Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/97/24. The contractual start date was in June 2015. The final report began editorial review in December 2016 and was accepted for publication in June 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Geoff Wong is a member of the Health Technology Assessment Primary Care, Community and Preventive Interventions Panel. Mark Pearson’s role was supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care South West Peninsula.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Papoutsi et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Background
A post-antibiotic era—in which common infections and minor injuries can kill—far from being an apocalyptic fantasy, is instead a very real possibility for the 21st century.
Antimicrobial resistance is a very real threat. If we have no suitable antibiotics to treat infection, minor surgery and routine operations could become high risk procedures.
The rise of antimicrobial resistance (AMR) has been described as a global crisis. Infections with bacteria such as Klebsiella pneumoniae, Staphylococcus aureus and Neisseria gonorrhoeae, which were once routine to treat, can now be untreatable. The urgency of this problem is reflected in policy developments and campaigns at an international level (e.g. World Antibiotic Awareness week). Recently, a United Nations declaration has garnered widespread commitment by countries to raise the level at which AMR is discussed politically and pave the way for an internationally co-ordinated approach. 3 The UK government has already taken action by establishing the Global AMR Research Innovation Fund together with China and contributing to the Fleming Fund for AMR surveillance in low- and middle-income countries, among other steps. 4–6
These steps followed initial recommendations by a high-profile AMR review, commissioned by the UK government, which estimated that there will be 10 million deaths a year globally as a result of drug resistance by 2050. 7 Beyond this very significant human cost in terms of morbidity and mortality from previously treatable infections, the consequences of drug resistance extend past patients who present with infections. Many surgical procedures (when antibiotics are given prophylactically in the hope of preventing infections) may be harder to justify as the risk and consequences of infection become more likely and serious. Cancer chemotherapy is potentially facing an equally significant burden because of AMR. 8
There is also a substantial financial cost resulting from increased use of expensive second- and third-line drugs, extended health-care stays and the inevitable complications of failed treatments. AMR has been estimated to cost US$21B–34B per annum in the USA. 1 The recently completed AMR review in the UK calculated that the cost of lost global production would amount to a total of US$100T by 2050 if no action is taken. 7 These numbers reinforce the argument that a focus on strategies to curtail the emergence and spread of AMR is vital.
In terms of suggested solutions, substantial emphasis is currently being placed on developing new antibiotic treatments and promoting access to diagnostic tests in a range of clinical settings. 7 With few new antibiotics currently in the pipeline or recently licensed, it is unlikely that we will encounter major developments in this area in the near future, despite new incentives for pharmaceutical firms, and resistance will redevelop quickly. 7 Diagnostic tests have been suggested as a solution that can help safeguard the effectiveness of antibiotics currently available. 7 It is assumed that better access and use of diagnostic tests will lead to better-informed decisions and more appropriate use of antimicrobial agents. However, studies in clinical settings show that this may not always be the case and a more nuanced understanding is needed. 9,10
Another way to achieve antimicrobial stewardship, that is, to promote optimal care for patients while preserving the effectiveness of antimicrobials and minimising the threat of drug resistance (see Glossary), has been through interventions in primary and secondary care. The aim of these interventions has been to ensure that health professionals are prescribing antimicrobials only when indicated, and that they are using the right drug, at the right time, at the right dose and for the right duration. 11,12 Antimicrobial prescribing interventions have been broadly classified into three categories according to the intervention strategy pursued (1) persuasive interventions mainly include educational and promotional strategies, (2) restrictive interventions refer to changes in the prescribing processes or efforts to introduce barriers such as approval processes and (3) structural interventions refer to changes in the way laboratory tests are provided and computerised systems are used in prescribing. 13 Given that up to 50% of antibiotic usage in hospitals is inappropriate, significant change is required by all specialties and professions involved in antimicrobial prescribing and administration. 14
In the UK, a broad range of such antimicrobial stewardship interventions have been implemented, including the Hospital Pharmacy Initiative15 and the Medical Schools Council’s Safe Prescribing Working Group. 16 Interventions have comprised distribution of educational materials,17–19 lectures and seminars,20,21 audit and feedback on performance19,22 and manual and automated reminders. 23,24 More recently, the TARGET toolkit has been introduced in primary care to influence prescribing choices, taking into account the role of patient expectations. 25,26 In secondary settings, the Start Smart Then Focus approach has been proposed to help prescribers make informed decisions and to encourage them to review their decisions when appropriate. 11,25 Top-down interventions aiming to invoke the power of social norms for behaviour change have also been employed,27 along with more grassroots approaches (e.g. the Antibiotic Guardian initiative). 28 The upcoming AMR Commissioning for Quality and Innovation payments framework will attempt to consolidate the impact of previous initiatives by monitoring hospital trust performance on a number of indicators and a similar benchmarking exercise is being carried out in primary care. 29
Previous systematic reviews have compared the effectiveness of different intervention strategies, favouring interventions that restrict prescribing options (e.g. compulsory order forms or expert approval) over purely educational or feedback programmes. 13 However, these reviews focus primarily on calculating effect sizes,13,30 rather than identifying how antimicrobial prescribing interventions work, for whom, how and why, so that they can be more effectively transferable across settings. When interventions have had variable levels of success, there was little explanation as to why. Qualitative studies on antimicrobial prescribing paid less attention to specific groups of prescribers, such as doctors in training. 31–33 With social norms and informal influences increasingly recognised as important in antimicrobial prescribing,34,35 uncertainty exists about which intervention types to implement for trainees and what refinements are needed for local circumstances. There is also less understanding of how antimicrobial prescribing interventions should be tailored to address the specific needs of doctors in training, as most studies assume that doctors are a uniform body of health professionals with similar needs. 36
Doctors in training and antimicrobial prescribing
After graduating from medical school in the UK, new doctors enter the 2-year foundation programme, which mostly takes place in hospital settings. They then undertake a further 5 years as a core/specialty trainee in hospitals or 3 years in general practice. Postgraduate trainees across all stages are classed as independent prescribers and will prescribe for patients, typically on a daily basis. In their first 2 years in clinical training, trainees rotate between hospitals and across specialties, commonly between every 3–6 months. In specialty training (after completion of the foundation programme), the duration of rotations varies depending on the area and the career path.
Doctors in training are an important target group, both as numerically the largest prescribers in the hospital setting in the UK and as a key part of a future generation of antimicrobial prescribers. 37 For many trainees, decisions around antimicrobial prescribing make up a significant part of their daily practice (e.g. general practice, paediatrics or emergency medicine training). Developing effective antimicrobial stewardship requires that we understand more about the antimicrobial prescribing behaviours of doctors in training.
The importance of education for prescribing behaviour change has been described as self-evident. 12 Evidence indicates that it is unclear if current educational prescribing behaviour change interventions have any consistent effect, particularly for new prescribers. 38 For example, a systematic review of prescribing behaviour change educational interventions for new prescribers in hospital settings found that the impact of particular types or combinations of interventions was highly variable as a result of the complex environments in which these interventions are embedded. 36,39 A systematic review focusing on behaviour change interventions in all prescriber types reported similar findings. 40 This raises the question as to why some prescribing interventions are successful in some contexts but not in others. Answering this question is important if we are to design interventions that are more effective. 12
This knowledge gap has partly come about because much of the current literature has not taken sufficient account of the wider context in which doctors in training prescribe antimicrobials. Prescribing is a complex mix of knowledge, skills and behaviours, with no simple relationship between them. 41,42 Prescribing the right antibiotic at the right time is not just about having the correct knowledge about, for example, local formularies, resistance patterns and dosages, but also understanding a patient’s expectations, concerns, comorbidities and social context. Hospital context and processes play an equally important role. 43 The antimicrobial prescribing challenges faced by foundation doctors include cognitive knowledge deficits (not knowing what to do in certain situations), practical issues of not knowing that local prescribing protocols exist on a ward, and professional challenges of having to ‘take sides’ when more senior health-care professionals disagree on prescribing decisions. 43 For example, Ross et al. 39 point out that doctors in training work within a strict medical hierarchy in complex organisations and that their prescriptions are often influenced by other doctors. McLellan et al. 44 report that a technical focus on isolated prescribing competencies is unlikely to support doctors in training to become safe prescribers.
The implication is that any review that seeks to understand antimicrobial prescribing interventions for doctors in training needs to look beyond just educational interventions and seek to make sense of the role of wider contexts. This review on IMProving Antimicrobial presCribing for doctors in Training (IMPACT) adds to a growing literature that acknowledges the importance of the wider context and attempts to explain how and why trainee prescribing practices differ under different circumstances.
Review questions
The IMPACT realist review aimed to understand how interventions to change antimicrobial prescribing behaviours of doctors in training produce their effects. The review was structured around the following objectives and review questions.
Objectives
-
To conduct a realist review to understand how interventions to change antimicrobial prescribing behaviours of doctors in training produce their effects.
-
To provide recommendations on the tailoring, implementation and design of strategies to improve antimicrobial prescribing behaviour change interventions for doctors in training.
Review questions
-
What are the mechanisms by which antimicrobial prescribing behaviour change interventions are believed to result in their intended outcomes?
-
What are the important contexts that determine whether or not the different mechanisms produce the intended outcomes?
-
In what circumstances are such interventions likely to be effective?
Chapter 2 Review methods
To make sense of the context in which antimicrobial prescribing decisions are made, we followed a realist approach for evidence synthesis. A realist review is an interpretive, theory-driven approach to synthesising evidence from qualitative, quantitative and mixed-methods research. Its main strength comes from providing findings that coherently and transferably explain how and why context can influence outcomes. This is particularly relevant to complex programmes characterised by significant levels of heterogeneity. The plan of investigation followed a detailed protocol based on Pawson’s five iterative stages for realist reviews: (1) locating existing theories, (2) searching for evidence, (3) selecting articles, (4) extracting and organising data and (5) synthesising the evidence and drawing conclusions. 45 To this, we have added an additional step 6: highlighting the importance of the write up in realist analysis and placing further emphasis on what counts as quality in realist research. The review ran for an 18-month period from June 2015 until November 2016. The protocol has been published in BMJ Open46 and the review has been registered with PROSPERO (CRD42015017802). 47 We were granted ethics clearance by the Central University Research Ethics Committee at the University of Oxford.
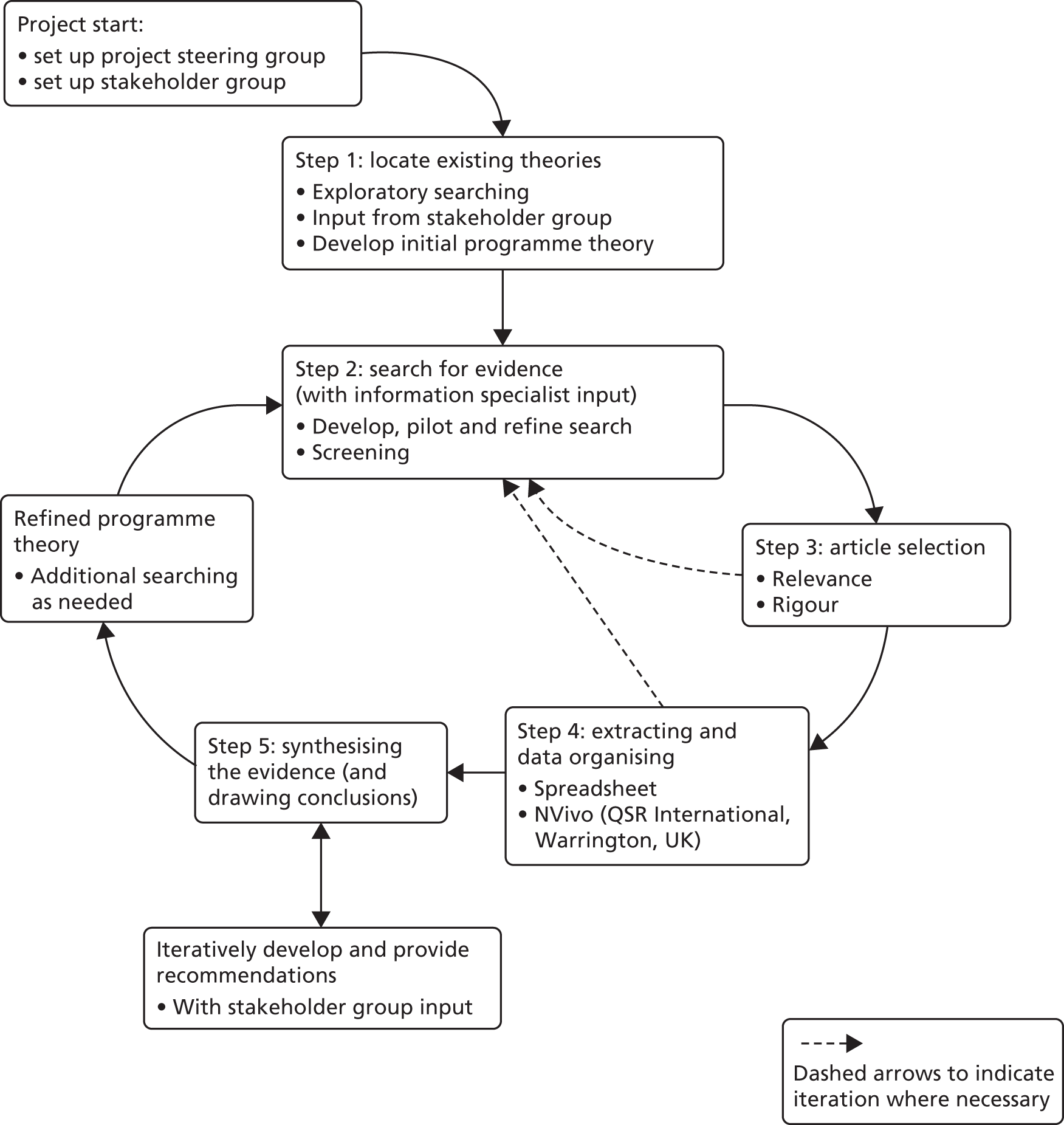
During the course of this project, the team sought to maximise learning from existing evidence to identify ‘what works, for whom, under what circumstances and why’, according to realist principles. This allowed increased emphasis on the mechanisms driving antimicrobial prescribing behaviour of doctors in training within specific contexts. Rather than defining effectiveness in terms of effect size, the review examined how the responses of doctors in training to the resources offered to them (mechanisms) were triggered in particular circumstances (contexts) to generate certain behaviours or outcomes for antimicrobial prescribing. In doing this, we focused first on developing an understanding of wider processes related to antimicrobial prescribing for doctors in training, rather than targeting and isolating particular interventions or groups of interventions for analysis. Having understood how the process of antimicrobial prescribing works for doctors in training, we then examined how particular families of interventions or intervention strategies may (or may not) address the contextual challenges identified. The review design and methodology is explained in more detail in the sections below and illustrated in Figure 1.
FIGURE 1.
Flow diagram of the project.
Stakeholder group
A diverse stakeholder group was recruited for the IMPACT review to provide content expertise for programme theory refinement. A total of 21 people were consulted throughout the review, including patient representatives/carers, consultants, doctors in training at different stages, pharmacists, microbiologists, academics and policy-makers. Consultations with stakeholder group members took place as part of 2-hour meetings at regular intervals throughout the project, but also through individual telephone calls if stakeholders were not able to attend meetings (n = 6) and e-mail exchange. Table 1 provides a detailed list of the meetings that took place, including the number of participants and the topics discussed.
| Date | Stakeholder group members | Key topics discussed |
|---|---|---|
| 17 September 2015 | Eleven participants:
|
Explored the role of social dynamics and informal influences in guiding prescribing behaviours for doctors in training, different conceptualisations of the problem of AMR, as well as the gap between patient expectations and the actual uncertainties of prescribing in practice |
| 3 December 2015 | Eight participants:
|
Discussed initial findings from the review of the literature and explored how these reflected stakeholders’ experiences with antibiotic prescribing |
| 18 March 2016 | Seven participants:
|
Continued the discussion of emerging findings from the review and started generating ideas on potential outputs from the project and optimal dissemination strategy |
| 17 June 2016 | Eight participants:
|
Finalised the programme theory and discussed actionable findings emerging from the review |
Following the first stakeholder meeting in September 2015, we carried out further recruitment to participant groups that were under-represented (e.g. junior doctors) in order to include a range of views and opinions on the topic. Although in the second and third stakeholder meetings we engaged fewer individuals in total (as per the numbers presented in Table 1), the diversity of the group was such that it allowed us to address the aspects of programme theory that were in need of refinement. Stakeholder meetings took place at the University of Exeter and usually started with a brief slide presentation by our project team to introduce stakeholders to the topic under discussion. Iterations of the programme theory were presented to the group in the form of statements, accompanied by relevant quotations from the literature, to obtain their feedback. Discussions were designed to be more open ended in the early stages of the review, but focused on particular aspects of the programme theory as the project progressed. Later stakeholder groups focused on actionable findings and dissemination of the study. Facilitation of the meetings ensured that everyone was able to contribute and voice their opinion, whether in agreement or disagreement. With the verbal consent of participants, discussions were audio-recorded and detailed minutes drafted, which were then shared with the stakeholder group. These data were used only to set direction for the review and to refine programme theory, rather than as primary data for analysis, and the report does not include any data excerpts from these meetings.
Discussions with stakeholders helped ground the review in the practical reality experienced by participants and the challenges they faced in their respective roles. ‘Translation’ of realist review terms into everyday language became necessary to avoid methodological jargon, while still adequately conveying the nuances of the review findings. Stakeholder involvement also contributed significantly to the development of actionable findings in a form that would be usable and engaging. More details on actionable findings emerging from the review are presented in Chapter 3.
Patient and public involvement
The stakeholder group included strong patient and public involvement (PPI) throughout the project. Mark Pearson led the PPI component of the review and invited patients and members of the public who would be part of the stakeholder group (n = 5 in total) to attend a preparation meeting, at which they discussed the terms of their involvement and any key issues that needed to be addressed to facilitate meaningful participation. In the stakeholder meetings, patients and members of the public provided significant input to programme theory development, often highlighting aspects and questioning assumptions that the rest of the group were taking for granted (e.g. how prescribing norms differ between hospitals). The Plain English summary for this report has been reviewed by two patient representatives from our stakeholder group.
Steering group
A separate steering group of three academics with expertise in realist review approaches was set up for the project. The steering group was updated about the progress of the study, provided scientific and budget oversight and made sure that the project was delivered as proposed in the protocol.
Step 1: locating existing theories
In the first stage of the review we carried out exploratory searching to identify initial literature sources on antimicrobial prescribing interventions and antimicrobial prescribing more generally. The aim of this initial search was to identify explanations about how antimicrobial prescribing interventions work for doctors in training at different levels and why they may work in particular circumstances and not in others. 48,49 In line with previous systematic reviews,36 this exploratory search identified a range of articles but found that few of those specifically discussed doctors in training. In this limited number of articles on doctors in training, antimicrobial prescribing interventions were often primarily educational, were not described in enough detail or were mainly evaluated using pre-/post-study designs. On their own, these articles did not provide enough information to adequately develop and refine a programme theory of antimicrobial prescribing interventions in a way that would generate an in-depth understanding of how the intervention components contributed to particular outcomes.
Therefore, we supplemented our focus on antimicrobial prescribing interventions for doctors in training with explaining how antimicrobial prescribing works for trainees as a process more generally. This enabled us to reach the same results through a less direct route: first looking at how antimicrobial prescribing is done and how specific mechanisms are driving particular antimicrobial prescribing behaviour in certain contexts, and then looking at whether or not current intervention strategies address these challenges. In this way, we were able to overcome limitations of poor reporting and lack of detail in the description and evaluation of interventions.
The exploratory searching of step 1 differs from the more formal search for data described in step 2, in that it aims to sample the literature to quickly identify the range of possible explanatory theories that may be relevant. We used methods such as keyword-, author- and project-based searches in MEDLINE/PubMed and Google Scholar (Google Inc., Mountain View, CA, USA), elicitation of key studies from expert recommendations, citation tracking and snowballing from relevant systematic reviews. 50 Keywords included ‘antimicrobial’, ‘prescribing’, ‘junior doctors’, ‘stewardship’ and synonymous terms. This was supplemented with grey literature searches [which identified reports and policy documents from key organisational websites such as Public Health England (PHE), WHO, UK government], along with searching for relevant theories based on the articles already retrieved. 51
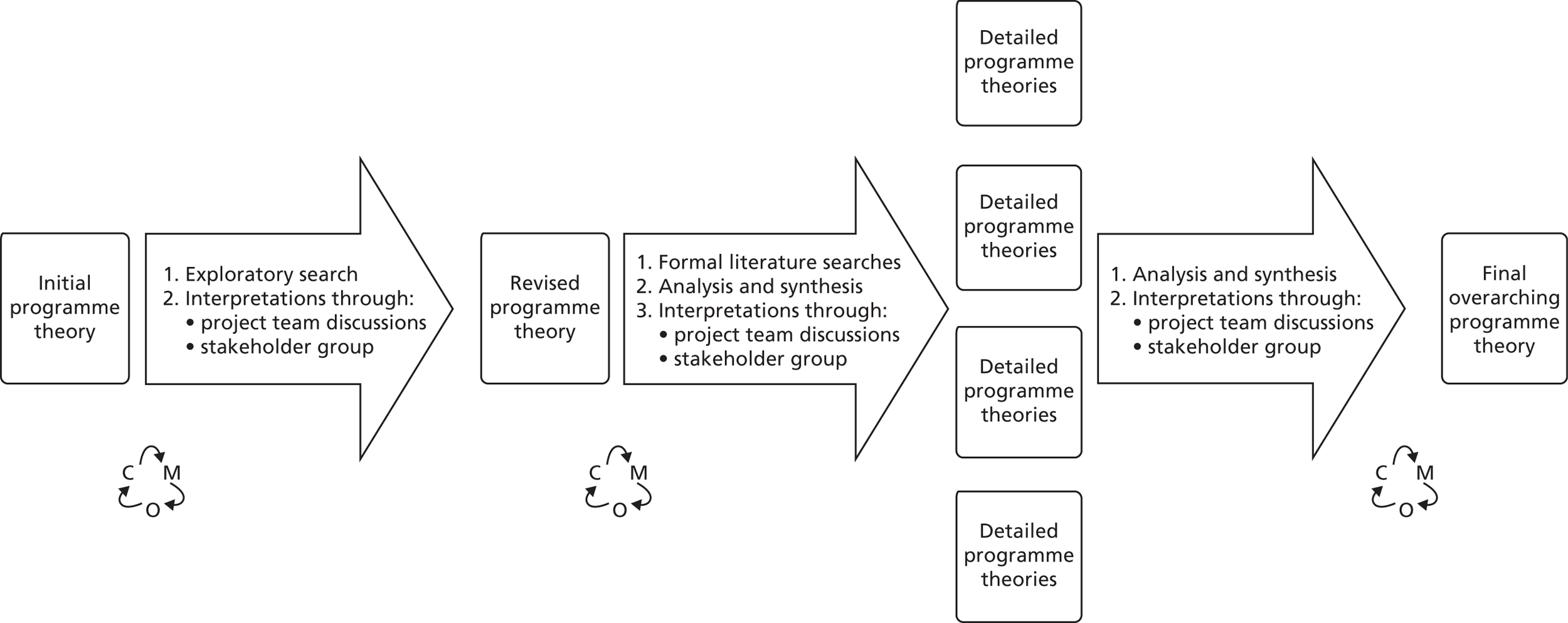
This initial search led to key documents that were used as a starting point to refine the initial programme theory devised at the outset of the project. Before any literature searching had taken place, Geoff Wong developed a ‘rough’ programme theory through experiential, professional and content knowledge. This initial programme theory included a number of assumptions about how the process of antimicrobial prescribing works for doctors in training and what mechanisms may interact with important contexts to produce certain outcomes. These initial assumptions were then discussed between the team at the outset of the project in order to develop a guide for literature searching and programme theory development (Figure 2 shows the process of programme theory development). For example, initial focus on ‘uncertainty’ as a potential core mechanism driving antimicrobial prescribing behaviour led to an informal review of relevant literature to examine whether or not and how this assumption could be embedded into the programme theory under development.
FIGURE 2.
Programme theory development. C, context; M, mechanism; O, outcome.
Building a programme theory required iterative discussions within the team to make sense of, interpret and synthesise the different components. We also consulted with key experts from our stakeholder group through face-to-face meetings, telephone calls and e-mail throughout the review (see Stakeholder group).
Step 2: searching for evidence
Main search
After completing initial exploratory searches and drafting a first version of the programme theory, we proceeded with more formal searches for relevant data in the research literature. The purpose of step 2 was to find a relevant ‘body of literature’ with which to further develop and refine the programme theory from step 1. Searching was designed, piloted and conducted by an information specialist (SB) with experience of conducting searches for complex systematic reviews. The search strategy was initially guided by a related systematic review by Brennan and Mattick36 on educational interventions to change the behaviour of new prescribers in the hospital setting. However, we needed to make modifications to the search strategy used by Brennan and Mattick to include search terms for doctors up until the end of their training and to focus specifically on antimicrobial prescribing. This resulted in a different body of literature that we analysed using a realist logic, as described in steps 3 and 4.
The search strategy was developed in MEDLINE (via Ovid) using an iterative process of adding, removing and refining search terms in order to retrieve a set of search results with an appropriate balance of sensitivity and specificity (i.e. the search was configured to retrieve a wide range of relevant literature and to minimise the retrieval of irrelevant literature). A combination of free text and indexing terms was used. Sample sets of results were screened by Chrysanthi Papoutsi as the search developed, which helped with the selection of relevant search terms. In addition, relevant studies identified by the review team through online keyword searching in Google Scholar and PubMed were used to benchmark or test the search strategy. The final search strategy used a range of search terms for the concepts ‘doctors in training’, ‘prescribing’ and ‘antimicrobial’, which were combined using the AND Boolean operator.
In September 2015, we searched the following nine bibliographic databases: EMBASE (via Ovid), MEDLINE (via Ovid), MEDLINE In-Process & Other Non-Indexed Citations (via Ovid), PsycINFO (via Ovid), Web of Science core collection limited to Science Citation Index Expanded (SCIE) and Conference Proceedings Citation Index – Science (CPCI-S) (via Thomson Reuters), Cochrane Central Register of Controlled Trials (CENTRAL), Cochrane Database of Systematic Reviews, the Health Technology Assessment (HTA) database (all via The Cochrane Library) and Applied Social Sciences Index and Abstracts (ASSIA) (via ProQuest). The search syntax and indexing terms were translated from the original MEDLINE search as appropriate for use in these databases. The search results were exported to EndNote X7 (Clarivate Analytics, Philadelphia, PA, USA) and deduplicated using the automatic deduplication feature and manual checking by the information specialist (SB). The search strategies for each database are reproduced in full in Appendix 1.
We also undertook forward citation chasing (using Google Scholar) and manually searched citations contained in the reference lists of important articles included in the review and in relevant grey literature. Google alerts were set up to update the literature with papers published after September 2015. Articles received from content experts were included in the data set for screening.
For the main search, our inclusion and exclusion criteria were broad as we sought to find quantitative, qualitative and mixed-methods studies.
Inclusion criteria
-
Aspects of antimicrobial prescribing: all studies that focused on one or more aspects of antimicrobial prescribing (or when combined with other types of prescribing). A comprehensive definition of prescribing proved challenging to identify in the existing literature. Therefore, we viewed prescribing as the act of determining what medication a patient should have and the correct dosage and duration of treatment. We also acknowledged how prescribing requires a ‘mixture of knowledge, skills and judgement’ as there is ‘no simple relationship between knowledge and behaviour’. 43
-
Study design: all study designs.
-
Types of settings: all studies that were conducted in hospital or primary care settings.
-
Types of participants: all studies that included doctors in training (any specialty and at any level).
-
Types of intervention: interventions that focus on changing/developing antimicrobial prescribing behaviour or studies discussing how doctors in training engage with antimicrobial prescribing.
-
Outcome measures: all prescribing-related outcome measures.
Exclusion criteria
-
Studies focusing only on drug administration (no prescribing decision).
All citations were reviewed by Chrysanthi Papoutsi to ensure that they matched the exclusion and inclusion criteria. A 10% random subsample was reviewed independently by Geoff Wong to ensure consistency around the application of the inclusion criteria. One small inconsistency was identified as a result of different interpretations of junior doctor roles, but this was easily resolved through discussion.
Additional search
An important process in realist reviews is searching for additional data to inform programme theory development and refinement. A second search was undertaken in January 2016 to allow the review to focus on issues that emerged as significant after the literature from the main search had been analysed. As outlined in the original protocol for the project, we anticipated that our programme theory would need to take into account the influence of the wider context in hospitals and primary care on the prescribing behaviour of doctors in training. During the course of the review, and through consultations with the stakeholder group, more specific contextual dynamics of hierarchies, teamworking and decision-making were identified as important in explaining how and why antimicrobial prescribing works in certain ways, for certain groups of doctors in training. Therefore, the supplementary search focused more specifically in those three areas: hierarchies, teamworking and decision-making.
Our approach to search-strategy development was similar to that used for the main search. A small set of articles was initially identified through hand-searching and expert opinion. These were then used by the information specialist (SB) to develop and pilot the search strategy for the additional search. The results of early versions of the search were discussed by e-mail between the project team and decisions were made on how best to refine the terms to be used in the search. This additional search was not intended to be exhaustive, but to purposefully draw together literature from different disciplines that could provide an explanatory backbone for the sociocultural influences identified as important. This also meant that the additional search did not focus on antimicrobial prescribing, per se, but in understanding the wider context in which doctors in training practise and prescribe.
The final search strategy used a wider range of search terms for the concepts ‘hierarchy’, ‘decision making’, ‘team work’ and ‘junior doctor’ – departing from a strict focus on the prescribing literature. A combination of free text and indexing terms were used for each concept. The search was developed in MEDLINE (via Ovid) and adapted for use in other databases, including (in toto) MEDLINE In-Process & Other Non-Indexed Citations (via Ovid), PsycINFO (via Ovid), CENTRAL, Cochrane Database of Systematic Reviews, the HTA database (all via The Cochrane Library) and ASSIA (via ProQuest). The search strategies for each database are reproduced in full in Appendix 1. The results of the searches were exported to EndNote X7 and deduplicated using automated and manual checking.
We also undertook forward citation searching (using Google Scholar) and manually searched citations contained in the reference lists of documents included in the review. Articles received from content experts were also screened for relevance. Google alerts were set up to update the literature with papers published after January 2016.
For the additional search, two members of the team (GW and CP) met to discuss inclusion and exclusion criteria, which were then confirmed in discussions with the rest of the group. Although we had a primary interest in qualitative studies that could provide rich contextual information on hierarchical and team dynamics, we did not exclude any study designs from the search.
Inclusion criteria
-
Studies discussing the role of hierarchies, teamwork and decision-making, in relation to doctors in training.
-
Study design: all study designs.
-
Types of settings: all studies that were conducted in hospital or primary care settings.
-
Types of participants: all studies that included doctors in training (any specialty and at any level).
Exclusion criteria
-
No prespecified exclusion criteria.
All citations were reviewed by Chrysanthi Papoutsi to ensure that they matched the inclusion criteria. A 10% random subsample was reviewed independently by Geoff Wong to ensure consistency in how the inclusion criteria were applied. There were no differences between reviewers.
Step 3: selecting articles
The selection process primarily focused on the extent to which articles included data that could contribute to the development and refinement of programme theory. Using Endnote X7, Chrysanthi Papoutsi screened the titles and abstracts of all articles resulting from the two searches in reverse chronological order, to exclude articles that did not contain information relevant to antimicrobial prescribing. Chronological order was important to be able to trace changes in the way medical education was delivered and to take into account the influence of culture.
Having completed the title and abstract screening, if the relevance of a reference could not be ascertained, the full text was obtained. Chrysanthi Papoutsi read the full texts of all remaining articles and classified them into categories of high and low relevance.
Articles from the main search were deemed to be of lower relevance when their findings were not as specific to the current situation in the NHS and the wider UK context, or if they were not specific enough for the target group of this review. For example, articles from the main search were classified as being of lower relevance when they:
-
referred to aspects of health care in low- and middle-income countries that are not as relevant to the way the health service is organised in the UK (but articles on low- and middle-income countries were included when of direct relevance to the review question)
-
referred to conditions that are not as common in the UK (e.g. tropical diseases)
-
involved all prescribers without making specific mention to doctors in training
-
fulfilled the search terms but were published before 1990 (as these articles were less likely to reflect recent changes to clinical training in the UK and contemporary challenges in clinical work).
Position or other background papers resulting from the main search were stored separately in case it was necessary to draw on them for additional data required for programme theory refinement.
For the additional theoretically driven search, articles were classified as being of lower relevance when they:
-
discussed hierarchies and teamwork but not in the context of junior–senior relationships, instead focusing primarily on interprofessional dynamics or on single non-medical professional groups (e.g. nurses, physiotherapists)
-
fulfilled the search terms but were published before 2000 (as cultural dynamics in the training environment would be better reflected in more recent literature, as identified after reviewing post-1990s papers resulting from the main search).
Directly relevant position or other background papers were included in the highly relevant category for the additional search, as the nature of the data in these position papers was much more useful for programme theory refinement, compared with the position papers emerging from the main search. This is likely because of the nature of the search, as the additional literature focused on sociocultural dynamics that are more likely to be discussed critically in position papers.
A random sample of 10% of documents selected was assessed and discussed between Chrysanthi Papoutsi and Geoff Wong to ensure that screening and selection decisions were made consistently.
At the point of inclusion based on relevance, the trustworthiness and rigour of each study were also assessed. 49 For example, if data had been generated using a questionnaire, then the trustworthiness of the data was considered to be greater if the questionnaire had been previously tested and shown to be reliable and valid, and had not been altered (or if alterations had been made, subsequent testing had been undertaken). Considerations of rigour and relevance were often inter-related, as papers were more likely to include data useful for programme theory refinement when they had followed their chosen methodology to the standard required. This means that studies were not excluded on the basis of rigour alone, but it was often the case that lack of rigour also meant lack of data useful enough for programme theory development. A qualitative study would provide richer data if a wide range of experiences were sought up to the point of data saturation (i.e. no new information would arise), and those experiences were analysed adequately and presented in detailed, contextualised quotations. Table 10 in Appendix 2 provides an overview of how particular aspects of the programme theory are supported by data from specific sources, and the strength of the arguments we were able to make based on our judgements about the trustworthiness of each study.
Step 4: extracting and organising data
Once article selection was finalised and the core data set was established, Chrysanthi Papoutsi reread the full texts of the included articles chronologically, starting with the most recent, and carried out initial manual coding. During this familiarisation stage, parallel notes were kept on potential contexts, mechanisms and outcomes, as well as their relationships with the initial programme theory, to prepare the ground for more in-depth work.
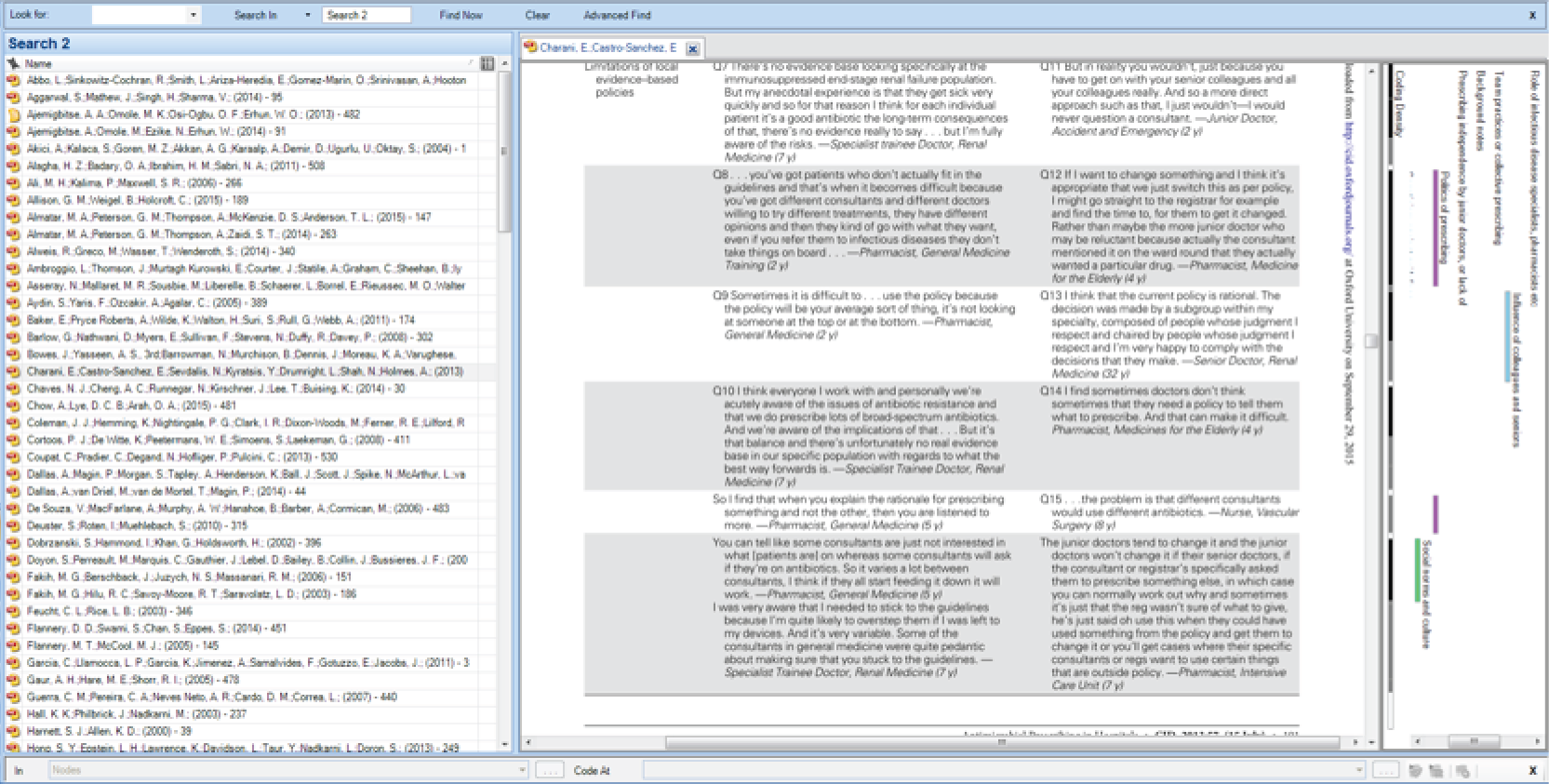
The electronic versions of the articles were then uploaded into NVivo 10 (QSR International, Warrington, UK) (qualitative data analysis software) for further analysis (see snapshot of NVivo coding in Figure 3). At this stage, the analysis focused on the richest sources, that is, articles that had been identified in the familiarisation stage as having the most potential to inform the programme theory. In some cases, the manual coding from the familiarisation stage was transferred into NVivo intact. In other cases, additional or different codes were applied to correspond to how the understanding of the literature had changed since the familiarisation process. The first rounds of coding focused on the conceptual level, classifying content in analytical categories, to be able to refine these further. We added this initial stage as we have found from past experience that it is easier to make sense of data when they have been categorised into related categories. This means that we did not immediately categorise data into contexts, mechanisms and outcomes, but approached coding with an open mind to understand what issues are coming up in the data (e.g. difficulties working with guidelines, time pressures, hierarchical environment). The data within these initial categories were reread and, when needed, recoded and reclassified. It was only after conceptual coding was completed that we started to consider whether or not each of these categories (or subcategories within them) included sections related to contexts, mechanisms and their relationships to outcomes. We continued refining the coding framework in NVivo and used relationships (a NVivo function) to create links between contexts, mechanisms and outcomes where possible across the NVivo data set, so that these links could be reviewed further.
FIGURE 3.
Screenshot from the analysis process in NVivo. Screenshot using NVivo version 10 software, reproduced with permission from QSR International Pty Ltd. NVivo Qualitative Data Analysis Software; QSR International Pty Ltd. Version 10, 2012. NVivo is a trademark and registered trademark of QSR International Pty Ltd. Patent pending, www.qsrinternational.com.
Coding followed both an inductive (codes emerging from the analysis of the literature) and a deductive (codes created in advance informed by the initial programme theory, stakeholder group discussions and exploratory literature searching) mode. The coding framework resulting from the analysis of the richest papers was subsequently applied to the rest of the articles, moving from more relevant and specific to less relevant and specific papers (from the most potential to contribute to programme theory refinement to least) [see Appendix 3 for an overview of the codes applied to each document (Tables 11–14)].
Having identified conceptual categories and, subsequently, potential contexts, mechanisms and outcomes, the analysis continued under a realist, explanatory logic. Starting from relevant outcomes, we sought to interpret and explain how different groups of doctors in training responded to resources available in their environment (the mechanisms) with regard to antimicrobial prescribing and to identify the specific contexts or circumstances when these mechanisms were likely to be ‘triggered’. For each step, we applied a realist logic of analysis, so as to explain how the (intermediate) outcome for each step might be achieved in realist terms, that is, what interaction between context(s) and mechanism(s) might lead to that outcome. For each step in the sequence, we sought to identify what mechanism(s) generates the outcome and in what contexts this mechanism might be triggered. Such an analysis was repeated throughout the review and enabled us to build sets of context–mechanism–outcome configurations (CMOCs) that explained the antimicrobial prescribing behaviours of doctors in training.
Realist reviews are used to synthesise data from qualitative, quantitative and mixed-methods studies. This means that different types of data were used to identify contexts, mechanisms and outcomes. Often, quantitative data illustrated the outcome patterns evident, such as error rates among different grades of doctors in training or proportions of trainees reporting use of guidelines to inform their decisions. Qualitative data were used to explain these patterns in more detail.
We compared and contrasted emerging CMOCs with the evolving programme theory, so as to understand the place of and relationships between each CMOC with the programme theory. As the review progressed, we iteratively refined the programme theory, driven by interpretations of the data included in the literature (see Figure 2 for process of programme theory development).
