Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/178/22. The contractual start date was in May 2014. The final report began editorial review in September 2016 and was accepted for publication in March 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Paul Aylin and Alex Bottle report that the Dr Foster Unit at Imperial College London is partially funded through a research grant by Dr Foster, a commercial health-care information company (wholly owned by Telstra Health) that provides health-care analytics solutions to NHS organisations. Paul Aylin and Alex Bottle are part-funded by a grant to the unit from Telstra Health (formerly Dr Foster Intelligence) outside the submitted work. Charles Vincent reports funding from the Health Foundation for research and from Haelo (a commercial innovation and improvement science organisation) for consultancy work.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Aylin et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Context
The purpose of Chapter 1 is to establish the context in which this evaluation of a national surveillance system for mortality alerts is set. It covers the background to the surveillance system, controversies around the use of hospital mortality and the rationale for the study.
Background
Background of the monthly mortality alerting system
The origins of the Imperial College monthly mortality alerting system lie in analyses commissioned by the Bristol Royal Infirmary Inquiry in 1999 examining paediatric cardiac surgical outcomes at Bristol Royal Infirmary. Our group confirmed serious concerns around the surgical outcomes at Bristol,1,2 and established the usefulness of routine administrative data [Hospital Episode Statistics (HES)] in helping to identify quality of care issues. In further research commissioned by the Shipman Inquiry and published in 2003,3,4 our group established the role that statistical process control charts [specifically, log-likelihood cumulative sum (CUSUM) charts], and other routinely collected data (from death certificates) could play in the continuous surveillance of health-care outcomes, and, in this specific case, the detection of unusual patterns of patient mortality within general practices. Since then, we have demonstrated that the coverage and completeness of routinely collected administrative data is comparable with (or better than) that of clinical audit data. 5,6 We have used mortality rates (because these are well recorded) as a potential reflection of quality of care, with the inference that possibly more, less serious complications underlie them. We have subsequently published other indicators on safety,7 stroke care8 and returns to theatre9 based on administrative data.
Our work on appropriate statistical techniques in mortality surveillance in general practice3 established the utility of statistical process control charts in surveillance of health-care performance. This led to the application of these methods to secondary care administrative data in the development of a surveillance system to detect high mortality rates, emergency readmission and long length of stay in 256 diagnosis groups and 120 surgical procedure groups in collaboration with a commercial company, Dr Foster (Dr Foster Limited, London, UK; www.drfoster.com). 10 The system is now used in 70% of acute hospital trusts in England. A similar system based on our work is in use in the Netherlands, the USA, Belgium and Italy.
Following the development of the surveillance system, it became apparent that we were identifying a number of alerts each month, some of which were generated in trusts that did not have access to Dr Foster analytical tools. In 2007, we created a system whereby, each month, we notified trusts by letter (regardless of whether or not they were Dr Foster customers) if they had alerted for a subset of diagnoses and conditions at a high alarm threshold (see Appendix 1 for an example of the alert letter). In this letter, we are explicit in the range of possible reasons for a signal, including random variation, poor data quality or coding problems and case-mix issues, and we emphasise that we draw no conclusions as to what lies behind the figures. We worked closely with the Healthcare Commission [which was to be taken over by the Care Quality Commission (CQC)] in setting up this mortality alerting and surveillance system (MASS), and agreed to notify them about the letters we sent. The Healthcare Commission subsequently set up their own alerting system, based on similar methods, but their data were originally less current and based around Healthcare Resource Groups. Within the first 8 months of running our monthly alerts, one hospital had a series of six mortality alerts in a range of conditions and procedures. This helped to trigger an inspection of care at Stafford Hospital, which was within Mid Staffordshire NHS Foundation Trust. The initial inspection team found ‘appalling’ failures of emergency care within the trust, and a number of inquiries, culminating in the public inquiry led by Robert Francis, confirmed a litany of failings. The inquiry report recognised the role that our surveillance system of mortality alerts had to play in identifying Mid Staffordshire as an outlier. 11 A key recommendation reflecting our unit’s work was that all health-care provider organisations should develop and maintain systems that give effective real-time information on the performance of each of their services, specialist teams and consultants in relation to mortality, patient safety and minimum quality standards.
Controversy in using hospital mortality in investigating quality of care
There is some controversy over the value of analyses looking at hospital mortality in relation to quality of care. Many arguments concern summary measures of hospital mortality such as the hospital-standardised mortality ratio (HSMR) and the summary hospital-level mortality indicator (SHMI),12,13 whereas the mortality alerting system we describe focuses on specific diagnosis and procedure groupings. Even Hogan et al. 14 acknowledge the value of standardised mortality ratios for specific groups of patients.
However, it is useful to review the criticisms of the use of mortality indicators (even if that criticism does tend to focus on summary measures of hospital mortality) in relation to quality of care. Several arguments have been made:
-
inconsistent relationship between mortality measures and quality of care
-
avoidable deaths
-
weak signals
-
case mix and coding.
Inconsistent relationship between mortality measures and quality of care
An often cited argument put forward by critics12,15,16 against the validity of mortality measures is that there is poor agreement between process measures and mortality outcomes. One widely quoted ‘systematic review’17 reviewed 36 studies and 51 processes of care and found a correlation between better quality of care and lower risk-adjusted mortality ‘in under half the relationships (26/51 51%) but the remainder showed no correlation (16/51 31%) or a paradoxical correlation (9/51 18%)’. 17 The authors concluded that the relationship between risk-adjusted mortality and quality of care was neither ‘consistent nor reliable’. Aside from an obvious point that 51% is not ‘under half’, the study undertakes no review of the quality of papers and makes no comment on sample size. Many of the studies in which no relationship was found were simply too small to detect an effect with any statistical significance. Additionally, it is entirely plausible that some process measures of care either are unrelated to mortality or have a relationship too small to detect without detracting from the validity of hospital mortality measures as an indicator of quality of care. Despite the weaknesses of the review, the paper has been cited many times in support of criticisms of the validity of mortality measures, even though there were a substantial number of studies that found a relationship. In our study, we have looked for relationships between some structure and process measures (agreed a priori in the study protocol) and alerting and non-alerting trusts.
Avoidable deaths
Although we have never made the claim that the MASS is a measure of avoidable deaths, it has been suggested that ‘avoidable deaths’ identified through case note reviews might be a more useful tool for exploring quality of care issues in relation to death; they have been proposed,14 and are being advocated,18 to be used routinely in NHS organisations. Case note reviews are by no means a gold standard. Studies trying to identify avoidable deaths find only low to moderate levels of agreement between reviewers19–21 with typical intraclass correlation coefficients in the range 0.4–0.6. Higher rates of reliability can be achieved by setting strict criteria for the reviewers as to what should be considered avoidable. However, the stricter the criteria, the more likely that important cases will be excluded. In one study,22 125 categories of avoidable death were listed, but there were still events that qualified as avoidable deaths that did not fall within them.
There is also some evidence that reviewers of case notes are less likely to classify avoidability among more sick and vulnerable patients. In a recent retrospective case note review of 1000 deaths, the observation was made that the fact that ‘patients were more likely to experience a problem in care if they were less functionally impaired, were elective admissions and had a longer life expectancy on admission was inconsistent with studies in other countries and might reflect a bias among reviewers towards discounting problems in the most frail, sick patients’. 23
The idea of avoidability as determined through a case note review is limited when considering the impact of quality of care on mortality. As an example, a study examining hospital admissions resulting from acute myocardial infarction (AMI)24 found that in-hospital mortality was lower with shorter door-to-needle times. Patients waiting > 45 minutes for fibrinolytic therapy had 37% higher odds of death than those waiting ≤ 30 minutes. There was no cut-off point at which delay becomes fatal, but on average a patient who waits longer for treatment is less likely to survive than one who is treated in < 30 minutes. It is rarely possible to say for any given patient that extra time waited contributed to their death. However, we know that, in aggregate, across a group of patients who wait longer, more of them will die and that some of them would have survived if treatment had been provided earlier.
Hogan et al. 14 attempted to relate estimates of avoidable deaths to HSMRs. Using only one reviewer per case, they looked at 34 hospital trusts, and reviewed 100 case notes in each. With an average of just over three ‘preventable’ deaths per hospital, with such small numbers, it is not surprising that they found no significant difference in the proportion of avoidable deaths across the trusts they examined. However, despite this, Hogan et al. 14 go on to examine the relationship of the tiny numbers of avoidable deaths in each trust with HSMRs. It is, again, no surprise, given the small numbers, that no significant relationship was found. In fact, one statistician commented that, given the study weaknesses, ‘the authors were trying to detect not just an implausibly large, but an impossibly large effect size’. 25 However, Hogan et al. 14 then make the bold assertion that ‘the absence of a significant association between hospital-wide standardised mortality ratios and avoidable death proportions suggests that neither metric is a helpful or informative indicator of the quality of a trust’. 14 As the same statistician commented, ‘robustly inferring the validity of hospital mortality indicators based on the findings of this study is impossible’. 25 To make any conclusion about the quality of other indicators based on case note reviews, particularly involving such small numbers, would seem to go way beyond the evidence in hand.
Weak signals
It is the low proportion of preventable deaths arising from these case note reviews that critics of mortality indicators use to argue that there are too few preventable deaths to account for the degree of variation in HSMRs. The extent to which any indicator is useful depends on the degree of ‘signal’ versus ‘noise’. With mortality measures, noise could be due to random variation or due to other factors such as unadjusted for case-mix or coding issues. The mortality alert surveillance system attempts to tackle the problem of random variation by setting high alarm thresholds, giving a very low false alarm rate as a result of simple random variation (probability of false alarm is < 0.001 over a 12-month period). Despite this high threshold, signals still arise.
The signal-to-noise ratio relates to the positive predictive value of an indicator. The true positive predictive value for HSMRs is unknown. There is some indication in the Keogh mortality review, where, of the 14 trusts inspected for quality of care on the grounds of high mortality rates by Sir Bruce Keogh in 2013,26 11 were regarded as being sufficiently poor to warrant being placed in special measures. This would equate to a positive predictive value of 0.79. This evidence is anecdotal and relates to HSMRs rather than to specific diagnosis and procedure mortality alerts. Part of the motivation to carry out this National Institute for Health Research-funded study was to go beyond anecdote and examine, more systematically, the relationship between mortality alerts and other external indicators, and to look at the findings and impact of our alerting system.
Case mix and coding
Case-mix adjustment based on administrative data has been criticised12,13,27 because for some variables it depends on the accuracy of clinical coding secondary diagnoses for comorbidity and palliative care. Some potentially valid theoretical concerns have been raised, particularly but not exclusively regarding case-mix adjustment, but little robust quantitative evidence has been presented as to the size of their effect. 28 The well-cited paper by Mohammed et al. ,27 which points to these methodological biases (specifically in HSMRs), uses a hypothetical example to illustrate the potential effect size. The paper focuses on at least two mechanisms that might contribute to this so-called ‘constant risk fallacy’: the first involves differential measurement error and the second involves inconsistent proxy measures of risk. In their analysis of real data, the authors argue that inconsistencies in risk of death for emergency admissions support their assertion. They suggest that large variations in the proportions of elective/non-elective patients with zero length of stay indicate that systematically different admission policies were being adopted across hospitals. Unfortunately, their data seemed to erroneously include day cases, which explains the low crude death rates and mean length of stay and affects the proportion of admissions that are emergencies. A paper published subsequently29 attempted to actually quantify the effect of coding and other concerns on the HSMR, including palliative care, short-stay observation patients, multiple admissions per patient and a failure to capture post-transfer or post-discharge deaths. The study concluded that, despite theoretical concerns about bias, HSMRs in most hospital trusts were in practice usually only modestly affected by the differences in the predictive models incorporated into this sensitivity analysis. There were a few notable exceptions, particularly relating to palliative care and timelier linkage with out-of-hospital deaths, although the paper also referred to improved coding guidelines that may address some of these issues.
Given the potential limitations to administrative data, the argument has been made for making better use of the increasing number of specialised sources of data, in particular those used to support national clinical audits. 13 Our group has carried out comparisons of administrative data with clinical audit data in the past, comparing risk prediction models and quality. One study compared the performance of risk prediction models for death in hospital based on administrative data with published results based on data derived from three clinical databases. 6 This concluded that routinely collected administrative data can be used to predict risk with similar discrimination to clinical databases, and that could be used to adjust for case mix for monitoring health-care performance. Two other papers looked at coverage and completeness of surgical procedures in colorectal surgery30 and vascular surgery5 in two clinical audit databases compared with hospital administrative data. They found between twice and four times as many cases recorded in the administrative data as in the audit data sets, suggesting significant under-recording. They also found that 39% of patients within the colorectal cancer database had missing data for risk factors used for risk adjustment. Although these papers were published in 2007 and 2008, more up-to-date reports from even well-established and reputable audits such as the Myocardial Ischaemia National Audit Project (MINAP) suggest that poor data quality, particularly on patient characteristics, renders the risk adjustment of mortality rates unreliable. 31 Given that the accuracy of administrative data appears to be improving and that clinical coding is now regarded as predominantly of good quality,32 the argument for abandoning it in favour of much more expensive, and often less complete, audit data seems rather less tenable.
Rationale for the study
The mortality alerting systems run by the CQC and the Imperial College London unit have already had some success in detecting hospitals delivering poor-quality care, such as the identification of problems at Mid Staffordshire NHS Foundation Trust. 1,11,33 Given the controversy, there is clearly still uncertainty about the sensitivity of systems based on the analysis of routinely collected hospital data and health-care providers’ responses following alerts. 14,34
As the mortality alerts provided by Imperial College London and CQC are for specific diagnoses or procedures, they are potentially more actionable than summary (overall) measures of mortality such as the HSMR or the SHMI. 35 The MASS demands significant resources from CQC and Imperial College London, and also from hospital staff following up the alerts; so although the CQC is continually evaluating its surveillance programme, this project will both complement and build on the CQC’s activity. 36
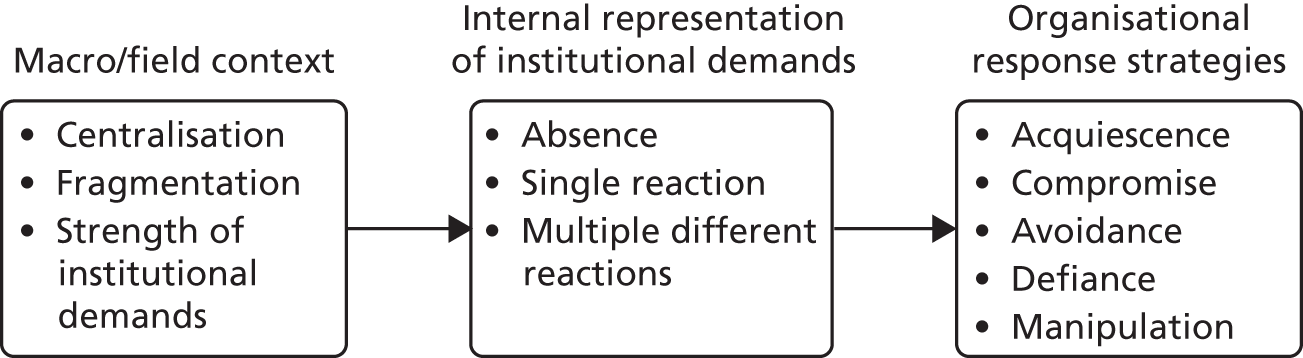
We based our evaluation of this MASS on the prior hypothesis that a mortality alert might be an indication of poor quality of care. By notifying a trust of a higher-than-expected death rate, we have made the assumption that efforts to investigate the alert resulting in changes to the structure and processes within the trust may result in improved outcomes. This hypothesised feedback mechanism triggered by a mortality alert is displayed in a simple theoretical model (Figure 1).
FIGURE 1.
Theoretical model displaying hypothesised feedback mechanism following mortality monitoring.
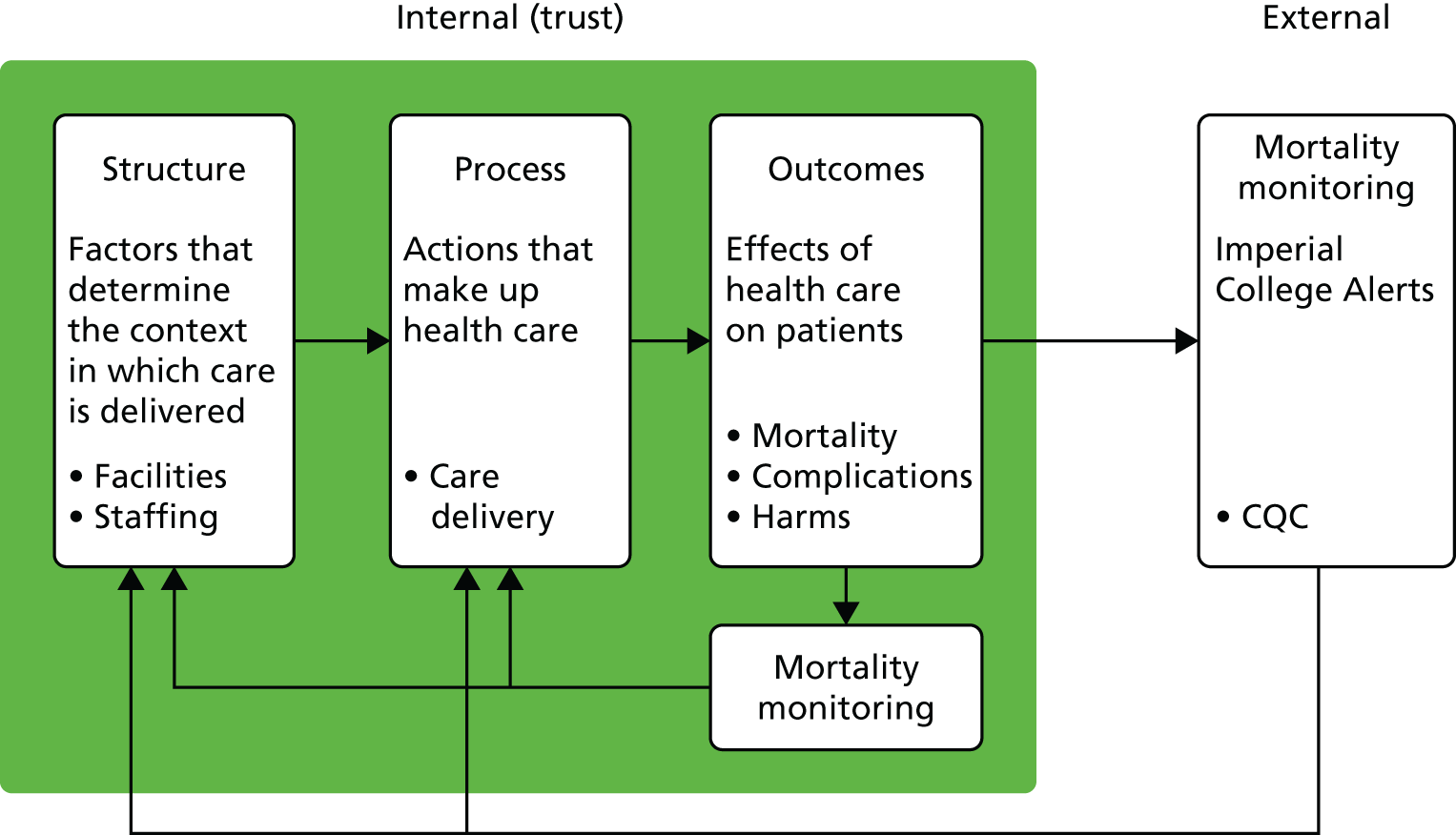
If a mortality alert is a reflection of quality of care issues, one might expect to see:
-
quality of care issues confirmed after further investigation
-
associations with factors related to care structure and processes within the trust that might impact on quality of care, including resources such as bed occupancy and staffing or care provision
-
associations with patient outcomes including patient satisfaction, harms or death
-
differences in care provided between frequently alerting trusts and trusts that rarely alert
-
a reduction in mortality following actions to improve quality of care.
According to CQC reports,37 500 mortality alerts were processed between 2007 and 2011 (approximately 100 each year38). However, there has been no systematic empirical research to determine whether the Imperial College London unit and the CQC joint national MASS is any better at detecting quality of care issues than other less focused approaches (e.g. HSMR or SHMI), or if alerts are associated with reductions in mortality rates. It is also unclear what the most appropriate actions are for trusts after they receive an alert.
Previous studies on effective interventions have tended to be small scale and descriptive, with methodological limitations restricting the control of confounding factors, interpretation of results or causality. Research evaluating interventions to reduce mortality has highlighted difficulties in attributing effects to specific interventions due to multiple concurrent schemes, and has produced equivocal results. 39–41 Similarly, internationally there is very little evaluation of other monitoring/regulatory systems on whether or not regulation (e.g. accreditation) leads to better outcomes. 42
National mortality surveillance could be potentially efficient to manage, as data are routinely collected. Computer algorithms are adaptable and can be refined more easily than employing additional staff and/or training for similar activities. The surveillance system requires minimal specialist equipment and it is not affected by potential delays due to policy changes in the provision or commissioning of health services.
Chapter 2 Research objectives
Chapter 2 outlines our research objectives and defines an overview of our approach to the evaluation of a national surveillance system for mortality alerts.
Through a detailed assessment of the Imperial College Unit/CQC mortality surveillance system, our project aims to improve understanding of mortality alerts and to evaluate their impact as an intervention to reduce mortality within English NHS hospital trusts. To achieve our aim, we focused on six objectives:
-
to describe the findings and impact of a national mortality surveillance system as a feedback mechanism for quality improvement
-
to determine the relationship of alerts to other potential indicators of quality
-
to determine the temporal patterns of alerts and whether or not they are associated with subsequent changes in mortality rates at trusts
-
to describe trusts’ responses to receiving mortality alerts and the impact on safety/quality improvements, including organisational and staff behaviour
-
to determine whether or not there are differences in the delivery of care between frequently alerting trusts and trusts that alert rarely for two conditions that commonly generate mortality alerts – AMI and sepsis
-
to determine, at trusts where mortality decreased after alerts, whether or not they were more likely to apply common safety/quality interventions than trusts that repeatedly alert.
Overview of approach
We applied a mixed-methods approach, which naturally fell into two workstreams: the first employed quantitative research methods and the second employed qualitative research methods.
In workstream 1, we described trends in mortality alerts and carried out a descriptive analysis of CQC investigations into the Imperial College mortality alerts (objective 1); examined the statistical relationships between mortality alerts and measures of quality of care that relate to the trust care structure, processes and outcomes (objective 2); and applied an interrupted time series model to examine the impact of mortality alerts on subsequent mortality, using national hospital administrative data on admissions (objective 3).
In workstream 2 we undertook in-depth qualitative case studies to understand the local impact of receiving an alert and the institutional behaviour that resulted. Adopting a realist evaluative stance, we aimed to generate rich descriptions of how the alerts, as a form of feedback intervention, instigated interactions between local context, institutional behaviour and institutional outcomes (objectives 1 and 4). We identified 11 sites that had alerted in one of two areas, sepsis or AMI, during the 2011–14 period, stratified by single or multiple alerting conditions and historical statistical trends in relative risk (objectives 5 and 6). We used principles of grounded theory and structured framework analysis to apply both inductive and deductive logic to our analysis and interpretation of the case study data, including a comprehensive review of organisational theory to ensure that our sense-making process was theoretically informed. A subanalysis of qualitative data was undertaken to support the development of an evaluative framework and survey instrument, which was subsequently used in a national cross-sectional survey of the perceptions of mortality leads at alerted trusts. The survey aimed to describe variance in organisational structures and processes concerning mortality governance (objective 1) and to capture evaluative perceptions concerning the efficacy of the current mortality surveillance and alerting system (objective 4).
Chapter 3 Literature review
In this chapter, we carry out a literature search and review to identify the current knowledge on the use of mortality surveillance systems as an indicator of quality. We then go on to review the literature for several areas of theory that are relevant to the institutional response to mortality alerts, namely institutional theory and neo-institutional theory, organisational readiness for change, absorptive capacity, normalisation process theory and sense-making, among others.
Mortality surveillance systems as an indicator of quality
Methods
In this project, we set out to understand how hospitals react to mortality alerts and whether or not outcomes improve as a consequence. We carried out an electronic literature search within three research databases to describe how our study fits into existing evidence. We aimed to identify literature that specifically examined clinical performance through hospital mortality assessment or monitoring.
The studies included people of any age who had been admitted for any hospital treatment living in an Organisation for Economic Co-operation and Development (OECD) country. The reason for excluding studies from non-OECD countries was partly to limit the search, and partly because non-OECD countries will have different health-care systems and, specifically, different health-care information systems. We limited the studies to only those written in English. We included exploratory, descriptive and quasi-experimental study designs.
Search strategy
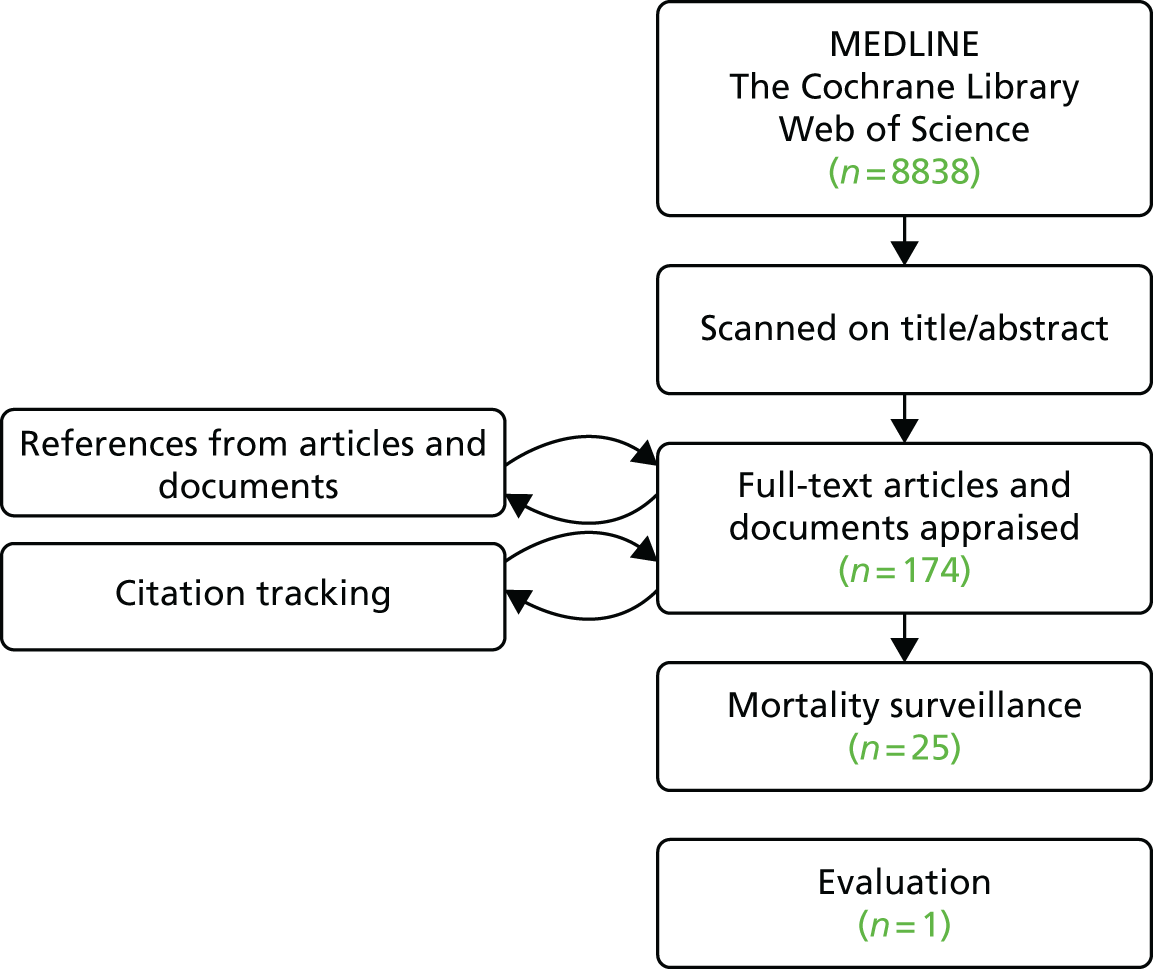
Our search terms (within the title and abstract) were Hospital AND (Monitor* OR Surveillance) AND (Death OR Mortality). We adapted our search for MEDLINE, The Cochrane Library and Web of Science. Literature was also retrieved using article references and citation tracking.
Data collection, analysis and reporting
We screened initially on the title; a second screen was on the abstract and the final screen was on the full papers. One reviewer carried out screening, a second reviewer checked the final screen and both reviewers reached a consensus on which studies to include in the review.
Results
There were > 8000 research papers/documents identified in MEDLINE, The Cochrane Library and Web of Science combined. We isolated 174 relevant articles and documents on the first two screenings. We appraised individual text articles/documents and identified further articles using referenced literature and citation tracking. Twenty-five studies were included for this final review. Figure 2 shows the flow chart for the process.
FIGURE 2.
Flow chart of process identifying articles and documents on hospital mortality surveillance evaluations.
Monitoring mortality is an integral part of health care43 and originally focused on specific departments such as the intensive care unit (ICU),44 or surgical procedures,45 for which data were collected through audits. Although our literature search focused on mortality monitoring using administrative data, we did include literature in which there was mortality monitoring using audit data.
Government bodies in the UK and USA have a long history of publishing mortality statistics. 46 One of the first articles that used routine hospital data to investigate hospital mortality and to suggest their use as a mechanism to identify patterns of potentially poor quality of care was a US report by the RAND Corporation and sponsored by the Health Care Financing Administration at the US Department of Health and Human Services, which was published in 1989. 47 In this study, admissions were extracted from hospital discharge data for all acute care hospitals treating Medicare patients. Admissions were over a 1-year period between October 1983 and September 1984, and included Medicare patients aged ≥ 65 years. The admissions were grouped by the diagnosis-related group and mortality rates were directly standardised for age, sex and race. The authors found that variation in hospital mortality rate was unlikely to have arisen through chance. The authors acknowledged that these large differences could have differed as a result of severity of the condition (the analysis did not adjust for comorbidity as they questioned the quality of the recording of secondary diagnoses) and highlighted that rates must be interpreted with caution. However, the authors did suggest that the data could be used as a screening tool to point to institutions or cases that appear to warrant more in-depth review.
Jarman et al.’s48 paper in 1999 was the first English study to use administrative, routinely collected data to investigate standardised hospital death rates. The authors were unable to adjust for severity but utilised a case-mix model (including a comorbidity score) as a proxy measure. The strength of this study was the population coverage. It used national public hospital administrative data in which the population was all patients admitted to NHS hospitals between April 1991 and March 1995. Previous mortality studies used regional, individual hospital or insurance-based populations. A major limitation with this study is that only inpatient deaths could be measured, as at that time there was no linkage to death registry data. This meant that the study missed deaths that occurred shortly after discharge but that may have been related to the hospital stay. The paper did, however, introduce a standardisation methodology that was to later be adapted (and further developed) for use by Dr Foster Intelligence, a commercial health-care information company that published performance indicators on NHS hospital services.
Table 1 lists the studies identified in the literature search on mortality surveillance as an indicator of quality. Hospital mortality monitoring studies were international, covering the UK,2,14,35,51,53 the USA,49,52,59,64,67,68,70 the Netherlands,57,63 Canada55,69 and Australia and New Zealand. 50,54,56,58,60–62,65,66 Studies were for a range of conditions and settings; these included surgical,2,51,59,64,66,70 intensive care,50,52,54,61,63,65 transplantation53,67,68 and all cause. 14,49,55,57,58,60
| Authors | Title | Year | Country | Condition |
|---|---|---|---|---|
| Hofer and Hayward49 | Identifying poor-quality hospitals. Can hospital mortality rates detect quality problems for medical diagnoses? | 1996 | USA | All cause |
| Aylin et al.2 | Comparison of UK paediatric cardiac surgical performance by analysis of routinely collected data 1984–96: was Bristol an outlier? | 2001 | UK | Surgical |
| Cook et al.50 | Monitoring the evolutionary process of quality: risk-adjusted charting to track outcomes in intensive care | 2003 | Australia | Intensive care |
| Aylin et al.51 | Paediatric cardiac surgical mortality in England after Bristol: descriptive analysis of hospital episode statistics | 2004 | England | Surgical |
| Afessa et al.52 | Evaluating the performance of an institution using an intensive care unit benchmark | 2005 | USA | Intensive care |
| Rogers et al.53 | Cumulative risk adjusted monitoring of 30-day mortality after cardiothoracic transplantation: UK experience | 2005 | UK | Cardiothoracic transplantation |
| Cook54 | Methods to assess performance of models estimating risk of death in intensive care patients: a review | 2006 | Australia | Intensive care |
| Canadian Institute for Health Information55 | HSMR: A New Approach for Measuring Hospital Mortality Trends in Canada; 2007 | 2007 | Canada | All |
| Bottle and Aylin35 | Intelligent information: a national system for monitoring clinical performance | 2008 | UK | 172 conditions/procedures |
| Coory et al.56 | Using control charts to monitor quality of hospital care with administrative data | 2008 | Australia | AMI |
| Heijink et al.57 | Measuring and explaining mortality in Dutch hospitals; the hospital standardised mortality rate between 2003 and 2005 | 2008 | Netherlands | All cause |
| Ben-Tovim et al.58 | Measuring and reporting mortality in hospital patients: Australian Institute of Health and Welfare; 2009 | 2009 | Australia | All cause |
| Hall et al.59 | Does surgical quality improve in the American College of Surgeons National Surgical Quality Improvement Program: an evaluation of all participating hospitals | 2009 | USA | Surgical |
| Ben-Tovim et al.60 | Routine use of administrative data for safety and quality purposes – hospital mortality | 2010 | Australia | All cause |
| Pilcher et al.61 | Risk-adjusted continuous outcome monitoring with an EWMA chart: could it have detected excess mortality among intensive care patients at Bundaberg Base Hospital? | 2010 | Australia | Intensive care |
| Cook et al.62 | Exponentially weighted moving average charts to compare observed and expected values for monitoring risk-adjusted hospital indicators | 2011 | Australia | AMI |
| Koetsier et al.63 | Performance of risk-adjusted control charts to monitor in-hospital mortality of intensive care unit patients: a simulation study | 2012 | Netherlands | Intensive care |
| Cohen et al.64 | Optimising ACS NSQIP modelling for evaluation of surgical quality and risk: patient risk adjustment, procedure mix adjustment, shrinkage adjustment, and surgical focus | 2013 | USA | Surgical |
| Moran and Solomon65 | Statistical process control of mortality series in the Australian and New Zealand Intensive Care Society (ANZICS) adult patient database: implications of the data generating process | 2013 | Australia/New Zealand | Intensive care |
| Smith et al.66 | Performance monitoring in cardiac surgery: application of statistical process control to a single-site database | 2013 | Australia | Cardiac surgery |
| Sun and Kalbfleisch67 | A risk-adjusted O-E CUSUM with monitoring bands for monitoring medical outcomes | 2013 | USA | Liver transplantation |
| Snyder et al.68 | New quality monitoring tools provided by the scientific registry of transplant recipients: CUSUM | 2014 | USA | Transplantation |
| Hogan et al.14 | Avoidability of hospital deaths and association with hospital-wide mortality ratios: retrospective case record review and regression analysis | 2015 | UK | All cause |
| Lesage et al.69 | A surveillance system to monitor excess mortality of people with mental illness in Canada | 2015 | Canada | Mental health |
| Cohen et al.70 | Improved surgical outcomes for ACS NSQIP hospitals over time: evaluation of hospital cohorts with up to 8 years of participation | 2016 | USA | Surgical |
Mortality monitoring methods
There are two types of methods reported in the literature for monitoring hospital mortality. The first uses a cross-sectional measurement of condition-specific standardised mortality ratios2 and HSMRs (all-cause mortality) in Canada,55 the Netherlands57 and Australia. 60 Using this method, assessment is achieved through benchmarking, whereby hospitals are assessed against set standards or using interhospital comparisons. The Australian Institute of Health and Welfare commissioned a report on measuring and reporting mortality in hospital patients to determine whether or not it was possible to produce accurate and valid indicators of in-hospital mortality using Australian administrative data. 58 Risk-adjusted modelling predicted or explained the variation in mortality rates to a similar extent as in international literature, and authors concluded that high or rising HSMRs could be used to signal a potential problem within a hospital.
The second method investigates cumulative measures over time using statistical process control charts. Steiner et al. ,71 in 2000, introduced the idea of using risk-adjusted CUSUM charts for monitoring mortality in patients undergoing cardiac surgery. Since then, there have been several international papers investigating the use of control charts to monitor the quality of hospital care in other settings;56,62,66,68 however, these studies were on clinical audit data and not on administrative hospital data. Bottle and Aylin35 published a paper in 2007 that investigated the use of statistical control charts for monitoring clinical performance, including in-hospital mortality. The methodology described was the basis for the national surveillance system for mortality alerts that is evaluated in this report. Pilcher et al. 61 investigated whether or not the use of a statistical process control chart could have detected the high death rate in the ICU at Bundaberg Base Hospital, around which there was considerable publicity because of perceived excess mortality between 2003 and 2005. The authors concluded that the methodology was able to detect fluctuations in relative risk of death in the Bundaberg ICU that were not apparent when standardised mortality ratios were used.
Validation
Two papers used the methodology to identify hospitals in which there were reported failings in quality as outliers. The paper by Aylin et al. 2 examined paediatric cardiac surgery and confirmed high mortality rates identified through surgical audits, and a large public inquiry, while Pilcher et al. 61 investigated the use of statistical process control chart methodology compared with previous reports of high death rates at an ICU, although it is not clear from their paper how the initially high rates were determined. Hogan et al. 14 attempted to use case note reviews as a gold standard. They reviewed 100 case notes of deceased patients in 34 hospital trusts. They found an average of just over three ‘preventable’ deaths per hospital. The authors then went on to examine the relationship of these small numbers of avoidable deaths in each trust with HSMRs. The study was woefully underpowered and no significant relationship was found. Despite this, the authors claimed that ‘the absence of a significant association between hospital-wide SMRs [standardised mortality ratios] and avoidable death proportions suggests that neither metric is a helpful or informative indicator of the quality of a trust’. 14
Evaluations
Many health-care systems internationally use routine administrative data to monitor quality indicators, including hospital mortality. Examples of these are the analytic toolkits, provided by commercial companies such as Dr Foster (UK), Telstra (Melbourne, VIC, Australia; www.telstra.com.au) and 3M (Maplewood, MN, USA; www.3m.com). However, we did not find published literature on evaluations of these toolkits.
Clinical audits (or databases) have been used for a number of years to monitor outcomes such as mortality in a range of settings and conditions, but particularly in surgery. 43,45 Audits involve data collection and analysis that is time-consuming and expensive to compile. However, we identified one evaluation of a study using clinical audit data in our literature search. The study was on the American College of Surgeons National Surgical Quality Improvement Program® (ACS NSQIP®). 64 ACS NSQIP collects data from participating hospitals and analyses them, and participating hospitals are provided with reports that permit risk-adjusted comparisons, including 30-day mortality, with a surgical quality standard. Cohen et al. 70 carried out an ‘evaluation’ of the surgical outcomes over time, and found a decreasing trend in mortality in 62% of participating hospitals and an average of 0.8% annual reduction in mortality rate. There are, however, limitations to this study. There are no control (non-ACS NSQIP participating) hospitals, and the reported trends could have been influenced by secular trends unrelated to ACS NSQIP. The authors do acknowledge this limitation, yet they still classify the article as an evaluation.
Limitations
We are aware that limiting the search to papers written in English may have resulted in some literature being missed; for example, one paper, by Stausberg et al.,72 was written in German. We also understand that not all evaluations are published in peer-reviewed journals; however, we feel that those studies that have been scrutinised by other experts in the same field are a more robust subset to include in our review.
Conclusions
Our literature search has highlighted that although there has been literature on the methodology for monitoring hospital mortality, there is little literature on evaluation, and the only study that attempted to evaluate a benchmarking system for surgical outcomes in the USA is weak. To our knowledge, there has never been an evaluation of a hospital mortality surveillance system using routinely collected administrative data. 2
Institutional theory
Institutional theory provides conceptual frameworks to analyse and compare the response of organisations working in the same field with demands placed on them by external institutions. 73–75 In this section, an overview of the relevant aspects of these theories is described in relation to hospital trusts (organisations) working in the English NHS (the field), considering their response to the demand placed on them from Imperial College London/Dr Foster and the CQC (external institutions) through the receipt of a mortality alert letter. We review several areas of theory that are relevant to the institutional response to mortality alerts, namely institutional theory and neo-institutional theory,74–78 organisational readiness for change,79–81 absorptive capacity,82–87 normalisation process theory88–90 and sense-making,91–93 among others. We include areas of institutional theory that were identified a priori in the initial research protocol, but have complemented these perspectives with a review of theories that emerged as relevant during the course of interaction with case study data. Rather than providing a comprehensive literature review, we consider each theory in terms of its specific relevance as a potential explanatory model for the operation of the MASS. In this sense, the following subsections define the theoretical lenses that will be used as frameworks in subsequent analyses and the parent theories from which we extract concepts to aid in the understanding and interpretation of the processes and mechanisms of interaction between the MASS and institutional behaviour in each of our case study sites.
Response to multiple competing influences
The structure and distribution of power among institutional actors at the field level within health-care systems is considered an important determinant of how organisations such as hospitals respond to external demands (Table 2). In fields such as health care, where there are multiple influential institutional actors, each without adequate power to clearly dominate but with enough power to constrain the actions of organisations, the leadership task in hospitals is considered even more complex. 95–97 Pache and Santos76 describe this external environment as a ‘moderately centralized field’. In health care, this is found where there are, for example, strong medical societies, government regulators and commissioners all making demands on health-care organisations.
| Field | Description |
|---|---|
| Highly centralised fields | Typically rely on one principal constituent whose authority in the field is both formalised and recognised.94 This principal constituent can resolve disagreements between disparate players and impose relatively coherent demands on organisations |
| Moderately centralised fields | Characterised by the competing influence of multiple and misaligned players whose influence is not dominant, yet is potent enough to be imposed on organisations |
| Decentralised fields | Institutional pressures are rather weak and, when incompatible, they can be easily ignored or challenged by organisations as the referents have little ability to monitor or enforce them |
NHS trusts have multiple competing influences from external institutions, not least from commissioners and financial regulators,98 and in this respect the English NHS can be described as a moderately centralised field. A broad range of external factors, such as policy-level initiatives, professional bodies seeking to change practice, local pressure from commissioning groups for service development and reconfiguration, and others, may influence the internal governance agenda within a health-care organisation, in addition to internal factors. Mortality alerts, therefore, compete with other priorities and demands placed on NHS trusts by external institutions, such as to reduce cancer and other waiting times, to improve infection control, to introduce standard operating procedures to reduce surgical ‘never events’ or to deliver specific local commissioning priorities. Investigating the local causes of mortality alerts, developing a formal response to regulators regarding the mortality trend and implementing actions to reduce avoidable mortality are all resource-intensive activities. Each has the potential to detract from effort and to divert resources that trusts may otherwise allocate to respond to these competing pressures.
Pache and Santos76 also suggest that the nature of external demands conditions the response of organisations. For example, responses may differ depending on whether the demands take the form of goals for the organisation to pursue or of the specific means or courses of action to achieve those goals. MASS letters take the form of information, indicating an area that the trust may wish to investigate. The letters are deliberately outcome focused, in that they focus on the observed significant trends in mortality without suggesting an underlying cause or course of action. The Imperial alert letters, therefore, do not set specific objectives for the response, and trusts are free to decide how they respond. When alerts are followed up by the CQC, the form of the response, its timescale and components are specified; however, the degree to which the focus of the planned actions is specified varies as a function of ongoing interactions between the alerting trust and the CQC and the results of local investigations into the origins of the alert.
Other institutional analysts have highlighted how organisational responses to external institutional pressures and resource dependencies may vary across contexts and how organisational leaders exercise a range of strategic choices. 99 A model outlining organisational responses to institutional demands and resource dependencies identified a continuum of organisational responses ranging from acquiescence, compromise and avoidance to defiance and manipulation (Box 1). 77
-
Acquiescence refers to how organisations comply with institutional demands whether consciously or unconsciously arising from habit, imitation or voluntary accession.
-
Compromise refers to when an organisation partially conforms to institutional demands by adjusting those institutional demands and/or adjusting internal organisational responses.
-
Avoidance strategies involve attempts by the organisation to adjust conditions so as to make it possible for the organisation to comply with institutional demands. Avoidance tactics include concealing non-conformity by pretending to acquiesce; by preventing technical monitoring of compliance (buffering); or by changing the organisational function so as to make compliance unnecessary (escaping).
-
A defiant strategy may occur when the organisation rejects at least one institutional demand and may be manifested as dismissal of a demand, overtly challenging a requirement or aggressively attacking the institutional demand.
-
A manipulation strategy refers to the deliberate attempt to actively change the content of institutional demands. Manipulation tactics include co-opting sources of institutional pressure, influencing norms by active lobbying and controlling the source of pressure.
Adapted from Oliver. 77
In relation to mortality alerts, acquiescence relates to trust accession to the institutional demand from the CQC or Dr Foster to accept the mortality alert as intended (i.e. as a valid and valuable signal worthy of investment of resources in a response). Compromise may take various forms in the context of the MASS, but may involve, for example, negotiation with the CQC over the components of the expected response itself or correcting erroneous coding of cases that it has been agreed are unduly affecting the ratio of observed to expected mortality. Avoidance strategies might include closing a problematic service or deliberately reducing monitoring in specific areas.
Defiance may see the trust actively challenging Imperial College/Dr Foster over the validity of the information content of the alert: the accuracy of the data themselves or the adequacy of the risk-adjustment model on which the alerts are based. Manipulation might include more deliberate attempts to recode cases so as to artificially reduce outliers.
The organisational (trust) response to the MASS may be governed, in part, by alignment between the alerting issue and parallel demands for organisational resources. In their analysis of how hospitals respond to competing demands for quality improvement and financial balance, Burnett et al. 98 grouped the responses into four categories. These ranged from (1) organisations that were more likely to respond to requests from regulators by using expedient, short-term measures, regardless of whether or not this would achieve sustainable change in the longer term, to (4) organisations that had invested in, and embedded, quality improvement into everyday work, and had worked with external institutions to align quality and cost requirements. Two factors were found to be important in this research: first, the organisational pre-conditions, and, second, the ability of senior leaders to align external demands with internal requirements into a coherent strategy that achieved both cost and quality requirements.
Legitimacy
Meyer and Rowan73 propose that organisations are more likely to respond to external demands, in ways that support the organisation’s legitimacy:
[O]rganisations are driven to incorporate the practices and procedures defined by prevailing rationalized concepts of organisational work and institutionalized in society. Organisations that do so increase their legitimacy and their survival prospects, independent of the immediate efficacy of the acquired practices and procedures.
Meyer and Rowan73
Meyer and Rowan73 propose that, in deciding how to respond, organisations adopt the practices of other organisations working in the same field, in a process of ‘ceremonial conformity’. They argue that this occurs regardless of whether or not the adopted practices conflict with the efficiency criteria or requirements of the other organisations. Organisations, it is argued, copy and incorporate these practices in order to gain legitimacy and enhance their survival prospects by being seen by external institutions to comply with current norms. Organisations seeking such legitimacy will conform to these practices, regardless of whether or not they are likely to achieve a desired outcome, and regardless of impact of these practices on other pressures and on costs. In this way, the practices spread, and organisations, and their structures, become isomorphic with the myths of the institutional environment. Applying this to mortality alerts, the question arises as to whether or not organisations’ responses to alert letters have become isomorphic over time, such that there is now an established way in which trusts are expected to respond. Furthermore, one may ask whether or not these new practices have the desired impact on reducing mortality and whether or not they are cost-effective. Alternatively, are they more ‘ceremonial’ so that trusts can be seen to be doing something, and hence complying with what is expected, regardless of the outcome?
Intraorganisational context and organisational change
Greenwood and Hinings100 proposed that the nature and pace of change within organisations in the same field varies because of the political dynamics among intraorganisational groups, and the degree to which organisations are socially and professionally embedded within their contexts. Pache and Santos76 build on these ideas to specify, more clearly, how the nature and degree of internal representation of, or support for, competing pressures within an organisation will result in mobilising the specific types of responses identified by Oliver. 77 For example, in hospitals, medical, nursing and managerial groups may have different priorities for, and conceptions of, the requirements in an alert letter, and here conflict may arise regarding what needs to be done and when. There may additionally be multiple interpretations of the validity of an alert, or the attributable causes of above-expected mortality rates. Pache and Santos76 suggest that when there is a single, common reaction shared across different internal groups this may lead to a unified resistance to an external pressure, for example in refuting the data in an alert letter or questioning coding. In contrast, when internal groups offer differing reasons for resisting an external pressure, they are likely to compete for their preferred course of action. In situations when there is an absence of internal representation or support, internal groups will usually exhibit indifferent commitment and the external pressures will tend to induce at least minimally compliant actions by the organisation. 76 This is summarised in Figure 3.
Neo-institutional theory
Neo-institutional theory is concerned with how organisations orientate themselves within the institutional environment and is concerned with three properties, or pillars, of organisational life, as follows:75,78,101–104
Institutions exhibit stabilising and meaning-making properties because of the processes set in motion by regulative, normative, and cultural-cognitive elements. These elements are the central building blocks of institutional structures, providing the elastic fibres that guide behaviour and resist change.
Scott,104 p. 57
Table 3 sets out the definitions of these elements in relation to each other and how they manifest themselves within organisations.
| Regulative | Normative | Cultural–cognitive | |
|---|---|---|---|
| Basis of compliance | Expedience | Social obligation | Taken-for-granted |
| Basis of order | Regulative rules | Binding expectations | Shared understanding |
| Mechanisms | Coercive | Normative | Constitutive schema |
| Logic | Instrumentality | Appropriateness | Mimetic |
| Indicators | Rules | Certification accreditation | Common beliefs |
| Laws | |||
| Sanctions | Shared logics of action | ||
| Affect | Fear guilt/innocence | Shame/honour | Certainty/confusion |
| Basis of legitimacy | Legally sanctioned | Morally governed | Comprehensible |
| Recognisable | |||
| Culturally supported |
Regulative influences on how trusts regard the Mortality Alerting and Surveillance System
The role of the CQC as the regulator is important in the MASS. Institutional theory suggests that the external institutions that are able to enforce their demands most effectively are usually those that possess greater power and influence over a particular set of organisations either through control of financial and material resources or through their authority over legal and professional sanctions. 75 Regulatory influences include rule-setting, monitoring and sanctioning activities,104 designed to impact on and influence the behaviour of an organisation. Theorists argue that the costliness of the sanctions governs how organisations will respond to regulative pressures. 105 Foucault introduced the concept of ‘governmentality’, whereby organisations self-govern in response to perceived surveillance and/or the coercive power of external organisations. 106
Applying these theoretical perspectives to the MASS, several factors are important. First, the CQC has considerable (actual) power over English NHS trusts through its role in licensing trusts to deliver health care. Institutional responses may, therefore, be governed by the threat of real sanctions or adverse repercussions for non-compliance. In addition, the subject of the letters (higher-than-expected death rates) has potential (if not real) implications for the reputation of the hospital (both locally and nationally) and the reputation of the medical professionals, not least the trust’s medical director.
Normative influences on how trusts respond to external pressures
Normative influences are related to social obligation, consisting of values and norms that develop over time and become embedded in organisational life as routines and roles. Norms relate to how things should be done, defining the legitimate means to achieving goals. Values relate to practices and actions that are considered desirable or preferred. 104 Normative influences, therefore, define the legitimate means of the pursuit of valued ends; for example, in this study, bundles for diagnosing and treating sepsis or for diagnosing or preventing AMI. Scott104 summarises this as:
The central imperative confronting actors is not ‘What choice is in my own best interests?’ but rather, ‘Given this situation, and my role within it, what is the appropriate behaviour for me to carry out?’
Scott,104 p. 65
Tendency towards specification of the response to mortality alerts may be regarded as a normative influence on institutional behaviour following an alert, just as the alerts themselves embody norms for risk-adjusted mortality across institutions.
Cultural–cognitive influences and sense-making
Cultural–cognitive influences focus on the meanings, beliefs and perception of people within the organisation and how they respond to these. Scott,104 in summarising extensive research by psychologists, describes how cognitive frames are part of the range information-processing activities, from determining what information will receive attention, and how it is encoded and retained in an organisation’s memory, to how it is interpreted. Together, these determine how an organisation will respond. In addition, Scott104 describes how cultural systems operate at multiple levels, from the shared definition of local situations to those that constitute an organisation’s culture. These cultural systems shape organisational life and, in our analysis, we examine these influences on how trusts respond to mortality alerts, for example the extent to which responses to the MASS are ‘taken for granted routines’, such as case note review: ‘the way we do things here’. This is built on in the next section on ‘sense-making’.
Sense-making
‘Sense-making’ is the process of giving meaning to experience. 91–93 Sense-making involves the ongoing development of plausible explanations that rationalise human behaviour when the current state of the world deviates from the expected state. 92 ‘Reasons’ or explanations for disruptions in the flow of activity are sought from frameworks such as institutional constraints, traditions, plans and acceptable justifications.
With regard to the MASS, we use this theory to consider how participants make sense of the alert letters, how they talk about them and how they rationalise the messages within. This leads to consideration of the actions taken in response to participants’ rationalisation of the messages in the alert letters.
Organisational receptivity and readiness for change
Responding to intelligence on avoidable mortality involves changes to the process of care delivery and, to a greater or lesser degree, organisational change. Organisational receptivity, or readiness for change, was found to be important in the course of change programmes that aimed to improve quality and safety of care. 81 Weiner et al. 107 frame organisational readiness for change (as opposed to individual readiness) as collective behaviour change in the form of systems redesign: multiple, simultaneous changes in staffing, workflow, decision-making, communication and reward systems. 29,30
Weiner et al. 107 set out the features of a receptive and non-receptive context for organisational change. Organisational readiness factors found to be important for successful change include senior management and board commitment, fostering receptivity to change, clinicians’ engagement in quality improvement, quality reporting processes and fostering processes for improvement that engaged frontline staff. 108–110 Other work has identified factors such as stakeholder support, team climate and individual attitudes and preferences. 111,112 Exemplars of past successful change are also considered important in giving those involved a sense of confidence that the proposed change can and will be achieved. 113
Research reported in 2006110 concluded that NHS organisations showed high variability in some of these important readiness factors, for example in the infrastructure for improvement and the use of improvement tools and techniques. The research also found financial targets to be the main drivers of improvement in the NHS, with these efforts largely project based and not part of routine operations.
Periods of uncertainty, for example trust mergers and management changes, have been found to have a negative influence on the course and success of change programmes. 114,115 Pettigrew et al. 97,116 described these as ‘receptive’ and ‘non-receptive’ contexts for change (Box 2).
Quality of ‘policy’ at the local level is important in terms of both the quality of analysis (e.g. importance of data in making argument) and the quality of the process (e.g. broad vision important).
Availability of key people leading changeNot individual, ‘heroic’ leadership, but leadership that is distributed and exercised in a more subtle and pluralist system. Continuity of leadership is very important and lack of continuity is highly detrimental.
Environmental pressure: intensity, scale and orchestrationCan be both positive and negative. Excessive pressure can drain energy from the system, but, if orchestrated skilfully, environmental pressure can produce movement (e.g. financial crisis can be seen as threat or can be leveraged to achieve change).
A supportive organisational culture‘Culture’ refers to deep-seated assumptions and values far below surface manifestations, officially espoused ideologies or even patterns of behaviour. The past can be very influential in shaping these values, which may be both a strength and a weakness. In health care, the array of subcultures is important. Aspects of culture found to be associated with high rate of change: flexible working across boundaries rather than formal hierarchies; open, risk-taking approach; openness to research and evaluation; strong value base giving focus to loose network; and strong positive self-image and sense of achievement.
Effective managerial/clinical relationsRelations better when negative stereotypes broken down (e.g. as a result of mixed roles such as hybrids). Important for managers to understand what clinicians value and have good understanding of health-care operational issues.
Co-operative interorganisational networksBetween health-care organisations and between health-care and other organisations. Most effective networks informal and purposeful, but vulnerable to turnover. Factors that can facilitate networks include financial incentives, shared ideologies or history and existence of boundary spanners.
Simplicity and clarity of goals and prioritiesA fewer number of priorities pursued over a long-time period associated with achieving change. Need to insulate from constantly shifting short-term pressures.
The fit between the change agenda and the localeHow factors in local environment, which may be outside control (e.g. nature of local population, presence or absence of teaching hospitals), are anticipated as potential obstacles of change.
Based on Pettigrew et al. 116
Organisational readiness factors are considered to be both psychological and behavioural. For example, those involved need to be motivated to implement the change,80 and they are often described as being dissatisfied with the status quo or believing that the change is beneficial either personally or to patients. A study of readiness to change in 58 general practice organisations in Australia found that staff were more ready to change when there was a low overall team climate. 117 They were also more ready to change when job satisfaction was considered low, supporting the findings elsewhere that staff are more ready to change if they are dissatisfied with the status quo.
In a recent targeted review examining which common implementation factors are associated with improving the quality and safety of care, eight success factors were found. 118 These included the preparations made for the change, staff capacity for implementation, and resources. Obstacles to implementation were the opposite: ‘for example, when people fail to prepare, have insufficient capacity for implementation or when the setting is resistant to change, then care quality is at risk, and patient safety can be compromised’. 118
Applied to the MASS, organisational readiness factors may affect the capacity of a trust to successfully implement change in care systems for key areas that are commonly alerted, such as sepsis or AMI, and to implement improvement actions more generally in response to mortality alerts. Specifically, organisational readiness for change theory would suggest that an optimal response requires the right culture, including teamwork, leadership and multiprofessional engagement, among other factors. Compatibility with existing goals and priorities, minimal resistance to change and effective intraorganisational communication may all be implicated in an effective organisational response.
Theories relating to implementation of quality improvement practices
Normalisation process theory
Normalisation process theory examines how new technology and routines become ‘normalised’ into the routine processes within an organisation. 88,119 It uses neo-institutional theory to explain how individuals in an organisation react to macro influences.
Normalisation process theory is described as a sociological ‘toolkit’ to understand the embedding of practices such as an innovation or the implementation of an innovation. Normalisation process theory is concerned with two areas:
-
process problems – about the implementation of new ways of thinking, acting and organising in health care
-
structural problems – about the integration of new systems of practice into existing organisational and professional settings.
Normalisation process theory focuses on the practices that occur through four generative mechanisms: coherence, cognitive participation, collective action and reflexive monitoring.
Coherence is defined as the sense-making that people do both individually and as a collective when they are faced with operationalising a particular set of practices. Coherence is divided into four subset processes including an examination of the work people do together to build a shared understanding of what is required. Cognitive participation is the relational work that people do to initiate change. This includes how key participants of the practice work to engage key participants and drive the change. Collective action is the operational work that people do to enact a set of practices. Finally, ‘reflexive monitoring’ is the appraisal work that individuals do to assess how the new or modified practices affect them and the people around them (note that this is not an appraisal of the practise itself but of the way it affects the individuals). Reflexive monitoring may lead attempts to redefine procedures or modify practice in the longer term.
Absorptive capacity
Absorptive capacity is concerned with the contribution of knowledge processes to organisational performance. 83–86 According to absorptive capacity theory, the success of an organisation is a result of the degree to which its internal processes are effective in aligning the organisation with its changing external environment. 84
Absorptive capacity has three components:83,84
-
Exploratory learning: the process through which new knowledge is recognised and understood. The capability of this process is based on prior knowledge in the organisation as well as value judgments.
-
Transformative learning: those processes that affect the way in which new knowledge is assimilated into and combined with prior knowledge.
-
Exploitive learning: how assimilated knowledge is translated into actions that will benefit the organisation. This includes the implementation of policies and plans.
The capacity for learning within an organisation will depend, according to absorptive capacity theory, on investment in these knowledge processes. Organisations that invest more in knowledge processes are considered more likely to increase their performance than those that fail to invest. Furthermore, those that fail to invest may find it hard to catch up and are likely to become ‘permanently failing organisations’. 120 The value of absorptive capacity as a theoretical framework lies in its focus on internal knowledge management within an organisation and organisational capacity to continuously embody that knowledge in its systems and processes. Failure to effectively manage knowledge to achieve this undermines the ability of public sector organisations to perform. 84
In the context of MASS, the mortality alerts represent externally generated intelligence on potentially harmful variations in care that, in turn, act as stimulus for internal investigation, monitoring and action. The process by which the organisation assimilates the information and knowledge generated is one of organisational learning governed by absorptive capacity. Furthermore, developing a repeatable process for responding to mortality alerts and understanding the local institutional value of a MASS involves processes of exploratory, transformative and exploitative learning.
Organising for quality
Organising for quality is a theoretical approach steeped in empirical evidence that aims to understand the processes involved in achieving quality. The theory is highly practical and was born out of an international study of European and US hospitals. Although the researchers found that there were many different paths by which quality improvement can be achieved, they identified unique unifying features that stretched across all of their case studies. Rather than focus on when things went right, organising for quality seeks to illustrate the challenges that are faced when implementing quality improvement. The approach recognises six unifying challenges to the process of organising for quality, shown in Box 3.
-
Structural: structuring, planning and co-ordinating quality efforts.
-
Political: addressing the politics and negotiating the buy-in, conflict and relationships of change surrounding any quality improvement effort.
-
Cultural: giving ‘quality’ a shared, collective meaning, value and significance within the organisation.
-
Educational: creating and nurturing a learning process that supports continuous improvement.
-
Emotional: inspiring, energising and mobilising people for the quality improvement effort.
-
Physical and technological: designing physical systems and technological infrastructures that support improvement and quality of care.
Added later in the QUASER research study:121
-
Leadership: providing clear, strategic direction.
-
External demands: responding to broader social, political and contextual factors.
Chapter 4 Data sources
This chapter focuses on external data sources relating to our evaluation. We first discuss HES, the data source used to create the mortality alert. We then consider other hospital indicators of quality of care used in our evaluation that relate to hospital (or trust) structure, process and outcomes. Data collected during the qualitative analysis (workstream 2) will be discussed in Chapter 5 (see Workstream 2).
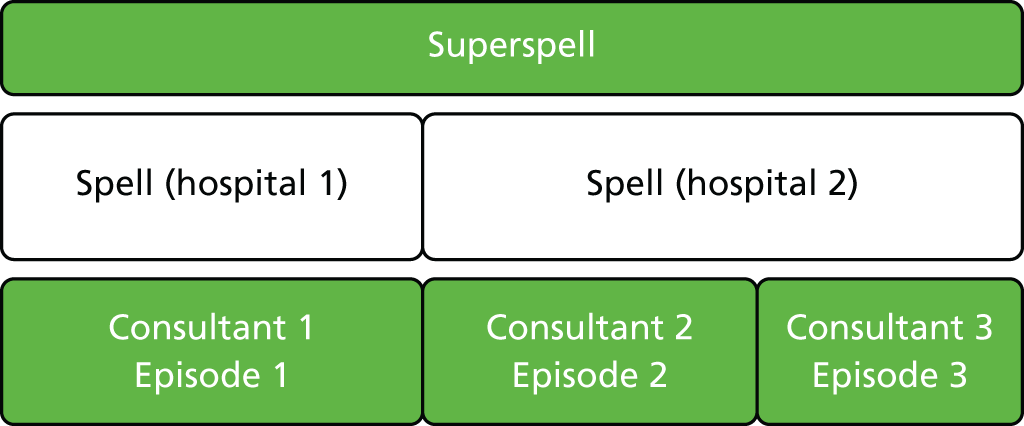
Hospital Episode Statistics data
Hospital Episode Statistics is a national administrative database containing information on all admissions to public (NHS) hospitals in England. 122 Each record in HES contains data on patient demographics, such as age, ethnicity and socioeconomic deprivation based on postcode of residence; data on the episode of care, such as hospital name, date of admission, date of discharge and discharge destination, which includes a code for death; and clinical information. 123 Diagnoses for each patient are recorded using the International Classification of Diseases, Tenth Edition (ICD-10),124 and the information is divided into the primary diagnosis (main problem treated) and various secondary diagnoses (including comorbidities and complications). Procedures performed during an episode are coded using the Office of Population, Censuses and Surveys Classification of Surgical Operations and Procedures, Fourth Revision (OPCS-4). 125 There is a unique identifier (HESID) for each patient in HES, which makes it possible to link a patient’s historical medical records. The Imperial College Unit holds provisional HES data provided monthly by NHS Digital. HES monthly data are used to generate the mortality alerts. The Imperial College Unit also holds the final annual publication of HES data. The data cover a financial year and the resulting snapshot of health-care activity will differ from the monthly HES extracts, as changes to the data may occur in the interim period. The Imperial College Unit combines episodes (periods of patient care under a single consultant) to form patient ‘spells’ to a single hospital; in turn, spells are linked together to account for interhospital transfers, creating ‘superspells’, as shown in Figure 4. In this report, we refer to a continuous period of care (whether a spell or superspell) as an admission.
FIGURE 4.
A patient’s stay in hospital (admission) in terms of episodes, spells and superspells.
Calculating risk of death
The Imperial College Unit calculates the probability of death using a logistic regression model based on national data and incorporating information on method of admission, patient age, patient gender, year of discharge, month of admission (for respiratory disease such as asthma), previous emergency admissions (in the last year), socioeconomic deprivation, comorbidities and palliative care. 126 The risk factors are further defined in Table 4. The relative risk for a specific diagnosis/procedure for each trust is the ratio of the observed number of deaths (the total number of finished provider admissions that resulted in a death) to the expected number of deaths (based on the probability of death from a risk-adjusted model).
| Risk factors | Definition |
|---|---|
| Method of admission | Elective or emergency |
| Patient age | Age at start of admission field in HES. Values were recoded to < 1, 1–4, 5–9 and 10–14 years, followed by 5-year bands |
| Patient gender | Gender |
| Year of discharge | The financial year of date of discharge at the end of the admission |
| Month of admission | The calendar month at the beginning of the admission |
| For respiratory diseases only | |
| Previous emergency admissions (in the last year) | From method of admission field in HES (values 21–28) in the admission records in the previous 365 days for the same patient |
| Socioeconomic deprivation | Carstairs and Morris127 |
| Comorbidities | Charlson score derived from secondary diagnosis fields of the admission128 |
| Palliative care | If any episode in the spell has the treatment function code 315 or contains Z515 in any of the diagnosis fields, then ‘palliative’; else, ‘non-palliative’ |
Alerts data
Since 2007, the Imperial College Unit has generated monthly mortality alerts on 122 diagnoses and procedures for all acute non-specialist NHS hospital trusts in England. 35 Diagnoses are determined from the primary diagnosis within an admission. The ICD-10 codes are combined into clinically meaningful groups using the agency for Healthcare Research and Quality’s Clinical Classification Software (CCS). 129 There is no similar grouping system for procedures. An OPCS grouping system was developed at the Imperial College Unit through an expert panel, a literature review and user input. 35 A list of the conditions and procedures covered by the alerting system is provided in Appendix 2.
Alerts are generated using statistical process control charts on monthly provisional HES extracts. This monitoring system applies log-likelihood CUSUM charts71 for specific conditions or procedures for each acute NHS trust, plotting a function of the difference between the actual outcome of patient survival or death and the case-mix adjusted probability or risk of death. 35 The strengths of this methodology have previously been reported. 130,131 The case-mix adjustment is given in Table 4. 128 After a sustained higher-than-expected level of monthly mortality within a trust, a set threshold is crossed, triggering a mortality alert. The threshold is set at a high level to ensure an estimated false alarm rate of 0.1% over a 12-month period of monitoring. This means that, given a hospital trust with a mortality rate equal to that expected based on national data, one could anticipate one alert every 1000 years to occur by chance. The threshold is tailored to the hospital’s annual volume and expected mortality rate. 128,132
Imperial College reviews each alert individually. Alerts are not sent to trusts if they represent small numbers of deaths (expected < 5), if they are repeat signals to which the trust has already been alerted to within the previous 9 months, or, following concerns raised by individual hospitals, if the validity of a particular procedure or diagnosis grouping has been brought in to question (as has happened with percutaneous transluminal coronary angioplasty). Imperial College notifies the chief executive of the alerting trust by a letter that details the rationale for the letter and also presents the statistical process control chart and statistics for the preceding 12 months (number of admissions, deaths, expected deaths, relative risk, C-statistic and the probability of the alert being a false alarm). An example alert letter can be found in Appendix 1. Imperial College keeps a database of all alerts, collecting information on the trust, the condition, the month and year of the alert and the statistics of the alert.
We examined all Imperial alerts and focused on two conditions commonly contributing to mortality alerts, AMI and septicaemia (except in labour), defined by the CCS codes ‘100’ and ‘2’, respectively. In this report, for simplicity, we will term septicaemia (except in labour) ‘sepsis’.
Other indicators of quality of care
A range of indicators based on other sources was identified a priori (see original proposal: www.journalslibrary.nihr.ac.uk/programmes/hsdr/1217822/#/) to examine the indicators’ relationship to mortality alerts. Indicators were all at a trust level. Information on the data source and time coverage is listed in Table 5 and we will then discuss each indicator individually.
| Data name | Data extracted/processed | Aggregation period | Data source | Data time coverage |
|---|---|---|---|---|
| Structure | ||||
| Bed availability and occupancy: overnight | Acute bed occupancy (%) | Quarter | NHS England | 2011–13 |
| NHS Workforce Statistics | Qualified nursing staff: FTE | Month | HSCIC | 2011–13 |
| Nurse-to-bed ratios | Qualified nursing staff/occupied beds | Quarter | Processed for analysis | 2011–13 |
| Trust financial data | Financial deficit (yes/no) | Financial year | Department of Health (freedom of information) and Monitor | 2011/12–2013/14 |
| GMC National Training Survey | Weighted combined satisfaction score (%) | Financial year | GMC | 2012/13–2013/14 |
| NHS Litigation Authority risk assessment | Assessment rating (level 1 vs. level ≥ 2) | Financial year | NHS Litigation Authority | 2011/12–2013/14 |
| Process | ||||
| MINAP | Percutaneous coronary intervention within 90 minutes of arrival (%) | Financial year | MINAP: UCL | 2011/12–2012/13 |
| Outcome | ||||
| The National Inpatient Survey | Overall satisfaction score (%) | Mid-year collection | NHS England | 2011–13 |
| The Patient Safety Thermometer | Patients harmed (%) | Month | HSCIC | 2012–13 |
| Hospital mortality: SHMI | SHMI | Financial year | HSCIC | 2011/12–2013/14 |
| Hospital mortality: HSMR | HSMR | Financial year | Dr Foster Good Hospital Guide | 2011/12–2012/13 |
Structure
Acute bed occupancy data
The bed availability and occupancy data are published quarterly by NHS England and identify, for each NHS Health Care Provider, the number of bed-days available for patients to have treatment or care. 133 For our analysis, we focused on the percentage of beds occupied over a 3-month period (a quarter) in general and acute wards. We analysed data for the calendar years 2011 to 2013, using the fourth-quarter data from the financial year 2010/11 and excluding the fourth-quarter data from the financial year 2013/14.
Nurse-to-bed ratio
NHS Workforce Statistics are available from NHS Digital. 134 The monthly publication is an accurate summary of the validated data extracted from the NHS’s human resources and payroll system. The data include full-time equivalent figures for all NHS hospital staff groups working in England. We used the mean number of full-time equivalent qualified nursing staff (over a 3-month period) as the numerator and quarterly bed availability as the denominator for each NHS trust. We analysed data for the calendar years 2011 to 2013.
Trust financial data
Annual financial NHS foundation trust data are provided by Monitor135 and we downloaded data for financial years 2011/12–2013/14 from the UK government information website. 17 For NHS trust financial data, we put in a freedom of information request to the Department of Health (reference 1041857) for the same years. As the two data sets are compiled from difference sources, we could not directly combine the data sets. We therefore created a binary variable to determine whether or not a trust was in deficit in a given year. We used the value for ‘surplus before impairments’ to determine whether or not a foundation trust was in deficit.
General Medical Council National Training Survey
The National Training Survey is carried out by the General Medical Council. 136 The aim of the survey is to ensure that medical education and training is meeting the standards set to support high-quality medical care and patient safety across the UK. In 2012, 51,316 doctors in training completed the survey out of 54,035 who were eligible, giving a response rate of 95.0%. The survey data cover over 12 questions or indicators, within 100 specialities/departments, in all NHS trusts in England. Data are available at a trust level from 2012/13; we used 2012/13 and 2013/14 data. Mean percentage satisfaction scores were presented only if there were more than three trainee respondents for a specific specialty and question within a trust. We created a weighted trust score across all indicators and all departments for each trust by year. To weight the hospital score, we needed to estimate the number of trainees (N) responding to a question. From the provided mean and 95% confidence interval (CI), we could calculate the standard error of the mean (SE):
We were also provided with the standard deviation (SD), and using:
we could calculate the number of trainees as:
The weighted mean is the sum of the partial means, which was calculated as the mean multiplied by the number of trainees (for a trust/specialty/question) divided by the total number of trust trainees:
where k denotes a single question answered by trainees within a single specialty for each trust.
NHS Litigation Authority
The NHS Litigation Authority is a not-for-profit part of the NHS that handles negligence and other claims against the NHS in England. 137 The NHS Litigation Authority conducts a risk-management assessment within each hospital and awards a rating basis against a set of risk management standards. The highest risk management assessment a trust can achieve is a level 3. The NHS Litigation Authority has been publishing factsheets on risk management assessment levels since 2002/3. The factsheets include data on the trust, the date of the last assessment and the level achieved. We used data from 2011/12–2013/14 and dichotomized trusts’ risk assessment achievement into those that had a risk management assessment level 1 versus those with levels 2 or 3 for each quarter over the 3 years.
Process
Myocardial Ischaemia National Audit Project
Myocardial Ischaemia National Audit Project is the national clinical audit of the management of heart attack. 138 MINAP captures information on all patients with a heart attack directly after treatment. All providers audited have common definitions of clinical important variables and common standards of good quality. In our analysis we focused on percutaneous coronary interventions (PCIs). National and international guidance recommend that in the emergency treatment of patients with ST-elevation myocardial infarction, a blockage in one of the heart’s major arteries, primary PCI should be performed within 90 minutes of arrival at the heart attack centre. Not all hospitals have the facility to perform primary PCI. We were unable to obtain information on which trusts provide PCI (independent of MINAP); we therefore included all trusts that provided primary PCI data in our analysis and assumed that the data were complete. We focused on the quality indicator ‘proportion of all patients who received primary PCI within 90 minutes from arrival at the heart attack centre’. We analysed data for years 2011/12 and 2012/13.
Outcome
National Inpatient Survey
The NHS Patient Survey Programme is run by Picker Institute Europe on behalf of the CQC. 139 The views of patients about the care they have recently received from all NHS health-care providers in England have been systematically gathered since 2005. Eligible patients for the survey were aged ≥ 16 years, had at least one overnight stay and were in hospital between June and August of the collection year. The questions cover four specific areas on access and waiting; on safe, high-quality co-ordinated care; on better information and more choice; and on building closer relationships. All questions are collated to give an overall patient experience score. We used annual National Inpatient Survey data for years 2011 and 2012.
NHS Safety Thermometer
The NHS Safety Thermometer is a tool designed to support patient safety and improvement. The tool focuses on four harms for which there is clinical consensus that they are largely preventable through good-quality patient care. These harms are pressure ulcers, falls, urinary tract infections in patients with a catheter, and new venous thromboembolisms. The prevalence of patient harms is recorded within each health-care setting, with the aim of providing information for performance monitoring. 140 NHS Safety Thermometer data are supplied by NHS Digital and are available, as monthly reports, from April 2012. For our analysis, we included all harms within an acute hospital ward setting, using data for the financial years 2012/13–2013/14.
Summary hospital-level mortality indicator
Summary hospital-level mortality indicator data were supplied by NHS Digital. 141 These annual standardised mortality statistics are generated using HES provider spells linked to the Office for National Statistics mortality data. The SHMI is a ratio of the observed number of deaths [the total number of finished provider spells for the trust that resulted in a death either in hospital or within 30 days (inclusive) of discharge from the trust] to the expected number of deaths for a trust adjusting for patient case mix. The SHMI risk model adjusts for age, gender, admission method, year index, Charlson Comorbidity Index and diagnosis grouping. 33 We used data for the financial years 2011/12 to 2013/14. There were no SHMI data for specialist trusts such as Birmingham Women’s and Children’s NHS Foundation Trust.
Hospital-standardised mortality ratio
Hospital-standardised mortality ratio data were accessed from Dr Foster Hospital Guides. 34 These annual standardised mortality statistics were generated by Dr Foster Intelligence using HES provider spells. The HSMR is a ratio of the observed number of deaths (the total number of finished provider spells for the trust that resulted in a death) to the expected number of deaths for a trust calculated from a risk-adjusted model, multiplied by 100. The risk model adjusted for various factors as in Table 4. 25 Data were available at an annual trust level for the financial 2011/12 and 2012/13.
Chapter 5 Methodology
This chapter outlines the methods applied in this mixed-methods evaluation of a national surveillance system for mortality alerts. We focus first on the methods for the quantitative component (workstream 1) and then on methods for the qualitative component (workstream 2).
Workstream 1
Research design overview
In workstream 1, we aimed to describe trends in mortality alerts and to carry out a descriptive analysis of CQC investigations into the Imperial College mortality alerts. We examined the relationships between mortality alerts and measures of quality of care that relate to the trust care structure, processes and outcomes, and applied an interrupted time series model to examine the impact of mortality alerts on subsequent mortality using national hospital administrative data on admissions.
Descriptive analysis of mortality alerts
Descriptive analysis of Imperial College mortality alerts
We investigated trends in alerts and frequency of alerts for specific diagnoses and procedures from the Imperial College alerts generated between April 2007 and December 2014.
We classified hospital trusts according to the number of alerts that they received between 2007 and 2014: single alerting trusts received one alert and multiple alerting trusts received two or more alerts.
Descriptive analysis of Care Quality Commission investigations into the Imperial College mortality alerts
Copies of all of the alerts, including those not sent to trusts, are sent to the CQC, the regulator of health and social care in England. The CQC has been running its own mortality alerting system using HES. 36 On the basis of either alerting system, the CQC may write to a trust to request a trust-level investigation and response. 36
On receipt of a trust response, a panel of clinicians and analysts reviews the information received. At this stage the CQC may close the case (and request follow-up by its regional teams) or request further information. The process chart outlining the CQC’s follow-up of mortality alerts is shown in Figure 5.
FIGURE 5.
Process chart outlining the CQC’s follow-up of mortality alerts.
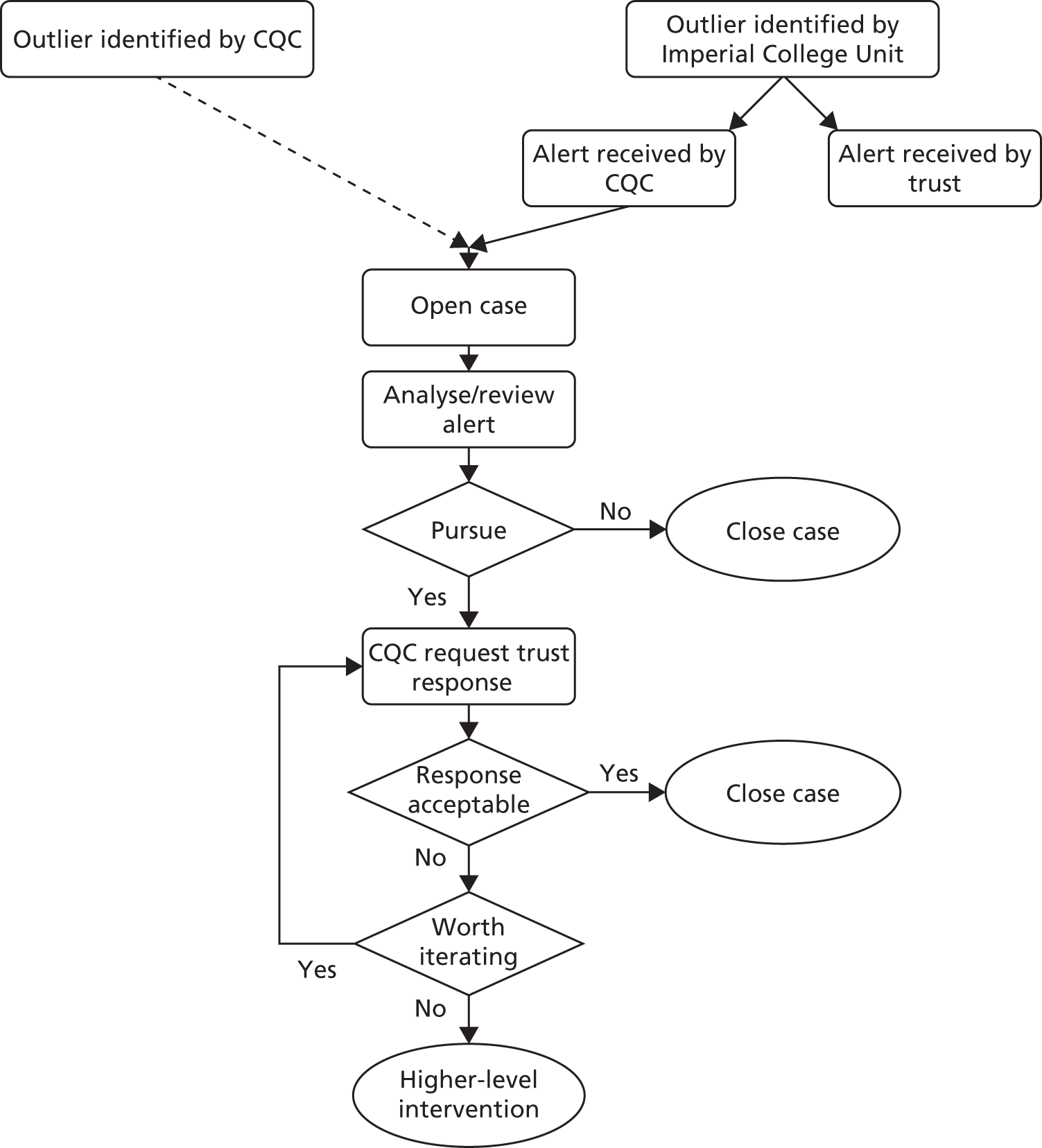
We systematically reviewed the documents held by the CQC for each mortality alert generated by Imperial College for a subset of total alerts between 2011 and 2013. This time period was chosen to enable us to investigate the CQC’s paper trail with the resources that we had available and, additionally, to allow time at the end of the period for investigations to be completed. The CQC documentation data were collected and compiled at the CQC site by one reviewer to protect the potentially sensitive information contained within the documents. Each alert leads to substantial communication between the CQC and the trusts, and the CQC checked the data collected before releasing them to Imperial College. Initially, the data collection comprised up to 121 pieces of data but, as we progressed with the data collection, we were able to limit the data to the 44 most relevant pieces from four document types during the collection process. Table 6 summarises the data and documents available at the CQC that related to mortality alert reviews.
| Document type | Document description | Number of items | Key data items |
|---|---|---|---|
| Analyst report | Created by CQC analysts. Collates CQC information for the trust and recent mortality data | 3 | Decision to pursue or close, and date report created |
| CQC information request | Letters sent to trusts from the CQC requesting information | 4 | Letter dates |
| Trust response | Letters received by the CQC from trusts containing responses to information request | 4 | Details of clinical audit and letter dates |
| CQC assessment of response | Summary document used by the CQC panel that summarises the case and the information received from the trust | 33 | Results of clinical audit, action plan status, panel recommendations and dates |
Summary information was predominantly located in documents used in the CQC panel meeting ‘CQC assessment of response’. The findings from trust investigations, summarised by the CQC analysts, were used to classify the trust’s conclusion as to the reasons for the alert. When the CQC analysts noted that trusts had identified deficiencies, we included these findings in our data collection. The broad classifications of findings were (1) no improvement required, (2) case mix, (3) coding, (4) care and (5) care and coding. When CQC analysts had not summarised the findings from a trust, the reviewer classified the trust response using information taken directly from ‘trust response’ documents. If the trust referred to plans to improve care or coding, then these were used to classify findings. The classifications of findings were subjective, but all decisions were made by one reviewer. Trusts did not always assess the likelihood of the findings affecting the outcome (the alert). When there was a reference to an outcome potentially being affected, we recorded this.
We developed a data collection form in Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA), which we piloted and refined during the data collection. Cases were eligible for inclusion if the case was opened by the CQC in response to an Imperial College mortality alert (i.e. not in response to a mortality alert generated internally at the CQC). We checked the quality of the data at various points in the data collection. As letter dates were predominantly sequential (i.e. trust responses should follow CQC data requests), dates were checked regularly to identify non-sequential letters. The final collated data set was shared with the CQC, which had an opportunity to comment.
We assessed trust findings across all diagnosis/procedure groups and focused on sepsis alerts. The number of AMI alerts between 2011 and 2013 was too small to assess separately.
Changes to coding following an alert
After receiving an alert letter, internal investigations are likely to occur, alongside an investigation by the CQC. We assume that an alerting trust will review its coding as an important mechanism in the investigation process. On the basis of these investigations, HES data submitted at the time of the alert may be recoded and resubmitted by the trust. We analysed coding changes for both AMI and sepsis alerts, comparing data contained within an alert letter (based on provisional monthly data) with data from the annual HES publication. Each alert letter indicates the trust and disease group triggering the alert; the defined period before the alert (covering 1 year); the number of admissions; the number of deaths (observed); and the relative risk of death over the defined period. We examined sent letters dated between April 2011 and December 2013 for AMI and sepsis, and extracted data from each alert letter. Using HES (annual publication), we extracted data covering the same date period and condition for those trusts that received mortality alerts. The risk adjustment model used to calculate relative risk was the same for both provisional and annual HES extracts. We described the coding changes between alert letter and annual HES data as a percentage change for admissions, deaths and relative risk.
Two calculations have been used to describe changes in the data:
-
absolute change = new data – old data
-
relative change = (new data – old data)/old data.
Investigation of mortality alerts and other measures of quality
For this objective, we aimed to explore whether or not mortality alerts reflect other indicators of quality of care; we specifically chose indicators that reflected the care structure, the care process and the patient outcomes within an acute NHS trust. We hypothesised that mortality alerts were highlighting broader quality issues in hospital care. We examined the relationship between frequently (≥ 2) alerting, single-alerting and non-alerting trusts and indicators of care quality.
Indicators relating to care structure included the provision of acute beds (bed occupancy), staffing levels (nurse-to-bed ratios), funding (trust financial data), staff training (General Medical Council National Training Survey) and risk assessment practices (NHS Litigation Authority risk assessment achievement level). MINAP data were an indicator of care process defined by guidelines. Indicators relating to patient outcomes were for patient satisfaction (National Inpatient Survey), patient harms (Patient Safety Thermometer) and death (SHMI and HSMR). All data were publicly available at a trust level. We analysed available data for the years 2011 to 2013 (calendar year) or 2011/12–2013/14 (financial year). Table 5 summarises the external quality measures used in our analysis with time periods analysed.
We used a cross-sectional study design of all NHS trusts in England between years 2011 and 2013 (when data were available). Each indicator was merged with mortality alerts data. We took the time period of the indicator to coincide with the date of the alert and examined whether a trust had alerted at the time of the indicator, had ever alerted during the study period (January 2011–December 2013) or had frequently alerted (twice or more) during the study period. For the continuous quality indicators, we used ordinary least squares regression, which estimates the mean in the baseline (no alert) with a parameter measuring the difference in mean in trusts with an alert. We also adjusted for year. We used robust standard errors to compensate for the clustering effect of repeated observations from the same NHS trust (ignoring clustering can overestimate an association between two variables). Ordinary least squares regression makes the assumption that the outcome is normally distributed, which was not always the case, and many of our outcomes were bounded (e.g. percentages are bounded by 0% and 100%); however, we had a large number of observations and the central limit theory states that the sampling distribution of the mean of any independent, random variable will be normal or nearly normal, if the sample size is large enough. We checked the distribution of model residuals for normality and outliers; we carried out sensitivity analyses on transformed data, when transformation normalises the distribution of the outcome and after the removal of outliers.
The linear model was as follows:
where α is the mean trust outcome at baseline (no alert/year 2011), β(alert) is the difference in means between the alerting and non-alerting trusts and β(year) is the difference in means between one year and the next.
NHS Litigation Authority assessment level achievement and trust financial data were binary outcomes, and we used logistic regression with robust standard errors to measure the association between mortality alerts and these outcomes. We adjusted for year. Logistic regression estimates log-odds ratios as well as the log-odds at baseline (in a non-alerting trust). We converted odds ratios into risk ratios (RR) using the following formula: risk = odds/(odds + 1).
We set the threshold value for p, the significance level of our hypothesis tests, at 0.05 (5%). The null hypothesis here was defined as no significant difference between the outcome in the alerting trusts and outcome in the non-alerting trusts, so that any observed difference would be due to random error. We calculated relative difference (%) as:
Controlling for false discovery rate
Our investigation of mortality alerts with other measures of quality involved the analysis of 11 outcomes. Multiple significance testing increases the probability of false-positive findings as a result of random chance alone. This is the false discovery rate (FDR). We controlled for the FDR using methodology described by Benjamini and Hochberg. 142
-
We ranked p-values (P) from each significance test from smallest to the largest: P1 ≤, P2 ≤ . . . ≤ Pm (where m is the total number of significant tests).
-
We denoted H(i) as the null hypothesis corresponding to P(i) (where i is the rank number).
-
We rejected H(i) if P(i) ≤imq∗ (where q* is 0.05, our set threshold for the p-value).
Analysing the association of an alert with trends in subsequent risk of death
We hypothesised that on receiving an alert the trust would investigate possible explanations within the trust, bringing about change (if needed) within the hospital setting, and as a result there would be a fall in mortality risk. We investigated the association between a mortality alert and subsequent mortality using an interrupted time series analysis.
We investigated alerts between January 2011 and December 2013. Our data included only trusts that had received a mortality alert. We investigated all alerts during the study period. The outcome was diagnosis/procedure-specific, trust-level relative risk, calculated as the number of deaths divided by the expected number of deaths. We matched the diagnosis/procedure of the outcome with the diagnosis/procedure of the alert for 12 months before an alert and 24 months post an alert.
Statistical methods
We used an interrupted time series design. Interrupted time series is the strongest quasi-experimental approach for evaluating longitudinal effects of interventions. 143 The design estimates a trend before an intervention, the impact of an intervention and the change in trend after the intervention. The start of the intervention was taken as the month of alert and the month after a 9-month lag. The 9-month lag is the hypothesised minimum time for a hospital trust to receive the mortality alert letter, to investigate the alert and to bring about change within the hospital setting, and was in part supported by workstream 2 findings.
After a high cumulative mortality rate, resulting in a mortality alert, rates may fall as a result of the phenomenon of regression to the mean. 137 Our analysis needed to differentiate between an immediate fall in trust mortality relative risk resulting from regression to the mean and a genuine fall resulting from improvement of care or amendments to coding. To achieve this, our investigation employed three models, graphically displayed in Figure 6.
FIGURE 6.
Interrupted time series analysis models. (a) Two parameters: a, pre slope and b, post-slope factor; (b) three parameters: a, pre slope, b, level change, and c, post-slope factor; and (c) three parameters: a, pre slope, b, level change (after lag period), and c, post-slope factor.
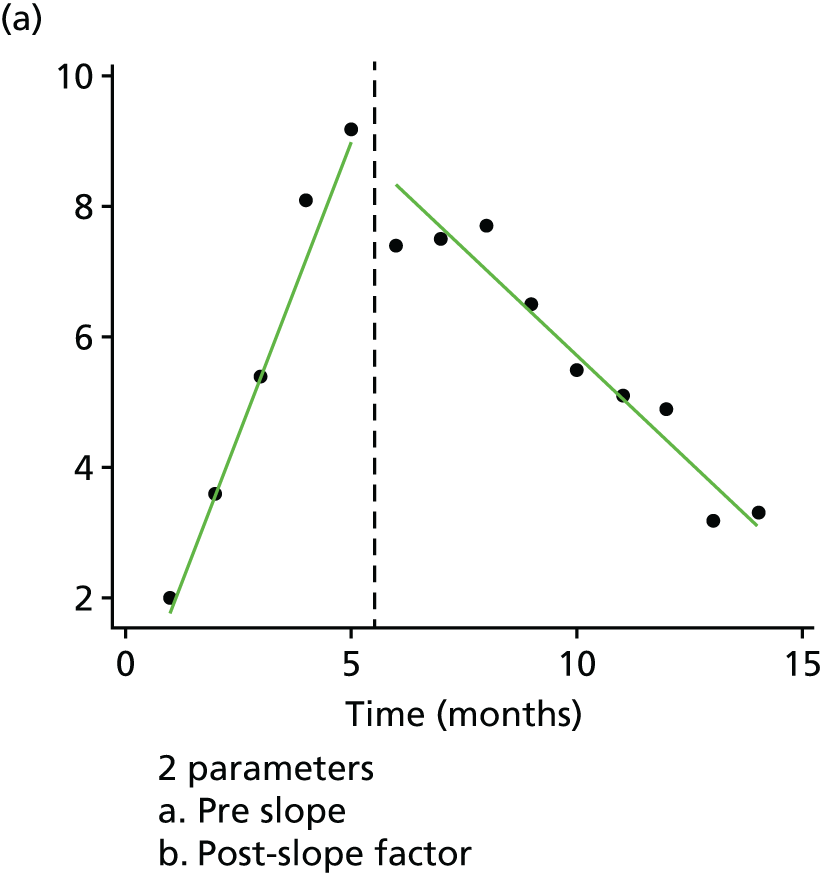
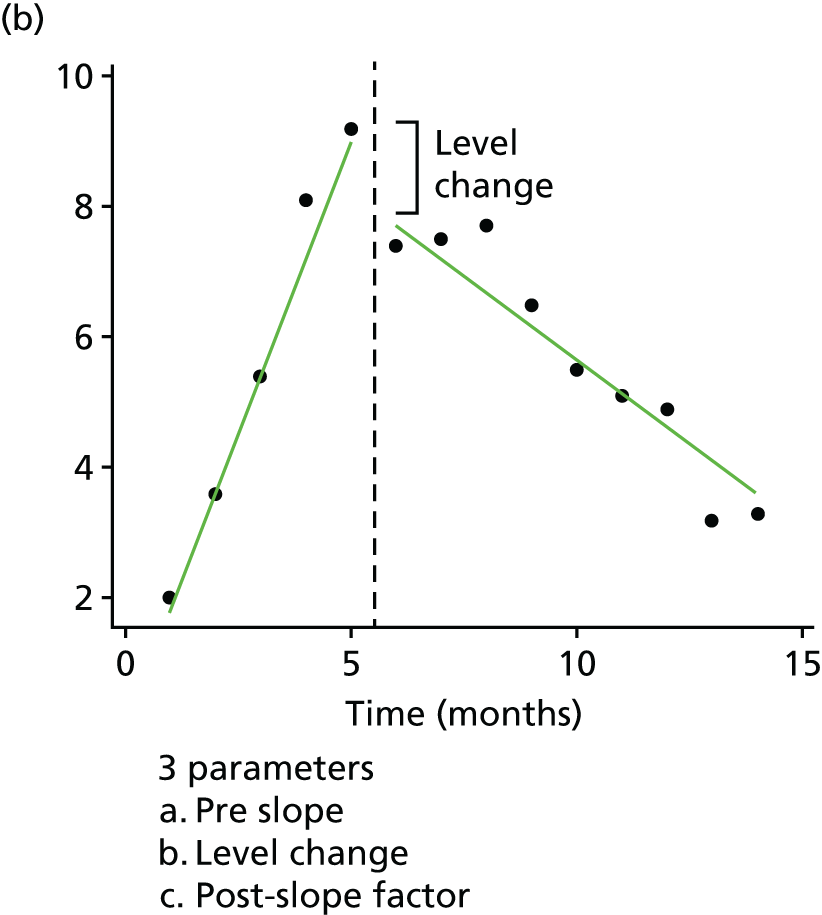
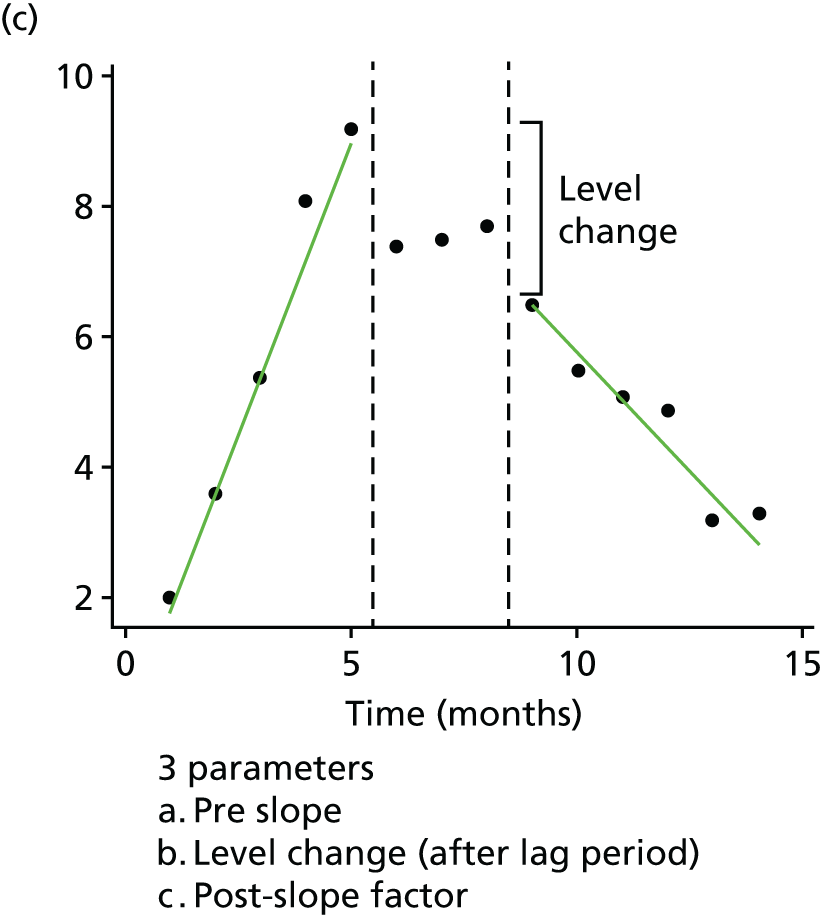
Model 1 (broken stick model) measured two parameters: the increasing slope in relative risk before a mortality alert (measured as a monthly increase) and the change in slope after. We restricted the data to 12 months before and 9 months of the lag period (the time we assumed the trust was investigating and implementing improvements to care or amendments to coding).
This model estimates the log relative risk as:
Model 2 measured three parameters: the increasing slope in relative risk before the mortality alert, a level (step) change after the mortality alert and the subsequent change in slope. Again, we restricted the data to 12 months before and the 9 months after an alert.
This model estimates the log relative risk as:
Model 3 ignored trends in the lag phase and measured three parameters: the increasing slope in relative risk before the mortality alert, a level (step) change after a 9-month lag period and the slope following the lag period.
This model estimates the log relative risk as:
(Data are excluded during the lag period.)
A more detailed description of the models’ parameters is given in Appendix 3.
A 12-month pre-alert increase was calculated as:
A monthly relative risk determining the trend after alert was calculated as:
We hypothesised that the decline in relative risks would be steeper after a lag period (model 3), when trusts have instigated improvement to care or amendments to coding, than during the lag period (models 1 and 2), when any decline would be influenced by a regression to the mean.
We modelled the data using generalised estimating equations based on a Poisson distribution. This semiparametric modelling compensates for the correlation between repeated measures of relative risk from individual trusts over the study period. It also allows for distribution assumptions of the data to be relaxed. Similar methodology assessed against a randomised controlled trial found the results to be concordant. 144 Generalised estimating equations calculates population-averaged parameter estimates.
We investigated all mortality alerts, AMI alerts and sepsis alerts. We carried out sensitivity analyses with lag periods of 3, 6 and 12 months. Further sensitivity analyses investigated crude risk (number of deaths over number of admissions).
Statistical analysis was carried out using the SAS 9.2 software package (SAS Institute, Cary, NC, USA) and Stata version 13 (StataCorp, College Station, TX, USA).
Workstream 2
Research design overview
Workstream 2 employed mixed methods to investigate the mechanisms by which mortality alerts were assimilated at local trust level, and the resulting organisational behaviour. It additionally sought to achieve a theoretically informed understanding of processes and mechanisms governing institutional responses to mortality alerts, drawing on institutional theory and a realist perspective that would account for the effects of institutional context on mechanism–outcome interactions. Workstream 2 comprised two complementary phases: (1) qualitative analysis of experience in responding to alerts at 11 hospital trusts, and (2) a national cross-sectional survey of alerted trusts. The survey study followed the institutional case study component, and the survey instrument itself was developed based on a qualitative analysis of key categories and themes derived from the interview data in order to ensure validity of the scales employed. The two-phase structure was designed to provide rich information on both the depth and the breadth of organisational responses to alerts, in order to provide a comprehensive investigation and evaluation of the current MASS and its interaction with local health-care organisations.
Institutional case studies
Eleven institutional case studies were undertaken based on interviews with key informants during 2-day site visits and follow-up documentary analysis. The case study design was selected because of its flexibility of focus, facility for in-depth investigation of mechanism and capacity to explore interactions between a phenomenon and its context (in 2001). The approach taken comprised descriptive and thematic analysis of individual organisational cases resulting in a series of case narratives describing the institutional responses to alerts received by the organisation in two target areas: sepsis and AMI. An integrative thematic and cross-case comparative analysis was then undertaken to draw evaluative inferences grounded in the qualitative data. This resulted in generalised themes that would serve as a basis for the development of the survey instrument used in the second phase of workstream 2 and to structure the analysis of the resulting quantitative data.
Case study site selection
Using stratified and theoretical sampling methods, case study sites were drawn from trusts alerted in two disparate clinical conditions, presumed to require local institutional responses of varying scope: sepsis and AMI. The target sample was 12 English acute care trusts, six in each condition area. Sites were selected from review of Imperial College’s historic alert data.
Trusts were selected and approached to participate in the study according to two sampling strata: (1) receipt of an alert in either sepsis or AMI in the 2011–14 period (six sites in each category), and (2) receipt of single or multiple alerts (i.e. single vs. repeat alerting sites: three sites within each category for both sepsis and AMI).
