Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/209/51. The contractual start date was in May 2014. The final report began editorial review in August 2016 and was accepted for publication in April 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Frances E Griffiths and Anne-Marie Slowther are funded for other research by the National Institute for Health Research (NIHR) Health Services and Delivery Research programme (14/156/20 and 13/10/14), the NIHR Programme Grants for Applied Research programme (RP-PG-1212-20018) and the NIHR Research Design Service (PR-RD-0312-1001).
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Griffiths et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Our overall research question was: what are the effects, impacts, costs and necessary safeguards for digital clinical communications (DCCs) for young people living with long-term conditions (LTCs) and engaging with specialist NHS providers?
Digital clinical communication
Our definition of DCC is one in which the clinician and/or young person is (or could be) mobile when sending or receiving the communication. It has two-way functionality and can be initiated by either party. It may be synchronous or asynchronous and is for the purpose of delivering or receiving clinical care. Examples of such digital communications take place using e-mail, text messaging, mobile phone, web portals or personal health record (PHR) systems (e.g. Patient Knows Best), voice over internet protocols (VoIPs) [typically Skype™ (Microsoft Corporation, Redmond, WA, USA) and FaceTime (Apple Inc., Cupertino, CA, USA)] and social media [e.g. Facebook (Facebook, Inc., Menlo Park, CA, USA) and Twitter (Twitter, Inc., San Francisco, CA, USA)].
The health burden of young people with long-term conditions and the health service factors
Young people living with LTCs are vulnerable to service disengagement and this endangers their long-term adult health. Poor transition between paediatric and adult services can lead to disengagement from health services and poorer health outcomes. 1–5 Among young renal transplant recipients, 35% had lost their transplants by 36 months after transfer to adult renal care and there is a large peak of graft loss between the ages of 20 and 24 years. 6 The introduction of transition co-ordinators for paediatric liver transplant recipients and integrated paediatric–adult clinical services for patients with kidney failure have led to improved outcomes in young people transitioning from paediatric to adult care. 7–9 Transition co-ordinators and integrated paediatric–adult clinical services have been associated with improved adherence and reduced rates of graft failure. 7,8 However, the use of these services at present is limited. A systematic review of 13 studies found that large numbers of young patients with congenital heart disease were lost to follow-up or experienced gaps in their care after transitioning from paediatric to adult cardiology services. 4 With sickle cell disease, during the period of transition to adult services, regular attendance at outpatient clinics and adherence to medical regimens, in particular penicillin prophylaxis, declines. 10–12 This is a worrying trend, especially because it is estimated that 25% of deaths reported in young people are linked to infection and poor compliance with penicillin prophylaxis. 13 Compared with adults, children and young people living with diabetes mellitus are less likely to have their glycated haemoglobin (HbA1c) levels measured. 14 Young people in their early twenties are less likely to have their HbA1c levels measured than those aged 10–19 years. 14 Furthermore, adolescents and young adults (aged 15–24 years) tend to have poorer diabetes mellitus control than younger children (aged 0–14 years). 15 This disengagement from services results in a considerable health burden for the young people and their families and an economic burden for the NHS. Health service factors affecting young people’s engagement with health care include poor patient–clinician communication, inflexible access to people and information, lack of person-centred health care and the need for continuity and relationship development. 4,16–19
Digital communication and its use for health care in the UK
In the UK, 66% of adults own a smartphone. Among young people aged 16–24 years smartphone ownership is 90% and almost all young people who own a smartphone use it to access the internet. 20 Although people of all ages use digital technologies in relation to health and health care,21–27 several studies have reported requests from young people for e-mail, text messages and social media communications with their health-care team. 16,28 At the start of the study we saw young people using the NHS as providing the best current opportunity for understanding how, why and with what effect, DCC can be used by NHS providers. At the time of initiating our research we were aware of a number of clinics using digital communication with young people. For example, clinical teams were using digital communication with young people with bipolar disorder29 and diabetes mellitus,30 and personal contacts confirmed use of e-mail, text messages or web portals in conditions including liver disease and sickle cell disease. These innovators provided opportunities to learn how to best harness digital communication in the NHS to the benefit of the young people for whom it provides care.
The research started at a time when UK policy and technological solutions were developing in relation to the use of digital communication in health care. Government policy on clinical information was to improve access to information31 and to have systems in place for digital communication between clinicians and patients by 2015. 31 One aspect of this was the NHSmail 2 project. 32 The then-ongoing Caldicott 2 review was seeking the appropriate balance between protection of personal information and sharing of information to improve care. 33 The imperative to digitalise the NHS has accelerated during our study. For example, in October 2015 the National Information Board’s Workstream Roadmaps was published. 34 NHSmail 2 was launched in July 2016, providing e-mail that is now secure for use with patients and Dame Fiona Caldicott published her review of data security, consent and opt-outs in the summer of 2016. 35 In the autumn of 2015, the National Information Board successfully negotiated, in the Treasury spending review, for £4.2B to digitalise the NHS. Professor Robert Wachter was appointed in November 2015 to chair a review of the NHS on its digital future and make recommendations. 36 This review was published in September 2016. 36
In his presentation to The King’s Fund Digital Health Congress in July 2016, Professor Wachter highlighted what is termed the productivity paradox – digitalisation has not resulted in a change in productivity – and suggested two factors for unlocking this for the NHS: the improvements in the technology and reimagining the work. 37
Professor Wachter’s review36 considered all aspects of digitalisation for the NHS, including electronic medical records, communication between clinicians and communication between clinicians and patients. Our study is limited to communication between clinicians and young people with LTCs about clinical issues. For our study, the key improvement in the technology is the smartphone, able to support all forms of digital communication: mobile phone infrastructure-supported voice and text communication (mobile phone and text messaging) and internet-supported voice and text communication (VoIP, such as Skype, e-mail and other social media), while people are on the move. Our study examines how clinicians have reimagined their work.
Evidence for the impact of digital clinical communication on health outcome
In the last two decades a wide range of digital communication systems have been developed in relation to health. There is a large research literature, including several dedicated peer-review journals and many reviews. In this section we discuss systematic reviews of evaluations of DCC and LTCs that were published prior to 2014 and so provided the rationale for our research. The evidence base has continued to grow and later evidence relevant to our research question is reviewed within this project report in Chapters 11–13. The published systematic reviews varied in how they defined their focus. Some focused on a specific technology (e.g. Ye et al. ,38 Blackburn et al. 39 and de Jongh et al. 40) and others specified both disease and technology (e.g. Holtz and Lauckner41). There were reviews in which the focus was the nature of the content of the communication, such as symptom reporting before a first appointment or between appointments (e.g. Johansen et al. 42) or the communication of diagnostic tests (e.g. Meyer et al. 43). Most reviews included studies from across all ages, except our own reviews on diabetes mellitus and mental health,44,45 which focus specifically on young people.
Evidence of the effectiveness of DCC from systematic reviews was equivocal, although all reviews reporting effects found either in favour of the intervention or no differences when compared with usual care. No trials reported poorer outcomes in the experimental digital communication arm. There was an almost unanimous finding from review authors of poor-quality intervention reporting alongside varying methodological quality of included studies. The reviews found study populations to be generally more educated, with higher socioeconomic status than population norms. 41,46,47 Several reviews found that patient engagement with health-care providers increased, as assessed by access data, contact data or health-care professional workload data (e.g. Ye et al. ,38 Sutcliffe et al. ,44 Martin et al. 45 and McLean et al. 48). A review that considered the possible impact of this increased engagement49 included 90 trials of synchronous and asynchronous communications in diabetes mellitus care. The authors found that the effect sizes of these interventions had remained static over the 16-year period covered by their review, despite increasing normalisation of the technologies across the populations and emphasis on higher-quality research designs. They found that asynchronous communications led to greater improvements in glycaemic control and self-care outcomes, with synchronous interventions being more user-friendly and more cost-effective for patient and provider. Combined interventions led to greatest quality-of-life improvements. Alongside these positive findings were negative impacts. Depression increased, parental relationships deteriorated and information overload was reported in some included studies.
Many reviews of the impact of DCC on health outcome also identified evidence gaps. To ensure that our research filled these gaps we systematically summarised these evidence gaps. We included in this summary reviews that (1) investigated asynchronous and/or synchronous communication between patients and clinicians using digital communication technologies; (2) had been published from 2010 onwards, as older reviews were unlikely to capture the types of digital communication usage patterns commonly experienced in 2014 when we wrote the summary; and (3) included children and young people or young adult populations only, or young people as well as older adults or if it concerned a condition commonly affecting young people. Seventeen published reviews were identified and their recommendations and justifications for future research were identified. We included one review from 2009 because of its focus on training and support for health professionals. Table 1 presents the list of research priorities identified along with details of the reviews and whether or not our research has tackled each one.
| Priority topics for future research identified in systematic reviews | Number of reviews recommending research on the topic | Research tackled topic: yes/no |
|---|---|---|
| Factors important to patients, public and clinicians | 940,41,43–46,49,51,52 | Yes: for patients and clinicians |
| Cost and/or cost-effectiveness/resource use | 838,40,42,44,46,51,53,54 | Yes |
| Research to identify moderators, mediators, active ingredients, theoretical basis for intervention and link with outcomes (MRC framework50) | 640,42,48,51,55,56 | Yes: qualitatively |
| Harms and risks (including privacy and data security) | 540,43,46,48,51 | Yes |
| Qualitative research designs | 443,46,48,49 | Yes |
| Research generic to multiple long-term-condition populations such as use of generic scales or outcomes of interest, measures to facilitate meta-analysis and/or comparisons across conditions (e.g. health economics, medication use, quality of life and service engagement) | 438,42,48,54 | Yes: a range of LTCs included with qualitative and health economics comparison; identification of a potential generic measure |
| Need for research to inform policy and practice in a range of digital communication aspects to inform implementation/roll out | 342,43,53 | Yes |
| Impact on contact frequency and on A&E attendance, hospitalisation and clinical outcomes | 344,49,53 | Yes: case based |
| Health-care professional–patient relationship within this digital communication context | 343,47,57 | Yes: via interviews |
| Broaden socioeconomic and ethnic diversity of research to assess access and inequalities and uptake/usage | 341,46,47 | Case studies include conditions common in ethnic minorities |
| Telephone counselling vs. e-mail counselling | 146 | Specific comparison not made, but one case study undertook text-based counselling |
| Function of communication (e.g. timely advice) in digital communications rather than technological mode of communication | 148 | Yes |
| Focus on widely used digital communication intervention not just future focused | 154 | Yes |
| Effects of age on use, impact, outcome | 144 | No: proposal is focused on young people |
| Patient and clinician training and preparation | 145 | Yes |
| Use in symptom monitoring | 145 | Symptoms monitoring not specifically studied but was talked about by participants |
| Investigation of the motivational/fun elements of health technology toys | 142 | No examples found |
| Smartphone applications to support web-based interventions | 149 | No specific examples found |
| Content of communication | 151 | Yes: via interviews |
Of the 17 reviews, nine mentioned the need to understand what was important to patients, the public and clinicians. 40,41,43–46,49,51,52 Eight reviews identified cost as a priority for research on DCC. 38,40,42,44,46,51,53,54 Specific areas identified were health-care resource use by patients and health professional workload. Several reviews reported increased communication with patients when digital communication channels were available. This led to concerns about the costs of meeting patient demand. 44,46 One of our own reviews44 identified clinician training and ongoing support as a potential hidden cost, as clinicians may not be as familiar with, and confident in, the use of these technologies as their younger patients. Five reviews indicated the importance of exploring risks and harms, information security and privacy issues. 40,43,46,48,51 Several reviews felt that it was time to develop an evidence base across conditions and clinical contexts38,42,48,54 as there are many commonalities across LTCs,42 but evidence was concentrated in a small number of LTCs, such as diabetes mellitus and asthma. Six reviews suggested the need for a deeper understanding of how these interventions work to produce the desired outcome40,42,48,51,55,56 and three specifically identified the relationship between the patient and clinician. 43,47,57 Outcomes suggested by three review teams were frequency of contact using the digital communication on offer, accident and emergency (A&E) attendance, hospitalisation and clinical outcome. 44,49,53 Several reviews indicated that the majority of research had been undertaken in more affluent, educated and ethnic majority populations. 41,46,47
Aims and objectives
In response to the identified evidence gaps we developed the following aims and objectives.
Aims
-
To evaluate the impacts and outcomes of DCCs for young people living with LTCs. Many young people disengage from health services between the ages of 16 and 24 years, resulting in poor health, but they are prolific users of digital communications. As such, young people using the NHS present the best current opportunity for addressing our second research aim.
-
To provide a critical analysis of the use of DCCs by NHS specialist care providers. DCCs are being widely embraced by clinicians working with young people, but the NHS is currently underserved by research evidence to prepare it for this development.
Objectives
-
To engage young people in the implementation of the research.
-
To observe and explore with young people with LTCs – and where appropriate a parent/carer, clinicians and managers – the use of DCC in the NHS for a variety of clinical conditions, how it is used and with what impact and issues related to ethics and patient safety.
-
To investigate the impact of DCCs on health outcomes for young people with LTCs and on their engagement with, and use of, health services.
-
To describe the cost of implementation and ongoing provision of DCC and how it varies across different clinical conditions, and to understand the value of this service to patients and clinicians.
-
To identify and explore the use of patient-reported outcome measures (PROMs) for future cost-effectiveness studies, which can be used across disease areas to capture the impact of DCC.
-
To evaluate and synthesise published evidence on the use of DCC by health professionals with young people with LTCs.
-
To develop and disseminate guidance for NHS providers and commissioners on the use of DCC, to provide insights for policy-makers from current NHS use of DCC and to consider the need for future research.
We chose not to specify a specific technology to study in order to future-proof the study and to avoid limiting the utility and validity of the results. The digital communication ecosystem is rapidly changing. 20 For example, the introduction of smartphones is changing the way people access information and use communication channels. The use of communication channels also evolves. For example, Twitter was initially used primarily for broadcasting, but then became used for communicating between individuals or within small groups. 58 We studied the use of DCC via whatever medium was being used by the patients and clinicians we studied, in order to draw out results that are transferable across technologies. This allowed us to learn from a small number of established systems for DCC for young people in the NHS, and from the informal, unregulated development of this means of communication between clinician and patient.
The research focused on young people (aged 16–24 years) who have LTCs such as diabetes mellitus, cancer, cystic fibrosis, sickle cell disease and other conditions that require engagement with specialist (secondary or tertiary) clinical services. We studied NHS providers of specialist clinical services. We were concerned with communication between patients and specialist (secondary or tertiary care) clinicians/clinic teams who have already been in contact with each other in the clinical setting, where communication was, or there was potential for it to be, in both directions – patient to clinician and clinician to patient. We did not include specifically the delivery of therapeutic interventions via digital communication media59 [such as cognitive–behavioural therapy (CBT)],60 nor digital communication that solely involves the delivery of information on disease prevention and health promotion. 61 However, where the use of a digitally delivered intervention or the delivery of disease prevention and health promotion information formed part of ongoing patient–clinical team communication, they were included.
Research questions
Our data collection, analysis and synthesis addressed the following prespecified research questions. These questions are grouped according to the approach to data analysis taken to answer the questions [or for Chapter 9 on information governance (IG), the perspective of the research participant]. These analysis approaches correspond to chapters in the report as indicated below.
Chapter 3: what works for whom, where, when and why?
-
What works for whom, where, when and why?
Chapter 4: ethical implications of using digital clinical communication to support young adults with long-term conditions
-
What concerns do patients and clinicians have about confidentiality in relation to DCC?
-
How does this form of communication affect the patient–clinician relationship and the clinician’s duty of care?
-
What regulatory framework is needed to reassure patients and clinicians regarding its use?
Chapter 5: patient safety
-
What are the significant risks to patient safety associated with the use of DCC in the context of supporting young people with chronic disease?
Chapter 6: health economic analysis
-
What value do patients place on DCC?
-
What are the direct resource use implications for the NHS of implementing it?
-
How does the direct resource use vary when used with different patient groups?
-
What are the resource implications for scaling up in the NHS?
Chapter 7: information governance
This chapter analyses the data from the interviews with IG officers with reference to the research questions for Chapters 4–6.
Chapter 8: impacts on health-related outcomes
-
How is the impact on the health status of patients currently evaluated?
-
Using existing clinical data, what is the impact on health status of patients?
Chapter 9: generic patient-reported outcome measures
-
What generic outcome measures are available to assess the impact of DCC?
-
In the future, how can its effectiveness be measured across health conditions?
Chapters 10–12: scoping reviews
-
What is the evidence in the literature to support, refute or add value to the case study findings?
Chapter 13: discussion
-
What are the risks to patients and to NHS specialist care providers from its use?
-
What policy and procedural changes are needed for gaining benefit and limiting harm?
-
In which clinical areas is benefit most likely and how is benefit most likely to be achieved?
-
What future evaluation is needed and how should it be undertaken?
In response to requests from NHS England and NHS Digital (formerly the Health and Social Care Information Centre) for assistance with the development of their policies and procedures, we undertook the analyses reported in Report Supplementary Material 1. The consensus conference, which also contributes to the above research questions, is also reported in Report Supplementary Material 1.
We tackled the following question through our internet search described in Chapter 3 in order to form our sampling frame.
-
How, and for what purpose, is this form of communication taking place (or not) in the UK?
We tackled the following question through maintaining awareness of developments in the ethical, legal, policy and governance landscapes relevant to DCC in the UK to ensure that our research took account of this.
-
What is the ethical, legal, policy and governance framework for DCC?
In Appendix 1, we provide a report on all our patient and public involvement (PPI) activity and the impact it had on the research, except for PPI activity linked to the identification of a generic outcome measure which is reported in Chapter 9. Our appendices also include copies of the quick reference guides produced in response to discussions with NHS Digital, from our data analysis. These are A4 leaflets available to freely download from www2.warwick.ac.uk/fac/med/research/hscience/sssh/research/lyncs/ (accessed 5 March 2017). The NHS Digital website carries a link to these guides.
Ethical considerations in planning this study
The key ethical issue in this study was confidentiality in both recruitment and data collection. During data collection we were asking clinic staff to reveal their clinical activities that may have been in breach of IG policies. This was a difficult issue, as these clinicians are rich sources of data. We drew up a protocol for action for serious breaches of confidentiality, but did not take action for activity that we found to be common practice. This approach was approved by the ethics committee (see Chapter 2). Data collection was planned across 20 different sites so preserving anonymity is possible.
Chapter 2 Methodology and methods of case studies and the characteristics of the cases
This chapter reports the methodology and methods for the case studies, and describes these case studies. Methods for the systematic scoping reviews, review of PROMs and consensus conference are reported in the relevant chapters.
The main empirical work for this study utilises a case study approach. Robert Yin describes a case study as ‘an empirical inquiry that investigates a contemporary phenomenon in depth and within its real-life context, especially when the boundaries between phenomenon and context are not clearly evident’ (p. 18). 62 In this research, the contemporary phenomenon we study is the use of DCC and the context is specialist NHS care provision for young people with LTCs. In-depth study allows us to simultaneously focus on several different elements of care provision, such as patient safety and ethical concerns. When conducting a case study, one of the first steps is to develop propositions to identify what to study. 62 Our propositions are that DCC fits with young people’s day-to-day mode of communication and, therefore, they would prefer it to other means of communication with their clinical team; and clinicians use DCC to encourage young people with LTCs to engage with their health care and improve their health outcomes (even if this puts other aspects of clinical service provision, such as record-keeping, at risk). Based on these propositions, we need to look for evidence to answer our research questions from the young people and clinical teams. The young person with a LTC in communication with their clinical teams (i.e. young person–communication–clinical team) is our unit of analysis. This unit of analysis is embedded within the wider clinic, the NHS and contemporary society. 62
Ethics and research governance permissions
The study was approved by the National Research Ethics Service Committee West Midlands, The Black Country on 5 March 2014 (reference number 14/WM/0066). A substantial amendment was granted on 26 February 2015 to allow the following changes to the invitation letters and participant information sheets: offer a £20 voucher as a thank you for participating in the study; include information regarding the study’s insurance and indemnity; and include information about whom participants should contact to make a complaint. In addition, the amendment approved a further two ‘invitation to interview’ letters specifically aimed at young people who did not attend (DNA) their appointments. A second amendment approved on 18 June 2015 covered the following amendments: (1) change to the protocol to make recruitment of parents/carers easier, enabling the researcher to contact a participant’s parent/carer directly once the consent of the participant was given; (2) taking the burden of recruitment away from research nurses by enabling the research team to contact the parent/carer; (3) extending the £20 voucher as a thank you for participation to parents/carers; (4) changes to the patient information leaflet to reflect the above changes; (5) changes to the recruitment poster to include information about the £20 voucher (which we had in error omitted from this participant information); (6) changing the term ‘long term’ to ‘health’ in patient information leaflets in cancer care clinics as the clinicians felt that the term ‘health condition’ would better reflect the patients’ view of their condition; and (7) request permission for a number of students undertaking health-related graduate and undergraduate studies to undertake data analysis. Research governance approvals were awarded by 16 participating NHS trusts hosting our 20 research sites. Details of these NHS trusts are withheld from this report to protect the identities of participating health professionals, many of whom were using digital communication methods at the time of interview under the radar of their NHS trust IG policies and procedures.
Clinical case site recruitment
Case site inclusion criteria
Inclusion criteria for clinical sites were as follows.
-
The clinic provided specialist care for young people with LTCs.
-
The LTC was currently expensive to the NHS.
-
The clinical team expressed interest in the use of two-way digital communications to a minimum, moderate or large extent.
We sampled clinical teams for diversity of long-term health conditions experienced by young people.
Case site recruitment
As a relatively large number of case sites were required, multiple recruitment strategies were used. An extensive internet search of grey literature was conducted to identify technology being used for clinical communications in the UK. An internet search using the search engine Google (Google Inc., Mountain View, CA, USA) was undertaken between December 2013 and February 2014. The keywords used were e-health, telehealth, telemedicine, digital communication, young people and young persons. Combined, the searches returned 24,626,063 hits. The first 35 pages of each search were scrutinised for relevance. In the case of potentially relevant projects, detailed information was sourced from individual trust websites, documents and reports. Further details were obtained by contacting key individuals and project leads. This search identified 71 projects involving DCC, running at 38 different NHS trusts, health-care organisations and universities. We tried to contact 14 sites that seemed eligible for participation (the search was not limited to young people with LTCs). Additionally, one clinical team was identified via the internet and approached.
Snowball recruitment was also used: the research co-applicants sent out recruitment e-mails to their colleagues and asked that they pass the information on to anyone else who may be interested; in addition, specific clinical teams were suggested by the research co-applicants, based on the known use of communication technology in their usual practice. The research team contacted 51 different clinical teams using this approach. Research team members attending academic and applied health conferences advertised the study with poster presentations and recruited potential case sites through networking sessions. Seven contacts were made this way. Finally, the research team was approached by seven NHS trusts that had seen the study listed in the National Institute for Health Research’s (NIHR’s) portfolio. A further 24 contacts were made after people already in discussion with the research team snowballed the study information to others they thought would be interested. Overall, we made initial contact with a total of 104 different clinical teams.
Interview participant recruitment
We aimed to conduct brief interviews with members of the clinical team, up to 15 patients aged 16–24 years and an IG officer at each site. Where the clinical team was < 15 patients, we aimed to interview all members of staff. Parents/carers/household members of young people with a LTC were also invited to participate in an interview.
Two weeks prior to fieldwork commencing, a research nurse from the local clinical research network or NHS trust identified eligible patients attending the clinic on days when a Long-term conditions Young people Networked Communication (LYNC) study researcher was present. These patients were sent (via post, or e-mail if appropriate) a study information sheet and given an option of contacting the researcher in advance to express interest in participating. Patients were also recruited by the researcher during their time in clinic, usually while waiting for their appointment. Patients were asked to bring examples of recent DCCs to inform interview discussion. The research nurse also identified patients who frequently DNA clinic appointments from clinic records and sent a separate recruitment letter to these patients. Young people were given a choice of medium for their interviews: in the clinic, over the telephone or via other technology chosen by the participant (including e-mail and Facebook). The researcher asked for consent either during recruitment or prior to commencement of the interview. For telephone interviews, consent was given verbally and a dated note was made by the researcher. All participants were offered a £20 high-street voucher as a thank-you token. At the end of the interview, researchers asked the patient if they were willing for their parent/carer/household member to be interviewed for the study. If they agreed, they provided contact details for the research nurse to send out an invitation letter. These interviews were conducted over the telephone, at a time convenient for the participant.
Clinic staff were recruited on an ad hoc basis during fieldwork. Prior to the start of fieldwork the researchers attended a team meeting to introduce themselves and the research, and to make staff aware of their presence on site. We aimed to interview any clinic staff who used (or would potentially use) DCC, such as nurses, doctors, professions allied to medicine and administrative staff. We specifically sampled for diversity of job role and experience of, and opinion about, DCC within each case study. Within each clinic we aimed to interview as many team members as were willing to participate, up to 15 members of staff. In small clinics we interviewed all relevant team members. In large clinics we aimed to get representation across all specialties and grades of staff. Interviews took place over the telephone, or in a location chosen by the participant (clinic space, offices, cafes, etc.). Participants were reassured that the information they provided would be confidential and that it would not be possible to identify specific clinics or staff members from our research report. It was also explained that if a concern arose about unethical or unsafe clinical practice, the researcher would need to report this to a principal investigator (PI) who would decide if it was necessary to initiate action through normal professional channels. However, no such practice was reported. During data collection we were asking clinic staff to reveal activities that may breach IG policies. This was a difficult issue, as these clinicians were likely to be rich sources of data. We therefore drew up a protocol of action for serious breaches of confidentiality (see Appendix 2). However, we did not expect to take action for activity that we found was common practice.
At each case site we aimed to interview a trust-wide IG officer. We aimed to conduct this interview prior to fieldwork commencing, so that the researcher would not inadvertently disclose clinic practices that may be out of step with trust IG policies. Additionally, this enabled an understanding of the local context in which the clinical staff operated. Interviews with IG officers took place on site in trust offices or over the telephone.
Data collection
Non-participant observation
Non-participant observation of the clinic and shadowing of clinic staff took place at each clinical site. Using an observation pro forma, the researchers noted how the clinic functioned, how DCC was used and monitored within the team and what evidence there was for more widespread use of digital communication within the clinic space (e.g. clinic staff using computers, patients using smartphones in waiting rooms). When shadowing members of the clinical team, the researchers reported if, and how, digital communication was used for clinical purposes, describing the context and content of the dialogue. Shadowing lasted for up to 2 hours, whereas clinic observation lasted for the duration of the clinic (up to 8 hours) and were designed to note the use of digital communications between appointments. When possible, observations preceded interviews. The researchers made patients and staff aware of their presence in the clinic by wearing a T-shirt identifying them as LYNC study researchers and putting up posters advertising the study. Observation schedules are available in Report Supplementary Material 1.
Semistructured interviews
All interview schedules focused on how digital communication was used for clinical purposes and the advantages and concerns participants had about this use, specifically identifying risk and ethical concerns. The interview schedules were a guide and we covered the part of the schedule relevant to each interviewee. Based on initial analysis of interviews we adjusted interview schedules to ensure that we obtained the richest possible data (e.g. altering question wording). During individual interviews we adjusted the words we used to refer to digital communication according to the words used by the interviewee in response to early questions.
Additional data on ethics, safety and the generic PROMs were collected from specific sites. Data from a cancer and liver conditions site were initially analysed with a focus on ethical concerns. Based on this analysis, the interview schedule was amended to focus on emerging ethical issues, such as equity in access, consent, privacy and confidentiality, risks/benefits to staff, patient–clinician relationship, patient autonomy and duty of care. This interview schedule was used to collect data from a further three sites (renal, cystic fibrosis and mental health). These sites were chosen based on their use of DCC and diversity in health condition. Additional data on safety were collected from two clinics (diabetes mellitus and cancer) which used DCC. The diabetes mellitus clinic was chosen as the self-management of diabetes mellitus involves the young person making decisions several times a day about their dose of insulin and errors in these decisions can quickly lead to adverse events. The cancer clinic was chosen as these young people are likely to be on medication with potentially serious side effects and are coping with psychological distress as a result of their life-threatening diagnosis. At these two sites, the interview schedule was amended to focus on important safety issues, such as risks, the importance of risks to patients, how risks are accepted or reduced, engagement with treatment regime, adverse events, unintended outcomes and benefits. In the later sites, the interview schedule was revised to focus on undertaking cognitive interviews to assess the two generic PROMs identified in the literature review and from PPI activity. This interview schedule was used with seven patients and seven clinicians.
A specific interview schedule was developed for use with IG officers, with input from our IG co-applicants. This focused on if, and how, technology was used within the trust for communication about clinical issues, what policies instruct the use of technology, recorded DCC-related incidents and their professional opinions on the use of digital technologies in their respective NHS trusts. When DCC was not used, the key professionals were asked whether or not there were any future ambitions to introduce these types of communication, and if there were any barriers to, and enablers of, this introduction. Interview schedules are available in Report Supplementary Material 1.
Collection of impact data
Data are broadly categorised in two groups: (1) the cross-clinic and condition outcome data and (2) clinic-specific outcomes. Cross-clinic outcomes are appointment status (attended, cancelled or not attended), A&E attendance and hospital admission. Such outcomes, from most sites, were obtained from the information technology (IT) departments of trusts, with contact initiated by the site contact (PI, consultant, etc.) or the service manager. For tertiary care case study sites, A&E attendance and hospital admission data for their clinic patients were not available, as the patients would attend their local A&E department or hospital for emergencies.
Clinic-specific outcomes are outcomes specific to the various health conditions and sites studied. These were identified in discussion with the clinical team as being key indicators of patients’ health. These outcomes were HbA1c and glucose levels for diabetes mellitus sites; body mass index (BMI); forced expiratory volume in 1 second (FEV1) as a percentage of predicted (FEV1% predicted); bed-days to receive intravenous (i.v.) therapy for cystic fibrosis sites; time to discharge for a dermatology site, where patients are discharged from the service when the skin condition is successfully treated; tacrolimus level for a liver cancer site; viral load for a human immunodeficiency virus (HIV) site; urine protein and serum creatinine levels for a renal site; and self-harm incidents and self-harm ward attendances for mental health sites. Tacrolimus level data from the liver cancer site, and BMI and FEV1% predicted data from one of the cystic fibrosis sites, were extracted by the clinic staff, whereas all the other clinic-specific outcomes were provided by IT specialists from trusts. These aggregated data were collected for all patients in the age range of our study on these cross-clinic and clinic-specific outcomes. Data collection periods were for the year prior to the escalation of DCC in each service and every year following to the point of fieldwork commencement.
Collection of economic data about the digital communication system
A structured questionnaire was developed to collect data on resource use associated with DCC (see Report Supplementary Material 1), during staff interviews. The questionnaire was based on initial case study observation and semistructured interviews with staff. All staff, at each case study site, who participated in an interview, and whose role involved any degree of contact with patients, were asked to complete the questionnaire. Where possible, the questionnaire was given during the interview, otherwise it was sent by e-mail after the interview had taken place. The questionnaire asked staff members to report the time they spent each day on DCC-related activities, broken down by the channel of communication used (e-mail, mobile phone calls, text messaging or other, such as VoIP). Staff were not asked to report a precise figure; instead they were asked to report usage for each channel by selecting from boxes corresponding to time intervals (e.g. 0–15 minutes, 15–30 minutes). The questionnaire also asked staff to report what technology they used for DCC (laptop, desktop personal computer, mobile phone or tablet) and who provided this equipment (i.e. whether it was provided by the clinic or themselves). Data were obtained from a site administrator, or suitable equivalent, at each site on the grade of each staff member and the number of days worked per week.
A further aim of the LYNC study was to explore, qualitatively and quantitatively, the value DCC provided service users, and how this value might be elicited. A number of ‘value’ questions were explored in the interview schedule, whereby patients at each site were asked how much they would hypothetically be willing to pay for a service which used DCC compared with one which did not. After interviews at the first two case sites, the question focusing on value to patients was changed from a willingness-to-accept format (as cited in the protocol) to a willingness-to-pay format, as patients struggled to understand the original question. An open-ended question was used, but where patients struggled to respond, we tried using prompts suggesting values ranging from £5 to £50 in order to understand what values respondents might consider plausible. In sites where technology was not used for clinical communication, clinic staff and patients were asked about how they currently communicated, how happy they were with the current situation and what DCC they would find useful in the future.
Documents collated
Current trust policies and procedures were collated with help from lead clinicians and IG managers. These documents were used to inform the IG interviews. IG managers were asked to tell us about any adverse events relating to the use of DCC.
Data management
All interviews were audio-recorded. At each case site, individual participants were given a unique code to identify all data collected from them. After each case site visit, field notes were typed up and interviews transcribed and anonymised. Qualitative data were managed by NVivo 11 (QSR International, Warrington, UK) and all files were stored on a secure server.
Impact data were supplied in Microsoft Excel® spreadsheets (Microsoft Corporation, Redmond, WA, USA). For each Excel file provided, a copy to be analysed was made. Both the original Excel files and analysed copies were stored in a secure project folder. Some analyses, such as computing the DNA appointment rates, involved computing rates in the Excel file copies. Other analyses consisted manipulating Excel files data using syntaxes written in the SPSS (version 23; IBM SPSS Statistics, IBM Corporation, Armonk, NY, USA) statistical program and this generated new formats of data. The generated data files were similarly stored in the secure project folders. Some plots were generated using the R statistical program (The R Foundation for Statistical Computing, Vienna, Austria). The R scripts written to make the plots were also stored securely.
Analysis
All qualitative data were initially coded in NVivo for the different analysis approaches within the project (what works for whom, where, when and why; ethics; patient safety; and health economics). The IG officer interviews were coded and analysed separately, as these interviews covered the use of DCC in the whole NHS trust in which the officer worked, not just the clinic we had studied. This provided a different perspective on our research questions. Further analysis of the qualitative data is described in the following sections on What works?, Ethics, Safety, Health economics and Information governance.
Survey and impact data were analysed as described in the following sections on analysis for Health economics and Impact.
Emerging findings from each analysis were discussed and shared with the project team and the Project Management Group (PMG).
What works?
Research question: what works for whom, where, when and why?
Qualitative interviews with patients and staff at 20 clinics across England and Wales, along with data from clinic observations, were analysed. This analysis stream focused on clinics’ current use of digital communications and did not consider that which was planned or wanted in the future. As per protocol, data from the first clinic were analysed line by line by using Pawson and Tilley’s configurations of context + mechanism > outcome, to produce a table which was further categorised into themes. 63 Attempting to identify these configurations at a ‘micro level’ (individual actions and interactions) was repetitive and distracted from understanding the variations in how DCC works. This led to the analysis team concluding that the idea of configurations of context + mechanism > outcome is useful, but at the level of the clinical team plus their patients. As a result, context was provided for each clinic through working with each site PI to capture the clinic purpose, mechanism became the main focus of this analysis and outcome was planned to be covered by the quantitative data derived from clinical outcome data.
Building on the codes identified in the first clinic, a coding structure was devised beneath the broad code of ‘what works’. These codes were refined with each subsequent clinic analysed, resulting in a structure with top-level codes under which was a series of subcodes that captured the similarities and differences between clinics. Codes were discussed and refined by team members (including a young PPI member of the PMG), working on the ‘what works’ analysis, at regular meetings as each subsequent clinic was analysed.
During the development of the initial coding structure, data from each clinic were coded by two members of the research team, who compared coding and discussed differences. This process enabled the team to reach consensus on the meaning and understanding of each code. After coding was completed for the first five clinics, one member of the research team took responsibility for coding the remaining sites.
Rather than develop propositions, as envisaged in the protocol, the analysis developed a number of key themes which answer the research question ‘What works for whom, where, when and why?’. Some themes focused on the perspectives of certain participants (e.g. clinicians or patients), others focused on time or technical differences in digital communication. The analysis incorporated context and outcome through comparison across clinics. The clinic-level approach gave us analytical gain that was missing when the first site was analysed for micro context + mechanism > outcome configurations. Rather than devise logic models from these configurations, one thread of the analysis analysed the data to produce scenarios illustrating which type of digital communications are most useful in the context of ‘what works for whom, where, when and why?’ These scenarios will be useful to clinicians who are proposing to use DCCs for the first time or who are planning to introduce different or new methods of communicating digitally.
Overall, 14 sites were analysed fully to produce the main themes in the ‘what works’ analysis. Data saturation had been reached by this point, meaning that no new substantive themes were identified in the data. The final six sites were analysed at the macro code level, with the data identified as ‘what works’ reviewed for differences from the case sites already analysed, or to give additional depth and understanding to the previously defined codes.
Ethics
Research questions: what concerns do patients and clinicians have about confidentiality in relation to DCC? How does it affect the patient–clinician relationship and the clinician’s duty of care? What regulatory framework is needed to reassure patients and clinicians regarding its use?
Data analysis followed the method described by Ives and Draper for ‘normative policy oriented empirical ethics’. 64 This approach recognises the need for ethical policy (in this case policy on the use of DCC) to be informed by both a theoretical analysis of the ethical concerns and the moral intuitions of the relevant stakeholders. Transcripts from two early sites were initially read to identify examples of explicit articulation of ethical issues; areas of conflict or disagreement; expressions of discomfort with current or perceived practice; or examples of avoidance of an ethical issue. A refined interview schedule focusing on prompts to elicit reflection on ethical issues was developed and used alongside the general interview schedule in a further three sites. The transcripts from these five sites were discussed in a series of five analysis meetings and initial themes relating to ethical concerns and issues were identified. All transcripts for these sites were coded against the initial themes with further discussion and refinement of the themes in analysis meetings in which consensus was reached on the ethical interpretation of the data. Ethical issues and values identified were then considered in relation to ethical, professional and legal normative frameworks. The discussions were recorded and transcribed to ensure that the range and nuance of the identified ethical issues were captured. The process was then repeated with a sample of transcripts from the remaining sites to look for any new themes/issues arising and to consolidate consensus on the initially agreed themes.
Safety
Research question: what are the main risks associated with the use of DCC in the context of young people with chronic conditions?
Data that had been macro coded as patient safety were analysed further in NVivo. These sections were first read in their entirety to allow familiarisation with the data.
Data were then coded using descriptive coding based on an established safety science framework for analysing and describing risk. 65 This framework describes risk qualitatively based on the hazard (i.e. a situation that carries risk); the potential consequences of the hazard; the potential causes that might lead to the hazard; and possible mitigation strategies to reduce the risk. Data were coded by two researchers.
In a second cycle of analysis, the descriptions of risk were clustered around similar hazards to identify the main risks. Clustering of hazards and identification of main risks were discussed and refined during 1- or 2-weekly analysis meetings. The findings were presented to members of the project team during methodology group meetings and to the wider advisory group during PMG meetings in order to validate the findings and to receive feedback.
Health economics
Research questions: what value do patients place on DCC? What are the direct resource use implications for the NHS of implementing it? How does the direct resource use vary when used with different patient groups? What are the resource implications for scaling up in the NHS?
Scope and aims of the health economic component of the Long-term conditions Young people Networked Communication study
The scope and aims of the LYNC study health economic component follow on from the design of the main study, which is an in-depth qualitative assessment of the use and impact of digital communications, defined broadly and evaluated across a diverse collection of case studies. This context does impose significant limitations on what could be achieved in terms of formal economic evaluation within the LYNC study. Specifically, the case studies provide cross-sectional data on current practice in diverse clinical settings, rather than information on specific interventions that could be subjected to economic evaluation. Furthermore, the scope of the LYNC study does not include longitudinal data collection or well-defined case and control groups that might be used to identify incremental costs and benefits. Given the restrictions imposed by the nature of the LYNC study, our aim was not to attempt estimation of the cost-effectiveness of digital communication use at each site, but instead to motivate future formal economic evaluations in this area and provide reflections that might be useful in the design of such studies. We aim to inform service delivery as well as research by considering what challenges might arise from the implementation and monitoring of practices around digital communication, and whether or not economic evidence might be required to inform decision-making around the adoption of digital communication in routine practice.
Data from the health economic questionnaire were used to calculate, for each respondent, the annual absolute costs associated with DCC usage. We refer to absolute cost as the data do not allow us to distinguish between additional activity occurring because of the adoption of digital communication usage, which is an incremental cost of digital communication, and activity which would have taken place even if digital communication had not been adopted, which is therefore not an incremental cost of digital communication. Time responses were converted into costs using the mid-point for the time interval and for the salary as given by the NHS Agenda for Change Pay Scales for 2014–15. 66 Costs for equipment were taken from price lists provided by IT services at the University of Warwick and annualised assuming a 3-year lifespan for the technology and a discount rate of 3.5%, in line with methods guidance from the National Institute for Health and Care Excellence (NICE). 67 A health services perspective was adopted for costing, which meant that equipment costs were only included if the equipment had been provided by the employer primarily to facilitate DCC. Where data were available on all staff members at a site who interacted with service users, this costing was used to estimate the total costs of DCC-related activity at the site. For sites where one or more staff did not complete the questionnaire, an attempt was made to identify a staff member in a similar role who had completed the questionnaire, from whom the missing information could be extrapolated. This was used to estimate the total clinic costs related to DCC activity, but only if the overall completion rate for the site was over 50% (if more than half the questionnaires were not completed at a site, no attempt was made to estimate clinic-level costs). For sites where it was possible to estimate annual DCC-related direct costs, information was sought from the clinic on the size of its patient list. Where this information was available, it was used to estimate the cost per patient supported by the service of DCC.
In order to identify the consequences of DCC use at each site in terms of the impact on patient health and well-being, and clinic costs and efficiency, the health economics team reviewed the transcripts of interviews carried out with staff members at each site. Quotes were extracted that provided information on the purpose and content of DCC between clinic staff and patients, either in terms of specific examples or general experience, the consequences that arose from such communications and the counterfactual (what would have happened if DCC was not available in this situation). The aim was to identify the route to impact on outcomes that were intrinsically valued by patients – this includes the health outcomes which the service is intended to improve, but could also include outcomes relating to patient well-being more broadly. It would also include outcomes related to service efficiency, utilisation and costs. Data were also extracted on intermediate or process impacts of DCC that could lead to such outcomes. Data extraction was carried out by one health economist for all transcripts. For each site, a sample of transcripts were reviewed independently by a second health economist and comparison made for quality assurance. Once data had been extracted from all transcripts at a site, the findings were compared to identify and combine, within a thematic analysis table, quotes relating to the same use of DCC. The health economics team reviewed this table to identify gaps in the information. A follow-up interview was carried out with a senior clinician at each site to elicit information on the consequences and counterfactuals of DCC examples identified from staff interviews, where the information provided at the initial interview was incomplete.
Information governance
All IG manager interviews were entered into NVivo 10 and analysed on the basis of systematic coding recommended by Saldana. 68 This method of analysis breaks down data to identify relevant patterns and, ultimately, groups coded segments into categories which are linked to overarching themes and concepts. Two investigators coded three interviews concurrently to develop preliminary codes. Subsequently, two transcripts and the preliminary codes were reviewed, discussed, amended and agreed between two IG co-investigators, a clinician, a member of the PPI and the researchers. These final codes were then applied to the remaining interview transcripts. Additional codes were developed and applied as appropriate and a 20% subset of all clinician and patient interviews were coded using these IG codes and contributed data to the analysis.
Inductive thematic analysis69 was adopted to identify themes that were strongly linked to the data (data driven) and equally served the purpose of eliminating the influence of the researcher’s analytic preconceptions. The identification of themes was explicitly achieved at a semantic level70 on the basis of the key patterned responses provided by the IG officers. Line-by-line analyses of transcripts were undertaken to identify recurring topics. These were then sorted, identifying similarities and differences. 71 The analysis provides a descriptive account of the emergent themes.
Impact
Research questions: how is impact of DCC on health status of patients currently evaluated? Using existing clinical data, what is the impact of DCC on health status of patients?
Analysing cross-clinic outcomes data
For the appointment status, DNA rates for each year were calculated to assess the trend over time. Most appointment data were provided in Excel spreadsheets giving a breakdown of how many were attended (attended), how many were cancelled (cancelled) and how many were not attended (DNA). DNA rates were calculated in Excel spreadsheets using the formula DNA/(attended + cancelled + DNA). In some sites, data were provided indicating appointment status for each individual appointment. In such instances, SPSS syntaxes were written to manipulate the data and calculate the DNA rate.
For A&E attendance, rates of at least one attendance in each year were calculated. These were used to assess trend over time. A&E attendances were reported for each episode. SPSS syntaxes were written to calculate A&E attendance rates. Hospital admission data were analysed similarly.
For all these cross-clinic impact outcomes, instances where there was a change associated with DCC use, or any other major change in practice, were noted so that their effects could be taken into account in interpretation.
Scatterplots and Pearson’s correlations (weighted and unweighted) between annual DNA rates and each of annual A&E attendance rates and hospital admission rates were used to assess if lowering DNA rates affects A&E rates and hospital admissions. Weights used for weighted correlations were proportional to the number of registered young persons.
Analysing clinic-specific impact data
Most clinic-specific outcomes were measurements taken continuously over time to monitor the management of a condition. For example, continuously monitoring viral load and HbA1c level for young people in HIV and diabetes mellitus sites, respectively. Change over time for such outcomes was assessed by plotting individual young patients’ profiles over time and also the mean profile. The profiles were compared with the target set by the site.
Time to discharge data have a different form, so these were summarised using Kaplan–Meier plots. To assess effect over time, patients were categorised into groups based on the period when they were registered in a clinic, with a Kaplan–Meier plot obtained for each category. An example of a clinic-specific outcome is i.v. infusion rates. For this outcome, rates of patients requiring at least one i.v. infusion per year were calculated.
Again, instances where there was a change associated with DCC use (or any other major change in practice) were noted, although, where possible, the impact of DNA rates on other outcomes was assessed using scatterplots and Pearson’s r correlations.
Additional analyses
In response to policy-maker requests (NHS Digital and NHS England), we undertook a thematic analysis of our qualitative data on the use of personalised medical records and on information governance managers regarding the use of Skype for clinician–patient communication. This is reported in Report Supplementary Material 1.
Consensus conference
We held a consensus conference to consider our key findings. This is reported in Report Supplementary Material 1.
Results
Description of case sites
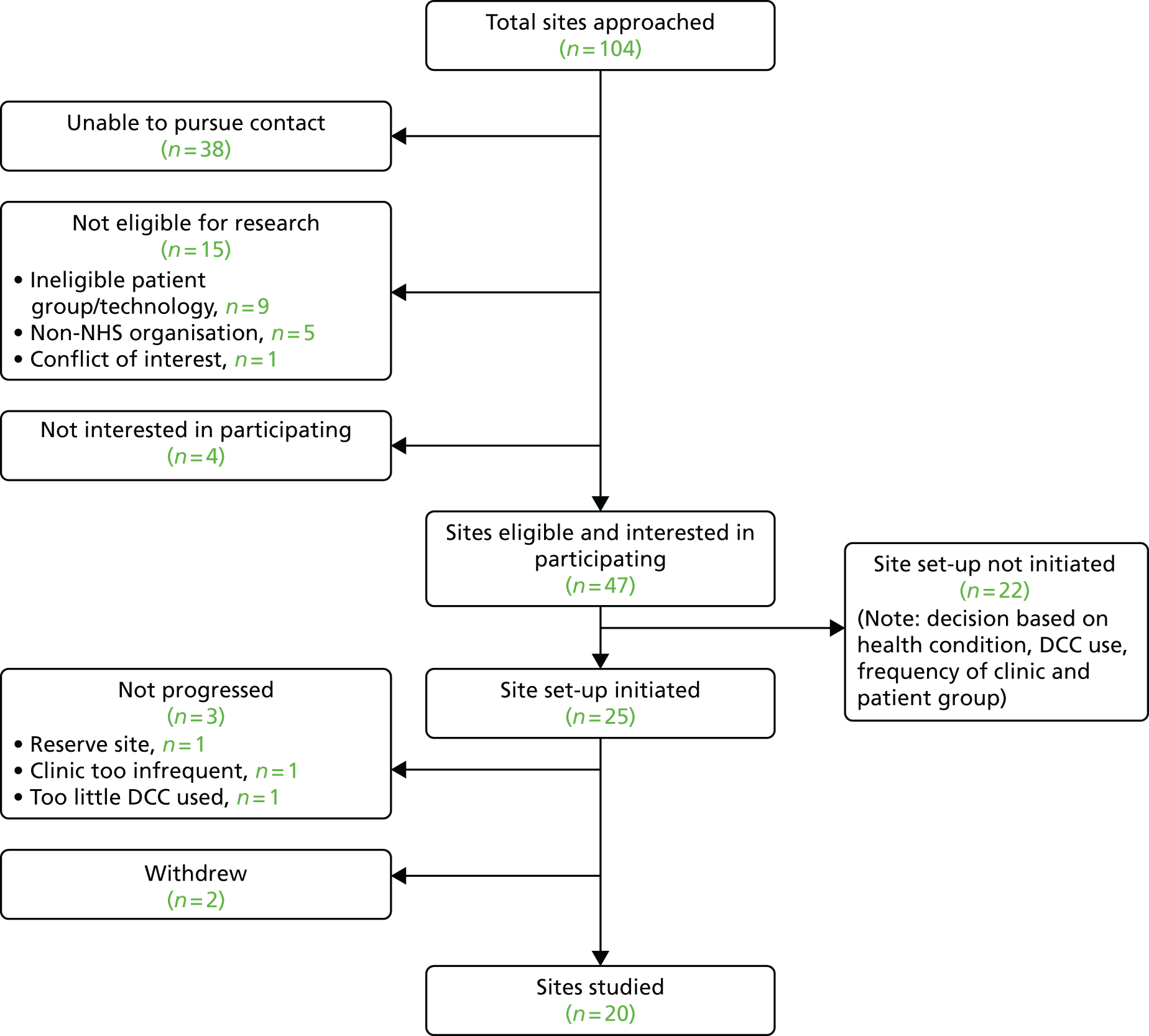
Of the 104 clinics contacted, 47 were eligible for the research and interested in participating (Figure 1). Sampling of eligible sites aimed to achieve diversity in health condition, DCC used, the frequency of the clinic, the size of the patient group cared for and geographical location, so that each case site was unique. We initiated site set-up at 25 sites. Of these, two withdrew and three were not progressed beyond initial set-up, giving a total of 20 case sites studied.
FIGURE 1.
Flow chart showing case site recruitment.
The case sites studied focused on 14 different health specialties: cancer, cystic fibrosis, dermatology, diabetes mellitus, HIV, inflammatory bowel disease (IBD), liver conditions, mental health [both Child and Adolescent Mental Health Services (CAMHS) and Early Intervention in Psychosis Teams (EIPTs)], renal conditions, rheumatology, sexual health, sickle cell disease (a condition experienced mostly by those from ethnic minorities) and a school nurse service which covered a range of different health conditions. Clinic populations varied from children and adolescent services, to transition populations, young adult services and adult services. Clinical teams were based in a range of locations around England and Wales: nine were in the south and east of England, seven were in the Midlands, three were in the north of England and one was in Wales. The types of geographical location served by the clinics included rural areas, major industrial cities, market towns, industrial towns and London. A range of DCCs was used in these clinics; some were heavy users, whereas others did not communicate digitally with patients in any way (Table 2 provides case study site descriptors).
| Site ID/health condition | Clinic population (as described by the clinic) | Patient age (years), range | Digital technology used in clinic |
|---|---|---|---|
| Liver conditions | Transition | 12–25 | Text messaging and e-mail |
| Sickle cell disease | Transition | 12–24 | Mobile phone and text messaging |
| Mental health 4 (early intervention) | Youth | 14–35 | Mobile phone, text messaging and e-mail |
| Cancer 1 | Teenage and young adult | 15–24 | Mobile phone, text messaging and e-mail |
| Diabetes mellitus 2 | Transition | 16–25 | Mobile phone and VoIP |
| IBD 1 | Adult | > 16 | Web portal and e-mail |
| IBD 2 | Adolescent | 13–23 | |
| HIV infection | Adult | > 18 | None |
| Sexual health | Adult and young people | > 16 | Testing kits ordered online |
| Cancer 2 | Teenage and young adult | 15–24 | Mobile phone, text messaging and e-mail |
| Diabetes mellitus 1 | Transition | 12–19 | Mobile phone, text messaging and e-mail |
| Mental health 1 (early intervention) | Age independent | > 16 | Mobile phone, text messaging and e-mail |
| Cystic fibrosis 1 | Adult | > 16 | |
| Dermatology | Adult | > 18 | |
| Mental health 2 (CAMHS) | Child and adolescent | < 18 | None |
| Mental health 3 (outreach team) | Child and adolescent | < 18 | Mobile phone, text messaging and VoIP |
| Arthritis | Transition | 16–25 | None |
| Paediatric | < 18 | None | |
| Cystic fibrosis 2 | Adult | > 16 | Mobile phone, text messaging and VoIP |
| School nurse service | Young people | 14–19 | Text messaging and VoIP (pilot) |
| Renal conditions | Young adult | 16–22 |
Description of interview participants
A total of 367 participants took part in an interview. Of these, 165 were patients, 173 were clinic staff, 13 were parents/carers and 16 were IG officers (Table 3).
| Health condition | Participants recruited (n) | |||||
|---|---|---|---|---|---|---|
| Case sites | Patients | Staff | Parents | IG officer | Staff shadowed | |
| Cancer | 2 | 23 | 18 | 3 | 2 | 11 |
| Cystic fibrosis | 2 | 15 | 16 | 1 | 1 | 4 |
| Dermatology | 1 | 7 | 4 | 1 | 0 | 2 |
| Diabetes mellitus | 2 | 23 | 14 | 0 | 2 | 7 |
| Mental health: CAMHS | 2 | 9 | 22 | 1 | 2 | 7 |
| Mental health: EIPT | 2 | 5 | 17 | 0 | 2 | 10 |
| HIV infection | 1 | 9 | 12 | 1 | 0 | 4 |
| IBD | 2 | 14 | 13 | 2 | 1 | 7 |
| Liver conditions | 1 | 15 | 12 | 2 | 2 | 7 |
| Renal conditions | 1 | 7 | 7 | 1 | 0 | 3 |
| Arthritis | 1 | 16 | 8 | 2 | 1 | 1 |
| Sexual health | 1 | 12 | 10 | 0 | 0 | 3 |
| Sickle cell disease | 1 | 10 | 13 | 0 | 2 | 9 |
| School nurse service | 1 | 0 | 7 | 0 | 1 | 4 |
| Total | 20 | 165 | 173 | 14 | 16 | 79 |
Patient recruitment ranged from 0 to 16 people per clinic. The largest number of patients was recruited from cancer and diabetes mellitus clinics. It was not possible to recruit any patients from the school nurse service and no patients who frequently DNA appointments volunteered to participate in the study. Only 16 patients chose to share examples of their digital communication with a clinician with us. Interviews with patients were primarily conducted over the telephone (n = 82), but also in person (n = 41), by e-mail (n = 35), via Facebook (n = 4), via Skype (n = 2) and by text messaging (n = 1). Synchronous interviews (taking place in person, or via telephone or Skype) took between 20 and 60 minutes, with most taking approximately 30 minutes. Asynchronous interviews took longer to complete; the longest, via e-mail, took 2 weeks. Overall, few parents/carers were recruited; none was recruited from 11 individual sites. Parent interviews took place primarily via telephone (n = 7), but also by e-mail (n = 4) and in person (n = 2).
Between 3 and 12 members of clinic staff were recruited from each site. The largest number of clinic staff were recruited from CAMHS teams and the fewest from dermatology. This reflects the size of the clinical teams being studied and the number of sites focusing on each health condition. Clinic staff had a range of clinical and clerical roles, including consultants, registrars, community nurses, advanced nurse practitioners, psychiatrists, psychologists, dietitians, physiotherapists, occupational therapists, pharmacists, secretaries and administrators. Interviews with staff took place in person (n = 148) or by telephone (n = 25). Interviews lasted up to 2 hours, but the majority took approximately 45 minutes. A total of 79 staff members were also shadowed across the clinical teams. Shadowing usually lasted between 1 and 2 hours, but lasted longer (the maximum was 7 hours) if the clinician felt that it was appropriate.
Information governance specialists and Caldicott Guardians were also interviewed. Two were interviewed in each of five trusts and one was interviewed at each of six trusts. It was not possible to interview an IG officer or Caldicott Guardian at nine sites. The majority of interviews were conducted in person (n = 10), with the remainder conducted by telephone. All interviews were audio-taped and lasted between 20 and 45 minutes.
In the results chapters that follow we include illustrative quotations from our qualitative data. These are each labelled with the condition the clinic manages, participant type and participant number. We present our analysis of qualitative data by thematic focus: ‘what works’, ethics and patient safety.
Chapter 3 ‘What works, for whom, where, when and why?’
In this chapter we report the thematic analysis of our case study data that addressed this research question. The context of the thematic analysis is the clinic and its purpose. This was described by each clinical team lead and is summarised in Table 4. The table includes a list of the digital communications that were in use in each clinic.
| Site ID/health condition | Clinic purpose | Use of digital communications |
|---|---|---|
| Diabetes mellitus 1 | Maintain good control of diabetes mellitus through maintaining blood glucose levels, with an aim to prevent or delay long-term complications. This is achieved through diet, exercise and insulin dosage | Mobile phone, text messaging and e-mail |
| Mental health 1 (early intervention) | Planned recovery approach following first episode of psychosis. Aim is to discharge after a maximum 3 years in the service. Care is through coping skills and medication monitored through CAARMS, which assesses mental health status | Mobile phone, text messaging and e-mail |
| Cystic fibrosis 1 and 2 | To maintain health status and prevent decline. This is achieved through regular clinic review to assess weight, diet, lung function and adherence to medication |
Cystic fibrosis 1 site: mobile phone Cystic fibrosis 2 site: mobile phone, text messaging and VoIP |
| Dermatology | To halt progression of condition and alleviate psychological distress. Regular reviews to monitor hair loss and blood monitoring for those on oral medication | |
| Mental health 2 (CAMHS) | Provides specialist assessment and treatment for young people with moderate to severe mental health needs and associated risks. Treatments include CBT, systemic and family therapy, psychodynamic therapy, art therapy and pharmacotherapy | None |
| Mental health 3 (outreach team) | Patient group is young people being discharged into the community from psychiatric care or on the verge of being admitted. Aim is to avoid admission and provide immediate help at a time of crisis. Deliver dialectic behavioural therapy through weekly meeting and telephone support. Also deal with young people displaying emotional or behavioural difficulties that are concerning to agencies | Mobile phone, text messaging and VoIP |
| Arthritis | Optimise health and well-being. This is achieved through regular reviews for physical and psychological health. No single measure of health as complex medical management. Regular checks of joint affected and regular eye checks are given | None |
| School nurse service | Service for 11- to 19-year-olds to get advice on health-related topics and as access point for services. Young people have the option to remain anonymous while accessing advice, but must give up anonymity to access services. The purpose is to provide information and advice and to provide a route to access services | Text messaging and VoIP (pilot) |
| Renal conditions | To preserve kidney function as long as possible. Regular monitoring of kidney function. Diet is particularly important as is psychological support. Rapid deterioration is a possibility | |
| Liver conditions | The aim is to improve young people’s self-management skills and, ultimately, improve health outcomes considering both physical health and psychological well-being. This is done through improving the process of transition from the paediatric to adult service for young people living with chronic liver disease. The service aims to achieve this through meeting young people’s development needs at this time | Text messaging and e-mail |
| Sickle cell disease | To empower young people to manage their care. This is done through imparting knowledge and giving skills to enable effective management of their condition in the community. The aim is to have fewer hospital admissions. Requires frequent blood monitoring | Mobile phone and text messaging |
| Mental health 4 (early intervention) | Aim to identify and treat as many people with the first episode of psychosis as possible. This is done through delivering a multidisciplinary package of care for up to 3 years | Mobile phone, text messaging and e-mail |
| Cancer 1 | This is a tertiary service the aim of which is to provide one environment where young people aged 16–24 years diagnosed with any form of cancer can come and get access to a multidisciplinary team. The service enables peer support and access to teenage cancer trusts | Mobile phone, text messaging and e-mail |
| Diabetes mellitus 2 | The aim is to assess, guide and support patients to attain and maintain good control of their diabetes mellitus. This is done through good maintenance of blood sugar levels aided by regular diet and lifestyle review. The purpose of the multidisciplinary team is to support and prepare individuals to live with diabetes mellitus. Regular reviews help to mitigate any untoward consequences and the team proactively intervenes to avoid hospital admission where possible | Mobile phone and VoIP |
| IBD 1 and 2 | To try and capture clinical remission measured as mucosal healing. From the patient perspective, the goal is to relieve symptoms and to avoid further flare-ups. Those who are considered stable enough are monitored remotely |
IBD 1 site: web portal and e-mail IBD 2 site: e-mail |
| HIV infection | The aim of the clinic is to maintain patients’ health and well-being. This is done by ensuring patients are aware of the condition and are encouraged to adhere to their treatment | None |
| Sexual health | The aim is to enable early and rapid diagnosis and treatment of sexually transmitted infections. A further aim is the prevention of unwanted conceptions | Testing kits ordered online |
| Cancer 2 | The aim is to enable access to expert care alongside up-to-date treatment. This is done through giving support to young people so they are more likely to comply with and complete their treatment. Overall, the aim is to enhance quality of life and quality of care | Mobile phone, text messaging and e-mail |
Timeliness
One of the key benefits of DCCs, highlighted by both patients and clinic staff, is its contribution to timely communication. Timeliness can be conceptualised as engaging with the right person, at the appropriate time, to enable effective condition management. Patients and staff held differing priorities in terms of timely communication and, similarly, emphasised differing benefits.
Both clinic staff and patients highlighted the role that DCCs played in saving them time. Time-saving has many facets depending on the type of digital technologies being used and their purpose. Getting in touch with individuals on the telephone using landlines, in the case of clinic staff, or through a NHS switchboard, in the case of patients, is time-consuming and frustrating. Clinic staff talked about difficulties faced in timing calls to landlines to reach patients when they were home, a task that frequently required multiple attempts. Furthermore, many patients were reluctant to answer their mobile phone when a call came from a ‘withheld’ number, which applies to NHS landlines. Similarly, for patients, getting hold of a member of a clinic team through a switchboard was time-consuming as they were frequently put on hold and transferred, all the more frustrating when a call is eventually put through to the right number to find the staff member away from their telephone. Both e-mail and text messaging were ways of overcoming these frustrations:
And I think the advantage of e-mail is that I can answer in my time, I don’t have to break off from a patient or I don’t have to spend time trying to phone back another patient and not getting through. We kind of have that exchange of message and that’s quite nice. It seems to be less frustrating having an e-mail conversation than it is having a voicemail conversation, playing telephone tennis. I don’t know why but it seems less frustrating.
Cystic fibrosis site, specialist nurse, 03
It was quick and easy, it meant that I didn’t have to sit, you know, find time in my day to sit and try and get hold of someone for 2 hours. I mean, the clinic that I’m with, the CFN [cystic fibrosis nurse specialist], I had tried to ring her first, and I just couldn’t get hold of her, and I couldn’t get hold of anyone.
Cancer 1 site, young person, 07
Beyond time-saving, timeliness was important in enabling both clinic staff and patients to be able to give measured responses to contacts made. For clinicians this means being able to compose a response without having to recall details of an individual’s case while on the telephone:
It does give you as a clinician a luxury that you don’t normally have, because normally your communication is face to face or over the phone and, therefore, it’s very instantaneous, you have to make an instantaneous decision or you have to very carefully make the patient wait while you go and find out other things. Whereas e-mail does give you that breathing space and that thinking space so that you can formulate a really strong response before doing so. So I really like it from that point of view. And also it means that the patient can take things in their own time and re-read things, whereas over the phone you’re never quite sure how much they’ve taken in or that they . . . that you’ve explained it in a clear or slow enough way.
Cystic fibrosis 1 site, specialist physiotherapist, 02
Patients value the asynchronous nature of these interactions as a way to enable them to think about both the questions they want to ask and the information they want to give. They also see it as a way to reduce their perceived burden on the health professionals they are contacting:
I think if I phoned her directly with, sort of, an issue, it’s not as simple as just over the phone resolving it. Once she’s sort of seen it in writing, she can have a little bit of time to think about it, look through my record and everything like that, and then get back to me appropriately . . . I don’t know if I’m just being silly, but I feel like if I’ve called someone up and put them on the spot, I think there’s a lot of pressure on her there and then to remember exactly what’s going on with my file and exactly what I’m on and things like that. So it’s probably easier for her as well for me to e-mail her, so she’s got it all in front of her . . . When I’ve put my question to her in an e-mail, I literally give her so much information about what time of day I’m taking medication, and what time of day I’ve done my, sort of, my blood pressure readings. But if I’m on the phone I just, kind of, you just quickly say, oh this is my reading.
Renal conditions site, young person, 05
Although the asynchronous nature of DCCs can be seen as advantageous to those initiating communications and responding in a measured rather than reactive manner, timeliness of communications also means initiating and responding at a time that suits you. Clinical team members value the ability to balance responding to DCCs with other workload commitments whether that be responding when they have a few minutes spare or allocating a time to answer a number of communications:
So it means you’re not interrupting your daily . . . that you can collect them all together and do them at a certain time. Obviously to be phoned when you’re in the middle of a patient consultation is really disruptive, so the great thing about e-mail is that you can do it . . . I can do it when I’ve got time, and then someone else can do it when they’ve got time and reply. So from that point of view it’s fantastic and much easier. I don’t know how . . . well things were just done much slower I think before.
Sickle cell disease site, consultant, 02
Young people value being able to initiate the communication when a question occurs to them or simply at a time that is convenient as a result of work or other commitments, rather than having to fit around the operating times of the clinic:
Timewise as well, especially if, you know, you are working. I don’t have time to find my own space and have a private conversation, because essentially what I’m talking to [name] about is private information, I don’t want people around me to hear. So, being able to send him a quick text is so helpful and yeah, I think that’s it.
Cancer 1 site, young person, 04
Patients often mentioned the speed of response to DCCs as one the greatest benefits of using them:
So, an e-mail is just quite a quick thing that you just want to say, you know, ‘this is what’s happened, can we do anything about it?’ It’s quick and easy because most people have like smartphones anyway and the internet’s on so like say if your appointment changes or you have to change it on the go, rather than going home and finding the number and ringing them, you can just kind of e-mail them quickly on the go like, you know, ‘can I change it to here?’
Cystic fibrosis 1 site, young person, 01
Getting advice between appointments also contributed to the theme of timeliness where young people were able to get quick answers to questions about their condition and its management. This was particularly useful for things the young people did not think important enough to make a telephone call about, but also it was not something that they would want to wait until their next appointment to have answered:
I have my phone on me most of the time, and like say I’m at college and something has gone wrong then I could text them . . .
Diabetes mellitus 1 site, young person, 01
I had one today [text message] saying, so and so, how many snacks should he have a day? And it’s just something little like that, to ring seems a bit, you know, a bit much. And it was fine saying, yes he should have this snack, this snack and this snack, and you can give that small bit of advice that isn’t urgent but you can give that quickly and then they’ve got the advice they want.
Diabetes mellitus 1 site, health-care assistant, 01
Digital clinical communications were not always considered to be time-saving, however, and some things are quicker to sort out over the telephone:
So if you’re sort of just speaking to someone over the phone you’re able to sort of have that and just free flowing conversation, so are there any particular days that are better for you, are there any particular times, I can do this time, can you do that time? Obviously if it is just text message by text message that could end up being sort of continuous, like, no I can’t do that time, can you do that time? Generally it’s not actually much of an issue, it’s fairly sort of straightforward, but you can see how it could get quite longwinded.
Mental health 4 (early intervention) site, assistant psychologist, 15
Young people also saw times when using DCCs would slow down contact:
You’re talking to someone that can answer your question directly, you don’t have to wait too long for them to reply. It’s just a lot more quick and direct. Rather than waiting around, you have to type out a text, they have to reply, you have to think about your reply and type out the reply. It’s just an unnecessary waste of time I think, with texting.
Cystic fibrosis 2 site, young person, 07
Although some members of the clinical team and patients could give examples of times when they felt that DCCs had slowed down contact, these examples could be seen as instances of the wrong technology being used to deal with the contact in question. Patients and clinical team members had clear views on which technologies should be used for which purpose.
Different types of digital clinical communication for different purposes
There were different types of DCCs used in individual clinics. Some used none, whereas others used a wide range, including text messaging, e-mail, VoIP and social media sites (e.g. Facebook). Only a few clinics used all the DCCs available, with most using one or two modes (see Table 4). Regardless of which, or how many, modes of communication were used, all teams recognised the importance of communicating to their patient group those that were available, how to access them and to outline parameters around their use ‘by having strict rules of communication actually everybody knows where they are’ (cancer 1 site, consultant, 01).
Telephone calls, whether to landline numbers or to mobile phone numbers, were considered most suitable for matters that required an urgent response or about a personal matter that a young person would not want to discuss in writing:
You just get advice straight away, and just you know, I don’t know . . . I don’t know if it’s reassurance or what it is, but it’s . . . you know, you’re doing this, or we’ll sort that, and they do it straight away.
Cystic fibrosis 2 site, young person, 01
Text messaging was used by many clinics to remind patients of appointments. Some were push text messages (that cannot be replied to), whereas others were sent out by team members as part of their attempts to improve attendance:
We have a texting service to remind our patients to attend clinic, so in the past specialist nurses have actually made the effort to text everybody just because there have been times in the past where attendances at clinics were quite variable. So this was really an attempt to ensure obviously that they do remember to come to clinic. So that’s I think another useful way of using the text service.
Cystic fibrosis 2 site, consultant, 05
Young people like text messages for making appointments and to make a quick contact or to ask a quick question. Clinicians reported using text messaging as a quick way to keep in touch with young people, often choosing to send a text message before they tried to call someone to let them know they were going to call, thus improving the chances of the young person picking up their phone. This was particularly useful when the phone call was going to be from a NHS landline, whose number would appear as ‘unknown’ or ‘withheld’. Another key issue for members of the clinical team was the flexibility of text messages. There could be a number of messages exchanged in a short period of time or it could be used in an asynchronous manner:
I think that the beauty of text messaging is that it is non-intrusive. If you phone somebody you never know what they’re doing and you’re intruding on what they’re doing. Whereas with a text message that gives the opportunity for the person who is receiving it to actually respond to it in their own time and they can make a judgement how quickly or slowly they do that. So I think that is why text is so good, and because people carry their phones with them the whole time, they know it is, you know, they know it’s easier to get hold of a person.
Cancer 1 site, consultant, 01
E-mail was seen as a more formal communication mechanism and was regarded by both patients and members of the clinical team as particularly useful for imparting complex or lengthy information. It was also seen as useful for giving patients and their parents information that they could refer to as required:
A number of parents say to me, ‘look when I talk on the phone I just get a bit flustered or I’m not really listening’ and it’s so much easier for me to return information, you know, in a calm way on e-mail and then, you know, I can always write back if anything is unclear.
Liver conditions site, consultant, 11
Some clinicians talked of ways that they use e-mail and the facility to attach photographs as an aid to diagnosis and treatment:
They actually phoned and said, I’ve got a rash, and then they said, actually I’ll e-mail you a picture, while they were on the phone, so they did a mixture of both, which was nice because I would say that that’s a more urgent query, so it was nice that they phoned and didn’t just rely on someone picking up the e-mail.
Cystic fibrosis 1 site, specialist physiotherapist, 02
Social media were used in fewer clinics, and were viewed primarily as means of patients communicating with other patients with the same condition for information and support. Where there was a social media presence, it was not used for communication between patients and clinical teams even where the clinical team was monitoring the posts and adding information to appropriate threads of conversation.
In-person communication retained relevance in all clinics and was seen as particularly important for conveying bad or potentially upsetting news: ‘so I think for the more serious conversations, good or bad, they need to be done face to face’ (cancer 1 site, dietitian, 03).
All clinics had an awareness of the particular uses they gave to different types of DCCs and conveyed their use to the young people in their service. For some, for example mental health services, therapies were delivered using DCCs. These clinics had very clear protocols for the use of DCCs, particularly to cover scenarios when the communication failed (e.g. a young person who was no longer answering their text messages). In this circumstance they would follow a protocol that involved making contact in another way or getting a trusted person to make contact with the young person.
Improving access to health-care teams using digital clinical communications
One of the key benefits of adopting DCCs, highlighted by both clinical team members and patients, was the numerous ways they enabled improved access to the service. None of the case study sites used all forms of DCC, and the emphasis of use and usefulness varied according to the particular clinical condition. However, access was seen to improve in various ways in clinics that adopted DCCs. Young people particularly liked the option to use digital communication methods they were used to. Being able to use a technology that they were familiar with was valued, as was the fact that they could access e-mail or text messages on their smartphones on the move at a time that suited them. Furthermore, using a text-based communication format was helpful for those young people who reported finding telephone calls difficult. Some young people simply do not like to talk on the telephone, whereas others used text messaging or e-mail to raise topics that were embarrassing or difficult to raise during their in-person interactions with their clinical team. This was often done in the knowledge that having mentioned the topic in a text message or an e-mail the health professional would raise it at their next meeting:
If I have got something important that I need to, like, try and talk about but I can’t talk about it, I can just text it over to them, and if they try to bring it up I can just say that I don’t want to talk about it but that is what happened or whatever. It’s easier because if you’ve got something like, it’s difficult to put into words sometimes and sometimes it’s easier to just type it out or write it out and then you can just give it to them but they don’t necessarily have to bring it up, they are just aware of it.
Mental health 3 (outreach team) site, young person, 02
I feel that over e-mail you can ask more personal questions. Like if you’re face to face with someone sometimes you can be like actually . . . chicken out about asking it. Whereas over e-mail there’s no embarrassment so you just ask it.
Diabetes mellitus 2 site, young person, 07
Clinicians also found it useful to use digital communications to get in touch with those who are hard to reach by conventional means (letter or telephone call), but who would respond to an e-mail or text message:
I’ve got one person, young person that I’ve been working with for quite some time now and I know he’s more likely to respond to a text than a phone call. I’m not really sure why, but if I text him he normally comes back within a couple of hours or so, but if I try and phone and leave a message, because I know it is his phone, sometimes I don’t get a reply at all.
Mental health 3 (outreach team) site, mental health practitioner, 04
Similarly, they knew that some young people would be unlikely to answer a call when it was initiated from a NHS landline:
They [landline initiated calls] are an impediment with young people . . . because if you contact them the number comes up as unrecognised and they just don’t answer the phone.
Sexual health site, nurse, 07
Digital clinical communications allow patients to access information and advice between appointments. Patients value having someone to contact with specialist knowledge of their case, who could give them advice or information, and clinicians value being able to send information using digital technologies, to give their patients information in a form they can access at a time they find suitable:
They can let me know if they’re concerned about something or letting them know information say for information about a support group for carers or something like that . . . kind of e-mails and then links and attachments and that kind of thing. So that usually works quite well.
Mental health 4 (early intervention) site, psychologist, 10
A further advantage of a mobile phone for clinical teams is that calls to the mobile phone are logged as missed calls, whereas calls to a landline are not logged unless the caller chooses to leave a message.
Improved and increased access was cited and appreciated by clinical teams and young people, with both groups also emphasising the need for clear expectations on response times to be communicated to patient groups. Clinicians are aware of the need to manage increased access. They define clear boundaries and actively manage their patient group’s expectations. Commonly adopted strategies are giving patients an information leaflet or sheet with contact details alongside hours of operation of services; bounce-back messages on e-mail and text message services; and answerphone messages. Additionally, it was important for clinical teams to talk to the young people in their service to reinforce information on hours of operation and expected response times and crucially under what circumstances they should make contact using each of the available modalities:
We have an automatic response from that e-mail to say, if your problem is urgent you need to phone da, da, da, da – and I can show you the response from here – and that all e-mails are responded to within 24–48 hours, so they can’t expect a . . . but if it’s office hours to be honest it usually is a fairly immediate response.
Cystic fibrosis 1 site, specialist physiotherapist, 02
I put that across at the very beginning, that it’s not for things that you need an immediate answer for and so they don’t have that expectation and I tell them I’m not responsible if I don’t answer it urgently, so I put that straight.
Liver conditions site, consultant, 02
Patients considered it important, for managing their expectations, to know how long they would have to wait for a reply. For example, one young person was asked to e-mail the consultant detailing the problems and received a reply within 2 days – a timescale he was happy with.
Inevitably, some service users will expect response times that are hard to achieve:
I’m sure [colleague] told you the story about the young person who thought we weren’t responding quickly enough, and when we asked . . . we said to her ‘oh really, that’s terrible, how long did it take?’ and she went, ‘oh it was awful, it was about 10 minutes’. And we were, that’s good, we think that’s amazing and very quick.
School nurse service, nurse, 03
Services depend on staff members following protocols and importantly understanding the technologies being used:
And it’s great having a work phone because I think one of the things it enables you to do is . . . we can . . . on our work phones as well, set up messages so that if we were on holiday or off or something, and a young person sends us a text message, it then sends them a message back so that they know you’re out of the office, so that they know their message isn’t going to be answered, and that sort of thing.
Cancer 1 site, young people worker, 04
For some services, particularly mental health services, stressing working hours and how to use the different DCCs was considered vital to the safety of the patients and to protect the clinical team:
Well what I do is reinforcing, when I speak to the young people or to the family member, how they get support out of hours. And I think it is important to reinforce even if it becomes very repetitive. So it’s in each communication we have. I normally finish off a phone conversation and say, if you need anything after 5 o’clock today or over the weekend you phone this number.
Mental health 3 (outreach team) site, mental health practitioner, 05
Enhancing patient engagement
The young patient population being served by the services in the study can be hard to engage with. There were a number of ways that DCCs were seen to help engage the young people in their care. Starting with the hard-to-reach patients, DCC was seen as a positive first step in encouraging engagement:
The main time that they’re not responsive is sometimes if we haven’t heard from someone for a while. So if they’ve DNA’d their clinics and they’ve not responded maybe to a follow-up letter or something, we might try dropping them an e-mail just sort of saying. We try and keep it fairly low key. We had someone recently actually who hadn’t responded to any DNA, automated DNA letters from clinic, so we just dropped her an e-mail saying, oh, you know, not heard from you for a bit, is everything OK, can we do anything, do you need anything? And she e-mailed us back so it was quite successful.
Cystic fibrosis 1 site, specialist physiotherapist, 02
There were a number of ways that, once engaged with the service, DCCs enhanced that engagement. Many clinicians talked of the ways that DCCs empowered their patients to take control of their care:
It’s not a huge amount of power for them, but in cancer, because we take away a lot of their independence, we take a lot of the control because we have to because of the treatment plans. Any tiny little thing that’s giving them a little bit of control back, even if it, well I’m not going to answer that text now, I’m going to answer it in 5 hours’ time, then that’s a little bit of control and a bit of empowerment that they have got.
Cancer 1 site, advanced nurse practitioner, 02
Through empowering patients to engage with their care, clinicians also felt that DCCs enabled patient activation, citing examples of young people starting to be more active in their own care:
First level of self-management that they at least know where to find somebody, where they probably wouldn’t call or turn up but they might e-mail and say, I can’t come or I haven’t come, or I’ve run out of medication, or can you organise this for me. So it’s almost like that first rung on the ladder of being able to do that and then help them think about, OK, what would you like to do next?
Liver conditions site, psychologist, 01
Furthermore, contacts made between appointments were seen to improve the clinical appointments both from the perspective of the clinical team and from the patients:
If I went away for 3 months at a time and came back, and then they’d have to ask me again about what I’d been doing in the 3 months. But if I’m constantly, sort of, keeping them up to date, then we’re all on the same page and everybody’s clued in as to what’s going on and how I feel. And then it can be straight down to the, well this is what I think we should do.
Renal conditions site, young person, 05
Being able to contact doctors and nurses has helped me trust them more as we have built a rapport and message so regularly that I feel more comfortable talking to them both in person and online. I think online communication has allowed us to feel more comfortable when we’re in person.
IBD 2 site, young person, 18
Clinicians felt the improved appointments were as a result of the relaxed style of DCCs encouraging contacts, which in turn helped them build relationships with their patient group which in turn improved their engagement:
If we can engage them via text then they’re more willing to engage with us in session I think.
Mental health 3 (outreach team) site, support worker, 03
The ultimate goal of these services is to produce better outcomes for their patients and many clinicians talk about the ways that DCC contribute to that objective.
Better outcomes for patients
What emerged from the data were many ways in which the use of DCCs could be conceptualised as enabling triage and, where appropriate, care escalation. A number of issues contributed to this enhanced care: the ability of patients to communicate with clinical teams between appointments; the perception that patients were receiving personalised care; the fact that clinicians’ ability to contact patients between appointments using DCC reduced anxiety in their patient group; the ability of clinicians to give advice between appointments, avoiding the need for additional clinic appointments; the use of DCC to diagnose minor issues or treat symptoms before they become serious; and the use of DCC to give advice on routine matters such as suitability of vaccinations for travel or how to use a particular medication. The young people in the study and members of the clinical teams felt that these issues contributed to an avoidance of negative health outcomes:
I’ve worked with a couple of young people that have had to access the emergency hormone contraceptive and if we hadn’t have acted in a timely manner . . . within the timeframe then obviously we would have been faced with an unwanted teenage pregnancy.
School nurse service, nurse, 08
I’m absolutely convinced it’s helped keep some people out of hospital, and in some cases I think it’s actually stopped people dying, a couple of really poorly people where we’ve been able to communicate quickly and been able to sort things really, really quickly.
Cystic fibrosis 1 site, specialist nurse, 03
It’s just a lot easier than waiting until the next day when they’re open and either phoning up and having to wait for a call back until he’s not with a patient, or having to phone up and get an appointment for like a week’s time as like an urgent one. And then a week later and you’re either even more ill or you’ve managed to work it out for yourself and you’re better.
Diabetes mellitus 2 site, young person, 07
It saved my life basically. And it’s made life more bearable for me not to do anything [self-harm], so . . . It’s made me open up more to my therapist and stuff, and people on the team. I need to know that they’re there and I can speak to them if I need it.
Mental health 3 (outreach team) site, young person, 01
In services where conditions can deteriorate rapidly, such as mental health and cystic fibrosis services, DCCs were seen to speed up access, which in turn reduced immediate negative outcomes. These communications modalities played different roles in different services, but all services saw some ways in which patient care was more responsive.
Impact of digital clinical communication on service staff workload
One of the concerns voiced by many clinical staff members we interviewed was around their worries that the use of DCCs would have a negative impact on their workload. Although workload, as a result of an increase in the volume of communications, was seen to increase, this was not necessarily viewed negatively:
So I think it is more work for us because we do get more communication from the patients who normally wouldn’t communicate with us at all. But then that’s a good thing. So, yes, it’s difficult to say, it probably does save time with some patients but it adds to our workload because some of the patients start to engage more.
Cystic fibrosis 1 site, specialist physiotherapist, 02
Some individual clinicians felt access to them was opened up with patients being able to use digital communications to bypass gatekeepers. Non-digital communications meant telephoning a clinic using a telephone number, usually for the consultant’s secretary, supplied on a letter, which enabled the channelling of communication to the appropriate person. However, changes enabled by digital communications were not always welcomed:
Having direct access to the consultant is, you know, great for the patient but it’s not so great for the consultant because these are things that I then have to deal with instead of someone else. So having them fielded would be great.
Sickle cell disease site, consultant, 02
Some of the increased workload arose from changes to record-keeping and the lack of clarity or systems to deal with logging DCCs. The lack of systems was seen as a potential risk if, for example, some communications were not logged on patient records.
Concerns that accompany increased use of digital clinical communication
Clinicians overall were very positive about the introduction, use and indeed expansion of DCCs. None wanted to go backwards; however, there was an awareness of associated risks with using these new technologies in a clinical setting. Some concerns focused on patient experience: were expectations being met, particularly where hours of operation were restricted? Was the use of DCCs consistent across the whole team within a clinic? Were urgent contacts missed as communications were made out of hours? And were DCCs being used as a shortcut in a stretched service rather than using traditional in-person consultation?
I guess part of the push for digital communication is partly for . . . well primarily hopefully for the young people, but also there’s usually a cost saving involved as well and manpower saving and . . . yeah, so from a cynical point of view I’d worry that it could be part of a streamlining process that would see less clinicians on the ground.
Mental health 3 (outreach team) site, mental health practitioner, 04
Communication issues were also raised: Were text-based communications always understood as intended? Were clinicians able to make assessments accurately without the added cues of tone of voice or body language? Were young people and, to some extent, clinicians able to be avoidant of difficult situations through the use of DCCs (e.g. cancelling appointments easily)? And how did clinicians ensure that they were communicating with the right person?
Many of these communications issues were articulated by a cancer nurse specialist explaining the differences between patient and clinician use of DCCs:
People feel that it’s easier to ask over text, but I think what’s harder to do is to actually answer them over text because it is, from a professional point of view that’s quite hard trying to [. . .] word the answers carefully enough to not, you know, be too distressing or, you know, not offensive [. . .] quite often if people text me and it is quite a difficult conversation then I would ring them back . . .
Cancer 2 site, teenage and young adult service cancer nurse specialist, 02
Other concerns included service issues: digital network coverage in some rural areas was described as patchy; the cost to young people of using digital-based communications on the go; and the concern that staff occasionally use their own mobile phone equipment for their clinical work.
Clinics not currently using digital clinical communication
Most of the clinics in the study used some type of DCC with their patients, although the volume and modalities differed. Only three clinics used no forms of DCC at the time of the study, with some of the clinical team in each advocating the introduction of some forms of DCC.
One service that is currently not using any DCC and which works with young people up to the age of 18 years saw the potential of using a means of communication that young people, especially those who are not happy talking, would be familiar and comfortable with, echoing some of the positives seen in the sites currently using these technologies:
We tend to rely on phone which is a challenge for young people, it’s not ideal and I can see it would be much nicer for many young people just to be able to send a text or something less stressful.
Arthritis site, specialist nurse, 05
Furthermore, this service saw DCC as a way of communicating directly with young people, rather than, as at present, through their parents. Concerns over increased workload, particularly record-keeping, were raised again, reflecting concerns originally held by clinics currently engaged in the use of DCC.
Another service not currently using any form of DCC was very keen to try and introduce such methods of communication. This service saw the benefits in terms of patient empowerment and activation as the key drivers of the use of new technologies:
I would quite like to use it for positive reinforcement, you know, like if I’ve just seen someone in clinic and we’ve discussed something, and you know, when you think about them the next day and you think, oh I wonder how they’re getting on, or just something to say, what we discussed yesterday, keep up the good work, or something like that.
Arthritis site, specialist nurse, 04
This service, too, was concerned about the increase in workload, but saw it as a positive move. Some of the young people served by this clinic had access to DCCs in the form of text messaging the drug service that delivered their biologic drugs. The service, which was independent of the health service clinic they attended, comprised the provision of a mobile phone number that they could text or call for advice. This facility was well liked but available only to those on specific medication. The value of the service is explained by this patient:
I just text the nurse, just giving her a brief description . . . and the nurse replied to me, within, I would say it was probably within the hour . . . with probably two quite big paragraphs and a good description. And to me it gave me everything I needed to know which was really useful.
Arthritis site, young person, 02
A consultant in a clinic not currently using digital communications was concerned over the potential increase in workload that would hit their service, which was already working beyond its service remit:
It’s easier to get to see us than their GP. So already we’re dealing with things that aren’t technically HIV related. Obviously we will try and help, but if we make it even easier to come to see us then with even more things that patients need to be dealt with, but they aren’t our prime area, therefore, we can’t take on all the health care of the patient.
Cancer 2 site, nurse consultant, 01
Summary of findings
Digital clinical communications can enhance service provision by offering timely access to information and advice. This is beneficial for members of clinical teams, patients and carers, albeit for differing reasons. Using digital communications gives patients time to construct questions, which they value, whereas, for clinicians, the asynchronous nature of these communications is a luxury, enabling them to gather all the information they need before responding. Furthermore, timely communications enable better time management by clinicians as they can respond when it best suits them, either when they have a few moments to spare or at a planned time during the day. Young people value being able to send communications as soon as a question occurs to them rather than being restricted to clinic opening times. Overall, timely communication enables young people to manage their condition by having questions or queries answered quickly, which some clinicians and young people identified as helping to prevent condition deterioration.
Improved access to clinical teams results in patient benefits that include greater engagement, enhanced activation and better self-management. Improved access leads to those patients who chose to use digital communications having more contacts with health-care staff. Both patients and clinical team members noted that this improved the relationship between patient and clinician. It was the improvement in relationships that enabled patients to take better control of their condition, and hence improved activation and self-management. This is crucial for patients in this age group, who are known to disengage with services as they transition from paediatric to adult services. Digital communications for clinical purposes are one way to enhance engagement, but are not a panacea.