With new iterations of the programme theory, already-included studies were rescrutinised to search for data relevant to the revised theory that may have been missed initially (e.g. three more papers were added to the core data set from the main search). Relevant articles cited in the included papers were followed up for additional data as described in Step 3: selecting articles. Memos and annotations were used to make sense of the data, especially in relation to inferring mechanisms and relationships between contexts, mechanisms and outcomes. We also coded articles for more descriptive categories, such as relevant background information, study characteristics and recommendations provided. The characteristics of the documents were extracted into a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet separately for the results of the main search, the additional search and studies identified outside the database searches (see Appendix 2). A sample of the coding for 10% of the papers included in the review was independently checked by Geoff Wong for consistency.
The aim of the analysis was to reach theoretical saturation, in that sufficient information had been captured to portray and explain the wide range of experiences of doctors in training with antimicrobial prescribing in primary and secondary care. Excerpts coded under specific concepts in NVivo were then exported into Microsoft Word (Microsoft Corporation, Redmond, WA, USA) documents. Drawing on the analysis of the literature done in NVivo, Word documents were used as coding reports, to provide a more flexible space to test the viability of different CMOCs and build the narrative of the synthesis. This included adding explanatory text through abductive and retroductive reasoning (see Step 5: synthesising the evidence and drawing conclusions). A diary was kept throughout the analytical stages to record processes followed and decisions made at different points during the review.
Step 5: synthesising the evidence and drawing conclusions
Lack of adequate reporting of intervention characteristics and implementation processes, along with limited measures of success, posed obstacles in directly comparing interventions against each other to understand how context had influenced outcomes. Instead, as explained in the beginning of Chapter 2, we focused on developing a programme theory of the antimicrobial prescribing experiences of doctors in training to try and understand how and why they made particular prescribing decisions. For instance, we compared the circumstances under which doctors in training may or may not be driven to comply with prescribing decisions made by their seniors without asking any questions.
To do this, we moved iteratively between the analysis of particular examples, stakeholder interpretations, refinement of programme theory and further iterative searching for data to test particular subsections of the programme theory. A realist logic of analysis was used to analyse and synthesise the data. During our analyses we developed and refined the initial programme theory by drawing on the coding carried out within and outside NVivo (e.g. Word document coding reports, memos, other notes) to configure relationships between contexts, mechanisms and outcomes. This entailed asking a series of questions and making judgements about the relevance and rigour of content within included articles, as set out below.
-
Relevance:
-
Are the contents of a section of text within an included document referring to data that might be relevant to programme theory development?
-
-
Judgements about trustworthiness and rigour:
-
Are these data sufficiently trustworthy to warrant making changes to the programme theory?
-
-
Interpretation of meaning:
-
If the section of text is relevant and trustworthy enough, do its contents provide data that may be interpreted as being context, mechanism or outcome?
-
-
Interpretations and judgements about CMOCs:
-
What is the CMOC (partial or complete) for the data?
-
Are there data to inform CMOCs contained within this document or other included documents? If so, which other documents?
-
How does this CMOC relate to CMOCs that have already been developed?
-
-
Interpretations and judgements about programme theory:
-
How does this (full or partial) CMOC relate to the programme theory?
-
Within this same document, are there data that inform how the CMOC relates to the programme theory? If not, are there data in other documents? Which ones?
-
In light of this CMOC and any supporting data, does the programme theory need to be changed?
-
Abductive reasoning (see Glossary) was employed at the analysis and synthesis stage, particularly to infer and elaborate on mechanisms (which often remained hidden or were not articulated adequately). This means that we followed a process of constantly moving from data to theory, in order to infer and refine explanations about why certain behaviours are occurring, and we tried to frame these explanations at a level of abstraction that they could cover a range of phenomena or patterns of behaviour.
Relationships between contexts, mechanisms and outcomes were sought not just within the same articles, but across sources (e.g. mechanisms inferred from one article could help explain the way contexts influenced outcomes in a different article). Synthesising data from different sources was often necessary to compile CMOCs, as not all parts of the configurations were always articulated in the same source.
In summary, the process of evidence synthesis was achieved by the following analytic processes, as modified from the original version:52
-
Juxtaposition of data sources – comparing and contrasting data presented in different articles. For example, data about prescribing experiences from an in-depth qualitative source enabled insights into how outcomes are achieved as described in a quantitative study.
-
Reconciling ‘contradictory’ or disconfirming data – when outcomes differ in apparently similar circumstances, further investigation was necessary to find explanations for why these different results occurred. This involved a closer consideration of context and what counts as context for different types of ‘problems’, in order to understand how the mechanisms triggered can explain differences in outcomes.
-
Consolidation of sources of evidence – when there are similarities between findings presented in different sources, a judgement needs to be made about whether these similarities are adequate to form patterns in the development of CMOCs and programme theory, or whether there are nuances that need to be highlighted, and to what end.
Engagement with substantive theory
Theory in realist research operates at a number of different levels to substantiate the inferences made about mechanisms, contexts, outcomes and the configurations between these elements. Theory is also useful in adjudicating findings with what is already known on the topic under research, to enhance the plausibility and coherence of the arguments made.
The first step we took in understanding what theoretical frameworks and ideas would be relevant to the review was to look at existing work on antimicrobial prescribing. Our starting point was the literature collected as part of the exploratory search in step 1, described in Chapter 2. This enabled us to consider a wide range of theoretical understandings that could be of potential relevance. We compiled a list of theories used in previous research and looked for updated frameworks that could further inform this work. As we retrieved literature more specific to the review questions from the main and additional literature searches in step 2, we focused on a smaller set of potentially relevant theories. Throughout the analysis and synthesis of data from the articles included in the review, we sought links between the different theoretical frameworks and emerging CMOCs. This was done with a view to extend the explanatory potential and usefulness of the overall programme theory developed out of the CMOCs.
Some of the theoretical ideas that informed the development of the programme theory derived from papers retrieved from the literature search – especially from the additional theoretically driven search (e.g. Broom et al.,53 who used Bourdieu’s practice theory). Other theoretical frameworks were sought specifically to cover particular aspects of the phenomena we were attempting to explain. For example, as it became evident that the need to belong in the clinical team emerged as an important mechanism driving antimicrobial prescribing behaviour, we sought substantive theory that would help us to think through what this mechanism means and how it can be conceptualised in the context of our data. This led us to group reference theory and its application from a realist perspective, which enabled us to both validate use of ‘group reference’ as a mechanism and to extend what this may mean by working across data and theory. 54 Substantive theory used in this work is further discussed in Chapter 3, Drawing on substantive theory.
Step 6: writing up and quality considerations
Writing up the results of the analysis and the CMOCs into programme theory has been an important step in fine-tuning our explanations. Our analyses (when we made interpretations by comparing data, evolving programme theory and substantive theoretical frameworks) were not abstract thought experiments, but involved drafting several diagrams and writing up numerous versions of the programme theory. We developed and refined several iterations of the CMOCs and narrative for the review, until we felt that all data were adequately accounted for and inferences were coherent with existing literature. Through drafting CMOCs and reviewing these between team members, along with supporting data, we were able to fine-tune our interpretations and achieve shared understanding of the arguments made. This process was necessary to unpack different assumptions and to distinguish between the nuances underpinning CMOCs. We found that simply verbally discussing our evolving interpretations did not enable us to fully engage with the data, their interpretation and the inferences made. Writing things down in detail and drawing diagrams enabled us to achieve greater explanatory depth in our analyses and resulted in recognition of more mechanisms than those immediately visible in the ‘raw’ data.
Each section in Chapter 3 of this report has been structured to provide:
-
a brief narrative on how and why doctors in training engage with antimicrobial prescribing
-
the realist analysis underlying each of these narratives, that is, the CMOC developed as the data from the literature was interpreted in realist terms
-
data excerpts from the literature that support the CMOC along with their reference and any additional explanatory text needed.
We have chosen to present text excerpts relevant to each CMOC to demonstrate the strength of the argument made in each of the sections and to increase the transparency of reporting (illustrative examples are included under each CMOC and all data extracted from the literature are available on request from the authors). Setting out the ‘raw’ data in this way allows closer scrutiny of the interpretations made to configure contexts, mechanisms and outcomes, which adds to the transparency and trustworthiness of the process undertaken.
Table 2 outlines how the review has fulfilled the quality standards for realist review according to the recently published RAMESES quality standards.
| Quality criteria | How the criteria were fulfilled |
|---|---|
| The research topic is appropriate for a realist approach | The review is focusing on antimicrobial prescribing for doctors in training, which is a complex issue as trainees have to navigate hierarchical dynamics, variability in prescribing practices and contradicting advice, as well as clinical uncertainty |
| The research question is constructed in such a way as to be suitable for a realist synthesis | The research question broadly asks how, why, to what extent, for whom and in what circumstances do interventions to improve antimicrobial prescribing work for doctors in training. To reach an in-depth understanding, this was extended in the process of the review to look at how trainees engage with antimicrobial prescribing more widely |
| The review demonstrates understanding and application of realist philosophy and realist logic that underpins a realist analysis | The data have been collected and analysed using a realist logic of analysis to provide explanations that contain CMOCs |
| The review question is sufficiently and appropriately focused | The review question was further focused in the first stages of the review, by specifically looking at hierarchical dynamics in more depth, led by initial findings in the literature |
| An initial realist programme theory is identified and developed | The first project meeting for the review discussed an initial programme theory, which was then further developed and refined |
| The search process is such that it would identify data to enable the review team to develop, refine and test programme theory or theories | The search strategy used terms that would maximise the potential for returning data relevant to the programme theory. The additional search performed was specifically driven by the programme theory |
| The selection and appraisal process ensures that sources relevant to the review containing material of sufficient rigour to be included are identified. In particular, the sources identified allow the reviewers to make sense of the topic area; to develop, refine and test theories; and to support inferences about mechanisms | Sources containing rich data and of adequate rigour were identified and allowed reviewers to configure CMOs and to support their inferences about relevant mechanisms. Illustrative quotations have been included in Chapter 3 to allow for transparency in the inferences made and in the way CMOCs have been developed. All quotations are available from the authors on request |
| The data extraction process captures the necessary data to enable a realist review | Data coding and extraction were iterative to enable all relevant data to be captured in support of specific CMOCs. As the programme theory developed, sources were revisited to ensure supporting or refuting data had not been missed |
| The realist synthesis is reported using the items listed in the RAMESES reporting standard for realist syntheses55 | This report and the publication planned out of this work have both followed the reporting standards for realist synthesis |
Results of the review
The process of screening and article selection resulted in 131 references. Of those, 81 references came from the main literature search and 35 references from the additional search. The remaining 15 articles resulted from citation tracking, targeted searches and expert suggestions, on the basis of relevance to programme theory.
Of the 131 references, 78 used quantitative methods, 37 used qualitative methods, 12 were mixed-methods papers and there were also three position papers and one report (for more details, see Appendix 2 on included studies).
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram (Figure 4) provides more detail on the screening and selection process.
FIGURE 4.
The PRISMA diagram.
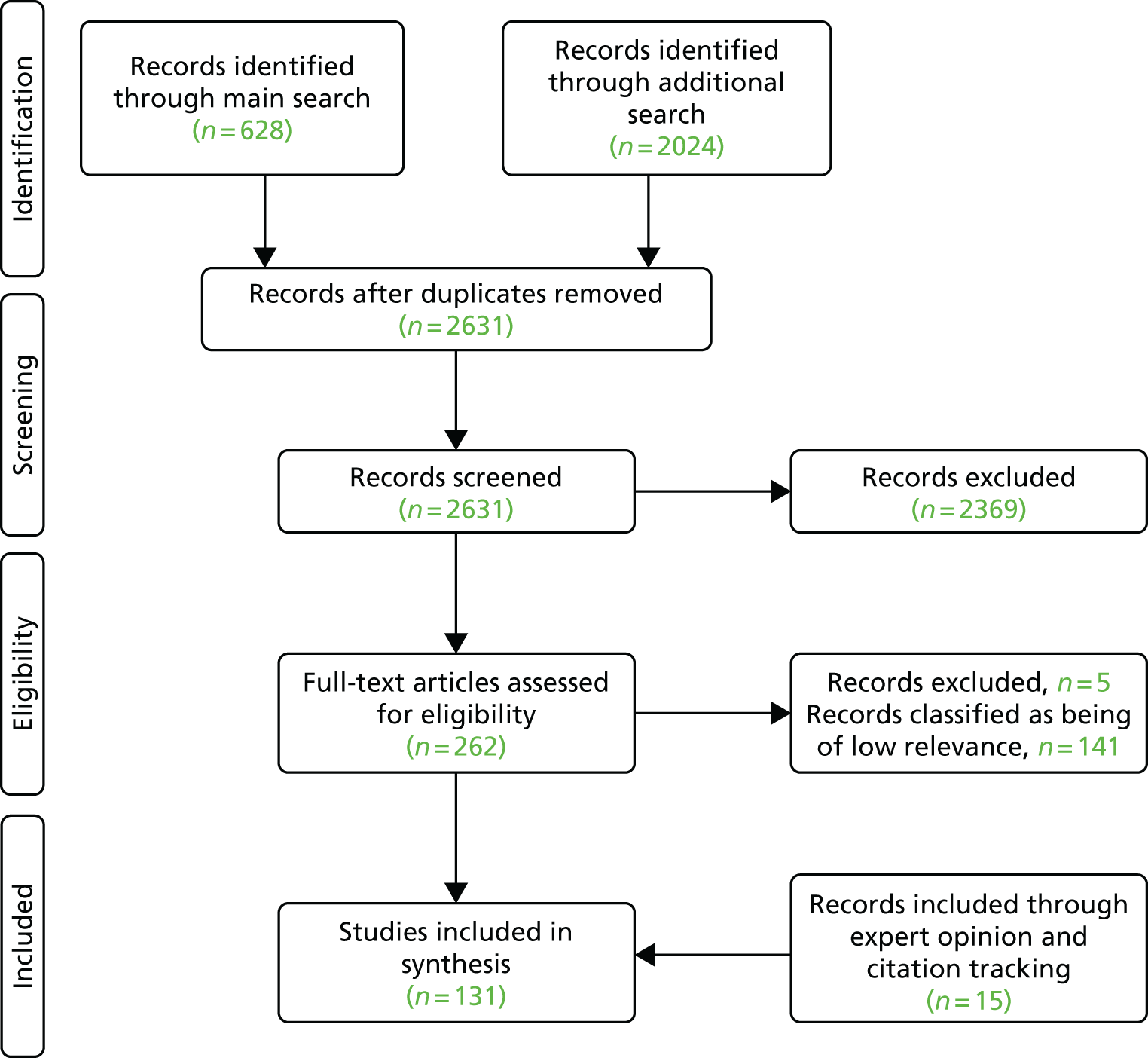
Main search
In more detail, the main literature search retrieved a total of 628 articles. Of those, 12 articles were duplicate records and 293 were not relevant to the purposes of this review. From the 81 titles accompanied only by conference abstracts, two full-text publications were identified, and these were already included in the data set. There were also 21 records for which the full text could not be retrieved. These records were saved separately to decide whether or not it was necessary to pursue other means of retrieving the full text. However, once the rest of the articles had been screened and analysed, it became obvious that these records had limited potential for informing programme theory and could be of questionable rigour. As theoretical saturation had been reached, a decision was made not to pursue full-text retrieval any further. Only studies published in English were included, to take account of the UK context. When non-English papers provided abstracts in English (in the majority of cases), these were reviewed by a member of the team who found that there was no clear mention of doctors in training or little relevance to programme theory development.
The screening process resulted in 97 papers being classified as being of low relevance to programme theory development and 81 articles being classified as comprising the core data set for the review. An additional 19 position and background papers were stored separately in case it became necessary to draw on them to supplement our interpretations of the data.
Additional search
From the additional, theory-driven search, a total of 2024 articles were identified. Of those, 1646 were excluded at title screening, and 302 at abstract screening, as irrelevant to the purposes of the review. Nine citations were already included in the data set from the main search and for two articles the full text was not available. As in the main search, a judgement was made about the potential added value of retrieving full texts when unavailable, which resulted in the decision that they would be of limited potential for informing programme theory. Another five articles were excluded as irrelevant at full-text screening.
The screening process for the additional search resulted in 25 papers classified as being of low relevance to programme theory development and 35 articles as core sources providing a necessary explanatory backbone to the review. Directly relevant position or other background papers (n = 3) were included in the highly relevant category for the additional search, as they were of sufficient relevance to inform the programme theory directly.
As explained in Chapter 2, two members of the team worked jointly to ensure consistency at different stages of the screening and coding process. For both searches, Geoff Wong independently reviewed a 10% random sample of the set of articles retrieved to ensure that they corresponded to the review aims, and a 10% sample of the articles selected to ensure that screening criteria were applied consistently. In addition, at the coding stage, Geoff Wong reviewed the coding for 10% of included papers out of both searches to ensure accuracy and consistency.
There were no major disagreements between the two reviewers (CP and GW). There was only one small discrepancy in the coding process, but this was easily resolved and ongoing discussions enriched data analysis.
Tables 7–9 in Appendix 2 provide more details on the characteristics of the studies included in the data set for the review.
Chapter 3 Findings
This realist review moves beyond identifying barriers of and facilitators to appropriate antimicrobial prescribing for doctors in training to reach an explanation of how and why trainees engage with antimicrobial prescribing differently under different circumstances. To do this, we focus on situations where antimicrobial prescribing decisions appear more challenging and there is increased uncertainty about what course of action to take (compared with when the diagnosis is clear-cut and it is widely accepted that an antimicrobial is appropriate – such as with a feverish patient with confirmed bacteraemia on blood cultures).
It is well recognised in the literature that doctors in training often find antimicrobial prescribing decisions challenging, either because of inherent diagnostic uncertainty, or because they have not yet developed relevant experience and knowledge. These barriers were discussed extensively in the set of articles included in this review. This has guided our focus in looking at what trainees do, in the presence of uncertainty, inexperience and lack of knowledge, to reach antimicrobial prescribing decisions. In other words, as guided by our data, we recognise that these factors will always limit prescribing decisions and place more emphasis on solutions that can work in the face of uncertainty, inexperience and lack of knowledge. For the same reasons, our analysis draws less attention to uncertainty about technical aspects of the process of prescribing,56–59 poor dissemination of information or conflicting guidelines and lack of awareness,43,60–65 and operational inefficiencies and pressures. 43,62,66–70 Instead, we are looking to understand what drives the behaviour of doctors in training in the presence of these limitations – namely uncertainty, inexperience and lack of knowledge.
The rest of this chapter sets out the findings from the analysis and synthesis of the literature reviewed. There are two parts to this findings chapter. Part A focuses primarily on antimicrobial prescribing decisions, use of guidelines and other decision support aids, receiving support from other health professionals and managing patient expectations. Part B presents data from the literature on seeking assistance and challenging decisions made by senior supervisors. In each of these two parts, there are a number of subsections organised as follows:
-
First, we provide a narrative of findings based on our analysis of the data found within the literature.
-
This is then followed by a detailed realist analysis that contains one or more CMOCs.
-
Illustrative data (i.e. extracts from manuscripts) that we have used to make our interpretations and inferences for each of the CMOCs are also provided in each of the subsections. Some of these data derive from quotations presented in relevant articles, other data come from interpretations or conclusions drawn by the authors of these articles (rather than being primary data), or data extracts are presented in other forms (e.g. survey results), depending on the study design. The full list of quotations extracted from the literature is available from the authors on request.
For some CMOCs there is a larger number of supporting quotations from the literature included in the review, while other CMOCs are supported by a smaller set of data. This would provide some indication of the strength with which arguments can be made out of the data included here, but quantity would not be the only consideration. The level of detail and depth within each of the quotations and the confidence with which we can draw inferences from the data also plays a role. Some articles presented a wealth of data (possibly because of reporting flexibility in some journals) whereas other articles were constrained in the data they could present, therefore limiting the number of data we had available to us to interpret. However, this does not mean that arguments cannot be made with adequate strength for CMOCs supported by a smaller set of data, especially when substantiated by relevant theory (see Chapter 3, Drawing on substantive theory).
In some of the CMOCs presented, lack of adequately detailed data in included papers means that we have not been able to fully determine the fine-grained relationships between contexts, mechanisms and outcomes. Limitations of the review are presented in more detail in Chapter 4.
Part A: making decisions about antimicrobial prescribing and prescribing support
Influence of the formal medical hierarchy
The literature describes hierarchies as a core and pervasive aspect of professional socialisation in medicine in the UK, particularly in the context of explicit and implicit role modelling of appropriate clinical and prescribing behaviours from senior to junior members of the clinical team. One of the professional values communicated through role modelling within hierarchical relationships by senior experienced practitioners is that of decision-making autonomy. More senior clinicians set the norms about what is appropriate prescribing in practice (i.e. what is and is not acceptable) and about how to manage conflicting priorities. Doctors in training largely comply with the specific prescribing etiquette(s) and behaviours considered legitimate by the formal prescribing hierarchy (medical ‘chain of command’) at any given instance. This compliance results primarily from fear of criticism and fear of individual responsibility for patients deteriorating, although inertia sometimes also plays a role in junior doctor responses. Some specialties are described as significantly hierarchical in the literature, such as surgery, in which status differences and authority gradients are particularly pronounced and continuously enacted (i.e. surgeons set the rules and permissions).
Doctors in training also try to sustain positive relationships and manage the impression of others, in the context of their seniors’ role in evaluating their performance and influencing career progression. They are fitting in with the teams they are working with by adopting an identity of a competent trainee (which often means that you do as you are told so that you are perceived as a ‘safe pair of hands’). As decision-making autonomy is understood to be an important professional marker of experienced practitioners, doctors in training try to balance their respect for the decision-making autonomy of their seniors with learning how to be a competent doctor themselves.
Realist analysis
Context–mechanism–outcome configuration 1
In a context of learning through role modelling within hierarchical relationships [context (C)], junior doctors passively comply with the prescribing habits and norms set by their seniors [outcome (O)], because of fear of criticism [mechanism (M)] and fear of individual responsibility for patients deteriorating (M).
Context–mechanism–outcome configuration 2
In a context in which career progression depends on hierarchical power relationships (C), junior doctors feel that they have to preserve their reputation and position in the hierarchy (fitting in) (M), by actively following the example of their seniors and avoiding conflict (O).
To provide one example of the process of interpreting data to develop CMOCs from the papers reviewed, we are drawing on Toulmin’s model of argumentation. 71 Toulmin suggests that an argument consists of a number of elements: a claim, which is the conclusion drawn; grounds for the claim, which are the data or evidence to support the claim; a warrant, which connects the evidence to the claim; backing, to support the warrant; a qualifier for the claim to show degree of certainty; and a rebuttal to recognise any limiting factors that apply to the claim being made. 71 On this basis, to develop a CMOC (what we have interpreted as being a claim in Toulmin’s model) we need a number of elements to substantiate our argument. For example, in CMOC 1 above:
-
The grounds for our claim are provided by data constituting context, mechanisms and outcome. From the data extracts below, quotation 1 provides evidence for ‘role-modelling within hierarchical relationships’ as a relevant context. Quotation 3 provides evidence for fear of criticism as a mechanism: ‘I actually have been criticized by a staff because of not covering somebody [with antibiotics . . . ]’70
-
And quotation 4 for fear of individual responsibility for patients deteriorating as a second mechanism: ‘Because if you make a mistake, it is going to be the primary concern of the patient, of course, and something bad is going to happen to them’. 70
-
A large number of quotations indicate the outcome, which is compliance with the prescribing habits and norms set by their seniors (e.g. quotation 9).
-
The warrant is what links data to the claim and, in the case of CMOCs, can be conceptualised as the relationships between the Cs, Ms and Os identified in the different quotations. This means that the warrant relates not to the individual data behind the claim, but to the connections between the data that allow the claim to be validated. For example, quotation 2 provides a warrant for the relationship between the context ‘Whatever attending [physician] you are with is the attending who you learn from . . .’70
-
and outcome ‘. . . and if I see them continuously not prescribe antibiotics over and over again, then I feel comfortable not prescribing antibiotics. But if they always do it, then I feel the need to do it.’70
-
Backing is provided by substantive theory, as discussed in Chapter 3, Drawing on substantive theory. Hierarchies are a pervasive aspect of medicine and have long been a topic of theoretical analysis.
-
Qualifiers link back to the strength of the argument and the degree of certainty we can have in the claim being made. CMOC 1 and CMOC 2 show that there is a fine difference between passive compliance and actively choosing to follow the decisions made by senior clinicians, which cannot be adequately resolved with the data included in this synthesis, although further CMOCs draw a more nuanced picture.
-
A rebuttal can be made in that, under some circumstances, or when doctors progress in their training, there is less fear of criticism, as trainees are more comfortable with understanding the prescribing practices in their context. This is further highlighted in CMOCs 27 and 28 towards the end of Chapter 3.
Relevant extracts from papers included in the review
‘I think it goes from the top down so everybody has to do the same thing. If the consultant or registrar doesn’t set a good example, the junior will certainly not follow it [the good example].’ (Specialist Trainee Doctor, Stroke)
‘Whatever attending [physician] you are with is the attending who you learn from, and if I see them continuously not prescribe antibiotics over and over again, then I feel comfortable not prescribing antibiotics. But if they always do it, then I feel the need to do it’. (Resident interview)
‘I actually have been criticized by a staff because of not covering somebody [with antibiotics . . . ] I was suspicious for endocarditis but they were clinically stable and so I wanted to get multiple blood cultures and monitor . . . The next morning I was pretty severely reamed out for not covering the patient [with antibiotics], although the person did fine and did not have a bad clinical result.’ (Resident interview)
‘Because if you make a mistake, it is going to be the primary concern of the patient, of course, and something bad is going to happen to them. And then you have your personal reputation to think about, too.’ (Resident interview)
The data [included in this paper] tell us, however, that junior doctors’ decisions and behaviours are also influenced by the prevailing culture of the organisation and the juniors’ perceptions of the hierarchy within which they work.
When focusing on the role of the supervisors, both internal medicine and surgical residents emphasized their importance as role models because supervisors’ practice strongly determined the subsequent prescribing behaviour of residents.
The most significant influence on prescribing practices was the opinion of more senior colleagues in the team to which the NCHD [Non-Consultant Hospital Doctor] was assigned. This was especially important in the earlier years of one’s medical career when doctors (particularly pre-registration house officers) have limited autonomy. [. . .] Instructions from seniors 1. ‘I did what I was told, like all interns do’ (Male Specialist Registrar, Anaesthesia) 2. ‘It’s a good system because he (Senior colleague) probably knows better than you; he may have a good reason’ (Male Registrar, Ear, Nose and Throat)
‘Some registrars described feeling undermined or criticised by their supervisors for their prescribing decisions. [. . .] ‘It’s a big power differential . . . You’re still at the mercy of the training provider coming and doing visits, and your supervisor giving input on if you do what you’re told or not’. (Registrar)
For some registrars, there are concerns that they need to ‘do what they’re told’ or fit in to a particular practice culture to prevent conflict and ensure career progression [. . .]
‘The origin of my practice came from supervisors during residency training, but the supervisors practised differently with respect to indication, dose, and number of doses. Thus, I chose to imitate the credible supervisors with good results of postoperative infection and my personal inclination.’ (Resident)
Influence of implicit and explicit rules or ‘norms’
When rotating in different environments, doctors in training encounter a number of different ‘rules’ or norms depending on the hierarchical relationships they become embedded within. According to the literature, junior doctors experience changes in prescribing norms not just between departments and hospitals, but also between different consultants in the same setting. Apart from differences between prescribing practices, the strength of norms may also differ according to how fluid or stable hierarchies are perceived to be (e.g. when doctors in training are members of multiple teams in different departments working on different wards vs. when doctors in training are primarily based within one department and on the same ward). At any given point in time, doctors in training seem to comply with the norms set by the consultants towards whom they feel most accountable.
Therefore, antimicrobial prescribing becomes situated – to respond to the norms and needs of particular situations – and relational – to respond to the requirements and norms of particular relationships within hierarchical and interprofessional modes of working.
The literature discusses particular examples of how norms are set in different specialties. For example, surgery is often referred to as a particularly hierarchical environment in which junior members of the team comply with the norms set by those at the top, as already mentioned. Yet the degree of supervision of antimicrobial prescribing decisions seems to be lower in surgery than in other specialties, signalling to doctors in training that they have permission to make their own decisions. 75,76
Realist analysis
Context–mechanism–outcome configuration 3
In contexts in which there are different prescribing norms and permissions set by different consultants/hierarchical relationships (C), doctors in training fit in with their teams and appear as knowledgeable and competent trainees (O) by accepting that they have to flexibly anticipate and adapt to the individual preferences (or non-preferences) of the senior clinician they are accountable to (M).
Relevant extracts from papers included in the review
‘When I was an SHO [Senior House Officer], you move around every six months and what you would have used, or what the consultant liked in one hospital, wouldn’t necessarily go in another hospital at all, you know? So to a certain extent you had to fit in a little bit with individual consultant preferences.’ (Female Specialist Registrar, Haematology/Medical Oncology)
‘[talking about having to sign orders one disagrees with] not like anybody was forcing my hand [but when you are] lower on a team [. . .] I guess this is what I order.’ [Consultant discussing experiences as a trainee]
Today interns, residents, and registrars work with many health professionals and seniors on a day to day basis and are required to understand and implement instructions from doctors above them. Registrars work for five or more consultants. They are expected to follow the usually unwritten rules of each of their ‘bosses’ and to take instructions. This results in inadequate communication, fragmented supervision, inadequate instructions, and more frequent suboptimal patient outcomes.
‘You can tell like some consultants are just not interested in what [patients are] on whereas some consultants will ask if they’re on antibiotics. So it varies a lot between consultants, I think if they all start feeding it down it will work.’ (Pharmacist, General Medicine)
In addition to learning about prescribing from protocols and from others, doctors were also required to learn about the preferences of particular consultants, even if these did not fit with the protocols they had just learned. One of our participants told us that, after drawing on her knowledge of therapeutics, she had taken a complex prescribing decision with which she was happy. However, she reported: ‘Yeah, whereas if it had been the other consultant I would probably have started antibiotics . . . Because he is for antibiotics so it just depends on who the consultant is, you have to know who you are working for. [Foundation Year 1 Doctor]
This participant went on to discuss how workplace culture had influenced him to prescribe suboptimally in certain circumstances. Although he was aware of how it should be done, the social environment made suboptimal prescribing acceptable: ‘I’ll still prescribe Tazocin because someone will just say Tazocin and all my colleagues just write Tazocin, and it’s just Tazocin . . . Everyone else does it so you do it . . . You actually have that written as Tazocin on the antimicrobial [guidelines] . . . maybe that’s why I’ve been influenced . . .’ (First-year junior doctor)
Influence of individual responsibility and accountability perceptions
As mentioned above, varying perceptions of individual responsibility and accountability influence the extent to which different norms are followed and sustained. Doctors at different levels of training perceive that they are accountable to their seniors as it is the seniors who bear ultimate responsibility for the patients. Therefore, they tend to follow the practices of the senior who carries responsibility for patient outcomes. A decision different from what would be more widely accepted and practised by seniors in a specific setting would mean that they assume more responsibility for the outcome than what they feel befits their role. Compliance towards senior prescribing patterns serves two functions for the doctor in training: (1) to preserve their own and their seniors’ role in the hierarchy (by acting as their agent) and (2) to limit their own responsibility from the consequences of their actions. However, trainees still felt that they had to do what would be considered ‘enough’ by their seniors before handing over (e.g. see quotations 6 and 7 below).
Realist analysis
Context–mechanism–outcome configuration 4
In a context in which trainees perceive that they have limited accountability over patient care (C), they comply with the decisions of their seniors or what they assume their decisions would be (O), because this is what they believe they are expected to do as part of their role in the hierarchy (M), and doing so limits their own responsibility for the consequences of their actions (M).
Relevant extracts from papers included in the review
While there was some role variation depending on the particular environment and supervisors, interns generally saw their primary role as providing clinical administration to the team, under supervision. The intern role was low status: ‘at the bottom of the food chain’, ‘a dogsbody’, ‘bottom of the bottom’.
In many cases, team members may feel less responsible for their own actions and will view themselves as just an ‘agent’ of their leader.
Residents described themselves as being in the role of a bystander. An example from the simulation scenario was a resident who considered that he hadn’t actually ‘given blood’ to the patient [when this was inappropriate to do]. Despite acknowledging that he spiked the bag of blood and hung it on the intravenous line, in his view, he was just doing what he was told and someone else made the decision.
One resident commented that the most important thing for him was that, if the regulatory bodies in Ontario investigated a case, he would never be found ultimately responsible for the case and would escape legal repercussions as he was following the directions of his attending. In his view, any real responsibility for a patient began once training was completed.
Trainees describe how leadership equates to clinical responsibility. The person who has ultimate clinical responsibility within a given situation was perceived to be the leader.
Although they considered themselves to be responsible solely for ensuring that a patient survived until senior help arrived, they also felt that they were abdicating responsibility if they did not attempt to assess, investigate, diagnose and treat a patient before calling for help.
In situations in which a resident physician was covering unfamiliar patients overnight, prescribing antibiotics was preferred when a patient’s clinical status declined; the expectation was that the primary team would de-escalate antibiotics at a later time if a bacterial infection was not present.
Role modelling prioritisation of conflicting goals
Role modelling from senior to junior levels of the hierarchy extends to how conflicting goals should be prioritised. For antimicrobial prescribing specifically, prescribing practices of senior members of staff indicate whether the primary consideration should be to predominantly address immediate patient needs (even when there is uncertainty around the value of antibiotics for specific clinical indications) or whether more long-term AMR is a consideration that merits direct attention in the clinical setting. In essence, the way that senior clinicians engage in decision-making illustrates how they would like their trainees to prioritise between more immediate short-term goals of patient recovery (e.g. from possible sepsis) and long-term goals of minimising AMR. Seniors also role model how to find a balance between the need for antimicrobial prescribing against the risk of side effects (e.g. Clostridium difficile infection) under different circumstances.
Realist analysis
Context–mechanism–outcome configuration 5
When balancing the potential shorter-term benefits of antimicrobials for a patient against longer-term issue (e.g. AMR) (C), junior doctors follow the way that seniors balance these considerations (O), out of fear of criticism and individual responsibility for the patient deteriorating while under their care (M).
Relevant extracts from papers included in the review
Antibiotic overuse is recognized but generally accepted. [This is one of the four themes identified by this paper on the culture of antibiotic prescribing.]
I think there is more pressure towards you are going to look bad if you missed something and did not treat it appropriately versus . . . giving people C[lostridium] difficile and diarrhea, [which] is a little more anonymous (resident interview). [. . .] While these participants’ sense of clinical competence was influenced by not missing an infection, they expressed less concern about their antibiotic prescribing decisions fostering C. difficile or an infection with ARB [antibiotic-resistant bacteria]. There may be several reasons why participants undervalued these adverse events. For example, these antibiotic-related adverse effects tend to be multifactorial; they may have a delayed manifestation; they may be difficult to attribute to a single physician’s decision, thereby providing a degree of anonymity for the prescribing physician.
Providers articulated that azithromycin prescriptions for upper respiratory prescription are perceived to be ‘like water’ and a ‘safe, cheap and effective’ choice and that they are thus given out ‘like candy’.
‘. . . I always think that there is feeling in all of doctors that antibiotics won’t do anything [harmful] “one or two doses of ceftriaxone won’t kill anyone” [. . .]’ (Resident)
Figure 5 consolidates CMOCs 1–5 described in the findings section so far and summarises the influence of hierarchical relationships on the prescribing decisions of doctors in training (presented as CMOCs). 10,35,56,60,62,63,66,69,70,72–76,78–98
FIGURE 5.
Partial programme theory (CMOCs 1–5).
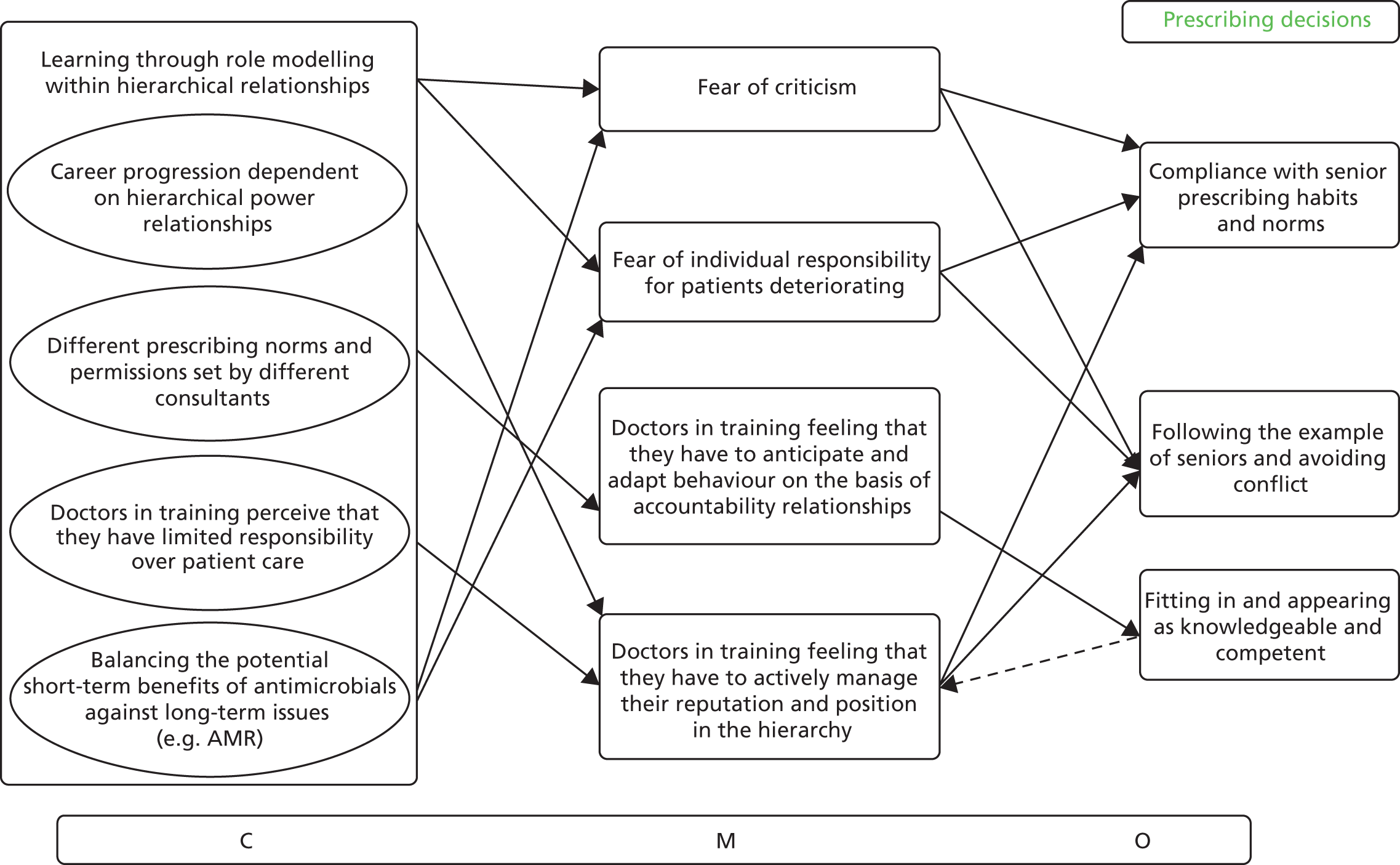
Influence of the hierarchy on using sources of support
In a context of learning through implicit or explicit role modelling within hierarchical relationships, junior doctors follow the example of seniors (out of fear of criticism and so as to appear to be competent trainees and good doctors) not just in their prescribing decisions, but also in what they count as legitimate sources of support for making prescribing decisions. Data from included studies indicate that doctors in training will be more inclined to follow guidelines when this is clearly signalled as appropriate behaviour by the senior clinical staff to whom they are accountable. The primary influence behind guideline use seems to be whether or not these are adopted and perceived as credible by senior colleagues. Acceptance will differ between settings and between teams, and might not always correspond to official organisational rules.
As doctors in training learn how to make sense of and navigate the social norms in different clinical environments, they also change the way they use decision aids. Early on in their careers, they rely more on guidelines to guide their prescribing decisions. There is also some evidence that trainees perceive guidelines as useful in the absence of other prescribing support or senior oversight. 99 However, this is likely to occur only when doctors in training perceive that such behaviour is acceptable to the senior clinicians to whom they are accountable. As doctors in training progress in their training, they become more experienced in reading and negotiating the prescribing etiquette around them so as to be able to strike a balance between evidence, experience and their identity as a competent doctor, making use of decision aids as considered appropriate in their environment.
Realist analysis
Context–mechanism–outcome configuration 6
In a context of learning through role modelling within hierarchical relationships in which norms are set by seniors to whom trainees are accountable (C), junior doctors comply not just with the prescribing behaviours of their seniors, but also with what seniors have signalled as being legitimate sources of support (including guidelines), as well as how and when these should be used (O), out of fear of criticism and so that they appear as competent trainees and good doctors (M).
Context–mechanism–outcome configuration 7
In contexts in which guidelines and local policy are not consistently used and have not been clearly approved by one’s peers and senior colleagues (C), doctors in training feel that to fit in with their team and avoid conflict (M) they should adhere to the prevailing prescribing practices of their seniors rather than following guidelines or local policy (O).
Context–mechanism–outcome configuration 8
In the context of having to make an antimicrobial prescribing decision when guidelines are available (C), doctors in training feel that to fit in with their team and avoid conflict (M), they should follow their seniors’ acceptance (or not) of guideline use (O).
Relevant extracts from papers included in the review
‘[. . .] what really is the law of the jungle is that whatever your senior says goes and that evidence and best practice (. . .) is never completely realised (. . .) that’s quite challenging.’ (Foundation Year 1 doctor)
A third theme in our interviews was the strong influence senior staff had on resident physicians’ antibiotic prescribing decisions. Studies from the United Kingdom, Ireland, and Belgium also identified senior opinion leaders as important determinants of antibiotic prescribing practices, superseding the influence of local policy.
Supervisor behaviour also impacts on this process. Some registrars see their supervisors prescribing contrary to guidelines, and find this a challenging dynamic to negotiate, mainly because of a differential of power and experience between registrar and supervisor. This tension between ‘experience and evidence’ and managing the complexities of relating within a hierarchical medical culture are a common experience for the doctor in training.