Application of sampling criteria 1 yielded 22 candidate sites, comprising six AMI and 16 sepsis. Of the 16 sepsis sites, one trust no longer existed as a result of a merger and was excluded. Of the remainder, eight sites were selected based on examination of a number of additional criteria applied to maximise variation across the final included case studies. These included single or repeat alert status, geographical location, trust size, how recent the last alert was, total number of historic alert letters sent to the site, availability of relative risk data and statistical trend in relative risk, gleaned from fitting interrupted time series models. Regarding the last criterion, time series models were fitted to individual trusts’ monthly relative risk data using segmented regression analysis with interrupts representing alert letter dates. Knowledge of the robustness and direction of apparent changes in trend were used to maximise variation across included sites. The final set of 14 target sites that were contacted with an invitation to participate in the study comprised six AMI sites (three single and three repeat alerting sites) and eight AMI sites (two single and six repeat alerting sites) (Table 7).
| Participated in study | Clinical condition | Number of target condition alert letters | Total number of alert letters | Single/multiple alerts | NHS cluster | Apparent statistical response in relative risk to alert letter |
|---|---|---|---|---|---|---|
| Yes | AMI | 4 | 10 | Multiple | Large acute trust | No effect/ambiguous |
| Yes | AMI | 1 | 5 | Single | Small acute trust | No effect/ambiguous |
| Yes | AMI | 2 | 6 | Multiple (recent) | Medium acute trust | Positive response |
| Declined | AMI | 1 | 11 | Single | Acute specialist trust [including acute specialist (children)] | No effect/ambiguous |
| Declined | AMI | 1 | 19 | Single | Acute teaching trust | Positive response |
| Yes | AMI | 2 | 9 | Multiple | Large acute trust | Positive response |
| Yes | Sepsis | 3 | 10 | Multiple | Medium acute trust | Positive response |
| Yes | Sepsis | 1 | 6 | Single | Medium acute trust | Positive response |
| Yes | Sepsis | 1 | 12 | Single | Large acute trust | Positive response |
| Yes | Sepsis | 3 | 5 | Multiple | Small acute trust | No effect/ambiguous |
| Yes | Sepsis | 3 | 11 | Multiple | Acute teaching trust | Positive response |
| Yes | Sepsis | 4 | 8 | Multiple (recent) | Large acute trust | No effect/ambiguous |
| Declined | Sepsis | 4 | 11 | Multiple | Large acute trust | No effect/ambiguous |
| Yes | Sepsis | 2 | 4 | Multiple | Large acute trust | Positive response |
Site recruitment
Recruitment and gaining approval for local data collection at the 14 identified sites involved contacting the medical director at each site with an invitation letter and details of the study (see Appendices 4 and 5) before seeking local research and development approval (Integrated Research Application System application) for the site visit itself. Once the research team received a letter of access, a preliminary telephone interview was conducted with the medical director or mortality lead, using a standard pro forma (see Appendix 6), to plan the site visit, including identifying key personnel for interview. Following initial contact, three sites declined to participate in the study, stating resource and personnel availability as the primary reasons.
The final research sample comprised four AMI sites (three multiple and one single alert site) and seven sepsis sites (two single and five multiple alert sites). The additional sampling characteristics of the final research sample are indicated in Table 6. The final sample was therefore achieved through a combination of stratified sampling, maximum variation sampling and, to a lesser degree, opportunistic availability.
Data collection
Workstream 2 qualitative case study data from the 11 included trusts were collected between February and December 2015, representing a total of 22 site visits and 72 separate face-to-face interviews with 73 informants. In addition, the research team undertook 11 preliminary telephone interviews with site leads.
For each site visit, a locally nominated site visit co-ordinator was contacted and key informants were agreed based on prior conversation with the medical director or mortality lead. These informants were to include (1) the chief executive officer (CEO), (2) the medical director, (3) the mortality lead (or relevant governance leads, as appropriate), (4) informatics and coding leads linked to mortality, (5) key leads and informants linked to mortality in the implicated clinical areas and (6) any other informants related to the trust’s programmes and structures relative to mortality reduction (e.g. patient safety, quality improvement and service development programmes). A schedule was developed for the site visit, giving individual interview timings (usually allowing at least 1 hour for each interview).
Before the site visit, invitation letters for participation (see Appendix 7), consent forms (see Appendix 8) and participant information forms (see Appendix 9) were circulated to all interviewees. Participants were assured of confidentiality and given the opportunity to ask questions at the start of each interview before they signed the consent form. Interviews lasted between 30 and 90 minutes (typically 50–60 minutes) and, with the participant’s consent, were recorded for later transcription. A small number (< 10) of participants were unavailable on the day of the site visit and these people were followed up with either subsequent visits or telephone interviews. One participant declined to have their interview recorded. Table 8 provides an overview of the site visit dates and the number of interviews conducted at each site.
| Site alert condition | Single/multiple alerts | Site visit dates | Number of interviews conducted |
|---|---|---|---|
| AMI | Multiple | 11 and 12 August 2015 | 7 |
| AMI | Single | 13 February and 1 July 2015 | 10 |
| AMI | Multiple | 9 March and 15 and 24 April 2015 | 6 |
| AMI | Multiple | 18 and 19 June 2015 | 7 |
| Sepsis | Multiple | 14 and 15 May 2015 | 8 |
| Sepsis | Single | 17 and 18 December 2015 | 5 |
| Sepsis | Single | 30 April and 21 July 2015 | 5 |
| Sepsis | Multiple | 12 March and 17 July 2015 | 4 |
| Sepsis | Multiple | 17 and 24 August 2015 | 7 |
| Sepsis | Multiple | 22 April 2015 | 4 |
| Sepsis | Multiple | 7 and 8 May 2015 | 8 |
Data collection followed standard practices for the conducting of semistructured qualitative research interviews. A comprehensive interview schedule was used as a guide during the interview (see Appendix 10), comprising 24 individual questions with prompts linked to the research questions and review of potential theoretical insights into institutional responses to mortality alerts. The interview started with broad introductory questions designed to frame the conversation and put respondents at ease. Subsequently, a chronological approach was taken to the discussion of the specific instances of alerts, starting with the context surrounding the first alert, the short-term response, longer-term developments following the alert(s) and finally the overall evaluation of mortality alerting from the respondent’s perspective. During the interview, care was taken not to lead the respondent, and a flexible approach was taken to the sequence and nature of topics explored in order to allow novel themes to emerge. Following initial responses to open questions, prompts were used to explore the themes raised in depth and to probe for relevance to mortality alerting mechanisms and processes. The site visit research team comprised two senior health service researchers with substantial experience in qualitative data collection and organisational research, and one junior researcher with expertise in medical sociology. The site visits and interviews were conducted with either one or two researchers present, and one or other of the senior researchers attended each site visit (95% of the interviews were conducted with a senior researcher present).
Data analysis
To fully explore the qualitative data related to institutional responses to mortality alerts at the case study sites, a number of parallel subanalyses were performed to address the main evaluative research questions, to explore themes linked to prior theory and to support the other areas of the study, such as the survey work. Figure 7 provides an overview of how the workstream 2 mixed-methods components and subanalyses inter-relate.
FIGURE 7.
Overview of the qualitative analysis process and main outputs from mixed-methods research, including input from multiple stakeholder perspectives into the interpretation of the cases and their theoretical significance, and the design of evaluative measures. DFI reps, Dr Foster Intelligence representatives.
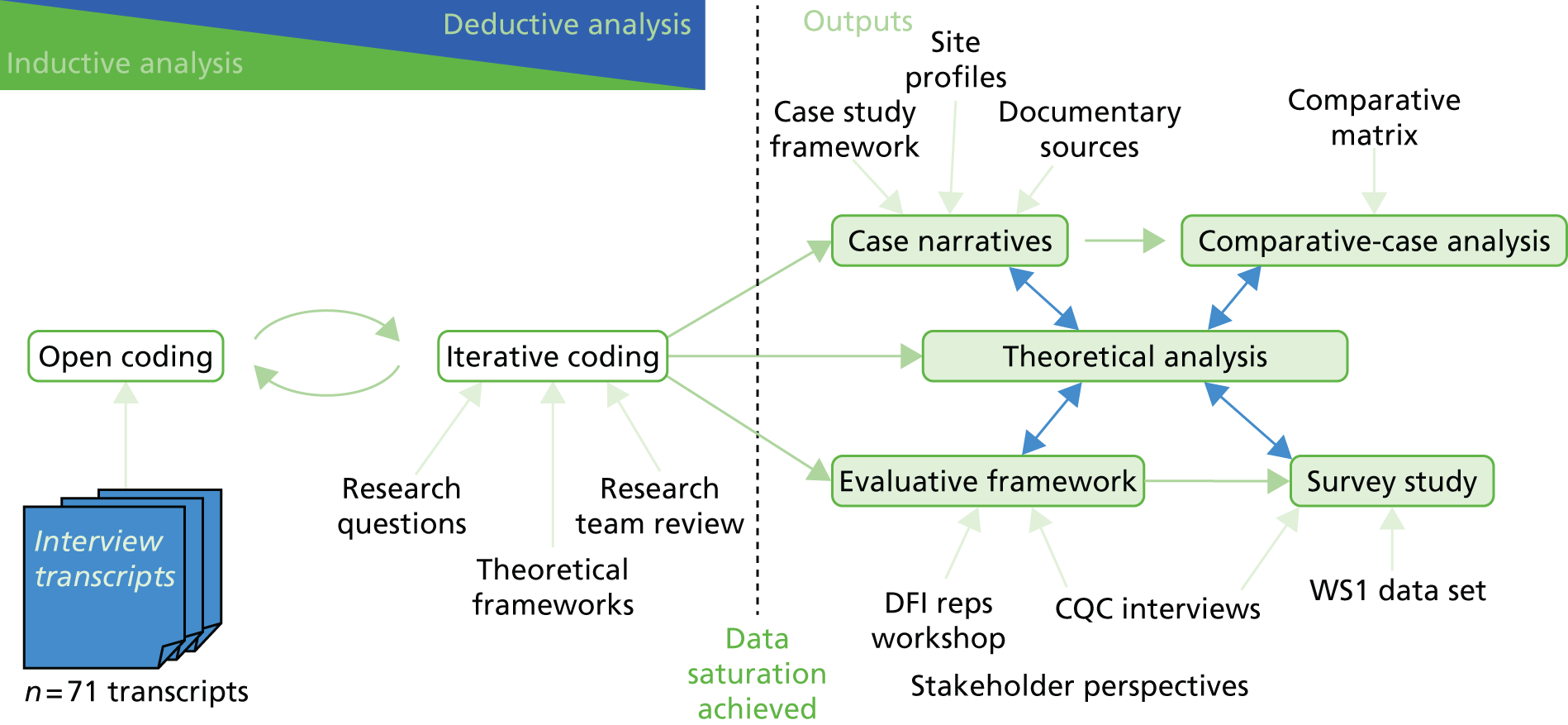
The main qualitative analysis work centred on the interpretation of the 11 institutional case studies conducted during the course of the programme. It was supported by input from five researchers with backgrounds in psychology, patient safety, sociology and health services research. Once the researchers were familiar with the data set, coding followed standard practices in qualitative research, drawing on grounded theory and framework analysis as methodological frame and the realist evaluative position as epistemological stance. Inductive open-coding was initially undertaken to thematically explore the data set and allow coding categories to emerge from the analysis (i.e. grounded in the data). Hierarchical categorisation was undertaken to begin to organise themes. As the coding framework moved towards data saturation (with fewer novel categories emerging), the coding incorporated increasingly iterative elements and deductive reasoning (i.e. established templates and frames developed in one area of the data set were applied to others), drawing on the constant comparative approach to iterate key definitions and distinctions. The later stages of refinement of coding were subject to repeated review and discussion among the broader research team, review of prior theory and structure imposed through the primary research questions and aims. NVivo software was used to support the initial and hierarchical coding, with some elements of the later stages of iterative refinement undertaken in word processor tables (using Microsoft Word;® Microsoft Corporation, Redmond, WA, USA).
Once iterative coding and category refinement had been initiated, the research team began to structure the data according to the key outputs required by the project. Adopting a realist evaluative stance, the aim of the analysis was to generate rich descriptions of how the alerts, as a form of feedback intervention, instigated interactions between local context, institutional behaviour and institutional outcomes (objectives 1 and 4). Initially, individual case narratives were produced that integrated testimony from informants within a single site in a historical narrative concerning the institutional response to the target alerts. A standardised template was used for the case narratives, including circumstances leading up to the first alert, short- and long-term responses and parallel evolution of the trust’s work on sepsis/AMI that was not directly attributable to the alert. Throughout the process, clinical, organisational and informatics perspectives were sought that had a focus on historical and factual content. A subsequent step was performing a thematic analysis of each case narrative in which the case was populated with salient quotations from the data set, as well as an interpretative researcher commentary, in preparation for comparative analysis.
Following the development of the individual case narratives, the analysis moved to an integrative mode in order to allow inference and interpretation to be drawn across the whole data set, and used a comparison of the cases to identify important areas of internal/external context and organisational behaviour relative to effective responses to signals in mortality data. Here, an evaluative perspective was gained through the reported perceptions and views of experienced informants concerning what worked in their organisations. The ‘effectiveness’ of specific characteristics was, therefore, inferred through reported links to mechanisms/processes and outcomes that were regarded by informants as representative of adaptive or capable organisational responses to signals in mortality data. The integrative analysis took two principal forms: (1) a cross-case comparative analysis in which case-based observations were combined and interpreted against the core sampling criteria (e.g. a comparison of sepsis and AMI alerting sites and a comparison of single and multiple alerting sites), and (2) the development and validation of an evaluative framework for institutional capacity to respond to signals in mortality data.
The evaluative framework analysis was based on the 73 interviews from the main qualitative study, with additional stakeholder engagement activity. The qualitative analysis approach used was deductive framework analysis so that potential evaluative dimensions for institutional behaviour could be described. In parallel to the interviews, workshops were conducted with Dr Foster Intelligence and the CQC to develop and refine understanding of the mortality alert process and to gain additional perspectives on the emergent findings: specifically, validation of the emergent framework and perspectives related to what constitutes mature and effective institutional arrangements for mortality governance and response to signals in mortality data. Qualitative data were analysed using the framework method, in which both inductive and deductive reasoning were combined to develop and iterate key themes and subthemes. Based on initial open-coding and the early-stage iterative refinement of categories, nine broad themes were identified to serve as a frame for further exploration in the data set. Multiple perspectives were incorporated throughout the analysis process through regular review and discussion across the research team, which consisted of two psychologists, a sociologist and a health-care manager with expertise in patient safety. The resulting thematic analysis was used to structure early versions of the survey instrument used within workstream 2 in order to ensure that response items and scales were both thematically balanced and theoretically grounded in the emerging perspectives on effective institutional responses.
To produce an integrated interpretation from the workstream 2 subanalyses, and to support practical outputs and guidance for future work in this area, the final stage in the analysis was to develop a model of MASSs as a complex intervention. A model framework was developed to accommodate key classes of variables (internal and external context, institutional preconditions, organisational behaviour, and intermediary and target outcomes). The overall approach to sense-making through the workstream 2 qualitative analysis was, therefore, to surface interactions between mechanisms (predominantly organisational behaviour), context (internal structure and external environment) and outcomes linked to institutional capacity for the reduction of avoidable mortality, in accordance with the realist position on complex interventions.
National cross-sectional survey
To provide insight into the broader patterns of organisational behaviour related to mortality and the institutional response to signals in mortality data, a national cross-sectional survey study was undertaken as the culmination of the workstream 2 research. The principal aims of the survey study were threefold:
-
to categorise and quantify organisational behavioural and contextual aspects of the response to alerts, specifically to explore the relationships between type and frequency of alerting, key contextual and organisational behavioural characteristics and intermediate outcomes
-
to identify and prioritise the main drivers of effective institutional responses to mortality alerts, as perceived by trust mortality leads
-
to quantify mortality lead perceptions of the current adequacy of the mortality surveillance and alerting system.
Design of the survey instrument
The survey instrument was developed based on insights from the qualitative case study data and with input from key stakeholders, including Dr Foster site co-ordinators, CQC mortality outlier programme leads, reviewers and analysts, and input from the research project strategic steering group, including feedback from the public and patient representatives. The analysis of the qualitative data was used to inform the development of a structured evaluative instrument. To do this, the core dimensions of the emergent evaluative framework were used to guide the formation of a number of candidate survey items. These items were iterated to address any issues associated with, for example, duplication and wording. This resulted in a number of iterations of the survey, which were continuously built on until the final survey instrument emerged.
The final survey contained both quantitative and free-text items. The quantitative items included categorical, ordinal and scale-based items, while the free-text items allowed for qualitative expansion and further detail. The survey was made up of seven sections, which are outlined in Table 9.
| Section | Description |
|---|---|
| Section 1: about you and your role | Basic demographic items about the individual completing the survey and their role within the trust |
| Section 2: organisational arrangements for mortality | Items on the trust’s governance structure for monitoring mortality |
| Section 3: coding, data and information for mortality | Items on the processes through which coding and information are used to support mortality |
| Section 4: mortality review | Items on the approach that a trust takes to reviewing mortality, both in response to a specific mortality alert and more generally |
| Section 5: responding to Imperial/CQC mortality alerts | Items on trust processes for developing actions and improvement mechanisms in response to an externally generated alert |
| Section 6: institutional capacity to respond to signals in mortality data | Scale items based on the evaluative framework to represent a trust’s overall capacity to respond to signals in mortality data |
| Section 7: evaluation of mortality alerts and surveillance | Items that allow respondents to express their overall views on the effectiveness of the mortality alerts and surveillance system |
Validation of the survey instrument
A piloting process was undertaken in which a number of key individuals were given the opportunity to comment on and contribute to the development of the survey items and the way in which these items were presented and structured for respondents. A number of methods were employed to support the piloting process, including the cognitive walkthrough/think-aloud method with a local mortality lead, the circulation of the survey by e-mail to key stakeholders and a focused discussion during project advisory and steering group meetings.
Data collection
Survey data collection opened on 11 May 2016 and closed on 10 June 2016. Only one response was required from each invited trust, with the target respondent the trust mortality lead or medical director. An initial personalised contact letter and a paper-based copy of the survey were circulated to all trusts that had received an Imperial College mortality alert (120 trusts). Multiple personalised follow-up e-mails were sent out directly to medical directors, and an electronic version of the survey was made available on request. A total of 78 survey responses were received, which represents a 65% response rate.
Analysis
All survey responses were entered manually into SPSS version 22 (IBM Corporation, Armonk, NY, USA) in preparation for analysis. To ensure that all research questions could be answered, a number of secondary metrics were created based on external data, and these were incorporated into the master database:
-
total number of Imperial College alerts sent (2007–16)
-
total number of CQC alerts sent (2011–13)
-
interval between information request date and first response date for most recent alert in CQC database
-
interval between information request date and last response date for most recent alert in CQC database
-
total length of investigation for most recent alert in CQC database
-
HSMR data (2012)
-
SHMI data (2015).
The following steps were then taken, in line with the research questions.
-
A missing data analysis was conducted to ensure that there were no significant differences between invited trusts that responded and invited trusts that did not.
-
Descriptive statistics were run to categorise and quantify organisational behavioural and contextual aspects of the response to alerts.
-
Aggregated scales were computed for specific sections of the survey (including subscales of the evaluative framework).
-
Inferential statistics were run to classify and quantify the relationships between type and frequency of alerting, key contextual and organisational behavioural characteristics and intermediate outcomes.
-
A simple thematic approach was employed to analyse the free-text data. All data fragments were grouped and categorised in relation to the key research questions.
Chapter 6 Results from workstream 1: quantitative analysis of alerts
This chapter reports results from workstream 1 of our mortality alert evaluation project. First, we focus on a descriptive analysis of the mortality alerts; next, we investigate the association of mortality alerts with other measures of quality; and, finally, we analyse the association of mortality alerts with subsequent trends in the risk of death.
Descriptive analysis of alerts
Descriptive analysis of the Imperial College mortality alerts
Between April 2007 and December 2014, 690 alerts were generated by the Imperial College mortality surveillance system, of which 532 (77%) were sent to alerting trusts. All alerts were sent to the CQC for information. On average, 66 alerts were sent each year and 18 were withheld. The number of alerts appears to have decreased over time, from an average of 80 in the first full 3 years (2008, 2009 and 2010) to 54 in the most recent 3 years (2012, 2013 and 2014). In 2014, only 40 alerts were sent. Of the 28 acute NHS trusts that never received an alert, three underwent a merger or closed during the lifetime of the mortality alert programme, so their time ‘at risk’ of an alert may be lower. Of the trusts that did receive an alert (n = 139), 27 (19.4%) were involved in mergers with other acute trusts or have closed. One hundred (18.8%) alerts were sent to trusts that had, at some point, been affected by a merger or closure.
‘Septicaemia (except in labour)’ was the most commonly alerting CCS group, with 72 alerts (61 sent) that accounted for 11.5% of all sent (Table 10). Some trusts received multiple alerts for the same diagnosis or procedure group. The most common source of repeat alerts was ‘coronary artery bypass graft (CABG) (other)’; one trust received five such alerts (‘other’ in this case means not first-time, isolated CABG and includes revisions and cases with heart valves involved in the procedure). A total of 61% (14/23) ‘CABG (other)’ alerts were repeat alerts. Repeat alerts constituted 67% (41/61) of the sepsis alerts. Urinary tract infections also resulted in a high number of repeat alerts, making up 56% of the 18 alerts for this diagnosis.
| Alerts, n (%) | |
|---|---|
| Diagnosis and procedure group | |
| Septicaemia (except in labour) | 61 (11.5) |
| Coronary atherosclerosis and other heart disease | 27 (5.1) |
| CABG (other) | 23 (4.3) |
| AMI | 18 (3.4) |
| Fluid and electrolyte disorders | 18 (3.4) |
| Liver disease alcohol related | 18 (3.4) |
| Urinary tract infections | 18 (3.4) |
| Intestinal obstruction without hernia | 17 (3.2) |
| Acute and unspecified renal failure | 15 (2.8) |
| Peripheral and visceral atherosclerosis | 15 (2.8) |
| Other groups | 302 (56.8) |
| Diagnosis or procedure | |
| Diagnosis | 406 (76.3) |
| Procedure | 126 (23.7) |
| Year | |
| 2014 | 40 (7.5) |
| 2013 | 57 (10.7) |
| 2012 | 65 (12.2) |
| 2011 | 84 (15.8) |
| 2010 | 62 (11.7) |
| 2009 | 101 (19.0) |
| 2008 | 76 (14.3) |
| 2007 | 47 (8.8) |
| Five top-alerting trusts | |
| A | 17 (3.2) |
| B | 13 (2.4) |
| C | 11 (2.1) |
| D | 11 (2.1) |
| E | 10 (1.9) |
Some trusts received multiple alerts. Thirty trusts received only one alert, 109 trusts received two or more alerts and 28 acute NHS trusts received no alerts.
Descriptive analysis of Care Quality Commission investigations into the Imperial College mortality alerts
There was a total of 206 alerts between 2011 and 2013. The alerts were first reviewed by CQC analysts, who compiled a report using CQC data on the trust. At this stage, 46 cases (22%) were not pursued by the CQC and these were closed; 154 cases (75%) were pursued by the CQC and requests were made for the trust to investigate the alert; six cases (3%) were trusts that were already being investigated; and one alert in 2012 appears to have been marked as sent by Imperial College and as not sent by the CQC, and was not pursued.
On average, cases were open with the CQC for 21 weeks, which is the number of weeks from the date on the mortality alert letter to the end of the CQC investigation. The longest case that we reviewed was 59 weeks, and the shortest case was pursued for 5 weeks. Ninety per cent (139/154) of pursued cases reported results of a clinical audit to the CQC. Most of the local investigations focused on the period during which the alert was generated. On average, these reports included details of 28 patients per alert. In total, 3856 sets of patient notes were reviewed between 2011 and 2013 as a result of the mortality alerting programme.
We found that investigations at the trusts were not standardised and that trusts investigated alerts according to local practice. Findings from the CQC investigations included themes relating to coding, case mix and quality of care. Areas of care were determined as ‘could be improved’ in 70% (108/154) of the alerts pursued by the CQC; however, when care was identified as a problem, only some trusts assessed that care was likely to have affected mortality. According to trust reports, deficiencies in care may have affected mortality in 27% (42/154) of the pursued alerts. Figure 8 displays findings from the CQC investigations. Overall, most trusts found areas that could be improved within their care pathways and, subsequently, started implementing action plans to address the issues. Full action plans were created in 64% (98/154) of the cases after the initial pursuit and in 77% (118/154) by the time the cases were closed. When care was identified as an issue, 85% of cases (92/108) resulted in an action plan.
FIGURE 8.
The CQC findings from alerts following trust reviews.
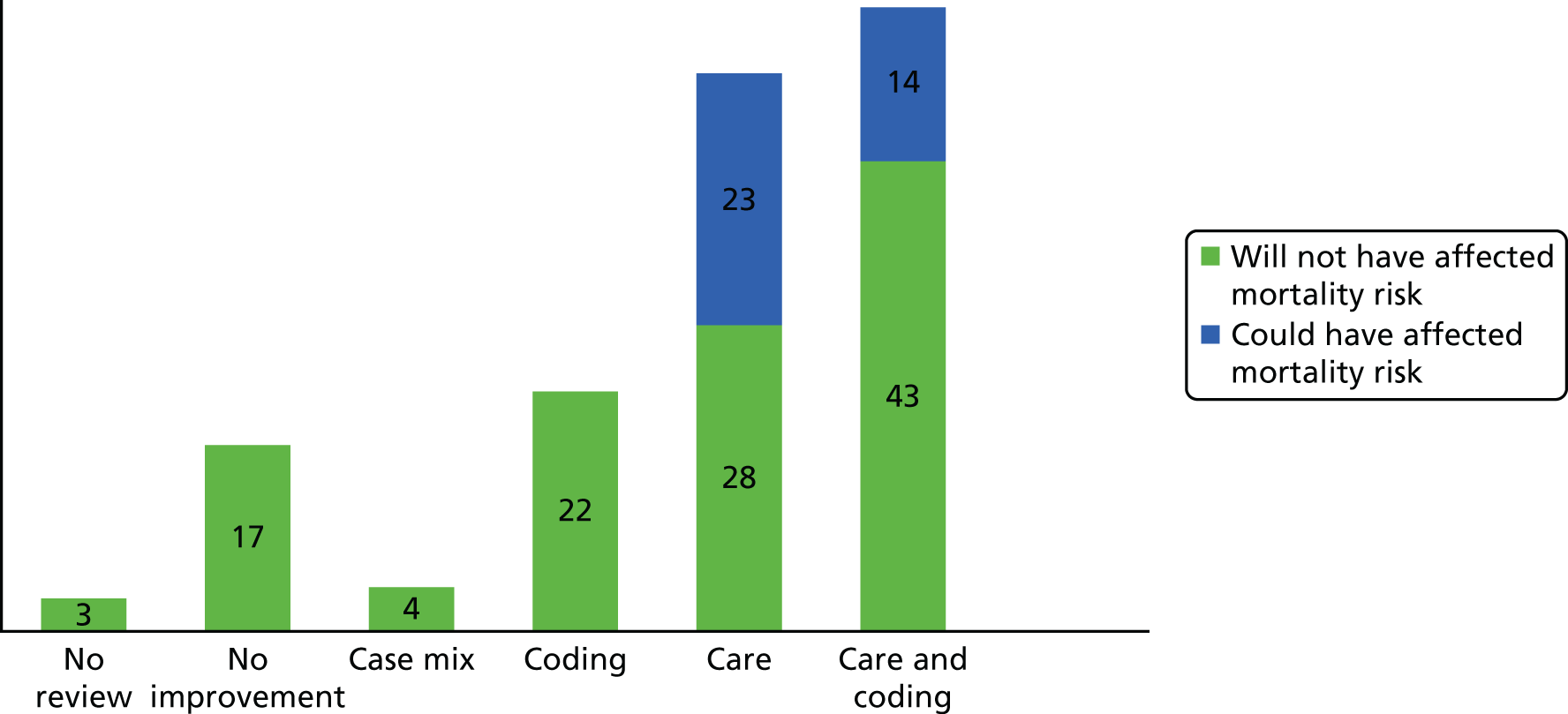
Trusts that alerted for sepsis were more likely to have had a trust assessment that identified care as problem within the trust than trusts that alerted for other diagnoses/procedures. Of the 19 alerts for sepsis, care was identified as a problem in 17 (89%) (Table 11), while for all other diagnosis/procedures care was identified in 67% of cases (91/135) (Pearson’s χ2 = 0.049).
| Type of alert | No review | No improvement required | Case mix | Coding | Care | Care and coding |
|---|---|---|---|---|---|---|
| Sepsis | 0 (0.0%) | 1 (5.3%) | 0 (0.0%) | 1 (5.3%) | 10 (52.6%) | 7 (36.8%) |
| Other | 3 (2.2%) | 16 (11.9%) | 4 (3.0%) | 21 (15.6%) | 41 (30.4%) | 50 (37.0%) |
Changes to coding following an alert
The previous section highlighted that coding was considered one of the major reasons for an alert. We investigated changes in trusts’ coding by comparing numbers recorded in alert letters with a further analysis of a finalised HES extract for the same period for AMI and sepsis.
A total of 11 alert letters for AMI, dated between April 2011 and December 2013, were sent to NHS trusts in England. All trusts that received a mortality alert letter appeared to amend their coded data. Five trusts increased the number of admissions for AMI and six trusts decreased the number. Table 12 shows descriptive statistics on the number of trust admissions; the number of deaths; the expected deaths and relative risks for AMI (and sepsis) before receipt of an alert letter; and the absolute and relative changes after an alert letter. There were more changes in the coding of an AMI admission when the outcome was death. There was, on average, a 2.9% fall in the number of deaths coded as AMI, compared with an average 0.3% fall in overall AMI coded admissions. The relative risk of AMI death increased, on average, by 1% in alerting trusts after changes in coding.
| AMI (n = 11) | Sepsis (n = 19) | |||
|---|---|---|---|---|
| Min., max. | Median (IQR) | Min., max. | Median (IQR) | |
| Admissions | ||||
| Counts: alert lettera | 144, 992 | 377 (331 to 497) | 52, 298 | 171 (112 to 231) |
| Counts: HESb extract | 149, 741 | 376 (268 to 545) | 52, 288 | 145 (103 to 217) |
| Absolute change | –251, 48 | –1 (–29 to 5) | –98, 3 | –6 (–14 to –1) |
| Relative change (%) | –26.5, 9.7 | –0.3 (–4.6 to 1.3) | –48.3, 1.7 | –3.4 (–11.5 to –0.4) |
| Deaths (observed) | ||||
| Counts: alert lettera | 22, 99 | 61 (52 to 78) | 29, 107 | 72 (44 to 82) |
| Counts: HESb extract | 18, 81 | 60 (45 to 76) | 25, 103 | 46 (34 to 81) |
| Absolute change | –23, 3 | –2 (–7 to 0) | –38, 2 | –3 (–12 to 0) |
| Relative change (%) | –36.1, 3.8 | –2.9 (–18.2 to 0.0) | –60.3, 2.7 | –3.7 (–21.1 to 0.0) |
| Deaths (expected)c | ||||
| Alert lettera | 12.4, 74.4 | 36.9 (34.1 to 52.4) | 15.2, 85.7 | 48.1 (32.8 to 67.2) |
| HESb extract | 12.4, 57.7 | 36.4 (30.0 to 48.9) | 14.1, 69.7 | 36.8 (21.9 to 57.0) |
| Absolute change | –17.8, 0.9 | –1.2 (–3.6 to 0.2) | –20.0, –0.6 | –6.4 (–13.5 to –3.3) |
| Relative change (%) | –26.8, 1.8 | –4.0 (–10.3 to 0.5) | –47.3, –1.1 | –15.6 (–19.8 to –7.1) |
| Relative riskd | ||||
| Alert lettera | 133, 177 | 156 (141 to 167) | 118, 191 | 134 (127 to 150) |
| HESb extract | 133, 173 | 147 (139 to 166) | 109, 205 | 141 (135 to 149) |
| Absolute change | –31, 10 | 1 (–7.9 to 3) | –37, 26 | 7 (0.3 to 19) |
| Relative change (%) | –17, 7 | 1 (–5.6 to 2) | –25, 18 | 5 (0.2 to 12) |
A total of 19 alert letters for sepsis, dated between April 2011 and December 2013, were sent to 17 trusts. Two trusts received two alert letters over the study period. Two trusts did not change their data; two trusts increased the number of admissions coded as sepsis; and 15 trusts decreased the number of admissions after receiving an alert letter. On average, the relative changes in coding were greater when the admission was coded as sepsis than when it was coded as AMI. The relative risk of sepsis death increased, on average, by 5% in alerting trusts after changes in coding.
The relative (%) changes are shown graphically in Figure 9. Although there was a decrease, on average, in the number of admissions and deaths coded as sepsis, the expected number of deaths also decreased, whereas the average relative risk of death increased.
FIGURE 9.
Relative (%) changes in AMI and sepsis coding between time of alert and time of annual publication of HES data for number of admissions, deaths and relative risk. (a) Relative changes for AMI; and (b) relative changes for sepsis.
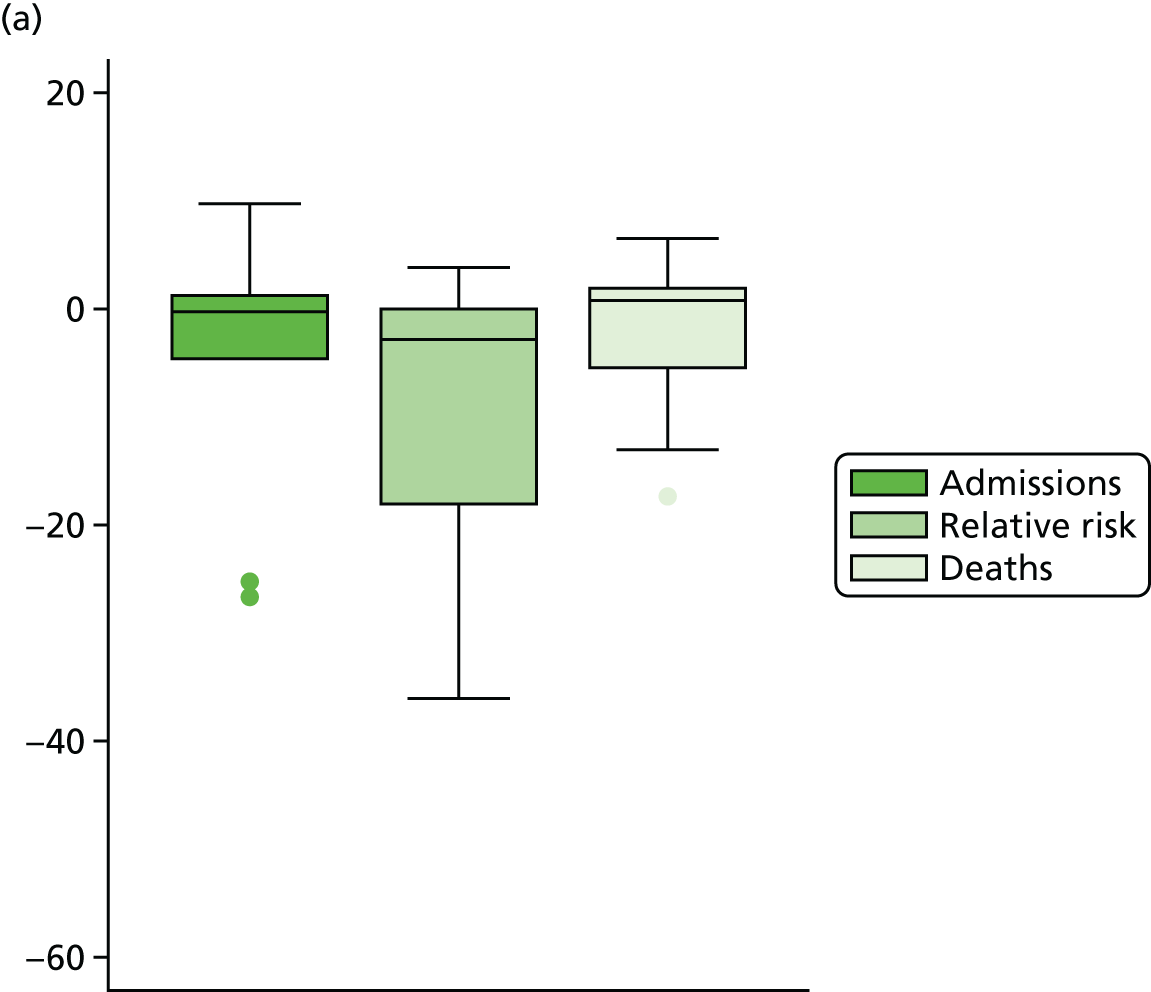
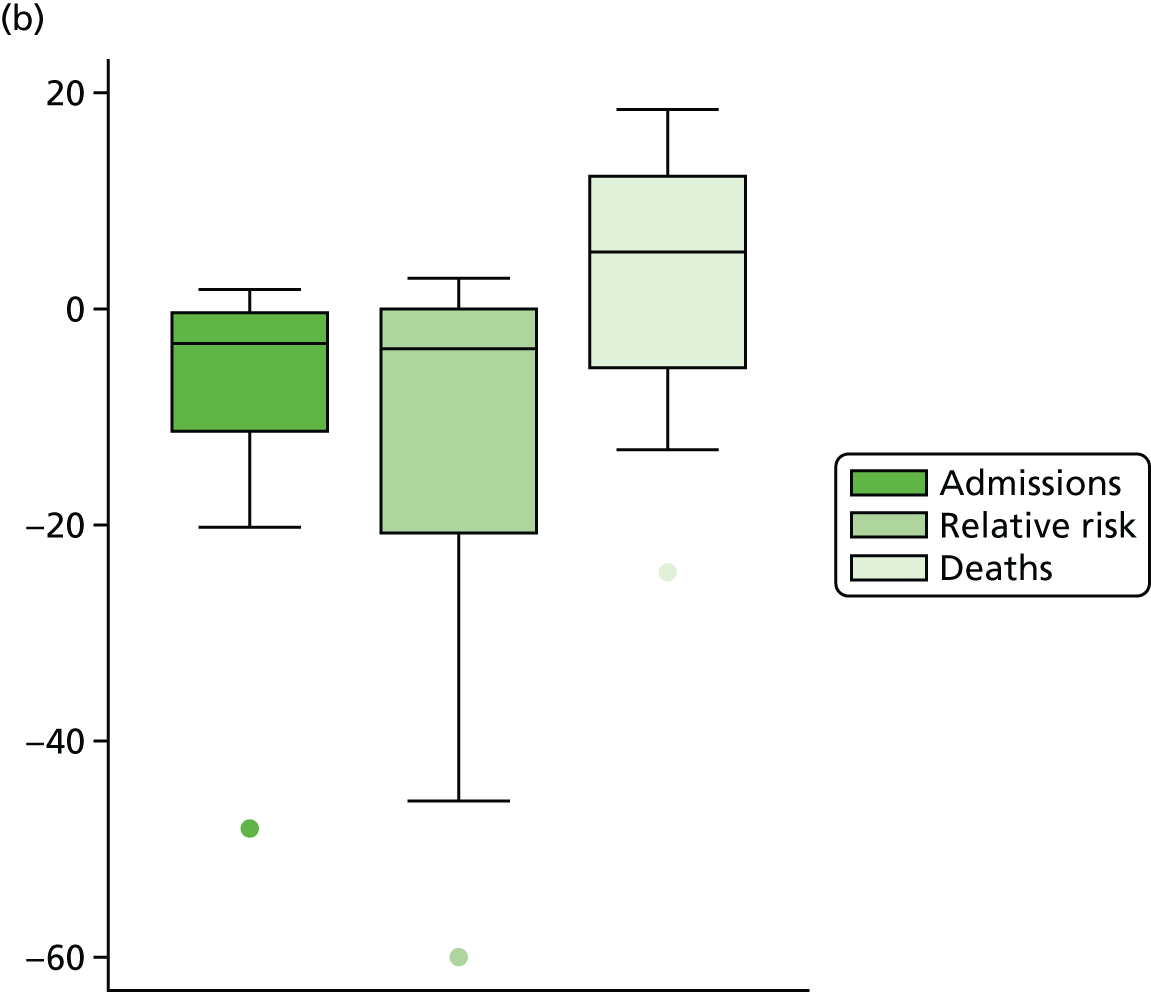
Investigation of mortality alerts and other measures of quality
We aimed to explore whether or not mortality alerts are associated with other indicators of quality of care. A priori, we chose a range of structure, process and outcome data that might be related to our alerts. We examined data for a total of 161 acute NHS trusts in England during the study period. There were 160 acute trusts in 2011, 161 acute trusts in 2012 and 158 acute trusts in 2013.
Acute bed occupancy
Data were available for 157 trusts (98%). The minimum proportion of trust beds occupied was 33% in the Birmingham Women’s and Children’s NHS Foundation Trust, and the maximum proportion was 100%, with a median (interquartile range) of 88 (83–92), highlighting the skewed nature of the data (Figure 10).
FIGURE 10.
Proportion of beds occupied overnight (by quarter) in general and acute wards, by trusts with a single and with multiple AMI and sepsis alerts, 2011–13, in England. (a) Single alert; (b) multiple alerts; (c) AMI; and (d) sepsis.
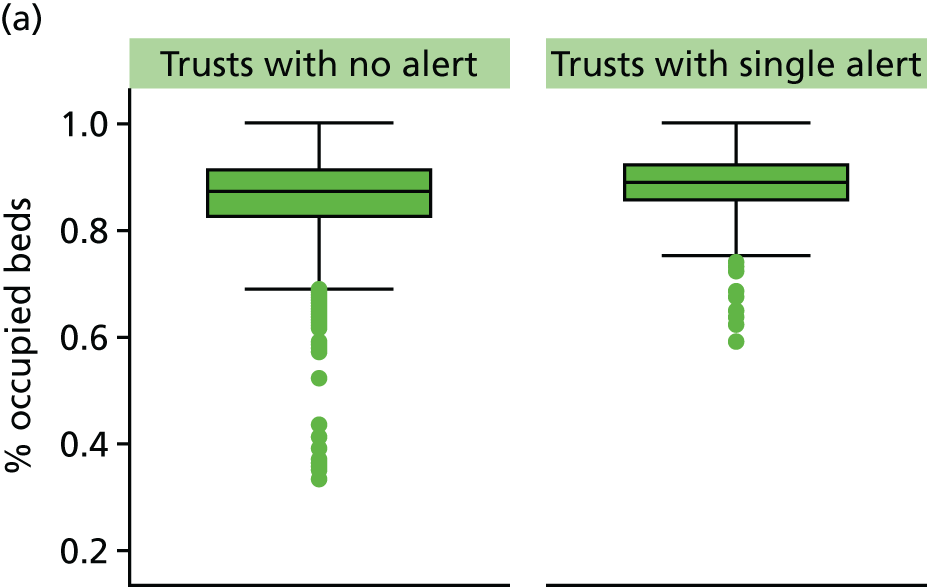
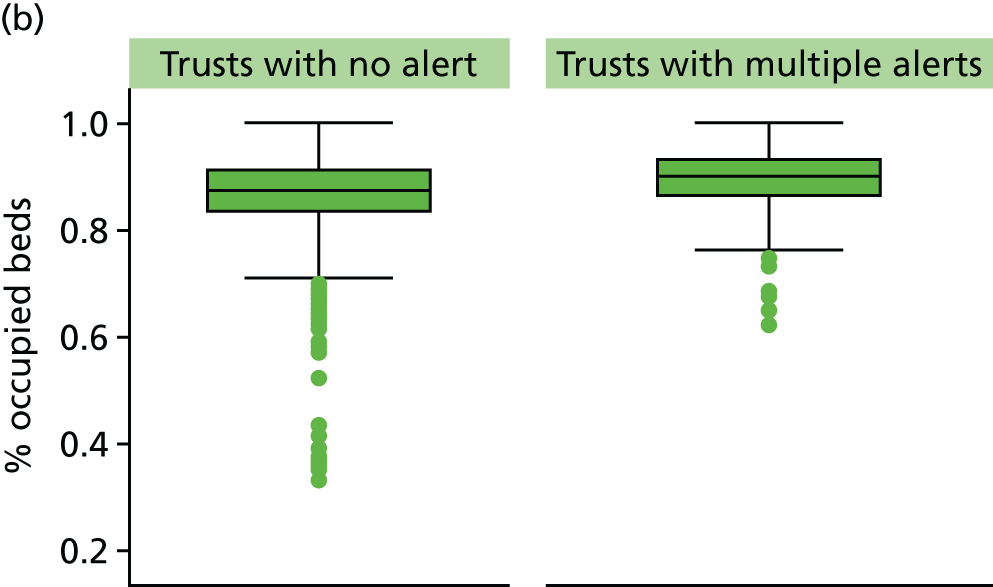
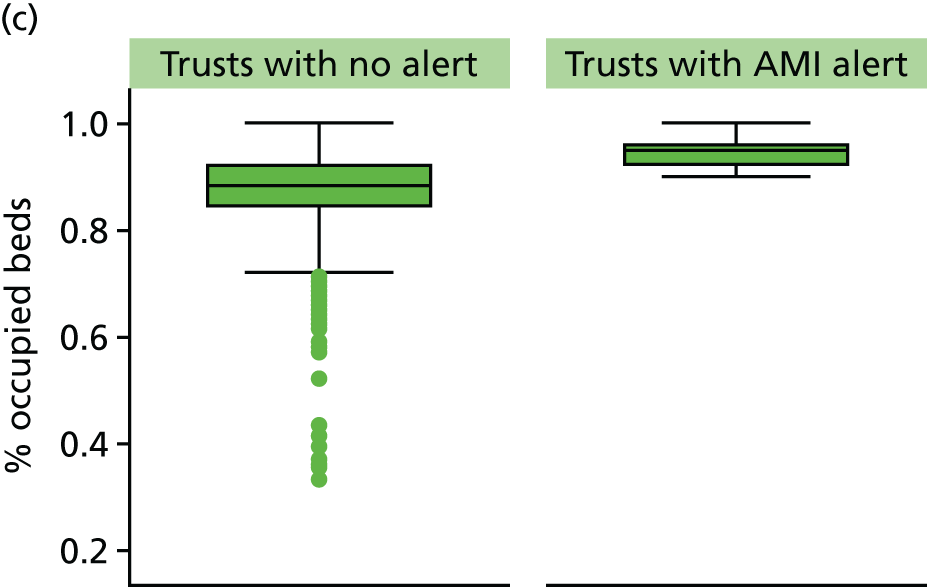
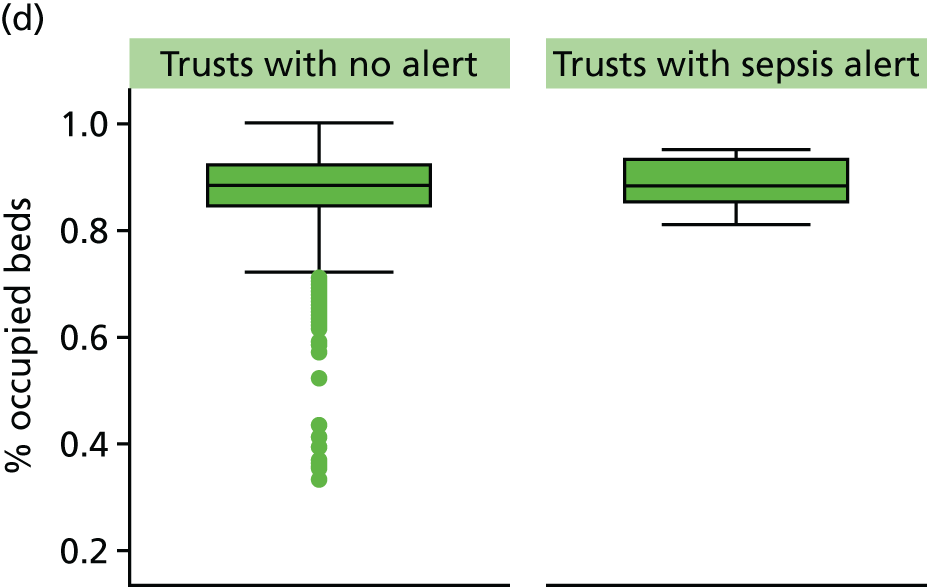
In the quarter when the alert occurred, trust-level acute bed occupancy rates were, on average, 2.2 percentage points higher in alerting than in non-alerting trusts (p = 0.001). In the same quarter as an AMI alert, acute bed occupancy rates were on average 7.7 percentage points higher (p < 0.001) in alerting than in non-alerting trusts. On average there was no strong evidence that trusts alerting for sepsis differed from non-alerting trusts (p = 0.063). Acute bed occupancy was on average 2.8 percentage points higher (p = 0.016) in single alerting and 2.7 percentage points higher (p = 0.001) in multiple alerting trusts than in trusts that had not had an alert during the study period. Cubic transformation, to normalise the distribution, found similar estimated differences.
Nurse-to-bed ratio
Nurse-to-bed ratio data were available for 157 trusts (98%). Trust-level nurse-to-bed ratios ranged from 0.3 to 6.6. The minimum value was an outlier; all other ratios were greater than one nurse to every bed. In the same quarter as an alert, nurse-to-bed ratios were on average 0.28 points lower in alerting than in non-alerting trusts (p < 0.001). Nurse-to-bed ratios were not, on average, lower in trusts with an alert for AMI; however, trusts alerting for sepsis had a nurse-to-bed ratio on average 0.38 points lower (p < 0.001). Nurse-to-bed ratios were on average 0.5 points lower in trusts with a single alert (p = 0.001) and 0.3 points lower in trusts with multiple alerts (p = 0.006) than in trusts that had not had an alert during the study period. Nurse-to-bed ratios increased over the study period by 0.08 points per year (p < 0.001). The box plots in Figure 11 graphically display the distribution of the trust nurse-to-bed ratios in alerting and non-alerting trusts.
FIGURE 11.
Nurse-to-bed ratio (by quarter), in acute trusts with a single, multiple, AMI and sepsis alerts, 2011–13, in England. (a) Single alert; (b) multiple alerts; (c) AMI; and (d) sepsis.
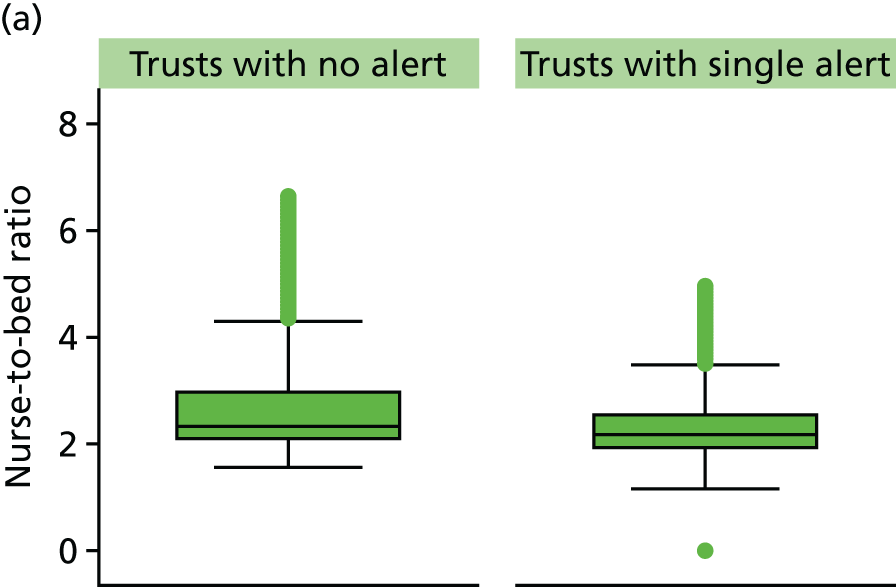
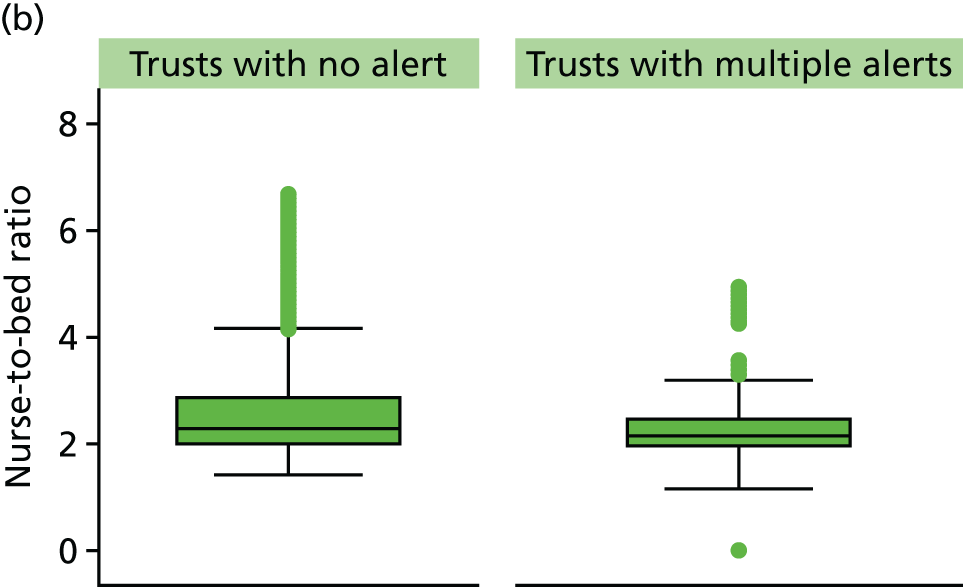
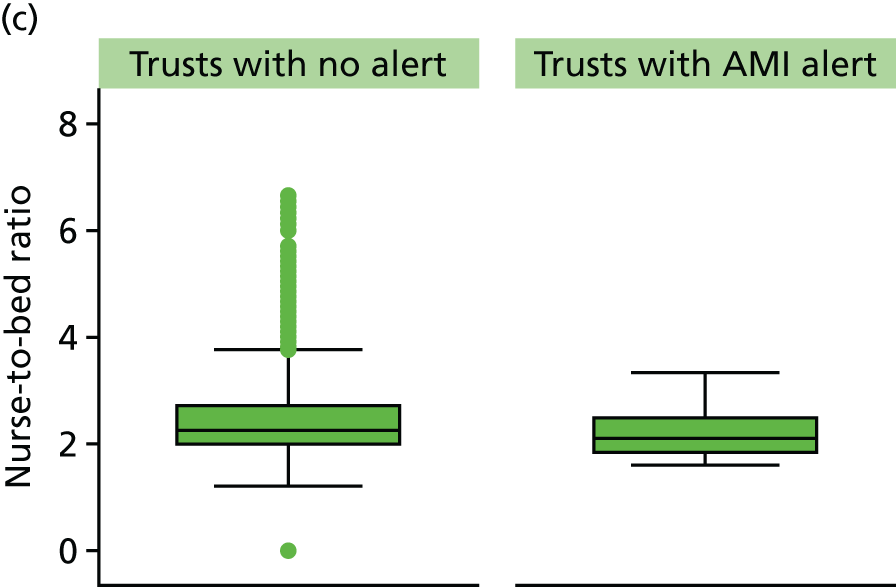
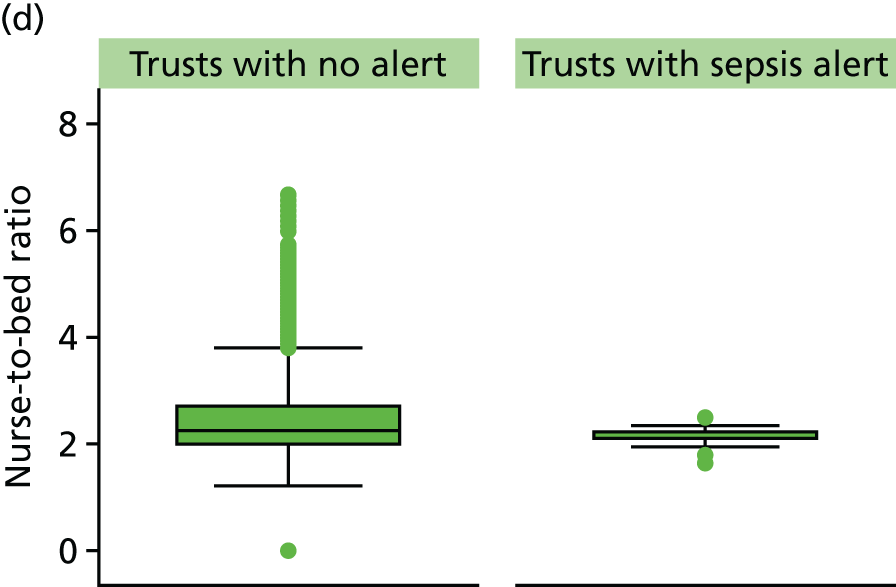
The model coefficients were exactly the same after a sensitivity analysis was carried out that removed the outlier.
Trust financial data
Trust financial data were available for 161 (100%) acute trusts. The number of trusts that were in deficit (by the end of the financial year) increased over the study period, from 14.4% (23/160) in 2011/12 to 34.2% (54/158) by 2013/14.
There was evidence of an association between alerting trusts and their financial position; 26% of trusts that had alerted during the study period were in deficit, while only those 13% of trusts that had never had an alert were in deficit. The RR of being in deficit if the trust had alerted, compared with those trusts that had not alerted, was 2.33 (95% CI 1.24 to 4.12; p = 0.009).
General Medical Council National Training Survey
General Medical Council National Training Survey data were available for 153 acute NHS trusts (95%).
Trust-level trainee satisfaction scores were on average lower in alerting than in non-alerting trusts. Variability was too high to establish a statistically significant difference between alerting and non-alerting trusts for all alerts; however, there was an association between trusts that alerted for AMI and non-alerting trusts.
NHS Litigation Authority
NHS Litigation Authority data were available for 156 acute NHS trusts (97%). There was no statistically significant evidence that risk assessment achievement differed between alerting and non-alerting trusts.
Myocardial Ischaemia National Audit Project
Data were available from 64 acute trusts on the proportion of patients who received PCI within 90 minutes of arrival. The proportion ranged from 78% to 100%. There was no evidence that the proportion of patients who received PCI within 90 minutes differed between alerting and non-alerting trusts. With only two AMI alerts between 2012 and 2013 in this study, we could not analyse the relation between AMI alerts and the proportion of patients receiving PCI within 90 minutes.
National Inpatient Survey
National Inpatient Survey data were available for 153 acute NHS trusts (95%). Trust-level patient satisfaction scores ranged from 67.4% to 88.2%. In the year of an alert, trust-level patient satisfaction scores were on average 1.3 percentage points lower in alerting than in non-alerting trusts (p = 0.002). There was no evidence of an association between the year of an AMI or sepsis alert and patient satisfaction scores (p = 0.065 and p = 0.085, respectively).
Patient satisfaction scores were on average 1.47 percentage points lower in trusts with a single alert (p = 0.015) and 1.58 percentage points lower in trusts with multiple alerts (p = 0.001) than in trusts that had not had an alert during the study period.
The box plots in Figure 12 graphically display the distribution of the trust patient satisfactions scores in alerting and non-alerting trusts.
FIGURE 12.
Patient satisfaction scores (%) in acute trusts with a single, multiple, AMI and sepsis alerts, 2011/12–2012/13, in England. (a) Single alert; (b) multiple alerts; (c) AMI; and (d) sepsis.
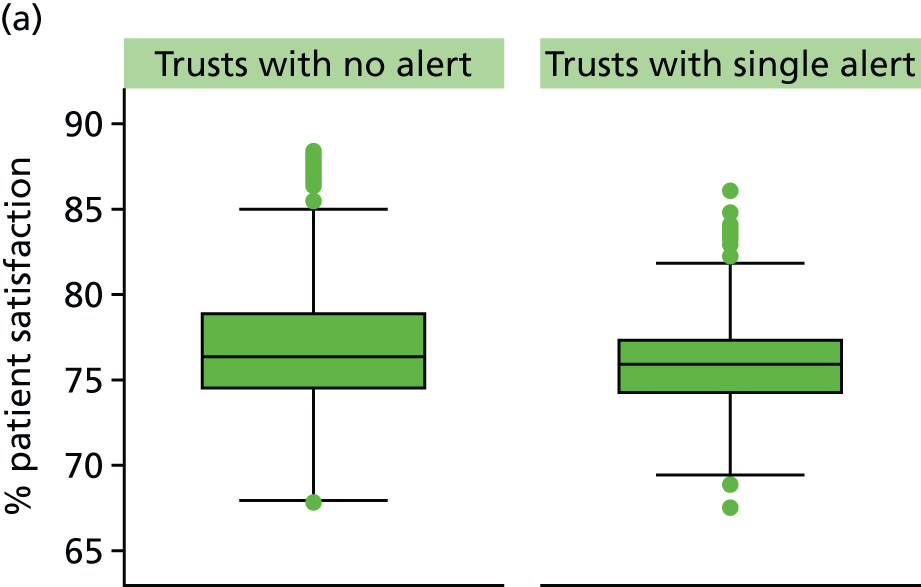
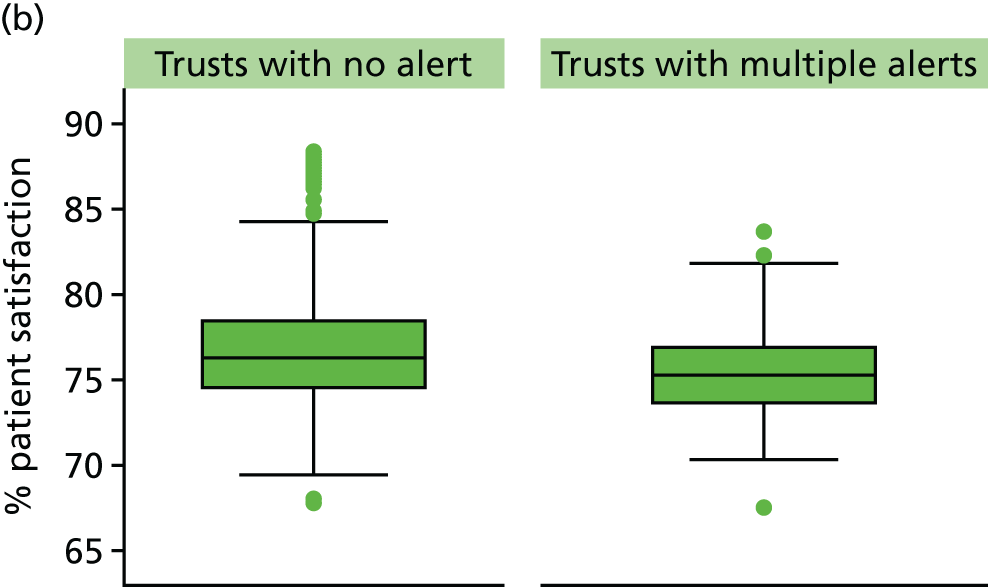
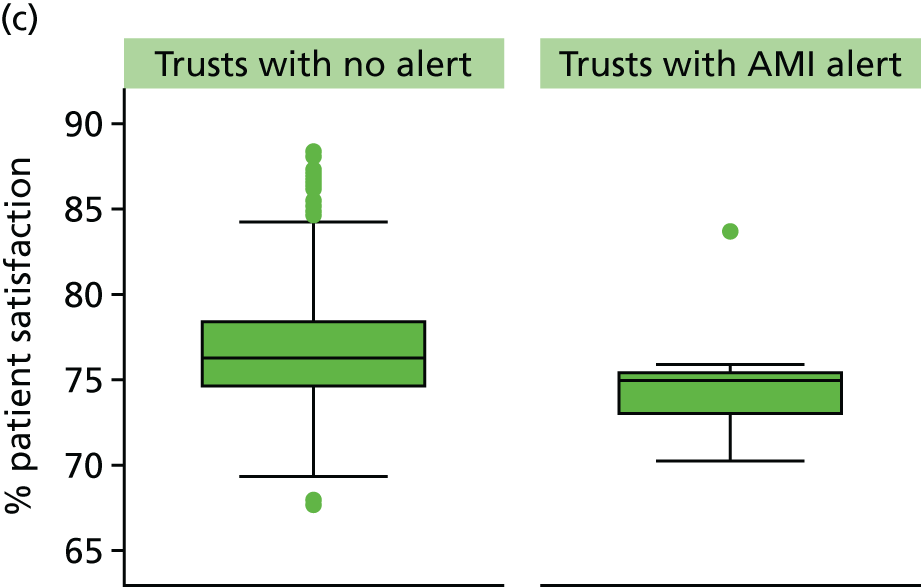
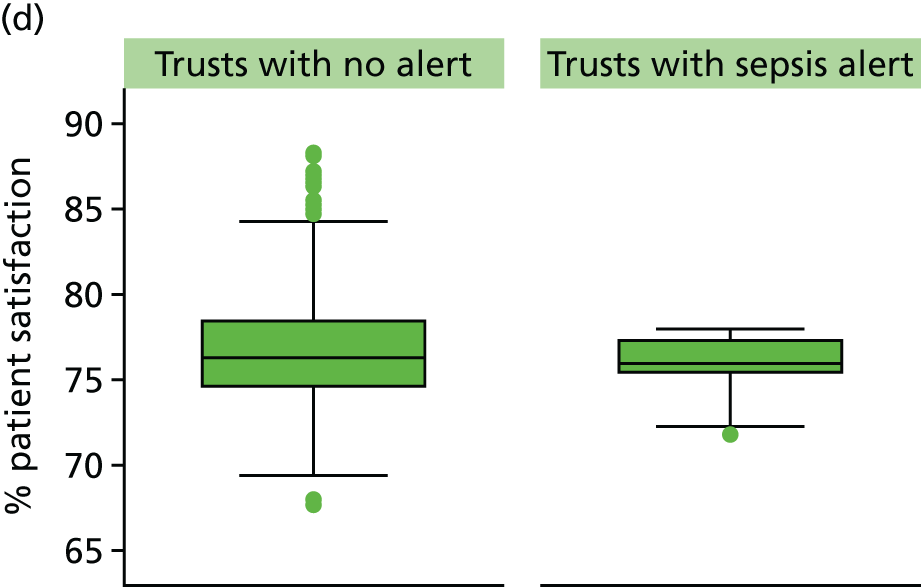
Patient Safety Thermometer
Patient Safety Thermometer data were available for 149 acute NHS trusts (92%). In these data, 62 trusts had received an alert in 2012/13 or 2013/14. However, only 56 trusts matched up with alert data. Data were missing for six trusts in the month of an alert. The proportion of patients harmed per month ranged from 0% to 54%. There was no evidence of a difference in the proportion of patients harmed between alerting and non-alerting trusts.
Standardised hospital mortality index
Standardised hospital mortality index data were available for 139 acute trusts (86%). Data were missing for specialist trusts, for example the Royal Brompton & Harefield NHS Foundation Trust, which specialises in cardiothoracic care. Trust-level SHMIs ranged from 0.62 to 1.25. In the year in which an alert occurred, trust-level SHMIs were, on average, 0.06 points higher in alerting than in non-alerting trusts (p < 0.001).
In the same year as an AMI alert, trust-level SHMI were, on average, 0.1 points higher (p = 0.022); however, after adjusting for FDR (see Multiple statistical testing), there ceased to be a statistically significant difference. In the year of a sepsis alert, trust-level SHMIs were, on average, 0.06 points higher than non-alerting trusts (p < 0.001).
The SHMI scores were, on average, 0.07 points higher in trusts with a single alert (p < 0.001) and 0.7 points higher in trusts with a multiple alerts (p < 0.001) than in trusts that had not had an alert over the study period. The box plots in Figure 13 graphically display the distribution of the trust SHMI scores in alerting and non-alerting trusts.
FIGURE 13.
Standardised hospital mortality indexes in acute trusts with a single, multiple, AMI and sepsis alerts, 2011/12–2013/14, in England. (a) Single alert; (b) multiple alerts; (c) AMI; and (d) sepsis.
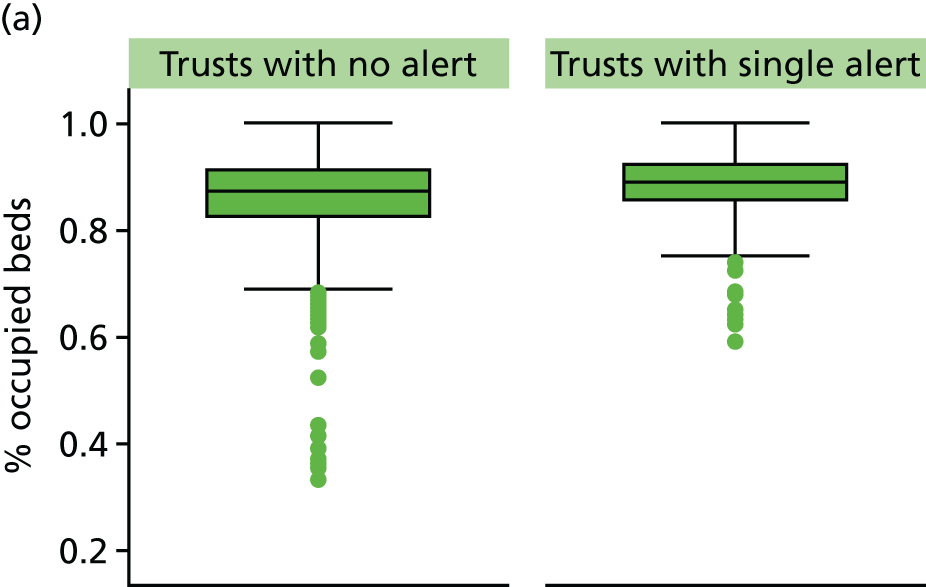
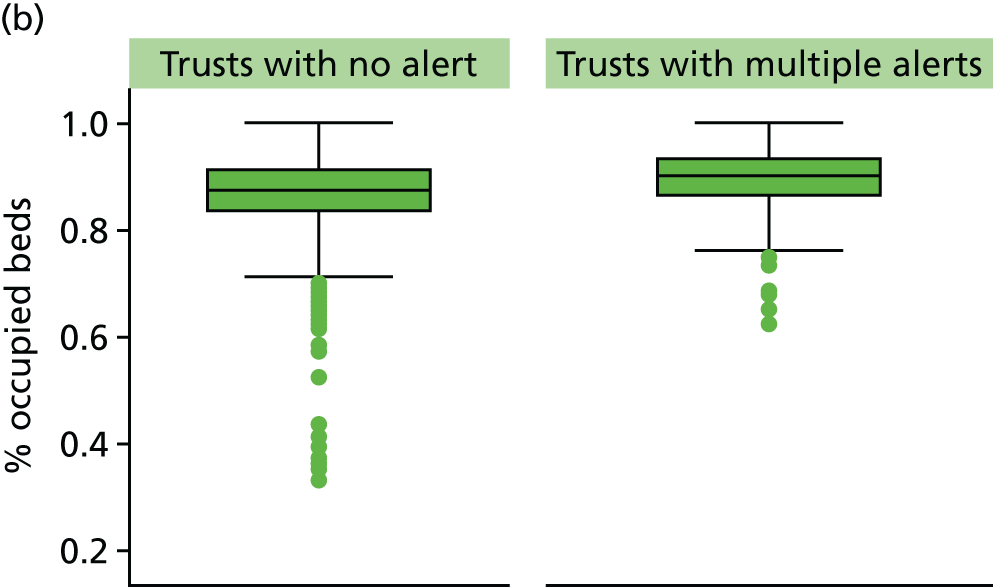
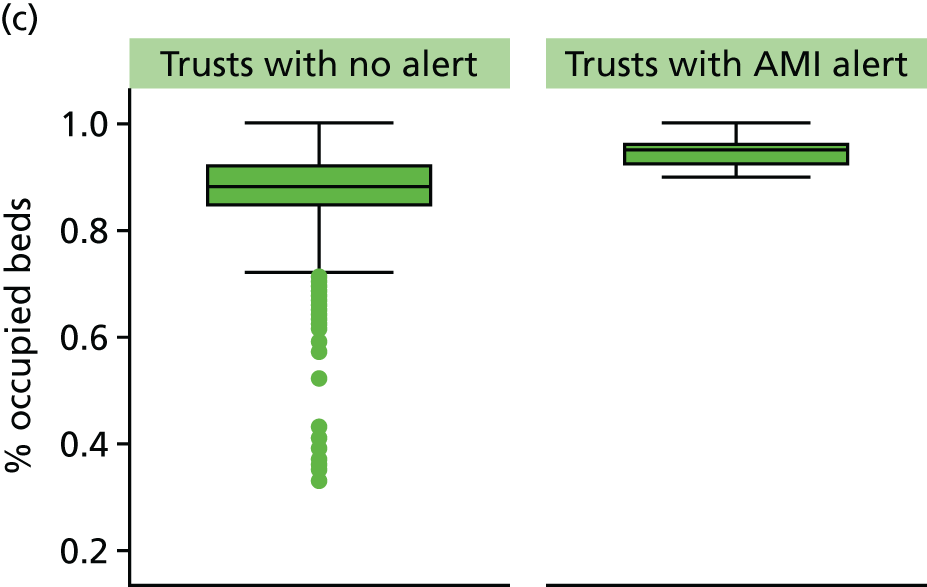
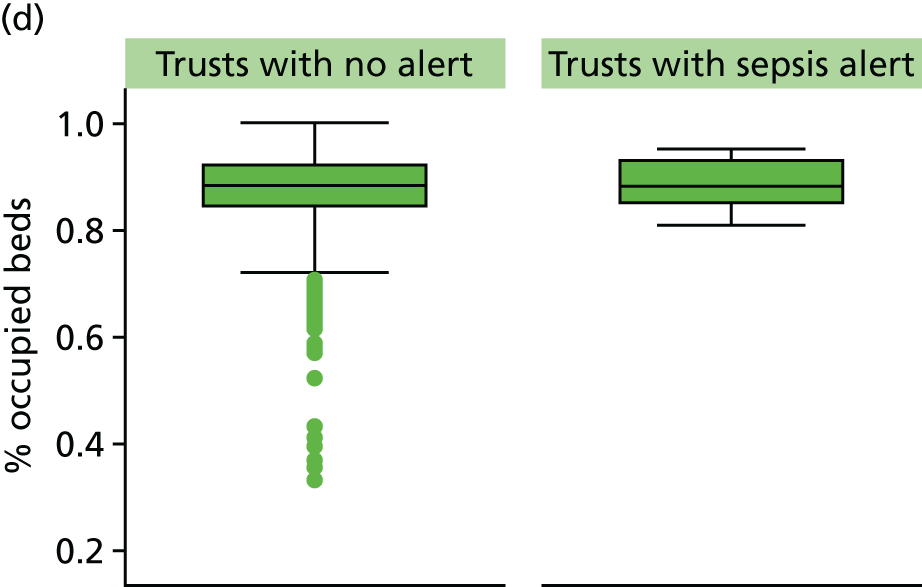
Hospital-standardised mortality ratio
Hospital-standardised mortality ratio data were available for 134 NHS acute trusts (83%). There were no data for specialist trusts. Trust-level HSMRs ranged from 57 to 120. In the year of an alert, trust-level HSMRs were, on average, 3.5 points higher in alerting than in non-alerting trusts (p = 0.003) (see Table 13).
There was no evidence of an association between the year of an AMI alert and HSMR; however, trust-level HSMRs were, on average, 6.2 points higher in alerting than in non-alerting trusts in the year of a sepsis alert (p = 0.009).
The HSMRs were, on average, 5.7 points higher in trusts with a single alert (p = 0.001) and 5.8 points higher in trusts with a multiple alerts (p = 0.0011) than in trusts that had not had an alert over the study period. The box plots in Figure 14 graphically display the distribution of the trust HSMR scores in alerting and non-alerting trusts.
FIGURE 14.
Hospital-standardised mortality ratios in acute trusts with single, multiple, AMI and sepsis alerts, 2011/12–2012/13, in England. (a) Single alert; (b) multiple alerts; (c) AMI; and (d) sepsis.
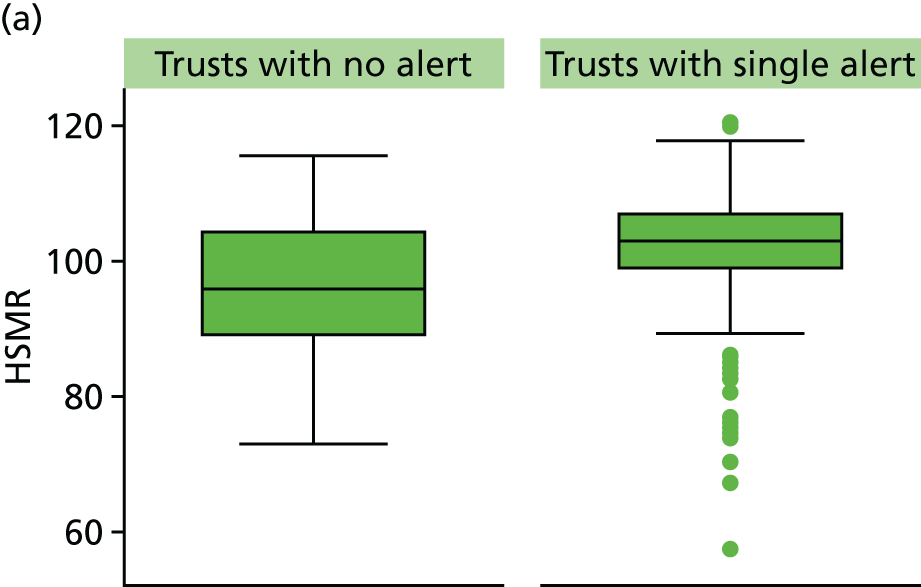
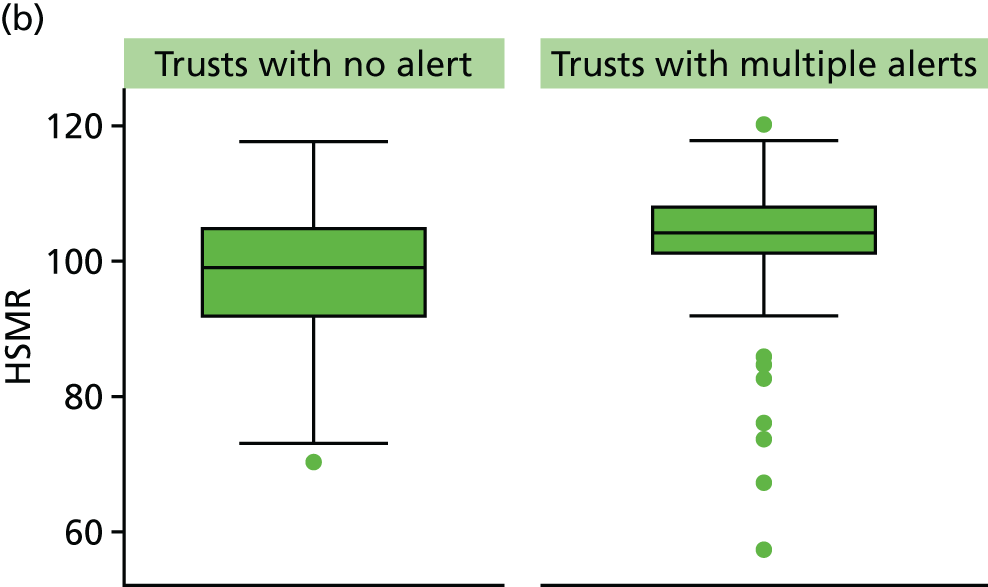
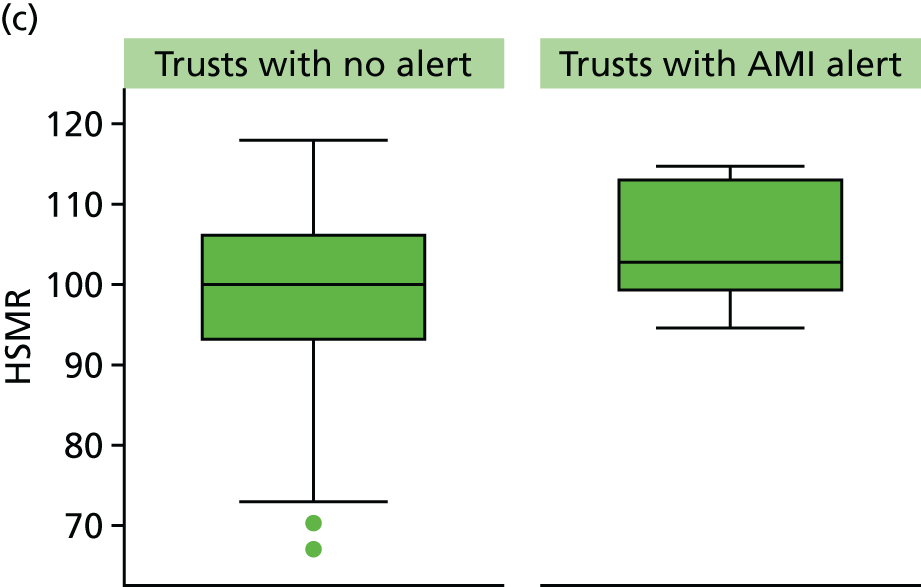
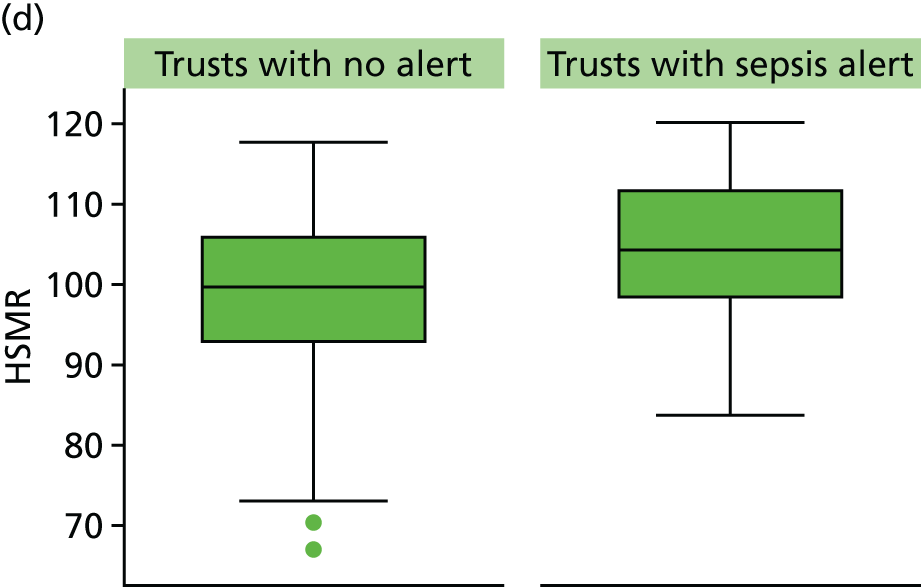
Summary tables
Table 13 summarises the descriptive statistics of the quality measures and the model-estimated difference in outcomes between non-alerting and alerting trusts for all diagnoses, AMI diagnoses and sepsis diagnoses; between trusts that had received a single alert during the study period; and for trusts that had received multiple alerts. Figure 15 displays the relative difference (%) and relative risks (with 95% CIs). The associations found between alerting trusts (compared with non-alerting trusts) and external indicators of quality were all in the hypothesised direction.
| Never alerted | Alert | AMI alert | Sepsis alert | Ever alerted | Frequent alerts | |
|---|---|---|---|---|---|---|
| Structure | ||||||
| Acute bed occupancy (%) | ||||||
| Trusts (number of alerts) | 68 | 85 (166) | 8 (11) | 16 (18) | 93 | 52 |
| Median (IQR) | 88 (83–92) | 90 (85–93) | 95 (92–96) | 88 (85–93) | 95 (92–96) | 90 (86–94) |
| Difference in mean (95% CI) | 2.2 (0.9 to 3.6) | 7.7 (5.6 to 9.8) | 2.0 (–0.1 to 4.2) | 2.8 (0.5 to 5.0) | 2.7 (1.1 to 4.3) | |
| p-value | p = 0.001 | p < 0.001 | p = 0.063 | p = 0.016 | p = 0.001 | |
| Nurse-to-bed ratio | ||||||
| Trusts (alerts) | 68 | 85 (166) | 8 (11) | 16 (18) | 93 | 52 |
| Median (IQR) | 2.2 (2.0–2.7) | 2.2 (1.9–2.4) | 2.1 (1.8–2.5) | 2.1 (2.1–2.2) | 2.2 (1.9–2.4) | 2.1 (1.9–2.5) |
| Difference in mean (95% CI) | –0.28 (–0.42 to –0.14) | –0.31 (–0.63 to 0.02) | –0.38 (–0.55 to –0.21) | –0.5 (–0.7 to –0.2) | –0.3 (–0.6 to –0.1) | |
| p-value | p < 0.001 | p = 0.064 | p < 0.001 | p = 0.001 | p = 0.006 | |
| Trust financial data (trusts in deficit vs. trusts in surplus) | ||||||
| Trusts (alerts) | 69 | 92 (189) | 8 (11) | 18 (21) | 92 | 51 |
| n (% trusts in deficit) | 49 (26) | 4 (45) | 7 (33) | 43 (47) | 17 (0.33) | |
| RR (95% CI) | 1.72 (1.02 to 2.76) | 2.52 (0.90 to 5.26) | 2.13 (0.93 to 4.13) | 2.33 (1.51 to 3.50) | 1.39 (0.92 to 2.06) | |
| p-value | p = 0.042 | p = 0.112 | p = 0.09 | p = 0.009 | p = 0.296 | |
| GMC National Training Survey trainee satisfaction % (weighted) | ||||||
| Trusts (alerts) | 73 | 69 (115) | 7 (9) | 12 (12) | 90 | 51 |
| Median (IQR) | 72.3 (70.8–73.5) | 72.1 (70.7–73.4) | 69.4 (67.7–70.8) | 72.3 (71.3–73.3) | 72.5 (71.1–73.6) | 72.3 (70.8–73.3) |
| Difference in meana (95% CI) | –0.14 (–0.90 to 0.62) | –2.7 (–4.50 to –0.90) | –0.28 (–1.50 to 0.94) | –0.32 (–1.07 to 0.42) | –0.29 (–0.96 to 0.38) | |
| p value | p = 0.721 | p = 0.004 | p = 0.650 | p = 0.393 | p = 0.4 | |
| NHS Litigation Authority risk assessment rating (level 1 vs. ≥ 2) | ||||||
| Trusts (alerts) | 64 | 92 (189) | 8 (11) | 18 (18) | 92 | 51 |
| n (% trusts with assessment rating 1) | 113 (69.8) | 8 (72.7) | 12 (57.7) | |||
| RRb (95% CI) | 1.20 (0.95–1.43) | 1.37 (0.63–1.76) | 1.07 (0.63–1.46) | 1.22 (0.89–1.52) | 1.19 (0.89–1.45) | |
| p-value | p = 0.111 | p = 0.316 | p = 0.754 | p = 0.201 | p = 0.223 | |
| Process | ||||||
| MINAP PCI within 90 minutes of arrival (%) | ||||||
| Trusts (alerts) | 16 | 33 (46) | 1 (2) | 1 (1) | 36 | 26 |
| Median (IQR) | 90 (88 to 95) | 93 (89–97) | 97 (93–100) | 83 (83–83) | 92 (90–96) | 92 (89–94) |
| Difference in meana (95% CI) | 0.46 (–1.86 to 2.79) | Insufficient data | Insufficient data | –0.41 (–3.22 to 2.39) | –0.41 (–3.22 to 2.39) | |
| p-value | p = 0.691 | p = 0.365 | p = 0.769 | |||
| Outcome | ||||||
| National Inpatient Survey: overall satisfaction (%) | ||||||
| Trusts (alerts) | 61 | 92 (189) | 8 (11) | 18 (21) | 92 | 51 |
| Median (IQR) | 76.2 (74.4–78.4) | 75.3 (73.9–77.1) | 74.9 (72.9–75.3) | 75.9 (75.2–77.2) | 75.3 (73.9–77.1) | 75.1 (73.5–76.9) |
| Difference in mean (95% CI) | –1.32 (–2.14 to –0.51) | –2.18 (–4.50 to 0.13) | –0.90 (–1.93 to 0.13) | –1.47 (–2.64 to –0.29) | –1.58 (–2.50 to –0.66) | |
| p-value | p = 0.002 | p = 0.065 | p = 0.085 | p = 0.015 | p = 0.001 | |
| Patient Safety Thermometer harms (%) | ||||||
| Trusts (alerts) | 93 | 56 (87) | 5 (6) | 8 (8) | 91 | 41 |
| Median (IQR) | 7.3 (5.4–9.3) | 7.8 (5.7–9.9) | 8.2 (6.5–10.3) | 7.6 (5.8–9.8) | 7.7 (5.9–9.6) | |
| Difference in meana (95% CI) | 0.33 (–0.34 to 1.00) | 0.76 (–0.92 to 2.44) | 0.48 (–1.40 to 2.37) | 0.32 (–0.44 to 1.08) | –0.17 (–1.12 to 0.78) | |
| p-value | p = 0.335 | p = 0.371 | p = 0.614 | p = 0.293 | p = 0.723 | |
| SHMI | ||||||
| Trusts (alerts) | 49 | 90 (186) | 7 (10) | 18 (21) | 90 | 50 |
| Median (IQR) | 1.00 (0.92–1.06) | 1.05 (0.99–1.11) | 1.09 (0.98–1.16) | 1.06 (1.02–1.08) | 1.05 (0.99–1.11) | 1.06 (1.00–1.11) |
| Difference in mean (95% CI) | 0.06 (0.04 to 0.09) | 0.10 (0.01 to 0.19) | 0.06 (0.03 to 0.09) | 0.07 (0.04 to 0.10) | 0.07 (0.04 to 0.11) | |
| p-value | p < 0.001 | p = 0.022 | p < 0.001 | p < 0.001 | p < 0.001 | |
| HSMR | ||||||
| Trusts (alerts) | 49 | 85 (113) | 5 (6) | 16 (18) | 90 | 50 |
| Median (IQR) | 100 (93–106) | 103 (98–107) | 103 (99–113) | 104 (98–112) | 103 (98–107) | 104 (101–108) |
| Difference (95% CI) | 3.5 (1.3 to 5.8) | 6.3 (–1.3 to 13.9) | 6.2 (1.5 to 10.8) | 5.7 (2.4 to 9.1) | 5.8 (2.3 to 9.2) | |
| p-value | p = 0.003 | p = 0.104 | p = 0.009 | p = 0.001 | p = 0.001 | |
FIGURE 15.
Relative difference (%) and relative risks, with 95% CIs, in outcomes comparing alerting trusts with non-alerting trusts. (a) All alerts; (b) AMI alerts; and (c) sepsis alerts. The green arrows display the hypothesised direction of association and the black lines represent the null values: 0 for relative differences and 1 for relative risks.
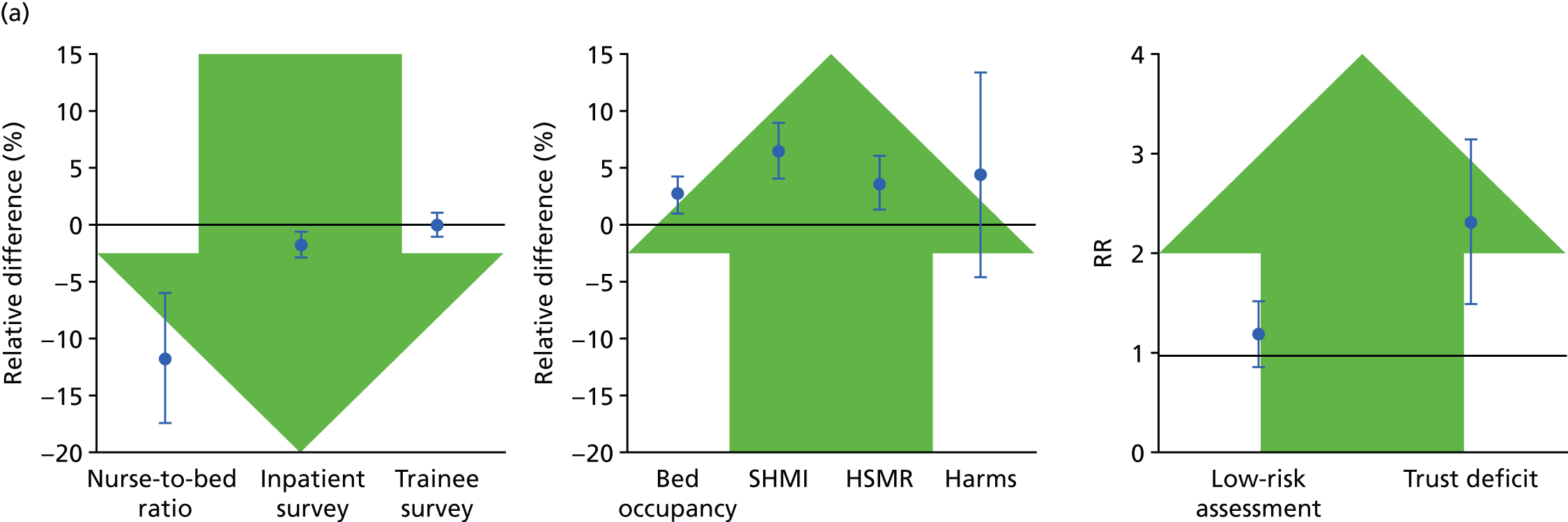
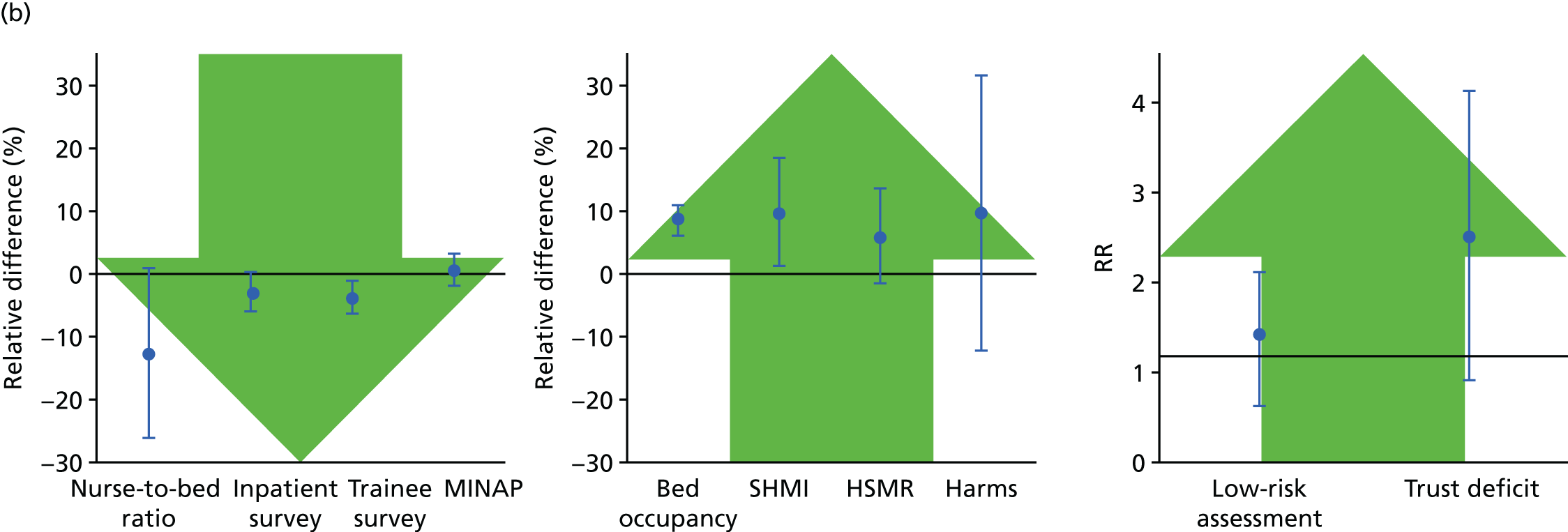
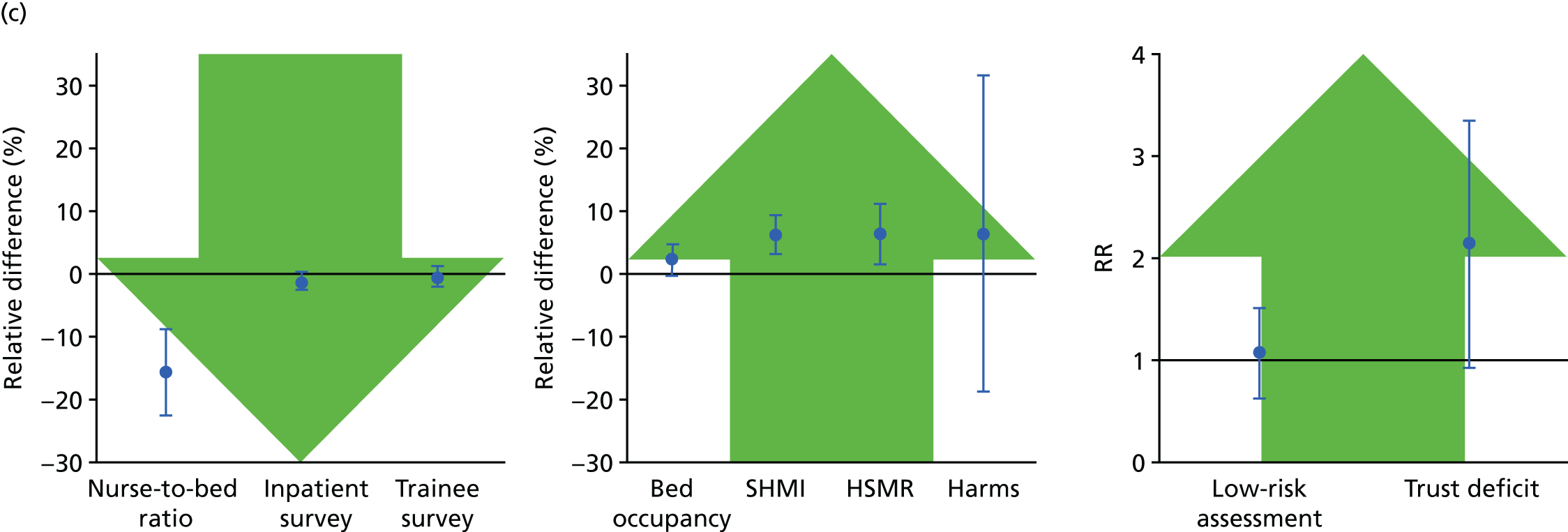
Multiple statistical testing
We attempted to control for multiple testing and FDR. We found that 23 of 48 (46%) of the external indicators of quality tests carried out had a statistical significance of p < 0.05, while 22 (45%) were still statistically significant after controlling for FDR (see Appendix 11 for more detail).
Analysing the association of an alert with trends in subsequent risk of death
We hypothesised that, on receiving an alert, the trust would investigate possible explanations within the trust, bringing about change (if needed) within the hospital setting and, as a result, there would be a fall in mortality risk. We investigated the association between a mortality alert and subsequent mortality using an interrupted time series analysis.
There were 92 first alerts (for a condition or procedure) sent to 65 trusts between 1 January 2012 and 31 December 2013. Of these alerts, six were for AMI and 10 were for sepsis.
Table 14 displays the relative risks from three models investigating trust-level tends in relative risk of death before and after alerts for any diagnosis, AMI and sepsis. Figure 16 graphically displays the model estimated trends in relative risk against the actual trust-level relative risks. For all models and diagnoses, the relative risk of death decreased immediately after an alert.
| Model | All diagnoses | AMI | Sepsis | |||
|---|---|---|---|---|---|---|
| RR (95% CI) | Significance | RR (95% CI) | Significance | RR (95% CI) | Significance | |
| 1 | ||||||
| Pre-alert trend | 1.01 (1.00 to 1.01) | * | 1.02 (1.01 to 1.04) | 1.02 (1.00 to 1.03) | ** | |
| Post-alert trend | 0.98 (0.97 to 0.99) | *** | 0.98 (0.96 to 1.00) | ** | 0.98 (0.96 to 0.99) | *** |
| 2 | ||||||
| Pre-alert trend | 1.04 (1.04 to 1.05) | *** | 1.05 (1.02 to 1.08) | *** | 1.04 (1.02 to 1.06) | *** |
| Level change | 0.64 (0.59 to 0.69) | *** | 0.70 (0.54 to 0.90) | ** | 0.83 (0.68 to 1.02) | |
| Post-alert trend | 0.99 (0.98 to 1.01) | 0.99 (0.94 to 1.04) | 0.96 (0.92 to 0.99) | *** | ||
| 3 | ||||||
| Pre-alert trend | 1.04 (1.04 to 1.04) | *** | 1.05 (1.02 to 1.08) | *** | 1.04 (1.02 to 1.06) | *** |
| Level change | 0.42 (0.37 to 0.47) | *** | 0.43 (0.28 to 0.67) | *** | 0.41 (0.29 to 0.59) | *** |
| Post-lag trend | 0.99 (0.98 to 1.01) | 0.99 (0.94 to 1.04) | 1.00 (0.96 to 1.05) | |||
FIGURE 16.
Trends in relative risk of death before a mortality alert, during 9-month lag period and after lag period, for (a) all diagnoses/procedures; (b) AMI; and (c) sepsis.
