Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/19/51. The contractual start date was in March 2015. The final report began editorial review in October 2016 and was accepted for publication in May 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Bee et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Foreword
Parent member, REfOCUS advisory panel
It’s simple, being the parent of a child with a long-term condition is tough. You watch your child struggle. You have very little to offer. It is their burden, and as a parent, you want to carry it. Doctors tell us what to do and what should happen. But it doesn’t really work that way. Families manage in unique ways. Sometimes, self-care is our only way to take control. We care for our kids, we look things up, we try alternative solutions and we do our best. Often, it’s not enough, and that can leave us frustrated. We are the ones awake at night, holding our children’s hands, giving them medication and contemplating their futures. Parents of children with long-term conditions want everything for their children. On good days, we are rational, we appreciate everything we are offered and we understand the limitations of a burdened health service. We understand our own role and we embrace our situation. During the tough times, we just want to carry the burden and we don’t know how. We know that ‘throwing money’ at the problem won’t solve it, but we are tired and sad, and we expect more. Using self-care support to reduce unnecessary health service use is important. Finding out which types of self-care support can reduce service use without compromising our own children’s health is crucial.
Terminology
Throughout this report, we use the term ‘parent’. This term is intended to cover a breadth of roles and has been chosen in preference to alternative and lengthier terms such as ‘parent/guardian’ or ‘adult caregiver’. We acknowledge that not all adults who are parenting children are biological parents.
Chapter 1 Background
Context
The global burden of disease is shifting to long-term conditions (LTCs)1 and there is increasing international emphasis on developing effective, efficient and person-centred models of service delivery to meet the needs of this client group. 2–4 Self-care support interventions constitute a central aspect of this agenda5–12 and are intended to empower individuals and enhance their self-care capacities and capabilities, while simultaneously reducing the fiscal burden on health-care systems. 13,14
The Department of Health defines a LTC as one ‘that cannot be cured but can be managed through medication and/or therapy’. 11 Underpinning the policy emphasis on self-care support for LTCs are a number of philosophical and patient-centred drivers. The shift in illness patterns from acute conditions to LTCs has coincided with a change in philosophy from ‘cure’ to ‘care’. Growing dissatisfaction with impersonal services, greater desire for personal control in health interactions and enhanced awareness of the potential impact of lifestyle on longevity and well-being have all complemented the drive to optimise health outcomes, without exacerbating rising health-care costs. 8,15 The English strategy for the NHS, the Five Year Forward View,3 emphasises the importance of health promotion, ill-health prevention and early intervention for sustainable health-care services, and mandates new models of care, including self-care, to facilitate efficiency savings alongside improved patient outcomes.
A global economic crisis means that substantial effort continues to be invested in improving the efficiency of health-care systems. Yet, despite self-care being advocated as a key way in which to increase efficiency, there remains uncertainty regarding the scale of the contribution that can be made. 16,17 Evidence for the success of self-care support has predominantly focused on individually centred outcomes of behavioural change and, until recently, ambiguity has surrounded the impact of these models on health service utilisation and costs. Initial reports of the effects of self-care support on health-care utilisation have not been consistently replicated across studies17–23 and the focus of interventions on enhancing intermediate outcomes such as self-efficacy has generated debate regarding the relevance of existing evidence to service commissioners. 24,25
A previous National Institute for Health Research-funded systematic review, REducing Care Utilisation thRough Self-management InterVEntions (RECURSIVE),26 successfully responded to this challenge by attempting to determine which models of self-care support were associated with significant reductions in health service utilisation without compromising the health outcomes of adults with LTCs. This review concluded that self-care support in adults is associated with small but significant improvements in quality of life (QoL) and, importantly, that only a minority of self-care support studies report reductions in health-care utilisation in conjunction with reductions in health status. However, patterns of health- and social-care utilisation in children and young people may be qualitatively and quantitatively very different from adults, and potential differences in the factors and systems influencing engagement in self-care support across the lifespan27–30 make it difficult to extrapolate these findings to younger populations. This review applies the approach employed by RECURSIVE26 to this different population. It builds on two previous National Institute for Health Research-funded reviews31,32 that investigated the effectiveness and acceptability of self-care support interventions for children and young people with long-term physical and mental health conditions, both updating and integrating them into a single data set.
Self-care and self-care support
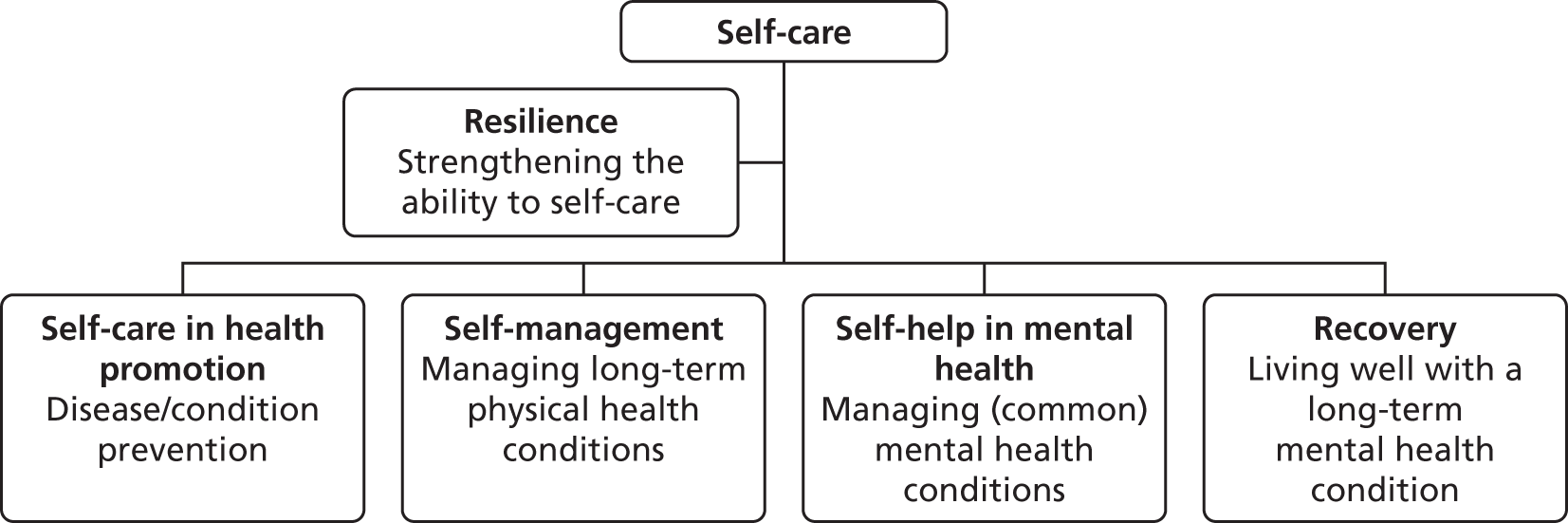
There is some conceptual blurring in the literature, with ‘self-care’ and ‘self-management’ often being used interchangeably in physical health, and terms such as ‘self-help’ and ‘recovery-centred care’ being preferred in mental health. 31–34 Resilience is often associated with self-care and is seen as a means of strengthening an individual’s capacity to self-care or as a buffer to the stresses associated with LTCs. 35 For the most part, however, self-care is regarded as the overarching term, with the alternative terms reflecting different variants of self-care or its influencing factors (Figure 1). A commonly accepted definition of self-care8 is:
The actions people take for themselves . . . to stay fit and maintain good physical and mental health; meet social and psychological needs; prevent illness or accidents; care for minor ailments and long-term conditions; and maintain health and wellbeing after an acute illness or discharge from hospital.
Department of Health. 8 © Crown copyright 2005. Contains public sector information licensed under the Open Government Licence v1.0
FIGURE 1.
Relationship of self-care concepts.
Whatever the terminology that is used, self-care ultimately refers to an approach in which control (and responsibility) shifts from the health-care professional (HCP) to the individual (or to the individual and their families/carers in the case of children and young people). This shift in control has implications for HCPs in that, within a philosophy of self-care, professionals work with patients, services users and their families as partners. 13
Partnership working introduces the notion of support for self-care (or self-care support). Support for self-care refers to HCPs (or other self-care support ‘agents’, such as a teachers or peers), supporting the individual and/or their families to take control of their health condition through developing their confidence, knowledge and skills. 8,36,37 This may occur via a variety of methods and techniques (e.g. information provision, psychoeducation and skills training) delivered in a variety of formats (e.g. online, face to face or by telephone) to individuals or groups. 8,32,33
In this study we have chosen to use the term self-care support rather than self-management support because this broader term incorporates self-management, self-help, recovery and resilience support. Furthermore, the term self-care support is more appropriate in describing the interventions examined.
Self-care support in children and young people
‘Whole-systems’ guidance advocates modernisation of the health-care system to improve the quality and efficiency of the services that children, young people and their families receive. 38 International childhood mortality data, combined with evidence of substantial variation in LTC management in this younger population, attest to how much additional effort is still required to achieve this goal. Compared with other nations, evidence points to a disproportionate number of UK children dying from non-communicable diseases and a rapid increase in the number of children and young people living with LTCs. 38,39 Fifteen per cent of children aged between 11 and 15 years experience long-term illness or disability and 10% have a mental health problem. 40–42 Over the last decade, child health policy has highlighted the vulnerability of these children and emphasised the need for health services to engage with them and support them effectively in self-care behaviours. 38,39,43–45
The case for early intervention in LTCs is compelling. Children diagnosed with LTCs face a lifetime of symptom management, and the extent to which they and their families negotiate this in childhood is likely to influence their longer-term health outcomes, life chances and subsequent patterns of health service utilisation. 31,39 Providing optimal, evidence-based support for self-care thus has the potential to make a significant and sustained contribution to NHS efficiency, as well as improving care quality and delivering direct benefits to patient health.
The role and effectiveness of different forms of self-care support in adults has been explored. An already extensive evidence base includes rigorous evaluations of the Expert Patients Programme and assistive technologies through the Whole System Demonstrator programme. To date, however, wholesale transfer of adult models to children and young people’s services has failed. 46,47 Comprehensive models of self-care48,49 argue that self-care cannot be divorced from the broader context in which it occurs. In children and young people, self-care knowledge, attitude and behaviour change50 are open to influence from health services, parents and peers. 51–53 Adolescence, in particular, is often characterised by increased risk-taking, lack of adherence to treatment regimens and a greater than normal deterioration in health status. 27,29,54–56 The importance of developing child- and young person-centred models that are developmentally appropriate and reflect the roles of parents and peers is increasingly being recognised. 31
Studies investigating the effectiveness of self-care support interventions designed for children and young people suggest positive effects on health status, QoL, self-efficacy, condition-related knowledge and coping. 31,32,57,58 For some interventions, acceptability has also been demonstrated. Qualitative studies reveal that children, young people and parents all value the opportunities that group-based self-care support provide to interact with others in similar situations to themselves. Interventions that use e-health methods to deliver self-care support have been judged to be feasible and applicable. 31,32
Yet, despite a developing body of evidence on the clinical effectiveness of self-care support interventions for children and young people, key knowledge gaps remain. There has been insufficient synthesis of quantitative data on health-care utilisation and the comparative effectiveness of different self-care support strategies. Previous reviews and meta-analyses have focused almost exclusively on intermediate or clinical outcomes, and rigorous evaluations of the cost-effectiveness of self-care interventions and their impact on health-care utilisation are lacking. Moreover, existing reviews do not explore associations between content and outcomes; they typically treat outcomes and costs as separate concepts and rarely have an explicit focus on the joint effects of outcomes and costs. This makes it difficult to identify technically efficient interventions capable of reducing unnecessary health-care use [such as avoidable emergency department (ED) visits and hospital admissions] without potentially compromising children and young people’s health.
Assessing the efficiency of self-care support
Commensurate with trends in the adult population, long-term physical and mental health conditions in children and young people are increasing. 59–61 Self-care support offers these young people and their families the opportunity to work collaboratively with professionals, actively participate in health-care decision-making and ensure that care is personalised to their needs. An implicit assumption underlying the use of self-care support is that it can successfully shift LTC management from health services to the patient, avoid unnecessary crises and prevent more extensive health services utilisation by managing patients’ problems more effectively. This has the potential to improving patient outcomes while simultaneously reducing resource utilisation and costs.
In health care, resource utilisation typically refers to as the number and type of health-care resources or services that are used, for example health professionals’ time, medicines, diagnostic tests/investigations and treatment appointments. Each aspect of resource utilisation incurs a cost. Rigorous and comprehensive evaluation of the effects of self-care support for children and young people thus demands concurrent evaluation of patient outcomes and health-care costs. As shown in Figure 2, plotting these effects against each other can identify models of self-care that are able to reduce costs without comprising outcomes for children and young people (quadrant A) and distinguish these from models that reduce both outcomes and costs (quadrant B), or improve outcomes at increased cost (quadrant C).
FIGURE 2.
Example matrix showing effects on utilisation and outcomes. Adapted from Panagioti et al. 26 Contains information licensed under the Non-Commercial Government Licence v2.0.
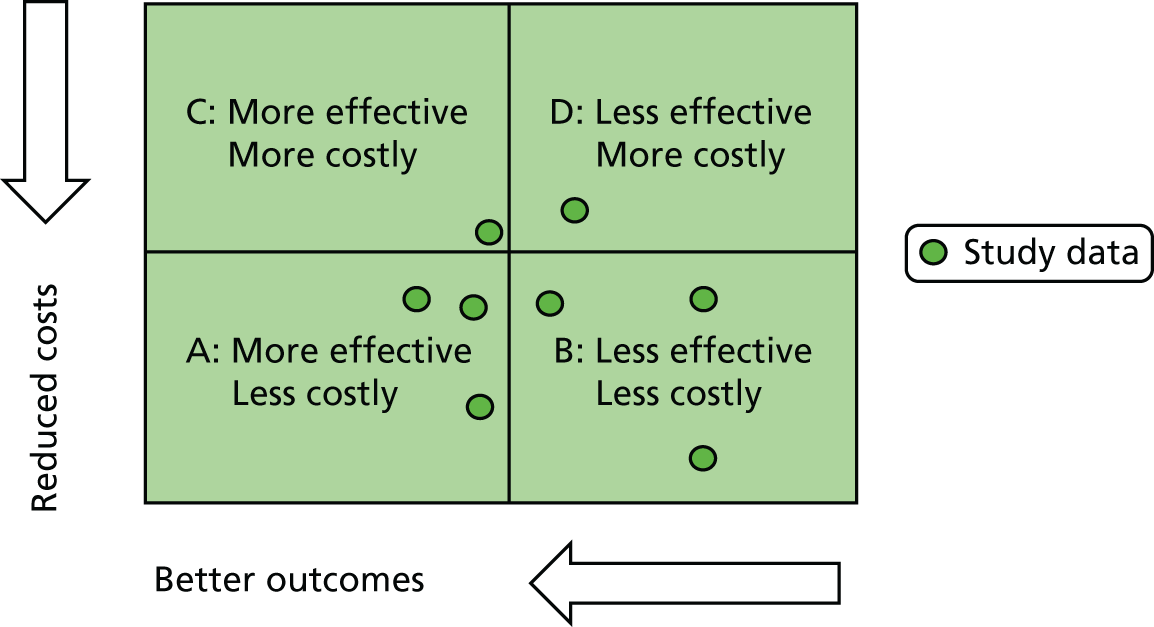
Systematic reviews and meta-analyses bear witness to the number of trials of self-care support for children and young people that have been conducted. Although not always designed to enable a full economic analysis, many present sufficient data to enable the intervention to be placed on the cost-effectiveness plane. Systematic synthesis of these data is required to inform evidence-based decision-making and the commissioning of high-quality, technically efficient services.
Review aim
The review reported here aimed to take account of health-care utilisation and costs in conjunction with health outcomes to provide evidence-based guidance on the provision of cost-effective self-care support for children and young people with long-term physical and mental health conditions.
Our objectives were to:
-
identify and integrate into one data set, eligible data from existing reviews on the clinical effectiveness and cost-effectiveness of self-care support interventions for children and young people with long-term physical and mental health conditions
-
update and expand existing search strategies to increase their sensitivity to a broader range of measures of health-care utilisation in children and young people
-
conduct a quantitative systematic review of the available evidence to identify those models of self-care support for children and young people that are associated with reductions in health services utilisation and cost, without compromising health outcomes
-
provide evidence-based recommendations for service commissioners regarding the optimal delivery models for self-care support interventions
-
provide key recommendations for research funding bodies on future research priorities.
Chapter 2 describes the review methods.
Chapter 2 Review methods
The review reported here was a quantitative systematic review that sought to answer three key questions:
-
What models of self-care support are associated with significant reductions in health-care utilisation without compromising health outcomes for children and young people with LTCs?
-
What are the key recommendations for service commissioners regarding the delivery of self-care support for LTCs in children and young people?
-
What are the priorities for research funding bodies regarding self-care support in children and young people?
Our review was conducted in line with current systematic review guidance. 62,63
Study eligibility criteria
Studies were assessed for inclusion in the review according to a standard set of eligibility criteria. These criteria are summarised in Box 1 and described in full below.
Children and young people aged 0–18 years with a long-term physical health condition evidenced through clinical diagnosis, contact with health services or scores above clinical cut-off points on validated screening measures.
InterventionSelf-care support delivered in a health, social care or educational setting.
ComparatorUsual care, including more intensive usual care (e.g. clinic or inpatient management).
OutcomesGeneric, HRQoL, or disease-specific symptom measures or events and health service utilisation (i.e. hospital visits and admissions, additional service use and costs).
DesignRandomised trials, non-randomised trials, CBAs, ITS designs.
Exclusion criteriaAt-risk populations or preventative interventions; self-care interventions lacking active support (e.g. pure self-care, passive instruction); intermediate health outcomes (e.g. self-efficacy, HbA1C levels, FEV recordings) and health outcomes of adult caregivers.
CBA, controlled before-and-after study; FEV, forced expiratory volume; HbA1c, glycated haemoglobin; HRQoL, health-related quality of life; ITS, interrupted time series.
Population
We defined children and young people as individuals aged < 18 years. Although the transition to adult services is not always immediate and key elements of development may continue beyond 18 years of age, this cut-off point aligned with our earlier reviews on the clinical effectiveness of self-care support interventions for children and young people. In accordance with the inclusion criteria of our previous reviews, we included studies with participants aged up to 25 years as long as the mean age of the sample, and/or the majority of participants, remained under the age of 18 years.
We restricted our review to LTCs. To be eligible for inclusion in the review, participants were required to have a diagnosis of a LTC, defined through clinical assessment, contact with health services or symptom scores above clinical cut-off points on validated screening instruments. We excluded preventative studies that looked at a population at ‘high risk’ of developing a LTC.
There is no definitive list of LTCs and hence we adopted the Department of Health’s generic definition of a LTC as one ‘that cannot be cured but can be managed through medication and/or therapy’. 11 We included studies recruiting patients with a mix of LTCs.
Both mental and physical health conditions were eligible for inclusion in the review. This included common conditions such as diabetes, asthma, coronary heart disease, depression, anxiety and psychosis. Comprehensive lists of eligible conditions are provided in Box 2. In line with the views of our patient and public involvement (PPI) advisory panel, we excluded autism spectrum disorder, intellectual disabilities, substance misuse (unless comorbid with another LTC) and cancer in long-term recovery or remission, as these conditions were deemed to fall outside our working definition of a long-term physical or mental health condition.
Asthma, diabetes, congenital heart disease, stroke, musculoskeletal disorders, epilepsy, chronic fatigue syndrome, sickle cell disease, cleft palate, cystic fibrosis, chronic skin conditions, inflammatory bowel disease, thalassaemia, HIV infection/AIDS.
Mental healthConduct disorder, ADHD, anxiety (including panic), phobia, school refusal/phobia, depression, OCD, traumatic stress (PTSD), self-harm, psychosis including schizophrenia, eating disorders (including anorexia and bulimia).
Ineligible for the reviewAutism spectrum disorder, intellectual disabilities, substance misuse, cancer in long-term recovery or remission, obesity.
ADHD, attention deficit hyperactivity disorder; AIDS, acquired immunodeficiency syndrome; HIV, human immunodeficiency virus; OCD, obsessive–compulsive disorder; PTSD, post-traumatic stress disorder.
Interventions
Self-care can be defined in different ways according to who engages in the self-care behaviour (e.g. individual, family, community) and the intervention context (e.g. health promotion, illness prevention, illness impact limitation or restoration of health). To meet the definition of self-care support, an intervention needs to include an agent other than the self, typically a health professional, peer group, voluntary sector representative or information technology platform.
The goal of self-care support has previously been defined as the enablement of patients to perform three discrete sets of tasks: medical management of their condition (e.g. taking medication); carrying out normal roles and activities; and managing the emotional impact of their condition. 64 For the purposes of our review, we defined a self-care support intervention as:
. . . any intervention primarily designed to develop the abilities of children and young people (and/or their adult carers) to undertake management of their long-term health condition through education, training and support to develop their knowledge, skills or psychological and social resources.
Example categories of self-care support of relevance to this review are outlined in Box 3. We included all formats and delivery methods for self-care support (e.g. group or individual, face to face or remote, professional or peer led). Interventions delivered in health, social care, educational or community settings were included. Interventions that targeted the child or young person, or their adult caregiver, were included.
Education or training, for example disease-specific education or behaviour change interventions for CYP and/or their adult caregivers. Education or training may be delivered online, paper based, face to face or through audio/visual technologies.
Decision support, for example support to help CYP and their families to make decisions about their treatment options.
Monitoring and feedback, for example real-time telephone or computer-based monitoring methods, with active monitoring from professionals, feedback response and potential access to a wider care team.
Environmental adaptations, for example supported living equipment or home modification.
Collaborative care planning, for example discussion and negotiation between professionals and CYP and/or their adult caregivers regarding illness and care management and goals.
Psychological support, for example face-to-face or online peer support, or formal counselling/therapy from a health professional.
CYP, children and young people.
Written action plans, developed in collaboration with children and young people or their families, were eligible for the review, but were excluded if there was no evidence of self-care discussion or negotiation. Self-care support, by definition, is designed to offer a more participatory approach to health care, with patients making a critical contribution to achieving health gain and making decisions to ensure that their care is personalised to their needs. We excluded all interventions where the target of the intervention was not actively engaged and/or remained a passive recipient of knowledge or instructions.
We excluded self-care undertaken without any input, guidance or facilitation by services. Although self-care can be, and often is, undertaken without service support, it is rarely the subject of intervention studies. We excluded studies where the effects of self-care support could not be distinguished from broader interventions for LTCs. We excluded studies evaluating service development or quality improvement initiatives in which self-care support was not the predominant component of the intervention.
Comparators
We included studies in which a self-care support intervention was additional to usual care and compared against usual care alone, or in which a self-care support intervention was compared against a more intensive usual care intervention (e.g. home- vs. clinic-based monitoring). We excluded studies in which two versions of self-care support were compared and the two interventions were of comparable intensity and content, because such comparisons did not allow for an assessment of the impact of self-care support per se.
Outcomes
To meet our research objectives, we required evidence of effectiveness of validated self-care support to reduce health-care utilisation without compromising children and young people’s outcomes. We restricted our analysis to studies of self-care support that reported quantitative data on patient outcomes and health-care utilisation, as these were the only studies that could answer our brief.
Eligible patient outcomes included standardised measures of health-related or generic QoL or disease-specific symptom measures or events. We excluded intermediate outcomes and measures of psychological or clinical variables that did not provide an assessment of subjective health status or QoL [e.g. self-care behaviours, self-efficacy, glycated haemoglobin (HbA1C) levels or forced expiratory volume recordings]. In adult populations, such variables are known to be unreliable indicators of health-related quality of life (HRQoL). 65 We extracted data on the health outcomes of the child/young person and excluded the health outcomes of adult caregivers.
Eligible outcomes for health-care utilisation comprised data on hospital visits and admissions, emergency care, primary care visits, other scheduled or unscheduled health-care use, patient costs and total costs. Our primary foci were comprehensive measures of health service costs (i.e. summed totals of multiple sources of cost) and/or major cost drivers (i.e. hospital admissions). Other, more minor, costs (such as medication use) were identified but not formally analysed. The rationale for this is discussed further in Data preparation and analysis.
Design
We included randomised controlled trials (RCTs), non-randomised controlled trials (nRCTs), controlled before-and-after studies (CBAs) and interrupted time series designs, as defined according to the Effective Practice and Organisation of Care (EPOC) criteria63 (Box 4). UK and non-UK studies were included. Translation of non-English-language studies was undertaken.
Investigators allocate participants to the different groups that are being compared using a method that is random. Randomisation ensures that participants in each comparison group should differ only in their exposure to the intervention. Randomisation can occur at an individual or cluster (site/region) level.
Non-randomised controlled trialsInvestigators allocate participants to the different groups that are being compared using a method that is not random.
Controlled before-and-after studiesDecisions about allocation to the different comparison groups are not made by the investigators. Outcomes of interest are measured in both the intervention and control groups before the intervention is introduced and again after the intervention has been introduced.
Interrupted time series designProvides a method of measuring the effect of an intervention when randomisation or identification of a control group are impractical. Multiple data points are collected before and after the intervention and the intervention effect is measured against the pre-intervention trend.
Search methods
In accordance with the review protocol, our search strategies included electronic database searches, reference list searches, targeted author searches and forward citation searching.
Electronic databases
We began the process of identifying eligible studies by checking published reviews, including those previously undertaken by the research team. 26,31,32 We complemented our searches of existing reviews with a primary search of multiple electronic databases, conducted in March 2015.
We updated and expanded our existing search strategies to ensure that they were sensitive to a broad range of health-care utilisation beyond formal cost-effectiveness analyses. Search terms relating to the key concepts of the review were identified by scanning the background literature and browsing the MEDLINE medical subject heading thesaurus, and through discussion with collaborating colleagues at the University of York’s Centre for Reviews and Dissemination.
A search strategy was developed in MEDLINE, using an iterative approach tested against a set of 15 studies known to be relevant to our review. This MEDLINE search strategy was adapted to run on all other databases designated in our protocol.
Electronic searches were undertaken on the following health and allied health databases:
-
MEDLINE (accessed 18 March 2015 via OvidSP; www.ovissp.ovid.com)
-
EMBASE (accessed 18 March 2015 via OvidSP; www.ovissp.ovid.com)
-
PsycINFO (accessed 17 March 2015 via OvidSP; www.ovissp.ovid.com)
-
Cumulative Index to Nursing and Allied Health Literature (CINAHL; accessed 19 March 2015 via EBSCOhost; www.search.ebscohost.com)
-
ISI Web of Science, including Social Sciences Citation Index (SSCI) and Science Citation Index Expanded (accessed 19 March 2015 via Web of Science; www.wos.mimas.ac.uk)
-
NHS Economic Evaluation Database (NHS EED) (accessed 18 March 2015 via Wiley Online Library)
-
The Cochrane Library, including Cochrane Database of Systematic Reviews (CDSR), Database of Abstracts of Reviews of Effects (DARE) and Cochrane Central Register of Controlled Trials (CENTRAL) (accessed 18 March 2015 via Wiley Online Library)
-
Health Technology Assessment database (accessed 18 March 2015 via Wiley Online Library)
-
Paediatric Economic Database Evaluation (PEDE) (accessed 31 March 2015 via http://pede.ccb.sickkids.ca/pede/index.jsp)
-
the IDEAS database of economic and finance research (accessed 31 March 2015 via http://ideas.repec.org).
All databases were searched from inception. No language or design restrictions were applied. Full details of the search strategies, search terms and the specific dates of individual searches are reported in Appendix 1.
Additional search strategies included scanning the bibliographies of all relevant retrieved articles, targeted author searches (for additional publications and/or unpublished data identified in conference abstracts) and forward citation searching. No studies were identified that had not been retrieved by other means.
Changes to the search protocol
All searches were conducted as specified in the original review protocol with the exception of the Health Economic Evaluations Database (HEED). HEED ceased publication prior to study commencement and was not searched as part of the final review. Coverage of the relevant economic evidence base was ensured through searches of the NHS EED, the Health Technology Assessment database, the PEDE and the IDEAS database of economic and finance research. The potential impact of this protocol change was judged to be minimal.
Study screening and selection
With the exception of the IDEAS database, all records retrieved from the electronic searches were imported into a bibliographic referencing software program (EndNote X5; Thomson Reuters, CA, USA) and duplicate references identified and removed. Review screening and eligibility judgements were managed in Covidence systematic review software (Veritas Health Innovation, Melbourne, VIC, Australia). Pairs of reviewers independently screened all titles and abstracts for eligibility using prespecified inclusion criteria described below. Additional economic abstracts located through IDEAS were managed as hard-copy records and independently screened for eligibility by two reviewers using identical eligibility criteria.
To be eligible for full-text screening, search records (titles and abstracts) had to fulfil three initial inclusion criteria:
-
RCT, nRCT or eligible quasi-experimental design
-
children or young people with a LTC as participants/possible participants
-
a potential self-care support intervention.
Where both reviewers agreed that the studies did not meet these criteria, studies were excluded from the review. When both reviewers agreed on inclusion, or when there was conflict, full-text articles were retrieved for review. All studies without abstracts were retained for full-text screening unless they could be reliably excluded on the basis of their title alone.
Two reviewers independently assessed all full-text articles against the review’s full list of eligibility criteria (see Box 1). Any remaining disagreements were resolved by third party discussion.
Data extraction and quality assessment
Data extraction used prespecified data extraction sheets designed and piloted specifically for this study. We extracted data on the study author, year of publication, study design and setting, and relevant characteristics of the population, intervention(s), comparison(s) and outcomes reported. We separately extracted data on the methods and economic perspective used in the subset of studies reporting formal cost-effectiveness, cost–utility or cost–benefit analyses. Where available, we extracted published data on the ‘reach’ of self-care interventions, defined according to Reach, Effectiveness, Adoption, Implementation, Maintenance (RE-AIM) guidance. 66 Intervention reach was defined in terms of (1) the proportion of eligible patients who did not take part in the study; and (2) the presence or absence of LTCs additional to the index condition in the study exclusion criteria.
Data extraction for study context was undertaken by one reviewer and independently verified by a second reviewer. Study outcomes were extracted independently by two reviewers using separate outcome extraction sheets. Discrepancies in the extracted data were resolved by referral to the original studies and, where necessary, arbitration by a third reviewer.
Where multiple outcomes were reported by the same study, we used a decision rule to determine, in advance, the most relevant outcome for meta-analysis. Our priority was on children and young people’s own subjective assessment of QoL. Where this was not reported, we extracted, in order of priority, parent-reported QoL, patient-reported symptoms or parent-reported symptoms. If two or more outcomes of equal priority were available, we selected the one with most complete reporting and prioritised continuous over dichotomous data.
When there were multiple publications for the same study, data were extracted from the most recent and complete publication. In cases where the duplicate publications reported additional relevant data, these data were also extracted.
Methodological quality appraisal
Methodological quality appraisals were undertaken by one reviewer and independently verified by a second reviewer. Studies were assessed for methodological quality using the Cochrane Collaboration Risk of Bias Assessment Tool for RCTs62 or the Cochrane guidance for non-randomised designs. 62 Economic studies were assessed using a critical appraisal checklist for economic evaluations. This checklist was based on Drummond’s checklist for assessing economic evaluations67 and was adapted to capture more fully the quality of economic evaluations in self-care support interventions (see Appendix 2).
Quality ratings for randomised studies were based on a dichotomous measure of allocation concealment (i.e. adequate or inadequate/unclear). Allocation concealment is the aspect of trial quality most consistently associated with treatment effect. 68,69 Other indicators may be less relevant in trials of behavioural interventions where participant, personnel and outcome blinding are often difficult to achieve.
Data preparation and analysis
The aim of our review was to establish which models of self-care support (if any) were associated with significant reductions in health service utilisation without compromising outcomes for children and young people with long-term physical or mental health conditions. To answer this question, studies needed to quantify the effect of an intervention on both costs and health outcomes.
Accurate placement of studies on a cost-effectiveness plane requires detailed data beyond a simple text description of statistical significance. We sought data that would enable the calculation of standardised effect sizes (ESs) for both health outcomes and costs. ES calculations are possible when primary research studies report appropriate statistics which can be translated into a common metric, such as a standardised mean difference. 70
We selected outcomes closest to a 12-month follow-up. Our choice of follow-up point was, to an extent, arbitrary, balancing analysis of longer-term effects with the consistency of data between studies. Continuous measures were translated to a standardised mean difference [the mean of the intervention group minus the mean of the control group, divided by the pooled standard deviation (SD)]. Outcomes were coded so that negative ESs always represented improvements for the intervention compared with control. Outcomes reported as dichotomous variables were translated to a standardised mean difference using the logit transformation.
We assumed a 70% follow-up from the number of participants randomised at baseline, where sample size could not be ascertained. This was an arbitrary imputation that sought to maximise the inclusion of data, using a value below that usually considered as an indicator of primary study quality (80%).
Where single parameters were missing (e.g. a SD), we imputed these where there was other comparable data in the review. We excluded studies that lacked data and where there were no other studies in the review to allow meaningful imputation. Calculation of ESs was not possible for all outcomes.
Measures of health-care utilisation (e.g. length of hospital stays) and costs can often demonstrate significant skew because many patients report low costs, but a small proportion can have disproportionately high levels of use. In line with other published reviews,26,71 we identified all outcomes where the SD multiplied by two was greater than the mean, as in these cases it is argued that the mean is not a good indicator of the centre of the distribution. 72
When studies reported multiple comparisons that were eligible for the same meta-analysis (e.g. two types of intervention vs. control), both comparisons were included, but sample sizes in the control group were halved to avoid ‘double counting’ of participants in the control group and thus inappropriate precision in the relevant meta-analysis. This method assumed independent ESs. We conducted the sample size modification in all cases where a study included two or more intervention groups compared with control and where more than one of those intervention groups was included in the same meta-analysis.
A minority of self-care support trials (n = 10) used cluster allocation to reduce bias associated with contamination. We identified cluster trials and adjusted the effective sample size (and thus the precision) of these comparisons using methods recommended by the EPOC group of the Cochrane Collaboration. 63 We assumed an intraclass correlation of 0.02.
Where sufficient data were reported for particular comparisons, and when populations and interventions were considered sufficiently homogeneous, we pooled effects. We pooled QoL and subjective symptom measures and did not explore differences in the effects of self-care support observed with different outcome measures.
Owing to marked heterogeneity in the interventions and outcomes, meta-analyses used random-effects modelling, with the I2 statistic to estimate heterogeneity. 73 We labelled ESs as minimal (an ES of < 0.2), small (an ES of 0.2 < 0.5), moderate (an ES of 0.5 < 0.8) or large (an ES of ≥ 0.8) and levels of heterogeneity as ‘low’ (I2 statistic 1–25%), ‘moderate’ (I2 statistic 26–74%) or ‘high’ (I2 statistic ≥ 75%). These categorisations are arbitrary distinctions. However, caution should be applied in the interpretation of pooled effects in meta-analyses where heterogeneity is ‘high’.
Small study bias
Funnel plots74 using standard errors75 and associated regression tests were used to explore small-study bias where sufficient data were available. The purpose of a funnel plot is to map standardised ESs from individual studies against their standard error (i.e. the underlying precision of the observed effect). A funnel plot is based on the premise that precision in an ES estimate will increase as sample size increases. Effect estimates from smaller studies with larger standard errors should, therefore, scatter more widely at the bottom of the plot. Larger studies with smaller standard error should display a narrower spread. Bias is suggested by an asymmetrical plot and statistical testing of a potential relationship between treatment effect and precision. An absence of smaller studies without statistically significant effects is an indicator of potential publication bias. In this situation, the effect calculated in a meta-analysis may overestimate the intervention effect.
Changes to the analytical protocol
Our analysis was designed to consider the ability of models of self-care to reduce health-care costs without compromising patient outcomes. Our primary analysis was on total costs. Our protocol stipulated that our secondary analyses would, where data allowed, consider all other major types of resource use and cost. This included inpatient, outpatient, primary care, community care and patient out-of-pocket expenditures.
Meaningful analysis requires that sufficient, comparable data are reported across the primary studies. Lack of consistent measurement and ambiguity in some of the outcomes that were reported prevented accurate demarcation of primary, secondary and community health-care costs. More usually, outcome data were presented as urgent (non-scheduled) compared with scheduled service use. Definitions of scheduled resource use varied according to illness type and context.
Our PPI advisory panel identified hospital admissions, ED visits and patient and families’ out-of-pocket expenses as the three outcomes that they would like to be prioritised in our review. An insufficient number of studies reported out-of-pocket expenses. Our secondary analyses thus focused on hospital admissions and ED use.
Hospital use represents a significant driver of total costs in most health-care systems. However, focusing on a single source of utilisation leaves the analysis vulnerable to cost shifting, where any benefits found in terms of reduced hospital use may mask increased costs elsewhere in the health-care system (such as in community care). Our primary analysis thus remained focused on total costs.
Data presentation
We present the results of included studies according to a permutation plot (see Chapter 1, Figure 2). The permutation plot presents data from all studies reporting both outcomes (i.e. QoL and total costs, QoL and hospital admissions, and QoL and emergency care). Each plot shows the pattern of results at the level of the individual study and gives a visual impression of the distribution of studies across the cost-effectiveness plane. The plot distinguishes between studies in the appropriate quadrant (i.e. those that reduce costs without compromising outcomes), from those in problematic quadrants (i.e. those that reduce costs but also compromise outcomes, or those that compromise both outcomes and costs).
We analysed data for included studies as a whole and then conducted meaningful subgroup analyses. A priori subgroup analyses were conducted for level of evidence quality (defined as the adequacy of allocation concealment) and the age of the children and young people. Subgroup analyses for age classified studies according to whether they delivered self-care support to children (aged < 13 years), adolescents (aged ≥ 13 years) or a mixed child–adolescent age group.
Additional subgroup analyses were conducted for the type of LTC and the setting and type of self-care support intervention that was evaluated (i.e. intervention target, format, delivery method and intensity). The subgroups that we used for these preplanned analyses were determined post hoc, based on the nature and distribution of the evidence.
Post hoc classification by long-term condition
We grouped different LTCs post hoc into four conceptually and clinically relevant categories. These categories were asthma, other (non-asthma) physical health conditions, behavioural disorders and mental health.
Our a priori intention was to also aggregate data across subtypes or ‘clusters’ of conditions, based on a similar typology to that developed by the Practical systematic RevIew of Self-Management Support for long-term conditions (PRISMS) study for adults with LTCs. 26 We did not aggregate our data in this way, as all but four studies focusing on behavioural disorders fell into the same condition cluster (cluster 1: LTCs with marked variability in symptoms over time).
Post hoc classification by intervention type
Existing typologies of self-care support for children and young people with LTCs highlight the importance of considering different aspects and characteristics of the intervention, including its target, location, facilitation and delivery methods. 31
We conducted subgroup analyses based on intervention target (child and/or young person, adult or both), format (individual, group or mixed) and delivery method (face to face, remote or mixed model). We also conducted subgroup analyses on intervention setting, defined as inpatient, outpatient/clinic, school or community, home or mixed location.
In line with our previous review of self-care support for adults with LTCs,26 we included interventions across the spectrum of care and distinguished post hoc between the different intensities and types of self-care support that were provided.
We used a similar approach to classify intervention intensity as we used in our previous review, with post hoc amendments to accommodate the level and type of intervention descriptions provided in our primary studies. Our final classification system was informed and approved by our PPI advisory panels and distinguished between four different categories of self-care support:
-
‘Pure’ self-care support for interventions providing self-care support through a stand-alone resource (e.g. interactive mobile application or educational online program).
-
Facilitated self-care support for interventions providing fewer than four sessions or < 2 hours of face-to-face or remote self-care support. Support is provided by a designated self-care agent (e.g. health professional or peer) and usually targets a single group (e.g. children or parents). The support provided will often be (but is not limited to) self-care education, feedback or care plan review.
-
Intensively facilitated self-care support for interventions providing regular and repeated contact exceeding more than four sessions or 2 hours’ support in total. Support is provided by a designated self-care agent health professional or peer and often targets multiple groups (e.g. children and parents or children and teachers). The support provided will often be multifaceted and may include some co-ordination of a patient’s primary or standard care.
-
Case management for interventions providing more than four sessions or 2 hours of additional support from a designated agent, with additional support from a multidisciplinary team and explicit referrals or care co-ordination as part of the intervention protocol.
Two authors independently assessed the type, and content, of each self-care support intervention. Disagreements were identified and resolved via team discussion.
Changes to the review protocol
The review protocol is available as part of the PROSPERO database: A Rapid Evidence synthesis of Outcomes and Care Utilisation following Self-care support for children and adolescents with long-term conditions (REfOCUS): reducing care utilisation without compromising health outcomes (registration number CRD42014015452). We have been explicit about any deviations from the published protocol in the relevant sections of this report. Deviations of the review from the protocol published in PROSPERO are summarised in Box 5.
We will search specialist economic databases including the NHS EED, the HEED, the Health Technology Assessment database, the PEDE and the IDEAS database of economic and finance research.
-
The HEED was not searched as part of the final review.
We will structure our synthesis according to the LTCs prioritised by previous reviews (i.e. diabetes, asthma, cystic fibrosis, anxiety and depression). We will include other LTCs in our synthesis where we identify eligible economic evidence (e.g. epilepsy, juvenile idiopathic arthritis, ADHD, eating disorders and self-harm).
-
We structured our synthesis according to the availability of data. We grouped studies in a way that was conceptually and clinically relevant.
Our primary analysis will be on total costs. We will repeat this analysis for all major types of costs (e.g. inpatients, outpatients, primary care, community care and out-of-pocket expenditure).
-
As stipulated, our primary analysis was on total costs. We only conducted secondary analyses where data allowed and where the costs were sufficiently similar to make meta-analyses appropriate and interpretable. Our secondary analysis focused on hospital admissions and urgent care.
We will extract data to assist in the quality assessment of primary studies according to the Cochrane risk-of-bias tool criteria for RCT and nRCT designs.
-
In line with other published reviews, we restricted our assessment of risk of bias to allocation concealment, independently assessed by two members of the research team.
We intend to aggregate data at several different levels (i.e. within a condition, across subtypes or ‘clusters’ of conditions and across all conditions).
-
We aggregated data across all conditions and within four post hoc categories of LTCs. Data did not allow for meaningful aggregation at the level of condition clusters.
We will distinguish between groups of interventions differing in content (e.g. psychological support, skills training, health monitoring and feedback).
-
We classified interventions post hoc into four broad categories of intervention types. Insufficient data were available to enable meaningful analysis at the level that was originally specified.
ADHD, attention deficit hyperactivity disorder.
Patient and public involvement
This review was conducted in collaboration with two PPI advisory panels: an adult panel composed of eight parents and health professionals working with children and young people with LTCs; and a children and young people’s panel composed of 12 young people living with a long-term physical or mental health condition. Panel members were recruited from local NHS trusts, children and young people’s physical and mental health services, user and carer organisations (e.g. YoungMinds, Asthma UK, Diabetes UK), allied organisations (e.g. the Mental Health Research Network’s Young Person’s Mental Health Advisory Group) and existing networks within the research team. All lay members were reimbursed for their time and travel expenses.
Four panel meetings were held for 1–2 hours on each occasion throughout the course of the review. Meetings took place on university premises and were attended by members of the research team. Two representatives from the children and young people’s panel attended the adult PPI panel meetings to provide a link between the two groups and ensure coherence and continuity in topic discussions.
The initial meeting for both panels was focused on establishing relationships, orientating panel members to the project, and developing and agreeing terms of reference for participation. The second meeting was led by the children and young people and was, at their own request, focused on developing a patient-centred logo and tagline for the project. The final logo and tagline, ‘Our Services, My Health’ were selected by PPI consensus and feature on all project resources and dissemination materials.
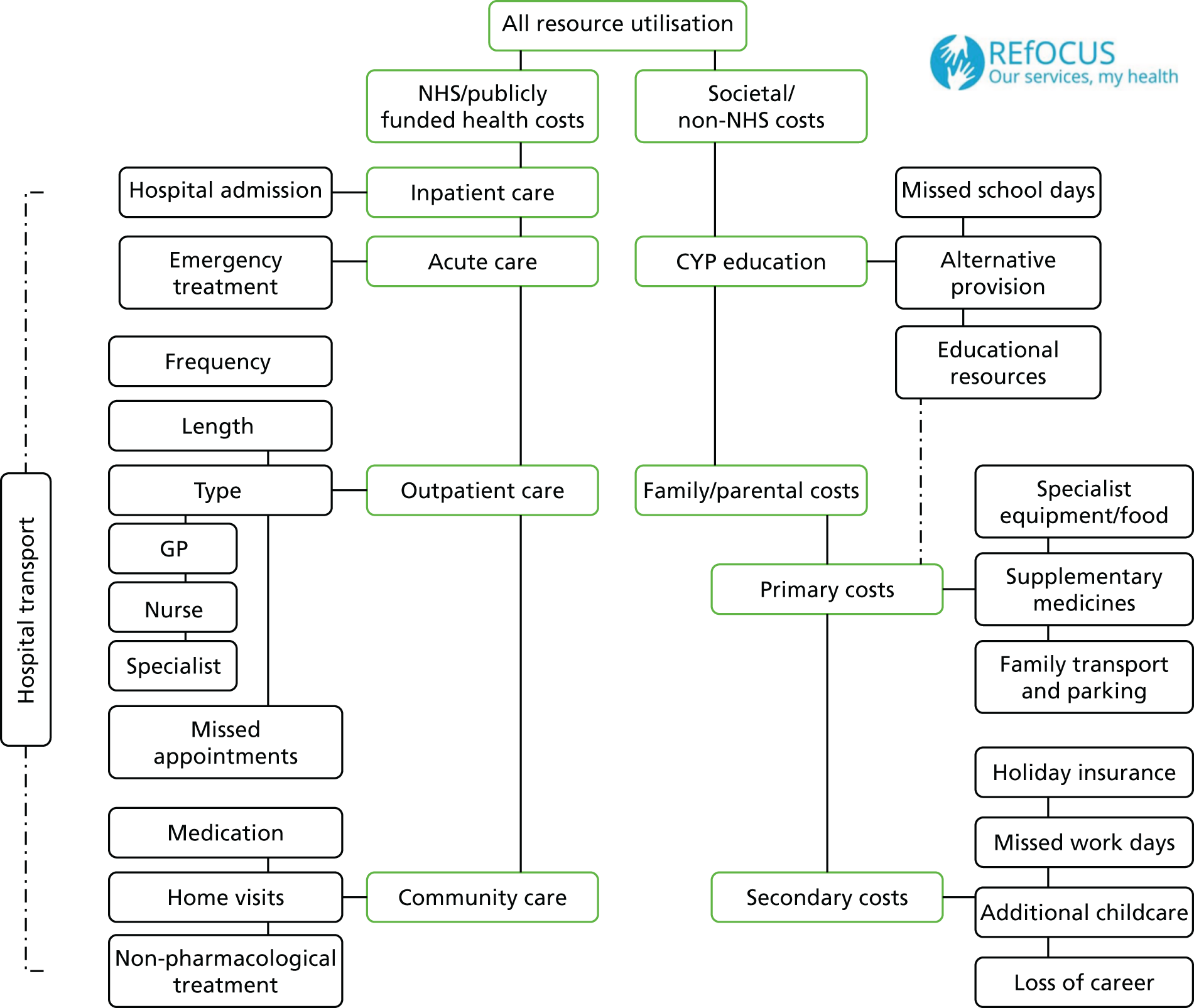
The third meeting was dedicated to developing the frameworks and priorities for the review. This process included PPI approval of the taxonomies used to classify self-care support interventions and the clusters of LTCs that fed through into the analyses. In collaboration with members of the research team, PPI panel members participated in an interactive discussion designed to explore lay interpretations of a systematic review simultaneously assessing patient outcomes and health-care costs. PPI panel members developed a framework depicting the impact of living with a LTC from the perspective of children, young people and their families (Figure 3). This was used to select meaningful patient-centred outcomes for extraction and analysis in the review and may be used to contextualise the remit and scope of this report within a broader sphere of the potential costs incurred by LTC management. This issue is discussed further in Chapter 4.
FIGURE 3.
Key determinants of resource utilisation in children and young people with long-term physical and mental health conditions: a PPI perspective. CYP, children and young people; GP, general practitioner.
At the fourth and final meeting, advisory panel members discussed the findings of the review and interpreted their meaning for services and for children, young people and their families. Panel members assisted in formulating and prioritising evidence-based recommendations for service commissioners and research funding bodies, ensuring that these remained relevant to stakeholder priorities. All recommendations arising from this review are detailed in Chapter 4.
Chapter 3 presents the review’s results.
Chapter 3 Results
Overview of the evidence base
We screened 36,493 unique records for eligibility; 127 papers reporting on 97 studies were included. 20,21,76–200 Figure 4 presents the flow of studies through the review. A full list of the included studies and their study reference details is provided in Appendix 3. Excluded studies and the reasons for their exclusion are provided in Appendix 4.
FIGURE 4.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram: flow of studies through the review. CYP, children and young people.
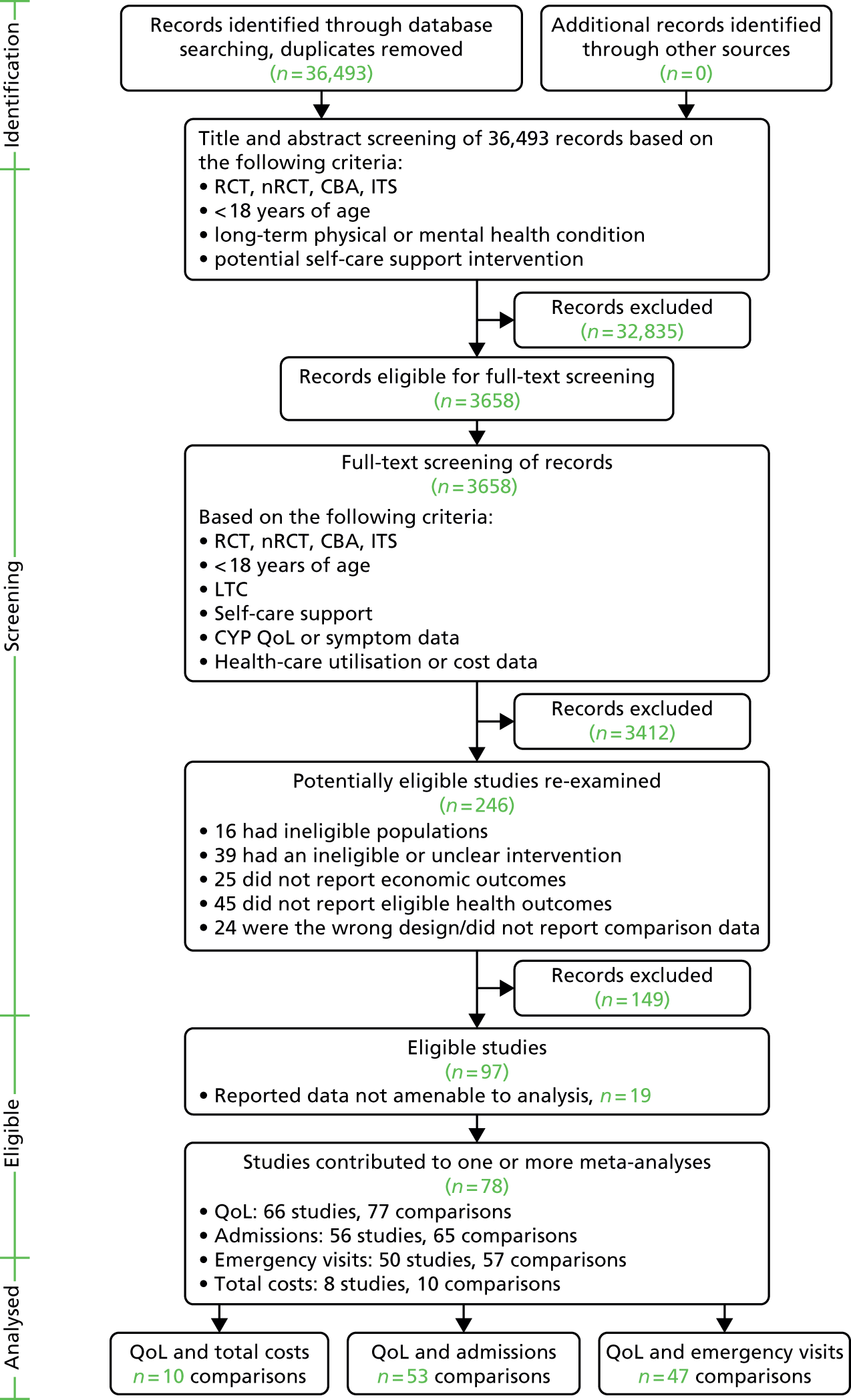
The included studies comprised 77 RCTs, 10 cluster RCTs, four nRCTs and six quasi-experimental (CBA) designs. Thirty-seven trials (38%) were rated as high quality (i.e. at low risk of bias) on the basis of adequate randomisation and allocation concealment procedures. Fourteen studies (14%) were conducted in the UK. Full details of the data extracted from individual studies (i.e. population characteristics, conditions, comparisons and design) are provided in Appendices 5–8 and summarised in Table 1. Formal economic analyses were reported by a subset of studies (n = 35, 36%). This subset is listed in Appendix 9, which provides detailed information on the design and quality of the economic analyses.
| Category | Characteristic | n (%) or mean (SD) |
|---|---|---|
| Study context | UK | 14 (14.4) |
| European | 18 (18.6) | |
| US/Canadian | 54 (55.7) | |
| Mixed/other | 11 (11.3) | |
| Baseline sample size | Mean (SD) | 215 (209) |
| Range | 10–1316 | |
| Quality rating | Adequate allocation concealment | 37 (38.1) |
| Population | Asthma | 66 (68.0) |
| Diabetes | 6 (6.2) | |
| Other physical health | 2 (2.1) | |
| Mental health | 18 (18.6) | |
| ADHD/behavioural difficulties | 5 (5.2) | |
| Children (aged 0–12 years) | 32 (33.0) | |
| Young people (aged 13–18 years) | 23 (23.7) | |
| Mixed children and young people | 42 (43.3) | |
| Mean (SD) CYP age (years) | 10.12 (3.9)a | |
| % CYP male | 53.4b | |
| Intervention contentc | Pure | 5 (4.3) |
| Facilitated | 26 (22.8) | |
| Intensively facilitated | 74 (64.9) | |
| Case managed | 9 (7.9) | |
| Intervention targetc | CYP | 32 (28.0) |
| Parents/adult caregivers | 9 (7.9) | |
| Mixed | 73 (64.0) | |
| Intervention settingc | Health (inpatient) | 6 (5.3) |
| Health (outpatient/clinic) | 49 (43.0) | |
| Home | 31 (27.2) | |
| School/community | 18 (15.8) | |
| Mixed | 10 (8.8) | |
| Intervention deliveryc | Face to face | 94 (82.5) |
| Remote | 13 (11.4) | |
| Mixed | 7 (6.1) | |
| Intervention formatc | Individual | 77 (67.5) |
| Group | 25 (21.9) | |
| Mixed | 12 (10.5) |
The vast majority of included studies recruited children and young people with physical health conditions (n = 77, 76%), predominantly asthma (n = 66, 68%). Long-term mental health conditions were also represented (n = 18, 19%), split between depression and anxiety (n = 6), psychosis or schizophrenia (n = 3), self-harm or suicide (n = 6) and eating disorders (n = 3). Most studies (n = 42, 43%) recruited across a broad age continuum (e.g. included both children and young people).
The majority of the interventions that were evaluated were intensively facilitated self-care support or case management, requiring more than four sessions or 2 hours of total contact from a health professional and/or other self-care agent. As might be expected in this population, the majority of interventions targeted adult caregivers, either together or in parallel with children and young people. Self-care support interventions were most typically delivered face to face to individuals or individual families, in either an outpatient setting or a patient’s home. Most studies delivered self-care support in addition to usual care and compared its effects with usual care alone.
Overall pattern of the results
Sixty-four studies, reporting on 77 comparisons, provided QoL outcome data in a form suitable for meta-analysis. The number of studies contributing data to a meta-analysis of health service costs was limited (n = 10 comparisons), restricting the utility of our primary analysis. A greater number of studies contributed data on hospital admissions (65 comparisons) and ED visits (57 comparisons), facilitating more meaningful interpretation of these outcomes (Table 2).
| Outcome | ES | 95% CI | I2 statistic (%) | Number of comparisons |
|---|---|---|---|---|
| QoL | –0.17 | –0.23 to –0.11 | 48 | 77 |
| Hospital admissions | –0.05 | –0.12 to 0.03 | 35 | 65 |
| Emergency visits | –0.11 | –0.17 to –0.04 | 38 | 57 |
| Total costs | –0.11 | –0.47 to 0.25 | 92 | 10 |
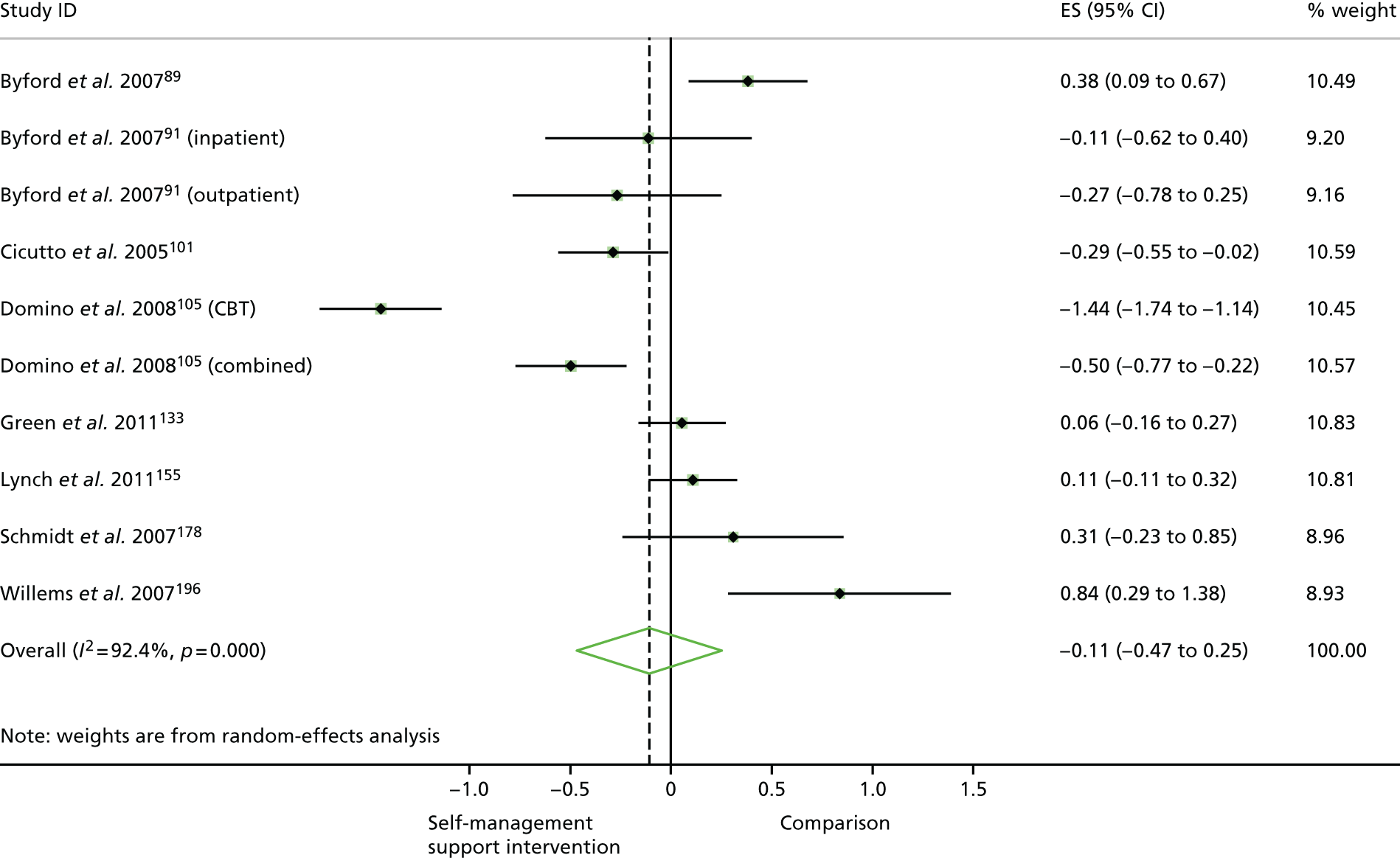
The meta-analysis of all study data demonstrated that self-care support was associated with statistically significant but minimal improvements in QoL [ES –0.17, 95% confidence interval (CI) –0.23 to –0.11], with moderate variation across trials (Figure 5). Self-care support was associated with minimal but statistically significant reductions in ED use (ES –0.11, 95% CI 0.17 to 0.04) (Figure 6). Meta-analyses showed minimal, statistically non-significant reductions in hospital admissions (ES –0.05, 95% CI –0.12 to 0.03) (Figure 7) and total health service costs (ES –0.11, 95% CI –0.47 to 0.25) (Figure 8). Pooled estimates for total health service costs were based on a small number of comparisons with high variation across trials. Subgroup analyses were used to explore the different characteristics of self-care support that may be associated with each of these outcomes (these are detailed in Analyses of different types of self-care support, Table 9).
FIGURE 5.
Forest plot: QoL. CBT, cognitive–behavioural therapy; CBTpA, Cognitive Behavioural Therapy for Adolescents with Psychosis; CC, care co-ordination; CIT, conventional insulin therapy; FACI, Facilitated Asthma Communication Initiative; FipA, family intervention in adolescent inpatients with psychosis; IIT, intensive insulin therapy; IVR, interactive voice response; PST, problem-solving skills training; ST, Sweet Talk.