[. . .] there is a dichotomy between the organizational expectation from juniors to follow official policy and the social and contextual norm of adhering to ‘prescribing etiquette’ set by one’s senior colleagues in their clinical groups, as the evidence in this study suggests.
Hospital policies aimed at influencing the antibiotic prescribing behaviours of junior physicians had limited effectiveness because of the social norm of adhering to the ‘prescribing etiquette’ set by one’s seniors.
Particularly unexpected was the finding that local knowledge sources, especially colleagues’ opinions, were perceived as more effective in modifying prescribing behavior than national guidelines. In fact, many providers cited specific individuals and explained how their research or opinions directly influenced their antibiotic prescription practices.
Peer approval is one of the essential rules in the successful implementation of interventions [. . .]. Whereas nurses and pharmacists reported a reliance on policy to help promote compliance of junior doctors to evidence-based practice, doctors reported adhering to policy only if it was endorsed by peers from their own specialties and clinical groups.
[. . .] locally developed guidelines for antimicrobial treatment are more useful than national guidelines. These perceptions suggest that guidelines promoted by ASPs [Antimicrobial Stewardship Programmes] are likely to meet with more success if they take into consideration local practices and patterns of resistance.
Less experienced doctors may prescribe more appropriately according to guidelines, but develop behaviours and prescribing habits similar to their supervisors as training progresses.
This demonstrates how prescribing protocols and evidence-based medicine do not always determine doctors’ performance. Sometimes a particular consultant’s preferences carry more weight than formal regulation. We termed this ‘contingent performance’.
Perceptions of guideline credibility and use
Within included documents, we found a number of other influences on doctors in training and senior perceptions of guideline credibility and use, such as, for example, previous experiences with patient outcomes when using guidelines, confidence in the process of guideline development, whether these are national or local, and whether or not the guidelines are seen as up to date. However, for doctors in training, the over-riding consideration seems to be what would be considered appropriate by the senior clinician(s) who they are accountable to, who signals whether guidelines should be followed or if a different balance between experience and evidence should be sought.
Realist analysis
Context–mechanism–outcome configuration 9
When deciding whether or not to follow a guideline on antimicrobial prescribing (O), senior clinicians make judgements (M) about guideline credibility, such as a rigorous development process (C), peer approval (C), source of the guideline (C), recency (C) and coherence with own experience (C).
Relevant extracts from papers included in the review
[. . .] determinants of why respondents trusted guidelines were: observing that the recommended practice worked, knowing that the developers had ‘looked into it, researched it, used evidence-based practice’ [. . .], observing more senior doctors using guidelines, and if the guideline was recent (i.e. in-date).
‘I think that the current policy is rational. The decision was made by a subgroup within my specialty, composed of people whose judgment I respect and chaired by people whose judgment I respect and I’m very happy to comply with the decisions that they make.’ (Senior Doctor, Renal Medicine)
Senior doctors will overrule policy as they consider it subordinate to their knowledge and clinical experience that is gained over their years of practice – this pattern only gets reversed if the policies have the clear endorsement of senior peers within their own clinical groups. This is indicative of the role of hierarchy in influencing practice [. . .]
The reported acceptance of noncompliance of senior staff with local policy is another element of prescribing etiquette. This noncompliance is justified first by recognition of the experience and expertise of senior staff and second, by a broader definition of ‘evidence base,’ which includes personal experience of individuals and the perception that policies are for the ‘average’ cases. Personal experience/expertise seems to win over evidence-based policies and guidelines.
A clear distinction between the antibiotic opinion leaders and other members of staff, together with clear communication on the reasons to divert from the guideline, is of primary importance and could be an effective intervention.
Consequently education about guideline content was unlikely to change behaviour unless it was accompanied by regular feedback about doctors’ adherence to key guideline recommendations.
Figure 6 consolidates the data presented in CMOCs 6–9 to summarise the influence of hierarchies on perceptions of guideline credibility and acceptability, and on the prescribing behaviours of doctors in training. 10,35,60,62,63,68,70,73,79,88,92,96,98–113
FIGURE 6.
Partial programme theory (CMOCs 6–9).
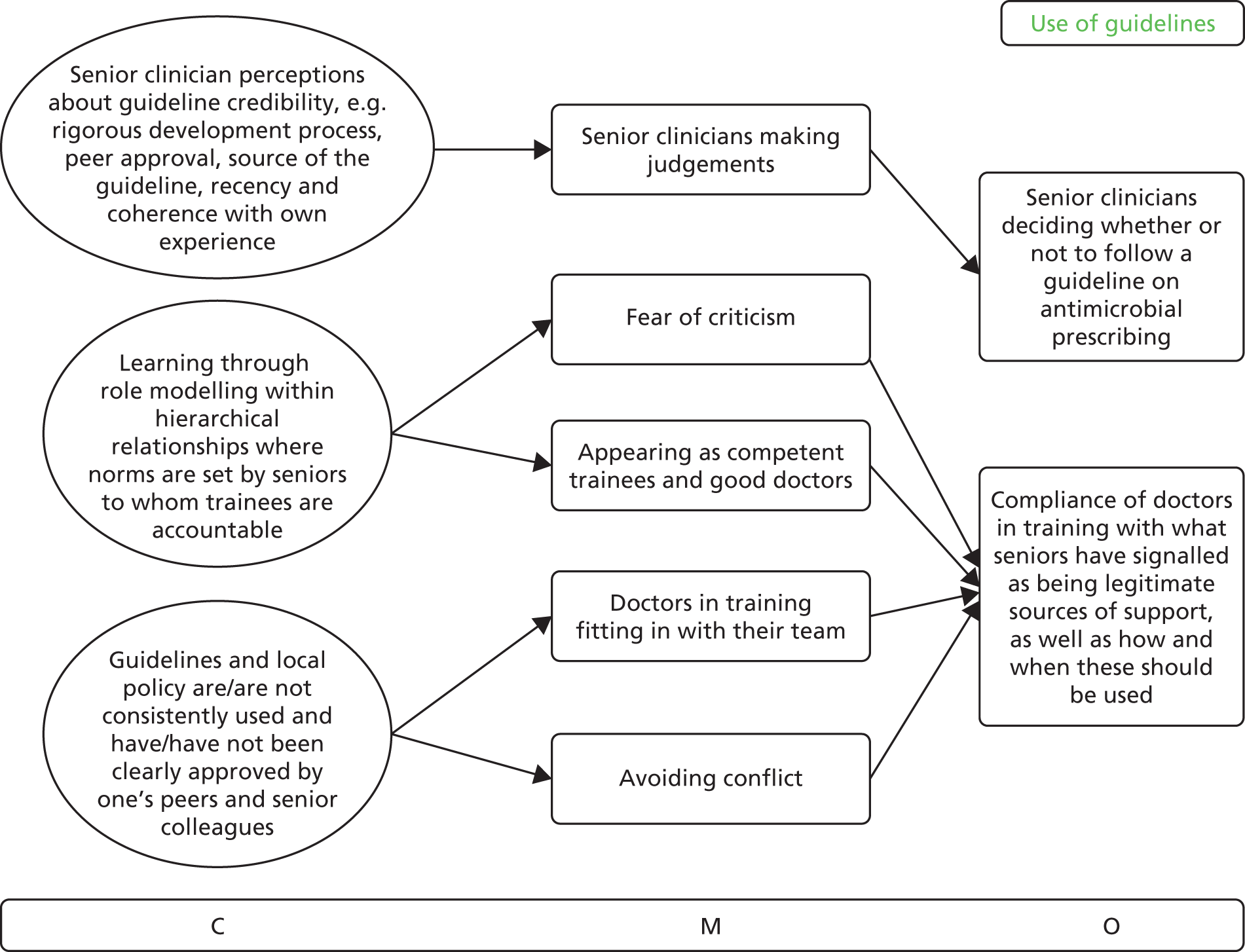
Influence of patient expectations
We found conflicting data in the literature about whether or not patient expectations influence the prescribing behaviour of doctors in training. 62,63 The way seniors negotiate patient expectations also seems to play an over-riding role in how doctors in training decide to respond to perceived patient pressures to prescribe antibiotics. When patients have received an antibiotic prescription for similar symptoms by the physician supervising the trainee, the ‘rules’ or norms for such consultations have been set so that the patient expects the same treatment. It would be perceived as challenging by the trainee to make a different decision and not comply with the prescribing behaviour of their superior. This dynamic appears to be more prevalent in primary care settings, in which relationships with patients are more direct and ongoing than in hospital-based care.
Realist analysis
Context–mechanism–outcome configuration 10
In a context of perceived patient pressures (C), junior doctors will follow the example of their seniors in the way they negotiate patient expectations and the rules already set by them in terms of what patients should expect (O), because of their need to be seen as equally as competent as their supervisors, fit in with their team and avoid creating conflict (M).
Relevant extracts from papers included in the review
There was evidence that participants sometimes felt under pressure to prescribe antibiotics, when they did not feel that they were necessary, from both nursing and other ward staff, and from patients and their relatives.
‘I do know one supervisor [in primary care] in particular will give his patients antibiotics even for something that sounds very viral, and therefore when I see his patients, I feel I’m expected to do that as well, because his patients have been seeing him for many years. So they expect it too, so I’m definitely more likely to give his patients antibiotics even when I don’t think it’s justified.’ (Registrar)
GP [general practitioner] registrars have been sent emails to say that they should prescribe antibiotics, because that’s what patients expect, but that’s coming down from the older generations. (Registrar)
‘We’ve created an expectation in the population. They come asking for antibiotics, ‘cause the last three times they came, they were told they needed them. So they come time number four and say, “I’m here for my antibiotic.” And we think they’re crazy. When in reality, it’s like no, we trained them to come back and get an antibiotic.’ (Attending, male, 11 years)
‘It’s almost like opiates. When the physician is just so beaten down that they don’t want to argue anymore with the patient. We all want to be that person who has that hard discussion and educates the patient, but sometimes it’s really hard to do that.’ (Attending, female)
[. . .] the pressure to ‘conform with perceived patient preferences’ rather than follow clinical guidelines [. . .]
[. . .] the patient has been given antibiotics in the past for similar presentations, thus the registrar questions their clinical acumen in the current situation.
Physicians report that they prescribe unwarranted antibiotics because patients expect to be prescribed antibiotics, because patients bounce from physician to physician if antibiotics are not prescribed, and because it is quicker to write a prescription than to explain why the antibiotics are not indicated.
Learning communication skills and confidence to build therapeutic relationships was perceived to improve also: ‘I think initially I was probably a lot less confident to say to patients no, and I think now it’s become a lot easier because I’m not afraid that they’re going to hate me and never come back’. (Registrar)
Influence of antimicrobial specialists
Besides the role of guidelines and patient expectations, senior doctors also role model how the opinions of other health professionals should be taken into account in terms of antimicrobial prescribing. By creating a legitimate role for other health professionals in the prescribing process, senior doctors signal to their trainees what is appropriate behaviour to follow, whose opinions count, in what cases and to what extent.
The literature describes cases in which doctors in training feel conflicted between the opinions of their seniors and other members of their interprofessional team or their own judgement, which becomes a difficult dynamic for them to handle. Our interpretation of the data in included documents was that junior doctors, especially in their early years, have not yet become familiar enough with the norms and conventions of the setting to know how to effectively reconcile different opinions or what the hierarchy indicates as the legitimate opinion to follow. Strategies that doctors in training appeared to employ in response were to follow/comply with the opinion of the person who is closest to them (i.e. a peer) or the person or team they feel they are most accountable to (at a given point in time or for the care of a specific patient).
Realist analysis
Context–mechanism–outcome configuration 11
In a context in which senior doctors set the norms about perceived legitimacy of antimicrobial prescribing advice from other health professionals (C), in an attempt to avoid conflict and be perceived as a competent trainee (M), doctors in training follow the example of their seniors in the way they take into account the professional opinions of others (O).
Context–mechanism–outcome configuration 12
When doctors in training find themselves in conflict about whose opinion to follow (C), they tend to follow the plan suggested by the person (O) to whom they feel most accountable (M) within the medical hierarchy.
Relevant extracts from papers included in the review
‘I had a similar case where a registrar prescribed a certain antibiotic and the pharmacist came up to me and said ‘these aren’t antibiotics that should be given’ and so I went and found the registrar and told him and he said ‘no keep them on’ but the pharmacist kept chasing me and I was like ‘no [laughs] do what the registrar says’. (Female Foundation Year 1 doctor)
This set of unwritten rules, or ‘prescribing etiquette,’ dictates not only the prescribing behavior of doctors but also how other healthcare professionals (i.e., pharmacists and nurses) view and exert influence on the antimicrobial prescribing, administration, and monitoring processes.
Senior doctors rely on their own professional judgment and the need to freely choose what they judge to be the most appropriate when prescribing antimicrobial prophylaxis or treatment [. . .]. This may involve making antimicrobial prescribing decisions that overrule infection specialist advice [. . .]
And the number of times you felt like a piggy in the middle. You were being batted backwards and forwards. At the end of the day you’re just trying to do the best for the patient who is outside your expertise. (Female, early-stage GP trainee)
Differences of opinion between senior colleagues on prescribing issues, usually consultants and other experts (e.g. microbiologists and pharmacists) disagreeing about an off-protocol drug, presented FY [Foundation Year] doctors with a dilemma: they often had to choose whose ‘side’ to take (12 mentions) and felt stuck in the middle (23 mentions [. . .]).
Interprofessional influence and support
The findings section has already established the importance of hierarchies in signposting what sources of support to use for antimicrobial prescribing, especially with regard to taking advice from other health professionals. As evidenced by the excerpts presented in the above sections, a large part of the literature argues that it is the opinion of the senior doctor that counts when it comes to antimicrobial prescribing decisions. There are, however, some contexts where interprofessional supervision (when relative status differences are more ambiguous) and contribution may also play an important role. For example, as the following quotations illustrate, newly qualified doctors who have not yet fully embraced the norms of their clinical setting may turn to the pharmacist as a source of support external to the medical hierarchy, as doctors in training will feel less fear of appearing ignorant or negative repercussions (e.g. see quotations 1–3). Pharmacists, nurses, microbiologists and infectious diseases specialists are deemed important, especially when it comes to ratifying decisions against local practice, deciding on de-escalation or rationalisation, or clarifying details about dose and duration. 35,58,62,70
Realist analysis
Context–mechanism–outcome configuration 13
If accountability relationships within the medical hierarchy do not specify what the rules or expectations are (C), or in cases where these rules have not yet been internalised by the doctor in training (C), there is greater willingness to seek help and/or advice from health professionals outside the immediate medical hierarchy (O), as doctors in training do not fear that their perceived ignorance might have an impact on their reputation and position in the hierarchy (M). This dynamic seems to be stronger when the input of other health professionals is legitimised by seniors in the medical hierarchy.
Relevant extracts from papers included in the review
‘[. . .] I mean I think the junior doctors actually are sometimes quite glad to see us because they often want advice on what to do with . . . how to prescribe certain drugs because they often don’t know, especially the brand-new qualified doctors [. . .].’ (Pharmacist, Respiratory Medicine)
Within the context of hierarchy and autonomous decision making, there may be a limited tacit influence on prescribing behaviors of doctors from nurses and pharmacists [. . .]. This influence may be transient, only limited to the behaviors of the more junior doctors, and only valid in situations where there is no conflict with the opinion or direction of senior medical staff, in which case the latter prevails: ‘Consultants. Those are the people who we listen to. It’s partly because we know the hierarchy, from the doctor’s side of things.’ Junior Doctor, Accident and Emergency.
[. . .] pharmacists were listed in the survey and acknowledged by the JMOs [Junior Medical Officers] as an important information source.
‘. . . although everyone was kind of looking at me . . . I noticed that one of the nurses was managing to get through to the patient and kind of getting him to listen . . . and I thought, I think ‘this is when I should be quiet and let this nurse deal with it’ and I just did what the nurse said . . .’ (Female, foundation trainee)
There exists a social network within which antimicrobial prescribing decisions are made, and healthcare professionals report awareness of the need to work within this network in their specialties. [. . .] The rule of ‘noninterference with the clinical decisions of others,’ despite the existence of local policies guiding antimicrobial prescribing, is an example of the influence of this social network on behaviors.
There is a clear sense of affiliation of healthcare professionals to clinical groups and specialties in which they work: that is, the local social network within specialties acts as a strong determinant of antimicrobial prescribing behaviors. Outside of their own autonomous decision making, healthcare professionals are happy to comply with practice that is a marker of their clinical group or identified social network [. . .].
Figure 7 provides an illustration of CMOCs 10–13 about responses to perceived patient pressures and to receiving conflicting advice from different health professionals. 10,35,43,56,58,59,62,63,69,70,73,79–81,91,97,98,114–116
FIGURE 7.
Partial programme theory (CMOCs 10–13).
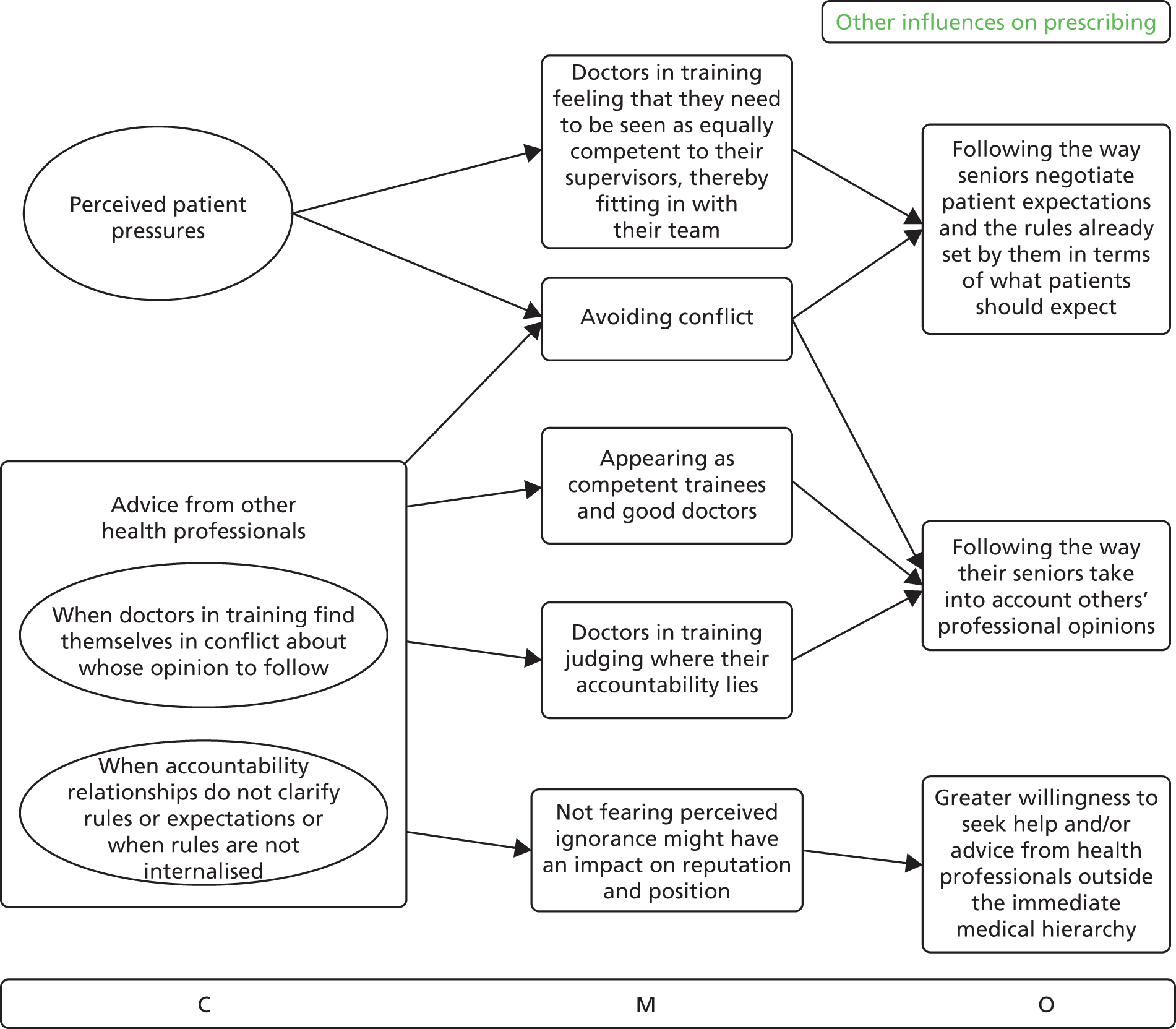
Influence of optimal role modelling
The literature further describes positive aspects of hierarchies as supporting junior doctor decision-making and contributing to effective care. Role modelling may result in positive learning when, for example, senior doctors follow appropriate prescribing behaviours and clearly explain the rationale of their decisions (e.g. how these correspond to the evidence base or why they diverge based on specific patient needs). This would allow trainees to make appropriate choices in their prescribing and draw useful learning to increase their confidence with using antibiotics.
Optimal role modelling also means explicitly setting the rules about how hierarchical relationships operate in different environments and how trainees should expect to be embedded within them. This extends to antimicrobial prescribing as role modelling and would signal how the rules of engagement operate, that is, how to go about making prescribing decisions and whom to consult. Clarity around sustaining positive relationships in the prescribing environment and around the antimicrobial prescribing responsibilities of doctors in training at different levels would provide additional support. This would involve setting explicit support processes, cognisant of the limitations and skills of doctors in training at different levels. Signalling how much a trainee would need to know at different stages of training appears to reduce uncertainty and result in a common and more productive understanding about rules of engagement and expectations. A wider emphasis on ongoing learning, recognising that even senior doctors require support to negotiate the boundaries of professional autonomy in their prescribing decisions (recognising fallibility and role modelling humility), would underpin optimal role modelling.
Realist analysis
Context–mechanism–outcome configuration 14
In the context of hierarchical relationships where the value of ongoing learning at all levels is emphasised (C), the rationale behind decisions is sufficiently explained (C) and the boundaries of knowledge and responsibility are clearly signposted (C), trainees feel less uncertainty about their role (M), are better able to gauge whose expectations to fulfil (M) and become more confident in how to approach antimicrobial prescribing (and other) decisions (O).
Relevant extracts from papers included in the review
. . . it’s all about the culture of teaching within the firms so it’s about all of the senior doctors not just rushing through a ward round and just shouting out “prescribe this, prescribe that” it’s about them saying “I am thinking of prescribing this and this is my rationale, what do you think” or “let’s go for this because of this – do you understand why I’ve done that?” ’ (Female Foundation Year 2 doctor)
‘The fact that I work in an academic facility with residents, fellows, faculty that are always going to ask why did you use that? Why couldn’t you have just used this? That is always staying in the back of my mind that I need to be able to clearly defend my decision to use an antibiotic in a given situation.’ (Attending)
Our study also highlighted the importance of feeling supported and appropriately supervised in building trainees’ confidence. The role of the trainer was pivotal here, with a positive and honest relationship fostering confidence through appropriate support and challenge while effective teaching supported the development of varied consultation skills [. . .]
Nineteen interviews discussed medical hierarchy, which sometimes worked well, with consultants leading important decision making but enabling juniors to take part.
Unarticulated rationales for senior clinicians’ prescribing decisions were enormously frustrating and sometimes time-wasting when F[oundation] Y[ear] doctors could not defend decisions made [. . .].
Clinical supervisors are key and should, we suggest, clarify their expectations in three ways. Firstly, consultants should be explicit about when and whom to ask for help. Secondly, supportive and constructive feedback on all decisions – good, bad and borderline – must accompany the omnipresent ‘reassurance’. Such discussions may lead to detection of near-misses and errors. Most juniors are motivated to learn from error and this reduces their distress. Thirdly, supervisors must ensure that juniors have an appropriate level of confidence and accept an appropriate level of responsibility for errors. Overconfident doctors with low self-criticism may lack insight, be unaware of their limitations and blame others when errors occur, whereas highly self-critical doctors may become disillusioned and depressed after error and grow increasingly detached from patients.
Suboptimal role modelling
Conversely, role modelling in hierarchical relationships may result in the reinforcement of suboptimal prescribing habits and prescribing etiquette(s) if rules remain implicit or are only enforced through authority and the rationale is not clarified to facilitate learning. This may result in trainees blindly following the decisions of their seniors (1) as a result of fear of criticism and reprimand or (2) because they believe that the productive relationship they have built with their senior on the basis of respect and trust may be jeopardised if they are seen as questioning decision-making autonomy.
Having to work under many different senior clinicians may have negative results when trainees feel uncertainty about how to manage relationships with multiple seniors in combination with their learning, but could also have positive results, as having multiple relationships with different people could lead to more opportunities to ask questions without thinking that this will have an impact on performance assessment.
The above points to the importance of explicitly and actively setting expectations when working with more junior members of a team, even if this will be only a brief relationship, signalling that trainees are expected to ask either their seniors or other health professionals about prescribing decisions rather than make assumptions.
Realist analysis
Context–mechanism–outcome configuration 15
In the context of role modelling within hierarchical relationships where rules remain implicit (C), trainees blindly follow the decisions of their seniors without asking about the rationale (O) because of fear of criticism and reprimand (M), or because they wish to avoid upsetting the relationship they have built with their supervisor (M).
Relevant extracts from papers included in the review
When confronted, staff members [senior clinicians] acknowledged being of great influence but sometimes giving bad examples [to junior clinicians . . .].
Another registrar described an interaction with her supervisor whom she had asked for advice regarding a diagnosis, and then was uncomfortable with their suggestion to prescribe an antibiotic: ‘I think in the back of my mind ‘I don’t know everything, maybe they’ve seen something like this before and it has been bacterial.’ I guess I’m just assuming that they have some kind of clinical knowledge that I don’t.’ (Registrar)
‘[Doctors] may have more information that I’m not yet aware of which may then mean that actually it is entirely appropriate.’ (Pharmacist, Medicines for the Elderly)
They [trainees] are expected to follow the usually unwritten rules of each of their ‘bosses’ and to take instructions. This results in inadequate communication, fragmented supervision, inadequate instructions, and more frequent suboptimal patient outcomes.
‘. . . a consultant who didn’t come up to the ward . . . when he did come up he was never that fussed if you were with him or not . . . he would just leave you a list of things to do . . . it was a bit disheartening . . . you were never . . . completely reassured about what you were doing . . . you never really get to grips with his actual overall plan . . . so you end up not feeling that important part in a team because it doesn’t matter if you were there or not . . . you’ve to follow blindly what he wrote . . .’ (Male, early-stage medical trainee)
Participants reported negative interactions with authority that resulted in a profound loss of commitment. Residents described experiences and personal interactions as profoundly negative, leading to an inability to function and a loss of joy and investment in their work. Also, participants voiced the desire for recognition. They reported their roles being perceived as insignificant, and they felt devalued.
Negative experiences included seniors not being supportive or available, being unnecessarily critical, having unreasonable expectations and undermining confidence [. . .] most comments about hierarchy were negative, with associated poor team relations and treatment delays [. . .].
‘On the first day of my residency I came in very early, drew up all the medications I thought would be appropriate for the first patient. My staff anesthesiologist came into the OR [Operating Room] and asked if those were my drugs, I said yes. He proceeded to throw them in the garbage and didn’t talk to me until after lunch. That was my first day of residency.’ (Resident)
The impact of service needs versus learning priorities
Hierarchical relationships, in which the rationale for prescribing decisions is rarely discussed, are often characterised by a culture of using doctors in training to provide service rather than prioritising their learning needs. Learning seems to be organised in ways that primarily fit in with the needs of the medical service and administrative work, that is, the needs of the hierarchy and the hospital structure, emphasising the short-term accomplishment of tasks against the long-term educational benefits for doctors in training. This communicates an understanding of what being a good doctor in training means: one who manages to provide care according to requirements (e.g. making fast and accurate decisions, processing quickly, remaining at the disposal of their seniors), rather than someone who manages their work in a way that fulfils their learning needs. In this context, expectations of doctors in training regarding their education are often not met adequately, which creates frustration and difficulties in managing the learner/practitioner role without appropriate support. This is particularly highlighted in more recent literature looking at the role of doctors in training in health-care settings.
Given this perceived gap between learning and service provision, explicitly supporting doctors in training in managing what appear to be conflicting priorities becomes critical. Explicitly explaining that learning is possible alongside service is important. For example, when doctors in training participate in patient care, senior clinicians can explicitly highlight learning opportunities when they provide their decision-making rationale and clarify that support is available without fear of reprimand.
Realist analysis
Context–mechanism–outcome configuration 16
In a context in which doctors in training perceive service needs to be prioritised over learning (C) and view routine patient care as separate from and in conflict with education (C), they experience difficulty and frustration with reconciling their dual learner/practitioner role within the hierarchy (M), which results in dissatisfaction (O).
Relevant extracts from papers included in the review
Yet, MRs [Medical Residents] argued that it is quite impossible to adequately combine the educational and the professional dimensions of their role. [. . .] Working overload thus makes it difficult to manage the learner and the professional role, and questions their planning efforts. This situation is all the more difficult that it is hardly acknowledged by other health care professionals [. . .].
Teaching sessions were seen as a conflicting priority for trainees and, while they are compulsory sessions, doctors often commented that the subject matter was not relevant to their needs. One doctor said that ‘I was quite disappointed with the teaching programme . . . much time was given over to audit, ethics, law, protocols etc. . . . insufficient time [was] spent on learning & developing clinically . . . ’[. . .]. Training was sometimes ‘interrupted by consultant bleeps [beeps/pager alerts] which you cannot reject’ [. . .]. One doctor remarked that the NHS treated junior doctors as ‘service providers, without investing any time in our welfare or future training’ [. . .]. Another felt that doctors ‘must be educated and given the opportunity to develop as doctors, not as a combined clerical and clinical support worker’ [. . .].
[Residents] expressed concerns about being placed in situations in which inappropriate expectations were being placed on the care that they were going to provide or in which the supervision was inappropriate [. . .].
Figure 8 provides an illustration of CMOCs 14–16 on optimal and suboptimal role modelling, including perceptions of trainees about their dual role as both practitioner and learner. 10,35,43,62,63,68,72,73,77,78,81,83,99,115,117–131
FIGURE 8.
Partial programme theory (CMOCs 14–16).
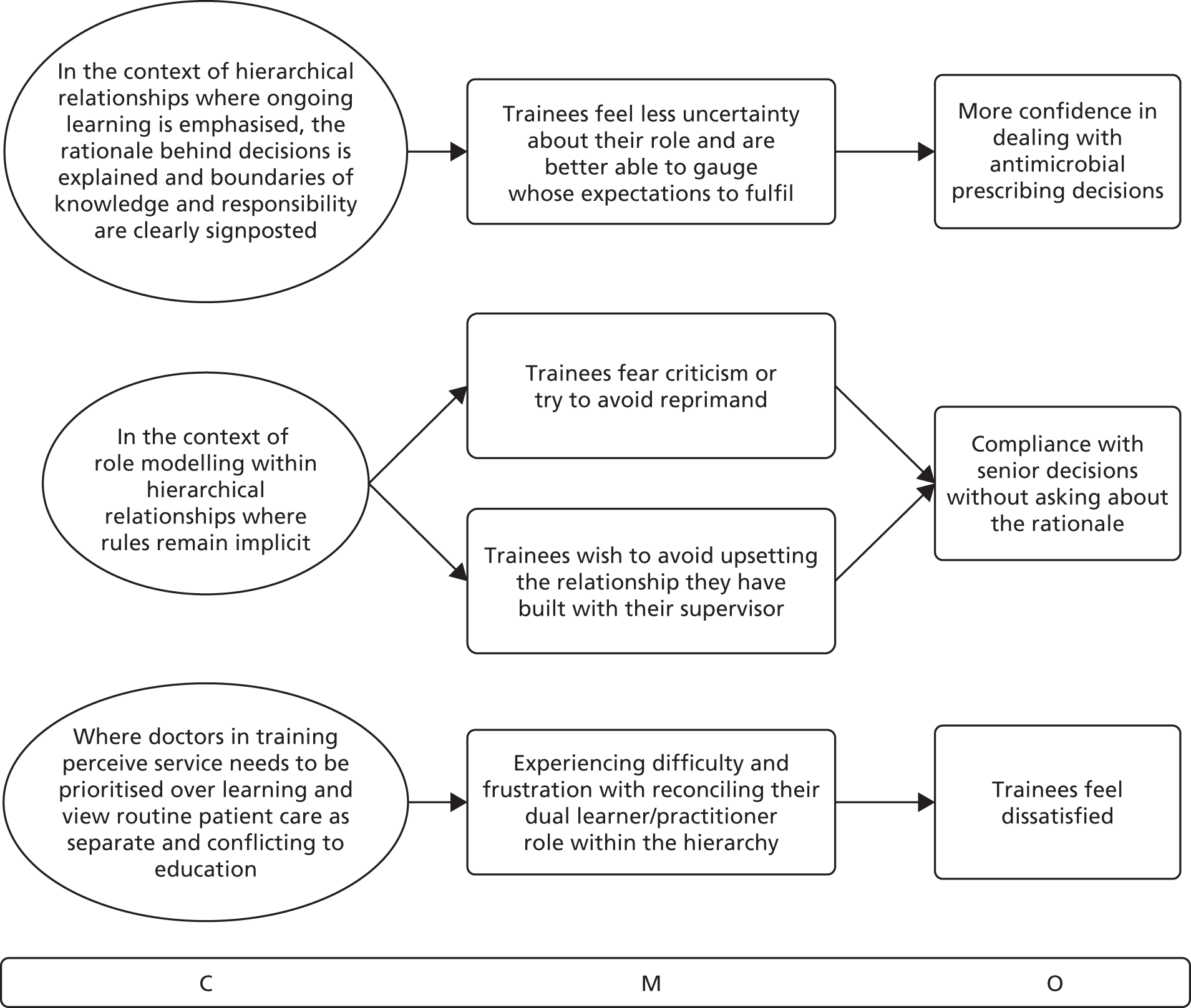
Part B: asking for advice and challenging decisions
Seeking assistance
In hierarchical environments, rules on how to interact with other health-care professionals, and on how to effectively apply knowledge to practice at different training levels, often remain implicit (or unspoken). As a result, doctors in training face difficulties navigating relationships with health professionals who could provide them with assistance. Asking for advice becomes particularly challenging when supervisors role model behaviours that rely on their own individual decision-making rather than engaging with other health professionals:
‘We’re not very good at asking each other for help, are we? . . . as a consultant I’m not good at asking for help; I’ve been in the resus [resuscitation] room and thought I could really do with a help and hadn’t realised it until really you’ve been with the patient too long.’ (Senior doctor)
The literature suggests that in cases where the condition of the patient is perceived as serious or unusual, doctors in training feel more justified in seeking assistance from their seniors. This is because it is clearer to the doctor in training that these cases exceed the boundaries of knowledge of a trainee, which means it would be appropriate behaviour to contact other (often more experienced) health professionals. In this way, doctors in training enact what they perceive to be their position in the hierarchy and show that they are competent enough to understand the boundaries of their knowledge and responsibility.
Literature sources also describe a ‘hierarchy of assistance’ whereby trainees make judgements about which health professionals they would be justified in contacting. 132 There is mention of trainees contacting health professionals for assistance with particular types of decision (e.g. antimicrobial selection), but relying on reference sources for questions such as dosing. This could indicate that trainees make judgements not just about whom to ask assistance from, but also about the types of questions that would be deemed justified in the context of their own abilities at different levels of training.
Having decided to seek assistance, doctors in training often find that they need to manage the way they ask questions carefully by employing ‘rhetorical strategies’, as described in the literature. 133 This is done in order to negotiate the norms of hierarchical clinical environments in which doctors in training perceive their performance to be assessed by means of appearing professionally autonomous. Trainees perceive that, to fulfil what is expected of them in the clinical setting, they need to manage their need to learn from their seniors in a way that fits in with the wider professional culture (e.g. not seeking help inappropriately or in ways that may be perceived by others as challenging decisions). This means that trainees often use specific communication strategies and rules of thumb to maintain their reputation as competent learners and team members. Such behaviours help them to sustain relationships with their seniors in the hierarchy without fear of appearing threatening, stupid or weak, or losing respect (e.g. ‘this may be a dumb question’: opening statement of a junior doctor when asking a senior for help). 116
Realist analysis
Context–mechanism–outcome configuration 17
In hierarchical relationships in which rules of engagement and boundaries of knowledge remain implicit (C), out of fear of appearing ignorant or incompetent (M) and fear of losing the respect of their seniors (M), doctors in training often avoid asking for assistance with patient management from seniors they are accountable to (O).
Context–mechanism–outcome configuration 18
When deciding whether to seek assistance and from whom within the medical hierarchy to seek it, (C), doctors in training make judgements (M) about: (1) the condition of the patient (e.g. if critical or unusual enough); (2) whether or not it falls within their remit of what they assume to be their responsibility and knowledge; and (3) the consequences of seeking assistance from particular colleagues, in order to preserve their position in the hierarchy (O) (which may result from asking or not asking for assistance).
Context–mechanism–outcome configuration 19
When deciding what to seek assistance on (C), doctors in training make judgements (M) about the types of questions they perceive as being justified to prioritise and against what they assume they are expected to be able to manage on their own according to the norms set by their seniors, in order to preserve their reputation and status in the hierarchy (O).
Context–mechanism–outcome configuration 20
When deciding how to seek assistance (C), doctors in training make judgements (M) about the types of strategies they perceive as being acceptable according to the norms set by seniors in different clinical settings, in order to avoid looking ignorant (O) and to preserve their status in the hierarchy (O).
Relevant extracts from papers included in the review
We found that residents in our study were concerned about appearing incompetent in front of those with more power and they were hesitant to communicate information that was unfavorable or negative to themselves. A resident does not want to appear ignorant about a patient. He or she wants to appear knowledgeable about the medical condition and about the patient in particular, and to present pertinent but not unnecessary information. [. . .] ‘You can’t be afraid to or ashamed to ask for help’. (Resident)
There may be uncertainty about local custom and practice, there may be a reluctance to admit ignorance and seek advice, there may be hierarchical obstacles to communication among medical colleagues and in the end the junior doctor may simply take a guess.
The protocol for phoning on-call staff was often unclear (e.g. who to call and what to check first) and sometimes resulted in a reprimand for phoning [. . .] ‘I went to the registrar who wasn’t a renal registrar he was the registrar on-call overnight and he didn’t know so he asked me to phone the microbiologist on-call and this was at about 5 o’clock in the morning and so I had a double check for half an hour and made sure there was nothing in there [the British National Formulary and guidelines] and eventually phoned the microbiologist and I think that she was incredibly angry with me over the phone about me the most junior member of the team was calling her at 5.30 in the morning to ask advice’. (Female Foundation Year 2 doctor)
The most common reason to use an external resource was for antimicrobial selection, and for this decision prescribers usually consulted with another physician or pharmacist (57 of 81, 70%). The second most common reason was to decide on the proper dose, and for this decision, prescribers usually consulted a nonhuman resource (38 of 55, 69%).
[. . .] lack of approachable senior support for inexperienced junior staff [. . .] when you’re starting, it’s really intimidating to try and find the Reg. [Registrar] on-call about what he thinks about their patient, so therefore you kind of leave it and wait for the ward round [. . .]
In managing uncertainty, residents report a ‘hierarchy of assistance’, using colleagues and literature for initial management, followed by senior residents, specialty fellows and, finally, the attending physician.
Trainees’ decisions about whether or not to seek clinical support were influenced by three issues: the clinical question (clinical importance, scope of practice), supervisor factors (availability, approachability), and trainee factors (skill, desire for independence, evaluation) [. . .] and the perceived impact of their request on their professional credibility.
Figure 9 summarises CMOCs 17–20, consolidating data on assistance-seeking behaviours by doctors in training. 43,58,59,66,68,72,80,81,94,95,116,118,123,124,132–138
FIGURE 9.
Partial programme theory (CMOCs 17–20).
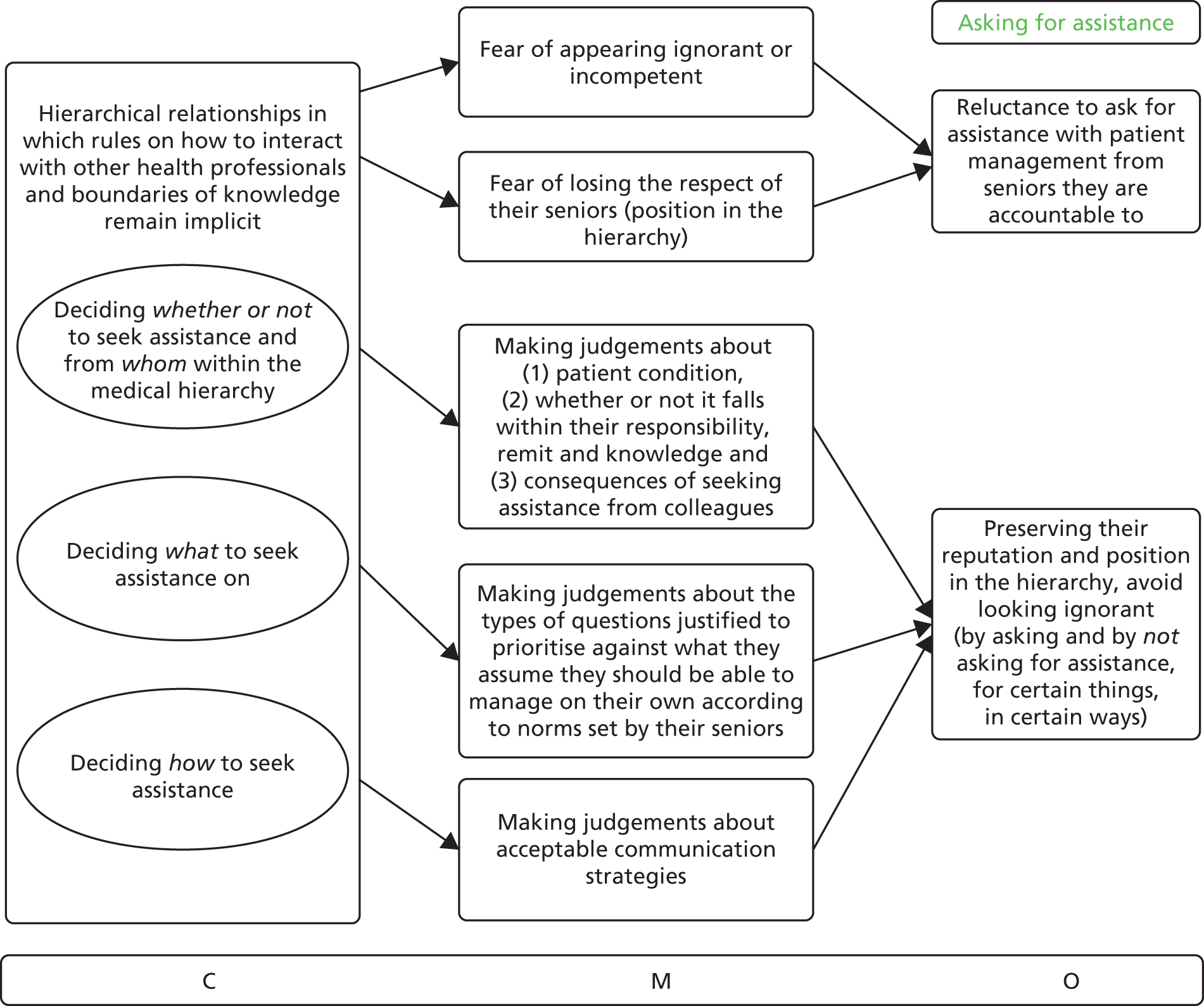
Challenging prescribing decisions
In hierarchical environments in which rules of engagement remain implicit, doctors in training are reluctant to challenge senior decisions about patient management, out of fear of rejection and embarrassment (e.g. ‘critiquing one’s colleagues can be awkward’,70 ‘fear of being stigmatized and being weak’119). The literature discusses how reluctance to challenge stems from the belief that it is unlikely that the consultant will change their decision, that any error would not be major enough to result in direct patient harm and that it would be more appropriate for someone else at a different position in the hierarchy to identify and intercept the error.
