or oxycodone or percocet or phencyclidine).ti,ab. (3310)
-
(poppers or pseudophedrine or psychotomimetic* or roofies or salvia divinorum or solvent*).ti,ab. (14,461)
-
(stimulant* or steroid abuse or street-drug* or tranquili?er* or valium or vicodin).ti,ab. (2886)
-
or/30-57 (121,553)
-
((physical$ or motor$) adj2 (activit$ or exerc$ or fitness)).ti,ab. (20,784)
-
exercis$.ti,ab. (24,780)
-
(physical$ adj5 (fit$4 or activ$3 or endur$4)).ti,ab. (18,908)
-
(exercis$3 adj5 (fit$4 or activ$3 or endur$4)).ti,ab. (2147)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$) adj5 physical$ activit$).ti,ab. (3481)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$) adj5 exercis$).ti,ab. (3743)
-
((self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$ or body image$) adj5 (physical activit$ or exercise$ or sport$)).ti,ab. (919)
-
((decreas$ or reduc$ or discourag$) adj5 sedentary).ti,ab. (236)
-
(pedomet* or step counter* or walk*).ti,ab. (8744)
-
(bicycl* or bike* or cycling or riding or rides).ti,ab. (4893)
-
((active or activity) adj5 (transport$1 or transportation or journey$)).ti,ab. (1711)
-
((active or activity) adj5 travel$).ti,ab. (136)
-
(travel$ adj5 (bike$ or walk$ or biking or cycle or cycling or bicycl$ or mode$1 or route$ or pattern$1 or plan$1 or planning or rollerblad$ or skateboard$ or scooter$ or rollerskat$)).ti,ab. (404)
-
((transport$1 or transportation) adj5 (bike$ or walk$ or biking or cycle or cycling or bicycl$ or mode$1 or route$ or pattern$1 or plan$1 or planning or rollerblad$ or skateboard$ or scooter$ or rollerskat$)).ti,ab. (1100)
-
(journey$ adj5 (bike$ or walk$ or biking or cycle or cycling or bicycl$ or mode$1 or rollerblad$ or skateboard$ or scooter$ or rollerskat$ or route$ or pattern$1 or plan$1 or planning)).ti,ab. (40)
-
(commut$ adj5 (bike$ or walk$ or biking or cycle or cycling or bicycl$ or mode$1 or route$ or pattern$1 or plan$1 or planning rollerblad$ or skateboard$ or scooter$ or rollerskat$)).ti,ab. (95)
-
(school$ adj5 (bike$ or walk$ or biking or cycle or cycling or bicycl$ or route$ or rollerblad$ or skateboard$ or scooter$ or rollerskat$)).ti,ab. (231)
-
((biking or cycle or cycling or bicycl$ or walk or walking or walks) adj1 route$).ti,ab. (28)
-
((travel$ or transport or transports or transportation or commut$ or journey$) and physical$ activ$).ti,ab. (552)
-
health club$1.ti,ab. (97)
-
(leisure adj5 (centre$1 or center$1 or facilit$)).ti,ab. (151)
-
(fitness adj5 (centre$1 or center$1 or facilit$)).ti,ab. (149)
-
parks.ti,ab. (1149)
-
(fitness club$1 or wellness centre$ or wellness center$).ti,ab. (60)
-
gym$1.ti,ab. (187)
-
(pitch or pitches).ti,ab. (328)
-
swimming pool$.ti,ab. (967)
-
gymnasia$1.ti,ab. (26)
-
health spa$1.ti,ab. (52)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (swim$ or walk$ or running or biking or bicycl$ or bike$ or cycling)).ti,ab. (1656)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (dance$1 or dancing or aerobics)).ti,ab. (56)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain) adj5 (sport$ or horse riding)).ti,ab. (491)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (football or rugby or netball or cricket or hockey or rounders or athletic*)).ti,ab. (193)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (rollerblading or rollerskating or skating or skateboard$)).ti,ab. (9)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (jump$1 or jumping)).ti,ab. (84)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (play$1 or playing or playfulness)).ti,ab. (2019)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (games or tennis or badminton or racquet sport$)).ti,ab. (114)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$ or maintain$ or sustain$ or self esteem or confidence or self efficacy or abilit$ or enjoy$ or learn$) adj5 (pilates or spinning or step$ class$)).ti,ab. (15)
-
physical education.ti,ab. (3394)
-
exercise/ (13,708)
-
physical fitness/ (2425)
-
physical activity/ (14,165)
-
exp sport/ (5463)
-
fitness/ (392)
-
health clubs/ (138)
-
exp sports facilities/ (1096)
-
recreational facilities/ or leisure centres/ or outdoor activity centres/ (257)
-
exp recreational activities/ (2270)
-
physical education/ (3541)
-
or/59-107 (67,655)
-
(immuni$ not innate immunity).ti,ab. (71,325)
-
(vaccin$ not vaccinia).ti,ab. (82,196)
-
((dtp or dtap or dpt) adj3 (vaccin$ or immuni$ or jab)).ti,ab. (800)
-
((diphtheria or tetanus or whooping cough or pertussis or polio* or hib) adj3 (vaccin$ or immuni$ or jab)).ti,ab. (9203)
-
(mmr vaccin$ or pluserix or priorix or trimovax or triviraten berna or virivac).ti,ab. (518)
-
(hpv vaccin$ or papillomavirus).ti,ab. (6637)
-
(anti-HBsAg or Engerix-B or Recombivax HB).ti,ab. (267)
-
((bcg or (bacillus and calmette and guerin)) and vaccine).ti,ab. (2435)
-
exp immunization/ (63,425)
-
immunization programmes/ (2314)
-
exp vaccines/ (50,476)
-
or/109-119 (138,219)
-
(screening or screen).ti,ab. (58,657)
-
exp screening/ (25,754)
-
121 or 122 (62,816)
-
(brief adj3 intervention*).ti,ab. (483)
-
counsel?ing.ti,ab. (8630)
-
((minimal or minimum or low) adj5 (intervention* or intensity)).ti,ab. (2534)
-
low-intensity.ti,ab. (785)
-
advice.ti,ab. (9435)
-
motivational.ti,ab. (1189)
-
opportunistic.ti,ab. (8348)
-
(self-help or self help).ti,ab. (621)
-
or/124-131 (29,985)
-
((risk* or harm*) adj3 reduc*).ti,ab. (19,623)
-
(safe* adj2 behavi*).ti,ab. (505)
-
risk reduction/ (3872)
-
or/133-135 (21,548)
-
lifestyle/ (6272)
-
lifestyle$.ti,ab. (14,166)
-
(inactivit$ or sedentary).ti,ab. (6359)
-
health behaviour/ (1667)
-
health behavior.ti,ab. (603)
-
health behaviour.ti,ab. (809)
-
obesity/ or overeating/ or overweight/ or thinness/ or weight reduction/ (54,899)
-
weight control/ or weight gain/ (13,239)
-
(weight adj3 (gain or loss or change*)).ti,ab. (41,341)
-
(overweight or over weight or overeat$ or over eat$).ti,ab. (17,666)
-
((bmi or body mass index) adj2 (gain or loss or change)).ti,ab. (770)
-
obes*.ti,ab. (57,424)
-
food habit$.ti,ab. (2184)
-
poor diet.ti,ab. (772)
-
healthy eating.ti,ab. (1635)
-
(fruit or vegetable$).ti,ab. (52,214)
-
leisure/ or enjoyment/ or free time/ or holidays/ or leisure activities/ or leisure behaviour/ or recreation/ (2378)
-
exp leisure activities/ or games/ or social activities/ or television/ (2728)
-
(leisure or relax* or holiday* or vacation* or recreation* or hobbies or hobby or play*).ti,ab. (82,508)
-
or/137-155 (241,266)
-
(annual report or annual report section or book or book chapter or bulletin or bulletin article or correspondence or orial or patent or standard).pt. (119,097)
-
5 and 17 and 29 (97)
-
158 not 157 (78)
-
limit 159 to (english language and yr=“1990 - 2010”) (54)
-
5 and 17 and 58 (334)
-
161 not 157 (264)
-
limit 162 to (english language and yr=“1990 - 2010”) (164)
-
5 and 17 and 108 (311)
-
164 not 157 (258)
-
limit 165 to (english language and yr=“1990 - 2010”) (156)
-
5 and 17 and 120 (616)
-
167 not 157 (488)
-
limit 168 to (english language and yr=“1990 - 2010”) (248)
-
5 and 17 and 123 (458)
-
170 not 157 (418)
-
limit 171 to (english language and yr=“1990 - 2010”) (309)
-
5 and 17 and 132 (511)
-
173 not 157 (426)
-
limit 174 to (english language and yr=“1990 - 2010”) (268)
-
5 and 17 and 136 (117)
-
176 not 157 (114)
-
limit 177 to (english language and yr=“1990 - 2010”) (101)
-
5 and 17 and 156 (690)
-
179 not 157 (581)
-
limit 180 to (english language and yr=“1990 - 2010”) (360)
-
160 or 163 or 166 or 169 or 172 or 175 or 178 or 181 (1186)
Cumulative Index to Nursing and Allied Health Literature Plus
Date range searched: 1990–2013.
Date of search: June 2013.
URL: https://www.ebscohost.com/
Search strategy
S1 (MH “Family Practice”) (13,315)
S2 (MH “Primary Health Care”) (27,954)
S3 (MH “Physicians, Family”) (8543)
S4 (MH “Community Health Nursing”) OR (MH “Family Nursing”) (22,009)
S5 (MH “Community Health Services+”) (231,870)
S6 (MH “Community Health Workers”) (712)
S7 (primary N1 care) or (primary N1 health*) or (community N1 care) or (community N1 health*) (91,150)
S8 (general n1 practice*) or (general N1 practitioner*) or (family N1 practice*) or (family N1 practitioner*) (24,448)
S9 (gp N1 service*) or (gp N1 practice*) or (gp N1 clinic) or (gp N1 clinics) (568)
S10 (practice N2 nurs*) or (communit* N2 nurs*) (78,933)
S11 health visitor* (2867)
S12 SO “family practice” (3309)
S13 (SO primary N1 care) or (SO primary N1 health*) (15,809)
S14 (SO general N1 practice) or (SO general N1 practitioner*) (5684)
S15 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 or S11 or S12 or S13 or S14 (353,441)
S16 (MH “United Kingdom+”) (204,333)
S17 (TI uk) or (TI united kingdom) or (TI britain) or (TI gb) or (TI gbr) or (TI british isles) (10,823)
S18 (AB uk) or (AB united kingdom) or (AB britain) or (AB gb) or (AB gbr) or (AB british isles) (20,559)
S19 (TI england) or (TI scotland) or (TI wales) or (TI ireland) (8810)
S20 (AB england) or (AB scotland) or (AB wales) or (AB ireland) (13,884)
S21 (TI nhs) or (AB nhs) or (TI national health service) or (AB national health service) (16,215)
S22 S16 or S17 or S18 or S19 or S20 or S21 (222,806)
S23 (MH “Smoking/PC/TH”) (4625)
S24 (MH “Tobacco+”) (3999)
S25 (MH “Tobacco Abuse (Saba CCC)”) (1)
S26 chewing tobacco (64)
S27 (pipe N2 smok*) (56)
S28 (cigar* or bidi* or kretek or paan or gutka or snuff or snus or betel) (8413)
S29 S23 or S24 or S25 or S26 or S27 or S28 (14,802)
S30 (quit* or stop* or giv* or ceas* or cessation or withdrawal) (108,214)
S31 S29 and S30 (4436)
S32 (MH “Tobacco Abuse Control (Saba CCC)”) (1)
S33 (MH “Smoking Cessation”) (9645)
S34 (MH “Smoking Cessation Programs”) (1183)
S35 smoking cessation (11,658)
S36 S31 or S32 or S33 or S34 or S35 (12,706)
S37 (MH “Substance Use Disorders+”) (75,086)
S38 (MH “Alcohol Drinking”) (12,143)
S39 overdos* or over-dos* or excessive use (3674)
S40 (drug N3 addict*) or (drug N3 dependen*) or (drug N3 abuse*) or (drug N3 misuse) or (drug N3 withdraw*) or (drug N3 intoxicat*) or (drug N3 abstinen*) or (drug N3 abstain*) or (substance N3 addict*) or (substance N3 dependen*) or (substance N3 abuse*) or (substance N3 misuse) or (substance N3 withdraw*) or (substance N3 intoxicat*) or (substance N3 abstinen*) or (substance N3 abstain*) or (alcohol* N3 addict*) or (alcohol* N3 dependen*) or (alcohol* N3 abuse*) or (alcohol* N3 misuse) or (alcohol* N3 withdraw*) or (alcohol* N3 intoxicat*) or (alcohol* N3 abstinen*) or (alcohol* N3 abstain*) (52,077)
S41 (alcohol* N3 consumption) or (alcohol* N3 drink*) (15,241)
S42 (MH “Amphetamines+”) (2084)
S43 (MH “Adrenergic Agents+”) (21,849)
S44 (MH “Antianxiety Agents+”) (6414)
S45 (MH “Antidepressive Agents+”) (12,177)
S46 (MH “Barbiturates+”) (1274)
S47 (MH “Cannabis”) (3112)
S48 (MH “Cocaine+”) (2696)
S49 (MH “Designer Drugs”) (93)
S50 (MH “Hallucinogens+”) (1045)
S51 (MH “Heroin”) (1438)
S52 (MH “Ketamine”) (1402)
S53 (MH “Lysergic Acid Diethylamide”) (138)
S54 (MH “Opium”) OR (MH “Methadone”) (2666)
S55 (MH “Street Drugs+”) (2559)
S56 alcohol or amphetamine* or angel dust or barbiturate* or cannabis or cocaine (40,635)
S57 designer drug* or dexedrine or diet pill* or dissociative drug* or doping or dxm (994)
S58 ephedra or ephedrine or ecstasy or hallucinogen* or hash oil* or hashish or heroin (4037)