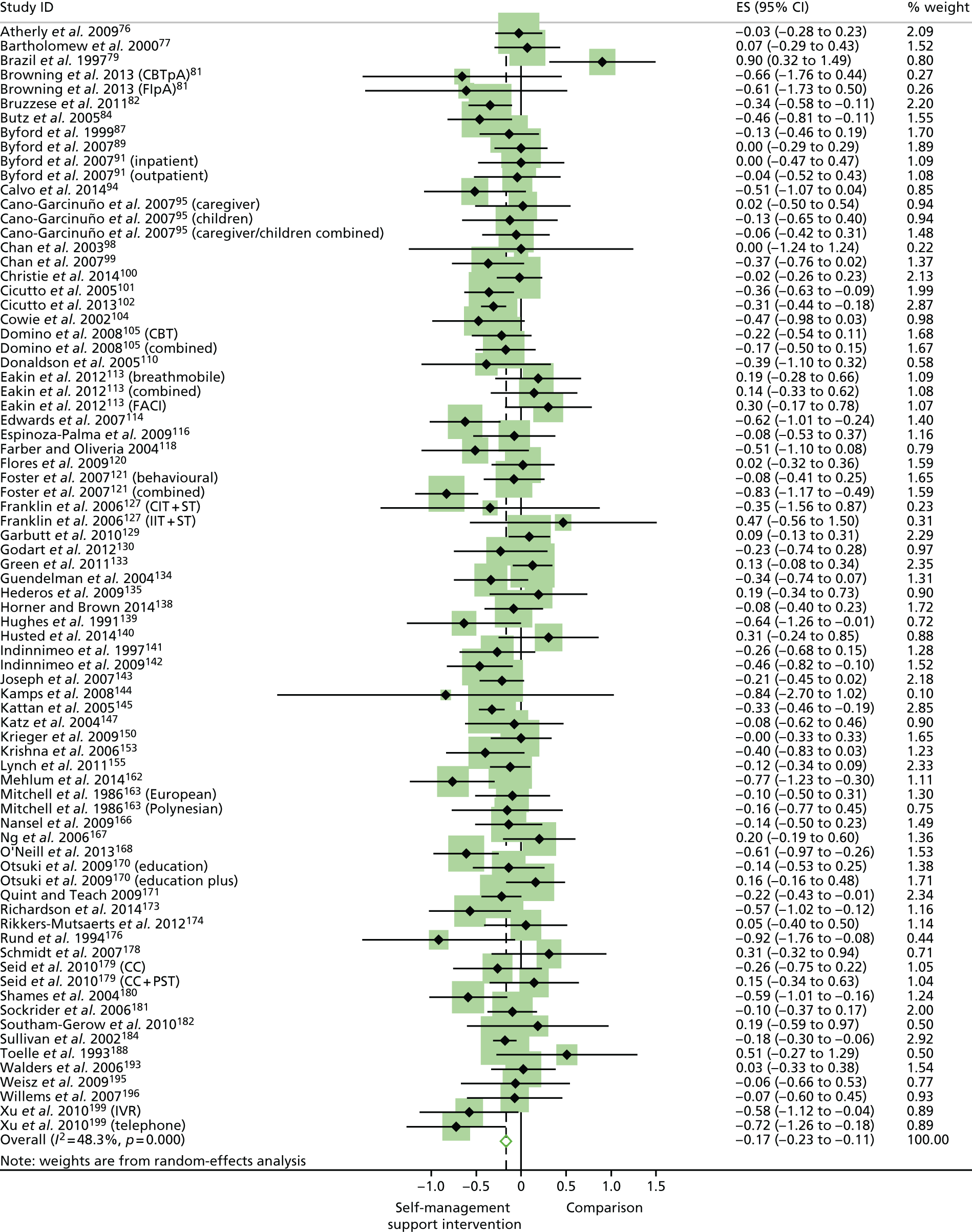
FIGURE 6.
Forest plot: emergency visits. CC, care co-ordination; CIT, conventional insulin therapy; FACI, Facilitated Asthma Communication Initiative; IIT, intensive insulin therapy; IVR, interactive voice response; PST, problem-solving skills training; ST, Sweet Talk.
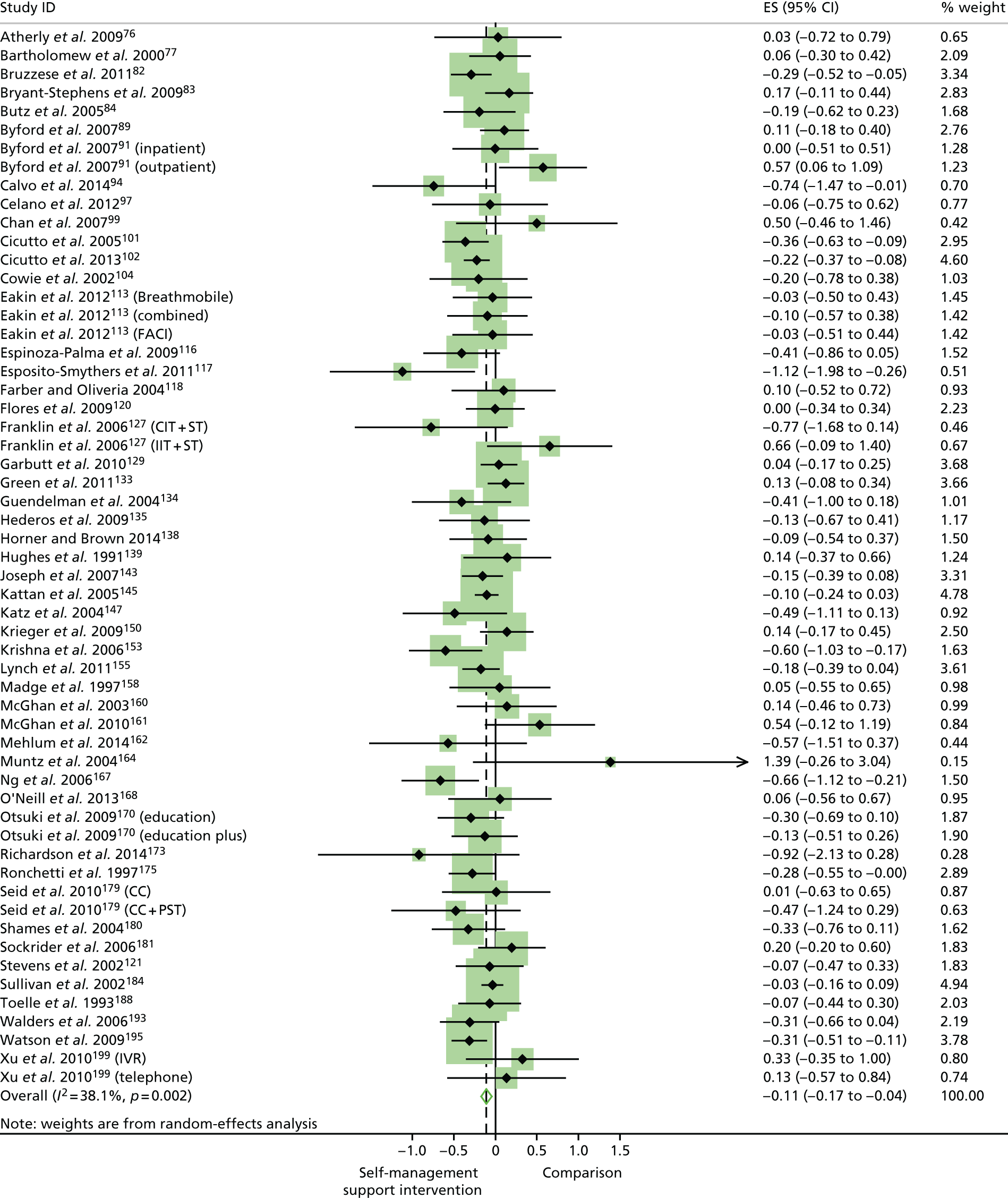
FIGURE 7.
Forest plot: hospital admissions. CC, care co-ordination; FACI, Facilitated Asthma Communication Initiative; IVR, interactive voice response; PST, problem-solving skills training.
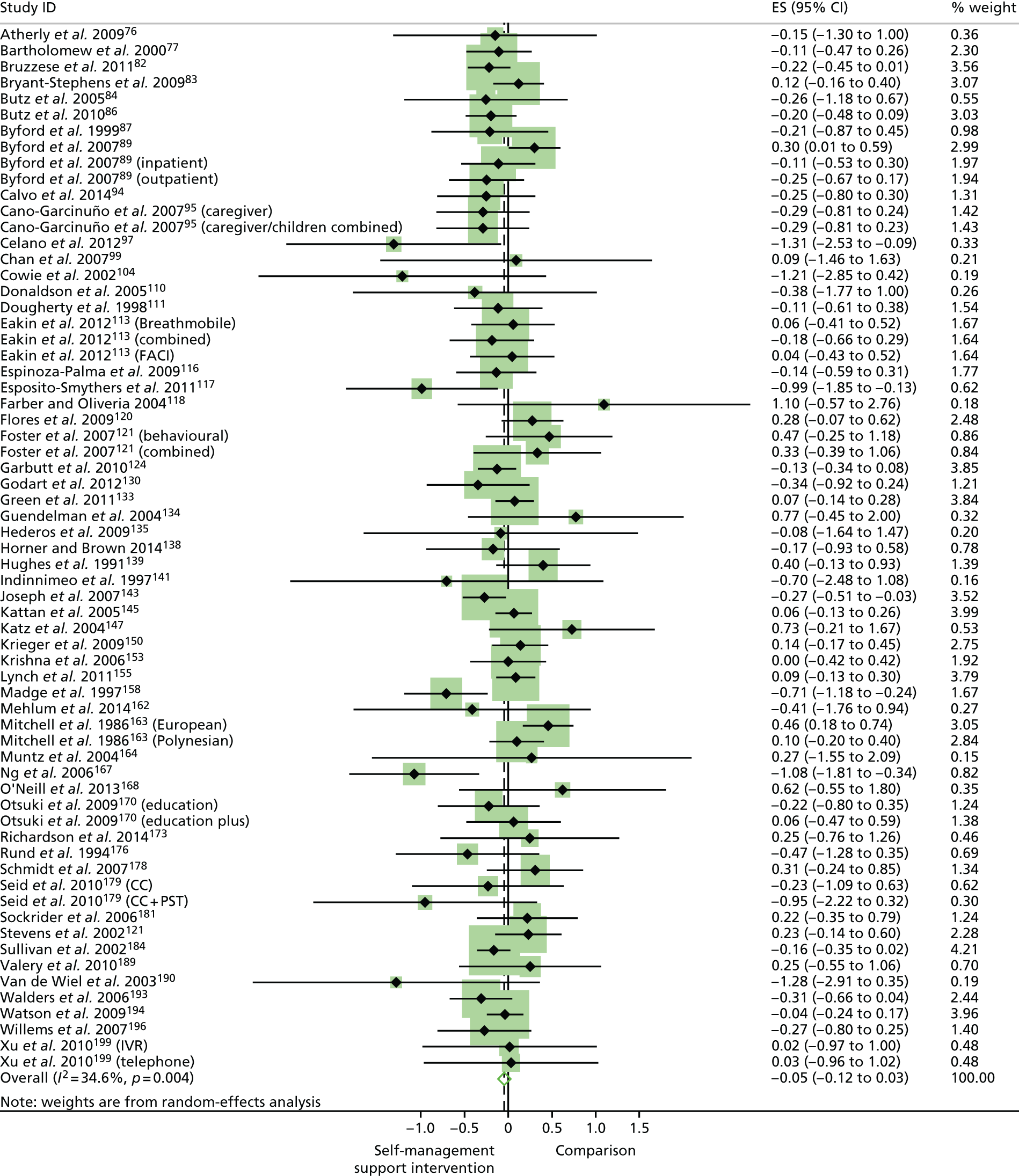
FIGURE 8.
Forest plot: total costs. CBT, cognitive–behavioural therapy.
Primary analysis: quality of life and total health service costs
Total health service costs were infrequently reported. Only eight studies reporting 10 comparisons were eligible for inclusion in a permutation plot that simultaneously charted the effects of self-care support on children and young people QoL and total health-care costs (Figure 9). Six of these comparisons were rated as being at a low risk of bias.
FIGURE 9.
Permutation plot of QoL and costs.
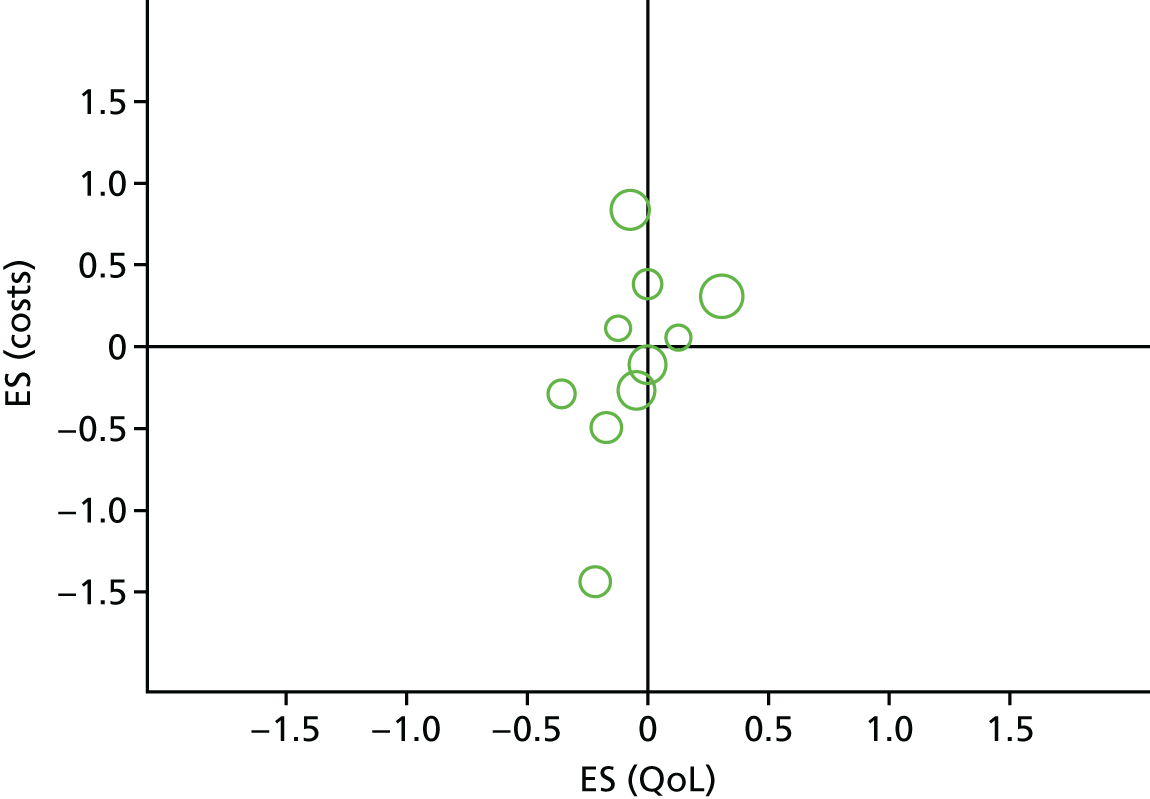
When effects were plotted against each other, the comparisons were primarily distributed across the left-hand quadrants of the plot, suggesting that self-care support interventions currently demonstrate high variability in terms of economic effect, but typically confer minimal to small improvements for QoL. This conclusion is based on limited data and must be treated with caution. The circles in the permutation plots are an illustrative indicator of their relative ‘weight’ in the analysis. Permutation plots do not consider uncertainty around individual study point estimates which, in some instances, may be marked. Almost all studies reporting total costs (eight comparisons) demonstrated significant skew in either control or intervention outcome data.
Quality of life and hospital admissions
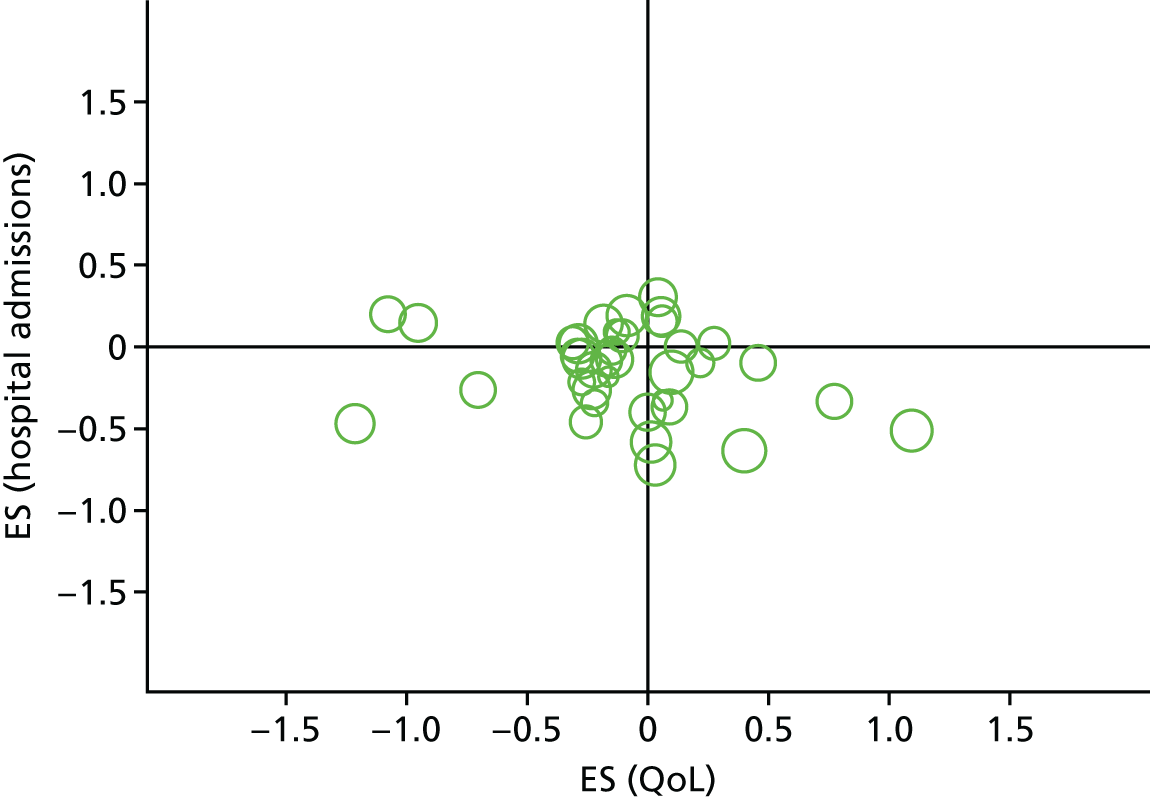
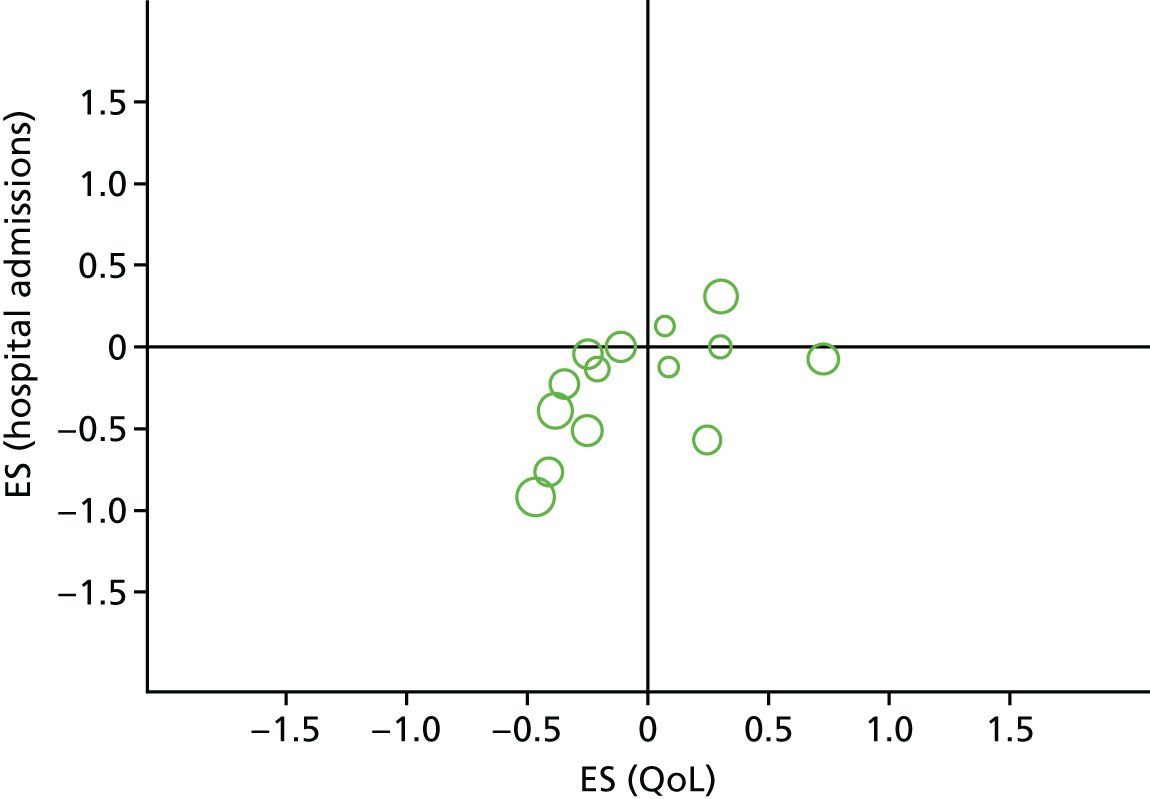
Fifty-three comparisons were eligible for inclusion in a permutation plot charting the effects of self-care support on QoL and hospital admissions (Figure 10); 29 of these comparisons originated from RCTs with adequate allocation concealment.
FIGURE 10.
Permutation plot of QoL and hospital admissions.
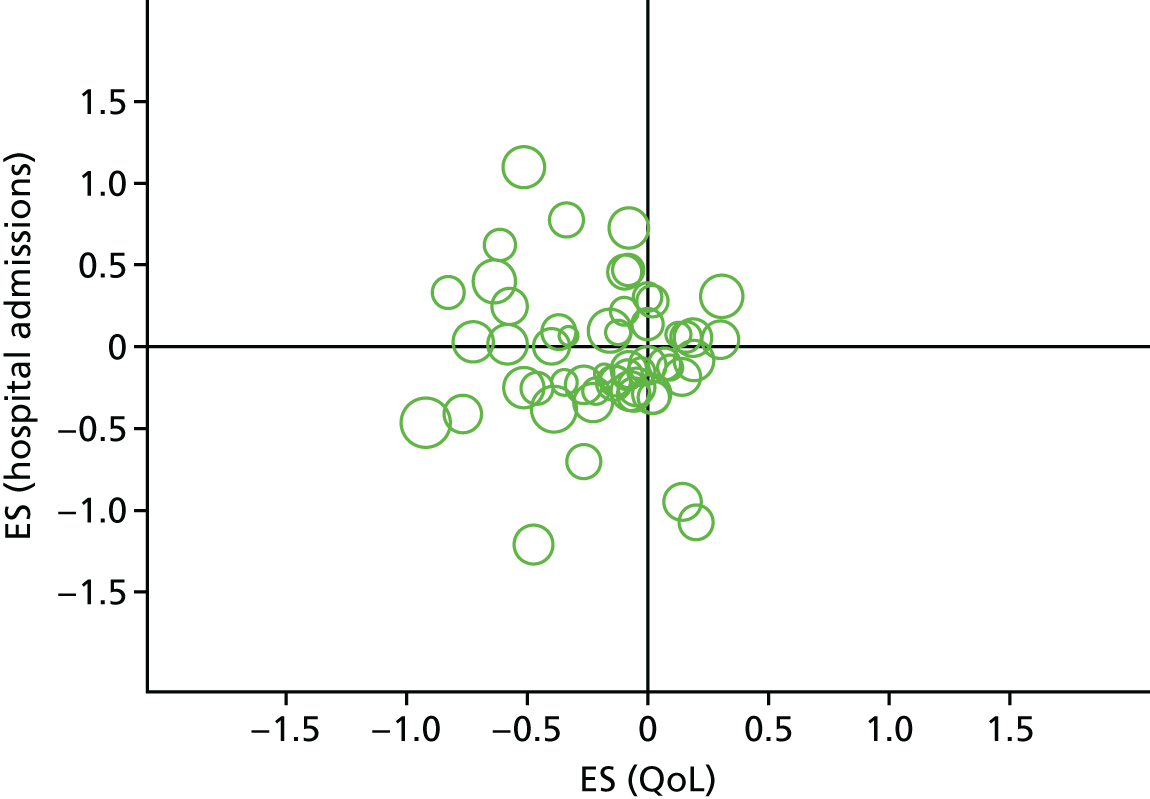
When hospital admissions were plotted against patient outcomes, most comparisons were distributed on the left-hand side, spanning both the lower and upper left-hand quadrants. This suggests that, on the basis of the available evidence, self-care support for children and young people is likely to be associated with improvements in QoL, but variable effects on hospital admissions. A minority of studies was located in the lower right-hand quadrant, suggesting reduced hospital admissions, but a marginally compromised QoL. As stated previously, permutation plots do not consider the magnitude of uncertainty around individual study point estimates and, for some studies in the current analysis, this uncertainty may be marked.
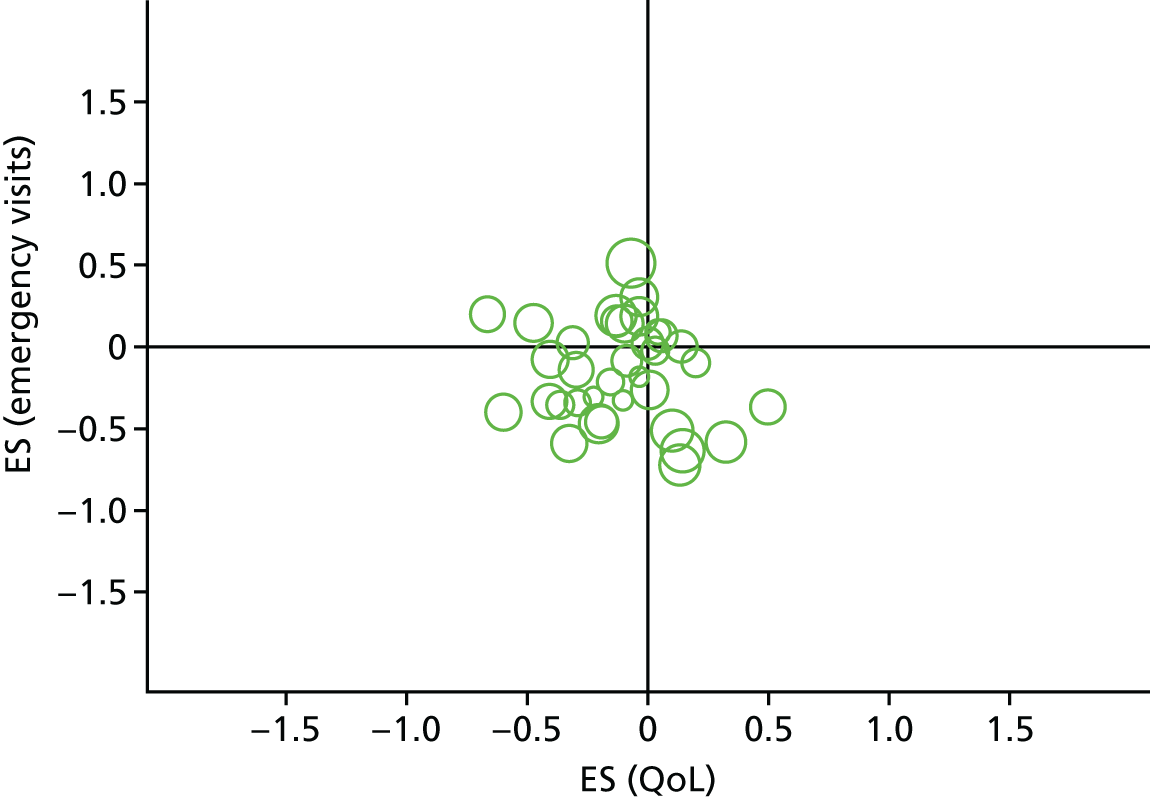
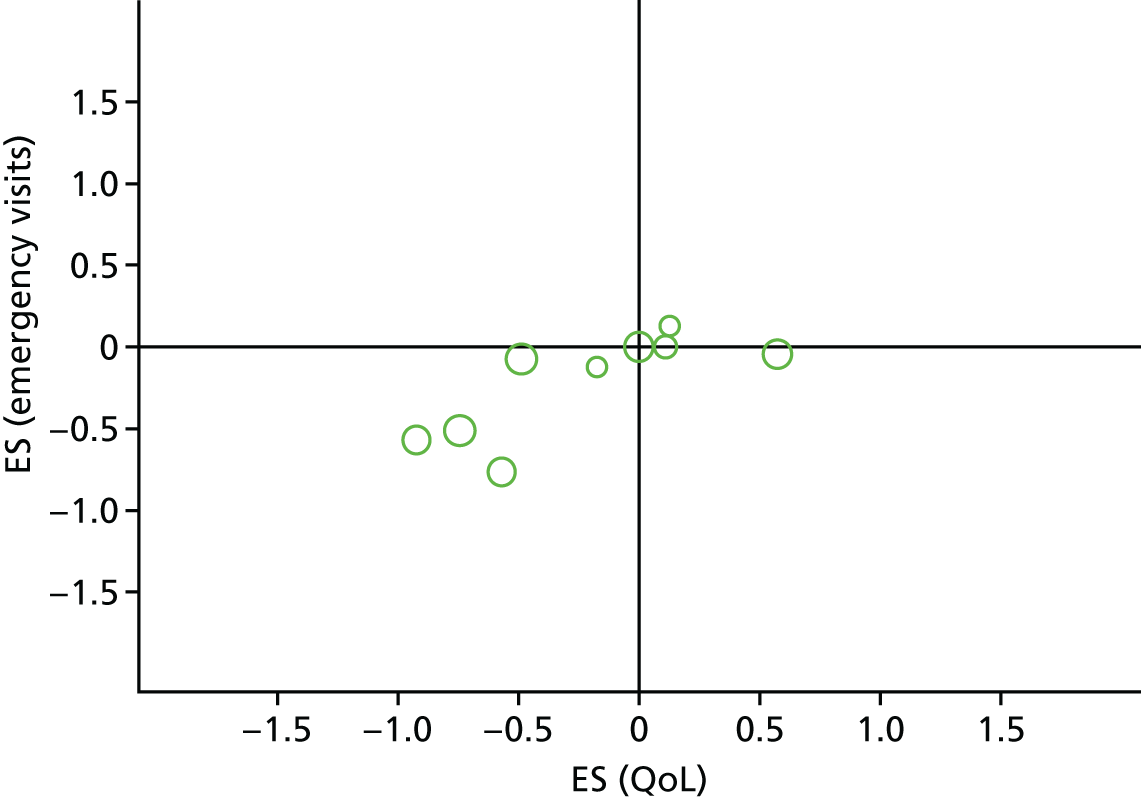
Quality of life and emergency department visits
Emergency department visits were identified by our PPI panel as a particularly important aspect of health service utilisation for children, young people and their parents. Forty-seven comparisons were eligible for inclusion in this permutation plot (Figure 11); 24 were from RCTs with adequate allocation concealment.
FIGURE 11.
Permutation plot of QoL and emergency visits.
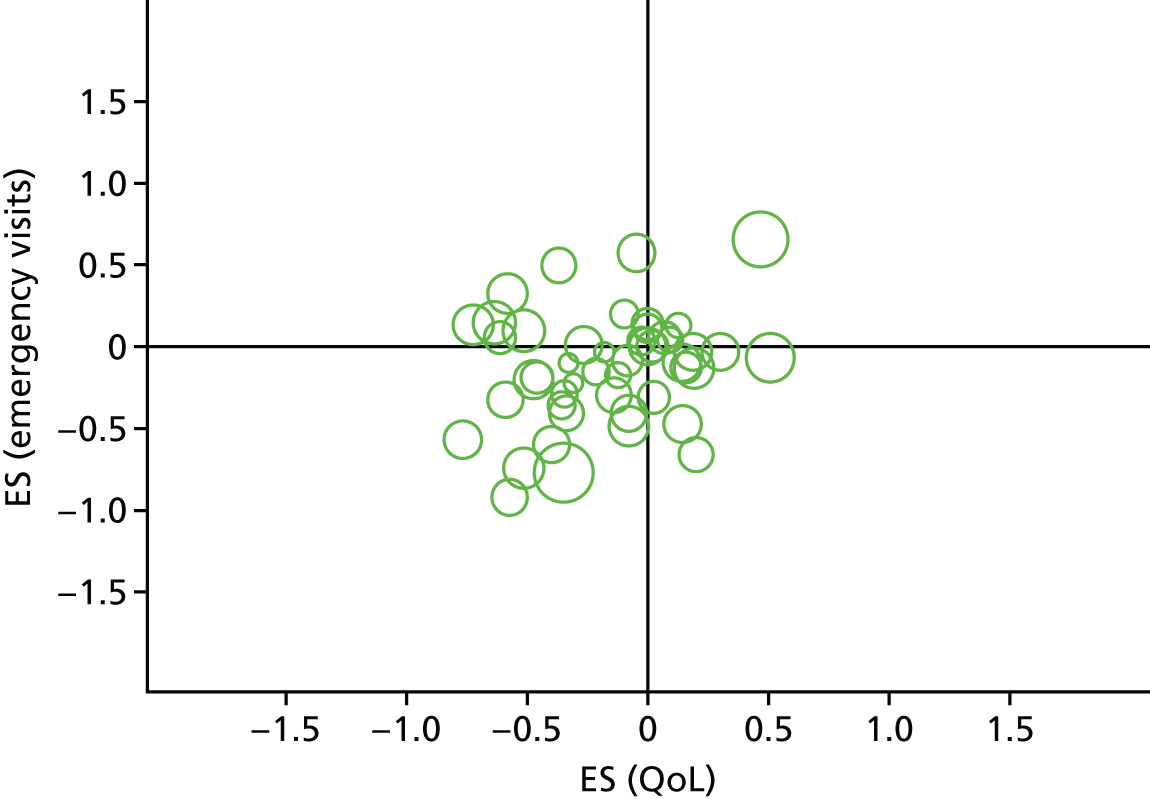
When emergency visits were plotted against patient outcomes, the majority of studies fell in the lower left-hand quadrant, demonstrating that self-care support can reduce ED use without routinely compromising children and young people’s QoL. Fewer studies report reduced emergency visits with decrements in QoL (lower right-hand quadrant) or significant improvements in QoL associated with increased service use (upper left-hand quadrant).
Analysis by long-term condition
Included studies were categorised into one of four broad groups based on the type of LTC: asthma, other physical health, mental health and behavioural difficulties. These groups were determined post hoc according to the nature of the evidence that was identified.
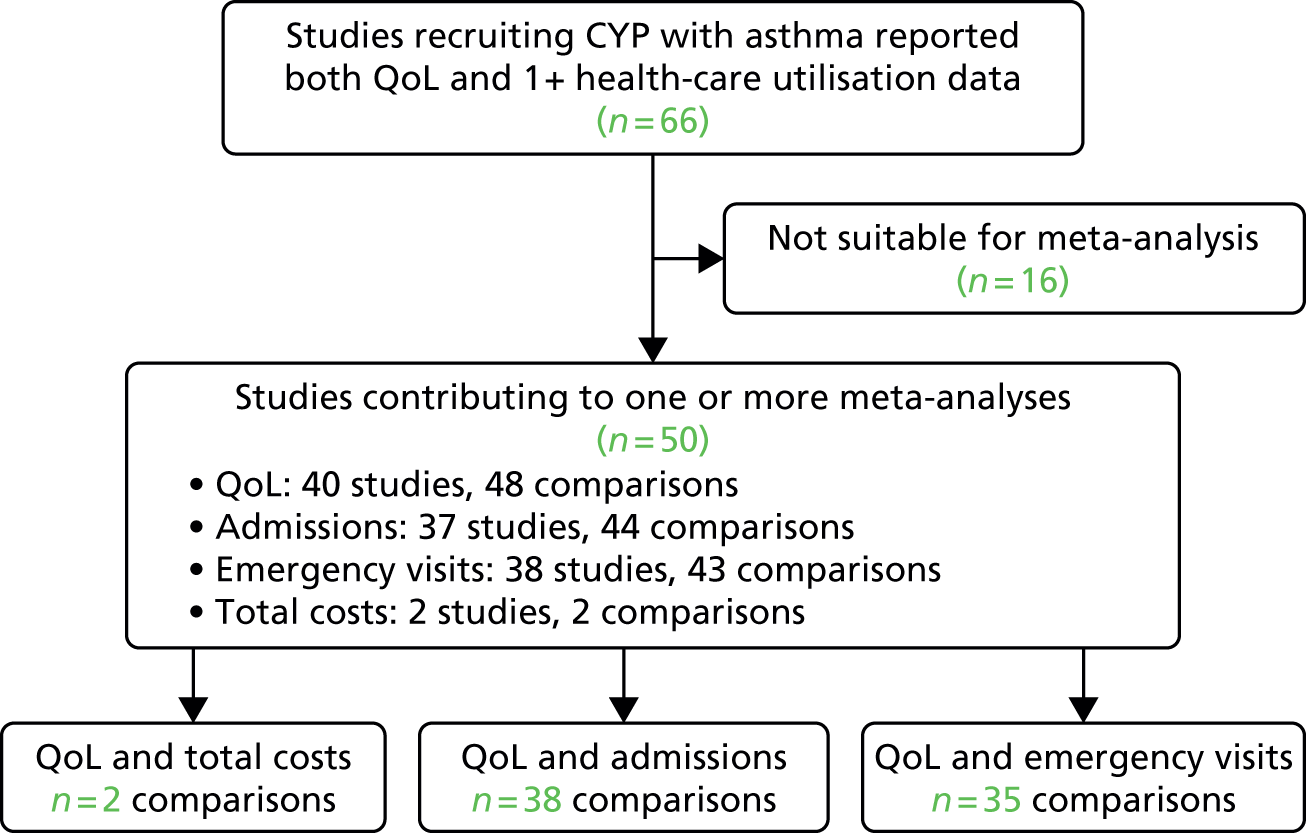
Asthma
Sixty-six studies evaluated self-care support for children and young people with asthma. The flow of studies through the review is depicted in Figure 12. Pooled effects for each outcome are reported in Table 3. Meta-analysis of all asthma studies demonstrated that self-care support was associated with minimal but statistically significant improvements in QoL, with moderate variation across trials. Self-care support was associated with minimal but statistically significant reductions in ED use, with low variation across the studies. Meta-analyses showed no significant effects on hospital admissions. Meaningful interpretation of total cost data was limited by the small number of comparisons (n = 2).
FIGURE 12.
Analyses of studies for patients with asthma. CYP, children and young people.
| Outcome | ES | 95% CI | I2 statistic (%) | Number of comparisons |
|---|---|---|---|---|
| QoL | –0.15 | –0.22 to –0.08 | 45 | 48 |
| Hospital admissions | –0.06 | –0.15 to 0.02 | 38 | 44 |
| Emergency visits | –0.12 | –0.18 to –0.06 | 22 | 43 |
| Total costs | 0.25 | –0.85 to 1.35 | 92 | 2 |
Owing to a lack of data, permutation plots were not calculated for total costs. Thirty-eight comparisons were eligible for inclusion in a permutation plot charting the effects of self-care support on QoL and hospital admissions for asthma (Figure 13); 16 of these comparisons originated from RCTs with adequate allocation concealment.
FIGURE 13.
Permutation plot of QoL and hospital admissions (asthma).
When hospital admissions were plotted against patient outcomes, most comparisons were distributed across the lower right- and left-hand quadrants. This suggests that self-care support interventions that reduce the number of hospital admissions for children and young people with asthma will not routinely compromise QoL but, on the basis of the current evidence, such compromises cannot be ruled out.
When emergency visits were plotted against QoL for children and young people with asthma (Figure 14), the majority of studies fell in lower left-hand quadrant, demonstrating that self-care support can reduce ED use without compromising children and young people’s QoL. A notable number of studies in other quadrants suggested that self-care support interventions may reduce emergency visits with decrements in QoL (lower right-hand quadrant) or improve in QoL but increase service use (upper left-hand quadrant).
FIGURE 14.
Permutation plot of QoL and emergency visits (asthma).
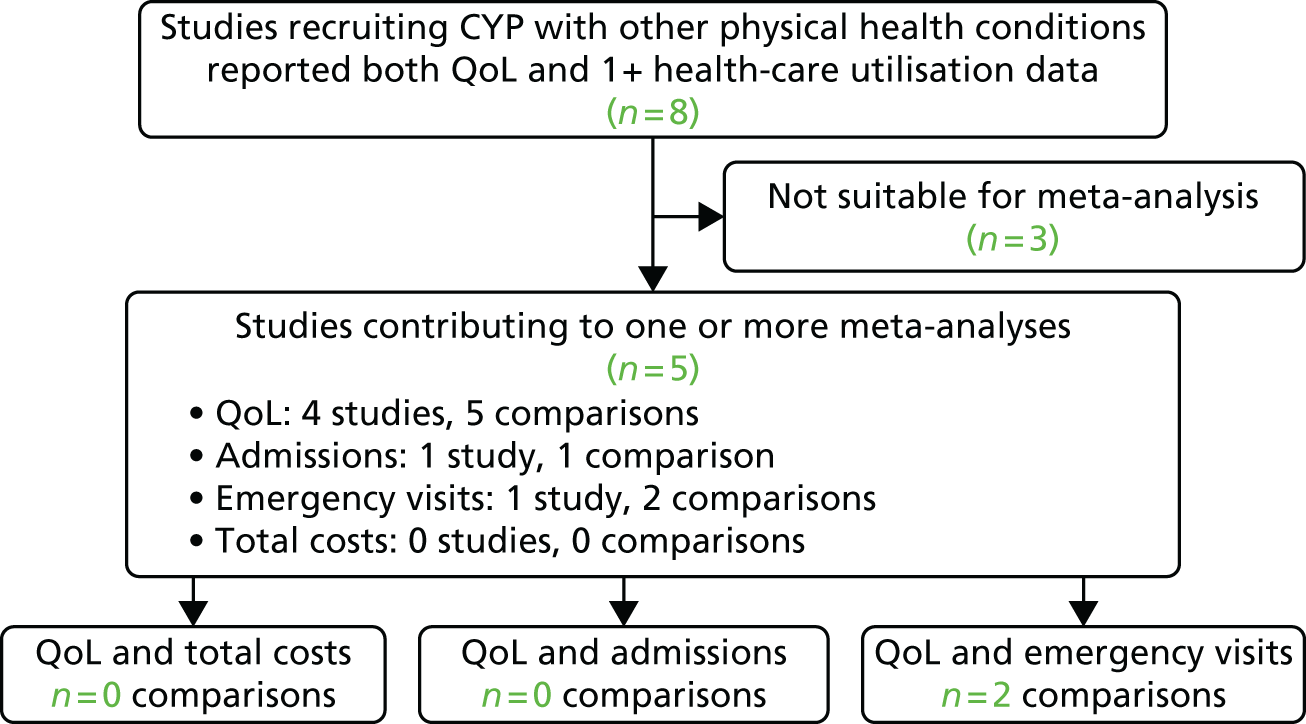
Other (non-asthma) physical health conditions
Eight studies evaluated self-care support for children and young people with other physical health conditions. The flow of studies through the review is depicted in Figure 15. Owing to the small number of data available for meta-analysis, meaningful interpretation of the evidence base for non-asthma physical health conditions is limited. Pooled ESs are presented in Table 4 for completeness. Permutation plots are not presented.
FIGURE 15.
Analyses of studies for patients with other (non-asthma) physical health conditions. CYP, children and young people.
| Outcome | ES | 95% CI | I2 statistic (%) | Number of comparisons |
|---|---|---|---|---|
| QoL | 0.00 | –0.18 to 0.19 | 0 | 5 |
| Hospital admissions | –0.11 | –0.61 to 0.38 | – | 1 |
| Emergency visits | –0.03 | –1.43 to 1.37 | 82 | 2 |
| Total costs | – | – | – | 0 |
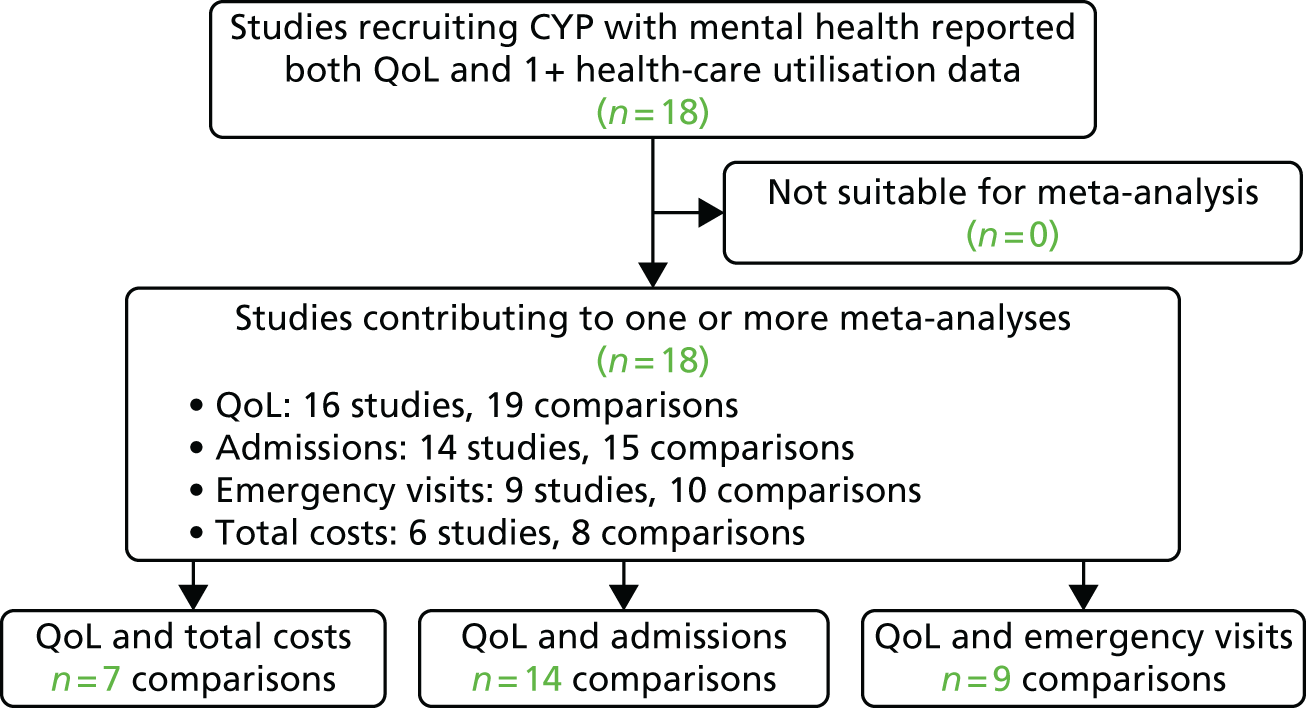
Mental health conditions
Eighteen studies evaluated self-care support for children and young people with mental health conditions. The flow of studies through the review is depicted in Figure 16. Pooled effects for each outcome are reported in Table 5. Meta-analysis of all mental health studies demonstrated that self-care support was associated with minimal but statistically significant improvements in QoL, with moderate variation across trials. The meta-analyses showed no significant effects on hospital admissions, ED visits or total costs. Meaningful interpretation of total cost data was limited by a small number of comparisons (n = 8) and high variation across trials.
FIGURE 16.
Analyses of studies for patients with mental health conditions. CYP, children and young people.
| Outcome | ES | 95% CI | I2 statistic (%) | Number of comparisons |
|---|---|---|---|---|
| QoL | –0.17 | –0.29 to –0.05 | 33 | 20 |
| Hospital admissions | –0.02 | –0.17 to 0.14 | 30 | 15 |
| Emergency visits | –0.15 | –0.39 to 0.09 | 64 | 10 |
| Total costs | –0.19 | –0.61 to 0.23 | 93 | 8 |
Owing to a lack of data, permutation plots were not calculated for total costs. Fourteen comparisons were eligible for inclusion in a permutation plot charting the effects of self-care support on QoL and hospital admissions for mental health (Figure 17); 10 of these comparisons originated from RCTs with adequate allocation concealment.
FIGURE 17.
Permutation plot of QoL and hospital admissions (mental health conditions).
When hospital admissions were plotted against patient outcomes, the majority of comparisons were located in the lower left-hand quadrant, suggesting that self-care support can reduce utilisation for children and young people with mental health conditions without compromising QoL. A minority of studies were located in the lower right-hand quadrant, suggesting reduced hospital admissions but a marginally compromised QoL. As stated previously, data were limited and findings must be treated with caution.
Nine comparisons were eligible for inclusion in a permutation plot charting ED visits against patient outcomes (Figure 18); seven were from RCTs with adequate allocation concealment. When emergency visits were plotted against patient outcomes, the majority of studies fell in lower left-hand quadrant, demonstrating that self-care support can reduce ED use without routinely compromising children and young people’s QoL. Limited data mean that these results must be treated with caution.
FIGURE 18.
Permutation plot of QoL and emergency visits (mental health conditions).
Behavioural difficulties
Five studies evaluated self-care support for children and young people with behavioural difficulties. The flow of studies through the review is depicted in Figure 19.
FIGURE 19.
Analyses of studies for patients with behavioural difficulties. CYP, children and young people.
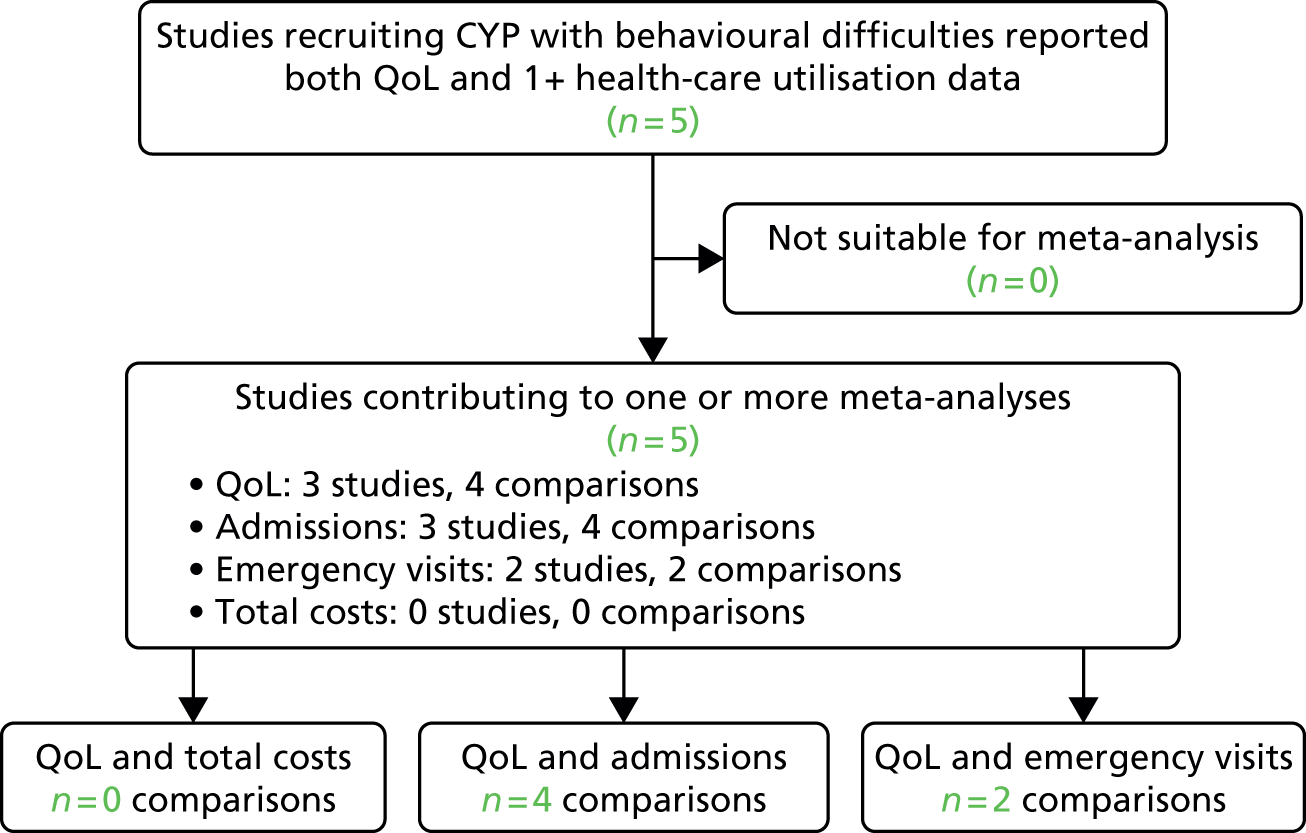
Owing to the small number of data available for meta-analysis, meaningful interpretation of the evidence base for non-asthma physical health conditions is limited. Pooled ESs are presented in Table 6 for completeness. Permutation plots are not presented. Table 7 summarises the results of all meta-analyses, presented according to LTC type.
| Outcome | ES | 95% CI | I2 statistic (%) | Number of comparisons |
|---|---|---|---|---|
| QoL | –0.53 | –0.86 to –0.20 | 71 | 4 |
| Hospital admissions | 0.30 | –0.14 to 0.75 | 3 | 5 |
| Emergency visits | 0.49 | –0.73 to 1.72 | 55 | 2 |
| Total costs | – | – | – | 0 |
| Outcome | LTC type | |||
|---|---|---|---|---|
| Asthma | Other physical health | Mental health | Behavioural disorders | |
| QoL | ||||
| Pooled ES | –0.15 | 0.00 | –0.17 | –0.53 |
| 95% CI | –0.22 to –0.08 | –0.18 to 0.19 | –0.29 to –0.05 | –0.86 to –0.20 |
| n | 48 | 5 | 20 | 4 |
| I2 statistic (%) | 45 | 0 | 33 | 71 |
| Hospital admissions | ||||
| Pooled ES | –0.06 | –0.11 | –0.02 | 0.30 |
| 95% CI | –0.15 to 0.02 | –0.61 to 0.30 | –0.17 to 0.14 | –0.14 to 0.75 |
| n | 44 | 1 | 15 | 5 |
| I2 statistic (%) | 38 | – | 30 | 3 |
| Emergency visits | ||||
| Pooled ES | –0.12 | –0.03 | –0.15 | 0.49 |
| 95% CI | –0.18 to –0.06 | –1.43 to 1.37 | –0.39 to 0.09 | –0.3 to 1.72 |
| n | 43 | 2 | 10 | 2 |
| I2 statistic (%) | 22 | 82 | 64 | 55 |
| Total costs | ||||
| Pooled ES | 0.25 | – | –0.19 | – |
| 95% CI | –0.85 to 1.35 | – | –0.61 to 0.23 | – |
| n | 2 | – | 8 | – |
| I2 statistic (%) | 92 | – | 93 | – |
Analysis by age
Subgroup analyses were carried out on the basis of children and young people’s age. Studies were categorised according to whether the self-care intervention targeted children (aged 0–12 years), adolescents (aged 13–18 years) or both (Table 8). Across all three age groups, self-care support had statistically significant but minimal effects (ES of < 0.2) on QoL. Self-care support was associated with a statistically significant but minimal reduction in ED use for children. Irrespective of the target age group, self-care support had no statistically significant effects on hospital admissions or total costs. Variation in the magnitude of ESs observed across the three subgroups will in part reflect differences in the number of studies available and the precision of the pooled estimates.
| Outcome | Age group | ||
|---|---|---|---|
| Children | Adolescents | Mixed | |
| QoL | |||
| Pooled ES | –0.19 | –0.17 | –0.13 |
| 95% CI | –0.30 to –0.08 | –0.28 to –0.07 | –0.23 to –0.04 |
| n | 23 | 23 | 31 |
| I2 statistic (%) | 66 | 40 | 27 |
| Hospital admissions | |||
| Pooled ES | –0.06 | –0.08 | –0.04 |
| 95% CI | –0.14 to 0.03 | –0.22 to 0.06 | –0.19 to 0.10 |
| n | 21 | 18 | 26 |
| I2 statistic (%) | 0 | 42 | 49 |
| Emergency visits | |||
| Pooled ES | –0.10 | –0.14 | –0.11 |
| 95% CI | –0.17 to –0.04 | –0.31 to 0.03 | –0.25 to 0.04 |
| n | 22 | 14 | 21 |
| I2 statistic (%) | 9 | 55 | 47 |
| Total costs | |||
| Pooled ES | –0.29 | –0.19 | 0.84 |
| 95% CI | –0.56 to –0.02 | –0.61 to 0.23 | 0.29 to 1.38 |
| n | 1 | 8 | 1 |
| I2 statistic (%) | – | 93 | – |
Analyses of different types of self-care support
When different intensities of self-care support were compared, intensive facilitation conferred limited benefit over and above other forms of self-care support (Table 9).
| Subgroup | Outcome | |||
|---|---|---|---|---|
| QoL | Hospital admission | Emergency visits | Total costs | |
| Intervention intensity | ||||
| Pure/facilitated | ||||
| Pooled ES | –0.20 | –0.08 | –0.12 | 0.84 |
| 95% CI | –0.29 to –0.10 | –0.24 to 0.09 | –0.29 to 0.05 | 0.29 to 1.38 |
| Number of comparisons | 22 | 17 | 16 | 1 |
| I2 statistic (%) | 25 | 38 | 44 | – |
| Intensive/case managed | ||||
| Pooled ES | –0.16 | –0.04 | –0.10 | –0.20 |
| 95% CI | –0.23 to –0.08 | –0.12 to 0.04 | –0.17 to –0.03 | –0.57 to 0.16 |
| Number of comparisons | 55 | 48 | 41 | 9 |
| I2 statistic (%) | 56 | 25 | 37 | 92 |
| Intervention target | ||||
| CYP | ||||
| Pooled ES | –0.09 | –0.00 | –0.12 | –0.11 |
| 95% CI | –0.20 to –0.02 | –0.18 to 0.17 | –0.28 to 0.04 | –0.61 to 0.38 |
| Number of comparisons | 23 | 12 | 12 | 7 |
| I2 statistic (%) | 37 | 49 | 51 | 95 |
| Parents | ||||
| Pooled ES | –0.20 | –0.05 | 0.02 | – |
| 95% CI | –0.57 to 0.17 | –0.22 to 0.12 | –0.15 to 0.19 | – |
| Number of comparisons | 5 | 6 | 5 | – |
| I2 statistic (%) | 48 | 0 | 38 | – |
| Mixed | ||||
| Pooled ES | –0.20 | –0.06 | –0.12 | 0.02 |
| 95% CI | –0.27 to –0.13 | –0.15 to –0.15 | –0.20 to –0.04 | –0.17 to 0.22 |
| Number of comparisons | 49 | 47 | 40 | 3 |
| I2 statistic (%) | 37 | 36 | 37 | 5 |
| Intervention format | ||||
| Individual | ||||
| Pooled ES | –0.16 | –0.02 | –0.09 | –0.10 |
| 95% CI | –0.22 to –0.09 | –0.10 to 0.06 | –0.18 to 0.00 | –0.59 to 0.39 |
| Number of comparisons | 54 | 55 | 40 | 8 |
| I2 statistic (%) | 29 | 34 | 37 | 94 |
| Group | ||||
| Pooled ES | –0.11 | –0.15 | –0.12 | –0.11 |
| 95% CI | –0.29 to 0.07 | –0.28 to –0.02 | –0.27 to 0.02 | –0.44 to 0.23 |
| Number of comparisons | 12 | 8 | 10 | 2 |
| I2 statistic (%) | 75 | 0 | 54 | 75 |
| Mixed/unclear | ||||
| Pooled ES | –0.25 | –0.70 | –0.13 | – |
| 95% CI | –0.42 to –0.09 | –1.77 to 0.37 | –0.25 to 0.00 | – |
| Number of comparisons | 11 | 2 | 7 | – |
| I2 statistic (%) | 64 | 44 | 13 | – |
| Intervention delivery | ||||
| Face to face | ||||
| Pooled ES | –0.17 | –0.04 | –0.11 | –0.20 |
| 95% CI | –0.24 to –0.11 | –0.13 to 0.05 | –0.17 to –0.04 | –0.57 to 0.16 |
| Number of comparisons | 62 | 48 | 46 | 9 |
| I2 statistic (%) | 51 | 40 | 32 | 92 |
| Remote | ||||
| Pooled ES | –0.20 | 0.01 | –0.13 | 0.84 |
| 95% CI | –0.38 to –0.03 | –0.16 to 0.17 | –0.33 to 0.07 | 0.29 to 1.38 |
| Number of comparisons | 10 | 8 | 8 | 1 |
| I2 statistic (%) | 41 | 21 | 46 | – |
| Mixed | ||||
| Pooled ES | –0.04 | –0.16 | 0.11 | – |
| 95% CI | –0.28 to 0.20 | –0.29 to –0.03 | –0.84 to 1.07 | – |
| Number of comparisons | 5 | 9 | – | – |
| I2 statistic (%) | 30% | 0% | 82% | – |
| Intervention setting | ||||
| Inpatient | ||||
| Pooled ES | –0.04 | –0.09 | –0.32 | –0.11 |
| 95% CI | –0.25 to 0.17 | –0.61 to 0.43 | –0.60 to –0.03 | –0.62 to 0.40 |
| Number of comparisons | 5 | 5 | 5 | 1 |
| I2 statistic (%) | 0 | 66 | 32 | – |
| Outpatient/clinic | ||||
| Pooled ES | –0.15 | –0.08 | –0.14 | –0.20 |
| 95% CI | –0.23 to –0.08 | –0.19 to 0.03 | –0.26 to –0.02 | –0.66 to 0.27 |
| Number of comparisons | 33 | 24 | 20 | 7 |
| I2 statistic (%) | 28 | 37 | 55 | 94 |
| School/community | ||||
| Pooled ES | –0.19 | –0.09 | –0.17 | –0.29 |
| 95% CI | –0.36 to –0.03 | –0.31 to 0.13 | –0.26 to –0.08 | –0.56 to –0.02 |
| Number of comparisons | 12 | 8 | 12 | 1 |
| I2 statistic (%) | 72 | 39 | 3 | – |
| Home | ||||
| Pooled ES | –0.13 | 0.02 | –0.02 | 0.84 |
| 95% CI | –0.25 to –0.01 | –0.10 to 0.13 | –0.13 to 0.09 | 0.29 to 1.38 |
| Number of comparisons | 20 | 21 | 16 | 1 |
| I2 statistic (%) | 40 | 25 | 16 | – |
| Mixed setting | ||||
| Pooled ES | –0.29 | 0.08 | 0.02 | – |
| 95% CI | –0.60 to 0.20 | –0.19 to 0.35 | –0.27 to 0.31 | – |
| Number of comparisons | 7 | 7 | 4 | – |
| I2 statistic (%) | 72 | 7 | 38 | |
Intensively facilitated or case-managed self-care support interventions produced statistically significant but minimal benefits in QoL (ES –0.16, 95% CI –0.23 to –0.08), with moderate variation across trials. Intensively facilitated or case-managed self-care support interventions were associated with statistically significant but minimal reductions in ED use (ES –0.10, 95% CI –0.17 to –0.03), but no statistically significant reductions in hospital admissions (ES –0.04, 95% CI –0.12 to 0.04) or total costs (ES –0.20, 95% CI –0.57 to 0.16). The lack of data for total costs prohibits meaningful interpretation of this outcome.
