Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/128/48. The contractual start date was in March 2014. The final report began editorial review in September 2016 and was accepted for publication in April 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Han et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2017 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Background
There are long-standing concerns that patients admitted to hospital outside normal working hours, when staffing levels are lower and some services are not available, suffer higher complication and mortality rates than patients admitted at times when the hospital is fully operational. 1–4 Although there is evidence for this phenomenon in all out-of-hours periods – principally at night and at weekends – it has become known as the ‘weekend effect’ because the seminal studies in this area concentrated on weekend admissions.
Payers and policy-makers have responded to these findings with health-care system reform on the assumption that reduced service provision underlies the higher risk of adverse outcomes at weekends and that more consistent hospital care throughout the week will reduce or remove the disparity. 5,6 In England, evidence on the weekend effect has been used to justify controversial attempts to introduce a ‘7-day service’ across the NHS, an approach that is supported by evidence suggesting that emergency weekend admission is not associated with poorer outcomes when there is consistent access to early diagnosis and treatments. 7–9
Although the weekend effect has been described internationally, it is of particular concern to the NHS, which was founded on fundamental principles of equity. Equity and Excellence: Liberating the NHS stated that the 2010 government’s long-term vision is of a NHS that eliminates discrimination and reduces inequalities in care. 10 If patients’ outcomes are strongly dependent on the time that they are admitted to hospital, and if time of presentation is partly socially determined, this has implications for equity across the service. Extending the hours for which the NHS is fully operational has the potential to improve access and outcomes for patients. However, extending fully operational hours could also decrease efficiency by raising input costs and providing services that are relatively underutilised.
However, although the weekend effect is well described it is poorly understood. Previous studies have been limited by the availability, completeness and content of routine admissions data, which has restricted investigations to day of admission and prevented direct measurement of severity of illness. It is therefore not clear whether or not the weekend effect extends to other out-of-hours periods, or how far excess mortality for out-of-hours admissions reflects a different presenting population with higher severity of illness, and how much is explained by poorer availability and quality of services. It is also not known if service changes could bring out-of-hours mortality rates down to levels comparable to daytime and weekday rates and what the cost implications of such changes would be. The NHS therefore faces difficult decisions in how it should respond to its responsibility to provide health care 24 hours a day, 7 days a week (24/7).
Research aims
Our original intention was to explore how extending fully operational hours affected costs and patient outcomes through a case study of an acute trust – Salford Royal NHS Foundation Trust (SRFT) – that had extended its hours of full operation, culminating in the provision of consultant-led care from 07.00 to 23.00 hours (see Appendix 1). This would enable us to determine whether or not rebalancing fully operational hours would represent a cost-effective use of NHS resources.
However, preliminary analyses of data from SRFT and interviews with local clinicians indicated that the population of patients admitted out of hours differed substantially from the population admitted on weekdays in terms of severity of illness. Furthermore, it was clear that standard risk adjustment models using routinely collected administrative data were not able to adequately adjust for these differences. If this pattern were repeated in other acute trusts, it would suggest that the weekend effect is strongly determined by selection into the admitted population and that our proposed analyses of patient outcomes would be biased.
Following consultation with the Study Steering Group, our research aims were reframed to address more fundamental questions about the causes of the weekend effect and the likely cost-effectiveness of restructuring NHS services to address excess mortality for out-of-hours admissions. We expanded the research to include all acute trusts in England, while continuing to use detailed data from SRFT. We also took advantage of newly emerging sources of data, which allowed for time of admission (and, therefore, out-of-hours mortality) to be measured more precisely.
Research questions
We conducted five linked studies addressing the following research questions.
-
What are the potential costs and benefits of introducing 7-day services?
-
Does the weekend effect extend to nights? Does it persist over time?
-
Do higher mortality rates for patients admitted to hospital out of hours reflect a lower probability of admission?
-
Are higher mortality rates for out-of-hours admissions explained by greater severity of illness?
-
What is the relationship between staffing levels and out-of-hours mortality?
Although variations in provision of care, patient characteristics and patient outcomes are also evident for elective admissions to hospital, examining these variations was beyond the scope of this study and we have therefore focused on emergency admissions.
Chapter 2 Methods
Material in this chapter has been reproduced with permission from Meacock R, Doran T, Sutton M. What are the costs and benefits of providing comprehensive seven-day services for emergency hospital admissions? Health Econ 2015;24:907–12 (copyright © 2015 John Wiley & Sons, Ltd);11 Meacock et al. 12 [this article is distributed under the terms of the Creative Commons Attribution-NonCommercial 3.0 License (http://www.creativecommons.org/licenses/by-nc/3.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed]; and Anselmi et al. 13 [this is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/].
Analysis of national data
For studies 1, 3 and 4, we used a combination of national patient-level data from Hospital Episode Statistics (HES) for patients attending accident and emergency (A&E) departments and all patients admitted to hospital in an emergency, in addition to data from the Office for National Statistics (ONS) on all-cause mortality within 30 days of admission.
Data sources and preparation
For study 1, we obtained data on all emergency admissions to hospital in England from HES between 1 April 2010 and 31 March 2011, linked to data from the ONS on all-cause mortality within 30 days of admission. We selected only the emergency admissions using the admission method field in HES. For studies 3 and 4 we used individual patient-level data on A&E attendances and emergency admissions from HES between 1 April 2013 and 31 March 2014. We analysed records from the first 11 months of this period so that each patient can be followed up for 30 days after attendance/admission. We restricted our analysis to attendances at type 1 units, which are consultant-led, multispecialty 24-hour services with full resuscitation facilities and designated accommodation for the reception of A&E patients. These units exclude single-specialty centres, minor injury units and walk-in centres, and account for 99% of emergency admissions via A&E.
The attendance records contain information on the patient’s age, gender, ethnic group, provider attended, diagnosis (38 major categories), arrival by ambulance or other mode, whether the attendance is a first or follow-up visit, where the incident occurred (home, work, educational establishment or other public place), the type of accident (including road traffic accident, assault, deliberate self-harm, sports injury), whether the attendance was patient initiated or recommended by a professional in another organisation, the time and date of attendance and whether the patient was admitted, discharged or died in the A&E department.
The admission records contain information on the patient’s age, sex, ethnic group, primary and secondary diagnosis classified using International Classification of Diseases, Tenth Edition (ICD-10), whether the patient was admitted from home or another institution, the date of admission and whether the patient was admitted via A&E or directly by a general practitioner (GP), through a bed bureau or by a consultant in a scheduled ambulatory clinic. Each record also contains a pseudonymised identifier for the consultant in charge of the patient’s care, the trust to which they were admitted and the date of death if the patient died in hospital.
Linked admission and A&E attendance record identifiers were provided by the Health and Social Care Information Centre (HSCIC) (now known as NHS Digital). 14 Admission records and attendance records were linked using a matching algorithm based on an encrypted person identifier, dates of discharge from A&E departments and dates of admission to hospital, as well as a set of criteria to prioritise conflicting information from the two data sources. 14 In cases of multiple episodes within an admission spell, the first episode was used. In cases of multiple attendances at A&E on the same day, the last attendance was used.
We analysed attendance and admission records from the 140 non-specialist acute trusts in England for which the HSCIC reports the summary hospital-level mortality indicator (SHMI). We linked these records using an encrypted patient identifier to the dates of death of all patients who had died in any hospital in England between 1 April 2013 and 31 March 2014. We focused on deaths within 30 days of attendance or admission. To allow a 30-day follow-up period for all patients over which to analyse mortality, we restricted the analysis to patients admitted to hospital between 1 April 2013 and 28 February 2014. We excluded all but the first admission in cases of multiple admissions in the last 30 days of life.
To control for deprivation, we attached the Index of Multiple Deprivation (IMD) 2010 score to the attendance and admission records using the patient’s lower-layer super output area (LSOA) of residence. England is divided into 32,844 LSOAs, with a mean population of 1500.
Statistical methods
Study 1: estimating the potential costs and benefits of introducing 7-day services
We estimated the loss in patient health associated with the weekend effect for emergency admissions to all hospitals in England between 1 April 2010 and 31 March 2011. We used data on inpatient episodes from HES linked to data from the ONS on all-cause mortality (both in and out of hospital) within 30 days of admission. We selected only the emergency admissions using the admission method field in HES.
We first estimated the number of excess deaths occurring among patients admitted at the weekend by applying the crude mortality rate observed for weekday admissions to the number of patients admitted during the weekend and subtracted this number of expected deaths from the number observed among weekend admissions.
As weekend admissions may represent a different case mix of patients, we then used risk-adjusted mortality rates. We used the risk-adjusted figures reported in the published studies that have been cited as support for the 7-day services initiative. We applied the inverse of the risk-adjusted odds ratios reported by Freemantle et al. 3 and by Aylin et al. 15 to the odds [p/(1 – p)] of mortality at weekends observed in our data. This represents the expected odds of mortality if weekend patients experienced the same death rate as those admitted during the week once we control for their risk characteristics. We calculated the risk-adjusted number of excess deaths by multiplying the number of weekend admissions by the risk-adjusted expected mortality rate and subtracting this number from the observed number of weekend deaths.
We then used a previously developed methodology to calculate the number of quality-adjusted life-years (QALYs) that could potentially be gained if the weekend effect were to be eradicated and these excess deaths were averted. This involved applying a discounted and quality-adjusted life expectancy tariff to the mortality records, which we developed for our evaluation of the advancing quality pay-for-performance programme16 and which is explained in detail in Meacock et al. 17 Using these estimated discounted QALY gains, we calculated the maximum amount that the NHS should be prepared to spend on averting these deaths using the standard threshold of £20,000 per QALY used by the National Institute for Health and Care Excellence (NICE) when assessing whether or not new technologies or interventions are cost-effective.
Study 3: examining selection of patients for admission at weekends
-
We separated patients by their route of admission to hospital, examining two distinct groups. The first group we examined were patients who access emergency services through A&E, which make up the majority of emergency admissions. To examine the importance of selection effects among the admitted population as a result of variations in clinical decisions to admit, we focused initially on the entire population of patients who attend A&E and then restricted the analysis to the subset who are selected for admission.
-
The second group consists of patients admitted directly to hospital in an emergency by GPs, through a bed bureau or by specialists in ambulatory clinics, termed ‘direct admissions’ (HES admission method codes 22, 23 and 24). The availability of these services is more limited at the weekends compared with during the week and we examined whether or not this leads to fewer direct admissions and whether or not there is a higher mortality rate among the restricted number of patients who are admitted via this route.
-
Within these groups we compared the mean number of A&E attendances, emergency admissions and deaths per day between each day of the week and between weekdays and weekend days using t-tests.
-
We used logistic regression to estimate the risk-adjusted probability of dying within 30 days for the entire population of patients attending A&E departments by day of the week. We then estimated the risk-adjusted probability of being admitted to hospital and the risk-adjusted probability of dying for the subset of patients who are selected for admission. The case-mix adjustment in these models included information taken from the A&E attendance records on age, gender, ethnicity, diagnosis, arrival mode, first or follow-up visit, incident location, accident type, referral source, deprivation quintile, month and hospital attended.
-
We also used logistic regression to estimate the risk-adjusted probability of dying within 30 days of direct admission by day of the week. The case-mix adjustment in these models included information taken from the admission records on age, gender, ethnicity, primary diagnosis (SHMI-grouped clinical classifications software category), Elixhauser (comorbidity) conditions, admission method, admission source, deprivation quintile, month and admitting hospital. SHMI-grouped clinical classifications software18 is a tool for grouping patients into a manageable number of clinically meaningful categories using ICD-10 diagnosis codes.
-
We compared each day with Wednesday and then estimated another model comparing weekend admissions to weekday admissions.
-
The analysis was undertaken using Stata version 13 (StataCorp LP, College Station, TX, USA). We clustered the error terms to account for the multiple observations of some individuals using the Stata command ‘robust cluster(id)’ and summarised the goodness-of-fit of the models using the c-statistic.
Study 4: estimating the impact of severity of illness
-
We used records for admitted patients with complete information and with matching A&E record. We first estimated each patient’s risk of mortality within 30 days to categorise patients into five quintiles based on their predicted risk of mortality. We used a logistic regression model that included risk adjustment for interaction between gender and age, ethnicity, primary diagnosis (based on ICD-10 classification and defined according to SHMI-grouped clinical classifications software),19 comorbidities measured using Elixhauser conditions,20–22 source of admission (home or another hospital provider or institution), deprivation in the patient’s area of residence (categorised in quintiles), admitting hospital and month of admission.
-
We then examined how the estimated risk of mortality varied by time of arrival at A&E and by mode of arrival. We classified time of arrival at A&E into 14 12-hour periods by dividing the week into seven daytime periods (07.00 to 18.59 hours) and seven night periods (19.00 to 06.59 hours the following day). We classified arrival mode as by ambulance, other or unknown (patients with missing information that could potentially be included in both categories). 19 Ambulance arrivals include all forms of ambulance, but > 98% are by emergency ambulance.
-
We finally used logistic regression models to analyse differences in the probability of death within 30 days of admission across the 14 12-hour time-of-arrival periods, with Wednesday daytime as the reference category. We used the risk adjustment detailed above and examined whether or not mortality was associated with the mode of arrival at A&E and whether or not the size of the estimated differences in mortality by day of the week and time of the day was affected by the inclusion of this factor in the set of risk adjusters or differed for patients arriving by ambulance or other mode.
-
Standard errors were clustered at the individual level to account for repeated admissions of each individual patient. We used the c-statistic to discriminate across models. Analyses were undertaken using Stata version 14.
Analysis of data from the Salford Royal NHS Foundation Trust
For studies 2 and 5, we used inpatient and staffing data derived from SRFT. SRFT is a large teaching NHS hospital in north-west England with a team of > 6000 staff to provide a comprehensive range of emergency care, specialist treatments and some community services. SRFT has a long-term commitment to improve equality in patient access and outcomes by delivering standardised safe care 7 days a week, particularly for emergency patients. Changes in the organisation of non-elective services have been implemented over time, including consultant presence ‘on the shop floor’ from 08.00 to midnight every day, acute physicians working in the emergency assessment unit from 08.00 to 20.00 hours 7 days a week, as well as radiology services available 24/7 for all core procedures.
Data sources and preparation
We extracted records for emergency patients admitted to SRFT between April 2004 and March 2014. This data set contains similar information to the national HES data. The patient records are originally collected on episode level, which is the period when a patient is treated by a consultant. Key information available at this level includes patient demographics, date and time of admission, method and source of admission, date of discharge, method and destination of discharge, primary and secondary diagnoses, as well as primary and secondary procedures. We created hospital spells by linking episodes from admission to discharge of a hospital stay. We excluded maternity spells of this period because of the service change implemented in November 2011. The majority of maternity services have been transferred elsewhere since this date except for early pregnancy care. Moreover, SRFT does not provide complete paediatric services. Children who attend A&E are assessed and stabilised before being transferred to other treatment centres. For this reason, we also dropped child patients (aged < 18 years) from our sample of analysis. There were a total of 244,639 emergency spells extracted for this period.
Owing to data limitations, most previous studies on the weekend effect have defined weekend admissions and procedures as those admitted or undergone procedures between 00.00 hours on Saturday and 23.59 hours on Sunday. However, concerns have been raised that this definition does not reflect the real pattern of service provision and staffing level between weekdays and weekend. Our patient records extracted from SRFT contain the hour and minute of admission, allowing us to categorise admissions over night-time and weekends accurately.
Statistical methods
For study 2, we estimated the association between patient outcomes and the precisely defined out-of-hours admissions for the entire study period, as well as for each individual year. For study 5 we considered multiple factors that might influence the poorer outcomes for out-of-hours admissions. We focused on the patients admitted to the acute stroke unit (ASU) in SRFT between January 2009 and July 2014 to closely examine the patterns in the number of admissions and the speed of initial treatments throughout the week. We intended to provide insights on whether or not fewer patients were selected for admission in out-of-hour periods, and for those out-of-hour admissions whether or not they had to wait longer for initial treatments. Moreover, we evaluated the impact of staffing level of nurses on the inequality in outcomes associated with out-of-hour admissions by linking admissions to the roster data of the admission hour.
Study 2: examining the relationship between out-of-hour admissions and patient mortality
Our primary outcome variable was mortality within 30 days of admission that occurred both in and out of hospital. As sensitivity checks, we also analysed mortality in 7 days and all in-hospital deaths. Our exposure variable, out-of-hours admission, was defined in three ways. First, we broadly defined out-of-hours admissions as those admitted at weekends and public holidays and compared their outcomes with admissions on weekdays. The weekend and holiday admission group consisted of emergency patients admitted from 19.00 hours on Friday through to 06.59 hours on Monday, which is a precise definition of weekend more closely reflecting the real pattern of service provision and staffing level. We expect hospital services on public holidays to have a similar arrangement as weekends. Therefore, we included in this group those patients admitted between 19.00 hours on the day before the holiday and 06.59 hours on the day after the holiday. Admissions outside these weekend and holiday periods were used as the reference group. Our second definition assigned each patient into one of the four admission groups: weekday day group (admissions between 07.00 and 18.59 hours, Monday to Friday), weekday night group (admissions between 19.00 hours and 06.59 hours of the next morning, Monday to Thursday), weekend day group (admissions between 07.00 and 18.59 hours, Saturday and Sunday) and weekend night group (admissions between 19.00 and 06.59 hours of the next morning, Friday to Sunday). Patient outcomes were used as the baseline if they were admitted to the hospital during normal working hours, defined as the daytime from Monday to Friday. Each out-of-hours admission group was compared with the reference looking for an independent impact of each out-of-hours period. We then took a closer examination on how patients’ probability of death varied across the week by applying our third grouping method. We divided each day into daytime (07.00–18.59 hours) and night-time (19.00–06.59 hours of the next day), and, therefore, each week into 14 12-hour admission groups. We followed the convention and used the daytime admissions on Wednesday as baseline by assuming that hospital services were provided at full capacity during this period. The other 13 admissions groups were compared with this group after adjusting for confounders.
We adjusted for the risk factors of mortality using information available in the administrative data of English hospitals. 21 We adjusted for patient characteristics using age on admission, gender, ethnicity and socioeconomic deprivation. We linked patients’ residential postcodes to the IMD at LSOA level and divided the deprivation scores into quintiles. 23 The first quintile, representing the most affluent neighbourhoods, was used as the baseline group. Without evidence suggesting that missing data were randomly distributed, we created an additional category in these variables to take into account those patients with missing observations.
We controlled for patient complexity associated with the current admissions using primary diagnosis groups, the total number of different diagnoses, the total number of different procedures, a dummy variable indicating whether or not the index spell involved palliative care, as well as the methods and sources of admission. The Charlson Comorbidity Index was included to account for the presence and the severity of comorbidities. 24 We updated the weights of included conditions according to their association with the risk of mortality estimated using the recent data from the UK. 15 The weights of dementia and human immunodeficiency virus have changed substantially: the former has much bigger impact on the risk of death than it did 25 years ago and the latter is having a reduced impact. Medical histories were assessed by calculating the total number of emergency admissions in the previous 365 days. We accounted for seasonal impact by including dummy variables for the months of admission. In the pooled analysis across the entire period, we included year-specific fixed effects to capture those unobserved factors that changed by financial year.
We fitted probit models to estimate the extent to which the probability of death was associated with our exposure variable after controlling for observed patient characteristics. In the pooled analysis across the study period, we assumed a latent propensity of death as a linear function of our exposure and controlling variables as outlined in Equation 1:
where yit* is the estimated propensity of death for spell i in year t; weekendit is a dummy variable indicating weekend and holiday admission; χit is a vector of variables measuring patient demographics and complexity; γt is a vector of year dummies controlling for unobserved year-specific fixed effect; the error term εit is assumed to follow a standard normal distribution and is independent from the explanatory variables. The observed outcome variable Yit depends on the value of yit*, so that:
We removed the year dummies γt from Equation 1 in the regression for each financial year, allowing the coefficients of explanatory variables to change with time. We applied variance–covariance matrices clustered by consultant to account for any correlation within the treatments of the same consultant. In this non-linear model, the estimated coefficients should not be interpreted as the size of impact. Therefore we reported the average marginal effects to compare the impact of predictors across regressions.
Study 5: examining the impact of staffing levels on mortality rates
In this study we considered multiple factors that vary across the week and might be associated with the observed pattern that outcome is worse for out-of-hours periods than normal working hours. Specifically, we took into account the possibility that (1) patients attending hospitals at weekends may represent a different mix of conditions and severity of illness and, therefore, the overall severity was different from the weekdays; (2) as a result of reduced staffing level and service provision over nights and weekends, fewer but sicker patients may be selected for admission during these periods; and (3) a different mix of medical staff are available during out-of-hours periods and, in particular, fewer senior staff are available.
To address points (1) and (2), we restricted our sample patients to those admitted to the ASU at SRFT as emergencies between January 2009 and July 2014, so that the overall composition of patients remained stable across the week. Moreover, we broke down a week into 14 periods with each day being divided into day (07.00–18.59 hours) and night (19.00–06.59 hours the next day), and compared the numbers of admissions and the speed of initial treatment across these periods. To address point (3), we first estimated a core model for the excess risk of death associated with out-of-hours periods of the week after adjusting for other risk factors of mortality. This model took a similar form to the equation in study 1 with only minor moderations, as outlined in Equation 3:
In this model, yit* is a latent propensity of death for admission i related to the observed outcome. We separately estimated three outcome variables, including the in-hospital mortality accounting for all death occurred during a hospital stay, as well as the 7-day and 30-day mortalities from admission accounting for both in- and out-of-hospital death. out-of-houri is the period of the week associated with admission i. We used the definition containing four categories to separate patients between weekdays and weekend, and between day and night. Each admission was assigned to one of the categories (weekday day group, weekday night group, weekend day group and weekend night group). χi represented a similar set of risk adjustment variables to study 1. These factors reflected patient demographics, socioeconomic status, complexity associated with the current admission, medical history, as well as the presence and severity of comorbidities. γyear is a vector of year dummies controlling for unobserved year-specific fixed effects. The error term εi is assumed to follow a standard normal distribution and is independent from the explanatory variables. We did not adjust for admission sources because the vast majority of our sample patients were admitted from their home addresses. We also dropped admission months from the equation because these dummy variables had an overall insignificant association with our dependent variables.
Second, we estimated an extended Equation 4 to examine whether or not the inequality in outcomes associated with out-of-hours admission can be reduced by taking into account the variations in the staffing level:
where nursesi,ASU reflects the staffing level of nurses in ASU in the first hour of admission i and patientsi,ASU adjusts for the workload to the medical staff on the admission day by counting the number of patients in the ward admitted both electively and as emergencies.
We fitted probit models for Equations 3 and 4 and reported the average marginal effects as the size of impact, as the estimated coefficients are difficult to interpret in this non-linear model. We focused on the comparison of β1, the coefficient of out-of-hours admission, between the core and extended models in terms of its significance and magnitude.
Patient and public involvement
To ensure that the aims of the study reflected patient priorities and outcomes of importance to patients, we regularly engaged with the public to ensure that findings were communicated to the groups most likely to be affected. Engagement was achieved through consultation with the Salford Royal NHS Foundation Trust Membership (SRFTM) and the Salford Citizen Scientist Project. The SRFTM has 14,545 patient members and 6179 staff members and provides feedback to clinicians, managers and researchers via surveys, focus groups, co-design events and public meetings. The Salford Citizen Scientist Project is a forum bringing together researchers and local residents to improve health research and health-related services.
We held regular engagement events, located at SRFT.
-
At month 3, we held an open day for patients, carers and staff to discuss study aims and objectives.
-
At month 15, we held two ‘Medicine for Members’ events to discuss emerging findings, priorities for members and potential changes to analyses:
-
a seminar for 60 SRFTM members with a floor debate
-
two ‘citizens’ juries’ with 15 SRFTM members, where members could put questions to two ‘expert witnesses’ (TD and RM).
-
-
At month 18, we held a focus group with 15 SRFTM members to disseminate preliminary findings and to elicit patient and public recommendations for providers.
Findings from these PPI events are detailed in Appendix 2.
Following the first event, two patient group representatives were recruited to sit on the Advisory Panel and attended three Advisory Group meetings during the course of the research programme.
Chapter 3 Results (study 1): estimated costs and benefits of 7-day services
Material in this chapter has been reproduced with permission from Meacock R, Doran T, Sutton M. What are the costs and benefits of providing comprehensive seven-day services for emergency hospital admissions? Health Econ 2015;24:907–1211 (copyright © 2015 John Wiley & Sons, Ltd).
Background
The English NHS is moving towards providing comprehensive 7-day hospital services in response to higher death rates for emergency weekend admissions. However, providing the same level of services every day of the week may not be the most cost-effective way of distributing limited health-care resources. It is not yet known whether or not changing to a 7-day service will improve outcomes and what the costs of any such reorganisation will be. In this study we examine the evidence base being used to support the case for 7-day services and, using national statistics and the results of published studies, we estimate the potential benefits of introducing such service extensions across England compared with the costs of doing so.
Recent evidence from England suggests that patients’ risk-adjusted probability of dying is increased by 11% [95% confidence interval (CI) 9% to 13%] if admitted to hospital on a Saturday and 16% (95% CI 14% to 18%) if admitted on a Sunday, compared with those admitted mid-week. 3 This weekend effect varies substantially by condition, from a zero additional risk for pneumonia to 16% for stroke, 28% for lung cancer and 37% for renal failure. 3 To interpret these weekend effects it is important to consider the baseline level of risk. In the review commissioned by the NHS Services, Seven Days a Week Forum,25 only one study, by Aylin et al. ,15 presented actual mortality rates for patients admitted at the weekend and during the week. Using data from 2005/6, Aylin et al. 15 reported in-hospital mortality rates for emergency admissions of 4.9% for weekday admissions and 5.2% for weekend admissions. This represents a 10% increase in relative risk, but only a 0.3 percentage point increase in absolute risk.
One of the main differences between hospital care at weekends compared with weekdays is the reduced availability of senior clinical staff; and this is often cited as an explanation for the observed weekend effect. 7,26 However, there is a lack of evidence that increasing the levels of consultant cover at weekends leads to reductions in mortality rates. 25
Available evidence on the impact of extending service provision comes from a small number of case studies of specific care pathways. For stroke, for example, improved outcomes, reduced length of stay and favourable evidence on cost-effectiveness have been found in specialised units configured to treat patients admitted for this condition every day of the week in London,27 though later work showed that the same results were not seen in another location, Greater Manchester. 28 The death rate within 7 days of admission is reported to have fallen from 10.0% to 7.3% for those admitted at the weekend after the reorganisation of stroke services in London. 25 However, these facilities provide a range of enhanced facilities in addition to 7-day services and it is therefore difficult to identify which aspects were responsible for the observed improvements in outcomes. In the London case study, the mortality rate for patients admitted during the week was reported to have fallen from 8.0% to 6.4%,25 meaning that the relative weekend effect was reduced but not eliminated.
Funding new interventions imposes costs on health systems, reducing the resources available for existing services and potentially resulting in a net loss of health benefits. The costs of extending normal operational hours must therefore be weighed against the predicted benefits. Increasing the level of consultant cover during the weekends will require a redistribution of the existing workforce and/or additional training and recruitment. Diverting consultant cover away from weekdays towards weekends would be expected to affect the quality of services and outcomes for patients admitted during the week. The introduction of 7-day services might therefore narrow the gap between weekday and weekend mortality, but at the cost of higher weekday rates.
Results
Summary statistics for emergency hospital admissions are given in Table 1. The crude 30-day mortality rate was 3.70% for patients admitted during the week and 4.05% for those admitted during the weekend, resulting in an excess death rate of 0.35 percentage points (Table 2). If the crude mortality rate observed during the week applied to patients admitted during the weekend, this would translate into an annual estimate of 4355 excess deaths occurring nationally at weekends (see Table 2). After applying the risk-adjusted odds ratio (OR) from Freemantle et al. ,3 this figure rose to an estimated 5353 excess deaths. The risk-adjusted OR reported in Aylin et al. 15 is very similar to that obtained using our crude mortality rates and produces a similar estimate of excess weekend deaths of 4376. Depending on the figures used, this translates into a potential health gain of between 29,727 and 36,539 QALYs per year if all excess deaths were to be averted. Using the NICE threshold, the NHS should spend no more than £595–731M to achieve a health gain of this size. Using the upper bound of the 95% CI for the OR reported by Freemantle et al. 3 of 1.145 increases these gains by 14%.
| Day of admission | Mean age of patients admitted (years) | Mean age of patients dying within 30 days of admission (years) | Total number of admissions | Crude 30-day mortality rate (%) |
|---|---|---|---|---|
| Monday | 50.5 | 77.1 | 816,742 | 3.79 |
| Tuesday | 50.8 | 77.4 | 793,807 | 3.68 |
| Wednesday | 50.8 | 77.3 | 777,685 | 3.65 |
| Thursday | 51.0 | 77.3 | 792,822 | 3.65 |
| Friday | 51.5 | 77.4 | 798,866 | 3.73 |
| Saturday | 50.8 | 80.0 | 618,666 | 4.01 |
| Sunday | 49.8 | 77.6 | 614,385 | 4.09 |
| Weekday | 50.9 | 77.3 | 3,979,922 | 3.70 |
| Weekend | 50.3 | 77.9 | 1,233,051 | 4.05 |
| Source of estimates | Death ratea | Excess deaths | ||||
|---|---|---|---|---|---|---|
| Weekday | Weekend | OR | Numberb | QALYsc | Maximum spend (£M)d | |
| Authors’ analysis of HES 2010/11 | 3.7% | 4.0% | 1.099 (crude) | 4355 | 29,727 | 595 |
| Freemantle et al. (2012)3 | Not reported | Not reported | 1.125e (risk adjusted) | 5353 | 36,539 | 731 |
| Aylin et al. (2010)15 | 4.9% | 5.2% | 1.100 (risk adjusted) | 4376 | 29,870 | 597 |
These calculations represent the maximum possible gains from introducing 7-day services for three reasons. First, they represent the number of deaths that would be averted if the weekend effect were to be completely eradicated by extending services. Second, the methodology probably overestimates the potential QALY gains from an averted death as it assumes that those surviving would enjoy the same quality of life and life expectancy as the general population, conditional on their age and sex. 17 Third, our calculations represent the scenario where benefits to patients admitted at the weekend are achieved without any detrimental effect on outcomes for those admitted during the week.