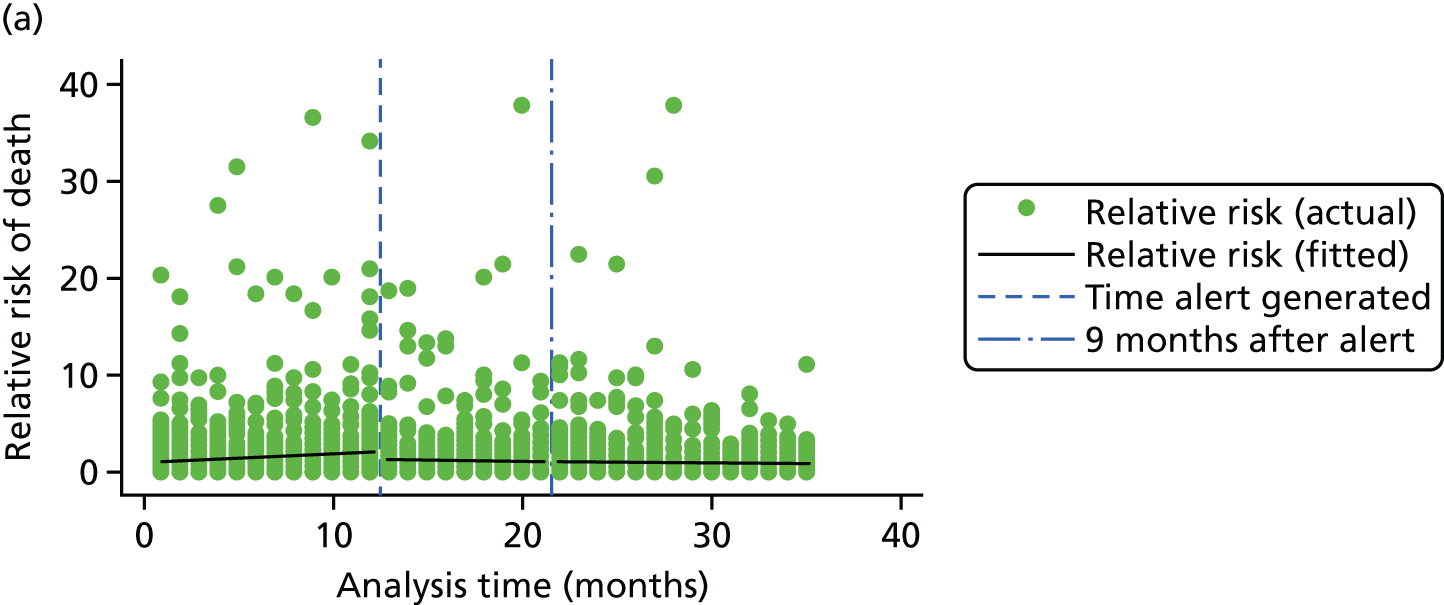
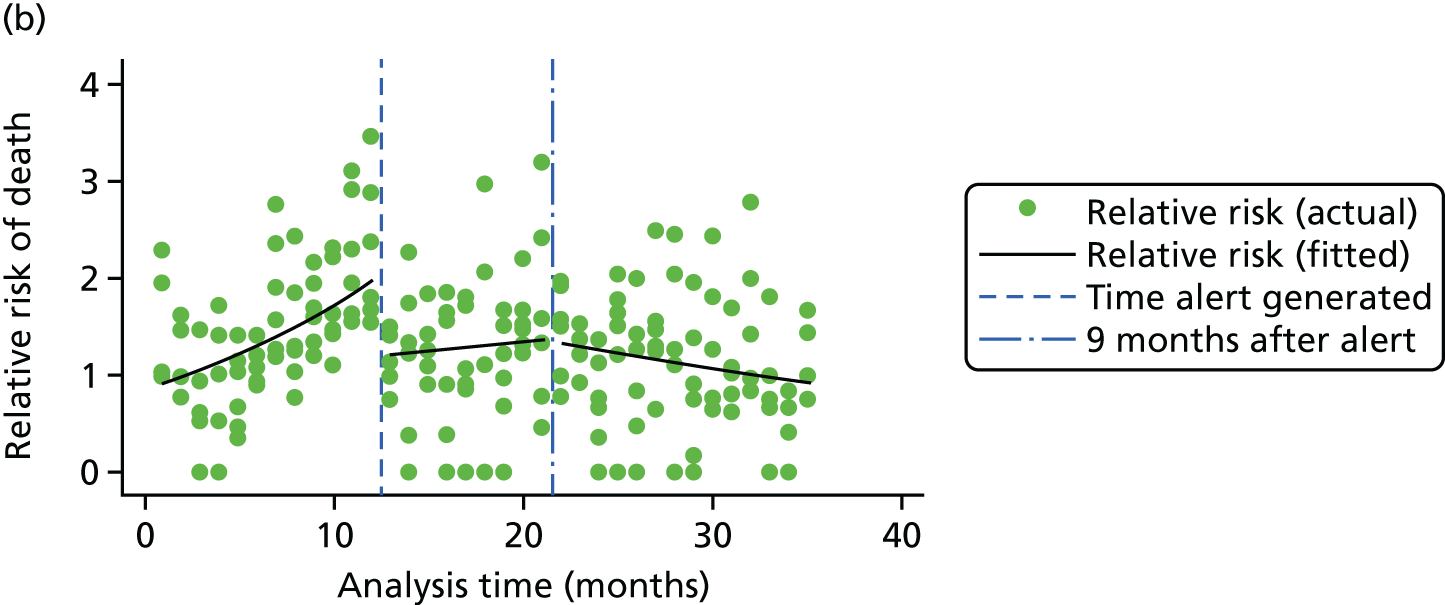
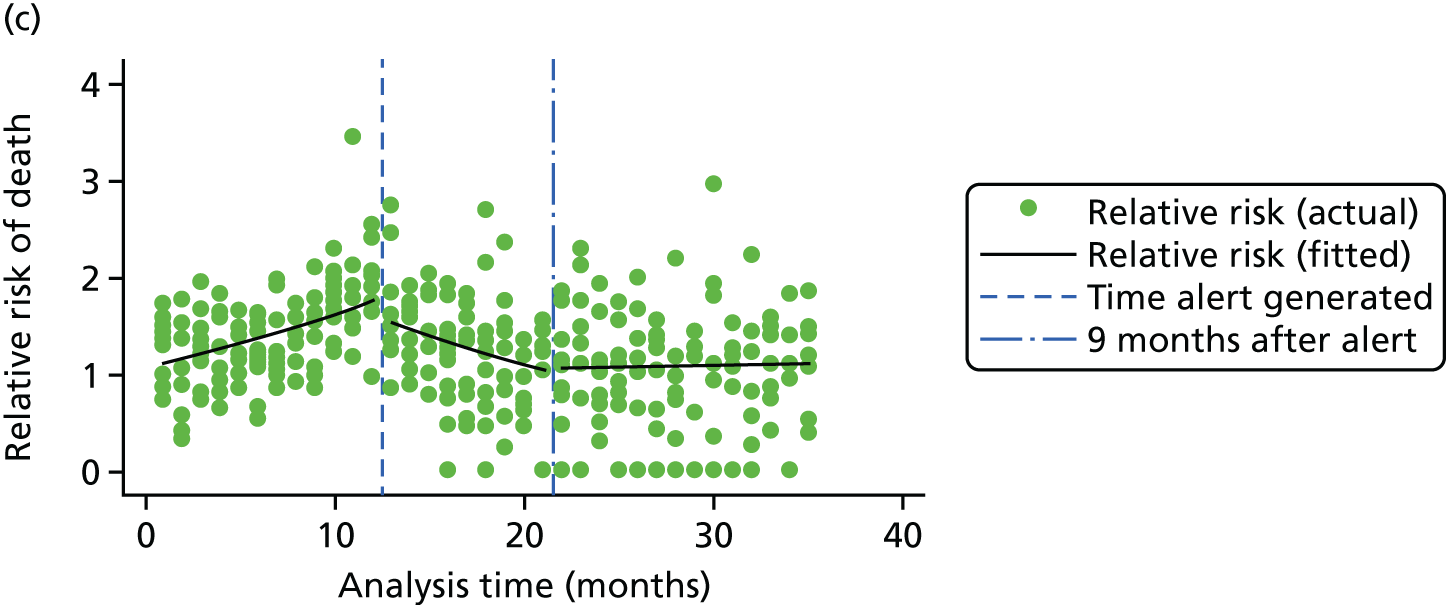
All diagnoses/procedure alerts
Model 1 estimated pre-alert and post-alert slopes, ignoring any lag that might occur as a result of processing and sending the alert letters. In this model, on average, there was a 1% increase in relative risk of death per month in the 12 months before an alert (RR 1.01), totalling a 13% increase. There was, on average, a 2% monthly fall (RR 0.98) after an alert, totalling a 38% fall over the following 24 months. Model 1 estimated that, on average, alerting trusts reduced their relative risk to an expected risk within 18 months of an alert.
Model 2 focused on modelling the reduction of relative risk in the lag period. It estimated a pre-alert slope, a level change at the time of the alert and a post-alert slope. This model showed, on average, a monthly increase in relative risk of 4% (RR 1.04) before an alert, representing a 60% increase in the 12 months before an alert. There was a 36% immediate fall (level change) in the following month (RR 0.64). Following this, there was a continued reduction (which was not statistically significant) of 1% per month, totalling 10% over the 9-month lag period. This model estimates that if trends were to continue after the lag period, alerting trusts would, on average, reduce their relative risk to an expected risk within 18 months of an alert.
Model 3 focused on modelling the reduction of relative risk after the lag period. It estimated a pre-alert slope, a level change during the lag period (ignoring the trends) and a post-alert slope. This model estimated an increase in relative risk of 60% in the 12 months (RR 1.04) before an alert, a 58% fall during the lag period (RR 0.42) and a continued reduction (non-statistically significant) of 1% per month (RR 0.99). This model suggested that, on average, alerting trusts reduced their relative risk to an expected risk within 18 months of an alert.
Sensitivity analyses, with a reduced lag time, estimated similar immediate falls in relative risk following an alert. Relative risks were similar when modelling crude risk to modelling relative risk (model 2: 0.62, 95% CI 0.59 to 0.64, vs. 0.64, 95% CI 0.59 to 0.69; and model 3: 0.37, 95% CI 0.34 to 0.40, vs. 0.42, 95% CI 0.37 to 0.47).
Acute myocardial infarction
As there were only six AMI alerts, the power of this analysis was restricted. This is graphically demonstrated in Figure 16. There is a clear increase in the relative risk of death before an alert but there is huge variability after an alert.
Sepsis
The increase in relative risk of death for sepsis, before an alert, fell during the 9-month lag, and then a levelling after the lag period is clearly displayed in Figure 16. There was no statistical evidence of a decrease in relative risk of death for sepsis after the 9-month lag period.
Chapter 7 Results from workstream 2: case studies
This chapter provides illustrative descriptions of the cases included in the analysis and then describes the results from the cross-case analysis. To better understand the factors contributing to perceived institutional capability for responding to signals in mortality data, we then describe an integrative analysis, independent of the case-based analysis and drawing on interview data collected across all case studies. Based on initial open-coding and early-stage iterative refinement of categories, nine broad themes were identified to serve as a frame for further exploration in the data set. The resulting thematic analysis was used to structure early versions of the survey instrument described in Chapter 8 in order to ensure that response items and scales were both thematically balanced and theoretically grounded in the emerging perspectives on effective institutional responses. An analysis of the nine core themes is reported, along with the emergent subthemes.
Case-based qualitative analysis of experience at 11 alerted NHS sites
Once the initial open coding and category refinement had been established for the emerging case-study data set, the initial stage in making sense of the rich qualitative information obtained from the 11 sites involved constructing case narratives. The aim of the case narratives was to produce an integrated summary of the historical and factual information concerning institutional experience of responding to the target alerts, along with contextual information obtained from documentary records provided during the site visits and external sources of contextual information and data. The case narratives were compiled in two stages. Initially, a standard template was used to establish the timeline of the alerts and response from three key perspectives, organisational, coding/informatics and clinical condition, drawing on key quotations from the data set. In a subsequent stage of the analysis, a second pass of the data set was made and the case narratives were analysed thematically as case studies of institutional behaviour. In this second stage, the case narratives were populated with quotations representing salient informant perspectives on mortality alerting and the local factors that had an impact on the institution’s approach to avoidable mortality, either directly attributable to the alerts or as a parallel evolution of institutional strategy and context. It was in the second stage of developing the case studies that the more subjective and interpretative perceptions and views of respondents were explored, in addition to the historical narrative of the organisation’s experience of responding to alerts. A thematic analysis was undertaken to identify themes relevant to the institutional response to the alert(s), structured in three high-level categories: (1) trust preconditions (before receipt of the alert), (2) reported institutional responses to the alert and (3) reported outcomes from institutional activity and initiatives to address mortality. In both the case narratives and the thematic analysis, one category was reserved for ‘parallel evolution of the institutional focus on the clinical condition’ (sepsis/AMI). The significance of this category is that information was coded within this category concerning institutional behaviour that was not attributed to the effects or outcomes of receiving a mortality alert during the interview.
The case narratives and subsequent thematic case-based comparative analysis generated a large number of structured data and researcher commentary. To reduce the burden on the reader, we have included in our write-up only the secondary case study descriptions, and only specific illustrative cases, before providing a deeper comparative analysis of the full case study data set. In reporting the case study results, in order to preserve confidentiality of the organisations and individuals who participated in the study, specifically identifiable site and respondent details have been removed, anonymised or replaced with coded descriptors. Salient contextual details for each case study site have been left in the case narratives so that the reader is presented with sufficient information to understand key variations between cases, and to illustrate the type of contextual features that the researchers were working with in interpreting each case.
Table 15 provides a list of the anonymised site identifiers that will be used from this point onwards in the report to refer to each individual case study site. For convenience, a naming convention has been used: sep = sepsis; AMI = acute myocardial infarction; -m = multiple alerting site; -s = single alerting site; and a unique numerical identifier (01–11).
| Anonymised site identifier | Site alert condition | Single/multiple alerts |
|---|---|---|
| AMI-s.01 | AMI | Single |
| AMI-m.02 | AMI | Multiple |
| AMI-m.03 | AMI | Multiple |
| AMI-m.04 | AMI | Multiple |
| Sep-s.05 | Sepsis | Single |
| Sep-s.06 | Sepsis | Single |
| Sep-m.07 | Sepsis | Multiple |
| Sep-m.08 | Sepsis | Multiple |
| Sep-m.09 | Sepsis | Multiple |
| Sep-m.10 | Sepsis | Multiple |
| Sep-m.11 | Sepsis | Multiple |
An abridged summary of each of the individual case study analyses is included in the report and appendices. Within the main text of the report, we have included an example of a single-alerting sepsis site (Sep-s.06) and a multiple-alerting AMI site (AMI-m.03) to illustrate our approach to the treatment of the case study data. The remaining nine case studies are reproduced in Appendix 12 along with extended examples of illustrative quotations linked to the themes derived from each analysis (see Appendix 13). In the summaries, for each case, an overview of the trust’s background and recent history, drawing on information such as the local health population, is provided, when this does not directly identify the trust. The trust’s relative risk profile is provided. By way of a concise overview, a condensed version of this case narrative template is then presented in table form, including salient information about the case in three areas: (1) relevant history and context at time of the first alert, (2) summary of response to first alert and (3) organisational learning and long-term response to alert(s). A brief thematic analysis for each case is then presented, drawing on the more comprehensive analysis compiled for the original case narratives. Further details from each case can be found in Appendix 13, which includes a summary of the roles of those interviewed at each site, each site’s alerting history and the illustrative quotations for the themes summarised in the main text of each case narrative summary in the main report.
Case study 03 (AMI-m.03) narrative summary
Overview
AMI-M.03 is a large acute trust with five hospital sites, serving a population of approximately 450,000. The trust has approximately 950 beds. The main site of AMI-M.03 hospital is a tertiary referral hospital. The trust was one of the 14 identified in the Keogh review. In recent years, it has had a new CEO and medical director, as well as a new lead for mortality.
Relative risk profile
Figure 17 displays the relative risk profile for site AMI-m-03 between January 2009 and January 2014. The green lines represent the date of an alert and the blue lines represent the date of the subsequent letter. Table 16 provides the summary.
FIGURE 17.
Time series displaying relative risk profile and alert (green)/letter (blue) dates for site AMI-m.03.
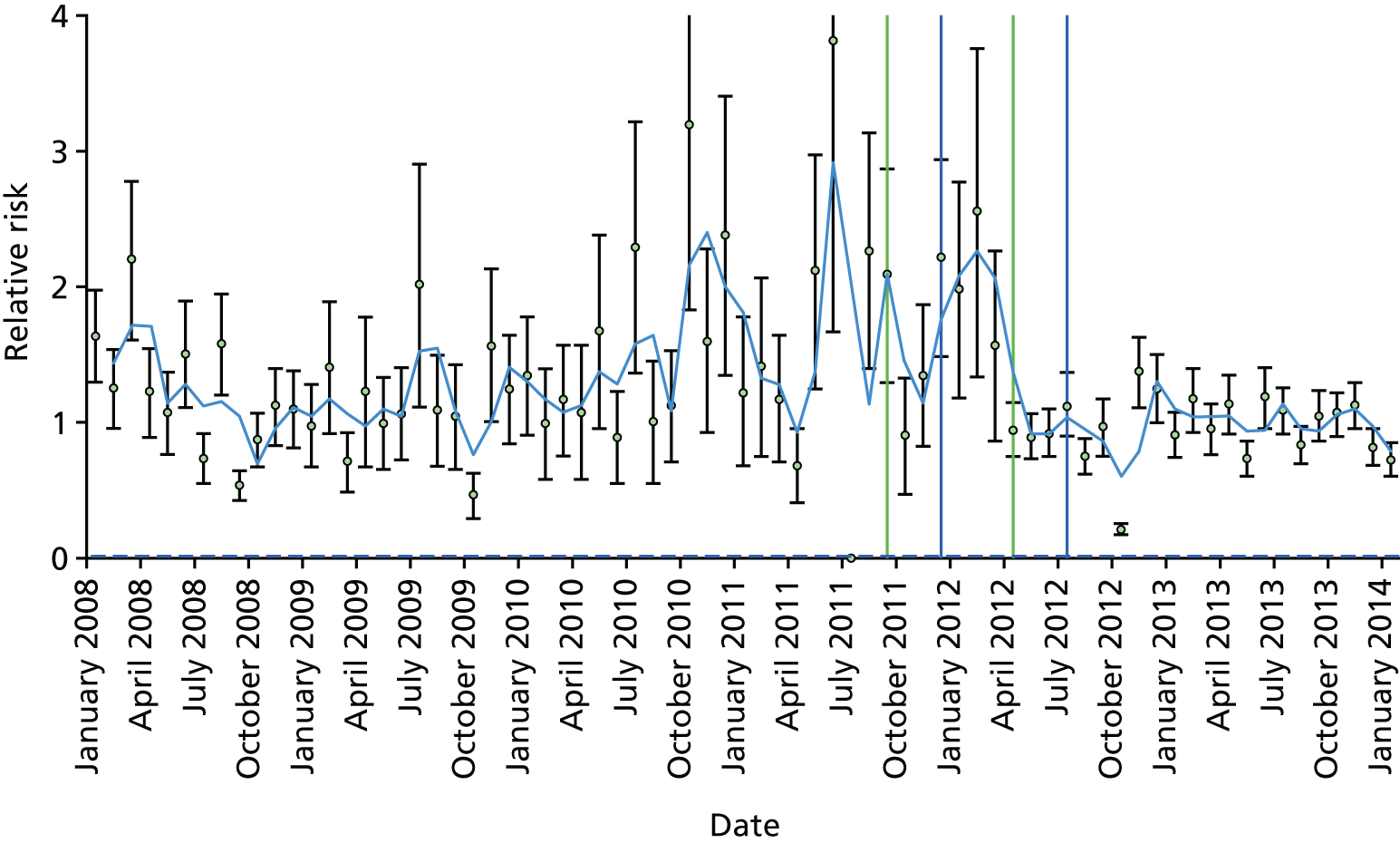
| Relevant history and context at time of first alert | The trust was aware of high mortality and had started a case note review of deaths. In addition, it had set up a mortality committee that was chaired by the CEO. It was considered that the mortality committee had too much information for people to digest and take action on. The trust had taken action through external reviews and joining the local quality network. The trust was identified in the Keogh review and had been criticised for trying to do too much and not doing anything effectively. The trust was using CHKS (Birmingham, UK) and tracking several mortality indices |
| There were no mortality review meetings in acute medicine. The trust had developed an AMI pathway, but this was considered too lengthy and implementation was not tracked in real time | |
| Summary of response to first alert | Departmental coding and comorbidity meetings were set up to review deaths and ensure that coding was accurate |
| The local quality network was brought in to help. An AMI pathway was introduced and an audit was undertaken. This found poor compliance with the pathway and variability in the implementation of the different aspects of the pathway. From this, ‘mission critical’ points were developed: clinical care that is evidence based and essential to the treatment of people with AMI | |
| Organisational learning and long-term response | There is now a weekly meeting to review all deaths that involves the medical director, the lead for mortality and the lead in informatics. The mortality meeting now takes place bimonthly and is attended by GPs, nurses and individual specialty leads. Every death is reviewed by the consultant who looked after the patient. The consultant is asked to highlight if there was anything preventable. If there was, a second consultant will review the death and there will be a ‘deep dive’. Each department has a mortality lead and holds mortality meetings |
| Making sure that the information is correct in the trust databases is now important. Consultants are now required to ‘OK’ the coding for their patients. The trust has purchased the HED tool and now has a wealth of information about mortality available. This enables early intervention. Concern still exists over the coding of comorbidities, especially in elderly patients | |
| The trust appointed a cardiologist who now leads the acute medicine mortality work. Two other cardiologists have also been appointed. The patient pathway has been developed and is now monitored in real time. The focus of this work has been on reducing variation in care. In parallel, there has been work to reduce harm in areas such as pressure ulcers, falls and MRSA |
AMI-m.03 thematic analysis
AMI-m.03 received repeat alerts for AMI in September 2011 and April 2012. An analysis is generated from interviews with five members of the trust executive team, plus one specialty manager and one manager responsible for coding, and is informed by trust documentary sources.
Trust preconditions before the first alert
Trust recognition of high acute myocardial infarction mortality triggering external engagement
One respondent, the current mortality lead, noted how staff were aware that the trust had a history of high levels of mortality before receiving the first AMI alert. He suggested that this knowledge had provided a trigger for the trust’s participation in the PRISM (Preventable Incidents, Survival and Mortality) national study. 23 This study aimed to examine avoidable deaths and develop a standard approach for local mortality review. It focused on the review of 1000 randomly selected case notes of patients who died either in hospital or within 30 days of discharge from hospital. It also involved training experienced hospital consultants to assess the preventability of adverse incidents and the effects of the adverse incidents on the subsequent clinical progress of the patients. It was reflected that participation in this study had indicated that the trust had no clear deficiencies in care.
Trust leaders’ informal engagement investigating mortality by case note review
It was reported that, around 2008, the medical director had asked one of his colleagues to help to review case notes of deaths. This was regarded as an informal weekly activity aimed at gaining a sense of mortality problems in the trust. After normal working hours, a review was undertaken of deaths that had occurred during that particular week. The deputy medical director conceded that ‘we didn’t know what we were looking for’ and that the exercise involved finding ‘out the current episode of patients’ journey and see whether they were actually managed properly and they had written the right diagnosis on the death certificate’.
Belief that trust catchments are not accurately accounted for in official mortality indices
Analysis suggests that trust staff perceived high mortality rates in the trust to be influenced by trust catchment characteristics and not by standards of care. Staff reported that these issues were related to high levels of social deprivation, poverty, a transient population (seasonal workers), an exceptionally unhealthy population (alcohol addiction and end-of-life care issues), inadequate services in the community to support this local population and difficulties in recruiting adequate staff. One senior clinician suggested that a case note review had already highlighted the extent of trust catchment influence on hospital mortality. Most respondents suggested that the risk adjustment weighting for these factors within mortality indicators was inaccurate. The chief nurse also linked high levels of mortality to staffing, as the trust catchment, geography and the profile of the local population were perceived to make recruitment difficult.
Mortality committee overwhelmed by information
Analysis suggests that, at the time of the first alert, the trust had a centralised senior team to oversee trust mortality. However, it was suggested that within divisions and some specialties mortality teams were often inactive, and it was noted that no mortality review meetings took place in the acute medicine department.
The CEO reported that she chaired the ‘mortality committee’ and that when she had first arrived at the trust it was operating poorly. She suggested that the trust had been overwhelmed by ‘reams of information’, which made it difficult to make sense of mortality. It is posited that this situation arose as a result of the absence of a supporting specialist infrastructure. The trust was at an early stage of tracking mortality using a CHKS system, which provided information on risk-adjusted mortality indicator (RAMI). The trust began to track RAMI, SHMI, HSMR and crude mortality. The director of nursing reflected that at the time of the first alert the trust was not as transparent as it later became, and this was due to a lack of good information.
Trust responses to an acute myocardial infarction alert
Engaging with an external organisation
In December 2011, the local quality network was commissioned to undertake a comprehensive review of the trust’s reported mortality rates. It focused on examining a range of factors that might explain the current and historically high mortality rates at the trust. This review centred on:
-
the implications of local population characteristics for the methodology used to calculate expected mortality rates
-
the impact of provision of services and quality of care both within the trust itself and in the wider community
-
the system and process that are employed within the trust.
The conclusions focused on the following:
-
Recognition of the trust’s strong track record in clinical quality improvement and that the non-mortality related quality indicators did not give concern.
-
Recognition that the trust’s standardised mortality rate (SHMI, HSMR or RAMI) was likely to be adversely affected by the way clinicians and the coding team interact and that the ‘expected deaths’ element of the standardised rate calculation can be affected by coding processes. They emphasised that this needs urgent attention.
-
Linking mortality reduction to other patient safety initiatives and developing a specific mortality reduction plan that cascades to divisions and departments and that reports to the trust board.
-
Improving clinical quality by adopting care bundles, reviewing staffing levels in high-risk areas and working with primary care to improve end-of-life care planning.
Developing an integrated structure linking the functions of the trust mortality committee with departmental mortality and morbidity meetings
The trust set up departmental coding and comorbidity meetings during which all consultants, under the instruction of the previous medical director, were to review deaths. These were then discussed during the mortality and morbidity meetings.
Acute myocardial infarction pathway audit launched
An AMI pathway audit was launched. Three areas were found: (1) compliance of AMI treatment was a major issue, (2) evidence of the success of the primary PCI integrated pathway was inconsistent and (3) the success of an in-house smoking cessation campaign was also inconsistent. Recommendations suggested that divisions should develop action plans addressing non-compliance and improvement, actions plans should be monitored via the clinical audit department and progress should be fed back to the mortality board. The mortality lead highlighted how, in developing the AMI pathway, ‘mission critical points of care’ should be identified. These identify areas of care that are evidence based and hence demonstrate how accumulated clinical learning transformed the AMI pathway.
A strategic focus on generating and using quality data
The trust leadership appeared to instigate a strategic focus on generating both quality data and analysis that could usefully inform decision-making. This involved the internal tracking of mortality as well as engaging with other trusts and comparing performance. Once an alert for AMI had been received, the trust began to look for other trusts with which to compare itself.
Trust responses to the second acute myocardial infarction alert
Senior leadership prioritising acute myocardial infarction mortality by investing in knowledge production, knowledge sharing and analysis focused on acute myocardial infarction mortality improvement
The AMI alert was instrumental in driving trust leadership to prioritise AMI mortality reduction. The mortality committee was recognised as a key structure for enabling knowledge sharing and analysis around AMI mortality. A general practitioner (GP) was seconded to inform the trust about improved primary care engagement and communication. Trust leaders ensured that consultants with a formal responsibility for monitoring and analysing AMI mortality attended and reported on mortality review, analysis and action plans and implemented actions in their specialties. Non-executive directors, information and coding specialists also provided input and support. It was noted that the GPs were also active in the Clinical Commissioning Group (CCG) as commissioners, so the dynamics of the mortality committee could be difficult at times.
The strategic resourcing of mortality analysis and review was achieved through investment in a new Healthcare Evaluation Data (HED) analysis system and the recruitment of more clinical staff specifically to support mortality review, action plans and the implementation of improved practice.
Resourcing greater clinical involvement in acute myocardial infarction mortality improvement
In resourcing greater involvement in AMI improvement, the trust appointed a consultant cardiologist and extended the role of consultants to validating and authorising coding. In 2012, a consultant cardiologist was appointed as the mortality lead in acute medicine. The trust also appointed two more consultants in cardiology. The role of consultants in coding was also extended to authorising and validating the coding of their patients.
A forensic and integrated approach to exploring mortality for acute myocardial infarction
Analysis suggests that the trust’s response to the AMI second alert was forensic and comprised three stages. The first was an administrative process whereby the information was checked to see if it was correct. The second stage focused on operational care patterns involving care pathways and other clinical-level processes. The third stage (described as the most difficult) related to system redesign.
Outcomes of acute myocardial infarction alerts
Acute myocardial infarction pathway guidance developed and improvements in acute myocardial infarction pathway implemented
In July 2013, the trust developed an AMI pathway to provide guidance to clinical staff working in the accident and emergency (A&E) department on how to treat a patient with a suspected AMI based on best evidence and agreed local practice. It is considered now that the pathways developed at this time were too complex and contained too much information to allow them to be followed properly. Consultant cardiologists have been instrumental changing the patients’ pathway across the area, acting as a tertiary centre.
Acute myocardial infarction alert as a tool for learning
The mortality lead at the trust is acutely aware of the value of the alerts as a learning tool. He recognises that their value lies in quality of care issues in general but that the specific target alerts allowed the trust to understand specific issues around AMI and chronic lung disease. The issue here is the understanding that chronic lung disease can be mistaken for AMI.
Parallel evolution of institutional focus on mortality reduction in acute myocardial infarction
In the analysis of data sources, it was difficult to attribute direct causality of the AMI alert. The mortality alerts sent from Dr Foster Intelligence did appear to have some impact on how mortality was organised in the trust, but it is also accepted that trust arrangements also developed in partial response to the Keogh Review and CQC inspections and occurred as natural progression of trust strategy.
Natural progression of trust strategy influencing mortality improvement
The natural progression of trust strategy appears to have influenced AMI mortality improvement. Examples of this relate to investment in the HED information technology (IT) tool and quality improvement work focused on falls, pressure ulcers and meticillin-resistant Staphylococcus aureus (MRSA). The HED tool is used by the lead in informatics to produce a ‘heat map’. Using the heat map, the medical director focused on the areas of concern and worked in these areas to develop pathways that are easily accessible on the trust’s intranet and monitored in real time.
Case study 06 (Sep-s.06) narrative summary
Overview
The Sep-s.06 NHS trust is an acute trust serving a population of circa 255,000. It was established in 2014 following a reorganisation of NHS trusts in the area and runs two acute hospitals. The trust received a single alert for septicaemia (except in labour) in October 2012. An analysis is generated from interviews with five members of the trust executive team, one specialty manager and one manager responsible for coding, and is informed by trust documentary sources.
Relative risk profile
Figure 18 displays the relative risk profile for site Sep-s.06 between January 2009 and January 2014. The green lines represent the date of an alert and the blue lines represent the date of the subsequent letter. Table 17 provides the summary.
FIGURE 18.
Relative risk profile and alert (green)/letter (blue) dates for site Sep-s.06.
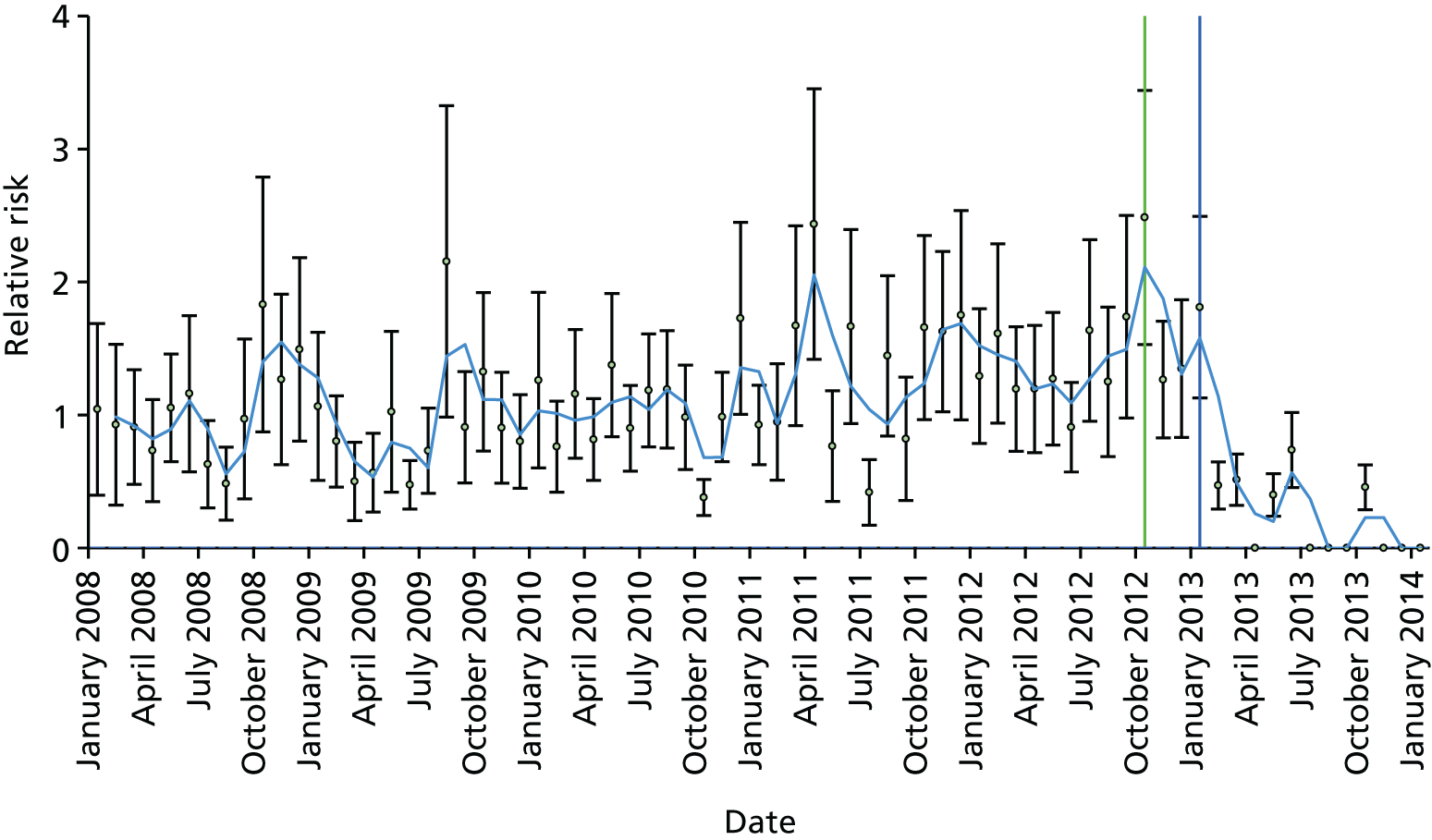
| Relevant history and context at time of first alert | Interviewees described the trust at the time of the first alert as administratively managed and reactive. HSMR was monitored but there was no reduction plan. There was a mortality review committee but morbidity and mortality meetings did not take place in every specialty, and when they did take place they were ‘cliquey’, with senior consultants in charge and no nurses or other allied professionals involved. Coding was not involved in the mortality review process |
| Sepsis had been identified as an issue in surgery alone; there had been no work on sepsis across the trust until the alert arrived. The surgical team had started to implement the sepsis bundle and had done a tremendous amount of work to collect data on the numbers of patients with sepsis in surgery. This work had not been supported financially until the alert arrived. As the surgical team had been working on sepsis, they were not surprised when the alert arrived | |
| Summary of response to first alert | The alert came to the CEO and was sent to the medical director and the head of quality, safety and compliance. With the help of Dr Foster, the patients were identified and their notes were pulled and reviewed using a standard template used in the region. From the case note review, 31 cases (roughly one-third) were found to have been wrongly coded. The case note review in surgery had found that patients were not being diagnosed and treated in a timely fashion. Some patients were found to have waited up to 27 hours for their antibiotics when these should have been given within 1 hour |
| The alert was used as evidence for change by the corporate team. A sepsis pathway working group was set up across the trust and specialties began working together on this | |
| Initially there was some scepticism about the data as some of the patients were coded on the death certificate as having died from cancer and yet the alert picked them up as having died from sepsis as this had been their initial diagnosis | |
| A large education programme began to train people on how to recognise and manage sepsis. Two new nurses were appointed to run this. The team started to collect data about the cases of sepsis and were able to monitor progress and show downwards trends in mortality from sepsis, which was very motivating to them and to other clinical teams in the trust | |
| Organisational learning and long-term response | All deaths are now coded from the case notes but the living patients are coded from discharge summaries, which the trust recognises do not pick up all comorbidities |
| The trust now has had a mortality review committee but the membership has changed over time. Now staff from the coding team attend along with senior consultants from across the trust. It is now chaired by a senior consultant. At least once per year every specialty has to present to the committee to show what they are doing to reduce mortality. The board wanted to implement a much stronger mortality review process across all specialties. Guidelines were issued as to what was expected from these meetings. In particular, they were to involve more nurses and physiotherapists | |
| The trust is now much more proactive in monitoring the data and seeing where the figures change and need investigating. There is also much more clinical engagement in the process and in management overall. Reducing mortality is now a key part of the trust’s plans and they have set an ambitious target to reduce the HSMR from 100 to 80 |
Sep-s.06 thematic analysis
Absence of clinical engagement in decision-making/an administrative approach
Before the receipt of the MASS sepsis alert, respondents reported that clinical engagement in trust decision-making was largely absent. Generally, it was suggested that managers displayed an administrative approach whereby they functioned in ’silos’ and failed to share and communicate information.
It was reported that some improvement work regarding sepsis was in place. However, this lacked a strategic direction and had arisen as a result of an individual clinician having a committed interest in addressing sepsis-related mortality. This had occurred after a nurse in the surgical department attended a conference and learnt about quality improvement focused on implementation of the ‘sepsis bundle six’ and, subsequently, managed to galvanise her colleagues to volunteer their time.
Fragmented structures and processes for mortality review and improvement; absence of leadership priority
Respondents reported that structures and processes supporting investigation of mortality were fragmented and lacked both integration and substance across organisational levels (corporate, divisional and specialties). At a corporate level a mortality committee existed, but strategic approaches in addressing mortality such as a ‘mortality reduction plan’ were absent. Likewise, even when they existed, trust specialty mortality meetings lacked strategic direction. Generally, it was recognised that there was lack of focus on investigating mortality.
Trust responses to sepsis alert
Clinical involvement and cultural ownership of trust mortality
The alert appeared to stimulate clinical ownership in divisional and specialty clinical leaders for improving mortality. Dispersed leadership of improvement around sepsis also concerned clinical champions operating as ‘opinion leaders’ encouraging ‘buy-in’ and stimulating the development of innovations within specialties. For example, in A&E a consultant was focusing on patient pathway analysis and improvement. He was instrumental in leading and developing a new technique (sepsis trolley) to facilitate the early treatment of sepsis. Similarly, dispersed clinical leadership was facilitated by a specialist ‘sepsis team’ led by an inspirational leader who was focusing on targeted interventions for improving sepsis. The CEO referred to this team currently tackling GP education around sepsis. Similarly, clinical champions operating as ‘boundary spanners’ made sense of how clinical diagnoses were coded and the implications of this for MASS alerts.
An integrated approach to tackling mortality for sepsis
It was reported that trust senior leaders were moving towards a more integrated approach, providing connecting structures and processes across corporate, divisional and specialty levels as instituted in response to the alert.
Trust divisions highlighted how the alert had prompted surgery and medical divisions to work together in developing the ‘sepsis working group’. It was reported that there were difficulties in achieving an integrated approach but that the divisions were moving forward.
Leadership priority and strategic interest in mortality around sepsis linked to regulator pressure
Analysis suggests that the alert for sepsis had stimulated the trust’s leadership to prioritise the improvement of mortality for sepsis. It was viewed that this, coupled with the CQC’s interest, had coerced and made the trust leadership ‘jump because you’ve got to’ as their ‘jobs were on the line’ if the trust ‘didn’t look good externally’. Hence, the response needed to be timely and effective.
A constructive approach in responding to the CQC inspection was demonstrated in how the ‘sepsis team’ engaged with the public and media at trust board meetings, where they talked openly about how they would tackle sepsis. In responding to the alert and CQC interest, the chief nurse conceded that the alert had focused attention on producing a strategic mortality reduction plan.
A universal approach
Respondents highlighted how the trust’s attention had focused on a universal approach to ‘insisting every doctor looks at their deaths’ (CEO Sep-s.06): ‘in medicine last year they were reviewing a random selection of cases, now we’re insisting every doctor looks at their deaths’. It was reported that this was implemented as a result of an external ‘dictat’ and that it had created an immense challenge for the trust. This was especially onerous in specialties focused on geriatric care. The medical director commented that this universal focus provided a broad understanding of trust mortality but did not provide depth. He also suggested that clinical judgement should dictate issues for which there appeared to be a problem and then investigate a random sample of case notes (Sep-s.06).
A forensic ‘big data’ approach: investigating mortality and targeting action
The alert appeared to have some part in stimulating the trust to apply a forensic approach to investigating mortality for sepsis. The engagement of an informal opinion leader in quality improvement initiatives around sepsis also appeared to have triggered a focus on mortality. As highlighted earlier, the use of the Sepsis 6 quality improvement initiative was ongoing before the alert, and after the alert it provided a detailed methodology for investigating the alert. 145 The alert was said to have provided a powerful trigger and urgency for focused action. Benchmarking HSMR trust performance data with those of other trusts was also considered useful.
Developing innovative tools to tackle sepsis mortality
During data collation for the case note review, respondents identified how the trust was starting to implement a ‘mortality pro forma’ that provided a standardised approach for reviewing case notes. It applied a grading (A–E) and identified the organisational level required for further detailed review. The forensic documenting of patient pathways also appeared to be a ‘powerful tool’ for nurses, as it provided evidence that they could use to persuade doctors that escalation of treatment for sepsis needed to take place.
Resourcing organisational capabilities enabling improvement in mortality
Analysis highlights how the trust investment in organisational capabilities such as IT infrastructure will support monitoring, awareness and education in addressing sepsis mortality. For example, escalating patient treatment early was identified as critical in limiting mortality for sepsis. Investing in an electronic awareness system for patient observation [modified early warning score (MEWS)] would enable greater awareness of patient deterioration and hence facilitate early treatment. Likewise, reference was made to the implementation of an ‘e-learning package’ aimed at facilitating awareness of sepsis.
Generally, it was perceived that the alert had encouraged the senior executive team to provide funding for staff to support investigation and problem-solving around sepsis.
Outcomes of sepsis alert
Trust outcomes of the alert are characterised as encouraging proactive engagement with the CQC: early intervention for ‘suspected sepsis’; increased trust confidence in delivering high-quality care and attention to increasing systemisation of care; and consultants taking a greater interest in their outcomes.
The trust-reported outcomes of the alert for sepsis highlight that the trust has adopted a proactive approach whereby internal review can highlight problems with mortality and the trust will engage proactively to notify the CQC. It was viewed that alerts were reducing as the trust was tackling problems in sepsis awareness. The CEO considered that the trust was reducing variation and increasing systemisation in care across the trust.
Increased trust confidence in delivering high-quality care
Trust leaders generally appeared confident about trust care and identified that any future alert would arise through coding problems as they were already addressing issues around sepsis awareness, early treatment; case note write-up by doctors and the involvement of clinicians in coding.
Overall, the CEO reported that mortality measures were ‘very helpful’ and that, although they had ‘pitfalls’, on balance these were ‘outweighed by their advantages’.
Consultants taking a greater interest in their outcomes
With the changes the trust has put in place it is considered that consultants are taking a much greater interest in their outcomes. Prior to the alert, the trust was described as looking only at the overall HSMR; now it is looking at ways of making improvements.
Parallel evolution of institutional focus on mortality reduction in sepsis
It was conceded that the improvement in mortality was not exclusively triggered by the alert but that other co-evolving strategies and cultural changes were also important. A matron identified that attention to investigating sepsis mortality ‘was already rolling’ and that the alert ‘gave us a bit of a spring board’. Clinical involvement and dispersed leadership was also recognised as a strategic direction for the trust and this was not specifically linked to the alert. The CEO also reported a strategic focus on integrating mortality review structures that linked to a cultural focus on patient safety and quality improvement organisational changes.
Trust respondents perceived that mortality had become part of the organisation’s guiding vision aimed at expounding core cultural values.
Criticism of external monitoring
Criticism was levelled at the extensive external monitoring of trust performance of mortality and safety. It was suggested that external organisations were all looking at the same data and performing much the same role. It was considered a distraction for the trust and that it was wasting both time and money. The medical director also criticised the validity of alerts. He suggested that there were flaws and inconsistencies in Dr Foster mortality data. The medical director was also convinced that trust coding practices had skewed Dr Foster data, as dead patients were coded differently (from case notes) from living patients (from discharge summaries). Hence, the alerts were inaccurate.
Cross-case comparative analysis
In order to maximise learning from variations in characteristics across the 11 case studies, comparative or cross-case analysis was undertaken. This approach aimed specifically to address the research objectives concerning the effects of multiple alerts within the same area and the implications of alerting in different clinical areas (i.e. sepsis and AMI) for the institutional response. The cross-case analysis built on the narrative and thematic case study analyses reported in the previous section, but sought to adopt an integrative perspective by systematically exploring salient common and divergent themes. The comparative analysis was performed at two levels within the data set. First it was based on the case narratives to identify the common and divergent surface features of the cases, and to guide a second, deeper pass of the case study data themselves. In the second pass, key categories were extracted linked to four high-level themes: (1) alert-relevant trust preconditions, (2) institutional responses to the alert(s), (3) perceived outcomes attributed to the alert and (4) parallel features of context, including evolution of the trust’s focus on mortality, that were not reported to be directly driven by the alert(s).
As in Chapter 6, we have elected not to include the full comparative analysis for editorial reasons and in the interest of reducing the burden placed on the reader. In the following subsections, we provide an abridged high-level commentary on emergent categories linked to the four aforementioned themes. The commentary is structured to address the key comparative research questions from our original research protocol, namely the questions of whether or not trusts with comparable mortality alert profiles vary in their response, whether or not responses vary depending on the number of alerts received by a trust in the same area (i.e. single vs. multiple alerters) and whether or not the focus of the alert influences the nature of the institutional response. In structure, our report therefore considers, in turn, (1) a comparison of sepsis single-alerting trusts, (2) a comparison of sepsis multiple-alerting trusts, (3) a comparison of AMI multiple-alerting trusts and (4) comparison of sepsis and AMI alerting trusts. Note that there is no separate analysis for single AMI alerting trusts, as only one such trust was available within the sampling framework. The final step in the comparative analysis was a synthesis of insights generated from the comparisons, the findings from which are summarised in Chapter 9.
Comparative analysis of sepsis single-alerting trust case studies
Two trusts (Sep-s.06 and Sep-s.05) received a single alert for sepsis during the sampling period.
Comparison of trust preconditions
A comparison of trust preconditions gave rise to a number of common themes. Both Sep-s.06 and Sep-s.05 appeared to have experienced:
-
problems with senior leadership
-
fragmented structures and processes for mortality review and improvement
-
poor engagement between clinicians and managers
-
individual clinicians championing improvements in sepsis awareness and treatment.
Problems with senior leadership
Important preconditions in both trusts included the experience of problems with senior leadership engagement in mortality review. In Sep-s.05, it was evident that clinicians felt much distrust of and antipathy towards the CEO. All respondents referred to poor clinical engagement with senior leaders and disagreement over the implementation of the IT-enabled patient records system:
And the chief executive at the time he wouldn’t listen to clinicians. [XXXX], he’s the one that implemented. He wouldn’t listen to us. He’d shout.
Consultant in critical care, Sep-s.05
It was a very dictatorial style. It was very much ‘my way or no way’. It was very much not including of the clinicians that were on the shop floor and disregard for much of the clinicians’ thoughts.
Associate medical director, Sep-s.05
Fragmented structures and processes for mortality review and improvement
Respondents in both Sep-s.06 and Sep-s.05 reported that structures and processes supporting the investigation of mortality were fragmented and lacked both integration and substance across organisational levels (corporate, divisional and specialties). In Sep-s.06, at corporate level a mortality committee existed but strategic approaches to addressing mortality, such as a ‘mortality reduction plan’, were absent:
We didn’t have a mortality reduction plan that was owned across the trust and we didn’t have embedded mortality, morbidity, meetings across specialties.
CEO, Sep-s.06
In Sep-s.05, respondents highlighted how the ‘mortality steering group’ did not always meet because of multiple changes in staff and that the trust’s routine attention to monitoring mortality was ‘ad hoc’ and had, at times, broken down:
There was no mortality steering group, the medics didn’t particularly look at their mortality and the data . . . was meaningless at most meetings . . . it has been a bit ad hoc, a bit unstandardised, various different departments doing what they felt was appropriate/not appropriate. There was no line of sight from the organisation about who was doing mortality reviews and how many mortality reviews were being done, and the outcome of those mortality reviews.
Associate medical director, Sep-s.05
Poor engagement between clinicians and managers
In both trusts, interviewees remarked on poor engagement between clinicians and management. In Sep-s.06 managers appeared to display an administrative approach, whereby they functioned in ’silos’ and failed to share and communicate information:
The organisation two and a half years ago was quite administratively managed; I think actually the idea of a manager’s good day wasn’t to see a doctor but to sit in offices and talk to other managers, and then worry about why we were so overspent, why we weren’t hitting the A&E target.
CEO, Sep-s.06
Individual clinicians championing improvements in sepsis awareness and treatment
In both trusts there were reports of a long history of quality improvement work in sepsis. However, often this lacked strategic direction and was undertaken by committed individual clinicians. In Sep-s.06, for example, one nurse in the surgical department had attended a conference and learnt about quality improvement focused on the implementation of the ‘sepsis bundle six’ and had managed to galvanise her colleagues to volunteer their time. This led to improvement in mortality around sepsis by applying quality improvement research and implementation techniques:
We worked for about 18 months to 2 years retrospectively looking at how patients with sepsis were managed and we were mortified if I’m honest. But I don’t think it was something that had really hit the radar at that point and I think we’d focused so much on clinical conditions that actually the secondary conditions like sepsis had gone by the wayside. So our research, the research that we did with the retrospective studies was really quite shocking.
Matron for general surgery, Sep-s.06
Comparison of trust responses to a single alert for sepsis
The comparison of trust responses to a single alert focused on the following themes:
-
regulator pressure coercing the trust response
-
useful as a trigger for a constructive approach
-
an integrated trust-wide response
-
a forensic approach in reviewing mortality
-
development of innovative tools
-
involvement of frontline clinicians.
Regulator pressure coercing the trust response
In both trusts there were reports that the alert for sepsis was a trigger for action. Sep-s.06 emphasised how the CQC intervention had coerced trust leaders to ‘jump because you’ve got to’ and ‘jobs were on the line’ if the trust did not look good externally. In Sep-s.05, it was also conceded that CQC intervention had directed the trust to investigate the alert and then develop action plans.
Useful as a trigger for a constructive approach
Staff in Sep-s.06 reported that the alert was a trigger for a constructive approach. This constructive approach in responding to CQC inspection was demonstrated in how the ‘sepsis team’ engaged with the public and media at trust board meetings, where they talked openly about how they would tackle sepsis:
Well there’s two things, one is you’ve got to do it because the CQC tells you you’ve got to do these things, but the other thing is, given that we’ve got to look at the data anyway, let’s use it to focus in a constructive way on things that we want . . . so the sepsis team, for example, have come to the trust board . . . And they talked openly in the trust board with the media there about what they’d done to cut deaths . . .
Trust mortality lead, Sep-s.06
A forensic approach in reviewing mortality
In both trusts, the alert and the CQC follow-up had led to a forensic approach to reviewing mortality. In Sep-s.05 this was entirely focused on the deaths highlighted in the alert. However, in Sep-s.06, it appeared to kickstart a ‘big data’ approach that linked back and informed quality improvement linked to Sepsis 6.
The impact to the sepsis bundle which was in response, partly in response to that alert, although not totally in response to that alert. But the alert gave us an opportunity to look in much more detail at those patients and we could look at patients whether they were in the medical division, in surgery or wherever, because we pulled all the notes and did a huge amount of work when that alert came out. So, you know, we looked at around 98 deaths.
Chief nurse, Sep-s.06
In Sep-s.06, the forensic investigation involved a case note review and the triangulation of data across hospitals, divisions and specialties, before reporting back to the CQC. Clinicians also undertook a routine universal case note review of all deaths. Likewise, in Sep-s.06, HSMR performance data was benchmarked against other trusts.
Information technology-enabled mortality review
In applying a forensic analysis of trust mortality, Sep-s.06 also developed an IT-enabled mortality review process. This used an e-mortality pro forma that set out a standard grading system for reviewing deaths and that graded deaths depending on whether the review needed trust-wide attention or was confined to specialty level.
An integrated trust-wide response
Both trusts reported an integrated trust-wide process for responding to the alerts. This focused on, first, the alert being validated and then a central structure (a mortality committee in Sep-s.06 and the clinical governance team in Sep-s.05) co-ordinating a trust-wide investigation. In Sep-s.05, respondents highlighted how the head of clinical governance asked the clinical director in the division implicated in the alert to recruit a senior clinician and task them with undertaking a case note review. This senior clinician produced a formal report, detailing action points, that formed the basis of the report sent to the CQC. In Sep-s.06 more detailed structures and roles were reported, involving the participation of a mortality lead and connecting structures such as regular mortality and morbidity groups at divisional levels.
Now we’ve had a big focus on getting a culture of morbidity and mortality meetings at divisional and directorate level. We’ve set some standards for those meetings.
CEO, Sep-s.06
Those in Sep-s.06 also highlighted how working groups assembled for medical and surgical divisions worked together to explore mortality following the alert. The outcomes of the mortality review were also fed into the trust’s quality improvement strategy process.
So we started a working group and from there it was – it’s unusual in this trust for the two divisions to work together. Surgery do their thing and medicine do their thing and never the twain shall meet. But with the sepsis working group it’s very much a core group of people who have taken this forward.
Matron for general surgery, Sep-s.06
Trust-wide awareness of the alert
Respondents in Sep-s.05 differed in their levels of awareness of the alert. The head of clinical governance suggested that those in trust divisions were aware that they were outliers for mortality and had been proactive in identifying problems to the CQC. However, the sepsis lead reported that he had not been aware of the alert, although he did concede that internal alerting systems were improving.
In Sep-s.06, a universal approach to reviewing patient deaths was in place. This promoted trust-wide awareness of mortality, as every doctor was responsible for reviewing each of their patient deaths:
In medicine last year they were reviewing a random selection of cases, now we’re insisting every doctor looks at their deaths.
CEO, Sep-s.06
Clinical engagement and cultural ownership of sepsis improvement
Sep-s.06 reported trust-wide intensive clinical engagement in mortality review. Clinicians also appeared to develop ownership of trust mortality. Opinion leaders in this trust, operating as informal sepsis champions, encouraged ‘buy-in’ and were instrumental in developing innovations within specialties.
The response in Sep-s.06 to the alert also appeared to prompt and motivate clinicians’ engagement by appealing to their implicit problem-solving epistemology mentality:
The other is then, you know, throughout the trust otherwise, every clinician wants to know how they’re doing and if mortality’s one of those measures, which it is, then if there’s something wrong, it motivates them to find out why . . . They all equally are animated when you get an alert, but that’s good because it engages them in the process. And then it engages them in the reduction plan as well, so an overarching mortality reduction plan, they all want to do the best they possibly . . . we use it in that way.
Chief nurse, Sep-s.06
Similarly, clinical champions in Sep-s.06, operating as boundary spanners, supported mortality review and made sense of how clinical diagnosis for sepsis was coded and the implications of this for alerts.
In contrast, in Sep-s.05 there appeared to be less focus on clinical involvement in the mortality review and investigation processes linked to the alert. For example, the sepsis lead acknowledged that there was a problem with coding for sepsis but conceded that he had not had any involvement in trying to address this problem, as he had not been asked for his input. Likewise, universal case note review by clinicians of all deaths was not undertaken.
In summary, the trusts differed in their responses in so far as Sep-s.05 limited its response to directly addressing the specific deaths highlighted in the alert. Sep-s.06 appeared to follow a more robust and clinically involved process of case note review but also started to develop a culture that encouraged an awareness of mortality linked to sepsis and ongoing improvements in sepsis care.
Comparative analysis of outcomes arising from the alert for sepsis
A comparative analysis of outcomes generated by the alert suggests that Sep-s.05 generated solutions directly related to problems arising from investigating the alert. These related to training junior doctors in writing up case notes and providing greater clarity in diagnosis and comorbidities. Junior doctors were also trained on greater awareness of sepsis and the importance of early intervention. However, cultural changes that supported ongoing improvement in sepsis awareness and routine case note review of all deaths appeared limited, although it was noted that more recently the new trust leaders had started to address clinician disengagement.
In contrast, Sep-s.06 addressed problems arising from alert investigations and went further in enabling the development of a trust culture that supported the routine clinical case note review of all deaths, improved sepsis awareness, the use of innovative IT-enabled technology to systemise routine case note review and monitoring of mortality and deterioration of patient condition. Sep-s.06 trust outcomes of the alert are characterised as encouraging proactive engagement with the CQC, encouraging early intervention for ‘suspected sepsis’, increasing trust confidence in delivering high-quality care and increasing systemisation of care.
Comparative analysis of parallel development of processes for sepsis mortality
Respondents in both Sep-s.05 and Sep-s.06 conceded that other factors influenced the evolution of trust mortality processes and improvement in sepsis mortality. The important emergent themes included:
-
regulatory pressures link to changes in trust leadership
-
engagement with external bodies
-
clinical engagement and dispersed leadership of mortality review and QI
-
integrated structures and processes
-
a culture supportive of mortality awareness
-
the use of data analysis tools to monitor mortality.
Regulatory pressures link to changes in trust leadership
Extensive organisational turbulence experienced in Sep-s.05 at the time of the alert prevented trust-wide engagement in mortality review. Regulatory pressures associated with Monitor and CQC intervention led to substantive changes in trust leadership. The resulting changes in trust leadership appear to have influenced improved clinical involvement in mortality review.
Engagement with external bodies
In Sep-s.05, consultants in critical care highlighted how their specialty had engaged for more than 5 years with the Intensive Care National Audit and Research Centre (ICNARC), whereby a specialist audit clerk inputs data into the ICNARC database and each quarter the critical care department receives a nationally produced report. They noted that this educates them in improvement on critical care practices and develops them professionally:
It gives us the opportunity to build on that which improves our professional fulfilments as doctors . . . And improves the care for our patients . . . So I’ve been emphasising the use of this from an education point of view.
Consultant, critical care, Sep-s.05
Similarly, both trusts were engaged with external bodies in clinical auditing specialty performance and participation in quality improvement initiatives for sepsis, and this appears to have played a part in improving the awareness and treatment of sepsis.
Clinical engagement in mortality review and dispersed leadership of mortality review and quality improvement
In Sep-s.06, a matron identified that attention to investigating sepsis mortality ‘was already rolling’ and that the alert ‘gave us a bit of a spring board’. Clinical involvement and dispersed leadership was also recognised as a strategic direction for the trust, and this was not specifically linked to the alert:
I think our deliberate approach to developing the organisation was based around getting the people who do the work, who are clever people, involved in leading services really. And I mean that’s a value and I have; it’s a value that the nurse and medical director have and their executives. So whilst there was a national impetus it’s kind of a no-brainer and the really successful organisations that excel have a number of characteristics – one of which is clinical excellence – and you only get that by effective clinical leadership. So it’s been deliberate from our point of view . . . And so I’ve tried to change it from quite a centralised cliquey sort of way of leading into a much more open transparent distributed way where people – I’m trying to give clinical leaders and execs clear role responsibilities really and their goals.
CEO, Sep-s.06
Integrated structures and processes
In Sep-s.05 it was suggested that major changes in trust structures had occurred as a result of Monitor intervention and that this had led to changes in trust senior leadership who had acted ‘as a new broom’ providing an ‘overhaul of trust governance’. The head of governance highlighted this as follows:
So a complete overhaul of all governance throughout the organisation starting at the board level and going downwards. Now clearly that includes mortality in terms of divisional governance, in terms of corporate governance, but also in terms of clinical governance. So that’s the impact. It makes you start again, basically.
Head of governance, Sep-s.05
The new medical director suggested that assurance of high-quality care needed to be facilitated, so divisional directors sit on the mortality review group:
We have five clinical divisions and they’re all represented on the mortality alerts group along with a few other people. We have [XXXX] who’s one of the senior nurses responsible for quality within the organisation. We have a representative from our coding unit. And normally Dr Foster will send along one of their team to assist and steer us through the data at the mortality alerts group.
Medical director, Sep-s.05
The three new associate director roles were created for standards, patient safety and revalidation. In the trust hierarchy, these sit beneath the medical director. One associate medical director responsible for standards, clinical effectiveness and research has responsibility for mortality review.
A culture supportive of mortality awareness
Trust respondents in Sep-s.06 perceived that mortality had become part of the organisation’s guiding vision aimed at expounding core cultural values:
Well it’s one of our, it’s one of our key strategic aims to reduce mortality, it’s explicit in our vision. And so the vision has lots of things in it, but one of the critical success factors is delivering excellence in quality and patient experience and mortality is a key element of that, so it’s clearly explicit throughout the document that everybody sees.
Chief nurse, Sep-s.06
In Sep-s.06, the CEO also reported a strategic focus on integrating mortality review structures that linked to a cultural focus on patient safety and quality improvement organisational changes:
I think we’ve had huge pressures with the A&E target and our performance on that has been awful, but actually the one thing that we’ve kept shape on is actually the quality. And I’ve just been with the CQC just now and actually they’re saying ‘Your A&E department is great’ despite the fact the patients are waiting long periods of time. And so I think we kind of kept our shape because we saw quality front and centre, and actually for us on the efficiency equation quality and efficiency are different sides of the same coin.
CEO, Sep-s.06
Comparative analysis of sepsis multiple-alerting trust case studies
Four trusts were reported as receiving repeat alerts for sepsis (Sep-m.07, Sep-m.11, Sep-m.09 and Sep-m.10).
Comparison of trust preconditions
Comparison of trust preconditions for receiving multiple alerts gave rise to the following common themes:
-
catchment characteristics
-
problems with coding mortality
-
fragmented organisational structures
-
financial and operational pressures
-
trust involvement in sepsis improvement work
-
leadership
-
sentinel events.
Catchment characteristics
It was commonly reported that catchment characteristics had an impact on trust mortality, and all trusts identified that deprivation and lower life expectancy had an impact on trust mortality. In Sep-m.09, trust staff highlighted that this related to immigration centres, alcohol and psychiatric diseases, and questioned whether the mortality calculations for the trust had taken account of this:
We’ve got lots of urban poverty . . . We have a lot of alcohol and psychiatric disease, and they score heavily in the 15–45 age group. And unless you know that we’re number three in the country for this particular problem, it’s hard to understand why we seem to have so many deaths, most of which happen outside and we can do nothing about because they’re just brought in and die in 24 hours on the intensive care unit.
Mortality lead, Sep-m.09.
Two trusts (Sep-m.07 and Sep-m.11) identified that poor community service provision in their catchment had an impact on trust mortality. Both trusts reported that terminally ill patients were being sent to the trust to die; the trusts reported limited palliative care systems and a lack of suitable staff:
We have a lot of young people dying of cancer who tend to die of cancer in the hospital rather than in the community. And we didn’t have very well-developed and palliative care systems, we didn’t have our own palliative care consultants.
Former medical director, Sep-m.07
That is a challenge for us compared to some other organisations where community services may be better developed and people have a choice to die outside of hospital. There was also a view that some of our community provision, our care home provision, was not as robust in this area as it is in some others. So, again, the choices for people are more limited. Now, again, all of those things might impinge on your HSMR.
Medical director, Sep-m.11
Problems with coding mortality
Both Sep-m.09 and Sep-m.10 reported issues with coding quality. In Sep-m.09, this was linked to shortages of skilled coders, and in Sep-m.10 respondents reported a lack of standardisation in coding mortality, as two of the trust hospitals adopted a different methodology:
The coders are organised – we’ve got coders on both of our main hospital sites and they have different models in each trust, in each of the hospitals. So in [B] the coders go to the wards and pick up the notes on discharge or death and will scrutinise them there, will take them back to their office if need be but sometimes they just take the details they need there and then so leave the notes in the system. At [A], the notes flow to the coding department.
Deputy head of information, Sep-m.10
In Sep-m.09, the mortality lead drew attention to limitations in trust capabilities for coding. These were linked to reductions in staffing allocation for non-clinical staff. It was noted that quality in coding was essential, as coding errors had had an impact on the usefulness and validity of alerts:
So if you put rubbish in, you get rubbish out. I understand that bit. Our chief coder, in the last few months, has gone onto retirement and is due to come back, so I don’t have a relationship with the new people. But my understanding seems to be that they’re short of people. We’re having a halt on recruitment, because we don’t want to spend money on non-clinical staff, so I kind of see this as a threat.
Mortality lead, Sep-m.09
Fragmented organisational structures
In two trusts (Sep-m.07 and Sep-m.10) it was emphasised that the structures and processes for addressing and recording mortality were fragmented. In Sep-m.07, although a central co-ordinating team or mortality review group examined trust mortality, respondents reported that mortality investigation was fragmented across the trust, and it was noted that senior leadership was disconnected and had not ensured that learning around mortality review was shared across the trust:
I think a lot of our mortality was, at that time, when I first came into post was most probably a little bit disconnected between the top of the organisation which the board would have numbers presented as a HSMR type data as part of a performance matrix, and then the mortality reviews, mortality and morbidity meetings which would be held within departments, and very often associated with all of this, and I think to be fair to say that there would be a differential between how good some of those mortality reviews were.
Former medical director, Sep-m.07
Likewise, the deputy head of information in Sep-m.10, who had worked in the trust for 25 years, said that before 2010 there was little knowledge about alerts in the trust and little interest in mortality data:
I’m not sure that we even knew that there were Dr Foster CQC alerts . . . they certainly didn’t come my way so if they arrived I don’t know to whom and I don’t know what was done with them.
Deputy head of information, Sep-m.10
Financial and operational pressures
In Sep-m.11, concern was raised about the impact of restructuring on finances and staff redundancies. Some trusts highlighted problems in specific care pathways. For example, in Sep-m.09, the chief nursing officer remarked that the trust was ‘stressed’ by challenges in the emergency pathway but also confirmed that there were no financial pressures, as the trust was in financial balance:
I mean the organisation was in financial balance, there were some challenges around the emergency pathway in delivering the 4-hour standard, other performance metrics were all pretty much online, so I wouldn’t have said the organisation was, other than the emergency pathway, stressed.
Chief nursing officer, Sep-m.09
Trust involvement in sepsis improvement work
All trusts referred to participation in external improvement programmes [Safer Patients Initiative (SPI) and ‘Think Sepsis’] related to sepsis. In Sep-m.11, Sep-m.09 and Sep-m.07, attention was focused on how trust champions or sepsis leads had implemented the sepsis care bundle and had undertaken work to promote the IT-enabled early identification of sepsis and patient escalation processes. It was noted that both Sep-m.07 and Sep-m.09 had developed IT-enabled systems for logging patient conditions. This enabled the visibility of patient deterioration and timely intervention.
In Sep-m.09, the trust sepsis lead recounted that the trust had been active for many years in responding to national campaigns focused on sepsis awareness. The move to a new hospital site in 2006 was linked to the implementation of the Electronic, Physiological Patient Observation Track and Trigger System (EPOTTS) in 2007:
In 2006 we moved into this hospital and 2007–8 we started working with an electronic system for track and trigger. So it was Electronic, Physiological Patient Observation Track and Trigger System, EPOTTS for short.
Mortality lead, Sep-m.09
This previous work on sepsis improvement appeared to focus primarily on the emergency department (ED) and critical care, as most sepsis leads were consultants in these specialties. For this reason, staff in most trusts (Sep-m.09, Sep-m.11 and Sep-m.07) were generally aware of sepsis problems. The associate medical director in Sep-m.11 said:
The alerts . . . have never told us anything we didn’t know already . . .
Associate medical director, Sep-m.11
Leadership
Many trusts drew attention to the way in which opinion leaders had been instrumental in addressing trust mortality. The medical director in Sep-m.07 had taken an interest in analysing mortality. In other trusts (Sep-m.09), champions working in particular specialties had led on sepsis work. It was noted that attention to sepsis mortality, and to mortality in general, was not reported as a trust-wide activity.
Sentinel events
One trust, Sep-m.09, reported that sentinel events or major patient safety failures linked to sepsis had driven a focus on improving trust-wide mortality. Two sentinel events were referred to as follows:
I started in the April of 2009 and I became aware of the alerts when we’d had two very serious cases of sepsis, or a failure to recognise sepsis within our emergency department, so we had a young girl who was 14 years of age and we had a young mum, I think, in the twenties or thirties, I can’t quite remember the full details. Anyway, and both of those cases went through a root cause analysis review following a serious incident.
Mortality lead, Sep-m.09
This was the only trust in which sentinel events were described in the context of preconditions for mortality alerts.
Comparison of trust responses to the alerts for sepsis
A comparative analysis of the trusts’ responses to multiple alerts for sepsis gave rise to the following common themes:
-
responses to first and subsequent alerts for sepsis
-
a centralised approach
-
clinical engagement in case note review
-
a forensic approach
-
the identification of problems
-
an action-focused approach linked to improvements.
Responses to first and subsequent alerts for sepsis
Difficulties arose in discriminating distinct responses to the individual alerts. Only one respondent in Sep-m.07 was able to identify the trust’s response to the first alert. In the other trusts, respondents highlighted how the trust leadership had increasingly prioritised attention as the number of alerts received increased. In Sep-m.11, Sep-m.09 and Sep-m.07, a forensic approach involved validating the alert, undertaking case note review, identifying problems with coding and care and developing corrective processes to address these issues. Sep-m.11 appeared to move faster in addressing problems, whereas Sep-m.09 and Sep-m.07 stepped up action to improve sepsis early identification and treatment only after the second alert. In Sep-m.09 in particular, interest in sepsis mortality was linked to investigation of sentinel events or major patient safety incidents linked to failures in identifying sepsis. Sep-m.10 appeared to also prioritise trust actions in responding to the alert but was still unable to complete the circle of identifying problems and then moving on to implementing solutions. Overall, Sep-m.10 appeared less clinically engaged.
A centralised approach
In some trusts (Sep-m.07 and Sep-m.11), the response to the first alert took a centralised approach. In Sep-m.07, the process started with the CEO who received the alert passing it to the medical director, who co-ordinated the response. A review process was initiated of 60 case notes by the head of coding and the medical director. Discussion and review of some of the case notes was undertaken by the mortality group, comprising consultants from ED, critical care, surgery, medicine and palliative care and a clinical audit lead. From this investigation was undertaken of coding and reports produced of review findings and action plans for the trust board, quality committee and clinical governance committee. The medical director would also send a report to all consultants explaining the alert, the results of the review and the action plan:
They come into the chief exec who then passes it onto me and I do the response, so I get people to help with some of the mortality reviews, we would do a report, look at some of the coding issues, put what we were doing, including a board report on mortality, we would go back to board to the quality committee and it would get sent to the consultants in terms of . . . so that would be the formal route, governance route that it would be reported to . . . So you have the board and then the quality committee. It’s slightly different now how they do it. And then it would’ve been reported to all as part of – I would do a medical director’s report to the consultants to say, ‘We’ve had this alert come’, etc.
Former deputy medical director, consultant critical care, Sep-m.07
A forensic approach
All trusts highlighted an increasingly forensic approach on receipt of the alerts. In Sep-m.07, this process was perceived as proactive, as the former medical director said that the trust had already identified a problem with mortality for sepsis before the alert (2013) and had already started to review case notes before receiving the CQC letter. The medical director reported that he had been monitoring trust mortality over a long period and had a lot of experience of using Dr Foster tools and the trust’s CHKS system:
I believe that the ITU [Intensive Therapy Unit] one, we noticed our figures were going up and we asked them to come in before we actually triggered, and we’d actually had the review and the report back by the time the CQC had picked up, and our figures were coming back down again. So that would have been 2013.
Former deputy medical director, consultant critical care, Sep-m.07
Emphasis was placed on thoroughly investigating the alert rather than immediately blaming it on poor coding. It was noted that some trusts appeared to respond to alerts by adjusting their coding and ‘manipulating the data’. This was viewed as an ‘unemotionally intelligent thing to do’ and in this trust the approach was to be ‘honest’ with coding. The approach was explained as follows:
To start with, he [former medical director] didn’t want to dismiss any of this as a coding issue and we’re not in a place where we can do that, we certainly weren’t back 3 years ago, because blaming the coding was just an unemotionally intelligent thing to do. And when you look at some trusts, I think, who’ve like hired kind of people to help them with it they’ve laid themselves open a little bit, I think, haven’t they, to sort of manipulating the data. So I can honestly say that, although our coding might not be as good as it can be, I think there’s every reason to assume that it’s actually honest.
Blaming it on the coding is just a blind alley, isn’t it, I mean, it’s pointless in a way because you just . . . you want to be absolutely sure that it’s not quality of care before you actually turn to the coding issue otherwise it just looks dismissive and . . . Plus the fact you miss an opportunity to actually improve things.
Interim medical director, Sep-m.07
In Sep-m.11, senior leaders highlighted the forensic examination of case notes, an analysis of care pathways, triangulation of data, production of action plans and implementation of new and improved practices:
We used to pounce on the monthly data from Dr Foster and go through it in enormous detail and we knew where we were heading in every single diagnostic group and we used to map them or we used to trend . . .
Associate medical director, Sep-m.11
This forensic approach to the alert was viewed as including review of 50 case notes, analysis, production of action plans and ‘spending time making sure those actions are embedded’ (head of governance). Respondents also commented that the process was very time-consuming and highlighted that it had not identified anything more than had already been covered in SPI-inspired improvement work:
The sepsis one, particularly the big one that we did, it was huge. It was myself, [XXXX] who’s the consultant nurse and another one of the . . . other consultants and I think I just cleared my diary for something like 6 weeks . . . do the analysis of it, come up with something, write an action plan and then spend the time making sure that those actions are imbedded is massive for an organisation and when it doesn’t really tell you anything at the end of it that you didn’t already know, it’s kind of like, ‘OK!’ . . .
Head of governance, Sep-m.11
Sep-m.09 also followed a systematic and forensic process. A working party was set up to review case notes of deaths occurring during the designated period of the alert. The head of nursing described how the sentinel events and the alert were joint drivers of a working party forensic investigation. This involved, first, validation of the alert by checking the coding and then the governance department identifying the time scale for the review process and instructing that a mortality review process was undertaken by the service that the alert related to. There was a peer review within that service and a report was presented to the mortality review committee. This report was then sent for scrutiny by senior trust leaders in the patient safety committee.
In Sep-m.10, respondents emphasised that validating the alert was necessary and drew parallels with Mid Staffordshire where ‘they didn’t trust HSMR data’. Sep-m.10 respondents stressed that, in responding to the alert, they were not trying to dismantle the alert but they were ‘healthily sceptical of it’. The deputy head of information also stressed that validating the alert comprised the following stages:
Right, let’s make sure (a) we understand what it’s telling us, (b) that we agree with what it’s telling us.
Deputy head of information, Sep-m.10
It was suggested that the trust needed to ‘prove’ that the alert was worth investigating and that, invariably, the alert ‘numbers matched’:
I think we start from a position of wanting to prove to ourselves that it’s something worth investigating which is why my first task is can I match the numbers? So, if we match the numbers and we almost invariably do, it’s relatively unusual to have a significant discrepancy.
Deputy head of information, Sep-m.10
The nursing director reported that validation of the alert was considered useful, as it made the trust ‘concentrate’ and ‘focus its’ attention and ‘dig down’ to identify problems. Overall, the alert was ‘a slap in the face’ that made the trust question how it was delivering care:
I think they do because I think we are doing all of this work and then something will come and slap you on the face and you find that the infection rates and the caesarean sections have gone up, but why?
Nursing director, Sep-m.10
Only after completing this process did they move to an indepth investigation of deaths linked to the alert. Hence, it was reported:
We’ll have a look anyway because it’s a good thing to audit your patients and see what’s happened.
Deputy head of information, Sep-m.10
Unlike the other repeat alerted trusts this process, Sep-m.10 lacked continuity, as it was reported that, initially, this information was forwarded to either the medical director or the director of clinical strategy. The medical director reported this inconsistent approach as follows:
They didn’t come to me and indeed what we’ve done in the organisation is maybe streamline that a little bit in that they would previously have probably gone to the information department for the first instance and then maybe have got to me eventually but not necessarily consistently.
Medical director, Sep-m.10
Identifying problems in coding
All trusts identified problems with coding arising from poor case note write-up. However, in one trust (Sep-m.10) intensive attention to identifying coding problems occurred only after the second alert.
In Sep-m.07 and Sep-m.11, case note review identified errors in coding for sepsis linked to palliative care. This related to elderly patients admitted from nursing homes with ‘multiple bed sores who were basically coming to the end of their lives’. The deaths of these patients were not preventable even when they had been treated well. The former medical director described this as follows:
When I looked at it they were a very desperate group, very desperate, and we did a bit of a coding thing with the chief coder, and I think we had something like 63 cases. I did about half of them the 30-odd cases . . . I don’t think sepsis was always the first choice that should’ve been when we were looking back at the coding, and some of them were, like I said, they were 90-year-olds from nursing homes with multiple bed sores who were basically coming to the end of their lives, so whether they were – I’m not particularly interested in the mortality ratios or whatever, what I want to see is where is the preventability of the death.
Former medical director, Sep-m.07
Overall, it was reported that there had not been any errors in the care of these patients:
I can’t remember seeing anything where there was poor care . . . I think sometimes I wonder whether this would be coded right or wrongly, and I think coding is an issue.
Former medical director, Sep-m.07
Errors in coding were widely acknowledged in all trusts; for example, in Sep-m.10, the medical director suggested:
There is nothing wrong with our clinical processes or our clinical care but still we’re an outlier and what we’ve narrowed it down to is things like coding.
Medical director, Sep-m.10
In Sep-m.10, the recording of primary diagnosis was perceived as ambiguous, as were failures in recording comorbidities:
Is there something about the way we’re coding primary diagnosis or comorbidities that would set us differently from everyone else? The other thing we thought, we’re one of the first trusts into the sepsis six bundle, care bundle programme.
Deputy head of information, Sep-m.10
The medical director also suggested that recording of comorbidities was low and that this failure to identify and code comorbidities could result in higher mortality indicators:
So we know we are numbers that the number of comorbidities per patient in our organisation is low.
In Sep-m.10, it was also mooted that the system for ‘capturing coding’ was different in the two main hospital sites. For example, mortality coding was high in the hospital site where the coding staff did not engage directly with clinicians on the wards:
We know that the process we’ve got for capturing coding is not very good. We know that the process we’ve got for capturing coding is different in [A] than in [B]. We know that our coding process is clinically linked in [A] because the coders go to the wards and sit down with the clinical staff and go through the coding with the clinical staff in [A] but they don’t in [B].
Medical director, Sep-m.10
Despite this highlighting of poor coding, it was emphasised that it was important to thoroughly investigated the alert rather than immediately blame it on poor coding. It was also noted that some trusts appeared to respond to alerts by adjusting their coding and ‘manipulating the data’. In Sep-m.07, this approach was explained as follows:
Blaming it on the coding is just a blind alley, isn’t it, I mean, it’s pointless in a way because you just . . . you want to be absolutely sure that it’s not quality of care before you actually turn to the coding issue otherwise it just looks dismissive and . . . Plus the fact you miss an opportunity to actually improve things.
Interim medical director, Sep-m.07
In Sep-m.11, attention also focused on whether or not patients should have been sent to the trust at all, and also on the nature of their primary diagnosis, with a focus on where they had developed sepsis:
Should they have come in the first place? Did they develop sepsis in this organisation? Because the problem with a lot of these is the primary diagnosis and they’re coming in with them so actually then you’re asking a different set of questions like did we treat them in a timely and the appropriate manner rather than could we have avoided them getting it in the first place.
Head of governance, Sep-m.11
In Sep-m.09, alerts were seen as smoke signals and something to prompt investigation, but it was conceded that in a complex organisation this can mean that irrelevant things are investigated, which could distract attention away from more pressing issues:
What they do is they’re a smoke signal of various sorts . . . So these alerts are useful. They tell us to go and look. The problem is, you can be distracted by certain alerts and you go looking at things that don’t warrant attention . . . So the clarity of the signalling is a problem.
Clinical lead for mortality, Sep-m.09
In Sep-m.10, the CQC’s involvement ‘gave teeth’ to alerts, which spurred trust leadership to address hospital mortality and forced them to drill down and explore sepsis mortality:
I suspect when the CQC itself started to generate the alerts I think that was probably the trigger for us because . . . I think the CQC gave it the teeth that people like chief executives started to say, ‘What’s going on here? We’ve got an alert. Are we killing people? We must know more about this’.
Deputy head of information, Sep-m.10
In so doing, Sep-m.10 investigated by completing a ‘full mortality audit’ and then identified a host of problems associated with high mortality for sepsis. These included problems with the writing up of case notes identifying comorbidities, the recording of primary diagnosis and the coding of mortality.
We have narrowed it down to things like coding, which is obviously a natural port of call. Is there something about the way we’re coding primary diagnosis or comorbidities that would set us differently from everyone else?
Head of information, Sep-m.10
Likewise, by drilling down and exploring the alerts forensically, Sep-m.10 also identified problems with junior doctors completing death certificates:
If you actually look at this hospital, there’s four, five deaths a day in the two hospital sites. Why don’t the consultants do it? Because it would be more accurate, wouldn’t it?
Consultant sepsis lead, Sep-m.10
Analysis suggests that the Sep-m.10 was comparing its mortality indicators with those of other trusts and identifying how its particular care pathways may be linked to it being recorded as an outlier in terms of mortality. It was noted that all unscheduled care patients were ‘fired at’ two acute care units and were assessed there for a short period, which may not be the model used in other trusts:
Almost all of our unscheduled care patients go into these two ACUs [acute care units], one on each site, that is again making us a bit different from the average in the country because although acute medical wards are not unusual, deliberately firing all your patients that way and then keeping them a relatively short amount of time may not be exactly the same model of care or pathway of care that other places have.
Deputy head of information, Sep-m.10
In Sep-m.09, problems with coding were also identified, as it was clear that the coders did not know how to code sepsis, and so guidelines were written to address these:
The other thing that was found is that the coders weren’t really clear at all, in what they should put into what codes because it wasn’t clear. So we wrote some common sense guidance forms to what counts as what [in terms of sepsis] . . . I’m not entirely sure I’m right on this, but at the time there wasn’t a code for septicaemia which is a bug in the blood and there wasn’t a code for sepsis syndrome, yeah, with the management, of that, a lot a people would put as sepsis was coded at septicaemia and that proved it was septicaemia and so we made a very sensible, I can’t remember what it was, a way for coders to be clear of what counts as what.
Deputy chief medical officer, Sep-m.09
An action-focused approach: implementation of the Sepsis 6 bundle
Most trusts identified errors in care and mobilised actions to implement the ‘Sepsis 6′ care bundle. In Sep-m.07 the alerts were seen as making clinical staff aware of the problem and then mobilising the trust to act effectively, as follows:
‘Look we have a problem, this is what we’re going to do about it’. So that was useful to gain people’s attention.
Sepsis lead, Sep-m.07
In Sep-m.07 a direct response to the sepsis alert was the implementation of the Sepsis 6 care bundle. The interim medical director reported this as follows:
We did introduce things like . . . the ‘sepsis bundle’, I think it is, and then he’s been [inaudible] doing that, and so we have responded to the alerts positively.
Interim medical director, Sep-m.07
In Sep-m.11, the case note review process highlighted known problems around sepsis care and contributed to initiating the application of care quality programme that brought together care bundles (sepsis, AMI, pressure ulcers). It was reported that the trust had already been investigating and monitoring sepsis mortality and had recognised that there was a problem.
Given the fact that the focus was on immediate response to sepsis and A&E was obviously a focus of a lot of the work that we did and a lot of the enthusiasm actually, and that’s not perfect yet either but that was reasonable.
Associate medical director, Sep-m.11
It was noted that the alert stimulated further investigation of sepsis mortality in A&E.
We did a lot of work and had already done a lot of work on the 2012 alert prior to it arriving. So we were already had done the investigation prior to the alert arriving. Then with the alert arriving we went, ‘Oh yeah, we know we have a problem’. We have done some investigation but then obviously we went through the formal mortality review investigation that they wanted us, which was fine because we had done a lot of investigation.
Nurse consultant, sepsis, Sep-m.11
In Sep-m.10, work on the Sepsis 6 care bundle started in 2012, after the second alert arrived (sepsis lead). When data collection started, the trust found that only 20% of patients were receiving the bundle on admission. In response, it stepped up implementation of the bundle.
But it’s gone originally from about 20% up to 80%. So within severe sepsis, the definition of severe sepsis being organ dysfunction and unwell, high lactate, that kind of thing, we do feel we’ve made an improvement.
Sepsis lead, Sep-m.10
It was noted that clinicians working within the ED had undertaken considerable efforts to implement the Sepsis 6 bundle that had led to a significant increase in the use of the bundle, from 16% in April 2012 to 91% coverage.
Despite the implementation of the Sepsis 6 care bundle after the alert, respondents in Sep-m.10 were keen to attribute problems to coding errors rather to than errors in care. It was suggested that care was appropriate and the patients concerned were ‘very frail’, had many comorbidities and had been admitted from nursing homes. It was noted that this cohort of patients deteriorated very quickly and died. It was suggested that doctors had queried sepsis in the case notes and the patient had received antibiotics so, as the first entry in the notes referred to sepsis, the cause of patient death was recorded as sepsis. Nevertheless, respondents suggested that patient care had been appropriate and that in this situation death was inevitable. This was cited as an ‘acceptable death’.
A cultural approach focused on high-quality care
All trusts set out to use quality improvement methodology to improve care for sepsis. One trust (Sep-m.11) emphasised a response focused on developing a culture focused on high-quality care rather than on chasing alerts. It was felt that by ‘chasing’ and dealing with each alert individually, the longer-term culture change needed would be lost:
I think that is where it was important for us to develop the care of the acutely ill action plan because it became really clear to us that you could just be chasing alerts. And even in HSMR, I think HSMR has I think 56 conditions or whatever else that sit within that, I think SHMI [Summary Hospital-Level Mortality Indicator] I think is 130-odd, you can get into the fixation of which this is. And we’ve done some of that. but the reason why we talked about having a plan per se rather than just chasing the lights is because we know that some of it is more than just the indicators themselves; it’s about culture, it’s about looking at the whole pathway and, therefore, if you just chase the lights what you do is you miss some of the real longer-term stuff that you have to do that eventually will improve the situation around alerting.
CEO, Sep-m.11
Alert driving clinical engagement
Leaders in Sep-m.09 identified how the alerts were used as a ploy to promote clinician engagement in case note review. It was suggested that when clinicians responded to the alert they became fully engaged in discovering if there had been errors and, if so, why. It was posited that clinicians were often less engaged in this process. The head of nursing (Sep-m.09) suggested that clinicians were ‘driven by outputs’, in this case the alert, and so became fully engaged in investigating the alert. This was referred to as follows:
But normally they are a difficult bunch. And I remember they weren’t a problem in terms of engaging with the work, primarily because outputs are quite, they’re quite driven by outputs anyway, so there were two reasons, one they wanted to prove it wasn’t true, or two if there was a problem they’d need to go away and fix it. So, yeah, I mean they weren’t really challenging but I mean it’s natural for clinicians where they’ve got a potentially mortality outlier to initially review the data from the perspective that there might be something wrong with the data rather than necessarily what’s wrong with the care.
Head of nursing, Sep-m.09
In Sep-m.11, the alerts were perceived as gaining the attention of clinicians:
Did it [CQC alert] get clinicians’ attention?
Oh god yes.
In Sep-m.11, every death is reviewed and the coding validated by the consultant concerned with the death, thereby ensuring that the coding is accurate. If it is not correct then the consultant will record why and, if necessary, put this information in the patient’s notes too. In this way any changes to the notes are documented separately on a sheet held in the coding department.
In Sep-m.10, trust-wide clinician involvement in case note review was inconsistent. Sep-m.10 respondents reported that clinical involvement in case not review as onerous and dependent on volunteers. The deputy head of information reported that it had been hard to find willing volunteers among the consultants to help with this. It was noted that clinicians were not automatically informed by the organisation about the receipt of a mortality alert specifically:
Yes. So the reality is – I’ve been here since 2004–5, so throughout all of these alerts I’ve been here. The reality is as a clinician I’m somewhat removed from that, you know. It comes into this central kind of management suite and various people are involved.
Consultant, Sep-m.10
Comparative analysis of outcomes from repeat alerts for sepsis
A comparison of the reported outcomes from multiple alerts yielded the following common themes:
-
implementation of Sepsis 6 care bundle
-
coding of acute kidney injury
-
increases in staffing of palliative care
-
changes in clinical practice regarding the diagnosis of sepsis
-
innovative sepsis training
-
challenging practice and rewarding good clinical practice
-
changes in coding guidelines
-
changes in service design
-
wider cultural change
-
a focus on resourcing data analysis.
Most trusts (Sep-m.11, Sep-m.09 and Sep-m.07) suggested that the alerts had led to a greater impetus in implementing the Sepsis 6 care bundle. Some trusts (Sep-m.07 and Sep-m.09) highlighted changes in coding, and one trust (Sep-m.09) identified extensive improvements in care processes and innovative practices as evidence of greater sepsis awareness. One trust (Sep-m.11) focused on a broader cultural approach, concentrating on quality improvement rather than on ‘chasing the alerts’. In one trust in particular (Sep-m.10) there were reflections on how only limited changes in the management of sepsis had arisen from the alerts:
Well yes but I don’t think that they’re – they’re helpful as a lever but I don’t think they’re helpful in terms of actually telling us where our problem is because I think certainly on the basis of the mortality alerts we’ve seen they haven’t said, ‘Oh my god in sepsis we’ve got a systematic problem with our management of sepsis’ because for instance we thought maybe we have got a systematic problem because we take too long to get the antibiotics in. We’re dramatically better at that now and we know that across the whole organisation and in some areas even better than others and our mortality hasn’t dropped. Now that’s not to say the care isn’t better and I’m absolutely convinced the care is better and there is people probably who aren’t dying now who did die previously or whatever, but it’s such a crude measure mortality as an indicator of the quality of care that you’ve got to be doing something really bad or really good to get your figures looking fantastic . . .
Medical director, Sep-m.10
In considering coding changes arising from the alerts, the Sep-m.10 medical director also suggested that many trusts had changed their coding in response to the alerts. In this way they suggested that many trusts were ‘gaming’ with their coding in order to fix their HSMR.
Implementation of Sepsis 6 care bundle
Implementation of the Sepsis 6 care bundle was recognised to be a direct consequence of the alert and the CQC letter (Sep-m.07). In Sep-m.09, the alerts required a case note review, and the second alert led to an overhaul of the sepsis campaign:
The second one I know my colleague had 56 sets of notes to go through. Which he did. To come out with learning from it. And at the same time there’s been a big sepsis campaign so there were two, there’s a big sepsis campaign within the trust. Which had been redone a year or so ago.
Deputy chief medical officer, Sep-m.09
The alerts were considered to have helped the further implementation of the Sepsis 6 work:
But the Sepsis 6 and those, the figures and all that kind of thing, which are now done on a regular basis and presented in grand round-type fora and in terms of outputs on the audits and that and people joining in with it, so some of that was generated from the septicaemia alerts.
Deputy chief medical officer, Sep-m.09
In Sep-m.10, respondents generally conceded that the mortality alerts may have heightened the profile of the sepsis group across the organisation:
Now if we hadn’t had mortality alerts would we have a sepsis group now in the trust is an interesting question because we’ve had a mortality alert around a sepsis and we do have a sepsis group. So it’s really difficult to un-know what you know isn’t it and I think we probably would have a sepsis group but whether it would’ve gained such a high profile in the trust if we hadn’t had a mortality alert I don’t know.
Medical director, Sep-m.10
Coding of acute kidney injury
The alert identified errors in sepsis coding, led to an awareness of sepsis and led to changes in coding; hence in correcting the coding mortality for sepsis the coding of acute kidney injury increased:
People come in with acute injury sepsis, it’s chicken and egg isn’t it? I think when there was a big concentration on sepsis I think if you look at our actual numbers I think they fell a bit, and then the acute kidney injury went up a bit because I think people saw that we’d coded things as acute kidney injury rather than sepsis. So there are silly patterns like that that you see that goes up and that goes down. Nothing deliberate it’s just some of these people may be aware that you’re looking at sepsis or something and they’re picking up, ‘Well the acute kidney injuries is the major component here rather than the sepsis'.
Former deputy medical director, Sep-m.07
Increases in staffing of palliative care
Case note review identified high numbers of patients in the palliative care pathway; as a result palliative care consultants were recruited and the trust was able to cope better. Nurses also offered a 7-day service in palliative care:
Now there’s certain groups, our SHMI is fine, actually our HSMR is as expected now. But it’s taken a while to come back down to that, and I think there’s several reason for that, and one is that we’re able to cope more of the palliative care that is going on because we’ve got palliative care consultants now, and they also offer 7-day week service, not the consultant but the nurses there.
Former deputy medical director, Sep-m.07
Changes in clinical practice regarding diagnosis of sepsis
It was generally understood that the early administering of antibiotics in the treatment of sepsis was necessary. However, diagnosis by doctors was difficult and could often take a long time. Changes were made that allowed the treatment of sepsis to proceed if there was a suspicion of sepsis rather than a definitive diagnosis. This allowed the wider health team to have input in deciding on treatment. It was suggested that because nursing staff spent more time with the patients on the wards, their monitoring input could facilitate more timely intervention:
But we made a couple of fundamental changes internally . . . so when [XXXX] and I were reviewing it internally in the organisation, one of the clear focuses was more about diagnosis, so it was seen as a medical issue. What [XXXX] and I tried to do was move it away from being a diagnosis to more suspect sepsis to draw upon the wider health-care team. So we worked on the principle it could be sepsis and anybody could raise sepsis as an issue, and then you would go through the sepsis protocol to determine whether or not it was. Most of the people who give their hands on hour-by-hour care are the nursing staff, so diagnosis wouldn’t necessarily fit within their remit, so what we try to do is shift the emphasis away from very specific defined outputs to a much more broader set of physiological presentations that would alert people to say sepsis could be occurring here, you need extra help, so what we did, we’ve broadened the base of people who would raise the concern around sepsis based on a number of very broad physiological criteria.
Nursing director, Sep-m.09
Innovative sepsis awareness training
A training programme, ‘Power Training’, was introduced. This used social movement theory to spread knowledge of sepsis awareness. A concise programme was devised that covered the main learning points, which were distilled into five or six Microsoft Powerpoint® (Microsoft Corporation, Redmond, WA, USA) slides. This was delivered in < 10 minutes. Those trained were then responsible for training 10 more staff. This led to 1000 staff being trained within 6 weeks. This ‘Power Training’ was referred to as follows:
So we did one thing we developed here which was actually quite innovative, is something that we call Power Training. We distilled down into no more than about five to six PowerPoint slides, the very, very key fundamentals, the information you’re trying to get across. You’re not allowed to go beyond 10 minutes. We set some, we tried to use social movement theory, so we tried to get, so we trained 10 people, those 10 people have got to go away and train another 10 people and those 10 people, so it was more of a catalyst to prompt so it was simple enough that I could give it to anybody as part of the clinical team and their responsibility was to go and find another 5 or 10 people and train them. So very rapidly over about a, I can’t remember, it was about a 6-week period, we trained nearly 1000 staff.
Nursing director, Sep-m.09
This programme was supported by more conventional marketing of sepsis awareness using posters, boards and leaflets:
At the same time as we did a lot of marketing so posters and boards and other types of training material went out and we made some fundamental changes in terms of how we documented sepsis to make people more aware of it.
Nursing director, Sep-m.09
Challenging clinical practice and rewarding good clinical practice
Senior clinicians checked that the environmental items facilitating the management of sepsis were in place. They also then verbally tested clinicians’ knowledge of sepsis training. This process was known as ‘Check and Challenge’:
So after about 3 months, yeah, we did something called Check and Challenge. So Check is, you go physically go the environment and check whether or not all the environmental things you expect to be in place to manage sepsis are in place, so pictures, boards, stickers, blood bottles, everything you would physically, so you know people could not come back to you and say, ‘Well, I didn’t know about it because there wasn’t a poster’, or people say, ‘Well there was no stickers available or there was no blood bottles’. So you physically check the environment . . . And then you challenge people’s knowledge on the power training, so you go, there was a, you take 5 or 10 people from a ward or environment, anybody who’s physically there, so on the labour ward, actually, the chief medical officer was there because he was a gynaecologist, and there were loads of doctors and there was a medical student and there were some midwives, so whoever’s there, you go through a set series of questions and you test out their knowledge as to how much they really understood what was in the programme.
Nursing director, Sep-m.09
Good performance in the ‘Check and Challenge’ process was rewarded in the form of an Outstanding Service Care Awards (OSCAs), and this often led to competition between wards:
We developed a sepsis award. So, we have something every year called the OSCAs, which is the Outstanding Service Care Awards . . . And it’s a way we get the very best of what happens in the organisation. We give them prizes and days out for people. And that year, because we’d had quite a challenge around sepsis, we had a sepsis award and it went to the maternity team. The maternity team were one of the people who had one of these sentinel events. But they trained, and they trained everybody in maternity, both community midwives and also inpatient midwives on sepsis, they go the best scores through the Check and Challenge process.
Nursing director, Sep-m.09
Changes in coding guidelines
From the alerts it became clear that the coders did not know how to code sepsis, and so guidelines were written:
The other thing that was found is that the coders weren’t really clear at all, in what they should put into what codes because it wasn’t clear. So we wrote some common sense guidance forms to what counts as what.
Deputy chief medical officer, Sep-m.09
Changes in service design
Changes in service design and the relationship between the ED and acute medicine were reported as an outcome of the alert and sentinel events. A holding area was created that allowing patients to be triaged from outside into this area, which enabled patients to be fast tracked. GPs sent patients to one area and ambulances to the other, thereby preventing patients waiting on trolleys in corridors and reducing patient waiting times.
The relationship between the acute medical unit and ED, and acute medicine, so two physical areas and arguably three teams, got sufficiently complicated that what they did was they created a new holding area. So they triaged patients from outside into this holding area, where they were seen as a fast-track arrangement, really. And the GPs were told to send the patients to either one or the other, and the ambulances to the other. So they got the waiting times more or less under control, but they’ve got more control of what goes on in each unit and less of the sort of lying in corridors scenario that we’re faced with.
Mortality lead, Sep-m.09
Wider cultural change
The alert for sepsis was recognised as a useful trigger and a focus for action on sepsis as well as for wider cultural change focusing on improvement in care pathways:
We talked about having a plan per se rather than just chasing the lights is because we know that some of it is more than just the indicators themselves; it’s about culture, it’s about looking at the whole pathway and, therefore, if you just chase the lights what you do is you miss some of the real longer term stuff that you have to do that eventually will improve the situation around alerting.
CEO, Sep-m.11
A focus on resourcing data analysis
It was noted that the alerts had resulted in investment in specialist analysis of trust mortality. In Sep-m.11, a specialist information manager was recruited and the number of coders increased:
Nowadays it’s not me doing that because we’ve got analysts who do all of that stuff . . . certainly we were a way ahead of the CQC letters when they came.
Associate medical director, Sep-m.11
Comparative analysis of parallel development of processes for sepsis mortality
It was conceded that the combined parallel evolution of trust structures, processes, culture and leadership contributed to improvements in sepsis mortality. Parallel evolution was reflected in the following common themes:
-
external intervention by regulatory authorities
-
routine use and triangulation of mortality indicators
-
difficulties in resourcing clinicians and triangulating information in case note review and analysis
-
developing a trust culture focused on shared learning to deliver high-quality care
-
engagement with external organisations for knowledge and expertise around sepsis improvement
-
differing clinical perception of care bundles leads to confusion and error (normative pressures)
-
universal case note review
-
integrated structures and processes supportive of sepsis mortality review
-
addressing poor clinical awareness of sepsis and difficulties in coding
-
persuading consultants to engage in mortality review
-
IT-enabled forensic mortality review and patient monitoring
-
senior leaders prioritising trust mortality reduction
-
clinical champions improve timeliness in administering first doses of antibiotics.
External intervention by regulatory authorities
It was suggested that Sep-m.07 had implemented many strategies to address both sepsis mortality and mortality in general. This was driven by a host of regularity pressures resulting from the trust being identified as an outlier for SHMI and HSMR mortality indicators. These included the Keogh Review (February 2013), Special Measures (2013) and CQC inspection (2014).
Respondents reported that this external scrutiny directed action towards addressing mortality failures. For some, this scrutiny was a distraction from looking at the key problems concerning quality of access for patients:
When there’s so much external scrutiny on an organisation you tend to start throwing a bit of resource at it and it gets more attention. It becomes a distraction more than anything I think. I’m not a great believer in HSMR, SHMI and you say that’s because you’re at the opposite end of the scale. What I really believe people should be doing – people say we have the quality of access to health care in this country, well we don’t, and quite clearly we don’t. You go to different hospitals and you’ll have different levels of care because each hospital has different types of services, different departments. Your outcome will be different where you go. So if you have an acute MI [myocardial infarction] and you come into a hospital like [Sep-m.07] where we don’t do acute PCIs. You would need to be put in the back of an ambulance and sent somewhere, and you’re outcomes and results are going be worse than if you went to a hospital that has that thing on site.
Deputy medical director, Sep-m.07
However, it was conceded that that external scrutiny ‘had raised our game in terms of actually understanding our services’ (deputy medical director) and it was noted that improvements in care had resulted from this scrutiny, especially in terms of understanding and using data:
I think has actually been extremely good for us raising our game in terms of actually understanding our services and being able to present them and report them.
Deputy medical director, Sep-m.07
Routine use and triangulation of mortality information
Sep-m.07 was viewed as becoming ‘data rich’, using IT-enabled CHKS, HED and Dr Foster tools and accessing internal trust data via Meditech (electronic patient records), the mortality monitoring system, safety thermometers, ward dashboards and score cards:
And it covers all of our dashboards and thermometers and serious incidents and so on, to reassure them effectively. It’s to reassure our commissioners from a quality perspective. And I think as an organisation, I mean, we are very data-rich, and I think a lot of what we’re trying to do generally, particularly with the mortality statistics and reports, is to try and describe them to the appropriate people in context where they can be assured that there aren’t any serious problems.
Interim medical director, Sep-m.07
A focus on accessing triangulating and using mortality information also drove improvements in mortality. Many respondents identified how they accessed Dr Foster data to identify trust mortality in depth and understand how coding fed into mortality indicators:
You can go on the system and you can look. At the moment I know there’s some things, something called Subcutaneous skin legions, we’re sky high on HSMR, very small numbers of deaths, but when you go onto them they’re all bed sores for people who are from nursing homes who are bed bound who are coming to the end of their life. So you can go on and you can look, and the other thing that we’re code high on is things like VF [ventricular fibrillation] arrests.
Deputy medical director, Sep-m.07
A comparison of mortality indicators across trusts also was useful for identifying trust problems in coding; for example:
From the SHMI where you have the comparative one, and you can compare trusts and you can look at how mortality how palliative care coding has changed. You have to have local trust and then look at them from a CCG point of view to have a look at your own coding because I was thinking, ‘I wonder if we’re coding things differently’ and that’s how I got interested in this pneumonia one because I thought, ‘Blimmin heck we’re just not coding pneumonia’.
Deputy medical director, Sep-m.07
Developing a trust culture focused on shared learning to deliver high-quality care
In Sep-m.11, leaders report a key strategic focus in developing a trust culture supportive of high-quality care through shared learning and staff engagement in continuous review and improvement in care pathways.
In addressing mortality, those at Sep-m.11 did not make an assumption that mortality was a result of coding but rather ensured that all aspects, including care and coding, were considered:
The assumption is that this is not coding, this is a quality issue until proven otherwise. We have quite a high percentage of people who die in hospital as well.
Medical director, Sep-m.11
Despite espousing this cultural shift, it was noted that it was difficult for the trust to resource coding and pathway investigation. The coding department was described as stretched, with 4.5 whole-time equivalent posts vacant.