Less intensive self-care interventions (i.e. facilitated or pure self-care support) showed small and significant improvements in QoL (ES –0.20, 95% CI –0.29 to –0.10), with low variation across trials. Facilitated or pure self-care support did not significantly reduce ED visits (ES –0.12, 95% CI –0.29 to 0.05) or hospital admissions (ES –0.08, 95% CI –0.24 to 0.09). The lack of data for total costs prohibited a meaningful analysis of this outcome.
Subgroup analyses additionally explored the effects of different intervention targets, formats, delivery modes and settings. ESs and 95% CIs for each of these subgroup analyses are shown in Table 8; results are highlighted where effects were statistically significant. In interpreting this table it is important to remember that any variation in the ESs observed for different subgroups will, in part, reflect differences in the number of studies available and the precision of the pooled estimates.
The existing evidence suggests that the effect of self-care support on children and young people’s QoL may be optimised by interventions that include the child or young person and deliver at least some of their content to an individual or individual family. Nonetheless, effects are likely to remain small. Minimal but statistically significant effects (ES of < 0.20) were observed across delivery modes (face to face and remote) and settings (outpatient, community and home).
With regard to hospital admissions, few positive effects were observed. Statistically significant but minimal benefits occurred with group-based interventions and mixed delivery models (i.e. those using a blend of face-to-face and remote facilitation). Both of these findings were based on limited data and must therefore be treated with caution.
Internal validity
Table 10 shows the effects of self-care support on the four core outcomes, for the whole sample and the subset of studies rated as being at low risk of bias on the basis of adequate allocation concealment. Studies rated as being at low risk of bias reported minimal benefits of self-care support on QoL and ED visits and no significant effects on hospital admissions or costs. The effects observed for the subset of studies rated as being at low risk of bias were analogous to the full data set, suggesting that our main analyses were robust.
| Outcome | All studies | Low risk of bias |
|---|---|---|
| QoL | ||
| Pooled ES | –0.17 | –0.15 |
| 95% CI | –0.23 to –0.11 | –0.25 to –0.06 |
| Number of comparisons | 77 | 34 |
| I2 statistic (%) | 48 | 59 |
| Hospital admissions | ||
| Pooled ES | –0.05 | –0.06 |
| 95% CI | –0.12 to 0.03 | –0.16 to 0.04 |
| Number of comparisons | 65 | 31 |
| I2 statistic (%) | 35 | 28 |
| Emergency visits | ||
| Pooled ES | –0.11 | –0.12 |
| 95% CI | –0.17 to –0.04 | –0.21 to –0.02 |
| Number of comparisons | 57 | 27 |
| I2 statistic (%) | 38 | 36 |
| Total costs | ||
| Pooled ES | –0.11 | 0.02 |
| 95% CI | –0.47 to 0.25 | –0.22 to 0.26 |
| Number of comparisons | 10 | 6 |
| I2 statistic (%) | 92 | 64 |
Small-study bias
The funnel plots for QoL and health utilisation outcomes are presented in Figures 20–23. A funnel plot is based on the premise that precision in the estimation of an ES will increase as sample size increases. Bias is suggested by the emergence of a non-symmetrical plot.
FIGURE 20.
Funnel plot: QoL. ESQoL, effect size QoL; SE, standard error.
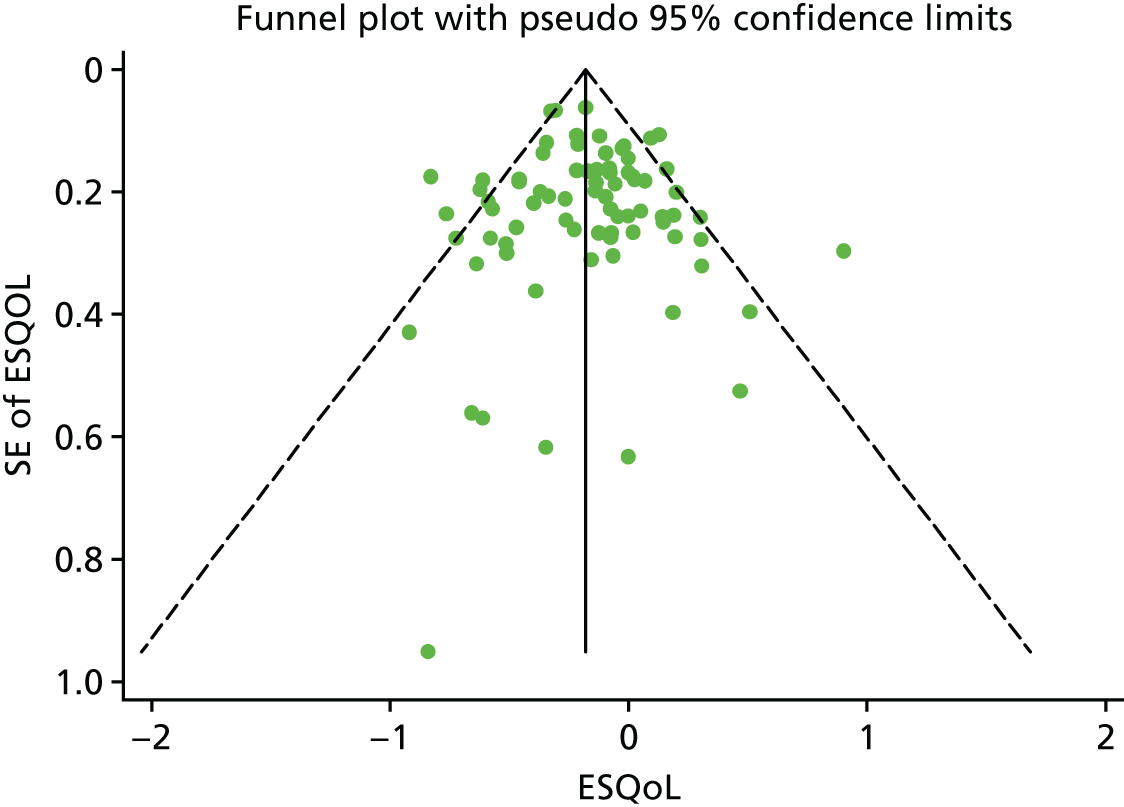
FIGURE 21.
Funnel plot: hospital admissions. ESADM, effect size hospital admissions.
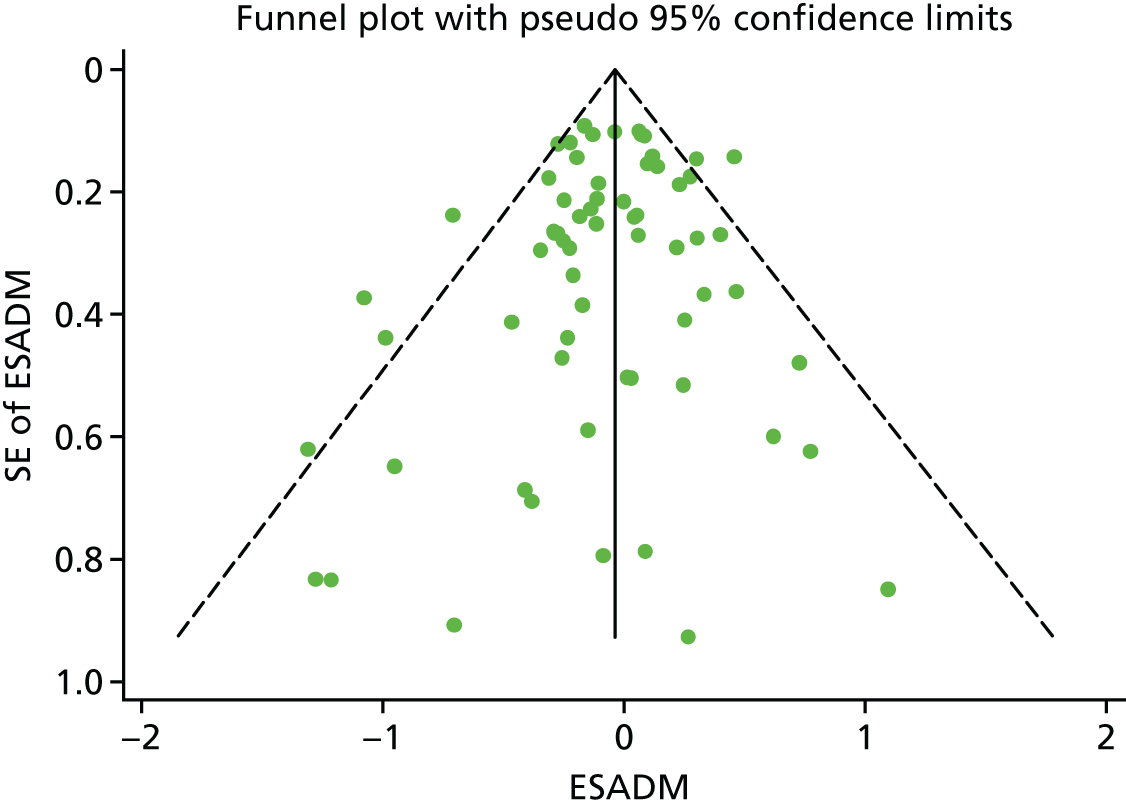
FIGURE 22.
Funnel plot: emergency visits. ESEmerg, effect size emergency visits.
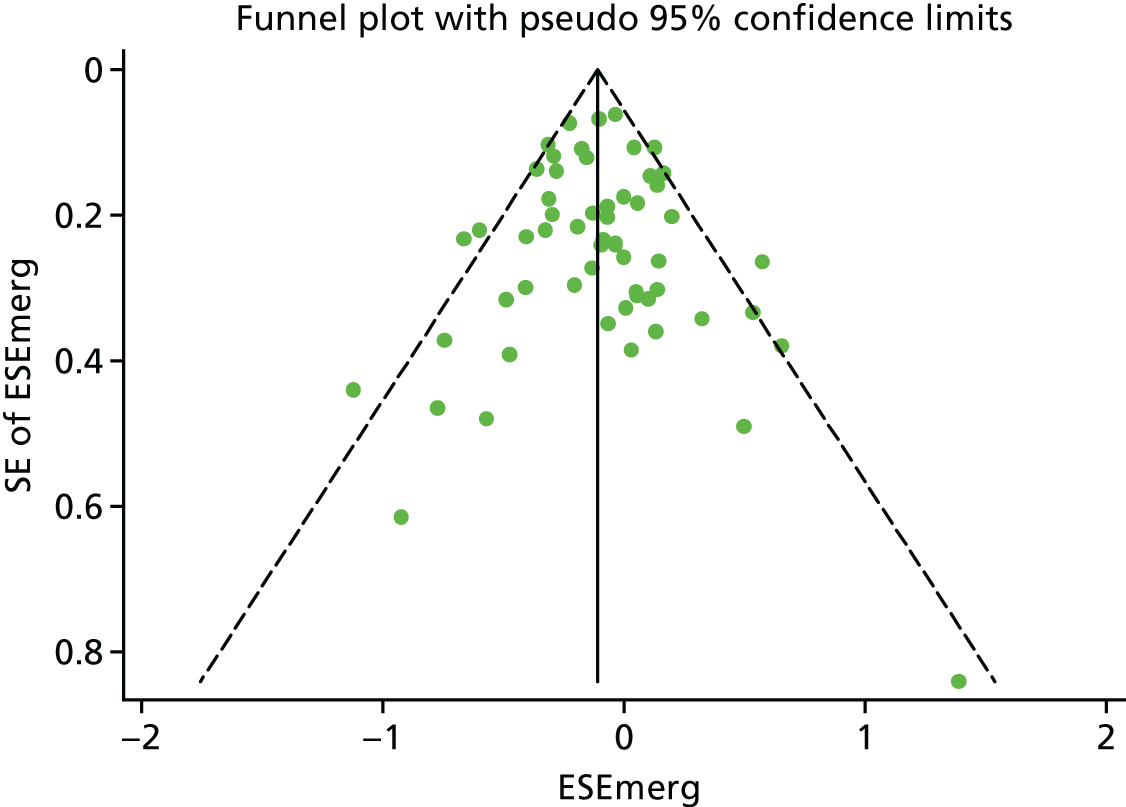
FIGURE 23.
Funnel plot: total costs. ESTot, effect size total costs.
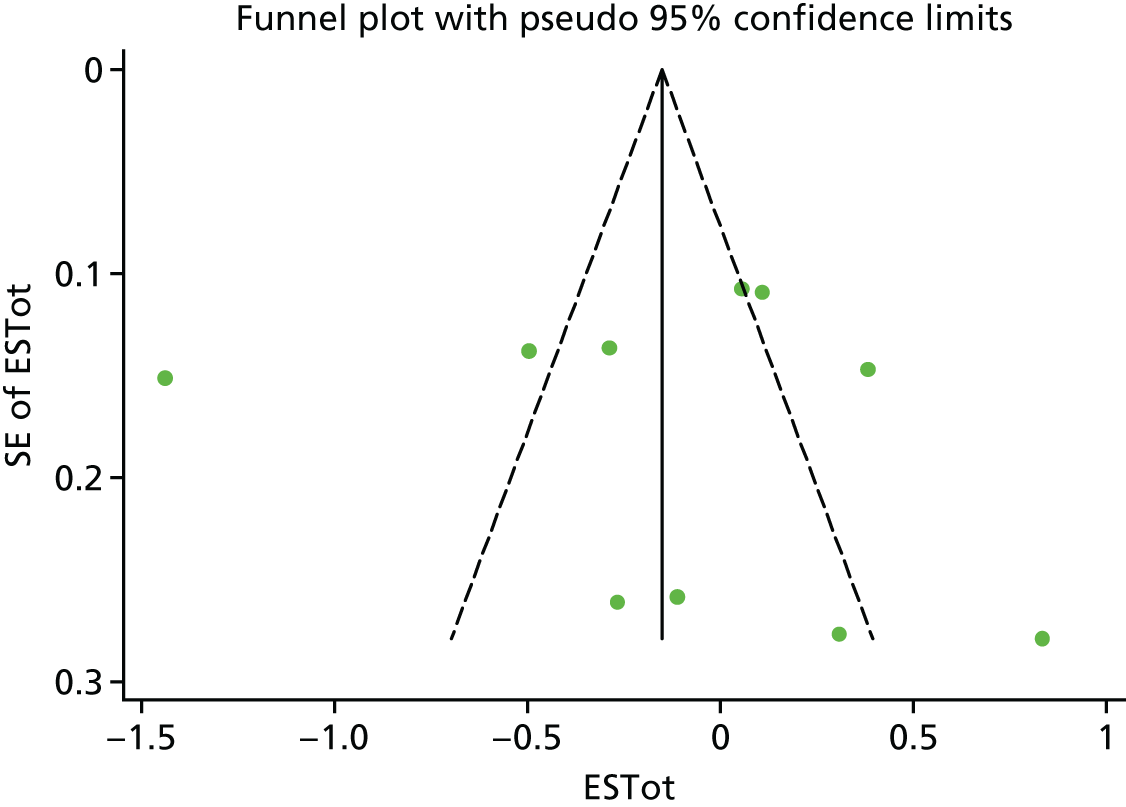
Potential for publication bias in QoL outcomes was observed (Egger’s bias 0.79, 95% CI 0.08 to 1.51; p = 0.03). This result is most likely influenced by a single study on the bottom left-hand side of the funnel plot. No evidence of publication bias was observed for hospital admissions (Egger’s bias 0.16, 95% CI –0.82 to 1.14; p = 0.74), emergency visits (Egger’s bias –0.19, 95% CI –1.00 to 0.62; p = 0.64) or total costs (Egger’s bias –3.40, 95% CI –15.25 to 8.46; p = 0.53), although the low power of this final test means that publication bias cannot definitely be ruled out.
Evidence context
The degree to which the results of a trial conducted in a particular setting can be generalised to a different setting (i.e. the external validity), is always an issue in the interpretation of findings of systematic reviews. The impact of variation in context may be greater when considering complex service-related interventions, which are designed to have an impact on individual behaviour, or when the focus is on utilisation outcomes, which may themselves reflect important differences in the context in which the study is run.
To explore this issue, we calculated overall ESs for QoL, hospitalisation, ED visits and total costs by country, to assess whether or not the effect of self-care interventions on these outcomes varied markedly between UK and non-UK settings. The results are shown in Table 11; analyses appear robust. The effects of self-care support on QoL are non-significant in the UK context, a difference that most likely reflects the smaller number of studies available and differences in precision of the pooled effects.
| Outcome | All studies | Study origin | |
|---|---|---|---|
| UK | Non-UK | ||
| QoL | |||
| Pooled ES | –0.17 | –0.13 | –0.18 |
| 95% CI | –0.23 to –0.11 | –0.31 to 0.04 | –0.24 to –0.11 |
| Number of comparisons | 77 | 13 | 64 |
| I2 statistic (%) | 48 | 53 | 47 |
| Hospital admissions | |||
| Pooled ES | –0.05 | 0.01 | –0.06 |
| 95% CI | –0.12 to 0.03 | –0.20 to 0.21 | –0.13 to 0.02 |
| Number of comparisons | 65 | 10 | 55 |
| I2 statistic (%) | 35 | 53 | 30 |
| Emergency visits | |||
| Pooled ES | –0.11 | –0.15 | 0.13 |
| 95% CI | –0.17 to –0.04 | –0.21 to –0.08 | –0.05 to 0.30 |
| Number of comparisons | 57 | 10 | 47 |
| I2 statistic (%) | 38 | 25 | 30 |
| Total costs | |||
| Pooled ES | –0.11 | –0.11 | –0.28 |
| 95% CI | –0.47 to 0.25 | –0.11 to 0.33 | –0.89 to 0.33 |
| Number of comparisons | 10 | 5 | 5 |
| I2 statistic (%) | 92 | 43 | 96 |
When analyses were limited to UK studies, self-care support continued to be associated with statistically significant reductions in ED visits; this result did not hold for studies conducted outside the UK. Direct comparison of the two is limited in the sense that many other factors may also differ between studies that are assigned to different groups on the basis of research origin.
Intervention implementation
The external validity of research studies can improve the sustainable adoption and implementation of effective, generalisable, evidence-based interventions. The RE-AIM framework65 identities five pieces of information that are necessary to translate research into action. These are:
-
reach
-
effectiveness
-
adoption
-
implementation
-
maintenance.
Reach
The reach of health behaviour interventions refers to the absolute number, proportion and representativeness of individuals who receive it. Generally, data on such issues are poorly reported in trials and often the data that are reported are not comparable between studies. We extracted data from trials on the proportion of eligible patients who did not take part, these data are presented in Appendix 10. Participation rates were unclear or not reported in 27 studies (28% of the data set). The average participation rate across the remaining studies was 70%, with a range of 13–100%. Interpretation of these data are difficult because of the variation and ambiguity in the exact recruitment procedures employed by each study involved for effective comparison. Sample representativeness was not reported in 39 studies; 50 studies reported study exclusion criteria, including acute and comorbid long-term health conditions.
Effectiveness
Effectiveness is defined as the impact of an intervention on important outcomes, including potential negative effects, QoL and economic outcomes. In this review, the effects of self-care are presented in forest and permutation plots, including any potential detrimental effects on QoL. The validity of the conclusions drawn at each stage remains dependent on the size of the evidence base and its scientific rigour. Limitations in the primary evidence base are considered, where appropriate, and a sensitivity analysis based on evidence quality has been carried out. Limitations in review procedures are discussed in the following chapter (see Chapter 4).
Adoption
The adoption of health behaviour interventions is dependent on the absolute number, proportion and representativeness of the settings and facilitators delivering a programme. Data relating to the proportion and representativeness of the settings used in the primary research studies were rarely reported. We have used subgroup analyses to compare the effects of self-care support delivered in different intervention settings. We extracted detailed information on intervention setting, size and facilitator expertise and present these data in Appendix 10. In our review, the vast majority of interventions (n = 95, 83%) were delivered by qualified health professionals or paraprofessionals (i.e. workers with formal tertiary education or training). Only four interventions were delivered by lay health workers (receiving only informal job-related training). One additional study included a lay health worker as part of a multidisciplinary team.
Implementation
Implementation refers to a study’s fidelity to an intervention protocol. This includes consistency of intervention delivery and the time and costs required to deliver the intervention as intended of the intervention. Twenty-four studies (25%) did not report any process measures. The majority of the remaining studies reported basic data on patient engagement. Lack of data pertaining to facilitator engagement and intervention fidelity means it is difficult to know the extent to which interventions were delivered as intended.
Maintenance
Maintenance in the RE-AIM framework refers to the long-term effects of an intervention on individual patient or organisational outcomes ≥ 6 months after intervention completion. Where multiple data points were reported in the primary studies, we selected outcomes closest to a 12-month follow-up. The mean (SD) follow-up duration for the data extracted for our review was 10.4 (SD 4.6) months.
Chapter 4 Discussion and conclusions
The review reported here aimed to take account of health-care utilisation and costs in conjunction with health outcomes to provide evidence-based guidance on the provision of cost-effective self-care support for children and young people with long-term physical and mental health conditions.
We identified evidence across a range of physical and mental health LTCs, although the vast majority of our included studies evaluated self-care support for asthma. Evidence was available for a range of self-care interventions, differing in nature, primary target (i.e. child or young person, parent or family) and the total amount of support provided. More often self-care support was ‘intensively facilitated,’ meaning that it exceeded four sessions or 2 hours in total. Most frequently, self-care support was delivered face to face by qualified HCPs who worked with individual patients or families at home or in outpatient settings.
A moderately sized evidence base enabled meaningful assessments of the impact of self-care support on children and young people’s QoL and hospital admissions. A total of 77 and 65 studies contributed data to meta-analyses of these outcomes, respectively. A comparable-sized evidence base (57 comparisons) permitted exploratory analyses of the effects of self-care support on emergency visits; this outcome was prioritised by patients in our PPI consultation. Comparatively fewer data demonstrated the effects of self-care support on total health service costs. Alternative forms of health-care use (e.g. primary care visits) were inconsistently reported and not amenable to meta-analysis.
The available evidence base was of moderate quality; almost half of all studies reported adequate methods to randomly allocate participants to treatment or control conditions and reported adequate allocation concealment. The mean baseline samples size was 215 (SD 209) participants.
In line with our protocol, we legitimately excluded studies that failed to report both clinical and economic outcomes. In this reduced data set, self-care support was associated with statistically significant, minimal benefits for QoL, but lacked clear benefit for hospital admissions and costs. This finding endured across different levels of evidence quality, intervention intensities and LTCs. Statistically significant but minimal reductions in ED use were observed.
Subgroup analyses revealed statistically significant, minimal reductions in ED use for children aged < 13 years, children and young people with asthma and children and young people receiving > 2 hours per four sessions of self-care support. Preliminary evidence suggests that interventions that include the child or young person, and deliver at least some content individually, may optimise QoL effects. Face-to-face delivery may be necessary to maximise impact on ED use. Limitations in the primary data demand that these results are treated with caution.
Review strengths and limitations
Our study was conducted and reported in line with current systematic review guidance. 62,63 Conceptual blurring within the literature means that self-care support is inconsistently defined. We deliberately used broad search criteria to maximise the likelihood that all relevant evidence was identified.
-
Designing effective search strategies for broadly defined concepts can be challenging and success invariably relies on the presence (or absence) of specific terms in the titles or abstracts of the papers that are identified. Although the risk is small, it is possible that some studies that met our definition of self-care support did not use any of our selected search terms and were thus not identified and included in our review. It is difficult to assess the bias that this may have generated. Self-care support is arguably more clearly defined in the physical health literature, where self-care typically focuses on education and illness management, than it is in the mental health literature, where support to develop problem-solving skills or address emotional challenges may also be framed as psychological therapy (e.g. guided self-help, parenting programmes or cognitive–behavioural therapy). Iterative and rigorous search development, tested against a set of known studies, enabled a comprehensive list of search terms to be compiled. Reference checking and forward citation searching provided further reassurance that relevant evidence had not been missed.
The broad scope of our search criteria, together with a relatively rapid time scale for our review, inevitably necessitated some methodological compromises. A higher number of studies than we expected was eligible for our review, which impacted on our assessment of evidence quality. We categorised our studies according to a recognised hierarchy of study designs and used a single parameter, allocation concealment, as a reliable indicator of trial quality. The Cochrane Collaboration advocates assessing risk of bias across multiple domains, but does not recommend that these assessments are summed to derive a single indicator of study quality. Sensitivity analyses necessitated grouping studies on the basis of one measure of study quality and allocation concealment is the aspect of trial quality most consistently associated with treatment effect. 68 We report other aspects of evidence quality, such as study design, in our detailed study tables (see Appendix 5).
Intervention descriptors, such as quality assessment, were largely dependent on the quantity and clarity of the information reported in the primary research papers. No definitive framework of self-care support interventions for children and young people exists. We thus adopted a generic definition of self-care support for screening purposes and worked with our project advisory panels to refine a post hoc typology of self-care support interventions. We used two independent researchers for all study eligibility decisions, including preliminary title and abstract screening. Intervention characteristics, categorisation and effects (i.e. outcome data) were also independently extracted. Any unidentified errors would be more likely to introduce imprecision than bias.
We adopted broad inclusion criteria for intervention eligibility and also adopted a broad approach to meta-analysis, using wide inclusion criteria to categorise intervention and patient groups. We combined data across different types and intensities of self-care support interventions and across different types of long-term mental health conditions. Consensus on how best to deal with clinically heterogeneous evidence is lacking. 62 We acknowledge that pooling more homogeneous groups of studies may have advantages. Where the size of an evidence base is sufficient to enable meaningful division, such analyses can usefully inform service design and decision-making. However, excessive splitting between intervention types and patient groups reduces precision, risks multiple testing problems and may overemphasise minor differences between study groupings. 201 It is also highly dependent on valid and reliable classifications of patients and interventions, which can be difficult both in principle (when consensus over such classification is lacking) and in practice (when reporting is suboptimal). We adopted a strategy that took a broad approach as the primary analysis, but we conducted subgroup analyses to identify possible intervention characteristics that may have influenced treatment effect.
Our approach sought to identify the maximum amount of quantitative evidence available relative to the aims of our brief and to balance this with meaningful analysis. Our emphasis was on children and young people’s own subjective assessments of QoL. Where these were not available, we used parent-reported QoL measures, or patient- or parent-reported symptom measures, as proxy indicators of children and young people’s QoL. HRQoL typically prioritises those domains of health and well-being that fall under the influence of health-care systems, policy-makers and providers,202 and is a particularly valuable tool in the assessment of behavioural and psychological interventions. However, the inherent subjectivity of QoL belies some unique challenges to its measurement. Limited evidence suggests that parental reports may be more accurate than those of health professionals,203 but empirical investigations of the level of agreement between parent and child appraisals yields mixed results. 204 Difficulties arise in establishing the levels of agreement between two parents,205,206 the potential for bias within parental ratings and the potential differences in the life priorities of parents and children. 207 We pooled health status and QoL measures, and did not explore differences in the effects of self-care support observed with different outcome measures or raters.
Our emphasis on meta-analytic models meant that a minority of studies with incomplete but potentially relevant data had to be excluded. Alternative models of synthesis could have used a more narrative approach, although the ability of this method to draw valid conclusions about the relationships between our outcome variables is questionable. We tabulated study findings, as reported by the study authors, in those instances where data were unsuitable for meta-analysis.
The requirement that data were reported in a way that was amenable to meta-analysis for two outcomes could potentially have caused selection effects. Studies that were not eligible for meta-analysis were, in broad terms, older and smaller in size. It is unclear how exclusion of these trials may have influenced the pooled-effects, as many provided little or no narrative of their findings. We were unable to formally test the differences in the outcomes of the two studies because, by definition, we were unable to calculate standardised ESs for studies that were not suitable for meta-analysis.
Our analyses of small-study bias across the studies did not find any evidence of bias in relation to health-care utilisation, but there was evidence of possible bias in the QoL data. Selective publication of positive studies is one potential reason for asymmetry in the funnel plot. If present, this bias would mean that smaller studies in the review had overestimated intervention effects. We conducted targeted author searches for additional publications and/or unpublished data identified in conference abstracts, but did not extend our searches to grey literature or ongoing trial registries.
Our focus on quantitative evidence meant that we gained insights into intervention effect. We categorised our ESs according to magnitude, using a commonly accepted, yet somewhat arbitrary, classification system. From a patient’s perspective, ‘small’ or ‘minimal’ effects may have greater or lesser meaning depending on the outcome to which they are attributed. ED visits were identified by our PPI panel as a particularly important aspect of health service utilisation for children, young people and their parents, and it is conceivable that very small reductions in ED use may be important and potentially more meaningful than equivalent effects on QoL. We did not conduct a mixed-methods or qualitative review, which may offer additional insights into the acceptability of self-care support to children, young people and their families, their preferred content and delivery formats and the meaning that they attribute to these very different outcomes.
Implications of the study for policy and practice
Self-care support interventions have small but statistically significant effects on children and young people’s quality of life
This review is the first to simultaneously examine the effect of self-care support for LTCs on patient outcomes and health service utilisation in children and young people. Pooled ESs suggest that self-care support has a positive but minimal effect on QoL (ES of 0.17). Evidence is most robust for children and young people with asthma (ES of 0.15) and long-term mental health conditions (ES of 0.17). Lack of evidence for other conditions (or condition clusters) prohibits meaningful assessments of effect.
A pooled effect of 0.17 aligns well with the results of our preceding review, which used identical methods to establish the effects of self-care support for LTCs in adults. 26 In adult populations, self-care support is associated with small but statistically significant effects on QoL (ES of 0.22). 26
Direct comparison of our findings with other reviews of self-care support for children and young people is limited by fundamental differences in remits and scope. A prior review of the clinical effectiveness of self-care support interventions for children and young people with physical health conditions31 reported positive impacts on QoL, but synthesised data narratively and did not present standardised ESs derived from a meta-analysis of intervention effects. The effect of self-care support on the health status of children and young people with mental health conditions has been studied separately; in this instance pooled ESs of 0.20 and 0.12 were reported at 6 and 12 months, respectively. 32
The size and the scope of the evidence base differ between different reviews. These differences are not unusual and reflect both practical and methodological variances. Earlier reviews31,32 adopted different search dates and applied different eligibility criteria, stemming from their need to address different research aims. In line with our protocol, we legitimately excluded studies that failed to report both clinical and economic outcomes. This was because our review was designed to identify those models of self-care support that could reduce health services utilisation and costs, without compromising outcomes for children and young people. Only studies reporting both forms of data could answer this brief. A number of trials of self-care support have reported children and young people’s subjective QoL assessments, but have not simultaneously quantified the impact of these interventions on health service costs. We acknowledge that some evidence with broader relevance to our population may have been excluded by these studies failing to meet our inclusion criteria.
Our up-to-date and comprehensive review makes an important and meaningful contribution to service development and commissioning debates. When QoL was plotted against health service utilisation data, relatively fewer studies reported reductions in both outcomes. This suggests that any intention to use self-care support to reduce utilisation should therefore not raise concerns that these interventions routinely compromise patients’ QoL.
In drawing this conclusion, it is important to remember that study effects are conventionally reported at the level of the group. The available data apply only to those participants consenting to take part in the included research studies. Where reported, study participation rates appeared typical of behavioural intervention trials, but explorations of sample representativeness were limited by inconsistent data and ambiguous reporting. Our review focused solely on children and young people’s QoL and did not consider the impact of self-care support on parental or family outcomes. Thus, it may be prudent for health professionals to monitor the individual impact of self-care support, including any potential effects on these broader contexts, during routine consultations with their patients.
Self-care support interventions lack clear benefits for health service utilisation and cost
Having established that self-care support does not routinely compromise children and young people’s QoL, it becomes necessary to consider its effect on health-care utilisation and costs. On the basis of the current evidence, we cannot reliably conclude that self-care support significantly reduces overall health-care costs.
Analysis of the impact of self-care support on total costs (our primary analysis) was limited by a lack of available data. Pooled ESs suggest a minimal effect (ES of –0.11) on ED visits and a non-significant effect on hospital admissions (ES of –0.06). Lack of a statistically significant effect on hospital admissions endured across different intervention intensities, evidence quality levels and LTCs.
Small reductions in the number of ED visits may well confer multiple advantages on children, young people and their families, not least because accessing emergency care can be associated with acute emotional and logistical stressors. However, at a population level, uncertainty remains regarding the extent to which minimal reductions in emergency use can offset the costs of delivering self-care support and ameliorate the fiscal burdens facing contemporary health-care systems. Our exploratory subgroup analyses suggest that effects may be more pronounced in UK than in non-UK settings and that more intensively facilitated self-care support interventions may be necessary to secure minimal benefits for ED use. In the absence of meta-regression, these subgroup analyses are limited by the fact that many other factors may also differ between study groups.
Any analysis focused on a single aspect of health-care utilisation is vulnerable to error. Single aspects of health-care utilisation represent ‘partial’ cost data, which, by definition, neglect costs and cost changes elsewhere in the system. Arguably, cost shifting may have been a greater risk had substantial reductions in health service utilisation been revealed. In this instance, it would have become crucial to ascertain whether the observed effects reflected genuine reductions in health service use or whether costs had simply been transferred to other health-care sectors or on to patients. With the exception of ED visits and hospital admissions, health service utilisation data were inconsistently reported by the primary studies in our review. This lack of transparent and standardised reporting means that we cannot be certain that other cost changes were not encountered.
Total cost outcome data are necessary to provide policy-makers and service providers with clear evidence of the efficiency (or otherwise) of self-care support. By definition, these data sum costs across all service sectors and include the costs of delivering the intervention that is intended to generate these cost changes. Few primary studies reported total cost data in the current review, prohibiting this more robust analysis.
Health utilisation outcomes rarely distinguish between ‘necessary’ and ‘avoidable’ service use. 26 Such distinctions are not common in the self-care support literature, partly because the difference is conceptually and logistically difficult to assess. 208 An implicit assumption underlying self-care support is that it reduces ‘avoidable’ health service contacts, either by improving a person’s overall health and/or by precipitating more effective crisis responses. Some of the studies in our review distinguished between scheduled and non-scheduled health service use, but did not report care appropriateness per se. We did not distinguish between elective and unplanned admissions in our analysis, nor did we distinguish between legitimate and inappropriate ED use. The effects of self-care support interventions on these different forms of health service utilisation may conceivably be very different.
The optimal assessment of the hypothesis underlying this review would have been to restrict our analysis to the most comprehensive assessment of costs, including those related to NHS service use, social care and other services (e.g. the cost of additional or alternative education for children and young people living with LTCs). Multiple family expenses may be incurred when a child or young person lives with a LTC and arguably the impact of self-care support on families’ out-of-pocket expenses and productivity need to be examined. There are inherent challenges in evaluating the economic effects of self-care support from this broader ‘societal perspective’.
From an operational perspective, it is difficult to foresee how self-care support interventions justified from a societal perspective will be implemented. 209 This is because the budgets for different service sectors are fixed and/or the financial transfers which would be needed between them are not always possible. Although any necessary reallocation of resources can be identified, transfers between sectors are not always considered desirable or feasible. 210 From an evaluative perspective, comprehensive costing of self-care support interventions is rare and generally restricted to formal economic analyses. Our review included 97 studies, of which only 35 reported formal economic analyses. The broader evidence base included in our review is reflective of a larger number of studies that report useful data on health service utilisation. Systematic assessment of this wider literature makes an important and much-needed contribution to policy and service development.
A global economic crisis means that substantial effort continues to be invested in improving the efficiency of health-care systems. Yet, despite self-care being advocated as a key method of increasing service efficiency, there remains uncertainty regarding the scale of the contribution that can be made. Although a previous review has suggested that self-care support interventions may reduce hospital use and total costs in adults, our study has demonstrated potentially smaller effects in children and young people. Understanding the reason for these differences may be an important focus for future research efforts.
Insufficient evidence of an effect of self-care support on children and young people’s health service utilisation raises important questions regarding the primary drivers for its use. Self-care support resonates with multiple policy strategies, including philosophical shifts towards partnership working and the delivery of personalised care. 33 In children and young people, self-care support may offer an early and otherwise unavailable opportunity to negotiate LTC management, maximise adult health outcomes and make a potentially longer-term, sustained contribution to service utilisation. 31,39 Consideration must thus be given to both its processes and outcomes, and the potential breadth of benefits that it will confer. Specific attention should be given to different stakeholder perspectives and whose views – population, policy, professional or patient – are the most important when minimal effects on QoL and health service utilisation are observed.
The impact of self-care support interventions may depend less on intervention intensity and more on its delivery mechanisms
Rigorous evaluation of the efficiency of self-care support interventions for children and young people with LTCs demands concurrent evaluation of patient well-being and health utilisation effects. The suggestion that self-care support may minimally benefit QoL, but not translate into marked benefits for health service use held, across different age groups, intervention intensities and settings. Constraints on the number of data underpinning these results demand some caution in their interpretation.
In line with our protocol and previous review,26 we categorised intervention intensity according to a broad typology and compared pure or facilitated self-care support with more intensively facilitated or case-managed care. The threshold for intensive facilitation took account of both amount of self-care support (> 2 hours or four sessions), as well as the nature of the support provided. This threshold was an arbitrary empirical threshold that provided a reasonable distribution of studies among the different categories.
Reductions in ED use were not consistent across LTCs or intervention type. Preliminary analyses suggest a significant reduction in emergency use for children aged < 13 years, children and young people with asthma and children and young people receiving more intensively facilitated self-care support interventions. However, the existing evidence base is of only moderate size and these different findings will, in part, reflect differences in the number of studies available and the precision of the pooled effects.
Pooled effects suggest a significant benefit for self-care support interventions for asthma that is not confirmed in mental health. Self-care support interventions for children and young people can vary considerably in the extent to which they target different service utilisation behaviours and this potential influence may be meaningful. It is plausible, for example, that, although written action plans to control asthma exacerbations may play a direct role in avoiding ED visits, self-care support for mental health may be more focused on longer-term recovery and patient empowerment. Notably, however, the potential burden of these different intervention models may also differ. Preliminary data in our permutation plots suggest that, although self-care support interventions can reduce utilisation for children and young people with asthma, compromises in their QoL cannot definitively be ruled out. Compromises in QoL were less evident for mental health conditions, although meaningful interpretation is currently limited by a lack of available data.
Our review did not explore differences in the effects of interventions with different content; this information was inconsistently reported by the primary studies in our review. Service developers might usefully explore the process and content of those interventions that did and did not compromise outcomes in the current review to assess the implications of this for future service design. Direct consideration of the aim and purpose of different self-care support interventions, including the rationale for delivering higher-intensity self-care support, may benefit service delivery.
Optimal assessment of the effects of more and less intensive self-care support demands a head-to-head comparison. Only six trials in our review adopted this design. 79,98,99,111,178,191 Meta-regression is possible, but has limited utility in moderate-to-small data sets as a result of a lack of available power. The variability that we observed in intervention descriptions also challenges its use. Lack of standardisation in the terminology and level of detail used to describe self-care support interventions meant that meta-regression had limited function in the context of the current evidence base.
The available evidence suggests that the effect of self-care support on children and young people’s QoL may be optimised by interventions that include the child or young person and deliver at least some of their content to an individual or individual family. Preliminary analyses suggest that face-to-face delivery may be necessary to secure minimal benefits for ED use but, at present, the evidence base does not discriminate between outpatient clinic or community settings. Further research is needed to confirm which approach works best, in what context and for what condition. Without evidence to suggest that health service utilisation is differentially impacted by different delivery models, decisions regarding where or how to deliver self-care may usefully be determined by patient and practitioner preferences and available service resources.
Differences in the magnitude and pattern of effects that were observed across children and young people’s QoL and hospital admissions are subject to multiple interpretations. One explanation is that the magnitude or nature of the improvement in QoL is insufficient to reduce this aspect of children and young people’s utilisation. Another is that children and young people’s subjective health assessments remain somewhat independent of their service use. Self-care in relation to children and young people is known to be complex and conceptually different from that of adult populations. This is, in part, attributable to the role that parents play in managing their child’s condition and the potentially different psychosocial consequences of LTC management for children, their parents and families. 210 Any policy mandates that seek to change children and young people’s health behaviours must consider children’s autonomy in the health-care system and the broader social and family contexts in which decision-making is occurring. Those developing and designing self-care support interventions might usefully consider the extent to which reductions in utilisation are an explicit goal of the intervention, the extent to which health professionals are prepared and willing to transfer responsibility to families211 and the extent to which parents and young people are willing to receive it. 51–53
Our review has identified a potential area of conflict in the delivery of self-care support interventions. Although effects on QoL and ED use may be optimised by delivering interventions to individuals, group-based interventions may be more likely to result in demonstrable reductions to hospital admissions. Group-based models of self-care support have previously been reported to normalise chronic illness, reduce social isolation and develop the social networks of children, young people and their parents,31 while also offering potential cost savings through higher staff-to-child ratios. Any notion that they may also confer benefits on health service utilisation may thus appeal to service providers. However, limitations in the current evidence base mean that this result must be treated with caution and further research is necessary to test this hypothesis prior to significant investment in service development.
Implications for research and future research funding
Our findings have clear implications for future research. NHS commissioning agendas emphasise the development of evidence-based services that can demonstrate adequate standards of care delivery, quality of care for patients and value for money. The design of new, rigorous studies of self-care support for children and young people with long-term health conditions is likely to be a vital part of the evidence-gathering process for this new commissioning agenda.
The size and scope of the evidence base should be expanded to ascertain the effects of self-care support across a wider range of long-term conditions
Our review identified a much smaller evidence base than our previous review, which used comparable methods to evaluate self-care support interventions for LTCs in adults. The smaller evidence base in this review is consistent with the recognition that the majority of self-care research has been conducted with adult populations. There has been a lack of a cumulative approach to learning from studies of self-care support with children and young people, especially in relation to the health economic and utilisation literature. Prior work has acknowledged a lack of synthesis of the effects of self-care support intervention across different long-term health conditions. 31,32
An important observation is that the majority of self-care support interventions included in our review were designed and delivered to children and young people with asthma. This is perhaps not surprising given its prevalence in the child population. However, the incidence and/or survival rates of other conditions (e.g. diabetes and cystic fibrosis) are also increasing;59–61 and meeting the needs and priorities of these children and young people, their families and NHS services is likely to constitute a crucial element of statutory service planning in the future. The generalisability of our findings to other long-term health conditions is not clear.
Our review identified a moderate evidence base for mental health conditions. This broad condition cluster encompassed a range of potential heterogeneous conditions, including (in relatively equal proportions) depression or anxiety, suicidality or self-harm, psychosis or schizophrenia and eating disorders. The decision to combine data across these different conditions was a methodological one, justified on the basis that this provided a reasonable number of studies for meta-analysis and permitted a broad cumulative assessment of the effects of self-care support interventions for mental health. A finer-grained analysis of the effects of self-care support on the different patient experiences and utilisation pathways that these conditions may precipitate demands the acquisition of a much bigger evidence base.
The generation of new evidence should adopt clear and consistent standards of data reporting, including comprehensive reporting of patient outcomes, utilisation and costs
Our review adopted a comprehensive and rigorous approach to study eligibility judgements and data synthesis. Our ability to conduct some of our analyses has been hampered by poor reporting of outcome data in primary studies. Although our typology of self-care support interventions was relatively simple, its application was complicated by variation in the amount of the detail provided, including lack of transparency regarding intervention personnel and the amount and nature of the support that they provided. More comprehensive, consistent and theory-led reporting of intervention content and processes would facilitate much more effective analyses of specific intervention ingredients.
We identified a notable number of studies (n = 19) that met our review inclusion criteria but failed to provide data amenable to meta-analysis. Deficiencies in outcome reporting are common and are not specific to our review, although the requirement that primary studies reported both QoL and utilisation outcomes meant that the impact of these deficiencies was inevitably more acute. More consistent and comprehensive reporting of data would enable more effective syntheses.
Our primary objective was to assess the ability of self-care support to reduce costs without compromising outcomes for children and young people. This objective does not map neatly onto conventional economic analyses, which focus on incremental cost-effectiveness ratios (ICERs) and associated net mean benefit statistics. Traditionally, interventions that increase costs, but provide significant health benefits for children, might attract support from decision-makers, who would then face decisions about which other interventions (with less attractive cost-effectiveness profiles) might be replaced. The current research aimed to establish whether or not cost savings could be made without comprising patient health.
The primary analysis identified in our protocol was on total costs. We applied liberal inclusion criteria to the cost outcomes included in our forest and permutation plots, and included data where it represented a composite measure of health service costs. However, inconsistencies in data reporting meant that not all studies included all sources of health service or intervention delivery costs. As such, some outcomes may have fallen short of what would conventionally be considered a comprehensive assessment of NHS costs. No clear relationship between patient outcomes and costs was evident in the permutation plot, although only a small number of comparisons was available for meta-analysis and variability across studies was high. Lack of data availability meant that we could not accurately assess the robustness of our secondary analyses, which we based on partial costs.
Our protocol stipulated that our secondary analyses would, where data allowed, sequentially explore the effect of self-care support on inpatient, outpatient, primary care and community care resources. We also intended to assess the effect of self-care support on prescribed medication and patients’ and families’ out-of-pocket expenditures. Lack of consistent measurement and ambiguity in the data available meant that these analyses could not be carried out.
From the patient perspective, any positive effect of self-care support on QoL is likely to be appraised and interpreted in the context of other gains and losses, including the costs incurred in engaging in self-care behaviours. Future studies should thus seek to establish which models of self-care support, if any, are associated with reduced service utilisation and explore, through the collection of comprehensive cost data, potential patterns of cost shifting between services and patients.
Potential differences in the shorter- and longer-term effects of self-care support for children and young people should be considered
Within the limits of the data available, our review suggests that self-care support may have minimal but positive impact on children’s QoL and lack clear benefits for health service utilisation. This finding is based on the short-term follow-up data reported by the primary studies in our review. Where multiple follow-up assessments were conducted, we extracted data closest to a 12-month assessment.
Self-care support for children and young people may have an early and valuable part to play in developing self-efficacy, empowering patients and promoting positive health behaviours for LTC management. Insights into the processes underlying utilisation can be derived from adult studies, which suggest that reductions in health service use may be facilitated by shifting conceptions of reliance on traditional services and translating the acquisition of skills and practices into everyday routines. 26 Prior experiences and methods of contact with services appear to need explicit attention to transition successfully to greater self-care. 212 Giving early legitimacy to personal self-care strategies and modifying perceptions of risk may thus be a key way to reduce later service utilisation. Further research may usefully establish if, and if so, which models of self-care support for children and young people have had longer-term effects on QoL and health utilisation. Modelling the long-term economic consequences of improved health outcomes may be necessary to assess these effects, given the logistical difficulties of prolonged follow-up in clinical trials. Qualitative research into the reasons underpinning sustained health service utilisation in children and young people may also afford valuable insights for future service design.
Our review has treated self-care support as a discrete form of health technology that is bounded and capable of being delivered in a standardised form. The primary studies in our review evaluated interventions that lasted for a limited amount of time (median total duration 5 hours delivered over 12 weeks). An implicit assumption driving many self-care support initiatives is that relatively short-term interventions will lead to permanent behaviour change and deliver cumulative linear benefits for health utilisation as professional support is reduced over time. 26,32 Self-care support in children and young people inevitably occurs in the context of many other transient influences, including critical influences from parents and peers. 51–53,213 Fluctuations and complexity in the transfer of responsibilities from parents to young people are routinely acknowledged in the self-care literature50,214 and introduce a level of uncertainty into the likely durability of intervention effects.
Our review suggested similar effects on QoL and hospital admissions irrespective of the intensity of the self-care support interventions. Intensively facilitated or case-managed self-care support interventions were associated with significant but minimal reductions in ED use. Augmented or ongoing support may thus be a possible method of optimising shorter- and longer-term service benefits, but a critical question then becomes whether or not this additional input is justified on the basis of the additional value it confers.
Clearly, further primary research is indicated to explore whether or not new models of self-care support can achieve more powerful and consistent effects on utilisation. This work should follow standard models for the development of complex interventions215 and draw on relevant behavioural and social science models of patient experience and care access in LTCs. Primary research and meta-synthesis of qualitative data31,32 has identified key elements of self-care support that may be essential for children and young people, including the acquisition of knowledge and skills, child-centred services, peer and professional support and positive beliefs about the effectiveness of their self-care regimes. Synthesising these data with new primary research may facilitate the timely development of new and effective evidence-based services.
Once adequate evidence of impact is achieved, research priorities should transition to the implementation of self-care support at a wider population level. The potential for effective models of self-care support for children and young people to be disseminated widely remains unclear. The studies included in our review typically evaluated the effects of self-care support in small or selected samples. Information pertaining the potential reach and adoption of different intervention models was limited and intervention fidelity inadequately reported. Most of the literature we examined originated from outside the UK. It is not clear how well an international evidence base, accumulated over the last three decades, translates to contemporary NHS settings and cultures. Rigorous research, drawing on implementation science methodologies is required to determine the effectiveness and feasibly of self-care support in the context of routine service provision.
The views of children, young people and their parents
Our review is the first to simultaneously examine the effect of self-care support for LTCs on patient outcomes and health service utilisation in children and young people. In doing so, it acknowledges the potentially different interests of different stakeholder groups.
Different stakeholder communities can differ in their motivations and experiences of different research topics and their expectations of the actions that should be taken by others. Traditionally, distinction has been drawn between high-stake, high-influence communities (e.g. Department of Health policy-makers and commissioners) and high-stake, lower-influence groups216 (in this case, front-line health professionals, parents and children and young people living with long-term physical and mental health conditions).
Professionals, parents, children and young people on our advisory panels were engaged in helping us to frame the outcomes of our review and in interpreting our findings. To ensure that our recommendations remain grounded in patient and professional priorities, the broader views of these individuals are documented in points 1–7 below. These views are those expressed by our PPI panel and are not limited to research recommendations arising from our review’s findings. Suggestions for future research effort are provided but are not presented in priority order.
-
The current evidence base is not sufficiently developed to fully inform health policy decision-making. Further research is required to ascertain the effect of self-care support across a broader range of LTCs and to confirm which intervention characteristics (if any) optimise patient- and service-level effects. Such evidence is best generated through rigorously conducted RCTs.
-
There is a need to co-develop with patients, and their families, new evidence-based models of self-care support. These interventions should be designed to maximise benefits at both patient and population level and should be rigorously evaluated to determine their clinical effectiveness and cost-effectiveness.
-
Self-care is a life skill. Further research is needed to determine the longer-term effects of self-care support for children and young people. Primary research should include well-designed cohort studies with sustained (10-year) follow-ups.
-
Current evidence is limited to those patients who have volunteered to take part in research studies. Self-care support services and health services researchers need to consider the likely uptake, acceptability and impact of self-care support interventions for marginalised groups. These groups include looked-after children and children and young people with learning disabilities. New research studies should adopt innovative methods of patient recruitment.
-
Access to self-care support is important. Further effort should be directed towards the development of digital health technologies to facilitate self-care support. Research should explore barriers to, and enablers of, the implementation of these technologies in statutory services and the concurrent effects of these interventions on patient well-being, health service resources and costs.
-
Self-care support is challenging when patients have more than one LTC. Whole-systems development is needed to facilitate the integrated delivery of self-care support services. Further research is required to identify which models of self-care support (if any) are effective for children and young people with multiple LTCs.
-
Self-care can be expensive and can impact differently on different families. The costs of self-care support to children, parents and families should be quantified. The effect of self-care support on children and young people’s school attendance should be assessed.
Acknowledgements
We would like to thank Kath Wright and the staff at Centre for Reviews and Dissemination, University of York, for their assistance with the searches. We thank Dr Katherine Stothard, Dr Gill Norman and Professor Karina Lovell for their help with abstract screening and study eligibility judgements and Irene Sanchez for her help with the quality appraisal of economic evaluations. We are grateful to Caitlin McWilliams for her help in preparing the report.
We especially thank the children and young people, parents and health professionals who gave up their time to join our PPI advisory panel and whose experiences, thoughts and recommendations have shaped and informed our review.
Contributions of authors
Penny Bee wrote the protocol for the study, managed the project, assessed studies for inclusion, extracted data on all studies, facilitated PPI contributions and had primary responsibility for writing the report.
Rebecca Pedley assessed studies for inclusion, extracted data on all studies, conducted analyses and wrote the report.
Amber Rithalia assessed studies for inclusion, extracted data on all studies and assisted with analyses.
Gerry Richardson contributed to the protocol for the study, extracted data on economic evaluations, advised on economic methodology and contributed to the writing of the report.
Steven Pryjmachuk contributed to the protocol for the study, assessed studies for inclusion and contributed to the writing of the report.
Susan Kirk contributed to the protocol for the study, assessed studies for inclusion, facilitated PPI contributions and contributed to the writing of the report.
Peter Bower contributed to the study protocol, guided review procedures, extracted study outcome data, led data analysis and contributed to the writing of the report.
Data sharing statement
This is a secondary research study and, therefore, no primary data have been generated. Further information can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Lopez AD, Murray CJ. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Boston, MA: Harvard School of Public Health on behalf of the World Bank; 1996.
- Epping-Jordan JE, Pruitt SD, Bengoa R, Wagner EH. Improving the quality of health care for chronic conditions. Qual Saf Health Care 2004;13:299-305. https://doi.org/10.1136/qhc.13.4.299.
- Five Year Forward View. Redditch: NHS England; 2014.
- The Mandate: A Mandate from the Government to the NHS Commissioning Board: April 2013 to March 2015. London: Department of Health; 2012.
- Choosing Health: Making Healthy Choices Easier. London: Her Majesty’s Stationery Office; 2004.
- The NHS Improvement Plan: Putting People at the Heart Of Public Services. London: Her Majesty’s Stationery Office; 2004.
- Supporting People with Long Term Conditions: An NHS and Social Care Model to Support Local Innovation and Integration. London: Her Majesty’s Stationery Office; 2005.
- Self Care: A Real Choice – Self-Care Support – A Practical Option. London: Her Majesty’s Stationery Office; 2005.
- Our Health, Our Care, Our Say: A New Direction for Community Services. London: Her Majesty’s Stationery Office; 2006.
- Supporting People with Long Term Conditions to Self Care: A Guide to Developing Local Strategies and Good Practice. London: Her Majesty’s Stationery Office; 2006.
- Long Term Conditions Compendium of Information. London: Department of Health; 2012.
- Equity and Excellence: Liberating the NHS. London: Her Majesty’s Stationery Office; 2010.
- Common Core Principles to Support Self-Care. London: Her Majesty’s Stationery Office; 2008.
- Wanless D. Securing Our Future Health: Taking a Long-Term View. London: Her Majesty’s Stationery Office; 2002.
- Supporting Self-Care: The Contribution of Nurses and Physicians. Ottawa, ON: Health Canada; 2002.
- Bury M, Newbould J, Taylor D. A Rapid Review of the Current State of knowledge Regarding Lay-Led Self-Management of Chronic Illness: Evidence Review. London: National Institute for Health and Care Excellence; 2005.
- Rogers A. Advancing the expert patient?. Prim Health Care Res Dev 2009;10:167-76. https://doi.org/10.1017/S1463423609001194.
- Lorig KR, Sobel DS, Stewart AL, Brown BW, Bandura A, Ritter P, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care 1999;37:5-14. https://doi.org/10.1097/00005650-199901000-00003.
- Griffiths C, Foster G, Ramsay J, Eldridge S, Taylor S. How effective are expert patient (lay led) education programmes for chronic disease?. BMJ 2007;334:1254-6. https://doi.org/10.1136/bmj.39227.698785.47.
- Guendelman S, Meade K, Benson M, Chen YQ, Samuels S. Improving asthma outcomes and self-management behaviors of inner-city children: a randomized trial of the Health Buddy interactive device and an asthma diary. Arch Pediatr Adolesc Med 2002;156:114-20. https://doi.org/10.1001/archpedi.156.2.114.
- Stevens CA, Wesseldine LJ, Couriel JM, Dyer AJ, Osman LM, Silverman M. Parental education and guided self-management of asthma and wheezing in the pre-school child: a randomised controlled trial. Thorax 2002;57:39-44. https://doi.org/10.1136/thorax.57.1.39.
- McPherson AC, Glazebrook C, Forster D, James C, Smyth A. A randomized, controlled trial of an interactive educational computer package for children with asthma. Pediatrics 2006;117:1046-54. https://doi.org/10.1542/peds.2005-0666.
- Wesseldine LJ, McCarthy P, Silverman M. Structured discharge procedure for children admitted to hospital with acute asthma: a randomised controlled trial of nursing practice. Arch Dis Child 1999;80:110-14. https://doi.org/10.1136/adc.80.2.110.
- Richardson G, Bojke C, Kennedy A, Reeves D, Bower P, Lee V, et al. What outcomes are important to patients with long term conditions? A discrete choice experiment. Value Health 2009;12:331-9. https://doi.org/10.1111/j.1524-4733.2008.00419.x.
- Kendall E, Rogers A. Extinguishing the social? State sponsored self-care policy and the Chronic Disease Self-management Programme. Disabil Soc 2007;22:129-43. https://doi.org/10.1080/09687590601141535.
- Panagioti M, Richardson G, Murray E, Rogers A, Kennedy A, Newman S, et al. Reducing Care Utilisation through Self-management Interventions (RECURSIVE): a systematic review and meta-analysis. Health Serv Deliv Res 2014;2.
- Skinner TC, John M, Hampson SE. Social support and personal models of diabetes as predictors of self-care and well-being: a longitudinal study of adolescents with diabetes. J Pediatr Psychol 2000;25:257-67. https://doi.org/10.1093/jpepsy/25.4.257.
- Kyngäs H, Rissanen M. Support as a crucial predictor of good compliance of adolescents with a chronic disease. J Clin Nurs 2001;10:767-74. https://doi.org/10.1046/j.1365-2702.2001.00538.x.
- Dashiff CJ, McCaleb A, Cull V. Self-care of young adolescents with type 1 diabetes. J Pediatr Nurs 2006;21:222-32. https://doi.org/10.1016/j.pedn.2005.07.013.
- Herrman JW. Children’s and young adolescents’ voices: perceptions of the costs and rewards of diabetes and its treatment. J Pediatr Nurs 2006;21:211-21. https://doi.org/10.1016/j.pedn.2005.07.012.
- Kirk S, Beatty S, Callery P, Milnes L, Pryjmachuk S. Evaluating Self-Care Support for Children and Young People with Long-Term Conditions. Southampton: NIHR, Service Delivery and Organisation Programme; 2010.
- Pryjmachuk S, Elvey R, Kirk S, Kendal S, Bower P, Catchpole R. Developing a model of mental health self-care support for children and young people through an integrated evaluation of available types of provision involving systematic review, meta-analysis and case study. Health Serv Deliv Res 2014;2. http://doi.org/10.3310/hsdr02180.
- Kirk S, Pryjmachuk S. Self-care of young people with long-term physical and mental health conditions. Nurs Child Young People 2016;28:20-8. https://doi.org/10.7748/ncyp.2016.e761.
- Gillard S, Edwards C, White S, White R, Adams K, Davies L, et al. The Barriers and Facilitators of Supporting Self Care in Mental Health NHS Trusts. Southampton: NIHR, Service Delivery and Organisation Programme; 2010.
- Yi JP, Vitaliano PP, Smith RE, Yi JC, Weinger K. The role of resilience on psychological adjustment and physical health in patients with diabetes. Br J Health Psychol 2008;13:311-25. https://doi.org/10.1348/135910707X186994.
- Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Patient Educ Couns 2002;48:177-87. https://doi.org/10.1016/S0738-3991(02)00032-0.
- Boger E, Ellis J, Latter S, Foster C, Kennedy A, Jones F, et al. Self-management and self-management support outcomes: a systematic review and mixed research synthesis of stakeholder views. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0130990.
- Improving Children and Young People’s Health Outcomes: A System Wide Response. London: Her Majesty’s Stationery Office; 2013.
- Chief Medical Officer’s Annual Report 2012: Our Children Deserve Better: Prevention Pays. London: Her Majesty’s Stationery Office; 2013.
- Green H, McGinnity Á, Meltzer H, Ford T, Goodman R. Mental Health of Children and Young People in Great Britain. A Survey Carried OUt by the Office for National Statistics on Behalf of the Department of Health and the Scottish Executive. Basingstoke: Palgrave Macmillan; 2004.