Chapter 4 Ethical implications of using digital clinical communication to support young adults with long-term conditions
Participants in this study believed that digital communication increases patient empowerment and autonomy; improves trust between patient and clinician; and reduces harm because of rapid access to clinical advice. However, concerns included difficulty with defining, and maintaining, boundaries of confidentiality; uncertainty regarding the level of consent required; and blurring of the limits of a clinician’s duty of care when unlimited access is possible. An overarching theme from the data was the need to redefine the patient–clinician relationship in the context of the use of digital communication. We discuss these findings in more detail below under four predominant themes: (1) autonomy and control, (2) communication and trust, (3) defining the limits of duty of care and (4) confidentiality.
Autonomy and control
The principle of respect for patient autonomy is a key element in professional regulatory frameworks and codes of practice. The concept of respect for autonomy is complex, including conceptions of self-determination and freedom from interference, and is actualised in a clinician’s duty of care by the requirement to obtain consent, to maintain confidentiality, and to support and enable patients to make informed choices in the management of their health. 72
Patient empowerment
The majority of clinicians agreed that digital communication increased patient autonomy by giving them more control in both the management of their condition and the way in which communication between them and the clinician was conducted. Questions can be formulated and feelings expressed, which the patient might otherwise find difficult to do. Young people also valued this opportunity:
Well I guess that’s saying, able to control their own illness but they feel in control if they’ve got a question, they’re not disenfranchised. They’ve got someone to ask about it so they can feel empowered to ask those questions and control their own health rather than don’t know who to ask or whether to come forward with things.
Cystic fibrosis 1 site, secretary, 04
. . . well I’ll just say that personally I think that method of communication is one that’s very important to people. It gives people another chance to explain their issues, you know, and it can even be good for things that maybe you’re not comfortable talking about in front of the person, you know. And e-mailing to, you know, to the person who is dealing with your care I think is an invaluable resource because you know, you can ask anything, you don’t have to wait, you can get an answer.
Liver conditions site, young person, 10
However, clinicians were also concerned that, in some cases, the availability of digital communication may discourage young people from taking responsibility for their own health. Easier access to advice about what to do in any situation could remove the need to think about the problem and develop their own management strategy. Some clinicians expressed a concern that this general dependence on easy access to a clinician could develop into a more personal dependence on a specific clinician:
I think . . . personally I do think it is too . . . I think it makes patients a little too dependent on you and you only, which we don’t like that to happen.
Diabetes mellitus 1 site, specialist nurse, 03
You know, they’re not going to have me forever to text, so they need to learn to manage these situations themselves.
Mental health 3 (outreach team) site, support worker, 03
Some clinicians observed that because of the ease of access, DCC makes it easier for young people to avoid engaging with health services:
Sometimes it makes you lazy and you text because you don’t want to have a conversation, well the same thing works for the young person because they actually remotely tell you, no I can’t make it, and then not answering if you call so you can’t have that conversation. So I guess it makes it easier for them to not turn up or to cancel stuff or to act avoidant if you like.
Mental health 3 (outreach team) site, mental health practitioner, 04
Person-centred care
Respect for autonomy in the context of health care includes a positive duty on the part of the health-care professional to support and enable a patient to make decisions that are consistent with his or her own preferences, values and ideas about how they wish to live their life. The emergence of the concept of person-centred care as fundamental to good clinical practice reflects this underlying ethical imperative. 73 The ability to have more frequent contact with a specific clinician who is known to the patient helps to build a more personal relationship and means the clinician is more likely to know that particular young person, their circumstances and what is important to them. Young people in our study more frequently identified benefits to this element of patient care from the use of digital communication than specific benefits to empowerment and control:
I think in some aspects it’s made [my relationship with the clinical team] stronger because I have more contact with them and more personal contact because I only ever e-mail like one person from the like clinical nurse specialist group if that makes sense [. . .] I think that because I have more contact now outside of clinic they kind of know me a bit better and I know them a little bit better, which is quite nice. So it doesn’t feel like I’m just ‘another patient’.
Liver conditions site, young person, 18
For me, it’s only every 3 months that you get to see a nurse . . . So when somebody’s been ill a long time, your relationship with that nurse, it’ a lot easier to contact them and they can help more with your issues because they know you there and they know your condition . . . They understand like how yours is different to everybody else’s.
Diabetes mellitus 1 site, young person, 04
Digital communication was perceived as enhancing person-centred care by our participants because it is a way of communication that young people are familiar with and use in their daily life. Communicating with them in this way can help to reduce the power imbalance in the patient–clinician relationship, with clinicians fitting into the young person’s world rather than the young person being expected to fit into the clinical world:
I think every case is individual, but on the whole if you had to rely on them ringing in the landline here and talk to you sort of through reception, nine times out of ten it wouldn’t happen because, you know, for a 14-year-old lad or whatever it’s too much like hard work . . . I suppose it’s bringing . . . not bringing yourself down but levelling . . . getting on the same level, the same wavelength.
Mental health 3 (outreach team) site, mental health practitioner, 04
Well again it’s like . . . it is like the texting and stuff because then they feel like . . . you know, that’s what they do in their everyday life, texting their friends, and I think having that contact with them through text makes them feel like we’re more on their sort of level.
Mental health 3 (outreach team) site, support worker, 03
Consent
Respect for autonomy requires clinicians to obtain consent from patients for all aspects of their care, including the use of their information. Communication by digital technology has risks as well as benefits, most notably risks related to breaches of confidentiality and data protection. Some clinician participants expressed concern at the lack of a formal consent process for the use of DCCs:
I think there probably needs to be some sort of formal conversation or information about the use of e-mail given to patients when they first attend for their first appointment, just to make sure that you’ve got their consent to communicate with e-mail. Because that doesn’t happen really, there isn’t any kind of terms of the use of . . . well there is information governance policies in the hospital but it doesn’t really translate to the clinic.
Dermatology site, consultant, 02
Because I think sometimes people might just say, oh do you have an e-mail address, and then people might not feel able to say no [. . .] so I think getting consent both to use e-mail, who can use e-mail and for what purposes, and consent for do they know about things like security of the link, so I think that’s a big one.
Liver conditions site, psychologist, 01
The practices of obtaining consent varied among clinicians in this study. A few clinicians said that they obtained written consent, some felt that it was sufficient that the patient understood the risks and others referred to implied consent to share test results:
For me times have moved on but as long as my responsibilities are professional, as long as I explain those risks to them before I use it, if they are well aware of the risks, well, the ball’s in their court.
Liver conditions site, consultant, 02
So in terms of asking them you know, about contacting them with their results the next day, they’re given an option of e-mail or telephone call . . . So I get them to e-mail me so their e-mail is coming into me rather than me e-mailing them, so that way I know that it’s their e-mail. I don’t think there’s any governance issues around it because in terms of risk or safety because the patient’s e-mailing you in and so you’ve already got implied consent at the point of the consultation we had the previous day and agreeing how would you like to get your results tomorrow [. . .] And so it’s their choice and it’s their consent.
Cystic fibrosis 1 site, specialist nurse, 03
Clinician autonomy
Discussion about respect for autonomy in health care usually focuses on patient autonomy. The traditional paternalistic role of doctors and the power differential between patients and all clinicians has required patient autonomy to be highlighted in recent discourse on good patient care. When a patient–clinician relationship changes to provide increased autonomy and control for the patient, the shifting relationship balance may mean less autonomy or control for the clinician. The use of digital communication raised some concerns about clinician autonomy in our participants. These concerns focused on setting limits on patients’ expectations and losing control over clinician information:
So that kind of electronic communication allows you to be much more accessible, which is a great thing, but on the other hand it also prevents you putting in normal professional boundaries, that allow you to exist as a clinician actually.
Mental health 1 (early intervention) site, consultant, 09
I discourage it [use of e-mail] a bit due to workload because they will just e-mail you all the time . . . I think for me the only time it doesn’t work well is if they persistently e-mail and you’ve already answered and very occasionally I have to say, ‘listen, I’ve had six e-mails about this issue now, we do have to meet face to face or have a telephone call to go through it in more detail’.
Liver conditions site, consultant, 02
So I’ve had text messages before where they just get a bit more friendly and they will sort of like put a kiss on the end and I just feel like it starts to get a bit more sort of friendly rather than professional, so it’s a bit more harder to sort of keep those boundaries in place with text messages.
Mental health 4 (early intervention) site, assistant psychologist, 15
Clinicians also described concerns regarding the use of clinician-initiated information where the content of the DCC was passed into the public domain by the patient without the consent of the clinician. This raises the question of whether or not the patient has a duty to respect the clinician’s privacy and the nature of the clinician–patient relationship with regard to sharing of, and control over, information.
I have had an issue last . . . oh a few months ago . . . when one young person decided to put texts that I’d been sending to her out on social media, which is inappropriate. She knew it was inappropriate . . . And although she’d removed my name on all of the texts it was my . . . you know, the girls [other patients] knew it was what I’d said.
Mental health 3 (outreach team) site, dialectical behaviour therapy co-ordinator, 10
There is perhaps another anxiety that, you know, my advice may then be e-mailed on to 30 other people, or put onto . . . look, this is what Dr [name] says about this, you know, on the group’s Facebook page. So I do have some anxieties about that.
Arthritis site, consultant, 10
Most clinicians who raised concerns about boundary setting and lack of control had developed strategies to deal with this. The key message was the need to set clear boundaries with patients when initiating the clinical digital communication pathway, setting out availability and what this method of communication could and should not be used for:
I will talk to them about that, but I will also say to them at that time, that yeah, you can contact me on all these things but you may not get an answer, because a) if you text and I’m in with somebody else for their one to one I’m not going to be answering you until that’s finished. They’re aware of that . . . And you know, if they’re in school I’m not going to be phoning them in the middle of a lesson, so you know, we do accept those boundaries at the beginning.
Mental health 3 (outreach team) site, dialectical behaviour therapy co-ordinator, 10
We’ve put a kind of a note on the bottom of our e-mails explaining that we will pick up our e-mails during working hours Monday to Friday and that if there is anything urgent, that they need to kind of go and see the GP [general practitioner] or their local health provider. And I think that was quite important for us to do that, because again there’s nothing much that tells us how to protect us from these things, and if something kind of goes wrong, whether you’re expected to check your e-mail at a certain time, and whether you’re OK not to pick them up.
Liver conditions site, consultant, 05
Communication and trust
In the context of health care, trust is considered a cornerstone of doctor–patient relationships. DCCs, as discussed earlier in the chapter, can increase patient autonomy and engagement, but it does not remove the need for trust. For some participants the use of digital communication enabled a trusting relationship to develop more easily:
So I know that she’s going to text me, so then I actually get some feedback on what we’ve actually just done and how we can move forward. So she is, she’s able . . . it enables her to be able to tell me how she’s feeling and what she needs and how she needs it and her true feelings, where she can’t do that when I’m sat in the room with her. So it’s a useful tool for her.
Mental health 3 (outreach team) site, dialectical behaviour therapy co-ordinator, 10
I think it’s knowing that I can contact her easily and that she’s so nice about it all the time, she’ll always send a really friendly reply. I think I have a lot more trust in her, I feel quite confident in her care.
Liver conditions site, young person, 07
However, both young people and clinicians expressed a view that the physical co-location, both during consultation and, even more importantly, when patients need direct care, is important. Direct contact can enhance trust from both a patient and clinician perspective:
I’m trusting these people with my life; literally trusting these people with you know, with your life. This isn’t just a question of, you know, you’re asking somebody to do something for you, write a letter for you or something like that. This is your health, this is, you know, this is important, there’s nothing more important than, you know, ultimately . . . and I think also there are so many things that you could fabricate in an e-mail or a text, you could say you feel fine when actually you’re not that fine . . . so I just don’t think you can replace that personal one on one sort of. Well I suppose from their perspective it’s they need to see you and I suppose from a patient perspective, you know . . . So from a patient perspective I quite like to know who is treating me, who is calling the shots, and yes to be able to just discuss with them properly why they’re doing the things that they’re doing, or you know, what other options there are.
Liver conditions site, young person, 16
So I mean from a more clinical point of view then if you were giving them, whether it’s good news or bad news or . . . I think that needs more of a face-to-face contact, you know, to be seen by the consultant. You know, you could never text someone, oh by the way, you’re progressed, because the way that it’s dealt with is obviously incredibly important, especially the way that they take to it psychologically and that kind of thing. So I think for the more serious conversations, good or bad, they need to be done face to face. And then like I said from my point of view just giving the advice that I would, it wouldn’t be appropriate to giving it by text or that kind of thing.
Cancer 1 site, dietitian, 03
Building and maintaining trust when using DCCs may therefore require renegotiation in the context of the clinician–patient relationship and a careful consideration of individual views of patients. Trust may depend on the patients’ needs and preferences and what they think is appropriate to communicate via digital means.
Defining the limits of a duty of care
The concept of a duty of care to an individual patient is enshrined in professional codes and common law. 74 However, the development of a more personalised relationship, together with a form of communication that is immediate and direct, creates uncertainty for both the patient and clinician about the understanding of the duty of care in this context. An intrinsic element of a clinician’s duty of care is to protect their patient from harm. Clinicians described facing difficult decisions when patients use text messaging or e-mail for communication relating to serious health concerns out of the clinic’s normal working hours:
I got an e-mail from in the middle of the night, so obviously I didn’t get it until the next day. [The patient] was telling me she was going to kill herself, which obviously nobody would get until the next day. And the next day I had to deal with that and escalate . . . But that really raises questions of where does that put me responsibility wise because that e-mail was sitting there not accessed, and she’d actually given me that information. If that was her calling in [by phone] saying that to me, obviously I’d be professionally obliged to do something significant with that.
Liver site, psychologist, 01
You know, if you get an e-mail, you know, it is a communication, you know, it would have to be acted on depending on what it said . . . that’s what sometimes makes it feel more anxiety provoking as you’ve just got this frozen snapshot, and then you’re like . . . and especially if . . . because e-mail, people could have sent it on an evening, on a night-time when we’re closed. You come in the following morning, you know [. . .] God, what happened . . . what happened to this person, you know . . . It sounds like things were pretty desperate at 11 o’clock, at midnight. And so I think it raises a lot of issues like that about duty of care and about, you know, when are people checking them, how often do we check them; what will we do with the information.
Mental health 2 (CAMHS) site, psychologist, 11
People can send an e-mail at any time in their lives and their time that might not really fit with the time that you are there. And then how do you kind of protect yourself that if somebody’s kind of putting their life in danger that you kind of . . . so in that situation you can’t really be expected to look at your e-mails 24 hours a day.
Liver conditions site, consultant, 05
We only work 9–5 Monday to Friday. If someone contacts you at 11 o’clock on Friday night to say I’m about to kill myself, where does our responsibility lie? So we have to be very, very clear on boundaries around that sort of thing . . . So if people go on holiday they leave their mobile phone with a secretary so we’re got a record of what’s going on but we don’t have to respond to them, and so it’s trying to keep the team safe as well as keeping the clients safe.
Mental health 1 (early intervention) site, community psychiatric nurse, 06
On this theme, our ‘what works’ analysis had determined that, although aware of these concerns, across all sites few interviewees were able to recall an instance where a patient had left an urgent communication that was not picked up in a timely manner. Some clinicians dealt with these concerns by having a strict rule about accessing their e-mails out of hours, arguing that the duty materialised only once they had received the information:
If I’d chosen to read my work e-mails, as some people do at, you know, 10 o’clock on Saturday night, that I would then be professionally obliged to do something with that knowledge I had but I wouldn’t be in working hours [. . .] So in a way, it sounds awful but for my professional responsibility the worst case would have been if that event had happened, but also if I’d accessed it out of working times.
Liver conditions site, psychologist, 01
This approach requires clinicians to make the limits of access and alternative sources of support clear to patients so that there is a joint understanding of the limits of the individual clinician’s duty of care.
Confidentiality
The professional duty of confidentiality is a key element of the patient–clinician relationship. There is an implied promise at the heart of this relationship that information disclosed to the clinician by the patient, or gained in the process of that patient’s care, will not be disclosed to others without the patient’s consent. Digital communication raises potential concerns regarding inadvertent breaches of confidentiality and data protection. Our data demonstrated that young patients varied in their level of understanding of, and concern about, confidentiality and privacy. Some expressed real concerns that e-mails could be intercepted or messages on the home screen of their mobile phone seen by others:
I’ve got my e-mail on my iPad, you know, if somebody’s . . . you know, even just my brother and sister could be playing on the iPad or on the phone, . . . I don’t particularly publicise the fact that I have an illness, so I wouldn’t really want somebody to find out accidentally, and I think that can definitely happen with e-mail, and even worse texts. I mean texts flash up on people’s phones and people, you know, press the lock screen to see the time or whatever and you know, there’s a text from the hospital it just . . . people are curious and would ask all sorts of questions and it’s not really my thing.
Liver conditions site, young person, 16
I think it’s quite private, like I said earlier, because it’s to do with my health and stuff. And especially when I’m e-mailing my psychologist it’s information that I’m only really comfortable sharing with a few people so I wouldn’t want just anybody to get hold of it.
Liver conditions site, young person, 18
Young people, in general, trusted clinicians to maintain confidentiality which they interpreted as not sending personal or sensitive information in e-mails or text messages. Others were not particularly concerned by potential breaches of confidentiality, placing less weight on the private nature of medical information than other personal information such as bank details:
I would have very little concerns about the sending the e-mails because with e-mails, I know that our security on our computer is quite up to date and I think that doctors on the whole, they wouldn’t send anything particularly sensitive over e-mail anyway . . . because I wouldn’t have put anything sensitive in what I was sending and I would have trusted them not to put anything sensitive, and I would have told [clinician’s name] not to. It’s just sort of general questions, ‘this has gone wrong with the pump, what do I do about it?’ Without any great . . . you didn’t get lots of information and stuff.
Liver conditions site, young person, 01
If someone gets their hands on that e-mail, just a random person reads it, I mean they’re not going to care, it’s not going to affect their life so, you know, I don’t . . . I wouldn’t have thought it would be much of an interest to anyone else. So I see that as really the only risk to be honest with e-mail intercepted by someone, really.
Liver conditions site, young person, 10
I mean, there’s nothing about, like, my bank details or things like that, it’s just, kind of, about my health. I’m not as worried about . . . if it was something like my bank details I probably wouldn’t send it over e-mail, but because it’s, sort of, my health and it’s specific to me. Like, it’s, no-one else is going to use that information. I like to think that, anyway.
Renal conditions site, young person, 05
Clinicians were usually cautious about sending confidential data digitally, and many distinguished between a clinician sending information to the patient (risk of breach of confidentiality) and the patient sending data to the clinician (patient’s choice and their responsibility):
Well I think you have to be mindful of confidentiality so you have to . . . when I’m sending the text messages and things I need to make sure that they’re going to the relevant people and not sort of mention . . . I have to make sure that it’s definitely going to [patient’s name], so you need to just be a little bit wary of what you’re doing and what you’re sending.
Cancer 1 site, advanced nurse practitioner, 02
If it’s your data and you’ve made the choice to send it, then that’s your look-out, and I think that’s why we’re very careful about not sending anything via e-mail. I suppose they’ve made the choice to send us the data by text and we would respond, but I wouldn’t give any data out by text, I would only give it over the phone, which I feel is more secure.
HIV site, consultant, 13
Digital communication enables correspondence about, and with, patients to be accessed outside the normal clinic environment. Some clinicians described accessing e-mail in public places, such as on the bus or train:
I tend to do e-mailing as I get on the train because my train’s a 40-minute train ride, and in the evening because I have to get out just after 5, and I’m not home until after 6, so I’ve got that time gap again, I can finish off stuff that isn’t urgent and I can do e-mail on my phone. So for me it’s very convenient. I fought against it for a while but it helps me a lot.
Liver conditions site, transplant co-ordinator, 04
This presents a significant risk to confidentiality as the communications could easily be observed by a fellow traveller. This risk was only identified by one participant and only in relation to telephone calls. It is possible that the risk to confidentiality from accessing e-mails and text messages in public places is not identified as readily by clinicians.
Summary of findings
The ethical implications of the introduction of digital communication are complex and go beyond concerns about confidentiality and consent to challenge clinicians to reconsider the nature and boundaries of the therapeutic relationship. Clinicians work within a legal and professional ethical framework that is determined by societal norms and in recent years there has been a shift in emphasis towards respect for patient autonomy and patient-centred care. A strong theme emerging from our data was that digital communication could potentially increase patient empowerment and autonomy. Clinicians described ways in which digital communication is altering their practices and supporting young patients in becoming autonomous and engaged. However, they also reported examples of increased patient dependence, with digital communication potentially disempowering some patients. Thus, there is a risk that rather than encouraging autonomy, digital communication might actually create a new kind of paternalism in which patients grow to rely on their clinicians because of the ease of access and the closeness it provides, rather than learning how to manage their disease themselves.
Chapter 5 Patient safety
This analysis aimed to identify what participants perceive as the main safety and security risks that might arise from the use of DCCs. From the analysis of the semistructured interviews with patients, clinicians and clinic managers, four key risks associated with DCC hazards were identified. The hazards and the associated risks identified were:
-
inadvertent disclosure of sensitive information
-
communication failures
-
failure to record the content of the digital communication
-
failure to consult the patient’s notes prior to engaging in DCC.
Below, each identified risk is analysed further following a standard safety science framework. 65 With the structure provided by this framework, each risk is described in terms of the DCC hazard, the potential consequences of the hazard, possible causes leading to the hazard and mitigation strategies described by participants. A summary of the identified risks is provided in Table 5.
| Hazard | Consequences | Causes | Mitigation |
|---|---|---|---|
| Inadvertent disclosure of sensitive information |
|
|
|
| Communication failures |
|
|
|
| Failure to record content of digital communication |
|
|
|
| Failure to consult patient’s notes prior to engaging in digital communication |
|
|
|
Inadvertent disclosure of sensitive information
Hazard
Digital clinical communication may include patient identifiers, condition-specific details (e.g. blood glucose levels), and other potentially sensitive and confidential information. Participants explained that such sensitive information might be inadvertently disclosed to parties other than the intended recipient.
In the following quotation, a patient attending a diabetes mellitus clinic emphasises the importance of considering inadvertent disclosure of sensitive information because there might be third parties seeking to benefit from unauthorised access to such data:
I’d like to think there wouldn’t be people out there that want to use people’s health information and stuff like that, but there probably are, that do want to kind of use that to their advantage. So, yeah, I think that [inadvertent disclosure] would be a big issue . . .
Diabetes mellitus 2 site, young person, 02
The following quotation, from a participant with an IG background, suggests that the scope of what should be regarded sensitive information might be broad, as it is possible to make inferences about the patient’s condition even if this is not explicitly communicated:
So, for example, we’ve probably had lots of communications that have gone on for quite a long time that could allow a third party to infer the clinical condition of a patient.
Diabetes mellitus 2 site, Caldicott Guardian, 01
In the following quotation, a clinician from a mental health clinic reveals that, in the past, sensitive information, such as patients’ names and their addresses, has sometimes been disclosed by mistake to unintended recipients:
There have been incidents and there still are incidents where clinical information gets sent to the wrong person [. . .] that can even be lists of patients names and addresses that meant to go there [i.e. were meant to be sent], but for whatever reason went to the wrong person. That does happen.
Mental health 4 (early intervention) site, case manager, 03
Consequences
Participants suggested that inadvertent disclosure of sensitive information could have negative effects on the patient’s mental health and on their well-being. It could also affect the trust between the patient and the health service.
In the following quotation, a patient attending a diabetes mellitus clinic reasons about potential adverse effects on patients resulting from the disclosure of their LTC. The quotation suggests that this might be a cause for concern, not only for conditions where known social stigmata might come into play (e.g. in relation to sexual health), but also for conditions such as diabetes mellitus, for which there might not be an obvious social stigma. Patients might perceive living with a LTC as something very personal, irrespective of the particular condition, and they might not wish to disclose this widely:
I think some people it may affect because I know like quite a few people who hide the fact that they’re diabetic.
Diabetes mellitus 1 site, young person, 13
This sentiment is echoed in the following quotation by a clinician from a different diabetes mellitus clinic. In the quotation the participant reasons about the breadth of factors as to why patients might not wish their condition to be disclosed, and about the potential impact on patients’ mental health and social relationships of disclosure:
Let’s say a patient doesn’t want anybody to know they have diabetes, you know, for whatever reason, cultural reasons, social reasons, and the world finds out they have diabetes. Well that can cause a lot of problems for them, socially acceptable, cause depression, so you know, there are those associated things.
Diabetes mellitus 2 site, consultant, 01
The patient providing the following quotation explores the potential adverse consequences on social relationships further. The patient argues that they would be most concerned about disclosure of their condition to colleagues at work. The patient expresses their concern that this might affect their relationship with colleagues or even their career:
Certain people that I work with [. . .] I suppose there would be that kind of thing, like, would that [inadvertent disclosure of the patient’s long-term condition] affect my relationship at work with them; would they think something different of me; would they always be like, ‘oh did you know this about [name], or did you blah blah blah?’ kind of thing. [. . .] I wouldn’t want it to affect my career or my job or my relationship with the people at work and stuff.
Diabetes mellitus 2 site, young person, 02
In the context of young patients, establishing a relationship between clinician and patient based on trust is particularly important. In the following quotation, a clinician from a cancer clinic argues that inadvertent disclosure of sensitive information might erode trust and jeopardise this relationship:
. . . it [inadvertent disclosure] would be a breakdown of relationship between the patient and yourself, which is probably the most dangerous part of it.
Cancer 2 site, consultant, 03
Causes
Participants suggested that potentially sensitive information might be disclosed inadvertently for a number of reasons, including hacking and interception of communication; loss or theft of mobile phones and computers; shared access to e-mail accounts and computers; forwarding or sending of e-mails to the wrong recipient; and excessive distribution of communication (e.g. copying a message to people who should not receive it).
In the following quotation, a patient expresses concern about inadvertent disclosure of sensitive information as a result of loss or theft by relating this to previous experience in other contexts:
Or if it was stored on some sort of device or something, and then as has happened for God knows how many years where people leave laptops on trains and it’s got people’s like, you know, their national insurance numbers on it and their tax codes and things like that, and their health, NHS numbers and things, that would be an issue.
Diabetes mellitus 2 site, young person, 02
Personal e-mail accounts and mobile devices can be shared easily between people. A clinician from a mental health clinic suggests that this might lead to inadvertent disclosure of information:
So for some young people it could be . . . there could be an element of risk if you’re sending stuff to phones or tablets if they leave them lying around. We don’t have many young people at all who don’t want their parents involved, for example in their care, but we do have some.
Mental health 2 (CAMHS) site, consultant, 02
Digital communication usually involves typing e-mail addresses or telephone numbers, or selecting a contact from a drop-down menu. Participants suggested that it was easy to make mistakes in these actions and to send information to the wrong recipient. A clinician from a cancer clinic describes such a scenario in the following quotation. The mistake was triggered by lack of familiarity with the mobile phone and – most likely – poor usability of the device:
I mean some of the problems that you have, and I’ve done it with another colleague’s phone, is texting . . . the hard bit is, as you say, with patient safety and confidentiality, is believing you’re texting the person when you’re not, you end up texting someone else.
Cancer 2 site, cancer nurse specialist, 11
Digital communication can be distributed easily to different recipients. There is the potential that unauthorised recipients are included by mistake or intentionally and that in this way information is disclosed to third parties. In the following quotation, a participant with an IG background suggests that such excessive distribution might breach the confidential nature of the communication between clinicians and patients:
And the other bit of that [risk of inadvertent disclosure] is the copying in of people. So suddenly this is no longer a confidential conversation between two people, there are other people, they can be forwarded. So there’s all that sort of worry from an information governance point of view.
Cancer 2 site, IG and data protection manager, 01
Mitigation
Participants described a number of strategies they adopt to prevent inadvertent disclosure of sensitive information. These included (1) limiting the use of DCCs; (2) implementing various barriers and safeguards, such as personal identification numbers (PINs), passwords and location-specific protection of devices; and (3) double-checking e-mail addresses and telephone numbers (to prevent wrong recipient errors). A further form of mitigation described was (4) explicit or implicit patient consent, where clinicians assume that the patient is willing to accept the risks when they engage in DCC.
In the following quotation, a clinician from a cancer clinic describes how they restrict the use of digital communication to sending appointment reminders. In this way, they aim to eliminate the risk of inadvertent disclosure of sensitive information:
If it was anything about say their diagnosis or deterioration in their condition, or if I had information like from our psychosocial, I would never share that on text, never, you know, it’s just . . . it’s very basic what I text and what they text me for generally. It’s more about appointments.
Cancer 2 site, social worker, 07
Some participants suggested they used passwords and PINs in order to keep the content of their digital communication secure. A patient attending a diabetes clinic describes this in the quotation below. The patient suggests that they felt reasonably well protected (in terms of security) because they were using passwords for their e-mail accounts and their phone, which were not shared:
I think I’m quite secure because I have a password that nobody knows and then I’ve got my phone encrypted as well, and I’ve also got a secure password on e-mail.
Diabetes mellitus 1 site, young person, 14
Awareness of the possibility that mistakes can be made when sending e-mails and text messages can prompt people to be particularly attentive to this action. A clinician from a cancer clinic describes, in the following quotation, how they pay particular attention when texting patients with similar or identical names in order to prevent mistakes:
I live in fear of sending the wrong text to the wrong person. So I’ve got a couple of people that are called [name] so when I have to text a [name] I make double, treble checks that I’ve got the right person.
Cancer 2 site, cancer nurse specialist, 08
Some clinicians described consenting patients as another strategy to deal with the risk of inadvertent disclosure of sensitive information. In the quotation below, a participant with an IG background highlights the importance of consenting patients, which implies that patients accept the risks associated with DCC. Although this might not prevent information from being disclosed inadvertently, the participant suggests that the organisation would be covered from a legal point of view:
. . . so we’d gain that consent from the beginning. Because once we’ve got that if the communication breaks down at least we’re covering our back as such to say well actually this was agreed with the patient.
Mental health 4 site, IG officer, 01
Communication failures
Hazard
Participants suggested that DCC could be subject to a broad range of communication failures, such as communication not taking place, delayed communication and misinterpretation of the communication content.
A patient attending a diabetes mellitus clinic described an example of failed communication. They described a situation where they were in need of urgent advice concerning the appropriate dose of insulin. They attempted contacting the clinic through different modalities, but were unsuccessful and did not receive any reply because the clinicians apparently did not receive any of these communication requests:
Yes, I think there was a time I was getting hypos [hypoglycaemia episodes] quite a few days in a row at the same times, and I must have rung actually, because normally if it’s a hypo they want to deal with that quite quickly, so I will try and ring. And if they . . . obviously if no one picked up so I’d text I think two of the nurses and I didn’t get a response, so I tried ringing again. And then no one picked up, so I think my mum tried texting them and ringing them and then after a few days they got back to us. But then when I said, I have tried to text and call you, they said, we haven’t got any texts or calls.
Diabetes mellitus 1 site, young person, 13
A clinician with an IG background raised similar concerns with respect to delayed communication. The clinician suggests that when patients are communicating urgent requests with clinicians using the latter’s designated contact details, then there is the risk that the response might be delayed if the clinician is away and the patient’s needs would potentially be left unaddressed:
One of the obvious risks is if for example we give a patient an e-mail address to use and it is mine as a clinician and they e-mail me and they’re in crisis and they choose to e-mail me whilst they go into crisis, and I’ve just gone on 2 weeks’ leave, who is going to pick that e-mail up?
Mental health 4 site, IG officer, 01
Some participants also expressed concerns about the possibility that digital communication can be ambiguous, or that it can be interpreted in ways different from what the sender intended. In the following quotation, a clinician from a diabetes mellitus clinic expresses such a concern about the possibility of patients misinterpreting e-mail and text message communications:
I do worry sometimes that information can be misinterpreted depending on how you phrase it in a text or an e-mail.
Diabetes mellitus 1 site, consultant, 07
A participant from a sickle cell disease clinic provided a more concrete example of possible misinterpretation of the content of digital communication. In the following quotation, the participant explains that there might be a failure to detect a critical detail when the examination and diagnosis are based on photos and images that were e-mailed by the patient:
There is always a risk that you will [miss] something that you would be able to pick up when you physically examine because you’re only as good as the photos that have been taken. And they’re two-dimensional rather than obviously in real life you can see far more perspective on it.
Sickle cell disease site, specialist registrar, 09
Consequences
Participants identified a large number of potential consequences of communication failures. These included, for example, delays in, or complete failure of, providing relevant clinical information and advice. Participants suggested that this might potentially discourage patients from seeking relevant advice. In the worst case, communication failures might require escalation to emergency services or even delay patients from seeking necessary help from emergency services. Participants suggested that communication failures could also contribute to anxiety and uncertainty for patients while they are waiting for a response from their clinician. Finally, participants pointed out that patients might react to communication failures in an abusive way, thereby negatively affecting the well-being of clinicians.
In the following quotation, a clinician from a diabetes mellitus clinic suggests that a critical consequence of the failure to establish communication with the relevant clinicians was that patients might give up seeking help even though they are in need of advice:
I guess the worst possible thing is that a patient doesn’t get the contact response that they want and give up, but really needs to speak to somebody. So you know, whichever method they use, they use, don’t get a response from us and just think, oh I don’t want to bother anybody; I won’t try again.
Diabetes mellitus 2 site, specialist nurse, 03
Some participants suggested that in the absence of advice as a result of communication failures patients might deteriorate. The following quotation is a continuation of a previous quotation given above. A patient attending a diabetes mellitus clinic described above that they had been unable to establish communication with their clinic when they were in need of advice about their insulin dose. When prompted by the interviewer about how the patient dealt with this situation, the patient suggested that they attempted to manage the critical situation themselves, but did so inadequately and, as a result, suffered a temporary deterioration in their well-being:
So how did you cope with them [hypoglycaemia episodes] while you were waiting for a response?
I just altered my insulin dose myself to how I thought it would be. Which actually turned out to be wrong, so it did leave an impact because obviously it took a good week to sort itself out.
A patient attending a sickle cell disease clinic describes, in the following quotation, an instance of communication failure that left them feeling very poorly and upset during an emergency admission to hospital. The patient describes that there had been a problem with medications and the patient was unable to contact the clinic to rectify the situation:
I went to hospital, when I was in the hospital I was taken to a ward and in that ward like I got like bad treatment, like I didn’t get the medication that I needed and stuff. And I was in pain all night, and they were prescribing me like paracetamol. Obviously I tried to call them on their mobile to say like what’s going on, but obviously their mobile phones were off because it was out of working hours. [. . .] I could have died. I could have died. I could have died. I could have died or I could have passed out or I could something. I could have even got angry and just started swearing or something, causing a disruption.
Sickle cell disease site, young person, 10
A clinician from a mental health clinic describes, in the following quotation, the importance of trust for the therapeutic relationship. When patients do not receive a prompt reply to their messages, they might feel ignored and this could have adverse consequences for the relationship between clinicians and patients:
Like if you did get to the stage where you use instant messenger kind of thing, that people can see when you’ve read that message, and I think that can be really harmful for like a therapeutic relationship if like a service user could see that a clinician had ignored . . . well not ignored, just hadn’t replied to their message but had read it and that kind of thing.
Mental health 4 (early intervention) site, occupational therapy student, 05
Finally, there might be a potentially negative impact on the well-being of staff. A clinician from a mental health clinic suggests, in the following quotation, that there have been instances where patients reacted to communication failures in an abusive way, which can put stress on staff:
My other biggest element is we work with families, where there are difficulties, and quite often lots of difficulties, more than often lots of difficulties. But also quite often within the parental side of things, there can be personality type difficulties, or just people who are not happy with the service. And I’ve seen, very early when I started here, I was on the receiving end, I think it had been forwarded to me rather than sent directly, but a very negative, very abusive complaint, basically unjustified I have to say. But from a parent who didn’t have the ability to reason or think or wait for a response, so it can become very problematic and can be very damaging to clinicians potentially.
Mental health 2 (CAMHS) site, psychologist, 14
Causes
Participants identified a multitude of potential causes for communication failures, including distraction (e.g. during Skype consultations); not answering/accepting communication from unknown numbers; not being able to establish the patient’s identity; delay in picking up/responding to messages (e.g. people working part-time, out-of-hours query, patient feeling too unwell to respond); inability to access the internet on mobile phones as a result of a lack of signal or credit; poor usability of devices; difficulty expressing clearly information requests in text messages; patients downplaying the severity of their condition in text messages; learning difficulties; and inability to check correct understanding of communication content in asynchronous communication.
Some participants suggested that their condition, for example cancer, could leave them feeling unwell for extended periods of time. During these periods they might prefer to avoid all social contact, and they might perceive e-mails and text messages as unwelcome disturbances and disregard these. In the following quotation, a patient attending a cancer clinic describes such situations, which put them in a different state of mind, and where they ignore messages sometimes for weeks while they are feeling unwell:
Like when I first came in I thought, I want to use my phone, but it’s like actually well I don’t want to use it [. . .] you end up leaving your phone for days. I mean the longest I’ve spent was I didn’t look at my phone for 2 weeks, and obviously when you look you get loads of messages and whatnot. And so using it when you want is one thing, you’ve just got to be able to be well enough to use it. Because sometimes your head is in another world and you’re just not sure when you want to use it or how to use it sometimes.
Cancer 2 site, young person, 03
In the following quotation, a clinician from a diabetes mellitus clinic describes how digital communication can create delays in getting advice across to patients as a result of its asynchronous nature. The clinician suggests that this was because a conversation sometimes requires additional information, and then there might be delays until a problem is resolved while messages are being read and replied to:
Whereas if it’s e-mail it’s then them responding to my message with another e-mail and then waiting for me to pick that up and respond again. So there’s a little bit of delay there whereas telephone, it’s quicker.
Diabetes mellitus 1 site, consultant, 07
Some participants contrasted textual DCC with in-person and telephone consultations. They concluded that the absence of additional cues about posture and tone might be a cause for communication failures, as it was easier to misinterpret information and to miss subtle details. In the following quotation, a clinician from a mental health clinic describes how this could adversely affect the therapeutic relationship because they might be less aware if a patient was struggling:
I suppose text messages it’s difficult to gauge, like I’ve said before, kind of subtleties in somebody’s tone of voice or, you can often from a person’s voice you can pick up on what might, you know . . . if there’s anything going on for them. And you can ask them questions about it, whereas you just don’t get that in a text message. So if that person is struggling then perhaps we might not be aware of that issue if and when we’re texting them.
Mental health 4 (early intervention) site, case manager, 06
Mitigation
Participants suggested that the risk of communication failures might be mitigated by (1) limiting the use of DCCs (e.g. using it for only simple things, such as appointment reminders), (2) providing training in asynchronous DCCs, (3) ensuring that enough time is set aside to write and read DCCs carefully (see Inadvertent disclosure of sensitive information), (4) using alternative means of seeking advice in an emergency and (5) following up DCCs by other means.
In the following quotation, a clinician from a cancer clinic describes that they restrict the use of text messaging, for example, to simple, unambiguous communication, such as arranging an appointment:
No, text is for the movement of small . . . it’s usually for the movement of a small fact, a small low-risk fact. ‘I know I said 9.30, but can it be 10.30?’ Or, ‘can you ring me this afternoon?’, or something like that. Text is fine for that.
Cancer 2 site, consultant, 03
The provision of training and guidance in the use of digital communication might increase the confidence of clinicians in managing and avoiding potential risks. A clinician from a mental health clinic explains in the following quotation that they required guidance in order to deal with new hazards that are introduced through the use of digital communication:
But then I think professionally to be given advice around what happens then [when digital clinical communication is used]; about sort of patients, what happens if somebody says at 12 a.m., maybe on our trust . . . for example if I’ve got a Facebook for mental health and I’m using it, what if they put on my Facebook or Twitter that I’m going to kill myself, what then, where do I go with that? It’s huge information.
Mental health 2 (CAMHS) site, consultant, 05
Some participants suggested that in the case of urgent queries, patients would not sit back and wait for a delayed response, but proactively seek out alternative means of communication in order to get advice. A clinician from a diabetes mellitus clinic describes, in the following quotation, a situation where they had been contacted by e-mail, but had not responded immediately. The patient’s parents then made contact by telephone fairly quickly:
Yes, because I had that when I received an e-mail while [colleague] was on annual leave, I received an e-mail from a parent. But before I’d actually seen the e-mail the parents rang me, so, you know, because I hadn’t responded the parents rang, so . . .
Diabetes mellitus 1 site, health-care assistant, 01
In the following quotation, a patient attending a diabetes mellitus clinic describes that they would follow up previous e-mail communication by a visit in person to ensure that there had been no communication failures:
Well I’d e-mailed her on the Saturday and then I popped in on the Monday or the Tuesday I think, to just kind of follow it up and say, ‘I’ve had a bit of nightmare kind of thing, did you get my e-mail?’
Diabetes mellitus 2 site, young person, 05
Failure to record the content of digital communication
Hazard
The clinicians at the different clinics used several information systems and they communicated with patients through a number of different media (e.g. telephone and various forms of DCC). Participants (clinicians) suggested that there was the potential that some of the content of these various conversations might not be recorded, or that it might be recorded in different places, and as a result some information might not be available to clinicians or patients, or they might not be aware of its existence.
In the following quotation, a clinician from a cancer clinic describes that they communicate digitally with patients while they are out of the clinic. The participant suggests that subsequently recording this information in the patient’s notes poses challenges:
I think the challenge is of actually ensuring that that communication gets in to the patient record. So I can be remote, and I can be responding to patient queries, but how that actually gets recorded into the patient record is a challenge.
Cancer 2 site, IG and data protection manager, 01
A participant from a mental health clinic describes the difference between guidelines for recording communication content and actual practice. The participant explains that although the guidelines require a record of every communication to be kept, in practice this is often not followed through:
Well technically we are supposed to write in the paper notes word for word every text message, every e-mail that we have. And I have to confess I’ve not always done that, in fact I frequently haven’t done.
Mental health 4 (early intervention) site, psychologist, 07
Consequences
Participants explained that failure to record that communication between a clinician and a patient had taken place, or to record what was said during the communication, could result in other clinicians working with the patient being unaware of this prior communication. Some participants suggested that, in consequence, this failure might lead to unnecessary duplication of questions and advice given to patients. Some participants also pointed out that failure to record what advice was given could leave gaps in the audit trail and that there was also the potential for subsequent disagreement between patients and clinicians about what was actually said.
In the following quotation, a clinician from a diabetes mellitus clinic describes how patients might interact with more than one clinician. The participant suggests that, if these interactions are not recorded, then there is no way of knowing what advice has already been provided and advice previously provided by another clinician might be repeated unnecessarily:
Say, for example, this patient saw a dietitian and I wouldn’t know unless somebody writes in there [electronic system]. So I will be able to read it if the patient has seen a dietitian or even a diabetic nurse before, so I know what kind of information they will have had from the diabetic nurse, so I can talk to my patients when I see them accordingly because otherwise I will just repeat the same thing what the diabetic nurses have said.
Diabetes mellitus 2 site, registrar, 06
A clinician from a mental health clinic recalls, in the quotation below, a recent incident where failure to record communication with a patient by text message over an extended period of time led to gaps in the documentation:
So the example that I can think of was a fairly recent death with a young person who was communicating with – a clinician was communicating with a young person a lot by text, but it wasn’t being entered into the paper records, because we don’t have electronic records throughout our system. And after the event there was lack of information readily available that was documented about that interaction.
Mental health 4 (early intervention) site, consultant, 01
Causes
Participants described a number of causes for the failure to record digital communication in patients’ notes. Participants suggested that mobile communication was not logged automatically, and the content of text messages was not as easily transferable to the patient’s notes as other forms of communication (e.g. e-mail). Some participants suggested that documenting e-mails also posed problems as these might not integrate easily with the patient’s notes and it could be a time-consuming activity. Devices have limited storage, and text messages and e-mails might have to be deleted even when they are not documented elsewhere. In addition, participants suggested that they needed to determine for themselves what kind of DCCs they deem reasonably relevant to document. This could lead to significant variation in practice.
A clinician from a cancer clinic describes, in the following quotation, that they are engaging in frequent digital communication with patients. The participant explains that they are struggling to record these interactions because there is no easy way to record text messages:
Because you’re doing it [texting] all the time during the day, you might sometimes text people four, five times in an hour, if not more. And you might text about 20 different patients a day, I think what I do find hard is having that ability to back it up, what I’ve done, and what my contact’s been with that patient.
Cancer 2 site, cancer nurse specialist, 11
A participant from a diabetes mellitus clinic indicated, in the following quotation, that they deleted all e-mails that they did not deem relevant. As this is a subjective assessment, there might be significant variation about what gets deleted and what is stored:
I wouldn’t necessarily keep hold of e-mails if they weren’t relevant to keep hold of.
Diabetes mellitus 2 site, dietitian, 04
Mitigation
Some participants suggested that treating every communication equivalent to an in-person consultation might mitigate the risk of not recording communication content. Risk could also be mitigated by limiting the use of DCC to forms that are more readily transferred to the patient’s notes (e.g. preferring e-mail over text messaging), or generally by restricting the use of digital communication to simple interactions with little or no clinical content.
In the following quotation, a clinician from a diabetes mellitus clinic explains that they recorded the clinically relevant content of digital communication to the same extent that they would if it had been a regular consultation:
Anything that’s clinically relevant I will cut and paste the conversation and put it in our electronic notes so that the rest of team are aware that I’ve done XY or Z in the same way that I would if there was a consultation, I do a summary of what that consultation is.
Diabetes mellitus 2 site, specialist nurse, 03
A different clinician from the same clinic describes in the following quotation that they preferred to use e-mails over text messages because recording of e-mails was easier:
I also like e-mails because of one simple reason; you’ve got a very nice little record to keep, and texts are not always easy to put back in the clinical notes. But e-mail you can clearly print off and put in the clinical notes, or scan it in. Texts, possible, there’s no reason you can’t, but I think technically it’s probably easier to do it this way.
Diabetes mellitus 2 site, consultant, 01
Restricting or avoiding the use of digital communication is described, in the following quotation by a clinician from a mental health clinic, as another strategy for reducing the risk of not recording clinically relevant information. The participant argues that there is a lack of clarity in the organisation’s guidelines about how digital communication should be recorded and for this reason the participant limited their use of these forms of communication:
So limited use actually of digital communication, and I guess mindfully really because some clinical incidents have happened when there’s been lack of clarity about how e-mails for example or texts are used and how they link with clinical recording of information. There isn’t clarity in our policies or processes at the moment, hence why personally I’m not using as much as I potentially could. Because of those issues.
Mental health 4 (early intervention) site, consultant, 01
Failure to consult the patient’s notes prior to engaging in digital clinical communication
Hazard
Patients can initiate digital communication at any time and they might have requests for urgent advice. Some participants (clinicians) reported that they sometimes respond to patients’ queries without consulting the patient’s notes.
In the following quotation, a clinician from a cancer clinic explains that they thought they did not need to refer to their patients’ notes because they were familiar with the patients and their history:
I might have 12, 15 service users that I work with at any one time, so I know their circumstances. I don’t need to refer to clinical notes, I retain everything.
Cancer 2 site, social worker, 07
A clinician from a diabetes mellitus clinic reflects on the nature of calls that patients are likely to make. The participant argues that mostly these would be requests for urgent advice and that, in such cases, consulting the patient’s history was not necessary as they were focusing on the immediate situation:
Those calls are, ‘I’m in an acute situation what should I do about this?’ And it doesn’t matter then what’s gone on before, it’s about ‘what do we do now to keep you safe?’ So I don’t need to access any notes at that stage.
Diabetes mellitus 2 site, specialist nurse, 03
Consequences
Some participants suggested that failure to consult the patient’s notes prior to engaging in DCC can result in the clinician’s reliance on an incomplete patient history, and they might duplicate or contradict advice given previously by a different clinician (see Failure to record the content of digital communication), or they might miss relevant pieces of information in their decision-making.
In the following quotation, a participant from a diabetes mellitus clinic points out that there might be gaps in their knowledge of the patient’s history if they do not consult the patient’s notes because other clinicians might have worked with the patient:
So I might have seen them, but you don’t always know what’s happened kind of in between.
Diabetes mellitus 2 site, dietitian, 04
Another clinician from the same clinic echoes this by explaining that they could not simply rely on what the patient relates at a particular moment in time and failure to check the notes might lead to critical pieces of information being overlooked:
It’s very, very common for patients not to report everything, because they know it, they’ve lived it, they tell you the bits they think are relevant but miss out something that’s quite critical.
Diabetes mellitus 2 site, specialist nurse, 03
Causes
Participants mostly identified perceived familiarity with the patient and frequency of contact with the patient as a reason for not consulting the patient’s notes. Some participants also identified the non-medical nature of many digital communications as a further reason for not consulting the patient’s notes. In addition, one participant suggested that, if a patient has an urgent query, it could be addressed independently of the patient’s history.
In the following quotation, a clinician from a diabetes mellitus clinic explains that whether or not they consulted the notes depended on how well they thought they knew the patient:
Generally speaking, if it’s a new person then I would, you know, definitely would like to refer back to the notes just to see who the patient is, because I wouldn’t just do it on the cuff. But most of the patients I would know who they are, so that sort of helps.
Diabetes mellitus 2 site, consultant, 01
A participant from a cancer clinic describes, in the following quotation, that they do not look up the patient’s notes in cases where they are communicating with a patient’s parent about a logistical matter:
And then another example for not having to look [up the notes] is trying to arrange a mum to pick up some tablets, so I know that the tablets will sort it, so it’s just a matter of texting her back and telling her to where to pick stuff up from.
Cancer 2 site, cancer nurse specialist, 08
Mitigation
Some participants perceived that they had a sufficiently high level of familiarity with the patient to mitigate patient safety being compromised by not referring to the patient’s notes. Some participants also described double-checking after the communication has taken place as mitigation.
In the following quotation, a clinician from a diabetes mellitus clinic explains that, even though they might engage in digital communication without having consulted the patient’s notes, they would afterwards double-check the notes in case they were worried or felt they did not have an up-to-date knowledge of the patient’s circumstances:
Yes, particularly if it’s someone I haven’t heard from for a while, I would go to my clinical notes to think, ‘have they had any contact with anyone else about this, and what have they said to them?’ Just to make sure that I didn’t go and contradict something that somebody else had previously said to them, or missed.
Diabetes mellitus 2 site, specialist nurse, 03
Limitations
Identification of patient safety and security risks is usually done through a systematic and structured risk analysis. This involves generating a clear representation of the system or the process and then considering the failure possibilities of each single component of the system or step in the process. Such a resource-intensive approach is usually indicated only for high-risk systems and processes. In this study, a less formal approach was adopted for pragmatic reasons. There is the possibility that the identification of potential risks was not as comprehensive as with a formal approach and that certain risks might have been missed. This less formal approach was justified because DCCs were not regarded as a high-risk activity (compared with, for example, surgery), and because of the diversity of the way DCCs were used across, and within, the different clinics, which made mapping of these very informal processes difficult.
Risk analysis sometimes involves both a qualitative description of risk and quantitative risk estimation. In this study no attempt was made at quantifying risk. This was justified because (1) the purpose of the study was to provide a rich and broad qualitative description of the potential risks associated with DCCs; and (2) no reliable data about the frequency of digital communication failures on which to base quantitative risk estimation were available.
Summary of findings
The descriptive analysis of interviews with patients, clinicians and clinic managers identified four main hazards of DCCs and associated risks: (1) inadvertent disclosure of sensitive information, (2) communication failures, (3) failure to record the content of DCCs and (4) failure to consult the patient’s notes prior to engaging in DCC.
All of the risks identified in this study appear to be predictable (i.e. they are not the result of some unexpected set of rare conditions and behaviours). Rather, the risks appear to be attributable to common failures and ordinary behaviours and, as such, could be identified readily and dealt with in a proactive fashion before a patient is harmed – if organisations are prepared to invest effort and resource in a proactive risk-management process. 75,76
Chapter 6 Health economic analysis
In this chapter we report the results of the health economic staff survey and the qualitative data analysis relevant to health economics.
Use of digital clinical communications
A total of 115 completed staff health economic questionnaires were received across 18 sites. The mean time spent by staff per day using DCCs to communicate with young people was 76 minutes (median 45 minutes, interquartile range 0–120 minutes). The mean and median times were not ‘typical’ levels of activity, which can be seen from Figure 2, illustrating the range of responses received. Thirty-three staff (29%) reported using DCC ‘rarely’ or ‘never’, whereas 25 staff (22%) reported using DCCs for over 2 hours per day.
FIGURE 2.
Breakdown of DCC use reported by staff (minutes per day). Note that minutes per day reported by 115 clinical team members.
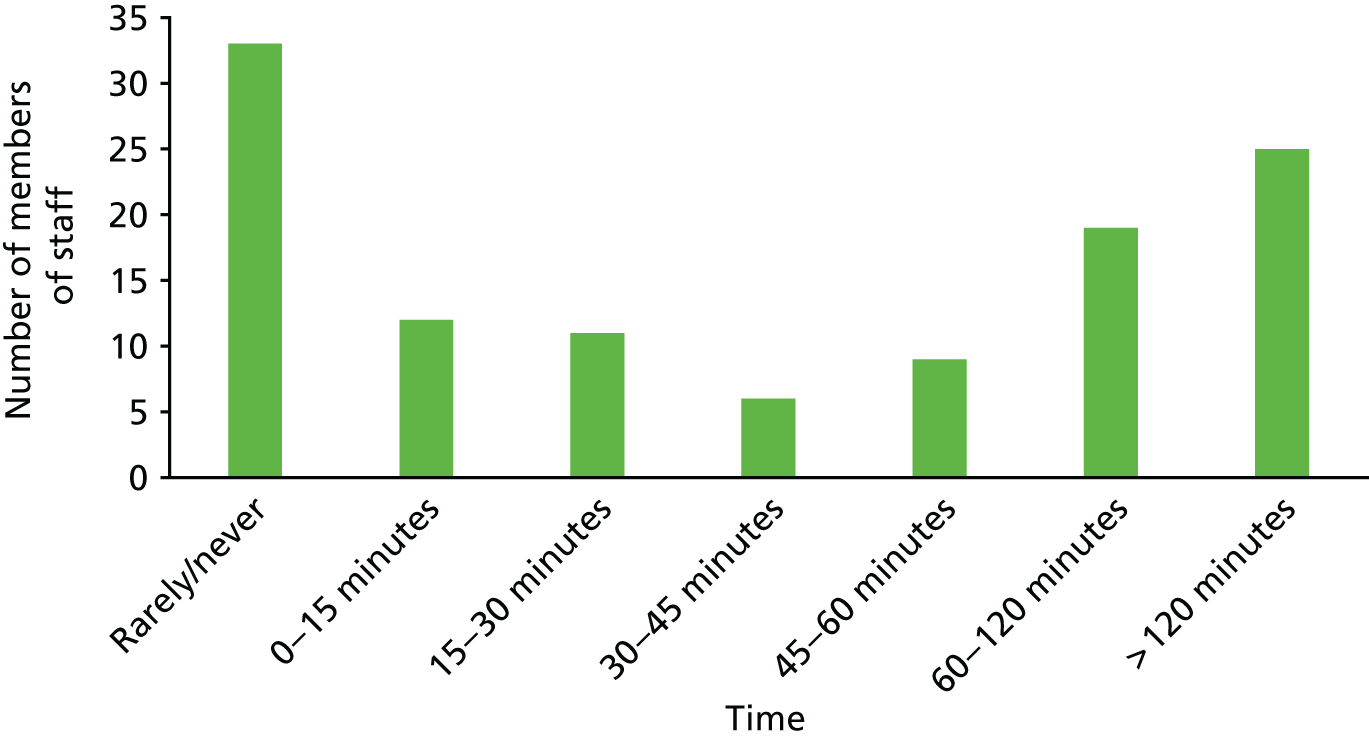
Figure 3 gives a breakdown of this activity by channel of DCC. The time spent using e-mail or mobile phone calls for DCC shows a similar pattern, with staff split equally between those who use these channels for DCC and those who do not. For text messaging, only 40 staff (37%) reported using this channel at all, of whom six (6%) reporting text message-based DCC took up > 60 minutes of their working day. Social media were used even less frequently: 11 staff (10%) reported using social media for DCC, and only one reported this activity involving > 1 hour per day.
FIGURE 3.
Breakdown by channel of time spent by staff in DCC with young people (minutes per day). (a) E-mail (n = 115); (b) text messaging (n = 115); (c) social media (n = 115); and (d) mobile phone (n = 115).
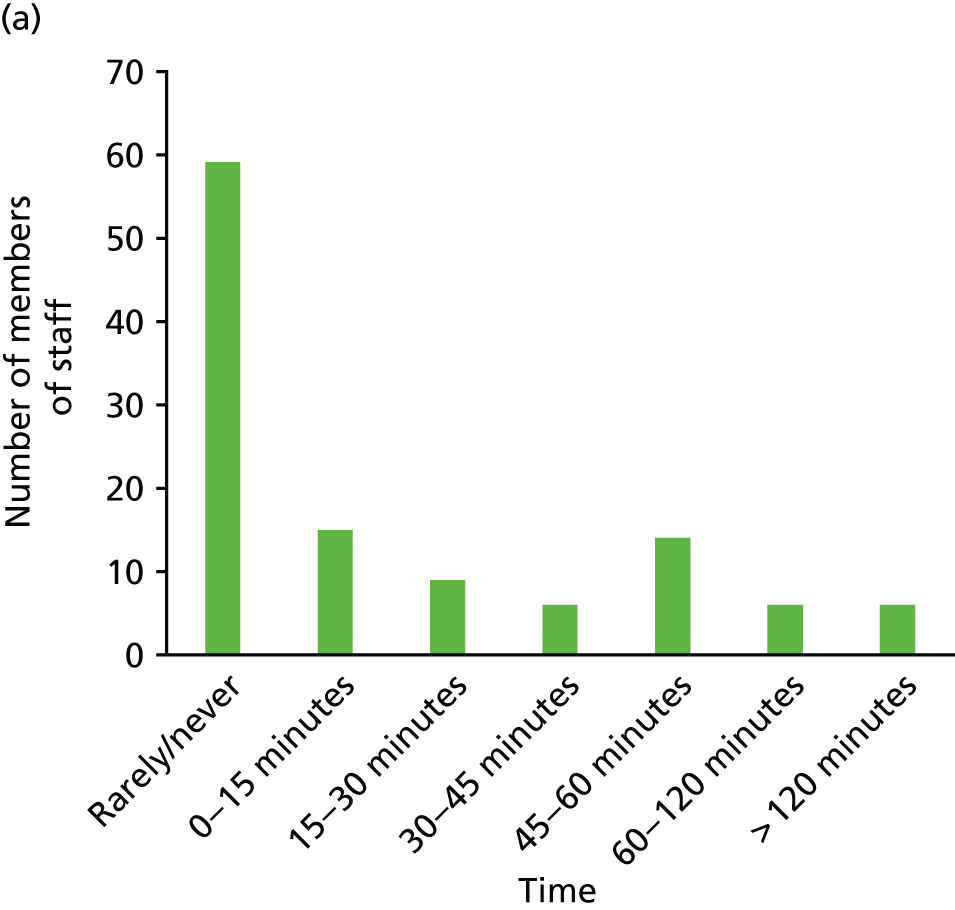
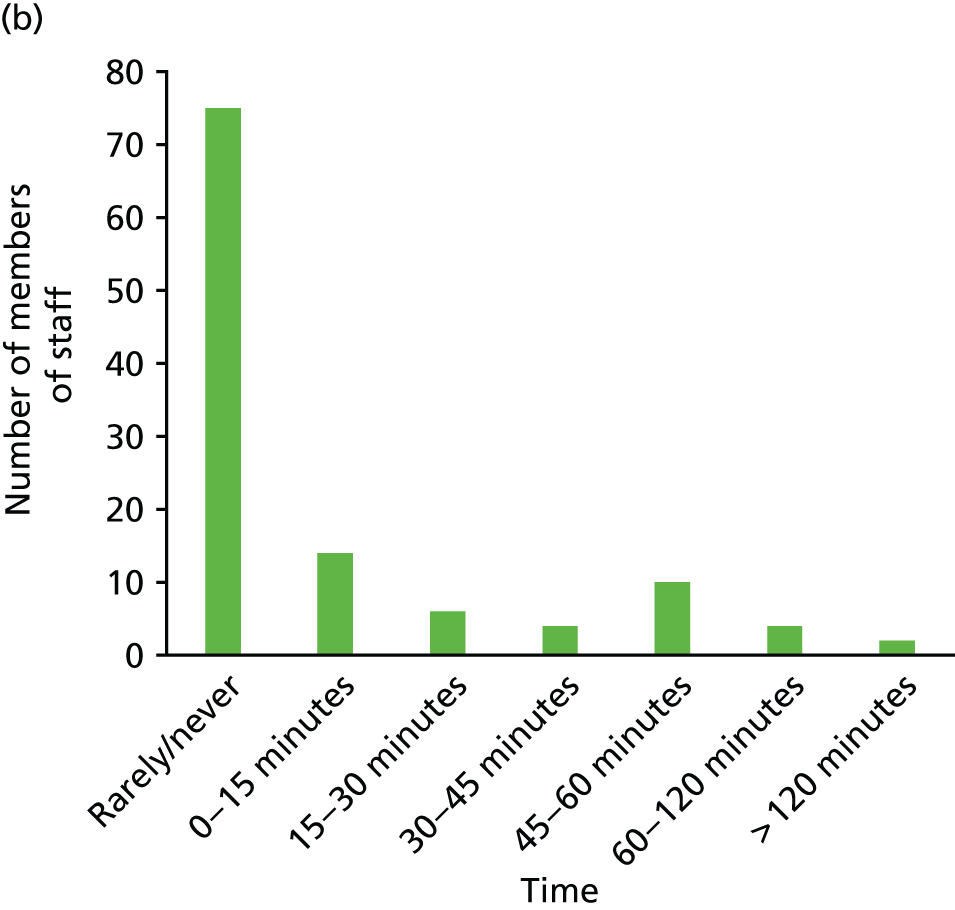
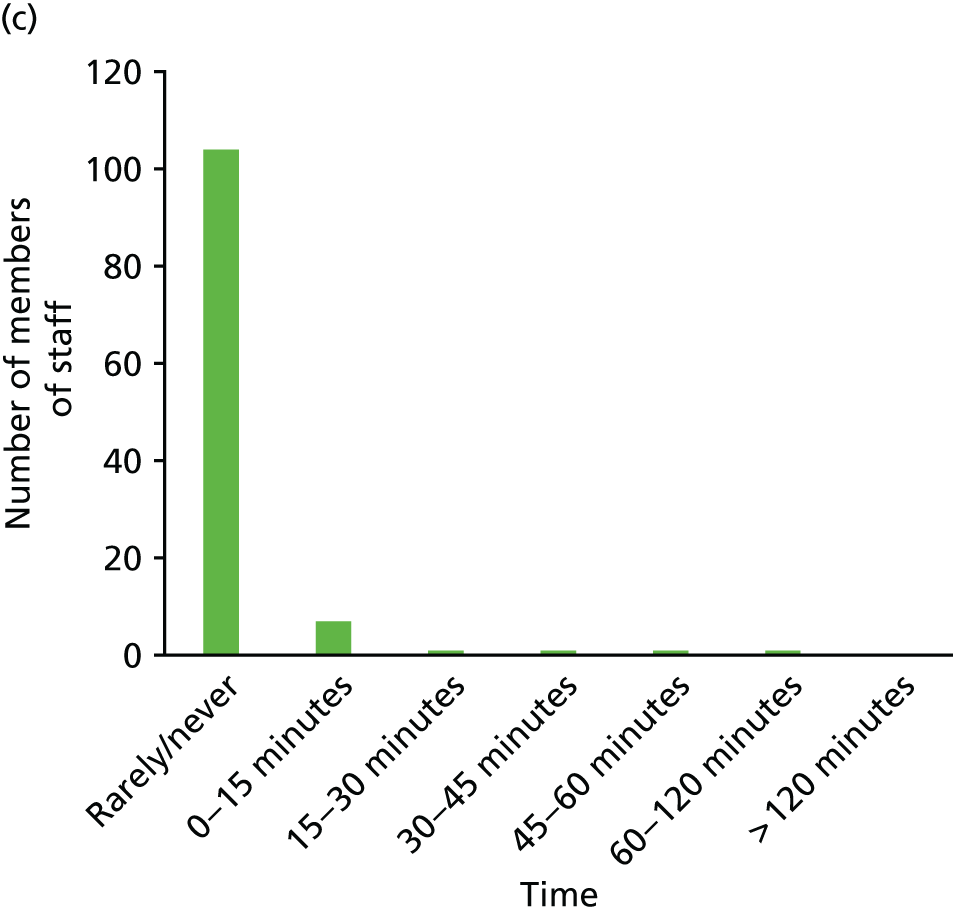
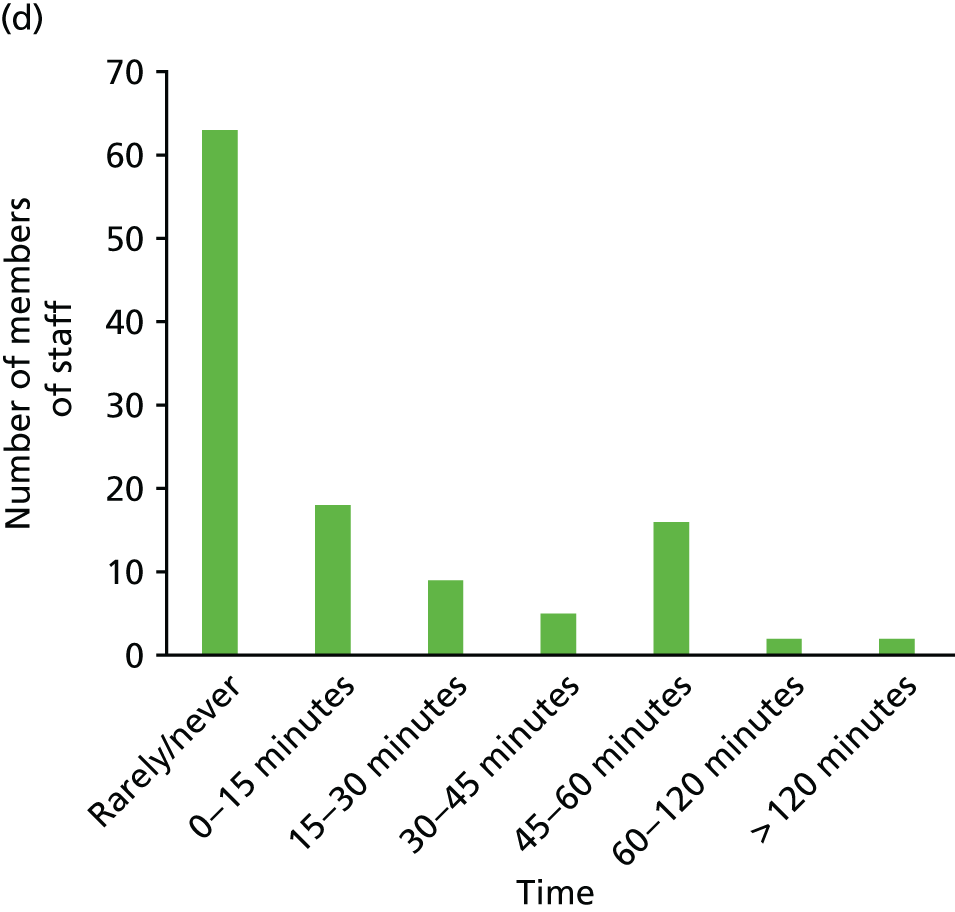
Table 6 gives further information about associations between the clinical condition being managed by the clinical team, and the role of the staff member and their grade, with the time spent in DCC with young people. The mean time per staff member spent varied substantially across conditions. The rheumatology service did not use DCC at all and the renal service reported an average of only 7 minutes per day. The most intensive use was by the sickle cell disease clinical team, with a mean time per day per staff member of > 2 hours. There was an apparent relationship between seniority and use, with those graded as medical consultants reporting significantly lower use of DCCs (32 minutes per day) than staff at grades 6 or 7, who reported a mean time of around 100 minutes per day. Those whose job was described as medical consultants reported substantially lower use (28 minutes per day) than nurses (120 minutes per day) and physiotherapists (120 minutes per day), but were broadly similar users of DCCs to dietitians (14 minutes per day) and psychologists (34 minutes per day).
| Staff completing health economic questionnaire | Number of sites | Total number of staff | Time per staff member per day (minutes) | ||
|---|---|---|---|---|---|
| Mean | Median | Interquartile range | |||
| 18 | 115 | 76 | 45 |
0 120 |
|
| Health condition | |||||
| Cancer | 2 | 16 | 94 | 90 | 18–154 |
| Cystic fibrosis | 2 | 14 | 63 | 38 | 0–120 |
| Dermatology | 1 | 2 | 28 | 28 | 26–29 |
| IBD | 2 | 11 | 79 | 15 | 0–165 |
| Renal conditions | 1 | 6 | 7 | 0 | 0–8 |
| Liver conditions | 1 | 7 | 104 | 60 | 38–98 |
| Mental health | 3 | 18 | 89 | 30 | 4–165 |
| Arthritis | 1 | 8 | 0 | 0 | 0–0 |
| Sexual health | 2 | 19 | 68 | 0 | 0–83 |
| Sickle cell disease | 1 | 6 | 133 | 113 | 56–169 |
| Diabetes mellitus | 2 | 8 | 41 | 53 | 15–60 |
| Grade | |||||
| 2–5 | 16 | 86 | 45 | 0–154 | |
| 6 | 22 | 98 | 68 | 10–120 | |
| 7 | 25 | 104 | 90 | 15–150 | |
| 8 | 19 | 69 | 30 | 8–68 | |
| Consultant | 29 | 32 | 15 | 0–45 | |
| Others | 4 | 69 | 60 | 0–120 | |
| Clinical role | |||||
| Nurse | 31 | 120 | 120 | 30–180 | |
| Psychologist | 11 | 34 | 30 | 0–30 | |
| Consultant | 31 | 28 | 15 | 0–45 | |
| Dietitian | 8 | 14 | 10 | 0–15 | |
| Physiotherapist | 4 | 120 | 135 | 101–154 | |
| Others | 30 | 105 | 60 | 4–169 | |
Costs associated with the use of digital clinical communications
Table 7 summarises the costs of DCCs for each of the 14 case study sites. There were insufficient data to calculate costs for the four remaining sites returning questionnaires.
| Health condition | Number of economic questionnaires completed | Cost per month (£) | |||
|---|---|---|---|---|---|
| Staff cost | Equipment cost | Total cost | Average cost per patient | ||
| Cancer 1 | 5 | 2920 | 97 | 3017 | NA |
| Mental health 3 | 8 | 9230 | 330 | 9560 | NA |
| Arthritis | 8 | 0 | 0 | 0 | 0 |
| Renal conditions | 6 | 135 | 26 | 161 | 16 |
| Diabetes mellitus 1 | 6 | 2648 | 85 | 2733 | 4 |
| Cystic fibrosis 1 | 11 | 5323 | 383 | 5706 | 73 |
| Sexual health | 10 | 3673 | 120 | 3793 | NA |
| HIV | 9 | 1055 | 51 | 1106 | NA |
| Cancer 2 | 11 | 6090 | 267 | 6357 | NA |
| Mental health 2 | 6 | 212 | 18 | 230 | 2 |
| Liver conditions | 7 | 3806 | 71 | 3877 | NA |
| IBD 1 | 7 | 3604 | 26 | 3630 | 3 |
| IBD 2 | 4 | 2672 | 63 | 2735 | NA |
| Cystic fibrosis 2 | 3 | 1490 | 69 | 1559 | 130 |
| Dermatology | 2 | ||||
| Mental health 4 | 4 | ||||
| Sickle cell disease | 6 | ||||
| Diabetes mellitus 2 | 2 | ||||
Young people’s willingness to pay for digital clinical communication
A total of 110 young people answered a question on their willingness to pay for a DCC service. The median willingness to pay was £5 per month (interquartile range £0–£16). Figure 4 gives a breakdown of the responses received to this question: 18 respondents were unable or unwilling to answer this question; 30 respondents stated that they would not be willing to pay extra for a DCC service; 27 respondents stated that they would be willing to pay £30 or more per month for such a service; and the maximum reported value was £120 per month. Additional information provided by respondents at interview provided insights into the reasons for these responses. Some respondents objected to the question on the basis that the service should be free or because of a perception that payment would be discriminatory if applied only in their service (mental health). Others thought that conventional communication channels were available that could be used just as well. There were respondents, however, who reported a wide range of reasons why they would assign a significant value to the availability of DCC. A young person attending the rheumatology clinic (arthritis site, young person, 02) described an issue with self-injection that was only resolved when they were able to directly communicate with a nurse using DCC. DCC was identified by a participant from a mental health clinic as enabling easier contact with a named clinician and so greater continuity of care [mental health 2 (CAMHS), young person, 01]. Two young people recruited from the diabetes mellitus clinics (diabetes mellitus 1 site, young person, 05; and diabetes mellitus 1 site, young person, 06) described sending blood sugar readings to their clinicians digitally, which saved them travelling to the clinic to provide this information.
FIGURE 4.
Willingness to pay for a DCC service (£ per month).
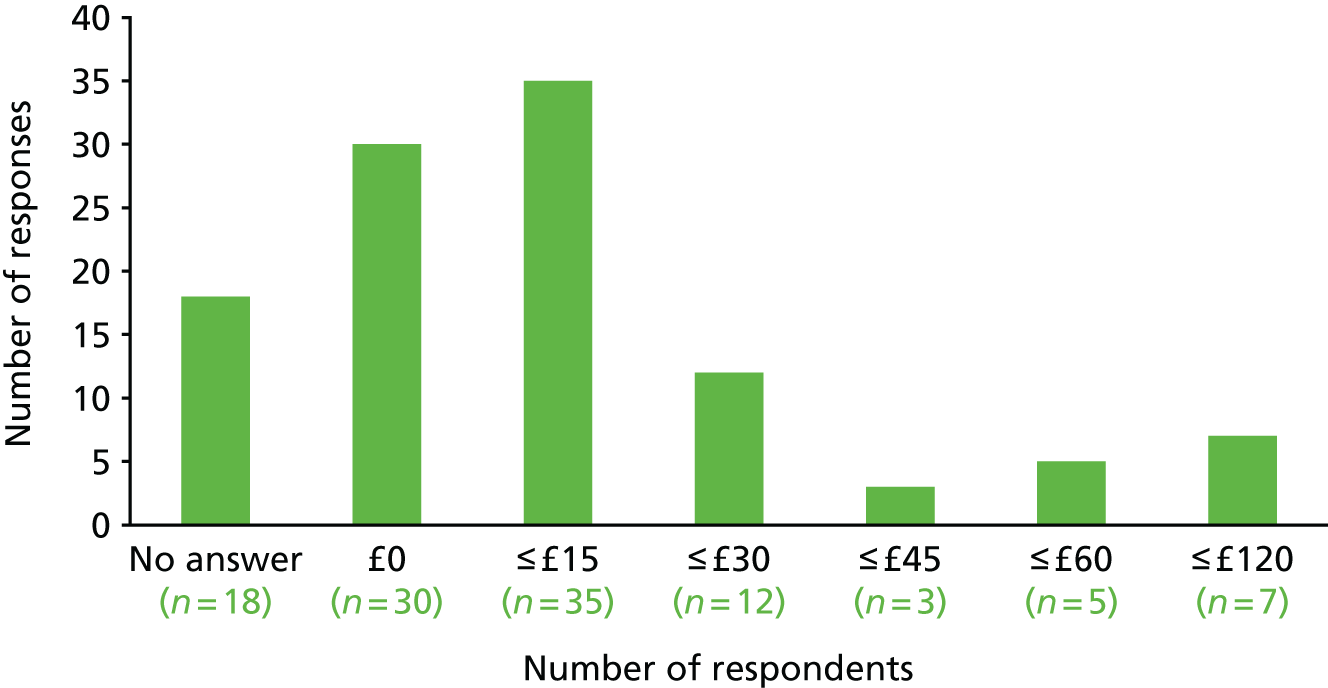
Pathways from digital clinical communication to costs and benefits
In previous chapters, a number of pathways have been identified through which the use of DCCs might affect patient health and well-being and/or health system resources. Follow-up health economic interviews provided further data about how the proximate impacts of DCC might translate into costs and benefits that would be relevant to an economic evaluation. These impacts could be categorised within four themes: (1) engagement with service users, (2) communication between appointments, (3) detection of acute health problems and (4) social and emotional support. Table 8 describes the consequences from each of these impacts, the disease areas in which they were reported and potential outcomes that could be measured to estimate the size of the impact.
| Impact themes from data | Disease areas | Consequence for health service | Consequence for patient health and well-being | Outcomes affected and which could be measured to assess cost-effectiveness |
|---|---|---|---|---|
| Improved engagement of young people, particularly those hard to reach because of their age, socioeconomic status, literacy |
|
|
|
|
| Improved communication between appointments |
|
|
|
|
| Earlier identification of acute complications |
|
|
|
|
| Improved social and emotional support of service users |
|
|
|
|
The specific nature of impacts and consequences depended on the condition being managed. For mental health, increased engagement may have happened because some young people were uncomfortable communicating with staff in person; the acute event might be a crisis requiring referral to inpatient mental health services. For cystic fibrosis, increased engagement might occur with a young person for whom English was a second language, making asynchronous communications more effective; the acute event might be a serious infection. The themes listed in Table 8 capture the underlying commonality of these impacts, which reflect the characteristics of DCC that give these impacts – synchronous or asynchronous communication, that is immediate and can be undertaken on the move. The impacts described above are also interdependent. Changes in the detection and management of adverse events are, for example, a consequence of improved engagement and communication between appointments. Table 8 lists outcomes for which data could be collected by clinical services or research groups in order to quantify the magnitude of impacts resulting from an intervention or service reconfiguration involving DCCs in a specific clinical setting.
In addition to the consequences for services and young people presented in Table 8, interviewees identified a number of ways in which DCC led to efficiencies at the clinic and savings for patients. DCC was used at a number of sites to manage appointments [mental health 3 (outreach team), cystic fibrosis 1, sickle cell disease, mental health 2 (CAMHS)], with staff at two sites suggesting that this had reduced the number of missed appointments [sickle cell disease, mental health 2 (CAMHS)]. At a cystic fibrosis clinic (cystic fibrosis 1), patients e-mailed the clinic when they needed replacement equipment, allowing the service to ensure that this was available at the next appointment. Staff at the liver conditions clinic reported that DCC improved the efficiency of communication through better planning and reducing the number of missed contacts. At this clinic, young people consulted with several members of staff. Clinicians were able to text patients when they were ready to see them, reducing waiting times. Several sites reported that DCC could replace visits in relation to routine queries and test results. At a diabetes mellitus clinic, it was estimated that DCC could save around 8–12 visits to the clinic per year (diabetes mellitus 1, health economics follow-up). At the sickle cell disease clinic, young people reported using DCC for queries that otherwise would have led them to visit A&E. This represents savings for the services, but also for the young people themselves. One young person attending the liver conditions clinic reported that DCC allowed them to avoid a clinic visit that involved 2 hours of travel time for the round trip (liver, young person, 18).
Despite these efficiencies, no staff reported that DCCs reduced their workload; many reported that DCCs had in fact increased their workload. This was partly a consequence of the increased engagement described in Table 8. Improved relationships between the young people and their clinicians, and the ease of communication, increased the demands placed by young people on services and changed their expectations of access. Staff at the liver conditions clinic reported that DCC made clinicians seem more accessible to young people (liver, consultant, 02), and young people reported feeling more likely to contact clinicians if it was via DCC, as they saw this as less of an imposition (liver, young person, 11). A clinician at the diabetes mellitus clinic reported that their workload had increased as young people expected prompt responses to e-mails (diabetes mellitus 2, consultant, 01). In a health economic follow-up interview, a clinician at a diabetes mellitus clinic (diabetes mellitus 1) reported that the service did not capture the impact of DCCs on workload. Clinicians were managing the DCC in their own time, which could lead to burnout. At the sickle cell disease clinic, staff reported that patients sometimes contact staff by digital means, in ways that are not always efficient or appropriate (e.g. bypassing a clinician’s personal assistant to request appointments). At the cancer clinic (cancer 1), it was noted that patients who expressed anxiety were likely to be seen more often, potentially increasing the number of visits.
Summary of findings
Limitations of the health economic component of the Long-term conditions Young people Networked Communication study
The LYNC study was an in-depth qualitative assessment of the use and impact of digital communications, defined broadly and evaluated across a diverse collection of case studies. Although this context yields numerous insights into current practice, it does impose significant limitations on what could be achieved in terms of formal economic evaluation within the LYNC study. We therefore begin with an acknowledgement of these limitations, and a clarification of the goals of the health economic data collection and analysis that was performed. As we explain in Chapter 2, the LYNC study was not designed to support formal economic evaluation of digital communication. Instead, our work might best be viewed as a feasibility study to motivate and inform future economic evaluations of specific interventions involving digital communication. We discuss the relevance of our findings to such evaluations below, but acknowledge fully that our results (qualitative and quantitative) should be seen as indicative rather than conclusive. Our collection of data on willingness to pay, for example, was never intended to provide precise and valid estimates of the value young people attach to the use by services of digital communication. Given that participants were recruited from diverse sites, with only a few participants per site, this would never have been possible. Instead, our aim was to use the opportunity afforded by the collection of qualitative data from service users to understand how they might interpret such questions, posed in different forms, and gain an indication of the range of values we might encounter. We discuss this experience in further detail below.
The challenge for any economic evaluation of DCC is that the term covers a broad range of practices, and the costs and benefits of these practices will vary according to aims of the clinic and the specific approaches involved when clinics adopt DCC. It is, therefore, not helpful to consider the cost-effectiveness of DCC in general terms, as any particular decision around the adoption of practices involving DCC would involve a specific economic evaluation, which was beyond the scope of this study. It may be helpful, however, to distinguish between two types of specific decision problem involving DCC. The first type would involve a well-defined intervention or practice for which the use of DCC is an integral component. There were some examples of this among our case studies, such as the delivery of dialectical behaviour therapy via text message. In such examples, it is more appropriate to consider an economic evaluation of the intervention as a whole, rather than of DCC in isolation. Such an evaluation would require a robust assessment of the incremental impact of the intervention relative to a suitable comparator, in terms of costs and benefits; however, it was not possible to obtain the data required for this within the study.
The second type involves the uptake and expansion of DCC as part of routine activities of a service. Our findings relate primarily to this second type of decision problem, although many of our findings are relevant to any economic evaluation of an intervention with a DCC component. However, the requirement for robust data on the incremental impact of the expansion of DCCs remains. The LYNC study was cross-sectional, rather than a before-and-after study, and did not include formally matched controls. It was therefore not possible to carry out any incremental analysis of the costs or benefits of changing practice regarding digital communication. The data on costs reflect total time spent on digital communication activities, which will include activities that would previously have been conducted using conventional communication channels, rather than the net impact of the adoption of digital communication on workload. Although staff commonly expressed the view that digital communication was more likely to have increased, rather than decreased, their workload, they were unable to quantify the net impact with any accuracy. This is understandable given that the adoption and impact of digital communication is a gradual process. It was, therefore, not possible to collect valid data on the incremental cost of digital communication within the LYNC study. Similarly, we did not collect primary data on outcomes and it was not possible to discern the incremental impact of digital communication on outcomes from the clinic data that were available, as would be possible in a study that was explicitly designed to evaluate the impact of a specific change in practice in a well-defined setting which involved collection of intervention and comparator data on costs and outcomes. However, the qualitative and quantitative data we collected provide substantial insights for such evaluations, which are discussed in the next section.
Insights for future economic evaluations
The first question to consider is whether or not an economic evaluation of the ongoing adoption of DCC in routine clinic practice is required. It might be thought that this is an inevitable evolution of clinical practice and that the cost implications of this change are likely to be immaterial, or even positive (cost saving). Our survey of staff shows significant variation in DCC use across sites and among respondents, and suggests that sites are making active choices about the adoption of DCC, with substantial cost implications. In particular, the key driver of cost is staff time, which typically accounts for > 90% of the direct costs associated with DCC use. Furthermore, we found a strong association between the use of DCC and the seniority of staff involved, with consultant-grade staff reporting substantially less time spent using DCC. This influences the total cost impact of DCC use, and may largely be a result of the different roles staff have in the clinic and the different relationships they have with service users. However, it is also possible that this reflects, at least in part, generational effects. As current young doctors become consultants, they may be more willing to engage with DCCs, and this may lead to an increase in DCC-related costs.
As we explain in Limitations of the health economic component of the Long-term conditions Young people Networked Communication study, the direct costs reported may well involve activities that were previously carried out using conventional channels of communication, rather than additional activities. When combined with efficiencies generated through the use of DCC, it is possible that the net impact of DCC might be to reduce staff burden and the cost associated with it. Examples of such efficiencies relate mainly to managing appointments and reducing missed appointments. There is the potential to replace in-person contacts for routine reviews. However, it is notable that no staff reported that DCC had reduced their workload overall, and many reported that it had in fact increased it. The importance of this finding is reinforced by those staff who perceived clinic managers to hold expectations that DCC would increase efficiency and reduce pressure on staff time, expectations which did not match reality for staff directly working with young people. It is the benefits of DCCs that cause the pressure. Respondents reported that DCC improved engagement with young people. There were examples provided of specific groups that responded favourably to DCCs, but there was also a general effect as young people preferred to use digital media. DCCs also improved relationships between young people and the clinicians, and made it easier for young people to contact staff between appointments. These are positive impacts, but dealing with this broadened and enriched engagement with young people took up considerable amounts of staff time. Furthermore, DCCs were in some cases reported to break down the professional/personal distinction in the relationship between young people and clinic staff, so that increased communication occurred that was not always directly related to clinical need.
When assigning costs to resource use implications in an economic evaluation, standard methodology requires that unit costs reflect the opportunity costs of the resource from the perspective of the decision-maker. 77 This has implications for costing the impact of DCCs in terms of reductions in appointments missed. This opportunity cost is likely to be high where staff are travelling to meet young people for appointments as considerable staff time will be wasted if the young person fails to turn up. In the case of clinic visits, however, the opportunity cost depends on how services respond to missed appointments. If the time is used to catch up on a backlog of attendees, or paperwork, then the opportunity cost of the missed appointment will be lower. The opportunity cost of reducing DNAs is, therefore, highly variable depending how a clinic operates and can be extremely difficult to quantify. It is clear, however, that missed appointments impose a cost because they restrict the ability of staff to use their time productively, and require resources to chase attendees and rearrange appointments. NHS England has estimated that the average cost of missed appointment is £103,78 although this is likely to be a considerable overestimate, as it assumes that the time that was allocated to the missed appointment is completely wasted. Nevertheless, there are likely to be considerable costs associated with missed appointments. A further implication of the standard costing approach relates to DCC carried out by staff in their own time, using their own equipment. From a health service perspective, this technically involves zero cost. Services need to be aware of the impact this is having on staff to avoid issues of burnout, absenteeism and staff turnover. It may be that services need to be reorganised to ensure that sufficient time is allowed for DCC, and investments need to be made in dedicated out-of-hours DCC services, which would have clear cost implications.
Although decision-makers need to be aware of these cost implications, and not expect DCC to be cost saving, they should take into account the potential benefits of effective use of DCCs. Although it was beyond the scope of this research to quantify such benefits, we have identified clear, consistent and credible pathways through which DCCs can lead to improved short- and long-term outcomes. Services cannot benefit young people unless they engage with them and DCC was widely perceived to improve this engagement. Although this does imply an increased clinic workload, this needs to be set against the benefits to young people who might otherwise not have engaged with services. The impact of DCCs across sites could be described as enabling a move from intermittent to continuous care, with improved monitoring and therapeutic interaction between appointments. A number of staff reported how this led to improved short- and long-term health outcomes. DCC also improved the richness of information available to staff, which was reported by several respondents to enable more personalised and responsive care, which would again lead to improved health outcomes.
The findings of our study highlight the importance of considering the benefits to young people of DCCs beyond the direct impact on their health. A recurring theme reported by respondents was that living with chronic health conditions negatively affected young people’s lives in ways that went beyond the clinical consequences of the condition itself. Young people reported a loss of control and independence as a result of the need to manage their condition. There was considerable anxiety reported as a result of the uncertainty around their health and the potential for it to deteriorate. In many conditions, young people are faced with challenges around learning to manage their health and their treatments. This can involve learning a complex task in a short period under considerable pressure. DCCs were reported to help young people with these challenges to their well-being. This has important implications for any economic evaluation because these benefits may be difficult to capture using standard preference-based health utility measures, such as the EuroQol-5 Dimensions, but are clearly highly valued by young people.