S59 illicit drug* or inhalant* or ketamine or lsd or lysergic-acid* or mescaline or Marihuana or marijuana (5973)
S60 mda or mdma or methadone or methcathinone or methamphetamine* or Narcotic (10,588)
S61 opioid* or opiate* or opium or oxycontin or oxycodone or percocet or phencyclidine (12,665)
S62 poppers or pseudophedrine or psychotomimetic* or roofies or salvia divinorum or solvent* (1547)
S63 stimulant* or steroid abuse or street-drug* or tranquili?er* or valium or vicodin (5183)
S64 S37 or S38 or S39 or S40 or S41 or S42 or S43 or S44 or S45 or S46 or S47 or S48 or S49 or S50 or S51 or S52 or S53 or S54 or S55 or S56 or S57 or S58 or S59 or S60 or S61 or S62 or S63 (159,167)
S65 (MH “Motor Activity”) (4522)
S66 (MH “Exercise+”) (48,670)
S67 (MH “Therapeutic Exercise+”) (25,350)
S68 (physical* N2 activit*) or (physical* N2 exerc*) or (physical* N2 fitness) or (motor* N2 activit*) or (motor* N2 exerc*) or (motor* N2 fitness) (35,855)
S69 exercis* (78,866)
S70 (physical* N5 fit*) or (physical N5 activ*) or (physical* endur*) (34,087)
S71 (exercis* N5 fit*) or (exercis* N5 activ*) or (exercis* endur*) (4368)
S72 (promot* N5 physical* activit*) (1249)
S73 (promot* N5 exercis*) or (uptak* N5 exercis*) or (encourag* N5 exercis*) or (increas* N5 exercis*) or (start* N5 exercis*) or (adher* N5 exercis*) or (maintain* N5 exercis*) or (sustain* N5 exercis*) (5780)
S74 (decreas* N5 sedentary) or (reduc* N5 sedentary) or (discourag* N5 sedentary) (179)
S75 pedomet* or step counter* or walk* (19,773)
S76 bicycl* or bike* or cycling or riding or rides (7102)
S77 (active N5 transport*) or (active N5 journey*) or (activity N5 transport*) or (activity N5 journey*) or (active N5 travel*) or (activity N5 travel*) (464)
S78 (travel* N5 walk*) or (travel* N5 biking) or (travel* N5 cycle) or (travel* N5 mode) or (travel* N5 modes) or (travel* N5 route) or (travel* N5 routes) or (travel* N5 pattern*) or (travel* N5 plan*) or (travel* N5 rollerblad*) or (travel* N5 skateboard*) or (travel* N5 scooter*) or (travel* N5 rollerskat*) (275)
S79 (transport* N5 walk*) or (transport* N5 biking) or (transport* N5 cycle) or (transport* N5 mode) or (transport* N5 modes) or (transport* N5 route) or (transport* N5 routes) or (transport* N5 pattern*) or (transport* N5 plan*) or (transport* N5 rollerblad*) or (transport* N5 skateboard*) or (transport* N5 scooter*) or (transport* N5 rollerskat*) (439)
S80 (journey* N5 walk*) or (journey* N5 biking) or (journey* N5 cycle) or (journey* N5 mode) or (journey* N5 modes) or (journey* N5 route) or (journey* N5 routes) or (journey* N5 pattern*) or (journey* N5 plan*) or (journey* N5 rollerblad*) or (journey* N5 skateboard*) or (journey* N5 scooter*) or (journey* N5 rollerskat*) (65)
S81 (commut* N5 walk*) or (commut* N5 biking) or (commut* N5 cycle) or (commut* N5 mode) or (commut* N5 modes) or (commut* N5 route) or (commut* N5 routes) or (commut* N5 pattern*) or (commut* N5 plan*) or (commut* N5 rollerblad*) or (commut* N5 skateboard*) or (commut* N5 scooter*) or (commut* N5 rollerskat*) (45)
S82 health club* (114)
S83 (leisure N5 centre*) or (leisure N5 center*) or (leisure N5 facilit*) or (fitness N5 centre*) or (fitness N5 center*) or (fitness N5 facilit*) (1048)
S84 parks (325)
S85 fitness club* or wellness centre* or wellness center* (142)
S86 gym* (1179)
S87 pitch or pitches (1171)
S88 swimming pool* (253)
S89 health spa* (104)
S90 (MH “Sports Facilities”) (13)
S91 swim* or walk* or running or biking or bicycl* or bike* or cycling or dance or dancing or aerobics sport* or horse riding or football or rugby or netball or cricket or hockey or rounders or athletic* or rollerblading or rollerskating or skating or skateboard* or play* or games or tennis or badminton or racquet sport* or pilates or spinning or step* class* or physical education (102,860)
S92 (MH “Physical Education and Training+”) (1471)
S93 (MH “Sports+”) (33,214)
S94 S65 or S66 or S67 or S68 or S69 or S70 or S71 or S72 or S73 or S74 or S75 or S76 or S77 or S78 or S79 or S80 or S81 or S82 or S83 or S84 or S85 or S86 or S87 or S88 or S89 or S90 or S91 or S92 or S93 (195,132)
S95 (MH “Immunization”) (11,351)
S96 (MH “Immunization Programs”) (2686)
S97 (MH “Vaccines+”) (22,241)
S98 vaccin* not vaccinia (27,290)
S99 immuni* not innate immunity (23,775)
S100 (dtp N3 immuni*) or (dtap N3 immuni*) or (dpt N3 immuni*) or (dtp N3 vaccin*) or (dtap N3 vaccin*) or (dpt N3 vaccin*) or (dtp N3 jab) or (dtap N3 jab) or (dpt N3 jab) (155)
S101 (diphtheria N3 vaccin*) or (diphtheria N3 immuni*) or (diphtheria N3 jab) (804)
S102 (tetanus N3 vaccin*) or (tetanus N3 immuni*) or (tetanus N3 jab) (953)
S103 (whooping cough N3 vaccin*) or (whooping cough N3 immuni*) or (whooping cough N3 jab) (49)
S104 (pertussis N3 vaccin*) or (pertussis N3 immuni*) or (pertussis N3 jab) (1232)
S105 (polio* N3 vaccin*) or (polio* N3 immuni*) or (polio* N3 jab) (1032)
S106 (hib N3 vaccin*) or (hib N3 immuni*) or (hib N3 jab) (469)
S107 mmr vaccin* or pluserix or priorix or trimovax or triviraten berna or virivac (305)
S108 hpv vaccin* or papillomavirus (4524)
S109 anti-HBsAg or Engerix-B or Recombivax HB (26)
S110 (bcg N3 vaccine) or (bacillus N5 vaccine) (673)
S111 S95 or S96 or S97 or S98 or S99 or S100 or S101 or S102 or S103 or S104 or S105 or S106 or S107 or S108 or S109 or S110 (42,373)
S112 (MH “Health Screening+”) (41,161)
S113 screening or screen (63,781)
S114 S112 or S113 (71,723)
S115 brief N3 intervention* (1593)
S116 counselling or counseling (28,756)
S117 (minimal N5 intervention*) or (minimum N5 intervention*) or (low N5 intervention*) or (minimal N5 intensity) or (minimum N5 intensity) or (low N5 intensity) (3477)
S118 low-intensity (1010)
S119 advice (13,453)
S120 motivational (3116)
S121 opportunistic (3704)
S122 self-help or self help (1939)
S123 S115 or S116 or S117 or S118 or S119 or S120 or S121 or S122 (53,326)
S124 (MH “Harm Reduction”) (1030)
S125 (risk* N3 reduc*) or (harm* N3 reduc*) (20,116)
S126 safe* N2 behavi* (717)
S127 S124 or S125 or S126 (20,746)
S128 (MH “Life Style+”) (95,547)
S129 lifestyle* (14,280)
S130 inactivit* or sedentary (5427)
S131 health behavior or health behaviour (21,084)
S132 (MH “Obesity+”) (36,187)
S133 (MH “Body Weight Changes+”) (44,713)
S134 (weight N3 gain) or (weight N3 loss) or (weight N3 change*) (20,770)
S135 (overweight or over weight or overeat* or over eat*) (8337)
S136 (bmi N2 gain) or (bmi N2 loss) or (bmi N2 change) or (body mass index N2 gain) or (body mass index N2 loss) or (body mass index N2 change) (552)
S137 obes* (43,293)
S138 food habit* or poor diet or healthy eating or fruit or vegetable* (15,932)
S139 (MH “Leisure Activities+”) (29,040)
S140 leisure or relax* or holiday* or vacation* or recreation* or hobbies or hobby or play* (71,526)
S141 S128 or S129 or S130 or S131 or S132 or S133 or S134 or S135 or S136 or S137 or S138 or S139 or S140 (246,835)
S142 Limiters - Publication Type: Accration, Advice and Referral Website, Algorithm, Anecdote, Audiovisual, Biography, Book, Book Chapter, Book Review, Care Plan, Cartoon, Chat Groups, Classification Term, Commentary, Commercial Website, Computer Program, Consumer/Patient Teaching Materials, Critical Path, Diagnostic Images, Directories, orial, Equations & Formulas, Exam Questions, Forms, Games, Glossary, Individual Testimonial Website, Information Website, Interview, Legal Cases, Letter, Listservs, Nurse Practice Acts, Obituary, Pamphlet, Pamphlet Chapter, Pictorial, Poetry, Questionnaire/Scale, Questions and Answers, Quick Lesson, Software, Standards, Teaching Materials, Tracings, Website (1,063,759)
S143 S15 and S22 and S36 (408)
S144 S143 not S142 (309)
S145 S143 not S142 Limiters - Published Date from: 19900101-20101231; Language: English (289)
S146 S15 and S22 and S64 (1911)
S147 S146 not S142 (1469)
S148 S146 not S142 Limiters - Published Date from: 19900101-20101231; Language: English (1338)
S149 S15 and S22 and S94 (2352)
S150 S149 not S142 (1798)
S151 S149 not S142 Limiters - Published Date from: 19900101-20101231; Language: English (1718)
S152 S15 and S22 and S111 (963)
S153 S152 not S142 (659)
S154 S152 not S142 Limiters - Published Date from: 19900101-20101231; Language: English (606)
S155 S15 and S22 and S114 (4304)
S156 S155 not S142 (3262)
S157 S155 not S142 Limiters - Published Date from: 19900101-20101231; Language: English (2992)
S158 S15 and S22 and S123 (2956)
S159 S158 not S142 (2263)
S160 S158 not S142 Limiters - Published Date from: 19900101-20101231; Language: English (2112)
S161 S15 and S22 and S127 (350)
S162 S161 not S142 (262)
S163 S161 not S142 Limiters - Published Date from: 19900101-20101231; Language: English (245)
S164 S15 and S22 and S141 (3716)
S165 S164 not S142 (2789)
S166 S164 not S142 Limiters - Published Date from: 19900101-20101231; Language: English (2582)
S167 S145 or S148 or S151 or S154 or S157 or S160 or S163 or S166 (6211)
Appendix 3 Potentially relevant Cochrane reviews identified
Buckley BS, Byrne MC, Smith SM. Service organisation for the secondary prevention of ischaemic heart disease in primary care. Cochrane Database Syst Rev 2010;3:CD006772.
Stead LF, Bergson G, Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst Rev 2008;5:CD000165.
Rice VH, Stead LF. Nursing interventions for smoking cessation. Cochrane Database Syst Rev 2008;8:CD001188.
Sinclair HK, Bond CM, Stead LF. Community pharmacy personnel interventions for smoking cessation. Cochrane Database Syst Rev 2004;1:CD003698.
Secker-Walker R, Gnich W, Platt S, Lancaster T. Community interventions for reducing smoking among adults. Cochrane Database Syst Rev 2002;2:CD001745.
Carson KV, Brinn MP, Labiszewki NA, Esterman AJ, Chang AB, Smith BJ. Community interventions for preventing smoking in young people. Cochrane Database Syst Rev 2011;7:CD001291.
Lumley J, Chamberlain C, Dowswell I, Oliver S, Oakly L, Watson L. Interventions for promoting smoking cessation during pregnancy. Cochrane Database Syst Rev 2009;3:CD001055.
Lai DTC, Cahill K, Qin Y, Tang J-L. Motivational interviewing for smoking cessation. Cochrane Database Syst Rev 2010;3:CD006936.
Kaner EF, Beyer F, Dickinson Ho, Pienaar E, Campbell F, Schlesinger C, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev 2007;2:CD004148.
Baker PRA, Francis DP, Soares J, Weightman Al, Foster C. Community wide interventions for increasing physical activity. Cochrane Database Syst Rev 2011;4:CD008366.
Bosch-Capblanch X, Abba K, Prictor M, Gamer P. Contracts between patients and healthcare practitioners for improving patients’ adherence to treatment, prevention and health promotion activities. Cochrane Database Syst Rev 2007;2:CD004808.
Smeeth LL, Iliffe S. Community screening for visual impairment in the elderly. Cochrane Database Syst Rev 2006;3:CD001054.
Flodgren G, Deane K, Dickinson HO, Kirk S, Alberti H, Beyer FR, et al. Interventions to change the behaviour of health professionals and the organisation of care to promote weight reduction in overweight and obese adults. Cochrane Database Syst Rev 2010;3:CD000984.
Jacobson Vann JC, Szilagyi P. Patient reminder and recall systems to improve immunization rates. Cochrane Database Syst Rev 2005;3:CD003941.
Norris SL, Zhang X, Avenell A, Gregg E, Schmid CH, Lau J. Long-term non-pharmacological weight loss interventions for adults with prediabetes. Cochrane Database Syst Rev 2005;2:CD005270.