Although the potential benefits of extending services appear large, they must be compared with the additional costs of doing so. The NHS Services, Seven Days a Week Forum estimated these costs for eight ‘successful Foundation Trusts with an interest in seven day services’. 29 The costs were estimated using a costing template and interviews with finance staff, managers and clinicians, followed by two workshops to agree methodology and overall findings. The cost estimates were highly variable across the trusts and included some cost savings associated with reduced length of stay and reduced readmissions where these were identified by the trusts. Caution was emphasised in generalising the results, but overall it was estimated that the costs of implementing 7-day services would be 1.5–2.0% of total hospital income, equivalent to a 5–6% increase in the cost of emergency admissions.
According to Department of Health (DH) accounts, national expenditure on hospitals was £71.3B in the financial year 2013/14. 30 Application of the estimates29 suggests that implementing 7-day services would cost between £1.07B and £1.43B per annum. This cost exceeds our estimates of the maximum amount that the NHS should spend to eradicate the weekend effect by a factor of 1.5 to 2.4, or between £339M and £831M.
Conclusion
Recent initiatives to extend normal hours of hospital operation and to provide more comprehensive 7-day services have been implemented in response to alarming statistics on the gap in mortality rates between patients admitted at the weekend and those admitted on weekdays. These statistics, however, are insufficient by themselves to justify a policy change towards extending normal hours of operation into the weekend. There is as yet no clear evidence that 7-day working will, in isolation, reduce the weekend death rate; that lower weekend mortality rates can be achieved without increasing weekday death rates; or that such reorganisation is cost-effective.
Our analysis indicates that the estimated cost of implementing 7-day services exceeds the maximum amount that NICE would recommend the NHS should be prepared to spend on eradicating the observed weekend effect. Comprehensive roll-out of 7-day services across the NHS is therefore unlikely to be a cost-effective use of resources, particularly as our estimates of potential health benefit represent the upper limit of what is achievable. Given the lack of evidence supporting the impact of service extension on patient outcomes, the benefits actually realised would likely be much lower. Furthermore, the consequences for patients admitted during the week also need to be considered, as care for these patients may deteriorate if resources are redistributed. Against that must be balanced other potential gains from a 7-day service, including improvements in morbidity, improvements in efficiency and overall improvements in mortality – rather than reductions in excess weekend mortality – as result of rebalancing of patient care across the week.
More – and more nuanced – evidence is required before a policy of providing full 7-day services can be supported. For example, our analysis considered only mortality and associated QALYs as an outcome, which are increasingly recognised as limited measures of outcomes. 31 There may be other detrimental effects on quality and outcomes for patients admitted at the weekend that improved weekend services could address. Although the policy debate to date has focused on the excess mortality rates observed for patients admitted in an emergency to hospitals during the weekend, there are likely to be wider consequences, such as the impact on elective activity currently undertaken during the week and the impact on primary and community services that are also limited at weekends. It is possible that selected service extensions – for specific specialties and at certain times of day – could prove to be cost-effective, but substantial commitments of NHS resources should not be made until these can be identified and robust evidence provided.
Chapter 4 Results (study 2): the relationship between out-of-hours emergency admission and patient mortality
Background
Admission to hospital at weekends has consistently been found to be associated with poorer patient outcomes, for both emergency and non-emergency conditions. 3,32–35 However, much of the evidence on the effect of weekend admission has been limited in key respects. First, it tends to be cross-sectional and there is therefore limited information on the trends in disparities over time. Second, it is often based on routinely available data that provides the day but not the hour of admission. As a result, weekends have effectively been defined as 00.00 hours Saturday to 23.59 hours Sunday (thereby excluding Friday evenings and Monday mornings) and separate analysis of night-time admissions has not been possible. This is an important omission, as it is likely that if reduced service availability at weekends adversely impact on outcomes, there is also an increased likelihood of adverse outcomes for patients admitted at night, when services are also reduced. Some studies have utilised specialist data to address this issue; for example, finding that at night there is an increased risk of mortality following in-hospital cardiac arrest36 or coronary artery bypass grafting,37 and a reduced chance of receiving timely intervention following stroke.
For this study, we analysed emergency admissions to SRFT, a large teaching hospital in north-west England providing a complete range of acute services, including specialist tertiary care. SRFT has maintained detailed electronic patient records since 2004, including precise time of admission, and has been a pioneer of extending normal hours of operation and providing enhanced weekend services. In 2011 it opened an ‘emergency village’, providing a consultant-led enhanced A&E service 7 days a week, and also extended services such as radiology, pathology and pharmacy across the weekend. 25
Using the enhanced data available from SRFT, we examined disparities in patient outcomes associated with out-of-hours admissions across the full range of clinical specialties. We aimed to answer the following three key questions:
-
Is the weekend effect found when weekends are more appropriately defined (i.e. 19.00 hours Friday to 06.59 hours Monday)?
-
Does the weekend effect vary over time?
-
Is there a ‘night-time’ effect, with increased risk of mortality for patients admitted at night-time compared with daytime?
Results
We extracted a total of 244,639 emergency spells admitted to SRFT between April 2004 and March 2014, excluding maternity patients and children. About one-third of these (80,971 spells) were admitted during weekends and holidays. Descriptive statistics, as shown in Table 3, suggested that patients in the weekday admission group had similar characteristics to the weekend and holiday admission group, in terms of age, gender, ethnicity distribution and socioeconomic composition. Each spell-level record was associated with around six different diagnosis codes (both primary and secondary diagnoses) and 1.5 operation codes (both primary and secondary procedures) in both groups. Each patient, on average, had one emergency admission in the past year, regardless when he/she was admitted. The Charlson Comorbidity Index, measured as a continuous variable, was only marginally higher for weekend and holiday admissions (5.15 for weekend and holiday admissions vs. 5.07 for weekday admissions).
| Characteristic | Time period | |
|---|---|---|
| Weekday | Weekend and holiday | |
| Number of admissions, n (%) | 163,668 (66.90) | 80,971 (33.10) |
| Average age (years) (SD) | 58.53 (20.98) | 58.51 (21.60) |
| Male, n (%) | 79,292 (48.45) | 39,913 (49.29) |
| White, n (%) | 147,294 (90.00) | 72,519 (89.56) |
| Most deprived quintile, n (%) | 29,197 (17.84) | 14,859 (18.35) |
| Average number of diagnoses (SD) | 5.99 (4.21) | 6.13 (4.20) |
| Average number of procedures (SD) | 1.47 (2.50) | 1.46 (2.54) |
| Average number of emergency admissions in the previous year (SD) | 0.96 (2.04) | 1.02 (2.17) |
| Average Charlson Comorbidity Index score (SD) | 5.07 (8.17) | 5.15 (8.25) |
| 30-day mortality, n (%) | 9363 (5.72) | 5172 (6.39) |
| 7-day mortality, n (%) | 3963 (2.42) | 2360 (2.91) |
| In-hospital mortality, n (%) | 7370 (4.50) | 4046 (5.00) |
The differences in crude mortality rates between the two groups were more noticeable. The weekend and holiday admission group had a higher unadjusted risk of death for each outcome measure. Within 7 days from admission, 2.91% of patients admitted out of hours were recorded as died (both in and out of hospital), compared with 2.42% of the weekday group. The probability of death in 30 days was 11.5% higher if the admission was outside normal working hours (6.39% for weekend and holiday admissions vs. 5.72% for weekday admissions). The result is similar when taking into account only in-hospital death. There was a 0.5 percentage point difference between our admission groups, representing a 10.6% higher risk of death for out-of-hour patients.
In Table 4 we report the association between the risk of death and weekend and holiday admissions after adjusting for patient characteristics and complexity. Each mortality rate was significantly higher for this admission group when averaged across the entire study period. The risk of dying in 30 days increased by 0.4 percentage points if the emergency patients were admitted at weekends or holidays, compared with if they were admitted in normal working hours. The risk of dying in 7 days and the risk of dying in hospital were both increased by 0.3 percentage points for the focal admission group.
| Variable | Mortality | |||||
|---|---|---|---|---|---|---|
| 30 days | SE | 7 days | SE | In hospital | SE | |
| Admission at weekend (and holiday) | 0.004*** | 0.001 | 0.003*** | 0.001 | 0.003*** | 0.001 |
| Case-mix variables | ||||||
| Age on admission | 0.002*** | 0.000 | 0.001*** | 0.000 | 0.001*** | 0.000 |
| Gender (female) | –0.003*** | 0.001 | –0.001 | 0.001 | –0.000 | 0.001 |
| Gender (not stated) | –0.009 | 0.015 | –0.002 | 0.011 | 0.001 | 0.015 |
| Ethnicity (mixed) | –0.012 | 0.010 | 0.003 | 0.007 | –0.009 | 0.009 |
| Ethnicity (Asian) | –0.013*** | 0.005 | –0.007*** | 0.003 | –0.013*** | 0.003 |
| Ethnicity (black) | –0.018*** | 0.006 | –0.011*** | 0.004 | –0.014*** | 0.005 |
| Ethnicity (other) | 0.017*** | 0.006 | 0.012*** | 0.004 | 0.020*** | 0.005 |
| Ethnicity (not stated) | 0.034*** | 0.008 | 0.021*** | 0.005 | 0.031*** | 0.006 |
| IMD quintile 2 | 0.002 | 0.002 | 0.001 | 0.001 | –0.000 | 0.001 |
| IMD quintile 3 | 0.003** | 0.001 | 0.002** | 0.001 | 0.001 | 0.001 |
| IMD quintile 4 | 0.003** | 0.001 | 0.001 | 0.001 | –0.000 | 0.001 |
| IMD quintile 5 (most deprived) | 0.005*** | 0.001 | 0.002** | 0.001 | 0.003** | 0.001 |
| IMD quintile (missing) | 0.014*** | 0.002 | 0.006*** | 0.001 | 0.011*** | 0.002 |
| Charlson Comorbidity Index | 0.002*** | 0.000 | 0.001*** | 0.000 | 0.001*** | 0.000 |
| Number of diagnoses | 0.002*** | 0.000 | 0.000 | 0.000 | 0.003*** | 0.000 |
| Number of procedures | –0.001** | 0.000 | –0.002*** | 0.000 | 0.001*** | 0.000 |
| Palliative care | 0.161*** | 0.013 | 0.039*** | 0.005 | 0.106*** | 0.009 |
| Number of emergency admissions in the previous 1 year (365 days) | 0.001*** | 0.000 | –0.000* | 0.000 | –0.001*** | 0.000 |
| Admission method (emergency transfer from other provider) | –0.017*** | 0.003 | –0.014*** | 0.002 | –0.014*** | 0.003 |
| Admission method (emergency domicile) | –0.007 | 0.018 | –0.026*** | 0.009 | ||
| Admission method (emergency GP refer) | 0.005** | 0.002 | –0.007*** | 0.002 | 0.002 | 0.003 |
| Admission method (emergency outpatient) | –0.021*** | 0.003 | –0.018*** | 0.002 | –0.017*** | 0.003 |
| Admission method (maternity antenatal) | 0.000 | 0.000 | ||||
| Admission method (postnatal) | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Admission method (non-emergency transfer from other provider) | –0.014*** | 0.005 | –0.015*** | 0.003 | –0.016*** | 0.004 |
| Financial year 2005/6 | –0.015*** | 0.004 | –0.003 | 0.002 | –0.015*** | 0.004 |
| Financial year 2006/7 | –0.013*** | 0.003 | –0.003* | 0.002 | –0.020*** | 0.003 |
| Financial year 2007/8 | –0.012** | 0.005 | 0.001 | 0.003 | –0.023*** | 0.006 |
| Financial year 2008/9 | –0.026*** | 0.004 | –0.006* | 0.003 | –0.042*** | 0.005 |
| Financial year 2009/10 | –0.033*** | 0.005 | –0.007** | 0.003 | –0.048*** | 0.005 |
| Financial year 2010/11 | –0.040*** | 0.004 | –0.011*** | 0.003 | –0.059*** | 0.005 |
| Financial year 2011/12 | –0.044*** | 0.004 | –0.013*** | 0.003 | –0.064*** | 0.005 |
| Financial year 2012/13 | –0.041*** | 0.004 | –0.012*** | 0.003 | –0.063*** | 0.005 |
| Financial year 2013/14 | –0.046*** | 0.005 | –0.014*** | 0.003 | –0.067*** | 0.005 |
| Diagnosis group dummies | Yes | Yes | Yes | |||
| Admission source dummies | Yes | Yes | Yes | |||
| Admission month dummies | Yes | Yes | Yes | |||
| c-statistic | 0.88 | 0.87 | 0.90 | |||
| Pseudo-R2 | 0.28 | 0.23 | 0.31 | |||
| Observations | 241,464 | 235,623 | 241,010 | |||
Consistent with the literature, patients’ age, gender and ethnic group were significant predictors for mortality. The risk of dying was increasing with each additional year of age when admitted. Male patients had higher probability of dying in 30 days than female patients. There was no significant difference between male and female patients for 7-day and in-hospital mortalities. Although white patients had a higher risk of death than Asian and black ethnicities, but had better outcome than the group containing all other ethnic backgrounds.
In general, more complex patients were associated with poorer outcomes. A 1-unit increase in the Charlson Comorbidity Index, representing a greater extent of comorbidity, would increase the risk of dying in 30 days by 0.2 percentage points when other confounders were held constant. This impact was 0.1 percentage point for the risk of dying in the first week and the risk of dying in hospital. More diagnosis codes and the inclusion of palliative care within an admission spell were found to be significant predictors for worse outcomes. However, the total number of procedures within a spell and the previous emergency admissions had varying impact across our mortality measures, although the estimated marginal effects were generally statistically significant.
We obtained a c-statistic of around 0.9 in the estimation of each mortality rate, suggesting that our model was a good prediction of our outcome measures. We examined the extent to which this weekend effect varied over time by analysing patients admitted in each financial year. The results in Table 5 show that admission at weekends and holidays were associated with a higher risk of 30-day mortality in 9 out of 10 years. However, in only 3 out of 10 years was this association statistically significant with a p-value of < 0.05. This may reflect a lack of power in the analysis, given the limited number of admissions in each year. These years include 2005/6, with a 0.7 percentage point marginal effect of out-of-hours admission, 2007/8, with a marginal effect of 0.5 percentage points, and 2012/13, with an marginal effect of 0.8 percentage points. The 7-day mortality rate was elevated for weekend and holiday admissions, at a statistical 95% confidence level in 2005/6, 2011/12 and 2012/13. A higher risk of dying in hospital was found for out-of-hours patients in 2011/12, with this impact only weakly significant at a 90% confidence level.
| Time period | Mortality | |||||
|---|---|---|---|---|---|---|
| 30 days | SE | 7 days | SE | In hospital | SE | |
| 2004/5 | ||||||
| Weekend and holiday | 0.004 | 0.004 | 0.005* | 0.003 | 0.003 | 0.003 |
| Observations | 20,898 | 18,404 | 20,303 | |||
| 2005/6 | ||||||
| Weekend and holiday | 0.007** | 0.003 | 0.005** | 0.002 | 0.004 | 0.003 |
| Observations | 20,521 | 17,535 | 20,070 | |||
| 2006/7 | ||||||
| Weekend and holiday | 0.005 | 0.003 | 0.001 | 0.003 | 0.003 | 0.002 |
| Observations | 21,174 | 18,732 | 20,479 | |||
| 2007/8 | ||||||
| Weekend and holiday | 0.005** | 0.003 | 0.002 | 0.002 | 0.003 | 0.003 |
| Observations | 21,626 | 19,202 | 21,591 | |||
| 2008/9 | ||||||
| Weekend and holiday | 0.004* | 0.002 | 0.003 | 0.002 | 0.002 | 0.00) |
| Observations | 21,506 | 19,688 | 20,998 | |||
| 2009/10 | ||||||
| Weekend and holiday | –0.001 | 0.003 | 0.001 | 0.002 | 0.004 | 0.003 |
| Observations | 22,101 | 20,245 | 21,701 | |||
| 2010/11 | ||||||
| Weekend and holiday | 0.005 | 0.004 | 0.001 | 0.003 | 0.003 | 0.002 |
| Observations | 23,802 | 21,787 | 22,939 | |||
| 2011/12 | ||||||
| Weekend and holiday | 0.004* | 0.002 | 0.005*** | 0.002 | 0.003* | 0.002 |
| Observations | 24,614 | 20,504 | 23,791 | |||
| 2012/13 | ||||||
| Weekend and holiday | 0.008*** | 0.003 | 0.005*** | 0.002 | 0.003 | 0.002 |
| Observations | 24,611 | 22,016 | 23,681 | |||
| 2013/14 | ||||||
| Weekend and holiday | 0.002 | 0.002 | 0.001 | 0.002 | 0.002 | 0.002 |
| Observations | 27,227 | 24,589 | 27,249 | |||
Applying our second definition of the exposure variable, we found evidence of inequality in the outcomes as each out-of-hours admission group had an independent and statistically significant association with higher risk of death (Table 6). Averaged across the study period, patients admitted on weekdays but after 19.00 hours were more likely to die by 0.3 percentage points than patients admitted during the day. This difference was constant across the three mortality variables. Weekend admissions during daytime had similar impact on the outcome variables compared with the same reference group. Adjusted 30-day mortality increased by 0.4 percentage points for this group, whereas both 7-day and in-hospital mortalities rose by 0.3 percentage points. Admissions to hospital overnight at weekends had the worst outcomes throughout the week. There was an additional 0.6 percentage point risk of dying in 30 days for these patients. The probability of dying in 7 days increased by 0.4 percentage points, whereas the chance of dying in hospital similarly increased by 0.5 percentage points.
| Variable | Mortality | |||||
|---|---|---|---|---|---|---|
| 30 days | SE | 7 days | SE | In hospital | SE | |
| Admission at weekday night | 0.003** | 0.001 | 0.003*** | 0.001 | 0.003*** | 0.001 |
| Admission at weekend day | 0.004*** | 0.001 | 0.003*** | 0.001 | 0.003** | 0.002 |
| Admission at weekend night | 0.006*** | 0.001 | 0.004*** | 0.001 | 0.005*** | 0.001 |
| Case-mix variables | ||||||
| Age on admission | 0.002*** | 0.000 | 0.001*** | 0.000 | 0.001*** | 0.000 |
| Gender (female) | –0.003*** | 0.001 | –0.001 | 0.001 | –0.000 | 0.001 |
| Gender (not stated) | –0.009 | 0.015 | –0.002 | 0.011 | 0.001 | 0.015 |
| Ethnicity (mixed) | –0.012 | 0.010 | 0.003 | 0.007 | –0.009 | 0.009 |
| Ethnicity (Asian) | –0.013*** | 0.005 | –0.007*** | 0.003 | –0.013*** | 0.003 |
| Ethnicity (black) | –0.018*** | 0.006 | –0.011*** | 0.004 | –0.014*** | 0.005 |
| Ethnicity (other) | 0.017*** | 0.006 | 0.012*** | 0.004 | 0.020*** | 0.005 |
| Ethnicity (not stated) | 0.034*** | 0.008 | 0.021*** | 0.005 | 0.031*** | 0.006 |
| IMD quintile 2 | 0.002 | 0.002 | 0.001 | 0.001 | –0.000 | 0.001 |
| IMD quintile 3 | 0.003** | 0.001 | 0.002** | 0.001 | 0.001 | 0.001 |
| IMD quintile 4 | 0.003** | 0.001 | 0.001 | 0.001 | –0.000 | 0.001 |
| IMD quintile 5 (most deprived) | 0.005*** | 0.001 | 0.002** | 0.001 | 0.003** | 0.001 |
| IMD quintile (missing) | 0.014*** | 0.002 | 0.006*** | 0.001 | 0.011*** | 0.002 |
| Charlson Comorbidity Index | 0.002*** | 0.000 | 0.001*** | 0.000 | 0.001*** | 0.000 |
| Number of diagnoses | 0.002*** | 0.000 | 0.000 | 0.000 | 0.003*** | 0.000 |
| Number of procedures | –0.001** | 0.000 | –0.002*** | 0.000 | 0.001*** | 0.000 |
| Palliative care | 0.161*** | 0.013 | 0.039*** | 0.005 | 0.106*** | 0.009 |
| Number of emergency admissions in the previous 1 year (365 days) | 0.001*** | 0.000 | –0.000* | 0.000 | –0.001*** | 0.000 |
| Admission method (emergency transfer from other provider) | –0.017*** | 0.003 | –0.013*** | 0.002 | –0.014*** | 0.003 |
| Admission method (emergency domicile) | –0.006 | 0.018 | –0.026*** | 0.009 | ||
| Admission method (emergency GP refer) | 0.006** | 0.003 | –0.007*** | 0.002 | 0.002 | 0.003 |
| Admission method (emergency outpatient) | –0.020*** | 0.003 | –0.018*** | 0.002 | –0.017*** | 0.003 |
| Admission method (maternity antenatal) | 0.000 | 0.000 | ||||
| Admission method (postnatal) | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Admission method (non-emergency transfer from other provider) | –0.014*** | 0.005 | –0.015*** | 0.003 | –0.016*** | 0.004 |
| Financial year 2005/6 | –0.015*** | 0.004 | –0.003 | 0.002 | –0.016*** | 0.004 |
| Financial year 2006/7 | –0.013*** | 0.003 | –0.003* | 0.002 | –0.020*** | 0.003 |
| Financial year 2007/8 | –0.012** | 0.005 | 0.001 | 0.003 | –0.023*** | 0.006 |
| Financial year 2008/9 | –0.026*** | 0.004 | –0.006* | 0.003 | –0.042*** | 0.005 |
| Financial year 2009/10 | –0.034*** | 0.005 | –0.008** | 0.003 | –0.049*** | 0.005 |
| Financial year 2010/11 | –0.041*** | 0.004 | –0.011*** | 0.003 | –0.059*** | 0.005 |
| Financial year 2011/12 | –0.044*** | 0.004 | –0.013*** | 0.003 | –0.064*** | 0.005 |
| Financial year 2012/13 | –0.042*** | 0.004 | –0.012*** | 0.003 | –0.063*** | 0.005 |
| Financial year 2013/14 | –0.047*** | 0.005 | –0.014*** | 0.003 | –0.067*** | 0.005 |
| Diagnosis group dummies | Yes | Yes | Yes | |||
| Admission source dummies | Yes | Yes | Yes | |||
| Admission month dummies | Yes | Yes | Yes | |||
| c-statistic | 0.88 | 0.87 | 0.90 | |||
| Pseudo-R2 | 0.28 | 0.23 | 0.31 | |||
| Observations | 241,464 | 235,623 | 241,010 | |||
Table 7 contains the results from the estimation of each financial year. There was evidence suggesting that, in most of these years, patients’ mortality was affected by which day of the week and what time of the day they were admitted. The pattern of this disparity, however, varied depending on the mortality variable as well as on the financial year under study. In general, patients’ chance of survival was more likely to be affected by the admission time and date in 2004/5, 2006/7 and 2012/13, with stronger correlation between higher mortality rates and out-of-hours admissions. However, these are not the only years that showed inequality in patient outcomes. In 2008/9, both 7-day and 30-day mortalities had a substantial increase for the weekend night admission group. In 2013/14, the highest risk of dying in 7 days and in hospital was observed for those admitted overnight on weekdays after adjusting for patient case mix.
| Time period | Mortality | |||||
|---|---|---|---|---|---|---|
| 30 days | SE | 7 days | SE | In hospital | SE | |
| 2004/5 | ||||||
| Weekday: night | 0.011*** | 0.003 | 0.008** | 0.003 | 0.009** | 0.004 |
| Weekend: day | 0.006 | 0.004 | 0.006* | 0.003 | 0.003 | 0.004 |
| Weekend: night | 0.010* | 0.005 | 0.009** | 0.004 | 0.008* | 0.005 |
| Observations | 20,898 | 18,404 | 20,303 | |||
| 2005/6 | ||||||
| Weekday: night | 0.001 | 0.004 | 0.002 | 0.003 | 0.004 | 0.005 |
| Weekend: day | 0.009* | 0.004 | 0.009** | 0.004 | 0.005 | 0.004 |
| Weekend: night | 0.007 | 0.005 | 0.004 | 0.003 | 0.007* | 0.004 |
| Observations | 20,521 | 17,535 | 20,070 | |||
| 2006/7 | ||||||
| Weekday: night | 0.009** | 0.004 | 0.008*** | 0.003 | 0.008* | 0.004 |
| Weekend: day | 0.001 | 0.004 | 0.000 | 0.004 | –0.000 | 0.004 |
| Weekend: night | 0.013*** | 0.004 | 0.007** | 0.003 | 0.010** | 0.004 |
| Observations | 21,174 | 18,732 | 20,479 | |||
| 2007/8 | ||||||
| Weekday: night | 0.001 | 0.003 | 0.002 | 0.003 | –0.002 | 0.003 |
| Weekend: day | 0.002 | 0.004 | 0.001 | 0.004 | 0.001 | 0.004 |
| Weekend: night | 0.008** | 0.004 | 0.003 | 0.003 | 0.003 | 0.003 |
| Observations | 21,626 | 19,202 | 21,591 | |||
| 2008/9 | ||||||
| Weekday: night | 0.005* | 0.003 | 0.002 | 0.003 | 0.003 | 0.003 |
| Weekend: day | 0.004 | 0.004 | –0.000 | 0.004 | 0.002 | 0.004 |
| Weekend: night | 0.009*** | 0.003 | 0.007** | 0.003 | 0.004 | 0.003 |
| Observations | 21,506 | 19,688 | 20,998 | |||
| 2009/10 | ||||||
| Weekday: night | –0.000 | 0.004 | 0.006** | 0.003 | 0.002 | 0.003 |
| Weekend: day | –0.001 | 0.007 | 0.003 | 0.003 | 0.005 | 0.006 |
| Weekend: night | –0.002 | 0.003 | 0.003 | 0.003 | 0.006* | 0.003 |
| Observations | 22,101 | 20,245 | 21,701 | |||
| 2010/11 | ||||||
| Weekday: night | 0.001 | 0.004 | 0.004* | 0.002 | 0.004 | 0.003 |
| Weekend: day | 0.007* | 0.004 | 0.002 | 0.002 | 0.004 | 0.003 |
| Weekend: night | 0.004 | 0.006 | 0.003 | 0.004 | 0.005 | 0.004 |
| Observations | 23,802 | 21,787 | 22,939 | |||
| 2011/12 | ||||||
| Weekday: night | –0.001 | 0.003 | –0.004 | 0.003 | –0.002 | 0.003 |
| Weekend: day | 0.001 | 0.005 | 0.003 | 0.003 | 0.002 | 0.004 |
| Weekend: night | 0.005** | 0.002 | 0.004 | 0.003 | 0.003 | 0.002 |
| Observations | 24,614 | 20,504 | 23,791 | |||
| 2012/13 | ||||||
| Weekday: night | 0.002 | 0.002 | –0.000 | 0.002 | –0.001 | 0.002 |
| Weekend: day | 0.010** | 0.004 | 0.006* | 0.003 | 0.004 | 0.003 |
| Weekend: night | 0.008** | 0.004 | 0.005* | 0.003 | 0.002 | 0.003 |
| Observations | 24,611 | 22,016 | 23,681 | |||
| 2013/14 | ||||||
| Weekday: night | 0.003 | 0.002 | 0.004** | 0.002 | 0.005** | 0.002 |
| Weekend: day | 0.003 | 0.003 | 0.002 | 0.003 | 0.005 | 0.003 |
| Weekend: night | 0.004* | 0.002 | 0.003 | 0.002 | 0.003 | 0.002 |
| Observations | 27,227 | 24,589 | 27,249 | |||
Dividing a week into 14 short periods, the results showed that patients admitted overnight were exposed to greater risk of mortality than day admissions (Table 8). The adjusted mortality rates were the highest for admissions overnight on Saturdays and Sundays, with the marginal effects on the risk of dying in 30 days being 0.8 and 0.6 percentage points, respectively. Moreover, emergency patients admitted overnight from Tuesdays to Fridays were also affected, although to a lesser extent. Among day admissions, only Sundays were associated with a higher risk of dying in 7 days than on Wednesdays, at 90% confidence level. We did not observe a similar association for any other day of the week.