In terms of antimicrobial prescribing, this reluctance to challenge also relates to perceptions about what constitutes harm in clinical settings. According to the data presented in the literature, the longer-term outcome of AMR is currently not prioritised as highly as other issues. Doctors in training believe that it would be futile to challenge antimicrobial prescribing decisions made by their seniors, first, because it would be unlikely that the decision would change and, second, because there would be little opportunity for feedback on whether or not they were right to challenge in the first place. The only opportunity to judge whether or not their challenge was right would be if certain side effects manifest, changing the short-term benefit/harm balance on an individual patient basis.
When it is difficult to judge whether or not a medical decision is correct (delayed consequences of an action or higher diagnostic uncertainty) or when doctors in training feel unsure about their own knowledge, a significant mechanism is the fear of being wrong in one’s challenge, which will result in embarrassment. Under these circumstances, data from included documents indicate that doctors in training are less likely to challenge the decisions of others, especially those higher in the hierarchy, which results in compliance with persisting prescribing patterns and reinforcement of the status quo.
When in long-standing hierarchical relationships with senior members of staff, trainees avoid challenging out of fear of upsetting established relationships and the perceived impact on their reputation, as some sources suggest. However, in other data it is noted that doctors in training would not question a consultant’s decision, even if that consultant was previously unknown to them. Respect for consultant authority is a prevalent norm of practice in clinical settings, and actively showing respect for seniors by not challenging their decisions allows doctors in training to avoid conflict and fit into the hierarchical culture.
Realist analysis
Context–mechanism–outcome configuration 21
In hierarchical environments where power relationships are emphasised and rules of engagement remain implicit (C), out of fear of rejection and embarrassment (Ms), doctors in training often avoid challenging senior decisions even if they know that something is wrong (O).
Context–mechanism–outcome configuration 22
When deciding whether or not to challenge a decision (C), doctors in training make judgements about the level of diagnostic uncertainty and the likelihood of being wrong in their challenge (M), to ensure that they do not upset professional relationships and lose their position in the hierarchy (O).
Relevant extracts from papers included in the review
‘If the attending wants him [the patient] to be on that antibiotic, usually I do not put [forth] a big argument unless I feel very, very strongly. Usually I ask, ‘Why? What is their rationale for being on that antibiotic?’ But if they give a reason I am not going to argue too much’. (Resident interview)
[M]any residents and staff physicians admitted that they would not provide direct critique of their colleagues’ antibiotic prescribing habits. One commonly cited obstacle to feedback was a respect for hierarchy: ‘If it is another resident in my equal level of training or somebody higher, I would be less inclined to question their antibiotic view’ (resident). [. . .] They did not want to ‘offend’ a colleague or harm a ‘good collegial relationship.’ While a physician’s decision to prescribe an antibiotic may seem questionable in hindsight, participants recognized that the clinical circumstances may have been less clear-cut at the time the decision was made to initiate antibiotics. In addition, critiquing one’s colleagues can be awkward: ‘You’re not going to teach someone who is senior faculty about MICs [minimum inhibitory concentrations] and sensitivities and specificities . . . or tell them to go back and read a book . . . It’s just not going to happen’. (Staff)
[. . .] a communication problem exists as a large proportion of residents indicated that their opinion had been discounted before by attendings and that they often would not speak up even though they knew something was wrong.
One resident told the interviewer of a conversation he had with his father (who was also an anaesthesiologist). Resident: ‘He said to me, the lesson I want you to always learn is that to swallow your pride, just go with whatever they [the consultant anaesthesiologists] say and don’t be argumentative. So, that is definitely always there in the back of my mind’.
[. . .] some saw hierarchy as protecting junior doctors, and therefore facilitating disclosure by some residents, whereas others highlighted how hierarchy inhibits residents from reporting errors committed by attending physicians.
Participants perceived a culture in which disagreement or open expression would be frowned on: ‘. . . surgery residency is similar to the military. Everything is really hush, hush. No one wants to tell the truth and be out in the open about what is going on. They want to say what directors want to hear for fear of being stigmatized and being weak. You cannot be seen as weak in a surgery residency, especially as a woman because they will chew you up and spit you out. But because of that you do not feel that you have anyone you can talk to’. (Surgical resident who had left the training programme)
The majority of medical students (85%) and postgraduate trainees (78%) reported difficulty questioning the decisions or actions of those with more authority and approximately two-thirds of medical students and one-third of postgraduate trainees did not feel they could approach someone engaging in unsafe patient care.
[. . .] the inability of trainees to intervene in a setting of a black-and-white scenario with repeated, obvious and life-threatening mistakes is alarming, and this behaviour could translate into ‘real-life’ errors of management.
The influence of issues such as desire for promotion, approval and appropriate respect for seniority makes it difficult to challenge a superior.
When issues around challenging authority arise during debriefing discussions, our course participants (anesthesiology residents) often describe perceived barriers to action, including (1) assumed hierarchy, (2) fear of embarrassment of self or others, (3) concern over being misjudged, (4) fear of being wrong, (5) fear of retribution, (6) jeopardizing an on-going relationship, (7) natural avoidance of conflict, and (8) concern for reputation. When these discussions involve the situation of a student challenging a teacher or a mentor, the related issues of (1) respect for the teacher/student relationship, (2) violation of a special trust, (3) high value placed on experience, and (4) concern over being negatively evaluated are often cited. In addition to the psychosocial constraints, our course participants report that not finding the appropriate words or phrasing inhibits their ability to challenge a decision when a concern over patient safety arises.
Challenging effectively
The literature included in this review does not contain adequate data to be able to fully identify under which contexts doctors in training feel more able to challenge decisions effectively. Sources remain at the descriptive level rather than trying to explain contexts where challenging is encouraged. One of the factors highlighted is the role of trust in junior–senior relationships where doctors in training feel comfortable to raise questions without thinking that this might have negative repercussions on their career and position in the hierarchy. This trust is often framed as deriving from the ‘personality’ and ‘approachability’ of the senior, and it influences whether or not doctors in training would be prepared to seek advice or challenge previous decisions. From our interpretations of the data, we inferred that ‘personality’ and ‘approachability’ refer to the extent to which the senior has explicitly signalled that they approve of receiving questions from more junior members of staff, thus setting the norms of behaviour and developing trust.
Beyond junior–senior relationships, there is one instance in the literature where handovers are described as an opportunity for sharing feedback on antibiotic prescribing between peers. This context may be more amenable to discussing prescribing decisions because it involves the sharing of responsibility, where one team has to follow the decisions made by someone else in the same level of hierarchy. In this case there may be less reluctance to challenge, since the new team will be held accountable for following a specific plan and need to be able to justify their decision.
Realist analysis
Context–mechanism–outcome configuration 23
When doctors at more senior levels of hierarchy have signalled that they would be prepared to be challenged on their decisions (C) and allowed adequate trust to develop in that there will be no repercussions from asking (C), trainees may feel more reassured about voicing questions and doubts on patient management (M), which could result in more effective communication dynamics and positive learning experiences (O).
Context–mechanism–outcome configuration 24
In situations where responsibility about a decision is being passed on from one team to another (e.g. handovers) (C), health professionals in similar hierarchical levels feel that they need to make an assessment about the extent to which they can support previous decisions (M), which leads to feedback on prescribing decisions among peers between teams being perceived as more justified and acceptable (O).
Relevant extracts from papers included in the review
[. . .] pre-existing relationships by themselves are not sufficient to create psychological safety on a team; another essential element is trust.
Other residents cited positive examples from their clinical training where an anesthesia staff was a clear and directive leader in a crisis situation but still listened to feedback and other ideas during the crisis and changed management appropriately as a consequence. They highlighted the importance for the team leader not to consider the challenges to the management plan as a challenge to their position in the hierarchy or to feel the need to become defensive.
Some staff physicians were willing to give feedback to their colleagues about antibiotic choices, but the forum had to be ‘appropriate.’ For example, changeovers were cited as a situation in which this feedback could be given. One staff physician thought the ‘academic’ environment was conducive to educating colleagues [. . .].
Person 1: ‘It also depends on the staff. The young ones who are fresh out of the system. They remember what it was like to be a resident, you know.’ Person 2: ‘And they’re approachable.’ Person 3: ‘Like, Dr. X. He’s set in his ways and I know I’m on tape [everybody laughs] but he’s not someone who’s going to be receptive to your feedback.’ [Focus group with pediatric residents]
Residents’ decisions to question or challenge are affected by the climate of their workplace. Universally, work environments that welcome and foster the ‘speaking up’ of residents encourage learning and a team approach to patient safety.
Issues related to relationship and personalities of superiors affected the willingness of residents to challenge; in fact, this was identified as the most important factor in NOT challenging in both countries.
Prevalence of collective norms
The importance of signalling trust and accessibility is, however, contradicted by other sources (albeit a limited number) that highlight collective hierarchical relationships as much more powerful. Regardless of whether or not seniors are perceived as approachable, in that they seem to have explicitly signalled that they are open to questions, some doctors in training would still refrain from asking for help and/or advice. This shows that the collective norms of medical training within the hierarchy are more powerful than just norms or rules set by individual senior doctors. Doctors in training may perceive that the benefit from asking is outweighed by the risk to their reputation, especially when certain topics may not be at the top of the agenda in specific situations, as is often the case with AMR. This was reinforced in one of the stakeholder meetings for the project, where one of the doctors in training commented on how the opportunities to ask questions are limited, which means that they have to prioritise what is deemed important.
Realist analysis
Context–mechanism–outcome configuration 25
When doctors in training decide whether or not to ask for advice or challenge decisions, even in situations where seniors have individually signalled their accessibility (C), they may still prioritise what is acceptable by the collective norms prevalent in the wider hierarchical environment (M) to avoid losing respect and their place in the hierarchy (O).
Relevant extracts from papers included in the review
[W]e found that other residents remained reluctant to seek advice despite simultaneously appreciating that attendings encouraged them to ask for assistance.
‘I don’t want to lose respect by asking a stupid question.’ (Resident)
‘I mean [the attending] said I could call him in the middle of the night if I needed anything but I am not going to do that . . . I am not going to wake him up . . .’ [Resident interview]
Our results showed no effect of OT [Operating Theatre] team behaviour on the quality of trainees’ challenges towards their consultant anaesthetist in a simulated crisis scenario. Personality type also did not correlate with the quality of the challenge.
Apart from the norms within the wider working and learning environment, the literature also discusses discrepancies between perceptions of doctors in training and consultants regarding accessibility and opportunities to ask questions freely. Senior doctors often seem to be unaware that communication boundaries exist and consider communication norms to be more open than they are perceived to be by doctors in training. They may also be sending contradictory messages between their words and actions. This resonates with the observation that doctors in training may avoid asking questions even if their seniors have signalled that this would be acceptable. Apart from implicit rules in the wider environment taking precedence over individual norms by single consultants, there may also be scope for improving the way accessibility is signalled and challenging is prioritised more concretely to change the overall balance.
Realist analysis
Context–mechanism–outcome configuration 26 (links back to context–mechanism–outcome configuration 22)
When doctors at more senior levels of hierarchy have signalled that they would be prepared to be challenged on their decisions but have not made this clear enough, (C) or have not allowed adequate trust to develop (C), out of fear for negative repercussions and losing their status in the hierarchy (M) trainees may be reluctant to act on their supervisors’ accessibility and refrain from pointing out communication barriers (O).
Relevant extracts from papers included in the review
In their review, Shreves and Moss reported that medical attending physicians were largely unaware of house staff concerns about patient management issues since these concerns were never brought forth, suggesting that residency directors need to encourage residents to discuss their ethical conflicts with attending physicians [. . .]. Interestingly, while the vast majority of attendings felt that they encouraged residents to speak up when they identified patient safety concerns only half of the residents perceived this to be the case (P < 0.001). In other words, even though attendings expressed the right attitude on this survey, they were not conveying this message clearly to their trainees which again identifies a communication issue.
The perceived patient safety culture varies between trainees and consultants, with more senior staff evaluating the safety culture to be safer than trainees. This effect is most marked between consultants and trainees [. . .] findings in this study suggest that more senior staff might over-estimate the safety of the clinical environment. [. . .] Perhaps most worrying of all is the response to the question ‘My safety concerns would be acted on if I expressed them to management’. Only 2.9% of trainees agreed strongly with this statement compared to 17.9% of consultants.
Senior doctors and trainee doctors also show a distinction in their perceptions of communication openness between doctors, with senior doctors reporting more positive perceptions.
Although the seniors did acknowledge the presence of a hierarchy, they felt that it was confined to surgical specialties, whereas the juniors described it as a barrier to seeking help in all contexts. [. . .] Senior doctors appreciated that juniors found acute situations stressful, but seemed to regard the emotional response as a transient, restrictive state rather than the pervasive, debilitating state described by their junior colleagues [. . .].
Figure 10 summarises CMOCs 21–26 on trainee decisions to challenge or not challenge the decisions made by others. 35,56,70,72,77,78,82,83,116,118,119,132,134,139–148
FIGURE 10.
Partial programme theory (CMOCs 21–26).
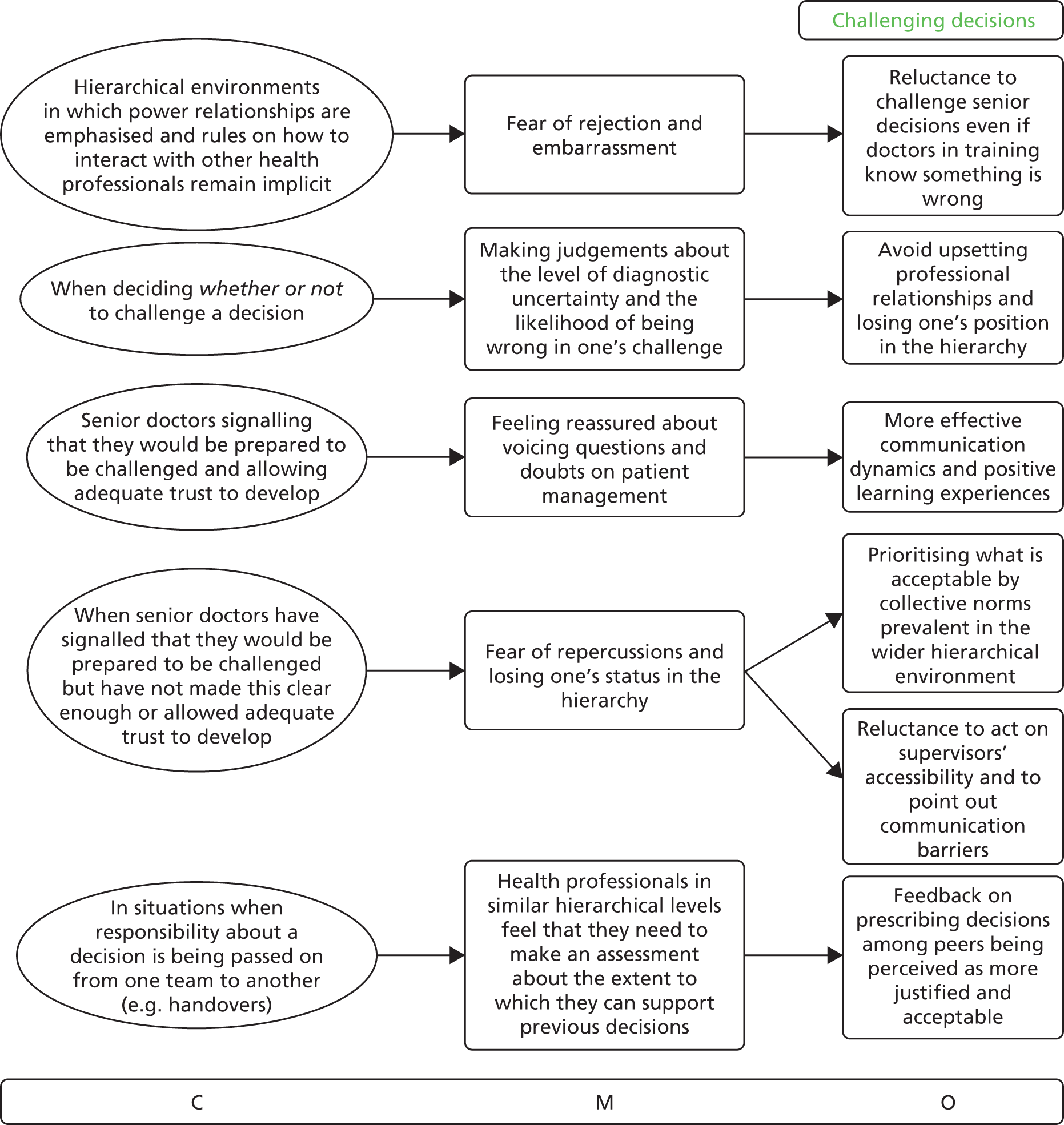
Changing contexts
As training progresses, doctors become more comfortable negotiating the boundaries of their responsibility and the level of knowledge they are expected to possess and apply to practice at different stages. Through professional socialisation in different environments, they learn how to operate under different rules set by the local hierarchies. Their ability to ask questions and confidently argue alternative positions changes over time as, with increasing seniority, they are expected to assume more autonomy and responsibility.
With prolonged exposure to multiple clinical settings, doctors in training learn how to carefully manage their identities as competent learners (the criteria for which change depending on where and for whom they are working and the stage of their training). They learn to employ indirect questioning strategies and diplomacy, for example the use of strategic language, delay tactics and circumvention (as also mentioned in CMOC 20), to manage their identities.
Realist analysis
Context–mechanism–outcome configuration 27
As training progresses (changing context) (C), doctors in training feel that they are expected to contribute more substantially to patient management and assume more responsibility for any decisions (M), which may result in less reluctance to challenge and ask questions (O).
Context–mechanism–outcome configuration 28
As training progresses (changing context) (C), doctors in training learn to make better judgements about what communication strategies work under different circumstances (M), which may lead them to adapt their approach accordingly to avoid conflict (O).
Relevant extracts from papers included in the review
‘Working constructively under somebody but if you’re something that you were completely thought was wrong then you don’t necessarily have to do it even though you’re not the leader of the team. Like, as long as you’ve you gone about it appropriately’ (female/medical/early-stage).
Diplomacy is necessary with patients, relatives and of course colleagues, who very often are older and more experienced than them: ‘You arrive as a MR [Medical Resident], you are young (. . . ). There is people here [the nurses] who have been working for 30 years, they could be your parents. You have to be very patient in the relationships, to show that you are the doctor and it’s your job to take decisions. But at the same time you don’t have to be too extreme and do things on your own. You need a balance. A lot of balance. (. . . ). You’d better not argue with them. (. . . ) You’d better have words in one ear and out from the other, otherwise you go crazy. This is stressing . . . You have to be tactful, patient.’ [Medical Resident, female]
‘It never happens to me; I always get approvals (smiling). Just change the fields (patients’ parameters) a bit and you know you get what you want.’ [Junior Medical Staff]
A delicate balance between taking responsibility and being supported was necessary to achieve the dual aims of intern development and patient care. This balance shifted over time, as the interns developed.
However, a number of participants reported that this anxiety around uncertainty decreased over time as they began to understand that managing uncertainty is a normal part of being a doctor: ‘I think there’s a lot of uncertainty and at first I think I found it quite difficult, you know wanting to find an answer for everything [. . .] but I know that it’s not possible and I think that’s fine to say that you don’t know [. . .] And I think, yeah I guess I am finding that easier [. . .] I think I am coming to realise that medicine is full of uncertainties.’ (Foundation Year 1 doctor)
However, the quality of challenges did improve with increasing level of training (PGY) [Postgraduate Year]. Final-year trainees’ challenges tended to be at a relatively high level, such as the use of an advocacy-inquiry technique, attempting to take over the case, or at least repeated use of advocacy or inquiry with initiation of discussion [. . .].
Figure 11 brings together the CMOCs for changing contexts, with the mechanisms and outcomes associated to training progression and willingness to negotiate prescribing decisions under certain circumstances. 63,76,77,81,84,98,116,120,136,145
FIGURE 11.
Partial programme theory (CMOCs 27 and 28).
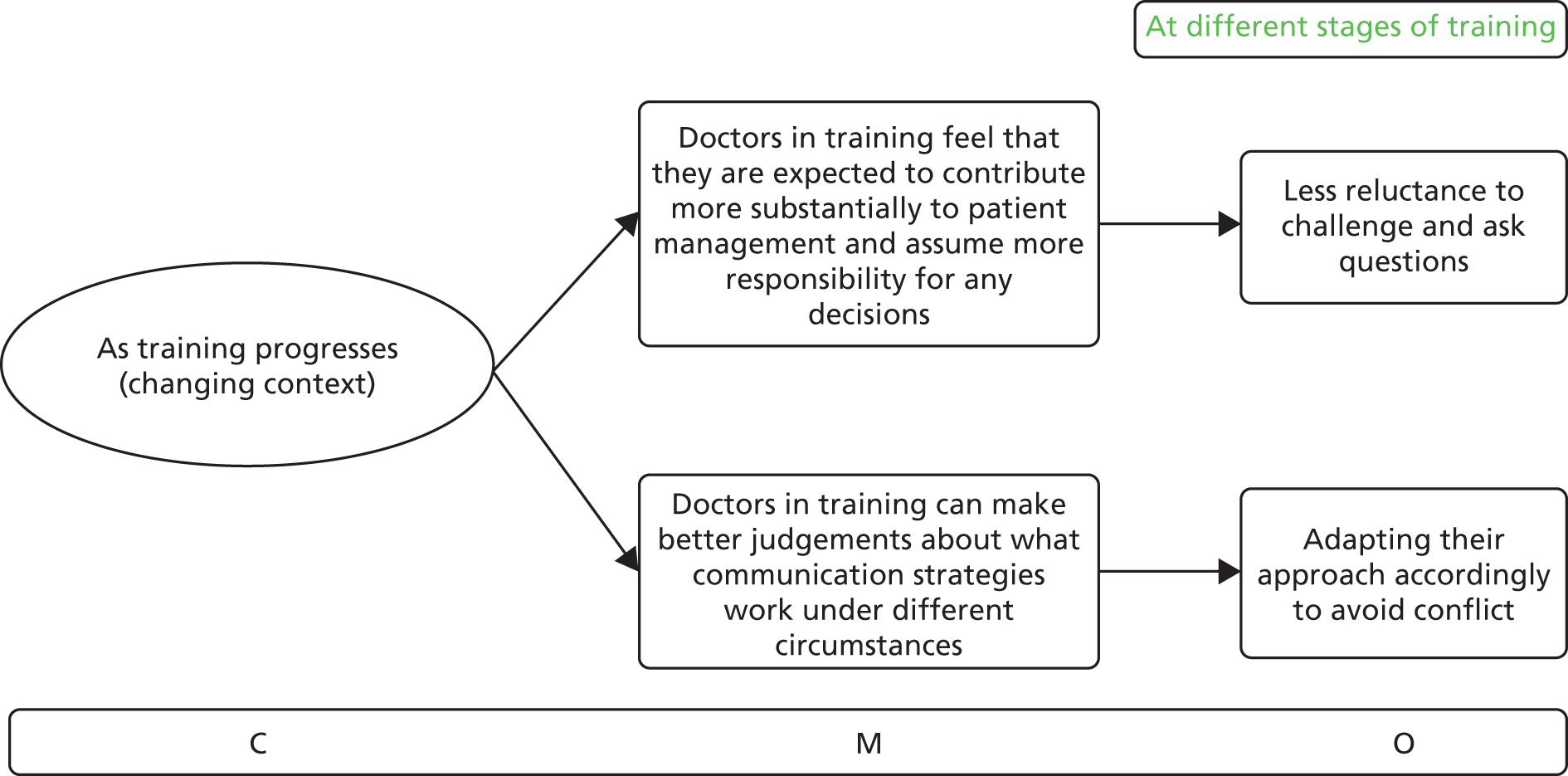
Overall programme theory
Figure 12 provides an overarching programme theory that consolidates the relationships between the 28 detailed CMOCs emerging from the data. The complex picture that has emerged from the analysis and synthesis of the data unavoidably includes overlaps and repetitions in an effort to capture and interpret all nuances of the literature included in the review. The overarching programme theory provides an overview of the data as organised around the various outcomes within the CMOCs. This has resulted from consolidation of important recurring contexts and mechanisms, and the relationships between them. These inter-relationships have been presented in a visual format to highlight useful insights and informing change.
FIGURE 12.
Overall programme theory.
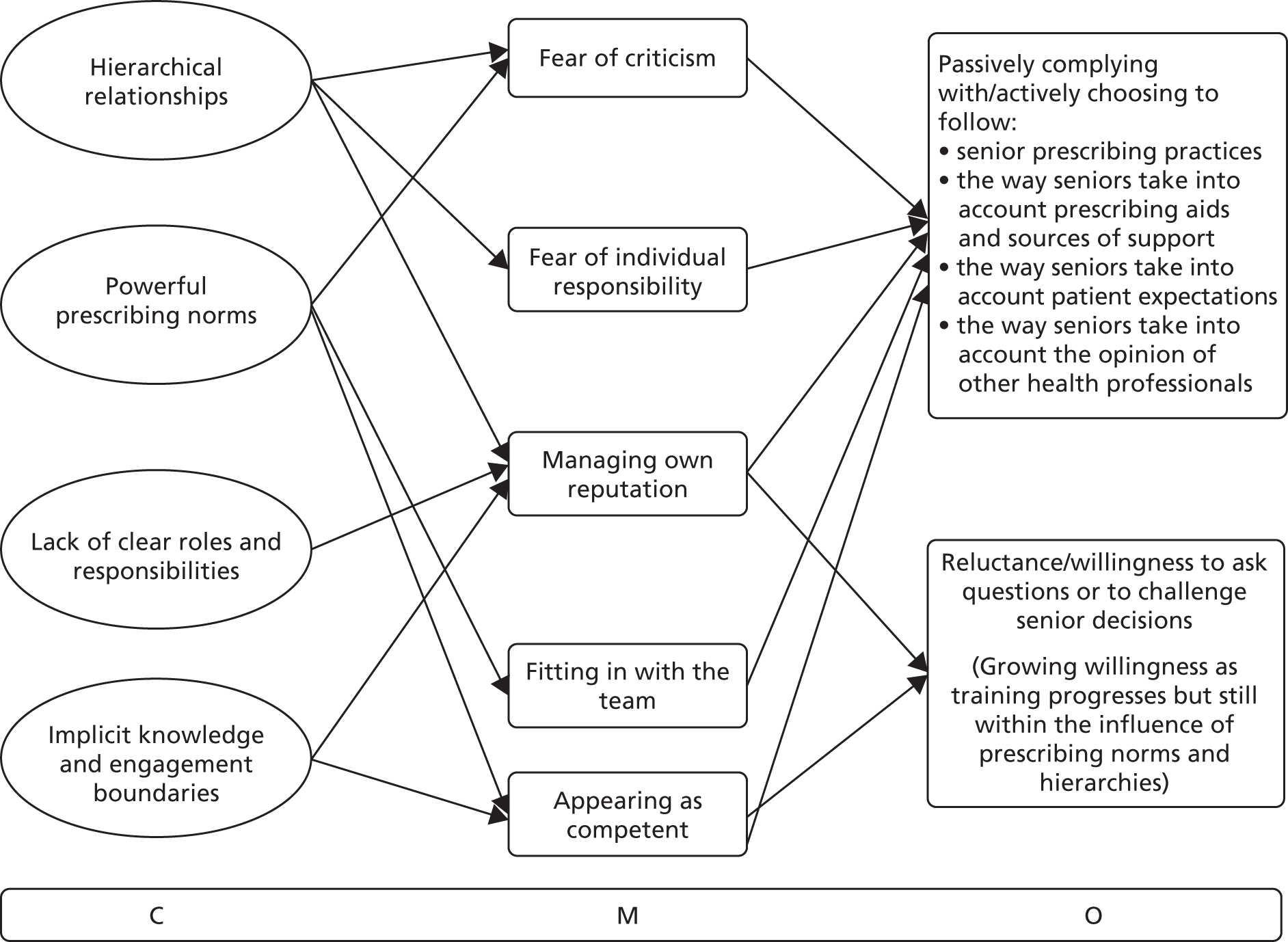
The overarching programme theory primarily focuses on antimicrobial prescribing behaviour from the perspective of doctors in training. This means that certain aspects of the CMOCs described in Chapter 3 have been subsumed under other CMOCs and are not presented here in detail (e.g. optimal and suboptimal role modelling).
The overarching programme theory explains how and why doctors in training decide to passively comply or actively follow their seniors’ prescribing habits (outcome 1), and the way they take into account prescribing aids (outcome 2), patient expectations (outcome 3) and the opinions of other health professionals (outcome 4). The programme theory also explains what drives reluctance or willingness to ask questions about antimicrobial prescribing (outcome 5) or to challenge the decisions made by seniors (outcome 6), as well as how this changes as training progresses (changing contexts). As discussed in the literature reviewed, these outcomes result from complex inter-relationships between the important contexts doctors in training are embedded in (i.e. hierarchical relationships, with powerful prescribing norms, where there is little clarity around roles and responsibilities and knowledge expectations, and how to put these into practice remain implicit) and the mechanisms triggered in these contexts (i.e. fear of criticism, fear of individual responsibility for patient outcomes, the need to manage one’s own reputation and position in the team and to appear competent).
Further work on the CMOCs and programme theory was carried out as described in Chapter 4 to develop implications and actionable findings from the review.
Drawing on substantive theory
As a form of theory-driven review, this work draws on a number of theoretical insights to explain antimicrobial prescribing of doctors in training, as explained in Step 5: synthesising the evidence and drawing conclusions in Chapter 2. Substantive theory was used to support configurations, to substantiate inferences about mechanisms, to validate interpretations of the literature and/or to contribute to the development of programme theory. This section specifies the theoretical ideas and frameworks that were used recursively throughout this review (during theory building and testing) to underpin the development of CMOCs and consolidate these into a programme theory.
Our review has highlighted how social capital influences the way antimicrobial prescribing decisions are made by doctors in training. This relates to the way doctors in training decide to prioritise questions and to challenge the decisions of their seniors. Consistent with explanations emerging from this realist review, Broom et al. 53 draw on Bourdieu’s practice theory to frame antibiotic prescribing ‘as [a] largely unconscious and habitual practice governed by forms of social interaction and social capital’. They discuss the crucial role of social capital in drawing in ‘players’ to the ‘social game’ of antimicrobial prescribing where ‘[. . .] decisions [. . .] are [. . .] governed less by stewardship initiatives, therapeutic guidelines and other techniques of bureaucratic routinisation, than by what constitutes appropriate behaviour within professional hierarchies, and the securing of professional reputation’. This is not only a result of particular prescribing habits being passed down the hierarchy, but derives from the complex ways in which doctors in training build and sustain their social capital through exhibiting competence, as judged by the context-specific norms and routines of each different clinical environment. Bourdieu’s practice theory as applied by Broom et al. 53 resonates with the findings of this review and particularly with CMOCs 1–3 on the role of hierarchies, CMOCs 6–8 on the role of guidelines and CMOCs 11–13 on the social network of prescribing. By thinking about social capital against the data emerging from the review, we have been able to identify mechanisms such as the need to preserve one’s professional reputation as key in driving prescribing behaviour and willingness to ask questions (see, for example, Chapter 3, Part B: asking for advice and challenging decisions). This mechanism was not always mentioned concretely in the literature analysed, but we have been able to infer its importance by comparing data on outcomes in specific contexts (e.g. compliance in hierarchical relationships) and drawing on substantive theory to develop interpretations about what mechanisms could be operating.
Along similar lines, Aveling et al. 149 emphasise the influence of context-specific norms over externally imposed standards in their study on individual accountability in patient safety, and argue for a better understanding of individual agency in how norms are reproduced. Although the authors acknowledge the importance of systemic, structural factors in framing spaces for ‘feasible action’, they also comment on how individuals condition their behaviour to fit these norms by merely accepting that ‘this is how things are done’. By considering this tension, we have been able to further interpret the literature on antimicrobial prescribing for doctors in training. The same principles apply to antimicrobial prescribing: as this realist review has emphasised, pre-existing norms and values condition the behaviour of new members of clinical teams. As doctors in training perceive their accountability to lie with their direct supervisors, they feel responsible for imitating accepted patterns of prescribing, which may not always reflect externally set rules of appropriate prescribing or even local guidelines. Their ability to exercise responsibility is thwarted by the structural conditions of the training environment they are embedded in (see Chapter 3, CMOC 4). Increased opportunities for being held accountable externally, beyond direct seniors with the power to influence career development, and clearly defined standards of care that individuals are responsible for upholding, would contribute to the ‘fostering of the conditions of moral community’, that is, opportunities to collectively engage in safe and responsible practice. 149 This notion of accountability and reproduction of norms has not only contributed to the development of CMOCs and programme theory, but served as a useful focus in suggesting areas for improvement (see Chapter 4).
Another theoretical framework that can help explain antimicrobial prescribing behaviour and the nuances of the mechanisms at play for doctors in training is that of group reference theory. 150 Group reference theory suggests that people make behavioural choices by comparing themselves to a group they perceive as salient. In the case of antimicrobial prescribing, doctors in training appear to compare their own prescribing with that of their consultant or of the team to which they are attached (e.g. CMOCs 1–3, 6–8 and 10). Prescribing according to local norms becomes not just a way to signify competence, but also a marker of belonging to and fitting in with the team and their established ways of doing things, which is a significant mechanism (in the realist sense) for driving outcomes.
Pawson has previously discussed group reference theory as an example of how middle-range theory building can be pursued from a realist perspective, to explain the outcomes of particular types of interventions. 54 In the case of antimicrobial prescribing, the group reference dynamics explained in the literature are summarised in Table 3. Doctors in training are ‘eligible for membership’ and ‘aspire to belong’ to a clinical team, and they are therefore more likely to follow locally agreed practices so that they can be perceived as equal members of the group. In circumstances where doctors in training do not perceive membership to the group as being important (‘indifferent to affiliation’), they are likely to avoid following particular practices and defer decisions to other members of the group.
| Attitude towards membership | Eligible for membership | Ineligible for membership |
|---|---|---|
| Aspire to belong |
1. Membership candidate Followership |
2. Marginal non-member Compliance |
| Indifferent to affiliation |
3. Potential member Avoidance |
4. Detached non-member Avoidance |
| Motivated not to belong |
5. Autonomous non-member Challenge |
6. Antagonistic non-member Resistance |
In a similar vein to group reference theory, the concept of legitimate peripheral participation has often been used to explain how clinical training evolves by gradually allowing participation in tasks of increasing difficulty and complexity. 151,152 This is reflected in the data on antimicrobial prescribing as trainees make judgements about their own position in the team and their roles and responsibilities in different contexts. When responsibility and knowledge boundaries are made clear by senior staff, it becomes easier to understand what constitutes legitimate participation and what decisions can be deferred to other members of the clinical team (see CMOCs 14 and 15). If seniors do not facilitate the participation of new members by legitimising responsibility and knowledge boundaries, then it becomes harder for trainees to know what to do in certain circumstances (e.g. to suggest whether or not antibiotics should be stopped). Therefore, antimicrobial prescribing is not just about prescribing knowledge, but also about creating legitimacy for trainees to learn to apply this knowledge while being active participants in their communities of practice. 153 As trainees are slowly accepted as members of their clinical communities (members of the in group) and training progresses, boundaries of responsibility and knowledge expectations grow and become better understood. This is, however, interrupted when trainees rotate in new teams and are faced with new norms, especially in terms of their role in antimicrobial prescribing. The process of learning through interaction and peripheral participation also involves observing how more senior trainees pose questions (or do not) and how they participate effectively in decision-making (or decide not to engage even if they think something wrong is happening) (see CMOC 23). Legitimate peripheral participation is also visible in the way rules of engagement change as training progresses (see CMOCs 27 and 28). Through interaction, trainees gradually come to understand what is expected of them by different members of the clinical team and they adapt to different circumstances as needed. This also increases their understanding of when and how it is considered legitimate to challenge decisions and to ask specific questions about patient management.
Last but not least, throughout the literature reviewed, antimicrobial prescribing behaviours are characterised by elements of impression management and symbolic interactionism. 154 Clinical teams operate on the basis of a working consensus about what antibiotics can be acceptably prescribed under different circumstances. There is also agreement about what questions are important to prioritise. Consensus is formed and sustained through back- and front-end interactions between members of the clinical teams. Doctors in training learn about these norms as they engage with different clinical teams and, accordingly, manage the way they present themselves to others so that their impression matches what is expected. In relation to antimicrobial prescribing, their decisions and actions are representative of the way they believe they are expected to engage with the clinical environment more widely. In this review, symbolic action and impression management were instrumental in developing an understanding of how trainees seek assistance and how they decide to frame challenging questions (see CMOCs 17–22, 25 and 26). As the data showed, doctors in training often actively manage whether or not to ask for help, when to do so, who is best to ask about certain things and how to frame these questions so that they do not appear ignorant or incompetent. For example, they may decide to approach different members of the clinical team (e.g. a pharmacist) if they believe that their question may be seen as naive by the consultant. Thinking about impression management, along with concepts of social capital and group reference mentioned above, we have been able to think through the data and develop CMOCs that unpack the nuances between different types of behaviour and the drivers behind them.
In summary, the theoretical perspectives above indicate how aspects of our findings are related to substantive theory. As others have noted previously, prescribing does not just encompass technical decisions, but conveys attention to group membership, involves decisions about one’s impression management and relates to accountability structures. 34,36,155 In our review, we have drawn on substantive theories that can specifically explain the antimicrobial prescribing behaviours of doctors in training and used these to draw further inferences for programme theory development and refinement. We have further highlighted that antimicrobial prescribing cannot be seen in isolation, but needs to be considered in the wider sociocultural context in which clinical training takes place. Chapter 4 elaborates on how the design and implementation of interventions can be tailored to take into account the sociocultural contexts relevant for doctors in training.
Chapter 4 Discussion
Summary of key findings
Several systematic reviews on antimicrobial prescribing have been carried out to understand the impact of antimicrobial stewardship programmes or to compare the effectiveness of different intervention strategies. 9,13,30,156–159 Yet little has been written on the relevance of such interventions for doctors who are still undergoing training but are already required to make antimicrobial prescribing decisions in the clinical setting (for an example, see Brennan and Mattick36). Given the widely recognised importance of social dynamics in driving prescribing behaviours,34,35 the role of doctors in training deserves explicit attention, as they often need to manage power and teamwork dynamics along with their learning and career progression, in ways different from their senior colleagues.
The IMPACT realist review attempts to expand our understanding of how trainees engage with antimicrobial prescribing and to explain the cognitive and sociocultural drivers behind their decision-making processes. Our intention was not to produce evidence about the relative advantage of different interventions against each other. Instead, we sought to explain how antimicrobial prescribing is done differently in different circumstances, for example by doctors at different levels of training or in different specialties, and why such differences are manifesting. Given that antimicrobial prescribing interventions for doctors in training are not adequately described in the literature, we decided to extend the remit of the review to be able to fully address our original aims. We have drawn on a wider set of studies to comprehensively explain the cultural, professional and organisational dynamics in which doctors in training prescribe antibiotics. This was necessary to explain how and why different types of interventions may or may not work in practice for trainees (e.g. if the intervention includes explicit senior support or not). Having identified the social and professional dynamics influencing the prescribing behaviour of doctors in training, in this section we discuss implications for intervention design.
Given the complexity and clinical uncertainty inherent in antimicrobial prescribing, it is likely that a combination of top-down and bottom-up multifaceted solutions and ongoing support would be required to improve practice. 160,161 Our priority in this review was not to present suggestions for the implementation of specific types of interventions, but to explain how interventions can be tailored effectively for doctors in training, taking into account the contexts and circumstances in which trainees negotiate antibiotic prescribing in practice.
In summary, from the synthesis of the published literature, we found that appropriately tailored interventions need to address challenges in the following key areas:
-
The significance of clinical hierarchies as a key influence in the complex decision-making processes associated with prescribing by doctors in training.
-
The critical role of senior supervisors in role modelling not just the ‘prescribing etiquette’, but also how trainees should engage with antimicrobial specialists, how they should manage patient expectations and how they should consult prescribing aids.
-
Lack of opportunities to meaningfully engage in dialogue about the prescribing rationale or to explain why prescribing choices may differ between environments.