Nield L, Summerbell CD, Hooper L, Whittaker V, Moore H. Dietary advice for the prevention of type 2 diabetes mellitus in adults. Cochrane Database Syst Rev 2008;3:CD005102.
Orozco LJ, Buchleitner AM, Gimenez-Perez G, Roque I Figuls M, Richter B, Mauricio D. Exercise or exercise and diet for preventing type 2 diabetes mellitus. Cochrane Database Syst Rev 2008;3:CD003054.
Renders CM, Valk GD, Griffin S, Wagner EH, Eijk JT, Assendelft WJ. Interventions to improve the management of diabetes mellitus in primary care, outpatient and community settings. Cochrane Database Syst Rev 2001;1:CD001481.
Boyle R, Solberg L, Fiore M. Use of electronic health records to support smoking cessation. Cochrane Database Syst Rev 2014;3:CD008743.
Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012;9:CD007146.
McClure RJ, Turner C, Peel N, Spinks A, Eakin E, Hughes K. Population-based interventions for the prevention of fall-related injuries in older people. Cochrane Database Syst Rev 2005;1:CD004441.
Hooper L, Bartlett C, Davey SG, Ebrahim S. Advice to reduce dietary salt for prevention of cardiovascular disease. Cochrane Database Syst Rev 2004;1:CD003656.
Ebrahim S, Taylor F, Ward K, Beswick A, Burke M, Davey Smith G. Multiple risk factor interventions for primary prevention of coronary heart disease. Cochrane Database Syst Rev 2011;1:CD001561.
Hillsdon M, Foster C, Thorogood M. Interventions for promoting physical activity. Cochrane Database Syst Rev 2005;1:CD003180.
Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2011;12:CD001871.
Oringanje C, Meremikwu MM, Eko H, Esu E, Meremikwu A, Ehiri JE. Interventions for preventing unintended pregnancies among adolescents. Cochrane Database Syst Rev 2009;4:CD005215.
Dyson L, McCormick F, Renfrew MJ. Interventions for promoting the initiation of breastfeeding. Cochrane Database Syst Rev 2005;2:CD001688.
Reviews which are in progress and thus only the protocol is currently available
Anderson P, Laurant M, Kaner EF, Wensing M, Grol R. Interventions to increase the use of screening and brief intervention programmes for hazardous alcohol consumption by patients in primary care settings. Cochrane Database Syst Rev 2004:7;CD004630.
Klein Woolthuis EP, de Grauw WJC, van der Laar FA, Akkermans RP. Screening for type 2 diabetes mellitus. Cochrane Database Syst Rev 2005;2:CD005266.
Noknoy S, Chamnan P, Anothaisintawee T. Theory based behavioural interventions for prediabetic state and people with diabetes mellitus. Cochrane Database Syst Rev 2009;4:CD008082.
Reviews set aside because it was decided the conditions are too specific
Dorresteijn JAN, Kriegsman DM, Assendelft WJ, Valk GD. Patient education for preventing diabetic foot ulceration. Cochrane Database Syst Rev 2014;12:CD001488.
Dorresteijn JAN, Kriegsman DMW, Valk GD. Complex interventions for preventing diabetic foot ulceration. Cochrane Database Syst Rev 2010;1:CD007610.
NB: A Cochrane systematic review Interventions to Implement Prevention in Primary Care (2001) was withdrawn in 2005 as the author did not have the resources to update it. This review was mainly concerned with educational interventions or outreach visits targeted at health professionals.
Appendix 4 Data extraction form
| 1. Name of reviewer performing data extraction | |
| 2. What country does the paper examine? | Please mark ‘X’ within the square brackets of only one answer: [ ] England, Northern Ireland, Scotland and/or Wales [ ] Multiple countries including non-UK and UK country(ies) [ ] Non-UK country(ies) [ ] Not applicable |
| 3. Is it primary care? | Please mark ‘X’ within the square brackets of only one answer: [ ] Yes [ ] No [ ] Partly |
| 4. Is it health improvement? (defined in this project as primordial, primary, secondary or tertiary prevention, and also encompassing health promotion) | Please mark ‘X’ within the square brackets of only one answer: [ ] Yes [ ] No |
| 5. What is the health topic? | Please mark ‘X’ within the square brackets of one or more answers: [ ] Alcohol [ ] Arthritis [ ] Asthma [ ] Breastfeeding [ ] Cancer screening [ ] Cardiovascular disease [ ] Child health [ ] Contraception [ ] COPD [ ] Diabetes [ ] Diet/nutrition [ ] Drugs [ ] Exercise [ ] Falls [ ] Maternity care [ ] Mental health [ ] Obesity [ ] Older adult health [ ] Osteoporosis [ ] Sexual health [ ] Smoking [ ] Stroke [ ] Vaccination [ ] No specific health topic [ ] Other (please specify in box below) |
| Other: | |
| 6. What type of paper is it? | Please mark ‘X’ within the square brackets of only one answer: [ ] Research [ ] Service description with evaluative component [ ] Service description without evaluative component [ ] Review [ ] Opinion piece/commentary [ ] Other (please specify in box below) |
| Other: | |
| 7. Is it related to service delivery or organisation? | Please mark ‘X’ within the square brackets of only one answer: [ ] Yes [ ] No [ ] Partly |
| 8. Based on the answers to questions 2–7 and your judgement, do you recommend including the paper, marking it as ‘of interest’, or rejecting it? | Please mark ‘X’ within the square brackets of only one answer: [ ] Include for evidence synthesis of approaches to delivery/organisation of health improvement [ ] Include because tells us about health improvement activities undertaken in primary care [ ] Mark as a paper ‘of interest’ [ ] Reject paper |
| If the recommendation is to reject the paper, the rest of the form does not have to be completed. If the paper is ‘of interest’, please complete parts of the form where possible. Please note useful information in the text box ‘Additional comments and notes’ at the end of the form if it doesn’t fit in any other boxes | |
|---|---|
| 9. Please describe the intervention (or service, if it was not an intervention study) | |
| 10. How does the intervention relate to service delivery or organisation? | |
| If the paper is a review, for the rest of the questions please select all answers that apply (e.g. if randomised controlled trials and controlled before/after studies were included in the review, please select both) | |
| 11. Was it a pilot/feasibility study? | Please mark ‘X’ within the square brackets of only one answer: [ ] Yes [ ] No |
| 12. What was the study design(s)? | Please mark ‘X’ within the square brackets of one or more answers: [ ] Randomised controlled trial – individual [ ] Randomised controlled trial – cluster [ ] Controlled before/after study/non-randomised controlled trial [ ] Uncontrolled before/after study [ ] Interrupted time series study [ ] Economic evaluation [ ] Cross-sectional study/survey [ ] Cohort study [ ] Case–control study [ ] Qualitative study [ ] Case study [ ] Other (please specify in box below) |
| Other: | |
| 13. If it was a qualitative study, what type of study was it? | Please mark ‘X’ within the square brackets of one or more answers: [ ] Focus group(s) [ ] Brief interview [ ] Extended interview [ ] Semi-structured interview [ ] Observation (passive/participant) [ ] Description of intervention [ ] Document analysis [ ] Other (please specify in box below) |
| Other: | |
| 14. What was the purpose of the study? | Please mark ‘X’ within the square brackets of one or more answers: [ ] Evaluation of practitioner role [ ] Evaluation of service delivery or organisation [ ] Evaluation/exploration of practitioner knowledge [ ] Evaluation of intervention [ ] Exploration of practitioner views or experiences [ ] Exploration of patient views or experiences [ ] Exploration of parent views or experiences [ ] Practitioner education programme [ ] Exploration of patient decision-making [ ] Description of intervention [ ] Other (please specify in box below) |
| Other: | |
| 15. What outcomes were measured? | Please mark ‘X’ within the square brackets of one or more answers: [ ] Changes in attendance to a service [ ] Hospital admissions [ ] Patient clinical outcomes [ ] Presence/absence of target disease [ ] Practitioner behaviour [ ] Practitioner knowledge/opinion [ ] Patient behaviour/decision [ ] Patient knowledge/opinion [ ] Identify barriers to care [ ] Cost effectiveness [ ] Not applicable [ ] Other (please specify in box below) |
| Other: | |
| 16. Where was the service delivered? | Please mark ‘X’ within the square brackets of one or more answers: [ ] General practice [ ] School [ ] Pharmacy [ ] Home [ ] Other community [ ] Other non-clinical setting [ ] Other clinical setting [ ] Not clear/not specified |
| Please provide further details of the service delivery location, if of interest: | |
| 17. Who provided the service? | Please mark ‘X’ within the square brackets of one or more answers: [ ] GP [ ] Practice nurse [ ] Community nurse/practitioner [ ] School nurse [ ] Health visitor [ ] Midwife [ ] Pharmacist [ ] Not clear/not specified [ ] Other (please specify in box below) |
| Other: | |
| 18. What was the population targeted? | Please mark ‘X’ within the square brackets of one or more answers: [ ] Older people [ ] Adults [ ] Children [ ] Adolescents [ ] Patients with ‘lifestyle’ risk factors [ ] Patients with other risk factors [ ] Patients with a specific disease [ ] All patients [ ] Mothers/parents [ ] Other (please specify in box below) |
| Other: | |
| 19. Please provide a summary of the results and conclusions | |
| Quality assessment Please assess the paper according to whether you have major, minor, or no concerns with the following five quality criteria, and then complete question 25. If the paper is a review please complete questions 25 and 26 | |
| 20. Quality of the sampling process (including sample size) | Please mark ‘X’ within the square brackets of only one answer: [ ] Major concern [ ] Minor concern [ ] No concerns [ ] Not possible to assess [ ] Not applicable |
| 21. Appropriateness of the analysis | Please mark ‘X’ within the square brackets of only one answer: [ ] Major concern [ ] Minor concern [ ] No concerns [ ] Not possible to assess [ ] Not applicable |
| 22. Comparability of the intervention and comparison groups (risk of selection bias, including bias with loss to follow up) | Please mark ‘X’ within the square brackets of only one answer: [ ] Major concern [ ] Minor concern [ ] No concerns [ ] Not possible to assess [ ] Not applicable |
| 23. Quality of the intervention delivery (was there risk of contamination? Was consistency of the intervention measured?) | Please mark ‘X’ within the square brackets of only one answer: [ ] Major concern [ ] Minor concern [ ] No concerns [ ] Not possible to assess [ ] Not applicable |
| 24. Outcome assessment (risk of measurement bias) | Please mark ‘X’ within the square brackets of only one answer: [ ] Major concern [ ] Minor concern [ ] No concerns [ ] Not possible to assess [ ] Not applicable |
| 25. Please rate the quality of the paper as A, B, C or D according to the following guidelines: A: no major or minor concerns. B: no major concerns but one or more minor concerns. C: one or more major concerns. D: reject paper due to major concerns or other quality issue(s) | Please mark ‘X’ within the square brackets of only one answer: [ ] A [ ] B [ ] C [ ] D |
| 26. If the paper is a review (or a study design for which several of the quality criteria above are not applicable) and you have major or minor concerns about its quality, please state your concerns | |
| 27. Additional comments and notes | |
Appendix 5 Papers included in evidence synthesis
Abayomi JC, Watkinson H, Boothby J, Topping J, Hackett AF. Identification of ‘hot spots’ of obesity and being underweight in early pregnancy in Liverpool. J Hum Nutr Diet 2009;22:246–54.
Abbott S, Hobby L. Impact on individual health of the provision of welfare advice in primary health care settings. Ment Health Learn Disabil Care 2000;3:260–2.
Abbott S, Hobby L. Welfare benefits advice in primary care: evidence of improvements in health. Public Health 2000;114:324–7.
Abbott S, Hobby L, Cotter S. What is the impact on individual health of services in general practice settings which offer welfare benefits advice? Health Soc Care Community 2006:14:1–8.
Abdullahi A, Copping J, Kessel A, Luck M, Bonell C. Cervical screening: perceptions and barriers to uptake among Somali women in Camden. Public Health 2009;123:680–5.
Adab P, Marshall T, Rouse A, Randhawa B, Sangha H, Bhangoo N. Randomised controlled trial of the effect of evidence based information on women's willingness to participate in cervical cancer screening. J Epidemiol Community Health 2003;57:589–93.
Adams CJ, Baeza JI, Calnan M. The new health promotion arrangements in general medical practice in England: results from a national evaluation. Health Educ J 2001;60:45–58.
Agomo CO. The role of community pharmacists in public health: a scoping review of the literature. J Pharm Health Serv Res 2012;3:25–33.
Ahern AL, Olson AD, Aston LM, Jebb SA. Weight Watchers on prescription: an observational study of weight change among adults referred to Weight Watchers by the NHS. BMC Public Health 2011;11:434.
Alazri MH, Heywood P, Neal RD, Leese B. UK GPs’ and practice nurses’ views of continuity of care for patients with type 2 diabetes. Fam Pract 2007;24:128–37.
Allan K, Hoddinott P, Avenell A. A qualitative study comparing commercial and health service weight loss groups, classes and clubs. J Hum Nutr Diet 2011;24:23–31.
Allcock D. Using a community respiratory service to reduce children’s hospital admissions. Nurs Times 2009;105:22–3.
Anderson C, Blenkinsopp A, Armstrong M. Feedback from community pharmacy users on the contribution of community pharmacy to improving the public’s health: a systematic review of the peer reviewed and non-peer reviewed literature 1990–2002. Health Expect 2004;7:191–202.
Anderson EM, Mandeville RP, Hutchinson SJ, Cameron SO, Mills PR, Fox R, et al. Evaluation of a general practice based hepatitis C virus screening intervention. Scott Med J 2009;54:3–7.