| Variable | Mortality | |||||
|---|---|---|---|---|---|---|
| 30 days | SE | 7 days | SE | In hospital | SE | |
| Admission: Monday/day | 0.002 | 0.003 | 0.000 | 0.001 | 0.000 | 0.002 |
| Admission: Monday/night | 0.003 | 0.002 | 0.002 | 0.001 | 0.003 | 0.002 |
| Admission: Tuesday/day | 0.002 | 0.004 | 0.001 | 0.002 | 0.001 | 0.002 |
| Admission: Tuesday/night | 0.004* | 0.002 | 0.003** | 0.002 | 0.003* | 0.002 |
| Admission: Wednesday/night | 0.002 | 0.002 | 0.003** | 0.001 | 0.002 | 0.002 |
| Admission: Thursday/day | –0.002 | 0.002 | –0.001 | 0.001 | –0.001 | 0.001 |
| Admission: Thursday/night | 0.004 | 0.002 | 0.003** | 0.001 | 0.005** | 0.002 |
| Admission: Friday/day | 0.001 | 0.002 | 0.000 | 0.001 | 0.002 | 0.002 |
| Admission: Friday/night | 0.006** | 0.003 | 0.002 | 0.001 | 0.005** | 0.002 |
| Admission: Saturday/day | 0.003 | 0.003 | 0.002 | 0.001 | 0.002 | 0.002 |
| Admission: Saturday/night | 0.008*** | 0.003 | 0.006*** | 0.002 | 0.006** | 0.003 |
| Admission: Sunday/day | 0.004 | 0.003 | 0.003* | 0.002 | 0.004 | 0.003 |
| Admission: Sunday/night | 0.006** | 0.003 | 0.004** | 0.002 | 0.004* | 0.002 |
| Case-mix variables | ||||||
| Age on admission | 0.002*** | 0.000 | 0.001*** | 0.000 | 0.001*** | 0.000 |
| Gender (female) | –0.003*** | 0.001 | –0.001 | 0.001 | –0.000 | 0.001 |
| Gender (not stated) | –0.009 | 0.015 | –0.002 | 0.011 | 0.001 | 0.015 |
| Ethnicity (mixed) | –0.012 | 0.010 | 0.003 | 0.007 | –0.009 | 0.009 |
| Ethnicity (Asian) | –0.013*** | 0.005 | –0.007*** | 0.003 | –0.013*** | 0.003 |
| Ethnicity (black) | –0.018*** | 0.006 | –0.011*** | 0.004 | –0.014*** | 0.005 |
| Ethnicity (other) | 0.017*** | 0.006 | 0.012*** | 0.004 | 0.020*** | 0.005 |
| Ethnicity (not stated) | 0.034*** | 0.008 | 0.021*** | 0.005 | 0.031*** | 0.006 |
| IMD quintile 2 | 0.002 | 0.002 | 0.001 | 0.001 | –0.000 | 0.001 |
| IMD quintile 3 | 0.003* | 0.001 | 0.002** | 0.001 | 0.001 | 0.001 |
| IMD quintile 4 | 0.003** | 0.001 | 0.001 | 0.001 | –0.000 | 0.001 |
| IMD quintile 5 (most deprived) | 0.005*** | 0.001 | 0.002** | 0.001 | 0.003** | 0.001 |
| IMD quintile (missing) | 0.014*** | 0.002 | 0.006*** | 0.001 | 0.011*** | 0.002 |
| Charlson Comorbidity Index | 0.002*** | 0.000 | 0.001*** | 0.000 | 0.001*** | 0.000 |
| Number of diagnoses | 0.002*** | 0.000 | 0.000 | 0.000 | 0.003*** | 0.000 |
| Number of procedures | –0.001** | 0.000 | –0.002*** | 0.000 | 0.001*** | 0.000 |
| Palliative care | 0.161*** | 0.012 | 0.039*** | 0.005 | 0.106*** | 0.009 |
| Number of emergency admissions in the previous 1 year (365 days) | 0.001*** | 0.000 | –0.000* | 0.000 | –0.001*** | 0.000 |
| Admission method (emergency transfer from other provider) | –0.017*** | 0.003 | –0.013*** | 0.002 | –0.014*** | 0.003 |
| Admission method (emergency domicile) | –0.006 | 0.018 | –0.026*** | 0.009 | ||
| Admission method (emergency GP refer) | 0.006** | 0.003 | –0.007*** | 0.002 | 0.002 | 0.003 |
| Admission method (emergency outpatient) | –0.020*** | 0.003 | –0.018*** | 0.002 | –0.017*** | 0.003 |
| Admission method (maternity antenatal) | 0.000 | 0.000 | ||||
| Admission method (postnatal) | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Admission method (non-emergency transfer from other provider) | –0.014*** | 0.005 | –0.015*** | 0.003 | –0.016*** | 0.004 |
| Financial year 2005/6 | –0.015*** | 0.004 | –0.003 | 0.002 | –0.016*** | 0.004 |
| Financial year 2006/7 | –0.013*** | 0.003 | –0.003* | 0.002 | –0.020*** | 0.003 |
| Financial year 2007/8 | –0.012** | 0.005 | 0.001 | 0.004 | –0.023*** | 0.006 |
| Financial year 2008/9 | –0.026*** | 0.004 | –0.006* | 0.003 | –0.042*** | 0.005 |
| Financial year 2009/10 | –0.034*** | 0.005 | –0.008** | 0.003 | –0.049*** | 0.005 |
| Financial year 2010/11 | –0.041*** | 0.004 | –0.011*** | 0.003 | –0.060*** | 0.005 |
| Financial year 2011/12 | –0.044*** | 0.004 | –0.013*** | 0.003 | –0.064*** | 0.005 |
| Financial year 2012/13 | –0.042*** | 0.004 | –0.012*** | 0.003 | –0.063*** | 0.005 |
| Financial year 2013/14 | –0.047*** | 0.005 | –0.014*** | 0.003 | –0.067*** | 0.005 |
| Diagnosis group dummies | Yes | Yes | Yes | |||
| Admission source dummies | Yes | Yes | Yes | |||
| Admission month dummies | Yes | Yes | Yes | |||
| c-statistic | 0.88 | 0.87 | 0.90 | |||
| Pseudo-R2 | 0.28 | 0.23 | 0.31 | |||
| Observations | 241,464 | 235,623 | 241,010 | |||
Conclusions
We found that, in addition to a weekend effect, there is a night-time effect; mortality rates are elevated for patients admitted at night and the highest risk of death is for patients admitted at night on weekends. We also found that the size of weekend and night-time effects varies over time. They are present in most years, but are not always statistically significant. However, this variation and lack of statistical significance may be attributable to a lack of power for analyses of individual years. Our finding of increased risk of mortality at night-times across the range of emergency admissions suggests that more patients may be affected by service variations across the week than estimated in previous studies based on weekend/weekday comparisons. However, as with previous studies, we cannot exclude the possibility that reduced capacity out of hours leads to the selection of a sicker patient population and that this explains increased risk of mortality for both weekend and night-time admissions. We explore the issue of patient selection in studies 3 and 4.
Chapter 5 Results (study 3): national emergency patient flows and evidence for patient selection at weekends
Material in this chapter has been reproduced from Meacock et al. 12 This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 3.0 License (http://www.creativecommons.org/licenses/by-nc/3.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Background
The finding that patients admitted to hospital in an emergency at the weekend have a higher rate of mortality than those admitted during the week is now well documented. 3,15,26 However, the cause of this weekend effect is not known. The phenomenon has been attributed to reduced availability of senior clinical staff and access to investigative services in hospitals at weekends,7 but there is no causal evidence establishing this link.
Differences in the severity of illness of patients admitted to hospital at the weekend compared with during the week may not be captured fully by the case-mix variables available in administrative data sets. 38 The number of patients admitted to hospital in an emergency is markedly reduced at weekends. 15,35 This may be because the population is less likely to seek emergency care, A&E departments are less likely to admit patients and/or the limited availability of services in the community leads to fewer direct admissions to hospital. Higher death rates among the restricted number of patients who are admitted at weekends might reflect a higher average severity of illness among those who are admitted rather than excess avoidable deaths caused by poorer quality of care on admission.
In this study we perform a detailed analysis of the variation by day of the week in the number of admissions and subsequent mortality, stratifying patients by their route of access to hospital. We exploit previously underutilised data on A&E attendances to investigate whether or not higher mortality among the population of patients admitted to hospital reflects a more stringent admission threshold. We then examine the extent to which the limited availability of services in the community at weekends leads to fewer direct admissions and whether or not there is a higher mortality rate among the restricted number of patients who are admitted via this route.
Results
Accident and emergency department attendances
The average number of people attending A&E is highest on Monday (41,417) and lowest on Friday (36,426) (Table 9). The average number of attendances on weekend days is similar to weekdays (38,254 vs. 37,812 attendances, difference = 442 attendances; 95% CI –148 to 1031 attendances). The characteristics of patients attending A&E on weekdays and at weekends are given in Table 10. A slightly higher proportion of patients attending A&E at the weekend are children or younger adults, but similar proportions are in the oldest age groups (aged > 90 years) on weekend days and weekdays. The proportions of patients with the most common presentations are similar on weekends and weekdays. Lower proportions of patients from the most deprived areas (quintiles 1 and 2) attend A&E at weekends.
| Day | Average number of | Mortality rate within 30 days following A&E attendance on this day of the week | ||
|---|---|---|---|---|
| A&E attendances per day on this day of the week | Deaths within 30 days following A&E attendance per day on this day of the week | Crude (%) | Risk-adjusted, OR (95% CI)a | |
| Monday | 41,416.8 | 402.9 | 0.97 | 1.034 (1.014 to 1.055) |
| Tuesday | 37,470.6 | 388.1 | 1.04 | 0.994 (0.974 to 1.014) |
| Wednesday | 36,932.9 | 375.6 | 1.02 | Reference |
| Thursday | 36,815.2 | 385.6 | 1.05 | 1.010 (0.989 to 1.030) |
| Friday | 36,425.6 | 389.4 | 1.07 | 0.996 (0.976 to 1.016) |
| Saturday | 37,165.9 | 374.9 | 1.01 | 0.997 (0.976 to 1.017) |
| Sunday | 39,341.8 | 381.1 | 0.97 | 1.037 (1.016 to 1.058) |
| Weekday | 37,812.2 | 388.3 | 1.03 | Reference |
| Weekend | 38,253.8 | 378.0 | 0.99 | 1.010b (0.997 to 1.022) |
| Difference (weekend – weekday) | 441.6 (–147.5 to 1030.8) | –10.3 (–22.3 to 1.8) | –0.04 (–0.076 to –0.001) | |
| Ratio (weekend : weekday) | 1.01 | 0.97 | 0.96 | |
| Variable | Time period | |||
|---|---|---|---|---|
| Weekday (n) | Weekend (n) | Weekday (%) | Weekend (%) | |
| n | 9,074,928 | 3,595,860 | 100.00 | 100.00 |
| Female | 4,518,407 | 1,786,423 | 49.79 | 49.68 |
| Age category (years) | ||||
| < 1 | 234,133 | 103,920 | 2.58 | 2.89 |
| 1–4 | 613,465 | 283,354 | 6.76 | 7.88 |
| 5–9 | 387,499 | 163,612 | 4.27 | 4.55 |
| 10–14 | 464,636 | 151,745 | 5.12 | 4.22 |
| 15–19 | 572,628 | 239,844 | 6.31 | 6.67 |
| 20–24 | 735,069 | 321,829 | 8.10 | 8.95 |
| 25–29 | 676,990 | 278,679 | 7.46 | 7.75 |
| 30–34 | 589,870 | 235,169 | 6.50 | 6.54 |
| 35–39 | 491,861 | 192,738 | 5.42 | 5.36 |
| 40–44 | 524,531 | 201,368 | 5.78 | 5.60 |
| 45–49 | 525,438 | 199,211 | 5.79 | 5.54 |
| 50–54 | 477,341 | 178,714 | 5.26 | 4.97 |
| 55–59 | 393,852 | 146,352 | 4.34 | 4.07 |
| 60–64 | 362,090 | 135,924 | 3.99 | 3.78 |
| 65–69 | 378,424 | 142,396 | 4.17 | 3.96 |
| 70–74 | 347,570 | 130,170 | 3.83 | 3.62 |
| 75–79 | 378,424 | 141,317 | 4.17 | 3.93 |
| 80–84 | 383,869 | 143,475 | 4.23 | 3.99 |
| 85–89 | 312,178 | 118,663 | 3.44 | 3.30 |
| 90–94 | 176,054 | 68,321 | 1.94 | 1.90 |
| 95–99 | 40,837 | 16,181 | 0.45 | 0.45 |
| ≥ 100 | 6352 | 2517 | 0.07 | 0.07 |
| Ethnic group | ||||
| Unknown | 1,247,803 | 509,893 | 13.75 | 14.18 |
| White | 6,565,710 | 2,591,536 | 72.35 | 72.07 |
| Mixed | 118,882 | 47,465 | 1.31 | 1.32 |
| Asian | 550,848 | 220,426 | 6.07 | 6.13 |
| Black | 336,680 | 125,136 | 3.71 | 3.48 |
| Other | 255,005 | 101,403 | 2.81 | 2.82 |
| Quintile of area deprivation | ||||
| 1 (most deprived) | 2,570,020 | 988,502 | 28.32 | 27.49 |
| 2 | 2,038,229 | 795,764 | 22.46 | 22.13 |
| 3 | 1,672,509 | 665,953 | 18.43 | 18.52 |
| 4 | 1,477,398 | 600,149 | 16.28 | 16.69 |
| 5 (least deprived) | 1,316,772 | 545,492 | 14.51 | 15.17 |
| Arrival mode | ||||
| By ambulance | 2,727,016 | 1,120,470 | 30.05 | 31.16 |
| Other | 6,308,890 | 2,463,524 | 69.52 | 68.51 |
| Not known | 38,115 | 11,866 | 0.42 | 0.33 |
| Incident location | ||||
| Home | 4,523,852 | 1,886,029 | 49.85 | 52.45 |
| Work | 343,940 | 64,366 | 3.79 | 1.79 |
| Educational establishment | 217,798 | 12,226 | 2.40 | 0.34 |
| Public place | 829,448 | 411,366 | 9.14 | 11.44 |
| Other | 2,333,164 | 897,527 | 25.71 | 24.96 |
| Not known | 826,726 | 324,706 | 9.11 | 9.03 |
| Referral source | ||||
| General medical practitioner | 664,285 | 84,143 | 7.32 | 2.34 |
| Self-referral | 5,447,679 | 2,302,429 | 60.03 | 64.03 |
| Local authority social services | 7260 | 3236 | 0.08 | 0.09 |
| Emergency services | 1,185,186 | 503,780 | 13.06 | 14.01 |
| Work | 63,524 | 11,507 | 0.70 | 0.32 |
| Educational establishment | 36,300 | 1798 | 0.40 | 0.05 |
| Police | 43,560 | 23,733 | 0.48 | 0.66 |
| Other health-care provider | 345,755 | 144,913 | 3.81 | 4.03 |
| Other | 1,183,371 | 485,441 | 13.04 | 13.5 |
| Not known | 98,917 | 34,880 | 1.09 | 0.97 |
| Diagnosis category | ||||
| Laceration | 302,195 | 138,441 | 3.33 | 3.85 |
| Contusion/abrasion | 251,376 | 93,852 | 2.77 | 2.61 |
| Soft-tissue inflammation | 299,473 | 110,033 | 3.30 | 3.06 |
| Head injury | 190,573 | 83,064 | 2.10 | 2.31 |
| Dislocation/fracture/joint injury/amputation | 444,671 | 176,916 | 4.90 | 4.92 |
| Sprain/ligament injury | 352,107 | 124,776 | 3.88 | 3.47 |
| Muscle/tendon injury | 128,864 | 46,027 | 1.42 | 1.28 |
| Nerve injury | 65,339 | 25,890 | 0.72 | 0.72 |
| Vascular injury | 5445 | 1798 | 0.06 | 0.05 |
| Burns and scalds | 42,652 | 18,698 | 0.47 | 0.52 |
| Electric shock | 5445 | 2158 | 0.06 | 0.06 |
| Foreign body | 68,062 | 23,733 | 0.75 | 0.66 |
| Bites/stings | 29,947 | 15,462 | 0.33 | 0.43 |
| Poisoning (including overdose) | 97,102 | 45,667 | 1.07 | 1.27 |
| Near drowning | 907 | 360 | 0.01 | 0.01 |
| Visceral injury | 2722 | 1079 | 0.03 | 0.03 |
| Infectious disease | 80,767 | 36,678 | 0.89 | 1.02 |
| Local infection | 118,882 | 51,780 | 1.31 | 1.44 |
| Septicaemia | 20,872 | 8630 | 0.23 | 0.24 |
| Cardiac conditions | 282,230 | 95,650 | 3.11 | 2.66 |
| Cerebrovascular conditions | 63,524 | 23,014 | 0.70 | 0.64 |
| Other vascular conditions | 43,560 | 13,664 | 0.48 | 0.38 |
| Haematological conditions | 24,502 | 7551 | 0.27 | 0.21 |
| Central nervous system conditions (excluding stroke) | 156,089 | 56,455 | 1.72 | 1.57 |
| Respiratory conditions | 297,658 | 125,136 | 3.28 | 3.48 |
| Gastrointestinal conditions | 417,447 | 162,892 | 4.60 | 4.53 |
| Urological conditions (including cystitis) | 178,776 | 72,996 | 1.97 | 2.03 |
| Obstetric conditions | 27,225 | 10,788 | 0.30 | 0.30 |
| Gynaecological conditions | 71,692 | 28,048 | 0.79 | 0.78 |
| Diabetes and other endocrinological conditions | 32,670 | 12,226 | 0.36 | 0.34 |
| Dermatological conditions | 39,930 | 19,418 | 0.44 | 0.54 |
| Allergy (including anaphylaxis) | 34,485 | 16,541 | 0.38 | 0.46 |
| Faciomaxillary conditions | 25,410 | 13,664 | 0.28 | 0.38 |
| ENT conditions | 111,622 | 50,342 | 1.23 | 1.40 |
| Psychiatric conditions | 87,119 | 34,161 | 0.96 | 0.95 |
| Ophthalmological conditions | 99,824 | 40,993 | 1.10 | 1.14 |
| Social problems (including chronic alcoholism and homelessness) | 22,687 | 10,068 | 0.25 | 0.28 |
| Diagnosis not classifiable | 1,349,442 | 531,468 | 14.87 | 14.78 |
| Nothing abnormal detected | 206,001 | 84,143 | 2.27 | 2.34 |
| Missing | 2,996,541 | 1,181,959 | 33.02 | 32.87 |
The average number of patients attending A&E on weekend days and dying within 30 days is similar to weekdays (378 vs. 388 patients, difference = –10 patients; 95% CI –22 to 2 patients). The crude death rate following an A&E attendance is significantly lower at the weekend than during the week (0.99% vs. 1.03%, difference = –0.04 percentage points; 95% CI –0.076 to –0.001 percentage points). The risk adjustment model was strongly predictive of mortality (c-statistic of 0.92). After adjusting for risk, attending A&E at the weekend is not associated with a significantly higher probability of mortality than attending during the week (OR 1.010, 95% CI 0.997 to 1.022). Examining the results for each day separately, attending A&E is associated with small but statistically significant higher probabilities of mortality for Sundays (OR 1.037, 95% CI 1.016 to 1.052) and Mondays (OR 1.034, 95% CI 1.014 to 1.055) than with Wednesday attendance. These increases in relative risk equate to absolute increases in the risk of death of 0.034 percentage points on Monday and 0.037 percentage points on Sunday, from a baseline of 1.02% on a Wednesday.
Admissions via accident and emergency departments
Results for the population of emergency patients who are admitted to hospital when they attend A&E are given in Table 11. A lower proportion of the patient population attending A&E at the weekend is admitted to hospital than during the week (27.5% vs. 30.0%, difference = –2.6 percentage points; 95% CI –3.0 to –2.1 percentage points). Consequently, the average number of admissions via A&E is 7% lower for weekend days than for weekdays (10,526 vs. 11,360, difference = –834; 95% CI –941 to –727).
| Day | Admission | Mortality rate within 30 days following admission via A&E on this day of the week | ||||
|---|---|---|---|---|---|---|
| Average number of admissions via A&E per day on this day of the week | Crude admission rate on this day of the week (%) | Risk-adjusted admission rate on this day of the week, OR (95% CI) | Crude (%) | Risk-adjusted (A&E records), OR (95% CI)a | Risk-adjusted (APC records), OR (95% CI)b | |
| Monday | 11,644.8 | 28.1 | 0.979 (0.974 to 0.984) | 3.46 | 1.032 (1.011 to 1.053) | 1.036 (1.012 to 1.060) |
| Tuesday | 11,401.0 | 30.4 | 0.990 (0.985 to 0.996) | 3.40 | 0.997 (0.977 to 1.018) | 1.000 (0.977 to 1.023) |
| Wednesday | 11,153.2 | 30.2 | Reference | 3.37 | Reference | Reference |
| Thursday | 11,241.3 | 30.5 | 1.009 (1.004 to 1.015) | 3.43 | 1.008 (0.987 to 1.029) | 1.019 (0.995 to 1.042) |
| Friday | 11,357.5 | 31.2 | 1.010 (1.005 to 1.016) | 3.43 | 0.981 (0.961 to 1.001) | 1.009 (0.986 to 1.033) |
| Saturday | 10,557.7 | 28.4 | 0.945 (0.940 to 0.951) | 3.55 | 1.037 (1.016 to 1.059) | 1.047 (1.023 to 1.072) |
| Sunday | 10,494.2 | 26.7 | 0.943 (0.937 to 0.948) | 3.63 | 1.081 (1.059 to 1.104) | 1.088 (1.063 to 1.114) |
| Weekday | 11,359.6 | 30.0 | Reference | 3.42 | Reference | Reference |
| Weekend | 10,525.9 | 27.5 | 0.946c (0.943 to 0.950) | 3.59 | 1.055 (1.042 to 1.068) | 1.054 (1.040 to 1.069) |
| Difference (weekend – weekday) | –833.6 (–940.6 to –726.7) | –2.6 (–3.0 to –2.1) | 0.17 (0.08 to 0.27) | |||
| Ratio (weekend : weekday) | 0.93 | 0.92 | 1.05 | |||
The risk adjustment model for the probability of admission had a c-statistic of 0.83. The adjusted admission rate of patients attending A&E at the weekend remains significantly lower than that of those attending during the week (OR 0.946, 95% CI 0.943 to 0.950). The risk adjustment model for the probability of mortality among the subset of patients who are admitted when attending A&E had a c-statistic of 0.91. Patients admitted at the weekend have a significantly higher probability of mortality than those admitted during the week (OR 1.054, 95% CI 1.040 to 1.069). These results are very similar regardless of whether risk adjustment variables are taken from the A&E or inpatient records. Examining the results for each day separately, admissions on Sundays (OR 1.088, 95% CI 1.063 to 1.114), Saturdays (OR 1.047, 95% CI 1.023 to 1.072) and Mondays (OR 1.036, 95% CI 1.012 to 1.060) are associated with higher mortality than Wednesday admissions. These are the days on which the patients who attend A&E have the lowest risk-adjusted probabilities of admission.
Direct admissions
The average number of direct admissions to hospital from services in the community is fairly stable across weekdays, but falls by 61% at weekends (average of 1317 admissions for weekend days compared with 3404 admissions for weekdays, difference = –2087 admissions; 95% CI –2174 to –1999 admissions) (Table 12). The characteristics of patients directly admitted to hospital on weekdays and weekends are given in Table 13. A higher proportion of patients directly admitted at the weekend are children, younger adults or very elderly (0–34 years or ≥ 90 years) than on weekdays. Very slightly higher proportions of patients from the most deprived areas (quintiles 1 and 2) are directly admitted at weekends. The most common primary diagnoses among patients directly admitted during the week are abdominal pain, influenza and headaches. For those directly admitted during the weekend, these are influenza, abdominal pain and intestinal infections. The population directly admitted at the weekend is less likely to have most of the Elixhauser conditions.
| Day | Admission | Mortality rate within 30 days following admission via A&E on this day of the week | ||
|---|---|---|---|---|
| Average number of admissions per day on this day of the week | Average number of deaths within 30 days of admission per day on this day of the week | Crude (%) | Risk-adjusted, OR (95% CI)a | |
| Monday | 3489.2 | 83.7 | 2.40 | 1.032 (0.982 to 1.085) |
| Tuesday | 3351.4 | 79.7 | 2.38 | 1.018 (0.968 to 1.071) |
| Wednesday | 3232.9 | 76.5 | 2.37 | Reference |
| Thursday | 3336.1 | 78.2 | 2.34 | 0.984 (0.935 to 1.035) |
| Friday | 3611.7 | 85.8 | 2.38 | 0.968 (0.922 to 1.018) |
| Saturday | 1397.5 | 36.7 | 2.63 | 1.154 (1.082 to 1.231) |
| Sunday | 1237.3 | 35.0 | 2.83 | 1.278 (1.196 to 1.366) |
| Weekday | 3404.3 | 80.8 | 2.37 | Reference |
| Weekend | 1317.4 | 35.9 | 2.72 | 1.212 (1.162 to 1.263) |
| Difference (weekend – weekday) | –2086.9 (–2174.4 to –1999.4) | –44.9 (–47.8 to –42.0) | 0.35 (0.24 to 0.46) | |
| Ratio (weekend : weekday) | 0.39 | 0.44 | 1.15 | |
| Variable | Time period | |||
|---|---|---|---|---|
| Weekday (n) | Weekend (n) | Weekday (%) | Weekend (%) | |
| Observations | 817,024 | 123,835 | 100.00 | 100.00 |
| Female | 441,520 | 67,180 | 54.04 | 54.25 |
| Age category (years) | ||||
| < 1 | 51,799 | 10,699 | 6.34 | 8.64 |
| 1–4 | 54,414 | 12,161 | 6.66 | 9.82 |
| 5–9 | 22,141 | 4520 | 2.71 | 3.65 |
| 10–14 | 19,037 | 2923 | 2.33 | 2.36 |
| 15–19 | 24,184 | 4235 | 2.96 | 3.42 |
| 20–24 | 34,887 | 6217 | 4.27 | 5.02 |
| 25–29 | 36,276 | 6056 | 4.44 | 4.89 |
| 30–34 | 35,704 | 5560 | 4.37 | 4.49 |
| 35–39 | 30,965 | 4594 | 3.79 | 3.71 |
| 40–44 | 34,805 | 4966 | 4.26 | 4.01 |
| 45–49 | 38,809 | 5201 | 4.75 | 4.2 |
| 50–54 | 39,871 | 5152 | 4.88 | 4.16 |
| 55–59 | 39,544 | 4842 | 4.84 | 3.91 |
| 60–64 | 45,672 | 5535 | 5.59 | 4.47 |
| 65–69 | 56,538 | 6811 | 6.92 | 5.5 |
| 70–74 | 55,639 | 6737 | 6.81 | 5.44 |
| 75–79 | 61,195 | 7517 | 7.49 | 6.07 |
| 80–84 | 60,215 | 8148 | 7.37 | 6.58 |
| 85–89 | 46,407 | 6972 | 5.68 | 5.63 |
| 90–94 | 23,612 | 4000 | 2.89 | 3.23 |
| 95–99 | 4739 | 879 | 0.58 | 0.71 |
| ≥ 100 | 572 | 124 | 0.07 | 0.1 |
| Ethnic group | ||||
| White | 698,147 | 105,074 | 85.45 | 84.85 |
| Mixed | 7435 | 1313 | 0.91 | 1.06 |
| Asian | 35,622 | 6068 | 4.36 | 4.9 |
| Black | 11,030 | 1474 | 1.35 | 1.19 |
| Other | 9069 | 1375 | 1.11 | 1.11 |
| Unknown | 55,721 | 8532 | 6.82 | 6.89 |
| Quintile of area deprivation | ||||
| 1 (most deprived) | 191,020 | 29,671 | 23.38 | 23.96 |
| 2 | 165,284 | 25,176 | 20.23 | 20.33 |
| 3 | 165,284 | 25,052 | 20.23 | 20.23 |
| 4 | 155,725 | 23,095 | 19.06 | 18.65 |
| 5 (least deprived) | 139,711 | 20,841 | 17.1 | 16.83 |
| Admission method | ||||
| GP | 633,275 | 102,709 | 77.51 | 82.94 |
| Bed bureau | 64,627 | 11,529 | 7.91 | 9.31 |
| Consultant clinic | 119,204 | 9597 | 14.59 | 7.75 |
| SHMI diagnosis group (138 in total, 10 most common on weekday and/or weekend listed) | ||||
| Abdominal pain | 48,531 | 8235 | 5.94 | 6.65 |
| Influenza and other upper respiratory infections | 41,913 | 8334 | 5.13 | 6.73 |
| Headache and eye disorders | 29,658 | 3740 | 3.63 | 3.02 |
| Complications of fertility and pregnancy | 29,331 | 4359 | 3.59 | 3.52 |
| Skin and subcutaneous infections | 26,390 | 4161 | 3.23 | 3.36 |
| Acute bronchitis | 25,164 | 4891 | 3.08 | 3.95 |
| Other connective tissue disease | 24,919 | 2340 | 3.05 | 1.89 |
| Non-specific chest pain | 24,592 | 2142 | 3.01 | 1.73 |
| Urinary tract infections | 23,040 | 5077 | 2.82 | 4.1 |
| Hepatitis and sexually transmitted infections | 22,386 | 4978 | 2.74 | 4.02 |
| Intestinal infections | 22,223 | 5275 | 2.72 | 4.26 |
| Pneumonia (excluding tuberculosis and sexually transmitted disease) | 22,141 | 4012 | 2.71 | 3.24 |
| Elixhauser conditions | ||||
| Congestive heart failure | 30,965 | 3926 | 3.79 | 3.17 |
| Cardiac arrhythmias | 78,598 | 10,514 | 9.62 | 8.49 |
| Valvular disease | 21,569 | 2365 | 2.64 | 1.91 |
| Pulmonary circulation disorders | 5392 | 582 | 0.66 | 0.47 |
| Peripheral vascular disorders | 16,831 | 1895 | 2.06 | 1.53 |
| Hypertension, uncomplicated | 179,827 | 22,340 | 22.01 | 18.04 |
| Hypertension, complicated | 980 | 124 | 0.12 | 0.1 |
| Paralysis | 4984 | 842 | 0.61 | 0.68 |
| Other neurological disorders | 26,717 | 4347 | 3.27 | 3.51 |
| Chronic pulmonary disease | 110,053 | 14,390 | 13.47 | 11.62 |
| Diabetes, uncomplicated | 85,216 | 11,294 | 10.43 | 9.12 |
| Diabetes, complicated | 9804 | 892 | 1.2 | 0.72 |
| Hypothyroidism | 32,599 | 4409 | 3.99 | 3.56 |
| Renal failure | 62,257 | 6353 | 7.62 | 5.13 |
| Liver disease | 14,788 | 1709 | 1.81 | 1.38 |
| Peptic ulcer disease excluding bleeding | 1797 | 248 | 0.22 | 0.2 |
| Lymphoma | 5066 | 854 | 0.62 | 0.69 |
| Metastatic cancer | 27,125 | 3913 | 3.32 | 3.16 |
| Solid tumour without metastasis | 35,541 | 5374 | 4.35 | 4.34 |
| Rheumatoid arthritis/collagen vascular diseases | 21,079 | 2650 | 2.58 | 2.14 |
| Coagulopathy | 4902 | 681 | 0.6 | 0.55 |
| Obesity | 14,461 | 1833 | 1.77 | 1.48 |
| Weight loss | 10,785 | 1090 | 1.32 | 0.88 |
| Fluid and electrolyte disorders | 34,233 | 5610 | 4.19 | 4.53 |
| Blood loss anaemia | 409 | 50 | 0.05 | 0.04 |
| Deficiency anaemia | 12,827 | 1560 | 1.57 | 1.26 |
| Alcohol abuse | 19,037 | 2402 | 2.33 | 1.94 |
The average number of patients directly admitted on weekend days and dying within 30 days is significantly lower than on weekdays (36 vs. 81 patients, difference = –45 patients; 95% CI –48 to –42 patients). However, as a result of the proportionally larger reduction in the average number of direct admissions at the weekend, the proportion of admissions that lead to death within 30 days is higher at weekends than on weekdays (2.72% vs. 2.37%, difference = 0.35%; 95% CI 0.21% to 0.46%).