Our willingness-to-pay exercise was an exploratory attempt to estimate the value of DCC for the young people, although the results must be interpreted with considerable caution, given the limitations to the study mentioned above. Our main aim was to explore how we might elicit this value and assess how young people might respond. We initially carried out this stated preference elicitation as a willingness-to-accept exercise to avoid the results being constrained by income. However, respondents found this perspective hard to relate to conceptually. We therefore revised our approach and asked a willingness-to-pay question. This was a more comfortable approach for respondents, as it was consistent with how they purchase the technology used for DCCs, but it did mean that responses reflect budgetary constraints. Where respondents still struggled to quantify the value they placed on digital communication, the interviewer was allowed to prompt the interviewee by offering suggested values. A range of £5–50 was used as prompt (although the most common value was £10). In addition, although it was explained that this was a hypothetical question, several respondents objected to having to pay for a service they considered themselves entitled to and their zero responses did not reflect their perceived value from DCCs. Such protest responses were, however, uncommon. The one site where protest votes were common was a mental health site, where the protests reflected a perception that this was another example of ongoing discrimination against mental health services.
Given the lack of consistency around approaches to the willingness-to-pay question, the use of prompts (which can lead to anchoring bias), the obvious difficulty many respondents had in answering the question, the diversity of contexts in which responses were collected and the small number of responses per site, the results presented can be considered only illustrative at best. However, they are consistent with many users placing a high value on the use of digital communication. When combined with the qualitative findings about the value users place on the non-health benefits associated with digital communication, our results suggest that a more robust estimation of this value would be an essential component of future formal economic evaluations of service delivery interventions involving digital communication. It may be that using an alternative approach, such as discrete choice experiments,79 in such an evaluation would give a more accurate estimate of the value young people experience from DCC.
Although we were unable to quantify the potential cost-effectiveness of DCCs across the study sites, cost-effectiveness evaluations of interventions in the conditions managed at the clinics illustrate the potential benefits that DCCs might achieve. In diabetes mellitus, for example, the potential benefit of reducing HbA1c levels from 7.5% to 6.5%, as recommended by NICE,80 via a structured education programme, was estimated to be around £3500 per patient. 81 The UK Prospective Diabetes Study 41 reported that improved blood glucose control reduced the mean cost of managing complications by £771 per patient. 82 The costs associated with a mental health crisis requiring inpatient stay have been estimated at £2900 per day. 83 These examples illustrate the potential magnitude of cost savings achievable, to be set alongside the gains in patient health. There is significant potential for DCCs to be cost saving overall when these costs are taken into account, although it must be noted that the savings do not necessarily accrue to the service incurring the DCC-related costs.
Chapter 7 Information governance
Analysis of the interviews with IG officers identified the following key themes: provision of patient-centred care, innovative health service delivery, policies, governance protocols and concerns. Subthemes were identified during this inductive thematic analysis.
Provision of patient-centred care
Data within this theme suggest that patients were central to IG officers’ thinking when they considered the use of DCCs in their organisations. They embraced the concept of new technologies and supported the idea of developing NHS systems that integrated current digital communication platforms.
Digital clinical communication as patients’ main requested method of communication
There was consensus among the IG officers that current society is technologically advanced and young patients have now adopted digital communication platforms as their main methods of communication. The IG officers were strongly in favour of the health-care sector using mainstream communication methods in order to deliver a high quality of service:
So, you know, we’re listening to what our service users are saying about how they, particularly the younger age group, how could this be part and parcel of how they communicate with each other on a day-to-day basis. And more and more, as individuals in our personal lives, we use digital communication, social media, so much more and actually we need to be able to respond to that within health.
School nurse service, IG lead, 01
A majority of the IG officers remarked that patients were increasingly making requests to engage with clinicians through digital communication and were resistant to receiving information relating to their health via conventional post:
But my personal view would be that particularly if you’re talking about young people, you know, their means of communication is not by letter and telephone, it is increasingly interactive with various forms of social media. And, therefore, to engage and to have relevance to those service users the organisation needs to use the tools and means best suited.
Mental health 2 (CAMHS) site, IG head, 01
Another incentive identified for establishing digital communication within the NHS was the recent Caldicott Review in 2013,33 which asserted that patients’ preferred methods of communication should be respected. The review was quoted by some of the IG officers:
But now we have it in the form of the Caldicott Review which you may be familiar with, and Dame Fiona Caldicott said it’s ridiculous that we’re not bending to patients’ demands for use of modern technology; the NHS needs to move into the 21st century and they concluded that it’s OK to communicate with patients by e-mail so long as the patient consented and they are aware of the risks.
Cystic fibrosis 1 site, IG lead, 01
Ten of the 16 IG officers interviewed indicated that responding to patients’ requests was essential and viewed DCCs as effective methods of communication. They gave examples of where it was better than using the postal service:
. . . It’s just kind of engaging with people in the way they want to be engaged with. We have a lot of people who are no fixed abode and they’re sofa surfing somewhere. Their life is on their smartphone.
Mental health 4 site, IG officer, 01
As a direct response to patient requests, a number of IG officers reported that their NHS trust was considering introducing text messaging and e-mailing facilities:
So, we’re beginning to allow e-mail communications with patients. It’s still in its infancy, policy change only happened a few months ago . . .
Diabetes mellitus 2 site, Caldicott Guardian, 01
We again, another development, we are looking at, at the request of patients really, an ability to use text messaging as a part of a keeping in contact. So, you know, a sort of checking up service, how are you today, you know, how are you feeling?
School nurse service, IG lead, 01
Digital clinical communication promotes patients’ access to their health records
The IG officers acknowledged policies to enable patients to have access to their own health records:
. . . The Caldicott Review is very supportive of new technologies. And there are lots of demands being made on trusts’ intent on the health service generally in terms of patients being able to access and manage their own care across the internet.
Cystic fibrosis 1 site, IG lead, 01
Eight IG officers said that their trusts were implementing, or had plans to implement, developments to achieve this goal:
. . . There’s obviously a requirement of any new provider of our clinical systems that they will have integral to them clinical interactive systems in that clinicians will be able to interact with the online clinical information out and about when they’re agile working. And that also there would be a patient portal so that patients could also be having access to certain aspects of their record and be able to input to their record . . .
Mental health 2 (CAMHS) site, IG head, 01
I mean there are isolated systems out in the trust and the one I can think of is renal patient use. So that’s online and it’s, you know, patients can access information about themselves and also clinicians can input into that system. So that’s an example of an online system that is accessed by both patient and clinicians managing their condition.
Sickle cell disease site, IG officer, 01
The popularity of e-mail communication as the principal option for meeting this goal emerged from the interviews:
. . . We would like to think we’d ultimately be able to use e-mails more securely so that we can provide patients with information about their care, electronic patient records, all these things will be not far away.
Diabetes mellitus 2 site, IG officer, 01
Yeah, ultimately I would like to think that we could e-mail patients copies of the letters and things like that from their outpatients. So at the moment we can send discharge summaries and stuff to GPs [general practitioners] but it would be nice one day if we could copy patients into the correspondence.
Diabetes mellitus 2 site, Caldicott Guardian, 01
Digital clinical communication improves patients’ service engagement
Six IG officers reported an improvement in young patients’ service engagement as a result of receiving either personalised or automated text messages:
We do phone patients to talk to them about appointments coming up and make sure that we improve DNA rates.
Liver conditions site, IG officer, 01
Sending text messages to patients was considered normal irrespective of its purposes across many of the NHS trusts where our participants worked:
Well we text a lot of patients, because we text them all prior to outpatients. We text them all prior to theatre to make sure they’re going to turn up.
Diabetes mellitus 2 site, IG officer, 01
We do use text services. Outpatients and orthopaedics use text services . . . We have our own in-house text servicing, so you can use it or not. I think some of the busier clinics do use text reminders.
Arthritis site, Caldicott Guardian, 01
Eight NHS trusts where our interviewees worked were implementing other digital communication systems in efforts to improve appointment attendance:
We are shortly due to implement a system called Lorenzo which enables us to collect e-mail addresses and things like that, and it works in a way which will enable e-mailing appointment letters to patients.
IBD 1 site, IG officer, 01
The use of social media would be both to promote the service and to engage the service user.
Mental health 2 (CAMHS) site, IG head, 01
Innovative health service delivery
All IG officers reported innovation within their own trust, which they thought would bring benefit to patients.
Innovative service proposals
The development of Skype clinics was reported from across more than half of participating trusts, although implementation was at varying stages in different NHS trusts:
So in the video world I’m aware there are people that [name] mentioned like speech therapy, paediatrics, who are doing some sort of Skype stuff. But mostly they’re people waiting for us to give them a solution that they can use it.
Sickle cell disease site, IG officer, 02
One IG officer reported that Skype clinics had been piloted in the wrong clinic, but the trust still remained interested in trying it out in a sexual health clinic:
They did pilot Skype clinics, in I think it was dermatology, but found that actually it was the wrong kind of clinic to run via Skype because dermatologists still need to be able to physically see and examine the conditions. So those were very quickly stopped.
Liver conditions site, IG officer, 01
A key motivation for initiating Skype clinics across different health conditions was to promote patient engagement with health services:
We‘re about to pilot two areas where we are going to Skype patients from clinic . . . Because we’re a specialist hospital, we have very specialist services, we have patients who travel over from [area], which is, you know, 100 miles. And so they want to try and do consultations by Skype.
Arthritis site, Caldicott Guardian, 01
One IG officer commented that sexual health clinics were leading innovation as they mostly served a younger population:
The trailblazers in this regard have been sexual health services, and I think that’s largely because of the particular cohort of patient they‘re dealing with, it will be teenagers very largely and under 25s . . .
Cystic fibrosis 1 site, IG lead, 01
As for consultations, obviously I mean we’ve all had a good laugh about the idea of the Skype consultation in sexual health and what that might consist of [laughs], you know, obviously the clinicians there are going to have to draw the line about how far they can take a consultation.
Cystic fibrosis 1 site, IG lead, 01
Being able to deliver care remotely and its use in triage were talked about as key advantages of video communication:
. . . Be able to put video by every intensive care bed in the trust, so that’s 60-something beds will be remotely supported by intensive care professionals sitting behind a computer. And we’re doing some other things in terms of being able to send diagnostic images from one location to an expert somewhere else.
Sickle cell disease site, IG officer, 02
You might not be able to get to see the dermatologist in person, but maybe you’ll be able to get to the point whereby you meet a specialist nurse in a video clinic who could press the button to record it at the right moment to escalate it through the process.
Sickle cell disease site, IG officer, 02
Perceived benefits to health-care service delivery
The IG officers identified a range of benefits from using DCCs.
Saving time and money for the patient, particularly those living in remote areas, and for the NHS was identified as a key benefit:
Telephone saves the patient a hell of a lot of bother. We also have . . . we provide services for patients from quite a wide geographical area, including the [place], so if it saves patients coming across the [place] then it’s a significant benefit . . . So you know we’re absolutely sold on modern technology.
Diabetes mellitus 2 site, Caldicott Guardian, 01
And, you know, it’s using these technologies to be able to provide that quality care to service users with maybe reduced service, if you know what I mean, reduced number of staff. So you might be able to see more patients, but your team might actually be smaller, because what you’re doing is you’re using other types of engagement methods with them.
School nurse service, IG lead, 01
Being able to provide services at the right time was also identified as a benefit:
So another benefit of e-mail . . . if a result comes through that means the patient needs to be reviewed, it’s much more instantaneous if you can phone them on a mobile or you can e-mail them, than sending a letter to be typed, getting that letter typed, putting in the mail. Mail is mainly second class now, so you know, there is inherent time delays.
Liver conditions site, IG officer, 01
Policies
Throughout each interview, the narrative of each IG officer turned to policies in between their enthusiastic comments about the benefits of using DCCs. This was to be expected given implementation of policy is a key part of their role.
Current digital clinical communication-related policies
Thirteen of the 16 IG officers reported the existence of policies in their organisations that were devised specifically to cover either text messaging, e-mailing, social media and/or the use of handheld mobile devices:
We have an e-mail policy, we have a mobile device policy, specifically for phones, and we have a social media policy for staff.
Arthritis site, Caldicott Guardian, 01
We‘ve got a large policy and protocol set and guidance set as part of IG, so there’s individual protocol for use of internet, use of e-mails, . . . and social networking, so you know, as these technologies come on board we create policies for them and sort of review the existing ones.
Sickle cell disease site, IG officer, 01
There was recognition that policies need to evolve as digital communication services evolve:
And if anything, my role as a Caldicott Guardian has been about saying to our information governance team, we can’t keep on with the same policies as we’ve had because we need to assure that there are these modes of communication for patients.
Cancer 2 site, Caldicott Guardian, 01
So I think our policies are beginning to acknowledge that where communication has come directly from the patient using e-mail, or where the patient has requested an e-mail correspondence, you know, these are the standards that we expect you to use.
Cancer 2 site, Caldicott Guardian, 01
One IG officer described how compliance with policies was monitored:
In terms of the Fair Processing Notice for individual projects we spot check them from time to time, and we don’t just spot check the new projects, we spot check elements within the trust. We will just walk into one department and say ‘hello we are from IG and let’s see what you’re doing’, which doesn’t make us very popular but it gives the organisation assurance and it gives our managers assurance.
Liver conditions site, IG officer, 01
Training courses during staff induction and mandatory refresher online courses were described among measures for enforcing policies related to DCCs.
Policies in development
A majority of IG officers reported having plans to develop digital specific policy for DCC:
They are currently working on guidance regarding e-mailing patients but this is very much in draft stage.
Liver conditions site, IG officer, 01
But I know the trust doesn’t currently have a policy for e-mailing patients because it’s a bit of a taboo subject within the NHS, there’s no national guidance on it, so . . . But it is something that the trust’s going to be embarking on anyway.
IBD 1 site, IG officer, 01
No existing policies
A few trusts did not permit DCCs, and there were no active policies in existence to cover such activities, but the IG officers in these trusts were aware that it was taking place. There were also no policies reported that covered clinicians giving out their contact details to patients, although most trusts were developing communication systems that enabled patients to e-mail clinicians:
Patients can obtain clinicians’ e-mail addresses from e-mail signatures and there is no policy that currently states that they cannot do it.
Liver conditions site, IG officer, 02
But anybody who has got any logical thought could work out an individual’s e-mail anyway in the organisation because it’s got corporate format.
Mental health team 3 (outreach team) site, IG head, 01
Generic policies that cover digital clinical communication activity
Eight IG officers referred to generic IG policies when discussing guidelines for DCC. The most commonly quoted were data protection and confidentiality policies:
Well under the information governance framework we have to have an overarching information governance policy which stipulates accountability, communications and overarching policies.
Cystic fibrosis 1 site, IG lead, 01
We also have a code of confidentiality for IT users . . . I’m not sure if that specifically talks about contact details, but it does talk about protecting confidential information, and certainly also the e-mail one talks about sending confidential information out. So there’s bits covered in different places. As I said before, it’s not necessarily patient centric at the moment, but certainly we do have four policies in place.
Liver conditions site, IG officer, 01
Digital clinical communication-related information governance protocols
All IG officers outlined protocols that clinicians were expected to adhere to when conducting DCCs. A detailed account was provided by each IG officer concerning the manner by which DCC was regulated within their NHS trusts. It is important to note that current data were collected prior to the formal implementation of NHSmail 2 and, therefore, responses provided by these key professionals illustrated solutions to issues that were not mainstream.
Protocols for digital clinical communication operationalisation
Consent had to be sought from patients to use DCCs, irrespective of whether the patient had initiated the communication or the clinician:
Some service users may request that communication is done via e-mail. If this is the case the following must happen: health professionals involved must inform the service user that e-mail is not a secure method of transferring information; ensure the service user is happy to accept the risk involved with using e-mail as a method of communication. This must be formally recorded in the service user’s record.
Mental health 2 (CAMHS) site, IG head, 01
All interviewees mentioned that patients had to be made aware of the risks involved with using private e-mails that were not secure:
So we tell clinicians that if the patient is happy to communicate in that way and they’ve been made aware of the risks it’s fine to do.
Sickle cell disease site, IG officer, 01
When the implementation of a new service was being considered, they considered the appropriateness of the patient group and undertook a privacy impact assessment:
There would be a clinical risk assessment of the appropriateness of providing care or service in that way.
Mental health team 3 (outreach team) site, IG head, 01
We do privacy impact assessments now. You know, we’re required to, you know, it’s part of the Data Protection Act we have to do . . . actually it’s not a legal requirement, but the Information Commission recommends that we do privacy impact assessments.
IBD 1 site, IG officer, 01
In NHS trusts where DCCs had not been formally implemented, exceptions were made to the rule to facilitate it and the IG officers detailed the procedures they followed:
We have a parent who has learning difficulties and she’s requested that we only communicate with her via e-mail because she’s got some special software on her computer that allowed her to be able to understand, read and listen to . . . We’ve responded to her and we’re putting in a particular measure to be able to communicate with her. The service have done a risk assessment to be able to do that . . .
School nurse service, IG lead, 01
A key issue that arose in discussion was about making an entry in a patient’s clinical notes after a patient–clinician digital interaction and payment for the clinical encounter:
So if we conduct an outpatient appointment with somebody on the telephone we will record that, so we get paid for it. So we record that it happens, but not necessarily the content of it.
Diabetes mellitus 2 site, Caldicott Guardian, 01
Payment, that’s probably the main one in an acute hospital. And of course we log the outcome of a discussion because that’s the patient safety record of what happened. So it’s imperative that something is recorded.
Diabetes mellitus 2 site, Caldicott Guardian, 01
The IG officers talked about the difficulties of logging patient consent:
Well I think one of the issues both for e-mail and for Skype is how do we effectively record someone’s consent and particularly for e-mail where it might be used a little bit more widely.
Diabetes mellitus 2 site, Caldicott Guardian, 01
E-mails . . . would tend to be printed out and stuck in the paper record and in the new system we have I guess the same will happen, it will be scanned in: printed out and scanned in like we’ve done with the e-mails. Texts are harder because you can’t print them out the same, and you have to write them down.
Mental health 4 site, consultant, 02
Protocol for incident management
Information governance specialists reported that the infrastructure for DCCs has to be adequate and secure. They wanted clinicians to use the software and hardware provided by the trust in order to minimise the occurrence of adverse incidents. Reinforcing the idea that clinicians had to apply encryption to e-mails sent to e-mail addresses that were considered not be secure was a priority across all NHS trusts:
But as soon as you start e-mailing patients, because I can’t, if I had to e-mail you a list of patients, I would have to apply encryption to it, so I’d have to do it as an attachment encrypt it, you know.
IBD 1 site, IG officer, 01
We’ve got a means of encryption e-mail to any e-mail address as it goes out. And so we’ve been using that, and so we can encrypt whatever we want to any organisation.
Mental health 4 site, IG officer, 01
Our interviewees also talked about management of mobile devices:
So we have all our mobile devices are managed through this mobile device management solution and it tracks where the devices are, if it goes out of a certain radius within the hospital it blocks itself and encrypts, so you can’t get into it . . . it becomes a brick, and we’ve adopted that.
Cancer 2 site, IG and data protection manager, 01
Essentially to access your smartphone with e-mail you must have a passcode that locks the screen. The screen locks after so many minutes . . . we’ve got setting in our e-mail servers that force that onto the device that you’re using.
Mental health 4 site, IG officer, 01
The majority of IG officers reported dealing with DCC incidents that involved sending text messages to the wrong number or more than one recipient and mistyping an e-mail address:
We had one incident where we had text reminders going to the wrong number, because the wrong number could have been typed in, in the first place, or the patient doesn’t use that phone anymore and they’ve given it to someone else.
IBD 1 site, IG officer, 01
Certainly we do have e-mails going to the wrong address. It’s usually human error, and that would come in through the information governance team in terms of incident reporting.
Mental health 2 (CAMHS) site, IG head, 01
Another example of an incident was the storage of patient data on personal mobile phones:
The only thing that we were aware of is that sometimes staff may take photos of patients using their personal mobile phones. So we tell people not to do this because it’s against trust policy, because obviously, you know you don’t want personal information belonging to a patient to be on a personal device belonging to a member of staff.
Sickle cell disease site, IG officer, 01
General concerns
The IG officers expressed a number of concerns regarding the use of digital communication systems. These could be categorised as clinical, technological, organisational and ethical issues.
Clinical concerns
Fears were expressed that clinicians would not check that their e-mail had been received and acted on, and that patients would expect responses when clinicians were not available:
With e-mail, I think the big danger with e-mail is that things get assumed. So you’ve sent an e-mail, you don’t get a response straight away, you assume that something’s happening and I think e-mail is probably the least useful tool between patient and a clinician, personally.
Arthritis site, Caldicott Guardian, 01
One of the obvious risks is if for example we give a patient an e-mail address to use and it is mine as a clinician and they e-mail me and they’re in crisis and they choose to e-mail me whilst they go into crisis and I’ve just gone on 2 weeks’ leave, who is going to pick that e-mail up?
Cancer 2 site, IG and data protection manager, 01
The IG officers pointed out the challenge they face to maintain the integrity of patient records:
There is . . . the integrity of the record . . . if information about a patient was going to be dissipated so that it’s no longer accessible in the way that we’ve worked hard to achieve, there will be a loss rather than a gain.
Mental health 4 site, IG officer, 01
I can be remote, and I can be responding to patient queries, but how that actually gets recorded into the patient record is a challenge, because we’re not working through an electronic patient record. So if the e-mail was coming in via the patient record, and you were responding, and that correspondence was all in the record, there would be an advantage to that. But there isn’t usually.
Cancer 2 site, Caldicott Guardian, 01
One interviewee was concerned about the quality of written communication:
. . . In days gone by, somebody would have written to you, you might have dictated a response which a secretary would have typed. They’d have picked up most of the typographical errors, some of the grammatical errors. And there’d have been some sort of quality assurance of the response. Even down to your secretary coming back to you and saying, did you really mean to say that, it sounds a bit, you know, rude or flippant, or whatever. Or even, perhaps the patient will be upset by that. Whereas that’s lost and you’ve got people, perhaps, entering into a dialogue where they’ve forgotten that they are having a formal communication.
Cancer 2 site, Caldicott Guardian, 01
Technological concerns
Information governance specialists were concerned that the technology could hinder effective health-care delivery:
Disadvantage of course is the internet is not, regardless of how good it is within an area, you know, is not a stable platform in the sense that you get the good strong continuous signal.
Mental health team 3 (outreach team) site, IG head, 01
You don’t have guarantee on delivery, because people can make mistakes with e-mail addresses.
Cancer 2 site, Caldicott Guardian, 01
There was some acknowledgement that clinicians required technological training in order to maximise the benefits of using these new digital communication platforms:
There’s a massive variation in IT literacy in the . . . staff base. I think we’ve probably got a few gaps in training, and I suppose, you know, the much younger generation is going to be by default more IT literate, but that’s generalising, that’s not always the case. So I think, you know, there’s going to be a large training requirement if we have to make these technologies usable so it’s going to have a design aspect as well.
Sickle cell disease site, IG officer, 01
Technology is, always we need proper training within the staff because if they are not trained properly it won’t do anything.
Liver conditions site, IG officer, 02
Reference was made to the difficulty of maintaining up-to-date digital contact details:
The predominant one for that is changing e-mail addresses. Certainly people are happy to change their e-mail addresses every time they change their internet service provider, they will have a new e-mail address because they don’t want to keep their old one. It’s similar if they don’t tell us they moved, but people are more akin to telling people, oh I’ve moved house, but e-mail addresses kind of, oh I’m with BT [British Telecom] now I used to be with Sky, or whatever it might be.
Mental health 4 site, IG officer, 01
Organisational concerns
Interviewees reported that funding allocated to new technologies was scarce and this impeded plans for technological advancement:
I think for me as well the other challenge on this is the cost. So funding in the NHS is tight. The funding goes as it should do, the priority goes to clinical care. The technology side of clinical care and especially the development side is something that can be extremely difficult to obtain the funding for.
Liver conditions site, IG officer, 01
There appeared to be a tug-of-war between IG officers and IT managers in relation to the development of digital communication systems. IG officers argued that digital innovations in the NHS needed to shift from being organisation centric to patient centric in order to provide best care:
So if, you know, I don’t go to Apple and say, look you know, we just want something for young people that Apple offers in their App Store, can we just do it with you? Why don’t they have apps that just do this, because they seem to work? Whereas when you ask our IT department to design something it suits the organisation not its population.
Mental health 4 site, IG officer, 01
One interviewee reported a lack of communication between the IT developers and IG officers and that new ideas were driven forward without seeking IG clearance:
I do think that developers of systems, you know, I think the NHS as a whole, and patients at the end of it, would benefit more and technology would move quicker in the NHS, if IG was involved at the very beginning. I think quite often IG isn’t involved quick enough, so you know, you’d generally get involved at development stage, you’ll get senior people within the NHS, Department of Health, and all these people, oh yeah, that’s good, yeah, yeah. A bit like Patient Knows Best, you know, it was . . . I can’t remember if it was Department of Health or NHS England, but, you know, really rated it, and they’d done their IG Toolkit and everything, but unfortunately it doesn’t tick all the boxes for IG; it doesn’t, you know.
IBD 1 site, IG officer, 01
Ethical concerns
Information governance was primarily concerned with patient confidentiality:
Also there’s risk of who is getting that e-mail; how is it being accessed? If it’s just on the computer and that’s their computer and they’ve got password protection on it, it’s probably quite safe to assume that only they’ve got access to it. But if it’s on your mobile phone or your tablet and you can just flick open the screen and your e-mail is presented, or if it’s an iPhone and it just pops up anyway on screen first time and you can see the first chunk of it, there are risks around that.
Mental health 4 site, IG officer, 01
And the other bit of that, is the copying in of people. So suddenly this is no longer a confidential conversation between two people, there are other people, they can be forwarded. So there’s all that sort of worry from an information governance point of view.
Cancer 2 site, IG and data protection manager, 01
Some interviewees talked about the impact of security breaches and the consequences these potentially posed on the lives of individuals:
You know, if you know that somebody’s got a long-term condition, they’ve got diabetes and they’ve got a respiratory problem, if that information’s sold to, you know, obtained and sold to insurance companies, you know, they could be exploited.
School nurse service, IG lead, 01
Summary of findings
Information governance specialists described a strong desire to introduce new technologies in health-care services that resembled the communication channels the general public were accustomed to using in their everyday life. They identified a number of benefits of DCCs to improve patient care. Patients were central to IG officers’ perspectives when considering the scope of utilising DCC systems in their organisations. IG officers reported a range of technologically enhanced ways in which services were being planned and in some cases delivered. Policy was central to their role in their NHS trust. From policy they derived protocols, documents that the IG officers developed with, and for, clinicians to support their digitally enhanced care. These included protocols around incident management. The IG officers were the only study participants to refer to training needs in rolling out these new modes of clinical communication. These interviewees shared similar concerns with their clinical colleagues regarding ethics but had some additional ones related to the reliability of the digital infrastructure on which care was being planned and delivered.
Chapter 8 Impacts on health-related outcomes
Introduction
During field work, sites were asked whether or not they had evaluated the impact of the use of DCCs through the analysis of patient data at the clinic level. No clinic had done this. We therefore requested routinely collected data from each of the case study sites.
This chapter reports the analysis of this routinely collected data to attempt to answer the research question: using existing clinical data, what is the impact of DCC on the health status of patients? We were limited by a lack of good comparators. We aimed to obtain data for periods before DCCs were used and when DCCs were being used. However, only one clinic was able to provide data from before and during use of DCCs. It was therefore not possible to assess the impact of DCCs within a site. It was also not possible to compare multiple sites with the same condition that were or were not using DCCs because of the diversity of conditions. Therefore, the impact of DCCs was assessed by descriptively comparing the trends for changes over time at sites that use DCCs and those that do not.
The analysis assessed two possible mechanisms for evaluating the impact of DCC on clinical outcomes. The first mechanism being that using DCCs affects outcomes directly because, for example, young people get an extra/alternative form of access to clinicians. This mechanism was assessed by analysing each outcome separately. The second mechanism is that DCC leads to fewer missed appointments and, consequently, better clinical outcomes. This mechanism was assessed through scatterplots and correlations between DNA rates and other clinical outcomes.
Data collected
For ethical reasons associated with protecting clinicians using DCCs without IG procedures in place, a decision was reached at a PMG meeting not to request data in one site. Therefore, data were requested from 19 out of the 20 planned sites. Eight sites provided a complete set of data requested and two sites provided no data, with the remainder providing some of the requested data.
Table 9 summarises data collection. An example of a case where data collection was not feasible is a site that offered drop-in services with no bookings made, so appointments data were not available. Another example is tertiary sites which receive patients from across the country. If these patients need to go to A&E, they will go to different hospitals and so it was impossible to collect A&E attendance and hospital admission data for such sites. To analyse A&E attendance and hospital admission data, clinic size was required. However, in some sites it was not possible to determine this. For example, in one site, the site registers patients into the wider service but not into a specific clinic. Therefore, we could not identify the number of patients who attend the clinic that was studied. In some sites, although number of A&E attendances and hospital admissions were provided, the clinic staff did not provide clinic size.
| Data | Number of sites providing data | Reasons for non-provision of specific data |
|---|---|---|
| Appointments | 16 | Ethical reasons (n = 1) |
| Not feasible (n = 1) | ||
| Non-response from clinic staff (n = 2) | ||
| Hospital admissions | 9 | Ethical reasons (n = 1) |
| Non-response from clinic staff (n = 2) | ||
| Tertiary sites (n = 2) | ||
| Not reasonable outcome (n = 2) | ||
| Not feasible (n = 2) | ||
| Unable to determine clinic size (n = 1) | ||
| Clinic size not given by staff (n = 1) | ||
| A&E attendances | 9 | Ethical reasons (n = 1) |
| Non-response from clinic staff (n = 2) | ||
| Tertiary sites (n = 2) | ||
| Not reasonable outcome (n = 2) | ||
| Not feasible (n = 2) | ||
| Unable to determine clinic size (n = 1) | ||
| Clinic size not given by staff (n = 1) | ||
| Clinic-specific outcome | 8 | Ethical reasons (n = 1) |
| Non-response from clinic staff (n = 11) |
Analysis of appointments data
The number of appointments and DNA rates in sites are given in Appendix 3. In general, the total number of appointments in each site is large so DNA rates have good precision. Exceptions are a cancer site (cancer 1) in year 2013, a cystic fibrosis site (cystic fibrosis 1) in year 2016 and all years for the renal conditions site (kidney). Three sites [mental health 2 (CAMHS), arthritis and HIV] do not have any form of DCC. For two of these sites (arthritis and HIV), generally, DNA rates do not increase over time. For the HIV site, there are substantial and sustained decreases in DNA rates. For mental health 2 (CAMHS), there is a small but sustained increase in DNA rates. To summarise results for three sites that do not use DCC, over time, DNA rates have increased in one site and have not increased in two sites.
The remaining 13 sites use DCCs. In four sites (diabetes mellitus 1, diabetes mellitus 2, sickle cell disease and cancer 1) there are sustained decreases in DNA rates, with the decreases in the two diabetes mellitus sites substantial (diabetes mellitus 1 and diabetes mellitus 2). In eight sites [liver conditions, mental health 3 (outreach team), mental health 2 (early intervention), dermatology, cystic fibrosis 1, cystic fibrosis 2, renal conditions and sexual health], DNA rates seem to have remained relatively stable over time. In one site (IBD 2), there has been a sustained increase in DNA rates. To summarise results for the 13 sites using DCCs, over time, DNA rates have increased in one site have not increased in 12 sites.
Comparing sites using DCCs and sites not using DCCs, in both cases, there was one site where DNA rates increased over time, with DNA rates in other sites decreasing or remaining approximately the same. Thus, over time, there were no clear differences in DNA rate profiles between sites using DCCs and sites not using DCCs.
In the liver site, when a new format for digital communication was introduced, there was a substantial drop in the DNA rate, but the rates over time increased to almost previous rates. For mental health 3 (outreach team), in 2016, although based on partial year data, the DNA rate went up by a substantial margin. A change in records system and of the clinic consultant occurred at this time.
Thus, there were no clear differences in DNA rate trends over time between sites using DCC and those not using. In addition, there did not seem to be differences in DNA rates for sites treating the same condition. Finally, when changes, such as change of a consultant, occurred in a site, substantial changes in DNA rates were observed.
Analysis of accident and emergency attendance data
The annual rates of young people with at least one A&E attendance (A&E attendance rate) are summarised in full in Appendix 3, Table 22.
For the arthritis site (this clinic does not use DCCs), A&E attendance rate in 2015 is lower than that in 2014. However, it should be noted that the number of young people at the arthritis site is small and, in both 2014 and 2015, data are not available for all months. For HIV (this clinic does not use DCCs), the A&E attendance rate increased by 1% in 2012, but remained relatively stable thereafter. To summarise A&E attendance rates for the two sites that do not use DCCs, over time, rates in one site remained stable and rates in the other site dropped.
The remaining four sites (diabetes mellitus 1, diabetes mellitus 2, IBD 2 and renal conditions) use DCCs. For the diabetes mellitus 1 site, in general, the A&E attendance rates are decreasing over time. However, the number of patients in 2009 is not large, and excluding the rate for this year, the A&E attendance rates remain relatively similar. For the diabetes mellitus 2 site, in general, the A&E attendance rates seem to be decreasing over time. For the IBD 2 site, the A&E attendance rates increase until 2009 and then, in general, rates decrease over time. Therefore, the A&E attendance rates for this IBD 2 site may be considered to have remained stable over time. In the renal conditions site, the A&E attendance rates increase over time, but the reason for this may be the very small number of young people. To summarise A&E attendance rates for sites using DCCs, over time, rates in one site remained stable, rates in two sites dropped and rates in one site (with very few young people) increased.
Comparing sites using DCCs and sites not using DCCs, in both categories there was one site where A&E attendance rates remained stable, with A&E attendance rates decreasing in other sites. Thus, over time, there were no clear differences in A&E attendance rate profiles between sites using DCCs and sites not using DCCs.
Results to assess if A&E attendance rates are influenced by DNA rates in sites that have sufficient data are summarised in Figure 5. For the HIV site (this clinic does not use DCCs), DNA and A&E attendance rates show a strong negative correlation, with the weighted correlation being –0.79 (see Figure 5a). This finding may be explained partly by qualitative data, which indicated that, following clinic appointments, A&E attendances may be booked for young people to get specialised treatment. For the diabetes mellitus 1 site (this clinic uses DCC), there does not appear to be a relationship between DNA and A&E attendance rates, with the weighted correlation being –0.02 (see Figure 5b). This finding may be explained by the fact that young people in the diabetes mellitus 1 site are able to send their results by e-mail so that if a young person misses appointments but engages through e-mail, they get advice which would improve other outcomes. For the IBD 1 site, there is a moderate correlation between DNA and A&E attendance rates, with the weighted correlation being –0.35 (see Figure 5c). No explanation could be found for this finding.
FIGURE 5.
Did-not-attend rates against A&E attendance rates for different sites. (a) DNA rate against A&E attendance rate for the HIV site; (b) DNA rate against A&E attendance rate for the diabetes mellitus 1 site; and (c) DNA rate against A&E attendance rate for the IBD 1 site.
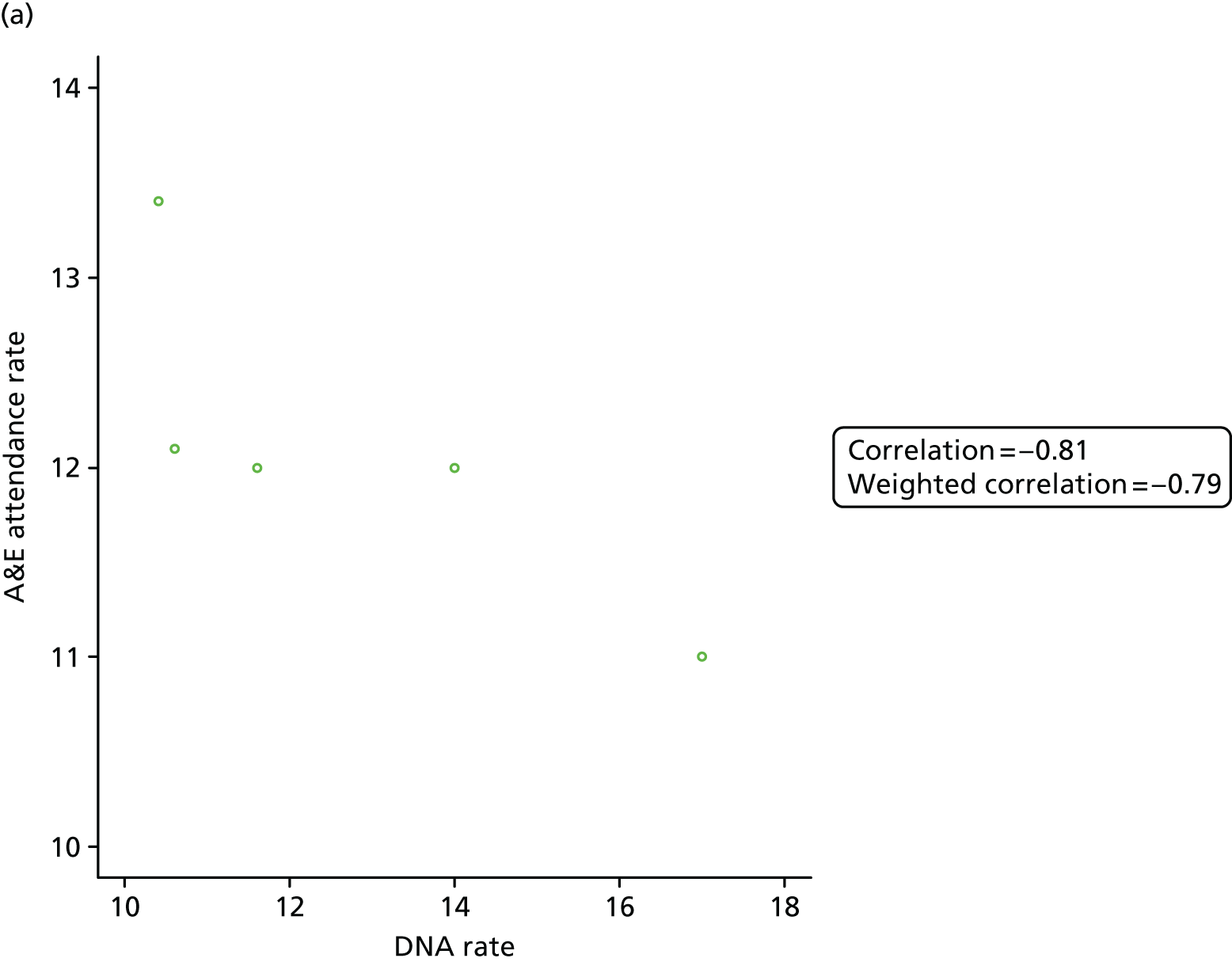
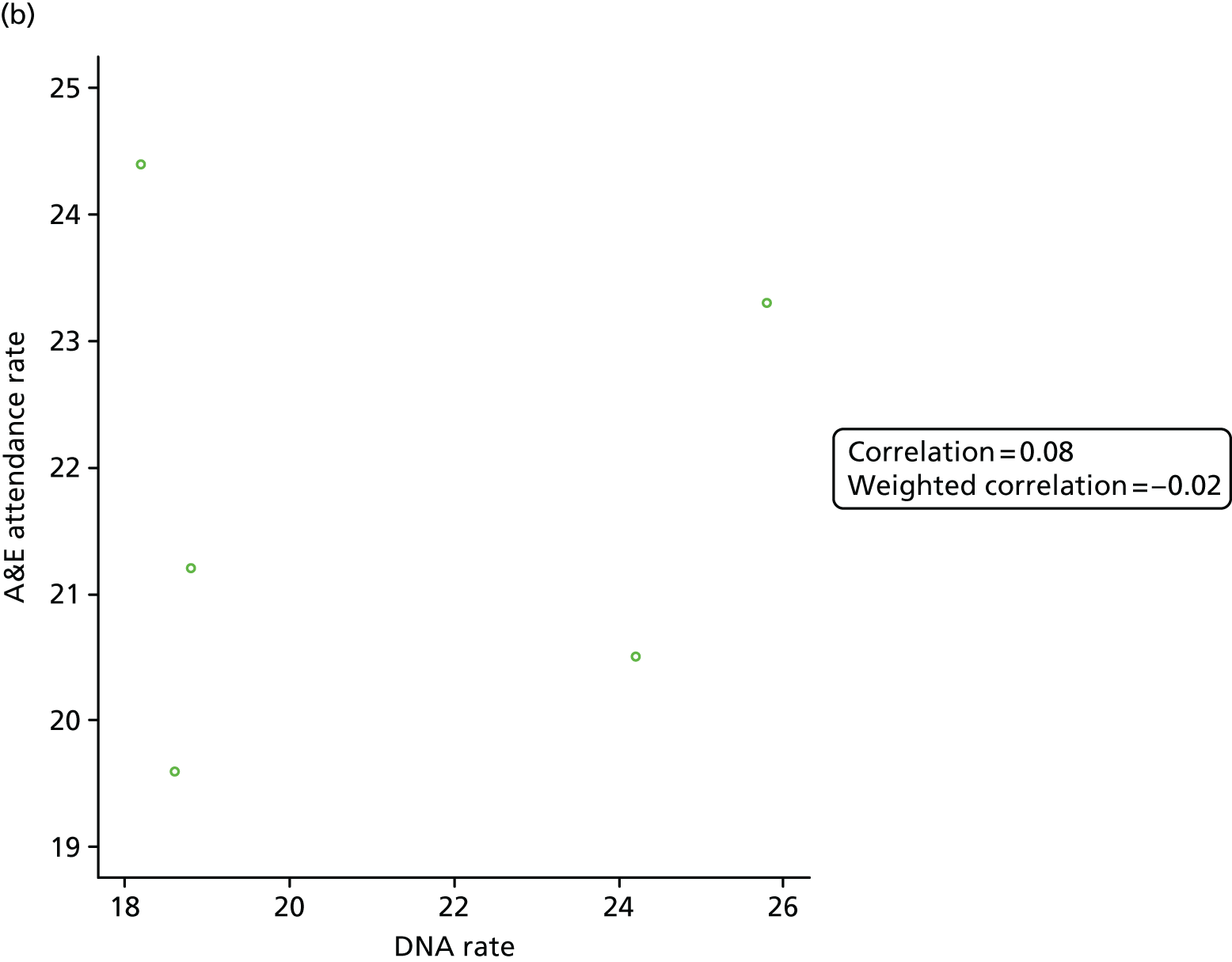
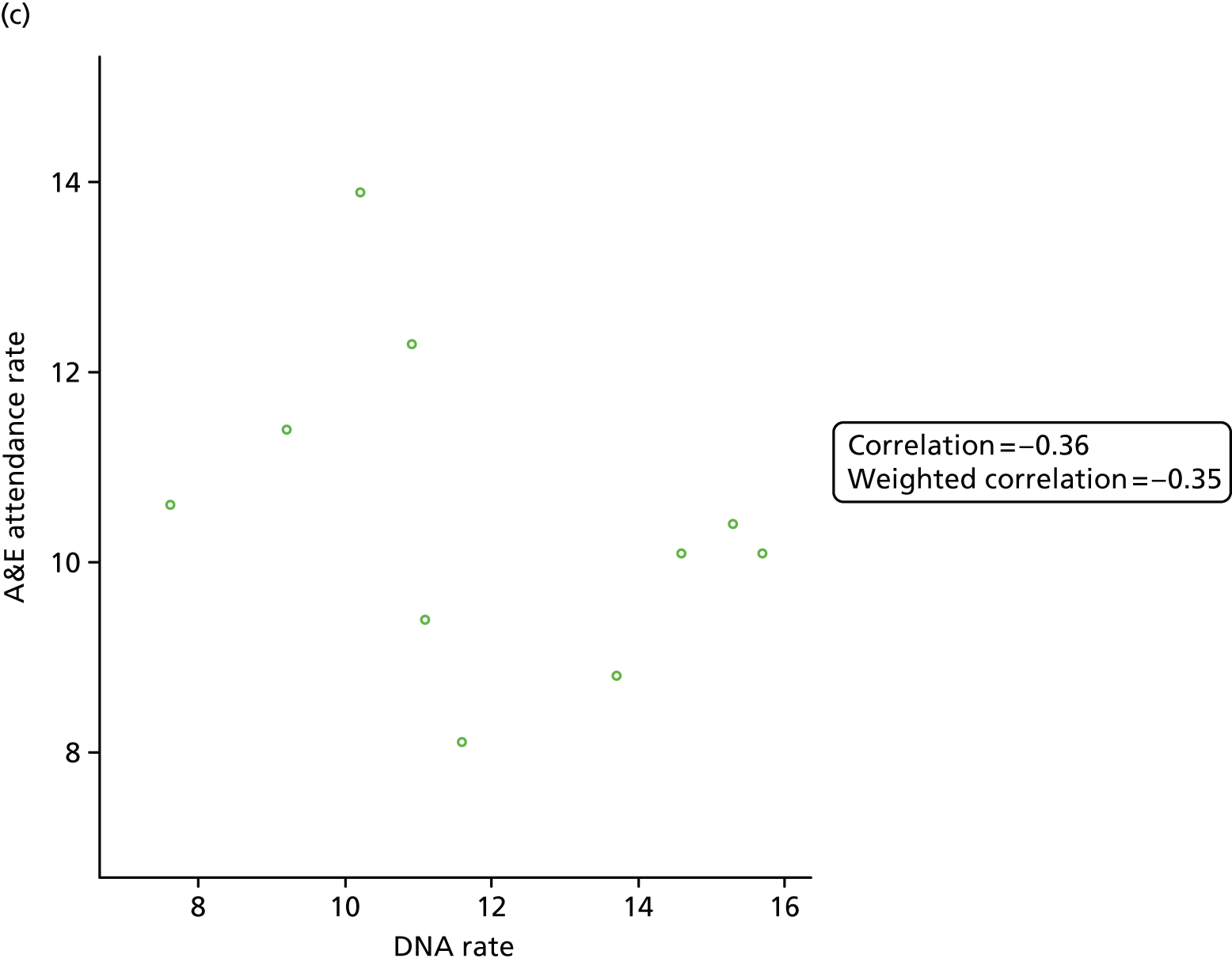
Analysis of hospital admission data
The annual rates of young people with at least one hospital admission are summarised in Appendix 3, Table 23. With the exception of the HIV site, the trends for A&E attendance and hospital admission rates are generally similar (compare Tables 22 and 23 in Appendix 3). For the HIV site, it was possible to identify emergency hospital admissions, and this may explain the difference between A&E attendance and hospital admission profiles.
As with A&E attendance rates, over time there were no clear differences in hospital admission rate profiles between sites using DCCs and sites not using DCCs.
Results to assess if hospital admission rates are influenced by DNA rates are summarised in Figure 6. For the HIV site (this clinic does not use DCCs), there is a strong positive relationship between DNA and hospital admission rates, with the correlation being 0.92 (see Figure 6a). This indicates that, if appointments are not missed, there are fewer emergency hospital admissions. For the diabetes mellitus 1 site (this clinic uses DCCs), there seems to be a weak positive relationship between DNA and hospital admission rates (see Figure 6b). Note that, although the weighted correlation is 0.6, this is largely influenced by one value which is very different from other values (an outlying value). For the IBD 1 site (this clinic uses DCCs), there is negative correlation between DNA and hospital admission rates, with the weighted correlation being –0.34 (see Figure 6c). This indicates that when DNA rate decreases, hospital admissions rise. No explanation could be found for this finding.
FIGURE 6.
Did-not-attend rates against hospital admission rates for different sites. (a) DNA rate against hospital admission rate for the HIV site; (b) DNA rate against hospital admission rate for the diabetes mellitus 1 site; and (c) DNA rate against hospital admission rate for the IBD 1 site.
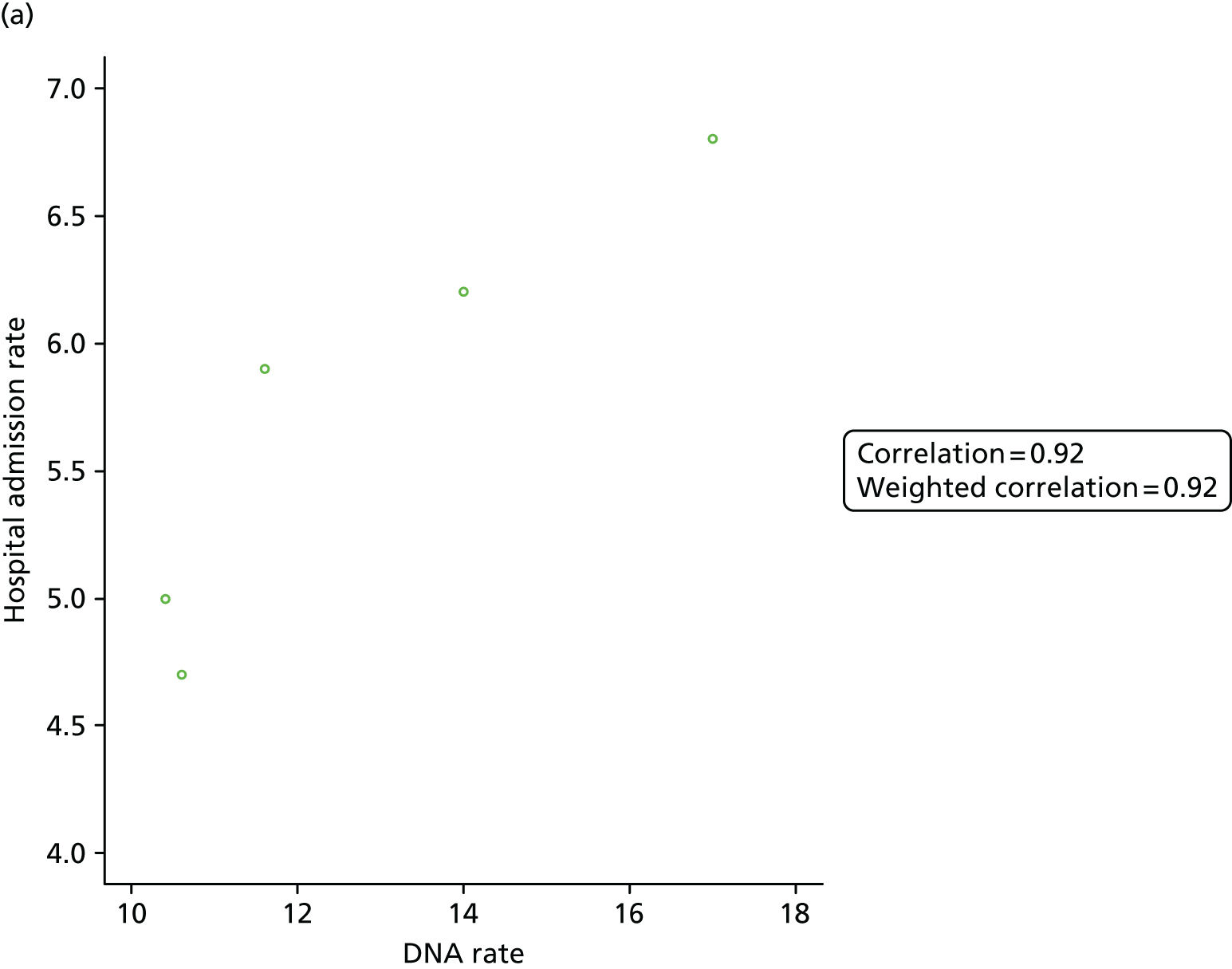
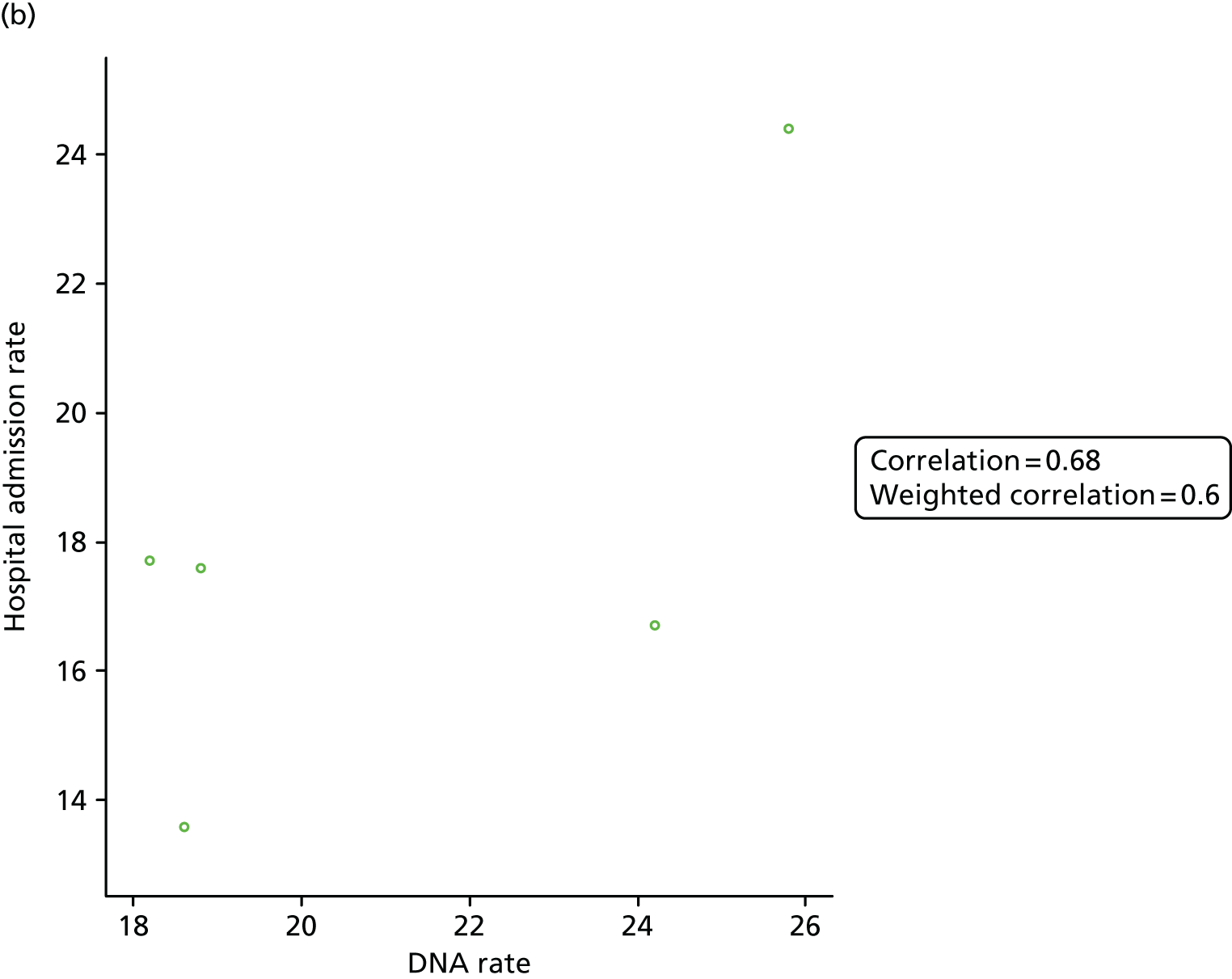
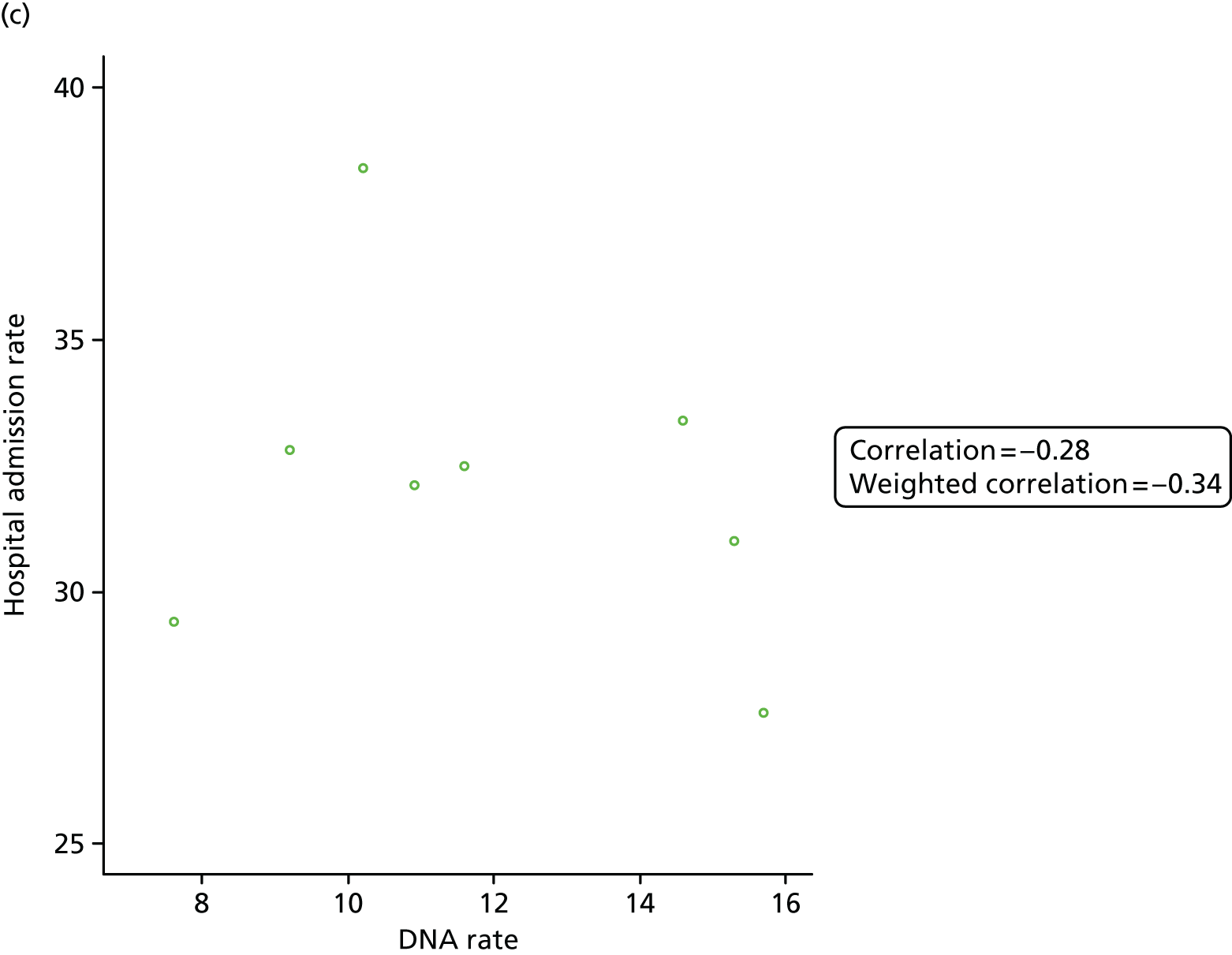
Analysis of clinic-specific outcomes
Clinic-specific outcomes were analysed for two sites that do not use DCCs [HIV and mental health 2 (CAMHS)] and six sites that use DCCs [diabetes mellitus 1, diabetes mellitus 2, dermatology, cystic fibrosis 2, sexual health and liver conditions). Results are presented for each site separately and later a section describes differences between sites using and sites not using DCCs (see Summary findings from analysis of clinic specific outcomes).
Human immunodeficiency virus site (does not use digital clinical communication)
The clinic-specific outcome for HIV infection is viral load. The threshold for a good/desired level of viral load is < 39 copies/ml. The viral load data provided are from 1851 young people collected between 1 November 2010 and 16 May 2016.
The profile for the percentage of young people with good viral loads is given in Figure 7a. In general, over time, the percentage of viral loads < 39 copies/ml has been increasing. For example, after January 2015, the percentage of good viral load measurements for most months is at least 80%. Thus, there seems to be improvements on viral load measurements over time.
FIGURE 7.
Profiles for percentage of viral load < 39 copies/ml for HIV-infected patients. (a) Profile of percentage of good viral load rates; and (b) DNA rate against good viral load rate for HIV-infected patients.
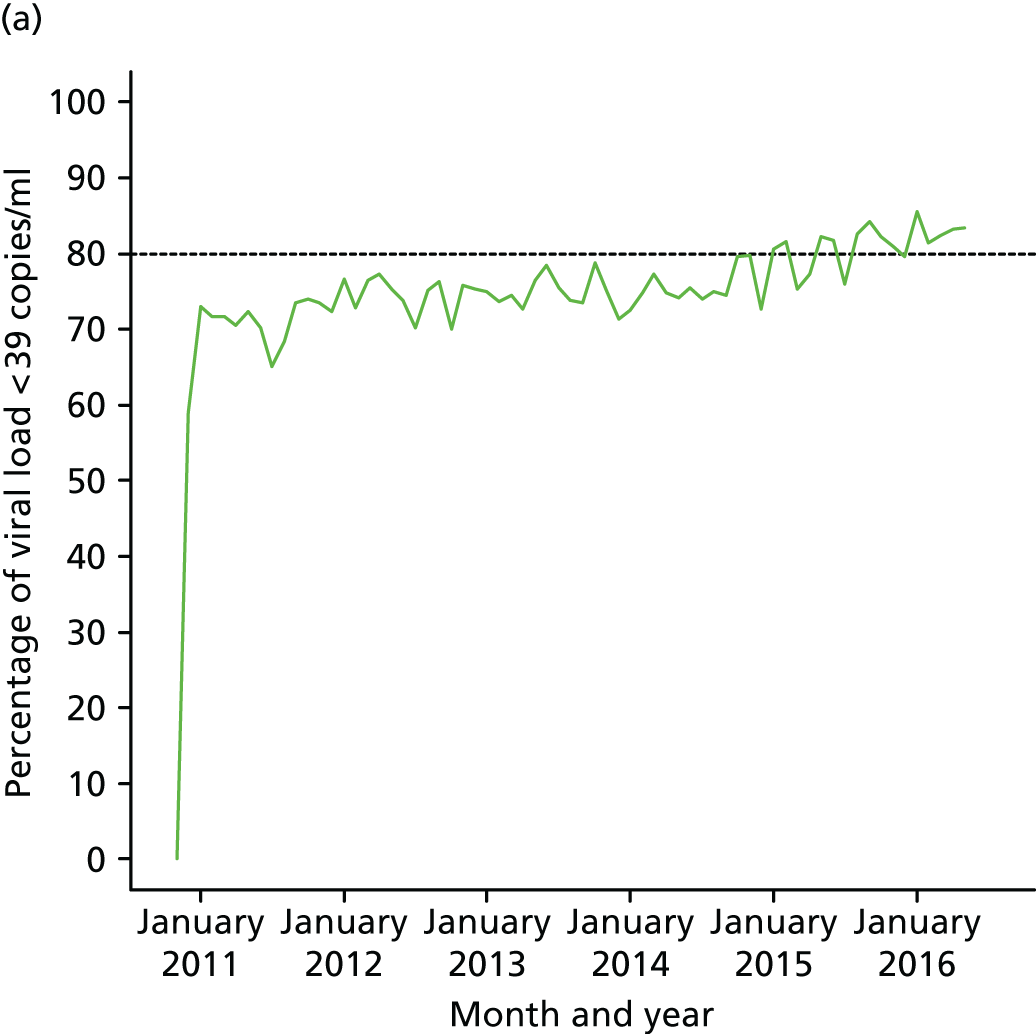
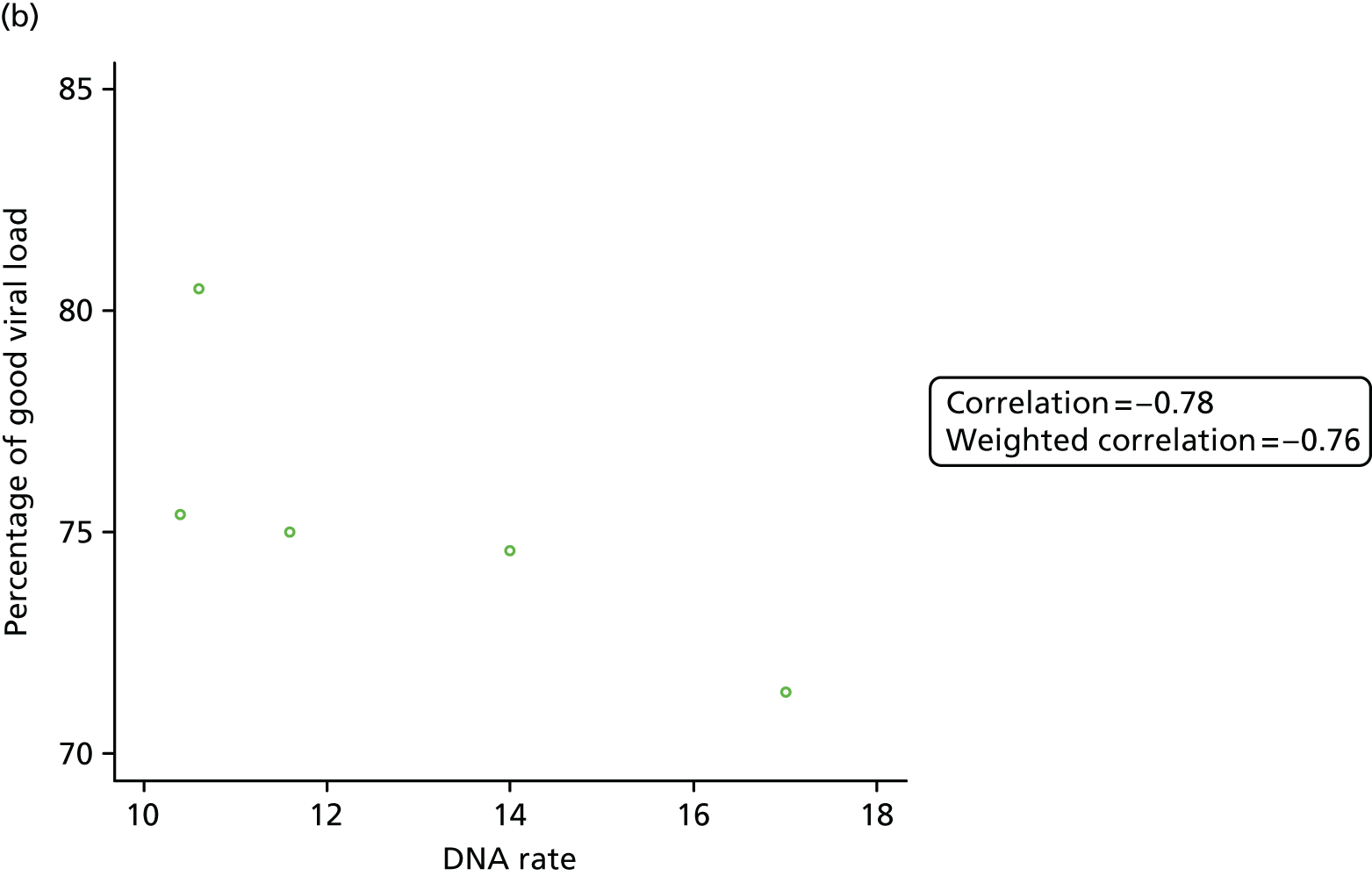
The results of assessments of where DNA rates influence viral load measurements are summarised in Figure 7b. The higher the DNA rate, the lower the percentage of good viral load rate, with the weighted correlation being –0.76. This indicates that, when DNA rates are low, young people’s viral loads are at desired levels.
Mental health 2 (CAMHS) site (does not use digital clinical communication)
Clinic-specific outcomes for the mental health 2 (CAMHS) site are self-harm incidents, self-harm ward attendances, Strengths and Difficulties Questionnaire (SDQ) scores and Health of the Nation Outcome Scale for Children and Adolescents (HoNOSCA) scores. SDQ scores have been recorded at enrolment only. Similarly, except for 11 young people, HoNOSCA scores available are for enrolment visits only. Therefore, SDQ scores and HoNOSCA scores cannot be used to assess trend over time.
From 2010 to 2015, the number of unique young people seen in each year was 659, 726, 633, 615, 472 and 244, respectively. These numbers are used to compute self-harm incident rates and self-harm ward attendance rates. From 2010 to 2015, the number (%) of young people with at least one self-harm incidence is 11 (1.7%), 9 (1.2%), 21 (3.3%), 65 (10.6%), 31 (6.6%) and 23 (9.4%), respectively, whereas the number (%) of young people with at least one self-harm ward attendance is 11 (1.7%), 9 (1.2%), 17 (2.7%), 39 (6.3%), 17 (3.6%) and 11 (4.5%), respectively.
Figure 8 shows results assessing if DNA rate influences self-harm rates and self-harm ward attendance rates. There are strong positive associations indicating that, when DNA rate increases, both the self-harm incidence and self-harm ward attendance rates increase.
FIGURE 8.
Did-not-attend rates against self-harm rates and self-harm ward attendance rates. (a) DNA rate against self-harm rate for the mental health 2 (CAMHS) site; and (b) DNA rate against self-harm ward attendance rate for mental health 2 (CAMHS) site.
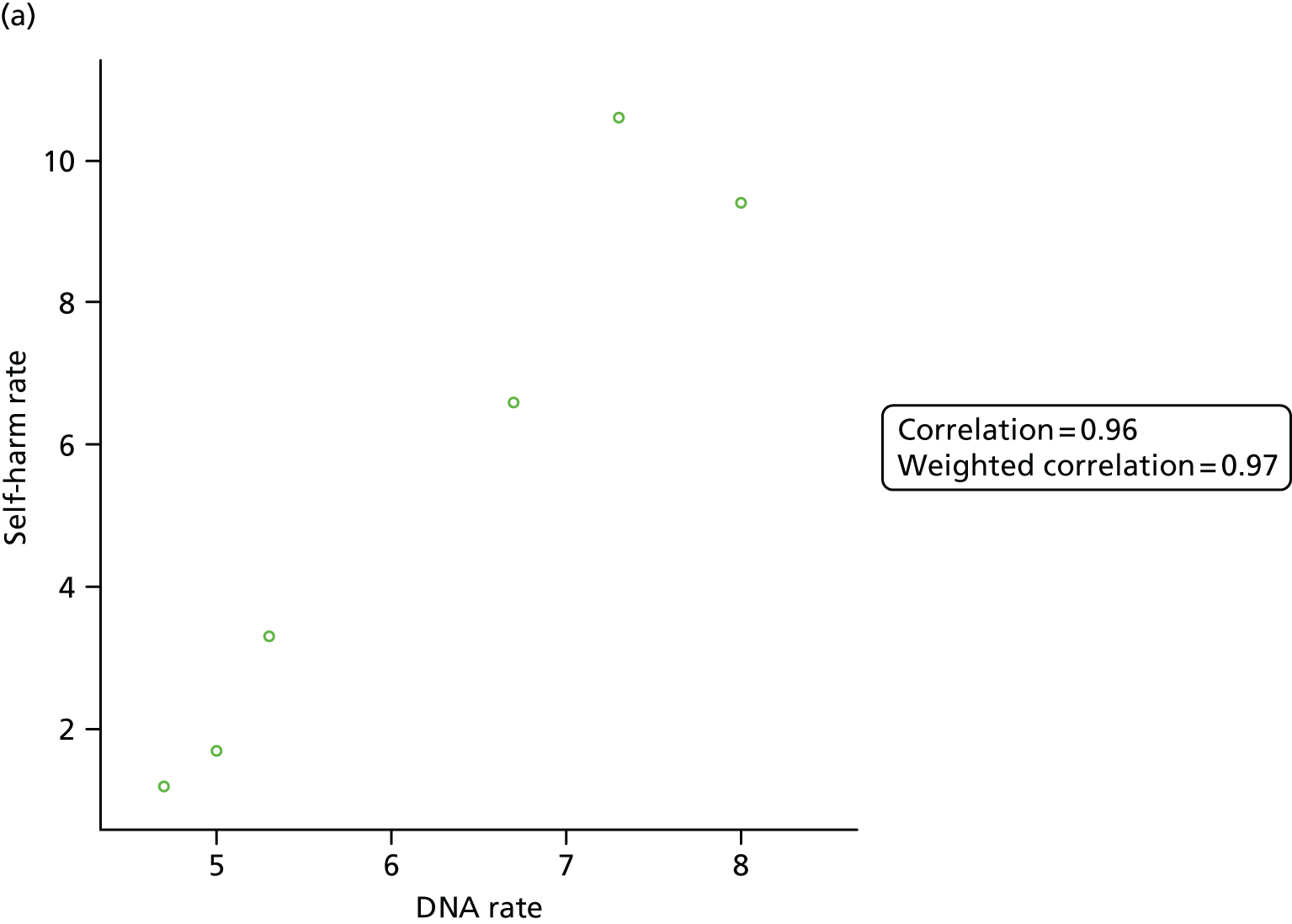
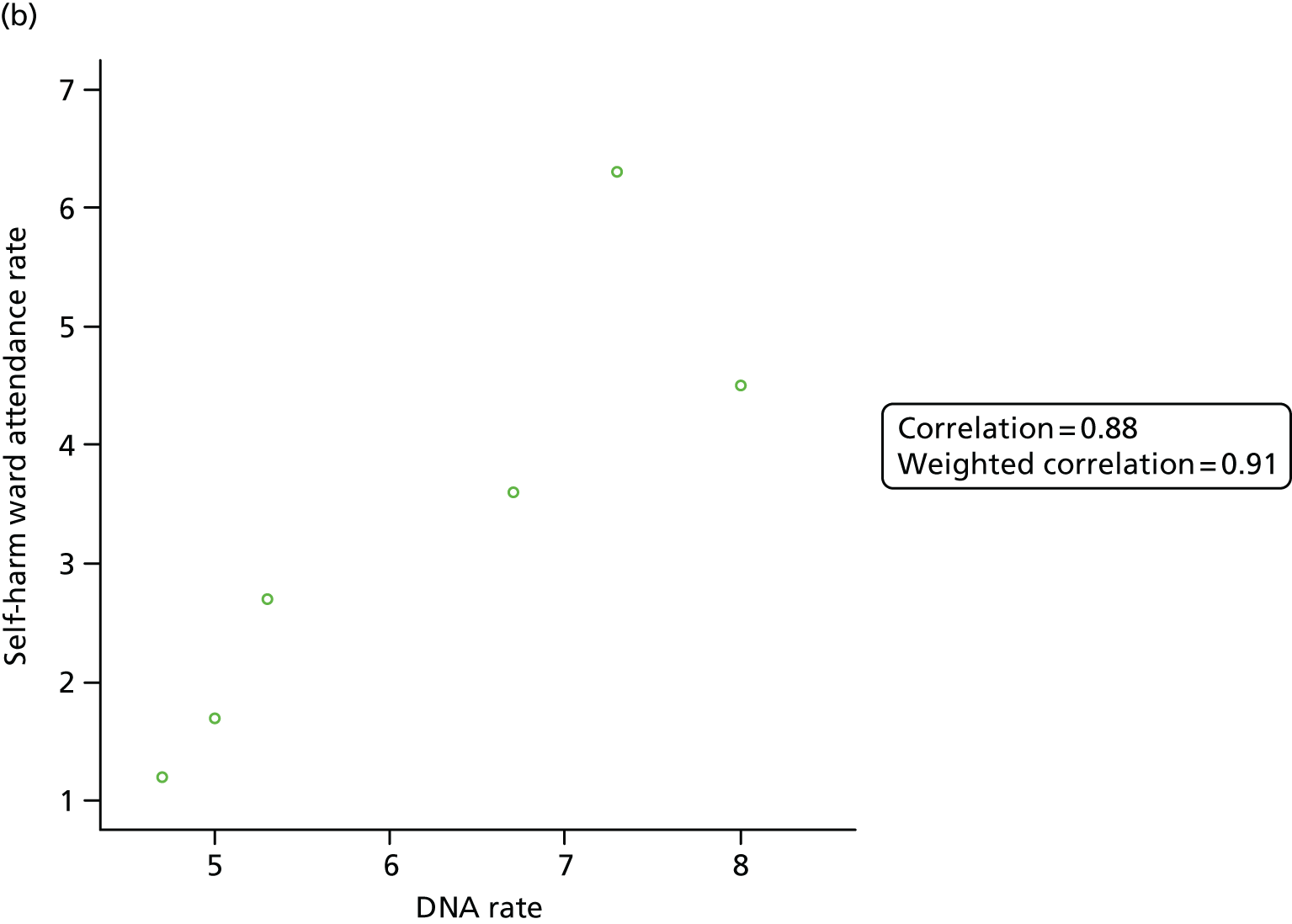
Diabetes mellitus 1 site (uses digital clinical communication)
Clinic-specific outcomes provided for diabetes mellitus 1 are HbA1c and glucose levels. However, there are no cut-off points to determine good or bad glucose levels and so these data were not analysed.
HbA1c levels are monitored over time, with the clinic staff using the average of the last three measurements taken to determine how good a young person’s HbA1c level is. Most young people have three measurements taken each year. For the analysis, to assess a young person’s HbA1c level, the average of up to the three most recent measurements in each year was calculated. Using the clinic’s definition, the ranges < 50 mmol/mol, 50–55 mmol/mol, 56–74 mmol/mol, 75–80 mmol/mol and > 80 mmol/mol correspond to low, good, borderline, at-risk and high-risk HbA1c levels, respectively.
Figure 9a shows the annual rates of young people with different dangerous HbA1c levels (low, at risk and high risk). The percentage of young people with low levels of HbA1c is small. The percentage of young people with high-risk HbA1c levels has been decreasing. Thus, there seems to be improvement of HbA1c levels over time.
FIGURE 9.
Profiles for different HbA1c levels and relationship between DNA rates and HbA1c levels for the diabetes mellitus 1 site. (a) Profiles of HbA1c levels and (b) DNA rates against percentage of high-risk HbA1c levels for the diabetes mellitus 1 site.
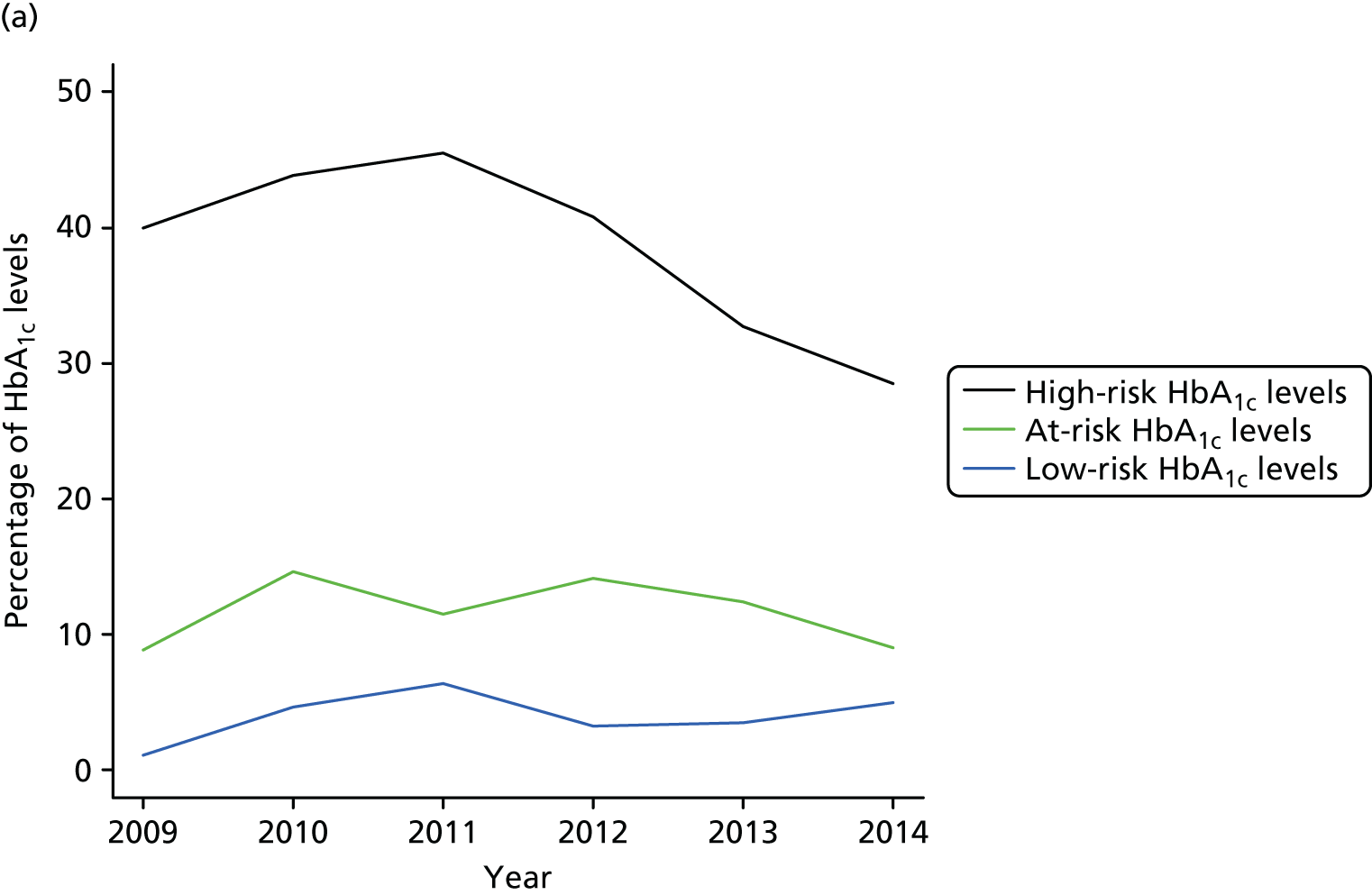
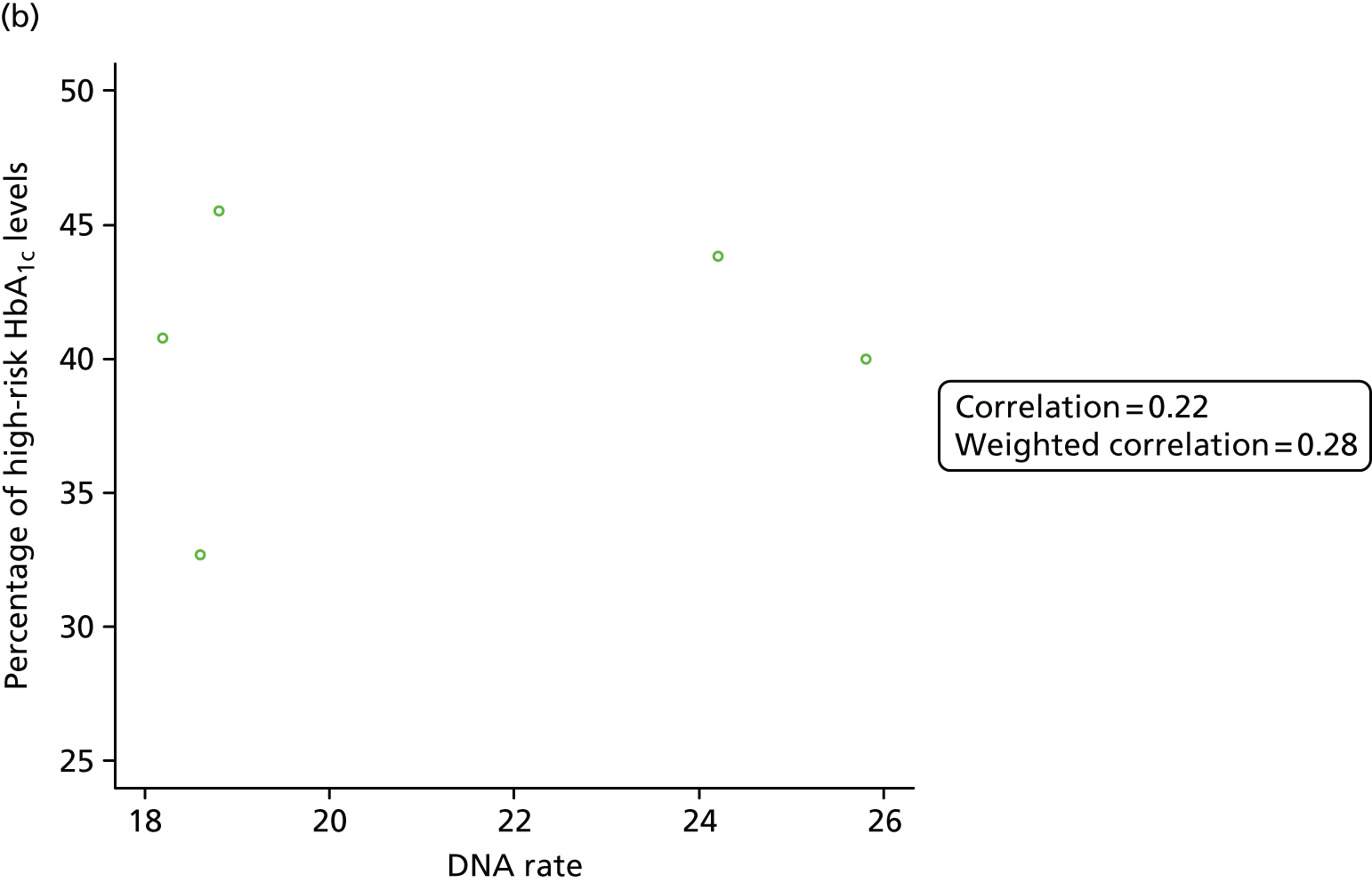
Figure 9b shows the relationship between DNA rates and the percentage of young people with high-risk HbA1c levels. There is weak positive relationship between the two rates, with a weighted correlation of 0.28. This indicates that when DNA rates increase, HbA1c rises to high-risk levels, but this association is weak.
Diabetes mellitus 2 (uses digital clinical communication)
The clinic-specific outcome for diabetes mellitus 2 was HbA1c level. Data were provided from April 2013 to March 2016. For most patients, in each year, one or two HbA1c measurements were taken.
The site did not provide us with cut-off points. The ranges defined by the diabetes mellitus 1 site were used to assess HbA1c levels over time. Annual rates of young people with low levels of HbA1c (< 50 mmol/mol), at-risk HbA1c levels (75–80 mmol/mol) and with high-risk HbA1c levels (> 80 mmol/mol) are shown in Figure 10a. The percentages of young people with low-risk and at-risk HbA1c levels are approximately the same across the 4 years. Over time, there is a decrease in the percentage of young people with high-risk HbA1c levels. Thus, in general, the percentage of young people with risky HbA1c levels has been decreasing.
FIGURE 10.
Profiles for different HbA1c levels and relationship between DNA rates and HbA1c levels for the diabetes mellitus 2 site. (a) Profiles of percentages of HbA1c levels in different ranges; and (b) DNA rates against percentage of high-risk HbA1c levels for the diabetes mellitus 2 site.