-
Lack of explicit recognition of AMR as an immediate threat, or at least not to the extent that trainees would perceive it as important to prioritise questioning the rationales underpinning antimicrobial prescribing decisions and approaches.
-
Uncertainty about the roles and responsibilities trainees are expected to assume in antimicrobial stewardship at different levels of training and the associated knowledge they are expected to exhibit.
-
Lack of co-ordination on antimicrobial prescribing, especially between teams in hospital settings, which drives further uncertainty about the best way to reconcile different prescribing decisions and approaches.
These findings point to a number of implications for how best to support trainees in antimicrobial prescribing. The following paragraphs outline findings and implications in a number of areas, before outlining more specific transferable principles for tailoring interventions to address the needs of doctors in training.
Implications
Education and feedback interventions
Currently, there is significant emphasis on educational interventions to improve antimicrobial prescribing for doctors in training. 10,64,67,74,76,88,92,101,105,107,108,162–164 This emphasis is underpinned by an assumption that, having identified misplaced beliefs and erroneous prescribing decisions, one can improve the knowledge ‘deficit’ by delivering targeted education (i.e. a teaching session on a specific aspect of antimicrobial prescribing). However, it appears that doctors in training often struggle to apply their knowledge in the practice setting and so addressing knowledge or skill ‘deficits’ may not lead to behaviour change or outcome change in practice. This theory–practice divide is well researched. 41 Some sources suggest a more nuanced approach to education, by promoting continuous learning for all health professionals in different settings. 10,165,166 This often takes the form of feedback interventions, drawing on principles of situated learning, as a targeted, context-specific way to improve prescribing practice. Feedback interventions can include informal ward-based teaching, one-to-one specialised education, repeated peer review or feedback during teaching rounds. 43,76,125,126,167–171 Consistent with wider literature on audit and feedback interventions, effectiveness is deemed to be associated with mode of delivery, source of feedback and whether or not feedback is tied to specific actions and targets. 172–174
When education and feedback interventions are disconnected from how prescribing decisions are made in the workplace, they are less likely to result in meaningful and sustainable change, as a result of the important influence of clinical hierarchies. Therefore, there is a need to incorporate an understanding of local prescribing norms and power dynamics in the design and delivery of context-sensitive education and feedback programmes. This would allow ‘persuasive interventions’13 to focus on the development of skills that would better equip trainees to productively engage with hierarchies and their ‘prescribing etiquette’. Previous literature has also suggested that education programmes need to be rethought to include training on teamwork, such as communication in hierarchical teams, as well as error awareness and management. 73,105,125,155 However, this has not yet translated into concrete changes to the way antimicrobial prescribing training is managed, as focus still primarily lies on technical knowledge, rather than on negotiating prescribing decisions and maximising learning from everyday interactions. 36
Competencies and supervision for collaborative prescribing
Organising principles for the education of doctors in training are often developed into competency statements, which can be used by trainees and their trainers to assess their abilities. 16,175 Although these provide a comprehensive picture of the abilities to be exhibited by trainees, they do not always differentiate between levels of training or specify required skills with sufficient detail. As mentioned previously on non-technical prescribing skills, it may be worth considering competencies that address the capacity to initiate dialogue about prescribing decisions and to co-ordinate teamwork productively. For example, antimicrobial prescribing competencies could take into account not just how trainees follow senior advice, but also how they capitalise on hierarchical relationships to achieve good antimicrobial prescribing and manage their own learning. Although doctor leadership has been widely discussed in the context of NHS improvement, little attention has been paid to how ‘leading from beneath’ – building leadership capabilities in the context of a hierarchical setting – could contribute to more appropriate antimicrobial prescribing decisions. 12,90,176,177
It may also be relevant to consider antimicrobial prescribing competencies for consultants (or for more senior doctors still in their training years) that could include how seniors consciously and deliberately role model prescribing practices for more junior staff or, when this is not feasible, how they facilitate assistance from antimicrobial specialists. Role modelling could also work across specialties, for example a medical registrar taking a leadership role in prescribing in surgery, or across professions, with pharmacists assuming a similar responsibility for other clinicians. Competencies could even extend to outline tasks relevant to antimicrobial prescribing that can be achieved as part of clinical supervision, that is, creating opportunities for doctors in training to take initiative in reviewing the necessity of antibiotics for certain patients or allowing discussions to explain the prescribing rationale when a case is less clear-cut. Characteristics of effective supervision that have been discussed elsewhere would need to be better embedded in training for appropriate antimicrobial prescribing (see, for example, Kilminster et al. 178). The concept of Entrustable Professional Activities provides a means to translate competencies into clinical practice, with appropriate supervision. 179
Input from other professional groups
Competencies for doctors in training currently mention the importance of building relationships with other health professionals, and learning to draw on and constructively use their advice,175,180 but it would be useful to further consider how to do this in the context of prescribing norms set by senior clinicians. The educational role of pharmacists43,60,64,125,171,181 and infectious disease specialists102 has been extensively discussed in the literature as critical for appropriate antimicrobial prescribing. Accepting antimicrobial prescribing more widely as ‘a specialised act’102 could significantly legitimise the input of antimicrobial specialists and contribute to their meaningful involvement. There is a recognised need to instil collaborative working between antimicrobial specialists and prescribers and to organise real-time, patient-centred specialist input to maximise relevance and usefulness. 70,162,181,182 Without senior involvement, however, it would be difficult to set an example for junior doctors in terms of role modelling and signposting appropriate assistance-seeking behaviours.
Antimicrobial prescribing support aids
Along with education and feedback interventions, the literature emphasises the necessity of readily available guidelines that present information that is locally relevant and in a format that allows direct clinical use. 62,163,183–185 This is particularly relevant to doctors in training, who often draw reassurance from guidelines when there is little senior support on prescribing, as this review has identified. The process of guideline development plays an equally important role in their acceptance. As this review has highlighted, it makes a difference to the perceived credibility of guidelines if they have been approved by peers, include up-to-date information from accepted sources and resonate with clinical experience. 35,60,68 The literature reviewed suggests that use of guidelines can be strengthened further through active senior support, better communication to health professionals including junior doctors and ongoing evaluation. 43,60,62,103,106
Apart from the use of guidelines for decision support, some articles also advocate the use of information technology to improve prescribing and decrease medication errors. 57,135,186 However, such arguments need to be treated with caution to avoid treating technology as a silver bullet. Introducing electronic systems and making them work in practice can be particularly challenging, as described in studies aiming to develop meaningful alerts for medication errors. 123,187,188 Significant work is needed in this area from a sociotechnical perspective to identify ways for information technology to complement human effort in addressing the problem of AMR.
Monitoring and accountability
The review has highlighted how accountability plays a role in antibiotic prescribing, in terms of following the practice of those seniors the trainee feels most accountable towards in different circumstances. Accountability relationships are easier to navigate in primary care, where supervision arrangements are usually much more direct and clear-cut. In secondary care, doctors in training work with and across multiple teams on a regular basis and they often enact ‘inherited’ decisions made by their seniors. 39 The analysis of the literature showed that clear accountability relationships in which expectations (e.g. for antimicrobial prescribing) are explicitly set help trainees to navigate hierarchical dynamics and interprofessional practice to maximise learning.
Establishing clear accountability relationships may be useful in combination with monitoring. A large body of literature refers to monitoring or ‘measurement for improvement’ as a way to drive changes in performance – for an overview see The King’s Fund. 189 However, when monitoring is delivered as a simple intervention on its own without a wider plan or capacity to implement change, it is less likely that the result will be sustainable in the longer term. 190,191 To monitor practice meaningfully, there is a need to combine both what is measurable quantitatively and what cannot be captured sufficiently in numbers. This would allow any learning that emerges from monitoring to be perceived as credible and directly relevant to practice, rather than be communicated through measures and messages that practitioners do not associate with. 192 Monitoring should not be perceived as a tool for performance management,193 but could be communicated as part of workplace-based feedback interventions if the right trust relationships have formed and the right circumstances of shared responsibility are in place.
Participatory design
Few antibiotic stewardship programmes report involving doctors in training in the design of strategies and interventions to improve prescribing. 43,98,194 Involving junior doctors in the development of competencies, workplace feedback programmes or other antimicrobial prescribing interventions could contribute to more targeted design and better-informed implementation efforts. Principles of participatory design195 would enable inclusivity, alignment of goals and continuous learning for all professional groups and training levels on the issue of AMR – when sensitively designed to address the issues of power and hierarchy. They would also allow teams to gain common ownership of the intervention, which would help to clarify expectations, increase engagement and strengthen collaboration. A theory-based approach to participatory design would promote local, context-sensitive solutions tailored to the needs of specific groups, instead of generic interventions to be ‘rolled out’ widely.
Table 4 provides an overview of potential short-, medium- and long-term goals that can be pursued to improve antimicrobial prescribing for doctors in training. These goals were developed by drawing on findings of this review, by reviewing detailed notes taken during consultations with stakeholders and by following discussions in the policy workshop organised towards the end of this project. The second column includes suggestions on the level of action required to introduce change effectively and sustainably.
| Goals | Level of action |
|---|---|
Short term:
|
Medical educators, clinical supervisors/trainers, intervention designers (i.e. any individual or group that seeks to develop an intervention to change the antimicrobial prescribing practice of doctors in training) |
Medium term:
|
Health organisations, medical educators, clinical supervisors/trainers, senior prescribers, intervention designers |
Long term:
|
Health organisations, clinical training programmes, clinical supervisors/trainers |
Knowledge-to-action framework
As set out in the project protocol, the review used the knowledge-to-action (KTA) framework to consider the implications of this research. The KTA framework graphically sets out the steps involved in attempting to bridge the knowledge-to-action gap: identify the problem; adapt knowledge to local context; assess barriers to knowledge use; select, tailor and implement interventions; monitor knowledge use; evaluate outcomes; and sustain knowledge use. 196
The IMPACT review has generated knowledge relevant to different contexts and explained findings at a level of abstraction so as to allow for transferability across settings and for different stakeholders. By discussing implications of the review and suggesting options for tailoring antimicrobial prescribing interventions to address the needs of doctors in training, we have also provided ways to adapt knowledge and tailor interventions to local contexts and users. Barriers to knowledge use have been identified and appropriate solutions considered (e.g. putting knowledge about appropriate antimicrobial prescribing in practice in the context of hierarchical relationships).
Producing stakeholder-relevant knowledge
Discussions with stakeholders (see Chapter 2, Stakeholder group for more details) helped to contextualise the knowledge acquired through the synthesis, taking into account barriers and facilitators that health professionals and patients had identified through their own experiences. For example, one of the things that was extensively discussed in the stakeholder meetings was disciplinary differences in prescribing habits and openness to receiving advice from other specialists. These discussions also helped in understanding how the training environment has recently changed for trainees (e.g. workload pressures or availability of guidelines in mobile applications) and how these changes have shaped their attitudes and practices.
Adapting knowledge to local context
The methodological approach used in this review (i.e. realist review) places primary emphasis on actionable findings that can lead to context-sensitive change. Departing from a one-size-fits-all approach, we developed high-level principles that can be tailored to different environments to fit different needs, using examples to help visualise possible scenarios. These principles were then presented in the form of non-academic outputs, aiming to help practitioners better tailor interventions for the specific needs of doctors in training, outlined as follows.
-
We have developed an infographic as a concise and visual decision support aid (Figure 13). This infographic points to the principles and processes that need to be considered when designing and implementing an antimicrobial prescribing intervention for doctors in training, as identified in this review. These principles are generic enough to allow local tailoring for different environments. Local stakeholders will be able to select knowledge that is relevant to their local context and to use the infographic as a guide to tailor and critically implement an intervention in a way that is context sensitive and appropriate for trainees at different levels. For example, the infographic asks if the intervention ‘makes AMR everyone’s business’. This means that the wider clinical team needs to be engaged with this issue, rather than just focusing on doctors in training. As a high-level principle, this will be implemented differently in different settings, but the aim would remain the same.
-
We have also developed an animation video (see Report Supplementary Material 1) that can be used as part of undergraduate or postgraduate training to trigger reflection and discussion on antimicrobial prescribing. Our stakeholder group identified hospital induction as a particular opportunity for more engaging ways of ‘setting a culture’ around ‘AMR being everyone’s business.’ Existing educational materials and training programmes cover a substantial amount of technical knowledge and address questions on local processes for prescribing, but do not refer to the sociocultural influences on the prescribing process. This video was developed to prepare doctors in training for engaging with the sociocultural dynamics and the hierarchies that characterise antimicrobial prescribing in different settings. It highlights situations where, for example, junior trainees may not understand what their consultant is prescribing and why, and invites them to consider what they would do to clarify the prescribing rationale and maximise their learning. Propositions made in the video summarise the findings of this review that are relevant to doctors in training and are intended as a useful background for discussion (with the ability to pause the video) tailored to the environment where the video is being used.
FIGURE 13.
High-level principles.
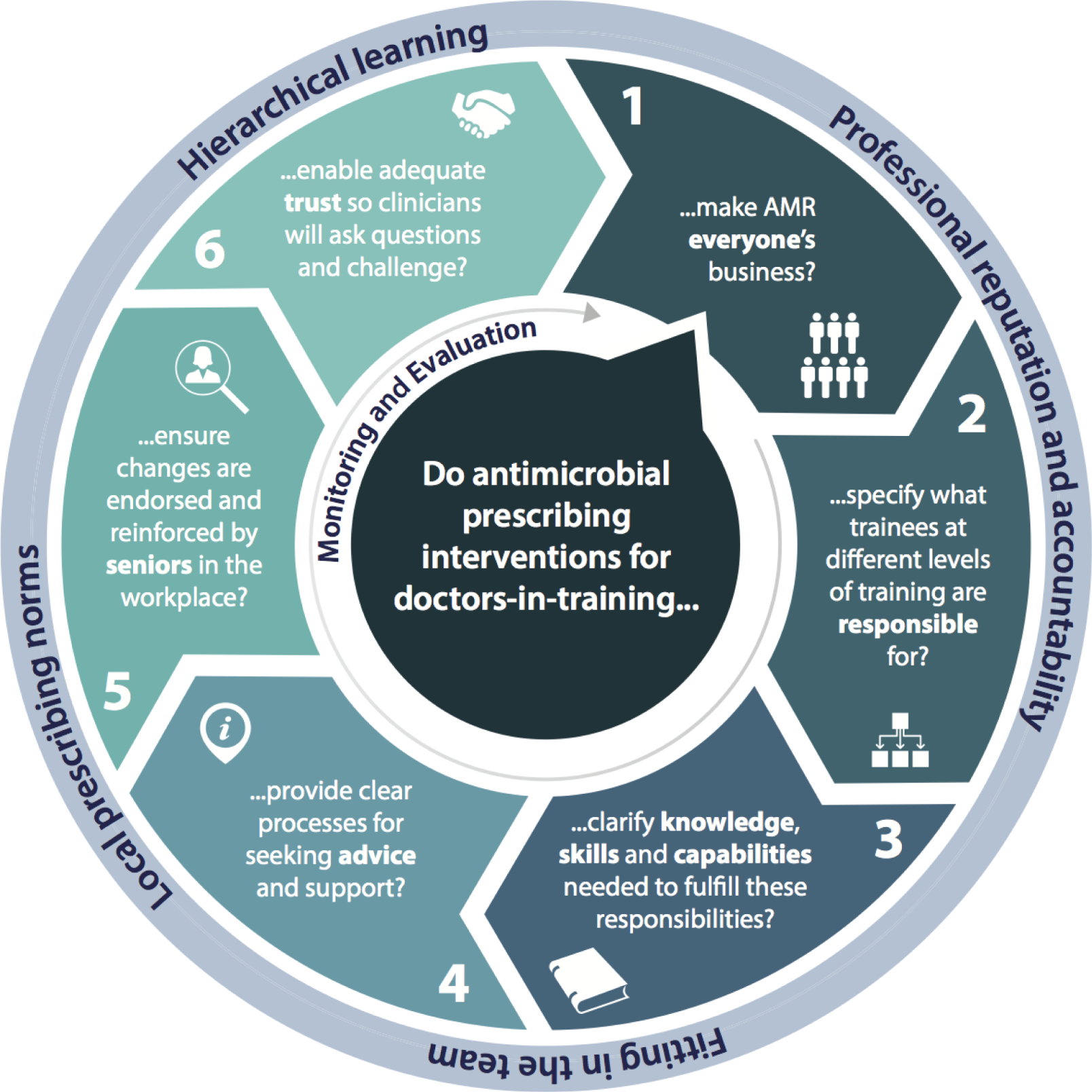
Assessing barriers to knowledge use
Through the review we have identified a number of barriers to knowledge use for the improvement of antimicrobial prescribing. One of the most important barriers to knowledge use is the influence of hierarchical dynamics on antimicrobial prescribing of doctors in training. Hence, we have primarily focused the review on how hierarchical dynamics influence doctors in training to follow the prescribing practices of their seniors. This includes following senior attitudes to guideline acceptance and responding to patient expectations. Although there is significant evidence on how to improve antimicrobial prescribing, it would be difficult to implement this in practice without meaningful and effective senior involvement and/or endorsement. To surface this issue and provide outputs that are simple enough yet also capture its complexities, we needed to develop accessible materials. Our infographic and animation video are intended as tools that can help to surface the importance of hierarchical dynamics for practitioners and give them the decision support or learning opportunities to tackle this issue, thus addressing one of the barriers to knowledge use. However, possible limitations remain as these resources are developed for use in advanced health-care systems, rather than in low- and middle-income countries where barriers to appropriate prescribing and training environments may differ radically.
The following sections discuss actionable findings emerging from the synthesis of the literature and present the dissemination materials developed as part of the IMPACT review for practitioners and policy-makers.
Actionable findings
Principles for tailoring antimicrobial prescribing interventions for doctors in training
So far in this report we have presented a number of implications and proposed areas for improvement emerging from this realist synthesis of the literature on antimicrobial prescribing for doctors in training. To translate these implications into actionable findings that are practical and feasible, we have focused on six key areas that need to be addressed in more depth if interventions are to be helpful for trainees.
The translation of our CMOCs and programme theory into actionable findings and implications was an iterative process that drew on the strengths of a theory-driven realist understanding and, to a significant degree, was guided by feedback from our stakeholder group. In the background of the KTA framework (as explained above), we focused on aspects of the programme theory where it would be more feasible to introduce change (e.g. on interactions within the clinical team rather than the way national training programmes are delivered). We then started developing propositions for actionable findings that were further refined and developed with the help of the stakeholder group.
For example, one set of CMOCs relates to how, in the absence of explicit roles and responsibilities for doctors in training to fulfil with regard to antimicrobial prescribing, trainees manage their position in the hierarchy by following the prescribing practices of their seniors. Although this is often a good way to transfer learning, when antimicrobial prescribing is done inappropriately, there is little opportunity for improvement. Drawing on this, we discussed the implications of this set of CMOCs and proposed that doctors in training could have explicitly set and agreed roles to fulfil, so that they can take responsibility for how antimicrobial prescribing is done within the different teams around which they rotate. Informed by other aspects of the programme theory, we also suggested that these roles need to be endorsed and encouraged by the formal medical hierarchy so trainees would be able to fulfil their responsibilities adequately. When considering this proposal with our stakeholder group, we discussed more specifically how doctors in training could play a role in day 3 medication review in hospital settings, including a review of whether antibiotics are still needed or if a change to a narrow-spectrum agent would be beneficial.
To consolidate applications of our findings, a policy workshop was organised in September 2016 with participation from Health Education England, the British Society for Antimicrobial Chemotherapy, NHS Improvement and patient representation. In this, we discussed actionable findings from the review and further developed our non-academic outputs to respond to the needs identified by policy. Additional meetings with policy stakeholders (e.g. PHE) led to the findings of the review being considered for inclusion in the guides produced by PHE for commissioners and for clinical trainers, as well as inclusion in the training presentations delivered by PHE representatives.
We have summarised the six key areas in an infographic aimed to help practitioners and policy-makers better tailor interventions for doctors in training (see Figure 13). The infographic guides readers to consider these six principles (middle circle numbered 1 to 6) when designing and implementing antimicrobial prescribing interventions.
The outer circle points to characteristics of the prescribing context (hierarchical learning, local prescribing norms) and relevant behaviour drivers (concern for professional reputation and fitting in the clinical team). As the context is likely to vary with time (e.g. with progress in training and when the composition of clinical teams changes) the arrow around the centre highlights the importance of continuously monitoring and evaluating how these six principles are considered when reviewing antimicrobial prescribing practices. This is consistent with a realist approach to emergence.
The rest of this section presents these six key areas in more detail and offers high-level principles to be considered when designing and implementing antimicrobial prescribing interventions for doctors in training.
-
Making AMR everyone’s ‘business’:
-
Establish antimicrobial prescribing as an important and immediate priority as part of wider culture change in clinical settings.
-
A wider cultural shift is necessary to address AMR by changing attitudes on antimicrobial prescribing across professional groups and levels of training. Given the importance of hierarchical dynamics in influencing prescribing decisions, it would not be adequate to implement interventions that target one specific group of prescribers, especially when this group is considered to have a lower status in the hierarchy.
Apart from differences between consultants and doctors in training, attention should also be paid to intragroup differences, such as the different needs of trainees at different levels. Currently, a significant number of interventions operate under the assumption that all doctors in training (or even all doctors) have similar needs. However, the review has shown that more junior doctors go through a period of adjustment to find their position in the hierarchy, to learn local prescribing norms and to become confident in their communication skills. Their needs will differ vastly from trainees at later stages who would have had more experience in managing prescribing norms and would be looking towards completion of specialist training and their transition into independent practice.
Making AMR relevant to everyone involved in clinical care, rather than just targeting new prescribers, would reinforce its importance as an immediate priority. In this respect, explicitly considering AMR in prescribing decisions would become a marker of good professional practice, rather than passively following prescribing habits as a way of exhibiting good learning, which is currently the norm. This means that doctors in training would be more likely to open a discussion on antimicrobial prescribing as it would be a behaviour that is rewarded and prioritised by seniors and colleagues from other professions. The ‘Antibiotic Guardian’ movement is a positive step towards this direction, although it would need to be further supported organisationally to achieve widespread impact. 28
It may also be worth reframing the way antimicrobial prescribing interventions are presented to their target groups and implemented in clinical settings. Most of the interventions included in this review attempt to improve antimicrobial prescribing in an episodic and isolated manner, restricted to the scope and duration of each intervention. Rather than presenting interventions as time-limited efforts to measure an impact on prescribing practice, a wider vision for ongoing change could be developed that accounts for contextual prescribing dynamics and depends on the participation of all professional groups and hierarchy levels. Strategic high-level endorsement could help to promote these changes, with named accountability starting at the senior executive board. There is also a need to reconcile potentially contradictory goals (e.g. between prioritisation of sepsis protocols and attention to antimicrobial prescribing).
-
Specifying what trainees at different levels of training are responsible for:
-
Set and communicate clear roles and explicit responsibilities in antimicrobial prescribing for trainees as appropriate at different levels (e.g. one explicit role for trainees could be to review the necessity of antibiotics).
-
In line with wider cultural change, the roles and responsibilities of trainees in antimicrobial prescribing could be further clarified as appropriate for different levels. At the moment, when responsibility for prescribing and reviewing antibiotics is not clear, or is assumed to lie only with the senior prescriber, it becomes more difficult for trainees to take up a particular role in the improvement of prescribing. Having a commonly agreed role and direct responsibility for appropriate antimicrobial prescribing would mean that doctors in training could be empowered to take initiative and address how antibiotic treatment could be optimised for each patient. For example, one of the roles that doctors in training could fulfil could be to review the necessity of continuing antibiotics as part of daily rounds – a role that has been suggested in discussions with the stakeholder group for this study.
Roles and responsibility structures would need to be explicitly communicated and formally endorsed by senior members of the clinical team (see point 5). This would clarify expectations among the team and would provide the legitimacy necessary for trainees to be able to fulfil their role. It would also reinforce attention to antibiotic prescribing as a marker of good professional practice, which could be reinforced through self-monitoring or in combination with clinical supervision.
-
Clarifying the knowledge, skills and capabilities needed to fulfil responsibilities:
-
Make explicit what levels of knowledge are expected to fulfil antimicrobial prescribing roles at different levels and how to apply this knowledge in practice, in the context of established workplace hierarchies and the ‘prescribing etiquette’.
-
In addition to setting particular roles and responsibilities for trainees in the context of antimicrobial prescribing, it would also be important to provide the appropriate knowledge and skills so that trainees can perform their roles effectively. The literature often cites knowledge gaps as responsible for suboptimal antimicrobial prescribing. This is reflected in trainees’ fears about whether or not the knowledge they have is sufficient to allow them to cope adequately with the demands of different prescribing environments. Uncertainty also exists in relation to what levels or aspects of knowledge are required at different stages in clinical training.
Explicitly circumscribing the boundaries of knowledge and capability deemed acceptable at various levels would provide trainees with confidence to practice antimicrobial prescribing, that is, understanding the extent to which they are supposed to prescribe on their own, or knowing what questions would be considered legitimate. It should also be highlighted that ongoing learning applies to all members of the clinical team, regardless of seniority, instead of assuming unquestioned autonomy in decision-making. However, as already mentioned, knowledge alone will not be sufficient to improve prescribing, as trainees will need to be enabled to translate knowledge into observable professional behaviours and appropriate decision-making in practice.
Interventions aiming at improving knowledge levels could provide part of the solution to this problem. However, they need to be sufficiently context sensitive to ensure that the knowledge imparted matches local antimicrobial prescribing practice and reflects good practice. As the review has shown, trainees often feel that they have to comply with or follow the prescribing practices of their seniors, which means that any knowledge they have will not be translated in practice if this is not what is considered acceptable in their clinical team.
-
Providing clear processes for seeking advice and support:
-
Provide trainees with easy access to a range of advice and support on antimicrobial prescribing, including senior consultants, antimicrobial pharmacists or other antimicrobial specialists, as well as guidelines or other decisions aids.
-
Another area of focus to improve antimicrobial prescribing for doctors in training relates to clarifying the ‘rules of engagement’ in every different rotation environment – in this case in relation to the range of advice and support that is perceived as legitimate. Even when trainees have commonly accepted roles in prescribing antibiotics and have acquired the locally relevant knowledge necessary to carry out these roles effectively, they would still occasionally need access to advice and resources as part of their learning.
The review of the literature highlighted that trainees make detailed judgements about (1) whether or not it would be acceptable to ask for assistance when making certain antimicrobial prescribing decisions, (2) what types of topics would be acceptable to ask about, (3) whom they should address their questions to and (4) how should they frame and communicate their questions. They make judgements on these points depending on the condition of the patient, whether or not they feel a case falls within their remit or knowledge and what they think the consequences of seeking assistance from particular colleagues would be. More attention could be paid to each of these decision points to adequately support trainees in their practice and in gaining transferable learning.
Developing explicit processes for seeking assistance, that is, commonly accepted procedures for seeking help from particular colleagues or seniors, would facilitate decision-making for doctors in training and would reduce barriers to seeking advice. There is a need to explicitly role model appropriate prescribing to junior doctors not just in terms of technical choices (what to prescribe), but also in terms of behaviour. This means communicating that it is considered good practice to ask when unsure and explicitly addressing the different aspects of assistance-seeking (whether, what, whom and how to ask). One application of role modelling assistance-seeking could be in relation to antimicrobial specialists. Through the review and stakeholder engagement, it was highlighted that different environments tend to legitimise the role of microbiologists or infectious disease specialists differently. Senior trainers could explicitly role model good practice by actively asking antimicrobial specialist opinion on particular prescribing decisions and by explaining how such engagement can have maximum value.
As commonly observed in the literature, receiving advice from different clinicians does not always facilitate the decision-making process, especially when senior colleagues offer contradicting opinions. 43 Processes that would allow trainees to prioritise and reconcile between conflicting sources of advice would be useful at the organisational level so that there is a commonly agreed strategy on how to approach difficult antimicrobial prescribing decisions or how to review decisions others have made. This could include helping trainees to develop the right communication strategies and language to discuss antimicrobial prescribing decisions and doubts effectively, as previous research has shown. 100,144
-
Ensuring changes are endorsed and reinforced by seniors in the workplace:
-
Establish senior support and ensure meaningful endorsement and reinforcement of antimicrobial prescribing interventions from influential seniors.
-
Any interventions that do not match or reconcile with accepted norms may not, in reality, translate to better practice. As the reviewed literature has highlighted, senior doctors play a significant role in setting prescribing norms and influencing junior members of the clinical team in hospitals. 35,66,111 Given their position higher up in the hierarchy, the attitudes and choices of senior clinicians set the tone for doctors in training in terms of how they should prioritise AMR as an issue and how this should be reflected in their prescribing decisions. This means that the role of doctors in training in antimicrobial prescribing, the knowledge levels and capabilities expected at different stages and the processes for seeking assistance need to be clearly accepted and supported by senior members of the clinical team.
Hierarchical relationships can have a constructive role when used productively to role model and reinforce appropriate prescribing behaviours. For example, senior doctors could consider explicitly discussing their prescribing rationale when making a decision to prescribe antibiotics, especially in less clear-cut cases. They could also initiate dialogue around prescribing choices, inviting critical questions and signposting to their doctors in training that they expect their prescription to be reviewed when necessary. Although hard to prioritise, this time investment will reap longer-term rewards given that junior doctors prescribe a large proportion of antibiotics.
-
Enabling adequate trust so that clinicians will ask questions and challenge:
-
Actively build and sustain adequate trust between senior and junior members of the clinical team so that there is a safe environment in which to ask questions about prescribing, rather than blindly following practice.
-
The review highlighted that doctors in training often associate competence with the ability to recognise and follow established prescribing norms. Seniors may assume that their team would be willing to ask questions or to challenge a particular decision, but this may not always be the case. Doctors in training are often reluctant to ask in case their questions show ignorance and result in consequences on their reputation or career progression. Being explicit about appropriate knowledge levels, skills and capabilities for different stages in training (see point 3) would be a necessary first step in building explicit boundaries around what questions are considered legitimate (what one is and is not expected to know). This may not be sufficient on its own, however, as there is a need to actively develop conditions in which doctors in training will feel safe to ask questions, feed back to their clinical teams and challenge decisions made by others. In policy studies, this has been described as ‘speaking truth to power’: an orientation towards a culture in which less senior team members overcome the obstacles of hierarchy to point out weaknesses in decision-making; in which team members are acting on the basis of shared accountability and responsibility; and in which there is learning from suboptimal practice, without attributing blame, while maintaining an open and honest dialogue. 197 It may be useful to explore how the principle of ‘speaking truth to power’ can support meaningful relationship building for the improvement of antimicrobial prescribing by paying more attention to how junior–senior interactions are negotiated, while being critical about how challenging in the context of power dynamics can work in different environments. 198
Dissemination
The infographic has been presented in conferences and revised as a result of the feedback received from the policy workshop for the review. We are currently in discussions with PHE, which is considering adding our findings, including the infographic, to its training guides. Further dissemination will include promotion through social media from the communications department of the lead site for this project (Department of Primary Care Health Sciences, University of Oxford, Oxford, UK), as well as through the professional networks of the project team. We have also disseminated this to our stakeholder group for further promotion to their own organisations and networks.
Animation video
To extend the reach of our work we have also developed an animation video together with a team of professional graphic designers in the USA (Kindea Labs, New York, NY, USA). The idea for this animation video came out of our stakeholder group when debating ways to influence junior doctors through non-academic outputs for wider dissemination. It was agreed that senior involvement would be crucial and trust induction would be a suitable way to set the tone for the attitudes of doctors in training (although the video is being developed for use in other contexts as well). A visually engaging way of grappling with the challenges of antimicrobial prescribing was deemed ideal to capture their interest.
The aim of the animation video is to trigger reflection and discussion, but not so much on the technical aspects of prescribing, such as when to prescribe or what antimicrobial to choose. Instead, our focus is on highlighting the hierarchical influences that junior doctors should expect when working that would influence their behaviours, as emphasised in our review. For example, we wanted to prepare junior doctors for instances where they might not understand why their consultant is prescribing an antibiotic or when they might find themselves receiving contradictory advice. Rather than being prescriptive, the animation provides opportunities to reflect on such instances and encourages viewers to pause and think about how the content presented may apply to their own circumstances and what the ‘solutions’ might be. Ideally, the video would be used in the context of an induction or other learning opportunity, together with senior clinicians, to discuss the best ways to overcome challenges with appropriate antimicrobial prescribing, as relevant to their own setting. We have been in discussions with clinicians at the Oxford John Radcliffe Hospital who are interested in reviewing this work further and would consider using it in practice. We are also exploring dissemination to clinicians based in Exeter. Members of our stakeholder group have also suggested they may be interested in trialling the video. The full video can be accessed at this link: https://vimeo.com/190717025 (see Report Supplementary Material 1).
Strengths and limitations
This is the first realist review on antimicrobial stewardship looking at the wider contextual drivers for the prescribing behaviours of doctors in training. In this review, we sought to inform the debate on appropriate prescribing support for doctors in training by looking beyond the technical aspects of prescribing and taking account of the context in which antimicrobial prescribing occurs. We followed systematic and transparent processes for the screening, analysis and synthesis of the data. To ensure consistency, we carried out checks between two reviewers. The CMOCs and programme theory are the results of in-depth, reflective discussions within and between the project team and the stakeholder group, rather than isolated data analysis.
Another key strength of the IMPACT review is the additional literature search we performed. Having completed the analysis of the articles resulting from the main search for data, we narrowed down the scope of the review to focus on what emerged as key influencing factors in prescribing behaviour, namely hierarchies and teamwork dynamics. The data retrieved from the additional search were not restricted to antimicrobial prescribing, but covered a wider range of sources, which allowed us to enhance the plausibility of our interpretations and the validity of our arguments.
Developing nuanced CMOCs that are supported by data and substantiated through theory has been an iterative process in order to reach an increased understanding. However, we do not treat this increased understanding as the end point of the review, as we sought ways to translate our CMOCs and programme theory into actionable findings. This allowed us to develop non-academic outputs for improving the design and implementation of a range of different types of prescribing interventions.
Apart from analysing and configuring the data in the literature, programme theory development was strongly influenced by the stakeholder group recruited for the IMPACT review. Stakeholder group involvement was particularly useful to refine the inferences and interpretations made from the data, particularly around mechanisms (in a realist sense) and in areas where the data were not adequate to develop a nuanced picture. The role of the group, which consisted of patients, health professionals and policy-makers, was significant in confirming and refining aspects of the programme theory. Initially, we intended to follow a uniform approach to stakeholder involvement in realist reviews (i.e. regular group meetings), but we soon realised that more ad hoc communications with different stakeholders would allow for increased input. We would advocate that, depending on the topic area of the review, there should be an explicit rationale for what different members of a stakeholder group can contribute at different stages of the review process, and in what ways interactions should be structured (e.g. through telephone calls or individual meetings) to gain maximum value.
The study also has a number of limitations. By definition, evidence syntheses are reliant on the evidence that is available. We found that interventions were often not described in enough detail to be able to draw conclusions on how their different aspects had operated to result in improved prescribing for doctors in training. Although this may have reduced the scope for analysing the role of intervention components per se, it has provided, at the same time, the opportunity to incorporate a wider body of literature on the social and professional influences on antimicrobial prescribing, thereby increasing transferable learning. Where the retrieved literature provided limited data for CMOC development, we have highlighted this as part of our interpretations and have been explicit about the strength of our arguments (see Table 10 in Appendix 2 for an indication of the data extracted for each CMOC). For example, the literature included in this review does not contain adequate data to be able to fully identify under which contexts doctors in training feel more able to challenge decisions effectively. We have also been unable to distinguish a hierarchy of mechanisms (i.e. which mechanisms may be more important than others) from the data available.
In addition, the majority of the articles presented studies in secondary care, rather than looking at trainees’ antimicrobial prescribing behaviour in general practice. This remains a limitation of the study, although our interpretations of the data attempted to account for differences between settings. Regardless of setting, many of our high-level findings are still applicable for primary care trainees and medical students in the UK and in countries where medical education and health services are organised in similar ways. This is because findings are at the level of commonly occurring mechanisms shared by doctors in training, rather than describing setting-specific barriers and facilitators. However, some aspects of antimicrobial prescribing analysed in this report may not apply in different settings (e.g. low- and middle-income countries) where the composition of the clinical team can be radically different, newly qualified doctors may operate alone and the lack of resources may pose different challenges.
Chapter 5 Conclusions
Previous research has discussed the importance of social relations, norms and hierarchies in shaping antibiotic prescribing. However, many of these studies have not provided a coherent and detailed picture of how, why and to what extent power dynamics and social influences affect the way doctors in training engage with different aspects of antibiotic prescribing.
The overarching programme theory of the IMPACT review explains how and why doctors in training decide in certain contexts to passively comply with or actively follow their seniors’ prescribing habits and the way they take into account prescribing aids and consult other health professionals, along with how they negotiate patient expectations (the most common outcomes in the data). The programme theory also explains what drives reluctance or willingness to ask questions about antimicrobial prescribing or to challenge the decisions made by seniors, as well as how this changes as training progresses. As discussed in the literature reviewed, these outcomes result from complex inter-relationships between the important contexts in which doctors in training are embedded (i.e. hierarchical relationships, with powerful prescribing norms, where there is little clarity around roles and responsibilities, and knowledge expectations and how to apply knowledge in practice remain implicit) and the mechanisms triggered in these contexts (i.e. fear of criticism, fear of individual responsibility, the need to manage one’s own reputation and position in the team and to appear competent).
Few interventions to change the antimicrobial prescribing practice of doctors in training are designed and implemented in a way that pays adequate attention to the influence of contexts and the ways that these change during clinical training. There is little scope for improvement if hierarchical and interprofessional dynamics remain unacknowledged. This review contributes to our understanding of how antimicrobial prescribing interventions can be better embedded in the hierarchical and interprofessional dynamics of different health-care settings. We have proposed areas for improvement to better support trainees with antimicrobial prescribing. This includes the development of multifaceted interventions that do not just focus on the prescribing of trainees, but take a wider approach to influence norms in hierarchical relationships and the wider environment in which trainees operate. Together with our stakeholder group, we have also designed dissemination materials to enable optimal tailoring, design and implementation of antimicrobial prescribing interventions targeted at doctors in training.
Future research
Significant research efforts and resources are currently being channelled towards tackling AMR and establishing appropriate stewardship. However, antimicrobial prescribing by doctors in training remains relatively under-researched, especially in primary care settings. The high-level principles presented in this review should be further developed for implementation in practice. Further research should also focus on the role of interprofessional support and learning to promote appropriate antimicrobial prescribing and stewardship (including the role of non-medical prescribers). Interdisciplinary engagement would benefit research in areas such as antimicrobial prescribing in the context of hierarchical working and the importance of role modelling for different training levels (e.g. how to challenge the decisions of seniors and how to have effective conversations). More ‘good’ practice examples of trainee decision-making, learning and communication are needed from clinical settings with good performance in their antimicrobial prescribing rates. This should also include an in-depth understanding of how clinicians manage competing priorities (e.g. sepsis/antimicrobial stewardship) in practice. Relevant organisational and behavioural theory (e.g. capability, opportunity, motivation – behaviour model, normalisation process theory) could be used to extend research on multifaceted antimicrobial prescribing interventions and improve practice in this area. 199,200
Acknowledgements
We would like to express our thanks to the members of our stakeholder group, those who attended the policy workshop and other individuals who offered their opinions through other means for their significant contributions to the programme theory and actionable findings emerging from the review (alphabetically): Cressida Auckland, Lucy Brooke, Isobel Eaton, Rose Gallagher, Julie Harvey, Philip Howard, Fran Husson, Alice Miller, Russell O’Brien, Hazel Parker, Rakesh Patel, Laura Piddock, John (Otto) Poole, Robert Porter, John Reynolds, Mohamed Sadak, Shirley Stevens, Lynn Tatnell, Mary Tully, Carwyn Watkins and Len Worsfold. We would also like to thank the members of the steering group (alphabetically): Rob Anderson, Peter Riou and Rod Sheaff.
Contributions of authors
Dr Chrysanthi Papoutsi (Health Services Researcher) carried out the exploratory literature search for the review, contributed to the formal search strategies, screened the resulting references, carried out the coding, applied a realist logic of analysis to the data, developed and refined the programme theory and CMOCs for the review, identified the theoretical ideas underpinning this analysis, facilitated the stakeholder meetings and drafted and revised this report.
Professor Karen Mattick (Professor, Medical Education) developed the research project, contributed to the formal search strategies and to the development and refinement of programme theory and CMOCs, provided relevant content and theoretical literature and revised the final report.
Dr Mark Pearson (Senior Research Fellow, Implementation Science) developed the research project, contributed to the formal search strategies and to the development and refinement of programme theory and CMOCs, provided methodological support and input, developed and facilitated PPI in the stakeholder group and revised the final report.
Dr Nicola Brennan (Research Fellow, Literature Reviews in Clinical Education) developed the research project, contributed to the formal search strategies and to the development and refinement of programme theory and CMOCs, provided relevant content literature and revised the final report.
Mr Simon Briscoe (Information Specialist) developed and conducted the main and additional search strategies and contributed to writing the literature search sections for the final report.
Dr Geoff Wong (General Practitioner, General Practitioner Trainer and Clinical Research Fellow, Realist Approaches) was the principal investigator and developed the research project. He contributed to the formal search strategies, carried out consistency checks on the literature retrieved from the formal searches, as well as consistency checks on the screening and coding process, applied a realist logic of analysis to the data, developed and refined the programme theory and CMOCs for the review, contributed theoretical ideas underpinning this analysis and drafted and revised this report.
Publications
Wong G, Brennan N, Mattick K, Pearson M, Briscoe S, Papoutsi C. Interventions to improve antimicrobial prescribing of doctors in training: the IMPACT (IMProving Antimicrobial presCribing of doctors in Training) realist review. BMJ Open 2015;5:e009059.
Papoutsi C, Mattick K, Pearson M, Brennan N, Briscoe S, Wong G. Social and professional influences on antimicrobial prescribing for doctors-in-training: a realist review. Journal of Antimicrobial Chemotherapy 2017;72(Suppl. 9):2418–30.