Anokye NK, Trueman P, Green C, Pavey TG, Hillsdon M, Taylor RS. The cost-effectiveness of exercise referral schemes. BMC Public Health 2011;11:954.
Ara R, Blake L, Gray L, Hernandez M, Crowther M, Dunkley A, et al. What is the clinical effectiveness and cost-effectiveness of using drugs in treating obese patients in primary care? A systematic review. Health Technol Assess 2012;16(5).
Arthur AJ, Matthews RJ, Jagger C, Clarke M, Hipkin A, Bennison DP. Improving uptake of influenza vaccination among older people: a randomised controlled trial. Br J Gen Pract 2002;52:717–18.
Ashenden R, Silagy C, Weller D. A systematic review of the effectiveness of promoting lifestyle change in general practice. Fam Pract 1997;14:160–76.
Bailey B. Parent–child relationships: developing a brief attachment-screening tool. Community Pract 2009;82:22–6.
Banks J, Shield JP, Sharp D. Barriers engaging families and GPs in childhood weight management strategies. Br J Gen Pract 2011;61:e492–7.
Baraitser P, Pearce V, Holmes J, Horne N, Boynton PM. Chlamydia testing in community pharmacies: evaluation of a feasibility pilot in south east London. Qual Saf Health Care 2007;16:303–7.
Barlow J, Whitlock S, Hanson S, Davis H, Hunt C, Kirkpatrick S, et al. Preventing obesity at weaning: parental views about the EMPOWER programme. Child Care Health Dev 2010:36:843–9.
Barr RJ, Stewart A, Torgerson DJ, Seymour DG, Reid DM. Screening elderly women for risk of future fractures: participation rates and impact on incidence of falls and fractures. Calcif Tissue Int 2005;76:243–8.
Basu S, Evans KL, Owen M, Harbottle T. Outcome of Newborn Hearing Screening Programme delivered by health visitors. Child Care Health Dev 2008;34:642–7.
Bauld L, Boyd KA, Briggs AH, Chesterman J, Ferguson J, Judge K, et al. One-year outcomes and a cost-effectiveness analysis for smokers accessing group-based and pharmacy-led cessation services. Nicotine Tob Res 2011;13:135–45.
Bazian Ltd. Advice about diet and lifestyle does not reduce blood pressure in people with hypertension. Evid Based Healthcare Public Health 2004;8:348–9.
Beake S, McCourt C, Rowan C, Taylor J. Evaluation of the use of health care assistants to support disadvantaged women breastfeeding in the community. Matern Child Nutr 2005;1:32–43.
Bebb C, Kendrick D, Stewart J, Coupland C, Madeley R, Brown K, et al. Inequalities in glycaemic control in patients with type 2 diabetes in primary care. Diabet Med 2005;22:1364–71.
Beckley A, Lees B, Collington S, de Bono A. Work-related health advice in primary care. Occup Med 2011;61:498–502.
Begh RA, Aveyard P, Upton P, Bhopal RS, White M, Amos A, et al. Promoting smoking cessation in Pakistani and Bangladeshi men in the UK: pilot cluster randomised controlled trial of trained community outreach workers. Trials 2011;12:197.
Bell A, Corfield M, Davies J, Richardson N. Collaborative transdisciplinary intervention in early years: putting theory into practice. Child Care Health Dev 2010;36:142–8.
Bell TS, Branston LK, Newcombe RG, Barton GR. Interventions to improve uptake of breast screening in inner city Cardiff general practices with ethnic minority lists. Ethn Health 1999;4:277–84.
Bell-Higgs AE, Brosnahan NT, Clarke AM, Dow MS, Haynes SM, Lyons GF, et al. The implementation of the Counterweight programme in Scotland, UK. Fam Pract 2012;29:i139–44.
Blenkinsopp A, Anderson C, Armstrong M. Systematic review of the effectiveness of community pharmacy-based interventions to reduce risk behaviours and risk factors for coronary heart disease. J Public Health Med 2003;25:144–53.
Bodenheimer T, Handley MA. Goal-setting for behavior change in primary care: an exploration and status report. Pat Educ Counsel 2009;76:174–80.
Boehler CE, Milton KE, Bull FC, Fox-Rushby JA. The cost of changing physical activity behaviour: evidence from a ‘physical activity pathway’ in the primary care setting. BMC Public Health 2011;11:370.
Bond M, Wyatt K, Lloyd J, Welch K, Taylor R. Systematic review of the effectiveness and cost-effectiveness of weight management schemes for the under fives: a short report. Health Technol Assess 2009;13(1).
Bowles H, Maher A, Sage R. Helping teenagers stop smoking: comparative observations across youth settings in Cardiff. Health Educ J 2009;68:111–18.
Boyd KA, Briggs AH. Cost-effectiveness of pharmacy and group behavioural support smoking cessation services in Glasgow. Addiction 2009;104:317–25.
Brabin L, Thomas G, Hopkins M, O’Brien K, Roberts SA. Delivery of chlamydia screening to young women requesting emergency hormonal contraception at pharmacies in Manchester, UK: a prospective study. BMC Womens Health 2009;9:7.
Brankin E, Mitchell C, Munro R, Lanarkshire Osteoporosis Service. Closing the osteoporosis management gap in primary care: a secondary prevention of fracture programme. Curr Med Res Opin 2005;21:475–82.
Brose LS, West R, McDermott MS, Fidler JA, Croghan E, McEwen A. What makes for an effective stop-smoking service? Thorax 2011;66:924–6.
Brown C, Hennings J, Caress AL, Partridge MR. Lay educators in asthma self management: reflections on their training and experiences. Pat Educ Couns 2007;68:131–8.
Brown ECF, Little P, Leydon GM. Communication challenges of HPV vaccination. Fam Pract 2010;27:224–9.
Brown K, Dormandy E, Reid E, Gulliford M, Marteau T. Impact on informed choice of offering antenatal sickle cell and thalassaemia screening in primary care: a randomized trial. J Med Screen 2011;18:65–75.
Brown KF, Long SJ, Ramsay M, Hudson MJ, Green J, Vincent CA, et al. UK parents’ decision-making about measles-mumps-rubella (MMR) vaccine 10 years after the MMR-autism controversy: a qualitative analysis. Vaccine 2012;30:1855–64.
Bryan S, Dormandy E, Roberts T, Ades A, Barton P, Juarez-Garcia A, et al. Screening for sickle cell and thalassaemia in primary care: a cost-effectiveness study. Br J Gen Pract 2011;61:e620–7.
Bull L. Smoking cessation intervention with pregnant women and new parents (part 2): a focus group study of health visitors and midwives working in the UK. J Neonatal Nurs 2007;13:179–85.
Burke D, Jennings M, McClinchy J, Masey H, Westwood D, Dickinson A. Community luncheon clubs benefit the nutritional and social well-being of free living older people. J Hum Nutr Diet 2011;24:278.
Burns VE, Ring C, Carroll D. Factors influencing influenza vaccination uptake in an elderly, community-based sample. Vaccine 2005;23:3604–8.
Burrows J, Baxter S, Baird W, Hirst J, Goyder E. Citizens advice in primary care: a qualitative study of the views and experiences of service users and staff. Public Health 2011;125:704–10.
Burt S, Whitmore M, Vearncombe D, Dykes F. The development and delivery of a practice-based breastfeeding education package for general practitioners in the UK. Matern Child Nutr 2006;2:91–102.
Buszewicz M, Rait G, Griffin M, Nazareth I, Patel A, Atkinson A, et al. Self management of arthritis in primary care: randomised controlled trial. BMJ 2006;333:879.
Cade JE, Kirk SFL, Nelson P, Hollins L, Deakin T, Greenwood DC, et al. Can peer educators influence healthy eating in people with diabetes? Results of a randomized controlled trial. Diabet Med 2009;26:1048–54.
Calvert MJ, McManus RJ, Freemantle N. The management of people with type 2 diabetes with hypoglycaemic agents in primary care: retrospective cohort study. Fam Pract 2007;24:224–9.
Campbell H, MacDonald S, McKiernan M. Promotion of cervical screening uptake by health visitor follow-up of women who repeatedly failed to attend. J Public Health Med 1996;18:94–7.
Campbell NC, Ritchie LD, Thain J, Deans HG, Rawles JM, Squair JL. Secondary prevention in coronary heart disease: a randomised trial of nurse led clinics in primary care. Heart 1998;80:447–52.
Campbell SM, Ludt S, Van Lieshout J, Boffin N, Wensing M, Petek D, et al. Quality indicators for the prevention and management of cardiovascular disease in primary care in nine European countries. Eur J Cardiovasc Prev Rehabil 2008;15:509–15.
Candy B, Taylor SJC, Ramsay J, Esmond G, Griffiths CJ, Bryar RM. Service implications from a comparison of the evidence on the effectiveness and a survey of provision in England and Wales of COPD specialist nurse services in the community. Int J Nurs Stud 2007;44:601–10.
Carey N, Courtenay M. Service delivery by nurse prescribers for diabetes care. Nurse Prescribing 2007;5:443–9.
Carlisle J, Lawton J, Goyder E, Peters J, Lacey EA. The role of healthcare assistants in screening for diabetes: a qualitative study. Qual Prim Care 2007;15:77–83.
Carnegie E, Kiger A. Developing the community environmental health role of the nurse. Br J Community Nurs 2010;15:298–305.
Carr S, Lhussier M, Forster N, Geddes L, Deane K, Pennington M, et al. An evidence synthesis of qualitative and quantitative research on component intervention techniques, effectiveness, cost-effectiveness, equity and acceptability of different versions of health-related lifestyle advisor role in improving health. Health Technol Assess 2011;15(9).
Caswell S, Anderson AS, Steele RJ. Bowel health to better health: a minimal contact lifestyle intervention for people at increased risk of colorectal cancer. Br J Nutr 2009;102:1541–6.
Chambers R, Chambers C, Campbell I. Exercise promotion for patients with significant medical problems. Health Educ J 2000;59:90–8.
Chapple A, Ziebland S, Hewitson P, McPherson A. What affects the uptake of screening for bowel cancer using a faecal occult blood test (FOBt): a qualitative study. Soc Sci Med 2008;66:2425–35.
Chauhan U, Kontopantelis E, Campbell S, Jarrett H, Lester H. Health checks in primary care for adults with intellectual disabilities: how extensive should they be? J Intellect Disabil Res 2010;54:479–86.
Chew-Graham C, Mole E, Evans L-J, Rogers A. Informed consent? How do primary care professionals prepare women for cervical smears: a qualitative study. Pat Educ Couns 2006;61:381–8.
Chiu LF, West RM. Health intervention in social context: understanding social networks and neighbourhood. Soc Sci Med 2007;65:1915–27.
Clamp M, Kendrick D. A randomised controlled trial of general practitioner safety advice for families with children under 5 years. BMJ 1998;316:1576–9.
Clark CE, Smith LFP, Taylor RS, Campbell JL. Nurse led interventions to improve control of blood pressure in people with hypertension: systematic review and meta-analysis. BMJ 2010;341:491.
Clark EM, Gould V, Morrison L, Ades AE, Dieppe P, Tobias JH. Randomized controlled trial of a primary care-based screening program to identify older women with prevalent osteoporotic vertebral fractures: Cohort for Skeletal Health in Bristol and Avon (COSHIBA). J Bone Miner Res 2012;27:664–71.
Cochrane T, Davey RC. Increasing uptake of physical activity: a social ecological approach. J R Soc Promot Health 2008;128:31–40.
Cockman P, Dawson L, Mathur R, Hull S. Improving MMR vaccination rates: herd immunity is a realistic goal. BMJ 2011;343:d5703.
Coleman T, Lewis S, Hubbard R, Smith C. Impact of contractual financial incentives on the ascertainment and management of smoking in primary care. Addiction 2007;102:803–8.
Coleman T, Wilson A, Barrett S, Wynne A, Lewis S. Distributing questionnaires about smoking to patients: impact on general practitioners’ recording of smoking advice. BMC Health Serv Res 2007;7:153.
Coleman T, Wynn AT, Barrett S, Wilson A, Adams S. Intervention study to evaluate pilot health promotion payment aimed at increasing general practitioners' antismoking advice to smokers. BMJ 2001;323:435–6.
Coleman T, Wynn AT, Stevenson K, Cheater F. Qualitative study of pilot payment aimed at increasing general practitioners’ antismoking advice to smokers. BMJ 2001;323:432–5.
Condon L. Do targeted child health promotion services meet the needs of the most disadvantaged? A qualitative study of the views of health visitors working in inner-city and urban areas in England. J Adv Nurs 2011;67:2209–19.
Connolly S, Holden A, Turner E, Fiumicelli G, Stevenson J, Hunjan M, et al. MyAction: an innovative approach to the prevention of cardiovascular disease in the community. Br J Cardiol 2011;18:171–6.
Copeland L, Robertson R, Elton R. What happens when GPs proactively prescribe NRT patches in a disadvantaged community. Scott Med J 2005;50:64–8.
Copello A, Templeton L, Orford J, Velleman R, Patel A, Moore L, et al. The relative efficacy of two levels of a primary care intervention for family members affected by the addiction problem of a close relative: a randomized trial. Addiction 2009;104:49–58.
Coppel DH, Packham CJ, Varnam MA. Providing welfare rights advice in primary care. Public Health 1999;113:131–5.
Counterweight Project, McQuigg M, Brown JE, Broom JI, Laws RA, Reckless JPD, et al. Engaging patients, clinicians and health funders in weight management: the Counterweight Programme. Fam Pract 2008;25:i79–86.
Cowley S, Caan W, Dowling S, Weir H. What do health visitors do? A national survey of activities and service organisation. Public Health 2007;121:869–79.