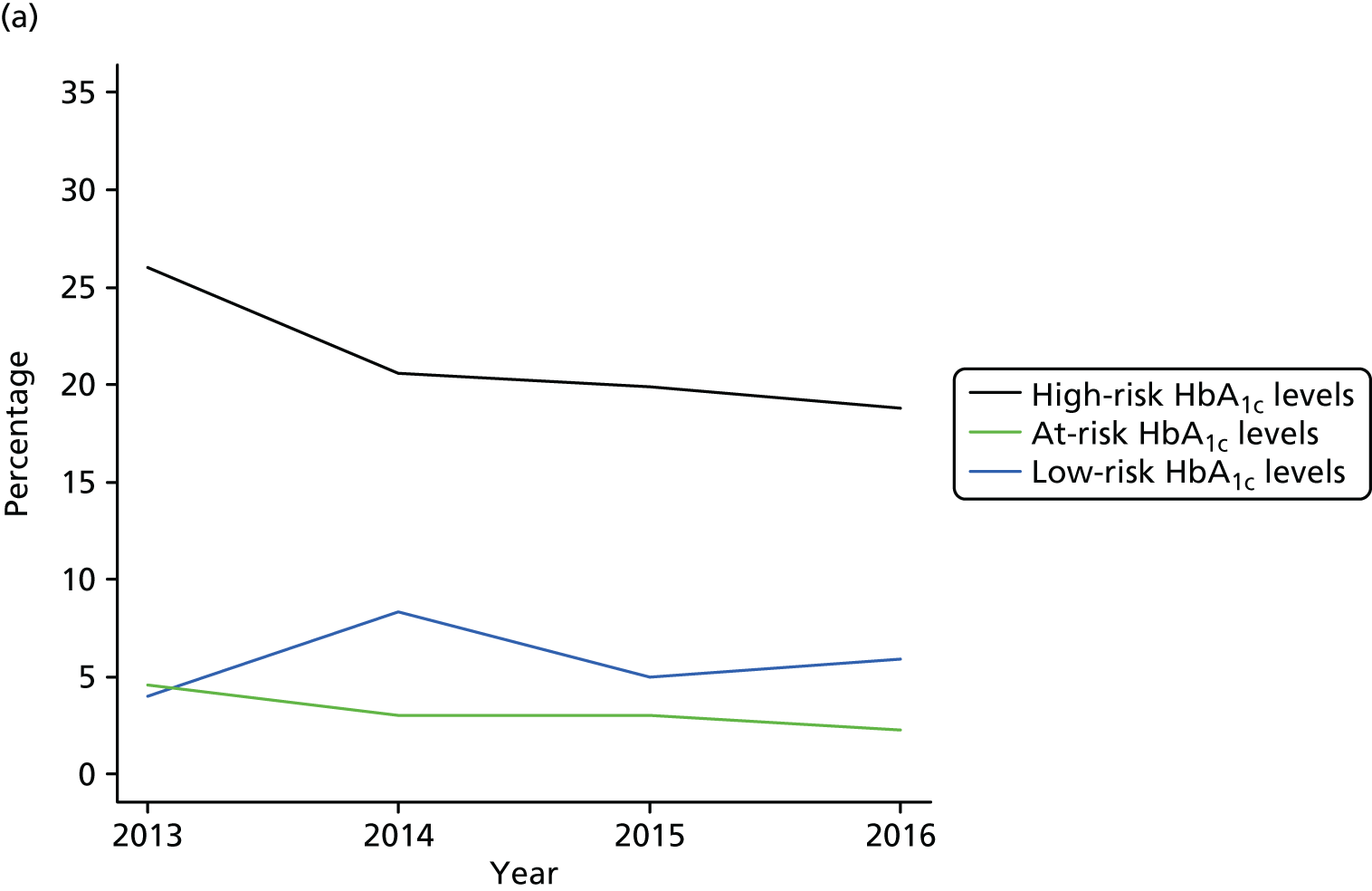
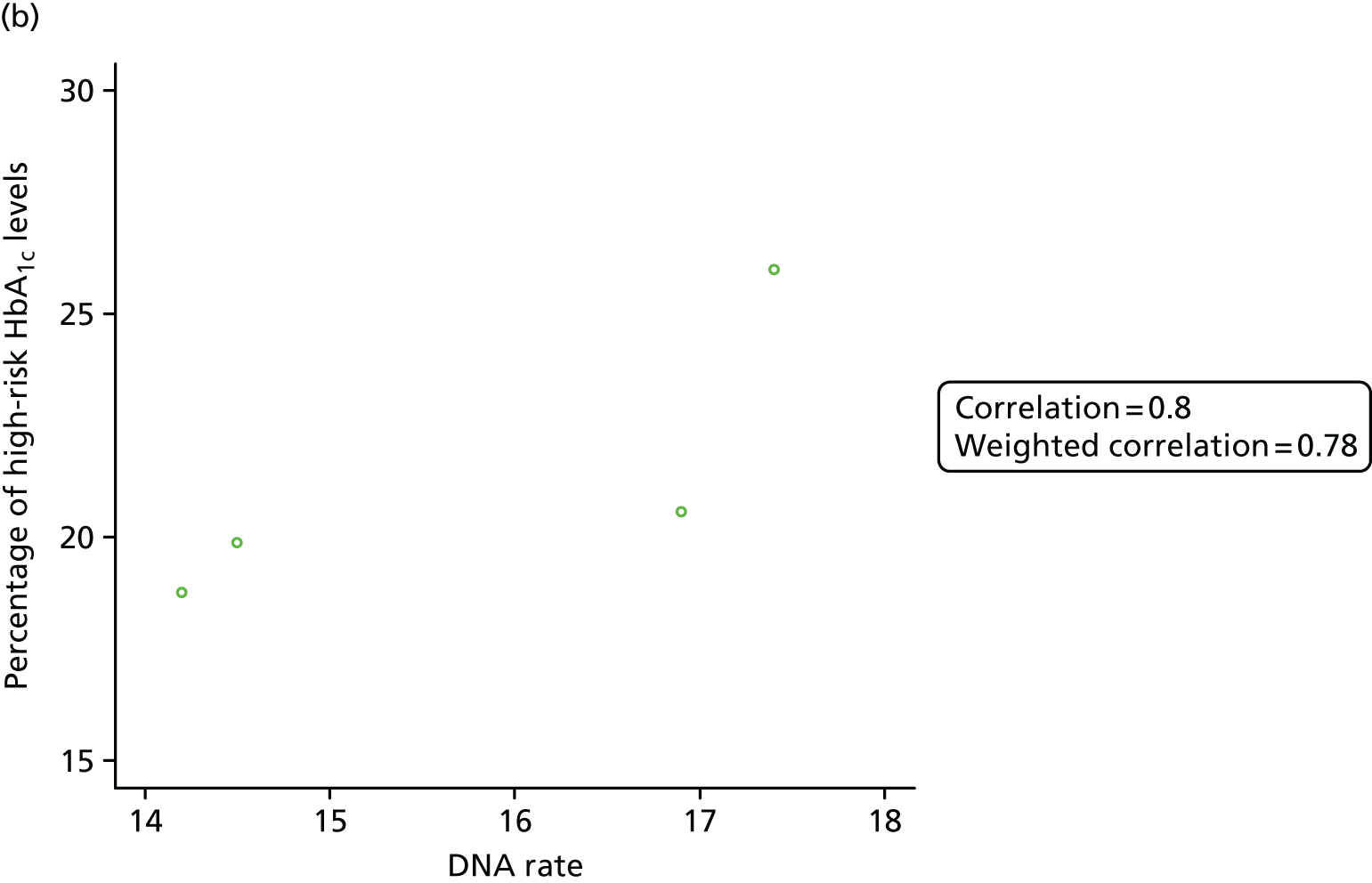
Results assessing if DNA rates affect the rates of young people with high-risk HbA1c levels are summarised in Figure 10b. There is a positive association, with the weighted correlation being 0.78. This correlation value indicates that high DNA rates lead to more patients with high-risk HbA1c levels.
Dermatology site (uses digital clinical communication)
Two clinical outcomes were provided by the dermatology site. These outcomes were whether or not a young person had been given a wig referral and time to discharge from the clinic (when young people are well, they are discharged). The clinic had not been established for long enough to provide enough information to analyse wig referral data.
To assess the effect of time, the young people in this site were categorised by three periods (December 2011–December 2013, January 2014–June 2014 and July 2014–February 2015) that were based on when they were referred/registered to the clinic. These periods were chosen based on the volume of referrals into the clinic during these times. The number of young people referred to the clinic in these periods was 76, 169 and 84, respectively.
Figure 11a shows the estimated probabilities of not being discharged from the clinic. Figure 11b provides more details for the time frame 0–15 months. The black, blue and green lines correspond to young people referred in periods December 2011–December 2013, January 2014–June 2014 and July 2014–February 2015, respectively. The short vertical ticks on the three lines correspond to young people who have not been discharged from the clinic (censored observations), with locations (on the x-axis) of the ticks giving durations the young people have been registered in the clinic so far. In general, the earlier the period of referral, the higher the line, meaning larger probabilities of not being discharged. This finding indicates that, over time, the time to discharge has been decreasing. In contrast, DNA rates remained relatively unchanged over time at this site. The difference between profiles for DNA rates and probabilities may be explained by qualitative research that has established that young people can e-mail images to get advice on their skin condition. Owing to the form of data, it was not possible to use scatterplots and Pearson’s r correlation to assess the association between DNA rates and clinic-specific outcomes in this clinic.
FIGURE 11.
Kaplan–Meier estimate for the probability of not being discharged. (a) Plot including all time points; and (b) a slice for the time between 0 and 15 months.
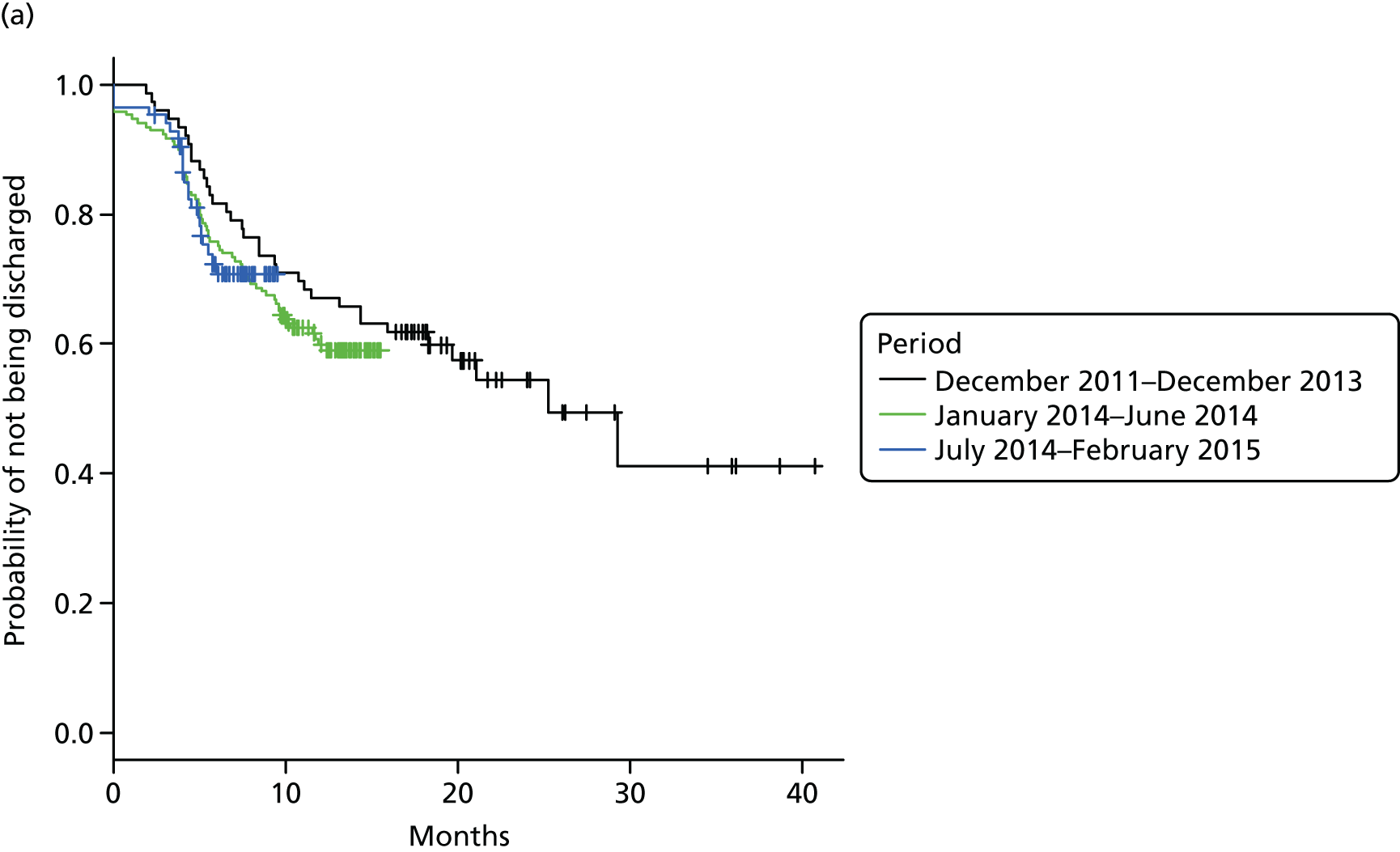
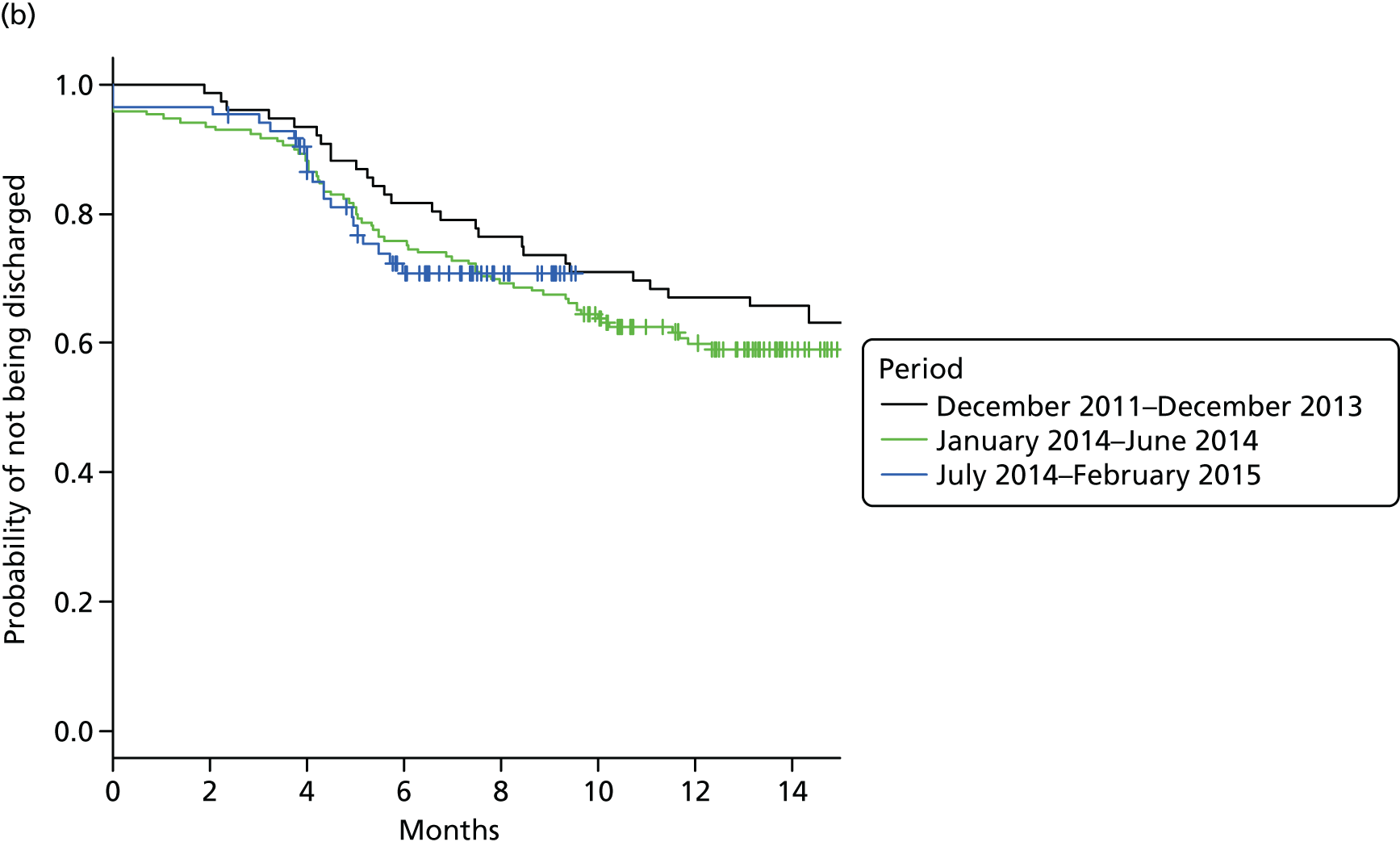
Cystic fibrosis 2 site (uses digital clinical communication)
Clinic-specific outcomes provided by the cystic fibrosis 2 site are days for i.v. therapy, annual review of BMI and annual review of FEV1% predicted.
The proportions of young people who required at least 1 day for i.v. therapy in 2014 and 2015 are 44.9% (35 in 78) and 52.6% (41 in 78), respectively. The difference in proportions is large (7.7%). However, the sample is relatively small (78 young people), which may be one explanation for the large observed difference. From 2014 to 2015, the mean BMI increased by 0.23 kg/m2 only (21.55 kg/m2 vs. 21.78 kg/m2), whereas mean FEV1 decreased by 0.40 litres only (74.81 vs. 74.41).
In general, comparing 2014 and 2015, there are only small differences in clinical outcomes for young people in the cystic fibrosis 2 site. This was always true for DNA rates (see Appendix 3). As we had data for only 2 years, it was not possible to use scatterplots and Pearson’s r correlation to assess association between DNA rates and clinic-specific outcomes in this clinic.
Sexual health site (uses digital clinical communication)
The clinic-specific outcome for the sexual health site is return to the clinic after a positive test, where positive means presence of a disease. The number of positive tests from 2011 to 2016 was 2135, 1887, 1841, 1789, 2386 and 1028, respectively. For 2016, the data were up to 31 March.
Figure 12 shows the profile for the percentages of young people who did not return to the clinic after a positive result. There was a decrease from 2011 to 2012, but there were increases in 2015 and 2016. In summary, outcomes have deteriorated over time.
FIGURE 12.
Profile for rates of not returning to the clinic after a positive test.
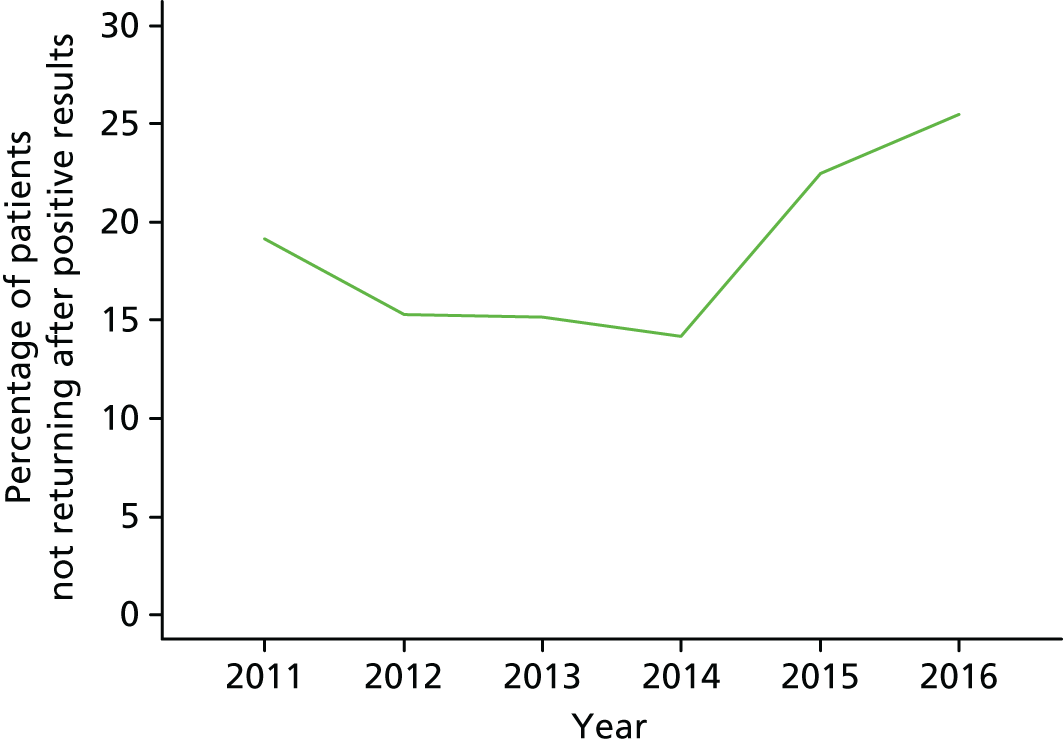
As appointments are not booked, it was not possible to calculate DNA rates. Consequently, it was not possible to assess the link between DNA rates and clinic-specific outcomes in this clinic.
Liver conditions site (uses digital clinical communication)
The clinic-specific outcome for the liver conditions site was tacrolimus levels in young people who have had a liver transplant. There is no threshold for good tacrolimus levels. The clinical objective is that tacrolimus measurements do not vary geatly over time. The consultant informed the project team that one way of summarising a young person’s tacrolimus measurements is calculating standard deviation. However, most young people had few measurements and so standard deviations were not used to summarise data. Annual mean profiles were used.
Figure 13 shows the mean annual profiles for young people. Young people have been categorised by the number of days post liver transplant. For young people up to 1000 days post liver transplant, there is variation up to year 2008. After year 2008, although there are increases in mean tacrolimus values over time, there is little variation. There is also less variation in the mean tacrolimus values after 2008 for young people 1001–2000 days post liver transplant. For young people 2001–3000 days post liver transplant, it is not clear whether or not there is less variation after 2008 because there had been increases in the mean levels over time and then a decrease for 2011.
FIGURE 13.
Tacrolimus mean profiles for patients post liver transplant.
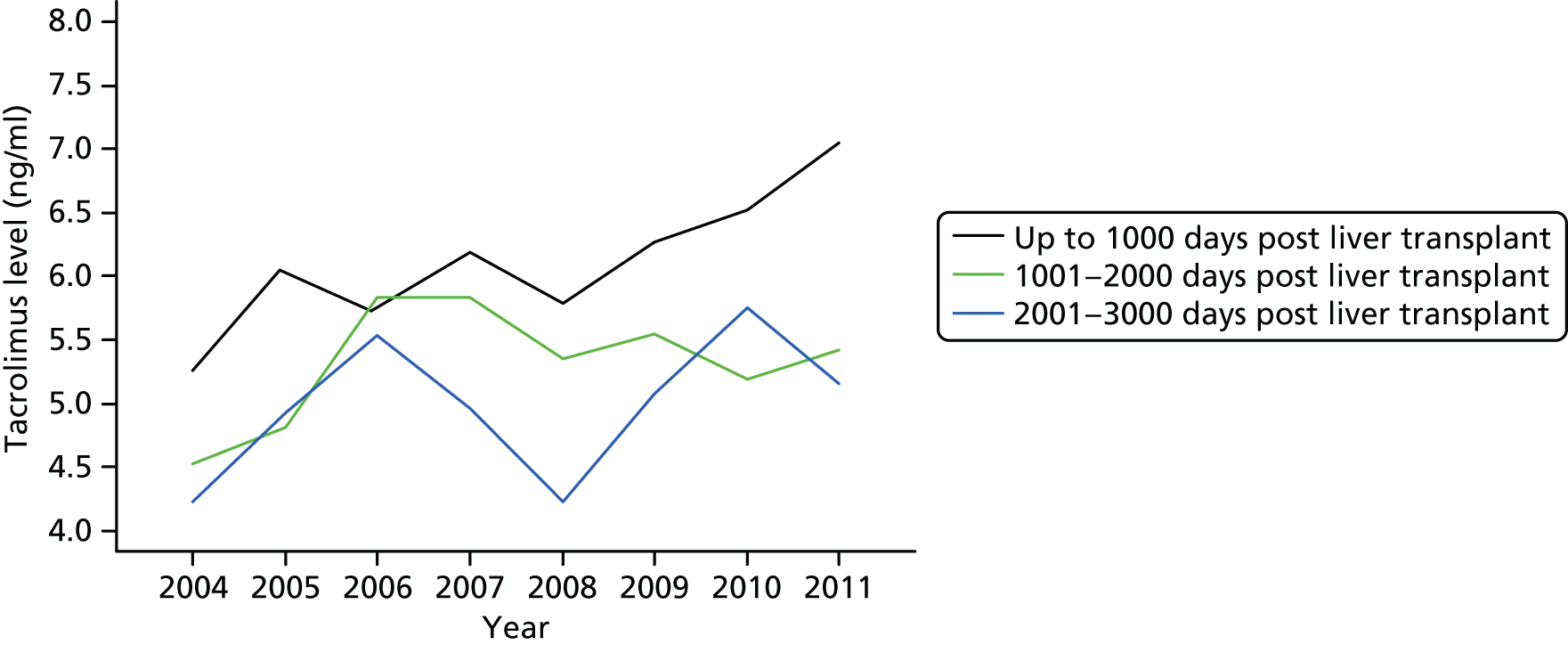
In summary, there is less variation in tacrolimus measurements from 2008. Noting that there was a change of DCC format, the stabilising of tacrolimus measurements from 2008 may be attributed to this change.
Owing to the form of data, it was not possible to use scatterplots and Pearson’s r correlation to assess association between DNA rates and clinic-specific outcomes in this clinic. However, it can be observed that DNA rates in years 2008 to 2011 were lower than in years 2004 to 2009 (see Appendix 3, Table 21). Therefore, it seems that lower DNA rates are associated with better outcomes.
Summary findings from analysis of clinic-specific outcomes
In the case of the two sites that do not use DCCs, over time, there was improvement in clinical outcomes in the HIV site and there was deterioration of outcomes in the mental health 2 (CAMHS) site. Among the six sites that use DCCs, there were improvements over time in clinical outcomes in four sites (diabetes mellitus 1, diabetes mellitus 2, dermatology, cystic fibrosis 2 and liver conditions) and deterioration of outcomes in the sexual health site. Thus, comparing sites that use DCCs and those that do not, over time, there are no clear differences in profiles for clinical outcomes.
The possible impact of DNA rates on clinic-specific outcomes was assessed using scatterplots and Pearson’s r correlation coefficients in two sites not using DCC [HIV and mental health 2 (CAMHS)] and two sites that use DCCs (diabetes mellitus 1 and diabetes mellitus 2). In all these sites, low DNA rates were associated with better clinic-specific outcomes. Thus, it seems to be the case that, if young people do not miss appointments, clinical outcomes improve. However, this association was weak in the diabetes mellitus 1 site. From qualitative data, it is known that patients in the diabetes mellitus 1 site send their glucose level results by e-mail. Therefore, it is possible they are getting clinical advice digitally when they miss appointments.
Discussion of data and analysis results
General findings
Based on all outcomes (DNA rates, A&E attendance rates, hospital admission rates and clinic-specific outcomes), there were no clear differences between sites using DCCs and sites that do not use DCCs. This finding may be attributable to the lack of good comparators.
Appointment status data
It could be expected that, in sites where DCCs are used, DNA rates would not increase and, in sites where they are not used, DNA rates would not decrease. This pattern was observed in all but two sites. In one site that does not use DCCs (the HIV site), DNA rates decreased continuously. In one site that uses DCCs (IBD 2), DNA rates increased over time. These unexpected trends may be a result of other changes in the sites. Overall, DCCs were linked to lower DNA rates.
Analysed data suggested that DNA rates are sensitive to changes of practice in sites. For example, in the liver conditions site, when a new digital communication format was introduced, DNA rates decreased. This indicates that the impact of digital communication can be assessed using DNA rates.
Appointments data were the most easy to obtain from sites and were well recorded, possibly because trusts record this information for the national audit. With the exception of sites that are drop-in services, if a site provided data, appointment status data were included. Appointment status data were analysed by computing annual ‘Did not attend and appointment rates’ (DNA rates). DNA rates were calculated using the formula DNA/(attended + cancelled + DNA). Having ‘cancelled’ in the denominator assumes that attended and cancelled appointments are equivalent in terms of young people receiving some form of advice. An alternative would be to have cancelled appointments in the numerator, but this assumes no advice is provided when an appointment is cancelled. Thus, appointments status data could be improved if additional information was available on whether advice was given digitally or via other means when an appointment was cancelled.
In summary, DNA rate is a good measure of the impact of DCCs. However, more information on actions taken following cancellation of appointments and possible confounders, such as other changes that may affect appointments data, need to be accounted for when assessing the impact of DCCs on DNA rates.
Accident and emergency attendance data
No differences between sites using DCCs and those not were demonstrated. However, this may be attributed to the fact that the comparison was made by contrasting profiles over time for clinics with different conditions.
It would be expected that low DNA rates would be associated with low A&E attendance rates. However, in all study sites where relationship between DNA and A&E attendance was assessed, this was not the case. For example, in the HIV site, there was a strong relationship between DNA and A&E attendance rates, with a low DNA rate associated with more A&E attendances. From qualitative data, this result could be explained by the fact that in this site, following a clinic visit, young people were booked an A&E visit to get specialised treatment. In other sites there was no substantial relationship between DNA and A&E attendance rates. Thus, no link was established between DNA and A&E attendance rates. Probably a link would be identified if additional information, such as whether or not an attendance was preceded by a DNA, were available.
Hospital admission data
There were no differences in hospital admission rates between sites using DCCs and those that did not. However, this may be attributed to the fact that the comparison was made by contrasting profiles over time for clinics with different conditions.
It would be expected that low DNA rates would be associated with low hospital admission rates in the three sites where this was assessed. This was the case in two sites (diabetes mellitus 1 and HIV) but not in the IBD 2 site, where a negative relationship was seen. A possible explanation for this surprising result in the IBD 2 site is that when young people are poorly, they do not miss clinic appointments and may also have hospital admissions. Thus, expected links were established between DNA and hospital admission rates in two sites and not in one. Like A&E attendance, expected links between DNA and hospital admission rates may be seen if additional information, such as whether or not an admission was preceded by a DNA, were available.
Clinic-specific outcomes data
Profiles of clinic-specific outcomes did not demonstrate clear differences between sites using DCCs and sites that did not. Improvement in outcomes was found in five of the six sites that use DCCs and in one of two sites that did not use DCCs. This difference may be because of the small number of sites studied, secular trends in patients’ health or differences in use of DCCs.
It is worth noting that, in one site (liver conditions), there were improvements in young people’s outcomes when a new format of digital communication was introduced. This suggests a benefit of using DCCs.
It would be expected that low DNA rates would improve clinical outcomes. This was the case in seven sites where associations between DNA rates and clinical outcomes were assessed. Thus, aiming to lower DNA rates in these sites would lead to better health outcomes for young people.
Limitations
Despite DNA rates being a good measure of the impact of DCC, the data analysed lacked good comparators. This was also a problem for all the other outcomes. In no site were data available for periods when DCC was being used and periods when it was not. Therefore, before-and-after comparisons could not be done. In addition, for a given condition, there were not multiple sites using and not using DCCs, so it was not possible to compare similar sites. Therefore, profiles for different conditions were compared and this may be the reason why possible impacts of digital communication were not demonstrated by the data.
Another limitation is that data in most sites were provided for a limited number of years. Therefore, correlation values may have poor precision and it is difficult to accurately assess associations between DNA rates and other outcomes.
Chapter 9 Generic patient-reported outcome measures
Evidence gaps identified in systematic reviews of DCC relevant to young people with LTCs are noted in Chapter 1. Among them was the need to undertake research across clinical populations in relation to the use of DCCs. Our research has addressed this by spanning 11 mental and physical health LTCs experienced by young people. In planning and undertaking interventional work across clinical populations aimed at achieving specified purposes, patient-reported outcomes (PROs) are of clear importance. Consequently, PROMs are required that will similarly span clinical conditions. This chapter presents the body of work undertaken to identify and evaluate PROs and PROMs that have been, or could be, used to evaluate the use of DCC across clinical populations and age profiles. First, we present a systematic review of outcome measures used to assess the impact of DCC. We then present further literature reviews, PPI activities and cognitive interviews of clinicians and young adult service users.
Patient-reported outcome measures used to assess the impact of digital clinical communication: a systematic review
Objectives
Using published peer-reviewed research literature, this systematic review aimed to identify and examine generic PROMs that have been used to assess the impact of DCC.
Methods
Search strategy
The scoping review of systematic reviews presented in Chapter 1, Table 1, which preceded the study, was used to inform the development of the search strategy and assess the volume and type of literature relating to the assessment question. An initial search strategy was developed for MEDLINE and was adapted and refined as appropriate for other databases. Keyword combinations and specific search terms were used. The following electronic bibliographic databases were searched to locate relevant published systematic reviews: The Cochrane Library (including Cochrane Systematic Reviews, Database of Abstracts of Reviews of Effects, Cochrane Central Register of Controlled Trials, NHS Economic Evaluation Database and Health Technology Assessment databases), MEDLINE, MEDLINE In-progress & Other Non-Indexed Citations, EMBASE, PsycINFO and Web of Science (including Science Citation Index and Conference Proceedings). Citations in eligible papers and previous reviews in the subject areas were examined for additional papers that meet the inclusion criteria for the present review. In addition, we undertook supplementary searches to find additional studies published since the systematic reviews, including scrutiny of references of included studies, citation-searching and searching relevant websites. References identified through the search were downloaded in EndNote X7 software (Thomson Reuters, CA, USA). All duplicate records were identified and removed.
Eligibility criteria
The following eligibility criteria have been applied.
Papers were selected for inclusion in this review if they met the following criteria. Systematic reviews that:
-
included at least one randomised controlled trial (RCT)
-
focused on any chronic health condition (including physical and mental)
-
included at least one PROM that assessed the impact of DCCs
-
included PROMs that could be assessed using either validated or non-validated scales
-
were published in English only
-
included studies with primary data
-
involved communication in both directions (patient to clinician and clinician to patient)
-
included the following technologies – e-mail, text messaging, social media and web-based patient portals, and VoIP (e.g. Skype and Google Talk), which can simultaneously transmit voice and other media such as text and images
-
involved the use of a digitally delivered intervention or the delivery of disease prevention and health promotion information forms as part of the ongoing patient–clinical team communication.
The search was not limited by date, populations or health conditions.
Study identification
One reviewer screened all identified bibliographic records for titles/abstracts and identified potential papers meeting the inclusion criteria. Two reviewers independently screened a portion of the records and any disagreements were resolved through discussion. Full texts were obtained for the relevant papers. The study identification process was split into two phases. Phase 1 included identification of relevant systematic reviews that met the eligibility criteria and phase 2 included the identification of relevant RCTs within the systematic reviews.
Data extraction
One reviewer extracted relevant data from the systematic reviews and RCTs on age groups, LTCs, digital interventions, generic and condition-specific outcome measures, validated PROMs (names, descriptions and full references) and RCT references into an Excel spreadsheet. Validated PROMs were those with a minimum of one paper assessing any aspect of the PROM validity (e.g. face construct, reliability). A second reviewer oversaw the process and disagreements were resolved through discussion. All relevant systematic reviews, RCTs, scales for validated generic PROMs and their references were retrieved.
Data synthesis
The extracted data were summarised in text and summary tables, as appropriate.
Results
A total of 3802 abstracts were identified from the electronic search. The title, abstract and full-text screening process reduced the potential number of systematic reviews to 56. A summary of the literature identified at each stage of the search process is provided in a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) study flow diagram (Figure 14). Thirty-seven systematic reviews out of the possible 56 were excluded because the RCTs described in them did not meet our eligibility criteria. A total of 19 systematic reviews covering 70 RCTs were assessed for inclusion of validated PROMs.
FIGURE 14.
The PRISMA study flow diagram.
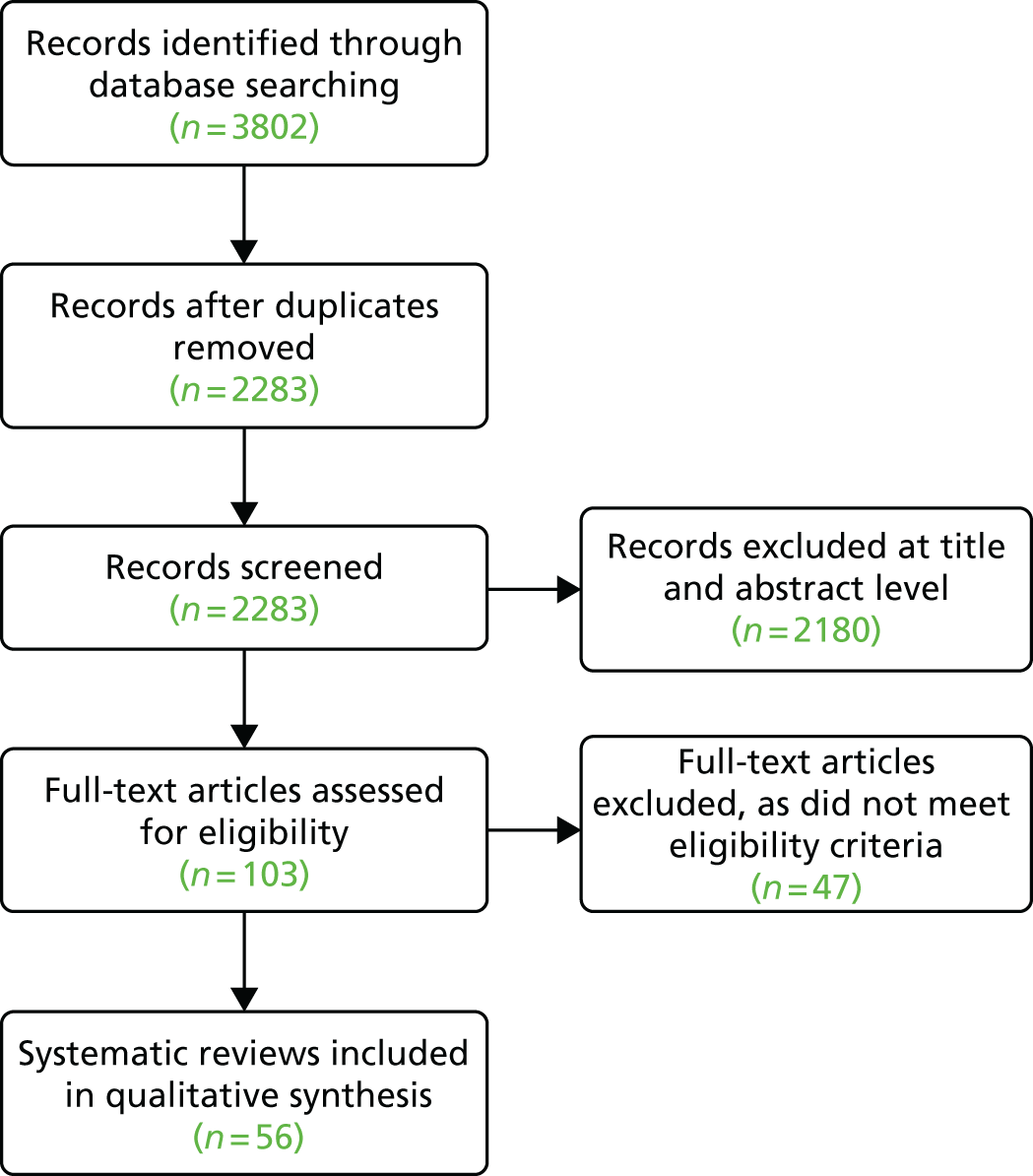
Patient-reported outcome measure selection
Thirty-five RCTs revealed 74 validated PROMs (Figure 15). The 74 validated PROMs were reviewed for relevance in accordance with our inclusion criteria of (1) no specific condition, symptoms or treatments stated in the PROM title, the PROM completion instructions or the items within the PROM; and (2) the PROM had been used in a population aged > 16 years. This resulted in 28 generic candidate PROMs (see Figure 15) for assessing the impact of DCCs across different LTC clinical populations.
FIGURE 15.
Flow diagram of candidate generic PROMs.
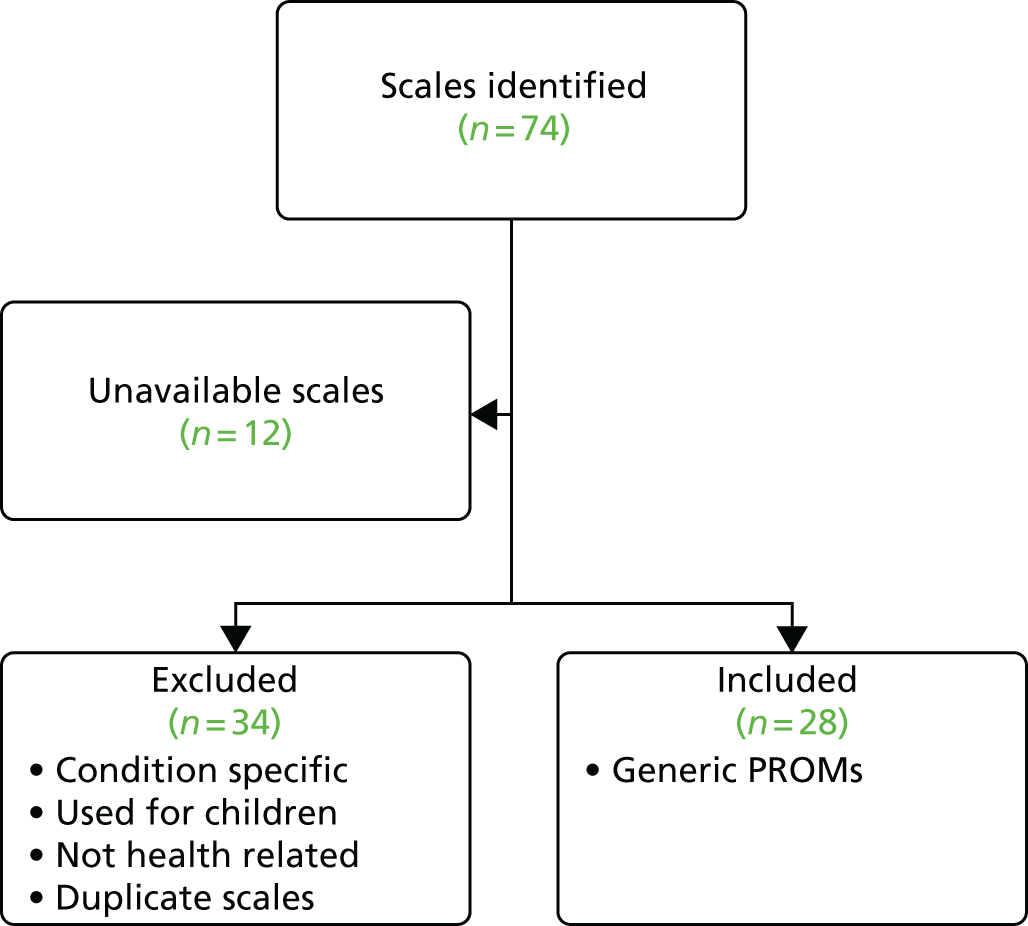
We present the identified PROMs which assess,first, patient-level factors (Table 10) and, second, care-level factors (Table 11).
| Outcome measure description | Scale name | Reference | |
|---|---|---|---|
| SR | RCT | ||
| Awareness | |||
| Health literacy | Health literacy | 84–86 | 87,88 |
| Knowledge of management strategies | Pulmonary rehabilitation knowledge test | 42,84,85 | 89 |
| Cognitive impact | |||
| Cognitive appraisal | Appraisal of Diabetes Scale | 90 | 91 |
| Empowerment | |||
| Decision-making confidence | Sanders and Courtney Scale | 92 | 93 |
| Patient empowerment | PAM | 85,86,94 | 95,96 |
| Patient Empowerment Scale | 94 | 95 | |
| Patient empowerment (self-care) | Heart Failure Self-Care Behaviour Scale | 84 | 97 |
| Self-confidence for communicating with providers | Perceived Efficacy in Patient–Physician Interactions | 98 | 42 |
| Self-efficacy | Cancer Behavior Inventory | 84 | 99 |
| General Self-Efficacy Scale | 100 | 101 | |
| Heart Failure Self-Efficacy Scale 30 | 102 | 103 | |
| Pain Self-Efficacy Questionnaire | 57,100 | 104 | |
| Self-efficacy instrument | 84 | 105 | |
| Diabetes Empowerment Scale | 42,84–86,94 | 87,88,106,107 | |
| Self-worth | Harter’s Self-Perception Profile for Adolescents | 85,108 | 109 |
| Health-related quality of life | |||
| Asthma | Modified Marks Asthma Quality of Life Questionnaire | 48 | 110 |
| Paediatric Asthma Caregiver’s Quality of Life Questionnaire | 48 | 111,112 | |
| Asthma Quality of Life Questionnaire | 42,48 | 113–120 | |
| Paediatric Asthma Quality of Life Questionnaire | 42,48 | 113,121–123 | |
| Cancer | Functional Assessment Of Cancer Therapy – Breast | 124 | 125 |
| Diabetes mellitus | Diabetes Distress Scale | 42 | 126 |
| Problem Areas in Diabetes-2 | 42,84,85,90,94 | 91,105,107,127,128 | |
| Diabetes Quality of Life for Youth | 44,90,101,129 | 90,130 | |
| Health related | Fifteen-dimensional Health-Related Quality of Life (15D) | 84 | 99 |
| Healthy Days Measure (Centers for Disease Control and Prevention Health-Related Quality of Life) | 42 | 98 | |
| Short Form questionnaire-36 items | 42,84,85,100,131 | 88,132–135 | |
| Short Form questionnaire-12 items | 94 | 136 | |
| Short Form questionnaire-6 Dimensions | 42 | 137 | |
| Personal Wellbeing Index | 100 | 101 | |
| EQ-5D | 42 | 137 | |
| Heart failure/cardiac | Minnesota Living with Heart Failure Questionnaire | 84,102 | 97,103 |
| Quality of Life Index-Cardiac Version | 102 | 103 | |
| Children | Pediatric Quality of Life Inventory 4.0 | 57 | 138 |
| EQ-5D Child Version: Quality of Life | 42 | 137 | |
| Mental health | |||
| Anxiety | State–Trait Anxiety Inventory | 57,100 | 104,139 |
| Depression | Beck Depression Inventory | 102,140,141 | 142 |
| Center for Epidemiological Studies Depression Scale | 57,84–86,90,92,100,102,131 | 93,104,107,135,139,143–145 | |
| Revised Children's Anxiety and Depression Scale | 57 | 146 | |
| Short-care | 84 | 105 | |
| Patient Health Questionnaire | 42,85,86,94,131 | 96,106,126–128,135,147 | |
| Depression, anxiety and stress | Depression Anxiety Stress Scales | 100 | 101 |
| HADS | 102 | 103 | |
| Distress | Memorial Symptom Assessment Scale | 84 | 99 |
| Health distress | 57,92,100,129 | 148 | |
| Medical Outcomes Study Health Distress Scale | 85,86 | 96,149 | |
| Mental health | Medical Outcomes Study Mental Health Inventory | 85,108 | 109 |
| Offer Self Image Questionnaire | 44,102,129 | 130 | |
| Physical impact | |||
| Activity participation | Australian version of the Activity Card Sort | 100 | 101 |
| Fatigue | Fatigue Impact Scale | 100 | 101 |
| Role function | Illness Intrusiveness Scale | 57,92,100,129 | 148 |
| Social impact | |||
| Family dynamics | Family Assessment Device | 57,102,129 | 130 |
| Responsibility for care | Parent–Child Responsibility Scale | 130 | 57,102,129 |
| Social acceptance | MacArthur Scale of Subjective Social Status | 85,108 | 109 |
| Social isolation | Instrumental–Expressive Social Support Scale | 92 | 93 |
| Social support | |||
| Diabetes Support Scale | 84,85,90 | 107,143 | |
| Medical Outcomes Study Social Support Scale | 42,84,85 | 89,145 | |
| Duke Social Support Index | 100 | 101 | |
| Outcome measure description | Scale name | Reference | |
|---|---|---|---|
| SR | RCT | ||
| Adherence to medical regimens | |||
| General Adherence Scale from the Medical Outcomes Study | 150 | 84,94,100,102,151 | |
| Hill-Bone Compliance to High Blood Pressure Therapy Scale | 87,88 | 84–86 | |
| Morisky Medication Adherence Scale | 150 | 84,94,100,102,151 | |
| Care satisfaction | |||
| Assessment of care | Patient Assessment of Chronic Illness Care | 95 | 94 |
| Doctor–patient communication | Art of Medicine Questionnaire | 150 | 84,94,100,102,151 |
| National Committee on Quality Assurance/American Diabetes Association provider recognition programme | 126 | 42 | |
| Patients’ perceptions of provider autonomy support | Modified Health Care Climate Questionnaire | 126 | 42 |
| Treatment acceptability and satisfaction | Treatment Evaluation Inventory-Short Form | 146 | 57 |
| Diabetes Treatment Satisfaction Questionnaire | 91,128 | 90,94 | |
| Consumer Assessment of Healthcare Providers and Systems | 95,128,136 | 94 | |
| Decision-making confidence | Sanders and Courtney Scale | 93 | 92 |
| Health-care utilisation | |||
| Ratings of outpatient visits | Visit satisfaction | 152 | 57 |
| Risk of readmission | Prediction of Rehospitalisation | 147 | 131 |
| ICT satisfaction | |||
| Client Satisfaction Questionnaire | 144 | 84,86,90,102 | |
| Home Care Client Satisfaction Instrument adapted for ICT | 154 | 132 | |
| Telemedicine Patient Satisfaction Survey | 91 | 90 | |
| Telemedicine Perception Questionnaire | 153 | 131 | |
| Internet use | Internet use | 152 | 57 |
Assessment of candidate patient-reported outcome measures
Twenty-eight PROMs met our inclusion criteria. Our aim at this stage was to identify appropriate topics of a PROM rather than a PROM itself prior to undertaking PPI work. We considered that exposing 28 PROMs to PPI communities for their assessment of relevance and face validity would be overwhelming, so we had to develop a method to condense the activity into a management task. Two investigators considered the purpose of the 28 PROMs using their titles, items and the completion instructions. Each PROM’s purpose was discussed, agreed and recorded, and we considered these purposes to be PROs [i.e. the purpose or aim of the PROM was to detect the presence or absence of something (an outcome)]. In our case this was a PRO. From the 28 PROMs, we formed six PRO topics (Table 12).
| PRO topic | Reference |
|---|---|
| Patient satisfaction with doctor–patient communication | 154–156 |
| Depression/anxiety/distress | 157–161 |
| Patient satisfaction with ICT | 162–165 |
| Social support/perception of support (from friends and family) | 166,167 |
| Quality of life | 168–176 |
| Patient empowerment/confidence | 177,178 |
Twenty-eight PROMs had been used in evaluations of DCCs and these 28 PROMs were clustered into six topics prior to their exposure to the PPI community to obtain some direction about the face validity of these topics as important outcomes for assessing the value to service users in general, and young people in particular, of DCC. As most of the included PROMs had not been developed specifically for measuring the effect of DCCs, their suitability remains unclear. For example, we do not know whether the outcomes reported included the effects of other additional in-person communication.
Summary of findings
Nineteen systematic reviews consisting of 70 RCTs were included in the review. Seventy-four validated PROMs were used in the included RCTs; most RCTs used more than one PROM at a time and some PROMs were used in multiple RCTs. Most validated PROMs were patient-focused, assessing quality of life, self-efficacy, depression or anxiety, and social impact. Some validated PROMs were also used to assess care-focused outcomes, such as adherence to medical regimens, doctor–patient communication and treatment acceptability or satisfaction. Finally, some PROMs were specifically developed for younger populations; however, the majority were aimed at adults. Thus, we are unsure whether they are suitable for use by younger people.
Measuring the effectiveness of digital clinical communications across health conditions
Methodological overview
The research approach taken combines (1) further scoping literature reviews, (2) a series of both personal and anonymous online public and patient engagement activities and (3) cognitive interviews with study participants. The reviewing (including the systematic review presented above) and the PPI activities are intertwined, and to aid understanding the methods are illustrated in Figure 16. For each activity, the method is presented first and the findings immediately below.
FIGURE 16.
Flow diagram depicting methods corresponding with research stages.
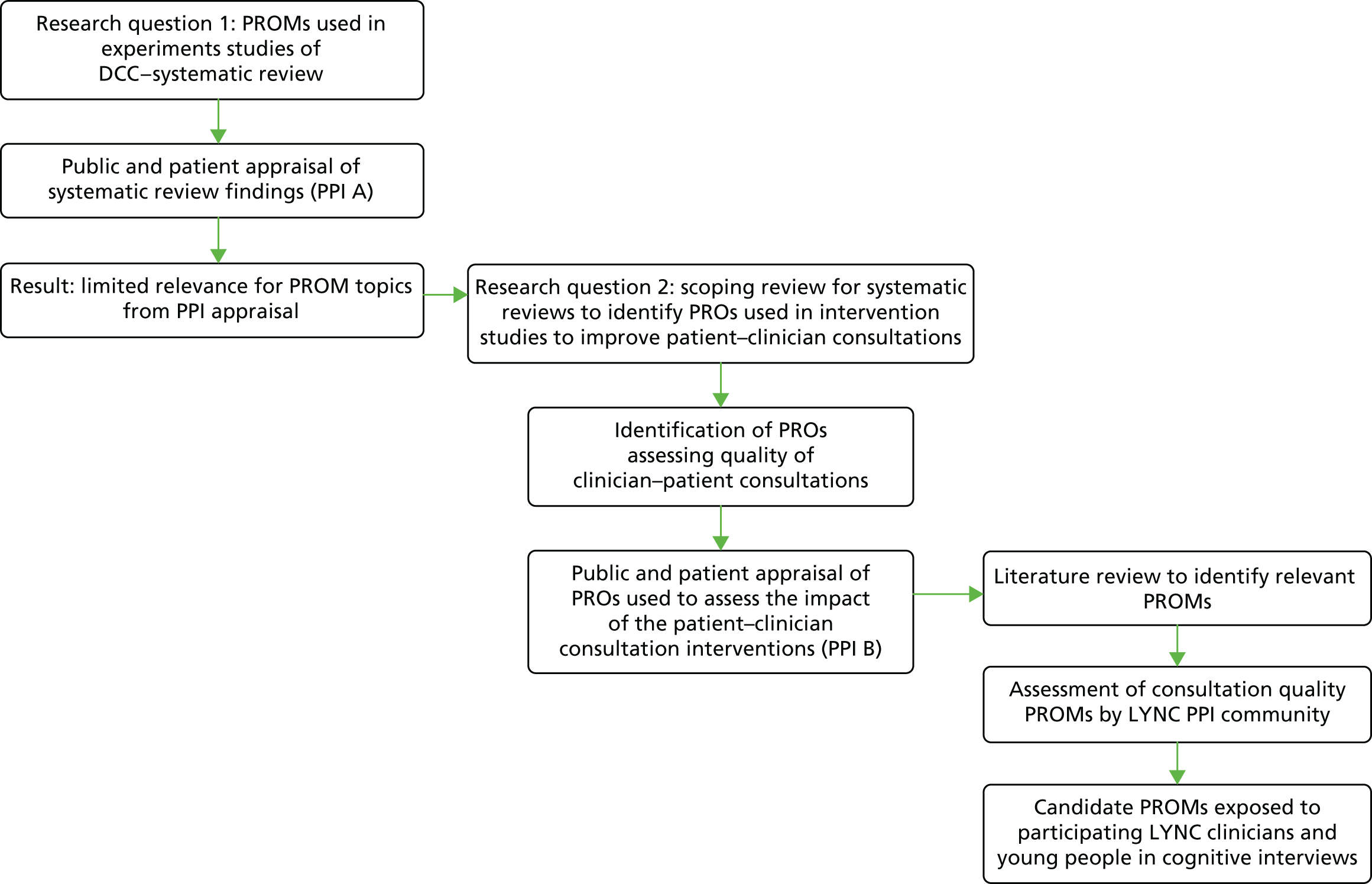
Public and patient appraisal of systematic review findings
Methods
To request feedback on the face validity of the PRO topics identified, we used the LYNC study social media activity as the mechanism to encourage engagement with, and appraisal of, the PRO cluster topics identified. The LYNC project social media presence operates via both Facebook and Twitter and these were mobilised to engage people with an interest in LTCs and, particularly, young people with LTCs in our project. The objective was to engage people in choosing one or more PRO cluster topics. The LYNC study Twitter profile and Facebook profile pages were enhanced with content and activity, and these were used to launch a SurveyMonkey® (Palo Alto, CA, USA) six-item questionnaire to ask people to rank the PRO cluster topics from most to least appropriate in the assessment of patient–clinician DCCs. We aimed to receive 50 SurveyMonkey PPI responses in 8 weeks (1 September 2015–31 December 2015). The six PRO cluster topics (see Table 12) were considered with our PPI co-investigator. During this process a stem vignette for introducing the survey was developed along with the survey format (see Appendix 4). Feedback from the PPI member was as follows.
-
The vignette made sense and it was easy to understand what was being asked.
-
Depression may not be appropriate as a PRO.
-
All of the six clusters are interrelated and there was an overlap among them, especially between (1) satisfaction with using information and communication technology (ICT) and level of satisfaction when communicating with the health-care provider; and (2) between experience of depression, anxiety and stress, and patient empowerment and confidence.
-
Exemplar questions or statements should be put next to the PRO cluster topics.
Following amendment, the draft online survey was circulated to five PPI members of the LYNC study PMG for specific consideration of the demographic questions, the completion instructions, the survey items and the LYNC study Facebook and Twitter accounts from where the online survey would be accessed. The following changes were made as a result.
-
A note was added to the completion instructions to say ‘ranking 1 is the most important and ranking 7 is the least important’.
-
If a new topic was suggested more than three times by PPI respondents, it will be added to the list of six topics for subsequent responders to assess.
-
The term ‘depression’ was replaced with ‘mood change’.
-
The topic title, ‘Impact of support from family and friends’, was not thought to match well with the example question that was given. The two PROMs included in this PRO topics were reviewed and found to have limited value for the study and were excluded. The topic cluster was still left in the questionnaire as DCCs may affect social interactions and relationships with parents and carers if the parents and carers become excluded from the relationship between the health-care professional and the young person as a consequence, and we wanted our PPI activity to confirm or refute the importance of this.
-
The PPI responder age range on the first page of the survey was further split to < 12 years and 13–15 years, with the thought that the view of those aged < 12 years would be discounted; however if anyone aged < 16 years found the survey and felt that they understood it and wanted to fill it out, their views were welcome.
-
The example question for the topic ’Patient empowerment and confidence’, did not capture the topic title. Four further possible exemplar questions were offered by the researchers and the PPI group chose ‘I am confident that I can take actions that will help prevent or minimise some symptoms or problems associated with my health condition’ [question 12, Patient Activation Measure (PAM) Short Form]. 178
-
The quality-of-life topic title was changed to ‘Impact of your health condition in your life’.
The final online survey was launched using SurveyMonkey in November 2014 via the LYNC study Facebook and Twitter sites. The relevant charities to our LYNC study population were contacted via their own online accounts and asked to promote the online survey. The charities included Diabetes Nottingham, Diabetes UK, Cystic Fibrosis Trust, CLIC Sargent (Childhood Cancer), Asthma UK, Teenage Cancer Trust, British Heart Foundation, American Diabetes Association, Diabetes.co.uk, Diabetes Support and Cystic Fibrosis Kids. We posted the following text on our Facebook LYNC study page:
Dear XXX, thanks for liking our Facebook page. We are looking for young people (16–24) who have a long-term health condition such as asthma or diabetes, their family, friends or health-care professionals involved in their care who would be willing to give us their advice on our research project. If you are interested please write back and I’ll send you the details. Just to note that although our study focuses on young people we are happy to have the views of all ages, for more information please see the ‘about’ section on the LYNC study Facebook page. Kind regards, XXX (on behalf of the LYNC study).
Online survey A findings
Online survey A resulted in 57 responses to the PRO cluster topics. There was no clear PRO topic preference, with only small differences between question scores resulting in the prioritisation of the following four PRO topics for evaluating the use of DCCs:
-
treatment satisfaction
-
mood
-
impact on health
-
patient empowerment.
However, although survey A PRO topics had all been used in PROMs evaluating some form of DCC, our LYNC study PPI members had found the PRO topics to be outdated and not fit for purpose. Our social media PPI respondents had found the topic appraisal difficult. We were additionally aware of limitations in the psychometric validity of many of them. Looking at PROs used in trials of interventions or care pathways which DCCs might seek to support was considered an appropriate next step in answering our research questions. This was informed by the fieldwork analysis that was under way and the early themes that were emerging about the impact of DCCs.
Scoping review for systematic reviews to identify patient-reported outcomes used in intervention studies to improve patient–clinician consultations
Following discussion at the October 2014 PMG meeting we undertook a scoping review of systematic reviews to identify PROs and PROMs used to evaluate interventions aimed at ‘bettering hospital appointments’. The rationale for this was that our early fieldwork indicated that in-person appointments were improved as a consequence of using DCCs in between the appointments. We determined this ‘better’ in relation to:
-
data availability for the consultation
-
timing of consultation
-
people involved: the right people for what the consultation needs to achieve
-
the place of the consultation.
The above criteria were used to identify relevant systematic reviews from which we used the reference lists to look at the included studies for the candidate PROs. In the light of evidence gathered from our clinical case sampling interviews and our first case study fieldwork, we focused our attention on looking for PROs that might indicate whether or not patients were having better hospital appointments as a consequence of the additional use of DCCs. Here we focus on the quality of the communication rather than the mode of communication. We scoped the literature to find systematic reviews with particular focus on interventions that aim to increase patient participation in consultations. 179,180 Patient activation PROMs had a good fit with the consultation dynamics, the management of LTCs and health policy directions around supporting self-management. The patient behaviours that these types of interventions target were:
-
increasing the number of questions patients ask in consultations
-
patients raising their own concerns
-
patients asking for clarification
-
patients checking their understanding.
Increases in these patient behaviours have been measured180 by:
-
immediate impacts (e.g. patient satisfaction and recall of information)
-
intermediate outcomes (e.g. agreeing with, and adherence to, recommendations)
-
long-term outcomes (could be changes in health status or lifestyle).
Harrington et al. 179 found that when interventions were used to increase patient activation and participation in consultations (none of the interventions was DCCs), the following range of immediate, intermediate and long-term outcomes were observed:
-
improvement in patient recall (immediate outcome)
-
increases in question asking (immediate outcome)
-
no change in consultation length (immediate outcome)
-
no change in patient treatment satisfaction (immediate outcome)
-
more participatory physician behaviour (immediate outcome)
-
reduced anxiety (intermediate outcome)
-
increased patient perception of control (intermediate outcome)
-
improved appointment attendance (long-term outcome)
-
increased medication adherence (long-term outcome)
-
increased perception of disease control (long-term outcome).
These outcomes were used to inform online PPI survey B.
Public and patient appraisal of patient-reported outcomes used to assess the impact of the patient–clinician consultation intervention (patient and public involvement survey B)
The social media methods developed in PPI survey A were repeated in relation to the findings from the scoping review of PROs. Online survey B was developed in consultation with LYNC study PPI members and was launched via SurveyMonkey and promoted by the LYNC study Facebook page and Twitter between December 2014 and February 2015. Our PRO topic question to potential PPI respondents in Table 13 asked them to prioritise outcomes identified in the Harrington et al. review. 179
| Instructions | |
|---|---|
|
Imagine that you have been communicating by e-mail/text message or Skype with your hospital doctor or nurse When you have hospital appointments now, you feel that you have ‘better hospital appointments’. You think they are better because . . . |
|
| PRO topics | Please place a number by each topic according to their importance to you (9 is most important, 1 is least important) |
| You remember more of the discussion when you leave (patient recall) | |
| You feel confident in asking more questions during it (question asking) | |
| Your consultation length seems the same (no change in consultation length) | |
| Your health professional seems more engaged with you and your condition (participatory health professional behaviour) | |
| You are calmer during, and at the end of, the appointment (anxiety) | |
| You feel more in control of your condition after your appointment (patient perception of control) | |
| You attend more of your scheduled appointments (attendance) | |
| You take your medication at the time and amount that you are prescribed after the appointment (medication adherence) | |
| Your condition is more under control and you feel well (disease control) | |
| Any additional outcome you think is important? | |
Response and completion rates for surveys A and B
In total, across both surveys, we received 143 responses and respondents could tick more than one category (e.g. if they had a LTC themselves and they also had a young family member with a LTC).
-
There were 56 respondents aged 16–24 years with a LTC.
-
There were 68 respondents aged > 24 years with a LTC.
-
Fifty-one respondents were family members of a young person with a LTC.
-
Twenty respondents were aged < 16 years or had no LTC.
-
No health-care professional responses were received.
The questions which asked PPI respondents to order topics according to priority as an appropriate PRO were often skipped, on both surveys (on survey A in 24/57 responses and on survey B in 33/86 responses). Survey B PROM question was skipped slightly less often. Of the 143 respondents, 67 reported using DCCs with their health professional (many of these responses were likely to be parents of young people aged < 18 years).
Online survey B findings
Survey B provided 53 responses to the PRO topic question. As with survey A, no outright preferred PRO was identified by our PPI respondents, but there were slightly greater score differences between the responses. The maximum score available to any topic was 9 and the lowest score for any PROM topic was 2.79 out of 9. The top four PRO topics in priority order were as follows.
-
You feel confident in asking more questions during your appointments (6.79/9.0).
-
Your health-care professional feels more engaged with you (6.53/9.0).
-
You remember more of the discussion when you leave the appointment (6.25/9.0).
-
You feel more in control of your condition (5.45/9.0).
The overlap in the PROM topics prioritised in surveys A and B is apparent in the data above.
Rapid scoping review to identify candidate patient-reported outcome measures to assess the patient-reported outcomes and final patient and public involvement assessment
Building on the four PPI survey B priorities we went back to the Harrington et al. review179 to identify the included studies that had assessed priorities a–d below.
-
Question asking: you feel confident in asking more questions during your appointments (see Table 3 in Harrington et al. 179).
-
Doctor encourages patient engagement: your clinician feels more engaged with you (see Table 3 in Harrington et al. 179).
-
Recall: you remember more of the discussion when you leave the appointment (see Table 4 in Harrington et al. 179).
-
Disease control: you feel more in control of your condition (see table 4 in Harrington et al. 179).
In response to the LYNC study PPI feedback regarding the datedness of the survey A topics and associated PROMs, our eligibility criteria applied an earliest publication date limit of 1995 for the included studies, given that the PROM will have been published prior to the publication of the study which used it. Three studies were potentially useful181–183 but on assessment none of them used a patient outcome measure to assess priorities a–d. A further search of the literature was subsequently undertaken to identify systematic reviews assessing clinician–patient communication interventions and patient activation interventions. The purpose of this activity was to identify PROMs used to assess PROs of interest (priorities a–d) associated with interventions to increase patient engagement with consultations. Using key words, Google Scholar (Google Inc., Mountain View, CA, USA) identified three further reviews (Table 14).
| Systematic reviews identified in the rapid scoping review | Included studies potentially relevant for assessing priorities a–d and full papers obtained | Studies confirmed as using a PROM to assess one or more of priorities a–d | PROM used |
|---|---|---|---|
| Search term: clinician/doctor/health professional + patient + communication | |||
| Rao et al. (2007)184 | 185–189 | Joos et al. (1996)189 | Krantz Health Opinion Survey190 |
| Beck et al. (2002)191 | None | n/a | n/a |
| Griffin et al. (2004)192 | 189,193–198 | Thom et al. (1999)196 | PHBQ;199 Trust in Physicians Scale200 |
Rao et al. 184 revealed one candidate PROM and Griffin et al. 192 revealed two candidate PROMs. The Krantz Health Opinion Survey,190 used by Joos et al. ,189 reported two subscales – desire for information (seven items scored 1–7) and behavioural involvement (nine items scored 1–9) – that were a close match to the PPI survey B priorities. Beck et al. 191 reviewed 22 studies about physician verbal and non-verbal communications. They looked at patient outcomes associated with the presence and absence of these verbal and non-verbal primary care communications. Analysis of the full text of the studies in Beck et al. 191 did not reveal PROMs addressing PRO priorities of our PPI work. Griffin et al. 192 identified seven studies to potentially reveal a candidate PROM. Thom et al. 196 used two potentially relevant scales: the Physicians’ Humanistic Behaviours Questionnaire (PHBQ) and their own Trust in Physicians Scale. 199,200
A scoping search of Google Scholar using patient + activation + outcome identified the Patient Activation Scale and the Patient Activation Short-Form Scale. 178,201 A search for patient activation systematic reviews identified the Griffin et al. review. 192 We consequently added the two PAMs and, therefore, had five candidate scales (Table 15) that assess aspects of our priorities: (a) patient question asking; (b) clinician engagement with patient; (c) post-consultation recall; and (d) patients feeling more in control of their own condition. Although these PROMs had not been linked in experimental studies to DCCs but instead to clinician–patient communications, they were nonetheless all themes that were emerging from our LYNC study fieldwork. Consequently, we appraised them as having topic validity to underpin further consultation with the LYNC study PPI members.
| PROM name; number of items; number of recent citations | Citation | Number of ‘fit-for-purpose’ PPI votes (n = 5) |
|---|---|---|
| PAM; 22 items; from scale publication date to June 2015 cited by 590; 82 citations in 2015 | Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 2004;39:1005–26201 | 3 |
| PAM Short Form; 13 items; from scale publication date to June 2015 cited by 371, 54 citations in 2015 | Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res 2005;40:1918–30178 | 2 |
| Krantz Health Opinion Survey; 16 items; from scale publication date to June 2015 cited by 350, four citations in 2015 | Krantz DS, Baum A, Wideman MV. Assessment of preferences for self-treatment and information in health care. J Pers Soc Psychol 1980;39:977–90190 | 1 |
| Trust in Physician Scale; 11 items; from scale publication date to June 2015 cited by 391, 14 citations in 2015 | Thom DH, Ribisl KM, Stewart AL, Luke DA. Further validation and reliability testing of the Trust in Physician Scale. The Stanford Trust Study Physicians. Med Care 1999;37:510–17200 | 2 |
| PHBQ; 25 items; from scale publication date to June 2015 cited by 70, no citations in 2015 or 11 citations since 2011 | Weaver MJ, Ow CL, Walker DJ, Degenhardt EF. A questionnaire for patients’ evaluations of their physicians’ humanistic behaviors. J Gen Intern Med 1993;8:135–9199 | 3 |
The PMG PPI members were consulted to assess the face validity of the PROMs for evaluating the effects of DCCs. They were asked for their fit-for-purpose votes as follows: (1) fit for purpose, (2) may be fit for purpose or (3) not fit for purpose. The full PAM201 and the PHBQ199 emerged as having the greatest face validity for assessing the impact of DCC-enhanced care (see Table 15).
Cognitive interviews with Long-term conditions Young people Networked Communication study case site clinicians and young people
Method
Cognitive interviews were used to assess the face validity and content validity of the two candidate PROMs for a population of young people using DCCs with their specialist clinicians. Cognitive interviews are an established method for the development of outcome measures202–205 and, although we were not developing an outcome measure, we were evaluating an existing measure for a new purpose and thus similar criteria for measure development applied. These criteria are that the items have clarity, relevance and are unambiguous for the new purpose. 202 Cognitive interviews use a concurrent interviewing approach, in which participants are asked to ‘think aloud’ as they consider and complete the measure, and/or a debriefing approach, in which participants are asked to consider their experience of answering the questions and completing the measure immediately after its completion. 202,203 We used both concurrent and debriefing approaches in order to understand the detailed cognitions of the participant as they were completing individual items and their overall experience of completing the PROM and its fitness for purpose in the use of DCCs. As we acknowledged that there may be clinician barriers to achieving, or facilitating, the candidate PROM items in a digital care context, we felt that it was important to expose the candidate PROMs to clinicians as well as young people. This would identify whether there are differences in perspectives between people receiving digitally enhanced care and those offering it.
The objective of the cognitive interviews was to establish if:
-
the PAM has face and content validity for capturing patient self-care outcomes related to use of DCCs
-
the PHBQ has face and content validity for patients to assess aspects of the clinician’s consultation performance via DCCs.
For cognitive interviews, clinicians were briefed on the purpose of the interview and the rationale for each candidate PROM. They were then asked to consider each item and articulate what they were considering as they read it. As both PROMs are aimed at patient completion and not clinician completion, the clinicians were asked to consider the extent to which they themselves performed or supported the behaviours and attitudes in the items and score themselves according to the scoring criteria. In doing so they would be prompted to consider the item’s relevance in a digital care context. To reduce participant burden, each clinician interviewed was asked to consider just one PROM.
Young people PROM cognitive interviews took place at the end of the regular case study interview. The young participants were briefed on the purpose of the interview and of the measure. To reduce participant burden, each young person was asked to consider, in rotation, one in three of the items in both measures. Where the measure comprises domains, we ensured that each domain was represented in each shortened measure. The rotation of items in a looped one, two, three sequence was documented in a separate worksheet. We expected that young people would find it difficult to separate out their in-person from their digitally enhanced care. Consequently, young people were asked to ‘think aloud’ as they completed the measure in relation to their own care and where necessary were prompted to think about digitally delivered care. They were asked to think aloud in relation to their own experience of digitally enhanced care and record a personal response to each item. All interviews were audio-recorded, transcribed and anonymised.
Analysis
For both young person and clinician interviews, a spreadsheet was developed to indicate, by item, if the participant could answer the question with ease, if it was considered relevant and if they had DCC examples as they thought aloud. We did not record whether the digital care-related thoughts and cognitions were spontaneous or interviewer prompted, as we were principally interested in whether or not the items, and the measure as a whole, could be understood in a digitally enhanced care context.
Findings
Cognitive interviews were completed with six young people and six clinicians.
Face and content validity assessments of the Patient Activation Measure
The assessments were made by six clinicians and six young people and each individual item was assessed eight times. All clinicians effectively evaluated the 22-item instrument and the majority of responses were in agreement that the item was relevant in appraising DCCs. Most clinicians interviewed were able to provide examples of the relevance of the item to digitally enhanced care in support of their assessment. However, the clinicians raised a number of issues in relation to some items. A young people’s community worker disagreed with the idea of the patient taking sole responsibility for their health condition (item 1) and reported that it took a joint effort to maintain good health outcomes for each patient. Some item similarities were observed in the instrument, specifically with reference to the following paired questions: items 1 and 2, 13 and 16, and 18 and 20, which made either item redundant. A paediatrics diabetes mellitus nurse commented that they struggled to establish the relevance of items 3 and 6 in relation to evaluating outcomes for DCCs and suggested that further clarification was required. The same health-care professional also remarked about the significant overlap between items 10 and 12 and other items in the instrument and emphasised the need for topics to be used once so that patients could understand the measure effectively. A clinical psychologist also found items 15 and 20 to be ambiguous and, therefore, could not provide a response. The health-care professional added that item 18 was condition specific and would yield different responses in various health conditions. One diabetes mellitus clinician reported that he was yet to encounter a patient who had successfully made changes in adopting a healthy lifestyle when considering item 16. Overall, the PAM has a satisfactory level of face and content validity notwithstanding the issues raised regarding some items.
Face and content validity assessments of the Physicians’ Humanistic Behaviours Questionnaire
Assessments were made by six clinicians and six young people and each individual item was assessed eight times. Similar to the PAM, the 25-item instrument achieved > 50% agreement among clinicians who assessed the relevance of each item in the measure in consideration of evaluating outcomes for DCCs. Clinicians were able to provide DCC cognitions in support of their responses. There were also queries raised with regard to the ambiguity of some items in the PHBQ. Although a paediatric consultant agreed with the relevance of item 1, which probed on clinicians’ ability to follow through on patients’ problems and provided DCC cognitions, they commented that some patients would potentially find the item difficult to comprehend. They also stated that the idea of making promises to patients (item 7) was uncomfortable and suggested that the item needed readjustment. A paediatric diabetes mellitus nurse reported that item 3, ‘is in a hurry’, required a context to be given in order to make the question clear for patients to respond. Item 11 was thought to be irrelevant with regard to evaluating DCCs by the same health professional; this idea was also supported by a consultant who, in addition, thought the same of item 16. These two professionals deemed item 17 to be inappropriate for a DCCs scenario and it was suggested that further clarification on the item was necessary. Three clinicians had queries regarding item 21. The professionals stated that they were already familiar with their patients and would know how they preferred to be addressed. A consultant further added that patients would already have experience in answering patient satisfaction surveys in relation to item 22 and also thought item 24 would yield interesting responses. In summary, all 25 items were appraised successfully with a good response rate.
Young people’s appraisal of the patient-reported outcome measures
Owing to limiting the research burden of this activity for the young participants, each item was reviewed by two young participants only. There was high agreement on the relevance of each item in both measures. Young people often required prompting to provide DCC cognitions and on some occasions could not elaborate any further beyond one-word responses. Unlike clinicians, young people were unable to critically analyse an item and made no further remarks beyond their scale responses. Some interviewees provided additional information around their responses; however, the majority failed to answer questions in the context of evaluating DCCs without prompting. This was particularly evident where DCCs would be spontaneously reported in a narrative that centred mostly on responding to items in the instrument in relation to their health conditions only. However, when prompted, the majority could provide examples that included DCCs.
Published psychometric evaluations of the patient-reported outcome measures
Physicians’ Humanistic Behaviours Questionnaire
The aim of the PHBQ instrument development was to understand what humanistic physician behaviours performed (or not) in the physician–patient interaction were important to patients and to develop a measure to assess for these behaviours in different medical contexts. 199 Participating patients were required to have previously consulted with a named physician on at least two previous occasions. During a process of structured interviews and questionnaires, patients were asked to define and give examples of behaviours that communicated, or not, integrity, respect and compassion. From these interviews the authors developed 96 items. Through a further process of face and content validity assessment with 96 patients and completion and statistical analyses on the data from a further 109 patients, the 25-item PHBQ was confirmed and administered along with the Medical Interview Satisfaction Scale206 to 119 inpatients and 111 outpatients to assess the humanistic behaviours of six junior physicians. A senior physician rated the humanistic behaviours of the junior physicians once during the study period. The study demonstrates convergent reliability in the close correlation between the PHBQ and the Medical Interview Satisfaction Scale in both settings (r = 0.87; p < 0.001), indicating that humanistic physician behaviour increases satisfaction with care evaluations by patients. This was similarly appraised in a systematic review which included the PHBQ. 207 Assessments of patients by the PHBQ and the Medical Interview Satisfaction Scale were higher in the clinic setting than in the hospital setting. The authors indicate that there are a number of possible for reasons for this: the physicians behave differently in the two settings, possibly because of organisational and workload pressures; and the patients have different expectations of their physicians in both settings. No further evaluations of this full scale have been identified in the literature, although a number of investigators have used items from the PHBQ in new outcome measures or used the PHBQ to undertake convergence validity assessments against the new measure. 208–210 In conclusion, the PHBQ evidences satisfactory face, content and convergence validity, but reports no reliability evidence. Research endeavour is required to address its psychometric properties relating to reliability.
The Patient Activation Measure
The measure development commenced with a literature review from which a Delphi-type expert consensus process was completed with 21 experts to consider what knowledge, belief and skills requirements were needed by service users to self-manage their LTC. 201 From their responses, six domains were developed, which were presented to 19 service users in two focus groups for discussion and further exploration. Using the six domains, a pool of 80 items was generated, following which three rounds of cognitive interviews were undertaken with 20 participants. This resulted in a 75-item measure. This was completed by 100 participants and Rasch analysis undertaken on the data. This resulted in a 21-item measure and reliability of 0.85 (real) and 0.87 (model) with α = 0.87. A test–retest reliability assessment conducted by 30 respondents 2 weeks after the initial interview found that 28 out of 30 respondents had a retest activation estimate within 95% confidence intervals (CIs) of their test activation estimate. The third stage of extending and refining the PAM achieved a Rasch person reliability of 0.85 (real), 0.88 (model) and α = 0.91. When tested with a national sample at stage 4, the Rasch person reliability was 0.87 (real) and 0.91 (model). 201 Criterion validity was examined with 10 respondents from the initial study selected based on recording lowest and highest responses. In-depth semistructured interviews were conducted with these participants with the aim of obtaining elaborate responses, and three judges who were blind to the participant’s measured activation independently reviewed and categorised each transcript as either ‘low’ or ‘high’. The results illustrated that the three independent judges’ classification of participants agreed with the measured activation level 83% of the time. Cohen’s kappa for measured activation and each judge’s classification were 0.80, 0.90 and 0.90. In a third stage, new items were added to challenge respondents at the top and bottom ends of the activation scale, resulting in a 22-item scale, and this was evaluated in a further 486 participants with and without a LTC. In a final stage, the PAM was delivered in a national probability sample of 1515 people aged > 45 years. The PAM demonstrated construct and criterion validity as individuals with higher activation reported significantly better health, as measured by the Short Form-8, and lower rates of doctor appointments, emergency room visits and hospital nights (r = –0.07; p < 0.01). Those with higher activation were also more likely to engage in healthy behaviours. 201
Patient Activation Measure validation studies
The PAM 22 has been cross-validated only once, in India, in a cross-sectional study conducted with 417 chronically ill patients visiting an outpatients clinic. 211 The measure was translated into Bengali and yielded a Rasch person reliability of 0.85 (real) and 0.89 (model), which was considered consistent with the original English version. Good model fits for the Rasch model and principal component analysis confirmed the unidimensionality of the construct. The PAM 13 was developed a year later,178 and, in contrast to the PAM 22, this has undergone close to 20 revalidations across countries, languages and clinical populations. The PAM 13 was reviewed less favourably than the PAM 22 by our LYNC study PPI colleagues and so the PAM 13 evidence will not be further presented here. Overall, the PAM 22 consistently yielded high reliability at all stages in the original study and these findings were closely mirrored in the Indian revalidation. 201,211
Discussion
Principal findings
This represents a large body of activity consisting of literature reviewing, PPI work and empirical research aimed at addressing our research questions. Research question 1 sought to identify existing measures that had been used to assess digitally enhanced care outcomes. We identified 28 such PROMs which our PPI activity consultation outcomes identified to be lacking in relevance and credibility. We answer question 1 by stating that the published evidence relating to previous evaluations of digitally enhanced services did not reveal a suitable outcome measure.
Research question 2 sought to look prospectively at future evaluations of digitally enhanced care using PPI-informed scoping reviews based on the emerging strengths of such care provision from the LYNC study fieldwork. This process resulted in the identification of two PROMs with potential clinical and research utility. Both measures were satisfactorily appraised by clinicians and patients as having sufficient degrees of face and content validity to proceed with further experimental use in a digitally enhanced service. Psychometrically, the PAM has stronger and more detailed validity in demonstrating clear face, content, construct and criterion validity and psychometric reliability. The PHBQ has less documented detail about the face and content validity. However, the cognitive interviews suggest that it has sufficient face and content validity to proceed to reliability testing in a DCC evaluation. Both scales have demonstrated themselves to be credible clinical evaluation measures. Subsequent research studies need to expose them to real clinical evaluations of digitally enhanced services to examine how they perform psychometrically.
Strengths and limitations: patient and public involvement activity and literature reviews
Particular strengths lie in the PPI activities, which have involved > 150 people with experience of living with a LTC and using specialist health services. Approximately 30% of these individuals have direct experience of receiving a digitally enhanced service, with the remainder reporting no experience of this. This offers a good spread of considerations of the PROM topics from across the NHS service user community. Systematic reviews very often do not incorporate PPI activity and this was the case in our initial systematic review. Interestingly, it was only when we began to incorporate PPI perspectives into our literature reviewing that we began to make some progress in answering our research questions. Our first evidence review was systematic and based on our previously published reviews44,45,212 and we are confident that we captured the available evidence. Our scoping reviews, intertwined with our PPI activities, were much less so and were more PPI question led. It is likely that we missed published PROMs that might be of future relevance for evaluating digitally enhanced services.
Strengths and limitations: cognitive interviews
The cognitive interviews provided in-depth analyses of two PROMs with both clinicians and patients. We recruited a broad range of health professional disciplines to participate and four of the six health professionals evaluated both measures and in this respect showed commitment to the endeavour. These health professionals were experienced users of digitally enhanced care and so were evaluating the measures’ real clinical relevance for use in a service evaluation or audit context. In relation to the young people, they were all receivers of digitally enhanced care and all patients evaluated some aspects of both measures.
There are a number of limitations, most important of which is that most young people and some clinicians did not understand the exercise of doing cognitive interviews. The interviewer had to work with the time and level of understanding that the participant presented. In this respect, it could be argued that some interviews were not sufficiently accessing cognitions on the topic, particularly those of young people; when they did, it was following considerable prompting from the researcher in an attempt to facilitate the young person’s understanding of the interview purpose. Only two young people answered each item on both measures as a result of an alternating strategy implemented to maximise response rates and the young people were recruited from just two clinical areas which might affect their views and experiences. With regard to health professional interviews, one participant was unable to provide cognitions for their PROM use in a digitally enhanced service. In addition, they sometimes answered the questions in the third person, on behalf of the patient and, consequently, did not truly represent the level of assessment that patients would make about the two instruments.
In the cognitive interviews, the PAM and the PHBQ have demonstrated both strengths and weaknesses. The weaknesses lie in the scale in general, and some items in particular, and not in their usefulness in assessing digitally enhanced care. The clinicians interviewed were looking at the PAM as a clinical tool and they had not been asked to do otherwise; this may have contributed to some negative appraisals regarding item or topic repetition within the scale. Asking the same question in different ways is often a strength in a research tool to enable the research team to tease out response congruity. In a clinical setting, where time for both clinicians and patients is at a premium, repetition may appear wasteful and irritating. The PAM is one of the few PROMs that serves twin purposes of performing well as both a clinical and research tool (URL: www.england.nhs.uk/2016/07/person-centred-care/; accessed 5 March 2017). The shorter 13-item PAM, which was slightly less well appraised by our LYNC study PPI team, has considerably more citations and psychometric validity studies, and its brevity as both a clinical and research tool may be the reason for the greater level of interest in it than in the full 22-item scale.
In concluding this chapter, it is important to remind ourselves of the increasing levels of interest across health economies in PROs. The US Food and Drug Administration213 has produced guidance on their use by the pharmaceutical industry in recognition that the evolution of science and health-care products and practices should not come at any price. Although this advice is specifically intended for the pharmaceutical industry, Speight and Barendse214 remind us that the principles underpinning the US Food and Drug Administration’s guidance applies across other contexts. Health care is awash with technological solutions and in the area of DCCs and the context of our LYNC study focus, NHSmail 2 is currently undergoing roll-out across the NHS with the specific objective of promoting secure DCCs. With such fundamental shifts in the way that health care will be delivered and received on the horizon, it is imperative that we ensure that we have clinically and scientifically fit-for-purpose PROMs available that have credibility with patients, clinicians, researchers and technological innovators.
Chapter 10 Rapid scoping reviews, methods and findings from a review of families and carers of children and young people with health conditions
We undertook six rapid scoping reviews on topics emerging from the study. Here we present the overarching methods for all the reviews and the specific methods and findings from one of the reviews. The specific methods and the findings of the remaining five reviews are presented in Chapters 12 and 13. The review topics were selected to support and add value to the case study findings and place the case study findings in a wider research context.
Rapid scoping reviews offer an alternative to a traditional systematic review. Varying definitions of the methodology exist, common to these is the concept of the reviews being comprehensive, but having a shorter time line. Their purpose is to aid emergent decisions in health-care settings. They should be transparent, rigorous and useful. 215,216
Rapid review topics
The reviews are all related to DCCs with young people with LTCs. The six topics chosen were:
-
mental health
-
diabetes mellitus
-
physical health conditions (excluding diabetes mellitus)
-
countries with/moving towards universal health coverage
-
parents and carers
-
internet video (VoIP).
Three reviews addressed conditions. Two of these are updates of reviews previously conducted and published by some of the team members and concern conditions or groups of conditions focused on the case study sites. One is about the use of DCCs for mental health conditions. The second is about the use of DCCs for diabetes mellitus.
The third condition-focused review examined physical health conditions (excluding diabetes mellitus). This reflected the use of DCCs observed in the remaining case study sites, where young people were attending clinics for varying physical health conditions (e.g. cystic fibrosis).
The other three reviews addressed varied issues. One refers to the use of DCC in international settings, specifically on research from middle- and high-income countries with (or moving towards) universal health-care systems.
Another relates to the period of transition between youth and adult services, identified during the fieldwork as being a crucial period for young people and a difficult time for parents.
The final review examined a specific form of DCC: internet video. During recruitment of case study sites it became apparent that, despite rhetoric about the use of video and the benefits for consultation, there were no sites using this and only a few considering its use. The aim of summarising evidence on the use of video was to provide an overview of how video is actually being used in health-care settings, by reviewing the existing published reviews available.
This chapter and Chapters 12 and 13 will present the methods and results for the six rapid scoping reviews.
Search method for all rapid reviews
A comprehensive search was undertaken in the electronic databases MEDLINE (via Ovid); MEDLINE In-Process & Other Non-Indexed Citations (via Ovid); EMBASE (via Ovid); PsycINFO (via ProQuest); and The Cochrane Library (via Wiley Online Library) for relevant literature appropriate to five of the six reviews (the searches for the internet videoconferencing review were slightly different and are described in Chapter 13). The search strategy was developed iteratively in MEDLINE by an information specialist (RC), with reference to previous systematic reviews44,45 and translated appropriately for the other databases. Initial scoping searches conducted in July 2015 indicated that a wide range of terminology is used by authors and in indexing in this topic area; therefore, a sensitive search was necessary. Free text and thesaurus terms for the concepts of ‘technology’, ‘clinical communication’ and ‘population’ were combined to gather related literature (see Appendix 5). All records were exported to bibliographic management software (EndNote X7), where duplicates were identified and removed.
For the rapid scoping review on international perspectives on LTCs, the Latin American and Caribbean Health Sciences Literature, IndMED and ISMEAR local databases were also searched for relevant articles to capture non-English-language articles published in these databases.
In order to provide these rapid scoping reviews in a timely and efficient way, a manageable subset of records for screening at the title/abstract level was isolated for each of the five reviews. The individual approach is reported with each specific review.
For the review on internet videoconferencing a slightly different set of searches was undertaken, as it was felt important to capture studies on the use of this specific technology for clinical communication irrespective of the age of study participants. The searches are detailed in Chapter 13, in which this review is reported.
The inclusion and exclusion criteria for each review were, in part, determined by the results of the case studies. Each review aimed to summarise the available literature from the previous 5-year period in tables with a narrative synthesis and discussion of findings.
Use of digital clinical communication for families and carers of children and young people with health conditions: a rapid scoping review
Background
The use of digital communication technologies has become ubiquitous in our societies over the last two decades. These technologies encompass a wide range of tools such as social networking sites [(e.g. Facebook, Myspace (Viant Technology, Beverly Hills, CA, USA)], mobile phones and smartphones, VoIP system (e.g. Skype), forums, e-mail, or short message services (SMSs).