- Brooks F, Magnusson J, Klemera E, Spencer N, Morgan A. HBSC England National Report: Health Behaviour in School-Aged Children (HBSC): World Health Organization Collaborative Cross National Study. University of Hertfordshire: Department of Health/NHS England; 2015.
- Future in Mind Promoting, Protecting and Improving Our Children and Young People’s Mental Health and Wellbeing. London: Department of Health; 2015.
- National Service Framework for Children, Young People and Maternity Services: Children and Young People Who Are Ill. London: Department of Health; 2004.
- Healthy Lives, Brighter Futures. London: Her Majesty’s Stationery Office; 2009.
- Report of the Children and Young People’s Health Outcomes Forum 2014/15. London: Department of Health; 2015.
- Hawley K. Report on the Pilot of the Expert Patient Programme for Children January 2004–January 2005. London: Expert Patient Programme; 2005.
- Milnes LJ, Callery P. The adaptation of written self-management plans for children with asthma. J Adv Nurs 2003;41:444-53. https://doi.org/10.1046/j.1365-2648.2003.02551.x.
- Kennedy A, Rogers A, Bower P. Support for self care for patients with chronic disease. BMJ 2007;335:968-70. https://doi.org/10.1136/bmj.39372.540903.94.
- Fisher EB, Brownson CA, O’Toole ML, Shetty G, Anwuri VV, Glasgow RE. Ecological approaches to self-management: the case of diabetes. Am J Public Health 2005;95:1523-35. https://doi.org/10.2105/AJPH.2005.066084.
- Giarelli E, Bernhardt BA, Mack R, Pyeritz RE. Adolescents’ transition to self-management of a chronic genetic disorder. Qual Health Res 2008;18:441-57. https://doi.org/10.1177/1049732308314853.
- Kirk S. Transitions in the lives of young people with complex healthcare needs. Child Care Health Dev 2008;34:567-75. https://doi.org/10.1111/j.1365-2214.2008.00862.x.
- Newbould J, Smith F, Francis SA. ‘I’m fine doing it on my own’: partnerships between young people and their parents in the management of medication for asthma and diabetes. J Child Health Care 2008;12:116-28. https://doi.org/10.1177/1367493508088549.
- Williams B, Mukhopadhyay S, Dowell J, Coyle J. From child to adult: an exploration of shifting family roles and responsibilities in managing physiotherapy for cystic fibrosis. Soc Sci Med 2007;65:2135-46. https://doi.org/10.1016/j.socscimed.2007.07.020.
- van Es SM, le Coq EM, Brouwer AI, Mesters I, Nagelkerke AF, Colland VT. Adherence-related behavior in adolescents with asthma: results from focus group interviews. J Asthma 1998;35:637-46. https://doi.org/10.3109/02770909809048966.
- Christian BJ, D’Auria JP, Fox LC. Gaining freedom: self-responsibility in adolescents with diabetes. Pediatr Nurs 1999;25:255-60.
- Bruzzese JM, Unikel L, Gallagher R, Evans D, Colland V. Feasibility and impact of a school-based intervention for families of urban adolescents with asthma: results from a randomized pilot trial. Fam Process 2008;47:95-113. https://doi.org/10.1111/j.1545-5300.2008.00241.x.
- Stinson J, Wilson R, Gill N, Yamada J, Holt J. A systematic review of internet-based self-management interventions for youth with health conditions. J Pediatr Psychol 2009;34:495-510. https://doi.org/10.1093/jpepsy/jsn115.
- Lindsay S, Kingsnorth S, Mcdougall C, Keating H. A systematic review of self-management interventions for children and youth with physical disabilities. Disabil Rehabil 2014;36:276-88. https://doi.org/10.3109/09638288.2013.785605.
- Dodge JA, Lewis PA, Stanton M, Wilsher J. Cystic fibrosis mortality and survival in the UK: 1947–2003. Eur Respir J 2007;29:522-6. https://doi.org/10.1183/09031936.00099506.
- Daley D, Jones K, Hutchings J, Thompson M. Attention deficit hyperactivity disorder in pre-school children: current findings, recommended interventions and future directions. Child Care Health and Dev 2009;35:754-66. https://doi.org/10.1111/j.1365-2214.2009.00938.x.
- Growing Up With Diabetes: Children and Young People with Diabetes in England. London: RCPCH; 2009.
- Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions (Version 5.0.1). London: The Cochrane Collaboration; 2009.
- EPOC Resources for Review Authors. Oslo: Norwegian Knowledge Centre for the Health Services; 2015.
- Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 2003;26:1-7. https://doi.org/10.1207/S15324796ABM2601_01.
- Tsiligianni I, Kocks J, Tzanakis N, Siafakas N, van der Molen T. Factors that influence disease-specific quality of life or health status in patients with COPD: a review and meta-analysis of Pearson correlations. Prim Care Respir J 2011;20:257-68. https://doi.org/10.4104/pcrj.2011.00029.
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999;89:1322-7. https://doi.org/10.2105/AJPH.89.9.1322.
- Drummond M, Stoddart G, Torrance G. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford Medical Publications; 1997.
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408-12. https://doi.org/10.1001/jama.1995.03520290060030.
- Pildal J, Hróbjartsson A, Jørgensen KJ, Hilden J, Altman DG, Gøtzsche PC. Impact of allocation concealment on conclusions drawn from meta-analyses of randomized trials. Int J Epidemiol 2007;36:847-57. https://doi.org/10.1093/ije/dym087.
- Lipsey M, Wilson D. Practical Meta-Analysis. Newbury Park, CA: Sage; 2001.
- Dieterich M, Irving CB, Park B, Marshall M. Intensive case management for severe mental illness. Cochrane Database Syst Rev 2010;10. https://doi.org/10.1002/14651858.CD007906.pub2.
- Altman DG, Bland JM. Detecting skewness from summary information. BMJ 1996;313. https://doi.org/10.1136/bmj.313.7066.1200.
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. https://doi.org/10.1136/bmj.327.7414.557.
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34. https://doi.org/10.1136/bmj.315.7109.629.
- Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol 2001;54:1046-55. https://doi.org/10.1016/S0895-4356(01)00377-8.
- Atherly A, Nurmagambetov T, Williams S, Griffith M. An economic evaluation of the school-based ‘power breathing’ asthma program. J Asthma 2009;46:596-9. https://doi.org/10.1080/02770900903006257.
- Bartholomew LK, Gold RS, Parcel GS, Czyzewski DI, Sockrider MM, Fernandez M, et al. Watch, discover, think, and act: evaluation of computer-assisted instruction to improve asthma self-management in inner-city children. Patient Educ Couns 2000;39:269-80. https://doi.org/10.1016/S0738-3991(99)00046-4.
- Bird SR, Noronha M, Kurowski W, Orkin C, Sinnott H. Integrated care facilitation model reduces use of hospital resources by patients with pediatric asthma. J Health Qual 2012;34:25-33. https://doi.org/10.1111/j.1945-1474.2011.00143.x.
- Brazil K, McLean L, Abbey D, Musselman C. The influence of health education on family management of childhood asthma. Patient Educ Couns 1997;30:107-18. https://doi.org/10.1016/S0738-3991(96)00913-5.
- Brown JV, Bakeman R, Celano MP, Demi AS, Kobrynski L, Wilson SR. Home-based asthma education of young low-income children and their families. J Pediatr Psychol 2002;27:677-88. https://doi.org/10.1093/jpepsy/27.8.677.
- Browning S, Corrigall R, Garety P, Emsley R, Jolley S. Psychological interventions for adolescent psychosis: a pilot controlled trial in routine care. Eur Psychiatry 2013;28:423-6. https://doi.org/10.1016/j.eurpsy.2013.05.008.
- Bruzzese JM, Sheares BJ, Vincent EJ, Du Y, Sadeghi H, Levison MJ, et al. Effects of a school-based intervention for urban adolescents with asthma. A controlled trial. Am J Respir Crit Care Med 2011;183:998-1006. https://doi.org/10.1164/rccm.201003-0429OC.
- Bryant-Stephens T, Kurian C, Guo R, Zhao H. Impact of a household environmental intervention delivered by lay health workers on asthma symptom control in urban, disadvantaged children with asthma. Am J Public Health 2009;99:S657-65. https://doi.org/10.2105/AJPH.2009.165423.
- Butz A, Pham L, Lewis L, Lewis C, Hill K, Walker J, et al. Rural children with asthma: impact of a parent and child asthma education program. J Asthma 2005;42:813-21. https://doi.org/10.1080/02770900500369850.
- Walker J, Winkelstein M, Land C, Lewis-Boyer L, Quartey R, Pham L, et al. Factors that influence quality of life in rural children with asthma and their parents. J Pediatr Health Care 2008;22:343-50. https://doi.org/10.1016/j.pedhc.2007.07.007.
- Butz A, Kub J, Donithan M, James NT, Thompson RE, Bellin M, et al. Influence of caregiver and provider communication on symptom days and medication use for inner-city children with asthma. J Asthma 2010;47:478-85. https://doi.org/10.3109/02770901003692793.
- Byford S, Harrington R, Torgerson D, Kerfoot M, Dyer E, Harrington V, et al. Cost-effectiveness analysis of a home-based social work intervention for children and adolescents who have deliberately poisoned themselves. Results of a randomised controlled trial. Br J Psychiatry 1999;174:56-62. https://doi.org/10.1192/bjp.174.1.56.
- Harrington R, Kerfoot M, Dyer E, McNiven F, Gill J, Harrington V, et al. Randomized trial of a home-based family intervention for children who have deliberately poisoned themselves. J Am Acad Child Adolesc Psychiatry 1998;37:512-18. https://doi.org/10.1016/S0890-8567(14)60001-0.
- Byford S, Barrett B, Roberts C, Wilkinson P, Dubicka B, Kelvin R, et al. Cost-effectiveness of selective serotonin reuptake inhibitors and routine specialist care with and without cognitive-behavioural therapy in adolescents with major depression. Br J Psychiatry 2007;191:521-7. https://doi.org/10.1192/bjp.bp.107.038984.
- Goodyer I, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al. Selective serotonin reuptake inhibitors (SSRIs) and routine specialist care with and without cognitive behaviour therapy in adolescents with major depression: randomised controlled trial. BMJ 2007;335. https://doi.org/10.1136/bmj.39224.494340.55.
- Byford S, Barrett B, Roberts C, Clark A, Edwards V, Smethurst N, et al. Economic evaluation of a randomised controlled trial for anorexia nervosa in adolescents. Br J Psychiatry 2007;191:436-40. https://doi.org/10.1192/bjp.bp.107.036806.
- Gowers SG, Clark A, Roberts C, Griffiths A, Edwards V, Bryan C, et al. Clinical effectiveness of treatments for anorexia nervosa in adolescents: randomised controlled trial. Br J Psychiatry 2007;191:427-35. https://doi.org/10.1192/bjp.bp.107.036764.
- Gowers SG, Clark AF, Roberts C, Byford S, Barrett B, Griffiths A, et al. A randomised controlled multicentre trial of treatments for adolescent anorexia nervosa including assessment of cost-effectiveness and patient acceptability – The TOuCAN trial. Health Technol Assess 2010;14. https://doi.org/10.3310/hta14150.
- Calvo A, Moreno M, Ruiz-Sancho A, Rapado-Castro M, Moreno C, Sánchez-Gutiérrez T, et al. Intervention for adolescents with early-onset psychosis and their families: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2014;53:688-96. https://doi.org/10.1016/j.jaac.2014.04.004.
- Cano-Garcinuño A, Díaz-Vázquez C, Carvajal-Urueña I, Praena-Crespo M, Gatti-Viñoly A, García-Guerra I. Group education on asthma for children and caregivers: a randomized, controlled trial addressing effects on morbidity and quality of life. J Invest Allerg Clin 2007;17:216-26.
- Carswell F, Robinson EJ, Hek G, Shenton T. A Bristol experience: benefits and cost of an ‘asthma nurse’ visiting the homes of asthmatic children. Bristol Med Chir J 1989;104:11-2.
- Celano MP, Holsey CN, Kobrynski LJ. Home-based family intervention for low-income children with asthma: a randomized controlled pilot study. J Fam Psychol 2012;26:171-8. https://doi.org/10.1037/a0027218.
- Chan DS, Callahan CW, Sheets SJ, Moreno CN, Malone FJ. An Internet-based store-and-forward video home telehealth system for improving asthma outcomes in children. Am J Health Syst Pharm 2003;60:1976-81.
- Chan DS, Callahan CW, Hatch-Pigott VB, Lawless A, Proffitt HL, Manning NE, et al. Internet-based home monitoring and education of children with asthma is comparable to ideal office-based care: results of a 1-year asthma in-home monitoring trial. Pediatrics 2007;119:569-78. https://doi.org/10.1542/peds.2006-1884.
- Christie D, Thompson R, Sawtell M, Allen E, Cairns J, Smith F, et al. Structured, intensive education maximising engagement, motivation and long-term change for children and young people with diabetes: a cluster randomised controlled trial with integral process and economic evaluation – the CASCADE study. Health Technol Assess 2014;18. https://doi.org/10.3310/hta18200.
- Cicutto L, Murphy S, Coutts D, O’Rourke J, Lang G, Chapman C, et al. Breaking the access barrier: evaluating an asthma center’s efforts to provide education to children with asthma in schools. Chest 2005;128:1928-35. https://doi.org/10.1378/chest.128.4.1928.
- Cicutto L, To T, Murphy S. A randomized controlled trial of a public health nurse-delivered asthma program to elementary schools. J School Health 2013;83:876-84. https://doi.org/10.1111/josh.12106.
- Clark NM, Gong M, Kaciroti N, Yu J, Wu G, Zeng Z, et al. A trial of asthma self-management in Beijing schools. Chronic Illn 2005;1:31-8. https://doi.org/10.1177/17423953050010010101.
- Cowie RL, Underwood MF, Little CB, Mitchell I, Spier S, Ford GT. Asthma in adolescents: a randomized, controlled trial of an asthma program for adolescents and young adults with severe asthma. Can Respir J 2002;9:253-9. https://doi.org/10.1155/2002/106262.
- Domino ME, Burns BJ, Silva SG, Kratochvil CJ, Vitiello B, Reinecke MA, et al. Cost-effectiveness of treatments for adolescent depression: results from TADS. Am J Psychiatry 2008;165:588-96. https://doi.org/10.1176/appi.ajp.2008.07101610.
- Domino ME, Foster EM, Vitiello B, Kratochvil CJ, Burns BJ, Silva SG, et al. Relative cost-effectiveness of treatments for adolescent depression: 36-week results from the TADS randomized trial. J Am Acad Child Adolesc Psychiatry 2009;48:711-20. https://doi.org/10.1097/CHI.0b013e3181a2b319.
- March J, Silva S, Vitiello B. TADS Team . The Treatment for Adolescents with Depression Study (TADS): methods and message at 12 weeks. J Am Acad Child Adolesc Psychiatry 2006;45:1393-403. https://doi.org/10.1097/01.chi.0000237709.35637.c0.
- March JS, Vitiello B. Clinical messages from the Treatment for Adolescents With Depression Study (TADS). Am J Psychiatry 2009;166:1118-23. https://doi.org/10.1176/appi.ajp.2009.08101606.
- Treatment for Adolescents with Depression Study (TADS) Team . The Treatment for Adolescents with Depression Study (TADS): demographic and clinical characteristics. J Am Acad Child Psy 2005;44:28-40. https://doi.org/10.1097/01.chi.0000145807.09027.82.
- Donaldson D, Spirito A, Esposito-Smythers C. Treatment for adolescents following a suicide attempt: results of a pilot trial. J Am Acad Child Adolesc Psychiatry 2005;44:113-20. https://doi.org/10.1097/00004583-200502000-00003.
- Dougherty GE, Soderstrom L, Schiffrin A. An economic evaluation of home care for children with newly diagnosed diabetes: results from a randomized controlled trial. Med Care 1998;36:586-98. https://doi.org/10.1097/00005650-199804000-00014.
- Dougherty G, Schiffrin A, White D, Soderstrom L, Sufrategui M. Home-based management can achieve intensification cost-effectively in type I diabetes. Pediatrics 1999;103:122-8. https://doi.org/10.1542/peds.103.1.122.
- Eakin MN, Rand CS, Bilderback A, Bollinger ME, Butz A, Kandasamy V, et al. Asthma in Head Start children: effects of the Breathmobile program and family communication on asthma outcomes. J Allergy Clin Immunol 2012;129:664-70. https://doi.org/10.1016/j.jaci.2011.10.013.
- Edwards RT, Céilleachair A, Bywater T, Hughes DA, Hutchings J. Parenting programme for parents of children at risk of developing conduct disorder: cost effectiveness analysis. BMJ 2007;334. https://doi.org/10.1136/bmj.39126.699421.55.
- Hutchings J, Gardner F, Bywater T, Daley D, Whitaker C, Jones K, et al. Parenting intervention in Sure Start services for children at risk of developing conduct disorder: pragmatic randomised controlled trial. BMJ 2007;334. https://doi.org/10.1136/bmj.39126.620799.55.
- Espinoza-Palma T, Zamorano A, Arancibia F, Bustos MF, Silva MJ, Cardenas C, et al. Effectiveness of asthma education with and without a self-management plan in hospitalized children. J Asthma 2009;46:906-10. https://doi.org/10.3109/02770900903199979.
- Esposito-Smythers C, Spirito A, Kahler CW, Hunt J, Monti P. Treatment of co-occurring substance abuse and suicidality among adolescents: a randomized trial. J Consult Clin Psychol 2011;79:728-39. https://doi.org/10.1037/a0026074.
- Farber HJ, Oliveria L. Trial of an asthma education program in an inner-city pediatric emergency department. Pediatr Asthma Aller 2004;17:107-15. https://doi.org/10.1089/0883187041269913.
- Flapper BC, Duiverman EJ, Gerritsen J, Postema K, van der Schans CP. Happiness to be gained in paediatric asthma care. Eur Respir J 2008;32:1555-62. https://doi.org/10.1183/09031936.00140407.
- Flores G, Bridon C, Torres S, Perez R, Walter T, Brotanek J, et al. Improving asthma outcomes in minority children: a randomized, controlled trial of parent mentors. Pediatrics 2009;124:1522-32. https://doi.org/10.1542/peds.2009-0230.
- Foster EM, Jensen PS, Schlander M, Pelham WE, Hechtman L, Arnold LE, et al. Treatment for ADHD: Is more complex treatment cost-effective for more complex cases?. Health Serv Res 2007;42:165-82. https://doi.org/10.1111/j.1475-6773.2006.00599.x.
- Swanson JM, Kraemer HC, Hinshaw SP, Arnold LE, Conners CK, Abikoff HB, et al. Clinical relevance of the primary findings of the MTA: success rates based on severity of ADHD and ODD symptoms at the end of treatment. J Am Acad Child Adolesc Psychiatry 2001;40:168-79. https://doi.org/10.1097/00004583-200102000-00011.
- Wells KC, Pelham WE, Kotkin RA, Hoza B, Abikoff HB, Abramowitz A, et al. Psychosocial treatment strategies in the MTA study: rationale, methods, and critical issues in design and implementation. J Abnorm Child Psychol 2000;28:483-505. https://doi.org/10.1023/A:1005174913412.
- Molina BS, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, et al. The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. J Am Acad Child Adolesc Psychiatry 2009;48:484-500. https://doi.org/10.1097/CHI.0b013e31819c23d0.
- Jensen PS, Garcia JA, Glied S, Crowe M, Foster M, Schlander M, et al. Cost-effectiveness of ADHD treatments: findings from the multimodal treatment study of children with ADHD. Am J Psychiatry 2005;162:1628-36. https://doi.org/10.1176/appi.ajp.162.9.1628.
- The MTA Cooperative Group . A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Arch Gen Psychiat 1999;56:1073-86. https://doi.org/10.1001/archpsyc.56.12.1073.
- Franklin VL, Waller A, Pagliari C, Greene SA. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabet Med 2006;23:1332-8. https://doi.org/10.1111/j.1464-5491.2006.01989.x.
- Galbreath AD, Smith B, Wood PR, Inscore S, Forkner E, Vazquez M, et al. Assessing the value of disease management: impact of 2 disease management strategies in an underserved asthma population. Ann Allergy Asthma Immunol 2008;101:599-607. https://doi.org/10.1016/S1081-1206(10)60222-0.
- Garbutt JM, Banister C, Highstein G, Sterkel R, Epstein J, Bruns J, et al. Telephone coaching for parents of children with asthma: impact and lessons learned. Arch Pediatr Adolesc Med 2010;164:625-30. https://doi.org/10.1001/archpediatrics.2010.91.
- Godart N, Berthoz S, Curt F, Perdereau F, Rein Z, Wallier J, et al. A randomized controlled trial of adjunctive family therapy and treatment as usual following inpatient treatment for anorexia nervosa adolescents. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0028249.
- Gorelick MH, Meurer JR, Walsh-Kelly CM, Brousseau DC, Grabowski L, Cohn J, et al. Emergency department allies: a controlled trial of two emergency department-based follow-up interventions to improve asthma outcomes in children. Pediatrics 2006;117:S127-34. https://doi.org/10.1542/peds.2005-2000J.
- Grainger-Rousseau TJ, Mc Elnay JC. A model for community pharmacist involvement with general practitioners in the management of asthma patients. J Appl Ther 1996;1:145-61.
- Green JM, Wood AJ, Kerfoot MJ, Trainor G, Roberts C, Rothwell J, et al. Group therapy for adolescents with repeated self harm: randomised controlled trial with economic evaluation. BMJ 2011;342. https://doi.org/10.1136/bmj.d682.
- Guendelman S, Meade K, Chen YQ, Benson M. Asthma control and hospitalizations among inner-city children: results of a randomized trial. Telemed J E Health 2004;10:6-14. https://doi.org/10.1089/1530562042632047.
- Hederos CA, Janson S, Hedlin G. Six-year follow-up of an intervention to improve the management of preschool children with asthma. Acta Paediatr 2009;98:1939-44. https://doi.org/10.1111/j.1651-2227.2009.01477.x.
- Hederos CA, Janson S, Hedlin G. Group discussions with parents have long-term positive effects on the management of asthma with good cost-benefit. Acta Paediatr 2005;94:602-8. https://doi.org/10.1080/08035250410023322.
- Homer C, Susskind O, Alpert HR, Owusu C, Schneider L, Rappaport LA, et al. An evaluation of an innovative multimedia educational software program for asthma management: report of a randomized, controlled trial. Pediatrics 2000;106:210-15.
- Horner SD, Brown A. Evaluating the effect of an asthma self-management intervention for rural families. J Asthma 2014;51:168-77. https://doi.org/10.3109/02770903.2013.855785.
- Hughes DM, McLeod M, Garner B, Goldbloom RB. Controlled trial of a home and ambulatory program for asthmatic children. Pediatrics 1991;87:54-61.
- Husted GR, Thorsteinsson B, Esbensen BA, Gluud C, Winkel P, Hommel E, et al. Effect of guided self-determination youth intervention integrated into outpatient visits versus treatment as usual on glycemic control and life skills: a randomized clinical trial in adolescents with type 1 diabetes. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-321.
- Indinnimeo L, Mercuri M, Marolla F, Raponi M, Ronchetti R. Asthma education program in outpatient children. Ital J Pediatr 1997;23:873-7.
- Indinnimeo L, Bonci E, Capra L, La Grutta S, Monaco F, Paravati F, et al. Clinical effects of a long-term educational program for children with asthma – Aironet. A 1-yr randomized controlled trial. Pediatr Allergy Immunol 2009;20:654-9. https://doi.org/10.1111/j.1399-3038.2009.00857.x.
- Joseph CL, Peterson E, Havstad S, Johnson CC, Hoerauf S, Stringer S, et al. A web-based, tailored asthma management program for urban African-American high school students. Am J Respir Crit Care Med 2007;175:888-95. https://doi.org/10.1164/rccm.200608-1244OC.
- Kamps JL, Rapoff MA, Roberts MC, Varela RE, Barnard M, Olson N. Improving adherence to inhaled corticosteroids in children with asthma: a pilot of a randomized clinical trial. Child Health Care 2008;37:261-77. https://doi.org/10.1080/02739610802437335.
- Kattan M, Stearns SC, Crain EF, Stout JW, Gergen PJ, Evans R, et al. Cost-effectiveness of a home-based environmental intervention for inner-city children with asthma. J Allergy Clin Immunol 2005;116:1058-63. https://doi.org/10.1016/j.jaci.2005.07.032.
- Morgan WJ, Crain EF, Gruchalla RS, O’Connor GT, Kattan M, Evans R, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med 2004;351:1068-80. https://doi.org/10.1056/NEJMoa032097.
- Katz LY, Cox BJ, Gunasekara S, Miller AL. Feasibility of dialectical behavior therapy for suicidal adolescent inpatients. J Am Acad Child Adolesc Psychiatry 2004;43:276-82. https://doi.org/10.1097/00004583-200403000-00008.
- Khan MS, O’Meara M, Stevermuer TL, Henry RL. Randomized controlled trial of asthma education after discharge from an emergency department. J Paediatr Child Health 2004;40:674-7. https://doi.org/10.1111/j.1440-1754.2004.00490.x.
- Khan MS, O’Meara M, Henry RL. Background severity of asthma in children discharged from the emergency department. J Paediatr Child Health 2003;39:432-5. https://doi.org/10.1046/j.1440-1754.2003.00183.x.
- Krieger J, Takaro TK, Song L, Beaudet N, Edwards K. A randomized controlled trial of asthma self-management support comparing clinic-based nurses and in-home community health workers: the Seattle-King County Healthy Homes II Project. Arch Pediat Adol Med 2009;163:141-9. https://doi.org/10.1001/archpediatrics.2008.532.
- Sunshine J, Song L, Krieger J. Written action plan use in inner-city children: is it independently associated with improved asthma outcomes?. Ann Allergy Asthma Immunol 2011;107:207-13. https://doi.org/10.1016/j.anai.2011.04.015.
- Krishna S, Francisco BD, Balas EA, König P, Graff GR, Madsen RW, et al. Internet-enabled interactive multimedia asthma education program: a randomized trial. Pediatrics 2003;111:503-10. https://doi.org/10.1542/peds.111.3.503.
- Krishna S, Balas EA, Francisco BD, Konig P. Effective and sustainable multimedia education for children with asthma: a randomized controlled trial. Child Health Care 2006;35:75-90. https://doi.org/10.1207/s15326888chc3501_7.
- Lewis CE, Rachelefsky G, Lewis MA, de la Sota A, Kaplan M. A randomized trial of A.C.T. (asthma care training) for kids. Pediatrics 1984;74:478-86.
- Lynch FL, Dickerson JF, Clarke G, Vitiello B, Porta G, Wagner KD, et al. Incremental cost-effectiveness of combined therapy vs medication only for youth with selective serotonin reuptake inhibitor-resistant depression: treatment of SSRI-resistant depression in adolescents trial findings. Arch Gen Psychiatry 2011;68:253-62. https://doi.org/10.1001/archgenpsychiatry.2011.9.
- Asarnow JR, Jaycox LH, Tang L, Duan N, LaBorde AP, Zeledon LR, et al. Long-term benefits of short-term quality improvement interventions for depressed youths in primary care. Am J Psychiatry 2009;166:1002-10. https://doi.org/10.1176/appi.ajp.2009.08121909.
- Brent D, Emslie G, Clarke G, Wagner KD, Asarnow JR, Keller M, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial. JAMA 2008;299:901-13. https://doi.org/10.1001/jama.299.8.901.
- Madge P, McColl J, Paton J. Impact of a nurse-led home management training programme in children admitted to hospital with acute asthma: a randomised controlled study. Thorax 1997;52:223-8. https://doi.org/10.1136/thx.52.3.223.
- Maslennikova GY, Morosova ME, Salman NV, Kulikov SM, Oganov RG. Asthma education programme in Russia: educating patients. Patient Educ Couns 1998;33:113-27. https://doi.org/10.1016/S0738-3991(97)00073-6.
- McGhan SL, Wong E, Jhangri GS, Wells HM, Michaelchuk DR, Boechler VL, et al. Evaluation of an education program for elementary school children with asthma. J Asthma 2003;40:523-33. https://doi.org/10.1081/JAS-120018785.
- McGhan SL, Wong E, Sharpe HM, Hessel PA, Mandhane P, Boechler VL, et al. A children’s asthma education program: Roaring Adventures of Puff (RAP), improves quality of life. Can Respir J 2010;17:67-73. https://doi.org/10.1155/2010/327650.
- Mehlum L, Tørmoen AJ, Ramberg M, Haga E, Diep LM, Laberg S, et al. Dialectical behavior therapy for adolescents with repeated suicidal and self-harming behavior: a randomized trial. J Am Acad Child Adolesc Psychiatry 2014;53:1082-91. https://doi.org/10.1016/j.jaac.2014.07.003.
- Mitchell EA, Ferguson V, Norwood M. Asthma education by community child health nurses. Arch Dis Child 1986;61:1184-9. https://doi.org/10.1136/adc.61.12.1184.
- Muntz R, Hutchings J, Edwards RT, Hounsome B, O’Céilleachair A. Economic evaluation of treatments for children with severe behavioural problems. J Ment Health Policy Econ 2004;7:177-89.
- Hutchings J, Appleton P, Smith M, Lane E, Nash S. Evaluation of two treatments for children with severe behaviour problems: child behaviour and maternal mental health outcomes. Behav Cogn Psychoth 2002;30:279-95. https://doi.org/10.1017/S1352465802003041.
- Nansel TR, Anderson BJ, Laffel LMB, Simons-Morton BG, Weissberg-Benchell J, Wysocki T, et al. A multisite trial of a clinic-integrated intervention for promoting family management of pediatric type 1 diabetes: feasibility and design. Pediatr Diabetes 2009;10:105-15. https://doi.org/10.1111/j.1399-5448.2008.00448.x.
- Ng D, Chow P, Lai W, Chan K, Chang B, So H. Effect of a structured asthma education program on hospitalized asthmatic children: A randomized controlled study. Pediatr Int 2006;48:158-62. https://doi.org/10.1111/j.1442-200X.2006.02185.x.
- O’Neill D, McGilloway S, Donnelly M, Bywater T, Kelly P. A cost-effectiveness analysis of the Incredible Years parenting programme in reducing childhood health inequalities. Eur J Health Econ 2013;14:85-94. https://doi.org/10.1007/s10198-011-0342-y.
- McGilloway S, Ni Mhaille G, Bywater T, Furlong M, Leckey Y, Kelly P, et al. A parenting intervention in childhood behavioural problems: a randomized controlled trial in disadvantaged community-based settings. J Consult Clin Psych 2012;80:116-27. https://doi.org/10.1037/a0026304.
- Otsuki M, Eakin MN, Rand CS, Butz AM, Hsu VD, Zuckerman IH, et al. Adherence feedback to improve asthma outcomes among inner-city children: a randomized trial. Pediatrics 2009;124:1513-21. https://doi.org/10.1542/peds.2008-2961.
- Quint DM, Teach SJ. IMPACT DC: reconceptualizing the role of the emergency department for urban children with asthma. Clin Pediatr Emerg Med 2009;10:115-21. https://doi.org/10.1016/j.cpem.2009.03.003.
- Teach SJ, Crain EF, Quint DM, Hylan ML, Joseph JG. Improved asthma outcomes in a high-morbidity pediatric population: results of an emergency department-based randomized clinical trial. Arch Pediat Adol Med 2006;160:535-41. https://doi.org/10.1001/archpedi.160.5.535.
- Richardson LP, Ludman E, McCauley E, Lindenbaum J, Larison C, Zhou C, et al. Collaborative care for adolescents with depression in primary care: a randomized clinical trial. JAMA 2014;312:809-16. https://doi.org/10.1001/jama.2014.9259.
- Rikkers-Mutsaerts ER, Winters AE, Bakker MJ, van Stel HF, van der Meer V, de Jongste JC, et al. Internet-based self-management compared with usual care in adolescents with asthma: a randomized controlled trial. Pediatr Pulmonol 2012;47:1170-9. https://doi.org/10.1002/ppul.22575.
- Ronchetti R, Indinnimeo L, Bonci E, Corrias A, Evans D, Hindi-Alexander M, et al. Asthma self-management programmes in a population of Italian children: a multicentric study. Italian Study Group on Asthma Self-Management Programmes. Eur Respir J 1997;10:1248-53. https://doi.org/10.1183/09031936.97.10061248.
- Rund BR, Moe L, Sollien T, Fjell A, Borchgrevink T, Hallert M, et al. The Psychosis Project: outcome and cost-effectiveness of a psychoeducational treatment programme for schizophrenic adolescents. Acta Psychiatr Scand 1994;89:211-18. https://doi.org/10.1111/j.1600-0447.1994.tb08094.x.
- Runge C, Lecheler J, Horn M, Tews JT, Schaefer M. Outcomes of a Web-based patient education program for asthmatic children and adolescents. Chest 2006;129:581-93. https://doi.org/10.1378/chest.129.3.581.
- Schmidt U, Lee S, Beecham J, Perkins S, Treasure J, Yi I, et al. A randomized controlled trial of family therapy and cognitive behavior therapy guided self-care for adolescents with bulimia nervosa and related disorders. Am J Psychiatry 2007;164:591-8. https://doi.org/10.1176/ajp.2007.164.4.591.
- Seid M, Varni JW, Gidwani P, Gelhard LR, Slymen DJ. Problem-solving skills training for vulnerable families of children with persistent asthma: report of a randomized trial on health-related quality of life outcomes. J Pediatr Psychol 2010;35:1133-43. https://doi.org/10.1093/jpepsy/jsp133.
- Shames RS, Sharek P, Mayer M, Robinson TN, Hoyte EG, Gonzalez-Hensley F, et al. Effectiveness of a multicomponent self-management program in at-risk, school-aged children with asthma. Ann Allergy Asthma Immunol 2004;92:611-18. https://doi.org/10.1016/S1081-1206(10)61426-3.
- Sockrider MM, Abraham S, Brooks E, Caviness AC, Pilney S, Koerner C, et al. Delivering tailored asthma family education in a pediatric emergency department setting: a pilot study. Pediatrics 2006;117:S135-44. https://doi.org/10.1542/peds.2005-2000K.
- Southam-Gerow MA, Weisz JR, Chu BC, McLeod BD, Gordis EB, Connor-Smith JK. Does cognitive behavioral therapy for youth anxiety outperform usual care in community clinics? An initial effectiveness test. J Am Acad Child Psy 2010;49:1043-52. https://doi.org/10.1016/j.jaac.2010.06.009.
- Staab D, von Rueden U, Kehrt R, Erhart M, Wenninger K, Kamtsiuris P, et al. Evaluation of a parental training program for the management of childhood atopic dermatitis. Pediatr Allergy Immunol 2002;13:84-90. https://doi.org/10.1034/j.1399-3038.2002.01005.x.
- Sullivan SD, Weiss KB, Lynn H, Mitchell H, Kattan M, Gergen PJ, et al. The cost-effectiveness of an inner-city asthma intervention for children. J Allergy Clin Immunol 2002;110:576-81. https://doi.org/10.1067/mai.2002.128009.
- Evans R, Gergen PJ, Mitchell H, Kattan M, Kercsmar C, Crain E, et al. A randomized clinical trial to reduce asthma morbidity among inner-city children: results of the National Cooperative Inner-City Asthma Study. J Pediatr 1999;135:332-8. https://doi.org/10.1016/S0022-3476(99)70130-7.
- Svoren BM, Butler D, Levine BS, Anderson BJ, Laffel LM. Reducing acute adverse outcomes in youths with type 1 diabetes: a randomized, controlled trial. Pediatrics 2003;112:914-22. https://doi.org/10.1542/peds.112.4.914.
- Szczepanski R, Gebert N, Hümmelink R, Könning J, Schmidt S, Runde B, et al. Outcome of structured asthma education in childhood and adolescence. Pneumologie 1996;50:544-8.
- Toelle BG, Peat JK, Salome CM, Mellis CM, Bauman AE, Woolcock AJ. Evaluation of a community-based asthma management program in a population sample of schoolchildren. Med J Aust 1993;158:742-6.
- Valery PC, Masters IB, Taylor B, Laifoo Y, O’Rourke PK, Chang AB. An education intervention for childhood asthma by Aboriginal and Torres Strait Islander health workers: a randomised controlled trial. Med J Australia 2010;192:574-9.
- Van de Wiel NMH, Matthys W, Cohen-Kettenis P, van Engeland H. Application of the Utrecht Coping Power Program and care as usual to children with disruptive behavior disorders in outpatient clinics: A comparative study of cost and course of treatment. Behav Ther 2003;34:421-36. https://doi.org/10.1016/S0005-7894(03)80028-X.
- Van Der Veek SMC, Derkx BHF, Benninga MA, Boer F, De Haan E. Cognitive behavior therapy for pediatric functional abdominal pain: a randomized controlled trial. Pediatrics 2013;132:e1163-e72. https://doi.org/10.1542/peds.2013-0242.
- Velsor-Friedrich B, Militello LK, Richards MH, Harrison PR, Gross IM, Romero E, et al. Effects of coping-skills training in low-income urban African-American adolescents with asthma. J Asthma 2012;49:372-9. https://doi.org/10.3109/02770903.2012.660296.
- Walders N, Kercsmar C, Schluchter M, Redline S, Kirchner HL, Drotar D. An interdisciplinary intervention for undertreated pediatric asthma. Chest 2006;129:292-9. https://doi.org/10.1378/chest.129.2.292.
- Watson WT, Gillespie C, Thomas N, Filuk SE, McColm J, Piwniuk MP, et al. Small-group, interactive education and the effect on asthma control by children and their families. CMAJ 2009;181:257-63. https://doi.org/10.1503/cmaj.080947.
- Weisz JR, Southam-Gerow MA, Gordis EB, Connor-Smith JK, Chu BC, Langer DA, et al. Cognitive-behavioral therapy versus usual clinical care for youth depression: an initial test of transportability to community clinics and clinicians. J Consult Clin Psych 2009;77:383-96. https://doi.org/10.1037/a0013877.
- Willems DCM, Joore MA, Hendriks JJE, Wouters EFM, Severens JL. Cost-effectiveness of a nurse-led telemonitoring intervention based on peak expiratory flow measurements in asthmatics: results of a randomised controlled trial. Cost Eff Resour Alloc 2007;5. https://doi.org/10.1186/1478-7547-5-10.
- Willems DC, Joore MA, Hendriks JJ, van Duurling RA, Wouters EF, Severens JL. Process evaluation of a nurse-led telemonitoring programme for patients with asthma. J Telemed Telecare 2007;13:310-17. https://doi.org/10.1258/135763307781644898.
- Willems DC, Joore MA, Hendriks JJ, Nieman FH, Severens JL, Wouters EF. The effectiveness of nurse-led telemonitoring of asthma: results of a randomized controlled trial. J Eval Clin Pract 2008;14:600-9. https://doi.org/10.1111/j.1365-2753.2007.00936.x.
- Xu C, Jackson M, Scuffham PA, Wootton R, Simpson P, Whitty J, et al. A randomized controlled trial of an interactive voice response telephone system and specialist nurse support for childhood asthma management. J Asthma 2010;47:768-73. https://doi.org/10.3109/02770903.2010.493966.
- Young NL, Foster AM, Parkin PC, Reisman J, MacLusky I, Gold M, et al. Assessing the efficacy of a school-based asthma education program for children: a pilot study. Can J Public Health 2001;92:30-4.
- Grimshaw J, McAuley LM, Bero LA, Grilli R, Oxman AD, Ramsay C, et al. Systematic reviews of the effectiveness of quality improvement strategies and programmes. Qual Saf Health Care 2003;12:298-303. https://doi.org/10.1136/qhc.12.4.298.
- Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA 1995;273:59-65. https://doi.org/10.1001/jama.1995.03520250075037.
- Barr RD, Pai MK, Weitzman S, Feeny D, Furlong W, Rosenbaum P, et al. A multiattribute approach to health-status measurement and clinical management illustrated by an application to brain tumors in childhood. Int J Oncol 1994;4:639-48. https://doi.org/10.3892/ijo.4.3.639.
- Matza LS, Swensen AR, Flood EM, Secnik K, Leidy NK. Assessment of health-related quality of life in children: a review of conceptual, methodological, and regulatory issues. Value Health 2004;7:79-92. https://doi.org/10.1111/j.1524-4733.2004.71273.x.
- Eiser C, Morse R. Quality-of-life measures in chronic diseases of childhood. Health Technol Assess 2001;5. https://doi.org/10.3310/hta5040.
- Landgraf JM, Abetz LN, Spilker B. Quality of Life and Pharmacoeconomics in Clinical Trials. Philadelphia, PA: Lippincott-Raven Publishers; 1996.
- Eiser C, Mohay H, Morse R. The measurement of quality of life in young children. Child Care Health Dev 2000;26:401-14. https://doi.org/10.1046/j.1365-2214.2000.00154.x.
- Roland M, Abel G. Reducing emergency admissions: are we on the right track?. BMJ 2012;345. https://doi.org/10.1136/bmj.e6017.
- Claxton K, Walker S, Palmer S, Sculpher M. Appropriate Perspectives for Health Care Decisions. CHE Research Paper 54. Centre of Health Economics, University of York; 2010.
- Kirk S, Glendinning C, Callery P. Parent or nurse? The experience of being the parent of a technology-dependent child. J Adv Nurs 2005;51:456-64. https://doi.org/10.1111/j.1365-2648.2005.03522.x.
- Thorne SE, Paterson BL. Health care professional support for self-care management in chronic illness: insights from diabetes research. Patient Educ Couns 2001;42:81-90. https://doi.org/10.1016/S0738-3991(00)00095-1.
- Rogers A, Lee V, Kennedy A. Continuity and change? Exploring reactions to a guided self-management intervention in a randomised controlled trial for IBS with reference to prior experience of managing a long term condition. Trials 2007;8. https://doi.org/10.1186/1745-6215-8-6.
- Schmidt C. Mothers’ perceptions of self-care in school-age children with diabetes. MCN Am J Matern Child Nurs 2003;28:362-70. https://doi.org/10.1097/00005721-200311000-00007.
- Buford TA. Transfer of asthma management responsibility from parents to their school-age children. J Pediatr Nurs 2004;19:3-12. https://doi.org/10.1016/j.pedn.2003.09.002.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Hewitt CE, Gilbody SM, Brealey S, Paulden M, Palmer S, Mann R, et al. Methods to identify postnatal depression in primary care: an integrated evidence synthesis and value of information analysis. Health Technol Assess 2009;13. https://doi.org/10.3310/hta13360.
- Juniper EF, Guyatt GH, Feeny DH, Ferrie PJ, Griffith LE, Townsend M. Measuring quality of life in children with asthma. Qual Life Res 1996;5:35-46. https://doi.org/10.1007/BF00435967.
- Bukstein DA, McGrath MM, Buchner DA, Landgraf J, Goss TF. Evaluation of a short form for measuring health-related quality of life among pediatric asthma patients. J Allergy Clin Immunol 2000;105:245-51. https://doi.org/10.1016/S0091-6749(00)90072-1.
Appendix 1 Search strategies
Cumulative Index to Nursing and Allied Health Literature Plus database (via EBSCOhost)
Date searched: 19 March 2015.
Date range searched: inception to 13 March 2015.
Records retrieved: 5330.
Search strategy
| # | Query | Results |
|---|---|---|
| S162 | S160 NOT S161 | 5330 |
| S161 | PT editorial or comment or letter | 394,243 |
| S160 | S151 OR S159 | 5362 |
| S159 | S152 OR S153 OR S154 OR S155 OR S156 OR S157 OR S158 | 208 |
| S158 | TI “friends program*” OR AB “friends program*” | 8 |
| S157 | TI “Triple P” OR AB “Triple P” | 97 |
| S156 | TI “Incredible Years” OR AB “Incredible Years” | 65 |
| S155 | TI “problem solving for life” OR AB “problem solving for life” | 3 |
| S154 | TI “Timid to Tiger” OR AB “Timid to Tiger” | 2 |
| S153 | TI “Sweet talk” OR AB “Sweet talk” | 27 |
| S152 | TI “Cool Kids” OR AB “Cool Kids” | 11 |
| S151 | S91 AND S116 AND S149 AND S150 | 5162 |
| S150 | S20 OR S84 | 874,894 |
| S149 | S117 OR S118 OR S119 OR S120 OR S121 OR S122 OR S123 OR S124 OR S125 OR S126 OR S127 OR S128 OR S129 OR S130 OR S131 OR S132 OR S133 OR S134 OR S135 OR S136 OR S137 OR S138 OR S139 OR S140 OR S141 OR S142 OR S143 OR S144 OR S145 OR S146 OR S147 OR S148 | 297,682 |
| S148 | TI (qaly* or “quality adjusted life” or “quality of life” or “life quality”) OR AB (qaly* or “quality adjusted life” or “quality of life” or “life quality”) | 53,176 |
| S147 | (MH “Quality-Adjusted Life Years”) | 2146 |
| S146 | TI ( hrql or hrqol or h-qol or hql or hqol ) OR AB ( hrql or hrqol or h-qol or hql or hqol ) | 2927 |
| S145 | TI ( hospitalisation* or hospitalization* or rehospitalisation* or rehospitalization* or re-hospitalisation* or re-hospitalization* ) OR AB ( hospitalisation* or hospitalization* or rehospitalisation* or rehospitalization* or re-hospitalisation* or re-hospitalization* ) | 22,851 |
| S144 | TI ( consultation* N2 (time or length) ) OR AB ( consultation* N2 (time or length) ) | 474 |
| S143 | TI ( (clinic or surgery or hospital or “accident and emergency”) N2 (work-flow or “work flow”) ) OR AB ( (clinic or surgery or hospital or “accident and emergency”) N2 (work-flow or “work flow”) ) | 6 |
| S142 | TI ( (uptake or access) W1 (service* or care or intervention*) ) OR AB ( (uptake or access) W1 (service* or care or intervention*) ) | 4262 |
| S141 | TI ( GP N1 (access or uptake or visit* or contact* or attendance* or admission* or episode*) ) OR AB ( GP N1 (access or uptake or visit* or contact* or attendance* or admission* or episode*) ) | 359 |
| S140 | TI ( surgery N1 (visit* or contact* or attendance* or admission* or episode*) ) OR AB ( surgery N1 (visit* or contact* or attendance* or admission* or episode*) ) | 240 |
| S139 | TI ( “primary care” N1 (visit* or contact* or attendance* or admission* or episode*) ) OR AB ( “primary care” N1 (visit* or contact* or attendance* or admission* or episode*) ) | 796 |
| S138 | TI ( number N2 (nights or days) ) OR AB ( number N2 (nights or days) ) | 2300 |
| S137 | TI ( (patient* or inpatient* or in-patient*) N1 (cost* or stay*) ) OR AB ( (patient* or inpatient* or in-patient*) N1 (cost* or stay*) ) | 5482 |
| S136 | TI “hospital day*” OR AB “hospital day*” | 827 |
| S135 | TI time N2 discharg* OR AB time N2 discharg* | 1206 |
| S134 | TI “hospital cost*” OR AB “hospital cost*” | 1254 |
| S133 | TI ( hospital N1 (access* or uptake or visit* or attendance* or admission* or admit* or episode*) ) OR AB ( hospital N1 (access* or uptake or visit* or attendance* or admission* or admit* or episode*) ) | 9825 |
| S132 | TI duration N2 stay OR AB duration N2 stay | 840 |
| S131 | TI length N2 stay OR AB length N2 stay | 11,520 |
| S130 | (MH “Health Resource Utilization”) OR (MH “Health Resource Allocation”) | 18,081 |
| S129 | (MH “Readmission”) | 5960 |
| S128 | (MH “Hospitalization”) OR (MH “Length of Stay”) OR (MH “Patient Admission”) | 48,675 |
| S127 | TI budget* OR AB budget* | 6666 |
| S126 | TI (value N1 money) OR AB (value N1 money) | 447 |
| S125 | TI (expenditure* not energy) OR AB (expenditure* not energy) | 5192 |
| S124 | TI ( econom* or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic* ) OR AB ( econom* or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic* ) | 112,768 |
| S123 | (MH “Health Care Costs+”) | 34,309 |
| S122 | (MH “Economic Aspects of Illness”) | 5807 |
| S121 | (MH “Economics, Dental”) | 96 |
| S120 | (MH “Economics, Pharmaceutical”) | 1694 |
| S119 | (MH “Economic Value of Life”) | 488 |
| S118 | (MH “Costs and Cost Analysis+”) | 75,720 |
| S117 | (MH “Economics”) | 9773 |
| S116 | S92 OR S93 OR S94 OR S95 OR S96 OR S97 OR S98 OR S99 OR S100 OR S101 OR S102 OR S103 OR S104 OR S105 OR S106 OR S107 OR S108 OR S109 OR S110 OR S111 OR S112 OR S113 OR S114 OR S115 | 398,552 |
| S115 | (MH “Mental Health”) | 17,397 |
| S114 | TI “school refusal” OR AB “school refusal” | 49 |
| S113 | (MH “Panic Disorder”) | 1597 |
| S112 | (MH “Phobic Disorders+”) | 3618 |
| S111 | (MH “Bipolar Disorder+”) | 7408 |
| S110 | (MH “Schizophrenia+”) | 16,421 |
| S109 | (MH “Eating Disorders+”) | 11,947 |
| S108 | (MH “Psychotic Disorders+”) | 77,469 |
| S107 | (MH “Stress Disorders, Post-Traumatic+”) | 13,346 |
| S106 | (MH “Obsessive-Compulsive Disorder+”) | 3756 |
| S105 | (MH “Affective Disorders+”) | 71,774 |
| S104 | (MH “Social Behavior Disorders+”) | 61,606 |
| S103 | (MH “Epilepsy+”) | 10,859 |
| S102 | (MH “Self-Injurious Behavior”) | 2371 |
| S101 | (MH “Injuries, Self-Inflicted”) | 1620 |
| S100 | (MH “Depression+”) | 68,027 |
| S99 | (MH “Anxiety+”) | 24,635 |
| S98 | (MH “Hyperkinesis”) | 313 |
| S97 | (MH “Child Behavior Disorders”) | 6047 |
| S96 | (MH “Attention Deficit Hyperactivity Disorder”) | 10,196 |
| S95 | (MH “Asthma+”) | 24,073 |
| S94 | TX mucoviscidosis | 7 |
| S93 | (MH “Cystic Fibrosis”) | 5069 |
| S92 | (MH “Diabetes Mellitus+”) | 100,829 |
| S91 | S85 OR S86 OR S87 OR S88 OR S89 OR S90 | 809,141 |
| S90 | TI ( parent* or mother* or father* or caregiver* or carer* or guardian* or advocate* or family ) OR AB ( parent* or mother* or father* or caregiver* or carer* or guardian* or advocate* or family ) | 206,010 |
| S89 | (MH “Caregivers”) | 20,984 |
| S88 | (MH “Parents+”) | 56,978 |
| S87 | TI ( child or children or schoolchild* or baby or babies or infant or infants or toddler* or teen* or teenager* or adolescen* or “young person*” or “young people” or youth or youngster* or juvenile* or paediatric or pediatric ) OR AB ( child or children or schoolchild* or baby or babies or infant or infants or toddler* or teen* or teenager* or adolescen* or “young person*” or “young people” or youth or youngster* or juvenile* or paediatric or pediatric ) | 362,291 |
| S86 | (MH “Adolescence+”) | 327,147 |
| S85 | (MH “Child+”) | 429,276 |
| S84 | S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52 OR S53 OR S54 OR S55 OR S56 OR S57 OR S58 OR S59 OR S60 OR S61 OR S62 OR S63 OR S64 OR S65 OR S66 OR S67 OR S68 OR S69 OR S70 OR S71 OR S72 OR S73 OR S74 OR S75 OR S76 OR S77 OR S78 OR S79 OR S80 OR S81 OR S82 OR S83 | 805,043 |
| S83 | TI “text messag*” OR AB “text messag*” | 694 |
| S82 | (MH “Reminder Systems”) | 1795 |
| S81 | (MH “Text Messaging”) | 514 |
| S80 | (MH “Wireless Communications”) | 9320 |
| S79 | (MH “Telephone”) | 12,992 |
| S78 | (MH “Patient Access to Records”) | 457 |
| S77 | (MH “Mindfulness”) | 566 |
| S76 | (MH “Communication+”) | 168,936 |
| S75 | (MH “Adaptation, Psychological”) | 21,027 |
| S74 | (MH “Coping”) | 20,654 |
| S73 | TI ( “skills training” or “coping skill*” or empower* ) OR AB ( “skills training” or “coping skill*” or empower*) | 13,751 |
| S72 | (MH “Problem Solving”) | 8019 |
| S71 | TI psychoeducat* OR AB psychoeducat* | 1274 |
| S70 | (MH “Psychoeducation”) | 1836 |
| S69 | (MH “Psychotherapy, Group”) | 4012 |
| S68 | (MH “Psychotherapy, Brief”) | 753 |
| S67 | TI ( (behavior* or behaviour*) N1 (manag* or modif*) ) OR AB ( (behavior* or behaviour*) N1 (manag* or modif*) ) | 3662 |
| S66 | (MH “Behavior Modification”) | 1651 |
| S65 | (MH “Behavior Therapy”) | 7714 |
| S64 | TI “parent* training” OR AB “parent* training” | 455 |
| S63 | (MH “Parenting”) | 10,162 |
| S62 | (MH “Social Media”) | 2963 |
| S61 | (MH “Blogs”) | 2147 |
| S60 | (MH “Internet”) | 33,921 |
| S59 | (MH “Bibliotherapy”) | 308 |
| S58 | TI ( “educational material*” or leaflet* or booklet* or toolkit* ) OR AB ( “educational material*” or leaflet* or booklet* or toolkit* ) | 5141 |
| S57 | (MH “Pamphlets”) | 2455 |
| S56 | (MH “Teaching Materials”) | 9621 |
| S55 | TI ( CBT or “cognitive therap*” or “cognitive behav*” ) OR AB ( CBT or “cognitive therap*” or “cognitive behav*” ) | 7897 |
| S54 | (MH “Cognitive Therapy”) | 12,009 |
| S53 | (MH “Motivational Interviewing”) | 1517 |
| S52 | (MH “Exercise+”) | 67,755 |
| S51 | (MH “Diet+”) | 71,326 |
| S50 | TI ( “goal set*” or “individual goal*” ) OR AB ( “goal set*” or “individual goal*” ) | 1364 |
| S49 | TI ( decision* N2 (shared or support* or aid or aids or making) ) OR AB ( decision* N2 (shared or support* or aid or aids or making) ) | 31,517 |
| S48 | (MH “Goal-Setting”) | 3952 |
| S47 | (MH “Decision Making”) | 29,422 |
| S46 | TI ( “contingent payment*” or “deposit contract*” ) OR AB ( “contingent payment*” or “deposit contract*” ) | 2 |
| S45 | TI ( ((financial or monetary or money) N2 (incentive* or competition* or contest* or lotter* or reward* or prize*)) ) OR AB ( ((financial or monetary or money) N2 (incentive* or competition* or contest* or lotter* or reward* or prize*)) ) | 1528 |
| S44 | (MH “Consumer Health Information”) | 9291 |
| S43 | TI nurse N2 educator* OR AB nurse N2 educator* | 3624 |
| S42 | TI ( (“consumer health” or patient) N1 information ) OR AB ( (“consumer health” or patient) N1 information ) | 3409 |
| S41 | TI ( patient N2 (educat* or advice or advis* or instruct* or instruct* or train* or coach*) ) OR AB ( patient N2 (educat* or advice or advis* or instruct* or instruct* or train* or coach*) ) | 11,053 |
| S40 | (MH “Patient Education”) | 49,243 |
| S39 | TI ( involv* or participat* or collaborat* ) OR AB ( involv* or participat* or collaborat* ) | 236,994 |
| S38 | (MH “Consumer Participation”) | 12,803 |
| S37 | TI ( “case manag*” or “action plan*” or “care plan*” or “care manag*” or “management plan*” or “management program*” or “care program*” or “goal setting” or “individual goal*” ) OR AB ( “case manag*” or “action plan*” or “care plan*” or “care manag*” or “management plan*” or “management program*” or “care program*” or “goal setting” or “individual goal*” ) | 27,900 |
| S36 | (MH “Case Management”) | 13,495 |
| S35 | TI ( (telephon* or remote or phone) N2 (follow* or support* or consult* or advice or advis* or intervention* or instruct* or assist* or educate or education or information or monitor*) ) OR AB ( (telephon* or remote or phone) N2 (follow* or support* or consult* or advice or advis* or intervention* or instruct* or assist* or educate or education or information or monitor*) ) | 4687 |
| S34 | (MH “Remote Consultation”) | 1196 |
| S33 | TI ( telemedicine or telecare or telenursing or telemonitor* or telehealth or ehealth ) OR AB ( telemedicine or telecare or telenursing or telemonitor* or telehealth or ehealth ) | 4913 |
| S32 | (MH “Telehealth”) | 3643 |
| S31 | (MH “Telenursing”) | 1624 |
| S30 | (MH “Telemedicine”) | 5638 |
| S29 | TI “health trainer*” OR AB “health trainer*” | 41 |
| S28 | TI ( befriend* or coach* or mentor* or buddy or buddies ) OR AB ( befriend* or coach* or mentor* or buddy or buddies ) | 12,215 |
| S27 | TI ( “expert patient*” or “virtual communit*” or “online communit*” ) OR AB ( “expert patient*” or “virtual communit*” or “online communit*” ) | 550 |
| S26 | TI ( (mutual or telephone) W1 support ) OR AB ( (mutual or telephone) W1 support ) | 592 |
| S25 | TI ( peer W1 (support* or advice or advis* or monitor* or intervention* or train* or instruct* or consult* or assist* or educat* or information) ) OR AB ( peer W1 (support* or advice or advis* or monitor* or intervention* or train* or instruct* or consult* or assist* or educat* or information) ) | 2726 |
| S24 | TI ( group W1 (support* or advice or advis* or monitor* or intervention* or train* or instruct* or consult* or assist* or educat* or information) ) OR AB ( group W1 (support* or advice or advis* or monitor* or intervention* or train* or instruct* or consult* or assist* or educat* or information) ) | 4948 |
| S23 | TI “social support*” OR AB “social support*” | 13,267 |
| S22 | (MH “Support Groups”) | 7557 |
| S21 | (MH “Support, Psychosocial”) | 44,816 |
| S20 | S1 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 | 123,653 |
| S19 | TI recovery OR AB recovery | 35,013 |
| S18 | TI ( collaborat* N1 (care or manag*) ) OR AB ( collaborat* N1 (care or manag*) ) | 1811 |
| S17 | TI ( self-treat* or selftreat* or self-cure* or selfcure* or self-curing or selfcuring ) OR AB ( self-treat* or selftreat* or self-cure* or selfcure* or self-curing or selfcuring ) | 442 |
| S16 | TI ( self-medicat* or selfmedicat* or self-remed* or selfremed* ) OR AB ( self-medicat* or selfmedicat* or self-remed* or selfremed* ) | 751 |
| S15 | (MH “Self Medication”) | 1270 |
| S14 | TI self-efficacy OR AB self-efficacy | 9551 |
| S13 | (MH “Self-Efficacy”) | 12,167 |
| S12 | TI self-initiat* OR AB self-initiat* | 237 |
| S11 | (MH “Blood Glucose Self-Monitoring”) | 2510 |
| S10 | TI ( self-diagnos* or selfdiagnos* or self-assess* or selfassess* ) OR AB ( self-diagnos* or selfdiagnos* or self-assess* or selfassess* ) | 4065 |
| S9 | TI ( self-help* or selfhelp* ) OR AB ( self-help* or selfhelp* ) | 2355 |
| S8 | TI ( self-monitor* or selfmonitor* or self-report* or selfreport* ) OR AB ( self-monitor* or selfmonitor* or self-report* or selfreport* ) | 34,036 |
| S7 | TI ( self-manag* or selfmanag* ) OR AB ( self-manag* or selfmanag* ) | 6324 |
| S6 | TI ( self-care* or selfcaring or selfcare* or selfcaring ) OR AB ( self-care* or selfcaring or selfcare* or selfcaring ) | 8332 |
| S5 | (MH “Self Care”) | 23,936 |
| S4 | S2 NOT S3 | 1589 |
| S3 | TI ( self-administer* N2 (questionnaire* or survey* or interview*) ) OR AB ( self-administer* N2 (questionnaire* or survey* or interview*) ) | 4926 |
| S2 | TI self-administer* OR AB self-administer* | 6515 |
| S1 | (MH “Self Administration+”) | 4246 |
The Cochrane Library (via Wiley Online Library)
Date searched: 18 March 2015.
The same search strategy was used across all five databases:
-
CDSR : issue 3 of 12, March 2015
-
DARE: issue 1 of 4, January 2015
-
CENTRAL: issue 2 of 12, February 2015
-
HTA database: issue 1 of 4, January 2015
-
NHS EED: issue 1 of 4, January 2015.
Records retrieved:
-
all results: 1894
-
CDSR: 124
-
DARE: 40
-
CENTRAL: 1596
-
HTA database: 8
-
NHS EED: 126.