Craigie AM, Barton KL, Macleod M, Williams B, van Teijlingen E, Belch JJ, et al. A feasibility study of a personalised lifestyle programme (HealthForce) for individuals who have participated in cardiovascular risk screening. Prev Med 2011;52:387–9.
Crilly M, Bundred P, Hu X, Leckey L, Johnstone F. Gender differences in the clinical management of patients with angina pectoris: a cross-sectional survey in primary care. BMC Health Services Res 2007;7:142.
Dabrera G, Pinson D, Whiteman S. Chlamydia screening by community pharmacists: a qualitative study. J Fam Plann Reprod Health Care 2011;37:17–21.
Dale J, Caramlau I, Sturt J, Friede T, Walker R. Telephone peer-delivered intervention for diabetes motivation and support: the telecare exploratory RCT. Pat Educ Couns 2009;75:91–8.
Daley A, Jolly K, MacArthur C. The effectiveness of exercise in the management of post-natal depression: systematic review and meta-analysis. Fam Pract 2009;26:154–62.
Dalia D, Palmer RM, Wilson RF. Management of smoking patients by specialist periodontists and hygienists in the United Kingdom. J Clin Periodontol 2007;34:416–22.
Davies JA, Damani P, Margetts BM. Intervening to change the diets of low-income women. Proc Nutr Soc 2009;68:210–15.
Daykin N, Naidoo J. Poverty and health promotion in primary health care: professionals’ perspectives. Health Soc Care Community 1997;5:309–17.
Deakin TA, Cade JE, Williams R, Greenwood DC. Structured patient education: the diabetes X-PERT Programme makes a difference. Diabet Med 2006;23:944–54.
Dickinson A, Horton K, Machen I, Bunn F, Cove J, Deepak J, et al. The role of health professionals in promoting the uptake of fall prevention interventions: a qualitative study of older people’s views. Age Ageing 2011;40:724–30.
Dinan S, Lenihan P, Tenn T, Iliffe S. Is the promotion of physical activity in vulnerable older people feasible and effective in general practice? Br J Gen Pract 2006;56:791–3.
Dixon A, Khachatryan A, Gilmour S. Does general practice reduce health inequalities? Analysis of quality and outcomes framework data. Eur J Public Health 2012;22;9–13.
Donyai P. Coronary heart disease risk screening: the community pharmacy Healthy Heart Assessment Service. Pharm World Sci 2009;31:643–7.
Dowell AC, Ochera JJ, Hilton SR, Bland JM, Harris T, Jones DR, et al. Prevention in practice: results of a 2-year follow-up of routine health promotion interventions in general practice. Fam Pract 1996;13:357–62.
Drennan V, Iliffe S, Haworth D, Tai SS, Lenihan P, Deave T. The feasibility and acceptability of a specialist health and social care team for the promotion of health and independence in ‘at risk’ older adults. Health Soc Care Community 2005;13:136–44.
Drennan V, Iliffe S, Tai SS, Lenihan P, Deave T. Can primary care identify an ‘at risk’ group in the older population. Br J Community Nurs 2007;12:142–8.
Dugdill L, Graham RC, McNair F. Exercise referral: the public health panacea for physical activity promotion? A critical perspective of exercise referral schemes; their development and evaluation. Ergon 2005;48:1390–410.
Dunkley A, Stone M, Squire I, Johnson T, Farooqi A, Khunti K. An audit of secondary prevention of coronary heart disease in post acute myocardial infarction patients in primary care. Qual Prim Care 2006;14:15–20.
Eborall H, Stone M, Aujla N, Taub N, Khunti K, Davies M. Influences on the uptake of diabetes screening: a qualitative study in primary care. Br J Gen Pract 2012;62:e204–11.
Egred M, Corr L. Establishment and feasibility of community-based general-practitioner-led cardiology clinics. Q J Med 2002;95:299–303.
Eilbert KW, Carroll K, Peach J, Khatoon S, Basnett I, McCulloch N. Approaches to improving breast screening uptake: evidence and experience from Tower Hamlets. Br J Cancer 2009;101:S64–S67.
Emmett CL, Redmond NM, Peters TJ, Clarke S, Shepstone L, Lenaghan E, et al. Acceptability of screening to prevent osteoporotic fractures: a qualitative study with older women. Fam Pract 2012;29:235–42.
Emond A, Pollock J, Deave T, Bonnell S, Peters TJ, Harvey I. An evaluation of the First Parent Health Visitor Scheme. Arch Dis Child 2002;86:150–7.
Evans MR, Prout H, Prior L, Tapper-Jones LM, Butler CC. A qualitative study of lay beliefs about influenza immunisation in older people. Br J Gen Pract 2007;57:352–8.
Fagan DM, Kiger A, Teijlingen E. A survey of faith leaders concerning health promotion and the level of healthy living activities occurring in faith communities in Scotland. Glob Health Promot 2010;17:15–23.
Farmer J, Iversen L, Peterkin G, Strachan P, Kelman H, Proctor K, et al. Acceptability and uptake of a community-based flu immunisation programme. Health Bull 2001;59:127–35.
Feder G, Davies RA, Baird K, Dunne D, Eldridge S, Griffiths C, et al. Identification and Referral to Improve Safety (IRIS) of women experiencing domestic violence with a primary care training and support programme: a cluster randomised controlled trial. Lancet 2011;378:1788–95.
Felce D, Baxter H, Lowe K, Dunstan F, Houston H, Jones G, et al. The impact of checking the health of adults with intellectual disabilities on primary care consultation rates, health promotion and contact with specialists. J Appl Res Intellect Disabil 2008;21:597–602.
Fisher B, Dowding D, Pickett KE, Fylan F. Health promotion at NHS breast cancer screening clinics in the UK. Health Promot Int 2007;22:137–45.
Foster G, Taylor SJ, Eldridge SE, Ramsay J, Griffiths CJ. Self-management education programmes by lay leaders for people with chronic conditions. Cochrane Database Syst Rev 2007;4;CD005108.
Foster JM, Hoskins G, Smith B, Lee AJ, Price D, Pinnock H. Practice development plans to improve the primary care management of acute asthma: randomised controlled trial. BMC Fam Pract 2007;8:23.
Gask L, Dixon C, May C, Dowrick C. Qualitative study of an educational intervention for GPs in the assessment and management of depression. Br J Gen Pract, 2005;55:854–9.
Gibbs HD, Broom J, Brown J, Laws RA, Reckless JPD, Noble PA, et al. Current approaches to obesity management in UK primary care: the Counterweight programme. J Hum Nutr Diet 2004;17:183–90.
Gilbert H, Nazareth I, Sutton S. Assessing the feasibility of proactive recruitment of smokers to an intervention in general practice for smoking cessation using computer-tailored feedback reports. Fam Pract 2007;24:395–400.
Gillam S, Joffe M, Miller R, Gray A, Epstein L, Plamping D. Community-oriented primary care: old wine in new bottles. J Interprof Care 1998;12:53–61.
Gillespie P, O’Shea E, Murphy AW, Byrne MC, Byrne M, Smith SM, et al. The cost-effectiveness of the SPHERE intervention for the secondary prevention of coronary heart disease. Int J Technol Assess Health Care 2010;26:263–71.
Glazebrook C, Garrud P, Avery A, Coupland C, Williams H. Impact of a multimedia intervention ‘Skinsafe’ on patients’ knowledge and protective behaviors. Prev Med 2006;42:449–54.
Goldsmith MR, Austoker J, Marsh G, Kehoe ST, Bankhead CR. Cervical screening result communication: a focus-group investigation of English women’s experiences and needs. Qual Saf Health Care 2008;17:334–8.
Gordon J, Dibble T, Adams C, McGee E. An evaluation of the long-term effectiveness of two adult community-based group weight management interventions. J Hum Nutr Diet 2011;24:388.
Goudie BM, Jarvis RI, Donnan PT, Sullivan FM, Pringle SD, Jeyaseelan S, et al. Screening for left ventricular systolic dysfunction using GP-reported ECGs. Br J Gen Pract 2007;57:191–5.
Goyder E, Carlisle J, Lawton J, Peters J. Informed choice and diabetes screening in primary care: qualitative study of patient and professional views in deprived areas of England. Prim Care Diabet 2009;3:85–90.
Goyder E, Wild S, Fischbacher C, Carlisle J, Peters J. Evaluating the impact of a national pilot screening programme for type 2 diabetes in deprived areas of England. Fam Pract 2008;25:370–5.
Graffy J, Grant J, Williams K, Cohn S, Macbay S, Griffin S, et al. More than measurement: practice team experiences of screening for type 2 diabetes. Fam Pract 2010;27:386–94.
Graffy J, Taylor J, Williams A, Eldridge S. Randomised controlled trial of support from volunteer counsellors for mothers considering breast feeding. BMJ 2004;328:26.
Graham RC, Dugdill L, Cable NT. Health professionals' perspectives in exercise referral: implications for the referral process. Ergon 2005;48:1411–22.
Graham RC, Dugdill L, Cable NT. Health practitioner perspectives in exercise referral: implications for the referral process. J Sports Sci 2006;24;636–7.
Greasley P. Welfare advice in general practice: a resource for community nurses. Br J Community Nurs 2005;10:368–72.
Greaves CJ, Middlebrooke A, O’Loughlin L, Holland S, Piper J, Steele A, et al. Motivational interviewing for modifying diabetes risk: a randomised controlled trial. Br J Gen Pract 2008;58:535–40.
Green SM, McCoubrie M, Cullingham C. Practice nurses’ and health visitors’ knowledge of obesity assessment and management. J Hum Nutr Diet 2000;13:413–23.
Griffin SJ, Borch-Johnsen K, Davies MJ, Khunti K, Rutten GE, Sandbæk A, et al. Effect of early intensive multifactorial therapy on 5-year cardiovascular outcomes in individuals with type 2 diabetes detected by screening (ADDITION-Europe): a cluster-randomised trial. Lancet 2011;378:156–67.
Griffiths C, Sturdy P, Brewin P, Bothamley G, Eldridge S, Martineau A, et al. Educational outreach to promote screening for tuberculosis in primary care: a cluster randomised controlled trial. Lancet 2007;369:1528–34.
Hall S, Marteau TM. Practice nurses’ self-reported opportunistic smoking cessation advice in three contexts. Nicotine Tob Res 2007;9:941–5.
Hall S, Vogt F, Marteau TM. A short report: survey of practice nurses' attitudes towards giving smoking cessation advice. Fam Pract 2005;22:614–16.
Hallam A. The effectiveness of interventions to address health inequalities during pregnancy: a review of relevant literature. Curr Womens Health Rev 2008;4:162–71.
Hampshire AJ, Blair ME, Crown NS, Avery AJ, Williams EI. Assessing the quality of preschool child health surveillance in primary care: a pilot study in one health district. Child Care Health Dev 2002;28:239–49.
Harari D, Iliffe S, Kharicha K, Egger M, Gillmann G, Renteln-Kruse W, et al. Promotion of health in older people: a randomised controlled trial of health risk appraisal in British general practice. Age Ageing 2008;37:565–71.
Harding R, Sherr L, Sherr A, Moorhead R, Singh S. Welfare rights advice in primary care: prevalence, processes and specialist provision. Fam Pract 2003;20:48–53.
Harding R, Sherr L, Singh S, Sherr A, Moorhead R. Evaluation of welfare rights advice in primary care: the general practice perspective. Health Soc Care Community 2002;10:417–22.
Harding S. Dietitians in primary care promote weight loss and glycated haemoglobin reductions. J Hum Nutr Diet 2011;24:389–90.
Harland J, White M, Drinkwater C, Chinn D, Farr L, Howel D. The Newcastle exercise project: a randomised controlled trial of methods to promote physical activity in primary care. BMJ 1999;319:828–32.
Harris DI. Implementation of chlamydia screening in a general practice setting: a 6-month pilot study. J Fam Plann Reprod Health Care 2005;31:109–12.
Harris H, Scotcher D, Hartley N, Wallace A, Craufurd D, Harris R. Pilot study of the acceptability of cystic fibrosis carrier testing during routine antenatal consultations in general practice. Br J Gen Pract 1996;46:225–7.
Harris TJ, Carey IM, Victor CR, Adams R, Cook DG. Optimising recruitment into a study of physical activity in older people: a randomised controlled trial of different approaches. Age Ageing 2008;37:659–65.
Hart AR, Barone TL, Gay SP, Inglis A, Griffin L, Tallon CA, et al. The effect on compliance of a health education leaflet in colorectal cancer screening in general practice in central England. J Epidemiol Community Health 1997;51:187–91.
Herbert R, Coleman T, Britton J. U.K. general practitioners’ beliefs, attitudes, and reported prescribing of nicotine replacement therapy in pregnancy. Nicotine Tob Res 2005;7:541–6.
Hewitson P, Ward AM, Heneghan C, Halloran SP, Mant D. Primary care endorsement letter and a patient leaflet to improve participation in colorectal cancer screening: results of a factorial randomised trial. Br J Cancer 2011;105:475–80.
Hickling J, Rogers S, Nazareth I. Barriers to detecting and treating hypercholesterolaemia in patients with ischaemic heart disease: primary care perceptions. Br J Gen Pract 2005;55:534–8.
Hillsdon M. Promoting physical activity: issues in primary health care. Int J Obes Relat Metab Disord 1998;22:S52–4.
Hilton S, Hunt K, Bedford H, Petticrew M. School nurses’ experiences of delivering the UK HPV vaccination programme in its first year. BMC Infect Dis 2011;11:226.
Hobbs FDR, Erhardt L. Acceptance of guideline recommendations and perceived implementation of coronary heart disease prevention among primary care physicians in five European countries: the Reassessing European Attitudes about Cardiovascular Treatment (REACT) survey. Fam Pract 2002;19:596–604.