Digital communication technologies have also been extensively implemented into health care because of their capacity to modernise and facilitate communication between health-care professionals and patients. As young people are prolific users of new technologies, a large number of studies have assessed the feasibility of DCC between young people with LTCs and health professionals as a way to meet the special needs of this population. Indeed, the management of young people with LTCs is challenging, as they tend to disengage from health services and experience poorer health outcomes when compared with the adult population with the same conditions. 217 Saywer et al. 218 have emphasised that this population of patients have distinct health needs. This is of particular importance during the transition from paediatric to adult health services. 219 Although promising and increasingly used, the effectiveness of digital communication technologies on young people’s outcomes remain unclear. 44 Some studies are currently ongoing to review the evidence of the effectiveness of mobile phone and tablet applications in this subset of patients. 220
For young people with health conditions, parental involvement and parent–health professional relationships are an important part of the treatment journey. At present, it is unclear what impact digital communication has on these relationships. Some authors have emphasised that parents play an important part in promoting the development of young people’s self-management skills in LTC management, but they may be less confident than young people in using technology. 221,222
There is an emerging body of literature on the use of digital communication for families and carers (e.g. childminders, home care workers) within the scope of management of children and young people with short-term conditions or LTCs (e.g. web-based consultations for parents of children with atopic dermatitis223 and the use of SMSs as a tool to reduce the social exclusion experienced by caregivers of people with disabilities224).
In order to bring more clarity to this area, this review aims to evaluate evidence on the impact of the use of DCCs between families/carers and health professionals.
Aim and objectives
The aim of this review was to evaluate evidence on the impact of the use of DCCs for the families and carers of young persons with LTCs.
Objectives were to:
-
describe existing DCC use in families and carers of young persons with LTCs
-
evaluate the feasibility of using DCCs with the families and carers of young persons with LTCs
-
evaluate the impact of using DCCs with the families and carers of young persons with LTCs.
Methods
Search strategy
Once the common search had been conducted, a series of terms relating to the concepts of ‘families’ and ‘carers’ were used to search within EndNote in the title field; sorting by publication date was then undertaken to select only those records published from 2009 onwards (see Appendix 5 for the list of terms). A check was performed on a large sample of records identified within EndNote by searching using the same terms in any field and found that only a very few were potentially relevant. In addition, citation searches and searches of reference lists of the included studies and any previously published reviews were performed.
Inclusion and exclusion criteria
Study type/language of publication
All types of study design published in the English language from January 2009 to August 2015, except conference abstracts and studies with fewer than five participants.
Participants
Family members and/or carers of young people/adolescents/children aged between 0 and 25 years.
Condition/disease
All conditions.
Intervention
All forms of communication technologies which involve two-way communication between families (including but not limited to parents, brothers and sisters), carers (including but not limited to childminders and child care workers), and health professionals (including but not limited to clinicians, nurses and psychologists). These include e-mail, social networking sites, mobile telephony, SMSs, videoconferencing and teleconferencing, forums and electronic monitoring. Technologies involving only one-way data transmission, parent/young people communication and parent–parent communication were excluded.
Comparator
None prespecified.
Outcomes
We have reported the following outcomes:
-
patient outcomes (e.g. treatment outcomes, health behaviours, health status and well-being, communication)
-
health professional outcomes (e.g. knowledge and understanding, consultation processes)
-
health service delivery outcomes (e.g. adverse events, health economic outcomes)
-
technical problems (e.g. text messages not being received).
Screening
Two independent reviewers screened all identified bibliographic records by title/abstract and then one reviewer read the full text. The final list of included studies at the full-text level was validated by two other reviewers. The study flow and reasons for exclusion of full-text papers were documented in a study flow diagram.
Data extraction strategy
One reviewer extracted relevant data from papers using a standardised data collection form. This extraction was checked by another reviewer.
Quality assessment
For RCTs, economic evaluations and qualitative research papers, we used the Critical Appraisal Skills Programme (CASP) checklists. 225 For pre–post intervention uncontrolled studies, individual study quality was assessed using a checklist published by the National Institutes of Health for before-and-after (pre–post) studies with no control group. This 12-item checklist enables an assessment of uncontrolled studies and provides an overall quality rating. Checklists published by the National Institutes of Health were also used for cross-sectional and observational studies and controlled intervention studies. 226 For both quantitative and qualitative studies, quality assessment was performed independently by two reviewers. Any disagreements between the two reviewers were resolved by a third reviewer. The overall quality of included studies was rated as poor, fair or good.
Data analysis and synthesis
Study, intervention, population and outcome characteristics were summarised narratively and in summary tables. The findings are presented in a narrative format.
The protocol of the rapid review was registered in the international PROSPERO database under the following number: CRD42016035467.
Results
Search
The search identified 1156 potentially relevant records. We removed 956 records that did not meet our inclusion criteria at title/abstract stage, leaving 200 articles to be examined at full text. Among these, 168 were excluded leading to a total of 32 publications meeting our inclusion criteria. The flow diagram describing the process of identifying relevant literature can be found in Figure 17, including the reasons for exclusion of papers at full-text level.
FIGURE 17.
Study PRISMA flow diagram.
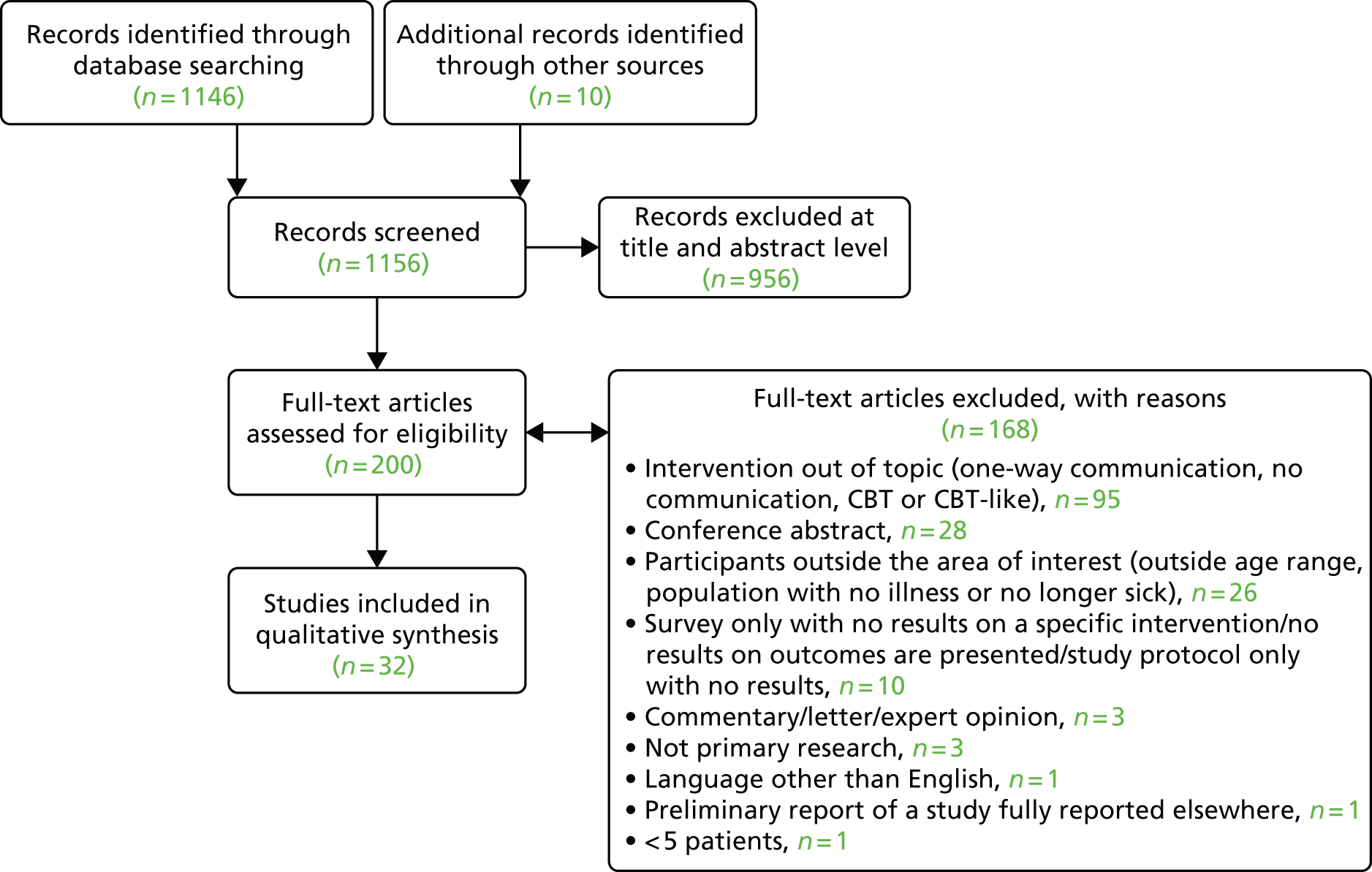
Characteristics of included studies
Of the 32 included publications (Table 16), 22 were quantitative research papers,223,227–229,235,236,238,240–247,249,250,252–256 four were qualitative224,230,237,251 and six were both quantitative and qualitative. 231–234,239,248 The majority of studies were conducted in the USA (17 studies 230,231,234,236,238–244,246,248,255); other main locations were Australia (three studies227,228,235), the Netherlands (three studies245,247,249), Sweden (three studies233,237,250) and the UK (two studies232,256).
| Author | Year of publication | Study design | Location | Participants | Technology | Intervention | Comparison |
|---|---|---|---|---|---|---|---|
| Barlott et al.224 | 2015 | Cross-sectional interview | Colombia | Eight parents of people with disabilities. Children aged 7–32 years | SMS | SMS messaging was used for parents of people with disabilities to receive information, ask questions and for social interaction | No comparison |
| Becker254 | 2011 | Pre–post intervention uncontrolled | USA |
63 parent/carers of healthy children. Child mean age was 6.5 years Phone call group, n = 33; and e-mail group, n = 30 |
A parent advice line, staffed by an on-call licensed psychologist and two doctoral students, was offered two nights per week. Parents could call or e-mail the service about common developmental problems (e.g. bed wetting, tantrums) | Parents who e-mailed the service were compared with those who contacted the service by telephone | |
| Bergmo et al.223 | 2009 | RCT | Norway |
Parents of 98 children with atopic dermatitis. The mean child age was 4.6 years in the intervention group and 5.3 years in the control group Intervention, n = 50; and control, n = 48 |
Web messaging | The intervention group received remote dermatology consultations where parents could send photographs of their child’s eczema with a written description of the condition. Based on this information, the specialist responded with treatment advice | A control group received usual care (i.e. they were encouraged to seek treatment through their GP or hospital visits) |
| Binford Hopf et al.255 | 2013 | Pre–post intervention uncontrolled | USA | 13 parents of 10 children aged 9–17 years with eating disorders | Web chat | Parents participated in 15 group web chat sessions with fellow parents and a clinical psychologist | Parents completed the Experience of Caregiving Inventory and the Eating Disorder Symptom Impact Scale before and after the intervention |
| Bradford et al.227 | 2014 | Economic model | Australia | 95 home video paediatric palliative care consultations | Video consultation | The actual cost of 95 home video consultations (home telehealth programme) were calculated. This was compared with the estimated cost of the consultations had they been conducted face to face | Costs of the home video consultations were compared with the estimated costs of face-to-face consultations |
| Bradford et al.228 | 2012 | Non-randomised controlled study | Australia |
14 parents of children (aged 0–18 years) referred to a PPCS Intervention, n = 6; control, n = 6; and not allocated, n = 2 |
Video consultation | Participants in the intervention group received a home telehealth consultation in addition to usual care. Home telehealth consultations included symptom management, discussions of changes in the patients and emotional support for caregivers | The intervention was compared with usual care, which included face-to-face care and the organisation of community nursing care services by PPCS staff |
| Braverman and Samsonov229 | 2011 | Cross-sectional study | Russia | 70 parents of children (aged 1 month–17 years) with kidney diseases | E-mails | An educational website for parents of children with kidney diseases allowed parents to ask questions, upload documents (e.g. medical summaries) and provide information about the child’s diagnosis | A paediatric nephrologist compared the information they received with the child’s diagnosis |
| Britto et al.230 | 2013 | Cross-sectional study | USA | 24 parents of 25 children with LTCs (cystic fibrosis, diabetes mellitus and juvenile idiopathic arthritis) | Web messaging | Condition-specific patient portals were developed. They provided access to medical record elements (e.g. test results) and allowed secure messaging with care providers | No comparison |
| Byczkowski et al.231 | 2014 | Cross-sectional study | USA | 126 parents of children with LTCs (cystic fibrosis, diabetes mellitus and juvenile idiopathic arthritis) who used the web-based portal and 15 parents who obtained an account for the portal but used it fewer than three times | Web messaging | Condition-specific patient portals were developed. They provided access to medical record elements (e.g. test results) and allowed secure messaging with care providers | No comparison |
| de Graaf et al.245 | 2013 | Cross-sectional study | Netherlands | 128 carers (127 parents and one grandparent) of children with infantile haemangioma | E-consults | Parents received an e-health intervention which included e-learning and e-consults. During e-consults, parents submitted a photograph of their child’s skin lesion and information about its growth pattern. A dermatologist provided advice on diagnosis and risk of complications and need to see a specialist by e-mail | No comparison |
| Epstein et al.248 | 2015 | Pre–post intervention uncontrolled with cross-sectional interview | USA | 26 parents of patients in the neonatal intensive care unit | Videoconferencing | Parents received daily Skype or FaceTime updates from the staff in the neonatal intensive care unit once a day for 5 days. The content of the updates was similar to those usually provided by telephone (feedings, events of the day, parents questions answered) | The Parents’ Understanding of Their Baby’s Care and Outcomes in the NICU Survey was completed before and after the intervention for comparison |
| Grover et al.256 | 2011 | RCT | UK |
64 carers of people with anorexia nervosa aged 12–44 years Intervention, n = 34; and control, n = 30 |
E-mails | Carers in the intervention group participated in web-based therapy sessions followed by e-mail or telephone support from a clinician | The intervention was compared with usual care |
| Grover et al.232 | 2011 | Pre–post intervention, with cross-sectional interview, uncontrolled | UK | 27 carers of people with anorexia nervosa aged 14–55 years | E-mails | Carers completed nine interactive workbooks designed for carers of people with anorexia nervosa. Clinician support of 20 minutes per week was also provided by e-mail or telephone | Five measures were compared at baseline, after the intervention and at the 10- to 12-week follow-up |
| Gulmans et al.249 | 2012 | Pre–post intervention uncontrolled | Netherlands | 30 parents of children with cerebral palsy aged between 4 and 8 years | Web messaging | A web-based system for parent–professional communication and interprofessional communication, where parents could ask questions and review their communication from professionals | Parents’ experience of parent–professional communication was compared before and after the intervention |
| Gund et al.233 | 2013 | RCT | Sweden |
34 families of preterm babies. Median infant gestational age = 33 weeks + 5 days Web application, n = 12; videoconferencing, n = 9; and control, n = 13 |
Web messaging or videoconferencing | The web application allowed families to communicate with health-care professionals via a web messaging service. In the videoconferencing intervention group families had videoconferences with nurses instead of telephone calls (standard home health care) | Web application and videoconferencing were compared with one another and a control group who received only standard home health care after discharge |
| Hanberger et al.250 | 2013 | RCT | Sweden |
474 families of children with type 1 diabetes mellitus. The mean child age in the intervention group was 13.2 years. The mean child age in the control group was 13.3 years Intervention, n = 244; and control, n = 230 |
Web messaging | The intervention included a web-based portal which provided diabetes mellitus-related information and allowed communication with diabetes mellitus peers and health-care professionals. All parents in the intervention group had access to the portal, as did children aged > 13 years | The intervention was compared with a control group who had no access to the web-based portal for the first year of the study |
| Haney and Tufts234 | 2012 | Pre–post intervention uncontrolled | USA | 19 parents and carers of children with various medical conditions (severe birth asphyxia, TBI, severe cerebral palsy, trisomy 18 . . .). The mean child age was 9.17 years | E-mails | Parents/caregivers communicated with nurses via e-mail. Nurses sent parent/caregivers a topic at the start of the week related to caring for a chronically ill child at home. Parents could send questions, comments and concerns | Well-being was compared before and after the intervention |
| Hanlon-Dearman et al.251 | 2014 | Cross-sectional study | Canada | 16 families of children diagnosed with fetal alcohol spectrum disorder | Videoconferencing | Families participated in diagnostic assessment and/or individual or group follow-up via telehealth | No comparison |
| Hopper et al.235 | 2011 | Observational study (survey of carers and consultation content) | Australia | 10 carers of children referred to a genetics service (children aged between 8 and 14 years) | Videoconferencing | Consultations with a genetic counsellor were video recorded, with a live feed of the session delivered to the clinical geneticist. DVDs of the session and still photos were also sent to the geneticist | Telemedicine consultations were compared with face-to-face consultations conducted with the same patients, carers, genetics counsellor and clinical geneticist |
| Lee et al.252 | 2010 | Cross-sectional study | USA | 42 parents of infants who underwent wide-field retinal imaging for retinopathy of prematurity | Web-based telemedicine system | Data from wide-field retinal imaging for retinopathy of prematurity was sent to a remote expert via telemedicine | No comparison |
| Looman et al.246 | 2015 | RCT | USA |
163 families of children with medical complexity receiving care from a special needs clinic (paediatric health-care home). Children were aged between 2 and 15 years at randomisation Intervention, n = 54; intervention + videoconferencing, n = 54; and control, n = 55 |
Videoconferencing | Participants in the intervention groups had access to an APRN care co-ordinator by telephone in one group and telephone and videoconferencing in the other | Two intervention groups (APRN telephone-delivered care co-ordination and APRN telephone care co-ordination + videoconferencing) were compared with a control group. Participants in the control group could contact the clinics general telephone number for care co-ordination |
| Mulgrew et al.236 | 2011 | Cross-sectional study | USA |
Parents of children who had received consultations for childhood obesity. Patients were aged between 4 and 11 years Telemedicine, n = 10; and face to face, n = 15 |
Unclear | Participants attending a rural/remote clinic received telemedicine consultations with a paediatrician specialising in weight management and a dietitian. A rural health-care provider was present with the patient and family during the consultation | Parent satisfaction was compared between those who received face-to-face consultations and those who received telemedicine consultations |
| Nordfeldt et al.237 | 2010 | Cross-sectional study | Sweden | 19 parents of children with type 1 diabetes mellitus and five children with type 1 diabetes mellitus aged between 11 and 18 years | Web messaging | A portal for patients and parents of patients with type 1 diabetes mellitus was launched. It provided diabetes mellitus information, blogs and message boards | No comparison |
| Petranovich et al.238 | 2015 | Clinical trial (randomised) | USA |
132 families of adolescents with traumatic brain injury. At baseline the mean patient age was 14.7 years in the counsellor-assisted problem-solving intervention group and 14.99 years in the internet resource comparison-programme group Counsellor-assisted problem-solving intervention group, n = 65; internet resource comparison programme group, n = 67 |
Videoconferencing | In the counsellor-assisted problem-solving intervention, families completed online modules and participated in Skype sessions with the therapist | The counsellor-assisted problem-solving intervention was compared with an internet resource comparison programme |
| Scharer et al.239 | 2009 | RCT | USA |
11 mothers (and maternal caregivers) of children with serious mental illness. Mean child age was 9.82 years Web-based support, n = 7; telephone support, n = 4 |
Web chat | In one group, patients received telephone social support on a one-to-one basis from a psychiatric nurse every 2 weeks. In the second group, a psychiatric nurse facilitated a chat room once a week for 1 hour (chats involving one mother and the nurse were analysed) | Web-based social support was compared with telephone social support |
| van Os-Medendorp et al.247 | 2012 | RCT | Netherlands |
90 parents of children with atopic dermatitis. The mean child age in the intervention group was 2.9 years. The mean child age in the control group was 2.7 years Intervention, n = 45; and control, n = 45 |
E-consultations | Patients in the intervention group had access to an eczema web portal which allowed e-consultations with a dermatology nurse and provided internet-guided monitoring and self-management training | The intervention was compared with a control group who received face-to-face consultations and monitoring and self-management training |
| Vismara et al.240 | 2013 | Pre–post intervention uncontrolled | USA | Parents of eight children with autism spectrum disorder. The mean child age was 27.5 months | Videoconferencing + e-mails | The intervention included videoconferencing with a therapist and a website allowing parents to access text- and video-based learning modules and message boards | Parent–child interaction was compared at baseline and after the intervention |
| Vismara et al.253 | 2012 | Pre–post intervention uncontrolled | USA | Parents of nine children with autism spectrum disorder. The mean child age was 28.89 months | Videoconferencing | The intervention included videoconferencing with a therapist and a parent intervention curriculum delivered by telehealth | Parent–child interaction was compared at baseline and after the intervention |
| Wade et al.241 | 2014 | Clinical trial (randomised) | USA |
132 families of adolescents with traumatic brain injury. At the time of injury, the mean patient age was 14.7 years in the internet resource comparison-programme group and 14.40 years in the counsellor-assisted problem-solving intervention group Counsellor-assisted problem-solving intervention group, n = 65; and internet resource comparison programme group, n = 67 |
Videoconferencing | In the counsellor-assisted problem-solving intervention group, families participated in online modules and Skype sessions with the therapist | The counsellor-assisted problem-solving intervention group was compared with an internet resource comparison programme (a home page with links to online resources) |
| Wade et al.242 | 2009 | Pre–post intervention uncontrolled | USA | Families of nine children aged between 3 and 8 years with traumatic brain injury | Videoconferencing | The intervention included videoconferencing and a website containing links to resources and self-guided session materials | Assessments (e.g. parent–child interaction and child behaviour) completed at baseline and at follow-up were compared |
| Wade et al.243 | 2012 | Clinical trial (randomised) | USA |
41 families of adolescents aged 11–18 years with TBI The TOPS group, n = 20; and the internet resource comparison-programme group, n = 21 |
Videoconferencing | The TOPS intervention included self-guided online modules and videoconferencing with a therapist | The TOPS intervention was compared with an internet resource comparison-programme (a home page with links to online resources) |
| Wade et al.244 | 2009 | Cross-sectional study | USA | Nine families of children with traumatic brain injury. The mean child age was 15.04 years | Videoconferencing | The TOPS intervention included self-guided online modules and videoconferencing with a therapist | No comparison |
The conditions of children/young people that were encountered included traumatic brain injury (five studies238,241–244), anorexia nervosa (three studies232,255,256), atopic dermatitis (two studies223,247), autism spectrum disorder (two studies240,253) and type 1 diabetes mellitus (two studies240,250). In two studies,227,228 children were receiving palliative care for different types of diseases. Three studies233,248,252 were related to the management of prematurity or some of its consequences. The range of mean age of children/young people with a condition was 24 days to 28 years (see Table 16).
The list of DCC tools that were used is reported in Table 16 and shows a broad range of tools across studies. However, as authors may have described similar technologies using different names, there may be some overlap between categories. Videoconferencing or video consultation was the most frequently used tool (14 studies 227,228,233,235,236,238,240–244,246,248,253), followed by e-mails or web messaging systems (13 studies223,229–232,234,237–239,245,247,249,250,254,256). Other categories were web chat (two studies239,255) and SMSs (one study224). The main categories of health-care professionals that were involved in the use of DCCs were therapists or CBT therapists (psychotherapist/psychologist) (11 studies235,238,240–244,251,253–255), physicians (eight studies223,227–229,232,236,245,256) and nurses (six studies233,234,239,248).
Stand-alone interventions comprised 13 studies,223,233,235,236,239,246,248,249,251,252,254–256 but in 19 studies224,227,229–234,237,238,240–245,247,250,253 the digital communication tool was included within a wider intervention such as a web-based therapy or web-based system (portal, telemedicine, telehealth, etc.), which allowed a two-way communication (e-mails, web messaging, videoconferencing, etc.) between health-care professionals and families/carers. The full list of included studies and their characteristics are reported in Table 16.
Quality assessment
The quality assessment of included studies is reported in Appendix 6, Table 24.
The majority of studies were rated as being fair or good, with only one study rated as being poor (see Appendix 6, Table 24). The main limitation of these studies was the uncertainty around whether or not the participants were representative of those who would be eligible for the intervention in the general population of interest.
Patient outcomes
Of the six studies that reported patients’ clinical outcomes,223,237,240,242,253,254 four found significant improvements for patients after the intervention compared with baseline. 223,240,253,254 Vismara et al. 253 found that the rate of child vocalisations and their joint attention increased, whereas Vismara et al. 240 found that child social communication behaviours improved. Both these studies used an intervention composed of videoconferencing and learning modules. Therefore, it cannot be concluded that the digital communication tool alone led to the improvement in patient outcomes. Becker254 found that the frequency and severity of the child’s disruptive behaviours was reduced at the 2-week follow-up compared with baseline. However, this difference was found in participants in both the digital communication group (e-mail) and the telephone group. Similarly, Bergmo et al. 223 found that the objective severity scoring of atopic dermatitis was improved at the 12-month follow-up in both the intervention group (remote dermatology consultations via web messaging) and the control group.
Two studies report patients’ perceptions of digital communication tools. 237,242 Digital communication tools were perceived positively by patients,242 and the majority found them easy to use. 237 Digital communication tools were also described by patients as helpful,242 and patients found advantages in their use (i.e. the availability of information in a diabetes mellitus portal). 237
Parent/carer outcomes
Several benefits of using digital communication tools were reported by parents/carers. These included the removal of barriers to communication, providing reassurance230 and feeling supported. 255 The majority of parents felt satisfied with the digital communication tools that they experienced. 235,251 The majority of parent/carers found them easy to use233,237,242,248 and the majority of parent/carers would recommend them to other parents. 245,251
No studies reported a difference in outcomes between the telehealth intervention and the control or alternative intervention group (e.g. telephone). 223,227,236,241,250,254
Six studies reported improvements for parents/carers after the intervention compared with baseline,223,227,240,241,253,255 whereas two studies reported no difference between baseline and follow-up. 234,248 Binford Hopf et al. 255 found an improvement in the score of the Eating Disorder Symptom Impact Scale after parents participated in web chat sessions with fellow parents and a clinical psychologist.
Vismara et al. 240,253 found that the Maternal Behaviour Rating Scale (designed to assess the quality of maternal interactive behaviour with children with learning difficulties) score increased from baseline to follow-up after interventions that included videoconferencing and a telehealth-delivered curriculum253 or online learning modules. 240 Wade et al. 241 found a reduction in caregiver distress after the intervention compared with baseline; Bradford et al. 227 found health-related quality of life improved after the intervention compared with baseline; and Bergmo et al. 223 found that the number of skin care treatments performed by parents improved. Of these six studies, three 223,227,241 found similar improvements in the control or alternative intervention group.
Mulgrew et al. 236 reported a disadvantage of digital communication tools. Parents rated telehealth consultation lower than face-to-face consultations when asked if the provider explained things about the child’s health in a way that is easy to understand.
Health-care professional outcomes
Two studies reported health-care professionals’ perceptions of digital communication tools. 233,248 Overall, their response was positive. In one study, 94% of 37 providers rated the ease of using videoconferencing as excellent or good and > 90% perceived videoconferencing to be reliable for updates in the neonatal intensive care unit. 248 Similarly, Gund et al. 233 found that most nurses were motivated to use the ICT; however, some were reluctant.
Health service delivery outcomes
Three studies224,229,231 described the use of digital communication tools. Two of the three studies reported the frequency of use, with one study finding 8.3 messages sent per participant over a 12-month period223 and one study finding 6.25 messages sent per participant over a 3-month period. 224 The content of digital communication was also described. Participants used SMSs for social interaction and to ask questions. 224 They used e-mail predominantly to provide information about common diseases and treatment. 229,231 One study231 found that 64% of 126 participants had used the portal instead of calling their health-care provider on at least one occasion.
Additionally, two studies227,247 reported economic benefits of using e-health compared with face-to-face consultations.
Technical problems
In three studies,237,253,255 participants reported experiencing technical problems when using digital communication tools. Vismara et al. 253 found that all nine participants recruited to their intervention experienced some degree of frustration when using the videoconferencing programme, including the audio or web cam not working or the internet connection freezing. Passwords were reported as a barrier to using the web portal and web messaging in Nordfeldt et al. ’s study,237 with the procedure for replacing lost passwords and creating your own password found to create problems. Finally, Binford Hopf et al. 255 found that 22.8% of 13 parents experienced technical problems during the web chat sessions with a therapist. However, the nature of these technical problems is not described.
Discussion
This review revealed an emerging body of literature on the use of DCC to improve families’ and carers’ involvement in the management of children and young people with short- or long-term illnesses. DCCs were found to be acceptable in most of the studies examined. Overall, parents/carers were satisfied with their experience of DCCs and found benefit in their use. Little difference was found between interventions that included DCCs and interventions that did not or where the control intervention was usual care. Two studies225,241 found economic benefits of using DCCs in comparison with in-person consultations. The included studies were mostly of fair to good quality and sampled families and carers of children and young people with a variety of illnesses.
Strengths and weaknesses
All the included studies presented results suggesting the feasibility of using DCCs, although several authors recognised these results to be preliminary and that they necessitated further confirmatory studies. Many studies within the review examined interventions composed of more than one component, making it difficult to determine whether the results were attributable to the use of DCCs or other aspects of the intervention. As we conducted a rapid review and not a systematic review, we were not able to undertake a grey literature search aimed to identify unpublished studies that could have failed to demonstrate the feasibility of such communication means. Consequently, we cannot exclude the absence of publication bias in this area. As the majority of included studies were conducted in the USA and overall came from only nine different countries, there is limited generalisability of the findings beyond these settings.
Comparison with other reviews
We are aware of a recently published systematic review that assessed telehealth tools and interventions to support family caregivers of paediatric, adult and older patients with chronic diseases. 257 This review, which included 64 articles published over the period 1997–2014, concluded that telehealth can positively affect care in family caregivers. Our work differs from the previous study as we were interested only in the impact of using DCCs for families or carers of young people with conditions and we excluded adults and older patients.
Conclusions
The review showed an emerging body of literature suggesting the feasibility of using digital clinical tools to enhance communication between families or carers of young people with conditions and health-care professionals. Further evaluations based on comparative studies with larger sample sizes are needed to confirm these preliminary results and should investigate the impact of using DCC in terms of quality and organisation of care, as well as the associated economic outcomes.
Chapter 11 Rapid reviews: findings
Here we present specific methodological features and findings of four rapid reviews:
-
the impact of communication technologies on clinical outcomes for young people with diabetes mellitus
-
effectiveness and impact of networked communication interventions in young people with mental health conditions
-
evaluation of the impacts and outcomes of digital communication technologies to promote access and engagement of young people with long-term physical conditions into health care
-
digital technology for communication between clinicians and young patients with LTCs in countries with or moving towards universal health coverage.
A rapid scoping review of the impact of communication technologies on clinical outcomes for young people with diabetes mellitus
Background
Diabetes mellitus is a common metabolic disorder. It affects > 3.2 million people in the UK, of whom approximately 35,000 are young people aged < 19 years. 258 NICE has recently lowered target HbA1C levels to 48 mmol/mol for children and young people in order to minimise risks of long-term complications. 259 However, in 2013–14, only 18.4% of children and young people with diabetes mellitus achieved the previous target for glycaemic control of < 58 mmol/mol, and 23.9% of children and young people have very poor glycaemic control (HbA1c levels of > 80 mmol/mol), predisposing them to dangerously high risks of health complications, such as diabetic ketoacidosis (DKA). 260 Research has indicated that clinical outcomes are worse in young diabetes mellitus patients than in older patients. 260,261 This has led to increased focus for the NHS as poor glycaemic control has been linked to increased risks of both microvascular and macrovascular complications. 260 Disorganised transition of patients from child to adult services also has a negative impact on clinical outcomes. The NHS identified the phenomenon and subsequently published a guide to facilitate a smoother transition from paediatric to adult services. 262
The use of communication technologies, such as mobile phones/smartphones, e-mail, SMSs/text messaging, VoIP (e.g. Skype) and social networks (e.g. Facebook and Twitter), has exploded in recent years. Now 90% of people in the UK own a mobile phone. 263 Among young adults aged 16–24 years, smartphone internet use has doubled over the past 5 years to 87%, and this age group is the highest subscriber (91%) to social networks. 264 Concurrently, digital communication systems are being increasingly developed specifically for health-care purposes. A Cochrane review of published evidence demonstrated the feasibility, and acceptability to patients, of establishing technologies in health care. 265 Evidence suggests that DCCs could help overcome some barriers to health-care access for marginalised groups. 266 These barriers include practical difficulties, such as travelling to a health-care centre and waiting for an appointment, and interpersonal difficulties, such as stigmatising and negative reactions to patients and lack of continuity of care. A review of the use of digital communication interventions between parents/carers of children with a LTC and health-care providers found that the technologies addressed issues of continuity of care, time constraints and geographical barriers. 55 The interventions commonly focused on medication management, education and physiological monitoring.
Several reviews have focused on the use of digital communication technologies in the management of diabetes mellitus in both children and adults. Telehealth is known to improve glycaemic control in adults,267 children and adolescents. 268 This can be facilitated through remote monitoring and treatment advice269 and diabetes mellitus self-management education. 270 Researchers have recently started to explore the use of more novel technologies in the care of diabetes mellitus patients. Text message (SMS)-based interventions have been used in the care of children and adolescents with diabetes mellitus to monitor blood glucose levels remotely and to send reminders and advice about medication and lifestyle choices. A review of such studies found that the impact of such interventions on glycaemic control and self-management was unclear. 271 Furthermore, although patients reported that using text messages was feasible and enjoyable, some did experience technical difficulties, resulting in data loss and affecting patient motivation. Applications on smartphones have been explored with adults with diabetes mellitus. Applications providing advice and assistance on how to manage diabetes mellitus help to improve glycaemic control. 272 There is, however, a lack of evidence for the impact of smartphones and applications on the glycaemic control of young adults and children with diabetes mellitus. 273 Studies exploring the use of social networking services have not yet studied well-known sites such as Facebook or Twitter, focusing instead on sites purposely designed for research. 274 Such interventions have provided secure messaging between patient and clinician (via e-mail or online chat rooms); self-management education; and a way of sharing medical records and blood glucose readings. A review of these studies reported that such interventions have a positive impact on glycaemic control and are a novel way of improving diabetes mellitus care. 274 Overall, digital communication technologies have the potential to positively affect the health of people with diabetes mellitus; however, the technology used must be appropriate to the patient group. 270
To date, only one review has focused on interventions that included two-way communications between clinicians and young adults with diabetes mellitus. 44 This review found that, although contact between clinician and patient increased, there was uncertainty about whether or not this led to improved clinical outcomes. As part of the wider LYNC study, this review will update this previous work.
Aim
The specific aim of this review is to present evidence for the effectiveness of digital communication technologies on clinical outcomes in young people with diabetes mellitus.
Methods
Search strategy
Please refer to Chapter 10 for details of the initial search conducted for five of the six rapid scoping reviews. Once the common search had been conducted, terms for the concept ‘diabetes’ were used to search within EndNote in any field and sorting by publication date was undertaken to select only those records published from 2009 onwards (see Appendix 5). In addition, searches of reference lists of the included studies were performed.
Inclusion and exclusion criteria
Study type/language of publication
All types of empirical study designs published in English, from May 2009 onwards were included.
Participants
Young people/adolescents (aged between 12 and 25 years) with diabetes mellitus (type 1 and 2). Mean/median age of the sample population of < 25 years were also included.
Condition/disease
We examined only diabetes mellitus type 1 and 2 and maturity-onset diabetes of the young. All other long-term illnesses were excluded. Patients with multiple long-term illnesses were excluded.
Intervention
All identified digital communication technologies involving two-way communication between patient and clinician were included. Examples include e-mails, SMSs, social networking websites, mobile telephony, videoconferencing and teleconferencing. Interventions that involve one-way data transmission were excluded. Clinicians included all health-care professionals.
Comparator
We compared the effectiveness of communication technology with traditional in-person intervention and, where relevant, telephone intervention.
Outcomes
All outcomes were included. We have reported the following outcomes:
-
patient outcomes [e.g. treatment outcomes (e.g. HbA1c levels), health behaviours, health status and well-being, communication]
-
health professional outcomes (e.g. knowledge and understanding, consultation processes)
-
health service delivery outcomes (e.g. adverse events, health economic outcomes)
-
technical problems (e.g. text messages not being received).
Screening
Two independent reviewers screened the identified papers at title and abstract stage and then four independent reviewers read the full text. Any discrepancies that arose between the reviewers were resolved by a fifth reviewer. The study flow and reasons for exclusion of full-text papers were documented in a study flow diagram.
Data extraction strategy
Two reviewers independently extracted relevant data from papers using a standardised data collection form.
Quality assessment
All included papers were assessed using the appropriate CASP instruments. 225 Studies with no flaws identified during this process were rated as being ‘good’. Studies with one or two limitations or uncertainties were rated as being ‘fair’ and any studies with three or more flaws were rated as ‘weak’.
Data analysis and synthesis
Study, intervention, population and outcome characteristics were summarised narratively and in summary tables. The findings are presented in a narrative format.
Results
Search
Initial searching yielded 775 unique records, of which 539 were removed based on their title and abstract. The full text of 236 was read and 223 were excluded: 120 did not meet the inclusion criteria, 68 were not full-text papers, 32 were not empirical papers and three were unobtainable in the time frame of the rapid review. To check reviewer agreement, 10% of papers were screened by two reviewers. Agreement was 94%. A total of 13 papers was included in the review (Figure 18).
FIGURE 18.
Study flow diagram.
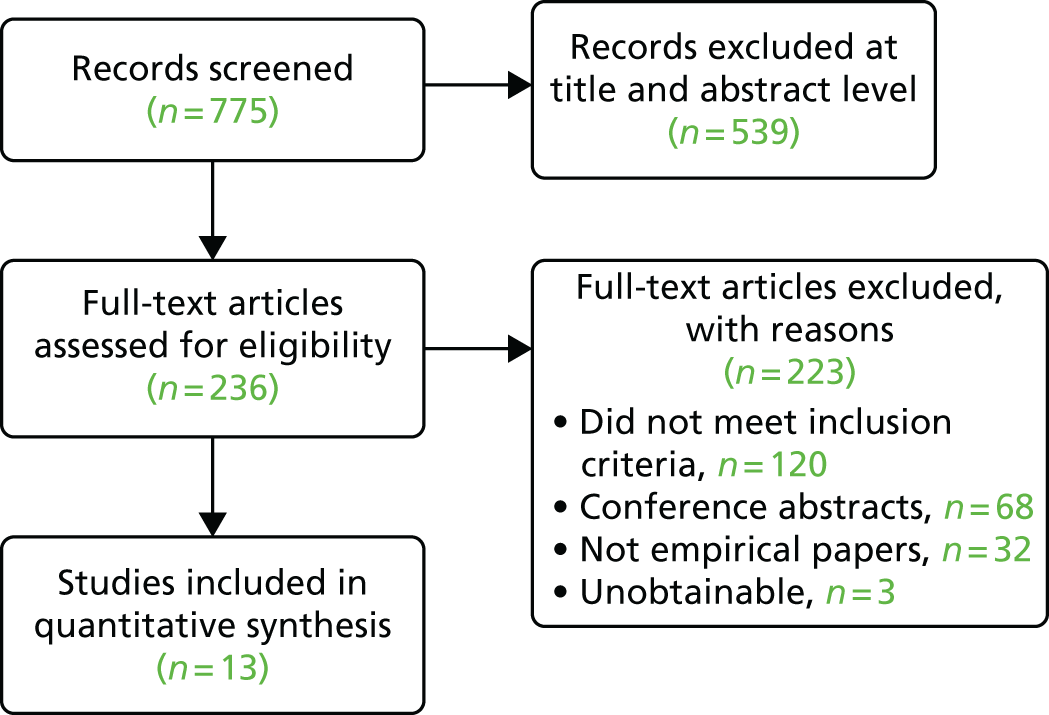
Characteristics of studies
Included studies were primarily RCTs (n = 7). Others were feasibility studies (n = 2), observational studies (n = 2), a pilot study (n = 1) and a retrospective study (n = 1). The studies were conducted in the USA (n = 6), Europe (n = 4), the Middle East (n = 2) and Australia (n = 1). None was conducted in the UK. A total of 1314 participants aged between 5 and 25 years participated in the studies. All studies examined the use of a digital intervention or digital service in diabetes mellitus care. Five studies used website-based interventions, three used videoconferencing/Skype, and the following technologies were utilised once: text messaging, e-mail, mobile telephony and mobile/web application (Table 17 contains more details on the included studies).
| Author | Year of publication | Study design | Location | Patients | Technology | Intervention | Comparison |
|---|---|---|---|---|---|---|---|
| Berndt et al.275 | 2014 | RCT with patient and health-care professional questionnaires | Germany |
68 children and teenagers aged between 8 and 18 years Intervention, n = 34; and control, n = 34 |
Mobile and web application | Application (Mobil Diab) where patients upload daily diabetes mellitus-related records. Medical staff (two diabetes mellitus specialists, two doctors, two nurses and one psychologist) can also access the app to analyse data and provide feedback | A control group received conventional therapy without the use of Mobil Diab |
| Boogerd et al.276 | 2014 | Feasibility study | Netherlands |
62 adolescents aged 11–21 years Intervention, n = 31; and control, n = 31 |
Online forum and messaging service | Sugarsquare is an online environment with four applications: (1) my diabetes, (2) chat, (3) forum and (4) carelink. Sugarsquare provides a message board for private discussion with professionals and individual treatment overview of basic diabetes mellitus data (e.g. HbA1c levels). Additionally, there is an opportunity to chat and read/contribute to forum posts with other members | A control group received care as usual without access to Sugarsquare |
| Carroll et al.277 | 2011 | Feasibility study | USA | 39 adolescents aged 13–18 years | Mobile glucose testing and text messaging | Glucophone is an integrated mobile phone and glucose metre. Individuals test their glucose levels through a mobile phone and the system uploads the measurement to a host computer. A nurse practitioner can then review data in the host computer, as can the parent/patient. Glucophone can also be used to text message or voice contact the nurse practitioner, who reviews data daily and can use text messaging to discuss blood glucose results, offer adjustments or suggest additional contact | NA |
| Choi et al.278 | 2013 | Retrospective study | USA | 31 young people aged 6–19 years with poorly controlled type 1 diabetes mellitus | A paediatric diabetes mellitus clinic relying almost exclusively on telemedicine. Adjustments to insulin regime (injections or pump) are done remotely. Patients and parents are provided with a messaging service comprising a group e-mail address for the diabetic team and paging access for emergencies. Patients and parents are encouraged to make all routine contact (e.g. prescriptions and routine questions) through e-mail. Clinic appointments were scheduled as needed | NA | |
| Farrell and Holmes-Walker279 | 2011 | Observational study | Australia |
A total of 350 patients aged between 15 and 25 years Group 1: clinic attendees without ketosis, n = 285; group 2: clinic attendees with ketosis accessing phone support, n = 31; group 3: clinic attendees not accessing mobile phone support presenting to hospital with ketoacidosis, n = 15; and group 4: non-clinic patients presenting to hospital with ketoacidosis, n = 19 |
Mobile phone | 24-hour mobile phone support for DKA by calling or text messaging a dedicated number for the diabetes mellitus transition support programme. Patients were encouraged to make contact for support with sick days if they self-tested high for ketosis and felt unwell, in order to prevent progression to ketoacidosis | A control group comprised clinic attendees without ketosis |
| Freeman et al.280 | 2013 | Observational study | USA |
71 patients aged 12–19 years with poorly controlled type 1 diabetes mellitus and at least one parent/guardian Intervention, n = 32; and control, n = 39) |
Skype | Ten sessions of BFST-D with trained therapists over 12 weeks via Skype. BFST-D is an intervention with four components: (1) problem-solving training, (2) communication skills training, (3) cognitive restructuring and (4) family systems intervention | A control group received clinic-based care |
| Frøisland et al.281 | 2012 | Pilot study with qualitative interviews | Norway | 12 patients aged 13–19 years (seven girls and five boys). All received the intervention | Mobile phone application and text messaging | A mobile phone-based diabetes mellitus diary Diamob and the diabetes mellitus message system, a text message service. Diamob is a camera-based tool used by adolescents with type 1 diabetes mellitus to document the food they ate. Diamob records blood glucose values before and after eating, insulin dose given and details about the patient’s physical activity. Secure text messaging was used between patient and two clinicians to discuss obstacles the patient faced in everyday life | NA |
| Hanberger et al.250 | 2013 | RCT with questionnaires | Sweden |
A total of 484 patients aged 0–18 years and their parents Year 1: intervention n = 244, control n = 230; year 2: intervention accepted by additional families in n = 254, previous control and newly diagnosed patients |
Web portal | Web 2.0 portal offered self-directed communication with health professionals, interaction with peers and access to information. It provides a service for prescription renewal, appointments and questions | A control group received no access to the Web 2.0 portal |
| Harris et al.282 | 2015 | RCT with questionnaires | USA |
90 young people aged 12–19 years Intervention, n = 46; and control, n = 44 |
Skype | Clinicians delivered BFST-D280 to adolescents and at least one caregiver via Skype. Patients received up to 10 therapy sessions over 12 weeks | A control group received the intervention in conventional clinic conditions |
| Izquierdo et al.283 | 2009 | RCT with questionnaires | USA |
41 participants aged 5–14 years Intervention, n = 23; and control, n = 18 |
Videoconference | Use of a portal supported by a V-connect application to facilitate communication between schools and the diabetes mellitus team. The portal allowed clinical data to be shared and monthly videoconferences between the school nurse, student (with or without a parent) and diabetes mellitus team to discuss management of the child’s diabetes mellitus | A control group received usual care (medical visits every 3 months and communication between school nurse and diabetes mellitus team by telephone as needed) |
| Landau et al.284 | 2012 | RCT | Israel |
70 adolescents aged 11–20 years Intervention, n = 36; and control, n = 34 |
Website | Use of the Medtronic CareLink website. Participants used the website to submit their blood glucose levels weekly to the diabetes mellitus care team during a 6-month period. A member of the clinical team contacted the parents by telephone if adjustments to medication were required | A control group received routine follow-up |
| Moattari et al.285 | 2013 | RCT | Iran |
48 participants aged 18–39 years Intervention, n = 24; and control, n = 24 |
Website and text messaging | Website-based educational intervention that also provided monitoring, a question–answer section and an opportunity for non-synchronous communication with clinicians (physician, nurse and nutritionist) via telephone and text messaging | A control group received standard educational advice |
| Pinsker et al.286 | 2011 | Observational study | USA | 16 participants who’s HbA1c level was above the American Diabetes Association guidelines. Intervention users (n = 9) mean age was 11.5 years; intervention non-users (n = 7) mean age was 10.9 years | Website | The Paediatric Diabetes Education Portal was designed to supplement the education delivered during clinic appointments and to improve access to care. The portal provided educational materials, and allowed users to post questions and read responses from their physician and diabetes mellitus education | NA |
Quality assessment
Overall, the quality of included papers was rated as being fair. Only three papers were rated as being good,285–287 whereas three were rated as being weak. 281,282,288 Weaknesses included the small sample size, lack of control group and poor analysis reporting (see Appendix 6, Table 26).
Patient outcomes
Improvements in intervention group HbA1c levels were seen in only four studies. 275,278,283,285 Of these, improvements were also seen in the control group,275 and no significant differences between the intervention and control were reported after 6 months. 283 Three studies reported no reduction in HbA1c levels following DCC interventions279,281,284 and five studies found no differences when the intervention was compared with a control. 250,276,282,284,286 Additionally, one study found that low-density lipoprotein cholesterol concentrations decreased significantly in the intervention arm and high-density lipoprotein cholesterol concentrations increased significantly in both the experimental and control groups. 285
Five studies reported positive impacts of DCC interventions on patients’ physical health (BMI and weight stabilised, whereas they increased in the control group,275 glucose testing increased,277 DKA admission rates decreased279 and the number of urgent clinic appointments decreased). 283 Findings were less clear regarding psychological outcomes, however. Two studies reported no differences in quality of life between the intervention and control groups. 250,276,283 There were also mixed findings in relation to self-efficacy: two studies found that self-efficacy and self-management increased in the intervention group,275,277 whereas one found no differences. 276
In the qualitative pilot study, patients reported benefits to the intervention. 281 The ability to contact their clinician via text message gave patients a sense of protection, as it was easy to ask questions and raise concerns about their health. They also appreciated the possibility of getting an immediate response to any concerns (rather than waiting for an appointment), and felt that using text messages made them feel closer to their clinician.
Health-care professional outcomes
Outcomes for health-care professionals were reported by only one study. 275 Berndt et al. 275 reported that health-care staff identified several benefits to their application, focusing on the daily diabetes mellitus-related records uploaded by patients: having regular data input creates a complete disease history, which is useful for developing individual therapy plans and minimising errors; having access to patients’ data from any time and location; and an automatic alarm message in case of critical data from a patient.
Health service delivery outcomes
Again, outcomes for health service delivery were reported by only one study. 275 Berndt et al. 275 reported that the intervention could delay and reduce complications, thereby minimising hospitalisation rates and reducing death rates. However, as this study reported improvements in the control arm of their study, as well as the intervention arm, these conclusions are speculative.
Adverse events
One study reports an episode of DKA in the intervention arm. 284 There was no discussion whether or not this episode was linked to the intervention. No other adverse events were reported.
Discussion
This review has explored the impact of DCCs on clinical outcomes in young people with diabetes mellitus. There was no clear indication as to how digital communication technologies affected glycaemic control; some studies reported decreased HbA1c levels in the intervention groups,275,278,283,285 whereas others reported no significant impact of DCCs on HbA1c levels. 250,276,279,281,282,284,286 Similarly, findings relating to psychological outcomes were mixed. There was a trend for reporting other benefits of the interventions, such as increased glucose testing277 and decreased admissions for DKA,279 but these were isolated findings not supported by other studies. These findings update a 2011 review exploring the use of communication technologies with young people with diabetes mellitus44 and support the authors’ original findings. Overall, there is no clear picture as to how DCCs affect clinical outcomes in young people with diabetes mellitus.
Potential benefits of DCC interventions for health-care professionals and health service delivery were described; however, these were not supported by data. 275 Advantages to the intervention described focused on the transmission of health records rather than two-way communication between the health professional and patient.
Comparison with other reviews
Previous reviews of the use of communication technology in the care of children and young adults with diabetes mellitus have produced conflicting conclusions. Similar to current findings, a review of the use of text messaging found that the impact of such interventions on glycaemic control and self-management was unclear,271 whereas other reviews have found that telehealth improves glycaemic control. 267,268 This confusing picture could be a result of the different patient groups targeted by interventions. Some of our included studies targeted young children and their parents, whereas others focused on teenagers or young adults. This difference could explain some of the variation in findings. Similarly, the variety of communication technologies used in different studies could account for the mixed findings. Each technology could hold different appeal to diverse population groups, and there will be different advantages and difficulties for the patient and staff groups using them. Additionally, the purposes of the technology-enhanced communication differed. For some the purpose was to increase patient knowledge of diabetes mellitus, for others it was to improve blood glucose monitoring or to improve glycaemic control. These differing purposes may alter what is communicated via these technological methods which may affect outcome.
Strengths and limitations
Overall, the research included in this review is not high quality. Three of the 13 included studies were rated as being weak, with very small sample sizes and poor reporting. 277,278,286 Higher-quality evidence is needed to produce a more complete picture of the impact of DCCs on diabetes mellitus care in young people.
This was a rapid review which has the advantage of synthesising evidence quickly in a changing technical environment; however, it does not include papers that are difficult to obtain.
Conclusion
This review analyses recent evidence for the impact of digital communication technologies on clinical outcomes in young people with diabetes mellitus. From the studies analysed, there is no clear benefit to the use of digital communication technology. However, the quality of the research is rated as moderate, highlighting the need for further research in this area.
Effectiveness and impact of networked communication interventions in young people with mental health conditions
Background
Worldwide, mental illness is a significant source of disease burden. 289 Its impacts are far-reaching and it negatively affects physical health, educational attainment, social capital and emotional well-being. 287,288,290 In young people, this is particularly significant. It is estimated that the economic cost amounts to £105B a year in the UK alone. 291
Most mental health problems begin in childhood or young adulthood,292 and their prevalence increases with age, affecting 7.7% of young people aged 5–10 years, 11.5% of young people aged 11–16 years 293 and around 23% of young people aged 18–20 years. 294 The prevalence of conditions such as depression increased among young people over the 20 years 1986–2006. 295 Early intervention and good care have been shown to be cost-effective and improve both short- and long-term outcomes. 296 Early intervention in psychosis, for example, has a reasonable evidence base297 and has been widely implemented in the UK.
There are a number of challenges associated with providing health care for young people, including barriers to access, behavioural issues such as risk-taking behaviour and problems associated with transitioning from paediatric to adult services. 298–300 This is particularly relevant in mental health, where there are significant differences between CAMHS and Adult Mental Health Services, and there is concern that young people may get lost as a result of the gaps in service provision. 301–303
The previous review, which examined diabetes mellitus, outlined the dramatic increase in utilisation of the communication technologies in recent years by young adults and the increasing development of digital communication systems for health-care purposes.
To date, systematic reviews focusing on two-way communication between clinician and young adults with mental health conditions are scarce. A previous review found that networked communication technologies can increase the opportunity for communication between patient and health-care professionals, but that limited improvements in quality of life and continuity of care were reported. 45 As part of the wider LYNC study, this review will update this previous work.
Aim
The aim of this review is to present evidence for the effectiveness of digital communication technologies on clinical and process outcomes.
Methods
Search strategy
Please refer to Chapter 11 for details of the initial search conducted for five of the six rapid scoping reviews. Once the common search had been conducted, search terms relating to mental health were used to search within EndNote and sorting by publication date was undertaken to select only those records published from 2009 onwards (see Appendix 5 for the list of terms). In addition, searches of reference lists of the included studies were performed.
Inclusion and exclusion criteria
Study type/language of publication
All types of study design published from May 2009 were included in the study. We excluded systematic reviews and literature reviews.
Participants
Adolescents and young adults (study mean age was 12–25 years) with any mental health disorder defined by the Diagnostic and Statistical Manual of Mental Disorders304 were included.
Condition/disease
We excluded studies that focused on neurodevelopmental disorders, such as attention deficit–hyperactivity disorder and autism, and non-chronic conditions, such as acute stress reaction.
Intervention
All digital communication technologies that allow for two-way communication between the patient and the health-care professional, such as e-mailing and social networking, were included. Those that allowed only one-way communication were excluded. Multifaceted interventions were also excluded. Studies evaluating computerised CBT were excluded from this review.
Comparator
Comparators were not prespecified.
Outcomes
All outcomes of communication technology as an intervention were included. The primary outcomes were clinical [e.g. measured by clinical scores such as the Beck Depression Inventory305 or Hospital Anxiety and Depression Scale (HADS)159]. Secondary outcomes included process outcomes (patient satisfaction, compliance, clinician satisfaction, cost) and cognitive outcomes (knowledge of condition, attitude, self-efficacy).
Screening
All titles and abstracts resulting from the initial search were screened for inclusion by one of two reviewers. A random selection of 20% were screened by both reviewers. A third reviewer resolved any disagreements. Reasons for exclusion were recorded. The full-text articles were screened by two reviewers. Any discrepancies over inclusion were resolved through discussion or with the help of a third reviewer. Literature in languages other than English was translated. The study flow and reasons for exclusion of full-text papers were documented in a study flow diagram.
Data extraction strategy
Two reviewers extracted relevant data from papers using a standardised data collection form.
Quality assessment
All included papers were assessed using the appropriate CASP instruments. 225 Studies with no flaws identified during this process were rated as ‘good’. Studies with one or two limitations or uncertainties were rated as ‘fair’ and any research with three or more flaws was rated as ‘weak’.
Data analysis and synthesis
The findings of this review were summarised using narrative synthesis and are presented in tables and text.
The protocol of the rapid review was registered in the International PROSPERO database under the following number: CRD42016038792.
Results
Search
The search resulted in 3503 papers. A total of 3281 were excluded based on title or abstract. Two hundred and twenty-two papers were read in full and a total of six papers met our inclusion criteria and form part of the review as presented in Figure 19.
FIGURE 19.
Study PRISMA flow diagram. CCBT, computerised cognitive–behavioural therapy.
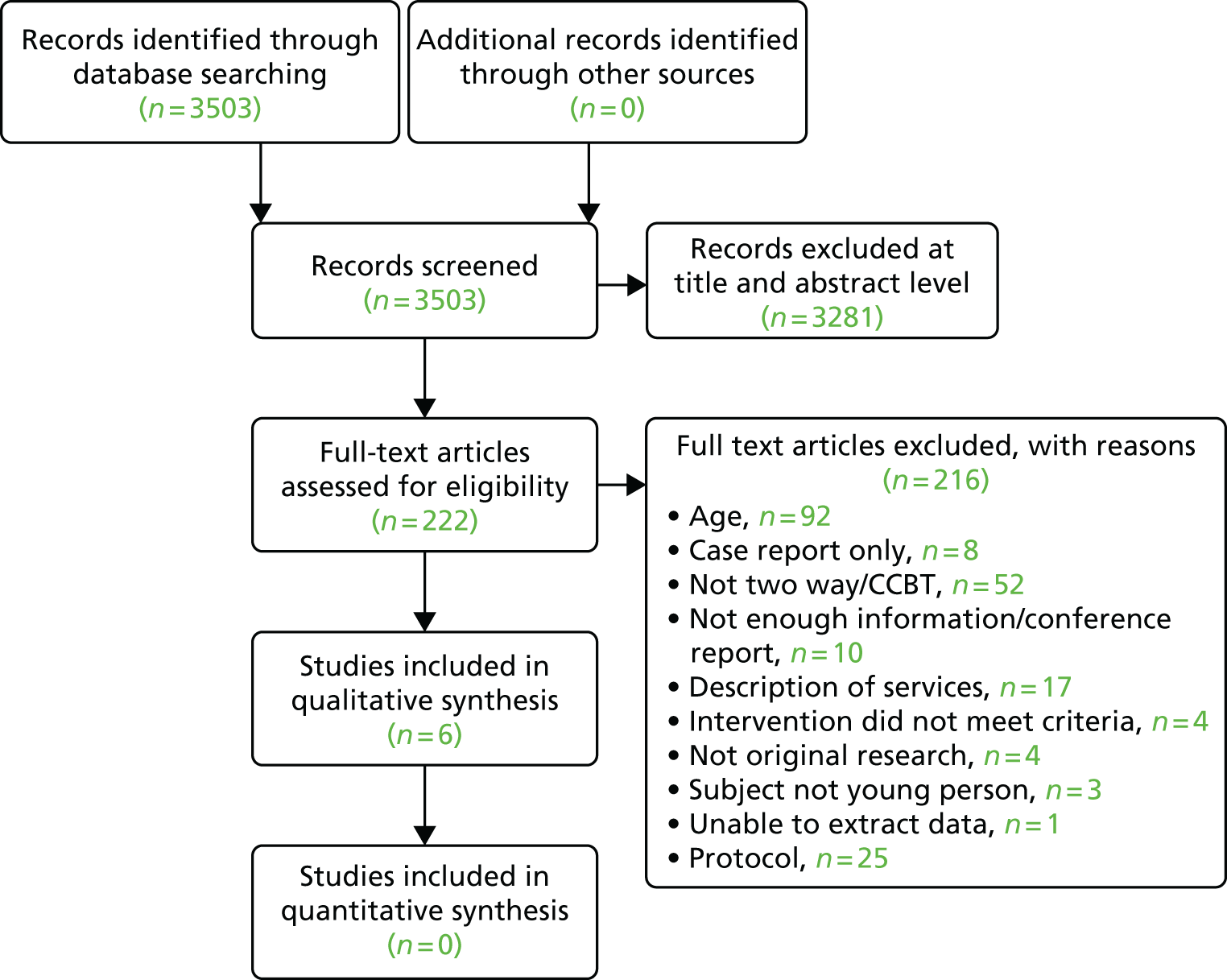
Characteristics of studies
The six studies306–311 comprised 637 young people, both male and female, with a range of mental health conditions [depression (n = 3), psychosis (n = 1), obsessive–compulsive disorder (n = 1) and mixed (n = 1)]. Sample sizes ranged from 11 to 263. Interventions included CBT, solution-focused brief therapy, psychiatric consultations and neuropsychiatric testing. One intervention was group based (in an online chat room) and all others were one to one. Studies were located in the USA, the UK, the Netherlands and Canada. All were published in English. Studies were published between 2010 and 2014 (note that studies published before 2009 were excluded). Four quantitative and two qualitative studies were included, as presented in Table 18.
| First author, date of publication, country | Study design | Population | Intervention | Outcomes |
|---|---|---|---|---|
| Williams, 2014, USA306 |
Quantitative and qualitative Aim: subsection of a study aiming to find out the feasibility and acceptability of web-based screening for depression Further details: students screening positive for depression in a web-based screening tool were invited to take part in telepsychiatric consultation |
Total, n: 17 Mean age (SD): not stated, college student Gender: M, n = 3; F, n = 14 Withdrawals, n: 52 Dropouts, n: NA Study groups, n: 1 Intervention group: n = 17 Comparison groups: n = 0 Recruitment area: universities in Massachusetts, USA Mental illness: depression |
Technologies used: videoconferencing |
Patient experience: satisfaction questionnaire Frequency of contact: once only |
| van der Zanden 2012, the Netherlands307 |
Quantitative Aim: to evaluate the effectiveness of a professionally facilitated online group-based CBT course [Grip op Je Dip (Master Your Mood)] delivered via a secure chat room, for people aged 16–25 years with depressive symptoms Further details: participants randomly allocated to either intervention or control (on waiting list for 14 weeks) |
Total, n: 244 Mean age (SD): not stated (16–25 years) Gender: M, n = 38; F, n = 106 Withdrawals: not stated Dropouts: 50 (at 12 weeks), 21 (at 12–24 weeks) Study groups, n: 2 Intervention group: n = 121 Comparison groups: n = 123 Recruitment area: advertising in general practices, educational institutions and online Mental illness: depression |
Technologies used: online chat room |
Primary: CES-D score Secondary: HADS, five-item mastery scale (sense of control) Frequency of contact: six sessions, 90 minutes each, once a week |
| Stain, 2011, Australia308 |
Quantitative Aim: to determine the feasibility of neuropsychological assessments via videoconferencing Further details: neuropsychological–Wechsler Test of Adult Reading; WMS-R Logical Memory Subtest; WAIS-III® Digit Span Subtest; and Controlled Oral Word Association Test. Clinical: Brief Psychiatric Rating Scale; Assessment of Quality of Life; Social and Occupational Functioning Assessment Scale; and Opiate Treatment Index |
Total, n: 11 Mean age (SD): 20 years Gender: M, n = 5; F, n = 6 Withdrawals, n: NA Dropouts: NA Study groups, n: 1 Recruitment area: mental health services within 170 km of Orange, New South Wales Mental illness: psychosis |
Technologies used: videoconferencing | Clinical: feasibility of testing |
| Turner, 2014, UK309 |
Quantitative Aim: to determine whether or not telephone CBT is as effective as face-to-face CBT for adolescents with OCD |
Total, n: 72 Mean age (SD): 14.19 years Gender: M, n = 40; F, n = 32 Dropouts: CBT, n = 3; telephone CBT, n = 3 Study groups, n: 2 Intervention group: n = 36 Comparison groups: n = 36 Recruitment area: referral from primary, secondary and tertiary care within the NHS Mental illness: OCD |
Technologies used: telephone |
Primary: Children’s Yale–Brown Obsessive-Compulsive Scale Secondary: depressive symptoms, self-report and parent-report of adolescent OCD symptoms, overall psychological health, global functioning and parental mental health symptoms Frequency of contact: 14 sessions over 17 weeks |
| Boydell, 2010, Canada310 |
Qualitative Aim: to explore the young person’s perspective on the experience of the psychiatric encounter, of receiving psychiatric services via televideo, and technological issues |
Total, n: 30 Mean age (SD): not stated, aged 7–18 years Gender: M, n = 17; F, n = 13 Study groups, n: 1 Recruitment area: rural and remote mental health organisations in Ontario Mental illness: mixed |
Technologies used: videoconferencing | Patient experience |
| Kramer, 2014, the Netherlands311 |
RCT Aim: to establish the effectiveness of solution-focused brief therapy delivered via a web-based chat room, for reducing depressive symptoms in young adults and adolescents Further details: participants randomly allocated to either the intervention or control (on a waiting list for 4.5 months) |
Total, n: 263 Mean age (SD): 19.5 years Gender: M, n = 56; F, n = 207 Study groups, n: 2 Intervention group: n = 131 Comparison groups: n = 132 Recruitment area: newspapers, websites and Facebook in the Netherlands Mental illness: depression |
Technologies used: secure chat room | Clinical: CES-D score |
Quality assessment
Overall, the quality of included papers was rated as fair. Only one paper was rated as good,308 whereas four were rated as fair307,309–311 and one was rated as weak. 306 Weaknesses included the small sample size, lack of control group and poor analysis reporting (see Appendix 6, Table 28).
Clinical outcomes
Four papers reported on clinical outcomes (see Table 18). 307–309,311 One study investigated online group CBT and found a statistically significant improvement in depressive symptoms, anxiety and mastery at both 12 weeks {depressive symptoms [as measured via the Center for Epidemiologic Studies Depression Scale (CES-D): d = 0.94, 95% CI 0.64 to 1.23], anxiety (as measured via the HADS anxiety: d = 0.49, 95% CI 0.24 to 0.75), and mastery (as measured by the 5-Item Mastery Scale: d = 0.44, 95% CI 0.19 to 0.70)} and 24 weeks [depressive symptoms (CES-D: d = 1.13, 95% CI 0.78 to 1.47), anxiety (HADS anxiety: d = 0.53, 95% CI 0.25 to 0.81), and mastery (5-Item Mastery Scale: d = 0.51, 95% CI 0.23 to 0.79)] compared with the control group. 307 Another study, looking at solution-focused brief therapy for depression delivered via web-based chat room, found an improvement in CES-D scores in the intervention group compared with the waiting list control at 9 weeks (d = 0.18, 95% CI –0.10 to 0.47) and 4.5 months (d = 0.79, 95% CI 0.45 to 1.08), but also that people in the intervention group who did not attend any chat sessions improved compared with controls (d = 1.79 vs. d = 0.93; p < 0.001). 311
Turner et al. 309 compared telephone CBT to face-to-face CBT. They found no significant clinical difference between the two groups following treatment after assessing the groups with a number of clinical scales, indicating the non-inferiority of telephone CBT compared with face to face.
The feasibility of neuropsychological testing via videoconferencing in adolescents with early psychosis was investigated by Stain et al. 308 They found that most tests demonstrated equivalence (Social and Occupational Functioning Assessment Scale, Wechsler Test of Adult Reading, the Controlled Oral Word Association Test, the Logical Memory subtest of the Wechsler Memory Scale and the Brief Psychiatric Rating Scale), indicating that they can reliably be carried out by videoconferencing. Difficulties were encountered when administering the quality-of-life measure because of the multiple-choice format.
Patient-level impacts
Two qualitative studies gave an insight into the patient experience of psychiatric consultations conducted by videoconferencing. 306,310 It is important to note that both these papers reported on patient experience after a single telepsychiatric consultation only. Participants generally found that the consultations were useful and they were reported to increase knowledge of mental illness and coping methods. Some participants appreciated the consultation taking place at home, where they are comfortable, and people appreciated the anonymity provided by not living in the same town as the clinician. Some of the younger group reported feeling a lack of control in the encounter, but excitement at the novelty. Some reported issues with sound or video quality.
Clinician satisfaction
One study reported that clinicians felt confident in making their diagnosis via videoconferencing. 306
Discussion
Based on this systematic review, it seems likely that networked communication technologies for the treatment of mental illness are generally acceptable to young people. It seems likely that interventions provided using these technologies may be effective, and the studies published between 2009 and 2016 are generally positive in their findings. Nevertheless, there is limited evidence available as far as young people are concerned and the effectiveness of most interventions for the majority of mental health conditions in this group has not yet been adequately investigated. Although we found a large number of studies resulting from our search, many of the articles focused on computerised CBT, perhaps indicating the current relative interest in this technology. Computerised CBT is an interactive programme of CBT delivered via computer that may or may not include therapist feedback. As it was not possible to extract the contribution of the therapist in relation to the computer program from these studies, these articles were excluded from this review.
Strengths and limitations of the review
Rapid reviews provide a timely approach to searching the relevant literature, useful in fields where change is ongoing (such as in the development of digital technologies). The search strategy covered a wide range of mental health conditions affecting younger people, included non-English-language papers and was developed by an information specialist. However, it excluded more time-consuming search processes, such as searching for grey literature. It is therefore possible that some relevant data may have been missed.
Comparison with other reviews
This systematic review is an update to a similar review based on articles published before 2009. Their findings were generally similar: although published data regarding networked communication technologies for the treatment of mental health were generally positive, limited evidence was available and thus it was difficult to draw robust conclusions. 45 Other systematic reviews have generally not limited their search to two-way communication and so provide different results but, again, they are mostly positive in their findings, for example Ye et al. ’s review into internet-based interventions for children with anxiety or depression312 and Aardoom et al. ’s review into treatments for eating disorders delivered by the internet. 313 These reviews were dominated by computerised CBT, but found that internet-delivered treatments were effective.
Conclusion
Networked communication technologies show promise in the treatment of mental health conditions, but further research is needed into a wider range of conditions and methods of treatment.
Evaluation of the impacts and outcomes of digital communication technologies to promote access and engagement of young people with long-term physical conditions into health care
Background
Adolescence is not normally characterised by ill health. The prevalence of chronic disease in this population is low, with the leading cause of death in middle- and high-income countries being road traffic accidents. 314 Nevertheless, one in five young people aged < 16 years must regularly take medications. 315 Many conditions for which medication is taken do not resolve quickly (e.g. some mental health conditions) or are permanent (e.g. diabetes mellitus); therefore, numerous young people will continue to take medication beyond the age of 16 years. The number of young people with LTCs has increased in recent years, mainly because of improvements in survival for previously fatal childhood conditions, such as cystic fibrosis314 and childhood cancers,316 and improved diagnosis of conditions, such as asthma. 317 At the same time, as children grow up, transition from paediatric to adult health services is a vulnerable time and can result in disengagement. 318
In this review we aim to evaluate new approaches to delivery of health care mediated by new communication technologies and the value of such technologies in aiding effective communication with health professionals and self-management of health care. The normal concerns about image and identity in the context of social development among the peer group in this age group319 and the transition to adult health services is an additional challenge. 318 It is hypothesised that the use of digital communication with health-care staff may help with the disengagement from health care often experienced by young patients at this time.
Aim
The specific aim of this review is to present evidence for the effectiveness of digital communication technologies in young people with long-term physical conditions.
Methods
Search strategy
Please refer to Chapter 11 for details of the initial search conducted for five of the six rapid scoping reviews. Once the common search had been conducted a selection of terms relating physical health conditions was used to search within EndNote and sorting by publication date was undertaken to select only those records published from 2009 onwards (see Appendix 5 for the terms). In addition, searches of reference lists of the included studies were performed.
Inclusion and exclusion criteria
Study type/language of publication
All types of study designs published in all languages, from 2009 onwards, were included.
Participants
Young people/adolescents (aged between 12 and 25 years). Studies where the mean/median age of the population was > 12 and < 25 years were included. Clinicians included all health-care professionals.
Condition/disease
Asthma, HIV infection, cancer (all types), cerebral palsy, Duchenne muscular dystrophy, physical disability, cystic fibrosis, juvenile rheumatoid arthritis, IBD, traumatic brain injury, chronic kidney disease, rheumatological condition, haemoglobinopathy, liver disease, dermatological condition, gynaecological condition, spina bifida, epilepsy and myalgic encephalopathy.
Intervention
All identified digital communication technologies involving two-way communication between patient and clinician were included. Examples include e-mails, SMSs, social networking websites, mobile telephony, videoconferencing and teleconferencing. When the intervention involved several components, such as health-care information transfer and access to websites for information, studies were included only if the two-way digital communication between patient and clinician was evaluated separately.
Comparator
We compared the effectiveness of communication technology with traditional in-person intervention and, where relevant, telephone intervention.
Outcomes
All outcomes were included. We reported the outcomes according to the following groupings:
-
patient outcomes (e.g. treatment outcomes, health behaviours, health status and well-being, communication)
-
health professional outcomes (e.g. knowledge and understanding, consultation processes)
-
health service delivery outcomes (e.g. adverse events, health economic outcomes).
Screening
One reviewer screened the identified papers at title and abstract stage, then two independent reviewers screened the full texts. Any discrepancies that arose between the reviewers were resolved by a third reviewer. The study flow and reasons for exclusion of full-text papers were documented in a study flow diagram (Figure 20).
FIGURE 20.
Study PRISMA flow diagram.
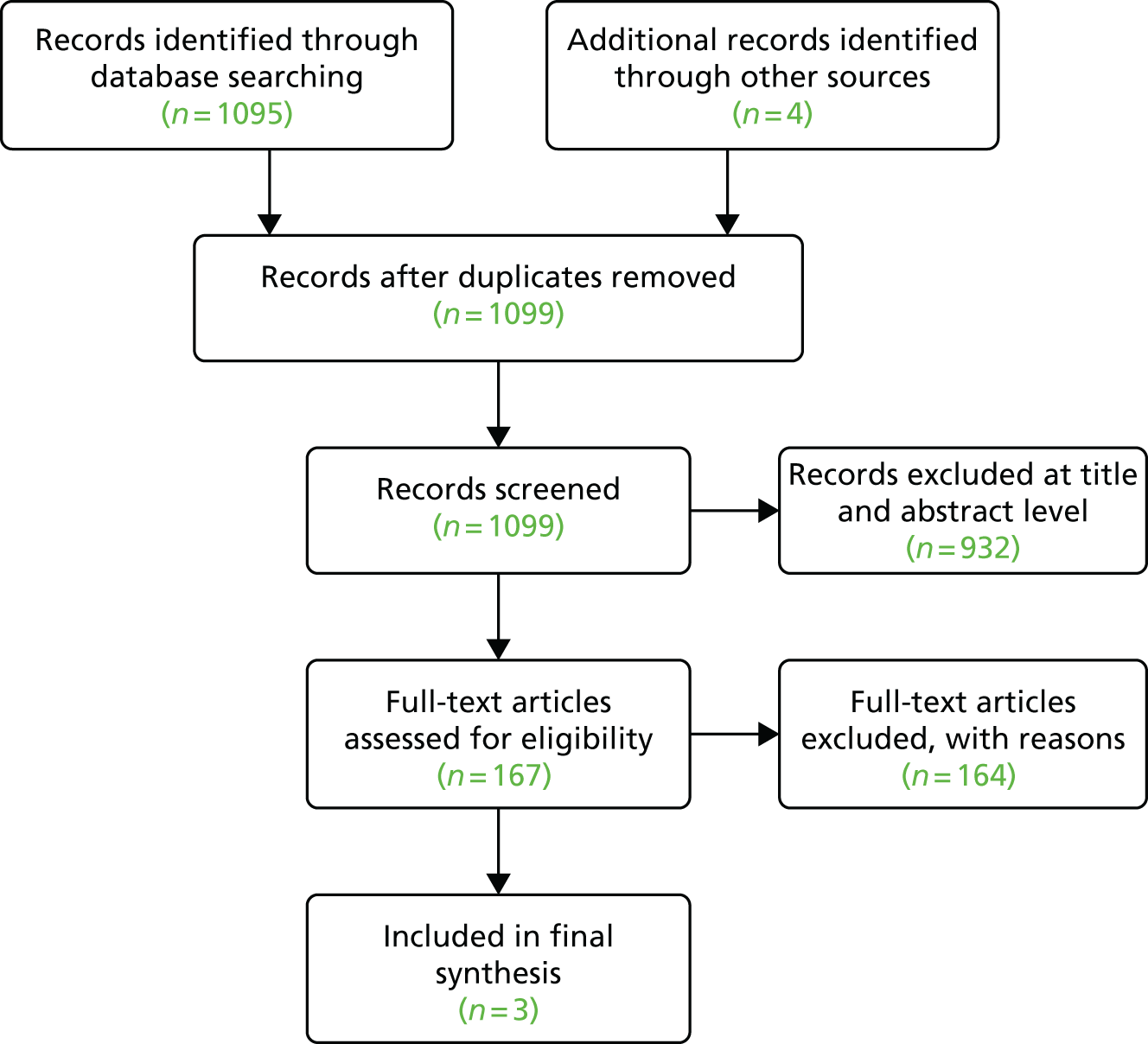
Data extraction strategy
Two reviewers independently extracted relevant data from all included studies using a standardised data collection form.
Quality assessment
All included papers were assessed using the appropriate CASP instruments. 225 Studies with no flaws identified during this process were rated as being ‘good’. Studies with one or two limitations or uncertainties were rated as being ‘fair’ and any research with three or more flaws was rated as ‘weak’.
Data analysis and synthesis
The findings of this review will be summarised using narrative synthesis. Findings will be presented in tables and via text.
Results
Characteristics of studies
Three studies met the inclusion criteria. 244,320,321 The conditions they focused on were acne,320 traumatic brain injury in childhood244 and asthma. 321 They were all RCTs, although one was a pilot RCT244 (Table 19).
| Author | Year of publication | Study design | Research type | Study location | Patients | Description of the intervention |
|---|---|---|---|---|---|---|
| Fruhauf et al.320 | 2015 | RCT | Quantitative | Austria | 69 people with facial acne, aged 13–37 years | Mobile teledermatology patients upload pictures and clinical information onto mobile phone and receive management, dose changes and requests for face-to-face appointments by dermatologist |
| Wade et al.244 | 2009 | Pilot trial (RCT) | Quantitative | USA | Nine adolescents (aged 12–18 years) who sustained a moderate to severe TBI in the previous 24 months and their families | TOPS: a novel online, manualised, treatment programme consisting of 10 web-based sessions providing information and interactive exercises on cognitive, social and behavioural skills typically affected by TBI. Web sessions were followed by synchronous videoconferences with a therapist to review target skills and apply problem-solving process to family goals |
| Wiecha et al.321 | 2015 | RCT | Quantitative | USA | 58 children with persistent-level asthma, aged 9–17 years | Boston Breathes is a website which allows participants to enter peak flow measurements, symptoms and medical events; complete educational activities and access information; participate in a discussion board with peers and participate in a discussion board with primary care provider |
Quality assessment
One study was rated as being of good quality,320 one as fair244 and the other as poor321 (see Appendix 6, Table 30). The study rated as poor reported outcomes selectively by combining the two intervention arms for analysis. As we were interested only in outcomes relating to the use of the messaging service in this study, and not in the results of the multifaceted intervention, this did not affect our interpretation of the data.
Patient outcomes
In patients with acne, clinical outcomes are measured using validated tools. Scores reported for clinical outcomes were similar in the teleconsultation and outpatient consultation groups: on the Global Acne Severity Scale, the teleconsultation group scored 2.25 and the outpatient consultation group scored 2 (p = 0.38), and for the total lesion count the teleconsultation group scored 89.08 and the outpatient consultation group 91.21 (p = 0.95). When patients were asked to self-report whether or not they experienced therapeutic benefits, only 50% (12/24) of the teleconsultation group did so, compared with 64% (18/28) in the outpatient group, despite the almost equivalent clinical results. 320 In the same study, the overall scores for patient satisfaction were high, with the overall mean acceptance at the end of the intervention being 73.9% in total (see Appendix 6, Table 31).
An online intervention for families and adolescents having experienced traumatic brain injury had a videoconferencing element. Families had videoconferences with a therapist after completing an online intervention. The majority of adolescents found the videoconferencing easy (5/8), helpful (7/8) and preferred it to a face-to-face consultation (5/8), but the sample size was very small244 (see Appendix 6, Table 31).
Health service delivery outcomes
When teleconsultation was compared with an outpatient appointment, it was observed that the teleconsultation group did not request any face-to-face outpatient appointments, even though they were free to do so. 320
A web-based asthma self-management system, Boston Breathes, had a component which offered communication between patients and health-care professionals. 321 This facility was utilised the most by the asthma nurses (38.7%, 235/607) and much less so by primary care physicians (16.5%, 100/607). The most frequent message content was the encouragement or enquiry about medication adherence. Socialising between patient and professional accounted for 10.1% of messages (61/607) (see Appendix 6, Table 31).
Discussion
In the limited number of studies identified, the use of DCCs was an acceptable method of communication with a health-care professional. In the one study in which clinical outcomes were assessed using clinical tools, teleconsultation provided clinical equivalence, but fewer patients perceived a benefit than in the control group. This highlights a possible gap between what is a clinically relevant benefit and what patients feel is a benefit. We did not identify any studies that reported health-care professional outcomes. The included studies had small sample sizes, which limits the reliability and generalisability of the findings.
We excluded studies in which the effect of the DCCs was not separately assessed, for example where DCCs were used to supplement a web-based intervention. It is possible that DCCs play an important role in the effectiveness of these interventions, but it is not possible to discern this in a multifaceted intervention.
Strengths and limitations of the review
Rapid reviews provide a timely approach to searching the relevant literature, useful in fields where change is ongoing, such as in the development of digital technologies. The search strategy covered a wide range of physical health conditions affecting younger people, including non-English-language papers, and was developed by an information specialist. However, it excluded more time-consuming search processes such as searching for grey literature. It is therefore possible that some relevant data may have been missed.
Conclusion
Digital clinical communication appears to be an acceptable method of communication for young people with LTCs. Conclusions about clinical outcomes cannot be drawn given the limited evidence base to date.
Digital technology for communication between clinicians and young patients with long-term conditions in countries with or moving towards universal health coverage
Background
Internationally, there is interest in using digital communication to improve access to health care, particularly in countries aiming to achieve universal health coverage. 322 Universal health coverage means that all people can use the promotive, preventative, curative, rehabilitative and palliative health services they need, of sufficient quality to be effective, while also ensuring that the use of these services does not expose the user to financial hardship. 323 Some countries, such as Brazil, are opting to use open-source software for digital health systems324 and Latin American countries have recognised the growing importance of DCCs by offering training in teleheath. 325 Although South American countries have universal health-care systems, they do not administer them universally and so are not classified as offering this coverage, being instead regarded as moving towards doing so. 326 In conducting this review we wanted to identify studies based in countries that were not already represented in our other reviews and might offer evidence over and above that already identified.
Aim
To identify the use of DCCs for young people in countries with or moving towards universal health coverage.
Methods
Search strategy
Please refer to Chapter 11 for details of the initial search conducted for five of the six rapid scoping reviews. Once the common search had been conducted, the search was limited to non-English-speaking middle- to high-income countries327 and Universal Healthcare System328 using a country name keyword search in EndNote X7.4. The country terms broadly captured any form of the country name (see Appendix 5 for list). (The exception to this inclusion criterion is Brazil, in which we had a special interest based on the level of telemedicine used in the nation.) In addition, searches of reference lists of the included studies were performed.
Inclusion and exclusion criteria
Study type/language of publication
All types of study designs published in all languages, from 2009 onwards, were included.
Setting
A study set in a country with or moving towards universal health coverage. Countries were identified according to the World Health Organization’s Global Health Observatory data. 329
Participants
Young people/adolescents (aged between 12 and 25 years). Mean/median age of the sample population of < 25 years or > 12 years were also included. Clinicians included all health-care professionals.
Condition/disease
We excluded mental health conditions, diabetes mellitus and long-term physical health conditions [asthma, HIV infection, cancer (all types), cerebral palsy, Duchenne muscular dystrophy, physical disability, cystic fibrosis, juvenile rheumatoid arthritis, IBD, traumatic brain injury, chronic kidney disease, rheumatological conditions, haemoglobinopathy, liver disease, dermatological conditions, gynaecological conditions, spina bifida, epilepsy and myalgic encephalopathy], as these were included in the other reviews.
Articles relating to health promotion or disease prevention were excluded. We excluded studies that focused on neurodevelopmental disorders, such as attention deficit–hyperactivity disorder and autism, and non-chronic conditions such as acute stress reaction.
Intervention
All identified digital communication technologies involving two-way communication between patient and clinician were included. Examples include e-mails, SMSs, social networking websites, mobile telephony, videoconferencing and teleconferencing. We excluded computerised CBT. Interventions allowing only one-way communication were excluded. Multifaceted interventions were also excluded.
Comparator
We were interested in comparisons with traditional in-person interventions and, when relevant, telephone interventions.
Outcomes
All outcomes were to be included. We intended to report outcomes according to the following groupings:
-
patient outcomes (e.g. treatment outcomes, health behaviours, health status and well-being, communication)
-
health professional outcomes (e.g. knowledge and understanding, consultation processes)
-
health service delivery outcomes (e.g. adverse events, health economic outcomes).
Screening
One reviewer screened the identified papers at title and abstract stage and the same reviewer read the full text. A second reviewer analysed 10% of the articles from each of the exclusion and inclusion lists. The study flow and reasons for exclusion of full-text papers were documented in a study flow diagram (Figure 21).
FIGURE 21.
Study PRISMA flow diagram. ISMEAR, Index Medicus for the South East Asia Region; LILACS, Latin American and Caribbean Health Sciences Literature.
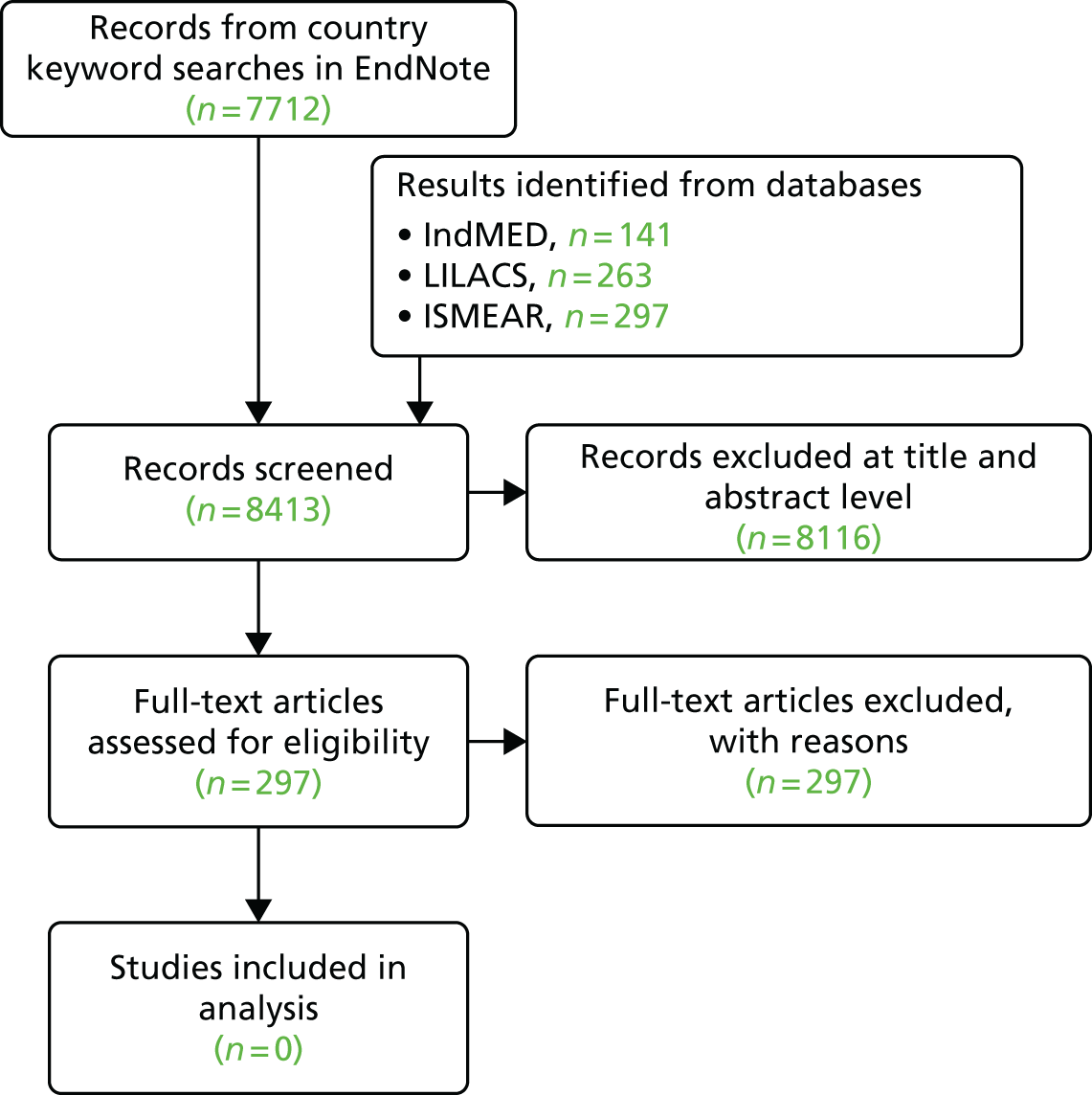
Results
After reviewing abstracts and titles against inclusion criteria, as described in Methods, 297 titles remained. After screening 297 full-text articles, none met the inclusion criteria. Six were already identified in the other reviews.