Sep-m.11 realised that it needed an organisational development strategy and a method for delivering culture change. Learning from other services, it adopted an approach involving four elements. Part of this involved developing coaching skills in the organisation so that different people could coach others on an improvement project: coaching circles. The view here is that by ‘chasing’ and dealing with each alert individually, the longer-term culture change that is needed will be lost:
I think that is where it was important for us to develop the care of the acutely ill action plan because it became really clear to us that you could just be chasing alerts. And even in HSMR, I think HSMR has I think 56 conditions or whatever else that sit within that, I think SHMI I think is 130-odd, you can get into the fixation of which this is. And we’ve done some of that. but the reason why we talked about having a plan per se rather than just chasing the lights is because we know that some of it is more than just the indicators themselves; it’s about culture, it’s about looking at the whole pathway and, therefore, if you just chase the lights what you do is you miss some of the real longer-term stuff that you have to do that eventually will improve the situation around alerting.
CEO, Sep-m.11
Knowledge of mortality was shared by the electronic sharing of case note reviews and coding knowledge was shared through the trust’s intranet. Hence all consultants can view data concerning all deaths reviewed:
It’s open access, you can search by consultant so you can have look at the reviews on patients under their care or you can look at what the reviewer’s found in the review. You can look at it by ward. There’s all sorts of ways you can cut the data . . . We said, ‘Well if we did them all upfront then actually we could pull through anything on COPD [chronic obstructive pulmonary disease]. Right let’s have a look at all the deaths that are reviewed on the patients that had a primary diagnosis of COPD or pneumonia’ and they just pull it and cohort it that way. So it’s much easier because the reviews have already been done.
Head of governance, Sep-m.11
Despite this trust’s drive for transparency and learning, it was suggested that the mortality and morbidity meetings were not always open learning environments, as junior doctors were scrutinised by senior doctors:
Perinatal people have always looked at theirs, but again it’s usually a case of a junior doctor presenting the case and the obstetrician sniping between one another to see what they do, it’s not a learning exercise particularly.
Associate medical director, Sep-m.11
Engagement with external organisations for knowledge and expertise around sepsis improvement
Sep-m.07 engaged in extensive external engagement that supported improvement in quality of care. Reviews focused on problems areas such as COPD, sepsis, ITU and mortality review. For example, reviews were undertaken by the Royal College of Surgery and local critical care networks. The trust called in experts on mortality statistics and reporting from academic institutions and experts in quality improvement specifically for sepsis:
So I’ve invited in external reviews, so over the time we’ve had one in respiratory looking particularly around COPD, we had an external review of the Royal College of Surgery by the Royal College of Surgery in [inaudible] and we also had – well the [XXXX] Critical Care Network came in and did a review of the ITU. All of these things were triggered by slightly different things, but it was an external assurance visit to really get an understanding of, ‘Is there a problem here that we should be highlighting’.
Former deputy medical director, Sep-m.07
In Sep-m.11, it was noted that ongoing sepsis improvement, stimulated by participation in the SPI national programme, had led to some improvement in mortality for sepsis and had also been a driver for action. A nurse consultant in the trust had been the sepsis lead for 5 or 6 years (so at approximately the time of the first alert), and the trust was also working on introducing the sepsis care bundle as part of its work for the SPI. Hence, the view was that the alert was not the sole driver of improvement for sepsis mortality:
There wasn’t anything major and I think that was quite evident. We already had a collaborative group looking at sepsis which was very active at the time and we’d already made some headway into our outcome targets around reducing mortality. We already had a step change so in a way, because we were looking back retrospectively, a way back, that’s when the data’s published, we were quite assured and obviously our local CCG were as well because we built that into the actual planning. Most of those were already in our driver diagram for that piece of work.
Sepsis lead, Sep-m.11
The continuing high HSMR prompted Sep-m.11 to review its coding, and it received an external review by a large consultancy company. Sep-m.10 also has an active programme of quality and safety improvement and has sent staff to the Institute for Healthcare Improvement international forum, with the chief nurse attending four times. This methodology was applied by junior doctors applying PDSA (Plan-Do-Study-Act) cycles and auditing implementation of sepsis bundles and antibiotic prescribing within ‘the golden hour’. Likewise, the trust also had plans to resort to further external engagement if the received more alerts.
Universal case note review
Routine case note review of all deaths was implemented across trusts; hence, when an alert was received there would be a review of the deaths contained in it.
You see we review all our deaths, so we know. So in terms of, you know, is there any excess work? No, there isn’t. So when the alert arrives, if an alert at that level arrives rather than just a red alert, if a CQC alert or an Imperial College alert which you copy to CQC, if that arrives then we look at it and we go, ‘What period does this cover? OK, this covers these 6 months’, and we know the numbers in those 6 months and over the last two occasions we’ve gone, ‘OK, well we’ve reviewed all the deaths in that period already’.
Chief medical officer, Sep-m.09
A report is produced every 2 weeks in Sep-m.09. This is discussed by the mortality committee, which meets every 2 weeks for 4 hours and scrutinises case note reviews, Dr Foster mortality data and other trust mortality indicators:
It’s been overall completely essentially because it used to be once a month for 1 hour. It’s now twice a month for 4 hours, so altogether we spend 4 hours talking about mortality in a meeting forum. We have a systematic way of approaching not just the HSMR but we look at our palliative care coding, we look at our comorbidity rates, we look at the alerts and we look at which alert needs investigating, we look at who’s going to investigate it, we look at the pathway, so if there’s an alert or high relative risk for say CCF, congestive cardiac failure, then we look at those number of notes, maybe 20 sets of notes, and we will work out whether there’s a problem pre hospital or post discharge or it is just in hospital care that’s causing the alert.
Deputy chief medical officer, Sep-m.09
The associate medical director of Sep-m.11 noted that the trust had been forensically examining mortality since 2006, so alerts were never a surprise. In December 2014, the trust implemented a two-tier review of mortality. Twenty people/teams are involved in this review process, which is two staged. Stage 1 examines key indicators, and, if any of these highlights a preventable death, a more detailed review (stage 2) is undertaken. If the first-level review finds any issues of concern, then a second-level and more in-depth review is undertaken; at this deeper level serious issues of preventability are highlighted but also any issues of quality of care are addressed.
So the current system, we have a two-level review and this has just been running since December where we have a ‘quick and dirty’, if you like, level 1 review where we look for some key indicators around preventability really. So that review is done by, it’s either a senior nurse or a senior doctor in the organisation who will look at them. If they have any concerns around either preventability but also quality of care issues, then they can refer them for a second-level review and a more detailed review until it’s then completed on a level 2 review.
General manager for governance, Sep-m.11
Integrated structures and processes supporting mortality review
Respondents in Sep-m.09 described the current review process, whereby mortality alerts come in to the CEO and are sent on to the chief medical officer (who refers it to the mortality lead and mortality review committee chairperson) and to the clinical effectiveness manager (who co-ordinates the reviews). There is also a parallel coding and case note review. The mortality review follows a detailed integrated and systematic process. The mortality review committee comprises the three assistant medical directors, the chief medical officer, the head of governance, the head of coding, the nursing director, the mortality lead, two mortality administrative staff, representatives from the divisions and specialties and the Dr Foster representative. It was noted that all clinical leads were expected to attend:
At the committee there’s the chief medical officer and her three deputy chief medical officers, deputy chief nurse, the director of governance, some other governance support, and then each specialty, there’s about five specialty-related mortality leads who come regularly, and every other specialty has a mortality lead who comes and presents either reports off investigations or a six-monthly update of where they’re at in their department. So it’s quite well, we could have more, more of a network around the one person trying to do it, but that’s taken several years to grow and kind of become embedded in the system.
Deputy chief medical officer, Sep-m.09
In Sep-m.09, mortality profiles are produced for each specialty from the Dr Foster data and these also include data on the time of day, day of week and staffing levels. These data are considered important as each specialty contributes in one way or another to the overall trust HSMR, and so the chief medical officer wants all specialties to work towards reducing mortality, not just those that have high levels:
. . . so we produce specialty mortality profiles for specialties, so we give them specialty-specific mortality data. So, on an ongoing basis we try to add definitions, etc., to all those charts, the relative risks, so if the clinician’s got any questions after looking at SMPs [Specialty Mortality Profiles] they can always just come back to us and if there are any blips we try to explain to them what these blips are, and can we just be statistical anomalies or not.
Clinical effectiveness manager, Sep-m.09
You can also cross-check them with other specialities. So for example, quite a lot of people die in the intensive care unit, so you get two points of opinion on that.
Mortality lead, Sep-m.09
In Sep-m.09, the CCG chairperson also now attends the mortality committee:
So if we feel that the referral was, or the patient came in a moribund state or, you know, what was going on in the community, how did we get to that stage? And also for palliative care in terms of getting people to their choice of place to die, the fast pathway, all of that, if it doesn’t work, or if somebody has a plan in place but they are referred in, in their last hours of their life, then that’s not good for the patient. So it’s not just about number, it’s about patient care.
Chief medical officer, Sep-m.09
The board Sep-m.09 receives a monthly report to the quality governance committee, which is a subcommittee of the board. There is then a 6-monthly detailed report to the board:
And one of the things we have done, that’s me and the director of quality, is we have made sure that the non-executive directors, we’ve sat down with them for an hour and a half, 2 hours, explaining everything because for someone who’s not of a medical background, understanding it to someone is not easy.
Chief medical officer, Sep-m.09
In Sep-m.11, there was concern that the alerts did not help to resolve clinical issues, so the mortality review process was considered a much better way of finding underlying clinical issues:
. . . my background beef with the HSMRs and how you can focus it down to diagnostic groups and say, ‘Oh my god we’ve got’ and which is why we’re trying to get mortality case note review that will argument as to what an HSMR means, but when you start dividing it down into specific diagnostic groups you can pop one up there and you hit that and then another pops and you hit that, and all you’ve done it slightly coded them differently and you think this is a game but did we gain anything from doing it and you can chase them around endlessly and we were doing that for years.
Associate medical director, Sep-m.11
Addressing poor clinical awareness of sepsis and difficulties in coding
In Sep-m.11, coding for sepsis on admission had been a difficult issue as not all doctors who admitted patients realised that they needed to write sepsis in the notes. As a result, the sepsis team introduced the use of a sticker on the notes to identify anyone complying with and being treated under the Sepsis 6 banner:
But if it’s not written down . . . So they have to see – and what we have been using I think is our sepsis boxes, so our stickers, they have taken that as a sepsis code.
Nurse consultant, Sep-m.11
Information technology-enabled forensic mortality review and patient monitoring
The entire mortality review process in Sep-m.09 is electronically enabled. When a patient dies, the IT-enabled mortality review process generates a primary e-review form that is sent to the consultant responsible for that patient. The consultant is expected to access the case notes and complete the form within 30 days. Follow-up e-mail reminders ensure that this happens. After reviewing the case notes, the consultant completes the e-mortality review form and grades the death on the scale A–E. A denotes a death that was entirely unavoidable, whereas E denotes a serious incident. Deaths in the grade E are tackled immediately by the serious incident group, with a full review undertaken and presented to the mortality review committee. If a death is graded B–D, then the case is examined in detail during the specialty-level mortality meetings. This grading was explained as follows:
And then that will be reported as an E death. It’ll go to the serious incident group, who will take action very much immediately because it’s the kind of thing that will end up in the newspapers if you don’t, but then it’ll also go in a slightly slower and more formal way to the MRC [Mortality Review Committee] group, who will then pretty commonly decide that a root cause analysis investigation is required, and then that follows that track, really. And then the outcome of the root cause analysis will be disseminated. We’ve just had a look at the last 27 E deaths and kind of bundled them together to date, and what we’re planning to do is come up with a presentation quite soon, probably next month when they grand round system comes back, to disseminate the findings in an educational way.
Clinical lead for mortality, Sep-m.09
In Sep-m.09, the clinical effectiveness manager oversees the mortality review process and ensures that local clinical guidelines are in place and comply with National Institute for Health and Care Excellence guidelines.
Continuous IT monitoring of patients in Sep-m.09, in real time, serves to communicate changes in patient condition and enables treatment to be escalated quickly. This was evidenced by clinicians regularly inputting into the NEWS (National Early Warning Score) and OPERA systems. The oversight of the NEWS system was conducted daily by the sepsis outreach team.
In Sep-m.10, it was hoped that the introduction of electronic patient records in the near future would further support improvements in coding and informatics:
So there’s an actual medication definition for septicaemia, which these patients perhaps didn’t fulfil, OK? But you have got them, if you like, labelled as having that and therefore it enters the mortality spike. So we have got concerns about that. We’re very hopeful that moving to an electronic patient record and our data collection and monitoring and assessment will be far superior in a year, 18 months, because we’ve got a huge IT project happening here called Smart Care, which is procuring a whole electronic patient record, etc., etc. So we’re hoping some of these issues will be flushed out with that.
Consultant oncologist, Sep-m.10
Senior leaders prioritise trust mortality reduction
In Sep-m.11, the analysis suggests that the trust board and the senior executive team appeared to prioritise mortality; those on the trust board were described as being very interested in mortality data and HSMR. They took an active interest and would ‘grill’ the executives; they ensured that mortality data were included in the monthly reports and every second month they received a report on the programme to improve care for the acutely ill patient.
Trust senior leaders in Sep-m.11 highlighted that they wanted more timely alerts, and they noted that the alerts arrived a long time after the trust became aware of the issue. They also suggested that they were trying to be more proactive by monitoring trends so that they could avoid the stage at which an alert would be received:
For me, if we are getting to an alert situation where statistical outlier, where we’ve failed in some way because we shouldn’t have got that far, so that’s why we are trying to be more proactive and pre-empt that. So if we see something that is moving or above average or is heading in the wrong direction then we will try and investigate that before we get an alert.
Medical director, Sep-m.11
In Sep-m.10, senior leaders visibly promoted quality improvement in their regular walkabouts and drop-in sessions. Every month senior nurses, including the chief nurse, completed clinical shifts followed by a debriefing session. A senior nurse also highlighted how trust leaders had resourced a ‘bottom-up approach’, enabling junior doctors’ engagement in implementing improvements in care. Hence, a ‘bright ideas’ group had been set up to mobilise these changes:
I think leadership. From right at the top, I think leadership. I think actually having the resource to actually focus it, being given permission, so for [safety lead]’s post to then go out and get all the junior doctors and be involved in that and, again, then getting the junior doctors to lead on it. So I think it’s definitely about the leadership and having the time to resource it.
Nursing and midwifery executive director, Sep-m.10
Similarly, ‘safety cafés’ were set up to promote clinical involvement in improving care. This was reported as follows:
A safety café is where you have different tables – you have to give them a cup of coffee – lots of tables, and you’ll have different speakers who will do mini presentations. So we get a lot of the consultants . . . lots of senior nurses, actually talking to them about actually new documentation in the group, so you can get a lot of people around in one go.
Nursing and midwifery executive director, Sep-m.10
Clinical champions improve timeliness in administering first doses of antibiotics
In Sep-m.10, a consultant oncologist reported on how clinical champions in the ED had implemented the ‘FAB 60’ project, which set out a quality standard that all first doses of antibiotics (FAB) should be given within 60 minutes of prescription:
Well, we approached it hospital wide and it’s been picked up very quickly, and successfully in ED and acute care areas, partly probably because I’ve had two very motivated consultants, from ED and acute medicine, who have been on our group, who have been very good at taking the message back and supporting that.
Consultant oncologist, Sep-m.10
This had moved on to implementation in wards and an auditing of this process to monitor the time to administration of the first dose of antibiotics:
Our next plan is to deliver a new quality standard in the hospital called FAB 60, OK? F-A-B, we’ve got some branding. There’s some branding with it [laughter] . . . And so first dose antibiotic . . . So all first doses of antibiotics, FAB, should be given within 60 minutes. And we have done a first-wave audit of every ward as to how many times that’s being delivered.
Consultant oncologist, Sep-m.10
In Sep-m.10 it was also reported that the scoring of FAB could be included in the future implementation of the electronic prescribing system, so a scoring could be set visibly within a ward ‘dashboard’ and hence prevent delays in the administration of antibiotics.
Comparative analysis of acute myocardial infarction multiple-alerting trust case studies
Three trusts, AMI-m.02, AMI-m.03 and AMI-m.04, received repeated alerts for AMI.
Comparison of trust preconditions
A comparative analysis of trust pre-conditions generated the following common themes:
-
recognition of high mortality for AMI
-
evidence of tracking mortality for AMI
-
changes in senior leadership
-
poor finances
-
external engagement to support learning around AMI mortality
-
catchment characteristics influencing high AMI mortality.
Recognition of high mortality for acute myocardial infarction
Respondents in both AMI-m.03 and AMI-m.04 recognised that the trust had high mortality levels for AMI. In AMI-m.03, the mortality lead noted that staff had known that the trust had a history of high levels of mortality before the first AMI alert. He suggested that this knowledge had provided a trigger for trust participation in PRISM. 23 This national study aimed to examine avoidable deaths, develop a standard approach for local mortality review and focus on the review of 1000 randomly selected case notes of patients who died either in hospital or within 30 days of discharge:
Well the trigger for that was an historical knowledge that there was an apparent mortality excess on the then measures, and as well as beginning to look in detail at various cases, it was felt that we should participate in the PRISM study as well, and that again didn’t really show any clear deficiencies in care, that we could attribute to historical apparent excess mortality.
Mortality lead, AMI-m.03
In AMI-m.04, data quality appeared to have been reasonable before the MASS alert, as the information project manager had been aware that the trust was going to receive an alert. He had informed senior members of staff and an investigation had been instigated:
. . . I think it was before – we were already investigating it before the CQC said that they were going to investigate it, I think. Yeah, because we already had that background data there.
Information project manager, AMI-m.04
Evidence of tracking mortality for acute myocardial infarction
The first alerts in AMI-m.02 arrived in 2008 and the trust was reported to be using the Dr Foster tools. However, the contract ended in around 2011; there was a gap before they implemented CHKS in 2012, and then in early 2015 they changed to the HED tool. AMI-m.03 was at an early stage of tracking mortality using a CHKS system, which provided information on RAMI. The trust began to track RAMI, SHMI, HSMR and crude mortality. In AMI-m.04, tracking of trust mortality appeared to be less efficient, as the trust was using a hybrid system of paper and electronic notes. This led to more time for coding and analysis as information was accessed on different systems.
Changes in senior leadership disrupt trust mortality review processes
AMI-m.02 had a difficult time for many years, with several changes in senior management. None of the interviewees was in post in 2008, when the first alert arrived, but some were able to comment on changes since. Respondents identified that the former medical director, who was in post before the first alert, had had limited involvement in clinical governance. The clinical outcomes manager also reported that the trust board members had changed many times and that this had limited their oversight of trust affairs:
We’ve had a very changeable board. The board we have in place now is very different to what we’ve had before. They’re much more involved in what we do.
Clinical outcomes manager, AMI-m.02
In AMI-m.04, it was reported that a change in CEO (in 2011) appeared to have been instrumental in changing how the trust approached mortality review. Hence, the trust had moved from a ‘command and control’ leadership style, which focused on ‘following the rules and meeting deadlines’ and producing only a superficial account of trust mortality, to empowering staff to engage in mortality review. The mortality lead reported this as:
. . . we’ve had a change of chief executive, probably 4 years ago now . . . but we had a very command and control attitude. There’s a palpable difference in atmosphere now . . . I think we would have, we’d have done everything by the rules. We would have produced a report; somebody would have cracked a whip to make sure that a report was produced by the deadline date. It might not have been a great report, it might not have really felt real.
Mortality lead, AMI-m.04
Fragmented approach to reviewing trust mortality
Respondents in AMI-m.04 identified that the trust dealt with mortality in silos. They suggested that mortality review lacked integration with clinical governance, safety and complaints structures. Similarly, the analysis of trust HSMR was not linked with either complaints data or safety data. Respondents described the trust as having a ‘tick-box’ governance system. Mortality review was confined to corporate level and was undertaken by the central mortality review group and the clinical audit department. Similarly, the coding of mortality lacked clinical oversight.
In AMI-m.03, it was reported that around 2008 the medical director had asked one of his colleague to help review case notes of deaths. This was regarded as an informal weekly activity aimed at gaining a sense of mortality problems in the trust. After normal working hours, a review was undertaken of deaths for that particular week. It was conceded that ‘we didn’t know what we were looking for’ (deputy medical director) and that the exercise involved finding ‘out the current episode of patients’ journey and see whether they were actually managed properly and they had written the right diagnosis on the death certificate’ (deputy medical director).
AMI-m.03 possessed a centralised senior team to oversee trust mortality. However, it was suggested that within divisions and some specialties mortality teams were often inactive and it was noted that no mortality meeting took place in acute medicine. The CEO (newly appointed) reported that she chaired the ‘mortality committee’ and that when she first had arrived at the trust it had operated poorly. She suggested the committee had been overwhelmed by ‘reams of information’ and, hence, this made it difficult to make sense of mortality in the trust. It is posited that this arose owing to the absence of a supporting specialist infrastructure.
Poor finances influencing resourcing of mortality review
In AMI-m.02, a reduction in finances appeared to have influenced a ‘culling’ of governance staff 4 years ago. It was recognised that more governance staff were needed to support mortality review, but this had not been remedied.
AMI-m.04 recorded a deficit of £17.4M in 2013/14 and had been expecting to end 2014/15 with a deficit of £2.9M. This later provoked an investigation by Monitor. The CEO highlighted that the trust was a private finance initiative hospital and that this led to an exorbitant mortgage payment:
It’s a PFI [private finance initiative] hospital, and because it’s a PFI hospital it’s always so – you know, most trusts do not have to pay a £20 million mortgage payment. And so the figures have always been quite tight in terms of finances, and particularly cash. Not just income and expenditure but the cash that underpins that. So we haven’t historically built up savings here, so we haven’t got big surpluses that we can live off while things are getting together . . . So it’s always been quite tight financially and quite close and up against it.
CEO, AMI-m.04
External engagement to support learning around acute myocardial infarction mortality
In AMI-m.04, efforts were also made to work with NCEPOD (National Confidential Enquiry into Patient Outcome and Death) and provide external awareness of the processes and issues surrounding hospital mortality. In AMI-m.04, trust governance was considered not up to standard as the new leadership had appointed Deloitte to undertake a governance review:
‘No, the governance of that’s not right.’ So I brought Deloitte’s in, in my first year . . . So we did a quality, governance review.
CEO, AMI-m.04
In AMI-m.02, cardiologists reported in to the national clinical audit (MINAP) and received reports back reviewing AMI mortality. It was suggested that this feedback was the main trigger for action concerning mortality.
AMI-m.03 participated in the PRISM study, which also involved training experienced hospital consultants to assess the preventability of adverse incidents and the effects of the adverse incidents on the subsequent clinical progress of the patients. It was reflected that participation in this study had indicated that the trust had no clear deficiencies in care:
Well the trigger for that was an historical knowledge that there was an apparent mortality excess on the then measures, and as well as beginning to look in detail at various cases, it was felt that we should participate in the PRISM study as well, and that again didn’t really show any clear deficiencies in care, that we could attribute to historical apparent excess mortality.
Mortality lead, AMI-m.03
Catchment characteristics influencing high acute myocardial infarction mortality
Respondents identified that trust catchment characteristics influenced high levels of AMI mortality. The catchment of AMI-m.02 was described as ‘very deprived’ and it was suggested that this limited progress in improving HSMR. The clinical outcomes manager reported this as follows:
The board at the time kept saying it had to be 90, it had to be – but I think – you know, this is quite a deprived area. We serve a big population . . . we’re one of the fourth biggest trusts in the country, you know, and we are in a fairly poor area. We do have – you know, our case mix is very, very different . . . I think the reaction in the past has been to justify where we are.
Clinical outcomes manager, AMI-m.02
The catchment of AMI-m.03 was described as having high incidence of alcoholism, end-of-life care issues and poor community care. The deputy medical director reported this as follows:
I know these are isolated cases but they make the biggest picture. These are the ones we picked up, so this was reported to the board meeting so the background came, lots of them with an alcohol problem and end-of-life care issues and then we realised the services in the community are not as good to manage these patients. Now I know every trust will say that but if you look at the profile and I’ve got the profile of [trust AMI-m.03] from 2008 and every annual one, I just find it really bad and I’ve been in [AMI-m.03] for 32 years [laughs]. I love it working here, but it is – the profile is very bad and it is evident as well when you go around.
Deputy medical director, AMI-m.03
In AMI-m.03, many respondents suggested that the risk adjustment weighting for these factors within mortality indicators was inaccurate:
We’ve got one of the most deprived electoral wards in the country, there is a huge rate of smoking, drug abuse, teenage pregnancy, all of those things, which I know the SHMI and HSMR say they correct for but I still can’t believe that they properly correct for all of those factors.
Medical director, AMI-m.03
AMI-m.04 was also noted as serving a population of 214,000, where deprivation is lower than average. A merger with a local community trust in 2011 also created disruption and pressure on existing structures and processes.
A comparative analysis identified the following divergent themes:
-
trust configuration and function influencing high AMI mortality
-
a closed trust culture
-
senior leaders’ participation in mortality review
-
staff shortages.
Trust configuration and function influencing high acute myocardial infarction mortality
In AMI-m.02, the configuration of services appeared to be linked to AMI mortality. Before 2014, cardiology was split between the two sites, meaning that the catheter laboratory was situated at hospital A and acute services were located at hospital B. This meant that there was a ‘split site mentality’ (divisional director for specialist medicine), which prevented an integrated approach to cardiology. Similarly, arrangements were in place for patients with suspected AMI to be taken directly to a central myocardial infarction centre rather than to this trust, indicating that most people who died as a result of AMI were inpatients and not patients arriving in the ED.
A closed trust culture
In AMI-m.03, the director of nursing reflected that at the time of the first alert the trust lacked transparency and this was due to a lack of good information:
We didn’t have the same I suppose transparency in terms of systems to see that that was maybe starting to be a cause for concern. So my recollection going back to 2011 and I think some of the conversations we had at the time and obviously we were a different exec team, was probably feeling a little bit frustrated that the alert would come but it didn’t feel we were able to have predicted that ourselves.
Director of nursing, AMI-m.03
Senior leaders’ informal participation in mortality review
Before the alert, senior leaders’ informal participation in mortality review was the sole type of mortality review undertaken in AMI-m.03. It was reported that around 2008 the medical director had asked one of his colleagues to help review case notes of deaths. This was regarded as informal weekly activity aimed at gaining a sense of mortality problems in the trust. After normal working hours, a review was undertaken of deaths during that particular week. The deputy medical director conceded that we didn’t know what we were ’looking for’ and that the exercise involved finding ‘out the current episode of patient’s journey and see whether they were actually managed properly and they had written the right diagnosis on the death certificate’ (deputy medical director).
Staff shortages
Staff shortages had been reported in AMI-m.02 before the alert. It was noted that reduced finances had influenced a ‘culling’ of governance staff. Although more governance staff were needed to support mortality review, the number of staff was described as not having changed much. The head of coding also highlighted difficulties in recruiting people who had specialist coding expertise:
In 2008 the coding department here was being managed by a contract manager due to difficulty to find [staff] . . .
Head of coding, AMI-m.04
Comparison of trust responses to multiple acute myocardial infarction alerts
Comparison of responses to the first alert for acute myocardial infarction
A comparative analysis showed that trust responses to the first AMI alert were characterised according to the following common themes:
-
a move towards greater trust-wide participation in mortality review
-
trust engagement with external organisations for support in mortality review
-
a focus on identifying errors in coding of AMI
-
gathering data and using data for AMI pathway analysis.
A move towards greater trust-wide participation in mortality review
Respondents suggested that their trusts were moving towards greater trust-wide participation in mortality review. AMI-m.03 had set up departmental coding and comorbidity meetings wherein all consultants, under the instruction of the previous medical director, were to review deaths. These deaths were then discussed during the mortality and morbidity meetings:
The steps we took were set up mortality and morbidity meetings within the departments. We asked – and I’ve got evidence to give you if you wish is by that previous medical director to say, ‘All deaths must be looked at by the consultants so that they can – the majority of them we won’t have any problem but some of them, if there are any issues, must be discussed in the mortality – M and M meeting and you should be also in charge of coding because there was an issue of coding’.
Deputy head of information, AMI-m.03
AMI-m.04 was empowering staff to engage in mortality review. The mortality lead reported this as:
. . . we’ve had a change of chief executive, probably 4 years ago now . . . but we had a very command and control attitude. There’s a palpable difference in atmosphere now.
Mortality lead, AMI-m.04
In AMI-m.02 there were mortality and morbidity meetings at a divisional level, but few of these were robust and the actions generated by them were limited. The divisional director reflected on this:
All the specialties I ensure that they have mortality and morbidity meetings which are documented, represented clearly and are all in ledger folders so that I actually can see what actions are. Few of them are more – well, put it this way, few of them are more robust, you will actually can articulate what the actions are out of those, few of them are not so robust.
Divisional director, specialist medicine, AMI-m.02
The medical director also reflected on the inadequacy of mortality review processes:
The way data was used when the alerts first came to the trust was not very good. Meetings surrounding mortality did not have a clear strategy, and nor was there a clear focus on how to improve areas that were clearly signalling a problem.
Medical director, AMI-m.02
Trust engagement with external organisation for support in mortality review
Engagement with external bodies for support in mortality review was a feature of one trust’s response. Respondents in AMI-m.03 suggested that a direct consequence of the alert was the commissioning of the Advancing Quality Alliance (AQuA) to undertake a comprehensive review of the trust’s mortality rates. This review focused on examining a range of factors that could explain the current and historically high mortality rates at the trust. This review centred on:
-
the implications of local population characteristics for the methodology used to calculate expected mortality rates
-
the impact of provision of services and quality of care both within the trust itself and in the wider community
-
the systems and processes that are employed within the trust.
The conclusions of AQuA focused on the following:
-
recognition of the trust’s strong track record in clinical quality improvement and that the non-mortality related quality indicators did not give concern
-
the trusts’ standardised mortality rates (SHMI, HSMR or RAMI) were likely to be adversely affected by the way clinicians and the coding team interact and that the ‘expected deaths’ element of the standardised rate calculation can be affected by coding processes (emphasising that this needs urgent attention)
-
a call for linking mortality reduction to other patient safety initiatives
-
the need to develop a specific mortality reduction plan that cascades to divisions and departments and which reports to the trust board
-
improving clinical quality by adopting care bundles, reviewing staffing levels in high risk areas, and working with primary care to improve end-of-life care planning.
A focus on identifying errors in coding of acute myocardial infarction
In responding to an alert, trusts focused on identifying errors in the coding of AMI mortality. In AMI-m.04 the first alert went to the clinical lead for mortality. The head of coding described being asked to pull the notes and examine the coding. An independent coder completed a review of case notes. Once this had been done, a ‘clinical investigation report’ was produced using all available data, including MINAP data and Draper and Dash [www.draperanddash.com (accessed 17 October 2017)]. This review identified that the inexperienced coders were coding using the death certificate rather than the admitting diagnosis. As a result, they were assuming that anyone who died from a myocardial infarction had been admitted with a myocardial infarction, which was incorrect. The head of coding highlighted this:
Because there were various signs and symptoms throughout the patient, the coders had then assumed that the reason for the admission was the MI, so they were not following the coding standards quite correctly due to their inexperience.
Head of coding, AMI-m.04
The coding review highlighted two further problems: (1) junior doctors were filling in the death certificates and not fully reviewing the notes and (2) junior coders were coding these deaths using the death certificate:
. . . the ones that were quite inexperienced were picking out something, like, in the death certificate. In this instance MI would have been recorded as cause of death. Because there were various signs and symptoms throughout the patient, the coders had then assumed that the reason for the admission was the MI, so they were not following the coding standards quite correctly due to their inexperience.
Head of coding, AMI-m.04
In response to the first alert, it became practice in AMI-m.04 for only experienced coders to code deaths:
Following that first alert, the decision was made in the trust that actually only the experienced coders would code deceased notes across the board. So we looked at then changing our practice and we have our band four coders, which are either ACC [Accredited Clinical Coder] or very, very experienced.
Head of coding, AMI-m.04
A system was also introduced in AMI-m.04 whereby coders would ask clinicians to check the coding for AMI. This process was followed if the coders lacked confidence with coding:
As a general theme within the trust, we actually put in a process where – if the coders were actually not overly confident about what they’ve actually coded for that patient . . . we then instigated a process whereby we would send a clinician responsible for that patient just a list of what we’d actually coded for that patient with a covering letter just to explain that this was a complicated patient and the coders weren’t definitely sure exactly what the main diagnosis treated was and could they just advise.
Head of coding, AMI-m.04
In AMI-m.03, coding errors were also highlighted. AQuA recommendations had indicated that the ‘expected deaths’ element of the SHMI, HSMR or RAMI can be affected by coding processes. They emphasised that coding was likely to be adversely affected by the way in which clinicians and the coding team interacted. It was suggested that coding processes needed urgent attention.
A strategy for using data analysis to identify problems in acute myocardial infarction care pathways
In AMI-m.03, and to a lesser extent in AMI-m.04, attention started to be focused on gathering and analysing data to inform the development of AMI care pathways. In AMI-m.03, leadership appeared to develop a strategic focus on generating both quality data and analysis that could usefully inform decision-making. This involved internally tracking mortality, auditing patient pathways and engaging with other trusts to compare performance. AMI-m.03 began to look for other trusts to compare itself with:
. . . so when we then start the investigations we’ll start to then look at quality metrics that are out there around the services that we have, and we start to look at activity patterns and we start to look at the type of services we run compared to other organisations and the fact that you’re a tertiary cardiac centre what does that mean, so again we wouldn’t just compare ourselves to everybody with AMI we would then start to look at trusts to perform tertiary services because again if we’re only getting the – if half are activities from the most acutely ill patients across the whole region, and we’re just getting them for primary PCI then our patient group is going to be different to a general DGH [District General Hospital] that doesn’t need those heavy interventions. It all forms part of that picture.
Deputy director of information, AMI-m.03
AMI-m.03 began to track mortality using CHKS, which provided information on RAMI. It also began to track RAMI, SHMI, HSMR and crude mortality:
When we produced the dashboards initially we used four measures and the idea was to look for correlation, so we put in there SHMI, HSMR, RAMI and crude mortality all the time, so you could actually then start to track through and see the word discrepancies and that’s another area to look.
Deputy director of information, AMI-m.03
In completing an AMI pathway audit, AMI-m.03 located three problem areas: (1) compliance of AMI treatment was a major issue, (2) evidence of the success of the primary PCI integrated pathway was inconsistent and (3) the success of an in-house smoking cessation campaign was also inconsistent. Recommendations suggested that divisions should develop action plans addressing non-compliance and improvement, actions plans should be monitored by the clinical audit department and progress should be fed back to the mortality board. The mortality lead also highlighted how, in developing the AMI pathway, ‘mission critical points of care’ should be identified. They identified areas of care that was evidence based and, hence, demonstrate how accumulated clinical learning transformed the AMI pathway:
We had a long-standing pathway for the treatment of cardiac chest pain, and before putting together a pathway, a revised pathway, there was a baseline audit conducted. The pathway wasn’t set up in a way that would allow you to identify what we now call ‘mission critical points of care’. You can take pathways for anything, you can pull together every bit of guidance that has come from every professional body on how you should or shouldn’t care for it . . . And having done a couple of audits on existing pathways, we looked at the pathway and tried to define them all in terms of what we have called ‘mission critical points’, that is things that are clearly known to make a . . . an evidence-based difference to the outcome . . . on the management of cardiac chest pain, against the existing pathway, we looked at every conceivable component of the care. It generated a suggested action plan and a report, and the cardiologists came in to comment on that. So this has occurred actually subsequent to, not concurrently, with the CQC response.
Mortality lead, AMI-m.03
In AMI-m.04, the generation and use of data to inform decision-making had been transformed. For example, the information provided to the trust board in the quality report appeared to have ‘improved out of all recognition’ (CEO). These data sources were included in the quality report, which revealed ‘trends and connections‘. The CEO highlighted how the trust now focused on detailed exploration of trends and triangulation of data:
Now you can see data, you can see trends, you can see connections . . . I think we only used to look at HSMR alerts, infection control rates, you know, a few indicators, but now we’re really into detail around trends and analysis and looking at different things. So comparing ones from early 2012 and early 2014, there’s a huge difference in the way that the reports now work.
CEO, AMI-m.04
In contrast, changes in leadership in AMI-m.02 prevented any strategic action to invest in mortality analysis tools. When the first alerts arrived in 2008, the trust was using the Dr Foster tools, but the contract ended in around 2011 and there was a gap before they moved to CHKS at some point in 2012. Then, around late 2014 they changed to using the HED tool.
Summary of trust responses to the first acute myocardial infarction alert
Some trusts demonstrated an initial corporate focus, with senior leaders delegating to senior clinicians in case note reviews of AMI patient deaths (AMI-m.02 and AMI-m.03) and a review of patient AMI deaths by a mortality committee led by the CEO (AMI-m.03 and AMI-m.02). Two trusts (AMI-m.02 and AMI-m.03) also appeared more integrated their response and appeared to engage beyond the senior leadership level by instituting specialty mortality and morbidity meetings. However, it seemed that these linkages appeared ad hoc and largely unstructured in AMI-m.02, whereas in AMI-m.03 coding and comorbidity meetings and reviews of deaths occurred regularly in specialty morbidity meetings. Only one trust (AMI-m.02) integrated the MASS alert with input into the quality and safety committee. In AMI-m.04 an administrative focus dominated. Here, most concern was given to checking and validating the alert by comparing trust data and checking coding. A clinical review of case notes appeared fragmented and patchy across the trust. Some trusts resourced coding, and AMI-m.02 funded a new head of coding. Similarly, AMI-m.03 resourced an AMI pathway audit and redesign, explored activity patterns and explored CHKS data using several quality metrics for mortality. Similarly, AMI-m.03 was described as engaging with external bodies (AQuA) and benchmarking with other trusts to evaluate and improve mortality for AMI.
Comparison of responses to the second and subsequent alerts for acute myocardial infarction
A comparison of responses to the second and subsequent alerts for AMI suggested that some trusts were surprised to receive a second alert, as they perceived that they had addressed problems in coding AMI. This ‘shock’ was referred to as follows:
We’d put a lot of work into place in the first one but we still alerted, so it was looking at what we also then needed to further do to make sure, you know, the alerts don’t occur any more. It was a particularly memorable one because, as I said, we’d done lots of different bits of work with – primarily it was probably down to the coding, the initial alert, but then going forward we’d addressed what we thought was the coding issue but we then alerted again.
Head of coding, AMI-m.04
In AMI-m.02, the CQC label at the top of the alert letter was said to make clinicians take notice and do the required work without challenging:
. . . particularly if an alert has come in through the CQC. There is something about having – you know, that banner on the page already will make people sit up and take notice. So they will buckle down and look at the cases and write their reviews and their patient summaries, and give their thoughts on where we are with it.
Clinical outcomes manager, AMI-m.02
The second alert appeared to drive trusts to drill down and improve mortality review processes, coding and acute myocardial infarction pathways
The analysis characterises common trust responses to the second and subsequent alerts for AMI as follows:
-
a forensic approach
-
boundary spanners address coding problems by facilitating clinical oversight of coding for AMI
-
joint clinical and coding involvement in case note review identifies errors in AMI diagnosis and problems in care pathways
-
trust leaders mobilise the mortality committee as ‘a boundary-spanning structure’
-
senior leadership prioritising AMI mortality by investing in knowledge production, knowledge sharing and analysis focused on AMI mortality improvement.
A forensic approach
In following a forensic approach, trusts attempted to ‘drill’ underneath and identify deep-seated problems with AMI mortality. On receipt of the alert in 2012, all cases in AMI-m.02 were reviewed and major issues were identified with coding of AMI:
With one of our MI alerts, and I think it might have been the earlier one, so maybe 2011, we looked at quite a big cohort of patients, about 70, and actually there were about 22 or 23 who actually had acute MI. So there were – so initially the focus would have been with the team. When we dug down into what the issues were, actually – obviously there are issues there, but it wasn’t so much the clinical team. It was more an issue of how we were coding, what we were writing.
Clinical outcomes manager, AMI-m.02
In undertaking this rigorous review of case notes, it emerged that only around one-third had been coded correctly for AMI. It was perceived that coding of case notes was the problem rather than the quality of care of patients with AMI.
The analysis in AMI-m.03 suggested that the trust’s response to the AMI second alert was also forensic and comprised three stages. The first was an administrative process whereby the information was checked to see if it was correct. The second stage focused on operational care patterns involving care pathways and other clinical-level processes. The third stage (described as the most difficult) was system redesign:
There are three stages to looking at improvement in terms of mortality so you’ve got that first stage in terms of the administrative process is making sure the information is correct is the first thing to do, and then you’ve got operational care patterns so pathway work, etc., etc., but the third one and the hardest one then is around system redesign.
Coding lead, AMI-m.03
The medical director also reported on how this staged process was integrated across the trust levels:
So we’ll have a stage 1 review where the parent consultant will go through the notes of each patient who’s died and make a judgement as to whether the care was in any way inadequate or the death potentially preventable or inevitable. If there is a feeling that the death was anything other than inevitable then we will go into a stage 2 review which will be done by a separate consultant where they will do a deeper dive on a fixed pro forma, and then on the back of that that finding is fed back into the departmental morbidity and mortality committee and the outputs from that are fed back to [mortality lead] so that they can be disseminated throughout the trust through the mortality committee but also through our clinical policy forum which is a monthly meeting of the heads of department and divisional directors.
Medical director
Boundary spanners address coding problems by facilitating clinical oversight of coding for acute myocardial infarction
Boundary spanners appeared to make sense of problems in coding AMI. They acted as sense-makers and sense-givers as they bridged both coding and clinical understanding of AMI. In AMI-m.02 the new head of coding acted as a boundary spanner, whereas in AMI-m.03 consultant cardiologists fulfilled this role.
In AMI-m.02, resourcing of coding was improved when a highly qualified head of coding was recruited in 2011. In attempting to bridge knowledge the head of coding started by speaking to every clinical director and clinical lead to ask for help with the data and to explain the issues relating to their recording in the notes and the national data. He set out to motivate clinicians by stressing that they should take ownership of their data (through case note write-up):
I met every clinical director or clinical lead and I asked them to help me help them with their data, and made it very clear, ‘This is not my data. This is your data. It’s going to be against your name. So if your patient is dying and then the primary diagnosis is a chest pain, and it’s going to show nationally’.
Head of coding, AMI-m.02
The head of coding recounted how clinical leads were very defensive about their coding, as they felt that it was correct. However, the new head of coding was able to demonstrate that they were making serious errors and developed a ‘double-coding policy’, whereby lead clinicians could authorise the head of coding to code their data.
The clinicians were described as being somewhat defensive at first, and some as being very aggressive:
Well, I’ve had a consultant storm in my office on the third day, one of the top consultants here, telling me how rubbish my work is. And I said, ‘I’m really sorry, Mr X, you know, but I didn’t know I could cause so much rubbish in 3 days. But please take a seat. Let’s go and let’s find out’ . . . ‘this is a fractured neck of femur, it’s all open, and that’s why the trust is not getting money’. And my next question was, ‘What kind of plate are you using? Is it three pin or six pin? What’s the size of the incision? Are you opening the fracture side?’ And they get gobsmacked. And I said, ‘Because . . .’ And this was not coming from the clinician, it was coming from coding knowledge . . . ‘It doesn’t show it in these fracture [notes] . . . are you doing this one or are you doing this one? Just clarify it to me. I’ll put it in a double coded policy. You sign it and I’ll code it. It’s your data, not my data.’ And that approach – but it was like that, you know. It turned out we were doing it right, actually.
Head of coding, AMI-m.02
In AMI-m.03, a consultant cardiologist was appointed mortality lead in 2012 and set out to improve coding by ensuring greater clinical involvement. For example, the role of consultants in coding was extended to authorising and validating the coding of their patients:
. . . the trusts have tried really hard to address this and I’m not aware that’s a major problem anymore by ensuring the consultants review all of the codes, so we get the notes or e-mails with, ‘Are you happy with this coding?’ and we say, ‘Yeah we’re happy or no please change this’ because some of the stuff you get put on is bizarre.
Consultant cardiologist, AMI-m.03
Joint clinical and coding involvement in case note review identifies errors in AMI diagnosis and problems in care pathways
In AMI-m.04, the clinical analysis of AMI coding highlighted that the number of patients admitted in the general medical intake and under the care of a general physician was high. It was suggested that these patients might have been admitted with a more pressing condition, such as stroke, and were treated in wards outside the cardiology department and without the oversight of a cardiologist:
Increased risk from myocardial infarction was not in patients under cardiology, it was in patients who were not under cardiology. And yet, we’ve got a direct admission policy that if you come in with ST elevation myocardial infarction you go straight to the cath lab and you have your PCI, and you’re under cardiology. So that immediately raised a bit of a question about, well, actually these clearly aren’t straight forward heart attack patients, that when you split the data between cardiology versus non-cardiology, the non-cardiology was where the excess death was. And actually with the benefit of hindsight, that was telling us quite an important piece of information that these weren’t straight forward heart attack patients.
Consultant cardiologist, AMI-m.04
Clinical case note review in AMI-m.04 also identified two types of myocardial infarction, one arising from the rupture of a coronary plaque and resulting in a heart attack, and another arising from another condition, such as sepsis, that leads to raised troponin levels and heart failure. It was suggested that, in the latter case, the root cause of the admission should be coded as sepsis and not as AMI:
So what we came out with at the end of that first review was an action plan that said we need to be better at coding, and there are type 1 or type 2, or is it type A and type B, myocardial infarctions. So there’s the myocardial infarction that happens because you rupture a coronary plaque and you have a heart attack. And then there’s the patient who’s septic who’s got profound hypotension, who might have got slightly abnormal coronary anatomy, they stop perfusing their heart very well and their troponin rises, but actually the root cause of the admission diagnosis is sepsis and it’s not a heart attack. And actually the journey that we’ve been on related to the alerts is that our acute medical team are very focused on the troponin because they set a bundle of tests. And actually the diagnosis is sometimes not that clear when you’re in the acute medical ward, and it only becomes clear when you move to the post-acute ward. But of course, when you move to the post-acute ward you’re in your second episode within the hospital spell, and Dr Foster only uses your first episode.
Mortality lead, AMI-m.03
In AMI-m.03, a consultant cardiologist was appointed and extended the role of consultants to validating and authorising coding. In 2012, a consultant cardiologist was appointed as the mortality lead in acute medicine and began to do work to improve cardiology services:
. . . so my whole appointment was actually partly in response presumably I wasn’t here at the time but maybe perhaps to the alerts from previously, and so when I started working one of the things that I started doing was restructuring how we did things, so we introduced extra pathways for people with chest pain, and we introduced a certain criteria where the patients just bypassed the medicine and came straight to the tertiary centre, so my understanding that from within 2 or 3 months I started off to with the Dr Foster stuff but the SHMI certainly dropped from over 100 to about a 100 and has continued to be low and so did the length of stay.
Consultant cardiologist, AMI-m.03
Trust leaders mobilise the mortality committee as ‘a boundary-spanning structure’
Across all trusts the centralised mortality committee co-ordinated with and linked to localised specialty mortality and morbidity groups. Notably, AMI-m.03 appeared to have made a lot of progress in using the mortality committee to enable knowledge sharing and analysis of AMI mortality.
In AMI-m.03, senior leadership drove mortality oversight by the mortality committee. The CEO chaired this committee and instructed that it met on a bimonthly basis. Likewise, trust leaders highlighted that they had prioritised an improved level of knowledge and understanding of AMI within this committee. Hence, a GP was seconded to inform the trust about improved primary care engagement and communication. It was perceived that this could inform trust clinicians in their diagnosis of AMI and link back to primary care delivery. Similarly, trust leaders ensured that consultants with a formal responsibility for monitoring and analysing AMI mortality attended reported on mortality review, analysis and action plans, and implemented actions in their specialties. Non-executive directors, information and coding specialists also provided input and support.
This strategic focus on improving knowledge generation and analysis of AMI mortality was reported:
. . . so are we getting the right information, what’s it telling us, where are these issues that we need to discuss, are there some new issues or not as the case may be, and then perhaps the most important thing is what we are seeing, hearing, discussion in this meeting going to drivers to materially change from the action plans that we’ve got, or do we believe that the action plans that go from workforce action plans perhaps to flow of patients through the building, action plans to pathways to equipment perhaps or whatever. Have we heard something today that really – have we got an action plans that’s addressing this or a piece of work, if not do we need one? If we’ve got an action plan is it the right actions, etc., etc.? That’s fundamentally and if we can keep to those three because you’ve got round the table public health, consultants, you’ve got GPs, you’ve got individual specialities and clearly usually we have, for example, one of the cardiologists you could obviously talk – we want a tertiary cardiologist service that there could be a 3-hour meeting on cardiology alone quite easily.
CEO, AMI-m.03
It was noted that the GPs were also active in the CCG as commissioners, so the dynamics of the mortality committee could be difficult at times:
. . . our new chief exec continues to chair the mortality committee, and we have representation there from non-exec directors as well, from the two CCGs and from public health, as well as the mortality reduction leads from each department in the trust, and that meets . . . It was meeting monthly but we’ve subsequently reduced that to bimonthly meetings.
Medical director, AMI-m.03
The CEO also conceded that managing this committee was challenging owing to the diverse vested interests of participants; however, he regarded it as useful and working well:
There is an element of having to strike a balance between, and manage the meeting around the job of the GPs and public health in the room and there is an element of contributing to the understanding and the solutions, but there’s an element of holding us to account and for want of a better term they are there as commissioners and the two GP reps that we’ve got are quite active in the CCG that they’re not just jobbing GPs if you like. So that’s a balance that you’ve got to, and occasionally that has dynamics that need managing, but I think overall it works pretty well.
CEO, AMI-m.03
Senior leadership prioritising acute myocardial infarction mortality by investing in knowledge production, knowledge sharing and analysis focused on acute myocardial infarction mortality improvement
In AMI-m.03, the AMI alert was instrumental in driving leadership to prioritise AMI mortality reduction by accessing and improving the content of knowledge concerning AMI mortality and increasing the frequency of leadership oversight of AMI mortality. It was perceived that in drawing from richer information sources the trust could improve the analysis that would inform trust decision-making.
The strategic resourcing of mortality analysis and review was accomplished by investment in a new HEDs data analysis system and more clinical staff recruited specifically to support mortality review, action plans and the implementation of improved practice:
Well I would say that this trust, compared to the last trust I was, this trust has a much more sophisticated, robust data set, weekly data that I get . . . that you can go to individual desks, etc., etc. [In my last trust] we developed a lot of info but we didn’t get anywhere near the mortality stuff that we do [here].
Coding lead, AMI-m.03
Summary of trust responses to acute myocardial infarction alerts
After repeated alerts, trusts’ responses to AMI MASS alerts generally became more urgent, and structures (mortality committee, service level mortality and morbidity groups) for investigating AMI mortality at corporate and service level become more robust (AMI-m.03, AMI-m.02 and AMI-m.04).
Senior leaders were more visibly engaging with responses to AMI MASS alerts (AMI-m.03). Consultants became more involved in investigation of AMI mortality and become responsible for coding patient deaths (AMI-m.03). Attention also focused on forensic identification and correction of errors in coding (AMI-m.03, AMI-m.04 and AMI-m.02). In AMI-m.02 a key champion (head of coding) acted as a boundary spanner, working across organisational levels and departments. Likewise, in AMI-m.04, a lead consultant cardiologist acted as a boundary spanner and identified two key issues: (1) common instances of wrong coding of AMI and (2) and that patients not referred to cardiology were more likely to suffer an AMI. This highlighted difficulties in escalating care and led to the development of real-time monitoring and an improved scoring system for deteriorating patients. Coding was internally and externally audited (AMI-m.04) and there was increased engagement with specialties to address problems with coding case notes (AMI-m.02 and AMI-m.04). An analysis across trusts focused on triangulating data from operational care pathways (AMI-m.02 and AMI-m.03) and MINAP data and Draper and Dash (AMI-m.04), and working closely with Dr Foster representatives (AMI-m.04).
Comparative analysis of outcomes from repeat alerts for acute myocardial infarction
The comparative analysis of trust outcomes from repeat alerts for AMI yielded the following common themes:
-
improvements in coding for AMI
-
identifying errors in diagnosing AMI
-
development of guidance for recognising AMI
-
changes made to the AMI pathway
-
tracking mortality and triangulating data
-
resourcing more cardiologists
-
promoting external engagement for knowledge acquisition.
Improvements in coding for acute myocardial infarction
Improvements in coding AMI were linked to the alert. More coding staff were resourced (AMI-m.02 and AMI-m.04). Clinical oversight and engagement has increased (AMI-m.02, AMI-m.03 and AMI-m.04). In AMI-m.04 coding of deaths was performed by a specialist coder who worked with the mortuary and with the clinicians to ensure that the codes were correct. They also assisted with mortality reviews:
For deceased patients, a change we put into place a few years ago is that the deceased coder actually goes down to the mortuary and reviews the notes in the mortuary, because what we were finding was sometimes notes were going for post mortems and we didn’t quite get the notes in time, or we didn’t have full access to all the episode history.
Head of coding, AMI-m.04
Identifying errors in diagnosing acute myocardial infarction
A forensic clinical case note review identified that myocardial infarction was being wrongly diagnosed. AMI-m.03’s specific target alerts allowed it to understand specific issues around AMI and chronic lung disease. It was noted that chronic lung disease could be mistaken for AMI:
I don’t know how good it is in terms of picking out avoidable mortality, because the frequency with which errors of omission and commission clearly contribute to a death is very low . . . One of the ones on acute myocardial infarction for example was the fact that in the absence of a diagnosis with the first 24 hours, if the traponin level, the heart enzyme that goes up if the heart has been damaged from a myocardial infarction, if the traponin level is elevated a bit, the working diagnosis will be a myocardial infarction. But in the elderly with chronic lung disease, with chronic renal disease, the traponin can be up a little bit anyway.
Mortality lead, AMI-m.03
Development of guidance for recognising acute myocardial infarction
AMI-m.03 developed an AMI pathway to provide guidance to clinical staff working in the A&E department on how to treat a patient with a suspected acute myocardial infarction based on best evidence and agreed local practice.
Changes made to the acute myocardial infarction pathway
An analysis of coding identified that AMI was occurring in medical wards and not in cardiology. It was understood that AMI was occurring in patients who had been admitted with other conditions and that in medical wards oversight by a cardiologist was limited. For example, in AMI-m.04, all patients under general medicine with suspected AMI would have a cardiologist review:
So the second alert, obviously we had a joint coding and clinical review, and it did highlight some areas where the processes we’d actually put into place probably weren’t working as well as they should . . . A cardiologist was involved, and he actually said, ‘Well no, that’s not quite right’. So what we then did was fine tune that process, and if we have any patients now that are under general medicine that don’t have a cardiologist input, we will send those to the cardiologist for a second review.
Head of coding, AMI-m.02
In AMI-m.03, consultant cardiologists had been instrumental changing the patients’ pathway across the area, acting as a tertiary centre:
So primary PCI is lots of data trials that show that basically instead of doing that if you just bring these people directly to a centre like us where we take them immediately to the cath lab and open up the artery physically and put a stent if necessary or just balloon and most of the time I put stents that’s better.
Consultant cardiologist, AMI-m.03
Focuses trust on researching mortality and improving care
In AMI-m.04, the head of information reported that the alerts had focused everyone’s attention and led to much internal research around improvement, which had improved, for example, palliative care arrangements:
I think they’re very effective. They certainly focus everyone’s attention. And it does mean that serious internal research is done as to why and what can be done to improve. And certainly in relation to palliative care as well, we’ve been – the local hospice, a clinician from there regularly attends the mortality group meeting as well, so it’s about getting better care for those patients that are going to die, because it’s an inevitable fact, isn’t it? It’s getting people to die in the right place and more appropriate place, comfortable place for them. I think that’s one of the positives that’s come from it.
Head of information, AMI-m.04
Comparative analysis of parallel development of processes for acute myocardial infarction mortality
A range of parallel contextual influences appeared to have an impact on changes in how AMI mortality was approached at trusts. Common emergent themes were:
-
external regulatory pressures drive mortality oversight (AMI-m.02 and AMI-m.03)
-
new trust leaders drive improvement (AMI-m.02, AMI-m.03 and AMI-m.04)
-
development of trust culture to improve clinician involvement and harness data (AMI-m.02, AMI-m.03 and AMI-m.04)
-
trust integrated structures and processes (AMI-m.02, AMI-m.03 and AMI-m.04)
-
resourcing of IT infrastructure (AMI-m.02 and AMI-m.04) monitoring
-
external engagement (AMI-m.04, AMI-m.02 and AMI-m.03) – trust involvement in safety-related improvement campaigns.
External regulatory pressures drive acute myocardial infarction mortality oversight
Care Quality Commission intervention and special measures were reported as forcing AMI-m.02 to address governance arrangements, A&E targets and finance, and set out priority areas for action. The CQC had visited again and reported some improvement but the trust remained in special measures at the end of data collection. It was noted that trust mortality levels were not covered specifically in the CQC review.
In AMI-m.03, the Keogh review and CQC inspections drove the trust to address improvement in mortality focused on the development of structures and processes to broadly address all trust mortality and, in some cases, AMI mortality specifically. Although the trust was one of the 14 identified in the Keogh review, it was not put into special measures after the review because it was deemed to be addressing the issues required to reduce mortality, and doing this well. Despite the trust having an internal process for reviewing mortality, the Keogh and CQC reviews found that this was not being applied uniformly across the trust, which had to be addressed:
[The CQC said] . . . ‘the process you’ve got for mortality reviews is a really good one but actually it’s not really robustly applied everywhere and you should be doing something about that’ so obviously we’ve been auditing that since.
CEO, AMI-m.03
The Keogh review suggested that the speed of any recognisable service change was unsatisfactory and that the pace of implementing improvements in patient care was at an unacceptable level. The review raised concerns about equipment safety checks, nurse staffing levels, incident review systems, shortage of medical staff, insufficient time for teaching, professional development and governance in specialties and inconsistent implementation of infection control. The Keogh review specifically criticised the trust’s AMI pathway as too long and complex.
The overarching message delivered to the trust was that it was attempting to implement too much and was, therefore, not doing anything effectively, which was borne out in the interviews:
One of the challenges back to us from the Keogh team was actually we were trying to do too much, so trying to grapple mortality reduction and safer care, the message that came back to us was, ‘You’ve got too many initiatives running and actually you need to narrow that down and focus’.
Chief nurse, AMI-m.03
In AMI-m.04, the Monitor intervention arising from poor financial management also led to regulatory oversight of trust activities and to a dramatic change in trust leadership.
New trust leadership drive improvements to improve quality of care and reduce mortality
Changes in senior leadership were common in all trusts. In AMI-m.04, they arose from the Monitor intervention. In AMI-m.02 and AMI-m.03 they arose after CQC and Keogh review investigations. New leaders were instrumental in prioritising the overhaul and integration of trust structures and processes to enable mortality review. A strategic focus was placed on mortality awareness and improved data quality across all divisions and specialties.
In AMI-m.02, the new management team gave managing avoidable mortality a new priority in the trust:
I just think it’s been given some clout and people realise how important it is now, and that because someone’s died that’s not actually the end of the story and, you know, that can impact on how we treat the next patient through the door, as opposed to, well, they’re dead so that’s kind of done . . . And it’s got some backing now, people that are interested in it. It’s kind of just growing and taking on a life of its own.
Clinical outcomes manager, AMI-m.02
In AMI-m.03, the CEO had been in post for 2 years, arriving just after the Keogh review, and the medical director had been in post for 3 years. The trust had also appointed a mortality lead 3 years previously who was a retired critical care consultant. All were appointed at the time of, or just after, the second AMI alert. It was suggested that these leaders brought unique skills and experience to tackling AMI mortality improvement. Similarly, it is possible that this new leadership team was in a position to start anew, unhindered by past decisions made around AMI mortality.
AMI-m.04 had a change of CEO in 2011 and a new medical director in 2014, and these changes were described as making a difference:
Soon after he [medical director] started one of the things he said was, ‘I don’t understand why we don’t put mortality first on our patient safety agenda. You know, isn’t it the most important that could possibly happen to anyone that comes into this hospital that they die? And so it needs to be top of the list’. And actually even this week, the chief exec, has sent out an e-mail . . . about the financial position that we’re in, a difficult financial position and Monitor helping us, but actually very strongly stating quality of care and outcomes being top of the list important priorities.
Mortality lead, AMI-m.04
Developing trust culture supportive of improving care, clinician involvement and harnessing data
In AMI-m.02, the focus was on developing a culture supportive of improving care and clinician involvement and harnessing data.
The clinical outcomes manager went on to say that as a result of this they had recognised how important it was for all clinicians to be involved in reviewing their patients’ notes and any death, and for this to be part of everyday working rather than a one-off event when an alert arrived:
So with our kind of day to day – trying to make this part of everyday business, really, mortality, as opposed to something that happens once a month that might tie in with a governance meeting. So everyone scurries around, doing a bit of M&M [morbidity and mortality review] and might present it at a governance meeting. It’s got to become part of everyday.
Clinical outcomes manager, AMI-m.02
The plan was also to specifically request that consultants review every one of their patients’ deaths, rather than asking junior doctors:
Your junior doctor is assessing the death of a patient under your care and passing judgement on the care your team delivered, are you comfortable with that?
Medical director, AMI-m.02
AMI-m.04 attempted to harness information to improve trust-wide understanding of mortality. This involved developing a narrative around mortality, the use of a mortality review process tool and developing an electronic database of mortality information. The idea of a narrative around mortality is deemed essential for understanding the entire process of mortality in the trust. The mortality report was said to be around 20 pages long but it was seen as too long for the general consultant population to read so work is now under way to condense it to four pages.
The mortality group met monthly and the information specialist provided a full report:
. . . there’s a monthly meeting, mortality group meeting, and I prepare a report for that that names any upcoming alerts and also links to things like the CUSUM charts that we review in the meeting to see if there’s anything coming up as well. And our Dr Foster rep is there as well normally.
Information specialist, AMI-m.04
The trust designed its own mortality review process and tool with a database to capture the information. Each department had the opportunity to amend the database to suit its own needs but there was a core set of data that everyone was required to complete. Clinical issues were added to the core data set to raise awareness of issues when clinicians were conducting mortality reviews:
. . . we’ve designed a pro forma for mortality reviews internally, we use the global trigger tool as our original template, we then embedded that review tool in a database that is a bespoke database.
Mortality lead, AMI-m.04
Part of the reason for this review and the database was to counter the fact that Dr Foster data were out of date by the time they arrived:
But one of the frustrations about Dr Foster is it’s always in arrears, it’s always such a long time ago that people have forgotten the cases, and learning should really be as soon after the event as possible when everyone in the team remembers what happened. As opposed to going back and looking at cases that some of which were 6 months old, and half the trainees have moved on.
Mortality lead, AMI-m.04
Resourcing information technology infrastructure
AMI-m.02 had a clinical outcomes manager with responsibility for the clinical harm review process and reviewing hospital mortality, and who worked closely with the medical director. A new system of mortality review was introduced. The previous system did not work as the death list came out 2 months in arrears. Now deaths were reviewed at the time when the death notification was completed. The clinical outcomes manager met with the associate medical directors to go through all of the deaths using the Hogan score23 as a trigger for avoidable deaths. From this, any information was fed back to the clinicians and to the mortality assurance group. The interviewees described the aim to be ahead of the curve in terms of knowing what is going on in the trust before an alert arrives.
Within the previous 6 months the trust had bought HED from Birmingham. Before this they had used CHKS. The reason for the change was that the clinicians wanted data that would help them to be more proactive:
I was really delighted when I came here that we’d bought HED because we’d used HED in my previous organisation when mortality was why that trust went into the Keogh special measures group up in [trust region]. So when we brought HED up in there, it just transformed the understanding of what the issues were because the richness of data was suddenly clinically useful.
Medical director, AMI-m.02
HQUIP also send data about mortality for those specialties contributing to national clinical audits.
AMI-m.03 uses the HED tools, and the lead in informatics produces a ‘heat map’ from the data to show which areas need to be focused on:
We also have a heat map which [XXXX] generates from our data which shows us areas of attention, and we are focusing on not so much the black squares but the big squares, so the areas where we’re seeing significant numbers of people with maybe a slightly elevated SHMI compared with very small numbers with a very significantly elevated SHMI . . .
Medical director, AMI-m.03
There has also been a focus on reducing harm from falls, pressure ulcers, MRSA and so on, and the medical director reflected that this overall focus on reducing harm had helped with the reduction in AMI mortality levels.
A focus on monitoring mortality
AMI-m.04 worked to understand the data better, as well as how alerts are generated:
We had a mortality group meeting last week, and we monitor things, and the other thing we did was we said, ‘Why didn’t we know this was about to happen again?’ Because we’d been monitoring the CUSUM chart, and actually what it turns out, I think, is that the CQC monitors at a different threshold. So you can set your threshold at 99% or 95% threshold on the CUSUM chart, and the CQC lowers their sensitivity, if you’ve had an alert they will look at a lower threshold for a future alert, whereas we were still looking a 99%, the CQC were looking at 95%.
Mortality lead, AMI-m.04
The trust now monitors deaths by day of the week and can show that there is no difference in the rate during the week and at weekends. Their HSMR is now around 90 and the SHMI is one of the best (top three) in the country. This was attributed to the work on sepsis and the triangulation of data to spot issues (gastroenterology was given as an example here).
There is a monthly conference call with the Dr Foster representative during which the current data are reviewed and any probable alerts are discussed so that staff can be proactive in spotting problems.
The coders sit with the clinicians when mortality reviews are undertaken and a joint mortality review is conducted:
Previously it had been a clinical review and a coding review and it wasn’t actually joined up. But since – not just as a result of that but since then we do a joint coding and clinical review, where myself and the coder go along with the clinical review and then we discuss the patients and look and make any changes or awareness actually at that review. So it’s more joined up and more fluent now.
Head of coding, AMI-m.04
The coding team has verified its coding of myocardial infarctions with the National Classification Centre for Clinical Coding:
So we’ve really sort of done a lot of work on making sure our coding met national standards, as I said, and with more experienced coders actually coding it and now the same coder coding, we’ve got the consistency in our coding.
Head of coding, AMI-m.04
The information specialist provided the medical director and the mortality lead with a spreadsheet detailing all of the patients who have died in the hospital. The information team also provides the clinical review team for mortality alerts with information about patients who have survived, in order to give a more complete picture.
Trust involvement in safety-related improvement campaigns
In AMI-m.04, the mortality lead’s engagement with NCEPOD allowed the trust to access useful information about how other trusts tackled mortality. It highlighted trust-wide approaches to reviewing deaths, frequency of meetings and techniques used. The head of mortality remarked on this:
It tells you, you know, by department and by hospital how many hospitals have got a trust-wide approach, or departments in hospitals what their approach is, frequency of meetings, a whole load of core data about what people are currently doing, there’s no narrative.
Head of mortality, AMI-m.04
The head of coding also identified how the trust audited practices against national standards:
The National Classification Centre for Clinical Coding, they advise us on coding issues. So that was part of that as well, because it was felt that, you know, the sequencing of coding from a clinical point of view wasn’t quite accurate, so we then confirmed that with our national standards and actually we were coding it to national standards. So we’ve really sort of done a lot of work on making sure our coding met national standards, as I said, and with more experienced coders actually coding it and now the same coder coding, we’ve got the consistency in our coding.
Head of coding, AMI-m.04
In AMI-m.02, coders were trained by the London Clinical Coding Academy, with two undergoing specific training to code mortality. By 2013 the coding was graded level 3 in the Information Governance national rating. This meant that they had around 95% accuracy across all coding, which is the top banding.
Summary of parallel evolution
The parallel evolution of AMI mortality was addressed by the real-time monitoring of AMI deaths (AMI-m.04), liaison with external networks for knowledge acquisition (MINAP, Dr Foster; AMI-m.04), resourcing cardiology by increasing staff (AMI-m.03), increasing staff involved in coding (AMI-m.02), investing in IT infrastructure (HED and training, mortality review database) (AMI-m.02, AMI-m.03), triangulating all data (AMI-m.04, AMI-m.03), developing a culture supportive of learning and problem-solving (e.g. CEO blogs, tweets, grand rounds; AMI-m.02) and developing a narrative around mortality (AMI-m.04).
Comparative analysis of single-alerting trust case studies for sepsis and acute myocardial infarction
Two trusts received a single alert for sepsis (Sep-s.06 and Sep-s.05) and one trust received a single alert for AMI. In the following commentary, we build on the description of themes emerging from the comparative analysis of the sepsis single-alerting trusts (reported in Comparative analysis of acute myocardial infarction multiple-alerting trust case studies), with a specific focus on AMI-s.01.
Comparison of trust preconditions
Comparison of trust preconditions focused on:
-
problems with senior leadership
-
fragmented structures and processes for mortality review and improvement
-
poor engagement between clinicians and managers
-
improvement work led by informal mortality champions
-
extreme regulatory pressures (CQC, Keogh review, quality accounts audit) creating organisational instability
-
learning gained from trust engagement with external organisations
-
trust culture characterised as ‘closed’, lack of awareness of mortality and limited staff engagement in addressing mortality.
Problems with senior leadership
Sep-s.06, Sep-s.05 and AMI-s.01 were reported as experiencing problems with senior leadership. In Sep-s.06, it appeared that senior leaders were disengaged and not prioritising mortality review. The matron recalled how:
In the beginning, being entirely honest with you, in the beginning I don’t think anybody was really that interested in what we were doing and why.
Matron for general surgery, Sep-s.06
Interest was limited to using HSMR statistics for insertion into trust documents:
I think before it was potentially just looking at the numbers and looking at ‘What’s the HSMR?’ and probably looking at it, I think as a lot of trusts probably did, when the hospital guide was due to be published and seeing what we were.
Head of quality, safety and compliance, Sep-s.06
In AMI-s.01, it was reported that trust leaders adopted a punitive and bullying approach as a senior clinician had been disciplined for engaging with the media and divulging severe problems with high mortality:
So because we knew this particular person had been disciplined because they had whistle-blown, it kind of made you think I’m not going to do that. So it was that kind of thing. If you stepped out of line or you made too much fuss that may be wasn’t the thing to do because it wasn’t going to get you anywhere.
Head of clinical audit, AMI-s.01
Leadership was also described as ‘command and control’. The newly appointed CEO suggested that staff failed to report incidents and also posited that this may have arisen because staff were fearful of the punitive consequences of reporting:
Nobody was engaged, it was very ‘command and control’, nobody – there were no incidents, nobody reported anything, so there were no incidents in the organisation, none. And there weren’t systems and processes for people to alert others and actually they wouldn’t alert others because they knew or were aware of those consequences.
CEO, AMI-s.01
Fragmented structures and processes for mortality review and improvement
In AMI-s.01, a fragmented and token approach was also suggested. Respondents highlighted that the trust leadership had failed to develop a strategic priority for investigating and tackling AMI mortality. Overall, they reported a fragmented and token approach that had failed to engage across divisions and specialties. It was suggested that mortality alerts went to the medical director who then sent them to the relevant consultants. The alerts were discussed at medical meetings but often the individual consultants argued that their care was good and then nothing else happened:
We didn’t really act on anything. We would get the information in, we’d see the report but nothing really happened. We would just note it, it would be minuted and then we would move on to the next thing.
Head of clinical audit, AMI-s.01
Poor engagement between clinicians and managers
In all trusts remarks were made about poor engagement between clinicians and management.
In Sep-s.06 managers appeared to display an administrative approach, whereby they functioned in silos and failed to share and communicate information. In AMI-s.01, limited clinical engagement in addressing mortality was reported. It was suggested that when senior consultants were made aware of mortality issues they attempted to shift the blame and argue about problems and solutions:
There was very much, ‘It’s not me, it must be someone else. So don’t ask me to improve my service because I’m alright and it must be somebody else that’s the problem’ . . . what would happen is the consultants would end up arguing over the problems so there didn’t seem to be a solution; it was all quite frustrating . . .
Head of clinical audit, AMI-s.01
Limited clinical engagement in addressing mortality was generally reported. The CEO highlighted this as ‘there was lack of engagement of clinicians’ and that this led to a ‘lack of noise in the system’.
Before receiving the alert, a lone clinician acting as a mortality consultant had reviewed case notes, but this had not generated any learning outcomes other than identifying that clinical coding was poor, and solutions had not been identified or implemented to correct this.
Improvement work led by informal mortality champions
Both Sep-s.06 and Sep-s.05 reported a long history of quality improvement work in sepsis and in AMI-s.01 a lone clinician was implementing care bundles. Across all trusts, this kind of improvement work often lacked strategic direction and was undertaken by committed individual clinicians.
AMI-s.01 was participating with AQuA, a NHS care quality improvement organisation, and implementing care bundles:
We did all of the [AQuA] programme which was AMI, heart failure, pneumonia, total hips and knees initially, stroke came online a few years ago . . .
Head of clinical effectiveness, AMI-s.01
However, this work was limited to a single clinician, who described this work as a ‘one-man band’.
Experience of severe operational pressures
Before receipt of the alert, Sep-s.05 in particular was experiencing much instability. This included a merger with the local community trust as well as major operational and financial pressures.
Sep-s.05 respondents emphasised how severe operational pressures had had an impact on trust mortality. This related to how, in winter, the crude mortality rate had doubled, there had been failures in identifying deteriorating patients and a failure to escalate patients, patient records were poorly written, the treatment of end-of-life patients was difficult and the discharge of patients was problematic as social care provision was poor. Hence, patients remaining in the hospital awaiting discharge were succumbing to hospital-acquired pneumonia:
Essentially it was the winter mortality rate. So our winter mortality rate, crude mortality had doubled, and essentially I then got the review.
Mortality lead, Sep-s.05
Sep-s.05 also reported staff shortages. In 2011, 60 redundancies were announced and a further 80 positions were made vacant. A critical care consultant referred to extensive staff losses:
Well we had clinicians leaving. You know we had some very good medical consultants leave and some very good surgical consultants leave. Only one anaesthetic consultant leave, probably not as a direct impact of that. But we did have . . . Certainly, we had clinicians leaving . . . Well the main problem we’ve got is probably the same as the lack of nursing staff on the wards is one of the main issues. So I think they haven’t got time to do it. And then the junior doctors seem to be too reluctant to call the seniors as well, is the other problem.
Critical care consultant, Sep-s.05
Extreme regulatory pressures (Care Quality Commission, Keogh review, quality accounts audit) creating organisational instability
Sep-s.05 and AMI-s.01 were experiencing extreme financial pressures. Sep-s.05 had overspent considerably on the implementation of an IT-enabled patient records system. The associate medical director reported this:
So probably around 2012. We were struggling for money. The chief exec was particularly – his managerial style was a particularly difficult one to deal with. We then got EPR which was electronic patient record which cost us £60 million which we have difficulty funding. So I think the downfall of our chief exec and our board was due to financial issues.
Associate medical director, Sep-s.05
These financial problems eventually led to Sep-s.05 being in breach of its financial obligations and to a Monitor intervention in 2013.
In AMI-s.01, financial pressure was seen as increasing, as the trust’s financial position had varied since 2010/11 from a surplus of £1.15M to a deficit of £4.77M. It was suggested that this had affected the resourcing of staff and prevented trust staff from attending meetings with regard to governance and mortality investigation. These intense financial pressures were also experienced by Sep-s.05, as the failed implementation of an IT-enabled patient records system had incurred costs of £60M and led to substantial staff redundancies.
AMI-s.01 was exposed to a host of regulatory pressures that sapped the energies of and demoralised staff. These pressures were described as emanating from the Quality accounts, Keogh review, CQC inspections and multiple alerts (Dr Foster):
I think the trust has been constantly under scrutiny for many years. I think the Keogh was the most high profile . . . But certainly when that report came out the morale within the trust obviously was quite poor because you’ve got nurses that are working very hard, doctors that are working very hard, and you’ve got really good areas and pockets of good practice. To be tarred with that brush it’s quite demoralising.
Head of clinical effectiveness, AMI-s.01
It was noted that the Keogh Review had identified real problems and that this pressure had caused much dissent in the trust executive team:
Keogh got it spot on and I will be very frank and honest because I’ve been with the Keogh team . . . on day 1 of the Keogh review the chief executive’s office is directly above me and on day 1 of the Keogh review the Keogh lead teams are sitting here, and the chief executive is calling and shouting at our medical director.
Head of clinical governance, AMI-s.01
In contrast, Sep-s.06 appeared to experience some regulatory pressure in CQC oversight of alerts but this pressure appeared to have had less of an impact than in either Sep-s.05 and AMI-s.01.
Learning gained from trust engagement with external organisations
It was generally accepted that AMI-s.01 was engaging with external bodies but not sharing knowledge and awareness of problems regarding mortality. For example, it was participating in the national audits for cardiac care. However, it was suggested that these audits were limited to particular questions and did not review overall care:
If, you’ve got a national audit . . . you are looking at specifics. So somebody would go through the case notes and say, ‘Has the patient had an echo within 24 hours or 2 weeks of discharge? Have we done an ECG? What was the initial ECG? Did the patient have a cardiac arrest? Yes, they had a cardiac arrest’. But you wouldn’t be doing that thorough review of the notes.
Consultant cardiologist, AMI-s.01
Clinicians had championed sepsis improvement in both Sep-s.06 and Sep-s.05 over many years and accessed knowledge and learning by participating in national programmes related to the Sepsis 6 care bundle. However, most activity was largely confined to critical care and ED departments.
Trust culture characterised as ‘closed’, lack of awareness of mortality and limited staff engagement in addressing mortality
In AMI-s.01 respondents generally reported that, before the AMI alert, the trust was ‘closed’ and lacked transparency. This was articulated by the director of quality and governance:
Having been able to compare it to other organisations, it was [limited] in its approach to transparency and openness. That inevitably had – and permeated through the whole way in which openness and transparency were seen.
Director of quality and governance, AMI-s.01
This echoed the closed culture reported in Sep-s.05 in which information was not shared, mortality review was ad hoc, and board meetings, before 2013, took place in private. This differed from the open culture reported in Sep-s.06.
Comparison of trust responses with a single alert for sepsis and acute myocardial infarction
Comparison of trust responses with a single alert for sepsis and AMI focused on the following themes:
-
a forensic approach to reviewing mortality
-
an integrated trust-wide response
-
clinical engagement and cultural ownership of sepsis improvement
-
a universal and timely response
-
a case note review identifying errors in coding.
A forensic approach in reviewing mortality
In all trusts, the alert and CQC follow-up had led to a forensic approach in reviewing mortality. In Sep-s.05 this was entirely focused on the deaths highlighted in the alert. In Sep-s.06, forensic investigation involved case note review and the triangulation of data across hospitals, divisions and specialties:
We would initiate an investigation and investigation would inevitably be a case note review of all the cases which is, you know, usually the most I’ve had is I think about 120 . . . You would go through all the notes and . . . it might be a condition where they’re all in one speciality, usually they’re across several specialities which is helpful so you can give them each a bunch, they look at them, they would get the data back to us, we would formulate it into a, you know, into a report, we would develop an action plan based on that and we would send that back to the CQC.
Medical director, Sep-s.06
In AMI-s.01, staff employed a forensic approach to responding to the AMI alert and CQC inspection. This comprised investigating, analysing problems and triangulating data. Attention focused on the trust’s critical care model and AMI pathway and on producing an action plan:
For cardiology obviously we had an alert and we also had a CQC visit which looked at critical care, and the model of critical care we had running here was very odd in that we have an upstairs intensive care unit which looked after level 3 – so the sickest ones – and surgical high-dependency patients and we had a medical health and [inaudible] downstairs which the critical care people were not involved with, which was run by physicians as a medical HDU [high-dependency unit].
Medical director, AMI-s.01
In AMI-s.01, respondents accepted that a problem with AMI mortality had been identified and they followed a forensic approach and produced a detailed action plan:
Seeing that alert, that acute myocardial infarction is not being dealt with correctly and in addition to this we have been asked to produce what patients’ plans were at [AMI-s.01] hospital with the chest pain, so we had to provide a detailed response.
Medical director, AMI-s.01
A clinician working with the mortality committee worked with another clinician to investigate and question all documentation that related to the AMI Alert. This included admitting condition, comorbidities and interventions, highlighted as follows:
I’ll usually sit down with a consultant and you’ll got through the actual documentation looking at obviously admitting condition, comorbidities, looking at interventions, were they appropriate, because at the end of the day these are patients who are a problem because they died, so we work through them, we’re just looking, has the right intervention occurred, have we missed anything.
Resus officer, AMI-s.01
If problems are identified in the case notes, then a mortality pro forma document is completed and this is forwarded to the division involved for further investigation:
But if there are issues they escalate, so the investigating officers, so the consultant and the nurse usually will then fill out the pro forma, and that will be escalated to the division where the issue has been raised and they need to take it further.
Resus officer, AMI-s.01
A similarly forensic approach was adopted in Sep-s.06, involving the mortality committee co-ordinating the trust’s case note review. An electric pro forma for mortality was completed and the case notes were graded A–E, thereby standardising the mortality review process, identifying comorbidities and directing the extent and level of case note review.
In AMI-s.01, the AMI alert was investigated by exploring the AMI pathway and generating an action plan to address problems. For example, problems were identified in failures of examination of patients by a cardiologist in wards outside cardiology; difficulties in the speed of identification of AMI using the existing patient at risk score (PARS) observation system; and incorrect coding of AMI. For example, a consultant reported how an action plan addressed the way in which infrastructure limitations had resulted in AMI patients being distributed to wards across the trust that did not have a cardiologist on site:
For cardiology obviously we had an alert and we also had a CQC visit which looked at critical care, and the model of critical care we had running here was very odd in that we have an upstairs intensive care unit which looked after level 3 – so the sickest ones – and surgical high-dependency patients and we had a medical health and [inaudible] downstairs which the critical care people were not involved with, which was run by physicians as a medical HDU [high-dependency unit].
Medical director, AMI-s.01
A forensic examination of the case notes in AMI-s.01 also identified problems with the speed of identification of AMI and early intervention in wards outside critical care and cardiology. Respondents highlighted that, in response, an action plan had been put forward, whereby every patient with suspected AMI was to be assessed by a consultant cardiologist:
So that we introduced, and also we showed that every patient that comes in with non-stemi is seen by a consultant cardiologist, he decides what is the best route in discussion with the patient and other colleagues if colleagues are involved.
Consultant cardiologist, AMI-s.01
An integrated trust-wide response
All trusts reported an integrated trust-wide process for responding to alerts. This focused on validating the alert and then a central structure (in Sep-s.06 a mortality committee, and in Sep-s.05 the clinical governance team) co-ordinating a trust-wide investigation. In AMI-s.01, the response to the AMI alert was characterised as integrated across corporate, divisional and speciality levels. The alert was sent to the executive team and then forwarded to the clinical governance unit. This unit comprised subunits that focused on patient safety, quality improvement, clinical audit and effectiveness, clinical governance, litigation, compliance, PALS (patient advice and liaison service), assurance and governance. Trust mortality leads demonstrated a key focus on improving data quality in mortality review. The clinical effectiveness subunit played an important role in generating supporting background data related to the alert. These data included information on the divisions affected, patient pathways, staff involved and history of alerts. This information fed into corporate teams, such as the mortality committee and coding teams, and was forwarded to the divisional mortality teams. At the divisional level the investigation involved case note review, review of coding, a patient pathway analysis and recommendations for improvements in care or coding that were forwarded to the mortality committee.
Clinical engagement and cultural ownership of sepsis improvement
Sep-s.06 reported trust-wide intensive clinical engagement in mortality review. Clinicians also appeared to develop ownership of mortality. Opinion leaders in this trust operated as informal sepsis champions, encouraged ‘buy-in’ and were instrumental in developing innovations within specialties. Clinical champions in Sep-s.06 and AMI-s.01 operated as boundary spanners, supported mortality review and made sense of how clinical diagnosis for sepsis was coded and the implications of this for Imperial College alerts. In AMI-s.01, a data analysis identified clinicians operating as boundary spanners, bridging knowledge areas and cognitive frames. A consultant cardiologist working with coders in the case note review was able to ‘bring the coders into the reality of medicine’ and helped the clinician make sense of how they worked:
There is a revolutionary drive in the trust running to try to bring the coders into the reality of medicine . . . every day, there are actually at least three notes, there’s one which are done, and the two are waiting. These are, the coders think that what’s in the note is not correct, so it’s sent to me as a lead for cardiology, I look into it, I follow the national guidance . . . I have been to, I’ve been brought into the coders’ mentality, how do they think, how do they work, so I can understand when I am right and the manager how to help them getting a resolution out of the confusion about specific cases.
Consultant cardiologist, AMI-s.01
Likewise, a senior nurse in critical care in AMI-s.01 identified how she had supported mortality investigation and acted as ‘the link between nursing and medics’:
I’d fit in ICU and initially I had a bit of resistance from both the nurses and the doctors, it was because the nurses saw me as, ‘Oh, who does she think she is?’ and I’m open with them, I know all that, and then the doctors were a bit like dubious, but then we had an external review 6 months from [external trust] and they felt that I needed to be on the unit full-time and since I’ve helped with the mortality, got the documentation, and I’m the link between nursing and medics, they’re looking to employ two more!
Senior nurse, AMI-s.01
In contrast, Sep-s.05 appears less focused on clinical involvement in mortality review and investigation processes linked to the alert. For example, the sepsis lead acknowledged that there was a problem with coding for sepsis but conceded that he had no involvement in trying to address this problem, as he had not been asked for input. Likewise, universal case note review by clinicians of all deaths was not reported.
AMI-s.01 respondents reported that, in responding to the AMI alert, there was increased involvement of clinicians in mortality review with the mortality committee and divisional mortality teams. The medical director highlighted that it was important for clinicians to volunteer to participate in these teams. He suggested that it was deemed important so as to ‘keep the process clean’, legitimate and free of scrutiny, although it was recognised that clinicians’ time and energy were limited:
I did it on a volunteer basis and that’s part of the struggle is that people are giving up their time and energy to do this, and it’s still done in that way . . . but it was done on a volunteering basis because that was the only way I could keep it clean. And, I wanted it to be, as much as I could, bomb proof in terms of critique that people might make of the process.
Medical director, AMI-s.01
A universal and timely response
In AMI-s.01, most staff reported that the trust response to the AMI alert was to have a review of case notes for every death. Hence, the head of clinical efficiency and effectiveness said:
We systematically reviewed every single death in patient death from February by panel.
Head of clinical efficiency and effectiveness, AMI-s.01
The CEO highlighted how these investigations fed into organisational changes:
The team then undertook a retrospective review of all deaths in the previous 2 years, all complaints, incidents, inquests, etc., and mapped the care delivery problems and the required actions onto an organisational development plan.
CEO, AMI-s.01
Importantly, clinicians involved in a mortality alert were excluded from the case note review process and attention focused on timely review of case notes. An internal target was set of a 14-day review period, which was managed directly by the clinical governance unit and ensured that clinicians recorded a clear memory of the patients involved.
Sep-s.06 also responded by instigating the universal case note review of all deaths by doctors. In [region], this was viewed as onerous, especially in specialties such as geriatrics that had many deaths.
Case note review identifying errors in coding
Across all trusts receiving a single alert, case note review identified errors in coding. For sepsis, this related to junior staff unable to identify a diagnosis early and writing up case notes in an ambiguous way, without highlighting the comorbidities and primary condition. For AMI, errors in coding arose from misdiagnosis and poor case note write-up. Problems were also identified in junior doctors’ ability to identify myocardial infarction.
Comparative analysis of outcomes arising from the alert for sepsis and acute myocardial infarction
A comparative analysis of outcomes generated by the alert suggests that Sep-s.05 and AMI-s.01 generated solutions directly related to problems arising from the investigation of the alert. These related to training junior doctors in writing up case notes and providing greater clarity in diagnosis and comorbidities.
AMI-s.01 appeared to have reported more outcomes related to the alert for AMI itself. These included improvements in escalation of deteriorating patients, and moving from a PARS system to a NEWS system thereby facilitating nursing engagement:
With the escalation process, yeah. That is there and it’s very clearly identified in the deteriorating patient policy now that if you don’t get it from Dr X then you go to Dr Y, and if all else fails you get the consultant. Where I think previously, yes, I think a junior nurse would probably not have gone straight to a consultant.
Head of clinical efficiency and effectiveness, AMI-s.01
In AMI-s.01, it was viewed that implementation of the MEWS system had had an impact on the number of cardiac arrests:
The number of cardiac arrests that has been influenced, has been, I’m absolutely convinced, has been influenced by the implementation of MEWS and early warning scores full stop. But I think the biggest reason why your crash calls are falling off is DNACPR [do not attempt cardiopulmonary resuscitation]. But that’s only a personal opinion.
Resus officer, head of clinical efficiency and effectiveness, AMI-s.01
AMI-s.01 was also reported as effective in changing patient pathways as work had been done to improve the use of the ‘do not attempt cardiopulmonary resuscitation’ policy. This involved introducing ‘ceilings of care’ into the patient case notes. Similarly, a reported outcome of the AMI alert was investment in trust infrastructure to redesign critical care and acute coronary care, with a ‘pacing room’ for the treatment of patients with confirmed AMI. Respondents reported how a mortality review arising from the AMI alert had identified that AMI mortality was high in wards outside critical care and cardiology. It was considered that non-specialist doctors were incorrectly diagnosing AMI in these wards, and in other cases not treating patients with AMI in a timely manner. Thus, changes were made to the AMI pathways allowing cardiology consultants to treat patients in the ‘pacing room’ and to diagnose their condition accurately in wards outside cardiology and critical care. A new protocol also set out that all patients with suspected AMI throughout the trust were to be assessed by a cardiologist.
A further outcome of the AMI alert was to include GP engagement in the mortality review process. The mortality pro forma was also changed to allow clinicians to identify whether or not the AMI had occurred outside the hospital.
Comparative analysis of parallel development of processes for sepsis and acute myocardial infarction mortality
Respondents in Sep-s.05, Sep-s.06 and AMI-s.01 conceded that other factors influenced the evolution of the mortality process. In Sep-s.05, extensive organisational turbulence experienced at the time of the alert prevented trust-wide engagement in mortality review. Regulatory pressures associated with Monitor and CQC intervention led to substantive changes in trust leadership. These resulting changes appeared to have influenced improved clinical involvement in mortality review. Engagement with external bodies was reported as influencing awareness of both sepsis and AMI. Clinical auditing of specialty performance and participation in quality improvement initiatives in both Sep-s.05 and Sep-s.06 appeared to have played a part in improving the awareness and treatment of sepsis. In AMI-s.01, engagement with AQuA and PRISM accessed learning about mortality review.
For AMI-s.01 regulatory pressures generated from the Keogh review were described as ‘giving teeth’ and urgency to trust-wide changes. A culture emerged that encouraged engagement, introduced structures supportive of learning, linked patient safety and QI ongoing processes, and fed into AMI awareness and mortality improvement.
Integrative analysis: towards an evaluative framework for institutional maturity
To better understand the factors contributing to the perceived institutional capability for responding to signals in mortality data, an integrative analysis was undertaken independently of the case-based analysis, drawing on interview data collected across all case studies. Based on initial open-coding and early-stage iterative refinement of categories, nine broad themes were identified to serve as a frame for further exploration in the data set. The resulting thematic analysis was used to structure early versions of the survey instrument used within workstream 2 in order to ensure that response items and scales were both thematically balanced and theoretically grounded in the emerging perspectives on effective institutional responses. Analyses of the nine core themes, along with emergent subthemes, are reported below.
Organisational structure for mortality governance
Key themes: presence of key committees, roles and processes for effective mortality governance; effective representation on mortality committees (both internal and external)
The role of the centralised mortality committee was emphasised. It was thought to be important to properly define the committee’s purpose and function, including leadership, membership and output:
And instead of the mortality committee being as small as it was, the chief executive began to take the chair, a little bit more direction on who should be represented at it, what sort of reports they should be producing . . .
Trust mortality lead
In terms of output from the centralised mortality committee, effective communication and dissemination to individual specialties was stressed. For example, this was sometimes achieved by inviting mortality chairpersons from individual departments to sit on the centralised committee and feed back, as well as conducting departmental-level mortality meetings:
We put a mortality chair for each and every department to collect the response for a whole mortality review, and make sure that minimum quarterly every department has a mortality meeting, and aim for 100% mortality reviews. Then once we set up that process then it became much easier for us to invite all mortality chairs to one mortality group meeting.
Trust mortality lead
Simultaneously, there was a strong need for intercommittee communication to ensure that key messages from mortality review reached the right people and to support broader organisational learning:
If there will be any cross-directed learning it will go to the governance committee. If there would be any trust-level issues, then the issues will be forwarded to HAC.
Trust mortality lead
Coding
Key themes: accuracy of mortality coding; investment in coding capability; provision of coding input to mortality review
Ensuring the quality of coding supported the effective use of the alert system and prevented false or misleading signals in the data:
. . . and I think getting the data quality right, along with palliative care, is what solves the coding, it solves the alert system. I don’t think there’s anything you can do in the alert system particularly, because if you send rubbish to Dr Foster it’ll come back as contaminated alerts.
Trust consultant anaesthetist
When we would look at the volume and compare to the volume with Dr Foster there was a big difference. And we were not alerting in Dr Foster but were alerting with the CQC.
Trust mortality lead
The recruitment of high-quality coders who were both experienced and permanent was also viewed to be a challenge that required rectifying:
So creating or hiring and recruiting, or training, more senior coders and putting them at the forefront of working with clinicians, I think it was a decision that was seen as promising at least.
Head of coding and data quality
What we’re lacking now is we’re lacking resources of senior coders. So what we need to do – and actually we’ve gone through this. What we need to do is more of this. So we know what we need to do and we have seen some results, but then we need a little bit more. And the clinical coding department hasn’t got the people, not because we haven’t got the money. We have the money.
Head of coding and data quality
In line with this view, coding-specific action plans were thought to be important to consider, and potentially execute, when a mortality alert was received:
So we put in place an action plan that was around improved coding and education.
Trust mortality lead
The other thing that was found is that the coders weren’t really clear at all, in what they should put into what codes because it wasn’t clear. So we wrote some common sense guidance forms to what counts as what.
Trust deputy chief medical officer
Use of information, monitoring and reporting
Key themes: effective organisational use of mortality data; analytic and predictive capacity; ability to detect and respond to signals and to drill down to identify priority areas based on available data
Proactive, as opposed to reactive, use of information was thought to be the key to anticipating potential alerts and acting on quality of care issues before they reached a pivotal stage. Not all participating organisations had been able to achieve this at the time of the interviews but it was often mentioned as something to strive for:
I wouldn’t say we definitely know they’re coming but they’re not always a surprise, because we know we’re getting close to a limit where we expect to be alerted.
Trust information project manager
And partly because actually we want to start collecting the data prospectively, rather than having a retrospective flag from Dr Foster . . .
Trust mortality lead
So if we can see that there’s going to be an alert because we’ve got the information, we would actually prospectively tell the CQC we were about to alert on it and we’re at this and we’re investigating and then just give them a plan of action.
Trust mortality lead
The availability of mortality data from various sources supported organisations in effective monitoring:
I think at [name of trust] we’ve got quite a rich amount of clinical data available online and that, in combination with some of the reporting we do, kind of helps you to get to the nub of the issues reasonably easily.
Trust information manager
The specificity of these available data was emphasised as being important:
And also being able to drill down to your specialty quickly would – I think that would make it more helpful.
Trust clinical lead for heart failure
Yeah, so we know the date range and we go and do our own analysis. Because in a sense what we can do very quickly is a much more detailed analysis down to very specifics that drive in that performance, and it isn’t there. We look at what it is, we look at the date range and we go and do our own analysis.
Trust head of coding
Alongside the availability of data, it was viewed to be of equal importance that an organisation has staff members, including clinicians, with the appropriate levels of analytical expertise to make optimal use of them:
I think there’s a lot of data there. I’d say the key thing is having sufficient expertise in terms of capacity and the knowledge to analyse what’s there. I’d say that’s probably – for us that would be the key challenge.
Trust information manager
And I would say it might be great to a statistician but if you want something that’s practically going to support you in a hospital, they’re trying to understand clinical care, outcomes and mortality, I think you need something a bit more user friendly, easy to understand, etc.
Trust information manager
The use of benchmarking and triangulation with other data sets was seen as useful for maximising the use of information:
If you look at our global HSMR it’s come down, we’ve improved in the last couple of years, certainly, and we rank ourselves, we present our data, we give the current year, the current month and then we do a 12-month rolling presentation of our mortality data. Partly 12-month rolling so that if we’re always improving we never overstate how much we’re improving, because it’s an improvement plan so you don’t want to rest on your laurels and say we’re really good, you want to make yourselves look as bad as you possibly can so that you’re always trying to improve more.
Trust mortality lead
I’d look on more sources of information like I go onto the head system, I go onto SHMI, I go onto HSMR and look at specific things, and analyse it.
Trust mortality lead
In terms of data presentation, some organisations had produced a mortality score card to explore mortality data more effectively:
I’m now managing to produce, you know, a proper mortality score card on the back of that, so that we can – you know, just that we can keep a snapshot of where we’re going, and what we’re seeing there, ties with what I’m looking at on head from our kind of data.
Trust mortality lead
Interviewees discussed the ways in which they identified triggers in mortality data for further investigation and/or improvement action. For example, one interviewee talked about the use of CIs to detect relative risk:
So originally we set up a monthly mortality report that we just looked at the list of top 90 diagnoses, or whatever it was, numerically the number of patients in each grouping, what was the relative risk with confidence intervals, and we would investigate something if the confidence intervals didn’t come to 100.
Trust mortality lead
It was emphasised that trends could be effectively used to both trigger and monitor improvement actions:
So we were able to then drill down to where the areas of concern were, show the information to the clinicians and say, ‘OK guys, we’re going to have to do something with this alert which is why we’re in trouble’. And they then started doing a really targeted piece of work on a cohort of patients. And it wasn’t data manipulation; it was improvement in systems and processes that actually took the organisation out of mortality risk picture, if that makes sense.
Trust medical director
Local investigation and mortality review process
Key themes: robustness of process; frequency of mortality review; ability to identify avoidable mortality; information technology support; reporting
Some organisations reported using a tool or defined system for comprehensive primary and secondary case note review:
Well, firstly there is a second-stage review so there’s a screening tool which is being used and if that highlights any areas then there’s a second-stage review. So probably about 10% of them end up in a second-stage review.
Trust medical director
So we put in a system whereby everyone gets reviewed, that is the aspiration. And that if on the basis of information available relating to the first 24 hours of admission, that includes previous history, if on the basis of that, survival was either thought probable or was expected, those cases then get a detailed review.
Trust medical director
The use of a systematic approach to reviewing was important to ensure standardisation and shared understanding of the process. This applied to both the process of case note review and the approach to classifying outcomes from it:
So previously it has been a bit ad hoc, a bit unstandardised, various different departments doing what they felt was appropriate/not appropriate. There was no line of sight from the organisation about who was doing mortality reviews and how many mortality reviews were being done, and the outcome of those mortality reviews.
Trust mortality lead
So one of the things that we’ve done with these secondary reviews, when we can get them back, is we have the outcomes of the findings classified under themes. So there are 11 themes that we’ve got . . . And then we try and see if we’ve got recurrent themes across places and so on.
Trust consultant anaesthetist
To ensure that the mortality review process was being executed sufficiently, quality monitoring processes were also employed. These included peer review, cross-checking across specialties, the development of guidelines and training, and reviews of random cases:
But actually one of the other principles for me is peer review. So one of the reasons I identified something when I did a review of acute and unspecified renal failure is because I’m not involved in that service. And it’s like doing a serious incident investigation, you get someone outside the department to do it because they see it with fresh eyes, they’re not constrained by the baggage of what happens in the department.
Trust mortality lead
The level of available support from IT and electronic systems was also thought to influence the effectiveness of mortality review. Interviewees associated better systems with better practice in this area:
Having gone to the NCEPOD review meeting 2 or 3 months ago on the way in which trusts engage with mortality reviews, it is clear that those who do it with least pain and with greatest efficiency have IT fully on board and the process electronic . . .
Trust mortality lead
Local improvement mechanisms
Key themes: capacity to translate learning from alerts into local actions for improvement and implement them using appropriate methodology; reporting and oversight of quality improvement projects to ensure they deliver
It was thought important to have a systematic and thorough evidence-based approach to developing improvement plans based on mortality alerts:
And actually if you’re going to have – you either do old style mortality reviews for the sake of it, or you make it part of your quality improvement process. And to be part of kind of a QI process, you have to learn from what you’re looking at.
Trust chief nurse
Once improvement plans had been executed, it was necessary to monitor and evaluate the impact that they had on quality of care. In some cases, actions required revision when they did not achieve their goals owing to either poor implementation or general ineffectiveness:
But also making sure that the clinicians are properly supported in terms of the QI methodology so that we can chart the things that we need to do, we can measure ourselves effectively against those and then we can complete the cycle in terms of what else needs to happen.
Trust CEO
Organisational culture
Key themes: attitude towards avoidability of mortality; willingness to investigate alerts as ‘valid’ signals; degree of open discussion on sensitive issues; sense of shared responsibility and accountability for avoidable mortality
The general approach taken to responding to mortality alerts was thought to be reflective of a broader organisational culture. Some organisations found it easier to exploit learning opportunities regardless of the underlying causes of an alert:
It may be that we are truly terrible or it may just be a little smouldering fire. You can’t ignore an alert, can you?
Trust consultant anaesthetist
. . . you could always do something, and there’s always learning, there is always something else that you could have thought of and done.
Trust CEO
This type of positive learning culture was often reflected in the integration of coding and clinical review and the avoidance of gaming through developing an open culture:
Absolutely not, the rule that I go by is that you have to have a coding and clinical review in parallel, and that every set of case notes that you open there is something that you can learn from them.
Trust mortality lead
Like we said, we’ve gone down the ‘let’s look at the quality’ and I’m aware that a lot of my other colleagues have gone down the ‘let’s look at the data’, maybe looking at the quality as well. We’ve assured ourselves that we are providing care to our patients and now we’re beginning to look at the data side of things as well and that aligns.
Trust mortality lead
A lot of organisations have come to problems because they assume this is down to coding and not down to quality of care. We have been very clear that we don’t make an assumption that this is a coding issue. So that’s the first thing I would say.
Trust medical director
We wanted to create a climate of openness and transparency and again part of the effort and space in the first instance is you build that by getting people to work together.
Trust CEO
It also required an organisation to attach sufficient significance to mortality as an indicator and increase and define its profile alongside competing priorities:
So with our kind of day to day – trying to make this part of everyday business, really, mortality, as opposed to something that happens once a month that might tie in with a governance meeting. So everyone scurries around, doing a bit of M&M [morbidity and mortality review], and might present it at a governance meeting. It’s got to become part of everyday.
Trust mortality lead
Interviewees expressed a need for organisations to devote greater time and resources to increasing clinicians’ engagement with mortality and ability to interpret and understand related data:
And I think the feeling was that generally the best trusts were those who were clinically led rather than managerially led, so the feeling was that there’s ambition in the trust to do the best for the local patients. So keen to provide a good service and to get everyone involved in doing that.
Trust mortality lead
An absence of clinical engagement could result in defensiveness from the front line, which was perceived as a barrier to effectively responding to mortality alerts:
And yes, it’s always difficult sometimes with clinicians to get them to believe and trust in the data. But once they do they normally become very sort of keen and interested in it.