Hoddinott P, Britten J, Pill R. Why do interventions work in some places and not others: a breastfeeding support group trial. Soc Sci Med 2010;70:769–78.
Hoddinott P, Britten J, Prescott GJ, Tappin D, Ludbrook A, Godden DJ. Effectiveness of policy to provide breastfeeding groups (BIG) for pregnant and breastfeeding mothers in primary care: cluster randomised controlled trial. BMJ 2009;338:a3026.
Hoddinott P, Pill R, Chalmers M. Health professionals, implementation and outcomes: reflections on a complex intervention to improve breastfeeding rates in primary care. Fam Pract 2007;24:84–91.
Hogan AH, Howell-Jones RS, Pottinger E, Wallace LM, McNulty CA. ‘. . . They should be offering it’: a qualitative study to investigate young people’s attitudes towards chlamydia screening in GP surgeries. BMC Public Health 2010;10:616.
Holden J, Tatham D, Wooff E. Delay pattern analysis of 368 patients with alcohol problems in one general practice. Eur J Gen Pract 2007;13:55–9.
Holt TA, Thorogood M, Griffiths F, Munday S, Friede T, Stables D. Automated electronic reminders to facilitate primary cardiovascular disease prevention: randomised controlled trial. Br J Gen Pract 2010;60:e137–43.
Hoskins RA, Smith LN. Nurse-led welfare benefits screening in a general practice located in a deprived area. Public Health 2002;116:214–20.
Howse JH, Jones S, Hungin AP. Screening and identifying diabetes in optometric practice: a prospective study. Br J Gen Pract 2011;61:436–42.
Howse JH, Jones S, Hungin AP. Screening for diabetes in unconventional locations: resource implications and economics of screening in optometry practices. Health Policy 2011;102:193–9.
Hughes AR, McLaughlin R, McKay J, Lafferty K, McKay T, Mutrie N. The B’Active programme for overweight primary school children in Glasgow: determining the prevalence of overweight and obesity and piloting an activity intervention. Br J Nutr 2007;97:204–9.
Hull S, Hagdrup N, Hart B, Griffiths C, Hennessy E. Boosting uptake of influenza immunisation: a randomised controlled trial of telephone appointing in general practice. Br J Gen Pract 2002;52:712–16.
Hunter D, McCartney G, Fleming S, Guy F. Improving the health of looked after children in Scotland: 2. The views of residential care workers on the promotion of health and well-being of the children they care for. Adoption Fostering 2008;32:57–63.
Hunter M, O’Dea I. An evaluation of a health education intervention for mid-aged women: five year follow-up of effects upon knowledge, impact of menopause and health. Pat Educ Couns 1999;38:249–55.
Ibbotson T, Wyke S, McEwen J, Macintyre S, Kelly M. Uptake of cervical screening in general practice: effect of practice organisation, structure, and deprivation. J Med Screen 1996;3:35–9.
Inskip HM, Crozier SR, Godfrey KM, Borland SE, Cooper C, Robinson SM, et al. Women’s compliance with nutrition and lifestyle recommendations before pregnancy: general population cohort study. BMJ 2009;338:b481.
Irvine L, Crombie IK, Clark RA, Slane PW, Feyerabend C, Goodman KE, et al. Advising parents of asthmatic children on passive smoking: randomised controlled trial. BMJ 1999;318:1456–9.
Jackson C, Cheater FM, Harrison W, Peacock R, Bekker H, West R, et al. Randomised cluster trial to support informed parental decision-making for the MMR vaccine. BMC Public Health 2011;11:475.
James JA, Laing GJ, Logan S, Rossdale M. Feasibility of screening toddlers for iron deficiency anaemia in general practice. BMJ 1997;315:102–3.
Jarvis A, McIntosh G. Carers' health clinic initiative in Edinburgh: pilot evaluation. Br J Community Nurs 2007;12:416–21.
Jebb SA, Ahern AL, Olson AD, Aston LM, Holzapfel C, Stoll J, et al. Primary care referral to a commercial provider for weight loss treatment versus standard care: a randomised controlled trial. Lancet 2011;378:1485–92.
Jit M, Aveyard P, Barton P, Meads CA. Predicting the life-time benefit of school-based smoking prevention programmes. Addiction 2010;105:1109–16.
Johnstone E, Hey K, Drury M, Roberts S, Welch S, Walton R, et al. Zyban for smoking cessation in a general practice setting: the response to an invitation to make a quit attempt. Addict Biol 2004;9:227–32.
Johnstone R, Nicol K, Donaghy M, Lawrie S. Barriers to uptake of physical activity in community-based patients with schizophrenia. J Ment Health 2009;18:523–32.
Jolly K, Lewis A, Beach J, Denley J, Adab P, Deeks JJ, et al. Comparison of range of commercial or primary care led weight reduction programmes with minimal intervention control for weight loss in obesity: Lighten Up randomised controlled trial. BMJ 2011;343:d6500.
Jones BJ, Mitra S, Price HC, Stratton IM. Factors affecting uptake of retinal screening in primary care. Diabet Med 2011;28:190.
Joshi UY, Dixon W. General practitioners’ views on the screening for genital Chlamydia trachomatis infection and partner notification. Int J STD AIDS 2000;11:588–91.
Joyce KE, Smith KE, Henderson G, Greig G, Bambra C. Patient perspectives of Condition Management Programmes as a route to better health, well-being and employability. Fam Pract 2010;27:101–9.
Kane K. Case-finding in the community: the results 2. Br J Community Nurs 2008;13:265–9.
Kaner E, Lock C, Heather N, McNamee P, Bond S. Promoting brief alcohol intervention by nurses in primary care: a cluster randomised controlled trial. Pat Educ Couns 2003;51:277–84.
Kaner EF, Heather N, Brodie J, Lock CA, McAvoy BR. Patient and practitioner characteristics predict brief alcohol intervention in primary care. Br J Gen Pract 2001;51:822–7.
Kaner EF, Lock CA, McAvoy BR, Heather N, Gilvarry E. A RCT of three training and support strategies to encourage implementation of screening and brief alcohol intervention by general practitioners. Br J Gen Pract 1999:49:699–703.
Keenan H, Campbell J, Evans PH. Influenza vaccination in patients with asthma: why is the uptake so low? Br J Gen Pract 2007;57:359–63.
Kendrick D, Marsh P. Injury prevention programmes in primary care: a high risk group or a whole population approach? Inj Prev 1997;3:170–5.
Kendrick D, Marsh P, Fielding K, Miller P. Preventing injuries in children: cluster randomised controlled trial in primary care. BMJ 1999;318:980–3.
Kenkre JE, Allan TF, Tobias RS, Parry DJ, Bryan S, Carter YH. Breaking bones, breaking budgets: a clinical and economic evaluation of a prospective, randomized, practice controlled, intervention study in the prevention of accidents in primary care. Fam Pract 2002;19:675–81.
Kennedy L. Benefits arising from lay involvement in community-based public health initiatives: the experience from community nutrition. Perspect Public Health 2010;130:165–72.
Kerr S, Whyte R, Watson H, Tolson D, McFadyen AK. A mixed-methods evaluation of the effectiveness of tailored smoking cessation training for healthcare practitioners who work with older people. Worldviews Evid Based Nurs 2011;8:177–86.
Kharicha K, Iliffe S, Harari D, Swift CG, Goodman C, Manthorpe J, et al. Feasibility of repeated use of the Health Risk Appraisal for Older people system as a health promotion tool in community-dwelling older people: retrospective cohort study 2001–05. Age Ageing 2012;41:128–31.
Khunti K, Stone M, Paul S, Baines J, Gisborne L, Farooqi A, et al. Disease management programme for secondary prevention of coronary heart disease and heart failure in primary care: a cluster randomised controlled trial. Heart 2007;93:1398–405.
Khunti K, Taub N, Webb D, Srinivasan B, Stockman J, Griffin SJ, et al. Validity of self-assessed waist circumference in a multi-ethnic UK population. Diabet Med 2012;29:404–9.
Kinmonth A-L, Wareham NJ, Hardeman W, Sutton S, Prevost AT, Fanshawe T, et al. Efficacy of a theory-based behavioural intervention to increase physical activity in an at-risk group in primary care (ProActive UK): a randomised trial. Lancet 2008;371:41–8.
Kiran T, Hutchings A, Dhalla IA, Furlong C, Jacobson B. The association between quality of primary care, deprivation and cardiovascular outcomes: a cross-sectional study using data from the UK Quality and Outcomes Framework. J Epidemiol Community Health 2010;64:927–34.
Kirkcaldy AJ, Robinson JE, Perkins ES, Forrest D. Older men's experiences of community-based health checks in Knowsley, UK. Global Public Health 2011;6:15–27.
Knussen C, Bingham D, Flowers P. The acceptability of health service and community-based venues for syphilis testing amongst men who have sex with men: the views of potential service users in Scotland. Public Health 2008;122:959–61.
Koopman J, Davey E, Thomas N, Wittkop T, Verschuure H. How should hearing screening tests be offered? Int J Audiol 2008;47:230–7.
Kumar J, Chambers R, Mawby Y, Leese C, Iqbal Z, Picariello L, et al. Delivering more with less? Making the NHS Health Check work in financially hard times: real time learning from Stoke-on-Trent. Qual Prim Care 2011;19:193–9.
Kyaw MH, Nguyen-Van-Tam JS, Pearson JC. Family doctor advice is the main determinant of pneumococcal vaccine uptake. J Epidemiol Community Health 1999;53:589–90.
Lamb SE, Bartlett HP, Ashley A, Bird W. Can lay-led walking programmes increase physical activity in middle aged adults? A randomised controlled trial. J Epidemiol Community Health 2002;56:246–52.
Lambert AM, Burden AC, Chambers J, Marshall T. Cardiovascular screening for men at high risk in Heart of Birmingham Teaching Primary Care Trust: the ‘Deadly Trio’ programme. J Public Health (Oxf) 2012;34:73–82.
Lamden KH, Gemmell I. General practice factors and MMR vaccine uptake: structure, process and demography. J Public Health (Oxf) 2008;30:251–7.
Lancaster T, Dobbie W, Vos K, Yudkin P, Murphy M, Fowler G. Randomized trial of nurse-assisted strategies for smoking cessation in primary care. Br J Gen Pract 1999;49:191–4.
Langham S, Thorogood M, Normand C, Muir J, Jones L, Fowler G. Costs and cost effectiveness of health checks conducted by nurses in primary care: the OXCHECK study. BMJ 1996;312:1265–8.
Lawlor DA, Hanratty B. The effect of physical activity advice given in routine primary care consultations: a systematic review. J Public Health Med 2001;23:219–26.
Laws R, Counterweight Project. A new evidence-based model for weight management in primary care: the Counterweight Programme. J Hum Nutr Diet 2004;17:191–208.
Lennox AS, Osman LM, Reiter E, Robertson R, Friend J, McCann I, et al. Cost effectiveness of computer tailored and non-tailored smoking cessation letters in general practice: randomised controlled trial. BMJ 2001;322:1396–400.
Levine AP, Mikhailidis DP, Moross T, Benson K, Gor M. Achieving vascular risk factor targets: a survey of a London general practice. Angiology 2008;59:36–46.
Litchfield J, Maronge A, Rigg T, Rees B, Harshey R, Keen J. Can a targeted GP-led clinic improve outcomes for street sex workers who use heroin? Br J Gen Pract 2010;60:514–16.
Little P, Kelly J, Barnett J, Dorward M, Margetts B, Warm D. Randomised controlled factorial trial of dietary advice for patients with a single high blood pressure reading in primary care. BMJ 2004;328:1054–7.
Logan L, McIlfatrick S. Exploring women's knowledge, experiences and perceptions of cervical cancer screening in an area of social deprivation. Eur J Cancer Care (Engl) 2011;20:720–7.
Lord J, Victor C, Littlejohns P, Ross FM, Axford JS. Economic evaluation of a primary care-based education programme for patients with osteoarthritis of the knee. Health Technol Assess 1999;3(23).
Low N, McCarthy A, Roberts TE, Huengsberg M, Sanford E, Sterne JAC, et al. Partner notification of chlamydia infection in primary care: randomised controlled trial and analysis of resource use. BMJ 2006;332:14–19.
Lowther M, Mutrie N, Scott EM. Promoting physical activity in a socially and economically deprived community: a 12 month randomized control trial of fitness assessment and exercise consultation. J Sports Sci 2002;20:577–88.
Lyte G, Milnes L, Keating P, Finke A. Review management for children with asthma in primary care: a qualitative case study. J Nurs Healthc Chronic Illn 2007;16:123–32.
Ma R, Clark A. Chlamydia screening in general practice: views of professionals on the key elements of a successful programme. J Fam Plann Reprod Health Care 2005;31:302–6.
Macpherson LM, McCann MF, Gibson J, Binnie VI, Stephen KW. The role of primary healthcare professionals in oral cancer prevention and detection. Br Dent J 2003;195:277–81.
Maguire TA, McElnay JC, Drummond A. A randomized controlled trial of a smoking cessation intervention based in community pharmacies. Addiction 2001;96:325–31.
Malin N, Morrow G. Evaluating the role of the Sure Start Plus Adviser in providing integrated support for pregnant teenagers and young parents. Health Soc Care Community 2009;17:495–503.
Mant J. Secondary prevention of coronary heart disease in primary care: the evidence. Br J Cardiol 2002;9:S6–10.
Marks L, Cave S, Wallace A, Mason A, Hunter DJ, Mason JM, et al. Incentivizing preventive services in primary care: perspectives on Local Enhanced Services. J Public Health (Oxf) 2011;33:556–64.
Marshall D, McConkey R, Moore G. Obesity in people with intellectual disabilities: the impact of nurse-led health screenings and health promotion activities. J Adv Nurs 2003;41:147–53.