Discussion
The review failed to identify any studies meeting the inclusion criteria, even when searching for articles published in languages other than English. This is due in part to having already identified relevant published literature in the other reviews. Rapid reviews do not search the grey literature; it may be that information and evidence about DCCs used in countries such as Brazil are published outside of the peer-reviewed literature (e.g. in policy documents and news sources). During the screening of the abstracts and titles, it was noticeable that a large number of studies did not meet the criterion of the mean age being ≤ 25 years. This may have led us to exclude articles that could provide us with knowledge useful for implementation of DCCs, based only on age. This is a disadvantage of the rapid review method, which utilises a focused question and, in this case, linked closely with the overall research question for the LYNC study. The setting of interest is likely to yield rich information on the use of DCCs, but at present this is not available in the published literature.
Chapter 12 Rapid reviews: videoconferencing
Background
Skype and other forms of videoconferencing are increasingly used in health-care settings, particularly to support contact with patients in remote and rural areas across the world. 330,331 Increasingly, policy-makers are encouraging the use of videoconferencing with patients in routine health-care settings,332 reflecting the normalisation of videoconferencing in society and current policy and the perceived benefits. 333,334 In the UK, software has been rolled out to allow Skype to be used in specialist clinical settings. 335 Previous studies of videoconferencing use have reported perceived benefits to patients in terms of increased convenience in consulting with clinicians from their own homes and clinicians have reported increased benefits in patient care. 308,336 For patients with LTCs, a potential role has been demonstrated for video consulting for follow-up consultations and in mental health conditions. 337,338
As this is a growing field, there are an increasing number of published reviews of the literature. We wanted to summarise the current literature relating to the use of videoconferencing with patients who have LTCs, so we conducted a review of existing review articles.
Aim
This review aims to give an up-to-date overview of the evidence concerning the use of videoconferencing between the clinician and patient from the patient’s own home (or mobile device), by summarising the existing reviews of the literature.
Methods
Search strategy
A set of searches was developed for this rapid scoping review aiming to capture reviews on the use of this specific technology for clinical communication, irrespective of the age of the study participants (see Appendix 5). First, the EndNote database of results from the review of systematic reviews undertaken to identify generic outcome measures populated in 2014 was searched using the terms ‘skype’, ‘videoconferenc*’, ‘Video-conferenc*’ and ‘Google AND (talk or hangouts)’ in any field and sorted by publication date to select only those records published from 2009 onwards (see Appendix 5). Second, an update search for systematic reviews of this specific technology was conducted in MEDLINE in January 2016 (see Appendix 5). Third, a search of MEDLINE combining thesaurus and free-text terms for the concepts of ‘internet videoconferencing technology’ and ‘clinical communication’ was conducted.
Inclusion and exclusion criteria
Study type/language of publication
This review included review articles only. We excluded reviews of reviews. We included English-language articles only, and only those published since 2009.
Intervention
We included interventions that comprised internet video use for a two-way communication.
Comparator
Comparators included any other forms of communication (face to face, telephone or e-mail).
Participants and condition
We included patients with long-term illnesses. Patients with multiple long-term illnesses were excluded.
Settings
We included reviews conducted in health-care settings where internet video use was with a patient in their own home or on a mobile device. We excluded reviews if some or all of the included studies were conducted in social care settings or with the use of video with the patient present in a health-care setting.
Outcomes
We did not restrict according to outcome. For the purposes of reporting we grouped outcomes in the following way:
-
patient outcomes (e.g. treatment outcomes, health behaviours, health status and well-being, communication)
-
health professional outcomes (e.g. knowledge and understanding, consultation processes)
-
health service delivery outcomes (e.g. adverse events, health economic outcomes).
Screening
One reviewer screened the identified papers at the title and abstract stage and two reviewers read and screened the full texts. Any issues were resolved by a third reviewer. The study flow is documented in Figure 22.
FIGURE 22.
Study PRISMA flow diagram.
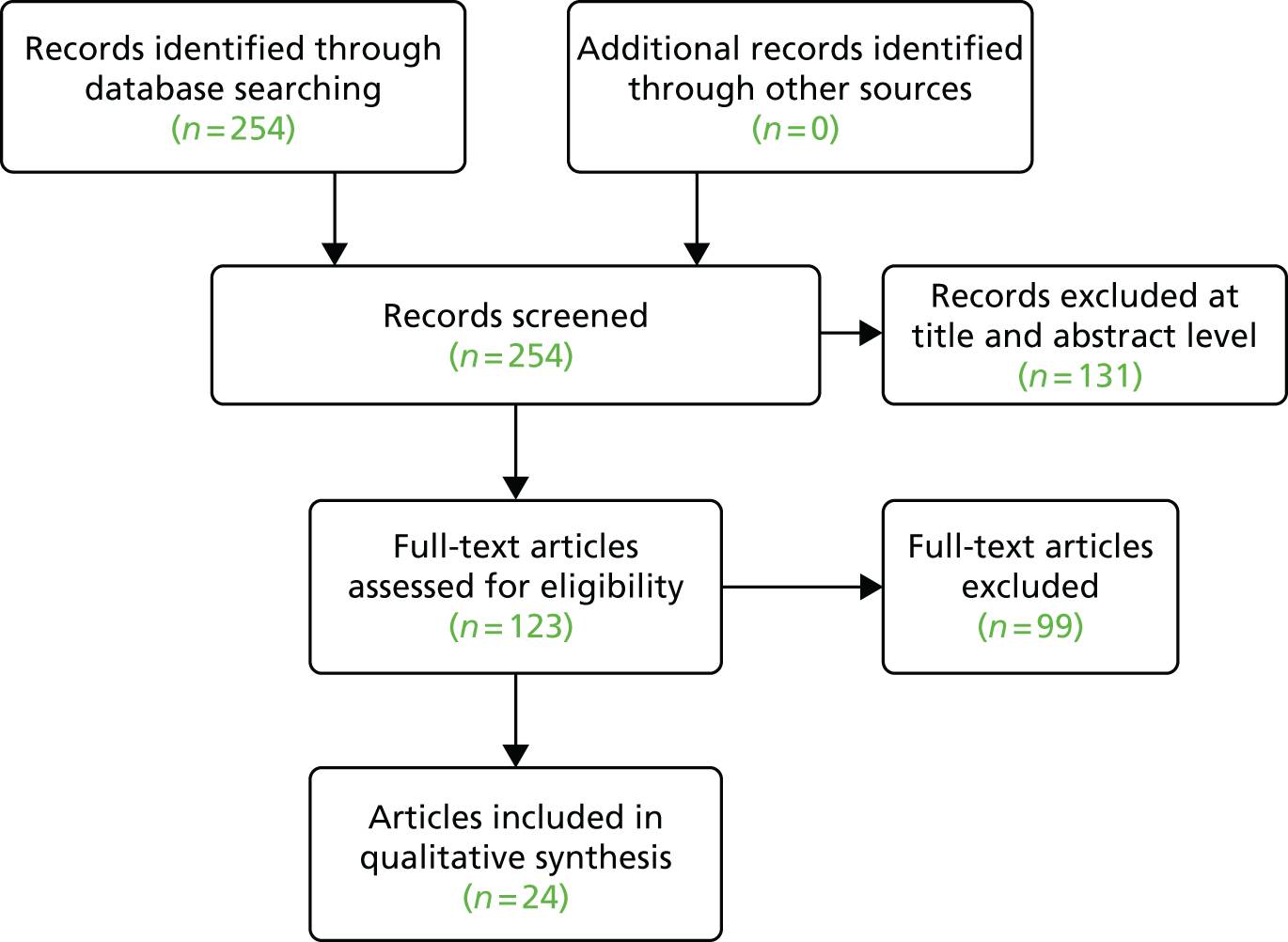
Data extraction strategy
One reviewer (CB) extracted relevant data from papers using a standardised data collection form.
Quality assessment
We used the Assessment of Multiple Systematic Reviews (AMSTAR) tool339 for assessing the methodological quality of systematic reviews, presenting a score for each review and taking the score into consideration in interpreting the results of the reviews. We have listed the point(s) on the AMSTAR checklist that each particular review has overlooked or excluded.
Data analysis and synthesis
The data are presented as a narrative synthesis of the findings of the identified reviews.
Results
Search
A total of 254 relevant studies were identified in the MEDLINE search, which included several systematic reviews. After screening, in total, 123 abstracts were selected for full-text review and 24 review articles were included in the review.
Characteristics of studies
A total of 24 reviews were included. The articles covered a wide range of LTCs, including heart failure, depression, schizophrenia, spinal cord injury and chronic pain. The majority of the articles were systematic reviews. Only seven reviews looked at videoconferencing exclusively, with the remainder looking at a range of telehealth interventions (including videoconferencing) (Table 20).
| Author | Year of publication | Review type | Participants and conditions | Intervention | Comparison |
|---|---|---|---|---|---|
| Backhaus et al.340 | 2012 | Systematic review | Patients with mental illness | Videoconferencing | Face-to-face consultation |
| Boisvert et al.341 | 2010 | Systematic review | Patients with autism spectrum disorder | Telepractice (communication technologies such as laptops, videoconferencing and the internet) | Face-to-face consultation |
| Conway et al.342 | 2014 | A subanalysis of a previously published systematic review and meta-analysis343,344 | Patients with heart failure | Four specific technologies (structured telephone calls, videophone, interactive voice response and telemonitoring) | Usual care |
| Dorstyn et al.345 | 2013 | Systematic review | Minority ethnic communities with depression | Telecounselling (counselling delivered by telephone, videoconferencing or the internet) | Usual care, face-to-face consultation, minimal support, waiting list |
| Dorstyn et al.346 | 2013 | Systematic review | Patients with spinal cord injury | Telecounselling (telephone and internet, including videoconferencing) | Information only, usual care |
| García-Lizana and Muñoz-Mayorga347 | 2010 | Systematic review | Patients with mental illnesses | Telepsychiatry (videoconferencing) | Face-to-face consultation |
| García-Lizana and Muñoz-Mayorga348 | 2010 | Systematic review | Patients with depression | Information communication technologies (e.g. website, internet programs, e-mail, videoconferencing and computer–telephone integrated system) | Face-to-face consultation |
| Kasckow et al.349 | 2014 | Systematic review | Patients with schizophrenia | Telepsychiatry (telephone, video or internet based) | Reduced telephone call exposure, usual care, treatment as usual, face-to-face multifamily groups |
| Kitamura et al.350 | 2010 | Systematic review | Patients with cancer | Video consultation | Face-to-face consultation |
| Mars et al.351 | 2012 | A review of the literature | Psychologists or psychiatrists dealing with prisoners with mental illnesses | Forensic telepsychiatry (videoconferencing) | Face-to-face consultation |
| Martin et al.45 | 2011 | Systematic review | Young people with mental illnesses | Networked communication interventions (e-mail-/web-based diary, videoconferencing or teleconferencing and virtual reality) | Waiting list controls, face-to-face consultation |
| McGeary et al.352 | 2013 | Meta-analysis | Patients with chronic pain | Telehealth (interactive and self-help websites, internet, telephone, internet and telephone, videoconferencing or teleconferencing, wireless biofeedback) | Face-to-face consultation, treatment as usual, waiting list controls |
| McLean et al.353 | 2010 | Systematic review | Patients with asthma | Telehealth (telephone, videoconferencing, internet, other networked technologies, SMSs, combination of SMSs and the internet) | Face-to-face consultation, educational approaches (e.g. leaflets), usual care plans |
| Neubeck et al.140 | 2009 | Systematic review | Patients with coronary heart disease | Telehealth interventions (telephone, internet) | Usual care |
| Peeters et al.354 | 2011 | Systematic review | Patients at home and patients with chronic conditions | Video communication | Usual care at home |
| Peterson355 | 2014 | Systematic review | Patients with type 1 diabetes mellitus | Mobile tools (internet, mobile, mobile and internet, telephone, videoconferencing and telephone) | Unspecified |
| Schlegl et al.356 | 2015 | Systematic review | Patients with anorexia and bulimia nervosa and their carers | Technology-based interventions (computer, videoconferencing, vodcasts, e-mail, mobile phone/SMSs, internet) | Waiting list controls, without intervention, face-to-face consultation, video or brochure controls, Beating Eating Disorders intervention |
| Sharp et al.357 | 2011 | A review of the literature | Patients with psychosis | Videoconferencing | Face-to-face consultation |
| Shore358 | 2013 | Review | Patients with psychiatric illnesses | Telepsychiatry (videoconferencing) | Face-to-face consultation |
| Siriwardena et al.359 | 2012 | A review of the literature | Patients with type 1 or 2 diabetes mellitus | Telemedicine (videoconferencing, mobile phone, telephone, feedback letters with or without telemonitoring) | Usual care, in-person health education, diabetes mellitus education group via videoconferencing with no follow-up, telemonitoring using web application to upload blood glucose levels, waiting list controls, no intervention, blood glucose levels communicated over the telephone, telemonitoring only |
| Sucala et al.360 | 2012 | Systematic review | Patients with mental illnesses | All text-based asynchronous and/or synchronous communicative e-therapies (e-mail, website postings, website exchanges, e-mail and chat, website postings and e-mail, chat) | Face-to-face consultation |
| van den Berg et al.131 | 2012 | Systematic review | Older patients | Telemedicine (telemedical devices to measure vital signs, telephone, short messages, videoconferencing and combinations of these, interactive systems only in combinations with the aforementioned modalities) | Usual care, face-to-face consultation, self-management, health education, manual approaches, additional controls relating to the specific included studies |
| Wile and Pringsheim361 | 2013 | Systematic review and meta-analysis | Patients with Tourette syndrome | Telehealth (videoconferencing) | Face-to-face consultation |
| Zhai et al.362 | 2014 | Systematic review and meta-analysis | Patients with type 2 diabetes mellitus | Telemedicine (websites, internet, videoconferencing, telephone based, internet transmissions) | Usual care, face to face, diabetes mellitus self-management programme |
Quality assessment
Table 32 in Appendix 6 provides a summary of the AMSTAR results. Only three reviews were methodologically strong,342,353,362 with the remaining 21 obtaining a score of ≤ 6, thus being rated as being of poor quality.
Mars et al. 351 and Shore358 provide limited details of included studies’ characteristics, such as clinical outcomes and participants’ demographics. Although McGeary et al. 352 searched for grey literature, they excluded it later without giving any reasons. This is significant as the authors note that unpublished material could have provided additional insights. 352 Although Peeters et al. 354 supply funding details, they do not specifically report any conflict of interest. For Conway et al. ’s342 subanalysis, full search terms, the inclusion of unpublished literature and list of excluded studies, and in-depth risk and publication assessments were appraised in the original systematic review and meta-analysis publication. 343
Patient outcomes
Almost all the reviews found evidence of increased patient satisfaction, and some found improvement in at least some health outcomes. A review related to mental health indicates that a good therapeutic alliance between clinician and patient is possible via video. 360 In a review of the use of telemedicine in diabetes mellitus, 23 of the 27 RCTs reported improved metabolic control. Twelve of these 23 studies produced significant results, whereas only two studies observed negative health outcomes. 359 The review of telepsychiatry analysed results from a total of 1054 patients with various mental illnesses. The 10 RCTs reviewed mostly included patients from psychiatric services. The conclusion of the review was that telepsychiatry is safe to use and may be a useful alternative when a face-to-face encounter is not possible, but there is not yet sufficient evidence regarding its effectiveness in routine management of mental illness. 347 In our own review of the use of digital communication between clinicians and young people requiring mental health care, 5 of the 12 studies concerned videoconferencing, but significant improvement in health outcome was seen only with e-mail contact and web-based technologies. 45 Although the review of videoconferencing in oncology included 19 studies, the authors found no conclusive evidence of a difference between video consultation and face-to-face consultation. 350 A review of telemedicine for asthma concluded that there was no improvement in asthma quality of life, but there was a reduction in hospital admissions. 353 There is also some evidence of increased satisfaction among individuals from minority ethnic communities. To illustrate, the review of telecounselling for depression pooled results from 498 adults of African-American, Spanish and Asian origin. 345 Three independent studies found significant short-term improvements with internet-mediated consultations. Limited data also pointed towards longer-term health benefits. 345 Some reviews found differences in outcome depending on the communication medium. For example, a review of telemedicine for heart failure concluded that videophone did not improve outcome but structured telephone follow-up and telemonitoring did improve health outcome, including all-cause mortality. 342 Furthermore, a review of information communication technologies for depression found that videoconferencing is as beneficial as in-person care. 348 The authors also concluded that, as self-help internet programs have shown to improve symptoms and quality of life, they could be utilised in situations when conventional health care is unavailable.
Health professional outcomes
Some of the reviews found that clinician satisfaction depended on the particular type of communication medium. A review of forensic telepsychiatry in mental illness351 reported that health-care staff were less satisfied with using videoconferencing than the prisoners they were treating. Martin et al., however, found that clinicians prefer e-mail and web-based approaches. 45 Despite the equivocal evidence for telemedicine, Shore358 argued that health-care professionals can feasibly implement this modality. Nevertheless, both reviews recommend that staff reflect on their communication styles in order to ensure they interact naturally with patients as they would during any face-to-face consultation. Shore358 has also maintained that psychiatrists should learn how to deal with the various clinical, regulatory and administrative issues surrounding videoconferencing which, if overlooked, could potentially compromise patient confidentiality and safety. In a review of technology-based interventions for anorexia and bulimia nervosa, only one study out of the 40 identified (outcomes noted in 45 publications), observed differences between the preferences of patients and health-care professionals. 356 The authors of the review concluded that videoconferencing provides little benefit for clinical staff in terms of cost or time savings, but may assist patients who live in remote places and find it difficult to access specialist psychological services.
Health service delivery outcomes
In the review of the use of telemedicine for older patients, 36 of the 50 studies (that included a medical end point) discussed various health service outcomes (i.e. cost, hospitalisation, health-care utilisation). 131 The conclusion of the review was that video consultation may be an effective method for decreasing health-care expenditure. The authors of a review focusing on telepsychiatry reported limited data supporting the cost-effectiveness of video technologies. 349 There is some evidence pointing towards the feasibility and acceptability of telemedicine in different sociocultural contexts. A review of telecounselling in minority ethnic communities concluded that it is a highly adaptable and appealing health-care medium that could be implemented in different spatial locations. 345 The evidence indicates that the impact of video consultation is a highly contested issue. Although the subanalysis342 of a larger systematic review and meta-analysis into heart disease343,344 found that structured telephone follow-up and telemonitoring reduced heart failure-related hospitalisation admittances, the authors found no conclusive evidence that this occurred with videophone. Furthermore, a review of the financial benefits of videoconferencing noted that eight of the nine included studies were methodologically weak and reported no advantages compared with usual care. 354 The remaining study, with the highest methodological quality, observed that video communication was more costly than conventional health care. Taking into consideration the limited data surrounding the financial implications of telemedicine, some reviews were unable to draw any meaningful conclusions. 45,140,362
Discussion
Patients were satisfied with the use of videoconferencing and this was the case even in minority groups. There was limited evidence that its use led to a change in health outcomes, either positive or negative. In some cases it compared unfavourably with other methods of communication, such as web- or telephone-based communication. Video consultation had a narrower remit than other methods examined in the same reviews (e.g. telephone). For example, video consulting can provide a practical solution in health-care settings (e.g. reducing the need for psychiatrists to travel to prisons to see patients in areas with low levels of specialist availability). Health-care professionals face challenges in adapting to the use of a new medium of consultation. Little is known about the impact of video consultation on health service time and costs, as there is insufficient evidence to draw conclusions. However, video consultation does appear to be a feasible and acceptable method of consultation particularly for patients.
The reviews included in this review were mostly rated as being of low quality. This has implications for researchers working in this field. With a proliferation of review articles to draw on, it can be difficult to discern the messages coming out of the data in a growing field. Focused reviews, using robust methods, are needed.
Strengths and limitations of the review
To our knowledge this is the first review of reviews conducted in this topic area. Conducting a review of existing reviews presents challenges in synthesising large amounts of information. We have aimed in this rapid review to summarise the existing literature, taking into account the quality of the reviews. However, we are conscious that summarising reviews can lead to loss of information and that our results are a high-level summary.
Several of the reviews looked at multiple telehealth interventions, which included videoconferencing. These reviews did not identify much evidence relating to videoconferencing. A review on diabetes mellitus included 35 RCTs, with videoconferencing being just one of a number of telehealth interventions included. 362
A review of telehealth for patients with heart disease found no studies that had examined the use of videoconferencing in this population. This limits the findings as we cannot be sure that they would hold for video alone.
Owing to the time restraints of a rapid review, we adapted point 11 on the AMSTAR checklist, ‘Was the conflict of interest reported?’. Ordinarily every included study within a review would be checked for a conflict of interest statement. This was not possible in our time frame and so we assessed conflict of interest in relation to the review itself.
Conclusions
The evidence base for the use of video for consultation between a health-care professional and patient is growing, but there is still a lack of evidence relating to the impact on time taken in consulting and cost. Information is also lacking on the safety of these consultations. Although video consulting appears to be feasible and acceptable to patients, there are unanswered questions about these other important implications.
Chapter 13 Discussion
Mobile digital communication technology and timely clinical communication between clinician and patient
Most young people predominantly use digital means of communication in their everyday life and older people are rapidly catching up. 20 With a smartphone, people can communicate from (almost) anywhere, even while on the move (where coverage allows), at home, work, while travelling, etc. This makes it technically straightforward for timely communication to take place between clinicians and young people living with LTCs.
Timely clinical communication connects the right people, at appropriate times and in appropriate depth, to enable effective condition management. Examples from our study include young people obtaining advice, requesting or offering information, and asking for support when they feel they need it; and clinicians contacting young people with results, queries and reminders about treatments, or to offer support in times of distress. The communication may be ad hoc, such as a young person with diabetes mellitus requesting advice on a problem with their insulin pump. It may also be planned, such as a young person sending in skin photographs or blood glucose results, or a clinician contacting a young person with depression to reinforce therapy. In our study most of the timely digital communication was not scheduled in advance by mutual agreement, although when clinicians initiated the contact, it was often planned. These communications are currently running in parallel with more traditional in-person consultations and therapy, and can complement this in-person contact.
Clinicians and young people emphasise different benefits, but agree that timely clinical communication improves the ability of young people to manage their condition. It also changes clinician–patient relationships and, at least initially, increases clinician workload. Clinicians and young people both claim positive impacts on health outcome, but clinical teams had not undertaken formal evaluations and we were unable to verify these claims in our study.
Provision for timely DCCs is occurring alongside a more general digitisation of NHS services for patients. 363 This digitisation brings the health service in line with how many individuals and businesses interact in an increasing range of circumstances and sectors. Clinicians and young people participating in our study use digital communication for clinical issues, at least in part because young people use digital communication to conduct the majority of their social and business interactions.
The digital communication taking place in the clinics we studied was mostly timely clinical communication, something clinicians and patients found difficult to achieve before the introduction of mobile phone technology. There was some evidence in our study sites of DCC being used as a straightforward replacement for traditional communication (e.g. providing a diet sheet electronically rather than on paper). It was also used as a replacement when there was potential to save time and money, particularly reducing travel for patients to appointments and for clinicians to visit patients, especially for patients who required frequent clinical review or lived in remote locations.
This study was designed to observe and explore current use of DCC in the NHS with young people with LTCs. At the time of the study most initiatives for using digital communication with patients were bottom up (i.e. developed and implemented by enthusiastic clinicians for their particular patient group). The clinicians were mostly choosing to use digital means to provide timely clinical communication for their patients and so most of our data are concerned with this. As a bottom-up development, many of our participating clinicians and young people were in the process of working out how best to use DCCs and reported their experiences. This included how they implemented the DCC, choosing the mode of communication used, understanding and mitigating risks, setting boundaries and managing clinician workload. Our data also provide insights on the costs of providing DCC and pathways through which patients may benefit and savings to the NHS can be achieved. The variation between clinics in access to timely DCC, and the absence of obvious correlated indicators of need, suggest a level of inequality of service provision during this initial phase of integration of its use that should be addressed as the practice matures and spreads.
All of the issues found in our data affect the digitisation of traditional clinical services more generally. However, our data suggest that these issues are more pressing in relation to timely DCC, which occurs outside traditional clinical appointment systems and patient–clinician interactions, where there are established processes, safeguards and boundaries already in place.
In using the term ‘timely DCC’, it could be argued that we are implying that traditional clinical appointments are not timely. They may well be timely, at least from the perspective of the initiating party, but the communication we studied displayed a different order of timeliness – anything from an immediate response to a response within a few days. In consequence, they were more likely to be ‘timely’ from the perspective of clinicians and patients alike.
Before considering further the experiences of young people and clinicians of using timely DCC, and the cost of providing it, we will consider its impact on the young people with LTCs.
The impact on young people with long-term conditions of timely digital clinical communication
The staff in each of our study clinics that used, or hoped to use, DCCs wanted to improve engagement of their young people with health care in order to ensure their best possible health outcomes. This fits with the evidence reported in Chapter 1 that young people who engage with their health-care providers achieve better outcomes that those who do not. The detail of what the timely engagement was for varied between clinics depending on the health condition and aims of treatment. Examples include changing treatment in response to symptoms in IBD; providing advice about the use of treatments; providing psychological support in times of distress; reminding young people of their treatment strategies; and encouraging attendance at follow-up appointments. Our qualitative data suggest that young people perceive this engagement as improving their ability to manage their health condition and so improve their health. This includes increased trust in the clinical team; increased self-efficacy in managing their condition; access to information at the time it is needed so information can be used effectively; and managing crises before they develop, thereby avoiding urgent admission or attendance at A&E. Clinicians gave similar examples of the positive impact of timely DCC. There was also evidence that young people who were resistant to contact with health services were prepared to communicate by digital means. There are credible pathways as to how the use of DCCs could lead to improved health outcome and so reduced cost to the NHS. Most of the savings are likely to be well in the future and not attributable to the clinic providing the DCC. For example, improved engagement with treatment by a young person may reduce hospital admissions for disease complications later in life.
There has been concern that digital communication can exclude people, but in this age group of people with LTCs it may lead to greater inclusion. Few negative impacts were reported, although there was concern about the potential for increased dependence on clinicians and the potential for intrusion of clinical communication into other aspects of life for the young people.
Young people and clinicians compared the use of mobile digital communication with previous attempts to provide timely access to clinical advice and support through landline telephones. For example, the opportunity to telephone a clinician directly was seen by young people as a great improvement from when they had to go via the hospital switchboard. With landline technology, contacting their clinical team might take half a day sitting by the telephone. Now they were often able to contact them directly and to do so while engaged in their everyday activities. This reduced their frustration with the health service and so they were more willing to engage.
None of the clinics we studied had undertaken its own evaluation of the impact of the use of DCC on patient care or health outcomes, a finding we found surprising. Our analysis of routinely collected hospital data does not distinguish between the use of digital media for timely clinical communication and their use as a replacement for traditional means of communication. For almost all study sites, we were unable to obtain routine hospital data relevant to the clinics and population we studied that covered both the time before the introduction of DCCs and after its introduction. We were therefore unable to examine trends in clinical and health service use outcomes over this period of change. We were unable to provide evidence of impact on these outcomes of DCC, recognising that even with relevant data the signal would be weak.
Our literature reviews indicate that the use of DCCs is mostly acceptable to patients, but there was no clear trend, positive or negative, in the health outcomes of young people for most health conditions, except for mental health, which exibited an overall positive trend.
Implementing timely digital clinical communication
The clinical teams we studied were early adopters364 of DCCs, motivated by their desire to see the best health outcomes for young people. They were providing the digital communication in parallel with traditional in-person contact. They were in the process of negotiating, with the young people within their service and with themselves, how to provide DCCs, particularly when this was what we are calling timely communication and so beyond standard clinical services. This process of developing and negotiating the use of digital communication can be considered an informal form of co-design, with front-line workers and patients influencing how it develops. This approach is advocated when implementing telecare. 365 Our data indicate that there were anxieties among some staff and young people during this process, many of which are explored in the following sections. A more formal co-design process has the potential to reduce this anxiety through providing a framework for the process. 366 Our interviews with IG officers indicate that they are keen to encourage this type of approach. It will also be important to consider whether or not the factors that draw clinicians and young people in to use DCC are the same as those that keep them using it. Their experience of using DCC may change their expectations as to its cost, benefits and the scale of necessary adjustments, including their behaviours for using. Our cross-sectional study was unable to tease this out.
Choosing the mode of communication
Each of the different digital modalities is particularly well suited to different purposes. Across the services we studied, patients and staff used telephones for urgent contact. E-mail was considered useful for giving complex or lengthy information and links to external sources, whereas text messaging was good for appointment changes or for quick queries. Upsetting news and complex issues would be discussed in person in a clinic appointment. PHRs were useful for sharing data prior to clinic appointments. There was little mention in our data of specific training in clinical communication using these communication modalities. 367,368 Our study participants considered the benefits, and limitations, of the use of the different modalities. For example, clinicians mentioned the loss of tone of voice, which may be important when assessing mental health, and young people mentioned that they preferred to raise embarrassing or sensitive issues with their clinician by e-mail or text message rather than in person. Young people liked to receive complex instructions by e-mail or text message so that they could refer back to them. Clinicians struggled with how to record their digital communication with young people in their clinical records. IG officers suggested that they would like to avoid dictating to patients the mode of communication to be used with the NHS.
Understanding and mitigating risks to patients from the use of timely digital clinical communication
Concern from clinicians about risk to patients varied across clinics depending on the health condition, the potential for harm to the patient in terms of how quickly harm might occur and the severity of the harm, and whether or not urgent care would normally be provided elsewhere (by a local hospital for young people attending a tertiary service). For example, those working in mental health were concerned about patients sending an e-mail out of hours when feeling suicidal and not getting a response. The young people who agreed to be interviewed did not echo this concern. The freedom to be able to write an e-mail when they want to was valued, but an immediate response out of hours was not expected. The young people interviewed described using different communication modalities according to the urgency of the health problem. Very few incidents could be recalled by patients or clinicians where the use of digital communication had adversely affected patient care.
However, the use of IT in health care does have its hazards that need to be addressed. 369 Unanticipated novel forms of hazards can occur. 370 For example, it has been shown that electronic prescription systems may improve the quality of prescribing, but also introduce new sources of error. 371,372 Hazards from the use of digital communication in health care include the manipulation of identity, the misinterpretation of digital information, breaching confidentiality and overreliance on digital communication as a means of communication at the detriment of traditional clinic visits. 372,373 The IG officers interviewed in our study recognised the importance of addressing these vulnerabilities. 374 Clinicians and young people described a number of mitigation strategies that they use to eliminate or reduce risks. Perhaps most importantly, timely DCCs were used between young people and clinicians who knew each other. There was a pre-existing relationship and a level of trust which was often enhanced through the use of this communication. This reshaping of relationships was identified in a realist review of telehealth interventions for self-management support for LTCs. 375 Participants also used common-sense strategies, such as seeking advice from other services (e.g. emergency department), when they required urgent help but communication with their clinic had failed (e.g. no response or delayed response). They limited or restricted the use of digital communication to reduce the risk of breaching confidentiality, for example by not including sensitive information in e-mails and text messages, or by using digital communication only for simple issues, such as rearranging an appointment. Not all the clinical teams we studied used communication systems with encryption. This is now becoming more widely available in the NHS providing a technological solution for this risk.
Most health-care professionals in our study strongly supported the need to inform patients of the risks of digital communication, although not all sought explicit consent from patients. Specific guidance for clinicians from their trusts on obtaining consent for the use of this form of communication was lacking in some places. This was a source of concern among clinicians. Young people tended to be less concerned about confidentiality than clinicians, but this may reflect their lack of awareness of the potential risks. Some young people were concerned about confidentiality of messages on their own mobile phones, whereas others were not.
The form of communication between clinician and patient does not change the ethical duty of clinicians to obtain informed consent and maintain confidentiality, or their legal obligations under the Data Protection Act. 376 However, General Medical Council guidance does not specifically consider the specific context of DCCs and it appears that few NHS trusts have clear policies to guide clinicians. Our data suggest that attention needs to be given not just to the obtaining of initial consent, but for confirmation of that consent over time as the health state and the life situation of the young person changes. What a young person finds acceptable to receive on their smartphone may change over time.
The importance of consent and confidentiality in using non-in-person communication has been highlighted in the literature, specifically in the context of e-mail communication,377 and the American Medical Association issued ethical guidelines for e-mail communication between patients and physicians in 2003. 378 In 2004, Car and Sheikh379 noted that ‘early email use in health care has grown without an adequate supporting infrastructure to address security issues’. They also noted the need for informed consent. 379 IG officers in our study varied in their views on the need for specific local guidance in addition to generic professional guidance about clinical communication and information. Professor Wachter has suggested that his report, published in September 2016,37 may encourage resistance to over-regulation of NHS IT. This would place the responsibility with individual clinicians and clinical teams to interpret generic professional guidance in this new context of DCC.
Setting the boundaries of timely digital clinical communication
Both clinical teams and young people talked about the importance of clear boundaries and achievable expectations when using timely DCC. These boundaries and expectations are likely to vary between clinics depending on the nature of the health condition. Of particular importance to clinicians and young people is clear communication about boundaries and continual reinforcement about the boundaries, particularly in clinical specialties dealing with young people who are at high risk (e.g. mental health). Young people wanted clear boundaries, but they also wanted a commitment from clinical teams that expectations would not only be clear but could be, and would be, met by the clinical team. This is important for effective service delivery and for patients to manage their anxiety. Patients and carers become anxious if communication is not received when expected, as they think it signifies complications or bad news.
Digital communication raises challenges for health-care professionals in relation to setting professional boundaries and understanding the implications for the professional duty of care. These challenges generated ethical discomfort in some of our participants. Boundary issues included their availability to respond to communications from patients, particularly out of work time, and the nature and content of these communications. This particular ethical concern related to the use of DCCs is less discussed in the literature. There is currently professional guidance for clinicians on maintaining professional boundaries with the use of social media,380 but not in relation to direct DCCs.
Managing the workload of clinicians providing timely digital clinical communication
Most clinical teams welcomed the ability to use digital communications, and none wanted them reduced or removed, even though they were using the digital communication in parallel with traditional in-person contact. However, the teams recognised real issues with workloads. Services that best managed this had planned systems in place. IG officers were anxious to ensure that all communication was logged so that their NHS trust would receive payment for all services provided. It is important to remember that most of the clinics we studied were providing care to young people who were known to the clinic, setting a limit on demand that would not be the case for a service providing care at first point of contact. In the clinics we studied, there was potential for time spent on responding to digital communication to be saved in other clinic activity, although our health economic analysis was unable to quantify this.
The costs of providing digital clinical communication
The early adopters364 we studied experienced costs, such as anxiety about patient safety and ethical discomfort in relation to professional boundaries, when providing timely DCCs. In this section, we discuss the economic value and cost of DCCs. Our economic evaluation did not distinguish between timely DCCs and replacement of traditional service provision.
Young people appear to value digital access to their clinical team. They gave examples of the opportunity costs and benefits for them from using DCCs. For the service provider the main cost was staff time. Most clinicians perceived the time they spent on DCCs as benefiting the young people. Only a few clinicians discussed other options for the use of the time they spent on DCCs.
The cost of the communication technology was relatively minor compared with staff time. However, we found examples of staff time being wasted because of the limitations of the communication technology they were having to use.
When assessing the cost of DCCs in relation to its benefits for young people with LTCs, it is important to consider any impact that goes beyond immediate health benefits. Most evaluations of the use of digital communication with patients reported in the literature are limited to a 1-year follow-up. However, improved engagement with health care may have health benefits well into the future. DCCs also have benefits for well-being beyond the health condition. For example, young people report reduced anxiety, a greater sense of control over their health and reduced impact of their condition on their lifestyle.
There are mechanisms through which DCC may lead to efficiencies and cost savings for services and the young people. These include replacing routine low-risk visits, reducing missed appointments, logistical efficiencies and triaging of queries. If DCC leads to improved health outcomes, savings may be made within the health service as a whole. However, for individual clinics it is likely that costs will, at least initially, increase if they implement timely DCCs as a result of the increased pressure on staff time. Reducing barriers to access between young people and the service is likely to increase the time young people spend contacting staff, and sometimes this may be for reasons which are not directly related to their care.
We found that the use of DCCs was higher among staff, such as nurses, than among the senior doctors in the clinical teams. Our qualitative data suggest that nurses are dealing with the majority of issues coming from young people via digital means. Where there is a more serious or complex problem, this is escalated to senior clinical staff, and, because it is more serious or complex, the use of digital communication becomes less appropriate.
The evolving use of timely digital clinical communication in a digital society
In-person interactions necessarily involve a simultaneous allocation of time by the clinician and the patient. Digital means of communication can, to an extent, relax this requirement. The constraints imposed by the need for synchronicity of time and serious attention are not static. As society and its use of electronic means of communication evolve, patients and clinicians each have increasingly complex and varied responsibilities and tasks. As a result, finding a time for mutual interaction becomes harder. This has distinct consequences for both parties. For clinicians, their relationship with each particular patient has to compete with an increasing range of other responsibilities with their own priorities and time frames. This affects continuity of care and the potential for achieving patient-centred care, working in partnership with patients to enhance their health and well-being. Achieving continuity of care and patient-centred care are costly in terms of time. DCCs, by reducing the amount and uncertainty of the time commitment involved, have the potential to facilitate further progress. For patients, communication with clinicians about their conditions must compete with the demands of life itself. This affects the time and awareness that they can bring to communications, and thus their ability and willingness to recall, report and discuss developments in their own experience of their condition. To the extent that DCC makes it easier to communicate in meaningful ways and to balance this with other life demands, it holds the potential to enable patients to both fully engage with the management of their condition while not allowing it to intrude unnecessarily on life generally. Our study data hints at this potential for DCCs, but could not capture it fully as we did not systematically collect data on the competing demands of practice and life, or the choice behaviour of clinicians and patients.
It is not possible to determine from our study whether the use of a particular digital medium was simply a historical accident, or because clinicians considered it the best available channel, or determined by an inability or reluctance to spend time developing a structured range of different channels. Nonetheless, clinicians and patients were able to suggest which channels worked well depending on what was being communicated. However, the digital landscape is changing, and this study provides only a snapshot of the evolution of DCC practices. Young people are learning how to use digital communication for clinical matters and this is influencing how clinicians choose to communicate with them. This study was unable to capture data on the pace and effectiveness of this mutual adjustment process. This would require a study of both clinician and patient learning, maturation and adjustment of digital communications use patterns. However, our study suggests that for young people DCC use is growing out of their existing ‘digital native’ approach to communication technology. For clinicians the chance or need to use DCC is shaping their learning and decisions about how to integrate electronic communications into their clinical practices.
The different types of digital communication and their associated behaviours, particularly whether or not it is synchronous, affect timeliness. How young people and clinicians conceive of timeliness can be different or very similar depending on the clinical context. The ideal would be for different mixes of communication channel and timeliness to be matched to both parties’ circumstances and adjusted as they learn to fit it into their other activities.
Most of the DCCs described in our study were prompted by an event (e.g. arrival of a blood test result or a change in symptoms). Here we consider these event-driven communications in terms of their type – whether it be ‘pushing’ or ‘pulling’ information – and who initiates them. Later in this section we consider flow-based information communication. Event-driven, timely, ‘push’ communication can be initiated by clinician or patient. Information flowing from clinicians to patients is timely if it (1) becomes available to the clinician (e.g. test results), (2) is relevant to the patient (e.g. advice on changes in treatment, diet, etc.), (3) can be ‘heard’ by the patient (who needs to be able and willing to give the message the appropriate level of time and attention) and (4) complements the rest of the clinician–patient relationship. Information flowing from patients to clinicians is timely when it (1) is communicated when it is noticed by patients (e.g. side effects, potentially significant changes in condition); and (2) can be captured and digested by clinicians. In particular, the relationship of the patient and the clinician via DCCs should lead to an answer to the question of what to do with information that would otherwise be overlooked, as it was not asked for and was not communicated during an appointment or consultation or in response to a question from a clinician. Similarly, event-driven, timely, ‘pull’ communication can be initiated by clinician or patient. Information elicited or requested by clinicians from patients (e.g. blood glucose monitoring data, symptom reports) is timely if the information is requested when it is required, the patient is able to provide it and the clinician has the opportunity to give it attention. Information requested by patients from clinicians (e.g. queries about medication, requests for advice) is timely if the information is requested when it is required, the clinician is able to provide it and the patient has the opportunity to give it attention.
We would suggest that the convergence of these different types of timeliness cannot be taken for granted. It is for this reason that it is important to take account of which party initiates the communication and the extent to which the purpose of the communication comes from the initiating message (push) or the response (pull). The different possibilities have not all been equally explored in our study, although we have evidence of each type. We would expect that the mixture of types of communication will evolve as young people and their clinicians become accustomed to using DCCs. A longitudinal study design would be required to capture this evolution.
We note here that there are concerns that arise from general norms and rules relating to privacy and information security, such as information minimisation, purpose limitation and retention limits. From the clinical perspective these are defined by patient needs and by the wishes of patients acting as data subjects, although the same information may also be useful for administrative, financial and other purposes, for which tighter limits are appropriate. The forms of DCCs examined in this study are not greatly affected by such considerations because they are mainly supplementary to other forms of communication and concerned with clinical matters, but this may change as the use of various forms of digital communication becomes more customary.
Digital communications are not simply electronic versions of their analogue forebears. As the flow of information between clinicians and patients increases in magnitude and pace, communication is practised and understood in different ways. One of the most significant developments concerns the emergence of real-time or flow-based information. 381 This is where cognitive information from one person (originator) passes to another, who receives the information (receiver), who may add to it (or not), then passes it on (as originator) to another person, who receives it (or back to the first originator) and so on, so there is an accumulation of information. Furthermore, the originators and receivers need not be people but some form of sensor and actuator (terms familiar from the internet of things, which will become increasingly important as a source of content for DCC). This form of communication involves continuous or regularly scheduled messages or information exchanges (in contrast to event-driven communication). It has different effects. For instance, it is not normally expected that each message will be noticed or given the same degree of attention by sender and receiver; instead it is understood that what are known as ‘lossy’ processes of paying attention and responding will identify the most mutually significant information and those areas where better communication is required, while preserving flexibility and proportionality. It is an open question whether or not this development in how information flows might prompt a new way of thinking about health care and its delivery. The entire corpus of information communicated through flows could, if captured, support the application of data analytics methods to shed light on how the use of communication itself evolves. However, it is important to recognise that digital natives, who typically send short but frequent messages, use channels that do not necessarily store messages for archival or analytic purposes [such as Snapchat (Snap Inc., Los Angeles, CA, USA) and other ‘ephemeral’ platforms]. They view digital communications in significantly different ways. The waning popularity of e-mail among young people provides evidence of this trend. It is suggested that the inhibitions attached to formal and recorded communications are relaxed in flow-based and ephemeral settings, allowing (in some cases) more honest and revealing communication, or more emotional or psychological subtext, although this has yet to be proven. However, our data suggest that some lowering of inhibitions between patient and clinician occurs with text-based digital communication, even when it can be stored. Our study and this discussion have not considered scheduled communications, such as routine appointment reminders. Overall, DCC lowers the bar for initiating exchanges and reduces the formality and size of messages. It can thus help (within limits) to resolve the problem of ‘double coincidence of time and attention’.
In addition to the distinction between event-driven and flow-based or scheduled communication, and between retained and ephemeral messaging, different types of DCCs offer differing degrees of ‘synchronicity’. Some channels (e-mail, Twitter, etc.) are fundamentally asynchronous – the recipient does not have to be connected at the same time as the sender and can respond at leisure or after reflection. This works particularly well for one-way delivery of information or when sender or receiver needs to reflect carefully on the content and meaning of the message. Others [e.g. phone, Skype and – to a lesser extent – WhatsApp (WhatsApp Inc., Menlo Park, CA, USA) and Instagram (Instagram, San Francisco, CA, USA)], are essentially synchronous. This works particularly well for situations where real-time or back-and-forth interaction is required (e.g. when the relationship aspect is at least as important as the content, or where incomplete information means that the parties have jointly to explore the situation to determine what should be communicated and to ensure common and effective understanding).
Our study suggests that improving young people’s ability to manage and live with their LTC depends on embedding DCCs in a long-term relationship. Continuity of communication, in the sense of a sustained awareness of the possibility for either side to open a channel of communication, though not necessarily actual real-time flows, is almost a necessary condition for continuity of care, especially when the two ‘sides’ have to juggle many outside competing demands for time and attention.
Strengths and limitations
Our study design limits the generalisability of our study findings, in large part because of two factors affecting any empirical study of practice-initiated behaviour: path dependence and endogeneity.
Path dependence
The cases we examined were empirical rather than experimental. As with most ‘bottom-up’ initiatives, the sample will tend to emphasise the most attractive and obvious situations and approaches. Therefore, the observed cases may not involve the most difficult issues, or may not seek to address them systematically. A well-designed quasi-experimental (RCT) approach can help to complete the picture, establish the robustness of the findings and identify specific characteristics that can help to inform decisions, such as if, and how, to implement DCC in other contexts.
Endogeneity
The data routinely collected for unrelated purposes had insufficient link to the DCCs. Interviews consisted of data that seemed significant to the participants in view of their motives for adopting DCCs, the time and attention needed to capture and record data, and the sensitivities that cause those involved to share and discuss their experiences or to keep them to themselves. These data reflect experiences with DCCs. Therefore, particularly ‘good’ or ‘bad’ (to a much lesser extent) experiences are more likely to be captured, which limits external validity.
Within the limitations of the study design, there were strengths of the study. It captured a wide range of perspectives obtained from both clinicians and young people from across different clinical specialties, from clinics of various sizes and from across the UK. The size of our data set ensured that we had a diversity of participants and reached data saturation for each of our major analysis approaches and in most clinics. The opportunity to develop focused interview schedules for ethics and patient safety for use in selected sites contributed to richness of these data. For the health economic analysis, we obtained a good response rate to the questionnaire from staff for quantifying the burden of DCCs. The qualitative data provided an in-depth understanding of the pathways by which DCC affects health, well-being and costs from a diverse range of sites. Our PPI activity gave us insight into the language related to health and digital communication that young people use which we incorporated into our data collection.
There were also limitations of the study. The young people who participated were recruited through their health-care provider. We were unable to recruit for interview young people who do not engage with their service so the voice of young people who have disengaged is missing from our data. These young people may be less positive about DCCs than those we interviewed, or do not have access to it. For example, they may not own a mobile phone, be unable to buy phone credit, live in a location with poor mobile phone coverage or have disabilities making the use of a mobile phone difficult.
We were surprised that health literacy did not arise as a theme from our data. It is possible that we failed to recruit young people for whom this is an issue. We did not directly ask clinicians about this issue.
In some of the small clinics we were unable to recruit for interview a diverse range of patients. We had no examples of Skype communication, as we were unable to identify any clinics using this during our recruitment phase. This was probably because there was still concern about security when using Skype, and NHSmail 2 which includes Skype as an option, had not yet started.
The main weakness of the study from an ethical analysis perspective was the difficulty in obtaining explicit ethical reflection from participants. The method of analysis allows us to look at implicit ethical concerns and issues, but in a study whose primary focus was ethics a Socratic approach to interviewing would be likely to elicit more nuanced ethical reflection.
Our study methodology did not permit a formal economic evaluation. We did not obtain quantitative data on the magnitude of impacts identified qualitatively. The missing responses to the questionnaire may disproportionately represent clinic staff whose engagement with DCCs is minimal, biasing the analysis of responses. Some staff found it difficult to quantify their time spent on DCCs. Some young people were reluctant to engage with the stated preference elicitation.
Most of the young people engaging in our PPI activities did not have a LTC, which may account for some of the contrasts between their views of DCC and that of the study participants.
Implications for practice and local service delivery
In this discussion we have distinguished between timely DCCs and digital communication that is a direct replacement of traditional clinical encounters. We recognise that clinics may use DCCs anyway on the continuum between these, but being clear about this distinction may help with planning service development.
A clinical team may want to introduce digital communication as direct replacement of traditional clinical encounters so patients are able to use the modality of their choice, in a way convenient to the patient and clinician, to save time spent travelling and waiting at clinics and to save travel cost. An expectation of improvement to clinical outcomes is not supported by our literature reviews and we suggest there is no mechanism by which this might occur. Digitalising traditional clinical encounters demands attention to:
-
cost and availability of the technology for the patient and health-care provider, the skills to use it and a suitable private space in which to use it
-
limitations on the ability to undertake a clinical assessment that the mode of communication imposes; for example, Skype limits physical examination to observation, e-mail and text messaging remove tone of voice and other patient safety issues
-
processes for gaining informed consent from the patient, including who will see/hear the consultation and how is it stored
-
communication skills particular to the mode of communication. 367,368
Issues such as expectations and boundaries need to be clear, but can be similar to those for the traditional service.
The provision of timely DCCs demands attention to all the above issues. However, as the communications are outside the systems for traditional clinical encounters, the service requires planning as a new or additional service with attention to issues such as workload, boundaries and expectations, and cost and price for the service. Arguably these and other issues such as consent, data security and safety need more attention for a service that is not within the traditional pattern of clinical encounters. For example, boundaries and consent need to be clear and continuously visible to the patient. Our study suggests that these issues are more easily resolved when the clinical team are clear on what they hope to achieve by providing this new or additional service in terms of the ability of the young person to manage their condition, their wider well-being and their health outcome. Evidence from the wider literature suggests the importance of a co-design approach, including shared understanding of what matters and what can be achieved along with flexibility and willingness to adapt. 365 Our study suggests that young people may take initiatives that clinicians do not think of as they see things differently.
The clinicians using DCC in our study were convinced of the need to ensure that the young people they care for continue to engage with the clinic, saw digital communication as a successful way of doing this and were able to give examples of where it had been successful. These clinicians did not need convincing of the benefits of implementing timely DCCs. 382 There is evidence that motivation and enthusiasm make a difference when implementing digital clinical interventions. 383 However, none of the clinics had undertaken an evaluation of the impact of implementing DCC and our own evaluation using routinely collected data was limited. Yet evaluation of the impact of technology-based communication is important for driving further development of the service365 and is best designed into the service.
However, evaluation requires a measurement tool. The routine data used in our study were too blunt an instrument for evaluating the impact of timely DCCs. What is probably needed are outcome measures more closely linked to purposes of the digital communication, which of course requires the clinical teams to define clear purpose. A range of potential types of outcomes relevant to communication interventions have been identified by a Cochrane review panel. 384 Our literature review and PPI consultation suggest the relevance of two measures for outcomes not directly identified on this list – patient activation and the humanistic behaviour of the clinician. These are generic outcomes, not specific to a particular disease, so there is potential for comparison of evaluation outcomes across disease areas.
Our study has focused on young people with LTCs. We suggest that our findings are transferable to other populations with LTCs in which there is a high rate of ownership/use of smartphones and there is an established relationship between the patient and clinical team. This could include patients with LTCs who receive their care from a general practice.
The same generic issues that we found in our study, for example deciding on the digital medium of communication to use, establishing boundaries and expectations, obtaining consent and mitigating risks, would apply to clinical services where patients do not have established relationships with the clinical team. However, without pre-existing relationships, these issues may be considerably more challenging to deal with. This might also apply to services, such as general practice, in which there is an established relationship between the clinical team and patient, but that relationship is not regularly exercised by some patients and could account for the reluctance to use DCCs other than telephone. 385
Implications for policy
Assessing the impacts of options for enhancing the use of DCCs rests on an understanding of three ‘decision gates’: (1) adopt DCCs, (2) retain timely DCCs and (3) adjust behaviour. Of particular importance is the degree to which these decisions are correlated with characteristics of the patients and clinicians, including the type of long-term medical condition and its trajectory, as this might influence clinical and other outcomes. Questions for policy-makers to consider include:
-
whether or not timely DCCs are, on balance, beneficial
-
whether the best way forward is to facilitate and build on local initiatives or there is instead a case for something more directive, uniform and even top down
-
whether or not the matching of patient and clinician characteristics to timely DCC trajectories is important enough to warrant restrictions, customisation or selective (rather than wholesale or liberal) introduction.
The present study establishes the relevance and significance of these questions, but cannot fully answer them because of its design. However, the results of the study establish that these questions are important to answer and could, in principle, be addressed by further research.
Further research
Test-relevant patient-reported outcome measures for use in evaluating digital clinical communication
The impact of the provision of timely clinical communication on young people with LTCs could potentially be evaluated using a non-disease-specific outcome measure. Our literature review and PPI consultation suggested two potential measures. As discussed in Chapter 1, there is evidence that young people with LTCs have improved health outcomes if they engage with health care. There is also evidence that young people are less likely to engage with health care where there is poor patient–clinician communication, inflexible access to people and information, lack of person-centred health care, and a lack of continuity and relationship development. 16–19 Many of these aspects of care are assessed by the Physicians’ Humanistic Behaviors Questionnaire. 199 There is growing evidence that patient activation, the other of our identified measures, is associated with improved health outcomes. 386 Given this evidence, these generic outcome measures may provide sufficient evidence of impact or not of timely DCCs.
Evaluate, with an experimental design, the impact of timely digital clinical communication for people living with long-term conditions
Our study provides a framework for clarifying the digital communication for testing. Based on current practice and commonly used technology, the intervention most likely to be acceptable to clinicians and patients is event-driven communication using communication technology, provided issues, such as confidentiality and linkage with clinical record, have been resolved. The design of such an evaluation would need to take account of the different ways in which digital communication has an impact on different LTCs.
Explore and evaluate the benefits and disbenefits of replacing traditional clinical consultations with digital communication
Our research suggests the type of issue that needs attention when setting up DCCs to replace traditional clinical encounters. Further research is needed on how this is undertaken most effectively and the benefits and disbenefits for patients and clinical teams evaluated. The IG officers interviewed in our study thought that Skype-type communication is the modality most likely to replace traditional clinical encounters.
Evaluate the impact of the changing digital landscape on how digital clinical communication can achieve continuity of care and patient-centred care in an ethical, safe and cost-effective way
The changing digital landscape offers the opportunity to rethink traditional ways of providing clinical care. What type of continuity of communication through digital channels would enhance continuity of care, and at what cost?
Conclusion
Timely DCCs are perceived as making a difference to the experience of health care and health outcomes for young people with LTCs, although this is not yet supported by evidence measuring health outcomes. This timely digital communication is running in parallel with traditional in-person contact. It is likely that evaluation of DCC requires measurement of modifiers of health outcome rather than health outcome itself, as impact on health outcome may be beyond the timescale of most studies.
The provision of timely DCCs is costly and challenging to provide. There are risks, many of which can be mitigated by relevant technology such as encrypted e-mail, clinical system design, clinical team protocols and training.
If clinical teams develop a business case for the use of digital communication, it is helpful to clarify the degree to which the digital communication will be additional to traditional provision or a replacement. As digital communication becomes the norm in society generally, replacement of some aspects of traditional clinical communication with digital may be important for maintaining health service access for the digital generations.
The manner in which information is shared through digital channels is evolving in society. At present, the use of digital communication between clinicians and patients is being operationalised to solve problems. These include non-engagement with health services of young people with LTCs, the cost of providing health services and costs to patients. There are now policy imperatives to use digital communication with patients as this form of communication is becoming the norm in society. However, there is opportunity to reconsider how we provide continuity of care through continuity of communication for people living with LTCs that demands a new way of thinking about health-care provision.
Acknowledgements
The LYNC study would like to thank all the young people, parents, carers and staff of our case study sites who participated in this research, through completing our surveys and/or being interviewed or observed as part of our fieldwork, or securing and preparing outcome data for us.
We would like to thank the following:
The members of our independent Study Steering Committee for their invaluable support and advice: chairperson, Paul Wallace; our PPI representatives, Debs Smith and Jane Whitehurst; and our specialist contributors, Paul Donachie, Catherine Exley, Martin Knapp and Janet McDonagh.
Sarah Christie and Obioma Orazulume, who provided very valuable assistance with the scoping reviews.
From NHS Digital: Mark Reynolds, Chris Dickson, Rebecca Jarratt and Mohammed Mayet, and Chris Gibbons and Corrine Baxter from Accenture, for their advice on the changing NHS technology and policy landscape and on dissemination.
Our PPI team, who attended our PMG meetings and contributed substantially to the development of the project throughout all its stages: Joe Fraser (chairperson of the PMG), Sandra Atkinson, Nidah Chaudhry, Joseph Eaton, Clare Martin and Bijal Trivedi.
Attendees of our Consensus Conference held in London on 12 July 2016: Grace Adjei-Chukwu, Jacqueline Allan, Anneka Appleton, Corinne Baxter, Nazia Begum, Annette Blackmore, Helen Blee, Peter Brown, Tim Burdsey, Sally Burnell, Kathrine Calder, Tim Callaghan, Sarah Collins, Jenny Cookson, Peter Davies, Savia de Souza, Chris Dickson, Alison Elderfield, Chris Gibbons, Richard Grant, Liz Green, Richard Green, Rabab Hashem, Diane Hubber, Rebecca Jarratt, Susan Johnson, Christopher Kaiyo, Mohammed Mayet, Diarmuid McCarthy, Nicola Murray, Luhanga Musumadi, Daniel Nyakutsey, Liz Odeh, Keisha Osmond-Joseph, Vish Papineni, Alan Peres, Frances Perrow, Julie Roberts, Claire Roden, Darren Sills, Magdalena Skrybant, Debs Smith, Amanda Tembedza, Iyamide Thomas, Erkal Topkara, Priya Warner, Jane Whitehurst, Lisa Whitley and Susan Williams.
Those who assisted with facilitation and taking notes at the Consensus Conference: Abi Buckle, Greg Chadburn, Hannah Krzyzanowski, Clare Martin, Bijal Trivedi and Ryadal Sturt.
Celia Janine Bernstein and Emma Phelps, who assisted with compiling the final report.
Our project administrators, Rebecca Rogers and Morna Woods, who provided support to the whole team throughout the project.
The anonymous reviewers of our project report.
Contributions of authors
Frances E Griffiths (Professor, Medical Sociology, Clinician) co-led the project with Jackie Sturt, conceived and designed the study, supervised all data collection, analysis and report writing, drafted the study introduction and discussion chapters, and editorially reviewed all chapters in the report.
Xavier Armoiry (Senior Visiting Fellow, Evidence Synthesis) conducted the scoping review on parents and carers.
Helen Atherton (Assistant Professor, Primary Care) oversaw the conduct and completion of the six scoping reviews, and drafted the three chapters on the reviews.
Carol Bryce (Research Fellow, Sociology) undertook data collection and preliminary analysis of data. She led the analysis and drafted the chapter on what works. She organised and co-delivered the second PPI research day.
Abigail Buckle (Medical Student) checked data for quality, coded data and contributed to analysis, and assisted with note-taking and analysis at the Consensus conference.
Jonathan AK Cave (Economist) advised the health economics team and other areas of the study in which policy, privacy and behaviour were paramount and contributed to the discussion chapter.
Rachel Court (Information Specialist) assisted with planning the literature reviews, developed and undertook searches, was the second reviewer for study selection in the diabetes mellitus rapid review and contributed to writing evidence review chapters.
Kathryn Hamilton (Research Associate, Health Psychology) contributed to case site selection and recruitment, data collection and preliminary analysis of data. She undertook the patient safety analysis and contributed to the chapter on patient safety. In addition, she contributed to the PPI research days.
Thandiwe R Dliwayo (Research Assistant, Psychiatric Research) contributed to data coding, conducted thematic analysis on the IG data and drafted the report chapter. She analysed cognitive interviews and contributed to the chapter on PROMs.
Melina Dritsaki (Senior Research Fellow, Health Economist) contributed to the design of the economic analysis, conducted follow-up health economic interviews and reviewed the health economics chapter.
Patrick Elder (Medical Student) assisted with qualitative ethical analysis of data and contributed to the ethics chapter.
Vera Forjaz (Research Assistant, Psychology) contributed to data collection and analysis, and drafted the PHRs and the IG chapters.
Joe Fraser (PPI) chaired the PMG, supervised the recruitment of PPI representatives for the PMG and independent Study Steering Committee, provided advice throughout the study, and edited the quick reference guides and Plain English summary.
Richard Goodwin (National Institute for Health Research Researcher, Specialist Paediatric Pharmacist) assisted with data collection, contributed to data coding and to the consensus meeting chapter.
Caroline Huxley (Senior Research Fellow, Health Psychology) contributed to case study selection and recruitment, led the first PPI activity, drafted the report chapters on methods and PPI activity, and contributed to scoping reviews.
Agnieszka Ignatowicz (Research Fellow) contributed to data collection, undertook ethical analysis of data and drafted the ethics chapter.
Eleni Karasouli (Senior Research Fellow, Health Psychology) conducted the review on generic measures available to assess the effects of DCC and drafted the report chapter.
Sung Wook Kim (Research Associate, Health Economics) undertook health economics data analysis.
Peter Kimani (Assistant Professor, Medical Statistics) requested quantitative outcome data from trusts, analysed them and drafted the chapter reporting outcome data analysis results.
Jason J Madan (Assistant Professor, Health Economics) contributed to the design of the study, led the health economic component and drafted the health economics section of the report.
Harjit Matharu (IG Manager) provided a NHS perspective from the NHS about IG, provided the study team with background policy documents and new policy as it emerged, and challenged the study team during analysis.
Mike May (Medical Student) undertook the international literature review and drafted the report.
Luhanga Musumadi (Lead Nurse, Adolescent Transition) assisted with case study access, advised on clinical issues during data collection and analysis, and contributed to the Consensus conference and the chapter reporting the conference.
Moli Paul (Consultant, Child and Adolescent Psychiatry) contributed to the conception and design of the study, negotiated access to mental health sites and service user organisations, advised on clinical issues during data collection and analysis, and contributed to the analysis of qualitative data.
Gyanu Raut (ICT Security Manager) guided the study team on issues related to NHS policy and ICT developments.
Sailesh Sankaranarayanan (Consultant and Honorary Assistant Professor, Endocrinology) contributed to the study concept and design, assisted with study site recruitment and advised on clinical issues during data collection and analysis.
Anne-Marie Slowther (Associate Professor, Clinical Ethics) contributed to the initial design of the study, led the ethical analysis package and contributed to writing the ethical analysis chapter.
Mark A Sujan (Associate Professor, Patient Safety) contributed to the development of the research design, led the safety and security analysis, and was lead author for the chapter on patient safety.
Paul A Sutcliffe (Senior Research Fellow, Evidence Synthesis) contributed to the study concept and design, developed and supervised the review of outcome measures, and contributed to the report chapter.
Isabelle Svahnstrom (Medical Student) contributed to coding and analysis of patient safety data.
Frances Taggart (Research Fellow, Evidence Synthesis) contributed to the design, conduct and writing-up of the six scoping reviews.
Ayesha Uddin (Medical Student) contributed to data collection and data analysis.
Alice Verran (Medical Student) undertook the mental health scoping review and wrote it up.
Leigh Walker (Medical Student) undertook data quality checks, coding and contributed to the analysis.
Jackie Sturt (Professor, Behavioural Medicine in Nursing) co-led the project with Frances E Griffiths, conceived and designed the study, supervised all data collection, analysis and report writing, drafted report chapters and editorially reviewed all chapters in the final report.
Publication
Griffiths FE, Atherton H, Barker JR, Cave JA, Dennick K, Dowdall P, et al. Improving health outcomes for young people with long-term conditions: the role of digital communication in current and future patient–clinician communication for NHS providers of specialist clinical services for young people–LYNC study protocol. Digital Health 2015;1:1–13.
Data sharing statement
Anonymised data from the empirical study is available to bona fide researchers on application to the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Dobbels F, Damme-Lombaert RV, Vanhaecke J, De Geest S. Growing pains: non-adherence with the immunosuppressive regimen in adolescent transplant recipients. Pediatr Transplant 2005;9:381-90. https://doi.org/10.1111/j.1399-3046.2005.00356.x.
- Annunziato RA, Emre S, Shneider B, Barton C, Dugan CA, Shemesh E. Adherence and medical outcomes in pediatric liver transplant recipients who transition to adult services. Pediatr Transplant 2007;11:608-14. https://doi.org/10.1111/j.1399-3046.2007.00689.x.
- Singh SP, Paul M, Ford T, Kramer T, Weaver T, McLaren S, et al. Process, outcome and experience of transition from child to adult mental healthcare: multiperspective study. Br J Psychiatry 2010;197:305-12. https://doi.org/10.1192/bjp.bp.109.075135.
- Heery E, Sheehan AM, While AE, Coyne I. Experiences and outcomes of transition from pediatric to adult health care services for young people with congenital heart disease: a systematic review. Congenit Heart Dis 2015;10:413-27. https://doi.org/10.1111/chd.12251.
- Chandra S, Luetkemeyer S, Romero R, Gupta NA. Growing up: not an easy transition—perspectives of patients and parents regarding transfer from a pediatric liver transplant center to adult care. Int J Hepatol 2015;2015. https://doi.org/10.1155/2015/765957.
- Watson AR. Non-compliance and transfer from paediatric to adult transplant unit. Pediatr Nephrol 2000;14:469-72. https://doi.org/10.1007/s004670050794.
- Annunziato RA, Baisley MC, Arrato N, Barton C, Henderling F, Arnon R, et al. Strangers headed to a strange land? A pilot study of using a transition coordinator to improve transfer from pediatric to adult services. J Pediatr 2013;163:1628-33. https://doi.org/10.1016/j.jpeds.2013.07.031.
- Harden PN, Walsh G, Bandler N, Bradley S, Lonsdale D, Taylor J, et al. Bridging the gap: an integrated paediatric to adult clinical service for young adults with kidney failure. BMJ 2012;344. https://doi.org/10.1136/bmj.e3718.
- Pape L, Lämmermühle J, Oldhafer M, Blume C, Weiss R, Ahlenstiel T. Different models of transition to adult care after pediatric kidney transplantation: a comparative study. Pediatr Transplant 2013;17:518-24. https://doi.org/10.1111/petr.12102.
- Witherspoon D, Drotar D. Correlates of adherence to prophylactic penicillin therapy in children with sickle cell disease. Child Health Care 2006;35:281-96. https://doi.org/10.1207/s15326888chc3504_1.
- Howard J, Woodhead T, Musumadi L, Martell A, Inusa BP. Moving young people with sickle cell disease from paediatric to adult services. Br J Hosp Med 2010;71:310-14. https://doi.org/10.12968/hmed.2010.71.6.48435.
- Musumadi L, Westerdale N, Appleby H. An overview of the effects of sickle cell disease in adolescents. Nurs Stand 2012;26:35-40. https://doi.org/10.7748/ns2012.02.26.26.35.c8973.
- Leikin SL, Gallagher D, Kinney TR, Sloane D, Klug P, Rida W. Mortality in children and adolescents with sickle cell disease. Cooperative Study of Sickle Cell Disease. Pediatrics 1989;84:500-8.
- National Paediatric Diabetes Audit Report 2010–11. London: Royal College of Paediatrics and Child Health; 2012.
- National Paediatric Diabetes Audit Report 2014–15. London: Royal College of Paediatrics and Child Health; 2016.
- Dovey-Pearce G, Hurrell R, May C, Walker C, Doherty Y. Young adults’ (16–25 years) suggestions for providing developmentally appropriate diabetes services: a qualitative study. Health Soc Care Community 2005;13:409-19. https://doi.org/10.1111/j.1365-2524.2005.00577.x.
- Kennedy A, Sloman F, Douglass JA, Sawyer SM. Young people with chronic illness: the approach to transition. Intern Med J 2007;37:555-60. https://doi.org/10.1111/j.1445-5994.2007.01440.x.
- Kreyenbuhl J, Nossel IR, Dixon LB. Disengagement from mental health treatment among individuals with schizophrenia and strategies for facilitating connections to care: a review of the literature. Schizophr Bull 2009;35:696-703. https://doi.org/10.1093/schbul/sbp046.
- Bell LE, Sawyer SM. Transition of care to adult services for pediatric solid-organ transplant recipients. Pediatr Clin North Am 2010;57:593-610. https://doi.org/10.1016/j.pcl.2010.01.007.
- The Communications Market Report. London: Ofcom; 2015.
- Menachemi N, Prickett CT, Brooks RG. The use of physician-patient email: a follow-up examination of adoption and best-practice adherence 2005–2008. J Med Internet Res 2011;13. https://doi.org/10.2196/jmir.1578.
- Byrne JM, Elliott S, Firek A. Initial experience with patient-clinician secure messaging at a VA medical center. J Am Med Inform Assoc 2009;16:267-70. https://doi.org/10.1197/jamia.M2835.
- Atkinson NL, Saperstein SL, Pleis J. Using the internet for health-related activities: findings from a national probability sample. J Med Internet Res 2009;11. https://doi.org/10.2196/jmir.1035.
- Liederman EM, Lee JC, Baquero VH, Seites PG. Patient–physician web messaging. The impact on message volume and satisfaction. J Gen Intern Med 2005;20:52-7. https://doi.org/10.1111/j.1525-1497.2005.40009.x.
- Nilsson C, Ohman M, Söderberg S. Information and communication technology in supporting people with serious chronic illness living at home – an intervention study. J Telemed Telecare 2006;12:198-202. https://doi.org/10.1258/135763306777488807.
- Sittig DF. Results of a content analysis of electronic messages (email) sent between patients and their physicians. BMC Med Inform Decis Mak 2003;3. https://doi.org/10.1186/1472-6947-3-11.
- Research Evidence on the Effectiveness of Self-Care Support. London: Department of Health and Social Care; 2007.
- Van Walleghem N, Macdonald CA, Dean HJ. Evaluation of a systems navigator model for transition from pediatric to adult care for young adults with type 1 diabetes. Diabetes Care 2008;31:1529-30. https://doi.org/10.2337/dc07-2247.
- Simon J, Budge K, Foster J, Bell S, Christensen J, Price J, et al. Impact of True Colours Mood Monitoring on Mental Health Service Utilisation n.d.
- Balasanthiran A, O’Shea T, Moodambail A, Woodcock T, Poots AJ, Stacey M, et al. Type 2 diabetes in children and young adults in East London: an alarmingly high prevalence. Practical Diabetes 2012;29:193-98a. https://doi.org/10.1002/pdi.1689.
- The Power of Information: Putting All of Us in Control of the Health and Care Information We Need. London: Department of Health and Social Care; 2012.
- Health and Social Care Information Centre . Vision 2013. http://systems.hscic.gov.uk/nhsmail/nhsmail2/vision (accessed 1 August 2016).
- Department of Health and Social Care . Information: To Share Or Not To Share? 2013. http://caldicott2.dh.gov.uk/ (accessed 1 August 2016).
- National Information Board . Workstream Roadmaps 2015. www.gov.uk/government/publications/national-information-boards-workstream-roadmaps (accessed 15 August 2017).
- Caldicott F. National Data Guardian for Health and Care: Review of Data Security, Consent and Opt-Outs. Leeds: National Data Guardian; 2016.
- NHS England . NHS Digital Technology: Wachter Review 2016. www.england.nhs.uk/digitaltechnology/info-revolution/wachter-review/ (accessed 5 March 2017).
- Wachter R. The Wachter Review of Health IT: Update and Insights. Digital Health and Care Congress 2016. London: The King’s Fund; 2016.
- Ye J, Rust G, Fry-Johnson Y, Strothers H. E-mail in patient-provider communication: a systematic review. Patient Educ Couns 2010;80:266-73. https://doi.org/10.1016/j.pec.2009.09.038.
- Blackburn S, Brownsell S, Hawley MS. A systematic review of digital interactive television systems and their applications in the health and social care fields. J Telemed Telecare 2011;17:168-76. https://doi.org/10.1258/jtt.2010.100610.
- de Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, Car J, Atun R. Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database Syst Rev 2012;12. https://doi.org/10.1002/14651858.CD007459.pub2.
- Holtz B, Lauckner C. Diabetes management via mobile phones: a systematic review. Telemed J E Health 2012;18:175-84. https://doi.org/10.1089/tmj.2011.0119.
- Johansen MA, Berntsen GK, Henriksen E, Horsch A. Electronic symptom reporting between patient and provider for improved health care service quality: a systematic review of randomized controlled trials. Part 1: state of the art. J Med Internet Res 2012;14. http://doi.org/10.2196/jmir.2214.
- Meyer B, Atherton H, Sawmynaden P, Car J. Email for communicating results of diagnostic medical investigations to patients. Cochrane Database Syst Rev 2012;8. http://doi.org/10.1002/14651858.CD007980.pub2.
- Sutcliffe P, Martin S, Sturt J, Powell J, Griffiths F, Adams A, et al. Systematic review of communication technologies to promote access and engagement of young people with diabetes into healthcare. BMC Endocr Disord 2011;11. https://doi.org/10.1186/1472-6823-11-1.
- Martin S, Sutcliffe P, Griffiths F, Sturt J, Powell J, Adams A, et al. Effectiveness and impact of networked communication interventions in young people with mental health conditions: a systematic review. Patient Educ Couns 2011;85:e108-19. http://doi.org/10.1016/j.pec.2010.11.014.
- Atherton H, Sawmynaden P, Sheikh A, Majeed A, Car J. Email for clinical communication between patients/caregivers and healthcare professionals. Cochrane Database Syst Rev 2012;11. http://doi.org/10.1002/14651858.CD007978.pub2.
- Osborn CY, Mayberry LS, Mulvaney SA, Hess R. Patient web portals to improve diabetes outcomes: a systematic review. Curr Diab Rep 2010;10:422-35. https://doi.org/10.1007/s11892-010-0151-1.
- McLean S, Protti D, Sheikh A. Telehealthcare for long term conditions. BMJ 2011;342. http://doi.org/10.1136/bmj.d120.
- Verhoeven F, Tanja-Dijkstra K, Nijland N, Eysenbach G, van Gemert-Pijnen L. Asynchronous and synchronous teleconsultation for diabetes care: a systematic literature review. J Diabetes Sci Technol 2010;4:666-84. https://doi.org/10.1177/193229681000400323.
- Medical Research Council Health Services, Public Health Research Board . A Framework for Development and Evaluation of RCTs Complex Interventions to Improve Health 2000.
- Gurol-Urganci I, de Jongh T, Vodopivec-Jamsek V, Car J, Atun R. Mobile phone messaging for communicating results of medical investigations. Cochrane Database Syst Rev 2012;6. http://doi.org/10.1002/14651858.CD007456.pub2.
- Gagnon MP, Legare F, Labrecque M, Frémont P, Pluye P, Gagnon J, et al. Interventions for promoting information and communication technologies adoption in healthcare professionals. Cochrane Database Syst Rev 2009;1. https://doi.org/10.1002/14651858.CD006093.pub2.
- Van Gaalen JL, Hashimoto S, Sont JK. Telemanagement in asthma: an innovative and effective approach. Curr Opin Allergy Clin Immunol 2012;12:235-40. https://doi.org/10.1097/ACI.0b013e3283533700.
- Valimaki M, Hatonen H, Lahti M, Kuosmanen L, Adams CE. Information and communication technology in patient education and support for people with schizophrenia. Cochrane Database Syst Rev 2012;10.
- Gentles SJ, Lokker C, McKibbon KA. Health information technology to facilitate communication involving health care providers, caregivers, and pediatric patients: a scoping review. J Med Internet Res 2010;12. http://doi.org/10.2196/jmir.1390.
- Johansen MA, Berntsen GKR, Schuster T, Henriksen E, Horsch A. Electronic symptom reporting between patient and provider for improved health care service quality: a systematic review of randomized controlled trials. Part 2: methodological quality and effects. J Med Internet Res 2012;14. http://doi.org/10.2196/jmir.2216.
- Bender JL, Radhakrishnan A, Diorio C, Englesakis M, Jadad AR. Can pain be managed through the Internet? A systematic review of randomized controlled trials. Pain 2011;152:1740-50. https://doi.org/10.1016/j.pain.2011.02.012.
- Graham T, Broersma M, Hazelhoff K, van ’t Haar G. Between broadcasting political messages and interacting with voters. Inf Commun Soc 2013;16:692-716. https://doi.org/10.1080/1369118X.2013.785581.
- Barak A, Klein B, Proudfoot JG. Defining internet-supported therapeutic interventions. Ann Behav Med 2009;38:4-17. https://doi.org/10.1007/s12160-009-9130-7.
- Carlbring P, Ekselius L, Andersson G. Treatment of panic disorder via the Internet: a randomized trial of CBT vs. applied relaxation. J Behav Ther Exp Psychiatry 2003;34:129-40. https://doi.org/10.1016/S0005-7916(03)00026-0.
- Sawmynaden P, Atherton H, Majeed A, Car J. Email for the provision of information on disease prevention and health promotion. Cochrane Database Syst Rev 2012;11. https://doi.org/10.1002/14651858.CD007982.pub2.
- Yin R. Case Study Research: Design and Methods. London: Sage; 2009.
- Pawson RT, Tilley N. Realist Evaluation. London: Sage; 1997.
- Ives J, Draper H. Appropriate methodologies for empirical bioethics: it’s all relative. Bioethics 2009;23:249-58. https://doi.org/10.1111/j.1467-8519.2009.01715.x.
- IEC 60812, Analysis Techniques for System Reliability-Procedure for Failure Mode and Effects Analysis (FMEA). Geneva: International Electrotechnical Commission; 2006.
- NHS England . Agenda for Change Pay Scales for 2014–2015 2014. www.nhsemployers.org/~/media/Employers/Documents/Pay%20and%20reward/AfC%20pay%20bands%20and%20points%20poster%202014.pdf (accessed 5 March 2017).
- Guide to the Methods of Technology Appraisal. London: National Institute for Health and Care Excellence; 2013.
- Saldana J. The Coding Manual for Qualitative Researchers. Thousand Oaks, CA: Sage; 2012.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Boyatzis RE. Transforming Qualitative Information: Thematic Analysis and Code Development. Thousand Oaks, CA: Sage; 1998.
- Ryan GW, Bernard HR. Techniques to identify themes. Field Methods 2003;15:85-109. https://doi.org/10.1177/1525822X02239569.
- Slowther A-M. The concept of autonomy and its interpretation in health care. Clin Ethics 2007;2:173-75. https://doi.org/10.1258/147775007783560166.
- Lee YY, Lin JL. Do patient autonomy preferences matter? Linking patient-centered care to patient–physician relationships and health outcomes. Soc Sci Med 2010;71:1811-18. https://doi.org/10.1016/j.socscimed.2010.08.008.
- The Duties of a Doctor Registered With the General Medical Council. London: General Medical Council; 2014.
- Sujan M, Spurgeon P, Cooke M, Weale A, Debenham P, Cross S. The development of safety cases for healthcare services: practical experiences, opportunities and challenges. Reliab Eng Syst Saf 2015;140:200-07. http://doi.org/10.1016/j.ress.2015.03.033.
- Sujan MA, Habli I, Kelly TP, Pozzi S, Johnson CW. Should healthcare providers do safety cases? Lessons from a cross-industry review of safety case practices. Saf Sci 2016;84:181-9. http://doi.org/10.1016/j.ssci.2015.12.021.
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated health economic evaluation reporting standards (CHEERS) statement. Cost Eff Resour All 2013;11. https://doi.org/10.1186/1478-7547-11-6.
- NHS England . NHS England Using Technology to Beat Cost of Missed Appointments 2016. www.england.nhs.uk/2014/03/missed-appts/ (accessed 5 March 2017).
- Ryan M, Gerard K. Using discrete choice experiments to value health care programmes: current practice and future research reflections. Appl Health Econ Health Policy 2003;2:55-64.
- National Institute for Health and Care Excellence . Diagnosis and Management of Type 1 Diabetes in Children, Young People and Adults: NICE Guidelines [CG15] 2004. www.nice.org.uk/Guidance/CG15 (accessed 5 March 2017).
- Costing Statement: Type 1 Diabetes in Adults Implementing the NICE Guideline on Type 1 Diabetes in Adults (NG17). London: National Institute for Health and Care Excellence; 2015.
- Gray A, Raikou M, McGuire A, Fenn P, Stevens R, Cull C, et al. Cost effectiveness of an intensive blood glucose control policy in patients with type 2 diabetes: economic analysis alongside randomised controlled trial (UKPDS 41). BMJ 2000;320:1373-8. https://doi.org/10.1136/bmj.320.7246.1373.
- Joint Commissioning Panel for Mental Health (JCPMH) . Commissioning Tools 2016. www.jcpmh.info/commissioning-tools/ (accessed 5 March 2017).
- Kuijpers W, Groen WG, Aaronson NK, van Harten WH. A systematic review of web-based interventions for patient empowerment and physical activity in chronic diseases: relevance for cancer survivors. J Med Internet Res 2013;15. https://doi.org/10.2196/jmir.2281.
- Stellefson M, Chaney B, Barry AE, Chavarria E, Tennant B, Walsh-Childers K, et al. Web 2.0 chronic disease self-management for older adults: a systematic review. J Med Internet Res 2013;15. https://doi.org/10.2196/jmir.2439.
- Cotter AP, Durant N, Agne AA, Cherrington AL. Internet interventions to support lifestyle modification for diabetes management: a systematic review of the evidence. J Diabetes Complications 2014;28:243-51. https://doi.org/10.1016/j.jdiacomp.2013.07.003.
- Glasgow RE, Kurz D, King D, Dickman JM, Faber AJ, Halterman E, et al. Outcomes of minimal and moderate support versions of an internet-based diabetes self-management support program. J Gen Intern Med 2010;25:1315-22. https://doi.org/10.1007/s11606-010-1480-0.
- Glasgow RE, Kurz D, King D, Dickman JM, Faber AJ, Halterman E, et al. Twelve-month outcomes of an Internet-based diabetes self-management support program. Patient Educ Couns 2012;87:81-92. https://doi.org/10.1016/j.pec.2011.07.024.
- Nguyen HQ, Donesky-Cuenco D, Wolpin S, Reinke LF, Benditt JO, Paul SM, et al. Randomized controlled trial of an internet-based versus face-to-face dyspnea self-management program for patients with chronic obstructive pulmonary disease: pilot study. J Med Internet Res 2008;10. https://doi.org/10.2196/jmir.990.
- Jackson CL, Bolen S, Brancati FL, Batts-Turner ML, Gary TL. A systematic review of interactive computer-assisted technology in diabetes care. Interactive information technology in diabetes care. J Gen Intern Med 2006;21:105-10. https://doi.org/10.1111/j.1525-1497.2005.00310.x.
- Izquierdo RE, Knudson PE, Meyer S, Kearns J, Ploutz-Snyder R, Weinstock RS. A comparison of diabetes education administered through telemedicine versus in person. Diabetes Care 2003;26:1002-7. https://doi.org/10.2337/diacare.26.4.1002.
- Kirsch SE, Lewis FM. Using the World Wide Web in health-related intervention research. A review of controlled trials. Comput Inform Nurs 2004;22:8-18. https://doi.org/10.1097/00024665-200401000-00005.
- Flatley-Brennan P. Computer network home care demonstration: a randomized trial in persons living with AIDS. Comput Biol Med 1998;28:489-508. https://doi.org/10.1016/S0010-4825(98)00029-8.
- Goldzweig CL, Orshansky G, Paige NM, Towfigh AA, Haggstrom DA, Miake-Lye I, et al. Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes: a systematic review. Ann Intern Med 2013;159:677-87. https://doi.org/10.7326/0003-4819-159-10-201311190-00006.
- Wagner PJ, Dias J, Howard S, Kintziger KW, Hudson MF, Seol YH, et al. Personal health records and hypertension control: a randomized trial. J Am Med Inform Assoc 2012;19:626-34. https://doi.org/10.1136/amiajnl-2011-000349.
- Lorig K, Ritter PL, Laurent DD, Plant K, Green M, Jernigan VB, et al. Online diabetes self-management program: a randomized study. Diabetes Care 2010;33:1275-81. https://doi.org/10.2337/dc09-2153.
- Artinian NT, Flack JM, Nordstrom CK, Hockman EM, Washington OG, Jen KL, et al. Effects of nurse-managed telemonitoring on blood pressure at 12-month follow-up among urban African Americans. Nurs Res 2007;56:312-22. https://doi.org/10.1097/01.NNR.0000289501.45284.6e.
- Leveille SG, Huang A, Tsai SB, Allen M, Weingart SN, Iezzoni LI. Health coaching via an internet portal for primary care patients with chronic conditions: a randomized controlled trial. Med Care 2009;47:41-7. https://doi.org/10.1097/MLR.0b013e3181844dd0.
- Mirkovic J, Kaufman DR, Ruland CM. Supporting cancer patients in illness management: usability evaluation of a mobile app. JMIR Mhealth Uhealth 2014;2. https://doi.org/10.2196/mhealth.3359.
- de Jong CC, Ros WJ, Schrijvers G. The effects on health behavior and health outcomes of internet-based asynchronous communication between health providers and patients with a chronic condition: a systematic review. J Med Internet Res 2014;16. https://doi.org/10.2196/jmir.3000.
- Ghahari S, Leigh Packer T, Passmore AE. Effectiveness of an online fatigue self-management programme for people with chronic neurological conditions: a randomized controlled trial. Clin Rehabil 2010;24:727-44. https://doi.org/10.1177/0269215509360648.
- García-Lizana F, Sarría-Santamera A. New technologies for chronic disease management and control: a systematic review. J Telemed Telecare 2007;13:62-8. https://doi.org/10.1258/135763307780096140.
- Benatar D, Bondmass M, Ghitelman J, Avitall B. Outcomes of chronic heart failure. Arch Intern Med 2003;163:347-52. https://doi.org/10.1001/archinte.163.3.347.
- Berman RL, Iris MA, Bode R, Drengenberg C. The effectiveness of an online mind-body intervention for older adults with chronic pain. J Pain 2009;10:68-79. https://doi.org/10.1016/j.jpain.2008.07.006.
- Trief PM, Teresi JA, Izquierdo R, Morin PC, Goland R, Field L, et al. Psychosocial outcomes of telemedicine case management for elderly patients with diabetes: the randomized IDEATel trial. Diabetes Care 2007;30:1266-8. https://doi.org/10.2337/dc06-2476.
- McCarrier KP, Ralston JD, Hirsch IB, Lewis G, Martin DP, Zimmerman FJ, et al. Web-based collaborative care for type 1 diabetes: a pilot randomized trial. Diabetes Technol Ther 2009;11:211-17. https://doi.org/10.1089/dia.2008.0063.
- Bond GE, Burr RL, Wolf FM, Feldt K. The effects of a web-based intervention on psychosocial well-being among adults aged 60 and older with diabetes: a randomized trial. Diabetes Educ 2010;36:446-56. https://doi.org/10.1177/0145721710366758.
- Smith AJ, Skow Á, Bodurtha J, Kinra S. Health information technology in screening and treatment of child obesity: a systematic review. Pediatrics 2013;131:e894-902. https://doi.org/10.1542/peds.2012-2011.
- Nguyen B, Shrewsbury VA, O’Connor J, Steinbeck KS, Lee A, Hill AJ, et al. Twelve-month outcomes of the Loozit randomized controlled trial: a community-based healthy lifestyle program for overweight and obese adolescents. Arch Pediatr Adolesc Med 2012;166:170-7. https://doi.org/10.1001/archpediatrics.2011.841.
- Donald KJ, McBurney H, Teichtahl H, Irving L, Browning C, Rubinfeld A, et al. Telephone based asthma management – financial and individual benefits. Aust Fam Physician 2008;37:272-5.
- de Jongste JC, Carraro S, Hop WC, Baraldi E. CHARISM Study Group . Daily telemonitoring of exhaled nitric oxide and symptoms in the treatment of childhood asthma. Am J Respir Crit Care Med 2009;179:93-7. https://doi.org/10.1164/rccm.200807-1010OC.
- Khan M, O’Meara M, Stevermuer T, Henry RL. Randomized controlled trial of asthma education after discharge from an emergency department. J Paediatr Child Health 2004;40:674-7. https://doi.org/10.1111/j.1440-1754.2004.00490.x.
- Willems DC, Joore MA, Hendriks JJ, Nieman FH, Severens JL, Wouters EF. The effectiveness of nurse-led telemonitoring of asthma: results of a randomized controlled trial. J Eval Clin Pract 2008;14:600-9. https://doi.org/10.1111/j.1365-2753.2007.00936.x.
- Van der Meer V, Bakker M, Van den Hout W, Rabe KF, Sterk PJ, Kievit J, et al. Internet-based self-management plus education compared with usual care in asthma: a randomized trial. Ann Intern Med 2009;151:110-20. https://doi.org/10.7326/0003-4819-151-2-200907210-00008.
- Clark NM, Gong ZM, Wang SJ, Lin X, Bria WF, Johnson TR. A randomized trial of a self-regulation intervention for women with asthma. Chest 2007;132:88-97. https://doi.org/10.1378/chest.06-2539.
- Gruffydd-Jones K, Hollinghurst S, Ward S, Taylor G. Targeted routine asthma care in general practice using telephone triage. Br J Gen Pract 2005;55:918-23.