The model used to predict the probability of mortality produced a c-statistic of 0.92. Adjusted mortality rates for directly admitted patients are lowest for Friday admissions (OR 0.968, 95% CI 0.922 to 1.018) and highest for those admitted on Sunday (OR 1.278, 95% CI 1.196 to 1.366). Compared with direct admissions on a weekday, the relative risk of mortality within 30 days was increased by 21.2% (OR 1.212, 95% CI 1.162 to 1.263) for direct admissions at the weekend. This equates to a 0.488 percentage point increase in the risk of death, from a baseline of 2.37% during the week.
Conclusions
Patients admitted to hospital as emergencies at the weekend are known to have a higher rate of death than patients admitted during the week. However, we did not find any increase in mortality rates for the whole population attending A&E departments at weekends. The weekend effect was only apparent in the subset of patients who are admitted to hospital and was far stronger for patients directly admitted from the community – who were admitted in far smaller numbers at weekends – than for patients admitted via A&E. These findings raise the strong possibility that a sicker population of patients is admitted to hospital at weekends and that this selection effect is at least partly responsible for the weekend effect.
Elevated mortality rates among the population of patients admitted to hospital in an emergency at weekends are driven by a reduction in the number of patients admitted to hospital at the weekend rather than an increase in the number of deaths. There was a 7% reduction in admission numbers through A&E at weekends, which was not fully explained by the patient characteristics that we could control for (although adjusting for patient characteristics did increase the effective odds of being admitted at the weekend – see notes in Table 11). Hospital staff appear to apply a more stringent admission threshold at weekends to patients seeking emergency care through A&E. This raises the possibility that the patient population admitted at weekends is, on average, more severely ill than the population admitted on weekdays and that this increased severity is not completely captured by standard risk adjustment using administrative data.
The weekend effect is greatest among the patients directly admitted to hospital, for whom the relative risk of mortality was 21% higher at the weekend. However, the number of admissions through this route was 61% lower at weekends than on weekdays and these admissions represent just 11% [1317/(1317 + 10,526)] of total emergency admissions on a typical weekend day. The decrease in the number of direct admissions at weekends is not matched by an increase in A&E attendances or admissions, indicating that patients are not simply switching between the two routes into hospital at weekends. The concentration of the weekend effect where we see a substantial restriction in the patient flows again raises the strong possibility that it is attributable to greater unmeasured severity of illness rather than lower quality of care at admission.
There may be concern that patients who are directly admitted could experience different quality of care on arrival at hospital. A small proportion (6%) of patients attending A&E have been referred there by a GP and they are therefore part of the same patient pool as direct admissions in that they initially sought GP care. However, on arrival at A&E these patients would be expected to receive the same care as those who self-refer to A&E. In an attempt to shed further light on our findings we performed some supplementary analysis on this group of patients. We found that the flows of patients referred to A&E by a GP behaved in much the same way as the direct admissions. The number of A&E attenders referred by a GP dropped by 68% at weekends, as did the number of admissions through A&E for this patient group. Attending A&E on a weekend following GP referral was associated with a significantly higher risk-adjusted probability of mortality (OR 1.168, 95% CI 1.096 to 1.245). These findings suggest that direct admission to hospital at the weekend is not a cause of elevated mortality, but instead an indicator of an inherently different patient group. If the cause of elevated weekend mortality among direct admissions was lower quality of care on admission rather than referral of sicker patients, we would not expect to see a weekend effect among patients referred to A&E by a GP.
The central findings of our analysis are (1) that there are fewer deaths following emergency hospital admission at the weekend; (2) that the mortality rate following an A&E attendance is the same regardless of whether patients present at the weekend or on a weekday; and (3) that, conditional on their characteristics as measured in HES, patients are less likely to be admitted to hospital at the weekend. Our interpretation of these findings is that the patients who are most likely to die form a larger proportion of the admitted patient population at the weekend. Hospitals apply more selective filters for admission at the weekend, admitting cases that are, on average, more urgent. Put differently, as we do not know what the appropriate level of admission is, hospitals have the capacity to admit more low-risk patients during the week.
An alternative interpretation could be that hospitals randomly select a smaller proportion of patients for admission at the weekend and the poorer quality of care that these patients receive on admission causes them to die at a higher rate. However, to generate the same overall death rate for all A&E attenders (both admitted and not admitted), this interpretation would require not only that hospitals effectively select the additional patients they choose not to admit at weekends at random (or based on criteria uncorrelated with severity of presentation), but also that the population of patients who present at weekends have a lower underlying risk of death. These offsetting phenomena would need to be even stronger for direct admissions. We think it more plausible that admission decisions at the weekend take some account of the severity and urgency of patients’ conditions. As described by McKee, the comparison of weekend to weekday admissions is ‘confounded by indication’. 38 There are some clues on this in the characteristics of patients attending A&E, including the higher proportion of patients arriving by ambulance at the weekend (see Figure 2).
Previous studies have consistently found higher mortality rates for patients admitted at weekends, both before and after risk adjustment. Although we have also found higher mortality rates among the patients who are admitted at weekends, our study differs in two important respects. First, we widened our focus to include all patients attending A&E departments, including those not admitted, in order to avoid possible selection effects in the admitted population. Second, we assessed direct admissions and admissions via A&E separately, in order to gain a better understanding of variations in patient flows throughout the week. Using this approach we found substantial falls in the number of patients admitted to hospital in an emergency on weekends, attributable to a 61% reduction in the number of direct admission and a 5% relative reduction in the risk-adjusted probability of admission following an A&E attendance. These increased thresholds for admission at weekends are likely to have biased previous studies on weekend mortality.
Chapter 6 Results (study 4): the effect of patient selection on national mortality rates for emergency hospital admissions
Material in this chapter has been reproduced from Anselmi et al. 13 This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/.
Background
Concerns about the adequacy of administrative data to account fully for fluctuations in the severity of patients admitted to hospital at different times of the week have been raised,39,40 suggesting that more accurate adjustment for severity of illness could explain the weekend effect. The majority of studies identifying a weekend effect have relied on analyses of routinely collected inpatient administrative databases and have therefore adjusted for patient risk accounting for demographic characteristics, primary diagnosis and comorbidity measures based on reported ICD-10 codes. 34 Although these risk adjustment models exhibit high explanatory power in predicting mortality, they cannot account fully for severity of illness. 41 Studies based on data from specialist clinical databases and audits for specific diseases or clinical departments have used richer risk adjustment models that account for variations in severity of illness within a diagnostic and comorbidity group. These studies have found little or no significant difference in death rates by day of admission. 42 However, these studies have focused on patients with specific conditions.
In this study, we use national administrative inpatient data merged with previously underutilised data on attendances at A&E departments. These contain information on whether or not the patient arrived by ambulance, an additional indicator of severity not available in the inpatient data. 43 Despite ambulance services being available 24 hours each day of the week, the proportion of patients arriving by ambulance varies substantially across the week. We examine how the inclusion of information on arrival by ambulance in the risk adjustment model affects the observed pattern of mortality across the week.
The attendance data also enable us to use information on the time of arrival at hospital, in addition to the day of arrival. Studies have shown that patterns of outcomes differ throughout the whole week and between daytime and night-time, and that either being admitted overnight or receiving care overnight tends to be associated with worse outcomes. 39,44 This suggests that the description of the weekly variation in care quality as a weekend effect is an oversimplification. If fluctuations in staffing levels are the cause of the weekend effect, we would expect to see the patterns of patient mortality align with the typical shift patterns worked by senior medical staff. We examined numbers and rates of hospital admissions and deaths across the week for patients presenting to emergency services through two routes: (1) hospital A&E departments, which are open throughout the week; and (2) services in the community, for which availability is more restricted at weekends.
Results
Association between crude risk of mortality and day and time of attendance
Of all 3,027,946 patients admitted to hospital following attendance at A&E, and for whom the admitted patient record can be matched with a corresponding A&E record, the majority (1,907,920; 63.0%) attended A&E during daytime, whereas the remaining 1,120,026 (37.0%) attended at night (Table 14). The crude mortality rates are higher for patients attending A&E during the day than at night. This reflects the higher proportions in the highest risk quintile (as measured using the standard risk adjustment model) among patients arriving during the day than for those arriving at night (Figure 1).
| Admission | Number of admitted patients | Crude mortality rate (%) | Model | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1: standard risk adjustment | 2: standard risk adjustment plus mode of arrival | 3: standard risk adjustment (mode of arrival: ambulance) | 4: standard risk adjustment (mode of arrival: non-ambulance) | ||||||||
| Total | Arrived by ambulance | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | ||
| Day and time | |||||||||||
| Wednesday day | 273,739 | 157,675 | 3.66 | Reference | Reference | Reference | Reference | ||||
| Wednesday night | 158,297 | 106,248 | 3.48 | 1.055 | 1.016 to 1.096 | 0.988 | 0.951 to 1.025 | 0.980 | 0.943 to 1.020 | 1.093 | 0.952 to 1.255 |
| Thursday day | 277,620 | 160,146 | 3.75 | 1.028 | 0.996 to 1.060 | 1.027 | 0.996 to 1.060 | 1.030 | 0.997 to 1.065 | 1.015 | 0.920 to 1.121 |
| Thursday night | 159,197 | 107,511 | 3.46 | 1.052 | 1.013 to 1.092 | 0.986 | 0.950 to 1.024 | 0.977 | 0.940 to 1.016 | 1.117 | 0.975 to 1.281 |
| Friday day | 278,570 | 159,339 | 3.71 | 1.001 | 0.970 to 1.033 | 1.007 | 0.976 to 1.039 | 1.006 | 0.973 to 1.041 | 1.015 | 0.921 to 1.120 |
| Friday night | 165,502 | 112,742 | 3.28 | 1.026 | 0.989 to 1.066 | 0.962 | 0.927 to 0.999 | 0.958 | 0.921 to 0.996 | 1.006 | 0.874 to 1.158 |
| Saturday day | 251,464 | 153,602 | 4.00 | 1.058 | 1.025 to 1.092 | 1.031 | 0.999 to 1.064 | 1.028 | 0.995 to 1.063 | 1.097 | 0.988 to 1.219 |
| Saturday night | 164,312 | 113,400 | 3.32 | 1.073 | 1.033 to 1.114 | 0.997 | 0.960 to 1.035 | 0.992 | 0.954 to 1.032 | 1.075 | 0.927 to 1.246 |
| Sunday day | 256,531 | 154,123 | 4.12 | 1.089 | 1.056 to 1.124 | 1.061 | 1.028 to 1.095 | 1.055 | 1.020 to 1.090 | 1.186 | 1.070 to 1.314 |
| Sunday night | 155,299 | 105,371 | 3.59 | 1.096 | 1.055 to 1.137 | 1.019 | 0.981 to 1.058 | 1.011 | 0.972 to 1.051 | 1.147 | 0.991 to 1.326 |
| Monday day | 294,526 | 164,155 | 3.72 | 1.010 | 0.979 to 1.042 | 1.017 | 0.986 to 1.049 | 1.014 | 0.981 to 1.048 | 1.056 | 0.960 to 1.161 |
| Monday night | 160,510 | 106,782 | 3.43 | 1.008 | 0.971 to 1.046 | 0.947 | 0.912 to 0.983 | 0.940 | 0.904 to 0.977 | 1.052 | 0.918 to 1.205 |
| Tuesday day | 275,470 | 157,148 | 3.68 | 1.004 | 0.973 to 1.036 | 1.007 | 0.975 to 1.039 | 1.008 | 0.975 to 1.043 | 0.994 | 0.901 to 1.097 |
| Tuesday night | 156,909 | 105,004 | 3.41 | 1.027 | 0.988 to 1.066 | 0.964 | 0.929 to 1.002 | 0.971 | 0.933 to 1.010 | 0.871 | 0.753 to 1.006 |
| Average | 216,282 | 133,089 | 3.66 | ||||||||
| Mode of arrival | |||||||||||
| Ambulance | 1,863,246 | 5.46 | Reference | ||||||||
| Non-ambulance | 1,152,854 | 0.78 | 0.339 | 0.330 to 0.348 | |||||||
| Unknown | 11,846 | 1.20 | 0.456 | 0.380 to 0.548 | |||||||
| n | 3,027,946 | 3,027,946 | 3,027,946 | 1,863,246 | 1,152,854 | ||||||
| c-statistic | 0.907 | 0.911 | 0.877 | 0.951 | |||||||
FIGURE 1.
Percentage of admissions by quintile of mortality risk and day and time of attendance. Figure reproduced from Anselmi et al. 13 This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/.
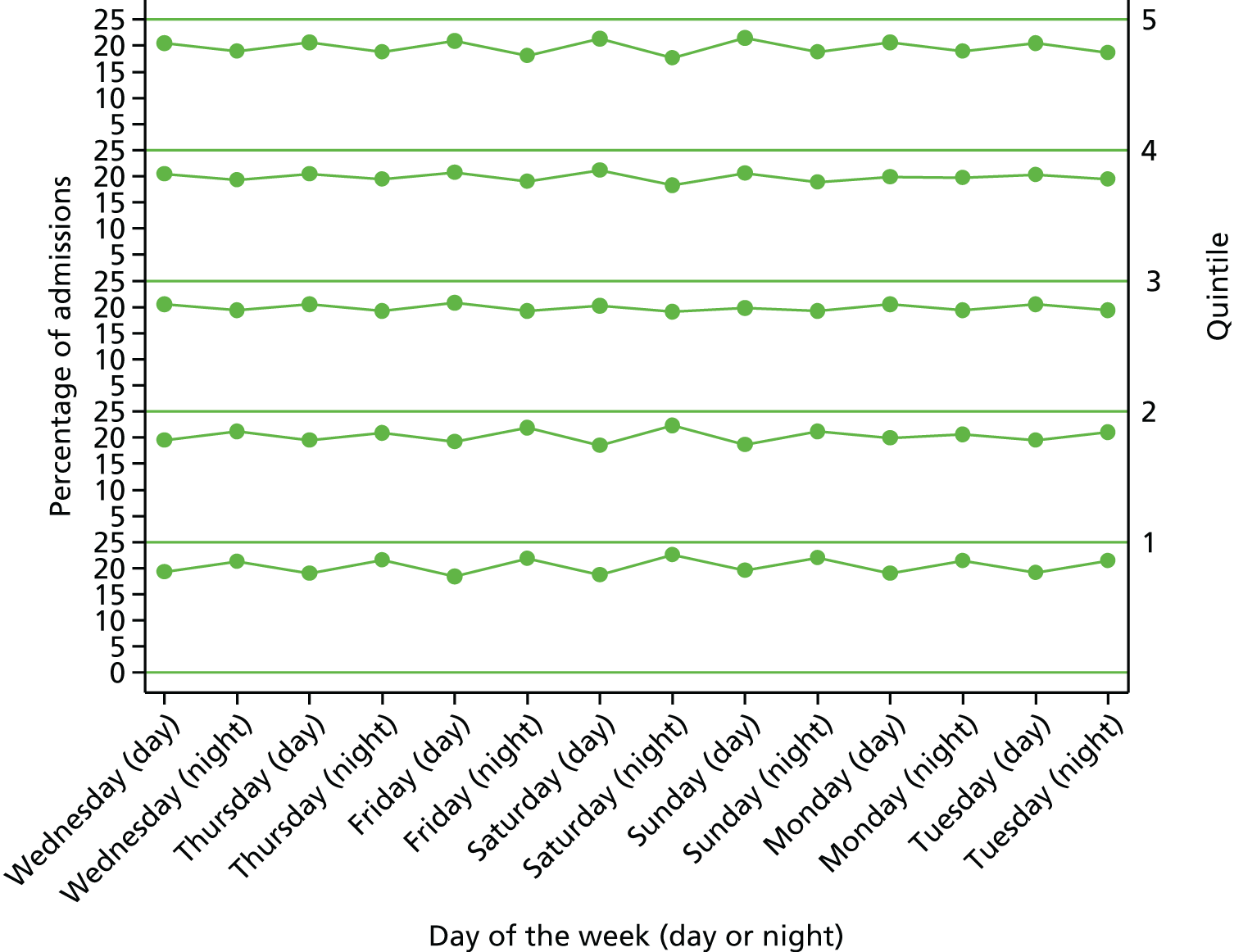
Over the whole week, 20.9% of daytime arrivals were in the highest risk quintile, compared with 18.5% for night-time arrivals. Daytime arrivals on Sundays contained the highest proportion of patients in the highest risk quintile (21.59%), followed by daytime arrivals on Saturdays (21.38%) and Fridays (20.89%). The proportions of patients in the highest risk quintile among those arriving at night-time were similar across the days of the week, with the highest proportions on Mondays (18.97%) and Wednesdays (18.9%) and the lowest proportion on Saturdays (17.62%).
As mortality is substantially higher for patients arriving by ambulance, and as the proportion of patients arriving by ambulance follows patterns similar to crude mortality rates, mode of arrival could be a proxy for severity of illness. The inclusion of a proxy for patient severity in the set of risk adjusters reduces the differences in risk-adjusted mortality throughout the week. After adjusting for ambulance arrival or when carrying out the analysis for the subsamples of patients arriving by ambulance or by other mode, mortality was significantly higher only for patients attending on Sunday daytime.
Association between risk of mortality and mode of arrival
The majority (1,863,246; 61.5%) of patients admitted to hospital after attendance at A&E were brought into hospital by ambulance (see Table 14). Patients admitted after being brought into A&E by ambulance were at a higher risk of death within 30 days: 27.4% of patients admitted after being brought into A&E by ambulance were in the highest risk quintile and 52.8% were in the two highest risk quintiles (Figure 2). Only 8.1% of patients who were admitted after arriving at A&E in other ways were in the highest risk quintile, whereas the majority were in the lowest risk quintile (31.9%) and over half of them (61.2%) were in the two lowest risk quintiles.
FIGURE 2.
Percentage of admissions by quintile of mortality risk and mode of arrival. Figure reproduced from Anselmi et al. 13 This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/.
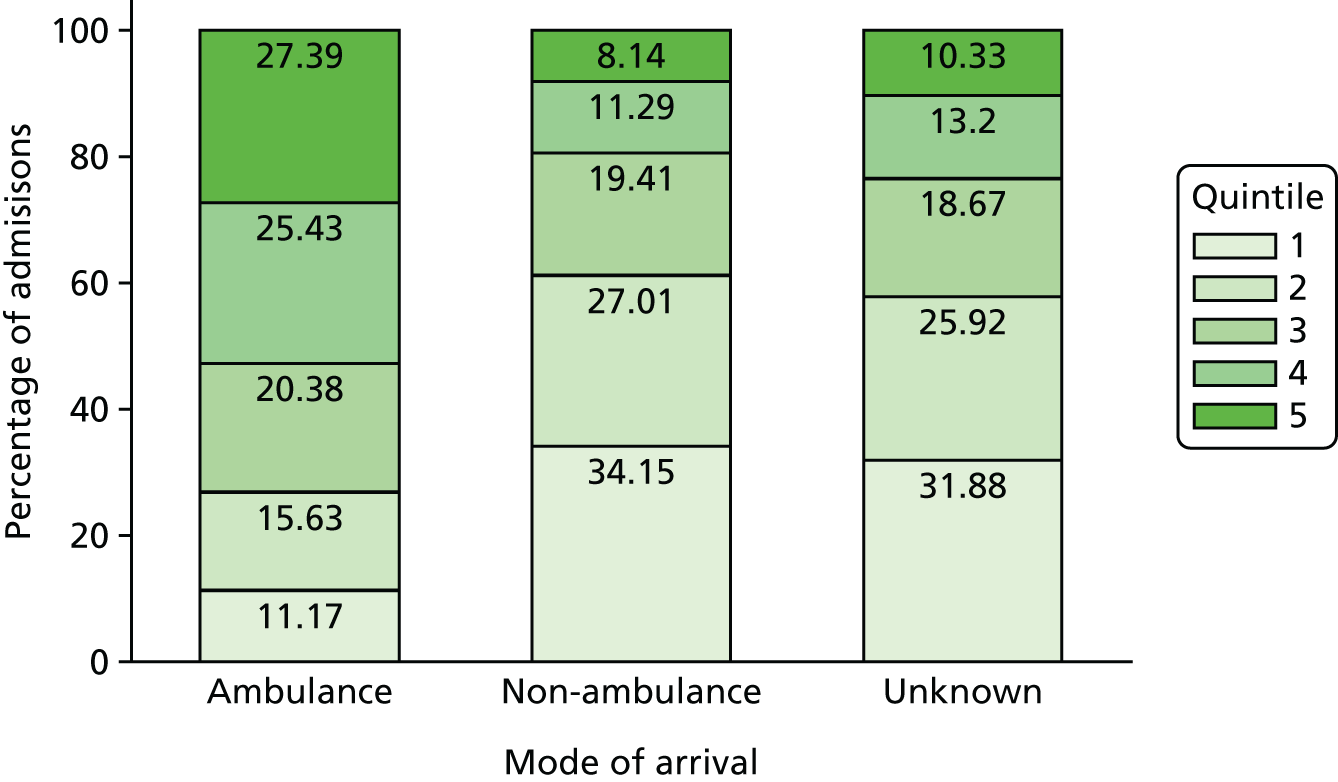
Association between day and time of attendance and mode of arrival
The proportion of admitted patients brought into A&E by ambulance was higher at night-time (average 67.6%) than daytime (average 57.1%), with the highest proportions on Saturday night (69.0%) and Friday night (68.1%) and the lowest proportion on Monday night (66.5%) (Figure 3). During daytime, the proportion of admitted patients brought in by ambulance was substantially higher on Saturdays (61.1%) and Sundays (60.1%), compared with other days of the week.
FIGURE 3.
Percentage of admissions by mode of arrival and day and time of attendance. Figure reproduced from Anselmi et al. 13 This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/.
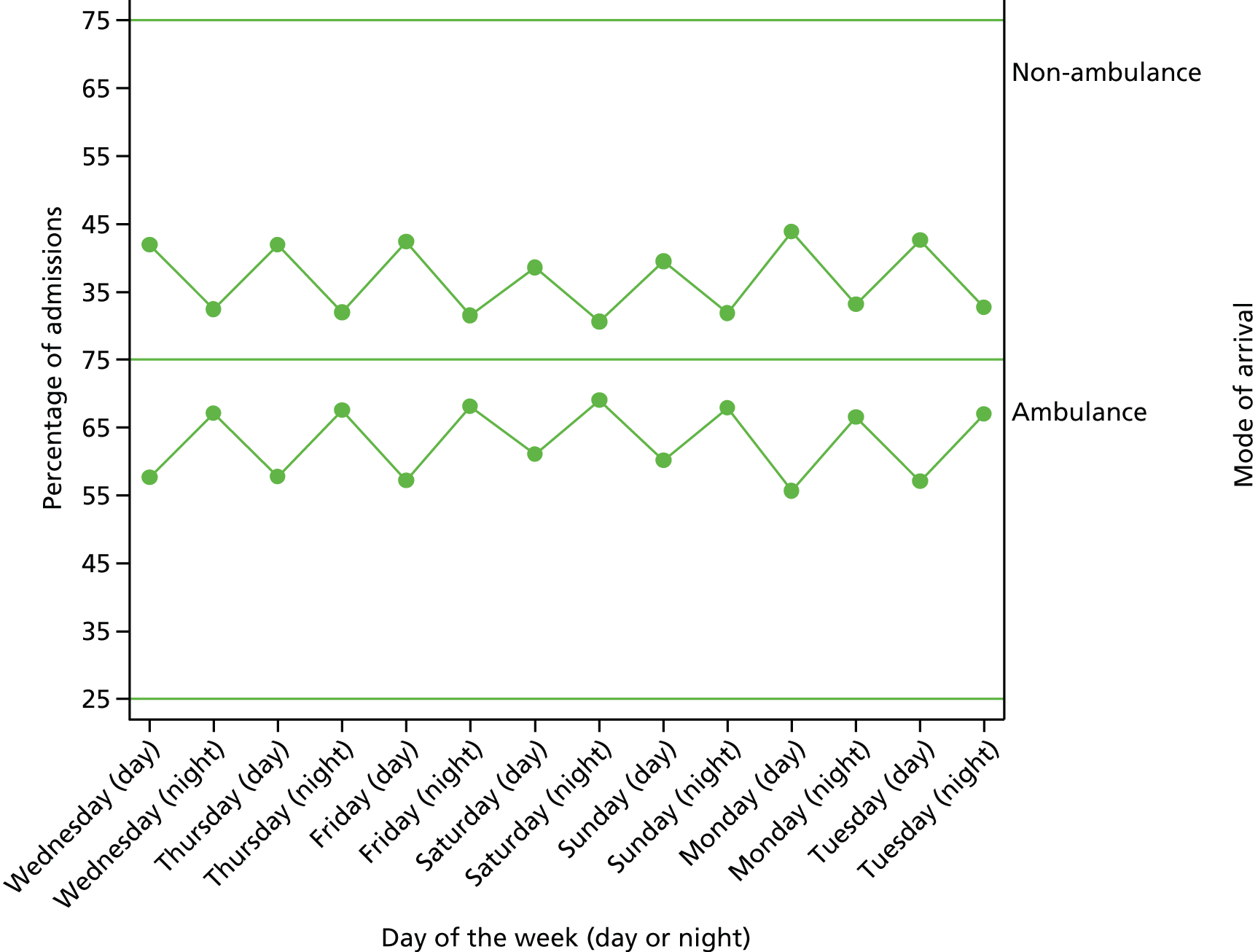
Association between risk-adjusted mortality and day and time of attendance
Using standard risk adjusters (excluding arrival mode), mortality was significantly higher than Wednesday daytime for patients arriving at A&E during the week at night-time on Wednesday (1.6 percentage points, OR 1.055, 95% CI 1.016 to 1.096) and Thursday (1.5 percentage points, OR 1.052, 95% CI 1.031 to 1.092) (model 1). Mortality increased through the weekend from Saturday daytime (1.6 percentage points, OR 1.058, 95% CI 1.025 to 1.092) to Sunday night-time (2.6 percentage points, OR 1.096, 95% CI 1.055 to 1.137). On every day, night-time arrival was associated with higher mortality. Mortality increased from Friday night-time to Sunday night-time before decreasing on Monday daytime.