Marshall T, Rouse A. Resource implications and health benefits of primary prevention strategies for cardiovascular disease in people aged 30 to 74: mathematical modelling study. BMJ 2002;325:197–202.
Marteau TM, Mann E, Prevost AT, Vasconcelos JC, Kellar I, Sanderson S, et al. Impact of an informed choice invitation on uptake of screening for diabetes in primary care (DICISION): randomised trial. BMJ 2010;340:c2138.
Mathews G, Alexander J, Rahemtulla T, Raj B. Impact of a cardiovascular risk control project for South Asians (Khush Dil) on motivation, behaviour, obesity, blood pressure and lipids. J Public Health (Oxf) 2007;29:388–97.
McCluskey S, Baker D, Percy D, Lewis P, Middleton E. Reductions in cardiovascular risk in association with population screening: a 10-year longitudinal study. J Public Health (Oxf) 2007;29:379–87.
McCormick R, Docherty B, Segura L, Colom J, Gual A, Cassidy P, et al. The research translation problem: alcohol screening and brief intervention in primary care - Real world evidence supports theory. Drugs Educ Prev Policy 2010;17:732–48.
McDonald P, Friedman EH, Banks A, Anderson R, Carman V. Pneumococcal vaccine campaign based in general practice. BMJ 1997;314:1094–8.
McDonald R, Campbell S, Lester H. Practice nurses and the effects of the new general practitioner contract in the English National Health Service: the extension of a professional project? Soc Sci Med 2009;68:1206–12.
McEwen A, Akotia N, West R. General practitioners’ views on the English national smoking cessation guidelines. Addiction 2001;96:997–1000.
McEwen A, West R. Smoking cessation activities by general practitioners and practice nurses. Tob Control 2001;10:27–32.
McIlfatrick S, Taggart L, Truesdale-Kennedy M. Supporting women with intellectual disabilities to access breast cancer screening: a healthcare professional perspective. Eur J Cancer Care (Engl) 2011;20:412–20.
McInnes RJ, Stone DH. The process of implementing a community-based peer breast-feeding support programme: the Glasgow experience. Midwifery 2001;17:65–73.
McIntosh J, Shute J. The process of health visiting and its contribution to parental support in the Starting Well demonstration project. Health Soc Care Community 2007;15:77–85.
McKay J, Wright A, Lowry R, Steele K, Ryde G, Mutrie N. Walking on prescription: the utility of a pedometer pack for increasing physical activity in primary care. Pat Educ Couns 2009;76:71–6.
McKenna J, Vernon M. How general practitioners promote ‘lifestyle’ physical activity. Pat Educ Couns 2004;54:101–6.
McMurdo MET, Sugden J, Argo I, Boyle P, Johnston DW, Sniehotta FF, et al. Do pedometers increase physical activity in sedentary older women? A randomized controlled trial. J Am Geriatr Soc 2010;58:2099–106.
McNaughton RJ, Oswald NTA, Shucksmith JS, Heywood PJ, Watson PS. Making a success of providing NHS Health Checks in community pharmacies across the Tees Valley: a qualitative study. BMC Health Serv Res 2011;11:222.
McNulty CAM, Freeman E, Bowen J, Shefras J, Fenton KA. Barriers to opportunistic chlamydia testing in primary care. Br J Gen Pract 2004;54:508–14.
McNulty CAM, Freeman E, Oliver I, Ford-Young W, Randall S. Strategies used to increase chlamydia screening in general practice: a qualitative study. Public Health 2008;122:845–56.
McNulty CAM, Thomas M, Bowen J, Buckley C, Charlett A, Gelb D, et al. Interactive workshops increase chlamydia testing in primary care: a controlled study. Fam Pract 2008;25:279–86.
McRobbie H, Hajek P, Feder G, Eldridge S. A cluster-randomised controlled trial of a brief training session to facilitate general practitioner referral to smoking cessation treatment. Tob Control 2008;17:173–6.
McWhirter J, McCann D, Coleman H, Calvert M, Warner J. Can schools promote the health of children with asthma? Health Educ Res 2008;23:917–30.
Misra A, Bachmann MO, Greenwood RH, Jenkins C, Shaw A, Barakat O, et al. Trends in yield and effects of screening intervals during 17 years of a large UK community-based diabetic retinopathy screening programme. Diabet Med 2009;26:1040–7.
Mitchell E. Prevention of falls in older people: the Weymouth and Portland project. Nurs Older People 2004;16:14–16.
Modell M, Wonke B, Anionwu E, Khan M, Tai SS, Lloyd M, et al. A multidisciplinary approach for improving services in primary care: randomised controlled trial of screening for haemoglobin disorders. BMJ 1998;317:788–91.
Moffat M, Cleland J, van der Molen T, Price D. Poor communication may impair optimal asthma care: a qualitative study. Fam Pract 2007;24:65–70.
Moher M, Yudkin P, Turner R, Schofield T, Mant D. An assessment of morbidity registers for coronary heart disease in primary care. ASSIST (ASSessment of Implementation STrategy) trial collaborative group. Br J Gen Pract 2000;50:706–9.
Moore H, Greenwood D, Gill T, Waine C, Soutter J, Adamson A. A cluster randomised trial to evaluate a nutrition training programme. Br J Gen Pract 2003;53:271–7.
Moore H, Summerbell CD, Greenwood DC, Tovey P, Griffiths J, Henderson M, et al. Improving management of obesity in primary care: cluster randomised trial. BMJ 2003;327:1085.
Morgan MZ, Evans MR. Initiatives to improve childhood immunisation uptake: a randomised controlled trial. BMJ 1998;316:1569–70.
Morgan S, Mant D. Randomised trial of two approaches to screening for atrial fibrillation in UK general practice. Br J Gen Pract 2002;52:373–480.
Morris S, Gravelle H. GP supply and obesity. J Health Econ 2008;27:1357–67.
Mountain G, Mozley C, Craig C, Ball L. Occupational therapy led health promotion for older people: feasibility of the Lifestyle Matters programme. Br J Occup Ther 2008;71:406–13.
Munro JF, Nicholl JP, Brazier JE, Davey R, Cochrane T. Cost effectiveness of a community based exercise programme in over 65 year olds: cluster randomised trial. J Epidemiol Community Health 2004;58:1004–10.
Murphy AW, Cupples ME, Smith SM, Byrne M, Byrne MC, Newell J. Effect of tailored practice and patient care plans on secondary prevention of heart disease in general practice: cluster randomised controlled trial. BMJ 2009;339:1186.
Murray J, Saxena S, Millett C, Curcin V, Lusignan S, Majeed A. Reductions in risk factors for secondary prevention of coronary heart disease by ethnic group in south-west London: 10-year longitudinal study (1998–2007). Fam Pract 2010;27:430–8.
Murray RL, Bauld L, Hackshaw LE, McNeill A. Improving access to smoking cessation services for disadvantaged groups: a systematic review. J Public Health (Oxf) 2009;31:258–77.
Murray RL, Coleman T, Antoniak M, Fergus A, Britton J, Lewis SA. The potential to improve ascertainment and intervention to reduce smoking in primary care: a cross sectional survey. BMC Health Serv Res 2008;8:6.
Nanchahal K, Power T, Holdsworth E, Hession M, Sorhaindo A, Townsend J, et al. Weight management in primary care: results from the Camden weight loss (Camwel) randomised controlled trial. Obes Rev 2011;12:60.
Ness AR, Ashfield-Watt PAL, Whiting JM, Smith GD, Hughes J, Burr ML. The long-term effect of dietary advice on the diet of men with angina: the diet and angina randomized trial. J Hum Nutr Diet 2004;17:117–19.
Nuttall D. The influence of health professionals on the uptake of the influenza immunization. Br J Community Nurs 2003;8:391–6.
Ohl M, Mitchell K, Cassidy T, Fox P. The Pyramid Club primary school-based intervention: evaluating the impact on children's social-emotional health. Child Adolesc Ment Health 2008;13:115–21.
O’Leary-Barrett M, Mackie CJ, Castellanos-Ryan N, Al-Khudhairy N, Conrod PJ. Personality-targeted interventions delay uptake of drinking and decrease risk of alcohol-related problems when delivered by teachers. J Am Acad Child Adolesc Psychiatry 2010;49:954–63.e1.
Packham C, Robinson J, Morris J, Richards C, Marks P, Gray D. Statin prescribing in Nottingham general practices: a cross-sectional study. J Public Health Med 1999;21:60–4.
Parkes G, Greenhalgh T, Griffin M, Dent R. Effect on smoking quit rate of telling patients their lung age: the Step2quit randomised controlled trial. BMJ 2008;336:598–600.
Patel JV, Gill PS, Chackathayil J, Ojukwu H, Stemman P, Sheldon L, et al. Short-term effects of screening for cardiovascular risk in the deaf community: a pilot study. Cardiol Res Pract 2011;2011:493546.
Patel JV, Gunarathne A, Lane D, Lim HS, Tracey I, Panja NC, et al. Widening access to cardiovascular healthcare: community screening among ethnic minorities in inner-city Britain – the Healthy Hearts Project. BMC Health Serv Res 2007;7:192.
Perkins E, Carlisle C, Jackson N. Opportunistic screening for chlamydia in general practice: the experience of health professionals. Health Soc Care Community 2003;11:314–20.
Pilnick A, Coleman T. ‘I'll give up smoking when you get me better’: patients’ resistance to attempts to problematise smoking in general practice (GP) consultations. Soc Sci Med 2003;57:135–45.
Pilnick A, Coleman T. Death, depression and ‘defensive expansion’: closing down smoking as an issue for discussion in GP consultations. Soc Sci Med 2006;62:2500–12.
Pilnick A, Coleman T. ‘Do your best for me’: the difficulties of finding a clinically effective endpoint in smoking cessation consultations in primary care. Health (Lond) 2010;14:57–74.
Pimenta JM, Catchpole M, Rogers PA, Perkins E, Jackson N, Carlisle C, et al. Opportunistic screening for genital chlamydial infection. I: Acceptability of urine testing in primary and secondary healthcare settings. Sex Transm Infect 2003;79:16–21.
Pinnock H, Fletcher M, Holmes S, Keeley D, Leyshone J, Price D, et al. Setting the standard for routine asthma consultations: a discussion of the aims, process and outcomes of reviewing people with asthma in primary care. Prim Care Respir J 2010;19:75–83.
Prost A, Griffiths CJ, Anderson J, Wight D, Hart GJ. Feasibility and acceptability of offering rapid HIV tests to patients registering with primary care in London (UK): a pilot study. Sex Transm Infect 2009;85:326–9.
Raftery JP, Yao GL, Murchie P, Campbell NC, Ritchie LD. Cost effectiveness of nurse led secondary prevention clinics for coronary heart disease in primary care: follow up of a randomised controlled trial. BMJ 2005;330:707.
Ramachandran S, Labib MH. Hyperlipidaemia and primary prevention of coronary heart disease: are the right patients being treated? J Cardiovasc Risk 2000;7:245–9.
Rapley T, May C, Frances Kaner E. Still a difficult business? Negotiating alcohol-related problems in general practice consultations. Soc Sci Med 2006;63:2418–28.
Read A, Ramwell H, Strorer H, Webber J. A primary care intervention programme for obesity and coronary heart disease risk factor reduction. Br J Gen Pract 2004;54:272–8.
Reading R, Steel S, Reynolds S. Citizens advice in primary care for families with young children. Child Care Health Dev 2002;28:39–45.
Redfern J, McKevitt C, Rudd AG, Wolfe CDA. Health care follow-up after stroke: opportunities for secondary prevention. Fam Pract 2002;19:378–82.
Reilly V, Cavanagh M. The clinical and economic impact of a secondary heart disease prevention clinic jointly implemented by a practice nurse and pharmacist. Pharm World Sci 2003;25:294–8.
Richards SH, Bankhead C, Peters TJ, Austoker J, Hobbs FDR, Brown J, et al. Cluster randomised controlled trial comparing the effectiveness and cost-effectiveness of two primary care interventions aimed at improving attendance for breast screening. J Med Screen 2001;8:91–8.
Ridout F, Charlton A, Hutchison I. Health risks information reaches secondary school smokers. Health Educ Res 2008;23:1039–48.
Ring N, Malcolm C, Wyke S, Macgillivray S, Dixon D, Hoskins G, et al. Promoting the use of Personal Asthma Action Plans: a systematic review. Prim Care Respir J 2007;16:271–83.
Ritchie D, Gnich W, Parry O, Platt S. ‘People pull the rug from under your feet’: barriers to successful public health programmes. BMC Public Health 2008;8:173.
Roderick P, Ruddock V, Hunt P, Miller G. A randomized trial to evaluate the effectiveness of dietary advice by practice nurses in lowering diet-related coronary heart disease risk. Br J Gen Pract 1997;47:7–12.
Romeo R, Knapp M, Morrison J, Melville C, Allan L, Finlayson J, et al. Cost estimation of a health-check intervention for adults with intellectual disabilities in the UK. J Intellect Disabil Res 2009;53:426–39.
Ross HM, Laws R, Reckless J, Lean M, McQuigg M, Noble P, et al. Evaluation of the Counterweight Programme for obesity management in primary care: a starting point for continuous improvement. Br J Gen Pract 2008;58:548–54.
Sachs M, Dykes F, Carter B. Feeding by numbers: an ethnographic study of how breastfeeding women understand their babies’ weight charts. Int Breastfeeding J 2006;1:29.
Sahota P, Rudolf MCJ, Dixey R, Hill AJ, Barth JH, Cade J. Evaluation of implementation and effect of primary school based intervention to reduce risk factors for obesity. BMJ 2001;323:1027–9.