- Pinnock H, Bawden R, Proctor S, Wolfe S, Scullion J, Price D, et al. Accessibility, acceptability, and effectiveness in primary care of routine telephone review of asthma: pragmatic, randomised controlled trial. BMJ 2003;326:477-9. https://doi.org/10.1136/bmj.326.7387.477.
- Pinnock H, Adlem L, Gaskin S, Harris J, Snellgrove C, Sheikh A. Accessibility, clinical effectiveness, and practice costs of providing a telephone option for routine asthma reviews: phase IV controlled implementation study. Br J Gen Pract 2007;57:714-22.
- Vollmer WM, Rand CS, Feldstein AC, Waterbury A, Dubanoski JP, Schneider J, et al. Use of automated phone calls to support inhaled corticosteroid (ICS) adherence. Am J Respir Crit Care Med 2009;179. https://doi.org/10.1164/ajrccm-conference.2009.179.1_MeetingAbstracts.A1089.
- Rasmussen LM, Phanareth K, Nolte H, Backer V. Internet-based monitoring of asthma: a long-term, randomized clinical study of 300 asthmatic subjects. J Allergy Clin Immunol 2005;115:1137-42. https://doi.org/10.1016/j.jaci.2005.03.030.
- Chan DS, Callahan CW, Sheets SJ, Moreno CN, Malone FJ. An internet-based store-and-forward video home telehealth system for improving asthma outcomes in children. Am J Health Syst Pharm 2003;60:1976-81.
- Chan DS, Callahan CW, Hatch-Pigott VB, Lawless A, Proffitt HL, Manning NE, et al. Internet-based home monitoring and education of children with asthma is comparable to ideal office-based care: results of a 1-year asthma in-home monitoring trial. Pediatrics 2007;119:569-78. https://doi.org/10.1542/peds.2006-1884.
- Guendelman S, Meade K, Benson M, Chen YQ, Samuels S. Improving asthma outcomes and self-management behaviors of inner-city children: a randomized trial of the Health Buddy interactive device and an asthma diary. Arch Pediatr Adolesc Med 2002;156:114-20. https://doi.org/10.1001/archpedi.156.2.114.
- Ryhänen AM, Siekkinen M, Rankinen S, Korvenranta H, Leino-Kilpi H. The effects of Internet or interactive computer-based patient education in the field of breast cancer: a systematic literature review. Patient Educ Couns 2010;79:5-13. https://doi.org/10.1016/j.pec.2009.08.005.
- Gustafson DH, Hawkins R, Pingree S, McTavish F, Arora NK, Mendenhall J, et al. Effect of computer support on younger women with breast cancer. J Gen Intern Med 2001;16:435-45. https://doi.org/10.1046/j.1525-1497.2001.016007435.x.
- Williams GC, Lynch M, Glasgow RE. Computer-assisted intervention improves patient-centered diabetes care by increasing autonomy support. Health Psychol 2007;26. https://doi.org/10.1037/0278-6133.26.6.728.
- Glasgow RE, Nutting PA, King DK, Nelson CC, Cutter G, Gaglio B, et al. Randomized effectiveness trial of a computer-assisted intervention to improve diabetes care. Diabetes Care 2005;28:33-9. https://doi.org/10.2337/diacare.28.1.33.
- Tang PC, Overhage JM, Chan AS, Brown NL, Aghighi B, Entwistle MP, et al. Online disease management of diabetes: engaging and motivating patients online with enhanced resources-diabetes (EMPOWER-D), a randomized controlled trial. J Am Med Inform Assoc 2013;20:526-34. https://doi.org/10.1136/amiajnl-2012-001263.
- Åkesson KM, Saveman BI, Nilsson G. Health care consumers’ experiences of information communication technology – a summary of literature. Int J Med Inform 2007;76:633-45. https://doi.org/10.1016/j.ijmedinf.2006.07.001.
- Marrero DG, Vandagriff JL, Kronz K, Fineberg NS, Golden MP, Gray Msn D, et al. Using telecommunication technology to manage children with diabetes: the Computer-Linked Outpatient Clinic (CLOC) Study. Diabetes Educ 1995;21:313-19. https://doi.org/10.1177/014572179502100409.
- van den Berg N, Schumann M, Kraft K, Hoffmann W. Telemedicine and telecare for older patients – a systematic review. Maturitas 2012;73:94-114. https://doi.org/10.1016/j.maturitas.2012.06.010.
- Nguyen HQ, Donesky D, Reinke LF, Wolpin S, Chyall L, Benditt JO, et al. Internet-based dyspnea self-management support for patients with chronic obstructive pulmonary disease. J Pain Symptom Manage 2013;46:43-55. https://doi.org/10.1016/j.jpainsymman.2012.06.015.
- Woodend AK, Sherrard H, Fraser M, Stuewe L, Cheung T, Struthers C. Telehome monitoring in patients with cardiac disease who are at high risk of readmission. Heart Lung 2008;37:36-45. https://doi.org/10.1016/j.hrtlng.2007.04.004.
- Whitten P, Mickus M. Home telecare for COPD/CHF patients: outcomes and perceptions. J Telemed Telecare 2007;13:69-73. https://doi.org/10.1258/135763307780096249.
- Gellis ZD, Kenaley B, McGinty J, Bardelli E, Davitt J, Ten Have T. Outcomes of a telehealth intervention for homebound older adults with heart or chronic respiratory failure: a randomized controlled trial. Gerontologist 2012;52:541-52. https://doi.org/10.1093/geront/gnr134.
- Green BB, Cook AJ, Ralston JD, Fishman PA, Catz SL, Carlson J, et al. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA 2008;299:2857-67. https://doi.org/10.1001/jama.299.24.2857.
- Willems DC, Joore MA, Hendriks JJ, Wouters EF, Severens JL. Cost-effectiveness of a nurse-led telemonitoring intervention based on peak expiratory flow measurements in asthmatics: results of a randomised controlled trial. Cost Effectiv Resource Alloc 2007;5. https://doi.org/10.1186/1478-7547-5-1.
- Hicks CL, von Baeyer CL, McGrath PJ. Online psychological treatment for pediatric recurrent pain: a randomized evaluation. J Pediatr Psychol 2006;31:724-36. https://doi.org/10.1093/jpepsy/jsj065.
- Devineni T, Blanchard EB. A randomized controlled trial of an internet-based treatment for chronic headache. Behav Res Ther 2005;43:277-92. https://doi.org/10.1016/j.brat.2004.01.008.
- Neubeck L, Redfern J, Fernandez R, Briffa T, Bauman A, Freedman SB. Telehealth interventions for the secondary prevention of coronary heart disease: a systematic review. Eur J Cardiovasc Prev Rehabil 2009;16:281-9. https://doi.org/10.1097/HJR.0b013e32832a4e7a.
- Eland-de Kok P, van Os-Medendorp H, Vergouwe-Meijer A, Bruijnzeel-Koomen C, Ros W. A systematic review of the effects of e-health on chronically ill patients. J Clin Nurs 2011;20:2997-3010. https://doi.org/10.1111/j.1365-2702.2011.03743.x.
- Southard BH, Southard DR, Nuckolls J. Clinical trial of an Internet-based case management system for secondary prevention of heart disease. J Cardiopulm Rehabil 2003;23:341-8. https://doi.org/10.1097/00008483-200309000-00003.
- Glasgow RE, Boles SM, McKay HG, Feil EG, Barrera M. The D-Net diabetes self-management program: long-term implementation, outcomes, and generalization results. Prev Med 2003;36:410-19. https://doi.org/10.1016/S0091-7435(02)00056-7.
- McKay HG, King D, Eakin EG, Seeley JR, Glasgow RE. The diabetes network internet-based physical activity intervention a randomized pilot study. Diabetes Care 2001;24:1328-34. https://doi.org/10.2337/diacare.24.8.1328.
- Ruland CM, Andersen T, Jeneson A, Moore S, Grimsbø GH, Børøsund E, et al. Effects of an internet support system to assist cancer patients in reducing symptom distress: a randomized controlled trial. Cancer Nurs 2013;36:6-17. https://doi.org/10.1097/NCC.0b013e31824d90d4.
- Palermo TM, Wilson AC, Peters M, Lewandowski A, Somhegyi H. Randomized controlled trial of an Internet-delivered family cognitive–behavioral therapy intervention for children and adolescents with chronic pain. Pain 2009;146:205-13. https://doi.org/10.1016/j.pain.2009.07.034.
- Bowles KH, Holland DE, Horowitz DA. A comparison of in-person home care, home care with telephone contact and home care with telemonitoring for disease management. J Telemed Telecare 2009;15:344-50. https://doi.org/10.1258/jtt.2009.090118.
- Lorig KR, Laurent DD, Deyo RA, Marnell ME, Minor MA, Ritter PL. Can a back pain e-mail discussion group improve health status and lower health care costs? A randomized study. Arch Intern Med 2002;162:792-6. https://doi.org/10.1001/archinte.162.7.792.
- Lorig K, Ritter PL, Plant K, Laurent DD, Kelly P, Rowe S. The South Australia health chronic disease self-management Internet trial. Health Educ Behav 2013;40:67-7. https://doi.org/10.1177/1090198112436969.
- Ross SE, Moore LA, Earnest MA, Wittevrongel L, Lin CT. Providing a web-based online medical record with electronic communication capabilities to patients with congestive heart failure: randomized trial. J Med Internet Res 2004;6. https://doi.org/10.2196/jmir.6.2.e12.
- Ammenwerth E, Schnell-Inderst P, Hoerbst A. The impact of electronic patient portals on patient care: a systematic review of controlled trials. J Med Internet Res 2012;14. https://doi.org/10.2196/jmir.2238.
- Sciamanna CN, Nicholson RA, Lofland JH, Manocchia M, Mui S, Hartman CW. Effects of a Website designed to improve the management of migraines. Headache 2006;46:92-100. https://doi.org/10.1111/j.1526-4610.2006.00312.x.
- Finkelstein SM, Speedie SM, Zhou X, Potthoff S, Ratner ER. Perception, satisfaction and utilization of the VALUE home telehealth service. J Telemed Telecare 2011;17:288-92. https://doi.org/10.1258/jtt.2011.100712.
- Rubin HR, Gandek B, Rogers WH, Kosinski M, McHorney CA, Ware JE. Patients’ ratings of outpatient visits in different practice settings. Results from the Medical Outcomes Study. JAMA 1993;270:835-40. https://doi.org/10.1001/jama.1993.03510070057036.
- Maly RC, Frank JC, Marshall GN, DiMatteo MR, Reuben DB. Perceived efficacy in patient–physician interactions (PEPPI): validation of an instrument in older persons. J Am Geriatr Soc 1998;46:889-94. https://doi.org/10.1111/j.1532-5415.1998.tb02725.x.
- Brown JB, Boles M, Mullooly JP, Levinson W. Effect of clinician communication skills training on patient satisfaction. A randomized, controlled trial. Ann Intern Med 1999;131:822-9. https://doi.org/10.7326/0003-4819-131-11-199912070-00004.
- Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977;1:385-401. https://doi.org/10.1177/014662167700100306.
- Brown TA, Chorpita BF, Korotitsch W, Barlow DH. Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behav Res Ther 1997;35:79-8. https://doi.org/10.1016/S0005-7967(96)00068-X.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996.
- Spielberger C, Gorsuch R, Lushene R. State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1970.
- Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann 1979;2:197-20. https://doi.org/10.1016/0149-7189(79)90094-6.
- Westra BL, Cullen L, Brody D, Jump P, Geanon L, Milad E. Development of the home care client satisfaction instrument. Public Health Nurs 1995;12:393-9. https://doi.org/10.1111/j.1525-1446.1995.tb00168.x.
- Telemedicine Clinical Consultation Patient Satisfaction Survey. Sacramento, CA: UC Davis Health; 1996.
- Demiris G, Speedie S, Finkelstein S. A questionnaire for the assessment of patients’ impressions of the risks and benefits of home telecare. J Telemed Telecare 2000;6:278-84. https://doi.org/10.1258/1357633001935914.
- Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med 1991;32:705-14. https://doi.org/10.1016/0277-9536(91)90150-B.
- Koenig HG, Westlund RE, George LK, Hughes DC, Blazer DG, Hybels C. Abbreviating the Duke Social Support Index for use in chronically ill elderly individuals. Psychosomatics 1993;34:61-9. https://doi.org/10.1016/S0033-3182(93)71928-3.
- Brooks R. EuroQol: the current state of play. Health Policy 1996;37:53-72. https://doi.org/10.1016/0168-8510(96)00822-6.
- Moriarty DG, Zack MM, Kobau R. The Centers for Disease Control and Prevention’s healthy days measures – population tracking of perceived physical and mental health over time. Health Qual Life Outcomes 2003;1. https://doi.org/10.1186/1477-7525-1-37.
- Cummins RA, Eckersley R, Pallant J, van Vugt J, Misajon RA. Developing a national index of subjective wellbeing: the Australian Unity Wellbeing Index. Soc Indic Res 2003;64:159-90. https://doi.org/10.1023/A:1024704320683.
- Ferrans CE, Powers MJ. Psychometric assessment of the Quality of Life Index. Res Nurs Health 1992;15:29-38. https://doi.org/10.1002/nur.4770150106.
- Farivar SS, Cunningham WE, Hays RD. Correlated physical and mental health summary scores for the SF-36 and SF-12 Health Survey, V.1. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-54.
- Sintonen H. The 15D instrument of health-related quality of life: properties and applications. Ann Med 2001;33:328-36. https://doi.org/10.3109/07853890109002086.
- Brazier J, Usherwood T, Harper R, Thomas K. Deriving a preference-based single index from the UK SF-36 Health Survey. J Clin Epidemiol 1998;51:1115-28. https://doi.org/10.1016/S0895-4356(98)00103-6.
- Devins GM, Mandin H, Hons RB, Burgess ED, Klassan J, Taub K, et al. Illness intrusiveness and quality of life in end-stage renal disease: comparison and stability across treatment modalities. Health Psychol 1990;9. https://doi.org/10.1037/0278-6133.9.2.117.
- Ware JE, Kosinski M, Keller S. SF-36 Physical and Mental Summary Scales: A User's Manual. Boston, MA: The Health Institute, New England Medical Center; 1994.
- Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Health 2004;11.
- Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res 2005;40:1918-30. https://doi.org/10.1111/j.1475-6773.2005.00438.x.
- Harrington J, Noble LM, Newman SP. Improving patients’ communication with doctors: a systematic review of intervention studies. Patient Educ Couns 2004;52:7-16. https://doi.org/10.1016/S0738-3991(03)00017-X.
- Pendleton D, Hasler J. Doctor–Patient Communication. London: Academic Press; 1983.
- McCann S, Weinman J. Encouraging patient participation in general practice consultations: effect on consultation length and content, patient satisfaction and health. Psychol Health 1996;11:857-69. https://doi.org/10.1080/08870449608400281.
- McGee DS, Cegala DJ. Patient communication skills raining for improved communication competence in the primary care medical consultation. J Appl Commun Res 1998;26:412-30. https://doi.org/10.1080/00909889809365517.
- Brown R, Butow PN, Boyer MJ, Tattersall MH. Promoting patient participation in the cancer consultation: evaluation of a prompt sheet and coaching in question-asking. Br J Cancer 1999;80:242-8. https://doi.org/10.1038/sj.bjc.6690346.
- Rao JK, Anderson LA, Inui TS, Frankel RM. Communication interventions make a difference in conversations between physicians and patients: a systematic review of the evidence. Med Care 2007;45:340-9. https://doi.org/10.1097/01.mlr.0000254516.04961.d5.
- Roter DL, Hall JA, Kern DE, Barker LR, Cole KA, Roca RP. Improving physicians’ interviewing skills and reducing patients’ emotional distress: a randomized clinical trial. Arch Intern Med 1995;155:1877-84. https://doi.org/10.1001/archinte.1995.00430170071009.
- Cegala DJ, McClure L, Marinelli TM, Post DM. The effects of communication skills training on patients’ participation during medical interviews. Patient Educ Couns 2000;41:209-22. https://doi.org/10.1016/S0738-3991(00)00093-8.
- Kim YM, Figueroa ME, Martin A, Silva R, Acosta SF, Hurtado M, et al. Impact of supervision and self-assessment on doctor-patient communication in rural Mexico. Int J Qual Health Care 2002;14:359-67. https://doi.org/10.1093/intqhc/14.5.359.
- Elwyn G, Edwards A, Hood K, Roblina M, Atwell C, Russel I, et al. Achieving involvement: process outcomes from a cluster randomized trial of shared decision making skill development and use of risk communication aids in general practice. Fam Pract 2004;21:337-46. https://doi.org/10.1093/fampra/cmh401.
- Joos SK, Hickam DH, Gordon GH, Baker LH. Effects of a physician communication intervention on patient care outcomes. J Gen Intern Med 1996;11:147-55. https://doi.org/10.1007/BF02600266.
- Krantz DS, Baum A, Wideman MV. Assessment of preferences for self-treatment and information in health care. J Pers Soc Psychol 1980;39:977-90. https://doi.org/10.1037/0022-3514.39.5.977.
- Beck RS, Daughtridge R, Sloane PD. Physician-patient communication in the primary care office: a systematic review. J Am Board Fam Pract 2002;15:25-38.
- Griffin SJ, Kinmonth AL, Veltman MW, Gillard S, Grant J, Stewart M. Effect on health-related outcomes of interventions to alter the interaction between patients and practitioners: a systematic review of trials. Ann Fam Med 2004;2:595-608. https://doi.org/10.1370/afm.142.
- Kinmonth AL, Woodcock A, Griffin S, Spiegal N, Campbell MJ. Randomised controlled trial of patient centred care of diabetes in general practice: impact on current wellbeing and future disease risk. The Diabetes Care From Diagnosis Research Team. BMJ 1998;317:1202-8. https://doi.org/10.1136/bmj.317.7167.1202.
- Pill R, Stott N, Rollnick S, Rees M. A randomized controlled trial of an intervention designed to improve the care given in general practice to type II diabetic patients: patient outcomes and professional ability to change behaviour. Fam Pract 1998;15:229-35. https://doi.org/10.1093/fampra/15.3.229.
- Peters T, Somerset M, Baxter K, Wilkinson C. Anxiety among women with mild dyskaryosis: a randomized trial of an educational intervention. Br J Gen Pract 1999;49:348-52.
- Thom DH, Bloch DA, Segal ES. An intervention to increase patients’ trust in their physicians. Stanford Trust Study Physician Group. Acad Med 1999;74:195-8. https://doi.org/10.1097/00001888-199902000-00019.
- Katon W, Von Korff M, Lin E, Walker E, Simon GE, Bush T, et al. Collaborative management to achieve treatment guidelines. Impact on depression in primary care. JAMA 1995;273:1026-31. https://doi.org/10.1001/jama.1995.03520370068039.
- Maly RC, Bourque LB, Engelhardt RF. A randomized controlled trial of facilitating information giving to patients with chronic medical conditions: effects on outcomes of care. J Fam Pract 1999;48:356-63.
- Weaver MJ, Ow CL, Walker DJ, Degenhardt EF. A questionnaire for patients’ evaluations of their physicians’ humanistic behaviors. J Gen Intern Med 1993;8:135-9. https://doi.org/10.1007/BF02599758.
- Thom DH, Ribisl KM, Stewart AL, Luke DA. Further validation and reliability testing of the Trust in Physician Scale. The Stanford Trust Study Physicians. Med Care 1999;37:510-17. https://doi.org/10.1097/00005650-199905000-00010.
- Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 2004;39:1005-26. https://doi.org/10.1111/j.1475-6773.2004.00269.x.
- Ahmed N, Bestall JC, Payne SA, Noble B, Ahmedzai SH. The use of cognitive interviewing methodology in the design and testing of a screening tool for supportive and palliative care needs. Support Care Cancer 2009;17:665-73. https://doi.org/10.1007/s00520-008-0521-2.
- Drennan J. Cognitive interviewing: verbal data in the design and pretesting of questionnaires. J Adv Nurs 2003;42:57-63. https://doi.org/10.1046/j.1365-2648.2003.02579.x.
- Rosal MC, Carbone ET, Goins KV. Use of cognitive interviewing to adapt measurement instruments for low-literate Hispanics. Diabetes Educ 2003;29:1006-17. https://doi.org/10.1177/014572170302900611.
- Knafl K, Deatrick J, Gallo A, Holcombe G, Bakitas M, Dixon J, et al. The analysis and interpretation of cognitive interviews for instrument development. Res Nurs Health 2007;30:224-34. https://doi.org/10.1002/nur.20195.
- Wolf MH, Putnam SM, James SA, Stiles WB. The medical interview satisfaction scale: development of a scale to measure patient perceptions of physician behavior. J Behav Med 1978;1:391-40. https://doi.org/10.1007/BF00846695.
- Boon H, Stewart M. Patient-physician communication assessment instruments: 1986 to 1996 in review. Patient Educ Couns 1998;35:161-76. https://doi.org/10.1016/S0738-3991(98)00063-9.
- Glaser KM, Markham FW, Adler HM, McManus PR, Hojat M. Relationships between scores on the Jefferson Scale of physician empathy, patient perceptions of physician empathy, and humanistic approaches to patient care: a validity study. Med Sci Monit 2007;13:CR291-CR94.
- Dine CJ, Ruffolo S, Lapin J, Shea JA, Kogan JR. Feasibility and validation of real-time patient evaluations of internal medicine interns’ communication and professionalism skills. J Grad Med Educ 2014;6:71-7. https://doi.org/10.4300/JGME-D-13-00173.1.
- She M, Li Z, Rau P. Physician communication behaviors that predict patient trust in outpatient departments. Lect Notes Comput Sci 2015;9181:361-73. https://doi.org/10.1007/978-3-319-20934-0_34.
- Saha S, Koley M, Mahoney ER, Hibbard J, Ghosh S, Nag G, et al. Patient activation measures in a government homeopathic hospital in India. J Evid Based Complementary Altern Med 2014;19:253-9. https://doi.org/10.1177/2156587214540175.
- Griffiths FE, Atherton H, Barker JR, Cave JAK, Dennick K, Dowdall P, et al. Improving health outcomes for young people with long term conditions: the role of digital communication in current and future patient–clinician communication for NHS providers of specialist clinical services for young people – LYNC study protocol. Digit Health 2015;1:1-13. https://doi.org/10.1177/2055207615593698.
- Patrick DL, Burke LB, Powers JH, Scott JA, Rock EP, Dawisha S, et al. Patient-reported outcomes to support medical product labeling claims: FDA perspective. Value Health 2007;10:125-37. https://doi.org/10.1111/j.1524-4733.2007.00275.x.
- Speight J, Barendse SM. FDA guidance on patient reported outcomes. BMJ 2010;340. https://doi.org/10.1136/bmj.c2921.
- Abrami PC, Borokhovski E, Bernard RM, Wade CA, Tamim R, Persson T, et al. Issues in conducting and disseminating brief reviews of evidence. Evid Policy 2010;6:371-89. https://doi.org/10.1332/174426410X524866.
- Featherstone RM, Dryden DM, Foisy M, Guise JM, Mitchell MD, Paynter RA, et al. Advancing knowledge of rapid reviews: an analysis of results, conclusions and recommendations from published review articles examining rapid reviews. Syst Rev 2015;4:1-8. https://doi.org/10.1186/s13643-015-0040-4.
- National Diabetes Audit 2010–2011 Report 1: Care Processes and Treatment Targets. Leeds: The Health and Social Care Information Centre; 2012.
- Sawyer SM, Afifi RA, Bearinger LH, Blakemore SJ, Dick B, Ezeh AC, et al. Adolescence: a foundation for future health. Lancet 2012;379:1630-40. https://doi.org/10.1016/S0140-6736(12)60072-5.
- Ambresin AE, Bennett K, Patton GC, Sanci LA, Sawyer SM. Assessment of youth-friendly health care: a systematic review of indicators drawn from young people’s perspectives. J Adolesc Health 2013;52:670-81. https://doi.org/10.1016/j.jadohealth.2012.12.014.
- Majeed-Ariss R, Hall AG, McDonagh J, Fallon D, Swallow V. Mobile phone and tablet apps to support young people’s management of their physical long-term conditions: a systematic review protocol. JMIR Res Protoc 2015;4. https://doi.org/10.2196/resprot.4159.
- Nightingale R, Sinha MD, Swallow V. Using focused ethnography in paediatric settings to explore professionals’ and parents’ attitudes towards expertise in managing chronic kidney disease stage 3–5. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-403.
- Swallow V. An exploration of mothers’ and fathers’ views of their identities in chronic-kidney-disease management: parents as students?. J Clin Nurs 2008;17:3177-86. https://doi.org/10.1111/j.1365-2702.2008.02642.x.
- Bergmo TS, Wangberg SC, Schopf TR, Solvoll T. Web-based consultations for parents of children with atopic dermatitis: results of a randomized controlled trial. Acta Paediatr 2009;98:316-20. https://doi.org/10.1111/j.1651-2227.2008.01033.x.
- Barlott T, Adams K, Díaz FR, Molina MM. Using SMS as a tool to reduce exclusions experienced by caregivers of people with disabilities in a resource-limited Colombian community. Disabil Rehabil Assist Technol 2015;10:347-54. http://doi.org/10.3109/17483107.2014.974223.
- Critical Appraisal Skills Programme UK . Critical Appraisal Skills Programme (CASP): Making Sense Of Evidence 2013. www.casp-uk.net/#!casp-tools-checklists/c18f8 (accessed 5 March 2017).
- National Heart, Lung, and Blood Institute . Quality Assessment Tool for Before–After (Pre–Post) Studies With No Control Group 2014. www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/before-after (accessed 1 August 2016).
- Bradford NK, Armfield NR, Young J, Smith AC. Paediatric palliative care by video consultation at home: a cost minimisation analysis. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-328.
- Bradford N, Young J, Armfield NR, Bensink ME, Pedersen LA, Herbert A, et al. A pilot study of the effectiveness of home teleconsultations in paediatric palliative care. J Telemed Telecare 2012;18:438-42. https://doi.org/10.1258/jtt.2012.GTH103.
- Braverman J, Samsonov DV. A study of online consultations for paediatric renal patients in Russia. J Telemed Telecare 2011;17:99-104. https://doi.org/10.1258/jtt.2010.100410.
- Britto MT, Hesse EA, Kamdar OJ, Munafo JK. Parents’ perceptions of a patient portal for managing their child’s chronic illness. J Pediatr 2013;163:280-. https://doi.org/10.1016/j.jpeds.2013.02.041.
- Byczkowski TL, Munafo JK, Britto MT. Family perceptions of the usability and value of chronic disease web-based patient portals. Health Informatics J 2014;20:151-62. https://doi.org/10.1177/1460458213489054.
- Grover M, Williams C, Eisler I, Fairbairn P, McCloskey C, Smith G, et al. An off-line pilot evaluation of a web-based systemic cognitive–behavioral intervention for carers of people with anorexia nervosa. Int J Eat Disord 2011;44:708-15. http://doi.org/10.1002/eat.20871.
- Gund A, Sjöqvist BA, Wigert H, Hentz E, Lindecrantz K, Bry K. A randomized controlled study about the use of eHealth in the home health care of premature infants. BMC Med Inform Decis Mak 2013;13. https://doi.org/10.1186/1472-6947-13-22.
- Haney T, Tufts KA. A pilot study using electronic communication in home healthcare: implications on parental well-being and satisfaction caring for medically fragile children. Home Healthc Nurse 2012;30:216-24. http://doi.org/10.1097/NHH.0b013e31824c28f2.
- Hopper B, Buckman M, Edwards M. Evaluation of satisfaction of parents with the use of videoconferencing for a pediatric genetic consultation. Twin Res Hum Genet 2011;14:343-6. http://doi.org/10.1375/twin.14.4.343.
- Mulgrew KW, Shaikh U, Nettiksimmons J. Comparison of parent satisfaction with care for childhood obesity delivered face-to-face and by telemedicine. Telemed J E Health 2011;17:383-7. https://doi.org/10.1089/tmj.2010.0153.
- Nordfeldt S, Hanberger L, Berterö C. Patient and parent views on a Web 2.0 Diabetes Portal – the management tool, the generator, and the gatekeeper: qualitative study. J Med Internet Res 2010;12. https://doi.org/10.2196/jmir.1267.
- Petranovich CL, Wade SL, Taylor HG, Cassedy A, Stancin T, Kirkwood MW, et al. Long-term caregiver mental health outcomes following a predominately online intervention for adolescents with complicated mild to severe traumatic brain injury. J Pediatr Psychol 2015;40:680-8. http://doi.org/10.1093/jpepsy/jsv001.
- Scharer K, Colon E, Moneyham L, Hussey J, Tavakoli A, Shugart M. A comparison of two types of social support for mothers of mentally ill children. J Child Adolesc Psychiatr Nurs 2009;22:86-98. https://doi.org/10.1111/j.1744-6171.2009.00177.x.
- Vismara LA, McCormick C, Young GS, Nadhan A, Monlux K. Preliminary findings of a telehealth approach to parent training in autism. J Autism Dev Disord 2013;43:2953-69. https://doi.org/10.1007/s10803-013-1841-8.
- Wade SL, Karver CL, Taylor HG, Cassedy A, Stancin T, Kirkwood MW, et al. Counselor-assisted problem solving improves caregiver efficacy following adolescent brain injury. Rehabil Psychol 2014;59:1-9. http://doi.org/10.1037/a0034911.
- Wade SL, Oberjohn K, Burkhardt A, Greenberg I. Feasibility and preliminary efficacy of a web-based parenting skills program for young children with traumatic brain injury. J Head Trauma Rehabil 2009;24:239-47. http://doi.org/10.1097/HTR.0b013e3181ad6680.
- Wade SL, Walz NC, Carey J, McMullen KM, Cass J, Mark E, et al. A randomized trial of teen online problem solving: efficacy in improving caregiver outcomes after brain injury. Health Psychol 2012;31:767-76. http://doi.org/10.1037/a0028440.
- Wade SL, Walz NC, Carey JC, Williams KM. Brief report: description of feasibility and satisfaction findings from an innovative online family problem-solving intervention for adolescents following traumatic brain injury. J Pediatr Psychol 2009;34:517-22. http://doi.org/10.1093/jpepsy/jsn081.
- de Graaf M, Totte J, Breugem C, van Os-Medendorp H, Pasmans S. Evaluation of the compliance, acceptance, and usability of a web-based ehealth intervention for parents of children with infantile hemangiomas: usability study. JMIR Res Protoc 2013;2. http://doi.org/10.2196/resprot.2897.
- Looman WS, Antolick M, Cady RG, Lunos SA, Garwick AE, Finkelstein SM. Effects of a telehealth care coordination intervention on perceptions of health care by caregivers of children with medical complexity: a randomized controlled trial. J Pediatr Health Care 2015;29:352-63. http://doi.org/10.1016/j.pedhc.2015.01.007.
- van Os-Medendorp H, Koffijberg H, Eland-de Kok PC, van der Zalm A, de Bruin-Weller MS, Pasmans SG, et al. E-health in caring for patients with atopic dermatitis: a randomized controlled cost-effectiveness study of internet-guided monitoring and online self-management training. Br J Dermatol 2012;166:1060-8. https://doi.org/10.1111/j.1365-2133.2012.10829.x.
- Epstein EG, Sherman J, Blackman A, Sinkin RA. Testing the feasibility of Skype and FaceTime updates with parents in the Neonatal Intensive Care Unit. Am J Crit Care 2015;24:290-6. https://doi.org/10.4037/ajcc2015828.
- Gulmans J, Vollenbroek-Hutten M, van Gemert-Pijnen L, van Harten W. A web-based communication system for integrated care in cerebral palsy: experienced contribution to parent–professional communication. Int J Integr Care 2012;12. https://doi.org/10.5334/ijic.672.
- Hanberger L, Ludvigsson J, Nordfeldt S. Use of a web 2.0 portal to improve education and communication in young patients with families: randomized controlled trial. J Med Internet Res 2013;15. https://doi.org/10.2196/jmir.2425.
- Hanlon-Dearman A, Edwards C, Schwab D, Millar MC, Longstaffe S. ‘Giving voice’: evaluation of an integrated telehealth community care model by parents/guardians of children diagnosed with fetal alcohol spectrum disorder in Manitoba. Telemed J E Health 2014;20:478-84. http://doi.org/10.1089/tmj.2013.0161.
- Lee JY, Du YE, Coki O, Flynn JT, Starren J, Chiang MF. Parental perceptions toward digital imaging and telemedicine for retinopathy of prematurity management. Graefes Arch Clin Exp Ophthalmol 2010;248:141-7. https://doi.org/10.1007/s00417-009-1191-6.
- Vismara LA, Young GS, Rogers SJ. Telehealth for expanding the reach of early autism training to parents. Autism Res Treat 2012;2012. https://doi.org/10.1155/2012/121878.
- Becker T. Effectiveness of parent call-in versus e-counseling services in treating pediatric behavior problems uncovered in a primary care medical encounter. Diss Abstr Int 2011;73.
- Binford Hopf RB, Le Grange D, Moessner M, Bauer S. Internet-based chat support groups for parents in family-based treatment for adolescent eating disorders: a pilot study. Eur Eat Disord Rev 2013;21:215-23. https://doi.org/10.1002/erv.2196.
- Grover M, Naumann U, Mohammad-Dar L, Glennon O, Ringwood S, Eisler I. A randomized controlled trial of an Internet-based cognitive-behavioural skills package for carers of people with anorexia nervosa. Psychol Med 2011;41:2581-91.
- Chi NC, Demiris G. A systematic review of telehealth tools and interventions to support family caregivers. J Telemed Telecare 2015;21:37-44. https://doi.org/10.1177/1357633X14562734.
- Diabetes: Facts and Stats. London: Diabetes UK; 2014.
- Diabetes (Type 1 and Type 2) in Children and Young People: Diagnosis and Management. London: National Institute for Health and Care Excellence; 2015.
- National Paediatric Diabetes Audit 2013–14. London: Royal College of Paediatrics and Child Health; 2015.
- Quah JH, Liu YP, Luo N, How CH, Tay EG. Younger adult type 2 diabetic patients have poorer glycaemic control: a cross-sectional study in a primary care setting in Singapore. BMC Endocr Disord 2013;13. https://doi.org/10.1186/1472-6823-13-18.
- Transition: Moving on Well. London: Department of Health; 2008.
- Media: Facts & Figures. London: Ofcom; 2015.
- Internet Access – Households and Individuals: 2014. London: Office for National Statistics; 2014.
- Currell R, Urquhart C, Wainwright P, Lewis R. Telemedicine versus face to face patient care: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2000;2. https://doi.org/10.1002/14651858.CD002098.
- Huxley CJ, Atherton H, Watkins JA, Griffiths F. Digital communication between clinician and patient and the impact on marginalised groups: a realist review in general practice. Br J Gen Pract 2015;65:e813-e21. https://doi.org/10.3399/bjgp15X687853.
- Pal K, Eastwood SV, Michie S, Farmer AJ, Barnard ML, Peacock R, et al. Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. Cochrane Database Syst Rev 2013;3. https://doi.org/10.1002/14651858.CD008776.pub2.
- Guljas R, Ahmed A, Chang K, Whitlock A. Impact of telemedicine in managing type 1 diabetes among school-age children and adolescents: an integrative review. J Pediatr Nurs 2014;29:198-204. https://doi.org/10.1016/j.pedn.2013.10.013.
- Russell-Minda E, Jutai J, Speechley M, Bradley K, Chudyk A, Petrella R. Health technologies for monitoring and managing diabetes: a systematic review. J Diabetes Sci Technol 2009;3:1460-71. https://doi.org/10.1177/193229680900300628.
- Fitzner K, Moss G. Telehealth – an effective delivery method for diabetes self-management education?. Popul Health Manag 2013;16:169-77. https://doi.org/10.1089/pop.2012.0054.
- Herbert L, Owen V, Pascarella L, Streisand R. Text message interventions for children and adolescents with type 1 diabetes: a systematic review. Diabetes Technol Ther 2013;15:362-70. https://doi.org/10.1089/dia.2012.0291.
- Franc S, Daoudi A, Mounier S, Boucherie B, Dardari D, Laroye H, et al. Telemedicine and diabetes: achievements and prospects. Diabetes Metab 2011;37:463-76. https://doi.org/10.1016/j.diabet.2011.06.006.
- Sheehy S, Cohen G, Owen KR. Self-management of diabetes in children and young adults using technology and smartphone applications. Curr Diabetes Rev 2014;10:298-301. https://doi.org/10.2174/1573399810666141010113050.
- Toma T, Athanasiou T, Harling L, Darzi A, Ashrafian H. Online social networking services in the management of patients with diabetes mellitus: systematic review and meta-analysis of randomised controlled trials. Diabetes Res Clin Pract 2014;106:200-11. https://doi.org/10.1016/j.diabres.2014.06.008.
- Berndt RD, Takenga C, Preik P, Kuehn S, Berndt L, Mayer H, et al. Impact of information technology on the therapy of type-1 diabetes: a case study of children and adolescents in Germany. J Pers Med 2014;4:200-17. https://doi.org/10.3390/jpm4020200.
- Boogerd EA, Noordam C, Kremer JA, Prins JB, Verhaak CM. Teaming up: feasibility of an online treatment environment for adolescents with type 1 diabetes. Pediatr Diabetes 2014;15:394-402. https://doi.org/10.1111/pedi.12103.
- Carroll AE, DiMeglio LA, Stein S, Marrero DG. Using a cell phone-based glucose monitoring system for adolescent diabetes management. Diabetes Educ 2011;37:59-66. https://doi.org/10.1177/0145721710387163.
- Choi YS, Berry-Cabän C, Nance J. Telemedicine in paediatric patients with poorly controlled type 1 diabetes. J Telemed Telecare 2013;19:219-21. https://doi.org/10.1258/jtt.2012.120506.
- Farrell K, Holmes-Walker DJ. Mobile phone support is associated with reduced ketoacidosis in young adults. Diabet Med 2011;28:1001-4. https://doi.org/10.1111/j.1464-5491.2011.03302.x.
- Freeman KA, Duke DC, Harris MA. Behavioral health care for adolescents with poorly controlled diabetes via Skype: does working alliance remain intact?. J Diabetes Sci Technol 2013;7:727-35. https://doi.org/10.1177/193229681300700318.
- Frøisland DH, Arsand E, Skårderud F. Improving diabetes care for young people with type 1 diabetes through visual learning on mobile phones: mixed-methods study. J Med Internet Res 2012;14. https://doi.org/10.2196/jmir.2155.
- Harris MA, Freeman KA, Duke DC. Seeing is believing: using Skype to improve diabetes outcomes in youth. Diabetes Care 2015;38:1427-34. https://doi.org/10.2337/dc14-2469.
- Izquierdo R, Morin PC, Bratt K, Moreau Z, Meyer S, Ploutz-Snyder R, et al. School-centered telemedicine for children with type 1 diabetes mellitus. J Pediatr 2009;155:374-9. https://doi.org/10.1016/j.jpeds.2009.03.014.
- Landau Z, Mazor-Aronovitch K, Boaz M, Blaychfield-Magnazi M, Graph-Barel C, Levek-Motola N, et al. The effectiveness of Internet-based blood glucose monitoring system on improving diabetes control in adolescents with type 1 diabetes. Pediatr Diabetes 2012;13:203-7. https://doi.org/10.1111/j.1399-5448.2011.00800.x.
- Moattari M, Hashemi M, Dabbaghmanesh MH. The impact of electronic education on metabolic control indicators in patients with diabetes who need insulin: a randomised clinical control trial. J Clin Nurs 2013;22:32-8. http://doi.org/10.1111/j.1365-2702.2012.04200.x.
- Pinsker JE, Nguyen C, Young S, Fredericks GJ, Chan D. A pilot project for improving paediatric diabetes outcomes using a website: the Pediatric Diabetes Education Portal. J Telemed Telecare 2011;17:226-30. https://doi.org/10.1258/jtt.2010.100812.
- Lee S, Tsang A, Breslau J, Aguilar-Gaxiola S, Angermeyer M, Borges G, et al. Mental disorders and termination of education in high-income and low- and middle-income countries: epidemiological study. Br J Psychiatry 2009;194:411-17. https://doi.org/10.1192/bjp.bp.108.054841.
- De Silva MJ, McKenzie K, Harpham T, Huttly SR. Social capital and mental illness: a systematic review. J Epidemiol Community Health 2005;59:619-27. https://doi.org/10.1136/jech.2004.029678.
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 2013;382:1575-86. https://doi.org/10.1016/S0140-6736(13)61611-6.
- Osborn DP. The poor physical health of people with mental illness. West J Med 2001;175:329-32. https://doi.org/10.1136/ewjm.175.5.329.
- Centre for Mental Health . The Economic and Social Costs of Mental Health Problems in 2009 10 2010. http://mhfe.org.uk/content/economic-and-social-costs-mental-health-problems-200910 (accessed 5 March 2017).
- Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustün TB. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry 2007;20:359-64. https://doi.org/10.1097/YCO.0b013e32816ebc8c.
- Green H, McGinnity A, Meltzer H, Ford T, Goodman R. Mental Health of Children and Young People in Great Britain, 2004. Norwich: National Statistics; 2005.
- Children and Young People’s Health Outcomes Forum . Report of the Children and Young People’s Health Outcomes Forum 2012. http://webarchive.nationalarchives.gov.uk/20130805113046/http://www.dh.gov.uk/health/files/2012/07/CYP-report.pdf (accessed 1 August 2016).
- Collishaw S, Maughan B, Natarajan L, Pickles A. Trends in adolescent emotional problems in England: a comparison of two national cohorts twenty years apart. J Child Psychol Psychiatry 2010;51:885-94. https://doi.org/10.1111/j.1469-7610.2010.02252.x.
- Khan L, Parsonage M, Stubbs J. Investing in Children’s Mental Health: A Review of Evidence on the Costs and Benefits of Increased Service Provision. London: Centre For Mental Health; 2014.
- Craig TK, Garety P, Power P, Rahaman N, Colbert S, Fornells-Ambrojo M, et al. The Lambeth Early Onset (LEO) Team: randomised controlled trial of the effectiveness of specialised care for early psychosis. BMJ 2004;329. https://doi.org/10.1136/bmj.38246.594873.7C.
- Klein JD, Slap GB, Elster AB, Schonberg SK. Access to health care for adolescents. A position paper of the Society for Adolescent Medicine. J Adolesc Health 1992;13:162-70. https://doi.org/10.1016/1054-139X(92)90084-O.
- Yonker LM, Zan S, Scirica CV, Jethwani K, Kinane TB. ‘Friending’ teens: systematic review of social media in adolescent and young adult health care. J Med Internet Res 2015;17. https://doi.org//jmir.3692.
- Jessor R. Problem behavior and developmental transition in adolescence. J Sch Health 1982;52:295-300. https://doi.org/10.1111/j.1746-1561.1982.tb04626.x.
- Bridging The Gaps: Healthcare For Adolescents. London: Royal College of Paediatrics and Child Health; 2003.
- Singh S, Paul M, Islam Z, Weaver T, Kramer T, McLaren S, et al. Transition from CAMHS to Adult Mental Health Services (TRACK): A Study of Service Organisation, Policies, Process and User and Carer Perspectives. London: National Institute for Health Research, Service Delivery and Organisation Programme; 2010.
- CAMHS Transition. London: YoungMinds; 2015.
- Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; 2000.
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry 1961;4:561-71. https://doi.org/10.1001/archpsyc.1961.01710120031004.
- Williams A, LaRocca R, Chang T, Trinh N-H, Fava M, Kvedar J, et al. Web-based depression screening and psychiatric consultation for college students: a feasibility and acceptability study. Int J Telemed Appl 2014;9. https://doi.org/10.1155/2014/580786.
- van der Zanden R, Kramer J, Gerrits R, Cuijpers P. Effectiveness of an online group course for depression in adolescents and young adults: a randomized trial. J Med Internet Res 2012;14. https://doi.org/10.2196/jmir.2033.
- Stain HJ, Payne K, Thienel R, Michie P, Carr V, Kelly B. The feasibility of videoconferencing for neuropsychological assessments of rural youth experiencing early psychosis. J Telemed Telecare 2011;17:328-31. https://doi.org/10.1258/jtt.2011.101015.
- Turner CM, Mataix-Cols D, Lovell K, Krebs G, Lang K, Byford S, et al. Telephone cognitive–behavioral therapy for adolescents with obsessive–compulsive disorder: a randomized controlled non-inferiority trial. J Am Acad Child Adolesc Psychiatry 2014;53:1298-307.e2. https://doi.org/10.1016/j.jaac.2014.09.012.
- Boydell KM, Volpe T, Pignatiello A. A qualitative study of young people’s perspectives on receiving psychiatric services via televideo. J Can Acad Child Adolesc Psychiatry 2010;19:5-11.
- Kramer J, Conijn B, Oijevaar P, Riper H. Effectiveness of a web-based solution-focused brief chat treatment for depressed adolescents and young adults: randomized controlled trial. J Med Internet Res 2014;16. https://doi.org/10.2196/jmir.3261.
- Ye X, Bapuji SB, Winters SE, Struthers A, Raynard M, Metge C, et al. Effectiveness of internet-based interventions for children, youth, and young adults with anxiety and/or depression: a systematic review and meta-analysis. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-313.
- Aardoom JJ, Dingemans AE, Spinhoven P, Van Furth EF. Treating eating disorders over the internet: a systematic review and future research directions. Int J Eat Disord 2013;46:539-52. https://doi.org/10.1002/eat.22135.
- World Health Organization . Genes and Human Disease: Mongenic Diseases 2016. www.who.int/genomics/public/geneticdiseases/en/index2.html#CF (accessed 5 March 2017).
- Elliott R, Watmough DE, Gray NJ, Glazebrook C, Conroy S, Lakhanpaul M, et al. Promoting Partnerships With Children and Adolescents in Medicine-Taking (Talking About Medicines; TABS) 2013. www.nottingham.ac.uk/~pazpps/ (accessed 5 March 2017).
- Cancer Research UK . Children’s Cancers Survival Statistics 2015. www.cancerresearchuk.org/health-professional/cancer-statistics/childrens-cancers/survival#heading-Two (accessed 5 March 2017).
- Anderson HR, Gupta R, Strachan DP, Limb ES. 50 years of asthma: UK trends from 1955 to 2004. Thorax 2007;62:85-90. https://doi.org/10.1136/thx.2006.066407.
- Viner R. Transition from paediatric to adult care. Bridging the gaps or passing the buck?. Arch Dis Child 1999;81:271-5. https://doi.org/10.1136/adc.81.3.271.
- Kroger J. Identity Development: Adolescence Through Adulthood. Newbury Park, CA: Sage; 2006.
- Fruhauf J, Krock S, Quehenberger F, Kopera D, Fink-Puches R, Komericki P, et al. Mobile teledermatology helping patients control high-need acne: a randomized controlled trial. J Eur Acad Dermatol Venereol 2015;29:919-24. http://doi.org/10.1111/jdv.12723.
- Wiecha JM, Adams WG, Rybin D, Rizzodepaoli M, Keller J, Clay JM. Evaluation of a web-based asthma self-management system: a randomised controlled pilot trial. BMC Pulm Med 2015;15. https://doi.org/10.1186/s12890-015-0007-1.
- Mehl G, Labrique A. Prioritizing integrated mHealth strategies for universal health coverage. Science 2014;345:1284-7. https://doi.org/10.1126/science.1258926.
- World Health Organization . What Is Universal Coverage? n.d. www.who.int/health_financing/universal_coverage_definition/en/ (accessed 1 September 2015).
- Webster PC. The rise of open-source electronic health records. Lancet 2014;377:1641-2. https://doi.org/10.1016/S0140-6736(11)60659-4.
- dos Santos Ade F, Alves HJ, Nogueira JT, Torres RM, Melo Mdo C. Telehealth distance education course in Latin America: analysis of an experience involving 15 countries. Telemed J E Health 2014;20:736-41. https://doi.org/10.1089/tmj.2013.0291.
- Fisher M. Here’s a Map of the Countries That Provide Universal Health Care (America’s Still Not on It) 2012. www.theatlantic.com/international/archive/2012/06/heres-a-map-of-the-countries-that-provide-universal-health-care-americas-still-not-on-it/259153/ (accessed 1 September 2015).
- The World Bank Group . World Bank Country and Lending Groups: Historical Classification By Income: 2015 n.d. http://databank.worldbank.org/data/download/site-content/OGHIST.xls (accessed 1 September 2015).
- Stuckler D, Feigl AB, Basu S, McKee M. The Political Economy of Universal Health Coverage. Background Paper for the First Global Symposium on Health Systems Research n.d.
- World Health Organization . Global Health Observatory (GHO) Data n.d. www.who.int/gho/en/ (accessed 1 August 2016).
- Taylor A, Morris G, Pech J, Rechter S, Carati C, Kidd MR. Home telehealth video conferencing: perceptions and performance. JMIR Mhealth Uhealth 2015;3.
- Raven M, Butler C, Bywood P. Video-based telehealth in Australian primary health care: current use and future potential. Aust J Prim Health 2013;19:283-6. https://doi.org/10.1071/PY13032.
- Del Signore AG, Dang R, Yerasi A, Iloreta AM, Malkin BD. Videoconferencing for the pre-operative interaction between patient and surgeon. J Telemed Telecare 2014;20:267-71. https://doi.org/10.1177/1357633X14537759.
- Video Conferencing. Coventry: NHS Institute for Innovation and Improvement; 2013.
- National Information Board . Personalised Health and Care 2020: Using Data and Technology to Transform Outcomes for Patients and Citizens – A Framework for Action 2014. www.gov.uk/government/uploads/system/uploads/attachment_data/file/384650/NIB_Report.pdf (accessed 1 August 2016).
- NHSmail 2. Leeds: Health and Social Care Information Centre; 2015.
- Wynn R, Bergvik S, Pettersen G, Fossum S. Clinicians’ experiences with videoconferencing in psychiatry. Stud Health Technol Inform 2012;180:1218-20.
- Edirippulige S, Levandovskaya M, Prishutova A. A qualitative study of the use of Skype for psychotherapy consultations in the Ukraine. J Telemed Telecare 2013;19:376-8. https://doi.org/10.1177/1357633X13506523.
- Good DW, Lui DF, Leonard M, Morris S, McElwain JP. Skype: a tool for functional assessment in orthopaedic research. J Telemed Telecare 2012;18:94-8. https://doi.org/10.1258/jtt.2011.110814.
- Shea BJ, Hamel C, Wells GA, Bouter LM, Kristjansson E, Grimshaw J, et al. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol 2009;62:1013-20. https://doi.org/10.1016/j.jclinepi.2008.10.009.
- Backhaus A, Agha Z, Maglione ML, Repp A, Ross B, Zuest D, et al. Videoconferencing psychotherapy: a systematic review. Psychol Serv 2012;9:111-31. https://doi.org/10.1037/a0027924.
- Boisvert M, Lang R, Andrianopoulos M, Boscardin ML. Telepractice in the assessment and treatment of individuals with autism spectrum disorders: a systematic review. Dev Neurorehabil 2010;13:423-32. https://doi.org/10.3109/17518423.2010.499889.
- Conway A, Inglis SC, Clark RA. Effective technologies for noninvasive remote monitoring in heart failure. Telemed J E Health 2014;20:531-8. https://doi.org/10.1089/tmj.2013.0267.
- Inglis SC, Clark RA, McAlister FA, Ball J, Lewinter C, Cullington D, et al. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev 2010;8. https://doi.org/10.1002/14651858.CD007228.pub2.
- Inglis SC, Clark RA, McAlister FA, Stewart S, Cleland JG. Which components of heart failure programmes are effective? A systematic review and meta-analysis of the outcomes of structured telephone support or telemonitoring as the primary component of chronic heart failure management in 8323 patients: Abridged Cochrane Review. Eur J Heart Fail 2011;13:1028-40. https://doi.org/10.1093/eurjhf/hfr039.
- Dorstyn DS, Saniotis A, Sobhanian F. A systematic review of telecounselling and its effectiveness in managing depression amongst minority ethnic communities. J Telemed Telecare 2013;19:338-46. http://doi.org/10.1177/1357633X13501767.
- Dorstyn D, Mathias J, Denson L. Applications of telecounselling in spinal cord injury rehabilitation: a systematic review with effect sizes. Clin Rehabil 2013;27:1072-83. https://doi.org/10.1177/0269215513488001.
- García-Lizana F, Muñoz-Mayorga I. What about telepsychiatry? A systematic review. Prim Care Companion J Clin Psychiatry 2010;12. https://doi.org/10.4088/PCC.09m00831whi.
- García-Lizana F, Muñoz-Mayorga I. Telemedicine for depression: a systematic review. Perspect Psychiatr Care 2010;46:119-26. http://doi.org/10.1111/j.1744-6163.2010.00247.x.
- Kasckow J, Felmet K, Appelt C, Thompson R, Rotondi A, Haas G. Telepsychiatry in the assessment and treatment of schizophrenia. Clin Schizophr Relat Psychoses 2014;8:21-27A. https://doi.org/10.3371/CSRP.KAFE.021513.
- Kitamura C, Zurawel-Balaura L, Wong RK. How effective is video consultation in clinical oncology? A systematic review. Curr Oncol 2010;17:17-2.
- Mars M, Ramlall S, Kaliski S. Forensic telepsychiatry: a possible solution for South Africa?. Afr J Psychiatry 2012;15:244-7. https://doi.org/10.4314/ajpsy.v15i4.31.
- McGeary DD, McGeary CA, Gatchel RJ, Allison S, Hersh A. Assessment of research quality of telehealth trials in pain management: a meta-analysis. Pain Pract 2013;13:422-31. https://doi.org/10.1111/j.1533-2500.2012.00601.x.
- McLean S, Chandler D, Nurmatov U, Liu J, Pagliari C, Car J, et al. Telehealthcare for asthma. Cochrane Database Syst Rev 2010;10. https://doi.org/10.1002/14651858.CD007717.pub2.
- Peeters JM, Mistiaen P, Francke AL. Costs and financial benefits of video communication compared to usual care at home: a systematic review. J Telemed Telecare 2011;17:403-11. http://doi.org/10.1258/jtt.2011.110405.
- Peterson A. Improving type 1 diabetes management with mobile tools: a systematic review. J Diabetes Sci Technol 2014;8:859-64. https://doi.org/10.1177/1932296814529885.
- Schlegl S, Burger C, Schmidt L, Herbst N, Voderholzer U. The potential of technology-based psychological interventions for anorexia and bulimia nervosa: a systematic review and recommendations for future research. J Med Internet Res 2015;17. https://doi.org/10.2196/jmir.3554.
- Sharp IR, Kobak KA, Osman DA. The use of videoconferencing with patients with psychosis: a review of the literature. Ann Gen Psychiatry 2011;10. https://doi.org/10.1186/1744-859X-10-14.
- Shore JH. Telepsychiatry: videoconferencing in the delivery of psychiatric care. Am J Psychiatry 2013;170:256-62. http://doi.org/10.1176/appi.ajp.2012.12081064.
- Siriwardena LS, Wickramasinghe WA, Perera KL, Marasinghe RB, Katulanda P, Hewapathirana R. A review of telemedicine interventions in diabetes care. J Telemed Telecare 2012;18:164-8. https://doi.org/10.1258/jtt.2012.SFT110.
- Sucala M, Schnur JB, Constantino MJ, Miller SJ, Brackman EH, Montgomery GH. The therapeutic relationship in e-therapy for mental health: a systematic review. J Med Internet Res 2012;14. https://doi.org/10.2196/jmir.2084.
- Wile DJ, Pringsheim TM. Behavior therapy for Tourette syndrome: a systematic review and meta-analysis. Curr Treat Options Neurol 2013;15:385-95. https://doi.org/10.1007/s11940-013-0238-5.
- Zhai YK, Zhu WJ, Cai YL, Sun DX, Zhao J. Clinical- and cost-effectiveness of telemedicine in type 2 diabetes mellitus: a systematic review and meta-analysis. Medicine 2014;93. https://doi.org/10.1097/MD.0000000000000312.
- NHS England . NHS Digital Technology: Harnessing the Information Revolution 2016. www.england.nhs.uk/digitaltechnology/info-revolution/ (accessed 5 March 2017).
- Berwick DM. Disseminating innovations in health care. JAMA 2003;289:1969-75. https://doi.org/10.1001/jama.289.15.1969.
- Greenhalgh T, Procter R, Wherton J, Sugarhood P, Hinder S, Rouncefield M. What is quality in assisted living technology? The ARCHIE framework for effective telehealth and telecare services. BMC Med 2015;13. https://doi.org/10.1186/s12916-015-0279-6.
- Point of Care Foundation . Experience-Based Co-Design Toolkit 2013. www.kingsfund.org.uk/projects/ebcd (accessed 5 March 2017).
- Medical Protection Society . Risks of Telephone Consultations. Secondary Risks of Telephone Consultations 2015 n.d. www.medicalprotection.org/uk/practice-matters-june-2015/risks-of-telephone-consultations (accessed 5 March 2017).
- Greenhalgh T, Collard A, Gutteridge C, Byrne E, Hodkinson I, Morris J, et al. HS&Amp;DR – 13 59 26: Virtual Online Consultations: Advantages and Limitations (VOCAL). A Qualitative Study of Micro, Meso and Macro Level Interactions 2015. www.nets.nihr.ac.uk/projects/hsdr/135926 (accessed 5 March 2017).
- Bath PA. Health informatics: current issues and challenges. J Inf Sci 2008;34:501-18. https://doi.org/10.1177/0165551508092267.
- Wears RL, Cook RI, Perry SJ. Automation, interaction, complexity, and failure: a case study. Reliab Eng Syst Saf 2006;91:1494-501. https://doi.org/10.1016/j.ress.2006.01.009.
- Donyai P, O’Grady K, Jacklin A, Barber N, Franklin BD. The effects of electronic prescribing on the quality of prescribing. Br J Clin Pharmacol 2008;65:230-7. https://doi.org/10.1111/j.1365-2125.2007.02995.x.
- Koppel R, Metlay JP, Cohen A, Abaluck B, Localio AR, Kimmel SE, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA 2005;293:1197-203. https://doi.org/10.1001/jama.293.10.1197.
- Househ M, Borycki E, Kushniruk A. Empowering patients through social media: the benefits and challenges. Health Informatics J 2014;20:50-8. https://doi.org/10.1177/1460458213476969.
- Sujan MA, Koornneef F, Chozos N, Pozzi S, Kelly T. Safety cases for medical devices and health IT: involving healthcare organisations in the assurance of safety. Health Informatics J 2013;19:165-82. https://doi.org/10.1177/1460458212462079.
- Vassilev I, Rowsell A, Pope C, Kennedy A, O’Cathain A, Salisbury C, et al. Assessing the implementability of telehealth interventions for self-management support: a realist review. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0238-9.
- Data Protection Act. London: The Stationery Office; 1998.
- Spielberg AR. On call and online: sociohistorical, legal, and ethical implications of e-mail for the patient-physician relationship. JAMA 1998;280:1353-9. https://doi.org/10.1001/jama.280.15.1353.
- Bovi AM. Council on Ethical and Judicial Affairs of the American Medical Association . Ethical guidelines for use of electronic mail between patients and physicians. Am J Bioeth 2003;3. https://doi.org/10.1162/152651603322874771.
- Car J, Sheikh A. Email consultations in health care: 2 – acceptability and safe application. BMJ 2004;329:439-42. https://doi.org/10.1136/bmj.329.7463.439.
- Doctors’ Use of Social Media. London: General Medical Council; 2013.
- Zhuge H. Workflow- and agent-based cognitive flow management for distributed team cooperation. Inf Manage 2003;40:419-29. https://doi.org/10.1016/S0378-7206(02)00061-7.
- Gagnon MP, Ngangue P, Payne-Gagnon J, Desmartis M. m-Health adoption by healthcare professionals: a systematic review. J Am Med Inform Assoc 2016;23:212-20. https://doi.org/10.1093/jamia/ocv052.
- O’Cathain A, Drabble SJ, Foster A, Horspool K, Edwards L, Thomas C, et al. Being human: a qualitative interview study exploring why a telehealth intervention for management of chronic conditions had a modest effect. J Med Internet Res 2016;18. https://doi.org/10.2196/jmir.5879.
- Cochrane Consumers and Communication . Outcomes of Interest to the Cochrane Consumers &Amp; Communication Group 2012. https://cccrg.cochrane.org/sites/cccrg.cochrane.org/files/public/uploads/Outcomes.pdf (accessed 1 August 2016).
- Brant H, Atherton H, Ziebland S, McKinstry B, Campbell JL, Salisbury C. Using alternatives to face-to-face consultations: a survey of prevalence and attitudes in general practice. Br J Gen Pract 2016;66:e460-6. https://doi.org/10.3399/bjgp16X685597.
- Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff 2013;32:207-14. https://doi.org/10.1377/hlthaff.2012.1061.
- Stewart AL. Measuring Functioning and Well-Being: The Medical Outcomes Study Approach. Durham, NC: Duke University Press; 1992.
Appendix 1 Patient and public involvement
Introduction
Patient and public involvement has been integral to this research, with significant input from a PPI co-applicant throughout the whole research process. Patients and members of the public were actively engaged in the research in two ways: first, through lay people’s involvement with the project management structures and, second, through patient and public engagement activities. This appendix reports PPI involvement in the project management structures and two PPI events involving school and college pupils.
Patient and public involvement in project management and data analysis
People were recruited to sit on the PMG and independent Study Steering Committee through a multipronged approach. Adverts seeking people who were either a young person aged 16–24 years, preferably with a long-term health condition, or a parent/carer/household member of a young person with a long-term health condition were sent out to the organisations University/User Teaching and Research Action Partnership (URL: www.warwick.ac.uk/go/untrap, accessed 5 March 2017) and Rethink Mental Illness (URL: www.rethink.org, accessed 5 March 2017), and to all medical students at the University of Warwick. Adverts provided a brief summary of the research and what participation in the management of the project would involve. Opportunistic recruitment also took place through networking at conferences and events: our PPI co-applicant who was involved in young people’s user groups distributed the advert to this group.
Two people responded through the University/User Teaching and Research Action Partnership, and both were recruited to the independent Study Steering Committee. One was an adult who had lived with a LTC since childhood and the other was the parent of a child with a LTC. Using the other recruitment methods, six people were recruited to the PMG. Of these, four were young people aged 16–25 years who had a LTC, one was the parent of a young person with a LTC and one was a young adult who has had a LTC since childhood. These lay members attended PMG meetings and provided ad hoc feedback throughout the duration of the project, giving input into research materials, site recruitment, analysis and outputs. At each PMG meeting, we had at least two PPI members participating and across the whole study collectively, there were 23 attendances. Our PPI co-investigator chaired each PMG. Each of our PPI members joined one of the five analysis approaches of ‘what works’ (young person), ethics (young person), patient safety (young person), health economics (PPI co-applicant) and IG (carer), and engaged in the coding development and interpretation of findings (one young person was unable to engage at this stage because of work load). Each analysis group met at least twice with its PPI member(s). PPI activity using social media linked with generic PROs research activities and analysis is reported separately in Chapter 10.
Patient and public engagement activities
Two events were held at the University of Warwick with young people aged 14–18 years, via the Warwick Young Researchers scheme. For both events, young people from schools and colleges were invited to undertake a survey on the topic of DCC. The LYNC study team provided research training and the young people recruited their peers to complete the survey. The aims of these events were to inform case study design, recruitment and research design, and analysis and dissemination.
Activity 1: project months 1 and 2
Method
Year 9 students (aged 14 and 15 years) from local schools were invited to take part in the Warwick Young Researchers scheme. Twenty students responded and 19 participated. During the first campus day, three LYNC study researchers trained the students in key research skills and discussed the topic under investigation. The students were asked to design a survey to use with their peers, on the use of digital communication technologies in health care. They were taught about the nature of research and why it is important; the importance of confidentiality and research ethics; what surveys and questionnaires are; and how to design a questionnaire using quantitative and qualitative questions. The 11 research teams (eight pairs, with three people working alone) each designed a questionnaire to use with their peers on the research topic. Questionnaires were limited to a maximum of eight questions in order to control the number of data that students would need to analyse and report. The research teams piloted their questionnaire with other young researchers before typing them up to either be printed and distributed manually, or completed online via SurveyMonkey. The first day ended with a discussion on recruitment strategies.
The students collected survey responses in between the two campus days. Each research team aimed to collect data from 30 fellow students (again, this was capped to ensure that the number of data produced was manageable). Hard copies of completed questionnaires were brought back to the second campus day.
During the second campus day, the students were taught how to analyse qualitative and quantitative data. They then entered their own data into Excel for analysis. Once the students had analysed their data, they were taught how to write up a research report. Copies of their reports were given to the LYNC study research team.
A LYNC study researcher synthesised the student reports. This involved identifying recruitment methods and the participant sample, and conducting a thematic analysis of their research findings.
Reports synthesis
Participants
Nine research teams used convenience sampling methods, one used a random sampling method and one purposively sampled for diversity in respondents. All students recruited peers from their school and social groups (such as scouts). Over 295 respondents participated in the surveys (two research teams were unclear as to precisely how many people completed their questionnaires). Ten participants in the whole sample were known to have a LTC, 83 were known to be female and 88 were known to be male.
Results
Although the students asked their participants a range of questions around the research topic, findings can be grouped around three common themes: (1) communication preferences, (2) advantages of the use of DCC in a clinical setting and (3) disadvantages of the use of DCC.
The research teams all reported what forms of communication their peers preferred, specifically in relation to contact with a clinician. Many participants preferred to communicate with a clinician in person rather than digitally:
83% of people preferred to speak to their clinicians face to face.
Research team 6
Among digital communication methods, text messages were preferred as it was considered ‘easy, reliable and instant’ (research team 5). Facebook was the most popular social media site and the ability to customise privacy settings was appreciated:
Most of the people we asked feel safer using ‘Facebook’ than any other social media. We think this is because you can choose if you want your account’s information to be private.
Research team 9
Disadvantages to DCC were discussed and centred on the comfort of the patient, security issues and the accuracy of diagnosis. Some people thought that it was easier to talk to people in person, whereas it was harder for them to explain their concern digitally:
[Some] would find it hard to discuss medical information with their clinicians if they weren’t face to face.
Research team 8
Security concerns focused on data security, with participants citing data leaks, hacking, technology failure (e.g. a text message failing to send) and the identity of the person they were talking to. One person said:
I think I might be worried if I was actually talking to a doctor or nurse.
Research team 3
The lack of physical cues created concerns over misdiagnosis:
Perhaps mistakes would be made due to lack of physical examination and it may be more difficult to diagnose conditions.
Research team 7
Advantages centred on the comfort of the patient, cost and time savings. Some people reported that digital communication was preferred by people who felt uncomfortable or embarrassed talking to a clinician. Communicating online, from a physical venue of choice, provided the patient with a sense of physical and psychological reassurance:
They think it is useful as the patient will have more confidence and they are able to communicate without having to leave their home.
Research team 5
Removing the need and cost to physically travel to a clinic and wait for an appointment was also highly valued:
It would be easier and quicker to discuss these matters over social media instead of booking an appointment and being forced to wait […] for something simple which can be solved in a simple discussion.
Research team 7
Young researcher reflections
The students were often surprised that their peers were not more keen for digital technology to be used for consultations, particularly as they were aware that, as a social group, they are heavy users of communication technology:
Overall most of them wouldn’t use [social media] to discuss their medical issues which is unexpected as I see young people using social media every day.
Research team 10
Researcher reflections
Additional learning from the event and reports focuses on the language adopted by the young people, the assumptions they made and comments from the young people about the technology they use.
Language
Two research teams commented that some of their participants were unclear what the word ‘clinician’ meant. This is not necessarily a word that young people use regularly, as the more specific terms ‘doctor’ and ‘nurse’ were used frequently in the reports, for example:
Most people would rather visit the doctor physically than online.
Research team 4
The young researchers used the term social media to mean digital communication:
We have also explored personal opinions about using social media for contacting doctors.
Research team 6
This term was used to refer to all forms of digital communication and online activity (including text messaging, VoIP, e-mail, Google and YouTube), both in the research reports and in group discussions on the day.
Assumptions
There was an assumption that young people use and understand social media more than adults:
As younger people use and understand social media more than adults, asking them which digital platform would be best to use when talking to clinicians can result in the experience being the best it could be.
Research team 3
There was also an assumption within one research team that face-to-face communication can occur via VoIP, as they linked preferences for face-to-face communication, with FaceTime being the most popular digital technology, ‘because people would feel more comfortable seeing their clinician’s face’ (research team 11). This was echoed by another research team, who found that ‘those who do prefer digital communication mostly want their conversation to be personal and still would like to see their clinician’s face’ (research team 2). For these young people, as long as a patient and clinician can see each other, then they could be having a face-to-face consultation, even if they are not physically in the same room.
There was an assumption that teenagers are embarrassed about discussing health concerns and can have difficulty communicating more generally. This was made explicit during the campus days (e.g. one person said that teenagers were self-conscious in waiting rooms as they feel that other people look at them), and in the research reports:
. . . this could be due to them feeling embarrassed talking face to face to a doctor or nurse or having difficulty with face-to-face communication in general e.g. confidence issues.
Research team 3
Technology
A wide range of social media sites are used by young people such as Snapchat, BBM (BlackBerry Ltd, ON, Canada), KIK (Kik Interactive, ON, Canada), 9GAG (9GAG Inc., Tsuen Wan, Hong, Kong), Tumblr (Tumblr Inc., NY, New York, USA) and Bebo (Bebo Inc., London, UK), as well as better-known sites such as Facebook, Twitter and Instagram. These different sites allow for different types of communication to take place, for example instant message, text message, live chat and photography.
Key learning from the event
-
Although text messaging is the most popular form of digital communication for these young people, they do use a wide range of communication media.
-
Young people can feel embarrassed talking to their clinicians.
-
Young people do have concerns over data security and accuracy of diagnosis via digital communication, although they are heavy users of technology and do see some advantages to communicating digitally with a health professional.
-
Young people use the term ‘social media’ to cover all forms of digital communication and do not necessarily understand terms such as ‘clinician’ and ‘LTC’.
Activity 2: project months 22 and 23
Method
Year 12 students (aged 16 and 17 years) from local schools and colleges were invited to take part in the Warwick Young Researchers scheme. Twenty-one students responded, 20 attended day 1; however, four students missed day 2 because of mock exams. The two campus days mirrored those of activity 1 in terms of introductions to the research topic and learning research and analysis skills.
Unlike the previous event, the students were tasked with devising one questionnaire that they could all take back to their peer groups. The group were asked to consider three main questions:
-
What is the value of digital communications to patients?
-
What are the safety and ethical issues around the illusion that digital communications create a 24-hour health service?
-
If you were a digital patient what would your expectations be of the response time of health-care professionals to digital communications?
The young researchers were split into three groups each focusing on one of these questions. Each group, facilitated by a LYNC study researcher, was tasked with devising three questions on their theme and the wording for either the introduction, consent or demographic questions. The group collectively approved the final survey. The questions were input into a single questionnaire using SurveyMonkey. Each participant received paper copies of the questionnaire and the link to the online version.
Students collected data in between the two campus days using a number of different recruitment strategies, aiming to achieve at least 15 responses each. The online responses were collated by the LYNC study researchers and downloaded into an Excel spreadsheet. Hard-copy responses were collected by individual students.
During the second campus day, the students worked in pairs and were allocated 15 hard-copy questionnaires to input to the Excel spreadsheet of online data. Each pair focused their analysis on three different questions, including at least one qualitative and one quantitative. Additionally, each pair was asked to write up their approach to recruitment and their completion rate. The second campus day was disrupted for 1 hour by a fire alarm.
By the end of campus day 2, each group had analysed their questions and described their recruitment methods. These brief reports were amalgamated by the LYNC study researchers. The team then combined the additional hard-copy responses input by each student pair into one database and re-ran the analyses undertaken by the students. The full data set mirrored the smaller data sets that had been used by the student pairs and the final report was compiled using text from the students along with tables re-run using the full data set. The report was circulated to the whole student group for comments. A number of students responded, with only one suggesting changes that were incorporated into the final version of the report.
Report
Participants
Four pairs used convenience sampling and four used purposive sampling methods. All students recruited peers from school/college and one leisure-based group. Overall, 177 responses were obtained, 111 hard copies and 66 online. The young researchers estimated that 124 hard copies of the questionnaires were distributed and 91 electronic links sent out. This gives response rates of 89.5% for hard copies, 72.5% for electronic copies and 82% overall. There were 73 male respondents and 101 female respondents, two did not complete that question and one preferred not to define their gender.
Results
Overall, 79 respondents had used digital communications to seek health advice, the majority of which had been over the telephone (it is not possible to know whether or not calls were between two mobile devices, but it is likely to have often been from a young person’s mobile device to a clinician’s landline). The telephone was considered a digital form of communication for young people, as they made all their calls on a mobile device, even if they were calling a landline.
When asked how quickly they would expect a response from a clinician they had contacted using digital communications, 72.5% expected a response within 2 hours. Only nine respondents expected a response to take ≥ 4 hours. The importance of a timely response was also noted by 89% of participants, who thought that they should be offered the possibility of digitally contacting their health-care professionals at any time.
Participants were asked about the reliability of advice sought digitally. Speed and ease of access were cited by those who rated the reliability of digital communications highly. However, some respondents were concerned over the technical reliability of the systems that would be used and others were not sure they would be confident the clinician was the person they said they were. The ability to diagnose digitally was a primary concern about reliability:
It would be more difficult to explain and show the issue over a phone or computer.
17-year-old female
Throughout the survey, participants were asked about seeking advice; however, respondents were concerned about diagnosis.
Participants were asked, ‘In what situation would you consider using digital communications to contact health-care professionals?’. Responses were coded into emergency and non-emergency circumstances, with no difference found between the two. Respondents were then asked how they would prefer to contact their health-care professional if they have, or have had, a LTC. The telephone was the most frequently chosen method of contact, with speed being cited as the main reason: ‘it’s the quickest way’ and ‘because it will be the quickest’. Others liked its direct nature and a feeling that you were less likely to be misinterpreted on the telephone.
Participants were finally asked, ‘Do you feel there is a need for a digital communication service?’. Overall, 65% of participants saw a need for such a service in health care. The young researchers concluded that this was likely to be as a result of the increasing use of technology and social media by young people who saw this as their primary means of communication. Therefore, it would be a convenient and easy way to receive health-care information. Only 8% of respondents did not see a need, and 27% were unsure. Unsure respondents were either happy with the current arrangements they had with their health-care teams or felt that the introduction of a digital service would overburden an already stretched service. Respondents who did see a need for such a service cited speed and the ability to raise issues they would be embarrassed to talk about in person as the main reasons.
Young researcher reflections
The young researchers reported that the young people surveyed saw a need for some form of digital communications with health-care professionals. They considered this to be a natural extension to the way young people currently communicate with peers and relatives. They also pointed to an awareness that the health service is stretched and that a digital service, particularly one in which there was an expectation of a quick response time, would stretch resources further. The young researchers saw a balance between awareness of issues of privacy and trust around personal information, speed of response and cost to the health service. They concluded that, as digital communications are part of their generation, it would be a natural progression for digital communications to be incorporated into the health service in some way, taking account of the challenges outlined.
Researcher reflections
Throughout the survey the young researchers used the term ‘phone’, by which they meant mobile phone. Therefore, when the young people talked about the importance of being able to talk to their health-care team on the ‘phone’ they assume that they are using their mobile device, even if they are calling a landline. To them, this constitutes digital communication.
Timeliness was important to survey participants, with most expecting a response to a digital communication within a 2-hour time period. When this was discussed among the group, most agreed that 2 hours was a very short time period and that it would be important to distinguish between urgent communications and those that were non-urgent and could be answered in a longer time frame. The group were aware that current health services face many pressures and opening up digital communications would add to these pressures, even if it was seen as a natural progression by a digitally literate cohort of patients. Discussing ways in which expectations, including response time, could be managed was a difficult concept for the young researchers to grasp. They were unsure how you could set up a service with caveats for use, as some of the benefits came from being able to send communications ‘out of hours’.
Key learning from the event
-
Young people see their mobile phone as a digital technology when it is being used for synchronous as well as asynchronous contact.
-
Young people value speed of contact with health-care professionals, which they consider would best be achieved by using their mobile phones.
-
The young researchers were able to reflect on realistic expectations of response times by health-care professionals, although they were unclear as to how these could be managed.
-
Young people value in-person communications for diagnosis and have some concerns over security and trust in health professionals.
Impact of the patient and public involvement activities
In accordance with the LYNC study project protocol, activity 1, conducted at the start of the study, had an impact on case study design, and research and recruitment design. Activity 2, conducted after data collection was complete, had an impact on interpretation of the data from young people.
Impact of activity 1
Activity 1 identified that many young people prefer text messaging over other forms of digital communication. Perceived advantages of DCC included patient comfort and a reduction in embarrassment about communicating with clinicians. These findings affected case study design, as we specifically sought sites that used text messages in order to communicate with patients. We also purposively sought clinical teams who cared for people with potentially stigmatising or embarrassing health conditions (such as HIV infection and sexually transmitted diseases) to further explore this issue. Furthermore, the research team were sensitive to the fact that some patients may be reluctant to engage with the research and might feel embarrassed about taking part in an interview.
Learning from activity 1 was also incorporated into the patient recruitment and data collection phases of the case studies, particularly in terms of the language used when talking to young people and how interview questions were framed. When describing the study to interview participants, the researchers explained what they meant by the term ‘digital communication.’ This explanation specifically included the term ‘social media’, as young people often understand this to cover a wide range of digital communication technologies. As some young people had expressed confusion over the term ‘clinician’, this was also clarified during the interview process. The terms ‘doctor’, ‘nurse’, ‘psychologist’, etc., were used as appropriate to each clinical team, to ensure that patients knew that we were referring to their health-care providers. The phrase ‘LTC’ was not used frequently in the interviews. As the interviews focused on the patient’s specific condition (e.g. diabetes mellitus), the relevant term was used during the interview.
Impact of activity 2
Overall, the findings of activity 2 support the themes that have emerged from analysis of the case studies. Both the main analysis and activity 2 identified timeliness and security as key issues. Timeliness in this context is being responded to by the right person at the right time. Although there were differences in what the young people saw as the purpose of digital communications (i.e. emergency purposes and non-urgent queries), timely responses were important to all. The security of DCC was also an issue. As was found in the case study data, young people are aware of issues of confidentiality and potential breaches from using digital communications, but these do not deter them. They were also wary of using non-visual digital communications for diagnosis purposes citing potential miscommunication as an issue. These findings mirror those found in the case studies in a number of ways, despite most of the survey respondents not having a LTC and not having had the experience of using digital communications for health care.
Appendix 2 Protocol for dealing with concerns about unethical practice revealed by participants during interviews for the Long-term conditions Young people Networked Communication study
Maintaining confidentiality of research participants
We will conduct interviews on the premise that participant confidentiality is a priority and would be breached only if we had reasonable concern that it was necessary in the public interest (i.e. a significant risk of serious harm to others was identified). This is in line with the General Medical Council guidance on confidentiality in clinical practice.
Procedure to be followed if a researcher is concerned that unethical or unsafe practice has been described by a research participant
If concern arises about unethical or unsafe clinical practice, the researcher will consult one of the PIs (Frances Griffiths or Jackie Sturt), who will decide if it is necessary to initiate action through normal professional channels. Concerns of this kind are likely to be extremely rare. If the PI considers further action is needed they will make appropriate enquiries (which may include contacting the research participant for further details). If the public interest test of a likelihood of significant risk of serious harm to others is fulfilled, the PI will inform the research participant of the need to disclose relevant information to the relevant organisation (NHS trust and/or professional regulatory body).
Disclosure of practice that is outside organisational policy on information governance
During data collection we are asking clinic staff to reveal activities that may breach IG policies. We do not expect to take action for activity that we find is common practice. However, if we discover a serious breach of confidentiality we will need to take action in line with the steps outlined below.
Procedure to be followed on identification of significant breaches of confidentiality or information governance
A significant breach of confidentiality is likely to involve disclosure of information to a third party without the patient’s consent. During the initial interview stage of the project, the research fellow will have regular debriefing meetings with the PIs or Anne Slowther (clinical ethicist) to discuss any possible breaches of IG identified in the interview data and to agree a level of breach that would warrant consideration of further action on the part of the research team. If the research fellow has a concern that an interview raises a question regarding a significant breach of IG they will inform the PI. The PI and Anne Slowther will listen to the interview recording and agree on whether or not the breach is sufficient to require further action. If further action is considered necessary, the PI will contact the participant to inform them of our concerns and advise them that we will need to inform the Trust IG officer. The PI will contact the Trust IG officer and advise them of our concerns.
Appendix 3 Additional tables of impacts on health-related outcomes
| Site | Health condition | DCC use/escalation notes | Number of appointments (percentage of DNA) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | |||
| CSW05IT | Mental health: CAMHS | No DCC | ND | ND | ND | ND | ND | ND | 4576 (5.0)a | 6150 (4.7) | 5549 (5.3) | 6041 (7.3) | 4321 (6.7) | 1438 (8.0)b | ND |
| CSW07 | Rheumatology | No DCC | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | 143 (13.3)c | 140 (8.6)b | ND |
| CSK08IT | HIV infection | No DCC | ND | ND | ND | ND | ND | ND | ND | 5417 (17.0) | 6062 (14.0) | 6138 (11.6) | 6301 (10.4) | 6421 (10.6) | 2204 (9.6)d |
| CSW01IT | Diabetes mellitus | Mobile phone since 2003 and e-mail since 2010 | ND | ND | ND | ND | ND | 364 (25.8) | 356 (24.2) | 372 (18.8) | 363 (18.2) | 349 (18.6) | 145 (11.0)e | ND | ND |
| CSK05IT | Diabetes mellitus | Mobile phone and VoIP. Used by two consultants | ND | ND | ND | ND | ND | ND | ND | ND | ND | 1082 (17.4)a | 1649 (16.9) | 1798 (14.5) | 413 (14.2)f |
| CSK02IT | Sickle cell disease | Mobile phone and text messaging | ND | ND | ND | ND | ND | 1032 (35.3) | 1155 (29.3) | 1091 (30.6) | 1232 (31.3) | 1250 (32.4) | 1470 (32.6) | ND | ND |
| CSK04Cl | Cancer | Mobile phone, text messaging and e-mail | ND | ND | ND | ND | ND | ND | ND | ND | ND | 45 (24.4)g | 229 (27.5) | 257 (16.0) | 114 (13.2)h |
| CSK01IT | Liver conditions | Text messaging and e-mail. New format introduced 1 January 2009 | 62 (19.4) | 125 (31.2) | 170 (22.4) | 200 (27.0) | 246 (24.4) | 375 (13.9) | 524 (17.0) | 569 (18.6) | 659 (24.9) | 619 (24.2) | 696 (22.1) | 687 (21.0) | ND |
| CSW06IT | Mental health: CAMHS | Mobile phone, text messaging and VoIP since 2010. Change in records system and consultant in 2015 | ND | ND | ND | ND | ND | ND | ND | 1295 (20.3)a | 1812 (9.6) | 2339 (8.9) | 2600 (7.0) | 2246 (9.8) | 472 (30.9)f |
| CSW02IT | Mental health: EIPT | Mobile phones since 2001. Smartphones introduced summer 2015 | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | 35 (48.6)i | 114 (35.1) | 27 (44.4)j |
| CSW04IT | Dermatology | Clinic existed since 2012 and e-mail has always been used | ND | ND | ND | ND | ND | ND | ND | ND | 210 (11.4)a | 414 (7.2) | 635 (11.5) | 162 (13.6)f | ND |
| CSW08Cl | Cystic fibrosis | Exercise specialist has used text messaging and VoIP since 2013. Basic mobile phone since 2013. New mobile phone 2015 – not smartphone | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | 532 (17.9) | 635 (16.2) | ND |
| CSW03IT | Cystic fibrosis | E-mail estimated use since 2012 | ND | ND | ND | ND | ND | ND | ND | ND | ND | 133 (5.3) | 176 (9.7) | 202 (6.4) | 71 (18.3)f |
| CSW12IT | Renal conditions | E-mail and text messaging used since clinic was set up in June 2014 | ND | ND | ND | ND | ND | ND | ND | ND | ND | 6 (33.3)k | 32 (12.5) | 19 (26.3)h | ND |
| CSK09IT | Sexual health | Testing kits ordered online | ND | ND | ND | ND | ND | ND | ND | 20,108 (29.0) | 19,312 (28.3) | 19,624 (28.8) | 18,987 (32.1) | 14,250 (30.9) | 2606 (10.0)f |
| CSK07IT | IBD | ND | ND | 183 (13.7) | 379 (11.1) | 393 (10.9) | 639 (10.2) | 778 (11.6) | 774 (7.6) | 827 (9.2) | 891 (14.6) | 872 (15.3) | 809 (15.7) | 274 (15.7)f | |
| Site | Health condition | DCC use notes | Number of patients (percentage with at least one A&E appointment) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | |||
| CSW07 | Rheumatology | No DCC | ND | ND | ND | ND | ND | ND | ND | ND | 64 (24.4)a | 88 (11.7)b | ND |
| CSK08 | HIV infection | No DCC | ND | ND | ND | ND | ND | 1548 (11.0) | 1684 (12.0) | 1851 (12.0) | 2019 (13.4) | 2199 (12.1) | 2265 (7.9)c |
| CSW01 | Diabetes mellitus | Mobile phone, text messaging and e-mail | ND | ND | ND | 86 (23.3) | 132 (20.5) | 170 (21.2) | 209 (24.4) | 235 (19.6) | 251 (20.7)d | ND | ND |
| CSK05 | Diabetes mellitus | Mobile phone and VoIP. Used by two consultants | ND | ND | ND | ND | ND | ND | ND | 373 (40.0)e | 578 (28.0) | 725 (23.0) | 755 (29.7)f |
| CSK07 | IBD | 80 (8.8) | 159 (9.4) | 227 (12.3) | 323 (13.9) | 431 (8.1) | 554 (10.6) | 685 (11.4) | 845 (10.1) | 993 (10.4) | 1103 (10.1) | 1168 (6.7)f | |
| CSW12 | Renal conditions | No formal DCC. Young people given e-mail and telephone contacts of staff | ND | ND | ND | ND | ND | ND | ND | 4 (0)g | 16 (12.5) | 20 (24.0)h | ND |
| Site | Health condition | DCC use notes | Number of patients (percentage with at least one hospital admission) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | |||
| CSW07 | Rheumatology | No DCC | ND | ND | ND | ND | ND | ND | 64 (52.5)a | 88 (29.2)b | ND |
| CSK08 | HIV infection | No DCC | ND | ND | ND | 5417 (6.8) | 6062 (6.2) | 6138 (5.9) | 6301 (5.0) | 6421 (4.7) | 2204 (2.5)c |
| CSW01 | Diabetes mellitus | Mobile phone, text messaging and e-mail | ND | 86 (24.4) | 132 (16.7) | 170 (17.6) | 209 (17.7) | 235 (13.6) | 251 (16.3)d | ND | ND |
| CSK05 | Diabetes mellitus | Mobile phone and VoIP. Used by two consultants | ND | ND | ND | ND | ND | 373 (8.9)e | 578 (8.3) | 725 (6.1) | 755 (10.6)f |
| CSK07 | IBD | 227 (32.1) | 323 (38.4) | 431 (32.5) | 554 (29.4) | 685 (32.8) | 845 (33.4) | 993 (31.0) | 1103 (27.6) | 1168 (12.2)f | |
| CSW12 | Renal conditions | No formal DCC. Young people given e-mail and telephone contacts of staff | ND | ND | ND | ND | ND | 4 (0)g | 16 (31.3) | 20 (24.0)h | ND |
Appendix 4 Amended format of online patient and public involvement patient-reported outcome survey A
The vignette
Just imagine that you are a young adult aged 16–24 years living with a long-term health condition. Over the past 18 months you have found it easy to e-mail your specialist nurse about your condition. You have sought their advice about your medication dose and you have also asked them questions about your condition. They usually respond within 24 hours, but they were on leave recently and you got the e-mail address of their colleague whom you could contact. In addition to being able to e-mail your nurse, the clinic is also about to start using Skype consultations; this means you won’t need to worry about taking time out of school or work to speak to someone. You have been asked to help evaluate their service and they would like to know which of the following topics the clinic should use to determine how useful you find these new DCCs.
-
Level of satisfaction when communicating with your health-care provider and services they provide, for example how confident are you in your ability to ask your doctor for more information if you don’t understand what he/she said? [Perceived Efficacy in Patient–Physician Interactions (PEPPI)155]
-
Experience of anxiety, depression and stress, for example during the past month were you frustrated by your health problems? (Health distress. 387)
-
Flexibility to meet friends and family, for example are you satisfied with how often you see your friends and relatives? (Koenig et al. and the Duke social support index. 167)
-
Quality of life, for example during the past 30 days, for about how many days did poor physical or mental health keep you from doing your usual activities, such as self-care, work, or recreation? [Centers For Disease Control And Prevention Health-Related Quality Of Life (CDC HRQOL) measure169]
-
Satisfaction with using ICT, for example can you be as satisfied talking to the nurse over Skype as talking in person? (Telemedicine Patient Questionnaire. 165)
-
Patient empowerment and confidence, for example ‘when all is said and done I’m the person who is responsible for managing my health condition’? (PAM Short Form. 178)
Are there other topics that you think we should consider as research outcomes?