Data sharing statement
All ‘raw’ data and the analyses performed can be obtained from the corresponding author. All data used to develop and refine the programme theory are included in the main body of the report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Antimicrobial Resistance: Global Report on Surveillance. Geneva: WHO; 2014.
- Department of Health and Social Care . Annual Report of the Chief Medical Officer: Infections and the Rise of Antimicrobial Resistance 2011. www.gov.uk/government/uploads/system/uploads/attachment_data/file/138331/CMO_Annual_Report_Volume_2_2011.pdf (accessed 10 April 2017).
- United Nations . Draft Political Declaration of the High-Level Meeting of the General Assembly on Antimicrobial Resistance 2016. www.un.org/pga/71/wp-content/uploads/sites/40/2016/09/DGACM_GAEAD_ESCAB-AMR-Draft-Political-Declaration-1616108E.pdf (accessed 10 April 2017).
- Department of Health and Social Care . UK and China Start Global Fund to Tackle Drug Resistant Infections n.d. www.gov.uk/government/news/uk-and-china-start-global-fund-to-tackle-drug-resistant-infections (accessed 10 April 2017).
- UK Mission to the United Nations Geneva . Statement by UK Public Health Minister on the First Day of the 68th Session of the World Health Assembly, Geneva n.d. www.gov.uk/government/world-location-news/statement-by-uk-public-health-minister-on-the-first-day-of-the-68th-session-of-the-world-health-assembly-geneva-18-may-2015 (accessed 10 April 2017).
- Department of Health and Social Care . UK Five Year Antimicrobial Resistance Strategy 2013 to 2018 2013. www.gov.uk/government/publications/uk-5-year-antimicrobial-resistance-strategy-2013-to-2018 (accessed 10 April 2017).
- HM Government . Tackling Drug-Resistant Infections Globally: Final Report and Recommendations 2016. https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf (accessed 10 April 2017).
- Teillant A, Gandra S, Barter D, Morgan DJ, Laxminarayan R. Potential burden of antibiotic resistance on surgery and cancer chemotherapy antibiotic prophylaxis in the USA: a literature review and modelling study. Lancet Infect Dis 2015;15:1429-37. https://doi.org/10.1016/S1473-3099(15)00270-4.
- Public Health England . Behaviour Change and Antibiotic Prescribing in Healthcare Settings: Literature Review and Behavioural Analysis 2015. www.gov.uk/government/uploads/system/uploads/attachment_data/file/405031/Behaviour_Change_for_Antibiotic_Prescribing_-_FINAL.pdf (accessed 10 April 2017).
- May L, Gudger G, Armstrong P, Brooks G, Hinds P, Bhat R, et al. Multisite exploration of clinical decision making for antibiotic use by emergency medicine providers using quantitative and qualitative methods. Infect Control Hosp Epidemiol 2014;35:1114-25. https://doi.org/10.1086/677637.
- Ashiru-Oredope D, Sharland M, Charani E, McNulty C, Cooke J. Improving the quality of antibiotic prescribing in the NHS by developing a new antimicrobial stewardship programme: Start Smart – Then Focus. J Antimicrob Chemother 2012;67:i51-i63. https://doi.org/10.1093/jac/dks202.
- Dryden M, Johnson AP, Ashiru-Oredope D, Sharland M. Using antibiotics responsibly: right drug, right time, right dose, right duration. J Antimicrob Chemother 2011;66:2441-3. https://doi.org/10.1093/jac/dkr370.
- Davey P, Marwick CA, Scott CL, Charani E, McNeil K, Brown E, et al. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Sys Rev 2017;2. https://doi.org/10.1002/14651858.CD003543.pub4.
- Davey P, Brown E, Fenelon L, Finch R, Gould I, Holmes A, et al. Systematic review of antimicrobial drug prescribing in hospitals. Emerging Infect Dis 2006;12:211-16. https://doi.org/10.3201/eid1202.050145.
- Hospital Pharmacy Initiative for Promoting Prudent Use of Antibiotics in Hospitals. London: Department of Health; 2003.
- Medical Schools Council . Outcomes of the Medical Schools Council Safe Prescribing Working Group 2007. www.medschools.ac.uk/publications/pages/safe-prescribing-working-group-outcomes.aspx (accessed 10 April 2017).
- Apisarnthanarak A, Srichomkwun P, Sutepvarnon A, Bailey TC, Fraser VJ. The long-term outcomes of an antibiotic control program with and without education. Clin Infect Dis 2007;45:1245-7. https://doi.org/10.1086/522279.
- Buyle F, Vogelaers D, Peleman R, Van Maele G, Robays H. Implementation of guidelines for sequential therapy with fluoroquinolones in a Belgian hospital. Pharm World Sci 2010;32:404-10. https://doi.org/10.1007/s11096-010-9384-y.
- Metlay JP, Camargo CA, MacKenzie T, McCulloch C, Maselli J, Levin SK, et al. Cluster-randomized trial to improve antibiotic use for adults with acute respiratory infections treated in emergency departments. Ann Emerg Med 2007;50:221-30. https://doi.org/10.1016/j.annemergmed.2007.03.022.
- Akter SF, Heller RD, Smith AJ, Milly AF. Impact of a training intervention on use of antimicrobials in teaching hospitals. J Infect Dev Ctries 2009;3:447-51. https://doi.org/10.3855/jidc.416.
- van Hees BC, de Ruiter E, Wiltink EH, de Jongh BM, Tersmette M. Optimizing use of ciprofloxacin: a prospective intervention study. J Antimicrob Chemother 2008;61:210-13. https://doi.org/10.1093/jac/dkm388.
- Angalakuditi M, Sunderland VB, Roberts MJ, Turner S, Lilley BJ. Impact of an educational program on antibiotic use in paediatric appendectomy procedures. J Pharm Pract Res 2005;35:21-4. https://doi.org/10.1002/j.2055-2335.2005.tb00295.x.
- Apisarnthanarak A, Danchaivijitr S, Khawcharoenporn T, Limsrivilai J, Warachan B, Bailey TC, et al. Thammasart University antibiotic management team. Effectiveness of education and an antibiotic-control program in a tertiary care hospital in Thailand. Clin Infect Dis 2006;42:768-75. https://doi.org/10.1086/500325.
- LeClaire AC, Lopez ID, Smith KM, Lewis DA, Rapp RP, Martin CA. Influence of a urinary tract infection empiric treatment pathway on physician prescribing in an academic medical center. Formulary 2006;41:74-81.
- Ashiru-Oredope D, Budd EL, Bhattacharya A, Din N, McNulty CAM, Micallef C, et al. Implementation of antimicrobial stewardship interventions recommended by national toolkits in primary and secondary healthcare sectors in England: TARGET and Start Smart Then Focus. J Antimicrob Chemother 2016;71:1408-14. https://doi.org/10.1093/jac/dkv492.
- Royal College of General Practitioners . TARGET Antibiotics Toolkit 2014. www.rcgp.org.uk/targetantibiotics/ (accessed 10 April 2017).
- Hallsworth M, Chadborn T, Sallis A, Sanders M, Berry D, Greaves F, et al. Provision of social norm feedback to high prescribers of antibiotics in general practice: a pragmatic national randomised controlled trial. Lancet 2016;387:1743-52. https://doi.org/10.1016/S0140-6736(16)00215-4.
- Bhattacharya A, Hopkins S, Sallis A, Budd EL, Ashiru-Oredope D. A process evaluation of the UK-wide Antibiotic Guardian campaign: developing engagement on antimicrobial resistance. J Public Health 2017;39:e40-e47.
- Public Health England . English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2016. www.gov.uk/government/uploads/system/uploads/attachment_data/file/575626/ESPAUR_Report_2016.pdf (accessed 10 April 2017).
- Arnold SR, Straus SE. Interventions to improve antibiotic prescribing practices in ambulatory care. Cochrane Database Syst Rev 2005;4. https://doi.org/10.1002/14651858.CD003539.pub2.
- Anthierens S, Tonkin-Crine S, Douglas E, Fernandez-Vandellos P, Krawczyk J, Llor C, et al. General practitioners’ views on the acceptability and applicability of a web-based intervention to reduce antibiotic prescribing for acute cough in multiple European countries: a qualitative study prior to a randomised trial. BMC Fam Pract 2012;13. https://doi.org/10.1186/1471-2296-13-101.
- Tonkin-Crine S, Yardley L, Coenen S, Fernandez-Vandellos P, Krawczyk J, Touboul P, et al. GPs’ views in five European countries of interventions to promote prudent antibiotic use. Br J Gen Pract 2011;61:e252-61. https://doi.org/10.3399/bjgp11X572445.
- Tonkin-Crine S, Yardley L, Little P. Antibiotic prescribing for acute respiratory tract infections in primary care: a systematic review and meta-ethnography. J Antimicrob Chemother 2011;66:2215-23. https://doi.org/10.1093/jac/dkr279.
- Charani E, Birgand G, Laundy M, Gilchrist M, Whitney L. Antimicrobial Stewardship. Oxford: Oxford University Press; 2016.
- Charani E, Castro-Sanchez E, Sevdalis N, Kyratsis Y, Drumright L, Shah N, et al. Understanding the determinants of antimicrobial prescribing within hospitals: the role of ‘prescribing etiquette’. Clin Infect Dis 2013;57:188-96. https://doi.org/10.1093/cid/cit212.
- Brennan N, Mattick K. A systematic review of educational interventions to change behaviour of prescribers in hospital settings, with a particular emphasis on new prescribers. Br J Clin Pharmacol 2013;75:359-72. https://doi.org/10.1111/j.1365-2125.2012.04397.x.
- Tully MP, Ashcroft DM, Dornan T, Lewis PJ, Taylor D, Wass V. The causes of and factors associated with prescribing errors in hospital inpatients. Drug Saf 2009;32:819-36. https://doi.org/10.2165/11316560-000000000-00000.
- Ross S, Bond C, Rothnie H, Thomas S, Macleod MJ. What is the scale of prescribing errors committed by junior doctors? A systematic review. Br J Clin Pharmacol 2009;67:629-40. https://doi.org/10.1111/j.1365-2125.2008.03330.x.
- Ross S, Hamilton L, Ryan C, Bond C. Who makes prescribing decisions in hospital inpatients? An observational study. Postgrad Med J 2012;88:507-10. https://doi.org/10.1136/postgradmedj-2011-130602.
- Gill PS, Mäkelä M, Vermeulen KM, Freemantle N, Ryan G, Bond C, et al. Changing doctor prescribing behaviour. Pharm World Sci 1999;21:158-67. https://doi.org/10.1023/A:1008719129305.
- Kennedy T, Regehr G, Rosenfield J, Roberts SW, Lingard L. Exploring the gap between knowledge and behavior: a qualitative study of clinician action following an educational intervention. Acad Med 2004;79:386-93. https://doi.org/10.1097/00001888-200405000-00006.
- McNulty CA, Boyle P, Nichols T, Clappison P, Davey P. Don’t wear me out – the public’s knowledge of and attitudes to antibiotic use. J Antimicrob Chemother 2007;59:727-38. https://doi.org/10.1093/jac/dkl558.
- Mattick K, Kelly N, Rees C. A window into the lives of junior doctors: narrative interviews exploring antimicrobial prescribing experiences. J Antimicrob Chemother 2014;69:2274-83. https://doi.org/10.1093/jac/dku093.
- McLellan L, Tully MP, Dornan T. How could undergraduate education prepare new graduates to be safer prescribers?. Br J Clin Pharmacol 2012;74:605-13. https://doi.org/10.1111/j.1365-2125.2012.04271.x.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist Synthesis: An Introduction. ESRC Research Methods Programme. Manchester: University of Manchester; 2004.
- Wong G, Brennan N, Mattick K, Pearson M, Briscoe S, Papoutsi C. Interventions to improve antimicrobial prescribing of doctors in training: the IMPACT (IMProving Antimicrobial presCribing of doctors in Training) realist review. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-009059.
- Booth A, Clarke M, Ghersi D, Moher D, Petticrew M, Stewart L. An international registry of systematic-review protocols. Lancet 2011;377:108-9. https://doi.org/10.1016/S0140-6736(10)60903-8.
- Pawson R, Owen L, Wong G. The Today Programme’s contribution to evidence-based policy. Evaluation 2010;16:211-3. https://doi.org/10.1177/1356389010369636.
- Pawson R. Evidence-Based Policy: A Realist Perspective. London: Sage; 2006.
- Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ 2005;331:1064-5. https://doi.org/10.1136/bmj.38636.593461.68.
- Booth A, Harris J, Croot E, Springett J, Campbell F, Wilkins E. Towards a methodology for cluster searching to provide conceptual and contextual ‘richness’ for systematic reviews of complex interventions: case study (CLUSTER). BMC Med Res Methodol 2013;13:1-14. https://doi.org/10.1186/1471-2288-13-118.
- Pawson R. The Science of Evaluation: A Realist Manifesto. London: Sage; 2013.
- Broom A, Broom J, Kirby E. Cultures of resistance? A Bourdieusian analysis of doctors’ antibiotic prescribing. Soc Sci Med 2014;110:81-8. https://doi.org/10.1016/j.socscimed.2014.03.030.
- Pawson R, Vaessen J, Leeuw F. Mind the Gap: Perspectives on Policy Evaluation and the Social Sciences. New Brunswick, NJ: Transaction Publishers; 2010.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-21.
- Ajemigbitse AA, Omole MK, Osi-Ogbu OF, Erhun WO. A qualitative study of causes of prescribing errors among junior medical doctors in a Nigeria in-patient setting. Ann Afr Med 2013;12:223-31. https://doi.org/10.4103/1596-3519.122691.
- Allison GM, Weigel B, Holcroft C. Does electronic medication reconciliation at hospital discharge decrease prescription medication errors?. Int J Health Care Qual Assur 2015;28:564-73. https://doi.org/10.1108/IJHCQA-12-2014-0113.
- Dobrzanski S, Hammond I, Khan G, Holdsworth H. The nature of hospital prescribing errors. Br J Clin Pharmacol 2002;7:187-93. https://doi.org/10.1108/14664100210438271.
- Hong SY, Epstein LH, Lawrence K, Davidson L, Taur Y, Nadkarni L, et al. Evaluation of programmatic changes to an antimicrobial stewardship program with house officer feedback. J Eval Clin Pract 2013;19:388-92. https://doi.org/10.1111/j.1365-2753.2012.01840.x.
- Ali MH, Kalima P, Maxwell SR. Failure to implement hospital antimicrobial prescribing guidelines: a comparison of two UK academic centres. J Antimicrob Chemother 2006;57:959-62. https://doi.org/10.1093/jac/dkl076.
- Alweis R, Greco M, Wasser T, Wenderoth S. An initiative to improve adherence to evidence-based guidelines in the treatment of URIs, sinusitis, and pharyngitis. J Community Hosp Intern Med Perspect 2014;4. https://doi.org/10.3402/jchimp.v4.22958.
- Cortoos PJ, De Witte K, Peetermans WE, Simoens S, Laekeman G. Opposing expectations and suboptimal use of a local antibiotic hospital guideline: a qualitative study. J Antimicrob Chemother 2008;62:189-95. https://doi.org/10.1093/jac/dkn143.
- De Souza V, MacFarlane A, Murphy AW, Hanahoe B, Barber A, Cormican M. A qualitative study of factors influencing antimicrobial prescribing by non-consultant hospital doctors. J Antimicrob Chemother 2006;58:840-3. https://doi.org/10.1093/jac/dkl323.
- Patel R, Green W, Martinez MM, Shahzad MW, Larkin C. A study of foundation year doctors’ prescribing in patients with kidney disease at a UK renal unit: a comparison with other prescribers regarding the frequency and type of errors. Eur J Hosp Pharm Sci Pract 2015;22:291-7. https://doi.org/10.1136/ejhpharm-2014-000620.
- Valerio M, Vena A, Bouza E, Reiter N, Viale P, Hochreiter M, et al. How much European prescribing physicians know about invasive fungal infections management?. BMC Infect Dis 2015;15. https://doi.org/10.1186/s12879-015-0809-z.
- Almatar MA, Peterson GM, Thompson A, Zaidi ST. Factors influencing ceftriaxone use in community-acquired pneumonia: emergency doctors’ perspectives. Emerg Med Australas 2014;26:591-5. https://doi.org/10.1111/1742-6723.12326.
- Baker E, Roberts AP, Wilde K, Walton H, Suri S, Rull G, et al. Development of a core drug list towards improving prescribing education and reducing errors in the UK. Br J Clin Pharmacol 2011;71:190-8. https://doi.org/10.1111/j.1365-2125.2010.03823.x.
- Barlow G, Nathwani D, Myers E, Sullivan F, Stevens N, Duffy R, et al. Identifying barriers to the rapid administration of appropriate antibiotics in community-acquired pneumonia. J Antimicrob Chemother 2008;61:442-51. https://doi.org/10.1093/jac/dkm462.
- Chaves NJ, Cheng AC, Runnegar N, Kirschner J, Lee T, Buising K. Analysis of knowledge and attitude surveys to identify barriers and enablers of appropriate antimicrobial prescribing in three Australian tertiary hospitals. Intern Med J 2014;44:568-74. https://doi.org/10.1111/imj.12373.
- Livorsi D, Comer A, Matthias MS, Perencevich EN, Bair MJ. Factors influencing antibiotic-prescribing decisions among inpatient physicians: a qualitative investigation. Infect Control Hosp Epidemiol 2015;36:1065-72. https://doi.org/10.1017/ice.2015.136.
- Toulmin SE. The Uses of Argument. New York: Cambridge University Press; 2003.
- Tallentire VR, Smith SE, Skinner J, Cameron HS. Understanding the behaviour of newly qualified doctors in acute care contexts. Med Educ 2011;45:995-1005. https://doi.org/10.1111/j.1365-2923.2011.04024.x.
- Dallas A, van Driel M, van de Mortel T, Magin P. Antibiotic prescribing for the future: exploring the attitudes of trainees in general practice. Br J Gen Pract 2014;64:e561-7. https://doi.org/10.3399/bjgp14X681373.
- Liabsuetrakul T, Chongsuvivatwong V, Lumbiganon P, Lindmark G. Obstetricians’ attitudes, subjective norms, perceived controls, and intentions on antibiotic prophylaxis in caesarean section. Soc Sci Med 2003;57:1665-74. https://doi.org/10.1016/S0277-9536(02)00550-6.
- Hoff TJ, Pohl H, Bartfield J. Teaching but not learning: how medical residency programs handle errors. J Organ Behav 2006;27:869-96. https://doi.org/10.1002/job.395.
- Navarro-San Francisco C, Del Toro MD, Cobo J, De Gea-Garcia JH, Vano-Galvan S, Moreno-Ramos F, et al. Knowledge and perceptions of junior and senior Spanish resident doctors about antibiotic use and resistance: results of a multicenter survey. Enferm Infecc Microbiol Clin 2013;31:199-204. https://doi.org/10.1016/j.eimc.2012.05.016.
- Hilliard R, Harrison C, Madden S. Ethical conflicts and moral distress experienced by paediatric residents during their training. Paediatr Child Health 2007;12:29-35. https://doi.org/10.1093/pch/12.1.29.
- Walton MM. Hierarchies: the Berlin Wall of patient safety. Qual Saf Health Care 2006;15:229-30. https://doi.org/10.1136/qshc.2006.019240.
- Kilminster S, Zukas M, Quinton N, Roberts T. Preparedness is not enough: understanding transitions as critically intensive learning periods. Med Educ 2011;45:1006-15. https://doi.org/10.1111/j.1365-2923.2011.04048.x.
- McLellan L, Dornan T, Newton P, Williams SD, Lewis P, Steinke D, et al. Pharmacist-led feedback workshops increase appropriate prescribing of antimicrobials. J Antimicrob Chemother 2016;71:1415-25. https://doi.org/10.1093/jac/dkv482.
- Bearman M, Lawson M, Jones A. Participation and progression: new medical graduates entering professional practice. Adv Health Sci Educ Theory Pract 2011;16:627-42. https://doi.org/10.1007/s10459-011-9284-5.
- Friedman Z, Hayter MA, Everett TC, Matava CT, Noble LM, Bould MD. Power and conflict: the effect of a superior’s interpersonal behaviour on trainees’ ability to challenge authority during a simulated airway emergency. Anaesthesia 2015;70:1119-29. https://doi.org/10.1111/anae.13191.
- Bould MD, Sutherland S, Sydor DT, Naik V, Friedman Z. Residents’ reluctance to challenge negative hierarchy in the operating room: a qualitative study. Can J Anaesth 2015;62:576-86. https://doi.org/10.1007/s12630-015-0364-5.
- Gordon LJ, Rees CE, Ker JS, Cleland J. Dimensions, discourses and differences: trainees conceptualising health care leadership and followership. Med Educ 2015;49:1248-62. https://doi.org/10.1111/medu.12832.
- Ajemigbitse AA, Omole MK, Ezike NC, Erhun WO. Assessment of the knowledge and attitudes of intern doctors to medication prescribing errors in a Nigeria tertiary hospital. J Basic Clin Pharm 2013;5:7-14. https://doi.org/10.4103/0976-0105.128244.
- Akici A, Kalaca S, Goren MZ, Akkan AG, Karaalp A, Demir D, et al. Comparison of rational pharmacotherapy decision-making competence of general practitioners with intern doctors. Eur J Clin Pharmacol 2004;60:75-82. https://doi.org/10.1007/s00228-004-0751-2.
- Conte H, Scheja M, Hjelmqvist H, Jirwe M. Exploring teams of learners becoming ‘WE’ in the Intensive Care Unit – a focused ethnographic study. BMC Med Educ 2015;15. https://doi.org/10.1186/s12909-015-0414-2.
- Fakih MG, Berschback J, Juzych NS, Massanari RM. Compliance of resident and staff physicians with IDSA guidelines for the diagnosis and treatment of streptococcal pharyngitis. Infec Dis Clin Prac 2006;14:84-8. https://doi.org/10.1097/01.idc.0000198462.55744.f8.
- Lee TC, Frenette C, Jayaraman D, Green L, Pilote L. Antibiotic self-stewardship: trainee-led structured antibiotic time-outs to improve antimicrobial use. Ann Intern Med 2014;161:53-8. https://doi.org/10.7326/M13-3016.
- Sculli GL, Fore AM, Sine DM, Paull DE, Tschannen D, Aebersold M, et al. Effective followership: A standardized algorithm to resolve clinical conflicts and improve teamwork. J Health Risk Manag 2015;35:21-30. https://doi.org/10.1002/jhrm.21174.
- Welch SA, Novy M, Preisz P, Quinn DI, Whicker SD, Brown SE, et al. Promoting rational prescribing by emergency department junior medical officers. Aust J Hosp Pharm 2000;30:262-7. https://doi.org/10.1002/jppr2000306262.
- Ziglam HM, Morales D, Webb K, Nathwani D. Knowledge about sepsis among training-grade doctors. J Antimicrob Chemother 2006;57:963-5. https://doi.org/10.1093/jac/dkl042.
- Hoff TJ. How work context shapes physician approach to safety and error. Qual Manag Health Care 2008;17:140-53. https://doi.org/10.1097/01.QMH.0000316992.94415.34.
- Illing J, Morrow G, Kergon C, Burford B, Spencer J, Peile E, et al. How Prepared Are Medical Graduates to Begin Practice: A Comparison of Three Diverse UK Medical Schools. Final Report for the GMC Education Commitee 2008.
- Stewart J. To call or not to call: a judgement of risk by pre-registration house officers. Med Educ 2008;42:938-44. https://doi.org/10.1111/j.1365-2923.2008.03123.x.
- Tell D, Engstrom S, Molstad S. Adherence to guidelines on antibiotic treatment for respiratory tract infections in various categories of physicians: a retrospective cross-sectional study of data from electronic patient records. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-008096.
- Tobaiqy M, McLay J, Ross S. Foundation year 1 doctors and clinical pharmacology and therapeutics teaching. A retrospective view in light of experience. Br J Clin Pharmacol 2007;64:363-72. https://doi.org/10.1111/j.1365-2125.2007.02925.x.
- Zaidi ST, Thursky KA. Using formative evaluation to improve uptake of a web-based tool to support antimicrobial stewardship. J Clin Pharm Ther 2013;38:490-7. https://doi.org/10.1111/jcpt.12093.
- Chow A, Lye DCB, Arah OA. Psychosocial determinants of physicians’ acceptance of recommendations by antibiotic computerised decision support systems: A mixed methods study. Int J Antimicrob Agents 2015;45:295-304. https://doi.org/10.1016/j.ijantimicag.2014.10.009.
- Vivekananda-Schmidt P, Vernon B. FY1 doctors’ ethicolegal challenges in their first year of clinical practice: an interview study. J Med Ethics 2014;40:277-81. https://doi.org/10.1136/medethics-2011-100391.
- Abbo L, Sinkowitz-Cochran R, Smith L, Ariza-Heredia E, Gomez-Marin O, Srinivasan A, et al. Faculty and resident physicians’ attitudes, perceptions, and knowledge about antimicrobial use and resistance. Infect Control Hosp Epidemiol 2011;32:714-8. https://doi.org/10.1086/660761.
- Asseray N, Mallaret MR, Sousbie M, Liberelle B, Schaerer L, Borrel E, et al. Antibiotherapy in hospital: evaluation of prescription habits within a hospital network. Med Mal Infect 2002;32:468-76. https://doi.org/10.1016/S0399-077X(02)00404-3.
- Almatar MA, Peterson GM, Thompson A, McKenzie DS, Anderson TL. Community-acquired pneumonia: why aren’t national antibiotic guidelines followed?. Int J Clin Pract 2015;69:259-66. https://doi.org/10.1111/ijcp.12538.
- Ambroggio L, Thomson J, Murtagh Kurowski E, Courter J, Statile A, Graham C, et al. Quality improvement methods increase appropriate antibiotic prescribing for childhood pneumonia. Pediatrics 2013;131:e1623-31. https://doi.org/10.1542/peds.2012-2635.
- Dallas A, Magin P, Morgan S, Tapley A, Henderson K, Ball J, et al. Antibiotic prescribing for respiratory infections: a cross-sectional analysis of the ReCEnT study exploring the habits of early-career doctors in primary care. Fam Pract 2015;32:49-55. https://doi.org/10.1093/fampra/cmu069.
- Doyon S, Perreault M, Marquis C, Gauthier J, Lebel D, Bailey B, et al. Quantitative evaluation of a clinical intervention aimed at changing prescriber behaviour in response to new guidelines. J Eval Clin Pract 2009;15:1111-7. https://doi.org/10.1111/j.1365-2753.2009.01259.x.
- Fakih MG, Hilu RC, Savoy-Moore RT, Saravolatz LD. Do resident physicians use antibiotics appropriately in treating upper respiratory infections? A survey of 11 programs. Clin Infect Dis 2003;37:853-6. https://doi.org/10.1086/377503.
- Gaur AH, Hare ME, Shorr RI. Provider and practice characteristics associated with antibiotic use in children with presumed viral respiratory tract infections. Pediatrics 2005;115:635-41. https://doi.org/10.1542/peds.2004-0670.
- Limbert C, Lamb R. Doctors’ use of clinical guidelines: two applications of the theory of planned behaviour. Psychol Health Med 2002;7:301-10. https://doi.org/10.1080/13548500220139377.
- Menéndez R, Torres A, Zalacaín R, Aspa J, Martín-Villasclaras JJ, Borderías L, et al. Guidelines for the treatment of community-acquired pneumonia: predictors of adherence and outcome. Am J Respir Crit Care Med 2005;172:757-62. https://doi.org/10.1164/rccm.200411-1444OC.
- Mincey BA, Parkulo MA. Antibiotic prescribing practices in a teaching clinic: comparison of resident and staff physicians. South Med J 2001;94:365-9. https://doi.org/10.1097/00007611-200194040-00001.
- Newham R, Thomson AH, Semple Y, Dewar S, Steedman T, Bennie M. Barriers to the safe and effective use of intravenous gentamicin and vancomycin in Scottish hospitals, and strategies for quality improvement. Eur J Hosp Pharm Sci Pract 2015;22:32-7. https://doi.org/10.1136/ejhpharm-2014-000483.
- Zallman L, Ma J, Xiao L, Lasser KE. Quality of US primary care delivered by resident and staff physicians. J Gen Intern Med 2010;25:1193-7. https://doi.org/10.1007/s11606-010-1456-0.
- Undeland DK, Kowalski TJ, Berth WL, Gundrum JD. Appropriately prescribing antibiotics for patients with pharyngitis: a physician-based approach vs a nurse-only triage and treatment algorithm. Mayo Clin Proc 2010;85:1011-15. https://doi.org/10.4065/mcp.2010.0382.
- Gordon LJ, Rees CE, Ker JS, Cleland J. Leadership and followership in the healthcare workplace: exploring medical trainees’ experiences through narrative inquiry. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-008898.
- Tamuz M, Giardina TD, Thomas EJ, Menon S, Singh H. Rethinking resident supervision to improve safety: from hierarchical to interprofessional models. J Hosp Med 2011;6:445-52. https://doi.org/10.1002/jhm.919.
- Wiener-Ogilvie S, Bennison J, Smith V. General practice training environment and its impact on preparedness. Educ Prim Care 2014;25:8-17. https://doi.org/10.1080/14739879.2014.11494236.
- Kroll L, Singleton A, Collier J, Rees Jones I. Learning not to take it seriously: junior doctors’ accounts of error. Med Educ 2008;42:982-90. https://doi.org/10.1111/j.1365-2923.2008.03151.x.
- Bongiovanni T, Yeo H, Sosa JA, Yoo PS, Long T, Rosenthal M, et al. Attrition from surgical residency training: perspectives from those who left. Am J Surg 2015;210:648-54. https://doi.org/10.1016/j.amjsurg.2015.05.014.
- Fiordelli M, Schulz PJ, Caiata Zufferey M. Dissonant role perception and paradoxical adjustments: an exploratory study on Medical Residents’ collaboration with senior doctors and head nurses. Adv Health Sci Educ 2014;19:311-27. https://doi.org/10.1007/s10459-013-9471-7.
- Maisonneuve JJ, Lambert TW, Goldacre MJ. Doctors’ views about training and future careers expressed one year after graduation by UK-trained doctors: questionnaire surveys undertaken in 2009 and 2010. BMC Med Educ 2014;14. https://doi.org/10.1186/s12909-014-0270-5.
- Hamui-Sutton A, Vives-Varela T, Gutierrez-Barreto S, Leenen I, Sanchez-Mendiola M. A typology of uncertainty derived from an analysis of critical incidents in medical residents: a mixed methods study. BMC Med Educ 2015;15. https://doi.org/10.1186/s12909-015-0459-2.
- Jaensch SL, Baysari MT, Day RO, Westbrook JI. Junior doctors’ prescribing work after-hours and the impact of computerized decision support. Int J Med Inform 2013;82:980-6. https://doi.org/10.1016/j.ijmedinf.2013.06.014.
- Lewis PJ, Ashcroft DM, Dornan T, Taylor D, Wass V, Tully MP. Exploring the causes of junior doctors’ prescribing mistakes: a qualitative study. Br J Clin Pharmacol 2014;78:310-19. https://doi.org/10.1111/bcp.12332.
- Simpson JH, Lynch R, Grant J, Alroomi L. Reducing medication errors in the neonatal intensive care unit. Arch Dis Child Fetal Neonatal Ed 2004;89:F480-2. https://doi.org/10.1136/adc.2003.044438.
- Steinke DT, Bain DJ, MacDonald TM, Davey PG. Practice factors that influence antibiotic prescribing in general practice in Tayside. J Antimicrob Chemother 2000;46:509-12. https://doi.org/10.1093/jac/46.3.509.
- Teunissen PW, Stapel DA, van der Vleuten C, Scherpbier A, Boor K, Scheele F. Who wants feedback? An investigation of the variables influencing residents’ feedback-seeking behavior in relation to night shifts. Acad Med 2009;84:910-7. https://doi.org/10.1097/ACM.0b013e3181a858ad.
- Ummenhofer W, Amsler F, Sutter PM, Martina B, Martin J, Scheidegger D. Team performance in the emergency room: assessment of inter-disciplinary attitudes. Resuscitation 2001;49:39-46. https://doi.org/10.1016/S0300-9572(00)00304-X.
- Jubraj B, Marvin V, Poots AJ, Patel S, Bovill I, Barnett N, et al. A pilot survey of junior doctors’ attitudes and awareness around medication review: time to change our educational approach?. European Journal of Hospital Pharmacy 2015;22:243-8. https://doi.org/10.1136/ejhpharm-2015-000664.
- Collins J. Foundation for Excellence: An Evaluation of the Foundation Programme 2010. www.agcas.org.uk/assets/download?file=2053&parent=793 (accessed 10 April 2017).
- Friedman SM, Sowerby RJ, Guo R, Bandiera G. Perceptions of emergency medicine residents and fellows regarding competence, adverse events and reporting to supervisors: a national survey. CJEM 2010;12:491-9. https://doi.org/10.1017/S1481803500012719.
- Farnan JM, Johnson JK, Meltzer DO, Humphrey HJ, Arora VM. Resident uncertainty in clinical decision making and impact on patient care: a qualitative study. Qual Saf Health Care 2008;17:122-6. https://doi.org/10.1136/qshc.2007.023184.
- Kennedy TJT, Regehr G, Baker GR, Lingard L. Preserving professional credibility: grounded theory study of medical trainees’ requests for clinical support. BMJ 2009;338. https://doi.org/10.1136/bmj.b128.
- Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: an insidious contributor to medical mishaps. Acad Med 2004;79:186-94. https://doi.org/10.1097/00001888-200402000-00019.
- Sellman JS, Decarolis D, Schullo-Feulner A, Nelson DB, Filice GA. Information resources used in antimicrobial prescribing. J Am Med Inform Assoc 2004;11:281-4. https://doi.org/10.1197/jamia.M1493.
- Brennan N, Corrigan O, Allard J, Archer J, Barnes R, Bleakley A, et al. The transition from medical student to junior doctor: today’s experiences of tomorrow’s doctors. Med Educ 2010;44:449-58. https://doi.org/10.1111/j.1365-2923.2009.03604.x.
- Garcia C, Llamocca LP, Garcia K, Jimenez A, Samalvides F, Gotuzzo E, et al. Knowledge, attitudes and practice survey about antimicrobial resistance and prescribing among physicians in a hospital setting in Lima, Peru. BMC Clin Pharmacol 2011;11. https://doi.org/10.1186/1472-6904-11-18.
- Kennedy TJ, Regehr G, Baker GR, Lingard LA. ‘It’s a cultural expectation.’ The pressure on medical trainees to work independently in clinical practice. Med Educ 2009;43:645-53. https://doi.org/10.1111/j.1365-2923.2009.03382.x.
- Belyansky I, Martin TR, Prabhu AS, Tsirline VB, Howley LD, Phillips R, et al. Poor resident-attending intraoperative communication may compromise patient safety. J Surg Res 2011;171:386-94. https://doi.org/10.1016/j.jss.2011.04.011.
- Coffey M, Thomson K, Tallett S, Matlow A. Pediatric residents’ decision-making around disclosing and reporting adverse events: the importance of social context. Acad Med 2010;85:1619-25. https://doi.org/10.1097/ACM.0b013e3181f046a6.
- Doyle P, VanDenKerkhof EG, Edge DS, Ginsburg L, Goldstein DH. Self-reported patient safety competence among Canadian medical students and postgraduate trainees: a cross-sectional survey. BMJ Qual Saf 2015;24:135-41. https://doi.org/10.1136/bmjqs-2014-003142.
- Pian-Smith MC, Simon R, Minehart RD, Podraza M, Rudolph J, Walzer T, et al. Teaching residents the two-challenge rule: a simulation-based approach to improve education and patient safety. Simul Health 2009;4:84-91. https://doi.org/10.1097/SIH.0b013e31818cffd3.
- van Schaik S, Plant J, O’Brien B. Challenges of interprofessional team training: a qualitative analysis of residents’ perceptions. Educ Health 2015;28:52-7. https://doi.org/10.4103/1357-6283.161883.
- Kobayashi H, Pian-Smith M, Sato M, Sawa R, Takeshita T, Raemer D. A cross-cultural survey of residents’ perceived barriers in questioning/challenging authority. Qual Saf Health Care 2006;15:277-83. https://doi.org/10.1136/qshc.2005.017368.
- Sydor DT, Bould MD, Naik VN, Burjorjee J, Arzola C, Hayter M, et al. Challenging authority during a life-threatening crisis: the effect of operating theatre hierarchy. Br J Anaesth 2013;110:463-71. https://doi.org/10.1093/bja/aes396.
- Bethune R, Canter R, Abrams P. What do surgical trainees think about patient safety culture, and is this different from their consultants?. Clin Risk 2012;18:52-7. https://doi.org/10.1258/cr.2012.011043.
- Reader TW, Flin R, Mearns K, Cuthbertson BH. Interdisciplinary communication in the intensive care unit. Br J Anaesth 2007;98:347-52. https://doi.org/10.1093/bja/ael372.
- Coats RD, Burd RS. Intraoperative communication of residents with faculty: perception versus reality. J Surg Res 2002;104:40-5. https://doi.org/10.1006/jsre.2002.6402.
- Aveling EL, Parker M, Dixon-Woods M. What is the role of individual accountability in patient safety? A multi-site ethnographic study. Sociol Health Illn 2016;38:216-32. https://doi.org/10.1111/1467-9566.12370.
- Merton R, Merton R. On Theoretical Sociology: Five Essays Old and New. New York, NY: Free Press; 1967.
- Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge: Cambridge University Press; 1991.
- Egan T, Jaye C. Communities of clinical practice: the social organization of clinical learning. Health 2009;13:107-25. https://doi.org/10.1177/1363459308097363.
- Wenger E. Communities of Practice: Learning, Meaning, and Identity. New York, NY: Cambridge University Press; 1998.
- Goffman E. The Presentation of Self in Everyday Life. London: Harmondsworth; 1978.
- Dearden E, Mellanby E, Cameron H, Harden J. Which non-technical skills do junior doctors require to prescribe safely? A systematic review. Br J Clin Pharmacol 2015;80:1303-14. https://doi.org/10.1111/bcp.12735.
- Arroll B, Kenealy T, Kerse N. Do delayed prescriptions reduce antibiotic use in respiratory tract infections? A systematic review. Br J Gen Pract 2003;53:871-7.
- Drekonja DM, Filice GA, Greer N, Olson A, MacDonald R, Rutks I, et al. Antimicrobial stewardship in outpatient settings: a systematic review. Infect Control Hosp Epidemiol 2015;36:142-52. https://doi.org/10.1017/ice.2014.41.
- Kaki R, Elligsen M, Walker S, Simor A, Palmay L, Daneman N. Impact of antimicrobial stewardship in critical care: a systematic review. J Antimicrob Chemother 2011;66:1223-30. https://doi.org/10.1093/jac/dkr137.
- Ranji SR, Steinman MA, Shojania KG, Gonzales R. Interventions to reduce unnecessary antibiotic prescribing: a systematic review and quantitative analysis. Med Care 2008;46:847-62. https://doi.org/10.1097/MLR.0b013e318178eabd.
- Hall KK, Philbrick J, Nadkarni M. Evaluation and treatment of acute bronchitis at an academic teaching clinic. Am J Med Sci 2003;325:7-9. https://doi.org/10.1097/00000441-200301000-00002.
- Pacheco GS, Viscusi C, Hays DP, Woolridge DP. The effects of resident level of training on the rate of pediatric prescription errors in an academic emergency department. J Emerg Med 2012;43:e343-e8. https://doi.org/10.1016/j.jemermed.2012.01.016.
- Feucht CL, Rice LB. An interventional program to improve antibiotic use. Ann Pharmacother 2003;37:646-51. https://doi.org/10.1345/aph.1C166.
- Guerra CM, Pereira CA, Neves Neto AR, Cardo DM, Correa L. Physicians’ perceptions, beliefs, attitudes, and knowledge concerning antimicrobial resistance in a Brazilian teaching hospital. Infect Control Hosp Epidemiol 2007;28:1411-4. https://doi.org/10.1086/523278.
- Nambiar S, Schwartz RH, Sheridan MJ. Antibiotic use for upper respiratory tract infections: how well do pediatric residents do?. Arch Pediatr Adolesc Med 2002;156:621-4. https://doi.org/10.1001/archpedi.156.6.621.
- Roumie CL, Halasa NB, Edwards KM, Zhu Y, Dittus RS, Griffin MR. Differences in antibiotic prescribing among physicians, residents, and nonphysician clinicians. Am J Med 2005;118:641-8. https://doi.org/10.1016/j.amjmed.2005.02.013.
- Rinke ML, Moon M, Clark JS, Mudd S, Miller MR. Prescribing errors in a pediatric emergency department. Pediatr Emerg Care 2008;24:1-8. https://doi.org/10.1097/pec.0b013e31815f6f6c.
- Flannery MT, McCool MJ. Community-acquired pneumonia guidelines and resident behavior. Am J Med 2005;118:929-30. https://doi.org/10.1016/j.amjmed.2005.01.053.
- Lee MJ, Kim M, Kim NH, Kim CJ, Song KH, Choe PG, et al. Why is asymptomatic bacteriuria overtreated?: A tertiary care institutional survey of resident physicians. BMC Infect Dis 2015;15. https://doi.org/10.1186/s12879-015-1044-3.
- Neumark T, Brudin L, Mölstad S. Antibiotic prescribing in primary care by international medical graduates and graduates from Swedish medical schools. Fam Pract 2015;32:343-7. https://doi.org/10.1093/fampra/cmv001.
- Pulcini C, Williams F, Molinari N, Davey P, Nathwani D. Junior doctors’ knowledge and perceptions of antibiotic resistance and prescribing: a survey in France and Scotland. Clin Microbiol Infect 2011;17:80-7. https://doi.org/10.1111/j.1469-0691.2010.03179.x.
- Solomon DH, Van Houten L, Glynn RJ, Baden L, Curtis K, Schrager H, et al. Academic detailing to improve use of broad-spectrum antibiotics at an academic medical center. Arch Intern Med 2001;161:1897-902. https://doi.org/10.1001/archinte.161.15.1897.