Risk-adjusted mortality was substantially lower for patients arriving by ‘other’ modes (–2.4 percentage points, OR 0.339, 95% CI 0.330 to 0.348) and unknown modes (–2.0 percentage points, OR 0.456, 95% CI 0.380 to 0.548) than for patients arriving by ambulance (model 2). Accounting for arrival mode changed the estimated effects of the time of arrival on mortality. After controlling for arrival mode, Sunday daytime was the only time period associated with a higher mortality risk (1.7 percentage points, OR 1.061, 95% CI 1.028 to 1.095) than Wednesday daytime.
The patterns of mortality among patients arriving by ambulance (model 3) were similar to those for all patients after adjusting for arrival mode. Among patients arriving by ambulance and patients arriving by other modes (model 3), mortality was only significantly higher for patients arriving on Sunday daytime (2.3 percentage points, OR 1.055, 95% CI 1.020 to 1.090; and 0.1 percentage points, OR 1.186, 95% CI 1.070 to 1.314, respectively).
Figure 4 shows how the estimated effects of time and day of arrival at A&E on mortality were affected by the addition of mode of arrival to the risk adjustment models. Once the mode of arrival is included in the model (Figure 5), the increase in risk of mortality associated with admission after attendance at weekend and at night-time reduced, compared with Wednesday daytime. The trend towards increased risk of mortality after night-time arrivals reversed, with lower mortality for patients arriving overnight from Monday to Saturday. Figure 6 shows that the same pattern is observed among patients arriving by ambulance. There is more variation in mortality among patients arriving by other modes, but only Sunday daytime differs significantly from Wednesday daytime. Additional work is needed to identify the reasons for the higher mortality rates for Sunday daytime admissions. Postponement of procedures and investigations until Monday for these patients, combined with the high number of handovers of care on Monday mornings, may mean that urgent care is delayed.
FIGURE 4.
Risk-adjusted mortality within 30 days of admission by day and time of attendance (standard risk adjustment). Logistic regression models including controls for age, gender, ethnicity, diagnosis, admission method, admission source, Elixhauser conditions, deprivation score, month and trust. Figure reproduced from Anselmi et al. 13 This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/.
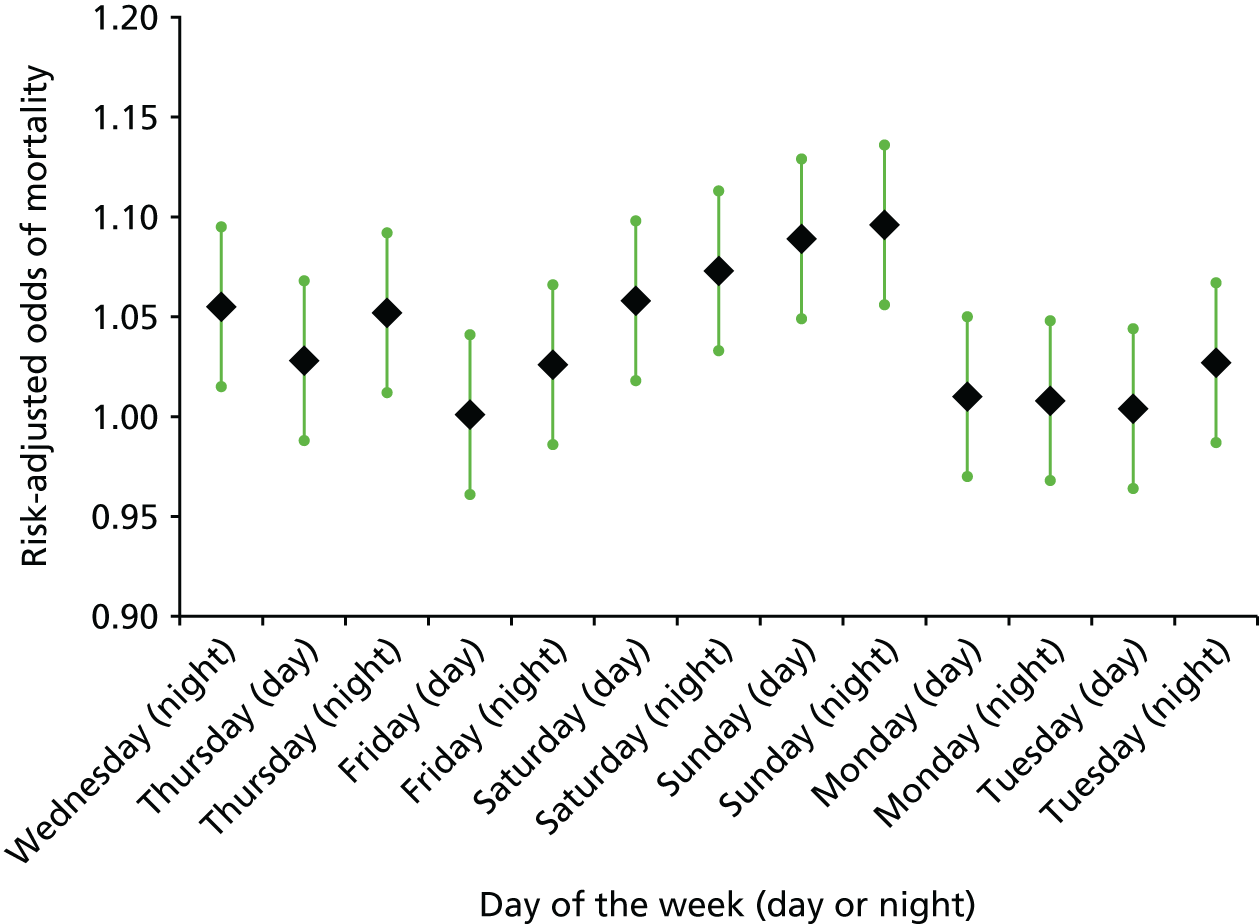
FIGURE 5.
Risk-adjusted mortality within 30 days of admission by day and time of attendance (standard risk adjustment plus mode of arrival). Logistic regression models including controls for age, gender, ethnicity, diagnosis, admission method, admission source, Elixhauser conditions, deprivation score, month, trust and mode of arrival. Figure reproduced from Anselmi et al. 13 This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/.
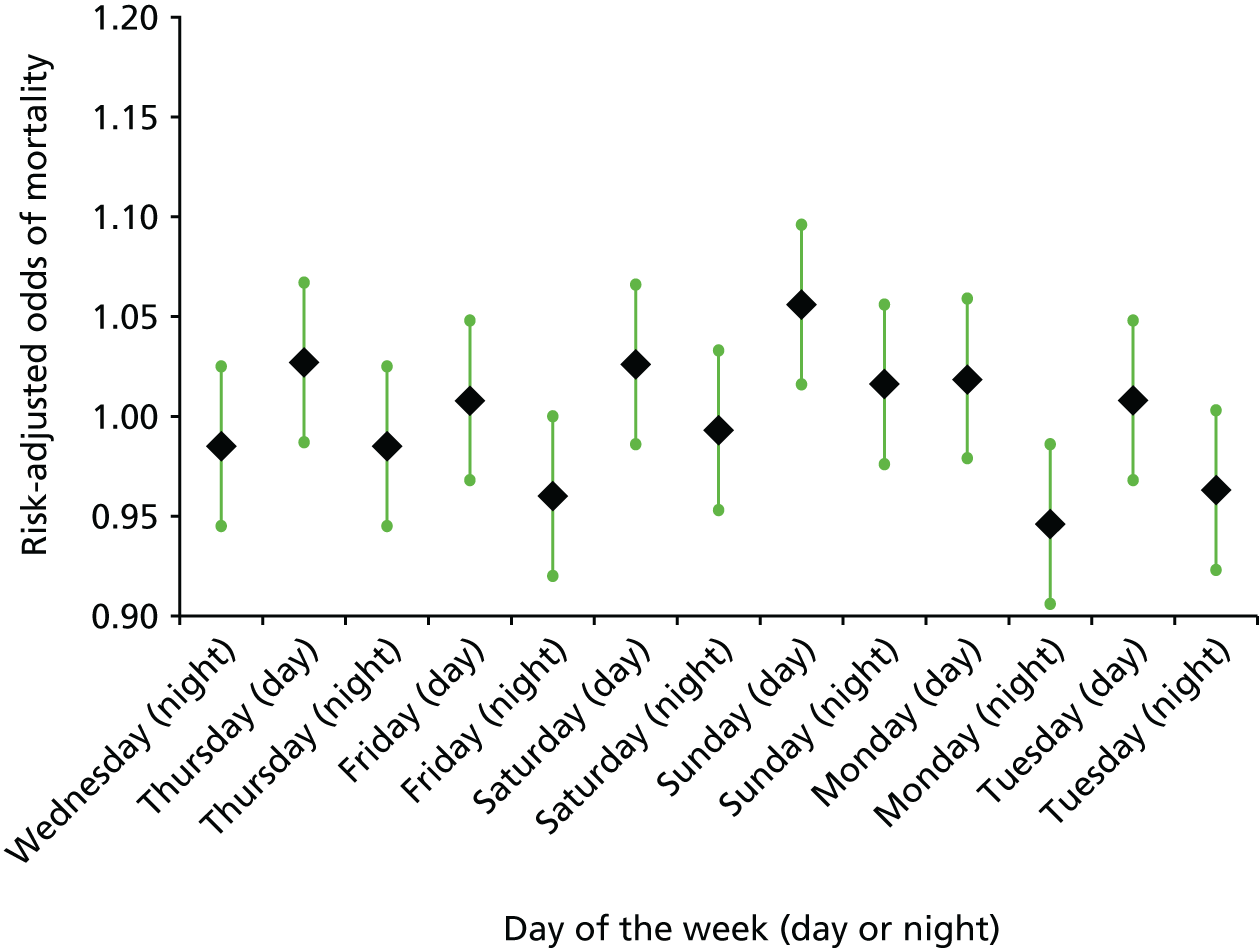
FIGURE 6.
Risk-adjusted mortality within 30 days of admission by day and time of attendance, by mode of arrival at A&E. Mode of arrival (a) ambulance; and (b) non-ambulance. Figure reproduced from Anselmi et al. 13 This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/.
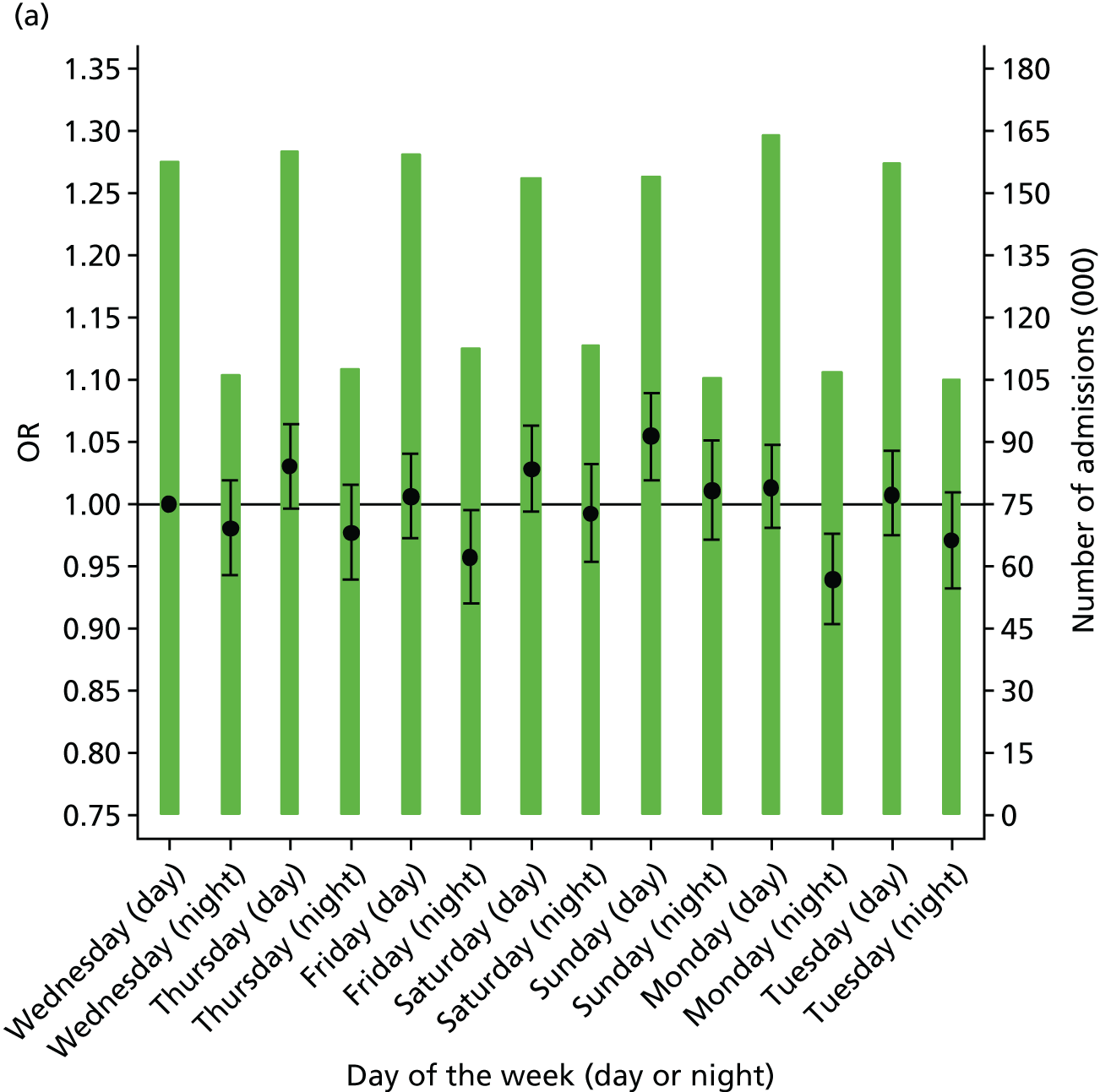
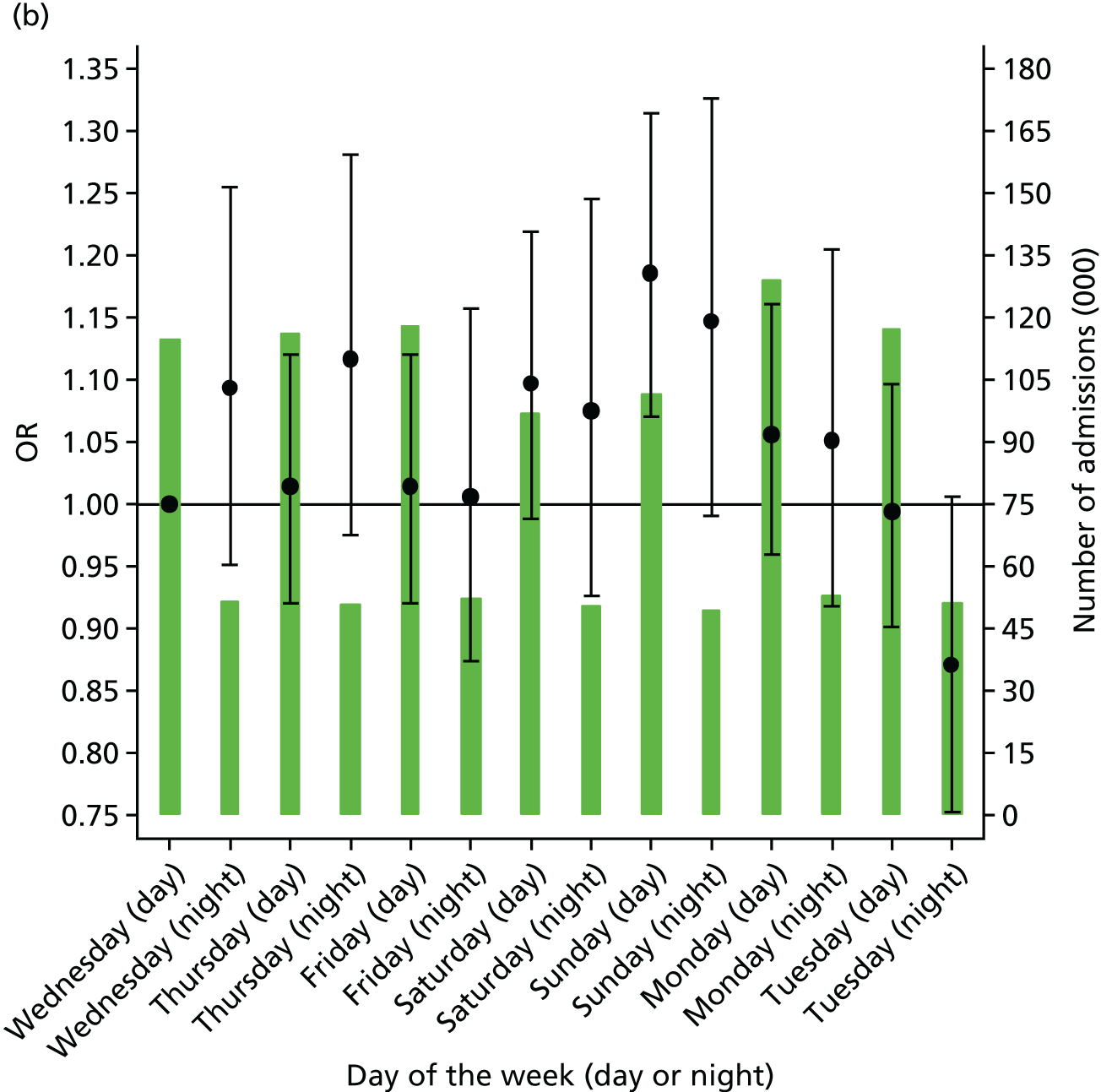
Comparison with other studies
For comparison with previous studies, which divide the week into week and weekend, we conducted pooled analyses comparing week with weekend, day with night and weekday daytime with other broad out-of-hours periods – weekday night-time, weekend daytime, weekend night-time (Table 15). These analyses show that the weekend effect is reduced from an OR of 1.059 (95% CI 1.044 to 1.075) to 1.036 (95% CI 1.021 to 1.052) when arrival mode is added to the regression model. This suggests that arrival by ambulance partly – but not entirely – explains the weekend effect. Dividing the week into four periods (weekday, weeknight, weekend day and weekend night) shows that this is largely attributable to the weekend daytime period, which retains an elevated mortality rate even after accounting for arrival by ambulance. This is in turn attributable to elevated mortality rates for Sunday daytime. The night-time effect is reduced from an OR of 1.020 (95% CI 1.006 to 1.035) to 0.959 (95% CI 0.946 to 0.973) when arrival mode is added to the regression model, which suggests that greater severity of illness for night-time admissions may explain the higher mortality rates for these patients.
| Day and time | Model | |||||||
|---|---|---|---|---|---|---|---|---|
| 1: standard risk adjustmenta | 2: standard risk adjustmenta plus arrival mode | 3: standard risk adjustmenta (patients arriving by ambulance) | 4: standard risk adjustmenta (patients arriving by other mode only) | |||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Daytime and night-time during week and at weekend | ||||||||
| Weekday day (base) | – | – | – | – | – | – | – | – |
| Weekday night | 1.025 | 1.007 to 1.042 | 0.958 | 0.942 to 0.974 | 0.954 | 0.937 to 0.971 | 1.009 | 0.948 to 1.075 |
| Weekend day | 1.065 | 1.045 to 1.085 | 1.034 | 1.015 to 1.054 | 1.030 | 1.010 to 1.050 | 1.122 | 1.055 to 1.195 |
| Weekend night | 1.075 | 1.050 to 1.101 | 0.996 | 0.973 to 1.020 | 0.990 | 0.966 to 1.014 | 1.093 | 0.993 to 1.203 |
| Week and weekend | ||||||||
| Weekday (base) | – | – | – | – | – | – | – | – |
| Weekend | 1.059 | 1.044 to 1.075 | 1.036 | 1.021 to 1.052 | 1.033 | 1.017 to 1.049 | 1.112 | 1.054 to 1.173 |
| Daytime and night-time | ||||||||
| Day (base) | – | – | – | – | – | – | – | – |
| Night | 1.020 | 1.006 to 1.035 | 0.959 | 0.946 to 0.973 | 0.956 | 0.942 to 0.970 | 0.996 | 0.944 to 1.052 |
In study 4 we noted that no weekend effect was apparent for all attenders at A&E, but our standard model included mode of arrival and referral sources as covariates. Excluding these covariates from the regression model made little difference to the odds of mortality (see footnote b, Table 9). This suggests that selection is only important for the admitted population and makes little difference to the population attending A&E.
Conclusions
We analysed the association between risk-adjusted mortality and day and time of arrival for patients admitted to hospital after attendance at A&E. When controlling only for the risk adjusters available in inpatient administrative records as in previous studies,3,15,26 mortality was found to be significantly higher for patients admitted to hospital throughout the weekend and on Wednesday and Thursday night-time. Patients arriving at A&E by ambulance had a higher risk of mortality. Higher proportions of patients admitted overnight and at weekends arrived by ambulance.
Accounting for mode of arrival substantially altered the temporal patterns of risk-adjusted mortality. Only admissions on Sunday daytime were associated with an increased risk of mortality than Wednesday daytime. Admissions on Monday and Friday night-time were associated with significantly lower mortality than Wednesday daytime. None of the night periods was associated with higher mortality.
Accident and emergency records are known to be less complete and accurate than inpatient records. 45 We relied mainly on the better-quality data extracted from inpatient records. We used only information on arrival time and mode of arrival from the A&E record. No specific concerns about these variables have been raised by the HSCIC in its audits of the quality of A&E records. We were restricted by data availability to deaths that occur in hospital and could not examine out-of-hospital deaths. However, > 80% of all deaths within 30 days of an emergency admission occur in hospital and the proportion is higher at weekends, leading to a small bias towards finding a weekend effect.
We used the time of attendance at A&E rather than the time of admission to hospital as our index time. We conducted a sensitivity analysis using the time of departure from A&E to approximate the time of admission to hospital (Table 16). The pattern of mortality across the week was largely unaffected, but admission on Sunday night-time became associated with a higher risk of mortality (OR 1.043, CI 1.005 to 1.081). We argue that the time of attendance is more appropriate, as this is the point at which hospitals become responsible for patient care. We used a classification of daytime versus night-time that was consistent with senior doctors’ working hours. We checked that our results were robust to using an alternative definition of daytime and night-time (08.00–19.59 hours and 20.00–07.59 hours the following day), as has been used in a previous study (Table 17). 36
| Admission | Model 2: standard risk adjustment plus mode of arrival | |||
|---|---|---|---|---|
| Time of attendance | Time of admission | |||
| OR | 95% CI | OR | 95% CI | |
| Day and time | ||||
| Wednesday day | Reference | Reference | ||
| Wednesday night | 0.988 | 0.951 to 1.025 | 1.005 | 0.970 to 1.042 |
| Thursday day | 1.027 | 0.996 to 1.060 | 1.021 | 0.986 to 1.057 |
| Thursday night | 0.986 | 0.950 to 1.024 | 1.018 | 0.982 to 1.055 |
| Friday day | 1.007 | 0.976 to 1.039 | 1.010 | 0.975 to 1.046 |
| Friday night | 0.962 | 0.927 to 0.999 | 0.982 | 0.947 to 1.017 |
| Saturday day | 1.031 | 0.999 to 1.064 | 1.033 | 0.998 to 1.070 |
| Saturday night | 0.997 | 0.960 to 1.035 | 1.021 | 0.984 to 1.059 |
| Sunday day | 1.061 | 1.028 to 1.095 | 1.061 | 1.025 to 1.099 |
| Sunday night | 1.019 | 0.981 to 1.058 | 1.043 | 1.005 to 1.081 |
| Monday day | 1.017 | 0.986 to 1.049 | 1.019 | 0.984 to 1.056 |
| Monday night | 0.947 | 0.912 to 0.983 | 1.007 | 0.972 to 1.043 |
| Tuesday day | 1.007 | 0.975 to 1.039 | 0.991 | 0.956 to 1.026 |
| Tuesday night | 0.964 | 0.929 to 1.002 | 0.998 | 0.962 to 1.034 |
| Mode of arrival | ||||
| Ambulance | Reference | Reference | ||
| Non-ambulance | 0.339 | 0.330 to 0.348 | 0.341 | 0.332 to 0.350 |
| Unknown | 0.456 | 0.380 to 0.548 | 0.458 | 0.381 to 0.550 |
| n | 3,027,946 | 3,027,946 | ||
| c-statistic | 0.911 | 0.911 | ||
| Admission | Model 2: standard risk adjustment plus mode of arrival | |||
|---|---|---|---|---|
| Daytime 07.00–18.59; night-time 19.00–06.59 | Daytime 08.00–19.59; night-time 20.00–07.59 | |||
| OR | 95% CI | OR | 95% CI | |
| Day and time | ||||
| Wednesday day | Reference | Reference | ||
| Wednesday night | 0.988 | 0.951 to 1.025 | 1.007 | 0.969 to 1.046 |
| Thursday day | 1.027 | 0.996 to 1.060 | 1.032 | 1.000 to 1.064 |
| Thursday night | 0.986 | 0.950 to 1.024 | 0.995 | 0.958 to 1.034 |
| Friday day | 1.007 | 0.976 to 1.039 | 1.008 | 0.977 to 1.040 |
| Friday night | 0.962 | 0.927 to 0.999 | 0.977 | 0.940 to 1.015 |
| Saturday day | 1.031 | 0.999 to 1.064 | 1.035 | 1.003 to 1.068 |
| Saturday night | 0.997 | 0.960 to 1.035 | 1.008 | 0.970 to 1.047 |
| Sunday day | 1.061 | 1.028 to 1.095 | 1.065 | 1.032 to 1.099 |
| Sunday night | 1.019 | 0.981 to 1.058 | 1.030 | 0.992 to 1.070 |
| Monday day | 1.017 | 0.986 to 1.049 | 1.024 | 0.993 to 1.056 |
| Monday night | 0.947 | 0.912 to 0.983 | 0.950 | 0.914 to 0.987 |
| Tuesday day | 1.007 | 0.975 to 1.039 | 1.015 | 0.984 to 1.048 |
| Tuesday night | 0.964 | 0.929 to 1.002 | 0.965 | 0.928 to 1.003 |
| Mode of arrival | ||||
| Ambulance | Reference | Reference | ||
| Non-ambulance | 0.339 | 0.330 to 0.348 | 0.339 | 0.330 to 0.348 |
| Unknown | 0.456 | 0.380 to 0.548 | 0.456 | 0.380 to 0.548 |
| n | 3,027,946 | 3,027,946 | ||
| c-statistic | 0.911 | 0.911 | ||
Previous studies have been constrained by the absence of information on patients’ time of arrival at hospital and have been forced to classify the weekend crudely by dates as 00.00 hours Saturday to 23.59 hours Sunday and have been unable to adjust for patient severity of illness. Including arrival mode in the risk adjustment accounted for most of the differences in mortality between different days and different times, leaving Sunday daytime as the only period associated with a higher risk of death. Our results are in line with previous studies which have used clinical audit data and concluded that the elevation of mortality at weekends disappears once indicators of severity are controlled for. 39,40 In contrast to these studies, however, we analysed a large national data set and considered all clinical causes of admissions. Nonetheless, arrival by ambulance is an imperfect proxy for severity of illness. It is likely that there are further aspects of severity affecting the risk of mortality and differing between patients admitted at different times of the week that remain unmeasured.