Appendix 5 Rapid review search strategy
The Long-term conditions Young people Networked Communication (LYNC) study rapid reviews: record of searches
Summary of database search results for the main search for five of the six rapid reviews
| Database | Number of results |
|---|---|
| MEDLINE | 15,042 |
| MEDLINE In-Process & Other Non-Indexed Citations (via Ovid) | 1938 |
| EMBASE | 22,140 |
| The Cochrane Library | 2781 |
| PsycINFO | 2957 |
| Total number | 44,858 |
Numbers for Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow chart for main search
| Total from databases | 44,858 |
| After duplicates removed | 27,696 |
| After duplicates removed 2009 onwards | 19,018 |
Record of main searches for five of the six rapid reviews
MEDLINE (via Ovid)
Date range searched: 1946 to August week 3 2015.
Date searched: 27 August 2015.
Search strategy
| 1 | Electronic Mail/ | 2038 |
| 2 | (email* or e-mail* or web-mail* or webmail* or internet-mail*).tw. | 7666 |
| 3 | Text Messaging/ | 887 |
| 4 | (text messag* or texting or multimedia message*).tw. | 1263 |
| 5 | ((mobile phone* or cellular phone* or cell phone*) and (message* or text* or sms or mms)).tw. | 819 |
| 6 | Social Media/ | 1923 |
| 7 | (social media or social networking or blog* or facebook or myspace or twitter).tw. | 3505 |
| 8 | ((internet* or web* or information or patient or health) adj2 (portal* or forum)).tw. | 1673 |
| 9 | (smartphone app* or smart phone app* or PDA app* or personal digital assistant app*).tw. | 331 |
| 10 | (video-conferenc* or videoconferenc* or videophone* or video-phone* or Voice over Internet Protocol or VoIP or skype or (google adj2 (talk or hangouts))).tw. | 1810 |
| 11 | Videoconferencing/ | 923 |
| 12 | digital interactive television.tw. | 5 |
| 13 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 | 17,838 |
| 14 | (digital or electronic or virtual or computer* or software* or internet* or online or on-line or web* or multimedia or multi-media or communication technolog* or telecommunication* or ICT or network* technolog* or telemedic* or telecare or telehealth* or telepsychiatr*).ti. | 163,183 |
| 15 | *computer communication networks/ or *internet/ | 37,023 |
| 16 | *telecommunications/ or *telemedicine/ or *remote consultation/ or *telepathology/ or *teleradiology/ or *cell phones/ or *modems/ or *wireless technology/ | 22,303 |
| 17 | 13 or 14 or 15 or 16 | 200,778 |
| 18 | exp *Professional-Patient Relations/ or exp *Professional-Family Relations/ | 62,797 |
| 19 | ((clinic* or center* or centre* or service* or hospital* or doctor* or physician* or clinician* or nurse* or pharmacist* or health worker* or professional* or provider* or practitioner* or therapist* or educator* or psychiatr* or patient* or outpatient* or out-patient* or inpatient* or in-patient* or client* or child* or teen* or paediatric* or pediatric* or boy* or girl* or youth* or schoolchild* or adoles* or minor or minors or under age* or juvenile* or schoolage* or school age* or young adult* or young person* or young people or student* or parent* or mother* or father* or brother* or sister* or sibling* or family or families or carer* or caregiver* or care giver*) adj4 (communicat* or relation* or interact* or convers* or discuss* or message* or feedback or respond* or response* or receive* or consult* or contact* or advice or advis* or counsel* or recommend* or monitor* or review* or diary or diaries or assess* or support* or educat* or train* or manage* or care or treat* or therapy or therapies or intervention* or report* or ongoing partnership)).tw. | 2,616,393 |
| 20 | 18 or 19 | 2,652,071 |
| 21 | 17 and 20 | 41,890 |
| 22 | Young Adult/ or Adolescent/ or Child/ or Students/ | 2,569,792 |
| 23 | (child* or teen* or paediatric* or pediatric* or boy* or girl* or youth* or schoolchild* or school child* or kid* or adoles* or minor or minors or under age* or juvenile* or pubescen* or secondary school* or highschool* or high school* or peer group* or schoolage* or school age* or young adult* or young person* or young people or student* or sixth form* or higher education or further education or undergraduate* or college* or universit*).tw. | 2,217,902 |
| 24 | 22 or 23 | 3,751,056 |
| 25 | 21 and 24 | 15,042 |
MEDLINE In-Process & Other Non-Indexed Citations (via Ovid)
Date range searched: to 2 September 2015.
Date searched: 3 September 2015.
Search strategy
| 1 | Electronic Mail/ | 0 |
| 2 | (email* or e-mail* or web-mail* or webmail* or internet-mail*).tw. | 1509 |
| 3 | Text Messaging/ | 0 |
| 4 | (text messag* or texting or multimedia message*).tw. | 457 |
| 5 | ((mobile phone* or cellular phone* or cell phone*) and (message* or text* or sms or mms)).tw. | 257 |
| 6 | Social Media/ | 0 |
| 7 | (social media or social networking or blog* or facebook or myspace or twitter).tw. | 1327 |
| 8 | ((internet* or web* or information or patient or health) adj2 (portal* or forum)).tw. | 306 |
| 9 | (smartphone app* or smart phone app* or PDA app* or personal digital assistant app*).tw. | 222 |
| 10 | (video-conferenc* or videoconferenc* or videophone* or video-phone* or Voice over Internet Protocol or VoIP or skype or (google adj2 (talk or hangouts))).tw. | 240 |
| 11 | Videoconferencing/ | 0 |
| 12 | digital interactive television.tw. | 1 |
| 13 | 2 or 4 or 5 or 7 or 8 or 9 or 10 or 12 | 3888 |
| 14 | (digital or electronic or virtual or computer* or software* or internet* or online or on-line or web* or multimedia or multi-media or communication technolog* or telecommunication* or ICT or network* technolog* or telemedic* or telecare or telehealth* or telepsychiatr*).ti. | 27,501 |
| 15 | 13 or 14 | 30,742 |
| 16 | ((clinic* or center* or centre* or service* or hospital* or doctor* or physician* or clinician* or nurse* or pharmacist* or health worker* or professional* or provider* or practitioner* or therapist* or educator* or psychiatr* or patient* or outpatient* or out-patient* or inpatient* or in-patient* or client* or child* or teen* or paediatric* or pediatric* or boy* or girl* or youth* or schoolchild* or adoles* or minor or minors or under age* or juvenile* or schoolage* or school age* or young adult* or young person* or young people or student* or parent* or mother* or father* or brother* or sister* or sibling* or family or families or carer* or caregiver* or care giver*) adj4 (communicat* or relation* or interact* or convers* or discuss* or message* or feedback or respond* or response* or receive* or consult* or contact* or advice or advis* or counsel* or recommend* or monitor* or review* or diary or diaries or assess* or support* or educat* or train* or manage* or care or treat* or therapy or therapies or intervention* or report* or ongoing partnership)).tw. | 252,369 |
| 17 | 15 and 16 | 5700 |
| 18 | (child* or teen* or paediatric* or pediatric* or boy* or girl* or youth* or schoolchild* or school child* or kid* or adoles* or minor or minors or under age* or juvenile* or pubescen* or secondary school* or highschool* or high school* or peer group* or schoolage* or school age* or young adult* or young person* or young people or student* or sixth form* or higher education or further education or undergraduate* or college* or universit*).tw. | 191,893 |
| 19 | 17 and 18 | 1938 |
EMBASE (via Ovid)
Date range searched: 1974 to week 35 2015.
Date searched: 2 September 2015.
Search strategy
| 1 | *e-mail/ | 1150 |
| 2 | (email* or e-mail* or web-mail* or webmail* or internet-mail*).tw. | 18,033 |
| 3 | *text messaging/ | 780 |
| 4 | (text messag* or texting or multimedia message*).tw. | 2242 |
| 5 | ((mobile phone* or cellular phone* or cell phone*) and (message* or text* or sms or mms)).tw. | 1469 |
| 6 | *social media/ | 2002 |
| 7 | (social media or social networking or blog* or facebook or myspace or twitter).tw. | 6596 |
| 8 | ((internet* or web* or information or patient or health) adj2 (portal* or forum)).tw. | 2702 |
| 9 | (smartphone app* or smart phone app* or PDA app* or personal digital assistant app*).tw. | 866 |
| 10 | (video-conferenc* or videoconferenc* or videophone* or video-phone* or Voice over Internet Protocol or VoIP or skype or (google adj2 (talk or hangouts))).tw. | 2742 |
| 11 | *videoconferencing/ | 576 |
| 12 | digital interactive television.tw. | 7 |
| 13 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 | 33,230 |
| 14 | (digital or electronic or virtual or computer* or software* or internet* or online or on-line or web* or multimedia or multi-media or communication technolog* or telecommunication* or ICT or network* technolog* or telemedic* or telecare or telehealth* or telepsychiatr*).ti. | 219,504 |
| 15 | *computer network/ or *internet/ | 34,588 |
| 16 | exp *telehealth/ or *teleconsultation/ or *mobile phone/ | 18,931 |
| 17 | 13 or 14 or 15 or 16 | 267,290 |
| 18 | *doctor patient relation/ or *nurse patient relationship/ | 47,263 |
| 19 | ((clinic* or center* or centre* or service* or hospital* or doctor* or physician* or clinician* or nurse* or pharmacist* or health worker* or professional* or provider* or practitioner* or therapist* or educator* or psychiatr* or patient* or outpatient* or out-patient* or inpatient* or in-patient* or client* or child* or teen* or paediatric* or pediatric* or boy* or girl* or youth* or schoolchild* or adoles* or minor or minors or under age* or juvenile* or schoolage* or school age* or young adult* or young person* or young people or student* or parent* or mother* or father* or brother* or sister* or sibling* or family or families or carer* or caregiver* or care giver*) adj4 (communicat* or relation* or interact* or convers* or discuss* or message* or feedback or respond* or response* or receive* or consult* or contact* or advice or advis* or counsel* or recommend* or monitor* or review* or diary or diaries or assess* or support* or educat* or train* or manage* or care or treat* or therapy or therapies or intervention* or report* or ongoing partnership)).tw. | 3,905,370 |
| 20 | 18 or 19 | 3,933,505 |
| 21 | 17 and 20 | 63,407 |
| 22 | exp student/ | 91,612 |
| 23 | (child* or teen* or paediatric* or pediatric* or boy* or girl* or youth* or schoolchild* or school child* or kid* or adoles* or minor or minors or under age* or juvenile* or pubescen* or secondary school* or highschool* or high school* or peer group* or schoolage* or school age* or young adult* or young person* or young people or student* or sixth form* or higher education or further education or undergraduate* or college* or universit*).tw. | 3,188,530 |
| 24 | limit 21 to (child <unspecified age> or school child <7 to 12 years> or adolescent <13 to 17 years>) | 8020 |
| 25 | 22 or 23 | 3,205,416 |
| 26 | 21 and 25 | 20,498 |
| 27 | 24 or 26 | 22,140 |
The Cochrane Library (via Wiley Online Library)
Date searched: 2 September 2015.
Search strategy
| #1 | MeSH descriptor: [Electronic Mail] this term only | 208 |
| #2 | (email* or e-mail* or webmail* or web-mail* or internet-mail*):ti,ab,kw | 1042 |
| #3 | MeSH descriptor: [Text Messaging] this term only | 161 |
| #4 | (text next messag* or texting or multimedia next message*):ti,ab,kw | 529 |
| #5 | ((mobile next phone* or cellular next phone* or cell next phone*) and (message* or text* or sms or mms)):ti,ab,kw | 334 |
| #6 | MeSH descriptor: [Social Media] this term only | 26 |
| #7 | (“social media” or “social networking” or blog* or facebook or myspace or twitter):ti,ab,kw | 190 |
| #8 | ((internet* or web* or information or patient or health) near/2 (portal* or forum)):ti,ab,kw | 110 |
| #9 | (smartphone next app* or “smart phone” next app* or PDA next app* or “personal digital assistant” next app*):ti,ab,kw | 69 |
| #10 | (video-conferenc* or videoconferenc* or videophone* or video-phone* or “Voice over Internet Protocol” or VoIP or skype or (google near/2 (talk or hangouts))):ti,ab,kw | 318 |
| #11 | MeSH descriptor: [Videoconferencing] this term only | 98 |
| #12 | “digital interactive television”:ti,ab,kw | 1 |
| #13 | #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 | 2260 |
| #14 | (digital or electronic or virtual or computer* or software* or internet* or online or on-line or web* or multimedia or multi-media or communication next technolog* or telecommunication* or ICT or network* next technolog* or telemedic* or telecare or telehealth* or telepsychiatr*):ti | 10,980 |
| #15 | [mh ^“computer communication networks” [mj]] or [mh ^internet [mj]] | 1045 |
| #16 | [mh ^telecommunications [mj]] or [mh ^telemedicine [mj]] or [mh ^“remote consultation” [mj]] or [mh ^telepathology [mj]] or [mh ^teleradiology [mj]] or [mh ^“cell phones” [mj]] or [mh ^modems [mj]] or [mh ^“wireless technology” [mj]] | 528 |
| #17 | #13 or #14 or #15 or #16 | 12,873 |
| #18 | [mh “Professional-Patient Relations” [mj]] or [mh “Professional-Family Relations” [mj]] | 1808 |
| #19 | ((clinic* or center* or centre* or service* or hospital* or doctor* or physician* or clinician* or nurse* or pharmacist* or health next worker* or professional* or provider* or practitioner* or therapist* or educator* or psychiatr* or patient* or outpatient* or out-patient* or inpatient* or in-patient* or client* or child* or teen* or paediatric* or pediatric* or boy* or girl* or youth* or schoolchild* or adoles* or minor or minors or under next age* or juvenile* or schoolage* or school next age* or young next adult* or young next person* or young next people or student* or parent* or mother* or father* or brother* or sister* or sibling* or family or families or carer* or caregiver* or care next giver*) near/4 (communicat* or relation* or interact* or convers* or discuss* or message* or feedback or respond* or response* or receive* or consult* or contact* or advice or advis* or counsel* or recommend* or monitor* or review* or diary or diaries or assess* or support* or educat* or train* or manage* or care or treat* or therapy or therapies or intervention* or report* or ongoing next partnership)):ti,ab,kw | 347,291 |
| #20 | #18 or #19 | 347,294 |
| #21 | #17 and #20 | 6476 |
| #22 | [mh ^"Young Adult"] or [mh ^Adolescent] or [mh ^Child] or [mh ^Students] | 78,701 |
| #23 | (child* or teen* or paediatric* or pediatric* or boy* or girl* or youth* or schoolchild* or school next child* or kid* or adoles* or minor or minors or under next age* or juvenile* or pubescen* or secondary next school* or highschool* or high next school* or peer next group* or schoolage* or school next age* or young next adult* or young next person* or young next people or student* or sixth next form* or higher next education or further next education or undergraduate* or college* or universit*):ti,ab,kw | 231,913 |
| #24 | #22 or #23 | 231,913 |
| #25 | #21 and #24 | 2781 |
All results (N = 2781):
-
Cochrane reviews (n = 39)
-
other reviews (n = 61)
-
trials (n = 2588)
-
methods studies (n = 67)
-
technology assessments (n = 6)
-
economic evaluations (n = 20)
-
Cochrane groups (n = 0).
PsycINFO (via ProQuest)
Date searched: 8 September 2015.
Note that the results exported from line S24 are limited to 2009 onwards as a result of ProQuest’s restrictions on the number of records that can be exported. Unable to export results from line S21.
Search strategy
| S24 |
S17 AND S22 Limited by: Publication date after 2009 |
2957* |
| S23 | S17 AND S22 | 4707* |
| S22 | S18Limits applied | 188,824* |
| S21 | S19 AND S20 | 9421* |
| S20 | TI,AB(child* OR teen* OR paediatric* OR pediatric* OR boy* OR girl* OR youth* OR schoolchild* OR school PRE/0 child* OR kid* OR adoles* OR minor OR minors OR under PRE/0 age* OR juvenile* OR pubescen* OR secondary PRE/0 school* OR highschool* OR high PRE/0 school* OR peer PRE/0 group* OR schoolage* OR school PRE/0 age* OR young PRE/0 adult* OR young PRE/0 person* OR young PRE/0 people OR student* OR sixth PRE/0 form* OR higher PRE/0 education OR further PRE/0 education OR undergraduate* OR college* OR universit*) | 1,245,671* |
| S19 | S17 AND S18 | 15,817* |
| S18 | TI,AB((clinic* OR center* OR centre* OR service* OR hospital* OR doctor* OR physician* OR clinician* OR nurse* OR pharmacist* OR health PRE/0 worker* OR professional* OR provider* OR practitioner* OR therapist* OR educator* OR psychiatr* OR patient* OR outpatient* OR out-patient* OR inpatient* OR in-patient* OR client* OR child* OR teen* OR paediatric* OR pediatric* OR boy* OR girl* OR youth* OR schoolchild* OR adoles* OR minor OR minors OR under PRE/0 age* OR juvenile* OR schoolage* OR school PRE/0 age* OR young PRE/0 adult* OR young PRE/0 person* OR young PRE/0 people OR student* OR parent* OR mother* OR father* OR brother* OR sister* OR sibling* OR family OR families OR carer* OR caregiver* OR care PRE/0 giver*) PRE/3 (communicat* OR relation* OR interact* OR convers* OR discuss* OR message* OR feedback OR respond* OR response* OR receive* OR consult* OR contact* OR advice OR advis* OR counsel* OR recommend* OR monitor* OR review* OR diary OR diaries OR assess* OR support* OR educat* OR train* OR manage* OR care OR treat* OR therapy OR therapies OR intervention* OR report* OR ongoing PRE/0 partnership)) | 642,259* |
| S17 | S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 | 84,172* |
| S16 | MJSUB.EXACT(“Online Therapy”) | 1492° |
| S15 | MJSUB.EXACT(“Telemedicine”) | 2614° |
| S14 | MJSUB.EXACT(“Internet”) | 19,034* |
| S13 | MJSUB.EXACT(“Cellular Phones”) | 2003° |
| S12 | MJSUB.EXACT(“Websites”) | 2602° |
| S11 | TI(digital OR electronic OR virtual OR computer* OR software* OR internet* OR online OR on-line OR web* OR multimedia OR multi-media OR communication PRE/0 technolog* OR telecommunication* OR ICT OR network* PRE/0 technolog* OR telemedic* OR telecare OR telehealth* OR telepsychiatr*) | 63,637* |
| S10 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 | 22,147* |
| S9 | MJSUB.EXACT.EXPLODE(“Electronic Communication”) | 10,148* |
| S8 | TI,AB(“digital interactive television”) | 4° |
| S7 | TI,AB(video-conferenc* OR videoconferenc* OR videophone* OR video-phone* OR “Voice over Internet Protocol” OR VoIP OR skype OR (google PRE/1 (talk OR hangouts))) | 1466° |
| S6 | TI,AB((smartphone PRE/1 app* OR “smart phone” PRE/1 app* OR PDA PRE/1 app* OR “personal digital assistant” PRE/1 app*)) | 169° |
| S5 | TI,AB((internet* OR web* OR information OR patient OR health) NEAR/1 (portal* OR forum)) | 745° |
| S4 | TI,AB(“social media” OR “social networking” OR blog* OR facebook OR myspace OR twitter) | 7850* |
| S3 | TI,AB((mobile PRE/0 phone* OR cellular PRE/0 phone* OR cell PRE/0 phone*) AND (message* OR text* OR sms OR mms)) | 766° |
| S2 | TI,AB(text PRE/0 messag* OR texting OR multimedia PRE/0 message*) | 1342° |
| S1 | TI,AB(email* OR e-mail* OR web-mail* OR webmail* OR internet-mail*) | 6408* |
Record of searching and sorting within EndNote for five of the six rapid reviews
Diabetes mellitus
Clicked on ‘Rapid reviews main search > All’ and in search panel selected ‘Search Whole Group’.
| Any field | Contains | diab* | |
| And | Year | Is greater than | 2008 |
Results saved to an EndNote group ‘Main search diabetes keyword 2009 onwards’.
Total: 774.
Families/carers
Clicked on ‘Rapid reviews main search > All’ and in search panel selected ‘Search Whole Group’.
| Title field | Contains | parent* | |
| Or | Title field | Contains | mother* |
| Or | Title field | Contains | father* |
| Or | Title field | Contains | sibling* |
| Or | Title field | Contains | brother* |
| Or | Title field | Contains | sister* |
| Or | Title field | Contains | family |
| Or | Title field | Contains | families |
| Or | Title field | Contains | carer* |
| Or | Title field | Contains | caregiver* |
| Or | Title field | Contains | care-giver* |
Total: 1479.
Total (2009 onwards): 1146.
Clicked on ‘Rapid reviews main search > All’ and in search panel selected ‘Search Whole Group’.
| Any field | Contains | parent* | 3283 | |
| Or | Any field | Contains | mother* | 974 |
| Or | Any field | Contains | father* | 190 |
| Or | Any field | Contains | sibling* | 122 |
| Or | Any field | Contains | brother* | 43 |
| Or | Any field | Contains | sister* | 50 |
| Or | Any field | Contains | family | 3235 |
| Or | Any field | Contains | families | 1339 |
| Or | Any field | Contains | carer* | 141 |
| Or | Any field | Contains | caregiver* | 655 |
| Or | Any field | Contains | care-giver* | 9 |
Total: 6767.
Then sorted this group by Year and kept records of articles published in 2009 or later.
Total remaining: 5125.
Mental health
Searched the group ‘All 2009 onwards’ in the group set ‘Rapid review main search’ within the EndNote library ‘LYNC WP2 lit reviews’.
| Term | Any field | Title field |
|---|---|---|
| General mental health | ||
| mental* | 401 | |
| psych* | 576 | |
| disorder* | 418 | |
| Specific mental health conditions | ||
| *depress* | 1053 | |
| Affective | 141 | |
| mood* | 339 | |
| manic* or mania* | 121 | |
| Bipolar | 64 | |
| cyclothymi* | 1 | |
| dysthymi* | 4 | |
| schizo* | 102 | |
| delusion* | 7 | |
| paranoi* | 16 | |
| autis* | 179 | |
| asperger* | 10 | |
| “eating disorder” | 122 | |
| “eating disorders” | 105 | |
| anorexi* | 43 | |
| bulimi* | 38 | |
| hyperkin* | 3 | |
| Hyperactivity | 140 | |
| ADHD | 128 | |
| attention-deficit | 57 | |
| “attention deficit” | 167 | |
| self-harm* | 36 | |
| “self harm” | 11 | |
| “self harms” | 0 | |
| “self harming” | 0 | |
| “self harmed” | 0 | |
| “self harmer” | 0 | |
| suicid* | 195 | |
| overdos* | 30 | |
| PTSD (n.b. Match Case ticked) | 50 | |
| post-traumatic | 56 | |
| Posttraumatic | 77 | |
| “post traumatic” | 3 | |
| anx* | 899 | |
| OCD (n.b. Match Case ticked) | 33 | |
| obsessi* | 61 | |
| compulsi* | 96 | |
| phobi* | 134 | |
| panic* | 357 | |
| “personality disorder” | 44 | |
| “personality disorders” | 15 | |
| “behavioural disorder” | 0 | |
| “behavioural disorders” | 0 | |
| “behavioral disorder” | 12 | |
| “behavioral disorders” | 10 | |
| “behaviour disorder” | 4 | |
| “behaviour disorders” | 0 | |
| “behavior disorder” | 149 | |
| “behavior disorders” | 128 | |
| “conduct disorder” | 18 | |
| “conduct disorders” | 1 | |
| “body dysmorphia” | 0 | |
| “body dysmorphic” | 3 | |
Totals
Note that many records will include more than one of the above terms. Therefore, the totals below are not the sum of the numbers above:
-
specific condition keywords in any fields: 2835
-
general mental health keywords in title: 1292
-
1 OR 2 = 3503 (final total for screening).
Long-term physical conditions
Searched the group ‘All 2009 onwards’ in the group set ‘Rapid review main search’ within the EndNote library ‘LYNC WP2 lit reviews’.
Note that phrase searching is only possible in quick search, which only searches any field.
Search strategy
| Term | Any field (not including full paper) |
|---|---|
| asthma* | 352 |
| carcinoma* | 100 |
| Cancer | 1486 |
| “cerebral palsy” | 134 |
| “cystic fibrosis” | 118 |
| Dermatitis | 55 |
| dermatol* | 318 |
| gynaecolog* OR gynecolog* | 395 |
| haemoglobinopath* OR hemoglobinopath* | 8 |
| “sickle cell” | 58 |
| thalassaemia OR thalassemia | 14 |
| “congenital heart” | 73 |
| epilep* | 189 |
| HIV (n.b. Match Words ticked) | 356 |
| “human immunodeficiency virus” | 173 |
| immunodeficien* | 189 |
| “kidney disease” | 228 |
| “kidney diseases” | 57 |
| “renal disease” | 81 |
| “renal diseases” | 8 |
| IBD (n.b. Whole Words ticked) | 65 |
| “inflammatory bowel disease” | 67 |
| “inflammatory bowel diseases” | 25 |
| “crohn’s disease” | 40 |
| “crohn disease” | 45 |
| “crohns disease” | 2 |
| “ulcerative colitis” | 37 |
| “colitis, ulcerative” | 10 |
| “liver disease” | 46 |
| “liver diseases” | 16 |
| “liver transplant” | 54 |
| Metabolic | 164 |
| “spina bifida” | 16 |
| “spinal dysraphism” | 10 |
| rheumatolog* | 345 |
| “juvenile rheumatoid arthritis” | 53 |
| “arthritis, juvenile” | 12 |
| “juvenile arthritis” | 12 |
| “juvenile chronic arthritis” | 0 |
| “juvenile idiopathic arthritis” | 57 |
| “chronic arthritis in children” | 0 |
| “chronic arthritis” | 2 |
|
Abstract/Title Contains arthritis AND Abstract/Title Contains child* |
114 |
|
Abstract/Title Contains arthritis AND Abstract/Title Contains juvenile |
83 |
| “brain injury” | 126 |
| “brain injuries” | 58 |
| “brain damage” | 22 |
|
Any Field/Abstract/Title Contains physical* AND Any Field/Abstract/Title Contains disab* |
145 |
| “duchenne” | 5 |
| “muscular dystrophy” | 8 |
| “muscular dystrophies” | 3 |
Totals
Note that many records will include more than one of the above terms. Therefore, the totals below are not the sum of the numbers above.
Total number for any terms (equivalent of asthma* OR carcinoma* OR cancer, etc.) searched for in any field (not including full paper): 4411 (added to EndNote group “3rd test”).
Searched within EndNote group “3rd test” for RCT/SR terms (RCT or random* or “clinical trial” or “clinical trials” or “controlled trial” or “controlled trials” or “systematic review” or “systematic reviews” or “systematically review” or “meta analysis” or “meta-analysis” or “meta analyse”) in Any Field (but not including full paper): 1096 (final total for screening).
International
Note that H = high-income country, LM = low- to middle-income country, UM = upper middle-income country.
| Country | Keyword(s) searched in any field | Results of search |
|---|---|---|
| Andorra, (H) | andorra* | 0 |
| Antigua, (H) | antigua* | 1 |
| Argentina, (H) | argentin* | 64 |
| Armenia, (LM) | armenia* | 0 |
| Austria, (H) | austria* | 206 |
| Azerbaijan, (UM) | azerbaijan* | 0 |
| Bahrain, (H) | bahrain* | 4 |
| Belarus, (UM) | belarus* | 1 |
| Belgium, (H) | belgi* | 242 |
| Bosnia and Herzegovina, (UM) | bosnia* OR herzegovin* | 17 |
| Botswana, (UM) | botswana* | 11 |
| Brazil, (UM) | brazil* OR brasil* | 256 |
| Brunei Darussalam, (H) | brunei* | 4 |
| Bulgaria, (UM) | bulgaria* | 16 |
| Chile, (H) | chile OR chilian | 46 |
| Costa Rica, (UM) | “costa rica” OR “costa rican” OR “Costa Rica” OR “Costa Rican” | 4 |
| Croatia, (H) | croat* | 33 |
| Cuba, (UM) | cuba* | 19 |
| Cyprus, (H) | cyprus OR cypriot* | 16 |
| Czech Republic, (H) | czech* | 79 |
| Denmark, (H) | denmark OR danish OR danes | 219 |
| Estonia, (H) | estonia* | 18 |
| Finland, (H) | finland* OR finnish* | 148 |
| France, (H) | france OR french | 747 |
| Germany, (H) | german* | 931 |
| Greece, (H) | greece* OR greek* | 117 |
| Hungary, (H) | hungar* | 61 |
| Iceland, (H) | iceland* | 18 |
| Israel, (H) | israel* | 200 |
| Italy, (H) | italy OR italia* | 512 |
| Japan, (H) | japan* | 302 |
| Kuwait, (H) | kuwait* | 14 |
| Luxembourg, (H) | luxembourg* | 6 |
| Moldova, (LM) | moldova* | 6 |
| Mongolia, (UM) | mongolia* | 6 |
| Netherlands, (H) | netherlands* OR holland OR dutch | 809 |
| Norway, (H) | norway OR norwegian | 149 |
| Oman, (H) | Oman* (n.b. match case ticked) | 11 |
| Panama, (UM) | panama* | 3 |
| Portugal, (H) | portug* | 238 |
| Romania, (UM) | romania* | 36 |
| Singapore, (H) | singapor* | 133 |
| Slovakia, (H) | slovakia* | 9 |
| Slovenia, (H) | slovenia* | 47 |
| South Korea, (H) | “south korea” OR “south korean” | 149 |
| Spain, (H) | spain OR spanish OR spaniard* | 710 |
| Sweden, (H) | sweden OR swedish OR swede* | 439 |
| Switzerland, (H) | switzerland OR swiss | 294 |
| Taiwan, (H) | taiwan* | 262 |
| Thailand, (UM) | thai* | 67 |
| Tunisia, (UM) | tunisia* | 7 |
| UAE, (H) | UAE (Match case and Match words ticked) OR united arab emirates | 19 |
| Ukraine, (LM) | ukrain* | 0 |
| Venezuela (H) | venezuela* | 6 |
Note that many records will include more than one of the above terms. Therefore, the total below is not the sum of the numbers above.
Total: 5726.
Other searches
International
India
IndMED.
Total: 141.
Advanced search
email OR e-mail OR mobile phone OR cell phone OR text message OR social media OR videoconferencing OR telemedicine OR telecare OR telehealth OR telecommunication OR digital OR electronic OR online OR internet OR web OR virtual
AND
communication OR communicate OR consultation OR consult OR interaction OR interact OR conversation OR relationship OR relations OR advice OR monitor OR counsel OR discuss OR respond OR response OR contact OR support
AND
clinician OR doctor OR physician OR nurse OR pharmacist OR health worker OR health professional OR healthcare provider OR therapist OR psychiatrist OR patient OR youth OR adolescent OR teenager OR young person OR young people
Latin America and the Caribbean
Latin American and Caribbean Health Sciences Literature.
Total: 390.
2009 onwards: 263.
Advanced form
Title Words (email OR e-mail OR mobile phone OR cell phone OR text message OR social media OR videoconferencing OR telemedicine OR telecare OR telehealth OR telecommunication OR digital OR electronic OR online OR internet OR web OR virtual)
AND
Words (communication OR communicate OR consultation OR consult OR interaction OR interact OR conversation OR relationship OR relations OR advice OR monitor OR counsel OR discuss OR respond OR response OR contact OR support)
AND
Country (Brazil)
South East Asia: Index Medicus for the South East Asia region (IMSEAR)
URL: http://imsear.li.mahidol.ac.th/
Total: 297.
Search strategy
Any field (communication OR communicate OR consultation OR consult OR interaction OR interact OR conversation OR relationship OR relations OR advice OR monitor OR counsel OR discuss OR respond OR response OR contact OR support) AND (clinician OR doctor OR physician OR nurse OR pharmacist OR worker OR professional OR provider OR therapist OR psychiatrist OR patient OR youth OR adolescent OR teenager OR young)
AND
Title: email OR e-mail OR mobile OR phone OR media OR videoconference OR videoconferencing OR telemedicine OR telecare OR telehealth OR telecommunication OR digital OR electronic OR online OR internet OR web OR virtual
AND
Date issued equals [2009 TO 2099]
Skype
Searched within results for review of systematic reviews
Date searched: 9 May 2014.
| Any field | Contains | skype | |
| Or | Any field | Contains | videoconferenc* |
| Or | Any field | Contains | Video-conferenc* |
| Or | Any field | Contains | Google AND (talk or hangouts) |
Total: 91.
Total 2009 onwards: 78.
Updated Skype element of search from review of systematic reviews
Ovid MEDLINE(R)
Date range searched: 1946 to November week 3 2015.
Date searched: 6 January 2016.
Search strategy
| 1 | (video-conferenc* or videoconferenc* or videophone* or video-phone* or Voice over Internet Protocol or VoIP or Skype or (google adj2 (talk or hangouts))).tw. | 1866 |
| 2 | Videoconferencing/ | 959 |
| 3 | 1 or 2 | 2202 |
| 4 | (metaanalys* or “meta analys*” or “meta-analys*”).tw. | 71,902 |
| 5 | “systematic* review*”.mp. | 63,126 |
| 6 | meta analysis.pt. | 62,613 |
| 7 | 4 or 5 or 6 | 127,154 |
| 8 | 3 and 7 | 49 |
| 9 | limit 8 to ed=20140510-20160106 | 11 |
Search for Skype terms and clinical communication terms
Ovid MEDLINE(R)
Date range searched: 1946 to November week 3 2015.
Date searched: 6 January 2016.
Search strategy
| 1 | (video-conferenc* or videoconferenc* or videophone* or video-phone* or Voice over Internet Protocol or VoIP or skype or (google adj2 (talk or hangouts))).tw. | 1866 |
| 2 | Videoconferencing/ | 959 |
| 3 | 1 or 2 | 2202 |
| 4 | remote consultation/ | 3890 |
| 5 | exp *Professional-Patient Relations/ or exp *Professional-Family Relations/ | 63,881 |
| 6 | ((clinic* or center* or centre* or service* or hospital* or doctor* or physician* or clinician* or nurse* or pharmacist* or health worker* or professional* or provider* or practitioner* or therapist* or educator* or psychiatr* or patient* or outpatient* or out-patient* or inpatient* or in-patient* or client* or child* or teen* or paediatric* or pediatric* or boy* or girl* or youth* or schoolchild* or adoles* or minor or minors or under age* or juvenile* or schoolage* or school age* or young adult* or young person* or young people or student* or parent* or mother* or father* or brother* or sister* or sibling* or family or families or carer* or caregiver* or care giver*) adj4 (communicat* or relation* or interact* or convers* or discuss* or message* or feedback or respond* or response* or receive* or consult* or contact* or advice or advis* or counsel* or recommend* or monitor* or review* or diary or diaries or assess* or support* or educat* or train* or manage* or care or treat* or therapy or therapies or intervention* or report* or ongoing partnership)).tw. | 2,682,183 |
| 7 | 4 or 5 or 6 | 2,720,173 |
| 8 | 3 and 7 | 1567 |
| 9 | limit 8 to yr = “2009 -Current” | 684 |
| 10 | limit 9 to english language | 673 |
| 11 | randomized controlled trial.pt. | 417,624 |
| 12 | (random* or “controlled trial*” or “clinical trial*” or rct).tw. | 899,985 |
| 13 | 11 or 12 | 1,003,125 |
| 14 | 10 and 13 | 134 |
| 15 | epidemiologic studies/ | 6465 |
| 16 | exp Case-Control Studies/ | 765,973 |
| 17 | exp Cohort Studies/ | 1,518,609 |
| 18 | case control.tw. | 83,075 |
| 19 | (cohort adj (study or studies)).tw. | 98,365 |
| 20 | cohort analy$.tw. | 4129 |
| 21 | (follow up adj (study or studies)).tw. | 38,541 |
| 22 | (observational adj (study or studies)).tw. | 49,321 |
| 23 | longitudinal.tw. | 147,760 |
| 24 | retrospective.tw. | 294,449 |
| 25 | cross sectional.tw. | 179,833 |
| 26 | Cross-Sectional Studies/ | 208,903 |
| 27 | 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 | 2,067,196 |
| 28 | 10 and 27 | 103 |
| 29 | 14 or 28 |
Appendix 6 Further details on studies included in the rapid reviews
| Study | Year of publication | Strength of research | Comments |
|---|---|---|---|
| Becker254 | 2011 | Fair | Unsure if study participants were representative of those who would be eligible in the general population. No blinded assessment of outcomes. Small sample size. Loss to follow-up after baseline > 20%, although the study duration was very short |
| Binford Hopf et al.255 | 2013 | Fair | Unsure if study participants were representative of those who would be eligible in the general population. No blinded assessment of outcomes. Small sample size |
| Bradford et al.228 | 2012 | Fair | Unsure if study participants were representative of those who would be eligible in the general population. Small sample size (study stopped prematurely before target sample size completed). Loss to follow-up after baseline > 20% (many deaths occurred – children receiving palliative care) |
| Epstein et al.248 | 2015 | Good | Unsure if study participants were representative of those who would be eligible in the general population. Outcome measures of interest not taken multiple times before the intervention and multiple times after the intervention |
| Grover et al.232 | 2011 | Fair | This study evaluated the intervention as a whole and not specifically the part of the intervention related to communication. Unsure if study participants were representative of those who would be eligible in the general population. Outcome measures of interest not taken multiple times before the intervention and multiple times after the intervention. Unsure whether or not the intervention delivered consistently, as participants completed workbooks in their own time without a rigid time limit set |
| Gulmans et al.249 | 2012 | Fair | Unsure if study participants were representative of those who would be eligible in the general population |
| Haney and Tufts234 | 2012 | Fair | Unsure if study participants were representative of those who would be eligible in the general population. No prespecified selection criteria. Patients who participated were only those interested in the use of technology. Small sample size |
| Vismara et al.253 | 2012 | Fair | Unsure if study participants were representative of those who would be eligible in the general population. Very small sample size (quasi-experimental study) |
| Vismara et al.240 | 2013 | Fair | Unsure if study participants were representative of those who would be eligible in the general population. Very small sample size (quasi-experimental study). No p-values for the pre–post changes after statistical analyses |
| Wade et al.244 | 2009 | Fair | Unsure if study participants were representative of those who would be eligible in the general population. Small sample size. No p-values for the pre–post changes after statistical analyses |
| Wade et al.242 | 2009 | Fair | Unsure if study participants were representative of those who would be eligible in the general population. Small sample size. No p-values for the pre–post changes after statistical analyses |
| Braverman and Samsonov229 | 2011 | Fair | Participation rate of eligible participants > 50%. Loss at follow-up < 20%. Sample size justification, power and effect sizes not reported. No blinded assessment of outcomes |
| Byczkowski et al.231 | 2014 | Fair | Participation rate of eligible participants > 50%. Loss at follow-up < 20%. Sample size justification, power and effect sizes not reported |
| de Graaf et al.245 | 2013 | Fair | Participation rate of eligible participants > 50%. Loss at follow-up < 20%. Sample size justification, power and effect sizes not reported |
| Hopper et al.235 | 2011 | Poor | No prespecified selection criteria. Patients who participated were only those interested in the use of technology. Results are provided with very few details. Very small sample size (10 patients) |
| Lee et al.252 | 2010 | Fair | Participation rate of eligible participants < 50%. Sample size justification, power and effect size not reported |
| Mulgrew et al.236 | 2011 | Fair | Sample size justification, power and effect size provided. Rate of eligible persons participating not reported |
| Bergmo et al.223 | 2009 | Good | No blinded assessment of outcomes. Baseline characteristics of patients unbalanced (control group more in urban location – uncertain effect) |
| Grover et al.232 | 2011 | Poor | This study evaluated the whole intervention and not specifically the part of the intervention related to communication. Patients were not blinded. No relevant clinical outcomes were reported. Estimate of the treatment effect was not precise |
| Gund et al.233 | 2013 | Fair | No blinded assessment of outcomes. Baseline characteristics of patients not provided. No measure of the intervention effect |
| Hanberger et al.250 | 2013 | Good | Intervention unblinded for patients but blinded to assessors. No effect was shown. Unsure if results can be applied in another context/local population |
| Looman et al.246 | 2015 | Good | No statement related to the randomisation procedure. Patients were not blinded. No relevant clinical outcomes were reported |
| Petranovich et al.238 | 2015 | Fair | This study evaluated the whole intervention and not specifically the part of the intervention related to communication. Interviewers were blinded, but there was a risk of unblinding following the discussion with patients. Loss to follow-up after baseline > 20% |
| Wade et al.243 | 2012 | Fair | No information related to the method of randomisation. No blinded assessment. Unbalanced rate of incomplete data. No relevant clinical outcomes were reported |
| Wade et al.241 | 2014 | Fair | This study evaluated the whole intervention and not specifically the part of the intervention related to communication. Although interviews/research assistants were masked, potential unblinding was possible during interviews. Sample size justification and power not reported |
| Barlott et al.224 | 2015 | Fair | Relationship between researcher and participants not adequately considered. Unsure if ethical issues been taken in to consideration |
| Britto et al.230 | 2013 | Good | Relationship between researcher and participants not adequately considered |
| Hanlon-Dearman et al.251 | 2014 | Good | Unsure if relationship between researcher and participants was adequately considered. Unsure if ethical issues been taken in to consideration |
| Nordfeldt et al.237 | 2010 | Good | Well-conducted study |
| Scharer et al.239 | 2009 | Good | Unsure if ethical issues been taken in to consideration |
| Bradford et al.227 | 2014 | Good | Costs not directly translatable to our setting but may be similar |
| van Os-Medendorp et al.247 | 2012 | Good | Limited time horizon (1 year) |
| Study | Year of publication | Results |
|---|---|---|
| Barlott et al.224 | 2015 |
Parent/carers outcomes: participation in the study provided caregivers with the possibility of a social support network, which gave them strength. Participation also showed caregivers the possibility of community participation and the possibility that their experience of disability could change, giving them optimism Health service outcomes: in total, 50 messages were sent by SMS (6.25/participant) over a 3-month period: 20 were question messages (2.5/participant; range 0–12 messages) and 30 were social interaction messages (3.75/participant; range 0–8 messages) |
| Becker254 | 2011 |
Patient outcomes: the Eyberg Child Behaviour Inventory (assessing the frequency and severity of disruptive behaviours) reduced from baseline to 2 weeks for both the e-mail and telephone groups, with no differences between the two groups Parents/carers outcomes: similarly, there were no differences between the e-mail and telephone groups on the Oral Outcome Rating Scale or the overall Parent Advice Line programme satisfaction score |
| Bergmo et al.223 | 2009 |
Patient outcomes: the objective severity scoring of atopic dermatitis at 12 months was improved in both groups compared with that at baseline, but there was no difference between the intervention and control groups Parent/carers outcomes: there was an improvement in both groups regarding the number of skin care treatments per week performed by the parents at 12 months, but no differences between the two groups were observed. The intervention did not affect family costs at 12 months or loss of employment at 12 months Health services outcomes: on average, the mean number of messages sent at 12 months was 8.3/participant. There were fewer health-care visits at 12 months in both groups compared with baseline, but no difference between the two groups |
| Binford Hopf et al.255 | 2013 |
Parents/carers outcomes: after chat session: 95.9% of participants felt supported by the therapist in today’s chat 85.6% of participants felt that the advice and guidance they received from the therapist in today’s chat was helpful 9.6% of participants felt that the technical environment limits their ability to express yourself or to self-disclose in today’s chat 22.8% of participants experienced technical problems (type of problem not reported) There was an improvement on the Eating Disorder Symptom Impact Scale total score (p = 0.02). There was also improvement on the stigma (p = 0.02) and dependency (p = 0.05) subscales of the Experience of Caregiving Inventory. There were no differences on the difficult behaviours (p = 0.30), negative symptoms (p = 0.44), problems with services (p = 0.33), effects on family (p = 0.06), need to backup (p = 0.59), loss (p = 0.55), positive personal experience (p = 0.58) or good aspects of relationship (p = 0.48) subscales |
| Bradford et al.227 | 2014 | Health services outcomes: the costs per consultation for the home telehealth programme, the outpatient consultation and the home visit were US$294, US$748, and US$1214, respectively |
| Bradford et al.228 | 2012 | Parent/carer outcomes: the health-related quality-of-life scores using the Life Threatening Illness-Family instrument improved in both groups compared with baseline, but there were no differences between video consultation and usual care |
| Braverman and Samsonov229 | 2011 |
Parent/carers outcomes: using a scale of 1–5, where 1 represents ‘definitely yes’, the majority of participants responded ‘1’ when asked about whether or not the consultation was useful (78%; 46/59) and if they trusted the consultation (54.2%; 32/59) Health service outcomes: the three main types of help provided by e-mail consultation were giving information about common diagnoses and treatment (89%), giving general information (59%) and giving recommendations about daily routine (30%). Half of the users engaged in short (one-message) correspondence (35/70), 43% of the users (30/70) engaged in longer correspondence (i.e. two or more e-mail messages on the same topic from the patient) and 10% of the users (7/70) returned to the physician 1–7 months after the initial correspondence |
| Britto et al.230 | 2013 | Parent/carers outcomes: parents reported benefits of using the portal, including removing barriers to communication, providing a sense of control and providing reassurance |
| Byczkowski et al.231 | 2014 |
Parent/carer outcomes: 62% of parents felt that the communication with the health professional was improved and 43% felt that the quality of relationship with the health professional was improved. 81% of parents agreed that the e-mail function was very useful, 74% declared that they received the information they needed, 71% reported that they received answers in a timely manner and 18% were sometimes concerned that e-mails/questions were sent to unintended recipients Health service outcomes: the proportion of parents that used the portal instead of calling their health-care provider sometimes was 58% and usually/always 6%; 39% of parents used the portal to send e-mails to their health-care professional |
| de Graaf et al.245 | 2013 | Parent/carer outcomes: after using the web-based e-health intervention, 89.9% of patients followed the advice of dermatologists and 98.4% would recommend the e-health intervention to other parents. 91.3% of parents perceived the e-health intervention as useful and 92.2% found the e-health intervention easy to use |
| Epstein et al.248 | 2015 |
Parent/carer outcomes: the videoconferencing system was rated as ‘good’ or ‘excellent’ by 100% of parents for ease of updates, and 78% for video and audio quality. > 90% of parents perceived the intervention to be reliable for updates in the NICU. At 5 days, there was no difference on parents’ understanding survey scores compared with baseline Health-care professional outcomes: > 90% of providers perceived the intervention to be reliable for updates in the NICU. 94% of providers rated the ease of using videoconferencing as excellent or good |
| Grover et al.232 | 2011 | Parent/carer outcomes: of the 33 carers randomised to the web intervention (overcoming anorexia online), 78.8% requested e-mail support as part of the package and 21.2% preferred telephone support |
| Grover et al.232 | 2011 | Parent/carer outcomes: of the 27 carers included, 59% requested e-mail support as part of the package and 41% preferred telephone support |
| Gulmans et al.249 | 2012 | Parent/carer outcomes: the web-based system for parent–professional communication was evaluated using a survey of 20 parents. 70% responded that the system considerably contributed to sufficient contact and 65% responded that it considerably contributed to timely information exchange; and 65% considered that the system considerably contributed to better accessibility for consultation. The consistency of information was rated using several items and rated as positive in 45% of responses, 10–25% did not know and 25–35% had a negative experience. Regarding the parents’ messenger/co-ordinator role, 45% had a positive experience, 10–25% did not know and 25–35% had a negative experience |
| Gund et al.233 | 2013 |
Parent/carer outcomes: Web-based system – 100% of parents found the experience extensive, 100% found the application easy to use, 83% found the application to be good or very good, 50% found that the webpage helped them to feel more confident in the care of the child at home and 33% found that the application reduced the need for home visits Skype – 100% of families found Skype easy to use, 100% were satisfied with the video calls, 87.5% found it easy to communicate with the nurse by video call, 75% found the answers or instructions received during the video calls useful, 50% found video calls less stressful than home visits, 100% found that the webpage helped them to feel more confident in the care of the child at home and 75% found that the application reduced the need for home visits Healthcare professional outcomes: most nurses were motivated to use the ICT, but one nurse reported seeing the study as a threat and avoided using the intervention |
| Hanberger et al.250 | 2013 |
Patient outcomes: the HbA1c level was 6.8% at baseline and 6.7% at 12 months in both groups (no significant differences). Although actual figures were not provided, no differences were reported between the intervention and control groups for severe self-reported hypoglycaemia, self-controlled blood glucose, health-related quality of life, satisfaction/acceptance and empowerment Parent/carer outcomes: although actual figures were not provided, no differences were reported between the intervention and control groups for health-related quality of life, satisfaction/acceptance and empowerment |
| Haney and Tufts234 | 2012 | Parent/carer outcomes: the Pediatric Quality of Life subscales family impact and health-care satisfaction were not statistically improved at 12 weeks compared with baseline |
| Hanlon-Dearman et al.251 | 2014 | Parent/carer outcomes: 81% of participants reported being happy with their experience of telehealth for diagnosis and follow-up support. All participants would recommend telehealth to another family |
| Hopper et al.235 | 2011 |
Parent/carer outcomes: 100% of respondents reported that they were satisfied with the telegenetic concept for clinics and agreed that they had enough opportunity to ask questions at the telemedicine and face-to-face appointment. 50% of respondents agreed that telemedicine was an effective medium to see a geneticist for the purpose of trying to ascertain a genetic diagnosis for their child. 25% of respondents felt that a face-to-face appointment was important for a first appointment with the clinical geneticist ‘because cameras don’t show everything’. 25% speculated that the effectiveness of telemedicine ‘depends on how a child deals with TV intrusion’ and that a follow-up appointment with the geneticist in person was important. All respondents were either satisfied or very satisfied with the telemedicine experience. Respondents were asked their opinion about improving the provision of telegenetics; however, no suggestions were made. All carers were given enough time to ask questions at both appointments and were happy with the information given at the telegenetic clinic. One parent commented that they ‘did not know what kind of questions to ask’ in the telemedicine appointment. The majority of participants (88%) agreed that telegenetics was an effective way of seeing a geneticist for assessment Health service outcomes: the measurements taken by the genetic counsellor and the geneticist varied slightly, but not sufficiently to affect the assessment and alter a diagnosis |
| Lee et al.252 | 2010 |
Parent/carer outcomes: using a five-point Likert scale (where 1 is strongly disagree, 3 is neutral and 5 is strongly agree), on average, parents agreed with the following statements: Digital pictures of my child’s eye findings will improve the quality of care from his/her doctor Digital pictures of my child’s eye findings will help me better understand his/her disease condition Digital pictures of my child’s eye findings could diagnose disease as accurately as an actual eye examination Digital pictures of my child’s retinopathy should be included in the permanent medical record Overall, technology will improve the quality of medical care for my child It is essential to meet face to face with my child’s doctor On average, parents did not agree or disagree with the following statements: Digital cameras and computers are reliable The potential benefits of sending these pictures electronically are worth the privacy risks Diagnosis by a far-away medical expert will make it easier to get the best possible health care for my child The quality of care from diagnosis by far-away medical experts is as good as the care from face-to-face medicine I could not trust a doctor that I did not personally meet On average, parents disagreed with the following statements: The quality of care from diagnosis by far-away medical experts is better than the care from face-to-face medicine I am worried that sending these pictures electronically will create risks for the privacy of my child’s medical information I am worried that a computer may not send the pictures correctly Overall, technology will make it harder for a patient and doctor to establish a good relationship |
| Looman et al.246 | 2015 | Health service outcomes: there was no statistically significant change between baseline and 24 months after, and no differences between the three groups regarding the following items: global rating of health care, family-centred care, getting needed care, getting care quickly, provider communication and help discrepancy (help needed–help received). Scores for personal doctor rating and adequacy of care co-ordination were rated higher in both intervention groups (telephone and video) than in the control group (p = 0.001 and p = 0.026, respectively) |
| Mulgrew et al.236 | 2011 | Parent/carer outcomes: there was no statistically significant difference between the intervention and control groups on overall parent satisfaction, satisfaction with the consulting health-care provider, satisfaction with appointment availability or in the parents’ comfort level in discussing health problems with provider. When asked whether or not the provider explained things about the child’s health in a way that is easy to understand, the rating of visits was lower for telehealth visits than for face-to-face visits (p = 0.01) |
| Nordfeldt et al.237 | 2010 |
Patient outcomes: patients had a positive attitude towards the portal, finding it easy to use. Advantages of the portal included the availability of information when it is needed and the ability to search and find information quickly. One patient reported that a more functional chat room was needed Parent/carer outcomes: parents had a positive attitude towards the portal, finding it easy to use. Advantages of the portal reported included peer–peer communication, the availability of information when it is needed and the ability to search for information. Barriers included the need for a password to access the portal |
| Petranovich et al.238 | 2015 | No outcomes related to the communication component of the programme were reported |
| Scharer et al.239 | 2009 | Parent/carer outcomes: mothers in the chat room intervention group had to be active in seeking support (e.g. by signing into the chat room to access the nurse). In the telephone intervention group both active and passive mothers received consistent support |
| van Os-Medendorp et al.247 | 2012 |
Patient outcomes: there was no significant differences between the intervention and control groups over time for the infants’ Dermatitis Quality of Life Index. The intensity of itching was not statistically different between the groups. The severity of atopic dermatitis differed significantly over time between the two groups (p = 0.04). However, the differences between the groups at each time point were not significant Health service outcomes: total costs (direct + indirect) at 12 months were €3378 for patients using individualised e-health and €3972 for patients with usual care (face-to-face care) |
| Vismara et al.240 | 2013 |
Patient outcomes: child behaviour – the rates of vocalidations and joint attention initiations increased from baseline to follow-up. The means of vocabulary production and comprehension also increased from baseline to follow-up Parent/carer outcomes: all eight parents agreed or strongly agreed that the website was easy to use, that there was enough information given to meet learning needs, that they were able to use the telehealth intervention to increase their child’s language, play and social engagement skills, they felt well supported by the intervention and would recommend it to other families. Only one person did not agree or strongly agree that the video conferencing sessions and online modules were the most helpful aspects of the intervention, or would feel confident teaching other caretakers to use the intervention with their child. The Maternal Behaviour Rating Scale (designed to assess the quality of maternal interactive behaviour with children with learning difficulties) score increased from baseline to follow-up (no p-value reported) |
| Vismara et al.253 | 2012 |
Patient outcomes: Child Social Communication Behaviours (spontaneous or prompted verbalisations, etc.) and the attention and initiation subscales of the Child Behaviour Rating Scale improved after the intervention Parent/carer outcomes: 88.9% of parents (8/9) expressed initial concerns about whether or not telehealth delivery would provide enough support to change behaviour and the logistics of using the software program. When asked if initial concerns were addressed by the end of the study, these parents felt reassured and perceived the distance coaching as informative and as valuable as live in-home or centre-based sessions delivered by professionals. All parents described some degree of frustration when using the videoconferencing program, such as the internet connection freezing in mid-conversation or the audio or web camera not working when first connecting with the therapist. Analysis of parent fidelity over time during treatment revealed significant increases from baseline to 12 weeks on the P-ESDM Fidelity Tool (0 no competent teaching to a score of 5 or extremely competent teaching). There were also increases on the Maternal Behaviour Rating Scale subscales of parent responsivity, parent affect, achievement-oriented behaviours and directive behaviour |
| Wade et al.241 | 2014 | Parent/carer outcomes: both the CAPS intervention and IRC intervention were associated with a reduction in caregiver distress. Participants who completed five or more CAPS sessions reported a greater reduction in depression than participants in the IRC intervention group |
| Wade et al.242 | 2009 | Parent/carer outcomes: 100% of parents found Skype videoconferences to be helpful |
| Wade et al.243 | 2012 | Parent/carer outcomes: no results were provided regarding the helpfulness of Skype videoconferences |
| Wade et al.244 | 2009 |
Patient outcomes: 62.5% of teenagers (5/8) considered the videoconferencing easy to use overall. 87.5% of teenagers (7/8) considered the videoconferencing helpful overall and 62.5% of teenagers (5/8) considered the videoconferencing helpful compared with face-to-face meetings Parent/carer outcomes: 57.1% of mothers (4/7) and 80% of fathers (4/5) considered the videoconferencing easy to use overall. 71.4% of mothers (5/7) and 60% of fathers (3/5) considered the videoconferencing helpful overall and 42.9% of mothers (3/7) and 60% of fathers (3/5) considered the videoconferencing helpful compared with face-to-face meetings |
| Study | Year of publication | Strength of research | Comments |
|---|---|---|---|
| Berndt et al.275 | 2014 | Fair | Health-care staff and researchers were not blinded to randomisation; however, this was not appropriate as the intervention involved clinicians accessing patient data and responding to patient queries. Small participant numbers |
| Boogerd et al.276 | 2014 | Fair | Health-care staff and researchers were not blinded to randomisation; however, this was not appropriate as the intervention involved two-way DCC between patient and clinician. Clinical outcomes were secondary to acceptability of the intervention |
| Carroll et al.277 | 2011 | Weak | No control group, very small sample size, statistics do not answer the questions on patient outcomes and have no significance/CIs |
| Choi et al.278 | 2013 | Weak | Small sample size, lack of control group, retrospective design |
| Farrell and Holmes-Walker279 | 2011 | Fair | The number of participants in the control group heavily outnumbered participants in the other groups |
| Freeman et al.280 | 2013 | Fair | The impact of the intervention on therapeutic alliance was given primacy and clinical outcomes were not analysed |
| Frøisland et al.281 | 2012 | Good | Only flaw is the lack of consideration between researchers and participants |
| Hanberger et al.250 | 2013 | Fair | There was little discussion of effect of intervention on HbA1c levels |
| Harris et al.282 | 2015 | Good | Health-care staff and researchers were not blinded to randomisation; however, this was not appropriate as the intervention involved patients receiving treatment via Skype |
| Izquierdo et al.283 | 2009 | Fair | Individual patients were not randomised, but their schools were. Small participant numbers |
| Landau et al.284 | 2012 | Fair | Health-care staff and researchers were not blinded to randomisation; however, this was not appropriate as the intervention involved remote blood glucose monitoring. Small participant numbers |
| Moattari et al.285 | 2013 | Good | Good design, but small participant numbers |
| Pinsker et al.286 | 2011 | Weak | Very small sample size, lack of randomisation, clinical outcomes not thoroughly considered |
| Study | Year of publication | Results |
|---|---|---|
| Berndt et al.275 | 2014 |
Patient outcomes: there was a significant reduction in HbA1c levels in both the intervention (p < 0.001) and control (p < 0.001) groups, and a significant improvement in diabetes mellitus self-efficacy in the intervention group (p = 0.04). Improved patient motivation and reduced check-up frequency was reported for the intervention group. In the control group there was a significant increase in BMI (p = 0.03) and weight (p = 0.04), but there was no change in the intervention group Health professional outcomes: reported benefits for health-care staff included complete and regular patient data input; minimisation of errors caused by lack of information; improvement of care process quality; and access to data independent of time and location Health service outcomes: reported benefits for the health service included delay and reduction of diabetes mellitus complications; minimised hospitalisation rates; and reduction in death rates |
| Boogerd et al.276 | 2014 |
Patient outcomes: there were no significant differences in change over time between the intervention and control group in terms of HbA1c levels (p = 0.69), confidence in diabetes mellitus self-management (p = 0.12), diabetes mellitus knowledge (p = 0.77) and health-related quality of life (p = 0.73). The intervention group did report improvement in evaluation of diabetes mellitus care (p = 0.03), which the control group did not. Health-related quality of life was measured by means of the Paediatric Quality of Life Inventory diabetes module (PedsQL-dm). This frequently used questionnaire is validated in Dutch paediatric diabetes mellitus care and consists of 28 items, which can be answered using a five-point Likert scale Technical problems: health professionals experienced problems with outdated browser software reducing processing speed and removing security certificates |
| Carroll et al.277 | 2011 |
Patient outcomes: the impact of the intervention on HbA1c levels was not reported. However, 94% of participants said receiving text messages from the nurse practitioner helped them to remember to check their blood sugar, 16% increased blood glucose testing as a result of the intervention, 71% reported feeling more independent in their diabetes mellitus management and 77% would use it after the study if they could Technical problems: there was limited mobile phone coverage, particularly in rural areas, and data would not upload unless there was good coverage. > 70% had to send their phone back for servicing during the study period |
| Choi et al.278 | 2013 | Patient outcomes: there was an improvement in HbA1c levels of 2% from baseline to the 3-month follow-up (p < 0.05); however, improvement stopped after 3 months |
| Farrell and Holmes-Walker279 | 2011 | Patient outcomes: HbA1c levels were significantly lower in the control group than in groups 2, 3 and 4 (p < 0.001). There were no differences in mean HbA1c level between patients with ketosis accessing the phone support intervention and those with DKA that did not (i.e. group 2 vs. 3 and 4). DKA admission rates in the phone support population was significantly lower than in the other groups (two in group 2 vs. 18 in group 3 and 19 in group 4) |
| Freeman et al.280 | 2013 | Patient outcomes: there was no significant relationship between therapeutic alliance and HbA1c level. There was no significant difference in therapeutic alliance between Skype and clinic groups (so Skype could be considered as effective as face-to-face contact) |
| Frøisland et al.281 | 2012 | Patient outcomes: overall, there was no significant change in follow-up HbA1c levels compared with baseline (metabolic control improved in seven participants, was unchanged in two participants and increased in three participants). Diamob helped patients to better understand self-management. Being able to text message their clinician gave patients a sense of protection, as it was easy to ask questions and raise concerns. They also appreciated the possibility of getting an immediate response and this improved their relationship with their physician |
| Hanberger et al.250 | 2013 | Patient outcomes: there were no differences between the intervention and control groups in all outcomes (including HbA1c levels, frequency of blood glucose self-control, health-related quality of life and empowerment). Visits to the website decreased over summer and Christmas periods. For health-related quality of life, we used the DISABKIDS Chronic Generic module, short form (12 items), adolescent and parent (as proxy) version combined with the diabetes mellitus-specific module (10 items) and adolescent and parent (as proxy) version. The items in the chronic-generic module were assigned to six dimensions: independence, emotion, social inclusion, social exclusion, limitation and medication. The items in the diabetes mellitus-specific module were assigned to treatment and impact on a five-point Likert scale, where a low value corresponds to low quality of life |
| Harris et al.282 | 2015 | Patient outcomes: there were no significant differences between the intervention and control groups for glycaemic control and diabetes mellitus self-management. When the Skype and face-to-face groups were collapsed the BFST-D was found to be effective in controlling HbA1c levels, when measured before intervention, after and at the 3-month follow-up (p = 0.01). There was a higher dropout rate in the intervention group (n = 17) than in the control (n = 9) |
| Izquierdo et al.283 | 2009 | Patient outcomes: during the first 6 months, when school was in session, there was an improvement in HbA1c levels in the intervention group (p = 0.02), whereas there was a non-significant increase in the control group. There was no difference in diabetes mellitus-related quality of life between the groups. Urgent visits to the school nurse for diabetes mellitus-related problems decreased over time in the intervention group, but not in the control group. The majority of participants (91%) in the intervention arm was satisfied with the telemedicine. Pediatric Diabetes Quality of Life Generic Module and the four subscale scores from the Pediatric Diabetes Quality of Life Diabetes Module |
| Landau et al.284 | 2012 |
Patient outcomes: at 6 months, there was no significant difference in HbA1c levels between the intervention and control groups (p = 0.54). There were high levels of non-compliance (12 out of 36 participants) among the intervention group. Participants in the compliant subgroup of the intervention arm reported that the intervention was useful in controlling blood glucose Adverse event: there was one episode of DKA in the intervention arm Technical problems: minor technical difficulties relating to uploading data were reported by five patients and these were resolved over the telephone |
| Moattari et al.285 | 2013 | Patient outcomes: HbA1c levels decreased significantly in intervention arm (p < 0.001), whereas there was a non-significant decrease in the control arm (p = 0.08). LDL cholesterol concentration decreased significantly in the intervention arm (p = 0.04), but not the control arm (p = 0.22). HDL cholesterol concentration increased significantly in the experimental and control groups (p = 0.03 and p = 0.01, respectively). Other metabolic control indicators did not significantly change |
| Pinsker et al.286 | 2011 | Treatment outcomes: there was no significant difference between baseline and follow-up HbA1c levels for users (p = 0.06) and non-users (p = 0.13) of the website intervention. However, comparison between the groups (users vs. non-users) showed a significant improvement in HbA1c levels for the user group (p = 0.03) |
| Study | Year of publication | Strength of research | Comments |
|---|---|---|---|
| Stain et al.308 | 2011 | Good | Crossover study – appropriate comparator for a neuropsychological test, although individual variation week to week is possible. Feasible explanation given for the test that did not correlate between the two methods. Bland–Altman plots showed significant bias only for WTAR. Small sample size |
| Turner et al.309 | 2014 | Fair | Unclear if participants are representative of the general population. Participants randomised to each intervention. Difference between CBT and tCBT consistently non-significant (95% CI). Higher loss to follow-up for tCBT at 31%. Non-inferiority margin of five points for CY-BOCS selected by researchers – has not been tested in this population |
| van der Zanden et al.307 | 2012 | Fair | Not blinded. Male population under-represented. Large loss to follow-up: 21% at 12 weeks; and a further 17% at 24 weeks. Improvement with intervention statistically significant compared with control |
| Williams et al.306 | 2014 | Weak | Self-selected group. No reasoning given for participant numbers. Male population under-represented. Qualitative methods not described, although data from this included. It appears qualitative data comes from discussion within the consultation – possible bias |
| Boydell et al.310 | 2010 | Fair | Clear goal and explanation for qualitative methods. No reasoning given for the process of participant recruitment. Little discussion around ethics. Large number of data with good explanation of methodology. Little discussion around bias or role of researcher |
| Kramer et al.311 | 2014 | Fair | Self-selected group. Males under-represented. High attrition rate, which was worse for those with higher depression scores. Missing values imputed for some statistical calculations |
| First author, date of publication, country | Main results |
|---|---|
| Williams, 2014, USA306 |
Patient satisfaction: Quantitative: most students (81.3%) found the interview useful in understanding their depressive symptoms. Fewer students (18.8%) found the interview useful in starting treatment for depression. Positive feedback (93.8%) on the likelihood that psychologists and psychiatrists could successfully see patients via web-based consultation service Qualitative: good for people who cannot get to hospital, able to connect with doctor from apartment where comfortable. Clinicians felt able to make a diagnosis. Preference for videoconferencing over audioconferencing as it allows eye contact and body language Technical problems: the majority of students reported that the sound (87.5%) and video (81.3%) quality of the consultation were clear |
| van der Zanden, 2012, the Netherlands307 | Clinical outcome: at 12 weeks the MYM group had a significantly greater improvement in depressive symptoms, anxiety and mastery than the control group. Depressive symptoms (CES-D d = 0.94, 95% CI 0.64 to 1.23), anxiety (HADS anxiety d = 0.49, 95% CI 0.24 to 0.75), mastery (d = 0.44, 95% CI 0.19 to 0.70). 56% (68/121) of the participants in the MYM group and 20% (24/123) in the control group showed a reliable and clinically significant change (a positive change of ≥ 5 points on the CES-D in combination with a score of < 22 points): significant between-group difference (χ2 1 = 35.0; p < 0.001). Number needed to treat of 2.7. The positive results achieved at 12 weeks were maintained at 24 weeks and mastery continued to improve |
| Stain, 2011, USA308 |
Clinical outcome: most tests demonstrated equivalence (Social and Occupational Functioning Assessment Scale, Wechsler Test of Adult Reading, the Controlled Oral Word Association Test, the Logical Memory subtest of the Wechsler Memory Scale and the Brief Psychiatric Rating Scale). Difficulties were encountered when administering the quality-of-life measure by videoconference because of the multiple-choice format Patient experience: participants reported that they felt comfortable and could understand the instructions. One in six participants said definitely that they did not prefer videoconferencing assessments |
| Turner, 2014, UK309 |
Clinical outcome: no significant difference, tCBT non-inferior to CBT. Clinician-rated global functioning – no significant difference Patient satisfaction: satisfaction between the two groups equal. Credibility ratings – no significant difference |
| Boydell, 2010, Canada310 | Patient satisfaction: some participants were uncomfortable with having others in the room, whereas others found it reassuring. Varying degrees of usefulness (only one consultation took place). Those who found it helpful found it increased knowledge around mental health and coping mechanisms. Some felt that they had a lack of control in the encounter. Excitement at novelty. Appreciated anonymity (e.g. not bumping into psychiatrist locally) |
| Kramer, 2014, the Netherlands311 | Clinical outcome: Depressive symptoms – CES-D scores:
|
| Study | Year of publication | Strength of research | Comments |
|---|---|---|---|
| Fruhauf et al.320 | 2015 | Good | The RCT was well conducted, all patients were accounted for and all outcomes identified and addressed |
| Wade et al.244 | 2009 | Fair | The methodological approach could have led to social desirability bias and a control group would have been beneficial to see any true benefit of the intervention |
| Wiecha et al.321 | 2015 | Poor | Post hoc decision to combine the two intervention arms for analysis led to asymmetrically sized intervention and control groups; any change observed could be attributable to either the educational content or communication with health-care team |
| Study | Year of publication | Results |
|---|---|---|
| Fruhauf et al.320 | 2015 |
Patient outcomes: where TCA and OCA were compared, there were no statistically significant differences observed between the groups. For the Global Acne Severity Scale the TCA group scored 2.25 and the OCA group scored 2 (p = 0.38). For the total lesion count the TCA group scored 89.08 and the OCA group scored 91.21 (p = 0.95). When self-reporting experiencing therapeutic benefit, just 50% (12/24) of TCA patients reported benefit from the intervention compared with 65% (18/28) in the OCA group, though there was no statistically significant difference between the groups. Patient satisfaction scores were calculated by asking patients to rate a series of statements from 0 to 4 for interaction, impact on daily life and usability. Results were presented as a percentage of the maximum possible score and measured at 12 and 24 weeks: interaction at 12 weeks, 72.2% acceptance; and interaction at 24 weeks, 74.5% acceptance. Impact on daily life at 12 weeks, 79.5% acceptance; and impact on daily life at 24 weeks, 72.9% acceptance. Usability at 12 weeks, 77.8% acceptance; and usability at 24 weeks, 74% acceptance. Total acceptance was 73% at 24 weeks across all domains Health services outcome: there were no additional consultations (face to face) requested by the TCA group |
| Wade et al.244 | 2009 | Patient outcomes: where information on the use of videoconferencing was reported separately from the outcomes for the main intervention, 63% (5/8) of the adolescents found the videoconferencing easy to use and 88% (7/8) found it helpful. 63% (5/8) of the adolescents preferred the videoconferencing to traditional face-to-face sessions |
| Wiecha et al.321 | 2015 | Health service delivery outcomes: the most frequent messaging activity (38.7%, 235/607) was between patients and the asthma nurse. The primary health-care providers of the research subjects used the discussion boards at a low level (16.5%, 100/607), highlighting the essential role of an active case manager in maintaining contact with the patient. The most frequent message content was encouragement of medication adherence (13.5%, 82/607) and encouraging patients to use the intervention website (12.9%, 78/607) |
| Study | Year of publication | AMSTAR score (n/11) | Comments |
|---|---|---|---|
| Backhaus et al.340 | 2012 | 3 | The authors refer to a protocol but do not provide a link to one; it is unclear whether or not the authors independently screened abstracts/titles and extracted data; a diagrammatic search strategy and publication dates were not provided; grey literature not included; there is some detail missing concerning the reference list of excluded studies; scientific quality not assessed or reported appropriately in the conclusion; and publication bias was not assessed |
| Boisvert et al.341 | 2010 | 2 | Protocol not provided; it is unclear whether or not the authors independently performed searches on supplementary material; a diagrammatic search strategy was not provided; grey literature not included; there is some detail missing concerning the reference list of excluded studies; scientific quality not assessed or reported appropriately in the conclusion; the authors have not adequately explained why they could not combine results; and publication bias was not assessed |
| aConway et al.342 | 2014 | 10 | The authors provide a non-accessible reference to their protocol |
| Dorstyn et al.345 | 2013 | 6 | Protocol not provided; it is unclear whether or not the authors independently screened titles and abstracts; excluded studies not referenced; publication bias was not assessed; and conflict of interest not stated |
| Dorstyn et al.346 | 2013 | 5 | Protocol not provided; it is unclear whether or not the authors independently screened abstracts/titles and only one author extracted data; the authors refer to an appendix supposedly containing details of key search terms but do not provide a link; grey literature not included; excluded studies not referenced; and publication bias not assessed |
| García-Lizana and Muñoz-Mayorga347 | 2010 (online) | 6 | Protocol not provided; independent duplicate assessments conducted on data extraction only; grey literature not included; excluded studies not referenced; and publication bias not assessed |
| García-Lizana and Muñoz-Mayorga348 | 2010 | 6 | Protocol not provided; independent duplicate assessments conducted on data extraction only; grey literature not included; excluded studies not referenced; and publication bias not assessed |
| Kasckow et al.349 | 2014 | 2 | Protocol not provided; it is unclear whether or not the authors independently extracted data; it is unclear whether or not the authors searched for supplementary material and they do not provide a diagrammatic search strategy; grey literature not included; excluded studies not referenced; scientific quality not assessed or reported appropriately in the conclusion; the authors have not adequately explained why they could not combine results; and publication bias not assessed |
| Kitamura et al.350 | 2010 | 2 | Protocol not provided; only one author screened titles/abstracts; diagrammatic search strategy not provided and supplementary material not searched; it is unclear whether or not the authors included grey literature; excluded studies not referenced; scientific quality not assessed or reported appropriately in the conclusion; publication bias not assessed; and conflict of interest not stated |
| Mars et al.351 | 2012 | 1 | Protocol not provided; it is unclear who screened titles/abstracts and extracted data and no information is provided about whether these activities were conducted independently or whether any disputes were resolved by a third reviewer; it is unclear whether or not the authors searched for supplementary material; publication dates and a diagrammatic search strategy not provided; grey literature not included; excluded studies not referenced; scientific quality not assessed or reported appropriately in the conclusion; the authors have not adequately explained why they could not combine results; publication bias not assessed; and conflict of interest not stated |
| Martin et al.45 | 2011 | 6 | Protocol not provided; it is unclear whether or not the authors independently screened titles/abstracts and extracted data; grey literature not included; there is some detail missing concerning the reference list of excluded studies; and publication bias not assessed |
| McGeary et al.352 | 2013 | 6 | The authors refer to an unpublished protocol but do not provide a link to one; it is unclear whether or not the authors independently screened titles/abstracts and independently extracted data; excluded studies not referenced; the authors mention using Egger’s regression to assess publication bias but do not provide any statistical data; and conflict of interest not stated |
| McLean et al.353 | 2010 | 11 | Study matched all the criteria on AMSTAR. There were no methodological limitations to report |
| Neubeck et al.140 | 2009 | 4 | Protocol not provided; search terms not provided; there is some detail missing concerning the reference list of excluded studies; the authors mention that they assessed methodological quality using the Jadad score in order to exclude studies with a rating of < 2, but do not provide scores for each of the included studies; scientific quality reported inappropriately in the conclusion; publication bias not assessed; and conflict of interest statement does not include details of any possible funding source(s) |
| Peeters et al.354 | 2011 | 5 | Protocol not provided; it is unclear whether or not the authors independently extracted data; grey literature not included; excluded studies not referenced; the authors have not adequately explained why they could not combine results; and publication bias not assessed |
| Peterson355 | 2014 | 3 | Protocol not provided; study selection and data extraction performed by one person only; supplementary material and grey literature not included; excluded studies not referenced; scientific quality not assessed for each included study or reported appropriately in the conclusion; and publication bias not assessed |
| Schlegl et al.356 | 2015 | 5 | Protocol not provided; it is unclear whether or not the authors independently screened titles/abstracts, independently extracted data and resolved disputes with a third reviewer; grey literature not included; excluded studies not referenced; publication bias not assessed; and conflict of interest statement does not include details of any possible funding source(s) |
| Sharp et al.357 | 2011 | 2 | Protocol not provided; it is unclear whether or not the authors independently screened titles/abstracts, independently extracted data and resolved disputes with a third reviewer; a diagrammatic search strategy not provided; grey literature not included; excluded studies not referenced; scientific quality not assessed for each included study or reported appropriately in the conclusion; publication bias not assessed; and conflict of interest statement does not include details of any possible funding source(s) |
| Shore358 | 2013 | 1 | Protocol not provided; no information is provided on study selection, data extraction, search strategy, the inclusion of grey literature or excluded studies; scientific quality not assessed for each included study or reported appropriately in the conclusion; no information is provided on how the author combined the results; publication bias not assessed; and conflict of interest statement does not include details of any possible funding source(s) |
| Siriwardena et al.359 | 2012 | 2 | Protocol not provided; it is unclear whether or not the authors independently screened titles/abstracts, independently extracted data and resolved disputes with a third reviewer; only one database search was performed and no supplementary material was searched; grey literature not included; excluded studies not referenced; scientific quality not assessed for each included study or reported appropriately in the conclusion; no information is provided on how the authors combined the results; and publication bias not assessed |
| Sucala et al.360 | 2012 | 5 | Protocol not provided; it is unclear whether or not the authors initially independently screened titles/abstracts (the authors report only doing this for 56 potentially eligible studies) and included supplementary material in their literature searches; grey literature not included; excluded studies not referenced; and publication bias not assessed |
| van den Berg et al.131 | 2012 | 1 | Protocol not provided; it is unclear whether or not the authors independently screened abstracts/titles, extracted data and searched for supplementary material; grey literature not included; excluded studies not referenced; scientific quality not assessed for each included study or reported appropriately in the conclusion; the authors do not provide enough detail for why a narrative synthesis was used to pool findings; publication bias not assessed; and conflict of interest statement does not include details of any possible funding source(s) |
| Wile and Pringsheim361 | 2013 | 3 | Protocol not provided; it is unclear whether or not the authors independently screened titles/abstracts; grey literature not included; excluded studies not referenced; the authors mention that they assessed methodological quality using the US Preventive Services Task Force Quality Rating Criteria for Randomized Trials in order to exclude low-quality studies, but do not provide scores for each of the included studies; scientific quality reported inappropriately in the conclusion; publication bias not assessed; and conflict of interest statement does not include details of any possible funding source(s) |
| Zhai et al.362 | 2014 | 9 | Protocol not provided; and grey literature not included |
| Study | Year of publication | Results |
|---|---|---|
| Backhaus et al.340 | 2012 |
Patient outcomes: patients are satisfied with using videoconferencing in order to discuss their mental health conditions with a professional Health service delivery outcomes: this modality is promising and feasible for those experiencing emotional disorders |
| Boisvert et al.341 | 2010 | Health service delivery outcomes: this modality is promising and feasible for patients with autism spectrum disorder |
| Conway et al.342 | 2014 | Patient outcomes: structured telephone follow-up and telemonitoring reduced heart failure-related hospitalisation admittances, but there was no conclusive evidence that this occurred with videophone |
| Dorstyn et al.345 | 2013 |
Patient outcomes: significant short-term improvements were associated with internet-based modalities. The evidence also indicates that in comparison with ‘information- or monitoring-only control conditions’, telecounselling is effective on its own. Limited data demonstrated longer-term improvements. However, this modality’s absolute effectiveness with in-person care is unknown Health service delivery outcomes: telecounselling is flexible, time-effective and appeals to a variety of ages. It also diversifies the treatments that patients receive |
| Dorstyn et al.346 | 2013 |
Patient outcomes: telecounselling is promising for improving patients’ physical (e.g. pain) and emotional (e.g. depression) health in the short term. The longer-term impact of this modality is unknown Health service delivery outcomes: telecounselling is time-efficient, practical and appealing to patients |
| García-Lizana and Muñoz-Mayorga347 | 2010 (online) |
Patient outcomes: patients are satisfied with using videoconferencing technology. The limited data also suggest it is effective for improving patients’ symptoms and adherence to treatment. Telepsychiatry is also safe to use Health service delivery outcomes: there is evidence to suggest that this modality improves service accessibility, provides educational services to patients, and saves time and money |
| García-Lizana and Muñoz-Mayorga348 | 2010 | Patient outcomes: video consulting increased patient satisfaction. The limited evidence suggests that this modality could improve symptoms when face-to-face care is unavailable |
| Kasckow et al.349 | 2014 |
Patient outcomes: telepsychiatry is promising and has shown to improve clinical outcomes in areas such as treatment adherence, symptoms, insight, perceived stress and social support Health service delivery outcomes: this modality is feasible, improves patient–staff communication, and decreases hospitalisation rates and visits to the emergency room. Limited data suggest that telepsychiatry is also cost-effective |
| Kitamura et al.350 | 2010 |
Patient outcomes: data suggest that videoconferencing is feasible and effective for assessing, monitoring and managing patients with cancer. Patient satisfaction was reported. However, the methodological quality of the supporting evidence was generally weak and limited by unmatched controls, small samples and inappropriate randomisation, thus making it difficult to ascertain the effectiveness of videoconferencing in this population Health service delivery outcomes: evidence points towards reductions in health-care expenditure and travel/waiting times |
| Mars et al.351 | 2012 |
Patient outcomes: although patient satisfaction for adjudicative competence has not been reported, there is evidence that prisoners are satisfied ‘with the use of videoconferencing for completing assessing tools’ (p. 245) Health professional outcomes: clinician satisfaction for adjudicative competence has not been reported. Health professionals are less satisfied with videoconferencing Health service delivery outcomes: telepsychiatry is cost-effective, ‘improve(s) access to scarce specialist skills and reduce(s) transport of prisoners’ (p. 244). This modality also reduces the risk of harm to clinicians by enabling them to assess prisoners without entering a prison |
| Martin et al.45 | 2011 |
Patient outcomes: patients expressed satisfaction with using videoconferencing. The data dealing with these modalities appear more rigorous and reliable. Although networked technologies:p. e112Health professional outcomes: health professionals felt satisfied with using e-mail and web-based technologies Health service delivery outcomes: limited data on financial implications makes it difficult to ascertain the cost-effectiveness of networked technologies |
| McGeary et al.352 | 2013 |
Patient outcomes: telehealth appears to produce beneficial results for patients undergoing pain treatment but exact benefits are unknown. The evidence also indicates that this modality reduces pain intensity Health service delivery outcomes: limited data suggest that telehealth is cost-effective |
| McLean et al.353 | 2010 |
Patient outcomes: telehealth does not appear to produce a desired impact on quality of life for those with mild asthma. There is evidence of symptom improvement in telehealth trial arms where symptoms are managed more rapidly than in the control arms Health service delivery outcomes: telehealth improves access to health-care services and may also reduce costs and hospital admission rates, particularly for those with more severe asthma who are managed in secondary health-care facilities |
| Neubeck et al.140 | 2009 |
Patient outcomes: telehealth produces beneficial effects on reducing risk factors associated with coronary heart disease Health service delivery outcomes: the scarce information provided by the reported trials on cost-effectiveness and delivery costs meant that the authors could not draw any conclusive statements |
| Peeters et al.354 | 2011 | Health service delivery outcomes: the authors found no evidence to suggest that administering video communication to patients at home is cost-effective |
| Peterson355 | 2014 | Patient outcomes: the limited data indicate that mobile tools including videoconferencing are a promising modality in the management of patients’ glycaemic levels |
| Schlegl et al.356 | 2015 |
Patient outcomes: technology-based interventions, including videoconferencing, may be beneficial for improving symptoms (e.g. purging) as well as treating and preventing eating disorders. This modality may also support carers looking after those with eating problems. No serious adverse effects were reported from using this modality Health professional outcomes: the limited data indicate that there are differences between patients and therapists ‘in terms of adherence to therapeutic tasks, adherence to therapeutic goals, and therapeutic bond’ (p. 9) Health service delivery outcomes: limited evidence suggests that the costs associated with telemedicine (including video) were lower, albeit still considerable. Cost-effectiveness was comparable with usual care |
| Sharp et al.357 | 2011 |
Patient outcomes: videoconferencing is relatively easy for patients with psychosis to use without exacerbating their symptoms. In fact, there is some evidence to suggest that the distance between patients and health professionals could reduce anxiety and oversimulation Health service delivery outcomes: the data indicate a reduction in travel time for patients and health professionals, decreased hospitalisation rates and an improvement in reaching those living in rural communities. It appears that videoconferencing produces more efficient health care |
| Shore358 | 2013 | Health professional outcomes: videoconferencing is feasible and has gained popularity within psychiatry. It is important that psychiatrists learn how to effectively implement this technology and develop an understanding of the clinical, regulatory and administrative issues associated with it. Psychiatrists should also generate an emergency protocol prior to caring for patients via videoconferencing and, if necessary, dialogue with them about their use or ownership of weapons and/or (il)legal substances. The psychiatrist should also reflect on their own communicative styles in order to ensure that they interact naturally with the patient as they would during face-to-face consultations |
| Siriwardena et al.359 | 2012 |
Patient outcomes: telemedicine (including video) is promising in the management of diabetes mellitus. Patients with non-insulin type 2 diabetes mellitus reported better clinical outcomes than insulin type 1 and type 2 patients. Although two studies revealed negative metabolic improvement, one demonstrated that patients still found it helpful to contact their health professional over the telephone. Overall, patient satisfaction was high with telemedicine Health service delivery outcomes: the data suggest that financial benefits are equal to usual care. This modality appears to reduce travel and in-clinic waiting times |
| Sucala et al.360 | 2012 |
Patient outcomes: three of the review’s included studies found that therapeutic alliance positively affected treatment outcomes and in some cases reduced anxiety-related symptoms Health service delivery outcomes: e-therapy (which includes video) provides promising results for the delivery of mental health services. This modality also appears equivalent to face-to-face care in terms of therapeutic alliance, albeit the limited data precludes any firm conclusions |
| van den Berg et al.131 | 2012 |
Patient outcomes: telemedicine (including video) aids self-management and leads to better behavioural changes (e.g. diet, exercise, self-efficacy) and quality of life. However, some studies (26/68) excluded patients with cognitive, visual and auditory impairments, making it difficult to generalise the findings of the review to these subpopulations Health service delivery outcomes: this modality appears economically beneficial in terms of reducing health-care costs and hospitalisation rates |
| Wile and Pringsheim361 | 2013 | Patient outcomes: telemedicine (including video) and in-person care improved tic severity compared with baseline measures for those living with Tourette syndrome. No conclusions could be made about the efficacy of each mode of treatment delivery or equivalence ‘due to lack of inactive control’ (p. 391) |
| Zhai et al362 | 2014 |
Patient outcomes: the authors observed a nominal but statistically significant effect on decreased levels of HbA1C for patients with type 2 diabetes mellitus. Although telemedicine (including video) appears promising for the management of this condition, the authors detected a high degree of publication bias Health service delivery outcomes: as a result of small samples and heterogeneous data, no conclusions about cost-effectiveness could be drawn |
Appendix 7 Quick reference guides
Reproduced with permission from University of Warwick and King’s College London.
List of abbreviations
- A&E
- accident and emergency
- AMSTAR
- Assessment of Multiple Systematic Reviews
- BMI
- body mass index
- CAMHS
- Child and Adolescent Mental Health Services
- CASP
- Critical Appraisal Skills Programme
- CBT
- cognitive–behavioural therapy
- CES-D
- Center for Epidemiologic Studies Depression Scale
- CI
- confidence interval
- DCC
- digital clinical communication
- DKA
- diabetic ketoacidosis
- DNA
- did not attend
- FEV1
- forced expiratory volume in 1 second
- HADS
- Hospital Anxiety and Depression Scale
- HbA1c
- glycated haemoglobin
- HIV
- human immunodeficiency virus
- HoNOSCA
- Health of the Nation Outcome Scale for Children and Adolescents
- IBD
- inflammatory bowel disease
- ICT
- information and communication technology
- IG
- information governance
- IT
- information technology
- i.v.
- intravenous
- LTC
- long-term condition
- LYNC
- Long-term conditions Young people Networked Communication
- NICE
- National Institute for Health and Care Excellence
- PAM
- Patient Activation Measure
- PHBQ
- Physicians’ Humanistic Behaviours Questionnaire
- PHR
- personal health record
- PI
- principal investigator
- PIN
- personal identification number
- PMG
- Project Management Group
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PRO
- patient-reported outcome
- PROM
- patient-reported outcome measure
- RCT
- randomised controlled trial
- SDQ
- Strengths and Difficulties Questionnaire
- SMS
- short message service
- SPSS
- Statistical Product and Service Solutions
- VoIP
- voice over internet protocol