Trust information project manager
So again, the power of data that becomes clinically relevant is the thing that engages clinicians to then being able to understand why they have a responsibility to engage. That’s the problem, it’s the engagement of the clinicians to the issues of mortality . . . we are failing them generally in connecting them to the number that comes in to what it means to them as a clinician.
Trust medical director
To achieve this, it was thought to be important for an organisation to engage in effective job/role planning and guarantee protected time to be devoted to mortality:
I think some of them would love to take it on but at the moment it’s proving difficult to get a handover because they’re so busy that they can’t free up the time to come and sit with me and go through it.
Trust mortality lead
Senior leadership and sponsorship
Key themes: strategic prioritisation of reducing avoidable mortality; senior presence on mortality review committees and action groups set up to address issues raised by mortality alerts; sponsorship of actions
Focused and engaged senior leadership who explicitly assign priority and resource to mortality alerts were thought to be vital to supporting the process:
I believe in people leading by example, and quality is a really big – and safety is a really big issue to the board now, whereas before I think they were seen as totally removed from it.
Trust mortality lead
It’s been a long time coming, and it’s coming because of the engagement of a very different type of medical director.
Clinical outcomes manager
And I think part of my responsibility is also to, with the medical director, nurse director, set the tone for the organisation around how seriously this is taken, the amount of time that is taken and part of my responsibility is also around providing some of the resource to support if we take the QI methodology and how we’re using that, so means of improving care to ensure the resource is there to support that methodology as well.
Trust CEO
Alongside high-level sponsorship, there was a need for senior leads to play an active role in the practical processes and to provide support for those who were responsible for overseeing mortality:
I feel like I’ve got a voice and I feel like I’ve got back-up now. I’ve got somewhere to escalate to so when things don’t go as they planned and when I’ve hit that brick wall I can escalate to [XXXX], I can escalate to [XXXX] and it will be done, and that is the change and it’s quite . . . yeah, it’s quite refreshing.
Trust mortality lead
Now the chief executive has put out a very clear summary of what he expects of those divisional and departmental representatives.
Trust medical director
The chief medical officer introduced a completed revision in the last 3 years around the mortality reviews . . . so we have much more openness and transparency in relation to how we deal with mortality alerts, mortality review, there is an upward track directly to board, so mortality data is reviewed monthly at board.
Trust mortality lead
Interprofessional collaboration
Key themes: frontline clinical and broad professional involvement in mortality review, investigation and action in response to alerts; clinical input into mortality review and coding
The integration between different professional groups was highlighted as key to a holistic understanding of and approach to mortality. Interviewees often referred to the integration of clinicians and coders as a key example of effective interprofessional collaboration:
It was dialogue, sitting together and working together, absolutely. And then we have consultants that are very receptive and they actually want to improve their data.
Head of coding
What we did do after the AMIs was I took a coding manager to lots of governance meetings with me . . . so we would try to get a case from that area and to show what their [clinicians’] perception of what happened was and what a coder read from the notes.
Trust medical director
However, even within professional groups, the integration of different levels of seniority was viewed as necessary, and achieving this required specific attention:
And we’ve struggled really to get the consultant body as a whole to take the leadership on that and tell them to engage with their juniors saying, ‘I expect the “bundle” to be done’. That’s a lot better now than it was though.
Trust mortality lead
I have a personal concern that because trainees may present in a public forum where their seniors are present, there may be concern about saying what they might truly think about care, which is why you need really consultant oversight to support them in their feelings, but I think most of the time, the issues do come out.
Trust Mortality Lead
Interviewees felt that information about mortality alerts required appropriate tailoring to its target audience(s) when it was to be disseminated across the organisation:
That’s designed by department across the hospital so that each department has the opportunity to adapt the database to make specific issues, or ask specific questions.
Trust consultant in respiratory and intensive care medicine/head of mortality
I think you’ve got to look at it in who is it designed for because I don’t think it’s actually designed to go straight down to our clinicians and to the ground floor.
Trust medical director
Multiple methods were employed to achieve effective dissemination, including presentations at grand rounds and other smaller forums, newsletters and magazines, and the sharing of key reports:
I often do the grand rounds and in my grand rounds I will put all the CQC alerts, what the trust had received, and what are the learning points.
Trust mortality lead
There is a new hospital magazine that includes lessons learnt, and I have a column in there, it has only been up for a couple of months where I will select three things from mortality review meetings that are of relevance trust wide.
Trust mortality lead
So we’ve got comms on board as well and that’s a huge part of managing sepsis, I think. And rather than me trying to do it on my laptop and trying to get messages out there and develop the comms myself . . . they’re designing the posters and they’re designing the comms and it’s on the intranet and it’s on the updated screen savers and there’s posters which change on a biweekly basis.
Trust sepsis lead
External environment
Key themes: availability of guidance, participation in national campaigns; pressure from public and regulatory bodies including the media
The association of mortality alerts with the CQC was thought to influence the ways in which organisations responded to them:
I think in any NHS trust, the CQC attached to something, my gut instinct is it makes people take notice of it. It just adds a little clout to it, I think. I don’t know. That’s my perception of it. I don’t think it’s a bad thing that they’re attached to it.
Trust mortality lead
And our chief exec’s never very impressed if it’s a CQC one. So there’s that element to it.
Trust service development/coding manager
Well there’s two things, one is you’ve got to do it because the CQC tells you you’ve got to do these things.
Trust mortality lead
The influence of public accountability and local reputation was also deemed to be important:
Yes, because in the press, the press were quite easy to knock us and . . . And we’re not perfect all the time but when listening to that, very, very powerful.
Trust mortality lead
. . . there was the exposure in the media around mortality and . . . I think that actually had a positive impact and one’s got to be careful around some of this because I think it’s very easy to jump to the wrong conclusions, but nevertheless, I think it galvanised a level of interest that perhaps it would have been difficult to generate otherwise.
Trust CEO
More specifically, the launch of broader clinical programmes encouraged organisations to engage in the mortality alert improvement process. For example, the Sepsis 6 national campaign was thought to have had a wide effect on professional practice:
And so we reckon we’re saving potentially 10 lives a month with the Sepsis 6 delivery. So there’s some workstreams, so changes in working practice that have been put in place in clinical practice that are probably contributing. And if I wanted to identify one that was the biggest hitter, it would be sepsis.
Trust consultant in respiratory and intensive care medicine/head of mortality
Chapter 8 Results from workstream 2: national evaluative survey on institutional responses to mortality alerts
This chapter reports the results from the evaluative survey study conducted within workstream 2 of the project. The instrument was developed based on insights from the qualitative case study data and with input from key stakeholders. We first report basic demographics and then describe the use of information, any local investigations, the institutional capacity to respond to alerts and the trusts’ evaluation of the alerting system.
Development of survey instrument
The survey instrument was developed based on insights from the qualitative case study data and had input from key stakeholders, including Dr Foster site co-ordinators and CQC mortality outlier programme leads, reviewers and analysts. There were three principal aims of the survey study:
-
to categorise and quantify organisational behavioural and contextual aspects of the response to alerts, specifically to explore the relationships between the type and frequency of alerting, key contextual and organisational behavioural characteristics and intermediate outcomes
-
to identify and prioritise the main drivers of effective institutional responses to mortality alerts, as perceived by trust mortality leads
-
to quantify mortality lead perceptions of the current adequacy of the mortality surveillance and alerting system.
The development of the survey instrument is detailed in Chapter 5 and the final version of the instrument is in Appendix 14. By way of an overview of the structure of the survey measures and the subsequently reported results, Table 18 provides a description of each survey section. The survey included both quantitative scale and categorical items, along with free-text items for respondents to expand on their ratings and provide elaborative information. In the following sections, a thematic description of the anonymised free-text responses is interspersed with the statistical results to illustrate individual respondent perspectives.
| Section | Description |
|---|---|
| Section 1: about you and your role | Basic demographic items about the individual completing the survey and their role within the trust |
| Section 2: organisational arrangements for mortality | Items on the trust’s governance structure for monitoring mortality |
| Section 3: coding, data and information for mortality | Items on the processes through which coding and information are used to support mortality |
| Section 4: mortality review | Items on the approach that a trust takes to reviewing mortality both in response to a specific mortality alert and more generally |
| Section 5: responding to Imperial College/CQC mortality alerts | Items on trust processes for developing actions and improvement mechanisms in response to an externally generated alert |
| Section 6: institutional capacity to respond to signals in mortality data | Scale items based on the evaluative framework to represent a trust’s overall capacity to respond to signals in mortality data |
| Section 7: evaluation of mortality alerts and surveillance | Items that allow respondents to express their overall views on the effectiveness of the mortality alerts and surveillance system |
Missing data analysis
A missing data analysis was conducted to look for any significant differences between responders and non-responders on the following key metrics:
-
trust type
-
total number of Imperial College alerts sent (2007–16)
-
HSMR data (2012)
-
SHMI data (2015).
No significant differences were found between responders and non-responders.
Demographics
Trust type
The pie chart in Figure 19 demonstrates that there was a relatively even split between the different trust types, except for acute specialist trusts, of which there was just one respondent.
FIGURE 19.
Pie chart of trust types in the observed survey sample.
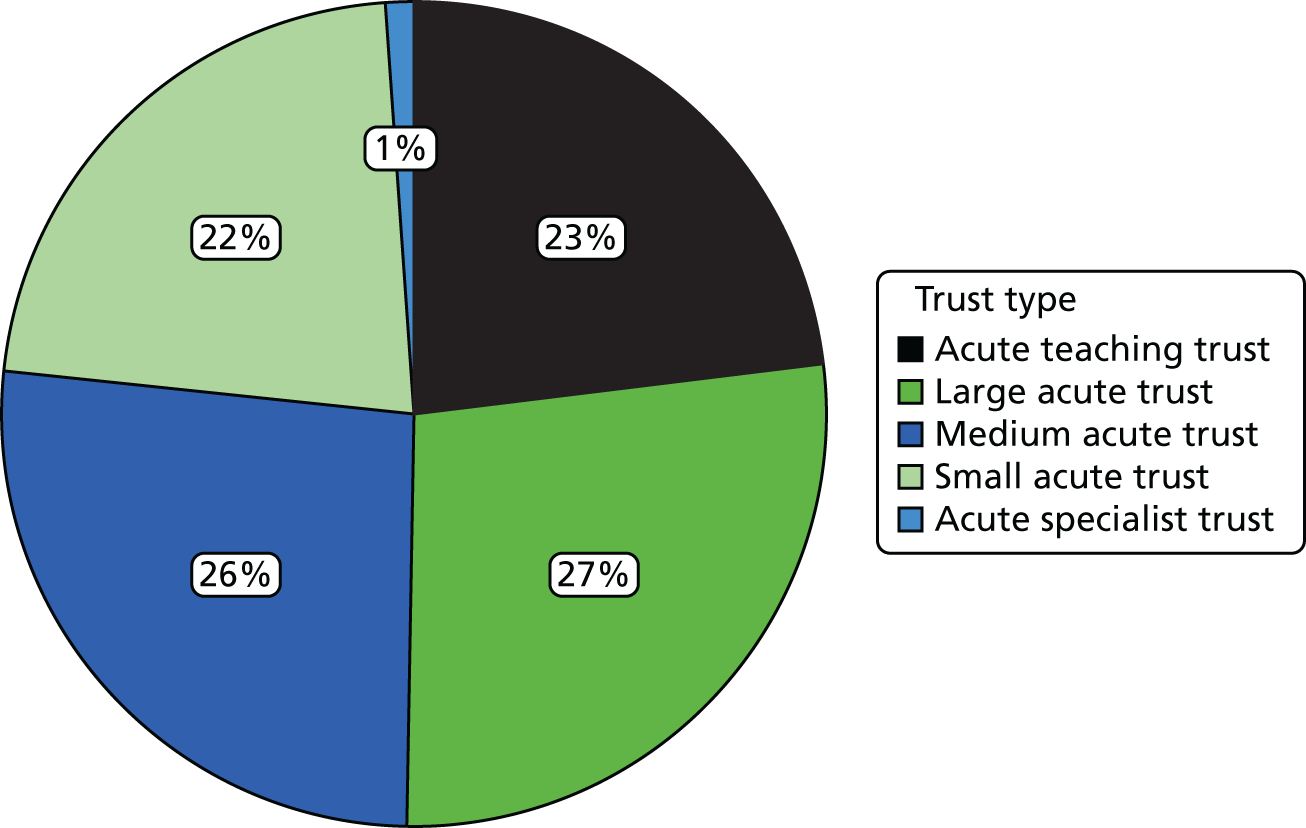
Profession of respondent
The pie chart in Figure 20 demonstrates that the majority (60%) of respondents described their profession as clinical, 38% described it as managerial/corporate and just 1% described it as informatics.
FIGURE 20.
Pie chart of respondent professional groups.
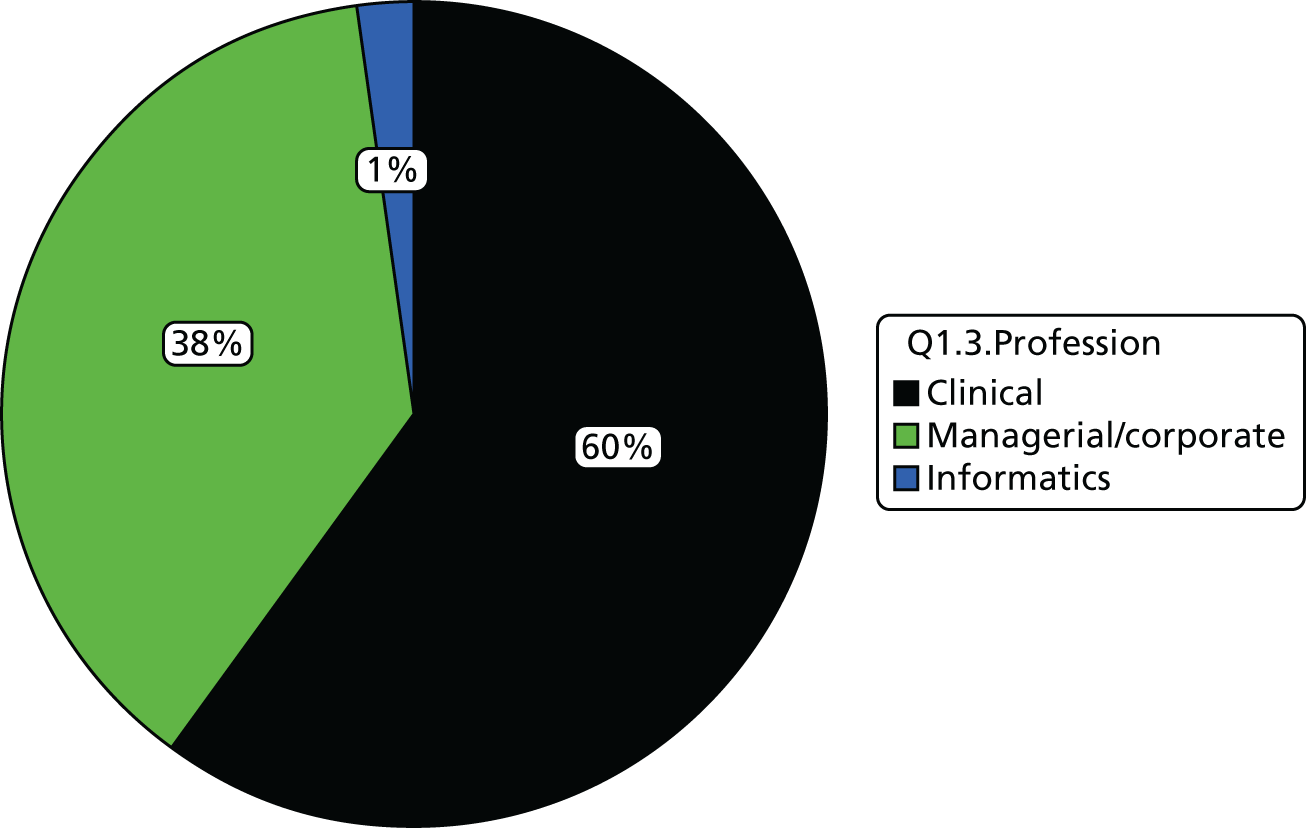
Role of respondent
The pie chart in Figure 21 demonstrates that the majority (73%) of respondents said that they had overall clinical responsibility for mortality reduction in their role.
FIGURE 21.
Pie chart of respondents’ professional roles.
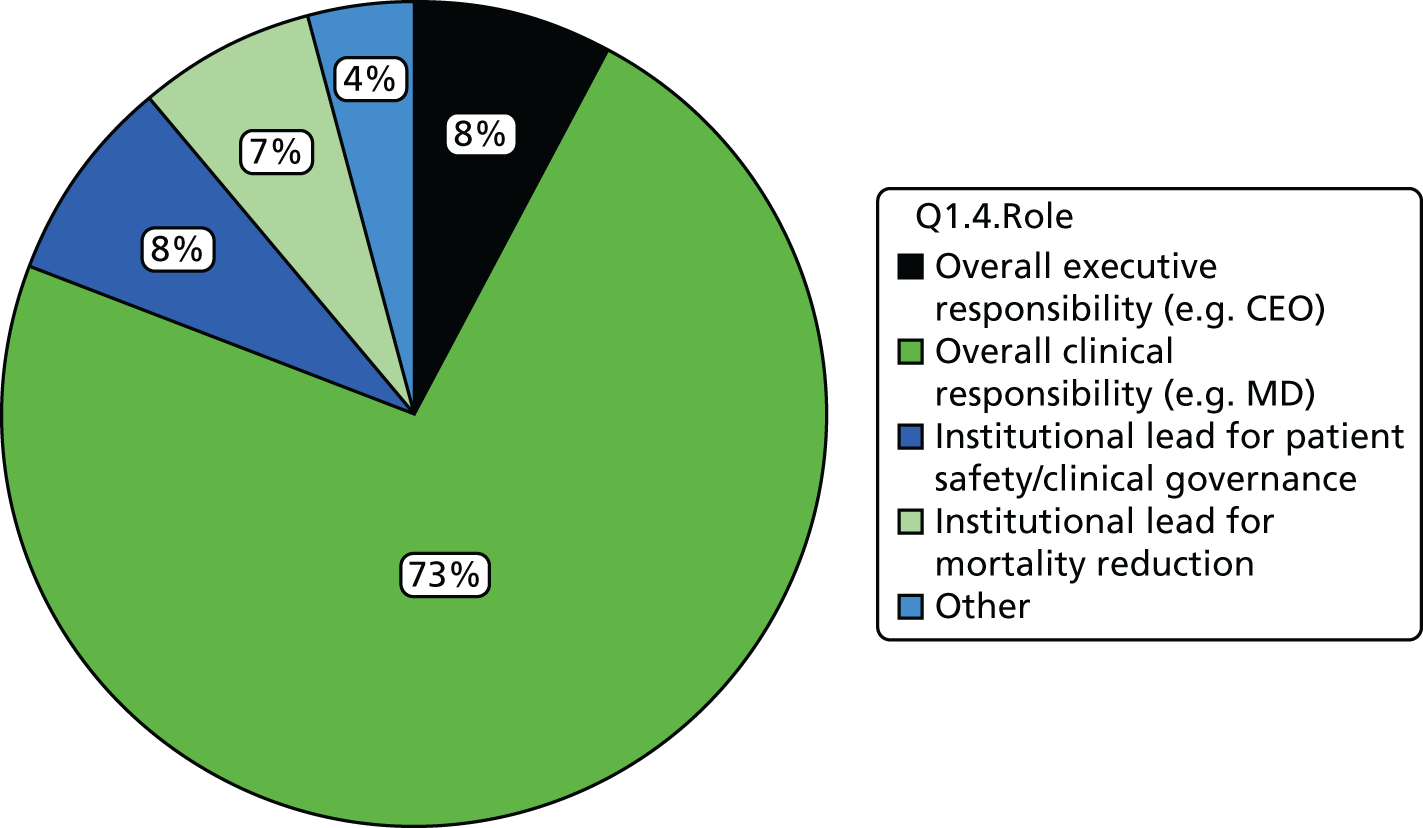
Descriptive analysis
Research question: to categorise and quantify organisational behavioural and contextual aspects of the response to alerts.
Organisational structure for mortality governance
A total of 86% of responding trusts had a dedicated trust-level lead for mortality reduction and 92% had a dedicated trust-level mortality group or committee in place. Seventy-seven per cent of those trusts said that the committee reviewed mortality on a monthly basis.
In terms of the appointment of mortality leads, 31% of responding trusts had these appointed at the individual division level, 30% had them appointed at the clinical directorate level and 41% had them appointed at the clinical specialty level.
Organisational structure for mortality governance (survey section 2 free-text analysis)
Out of the 78 trusts that responded to the survey, only nine did not have dedicated trust-level mortality group or committee. These nine, however, had a group or body that was responsible for mortality reviews and responses to alerts. These groups varied from a specialty-level group (e.g. the cardiology department for AMI alerts) to a patient safety panel.
All of the trusts had someone chairing the group, whether that group was a dedicated mortality group or one of the nine discussed above. The majority of these chairpersons were senior clinical staff; over half (56%) were medical directors and around one-third (27%) were a deputy or associate medical director. Only a very small number of trusts (n = 5) had a dedicated mortality lead chairing the group.
Use of information, monitoring and reporting
Ninety-six per cent of responding trusts routinely used SHMI to monitor variations in mortality and 90% used HSMR. A total of 82% of responding trusts reported using crude unadjusted data to monitor variations in mortality and 23% of responding trusts routinely used RAMI. In terms of subscriptions to toolsets, 97% of responding trusts reported subscribing to at least one toolset, with 54% subscribing to the Dr Foster Toolset, 28% to HED, 24% to CHKS and 10% to CRAB.
Thirty-seven per cent of trusts reported that specialty-level mortality data were reviewed by the trust board as part of the organisation’s key performance indicators.
Local investigation and mortality review process
Sixty-nine per cent of responding trusts reported that they routinely reviewed all deaths, in addition to the reviews instigated in response to alerts. The mean proportion of deaths being reviewed at any one time across the sample was 60%, as demonstrated by the histogram in Figure 22.
FIGURE 22.
Histogram of respondent-estimated percentage of deaths reviewed.
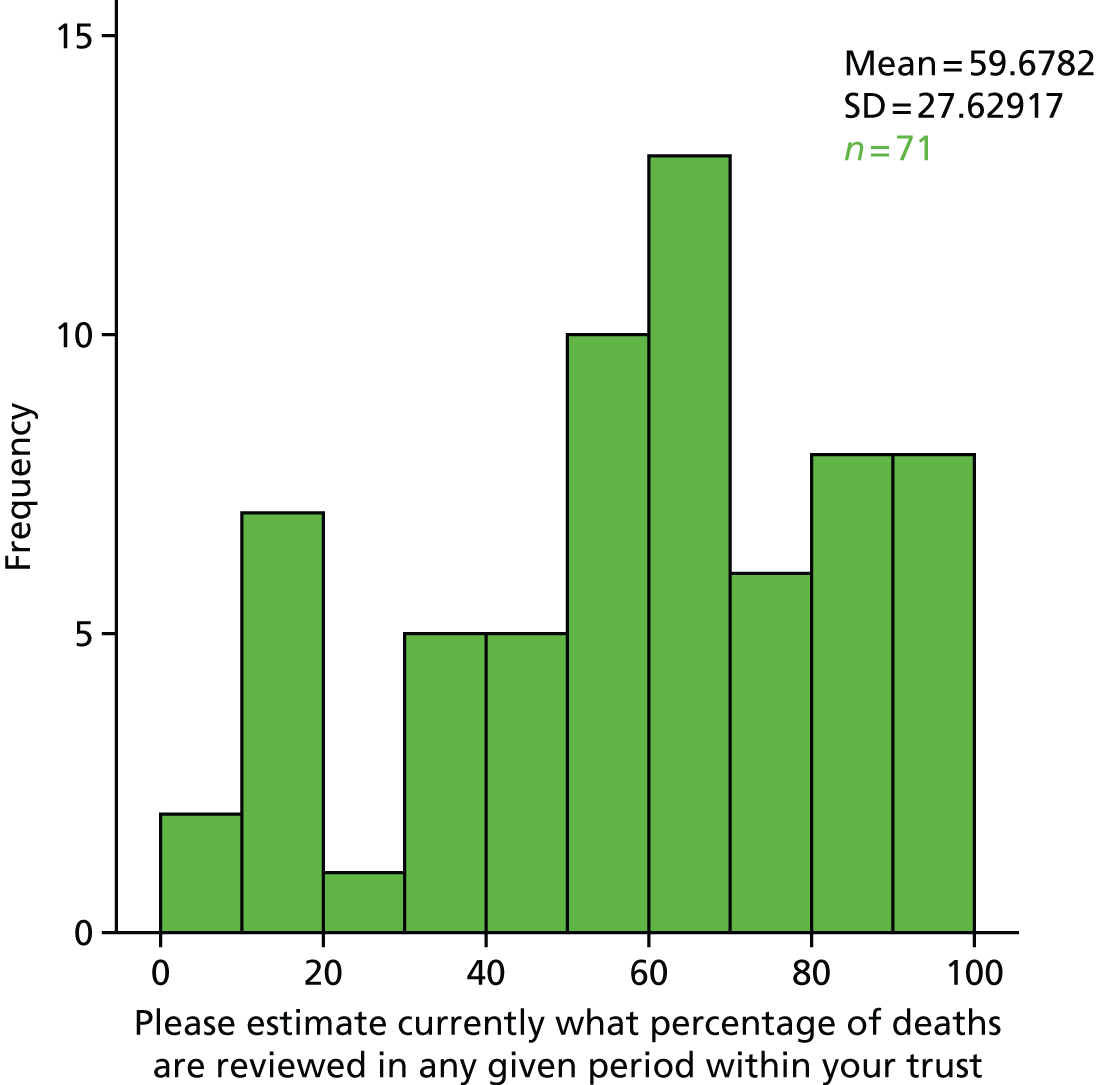
Eighty-five per cent of responding trusts stated that case notes were reviewed by someone independent of those responsible for the care of the patient.
Local investigation and mortality review process (survey sections 4 and 5 free-text analysis)
Trusts tended to use a standardised process for mortality reviews but there was variation in these processes between trusts. A significant number used external methodologies such as NCEPOD’s classificatory system or a variation of PRISM’s methodology.
Following case note reviews, trusts would formally report their results to some form of mortality meeting or group within the trust. These groups tended to be either mortality and morbidity meetings or a mortality committee. A small number would report to patient safety committees.
There was a higher level of variation in how the results of case note reviews were disseminated across the trust. A large number of trusts did this through some form of mortality review group. However, answers varied from disseminating results through global e-mails to newsletters. More descriptive answers to this question involved listing specific groups within the organisation.
When trusts first received a mortality alert there was a degree of inconsistency in the initial action undertaken across trusts. They tended to review the coding or the clinical notes but they also undertook other measures; for example, trusts reported that they either exclusively reviewed coding or did so with a number of other actions.
When a mortality review is undertaken, part of this process is case note review. The relevant specialty lead associated with the alert condition is predominantly the person responsible for the case note reviews when a mortality review is undertaken. A very small number of these are coupled with either clinical coders or the mortality lead at the trust.
Following an alert, a trust will generally develop certain actions in order to address it. The groups largely responsible for ensuring that these actions are put into place are dedicated mortality groups such as a mortality assurance group or mortality review committee. However, for a small number of trusts this was the sole responsibility of the medical director.
Institutional capacity to respond to signals in mortality data
Figure 23 shows the aggregated item responses for ratings of local institutional capacity to respond to signals in mortality data.
FIGURE 23.
Bar chart of aggregated item responses for institutional capacity to respond to signals in mortality data.
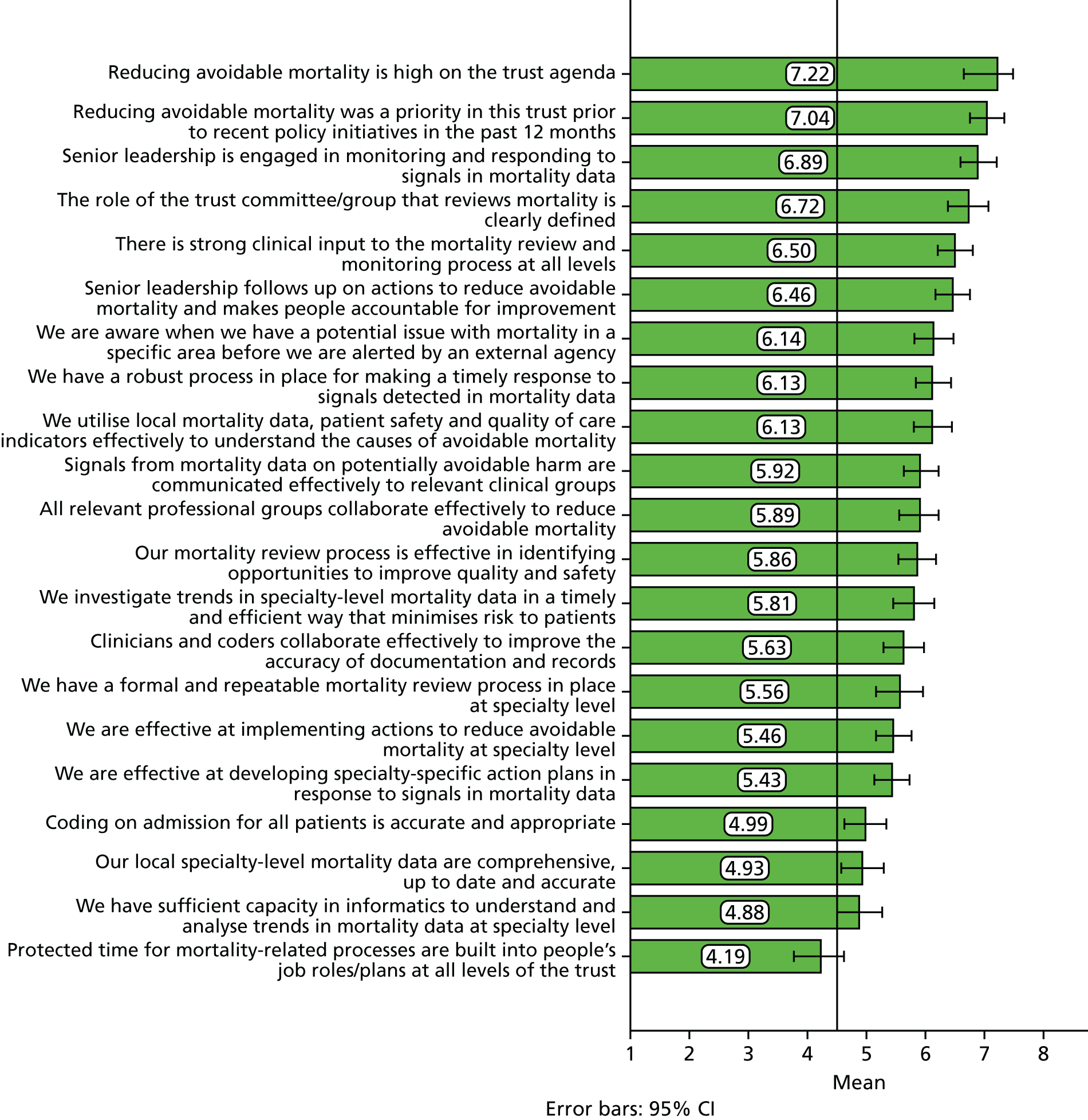
The items with the strongest level of agreement were associated with the organisational culture in terms of mortality having a strong profile and being viewed as a priority across the institution. The item with the lowest level of agreement was related to the extent to which mortality is successfully built into people’s job roles and plans rather than being additional work.
Evaluation of mortality alerts and surveillance
Figure 24 depicts the aggregated responses for items designed to capture evaluative views on the current arrangements for mortality surveillance.
FIGURE 24.
Bar chart of aggregated scale responses for evaluation of mortality alerts and surveillance.
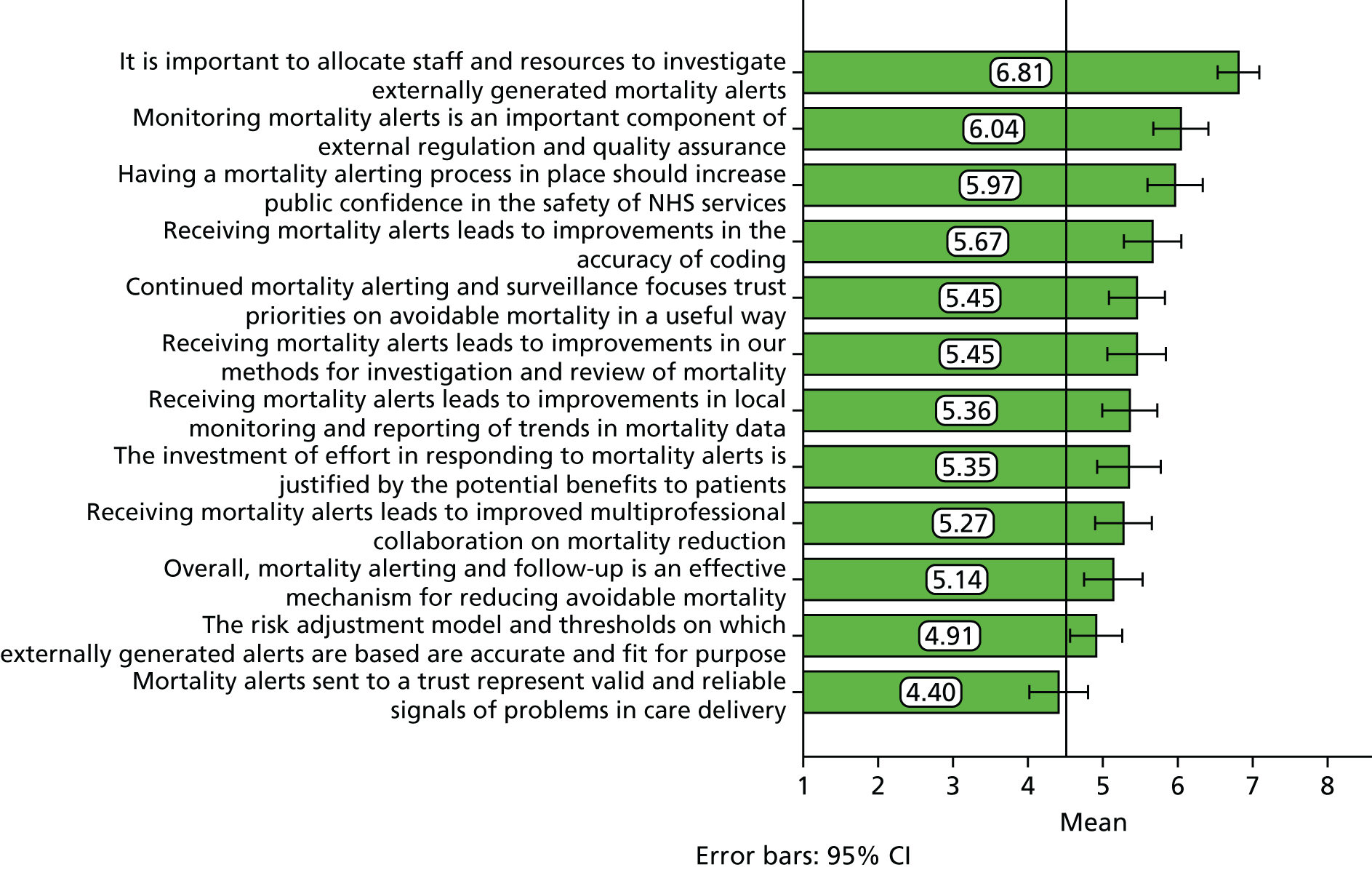
The items with the strongest level of agreement were around the importance of trusts devoting staff and resources to investigating externally generated mortality alerts and the role of monitoring mortality alerts as an important component of quality assurance. The items with the lowest level of agreement were around the accuracy of the risk adjustment model on which the alerts are based and the fact that they represent valid and reliable signals of problems in care delivery.
Figure 25 depicts the aggregated item responses for various barriers to effective reduction in avoidable mortality. Respondents were asked to rate each factor in terms of which were the largest barriers to effective reduction of avoidable mortality in their trust.
FIGURE 25.
Bar chart of aggregated scale responses for barriers to effective reduction of avoidable mortality.
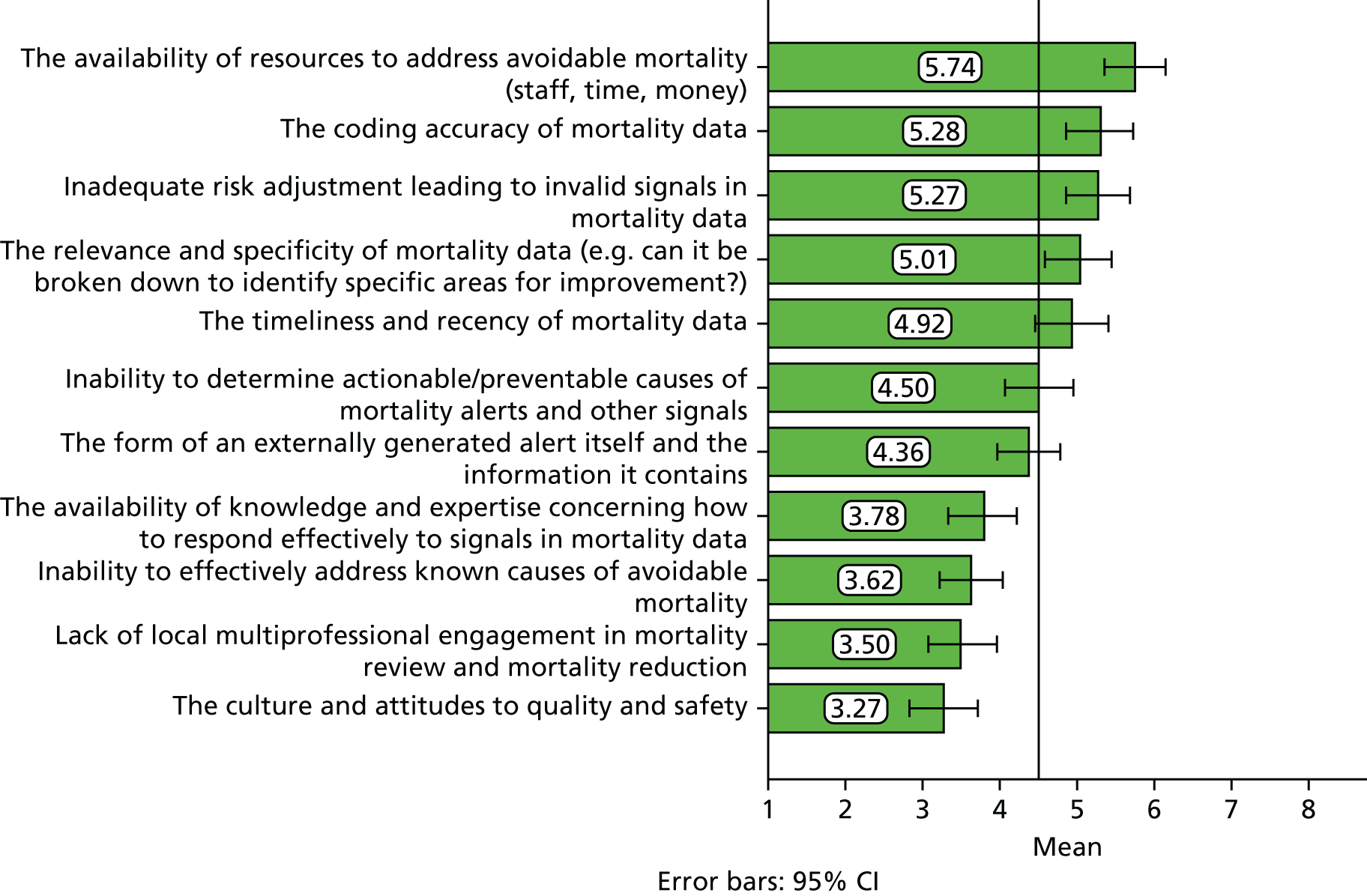
The results demonstrate that the biggest barriers to effective reduction of avoidable mortality are the availability of resources to investigate and take action, the coding accuracy and the risk adjustment that determines the signals in mortality data. The smallest barriers were perceived to be the local multiprofessional engagement and the general culture and attitudes towards quality and safety across the organisation.
Figure 26 depicts the aggregated scale responses elicited in response to the question: ‘How influential are the following in governing the level of priority allocated to investigating and responding to mortality alerts within your trust?’
FIGURE 26.
Bar chart of aggregated scale responses for priority factors for investigating and responding to mortality alerts.
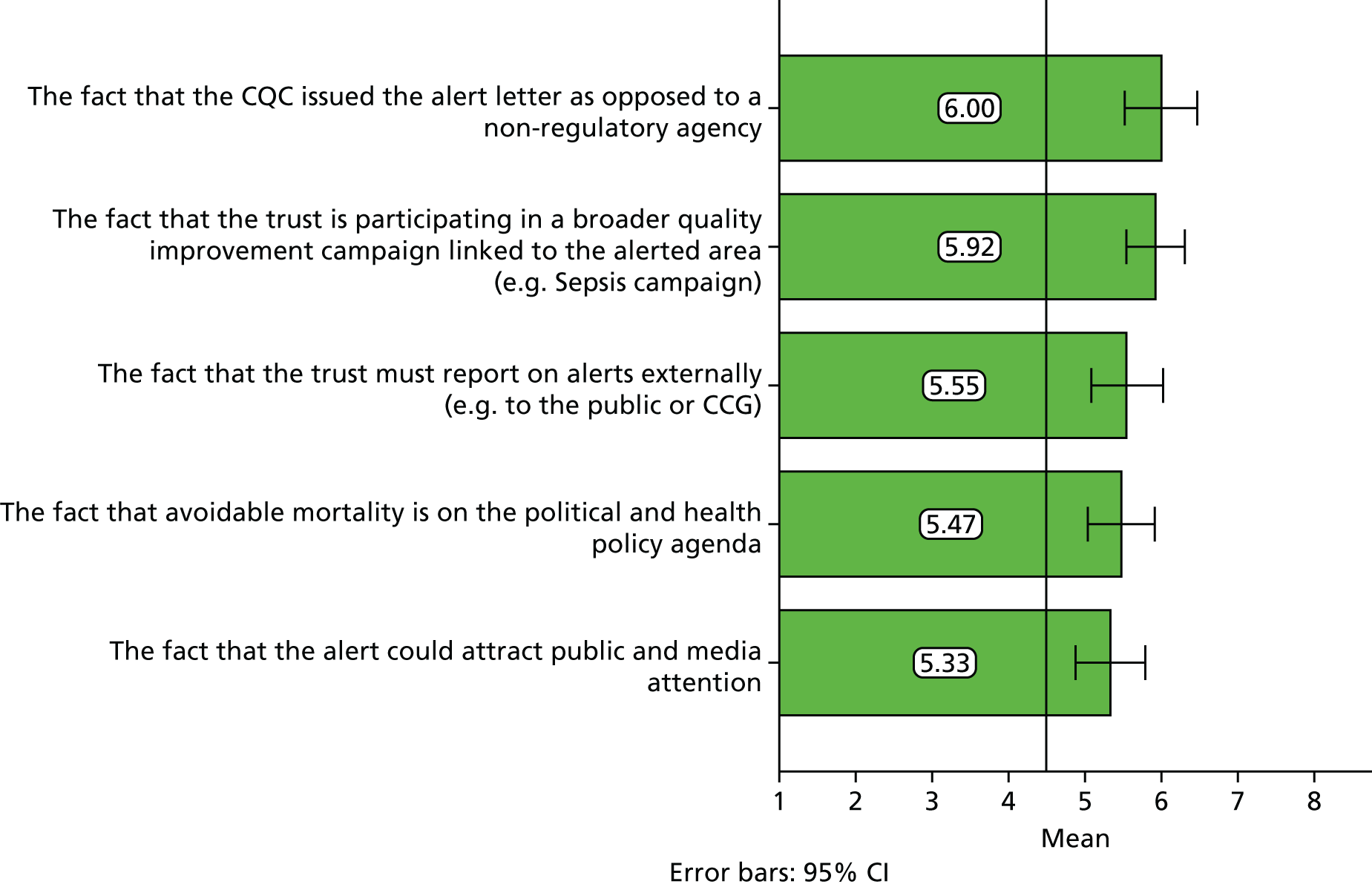
The fact that the CQC issues the alert letters was viewed to be the most influential factor in governing the level of priority allocated to investigating and responding to mortality alerts. It is worth noting, however, that all of the means for these items fall above the mid-point and therefore all factors were perceived to be influential to some extent.
Free-text analysis of survey section 7 items
In reporting the results of the analysis of the free-text responses to the qualitative items in the survey, we provide the following commentary, which describes the range of views expressed and presents examples of actual responses when the researchers considered these to be representative of either commonly held views or important insights.
In your view, what are the most important factors that influence the quality of your trust’s responses to externally-generated mortality alerts?
There was a wide range of responses regarding what were considered the most important factors influencing the trust’s responses to the alerts. These factors were seen as negative or positive influences and were generated by factors related to either the alerting process itself (such as methodological issues of the alerts) or internal factors related to the trust’s internal standards of health care (such as patient safety concerns).
One of the most prevalent responses related to issues regarding time. Trusts viewed the alerts as too retrospective in their ability to provide an indication of what was occurring in the trust due the alert-to-letter time lag. Trusts also viewed the time constraint on responding to the CQC as a factor affecting the quality of response.
Another factor was in the ability of trusts to determine whether or not the alert possessed accurate data. This related to a number of factors, but was primarily due the issue of coding accuracy:
Too many of the alerts, when the case notes are pulled turn out to be coding error. We seem to struggle to correct this, but repeated coding based alerts destroy the credibility of the process.
The factor of coding accuracy was therefore said to undermine the entire process of the alerting system. This related to resource issues around to the quality of coding staff.
Case note reviews were said to have an impact on the quality of the response in terms of data validation:
I think our responses have been thorough and high quality but often there is little to report because case note reviews have demonstrated that deaths identified as being excessive or potentially avoidable by Dr Foster have been confirmed as being expected and unavoidable on case note review.
Alongside the issue of recruiting adequate coding staff, clinical engagement with the process was a factor that influenced the quality of trust responses. If clinicians engaged with the process, there was likely to be a high-quality response:
High-level clinical engagement to external alerts leads to a good out outcome.
The quality of response was also related to the ownership of the alerts.
Alongside issues related to data validity and clinical engagement, an important factor was the trust board and senior clinical leadership.
How effective do you think externally generated mortality alerts are for driving improvement in your trust and why?
Responses varied from ineffective to moderately effective to extremely effective. Many of the responses suggested that the alerts were extremely effective in allowing trusts to review problems that arise with data, and therefore improve data quality. However, there was little to suggest that the alerts spoke to any clinical improvement.
The alerts could be a method of focusing the trust board’s priorities in terms of resources:
Extremely effective – trust exec and board more focussed and more likely to identify/support resources required.
Because the alerts were generated by the CQC and carried its authority, they could also be used to influence the staff within the trust, not just the board and senior clinical staff:
It is useful to some extent. The fact that the alert is issued by CQC provides some weight to it and provides a lever in getting clinicians to discuss the alert and to develop action plans. This is useful as it is an avenue to raise the profile of mortality reviews and quality of care reviews with the alerts can sometimes be less specific and local clinical ownership can be difficult to identify and this makes it difficult to drive improvement as a result of the alert. In addition, alerts are not always caused by a deterioration in quality.
Here we can see an indirect result of the mortality alerting surveillance system’s effects. Owing simply to the authority that is carried by the CQC, the alert can make clinical teams take notice and become more aware of mortality and the required review process.
Although the trusts once viewed the alerts as having significance, the priority that mortality now had meant that they were less effective. They were also seen as a driver for reviews and allowing an interrogation of data. This tended to flag up areas other than a need for clinical improvement. They were also effective at showing the difference in coding and data quality, and mortality improvements can be seen.
What practical changes would increase the value of a mortality monitoring and alerting service to your organisation and the NHS?
Regarding the practical changes that would increase the value of a mortality monitoring and alerting service to the organisation and the NHS, these responses, in the main, related to the alerting process or the data inherent with the alerts. Alongside this, responses suggested that a system owned by the NHS and standardised across the health service would be appropriate and increase its value.
The sensitivity of the system would also increase its value. Coding accuracy and its implications for data validity were again issues, as was the time lag of the alerts. Specific conditions that had an affect related to the alerting system’s insensitivity to paediatric or neonatal mortality.
Data accuracy and validity, again, was important to respondents here and would affect any practical changes.
There were also suggestions about the role of the CQC. These tended to suggest that the CQC induces negative behaviour in the sense of making the responses to the alerts untrue and superficial, with one respondent describing the alert response as ‘a data management beauty pageant’ and ‘that the requirement to report the responses to the CQC is highly counterproductive and induces defensive behaviours’.
One issue that also tended to occur was the insensitivity of the risk-adjusted model. One respondent argued that the poor benchmarking of the risk-adjusted model related to a non-standardised system within the NHS:
If the monitoring/alerting system was NHS funded would save money and ensure all trusts are using the same risk adjustment model for data comparison. Increase in patient safety (non-mortality) alerts.
The idea of a national standardised alerting system was an important point raised by the respondents, for example sharing the quality of trusts’ use of the system and creating a national system of best practice responses to alerts. The use of mortality was seen as needing to change as it was viewed as too narrow an indicator of quality.
Additional comments
Respondents were invited to provide any additional comments to their responses. These varied to a degree and explored points made throughout the survey in more detail.
One issue that was raised constantly was the retrospective character of the alert; this appeared to be a very important weakness of the system, and one respondent explained the issue in detail:
The alerts are helpful and informative but do not accurately reflect the mortality data at the time of the alert. Therefore, once the reviews have been submitted the frequent follow-ups regarding cases which are often two years’ old result in a delay in dealing with current issues as we have very small teams. For example, our current HSMR for COPD is 99 but I am still receiving multiple queries regarding the alert for COPD which referred to 2014. It would also be helpful for some context in terms of type of organisation. For example, we are an integrated trust with 4 community hospitals in addition to a district general hospital. Often as a result of lack of availability of social care, elderly patients spend several months in a community hospital and may die within of 30 days of discharge from a condition entirely unrelated to their initial admission. This adversely affects SHMI.
This issue also reflected issues of the wider health economy and the problems associated with the risk-adjusted model.
There appeared to be too much emphasis on the alerts as a self-contained system that did not warrant the specificity of responding to the CQC based on their data as indicated by the perceived flaws of the risk-adjusted model. In addition to this overemphasis on the alerts, respondents claimed that there were factors that related to the priority of mortality, such as the Keogh Review:
As a Keogh trust we have done a great deal of work to ensure our mortality data is accurate and timely. We monitor mortality by diagnostic group and assign a lead clinician to formulate an action plan if a diagnostic group is alerting or if the lower confidence interval is greater than 90. In this way we have a number of diagnostic groups with specific action plans which are monitored monthly until the alert is no longer generated and lower confidence interval is below 90. Many of these reviews have resulted in specific quality improvement projects or formulation of specific care bundles.
This response illustrated the wider picture of mortality review process including where that alert fitted into the processes it generated, and could be said to show the importance to the mortality review processes of trusts of spending time and making sure that data are accurate and timely.
The comments of this section also highlighted issues of coding accuracy:
Numerous investigations into alerts in cerebrovascular and leukaemia deaths in three trusts have led me to the conclusion that these codes are not fit for use. Which in turn leads me to not be as concerned if one of these is alerting though we still investigate.
This respondent is illustrating the problem of inaccurate coding data, and how this would lead to a false positive and a potential misallocation of resources when investigating an alert.
Other comments were not as detailed as this, but they referenced the time-consuming process of reviewing deaths and the iterative and evolutionary character of mortality review process improvements at trusts.
Development of aggregated scales and subscales
Institutional capacity to respond to signals in mortality data
The Cronbach’s alpha for all individual items in section 6 of the survey was 0.907. The mean value for the aggregated scale representing institutional capacity to respond to signals in mortality data was 5.96, which indicates a relatively high level of capacity based on our evaluative framework (Table 19).
| Dimension of the evaluative framework | Items from the survey that were combined to form the subscale | Reliability checks |
|---|---|---|
| Organisational structure for mortality governance | 6.1 The role of the trust committee/group that reviews mortality is clearly defined | Cronbach’s alpha = 0.032 |
| 6.14 Protected time for mortality-related processes are built into people’s job roles/plans at all levels of the trust | Correlation = 0.017 | |
| Coding | 6.2 Coding on admission for all patients is accurate and appropriate | This subscale has only one item |
| Use of information, monitoring and reporting | 6.3 We have sufficient capacity in informatics to understand and analyse trends in mortality data at specialty level | Cronbach’s alpha = 0.683 |
| 6.4 Our local specialty-level mortality data are comprehensive, up to date and accurate | ||
| 6.5 We are aware when we have a potential issue with mortality in a specific area before we are alerted by an external agency | ||
| 6.6 We utilise local mortality data, patient safety and quality of care indicators effectively to understand the causes of avoidable mortality | ||
| 6.13 Signals from mortality data on potentially avoidable harm are communicated effectively to relevant clinical groups | ||
| Local investigation and mortality review process | 6.7 We investigate trends in specialty-level mortality data in a timely and efficient way that minimises risk to patients | Cronbach’s alpha = 0.714 |
| 6.8 We have a formal and repeatable mortality review process in place at specialty level | ||
| 6.9 Our mortality review process is effective in identifying opportunities to improve quality and safety | ||
| Local improvement mechanisms | 6.10 We have a robust process in place for making a timely response to signals detected in mortality data | Cronbach’s alpha = 0.795 |
| 6.11 We are effective at developing specialty-specific action plans in response to signals in mortality data | ||
| 6.12 We are effective at implementing actions to reduce avoidable mortality at specialty level | ||
| Senior leadership and sponsorship | 6.15 Senior leadership is engaged in monitoring and responding to signals in mortality data | Cronbach’s alpha = 0.899 |
| 6.16 Senior leadership follows up on actions to reduce avoidable mortality and makes people accountable for improvement | ||
| 6.17 Reducing avoidable mortality is high on the trust agenda | ||
| 6.18 Reducing avoidable mortality was a priority in this trust before recent policy initiatives in the last twelve months | ||
| Interprofessional collaboration | 6.19 All relevant professional groups collaborate effectively to reduce avoidable mortality | Cronbach’s alpha = 0.696 |
| 6.20 There is strong clinical input to the mortality review and monitoring process at all levels | ||
| 6.21 Clinicians and coders collaborate effectively to improve the accuracy of documentation and records |
Figure 27 depicts the frequencies of scale scores for the overall institutional capacity to respond to signals in mortality data.
FIGURE 27.
Frequency histogram of scale scores for institutional capacity to respond to signals in mortality data.
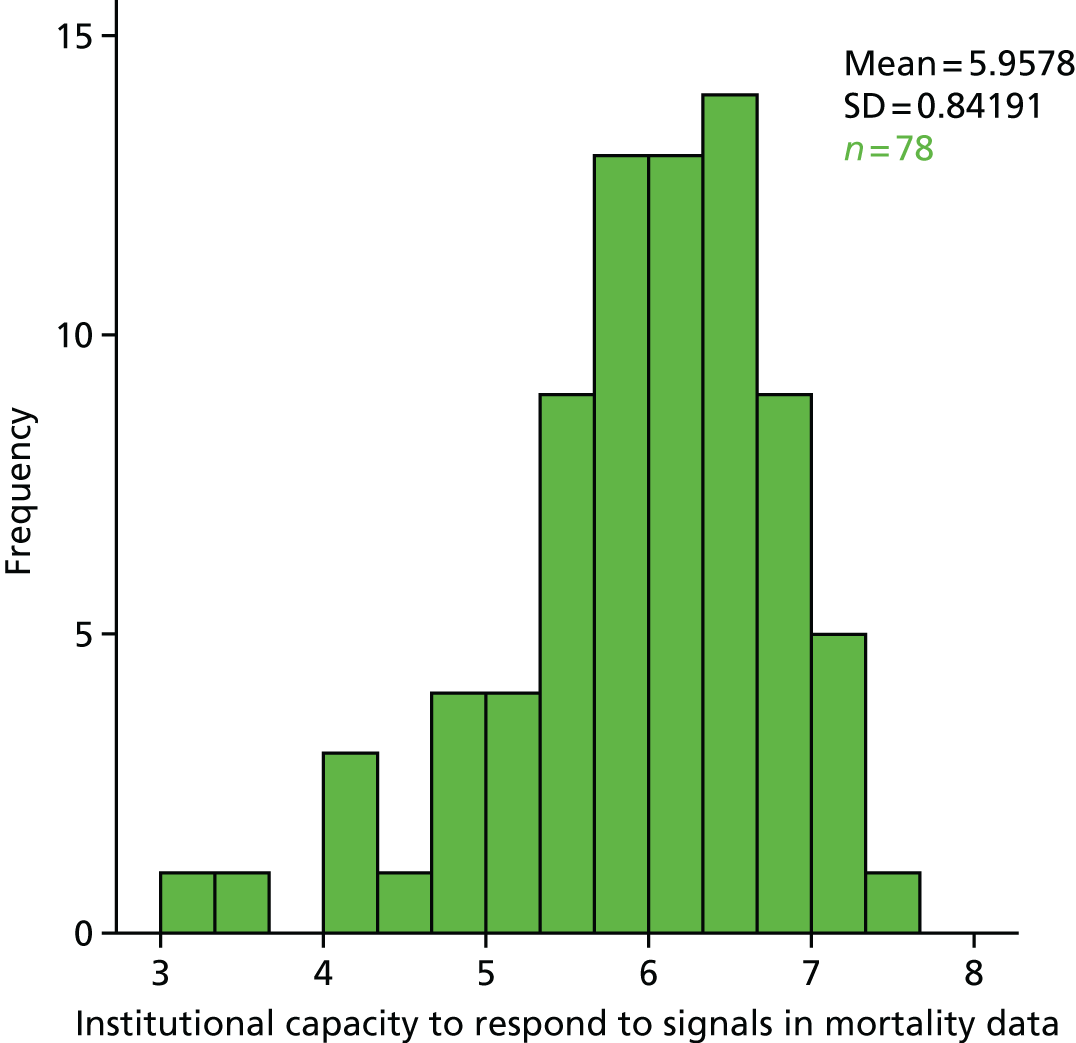
Evaluation of mortality alerts and surveillance
The Cronbach’s alpha for items 1–12 in section 7 of the survey was 0.937. The mean value for the aggregated scale representing the evaluation of mortality alerts and surveillance was 5.48, which overall indicates positive agreement.
Figure 28 depicts the frequencies of scale scores for the overall evaluation of the current MASS.
FIGURE 28.
Frequency histogram of scale scores for overall evaluation of mortality alerts and surveillance system.
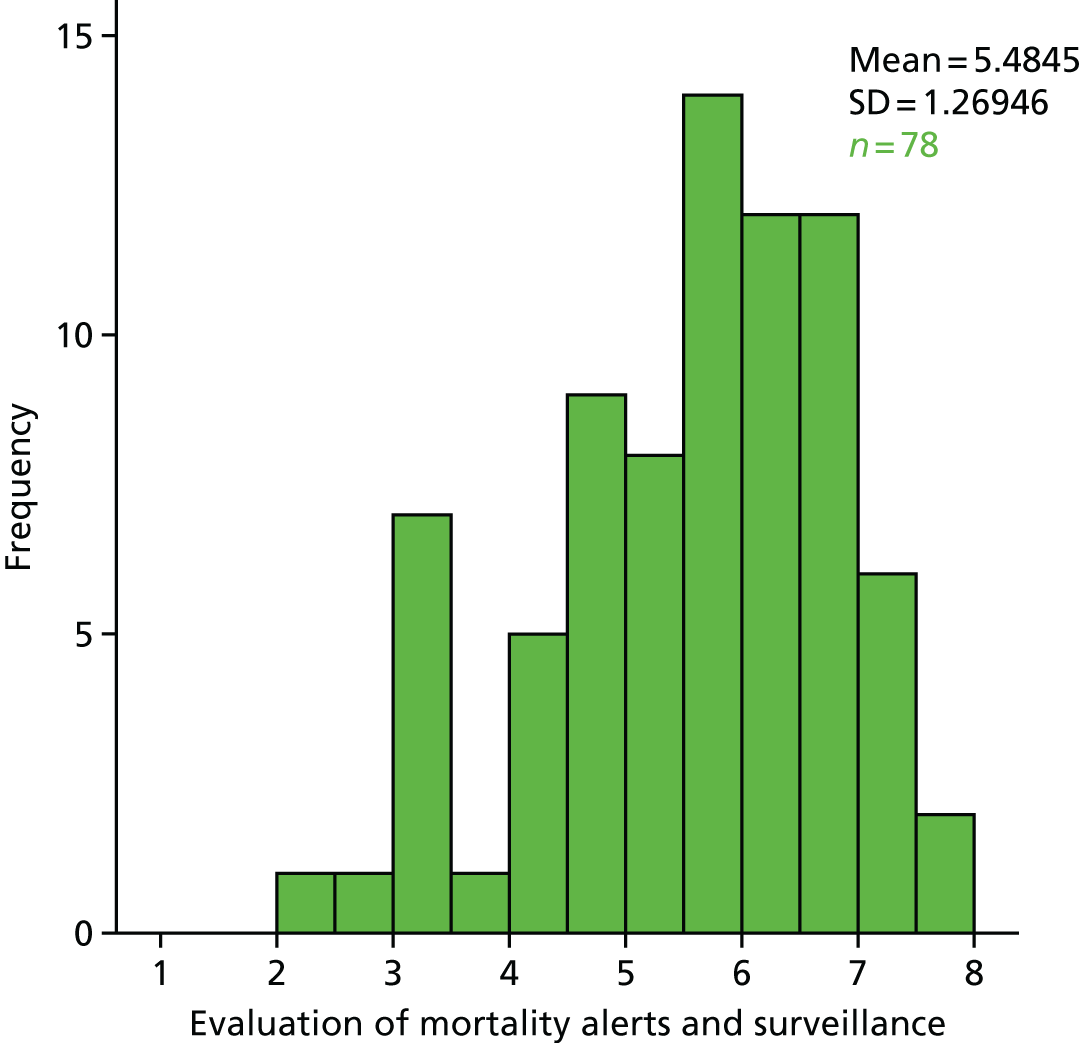
Figure 29 depicts the frequency of specific scale scores for organisational structure for mortality governance. The mean value for the aggregated subscale representing organisational structure for mortality governance was 5.46.
FIGURE 29.
Frequency histogram of scale scores for organisational structure for mortality governance dimension.
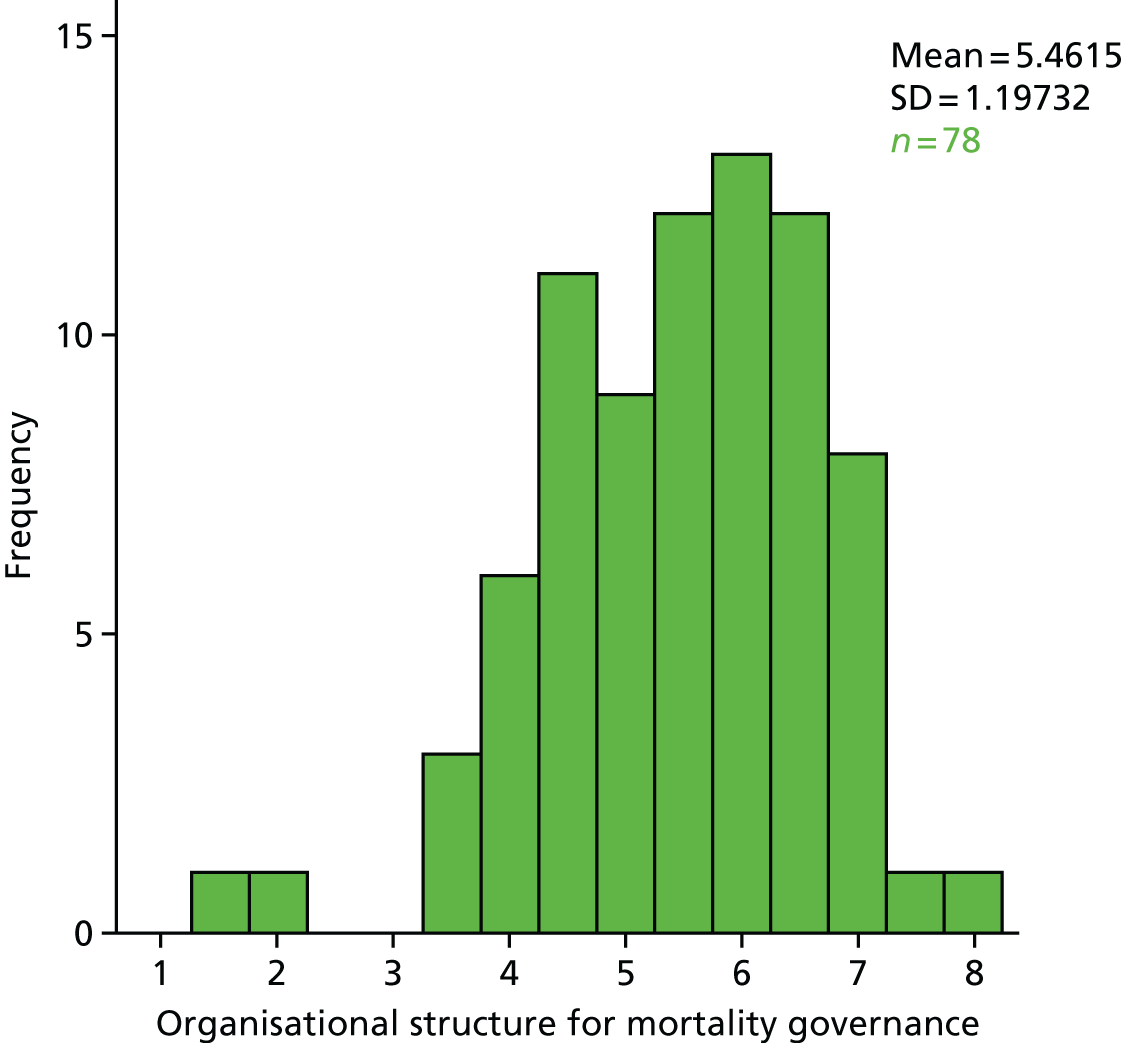
Figure 30 depicts the frequency of individual scale scores for the coding dimension of the evaluative framework for institutional capability to respond to signals in mortality data. The mean value for the individual item representing coding was 5.04.
FIGURE 30.
Frequency histogram of scale scores for coding dimension.
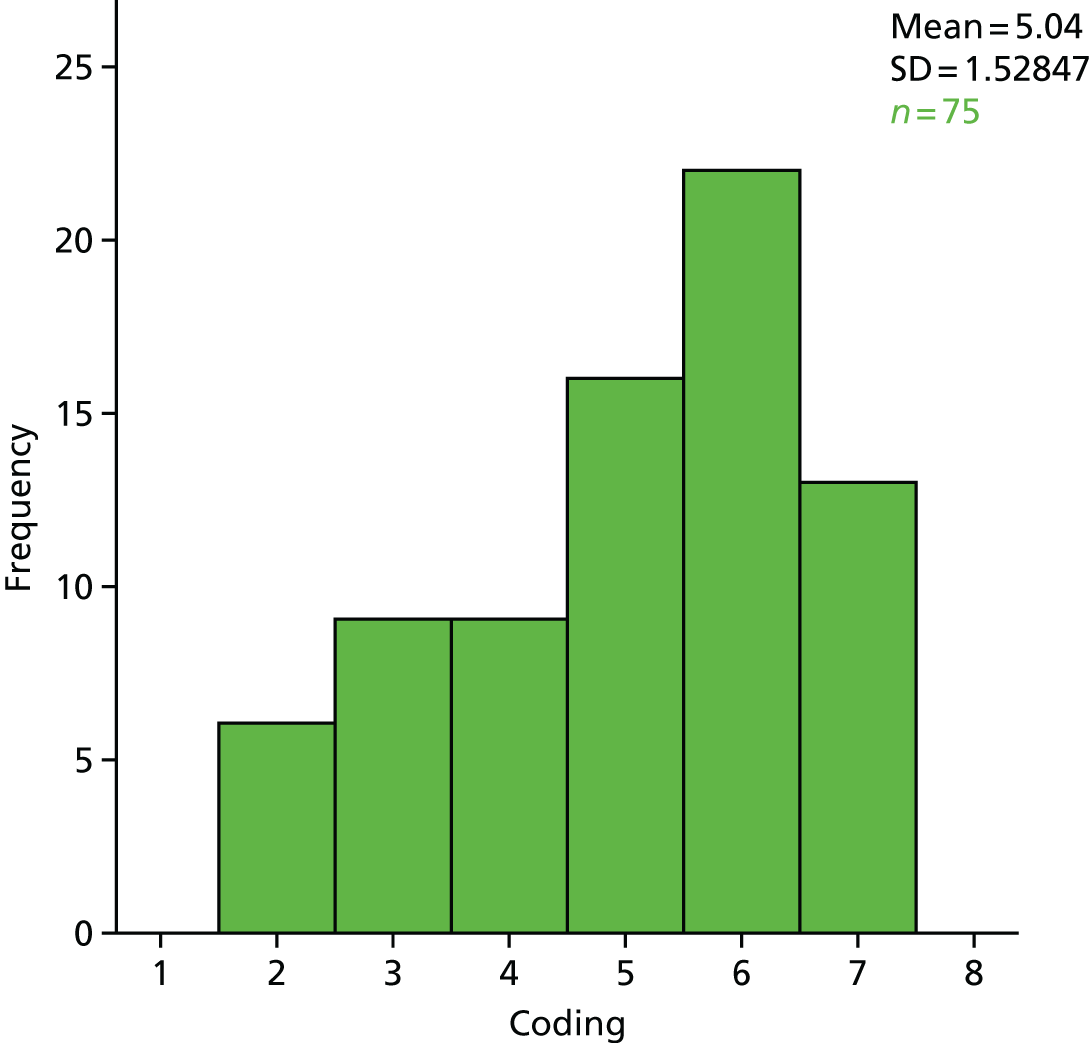
Figure 31 depicts the frequency of individual scale scores for the use of information, monitoring and reporting dimension of the evaluative framework for institutional capability to respond to signals in mortality data. The mean value for the aggregated subscale representing use of information, monitoring and reporting was 5.71.
FIGURE 31.
Frequency histogram of scale scores for use of information, monitoring and reporting dimension.
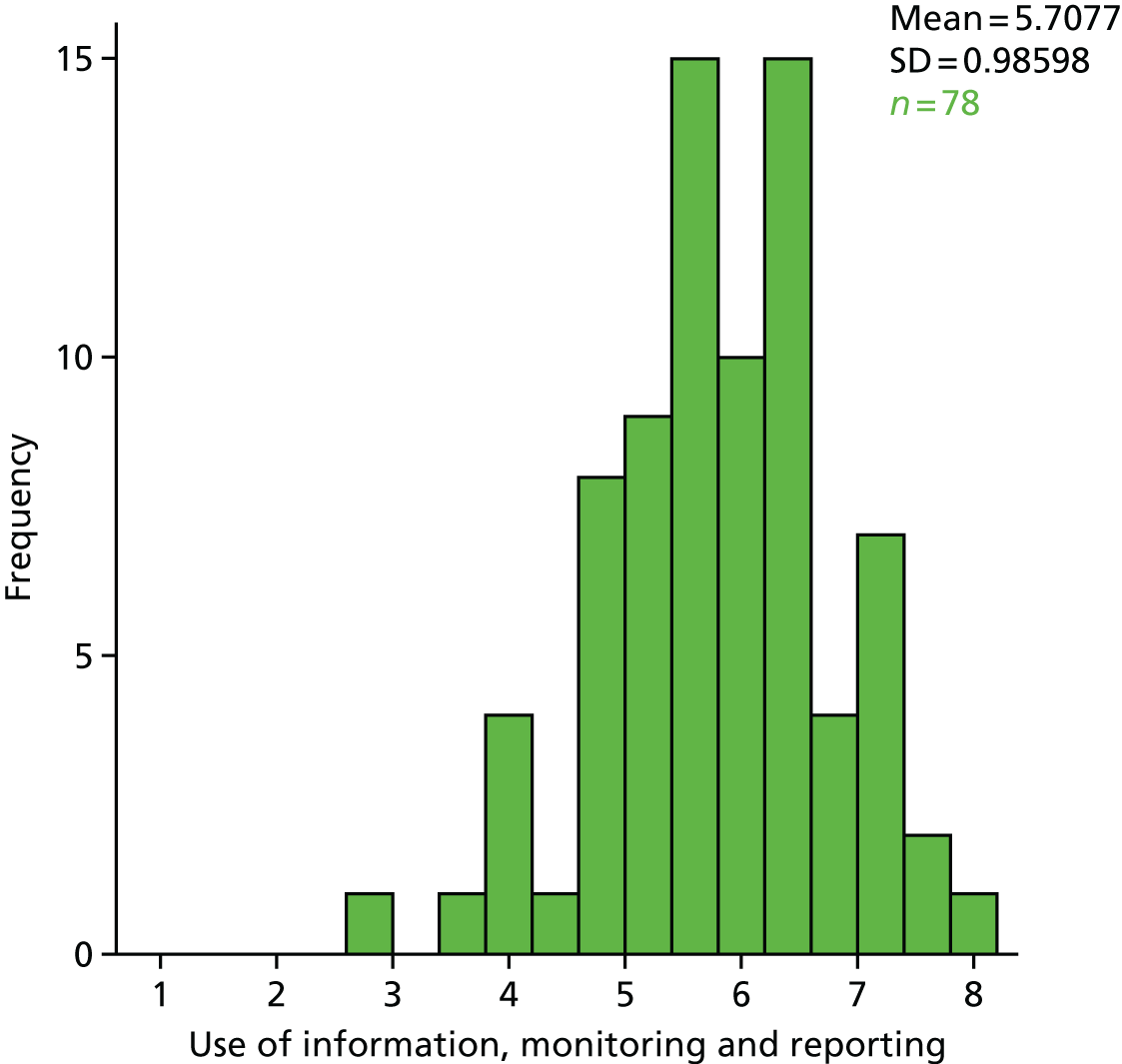
Figure 32 depicts the frequency of individual scale scores for the local investigation and mortality review process dimension of the evaluative framework for institutional capability to respond to signals in mortality data. The mean value for the aggregated subscale representing local investigation and mortality review process was 5.82.
FIGURE 32.
Frequency histogram of scale scores for local investigation and mortality review process dimension.
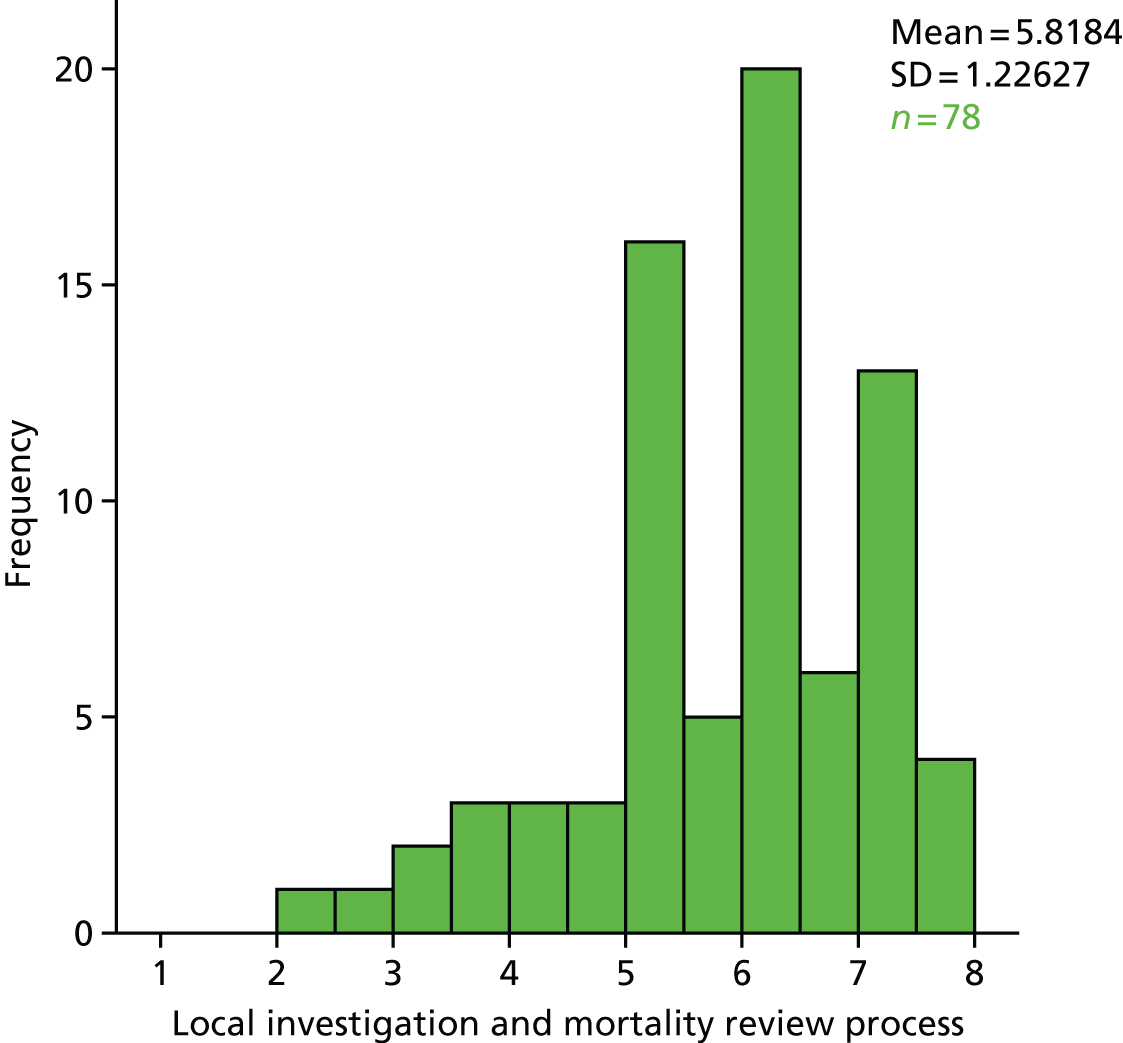
Figure 33 depicts the frequency of individual scale scores for the local improvement mechanisms dimension of the evaluative framework for institutional capability to respond to signals in mortality data. The mean value for the aggregated subscale representing local improvement mechanisms was 5.71.
FIGURE 33.
Frequency histogram of scale scores for local improvement mechanisms dimension.
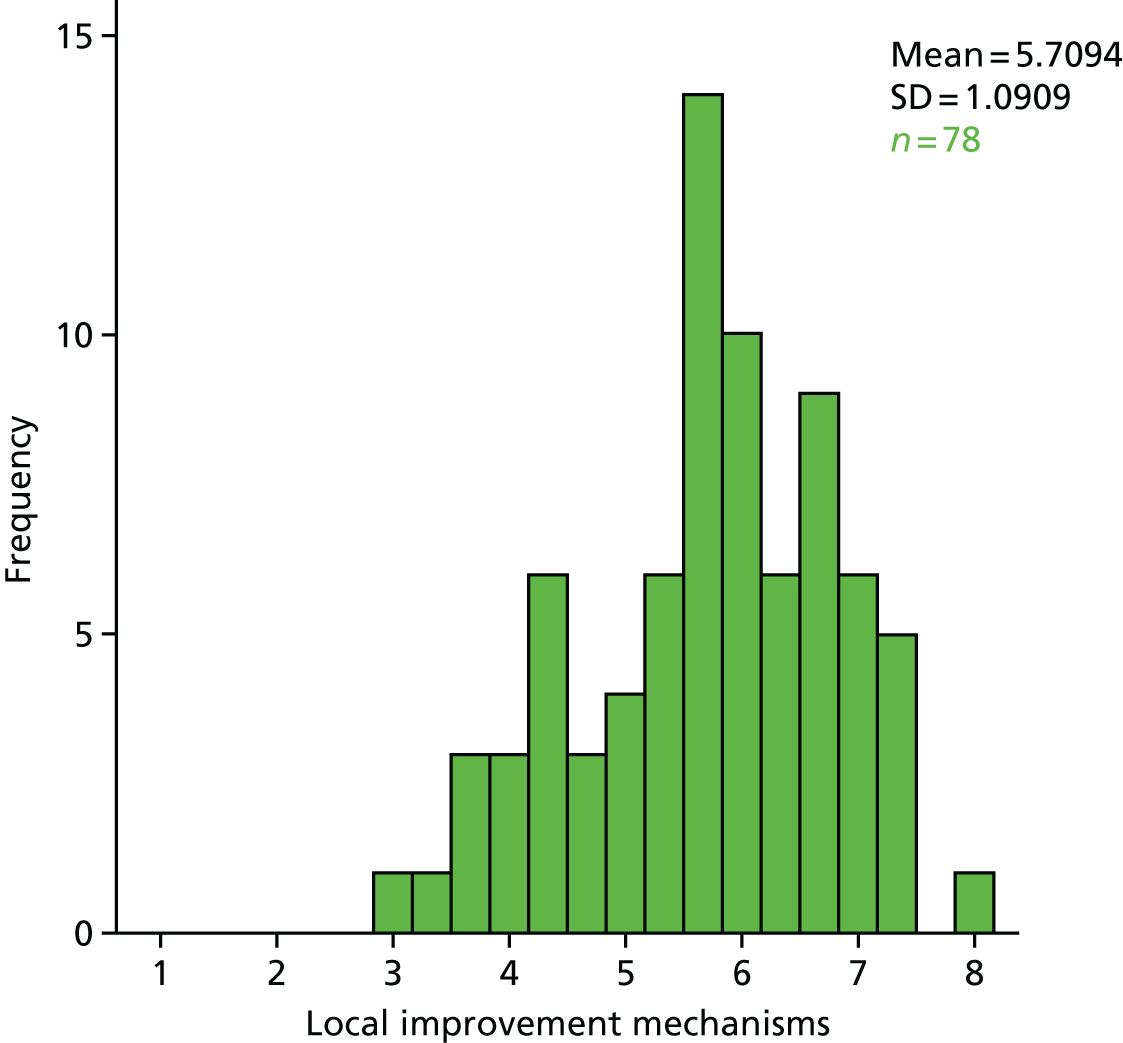
Figure 34 depicts the frequency of individual scale scores for the senior leadership and sponsorship dimension of the evaluative framework for institutional capability to respond to signals in mortality data. The mean value for the aggregated subscale representing senior leadership and sponsorship was 6.96.
FIGURE 34.
Frequency histogram of scale scores for senior leadership and sponsorship dimension.
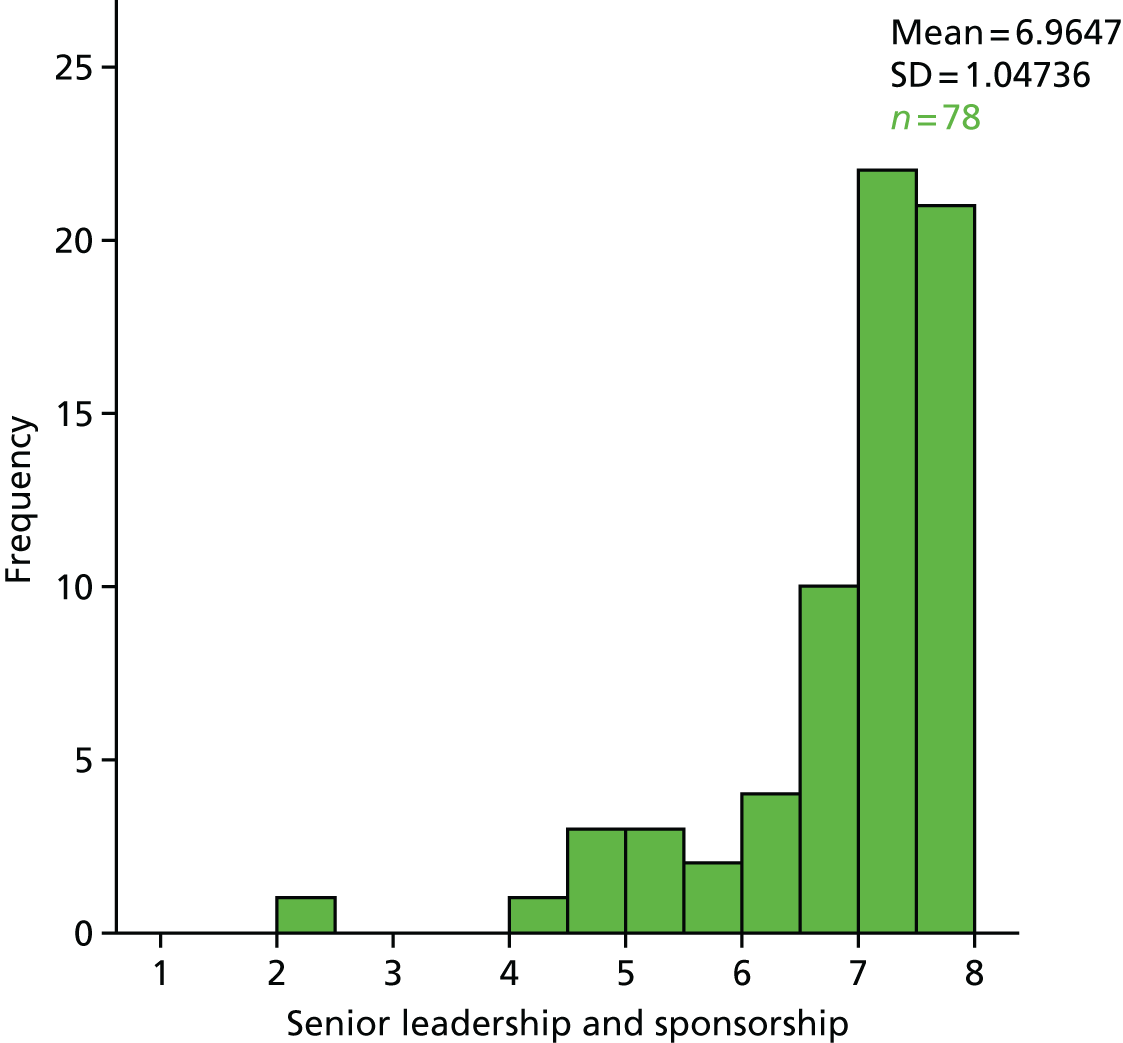
Figure 35 depicts the frequency of individual scale scores for the inter-professional collaboration dimension of the evaluative framework for institutional capability to respond to signals in mortality data. The mean value for the aggregated subscale representing interprofessional collaboration was 4.15.
FIGURE 35.
Frequency histogram of scale scores for inter-professional collaboration dimension.
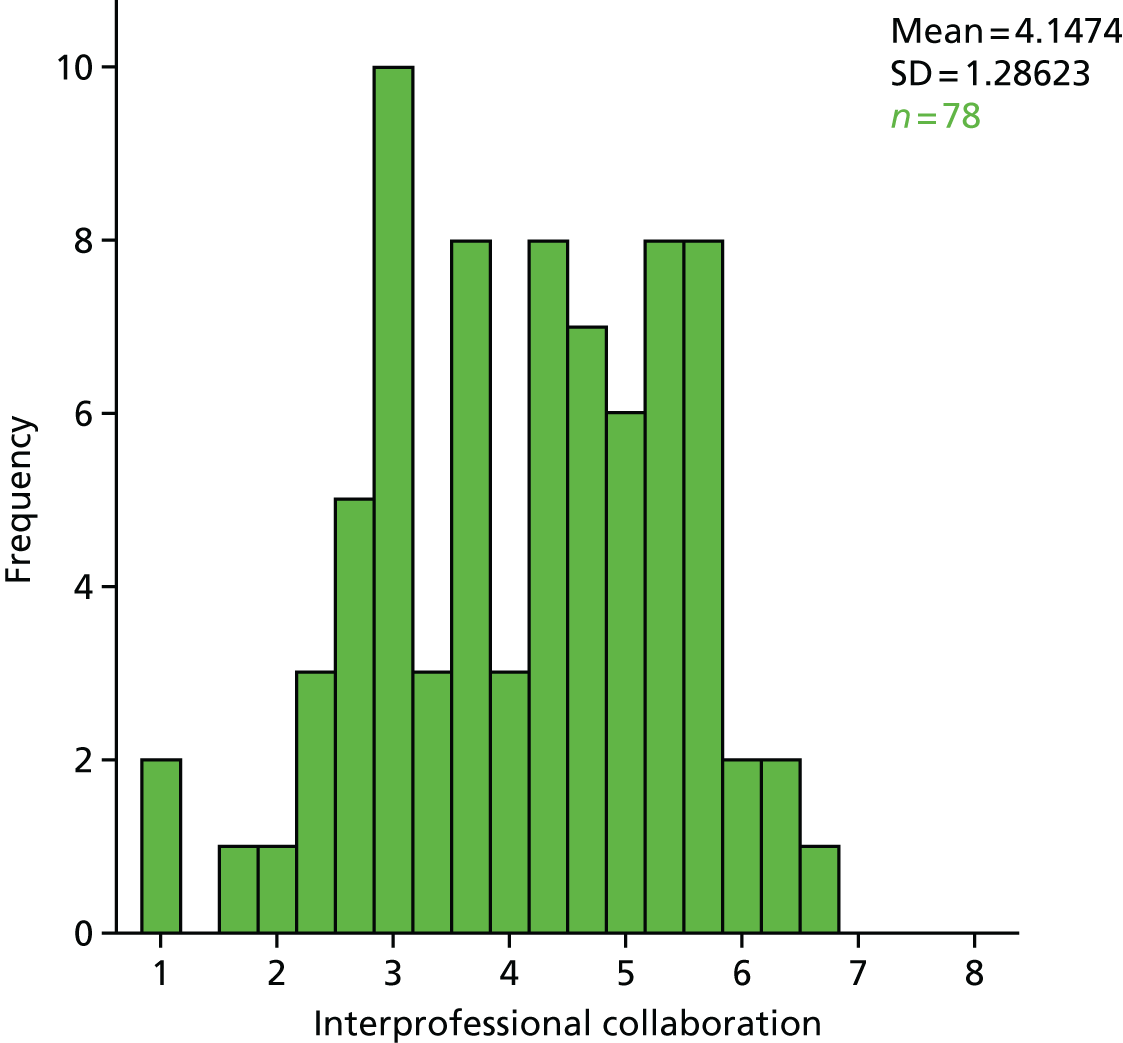
Inferential analysis
Research question: to explore the relationships between type and frequency of alerting, key contextual and organisational behavioural characteristics and intermediate outcomes.
t-tests were run to explore the differences in institutional capability (section 6 aggregated scale) between various groups.
Trust-type differences
No significant difference was found between large and small trusts.
No significant difference was found between teaching and non-teaching trusts.
Is there a dedicated trust-level lead for mortality reduction in your trust?
No significant difference was found between trusts that did and trusts that did not have a trust-level lead for mortality reduction.
Are there specific mortality leads appointed in the following areas in your trust?
No significant difference was found between trusts that did and trusts that did not have specific mortality leads appointed at the individual division level.
No significant difference was found between trusts that did and trusts that did not have specific mortality leads appointed at the clinical directorate level.
No significant difference was found between trusts that did and trusts that did not have specific mortality leads appointed at the clinical specialty level.
Does your trust have a dedicated trust-level mortality group or committee in place currently?
No significant difference was found between trusts that did and did not have a dedicated trust-level mortality group or committee in place currently.
Does the mortality group report to the trust board?
No significant difference was found between trusts that did and did not have a mortality group that reported directly to the trust board.
Are specialty-level mortality data reviewed by the trust board as part of the organisation’s key performance indicators?
There is a significant difference between trusts that reported that specialty-level mortality data are reviewed by the trust board as part of the organisation’s key performance indicators [t(74) = 2.65, p = 0.01]. Trusts in which specialty-level mortality data are reviewed by the trust board reported significantly higher institutional capacity to respond to signals in mortality data (mean 6.28, SD 0.67) than those in which they are not (mean 5.77, SD 0.88). Figure 36 compares the mean institutional capacity to respond to signals in mortality data between trusts that report the review of specialty-level mortality data as part of key performance indicators and trusts that do not.
FIGURE 36.
Bar chart showing rated institutional capacity by presence of specialty-level trust board mortality data review.
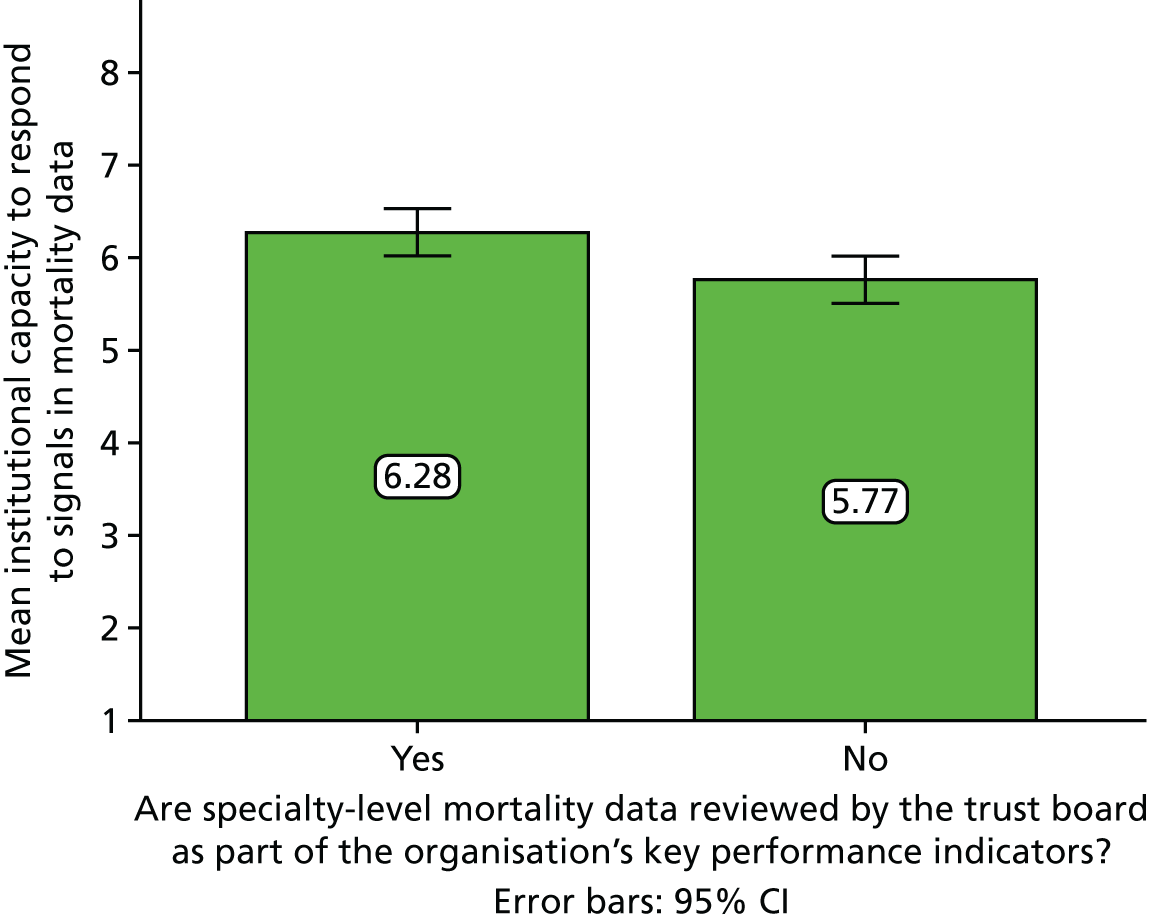
Are case notes reviewed by someone independent of those responsible for the care of the patient?
No significant difference was found between trusts that did and trusts that did not report that case notes are reviewed by someone independent of those responsible for the care of the patient.
How are reviews of death instigated in your trust?
No significant difference was found between trusts that review deaths in response to both external alerts and alerts from their internal systems and trusts that routinely review all deaths in addition to carrying out reviews in response to alerts.
Correlations between internal survey metrics
Correlations were run to explore the internal validity of our survey metrics by looking at the relationship between various scale items. The findings demonstrate the following significant correlations.
-
A positive correlation between the length of time that the mortality group has been in place and the length of time that the trust lead for mortality has been in post (R = 0.439; p < 0.0001).
-
A positive correlation between the length of time that the current arrangements for mortality have been in place and the length of time that the mortality group has been in place (R = 0.367; p = 0.002).
-
A positive correlation between the percentage of deaths that are reviewed in any given period and the percentage of specialties in the trust that reliably review all deaths (R = 0.684; p ≤ 0.0001).
-
A positive correlation between institutional capacity to respond to signals in mortality data and the length of time that the current arrangements for mortality have been in place (R = 0.237; p = 0.048).
-
A positive correlation between institutional capacity to respond to signals in mortality data and the percentage of specialties in the trust that reliably review all deaths (R = 0.345; p = 0.046).
-
A positive correlation between institutional capacity to respond to signals in mortality data and the percentage of deaths that are reviewed in any given period (R = 0.406; p < 0.0001).
-
A positive correlation between institutional capacity to respond to signals in mortality data and evaluation of mortality alerts and surveillance (R = 0.307; p = 0.006).
-
A positive correlation between the use of information, monitoring and reporting subscale and the length of time that the current arrangements for mortality have been in place (R = 0.270; p = 0.024).
-
A positive correlation between the local investigation and mortality review process subscale and the percentage of specialties in the trust that reliably review all deaths (R = 0.427; p = 0.012).
-
A positive correlation between the local investigation and mortality review process subscale and the percentage of deaths that are reviewed in any given period (R = 0.491; p < 0.0001).
-
A positive correlation between the local investigation and mortality review process subscale and the length of time that the current arrangements for mortality have been in place (R = 0.258; p = 0.031).
-
A positive correlation between the local investigation and mortality review process sub-scale and the length of time that the current arrangements for mortality have been in place (R = 0.258; p = 0.031).
-
A positive correlation between the local improvement mechanisms subscale and the percentage of specialties in the trust that reliably review all deaths (R = 0.372; p = 0.030).
-
A positive correlation between the local improvement mechanisms subscale and the percentage of deaths that are reviewed in any given period (R = 0.305; p = 0.010).
-
A positive correlation between the local improvement mechanisms subscale and the percentage of deaths that are reviewed in any given period (R = 0.305; p = 0.010).
-
A positive correlation between the senior leadership and sponsorship subscale and the percentage of deaths that are reviewed in any given period (R = 0.300; p = 0.011).
-
A negative correlation between the interprofessional collaboration subscale and the percentage of specialties in the trust that reliably review all deaths (R = –0.344; p = 0.047).
-
A negative correlation between the interprofessional collaboration subscale and the percentage of deaths that are reviewed in any given period (R = –0.238; p = 0.046).
-
A positive correlation between the coding subscale and the length of time that the mortality group has been in place (R = 0.349; p = 0.003).
Correlations between survey and external metrics
-
These correlations explore the relationship between organisational response and measures of mortality including numbers of alerts.
-
A negative correlation between the use of information, monitoring and reporting subscale and the CQC total length of investigation time (R = –0.327; p = 0.018).
-
A negative correlation between the use of information, monitoring and reporting subscale and HSMR (R = –0.246; p = 0.031).
Chapter 9 Discussion
In this chapter we summarise the main results (see Key findings), discuss the findings in relation to previous studies and consider the strengths and limitations to our analyses within each workstream.
Workstream 1
Key findings
Between April 2007 and December 2014, 690 alerts were generated by the Imperial College mortality surveillance system, 532 of which (77%) were sent to trusts. The numbers of annual mortality alerts have been falling since the beginning of the surveillance programme. Sepsis accounted for 11.5% (61/532) and AMI for 3.4% (18/532) of all alerts. The CQC pursued 75% (154/206) of mortality alerts from Imperial College letters sent between 2011 and 2013. CQC investigations found issues relating to coding, case mix and quality of care within the trust. Care was cited as a factor in 70% (108/154) of all investigations but was particularly an issue in sepsis alerts [89% (17/19)]; for all patient groups combined, care was considered by the trusts themselves to have contributed to elevated mortality in 27% (42/154) of alerts. CQC investigations resulted in action plans in 77% (118/154) of pursued cases. The majority of trusts appeared to have made some changes to their data after a sepsis or an AMI alert.
Mortality alerts were associated with other indicators of quality, including structure and outcome measures. Acute bed occupancy and all hospital mortality were higher in hospitals that had a mortality alert, while nurse-to-bed ratio, patient and trainee satisfaction were lower. Alerting trusts were more likely to be in deficit than non-alerting trusts.
On average, the risk of death fell by 36% in the month following an alert and then declined more slowly, reaching the level of expected risk within 18 months of the alert.
Findings in relation to other studies
Monitoring health-care performance is a complicated, and potentially expensive, procedure, so it is important to assess whether or not the monitoring is effective in improving performance. However, it is also important to ensure that there are no unintended consequences of monitoring. There are plenty of examples of evaluations of accreditations within health-care providers that mainly focus on care processes. 146 However, there are few studies that investigate the monitoring of a surveillance programme, and the information held within these reports is limited. 36–38 The evaluation of the Imperial College mortality alerting system is the first in-depth analysis of a national hospital mortality alerting system, and it provides a description of the system that has been operating since 2007.
Our investigation of mortality alerts and other measures of quality found that mortality alerts were strongly associated with nurse-to-bed ratio. A link between hospital nurse staffing and patient mortality has previously been reported. 147 The association of nurse-to-bed ratio and sepsis mortality alerts was particularly strong. Understandably, the higher the nurse-to-bed ratio, the more time a nurse has to assess their patients for the early identification and treatment of sepsis. 148 Interestingly, this finding is consistent with our descriptive analysis of CQC investigations into the Imperial College mortality alerts (objective 1), where care was cited by the trust as an issue in a statistically significantly higher proportion of sepsis alerts (89%) than of all other alerts (70%). Overcrowding and understaffing have been described as important determinants in MRSA transmission. 149 The association between bed occupancy and mortality has also been previously reported. 48 Studies investigating the relationship between patient satisfaction and mortality are mixed. Fenton et al. 150 found that there was a higher mortality rate in more satisfied patients. However, this is an American study and its results are difficult to generalise to the UK setting.
Strengths and limitations
Our mixed-method research, carried out by an experienced team of researchers, is of interest to patients, health professionals and policy-makers. Our methodology combines elements of qualitative and quantitative research approaches that provide a wide understanding and corroboration of findings. 151 We applied a quasi-experimental time series study design. This strong statistical approach has been verified against randomised controlled trails with comparative findings. 144 However, there are also some limitations to our study that need to be highlighted.
Descriptive analysis of the Imperial College mortality alerts
Our analysis found that there has been a fall in the number of mortality alerts over the study period; however, there has been a corresponding fall in national mortality rates. 152,153 This in itself would not lead to a reduction in the number of alerts, as they take into account national trends, but the reduction in number might reflect a reduction in variation between hospital trusts.