Search strategy
#1 MeSH descriptor: [Self Administration] this term only (653)
#2 self next administer*:ti,ab,kw (2287)
#3 (self next administer* near/2 (questionnaire* or survey* or interview*)):ti,ab,kw (792)
#4 #2 not #3 (1495)
#5 MeSH descriptor: [Self Care] this term only (2833)
#6 (self next care* or selfcaring or selfcare* or selfcaring):ti,ab,kw (4256)
#7 (self next manag* or selfmanag*):ti,ab,kw (2420)
#8 (self next monitor* or selfmonitor* or self report* or selfreport*):ti,ab,kw (18,030)
#9 (self next help* or selfhelp*):ti,ab,kw (1870)
#10 (self next diagnos* or selfdiagnos* or self next assess* or selfassess*):ti,ab,kw (2006)
#11 MeSH descriptor: [Blood Glucose Self-Monitoring] this term only (495)
#12 self next initiat*:ti,ab,kw (79)
#13 MeSH descriptor: [Self Efficacy] this term only (1599)
#14 self next efficacy:ti,ab,kw (3692)
#15 MeSH descriptor: [Self Medication] this term only (81)
#16 (self next medicat* or selfmedicat* or self next remed* or selfremed*):ti,ab,kw (247)
#17 (self next treat* or selftreat* or self next cure* or selfcure* or self next curing or selfcuring):ti,ab,kw (218)
#18 (collaborat* next (care or manag*)):ti,ab,kw (366)
#19 recovery:ti,ab,kw (25,073)
#20 #1 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 (52,340)
#21 MeSH descriptor: [Social Support] this term only (2441)
#22 social next support*:ti,ab,kw (3863)
#23 (group next (support* or advice or advis* or monitor* or intervention* or train* or instruct* or consult* or assist* or educat* or information)):ti,ab,kw (2670)
#24 (peer next (support* or advice or advis* or monitor* or intervention* or train* or instruct* or consult* or assist* or educat* or information)):ti,ab,kw (515)
#25 ((mutual or telephone) next support):ti,ab,kw (294)
#26 (expert next patient* or virtual next communit* or online next communit*):ti,ab,kw (45)
#27 (befriend* or coach* or mentor* or buddy or buddies):ti,ab,kw (1348)
#28 health next trainer*:ti,ab,kw (5)
#29 MeSH descriptor: [Telemedicine] this term only (1013)
#30 (telemedicine or telecare or telenursing or telemonitor* or telehealth or ehealth):ti,ab,kw (1776)
#31 MeSH descriptor: [Remote Consultation] this term only (333)
#32 ((telephon* or remote or phone) near/2 (follow* or support* or consult* or advice or advis* or intervention* or instruct* or assist* or educate or education or information or monitor*)):ti,ab,kw (2831)
#33 MeSH descriptor: [Case Management] this term only (652)
#34 (case next manag* or action next plan* or care next plan* or care next manag* or management next plan* or management next program* or care next program* or goal next setting or individual next goal*):ti,ab,kw (6445)
#35 MeSH descriptor: [Patient Participation] this term only (890)
#36 (involv* or participat* or collaborat*):ti,ab,kw (72,418)
#37 MeSH descriptor: [Patient Education as Topic] this term only (6657)
#38 patient next education:ti,ab,kw (8086)
#39 (patient near/2 (educat* or advice or advis* or instruct* or train* or coach*)):ti,ab,kw (8784)
#40 ((consumer next health or patient) next information):ti,ab,kw (553)
#41 (nurse near/2 educator*):ti,ab,kw (73)
#42 ((financial or monetary or money) near/2 (incentive* or competition* or contest* or lotter* or reward* or prize*)):ti,ab,kw (513)
#43 (contingent next payment* or deposit next contract*):ti,ab,kw (17)
#44 MeSH descriptor: [Decision Making] this term only (1692)
#45 (decision* near/2 (shared or support* or aid or aids or making)):ti,ab,kw (7150)
#46 (goal next set* or individual next goal*):ti,ab,kw (446)
#47 MeSH descriptor: [Diet] explode all trees (12,385)
#48 MeSH descriptor: [Exercise] explode all trees (14,181)
#49 MeSH descriptor: [Motivational Interviewing] this term only (136)
#50 MeSH descriptor: [Cognitive Therapy] this term only (5146)
#51 (CBT or cognitive next therap* or cognitive next behav*):ti,ab,kw (9693)
#52 MeSH descriptor: [Teaching Materials] this term only (383)
#53 MeSH descriptor: [Pamphlets] this term only (623)
#54 (educational next material* or leaflet* or booklet* or toolkit*):ti,ab,kw (1977)
#55 MeSH descriptor: [Bibliotherapy] this term only (105)
#56 MeSH descriptor: [Internet] explode all trees (1900)
#57 MeSH descriptor: [Parenting] this term only (669)
#58 parent* next training:ti,ab,kw (382)
#59 MeSH descriptor: [Behavior Therapy] this term only (3633)
#60 ((behavior* or behaviour*) next (manag* or modif*)):ti,ab,kw (950)
#61 MeSH descriptor: [Psychotherapy, Brief] this term only (708)
#62 MeSH descriptor: [Psychotherapy, Group] this term only (1533)
#63 psychoeducat*:ti,ab,kw (1071)
#64 MeSH descriptor: [Problem Solving] this term only (1209)
#65 (skills next training or coping next skill* or empower*):ti,ab,kw (2354)
#66 MeSH descriptor: [Adaptation, Psychological] this term only (3112)
#67 MeSH descriptor: [Communication] explode all trees (9893)
#68 MeSH descriptor: [Mindfulness] this term only (32)
#69 MeSH descriptor: [Patient Access to Records] this term only (17)
#70 MeSH descriptor: [Cell Phones] this term only (323)
#71 MeSH descriptor: [Telephone] this term only (1409)
#72 MeSH descriptor: [Text Messaging] this term only (144)
#73 MeSH descriptor: [Reminder Systems] this term only (618)
#74 text next messag*:ti,ab,kw (427)
#75 {or #21-#74} (136,490)
#76 MeSH descriptor: [Child] explode all trees (151)
#77 MeSH descriptor: [Adolescent] this term only (77,091)
#78 (child or children or schoolchild* or baby or babies or infant or infants or toddler* or teen* or teenager* or adolescen* or young next person* or young next people or youth or youngster* or juvenile* or paediatric or pediatric):ti,ab,kw (163,314)
#79 MeSH descriptor: [Parents] explode all trees (2723)
#80 MeSH descriptor: [Caregivers] this term only (1265)
#81 (parent* or mother* or father* or caregiver* or carer* or guardian* or advocate* or family):ti,ab,kw (40,218)
#82 #76 or #77 or #78 or #79 or #80 or #81 (182,717)
#83 MeSH descriptor: [Diabetes Mellitus] explode all trees (16,726)
#84 MeSH descriptor: [Cystic Fibrosis] this term only (1102)
#85 mucoviscidosis:ti,ab,kw (33)
#86 MeSH descriptor: [Asthma] explode all trees (9404)
#87 MeSH descriptor: [Attention Deficit and Disruptive Behavior Disorders] explode all trees (1865)
#88 MeSH descriptor: [Hyperkinesis] this term only (168)
#89 MeSH descriptor: [Anxiety] explode all trees (5226)
#90 MeSH descriptor: [Depression] this term only (5541)
#91 MeSH descriptor: [Depressive Disorder] this term only (4754)
#92 MeSH descriptor: [Self Mutilation] this term only (25)
#93 MeSH descriptor: [Self-Injurious Behavior] this term only (205)
#94 MeSH descriptor: [Epilepsy] explode all trees (2311)
#95 MeSH descriptor: [Conduct Disorder] explode all trees (179)
#96 MeSH descriptor: [Mood Disorders] explode all trees (9310)
#97 MeSH descriptor: [Obsessive-Compulsive Disorder] explode all trees (662)
#98 MeSH descriptor: [Stress Disorders, Post-Traumatic] this term only (972)
#99 MeSH descriptor: [Psychotic Disorders] explode all trees (1562)
#100 MeSH descriptor: [Eating Disorders] explode all trees (838)
#101 MeSH descriptor: [Schizophrenia] explode all trees (4966)
#102 MeSH descriptor: [Bipolar Disorder] explode all trees (1601)
#103 MeSH descriptor: [Phobic Disorders] this term only (847)
#104 MeSH descriptor: [Panic Disorder] this term only (758)
#105 school next refusal:ti,ab,kw (14)
#106 MeSH descriptor: [Mental Health] this term only (689)
#107 {or #83-#106} (57,988)
#108 MeSH descriptor: [Economics] this term only (58)
#109 MeSH descriptor: [Costs and Cost Analysis] explode all trees (23,270)
#110 MeSH descriptor: [Value of Life] this term only (144)
#111 MeSH descriptor: [Economics, Hospital] explode all trees (1655)
#112 MeSH descriptor: [Economics, Medical] this term only (38)
#113 MeSH descriptor: [Economics, Nursing] this term only (17)
#114 MeSH descriptor: [Economics, Pharmaceutical] this term only (236)
#115 MeSH descriptor: [Economics, Dental] this term only (3)
#116 (econom* or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic*):ti,ab,kw (48,142)
#117 (expenditure* not energy):ti,ab (762)
#118 (value next money):ti,ab,kw (2)
#119 budget*:ti,ab,kw (418)
#120 MeSH descriptor: [Hospitalization] this term only (4574)
#121 MeSH descriptor: [Length of Stay] this term only (6734)
#122 MeSH descriptor: [Patient Admission] this term only (578)
#123 MeSH descriptor: [Patient Readmission] this term only (811)
#124 MeSH descriptor: [Health Resources] this term only (513)
#125 (length near/2 stay):ti,ab,kw (10,176)
#126 (duration near/2 stay):ti,ab,kw (372)
#127 (hospital next (access* or uptake or visit* or attendance* or admission* or admit* or episode*)):ti,ab,kw (3243)
#128 hospital next cost*:ti,ab,kw (2548)
#129 (time near/2 discharg*):ti,ab,kw (896)
#130 hospital next day*:ti,ab,kw (508)
#131 ((patient* or inpatient* or in-patient*) next (cost* or stay*)):ti,ab,kw (772)
#132 (number near/2 (nights or days)):ti,ab,kw (1889)
#133 (primary next care next (visit* or contact* or attendance* or admission* or episode*)):ti,ab,kw (139)
#134 (surgery next (visit* or contact* or attendance* or admission* or episode*)):ti,ab,kw (36)
#135 (GP next (access or uptake or visit* or contact* or attendance* or admission* or episode*)):ti,ab,kw (65)
#136 ((uptake or access) next (service* or care or intervention*)):ti,ab,kw (39)
#137 ((clinic or surgery or hospital or “accident and emergency”) near/2 (work-flow or work next flow)):ti,ab,kw (2)
#138 (consultation* near/2 (time or length)):ti,ab,kw (116)
#139 (hospitalisation* or hospitalization* or rehospitalisation* or rehospitalization* or re-hospitalisation* or re-hospitalization*):ti,ab,kw (15,517)
#140 (hrql or hrqol or “h qol” or h-qol or hql or hqol):ti,ab,kw (1887)
#141 MeSH descriptor: [Quality-Adjusted Life Years] this term only (3773)
#142 (qaly* or “quality adjusted life” or “quality of life” or “life quality”):ti,ab,kw (37,642)
#143 {or #108-#142} (97,676)
#144 #20 or #75 (169,797)
#145 #144 and #82 and #107 and #143 (1739)
#146 “Cool Kids”:ti,ab,kw (3)
#147 “Sweet talk”:ti,ab,kw (2)
#148 “Timid to Tiger”:ti,ab,kw (0)
#149 “problem solving for life”:ti,ab,kw (2)
#150 “Incredible Years”:ti,ab,kw (67)
#151 “Triple P”:ti,ab,kw (77)
#152 friends next program*:ti,ab,kw (12)
#153 #146 or #147 or #148 or #149 or #150 or #151 or #152 (162)
#154 #145 or #153 (1894)
EMBASE (via OvidSP)
Date searched: 18 March 2015.
Date range searched: 1974 to 17 March 2015.
Records retrieved: 17,780.
Search strategy
-
self administer*.ti,ab. (30,354)
-
(self administer$ adj2 (questionnaire$ or survey$ or interview$)).ti,ab. (18,534)
-
1 not 2 (11,820)
-
self care/ (33,623)
-
(self care$ or selfcaring or selfcare$ or selfcaring).ti,ab. (14,723)
-
(self manag$ or selfmanag$).ti,ab. (13,745)
-
(self monitor$ or selfmonitor$ or self report$ or selfreport$).ti,ab. (120,139)
-
(self help$ or selfhelp$).ti,ab. (6234)
-
(self diagnos$ or selfdiagnos$ or self assess$ or selfassess$).ti,ab. (14,481)
-
blood glucose self-monitoring/ (9642)
-
self initiat$.ti,ab. (1171)
-
self concept/ (65,378)
-
self efficacy.ti,ab. (17,042)
-
Drug self administration/ (8067)
-
(self medicat$ or selfmedicat$ or self remed$ or selfremed$).ti,ab. (4434)
-
(self treat$ or selftreat$ or self cure$ or selfcure$ or self curing or selfcuring).ti,ab. (2748)
-
(collaborat$ adj (care or manag$)).ti,ab. (1749)
-
recovery.ti,ab. (399,435)
-
3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 (666,873)
-
social support/ (60,564)
-
social support$.ti,ab. (29,089)
-
(group adj (support$ or advice or advis$ or monitor$ or intervention$ or train$ or instruct$ or consult$ or assist$ or educat$ or information)).ti,ab. (7925)
-
(peer adj (support$ or advice or advis$ or monitor$ or intervention$ or train$ or instruct$ or consult$ or assist$ or educat$ or information)).ti,ab. (4169)
-
((mutual or telephone) adj support).ti,ab. (1115)
-
(expert patient$ or virtual communit$ or online communit$).ti,ab. (914)
-
(befriend$ or coach$ or mentor$ or buddy or buddies).ti,ab. (20,445)
-
health trainer$.ti,ab. (65)
-
telemedicine/ (12,152)
-
(telemedicine or telecare or telenursing or telemonitor$ or telehealth or ehealth).ti,ab. (11,512)
-
teleconsultation/ (6439)
-
((telephon$ or remote or phone) adj2 (follow$ or support$ or consult$ or advice or advis$ or intervention$ or instruct$ or assist$ or educate or education or information or monitor$)).ti,ab. (13,807)
-
case management/ (8130)
-
(case manag$ or action plan$ or care plan$ or care manag$ or management plan$ or management program$ or care program$ or goal setting or individual goal$).ti,ab. (66,439)
-
Patient Participation/ (17,929)
-
(involv$ or participat$ or collaborat$).ti,ab. (2,443,918)
-
patient education/ (88,903)
-
patient education.ti,ab. (16,471)
-
(patient adj2 (educat$ or advice or advis$ or instruct$ or instruct$ or train$ or coach$)).ti,ab. (24,060)
-
((consumer health or patient) adj information).ti,ab. (7877)
-
(nurse adj2 educator$).ti,ab. (2777)
-
((financial or monetary or money) adj2 (incentive$ or competition$ or contest$ or lotter$ or reward$ or prize$)).ti,ab. (5470)
-
(contingent payment$ or deposit contract$).ti,ab. (33)
-
decision making/ (149,178)
-
(decision$ adj2 (shared or support$ or aid or aids or making)).ti,ab. (112,354)
-
(goal set$ or individual goal$).ti,ab. (3176)
-
exp Diet/ or exp exercise/ (433,362)
-
Motivational Interviewing/ (1362)
-
Cognitive therapy/ (35,839)
-
(CBT or cognitive therap$ or cognitive behav$).ti,ab. (28,386)
-
Teaching/ or Publication/ (194,835)
-
(educational material$ or leaflet$ or booklet$ or toolkit$).ti,ab. (31,734)
-
Bibliotherapy/ (68)
-
Internet/ or Social Media/ (80,342)
-
exp Child Parent Relations/ (68,127)
-
(parenting or parent$ training).ti,ab. (13,012)
-
exp Behavior Therapy/ (37,925)
-
((behavior$ or behaviour$) adj (manag$ or modif$)).ti,ab. (6548)
-
exp Psychotherapy/ (195,095)
-
Group therapy/ (18,204)
-
psychoeducat$.ti,ab. (4261)
-
Problem Solving/ (27,244)
-
(skills training or coping skill$ or empower$).ti,ab. (25,022)
-
Adaptative Behavior/ (0)
-
exp interpersonal communication/ (417,154)
-
Mindfulness/ (1015)
-
exp Patient Right/ (91,293)
-
mobile phone/ or telephone/ or Text Messaging/ or Reminder System/ (37,748)
-
text messag$.ti,ab. (1632)
-
or/20-68 (4,059,777)
-
exp Child/ (2,160,034)
-
exp juvenile/ (2,820,035)
-
(child or children or schoolchild$ or baby or babies or infant or infants or toddler$ or teen$ or teenager$ or adolescen$ or young person$ or young people or youth or youngster$ or juvenile$ or paediatric or pediatric).ti,ab. (1,761,362)
-
exp Parent/ (168,626)
-
Caregiver/ (43,942)
-
(parent$ or mother$ or father$ or caregiver$ or carer$ or guardian$ or advocate$ or family).ti,ab. (1,237,658)
-
70 or 71 or 72 or 73 or 74 or 75 (4,140,594)
-
exp Diabetes Mellitus/ (642,426)
-
Cystic Fibrosis/ (50,945)
-
mucoviscidosis.mp. (1548)
-
exp Asthma/ (196,806)
-
Attention Deficit Disorder/ (39,064)
-
Hyperkinesia/ (4305)
-
exp Anxiety/ (129,925)
-
Depression/ (260,270)
-
Automutilation/ (11,299)
-
exp Epilepsy/ (181,678)
-
exp Conduct Disorder/ (4717)
-
exp Mood Disorders/ (361,339)
-
exp Obsessive-Compulsive Disorder/ (29,047)
-
Posttraumatic Stress Disorder/ (37,336)
-
exp Psychosis/ (227,323)
-
exp Eating Disorder/ (37,814)
-
exp Schizophrenia/ (148,365)
-
exp Bipolar Disorder/ (42,348)
-
exp Phobia/ (22,859)
-
Panic/ (18,214)
-
school refusal.ti,ab. (310)
-
exp Mental Health/ (90,904)
-
77 or 78 or 79 or 80 or 81 or 82 or 83 or 84 or 85 or 86 or 87 or 88 or 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98 (1,802,468)
-
exp economics/ (222,944)
-
exp Cost/ (265,768)
-
Health care planning/ (80,549)
-
(econom$ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab. (653,899)
-
(expenditure$ not energy).tw. (25,636)
-
(value adj money).tw. (6)
-
budget$.tw. (25,819)
-
hospitalization/ or “length of stay”/ or patient admission/ or patient readmission/ (401,452)
-
((healthcare or health) adj resource$).ti,ab. (8383)
-
(length adj2 stay).ti,ab. (50,442)
-
(duration adj2 stay).ti,ab. (3162)
-
(hospital adj (access$ or uptake or visit$ or attendance$ or admission$ or admit$ or episode$)).ti,ab. (39,882)
-
hospital cost$.ti,ab. (7701)
-
(time adj2 discharg$).ti,ab. (6339)
-
hospital day$.ti,ab. (6826)
-
((patient$ or inpatient$ or in-patient$) adj (cost$ or stay$)).ti,ab. (8915)
-
(number adj2 (nights or days)).ti,ab. (12,521)
-
(primary care adj (visit$ or contact$ or attendance$ or admission$ or episode$)).ti,ab. (1236)
-
(surgery adj (visit$ or contact$ or attendance$ or admission$ or episode$)).ti,ab. (342)
-
(GP adj (access or uptake or visit$ or contact$ or attendance$ or admission$ or episode$)).ti,ab. (614)
-
((uptake or access) adj (service$ or care or intervention$)).ti,ab. (1011)
-
((clinic or surgery or hospital or “accident and emergency”) adj2 (work-flow or work flow)).ti,ab. (13)
-
(consultation$ adj2 (time or length)).ti,ab. (1466)
-
(hospitalisation$ or hospitalization$ or rehospitalisation$ or rehospitalization$ or re-hospitalisation$ or re-hospitalization$).ti,ab. (152,093)
-
(hrql or hrqol or h qol or hql or hqol).ti,ab. (16,145)
-
quality adjusted life year/ (13,443)
-
(qaly$ or quality adjusted life or quality of life or life quality).tw. (242,535)
-
100 or 101 or 102 or 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114 or 115 or 116 or 117 or 118 or 119 or 120 or 121 or 122 or 123 or 124 or 125 or 126 (1,622,052)
-
19 or 69 (4,503,231)
-
128 and 76 and 99 and 127 (21,601)
-
Cool Kids.ti,ab. (10)
-
Sweet talk.ti,ab. (18)
-
Timid to Tiger.ti,ab. (0)
-
“problem solving for life”.ti,ab. (11)
-
Incredible Years.ti,ab. (109)
-
Triple P.ti,ab. (171)
-
friends program$.ti,ab. (17)
-
130 or 131 or 132 or 133 or 134 or 135 or 136 (327)
-
129 or 137 (21,901)
-
(editorial or comment or letter).pt. (1,340,488)
-
138 not 139 (21,728)
-
limit 140 to embase (17,780)
IDEAS database of Economic and Finance Research
Date searched: 31 March 2015.
The IDEAS search interface is only suitable for one-word or phrase searching, so a number of small searches were conducted to identify potentially relevant records (e.g. children AND diabetes, children AND asthma and so on). The search results were cut and pasted into word documents to enable scanning.
Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations and Ovid MEDLINE(R)
Date searched: 18 March 2015.
Date range searched: 1946 to present.
Records retrieved: 10,870 records.
Search strategy
-
self administration/ (9309)
-
self administer*.ti,ab. (24,903)
-
(self administer$ adj2 (questionnaire$ or survey$ or interview$)).ti,ab. (15,609)
-
2 not 3 (9294)
-
self care/ (24,322)
-
(self care$ or selfcaring or selfcare$ or selfcaring).ti,ab. (10,990)
-
(self manag$ or selfmanag$).ti,ab. (9689)
-
(self monitor$ or selfmonitor$ or self report$ or selfreport$).ti,ab. (95,133)
-
(self help$ or selfhelp$).ti,ab. (4821)
-
(self diagnos$ or selfdiagnos$ or self assess$ or selfassess$).ti,ab. (10,513)
-
blood glucose self-monitoring/ (4401)
-
self initiat$.ti,ab. (955)
-
self efficacy/ (12,604)
-
self efficacy.ti,ab. (14,136)
-
self medication/ (4026)
-
(self medicat$ or selfmedicat$ or self remed$ or selfremed$).ti,ab. (2938)
-
(self treat$ or selftreat$ or self cure$ or selfcure$ or self curing or selfcuring).ti,ab. (2268)
-
(collaborat$ adj (care or manag$)).ti,ab. (1381)
-
recovery.ti,ab. (315,800)
-
1 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 (495,898)
-
social support/ (52,876)
-
social support$.ti,ab. (23,715)
-
(group adj (support$ or advice or advis$ or monitor$ or intervention$ or train$ or instruct$ or consult$ or assist$ or educat$ or information)).ti,ab. (5138)
-
(peer adj (support$ or advice or advis$ or monitor$ or intervention$ or train$ or instruct$ or consult$ or assist$ or educat$ or information)).ti,ab. (3223)
-
((mutual or telephone) adj support).ti,ab. (809)
-
(expert patient$ or virtual communit$ or online communit$).ti,ab. (662)
-
(befriend$ or coach$ or mentor$ or buddy or buddies).ti,ab. (16,424)
-
health trainer$.ti,ab. (45)
-
telemedicine/ (11,775)
-
(telemedicine or telecare or telenursing or telemonitor$ or telehealth or ehealth).ti,ab. (9452)
-
remote consultation/ (3667)
-
((telephon$ or remote or phone) adj2 (follow$ or support$ or consult$ or advice or advis$ or intervention$ or instruct$ or assist$ or educate or education or information or monitor$)).ti,ab. (9595)
-
case management/ (8506)
-
(case manag$ or action plan$ or care plan$ or care manag$ or management plan$ or management program$ or care program$ or goal setting or individual goal$).ti,ab. (50,370)
-
Patient Participation/ (18,448)
-
(involv$ or participat$ or collaborat$).ti,ab. (2,006,956)
-
patient education as topic/ (71,385)
-
patient education.ti,ab. (12,012)
-
(patient adj2 (educat$ or advice or advis$ or instruct$ or instruct$ or train$ or coach$)).ti,ab. (17,109)
-
((consumer health or patient) adj information).ti,ab. (5353)
-
(nurse adj2 educator$).ti,ab. (2644)
-
((financial or monetary or money) adj2 (incentive$ or competition$ or contest$ or lotter$ or reward$ or prize$)).ti,ab. (4578)
-
(contingent payment$ or deposit contract$).ti,ab. (25)
-
decision making/ (70,170)
-
(decision$ adj2 (shared or support$ or aid or aids or making)).ti,ab. (87,782)
-
(goal set$ or individual goal$).ti,ab. (2251)
-
exp Diet/ or exp exercise/ (313,869)
-
Motivational Interviewing/ (393)
-
Cognitive therapy/ (16,603)
-
(CBT or cognitive therap$ or cognitive behav$).ti,ab. (19,378)
-
Teaching Materials/ or Pamphlets/ (8753)
-
(educational material$ or leaflet$ or booklet$ or toolkit$).ti,ab. (24,101)
-
Bibliotherapy/ (342)
-
Internet/ or Blogging/ or Social Media/ (52,994)
-
Parenting/ (10,836)
-
parent$ training.ti,ab. (778)
-
Behavior Therapy/ (23,664)
-
((behavior$ or behaviour$) adj (manag$ or modif$)).ti,ab. (5083)
-
Psychotherapy, Brief/ (2781)
-
Psychotherapy, Group/ (11,975)
-
psychoeducat$.ti,ab. (2827)
-
Problem Solving/ (21,273)
-
(skills training or coping skill$ or empower$).ti,ab. (19,438)
-
Adaptation, Psychological/ (76,111)
-
exp Communication/ (374,050)
-
Mindfulness/ (345)
-
Patient Access to Records/ (871)
-
Cell Phones/ or Telephones/ or Text Messaging/ or Reminder Systems/ (16,546)
-
text messag$.ti,ab. (1261)
-
or/21-69 (3,069,577)
-
exp Child/ (1,568,167)
-
Adolescent/ (1,639,965)
-
(child or children or schoolchild$ or baby or babies or infant or infants or toddler$ or teen$ or teenager$ or adolescen$ or young person$ or young people or youth or youngster$ or juvenile$ or paediatric or pediatric).ti,ab. (1,420,691)
-
exp Parents/ (74,561)
-
Caregivers/ (22,451)
-
(parent$ or mother$ or father$ or caregiver$ or carer$ or guardian$ or advocate$ or family).ti,ab. (1,021,910)
-
71 or 72 or 73 or 74 or 75 or 76 (3,693,299)
-
exp Diabetes Mellitus/ (322,132)
-
Cystic Fibrosis/ (28,835)
-
mucoviscidosis.mp. (1399)
-
exp Asthma/ (107,539)
-
exp “Attention Deficit and Disruptive Behavior Disorders”/ (23,586)
-
Hyperkinesis/ (3695)
-
exp Anxiety/ (57,586)
-
Depression/ (79,319)
-
Depressive Disorder/ (59,030)
-
Self Mutilation/ or Self-Injurious Behavior/ (8004)
-
exp Epilepsy/ (131,823)
-
exp Conduct Disorder/ (2286)
-
exp Mood Disorders/ (117,649)
-
exp Obsessive-Compulsive Disorder/ (11,558)
-
Stress Disorders, Post-Traumatic/ (21,973)
-
exp Psychotic Disorders/ (39,064)
-
exp Eating Disorders/ (22,708)
-
exp Schizophrenia/ (86,432)
-
exp Bipolar Disorder/ (32,171)
-
Phobic Disorders/ (9386)
-
Panic Disorder/ (6032)
-
school refusal.ti,ab. (207)
-
Mental Health/ (22,673)
-
78 or 79 or 80 or 81 or 82 or 83 or 84 or 85 or 86 or 87 or 88 or 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98 or 99 or 100 (1,006,004)
-
economics/ (26,582)
-
exp “Costs and Cost Analysis”/ (185,512)
-
value of life/ (5422)
-
exp economics, hospital/ or economics, medical/ or economics, nursing/ or economics, pharmaceutical/ or economics, dental/ (36,516)
-
(econom$ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab. (507,710)
-
(expenditure$ not energy).tw. (19,526)
-
(value adj money).tw. (5)
-
budget$.tw. (19,998)
-
hospitalization/ or “length of stay”/ or patient admission/ or patient readmission/ (148,295)
-
health resources/ (9102)
-
(length adj2 stay).ti,ab. (30,699)
-
(duration adj2 stay).ti,ab. (2182)
-
(hospital adj (access$ or uptake or visit$ or attendance$ or admission$ or admit$ or episode$)).ti,ab. (27,387)
-
hospital cost$.ti,ab. (5555)
-
(time adj2 discharg$).ti,ab. (4083)
-
hospital day$.ti,ab. (4364)
-
((patient$ or inpatient$ or in-patient$) adj (cost$ or stay$)).ti,ab. (5452)
-
(number adj2 (nights or days)).ti,ab. (8981)
-
(primary care adj (visit$ or contact$ or attendance$ or admission$ or episode$)).ti,ab. (953)
-
(surgery adj (visit$ or contact$ or attendance$ or admission$ or episode$)).ti,ab. (232)
-
(GP adj (access or uptake or visit$ or contact$ or attendance$ or admission$ or episode$)).ti,ab. (407)
-
((uptake or access) adj (service$ or care or intervention$)).ti,ab. (721)
-
((clinic or surgery or hospital or “accident and emergency”) adj2 (work-flow or work flow)).ti,ab. (6)
-
(consultation$ adj2 (time or length)).ti,ab. (1013)
-
(hospitalisation$ or hospitalization$ or rehospitalisation$ or rehospitalization$ or re-hospitalisation$ or re-hospitalization$).ti,ab. (101,245)
-
(hrql or hrqol or h qol or hql or hqol).ti,ab. (10,897)
-
quality adjusted life year/ (7363)
-
(qaly$ or quality adjusted life or quality of life or life quality).tw. (163,414)
-
102 or 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114 or 115 or 116 or 117 or 118 or 119 or 120 or 121 or 122 or 123 or 124 or 125 or 126 or 127 or 128 or 129 (993,754)
-
20 or 70 (3,436,791)
-
131 and 77 and 101 and 130 (10,689)
-
Cool Kids.ti,ab. (7)
-
Sweet talk.ti,ab. (15)
-
Timid to Tiger.ti,ab. (1)
-
“problem solving for life”.ti,ab. (9)
-
Incredible Years.ti,ab. (95)
-
Triple P.ti,ab. (136)
-
friends program$.ti,ab. (11)
-
133 or 134 or 135 or 136 or 137 or 138 or 139 (266)
-
132 or 140 (10,943)
-
animals/ not humans/ (3,907,576)
-
141 not 142 (10,938)
-
(editorial or comment or letter).pt. (1,386,778)
-
143 not 144 (10,870)
Paediatric Economic Database Evaluation
URL: http://pede.ccb.sickkids.ca/pede/index.jsp
Date searched: 31 March 2015.
The PEDE search interface is only suitable for one word or phrase searching so a number of small searches were conducted to identify potentially relevant records (e.g. self, diabetes, asthma, depression and so on). A total of 480 potentially relevant records were downloaded.
PsycINFO (via OVIDSP)
Date searched: 17 March 2015.
Date range searched: 1806 to March week 2 2015.
Records retrieved: 4620.
Search strategy
-
Drug self administration/ (1547)
-
self administer*.ti,ab. (10,130)
-
(self administer$ adj2 (questionnaire$ or survey$ or interview$)).ti,ab. (5254)
-
2 not 3 (4876)
-
self care skills/ (3532)
-
(self care$ or selfcaring or selfcare$ or selfcaring).ti,ab. (6125)
-
(self manag$ or selfmanag$).ti,ab. (6074)
-
(self monitor$ or selfmonitor$ or self report$ or selfreport$).ti,ab. (87,437)
-
(self help$ or selfhelp$).ti,ab. (6904)
-
(self diagnos$ or selfdiagnos$ or self assess$ or selfassess$).ti,ab. (6241)
-
blood glucose self-monitoring/ (0)
-
self initiat$.ti,ab. (1179)
-
self efficacy/ (15,881)
-
self efficacy.ti,ab. (25,391)
-
self medication/ (562)
-
(self medicat$ or selfmedicat$ or self remed$ or selfremed$).ti,ab. (1279)
-
(self treat$ or selftreat$ or self cure$ or selfcure$ or self curing or selfcuring).ti,ab. (383)
-
(collaborat$ adj (care or manag$)).ti,ab. (835)
-
recovery.ti,ab. (46,680)
-
1 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 (189,281)
-
social support/ (28,230)
-
social support$.ti,ab. (34,367)
-
(group adj (support$ or advice or advis$ or monitor$ or intervention$ or train$ or instruct$ or consult$ or assist$ or educat$ or information)).ti,ab. (6330)
-
(peer adj (support$ or advice or advis$ or monitor$ or intervention$ or train$ or instruct$ or consult$ or assist$ or educat$ or information)).ti,ab. (3732)
-
((mutual or telephone) adj support).ti,ab. (868)
-
(expert patient$ or virtual communit$ or online communit$).ti,ab. (1488)
-
(befriend$ or coach$ or mentor$ or buddy or buddies).ti,ab. (22,379)
-
health trainer$.ti,ab. (17)
-
telemedicine/ (2763)
-
(telemedicine or telecare or telenursing or telemonitor$ or telehealth or ehealth).ti,ab. (1937)
-
(remote consult$ or teleconsult$).ti,ab. (105)
-
((telephon$ or remote or phone) adj2 (follow$ or support$ or consult$ or advice or advis$ or intervention$ or instruct$ or assist$ or educate or education or information or monitor$)).ti,ab. (3067)
-
exp case management/ (2944)
-
(case manag$ or action plan$ or care plan$ or care manag$ or management plan$ or management program$ or care program$ or goal setting or individual goal$).ti,ab. (22,094)
-
Client participation/ (1459)
-
(involv$ or participat$ or collaborat$).ti,ab. (550,207)
-
client education/ (3154)
-
patient education.ti,ab. (2186)
-
(patient adj2 (educat$ or advice or advis$ or instruct$ or instruct$ or train$ or coach$)).ti,ab. (3416)
-
((consumer health or patient) adj information).ti,ab. (745)
-
(nurse adj2 educator$).ti,ab. (684)
-
((financial or monetary or money) adj2 (incentive$ or competition$ or contest$ or lotter$ or reward$ or prize$)).ti,ab. (3247)
-
(contingent payment$ or deposit contract$).ti,ab. (31)
-
exp decision making/ (70,405)
-
(decision$ adj2 (shared or support$ or aid or aids or making)).ti,ab. (64,722)
-
(goal set$ or individual goal$).ti,ab. (4646)
-
exp Diets/ or exp exercise/ (26,852)
-
Motivational Interviewing/ (1454)
-
Cognitive therapy/ (11,872)
-
(CBT or cognitive therap$ or cognitive behav$).ti,ab. (34,514)
-
exp Instructional Materials/ (0)
-
(educational material$ or leaflet$ or booklet$ or toolkit$).ti,ab. (4797)
-
Bibliotherapy/ (610)
-
Internet/ or Social Media/ (24,179)
-
exp Parenting/ (76,945)
-
parent$ training.ti,ab. (2578)
-
exp Behavior Therapy/ (17,292)
-
((behavior$ or behaviour$) adj (manag$ or modif$)).ti,ab. (7480)
-
Psychotherapy, Brief/ (0)
-
exp Group therapy/ (20,117)
-
psychoeducat$.ti,ab. (6489)
-
exp Problem Solving/ (28,843)
-
(skills training or coping skill$ or empower$).ti,ab. (28,916)
-
Adaptative Behavior/ (0)
-
exp Communication/ (191,116)
-
Mindfulness/ (4018)
-
Client Records/ (677)
-
Cellular Phones/ or Telephone Systems/ or Messages/ (9003)
-
text messag$.ti,ab. (940)
-
or/21-69 (1,048,326)
-
childhood birth 12 yrs.ag. (431,936)
-
adolescence 13 17 yrs.ag. (340,365)
-
(child or children or schoolchild$ or baby or babies or infant or infants or toddler$ or teen$ or teenager$ or adolescen$ or young person$ or young people or youth or youngster$ or juvenile$ or paediatric or pediatric).ti,ab. (686,296)
-
exp Parents/ (74,045)
-
Caregivers/ (20,108)
-
(parent$ or mother$ or father$ or caregiver$ or carer$ or guardian$ or advocate$ or family).ti,ab. (474,588)
-
71 or 72 or 73 or 74 or 75 or 76 (1,087,542)
-
Diabetes Mellitus/ (4020)
-
Cystic Fibrosis/ (687)
-
mucoviscidosis.mp. (4)
-
Asthma/ (3816)
-
exp Attention Deficit Disorder/ (19,781)
-
Hyperkinesis/ (7565)
-
exp Anxiety/ (53,810)
-
Depression/ (22,138)
-
exp Major Depression/ (97,934)
-
Self-Injurious Behavior/ (2077)
-
exp Epilepsy/ (20,442)
-
Conduct Disorder/ (3575)
-
exp Affective Disorders/ (125,594)
-
Obsessive Compulsive Disorder/ (10,627)
-
Posttraumatic Stress Disorder/ (23,065)
-
exp Psychosis/ (95,067)
-
exp Eating Disorder/ (24,088)
-
exp Schizophrenia/ (74,719)
-
exp Bipolar Disorder/ (20,574)
-
exp Phobias/ (11,206)
-
Panic Disorder/ (6929)
-
school refusal.ti,ab. (478)
-
exp Mental Health/ (44,641)
-
78 or 79 or 80 or 81 or 82 or 83 or 84 or 85 or 86 or 87 or 88 or 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98 or 99 or 100 (422,609)
-
exp economics/ (18,357)
-
exp costs/ (19,890)
-
(econom$ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab. (163,542)
-
(expenditure$ not energy).tw. (5744)
-
(value adj money).tw. (11)
-
budget$.tw. (6378)
-
hospitalization/ or “length of stay”/ or patient admission/ or patient readmission/ (8465)
-
((healthcare or health) adj resource$).ti,ab. (1564)
-
(length adj2 stay).ti,ab. (3614)
-
(duration adj2 stay).ti,ab. (240)
-
(hospital adj (access$ or uptake or visit$ or attendance$ or admission$ or admit$ or episode$)).ti,ab. (3798)
-
hospital cost$.ti,ab. (252)
-
(time adj2 discharg$).ti,ab. (578)
-
hospital day$.ti,ab. (388)
-
((patient$ or inpatient$ or in-patient$) adj (cost$ or stay$)).ti,ab. (911)
-
(number adj2 (nights or days)).ti,ab. (1891)
-
(primary care adj (visit$ or contact$ or attendance$ or admission$ or episode$)).ti,ab. (360)
-
(surgery adj (visit$ or contact$ or attendance$ or admission$ or episode$)).ti,ab. (11)
-
(GP adj (access or uptake or visit$ or contact$ or attendance$ or admission$ or episode$)).ti,ab. (102)
-
((uptake or access) adj (service$ or care or intervention$)).ti,ab. (331)
-
((clinic or surgery or hospital or “accident and emergency”) adj2 (work-flow or work flow)).ti,ab. (1)
-
(consultation$ adj2 (time or length)).ti,ab. (252)
-
(hospitalisation$ or hospitalization$ or rehospitalisation$ or rehospitalization$ or re-hospitalisation$ or re-hospitalization$).ti,ab. (21,193)
-
(hrql or hrqol or h qol or hql or hqol).ti,ab. (3414)
-
(qaly$ or quality adjusted life or quality of life or life quality).tw. (45,441)
-
102 or 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114 or 115 or 116 or 117 or 118 or 119 or 120 or 121 or 122 or 123 or 124 or 125 or 126 (246,148)
-
20 or 70 (1,167,628)
-
128 and 77 and 101 and 127 (4155)
-
Cool Kids.ti,ab. (20)
-
Sweet talk.ti,ab. (5)
-
Timid to Tiger.ti,ab. (3)
-
“problem solving for life”.ti,ab. (25)
-
Incredible Years.ti,ab. (160)
-
Triple P.ti,ab. (231)
-
friends program$.ti,ab. (38)
-
130 or 131 or 132 or 133 or 134 or 135 or 136 (474)
-
129 or 137 (4620)
Science Citation Index and Social Science Citation Index (Searched using Web of Science)
Date searched: 19 March 2015.
Date range searched: Science Citation Index – 1900 to present.
Date range searched: SSCI – 1956 to present.
Records retrieved from both databases: 12,737 records.
Search strategy
| #36 | 12,737 |
#34 not #35 Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #35 | 2,992,107 |
TI=(rat or rats or mouse or mice or hamster or hamsters or dog or dogs or cat or cats or feline or bovine or sheep or fly or flies or fish or fishes or fisheries or horse or horses or equine or bat or bats or bee or bees or grass or grasses or bird or birds or avian or fossil or fossils or lichen or lichens or mushroom or mushrooms or rabbit or rabbits or moss or mosses or fungus or fungi or cow or cattle or bovine or livestock or swine or poultry or genera or species or fauna or habitat or marine or ecology) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #34 | 12,774 |
#33 OR #32 Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #33 | 505 |
TS=(“Cool Kids” or “Sweet talk” or “Timid to Tiger” or “problem solving for life” or “Incredible Years” or “Triple P” or “friends program*”) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #32 | 12,295 |
#31 AND #30 AND #18 AND #17 Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #31 | 4,194,119 |
#16 OR #5 Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #30 | 1,789,043 |
#29 OR #28 OR #27 OR #26 OR #25 OR #24 OR #23 OR #22 OR #21 OR #20 OR #19 Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #29 | 211,979 |
TS=(hrql or hrqol or h-qol or hql or hqol or qaly* or “quality adjusted life” or “quality of life” or “life quality”) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #28 | 1361 |
TS=(consultation* near/2 (time or length)) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #27 | 5 |
TS=(“accident and emergency” SAME (work-flow or work flow)) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #26 | 12 |
TS=((clinic or surgery or hospital) near/2 (work-flow or “work flow”)) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #25 | 86,270 |
TS=(“primary care visit*” or “primary care contact*” or “primary care attendance*” or “primary care admission*” or “primary care episode*” or “surgery visit*” or “surgery contact*” or “surgery attendance*” or “surgery admission*” or “surgery episode*” or “GP access” or “GP uptake” or “GP visit*” or “GP contact*” or “GP attendance*” or “GP admission*” or “GP episode*” or “uptake service*” or “uptake care” or “uptake intervention*” or “access service*” or “access care” or “access intervention*” or hospitalisation* or hospitalization* or rehospitalisation* or rehospitalization* or re-hospitalisation* or re-hospitalization*) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #24 | 18,204 |
TS=(number near/2 (nights or days)) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #23 | 7480 |
TS=(time near/2 discharg*) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #22 | 4626 |
TS=(duration near/2 stay) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #21 | 38,610 |
TS=(length near/2 stay) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #20 | 34,617 |
TS=(expenditure* not energy) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #19 | 1,480,654 |
TS=(econom* or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic* or “value for money” or budget* or “hospital access*” or “hospital uptake” or “hospital visit*” or “hospital attendance*” or “hospital admission*” or “hospital admit*” or “hospital episode*” or “hospital cost*” or “hospital day*” or “patient* cost*” or “inpatient* cost*” or “in-patient* cost*” or “patient* stay*” or “inpatient* stay*” or “in-patient* stay”) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #18 | 1,075,262 |
TS=(“Diabetes Mellitus” or “Cystic Fibrosis” or mucoviscidosis or Asthma or “Attention Deficit disorder*” or “Disruptive Behaviour disorder*” or “Disruptive Behavior disorder*” or Hyperkinesis or Anxiety or Depression or “Depressive Disorder*” or Epilepsy or “Conduct Disorder*” or “Mood Disorder*” or “Obsessive-Compulsive Disorder*” or “Post-Traumatic Stress Disorder*” or “Psychotic Disorder*” or “Eating Disorder*” or Schizophrenia or “Bipolar Disorder*” or “Phobic Disorder*” or “Panic Disorder*” or “school refusal” or “Mental Health” or “Self Mutilation” or “Self-Injurious Behavior*” or “Self-Injurious Behaviour*”) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #17 | 2,818,271 |
TS=(child or children or schoolchild* or baby or babies or infant or infants or toddler* or teen* or teenager* or adolescen* or “young person*” or “young people” or youth or youngster* or juvenile* or paediatric or pediatric or parent* or mother* or father* or caregiver* or carer* or guardian* or advocate* or family) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #16 | 3,686,708 |
#15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 OR #8 OR #7 OR #6 Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #15 | 1,215,905 |
TS=(diet or exercise or “Motivational Interviewing” or CBT or “cognitive therap*” or “cognitive behav*” or “teaching material*” or pamphlet* or “educational material*” or leaflet* or booklet* or toolkit* or Bibliotherapy or Internet or Blogging or Social Media or “parent* training” or “Behavior Therapy” or “Behaviour Therapy” or “behavior* manag*” or “behaviour* manag*” or “behavior* modif*” or “behaviour* modif*” or psychoeducat* or “Problem Solving” or “skills training” or “coping skill*” or empower* or communication or Mindfulness or “patient access to records” or “Cell Phones” or Telephones or “Text Messaging” or “Reminder Systems” or “text messag*”) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #14 | 1132 |
TS=(Adaptation near/2 Psychological) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #13 | 6107 |
TS=(Psychotherapy near/2 (Brief or group)) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #12 | 216,156 |
TS=(decision* near/2 (shared or support* or aid or aids or making)) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #11 | 7395 |
TS=((financial or monetary or money) near/2 (incentive* or competition* or contest* or lotter* or reward* or prize*)) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #10 | 1796 |
TS=(nurse near/2 educator*) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #9 | 33,339 |
TS=(patient near/2 (educat* or advice or advis* or instruct* or instruct* or train* or coach*)) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #8 | 2,406,262 |
TS=(“case manag*” or “action plan*” or “care plan*” or “care manag*” or “management plan*” or “management program*” or “care program*” or “goal setting” or “individual goal*” or involv* or participat* or collaborat* or “patient education” or “consumer health information” or “patient information” or “contingent payment*” or “deposit contract*” or “goal set*” or “individual goal*”) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #7 | 15,609 |
TS=((telephon* or remote or phone) near/2 (follow* or support* or consult* or advice or advis* or intervention* or instruct* or assist* or educate or education or information or monitor*)) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #6 | 87,375 |
TS=(“social support*” or “group support*” or “group advice” or “group advis*” or “group monitor*” or “group intervention*” or “group train*” or “group instruct*” or “group consult*” or “group assist*” or “group educat*” or “group information” or “peer support*” or “peer advice” or “peer advis*” or “peer monitor*” or “peer intervention*” or “peer train*” or “peer instruct*” or “peer consult*” or “peer assist*” or “peer educat*” or “peer information” or “mutual support” or “telephone support” or “expert patient*” or “virtual communit*” or “online communit*” or befriend* or coach* or mentor* or buddy or buddies or “health trainer*” or telemedicine or telecare or telenursing or telemonitor* or telehealth or ehealth) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #5 | 651,796 |
#4 OR #3 Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #4 | 645,267 |
TS=(self-care* or selfcaring or selfcare* or selfcaring or self-manag* or selfmanag* or self-monitor* or selfmonitor* or self-report* or selfreport* or self-help* or selfhelp* or self-diagnos* or selfdiagnos* or self-assess* or selfassess* or self-initiat* or self-efficacy or self-medicat* or selfmedicat* or self-remed* or selfremed* or self-treat* or selftreat* or self-cure* or selfcure* or self-curing or selfcuring or “collaborat* care” or “collaborat* manag*” or recovery) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #3 | 7269 |
#1 not #2 Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #2 | 14,320 |
TS=(self-administer* near/2 (questionnaire* or survey* or interview*)) Indexes=SCI-EXPANDED, SSCI Timespan=All years |
| #1 | 21,589 |
TS=self-administer* Indexes=SCI-EXPANDED, SSCI Timespan=All years |
Appendix 2 Economic checklist template
Question 1: study clarity.
Question 2: comprehensive description of competing alternatives.
Question 3: perspective.
1 = Societal.
2 = Health-care system and patient.
3 = Health-care system.
4 = Not clear.
Question 4: study design.
5 = RCT
6 = Case–control trial.
7 = Before and after.
8 = Decision model.
Question 5: economic study design.
9 = Cost-effectiveness analysis.
10 = Cost–consequence analysis.
11 = Cost–utility analysis.
Question 6: design adequacy given study type.
Question 7a: relevant costs identified.
Question 7b: relevant consequences identified.
Question 8a: costs measured accurately.
Question 8b: consequences measured adequately.
Question 9: statistical analysis appropriateness given the design.
Question 10a: subgroup analysis.
Question 10b: subgroups prespecified.
Question 11: discounting.
Question 12: incremental analysis.
Question 13: allowance for uncertainty.
Question 14: missing data handled appropriately.
Question 15a: economic model.
Question 15b: appropriateness of economic model.
Question 16: funder stated (yes/no).
Question 16a: type of funder.
12 = public/voluntary sector.
13 = private sector.
14 = do not state.
Question 16b: generalisability.
Question 16c: presentation and discussion of key results.
Appendix 3 List of included studies
Indented studies denote additional papers associated with the same top-line study.