- Jamtvedt G, Young JM, Kristoffersen DT, O’Brien MA, Oxman AD. Audit and feedback: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2006;2. https://doi.org/10.1002/14651858.CD000259.pub2.
- Foy R, Eccles MP, Jamtvedt G, Young J, Grimshaw JM, Baker R. What do we know about how to do audit and feedback? Pitfalls in applying evidence from a systematic review. BMC Health Serv Res 2005;5. https://doi.org/10.1186/1472-6963-5-50.
- Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2012;6. https://doi.org/10.1002/14651858.CD000259.pub3.
- Advisory Committee on Antimicrobial Resistance and Healthcare Associated Infections (ARHAI) and Public Health England (PHE) . Antimicrobial Prescribing and Stewardship Competencies 2013. www.gov.uk/government/uploads/system/uploads/attachment_data/file/253094/ARHAIprescrcompetencies__2_.pdf (accessed 10 April 2017).
- General Medical Council . Leadership and Management for All Doctors 2012. www.gmc-uk.org/Leadership_and_management_for_all_doctors___English_1015.pdf_48903400.pdf (accessed 10 April 2017).
- Wilkie V. Leadership and management for all doctors. Br J Gen Pract 2012;62:230-1. https://doi.org/10.3399/bjgp12X636290.
- Kilminster SM, Jolly BC. Effective supervision in clinical practice settings: a literature review. Med Educ 2000;34:827-40. https://doi.org/10.1046/j.1365-2923.2000.00758.x.
- Ten Cate O. Nuts and bolts of entrustable professional activities. J Grad Med Educ 2013;5:157-8. https://doi.org/10.4300/JGME-D-12-00380.1.
- Medical Schools Council Safe Prescribing Working Group . Outcomes of the Medical Schools Council Safe Prescribing Working Group 2007. www.medschools.ac.uk/publications/pages/safe-prescribing-working-group-outcomes.aspx (accessed 10 April 2017).
- Thorpe JM, Smith SR, Trygstad TK. Trends in emergency department antibiotic prescribing for acute respiratory tract infections. Ann Pharmacother 2004;38:928-35. https://doi.org/10.1345/aph.1D380.
- McCarthy RM, Hilmer SN. Teaching Junior Medical Officers safe and effective prescribing. Intern Med J 2013;43:1250-3. https://doi.org/10.1111/imj.12279.
- Aggarwal S, Mathew J, Singh H, Sharma V. Attitude and perception of junior resident doctors’ regarding antibiotic resistance – a pilot study. J Acute Dis 2014;3:6-9. https://doi.org/10.1016/S2221-6189(14)60002-0.
- Deuster S, Roten I, Muehlebach S. Implementation of treatment guidelines to support judicious use of antibiotic therapy. J Clin Pharm Ther 2010;35:71-8. https://doi.org/10.1111/j.1365-2710.2009.01045.x.
- Parker HM, Mattick K. The determinants of antimicrobial prescribing among hospital doctors in England: a framework to inform tailored stewardship interventions. Br J Clin Pharmacol 2016;82:431-40. https://doi.org/10.1111/bcp.12953.
- Levinsky Y, Mimouni FB, Fisher D, Ehrlichman M. Chest radiography of acute paediatric lower respiratory infections: experience versus interobserver variation. Acta Paediatr 2013;102:e310-4. https://doi.org/10.1111/apa.12249.
- Oppenheim MI, Vidal C, Velasco FT, Boyer AG, Cooper MR, Hayes JG, et al. Impact of a computerized alert during physician order entry on medication dosing in patients with renal impairment. Proceedings of American Medical Informatics Association Annual Symposium 2002:577-81.
- Weingart SN, Toth M, Sands DZ, Aronson MD, Davis RB, Phillips RS. Physicians’ decisions to override computerized drug alerts in primary care. Arch Intern Med 2003;163:2625-31. https://doi.org/10.1001/archinte.163.21.2625.
- The King’s Fund . Getting the Measure of Quality: Opportunities and Challenges 2010. www.kingsfund.org.uk/sites/files/kf/Getting-the-measure-of-quality-Veena-Raleigh-Catherine-Foot-The-Kings-Fund-January-2010.pdf (accessed 10 April 2017).
- Berwick DM, James B, Coye MJ. Connections between quality measurement and improvement. Med Care 2003;41:I30-8. https://doi.org/10.1097/00005650-200301001-00004.
- Mannion R, Braithwaite J. Unintended consequences of performance measurement in healthcare: 20 salutary lessons from the English National Health Service. Intern Med J 2012;42:569-74. https://doi.org/10.1111/j.1445-5994.2012.02766.x.
- Waring JJ. Constructing and re-constructing narratives of patient safety. Soc Sci Med 2009;69:1722-31. https://doi.org/10.1016/j.socscimed.2009.09.052.
- Dixon-Woods M, McNicol S, Martin G. Ten challenges in improving quality in healthcare: lessons from the Health Foundation’s programme evaluations and relevant literature. BMJ Qual Saf 2012;21:876-84. https://doi.org/10.1136/bmjqs-2011-000760.
- Thursky KA, Mahemoff M. User-centered design techniques for a computerised antibiotic decision support system in an intensive care unit. Int J Med Inform 2007;76:760-8. https://doi.org/10.1016/j.ijmedinf.2006.07.011.
- Simonsen J, Robertson T. Routledge International Handbook of Participatory Design. New York, NY: Routledge; 2012.
- Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, et al. Lost in knowledge translation: time for a map?. J Contin Educ Health Prof 2006;26:13-24. https://doi.org/10.1002/chp.47.
- Wildavsky AB. Speaking Truth to Power: The Art and Craft of Policy Analysis. New Brunswick, NJ: Transaction Publishers; 1989.
- Haas P. When does power listen to truth? A constructivist approach to the policy process. J Eur Public Policy 2004;11:569-92. https://doi.org/10.1080/1350176042000248034.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-42.
- Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med 2010;8. https://doi.org/10.1186/1741-7015-8-63.
- Alagha HZ, Badary OA, Ibrahim HM, Sabri NA. Reducing prescribing errors in the paediatric intensive care unit: an experience from Egypt. Acta Paediatr 2011;100:e169-74. https://doi.org/10.1111/j.1651-2227.2011.02270.x.
- Aydin S, Yaris F, Ozcakir A, Agalar C. Most common infections and antibiotic prescribing habits of residents: experience of three university hospitals. Turk J Med Sci 2005;35:169-73.
- Bowes J, Yasseen AS, Barrowman N, Murchison B, Dennis J, Moreau KA, et al. Antimicrobial stewardship in pediatrics: focusing on the challenges clinicians face. BMC Pediatr 2014;14. https://doi.org/10.1186/1471-2431-14-212.
- Coleman JJ, Hemming K, Nightingale PG, Clark IR, Dixon-Woods M, Ferner RE, et al. Can an electronic prescribing system detect doctors who are more likely to make a serious prescribing error?. J R Soc Med 2011;104:208-18. https://doi.org/10.1258/jrsm.2011.110061.
- Coupat C, Pradier C, Degand N, Hofliger P, Pulcini C. Selective reporting of antibiotic susceptibility data improves the appropriateness of intended antibiotic prescriptions in urinary tract infections: a case-vignette randomised study. Eur J Clin Microbiol Infect Dis 2013;32:627-36. https://doi.org/10.1007/s10096-012-1786-4.
- Flannery DD, Swami S, Chan S, Eppes S. Prescriber perceptions of a pediatric antimicrobial stewardship program. Clin Pediatr (Phila) 2014;53:747-50. https://doi.org/10.1177/0009922814528279.
- Harnett SJ, Allen KD. Antibiotic policy use amongst junior doctors in a Merseyside hospital. J Hosp Infect 2000;46:239-40. https://doi.org/10.1053/jhin.2000.0825.
- Oshikoya KA, Senbanjo IO, Amole OO. Interns’ knowledge of clinical pharmacology and therapeutics after undergraduate and on-going internship training in Nigeria: a pilot study. BMC Med Educ 2009;9. https://doi.org/10.1186/1472-6920-9-50.
- Purcell K, Fergie J. Effect of an educational program on the treatment of RSV lower-respiratory-tract infection. Am J Health Syst Pharm 2003;60:759-67.
- Salomon L, Levu S, Deray G, Launay-Vacher V, Brücker G, Ravaud P. Assessing residents’ prescribing behavior in renal impairment. Int J Qual Health Care 2003;15:235-40. https://doi.org/10.1093/intqhc/mzg034.
- Seemungal IA, Bruno CJ. Attitudes of housestaff toward a prior-authorization-based antibiotic stewardship program (research brief). Infect Control Hosp Epidemiol 2012;33:429-31. https://doi.org/10.1086/664769.
- Stone S, Gonzales R, Maselli J, Lowenstein SR. Antibiotic prescribing for patients with colds, upper respiratory tract infections, and bronchitis: a national study of hospital-based emergency departments. Ann Emerg Med 2000;36:320-7. https://doi.org/10.1067/mem.2000.109341.
- Cosby KS, Croskerry P. Profiles in patient safety: authority gradients in medical error. Acad Emerg Med 2004;11:1341-5. https://doi.org/10.1111/j.1553-2712.2004.tb01925.x.
- Lingard L, Reznick R, Espin S, Regehr G, DeVito I. Team communications in the operating room: talk patterns, sites of tension, and implications for novices. Acad Med 2002;77:232-7. https://doi.org/10.1097/00001888-200203000-00013.
- Rosenbaum JR, Bradley EH, Holmboe ES, Farrell MH, Krumholz HM. Sources of ethical conflict in medical housestaff training: a qualitative study. Am J Med 2004;116:402-7. https://doi.org/10.1016/j.amjmed.2003.09.044.
- Stack SJ, Watson MJ. Enriching the resident–faculty relationship. Ann Emerg Med 2001;38:336-8. https://doi.org/10.1067/mem.2001.117954.
Appendix 1 Literature searches
Main literature search strategies
Database: MEDLINE
Host: Ovid.
Data parameters: 1946 to September Week 3 2015.
Date searched: 28 September 2015.
Searcher: Simon Briscoe.
Hits: 201.
Strategy
-
((junior or train*) adj2 (doctor* or medic* or physician*)).tw.
-
(“foundation year 1” or “foundation year 2” or “foundation year one” or “foundation year two” or registrar* or “new prescriber*”).tw.
-
((f1 or f2 or fy1 or fy2) adj3 (doctor* or medic* or physician*)).tw.
-
(foundation adj3 (doctor* or medic* or physician*)).tw.
-
((SpR or SpRs) adj10 (doctor* or medic* or physician*)).tw.
-
GPST.tw.
-
(“pre-registration house officer*” or “senior house officer*” or “house officer*”).tw.
-
((resident* or residenc*) adj2 (doctor* or medic* or physician*)).tw.
-
PRHO.tw.
-
((HO or SHO) adj3 (doctor* or medic* or physician*)).tw.
-
((intern or interns or internship*) and (doctor* or medic* or physician*)).tw.
-
“Internship and Residency”/
-
or/1-12
-
(prescrib* or prescrip*).tw.
-
((drug* or medicine* or medication*) adj2 (administ* or utili?ation or error*)).tw.
-
exp prescription/
-
exp Drug Utilization/
-
Prescription Drugs/
-
Drug Prescriptions/
-
Medication Errors/
-
or/14-20
-
(antimicrobial* or “anti microbial*” or antibiotic* or “anti biotic*” or antibacterial* or “anti bacterial*” or antiviral* or “anti viral*” or antifungal* or “anti fungal*” or “antiinfective*” or “anti infective*” or antiparasitic* or “anti parasitic*”).tw.
-
anti-infective agents/
-
exp anti-bacterial agents/
-
exp antifungal agents/
-
exp anti-infective agents, urinary/
-
exp antiparasitic agents/
-
exp antiviral agents/
-
or/22-28
-
13 and 21 and 29
Database: MEDLINE In-Process & Other Non-Indexed Citations
Host: Ovid.
Data parameters: September 25, 2015.
Date searched: 28 September 2015.
Searcher: Simon Briscoe.
Hits: 30.
Strategy
-
((junior or train*) adj2 (doctor* or medic* or physician*)).tw.
-
(“foundation year 1” or “foundation year 2” or “foundation year one” or “foundation year two” or registrar* or “new prescriber*”).tw.
-
((f1 or f2 or fy1 or fy2) adj3 (doctor* or medic* or physician*)).tw.
-
(foundation adj3 (doctor* or medic* or physician*)).tw.
-
((SpR or SpRs) adj10 (doctor* or medic* or physician*)).tw.
-
GPST.tw.
-
(“pre-registration house officer*” or “senior house officer*” or “house officer*”).tw.
-
((resident* or residenc*) adj2 (doctor* or medic* or physician*)).tw.
-
PRHO.tw.
-
((HO or SHO) adj3 (doctor* or medic* or physician*)).tw.
-
((intern or interns or internship*) and (doctor* or medic* or physician*)).tw.
-
or/1-11
-
(prescrib* or prescrip*).tw.
-
((drug* or medicine* or medication*) adj2 (administ* or utili?ation or error*)).tw.
-
or/13-14
-
(antimicrobial* or “anti microbial*” or antibiotic* or “anti biotic*” or antibacterial* or “anti bacterial*” or antiviral* or “anti viral*” or antifungal* or “anti fungal*” or “antiinfective*” or “anti infective*” or antiparasitic* or “anti parasitic*”).tw.
-
12 and 15 and 16
Database: EMBASE
Host: Ovid.
Data parameters: 1974 to 2015 September 25.
Date searched: 28 September 2015.
Searcher: Simon Briscoe.
Hits: 548.
Strategy
-
((junior or train*) adj2 (doctor* or medic* or physician*)).tw.
-
(“foundation year 1” or “foundation year 2” or “foundation year one” or “foundation year two” or registrar* or “new prescriber*”).tw.
-
((f1 or f2 or fy1 or fy2) adj3 (doctor* or medic* or physician*)).tw.
-
(foundation adj3 (doctor* or medic* or physician*)).tw.
-
((SpR or SpRs) adj10 (doctor* or medic* or physician*)).tw.
-
GPST.tw.
-
(“pre-registration house officer*” or “senior house officer*” or “house officer*”).tw.
-
((resident* or residenc*) adj2 (doctor* or medic* or physician*)).tw.
-
PRHO.tw.
-
((HO or SHO) adj3 (doctor* or medic* or physician*)).tw.
-
((intern or interns or internship*) and (doctor* or medic* or physician*)).tw.
-
“interns and residents”/
-
residency education/
-
or/1-13
-
(prescrib* or prescrip*).tw.
-
((drug* or medicine* or medication*) adj2 (administ* or utili?ation or error*)).tw.
-
prescription/
-
drug utilization/
-
Prescription Drugs/
-
Drug Prescriptions/
-
medication error/
-
or/15-21
-
(antimicrobial* or “anti microbial*” or antibiotic* or “anti biotic*” or antibacterial* or “anti bacterial*” or antiviral* or “anti viral*” or antifungal* or “anti fungal*” or “antiinfective*” or “anti infective*” or antiparasitic* or “anti parasitic*”).tw.
-
exp antiinfective agent/
-
or/23-24
-
14 and 22 and 25
Database: PsycINFO
Host: Ovid.
Data parameters: 1806 to September Week 4 2015.
Date searched: 28 September 2015.
Searcher: Simon Briscoe.
Hits: 10.
Strategy
-
((junior or train*) adj2 (doctor* or medic* or physician*)).tw.
-
(“foundation year 1” or “foundation year 2” or “foundation year one” or “foundation year two” or registrar* or “new prescriber*”).tw.
-
((f1 or f2 or fy1 or fy2) adj3 (doctor* or medic* or physician*)).tw.
-
(foundation adj3 (doctor* or medic* or physician*)).tw.
-
((SpR or SpRs) adj10 (doctor* or medic* or physician*)).tw.
-
GPST.tw.
-
(“pre-registration house officer*” or “senior house officer*” or “house officer*”).tw.
-
((resident* or residenc*) adj2 (doctor* or medic* or physician*)).tw.
-
PRHO.tw.
-
((HO or SHO) adj3 (doctor* or medic* or physician*)).tw.
-
((intern or interns or internship*) and (doctor* or medic* or physician*)).tw.
-
medical internship/
-
medical residency/
-
or/1-13
-
(prescrib* or prescrip*).tw.
-
((drug* or medicine* or medication*) adj2 (administ* or utili?ation or error*)).tw.
-
prescription drugs/
-
exp “Prescribing (Drugs)”/
-
or/15-18
-
(antimicrobial* or “anti microbial*” or antibiotic* or “anti biotic*” or antibacterial* or “anti bacterial*” or antiviral* or “anti viral*” or antifungal* or “anti fungal*” or “antiinfective*” or “anti infective*” or antiparasitic* or “anti parasitic*”).tw.
-
14 and 19 and 20
Database: Web of Science
Host: Thomson Reuters.
Data parameters: SCIE (1900-present); Social Sciences Citation Index (SSCI) (1956-present); CPCI-S (1990-present); Conference Proceedings Citation Index – Social Sciences & Humanities (CPCI-SSH) (1990-present).
Date searched: 28 September 2015.
Searcher: Simon Briscoe.
Hits: 134.
Strategy
-
TOPIC: ((junior or train*) near/1 (doctor* or medic* or physician*))
-
TOPIC: (“foundation year 1” or “foundation year 2” or “foundation year one” or “foundation year two” or registrar* or “new prescriber*”)
-
TOPIC: ((f1 or f2 or fy1 or fy2) near/2 (doctor* or medic* or physician*))
-
TOPIC: (foundation near/2 (doctor* or medic* or physician*))
-
TOPIC: ((SpR or SpRs) near/9 (doctor* or medic* or physician*))
-
TOPIC: (GPST)
-
TOPIC: ((“pre-registration house officer*” or “senior house officer*” or “house officer*”))
-
TOPIC: ((resident* or residenc*) near/1 (doctor* or medic* or physician*))
-
TOPIC: (PRHO)
-
TOPIC: ((HO or SHO) near/2 (doctor* or medic* or physician*))
-
TOPIC: ((intern or interns or internship*) and (doctor* or medic* or physician*))
-
#11 OR #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1
-
TOPIC: ((prescrib* or prescrip*))
-
TOPIC: ((drug* or medicine* or medication*) near/1 (administ* or utili?ation or error*))
-
#14 OR #13
-
TOPIC: (antimicrobial* or “anti microbial*” or antibiotic* or “anti biotic*” or antibacterial* or “anti bacterial*” or antiviral* or “anti viral*” or antifungal* or “anti fungal*” or “antiinfective*” or “anti infective*” or antiparasitic* or “anti parasitic*”)
-
#16 AND #15 AND #12
Database: The Cochrane Library
Host: Cochrane Collaboration.
Data parameters: CENTRAL: Issue 8 of 12, August 2015; Cochrane Database of Systematic Reviews (CDSR): Issue 9 of 12, September 2015; HTA: Issue 3 of 4, July 2015.
Date searched: 28 September 2015.
Searcher: Simon Briscoe.
Hits: CENTRAL: 10; CDSR: one; HTA: one.
Strategy
-
((junior or train*) near/2 (doctor* or medic* or physician*)):ti or ((junior or train*) near/2 (doctor* or medic* or physician*)):ab
-
(“foundation year 1” or “foundation year 2” or “foundation year one” or “foundation year two” or registrar* or “new prescriber*”):ti or (“foundation year 1” or “foundation year 2” or “foundation year one” or “foundation year two” or registrar* or “new prescriber*”):ab
-
((f1 or f2 or fy1 or fy2) near/3 (doctor* or medic* or physician*)):ti or ((f1 or f2 or fy1 or fy2) near/3 (doctor* or medic* or physician*)):ab
-
(foundation near/3 (doctor* or medic* or physician*)):ti or (foundation near/3 (doctor* or medic* or physician*)):ab
-
((SpR or SpRs) near/10 (doctor* or medic* or physician*)):ti or ((SpR or SpRs) near/10 (doctor* or medic* or physician*)):ab
-
GPST:ti or GPST:ab
-
(“pre-registration house officer*” or “senior house officer*” or “house officer*”):ti or (“pre-registration house officer*” or “senior house officer*” or “house officer*”):ab
-
((resident* or residenc*) near/2 (doctor* or medic* or physician*)):ti or ((resident* or residenc*) near/2 (doctor* or medic* or physician*)):ab
-
PRHO:ti or PRHO:ab
-
((HO or SHO) near/3 (doctor* or medic* or physician*)):ti or ((HO or SHO) near/3 (doctor* or medic* or physician*)):ab
-
((intern or interns or internship*) and (doctor* or medic* or physician*)):ti or ((intern or interns or internship*) and (doctor* or medic* or physician*)):ab
-
MeSH descriptor: [Internship and Residency] this term only
-
or #1-#12
-
(prescrib* or prescrip*):ti or (prescrib* or prescrip*):ab
-
((drug* or medicine* or medication*) near/2 (administ* or utili?ation or error*)):ti or ((drug* or medicine* or medication*) near/2 (administ* or utili?ation or error*)):ab
-
MeSH descriptor: [Prescriptions] explode all trees
-
MeSH descriptor: [Drug Utilization] explode all trees
-
MeSH descriptor: [Prescription Drugs] this term only
-
MeSH descriptor: [Drug Prescriptions] this term only
-
MeSH descriptor: [Medication Errors] this term only
-
or #14-#20
-
(antimicrobial* or “anti microbial*” or antibiotic* or “anti biotic*” or antibacterial* or “anti bacterial*” or antiviral* or “anti viral*” or antifungal* or “anti fungal*” or “antiinfective*” or “anti infective*” or antiparasitic* or “anti parasitic*”):ti or (antimicrobial* or “anti microbial*” or antibiotic* or “anti biotic*” or antibacterial* or “anti bacterial*” or antiviral* or “anti viral*” or antifungal* or “anti fungal*” or “antiinfective*” or “anti infective*” or antiparasitic* or “anti parasitic*”):ab
-
MeSH descriptor: [Anti-Infective Agents] this term only
-
MeSH descriptor: [Anti-Bacterial Agents] 1 tree(s) exploded
-
MeSH descriptor: [Antifungal Agents] 1 tree(s) exploded
-
MeSH descriptor: [Anti-Infective Agents, Urinary] explode all trees
-
MeSH descriptor: [Antiparasitic Agents] 1 tree(s) exploded
-
MeSH descriptor: [Antiviral Agents] 1 tree(s) exploded
-
77-#28
-
#13 and #21 and #29
Database: ASSIA
Host: ProQuest.
Data parameters: not applicable.
Date searched: 28 September 2015.
Searcher: Simon Briscoe.
Hits: five.
Strategy
-
TI,AB(((junior OR train*) NEAR/1 (doctor* OR medic* OR physician*)) OR “foundation year 1” OR “foundation year 2” OR “foundation year one” OR “foundation year two” OR registrar* OR “new prescriber*” OR ((f1 OR f2 OR fy1 OR fy2) NEAR/2 (doctor* OR medic* OR physician*)) OR (foundation NEAR/2 (doctor* OR medic* OR physician*)) OR ((SpR OR SpRs) NEAR/9 (doctor* OR medic* OR physician*)) OR GPST OR “pre-registration house officer*” OR “senior house officer*” OR “house officer*” OR ((resident* OR residenc*) NEAR/1 (doctor* OR medic* OR physician*)) OR PRHO OR ((HO OR SHO) NEAR/2 (doctor* OR medic* OR physician*)) OR ((intern OR interns OR internship*) AND (doctor* OR medic* OR physician*))) OR SU.EXACT.EXPLODE(“House officers” OR “Preregistration house officers” OR “Senior house officers”) OR SU.EXACT(“Senior registrars”) OR SU.EXACT(“Registrars”)
-
TI,AB((prescrib* OR prescrip*) OR (drug* OR medicine* OR medication*) NEAR/1 (administ* OR utili?ation OR error*)) OR SU.EXACT(“Prescriptions”)
-
TI,AB(antimicrobial* or “anti microbial*” or antibiotic* or “anti biotic*” or antibacterial* or “anti bacterial*” or antiviral* or “anti viral*” or antifungal* or “anti fungal*” or “antiinfective*” or “anti infective*” or antiparasitic* or “anti parasitic*”) OR SU.EXACT(“Antibiotics”) OR SU.EXACT(“Antiviral drugs”) OR SU.EXACT.EXPLODE(“Anthelmintics” OR “Antiparasitic agents”)
-
1 AND 2 AND 3
| Database | Hits |
|---|---|
| MEDLINE | 201 |
| MEDLINE In-Process | 30 |
| EMBASE | 548 |
| PsycINFO | 10 |
| Web of Science | 134 |
| CENTRAL | 10 |
| CDSR | 1 |
| HTA | 1 |
| ASSIA | 5 |
| Total records | 940 |
| Duplicate records | 312 |
| Total unique records | 628 |
Additional literature search strategy
Database: MEDLINE
Host: Ovid.
Data parameters: 1946 to December Week 5 2015.
Date searched: 13 January 2016.
Searcher: Simon Briscoe.
Hits: 968.
Strategy
-
(authority or “senior staff” or “senior doctor*” or hierarch* or nonhierarch*).tw.
-
Hierarchy, Social/
-
or/1-2
-
(team* or interpersonal* or interprofessional*).tw.
-
(role* adj2 responsibil*).tw.
-
Interprofessional Relations/
-
Interpersonal Relations/
-
or/4-7
-
decision*.tw.
-
exp Decision Making/
-
or/9-10
-
8 or 11
-
(trainee* or (train* adj2 program*)).tw.
-
(“junior doctor*” or intern* or residen*).tw.
-
“Internship and Residency”/
-
or/13-15
-
3 and 12 and 16
Database: MEDLINE(R) In-Process & Other Non-Indexed Citations
Host: Ovid.
Data parameters: January 12, 2016.
Date searched: 13 December 2016.
Searcher: Simon Briscoe.
Hits: 91.
Strategy
-
(authority or “senior staff” or “senior doctor*” or hierarch* or nonhierarch*).tw.
-
(team* or interpersonal* or interprofessional*).tw.
-
(role* adj2 responsibil*).tw.
-
or/2-3
-
decision*.tw.
-
4 or 5
-
(trainee* or (train* adj2 program*)).tw.
-
(“junior doctor*” or intern* or residen*).tw.
-
7 or 8
-
1 and 6 and 9
Database: PsycINFO
Host: Ovid.
Data parameters: 1809 to January Week 2 2016.
Date searched: 13 January 2016.
Searcher: Simon Briscoe.
Hits: 1062.
Strategy
-
(authority or “senior staff” or “senior doctor*” or hierarch* or nonhierarch*).tw.
-
dominance hierarchy/
-
or/1-2
-
(team* or interpersonal* or interprofessional*).tw.
-
(role* adj2 responsibil*).tw.
-
interpersonal relationships/
-
or/4-6
-
decision*.tw.
-
exp Decision Making/
-
or/8-9
-
7 or 10
-
(trainee* or (train* adj2 program*)).tw.
-
(“junior doctor*” or intern* or residen*).tw.
-
medical internship/
-
medical residency/
-
or/12-15
-
3 and 11 and 16
Database: The Cochrane Library (CENTRAL, CDSR, HTA)
Host: Cochrane Collaboration.
Data parameters: CENTRAL = Issue 12 of 12, December 2015; CDSR = Issue 1 of 12, January 2016; HTA = Issue 4 of 4, October 2015.
Date searched: 13 January 2016.
Searcher: Simon Briscoe.
Hits: CENTRAL = 20; CDSR = zero; HTA = zero.
Strategy
-
authority or “senior staff” or “senior doctor*” or hierarch* or nonhierarch*:ti or authority or “senior staff” or “senior doctor*” or hierarch* or nonhierarch*:ab in Cochrane Reviews (Reviews and Protocols), Trials and Technology Assessments
-
MeSH descriptor: [Hierarchy, Social] explode all trees
-
#1 or #2
-
team* or interpersonal* or interprofessional*:ti or team* or interpersonal* or interprofessional*:ab in Cochrane Reviews (Reviews and Protocols), Trials and Technology Assessments
-
role* near/2 responsibil*:ti or role* near/2 responsibil*:ab in Cochrane Reviews (Reviews and Protocols), Trials and Technology Assessments
-
MeSH descriptor: [Interprofessional Relations] explode all trees
-
MeSH descriptor: [Interpersonal Relations] explode all trees
-
(57-#7)
-
decision*:ti or decision*:ab in Cochrane Reviews (Reviews and Protocols), Trials and Technology Assessments
-
MeSH descriptor: [Decision Making] explode all trees
-
#9 or #10
-
#8 or #11
-
trainee* or (train* near/2 program*):ti or trainee* or (train* near/2 program*):ab in Cochrane Reviews (Reviews and Protocols), Trials and Technology Assessments
-
“junior doctor*” or intern* or residen*:ti or “junior doctor*” or intern* or residen*:ab in Cochrane Reviews (Reviews and Protocols), Trials and Technology Assessments
-
MeSH descriptor: [Internship and Residency] this term only
-
{or #13-#15}
-
#3 and #12 and #16
Database: ASSIA
Host: ProQuest.
Data parameters: not applicable.
Date searched: 13 January 2016.
Searcher: Simon Briscoe.
Hits: 206.
Strategy
(ti(authority OR “senior staff” OR “senior doctor*” OR hierarch* OR nonhierarch*) OR ab(authority OR “senior staff” OR “senior doctor*” OR hierarch* OR nonhierarch*)) AND (((ti(team* OR interpersonal* OR interprofessional*) OR ab(team* OR interpersonal* OR interprofessional*)) OR (ti(role* NEAR/1 responsibil*) OR ab(role* NEAR/1 responsibil*)) OR SU.EXACT(“Interpersonal relationships”)) OR ((ti(Decision*) OR ab(Decision*)) OR SU.EXPLODE(“Decision making”))) AND ((ti(trainee* OR (train* NEAR/1 program*)) OR ab(trainee* OR (train* NEAR/1 program*))) OR (ti(“junior doctor*” OR intern* OR residen*) OR ab(“junior doctor*” OR intern* OR residen*)) OR SU.EXACT(“Internships”) OR SU.EXPLODE(“House officers”))
| Database | Hits |
|---|---|
| MEDLINE | 968 |
| MEDLINE In-Process & Other Non-Indexed Citations | 91 |
| PsycINFO | 1062 |
| CENTRAL | 20 |
| CDSR | 0 |
| HTA | 0 |
| ASSIA | 206 |
| Total records | 2347 |
| Duplicate records | 323 |
| Total unique records | 2024 |
Appendix 2 Characteristics of all studies included in the review
| Authors | Year | Country | Type of paper | Study design/methods | Sample/setting | Objectives |
|---|---|---|---|---|---|---|
| Abbo L, Sinkowitz-Cochran R, Smith L, Ariza-Heredia E, Gomez-Marin O, Srinivasan A, Hooton TM101 | 2011 | USA | Research | Web-based survey questionnaire | Faculty and residents in one teaching hospital | To assess attitudes, perceptions and knowledge about antimicrobial use and resistance |
| Aggarwal S, Mathew J, Singh H, Sharma V183 | 2014 | India | Research | Cross-sectional e-mail-based survey questionnaire | Junior residents in two tertiary care centres | To examine junior doctor perceptions and attitudes on antibiotic resistance |
| Ajemigbitse AA, Omole MK, Osi-Ogbu OF, Erhun WO56 | 2013 | Nigeria | Research | Prospective review of medication orders and semistructured interviews | Doctors at different levels of training and from different specialties in a 200-bed tertiary referral hospital | To understand causes of prescribing errors, including antimicrobial prescribing |
| Ajemigbitse A, Omole M, Ezike N, Erhun W85 | 2013 | Nigeria | Research | Cross-sectional survey questionnaire | Interns in a federal government-funded tertiary care hospital | To assess knowledge and attitudes of interns on medication prescribing errors |
| Akici A, Kalaca S, Goren MZ, Akkan AG, Karaalp A, Demir D, Ugurlu U, Oktay S86 | 2004 | Turkey | Research | Clinical examination on prescribing and survey questionnaire | Interns (final-year medical students working in hospitals) and GPs working at primary health-care centres | To examine the impact of rational pharmacotherapy education |
| Alagha HZ, Badary OA, Ibrahim HM, Sabri NA201 | 2011 | Egypt | Research (intervention study) | Pre–post study of prescribing errors from review of medication orders written by residents | 12-bed paediatric ICU | To assess the impact of multiple pharmacist-led interventions on the rate of prescribing errors |
| Ali MH, Kalima P, Maxwell SR60 | 2006 | UK | Research | Questionnaire with free-text answers to clinical scenarios | Doctors at different grades across four NHS teaching hospitals | To investigate which antimicrobial drugs were chosen by hospital doctors faced with presentations of two common infections, whether or not these choices were in line with local guidance and which factors were most influential in guiding antimicrobial choice |
| Allison GM, Weigel B, Holcroft C57 | 2015 | USA | Research (intervention study) | Retrospective review of discharge orders for antibiotic errors | 415-bed, academic tertiary care hospital where house officers order discharge medications | To assess the impact of an electronic discharge medication reconciliation tool on antibiotic prescribing errors at hospital discharge |
| Almatar MA, Peterson GM, Thompson A, McKenzie DS, Anderson TL103 | 2015 | Australia | Research | Retrospective review of medical records and survey questionnaire | Doctors in general medical and EDs in a 550-bed major referral and teaching hospital | To assess adherence to guidelines for community-acquired pneumonia and explore barriers to adherence. |
| Almatar MA, Peterson GM, Thompson A, Zaidi ST66 | 2014 | Australia | Research | Qualitative interview study | ED doctors at different levels of training in a tertiary public hospital | To explore the perceptions of ED doctors regarding the use of ceftriaxone in patients with community-acquired pneumonia |
| Alweis R, Greco M, Wasser T, Wenderoth S61 | 2014 | USA | Research (intervention study) | Pre–post study (survey questionnaire and medication chart review) | University-affiliated community hospital internal medicine residency programme | To increase treatment guideline adherence rates for acute sinusitis, pharyngitis and upper respiratory infection through a quality improvement initiative |
| Ambroggio L, Thomson J, Murtagh Kurowski E, Courter J, Statile A, Graham C, Sheehan B, Iyer S, Shah SS, White CM104 | 2013 | USA | Research (intervention study) | Pre–post study (statistical analysis on prescribing decisions from medical records) | ED and hospital medicine resident teams | To evaluate if quality improvement methods could improve appropriate antibiotic prescribing in a setting without a formal antimicrobial stewardship programme |
| Asseray N, Mallaret MR, Sousbie M, Liberelle B, Schaerer L, Borrel E, Rieussec MO, Walter B, Guimier C, Buffet X, Soule H, Croize J, Stahl JP102 | 2002 | France | Research | Review of antibiotic prescriptions (for past 7 days) | Seven health-care institutions with various wards, both short stay (medicine, surgery, maternity, emergency, intensive care) and long stay (post-operative care or rehabilitation) | To assess rates of antibiotic prescribing |
| Aydin S, Yaris F, Ozcakir A, Agalar C202 | 2005 | Turkey | Research | Survey questionnaire | Residents in three university hospitals | To identify common infections and antibiotic prescribing choices, including role of laboratory testing |
| Baker E, Pryce Roberts A, Wilde K, Walton H, Suri S, Rull G, Webb A67 | 2011 | UK | Research | Retrospective analysis of prescribing data and survey questionnaire | Data from primary care and two teaching hospitals/foundation year 1 doctors from 39 NHS trusts across London | To develop a core list of commonly used medicines |
| Barlow G, Nathwani D, Myers E, Sullivan F, Stevens N, Duffy R, Davey P68 | 2008 | UK | Research (intervention study) | Controlled before-and-after study (quantitative survey, semistructured interviews, field notes and review of medical records) | Junior doctors in acute medicine | To identify determinants of and barriers to appropriate antibiotic use in community-acquired pneumonia |
| Bowes J, Yasseen AS, Barrowman N, Murchison B, Dennis J, Moreau KA, Varughese N, Le Saux N203 | 2014 | Canada | Research | Cross-sectional prospective survey questionnaire | Staff and trainee physicians at a single tertiary care paediatric hospital | To identify knowledge levels and challenges in antimicrobial use in paediatrics |
| Charani E, Castro-Sanchez E, Sevdalis N, Kyratsis Y, Drumright L, Shah N, Holmes A35 | 2013 | UK | Research | Qualitative interview study | Doctors, pharmacists, nurses and midwives from four hospitals in a multisite, 1500-bed health-care delivery organisation | To investigate social determinants of antimicrobial prescribing in the hospital setting |
| Chaves NJ, Cheng AC, Runnegar N, Kirschner J, Lee T, Buising K69 | 2014 | Australia | Research | Paper- and web-based survey questionnaires | Doctors at different training levels in three university teaching hospitals | To assess the knowledge and attitudes of Australian hospital doctors to antibiotic use |
| Chow A, Lye DCB, Arah OA99 | 2015 | Singapore | Research (intervention study) | Mixed methods (focus groups, followed by a cross-sectional survey) | Junior and senior physicians from all clinical specialties in a 1500-bed adult tertiary care centre | To evaluate physician acceptance and attitudes towards antibiotic computerised decision support systems |
| Coleman JJ, Hemming K, Nightingale PG, Clark IR, Dixon-Woods M, Ferner RE, Lilford RJ204 | 2011 | UK | Research (intervention study) | Retrospective analysis of prescribing | Junior doctors in a large teaching hospital across two sites | To assess the potential for an electronic system to detect likelihood of serious prescribing errors |
| Cortoos PJ, De Witte K, Peetermans WE, Simoens S, Laekeman G62 | 2008 | Belgium | Research | Qualitative focus group study | Physicians at different levels of training from internal medicine and surgery in a 1900-bed tertiary care university teaching hospital | To identify barriers to and facilitators of using local antibiotic guidelines |
| Coupat C, Pradier C, Degand N, Hofliger P, Pulcini C205 | 2013 | France | Research (intervention study) | Prospective randomised controlled case vignette study (survey questionnaire) | Residents training in general practice | To examine the role of reporting antibiotic susceptibility data in improving appropriate prescribing in urinary tract infections |
| Dallas A, Magin P, Morgan S, Tapley A, Henderson K, Ball J, Scott J, Spike N, McArthur L, van Driel M105 | 2015 | Australia | Research | Cross-sectional analysis of documented consultations from a prospective cohort study | GP trainees participating in the multicentre ReCEnT study | To establish prevalence and determinants of antibiotic prescribing for respiratory infections |
| Dallas A, van Driel M, van de Mortel T, Magin P73 | 2014 | Australia | Research | Qualitative interview and focus group study | Vocational trainees in general practice in rural and urban areas | To understand trainee attitudes and influences on antibiotic prescribing |
| De Souza V, MacFarlane A, Murphy AW, Hanahoe B, Barber A, Cormican M63 | 2006 | Ireland | Research | Qualitative interview study | Non-consultant hospital doctors in a university teaching hospital | To establish factors influencing antimicrobial prescribing |
| Deuster S, Roten I, Muehlebach S184 | 2010 | Switzerland | Research (intervention study) | Pre–post study with additional follow-up (chart review) | 550-bed tertiary care teaching hospital | To determine the role of treatment guidelines in changing antibiotic prescribing practice |
| Dobrzanski S, Hammond I, Khan G, Holdsworth H58 | 2002 | UK | Research | Prospective recording of medication errors | Wards and dispensaries in one NHS trust | To establish causes of prescribing error |
| Doyon S, Perreault M, Marquis C, Gauthier J, Lebel D, Bailey B, Collin J, Bussieres JF106 | 2009 | Canada | Research (intervention study) | Pre–post study (review of medical records against prescription compliance) | Tertiary care paediatric hospital, including emergency and general wards and prescribers at different levels of training | To examine the impact of community-acquired pneumonia management guidelines |
| Fakih MG, Berschback J, Juzych NS, Massanari RM88 | 2006 | USA | Research | Audit of patient records | ED of a 609-bed tertiary care hospital | To evaluate resident and staff compliance with Infectious Disease Society of America guidelines for group A streptococcal pharyngitis |
| Fakih MG, Hilu RC, Savoy-Moore RT, Saravolatz LD107 | 2003 | USA | Research | Survey questionnaire | 379 residents responded from 11 primary care programmes | To assess resident views on treatment of upper respiratory tract illnesses, appropriate antibiotic use and AMR |
| Feucht CL, Rice LB162 | 2003 | USA | Research (intervention study) | Pre–post study (review of medical records and cost analysis) | Veterans Affairs Medical Centre | To assess the impact of an interventional programme on antibiotic use |
| Flannery DD, Swami S, Chan S, Eppes S206 | 2014 | USA | Research (intervention study) | Online survey | Paediatric tertiary care centre in a teaching hospital | To examine perceived usefulness and acceptance of an antimicrobial stewardship programme |
| Flannery MT, McCool MJ167 | 2005 | USA | Letter describing research results (intervention study) | Small-scale controlled study (chart review) | Rotating general medicine ward residents at a university teaching hospital | To examine the impact of guideline education on resident prescribing in community-acquired pneumonia |
| Garcia C, Llamocca LP, Garcia K, Jimenez A, Samalvides F, Gotuzzo E, Jacobs J137 | 2011 | Peru | Research | Cross-sectional survey questionnaire | Physicians at different levels of training in two large public hospitals | To establish knowledge, attitudes and antimicrobial prescribing practices |
| Gaur AH, Hare ME, Shorr RI108 | 2005 | USA | Research | Cross-sectional study drawing on data collected as part of a national survey on patient encounters | Outpatient departments included in the US National Hospital Ambulatory Medical Care Survey database | To evaluate provider and facility characteristics associated with antibiotic overuse in children with presumed viral respiratory tract infections |
| Guerra CM, Pereira CA, Neves Neto AR, Cardo DM, Correa L163 | 2007 | Brazil | Communication piece describing research results | Cross-sectional survey questionnaire | Physicians at different training levels (majority residents) in a 700-bed tertiary care teaching hospital | To assess perceptions and knowledge on AMR and antimicrobial prescribing practices |
| Hall KK, Philbrick J, Nadkarni M160 | 2003 | USA | Research | Review of patient charts | Teaching clinic for internal medicine residents | To determine prescribing decisions for treatment of acute bronchitis |
| Harnett SJ, Allen KD207 | 2000 | UK | Letter describing research results (intervention study) | Interview study | Senior and junior house officers from different specialties in one NHS hospital | To assess use of hospital antibiotic policy and alternative sources of information among junior doctors |