Using arrival by ambulance as a measure of severity, we have shown that much of the weekend effect identified in previous studies is instead explained by variations in patient severity. With the exception of Sunday daytime, elevated mortality among admissions at weekends reflects a higher proportion of patients arriving by ambulance.
Chapter 7 Results (study 5): the impact of staffing levels on mortality rates at Salford Royal NHS Foundation Trust
Background
Most staffing studies focus on nurses because of their well-documented work shifts. Higher levels of nurse staffing (as measured by the number of nurses per bed or patient-to-nurse ratio) is generally associated with better quality of care and patient outcomes. 46–48 Bond and Raehl49 investigated mortality rates in relation to hospital-based clinical pharmacy services and pharmacy staffing in 885 US hospitals. After controlling for the severity of illness, they found that the presence of a number of pharmacy services was associated with lower mortality rates. Bond et al. 50 examined the impact of staffing levels of a variety of health professional groups and found lower mortality rates were associated with higher staffing levels of medical residents, registered nurses, registered pharmacists, medical technologists and total hospital personnel. Conversely, higher mortality rates were associated with higher levels of hospital administrators and licensed practical/vocational nurses per occupied bed.
There is a lack of evidence, however, on the interaction between staffing levels and out-of-hours periods, that is, whether or not reduced staffing levels is partly responsible for the weekend effect. In this study, we aimed to estimate the impact of staffing level of nurses, both qualified and unqualified, on variation in patient outcomes associated with out-of-hours admissions.
Results
Stroke admissions
We assessed 7286 patients admitted to the ASU at SRFT as emergencies between January 2009 and July 2014. We initially divided patients into four admission groups: weekday day, weekday night, weekend day and weekend night. Characteristics of admitted patients are given in Table 18. Sixty-eight per cent of patients were out-of-hours admissions, with only one-third admitted through normal working hours (07.00–18.59 hours, Monday to Friday). Admissions during the day at weekends had the highest average age (71.7 years), were more likely to be female (52.9%) and white (83.8%), and less likely to reside in the most deprived one-fifth of neighbourhoods (11.5%).
| Variable | Time period | |||
|---|---|---|---|---|
| Weekday day | Weekday night | Weekend day | Weekend night | |
| Number of admissions (%) | 2360 (32.39) | 1918 (26.32) | 1375 (18.87) | 1633 (22.41) |
| Age on admission (years) (SD) | 69.72 (16.14) | 68.77 (16.62) | 71.68 (15.16) | 69.03 (16.55) |
| Male, n (%) | 1143 (48.43) | 932 (48.59) | 647 (47.05) | 800 (48.99) |
| White, n (%) | 1962 (83.14) | 1547 (80.66) | 1153 (83.85) | 1360 (83.28) |
| IMD quintile = 5 (most deprived), n (%) | 332 (14.07) | 284 (14.81) | 158 (11.49) | 207 (12.68) |
| Number of diagnoses (SD) | 6.24 (3.31) | 6.06 (3.22) | 6.02 (3.17) | 5.99 (3.20) |
| Number of procedure (SD) | 3.01 (2.07) | 2.72 (1.91) | 2.92 (1.92) | 2.66 (1.78) |
| Number of emergency admissions in the previous 365 days (SD) | 0.30 (0.83) | 0.21 (0.66) | 0.25 (1.17) | 0.23 (0.87) |
| Charlson Comorbidity Index score (SD) | 6.58 (8.42) | 5.94 (7.88) | 6.45 (8.49) | 6.14 (8.17) |
| 7-day mortality, n (%) | 124 (5.25) | 133 (6.93) | 104 (7.56) | 112 (6.86) |
| 30-day mortality, n (%) | 237 (10.04) | 219 (11.42) | 179 (13.02) | 188 (11.51) |
| In-hospital mortality, n (%) | 154 (6.53) | 140 (7.30) | 115 (8.36) | 112 (6.86) |
Patients admitted during normal working hours (07.00–18.59 hours, Monday to Friday) had the most diagnoses and procedures during a hospital stay, the most emergency admissions in the last year and the highest Charlson Comorbidity Index score among the four admission groups, although the absolute differences were marginal. On average, each spell in the weekday day group had 6.2 different diagnosis codes and 3.0 operation codes. Patients in this group had an average of 0.3 previous emergency admission and an average Charlson Comorbidity Index score of 6.58. Patients in the weekend night group had the fewest diagnoses (5.9) and procedures (2.6). Patients in the weekday night group had the fewest average previous emergency admissions (0.2) and the lowest average Charlson Comorbidity Index score (5.9).
Unadjusted mortality rates were highest for the weekend day group; 7.5% of these patients died within 7 days from admission, 13.0% died in 30 days and 8.3% died in hospital. Mortality rates were lowest for weekday day admissions; the 30-day mortality rate for these patients was 10.0%, the 7-day mortality rate was 5.2% and the in-hospital mortality rate was 6.5%.
We further divided the week into 14 12-hour periods. The total number of emergency admissions of each 12-hour period was stable across the week (Table 19), as was the number of admissions through A&E. In general, more patients were admitted overnight than during the daytime from Monday to Friday. This pattern was reversed for Saturdays and Sundays, which had a higher numbers of admissions than on weekdays. The two busiest periods were Saturday and Sunday daytimes; 9.2% and 8.6% of patients were admitted during these periods, respectively.
| Day | Admission (%) | ||||
|---|---|---|---|---|---|
| Number of | Via A&E | With the earliest main procedure on the same day of admission | With the earliest main procedure on the next day of admission | With earliest main procedure on the same day or on the next day of admission | |
| Monday | |||||
| Day | 484 (6.64) | 472 (6.66) | 432 (89.25) | 16 (3.30) | 448 (92.56) |
| Night | 507 (6.96) | 496 (7.00) | 423(83.43) | 36 (7.10) | 459 (90.53) |
| Tuesday | |||||
| Day | 452 (6.20) | 437 (6.17) | 392 (86.72) | 20 (4.42) | 412 (91.15) |
| Night | 490 (6.73) | 469 (6.62) | 419 (85.51) | 28 (5.71) | 447 (91.22) |
| Wednesday | |||||
| Day | 476 (6.53) | 464 (6.55) | 420 (88.23) | 29 (6.09) | 449 (94.32) |
| Night | 475 (6.52) | 456 (6.44) | 404 (85.05) | 27 (5.68) | 431 (90.73) |
| Thursday | |||||
| Day | 509 (6.99) | 490 (6.92) | 453 (88.99) | 23 (4.51) | 476 (93.51) |
| Night | 530 (7.27) | 519 (7.33) | 447 (84.33) | 30 (5.66) | 477 (90.00) |
| Friday | |||||
| Day | 511 (7.01) | 492 (6.95) | 449 (87.86) | 16 (3.13) | 465 (90.99) |
| Night | 519 (7.12) | 505 (7.13) | 436 (84.00) | 43 (8.28) | 479 (92.29) |
| Saturday | |||||
| Day | 673 (9.24) | 653 (9.22) | 605 (89.89) | 26 (3.86) | 631 (93.75) |
| Night | 501 (6.88) | 493 (6.96) | 417 (83.23) | 29 (5.78) | 446 (89.02) |
| Sunday | |||||
| Day | 630 (8.65) | 616 (8.70) | 569 (90.31) | 28 (4.44) | 597 (94.76) |
| Night | 529 (7.26) | 520 (7.34) | 454 (85.82) | 24 (4.53) | 478 (90.35) |
| Total | 7286 | 7082 | 6320 | 375 | 6695 |
Across the week, > 80% of patients had their earliest main operation on the day of admission. Compared with the patients admitted during daytime, patients were less likely to have the first main operation on the same day of admission if they were admitted overnight, but we lacked precise timings for procedures and so could not assess whether or not there was genuine delay for patients admitted overnight. We therefore also compared the proportion of patients who had their main procedure on the same day or on the next day of admission. Over 90% of patients had the earliest main procedure within 2 days’ time, with a slightly lower proportion of overnight admitted patients receiving same or next day first procedures.
Staffing patterns
Roster data contained the number of nurses, both qualified and unqualified, working in the ASU for each hour of the day and each day of the study period. In Figures 7–10 the level of nurses by daytime and night-time for each day of the week are plotted over time. Overall staffing levels increased over time, with the largest increase for qualified nurses during the day. As expected, daytimes had the highest level of qualified nurses and levels during the daytime were higher during the week than at the weekend. The lowest level of qualified nurses was observed for night periods, with no significant difference between weekdays and weekend. The pattern was broadly similar for unqualified nurses.
FIGURE 7.
Staffing level of nurses: January 2009–July 2014 (qualified, daytime).
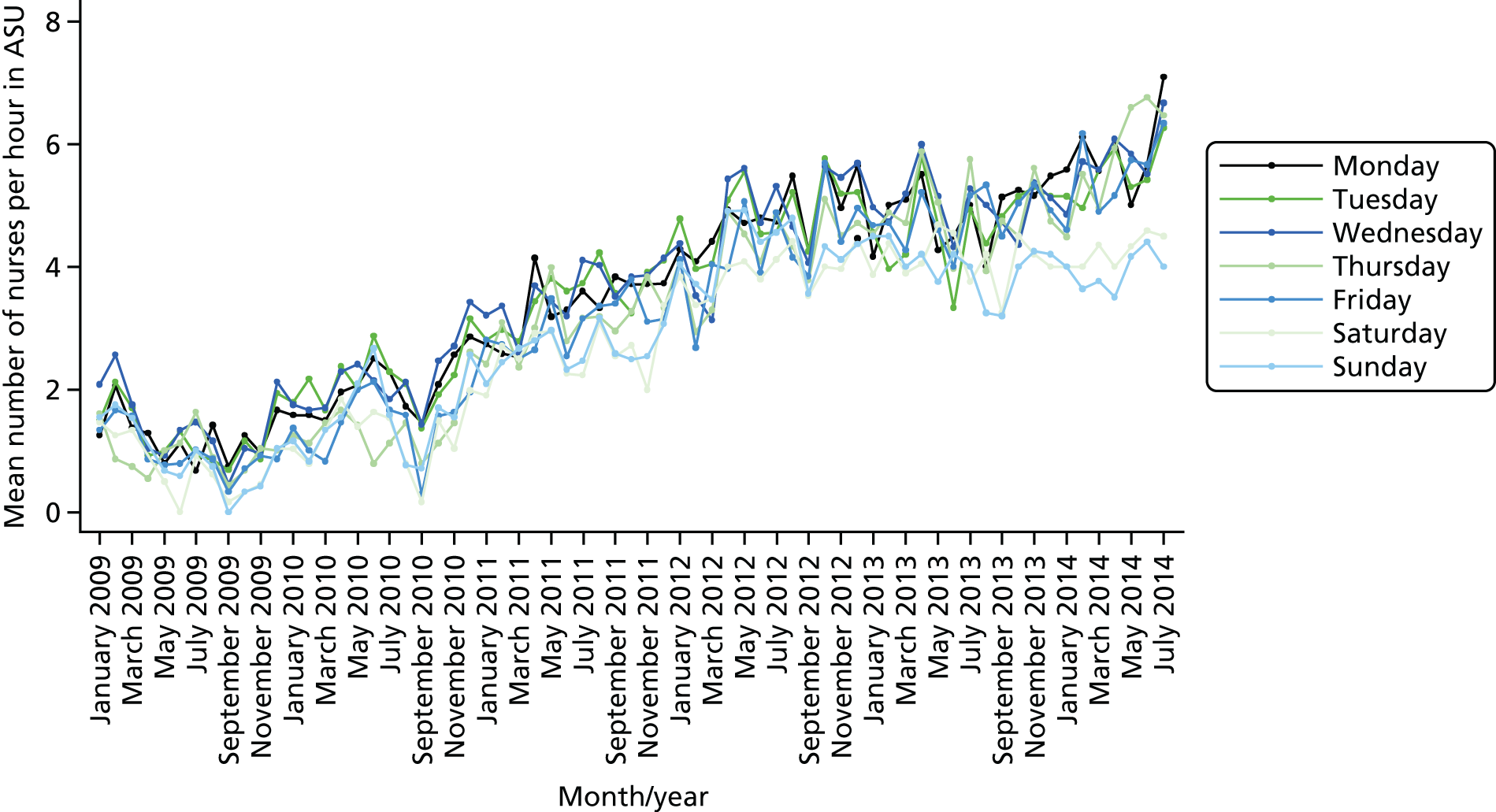
FIGURE 8.
Staffing level of nurses: January 2009–July 2014 (qualified, night-time).
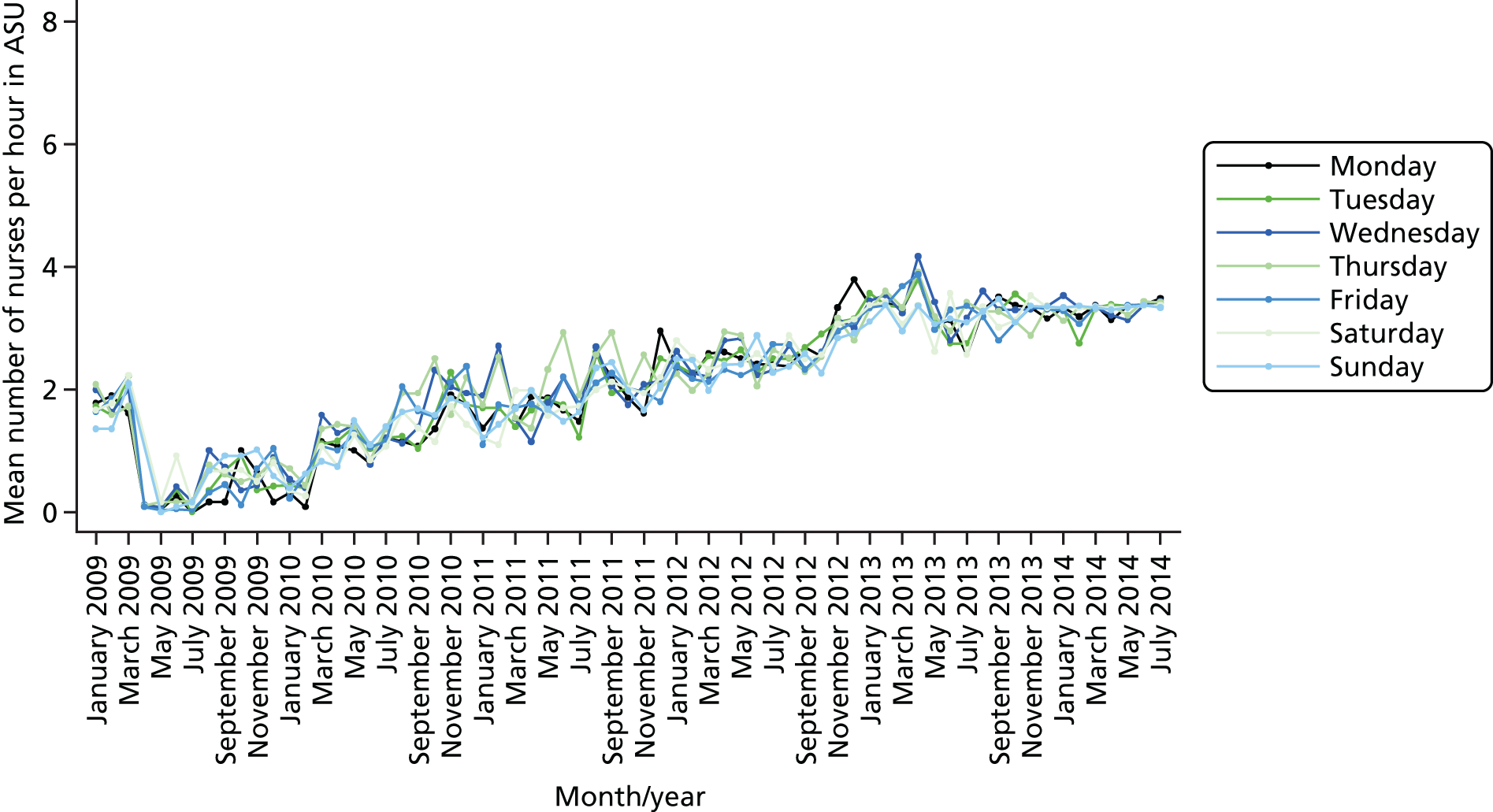
FIGURE 9.
Staffing level of nurses: January 2009–July 2014 (unqualified, daytime).
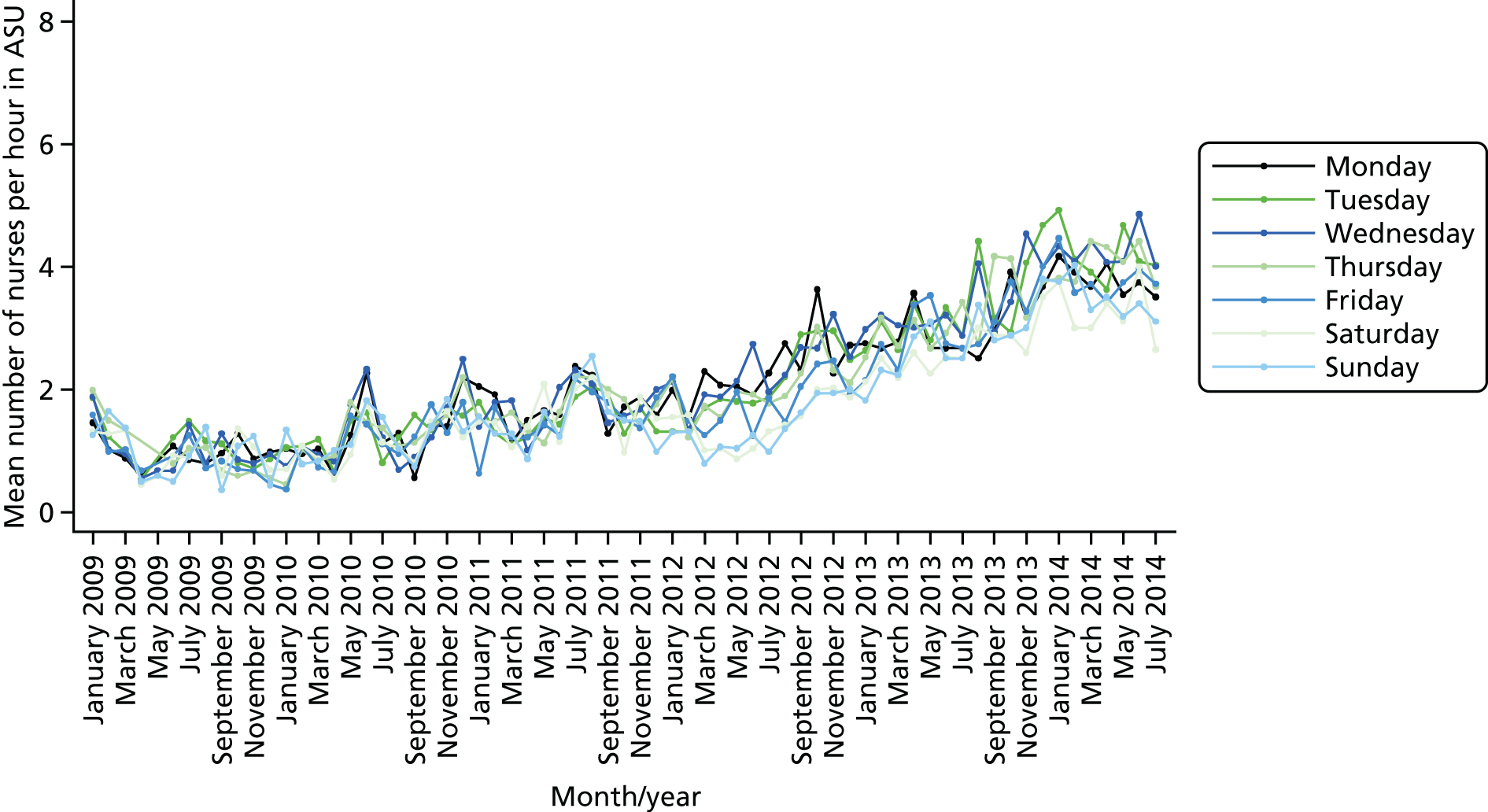
FIGURE 10.
Staffing level of nurses: January 2009–July 2014 (unqualified, night-time).
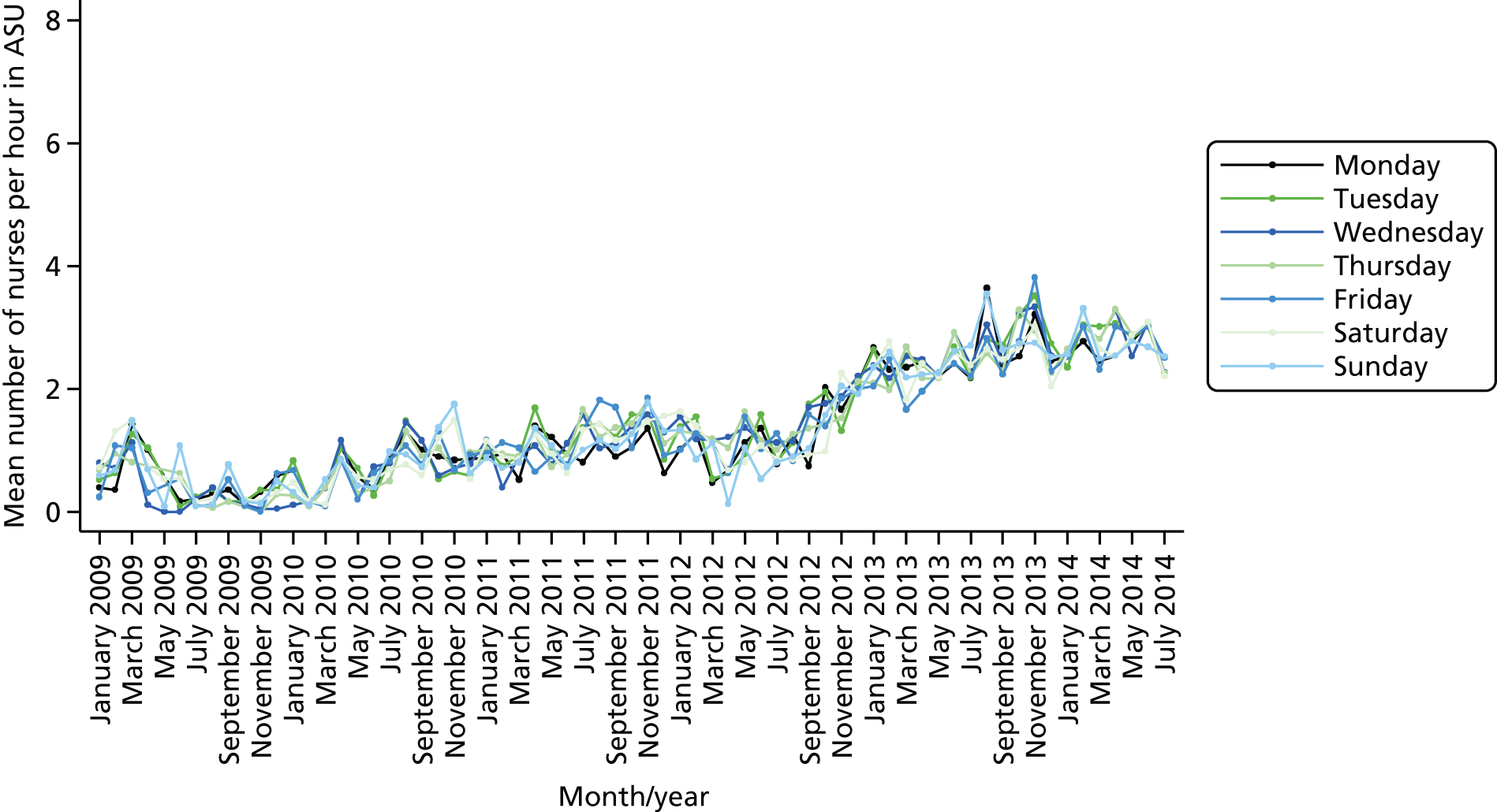
Patterns of mortality
We estimated three models for each of the mortality outcomes (7-day, 30-day and in-hospital mortality). First, we estimated a core model (including out-of-hours admission periods) and standard risk predictors (including demographics, socioeconomic status, complexity of the current spell, medical history and comorbidities). Second, we extended the core model by adding the number of nurses in the admission hour and the number of patients in the same ward on the admission day. The aim was to estimate the impact of the staffing level of nurses on patient survival, as well as its impact on the association between out-of-hours admissions and mortality.
In the core model (Tables 20–22), higher risk of death was associated with increasing age and episodes of palliative care (39.3 percentage point increase risk of dying in 7 days, 55.7 percentage point for 30 days and 67.5 percentage point for dying in hospital). Mortality rates also increased with comorbidity, although not for in-hospital mortality. Adjusted risk of dying in 7 days varied substantially across the week (see Table 20). Compared with weekday day admissions, mortality was 1.8 percentage points higher for weekday night admissions, 1.6 percentage points higher weekend day admissions and 1.5 percentage points higher for weekend night admissions. There were similar patterns for 30-day and in-hospital mortality, although the increased risk for weekend night admissions was non-significant for these outcomes.