| Study | Reference number |
|---|---|
| Atherly A, Nurmagambetov T, Williams S, Griffith M. An economic evaluation of the school-based ‘power breathing’ asthma program. J Asthma 2009;46:596–9 | 76 |
| Bartholomew LK, Gold RS, Parcel GS, Czyzewski DI, Sockrider MM, Fernandez M, et al. Watch, discover, think, and act: evaluation of computer-assisted instruction to improve asthma self-management in inner-city children. Patient Educ Couns 2000;39:269–80 | 77 |
| Bird SR, Noronha M, Kurowski W, Orkin C, Sinnott H. Integrated care facilitation model reduces use of hospital resources by patients with pediatric asthma. J Healthc Qual 2012;34:25–33 | 78 |
| Brazil K, McLean L, Abbey D, Musselman C. The influence of health education on family management of childhood asthma. Patient Educ Couns 1997;30:107–18 | 79 |
| Brown JV, Bakeman R, Celano MP, Demi AS, Kobrynski L, Wilson SR. Home-based asthma education of young low-income children and their families. J Pediatr Psychol 2002;27:677–88 | 80 |
| Browning S, Corrigall R, Garety P, Emsley R, Jolley S. Psychological interventions for adolescent psychosis: a pilot controlled trial in routine care. Eur Psychiatry 2013;28:423–6 | 81 |
| Bruzzese JM, Sheares BJ, Vincent EJ, Du Y, Sadeghi H, Levison MJ, et al. Effects of a school-based intervention for urban adolescents with asthma. A controlled trial. Am J Respir Crit Care Med 2011;183:998–1006 | 82 |
| Bryant-Stephens T, Kurian C, Guo R, Zhao H. Impact of a household environmental intervention delivered by lay health workers on asthma symptom control in urban, disadvantaged children with asthma. Am J Public Health 2009;99(Suppl. 3):S657–65 | 83 |
| Butz A, Pham L, Lewis L, Lewis C, Hill K, Walker J, et al. Rural children with asthma: impact of a parent and child asthma education program. J Asthma 2005;42:813–21 | 84 |
| Walker J, Winkelstein M, Land C, Lewis-Boyer L, Quartey R, Pham L, et al. Factors that influence quality of life in rural children with asthma and their parents. J Pediatr Health Care 2008;22:343–50 | 85 |
| Butz A, Kub J, Donithan M, James NT, Thompson RE, Bellin M, et al. Influence of caregiver and provider communication on symptom days and medication use for inner-city children with asthma. J Asthma 2010;47:478–85 | 86 |
| Byford S, Harrington R, Torgerson D, Kerfoot M, Dyer E, Harrington V, et al. Cost-effectiveness analysis of a home-based social work intervention for children and adolescents who have deliberately poisoned themselves. Results of a randomised controlled trial. Br J Psychiatry 1999;174:56–62 | 87 |
| Harrington R, Kerfoot M, Dyer E, McNiven F, Gill J, Harrington V, et al. Randomized trial of a home-based family intervention for children who have deliberately poisoned themselves. J Am Acad Child Adolesc Psychiatry 1998;37:512–18 | 88 |
| Byford S, Barrett B, Roberts C, Wilkinson P, Dubicka B, Kelvin R, et al. Cost-effectiveness of selective serotonin reuptake inhibitors and routine specialist care with and without cognitive-behavioural therapy in adolescents with major depression. Br J Psychiatry 2007;191:521–7 | 89 |
| Goodyer I, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al. Selective serotonin reuptake inhibitors (SSRIs) and routine specialist care with and without cognitive behaviour therapy in adolescents with major depression: randomised controlled trial. BMJ 2007;335:142 | 90 |
| Byford S, Barrett B, Roberts C, Clark A, Edwards V, Smethurst N, et al. Economic evaluation of a randomised controlled trial for anorexia nervosa in adolescents. Br J Psychiatry 2007;191:436–40 | 91 |
| Gowers SG, Clark A, Roberts C, Griffiths A, Edwards V, Bryan C, et al. Clinical effectiveness of treatments for anorexia nervosa in adolescents: randomised controlled trial. Br J Psychiatry 2007;191:427–35 | 92 |
| Gowers SG, Clark AF, Roberts C, Byford S, Barrett B, Griffiths A, et al. A randomised controlled multicentre trial of treatments for adolescent anorexia nervosa including assessment of cost-effectiveness and patient acceptability – the TOuCAN trial. Health Technol Assess 2010;14(15) | 93 |
| Calvo A, Moreno M, Ruiz-Sancho A, Rapado-Castro M, Moreno C, Sánchez-Gutiérrez T, et al. Intervention for adolescents with early-onset psychosis and their families: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2014;53:688–96 | 94 |
| Cano-Garcinuño A, Díaz-Vázquez C, Carvajal-Urueña I, Praena-Crespo M, Gatti-Viñoly A, García-Guerra I. Group education on asthma for children and caregivers: a randomized, controlled trial addressing effects on morbidity and quality of life. J Invest Allerg Clin 2007;17:216–26 | 95 |
| Carswell F, Robinson EJ, Hek G, Shenton T. A Bristol experience: benefits and cost of an ‘asthma nurse’ visiting the homes of asthmatic children. Bristol Med Chir J 1989;104:11–12 | 96 |
| Celano MP, Holsey CN, Kobrynski LJ. Home-based family intervention for low-income children with asthma: a randomized controlled pilot study. J Fam Psychol 2012;26:171–8 | 97 |
| Chan DS, Callahan CW, Sheets SJ, Moreno CN, Malone FJ. An Internet-based store-and-forward video home telehealth system for improving asthma outcomes in children. Am J Health Syst Pharm 2003;60:1976–81 | 98 |
| Chan DS, Callahan CW, Hatch-Pigott VB, Lawless A, Proffitt HL, Manning NE, et al. Internet-based home monitoring and education of children with asthma is comparable to ideal office-based care: results of a 1-year asthma in-home monitoring trial. Pediatrics 2007;119:569–78 | 99 |
| Christie D, Thompson R, Sawtell M, Allen E, Cairns J, Smith F, et al. Structured, intensive education maximising engagement, motivation and long-term change for children and young people with diabetes: a cluster randomised controlled trial with integral process and economic evaluation – the CASCADE study. Health Technol Assess 2014;18(20) | 100 |
| Cicutto L, Murphy S, Coutts D, O’Rourke J, Lang G, Chapman C, et al. Breaking the access barrier: evaluating an asthma center’s efforts to provide education to children with asthma in schools. Chest 2005;128:1928–35 | 101 |
| Cicutto L, To T, Murphy S. A randomized controlled trial of a public health nurse-delivered asthma program to elementary schools. J School Health 2013;83:876–84 | 102 |
| Clark NM, Gong M, Kaciroti N, Yu J, Wu G, Zeng Z, et al. A trial of asthma self-management in Beijing schools. Chronic Illn 2005;1:31–8 | 103 |
| Cowie RL, Underwood MF, Little CB, Mitchell I, Spier S, Ford GT. Asthma in adolescents: a randomized, controlled trial of an asthma program for adolescents and young adults with severe asthma. Can Respir J 2002;9:253–9 | 104 |
| Domino ME, Burns BJ, Silva SG, Kratochvil CJ, Vitiello B, Reinecke MA, et al. Cost-effectiveness of treatments for adolescent depression: results from TADS. Am J Psychiatry 2008;165:588–96 | 105 |
| Domino ME, Foster EM, Vitiello B, Kratochvil CJ, Burns BJ, Silva SG, et al. Relative cost-effectiveness of treatments for adolescent depression: 36-week results from the TADS randomized trial. J Am Acad Child Adolesc Psychiatry 2009;48:711–20 | 106 |
| March J, Silva S, Vitiello B, TADS Team. The Treatment for Adolescents with Depression Study (TADS): methods and message at 12 weeks. J Am Acad Child Adolesc Psychiatry 2006;45:1393–403 | 107 |
| March JS, Vitiello B. Clinical messages from the Treatment for Adolescents With Depression Study (TADS). Am J Psychiatry 2009;166:1118–23 | 108 |
| Treatment for Adolescents with Depression Study (TADS) Team. The Treatment for Adolescents with Depression Study (TADS): demographic and clinical characteristics. J Am Acad Child Psy 2005;44:28–40 | 109 |
| Donaldson D, Spirito A, Esposito-Smythers C. Treatment for adolescents following a suicide attempt: results of a pilot trial. J Am Acad Child Adolesc Psychiatry 2005;44:113–20 | 110 |
| Dougherty GE, Soderstrom L, Schiffrin A. An economic evaluation of home care for children with newly diagnosed diabetes: results from a randomized controlled trial. Med Care 1998;36:586–98 | 111 |
| Dougherty G, Schiffrin A, White D, Soderstrom L, Sufrategui M. Home-based management can achieve intensification cost-effectively in type I diabetes. Pediatrics 1999;103:122–8 | 112 |
| Eakin MN, Rand CS, Bilderback A, Bollinger ME, Butz A, Kandasamy V, et al. Asthma in Head Start children: effects of the Breathmobile program and family communication on asthma outcomes. J Allergy Clin Immunol 2012;129:664–70 | 113 |
| Edwards RT, Céilleachair A, Bywater T, Hughes DA, Hutchings J. Parenting programme for parents of children at risk of developing conduct disorder: cost effectiveness analysis. BMJ 2007;334:682 | 114 |
| Hutchings J, Gardner F, Bywater T, Daley D, Whitaker C, Jones K, et al. Parenting intervention in Sure Start services for children at risk of developing conduct disorder: pragmatic randomised controlled trial. BMJ 2007;334:678 | 115 |
| Espinoza-Palma T, Zamorano A, Arancibia F, Bustos MF, Silva MJ, Cardenas C, et al. Effectiveness of asthma education with and without a self-management plan in hospitalized children. J Asthma 2009;46:906–10 | 116 |
| Esposito-Smythers C, Spirito A, Kahler CW, Hunt J, Monti P. Treatment of co-occurring substance abuse and suicidality among adolescents: a randomized trial. J Consult Clin Psychol 2011;79:728–39 | 117 |
| Farber HJ, Oliveria L. Trial of an asthma education program in an inner-city pediatric emergency department. Pediatr Asthma Aller 2004;17:107–15 | 118 |
| Flapper BC, Duiverman EJ, Gerritsen J, Postema K, van der Schans CP. Happiness to be gained in paediatric asthma care. Eur Respir J 2008;32:1555–62 | 119 |
| Flores G, Bridon C, Torres S, Perez R, Walter T, Brotanek J, et al. Improving asthma outcomes in minority children: a randomized, controlled trial of parent mentors. Pediatrics 2009;124:1522–32 | 120 |
| Foster EM, Jensen PS, Schlander M, Pelham WE Jr, Hechtman L, Arnold LE, et al. Treatment for ADHD: Is more complex treatment cost-effective for more complex cases? Health Serv Res 2007;42:165–82 | 121 |
| Swanson JM, Kraemer HC, Hinshaw SP, Arnold LE, Conners CK, Abikoff HB, et al. Clinical relevance of the primary findings of the MTA: success rates based on severity of ADHD and ODD symptoms at the end of treatment. J Am Acad Child Adolesc Psychiatry 2001;40:168–79 | 122 |
| Wells KC, Pelham WE, Kotkin RA, Hoza B, Abikoff HB, Abramowitz A, et al. Psychosocial treatment strategies in the MTA study: rationale, methods, and critical issues in design and implementation. J Abnorm Child Psychol 2000;28:483–505 | 123 |
| Molina BS, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, et al. The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. J Am Acad Child Adolesc Psychiatry 2009;48:484–500 | 124 |
| Jensen PS, Garcia JA, Glied S, Crowe M, Foster M, Schlander M, et al. Cost-effectiveness of ADHD treatments: findings from the multimodal treatment study of children with ADHD. Am J Psychiatry 2005;162:1628–36 | 125 |
| The MTA Cooperative Group. A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Arch Gen Psychiat 1999;56:1073–86 | 126 |
| Franklin VL, Waller A, Pagliari C, Greene SA. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabet Med 2006;23:1332–8 | 127 |
| Galbreath AD, Smith B, Wood PR, Inscore S, Forkner E, Vazquez M, et al. Assessing the value of disease management: impact of 2 disease management strategies in an underserved asthma population. Ann Allergy Asthma Immunol 2008;101:599–607 | 128 |
| Garbutt JM, Banister C, Highstein G, Sterkel R, Epstein J, Bruns J, et al. Telephone coaching for parents of children with asthma: impact and lessons learned. Arch Pediatr Adolesc Med 2010;164:625–30 | 129 |
| Godart N, Berthoz S, Curt F, Perdereau F, Rein Z, Wallier J, et al. A randomized controlled trial of adjunctive family therapy and treatment as usual following inpatient treatment for anorexia nervosa adolescents. PLOS ONE 2012;7:e28249 | 130 |
| Gorelick MH, Meurer JR, Walsh-Kelly CM, Brousseau DC, Grabowski L, Cohn J, et al. Emergency department allies: a controlled trial of two emergency department-based follow-up interventions to improve asthma outcomes in children. Pediatrics 2006;117:S127–34 | 131 |
| Grainger-Rousseau TJ, Mc Elnay JC. A model for community pharmacist involvement with general practitioners in the management of asthma patients. J Appl Ther 1996;1:145–61 | 132 |
| Green JM, Wood AJ, Kerfoot MJ, Trainor G, Roberts C, Rothwell J, et al. Group therapy for adolescents with repeated self harm: randomised controlled trial with economic evaluation. BMJ 2011;342:d682 | 133 |
| Guendelman S, Meade K, Benson M, Chen YQ, Samuels S. Improving asthma outcomes and self-management behaviors of inner-city children: a randomized trial of the Health Buddy interactive device and an asthma diary. Arch Pediatr Adolesc Med 2002;156:114–20 | 20 |
| Guendelman S, Meade K, Chen YQ, Benson M. Asthma control and hospitalizations among inner-city children: results of a randomized trial. Telemed J E Health 2004;10(Suppl. 2):6–14 | 134 |
| Hederos CA, Janson S, Hedlin G. Six-year follow-up of an intervention to improve the management of preschool children with asthma. Acta Paediatr 2009;98:1939–44 | 135 |
| Hederos CA, Janson S, Hedlin G. Group discussions with parents have long-term positive effects on the management of asthma with good cost-benefit. Acta Paediatr 2005;94:602–8 | 136 |
| Homer C, Susskind O, Alpert HR, Owusu C, Schneider L, Rappaport LA, et al. An evaluation of an innovative multimedia educational software program for asthma management: report of a randomized, controlled trial. Pediatrics 2000;106:210–15 | 137 |
| Horner SD, Brown A. Evaluating the effect of an asthma self-management intervention for rural families. J Asthma 2014;51:168–77 | 138 |
| Hughes DM, McLeod M, Garner B, Goldbloom RB. Controlled trial of a home and ambulatory program for asthmatic children. Pediatrics 1991;87:54–61 | 139 |
| Husted GR, Thorsteinsson B, Esbensen BA, Gluud C, Winkel P, Hommel E, et al. Effect of guided self-determination youth intervention integrated into outpatient visits versus treatment as usual on glycemic control and life skills: a randomized clinical trial in adolescents with type 1 diabetes. Trials 2014;15:321 | 140 |
| Indinnimeo L, Mercuri M, Marolla F, Raponi M, Ronchetti R. Asthma education program in outpatient children. Ital J Pediatr 1997;23:873–7 | 141 |
| Indinnimeo L, Bonci E, Capra L, La Grutta S, Monaco F, Paravati F, et al. Clinical effects of a long-term educational program for children with asthma – Aironet. A 1-yr randomized controlled trial. Pediatr Allergy Immunol 2009;20:654–9 | 142 |
| Joseph CL, Peterson E, Havstad S, Johnson CC, Hoerauf S, Stringer S, et al. A web-based, tailored asthma management program for urban African-American high school students. Am J Respir Crit Care Med 2007;175:888–95 | 143 |
| Kamps JL, Rapoff MA, Roberts MC, Varela RE, Barnard M, Olson N. Improving adherence to inhaled corticosteroids in children with asthma: a pilot of a randomized clinical trial. Child Health Care 2008;37:261–77 | 144 |
| Kattan M, Stearns SC, Crain EF, Stout JW, Gergen PJ, Evans R, et al. Cost-effectiveness of a home-based environmental intervention for inner-city children with asthma. J Allergy Clin Immunol 2005;116:1058–63 | 145 |
| Morgan WJ, Crain EF, Gruchalla RS, O’Connor GT, Kattan M, Evans R, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med 2004;351:1068–80 | 146 |
| Katz LY, Cox BJ, Gunasekara S, Miller AL. Feasibility of dialectical behavior therapy for suicidal adolescent inpatients. J Am Acad Child Adolesc Psychiatry 2004;43:276–82 | 147 |
| Khan MS, O’Meara M, Stevermuer TL, Henry RL. Randomized controlled trial of asthma education after discharge from an emergency department. J Paediatr Child Health 2004;40:674–7 | 148 |
| Khan MS, O’Meara M, Henry RL. Background severity of asthma in children discharged from the emergency department. J Paediatr Child Health 2003;39:432–5 | 149 |
| Krieger J, Takaro TK, Song L, Beaudet N, Edwards K. A randomized controlled trial of asthma self-management support comparing clinic-based nurses and in-home community health workers: the Seattle-King County Healthy Homes II Project. Arch Pediat Adol Med 2009;163:141–9 | 150 |
| Sunshine J, Song L, Krieger J. Written action plan use in inner-city children: is it independently associated with improved asthma outcomes? Ann Allergy Asthma Immunol 2011;107:207–13 | 151 |
| Krishna S, Francisco BD, Balas EA, König P, Graff GR, Madsen RW, et al. Internet-enabled interactive multimedia asthma education program: a randomized trial. Pediatrics 2003;111:503–10 | 152 |
| Krishna S, Balas EA, Francisco BD, Konig P. Effective and sustainable multimedia education for children with asthma: a randomized controlled trial. Child Health Care 2006;35:75–90 | 153 |
| Lewis CE, Rachelefsky G, Lewis MA, de la Sota A, Kaplan M. A randomized trial of A.C.T. (asthma care training) for kids. Pediatrics 1984;74:478–86 | 154 |
| Lynch FL, Dickerson JF, Clarke G, Vitiello B, Porta G, Wagner KD, et al. Incremental cost-effectiveness of combined therapy vs medication only for youth with selective serotonin reuptake inhibitor-resistant depression: treatment of SSRI-resistant depression in adolescents trial findings. Arch Gen Psychiatry 2011;68:253–62 | 155 |
| Asarnow JR, Jaycox LH, Tang L, Duan N, LaBorde AP, Zeledon LR, et al. Long-term benefits of short-term quality improvement interventions for depressed youths in primary care. Am J Psychiatry 2009;166:1002–10 | 156 |
| Brent D, Emslie G, Clarke G, Wagner KD, Asarnow JR, Keller M, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial. JAMA 2008;299:901–13 | 157 |
| Madge P, McColl J, Paton J. Impact of a nurse-led home management training programme in children admitted to hospital with acute asthma: a randomised controlled study. Thorax 1997;52:223–8 | 158 |
| Maslennikova GY, Morosova ME, Salman NV, Kulikov SM, Oganov RG. Asthma education programme in Russia: educating patients. Patient Educ Couns 1998;33:113–27 | 159 |
| MeGhan SL, Wong E, Jhangri GS, Wells HM, Michaelchuk DR, Boechler VL, et al. Evaluation of an education program for elementary school children with asthma. J Asthma 2003;40:523–33 | 160 |
| McGhan SL, Wong E, Sharpe HM, Hessel PA, Mandhane P, Boechler VL, et al. A children’s asthma education program: Roaring Adventures of Puff (RAP), improves quality of life. Can Respir J 2010;17:67–73 | 161 |
| Mehlum L, Tørmoen AJ, Ramberg M, Haga E, Diep LM, Laberg S, et al. Dialectical behavior therapy for adolescents with repeated suicidal and self-harming behavior: a randomized trial. J Am Acad Child Adolesc Psychiatry 2014;53:1082–91 | 162 |
| Mitchell EA, Ferguson V, Norwood M. Asthma education by community child health nurses. Arch Dis Child 1986;61:1184–9 | 163 |
| Muntz R, Hutchings J, Edwards RT, Hounsome B, O’Céilleachair A. Economic evaluation of treatments for children with severe behavioural problems. J Ment Health Policy Econ 2004;7:177–89 | 164 |
| Hutchings J, Appleton P, Smith M, Lane E, Nash S. Evaluation of two treatments for children with severe behaviour problems: child behaviour and maternal mental health outcomes. Behav Cogn Psychoth 2002;30:279–95 | 165 |
| Nansel TR, Anderson BJ, Laffel LMB, Simons-Morton BG, Weissberg-Benchell J, Wysocki T, et al. A multisite trial of a clinic-integrated intervention for promoting family management of pediatric type 1 diabetes: feasibility and design. Pediatr Diabetes 2009;10:105–15 | 166 |
| Ng D, Chow P, Lai W, Chan K, Chang B, So H. Effect of a structured asthma education program on hospitalized asthmatic children: A randomized controlled study. Pediatr Int 2006;48:158–62 | 167 |
| O’Neill D, McGilloway S, Donnelly M, Bywater T, Kelly P. A cost-effectiveness analysis of the Incredible Years parenting programme in reducing childhood health inequalities. Eur J Health Econ 2013;14:85–94 | 168 |
| McGilloway S, Ni Mhaille G, Bywater T, Furlong M, Leckey Y, Kelly P, et al. A parenting intervention in childhood behavioural problems: a randomized controlled trial in disadvantaged community-based settings. J Consult Clin Psych 2012;80:116–27 | 169 |
| Otsuki M, Eakin MN, Rand CS, Butz AM, Hsu VD, Zuckerman IH, et al. Adherence feedback to improve asthma outcomes among inner-city children: a randomized trial. Pediatrics 2009;124:1513–21 | 170 |
| Quint DM, Teach SJ. IMPACT DC: reconceptualizing the role of the emergency department for urban children with asthma. Clin Pediatr Emerg Med 2009;10:115–21 | 171 |
| Teach SJ, Crain EF, Quint DM, Hylan ML, Joseph JG. Improved asthma outcomes in a high-morbidity pediatric population: results of an emergency department-based randomized clinical trial. Arch Pediat Adol Med 2006;160:535–41 | 172 |
| Richardson LP, Ludman E, McCauley E, Lindenbaum J, Larison C, Zhou C, et al. Collaborative care for adolescents with depression in primary care: a randomized clinical trial. JAMA 2014;312:809–16 | 173 |
| Rikkers-Mutsaerts ER, Winters AE, Bakker MJ, van Stel HF, van der Meer V, de Jongste JC, et al. Internet-based self-management compared with usual care in adolescents with asthma: a randomized controlled trial. Pediatr Pulmonol 2012;47:1170–9 | 174 |
| Ronchetti R, Indinnimeo L, Bonci E, Corrias A, Evans D, Hindi-Alexander M, et al. Asthma self-management programmes in a population of Italian children: a multicentric study. Italian Study Group on Asthma Self-Management Programmes. Eur Respir J 1997;10:1248–53 | 175 |
| Rund BR, Moe L, Sollien T, Fjell A, Borchgrevink T, Hallert M, et al. The Psychosis Project: outcome and cost-effectiveness of a psychoeducational treatment programme for schizophrenic adolescents. Acta Psychiatr Scand 1994;89:211–18 | 176 |
| Runge C, Lecheler J, Horn M, Tews JT, Schaefer M. Outcomes of a Web-based patient education program for asthmatic children and adolescents. Chest 2006;129:581–93 | 177 |
| Schmidt U, Lee S, Beecham J, Perkins S, Treasure J, Yi I, et al. A randomized controlled trial of family therapy and cognitive behavior therapy guided self-care for adolescents with bulimia nervosa and related disorders. Am J Psychiatry 2007;164:591–8 | 178 |
| Seid M, Varni JW, Gidwani P, Gelhard LR, Slymen DJ. Problem-solving skills training for vulnerable families of children with persistent asthma: report of a randomized trial on health-related quality of life outcomes. J Pediatr Psychol 2010;35:1133–43 | 179 |
| Shames RS, Sharek P, Mayer M, Robinson TN, Hoyte EG, Gonzalez-Hensley F, et al. Effectiveness of a multicomponent self-management program in at-risk, school-aged children with asthma. Ann Allergy Asthma Immunol 2004;92:611–18 | 180 |
| Sockrider MM, Abraham S, Brooks E, Caviness AC, Pilney S, Koerner C, et al. Delivering tailored asthma family education in a pediatric emergency department setting: a pilot study. Pediatrics 2006;117:S135–44 | 181 |
| Southam-Gerow MA, Weisz JR, Chu BC, McLeod BD, Gordis EB, Connor-Smith JK. Does cognitive behavioral therapy for youth anxiety outperform usual care in community clinics? An initial effectiveness test. J Am Acad Child Psy 2010;49:1043–52 | 182 |
| Staab D, von Rueden U, Kehrt R, Erhart M, Wenninger K, Kamtsiuris P, et al. Evaluation of a parental training program for the management of childhood atopic dermatitis. Pediatr Allergy Immunol 2002;13:84–90 | 183 |
| Stevens CA, Wesseldine LJ, Couriel JM, Dyer AJ, Osman LM, Silverman M. Parental education and guided self-management of asthma and wheezing in the pre-school child: a randomised controlled trial. Thorax 2002;57:39–44 | 21 |
| Sullivan SD, Weiss KB, Lynn H, Mitchell H, Kattan M, Gergen PJ, et al. The cost-effectiveness of an inner-city asthma intervention for children. J Allergy Clin Immunol 2002;110:576–81 | 184 |
| Evans R III, Gergen PJ, Mitchell H, Kattan M, Kercsmar C, Crain E, et al. A randomized clinical trial to reduce asthma morbidity among inner-city children: results of the National Cooperative Inner-City Asthma Study. J Pediatr 1999;135:332–8 | 185 |
| Svoren BM, Butler D, Levine BS, Anderson BJ, Laffel LM. Reducing acute adverse outcomes in youths with type 1 diabetes: a randomized, controlled trial. Pediatrics 2003;112:914–22 | 186 |
| Szczepanski R, Gebert N, Hümmelink R, Könning J, Schmidt S, Runde B, et al. [Outcome of structured asthma education in childhood and adolescence.] Pneumologie 1996;50:544–8 | 187 |
| Toelle BG, Peat JK, Salome CM, Mellis CM, Bauman AE, Woolcock AJ. Evaluation of a community-based asthma management program in a population sample of schoolchildren. Med J Aust 1993;158:742–6 | 188 |
| Valery PC, Masters IB, Taylor B, Laifoo Y, O’Rourke PK, Chang AB. An education intervention for childhood asthma by Aboriginal and Torres Strait Islander health workers: a randomised controlled trial. Med J Australia 2010;192:574–9 | 189 |
| Van de Wiel NMH, Matthys W, Cohen-Kettenis P, van Engeland H. Application of the Utrecht Coping Power Program and care as usual to children with disruptive behavior disorders in outpatient clinics: A comparative study of cost and course of treatment. Behav Ther 2003;34:421–36 | 190 |
| Van Der Veek SMC, Derkx BHF, Benninga MA, Boer F, De Haan E. Cognitive behavior therapy for pediatric functional abdominal pain: a randomized controlled trial. Pediatrics 2013;132:e1163–e72 | 191 |
| Velsor-Friedrich B, Militello LK, Richards MH, Harrison PR, Gross IM, Romero E, et al. Effects of coping-skills training in low-income urban African-American adolescents with asthma. J Asthma 2012;49:372–9 | 192 |
| Walders N, Kercsmar C, Schluchter M, Redline S, Kirchner HL, Drotar D. An interdisciplinary intervention for undertreated pediatric asthma. Chest 2006;129:292–9 | 193 |
| Watson WT, Gillespie C, Thomas N, Filuk SE, McColm J, Piwniuk MP, et al. Small-group, interactive education and the effect on asthma control by children and their families. CMAJ 2009;181:257–63 | 194 |
| Weisz JR, Southam-Gerow MA, Gordis EB, Connor-Smith JK, Chu BC, Langer DA, et al. Cognitive-behavioral therapy versus usual clinical care for youth depression: an initial test of transportability to community clinics and clinicians. J Consult Clin Psych 2009;77:383–96 | 195 |
| Willems DCM, Joore MA, Hendriks JJE, Wouters EFM, Severens JL. Cost-effectiveness of a nurse-led telemonitoring intervention based on peak expiratory flow measurements in asthmatics: results of a randomised controlled trial. Cost Eff Resour Alloc 2007;5(10) | 196 |
| Willems DC, Joore MA, Hendriks JJ, van Duurling RA, Wouters EF, Severens JL. Process evaluation of a nurse-led telemonitoring programme for patients with asthma. J Telemed Telecare 2007;13:310–17 | 197 |
| Willems DC, Joore MA, Hendriks JJ, Nieman FH, Severens JL, Wouters EF. The effectiveness of nurse-led telemonitoring of asthma: results of a randomized controlled trial. J Eval Clin Pract 2008;14:600–9 | 198 |
| Xu C, Jackson M, Scuffham PA, Wootton R, Simpson P, Whitty J, et al. A randomized controlled trial of an interactive voice response telephone system and specialist nurse support for childhood asthma management. J Asthma 2010;47:768–73 | 199 |
| Young NL, Foster AM, Parkin PC, Reisman J, MacLusky I, Gold M, et al. Assessing the efficacy of a school-based asthma education program for children: a pilot study. Can J Public Health 2001;92:30–4 | 200 |
Appendix 4 Excluded studies list
| Study ID | Reason for exclusion |
|---|---|
| Agras WS, Lock J, Brandt H, Bryson SW, Dodge E, Halmi KA, et al. Comparison of 2 family therapies for adolescent anorexia nervosa: a randomized parallel trial. JAMA Psychiatry 2014;71:1279–86 | Absent/ineligible comparator |
| Allen HF, Yarnie S, Murray MA, Reiter EO. Personnel costs and perceived benefit of telephone care in the management of children with type 1 diabetes. Pediatr Diabetes 2002;3:95–100 | Ineligible intervention |
| Al-sheyab N, Gallagher R, Crisp J, Shah S. Peer-led education for adolescents with asthma in Jordan: a cluster-randomized controlled trial. Pediatrics 2012;129:e106–12 | No eligible economic outcomes |
| Andrade WCC, Camargos P, Lasmar L, Bousquet J. A pediatric asthma management program in a low-income setting resulting in reduced use of health service for acute asthma. Allergy 2010;65:1472–7 | No eligible health outcomes |
| Arga M, Sahbaz H, Bakirtas A, Turktas I, Demirsoy MS. Does self-monitoring by means of symptom diaries improve asthma control in children? J Asthma 2014;51:299–305 | Ineligible intervention |
| Asarnow JR, Jaycox LH, Duan N, LaBorde AP, Rea MM, Murray P, et al. Effectiveness of a quality improvement intervention for adolescent depression in primary care clinics: a randomized controlled trial. JAMA 2005;293:311–19 | Ineligible intervention |
| Asarnow JR, Jaycox LH, Tang L, Duan N, LaBorde AP, Zeledon LR, et al. Long-term benefits of short-term quality improvement interventions for depressed youths in primary care. Am J Psychiatry 2009;166:1002–10 | Ineligible intervention |
| Au A, Lau K-M, Wong AH-C, Lam C, Leung C, Lau J, et al. The efficacy of a group Triple P (positive parenting program) for Chinese parents with a child diagnosed with ADHD in Hong Kong: a pilot randomised controlled study. Aust Psychol 2014;49:151–62 | No eligible economic outcomes |
| Bartholomew LK, Sockrider M, Abramson S, Swank PR, Czyzewski D, Tortolero SR, et al. Partners in school asthma management: evaluation of a self-management program for children with asthma. J Sch Health 2006;76:283–90 | No clinical diagnosis, ineligible intervention |
| Beebe A, Gelfand EW, Bender B. A randomized trial to test the effectiveness of art therapy for children with asthma. J Allergy Clin Immunol 2010;126:263–6 | No eligible economic outcomes |
| Bhaumik U, Norris K, Charron G, Walker SP, Sommer SJ, Chan E, et al. A cost analysis for a community-based case management intervention program for pediatric asthma. J Asthma 2013;50:310–17 | No eligible health outcomes |
| Bodden DHM, Dirksen CD, Bogels SM, Nauta MH, De Haan E, Ringrose J, et al. Costs and cost-effectiveness of family CBT versus individual CBT in clinically anxious children. Clin Child Psychol Psychiatry 2008;13:543–64 | Absent/ineligible comparator |
| Boogerd EA, Noordam C, Kremer JA, Prins JB, Verhaak CM. Teaming up: feasibility of an online treatment environment for adolescents with type 1 diabetes. Pediatr Diabetes 2014;15:394–402 | No eligible economic outcomes |
| Bowen F. Asthma education and health outcomes of children aged 8 to 12 years. Clin Nurs Res 2013;22:172–85 | No eligible economic outcomes |
| Brandao HV, Cruz CM, Santos Ida S Jr, Ponte EV, Guimaraes A, Augusto Filho A. Hospitalizations for asthma: impact of a program for the control of asthma and allergic rhinitis in Feira de Santana, Brazil. J Bras Pneumol 2009;35:723–9 | Ineligible population, adult/child data mixed |
| Brandt S, Gale S, Tager I. The value of health interventions: evaluating asthma case management using matching. Appl Econ 2012;44:2245–63 | No eligible health outcomes |
| Brandt S, Gale S, Tager I. Estimation of Treatment Effect of Asthma Case Management Using Propensity Score Methods. Amherst, MA: University of Massachusetts, Department of Resource Economics; 2009 | No eligible health outcomes |
| Bratton DL, Price M, Gavin L, Glenn K, Brenner M, Gelfand EW, et al. Impact of a multidisciplinary day program on disease and healthcare costs in children and adolescents with severe asthma: a two-year follow-up study. Pediatr Pulmonol 2001;31:177–89 | Absent/ineligible comparator |
| Brent DA, Holder D, Kolko D, Birmaher B, Baugher M, Roth C, et al. A clinical psychotherapy trial for adolescent depression comparing cognitive, family and supportive therapy. Arch Gen Psychiatry 1997;54:877–85 | No eligible economic outcomes |
| Brent DA, Kolko DJ, Birmaher B, Baugher M, Bridge J. A clinical trial for adolescent depression: predictors of additional treatment in the acute and follow-up phases of the trial. J Am Acad Child Adolesc Psychiatry 1999;38:263–70 | No eligible economic outcomes |
| Brent DA, Holder D, Kolko D, Birmaher B, Baugher M, Roth C, et al. A clinical psychotherapy trial for adolescent depression comparing cognitive, family and supportive therapy. Arch Gen Psychiatry 1997;54:877–85 | No eligible economic outcomes |
| Britto MT, Vockell AL, Munafo JK, Schoettker PJ, Wimberg JA, Pruett R, et al. Improving outcomes for underserved adolescents with asthma. Pediatrics 2014;133:e418–27 | Absent/ineligible comparator |
| Broquet Ducret C, Verga ME, Stoky-Hess A, Verga J, Gehri M. [Impact of a small-group educational intervention for 4- to 12-year-old asthmatic children and their parents on the number of healthcare visits and quality of life.] Arch Pediatr 2013;20:1201–5 | Absent/ineligible comparator |
| Brown MD, Reeves MJ, Meyerson K, Korzeniewski SJ. Randomized trial of a comprehensive asthma education program after an emergency department visit. Ann Allergy Asthma Immunol 2006;97:44–51 | No eligible health outcomes |
| Bruzzese JM, Markman LB, Appel D, Webber M. An evaluation of open airways for schools: using college students as instructors. J Asthma 2001;38:337–42 | Absent/ineligible comparator |
| Bruzzese JM, Evans D, Wiesemann S, Pinkett-Heller M, Levison MJ, Du YL, et al. Using school staff to establish a preventive network of care to improve elementary school students’ control of asthma. J Sch Health 2006;76:307–12 | Ineligible intervention |
| Bruzzese JM, Unikel L, Gallagher R, Evans D, Colland V. Feasibility and impact of a school-based intervention for families of urban adolescents with asthma: results from a randomized pilot trial. Fam Process 2008;47:95–113 | No eligible economic outcomes |
| Buchner DA, Butt LT, De Stefano A, Edgren B, Suarez A, Evans RM. Effects of an asthma management program on the asthmatic member: patient-centered results of a 2-year study in a managed care organization. Am J Manag Care 1998;4:1288–97 | No comparator; adult/child mixed data |
| Buelow JM, Johnson CS, Perkins SM, Austin JK, Dunn DW. Creating Avenues for Parent Partnership (CAPP): an intervention for parents of children with epilepsy and learning problems. Epilepsy Behav 2013;27:64–9 | No eligible economic outcomes |
| Butz AM, Malveaux FJ, Eggleston P, Thompson L, Schneider S, Weeks K, et al. Use of community health workers with inner-city children who have asthma. Clin Pediatr 1994;33:135–41 | Absent/ineligible comparator |
| Bynum A, Hopkins D, Thomas A, Copeland N, Irwin C. The effect of telepharmacy counseling on metered-dose inhaler technique among adolescents with asthma in rural Arkansas. Telemed J E Health 2001;7:207–17 | No eligible economic outcomes |
| Bywater T, Hutchings J, Linck P, Whitaker C, Daley D, Yeo ST, et al. Incredible Years parent training support for foster carers in Wales: a multi-centre feasibility study. Child Care Health Dev 2011;37:233–43 | Population |
| Cabral ALB, Carvalho WAF, Chinen M, Barbiroto RM, Boueri FMV, Martins MA. Are International Asthma Guidelines effective for low-income Brazilian children with asthma? Eur Respir J 1998;12:35–40 | Study design |
| Catov JM, Marsh GM, Youk AO, Huffman VY. Asthma home teaching: two evaluation approaches. Dis Manag 2005;8:178–87 | No eligible health outcomes |
| Charlton I, Charlton G, Broomfield J, Mullee MA. Audit of the effect of a nurse run asthma clinic on workload and patient morbidity in a general practice. Br J Gen Pract 1991;41:227–31 | No eligible health outcomes |
| Chase HP, Crews KR, Garg S, Crews MJ, Cruickshanks KJ, Klingensmith G, et al. Outpatient management vs. in-hospital management of children with new-onset diabetes. Clin Pediatr 1992;31:450–6 | Absent/ineligible comparator |
| Chen SH, Yeh KW, Chen SH, Yen DC, Yin TJ, Huang JL. The development and establishment of a care map in children with asthma in Taiwan. J Asthma 2004;41:855–61 | No eligible health outcomes |
| Chen S-H, Huang J-L, Yeh K-W, Tsai Y-F. Interactive support interventions for caregivers of asthmatic children. J Asthma 2013;50:649–57 | No eligible health outcomes |
| Chiang LC, Ma WF, Huang JL, Tseng LF, Hsueh KC. Effect of relaxation-breathing training on anxiety and asthma signs/symptoms of children with moderate-to-severe asthma: a randomized controlled trial. Int J Nurs Stud 2009;46:1061–70 | Ineligible intervention |
| Clark NM, Feldman CH, Evans D, Levison MJ, Wasilewski Y, Mellins RB. The impact of health education on frequency and cost of health care use by low income children with asthma. J Allergy Clin Immunol 1986;78:108–15 | No eligible health outcomes |
| Cottrell CK, Young GA, Creer TL, Holroyd KA, Kotses H. The development and evaluation of a self-management program for cystic fibrosis. Pediatr Asthma Allergy Immunol 1996;10:109–18 | No eligible economic outcomes |
| Coughey K, Klein G, West C, Diamond JJ, Santana A, McCarville E, et al. The child asthma link line: a coalition-initiated, telephone-based, care coordination intervention for childhood asthma. J Asthma 2010;47:303–9 | No eligible health outcomes |
| Creer TL, Backial M, Burns KL, Leung P, Marion RJ, Miklich DR, et al. Living with asthma. I. Genesis and development of a self-management program for childhood asthma. J Asthma 1988;25:335–62 | Absent/ineligible comparator |
| Cummings CM, Fristad MA. Medications prescribed for children with mood disorders: effects of a family-based psychoeducation program. Exp Clin Psychopharmacol 2007;15:555–62 | No eligible health outcomes |
| DePue JD, McQuaid EL, Koinis-Mitchell D, Camillo C, Alario A, Klein RB. Providence school asthma partnership: school-based asthma program for inner-city families. J Asthma 2007;44:449–53 | Wrong study design |
| Ducharme FM, Zemek RL, Chalut D, McGillivray D, Noya FJD, Resendes S, et al. Written action plan in pediatric emergency room improves asthma prescribing, adherence, and control. Am J Respir Crit Care Med 2011;183:195–203 | Ineligible intervention |
| Ellis DA, Naar-King S, Frey M, Templin T, Rowland M, Greger N. Use of multisystemic therapy to improve regimen adherence among adolescents with type 1 diabetes in poor metabolic control: a pilot investigation. J Clin Psychol Med Settings 2004;11:315–24 | No eligible health outcomes |
| Ellis DA, Templin T, Naar-King S, Frey MA, Cunningham PB, Podolski CL, et al. Multisystemic therapy for adolescents with poorly controlled type I diabetes: stability of treatment effects in a randomized controlled trial. J Consult Clin Psychol 2007;75:168–74 | No eligible health outcomes |
| Ellis D, Naar-King S, Templin T, Frey M, Cunningham P, Sheidow A, et al. Multisystemic therapy for adolescents with poorly controlled type 1 diabetes: reduced diabetic ketoacidosis admissions and related costs over 24 months. Diabetes Care 2008;31:1746–7 | No eligible health outcomes |
| Ellis DA, Frey MA, Naar-King S, Templin T, Cunningham P, Cakan N. Use of multisystemic therapy to improve regimen adherence among adolescents with type 1 diabetes in chronic poor metabolic control: a randomized controlled trial. Diabetes Care 2005;28:1604–10 | No eligible health outcomes |
| Ellis DA, Naar-King S, Frey M, Templin T, Rowland M, Cakan N. Multisystemic treatment of poorly controlled type 1 diabetes: effects on medical resource utilization. J Pediatr Psychol 2005;30:656–66 | No eligible health outcomes |
| Enebrink P, Hogstrom J, Forster M, Ghaderi A. Internet-based parent management training: a randomized controlled study. Behav Res Ther 2012;50:240–9 | No eligible economic outcomes |
| Fanelli A, Cabral ALB, Neder JA, Martins MA, Carvalho CRF. Exercise training on disease control and quality of life in asthmatic children. Med Sci Sports Exerc 2007;39:1474–80 | Ineligible intervention |
| Findley SE, Thomas G, Madera-Reese R, McLeod N, Kintala S, Andres Martinez R, et al. A community-based strategy for improving asthma management and outcomes for preschoolers. J Urban Health 2011;88:85–99 | Wrong study design |
| Fireman P, Friday GA, Gira C, Vierthaler WA, Michaels L. Teaching self-management skills to asthmatic children and their parents in an ambulatory care setting. Pediatrics 1981;68:341–8 | Wrong study design |
| Fischl AF, Herman WH, Sereika SM, Hannan M, Becker D, Mansfield MJ, et al. Impact of a preconception counseling program for teens with type 1 diabetes (READY-Girls) on patient–provider interaction, resource utilization, and cost. Diabetes Care 2010;33:701–5 | No eligible health outcomes |
| Fisher EB, Strunk RC, Sussman LK, Sykes RK, Walker MS. Community organization to reduce the need for acute care for asthma among African American children in low-income neighborhoods: the Neighborhood Asthma Coalition. Pediatrics 2004;114:116–23 | No eligible health outcomes |
| Forsander GA, Sundelin J, Persson B. Influence of the initial management regimen and family social situation on glycemic control and medical care in children with type 1 diabetes mellitus. Acta Paediatr 2000;89:1462–8 | No eligible health outcomes |
| Foster EM, Jones D, Conduct Problems Prevention Research Group. Can a costly intervention be cost-effective? An analysis of violence prevention. Arch Gen Psychiatry 2006;63:1284–91 | Ineligible population |
| Foster EM. Costs and effectiveness of the fast track intervention for antisocial behavior. J Ment Health Policy Econ 2010;13:101–19 | Ineligible population |
| Foulds JL, Vanderloo SE, Marks SD, Johnson JA. Healthcare costs for initial management of children with new-onset type 1 diabetes mellitus in central and northern Alberta. Can J Diabetes 2012;36:128–32 | No eligible health outcomes |
| Franklin BE, Crisler SC Jr, Shappley R, Armour MM, McCommon DT, Ferry RJ Jr. Real-time support of pediatric diabetes self-care by a transport team. Diabetes Care 2014;37:81–7 | Ineligible intervention |
| Garcia-Perez L, Perestelo-Perez L, Serrano-Aguilar P, Del Mar Trujillo-Martin M. Effectiveness of a psychoeducative intervention in a summer camp for children with type 1 diabetes mellitus. Diabetes Educ 2010;36:310–17 | No eligible health outcomes |
| Geist R, Heinmaa M, Stephens D, Davis R, Katzman DK. Comparison of family therapy and family group psychoeducation in adolescents with anorexia nervosa. Can J Psychiatry 2000;45:173–8 | Absent/ineligible comparator |
| Gerald LB, Redden D, Wittich AR, Hains C, Turner-Henson A, Hemstreet MP, et al. Outcomes for a comprehensive school-based asthma management program. J Sch Health 2006;76:291–6 | No eligible health outcomes |
| Gerald LB, Redden D, Wittich AR, Hains C, Turner-Henson A, Hemstreet MP, et al. Outcomes for a comprehensive school-based asthma management program. J Sch Health 2006;76:291–6 | Ineligible intervention |
| Gillies J, Barry D, Crane J, Jones D, MacLennan L, Pearce N, et al. A community trial of a written self management plant for children with asthma. N Z Med J 1996;109:30–3 | Ineligible intervention |
| Greer D, Grasso DJ, Cohen A, Webb C. Trauma-focused treatment in a state system of care: is it worth the cost? Adm Policy Ment Health Ment Health Serv Res 2014;41:317–23 | No eligible health outcomes |
| Greineder DK, Loane KC, Parks P. A randomized controlled trial of a pediatric asthma outreach program. J Allergy Clin Immunol 1999;103:436–40 | No eligible health outcomes |
| Grey M, Boland EA, Davidson M, Li J, Tamborlane WV. Coping skills training for youth with diabetes mellitus has long-lasting effects on metabolic control and quality of life. J Pediatr 2000;137:107–13 | No eligible economic outcomes |
| Griffiths JD, Martin PR. Clinical- versus home-based treatment formats for children with chronic headache. Br J Health Psychol 1996;1:151–66 | No eligible economic outcomes |
| Grimes KE, Schulz MF, Cohen SA, Mullin BO, Lehar SE, Tien S. Pursuing cost-effectiveness in mental health service delivery for youth with complex needs. J Ment Health Policy Econ 2011;14:73–83 | No eligible health outcomes |
| Guglani L, Havstad SL, Johnson CC, Ownby DR, Joseph CL. Effect of depressive symptoms on asthma intervention in urban teens. Ann Allergy Asthma Immunol 2012;109:237–42 | No eligible economic outcomes |
| Gustafson D, Wise M, Bhatacharya A, Pulvermacher A, Shanovich K, Philips B, et al. The effects of combining web-based eHealth with telephone nurse case management for pediatric asthma control: a randomized controlled trial. J Med Internet Res 2012;14:41–59 | No eligible economic outcomes |
| Halterman JS, Fagnano M, Tremblay PJ, Fisher SG, Wang H, Rand C, et al. Prompting Asthma Intervention in Rochester-Uniting Parents and Providers (PAIR-UP): a randomized trial. JAMA Pediatrics 2014;168:e141983 | Ineligible intervention |
| Harish Z, Bregante AC, Morgan C, Fann CS, Callaghan CM, Witt MA, et al. A comprehensive inner-city asthma program reduces hospital and emergency room utilization. Ann Allergy Asthma Immunol 2001;86:185–9 | No eligible health outcomes |
| Harrington R, Peters S, Green J, Byford S, Woods J, McGowan R. Randomised comparison of the effectiveness and costs of community and hospital based mental health services for children with behavioural disorders. BMJ 2000;321:1047–50 | Absent/ineligible comparator |
| Honeycutt AA, Khavjou OA, Jones DJ, Cuellar J, Forehand RL. Helping the noncompliant child: an assessment of program costs and cost-effectiveness. J Child Fam Stud 2015;24:499–504 | No eligible economic outcomes |
| Hudson A, Cameron C, Matthews J. The wide-scale implementation of a support program for parents of children with an intellectual disability and difficult behaviour. J Intellect Dev Disabil 2008;33:117–26 | Ineligible population |
| Hui SHL, Leung TF, Ha G, Wong E, Li AM, Fok TF. Evaluation of an asthma management program for Chinese children with mild-to-moderate asthma in Hong Kong. Pediatr Pulmonol 2002;33:22–9 | Wrong study design |
| Izquierdo R, Morin PC, Bratt K, Moreau Z, Meyer S, Ploutz-Snyder R, et al. School-centered telemedicine for children with type 1 diabetes mellitus. J Pediatr 2009;155:374–9 | Ineligible intervention |
| Kamps AWA, Brand PLP, Kimpen JLL, Maille AR, Overgoor-Van De Groes AW, Van Helsdingen-Peek LCJAM, et al. Outpatient management of childhood asthma by paediatrician or asthma nurse: randomised controlled study with one year follow up. Thorax 2003;58:968–73 | Ineligible intervention |
| Karnick P, Margellos-Anast H, Seals G, Whitman S, Aljadeff G, Johnson D. The pediatric asthma intervention: a comprehensive cost-effective approach to asthma management in a disadvantaged inner-city community. J Asthma 2007;44:39–44 | No eligible health outcomes |
| Kelly CS, Morrow AL, Shults J, Nakas N, Strope GL, Adelman RD. Outcomes evaluation of a comprehensive intervention program for asthmatic children enrolled in Medicaid. Pediatrics 2000;105:1029–35 | No eligible health outcomes |
| King CA, Klaus N, Kramer A, Venkataraman S, Quinlan P, Gillespie B. The youth-nominated support team-version ii for suicidal adolescents: a randomized controlled intervention trial. J Consult Clin Psychol 2009;77:880–93 | No eligible economic outcomes |
| Laffel LM, Wentzell K, Loughlin C, Tovar A, Moltz K, Brink S. Sick day management using blood 3-hydroxybutyrate (3-OHB) compared with urine ketone monitoring reduces hospital visits in young people with T1DM: a randomized clinical trial. Diabet Med 2006;23:278–84 | Ineligible intervention |
| Lara M, Ramos-Valencia G, Gonzalez-Gavillun JA, Lopez-Malpica F, Morales-Reyes B, Marin H, et al. Reducing quality-of-care disparities in childhood asthma: La red de asma infantil intervention in San Juan, Puerto Rico. Pediatrics 2013;131:S26–37 | Wrong study design |
| Lawson ML, Cohen N, Richardson C, Orrbine E, Pham B. A randomized trial of regular standardized telephone contact by a diabetes nurse educator in adolescents with poor diabetes control. Pediatr Diabetes 2005;6:32–40 | Ineligible intervention |
| Letz KL, Schlie AR, Smits WL. A randomized trial comparing peak expiratory flow versus symptom self-management plans for children with persistent asthma. Pediatr Asthma Allergy Immunol 2004;17:177–90 | Ineligible intervention |
| Levy M, Heffner B, Stewart T, Beeman G. The efficacy of asthma case management in an urban school district in reducing school absences and hospitalizations for asthma. J Sch Health 2006;76:320–4 | No eligible health outcomes |
| Lipman TH. Length of hospitalization of children with diabetes: effect of a clinical nurse specialist. Diabetes Educ 1988;14:41–3 | No eligible health outcomes |
| Lock J, Le Grange D, Agras WS, Moye A, Bryson SW, Jo B. Randomized clinical trial comparing family-based treatment with adolescent-focused individual therapy for adolescents with anorexia nervosa. Arch Gen Psychiatry 2010;67:1025–32 | Absent/ineligible comparator |
| Lynch FL, Dickerson JF, Saldana L, Fisher PA. Incremental net benefit of early intervention for preschool-aged children with emotional and behavioral problems in foster care. Child Youth Serv Rev 2014;36:213–19 | Ineligible population |
| Mandhane PJ, McGhan SL, Sharpe HM, Wong E, Hessel PA, Befus AD, et al. A child’s asthma quality of life rating does not significantly influence management of their asthma. Pediatr Pulmonol 2010;45:141–8 | No eligible economic outcomes |
| Mangione-Smith R, Schonlau M, Chan KS, Keesey J, Rosen M, Louis TA, et al. Measuring the effectiveness of a collaborative for quality improvement in pediatric asthma care: does implementing the chronic care model improve processes and outcomes of care? Ambul Pediatr 2005;5:75–82 | Ineligible intervention |
| Mann NP, Noronha JL, Johnston DI. A prospective study to evaluate the benefits of long-term self-monitoring of blood glucose in diabetic children. Diabetes Care 1984;7:322–6 | No eligible health outcomes |
| Marrero DG, Vandagriff JL, Kronz K, Fineberg NS, Golden MP, Gray D, et al. Using telecommunication technology to manage children with diabetes: the Computer-Linked Outpatient Clinic (CLOC) study. Diabetes Educ 1995;21:313–19 | Ineligible intervention |
| Massie J, Efron D, Cerritelli B, South M, Powell C, Haby MM, et al. Implementation of evidence based guidelines for paediatric asthma management in a teaching hospital. Arch Dis Child 2004;89:660–4 | Ineligible intervention |
| McGorry PD, Edwards J. The feasibility and effectiveness of early intervention in psychotic disorders: the Australian experience. Int Clin Psychopharmacol 1998;13:S47–52 | Ineligible population |
| McPherson AC, Glazebrook C, Forster D, James C, Smyth A. A randomized, controlled trial of an interactive educational computer package for children with asthma. Pediatrics 2006;117:1046–54 | No eligible health outcomes |
| Meng YY, Pourat N, Cosway R, Kominski GF. Estimated cost impacts of law to expand coverage for self-management education to children with asthma in California. J Asthma 2010;47:581–6 | Ineligible intervention |
| Mihalopoulos C, McGorry PD, Carter RC. Is phase-specific, community-oriented treatment of early psychosis an economically viable method of improving outcome. Acta Psychiatr Scand 1999;100:47–55 | Ineligible intervention |
| Moran G, Fonagy P, Kurtz A, Bolton A, Brook C. A controlled study of the psychoanalytic treatment of brittle diabetes. J Am Acad Child Adolesc Psychiatry 1991;30:926–35 | No eligible health outcomes |
| Murphy HR, Wadham C, Hassler-Hurst J, Rayman G, Skinner TC, Families and Adolescents Communication and Teamwork Study (FACTS) Group. Randomized trial of a diabetes self-management education and family teamwork intervention in adolescents with type 1 diabetes. Diabet Med 2012;29:e249–54 | No eligible economic outcomes |
| Nelson KA, Highstein GR, Garbutt J, Trinkaus K, Fisher EB, Smith SR, et al. A randomized controlled trial of parental asthma coaching to improve outcomes among urban minority children. Arch Pediatr Adolesc Med 2011;165:520–6 | No eligible health outcomes |
| Ngo VK, Asarnow JR, Lange J, Jaycox LH, Rea MM, Landon C, et al. Outcomes for youths from racial-ethnic minority groups in a quality improvement intervention for depression treatment. Psychiatr Serv 2009;60:1357–64 | Ineligible intervention |
| Nguyen KH, Boulay E, Peng J. Quality-of-life and cost–benefit analysis of a home environmental assessment program in Connecticut. J Asthma 2011;48:147–55 | Wrong study design |
| Nunn E, King B, Smart C, Anderson D. A randomized controlled trial of telephone calls to young patients with poorly controlled type 1 diabetes. Pediatr Diabetes 2006;7:254–9 | No eligible economic outcomes |
| Oishi T, Narita M, Morisawa Y, Watanabe H, Fukuie T, Akashi M, et al. The written action plan in childhood asthma can reduce unscheduled physician visits. Allergy 2013;68:377 | Ineligible intervention |
| Patel B, Sheridan P, Detjen P, Donnersberger D, Gluck E, Malamut K, et al. Success of a comprehensive school-based asthma intervention on clinical markers and resource utilization for inner-city children with asthma in Chicago: the Mobile C.A.R.E. Foundation’s asthma management program. J Asthma 2007;44:113–18 | Ineligible intervention |
| Persaud DI, Barnett SE, Weller SC, Baldwin CD, Niebuhr V, McCormick DP. An asthma self-management program for children, including instruction in peak flow monitoring by school nurses. J Asthma 1996;33:37–43 | No eligible health outcomes |
| Polisena J, Tam S, Lodha A, Laporte A, Coyte PC, Ungar WJ. An economic evaluation of asthma action plans for children with asthma. J Asthma 2007;44:501–8 | Ineligible intervention |
| Reagan MM, DeBaun MR, Frei-Jones MJ. Multi-modal intervention for the inpatient management of sickle cell pain significantly decreases the rate of acute chest syndrome. Pediatr Blood Cancer 2011;56:262–6 | Ineligible intervention |
| Rhee H, Pesis-Katz I, Xing J. Cost benefits of a peer-led asthma self-management program for adolescents. J Asthma 2012;49:606–13 | Absent/ineligible comparator |
| Rhee H, Belyea MJ, Hunt JF, Brasch J. Effects of a peer-led asthma self-management program for adolescents. Arch Pediatr Adolesc Med 2011;165:513–19 | Absent/ineligible comparator |
| Robling M, McNamara R, Bennert K, Butler CC, Channon S, Cohen D, et al. The effect of the Talking Diabetes consulting skills intervention on glycaemic control and quality of life in children with type 1 diabetes: cluster randomised controlled trial (DEPICTED study). BMJ 2012;344:e2359 | Ineligible intervention |
| Rushton A, Monck E, Leese M, McCrone P, Sharac J. Enhancing adoptive parenting: a randomized controlled trial. Clin Child Psychol Psychiatry 2010;15:529–42 | Ineligible population |
| Sanders MR, Baker S, Turner KM. A randomized controlled trial evaluating the efficacy of Triple P Online with parents of children with early-onset conduct problems. Behav Res Ther 2012;50:675–84 | No eligible economic outcomes |
| Schauerte G, Fendel T, Schwab S, Bredl C. [Children with bronchial asthma: effects of an integrated health-care programme.] Pneumologie 2010;64:73–80 | Ineligible intervention |
| Schmidt S, Konning J, Szczepanski R, Hummelink R, Gebert N, Wahn U. [Cost effectiveness of asthma education in clinic and practice.] Prav Rehabil 1994;6:27–32 | Ineligible intervention |
| Schneiderman-Walker J, Pollock SL, Corey M, Wilkes DD, Canny GJ, Pedder L, et al. A randomized controlled trial of a 3-year home exercise program in cystic fibrosis. J Pediatrics 2000;136:304–10 | No eligible health outcomes |
| Schulze J, Riel B, Wolfraum B, Fischer S, Lecheler J, Hofmann D. [Improvement of the quality of life by asthma training.] Prav Rehabil 2000;12:91–8 | Ineligible intervention |
| Scott S, Sylva K, Doolan M, Price J, Jacobs B, Crook C, et al. Randomised controlled trial of parent groups for child antisocial behaviour targeting multiple risk factors: the SPOKES project. J Child Psychol Psychiatry 2010;51:48–57 | Ineligible population |
| Shah S, Peat JK, Mazurski EJ, Wang H, Sindhusake D, Bruce C, et al. Effect of peer led programme for asthma education in adolescents: cluster randomised controlled trial. BMJ 2001;322:583–5 | Ineligible population |
| Sharac J, McCrone P, Rushton A, Monck E. Enhancing adoptive parenting: a cost-effectiveness analysis. Child Adolesc Ment Health 2011;16:110–15 | Ineligible population |
| Sheidow AJ, Bradford WD, Henggeler SW, Rowland MD, Halliday-Boykins C, Schoenwald SK, et al. Treatment costs for youths receiving multisystemic therapy or hospitalization after a psychiatric crisis. Psychiatr Serv 2004;55:548–54 | Ineligible intervention |
| Siminerio LM, Charron-Prochownik D, Banion C, Schreiner B. Comparing outpatient and inpatient diabetes education for newly diagnosed pediatric patients. Diabetes Educ 1999;25:895–906 | No eligible health outcomes |
| Simon E, Dirksen C, Bogels S, Bodden D. Cost-effectiveness of child-focused and parent-focused interventions in a child anxiety prevention program. J Anxiety Disord 2012;26:287–96 | Ineligible population |
| Simon E, Dirksen CD, Bogels SM. An explorative cost-effectiveness analysis of school-based screening for child anxiety using a decision analytic model. Eur Child Adolesc Psychiatry 2013;22:619–30 | Ineligible population |
| Stallard P, Phillips R, Montgomery A, Spears M, Anderson R, Taylor J, et al. A cluster randomised controlled trial to determine the clinical effectiveness and cost-effectiveness of classroom-based cognitive–behavioural therapy (CBT) in reducing symptoms of depression in high-risk adolescents. Health Technol Assess 2013;17 | Ineligible population |
| Suh DC, Shin SK, Voytovich RM, Zimmerman A. Economic impact of an asthma education programme on medical care utilisation. Dis Manag Health Outcomes 2000;8:159–70 | Ineligible intervention |
| Sullivan SD, Lee TA, Blough DK, Finkelstein JA, Lozano P, Inui TS, et al. A multisite randomized trial of the effects of physician education and organizational change in chronic asthma care: cost-effectiveness analysis of the Pediatric Asthma Care Patient Outcomes Research Team II (PAC-PORT II). Arch Pediatr Adolesc Med 2005;159:428–34 | Ineligible intervention |
| Tiberg I, Katarina SC, Carlsson A, Hallstrom I. Children diagnosed with type 1 diabetes: a randomized controlled trial comparing hospital versus home-based care. Acta Paediatr 2012;101:1069–73 | No eligible health outcomes |
| Tieffenberg JA, Wood EI, Alonso A, Tossutti MS, Vicente MF. A randomized field trial of ACINDES: a child-centered training model for children with chronic illnesses (asthma and epilepsy). J Urban Health 2000;77:280–97 | No eligible health outcomes |
| Tinkelman D, Wilson S. Asthma disease management: regression to the mean or better? Am J Manag Care 2004;10:948–54 | No eligible health outcomes |
| Tolomeo C, Savrin C, Heinzer MM. Impact of asthma self-management on pediatric emergency department visits and hospitalizations. J Asthma Allergy Educ 2010;1:61–70 | No eligible health outcomes |
| Turcotte DA, Alker H, Chaves E, Gore R, Woskie S. Healthy homes: in-home environmental asthma intervention in a diverse urban community. Am J Pub Health 2014;104:665–71 | Wrong study design |
| von Sengbusch S, Müller-Godeffroy E, Häger S, Reintjes R, Hiort O, Wagner V. Mobile diabetes education and care: intervention for children and young people with type 1 diabetes in rural areas of northern Germany. Diabet Med 2006;23:122–7 | Wrong study design |
| Wade SL, Walz NC, Carey J, McMullen KM, Cass J, Mark E, et al. A Randomized trial of teen online problem solving: efficacy in improving caregiver outcomes after brain injury. Health Psychology 2012;31:767–76 | No eligible economic outcomes |
| Webb C, Hayes AM, Grasso D, Laurenceau J-P, Deblinger E. Trauma-focused cognitive behavioral therapy for youth: effectiveness in a community setting. Psychol Trauma 2014;6:555–62 | No eligible health outcomes |
| Weiss B, Han S, Harris V, Catron T, Ngo VK, Caron A, et al. An independent randomized clinical trial of multisystemic therapy with non-court-referred adolescents with serious conduct problems. J Consult ClinPsychol 2013;81:1027–39 | Ineligible population |
| Weng HC, Yuan BC, Su YT, Perng DS, Chen WH, Lin LJ, et al. Effectiveness of a nurse-led management programme for paediatric asthma in Taiwan. J Paediatr Child Health 2007;43:134–8 | No eligible health outcomes |
| Wensley D, Silverman M. Peak flow monitoring for guided self-management in childhood asthma: a randomized controlled trial. Am J Respir Crit Care Med 2004;170:606–12 | Ineligible intervention |
| Wesseldine LJ, McCarthy P, Silverman M. Structured discharge procedure for children admitted to hospital with acute asthma: a randomised controlled trial of nursing practice. Arch Dis Child 1999;80:110–14 | No eligible health outcomes |
| Williams SG, Brown CM, Falter KH, Alverson CJ, Gotway-Crawford C, Homa D, et al. Does a multifaceted environmental intervention alter the impact of asthma on inner-city children? J Natl Med Assoc 2006;98:249–60 | Ineligible intervention |
| Wilson SR, Yamada EG, Sudhakar R, Roberto L, Mannino D, Mejia C, et al. Occupational and environmental lung disease. A controlled trial of an environmental tobacco smoke reduction intervention in low-income children with asthma. Chest 2001;120:1709–22 | Ineligible intervention |
| Wong SS, Nathan AM, de Bruyne J, Zaki R, Mohd Tahir SZ. Does a written asthma action plan reduce unscheduled doctor visits in children? Indian J Pediatr 2013;80:590–5 | Ineligible intervention |
| Wysocki T, Harris MA, Buckloh LM, Mertlich D, Lochrie AS, Mauras N, et al. Randomized trial of behavioral family systems therapy for diabetes: maintenance of effects on diabetes outcomes in adolescents. Diabetes Care 2007;30:555–60 | No eligible economic outcomes |
| Zatzick D, Russo J, Lord SP, Valery C, Wang J Berliner L et al. Collaborative care intervention targeting violence risk behaviors, substance use, and posttraumatic stress and depressive symptoms in injured adolescents a randomized clinical trial. JAMA Pediatrics 2014;168:532–9 | Ineligible population |
Appendix 5 Details of individual studies: context
| Study (first author and year of publication) | Country | Baseline completion (n) | Design | Other LTCs excluded | Measures of effectiveness | Health utilisation outcomes | Costs |
|---|---|---|---|---|---|---|---|
| Atherly et al., 200976 | USA | Unclear (minimum, 458; maximum, 524) | Cluster RCT | N/S | Asthma-related QoL (measure not specified) and number of days with asthma symptoms | ED visits and hospitalisations | Intervention costs and direct medical care costs used to calculate cost per symptom-free day |
| Bartholomew et al., 200077 | USA | 171 | RCT | Yes | Functional status (FS II-R) and symptoms (Usherwood Symptom Questionnaire) | Hospitalisation and ED visits | No costs reported |
| Bird et al., 201278 | Australia | 295 | Quasi-experimental | N/S | QoL (PAQLQ – for participants aged > 6 years) | ED visits, hospital admissions and hospital bed-days | Hospital service costs (including ED presentations, admissions and bed-days) |
| Brazil et al., 199779 | Canada | 50 | Quasi-experimental | N/S | Number of asthma attacks | Scheduled physician visits, emergency or unscheduled physician visits and hospitalisations | No costs reported |
| Brown et al., 200280 | USA | 101 | RCT | N/S | Number of symptom-free days and QoL (PAQLQ symptom subscale) | Medical visits for acute asthma exacerbations | No costs reported |
| Browning et al., 201381 | UK | 30 | nRCT | N/S | Symptoms (BPRS) and global functioning (CGAS) | Length of hospital stay | No costs reported |
| Bruzzese et al., 201182 | USA | 345 | RCT | N/S | QoL (PAQLQ), number of symptom days, night awakenings and days with activity restriction as a result of asthma | Acute medical visits, ED visits, hospitalisations and use of controller medication | No costs reported |
| Bryant-Stephens et al., 200983 | USA | 264 | RCT | N/S | Daytime and night-time coughing and wheezing | ED visits, hospitalisations and medication usage | Intervention costs |
| Butz et al., 2005;84 and Walker et al., 200885 | USA | 221 | Cluster RCT | Yes | QoL (PAQLQ) and asthma symptom severity | Hospitalisations, ED visits, preventative visits, specialty care visits and asthma medication use | Intervention costs |
| Butz et al., 201086 | USA | 231 | RCT | N/S | Number of symptom days/nights, activity limitation and asthma symptom severity | ED visits, clinician visits, hospitalisations and pharmacy-based asthma medication use | No costs reported |
| Byford et al., 1999;87 and Harrington et al., 199888 | UK | 162 | RCT | Yes | Suicidal ideation (SIQ), family functioning (FAD) and episodes of self-harm | Inpatient days, day patient days, intensive care days, outpatient attendance, GP visits, school doctor contacts, CPN contacts, counselling sessions, education contacts, social services contacts and voluntary service contacts | Health service costs, education costs, social services costs, residential care costs, voluntary services and intervention costs |
| Byford et al., 2007;89 and Goodyer et al., 200790 | UK | 208 | RCT | Yes | Global functioning (HoNOSCA, CGAS and CGI-I), depressive symptoms (CDRS-R and MFQ), suicidality and self harm, and QoL (EQ-5D), QALYs | Hospitalisations, outpatient contacts, day patient contacts, ED visits, community care contacts, voluntary sector contacts, private sector contacts and social services contacts | Total health services costs (intervention costs, hospital service costs, community health service costs and medication), education costs, social services costs, voluntary sector services costs, private sector and social services costs |
| Byford et al., 2007;91 and Gowers et al., 200792 and 201093 | UK | 167 | RCT | Yes | Eating disorder symptoms and severity (MRAOS, EDI-2) global functioning (HoNOSCA self-rated and clinician rated), depressive symptoms (MFQ) and family functioning (FAD) | Hospitalisations, outpatient appointments, day patient contacts, ED contacts, community contacts and social services contacts | Total costs (health service costs, social services costs, education costs and voluntary/private sector costs) |
| Calvo et al., 201494 | Spain | 55 | RCT | Yes | Symptoms (PANSS) and global functioning (CGAS) | Hospital admissions, ED visits and antipsychotic usage | No costs reported |
| Cano-Garcinuño et al., 200795 | Spain, Cuba and Uruguay | 245 | RCT | N/S | QoL (PAQLQ – Spanish version) and number of asthma attacks | Hospital admissions | No costs reported |
| Carswell et al.,198996 | UK | 86 | RCT | N/S | Daily symptom score | Visits to surgery, hospital visits and family practitioner home visits | Intervention costs (cost of nurse) and medication costs |
| Celano et al., 201297 | USA | 43 | RCT | Yes | Asthma symptom days | ED visits and hospitalisations | No costs reported |
| Chan et al., 200398 | USA | 10 | RCT | N/S | QoL (PAQLQ), symptom-free days and symptom diary score | ED visits, hospitalisations, unscheduled visits for asthma and medication use | No costs reported |
| Chan et al., 200799 | USA | 120 | RCT | N/S | QoL (PAQLQ), symptom-free days and lung functioning | ED visits, hospitalisations, unscheduled acute visits and medication use | No costs reported |
| Christie et al., 2014100 | UK | 362 | Cluster RCT | Yes | Hypoglycaemic episodes, QoL (PedsQL – general and diabetes specific), and behaviour and well-being (SDQ), QALYs | Clinic utilisation/contacts with diabetes nurse specialists and diabetes teams, and hospitalisations | Intervention costs and health service costs |
| Cicutto et al., 2005101 | Canada | 256 | Cluster RCT | Yes | QoL (PAQLQ) | Urgent health-care visits (including ED visits, walk-in clinic and same-day physician visits) and follow-up visits | No costs reported |
| Cicutto et al., 2013102 | Canada | 1316 | Cluster RCT | Yes | QoL (PAQLQ) | ED visits, unscheduled physician office visits, walk-in clinics and unscheduled community clinic visits | No costs reported |
| Clark et al., 2005103 | China | 639 | Cluster RCT | N/S | Number of symptom days | Hospitalisations, ED visits and medicines use | No costs reported |