Analysis of Care Quality Commission investigations into the Imperial College mortality alerts
The CQC’s purpose is to maintain and improve standards of care in NHS trusts and it uses the mortality alerting system as part of its risk assessment profiles. We systematically reviewed all evidence held within the CQC, including its communications with trusts, resulting in full data capture during the study period. However, the reviewer of CQC information was not blinded to the aims and objectives of the study question, and although efforts were taken to standardise the data collection, bias may still have been introduced. Our review found that most trusts were able to identify areas that could be improved within their care pathways, and implemented action plans to address these issues. Action plans were created in 64% (99/154) of CQC cases after the initial investigation but 77% (118/154) by the time the cases were closed. This suggests that the CQC may be more likely to pursue the case until an action plan is created. We are unable to associate the creation of action plans with Imperial College mortality alerts, as we cannot disentangle the effect of the mortality alert letter from the input of the CQC. The creation of action plans to improve care in ‘outlier’ trusts is highlighted in the CQC annual reports. 36,38 In addition, we noted that there was variation in the clinical audit standards used by the trusts in their responses. For example, some trusts identified potential causes for the increased mortality, whereas others consistently failed to do this.
Changes to coding following an alert
We found that, following an AMI or sepsis alert, the majority of trusts made some changes to their data, possibly as a consequence of coding reviews. On average, the number of admissions and deaths with these diagnoses fell in alerting trusts following our reanalysis. However, we had no control group (non-alerting trusts) to investigate. The CQC mandates yearly audits of individual trust data quality, which will trigger an audit of coding within the trust;153 as a result, clinical coding is predominantly good quality. 32 However, such auditing could also explain the changes in coding that we found. Gaming seems to be an unlikely explanation, as there was actually an increase in the relative risks following sepsis changes in the data.
Investigation of mortality alerts and other measures of quality
Ours was an observation study that does not allow causality to be established, but it did allow us to investigate associations. Mortality alerts were associated with other indicators of quality such as patient satisfaction, overcrowding (% acute bed occupancy), staff resources (nurse-to-bed ratio) and trust deficit. We carried out significance tests to a significance level of 0.05, used cluster-robust standard errors and controlled for FDR. We hypothesised that mortality alerts were associated with our measures of quality and found associations in some of the indicators. AMI and sepsis analyses were underpowered owing to the small number of alerts. We matched time points, some of which were annual and others were monthly or quarterly. When outcomes cover wide time periods, this may affect the sensitivity of the analysis. Missing data were difficult to determine. In the absence of a consistent authoritative list of trusts in existence in each year of analysis, we compiled our own comprehensive list of acute hospital trusts (and their provider codes) from a range of sources, including the mortality alerts database, updating the status depending on trust closures and mergers. However, quality measures were not always complete; for example, measures of hospital mortality measurements did not include specialist NHS trusts. We assume that MINAP data are complete but do not have a comprehensive list of NHS trusts that provide PCI treatment. Most of our quality indicators are objective, which limits bias; however, NHS thermometer data on harms are self-reported. This could introduce bias, as trusts with poor care may also have poor reporting.
Analysing the association of an alert with trends in subsequent risk of death
Interrupted time series is a strong quasi-experimental study design (one of the strongest after randomised controlled trials). There are some factors that need to be noted. After extreme measurements subsequent measurements are likely to fall. This is termed regression to the mean. The Imperial College alerts are triggered by a sustained increase in relative mortality risk with a threshold set at a high level to ensure an estimated false alarm rate of 0.1% over a 12-month period of monitoring. It is, therefore, unlikely that the sustained high relative mortality risks are due to chance and that the subsequent falls are due to chance. However, our three models all found that trust-level relative risks of mortality fell after an alert and the majority of the decrease took place within the lag period, the period we hypothesised that it would take for the trust to be notified by an alert letter and implement changes to reduce mortality. Given these results, it is difficult to determine the true effect of the surveillance system, but these findings could indicate that trusts are monitoring their own mortality statistics and taking action before the alert letter. We found that the unadjusted risk of mortality fell after an alert to a similar extent as relative risk. Given that it is unlikely that case mix will drastically alter, over time, in a typical acute unit, we would expect effect sizes to be similar in adjusted and unadjusted models. This finding suggests that changes in coding after an alert contribute minimally to the fall.
Workstream 2
Key findings
Qualitative case-based analysis
Workstream 2 aimed to employ mixed methods to investigate the mechanisms by which mortality alerts were assimilated at the local trust level and influenced organisational behaviour through investigation of 11 in-depth case studies (objectives 1 and 4). Using a realist framework and theoretical insights from institutional theory, the analysis sought to describe interactions between the alerts (as feedback intervention), institutional context, organisational behaviour and outcomes. Using a cross-case analysis, we sought to achieve comparative perspectives on the effects of alerts in two diagnoses (sepsis and AMI) and the effects of single versus repeat alerts within these diagnoses in order to enrich our understanding of potential intervention mechanisms (objectives 5 and 6).
An integrative analysis across the reported case studies focused on a comparison of AMI-alerted and sepsis-alerted trusts, and of single- and repeat-alerted trusts, in accordance with the original research objectives, in order to identify common and divergent themes. The resulting analysis developed a deep insight into the ways in which trusts responded to AMI and sepsis alerts, and the institutional contextual and behavioural processes that support or regulate the response. The key findings from this analysis are summarised as follows and discussed subsequently.
-
Alerts are considered useful in providing focus for trust intervention in addressing mortality.
-
Case note review was the common response to alerts across all 11 sites.
-
A forensic approach that completes the circle of problem identification, problem analysis, triangulation of data, identification of solutions and implementation of new ways of working.
-
Use of innovative techniques to improve connectivity and knowledge sharing across trusts focused on tackling mortality (boundary spanners, boundary objects and electronic information sharing).
-
Degree of clinical involvement in responding to alerts for sepsis and AMI.
-
Senior clinicians identifying problems in the coding of sepsis and AMI diagnosis.
In addition to the outcomes and behaviours that were attributable to the mortality alert, as stimulus or intervention, a comparative qualitative analysis of cases revealed a range of institutional processes centred on the implicated mortality area that were not directly attributable to the alert as intervention, and hence were classified as parallel evolution of the trust’s focus on managing avoidable mortality within the area:
-
changes in trust leaders and sentinel events
-
an emphasis on building a trust culture focused on improving quality of care
-
engagement with external organisations to provide knowledge and learning about mortality
-
the development of integrated structures linking trust organisational levels (corporate, division and specialty).
The analysis suggests that the alerts for both AMI and sepsis did instigate institutional responses across all the case study sites. These responses were characterised as follows: the alert served as a trigger for action; a universal case note review response; a forensic approach to identifying problems, identifying solutions and implementing actions; the development of some innovative techniques in developing sepsis and AMI awareness; senior clinical involvement in case note review, coding of deaths and diagnosis identification. It was reported that these responses resulted in the following outcomes: case note review and coding improvements, specific changes in patient pathways, changes in diagnosis of sepsis and AMI, training of clinical staff in case note write-up and coding, greater transparency in patient deterioration and resourcing of some infrastructure changes. The results suggested that trusts receiving repeat alerts for sepsis and AMI appeared to demonstrate a slightly different approach and response from those trusts receiving a single alert for AMI and sepsis, but that the exact nature of variations in response were context-dependent. In some trusts, this difference was a slower movement or reaction to the alert than that in trusts that had received previous alerts in the same area. It is noted that this slow movement was often boosted by intervention from the regulator (CQC, Keogh review and Monitor), and it was this combination of interventions, information and regulation that appeared to link with a turnaround in how mortality was tackled. In many trusts, this coincided with a complete overhaul of the executive team and the development of a new regime for addressing mortality as a result of external pressure and scrutiny.
The comparative analysis of case studies not only revealed patterns of institutional behaviour that were directly attributable to the alert, but emphasised the important role that local contextual circumstances and parallel developmental processes and strategies, instigated by the trust in relation to sepsis and AMI mortality reduction, played in interacting with the response to alerts and regulatory follow-up. In contrast with directly attributable institutional responses, the parallel evolution of trust culture and processes was recognised across all trusts and often made it difficult for the research team to attribute causality in how the alerts influenced trust responses. This finding illustrates the complex nature of institutional behaviour around mortality governance and the role of mortality surveillance and alerting in that process. In those trusts that demonstrated mature mortality monitoring and reporting processes, the receipt of a mortality alert was often predicted from local review of dashboard indicators and use of subscription-based statistical tool packages. Investigation into the causes of abnormal trends in risk-adjusted mortality was often already under way at the time of the receipt of the alert letter, greatly facilitating the speed with which the institution could respond to the CQC requests for follow-up or engage with the Imperial College alerts team to seek clarification. As a result of previous scrutiny in response to above-expected mortality, several trusts had completely overhauled their organisational governance structures for mortality reduction and these substantial changes in organisational structure and behaviour were not directly attributable to the effect of a single alert or string of alerts within any particular area. Interestingly, several mortality and executive leads reported that the trust had been pursuing a long-term mortality-reduction agenda when the alert letter was received and they were subsequently able to use that alert letter to bolster local support, renew institutional commitment or engage dissenting staff groups in support of the programme. The information that the alert represented was, therefore, not as important as its symbolic representation of external scrutiny and the need for continuous remedial effort.
Taking the findings from the case-based analysis concerning the extent of locally-reported behaviour that we were able to attribute directly to the effects of the alerts, our experience in this study is relevant to understanding the extent of evaluation that is possible for a complex, institutional-level intervention such as the mortality alerting system. Our findings are more broadly relevant to any attempt to evaluate the impact of a complex informatics intervention, such as surveillance and feedback. First, for any such intervention, a large component of the active ingredients are context-specific and locally-determined. Information may be fed to a system (with or without guidance for how to act on it), but the system changes that arise (organisational structure and behaviour; quality improvement actions and processes) are not specified as part of the intervention, mainly because the alert is akin to a smoke signal, with the exact origin of the fire unknown. Second, in the absence of clear causality, the contribution of any one component of the system (i.e. the alert) to variance in the outcome of interest (mortality reduction) becomes difficult to ascertain without the benefit of the type of experimental controls that it is difficult to achieve when the units of analysis are themselves complex organisational systems. Finally, the opportunity for evaluation lies in identification and dissemination of what are judged to be adaptive intermediary processes and mechanisms, rather than the dose–response relationship with outcome.
This study has described the nuanced behavioural responses of institutions to intelligence on potentially avoidable mortality. A key message from our work is that it is as important to understand the local preconditions for effective responses – how maturity in institutional mortality monitoring, review and action processes can be achieved – as it is to seek the design of an optimum analytic toolset, set of metrics or mode of alerting. An important developmental step towards enhancing local capability to generate, understand and respond to signals in mortality data is, therefore, to provide guidance and evidence to promote institutional responses that are in the best interests of patient safety. We believe that this current study is an important step in that direction.
To present a more complete discussion and interpretation of the higher-level themes that emerged from the comparative case study analysis, the following sections provide meta-synthesis and review, drawing on knowledge gained across the separate subanalyses.
Key themes from integrated case analysis: institutional behaviour attributable to the alert as intervention
Alerts are considered useful in providing focus for trust intervention in addressing mortality
All trusts recognised that alerts for both AMI and sepsis were useful in providing focus for identifying problems around mortality. In some trusts, alerts were described as ‘smoke signals’ that highlighted problems requiring intensive investigation. However, some also described how they knew that they had problems with sepsis and AMI and that the alerts only served to confirm these problems. Most respondents in repeat-alerting trusts were surprised to receive the second alert, as they felt that they had already tackled the relevant problems; for them, intensive investigation of trust mortality was often boosted by regulator intervention that set out how they needed to improve mortality. Some respondents in repeat-alerting trusts reported that responding to the alerts had expended massive resources in time and staff capacity and reflected that this was wasteful. A few repeat-alerting trusts reflected that the case note investigations arising from the alerts had not told them anything that they had not already known. Some repeat-alerting trusts were confident that they had addressed problems with both AMI and sepsis mortality, but they recognised that case note write-up by doctors for both conditions was not being picked up accurately in coding.
Case note review was the common response to alerts across all 11 sites
All respondents recognised that case note review was the immediate response that trusts undertook. In a few repeat-alerting trusts, for both AMI and sepsis the initial approach was to undertake a review of a sample of relevant case notes. One trust characterised this process as ‘administrative’ and explained that it involved non-clinical staff validating and checking the relevant cases alluded to by the alerts. Senior executives then compiled an action plan outlining their actions in response to the alert. However, in most trusts time and resources were set aside to undertake a case note review in which senior clinicians participated. In some repeat-alerting trusts, this review involved looking at a sample of case notes, and in others a universal case note review of all patient deaths for the relevant sepsis or AMI alert was undertaken. Despite this universal review, it is posited that these trusts often failed to engage with staff across divisions and specialties and, hence, case note review was contained within the senior management level. However, it is conceded that a few trusts did engage across levels and undertook a universal case note review. Hence, they reflected on how local ‘mortality and morbidity teams’ at the divisional and specialty levels were reporting back to the trust mortality committee.
A forensic approach that completes the circle of problem identification, problem analysis, triangulation of data, identification of solutions and implementing new ways of working to mitigate sepsis and acute myocardial infarction mortality
An increasingly forensic approach to responding to the alert was identified by all respondents. For some repeat-alerting trusts, this was articulated as completing the circle and included problem identification, problem analysis, triangulation of data, identification of solutions and implementation of new ways of working. An analysis of repeat-alerting trusts identified a stark movement in this positive direction. In many of these trusts the alert was accompanied by regulator intervention (CQC, Keogh review, Monitor) that set out actions that the trusts had to make in addressing mortality. In tackling mortality, these leaders focused on implementing a strategic trust-wide approach. This involved stepping up engagement of leaders in the mortality committee, improving the oversight of the trust board in reporting mortality, increasing involvement in divisional mortality and morbidity teams, and linking problem-solving of mortality issues to implementing new ways of working. In this way the response to the alert was linked to the ongoing patient safety and quality improvement strategy. In applying this forensic approach, trust leaders focused on investing in staff and IT resources to improve data quality.
It is noted that a few repeat-alerting trusts were making great strides in addressing AMI and sepsis mortality by following this forensic approach. However, others were either limited by resource constraints in resourcing this forensic approach or more focused on taking a strategic cultural approach that focused on broader quality improvement in care. For some, it was not useful in expending resources in ‘chasing alerts’ but more effective to use resources improving quality of care. Some respondents argued that, in this way, trust mortality would also be addressed. One CEO argued that doing both, forensically undertaking case note reviews and following a strategic cultural approach to improve quality of care, would have been the most useful, but in this current resource-constrained environment he was able to focus only on improving quality of care.
Use of innovative techniques to improve connectivity and knowledge sharing across trusts focused on tackling acute myocardial infarction and sepsis mortality (boundary spanners, boundary objects and electronic information sharing)
Most repeat-alerting trusts highlighted how they set out to improve connectivity and knowledge sharing across their organisations. Many employed specialist information experts that implemented techniques aimed at improving data quality and visibility of potential problems. Hence, they invested in an increasing range and combination of IT solutions (HEDS, electronic escalation software NEWS, electronically enabled mortality case note review pro forma processes). Within specialties, senior consultants operated as ‘boundary spanners’, working within the coding team to ‘understand the reality of coders’. In addition, coding team members worked within specialty mortality teams.
Attention was focused on improving the spread of organisational learning about mortality. This involved improving the way in which staff sensed problems and gave sense to these problems. Implicitly, trusts recognised that it was difficult to share knowledge across staff drawn from different areas of expertise. Staff operated within professional knowledge domains, used differing cognitive frames and expressed their understanding using complex and often impenetrable language. The awareness of mortality issues were improved by sharing knowledge gained from case note review, and hence some trusts produced a ‘mortality pro forma’ electronic form that could be updated and accessed by staff involved in mortality investigation. Likewise, case note review investigations were made available on the trust-wide intranet. Intranet portals and learning cafés also provide virtual training support for staff in A&E. Boundary objects were identified that enabled staff to interpret patient deterioration. In one trust, a document was produced that enabled all members of the care team to oversee. It was suggested that this document provided official oversight and gave nursing staff the confidence and evidence to approach medical staff and promote escalation of patient treatment. Additionally, information specialists and coding specialists were enlisted in local teams focused on mortality investigation. Analysis suggests that repeat-alerting trusts had moved the furthest in addressing these issues around knowledge transfer.
Degree of clinical involvement in responding to alerts for sepsis and acute myocardial infarction
Case note review was undertaken in response to the alerts. For a first alert, trust-wide clinical engagement in the review of case notes was absent for some trusts. In some trusts, focus was on administrative validation of the alert and then a review of case notes by designated senior clinician or group of clinicians. Repeat-alerting trusts were often shocked by a second and subsequent alert as they felt that they had addressed issues around either sepsis or AMI. In some this led to greater involvement of clinicians at the divisional and specialty levels. In others, focus was on training junior doctors to write up case notes and consultant authorisation of death certificates. Some trusts’ clinicians championed sepsis and AMI improvement processes within specialties. Some consultants operated as boundary spanners, bridging knowledge domains. For example, in some trusts cardiologists worked with coders to learn ‘their reality’ and, hence, understand how coders interpreted case notes.
Senior clinicians as ‘sense-makers’ identifying problems in coding of sepsis and acute myocardial infarction diagnoses
Reviewing case notes identified major difficulties in the coding of case notes. All trusts identified that junior doctors were not writing up case notes accurately and hence coders had coded for sepsis and AMI incorrectly. Case note reviews by senior clinicians identified that AMI was sometimes an incorrect diagnosis written in the case notes and that incorrect care had resulted. Attention in all AMI alerted trusts focused on training junior doctors in AMI diagnosis and writing up case notes. Most trusts ensured that all patients with suspected AMI and heart problems were assessed by a cardiologist early in the patient journey. Likewise, consultant cardiologists in some trusts were employed to authorise all coding of AMI. In many trusts case notes review resulting from the AMI alert had led to a re-examination of patient pathways for AMI. In some cases, AMI pathways were improved, but it was noted that this had not always been useful. In one trust AMI pathways were changed but later reviews by CQC and Keogh highlighted that these were still too complex and needed further improvement. In this case, the resourcing of new infrastructure enabled a new ‘pacing ward’ for patients drawn from other wards to be monitored by a specialist team. Senior consultants involved in coding also identified that some patients coded for AMI as cause of death were ‘elderly’ and in some cases these patients should have been taken out of the mortality coding of AMI as they followed a ‘do not resuscitate’ protocol. This problem also led to engagement in adjustment of this protocol across the NHS.
Senior consultants undertaking case note review in response to the alert were also responsible for identifying problems with sepsis diagnosis. Junior doctors’ case note write-up was again seen to be problematic. It was suggested that happened because sepsis diagnosis was difficult, emerged over time and arose from a number of conditions. Respondents highlighted that often junior doctors failed to write up the primary condition and sometimes queried sepsis. Similarly, junior doctors often wrote up death certificates and attributed sepsis as the cause of death when in fact the patient had been admitted with a different primary condition. Trust responses to this problem focused mainly on training junior doctors in case note write-up. Some trusts invested in the use of IT-enabled recording of patient observations (NEWS) to enable speeding identification of patient deterioration occurred and the use of IT-enabled patient record systems that provided coders with a real-time record of comorbidities.
It was generally recognised that early intervention for sepsis was critical, and hence in some trusts a patient diagnosed with suspected sepsis was automatically treated for sepsis. It was this early intervention that had a significant influence on sepsis mortality in one trust. In another, a senior consultant in A&E, recognising the importance of early intervention, had set up a ‘sepsis trolley’ containing all necessary medication and equipment to support early intervention for sepsis. In some trusts, clinicians identified that coding of patient deaths was problematic. They recognised that some elderly and terminally ill patients, admitted from care homes with serious conditions, also were suffering from sepsis and, therefore, sepsis recorded on the death certificate had not reflected care in the trust. This led to death certificates being written by consultants and specialist coders of patient deaths. In one trust greater engagement with community care was undertaken and led to a GP sitting on the ‘mortality committee’.
Consultant involvement in coding of case notes around sepsis, also identified that junior doctors were sometimes confused about how to apply the appropriate care bundle. It was noted that care bundles were often confusing and overlapping. This led to improvements in the training in the use of care bundles and further development of care bundles. Overall, senior clinical involvement in case note review and coding led to important changes in coding of case notes, training of junior doctors in recognising AMI and sepsis, and changes in AMI and sepsis treatment.
Parallel evolution of the trust’s focus on avoidable mortality (not attributed to the effects of the alert)
Changes in leadership and sentinel events
It is noted that intervention from the regulator (CQC, Keogh Review and Monitor) appears to precipitate a turnaround in how mortality is tackled. In many trusts, this coincided with a complete overhaul of the executive team and then the institution of a new regime for addressing mortality. Likewise, in one trust two sentinel events (deaths of young patients experiencing poor care) appear to link to a complete change in how mortality was addressed.
Emphasis on building a trust culture focused on improving quality of care
Across all trusts senior leaders reported on the priority of developing a transparent, open and learning-focused culture. In some trusts, they highlighted that before the alert the culture was closed, and communication and learning around mortality occurred in silos. In these trusts, investigation of mortality was not integrated across organisational levels. In one trust it was highlighted that staff were unaware of mortality and that a bullying culture was present.
Changes in leadership appeared to be a key driver in changing trust culture. All trusts, except one, had experienced major changes in leadership. Some of these changes arose as a natural progression but most occurred after repeated interventions by one or more of the following organisations: the CQC, Keogh Review, Special Measures, Provider investigation and Monitor. Trusts experiencing these major overhauls in leadership appeared to actively promote development of a culture focused on transparency, learning and enabling high-quality care. Some were very effective in achieving this by investing in IT-enabled mortality review, patient records, patient escalation systems, training in sepsis and AMI treatment; in addition, they were improving care pathways for AMI and sepsis, enabling knowledge transmission at the front line (e.g. learning cafes, walkrounds, grand rounds, learning portals) and accessing knowledge and learning around improvement from engagement with external organisations (PRISM, AQuA, MINAP, SPI). Other trusts appeared to report this focus but were less committed to engaging more widely.
Most trusts reported that they were focusing on developing a proactive culture in which alerts could be anticipated. For some this was only an aspiration, but others demonstrated that they were making great strides towards achieving this goal. In one trust it was highlighted that it intended to proactively alert the CQC if it anticipated high levels of mortality.
Engagement with external organisations to provide knowledge and learning regarding mortality
Improved knowledge acquisition and sharing was exhibited in some repeat-alerting trusts. Respondents also identified how mortality performance indicators were triangulated and analysed to unpick mortality problems. One trust highlighted how it was engaged in comparing performance of others with similar numbers of hospital sites and catchment characteristics. Similarly, many trusts reflected on intensive engagement with external bodies. These included national programmes and professional bodies committed to quality improvement, patient safety and mortality improvement (AQuA, SPI, MINAP, PRISM). In this way they usefully accessed new knowledge, learning and new practices aimed at improving trust mortality. For example, the Sepsis 6 bundle was introduced and developed in most trusts. In one, new procedures developed for the DNR protocol were transmitted back to the professional body to inform the development of national guidance.
Development of integrated structures linking trust organisational levels (corporate, division and specialty)
All trusts identified some changes in structures and processes aimed at improving connectivity. For example, ‘trust mortality committees’ comprised senior trust leaders (CEO, medical director, director of nursing), senior clinicians and information specialists. Sepsis teams co-ordinating actions around sepsis mortality also fed into both the mortality committee and the local/specialty mortality and morbidity teams that comprised clinicians (doctors and nurses) and specialist coding staff and were led by a senior clinical lead. Specialist departments also engaged in data analysis comparing trust sites, divisions and specialty performance regarding mortality and fed back good practice to local divisional and specialty teams. Some trusts highlighted how the mortality committee sat within the clinical governance directorate. Representatives of the mortality committee also led the other clinical governance subteams and, in this way, its actions fed into patient safety, quality improvement, professional governance and information services (including coding). Hence, mortality review of AMI and sepsis fed into patient pathway analysis and redesign for AMI and sepsis. Many trusts referred to how mortality review findings fed into quality improvement and patient safety but did not allude to this structural connection.
National cross-sectional survey
The national cross-sectional survey employed scales developed through the qualitative analysis of evaluative dimensions for institutional responses to mortality alerts, along with free-text items designed to capture elaborative information from respondents. The survey study sought to analyse variance in organisational structural and behavioural characteristics relative to mortality governance, to identify the main drivers of effective institutional responses and to capture mortality leads’ views of the current adequacy of the MASS.
The survey data suggested that 86% of responding trusts had a dedicated trust-level lead for mortality reduction and 92% had a dedicated trust-level mortality group or committee in place. These are high proportions and fall in line with recent policy development geared towards improving mortality monitoring and review processes within trusts. Over half of the mortality committees were chaired by a senior clinical member, who was the trust medical director in 56% of cases.
In addition to a high proportion of dedicated mortality groups, the majority of trusts (97%) subscribed to one or more commercially available data analytic tools to support mortality monitoring. Over 90% of trusts reported routinely using one or other of the common trust-level mortality indicators, HSMR and SHMI. Although trust-level investment in mortality monitoring and analytics was strong, the practice of review of granular mortality data at board level was more variable, with only 37% of trusts reporting that specialty-level mortality data were reviewed by the board as part of the organisation’s key performance indicators. The implication is that although trusts are clearly investing in informatics capabilities around mortality monitoring, analytics and reporting, they may lag behind in maximising the local use of these systems as a means of internal regulation of mortality and as a means of achieving granular prioritisation of areas for remedial action.
In terms of the intensity of local mortality review, on average 60% of deaths were reviewed for any given period by responding trusts, with 69% of responding trusts reporting that they routinely reviewed all deaths. Clearly, some variation in practice exists for the extent of mortality review undertaken and the specific methodologies used. Testimonies from the case study site visits suggested that, for some trusts, instigating mortality review processes to respond to a specific query was a challenging process, involving changes to roles and responsibilities, staffing time allocations, organisational and reporting structures, and information technologies. When reliable mortality review processes were in place and the process did not need to be configured in an ad hoc manner in response to a CQC request for local investigation, invariably interviewees reported a more effective response.
An examination of the responses to individual survey items within the institutional capacity to respond to signals in mortality data scale revealed stronger and weaker areas of practice. Across the sample, high agreement was recorded for the trust priority assigned to mortality reduction and senior leadership support for mortality monitoring. The weakest areas reported concerned accuracy of coding, the quality of specialty-level mortality data and understanding trends in specialty-level mortality data. The only item to achieve a negative response, on average, was the provision of protected time in people’s job plans for mortality-related work.
During the case study analysis, it became clear that the recipient’s perception of the validity of the alert as a function of data quality, coding accuracy and adequacy of the risk adjustment was an important moderator for the institutional response. The perception of the recipient in this case might be a collective institutional sense of identity or justice, or the judgement of one or more powerful individuals within the organisation who provided an accepted ‘local interpretation’ of the information the alert contained, which was then accepted by colleagues or used to shape the form of the initial response. During stakeholder consultation with the CQC, for example, it became apparent that often the CQC’s role was to attempt to focus the alerted trust on making an investigative response, following the rejection of an initial attempt by the organisation to dismiss the alert as non-valid or unreliable. The perception of data quality, coding and statistical accuracy of the analytics underpinning the alerts, as measured by our survey, is therefore a key area for development, given the relatively low maturity reported in this area.
On average, respondents felt that senior commitment to a mortality reduction agenda was a strong feature of current trust activities in this area, but that there was room for improvement in data accuracy and comprehension. Having dedicated time to work on mortality was a commonly reported issue and echoed opinions expressed consistently during site visits. Experience during the case study site visits additionally highlighted the complexity involved in making sense of locally available data and analytics related to mortality. Often, individuals with a specific interest in the area would dedicate significant amounts of unofficial time in studying and monitoring available data outputs in order to achieve an understanding of key metrics and analyses in an attempt to guide the trust’s work.
An important contribution of the current study lies in the formalisation of an evaluative framework for institutional capability to respond to signals in mortality data, based on extensive empirical qualitative work and the development, refinement and testing of associated scale measures. A qualitative framework analysis of testimony across the 11 case study sites elicited the following nine evaluative dimensions for understanding variance in institutional capability to respond to signals in mortality data.
-
Organisational structure for mortality governance. Key themes: presence of key committees, roles and processes for effective mortality governance; effective representation on mortality committees (both internal and external).
-
Coding. Key themes: accuracy of mortality coding; investment in coding capability; provision of coding input to mortality review.
-
Use of information, monitoring and reporting. Key themes: effective organisational use of mortality data; analytic and predictive capacity; ability to detect and respond to signals and to drill down to identify priority areas based on available data.
-
Local investigation and mortality review process. Key themes: robustness of process; frequency of mortality review; ability to identify avoidable mortality; IT support; reporting.
-
Local improvement mechanisms. Key themes: capacity to translate learning from alerts into local actions for improvement and implement them using appropriate methodology; reporting and oversight of quality improvement projects to ensure they deliver.
-
Organisational culture. Key themes: attitude towards avoidability of mortality; willingness to investigate alerts as ‘valid’ signals; degree of open discussion on sensitive issues; sense of shared responsibility and accountability for avoidable mortality.
-
Senior leadership and sponsorship. Key themes: strategic prioritisation of reducing avoidable mortality; senior presence on mortality review committees and action groups set up to address issues raised by mortality alerts; sponsorship of actions.
-
Interprofessional collaboration. Key themes: frontline clinical and broad professional involvement in mortality review, investigation and action in response to alerts; clinical input into mortality review and coding.
-
External environment. Key themes: availability of guidance; participation in national campaigns; pressure from public and regulatory bodies including the media.
An interesting feature of the evaluative dimensions for institutional capability to respond to signals in mortality data is that only two of the nine dimensions are directly related to informatics. The remainder of the dimensions address organisational structure and other aspects of internal and external context from a sociotechnical perspective. The implication of the breadth of dimensions found to be relevant is that although the validity of information content in the signal and its comprehension and interpretation on the part of the receiving trust are important, ultimately the success of the system as a holistic intervention is dependent on a range of additional local factors concerning how the signal is translated into actions/behaviour and how robustly those actions are implemented. Local action in response to signals in mortality data is, therefore, governed by the adequacy of responsible organisational structures and processes, local investigative mechanisms, the local culture and climate for interprofessional collaboration and openness to feedback on quality of care, strategic prioritisation for reducing avoidable mortality and external support.
In the final version of the survey instrument, an aggregated scale was developed to test the latent construct: institutional capability to respond to signals in mortality data, comprising 21 individual items derived from the qualitative definitions of the evaluative dimensions. The 21 items corresponded to seven of the evaluative dimensions (with the remaining two, culture and external factors, tested elsewhere in the survey instrument). The seven subscales tested were organisational structure for mortality governance, coding, use of information monitoring and reporting, local investigation and mortality review process, local improvement mechanisms, senior leadership and sponsorship, and interprofessional collaboration.
A correlational analysis of the evaluative dimensions revealed several interesting findings. First, the overall institutional capability scale achieved moderate positive correlations with three other variables tested within the survey: the length of time that current arrangements for mortality have been in place, the percentage of specialties within the trust that reliably review all deaths and the overall percentage of deaths that are reviewed by the trust in any given period. The last variable approached a large correlation (r = 0.406; p > 0.0001), demonstrating a particularly robust observed association. Clearly, the development of a trust’s capacity for response occurs over a period of time, and the rapid deployment of measures for sustained management of avoidable mortality may not be immediately effective. The observed association between overall institutional capability to respond to mortality alerts and the capacity of a trust to maintain comprehensive mortality review processes in all clinical areas is suggestive of the importance of having reliable and continuous institutional mortality review processes in place, in order for signals of potential patient safety vulnerabilities to be addressed in a timely and effective manner. The direction of causal inference here becomes important. Both the notion that establishing comprehensive trust-wide mortality review leads to alignment of other organisational areas for effective mortality governance and the converse, that investment in conducive organisational structure and context is a prerequisite for effective mortality review processes, are viable. The results from our qualitative analyses would favour the latter explanation, as the dependency of effective mortality review processes on broad cross-specialty engagement, interprofessional collaboration (e.g. coders working with clinicians) and effectively chaired review committees supported by capable data analytics was demonstrated repeatedly during our site visits.
Regarding the specific subscales employed to test the evaluative framework dimensions within the institutional capability scale, it is interesting to note that the percentage of deaths reviewed in any given period was positively associated with the capacity for local investigation and mortality review processes, robustness of improvement mechanisms and senior leadership support. The implication is that comprehensive internal mortality monitoring requires effective local action mechanisms and sustained senior-level priority within a health-care organisation. The qualitative case study results demonstrate the potential value of institutional investment in comprehensive, clinician-led, ongoing mortality review, if queries raised by alerts representing potential escalating risk to patient safety are to be resolved quickly and effectively.
When respondents were asked to evaluate the current arrangements for mortality alerting and surveillance directly, responses overall and for the vast majority of individual evaluative items were positive. The highest level of agreement was achieved for statements concerning willingness to invest staff and resources in responding to alerts and the role of mortality alerting in regulatory processes and public assurance. Overall, respondents agreed that continuous alerting and surveillance focused trusts on avoidable mortality in a constructive way, a viewpoint echoed by the majority of senior staff interviewed during site visits, who acknowledged that, even in the absence of a clear clinical service implication, the institutional process of investigating statistically abnormal mortality within an area had additional benefits in terms of the lessons learnt for improving coding accuracy and focusing staff and units on patient safety and quality of care. The survey responses additionally indicated that, taken as a whole, respondents felt to a modest degree that mortality alerts led to improvements in local review processes, data monitoring and reporting and multiprofessional engagement in mortality reduction, all sentiments that were expressed to the research team during site visits. The only area that received a slightly negative response, on average, was the perception that mortality alerts represented valid and reliable signals of problems in care delivery.
It is particularly interesting to note that respondents held positive views of the value of mortality surveillance and alerting despite lacking surety in the validity and reliability of the alerts as signals of problems in care. This was a somewhat surprising finding but, as previously mentioned, testimonies from key informants during the case study site visits would support the notion that the alerting system served multiple parallel functions and supported varied intermediary outcomes for the receiving institution, such as focusing attention, improving documentation or securing investment in improved informatics. The notion was expressed on multiple occasions that a diligent response to a mortality alert was synonymous with professionalism in clinical care and symbolic of the trust’s commitment to mortality reduction and high standards of patient care. When mortality alerts are found to be attributable to underlying data quality issues rather than to problems in clinical care, the actions that trusts take to improve coding and data accuracy should improve the reliability of future signals and reduce false positives.
When considering the barriers to reduction of avoidable mortality, respondents indicated that resource availability was a primary concern, followed by coding accuracy, risk adjustment adequacy and specificity and recency of mortality data. Other issues also received moderate attention, such as the availability of knowledge of and expertise in how to respond effectively to the alert. These findings are in accordance with existing research on the characteristics of effective feedback from quality indicators and medical registries, which holds that feedback must be continuous, relevant, timely and accompanied by guidance on remedial actions if it is to be maximally effective in improving outcomes.
Regarding the reported drivers for local institutional responses to mortality alerts, on average, respondents identified CQC involvement in mortality alerting and involvement in national programmes and campaigns in related areas as moderately strong motivating factors, followed by external reporting on mortality alerts received by the trust. Clearly, the external regulatory and public environment is an important consideration for trust leads when it comes to mortality, particularly being seen to respond to regulatory scrutiny and being able to present a strong track record to the public. It is encouraging that trust involvement in national campaigns, such as recent sepsis reduction programmes, is additionally a strong motivator in the level of resources a trust is willing to invest in responding to signals that may herald problems with care.
Strengths and limitations
The broad aim of workstream 2, to understand and describe the mechanisms underpinning the institutional response to mortality alerts and the lack of prior research in this area, necessitated an exploratory approach. The mixed-methods framework developed to guide the investigation in this workstream was, therefore, a considerable strength of the overall design, allowing inductive qualitative analysis based on systematically sampled cases to feed into deductive, framework-driven interpretations of the dataset and cross-sectional measurement using surveys. The substantial effort expended in data collection at 11 sites and the depth of analysis this afforded was another asset of the study design. The current study should, therefore, serve as a firm basis for future research to investigate the efficacy of specific organisational configurations for responding to signals in mortality data using more deductive models and hypotheses.
Qualitative study
In qualitative research, the opportunities afforded for sense-making and interpretation in the pursuit of depth of useful understanding of the mechanisms governing a phenomenon in one or more context-specific cases are favoured over traditionally experimental notions of generalisability and repeatability. Given the socially situated nature of the testimony provided by case study informants, along with the subjectively constructed nature of their narratives, our qualitative investigation of the institutional response to mortality alerts was, inevitably, possessed of subjectivity and bias in various forms. Subjectivity was inherent in the recall of our participants, the social context for data collection (interviews) and the preconceptions and perspectives of the researchers involved in the analysis and interpretation. The sensitive nature of the topic area may well have led certain respondents to adjust their accounts to present the institutional track record in this area in a positive light, or to omit other important details that they felt might have led to negative construction. The institutional responses to signals in mortality data were themselves often long-term institutional programmes involving multiple stakeholders, multiple analytic steps, service change and negotiations with external entities. As such, the institutional experience is often constructed at the individual level, with or without the benefit of hindsight, and events are subject to reinterpretation and post hoc reconstruction. As a consequence of complexity and subjectivity, a key issue experienced by the research team concerned the ability to link the organisational behaviour around local mortality governance described by informants, to the effects of receiving an alert (or the specific alert in question). Essentially, it was often difficult to make a causal attribution, for a reported behaviour, to the mortality alert, effectively framing the latter as stimulus or intervention. This effect was compounded when the time since the original alert instance was longer and spanned what were sometimes multiple changes in trust leadership and structure.
The preconceptions and position of the researcher(s) undertaking the inquiry may influence the course and outcomes of that inquiry, leading to subjectivity in interpretations of data. This is an acknowledged limitation of all qualitative research, and in the present study we took a variety of steps to maximise objectivity and usefulness in our interpretations.
An important consideration when appraising the research reported here concerns the critical distance of the qualitative research team and the opportunity for bias in interpretation of the data afforded by the researcher’s position as academics working at Imperial College London, the host organisation for the Dr Foster mortality alerting system. Despite this connection, the research team, under the guidance of its independently chaired steering committee, designed as part of the peer-reviewed funding application process a systematic and evaluation-driven approach to data collection and analysis that employed best practices in qualitative research. Furthermore, the qualitative research team responsible for visiting sites and collecting data were from a different department within Imperial College from the Dr Foster academic unit (surgery and cancer as opposed to public health) and, therefore, had limited experience of the alerting system and few prior conceptions concerning the value of such a system, other than a genuine desire to capture and describe service-level perceptions of this type of surveillance. The qualitative research team was therefore well placed to elicit balanced and systematic evaluative data. The resulting data, as demonstrated through the detailed case narratives and thematic analysis, contains both positive and negative viewpoints expressed by informants and that were subsequently synthesised into categories within the analytic process.
In the qualitative data collection activity, it was additionally important to be clear about which perspective the visiting research team represented, so as to not bias responses as a result of perceived demand characteristics. During the course of the study it was made clear to each interview respondent at the start of the interview that the interview team was independent of the alert-issuing academic unit at Imperial College, of the Dr Foster corporate entity and of the CQC itself, although it was pointed out that all of these organisations were key stakeholders of the results of the research. The interviewees were provided the opportunity to ask questions concerning this aspect and the standard information provided before they consented to the interview.
At the level of the individual case study sites, bias may have occurred in the presentation of key roles to provide information concerning institutional perspectives on mortality. This may also have led to the misrepresentation or omission of key perspectives, including that of the clinical front line, on the local institutional arrangements. The research team attempted to address these limitations in a number of ways through the design of sampling and recruitment at each site. Following site recruitment, the researchers held preliminary telephone meetings with each site lead (usually the mortality lead or medical director) to obtain information concerning whom to interview during the visit, in order to obtain the most comprehensive and balanced view of the site context. Sampling was also driven by a quota of defined roles that were linked to the research aims. Individuals’ availability for interview on the day was an issue in only a small minority of cases. This approach ensured that a diagonal cross-section of the organisation was sampled (i.e. key functional areas at different levels). We sought predominantly senior roles, as these were the levels at which the response to mortality alerts was overseen and these individuals sat on or chaired the committees that had the responsibility for mortality review and action planning. Frontline representation was also sought, however, in the form of the clinical leads responsible for the implicated clinical areas. Conversations with these individuals demonstrated sensitivity to frontline perspectives on mortality and mortality governance.
Throughout the study, many steps were taken to ensure that the data collection and analysis proceeded as systematically as possible (e.g. standardised data collection, systematic approach to sampling) and, in accordance with best practice in qualitative work, interpretations were iterated extensively and subject to peer review and reinterpretation by multiple researchers and advisors who had varying perspectives and expertise. Further objectivity was introduced through a phased approach to data analysis in which qualitative data was first processed on a case-by-case basis before comparative and integrative approaches were employed to establish robust themes across cases and surface critical differences. Despite these efforts, generalisation from the causal mechanisms and processes reported here should be undertaken only with the usual caveats that apply to case study research. Although many aspects of intervention–context–outcome interactions reported here for the institutional response to mortality alerts are tied to the potentially idiosyncratic features and histories of the organisations visited during the course of the study, we believe that there are valid and useful generalisable lessons to be learnt from the experiences of our 11 case study sites at many levels.
Survey study
Regarding the survey measure that was employed in the cross-sectional study, a considerable strength of the design was the extensive qualitative analysis that underpinned development of the items used within the measure itself, including the steps taken to gain broader stakeholder input into the development of the evaluative framework and the refinement and validation of the measurement instrument itself. Although internal consistency as indicated by examination of scale reliability metrics was deemed acceptable for a new measurement tool in a novel area of research, the achieved sample size was prohibitive of further psychometric analysis and exploratory factor analysis is advisable to support any further refinement and application of the measure.
Aside from the reliability and validity of the measurement tool, the usual caveats and threats to external validity for generalisation of survey research findings apply. The 65% response rate achieved, although good for an unincentivised national survey of this type, still omitted 35% of trusts approached to participate. Although variance was observed in both the responses to individual scale items in the survey and the qualitative views expressed, the possibility of the operation of response bias (i.e. systematic rather than random missing data) cannot be ruled out. It might be the case, for example, that trust leads who were aware of less capable local institutional arrangements for responding to mortality alerts, or who held negative views concerning the current arrangements for mortality surveillance, were less inclined to respond. The nature of the approach to sampling, targeting medical directors and mortality leads as representatives of the institutional stance on managing avoidable mortality, also had strengths and weaknesses. Our qualitative research suggested that only people in these particular roles who possessed the requisite oversight and experience to comment on the mechanics of local organisational arrangements for mortality governance. However, the possibility exists that bias entered the survey responses owing to a desire on the part of senior leads to present their organisation in a positive light. It was notable that respondents rated several leadership dimensions within the survey scales as some of the strongest aspects of the local system, and this result should, therefore, be interpreted with explicit knowledge of the sampling framework employed.
In the survey analysis, the novel nature of the research focus and associated lack of prior research to support clear causal hypotheses necessitated an exploratory analytic frame, which led to a larger number of statistical tests and an associated inflated family-wise error rate. Although the results from correlational analysis of the scale items are interpretable, possess face validity and represent interesting insight into the research questions, any specific inferences should be subject to further investigation and replication.
Finally, the timing of the survey study should be acknowledged in the context of broader NHS England policy concerning local mortality review and mortality governance. Consultation with trusts on the development of national guidance and compulsory practices for local mortality governance had taken place in early 2016, concluding some 2 months before the survey administration. Respondents, therefore, may have been primed to make aspirational responses or may have undertaken rapid recent development in local mortality governance processes in anticipation of the implementation of new guidance. Both eventualities would render aspects of the survey response unrepresentative of the state of local institutional capability 6 months previously, that is, at the time of the site visits. The research team were aware of this risk and steps were taken to accommodate this within the definition of the survey measures, which were adjusted to refer specifically to the previous 12-month period, rather than reflecting more recent developments.
Chapter 10 Conclusions
In this chapter we describe the implications for practice, recommendations for future research and our proposed dissemination activity.
Mortality alerts appear to reflect some aspects of quality of care. Prompted by the CQC, the investigations carried out by the alerting trusts themselves cited quality of care as a factor in 70% of all investigations and particularly an issue in sepsis alerts (89%). We found that mortality alerts were associated with other indicators of quality of care in the direction expected, supporting our theoretical model of mortality alerts being a signal related to quality and safety of care in general. Mortality rates also fell over the 9-month period following an alert, and on average, approximating the expected rate at 18 months. The use of time series analysis and statistical process control charts to examine sustained changes in mortality makes regression to the mean an unlikely explanation. However, the fall in mortality in many cases appeared to precede any reasonable time lag for action given the lag in issuing and investigating alert letters. However, in many of its case studies and in its survey workstream 2 has found that hospitals already have their own internal processes for monitoring mortality, and some trusts described how they already knew that they had areas of concern, and that the alerts only served to confirm these problems.
Trust staff held positive views of the value of mortality surveillance and alerting despite lacking surety in the validity and reliability of the alerts as signals of problems in care. Alerts were also considered useful in providing a focus for trust interventions and for identifying problems around mortality. Some described alerts as ‘smoke signals’, highlighting problems that required intensive investigation. Key informants during the case study site visits supported the notion that the alerting system served multiple parallel functions and supported varied intermediary outcomes for the receiving institution, such as focusing attention, improving documentation and securing investment in improved informatics. The notion was also expressed on multiple occasions that a diligent response to a mortality alert was synonymous with professionalism in clinical care and symbolic of the trust’s commitment to mortality reduction and high standards of patient care.
Our analysis suggests that the alerts for both AMI and sepsis did appear to link with institutional responses. These responses were characterised as a trigger for action; universal case note review; a forensic approach in identifying problems, identifying solutions and implementing actions; the development of some innovative techniques in developing sepsis and AMI awareness; senior clinical involvement in case note review; and coding of deaths and diagnosis identification.
Implications for health care
Given that there does appear to be a relationship between mortality alerts and other external indicators of quality of care, that significant decreases in mortality occur post alert, and the generally positive views of respondents on the value of mortality surveillance, there does appear to be value in continuing with a mortality alert and surveillance system in some form.
There is some doubt among trust staff as to the validity and reliability of the alerts as signals of problems in care. It will be important to make our findings accessible to a wide audience in order to assist trusts in their interpretation of the alerts. We intend to do this through academic publications, but also see a way to include some of this study’s findings in the material included in the alert letters themselves.
There are practices described by some of the site visits and through the national survey, such as the use of innovative techniques to improve connectivity and knowledge sharing across trusts (e.g. boundary spanners, boundary objects and electronic information sharing), and the degree of clinical involvement in responding to alerts that may be useful for other trusts. All respondents identified an increasingly forensic approach to responding to alerts, which could perhaps be formalised.
The survey data suggested that 86% of responding trusts had a dedicated trust-level lead for mortality reduction and 92% had a dedicated trust-level mortality group or committee in place. These are high proportions and fall in line with recent policy development geared towards improving mortality monitoring and review processes within trusts.
The weakest areas reported concerned the accuracy of coding, the quality of specialty-level mortality data and the understanding of trends in specialty-level mortality data. The only item to achieve a negative response, on average, was the provision of protected time in people’s job plans for mortality-related work. On average, respondents felt that senior commitment to a mortality reduction agenda was a strong feature of current trust activities in this area, but that there was room for improvement in data accuracy and comprehension.
The development of a trust’s capacity for response occurs over a period of time, and the rapid deployment of measures for sustained management of avoidable mortality may not be immediately effective. The observed association between overall institutional capability to respond to mortality alerts and the capacity of a trust to maintain comprehensive mortality review processes in all clinical areas is suggestive of the importance of having reliable and continuous institutional mortality review processes in place in order for signals of potential patient safety vulnerabilities to be addressed in a timely and effective manner.
We held a workshop with CQC on 8 December 2016 to discuss the findings of the report and the implications for practice. The following points were covered.
-
The composition of any alert investigation panel was important, particularly around ownership of the problem, as was being able to take a wider perspective on clinical pathways within a trust. This related to the ownership of a specific diagnosis or condition by a specialty or an individual.
-
Circumstances external to the trust in terms of community are also important to consider.
-
In the CQC’s view, a delayed response to an alert was often an indication of governance issues within the trust (organisational). This was backed up by our interviews.
Some practical actions/implications arising from our workshop are as follows.
-
Be clearer from the outset regarding any response required. This might include a more positive framing of the multiple potential local benefits to the trust of engaging with the alert and its response.
-
Provide more generally available information as a learning resource via websites and other means, concerning response practices, case studies and examples of local innovation and best practice (perhaps linking to the outliers’ programme on CQC website).
-
Guidance on who might make up the investigation panel, making it more independent from the specialty in question.
-
Consider community issues (either inappropriate admissions or delayed discharge).
-
There are CPD opportunities for clinical trainees.
-
Feedback given in subsequent follow-up letters from CQC when the initial response from the trust is regarded as inadequate could be provided in the first letter, along with examples of good practice.
-
Trusts should involve coders in the review of cases, given their valuable input and potential independence.
-
Encourage development of local data/analytic/information maturity to decrease reliance on alerts and move trusts from responsive to proactive modes of functioning, especially leveraging existing information assets (audits/local record systems/databases) to triangulate evidence to inform the response.
Recommendations for further research
From the literature review, there is a paucity of evidence on validating surveillance systems such as the MASS. In our original proposal, we proposed a case note review of patients in non-alerting hospitals, compared with alerting hospitals. We wanted to look at quality of care in case notes in patients that had survived their hospital admission, as well as in patients who had died. We wanted to go beyond the limited avoidable deaths approach. Unfortunately, this workstream was not funded, but we still feel this approach might be the only way to validate the alerting system.
An important contribution of the study lies in the formalisation of an evaluative framework for institutional capability to respond to signals in mortality data, based on extensive empirical qualitative work and the development, refinement and testing of associated scale measures. A qualitative framework analysis of testimony across the 11 case study sites elicited nine evaluative dimensions for understanding variance in institutional capability to respond to signals in mortality data. There is potential for application of this framework to other areas.
Given the enormous number and richness of data collected, further analysis of site visits and survey material is certainly merited.
Dissemination activity
-
At the time of publication of this report, we have a number of scientific papers in preparation for dissemination in peer-reviewed academic journals. We currently have three papers, based on workstream 1 research, under review and two drafts in preparation, based on workstream 2 findings.
-
We have disseminated findings from this project at several International scientific meetings, including the following:
-
We presented an overview of the project at the Applied Epidemiology Scientific Meeting, Warwick University, March 2015. 154
-
We have presented some of the quantitative findings at the International Society for Quality in Health Care conference, London, October 2017. 155
-
We presented qualitative research findings at the International Society for Quality in Healthcare Annual Conference. 156
-
-
We held a workshop on our findings with data analysts, senior inspectors and other stakeholders from the CQC and discussed a range of implications and potential further work to build on our report. Some of these are mentioned in Implications for health care.
-
Some of our findings will be included in new revised material to accompany mortality alert letters.
-
Other groups to target for dissemination:
-
Royal College of Physicians
-
Academy of Medical Royal Colleges
-
Royal College of Surgeons
-
NHS Coders organisation.
-
Acknowledgements
Contributions of authors
Paul Aylin (Professor of Epidemiology and Public Health) was the principal investigator. He conceived the project and contributed to the design and management of the project, the collection of data and the drafting of the report. He also led workstream 1.
Alex Bottle (Reader, Medical Statistics) helped to conceive the project, contributed to the design and the management of the project, provided statistical advice and contributed to the drafting of the report.
Susan Burnett (Researcher in Patient Safety) contributed to the design, collection and analysis of the workstream 2 qualitative data and the drafting of the workstream 2 qualitative sections of the report.
Elizabeth Cecil (Research Assistant, Medical Statistics) collated publicly available data on external indicators, provided the statistical analysis in workstream 1 and was responsible for drafting the workstream 1 contribution to the report.
Kathryn L Charles (Researcher in Organisational Science) contributed to the analysis of the workstream 2 qualitative data and the drafting of the workstream 2 qualitative section of the report.
Paul Dawson (Research Associate in Patient Safety) contributed to the collection and analysis of the workstream 2 qualitative data.
Danielle D’Lima (Research Associate in Patient Safety) contributed to the collection and analysis of the workstream 2 survey data, the analysis of the workstream 2 qualitative data and the drafting of the workstream 2 qualitative and survey sections of the report.
Aneez Esmail (Professor of General Practice) contributed to the design and management of the project and the drafting of the report.
Charles Vincent (Professor of Clinical Safety Research) contributed to the design and management of the project and the drafting of the report.
Samantha Wilkinson (Research Assistant, Health Service Research) contributed to the design of the project, was responsible for collating data from CQC investigations into the mortality alerts and contributed to the drafting of the report.
Jonathan Benn (Lecturer in Quality Improvement in Healthcare) helped to conceive the project and contributed to the design and management of the project. He led workstream 2, including the collection and analysis of qualitative and survey data, and the drafting of the workstream 2 sections of the report.
Patient and public involvement
We had two patient representative members of the Scientific Advisory Group, Geoffrey Roughton and Julie Carmen. We would like to thank them for their insightful contributions to the meetings.
Data sharing statement
This is a mixed-methods study. Requests for access to aggregated workstream 1 data, the quantitative component, should be addressed to the corresponding author. The raw data generated in workstream 2, the qualitative component, may not be suitable for sharing, beyond those contained within the report, because of confidentiality concerns. Further information can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Kennedy I. Learning from Bristol: The Report of the Public Inquiry into Children’s Heart Surgery at the Bristol Royal Infirmary 1984–1995 2001. http://webarchive.nationalarchives.gov.uk/20090811143745/http://www.bristol-inquiry.org.uk/final_report/the_report.pdf (accessed 13 January 2017).
- Aylin P, Alves B, Best N, Cook A, Elliott P, Evans SJ, et al. Comparison of UK paediatric cardiac surgical performance by analysis of routinely collected data 1984–96: was Bristol an outlier?. Lancet 2001;358:181-7. https://doi.org/10.1016/S0140-6736(01)05404-6.
- Aylin P, Best N, Bottle A, Marshall C. Following Shipman: a pilot system for monitoring mortality rates in primary care. Lancet 2003;362:485-91. https://doi.org/10.1016/S0140-6736(03)14077-9.
- Hewitt P, McNulty T, Harman H. Learning from Tragedy, Keeping Patients Safe: Overview of the Government’s Action Programme in Response to the Recommendations of the Shipman Inquiry 2007. www.gov.uk/government/uploads/system/uploads/attachment_data/file/228886/7014.pdf (accessed 13 January 2017).
- Aylin P, Lees T, Baker S, Prytherch D, Ashley S. Descriptive study comparing routine hospital administrative data with the Vascular Society of Great Britain and Ireland’s National Vascular Database. Eur J Vasc Endovasc Surg 2007;33:461-5. http://dx.doi.org/10.1016/j.ejvs.2006.10.033.
- Aylin P, Bottle A, Majeed A. Use of administrative data or clinical databases as predictors of risk of death in hospital: comparison of models. BMJ 2007;334. https://doi.org/10.1136/bmj.39168.496366.55.
- Bottle A, Aylin P. Application of AHRQ patient safety indicators to English hospital data. Qual Saf Health Care 2009;18:303-8. https://doi.org/10.1136/qshc.2007.026096.
- Palmer WL, Bottle A, Davie C, Vincent CA, Aylin P. Dying for the weekend: a retrospective cohort study on the association between day of hospital presentation and the quality and safety of stroke care. Arch Neurol 2012;69:1296-302. https://doi.org/10.1001/archneurol.2012.1030.
- Bottle A, Aylin P, Loeffler M. Return to theatre for elective hip and knee replacements: what is the relative importance of patient factors, surgeon and hospital?. Bone Joint J 2014;96-B:1663-8. https://doi.org/10.1302/0301-620X.96B12.34002.
- Minne L, Eslami S, de Keizer N, de Jonge E, de Rooij SE, Abu-Hanna A. Statistical process control for monitoring standardized mortality ratios of a classification tree model. Methods Inf Med 2012;51:353-8. http://dx.doi.org/10.3414/ME11-02-0044.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry – Executive Summary 2013. http://webarchive.nationalarchives.gov.uk/20150407084003/http://www.midstaffspublicinquiry.com/sites/default/files/report/Executive%20summary.pdf (accessed 13 January 2017).
- Lilford R, Pronovost P. Using hospital mortality rates to judge hospital performance: a bad idea that just won’t go away. BMJ 2010;340. https://doi.org/10.1136/bmj.c2016.
- Black N. Assessing the quality of hospitals. BMJ 2010;340. https://doi.org/10.1136/bmj.c2066.
- Hogan H, Zipfel R, Neuburger J, Hutchings A, Darzi A, Black N. Avoidability of hospital deaths and association with hospital-wide mortality ratios: retrospective case record review and regression analysis. BMJ 2015;351. https://doi.org/10.1136/bmj.h3239.
- Mohammed MA, Lilford R, Rudge G, Holder R, Stevens A. The findings of the Mid-Staffordshire Inquiry do not uphold the use of hospital standardized mortality ratios as a screening test for ‘bad’ hospitals. QJM 2013;106:849-54. https://doi.org/10.1093/qjmed/hct101.
- Hogan H, Healey F, Neale G, Thomson R, Vincent C, Black N. Relationship between preventable hospital deaths and other measures of safety: an exploratory study. Int J Qual Health Care 2014;26:298-307. http://dx.doi.org/10.1093/intqhc/mzu049.
- Pitches DW, Mohammed MA, Lilford RJ. What is the empirical evidence that hospitals with higher-risk adjusted mortality rates provide poorer quality care? A systematic review of the literature. BMC Health Serv Res 2007;7. http://dx.doi.org/10.1186/1472-6963-7-91.
- British Broadcasting Corporation (BBC) . NHS ‘must Be More Open on Preventable Patient deaths’ 2016. www.bbc.co.uk/news/health-38305033 (accessed 13 January 2017).
- Hayward RA, Hofer TP. Estimating hospital deaths due to medical errors: preventability is in the eye of the reviewer. JAMA 2001;286:415-20. https://doi.org/10.1001/jama.286.4.415.
- Lilford R, Edwards A, Girling A, Hofer T, Di Tanna GL, Petty J, et al. Inter-rater reliability of case-note audit: a systematic review. J Health Serv Res Policy 2007;12:173-80. https://doi.org/10.1258/135581907781543012.
- Hutchinson A, Coster JE, Cooper KL, McIntosh A, Walters SJ, Bath PA, et al. Assessing quality of care from hospital case notes: comparison of reliability of two methods. Qual Saf Health Care 2010;19. https://doi.org/10.1136/qshc.2007.023911.
- Dubois RW, Rogers WH, Moxley JH, Draper D, Brook RH. Hospital inpatient mortality. Is it a predictor of quality?. N Engl J Med 1987;317:1674-80. https://doi.org/10.1056/NEJM198712243172626.
- Hogan H, Healey F, Neale G, Thomson R, Vincent C, Black N. Preventable deaths due to problems in care in English acute hospitals: a retrospective case record review study. BMJ Qual Saf 2012;21:737-45. https://doi.org/10.1136/bmjqs-2011-001159.
- McNamara RL, Herrin J, Wang Y, Curtis JP, Bradley EH, Magid DJ, et al. Impact of delay in door-to-needle time on mortality in patients with ST-segment elevation myocardial infarction. Am J Cardiol 2007;100:1227-32. https://doi.org/10.1016/j.amjcard.2007.05.043.
- Abel GA. Re: avoidability of hospital deaths and association with hospital-wide mortality ratios: retrospective case record review and regression analysis. BMJ 2015. www.bmj.com/content/351/bmj.h3239/rr-6 (accessed 13 January 2017).
- Keogh B. Review into the Quality of Care and Treatment Provided by 14 Hospital Trusts in England: Overview Report. 2013. www.nhs.uk/NHSEngland/bruce-keogh-review/Documents/outcomes/keogh-review-final-report.pdf (accessed 13 January 2017).
- Mohammed MA, Deeks JJ, Girling A, Rudge G, Carmalt M, Stevens AJ, et al. Evidence of methodological bias in hospital standardised mortality ratios: retrospective database study of English hospitals. BMJ 2009;338. https://doi.org/10.1136/bmj.b780.
- Nicholl J. Case-mix adjustment in non-randomised observational evaluations: the constant risk fallacy. J Epidemiol Community Health 2007;61:1010-13. https://doi.org/10.1136/jech.2007.061747.
- Bottle A, Jarman B, Aylin P. Hospital standardized mortality ratios: sensitivity analyses on the impact of coding. Health Serv Res 2011;46:1741-61. http://dx.doi.org/10.1111/j.1475-6773.2011.01295.x.
- Garout M, Tilney HS, Tekkis PP, Aylin P. Comparison of administrative data with the Association of Coloproctology of Great Britain and Ireland (ACPGBI) colorectal cancer database. Int J Colorectal Dis 2008;23:155-63. http://dx.doi.org/10.1007/s00384-007-0390-z.
- Myocardial Ischaemia National Audit Project . How the NHS Cares for Patients With Heart Attack. Annual Public Report April 2013–March 2014 2014. www.ucl.ac.uk/nicor/audits/minap/documents/annual_reports/minap-public-report-2014 (accessed 13 January 2017).
- Burns EM, Rigby E, Mamidanna R, Bottle A, Aylin P, Ziprin P, et al. Systematic review of discharge coding accuracy. J Public Health 2012;34:138-48. https://doi.org/10.1093/pubmed/fdr054.
- CQC . University Hospitals Birmingham NHS Foundation Trust: Queen Elizabeth Medical Centre Quality Report 2015. www.cqc.org.uk/sites/default/files/new_reports/AAAE8393.pdf (accessed 13 January 2017).
- Taylor P. Standardized mortality ratios. Int J Epidemiol 2013;42:1882-90. http://dx.doi.org/10.1093/ije/dyt209.
- Bottle A, Aylin P. Intelligent information: a national system for monitoring clinical performance. Health Serv Res 2008;43:10-31. http://dx.doi.org/10.1111/j.1475-6773.2007.00742.x.
- CQC . Annual Report and Accounts 2013 14 2014. www.cqc.org.uk/sites/default/files/20140708-cqc-annual-report-web-final.pdf (accessed 13 January 2017).
- CQC . Annual Report and Accounts 2011 12 2012. www.cqc.org.uk/sites/default/files/documents/cqc_annualreport_2012_tagged.pdf (accessed 13 January 2017).
- CQC . Annual Report and Accounts 2012 13 2013. www.cqc.org.uk/sites/default/files/documents/annual_report_2012_2013.pdf (accessed 13 January 2017).
- Wright J, Dugdale B, Hammond I, Jarman B, Neary M, Newton D, et al. Learning from death: a hospital mortality reduction programme. J R Soc Med 2006;99:303-8. https://doi.org/10.1258/jrsm.99.6.303.
- Rogers H. Reducing avoidable deaths in hospital. Clinical Risk 2008;14:174-8. http://dx.doi.org/10.1258/cr.2008.080068.
- Jarman B, Bottle A, Aylin P, Browne M. Monitoring changes in hospital standardised mortality ratios. BMJ 2005;330. https://doi.org/10.1136/bmj.330.7487.329.
- Falstie-Jensen AM, Larsson H, Hollnagel E, Nørgaard M, Svendsen MLO, Johnsen SP. Compliance with hospital accreditation and patient mortality: a Danish nationwide population-based study. Int J Qual Health Care 2015;27:165-74. https://doi.org/10.1093/intqhc/mzv023.
- Spiegelhalter DJ. Surgical audit: statistical lessons from Nightingale and Codman. J R Stat Soc Ser A Stat Soc 1999;162:45-58. http://dx.doi.org/10.1111/1467-985X.00120.
- Pronovost PJ, Miller MR, Dorman T, Berenholtz SM, Rubin H. Developing and implementing measures of quality of care in the intensive care unit. Curr Opin Crit Care 2001;7:297-303. https://doi.org/10.1097/00075198-200108000-00014.
- Russell EM, Bruce J, Krukowski ZH. Systematic review of the quality of surgical mortality monitoring. Br J Surg 2003;90:527-32. https://doi.org/10.1002/bjs.4126.
- Hartz AJ, Krakauer H, Kuhn EM, Young M, Jacobsen SJ, Gay G, et al. Hospital characteristics and mortality rates. N Engl J Med 1989;321:1720-5. https://doi.org/10.1056/NEJM198912213212506.
- Chassin MR, Park RE, Lohr KN, Keesey J, Brook RH. Differences among hospitals in Medicare patient mortality. Health Serv Res 1989;24:1-31.
- Jarman B, Gault S, Alves B, Hider A, Dolan S, Cook A, et al. Explaining differences in English hospital death rates using routinely collected data. BMJ 1999;318:1515-20. http://dx.doi.org/10.1136/bmj.318.7197.1515.
- Hofer TP, Hayward RA. Identifying poor-quality hospitals. Can hospital mortality rates detect quality problems for medical diagnoses?. Med Care 1996;34:737-53. https://doi.org/10.1097/00005650-199608000-00002.
- Cook DA, Steiner SH, Cook RJ, Farewell VT, Morton AP. Monitoring the evolutionary process of quality: risk-adjusted charting to track outcomes in intensive care. Crit Care Med 2003;31:1676-82. https://doi.org/10.1097/01.CCM.0000065273.63224.A8.
- Aylin P, Bottle A, Jarman B, Elliott P. Paediatric cardiac surgical mortality in England after Bristol: descriptive analysis of hospital episode statistics 1991–2002. BMJ 2004;329. http://dx.doi.org/10.1136/bmj.329.7470.825.
- Afessa B, Keegan MT, Hubmayr RD, Naessens JM, Gajic O, Long KH, et al. Evaluating the performance of an institution using an intensive care unit benchmark. Mayo Clin Proc 2005;80:174-80. https://doi.org/10.4065/80.2.174.
- Rogers CA, Ganesh JS, Banner NR, Bonser RS. Steering Group . Cumulative risk adjusted monitoring of 30-day mortality after cardiothoracic transplantation: UK experience. Eur J Cardiothorac Surg 2005;27:1022-9. https://doi.org/10.1016/j.ejcts.2005.02.033.
- Cook DA. Methods to assess performance of models estimating risk of death in intensive care patients: a review. Anaesth Intensive Care 2006;34:164-75.
- HSMR: A New Approach for Measuring Hospital Mortality Trends in Canada. Ottawa, ON: Canadian Institute for Health Information; 2007.
- Coory M, Duckett S, Sketcher-Baker K. Using control charts to monitor quality of hospital care with administrative data. Int J Qual Health Care 2008;20:31-9. https://doi.org/10.1093/intqhc/mzm060.
- Heijink R, Koolman X, Pieter D, van der Veen A, Jarman B, Westert G. Measuring and explaining mortality in Dutch hospitals; the Hospital Standardized Mortality Rate between 2003 and 2005. BMC Health Serv Res 2008;8. http://dx.doi.org/10.1186/1472-6963-8-73.
- Ben-Tovim D, Woodman R, Harrison JE, Pointer SC, Hakendorf PH, Henley G. Measuring and Reporting Mortality in Hospital Patients. Australian Institute of Health and Welfare; 2009.
- Hall BL, Hamilton BH, Richards K, Bilimoria KY, Cohen ME, Ko CY. Does surgical quality improve in the American College of Surgeons National Surgical Quality Improvement Program: an evaluation of all participating hospitals. Ann Surg 2009;250:363-76. http://dx.doi.org/10.1097/SLA.0b013e3181b4148f.
- Ben-Tovim DI, Pointer SC, Woodman R, Hakendorf PH, Harrison JE. Routine use of administrative data for safety and quality purposes – hospital mortality. Med J Aust 2010;193:100-3.
- Pilcher DV, Hoffman T, Thomas C, Ernest D, Hart GK. Risk-adjusted continuous outcome monitoring with an EWMA chart: could it have detected excess mortality among intensive care patients at Bundaberg Base Hospital?. Crit Care Resusc 2010;12:36-41.
- Cook DA, Coory M, Webster RA. Exponentially weighted moving average charts to compare observed and expected values for monitoring risk-adjusted hospital indicators. BMJ Qual Saf 2011;20:469-74. http://dx.doi.org/10.1136/bmjqs.2008.031831.
- Koetsier A, de Keizer NF, de Jonge E, Cook DA, Peek N. Performance of risk-adjusted control charts to monitor in-hospital mortality of intensive care unit patients: a simulation study. Crit Care Med 2012;40:1799-807. https://doi.org/10.1097/CCM.0b013e31824e0ff9.
- Cohen ME, Ko CY, Bilimoria KY, Zhou L, Huffman K, Wang X, et al. Optimizing ACS NSQIP modeling for evaluation of surgical quality and risk: patient risk adjustment, procedure mix adjustment, shrinkage adjustment, and surgical focus. J Am Coll Surg 2013;217:336-46. http://dx.doi.org/10.1016/j.jamcollsurg.2013.02.027.
- Moran JL, Solomon PJ. Statistical process control of mortality series in the Australian and New Zealand Intensive Care Society (ANZICS) adult patient database: implications of the data generating process. BMC Med Res Methodol 2013;13. http://dx.doi.org/10.1186/1471-2288-13-66.
- Smith IR, Gardner MA, Garlick B, Brighouse RD, Cameron J, Lavercombe PS, et al. Performance monitoring in cardiac surgery: application of statistical process control to a single-site database. Heart Lung Circ 2013;22:634-41. http://dx.doi.org/10.1016/j.hlc.2013.01.011.
- Sun RJ, Kalbfleisch JD. A risk-adjusted O-E CUSUM with monitoring bands for monitoring medical outcomes. Biometrics 2013;69:62-9. https://doi.org/10.1111/j.1541-0420.2012.01822.x.
- Snyder JJ, Salkowski N, Zaun D, Leppke SN, Leighton T, Israni AK, et al. New quality monitoring tools provided by the scientific registry of transplant recipients: CUSUM. Am J Transplant 2014;14:515-23. http://dx.doi.org/10.1111/ajt.12628.
- Lesage A, Rochette L, Émond V, Pelletier É, St-Laurent D, Diallo FB, et al. A Surveillance System to Monitor Excess Mortality of People With Mental Illness in Canada. Can J Psychiatry 2015;60:571-9. https://doi.org/10.1177/070674371506001208.
- Cohen ME, Liu Y, Ko CY, Hall BL. Improved surgical outcomes for ACS NSQIP hospitals over time: evaluation of hospital cohorts with up to 8 years of participation. Ann Surg 2016;263:267-73. https://doi.org/10.1097/SLA.0000000000001192.
- Steiner SH, Cook RJ, Farewell VT, Treasure T. Monitoring surgical performance using risk-adjusted cumulative sum charts. Biostatistics 2000;1:441-52. https://doi.org/10.1093/biostatistics/1.4.441.
- Stausberg J, Jungen T, Bartels C, Scheu C. Robustness of hospital benchmarking with the Hospital Standardized Mortality Ratio (HSMR): an analysis of secondary data from 37 German hospitals. Gesundheitswesen 2016;78:637-44. http://dx.doi.org/10.1055/s-0035-1548818.
- Meyer JW, Rowan B. Institutionalized organizations: formal structure as myth and ceremony. AJS 1977;83:340-63. https://doi.org/10.1086/226550.
- Scott WR. The adolescence of institutional theory. Adm Sci Q 1987:493-511. https://doi.org/10.2307/2392880.
- Scott WR. Institutional theory. Encycl Soc Theory 2004;4:408-14.
- Pache A-C, Santos F. When worlds collide: the internal dynamics of organizational responses to conflicting institutional demands. Acad Manag Rev 2010;35:455-76. https://doi.org/10.5465/AMR.2010.51142368.
- Oliver C. Strategic responses to institutional processes. Acad Manag Rev 1991;16:145-79. http://dx.doi.org/10.5465/AMR.1991.4279002.
- Powell WW, DiMaggio PJ. The New Institutionalism in Organizational Analysis. Chicago, IL: University of Chicago Press; 2012.
- Weiner BJ. A theory of organizational readiness for change. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-67.
- Weiner BJ, Amick H, Lee SY. Conceptualization and measurement of organizational readiness for change: a review of the literature in health services research and other fields. Med Care Res Rev 2008;65:379-436. https://doi.org/10.1177/1077558708317802.
- Burnett S, Benn J, Pinto A, Parand A, Iskander S, Vincent C. Organisational readiness: exploring the preconditions for success in organisation-wide patient safety improvement programmes. Qual Saf Health Care 2010;19:313-17. https://doi.org/10.1136/qshc.2008.030759.
- Cohen WM, Levinthal DA. Absorptive capacity: a new perspective on learning and innovation. Adm Sci Q 1990:128-52. https://doi.org/10.2307/2393553.
- Harvey G, Jas P, Walshe K, Skelcher C. Analysing organisational context: case studies on the contribution of absorptive capacity theory to understanding inter-organisational variation in performance improvement. BMJ Qual Saf 2015;24:48-55. http://dx.doi.org/10.1136/bmjqs-2014-002928.
- Harvey G, Skelcher C, Spencer E, Jas P, Walshe K. Absorptive capacity in a non-market environment: a knowledge-based approach to analysing the performance of sector organizations. Public Manag Rev 2010;12:77-9. https://doi.org/10.1080/14719030902817923.
- Lane PJ, Koka BR, Pathak S. The reification of absorptive capacity: a critical review and rejuvenation of the construct. Acad Manag Rev 2006;31:833-63. http://dx.doi.org/10.5465/AMR.2006.22527456.
- Lane PJ, Salk JE, Lyles MA. Absorptive capacity, learning, and performance in international joint ventures. Strateg Manag J 2001;22:1139-61. http://dx.doi.org/10.1002/smj.206.
- Zahra SA, George G. Absorptive capacity: a review, reconceptualization, and extension. Acad Manag Rev 2002;27:185-203. http://dx.doi.org/10.5465/AMR.2002.6587995.
- May C, Finch T. Implementing, embedding, and integrating practices: an outline of normalization process theory. Sociology 2009;43:535-54. http://dx.doi.org/10.1177/0038038509103208.
- May CR, Mair F, Finch T, MacFarlane A, Dowrick C, Treweek S, et al. Development of a theory of implementation and integration: normalization process theory. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-29.
- McEvoy R, Ballini L, Maltoni S, O’Donnell CA, Mair FS, MacFarlane A. A qualitative systematic review of studies using the normalization process theory to research implementation processes. Implement Sci 2014;9. http://dx.doi.org/10.1186/1748-5908-9-2.
- Weick KE. Sensemaking in Organizations. Thousand Oaks, CA: Sage; 1993.
- Weick KE, Sutcliffe KM, Obstfeld D. Organizing and the process of sensemaking. Organ Sci 2005;16:409-21. https://doi.org/10.1287/orsc.1050.0133.
- Gioia DA, Chittipeddi K. Sensemaking and sensegiving in strategic change initiation. Strateg Manag J 1991;12:433-48. https://doi.org/10.1002/smj.4250120604.
- Meyer J, Scott WR, Strang D. Centralization, fragmentation, and school district complexity. Adm Sci Q 1987:186-201. https://doi.org/10.2307/2393125.
- Ruef M, Scott WR. A multidimensional model of organizational legitimacy: hospital survival in changing institutional environments. Adm Sci n.d.:877-904. https://doi.org/10.2307/2393619.
- Thompson JD. Organizations in Action: Social Science Bases of Administrative Theory. Piscataway, NJ: Transaction Publishers; 2011.
- Thompson JD, Shafritz JM, Ott JS, Jang YS. Classics of Organization Theory. Andover: Cengage Learning; 1967.
- Burnett S, Mendel P, Nunes F, Wiig S, van den Bovenkamp H, Karltun A, et al. Using institutional theory to analyse hospital responses to external demands for finance and quality in five European countries. J Health Serv Res Policy 2016;21:109-17. http://dx.doi.org/10.1177/1355819615622655.
- Clemens ES, Cook JM. Politics and institutionalism: explaining durability and change. Annu Rev Sociol 1999;25:441-66. https://doi.org/10.1146/annurev.soc.25.1.441.
- Greenwood R, Hinings CR. Understanding radical organizational change: bringing together the old and the new institutionalism. Acad Manag Rev 1996;21:1022-54.
- Scott WR, Ruef M, Mendel P, Caronna C. Institutional Change and Healthcare Organizations: From Professional Dominance to Managed Care. Chicago, IL: University of Chicago Press; 2001.
- Suddaby R. Challenges for institutional theory. J Manag Inquiry 2010;19:14-20. https://doi.org/10.1177/1056492609347564.
- Thornton PH, Ocasio W, Lounsbury M. The Institutional Logics Perspective: A New Approach to Culture, Structure, and Process. Oxford University Press; 2012.
- Scott WR. Institutions and Organizations: Ideas, Interests, and Identities. Thousand Oaks, CA: Sage Publications; 2013.
- North DC. Institutions, Institutional Change and Economic Performance. Cambridge: Cambridge University Press; 1990.
- Foucault M, Burchell G, Gordon C, Miller P. The Foucault Effect: Studies in Governmentality. Chicago, IL: University of Chicago Press; 1991.
- Weiner BJ, Amick H, Lee SY. Review: conceptualization and measurement of organizational readiness for change: a review of the literature in health services research and other fields. Med Care Res Rev 2008;65:379-436. https://doi.org/10.1177/1077558708317802.
- Gollop R, Whitby E, Buchanan D, Ketley D. Influencing sceptical staff to become supporters of service improvement: a qualitative study of doctors’ and managers’ views. Qual Saf Health Care 2004;13:108-14. https://doi.org/10.1136/qshc.2003.007450.
- Vaughn T, Koepke M, Kroch E, Lehrman W, Sinha S, Levey S. Engagement of leadership in quality improvement initiatives: executive quality improvement survey results. J Patient Saf 2006;2:2-9.
- Walley P, Rayment J, Cooke M. Clinical Systems Improvement in NHS Hospital Trusts and their PCTs: A Snapshot of Current Practice. Institute for Innovation and Improvement, University of Warwick; 2006.
- Hamilton S, McLaren S, Mulhall A. Assessing organisational readiness for change: use of diagnostic analysis prior to the implementation of a multidisciplinary assessment for acute stroke care. Implement Sci 2007;2. https://doi.org/10.1186/1748-5908-2-21.
- Eby LT, Adams DM, Russell JE, Gaby SH. Perceptions of organizational readiness for change: factors related to employees’ reactions to the implementation of team-based selling. Hum Relations 2000;53:419-42. https://doi.org/10.1177/0018726700533006.
- Kotter JP. Leading Change. Boston, MA: Harvard Business Press; 1996.
- Wezel FC, Saka-Helmhout A. Antecedents and consequences of organizational change: ’institutionalizing’ the behavioral theory of the firm. Organ Stud 2006;27:265-86. https://doi.org/10.1177/0170840605057670.
- Fulop N, Protopsaltis G, King A, Allen P, Hutchings A, Normand C. Changing organisations: a study of the context and processes of mergers of health care providers in England. Soc Sci Med 2005;60:119-30. https://doi.org/10.1016/j.socscimed.2004.04.017.
- Pettigrew A, Ferlie E, McKee L. Shaping strategic change – the case of the NHS in the 1980s. Public Money Manag 1992;12:27-31. https://doi.org/10.1080/09540969209387719.
- Christl B, Harris MF, Jayasinghe UW, Proudfoot J, Taggart J, Tan J. Teamwork Study Group . Readiness for organisational change among general practice staff. Qual Saf Health Care 2010;19. https://doi.org/10.1136/qshc.2009.033373.
- Braithwaite J, Marks D, Taylor N. Harnessing implementation science to improve care quality and patient safety: a systematic review of targeted literature. Int J Qual Health Care 2014;26:321-9. https://doi.org/10.1093/intqhc/mzu047.
- May C. Towards a general theory of implementation. Implement Sci 2013;8. https://doi.org/10.1186/1748-5908-8-18.
- Meyer MW, Zucker LG. Permanently Failing Organizations. Thousand Oaks, CA: Sage Publications; 1989.
- Burnett S, Renz A, Wiig S, Fernandes A, Weggelaar AM, Calltorp J, et al. Prospects for comparing European hospitals in terms of quality and safety: lessons from a comparative study in five countries. Int J Qual Health Care 2013;25:1-7. https://doi.org/10.1093/intqhc/mzs079.
- NHS Digital . Hospital Episode Statistics n.d. http://content.digital.nhs.uk/hes (accessed 13 January 2017).
- Aylin P, Williams S, Bottle A, Jarman B. Counting hospital activity: spells or episodes?. BMJ 2004;329. https://doi.org/10.1136/bmj.329.7476.1207.
- International Statistical Classification of Diseases. Geneva: World Health Organization; 1990.
- OPCS Classification of Interventions and Procedures . OPCS-4. n.d. http://isd.digital.nhs.uk/trud3/user/guest/group/0/pack/37 (accessed 13 January 2017).
- Aylin P, Bottle A, Jen MH, Middleton S. HSMR Mortality Indicators 2009. www.nhs.uk/NHSEngland/Hospitalmortalityrates/Documents/090424%20MS(H)%20-%20NHS%20Choices%20HSMR%20Publication%20-%20Presentation%20-%20Annex%20C.pdf (accessed 13 January 2017).
- Carstairs V, Morris R. Deprivation and health in Scotland. Health Bull 1990;48:162-75.
- Bottle A, Aylin P. Comorbidity scores for administrative data benefited from adaptation to local coding and diagnostic practices. J Clin Epidemiol 2011;64:1426-33. https://doi.org/10.1016/j.jclinepi.2011.04.004.
- Agency for Health Care Policy and Research . Clinical Classifications Software for ICD-10 Data n.d. www.ahrq.gov/research/data/hcup/icd10usrgd.html (accessed 13 January 2017).
- Moustakides GV. Optimality of the CUSUM procedure in continuous time. Ann Stat n.d.:302-15.
- Marshall C, Best N, Bottle A, Aylin P. Statistical issues in the prospective monitoring of health outcomes across multiple units. J R Stat Soc Ser A Stat Soc 2004;167:541-59. http://dx.doi.org/10.1111/j.1467-985X.2004.apm10.x.
- Bottle A, Aylin P. Predicting the false alarm rate in multi-institution mortality monitoring. J Oper Res Soc 2011;62:1711-8. https://doi.org/10.1057/jors.2010.121.
- NHS England . Statistics n.d. www.england.nhs.uk/statistics/statistical-work-areas/bed-availability-and-occupancy/bed-data-overnight/ (accessed 13 January 2017).
- NHS Digital . NHS Workforce – Monthly Workforce Statistics n.d. www.digital.nhs.uk/article/4304/Workforce/ (accessed 13 January 2017).
- Monitor . NHS Foundation Trusts: Consolidated Accounts 2013 14 2014. www.gov.uk/government/uploads/system/uploads/attachment_data/file/331166/Consolidated_Accounts_2013-14.pdf (accessed 13 January 2017).
- General Medical Council . National Training Survey for Doctors in Training n.d. http://www.gmc-uk.org/education/national_trainee_survey.asp (accessed 13 January 2017).
- Jones HE, Spiegelhalter DJ. Accounting for regression-to-the-mean in tests for recent changes in institutional performance: analysis and power. Stat Med 2009;28:1645-67. https://doi.org/10.1002/sim.3583.
- Myocardial Ischaemia National Audit Project. Datasets and User Guides n.d. http://www.ucl.ac.uk/nicor/audits/minap/datasets (accessed 13 January 2017).
- Care Quality Commission. Surveys n.d. http://www.cqc.org.uk/publications/surveys/surveys (accessed 17 June 2017).
- Health and Social Care Information Centre . NHS Safety Thermometer: Annual Publication, Patient Harms and Harm Free Care, England April 2012–March 2014, Official Statistics 2014. http://content.digital.nhs.uk/catalogue/PUB14502/nhs-safe-ann-rep-apr-2012-mar-2014.pdf (accessed 13 January 2017).
- NHS Digital . Summary Hospital-Level Mortality Indicator n.d. https://www.digital.nhs.uk/SHMI (accessed 17 June 2017).
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B Methodol 1995:289-300.
- Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther 2002;27:299-30. https://doi.org/10.1046/j.1365-2710.2002.00430.x.
- Fretheim A, Soumerai SB, Zhang F, Oxman AD, Ross-Degnan D. Interrupted time-series analysis yielded an effect estimate concordant with the cluster-randomized controlled trial result. J Clin Epidemiol 2013;66:883-7. http://dx.doi.org/10.1016/j.jclinepi.2013.03.016.
- Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock. Intensive Care Med 2008;34:17-60. http://dx.doi.org/10.1007/s00134-007-0934-2.
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA 2002;288:1987-93. https://doi.org/10.1001/jama.288.16.1987.
- McClelland H, Moxon A. Early identification and treatment of sepsis. Nurs Times 2014;110:14-7.
- Clements A, Halton K, Graves N, Pettitt A, Morton A, Looke D, et al. Overcrowding and understaffing in modern health-care systems: key determinants in meticillin-resistant Staphylococcus aureus transmission. Lancet Infect Dis 2008;8:427-34. http://dx.doi.org/10.1016/S1473-3099(08)70151-8.
- Fenton JJ, Jerant AF, Bertakis KD, Franks P. The cost of satisfaction: a national study of patient satisfaction, health care utilization, expenditures, and mortality. Arch Intern Med 2012;172:405-11. https://doi.org/10.1001/archinternmed.2011.1662.
- Johnson RB, Onwuegbuzie AJ, Turner LA. Toward a definition of mixed methods research. J Mix Methods Res 2007;1:112-33. http://dx.doi.org/10.1177/1558689806298224.
- Office for National Statistics . Deaths Registered in England and Wales: 2014 2015. www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsregistrationsummarytables/2015-07-15 (accessed 13 January 2017).
- Nichols M, Townsend N, Scarborough P, Rayner M. Cardiovascular disease in Europe 2014: epidemiological update. Eur Heart J 2014;35:2950-9. http://dx.doi.org/10.1093/eurheartj/ehu299.
- CQC . Care Quality Commission n.d. www.cqc.org.uk/ (accessed 13 January 2017).
- Wilkinson S, Bottle A, Aylin P. Evaluation of a National Surveillance System of Mortality Alerts n.d.
- Cecil E, Bottle A, Aylin P. International Society for Quality in Health Care Annual conference . Are Mortality Alerts Associated With Other Indicators of Hospital Quality in England? A National Cross-Sectional Study n.d.
- Benn J, D’Lima D, Burnett S, Dawson P, Aylin P. The Institutional Response to Mortality Alerts: An Evaluative Framework n.d.
Appendix 1 Sample letter
Appendix 2 List of diagnoses and procedures in mortality alerting system
| Group number | Description |
|---|---|
| Diagnoses | |
| 2 | Septicaemia (except in labour) |
| 49 | Diabetes mellitus without complication |
| 50 | Diabetes mellitus with complications |
| 55 | Fluid and electrolyte disorders |
| 59 | Deficiency and other anaemia |
| 66 | Alcohol-related mental disorders |
| 67 | Substance-related mental disorders |
| 69 | Affective disorders |
| 70 | Schizophrenia and related disorders |
| 71 | Other psychoses |
| 72 | Anxiety, somatoform, dissociative, and personality disorders |
| 83 | Epilepsy, convulsions |
| 96 | Heart valve disorders |
| 100 | Acute myocardial infarction |
| 101 | Coronary atherosclerosis and other heart disease |
| 103 | Pulmonary heart disease |
| 106 | Cardiac dysrhythmias |
| 109 | Acute cerebrovascular disease |
| 114 | Peripheral and visceral atherosclerosis |
| 115 | Aortic, peripheral, and visceral artery aneurysms |
| 125 | Acute bronchitis |
| 127 | COPD and bronchiectasis |
| 128 | Asthma |
| 130 | Pleurisy, pneumothorax, pulmonary collapse |
| 144 | Regional enteritis and ulcerative colitis |
| 145 | Intestinal obstruction without hernia |
| 148 | Peritonitis and intestinal abscess |
| 149 | Biliary tract disease |
| 150 | Liver disease, alcohol related |
| 153 | Gastrointestinal haemorrhage |
| 154 | Non-infectious gastroenteritis |
| 157 | Acute and unspecified renal failure |
| 158 | Chronic renal failure |
| 159 | Urinary tract infections |
| 196 | Normal pregnancy and/or delivery |
| 197 | Skin and subcutaneous tissue infections |
| 199 | Chronic ulcer of skin |
| 205 | Spondylosis, intervertebral disc disorders, other back problems |
| 218 | Liveborn |
| 226 | Fracture of neck of femur (hip) |
| 233 | Intracranial injury |
| 237 | Complication of device, implant or graft |
| 238 | Complications of surgical procedures or medical care |
| Procedure | |
| 2 | Operations on peptic ulcer |
| 3 | Excision of stomach (non-bariatric) |
| 4 | Therapeutic operations on jejunum and ileum |
| 5 | Appendicectomy |
| 8 | Laparascopic cholecystectomy |
| 9 | Total excision of spleen |
| 10 | Transplantation of kidney |
| 11 | Placement of ambulatory apparatus for compensation for renal failure |
| 12 | Graft of bone marrow |
| 13 | Amputation of leg |
| 14 | Excision of lung |
| 15 | Plastic repair of mitral valve (adult without CABG) |
| 16 | Plastic repair of aortic valve (adult without CABG) |
| 19 | Excision of oesophagus ± stomach |
| 20 | Excision of larynx or pharynx |
| 21 | Excision of tongue |
| 23 | Excision of pancreas or head of pancreas |
| 24 | Partial excision of liver |
| 25 | Total excision of kidney |
| 26 | Abdominal excision of uterus |
| 27 | Total excision of bladder |
| 28 | Hip replacement |
| 29 | Knee replacement |
| 30 | Iliac bypass (without transluminals) |
| 31 | Coronary angioplasty (PTCA) |
| 35 | Reconstruction of carotid artery |
| 39 | Craniotomy for trauma |
| 40 | Clip and coil aneurysms |
| 47 | CABG (isolated first time) |
| 201 | Extirpation of lesion of meninges of brain |
| 202 | Shunting for hydrocephalus |
| 203 | Primary neck procedures |
| 507 | Transurethral resection of bladder tumour |
| 601 | Destruction of lesion of retina |
| 602 | Extraction of tooth |
| 606 | Cardiac pacemaker or defibrillator introduced through the vein |
| 608 | Vaginal excision of uterus (without repair of prolapse) |
| 610 | Therapeutic endoscopic procedures on upper GI tract |
| 613 | Therapeutic endoscopic procedures on lower GI tract |
| 614 | Repair of umbilical hernia |
| 616 | Therapeutic endoscopic procedures on biliary tract |
| 620 | Primary repair of tendon |
| 622 | Reduction of fracture of bone (upper/lower limb) |
| 623 | Excision of breast |
| 624 | Therapeutic endoscopic procedures on ureter |
| 626 | Endoscopic resection of outlet of male bladder |
| 629 | Excision of cervix uteri |
| 630 | Vaginal prolapse repair ± hysterectomy |
| 632 | Termination of pregnancy (other) |
| 633 | Delivery |
| 634 | Head of femur replacement |
| 646 | Transluminal operations on femoral artery |
| 649 | Paediatric open heart operations (excl. transplants) |
| 651 | Lumbar spine procedures |
| 671 | Transplantation of lung |
| 672 | Transplantation of liver |
| 674 | Transplantation of heart ± lung |
| 677 | Repair of abdominal aortic aneurysm |
| 680 | Electroconvulsive therapy |
| 699 | Repair of thoracic or unspecified aortic aneurysm |
| 700 | Infra-inguinal bypass |
| 701 | Other femoral bypass |
| 702 | Correction of deformity of eyelid or ptosis |
| 703 | Other destruction of haemorrhoid |
| 705 | Primary repair of femoral hernia |
| 707 | Excision of thyroid gland |
| 708 | Repair of other hernia of abdominal wall |
| 709 | Other excision of gall bladder |
| 710 | Excision of colon and/or rectum |
| 711 | CABG (other) |
| 714 | Excision of ovary and/or fallopian tube (without hysterectomy) |
| 716 | Percutaneous transluminal ablation of heart |
| 728 | Therapeutic endoscopic operations on urethra |
| 731 | Vaginal operations to support outlet of female bladder |
| 739 | Primary repair of incisional hernia |
| 751 | Reduction of fracture of neck of femur |
| 752 | Therapeutic transluminal operations on iliac artery |
| 753 | Therapeutic endoscopic operations on larynx |
| 755 | Bariatric operations |
Appendix 3 Interrupted time series analysis models
Model 1:
Model 2:
Model 3:
(Data are excluded during the lag period.)
Where:
α = log(relative risk) when analysis time is 0 (12 months before the alert).
β(analysis slope) = the slope parameter. This is the increase in log(relative risk) with each month (before an alert).
X1 is the analysis time. The analysis time is coded as 0 at the beginning of the follow-up time (12 months before an alert) and increases by one for each progressive month of the follow-up time.
β(alert) = the step change parameter. This is the fall in log(relative risk) directly following an alert.
X2 is alert indicator coded as a 0 before an alert and 1 after an alert.
β(post-alert factor) = the slope change parameter. This factor added β(analysis slope) parameter estimates the increase in the log(relative risk) with each month (after an alert).
X3 is the post-analysis time. Post-analysis time is coded as a 0 before an alert and then increases by one for each progressive month following an alert.
β(9month lag) = the lagged step change parameter. This is the fall in log(relative risk) following a 9-month lag.
X4 is lag indicator coded as a 0 before the lag period and 1 after the lag period.
β(post-lag factor) = the slope change parameter. This factor added to β(analysis slope) parameter estimates the increase in the log(relative risk) with each month (after the lag period).
X5 is the post lag time. Post lag time is coded as a 0 before an alert and then increases by one for each progressive month following the lag period.
Appendix 4 Site recruitment letter
Appendix 5 Information for trusts
Appendix 6 Preliminary telephone interview pro forma
-
What has been your experience of mortality alerts in septicaemia/AMI and in other areas?
-
Which functions/structures within your organisation are responsible for managing mortality risk and/or responding to mortality alerts?
-
Have there been any working groups or committees set up in response to a mortality alert?
-
Have you been involved in any campaigns or programmes to reduce mortality due to septicaemia/AMI?
-
-
Who would it be important for us to speak to, to understand how your organisation responded to the mortality alert? [Record name and position in order to follow up and obtain contact details]
-
At board/senior level
-
At middle/directorate level?
-
At frontline/clinical level?
-
-
Has management and organisation been stable in the trust over the last five years?
-
Have there been any major events that might have influenced how much attention the trust has paid to quality issues, generally and in AMI/sepsis areas? What/how?
-
Over the last 5 years has the trust had particular pressures imposed from external organisations – such as financial pressures to save money? Particular issues with the CQC? Requirements emanating from the Mid Staffordshire enquiry? Etc.
-
Are there any patient liaison groups associated with the trust (e.g. Healthwatch group) that could provide a patient perspective on the trust’s response to mortality alerts?
Appendix 7 Interviewee invitation letter
Appendix 8 Interviewee consent form
Appendix 9 Interviewee participant information sheet
Appendix 10 Site visit interview questions (generic)
Appendix 11 False discovery rate analysis
We attempted to control for multiple testing and FDR. We found that 23 out of 48 (46%) of the external indicators of quality tests carried out had statistical significance of p < 0.05, while 22 (45%) were still statistically significant after controlling for FDR. This table lists the external quality indicator, the alert being measured, the significance test p-value (for test with a p-value of < 0.1), the rank of the p-value (lowest to highest), the FDR-adjusted p-value and the hypothesis test outcome.
| External quality indicator | Alert type | p-valuea | Rank | Adjusted thresholdb | Null hypothesis |
|---|---|---|---|---|---|
| SHMI | Alert | p < 0.0001 | 1 | p = 0.0010 | Reject |
| SHMI | Frequent alerter | p < 0.0001 | 2 | p = 0.0021 | Reject |
| Acute bed occupancy | AMI alert | p < 0.0001 | 3 | p = 0.0031 | Reject |
| Nurse-to-bed ratio | Sepsis alert | p < 0.0001 | 4 | p = 0.0042 | Reject |
| SHMI | Alert over study | p < 0.0001 | 5 | p = 0.0052 | Reject |
| SHMI | Sepsis alert | p < 0.0001 | 6 | p = 0.0063 | Reject |
| Nurse-to-bed ratio | Alert | p < 0.0001 | 7 | p = 0.0073 | Reject |
| Acute bed occupancy | Frequent alerter | p < 0.0001 | 8 | p = 0.0083 | Reject |
| HSMR | Alert over study | p = 0.001 | 9 | p = 0.0094 | Reject |
| Inpatient satisfaction | Frequent alerter | p = 0.001 | 10 | p = 0.0104 | Reject |
| Acute bed occupancy | Alert | p = 0.001 | 11 | p = 0.0115 | Reject |
| Nurse-to-bed ratio | Alert over study | p = 0.001 | 12 | p = 0.0125 | Reject |
| HSMR | Frequent alerter | p = 0.001 | 13 | p = 0.0135 | Reject |
| Inpatient satisfaction | Alert | p = 0.002 | 14 | p = 0.0146 | Reject |
| HSMR | Alert | p = 0.003 | 15 | p = 0.0156 | Reject |
| Training survey | AMI alert | p = 0.004 | 16 | p = 0.0167 | Reject |
| Nurse-to-bed ratio | Frequent alerter | p = 0.006 | 17 | p = 0.0177 | Reject |
| Trust financial data | Alert over study | p = 0.009 | 18 | p = 0.0188 | Reject |
| HSMR | Sepsis alert | p = 0.001 | 19 | p = 0.0198 | Reject |
| Inpatient satisfaction | Alert over study | p = 0.015 | 20 | p = 0.0208 | Reject |
| Acute bed occupancy | Alert over study | p = 0.016 | 21 | p = 0.0219 | Reject |
| SHMI | AMI alert | p = 0.022 | 22 | p = 0.0229 | Reject |
| Trust financial data | Alert | p = 0.042 | 23 | p = 0.0240 | Accept |
| Acute bed occupancy | Sepsis alert | p = 0.063 | 24 | p = 0.0250 | Accept |
| Nurse-to-bed ratio | AMI alert | p = 0.064 | 25 | p = 0.0260 | Accept |
Appendix 12 Full descriptive summaries for nine case study sites
Note that the additional two case studies appear in Chapter 7 of the report main text as illustrative examples.
Case study 01 (AMI-s.01) narrative summary
Overview
The trust has one main hospital of circa 500 beds, a budget of £160M, and 2500 staff. In 2013 the trust was included in the Keogh review. The report from this review highlighted particular problems in dealing with medical emergencies and medical patients once they had been admitted.
The trust received a single AMI alert.
Relative risk profile
Figure 37 displays the relative risk profile for AMI-m-01 between January 2009 and January 2014. The green lines represent the date of an alert and the blue lines represent the date of the subsequent letter.
FIGURE 37.
Time series displaying relative risk profile and alert (green)/letter (blue) dates for site AMI-s.01.
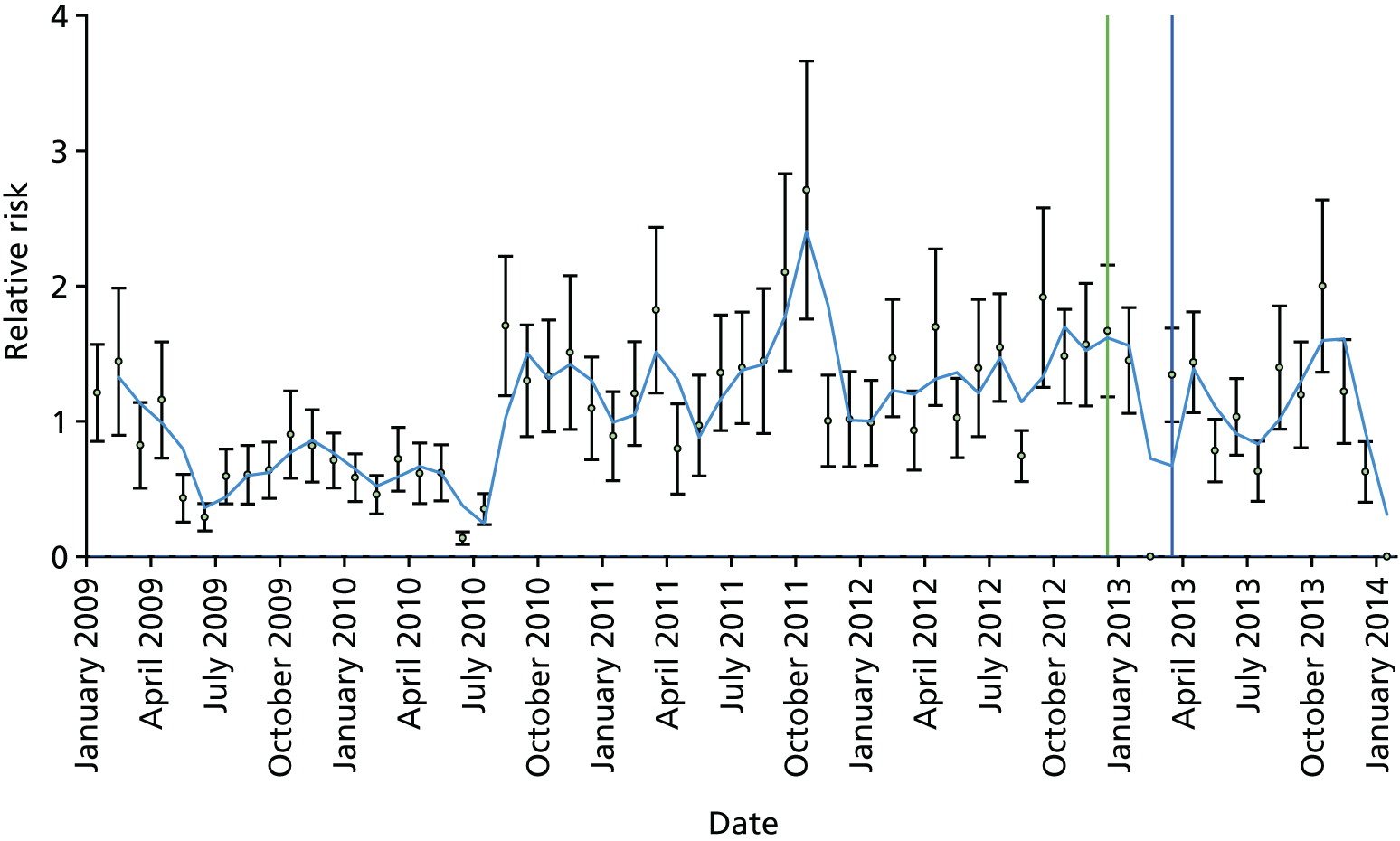
Chronology of key events
-
Alert arrives in 2008: retired cardiology consultant asked to review case notes and finds it is related to coding.
-
PARS early warning scoring system introduced but no outreach team.
-
Target alert and Keogh review in 2013; new senior leadership team appointed.
-
New governance arrangements put in place with emphasis on improving quality of care.
-
Lead consultant cardiologist reviews deaths.
-
New early warning scoring system introduced across the trust; outreach team appointed who see all patients with elevated early warning scores every day.
-
New cardiac consultants appointed; new critical care area set up; new patient pathway introduced for chest pain.
-
All cardiac death coding now reviewed by consultant cardiologists.