| Variable | Model | |||||
|---|---|---|---|---|---|---|
| 1: 7-day mortality | 2: 7-day mortality | 3: 7-day mortality | ||||
| AME | SE | AME | SE | AME | SE | |
| Admission at weekday night | 0.018** | 0.008 | 0.010 | 0.010 | 0.009 | 0.009 |
| Admission at weekend day | 0.016* | 0.009 | 0.014 | 0.009 | 0.014 | 0.009 |
| Admission at weekend night | 0.015* | 0.008 | 0.007 | 0.010 | 0.006 | 0.010 |
| Number of patients in ASU on admission day | 0.001 | 0.001 | 0.001 | 0.001 | ||
| Number of nurses on duty at admission hour | –0.003* | 0.002 | ||||
| Number of qualified nurses on duty at admission hour | –0.005** | 0.003 | ||||
| Case-mix variables | ||||||
| Age on admission | 0.001*** | 0.000 | 0.001*** | 0.000 | 0.001*** | 0.000 |
| Gender (female) | –0.003 | 0.006 | –0.003 | 0.006 | –0.002 | 0.006 |
| Gender (not stated) | –0.051* | 0.029 | –0.051* | 0.030 | –0.050* | 0.030 |
| Ethnicity (mixed) | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Ethnicity (Asian) | 0.016 | 0.026 | 0.016 | 0.026 | 0.016 | 0.026 |
| Ethnicity (black) | 0.048 | 0.055 | 0.048 | 0.055 | 0.051 | 0.055 |
| Ethnicity (other) | –0.011 | 0.015 | –0.010 | 0.015 | –0.009 | 0.015 |
| Ethnicity (not stated) | –0.015* | 0.009 | –0.015* | 0.009 | –0.015* | 0.009 |
| IMD quintile 2 | 0.020** | 0.010 | 0.020** | 0.010 | 0.021** | 0.010 |
| IMD quintile 3 | 0.005 | 0.009 | 0.004 | 0.009 | 0.002 | 0.009 |
| IMD quintile 4 | –0.002 | 0.010 | –0.001 | 0.010 | –0.001 | 0.010 |
| IMD quintile 5 (most deprived) | –0.005 | 0.010 | –0.005 | 0.010 | –0.006 | 0.010 |
| IMD quintile (missing) | 0.028** | 0.013 | 0.029** | 0.014 | 0.027* | 0.014 |
| Charlson Comorbidity Index | 0.001** | 0.000 | 0.001** | 0.000 | 0.001** | 0.000 |
| Number of diagnoses | –0.001 | 0.001 | –0.001 | 0.001 | –0.001 | 0.001 |
| Number of procedures | –0.012*** | 0.003 | –0.012*** | 0.003 | –0.011*** | 0.003 |
| Palliative care | 0.393*** | 0.033 | 0.395*** | 0.033 | 0.396*** | 0.033 |
| Number of emergency admissions in the previous year | 0.001 | 0.004 | 0.000 | 0.005 | –0.001 | 0.005 |
| Financial year 2009/10 | 0.025 | 0.025 | 0.029 | 0.024 | 0.027 | 0.023 |
| Financial year 2010/11 | 0.019 | 0.023 | 0.025 | 0.022 | 0.025 | 0.021 |
| Financial year 2011/12 | 0.024 | 0.023 | 0.032 | 0.021 | 0.035* | 0.021 |
| Financial year 2012/13 | 0.004 | 0.023 | 0.017 | 0.021 | 0.020 | 0.021 |
| Financial year 2013/14 | 0.009 | 0.023 | 0.026 | 0.022 | 0.026 | 0.021 |
| Financial year 2014/15 | –0.005 | 0.025 | 0.012 | 0.024 | 0.012 | 0.023 |
| Diagnosis group dummies | Yes | Yes | Yes | |||
| Admission method dummies | Yes | Yes | Yes | |||
| Observations | 6274 | 6231 | 6163 | |||
| c-statistic | 0.785 | 0.784 | 0.783 | |||
| Pseudo-R2 | 0.183 | 0.184 | 0.183 | |||
| Variable | Model | |||||
|---|---|---|---|---|---|---|
| 1: 30-day mortality | 2: 30-day mortality | 3: 30-day mortality | ||||
| AME | SE | AME | SE | AME | SE | |
| Admission at weekday night | 0.016* | 0.009 | 0.013 | 0.011 | 0.015 | 0.011 |
| Admission at weekend day | 0.016* | 0.010 | 0.016 | 0.010 | 0.016 | 0.010 |
| Admission at weekend night | 0.015 | 0.009 | 0.011 | 0.011 | 0.012 | 0.011 |
| Number of patients in ASU on admission day | 0.001 | 0.001 | 0.001 | 0.001 | ||
| Number of nurses on duty at admission hour | –0.001 | 0.002 | ||||
| Number of qualified nurses on duty at admission hour | –0.001 | 0.003 | ||||
| Case-mix variables | ||||||
| Age on admission | 0.003*** | 0.000 | 0.003*** | 0.000 | 0.003*** | 0.000 |
| Gender (female) | 0.006 | 0.007 | 0.006 | 0.007 | 0.006 | 0.007 |
| Gender (not stated) | –0.063** | 0.025 | –0.064** | 0.025 | –0.063** | 0.025 |
| Ethnicity (mixed) | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Ethnicity (Asian) | –0.006 | 0.028 | –0.006 | 0.028 | –0.007 | 0.028 |
| Ethnicity (black) | 0.055 | 0.059 | 0.056 | 0.060 | 0.057 | 0.060 |
| Ethnicity (other) | –0.011 | 0.018 | –0.010 | 0.018 | –0.008 | 0.018 |
| Ethnicity (not stated) | –0.021** | 0.010 | –0.021** | 0.011 | –0.021** | 0.011 |
| IMD quintile 2 | 0.018* | 0.011 | 0.018* | 0.011 | 0.019* | 0.011 |
| IMD quintile 3 | 0.011 | 0.010 | 0.011 | 0.010 | 0.010 | 0.010 |
| IMD quintile 4 | 0.016 | 0.012 | 0.014 | 0.012 | 0.014 | 0.012 |
| IMD quintile 5 (most deprived) | –0.011 | 0.011 | –0.012 | 0.011 | –0.011 | 0.011 |
| IMD quintile (missing) | 0.035** | 0.015 | 0.037** | 0.015 | 0.037** | 0.015 |
| Charlson Comorbidity Index | 0.002*** | 0.000 | 0.002*** | 0.000 | 0.002*** | 0.000 |
| Number of diagnoses | –0.000 | 0.001 | –0.000 | 0.001 | –0.000 | 0.001 |
| Number of procedures | –0.014*** | 0.003 | –0.014*** | 0.003 | –0.014*** | 0.003 |
| Palliative care | 0.557*** | 0.031 | 0.557*** | 0.031 | 0.558*** | 0.032 |
| Number of emergency admissions in the previous year | 0.008** | 0.004 | 0.008** | 0.004 | 0.008** | 0.004 |
| Financial year 2009/10 | 0.028 | 0.028 | 0.052* | 0.027 | 0.049* | 0.028 |
| Financial year 2010/11 | 0.034 | 0.027 | 0.053** | 0.025 | 0.053** | 0.025 |
| Financial year 2011/12 | 0.049* | 0.027 | 0.068*** | 0.024 | 0.067*** | 0.025 |
| Financial year 2012/13 | 0.016 | 0.026 | 0.035 | 0.024 | 0.033 | 0.024 |
| Financial year 2013/14 | 0.004 | 0.026 | 0.025 | 0.024 | 0.022 | 0.024 |
| Financial year 2014/15 | –0.016 | 0.028 | 0.006 | 0.026 | 0.002 | 0.026 |
| Diagnosis group dummies | Yes | Yes | Yes | |||
| Admission method dummies | Yes | Yes | Yes | |||
| Observations | 6887 | 6836 | 6761 | |||
| c-statistic | 0.825 | 0.826 | 0.824 | |||
| Pseudo-R2 | 0.245 | 0.245 | 0.244 | |||
| Variable | Model | |||||
|---|---|---|---|---|---|---|
| 1: in-hospital mortality | 2: in-hospital mortality | 3: in-hospital mortality | ||||
| AME | SE | AME | SE | AME | SE | |
| Admission at weekday night | 0.017* | 0.010 | 0.011 | 0.011 | 0.010 | 0.011 |
| Admission at weekend day | 0.019* | 0.011 | 0.017 | 0.011 | 0.016 | 0.011 |
| Admission at weekend night | 0.010 | 0.010 | 0.004 | 0.012 | 0.003 | 0.011 |
| Number of patients in ASU on admission day | 0.001 | 0.001 | 0.001 | 0.001 | ||
| Number of nurses on duty at admission hour | –0.002 | 0.002 | ||||
| Number of qualified nurses on duty at admission hour | –0.003 | 0.003 | ||||
| Case-mix variables | ||||||
| Age on admission | 0.002*** | 0.000 | 0.002*** | 0.000 | 0.002*** | 0.000 |
| Gender (female) | 0.000 | 0.008 | –0.001 | 0.008 | –0.001 | 0.008 |
| Gender (not stated) | –0.003 | 0.044 | –0.004 | 0.043 | –0.002 | 0.044 |
| Ethnicity (mixed) | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Ethnicity (Asian) | 0.014 | 0.032 | 0.014 | 0.032 | 0.014 | 0.032 |
| Ethnicity (black) | 0.054 | 0.065 | 0.055 | 0.066 | 0.056 | 0.066 |
| Ethnicity (other) | –0.016 | 0.019 | –0.015 | 0.019 | –0.014 | 0.019 |
| Ethnicity (not stated) | –0.036*** | 0.010 | –0.036*** | 0.010 | –0.036*** | 0.010 |
| IMD quintile 2 | 0.017 | 0.011 | 0.016 | 0.011 | 0.017 | 0.011 |
| IMD quintile 3 | 0.018 | 0.011 | 0.017 | 0.011 | 0.015 | 0.011 |
| IMD quintile 4 | 0.014 | 0.012 | 0.013 | 0.012 | 0.013 | 0.012 |
| IMD quintile 5 (most deprived) | –0.001 | 0.012 | –0.002 | 0.012 | –0.003 | 0.012 |
| IMD quintile (missing) | 0.040** | 0.016 | 0.041** | 0.017 | 0.039** | 0.016 |
| Charlson Comorbidity Index | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Number of diagnoses | 0.006*** | 0.001 | 0.006*** | 0.001 | 0.006*** | 0.001 |
| Number of procedures | –0.004* | 0.003 | –0.004* | 0.003 | –0.004 | 0.003 |
| Palliative care | 0.675*** | 0.035 | 0.675*** | 0.035 | 0.677*** | 0.035 |
| Number of emergency admissions in the previous year | 0.011** | 0.005 | 0.010** | 0.005 | 0.010* | 0.005 |
| Financial year 2009/10 | –0.008 | 0.036 | 0.022 | 0.034 | 0.019 | 0.034 |
| Financial year 2010/11 | –0.018 | 0.035 | 0.011 | 0.031 | 0.009 | 0.031 |
| Financial year 2011/12 | –0.020 | 0.035 | 0.010 | 0.031 | 0.010 | 0.031 |
| Financial year 2012/13 | –0.046 | 0.035 | –0.015 | 0.031 | –0.014 | 0.031 |
| Financial year 2013/14 | –0.041 | 0.035 | –0.007 | 0.031 | –0.009 | 0.031 |
| Financial year 2014/15 | –0.051 | 0.036 | –0.016 | 0.033 | –0.018 | 0.033 |
| Diagnosis group dummies | Yes | Yes | Yes | |||
| Admission method dummies | Yes | Yes | Yes | |||
| Observations | 5132 | 5098 | 5041 | |||
| c-statistic | 0.782 | 0.784 | 0.782 | |||
| Pseudo-R2 | 0.215 | 0.217 | 0.218 | |||
After including the number of nurses in the model, mortality rates for out-of-hours admissions remained higher, but the difference was no longer statistically significant. Compared with weekday day admissions, mortality was 1.0 percentage points higher for weekday night admissions, 1.4 percentage points higher for weekend day admissions and 0.7 percentage points higher for weekend night admissions, a reduction of 0.8 to 0.2 and 0.8 percentage points in the respective periods compared with model 1. Over the week, each additional nurse reduced the risk of 7-day mortality by 0.3 percentage points. Qualified nurses, estimated in the third model, were associated with a greater marginal effect: mortality rates were reduced by 0.5 percentage points for each additional qualified nurse on site during the first hour of admission. There were similar results in-hospital mortality (see Table 22), but for 30-day mortality (see Table 21), including number of nurses in the model did significantly increase survival.
Conclusions
In this study we found no evidence that patients admitted out of hours were processed more slowly than patients admitted during normal working hours, although they tended to receive fewer diagnoses and procedures. In general, there were more overnight admissions during the week and more daytime admissions at the weekend. The highest number of admissions was during the daytime on Saturdays and Sundays, and these periods carried the highest unadjusted risk of mortality.
Risk-adjusted mortality rates were higher for all out-of-hours periods, with the risk marginally higher for weekday night admissions. This is slightly different pattern from that observed for all emergency admissions (see Table 7), for which the weekend night period carried the highest risk of mortality. The increased out-of-hours mortality risk was reduced for 7-day and in-hospital mortality after adjusting for the number of nurses present in the first hour of admission. The marginal effect was greater for qualified nurses. This suggests that the increased risk of mortality for out-of-hours stroke admissions could be partly attributable to a reduced number of qualified nurses during those periods. Our analysis was, however, restricted by a lack of data on other clinical staff and information on availability of diagnostic services, so were unable to determine whether or not other staffing factors are associated with out-of-hours mortality. It is also worth noting that we assessed relative differences in survival across the week and their relationship to staffing levels, rather than the absolute effect of staffing levels on survival.
Chapter 8 Overarching discussion
Summary of results
Study 1: costs and benefits of 7-day services
-
The estimated cost of implementing 7-day services nationally is £1.1–1.4B per year. This exceeds the maximum amount that NICE would recommend the NHS should spend on eradicating the observed weekend effect (£0.6–0.7B per year).
-
There is as yet no evidence that (1) 7-day working can and will reduce the weekend effect, (2) lower weekend mortality rates can be achieved without increasing weekday death rates and (3) reorganising services to be fully operational over 7 days would be cost-effective.
Study 2: persistence of the weekend effect and night-time effects
-
In addition to a weekend effect, there is a night-time effect. Mortality rates are elevated for patients admitted at night and the highest risk of death is for patients admitted at night on weekends.
-
The size of weekend and night-time effects varies substantially over time. They are present in most years, but are not always statistically significant.
Study 3: admission thresholds at weekends
-
There are fewer people admitted to hospital at weekends in an emergency and fewer deaths.
-
There is a higher threshold for emergency admission at weekends. Fewer patients are admitted and, on average, they are sicker than patients admitted on weekdays.
-
Higher mortality rates at weekends are found only among the subset of patients who are admitted to hospital.
Study 4: severity of illness at weekends
-
Arrival at hospital by ambulance is a proxy for severity of illness. Compared with weekday admissions, a higher proportion of patients admitted to hospital at night and on weekends arrive by ambulance.
-
Using standard risk adjustment, mortality is higher for patients admitted to hospital at weekends, and on Wednesday and Thursday nights, than Wednesday daytime.
-
After accounting for arrival by ambulance, mortality rates are not elevated for patients admitted at nights and at weekends, with the exception of Sunday daytime.
-
Elevated mortality rates for patients admitted at weekends and at night reflects higher average severely of illness.
Study 5: the impact of staffing levels
-
After adjusting for the staffing level of nurses, elevated mortality for patients admitted with stroke at weekends and nights were substantially reduced.
-
Having higher numbers of nurses on site immediately following admission is associated with increased patient survival in the first week, but not over longer periods. This effect is stronger for qualified nurses.
Conclusions
As well as patients admitted at the weekend, patients admitted at night also experience higher mortality rates. This effect was reduced for stroke patients in a large teaching hospital when more – and more experienced – nursing staff were present during the first hour of admission. Nationally, looking at all emergency admissions, we found that excess mortality out of hours was largely explained by a sicker population of patients being selected for admission. However, mortality rates were still higher than expected on Sunday daytimes when we accounted for severity of patient illness. We also found that the estimated cost of implementing 7-day services exceeds the maximum amount that NICE would recommend the NHS should spend on eradicating excess mortality at weekends.
Through our patient engagement work, we found that patient groups expressed concerns about potential variations in quality of care throughout the week and also expressed a strong preference for having the most experienced staff available outside normal working hours. However, after examining the evidence on cost-effectiveness of extending normal hours of operation and considering the potential unintended effects of such extensions, they also expressed reservations about implementing radical changes to current working arrangements in the absence of clear evidence for patient benefit. There was also a consensus that the NHS had greater priorities than providing 7-day services and that this issue had become unnecessarily politicised.
Implications for management and practice
The move towards 7-day services has begun with local implementation in acute trusts; hospitals are required to implement new clinical standards for ‘7-day services’, which include providing emergency admissions with a thorough clinical assessment by a suitable consultant within 14 hours of arrival and timely 24-hour access to consultant-directed interventions. These moves are being supported by other initiatives, including longer nursing shifts, extended contracts for community pharmacies and the opening of GP surgeries at evenings and weekends. The costs and benefits of these initiatives are largely unknown. Extending normal hours of operation could be cost-effective if it leads to improved access and better patient outcomes, particularly if these improvements benefit groups that are traditionally underserved and suffer worse health as a result.
Current initiatives to move towards 7-day hospital services are only likely to be successful in reducing mortality if reduced availability of services in hospitals on the day of admission is the major cause of the weekend effect. We have found some evidence that nursing levels may explain some of the excess mortality for stroke patients admitted during out-of-hours periods, and the potential cost-effectiveness of increasing staffing levels for these periods and for all types of staff should therefore be investigated. However, unless there is substantial investment in training and recruitment, increasing the level of nursing and clinician cover during the weekends will require a redistribution of the existing workforce, diverting cover away from weekdays.
Our findings at the national level across all indications for admission cast significant doubt over whether or not quality and availability of services is the major driver of excess out-of-hours mortality. Patients who attend A&E on weekends are at no higher mortality risk than patients who attend A&E on weekdays. A smaller proportion of attending patients are admitted at the weekend, and this higher threshold for admission is likely to mean that patients who are admitted via A&E at the weekend have, on average, greater severity of illness than patients admitted during the week. Reduced availability of primary care services at weekends means that a much smaller number of patients are admitted to hospital via this route and these patients are also likely to have greater severity of illness than their counterparts admitted during the week. When we accounted for mode of arrival at hospital – whether or not the patient arrived by ambulance – patterns of mortality changed substantially and most out-of-hours periods no longer carried an increased risk of mortality. However, admissions on Sunday daytime were still associated with an increased risk of mortality compared with Wednesday daytime. The reasons for this warrant further investigation.
Seven-day services, as currently defined, do not extend to a full 24/7 service (i.e. the government proposes to extend normal hours of operation to weekends but not to night-times). In addition to the previously described weekend effect, we found similarly elevated mortality rates for overnight admissions. A consistent policy approach would therefore involve extensions of normal hours of operation into night-time periods. However, the same issues of selection and lack of cost-effectiveness (if reducing mortality is the primary aim) would affect such extensions.
It should be noted that our analyses focused on the hospital setting and that other parts of the patient pathway – including primary care and social care settings – will have an impact on variations in mortality across the week and have a vital role to play in a co-ordinated response to extending normal hours of service operation.
Patient and public involvement
We aimed to ensure that the aims and objectives of the study reflected patient and public priorities and engaged with the public in order to communicate findings to the groups most likely to be affected. This public engagement activity benefited the research programme by ensuring that (1) it addressed questions that matter to service users, (2) interpretations of results and findings were plausible and (3) dissemination was in appropriate formats.
Patients, medical staff and members of the public were involved in the development and dissemination stages of this research. We engaged throughout the project with the SRFTM (an advisory body of 20,000 patients and staff members); we recruited two lay members to the Project Advisory Group; we convened focus groups drawn from patients, carers and staff, at critical points of the project; and we hosted a public engagement day at SRFT (see Appendix 2). We held a final public engagement exercise in November 2016 to feed findings back to the membership.
Chapter 9 Recommendations
Implications for practice
In light of our findings, we have the following recommendations.
-
Caution should be exercised when interpreting trends in mortality following recent changes to weekend service provision. Extending services in hospitals and in the community at weekends may increase the number of emergency admissions, particularly for patients with less severe illness, and this could have the desired effect of securing lower hospital mortality rates. However, this would be a statistical phenomenon rather than a clinically meaningful improvement, as it would be achieved by admitting a less severely ill mix of patients rather than by reducing the absolute number of deaths.
-
There are many important aspects of care quality beyond mortality. Indicators of quality, such as the time taken to receive necessary scans and procedures, have been shown to exhibit temporal variation throughout the week in condition-specific studies using clinical audit data. Temporal variations in quality indicators beyond mortality warrant further investigation.
-
In addressing variations in patient outcomes across the week, a more nuanced approach, extending services for key specialties over critical periods – rather than implementing whole-system changes – is likely to be the most cost-effective.
Implications for research
In advancing the research agenda in relation to out-of-hours mortality and 7-day services we have the following recommendations.
-
Most of the debate on 7-day services has focused on weekend care. A more granular approach to time classification is needed to fully capture the variations in the flow of patients and the services offered across times of the day in addition to days of the week (see studies 2 and 4). In particular, emergency admissions on Sunday daytime appear to have an increased risk of mortality that is not fully explained by the patient characteristics we could control for.
-
In addition to the patient’s mode of arrival at hospital (see study 4), other information on the services that patients have accessed prior to their arrival at hospital should be included in future studies to further understand mortality risk. Such proxies will, however, always be inferior to direct measurement of severity of illness, which is required in order for clinicians and policy-makers to make valid comparisons of outcomes over time and across providers. Our results, therefore, add to the increasing body of evidence highlighting the limitations of the risk adjusters available in inpatient records when standardised mortality rates are interpreted as an indicator of hospital quality.
-
Although we have found that mortality is not significantly increased for patients who are admitted during most out-of-hours periods once selection effects are accounted for (see studies 3 and 4), it is possible that risks are elevated for patients who are already in hospital and who deteriorate or require critical interventions during out-of-hours periods. Further research on critical periods other than the time of admission is required.
-
In order to improve understanding of the underlying reasons behind variations in mortality across the week, more detailed analysis of mortality by cause and by patient group are required.
-
Fewer than 4% of patients admitted to hospital die during their admission and most of these deaths are unavoidable. Focusing on mortality, therefore, tells us little about the care that most patients receive and other indicators of quality of care should be included in future studies of out-of-hours care.
-
In light of our finding in study 1 on the likely failure of service-wide extensions to be cost-effective, future research should aim to identify candidate specialties and critical periods for which extending services is likely to be cost-effective.
Acknowledgements
Contributions of authors
Lu Han (Research Associate, Health Services Research), co-investigator, was responsible for data extraction and preparation, study design, statistical analysis, and preparation of reports and manuscripts.
Rachel Meacock (Research Associate, Health Economics), co-investigator, was responsible for data extraction and preparation, study design, statistical analysis, and preparation of reports and manuscripts.
Laura Anselmi (Research Associate, Health Economics), co-investigator, was responsible for data extraction and preparation, study design, statistical analysis, and preparation of reports and manuscripts.
Søren R Kristensen (Research Associate, Health Economics), co-investigator, was responsible for data extraction and preparation, study design, statistical analysis, and preparation of reports and manuscripts.
Matt Sutton (Professor of Health Economics) co-investigator, was responsible for design of the study and editing of reports and manuscripts.
Tim Doran (Professor of Health Policy), principal investigator, was responsible for overall management of the project, design of the study and editing of reports and manuscripts.
Stuart Clough (Programme Manager, SRFT) was responsible for securing data access and liaising with clinical and managerial staff.
Maxine Power (Director of Innovation and Improvement Science, SRFT) was responsible for project management at SRFT.
Publications
Meacock R, Doran T, Sutton M. What are the costs and benefits of providing comprehensive seven-day services for emergency hospital admissions? Health Econ 2015;24:907–12.
Meacock R, Anselmi L, Kristensen S, Doran T, Sutton M. Higher mortality rates amongst emergency patients admitted to hospital at weekends reflect a lower probability of admission. J Health Serv Res Pol 2016;22:12–19.
Anselmi L, Meacock R, Kristensen SR, Doran T, Sutton M. Arrival by ambulance explains variation in mortality by time of admission: retrospective study of admissions to hospital following emergency department attendance in England. Br Med J Qual Saf 2016;26:613–21.
Han L, Sutton M, Clough S, Warner R, Doran T. The impact of out-of-hours admission on patient mortality: longitudinal analysis in a tertiary acute hospital [published online ahead of print September 28 2017]. BMJ Qual Saf 2017.
Presentations
Meacock R, Anselmi L, Kristensen S, Doran T, Sutton M. Is Elevated Mortality at Weekends a Supply or a Demand Side Phenomenon? Health Economists’ Study Group, Lancaster, UK, June 2015.
Meacock R, Doran T, Sutton M. What Are the Costs and Benefits to the NHS of Providing Comprehensive Seven Day Hospital Services? Health Services Research Network Symposium, Nottingham, UK, June 2015.
Anselmi L, Meacock R, Kristensen S, Doran T, Sutton M. Effect of Day and Time of Attendance to A&E on the Probability of Admission, Short-Stay and 30 Day Mortality in England. European Health Economics Association PhD Student-Supervisor Conference, Paris, France, September 2015.
Meacock R, Doran T, Sutton M. How Much Should We Spend on Providing Comprehensive Hospital Services Seven Days a Week? International Health Economics Association World Congress, Milan, Italy, July 2015.
Meacock R, Anselmi L, Kristensen S, Doran T, Sutton M. Is Elevated Mortality at Weekends a Supply or a Demand Phenomenon? Nordic Health Economists’ Study Group, Uppsala, Sweden, August 2015.
Meacock R. Is Elevated Hospital Mortality at Weekends a Selection Issue? Health Economics Unit, University of Birmingham, Birmingham, UK, October 2015.
Meacock R. Is Elevated Hospital Mortality at Weekends a Selection Issue? Department of Health Sciences, University of York, York, UK, November 2015.
Meacock R. Evaluating the Cost-Effectiveness of Changes to Health Services Organisation and Delivery. CLAHRC Health Economics of Service Delivery Research Workshop, King’s College London, London, UK, January 2016.
Meacock R. Unpicking the Weekend Effect. British Medical Association Clinical Trainees Seminar, London, UK, February 2016.
Meacock R. Is Elevated Mortality at Weekends a Selection Issue? Health Economics Group, University of Nottingham, Nottingham, UK, March 2016.
Doran T. Quality, Selection and Out-of-Hours Mortality. Health Economics Group, Odense University, Odense, Denmark, March 2016.
Doran T. Death at the Weekend. What Lies Behind the Weekend Effect? Centre for Health Economics, University of York, York, UK, May 2016.
Meacock R, Anselmi L, Kristensen S, Doran T, Sutton M. Is Elevated Mortality at Weekends a Selection Issue? American Society of Health Economists 6th Biennial Conference, Philadelphia, PA, USA, June 2016.
Meacock R, Anselmi L, Kristensen S, Doran T, Sutton M. Is Elevated Mortality Following Emergency Hospital Admission at Weekends a Selection Issue? Academy Health Annual Scientific Meeting, Boston, MA, USA, June 2016.
Han L, Doran T. The Impact of Out-of-Hour admission on Patient Mortality: A Longitudinal Analysis in a Major Acute Hospital. Society for Social Medicine 60th Annual Scientific Meeting, University of York, York, UK, September 2016.
Media
Doran T. Seven Day Services. Five Live Daily, BBC Radio Five Live. October 2015. URL: www.bbc.co.uk/radio/player/b06j0c28 (accessed 5 November 2015).
Doran T. Seven Day NHS Services. Equipoise No.5. December 2015.
Meacock R. 7 Day NHS. The Report, BBC Radio 4. February 2016. URL: www.bbc.co.uk/programmes/b070hns3 (accessed 3 March 2016).
Meacock R. The Weekend Effect – What’s (Un)knowable, and What Next? BMJ Talk Medicine Podcast. May 2016.
Doran T. Weekend Mortality. BBC News Channel. May 2016.
Meacock R, Sutton M. The ‘Weekend Effect’ is About Admissions as Much as Mortality Rates. Health Service Journal, 6 May 2016. URL: www.hsj.co.uk/topics/quality-and-performance/the-weekend-effect-is-about-admissions-as-much-as-mortality-rates/7004527.article (accessed 8 May 2016).
Meacock R. 7 Day NHS Statistics. Science Media Centre Background Briefing. July 2016.
Invited blogs
The NHS has rushed to fix a weekend problem that doesn’t exist. Manchester Policy Blogs. May 2016. URL: http://blog.policy.manchester.ac.uk/posts/2016/05/the-nhs-has-rushed-to-fix-a-weekend-problem-that-doesnt-exist/ (accessed 1 August 2016).
The economics of a 7-day NHS. The Academic Health Economists’ Blog. June 2015. URL: http://aheblog.com/2015/06/04/the-economics-of-a-7-day-nhs/ (accessed 9 July 2015).
The economics of elevated hospital mortality at weekends. Office of Health Economics News Blog. July 2015. URL: www.ohe.org/news/guest-post-economics-elevated-hospital-mortality-weekends (accessed 1 August 2016).
Data sharing statement
Requests for access to data should be addressed to the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Ensminger SA, Morales IJ, Peters SG, Keegan MT, Finkielman JD, Lymp JF, et al. The hospital mortality of patients admitted to the ICU on weekends. Chest 2004;126:1292-8. https://doi.org/10.1378/chest.126.4.1292.
- Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Med Care 2007;45:1195-204. https://doi.org/10.1097/MLR.0b013e3181468ca3.
- Freemantle N, Richardson M, Wood J, Ray D, Khosla S, Shahian D, et al. Weekend hospitalization and additional risk of death: an analysis of inpatient data. J R Soc Med 2012;105:74-8. https://doi.org/10.1258/jrsm.2012.120009.
- Palmer WL, Bottle A, Davie C, Vincent CA, Aylin P. Dying for the weekend: a retrospective cohort study on the association between day of hospital presentation and the quality and safety of stroke care. Arch Neurol 2012;69:1296-302. https://doi.org/10.1001/archneurol.2012.1030.
- A Promise to Learn – A Commitment to Act: Improving the Safety of Patients in England. London: The National Advisory Group on the Safety of Patients in England; 2013.
- Consultant Delivered Care: An Evaluation of New Ways of Working in Paediatrics. London: Royal College of Paediatrics and Child Health; 2012.
- Schmulewitz L, Proudfoot A, Bell D. The impact of weekends on outcome for emergency patients. Clin Med 2005;5:621-5. https://doi.org/10.7861/clinmedicine.5-6-621.
- Albright KC, Raman R, Ernstrom K, Hallevi H, Martin-Schild S, Meyer BC, et al. Can comprehensive stroke centers erase the ‘weekend effect’?. Cerebrovasc Dis 2009;27:107-13. https://doi.org/10.1159/000177916.
- McKinney J, Deng Y, Kasner S, Kostis J. Myocardial Infarction Data Acquisition System Study Group . Comprehensive stroke centers overcome the weekend versus weekday gap in stroke treatment and mortality. Stroke 2011;42:2403-9. https://doi.org/10.1161/STROKEAHA.110.612317.
- Equity and Excellence: Liberating the NHS. London: Department of Health; 2010.
- Meacock R, Doran T, Sutton M. What are the costs and benefits of providing comprehensive seven-day services for emergency hospital admissions?. Health Econ 2015;24:907-12. https://doi.org/10.1002/hec.3207.
- Meacock R, Anselmi L, Kristensen S, Doran T, Sutton M. Higher mortality rates amongst emergency patients admitted to hospital at weekends reflect a lower probability of admission. J Health Serv Res Policy 2016. https://doi.org/10.1177/1355819616649630.
- Anselmi L, Meacock R, Kristensen SR, Doran T, Sutton M. Arrival by ambulance explains variation in mortality by time of admission: retrospective study of admissions to hospital following emergency department attendance in England. BMJ Qual Saf 2016;26:613-21. https://doi.org/10.1136/bmjqs-2016–005680.
- HES Accident & Emergency (A&E) to Admitted Patient Care (APC) Linkage Methodology. Leeds: HSCIC; 2011.
- Aylin P, Yunus A, Bottle A, Majeed A, Bell D. Weekend mortality for emergency admissions. A large, multicentre study. Qual Saf Health Care 2010;19:213-7. https://doi.org/10.1136/qshc.2008.028639.
- Kristensen SR, Meacock R, Turner AJ, Boaden R, McDonald R, Roland M, et al. Long-term effect of hospital pay for performance on mortality in England. N Engl J Med 2014;371:540-8. https://doi.org/10.1056/NEJMoa1400962.