| Cowie et al., 2002104 | Canada | 93 | RCT | N/S | Night-time asthma symptoms (frequency) and QoL (PAQLQ) | ED visits, hospitalisations (including number of admissions and number of patients admitted), medication usage and number of intensive care admissions | No costs reported |
| Domino et al., 2008,105 2009;106 March et al., 2006107 and 2009;108 and Treatment for Adolescents with Depression Study Team, 2005109 | USA | 327 | RCT | Yes | Depression symptoms [CDRS-R (used to calculate depression-free days and QALYs) and RADS], responder status (CGI-I), suicidal ideation (SIQ-Junior High School Version), QoL (PQ-LES-Q), health and social functioning (HoNOSCA) and remission rate | Service use (ED, hospitalisation, primary care, other medical visits, school-based services and criminal justice courts) | Total health-care costs [intervention costs (CBT, medication, medication management, adjunctive service and attrition prevention services, time and travel) and additional health-care services costs (service, time and travel)] |
| Donaldson et al., 2005110 | USA | 39 | RCT | Yes | Suicidal ideation (SIQ) and depressive symptoms (CES-D) | Hospitalisations and medication use (including percentage of adolescents taking medication and the number of sessions taking medication) | No costs reported |
| Dougherty et al., 1998111 and 1999112 | Canada | 63 | RCT | N/S | Diabetes-related adverse events (e.g. hypoglycaemia) | Hospitalisations, clinic visits, ED visits, services used and medication use | Health service costs (hospital services, medication and physician contacts), parent costs (expenses and parental time cost) |
| Eakin et al., 2012113 | USA | 321 | RCT and cluster | N/S | Symptom-free days | Hospitalisations, ED visits and medication use | No costs reported |
| Edwards et al., 2007;114 and Hutchings et al., 2007115 | UK | 153 | RCT | N/S | Problem behaviour (ECBI, SDQ, Conners Abbreviated Parent/Teacher Rating Scale and Kendall Self-Control Rating Scale) | Health, social and special educational service use (CSRI) | Total costs [intervention costs (detailed), health service costs (primary care costs and hospital services costs), social services costs and special educational costs] |
| Espinoza-Palma et al., 2009116 | Chile | 88 | RCT | Yes | Number of exacerbations | Hospitalisations, medication use and ED visits | No costs reported |
| Esposito-Smythers et al., 2011117 | USA | 40 | RCT | Yes | Mental health symptoms (RADS-2, SCARED, BASC), suicide attempts (K-SADS-PL depression module), suicidal ideation (SIQ), global impairment (CIS) and alcohol/marijuana use (TLFB) | Hospitalisations, ED visits and number participants prescribed medication | No costs reported |
| Farber and Oliveria, 2004118 | USA | 56 | RCT | Yes | Asthma severity (Asthma Functional Severity Scale) | ED visits, hospital admissions and medication use | No costs reported |
| Flapper et al., 2008119 | The Netherlands | 36 | RCT | Yes | QoL [DUX-25, TACQOL (generic version and asthma-specific version)] and number of asthma attacks | GP visits, ED visits, hospital visits, paediatrician visits and medication use | No costs reported |
| Flores et al., 2009120 | USA | 220 | RCT | Yes | Asthma symptoms, asthma exacerbations, QoL (PedsQL) | ED visits, hospitalisations and doctor visits | Intervention costs, health service costs (ED, hospitalisation, physician visit, home care, medical equipment costs and other asthma-related claims) and parental costs (income) |
| Foster et al., 2007;121 Swanson et al., 2001;122 Wells et al., 2000;123 Molina et al., 2009;124 Jensen et al., 2005;125 and the MTA Cooperative Group, 1999126 | USA | 579 | RCT | Yes | Symptoms (SNAP), functional impairment (CIS), depression (CDI), anxiety (Multidimensional Anxiety Scale for Children), severity of delinquent behaviour, and aggression and conduct | Hospitalisations, medication use, school-based services and police services (SCAPI) | Total treatment costs (medication costs, medication visit costs and psychosocial therapy costs) |
| Franklin et al., 2006127 | UK | 92 | RCT | Yes | Acute complications (including diabetic ketoacidosis and severe hypoglycaemia) | Clinic visits and emergency hotline contacts | No costs reported |
| Galbreath et al., 2008128 | USA | 473 | RCT | N/S | Asthma symptoms and QoL (PAQLQ) | Admissions, ED visits, urgent office visits and medication usage | No costs reported |
| Garbutt et al., 2010129 | USA | 362 | RCT | N/S | QoL (PAQLQ) and asthma symptoms | Urgent office visits, after-hours calls and ED visits | No costs reported |
| Godart et al., 2012130 | France | 60 | RCT | Yes | Eating disorder symptoms and severity (EDI, Morgan–Russell Outcome Category and GOAS) | Hospitalisations | No costs reported |
| Gorelick et al., 2006131 | USA | 352 | RCT | Yes | QoL (ITG-CASF) | ED visit, medication use and hospitalisations | No costs reported |
| Grainger-Rousseau and McElnay, 1996132 | UK | 152 | RCT | Yes | QoL (QWB) and asthma symptoms (frequency) | Hospitalisations | No costs reported |
| Green et al., 2011133 | UK | 366 | RCT | Yes | Frequency and severity of self-harm, depressive symptoms (MFQ), suicidal ideation (SIQ) and global functioning (HoNOSCA) | Hospitalisations, CAMHS/outpatient appointments, ED visits and community care/social service contacts (GP, practice nurse, CPN, health visitor, psychologist, counselling, family therapist, drug and alcohol worker, dietitian, physiotherapist, occupational therapist, walk-in centre, social worker, support worker, school doctor and voluntary sector) | Health service costs (intervention costs, hospital costs, community health service costs and medication costs), social care costs, education costs, criminal justice service costs and costs to family/carers (including productivity losses) |
| Guendelman et al., 200220 and 2004134 | USA | 134 | RCT | Yes | Asthma symptoms, limitation in activity | Hospitalisations, ED visits and urgent calls to hospital | Intervention costs |
| Hederos et al., 2009135 and 2005136 | Sweden | 60 | RCT | Yes | QoL (PAQLQ), asthma control (ACQ) and symptom exacerbations | Hospitalisation, emergency visits, outpatient visits (doctor and nurse) and telephone consultations | Cost in terms of parental sickleave |
| Homer et al., 2000137 | USA | 137 | RCT | Yes | Asthma severity and functional status (CHQ-PF50) | ED visits and acute office visits | No costs reported |
| Horner and Brown, 2014138 | USA | 183 | Cluster RCT | Yes | QoL (PAQLQ) | Hospitalisations and ED visits | No costs reported |
| Hughes et al., 1991139 | Canada | 95 | RCT | Yes | Asthma severity and symptoms | Clinic/GP/paediatrician visits, ED visits and hospitalisations | No costs reported |
| Husted et al., 2014140 | Denmark | 71 | RCT | Yes | Hypoglycaemic episodes and emotional well-being (WHO5) | Hospitalisations | No costs reported |
| Indinnimeo et al., 1997141 | Italy | 120 | RCT | N/S | Number of asthma episodes and children’s level of anxiety (assessed by parents, measure not specified) | Number of emergency visits and number of patients admitted | None reported |
| Indinnimeo et al., 2009142 | Italy | 123 | nRCT | N/S | Number of asthma attacks | Medication use, GP and ED visits, and hospitalisations | No costs reported |
| Joseph et al., 2007143 | USA | 314 | RCT | N/S | Asthma symptoms (number of symptom days, symptom nights, days of restricted activity and days of changed plans), QoL217 | ED visits and hospitalisations | Intervention cost (cost of referral co-ordinator) |
| Kamps et al., 2008144 | USA | 15 | RCT | N/S | QoL (PedsQL generic and asthma module) | None reported | Costs incurred by parents (expenses) |
| Kattan et al., 2005;145 and Morgan et al., 2004146 | USA | 937 | RCT | Yes | Asthma symptoms (days with symptoms, nights with disturbed sleep and days of limited play) | Health-care use (hospitalisations, ED visits, clinic visits) and medication use | Intervention costs and total direct medical costs |
| Katz et al., 2004147 | Canada | 62 | nRCT | Yes | Symptoms of depression, hopelessness and suicidal ideation (BDI, KHS and SIQ) | ED visits and hospitalisations | No costs reported |
| Khan et al., 2004148 and 2003149 | Australia | 310 | RCT | Yes | Number of days wheezing in the last 3 months and asthma attacks in the last 6 months | Use of preventer medication, number of visits to GP/paediatricians, ED visits and hospital admissions with asthma in the previous 6 months | None reported |
| Krieger et al., 2009;150 and Sunshine et al., 2011151 | USA | 309 | RCT | N/S | Symptom-free days, activity limitation and number of asthma attacks | Urgent health care use (ED, hospital and clinic) and medication use | No costs reported |
| Krishna et al., 2003152 and 2006153 | USA | 246 | RCT | Yes | Asthma symptoms (days with asthma symptoms, days of activity limitation and nights of disturbed sleep) and QoL (PAQLQ) | ED visits, hospitalisation (including duration of stay), urgent GP visits and medication use | No costs reported |
| Lewis et al., 1984154 | USA | 103 | RCT | N/S | Asthma severity (National Health Insurance Study System) | ED visits, hospitalisation (events and duration) | Intervention costs, cost of hospital stay and ED use |
| Lynch et al., 2011;155 Asarnow et al., 2009;156 and Brent et al., 2008157 | USA | 334 | RCT | Yes | Symptoms assessed at interview (CGI-I and CDRS-R), self-rated symptoms (BDI and SIQ-Junior version), functional status (CGAS), depression-free days, QALYs and depression-improvement days | Service use (including hospitalisation, ED visits and medication use) | Intervention costs, non-protocol services (health care and others) costs and costs incurred by parents |
| Madge et al., 1997158 | UK | 201 | RCT | N/S | Asthma symptoms days, and night and disability scores (Usherwood Index) | Hospitalisation, ED visits and GP visits | No costs reported |
| Maslennikova et al., 1998159 | Russia | 252 | RCT | N/S | Asthma symptom score | Visits to doctor and medication use | No costs reported |
| McGhan et al., 2003160 | Canada | 162 | Cluster RCT | N/S | QoL (PAQLQ and Childhood Asthma Pictorial Scale), asthma symptoms and asthma severity (parent rated) | Health-care use (unscheduled doctor visits and ED visits) and medication use | No costs reported |
| McGhan et al., 2010161 | Canada | 266 | Cluster RCT | N/S | QoL (PAQLQ) and global asthma ratings of change (including symptoms) | Health-care use (unscheduled doctor visits and ED visits) and medication use | No costs reported |
| Mehlum et al., 2014162 | Norway | 77 | RCT | Yes | Self-harm episodes, suicidal ideation (SIQ-junior version), depression (SMFQ, MADRS), hopelessness (BHS) and borderline symptoms (BSL) | Hospitalisations and ED visits | No costs reported |
| Mitchell et al., 1986163 | New Zealand | 368 | RCT | N/S | Severe asthma attacks (requiring more than treatment at home) | Hospitalisations (admissions, duration of stay) and medication use | No costs reported |
| Muntz et al., 2004;164 and Hutchings et al., 2002165 | UK | 41 | RCT | Yes | Child behaviour (CBCL) and general health (GHQ) | Health, educational and social service use (CSRI) | Health, educational and social service costs, costs to parents (loss of earnings) and intervention costs |
| Nansel et al., 2009166 | USA | 122 | RCT | Yes | QoL (PedsQL core generic module and diabetes module, DFRQ and DFCS), mental health (BYI and CDI) and episodes of hypoglycaemia requiring treatment | Hospitalisations and ED visits | No costs reported |
| Ng et al., 2006167 | China | 100 | RCT | N/S | Number of asthma attacks and number of nocturnal symptoms | Hospitalisations, ED visits and GP visits | Hospitalisation cost and intervention cost (nurse time) |
| O’Neill et al., 2013;168 and McGilloway et al., 2012169 | Ireland | 149 | RCT | N/S | Child problem behaviour (ECBI), behaviour and well-being (SDQ), hyperactive inattentive behaviour (CAPRS) and child social functioning (SCS) | Health, educational and social service use (CSRI) | Health service costs and intervention costs |
| Otsuki et al., 2009170 | USA | 250 | RCT | N/S | Asthma symptoms and night-time awakenings | Hospitalisations, ED visits and medication use | No costs reported |
| Quint and Teach, 2009;171 and Teach et al., 2006172 | USA | 488 | RCT | Yes | Asthma QoL (measure from Bukstein et al.218) and asthma symptoms (NCICAS) | Hospitalisations, ED visits, medication use and GP visits | No costs reported |
| Richardson et al., 2014173 | USA | 101 | RCT | Yes | Symptoms (Patient Health Questionnaire and CDRS-R) and functional status (CIS) | ED visits and psychiatric hospitalisation | Intervention costs |
| Rikkers-Mutsaerts et al., 2012174 | The Netherlands | 90 | RCT | Yes | QoL (PAQLQ), and asthma symptoms and control (ACQ, symptom-free days and exacerbations) | Physician visits and medication use | No costs reported |
| Ronchetti et al., 1997175 | Italy | 312 | RCT | N/S | Number of asthma attacks | Emergency treatment, hospitalisations and medication use | No costs reported |
| Rund et al., 1994176 | Norway | 24 | Quasi-experimental | N/S | Relapses and psychosocial functioning (GAS) | Hospitalisation | Direct costs (inpatient treatment, home visits, consultations with medical doctor/psychologist, social welfare services and seminars for parents) |
| Runge et al., 2006177 | Germany | 358 | Quasi-experimental | N/S | QoL (KINDL®) | Hospitalisations, visits to GP or specialist, ED visits and use of rescue medication | Direct medical costs (health-care services and intervention), direct non-medical costs (transportation and internet) and indirect costs (loss of workdays) |
| Schmidt et al., 2007178 | UK | 85 | RCT | Yes | Eating disorder symptoms (EATATE) and short evaluation of eating disorders | Health service use (CSRI) | Intervention costs, public sector services costs (education, hospital, primary care, specialist services, medication and social care), and family and patient costs (lost employment and out-of-pocket expenses) |
| Seid et al., 2010179 | USA | 252 | RCT | Yes | Child-reported and parent-reported QoL (PedsQL 4.0), and asthma symptoms (PedsQL 3.0 asthma module) day and night | ED visits, hospitalisation or urgent doctor service use | No costs reported |
| Shames et al., 2004180 | USA | 119 | RCT | Yes | Asthma symptoms and symptom days, asthma attacks and QoL (CHSA) | ED visits, hospitalisations and unscheduled physician visits | No costs reported |
| Sockrider et al., 2006181 | USA | 464 | RCT | Yes | Asthma symptoms and QoL (ITG-CASF) | ED visits, hospitalisations and well asthma visits | No costs reported |
| Southam-Gerow et al., 2010182 | USA | 48 | RCT | Yes | Symptoms (DISC version 4.0, STAIC-T, STAIC-P-T and CBCL) | Health service use (SACA) | Intervention costs |
| Staab et al., 2002183 | Germany | 204 | RCT | N/S | Eczema symptoms (SCORAD) | None reported | Direct treatment costs (medical consultation and prescriptions covered by public health insurance) |
| Stevens et al., 200221 | UK | 200 | RCT | N/S | Asthma symptoms (IPSAC and symptom diaries) | GP visits, hospitalisations, ED visits and GP prescriptions written | Intervention costs |
| Sullivan et al., 2002;184 and Evans et al., 1999185 | USA | 1033 | RCT | N/S | Asthma symptom days (wheeze, loss of sleep, and reduction in play activity caused by asthma) | Days in hospital (including intensive care unit), ED visits, scheduled and unscheduled clinic visits | Intervention costs and health-care costs |
| Svoren et al., 2003186 | USA | 299 | RCT | Yes | Hypoglycaemic events | ED visits and hospitalisation | No costs reported |
| Szczepanski et al., 1996187 | Germany | 84 | Quasi-experimental | N/S | Asthma symptoms and severity | Emergency visits to hospital, emergency visits to GP and hospitalisations | No costs reported |
| Toelle et al., 1993188 | Australia | 132 | nRCT | N/S | Asthma symptoms (wheeze, night cough and symptoms limiting activity) | Doctor or emergency room visits and medication use | No costs reported |
| Valery et al., 2010189 | Australia | 113 | RCT | N/S | QoL (PAQLQ), functional severity index and episodes of asthma | Hospital visits, doctor visits and hospitalisations | No costs reported |
| Van de Wiel et al., 2003190 | The Netherlands | 77 | RCT | N/S | Parent-reported behaviours (Parent Daily Report, Interview for Antisocial Behaviour, CBCL, MESSY) and teacher-reported behaviours (Child Behaviour Checklist – Teacher Report Form) | Use of inpatient psychiatric or residential care | Intervention cost |
| Van Der Veek et al., 2013191 | The Netherlands | 104 | RCT | Yes | QoL (KIDSCREEN-27), physical symptoms (Abdominal Pain Index and Children’s Somatization Inventory), functional disability (Functional Disability Inventory), anxiety and depression (Revised Child Anxiety and Depression Scale), frequency and duration and intensity of pain | Health-care use | No costs reported |
| Velsor-Friedrich et al., 2012192 | USA | 137 | Cluster-RCT | Yes | QoL (PAQLQ) and number of symptom days | ED visits, hospitalisations and use of rescue medicine | No costs reported |
| Walders et al., 2006193 | USA | 175 | RCT | Yes | Asthma symptoms (number of days with wheeze or asthma attack in previous month, symptom score) and QoL (CHSA) | ED visits and hospitalisations | No costs reported |
| Watson et al., 2009194 | Canada | 398 | RCT | Yes | QoL (PAQLQ) | ED visits, hospital admissions and use of oral corticosteroid therapy for exacerbations of asthma | No costs reported |
| Weisz et al., 2009195 | USA | 57 | RCT | Yes | Depression symptoms [DISC (version 4.0), CDI, CDI Parent Form and CBCL] | Parent-reported service use (outpatient, inpatient and other) (SACA) | Intervention cost |
| Willems et al., 2007196,197 and 2008198 | The Netherlands | 56 | RCT | Yes | QoL (PAQLQ and EQ-5D) and self-reported clinical symptoms (coughing, production of sputum and shortness of breath/wheezing in morning and evening) | Medication use, contact with HCPs (GP, GP assistant, nurse practitioner, lung specialist, paediatrician and asthma nurse), ED visits and hospitalisation | Health-care costs (hospital care, GP, other HCPs, prescribed medication, professional home care and intervention), patient/family costs (over-the-counter medication, informal care) and costs of school absenteeism |
| Xu et al., 2010199 | Australia | 121 | RCT | N/S | QoL (PAQLQ and PedsQL) | Health-care utilisation (GP visits, ED presentations and hospital admissions) and use of oral steroid rescue | Health-care resource costs and intervention costs |
| Young et al., 2001200 | Canada | 32 | nRCT | N/S | QoL (PAQLQ) | Use of health services (including doctor visits and days of hospitalisation) | No costs reported |
Appendix 6 Details of individual studies: participants
| Study (first author and year of publication) | LTC | Males (%) | Mean age (years) | Age category | % eligible patients not taking part |
|---|---|---|---|---|---|
| Atherly et al., 200976 | Asthma | 54.6 | 13.7 | Adolescents | NR |
| Bartholomew et al., 200077 | Asthma | 65.5 | 10.9 | Mixed | 11.4 |
| Bird et al., 201278 | Asthma | 60.3 | 5.3 | Mixed | NR |
| Brazil et al., 199779 | Asthma | 70.0 | 9.5 | Mixed | NR |
| Brown et al., 200280 | Asthma | 61.0a | 4.3a | Children | 29.9 |
| Browning et al., 201381 | Psychosis | 53.3 | 16.9 | Adolescents | 0.0 |
| Bruzzese et al., 201182 | Asthma | 29.6 | 15.1 | Adolescents | 27.5 |
| Bryant-Stephens et al., 200983 | Asthma | 66.0 | 6.0 | Mixed | NR |
| Butz et al., 2005;84 and Walker, 200885 | Asthma | 62.0 | 8.0 | Children | 23.3 |
| Butz et al., 201086 | Asthma | 60.6 | 8.0 | Children | 30.2 |
| Byford et al., 1999;87 and Harrington et al., 199888 | Self-harm | 10.5 | 14.5 | Mixed | 43.8 |
| Byford et al., 2007;89 and Goodyer et al., 200790 | Depression | 26.0 | 14 (median) | Adolescents | 38.6 |
| Byford et al., 2007;91 and Gowers et al., 200792 and 201093 | Anorexia nervosa | 8.4 | 14.9 | Adolescents | 31.6 |
| Calvo et al., 201494 | Psychosis | 61.8 | 16.5 | Adolescents | 36.8 |
| Cano-Garcinuño et al., 200795 | Asthma | 64.8 | 11.0 | Mixed | 9.3 |
| Carswell et al., 198996 | Asthma | 68.6 | 11.2 | Mixed | 24.6 |
| Celano et al., 201297 | Asthma | 63.0 | 10.5 | Mixed | 77.4 |
| Chan et al., 200398 | Asthma | 50.0 | 7.6 | Mixed | NR |
| Chan et al., 200799 | Asthma | 62.5 | 9.6 | Mixed | 4.8 |
| Christie et al., 2014100 | Diabetes | 44.6a | 13.2a | Mixed | 73.0 |
| Cicutto et al., 2005101 | Asthma | 59.0 | 8.6 | Children | 13.8 |
| Cicutto et al., 2013102 | Asthma | 57.5 | 8.2 | Children | 47.4 |
| Clark et al., 2005103 | Asthma | NR | NR | Children | NR |
| Cowie et al., 2002104 | Asthma | 29.0a | 17.2a | Adolescents | 63.4 |
| Domino et al., 2008105 and 2009;106 March and Vitiello 2006107 and 2009;108 and the Treatment for Adolescents with Depression Study Team, 2005109 | Depression | 45.0 | 14.6 | Adolescents | Unclear |
| Donaldson et al., 2005110 | Suicide attempt | 17.9 | 15.0 | Adolescents | 11.4 |
| Dougherty et al., 1998111 and 1999112 | Diabetes | 44.4 | 10.3 | Mixed | 0.0 |
| Eakin et al., 2012113 | Asthma | 53.3 | 4.0 | Children | 24.8 |
| Edwards et al., 2007;114 and Hutchings et al., 2007115 | Conduct disorder | 58.2 | 3.8 | Children | 6.7 |
| Espinoza-Palma et al., 2009116 | Asthma | 62.5 | 8.0 | Mixed | 0.0 |
| Esposito-Smythers et al., 2011117 | Suicidality | 33.3a | 15.7a | Adolescents | 24.5 |
| Farber and Oliveria 2004118 | Asthma | NR | 7.5 | Mixed | NR |
| Flapper et al., 2008119 | Asthma | 53.0 | 10.0 | Children | 26.5 |
| Flores et al., 2009120 | Asthma | 56.4 | 7.2 | Mixed | 35.5 |
| Foster et al., 2007;121 Swanson et al., 2001;122 Wells et al., 2000;123 Molina et al., 2009;124 Jensen et al., 2005;125 and the MTA Cooperative Group, 1999126 | ADHD | 80.0 | 8.5 | Children | Unclear |
| Franklin et al., 2006127 | Diabetes | 53.8a | 13.2a | Mixed | 27.0 |
| Galbreath et al., 2008128 | Asthma | 59.4 | 9.5 | Mixed | 33.4 |
| Garbutt et al., 2010129 | Asthma | 61.9 | 7.8 | Children | 25.1 |
| Godart et al., 2012130 | Anorexia nervosa | 0.0 | 16.5 | Adolescents | 21.1 |
| Gorelick et al., 2006131 | Asthma | 65.5a | 6.8a | Mixed | 73.9 |
| Grainger-Rousseau et al., 1996132 | Asthma | 51.3 | 16.8 | Adolescents | NR |
| Green et al., 2011133 | Self-harm | 11.5 | NR | Adolescents | 7.1 |
| Guendelman et al., 200220 and 2004134 | Asthma | 57.5 | 12.1 | Mixed | 1.5 |
| Hederos et al., 2009135 and 2005136 | Asthma | 60.0 | 2.3 | Children | 9.1 |
| Homer et al., 2000137 | Asthma | 69.3 | 7.4 | Children | 70.9 |
| Horner and Brown, 2014138 | Asthma | NR | 8.8 | Children | 24.4 |
| Hughes et al., 1991139 | Asthma | 63.2 | 9.7 | Mixed | 57.6 |
| Husted et al., 2014140 | Type 1 diabetes | 39.4 | 14.8 | Adolescents | 47.8 |
| Indinnimeo et al., 1997141 | Asthma | 61.0 | 5.9 | Children | NR |
| Indinnimeo et al., 2009142 | Asthma | 58.5 | 8.8 | Mixed | NR |
| Joseph et al., 2007143 | Asthma | 36.6 | 15.3 | Adolescents | 73.9 |
| Kamps et al., 2008144 | Asthma | 66.7 | 9.0 | Children | 55.9 |
| Kattan et al., 2005;145 and Morgan et al., 2004146 | Asthma | 62.7 | 7.6 | Children | 5.7 |
| Katz et al., 2004147 | Suicide attempts | 16.1 | 15.4 | Adolescents | NR |
| Khan et al., 2004148 and 2003149 | Asthma | 65.5 | 4.9 | Mixed | 33.8 |
| Krieger et al., 2009;150 and Sunshine et al., 2011151 | Asthma | 63.7 | 8.0 | Children | 55.0 |
| Krishna et al., 2003152 and 2006153 | Asthma | 64.9a | NR | Mixed | 1.2 |
| Lewis et al., 1984154 | Asthma | 68.5 | 10.3 | Children | 22.6 |
| Lynch et al., 2011;155 Asarnow et al., 2009;156 and Brent et al., 2008157 | Depression | 30.2 | 15.9 | Adolescents | 15.2 |
| Madge et al., 1997158 | Asthma | 61.7 | I, 6; C, 4.23 (median) | Mixed | 29.0 |
| Maslennikova et al., 1998159 | Asthma | 63.5 | 9.5 | Mixed | 31.5 |
| McGhan et al., 2003160 | Asthma | 59.3 | NR | Children | 74.9 |
| McGhan et al., 2010161 | Asthma | 62.4 | 8.6 | Children | 7.3 |
| Mehlum et al., 2014162 | Suicidal/self-harm behaviour | 11.7 | 15.6 | Adolescents | 59.3 |
| Mitchell et al., 1986163 | Asthma | 59.8 | 5.8 | Mixed | NR |
| Muntz et al., 2004;164 and Hutchings et al., 2002165 | Conduct disorder | 85.4 | 6.0 | Children | 12.8 |
| Nansel et al., 2009166 | Diabetes | NR | 11.5 | Mixed | 26.9 |
| Ng et al., 2006167 | Asthma | 74.0 | NR | Mixed | NR |
| O’Neill et al., 2013;168 and McGilloway et al., 2012169 | Behavioural | 62.4 | 4.8 | Children | NR |
| Otsuki et al., 2009170 | Asthma | 62.0 | 7.0 | Children | 45.2 |
| Quint and Teach, 2009;171 and Teach et al., 2006172 | Asthma | 63.9 | NR | Mixed | 6.3 |
| Richardson et al., 2014173 | Depression | 27.7 | 15.3 | Adolescents | 3.8 |
| Rikkers-Mutsaerts et al., 2012174 | Asthma | 49.8 | 13.6 | Adolescents | 86.9 |
| Ronchetti et al., 1997175 | Asthma | 64.0 | 9.6 | Mixed | NR |
| Rund et al., 1994176 | Schizophrenia | 66.7 | 16.0 | Adolescents | NR |
| Runge et al., 2006177 | Asthma | 64.0a | 12.3a | Mixed | Unclear |
| Schmidt et al., 2007178 | Bulimia nervosa | 2.4 | 17.6 | Adolescents | 38.8 |
| Seid et al., 2010179 | Asthma | 61.1 | 7.4 | Mixed | 26.7 |
| Shames et al., 2004180 | Asthma | 58.0 | 8.0 | Children | NR |
| Sockrider et al., 2006181 | Asthma | 63.4 | 6.6 | Mixed | NR |
| Southam-Gerow et al., 2010182 | Anxiety | 43.8 | 10.9 | Mixed | 63.4 |
| Staab et al., 2002183 | Atopic dermatitis | NR | 3.1a | Children | NR |
| Stevens et al., 200221 | Asthma | 67.0 | 2.7 | Children | NR |
| Sullivan et al., 2002;184 and Evans et al., 1999185 | Asthma | 64.1 | 7.6 | Children | 13.6 |
| Svoren et al., 2003186 | Diabetes | 43.6 | 11.9 | Mixed | Unclear |
| Szczepanski et al., 1996187 | Asthma | NR | NR | Mixed | NR |
| Toelle et al., 1993188 | Asthma | 68.8a | 9.2a | Children | NR |
| Valery et al., 2010189 | Asthma | 69.3a | 7.0a | Mixed | 3.4 |
| Van de Wiel et al., 2003190 | Disruptive behaviour | 88.3 | 10.1 | Children | NR |
| Van Der Veek et al., 2013191 | Abdominal pain | 27.9 | 11.9 | Mixed | 25.2 |
| Velsor-Friedrich et al., 2012192 | Asthma | 30.7 | 15.8 | Adolescents | 7.4 |
| Walders et al., 2006193 | Asthma | 72.0 | 7.3 | Children | 46.5 |
| Watson et al., 2009194 | Asthma | 66.8 | 7.4 | Mixed | 60.1 |
| Weisz et al., 2009195 | Depression | 44.0 | 11.8 | Mixed | 31.3 |
| Willems et al., 2007196,197 and 2008198 | Asthma | 64.3 | 10.7 | Mixed | Unclear |
| Xu et al., 2010199 | Asthma | 52.9 | 7.0 | Mixed | 46.0 |
| Young et al., 2001200 | Asthma | NR | 8.6 (asthma group only) | Children | 27.3 |
Appendix 7 Details of individual studies: interventions
| Study (first author and year of publication) | Content of intervention | Content of control | Intensity |
|---|---|---|---|
| Atherly et al., 200976 | School-based educational intervention ‘Power Breathing’. Group sessions for CYP covering asthma education, asthma control strategies and development of constructive coping strategies | Usual care | Three 90-minute sessions |
| Bartholomew et al., 200077 | An interactive multimedia computer game to enhance self-management skills, played by CYP while attending usual care asthma appointments. Written asthma plan also provided | Usual care | Before usual clinic appointments –schedule not reported |
| Bird et al., 201278 | Participants allocated a care facilitator who assessed individual needs to develop an individual care plan (with multidisciplinary team), delivered self-management education and assisted with access to health and other services | Usual care (historical) | Four to seven sessions (no time length indicated) |
| Brazil et al., 199779 | Day camp for CYP aimed at improving self-management skills and emotional adjustment. The programme incorporated sports, outdoor recreation, drama, creative activities and community outings, as well as formal sessions with physiotherapists (breathing techniques and energy conservation), nurses (education about medication) and social workers (social and emotional issues) | Inpatient programme: 3-month intensive programme for children. Parents received monthly teaching sessions with weekly reinforcement | 3-week day camp |
| Brown et al., 200280 | Home-based educational sessions aimed at parent and CYP. Subsequent sessions based on family’s responses. Printed material, videos and homework | Usual care | Eight 90-minute sessions (median 10 weeks, range 1.9–24.4 weeks) |
| Browning et al., 201381 | Two intervention groups:
|
Usual care (medication, nursing care plan, group activity programme and on-site education) |
|
| Bruzzese et al., 201182 | School-based educational intervention for CYP. Group sessions teaching asthma management skills and ways to cope with asthma plus encouragement to see medical providers. Individual sessions reinforced educational sessions and helped students identify and overcome barriers to management | Waiting list | Three 45- to 60-minute weekly group sessions, individual sessions once a week for 5 weeks |
| Bryant-Stephens et al., 200983 | Educational home-based intervention aimed at families conducted by trained lay health educators covering asthma pathophysiology, recognition of symptoms, recognition and avoidance of triggers, appropriate treatment | Delayed intervention (crossover design study): control group received one visit each month for 6 months to collect asthma diaries and carry out bedroom assessments | Five sessions |
| Butz et al., 2005;84 and Walker et al., 200885 | School/community library-based education intervention for groups of parents and children separately. Parents received a 1-hour education session covering early warning signs of asthma exacerbations, levels of asthma severity, avoidance of rural environmental exposures, types of asthma medications, how to obtain and use an asthma action plan and use of cue cards to communicate with their child’s health-care provider. Interactive demonstrations. Quarterly newsletters. Children received 4 hours of interactive instruction aimed at appropriate developmental level, a peak flow meter, spacer device and colouring book | Usual care plus quarterly newsletter and written asthma guide | Parents: one 1-hour session; children: two 2-hour sessions |
| Butz et al., 201086 | Asthma education (triggers, medication, device training, reducing barriers to regular asthma care), plus home-based communication skills training, assistance arranging clinician appointments, attendance by the nurse/health educator at the child’s clinic visits and reinforcement of medication device technique from nurse/health educator | Asthma education only: delivered in three 30-minute home visits | Four 30-minute home visits |
| Byford et al., 1999;87 and Harrington et al., 199888 | Family focused home-based intervention. Action-oriented intervention was targeted towards intrafamilial communication, behavioural techniques and problem-solving | Usual care (routine psychiatric aftercare and no home-based family interventions) | Five sessions |
| Byford et al., 2007;89 and Goodyer et al., 200790 | CBT for CYP in clinic setting | Usual care (fluoxetine and nine 30-minute outpatient visits over 28 weeks) | One 55-minute session weekly for 12 weeks plus six maintenance sessions every 2 weeks and a final session at 28 weeks |
| Byford et al., 2007;91 and Gowers et al., 200792 and 201093 | Two intervention groups:
|
Usual care (community mental health services) |
|
| Calvo et al., 201494 | Two groups:
|
Attention control (support groups for patients or parents, following same schedule as intervention, no written material and no structure) | (1) and (2): three 50-minute individual sessions, then 12 90-minute group sessions, every 15 days |
| Cano-Garcinuño et al., 200795 | Three intervention groups:
|
Not reported | Three 45- to 60-minute sessions, 2 weeks apart |
| Carswell et al., 198996 | Nurses visited homes to discuss the child’s asthma and treatment and appropriate methods of preventing or curtailing attacks | Usual care | Variable, based on judgement of family need by visiting nurse |
| Celano et al., 201297 | Home-based family intervention. Trained asthma counsellors worked with families to identify challenges from baseline assessment, with goal-setting, family processes addressed and written action plans developed if necessary | Enhanced treatment as usual (one home visit – feedback on lung functioning and inhaler use and action plan) | Four to six home visits over a 4-month period |
| Chan et al., 200398 | Internet-based education. All participants were given a home computer, camera and internet access and instructed in their use. CYP received education online via a website and recorded daily symptom diaries online. Case manager contact available at any time via telephone or e-mail | Office-based care: received education in office visits (same schedule as intervention) and recorded symptoms in hard-copy diary | Visits via website at 2 weeks, 6 weeks, 3 months and 6 months |
| Chan et al., 200799 | Internet- and outpatient clinic-based intervention. CYP and parents received in-depth asthma education from the case manager, determined by an asthma educational pathway. Half of the visits were virtual via a study-provided home computer system, camera and internet access. Virtual visits included asthma education, a video recording of peak flow meter and inhaler use forwarded to the website, daily asthma diaries and communication with the case manager electronically via the website. Access was 24 hours/7 days to their case manager through the internet or telephone | Office-based care: as per intervention group, but all visits at clinic and case manager contact by telephone | Clinic visits at 0, 26 and 52 weeks. Virtual visits at 2, 6 and 12 weeks. Plus daily diary |
| Christie et al., 2014100 | Structured group education intervention. CASCADE consists of four group education sessions (three or four families per group), led by a paediatric diabetes specialist nurse with another team member | Usual care | Average one session per month for 4 months |
| Cicutto et al., 2005101 | School-based intervention run by trained asthma educators. Roaring Adventures of Puff: asthma education, goal-setting, monitoring, medications and correct use of, lifestyle, managing asthma episode and sharing information with others. Child focused with parents attending last session. Teaching strategies including puppetry, role-playing, model building, homework, etc. | Usual care | Six 50- to 60-minute sessions over 6 weeks |
| Cicutto et al., 2013102 | School-based intervention run by trained asthma educators. Roaring Adventures of Puff: asthma education, goal-setting, monitoring, medications and correct use of, lifestyle, managing asthma episode and sharing information with others. Child focused with parents attending last session. Teaching strategies including puppetry, role-playing, model building, homework, etc. Plus Creating Asthma Friendly Schools resource kit for the broader school community | Usual asthma care: schools on waiting list for intervention | Six 50- to 60-minute sessions over 6 weeks |
| Clark et al., 2005103 | School-based CYP group intervention led by trained teachers. Open Airways for School programme, developed in the USA. 20–25 children grouped by age. Social cognitive theory/self-regulation focused. Sessions on asthma symptoms, triggers and management techniques. Teaching involved activities, homework to be completed with parents, games and discussion | Usual care | Five sessions over 5 weeks |
| Cowie et al., 2002104 | CYP group intervention at outpatient site. Inhalation technique assessed and instructions given. General asthma information and management. Action plan development. Adjustment of therapy where appropriate. Discussion of asthma in relation to career | Usual care (spirometry before and after bronchodilator; therefore, received instruction on inhaler technique) | 90- to 120-minute session. Follow-up visit |
| Domino et al., 2008105 and 2009;106 March et al., 2006107 and 2009;108 and Treatment for Adolescents with Depression Study Team, 2005109 | CBT (alone, or with fluoxetine). CBT focused on cognitive restructuring, behavioural activations and behavioural family therapy. Individual sessions, parent-only sessions (two sessions) and family sessions (1–3 sessions) | Usual care (placebo or fluoxetine medication alone – six 20- to 30-minute medication visits) | Six 20- to 30-minute medication visits. CBT: 15 50- to 60-minute sessions over 12 weeks |
| Donaldson et al., 2005110 | Therapist-led individual therapy intervention with CYP at outpatient clinic. Parents attended the start of each session and family sessions if required. Intervention was a skills-based treatment focused on problem-solving and affect management skills. Each session included an assessment of suicidality, skill education and skill practice (both in-session and homework assignments) | Attention control (supportive relationship treatment on same schedule as intervention. Specific skills were not taught and homework assignments were not given) | Six individual sessions and one family session in first 3 months, then 3-monthly sessions (two additional family sessions and two crisis sessions if necessary) |
| Dougherty et al., 1998111 and 1999112 | Home care at diagnosis from diabetes nurse. Visits once or twice for first 3 days after diagnosis to carry out flexible education sessions and supervise practical and theoretical aspects of treatment. Access to 24-hour telephone line to nurse/physician. Two clinic visits with diabetologist and dietitian. Flexible and paced at family’s needs | Usual care (hospital inpatient treatment, then outpatient clinic) | One or two daily home visits for 3 days after diagnosis, then as required |
| Eakin et al., 2012113 | Three intervention groups:
|
Usual care |
|
| Edwards et al., 2007;114 and Hutchings et al., 2007115 | Community-based positive parenting group programme using role-playing, modelling, discussion and analysis of video material | Waiting list control | 12 weekly 2.5-hour sessions |
| Espinoza-Palma et al., 2009116 | Hospital-based self-management intervention in addition to the standard education programme (general education about aetiology, triggers, types, severity, treatment of asthma and correct use of spacers with inhalers plus booklet). The self-management intervention included written information, scenario-based teaching by a nurse and a puzzle game | Usual care (standard education programme, one 30-minute session while admitted to hospital) | One 30-minute session while admitted to hospital |
| Esposito-Smythers et al., 2011117 | Psychiatrist-led outpatient clinic-based integrated CBT intervention. This included individual sessions for CYP, plus family and parent training sessions | Enhanced treatment as usual (diagnostic evaluation report and medication management by study psychiatrist) | Weekly sessions for 6 months, biweekly sessions for 3 months then monthly sessions for 3 months |
| Farber and Oliveria, 2004118 | Inpatient education and management intervention involving asthma education and discussion, a self-management plan, inhaler and medication. Follow-up telephone calls to reinforce asthma management skills | Usual care (referral back to community resources with no input from research staff) | Initial session during ED visit (or hospital stay if admitted from ED) then follow-up telephone calls at 1–2 weeks, 4–6 weeks and 3 months |
| Flapper et al., 2008119 | Group interventions for parents and children separately at outpatient clinic. Education–exercise programme for groups of 8–10 children. Education sessions for parents and teachers | Usual care | Children: 10-weekly 2.5-hour sessions, follow-up session at 6 months. Parents: five 1.5-hour education sessions every 2 weeks |
| Flores et al., 2009120 | Home- and community-based intervention with trained peer mentors supporting families with asthma self-management in terms of education, hospital appointments and other unmet health needs. 24-hour availability by telephone (additional cover by asthma nurse) | Usual care | Monthly family group meetings and telephone calls, two home visits over 12 months |
| Foster et al., 2007;121 Swanson et al., 2001;122 Wells et al., 2000;123 Molina et al., 2009;124 Jensen et al., 2005;125 and the MTA Cooperative Group, 1999126 | Three intervention groups:
|
Usual care (in community) |
|
| Franklin et al., 2006127 | Two intervention groups:
|
Usual care (conventional insulin therapy, 3- to 4-monthly clinic visits and access to an emergency hotline) | Daily text message, plus weekly reminder of clinic goals and occasional newsletters |
| Galbreath et al., 2008128 | Two intervention groups:
|
Usual care |
|
| Garbutt et al., 2010129 | Telephone coaching programme providing education and support to parents to help with day-to-day management. Targeting four areas:
|
Usual care | First call within 2 weeks, then monthly calls but flexible depending on need, over 12 months |
| Godart et al., 2012130 | Outpatient clinic family therapy intervention in addition to usual care. Family therapy aimed to construct therapeutic alliance, identify areas of individual responsibility, support family, enable appropriate expression and management of conflict, develop patient’s autonomy and restore sense of family identity | Usual care (individual consultations with psychiatrist, parent interviews and psychotherapy and nutritional advice if required) | 1.5-hour sessions every 3–4 weeks for 18 months (flexible) |
| Gorelick et al., 2006131 | Two intervention groups:
|
Usual care (asthma education and discharge planning) | Telephone contact over 2 weeks, then case manager group received up to six home visits over 6 months |
| Grainger-Rousseau and McElnay, 1996132 | Three community pharmacist-delivered intervention groups:
|
Usual care | Not reported |
| Green et al., 2011133 | Therapist-led outpatient intervention. Developmental group therapy based on CBT, dialectical behavioural therapy and group psychotherapy. Group goals based around peer relationships, bullying and family problems. Strategies were developed for these situations | Usual care (treatments as judged most appropriate, but excluding group interventions) | 6-weekly sessions followed by weekly sessions as long as needed |
| Guendelman et al., 2002,20 2004134 | Education session (including instructions on using peak flow reading), plus Health Buddy (a personal and interactive communication device that connects to a home telephone). Nurse co-ordinator sends daily queries and the Health Buddy presents questions and records/processes responses. For use by children with parental supervision | Education session plus daily use of written asthma diary to record symptoms and peak flow | Daily use of Health Buddy for 90 days |
| Hederos et al., 2009135 and 2005136 | Outpatient group sessions for parents in addition to usual care (basic education about asthma, medication guidance, written treatment plan). Group sessions had specific topics and involved teaching, dialogue and peer education and sharing of personal experiences | Usual care | Three 1.5-hour meetings soon after baseline, fourth meeting at 6 months |
| Homer et al., 2000137 | Interactive educational computer program (Asthma Control) designed to teach about asthma and its management. Game with simulated daily events emphasising monitoring, allergen identification, use of medications, use of health services and maintenance of normal activity | Written asthma education materials (reviewed with research assistant) and non-educational computer game (three visits) | Three visits over 1 year |
| Horner and Brown, 2014138 | Asthma self-management educational intervention for children and parents. Children were given group sessions during lunch break at school involving problem-solving exercises, activities to enhance coping, education (such as recognising symptoms and avoiding triggers) and practising inhaler technique. Parents received a home visit where they were given individualised family education. A written asthma action plan was completed and discussed with the parents | Attention-control intervention: same schedule as asthma self-management intervention but focused on general health promotion (e.g. nutrition, safely exercising, hygiene) | 16 sequential sessions of 15 minutes duration (4 hours total), 3 days a week for 5.5 weeks |
| Hughes et al., 1991139 | Outpatient clinic and home-based intervention. Seen by same physician/nurse, individualised asthma plan, inhalation technique and trigger factors discussed, asthma teaching programme plus written information and home visits by nurse to discuss environmental factors | Usual care | 3-monthly clinic visits, with more if required and two home visits over 1 year |
| Husted et al., 2014140 | Guided self-determination for adolescents and parents. Outpatient-based intervention. This is a life skills approach aimed at facilitating shared decision-making, and involved discussion of ‘reflection sheets’ completed by children and parents. Opportunity for joint adolescent–parent sessions, as well as individual sessions. Health-care providers could refer to dietitian depending on need | Usual care (eight sessions consisting of typical outpatient care including parental involvement as per intervention) | Eight 1-hour sessions scheduled over an 8- to 12-month period |
| Indinnimeo et al., 1997141 | Outpatient clinic-based asthma self-management education intervention for families, delivered before routine appointment. Education session followed by 30 minutes discussion. Plus usual care | Usual care | One session |
| Indinnimeo et al., 2009142 | Outpatient clinic-based self-management education intervention for children and parents. Personalised treatment and symptom diary plus a 1-hour education session, then a 30-minute group discussion session. Education used age-targeted games | Usual care (including personalised treatment plan and symptom diary) | Two 1.5-hour sessions: one at baseline and one 2 months later |
| Joseph et al., 2007143 | Internet-based asthma management program (Puff City) focusing on three core behaviours:
|
Access to existing asthma management websites, four sessions as per intervention group | Four sessions within 180 days of baseline |
| Kamps et al., 2008144 | Home-based education and behavioural intervention targeted at improving adherence to medication. Sessions involved focused education, monitoring, contingency management and discipline techniques. Interactive computer program and written materials used. Adherence data reviewed with children and parents | General asthma education programme (six 1-hour home-based sessions) | 6-weekly 1-hour sessions |
| Kattan et al., 2005;145 and Morgan et al., 2004146 | Trained environmental counsellors made home visits to discuss six environmental modules including education and demonstration of environmental remediation techniques. Families were also given equipment to address environmental triggers | Usual care | Five visits (plus two optional visits) over 12 months |
| Katz et al., 2004147 | Inpatient therapy-based intervention. DBT – principle-based psychotherapy that attempts to change behaviours by balancing skills-enhancing change strategies with validation | Usual care (daily psychodynamic psychotherapy group, weekly individual psychotherapy) | 10 daily DBT sessions over 2 weeks, plus twice weekly individual DBT psychotherapy review |
| Khan et al., 2004,148 2003149 | Education via telephone, in addition to usual care. Telephone consultation reviewed hospital care, in particular whether or not there was a written action plan, the medication prescribed and arrangements made for follow-up. Advice was reinforced | Usual care | One telephone consultation averaging 13 minutes (range 5–44 minutes) within 2 weeks of receipt of baseline data |
| Krieger et al., 2009;150 and Sunshine et al., 2011151 | Home visits by CHW in addition to asthma education and support in clinic from asthma nurse. CHW developed protocol-driven client and CHW actions, assessed progress, reviewed asthma education and provided support, advocacy and equipment to reduce allergens in participants’ homes. CHW and nurse communicated to co-ordinate care | Usual care (including asthma education and support in clinic with nurse, allergen-impermeable bedding encasements) | Five visits over a year |
| Krishna et al., 2003152 and 2006153 | Interactive multimedia education intervention at usual care clinic visits (in waiting room before appointments). 44 short (1-minute) cartoons covering asthma education ending with game to find triggers in home environment. Programme tracks learners’ progress and repeats information if not understood based on tests of knowledge. Interactive and provides immediate feedback | Usual care | At clinic visits (average 15–30 minutes per visit) |
| Lewis et al., 1984154 | Outpatient clinic-based group session intervention (A.C.T for Kids). Children and parents in different groups for the first 45 minutes, then together for last 15 minutes. Focus on children taking responsibility for their asthma management, input from asthma physician in third session. Asthma physiology, triggers, medication and decision-making skills. Groups of 5–7 children | Same content as intervention delivered in three 1.5-hour lectures held weekly (6–12 families) | 5-weekly 1-hour sessions |
| Lynch et al., 2011;155 Asarnow et al., 2009;156 and Brent et al., 2008157 | CBT intervention in addition to family psychotherapy (three sessions, at start, and at 6 and 12 weeks) and medication change. There were CBT sessions for children alone and with parents | Family psychotherapy and medication change | Up to 12 CBT sessions over 12 weeks, 3–6 sessions including parents (mean 8.3 sessions) |
| Madge et al., 1997158 | Outpatient clinic-based intervention. Trained specialist asthma nurse delivered review discussion sessions, (highly visual) written information and advice, subsequent follow-up and telephone advice. Individual management plan agreed and provided on credit card-sized card. In addition to usual clinical care with paediatrician | Usual care | Visit within 24 hours then two 45-minute sessions |
| Maslennikova et al., 1998159 | Outpatient-based group education intervention for parents and children separately. Asthma education sessions (using either the Open Airways or Air Power programme), focused on physiology, triggers, medication and handling problems. Designed to develop, enhance and encourage self-management skills. Plus asthma care and medication provided by research investigators | Usual care (with access to the same medication as the intervention group) | Four 1- to 1.25-weekly sessions |
| McGhan et al., 2003160 | Child-centred school-based education intervention. Roaring Adventures of Puff, designed using principles of social cognitive theory and appropriate child education approaches: asthma education, goal-setting, monitoring, medications, lifestyle, managing asthma episode and sharing information with others. Teaching strategies including puppetry, role-playing, model building, homework, etc. Parents attended last session and pre-intervention event | Usual care | Six 45- to 60-minute weekly sessions |
| McGhan et al., 2010161 | Child-centred school-based education intervention. Roaring Adventures of Puff, a programme designed using the principles of social cognitive theory and appropriate child education approaches: asthma education, goal-setting, monitoring, medications and correct use of, lifestyle, managing asthma episode and sharing information with others. Teaching strategies including puppetry, role-playing, model building, home work, etc. Parents attended last session and a pre-intervention information event | Usual care | Six 45- to 60-minute weekly sessions |
| Mehlum et al., 2014162 | Therapist-led outpatient clinic-based individual and family intervention. DBT for adolescents | Enhanced usual care (at least one weekly treatment session to match intervention frequency) | One 60-minute individual training session, one 120-minute family skills training session every week for 19 weeks (plus family therapy and telephone coaching if required) |
| Mitchell et al., 1986163 | Community-based, family focused home visit intervention. Child health nurse visits involved education about the pathophysiology of asthma, triggers, medication, a check of drug compliance and encouragement to attend follow-up treatment and communication with HCPs | Usual care | Monthly visits for 6 months |
| Muntz et al., 2004;164 and Hutchings et al., 2002165 | Home- and clinic-based parent training intervention led by trained specialists. Intensive specialist unit-based intervention used video-taped recordings of parent–child interactions to give feedback to parent. Therapist used bug-in-the-ear equipment to deliver advice, praise and encouragement to parents during observations. All 10 behavioural strategies were used. Home visits were used to help parents generalise skills to the home situation | Usual care [various standard interventions, including behavioural strategies (average five) delivered by CAMHS team at home and in clinic] | Three 5-hour unit-based sessions, plus at least one home visit |
| Nansel et al., 2009166 | Research assistant (health advisor)-led family focused outpatient clinic-based education intervention. Health advisor met with parent and child at their regular clinic visit to identify and address areas of difficulty with diabetes management, set goals to improve management, facilitate family discussion and provide guidance through problem-solving process with written materials. Health advisor contacted families prior to clinic visits to remind them of the appointment | Usual care (with health advisor reminders prior to clinic visits) | Three sessions over maximum 12 months |
| Ng et al., 2006167 | Intensive asthma education programme:
|
Standard asthma education programme (1 hour in total):
|
2 hours in total |
| O’Neill et al., 2013;168 and McGilloway et al., 2012169 | Community-based parent-focused group intervention (Incredible Years BASIC parenting programme). Involves discussions and role-play, videos to illustrate parenting and discipline strategies and promoting positive parenting styles | Waiting list control – care as usual | 14 2-hour weekly sessions |
| Otsuki et al., 2009170 |
Two intervention groups: Education – home-based education with five components:Education and feedback – as per education plus objective feedback of medication adherence, goal-setting, reinforcement for attaining adherence goals and strategies for self-monitoring medication use |
Usual care (plus asthma education booklet) | Five 30- to 45-minute sessions at 1, 2, 3, 4 and 8 weeks |
| Quint and Teach 2009;171 and Teach et al., 2006172 | Outpatient clinic-based intervention. Each family met with an asthma educator and a physician. Education delivered on physiology, self-monitoring and management, and environmental triggers along with provision of hypoallergenic bed encasings. The physician completed an individual medical action plan, prescribed medication and provided device teaching. A report was sent to the child’s PCP and follow-up appointment scheduled | Usual care (plus asthma education booklet) | One 60- to 90-minute appointment, within 2–15 days of ED discharge |
| Richardson et al., 2014173 | Outpatient clinic-based, individual intervention. Initial education and engagement session with DCM during which patients had a choice of CBT with the DCM, antidepressant medication or both. DCMs followed up every 1–2 weeks (telephone or in person) to assess treatment progress. Lack of improvement led to stepped-care process | Enhanced usual care (treatment recommendation and access to mental health care) | DCM contact every 1–2 weeks (plus optional CBT, two four-session modules) |
| Rikkers-Mutsaerts et al., 2012174 | Internet-based self-management comprising four components:
|
Usual care | Two education sessions, weekly self-monitoring for a year |
| Ronchetti et al., 1997175 | Two intervention groups as clinics were randomised to deliver one of two different asthma management educational programmes for groups of CYP and parents:
|
Usual care | Weekly 1-hour sessions. Phase 1 eight sessions; and phase 2 four sessions |
| Rund et al., 1994176 | Inpatient and outpatient family-focused intervention. Three phases of psychoeducational approach:
|
Usual care at earlier time – historical case controls | Hospitalisation: family treatment every 2 weeks, duration several months to 1 year +. Rehabilitation: monthly sessions. Follow-up sessions every 2 months |
| Runge et al., 2006177 | Two intervention groups
|
Waiting list for education programme | Five 2-hour sessions plus computer access for internet-based education program |
| Schmidt et al., 2007178 | Outpatient clinic-based therapist-led intervention. Guided self-care: manual-led CBT with homework. Problem focused with self-monitoring of thoughts, feelings and behaviours. Goal-setting. Therapist guides and motivates patient through manual | Family therapy: up to 13 sessions with close others and two individual sessions over 6 months | Guided self-care: 10-weekly sessions, 3-monthly follow-up sessions, two optional sessions with close other |
| Seid et al., 2010179 | Two groups:
|
Usual care (ongoing asthma care and waiting list for intervention after trial) |
|
| Shames et al., 2004180 | Outpatient clinic-based intervention. Children/families were assigned a case manager who helped co-ordinate medical appointments, made follow-up telephone calls to evaluate progress and provide self-management counselling and delivered asthma self-management education sessions. They also received a games console and video game based on asthma self-management skills, had visits with allergist/immunologist who developed asthma action plan and had access to free telephone helpline staffed by paediatric nurses with access to individual treatment plans | Usual care plus games console and non-asthma-related video game | Three education sessions, two allergist visits (weeks 2 and 4) and calls from case manager (to week 32) |
| Sockrider et al., 2006181 | Asthma educator-led intervention at ED visit. Computer-based resource with universal and tailored content that the educator navigates according to the individual child/family’s needs and questions. Written asthma plan developed and report sent to PCP. Follow-up telephone call 1–2 weeks later to reinforce the action plan, address concerns and make referrals if necessary. A free 24-hour telephone service was also available for general asthma questions, answered by project physician | Usual care | Session at recruitment, then follow-up telephone call 1–2 weeks later |
| Southam-Gerow et al., 2010182 | Outpatient clinic-based therapist-led intervention, the Coping Cat CBT programme for childhood anxiety disorders which emphasises anxiety management skills training | Usual care (randomly assigned therapists used their usual treatment procedures) | Coping Cat is a 16- to 20-session programme |
| Staab et al., 2002183 | Multidisciplinary team at an outpatient clinic led a parent group training intervention. Medical, psychological and nutritional topics were presented and the group was encouraged to share personal experience and to exercise newly learned skills | Waiting list control | Six 2-hour sessions over 6 weeks |
| Stevens et al., 200221 | Children and parents received an educational booklet, a written self-management plan and one-to-one structured educational sessions on asthma and self-management with a nurse | Usual care | Two 20-minute sessions: the first within 2 weeks of recruitment and the second 1 month later |
| Sullivan et al., 2002;184 and Evans et al., 1999185 | Asthma counsellors met with children’s care providers to improve contact with the primary care physician, ensured a care plan was obtained from or constructed with the PCP and understood by care providers, delivered group asthma education sessions to adults and children separately and referred care providers to other community resources where appropriate. Environmental intervention (advice and equipment to reduce asthma symptom triggers) | Usual care | One individual meeting plus two adult education sessions in first 2 months, then two child education sessions in next 2 months and at minimum contact every month (individual meetings/telephone calls alternating) |
| Svoren et al., 2003186 | Two intervention groups:
|
Usual care | Eight clinic visits over 24 months (care ambassador 5–10 minutes per visit; care ambassador + 20–40 minutes per visit), plus between-clinic contact via telephone/mail if necessary |
| Szczepanski et al., 1996187 | Two intervention groups:
|
Usual care at asthma clinic |
|
| Toelle et al., 1993188 | School-based education sessions for children and parents covering asthma basics with focus on self-management of asthma. Management plans were produced and shared with the child’s doctor. Doctors, pharmacists, community nurses and teachers in the intervention area also received education sessions. All those who did not attend education sessions were sent education materials by mail | Usual care | Two 2-hour sessions over 2 weeks |
| Valery et al., 2010189 | Initial asthma education session using paediatric asthma education resources adapted for local culture and three further sessions at 1, 3 and 6 months | Initial asthma education session only | Four sessions: baseline, and at 1, 3 and 6 months |
| Van de Wiel et al., 2003190 | School-based intervention, adapted from the preventative Coping Power Programme for parents and children. Parents attended sessions in groups of 4–8, involving teaching and advice on behaviour and stress management and family problem-solving. Children attended sessions on communication, handling emotions and social problem-solving and these were also used to inform the parent sessions | Usual outpatient clinic care (e.g. family therapy, psychoanalytic psychotherapy, play therapy) | Parents: 15 1.5-hour sessions; children: 23 weekly 1.15-hour sessions [mean duration of treatment 8 months (SD 1.4 months)] |
| Van Der Veek et al., 2013191 | Outpatient clinic-based individually tailored CBT for CYP and parents (as age appropriate). CBT protocol had one standard and three optional modules that the therapist could select according to the child’s needs | Intensified usual care (consultations with paediatricians who gave education/advice/medication as appropriate, six 20- to 30-minute sessions over 6 weeks) | Six 45-minute weekly CBT sessions |
| Velsor-Friedrich et al., 2012192 | School-based education intervention for CYP
|
Asthma education as per intervention group (but no coping skills training) | Six 45-minute coping skills sessions over 6 weeks (in addition to education sessions received by all participants) |
| Walders et al., 2006193 | Outpatient clinic-based, family focused intervention. Baseline visit and run-in visit that included written treatment plan and a 1-hour education session. Psychologists identified biopsychosocial barriers to effective asthma management for each family and these were addressed with participants at a third study visit. Following this, families had access to a 24-hour nurse advice line | Usual care (including baseline visit and run-in visit with written treatment plan) | Three study visits |
| Watson et al., 2009194 | Outpatient clinic-based group educational intervention aimed at the parent, child or both, as appropriate for child’s age. The programme was delivered to groups of 6–8 participants by a nurse educator and respiratory therapist. Key educational messages were also posted to participants 2, 4, 6 and 12 months after enrolment | Usual care (via primary care physician) plus basic information booklet | Weekly 1.5-hour sessions over 4 weeks |
| Weisz et al., 2009195 | Outpatient clinic-based therapist-led CBT intervention. CBT for youth depression using the PASCET programme (detailed plans for 10 sessions, outlines for five more, but treatment can extend to > 15 sessions if necessary) | Usual care (outpatient therapy) | Number of therapy sessions and duration of treatment as required [mean 16.45 sessions (SD 6.07 sessions); mean duration 25.20 weeks (SD 15.40 weeks)] |
| Willems et al., 2007196,197 and 2008198 | Nurse-led telemonitoring programme: participants received an asthma monitor to use at home, with which to perform daily lung function tests and pass on data to a hospital-based nurse practitioner for monitoring and treatment adjustment if required | Usual care (outpatient) | Not reported |
| Xu et al., 2010199 | Two groups:
|
Usual care (including initial education with specialist nurse) |
|
| Young et al., 2001200 | Air Force asthma education programme designed to educate children and parents about asthma and its management. Evening session for children and parents: video followed by discussion with nurse facilitator (children) and presentation plus Q&A with paediatric asthma specialist (parents). Once a week for 4 weeks | Usual care (plus educational pamphlets) | Evening session once a week for 4 weeks |
Appendix 8 Details of individual studies: quality
| Study (first author and year of publication) | Design | Baseline sample (n) | Unit of allocation | Risk of bias | |
|---|---|---|---|---|---|
| Random allocation | Allocation concealment | ||||
| Atherly et al., 200976 | Cluster RCT | Unclear | School | Unclear | Unclear |
| Bartholomew et al., 200077 | RCT | 171 | Individual | Unclear | Unclear |
| Bird et al., 201278 | Quasi-experimental | 295 | N/A | High | N/A |
| Brazil et al., 199779 | Quasi-experimental | 50 | N/A | High | N/A |
| Brown et al., 200280 | RCT | 101 | Individual | Unclear | Unclear |
| Browning et al., 201381 | nRCT | 30 | Individual | High | High |
| Bruzzese et al., 201182 | RCT | 345 | Individual | Low | Low |
| Bryant-Stephens et al., 200983 | RCT | 264 | Individual | Unclear | Unclear |
| Butz et al., 2005;84 and Walker et al., 200885 | Cluster RCT | 221 | County | Unclear | Unclear |
| Butz et al., 201086 | RCT | 231 | Individual | Unclear | Low |
| Byford et al., 1999;87 and Harrington et al., 199888 | RCT | 162 | Individual | Low | Low |
| Byford et al., 2007;89 Goodyer et al., 200790 | RCT | 208 | Individual | Low | Low |
| Byford et al., 2007;91 and Gowers et al., 200792 and 201093 | RCT | 167 | Individual | Low | Low |
| Calvo et al., 201494 | RCT | 55 | Individual | Low | Unclear |
| Cano-Garcinuño et al., 200795 | RCT | 245 | Individual | Low | Unclear |
| Carswell et al., 198996 | RCT | 86 | Individual | Low | Unclear |
| Celano et al., 201297 | RCT | 43 | Individual | Unclear | Unclear |
| Chan et al., 200398 | RCT | 10 | Individual | Low | Unclear |
| Chan et al., 200799 | RCT | 120 | Individual | Low | Unclear |
| Christie et al., 2014100 | Cluster RCT | 362 | Clinic | Low | Low |
| Cicutto et al., 2005101 | Cluster RCT | 256 | School | Low | Low |
| Cicutto et al., 2013102 | Cluster RCT | 1316 | School | Low | Unclear |
| Clark et al., 2005103 | Cluster RCT | 639 | School | Unclear | Unclear |
| Cowie et al., 2002104 | RCT | 93 | Individual | Low | Low |
| Domino et al., 2008105 and 2009;106 March et al., 2006107 and 2009;108 and the Treatment for Adolescents with Depression Study Team, 2005109 | RCT | 327 | Individual | Low | Unclear |
| Donaldson et al., 2005110 | RCT | 39 | Individual | Unclear | Unclear |
| Dougherty et al., 1998111 and 1999112 | RCT | 63 | Individual | Unclear | Unclear |
| Eakin et al., 2012113 | RCT and cluster | 321 | Individual and sites | Low | Low |
| Edwards et al., 2007;114 and Hutchings et al., 2007115 | RCT | 153 | Individual | Low | Low |
| Espinoza-Palma et al., 2009116 | RCT | 88 | Individual | Low | Low |
| Esposito-Smythers et al., 2011117 | RCT | 40 | Individual | Low | Low |
| Farber and Oliveria, 2004118 | RCT | 56 | Individual | Low | Low |
| Flapper 2008119 | RCT | 36 | Individual | Low | Unclear |
| Flores 2009120 | RCT | 220 | Individual | Low | Unclear |