Sahota P, Rudolf MCJ, Dixey R, Hill AJ, Barth JH, Cade J. Randomised controlled trial of primary school based intervention to reduce risk factors for obesity. BMJ 2001;323:1029–32.
Salisbury C, Macleod J, Egger M, McCarthy A, Patel R, Holloway A, et al. Opportunistic and systematic screening for chlamydia: a study of consultations by young adults in general practice. Br J Gen Pract 2006;56:99–103.
Santer M, Warner P, Wyke S, Sutherland S. Opportunistic screening for chlamydia infection in general practice: can we reach young women? J Med Screen 2000;7:175–6.
Santer M, Wyke S, Warner P. Women’s experiences of chlamydia screening: qualitative interviews with women in primary care. Eur J Gen Pract 2003;9:56–61.
Sargeant LA, Simmons RK, Barling RS, Butler R, Williams KM, Prevost AT, et al. Who attends a UK diabetes screening programme? Findings from the ADDITION-Cambridge study. Diabet Med 2010;27:995–1003.
Schedlbauer A, Schroeder K, Fahey T. How can adherence to lipid-lowering medication be improved? A systematic review of randomized controlled trials. Fam Pract 2007;24:380–7.
Schroeder K, Fahey T, Hollinghurst S, Peters TJ. Nurse-led adherence support in hypertension: a randomized controlled trial. Fam Pract 2005;22:144–51.
Senok A, Wilson P, Reid M, Scoular A, Craig N, McConnachie A, et al. Can we evaluate population screening strategies in UK general practice? A pilot randomised controlled trial comparing postal and opportunistic screening for genital chlamydial infection. J Epidemiol Community Health 2005;59:198–204.
Sharp DJ, Peters TJ, Bartholomew J, Shaw A. Breast screening: a randomised controlled trial in UK general practice of three interventions designed to increase uptake. J Epidemiol Community Health 1996;50:72–6.
Sinclair A, Alexander HA. Using outreach to involve the hard-to-reach in a health check: what difference does it make? Public Health 2012;126:87–95.
Siriwardena AN, Rashid A, Johnson MRD, Dewey ME. Cluster randomised controlled trial of an educational outreach visit to improve influenza and pneumococcal immunisation rates in primary care. Br J Gen Pract 2002;52:735–40.
Smith CJP, Gribbin J, Challen KB, Hubbard RB. The impact of the 2004 NICE guideline and 2003 General Medical Services contract on COPD in primary care in the UK. Q J Med 2008;101:145–53.
Spice CL, Morotti W, George S, Dent THS, Rose J, Harris S, et al. The Winchester falls project: a randomised controlled trial of secondary prevention of falls in older people. Age Ageing 2009;38:33–40.
Springett J, Owens C, Callaghan J. The challenge of combining ‘lay’ knowledge with ‘evidence-based’ practice in health promotion: Fag Ends Smoking Cessation Service. Critical Public Health 2007;17:243–56.
Standing P, Deakin H, Norman P, Standing R. Hypertension: its detection, prevalence, control and treatment in a quality driven British general practice. Br J Cardiol 2005;12:471–6.
Stapleton JA, Sutherland G. Treating heavy smokers in primary care with the nicotine nasal spray: randomized placebo-controlled trial. Addiction 2011;106:824–32.
Steptoe A, Doherty S, Kendrick T, Rink E, Hilton S. Attitudes to cardiovascular health promotion among GPs and practice nurses. Fam Pract 1999;16:158–63.
Stone MA, Taub N, Aujla N, Davies MJ, Farooqi A, Khunti K. The MY-WAIST diabetes screening programme in primary care: key quantitative findings from the final data set. Diabet Med 2011;28:75.
Sutton S, Gilbert H. Effectiveness of individually tailored smoking cessation advice letters as an adjunct to telephone counselling and generic self-help materials: randomized controlled trial. Addiction 2007;102:994–1000.
Syson-Nibbs L, Peters J, Saul C. Can health visitor intervention change sun safety policies and practice in preschool establishments? A randomised controlled study. Health Educ J 2005;64:129–41.
Taggart L, Truesdale Kennedy M, McIlfatrick S. The role of community nurses and residential staff in supporting women with intellectual disability to access breast screening services. J Intellect Disabil Res 2011;55:41–52.
Tappin D, Britten J, Broadfoot M, McInnes R. The effect of health visitors on breastfeeding in Glasgow. Int Breastfeeding J 2006;1:11.
Taylor AH, Fox KR. Effectiveness of a primary care exercise referral intervention for changing physical self-perceptions over 9 months. Health Psychol 2005;24:11–21.
Taylor CA, Shaw RL, Dale J, French DP. Enhancing delivery of health behaviour change interventions in primary care: a meta-synthesis of views and experiences of primary care nurses. Pat Educ Couns 2011;85:315–22.
Taylor E. Project based approach to increasing uptake of influenza vaccine in an underachieving GP practice. Br J Infect Control 2007;8:8–12.
Telford R, Rogers A. What influences elderly peoples' decisions about whether to accept the influenza vaccination? A qualitative study. Health Educ Res 2003;18:743–53.
Thomas P, Oni L, Alli M, St Hilaire J, Smith A, Leavey C, et al. Antenatal screening for haemoglobinopathies in primary care: a whole system participatory action research project. Br J Gen Pract 2005;55:424–8.
Thompson KA, Parahoo AK, Blair N. A nurse-led smoking cessation clinic: quit rate results and views of participants. Health Educ J 2007;66:307–22.
Thorburn R, Roland M. The effectiveness of preschool vision screening by health visitors. Br J Community Nurs 2000;5:41–4.
Trueman P, Haynes SM, Lyons GF, McCombie EL, McQuigg MSA, Mongia S, et al. Long-term cost-effectiveness of weight management in primary care. Int J Clin Pract 2010;64:775–83.
Tsianakas V, Calnan M, Atkin K, Dormandy E, Marteau TM. Offering antenatal sickle cell and thalassaemia screening to pregnant women in primary care: a qualitative study of GPs’ experiences. Br J Gen Pract 2010;60:822–8.
Tulloch H, Fortier M, Hogg W. Physical activity counseling in primary care: who has and who should be counseling? Pat Educ Couns 2006;64:6–20.
Ulbricht S, Meyer C, Schumann A, Rumpf HJ, Hapke U, John U. Provision of smoking cessation counseling by general practitioners assisted by training and screening procedure. Pat Educ Couns 2006;63:232–8.
Vogt F, Hall S, Hankins M, Marteau TM. Evaluating three theory-based interventions to increase physicians' recommendations of smoking cessation services. Health Psychol 2009;28:174–82.
Vogt F, Hall S, Marteau TM. General practitioners’ beliefs about effectiveness and intentions to prescribe smoking cessation medications: qualitative and quantitative studies. BMC Public Health 2006;6:277.
Vogt F, Hall S, Marteau TM. Hypertension: its detection, prevalence, control and treatment in a quality driven British general practice. BMC Fam Pract 2007;8:39.
Walker L, Jamrozik K. Effectiveness of screening for risk of medical emergencies in the elderly. Age Ageing 2005:34:238–42.
Walker Z, Townsend J, Oakley L, Donovan C, Smith H, Hurst Z, et al. Health promotion for adolescents in primary care: randomised controlled trial. BMJ 2002;325:524.
Waller J, Bartoszek M, Marlow L, Wardle J. Barriers to cervical cancer screening attendance in England: a population-based survey. J Med Screen 2009;16:199–204.
Warren JM, Henry CJK, Lightowler HJ, Bradshaw SM, Perwaiz S. Evaluation of a pilot school programme aimed at the prevention of obesity in children. Health Promot Int 2003;18:287–96.
Watson M, Kendrick D, Coupland C, Woods A, Futers D, Robinson J. Providing child safety equipment to prevent injuries: randomised controlled trial. BMJ 2005;330:178.
Watson MC, Inch J, Jaffray M, Stewart D. Screening and brief interventions for alcohol misuse delivered in the community pharmacy setting: a pilot study. Int J Pharm Pract 2011;19:5.
Watt G, O’Donnell C, Sridharan S. Building on Julian Tudor Hart’s example of anticipatory care. Prim Health Care Res Dev 2011;12:3–10.
White M, Bush J, Kai J, Bhopal R, Rankin J. Quitting smoking and experience of smoking cessation interventions among UK Bangladeshi and Pakistani adults: the views of community members and health professionals. J Epidemiol Community Health 2006;60:405–11.
Wilkes S, Evans A, Henderson M, Gibson J. Pragmatic, observational study of bupropion treatment for smoking cessation in general practice. Postgrad Med J 2005;81:719–22.
Williams NH. ‘The wise, for cure, on exercise depend’: physical activity interventions in primary care in Wales. Br J Sports Med 2009;43:106–8.
Williams NH, Hendry M, France B, Lewis R, Wilkinson C. Effectiveness of exercise-referral schemes to promote physical activity in adults: systematic review. Br J Gen Pract 2007;57:979–86.
Wilson A, Agarwal S, Bonas S, Murtagh G, Coleman T, Taub N, et al. Management of smokers motivated to quit: a qualitative study of smokers and GPs. Fam Pract 2010;27:404–9.
Wilson A, Sinfield P, Rodgers S, Hammersley V, Coleman T. Drugs to support smoking cessation in UK general practice: are evidence based guidelines being followed? Qual Saf Health Care 2006;15:284–8.
Wilson GB, Lock CA, Heather N, Cassidy P, Christie MM, Kaner EFS. Intervention against excessive alcohol consumption in primary health care: a survey of GPs’ attitudes and practices in England 10 years on. Alcohol Alcohol 2011;46:570–7.
Wolfe CDA, Redfern J, Rudd AG, Grieve AP, Heuschmann PU, McKevitt C. Cluster randomized controlled trial of a patient and general practitioner intervention to improve the management of multiple risk factors after stroke: stop stroke. Stroke 2010;41:2470–6.
Woodrow C, Rozmovits L, Hewitson P, Rose P, Austoker J, Watson E. Bowel cancer screening in England: a qualitative study of GPs’ attitudes and information needs. BMC Fam Pract 2006;7:53.
Yardley L, Kirby S, Ben-Shlomo Y, Gilbert R, Whitehead S, Todd C. How likely are older people to take up different falls prevention activities? Prev Med 2008;47:554–8.
Glossary
- Coproduction
- Production of solutions (e.g. design of services) by the people who may use them alongside those who have traditionally provided or arranged them. The concept of coproduction assumes that people have assets to contribute rather than simply needs which must be met.
- County council
- Authority covering the whole county and providing 80% of services in the areas, including children’s services and adult social care.
- Director of public health
- Appointed through local authorities and Public Health England (on the Secretary of State’s behalf), acting jointly, directors of public health provide leadership and direction to local collaborative discussions about the best use of the local ring-fenced public health budget. There is a director of public health for each upper-tier local authority, although one director of public health may cover more than one local authority.
- General Medical Services
- Contract negotiated nationally which is held with each general practice.
- Health and Wellbeing Board
- A statutory committee of a local authority which leads and advises on work to improve health and reduce health inequalities among the local population. It has a performance-monitoring role in relation to NHS Clinical Commissioning Groups, public health and social care. Members include councillors, general practitioners, health and social care officers, and representatives of patients and the public, including local HealthWatch.
- Health promotion
- The process of enabling people to increase control over, and to improve, their health.
- National Institute for Health and Care Excellence
- The body responsible for providing research, evidence and guidance on what medication and treatments should be available on the NHS.
- NHS Commissioning Board
- An organisation established in shadow form to take on national commissioning of health care and regulate Clinical Commissioning Groups. It became NHS England from 2013.
- NHS England
- The body that holds the ‘contract’ for the NHS (the NHS Mandate). Its role includes supporting, developing and holding to account the system of Clinical Commissioning Groups, as well as being directly responsible for some specialist commissioning.
- Outcomes Framework
- A national framework which sets out the outcomes and corresponding indicators against which achievements in health and social care will be measured. There are three outcome frameworks: for the NHS, for adult social care and for public health.
- Personal Medical Services
- A variance on the General Medical Services contract which has additional agreed elements.
- Practice-based commissioning
- Where general practices advised on or undertook commissioning of health-care services with primary care trusts.
- Primary care trust
- Key local health-commissioning agency and provider of public health until March 2013.
- Public health
- The science and art of promoting and protecting health and well-being, preventing ill-health and prolonging life through the organised efforts of society.
- Public Health England
- The new national public health service, which integrates the work of a large number of disparate public health organisations into a single, expert body providing advice and services across the range of public health. It allocates ring-fenced funding to local authorities and also acts on behalf of the Secretary of State in the process of appointing directors of public health at the local authority level.
- Quality and Outcomes Framework
- A voluntary reward and incentive programme for all general practice surgeries in England, detailing practice achievement results.
- Strategic health authority
- Regional health agency until March 2013, providing local co-ordination and oversight.
- Unitary authority
- Just one level of local government responsible for all local services; it can be called a city council (e.g. Nottingham City Council), a borough council (e.g. Reading Borough Council) or simply a council (e.g. Medway Council).
List of abbreviations
- ADDITION
- Anglo-Danish-Dutch Study of Intensive Treatment in People with Screen Detected Diabetes in Primary Care
- CCG
- Clinical Commissioning Group
- CHD
- coronary heart disease
- COPD
- chronic obstructive pulmonary disease
- CVD
- cardiovascular disease
- DH
- Department of Health
- ERS
- exercise referral scheme
- GMS
- General Medical Services
- GP
- general practitioner
- HWB
- Health and Wellbeing Board
- LA
- local authority
- LES
- Local Enhanced Service
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OXCHECK
- Oxford and Collaborators Health CHECK
- PCT
- primary care trust
- PHE
- Public Health England
- QOF
- Quality and Outcomes Framework
- RCT
- randomised controlled trial
- SDO
- Service Delivery and Organisation