- Meacock R, Kristensen SR, Sutton M. The cost-effectiveness of using financial incentives to improve provider quality: a framework and application. Health Econ 2014;23:1-13. https://doi.org/10.1002/hec.2978.
- Beta Classifications Software (CCS) for Mortality Reporting. 2017.
- HES Data Dictionary: Accident and Emergency – Accident and Emergency (A&E) Hospital Episodes Statistics (HES) Data Dictionary. Version 2.0. Leeds: HSCIC; 2015.
- Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43:1130-9. https://doi.org/10.1097/01.mlr.0000182534.19832.83.
- Bottle A, Gaudoin R, Goudie R, Jones S, Aylin P. Can Valid and Practical Risk-Prediction or Case-Mix Adjustment Models, Including Adjustment for Comorbidity, be Generated from English Hospital Administrative Data (Hospital Episode Statistics)? A National Observational Study. Southampton: Health Services and Delivery Research; 2014.
- Gutacker N, Bloor K, Cookson R. Comparing the performance of the Charlson/Deyo and Elixhauser comorbidity measures across five European countries and three conditions. Eur J Public Health 2015;25:15-20. https://doi.org/10.1093/eurpub/cku221.
- Department of Communities and Local Government . The English Indices of Deprivation 2010 2011. www.gov.uk/government/statistics/english-indices-of-deprivation-2010 (accessed 4 February 2015).
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-83. https://doi.org/10.1016/0021-9681(87)90171-8.
- Costing Seven Services: The Financial Implications of Seven Day Services for Acute Emergency and Urgent Services and Supporting Diagnostics. London: NHS England; 2013.
- Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med 2001;345:663-8. https://doi.org/10.1056/NEJMsa003376.
- Hunter RM, Davie C, Rudd A, Thompson A, Walker H, Thomson N, et al. Impact on clinical and cost outcomes of a centralized approach to acute stroke care in London: a comparative effectiveness before and after model. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0070420.
- Morris S, Hunter R, Ramsay A, Boaden R, McKevitt C, Perry C, et al. Impact of centralising acute stroke services in English metropolitan areas on mortality and length of hospital stay: difference-in-differences analysis. BMJ 2014;349. https://doi.org/10.1136/bmj.g4757.
- NHS Services, Seven Days a Week Forum . Costing Seven Day Services n.d. www.england.nhs.uk/wp-content/uploads/2013/12/costing-7-day.pdf (accessed 4 June 2015).
- Department of Health . Annual Report and Accounts 2013–14 2014. www.gov.uk/government/ uploads/system/uploads/attachment_data/file/335166/DH_annual_accounts_2013–14.pdf (accessed 4 June 2015).
- Coast J. Is economic evaluation in touch with society’s health values?. BMJ 2004;329:1233-6. https://doi.org/10.1136/bmj.329.7476.1233.
- Aylin P, Alexandrescu R, Jen M, Mayer E, Bottle A. Day of week of procedure and 30 day mortality for elective surgery: retrospective analysis of hospital episode statistics. BMJ 2013;346. https://doi.org/10.1136/bmj.f2424.
- McIsaac DI, Bryson GL, van Walraven C. Elective, major noncardiac surgery on the weekend: a population-based cohort study of 30-day mortality. Med Care 2014;52:557-64. https://doi.org/10.1097/MLR.0000000000000137.
- Perez Concha O, Gallego B, Hillman K, Delaney G, Coiera E. Do variations in hospital mortality patterns after weekend admission reflect reduced quality of care or different patient cohorts? A population-based study. BMJ Qual Saf 2014;23:215-22. https://doi.org/10.1136/bmjqs-2013-002218.
- Freemantle N, Ray D, McNulty D, Rosser D, Bennett S, Keogh BE, et al. Increased mortality associated with weekend hospital admission: a case for expanded seven day services?. BMJ 2015;351. https://doi.org/10.1136/bmj.h4596.
- Robinson E, Smith G, Power S, Harrison D, Nolan J, Soar J, et al. Risk-adjusted survival for adults following in-hospital cardiac arrest by day of week and time of day: observational cohort study. BMJ Qual Saf 2015.
- Coumbe A, John R, Kuskowski M, Agirbasli M, McFalls EO, Adabag S. Variation of mortality after coronary artery bypass surgery in relation to hour, day and month of the procedure. BMC Cardiovasc Disord 2011;11. https://doi.org/10.1186/1471-2261-11-63.
- McKee M. Is the UK government right that seven day working in hospitals would save 6000 lives a year?. BMJ 2015;351. https://doi.org/10.1136/bmj.h4723.
- Bray BD, Cloud GC, James MA, Hemingway H, Paley L, Stewart K, et al. Weekly variation in health-care quality by day and time of admission: a nationwide, registry-based, prospective cohort study of acute stroke care. Lancet 2016;388:170-7. https://doi.org/10.1016/S0140–6736(16)30443–3.
- Mohammed MA, Faisal M, Richardson D, Howes R, Beaston K, Speed K, et al. Adjusting for illness severity shows there is no difference in patient mortality at weekends or weekdays for emergency medical admissions. QJM 2017;110:e1-8.
- Black N. Is hospital mortality higher at weekends? If so, why?. Lancet 2016;388:108-11. https://doi.org/10.1016/S0140–6736(16)30505–0.
- Li L, Rothwell PM. Oxford Vascular Study . Biases in detection of apparent ‘weekend effect’ on outcome with administrative coding data: population based study of stroke. BMJ 2016;353. https://doi.org/10.1136/bmj.i2648.
- Hospital Episode Statistics, Accident and Emergency (A&E), England 2013–2014: Summary Report. Leeds: HSCIC; 2015.
- Vest-Hansen B, Riis AH, Sørensen HT, Christiansen CF. Out-of-hours and weekend admissions to Danish medical departments: admission rates and 30-day mortality for 20 common medical conditions. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014–006731.
- HES 2013–2014 Annual A&E Data Quality Note (Version 2). Leeds: HSCIC; 2015.
- Aiken LH, Clarke SP, Sloane DM. International Hospital Outcomes Research Consortium . Hospital staffing, organization, and quality of care: cross-national findings. Int J Qual Health Care 2002;14:5-13. https://doi.org/10.1093/intqhc/14.1.5.
- Rafferty AM, Clarke SP, Coles J, Ball J, James P, McKee M, et al. Outcomes of variation in hospital nurse staffing in English hospitals: cross-sectional analysis of survey data and discharge records. Int J Nurs Stud 2007;44:175-82. https://doi.org/10.1016/j.ijnurstu.2006.08.003.
- Griffiths P, Jones S, Bottle A. Is ‘failure to rescue’ derived from administrative data in England a nurse sensitive patient safety indicator for surgical care? Observational study. Int J Nurs Stud 2013;50:292-300. https://doi.org/10.1016/j.ijnurstu.2012.10.016.
- Bond CA, Raehl CL. Clinical pharmacy services, pharmacy staffing, and hospital mortality rates. Pharmacotherapy 2007;27:481-93. https://doi.org/10.1592/phco.27.4.481.
- Bond C, Raehl C, Pitterle M, Franke T. Health care professional staffing, hospital characteristics, and hospital mortality rates. Pharmacotherapy 1999;19:130-8. https://doi.org/10.1592/phco.19.3.130.30915.
Appendix 1 Original research aims
The research aims for this project changed when it became apparent that there might be differences in severity of illness between patients admitted during normal hours and out of hours, which are not captured by standard risk adjustment. This appendix provides the original research aims and our reasons for changing them.
Original rationale
There are long-standing concerns that patients admitted to hospital at night and at weekends, when staffing levels are lower and some services are not available, suffer higher complication and mortality rates than patients admitted at times when the hospital is fully operational. It is not known, however, what service changes would be required to bring these rates down to levels comparable with daytime and weekday rates, and what the cost implications of such changes would be. The NHS therefore faces difficult decisions in how it should respond to its responsibility to provide health care 24/7. These decisions include the external margin (e.g. when services are open to patients) and the internal margin (e.g. when facilities are fully operational).
Extending availability increases overall costs and, at a time of resource constraint, these investment decisions must recognise the opportunity costs. 24/7 care could be cost-effective if it leads to improved access and better patient outcomes, particularly if these improvements are experienced by population and patient groups that are traditionally underserved and suffer worse health as a consequence. The evidence on equity in service use suggests that more deprived populations make greater use of unplanned services and less use of planned services. It is therefore feasible that extending opening hours differentially benefits the poor and may contribute towards reducing inequalities in health.
Original research aims and objectives
We aim to answer four key questions:
-
What is the impact of changes to fully operational hours on access to services for different population and patient groups?
-
How do service reconfigurations affect quality of care and patient outcomes for different population and patient groups?
-
How should staff be best deployed to deliver care throughout the week?
-
What balance of fully operational hours represents the most cost-effective use of NHS resources?
Reasons for changing research aims
Our original research aims were based on the assumption that one or more aspects of quality of care at the time of admission varied substantially throughout the week and that these variations were the primary cause of the higher rates of mortality observed for weekend admissions in previous studies. The assumptions were challenged during interviews with clinical staff at SRFT, who indicated that the population of patients admitted out of hours differed substantially from the population admitted on weekdays in terms of severity of illness. On inspection of the standard risk adjustment models used in previous studies, it was clear that several key markers of severity (e.g. pulse, blood pressure, respiratory rate, level of consciousness in most cases) were not included, because these variables are not routinely included in the administrative data used to construct these risk adjustment models. These data were also absent from the data we had collected from SRFT.
The hypothesis that studies on the weekend effect could be confounded by severity of illness received support from new studies published during this project. 39,40 We therefore reframed our research questions to address more fundamental questions about the patterns of mortality for emergency admissions throughout the week, the causes of the weekend effect and the likely cost-effectiveness of restructuring NHS services to address excess mortality for out-of-hours admissions.
Our first question aimed to establish a baseline for the potential cost-effectiveness of extending services if the weekend effect was entirely attributable to service provision and if moving to 7-day services could eliminate the effect:
-
What are the potential costs and benefits of introducing 7-day services?
Our rationale was that if this ‘maximum effect’ estimate fell short of NICE’s cost-effectiveness threshold, then even if severity of illness had no impact on the weekend effect moving towards a full 7-day service would not be cost-effective if the purpose of the change was to eliminate the weekend effect.
Our second question addressed the issue of other out-of-hours periods:
-
Does the weekend effect extend to nights? Does it persist over time?
Our third and fourth questions addressed the issue of unmeasured severity of illness:
-
Do higher mortality rates for patients admitted to hospital out of hours reflect a lower probability of admission?
-
Are higher mortality rates for out-of-hours admissions explained by greater severity of illness?
Our findings for these four questions suggested that system-wide service reconfiguration was unlikely to be cost-effective under any circumstances (see Table 2) and that unmeasured severity of illness was a key contributor to the weekend effect (compare, for example, Figures 4 and 5). We therefore concluded that pursuing our original research questions would be unproductive. However, we were aware that we had not incorporated staffing levels in our first four studies, and concluded that this issue – central to our third original research question – warranted further investigation. We therefore returned to the SRFT data to address a fifth research question:
-
What is the relationship between staffing levels and out-of-hours mortality?
The decision to move from our original research questions to the new research questions was not a single, discrete choice. Our aims evolved over time in light of emerging findings from our research programme and it was our intention to return to the original research questions if they remained relevant. However, as the research progressed it became clear that pursuing the original research questions would be unproductive. We discussed these issues with the Advisory Group, which supported our decisions to move towards the new research questions.
Appendix 2 Outputs from patient and public involvement
National Institute for Health Research patient and public involvement event: Medicine for Members, 14 July 2015
Debate questions
Expert witness number 1: Professor Tim Doran
(1) Illness versus accident? Difference may not be hospital’s fault
Professor Tim Doran: the research team have been looking at emergency admissions; there is an assumption that some patients’ lives could not be saved because of the severity of admission cause. Inpatient mortality rate shows a gap between weekend and weekday; however, this gap is closing. The British Medical Journal is to release a paper that was undertaken by the Imperial College London, which studied mortality rates and avoidable deaths and was a fine case note study. Ninety-six per cent to 97% were not preventable deaths, therefore only 3–4% we viewed as something further could have been done.
(2) Errors causing death?
Professor Tim Doran: all data received were anonymised; to some extent the data can show story of the patient journey, but this is only an indication. There are indicators throughout the data, for example speed of pathway and infection types, which could show error. No case notes have been used throughout the study, therefore it’s very difficult to obtain errors that have led to death.
(3) Salford Royal NHS Foundation Trust costs over a longer period/efficiency affecting smaller hospitals? Query of quality-performing trusts affecting smaller trusts performing less well?
Professor Tim Doran: the difference between urgent and routine services. Extension of services of this nature often see a benefit on Mondays and Tuesdays, as services are more manageable (e.g. patients are not discharged on a Saturday and Sunday, therefore wait for ‘normal’ hours on Monday, which causes a bit of a bottle neck). However, any extensions or attempts at extending services also need to be aligned with community services and they need to work in tandem, for example discharge on a Saturday would need GP services available Saturday and Sunday.
(4) Cost: 1.5–2% query?
Professor Tim Doran: confirmation that to extend services into the weekend will increase operational cost. The percentage described is a cost from London. The DH tried to broaden this percentage outside and came up with the 1.5–2%; it is its estimate.
(5) What is meant by 24/7?
Professor Tim Doran: this means different things to different people. Some people may suggest NHS services are 24/7 already; purely down to A&E services operating that way. Some people describe a 7-day service as a ward round on the Saturday and Sunday; however, it is unlikely that full services could be replicated for every day of the week. 24/7 means every minute of every day not just flexible service extension.
(6) Locations of patients been referred in?
Professor Tim Doran: this element will be looked into, but we have not looked where the referral has gone thus far. We have the source of the Salford admission, but this will be undertaken in time.
(7) £595M meaning?
Professor Tim Doran: NICE was formed back in 1998 to answer questions such costs of mortality, etc., QALYS are an example. NICE put a £20,000 threshold on cost of treatment per patient. Current evidence would suggest that it is not worth spending the fees on the full extensions of service; however, it is suggested that NHS trusts should now look at where services are best deployed to spend their money.
(8) Mortality 3.7–4% at the weekend? Is it worth it?
Professor Tim Doran: there will be a probable reduction; however, national data shows that it would actually not be worth it. Actual cost to do it would be nearer £1B; NICE say that it would cost £595M to fully extended services. However, it is perceived that there are better ways to spend the money than to fully extend.
(9) Costs for young and old?
Professor Tim Doran: this could certainly be looked at; patient differences, and this could explain the gap. It may not be that mortality is the fault of the hospital, it may be more due to patient illness.
Medicine for Members: first session – 14.00–16.00, 21 July 2015
Part 1: citizens’ jury
Expert witness number 1: Professor Tim Doran
Professor Tim Doran presented the case for 24/7 health care from a government perspective, outlining why the government is proposing this as a way forward – potential reductions in mortality rate (i.e. mitigating what has been widely cited as the ‘weekend effect’).
Professor Tim Doran emphasised the current political climate and the recognition that 24/7 health care has had recently.
Professor Tim Doran outlined the founding principles of the NHS: comprehensive treatment; universal access; services delivered free at the point of delivery; provision of equitable access – care provided on basis of need, not on ability to pay.
Various studies have shown that there are significant variations in patient outcomes and service arrangements depending on whether it is a weekday or weekend. It is suggested that at the weekend there are fewer senior staff on duty, therefore (the government position is that) a reduced service provision leads to a reduction in diagnosis rates and ultimately an increase in mortality, thereby violating the premise of equity.
Professor Tim Doran presented a slide detailing the levels of service provision – level 0 to level 4 – and presented national and local results from 2010 and 2006. Professor Tim Doran explained how these data could be presented in terms of relative and absolute risk, which could lead to the actual increase in mortality being exaggerated.
Professor Tim Doran also highlighted that there had been no discussion about the differences between day and night mortality (i.e. whether or not there is a greater risk of a patient dying if she/he is admitted during the day or during the night).
After ‘expert witness number 1’, there were questions from the floor
Question: what does ‘24/7 health care’ mean? Lots of figures/statistics have been presented (referring to slides in Professor Tim Doran’s presentation), but they all indicate different things – it seems as if ‘you’ do not know the numbers?
Professor Tim Doran: depends on what type of data are being presented; some are national data, some are local/regional data. It also depends on the types of patients/specialties; lots of different figures can be used depending on what narrative/emphasis/point of view is being made. Also, over time, chances of surviving in hospital increases as a result of improvements in care and medicine – data do not also represent whether or not patients are suffering from certain conditions (i.e. myocardial infarction, pneumonia), which can also impact on survival rates.
Question: there are huge sums of money involved, but it appears that we do not know where we are starting from.
Professor Tim Doran: I think that this question would be best answered by my colleague, Rachel Meacock.
Question: what does it mean to have full 24/7 health-care provision? (In terms of how it is being expressed/used by the government recently.)
Professor Tim Doran: when ‘full 24/7 health care’ is mentioned, it refers to appropriate provision of routine services, specialty dependent. After all, is it appropriate for all services to run 24/7? It would not mean that all specialties would be available 24/7.
Question: is there any time frame associated with the government’s aim to provide ‘24/7 health care’?
Professor Tim Doran: the framework for service-appropriate 24/7 provision of health care states that it will be in place by 2020. I (Professor Tim Doran) would be very surprised if we (England and Wales) gets anywhere close to this.
Expert witness number 2: Rachel Meacock
Rachel Meacock referred to the previous statistics in Professor Tim Doran’s evidence – these are the studies on which current policies (to implement 24/7 health care) are based. Rachel Meacock explained that her studies have included considering what the costs and benefits of 24/7 health care would be – what would the costs be and would this improve patient health? Are there any other options?
Rachel Meacock posed the question ‘what is causing higher mortality?’ Is staffing key to mortality? There is no evidence for causation (i.e. that decreased/increased staffing would directly increase/decrease mortality), and the only studies have been small scale and in specific specialties – the problem (of whether or not to provide 24/7 health care) is actually more complicated than initially presented.
Rachel Meacock emphasised that the NHS has limited resources and there must be value for each service the NHS provides. There has been no appreciation (in the rhetoric about 24/7 health care) of whether or not the extension of services at the weekend would impact on patients during the week – what will happen during the week if consultants are working over the weekend? It could be that the gap between weekday/weekend mortality would be narrowed through weekday morality increasing.
Rachel Meacock outlined how she had begun to understand whether or not there would be value (in both financial costs and patient costs) in providing 24/7 health care. Rachel Meacock’s preliminary work was:
-
to estimate the number of lives that could be potentially saved if the weekend mortality was decreased to align with weekday mortality
-
this estimate was then converted into QALYs, and from this, an estimate of how much NICE would recommend to be spent (to achieve this)
-
to estimate whether or not (in light of how much 24/7 health care would cost), such a level of service provision would represent value.
Rachel Meacock’s figures relate to emergency admissions and the data are taken from HES.
A crude 30-day mortality rate was 3.70% for weekday admissions and 4.05% for weekend admissions; these data would suggest that the excess weekend death rate = 4355 (which was risk adjusted to 5353) per year. The estimated health gain would be 29–727 or 36–539 QALYs per year, dependent on the assumptions made in the analysis. NICE’s threshold (for said level of QALYs) would be £595–731M; however, the estimated cost of implementing 24/7 health care nationally would be £1.07–1.43B, which exceeds NICE’s own estimates by £339–831M.
Rachel Meacock highlighted that there are lots of gaps in the evidence. We know that mortality increases at the weekend, but we do not know why. There is no evidence that moving to a 7-day service would not affect weekday patients or that it would reduce weekend deaths.
After ‘expert witness number 2’, there were questions from the floor
Question: taking the figures presented (risk-adjusted number of deaths and lowest figure for 24/7 health care) would roughly = £31M per death. Is it really worth it? Even if a mid-range estimate of NICE’s threshold (say £600M) were used instead of the actual costs, this would = £120,000/death – is it really worth it?
Rachel Meacock: our study is not trying to provide answers, we are trying to spark debate about whether or not this is the right course of action for the government to be pursuing.
Question: what has happened with the reversal of waiting times (since 2010)? Is not it better to focus on other things than just going after 24/7 health care? Computerised tomography scans are needed on a Friday evening.
Rachel Meacock: you’re right, nothing happens in isolation.
Question: £1–1.43B – does it include staff wages/training, etc.?
Professor Tim Doran: costs are per hospital; unsure whether or not training costs are captured.
Rachel Meacock: costs have come from foundation trusts.
Question: costs increase all the time, we do not know that it will only be £1–1.43B. What about community costs? It’s not worth it, the government is not listening.
Professor Tim Doran: (explained some of the background to 24/7 health care;) Sir Bruce Keogh instigated the push for 24/7 health care as he considered the variation between weekend and weekday mortality an equity issue. The government has jumped the gun and instead of waiting for more evidence is rolling this into practice. Depending on how far down this road the DH pushes the NHS, it may be very difficult to reverse.
Part two: discussion
Professor Tim Doran: remember, the discussion (here, in the press, etc.), is all about weekends, but we need to start talking about differences between day and night.
Question: recent patient experience with weekend services – was an emergency admission and presented with an unusual condition that required more specialist opinion. There was difficulty on Saturday and Sunday and there was no specialist around to confirm a diagnosis. During the weekend the patient felt that nothing happened and that certain diagnostic tests were not available. Patient comments – ‘It’s great that (when talking about 24/7 health care) we talk about having the right levels of skills and training available (i.e. only having certain specialties staffed 24/7), but the problem is that you don’t know what the right skills and training are’. What has happened with people (clinicians) on call?
Professor Tim Doran: they (clinicians, consultants) are, but they may not be as visible – they may not be physically located at the hospital; junior doctors may have to telephone them, but a more experienced member of staff will be contactable.
Question: there’s confusion about what 24/7 means – is actually 24/7 going to be available?
Professor Tim Doran: there needs to be clarity – does 7-day services mean that you’ll get the same services Saturday and Sunday as you would do Monday–Friday? 24/7 implies services around the clock, night and day, whereas a 7-day service could mean that there would be a service (i.e. outpatient clinic, available 08.00–20.00), with emergency admissions as night.
Question: what about discharge? Does that mean that you could be discharged on a Sunday?
Professor Tim Doran: yes, and what about community and social services? GPs would have to work (corresponding hours).
Question: why look at 24/7 when we have not got 24/5 now?
Professor Tim Doran: (explains that there is a knock on from the weekend) Monday is very busy because people are catching up from the weekend. If we had 7-day services people could not be catching up.
Question: why do specialists need the weekend off? We should scrap bank holidays for clinicians, etc.
Professor Tim Doran: patient outcomes for the Monday/Tuesday after a bank holiday are very similar to the weekend.
Question: but there’s no guarantee of survival any day of the week?
Question: public services have not moved on with a changing society – this should have been addressed earlier.
Professor Tim Doran: (mentioned real trials that have been performed in Whitby, etc.) focus groups get together and say ‘this is what we want’, ‘we’d like/we’d use 7-day services’, but then people do not take advantage.
Question: what about the critical care aspect? There are now many specialist centres of excellence which mean that you have to travel.
Professor Tim Doran: other inequalities exist in the NHS – services are locality dependent. It’s a trade-off to try to end some inequalities in outcome – centres of excellence exist, but it results in people being less tolerant of travel.
Professor Tim Doran: part of the issue is A&E, which provides 24-hour services but does not provide specialists. Which of the specialties should be prioritised? Further explanation is needed to provide context and narrative – qualitative research needs to be conducted.
Question: why not take one, fairly standard (typical) hospital, give them money to make this happen and use it as a prototype; gather as much data as possible both before and after and compare baseline with results afterwards. Start small and then scale up (and out).
Professor Tim Doran: hallelujah!
Rachel Meacock: there are 13 sites that have been labelled ‘early adopters’ – that’s why there’s an evaluation of the services in Salford . . . we are taking advantage of a natural experiment.
Professor Tim Doran: the medical profession is great at performing randomised controlled trials on drugs, etc., but not on itself. It would be much better if we could implement the interventions and then see – compare the hospital to itself, and see comparators. Take advantage of natural experiments.
Question: can we look at a hospital in isolation? Hospitals depend on other community/tertiary/GP support.
Question: very difficult to perform experiments – constraints due to patient size (i.e. of hospital).
Professor Tim Doran: we can account for cross-border effects and adjust to an extent.
Question: who would make the decision?
Professor Tim Doran: the DH would make the main decision to go 24/7; however, it would be up to the Royal College of Psychiatrists/the Royal College of Nursing/the British Medical Association.
General conversation followed – the health- and social-care devolution deal for Greater Manchester was mentioned; this would be a prime situation for the implementation of (some form of) 24/7 services. It was also mentioned that it would be interesting to see where the demand for services comes from – who are the consultants ‘on call’ most requested? (Though this may be presuming that it is consultants who would make a difference to the weekend/weekday mortality rates.) It would also be interesting to see where the demand comes from in terms of patient groups (i.e. patient demographic admitted who require certain services that are not available). There was also some discussion around the possibilities afforded by telehealth and technology.
Medicine for Members: second session – 14.00–16.00, 15 November 2015
24/7 patient and public involvement discussion group
-
Would it be acceptable to reduce services during the week in order to improve services at the weekend?
-
no × 4
-
no, that seems to be just shifting the problem
-
on the subject of hospital-based services being operational 24/7, yes for certain types of services and procedures but no for others
-
for me, my number one priority for attending hospital-based services outside normal hours would be being certain that whoever I was being seen by, particularly if it was not my usual doctor or nurse, knew my details and understood my unique requirements.
-
-
Would you be willing to pay more in tax in order to fund improved weekend and evening services?
-
yes
-
who would say the NHS would have the extra finance, cannot trust the government
-
yes, as long as it was clear that the increase was channelled into this
-
yes, but other taxes dedicated to an issue have failed to deliver.
-
-
Should hospital inpatients, be reviewed by the most senior doctor every day, including at weekends?
-
no
-
no, if it is not clinically required.
-
-
Should all NHS staff be expected to work routinely at evenings and weekends?
-
yes
-
expectation should not mean ‘forced’
-
no, needs to take account of preferences of staff involved
-
this has potential to affect staff morale, sickness rates and impact weekly provision of services.
-
-
Should the NHS make reducing the variations in patient outcomes by day and time of admission one of its top priorities?
-
not if the absolute difference is too small – costs do not seem to be justified by the potential benefit
-
do not know what current top priorities are.
-
-
Should routine NHS services (e.g. general practice and outpatients) be available 7 days a week?
-
yes, but not 24 hours per day
-
yes, maybe to start implementing now
-
yes, to provide services to match people’s lifestyle and commitments – but not 24 hour.
-
-
Should hospital-based services be operational 24/7?
-
eventually, yes
-
maybe 12/7 is a more realistic target
-
no too expensive, detrimental to current services
-
7 days yes, extended hours yes, 24 hours no.
-
-
What would your number one priority be when accessing hospital-based services outside standard working hours?
-
to have the best care and treatment
-
quality of care
-
quality and speed of treatment
-
education about how to use services
-
same as within standard hours: competent staff; efficient running of services (e.g. being seen on time); access to necessary support services.
-
-
Does it matter to you who you see, providing they have the right skills and training to accurately diagnose and/or treat your condition?
-
managing patient expectations, would be happy to be seen by any clinically competent professional
-
it would not matter to me whether or not I saw a doctor, nurse or nurse practitioner as long as the person had got the correct training, skills and understanding to see, assess and treat me appropriately and properly, so no it would not be a problem for me.
-
Appendix 3 Project Advisory Group membership
| Name | Position and organisation |
|---|---|
| David Buck | Health Policy Analyst, The King’s Fund |
| John Davies | Lay member |
| Sue Jacques | Chief Executive, Darlington Memorial Hospital |
| Roger Laitt | SRFT |
| Elizabeth Page | Lay member |
| Beth Shaw | Associate Director for Methodology, National Institute for Health and Clinical Excellence |
| Hamish Stedman | Chairperson, NHS Salford Clinical Commissioning Group |
| Frank Windmeijer | Professor of Health Economics, University of Bristol |
List of abbreviations
- 24/7
- 24 hours a day, 7 days a week
- A&E
- accident and emergency
- ASU
- acute stroke unit
- CI
- confidence interval
- DH
- Department of Health
- GP
- general practitioner
- HES
- Hospital Episode Statistics
- HSCIC
- Health and Social Care Information Centre
- ICD-10
- International Classification of Diseases, Tenth Edition
- IMD
- Index of Multiple Deprivation
- LSOA
- lower-layer super output area
- NICE
- National Institute for Health and Care Excellence
- ONS
- Office for National Statistics
- OR
- odds ratio
- QALY
- quality-adjusted life-year
- SHMI
- summary hospital-level mortality indicator
- SRFT
- Salford Royal NHS Foundation Trust
- SRFTM
- Salford Royal NHS Foundation Trust Membership