| Foster et al., 2007;121 Swanson et al., 2001;122 Wells et al., 2000;123 Molina et al., 2009;124 Jensen et al., 2005;125 and the MTA Cooperative Group 1999126 | RCT | 579 | Individual | Low | Low |
| Franklin et al., 2006127 | RCT | 92 | Individual | Low | Unclear |
| Galbreath et al., 2008128 | RCT | 473 | Individual | Low | Low |
| Garbutt et al., 2010129 | RCT | 362 | Individual | Low | Low |
| Godart et al., 2012130 | RCT | 60 | Individual | Low | Low |
| Gorelick et al., 2006131 | RCT | 352 | Individual | Low | Low |
| Grainger-Rousseau et al., 1996132 | RCT | 152 | Individual | Unclear | Unclear |
| Green et al., 2011133 | RCT | 366 | Individual | Low | Low |
| Guendelman et al., 200220 and 2004134 | RCT | 134 | Individual | Unclear | Low |
| Hederos et al., 2009135 and 2005136 | RCT | 60 | Individual | Unclear | Unclear |
| Homer et al., 2000137 | RCT | 137 | Individual | Low | Low |
| Horner and Brown, 2014138 | Cluster RCT | 183 | Schools | Low | High |
| Hughes et al., 1991139 | RCT | 95 | Individual | Low | Unclear |
| Husted et al., 2014140 | RCT | 71 | Individual | Low | Low |
| Indinnimeo et al., 1997141 | RCT | 120 | Individual | Unclear | Unclear |
| Indinnimeo et al., 2009142 | nRCT | 123 | Individual | High | High |
| Joseph et al., 2007143 | RCT | 314 | Individual | Low | Low |
| Kamps et al., 2008144 | RCT | 15 | Individual | Low | Unclear |
| Kattan et al., 2005;145 and Morgan et al., 2004146 | RCT | 937 | Individual | Unclear | Unclear |
| Katz et al., 2004147 | nRCT | 62 | Individual | High | High |
| Khan et al., 2004,148 2003149 | RCT | 310 | Individual | Low | Low |
| Krieger et al., 2009;150 and Sunshine et al., 2011151 | RCT | 309 | Individual | Low | Low |
| Krishna et al., 2003152 and 2006153 | RCT | 246 | Individual | Unclear | Unclear |
| Lewis et al., 1984154 | RCT | 103 | Individual | Low | High |
| Lynch et al., 2011;155 Asarnow et al., 2009;156 and Brent et al., 2008157 | RCT | 334 | Individual | Low | Unclear |
| Madge et al., 1997158 | RCT | 201 | Individual | Low | High |
| Maslennikova et al., 1998159 | RCT | 252 | Individual | Unclear | Unclear |
| McGhan et al., 2003160 | Cluster RCT | 162 | Schools | Unclear | Unclear |
| McGhan et al., 2010161 | Cluster RCT | 266 | Schools | Low | Unclear |
| Mehlum et al., 2014162 | RCT | 77 | Individual | Low | Low |
| Mitchell et al., 1986163 | RCT | 368 | Individual | Unclear | Unclear |
| Muntz et al., 2004;164 and Hutchings et al., 2002165 | RCT | 41 | Individual | Unclear | High |
| Nansel et al., 2009166 | RCT | 122 | Individual | Unclear | Unclear |
| Ng et al., 2006167 | RCT | 100 | Individual | Low | Unclear |
| O’Neill et al., 2013;168 and McGilloway et al., 2012169 | RCT | 149 | Individual | Low | Low |
| Otsuki et al., 2009170 | RCT | 250 | Individual | Low | Low |
| Quint and Teach, 2009;171 and Teach et al., 2006172 | RCT | 488 | Individual | Low | Low |
| Richardson et al., 2014173 | RCT | 101 | Individual | Low | Low |
| Rikkers-Mutsaerts et al., 2012174 | RCT | 90 | Individual | Low | Low |
| Ronchetti et al., 1997175 | RCT | 312 | Individual/centres | Low | Low |
| Rund et al., 1994176 | Quasi-experimental | 24 | N/A | High | N/A |
| Runge et al., 2006177 | Quasi-experimental | 358 | N/A | High | N/A |
| Schmidt et al., 2007178 | RCT | 85 | Individual | Low | Low |
| Seid et al., 2010179 | RCT | 252 | Individual | Low | Low |
| Shames et al., 2004180 | RCT | 119 | Individual | Low | Unclear |
| Sockrider et al., 2006181 | RCT | 464 | Individual | Unclear | Unclear |
| Southam-Gerow et al., 2010182 | RCT | 48 | Individual | Low | Unclear |
| Staab et al., 2002183 | RCT | 204 | Individual | Unclear | Unclear |
| Stevens et al., 200221 | RCT | 200 | Individual | Low | Low |
| Sullivan et al., 2002;184 and Evans et al., 1999185 | RCT | 1033 | Individual | Low | Unclear |
| Svoren et al., 2003186 | RCT | 299 | Individual | Unclear | Unclear |
| Szczepanski et al., 1996187 | Quasi-experimental | 84 | N/A | High | N/A |
| Toelle et al., 1993188 | nRCT | 132 | N/A | High | High |
| Valery et al., 2010189 | RCT | 113 | Individual | Low | Unclear |
| Van de Wiel et al., 2003190 | RCT | 77 | Individual | Low | Unclear |
| Van Der Veek et al., 2013191 | RCT | 104 | Individual | Low | Low |
| Velsor-Friedrich et al., 2012192 | Cluster RCT | 137 | Schools | Unclear | Unclear |
| Walders et al., 2006193 | RCT | 175 | Individual | Low | Low |
| Watson et al., 2009194 | RCT | 398 | Individual | Low | Unclear |
| Weisz et al., 2009195 | RCT | 57 | Individual | Unclear | Unclear |
| Willems et al., 2007196,197 and 2008198 | RCT | 56 | Individual | Low | Unclear |
| Xu et al., 2010199 | RCT | 121 | Individual | Low | Unclear |
| Young et al., 2001200 | nRCT | 32 | Schools | High | High |
Appendix 9 Details of individual studies: economic analyses
Economic analyses: quality
| Study (first author and year of publication) | Question | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7a | 7b | 8a | 8b | 9 | 10a | 10b | 11 | 12 | 13 | 14 | 15a | 15b | 16 | 16a | 16b | 16c | |
| Atherly et al., 200976 | ✓ | ✓ | 1 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Butz et al., 2005;84 and Walker et al., 200885 | ✓ | ✓ | 4 | 5 | – | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✗ | ✓ | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Byford et al., 1999;87 and Harrington et al., 199888 | ✓ | ✓ | 3 | 4 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✗ | ✓ | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Byford et al., 2007;89 and Goodyer et al., 200790 | ✓ | ✓ | 3 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✗ | ✓ | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Byford et al., 2007;91 and Gowers et al., 200792 and 201093 | ✓ | ✓ | 4 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Carswell et al., 198996 | ✓ | ✓ | 3 | 5 | 10 | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Christie et al., 2014100 | ✓ | ✓ | 3 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 12 | ✓ | ✓ | ✓ |
| Cicutto et al., 2005101 | ✓ | ✓ | 1 | 5 | ✗ | ✓ | ✗ | ✓ | – | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ | – | 14 | ✓ | ✓ | ✓ |
| Domino et al., 2008105 and 2009;106 March et al., 2006107 and 2009;108 and the Treatment for Adolescents with Depression Study Team, 2005109 | ✓ | ✓ | 1 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 12 | ✓ | ✓ | ✓ |
| Dougherty et al., 1998111 and 1999112 | ✓ | ✓ | 1, 2 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✗ | ✗ | ✓ | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Edwards et al., 2007;114 and Hutchings et al., 2007115 | ✓ | ✓ | 1 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | – | 14 | ✓ | ✓ | ✓ |
| Flores et al., 2009120 | ✓ | ✓ | 3 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✗ | ✓ | ✗ | – | 14 | ✓ | ✓ | ✓ |
| Foster et al., 2007;121 Swanson et al., 2001;122 Wells et al., 2000;123 Molina et al., 2009;124 Jensen et al., 2005;125 and the MTA Cooperative Group, 1999126 | ✓ | ✓ | 3, 1 | 8 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✗ | ✓ | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Galbreath et al., 2008128 | ✓ | ✓ | 3 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✓ | 12 | ✓ | ✓ | ✓ |
| Green et al., 2011133 | ✓ | ✓ | 4 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | – | ✗ | ✓ | ✗ | ✓ | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Hederos et al., 2009135 and 2005136 | ✓ | ✓ | 1 | 5 | 9 | ✓ | ✗ | ✓ | ✗ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ | – | – | ✓ | ✓ | ✓ |
| Joseph et al., 2007143 | ✓ | ✓ | 3 | 5 | – | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Kattan et al., 2005;145 and Morgan et al., 2004146 | ✓ | ✓ | 3 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✗ | ✓ | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Lewis et al., 1984154 | ✓ | ✗ | 4 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | – | ✗ | – | 12 | ✓ | ✗ | ✓ |
| Lynch et al., 2011;155 Asarnow et al., 2009;156 and Brent et al., 2008157 | ✓ | ✓ | 1 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✗ | – | 14 | ✓ | ✓ | ✓ |
| Muntz et al., 2004;164 and Hutchings et al., 2002165 | ✓ | ✓ | 3 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Ng et al., 2006167 | ✓ | ✓ | 4 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | – | ✗ | – | 14 | ✓ | ✓ | ✓ |
| O’Neill et al., 2013;168 and McGilloway et al., 2012169 | ✓ | ✓ | 4 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✓ | ✓ | ✓ | ✗ | – | 14 | ✓ | ✓ | ✓ |
| Rund et al., 1994176 | ✓ | ✓ | 1 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Runge et al., 2006177 | ✓ | ✓ | 2, 1 | 6 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✗ | – | 14 | ✓ | ✓ | ✓ |
| Schmidt et al., 2007178 | ✓ | ✓ | 3 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Southam Gerow et al., 2010182 | ✓ | ✓ | 4 | 5 | 10 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✓ | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Staab et al., 2002183 | ✓ | ✓ | 4 | 5 | 10 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | – | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Stevens et al., 200221 | ✓ | ✓ | 4 | 5 | 10 | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✓ | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Sullivan et al., 2002;184 and Evans et al., 1999185 | ✓ | ✓ | 3 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✗ | – | 14 | ✓ | ✓ | ✓ |
| Svoren et al., 2003186 | ✓ | ✓ | 3 | 5 | 10 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | – | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Van de Wiel et al., 2003190 | ✓ | ✓ | 3 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✓ | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Weisz et al., 2009195 | ✓ | ✓ | 3 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✗ | – | 12 | ✓ | ✓ | ✓ |
| Willems et al., 2007196,197 and 2008198 | ✓ | ✓ | 1, 3 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✗ | – | 14 | ✓ | ✓ | ✓ |
| Xu et al., 2010199 | ✓ | ✓ | 3 | 5 | 9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✗ | ✓ | ✗ | – | 12 | ✓ | ✓ | ✓ |
Economic analyses: summary overview
| Study (first author and year of publication) | Population setting | Intervention and comparison | Perspective and time horizon | Outcomes and costs | Outcomes reported (including ICERs and uncertainty) | Author conclusion/additional comments |
|---|---|---|---|---|---|---|
| Atherly et al., 200976 |
USA Adolescents in grades 6–12 |
Implementation of asthma programme vs. control group | Societal 3 months follow-up | Change in symptom-free days for treated and non-treated and cost of intervention | Cost of the intervention is US$3.90 per symptom-free day (0.34 days per participant per 2 weeks) gained | The intervention is cost-effective only for adolescents who have symptoms of asthma at baseline |
| Butz et al., 2005;84 and Walker et al., 200885 |
USA Children aged 6–12 years with asthma |
Educational asthma intervention vs. control | N/A | Parent/child asthma knowledge, self-efficacy and QoL. Costs of the intervention (nurse time, colouring books, peak flow meters, food and travel expenses) | Means and QoL | Knowledge and self-efficacy significantly higher for intervention group at follow-up. QoL parents 6.49 intervention vs. 6.38 control; QoL children 5.50 intervention vs. 4.81 for control |
| Byford et al., 1999;87 and Harrington et al., 199888 |
UK Children aged ≤ 16 years who have self-poisoned |
Routine care plus social work intervention vs. routine care only | CEA | Suicidal Ideation Questionnaire and Hopelessness Scale. Costs: hospital services, GP, social worker and nurse. Costs per assessment session | Means | Cost intervention group is £1455 vs. cost control group £1751 |
| Byford et al., 2007;89 and Goodyer et al., 200790 |
UK 11- to 17-year-old adolescents with major depression |
Combination therapy (SSRIs and CBT) vs. therapies alone | CEA | QALYs using EQ-5D, ICER and acceptability curves | 26% probability that combination therapy is more cost-effective than single therapy. Increase in QALY of 4% | The combination therapy is not cost-effective compared with single therapies |
| Byford et al., 2007;91 and Gowers et al., 200792 and 201093 |
UK Adolescents aged 12–18 years with anorexia nervosa |
Inpatient psychiatric treatment, specialist outpatient treatment and general outpatient treatment | Broad service-providing perspective (includes both health and social costs) | Morgan–Russell Average Outcome Scale. Costs: health, social services, education, and voluntary and private sectors | ICER and CEACs | Specialist outpatient group is more cost-effective (£26,738) than the inpatient (£34,531) and general outpatient treatment (£40,794), but results are not statistically significant |
| Carswell et al., 198996 |
UK Families with asthmatic children aged 5–15 years |
Asthma nurse visiting homes vs. no asthma nurse | N/A | Peak expiratory flow rate, asthma knowledge, parents’ time off work, child’s school absence and nurses | Cost of the asthma nurse £15 patient/6 months | Health authority nurses sent into homes with children with asthma can improve child’s physical asthma disability |
| Christie et al., 2014100 |
UK Children aged 8–16 years with type 1 diabetes diagnosed for > 12 months |
Clinic-based structured education vs. current NHS practice | Health care | Long-term glycaemic control, QoL and psychosocial functioning. Cost of the intervention | QALY = 14.43. Incremental cost of intervention = £422 | Cost of intervention is £683 per child. Intervention did not improve glycaemic control and it costs more than current NHS practice. Therefore, it is not cost-effective |
| Cicutto et al., 2005101 |
Toronto, ON, Canada Children in grades 2–5 with asthma and their parents |
Asthma education programme vs. usual care for control group | Societal | Asthma QoL, self-efficacy for managing asthma, school absenteeism, days of interrupted activity, health services use and parental loss of time for work | Means and SD | Asthma education programme was able to increase QoL, improve efficacy for the treated and fewer used urgent health care at 1 year |
| Domino et al., 2008105 and 2009;106 March et al., 2006107 and 2009;108 Treatment for Adolescents with Depression Study Team, 2005109 |
USA Outpatients aged 12–18 years with a diagnosis of major depression |
Treatment of CBT, fluoxetine, CBT combined with fluoxetine on children with depressive disorder vs. placebo | Societal | QALYs, ICERs, cost-effectiveness acceptability curve and differential cost-effectiveness for subgroups. Total costs of health-care services | ICERs and CEACs. Incremental cost over placebo from US$24,000/QALY for treatment with fluoxetine to US$123,000/QALY for combination therapy treatment | Combination treatment is cost-effective |
| Dougherty et al., 1998111 and 1999112 |
Montreal, QC, Canada Children newly diagnosed with type 1 diabetes |
Home care treatment vs. inpatient hospital care | Focus mainly on societal but also presents health care | Hospital use, metabolic and psychosocial outcomes, use of hospitals, counselling and nursing hours. Hospital stay, site and timing of initial teaching, hospital costs, government costs and social costs | Parents and hospital cost data. Means and SD | Societal cost was CA$48 higher when using home care. The results are sensitive to how parental time is valued. Health-care services cost was CA$768 with home care, but it was offset by the parental cost savings of CA$720. Home care improved children’s outcomes without increasing the societal cost significantly |
| Edwards et al., 2007;114 and Hutchings et al., 2007115 |
UK Children at risk of developing conduct disorder |
Training programme for parents with children with conduct disorder compared with control group | Societal | ICER cost-effectiveness acceptability curve | ICER £73 (95% CI £42 to £140) | The parenting programme improves child behaviour. The programme is cost-effective |
| Flores et al., 2009120 |
USA Urban minority children with asthma |
Parents mentor intervention vs. traditional asthma care | Health-care system | Pediatric Quality of Life Inventory and parent-reported health QoL. Costs of whole intervention | ICER and QoL | ICER for intervention, US$597.10. Average monthly cost of intervention, US$60.42 vs. net savings US$40.26. Overall cost savings |
| Foster et al., 2007;121 Swanson et al., 2001;122 Wells et al., 2000;123 Molina et al., 2009;124 Jensen et al., 2005;125 and the MTA Cooperative Group 1999126 |
USA Children aged 7–10 years with diagnosed ADHD |
Four-treatment comparison:
|
Health care and societal | CIS and all costs. Composite outcome measure of treatment success based on overall parents and teachers ratings. Direct costs of each treatment | ICER and CEAC | Cost-effective treatment varies as a function of the child’s comorbidity and of the policy-maker’s willingness to pay. Medical management not as effective as combined treatment but it is more likely to be more cost-effective |
| Galbreath et al., 2008128 |
USA Children and adults with asthma |
DM and augmented DM programmes vs. routine care | Health-care system | Asthma symptoms and QoL | QoL | No significant differences among interventions. The study is not limited to children but also includes adults |
| Green et al., 2011133 |
UK Adolescents aged 12–17 years with past episodes of self-harm |
Group therapy with routine care vs. routine care | Not clear | Frequency of episodes of self-harm, severity, mood disorder, suicidal ideation and global functioning. Costs of health, social care, education and criminal justice, and family-related costs | Incremental mean costs and effects, and odds ratio | No evidence of cost-effectiveness |
| Hederos et al., 2009135 and 2005136 | Parents of preschool children recently diagnosed with asthma | Intervention though extra parental support vs. control | Societal | Adherence, children’s symptoms and medication. Cost in terms of parental sick leave | Means | Programme helps to reduce the number of children with exacerbation days. The intervention would save, on average, 42.5 working days to parents. The authors conclude that intervention is not cost-effective, as they say those are few days saved |
| Joseph et al., 2007143 |
USA Urban African-American youth aged 15–19 years |
Multimedia web-based asthma management program vs. generic asthma websites | Health-care system | Number of symptoms days and QoL. Cost of program delivery | QoL, CI and cost estimates | More positive behaviours of children receiving treatment. Does not compare costs between treated and non-treated |
| Kattan et al., 2005;145 and Morgan et al., 2004146 |
USA Children aged 5–11 years with asthma |
Home environmental allergen asthma intervention vs. control | Health care | Maximum number of days with symptom, levels of allergens at home and costs of intervention | ICERs and acceptability curves. Coefficients of a linear fixed-effects mixed model | The intervention is cost-effective, but likelihood that the intervention is cost-saving over the 2-year follow-up period is very small (0.5%). The intervention led to 21.3 fewer days with symptoms/year, 4.4 missed school days/year and 2.1 fewer unscheduled visits. The intervention might not be cost-effective from a health-care point of view, but it is from a societal perspective |
| Lewis et al., 1984154 |
USA Children aged 8–12 years with severe asthma |
Treatment offered in small groups vs. larger groups | N/A | Number of visits to the emergency room, hospitalisation days and cost of each experimental group | ANCOVA (covariances) | Reductions on the number of hospital visits and emergency room in the treatment group and save in costs, so the programme is cost-effective |
| Lynch et al., 2011;155 Asarnow et al., 2009;156 and Brent et al., 2008157 |
USA Children aged 12–18 years with depression |
Combined CBT plus medication vs. medication only | Societal | Depression-free days, depression-improvement days and QALYs. Cost of intervention and non-protocol services | QALYs, ICER and CEACs | ICER for depression-free days is US$188, for depression-improvement days is US$142 and for QALYs US$78,948. The CEAC suggests that there is a 61% probability of combined treatment is more cost-effective (at very high threshold of US$100,000 per QALY) |
| Muntz et al., 2004;164 and Hutchings et al., 2002165 |
UK Children aged 2–10 years with behavioural problems |
Intense vs. standard practice-based treatment | Multisectoral service | Child Behaviour Checklist, ICERs and CEACs | ICERs and CEACs | The ICER is £224 and the CEAC shows that 89.6% of the cost-effectiveness is saved in the controls group, whereas 99.9% applies to intense treatment. Then, the intense treatment does not significantly differ from the standard treatment |
| Ng et al., 2006167 |
Hong Kong Children aged 2–15 years with an acute attack of asthma |
Intensive asthma education programme vs. standard asthma education programme | N/A | Number of visits to the ED and the number of hospitalisations for asthma. Cost of ward services, hospitalisation costs and nursing costs | Medians | Applying the intervention reduces the costs and brings to a net saving of HK$969 |
| O’Neill et al., 2013;168 and McGilloway et al., 2012169 |
Ireland Children aged 3–7 years with behaviour problems |
Incredible Years parenting programme vs. control group | N/A | Child Behaviour Inventory, use of health, educational and social services, and cost per parent | ICERs and CEACs | ICER is €87. The probability of the programme being cost-effective would exceed 90% (at a willingness-to-pay threshold of at least €137). The authors conclude that the intervention is cost-effective |
| Rund et al., 1994176 |
Norway Adolescents aged 12–18 years with schizophrenia |
Psychoeducational programme vs. standard treatment | Societal | Relapses during the 2-year programme and changes in psychosocial functioning. Costs of treatment: inpatient treatment, home visits, consultations with doctors, social welfare service costs and seminars for parents | Means and SDs | Costs are higher for the control group than for the treatment group. The intervention is successful. Only 12 patients in every group, so results cannot be generalised to the whole population |
| Runge et al., 2006177 |
Germany Children aged 8–16 years with asthma |
Internet-based education programme vs. standardised programme and vs. control group | Health care and societal | Utilisation of several health care services. Direct medical and non-medical costs and indirect costs | Benefit–cost ratio and QoL | Utilisation of health-care services reduced in both intervention groups. Benefit–cost ratio improves (0.79) when adding the internet-based education program as opposed to the standardised programme (0.55). It is a non-randomised trial |
| Schmidt et al., 2007178 |
UK Adolescents with bulimia nervosa or eating disorders |
Family therapy vs. CBT | Health care | Abstinence from binge eating and vomiting. Cost of treatments | Mean cost comparisons | CBT has advantages as a family therapy as it decreases binging and it has a lower cost |
| Southam Gerow et al., 2010182 |
USA Youth aged 8–15 years with anxiety (Caucasian, Latino, African-American) |
CBT vs. usual care | N/A | Clinical outcomes and treatment durations. Cost of treatment, therapist time and medication | ANCOVA and estimated coefficients | CBT did not produce better clinical outcomes than usual care. The study was based in a small sample. There were no differences in costs between intervention and control |
| Staab et al., 2002183 |
Germany Children aged 5 months to 12 years with atopic dermatitis |
Intervention educational programme vs. control | N/A | Severity of eczema, treatment habits, treatment costs, QoL and coping strategies | Coefficients from logistic regressions | Outcomes were improved for applying intervention: less severity of eczema and a reduction of treatment costs |
| Stevens et al., 200221 |
UK Children aged 18 months to 5 years with asthma |
Parental educational intervention and written guided self-management plan vs. usual care | N/A (possibly health care) | GP consultation rates, hospital readmissions, QoL and parent’s asthma knowledge. Cost of intervention | t-test | No differences between groups |
| Sullivan et al., 2002;184 and Evans et al., 1999185 |
USA Asthmatic children living in rural areas |
Social worker-based education programme and environmental control vs. standard care | Health care | Symptom-free days, cost per symptom-free day gained and annual costs of asthma morbidity | ICER | Intervention improves outcomes and has an average additional cost of US$9.20 (ICER) per symptom-free day gained. The intervention is more cost-effective in children with asthma severity |
| Svoren et al., 2003186 |
USA Youths aged 7–16 years with type 1 diabetes |
Care ambassador, care ambassador and psychoeducational modules vs. standard diabetes care | Health care | Number of medical visits, frequency of hypoglycaemic events, hospital/ED utilisation and HbA1c levels | Means and SDs | Estimated annual cost savings of US$80,000–90,000 when using care ambassador plus intervention. In addition, there were reduced EDs and rates of hypoglycaemia. Therefore, non-medical case management seems to be cost-effective |
| Van de Wiel et al., 2003190 |
Amsterdam, the Netherlands Children aged 8–13 years with disruptive behaviour disorders |
Parent management and social problem-solving skills training vs. usual care | Health care | Therapist experience, and number of sessions and duration. Cost of treatment and usual care | Means and SDs | The intervention was 49% cheaper than usual care when attaining the same improvement in behaviour, so the treatment is cost-effective |
| Weisz et al., 2009195 |
USA Youths aged 8–15 years with depression, low-income families |
CBT vs. usual clinical care | Health care | Depressive symptom measures, parent-rated therapeutic alliance and additional services. Cost of treatment | Means and SDs | No differences in the number of depressive symptoms between treatment and control, but CBT was superior in parent-rated therapeutic alliance (i.e. it was less likely to require additional services and was less costly) |
| Willems et al., 2007196,197 and 2008198 |
The Netherlands Children and adults with asthma |
Nurse-led telemonitoring programme vs. usual care | Societal and health care | EQ-5D and SF-6D, health care, and patient and family costs | QALY and ICERs | There were no differences between groups regarding QALYs and the mean health-care costs per patient were higher in the intervention group. There was a limited cost-effectiveness from a health-care perspective. From a societal perspective, the probability of the programme being cost-effective is 85% (at a very high threshold of €80,000/QALY) |
| Xu et al., 2010199 |
Australia Children aged 3–16 years with doctor-diagnosed asthma |
IVR and specialist nurse vs. usual care | Health care | Health-care utilisation, use of oral steroid rescue and HRQoL | ICER: AUS$225.73 per child for nurse support and AUS$451.45 per child for IVR | Both IVR and support interventions are cost savings |
Appendix 10 RE-AIM framework for included studies
| Study (first author and year of publication) | Participation ratea | Representativeness of sampleb | Intervention | Process measuresd | Follow-up measure timingse | |
|---|---|---|---|---|---|---|
| Setting and size | Expertisec | |||||
| Atherly et al., 200976 | Not reported | Not reported | School, 10 middle and high schools in two US sites | Not explicitly reported (programme facilitators, school nurses and teachers mentioned in costs) | Not reported | 3 months post intervention |
| Bartholomew et al., 200077 | 0.89 | Other ‘chronic’ disease excluded | Outpatient, four inner-city asthma clinical sites (two asthma clinics at hospitals and two community paediatric practices) | Self-guided (research assistants were available to support children if required) | Return rate to clinic was 66% (exceeding general return rate of 47%). 84% of children usually or always engaged in the game during sessions. 94% of children required some assistance from research assistant | Mean 7.9 months (SD 3.5 months, range 4–15.6 months) |
| Bird et al., 201278 | Not reported | Not reported | Home (or sometimes GP surgery/outpatient if more appropriate) | Care facilitator (with professional experience in nursing and asthma education) | Not reported | Post intervention (mean 186 days, range 29–919 days) |
| Brazil et al., 199779 | Not reported | Not reported | Day camp, children’s rehabilitation centre | Day camp: teaching by physiotherapist, nurses and social worker | Not reported | Post intervention (participants had received intervention in previous 24 months) |
| Brown et al., 200280 | 0.70 | Not reported | Home, recruitment from three asthma clinics and some primary care paediatricians serving low-income children in Atlanta, GA, USA | Trained registered nurses. Nurses documented the extent to which session objectives were met. Supervisory meetings and ongoing training | 39/55 completed all sessions, four did not complete any | 3 and 12 months |
| Browning et al., 201381 | 1.00 | No exclusions | Outpatient, 10-bed adolescent psychiatric unit in an inner-city location | CBT delivered by unit clinical psychologist. Family intervention delivered by two co-therapists | Psychological interventions received more ‘very satisfied’ ratings than usual care | At discharge (median 76 days, range 8–358 days) |
| Bruzzese et al., 201182 | 0.72 | No difference in asthma classification, but more female (68%) enrolled students than non-enrolled (58%) | School, five high schools | Trained health educators – no further details | 157/175 (90%) attended all three group workshops and 11 (6%) attended none. 137/175 (78%) met 4–6 times for individual coaching and 13 (7%) received none | 6 and 12 months |
| Bryant-Stephens et al., 200983 | Not reported | Not reported | Home | Trained lay health educators supervised by experienced practitioner until competent | 77% of participants completed the project | 6 months (with biweekly assessments) |
| Butz et al., 2005;84 and Walker et al., 200885 | 0.77 | Comorbid pulmonary conditions excluded | School/community library, elementary schools in seven rural counties in Maryland, USA | Trained nurse/health educator | 81% of parents completed evaluation forms and most reported positive evaluations | 10 months |
| Butz et al., 201086 | 0.70 | 12 families who were eligible but dropped out before randomisation did not differ by sociodemographic characteristics from enrolled group | Home, recruitment from paediatric ED records and community paediatric practices in Baltimore, MA, USA | Trained nurse/health educators | Intervention caregivers received a mean 3.29 (SD 1.2) of 4 home visits. Clinician visit rates were low for the intervention group, 60% completed one clinician visit in 6 months and 27% completed two | 12 months |
| Byford et al., 1999;87 and Harrington et al., 199888 | 0.56 | Severe mental illness, current psychiatric patient or severely suicidal, significant learning disability and other self-harm behaviours excluded | Home, recruitment from child mental health team referrals in four Manchester hospitals | Two trained child psychiatric social workers, supervised by consultant child psychiatrist | 22/85 (26%) missed one or more of the five intervention sessions | 2 and 6 months |
| Byford et al., 2007;89 and Goodyer et al., 200790 | 0.61 | Schizophrenia, bipolar disorder, global learning disability, sensitivity/allergy to SSRI, medical contraindication, previous combined optimal treatment with a SSRI and CBT with no effect and rapidly remitting depression excluded | Outpatient, two study centres in different cities in UK | Psychiatrist or CBT therapist (pre-agreed competency reached and supervised by fully accredited CBT supervisor). Quality of CBT rated for 86% cases and found to be acceptable | Not reported | 6, 12 and 28 weeks |
| Byford et al., 2007;91 and Gowers et al., 200792 and 201093 | 0.68 | Severe learning difficulties, severe and chronic physical conditions affecting digestion and/or metabolism excluded | Inpatient recruitment from child or adolescent psychiatric units, outpatient recruitment from 35 community CAMHS in north-west England | Outpatient treatment delivered by trained member of eating disorder team, trained dietitian. Checks of fidelity made at weekly meetings between clinical and research teams | 67% adherence to allocated treatment (49.1% to inpatient, 76.5% to outpatient and 71.1% to general CAMHS) | 1, 2 and 5 years |
| Calvo et al., 201494 | 0.63 | Neurological developmental disorder and drug abuse or dependency excluded | Outpatient, one hospital clinic, Spain | The same therapists delivered both programmes, externally supervised. Sessions were recorded for weekly review. Fidelity to treatment assessed with adherence questionnaire | Mean sessions attended by:
|
Within 1 month of intervention (9 months post baseline if participant discontinued treatment) |
| Cano-Garcinuño et al., 200795 | 0.91 | Not reported | Outpatient, 13 primary health-care centres in Spain, Cuba and Uruguay | Paediatricians and paediatric nurses, experienced in paediatric asthma education. Website and discussion forum for standardisation of intervention | 85.8% children attended all sessions and 80.5% caregivers attended all sessions | 1 and 6 months post intervention |
| Carswell et al., 198996 | 0.75 | Not reported | Home, recruitment from two family group practices | District health authority nurses (full-time working community nurses) trained for 1 week in paediatric asthma management | All families reported a benefit of nurse visits | 6 months (4 weeks of PEF readings – not stated when) |
| Celano et al., 201297 | 0.23 | Non-atopic, non-psychiatric illnesses needing daily medication excluded. No differences in characteristics between participants and those who withdrew after screening (n = 8) | Home, recruited from an urban hospital and asthma camp | Two trained asthma counsellors (a postdoctoral fellow in psychology and a respiratory therapist). 16% sessions recorded and rated by supervisors to assess treatment fidelity. Mean 70% (range 22–100%) adherence to curriculum | All families received at least one visit, mean 4.6 (SD 1.2) and 86% received 4–6 visits | Post intervention and 6 months later |
| Chan et al., 200398 | Not reported | Not reported | Home (via internet) | Case manager (pharmacist) delivered education | In the first 90 days 70.0% inhaler videos were submitted, 69.2% peak flow meter use videos were submitted and 18.7% symptom diary entries were completed. For days 90–180 these figures were 54.2%, 45.0% and 6.7%, respectively | 90 and 180 days |
| Chan et al., 200799 | 0.95 | Not reported | Home (via internet), Oahu, HI, USA | Case manager (nurse or clinical pharmacist) | Electronic submission of peak flow only 1 out of 4 of that directed by protocol and symptom diaries were completed every 2.8 days on average | 6 and 12 months |
| Christie et al., 2014100 | 0.27 | Comorbid chronic illness that was likely to impact on HbA1c levels, ongoing psychiatric/psychological therapy or significant learning disability excluded | Outpatient, 14 paediatric diabetes services, England, UK | Paediatric diabetes specialist nurse with another team member. Training was through two 1-day workshops. Some sessions were delivered by an untrained second educator. Self-reported fidelity was 100%, observers scored it lower although still high | 68% of possible groups were run. 53% of families attended at least one session | 12 and 24 months |
| Cicutto et al., 2005101 | 0.86 | Second major chronic illness with a pulmonary component (e.g. cystic fibrosis) excluded | School, elementary schools (26 in total, unclear how many received intervention) in Toronto, ON, Canada | Certified asthma educators (6 months training), trained specifically in RAP with 2-day workshop | 9/132 children did not receive intervention as they had other lunchtime activities | 2 months (QoL), 3, 6, 9 and 12 months |
| Cicutto et al., 2013102 | 0.53 | Chronic conditions that could mimic asthma (e.g. cystic fibrosis) excluded | School, 85 elementary schools | Public health nurses (attended RAP training workshop) and a certified asthma educator | 29–45% increase in the use of comprehensive school asthma plans (school personnel report) | 7–9 weeks, 12 months (some data collected every 3 months) |
| Clark et al., 2005103 | Not reported | Not reported | School, 21 elementary schools in one industrial and one agricultural area in China | Teachers, trained in a 2-day workshop by trainer from the US programme team | Not reported | 12 months |
| Cowie et al., 2002104 | 0.37 | Not reported | Outpatient, single site in Calgary, AB, Canada | Asthma educators, respiratory therapists, respiratory physician or paediatrician | 81% of programme attendees returned for the second visit | 3 and 6 months |
| Domino et al., 2008105 and 2009;106 March et al., 2006107 and 2009;108 and the Treatment for Adolescents with Depression Study Team, 2005109 | Unclear |
Bipolar disorder, conduct disorder, thought disorder, developmental disorder, substance abuse or dependency, treatment with psychotropic medication and confounding medical conditions excluded Comparison with national survey data shows study sample is similar to adolescent population treated for depression in male-to-female ratio, but higher percentage of African-American and Hispanic adolescents in study sample |
Outpatient, 13 academic and community clinics in the USA | Pharmacotherapist and CBT therapist | 87/111 CBT alone group and 92/107 CBT + fluoxetine group completed 12 weeks. Mean 11/15 (median 12/15) CBT sessions attended for both CBT alone and with fluoxetine groups | 12 and 36 weeks |
| Donaldson et al., 2005110 | 0.89 | Psychosis or intellectual functioning judged by a clinician to preclude engagement in psychotherapy excluded | Outpatient | Therapists (with doctorate in clinical psychology, or masters degree in psychology or social work) trained in both interventions. All sessions audio-taped and performance reviewed during weekly supervision meetings, with a random 44% rated for session adherence and therapist competence | 6/21 dropped out of SBT treatment and 2/18 dropped out of SRT. 77% of participants attended six or more sessions | 3 and 6 months |
| Dougherty et al., 1998111 and 1999112 | 1.00 | Not reported | Home-based, recruitment from children’s hospital in Montreal, QC, Canada | Diabetes treatment nurse conducted home visits. Usual outpatient care provided by diabetologists, psychologist and social worker. Telephone line manned by nurse or physician | Mean 20.0 hours home visits and telephone consultations in month 1, 31.0 hours in months 2–20 | 24 months |
| Eakin et al., 2012113 | 0.75 | Not reported | Community (Breathmobile) and home (FACI) in Baltimore, MD, USA |
Breathmobile: specially trained nurse practitioner, allergist, nurse and assistant FACI: asthma educator |
19% of Breathmobile-only participants completed a Breathmobile visit, 64% of FACI-only patients completed both FACI visits, 65% of combined Breathmobile and FACI patients completed both FACI visits and 22% completed a Breathmobile visit | 6 and 12 months |
| Edwards et al., 2007;114 and Hutchings et al., 2007115 | 0.93 | Not reported | Community, 11 Sure Start areas in Wales, UK | Two trained leaders (social workers, Barnardo’s project workers, health visitors, psychologists). Random videotapes were evaluated by an independent programme trainer to assess treatment fidelity | 71% attended seven or more sessions, mean attendance: 9.2 (SD 3.2) sessions | 6 months |
| Espinoza-Palma et al., 2009116 | 1.00 | Other lung diseases (e.g. cystic fibrosis, ciliary dyskinesia, chronic lung injury secondary to aspiration, bronchopulmonary dysplasia, foreign body, bronchiolitis obliterans, cardiopulmonary malformation or neurological alterations) excluded | Inpatient, inner-city children’s hospital in Chile | Research nurse | Not reported | 3, 6, 9 and 12 months |
| Esposito-Smythers et al., 2011117 | 0.75 | Actively psychotic, bipolar disorder excluded | Outpatient | Therapists (clinical psychologists, clinical psychology postdoctoral trainees, masters level clinician) trained and experienced in CBT. The first two sessions and random session audiotapes were rated for fidelity | 74% of adolescents, 90% of parents and 74% of families completed an acute dose of treatment (24 sessions for adolescents and 12 for parents) | 18 months |
| Farber and Oliveria 2004118 | Not reported | Other clinically significant (i.e. moderate to severe chronic illness) conditions excluded | Inpatient, inner-city paediatric ED in New Orleans, LA, USA | Research staff (a paediatric pulmonary fellow and a research nurse) | 27/28 received the education intervention, 8/28 completed all three follow-up calls and 23/28 completed at least one call | 1 and 6 months |
| Flapper et al., 2008119 | 0.73 | Other causes of low HRQoL or cognitive level of < 7 years excluded | Outpatient | Paediatric nurse and child physiotherapist, trained in the programme | Attendance was 84.5% for children and 79.4% for parents | 3, 6 and 9 months |
| Flores et al., 2009120 | 0.65 | Significant comorbidities (including other pulmonary conditions, cardio-pathologies, renal abnormalities, diabetes or epilepsy) were excluded | Community centres and homes based in Milwaukee, WI, USA | Parent mentors, experienced African-American or Latino parents of children with asthma, living in the same community as participants, received a 2.5-day training session with a nurse specialist and programme co-ordinator | 60% participants remained in study for 12 months and 24% of these had high participation (attended > 25% meetings, completed > 50% telephone calls) | Monthly for 12 months |
| Foster et al., 2007;121 Swanson et al., 2001;122 Wells et al., 2000;123 Molina et al., 2009;124 Jensen et al., 2005;125 and the MTA Cooperative Group, 1999126 | Unclear | Bipolar disorder, psychosis or personality disorder; chronic serious tics/Tourette syndrome; OCD requiring separate treatment; major neurological or medical illness; suicidal/homicidal; score of < 80 on Wechsler Intelligence Scale for children – third edition excluded | Outpatient clinic, recreational settings and school, six sites | A therapist consultant delivered parent training. The summer treatment programme and school-based treatment was delivered by counsellors/aides (behaviourally trained paraprofessionals) supervised by the therapist consultant. Medication management visits with pharmacotherapist. All sessions were audio-taped and there was regular supervision and meetings of pharmacotherapists and psychotherapists | Families attended mean 77.8% parent training sessions and 36.2/40 summer treatment programme days. At school the mean was 47.6/60 days work with classroom aides | 14 months, 6 and 8 years |
| Franklin et al., 2006127 | 0.73 | Serious social problems, severe learning difficulties, needle phobia excluded | Home, Tayside, Scotland, UK | Not applicable | At the end of the study 90% wanted to continue receiving messages | 12 months |
| Galbreath et al., 2008128 | 0.67 | Not reported | Home, TX, USA | DM delivered by registered nurses trained in respiratory care., Augmented DM home visits by respiratory therapists | Not reported | 6 and 12 months |
| Garbutt et al., 2010129 | 0.75 | Not reported | Home | Coaches were call centre nurses with ≤ 2 years paediatric nursing experience, trained over ≤ 2 weeks. Group meetings every 6 weeks | 92% participants had at least one call with coach, 15% had nine or more calls | 12 months |
| Godart et al., 2012130 | 0.79 |
Metabolic pathology interfering with eating or digestion (e.g. diabetes, psychotic disorder) excluded Patients and parents who refused to participate did not differ from those included in sociodemographic variables or clinical status on entry and at discharge |
Outpatient | Two experienced co-therapists delivered FT. Weekly meetings with other practitioners, meetings with research team every 2–3 months to ensure consistency | 29/30 received intervention, attending an average of 11.8 (SD 5.7) FT sessions | 18 months |
| Gorelick et al., 2006131 | 0.26 |
Other chronic pulmonary disease, presence of a tracheostomy excluded Those who were eligible but did not take part were similar to those who participated in age, ED visits and percentage with persistent asthma |
|
Study co-ordinator liaised between participants and primary care provider. Case management intervention delivered by nurse or social worker case manager | In case manager intervention, 72% participants had at least one home care visit | 1, 3 and 6 months |
| Grainger-Rousseau et al., 1996132 | Not reported | Significant pulmonary disease, pathology that would hinder pulmonary function tests or completion of the assessment questionnaires excluded | Pharmacy, health centre community pharmacy in Northern Ireland | Pharmacist | GP acceptance of pharmacist recommendations was 87%, 95% participants found the service convenient to attend | 6 months |
| Green et al., 2011133 | 0.93 | Low-weight anorexia, current psychosis, attendance at a special learning disability school excluded | Outpatient, eight CAMHS centres in north-west England, UK | Experienced therapists, trained by programme developers and the researchers. Protocol adherence measured from video-taped sessions (four per site per year) by independent experts | 144/183 attended four or more sessions, mean attended was 10.2 (SD 10.1) sessions | 6 and 12 months |
| Guendelman et al., 200220 and 2004134 | 0.99 | Mental or physical challenges that could make it difficult to use Health Buddy. Comorbid conditions that could affect QoL excluded | Home | Nurse co-ordinator | 89% used Health Buddy ≥ 3 days a week on average, use decreased over time | 12 weeks |
| Hederos et al., 2009135 and 2005136 | 0.91 | Primary ciliary dysfunction, autism (excluded post recruitment) excluded | Outpatient | Nurses, psychologists and paediatricians | 70% participation in initial three sessions and 40% participation in session 4 | 18 months, 6 years |
| Homer et al., 2000137 | 0.29 |
Major chronic illness with a pulmonary component (e.g. cystic fibrosis) excluded No difference in age or proportion covered by private insurance between those who enrolled and those who did not |
Outpatient | Not applicable (guidance by research assistant if necessary) | 63% of participants returned for more than one visit. All children reported enjoying using the game, parents enjoyed educational videos but not playing the game | 12 months |
| Horner et al., 2014138 | 0.76 |
Significant comorbidity that would preclude participation in classes excluded No differences between study participants and non-participants from original sample in gender, grade level or ethnicity |
School and home in rural Texas, USA | School nurses, assisted by health aides or licensed vocational nurse | 96/101 received intervention | 1, 4 and 7 months post intervention (whole data collection period including intervention = 12 months) |
| Hughes et al., 1991139 | 0.42 | Other major medical problems excluded | Outpatient (one children’s hospital) and home | Paediatric respirologist and nurse in clinic, home visits by nurse | 100% satisfied with medical care (84% of control) and 91% found home visits beneficial | 6 and 12 months, and 2 years |
| Husted et al., 2014140 | 0.52 | Mental health problem/undergoing psychiatric or psychological treatment excluded | Outpatient, two hospital paediatric clinics in Denmark | Paediatric physicians, diabetes nurses and dieticians with at least 1 year’s experience in diabetes paediatric outpatient clinic, GSD-Y trained. Fidelity of treatment assessed | 26/37 completed eight sessions | 6 months post treatment [treatment duration mean 608 (SD 125) days] |
| Indinnimeo et al., 1997141 | Not reported | Not reported | Outpatients in Italy | Trained doctor | Not reported | 12 months |
| Indinnimeo et al., 2009142 | Not reported | Not reported | Outpatient, six specialist paediatric asthma clinics in Italy | Resident physicians and trained nurses | Not reported | 2, 4 and 12 months |
| Joseph et al., 2007143 | 0.26 | Participants were more likely than non-participants to be female, have a physician diagnosis of asthma, have missed school in previous 30 days and be classified as having mild, persistent asthma | School, six high schools in Detroit, MI, USA | Not applicable | 8% did not complete any sessions and 74.1% completed all four sessions | 12 months |
| Kamps et al., 2008144 | 0.44 | Not reported | Home, recruitment from two asthma clinics | Two psychologists and two masters-level graduate students in psychology. Fidelity ensured by use of checklist of tasks and regular meetings | All participants completed intervention | 12 months |
| Kattan et al., 2005;145 and Morgan et al., 2004146 | 0.94 | Other serious chronic illnesses excluded | Home, seven low-income urban areas in the USA | Two environmental counsellors per visit (high-school graduates from the community, trained using centralised training sessions) | Not reported | 1 and 2 years |
| Katz et al., 2004147 | Not reported | Mental retardation, psychosis, bipolar affective disorder and severe learning difficulties excluded | Inpatient, two psychiatric inpatient units | Psychiatrist with 2 years adolescent DBT training, supervised by intensively trained DBT therapist. Regular consultation meetings to increase adherence to treatment | All DBT participants completed treatment | 12 months |
| Khan et al., 2004;148 and Khan 2003149 | 0.66 | Children with bronchitis where it was unclear whether or not the main diagnosis was asthma were excluded | Home, participants recruited from ED of Sydney Children’s Hospital, Sydney, NSW, Australia | Trained asthma educators, registered nurses who had attended an Asthma Educators Association course | Not reported | 6 months |
| Krieger et al., 2009;150 and Sunshine et al., 2011151 | 0.45 | Not reported | At home in Washington, DC, USA | Community health workers who had personal/family experience of asthma and shared ethnic background with participant | 133/156 received the full intervention (all received first CHW visit and 153 had at least one follow-up visit) | 12 months |
| Krishna et al., 2003152 and 2006153 | 0.99 | Cystic fibrosis, bronchopulmonary dysplasia or other chronic lung disease excluded | Outpatient, paediatric pulmonary clinic, in the USA | Not applicable (self-guided) | Children rated computers as their preferred method of receiving information | 3 and 12 months |
| Lewis et al., 1984154 | 0.77 | Not reported | Outpatient, two allergy clinics in Los Angeles, CA, USA | Physician and other educators (programme designed to be delivered by teachers, health educators or nurses) | 48/62 intervention group attended three or more sessions | 3, 6 and 12 months |
| Lynch et al., 2011;155 Asarnow et al., 2009;156 and Brent et al., 2008157 | 0.85 | Bipolar spectrum disorders, psychosis, pervasive developmental disorder, autism, eating disorders, substance abuse or dependence and hypertension were excluded | Outpatient, six academic and community clinics in the USA | CBT delivered by experienced therapists with at least a masters degree in a mental health field, 2-day training at the beginning and mid-point of the study. Sessions were taped and 92.8% pharmacotherapy sessions rated as acceptable quality. Between 93.9% and 94.9% CBT sessions were rated acceptable | 110/166 completed the treatment protocol. 7/166 completed two or more CBT sessions | 6, 12 and 24 weeks |
| Madge et al., 1997158 | 0.71 | Demographic and clinical data show the children who did not take part were very similar to those who did | Outpatient, large children’s hospital in Glasgow, UK | A trained specialist asthma nurse | Not reported | 2–14 months |
| Maslennikova et al., 1998159 | 0.68 | Not reported | Outpatient, research centre for preventative medicine in Moscow, Russia | The investigators and paediatricians from the research centre delivered education sessions | Not reported | 10–12 months |
| McGhan et al., 2003160 | 0.25 | Not reported | School, 18 elementary schools in total (unclear how many received the intervention) in Edmonton, AB, Canada | Nursing and pharmacy students trained in a 2-day workshop, under guidance of supervisor | 85–100% attendance rate for the child sessions. Parent and teacher attendance was 10–80% | 9 months |
| McGhan et al., 2010161 | 0.93 | Not reported | School, 34 schools in total (unclear how many received the intervention) in three health regions of Alberta, Canada | Instructors (four respiratory therapists, one community health nurse) trained in a 2-day workshop | None of the children dropped out of the intervention once it commenced | 6 and 12 months |
| Mehlum et al., 2014162 | 0.41 | Bipolar disorder, schizophrenia, schizoaffective disorder, psychotic disorder not otherwise specified, intellectual disability and Asperger syndrome were excluded | Outpatient, 10 child and adolescent psychiatric clinics | Eight therapists (psychiatrists, clinical psychologists and an educational psychologist) recruited and trained for the trial with a 80-hour seminar and 12 months supervised practice. Only therapists with consistent adherence to treatment during training took part. Sessions were independently rated | Participants attended mean 13.8 (SD 6.9) individual sessions and 11.2 (SD 5.9) family sessions | 9, 15 and 19 weeks |
| Mitchell et al., 1986163 | Not reported | Not reported | Home, living in Auckland, New Zealand | Community child health nurses | 68% had all six visits and 26% had 1–5 visits | 6 and 18 months |
| Muntz et al., 2004;164 and Hutchings et al., 2002165 | 0.87 | Significant intellectual or physical deficit excluded | Home and outpatient, specialist unit | Two consultant clinical psychologists | Not reported | 6 months, 4 years |
| Nansel et al., 2009166 | 0.73 | Major chronic disease or psychological problems, substance abuse excluded | Outpatient, four major medical centres | College-educated research assistants were specially trained as health advisors. Study investigators supervised and checked fidelity of intervention delivery. All sessions were fully or partially completed in each compulsory domain | Average of 2.85 clinic visits. Participating caregivers rated as ‘completely’ or ‘somewhat’ involved except one caregiver at one session. In total, > 91% youth and 97.7% parents agreed or strongly agreed that health advisors ‘helped us learn new ways to solve problems’ | Mid-point and post intervention |
| Ng et al., 2006167 | Not reported | Not reported | Inpatient, paediatric ward in a general hospital in Hong Kong | Asthma nurse | Significantly more parents satisfied with intervention (52/55) than control (36/45) | 3 months |
| O’Neill et al., 2013;168 and McGilloway et al., 2012169 | Not reported | Not reported | Community, various community centres in four disadvantaged urban areas | 11 trained group facilitators (various backgrounds, including psychology, counselling, education) and two per group. Facilitators received weekly supervision from an independent programme trainer. Video-taped sessions were randomly reviewed by the trainer | 60% completed seven or more sessions | 6 months |
| Otsuki et al., 2009170 | 0.55 | Not reported | Home, recruited from paediatric ED in Baltimore City, MD, USA | Trained asthma educators | 71% of education group completed all five visits [mean 4.0 (SD 1.7) visits]. 63% of education and feedback group completed all five visits [mean 3.8 (SD 1.8) visits] | 6, 12 and 18 months |
| Quint and Teach 2009;171 and Teach et al., 2006172 | 0.94 | Significant medical comorbidities affecting the cardiorespiratory system were excluded | Outpatient, specialised asthma clinic in urban paediatric ED | Asthma educator and physician | High adherence and engagement (use of medical action plan, medication and inhalers and bed casings, etc. at follow-up) | 1, 3 and 6 months |
| Richardson et al., 2014173 | 0.96 | Alcohol/drug misuse, suicidal plan or recent attempt, bipolar disorder or developmental delay were excluded | Outpatient, nine clinics in three urban areas in Washington State, DC, USA | Delivery by masters-level clinicians (depression care managers) trained by the study psychologist, with weekly clinical supervision | All had at least one in-person visit with a DCM, mean 14 (SD 8.2) in-person visits, 7 (SD 5.1) telephone sessions | 6 and 12 months |
| Rikkers-Mutsaerts et al., 2012174 | 0.13 | Relevant comorbidity excluded | Home/outpatient, participants from 35 GPs and eight hospital outpatient clinics in the Netherlands | A specialist asthma nurse delivered education sessions and was available to contact | 27/46 attended first and 10/46 second educational session, six were lost to follow-up and five withdrew consent before the end of the intervention at 12 months. The average number was 4.6 online contacts with an asthma nurse | 3 and 12 months |
| Ronchetti et al., 1997175 | Not reported | Not reported | Outpatient, 14 medical centres from across Italy | Physicians (and a psychologist and a social worker) were trained in a 3-day seminar | Not reported | 12 months |
| Rund et al., 1994176 | Not reported | Not reported | Inpatient/outpatient, national child and adolescent psychiatry unit in Norway | Not explicitly reported (presumably professionals working in the unit) | All but two sets of parents reported satisfaction with the psychoeducational treatment programme | 2 years |
| Runge et al., 2006177 | Unclear | Not reported | Outpatient and home/school (for internet intervention) and 36 study centres (GP, specialist offices, hospital asthma outpatient clinics) | Not reported | Not reported | 6 months (all groups) and 12 months (intervention groups only) |
| Schmidt et al., 2007178 | 0.61 | Learning disability, severe mental illness or substance dependence excluded | Outpatient, four NHS eating disorder services in the UK | 23 experienced therapists trained in FT and guided self-care, who received weekly supervision. Three experienced supervisors provided regular ‘live’ supervision of FT and taped sessions were checked | 29/41 received four or more FT sessions and 31/44 received all self-care sessions. One switched from family to self-care therapy | 6 and 12 months |
| Seid et al., 2010179 | 0.73 |
Comorbid conditions that could affect care or outcomes were excluded No difference between participants and those eligible but refused on child age or gender, referral source or asthma severity |
Home, San Diego, CA, USA | CC delivered by bachelor- level asthma home visitors. Problem-solving skills training delivered by masters-level health educators. All received 2 weeks of training. All sessions audio-taped and used in weekly supervision meetings, and a random 10% were rated. Treatment fidelity was 98.4% for CC and 97.5% for CC+ problem-solving skills training | 91.6% sessions were delivered for CC and 71.8% for CC+ problem-solving skills training (23.8% received no problem-solving skills training, 52.4% all) | 3 and 9 months |
| Shames et al., 2004180 | Not reported | Those under the care of an allergist or pulmonologist were excluded | Outpatient, three study centres at hospitals in and around San Francisco and San Jose, CA, USA | Case manager delivered education sessions – no details on expertise or training | 73% of the intervention group completed all study visits | 8, 32 and 52 weeks |
| Sockrider et al., 2006181 | Not reported | Other chronic lung or cardiovascular disease were excluded | ED, four EDs in the greater Houston–Galveston area, TX, USA | Asthma educators (nurses, respiratory care practitioners, a physician and a layperson) were trained in intervention delivery | Five calls were made to the 24-hour telephone line | 9 months |
| Southam-Gerow et al., 2010182 | 0.37 | Pervasive developmental disorder, psychotic disorder or intellectual disability were excluded | Outpatient, six public, urban, community mental health clinics | Experienced therapists who received 1 day of training in the Coping Cat programme plus weekly supervision by a psychologist with Coping Cat expertise. Therapists were randomly assigned to Coping Cat or usual care. Sample testing found 98.9% Coping Cat sessions contained expected procedures | 54% Coping Cat group received 16 or more sessions | Post intervention |
| Staab et al., 2002183 | Not reported | Not reported | Outpatient | Different sessions were delivered by a paediatrician, psychologist, dietitian or paediatrician and psychologist together | Not reported | 12 months |
| Stevens et al., 200221 | Not reported | Not reported | Outpatient (or first session on the ward if recruited as an inpatient), two children’s hospitals in England, UK | Specialist respiratory nurse with a diploma in asthma care | Not reported | 3, 6 and 12 months |
| Sullivan et al., 2002;184 and Evans et al., 1999185 | 0.86 | Eligible children who did not participate did not differ from study participants in age, sex, health-care use and symptoms, but enrolled participants used more asthma medications | Outpatient, eight sites in seven inner-city urban areas in the USA | Asthma counsellors were master’s-level social workers, trained in three 2.5-day sessions and with 2 weeks’ asthma clinic experience | Not reported | 1 and 2 years |
| Svoren et al., 2003186 | Unclear |
Major psychiatric problems excluded Those who declined to participate were slightly older and had slightly longer duration of diabetes than, but similar glycaemic control to, participants |
Outpatient, paediatric unit of a diabetes centre in New York, NY, USA | Care ambassadors were college graduates with no formal medical education, trained by research and medical staff | Mean clinic visits was 7.3 (SD 2.06) for care ambassador and 7.5 (SD 2.02) for care ambassador+ compared with 5.4 (SD 2.62) for control. Total range was 1–14 clinic visits | 24 months |
| Szczepanski et al., 1996187 | Not reported | Not reported | Inpatient (initial intervention) and outpatient (with two home visits during intensive aftercare), two asthma centres in Germany | Interdisciplinary – sessions conducted by professionals jointly | Not reported | 6 and 12 months |
| Toelle et al., 1993188 | Not reported | Not reported | School, primary schools in Sydney, NSW, Australia | Not reported | 54 (74%) intervention families attended the sessions. A total of 38 children suggested a change in management and 11 accepted the new ‘plan’ | 3 and 6 months |
| Valery et al., 2010189 | 0.97 | Not reported | Home, Torres Strait region, QLD, Australia | Trained indigenous health-care workers (received specialist training in a 3-day asthma education workshop and specialist clinic experience) | Protocol was for four visits post baseline assessment, median of 2 (range 0–4) visits were actually received | 12 months |
| Van de Wiel et al., 2003190 | Not reported | Not reported | School | Clinically inexperienced therapists (with a psychology masters degree) received 6 months training prior to the study and regular supervision meetings | 4/38 intervention participants and 5/39 control participants did not complete the programme | 9 and 15 months |
| Van Der Veek et al., 2013191 | 0.75 | Those with evidence of an inflammatory, anatomic, metabolic, or neoplastic process cause of symptoms, or psychiatric disorder requiring treatment first were excluded | Outpatient, hospital outpatient clinic in the Netherlands | Psychology masters students or psychologists, trained and supervised by an experienced children’s psychotherapist. Biweekly supervision | 6/52 did not complete CBT, two of these found an alternative treatment. 4/52 did not complete intensive medical care and one of these requested CBT instead | 6 and 12 months |
| Velsor-Friedrich et al., 2012192 | 0.93 | Significant chronic illnesses excluded | School, five high schools in low-income and high African-American areas of Chicago, IL, USA | Doctoral student, trained in delivering coping skills by the principal investigator. Audio-taped sessions reviewed by principal investigator to assess fidelity | Not reported | 2, 6 and 12 months |
| Walders et al., 2006193 | 0.54 | Serious comorbid chronic health conditions were excluded | Outpatient, an urban academic tertiary care medical centre in the USA | A paediatric pulmonologist prepared a treatment plan. Education session delivered by nurse or asthma social worker. Psychologists identified content for session 3. Nurses provided telephone advice | 6/89 families did not return for third visit. 26% of families used nurse advice telephone line | 6 and 12 months |
| Watson et al., 2009194 | 0.40 | Other serious chronic illnesses, including respiratory illnesses, were excluded | Outpatient, a children’s hospital in an urban setting in Canada | Experienced nurse educator and respiratory therapist | Not reported | 12 months |
| Weisz et al., 2009195 | 0.69 | Psychotic or developmental disorders excluded | Outpatient, seven public urban community mental health clinics in a US county | Community clinic therapists, trained in PASCET by experienced clinical psychologists. 1-day training. 30 minutes weekly supervision. Sessions were video-taped and a random 50% cases were coded. Mean 98% required elements were present in the sessions | Mean cancelled sessions were 2.25 (SD 2.28) sessions and no shows were 1.66 (2.98) sessions | End of treatment (mean duration was 25.2 weeks for intervention and 39.26 weeks for control) |
| Willems et al., 2007196,197 and 2008198 | Unclear | Severe comorbidity (such as cystic fibrosis or congenital lung abnormalities) excluded | Home, recruitment from single hospital outpatient department in the Netherlands | Hospital-based nurse practitioner | After baseline, 85–92% questionnaires and 81–90% diary entries were completed. The average number of PEF tests completed per day was 1.3 (protocol specified 2). Most children responded ‘maybe’ when asked if they wanted to continue with monitor use | 4, 8 and 12 months |
| Xu et al., 2010199 | 0.54 | Not reported | Home (telephone based) | Specialist nurse or automated system | IVR: successful call rate 63%, 19/25 reported IVR system very worthwhile, 4/25 not very worthwhile. Nurse support: 56% successful calls, 53% successful e-mails, 19/25 reported support worthwhile, 1/25 not worthwhile | 6 months |
| Young et al., 2001200 | 0.73 | Not reported | School, two elementary schools in Toronto, ON, Canada | Nurse facilitator and paediatric asthma specialists | 17/24 received the intervention. Those who attended were satisfied (33%) or very satisfied (66%) | 6 weeks post intervention |
List of abbreviations
- CBA
- controlled before-and-after study
- CDSR
- Cochrane Database of Systematic Reviews
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CI
- confidence interval
- DARE
- Database of Abstracts of Reviews of Effects
- ED
- emergency department
- EPOC
- Effective Practice and Organisation of Care
- ES
- effect size
- HbA1c
- glycated haemoglobin
- HCP
- health-care professional
- HEED
- Health Economic Evaluations Database
- HRQoL
- health-related quality of life
- ICER
- incremental cost-effectiveness ratio
- LTC
- long-term condition
- NHS EED
- NHS Economic Evaluation Database
- nRCT
- non-randomised controlled trial
- PEDE
- Paediatric Economic Database Evaluation
- PPI
- patient and public involvement
- QoL
- quality of life
- RCT
- randomised controlled trial
- RE-AIM
- Reach, Effectiveness, Adoption, Implementation, Maintenance
- RECURSIVE
- REducing Care Utilisation thRough Self-management InterVEntions
- SD
- standard deviation
- SSCI
- Social Sciences Citation Index