AMI-s.01 thematic analysis
There were 10 interviewees, including the CEO, the medical director and a range of frontline staff engaged in safety and improvement work related to mortality (Table 21).
| Relevant history and context at time of first alert | Very poor communication between the executive team and the frontline clinicians. The trust had a mortality committee chaired by the medical director but it only appeared to note alerts. Members of the committee thought that nothing happened with them. One clinician had been disciplined for speaking out about poor care. Alerts were seen as criticisms of individual clinicians. Coding was considered poor, especially the coding of comorbidities. The trust participated in national clinical audits for AMI but these focused on whether or not the specific aspects of care had been delivered and did not identify poor care or poor outcomes caused by poor care. Clinicians kept their own data to themselves. The trust had introduced an early warning scoring system. There was no outreach team from critical care |
| Summary of response to first alert | The committee arrangements were overhauled and a new mortality committee was set up. Every death was reviewed. Work was done to improve coding. Coding was overhauled with clinicians becoming involved; all cardiac deaths coding now involves cardiologists. Lead cardiology consultant reviewed all deaths and found that many were related to coding but that there were care issues to address. A chest pain pathway was introduced across the trust. A business case was written for an outreach team and new coronary care facilities and more consultants were all approved |
| Organisational learning and long-term response | There is a mortality committee chaired by the medical director that has nurses and a GP as members. Every death in the hospital is now reviewed. When an alert comes in, the governance team provides a report to the specialty concerned, which is then required to conduct a full review and report. Coding has been completely changed since, with clinicians much more involved. All cardiac-related deaths in the hospital are seen by the lead consultant cardiologist to review and sign off the coding. Lead consultant cardiologist reviews deaths – many related to coding elevated troponin levels. New early warning scoring system introduced across the trust. Outreach team appointed. New cardiac consultants appointed. New critical care area set up. New patient pathway introduced for chest pain. Work done to improve how ‘do not attempt’ orders are given, including new approach using ‘ceilings of care’. All cardiac death coding now reviewed by consultant cardiologists |
Trust preconditions before the alert
A trust culture characterised as ‘closed’, lacking awareness of mortality and limited staff engagement in addressing of trust mortality
Respondents generally reported that before the AMI alert the trust was ‘closed’ and lacked transparency. Trust participants reported varying degrees of awareness regarding mortality. In one specialty clinical staff reported worry concerning mortality rates, whereas in other areas there was no awareness. However, clinical staff did appear to hold a general view that trust mortality had been a problem for many years. A punitive and bullying approach was described, as a senior clinician had been disciplined for engaging with the media about severe problems around high mortality, and this led to others being unwilling to speak up.
Limited learning gained from trust engagement with external organisations
It was generally accepted that the trust was engaging with external bodies but not sharing its knowledge and awareness of problems regarding mortality. For example, the trust was participating with a NHS care quality improvement organisation and implementing care bundles as far as possible. However, this work was limited to a single clinician, who described this work as a ‘one-man band’. Staff described how the knowledge gained through this external engagement was either not shared or not followed up.
Limited in clinical engagement in addressing mortality: senior clinicians denying responsibility for acute myocardial infarction mortality
Limited clinical engagement in addressing mortality was generally reported. It was suggested that when senior consultants were made aware of mortality issues they attempted to shift the blame and argue about problems and solutions with each other.
Extreme regulatory pressures (Care Quality Commission, Keogh Review, Quality Accounts Audit) create organisational instability and fatigue but also provide a new and improved way forward
It was conceded that the trust was exposed to a host of regulatory pressures that sapped its energies and demoralised staff. The CQC inspections were said to have laid bare how the trust was failing. It was posited that Imperial College alerts were less coercive when not followed up by a CQC inspection. However, in themselves these alerts (for multiple conditions) were seen as useful but still created organisational turbulence and fatigue, as time was limited to address each one. Respondents highlighted how the Keogh investigation had allowed the trust ‘to wipe the slate clean’.
Financial pressures limit resources
The trust’s financial position has varied since 2010/11 between a surplus of £1.15M and a deficit of £4.77M. It was suggested that this had affected the resourcing of staff and prevented the trust from attending meetings about governance and mortality investigation.
A fragmented and token approach to mortality that fails to engage trust divisions and specialities
Respondents suggested that the trust’s leadership had failed to develop a strategic priority for investigating and tackling AMI mortality. Overall, they reported a fragmented and token approach that had failed to engage across divisions and specialties.
Trust responses to acute myocardial infarction alert
An integrated approach linking trust levels and ensuring generation of high-quality data and improved ways of working
Trust response to the AMI alert was characterised now as integrated across corporate, divisional and specialty levels. The CEO highlighted how mortality investigations now feed into organisational changes. At divisional level investigation involves case note review, review of coding, patient pathway analysis and recommendations for improvements in care or coding. This information is all forwarded to the mortality committee for discussion, decision and action.
A universal and timely approach
An internal target is set for a 14-day post-death review period. Importantly, clinicians involved in a mortality alert are excluded from the case note review process. This is managed directly by the clinical governance unit.
A forensic approach: reviewing case notes and acute myocardial infarction pathways
It was reported that staff employed a forensic approach in responding to the alert and CQC inspection. This comprised investigating, analysing problems and triangulating data. Attention focused on the trust’s critical care model and AMI pathway and producing an action plan. A clinician on the mortality committee worked with another clinician to investigate and question all documentation that related to the AMI alert. This includes admitting condition, comorbidities and interventions.
Improved clinical engagement in responding to acute myocardial infarction alert
In responding to the alert respondents reported increased involvement of clinicians in mortality review with the mortality committee and divisional mortality teams. The medical director highlighted how it was important for clinician to volunteer in participating in these teams.
Clinicians as boundary spanners
Data analysis identified clinicians operating as boundary spanners, bridging knowledge areas and cognitive frames. A consultant cardiologist working with coders in case note review was able to ‘bring the coders into the reality of medicine’ and helped the clinician make sense of how they worked.
Outcomes of acute myocardial infarction alert
Changes in patient escalation processes
Changes were made in the early warning scoring system for escalating deteriorating patients.
Changes in patient pathways
Work was also done to improve the use of the ‘do not attempt cardio-pulmonary resuscitation’ policy. This involved introducing ‘ceilings of care’ being written into the patient case notes, which was reported as an outcome of the alert investigation.
Engagement with primary care
Difficulties were also identified regarding AMI originating in primary care. Hence, a key outcome of the alert was to include GP engagement in the mortality review process. The mortality pro forma was also changed to allow clinicians to identify whether the AMI had occurred outside the hospital.
Investment in infrastructure
A reported outcome of the alert was investment in trust infrastructure to redesign critical care and acute coronary care, with a ‘pacing room’ for treatment of patients with confirmed AMI. Respondents reported how mortality review arising from the alert had identified that AMI mortality was high in wards outside critical care and cardiology. Thus, changes were made in the AMI pathways.
Coding changes
Coding completely changed since the alert, with clinicians now much more involved. All cardiac-related deaths in the hospital were seen by the lead consultant cardiologist to review and validate the coding.
Training of staff
In addressing errors in case note write-up, incorrect diagnosis and early intervention for AMI treatment, trust staff reported much investment in training and wider quality improvement.
Parallel evolution of institutional focus on mortality reduction in acute myocardial infarction
Leadership priority for culture change focused on quality improvement and patient safety
Trust leaders described how chasing the alerts was not productive. Instead, a broader priority to improve culture by focusing on quality and patient safety was more effective.
Changes in trust culture influencing mortality
Cultural change appeared to have stimulated how the trust approached mortality. Trust priorities were now driven by a cultural focus on patient safety and quality improvement. Frontline clinicians reported the culture as ‘more open’ and encouraging of staff engagement as ‘people feel that they can speak up more’.
Engagement with external organisations in benchmarking care and accessing knowledge and practices to improve mortality
Respondents identified how engagement with national quality improvement mortality programmes, national clinical audits and other trusts had supported changes both in mortality investigations of alerts and improved care. Engagement with other trusts was also reported as influencing changes in the new critical care model. The culture was described as now being more open and welcoming of new ideas from outside the trust.
Changes in structures and processes linked to improved connectivity between learning and improvement
The head of clinical audit described how structures and processes were very different since the Keogh review. They described as clinical governance integrating and providing reporting connectivity between learning from patient safety and complaints processes to ‘feeding back’ to frontline staff: ‘Nothing is the same . . . It’s all completely different’.
Investment in organisational capabilities (IT infrastructure: electronic incident reporting, mortality pro forma and electronic patient record and MEDICUS)
It was suggested that investment in IT infrastructure had improved data quality, enabling trust feedback and leading to improved knowledge for decision-making. The trust had recently implemented a new electronic incident reporting system, which had dramatically improved the reporting of incidents. The medical director referred to the use of an electronic database containing an audit of patient mortality from AMI.
Universal and timely review of all deaths
Respondents confirmed that a retrospective review of all deaths in the previous 2 years, including all complaints, incidents and inquests, was instituted by the senior leadership team. Care delivery problems were identified and the required actions were linked to an organisational development programme.
Case study 02 (AMI-m.02) narrative summary
Overview
The trust serves a population of approximately 200,000. It has two sites with one worse on mortality than the other. It was sampled as a repeat alerter, with a positive but not significant response for AMI with two alerts in 2008, one in 2012 and one in 2013 (Table 22).
| Relevant history and context at time of first alert |
The trust went through a lot of management changes and this disrupted work on reducing mortality. They also had financial problems that led to a ‘cull’ of staff in the governance team. Previously the view was that the trust tried to justify its position as being a result of the deprived local population rather than trying to understand why there was a problem The CEO would receive the alerts and give them to the director of clinical governance to investigate. This person asked the head of clinical outcomes to pull the notes and ask a clinician to review things and report. The report went to the quality and safety committee, a committee that reported in to the board. It was unclear how long the mortality review committee had been in place Initially, the trust was described as being in denial about problems in clinical care, focusing attention on and blaming poor coding. There were only three people in the coding department in 2011 and there was little clinical engagement in coding. When the current head of coding started to speak to clinicians they were said to have been very defensive The cardiologists reported in to the national audit MINAP and used these data, not the local data, to keep informed about the quality of their service. The cardiac services were split between two sites and were described as having a ‘split-site mentality’ that prevented integration |
| Summary of response to first alert | The CQC heading at the top of the alert was said to have made clinicians sit up and take notice. When the alert arrived in 2011 there was a review of the case notes and it was considered that the cause was more of a coding issue. However, there was little recollection as to any action arising from this alert |
| Organisational learning and long-term response |
Managing avoidable mortality has been given priority in the trust with the new management team. Mortality alerts now go to the medical director and then to the mortality review group. They are disseminated to relevant people in the group with each being given an action list – so the coders will be told to review certain cases alongside the clinicians reviewing care, etc. Now coding is reviewed routinely for all alerts that arrive. However, the head of coding said that coding was not considered the main issue for alerts but rather the clinical care pathway was reviewed first and coding sorted later if necessary The trust now has a clinical outcomes manager with responsibility for the clinical harm review process and reviewing hospital mortality. They work closely with the medical director. A new system of mortality review has just been introduced. The previous system did not work as the death list came out 2 months in arrears. Now deaths are reviewed at the point of completing the death notification in the bereavement office. The Hogan score23 is used as a trigger for avoidable deaths. From this any information is fed back to the clinicians and to the mortality assurance group. The interviewees described the aim to be ahead of the curve in terms of knowing what is going on in the trust before an alert arrives There are morbidity and mortality meetings in departments and one clinician from each sits on the trust’s morbidity and mortality assurance group, which takes place every month. There is a weekly patient safety summit meeting at which all serious incidents and unexpected deaths are reported The trust now uses the HED tool to look at data more in real time. The coding team has been expanded to 30 people who have all been trained through an academy. There are dedicated coders for deaths. The aim in the trust has been to get the coding accurate so that they can monitor trends examine issues without having to question the coding. However, this has been difficult to achieve as a result of the doctor not recording diagnosis and comorbidities. To improve coding the coders now go and work with the clinicians to validate their coding Services for myocardial infarction have been reorganised in the region and ambulances now pass the trust’s doors to take chest pain to the regional centre |
Relative risk profile
Figure 38 displays the relative risk profile for AMI-m-02 between January 2008 and January 2014. The green lines represent the date of an alert and the blue lines represent the date of the subsequent letter.
FIGURE 38.
Relative risk profile with alert (green)/letter (blue) dates for site AMI-m.02.
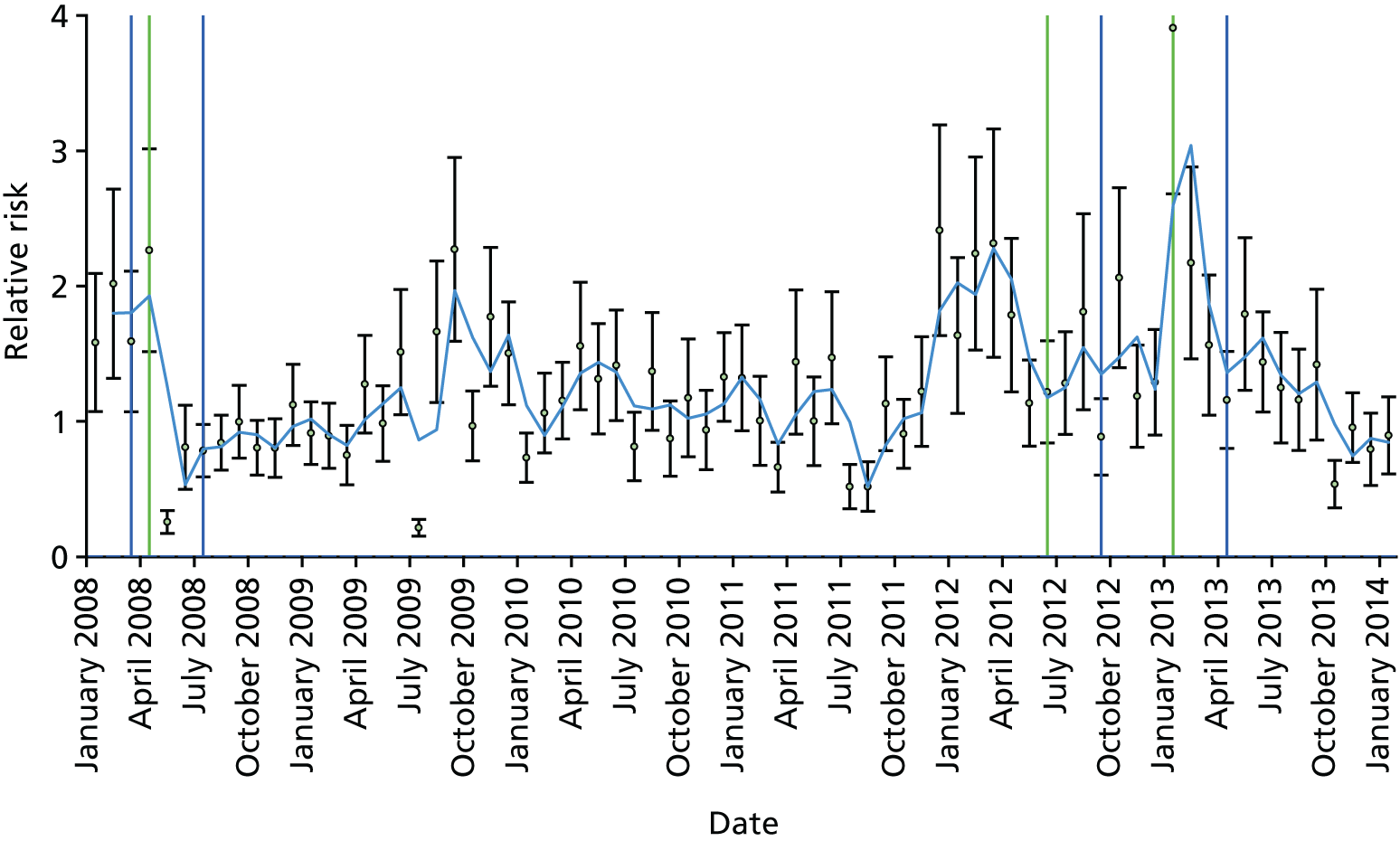
AMI-m.02 thematic analysis
The trust had a CQC review in 2013 and was put into special measures. The review looked at the trust’s governance arrangement, A&E targets and finance (large overspend). The CQC visited again and reported an improvement, but at the time the trust remained in special measures. In March 2014, the trust forecasted a deficit of > £30M.
AMI-m.02 received multiple alerts, alerting four times for AMI (twice in 2008, once in 2012 and once in 2013), although two of these alerts letters were withheld. Analysis is generated from interviews with two senior leaders, one coding manager, one information manager and one clinical lead (A&E).
Trust preconditions before the first alert
Catchment characteristics limit improvement in HSMR
The board at the time of the alerts in 2011 had wanted the HSMR down to 90 from 115 but they considered that the trust catchment described as ‘very deprived’ limited the progress they could make in improving HSMR.
Changes in leadership and financial difficulties create disruption in mortality review
The trust has had a difficult time for many years with several changes in senior management. None of the interviewees was in post in 2008 when the first alert arrived; however, some were able to comment on changes since. Respondents identified that the former medical directors in post before the first alert were not very involved in clinical governance. The clinical outcomes manager reported that the board members had changed many times and as a result they had limited involvement in trust affairs. Changes in ‘upper management’ were perceived by interviewees as ‘a little bit of a hindrance’ and a ‘break in the continuity of the mortality review group’. Financial problems resulted in a ‘culling’ governance and coding staff 4 years previously.
Discontinuity in tools used to support mortality review
When the first alerts arrived in 2008 the trust was using the Dr Foster tools, but the contract was ended in around 2011 and there was a gap before they went with CHKS in 2012. This has changed again and now the trust uses the HED tool.
Cardiology/acute myocardial infarction services
Before 2014, cardiology was split between the two sites, meaning that the catheter laboratory was situated at hospital A and acute services were located at hospital B. This was described as resulting in a ‘split-site mentality’ that prevented an integrated approach to cardiology.
For around 5 years there have been arrangements for patients with AMI to be taken directly to a central myocardial infarction centre rather than to local hospitals. This would suggest that the admission diagnosis of AMI at this trust was not clear-cut when such patients were collected by the ambulance service.
The cardiologists reported in to the national clinical audit (MINAP) and received reports back. These were the main triggers for action.
Trust responses to acute myocardial infarction alert
Lack of trust-wide involvement in trust response
At the time of the first alerts, these would arrive to the CEO and be given to the director of clinical governance, who would ask the clinical outcomes manager to get the notes and select a clinician to ask to review these and write a summary. The results would then go to the quality and safety committee, which reported to the board. It was unclear how long the mortality review committee had been in place, but it was described as having no clear focus or strategy. The head of coding identified how the mortality review group had stopped a couple of times owing to senior management changes.
It was suggested that changes in leadership had led to a lack of strategic direction in addressing mortality. This failure is demonstrated by changes and time lapses in purchasing new mortality analysis IT tools.
Trust responses to the subsequent acute myocardial infarction alerts (2012–13)
Universal case note review
When the AMI alert arrived in 2012 all cases were reviewed and major issues were identified with the coding of AMI. In undertaking this rigorous review of case notes it emerged that only around one-third had been coded correctly for AMI. It was perceived that coding of case notes was the problem, rather than quality of care for patients with AMI.
Poor structures and processes for mortality review limit long-term learning
There appeared to be no long-term learning from the target alerts. The medical director reported that when he was appointed < 1 year previously, the mortality review systems were limited. He explained that he did not receive the mortality alerts, that there was confusion around the process and that he did not have confidence that the institutional response was adequate. The way the data were presented was also said to be very poor, lacking ‘rhythm’. A divisional director also conceded that although there were mortality and morbidity meetings at divisional level, few were robust and the actions generated as a result of them were limited.
The medical director articulated that the plan now is to get the data down to divisional level and then to service level and to have ownership of the data by the clinicians. Work is under way to increase use of the HED tool and provide training in the use of it.
Newly recruited of head of coding motivates trust-wide clinical ownership and improvement in coding
When appointed to the role in 2011, the head of coding started by speaking to every clinical director and clinical lead to ask for help with the data and to explain the issues relating to their recording in the notes and the national data. They set out to motivate clinicians by stressing that that they should take ownership of their data (through case note write-up).
It was noted that clinical leads, at first, were very defensive with regard to their coding, as they felt that their coding was correct. However, the new head of coding was able to demonstrate that they were making serious errors and developed a ‘double-coding policy’. The clinicians were described as being somewhat defensive at first, with some being very aggressive. From this work, new systems were developed, including a validation programme whereby each year every specialty randomly selected 50 sets of notes and went through them with the coder to pick out issues and develop learning points to disseminate within their clinical department.
Care Quality Commission association with the alert triggering greater urgency
Having the CQC label at the top of the alert letter was said to make clinicians take notice and do the required work without challenge. The trust had a CQC review in 2013 and was put into special measures. The review looked at their governance arrangement, A&E targets and finance (large overspend) but did not specifically address AMI. The CQC visited again subsequently and reported improvement but the trust remained in special measures.
Outcomes of acute myocardial infarction alerts
A focus on producing quality data
Case note review resulting from the alert for AMI highlighted that only one-third of the case notes had been coded correctly for AMI. Thus, greater attention was placed to improve coding of case notes. A broad strategic drive was instituted to improve coding for mortality. A new head of coding was recruited and engaged systematically with consultants in specialities to validate their coding of mortality. There were only three people in the coding team in 2011 and by 2014 this expanded to 30. Despite the management changes and the difficulty recruiting, coding was said to have not been disrupted since they were following national guidance, despite using temporary staff.
Trust staff reflected that some progress had been made regarding improving the quality of trust data by recruiting specialist coding staff but that more needs to be achieved in improving case note coding and embedding greater clinical awareness of AMI and how it is coded.
Limited learning gained from mortality review
It was reported that limited learning had been gained from mortality review in response to the alerts for AMI. This had occurred as existing mortality review structures and processes lacked integration across trust levels.
Parallel evolution of institutional focus on mortality reduction in acute myocardial infarction
Most respondents remarked that the trust was moving forward in addressing AMI mortality but that this was only part of a campaign focused on addressing mortality more broadly. It was recognised that this had been driven by a number of co-evolving factors that related to:
-
new trust leadership drive improvements to improve quality of care and reduce mortality, developing a culture where mortality review is part of every clinician’s role
-
strategic focus to integrate structures and processes across the trust to support mortality review, analysis and improvement
-
investing in specialist staff and IT infrastructure to support mortality review
-
investing in coding staff and tackling problems with coding.
Managing avoidable mortality has been given a new priority in the trust by the new management team. In driving mortality awareness, the medical director has started communicating about mortality through a blog, tweeting and presenting at the grand rounds. The clinical outcomes manager went on to say that as a result of this they have recognised how important it is for all clinicians to be involved in reviewing their patients’ notes and any deaths. Consultants are asked to review every one of their own deaths, rather than leaving it to the juniors, and to make this part of everyday working rather than a one-off event when an alert arrives.
Trust leadership striving to provide strategic focus in tackling mortality awareness
The new leadership team has set a clear strategy for improving awareness of mortality at service level, generating meaningful data for use in improving services and instituting trust-wide structures and processes to support mortality review and improvement. In improving awareness of mortality, there has been a focus on standardising data generation and presentation. Trust leaders also highlighted their plan to give ownership of mortality data to clinicians and integrate sharing of mortality data across divisions and specialities. In doing so, they set out to train all clinical staff in using the HED software.
Focus on integrating structures and processes across the trust to support mortality review, analysis and improvement
There is a mortality assurance group that should have representation from each division but the medical director has had difficulty getting this representation. There are morbidity and mortality meetings in departments and one clinician from each sits on the trust’s morbidity and mortality assurance group which takes place every month. There is a weekly patient safety summit at which all serious incidents and unexpected deaths are reported.
Mortality alerts now go to the medical director and then to the mortality review group. They are disseminated to relevant people on the group with each being given an action list. Hence coders will be told to review certain cases alongside the clinicians reviewing care, etc. However, the head of coding said that, now, coding was not considered the main issue for alerts but rather the clinical care pathway was reviewed first and coding sorted later if necessary. The senior managers are given quarterly reports for key specialities. If there is a trigger for anything of concern, then this is how the trust alerts, rather than through external alerts.
Investing in specialist staff and information technology infrastructure to support timely mortality review
The trust now has a clinical outcomes manager, with responsibility for the clinical harm review process and reviewing hospital mortality. They work closely with the medical director. A new system of mortality review has just been introduced. Now deaths are reviewed at the point of completing the death notification in the bereavement office. The Hogan score23 is used as a trigger for avoidable deaths. From this any information is fed back to the clinicians and to the mortality assurance group. The interviewees described the aim to be ahead of the curve in terms of knowing what is going on in the trust before an alert arrives. The plan now is to automate the death review process, make it an electronic system and create a database – currently it is on paper records.
Case study 04 (AMI-m.04) narrative summary
Overview
This is a large acute trust with seven hospitals sites formed from a merger 5 years ago and serving a population of around 220,000. The trust recorded a deficit of approximately £18M in 2013/14 and was expecting to end 2014/15 with a £3M deficit. The trust received three alerts for AMI mortality between 2011 and 2013 (Table 23).
| Relevant history and context at time of first alert | The trust was described as having a ‘tick-box’ governance system before the alert, although they did have a mortality lead and a mortality committee. On the appointment of the new CEO in 2011 there was a review of governance arrangements and a review and change to nurse leadership across the trust to put patient experience and patient safety central. Information to the board was described as poor in the past |
| The head of mortality recognised that the clinical side of mortality reviews had always been patchy. There were certain areas that had good engagement such as palliative care, anaesthetics, and surgery but other areas were less engaged | |
| The trust was aware of the mortality for AMI ‘creeping up’ before the alert and an investigation had begun | |
| Summary of response to first alert | The initial response to the first alert centred on the perspective that the alerts were generated by inaccurate coding and there was a review of the case notes by an independent expert coder. This review picked up that the inexperienced coders were coding using the death certificate and not the admitting diagnosis. As a result, they were assuming that anyone who died from a myocardial infarction had been admitted with this, which was wrong. There was no clinical review for the first alert. From this the coding system was changed from all coders coding deaths to only the experienced coders. They also introduced a system whereby coders would ask clinicians to check the coding if they were not confident from the notes – this started with myocardial infarction deaths but has now spread to all deaths |
| The view was that the second alert included data from the tail of the first alert so the actions the trust had put in place had not come into full effect by then. A clinical review took place for the second alert and involved a cardiologist who highlighted that many cases were not myocardial infarctions – the complexity of raised troponin levels meant that doctors were querying an myocardial infarction on admission but this was later found not to be the case. The problem identified was with patients admitted through the general medical take and not referred to cardiology | |
| Organisational learning and long-term response | The trust has introduced a template that is used to review every death. From these reviews, there is an action plan – also drawing from other data in the trust about the clinical area. There is a coding review conducted alongside a case note review for all alerts. In addition, other information is reviewed to triangulate and set the alert in context. The trust has designed its own mortality review process and tool with a database to capture the information. Each department has had the opportunity to amend the database to suit their own needs but there is a core set of data that everyone has to complete. Clinical issues are added to the core dataset to raise awareness of issues when clinicians are conducting mortality reviews. The CEO emphasised how important it is to look at all the data and not just mortality, and how the trust is now more able to anticipate problems and alerts. The CEO also reflected on how difficult it is to keep on top of all the action plans arising out of the reviews of care |
| The trust now monitors deaths by day of week and can show that there is no difference in the rate during the week compared with weekends. There is a monthly conference call with the Dr Foster representative where the current data is reviewed and any likely alerts are discussed in order to be proactive in spotting problems arising. The information team also provide the clinical review team for mortality with information about patients who have survived, in order to give a more complete picture. The trust is now involved in a range of safety related campaigns including for sepsis |
Relative risk profile
Figure 39 displays the relative risk profile for AMI-m-03 between January 2008 and January 2014. The green lines represent the date of an alert and the blue lines the date of the subsequent letter.
FIGURE 39.
Relative risk profile and alert (green)/letter (blue) dates for AMI-m.04.
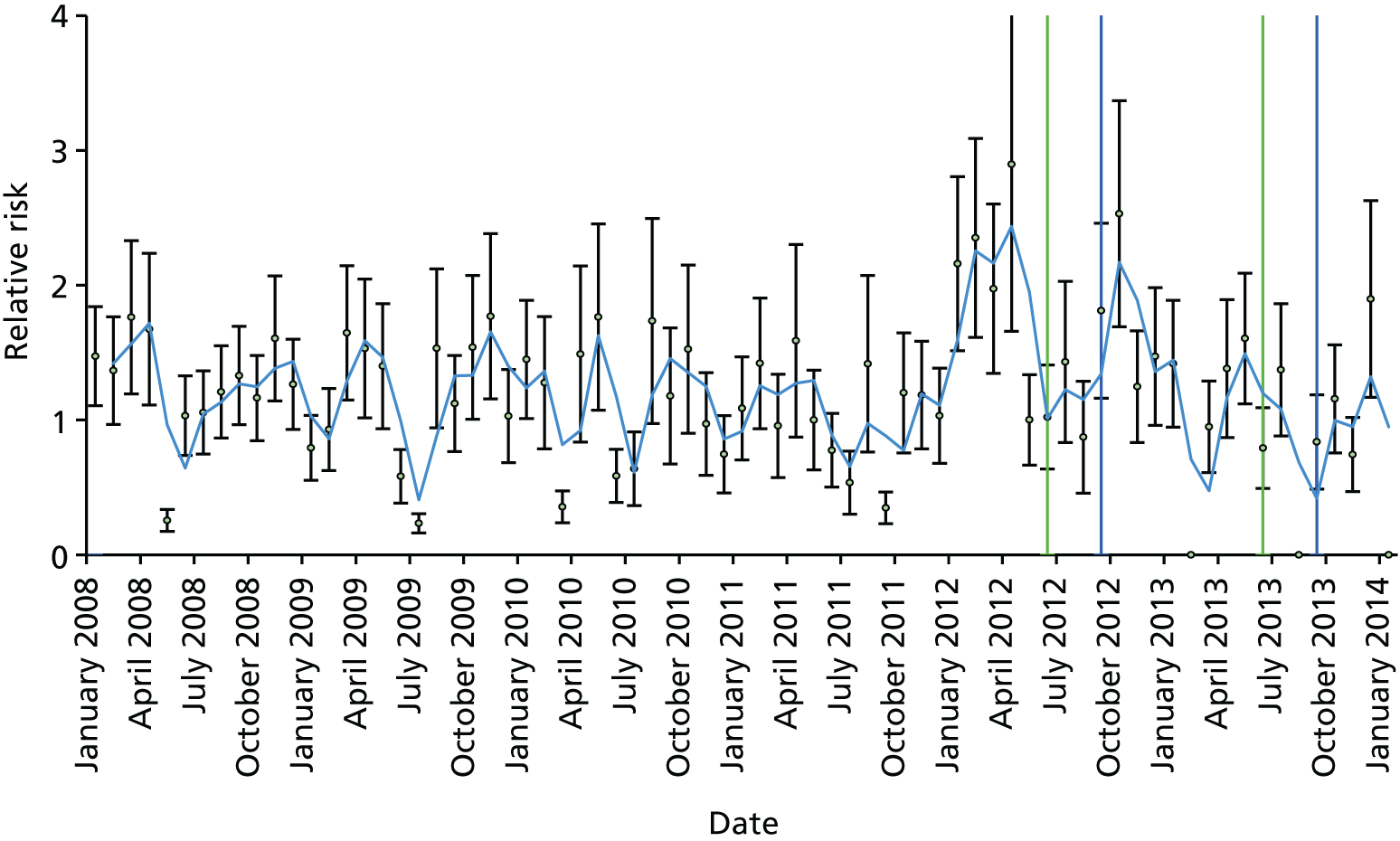
AMI-m.04 thematic analysis
Analysis is generated from interviews with two senior executive leaders, three consultant leads, one head of coding, one information lead and one deputy director of governance.
Trust preconditions before the first alert
Fragmented approach to acute myocardial infarction alert
Respondents identified that the trust dealt with mortality in silos as it was not linked to governance, safety or complaints structures. Similarly, HSMR was not linked with complaints data or safety data. Those interviewed described the trust as having a tick-box governance system. Mortality review was confined to corporate level and undertaken by the mortality review group and the clinical audit department. Coding also lacked clinical oversight.
Changes in leadership influenced trust approach to reviewing mortality
It was reported that a change in CEO was instrumental in changing how the trust approached mortality review. Hence, the trust had moved from a ‘command and control’ leadership style which focused on ‘following the rules and meeting deadlines’ and only producing superficial account of trust mortality to empowering staff to engage in mortality review.
Senior leaders instigate improvement in trust structures and processes by commissioning external oversight
It was recognised that the trust had had a mortality group for over 6 years. Respondents identified that trust structures and processes concerning mortality had recently improved. Efforts were also made to work with NCEPOD and provide external awareness of the processes and issues surrounding hospital mortality. It was also accepted that there was good engagement from departments such as palliative care, anaesthetics, surgery and gastroenterology. However, some shortfalls in trust processes were acknowledged. These included the coding team failing to have a separate arrangement for coding deaths.
The new trust leadership appointed an external consultancy company to undertake a governance review. Outcomes of the governance review were a change to nurse leadership to make patient experience and patient safety central and a change to the committee structures reporting to the board.
Poor standards of care before alert
The CEO noted that on his arrival in 2011, the trust had low standards of care. Patients were ‘crammed into four bedded bays’, ‘without patient privacy, without lockers’, ‘there were lots of falls’ and ‘high infection rates’, breaches of C. diff [Clostridium difficile] targets’ and ‘a bad CQC inspection of care’.
Expecting acute myocardial infarction alert
Data quality appears reasonable before the alert as the information project manager was aware that the trust was going to alert and had informed senior people and an investigation had been instigated. However, recently information around mortality was said to have improved considerably. For example, the information provided to the trust board in the quality report was said to have ‘improved out of all recognition’ (CEO). The CEO highlighted how the trust now focused on detailed exploration of trends and triangulation of data.
Trust responses to acute myocardial infarction alert
Trust response to acute myocardial infarction alert highlights errors in coding deaths and led to only experienced coders coding deaths
The first alert went to the clinical lead for mortality in the trust. The head of coding described being asked to pull the notes and examine the coding. A review of case notes was completed by an independent coder. Once this was done, a ‘clinical investigation report’ was produced using all available data, including MINAP data. The coding review also highlighted that there were two problems: (1) junior doctors were filling in the death certificates and not fully reviewing the notes and (2) junior coders were coding these deaths using the death certificate. In response to the first alert it became trust practice for only experienced coders to code deaths.
It was suggested that there was shock felt by staff on receiving the second AMI alert as they considered coding problems had been addressed. A consultant reported that staff felt depressed as they thought that this problem had been addressed. This led to coding for all myocardial infarctions to be confirmed by the cardiologist.
Joint clinical and coding involvement in case note review identifies errors in myocardial infarction diagnosis and problems in care
A coding and clinical review was instigated. A cardiologist reviewed relevant cases and identified that many had been coded inaccurately to AMI and also that AMI mortality was high in wards other than cardiology, thereby indicating potential problems in patient care. An example of erroneous coding on admission was identified by a cardiologist who reported that the complexity of raised troponin levels had led to doctors querying myocardial infarction on admission but this was later found not to be the case.
Analysis of coding of AMI, highlighted that patients admitted in the general medical intake and under the care of a general physician was high. It was suggested that these patients may have been admitted with a more pressing condition, such as stroke and were treated in wards out with cardiology and without oversight of a cardiologist.
Two alerts close together provide data overlap
The clinical investigation report produced after the first alert highlighted the areas where action was needed. The view was that the second alert included data from the tail of the first alert so the actions the trust had put in place had not come into full effect by then.
Outcomes of acute myocardial infarction alerts
Changes in coding deaths
The trust has a team of 14 coders, one of whom is an expert in coding deaths. This coder works with the mortuary and with the clinicians to ensure that the codes are correct. They also assist with mortality reviews. The head of coding sits on the mortality review group. For each mortality review they look at the coding to see if there is an obvious issue. The information lead said that he had had to work with clinicians to help them understand that the data used by Dr Foster was trust data and related to their cases, so they needed to be involved in coding correctly.
External auditing of coding
Coding is audited internally by the head of coding and externally by the auditors examining Payment By Results and those assessing the Information Governance Toolkit. The head of coding identified how the National Classification Centre for Clinical Coding also advises on coding issues.
Identification of trust need to implement electronic monitoring of deteriorating patients
A consultant cardiologist highlights that the alerts had identified the importance of monitoring patients in a timely fashion and this had in part stimulated efforts in implementing an electronic scoring system for deteriorating patients. However, it was also noted that the trust financial pressures were likely to prevent this happening in the near future.
Consultant cardiologist oversight of all patients with suspected myocardial infarction
The lessons from the investigations into the AMI alerts has highlighted that patients are more at risk if they are not referred to the cardiologists on admission. However, it was unclear what the trust has done to address this. In theory, all patients under general medicine with suspected AMI should now have cardiologist review but interviewees recognised that this relies on junior doctors in the admissions area recognising a potential myocardial infarction and referring the patient to the cardiology team.
Focuses trust on researching mortality
The head of information reported that the alerts had focused everyone’s attention and led to much internal research around improvement that had improved, for example, palliative care arrangements.
Parallel evolution of institutional focus on mortality reduction in acute myocardial infarction
Changes in trust senior leadership driving improvement in mortality
The mortality alerts sent from Dr Foster Intelligence did appear to have some impact on how mortality is organised in the trust, but it is also accepted that trust arrangements have also developed in partial response to changes in the CEO and medical director; and the financial deficit resulting in a Monitor review; and as natural progression of trust strategy. Reducing avoidable mortality is now a top priority for the trust. There was a view that quality and safety received more attention at board and senior management level now than finance – and that this is possibly one reason why they were overspent that year. Information to the board had also improved.
Trust senior leaders drive clinician inspired improvement
The new medical director has adopted a very different approach to QI through encouraging clinicians to work on areas of interest to them, and by giving these clinical leaders as much support as possible. One area described was sepsis, where a clinician came forward and said they wanted to work on early identification and treatment of sepsis. A huge amount of work has now been done on this and the results are showing up in the HSMR and other quality indicators. The trust has introduced a template that is used to review every death. From these reviews, there is an action plan – also drawing from other data in the trust about the clinical area.
Focus on understanding contextual factors influencing alerts and anticipating alerts
The alerts come to the CEO who passes them to the lead for mortality and the clinical governance team for a joint investigation. There is a coding review conducted alongside a case note review for all alerts. In addition, other information is reviewed to set the alert in context. The CEO reflected how they are much better now at dealing with alerts. The CEO emphasised how important it is to look at all the data and not just mortality, and how the trust is now more able to anticipate problems and alerts.
External engagement with organisations to triangulate data and audit coding practices
Engagement with the National Confidential Enquiry into Patient Outcome and Death by the mortality lead allows the trust to access useful information regarding how other trusts tackle mortality. It highlights trust-wide approaches to reviewing deaths, frequency of meetings and techniques used.
Harnessing information to improve trust-wide understanding of mortality
The trust attempts to harness information to improve trust-wide understanding of mortality. This involves developing a narrative around mortality, use of a mortality review process tool and developing an electronic data base of mortality information. The idea of a narrative around mortality is deemed essential for understanding the entire process of mortality within the trust. The mortality group meets monthly and the information specialist provides a full report.
The trust has designed its own mortality review process and tool with a database to capture the information. Each department has had the opportunity to amend the database to suit their own needs but there is a core set of data that everyone has to complete. Clinical issues are added to the core data set to raise awareness of issues when clinicians are conducting mortality reviews. Part of the reason for this review and the database are to counter the fact that Dr Foster data are out of date by the time they arrives.
The mortality review process has developed, and the mortality lead described one recent review that had been undertaken by a cross-specialty team. The CEO also reflected on how difficult it is to keep on top of all the action plans arising out of the reviews of care.
Monitoring mortality
The trust now monitors deaths by day of week and can show that there is no difference in the rate during the week compared with weekends. Their HSMR is now around below 100 and the SHMI is one of the best. This was attributed to the work on sepsis and the triangulation of data to spot issues.
There is a monthly conference call with the Dr Foster representative where the current data is reviewed and any likely alerts are discussed to be proactive in spotting problems arising. The coders now sit with the clinicians when mortality reviews are undertaken and a joint mortality review is conducted. The information specialist now provides the medical director and the mortality lead with a spreadsheet of all the patients that have died in the hospital. The team also provide the clinical review team for mortality alerts with information about patients who have survived, in order to give a more complete picture.
Case study 05 (Sep-s.05) narrative summary
Overview
Sep-s.05 is an acute NHS trust serving a population of approximately 260,000. It has one site, Sep-s.05 general hospital. The trust has approximately 4000 employees and 100 consultants. It had severe financial problems from 2013 onwards and is still at a high risk with regard to finances. In 2013, Monitor began regulation after identifying some governance issues. The trust was seen to be in breach of its provider licence around three issues relating to its electronic patient records, the effectiveness of the board of directors, and the trust’s financial planning. In 2015 a CQC inspection said the trust ‘requires improvement’ (Table 24).
| Relevant history and context at time of first alert | Over the previous 5 years the trust had experienced a period of managerial turbulence and financial difficulty, with several interim chief executives, several medical directors and many changes in the informatics staff. The culture was described as being ‘bullyish’ – with some interim CEOs pushing changes through and ignoring the opinion of the doctors |
| One of the interim medical directors during this period realised that the trust was over coding palliative care. This was corrected and as a result the trust’s HSMR rose very quickly. The board became very concerned but the clinical staff did not believe there was a problem since they had not changed practice and only a few months earlier, and for over 10 years, the HSMR had been low. That medical director departed and those following (until now) have had difficulty getting the clinicians to believe that there is a problem. There was no mortality committee until 2014 and it was considered that medics did not look at their mortality routinely | |
| Work had been under way on sepsis for many years before the alert arrived. This was mainly focused around twice yearly training. There was a sepsis screening tool in A&E but this was not being used properly. The clinicians had wanted an electronic early warning scoring system for deteriorating patients but problems with implementing the electronic patient records meant that this did not happen. The trust has had an outreach team for deteriorating patients for 15 years. This team picked up that sepsis was not being recognised early enough and over the last 10 years they have put in place a campaign to improve this. However, it was known that the screening tools were not being used effectively | |
| Summary of response to first alert | There was a full investigation and an action plan was produced for the CQC. This had five action points including increased clinical engagement, improving coding and redesigning the discharge summary to enhance the coding of deaths. The CQC were not convinced and came back asking for more information, in particular that the trust had completed a case note review and evidence that the actions described in the plan had actually been implemented |
| Organisational learning and long-term response | The new medical director has been working to change the culture. In particular, challenging clinicians about their outcomes and their data, asking them if they want to defend mediocrity or actually improve care. The new CEO and the board have put mortality as a top priority for the trust |
| There is now a mortality lead who is an associate medical director, a mortality steering group, chaired by the mortality lead, and data were said to be getting better. Attendance at these meetings by clinical directors and leads has been made mandatory and linked to the consultant appraisal process. Attendance is now good. The trust has recently introduced a standardised approach to mortality reviews based on the approach adopted across the region. This uses the PRISM method and the NCEPOD scoring system. Consultants do not review their own deaths, but they review those of a colleague | |
| Coding has improved and so has belief in the data, although this has been hard won; indeed, some think that the trust is still blaming coding for the death rates being high. Now the coders work more closely with the consultants. The new medical director has started to work with Dr Foster to review and understand their mortality data including the CUSUM charts and to be ahead of the curve in anticipating alerts. The clear view is that the trust has not been using data well and therefore has not been aware of when mortality began to rise | |
| There is poor data about the implementation of the sepsis bundle (there is a twice-yearly audit but no regular data) so the medical director is now using a case-by-case approach to go through with staff to encourage them to see where things went wrong and to make improvements |
Relative risk profile
Figure 40 displays the relative risk profile for Sep-s.05 between January 2009 and January 2014. The green lines represent the date of an alert and the blue lines the date of the subsequent letter.
FIGURE 40.
Relative risk profile with alert (green)/letter (blue) dates for site for Sep-s.05.
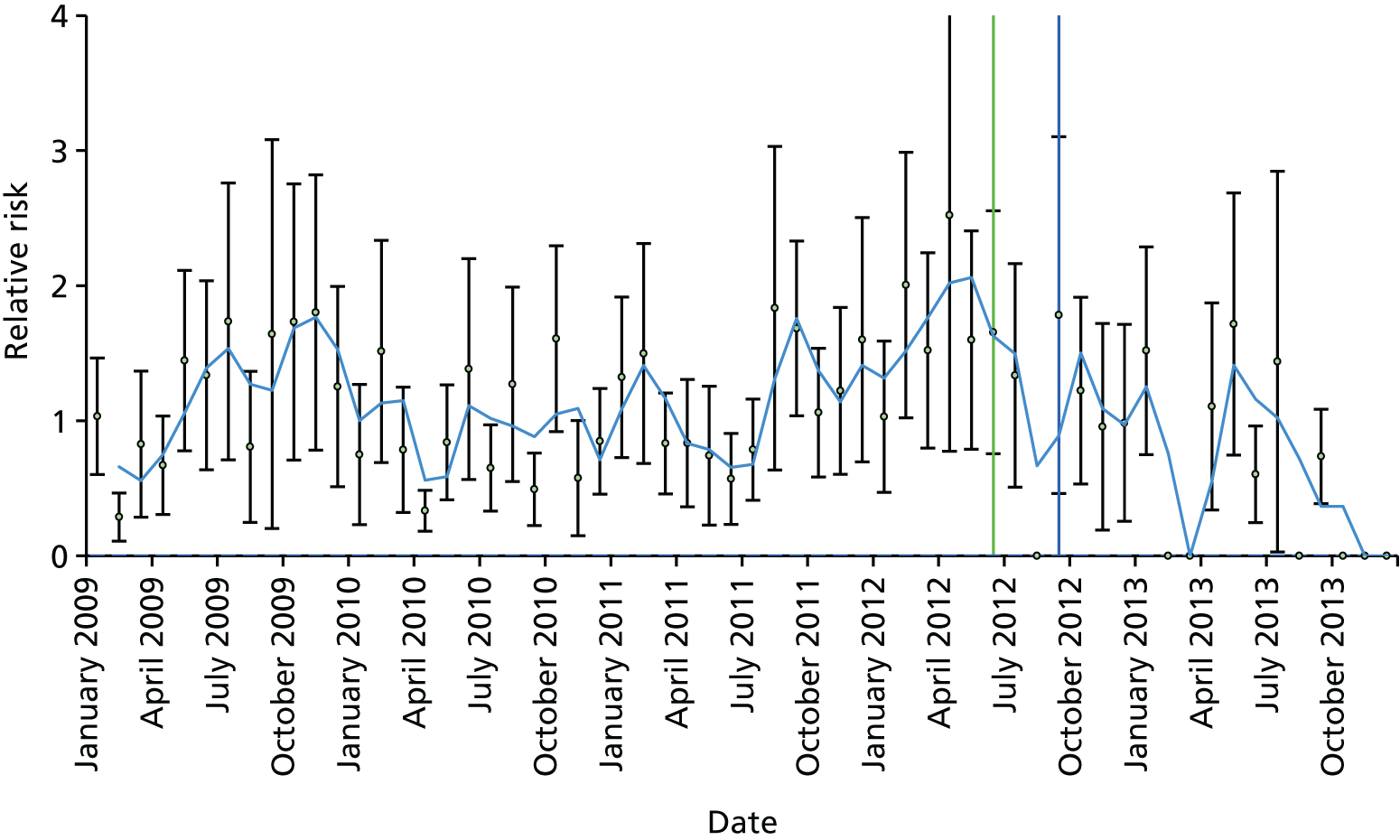
Sep-s.05 thematic analysis
Sep-s.05 is an acute NHS trust and had one alert for sepsis in June 2012. Analysis is generated from interviews with four members of the senior executive team and a consultant in critical care.
Trust preconditions before the alert
The trust had a very stable executive team and board for many years but around 2011 the CEO and medical director left. The trust then went through a period of turbulence until late 2014 and into 2015. During this period the trust had several CEOs, four medical directors and several different leads for informatics. The HSMR had been low for many years but one of the interim medical directors realised that palliative care was being over coded and he changed this. This led to a fast rise in HSMR and the clinicians did not believe it was a clinical problem, since all that had changed was coding. This led to a period of difficulty getting clinicians engaged in mortality data and mortality reviews. This is now beginning to change.
The trust’s financial difficulties led, in 2011, to 60 redundancies and a further 80 positions made vacant. A critical care consultant explained that at that time many good medical consultants left the organisation.
Information technology implementation failures
In the period running up to the alert, the trust experienced failures in implementing the electronic patient records system owing to persistent serious issues with usability. The trust’s annual report for 2012/13 indicated that this failure had had a significantly negative impact on the finances, staff workload and patient experience of care.
A critical care consultant highlighted that the patient records system had ‘failed appallingly’ and it had ‘cost lost a lot of money’. It was suggested that it had been introduced ‘in one go’ and that many clinicians had raised concerns about it before implementation but these were ignored and it was implemented anyway. At the time of data collection, the trust had no link between the PARS deteriorating patient system and the electronic patient records system.
Trust leadership culture
Most leadership changes arose after the alert, as the CEO, medical director, head of informatics and nursing director all stepped down. It was evident that in the period before this there was much distrust and antipathy towards the CEO. All respondents referred to poor clinical engagement with senior leaders and disagreement over the implementation of the IT-enabled patient records system. The associate medical director referred to the former CEO’s ‘dictatorial style’ and how he had indicated ‘it’s my way or no way’ and how that there was a general ‘disregard of what clinicians thought’.
Respondents acknowledged that the culture was closed, as communication, transparency of information and sharing of knowledge had been largely absent. The new nursing director drew attention to how from April 3013 board meetings were open to the public but that before 2013 they had been conducted in private. Newly appointed staff remarked on the lack of priority given to mortality. They highlighted how the ‘mortality steering group’ did not always meet owing to multiple changes in staff, and that trust routine attention to monitoring mortality was ‘ad hoc’ and had at times broken down. Reports to the board regarding mortality HSMR were perceived as inaccurate: ‘Then [the interim] medical director said oh I don’t know what you’ve been told in the past but that’s not true. HSMR is now 112. And so, you can imagine that the board’s anxiety was you know who do I believe and what on earth is going on here with mortality’ (nursing director).
A history of improvement work on sepsis
Respondents reported that the trust had commenced sepsis improvement work 14 years earlier. During this period consultants in critical care had championed these activities. More than 5 years before the first alert, sepsis improvements had been implemented on all wards and in A&E. It was conceded that some work was still needed in satisfactory use of the sepsis screening tool. However, much attention had been given to training staff about awareness and treatment of sepsis via a study day for staff every 6 months.
Trust experiencing severe operational pressures
In recounting the intense operational pressures, the associate medical director referred to how during the winter months the crude mortality rate had doubled, there had been failures in identifying deteriorating patients, failure to escalate patients, patient records were poorly written, the treatment of end-of-life patients was difficult and the discharge of patients was problematic as social care provision was poor. Hence, patients remaining in the hospital awaiting discharge were succumbing to hospital-acquired pneumonia.
Trust responses to sepsis alert
Mortality review after the alert
Only one respondent, the head of governance, present at the time of the alerts, was able to recount actions specific to the alert for sepsis and the subsequent response to the CQC letter. A critical care consultant working at the time of the alert recounted that he had been unaware of the alert.
The alert was received by the head of governance and validated by the business intelligence department using Dr Foster and CHKS analysis tools. An investigation took place and an action plan was produced. Specific actions identified in the trust response included: implementing the training of coders and junior doctors, improving quality of trust information and ensuring ongoing review of actions ensuring awareness, treatment and coding of sepsis. One of the actions included increasing clinical engagement in the coding of sepsis, training sessions for coders in assessing cause of death and using the electronic patient record, redesign of the discharge summaries to ensure all deaths have appropriate details of primary diagnosis. Teaching sessions were implemented for every new intake of junior doctors on coding for sepsis, awareness and treatment of sepsis and a review of each case of sepsis and production of a monthly ongoing action plan.
The CQC followed up on the trust’s response by asking for more assurance on actions taken in response to specific failings identified in the initial case note review. Hence, the trust was asked to identify actions taken in respect of the methodology they had used to identify problems in care. The trust was also asked to supply more detailed evidence on delays in treatment of sepsis, provision of medication and how the trust now complies with national guidelines in the treatment of sepsis.
Fragmented awareness of problems around mortality
The head of governance suggested that the trust divisions were aware of being outliers for mortality and, in some cases, had proactively identified these issues to the CQC. It was posited that the existing CHKS system was capable of identifying these problems. Hence, internal alerts were occurring. Despite this, some specialties noted very limited engagement. Notably, the sepsis lead indicated that she had been unaware of the MASS sepsis alert. However, more recently she did concede that internal systems and mortality review processes were identifying internal alerts.
Problems with trust-wide clinical engagement in mortality review
Clinicians generally highlighted limited engagement in mortality review. Although the alert and CQC follow-up had forced the trust to develop specific action plans and identify problems, clinicians generally appeared not to routinely engage in mortality review. The new medical director suggested that this was a result of their historically poor relationship and respect for past senior leaders.
Outcomes of sepsis alert
Changes in training of junior doctors focused on improving awareness of sepsis and improving clarity in case note write-up appear as a direct result of the alert response. However, attempts to improve and integrate the mortality review process appeared not to have been affected by the alert. Clinical engagement in mortality review was not affected by the alert as clinicians generally appeared disenfranchised owing to their relationship with senior management.
Parallel evolution of institutional focus on mortality reduction in sepsis
It was suggested that major structural changes had occurred in the trust as a result of intervention by Monitor. This had led to changes in senior leadership, who had acted ‘as a new broom’ providing an ‘overhaul of trust governance’. The new medical director suggested that assurance of high-quality care needed to be facilitated so divisional directors now sit on the mortality review group. Likewise, clinical directors are invited to the trust board meetings to provide assurance and contextual understanding of mortality and trust processes. The overhaul of governance led to the creation of five directors of clinical services with service managers and clinical leads for specialities sitting beneath them.
The three new associate director roles were created for standards, patient safety and revalidation. In the trust hierarchy, these sit beneath the medical director. One associate medical director, responsible for standards, clinical effectiveness and research, has responsibility for mortality review. Challenging clinicians with the data has been used as a method from forcing clinicians to engage and take ownership of mortality.
Critical care consultants championing sepsis improvement
Consultants in critical care highlighted how their speciality had engaged for more than 5 years with ICNARC. They noted that their participation educated them regarding improvement on critical care practices and developed them professionally. The critical care consultants appeared to be the spearheads for improvements in sepsis awareness and treatment. They had worked for many years in isolation without substantive leadership support. Only recently has this changed. They identified core problems in trying to gain early intervention of antibiotics related to a shortage of nurses on the wards and with junior doctors afraid to report effectively to their consultant their early suspicion of sepsis.
Case study 07 (Sep-m.07) narrative summary
Overview
Sep-m.08 is an acute trust serving a population of approximately 900,000. It had three sepsis alerts, in November 2009, September 2011 and February 2012. Analysis is generated from interviews with one former medical director, an interim medical director, one information manager and two critical care consultants and is informed by trust documentary sources (Table 25).
| Relevant history and context at time of first alert | The trust was involved in the Keogh review. It was considered by interviewees that this was misunderstood as an investigation purely into mortality. It was suggested that, before the alerts, a central co-ordinating team or mortality review group examined trust mortality. Despite this, respondents reported that mortality investigation was fragmented across the trust and it was noted that senior leadership was disconnected and had not ensured that learning around mortality review was shared across the trust |
| Summary of response to first alert | The alert would be passed on to the medical director from the CEO. The medical director would undertake a case note review and then pass the findings onto the board and then the quality committee and finally to all of the trust’s consultants. The coding team would review its own coding and feed this back to the medical director. For the sepsis alerts this raised issues surrounding over coding of the condition. There was no sepsis lead in post at the time but retrospectively the sepsis lead feels that the case note reviews of the medical director did not provide enough information. The Sepsis 6 bundle was implemented as result of the alerts. The sepsis lead felt that previous case note reviews were not adequate regarding sepsis |
| Organisational learning and long-term response |
A mortality review assurance group was set up as a response to the Keogh review and general issues associated with mortality, chaired by the CEO. External reviews have been undertaken in a number of clinical areas so to provide assurance and identify problematic areas There has been an increase in available mortality data for review and analysis. A mortality dashboard is now in use in a supportive function. A coding review group has been set up by the medical director in order to understand any issues with coding (e.g. overcoding). The sepsis bundle has been implemented |
Relative risk profile
Figure 41 displays the relative risk profile for Sep-m.07 between January 2008 and January 2014. The green lines represent the date of an alert and the blue lines the date of the subsequent letter.
FIGURE 41.
Relative risk profile and alert (green)/letter (blue) dates for Sep-m.07.
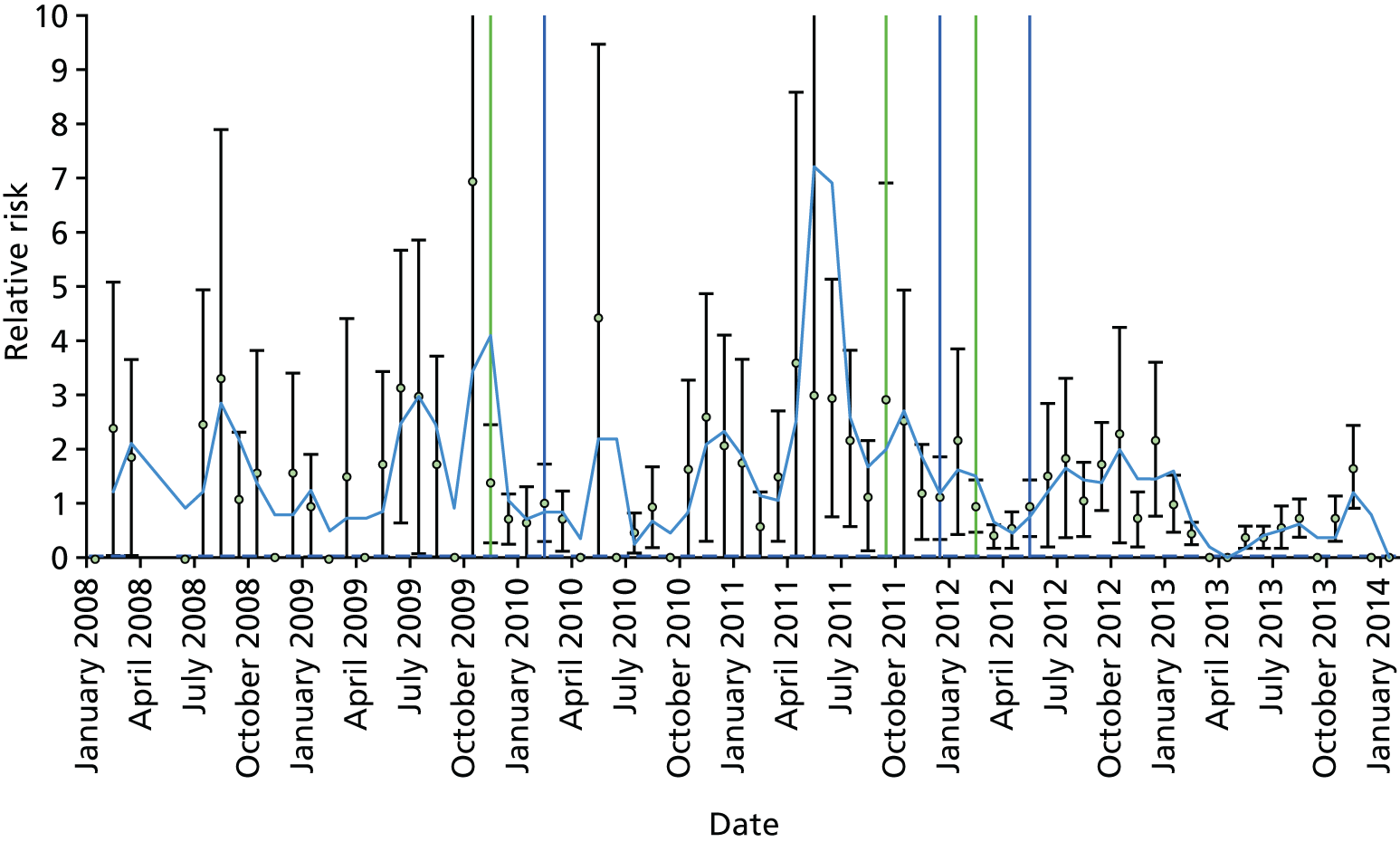
Sep-m.07 thematic analysis
Fragmented structures and processes across trust levels
It was suggested that, before the alerts, a central co-ordinating team or mortality review group examined trust mortality. Despite this, respondents reported that mortality investigation was fragmented across the trust and it was noted that senior leadership was disconnected and had not ensured that learning around mortality review was shared across the trust. Most review work occurred in certain specialities such as critical care, ED and the surgical division. While in medical wards there was less exploration and attention given to mortality. The mortality review group selected random case notes per month and reviewed them using a standard template or pro forma.
Catchment
Most respondents highlighted how community care processes had impacted on mortality. They suggested that terminally ill patients were sent to the hospital to die. They highlighted that the trust lacked a developed palliative care system staffed by palliative care consultants. A critical care consultant drew attention to how the hospital was not supposed to be a hospice and that patients were admitted with ‘do not resuscitate’ orders and they died within 24 hours, which had implications for the coding of mortality.
Role of informal opinion leader championing mortality investigation
All respondents remarked on how the former medical director, now a consultant in critical care, had worked alone over many years promoting and investigating trust mortality. The trust has developed IT-enabled systems for logging patient conditions. This enabled visibility of patient deterioration and timely intervention.
Retention and recruitment problems
Retention and recruitment problems were widely reported. It was suggested that there were not enough specialist doctors and consultants. Difficulties also arose in recruiting clinical coders as they needed to have complex competencies in understanding clinical conditions and coding procedures. It was considered by interviewees that the trust was bottom of the ‘feeding chain’ as far as resourcing of care was concerned. The plight of the trust was compared with teaching hospitals that were better resourced as a far as medical staff.
Trust responses to sepsis alerts
It was difficult to identify responses to each alert for sepsis as only one respondent was able to recall the trust response specifically to only one alert. This occurred because of changes in staffing over the last 5 years. Increased awareness of mortality was closely linked to the CQC inspection and special measures investigation. Hence, cumulative regulatory pressures worked in concert to drive trust strategy in addressing mortality. In identifying reported responses to the alerts for sepsis, it is conceded that these responses were suggested by only one respondent and was reported as follows.
Proactive monitoring of mortality
The former medical director identified that the trust had already identified that there was a problem with mortality for sepsis before the last alert (2013) and had already started to review case notes before receiving the CQC letter. He reported that he had been monitoring trust mortality over a long period and had much experience of using Dr Foster tools and the trust CHKS system.
A centralised approach
A centralised response process was described, whereby the review of case notes was confined to the mortality committee members and information concerning outcomes of the response were passed to the consultants across all specialities. The process started with the CEO receiving the alert passing it to the medical director who co-ordinated the response. A review process was initiated of 60 cases notes by the head of coding and the medical director. Discussion and review of some of the case notes was undertaken by the mortality group, comprising consultants from ED, critical care, surgery, medicine, palliative care and a clinical audit lead. From this investigation was undertaken of coding and a reports produced of review findings and action plans for the trust board, quality committee and clinical governance committee. A report would also be sent by the medical director to all consultants explaining the alert, the results of the review and the actions plan.
Identifying problems with coding and care
Case note review identified errors in coding for sepsis and problems in palliative care. This related to elderly patients admitted from nursing homes with ‘multiple bed sores who were basically coming to the end of their lives’. Death was thought not to be preventable even when they were treated well. Overall, it was reported that there had not been any errors in care of these patients.
Emphasis was placed on thorough investigation of the alert rather than immediately blaming it on poor coding. It was noted that some trusts appeared to respond to alerts by adjusting their coding and ‘manipulating the data’. It was viewed as an ‘unemotionally intelligent thing to do’ and in this trust the approach was to be ‘honest’ with coding. An action-focused approach was recognised as the most useful. The alerts were seen as making clinical staff aware of the problem and then mobilising the trust to act effectively.
Outcomes of sepsis alerts
The alert identified errors in coding sepsis and led to awareness of sepsis and led to changes in coding, and hence in correcting the coding mortality for sepsis the coding of acute kidney injury went up. Implementation of the Sepsis 6 care bundle was recognised as a direct consequence of the alert and CQC letter. Case note review identified high numbers of patients in the palliative care pathway. As result palliative care consultants were recruited and the trust was able to cope better with in the palliative care pathway. Nurses also offered a 7-day service in palliative care.
Parallel evolution of institutional focus on mortality reduction in sepsis
It was suggested that the trust had implemented many strategies in addressing sepsis mortality and mortality in general. This was driven by a host of regularity pressures resulting from the trust being identified as an outlier for SHMI and HSMR mortality indicators. These included the Keogh review (2013), special measures (2013) and CQC inspection (2014). Respondents reported how this external scrutiny directed action on addressing mortality failures. For some this scrutiny was a distraction away from looking at key problems concerning quality of access for patients. However, it was conceded that that external scrutiny ‘had raised our game in terms of actually understanding our services’ (deputy medical director) and it was noted that improvements in care had resulted from this scrutiny, especially in understanding and using data. However, it was felt that intensive media interest was demoralising and unfair.
A drive in providing information technology-enabled quality information for trust decision-making and reporting
It was as noted that the focus on information was also driven by a host of statutory reporting. Gathering data and undertaking analysis of mortality has become routine. It was viewed that the trust was becoming ‘data rich’ using IT-enabled CHKS, HED and Dr Foster tools and accessing internal trust data via the electronic patient record, the mortality monitoring system, safety thermometers, ward dashboards and scorecards.
External engagement providing expertise and oversight in tackling trust mortality
The trust engaged in extensive external engagement that supported improvement in quality of care. The reviews focused on problems areas such as COPD, sepsis, ITU and mortality review. For example, reviews were undertaken by the Royal College of Surgeons and the local critical care network. In addition, experts on mortality statistics and reporting from academic institutions and experts in quality improvement specifically for sepsis were called in to help. It was suggested that external reviews of ITU had changed handover procedures and the writing of case notes.
Accessing, triangulating and comparing Dr Foster mortality information
A focus on accessing triangulating and using mortality information also drove improvement in mortality. Interviewees identified how they accessed Dr Foster data to identify in-depth mortality and understand how coding fed into mortality indicators. Comparison of mortality indicators across trusts also was useful in identifying trust problems in coding, for example. Likewise, other trusts that had achieved a massive turnaround in mortality could be identified and approached so as their learning could be accessed. In exploring data across a number of trusts, one respondent reported that they thought that it was evident that some trusts were ‘gaming’ the coding of mortality.
It was interesting to note that one clinician highlighted that accessing Dr Foster data had not been promoted by the trust and he had accessed them because of his own interest.
Senior leadership prioritising the development of formal structures and systematic processes to support mortality review of all deaths
Trust leaders were reported as playing a key part in prioritising the development of formal structures to support mortality review of all deaths. The mortality review group was set up, chaired by the CEO. This had representation from across trust divisions and external bodies.
A system was developed whereby every death was reviewed and graded according to three levels. Level 1 considered the death certificate, coding, coroner report, palliative care involvement, end-of-life pathway and the predictability of the death. Level 2 focused deeper and considered, for example, diagnosis, elective/non-elective admission and patient safety incidents. Level 3 was an alert and CQC letter requiring a detailed review.
Strategy for information technology-enabled monitoring of mortality and tracking of sepsis driven by informal champions
A host of factors including external pressures, exploration of how other trusts monitored mortality and the actions of individual committed senior clinicians led to the development of an IT-enabled mortality monitoring system or mortality dashboard. This drew from existing IT systems and facilitated trust-wide awareness of deaths and investigations. It was suggested that this drove clinician involvement as it also provided surveillance of their role in the patient pathway. The trust is also developing an IT-enabled system for tracking patients with sepsis.
Case study 08 (Sep-m.08) narrative summary
Overview
Sep-m.08 is a NHS foundation trust that alerted three times for sepsis during our sampling framework, in 2008, 2011 and 2012 (Table 26).
| Relevant history and context at time of first alert | Leading up to the first alert the trust explained high mortality as being due to the age of the patients and the deprivation in the local population; clinicians in the organisation were not made aware of alerts; poor care was known about by clinicians but not spoken about. The findings in the CQC inspection report, conducted owing to high mortality figures for the trust, did not come as a surprise to most clinicians. At that time there was no clinical engagement in coding. A sepsis group was set up around the time of the first alert but was not seen as particularly effective |
| Summary of response to first alert |
A mortality group was in existence in 2009 and there had been a review of 62 deaths. Alerts would come in to the CEO, who would discuss them with the medical director, who would talk to the clinical director of the area concerned. The approach was described as trying to explain why a patient died rather than to identify areas for improvement. Only a few senior clinicians were involved in the mortality group so what it did was not widely known about After the second alert an external nurse consultant was brought in to advise and help with sepsis reduction. Around this time the chairperson of the sepsis group changed and a whole new approach started |
| Organisational learning and long-term response |
There have been many changes since 2013, including a new medical director; the start of external reviews of mortality; a new quality improvement programme; a programme to change the culture of the organisation; and much more focus on mortality from the board. Alerts now undergo a review of coding and, simultaneously, a review of clinical care through case note review. When the second alert came, 20 cases were reviewed and deficiencies were identified There are morbidity and mortality leads in each specialty. The mortality group is well attended by these leads. There is a trust mortality lead who looks at the data regularly and is now able to anticipate alerts so that case notes can be reviewed in advance and improvements can be made A huge amount of work has been done to improve sepsis identification and care. A quality improvement programme has been under way for some time using PDSA cycles An e-mortality form is now completed for all deaths by the consultant responsible for the care of the patient. The coding manager then codes all deaths from electronic records, pre-populated with comorbidities. There is still a view that the high mortality locally is due to the local population and the fact that the trust has a palliative care unit |
Relative risk profile
Figure 42 displays the relative risk profile for Sep-m.08 between January 2009 and January 2014. The green lines represent the date of an alert and the blue lines the date of the subsequent letter.
FIGURE 42.
Relative risk profile and alert (green)/letter (blue) dates for Sep-m.08.
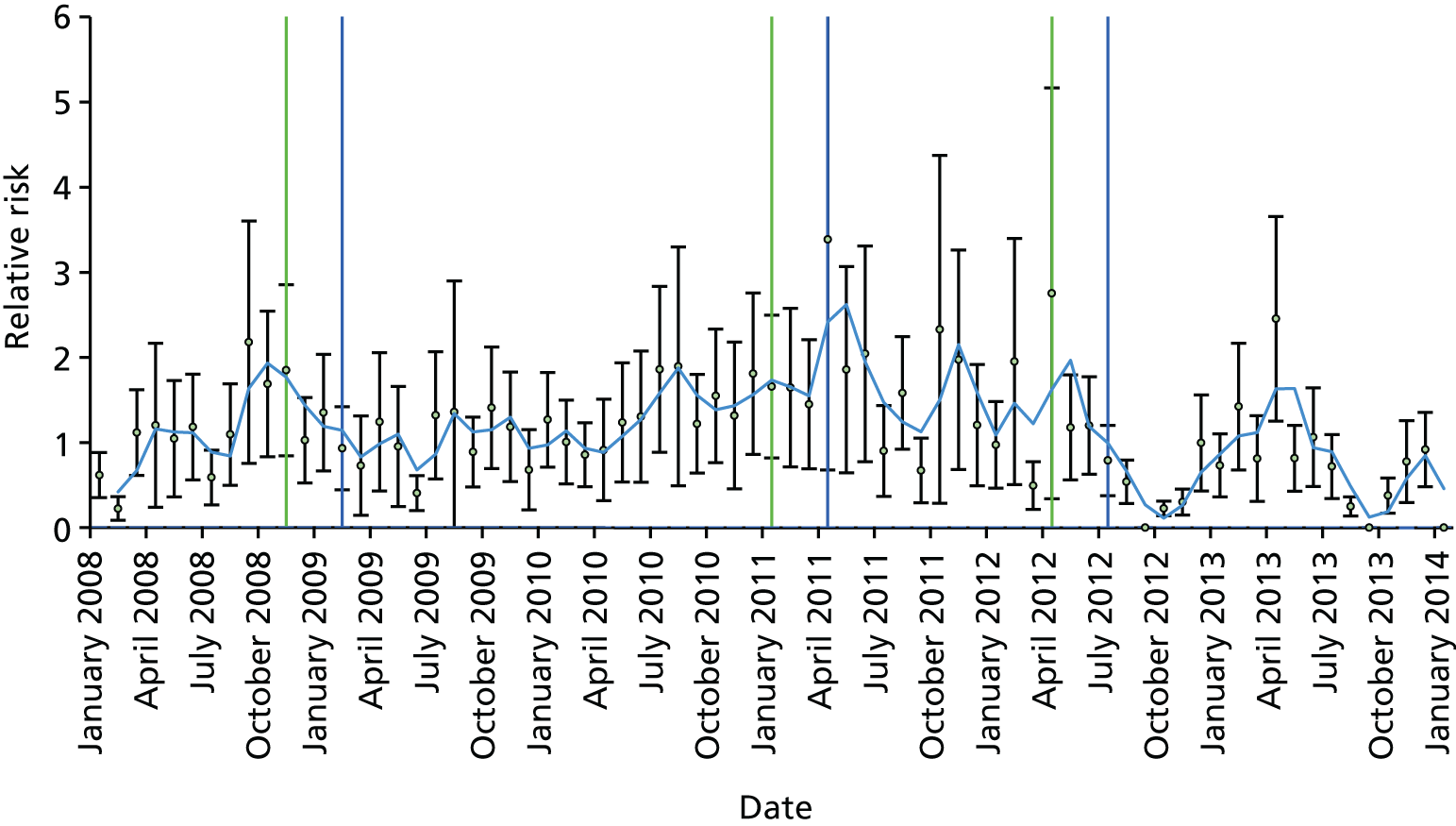
Sep-m.08 thematic analysis
Analysis is generated from interviews with three members of the executive team, three clinicians specifically tasked with sepsis improvement, the mortality lead and the coding manager. It is also informed by trust documentary sources.
Trust preconditions before the first alert
Issues relating to the trust
Senior leaders described being surprised by receiving the target alerts and said how it was considered that the local population age demographic was an important influence on the trust receiving the alert for sepsis. The trust had been involved in a planned merger with a neighbouring trust, and a lot of work was done in the lead-up to this. However, in November 2011 the merger was blocked. In 2013/14 the trust had to find £10M of savings. In the year before this it had been in financial balance.
Regulatory pressures
This trust experienced strong regulatory pressures from the Keogh Review and CQC. It was placed in the highest risk category by the Keogh review in 2013 but was not included in the top 14 visited by the Keogh team. The trust has been inspected five times by CQC since it was registered in October 2011. The medical director identified that the CQC inspectors had produced a ‘damning report’. Trust clinical directors were reported as perceiving this as a ‘light bulb moment’ stimulating a major turnaround.
Trust infrastructure to support sepsis improvement work
The medical director highlighted that quality improvement work had been very informal before the first alert. However, the process of mortality review had actually started before the CQC visit and had been part of a quality improvement project that had been presented nationally. The trust had implemented an IT system (Vitalpac, London, UK; http://vitalpac.com) to support the recording of patient observations. This enabled the identification of patients who are deteriorating (sepsis and other conditions) and requiring of critical care outreach services. Interviewees were aware that there was a sepsis group set up and chaired by a surgeon at sometime around 2009. It was noted that focus was placed on identifying problems around sepsis rather than following through in developing solutions. It was viewed that some plans had been actioned but that these were ‘ad hoc’ and not part of a systemised approach.
Absence of clinical engagement in coding and lack of standardisation in coding
The coding manager highlighted how there was no clinical engagement in coding around the time of the first alerts. Likewise, coding generally was perceived as an issue and lacked rigour. Poor attention and lack of standardisation of coding meant that the trust has had phases when particular causes of death were regularly put on the death certificates.
Trust responses to sepsis alerts
Senior leaders prioritise case note review and start to formalise up mortality group activities
A mortality group comprising the medical director, the associate medical director, the risk manager and the audit manager led a review of 62 sets of case notes. Relevant specialists were also asked to present to the mortality group regarding learning points and potential areas of improvement. Initially, the trust used the Global Trigger Tool and there was a sense of urgency in needing to know why the organisation was alerting and what this meant for patient care.
Clinical trust-wide engagement in case note review
Senior leaders in the mortality group assigned clinical reviews to clinicians, as well as reviewing the report against the number of expected deaths. Clinicians then presented recommendations back to the group and the identified issues are forwarded on to other relevant committees across the trust. Mortality leads within specialities were responsible for disseminating information across their clinical department. External reviews would also take place as a response to an alert.
Greater emphasis on the sepsis group and operationalising the action plan
In response to the second alert for sepsis (2011), there appeared a greater emphasis on operationalising and resourcing the action plan. Again, a review was undertaken, this time of 20 case notes. An action plan was identified. The sepsis group was reformed with a new lead clinician and an external nurse consultant was brought in to help formulate an action plan and help with education. This started new approach in tackling mortality around sepsis.
Greater integration of mortality group activities with trust-wide committees, quality improvement processes and external engagement
The medical director now chairs a mortality group which feeds in to the health-care assurance committee, which is a subcommittee of the board. Alongside the mortality group is an improvement group. Quality improvement methodology has been applied to sepsis as a result of the target alerts. This was thought to be a more systematic way of approaching things. The clinical management board reviewed the work being done in relation to sepsis. There have been noted improvements in HSMR since these changes were implemented.
Senior clinical involvement in mortality review and improvement work around sepsis
It was thought that alerts now receive attention and engagement from senior clinicians. It was noted that there was a need for more nursing involvement in mortality meetings in order to increase wider engagement. Time allocation for mortality review by clinicians was considered onerous especially in some specialities. It was noted that time for this needed to be factored into formal work load allocation. Consultant engagement in coding was reported as greatly improved especially since the CQC inspection.
Mobilising trust-wide learning using sepsis alerts
Efforts were made to mobilise learning throughout the trust by using MASS sepsis alerts as a focus for learning. Overall, respondents suggested that there was a need for more education on the front line in order to change practice. The CEO believed that there was a need to spread learning from mortality alerts across the NHS. For example, learning from other hospitals that have alerted in the same areas could provide great learning opportunities. Despite all the efforts to disseminate information generated from the e-mortality review form in the newsletters, undertaking grand rounds and training, it was considered difficult to ‘land the learning’.
A strategic commitment to developing improved data quality
A commitment to developing improved data quality around sepsis mortality reporting became a priority. This involved improving coding criteria, triangulating data and systemising monitoring of suspected sepsis in the care pathway. Difficulties in the coding of sepsis were tackled as the coding manager described standard methods for coding of sepsis. Validation of coding for sepsis arose only if the patients’ blood results identified that there is sepsis and the doctor confirmed this in the case notes.
A focus on long-term improvement actions rather than focusing solely on alerts
Overall, trust staff reported a focus on long-term improvement actions rather than just focusing on alerts. The process of comparing actual alerts with expected alerts was introduced as a result of receiving the alerts. It was accepted that mortality alert numbers were important as they affected the trust’s reputation. However, it was also highlighted that long-term improvement work that should be prioritised. The later alerts appear to have influenced the complete overhaul of the sepsis group and sepsis campaign.
Outcomes of sepsis alerts
Alerts for sepsis provide a focus on use of QI methodology applied to sepsis
QI methodology has been applied to sepsis as a result of the target alerts. This was thought to be a more systematic way of approaching things.
Improvements in mortality review processes
All deaths are now reviewed. The medical director remarked on how trust mortality review processes had improved over the last year. Similarly, follow-up after the review was deemed effective. Now doctors are stopped from working if there are concerns following a mortality review.
Parallel evolution of institutional focus on mortality reduction in sepsis
Although the alerts for sepsis appeared to provide focus on sepsis mortality review, it was also noted that other influences drove a parallel evolution of improvement in mortality for sepsis.
The cumulative effect of external pressures and changes in trust leadership influence development of a proactive cultural change in tackling hospital mortality
Overall, mortality alerts in general and the actions of other external organisations (CQC, CQUIN, ombudsman, Mid Staffordshire NHS Foundation Trust and media exposure) were thought to have contributed to a cultural change and new proactive approach to dealing with mortality.
Engagement with external organisations to access knowledge and learning of QI around sepsis
The CQC identified that the trust was ‘particularly defensive’ concerning mortality and suggested that the trust ‘don’t rely on your own clinicians to review mortality’ (medical director). This prompted the trust to engage with external organisations to review trust services, for example external review of the heart failure service together with an internal examination of the service against national standards. It was believed that mortality alerts form just one part of intelligent monitoring.
Investment in QI methodology
The CQC negative report also appears to have galvanised a coalition of trust leaders to actively promote and champion the use of QI methodology to enable continuous improvement in care. The trust has defined their QI methodology and has appointed a director for improvement and a director for organisational development (the latter working on culture change). Their aim is to move from having ‘champions’ for a topic area to having active improvement work everywhere. QI methodology is now in use across the board. A systematic approach was thought to be important as, unfortunately, enthusiastic individuals alone are not enough to make a lasting change to mortality. The communications team has become more involved in the improvement process and this has been viewed positively.
Investment in IT infrastructure improving: coding, communication, monitoring and information sharing for development of high quality mortality data
The trust has focused on improving IT infrastructure by developing an e-mortality form that is generated for every death and sent to the relevant consultant to fill in. It was noted that coding of mortality is generated from the electronic record which is pre-populated with comorbidities and not from case notes. This process for coding has been externally audited. The coding manager reported that coding has improved as a result of updating to electronic forms.
Integrated structures and processes supporting mortality review
The mortality review process has been overhauled. Now every death is reviewed by the clinician who cared for the patient and an e-mortality form is completed. The LIPS project and e-mortality review form led to the introduction of a mortality lead for each department, quarterly mortality meetings for each department and involvement of the chairs in the trust mortality group meetings. Irrespective of alerts, different specialties review clinical care and present findings to the mortality group.
Case study 09 (Sep-m.09) narrative summary
Overview
Sep-m.09 is a large acute teaching hospital. The trust comprises two hospitals.
Relative risk profile
Figure 43 displays the relative risk profile for Sep-m.09 between January 2009 and January 2014. The green lines represent the date of an alert and the blue lines the date of the subsequent letter.
FIGURE 43.
Relative risk profile and alert (green)/letter (blue) dates for Sep-m.09.
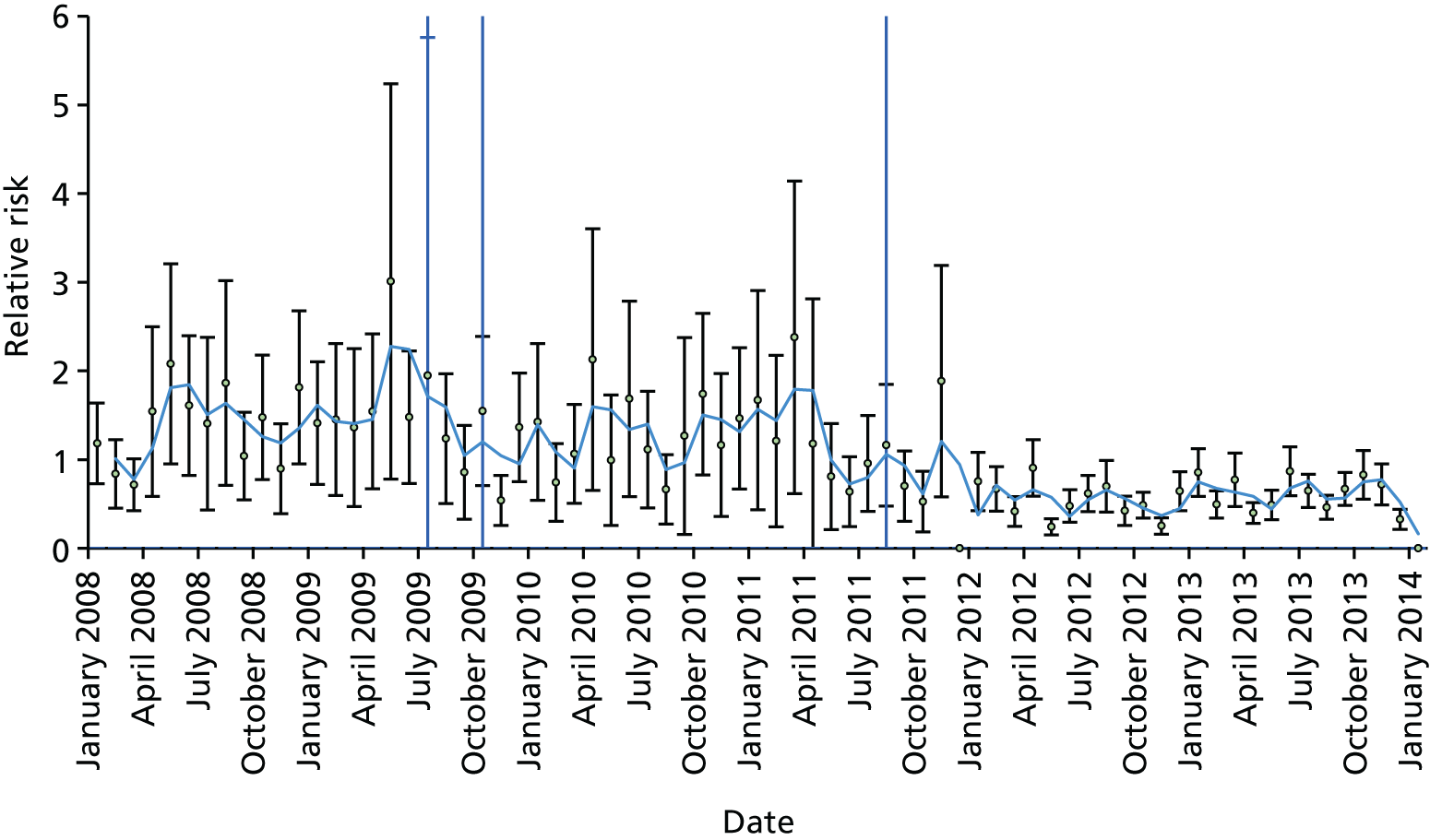
Sep-m.09 thematic analysis
Sep-m.09 is a large acute teaching NHS trust comprising two hospital sites. The trust alerted three times, most recently in August 2011. They had alerted twice before this period in April 2009 and July 2009 (although the second letter was withheld owing to its proximity to the April alert). Analysis is generated from interviews with three members of the senior executive team, one coding manager, the clinical effectiveness manager, one clinician responsible for mortality review and one clinician with responsibility for sepsis improvement (Table 27).
| Relevant history and context at time of first alert | The trust had two serious incidents of young patients dying from sepsis in 2009 and this kickstarted a whole programme of work around sepsis. Coding was seen as a backwater and no one took any interest until it was linked to the trust’s income. In 2014 the trust had a deficit of £4M |
| Summary of response to first alert | After the deaths from sepsis, a working party was put together (same time as the alert) and the sepsis trust was brought in to also help with the action plans and implementation. A sepsis campaign was developed. There was a case note review and a review of coding. A protocol was written that shifted sepsis away from being a definitive diagnosis but rather to suspected sepsis. This allowed the principle that sepsis could be identified by anybody among the health-care team, and not just clinicians who were primarily involved in diagnosing |
| Organisational learning and long-term response |
The trust has had a mortality review committee for about 7 years. Following an overhaul, the committee now it meets for 4 hours twice per month. There is also a clinical lead for mortality and mortality leads in each division and specialty. All deaths are now reviewed by a consultant in the specialty who grades the death using the NCEPOD categories from A to E. In code A the care is deemed adequate and, at the other end of the spectrum, E means there was a serious failure of care. All those graded E have a full investigation at trust level and are reported to the mortality committee. Those graded B–D are reviewed in the specialty/division and action for improvement is taken locally The mortality team look at the alerts and the surrounding data: days of the week, pre-hospital care, availability of post-hospital placements, discharge procedures, etc. However, sometimes it is hard to find the cause of high mortality. The clinical lead for mortality explained how important he felt it was to understand the mortality figures in relation to the pattern of services the trust offered and the make-up of the local population. In the last 18 months the view represented was that the majority of alerts were coding and not care issues The trust has implemented the Sepsis 6 bundle. Information is regularly presented at the grand rounds. A new approach called ‘check and challenge’ has been introduced to check and challenge staff on their knowledge about sepsis, to keep it at the forefront |
Trust preconditions before the alert
Catchment characteristics
Respondents identified major deprivation in the trust catchment population. It was noted that the trust was one of the busiest major trauma centres in the country, taking many tertiary referrals. Interviewees described how these two factors drove up their HSMR. For example, this hospital never closes its doors, and takes all cases when other hospitals are full.
Coding
Coding was described as being a backwater, with no one interested in what went on in the coding department. It was seen as useful for information purposes when it was tied to funding. The mortality lead drew attention to difficulties in trust capabilities in coding. This was linked to reductions in staffing. It was noted that quality in coding was essential as coding errors had an impact on the usefulness and validity of alerts.
Long-term engagement in sepsis improvement work
The trust sepsis lead recounted that the trust had for many years been active in responding to national campaigns focused on sepsis awareness. Moving to a new hospital site in 2006 was linked to the implementation of an electronic, physiological patient observation system. The trust participated in the ‘Think Sepsis’ campaign.
Sentinel events leading to a systematic and forensic process
Coinciding with the first alert in 2009 the trust experienced two sentinel events linked to failings in recognising sepsis in the ED. These events and the alert led to organisation of a working party to review these deaths and, after this, the implementation of a system to review all deaths.
Trust responses to sepsis alerts
Only two respondents knew about the trust response to the alert in 2009. Other respondents identified the generic processes regarding how alerts were handled.
Mortality alerts a ‘smoke signal’ promoting investigation
The alerts were seen as ‘smoke signals’ and something to promote investigation, but it was conceded that in a complex organisation this can mean that things are looked into that are not relevant: ‘The problem is, you can be distracted by certain alerts and you go looking at things that don’t warrant attention, but you’ve still got all the stuff that does warrant attention in the midst of it. So the clarity of the signalling is a problem’ (clinical lead for mortality).
Alerts used as a way to promote clinician engagement in case note review
It was suggested that clinicians in responding to the specific alert were fully engaged in discovering if there had been care problems, and if so, why these had happened. However, clinicians were often less engaged in case note review overall, which interviewees attributed to doctors having problems in accepting the validity of mortality data. It was suggested that presenting the alert as ‘a warning or a flag’ was a useful way for gaining clinician engagement in mortality review.
Difficulties in time allocation to case note review
Respondents suggested that the alerts had mainly identified problems in coding and that the process of case note review and investigation was resource intensive. Formally responding to these alerts and other regulatory organisations was considered onerous.
Outcomes of sepsis alerts
Changes in clinical practice regarding diagnosis
It was generally understood that early intervention of antibiotics in treatment of sepsis was necessary; however, diagnosis by doctors was difficult and often slow. Changes were made which allowed treatment of sepsis to proceed if there was a suspicion of sepsis rather than a definitive diagnosis. This allowed the wider health team to have input in deciding on treatment. It was suggested that as nursing staff spent more time with the patients on the wards, then their monitoring input could facilitate more timely intervention.
Innovative sepsis awareness training
A training programme was introduced. This used social movement theory to spread knowledge around sepsis awareness. A concise programme was devised covering the main learning points and distilled into five or six power point slides. This was delivered in less than 10 minutes. Those trained were then responsible for training 10 more staff. This led to 1000 staff being trained within 6 weeks. The programme was supported by more conventional marketing of sepsis awareness using posters, boards and leaflets.
Challenging clinical practice and rewarding good clinical practice
Senior clinicians checked that the environmental items facilitating the management of sepsis were in place. They also then orally tested clinicians’ knowledge of sepsis training. This process was known as ‘Check and Challenge’. Good performance in this process was rewarded in the form of awards for outstanding care. This often led to competition between wards.
Changes in service design relationship between the emergency department and acute medicine
Changes in service design and the relationship between the ED and acute medicine were reported as an outcome of the alert and sentinel events. A holding area was created allowing patients to be triaged from outside into this holding area was put in place. This enabled patients to be fast tracked. GPs sent patients to one area and ambulances to the other, preventing trolleys with patients waiting in corridors and reducing patient waiting times.
Changes in coding guidelines
As a result of the alerts, it became clear that the coders did not know how to code sepsis, and so guidelines on this were written.
Parallel evolution of institutional focus on mortality reduction in sepsis
Universal case note review a routine process
Routine case note review of all deaths has been implemented. A report is produced every 2 weeks. These are discussed in the mortality committee, which meets every 2 weeks for 4 hours and scrutinises case note reviews, Dr Foster mortality data and other trust mortality indicators.
Trust-wide integration of mortality review processes
Respondents identified the current review process where mortality alerts come in to the CEO and are sent on to the chief medical officer (who refers it to the mortality lead and mortality review committee chair) and to the clinical effectiveness manager (who co-ordinates the reviews). There is also a parallel coding and case note review. Mortality review follows a detailed integrated and systematic process. The mortality review committee comprised the three assistant medical directors, the medical director, the head of governance, the head of coding and the nursing director, the mortality lead, two mortality administrative staff, representatives from the divisions and specialties and the Dr Foster representative. It was noted that all clinical leads were expected to attend. The CCG chairperson also attends the mortality committee.
Mortality profiles are produced for each specialty from the Dr Foster data and these also include data on the time of day, day of week and staffing levels, etc. These are considered important as each specialty contributes in one way or another to the overall trust HSMR so the chief medical officer wants all specialties to work to reduce mortality, not just those that are high.
There is a monthly report to the quality governance committee, which is a subcommittee of the board. There is then a 6-monthly detailed report to the board.
Persuading consultants to engage in mortality review
Consultants pay an important role in mortality review. Gaining their participation was viewed as problematic as it was felt that they should not review their own deaths. It was noted that surgeons were the most recalcitrant in doing this. However, using allocating SPA (Supporting Professional Activity – payment for non-clinical activity) was a way of maintaining their support.
Information technology-enabled forensic mortality review and patient monitoring
The entire mortality review process is electronically enabled. When a patient dies, the IT-enabled mortality review process generates a primary e-review form that is sent to the consultant responsible for the patient. The consultant is expected to access the case notes and complete the form within 30 days. Follow-up e-mail reminders ensure that this happens. After reviewing the case notes the consultant completes the e-mortality review form and grades the death A–E: A if the death was entirely unavoidable, to E, which denotes a serious incident. E is tackled immediately by the serious incident group and a full review is undertaken and presented to the mortality review committee. If care is graded B to D then the case is looked at in detail at the specialty-level mortality meetings. The clinical effectiveness manager oversees the mortality review process and ensures that local clinical guidelines are in place and comply with National Institute for Health and Care Excellence guidelines.
Continuous IT monitoring of patients in real-time serves to communicate changes in patient condition enables speedy escalation in treatment. This was evidenced by clinicians regularly imputing into the NEWS and OPERA systems. Oversight of NEWS is conducted daily by the sepsis outreach team.
Continuous progress with sepsis improvement
The trust continuously updates its sepsis campaign and liaises externally through CQUIN support. Recent attention focused on development of the ‘do you speak sepsis’ campaign. Key to identifying sepsis early is now the identification of ‘altered mental states’.
Case study 10 (Sep-m.10) narrative summary
Trust overview
Sep-m.10 is an acute NHS trust that covers three sites, including the two main hospital sites: Sep-m.10 hospital 1 and Sep-m.10 hospital 2. The top team was stable before and during the alerting period. The current CEO has been in post since 2008 and the medical director since 2005. The trust serves a population of approximately 610,000. It has had four alerts for sepsis since 2010.
Relative risk profile
Figure 44 displays the relative risk profile for Sep-m.10 between January 2009 and January 2014. The green lines represent the date of an alert and the blue lines the date of the subsequent letter.
FIGURE 44.
Relative risk profile and alert (green)/letter (blue) dates for Sep-m.10.
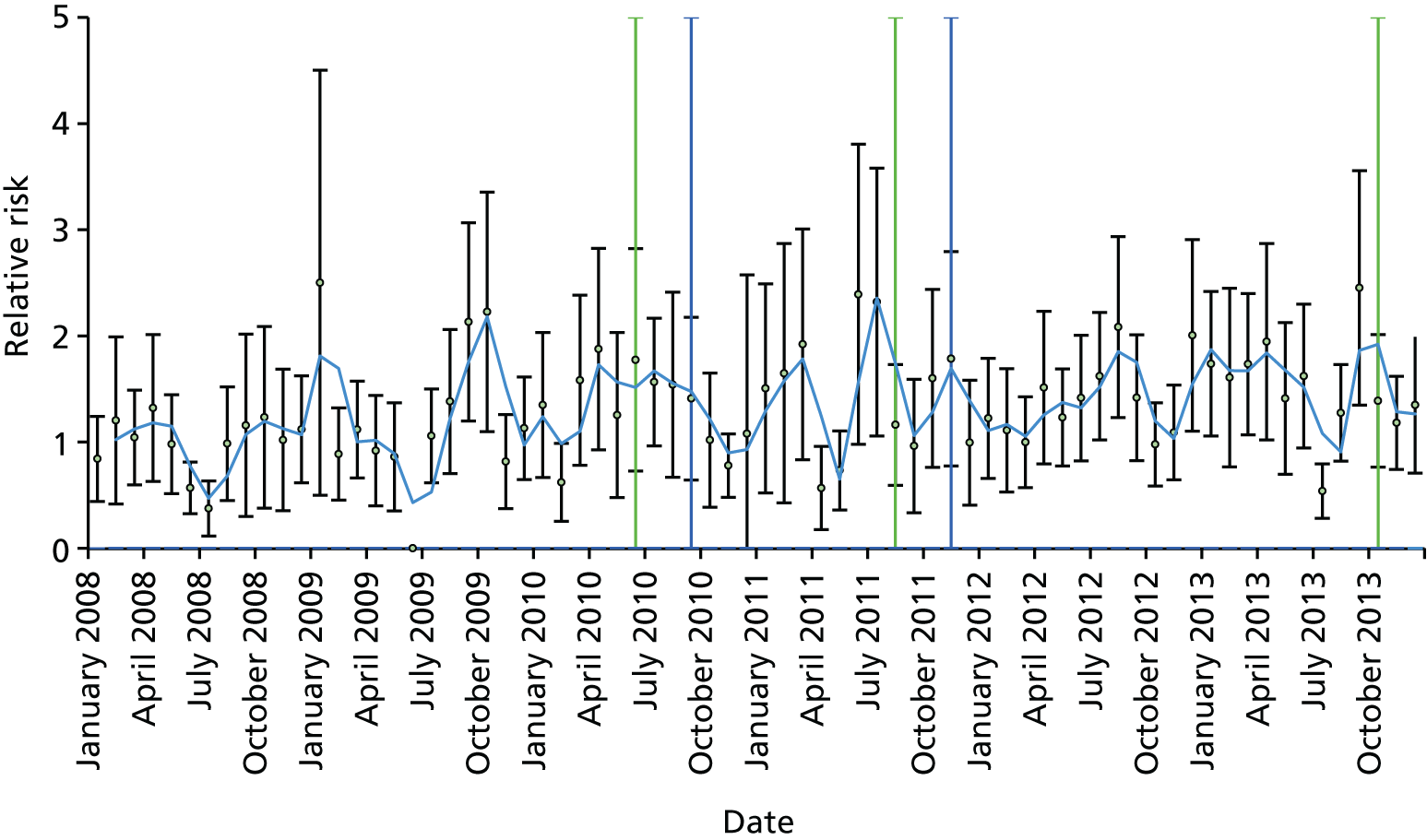
Sep-m.10 thematic analysis
Sep-m.10 is a NHS foundation trust. It was a repeat alerter, alerting four times for sepsis, in June 2001, August 2011, October 2014 and February 2014. The trust was described as having a small improvement effect. Analysis is generated from interviews with three members of the executive team: one consultant and the Deputy head of information (lead for mortality in this team). The analysis was also informed by trust documentary sources. The top team was stable before and during the alerting period: all had been in post for over 8 years (Table 28).
| Relevant history and context at time of first alert |
Leading up to the first alerts, there was little interest in mortality statistics in the trust and few people were aware that the trust had received alerts. Since then there has been a big increase in awareness and interest in mortality data. There was shock when the second alert arrived There are two hospitals in the trust, which used to be separate organisations. Each hospital has its own inherited ways of working – including how it codes deaths |
| Summary of response to first alert |
Arrangements for dealing with alerts have not been clear – sometimes the medical director gets them but at other times it is the director of strategy. On each occasion the alerts go to the information department first to look at the data and to review coding, and then a clinical review takes place It appears that work on Sepsis 6 started after the second alert – so there were no special arrangements in place for sepsis when the first alert arrived. When data collection began for Sepsis 6 it was found that only 20% of cases were getting the bundle |
| Organisational learning and long-term response |
The process for dealing with alerts was described as still unclear. There is a case note review, which until now had been done by one consultant. There is now a quarterly mortality indicators group, chaired by the medical director with representation from each division, to look at the data In examining each alert that has come in, the trust realises that sepsis is incredibly complex and that it cannot pick up problems in clinical care from case note review; as a result the view is that this has to be due to the cohort of patients and to coding comorbidities It was recognised that the alerts has enabled the profile of the work on sepsis to be increased in the trust. The trust has been focusing on improving care rather than looking at the mortality data. There was a strong view that the alerts were a distraction and did not help to improve care – in fact they were seen as promotion for Dr Foster Intelligence. There was also a strong view that many other trusts were controlling their coding of comorbidities to get their HSMR down |
Limited awareness of alerts
Interviewees said that before 2010 there was little knowledge about alerts in the trust and little interest in mortality data. The information manager reported that mortality information had gravitated to him and he had started to use it and ‘do interesting things with it’. He noted that generally leaders and most staff were disinterested. Eventually, the information manager used mortality data to express concern around hospital mortality. A patient safety lead was then appointed and it was reported that he had started to ask questions around SHMI and HSMR indicators which triggered greater interest.
Analysis suggested that the trust divisions were analysing a host of data. However, this was confined to the specialities and synthesis of this information was not shared or used centrally.
Mid Staffordshire experience influences trust response of validating the alert data
Respondents emphasised that validating the alert was necessary and drew parallels with Mid Staffordshire where ‘they didn’t trust HSMR data’. Sep-m.10 respondents stressed that in responding to the alert, they were not trying to dismantle the alert but they were ‘healthily sceptical of it’. The deputy head of information also stressed that validation of the alert was the first thing that was done – ‘proving’ that it was worth investigating and that the alert ‘numbers matched’. The nursing director reported that validation of the alert was considered useful as it made the trust ‘concentrate’ and ‘focus’ its attention and ‘dig down’ to identify problems. Overall, the alert was ‘a slap in the face’ that made the trust question how it was delivering care. Only after completing this process did it move to a depth investigation of deaths linked to the alert.
Process for handling alerts lacks continuity
Trust response to the first alert for sepsis lacked continuity and urgency. It was reported alerts are received by the information team. They checked details of the alert and extracted relevant patient data. It was reported that initially this information was forwarded to either the medical director or the director of clinical strategy. The medical director reported this inconsistent approach.
Care Quality Commission involvement ‘give teeth’ to alert that spurred trust leadership action to address hospital mortality
Interviewees described how mortality and HSMR became more important once the CQC became involved in the alerting process. Around that time the clinicians in the trust began to be more interested generally in outcome data and since then interest has grown considerably.
The alert created urgency to investigate and identify why the trust has recorded high mortality for sepsis
The second and subsequent alert’s created urgency to thoroughly investigate and then identify why the trust has recorded high mortality for sepsis. The medical director acknowledged that the alerts were helpful but not specific enough to identify the problem: ‘They’re helpful as a lever but I don’t think they’re helpful in terms of actually telling us where our problem is’.
Increasing standardisation and integration of trust structures and processes to identify mortality issues and generate trust-wide solutions
Respondents identified increasing standardisation and integration of trust structures and processes to address the investigation of the alerts. Oversight of this process is undertaken by the patient safety lead and the head of clinical strategy. A new quarterly mortality indicators group led by the medical director was implemented. The aim of this meeting was to ‘discuss the latest things that are cropping up, the “latest alerts” engage with the Dr Foster representative and ask questions such as “Can we assure ourselves that that’s not a problem? Can we assure ourselves that it is a problem and we’re doing something about it?” ’ (deputy head of information).
Exploration of alerts identifying problems in coding, death note completion and case note write-up
Most respondents highlighted problems with case note write-up identifying comorbidities, recording of primary diagnosis and coding of mortality. ‘There is nothing wrong with our clinical processes or our clinical care but still we’re an outlier and what we’ve narrowed it down to is things like coding’ (medical director). A new head of coding was appointed to try to unravel these complex problems.
Analysis suggests that the trust was comparing its mortality indicators with other trusts and identifying how its particular care pathways may be linked to it being recorded as an outlier in terms of mortality. It was noted that all unscheduled care patients are admitted to one of the two acute care units and are assessed for a short period and this may not be the model used in other trusts. Likewise, by drilling down exploring the alerts forensically, problems associated with junior doctors completing death certificates were identified.
In comparing differing coding practices in two hospital sites, the medical director reported that coding was definitely the main issue and not clinical care. The hospital site where coders actively engaged with clinicians on the wards appeared to have lower SHMI indicators. The view was also put forward that the alerts had led many trusts around the country to game or play with their coding to get it right in terms of HSMR.
Elderly cohort of patients of ‘very frail patients’ and coding of primary diagnosis blamed for high mortality and not clinical performance
Respondents were keen to deny any link of high mortality to poor care. It was suggested that care was appropriate and the patients concerned were ‘very frail’, had many comorbidities and had been admitted from nursing homes. It was noted that this cohort of patients deteriorated very quickly and died. It was suggested that doctors had queried sepsis in the case notes and the patient had received antibiotics. However, respondents suggested that patient care had been appropriate and that in this situation death was inevitable, as this was an ‘acceptable death’. Similarly, a consultant also confirmed that the alerts for sepsis did not link to poor clinical performance as the Sepsis 6 care bundle was being implemented.
Clinical involvement in case note review
One clinician has been reviewing case notes but regards it as onerous. Interviewees reported that it has been hard to get willing volunteers among the consultants to help with this. It was noted that clinicians are not automatically informed by the organisation about the receipt of a mortality alert specifically. They are considering how to resource this to get more involved.
Raising awareness of sepsis and implementation of the Sepsis 6 care bundle
Trust work on the Sepsis 6 care bundle started in 2012, after the second alert arrived. When data collection started they found that only 20% of patients were getting the bundle on admission. In response the trust stepped up implementation of the Sepsis 6 care bundle, which has led to significant improvements: from 16% in April 2012 to over 90% coverage now. In raising awareness of sepsis a publicity campaign (newsletter) was pursued that aimed to highlight trust concerns over sepsis mortality; increase the profile of the sepsis 6 care bundle and facilitate access to an electronic form explaining the Sepsis 6 care bundle. However, it was reported that these articles were not linked explicitly to the alert.
No impact on sepsis mortality
Respondents felt that any clinical changes that had been put into place as a result of the alerts (owing to a greater organisational focus on sepsis) had had a positive influence on patient care but yet did not result in a reduction in the mortality statistics over time. Overall, the view in the trust from the CEO and the medical director was that the alerts are not particularly helpful, as they appear to highlight lack of clarity in recording patient observations in case notes and that take resources away from delivering care. Respondents working in sepsis generally conceded that the mortality alerts may have enabled heightened the profile of the sepsis group across the organisation.
Senior trust leaders employed diverse methods in promoting frontline clinician involvement in improving care
It was suggested that senior leaders visibly promoted quality improvement in their regular walkabouts and drop in sessions. Senior nurses, including the chief nurse, completed clinical shifts every month followed by a debriefing session. A senior nurse also highlighted how trust leaders had also resourced a ‘bottom-up approach’ enabling junior doctors’ engagement in implementing improvements in care.
The trust has an active programme of quality and safety improvement and has sent staff to the Institute for Healthcare Improvement international forum. The chief nurse has been to the Institute for Healthcare Improvement four times. This methodology was applied by junior doctors applying PDSA cycles and auditing implementation of sepsis bundles and antibiotic prescribing within ‘the golden hour’.
Case study 11 (Sep-m.11) narrative summary
Trust overview
Sep-m.11 is an acute NHS trust and runs the two main hospitals in the area. The trust employs approximately 6000 staff including 170 consultants. It alerted twice for septicaemia.
Relative risk profile
Figure 45 displays the relative risk profile for site Sep-m.11 between January 2009 and January 2014. The green lines represent the date of an alert and the blue lines the date of the subsequent letter.
FIGURE 45.
Relative risk profile and alert (green)/letter (blue) dates for site Sep-m.11.
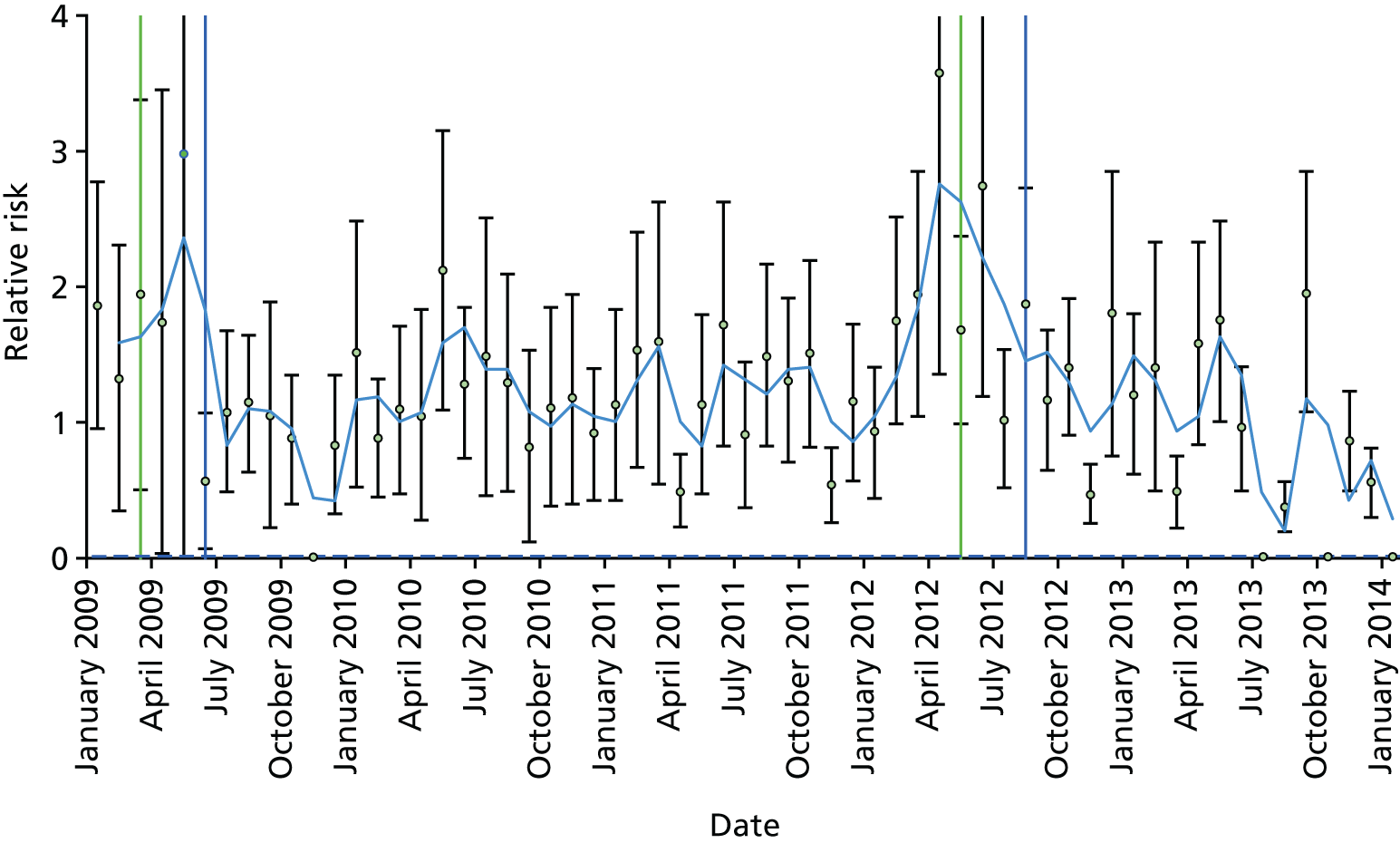
Key events
-
The trust took part in the SPI so from 2006 it started working on improving care for sepsis and on reviewing its mortality figures and taking action.
-
The current CEO started in 2012. The trust has a forecast deficit of £2.4M and there is a programme of redundancies under way to save money in the longer term.
-
The trust subscribes to and uses the HED information tools.
Sep-m.11 thematic analysis
Sep-m.11 received two alerts for sepsis, in 2009 and 2012. Analysis is generated from interviews with four senior leaders, one coding manager, one information manager and two clinicians (one sepsis lead) (Table 29).
| Relevant history and context at time of first alert | The trust was a SPI site so from 2006 it took part in a large-scale intervention to implement a range of safety measures, led by the Institute for Healthcare Improvement in the USA and funded by the UK Health Foundation. As a result of this work the trust was aware of its rates of mortality, including for sepsis, so the alert was not a surprise. The trust started implementing the sepsis care bundle in 2006/7 as part of SPI. In 2009 the compliance with the sepsis care bundle was examined. There was a report produced, as well as an action plan |
| Summary of response to first alert | The trust reviewed over 50 sets of case notes. There was already a group looking at sepsis and the review did not find anything that the trust was not already aware of. The time taken for the review was said to be considerable. A case note review was also undertaken for the alert in 2012 and again it did not find anything of surprise |
| Organisational learning and long-term response | The trust has recently introduced case note review for all deaths – the outcomes of these reviews are posted on the intranet for all staff to see. The process has two stages. Stage 1 looks at key indicators and if any of these highlight a preventable death, then a second stage, more detailed review, is undertaken. There was a view that other priorities took hold in the period between the two alerts. As a result of this, when the second alert arrived the bundle work was reviewed and it was decided to put them all together into a programme of work for the ‘acutely ill patient’ (AMI, sepsis, pressure ulcers, VTE, etc.). This has been combined with a programme to develop a supportive, learning culture in the organisation |
External engagement in national patient safety programme
The trust has had long-term engagement with the SPI from 2006. This involved a large-scale intervention to implement a range of safety measures, led by the Institute for Healthcare Improvement in the USA and funded by the UK Health Foundation. From 2006 the trust had a sepsis group. It was also working on implementation of the implementation of care bundles, developing quality metrics and care bundle compliance in many areas (including sepsis). In 2009, the compliance with the sepsis care bundle was examined and this led to a report and an action plan, including the recruitment of a specialist nurse consultant for sepsis. As a result of this work, the trust became aware of their high rates of sepsis, and hence the alerts were not a surprise.
Senior leadership priority and involvement in case note review and examination of Dr Foster mortality data
It was noted that examination of case notes at the outset in 2006 was confined to a few senior level staff. Wider trust involvement across divisions and specialties other than A&E came much later. With the sepsis alert requiring 50 notes to be reviewed, the time taken was said to be considerable, and this did not tell it anything that it did not already know.
Forensic examination of case notes, analysis, production of action plans and embedding new practices
Senior leaders highlighted the forensic examination of case notes, analysis of care pathways, triangulation of data, production of action plans and implementation of new improved practices. The associate medical director remarked on how they ‘pounced on all monthly data from Dr Foster’ and used them to map mortality across every diagnostic group. This forensic approach was also employed in response to the alert for sepsis.
Senior clinical engagement in case note review and coding validation
The alerts with the CQC heading were said to have gained the clinicians attention. Now every death is reviewed by the consultant concerned with the death to validate the coding. If it is not correct, the consultant will record why and, if necessary, put this in the patients’ notes too. In that way any changes to notes are documented separately on a sheet held in the coding department.
Universal case note review highlights sepsis as multifactorial and drives a broad approach for improving quality in care pathways
Generally, staff reported that the alert (2008) had some influence on ‘kick-starting’ work exploring care pathways. The initial universal case note review had highlighted that sepsis was driven by many factors and that attention should focus on addressing care of patients more broadly. Hence, work on addressing sepsis was integrated into a much larger project focused on care of the acutely ill patient.
Trust attention focuses on accident and emergency investigation and sepsis pathway improvement
It was reported that the trust had already been investigating and monitoring sepsis mortality and had recognised that there was a problem. It was noted and that the alert stimulated further investigation of sepsis mortality in A&E. However, in response to both the ongoing SPI improvement work and the alert, the trust focused its attention on screening for sepsis in A&E. This involved process mapping and identifying ‘who can do it . . . and how they can do it’ (nurse consultant sepsis).
Trust operational pressures reduce priority for responding to the alert
There was a view that other priorities took hold in the period between the two alerts. So, mortality dropped down the list and there was more focus on admissions, so while the sepsis work was still ongoing, other things took priority. For example, admissions took precedence over mortality.
Trust reported responses to the second alert for sepsis (2012)
A combined response focusing on formal case note review process and application of care quality and culture change programme that brought together care bundles (sepsis, acute myocardial infarction, pressure ulcers)
The trust had been working to implement care bundles, including the bundle for sepsis, but there was frustration that things were not happening in a standard, routine way. In addition, there was a concern that chasing every single alert was not productive. As a result, a group was set up to look at all the bundles in the trust and realised that the bundles did not always agree; for example, the bundle for pneumonia did not agree with what was required for sepsis. This was causing confusion for the junior doctors as they were not sure which bundle to use. From this, the trust set up a workstream to look at the care of the acutely ill patient in order to combine all bundles. It has also begun a culture change programme to improve learning and improve safety.
Trigger for action in improving sepsis mortality
The alert for sepsis was recognised as useful trigger and focus for action on sepsis and wider cultural change focusing on improvement in care pathways. It augmented existing universal case note review and identified problems in pathways. In focusing on mapping patient pathways it located problems in clinical perception of care bundles and clinician knowledge of underlying clinical issues.
A focus on resourcing data analysis and generating information to inform decisions
It was noted that investment in specialist analysis of trust mortality had resulted from the alerts. A specialist information manager was recruited and the number of coders was increased.
Parallel evolution of institutional focus on mortality reduction in sepsis
Focus on forensic universal case note review
In December 2014, the trust implemented a two-tier review of mortality. Twenty people/teams are involved in this review process. Stage 1 looks at key indicators, and if any of these highlight a preventable death, then a second stage, more detailed review is undertaken. About 10% were said to get through to a second stage. It was suggested that before they were ‘jumping around’ only looking at the notes of the patients that had triggered and this was not considered the best way of finding clinical issues. These reviews do not include information surrounding the death, for example the staffing and skills mix on the ward at the time, and factors that might be related to the death that are not in the case notes.
The consultant involved in the care of the deceased now authorises the coding of mortality, for accuracy. If it is not correct the consultant will record why and if necessary put this in the patients’ notes too. In that way any changes to notes are documented separately on a sheet held in the coding department.
Monitoring and triangulating data
The HSMR is still 109 despite all the trust’s efforts and it is uncertain as to why, even with universal review of deaths. Crude mortality is monitored: how many people are dying in the trust every month (around 150 people). Now the trust is focusing more on SHMI. The difficulty in finding out why the HSMR is high has led to some discussion about the local services, particularly in nursing homes and for palliative care. The trust has started to try to work with the CCGs to look at 30-day post-discharge deaths, but this has been very difficult.
Developing a trust culture focused on shared learning to deliver high-quality care
Trust leaders report a key strategic focus in developing a culture supportive of high-quality care via shared learning and staff engagement in continuous review and improvement in care pathways. The board and senior executive team now prioritise mortality.
Trust work on sepsis
Sepsis is still seen by some as a condition that is so severe that it has to be treated in ICU, whereas the message that the team are trying to get across is that it is a spectrum from a systemic response to an infection to septic shock. A registrar conducted a review of patients who had a diagnosis of sepsis on admission and found that all but 1.5% were correct diagnoses. This has helped to counter the view of some doctors that ‘everything is sepsis these days’ (nurse consultant). Of those with a sepsis diagnosis the death rate has come down from 40% to 23%. There has been concern from the doctors about the clash of sepsis guidelines with other guidelines, such as for giving oxygen to elderly people. The clinical lead has done a lot of work to resolve these issues. The rotation of junior doctors was raised as an issue in terms of them having to be trained on the way of working in every new organisation they went to work in, despite the sepsis bundle being implemented across the UK.
As part of the work on sepsis, the trust now has all the drugs available in all entry points of the hospital. They also have machines to do full blood counts and venous gas measurements in their EDs.
Appendix 13 Details of cases
Case study 01 (AMI-s.01)
Interviewees
-
CEO.
-
Medical director.
-
Director of quality and governance.
-
Head of assurance and governance.
-
Head of clinical effectiveness.
-
Chairperson of the trust clinical effectiveness and audit group.
-
Director of performance and informatics.
-
Advanced nurse practitioner in critical care.
-
Consultant cardiologist and lead for cardiology.
-
Resuscitation officer.
Mortality context
| Condition | Alert date | Letter date |
|---|---|---|
| Septicaemia | April 2007 | 3 July 2007 |
| Intestinal obstruction without hernia | April 2007 | 10 March 2008 |
| Cardiac arrest and ventricular fibrillation | December 2007 | November 2008 |
| Coronary atherosclerosis and other heart disease | August 2008 | 17 August 2010 |
| AMI | December 2012 | 4 March 2013 |
Illustrative quotations
A trust culture characterised as ‘closed’, a lack of awareness of mortality and limited staff engagement in addressing of trust mortality
Having been able to compare it to other organisations, it was [limited] in its approach to transparency and openness. That inevitably had – and permeated through the whole way in which openness and transparency were seen.
Governance team
So before the Keogh review, did you know the trust had a high SHIMI and a high HSMR?
No.
Governance team
Limited learning gained from trust engagement with external organisations
We thought we were doing, because, you know, it’s like everything, if you don’t go outside you don’t know what’s happening so we were continuing and people were reading and they were bringing back good things that they’d been reading, but we weren’t aware that they’d moved on [elsewhere].
Senior nurse
Limited in clinical engagement in addressing mortality: senior clinicians denying responsibility for acute myocardial infarction mortality
There was very much, ‘It’s not me, it must be someone else. So don’t ask me to improve my service because I’m all right and it must be somebody else that’s the problem’ . . . what would happen is the consultants would end up arguing over the problems so there didn’t seem to be a solution; it was all quite frustrating . . .
Quality and audit team
Financial pressures limit resources
I think we’d stopped going to some of the meetings, because we were short staffed and you know what it gets like? That doesn’t become a priority and I think everything sort of drifted out and we sort of lost track, but now we’ve got designated people that are responsible . . .
Nurse practitioner
An integrated approach linking trust levels and ensuring generation of high-quality data and improved ways of working
There is a clinical governance system, as I said, there are clinical audit system, where we actually drive the changes. We ourselves, clinician as well, have our own settings where we drive the changes, for example there is a monthly cardiology, we call that business group meeting, which means nurses in cardiology, physiologists in cardiology, junior doctors in cardiology, consultant cardiologists, management, these are all sitting every month with an agenda for one hour and a half, discussing where . . . and secondly developing pathways, developing ideas.
Consultant
Clinicians as boundary spanners
There is a revolutionary drive in the trust running to try to bring the coders into the reality of medicine . . . every day, there are actually at least three notes, there’s one which are done, and the two are waiting. These are, the coders think that what’s in the note is not correct, so it’s sent to me as a lead for cardiology, I look into it, I follow the national guidance . . . I have been to, I’ve been brought into the coders’ mentality, how do they think, how do they work, so I can understand when I am right and the manager how to help them getting a resolution out of the confusion about specific cases.
Consultant cardiologist
Changes in trust culture influencing mortality
We’ve got the learning from experience group where all this information of shared learning goes to and this is what we’ve done and this is the improvement that we’ve had. We’ve got a results group that’s just gone on to the patient safety where we are looking at data that’s coming in, analysing and finding outcomes from that as well. We’ve got the aggregated learning as well . . .
Head of clinical effectiveness
Changes in structures and processes linked to improved connectivity between learning and improvement
So there was a new process developed which has taken a few months to get going but it’s now clear what happens and where things go. So that has been a major change. There has been a lot of learning from serious incidents and complaints that’s now fed into the governance structures and fed back to staff because that wasn’t happening before.
Head of clinical audit
Investment in organisational capabilities
We’ve launched the new electronic incident reporting system and we’ve gone from being a zero reporter of SIs and incidents to quite respectably up.
Medical director
Case study 02 (AMI-m.02)
Interviewees
-
Medical director.
-
Clinical lead ED.
-
Head of clinical coding.
-
Divisional director specialist medicine.
-
Clinical outcomes manager.
Mortality context
| Condition | Alert date | Letter date |
|---|---|---|
| AMI | December 2007 | 10 March 2008 |
| AMI | April 2008 | 11 July 2008 |
| Diabetes mellitus with complications | January 2010 | 30 April 2010 |
| Complication of device, implant or graft | May 2010 | 17 August 2010 |
| Peritonitis and intestinal abscess | April 2011 | 5 July 2011 |
| Shunting for hydrocephalus | December 2011 | 1 March 2012 |
| AMI | June 2012 | 6 September 2012 |
| Shunting for hydrocephalus | November 2012 | 4 February 2013 |
| AMI | January 2013 | 3 April 2013 |
| AMI | June 2013 | 16 September 2013 |
Illustrative quotations
The board at the time kept saying it had to be 90, it had to be – but I think – you know, this is quite a deprived area. We serve a big population . . . we’re one of the biggest trusts in the country, you know, and we are in a fairly poor area. We do have – you know, our case mix is very, very different . . .
Clinical outcomes manager
We’ve had a very changeable board. The board we have in place now is very different to what we’ve had before. They’re much more involved in what we do.
Clinical outcomes manager
[The mortality review group] has started and stopped a couple of times because our trust has gone through a lot of changes, especially in the upper management. When I started I was reporting to a director that’s not here any more, and even the one that replaced the director has already gone. So I have been 3 years here and I think I’ve seen certainly two layers of upper management, if I can put it that way . . . So every time this has happened we have had a little bit of a hindrance and we have had some break on the continuity of the mortality review group.
Head of coding
The way data was used when the alerts first came to the trust was not very good. Meetings surrounding mortality did not have a clear strategy, and nor was there a clear focus on how to improve areas that were clearly signalling a problem.
Medical director
With one of our MI alerts, and I think it might have been the earlier one, so maybe 2011, we looked at quite a big cohort of patients, about 70, and actually there were about 22 or 23 who actually had acute MI. So there were – so initially the focus would have been with the team. When we dug down into what the issues were, actually – obviously there are issues there, but it wasn’t so much the clinical team. It was more an issue of how we were coding, what we were writing.
Clinical outcomes manager
. . . when I sat on the first mortality assurance group, I got a sense that people were really frustrated because there was an absence of leadership at the mortality assurance group. So nobody was really setting the direction . . .
Medical director
So I was concerned about it and the actual data presentation, as much as the narrative in the report wasn’t really to standard . . . But they’ve been struggling for a long time about extracting the value back into the organisation on what mortality means to people day in, day out. There was no grand, round presentation of mortality. Services had no idea of their mortality, really. OK, so for me this was about leadership, infrastructure process and how data is presented . . .
Medical director
All the specialties I ensure that they have mortality and morbidity meetings which are documented, represented clearly and are all in ledger folders so that I actually can see what actions are. Few of them are more – well, put it this way, few of them are more robust, you will actually can articulate what the actions are out of those, few of them are not so robust.
Divisional director specialist medicine
. . . the power of data that becomes clinically relevant is the thing that engages clinicians to then being able to understand why they have a responsibility to engage.
Medical director
I met every clinical director or clinical lead and I asked them to help me help them with their data, and made it very clear, ‘This is not my data. This is your data. It’s going to be against your name. So if your patient is dying and then the primary diagnosis is a chest pain, and it’s going to show nationally . . .’
Head of coding
Well, I’ve had a consultant storm in my office on the third day, one of the top consultants here, telling me how rubbish my work is. And I said, ‘I’m really sorry, Mr X, you know, but I didn’t know I could cause so much rubbish in 3 days. But please take a seat. Let’s go and let’s find out . . . this is a fractured neck of femur, it’s all open, and that’s why the trust is not getting money’. And my next question was, ‘What kind of plate are you using? Is it three pin or six pin? What’s the size of the incision? Are you opening the fracture side?’ And they get gobsmacked. And I said, ‘Because . . .’ And this was not coming from the clinician, it was coming from coding knowledge . . . ‘It doesn’t show it in these fracture [notes] . . . are you doing this one or are you doing this one? Just clarify it to me. I’ll put it in a double coded policy. You sign it and I’ll code it. It’s your data, not my data’. And that approach – but it was like that, you know. It turned out we were doing it right, actually.
Head of coding
And then we developed a validation programme, which we did with every specialty at least once a year, because we don’t have the capacity. We would ask one of the clinicians to choose 50 patients in one of the specialties, or we could choose them for the clinician, and go through these 50 patients, find out where the issues with coding are, find out where the issues with clinical recording are and then find out where the opportunities are. And then we’d create a spreadsheet together and then they would invite me or the team leader to do a presentation, believe it or not, as part of their clinical learning. So they’ve been so receptive . . .
Head of coding
. . . particularly if an alert has come in through the CQC. There is something about having – you know, that banner on the page already will make people sit up and take notice. So they will buckle down and look at the cases and write their reviews and their patient summaries, and give their thoughts on where we are with it.
Clinical outcomes manager
I’ve not mentioned money and it’s got nothing to do with money. If we’re not here to deliver safe care then we might as well shut the doors.
Medical director
We turned things around from it being three permanent members of staff and everyone else contractor to having a team of 22, with three or four contractors only in the last couple of years. So in a difficult period on recruiting coders nationally, we had some success in that. And I think we have had a little bit of improvement on the data as well, but a lot of work needs to be done.
Head of clinical coding
I believe in people leading by example, and quality is a really big – and safety is a really big issue to the board now, whereas before I think they were seen as totally removed from it . . . there’s been here a very clear divide in the past between clinicians and managers . . . I do believe it is changing. I’m more confident in what we’re doing now than I have been for, you know, a long time.
Clinical outcomes manager
We’ve had one grand round, so we’ve set a rhythm now for the grand round. So every quarter, there is a grand round. So the first one was really scene setting and talking about sepsis. Fantastic attendance, the highest number of consultants ever attended to a grand round, it was about mortality about them and the second one is going to be more about the data, more about our strategy . . .
Medical director
So with our kind of day to day – trying to make this part of everyday business, really, mortality, as opposed to something that happens once a month that might tie in with a governance meeting. So everyone scurries around, doing a bit of M&M, and might present it at a governance meeting. It’s got to become part of everyday.
Clinical outcomes manager
All the specialties I ensure that they have mortality and morbidity meetings which are documented, represented clearly and are all in ledger folders so that I actually can see what actions are. Few of them are more – well, put it this way, few of them are more robust, you will actually can articulate what the actions are out of those, few of them are not so robust.
Divisional director specialist medicine
. . . we’ve got a dedicated mortality coder that makes sure that all the data is coded accurately. That doesn’t mean that our data is brilliant. That doesn’t mean that our data is perfect. But it was a measure to sort of improve a little bit.
Head of coding
Let’s say if the patient had a UTI [urinary tract infection] and pneumonia. You’ve got one SpR [specialist registrar] comes and says, ‘pneumonia, UTI. Patient is on treatment for pneumonia and treatment for a UTI’. Then the other one records, ‘UTI and pneumonia’. Then it becomes pneumonia, UTI, UTI, pneumonia. The difficulty is deciding what the primary diagnosis is . . .
Head of coding
It’s like for – you see that people are on insulin and everyone would know that if someone is on insulin they’re diabetic. We cannot code diabetes unless the clinician has recorded diabetes, although we know he’s a diabetic patient, but such are the coding rules.
Head of coding
Well, that is probably a trick up my sleeve that I use in my presentations to threaten clinicians to cooperate, sorry [laughter], if I can put it that way. The idea is they need to know that the data is recorded against consultant, and if this consultant is getting T810 codes every time, it means his patients are getting infected every time. Or if the one is doing an angioplasty and he’s getting haemorrhage post angioplasty, every single one, something is wrong. Either his junior is not holding the hand enough for the patient’s groin to keep it from bleeding, or he is damaging the artery, and there is an issue there . . . So by just making them aware, letting them know how the data affects them . . . it probably made them a little bit more co-operative. It made them work closer with us.
Head of coding
Case study 03 (AMI-m.03)
Interviewees
-
Deputy medical director.
-
Director of nursing and quality.
-
Trust mortality reduction lead.
-
Deputy director of information.
-
Consultant cardiology/medicine.
-
Chief executive.
-
Organisational description/institutional overview.
Mortality context
The trust received two target alert letters for AMI and has been sampled as a repeat alerter. The statistical trend for its response is significant and positive.
| Condition | Alert date | Letter date |
|---|---|---|
| Intestinal obstruction without hernia | May 2009 | 19 August 2009 |
| Chronic renal failure | November 2009 | 4 February 2010 |
| Chronic renal failure | December 2009 | 5 March 2010 |
| Coronary angioplasty (PTCA) | November 2010 | 2 February 2011 |
| AMI | September 2011 | 5 December 2011 |
| Deficiency and other anaemia | November 2011 | 2 February 2012 |
| Acute and unspecified renal failure | January 2012 | 11 April 2012 |
| AMI | April 2012 | 4 July 2012 |
| Urinary tract infections | November 2013 | 11 February 2014 |
Illustrative quotations
We’ve got one of the most deprived electoral wards in the country, there is a huge rate of smoking, drug abuse, teenage pregnancy, all of those things, which I know the SHMI and HSMR say they correct for but I still can’t believe that they properly correct for all of those factors.
Medical director
We do have recruitment challenges here in this part of the geography of [region] and obviously we know that that’s going to become harder in terms of the national directions around temporary staffing and agency, etc., but for me that’s still a critical point that we have safe staffing.
Chief nurse
When we produced the dashboards initially we used four measures and the idea was to look for correlation, so we put in there SHMI, HSMR, RAMI and crude mortality all the time, so you could actually then start to track through and see the word discrepancies and that’s another area to look.
Deputy director of information
We didn’t have the same I suppose transparency in terms of systems to see that that was maybe starting to be a cause for concern. So my recollection going back to 2011 and I think some of the conversations we had at the time and obviously we were a different exec team, was probably feeling a little bit frustrated that the alert would come but it didn’t feel we were able to have predicted that ourselves . . .
Director of nursing
The steps we took were set up mortality and morbidity meetings within the departments. We asked – and I’ve got evidence to give you if you wish is by that previous medical director to say, ‘All deaths must be looked at by the consultants so that they can – the majority of them we won’t have any problem but some of them, if there are any issues, must be discussed in the Mortality – M&M [mortality and morbidity] meeting and you should be also in charge of coding because there was an issue of coding’.
Deputy head of information
We had a long-standing pathway for the treatment of cardiac chest pain, and before putting together a pathway, a revised pathway, there was a baseline audit conducted. The pathway wasn’t set up in a way that would allow you to identify what we now call ‘mission critical points of care’. You can take pathways for anything, you can pull together every bit of guidance that has come from every professional body on how you should or shouldn’t care for it . . . And having done a couple of audits on existing pathways, we looked at the pathway and tried to define them all in terms of what we have called ‘mission critical points’, that is things that are clearly known to make a . . . an evidence based difference to the outcome . . . on the management of cardiac chest pain, against the existing pathway, we looked at every conceivable component of the care. It generated a suggested action plan and a report, and the cardiologists came in to comment on that. So this has occurred actually subsequent to, not concurrently, with the CQC response.
Mortality lead
. . . our new chief exec continues to chair the mortality committee, and we have representation there from non-exec directors as well, from the two CCGs and from public health, as well as the mortality reduction leads from each department in the trust, and that meets . . . It was meeting monthly but we’ve subsequently reduced that to bimonthly meetings.
Medical director
There is an element of having to strike a balance between, and manage the meeting around the job of the GPs and public health in the room and there is an element of contributing to the understanding and the solutions, but there’s an element of holding us to account and for want of a better term they are there as commissioners and the two GP reps that we’ve got are quite active in the CCG that they’re not just jobbing GPs if you like. So that’s a balance that you’ve got to, and occasionally that has dynamics that need managing, but I think overall it works pretty well.
CEO
. . . so my whole appointment was actually partly in response presumably I wasn’t here at the time but maybe perhaps to the alerts from previously, and so when I started working one of the things that I started doing was restructuring how we did things, so we introduced extra pathways for people with chest pain, and we introduced a certain criteria where the patients just bypassed the medicine and came straight to the tertiary centre, so my understanding that from within 2 or 3 months I started off to with the Dr Foster stuff but the SHMI certainly dropped from over 100 to about 100 and has continued to be low and so did the length of stay.
Consultant cardiologist
. . . the trusts have tried really hard to address this and I’m not aware that’s a major problem any more by ensuring the consultants review all of the codes, so we get the notes or e-mails with, ‘Are you happy with this coding?’ and we say, ‘Yeah we’re happy or no please change this’ because some of the stuff you get put on is bizarre.
Consultant cardiologist
So we’ll have a stage 1 review where the parent consultant will go through the notes of each patient who’s died and make a judgement whether the care was in any way inadequate or the death potentially preventable or inevitable. If there is a feeling that the death was anything other than inevitable then we will go into a stage 2 review which will be done by a separate consultant where they will do a deeper dive on a fixed pro forma, and then on the back of that that finding is fed back into the departmental morbidity and mortality committee and the outputs from that are fed back to [mortality lead] so that they can be disseminated throughout the trust through the mortality committee but also through our clinical policy forum which is a monthly meeting of the heads of department and divisional directors.
Medical director
. . . what we had were too many pathways that were too long that were not really being tracked in real time and not really driving improvement that weren’t really focused on mission critical things but had loads of bad definition, and the reason why they were too long was because they probably had just too much in them.
CEO
[The CQC said] ‘the process you’ve got for mortality reviews is a really good one but actually it’s not really robustly applied everywhere and you should be doing something about that’ so obviously we’ve been auditing that since.
CEO
. . . because what we could’ve done is just get our existing pathways and just take a few pages out and tick the box, but to be fair it’s not really me but [medical director] and some of the other people really put some effort into let’s get this 50-page document, and let’s say what we we’re really, really all about, and let’s try and get into some of those issues of variation in clinical practice and the way people like to do things because there is quite a lot of variation, and let’s come up with a way of actually launching them and let’s put some real energy into that and then let’s get real-time information on them when we launch them, so we really get them going in the organisation as opposed to we’ll do an audit in 6 months of data that’s 6 months old, etc., etc., and we’ll see how we get on, and like I say of all the meetings that I’ve been to in the time that I’ve been here they’ve been one of the most well attended, most energetic if you like, and I think it’s worked well . . . What we do is we have a cycle, so when we launch the pathway we have a small team of people that are going around the hospital everyday finding patients that are on it or should be on it and making sure their data’s up to date and sticking on the internet.
CEO
. . . we also have a heat map which [individual] generates from our data which shows us areas of attention, and we are focusing on not so much the black squares but the big squares, so the areas where we’re seeing significant numbers of people with maybe a slightly elevated SHMI compared with very small numbers with a very significantly elevated SHMI. So if we look at carcinoma in the rectum or whatever it is, we may have a very high SHMI but it’s only two cases, whereas if we look at COPD we have a slightly elevated SHMI but a hundred cases.
Medical director
Case study 04 (AMI-m.04)
Interviewees
-
CEO.
-
Consultant cardiologist.
-
Information project manager.
-
Head of coding.
-
Consultant respiratory medicine and intensive care and clinical lead for quality.
-
Consultant physician (ED).
-
Deputy director of quality governance.
-
Associate medical director.
Mortality context
Summary of mortality alert profile (number of category-specific alerts, total number of alerts, dates of alerts).
| Condition | Alert date | Letter date |
|---|---|---|
| Acute and unspecified renal failure | September 2010 | 2 December 2010 |
| AMI | June 2012 | 6 September 2012 |
| AMI | June 2013 | 11 February 2013 |
| AMI (withheld) | October 2013 | 8 January 2013 |
Illustrative quotations
We’ve had a change of chief executive, probably 4 years ago now . . . but we had a very command and control attitude. There’s a palpable difference in atmosphere now . . . I think we would have, we’d have done everything by the rules. We would have produced a report; somebody would have cracked a whip to make sure that a report was produced by the deadline date. It might not have been a great report, it might not have really felt real, and now I think we would be much more inclined to say, ‘Actually, we’ve done most of this for you, can you give us an extra few days because you’ll get a much better response and our actions might be more effective’.
Mortality lead
I mean, if you look at the quality report to the board, it really has improved out of all recognition in the last 12 months. So in the past it gave information. Now you can see data, you can see trends, you can see connections . . . I think we only used to look at HSMR alerts, infection control rates, you know, a few indicators, but now we’re really into detail around trends and analysis and looking at different things. So comparing ones from early 2012 and early 2014, there’s a huge difference in the way that the reports now work.
CEO
Because there were various signs and symptoms throughout the patient, the coders had then assumed that the reason for the admission was the MI, so they were not following the coding standards quite correctly due to their inexperience . . . Following that first alert, the decision was made in the trust that actually only the experienced coders would code deceased notes across the board. So we looked at then changing our practice and we have our band 4 coders, which are either ACC [Accredited Clinical Coder] or very, very experienced.
Head of coding
So we want to get the coding right because what we were anxious about, we were anxious that everything gets called ‘coding’ and we may be actually missing real deaths due to other things, they go, ‘Oh, it’s coding, it’s coding, we don’t have to worry about anything, it’s coding’.
Associate medical director
And then we got the second alert. And that’s really depressing, that the same issues, that our action plan the first time around had not solved the issues. And so the solution was to send the notes to the cardiologists every time we were coding for an MI, so we put in place an action plan that was around improved coding and education.
Consultant intensive care
Because it was felt that sometimes the raised levels of troponin were indicative, it could be an MI, so the clinicians were putting query MI, etc. So when we coded and they’d put on the cause of death, it was an MI. It may not have been the case. The troponin level could have been due to something else.
Head of coding
Increased risk from myocardial infarction was not in patients under cardiology, it was in patients who were not under cardiology. And yet, we’ve got a direct admission policy that if you come in with ST elevation myocardial infarction you go straight to the cath lab and you have your PCI, and you’re under cardiology. So that immediately raised a bit of a question about, well, actually these clearly aren’t straight forward heart attack patients, that when you split the data between cardiology versus non-cardiology, the non-cardiology was where the excess death was. And actually with the benefit of hindsight, that was telling us quite an important piece of information that these weren’t straight forward heart attack patients.
Associate medical director
For deceased patients, a change we put into place a few years ago is that the deceased coder actually goes down to the mortuary and reviews the notes in the mortuary, because what we were finding was sometimes notes were going for post mortems and we didn’t quite get the notes in time, or we didn’t have full access to all the episode history. A few years ago the onus was that the coders had to look through the whole of the notes for any information. That’s changed now. The standards have changed. It’s only documentation that’s relevant to that current spell. So that’s actually eased it slightly. But we like to make sure that we get the information as soon as we can. The other thing with deceased patients is once the information has been looked at in the mortuary, the notes get married up with the loose history by the deceased notes clerk and then the notes are then sent back to us so we can just make sure everything’s in there and contained, coding amended if required, prior to us sending them for a clinical review of the coding if required.
Head of coding
The main thing at the moment is escalation of care and rescuing sick patients, and bringing in a new system, looking how we do that and incorporating other things such as urine output and so on, which sounds quite small but in fact it makes a big difference to how you look after people. And trying to bring that out, and then make sure it’s accurately scored. And one of the things we’re all trying to do is get electronic scoring systems in, but we’ve no money to do it, so it’s also trying to achieve that by various negotiations with System C, who supply the software which runs the hospital clinical system, to see if their next version will have that and trying to see where we can embed that without having to spend any money, because we haven’t got any money to do that.
Consultant cardiologist
So the second alert, obviously we had a joint coding and clinical review, and it did highlight some areas where the processes we’d actually put into place probably weren’t working as well as they should . . . A cardiologist was involved, and he actually said, ‘Well no, that’s not quite right’. So what we then did was fine tune that process, and if we have any patients now that are under general medicine that don’t have a cardiologist input, we will send those to the cardiologist for a second review, mean, the AMI ones are quite interesting. I think a lot of it’s about how we capture them . . . They’ll have been seen by juniors in kind of the general take and got into cardiology . . . so once the cardiologist get them, we absolutely know we’re pucker on them. It’s when the juniors for the general medical take is when we start to worry.
CEO
I think they’re [the MASS alerts] very effective. They certainly focus everyone’s attention. And it does mean that serious internal research is done as to why and what can be done to improve. And certainly in relation to palliative care as well, we’ve been – the local hospice, a clinician from there regularly attends the mortality group meeting as well, so it’s about getting better care for those patients that are going to die, because it’s an inevitable fact, isn’t it? It’s getting people to die in the right place and more appropriate place, comfortable place for them. I think that’s one of the positives that’s come from it.
Head of information
Soon after he [medical director] started one of the things he said was, ‘I don’t understand why we don’t put mortality first on our patient safety agenda. You know, isn’t it the most important that could possibly happen to anyone that comes into this hospital that they die? And so it needs to be top of the list’. And actually even this week, the chief exec, has sent out an e-mail . . . about the financial position that we’re in, a difficult financial position and Monitor helping us, but actually very strongly stating quality of care and outcomes being top of the list important priorities.
Mortality lead
I mean, if you look at the quality report to the board, it really has improved out of all recognition in the last 12 months . . . now we’re really into detail around trends and analysis and looking at different things. So comparing ones from early 2012 and early 2014, there’s a huge difference in the way that the reports now work.
CEO
And I think we used to get [alerts], we used to answer them and we would respond and they’d be closed off. These days we get them, we look at them. We understand the context. Are there other indicators that are coming out around those alerts? . . . Have we closed off the actions from there to make sure that the alerts are being properly dealt with and do we really have a problem?
CEO
. . . the hospital’s been – like everywhere else, really, but it’s been incredibly busy over the last couple of years, so we’ve seen a 35% increase in emergency admissions into the hospital, which just is absolutely killing us. And so we’ve got really sensitive to the mortality scores, because one of the key indicators for us would be where mortality is. We started to drift out in the [region] about December last year, and we’ve done a load of work to really start to focus in on mortality.
CEO
So mortality gives you some indicators. Your complaints give you some indicators. Some of the things that you’ll see coming out of the nursing falls – you start to get a picture as to – and you try and get that portrayed for the board so the board can see it, so that you can spot things going wrong before they become major disasters.
CEO
The National Classification Centre for Clinical Coding, they advise us on coding issues. So that was part of that as well, because it was felt that, you know, the sequencing of coding from a clinical point of view wasn’t quite accurate, so we then confirmed that with our national standards and actually we were coding it to national standards. So we’ve really sort of done a lot of work on making sure our coding met national standards, as I said, and with more experienced coders actually coding it and now the same coder coding, we’ve got the consistency in our coding.
Head of coding
. . . we’ve designed a pro forma for mortality reviews internally, we use the global trigger tool as our original template, we then embedded that review tool in a database that is a bespoke database.
Mortality lead
But one of the frustrations about Dr Foster is it’s always in arrears, it’s always such a long time ago that people have forgotten the cases, and learning should really be as soon after the event as possible when everyone in the team remembers what happened. As opposed to going back and looking at cases that some of which were 6 months old, and half the trainees have moved on.
Mortality lead
So we’re keeping an eye on action plans. Because the place has more bloody action plans than you can shake a stick at, so it’s really making sure that those action plans are then followed through and that we’re closing it off. And that’s the work within the last 18 months that we’ve been doing.
CEO
So we’ve really sort of done a lot of work on making sure our coding met national standards, as I said, and with more experienced coders actually coding it and now the same coder coding, we’ve got the consistency in our coding.
Head of coding
. . . we had a high crude mortality rate, the last month of data, 3 months ago. So we had a high crude mortality rate, but our HSMR was low. And we queried it with Dr Foster and said, how come? And they said, ‘No, it’s accurate, you know, there’s no question about it’, they went over the data again. Other trusts have had a high mortality rate because over the winter months nationally there was a 30% increase in deaths over the winter months with flu vaccine not working, and in intensive care we’ve seen way more cases of influenza than we have seen in my memory actually. So high crude mortality but our HSMR didn’t go up . . . I’m worried now because of the more detailed explanation I was given which is that actually most of the people that died didn’t fall in the 80% basket that HSMR encompasses.
Mortality lead
We have, in the last 7 years, our rates of C. diff [Clostridium difficile] have gone down, so clostridium infections have gone down from 250 a year to about 16 a year. 20% of patients with C. diff die. Our MRSA rates, bacteraemia rates are very low. We’ve established a cardiopulmonary exercise testing service to stratify risk pre-abdominal surgery, and to admit patients electively to HDU [high-dependecy unit] post-op. We’ve established a sepsis group and are delivering sepsis 6, and we know that our antibiotics within 1 hour have improved from 7% to 60% . . . And so we reckon we’re saving potentially 10 lives a month with the sepsis 6 delivery. So there’s some workstreams, so changes in working practice that have been put in place in clinical practice that probably contributing. And if I wanted to identify one that was the biggest hitter, it would be sepsis.
Mortality lead
So the sign up to safety’s something we’re doing. So we’re changing the observation charts, so we’re bringing in new charts. We’ve got a sepsis campaign, giving appropriate antibiotics and so on quickly, looking at renal function. So everything is geared to trying to improve the care of the patient as much as possible within the resources and so on.
Consultant cardiologist
Case study 05 (Sep-s.05)
Interviewees
-
Head of governance and assurance.
-
Chief nurse.
-
Associate medical director.
-
Medical director.
-
Consultant anaesthetist.
Mortality context
| Condition | Alert date | Letter date |
|---|---|---|
| Cardiac arrest and ventricular fibrillation (withheld) | December 2007 | 10 March 2008 |
| Peripheral and visceral atherosclerosis | September 2009 | 10 December 2009 |
| Pleurisy, pneumothorax, pulmonary collapse | September 2009 | 10 December 2009 |
| Excision of colon and/or rectum (withheld) | June 2011 | 19 September 2011 |
| Peripheral and visceral atherosclerosis (withheld) | June 2011 | 19 September 2011 |
| Septicaemia (except in labour) | June 2012 | 6 September 2012 |
Illustrative quotations
It had been quite stable for a long period of time. But then the chief executive changed and the trust ran into some difficulties financially. And at that point a health care consultancy company were brought into as a recovery team.
Medical director
We were struggling for money. The chief exec was particularly – his managerial style was a particularly difficult one to deal with. We then got EPR which was electronic patient record which cost us £60 million which we have difficulty funding. So I think the downfall of our chief exec and our board was due to financial issues.
Associate medical director
Well we had clinicians leaving. You know we had some very good medical consultants leave and some very good surgical consultants leave . . . probably not as a direct impact of that. But we did have . . . Certainly, we had clinicians leaving . . . So we had four [XXXX consultants] now we’ve got two locums.
Critical care consultant
They introduced it [a new electronic patient record system] trust-wide in one go. We wrote . . . a 46-page document to the trust saying our concerns for it. And they implemented it anyway. A&E came . . . Ground to a halt . . .
Consultant critical care
It was a very dictatorial style. It was very much ‘my way or no way’. It was very much not including of the clinicians that were on the shop floor and disregard for much of the clinicians’ thoughts.
Associate medical director
In June 2013 there was a . . . The departure of the chairman and departure of the chief exec, the chief operating officer and the chief nurse. In July there was a departure of three non-executive directors and that’s when I arrived in the trust. There was an interim chief executive appointed, an interim chair appointed, a change of interim chief executive in November 2013, a change of chairman in January 2014.
Chief nurse
I’ve been here 9 years. Obviously the whole surviving sepsis campaign kicked up what 14 years ago, 13 years ago. So I know they were developing stuff before outreach has been developed . . . For the last 16, 17 years here they’d been doing study data on all sort of, of different things since then. Specifically in the last 9 years we’ve got the sepsis 6 highlighted on all the wards and A&E. And they’re meant to be using sepsis screening tool in A&E as well. Which is one of the things I think they’re not using properly. They’ve also developed twice yearly sepsis . . . A pure sepsis study day [background noise] which is open to everyone. And that’s twice a year. And that’s what we developed 7 years ago because we’re running it for the last 7 years.
Critical care consultant
Our outreach team is fantastic, so we’ve got three outreach nurses, all very senior nurses, who run a fantastic service connected to the intensive care unit and they tirelessly – I think they’ve brought in our PAS scores which is our patient at-risk score for the last 15 years, and tirelessly worked to try and get our deteriorated patient on the ward better.
Associate medical director
I think the culture of the organisation was information being power and they were really not sharing information with a lot of the work force. And they really weren’t respecting or valuing the clinical knowledge of the senior workforce, is my impression, and that’s certainly the impression of the clinicians here.
Medical director
They only started holding board meetings in public in April 2013. So to that point all of the board meetings were in private . . . So the concept of transparency here in this trust is relatively new.
Chief nurse
There was no mortality steering group, the medics didn’t particularly look at their mortality and the data that was presented was always poorly presented from our business intelligence unit, so it was meaningless at most meetings . . . So previously it has been a bit ad hoc, a bit unstandardised, various different departments doing what they felt was appropriate/not appropriate. There was no line of sight from the organisation about who was doing mortality reviews and how many mortality reviews were being done, and the outcome of those mortality reviews.
Associate medical director
And a number of clinicians believed that (a) the trust didn’t have a problem with mortality and (b) they certainly, as clinicians didn’t have a problem with mortality . . . And then we had a change of medical director who said, yeah looked at it, really comfortable with that. That’s absolutely accurate.
Nursing director
We will [now] launch an investigation which is where the actual clinical divisions come in once we’ve drilled down to find out which division we’re dealing with that the source of the alert, we’ll deal with the clinical director of that division and ask them to engage the appropriate clinician to lead a full investigation of our outlier stats. We will require the investigation to be written up into a formal report which then can then be sent back to the Care Quality Commission.
Head of governance
And we will require a full action plan with smart actions with a lead assigned to each action and a time scale assigned to each action to also accompany that report. That report and a covering letter from us will then be sent back to the Care Quality Commission who will then assess whether or not they’re assured that we’ve done sufficient . . . And to close the action . . . Because to close the alert down at that stage or to continue monitoring at periodic intervals in the future.
Head of governance
We had another action around the coding of septicaemia should be included as a specific topic in the teaching session for junior doctors, every new intake . . . And then the fifth action was continued review of each case of septicaemia and action plan on a month-by-month basis.
Head of governance
We then had further correspondence at the beginning of January. So the 2nd of January 2013 and the CQC requested details of a case note review at individual patient level to show how we judge the quality of care in each case. They wanted details of how the issues identified in the investigation that we had done previously which were around delays in treatment and provision of medication will be addressed. And they wanted to know what national guidance the trust follows for the management of septicaemia patients.
Head of governance
And quite often [now] we’re already aware of it. I mean I’ve got a number of occasions where we proactively contact the outlier department of CQC and say, oh we’ve noticed this so before you send us an alert kind of just like know what we’re doing kind of thing . . . As I say in the vast majority of cases we’ve already known that we’ve got an issue with a certain area. And we’re already on it. We use, obviously CHKS and things like that to keep an eye on our mortality rates and any outlier statuses . . . So when I’ve approached people because I’ve received the letter from the CQC it’s never been a complete, bloody hell where’s that come from kind of conversation. It’s always been oh yeah right, yeah OK we know about his. We’ve got an investigation ongoing.
Head of governance
I’ve taken over the mortality in the last 18 months and it’s been a fairly significant battle to get engagement by clinicians because we’ve had a lot of mistrust with our coding, with our data, they haven’t felt that it was our problem/their problem or that we had a problem.
Associate medical director
So a complete overhaul of all governance throughout the organisation starting at the board level and going downwards. Now clearly that includes mortality in terms of divisional governance, in terms of corporate governance, but also in terms of clinical governance. So that’s the impact. It makes you start again, basically.
Head of governance
So what I’ve been doing over the last 6 months is to really bring the . . . For example, using the mortality data. I very much brought the clinicians into it going through the data. I had done some quite in-depth analysis which I’ve shared with them to create a picture of where they were, why they were there, what we could do about it. With the aim of getting them to take some ownership. And I’m starting to craft some clinical leaders who are actually taking ownership of it. And that’s really . . . You know my impression that’s actually . . . What’s not been happening for quite a few years.
Medical director
Well I’ve gone to them with the data and I’ve publicised the data in a number of areas and it’s obviously gone to the board. It went to the medical staff committee. It went to the mortality alerts group. I came up with some hypothesis. I challenged people with what they were doing. People wanted to hide behind the coding issue. And there clearly was a coding issue. But I challenged them. Did they want to defend the mediocrity or did they actually want to make a significant difference to what they were doing?
Medical director
I have a scientific approach. You provide people with data, you need valid data. You need to explain how it’s derived and you give the data to people. And that will bring some people over the line. It won’t bring everybody over the line but it’s the first-off approach. Then my second phase is sort of, an emotional phase. A lot of people don’t want to hear that and they go into a bit of a grief . . . Grieving process. And we’ve seen that here with . . . We’ve seen . . . Well the first thing is the data’s wrong. It’s denial. And then the next thing here is it’s not fair . . . You know it doesn’t apply to our patients because our patients are really sick. There’s anger. And I’m just trying to get them to accept and so you know Kübler-Ross stages of grief. So I’m working through that process. And then the third phase, some people you just have to very direct and say just do it. But we . . . So it’s absolutely vital, I think to start with some good robust data that you understand that you can rely on. Because doctors are intelligent people. They’re clinicians. You can approach them with a valid argument and some people will come round.
Medical director
The local focus is to get in early antibiotics. Early monitoring and early referral to ITU/HTU. So antibiotics is the main thing . . . Is what we’re doing. We’re trying to drum that into everyone . . . Two outreach nurses. They’ve done the twice-yearly audits on the PARS scoring and into that they also take into account whether people have been using Sepsis 6 boxes on the front as well. And the PARS scoring is used terribly despite teaching. And Sepsis 6 is used variably . . . Well the main problem we’ve got is probably the same as the lack of nursing staff on the wards is one of the main issues. So I think they haven’t got time to do it. And then the junior doctors seem to be too reluctant to call the seniors as well.
Critical care consultant
Case study 06 (Sep-s.06)
Interviewees
-
CEO.
-
Chief nurse.
-
Deputy medical director.
-
Head of quality, safety and compliance.
-
Matron for general surgery.
-
Data quality and clinical coding manager.
-
Medical director.
Mortality context
| Condition | Alert date | Letter date |
|---|---|---|
| CABG (isolated first time) | November 2009 | 4 February 2010 |
| CABG (isolated first time) | December 2009 | 5 March2010 |
| Deficiency and other anaemia | January 2011 | 4 April 2011 |
| Cardiac pacemaker or defibrillator introduced through the vein | May 2011 | 16 August 2011 |
| COPD and bronchiectasis | June 2011 | 19 September 2011 |
| Therapeutic endoscopic procedures on biliary tract | June 2011 | 19 September 2011 |
| Coronary angioplasty (PTCA) | August 2011 | 10 November 2011 |
| Acute and unspecified renal failure | September 2011 | 05 December 2011 |
| Biliary tract disease | September 2011 | 05 December 2011 |
| Septicaemia (except in labour) | October 2012 | 08 January 2013 |
| Liver disease, alcohol-related | November 2013 | 11 February 2014 |
Illustrative quotations
The organisation 2 and a half years ago was quite administratively managed; I think actually the idea of a manager’s good day wasn’t to see a doctor but to sit in offices and talk to other managers, and then worry about why we were so overspent, why we weren’t hitting the A&E target.
CEO
We worked for about 18 months to 2 years retrospectively looking at how patients with sepsis were managed and we were mortified if I’m honest. But I don’t think it was something that had really hit the radar at that point and I think we’d focused so much on clinical conditions that actually the secondary conditions like sepsis had gone by the wayside. So our research, the research that we did with the retrospective studies was really quite shocking.
Matron for general surgery
We didn’t have a mortality reduction plan that was owned across the trust and we didn’t have embedded mortality, morbidity, meetings across specialties.
CEO
A group of a few, ‘wise men’, senior clinicians, the odd nurse who professed to be experts on this and took an interest, but didn’t have a clear structure of controlling and influencing the organisation.
Medical director
In the beginning, being entirely honest with you, in the beginning I don’t think anybody was really that interested in what we were doing [around sepsis] and why.
Matron for general surgery
I think before it was potentially just looking at the numbers and looking at ‘What’s the HSMR?’ and probably looking at it, I think as a lot of trusts probably did, when the hospital guide was due to be published and seeing what we were.
Head of quality, safety and compliance
I was hoping this year/end of last year that we’d get to a situation where the clinical director and the leads for the mortality and morbidity meetings would sign off a self-declaration of ‘this is my governance’ just like I do for the finance – and we’ve not got there yet but actually that’s part of our journey, we will do that so that at the end of this year I’m hoping that with our new divisional structure which we’ve implemented in August last year – we had a big debate about what good clinical leadership looks like beforehand, I did all the kinds of things you’d expect: sort of describing what it meant, consulting on it, and then going back and re-consulting on structures and things. So I’m looking to try and do that. In terms of mortality reduction plan we’re now in our second year of mortality reduction plans.
CEO
The sepsis team are looking at GP education at the moment. So the lead, who is an inspirational anaesthetist, was at the awards – we won awards and ‘well done’ at the trust board for these reductions, but he was raising – their big challenge is educating the GPs and they were going to look at that as part of their intervention.
CEO
The other is then, you know, throughout the trust otherwise, every clinician wants to know how they’re doing and if mortality’s one of those measures, which it is, then if there’s something wrong, it motivates them to find out why . . . They all equally are animated when you get an alert, but that’s good because it engages them in the process. And then it engages them in the reduction plan as well, so an overarching mortality reduction plan, they all want to do the best they possibly, it’s kind of, we use it in that way anyway.
Chief nurse
So we started a working group and from there it was – it’s unusual in this trust for the two divisions to work together. Surgery do their thing and medicine do their thing and never the twain shall meet. But with the sepsis working group it’s very much a core group of people who have taken this forward really.
Matron for general surgery
We’ve sharpened up our whole quality strategy at the board.
CEO
You know, if we get an external from some kind of regulator, you know, I think any NHS trust will, or, you know? You know, foundation trust, I think, you know, we’ll jump because you’ve got to, that’s the, you know, we are – And we’re, you know, managers of, you know NHS organisations, you know believe that their jobs are on the line if it doesn’t look good externally. You know? Massively important and very different.
CEO
Well there’s two things, one is you’ve got to do it because the CQC tells you you’ve got to do these things, but the other thing is, you know, given that we’ve got to look at the data anyway, let’s use it to focus in a constructive way on things that we want to put I think when we’ve done particularly certain things well; so the sepsis team, for example, have come to the trust board, I saw what they did, I met the team, we talked through what they were doing to reduce it, and direct benefits – there are masses of that of course not just in terms of mortality but in terms of beds. And they talked openly in the trust board with the media there about what they’d done to cut deaths and so the board is quite open.
CEO
It would be more sensible to do two things, one, look at the cases where you think there was an issue, and secondly do a random sample and see what problems you identify so you’re getting some broad coverage of what the problems are, so that would be the system.
Medical director
The impact to the sepsis bundle which was in response, partly in response to that alert, although not totally in response to that alert. But the alert gave us an opportunity to look in much more detail at those patients and we could look at patients whether they were in the medical division, in surgery or wherever, because we pulled all the notes and did a huge amount of work when that alert came out. So, you know, we looked at around 98 deaths.
Chief nurse
But for the juniors, the registrars, they really have no choice but to listen to us. The pathway is very prescriptive and if you don’t fill the pathway in that sends out more alerts to us. So it is literally, ‘Can you tick this box?’ ‘Yes, I can tick that box’ therefore the patient is septic. ‘What are you going to do about it?’ and it is very powerful for nurses to have something that says on paper, ‘If this, this, this and this happens, your patient in septic, you need to do this. You’ve got an hour’. And it’s very powerful for nurses to be able to use that and have the confidence to walk up to a very senior clinician and say, ‘I believe my patient is septic because this piece of paper tells me so’. And that’s quite a powerful tool.
Matron for general surgery
The IT department are developing an electronic MEWS which is going to be an awful lot easier. So what will happen is patients who score 4 or more will alert my nurse with a pager. But we’re not quite there yet so we’re still going to have to do the daily walk. She’s going to love me! But we’re still going to have to do the ward walking.
Matron for general surgery
We’ve even developed an e-learning package as well and there has been lots and lots of education. It was the fact that people didn’t take it seriously I think, was the biggest challenge for us. But there was education that was needed all the way through.
Education is the biggest part. Sepsis, for whatever reason, at that point in time was something that people used to use the word and never understood the term. We’ve put in a whole remit of education that goes from nursing students’ right through to we attend the clinical audits for the consultants and all the way through the chain we’ve done ward-based and audit-based education.
CEO
If we have a negative alert identified from our own review we’ll notify the chief nurse. And we’ve done it that we pre-notify the CQC so we’ll say ‘We’ve identified this; we’re investigating it’ and we then alert the clinical director and the director, so the director at M&M [morbidity and mortality] can look at that if it fits within a particular directorate.
Head of quality, safety and compliance
It was about identifying early and suspecting sepsis even if the patient clinically probably wasn’t septic but actually it’s pre-empt it right through to how we treat it appropriately with the six-stage process. So for us, the challenge was getting the clinicians in particular alerted to the fact that it might be sepsis. We took the approach of, ‘Well, let’s assume it’s sepsis until we’re proven otherwise’ and that’s how we run.
Matron for general surgery
And 2 years ago it may have been data or it may have been something quite serious; now when we get them we think it’s got to be the data, it can’t be the underlying service.
CEO
So I think this has been an additional force for them to be able to look at their own information. The fact that when we go and we go to the presentation and they go to the surgical meeting and we’ve got the mortality leads for the different specialties within general surgery and we’ll go there, and I’ll go with the laptop and have Dr Foster and say ‘OK, we’re showing high within upper GI’ and we’ll click on it.
Head of quality, safety and compliance
I think we’ve had huge pressures with the A&E target and our performance on that has been awful, but actually the one thing that we’ve kept shape on is actually the quality. And I’ve just been with the CQC just now and actually they’re saying ‘Your A&E department is great’ despite the fact the patients are waiting long periods of time. And so I think we kind of kept our shape because we saw quality front and centre, and actually for us on the efficiency equation quality and efficiency are different sides of the same coin.
CEO
I have to say I find it annoying actually because I think actually, you know, why, my first question is why are these organisations wasting their money doing variations on the theme, because actually they come out with rather similar results, they don’t, they’re not very different, they’re all using the same data.
Medical director
The alert for us made engaging with the corporate team an awful lot easier. People were much more interested in our work. It certainly got us off the ground and obviously it’s enabled us to get the funding for those two posts as well.
Matron for general surgery
Case study 07 (Sep-m.07)
Interviewees
-
Mortality lead and previous medical director.
-
Sepsis lead.
-
Head of information governance.
-
Current medical director.
Mortality context
| Condition | Alert date | Letter date |
|---|---|---|
| Acute and unspecified renal failure | October 2008 | 20 January 2009 |
| Septicaemia | November 2009 | 4 February 2010 |
| Septicaemia | September 2011 | 5 December 2011 |
| Septicaemia | February 2012 | 9 May 2012 |
| Acute and unspecified renal failure | July 2013 | 1 October 2013 |
Illustrative quotations
If I’m being honest with you, I think a lot of our mortality was, at that time, when I first came into post was most probably a little bit disconnected between the top of the organisation which the board would have numbers presented as a HSMR-type data as part of a performance matrix, and then the mortality reviews, mortality and morbidity meetings which would be held within departments, and very often associated with all of this, and I think to be fair to say that there would be a differential between how good some of those mortality reviews were.
Former medical director
I think there’s always been a much more of a push on the surgical side to look at mortality rather than the medical side where I think quite often you can have a 90-year-old come in who’s bed bound and come in with sepsis from a nursing home, and people say . . . and you could well find that they weren’t given antibiotics so quickly and all the rest of it. So I don’t think we were very strong on the medical side really at that point in time.
Former medical director
We have a lot of young people dying of cancer who tend to die of cancer in the hospital rather than in the community. And we didn’t have very well developed and palliative care system, we didn’t have our own palliative care consultants.
Former medical director
But we’re not supposed to be a hospice, we’re supposed to be an acute hospital. But let’s say, for example . . . because you can give very good end-of-life care but you’ll have 100% mortality. I know that’ll be reflected in the palliative care coding.
Critical care consultant
The coders, unfortunately it’s quite difficult to employ coders, they’re probably a little bit like cervical screeners in the past where, you know, they’re desperately well paid and it can be quite a tedious job.
Interim medical director
Funding – bottom of the chain. And people don’t really look, but 50%, almost 50% of the training numbers in this country are based in the London teaching hospitals. They’re much less reliant on things like tariff or the money . . . And they have a lot more senior doctors most probably, and the junior doctors tend to be more senior, so teaching hospitals tend to have more proper trainee doctors that tend to be more senior, and there’s a feeding chain that goes down . . .
Consultant critical care
When I looked at it they were a very desperate group, very desperate, and we did a bit of a coding thing with the chief coder, and I think we had something like 63 cases. I did about half of them the 30-odd cases . . . and some of them were, like I said, they were 90-year-olds from nursing homes with multiple bed sores who were basically coming to the end of their lives, so whether they were – I’m not particularly interested in the mortality ratios or whatever, what I want to see is where is the preventability of the deaths . . . That’s not saying that the 90-year-old that comes with sepsis or acute kidney injury because you could treat them, but it may be that the death isn’t preventable even if you treat them very well or even if you don’t treat them very well, i.e. you don’t get the antibiotics just because of all of the other comorbidity that they almost certainly would have if they’re very elderly.
Former medical director
I can’t remember seeing anything where there was poor care . . . I think sometimes I wonder whether this would be coded right or wrongly, and I think coding is an issue, and because basically all of these mortality ratios the basis that you go into whatever stent you go into is based on the code, and then it’s split up by sex, your postcode, your age groups and all the rest of it . . . So the foundation of everything is the code, and palliative care coding that’s the obviously thing.
Former medical director
To start with he [doctor] didn’t want to dismiss any of this as a coding issue and we’re not in a place where we can do that, we certainly weren’t back 3 years ago, because blaming the coding was just an unemotionally intelligent thing to do. And when you look at some trusts, I think, who’ve like hired kind of people to help them with it they’ve laid themselves open a little bit, I think, haven’t they, to sort of manipulating the data. So I can honestly say that, although our coding might not be as good as it can be, I think there’s every reason to assume that it’s actually honest.
Interim medical director
We did introduce things like . . . the ‘sepsis bundle’ . . . and so we have responded to the alerts positively.
Interim medical director
People come in with acute injury sepsis, it’s chicken and egg isn’t it? I think when there was a big concentration on sepsis I think if you look at our actual numbers I think they fell a bit, and then the acute kidney injury went up a bit because I think people saw that we’d coded things as acute kidney injury rather than sepsis. So there are silly patterns like that that you see that goes up and that goes down. Nothing deliberate it’s just some of these people may be aware that you’re looking at sepsis or something and they’re picking up, ‘Well the acute kidney injuries is the major component here rather than the sepsis’.
Former deputy medical director
When there’s so much external scrutiny on an organisation you tend to start throwing a bit of resource at it and it gets more attention. It becomes a distraction more than anything I think. I’m not a great believer in HSMR, SHMI and you say that’s because you’re at the opposite end of the scale. What I really believe people should be doing – people say we have the quality of access to health care in this country, well we don’t, and quite clearly we don’t. You go to different hospitals and you’ll have different levels of care because each hospital has different types of services, different departments. You’re outcome will be different where you go. So if you have an acute MI and you come into a hospital like [Sep-m.07] where we don’t do acute PCIs. You would need to be put in the back of an ambulance and sent somewhere, and you’re outcomes and results are going be worse than if you went to a hospital that has that thing on-site.
Deputy medical director
I mean, just across the board, I think to start with people were a bit dismayed that we were put in Special Measures, I mean, you don’t want to turn the television on . . . But the way it was sold by the media, I think, was that we had high mortality, it was just a simple headline thing to go for. You know, people would certainly be a lot more attuned to that than . . . they probably continued to watch the television on the basis of mortality for a lot longer than they would just because a few old people had fallen over. So it was a good gold standard from their point. So I think to start with there was a feeling, yeah, that it probably was unfair.
Interim medical director
So I would go on each morning and have a look at the deaths overnight, and I could identify them very quickly, and have a quick scan through some of the records and see if there’s anything then that I wasn’t happy about or weren’t sure about. And we would then potentially follow that if there was something that I thought looked a bit unusual and I’d ask people to follow up as part of an SI or part of a clinical incident like response. We would have quality reports, so the clinical quality review mechanism with the CCGs, so we used to have monthly meetings with them and mortality would be a standing agenda item.
Deputy medical director
And it covers all of our dashboards and thermometers and serious incidents and so on, to reassure them effectively. It’s to reassure our commissioners from a quality perspective. And I think as an organisation, I mean, we are very data-rich, and I think a lot of what we’re trying to do generally, particularly with the mortality statistics and reports, is to try and describe them to the appropriate people in context where they can be assured that there aren’t any serious problems and current underlying.
Interim medical director
So I’ve invited in external reviews, so over the time we’ve had one in respiratory looking particularly around COPD, we had an external review of the Royal College of Surgery by the Royal College of Surgery in [inaudible] and we also had – well the East Midlands Critical Care Network came in and did a review of the ITU. All of these things were triggered by slightly different things, but it was an external assurance visit to really get an understanding of, ‘Is there a problem here that we should be highlighting’.
Former deputy medical director
I could tell you know [XXXX] trust had very high HSMR and he’s got low HSMR now. Why is that? Has their case mix changed? Have they put in lots and lots of different processes? Are they coding differently? Have their coding changes? That would be really interesting, ‘So why has their HSMR dropped from there to there?’ . . . The reason why I know about [XXXX] is that we base some of our response to the CQC on how they responded. I asked them, ‘How did you respond to the CQC when I had one’. So I use that. They sent me all the pro formas. This is what we do, we do case note and we go through the coding and look at what we’re going to do and we put in an action plan, so it was like a skeleton type response.
Deputy medical director
I just was aware Dr Foster existed, googled their website and then managed – through whatever mechanism, I don’t recall, managed to get a user access into Dr Foster and looked at the graphs.
I’ve gone on the website and subscribed as a user in order to get certain pieces of data out of it, but the senior medical team haven’t come to me and said, ‘This is our problem’. As I say it was me bottom up rather than top down.
Consultant in critical care
I always wanted and was to have a system where people where every death was looked at some level, and what we’ve gone for is something we call level 1, level 2, and level 3, and level 3 is a bit different. Level 3 would be a Dr Foster alert, CQC alert. So a level 1 . . . It’s very simple, a patient came in, this is what we thought was wrong with them, this is the final thing that was wrong with them, it’s all linked into our hospital systems so we get – if you look at the coding what’s been coded is there any inaccuracies, what was on the death certificate and has it been referred to the coroner, palliative care involved, end-of-life pathway, do we think there it was a predictable death? And then we say there’s a question, do you need a level 2 review? So the level 2 review is a much deeper review, and there’s certain categories the cases now that we would have to, so if you think there’s anything wrong, if somebody’s had a cardiac arrest, if it’s an elective admission, if it’s paediatric it’s obstetrics or there was an SI.
Former deputy medical director
[W]e do a high intensity mortality review on every patient who dies on the critical care unit, I should make that clear, to learn – obviously learn from mistakes and learn from what we’re doing as a critical care consultant . . .
Sepsis lead
The only thing that isn’t electronic would be like the doctors’ notes, so all the admin-type stuff is on there, all the nursing notes are on there, all the clinical letters for inpatients and outpatients are on the system. So there’s all the test results, etc., so there’s a lot you can do without having to get the case notes but obviously the case notes are like a fuller record in some respects because they’ve got doctors’ notes and op notes and things like that in there.
Information manager
[XXXX] was already working on the database which we then could obviously track the septic patients from and then go back and subsequently analyse that. So that’s what he was doing. I kind of joined in and said, ‘Yeah that’s a great idea, have you thought about the shop floor sepsis care pathway?’ Then we looked through the Sepsis 6 document, as published by [XXXX] and looked through the other trust’s sepsis boxes and sepsis care pathways and whether we wanted to do that, so whether that’s a tool we could use to keep sepsis in the shop floor staff’s brain.
Consultant critical care
Case study 08 (Sep-m.08)
Interviewees
-
Coding manager.
-
Director of nursing.
-
Medical director.
-
Chair of sepsis group.
-
CEO.
-
Sepsis specialist nurse.
-
Trust mortality lead.
-
Manager of sepsis group.
Mortality context
Summary of mortality alert profile (number of category-specific alerts, total number of alerts, dates of alerts).
| Condition | Alert date | Letter date |
|---|---|---|
| Peritonitis and intestinal abscess | April 2008 | 11 July 2008 |
| Septicaemia (except in labour) | November 2008 | 16 February 2009 |
| Pulmonary heart disease | November 2009 | 4 February 2010 |
| Pulmonary heart disease | December 2009 | 5 March 2010 |
| Coronary atherosclerosis and other heart disease | September 2010 | 2 December 2010 |
| Septicaemia (except in labour) | January 2011 | 4 April 2011 |
| Peritonitis and intestinal abscess | August 2011 | 10 November 2011 |
| Septicaemia (except in labour) | April 2012 | 4 July 2012 |
| Chronic renal failure | April 2013 | 1 July 2013 |
Illustrative quotations
So our demographics are that we have the highest density of residents aged over 85 in England . . . so when we would look at some of these alerts in detail, they’d be patients in their 90s and patients over 100 and therefore part of the explanation coming back was, actually they were elderly patients.
CEO
This was before we had actually formalised our quality improvements, our practices, within the trust, which I regret to say is sort of only in the last 8 months, really . . . The process of mortality review had actually started before the CQC visit, so that had been done as a quality improvement project. And had been presented nationally.
Medical director
Obviously we had M&M [morbidity and mortality] meetings, I mean I am a surgeon and we have always had M&M meetings, but there is something about if you look at individual deaths, then that is one aspect. If as an organisation you collectively look at deaths, then you actually get more powerful in-depth information about how your organisation is working.
Medical director
And that was because we didn’t have clinical engagement so people weren’t telling us what was wrong with the patient, so we’ve worked, or I have worked on that, and, you know, covered that one . . . People were just putting on the death certificates septicaemia if they didn’t know what was wrong with the patient . . . We went through another phase where they put old age . . . Then there was a phase where they were putting stroke . . .
Coding manager
So in terms of dealing with the mortality group, upped the ante on the mortality group, and took a very cold, hard look at things, and made it absolutely abundantly clear in the organisation that if we were doing mortality reviews, or . . . so if we got an alert, we would not be doing our mortality review correctly in response to that alert if we did not find problems.
Medical director
We would tend to do a review of patient notes to see the care that was provided and to evaluate whether there were issues that meant that there were shortcomings in terms of the quality of care. My sense is at the time we tended to have more of an approach which [was] to explain why patients had died rather than necessarily to stand back and say ‘actually we’ve got a problem here and we need to do something about it’.
CEO
Then coming back, sort of bringing that really up to date, the QI bit, which is the latest manifestation of our sepsis work, so you’ve probably heard of this already so, but anyway, quality improvement programme, PDSA, TQM if you remember back to total quality improvement, all sorts of phrases that have been . . . all that sort of stuff from the past, I think has sort of landed here and I think we’ve got five, well we have got, we’ve got five projects which are being dealt with under the new QI banner, these are being resourced better than these things have been in the past I would say, and so sepsis is one of them.
Associate director of service department
[S]o the peer review process by CQC I think has been very beneficial to this organisation, and the process of care for patients, so I see it as a difficult but very positive process to have gone through. So you could say that mortality alerts were absolutely crucial to precipitating the process.
Coding manager
So currently it is reviewed by the clinician who has actually looked after the deceased patient. There are some advantages to that, and some disadvantages. The important thing for me has been to actually get that process in place, so that individual clinicians are actually reviewing mortality . . . we have a data set that shows us which individual consultants are, or are not, reviewing their deaths. That is pretty powerful data, and that has been reported to board with clear visibility of which consultants are not complying with the process.
Medical director
I think we’ve now got complete engagement from all consultants. They’re completely aware of what it is to do with coding, because obviously initially it’s the income but it’s not just income, it’s to show quality, safety and everything else, and they want the right data against their name.
Head of coding
From being perhaps very heavily data centric to we’ve moved, I think massively, to being more the improvement side of things. And I think that mortality improvements piece, which I report on and it’s been taken to the board every quarter, has really demonstrated that it is all about, you know, the mortality improvements. You know, what we’re doing in practice is improving the data, I think I absolutely can see that, so there’s been a very strong focus on practice, rather than just looking at the data.
Director of nursing and midwifery
Because that’s what the mortality meeting’s all about is to look and see what’s, is there anything that’s possibly going to alert, do we need to do a notes review before that, so there, you know, the whole team pre-empt it rather than, so when a CQC ones, we’ve failed really because we haven’t pre-empted that there’s a problem coming up.
Coding manager
So if something is raising itself as an issue, then it is going to require actions, and there would be a range of ways of getting into that, but one of the ways would be along a quality improvement project.
Medical director
Then coming back, sort of bringing that really up to date, the QI bit, which is the latest manifestation of our sepsis work, so you’ve probably heard of this already so, but anyway, quality improvement programme, PDSA, TQM if you remember back to total quality improvement, all sorts of phrases that have been . . . all that sort of stuff from the past, I think has sort of landed here and I think we’ve got five, well we have got, we’ve got five projects which are being dealt with under the new QI banner, these are being resourced better than these things have been in the past I would say, and so sepsis is one of them.
Associate director of service department
When we track where we are with HSMR and with SHMI, it has actually been gratifying to watch that over the year, and then I asked the group was that an accident or was . . . had that occurred because we had made changes? And as a group, we were pretty confident that we had effective change.
Medical director
We in a different place to where we were 12 months ago? Yes, very definitely. So you could say that mortality alerts were absolutely crucial to precipitating the [improvement] process. If the pre-existing process had been in place then nothing would necessarily have happened.
Medical director
I think there’s a bit both actually, so I wouldn’t necessarily want to put a percentage on one and then the other and but, so . . . I think often with these things, it isn’t a single event that help shape the future, it’s a combination of events, so I think the two, I think the change in terms of focus from medical director, I think from my point of view, and others, quite a distinct and different shift in terms of actually picking this up and actually wanting to properly get underneath it as well, and all of those combining, I think, were helpful.
Chief executive
The other thing I would say as well as a measurement, you mentioned, was the communications part of it, so we’ve involved the comms department, the T-shirts, the branding which I think is really strong, so I actually, there are things where, you know, if you go back 5 years, the medical education would never even have thought about doing that, but actually, you know, the logo that we got I think is really good. And it, you know, I just think it helps add to the kind of how seriously this is taken throughout the organisation, well I certainly hope that that’s the case.
Associate director of service department
. . . we are not actually finding as much preventable deaths as we should be doing but I think this is down to the binary question . . . ‘was this death preventable? Yes/No?’ And clearly depending on whether you use Hogan or you use something else, there is a whole range of shades of grey . . . so you could say to me am I fully secure at this moment that the processes are completely robust? No. Are we in a different place to where we were 12 months ago? Yes, very definitely . . .
Medical director
And our coding’s improved and improved and improved . . . because we’ve made sure that the documents we use have improved as we go along.
Coding manager
This patient’s died, you need to complete the e-mortality form and the, what’s written on the death certificate and what we’ve coded is on that . . . And then they have to sign it off that that’s not untoward or anything else, and then that goes to the M&M [morbidity and mortality] lead who agrees or disagrees with them. So there’s quite a tight process in place that . . .
Head of coding
Case study 09 (Sep-m.09)
Interviewees
-
Medical director.
-
Deputy chief executive officer.
-
Chief nursing officer.
-
Clinical mortality lead.
-
Lead for sepsis.
-
Clinical coding supervisor.
-
Clinical effectiveness manager.
Mortality context
| Condition | Alert date | Letter date |
|---|---|---|
| Other operations on heart | May 2008 | 18 August 2008 |
| Other operations on heart | November 2008 | 16 February 2009 |
| Septicaemia (except in labour) | April 2009 | 10 July 2009 |
| Septicaemia (except in labour) | July 2009 | 27 October 2009 |
| Liveborn | December 2009 | 5 March 2010 |
| Diabetes mellitus without complication | October 2010 | 11 January 2011 |
| Septicaemia (except in labour) | May 2011 | 16 August 2011 |
| Craniotomy for trauma | June 2012 | 6 September 2012 |
| Clip and coil aneurysms | January 2013 | 3 April 2013 |
| Intracranial injury | July 2013 | 1 October 2013 |
| Craniotomy for trauma | September 2013 | 4 December 2013 |
Illustrative quotations
We’ve got lots of urban poverty . . . in 2008 the council reported that there were 75 different languages spoken in [local] schools. And it’s always been like that, but they bring a pattern of disease with them that is worth knowing. We have a lot of alcohol and psychiatric disease, and they score heavily in the 15 to 45 age group. And unless you know that we’re number three in the country for this particular problem, it’s hard to understand why we seem to have so many deaths, most of which happen outside and we can do nothing about because they’re just brought in and die in 24 hours on the intensive care unit.
Mortality lead
So these are all the kind of epidemiological things that I’ve kind of learnt from doing my job, but also made me think, I’m not sure that I trust what I’m looking at, because I know that there’s more to a story when you see these alerts. So for example, if a hospital stops receiving, its work comes to us. If the [hospital] decides to stop taking head trauma, the helicopters just fly straight over because it’s only 8 minutes . . . We’re getting kidney patients from all over the country because we do a rather special transplant programme. We’ve had trauma patients from [city], which is bizarre when you think that [city] is so far away and they’re surrounded by the three major [regional] hospitals.
Clinical lead for mortality
. . . when I first started coding it was . . . kind of a, almost where people went out to pasture kind of job. Nobody’s interested. It was only for information purposes . . . And it wasn’t until they tied us into the finance . . . that the reimbursement of the hospital had become via our coding, so all of sudden, aha! . . . The spotlight, a way to get something, you know?
Clinical coding supervisor
So if you put rubbish in, you get rubbish out. I understand that bit. Our chief coder, in the last few months, has gone onto retirement and isn’t due to come back, so I don’t have a relationship with the new people. But my understanding seems to be that they are short of people. We’re having a halt on recruitment, because we don’t want to spend money on non-clinical staff, so I kind of see this as a threat.
Mortality lead
And one of those occurred in my area that I looked after within the organisation. And well obviously both patients died as a result of a failure to recognise sepsis. And as part of a working party that was organised within the organisation in relation to these two deaths, and also the septicaemia alerts, I became aware, obviously, I’d known about Dr Foster alerts before, however, it’s the first one I was aware on a senior leadership position and also directly related to impacts in terms of the organisation.
Chief nursing officer
. . . so I think there was a recognition that we could do sepsis better, so we had enough what I would say collateral information so we had enough information around our compliance against sepsis bundles and other types of monitoring feedback that we had, alongside the alert itself as well as also the SUI cases, the serious untoward incident cases, to know that there was a particular challenge.
Nursing director
Even if there is a coding issue and there’s nothing really to explore, it still involves a huge amount of management because lots of the organisations such as the TDA [Trust development authority] request a formalised response and that, which is fine, I haven’t got a problem with the regulators being involved in it, but sometimes they don’t understand the nuances of it because they’re not close enough to the clinical coalface to understand what the difference is between a, you know, an expected death of eight and you’ve had nine and, you know, might kick off an alert and the root cause review process that gets involved in that.
Nursing director
Most of the people who give their hands on hour-by-hour care are the nursing staff, so diagnosis wouldn’t necessarily fit within their remit, so what we try to do is shift the emphasis away from very specific defined outputs to a much more broader set of physiological presentations that would alert people to say sepsis could be occurring here, you need extra help, so what we did, we’ve broadened the base of people who would raise the concern around sepsis based on a number of very broad physiological criteria.
Nursing director
So we did one thing we developed here which was actually quite innovative, is something that we call [XXXX] training. We distilled down into no more than about five to six PowerPoint slides, the very, very key fundamentals, the information you’re trying to get across. You’re not allowed to go beyond 10 minutes. We set some, we tried to use social movement theory, so we tried to get, so we trained 10 people, those 10 people have got to go away and train another 10 people and those 10 people, so it was more of a catalyst to prompt so it was simple enough that I could give it to anybody as part of the clinical team and their responsibility was to go and find another five or 10 people and train them. So very rapidly over about a, I can’t remember, it was about a 6-week period, we trained nearly 1000 staff.
Nursing director
We developed a sepsis award . . . And it’s a way we get the very best of what happens in the organisation. We give them prizes and days out for people. And that year, because we’d had quite a challenge around sepsis, we had a sepsis award and it went to the maternity team. The maternity team were one of the people who had one of these sentinel events. But they trained, and they trained everybody in maternity, both community midwives and also inpatient midwives on sepsis, they go the best scores.
Nursing director
The other thing that was found is that the coders weren’t really clear at all, in what they should put into what codes because it wasn’t clear. So we wrote some common sense guidance forms to what counts as what [in terms of sepsis] . . . I’m not entirely sure I’m right on this, but at the time there wasn’t a code for septicaemia which is a bug in the blood and there wasn’t a code for sepsis syndrome, yeah, with the management, of that, a lot a people would put as sepsis was coded at septicaemia and that proved it was septicaemia and so we made a very sensible.
Medical director
. . . so we produce specialty mortality profiles for specialties, so we give them specialty-specific mortality data. So, on an ongoing basis we try to add definitions, etc., to all those charts, the relative risks, so if the clinician’s got any questions after looking at SMPs [Specialty Mortality Profiles] they can always just come back to us and if there are any blips we try to explain to them what these blips are, and can we just be statistical anomalies or not.
Clinical effectiveness manager
We still have some recalcitrant people who I’m working on. They’re essentially surgical. Pretty much most of the surgeons don’t do each other’s reports, and they kick up a fuss about it. But that’s why I’m the clinical lead for mortality, because my job is to help these people see things in the way we want them to be.
Mortality lead
Case study 10 (Sep-m.10)
Interviewees
-
CEO.
-
Medical director.
-
Chief nurse.
-
Consultant oncologist.
-
Deputy head of information.
Mortality context
| Condition | Alert date | Letter date |
|---|---|---|
| Pleurisy, pneumothorax, pulmonary collapse | September 2008 | 10 December 2008 |
| Pleurisy, pneumothorax, pulmonary collapse | January 2009 | 6 April 2009 |
| Coronary atherosclerosis and other heart disease | June 2009 | 14 September 2009 |
| Septicaemia (except in labour) | June 2010 | 15 September 2010 |
| Septicaemia (except in labour) | August 2011 | 10 November 2011 |
| Reduction of fracture of bone (upper/lower limb) | July 2012 | 2 October 2012 |
| Septicaemia (except in labour) | October 2013 | 6 January 2014 |
| Septicaemia (except in labour) | February 2014 | 1 May 2014 |
Illustrative quotes
I was a little lone voice in the corner pulling the data, doing interesting things with it. I remember thinking, ‘What do I do with this?’ and nobody was really interested. The first glimmer of interest was when we appointed a director of what was then ‘patient safety’. . . And he came and started to ask these sorts of questions about, ‘Do we know how many patients die in the hospital?’ and of course, that’s a, ‘Yeah, I actually have that’. So I was looking at crude mortality and total deaths in the trust for a couple of years, bit of a voice in the wilderness, saw some things, may have slightly concerned me but didn’t really know what to do with them and eventually found a root to say, ‘Look, I’m a bit worried about this. What do you think?’
Information manager
I think we start from a position of wanting to prove to ourselves that it’s something worth investigating which is why my first task is can I match the numbers? So, if we match the numbers and we almost invariably do, it’s relatively unusual to have a significant discrepancy.
Information manager
They didn’t come to me and indeed what we’ve done in the organisation is maybe streamline that a little bit in that they would previously have probably gone to the information department for the first instance and then maybe have got to me eventually but not necessarily consistently.
Medical director
Yes. So the reality is – I’ve been here since 2004–05, so throughout all of these alerts I’ve been here. The reality is as a clinician I’m somewhat removed from that, you know. It comes into this central kind of management suite and various people are involved, and, yeah, I’ll probably get to know about them. I don’t know what time delay or whatever, yeah, but, yeah.
Consultant oncologist
I suspect when the CQC itself started to generate the alerts I think that was probably the trigger for us because – I forget who their predecessor organisations were, but I think the CQC gave it the teeth that people like chief executives started to say, ‘What’s going on here? We’ve got an alert. Are we killing people? We must know more about this’ and I think that coincided with, generally speaking, a beginning of interest in clinical information.
Information manager
So therefore when a mortality alert comes in, we were somewhat shocked, upset, confused, various adjectives like that [laughter], OK? And that led us to do a full mortality audit of those patients. So as many sets of notes – we did this about 18 months ago . . . So we looked in detail at the sets of notes. Several clinicians did it, ED clinicians, microbiologists, myself, acute physicians, a sort of committee of us, we all looked at them independently . . .
Sepsis lead
We have narrowed it down to things like coding, which is obviously a natural port of call. Is there something about the way we’re coding primary diagnosis or comorbidities that would set us differently from everyone else?
Information manager
. . . it does paint an interesting picture in that the mortality in [B] the SHMI is about 92 I think and the SHMI in [A] is about 115 or something, and we are pretty confident because if you look at the differential in coding figures it’s also very similarly skewed, so we think it’s all a coding issue.
Medical director
. . . And there was a real flavour from this audit that a patient arrives who’s very sick, from frailty, comorbidities, deterioration, and is question mark sepsis. So you write down question mark sepsis – you know where this is going. This is going to a coding issue, isn’t it? So you write question mark sepsis in the notes. They’re given a shot of antibiotics in ED, resus, and then a few hours later they die on the ward, having what we felt was appropriate care, no escalation of their care, because it wasn’t appropriate, the family being spoken to, etc., etc., and they died, and we felt that was an acceptable death. If you look at that set of notes, the first entry is sepsis, so it gets coded as septicaemia. There’s so many different codes, aren’t they, for sepsis? One of them is septicaemia. One of our alerts has been about septicaemia per se, that code. I think it’s A419 or something?
Sepsis lead
If we meet Sepsis 6, surely, surely, we won’t have another one. If we do, as we have done, then I’m not sure it’s down to the – it’s not a clinical performance issue, would be my argument.
Consultant oncologist
But it’s gone originally from about 20% up to 80%. So within severe sepsis, the definition of severe sepsis being organ dysfunction and unwell, high lactate, that kind of thing, we do feel we’ve made an improvement.
Sepsis lead
Honestly, I don’t think they are really. In a sense that I think they allow us to say there might be something there, let’s have a look at it, but as yet and we’ve done quite a lot of work on each of the alerts in terms of the number of hours of person time to do notes audits and look in detail at what it is and develop an action plan, etc., and if I honestly had to say the 10 things you have learnt or five things that you have learnt from those reviews are what? I think the honest truth is a whole load of noise in those patient’s notes, no clear messages.
Medical director
Now if we hadn’t had mortality alerts would we have a sepsis group now in the trust is an interesting question because we’ve had a mortality alert around a sepsis and we do have a sepsis group. So it’s really difficult to un-know what you know isn’t it and I think we probably would have a sepsis group but whether it would’ve gained such a high profile in the trust if we hadn’t had a mortality alert I don’t know.
Medical director
I frankly think there are a lot of trusts around the country playing games around mortality and making sure they get the coding right to make sure their mortality looks as good as it possibly can, and we know because we’ve looked if we were more rigorous about coding we would have a huge impact on our mortality, but it would not make a jot of difference in its own right to how the experience of care, the safety of care, the effectiveness of care that we delivered in its own right . . . we could fix our mortality figures and get them down to 85 tomorrow if we just employ 10 coding clerks and shove them in the organisation and say, ‘Get every bit of comorbidity in’ and particularly the ones that have a big impact on Dr Foster’s mortality figures, and let’s get the mortality down to 85 and everybody will be off our backs so we can forget it and actually we can then not bother about doing anything about quality of care . . .
Medical director
Well, we approached it hospital wide and it’s been picked up very quickly, and successfully in ED and acute care areas, partly probably because I’ve had two very motivated consultants, from ED and acute medicine, who have been on our group, who have been very good at taking the message back and supporting that.
Consultant oncologist
Case study 11 (Sep-m.11)
Interviewees
-
CEO.
-
Medical director.
-
Chief nurse.
-
Sepsis lead.
-
Information manager.
-
General manager CGSU.
-
Associate medical director.
-
Clinical coding lead.
Mortality context
| Condition | Alert date | Letter date |
|---|---|---|
| Septicaemia (except in labour) | May 2012 | 6 August 2012 |
| Septicaemia (except in labour) | March 2009 | 9 June 2009 |
| Intracranial injury | May 2012 | 6 August 2012 |
| Peripheral and visceral atherosclerosis | June 2013 | 16 September 2013 |
Illustrative quotations
The trust knew about the poor outcomes in mortality including for sepsis
The alerts . . . have never told us anything we didn’t know already . . .
Associate medical director
. . . we did a lot of work and had already done a lot of work on the 2012 alert prior to it arriving . . . Then with the alert arriving we went, ‘Oh yeah, we know we have a problem’. We have done some investigation but then obviously we went through the formal mortality review investigation that they wanted us, which was fine because we had done a lot of investigation.
Nurse consultant, sepsis
Nowadays it’s not me doing that because we’ve got analysts who do all of that stuff . . . certainly we were a way ahead of the CQC letters when they came.
Associate medical director
Trust catchment and limitation in community services
We have quite a high percentage of people who die in hospital as well. I think it was over 65% of deaths. That is a challenge for us compared to some other organisations where community services may be better developed and people have a choice to die outside of hospital. There was also a view that some of our community provision, our care home provision, was not as robust in this area as it is in some others . . . Now, again, all of those things might impinge on your HSMR.
Medical director
Only one person conducts case note review at the outset
It was myself, [XXXX] and another one of the – . . . other consultants and I think I just cleared my diary for something like 6 weeks . . . do the analysis of it, come up with something, write an action plan and then spend the time making sure that those actions are imbedded is massive for an organisation and when it doesn’t really tell you anything at the end of it that you didn’t already know, it’s kind of like, ‘OK!’.
Head of governance
Learning from case note review
There were some general quality of care stuff but again, it was around were the patients – should they have come in the first place? Did they develop sepsis in this organisation? Because the problem with a lot of these is the primary diagnosis and they’re coming in with them so actually then you’re asking a different set of questions like did we treat them in a timely and the appropriate manner rather than could we have avoided them getting it in the first place.
Head of governance
Trust operational pressures reduce priority for responding to the alert
Between 2009 and 2012 it went off the boil. The work was carrying on and the group was still meeting and we were still doing it and as a trust priority ‘bundles’ and well sepsis particularly, but ‘bundles’ in general and that sort of thing dropped down the list a bit and there was more focus on other things like readmissions and what not, so generally mortality work dropped down the list a little bit and other stuff moved up.
Associate medical director
The need for culture change too
I think that is where it was important for us to develop the care of the acutely ill action plan because it became really clear to us that you could just be chasing alerts . . . but the reason why we talked about having a plan per se rather than just chasing the alerts is because we know that some of it is more than just the indicators themselves; it’s about culture, it’s about looking at the whole pathway and, therefore, if you just chase the alerts what you do is you miss some of the real longer-term stuff that you have to do that eventually will improve the situation around alerting.
CEO
The need for universal case note review for all deaths
But again we had this feeling we were jumping around and dealing with this condition and this condition and this condition, but actually when you looked at the case notes for this condition and that condition, you found Mrs Smith was all of them and it was the same small group of patients that had all of these things and I thought, ‘Is this really the way to do it,’ so we thought no let’s not use that as the trigger, let’s try and select our mortality cases in a better way so we’re trying to look at other ways of triggering mortality reviews and then we thought well actually shouldn’t we be doing them all anyway . . .
Associate medical director
Involvement of primary care
We’ve got a project running, albeit it’s slowly with the CCGs to do some reviews of the 30-day post-discharge bit, and now that’s been an uphill struggle because we’ve not been able to do that . . . where they just went home and we don’t know what happened, we don’t know what they died of and we don’t have access to that data, there’s all sorts of data protection stuff about this that we’ve no ability to access that. We’ve had a huge uphill task, even just to get cause of death of these people, certified cause of death.
Associate medical director
Transparency in case note review outcomes
It’s open access, you can search by consultant so you can have look at the reviews on patients under their care or you can look at what the reviewer’s found in the review. You can look at it by ward. There’s all sorts of ways you can cut the data . . . We said, ‘Well if we did them all upfront then actually we could pull through anything on COPD. Right let’s have a look at all the deaths that are reviewed on the patients that had a primary diagnosis of COPD or pneumonia’ and they just pull it and cohort it that way. So it’s much easier because the reviews have already been done . . .
Head of governance
Conflicts in coding sepsis
. . . that’s interesting isn’t it, because on the one hand the work that’s going on on sepsis they want the clinicians to code more as sepsis to actually be able to pick it up to see – to pull the notes and see whether it’s being treated appropriately, but from a coding point of view you want to go the other way and actually code the pneumonias and the UTIs and what have you and then the secondary diagnosis of sepsis. So you’ve got these conflicting things going on.
Clinical coding lead
There has been understandable resistance to some aspects of the Sepsis 6 bundle
So for instance in the elderly population there is always hesitance about giving too much intravenous fluid. . . . another one of course which is we recommend high-flow oxygen within the care bundle but obviously the British Thoracic Society Guidelines don’t and clearly recommend not giving patients high-flow oxygen and giving them targeted oxygen. So we know there’s a little bit of internal – and indeed national confusion with that because of two perfectly well meaning but differently applied pieces of guidance. We had issues with our general surgical colleagues who felt that in certain acute surgical conditions, blindly giving antibiotics early actually they felt masked the evolution of surgical conditions. So the classic one in their case is acute appendicitis in that in some cases what patients would need to have is a period of observation and then a trip to theatre for their appendix taking out because things were allowed to evolve but actually the sepsis guidelines were suggesting that these patients needed broad-spectrum antibiotics within an hour and they felt that there were some of these patients that were settling enough to not declare themselves as needing an operation. So they’d go home and then represent a few weeks later with the same problem again as an untreated case. Now we’ve worked with them and I think we’ve worked round to the situation whereby they’ve got a better understanding of what we’re trying to do with sepsis and say that what we’re trying to do is save lives.
Clinical lead, sepsis
Appendix 14 Evaluative survey
Glossary
- Case mix
- Patient factors that are often associated with the outcome of interest, such as age and comorbidity, and that therefore need to be accounted for when comparing performance by hospital.
- Clinical Classifications Software
- A classification system that aggregates individual diagnosis, recorded as International Classification of Diseases, Tenth Edition codes, into broad diagnosis groups to facilitate statistical analysis and reporting with mortality data.
- Hospital Episode Statistics
- An administrative database covering the main types of patient-level NHS hospital activity.
- International Classification of Diseases, Tenth Edition
- The standard diagnostic tool for diseases and other health problems.
- Mortality alert
- A signal triggered from statistical process control charts when accumulative mortality surpasses a set threshold.
- Office of Population, Censuses and Surveys Classification of Surgical Operations and Procedures, 4th revision
- A standard classification system for operations procedures and interventions.
- Relative risk
- A relative measure of mortality calculated as the observed number of deaths divided by the expected (risk-adjusted) number of deaths.
- Statistical process control chart
- A tool for monitoring processes by means of time series plots.
- Superspell
- A spell ending in transfer to another NHS hospital that is linked with the succeeding spell to create a continuous period of care.
- Surveillance system
- The systematic collection, consolidation, analysis and dissemination of mortality data.
List of abbreviations
- A&E
- accident and emergency
- ACS NSQIP
- American College of Surgeons National Surgical Quality Improvement Program
- AMI
- acute myocardial infarction
- AQuA
- Advancing Quality Alliance
- CABG
- coronary artery bypass graft
- CCG
- Clinical Commissioning Group
- CCS
- Clinical Classification Software
- CEO
- chief executive officer
- CI
- confidence interval
- COPD
- chronic obstructive pulmonary disease
- CQC
- Care Quality Commission
- CUSUM
- cumulative sum
- ED
- emergency department
- FDR
- false discovery rate
- GP
- general practitioner
- HED
- Healthcare Evaluation Data
- HES
- Hospital Episode Statistics
- HSMR
- hospital-standardised mortality ratio
- ICD-10
- International Classification of Diseases, Tenth Edition
- ICNARC
- Intensive Care National Audit and Research Centre
- ICU
- intensive care unit
- IT
- information technology
- ITU
- intensive therapy unit
- MASS
- mortality alerting and surveillance system
- MEWS
- modified early warning score
- MINAP
- Myocardial Ischaemia National Audit Project
- MRSA
- meticillin-resistant Staphylococcus aureus
- NCEPOD
- National Confidential Enquiry into Patient Outcome and Death
- NEWS
- National Early Warning Score
- OECD
- Organisation for Economic Co-operation and Development
- OPCS-4
- Office of Population, Censuses and Survey Classification of Surgical Operations and Procedures, Fourth Edition
- PARS
- patient at risk score
- PCI
- percutaneous coronary intervention
- PDSA
- Plan-Do-Study-Act
- PRISM
- Preventable Incidents, Survival and Mortality
- RAMI
- risk-adjusted mortality indicator
- RR
- risk ratio
- SD
- standard deviation
- SE
- standard error of the mean
- SHMI
- summary hospital-level mortality indicator
- SPI
- Safer Patients Initiative