| Hong SY, Epstein LH, Lawrence K, Davidson L, Taur Y, Nadkarni L, Doron S59 | 2013 | USA | Research (intervention study) | Pre–post study (web-based survey questionnaire) | House officers at an academic medical centre | To understand experiences of house officers with an antimicrobial stewardship programme |
| Jaensch SL, Baysari MT, Day RO, Westbrook JI123 | 2013 | Australia | Research (intervention study) | Shadowing and recording of prescribing information | Twelve junior doctors at a 350-bed teaching hospital | To assess the impact of partial implementation of Computerised Provider Order Entry on junior doctors’ prescribing work after hours |
| Lee MJ, Kim M, Kim NH, Kim CJ, Song KH, Choe PG, Park WB, Bang JH, Kim ES, Park SW, Kim NJ, Oh MD, Kim HB168 | 2015 | Korea | Research | Retrospective review of treatment decisions and cross-sectional survey questionnaire | Adult inpatients in 900-bed university-affiliated tertiary care hospital/resident physicians surveyed | To determine rates of asymptomatic bacteriuria overtreatment and perceptions of residents |
| Lee TC, Frenette C, Jayaraman D, Green L, Pilote L89 | 2014 | Canada | Research (Intervention study) | Pre–post study (statistical analysis on costs and antibiotic use) | Two 23-bed internal medicine clinical teaching units in the Montreal General Hospital, a 417-bed tertiary care hospital | To examine the role of education and trainee-led timeout audits on antibiotic use and costs |
| Levinsky Y, Mimouni FB, Fisher D, Ehrlichman M186 | 2013 | Israel | Research | Prospective review of chest radiographs (statistical analysis on strength of agreement between case-based interpretations) | Paediatric residents, board-certified paediatricians, paediatric pulmonologists and a paediatric radiologist in a paediatric ED | To compare interpretations of chest readings for children with acute respiratory disease between clinicians with different levels of experience and differences in antibiotic treatment decisions |
| Liabsuetrakul T, Chongsuvivatwong V, Lumbiganon P, Lindmark G74 | 2003 | Thailand | Research | Qualitative interview study and survey questionnaire | Resident and faculty obstetricians from three hospitals (university, regional and general) | To examine the relative influence of attitudes, subjective norms and perceived controls on antibiotic prophylaxis in caesarean section |
| Livorsi D, Comer A, Matthias MS, Perencevich EN, Bair MJ70 | 2015 | USA | Research | Qualitative interview study | Physicians at different levels of training in two acute care hospitals | To understand the context of antibiotic prescribing and influences on prescribing decisions |
| Mattick K, Kelly N, Rees C43 | 2014 | UK | Research | Qualitative interview study | FY1 and FY2 doctors in two hospitals | To provide an understanding of junior doctors’ antimicrobial prescribing experiences on hospital wards |
| May L, Gudger G, Armstrong P, Brooks G, Hinds P, Bhat R, Moran GJ, Schwartz L, Cosgrove SE, Klein EY, Rothman RE, Rand C10 | 2014 | USA | Research | Survey questionnaire, in-depth interviews and observation | ED providers recruited from 8 sites in three cities/observations in one of the ED sites | To explore antimicrobial prescribing practices and decision-making |
| McCarthy RM, Hilmer SN182 | 2013 | Australia | Research (intervention study) | Pre–post study (assessing knowledge levels through mock medication charts and a questionnaire) | Junior medical officers working in adult surgical or medical teams at a large tertiary referral hospital | To assess ability to detect medication prescribing errors before and after the teaching session |
| Menéndez R, Torres A, Zalacaín R, Aspa J, Martín-Villasclaras JJ, Borderías L, Benitez-Moya JM, Ruiz-Manzano J, de Castro FR, Blanquer J, Perez D, Puzo C, Sanchez-Gascon F, Gallardo J, Alvarez C, Molinos L, Group Neumofail110 | 2005 | Spain | Research | Observational prospective study (review of antibiotic decisions and prescriber characteristics) | Multicentre in the pneumology service of 15 hospitals | To identify factors influencing adherence to guidelines for empirical treatment of community-acquired pneumonia |
| Mincey BA, Parkulo MA111 | 2001 | USA | Research | Review of prescriptions for acute sinusitis | Community internal medicine practice | To compare prescribing choices between residents at different levels of training and senior physicians |
| Nambiar S, Schwartz RH, Sheridan MJ164 | 2002 | USA | Research | Survey questionnaire | Paediatric residency programmes | To assess awareness and compliance with guidelines |
| Navarro-San Francisco C, Del Toro MD, Cobo J, De Gea-Garcia JH, Vano-Galvan S, Moreno-Ramos F, Rodriguez-Bano J, Pano-Pardo JR76 | 2013 | Spain | Research | Cross-sectional web-based survey questionnaire | Resident doctors in five teaching hospitals | To explore resident perceptions about antibiotic use and resistance |
| Neumark T, Brudin L, Mölstad S169 | 2015 | Sweden | Research | Retrospective study with matched control group (review of infection diagnosis and prescribing decisions) | GPs or residents in general practice | To examine differences in antibiotic prescribing decisions between physicians depending on country of undergraduate training |
| Newham R, Thomson AH, Semple Y, Dewar S, Steedman T, Bennie M112 | 2015 | UK | Research | Qualitative focus group study | Junior doctors and clinical pharmacists in two moderately sized (500–600 beds) and two large (> 800 beds) hospitals | To understand barriers to effective use of guidelines when prescribing and monitoring gentamicin and vancomycin |
| Oppenheim MI, Vidal C, Velasco FT, Boyer AG, Cooper MR, Hayes JG, Frayer WW187 | 2002 | USA | Conference proceedings (intervention study) | Review of medication orders during the study period | Tertiary care academic medical centre | To evaluate the role of automatic renal dosing adjustment calculation for antimicrobials and the impact of computerised alerts to correcting errors |
| Oshikoya KA, Senbanjo IO, Amole OO208 | 2009 | Nigeria | Research | Survey questionnaire | Interns from five hospitals (teaching, specialist and general) | To identify levels of knowledge in clinical pharmacology and therapeutics following undergraduate training |
| Pacheco GS, Viscusi C, Hays DP, Woolridge DP161 | 2012 | USA | Research | Retrospective review of computer-based prescriptions | Residents from emergency medicine, paediatrics, and family medicine residencies in an academic ED | To compare paediatric prescription errors based on resident level of training |
| Patel R, Green W, Martinez MM, Shahzad MW, Larkin C64 | 2015 | UK | Research | Retrospective review of medication charts | Foundation year doctors and other prescribers in four inpatient wards of a tertiary centre renal unit at a teaching hospital | To compare prescribing choices of foundation year doctors prescribing for patients with kidney disease with other prescribers |
| Pulcini C, Williams F, Molinari N, Davey P, Nathwani D170 | 2011 | France/UK | Research | Survey questionnaire | Postgraduate doctors still in training at two university teaching hospitals, in Nice (France) and Dundee (Scotland, UK) | To assess junior doctor perceptions of their antibiotic prescribing practice and of bacterial resistance |
| Purcell K, Fergie J209 | 2003 | USA | Research (intervention study) | Pre–post study (chart review and cost analysis) | 200-bed, tertiary care paediatric teaching hospital | To determine effectiveness of an educational programme in reducing antimicrobial prescribing rates and costs |
| Rinke ML, Moon M, Clark JS, Mudd S, Miller MR166 | 2008 | USA | Research | Retrospective chart and ambulatory prescription review | Urban tertiary care academic paediatric ED | To determine the frequency, prescriber and type of prescribing errors |
| Roumie CL, Halasa NB, Edwards KM, Zhu Y, Dittus RS, Griffin MR165 | 2005 | USA | Research | Cross-sectional study drawing on data collected as part of two national surveys on service utilisation | Physicians, residents and on-physician clinicians in office practices, hospital practices and EDs | To compare outpatient antibiotic prescribing by practising physicians, non-physician clinicians and resident physicians |
| Salomon L, Levu S, Deray G, Launay-Vacher V, Brucker G, Ravaud P210 | 2003 | France | Research | Prospective criterion-referenced vignette study | Residents in a 2070-bed tertiary care teaching hospital | To assess residents’ prescribing practices for renal impairment (including antimicrobials) |
| Seemungal IA, Bruno CJ211 | 2012 | USA | Research (intervention study) | Survey questionnaire | House staff in a 496-bed academic tertiary care hospital | To investigate attitudes towards an antibiotic stewardship programme including prior authorisation |
| Sellman JS, Decarolis D, Schullo-Feulner A, Nelson DB, Filice GA135 | 2004 | USA | Research | Brief telephone questionnaire with prescribers after making antimicrobial prescribing decisions and review of medical records | Physicians at different training levels and from different specialties in a 280-bed university-affiliated tertiary care hospital | To describe resources clinicians use when they prescribe antimicrobials |
| Simpson JH, Lynch R, Grant J, Alroomi L125 | 2004 | UK | Research (intervention study) | Pre–post study (critical incident reporting and statistical analysis of medication errors) | Large, tertiary referral neonatal ICU | To assess the impact of interventions in reducing medication errors (including antimicrobial prescribing) |
| Solomon DH, Van Houten L, Glynn RJ, Baden L, Curtis K, Schrager H, Avorn J171 | 2001 | USA | Research (intervention study) | Randomised controlled trial (review of patient records) | 697-bed academic medical centre | To test the efficacy of academic detailing in improving appropriate broad-spectrum antibiotic use |
| Steinke DT, Bain DJ, MacDonald TM, Davey PG126 | 2000 | UK | Research | Retrospective review of prescriptions | Non-training and training GP practices | To identify differences between primary care practices and association to antibiotic prescribing patterns |
| Stone S, Gonzales R, Maselli J, Lowenstein SR212 | 2000 | USA | Research | Cross-sectional study drawing on data from a national survey | Hospital-based ED visits for patients with colds, upper respiratory tract infections and bronchitis | To examine antibiotic prescription rates and patterns |
| Tell D, Engstrom S, Molstad S96 | 2015 | Sweden | Research | Retrospective cross-sectional study of structured data from electronic patient records | Physicians working in primary care health centres and out-of-hours units | To study antibiotic guideline adherence for respiratory tract infections and differences between physicians at different levels |
| Thorpe JM, Smith SR, Trygstad TK181 | 2004 | USA | Research | Cross-sectional study drawing on data from a national survey | ED | To estimate potentially inappropriate antibiotic prescribing for acute respiratory tract infections and associations to patient/provider characteristics |
| Thursky KA, Mahemoff M194 | 2007 | Australia | Research | Observational study with unstructured interviews and participatory design processes | 21-bed mixed medical/surgical ICU of a tertiary referral and teaching hospital (key users: residents, registrars and unit pharmacist) | To discuss user-centred design techniques including flow models) in the development of an antibiotic decision support tool |
| Tobaiqy M, McLay J, Ross S97 | 2007 | UK | Research | Survey questionnaire | FY1 doctors in teaching hospital | To examine perceptions about whether the undergraduate programme in clinical pharmacology and therapeutics has provided enough skills for safe and rational prescribing |
| Undeland DK, Kowalski TJ, Berth WL, Gundrum JD114 | 2010 | USA | Research | Retrospective cohort study on diagnosed cases of pharyngitis | Large multispecialty health-care system | To compare the safety and appropriateness of antibiotic use between nurse-only triage and treatment algorithm and physician-directed evaluation |
| Valerio M, Vena A, Bouza E, Reiter N, Viale P, Hochreiter M, Giannella M, Munoz P, Comic study group65 | 2015 | Spain/Germany/Denmark/Italy | Research | Cross-sectional multicentre survey questionnaire | Attending physicians and residents from different specialisms | To assess the knowledge of European prescribing physicians on invasive fungal infections management |
| Weingart SN, Toth M, Sands DZ, Aronson MD, Davis RB, Phillips RS188 | 2003 | USA | Research | Retrospective review of drug interaction and drug allergy alerts | 5 adult primary care practices in a teaching hospital (employing attending physicians and house officers) | To identify factors associated with decisions to over-ride medication alert and possible adverse drug events |
| Welch SA, Novy M, Preisz P, Quinn DI, Whicker SD, Brown SE, Day RO91 | 2000 | Australia | Research (intervention study) | Pre–post study (prescription review and survey questionnaire) | Junior medical officers in the ED | To assess the impact of an educational and feedback intervention for rational antibiotic and analgesic prescribing |
| Zaidi ST, Thursky KA98 | 2013 | Australia | Research (intervention study) | Formative evaluation/qualitative interviews | Junior and senior doctors and pharmacists at a university teaching hospital | To assess the impact of a formative evaluation on the uptake of a web-based antibiotic computerised decision support system |
| Zallman L, Ma J, Xiao L, Lasser KE113 | 2010 | USA | Research | Cross-sectional analysis drawing on data from a national survey | Resident and staff physicians in outpatient care | To assess the quality of outpatient care delivered by resident and staff physicians |
| Ziglam HM, Morales D, Webb K, Nathwani D92 | 2006 | UK | Research (intervention study) | Cross-sectional questionnaire- and interview-based knowledge surveys | Training grade doctors in a teaching hospital | To determine knowledge levels on sepsis, awareness of local antimicrobial prescribing information sources and cost differences between intravenous and oral antibiotics |
| Authors | Year | Country | Type of paper | Study design/methods | Sample/setting | Objectives |
|---|---|---|---|---|---|---|
| Belyansky I, Martin TR, Prabhu AS, Tsirline VB, Howley LD, Phillips R, Sindram D, Heniford BT, Stefanidis D139 | 2011 | USA | Research | Survey questionnaire | Residents and attendings in general surgery, gynaecology, orthopaedic surgery | Impact of the surgical hierarchy on reporting patient safety concerns |
| Bethune R, Canter R, Abrams P146 | 2012 | UK | Research | Web-based survey questionnaire | Surgical trainees and consultant surgeons | Differences in perceptions of patient safety culture between trainees and consultants |
| Bongiovanni T, Yeo H, Sosa JA, Yoo PS, Long T, Rosenthal M, Berg D, Curry L, Nunez-Smith M119 | 2015 | USA | Research | Qualitative interview study | Surgical residents who had left their training programme | To examine the reasons behind attrition from surgical residency training |
| Bould MD, Sutherland S, Sydor DT, Naik V, Friedman Z83 | 2015 | Canada | Research | Simulation scenario and qualitative interview study | Anaesthesia residents | How hierarchy influences reluctance to challenge authority |
| Coffey M, Thomson K, Tallett S, Matlow A140 | 2010 | Canada | Research | E-mail questionnaire and focus group study | First to fourth year paediatric residents | Knowledge and attitudes about disclosure of medical errors |
| Conte H, Scheja M, Hjelmqvist H, Jirwe M87 | 2015 | Sweden | Research | Focused ethnographic methods (observation and interviews) | Teams of ‘learners’ (resident, specialist nurse student, supervisors) in intensive care | Exploring collaboration in an interprofessional education unit |
| Cosby KS, Croskerry P213 | 2004 | USA/Canada | Position paper | N/A | Emergency medicine | Discussing the role of the ‘authority gradient’ in clinical practice and its influence on medical errors |
| Doyle P, VanDenKerkhof EG, Edge DS, Ginsburg L, Goldstein DH141 | 2015 | Canada | Research | Survey questionnaire | Medical students and postgraduate trainees at different stages | To examine perceived patient safety competence and how this changes depending on levels of training |
| Farnan JM, Johnson JK, Meltzer DO, Humphrey HJ, Arora VM132 | 2008 | USA | Research | Qualitative interview study | Internal medicine residents in a tertiary care institution | To examine how residents perceive and manage uncertainty in clinical care |
| Fiordelli M, Schulz PJ, Caiata Zufferey M120 | 2014 | Switzerland | Research | Focus group study | Medical residents, senior doctors and head nurses in a small peripheral and non-teaching hospital | Differences in perceptions about the role of medical residents and impacts on interprofessional collaboration |
| Friedman SM, Sowerby RJ, Guo R, Bandiera G131 | 2010 | Canada | Research | Web-based survey questionnaire | Residents and fellows in emergency medicine | Exploring perceptions of own competence and barriers to reporting to supervisors |
| Friedman Z, Hayter MA, Everett TC, Matava CT, Noble LM, Bould MD82 | 2015 | Canada | Research | Simulation scenario and debrief | Second year anaesthesia trainees | How status asymmetry influences communication failures |
| Gordon LJ, Rees CE, Ker JS, Cleland J115 | 2015a | UK | Research | Qualitative narrative interview study (group and individual) | Trainees across different stages of training and across specialties | How trainees experience ‘leadership’ and ‘followership’ in the workplace |
| Gordon LJ, Rees CE, Ker JS, Cleland J84 | 2015b | UK | Research | Qualitative interview study | Trainees across different stages of training and across specialties | To understand trainee conceptions of ‘leadership’ and ‘followership’ |
| Hamui-Sutton A, Vives-Varela T, Gutierrez-Barreto S, Leenen I, Sanchez-Mendiola M122 | 2015 | Mexico | Research | Mixed methods (critical incident analysis and survey questionnaire) | Trainees across different stages of training | To build a typology of uncertainty and examine impacts on decision-making |
| Hilliard R, Harrison C, Madden S77 | 2007 | Canada | Research | Focus group study | Paediatric residents representing a range of training levels | To identify ethical issues faced by paediatric residents during training |
| Hoff TJ93 | 2008 | USA | Research | Observation and interviews | Medical residency teams in the ED, surgery and medical ICU | To examine differences between settings in terms of patient safety and learning from error |
| Kobayashi H, Pian-Smith M, Sato M, Sawa R, Takeshita T, Raemer D144 | 2006 | USA | Research | Survey questionnaire | US and Japanese residents | Cross–cultural barriers to challenging seniors and questioning authority |
| Limbert C, Lamb R109 | 2002 | UK | Research | Qualitative interviews and survey questionnaires | Trainees and senior doctors at different levels and from a range of specialties including surgery and emergency medicine | Factors influencing the use of clinical guidelines (antibiotics and asthma) |
| Lingard L, Reznick R, Espin S, Regehr G, DeVito I214 | 2002 | Canada | Research | Observation and unstructured interviews | Procedures in four surgical divisions (general surgery, urology, otolaryngology, cardiac surgery) | To examine patterns of team communication in operating rooms and implications for trainees |
| Maisonneuve JJ, Lambert TW, Goldacre MJ121 | 2014 | UK | Research | Postal and e-mail questionnaires, with free-text comments | UK medical graduates in their first year of the foundation programme | Views on quality of clinical training and career progression |
| Pian-Smith MC, Simon R, Minehart RD, Podraza M, Rudolph J, Walzer T, Raemer D142 | 2009 | USA | Research (intervention study) | Simulated scenarios and feedback | Anaesthesia residents at different training levels | Study of a debriefing intervention (two-challenge rule) to improve the way trainees challenge decisions made by seniors |
| Reader TW, Flin R, Mearns K, Cuthbertson BH147 | 2007 | UK | Research | Survey questionnaire | Doctors (senior and junior) and nurses in four ICUs | Perceptions of interdisciplinary communication in ICU |
| Rosenbaum JR, Bradley EH, Holmboe ES, Farrell MH, Krumholz HM215 | 2004 | USA | Research | Qualitative interview study | Internal medicine residents at different training levels in tertiary care and community hospitals | Ethical conflicts faced by trainees in medicine |
| Sculli GL, Fore AM, Sine DM, Paull DE, Tschannen D, Aebersold M, Seagull FJ, Bagian JP90 | 2015 | USA | Research (intervention study) | Survey questionnaire, pre- and post-teamwork scales | Residents and nurses in paediatric and adult operating rooms | Describes a tool to improve communication skills and to develop techniques to challenge authority |
| Stack SJ, Watson MJ216 | 2001 | USA | Commentary | N/A | Emergency medicine | Reflecting on the residency experience and relationships between senior and junior staff |
| Sutcliffe KM, Lewton E, Rosenthal MM134 | 2004 | USA | Research | Qualitative interview study | Range of training levels across three residency programmes (surgery, medicine and obstetrics/gynaecology) | To understand how communication failures contribute to medical error |
| Sydor DT, Bould MD, Naik VN, Burjorjee J, Arzola C, Hayter M, Friedman Z145 | 2013 | Canada | Research | Simulation scenario and qualitative interview study | Anaesthesia residents at different training levels | The role of hierarchy in the operating team and impacts on challenging decisions |
| Tallentire VR, Smith SE, Skinner J, Cameron HS72 | 2011 | UK | Research | Focus group study | FY1, FY2, SpR and consultant doctors in acute care | Factors that influence the behaviour of newly qualified doctors in acute care contexts |
| Tamuz M, Giardina TD, Thomas EJ, Menon S, Singh H116 | 2011 | USA | Research | Qualitative interview study | ICU in tertiary care | Hierarchical and interprofessional models of supervision on medication safety |
| Ummenhofer W, Amsler F, Sutter PM, Martina B, Martin J, Scheidegger D128 | 2001 | Switzerland | Research | Survey questionnaire | Emergency medicine clinicians, including internal medical, surgery and anaesthesia residents | Interdisciplinary attitudes on team performance in the emergency room |
| van Schaik S, Plant J, O’Brien B143 | 2015 | USA | Research | Secondary analysis of interviews taken following a simulation scenario | Paediatric residents and nursing staff | Resident perceptions of interprofessional team training |
| Vivekananda-Schmidt P, Vernon B100 | 2014 | UK | Research | Qualitative interview study | Doctors in their first year of the foundation programme | Ethical and legal challenges faced by newly qualified doctors in their clinical practice |
| Walton MM78 | 2006 | Australia | Commentary | N/A | N/A | Discussing the role of hierarchies in patient safety |
| Wiener-Ogilvie S, Bennison J, Smith V117 | 2014 | UK | Research | Qualitative interview study | Newly qualified GPs and GP trainees | Focused on how workplace learning in primary care prepares trainees for their future role |
| Authors | Year | Country | Type of paper | Study design/methods | Sample/setting | Objectives |
|---|---|---|---|---|---|---|
| Bearman M, Lawson M, Jones A81 | 2011 | Australia | Research | Qualitative interview study | Interns and supervisors in major metropolitan hospitals | To explore views on participation and professional development in clinical practice |
| Brennan N, Corrigan O, Allard J, Archer J, Barnes R, Bleakley A, Collett T, Bere D, Regan S136 | 2010 | UK | Research | Qualitative interviews and audio diary recordings | Newly qualified doctors from five hospital sites | Experiences of the transition from undergraduate to postgraduate medical training |
| Coats RD, Burd RS148 | 2002 | USA | Research | Survey questionnaire | Residents and faculty in surgery and seven subspecialties | To identify levels of comfort in discussing decisions made by faculty |
| Collins J130 | 2010 | UK | Policy report | Evidence from 67 organisations, review of publications, stakeholder input | Medical students and trainees, trainers and others involved in the delivery of the foundation programme | Strengths and limitations of the foundation programme |
| Hoff TJ, Pohl H, Bartfield J75 | 2006 | USA | Research | Nested case study design, using observation and interviews | Residents in trauma surgery and internal medicine | Exploring how residents develop the capability to learn from error in everyday work |
| Illing J, Morrow G, Kergon C, Burford B, Spencer J, Peile E, Davies C, Baldauf B, Allen M, Johnson N94 | 2008 | UK | Research (published as a report) | Multimethod, prospective, cross-sectional study, including interviews, focus groups, questionnaires and assessment data | Foundation year 1 doctors, undergraduate tutors, educational supervisors, key managers and members of clinical teams | To compare three UK medical schools on the basis of the preparedness of their graduates for practice |
| Jubraj B, Marvin V, Poots AJ, Patel S, Bovill I, Barnett N, Issen L, Bell D129 | 2015 | UK | Research | Web-based survey questionnaire | FY1 doctors in one hospital trust | To assess junior doctor attitudes towards awareness of medication review |
| Kennedy TJT, Regehr G, Baker GR, Lingard L133 | 2009 | Canada | Research | Qualitative interviews and observations | Internal and emergency medicine teaching teams, including attendings, residents and medical students | To examine trainees’ rationale about whether to seek clinical support or not |
| Kennedy TJT, Regehr G, Baker GR, Lingard LA138 | 2009 | Canada | Research | Qualitative interviews and observations | Internal and emergency medicine teaching teams, including attendings, residents and medical students | To theoretically explore cultural expectations of independent working and impacts on patient safety |
| Kilminster S, Zukas M, Quinton N, Roberts T79 | 2011 | UK | Research | Literature review, interviews and observation | FY1 doctors and specialist trainees, as well as supplementary interviews with other members of the clinical team | To analyse challenges faced by junior doctors in their transition from medical school and between settings, and how this can affect performance |
| Kroll L, Singleton A, Collier J, Rees Jones I118 | 2008 | UK | Research | Qualitative interview study | Pre-registration house officers in 10 hospitals | To examine junior doctor challenges with reporting errors and learning from their experiences |
| Lewis PJ, Ashcroft DM, Dornan T, Taylor D, Wass V, Tully MP124 | 2014 | UK | Research | Interview study using the critical incident technique | Newly qualified doctors FY1 across a range of medical schools and hospitals | To explore the perceived causes of junior doctors’ prescribing mistakes |
| McLellan L, Dornan T, Newton P, Williams SD, Lewis P, Steinke D, Tully MP80 | 2016 | UK | Research (intervention study) | Intervention study using pharmacist feedback – data collected from audit of prescriptions (plus contextual data) and qualitative interviews | Junior doctors in their first year of training | To investigate whether or not and how structured feedback sessions can increase appropriate antimicrobial prescribing |
| Stewart J95 | 2008 | UK | Research | Qualitative interview study including observations | Doctors in their first year of postgraduate practice from a range of hospitals | To identify influences on whether or not junior doctors choose to seek senior assistance |
| Teunissen PW, Stapel DA, van der Vleuten C, Scherpbier A, Boor K, Scheele F127 | 2009 | The Netherlands | Research | Survey questionnaire | Obstetrics/gynaecology residents at different levels of training | To examine residents’ feedback-seeking behaviour in relation to individual and situational variables |
Table 10 shows the number of quotations extracted from each of the documents to contribute to CMOC development. The number of quotations does not necessarily capture the richness or extent of support that each quotation provides for the CMOC. This table provides only a crude measure of the interpretation process and should be read together with the methodology section in this report, to provide a better picture of the analytical processes involved. All quotations are available from the authors on request.
| Authors (year) | CMOC | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 and 2 | 3 | 4 | 5 | 6–8 | 9 | 10 | 11 and 12 | 13 | 14 | 15 | 16 | 17–20 | 21 and 22 | 23 and 24 | 25 | 26 | 27 and 28 | |
| Abbo L, Sinkowitz-Cochran R, Smith L, Ariza-Heredia E, Gomez-Marin O, Srinivasan A, Hooton TM (2011)101 | 1 | |||||||||||||||||
| Aggarwal S, Mathew J, Singh H, Sharma V (2014)183 | ||||||||||||||||||
| Ajemigbitse A, Omole M, Ezike N, Erhun W (2014)85 | 1 | |||||||||||||||||
| Ajemigbitse AA, Omole MK, Osi-Ogbu OF, Erhun WO (2013)56 | 1 | 1 | 1 | |||||||||||||||
| Akici A, Kalaca S, Goren MZ, Akkan AG, Karaalp A, Demir D, Ugurlu U, Oktay S (2004)86 | 1 | |||||||||||||||||
| Alagha HZ, Badary OA, Ibrahim HM, Sabri NA (2011)201 | ||||||||||||||||||
| Ali MH, Kalima P, Maxwell SR (2006)60 | 1 | 1 | 2 | |||||||||||||||
| Allison GM, Weigel B, Holcroft C (2015)57 | ||||||||||||||||||
| Almatar MA, Peterson GM, Thompson A, Zaidi ST (2014)66 | 1 | 3 | ||||||||||||||||
| Almatar MA, Peterson GM, Thompson A, McKenzie DS, Anderson TL (2015)103 | 2 | |||||||||||||||||
| Alweis R, Greco M, Wasser T, Wenderoth S (2014)61 | ||||||||||||||||||
| Ambroggio L, Thomson J, Murtagh Kurowski E, Courter J, Statile A, Graham C, Sheehan B, Iyer S, Shah SS, White CM (2013)104 | 1 | |||||||||||||||||
| Asseray N, Mallaret MR, Sousbie M, Liberelle B, Schaerer L, Borrel E, Rieussec MO, Walter B, Guimier C, Buffet X, Soule H, Croize J, Stahl JP (2002)102 | 1 | |||||||||||||||||
| Aydin S, Yaris F, Ozcakir A, Agalar C (2005)202 | ||||||||||||||||||
| Baker E, Pryce Roberts A, Wilde K, Walton H, Suri S, Rull G, Webb A (2011)67 | ||||||||||||||||||
| Barlow G, Nathwani D, Myers E, Sullivan F, Stevens N, Duffy R, Davey P (2008)68 | 1 | 1 | 2 | 1 | ||||||||||||||
| Bearman M, Lawson M, Jones A (2001)81 | 1 | 2 | 1 | 1 | 1 | |||||||||||||
| Belyansky I, Martin TR, Prabhu AS, Tsirline VB, Howley LD, Phillips R, Sindram D, Heniford BT, Stefanidis D (2011)139 | 1 | 2 | 3 | |||||||||||||||
| Bethune R, Canter R, Abrams P (2012)146 | 3 | |||||||||||||||||
| Bongiovanni T, Yeo H, Sosa JA, Yoo PS, Long T, Rosenthal M, Berg D, Curry L, Nunez-Smith M (2015)119 | 1 | 2 | 1 | |||||||||||||||
| Bould MD, Sutherland S, Sydor DT, Naik V, Friedman Z, (2015)83 | 1 | 3 | 1 | 1 | 2 | 4 | 1 | |||||||||||
| Bowes J, Yasseen AS 3rd, Barrowman N, Murchison B, Dennis J, Moreau KA, Varughese N, Le Saux N (2014)203 | ||||||||||||||||||
| Brennan N, Corrigan O, Allard J, Archer J, Barnes R, Bleakley A, Collett T, Bere D, Regan S (2010)136 | 1 | 1 | ||||||||||||||||
| Charani E, Castro-Sanchez E, Sevdalis N, Kyratsis Y, Drumright L, Shah N, Holmes A (2013)35 | 4 | 1 | 5 | 3 | 9 | 2 | 3 | |||||||||||
| Chaves NJ, Cheng AC, Runnegar N, Kirschner J, Lee T, Buising K (2014)69 | 1 | 1 | ||||||||||||||||
| Chow A, Lye DCB, Arah OA (2015)99 | 3 | 1 | ||||||||||||||||
| Coats RD, Burd RS (2002)148 | 1 | |||||||||||||||||
| Coffey M, Thomson K, Tallett S, Matlow A (2010)140 | 1 | 1 | ||||||||||||||||
| Coleman JJ, Hemming K, Nightingale PG, Clark IR, Dixon-Woods M, Ferner RE, Lilford RJ (2011)204 | ||||||||||||||||||
| Collins J (2010)130 | 1 | |||||||||||||||||
| Conte H, Scheja M, Hjelmqvist H, Jirwe M (2015)87 | 1 | 1 | ||||||||||||||||
| Cortoos PJ, De Witte K, Peetermans WE, Simoens S, Laekeman G (2008)62 | 1 | 1 | 5 | 1 | 1 | 1 | 1 | 1 | 2 | |||||||||
| Cosby KS, Croskerry P (2004)213 | ||||||||||||||||||
| Coupat C, Pradier C, Degand N, Hofliger P, Pulcini C (2013)205 | ||||||||||||||||||
| Dallas A, Magin P, Morgan S, Tapley A, Henderson K, Ball J, Scott J, Spike N, McArthur L, van Driel M (2015)105 | 1 | |||||||||||||||||
| Dallas A, van Driel M, van de Mortel T, Magin P (2014)73 | 2 | 1 | 1 | 3 | 2 | |||||||||||||
| De Souza V, MacFarlane A, Murphy AW, Hanahoe B, Barber A, Cormican M (2006)63 | 2 | 3 | 1 | 1 | 1 | 1 | 2 | |||||||||||
| Deuster S, Roten I, Muehlebach S (2010)184 | ||||||||||||||||||
| Dobrzanski S, Hammond I, Khan G, Holdsworth H (2002)58 | 1 | 1 | ||||||||||||||||
| Doyle P, VanDenKerkhof EG, Edge DS, Ginsburg L, Goldstein DH (2015)141 | 1 | |||||||||||||||||
| Doyon S, Perreault M, Marquis C, Gauthier J, Lebel D, Bailey B, Collin J, Bussieres JF (2009)106 | 1 | |||||||||||||||||
| Fakih MG, Hilu RC, Savoy-Moore RT, Saravolatz LD (2003)107 | 1 | |||||||||||||||||
| Fakih MG, Berschback J, Juzych NS, Massanari RM (2006)88 | 1 | 1 | ||||||||||||||||
| Farnan JM, Johnson JK, Meltzer DO, Humphrey HJ, Arora VM (2008)132 | 4 | 1 | ||||||||||||||||
| Feucht CL, Rice LB (2003)162 | ||||||||||||||||||
| Fiordelli M, Schulz PJ, Caiata Zufferey M (2014)120 | 1 | 4 | 1 | |||||||||||||||
| Flannery DD, Swami S, Chan S, Eppes S (2014)206 | ||||||||||||||||||
| Flannery MT, McCool MJ (2005)167 | ||||||||||||||||||
| Friedman SM, Sowerby RJ, Guo R, Bandiera G (2010)131 | 1 | |||||||||||||||||
| Friedman Z, Hayter MA, Everett TC, Matava CT, Noble LM, Bould MD (2015)82 | 1 | 2 | 1 | |||||||||||||||
| Garcia C, Llamocca LP, Garcia K, Jimenez A, Samalvides F, Gotuzzo E, Jacobs J (2011)137 | 2 | |||||||||||||||||
| Gaur AH, Hare ME, Shorr RI (2005)108 | 1 | |||||||||||||||||
| Gordon LJ, Rees CE, Ker JS, Cleland J (2015a)115 | 1 | 1 | 1 | 2 | ||||||||||||||
| Gordon LJ, Rees CE, Ker JS, Cleland J (2015b)84 | 2 | 1 | 1 | |||||||||||||||
| Guerra CM, Pereira CA, Neves Neto AR, Cardo DM, Correa L (2007)163 | ||||||||||||||||||
| Hall KK, Philbrick J, Nadkarni M (2003)160 | ||||||||||||||||||
| Hamui-Sutton A, Vives-Varela T, Gutierrez-Barreto S, Leenen I, Sanchez-Mendiola M (2015)122 | 1 | |||||||||||||||||
| Harnett SJ, Allen KD (2000)207 | ||||||||||||||||||
| Hilliard R, Harrison C, Madden S (2007)77 | 1 | 1 | 1 | 1 | ||||||||||||||
| Hoff Timothy J, Pohl H, Bartfield J (2006)75 | 1 | |||||||||||||||||
| Hoff TJ (2008)93 | 1 | |||||||||||||||||
| Hong SY, Epstein LH, Lawrence K, Davidson L, Taur Y, Nadkarni L, Doron S, (2013)59 | 1 | 1 | ||||||||||||||||
| Illing J, Morrow G, Kergon C, Burford B, Spencer J, Peile E, Davies C, Baldauf B, Allen M, Johnson N (2008)94 | 1 | 1 | ||||||||||||||||
| Jaensch SL, Baysari MT, Day RO, Westbrook JI (2013)123 | 1 | 1 | ||||||||||||||||
| Jubraj B, Marvin V, Poots AJ, Patel S, Bovill I, Barnett N, Issen L, Bell D (2015)129 | 1 | |||||||||||||||||
| Kennedy TJT; Regehr G, Baker GR, Lingard L (2009)133 | 1 | |||||||||||||||||
| Kennedy TJT, Regehr G, Baker GR, Lingard LA (2009)138 | 1 | |||||||||||||||||
| Kilminster S, Zukas M, Quinton N, Roberts T (2011)79 | 1 | 1 | 1 | |||||||||||||||
| Kobayashi H, Pian-Smith M, Sato M, Sawa R, Takeshita T, Raemer D (2006)144 | 2 | 2 | ||||||||||||||||
| Kroll L, Singleton A, Collier J, Rees Jones I (2008)118 | 1 | 1 | 2 | |||||||||||||||
| Lee MJ, Kim M, Kim NH, Kim CJ, Song KH, Choe PG, Park WB, Bang JH, Kim ES, Park SW, Kim NJ, Oh MD, Kim HB (2015)168 | ||||||||||||||||||
| Lee TC, Frenette C, Jayaraman D, Green L, Pilote L (2014)89 | 1 | |||||||||||||||||
| Levinsky Y, Mimouni FB, Fisher D, Ehrlichman M (2013)186 | ||||||||||||||||||
| Lewis PJ, Ashcroft DM, Dornan T, Taylor D, Wass V, Tully MP (2014)124 | 1 | 2 | ||||||||||||||||
| Liabsuetrakul T, Chongsuvivatwong V, Lumbiganon P, Lindmark G (2003)74 | 1 | |||||||||||||||||
| Limbert C, Lamb R (2002)109 | 1 | |||||||||||||||||
| Lingard L, Reznick R, Espin S, Regehr G, DeVito I (2002)214 | ||||||||||||||||||
| Livorsi D, Comer A, Matthias MS, Perencevich EN, Bair MJ (2015)70 | 6 | 1 | 1 | 2 | 2 | 1 | 4 | 1 | ||||||||||
| Maisonneuve JJ, Lambert TW, Goldacre MJ (2014)121 | 2 | 1 | ||||||||||||||||
| Mattick K, Kelly N, Rees C (2014)43 | 3 | 1 | 5 | 1 | 2 | |||||||||||||
| May L, Gudger G, Armstrong P, Brooks G, Hinds P, Bhat R, Moran GJ, Schwartz L, Cosgrove SE, Klein EY, Rothman RE, Rand C (2014)10 | 1 | 1 | 1 | 2 | 4 | 1 | ||||||||||||
| McCarthy RM, Hilmer SN (2013)182 | ||||||||||||||||||
| McLellan L, Dornan T, Newton P, Williams SD, Lewis P, Steinke D, Tully MP (2016)80 | 1 | 1 | 2 | |||||||||||||||
| Menendez R, Torres A, Zalacain R, Aspa J, Martin-Villasclaras JJ, Borderias L, Benitez-Moya JM, Ruiz-Manzano J, de Castro FR, Blanquer J, Perez D, Puzo C, Sanchez-Gascon F, Gallardo J, Alvarez C, Molinos L, Neumofail Group (2005)110 | 2 | |||||||||||||||||
| Mincey BA, Parkulo MA (2001)111 | 1 | |||||||||||||||||
| Nambiar S, Schwartz RH, Sheridan MJ (2002)164 | ||||||||||||||||||
| Navarro-San Francisco C, Del Toro MD, Cobo J, De Gea-Garcia JH, Vano-Galvan S, Moreno-Ramos F, Rodriguez-Bano J, Pano-Pardo JR (2013)76 | 1 | 1 | ||||||||||||||||
| Neumark T, Brudin L, Molstad S (2015)169 | ||||||||||||||||||
| Newham R, Thomson AH, Semple Y, Dewar S, Steedman T, Bennie M (2015)112 | 1 | |||||||||||||||||
| Oppenheim MI, Vidal C, Velasco FT, Boyer AG, Cooper MR, Hayes JG, Frayer WW (2002)187 | ||||||||||||||||||
| Oshikoya KA, Senbanjo IO, Amole OO (2009)208 | ||||||||||||||||||
| Pacheco GS, Viscusi C, Hays DP, Woolridge DP (2012)161 | ||||||||||||||||||
| Patel R, Green W, Martinez MM, Shahzad MW, Larkin C (2015)64 | ||||||||||||||||||
| Pian-Smith MC, Simon R, Minehart RD, Podraza M, Rudolph J, Walzer T, Raemer D (2009)142 | 2 | |||||||||||||||||
| Pulcini C, Williams F, Molinari N, Davey P, Nathwani D (2011)170 | ||||||||||||||||||
| Purcell K, Fergie J (2003)209 | ||||||||||||||||||
| Reader TW, Flin R, Mearns K, Cuthbertson BH (2007)147 | 1 | |||||||||||||||||
| Rinke ML, Moon M, Clark JS, Mudd S, Miller MR (2008)166 | ||||||||||||||||||
| Rosenbaum JR, Bradley EH, Holmboe ES, Farrell MH, Krumholz HM (2004)215 | ||||||||||||||||||
| Roumie CL, Halasa NB, Edwards KM, Zhu Y, Dittus RS, Griffin MR (2005)165 | ||||||||||||||||||
| Salomon L, Levu S, Deray G, Launay-Vacher V, Brucker G, Ravaud P (2003)210 | ||||||||||||||||||
| Sculli GL, Fore AM, Sine DM, Paull DE, Tschannen D, Aebersold M, Seagull FJ, Bagian JP (2015)90 | 1 | |||||||||||||||||
| Seemungal IA, Bruno CJ (2012)211 | ||||||||||||||||||
| Sellman JS, Decarolis D, Schullo-Feulner A, Nelson DB, Filice GA (2004)135 | 1 | |||||||||||||||||
| Simpson JH, Lynch R, Grant J, Alroomi L (2004)125 | 1 | |||||||||||||||||
| Solomon DH, Van Houten L, Glynn RJ, Baden L, Curtis K, Schrager H, Avorn J (2001)171 | ||||||||||||||||||
| Stack SJ, Watson MJ (2001)216 | ||||||||||||||||||
| Steinke DT, Bain DJ, MacDonald TM, Davey PG (2000)126 | 2 | |||||||||||||||||
| Stewart J (2008)95 | 1 | 1 | ||||||||||||||||
| Stone S, Gonzales R, Maselli J, Lowenstein SR (2000)212 | ||||||||||||||||||
| Sutcliffe KM, Lewton E, Rosenthal MM (2004)134 | 2 | 3 | ||||||||||||||||
| Sydor DT, Bould MD, Naik VN, Burjorjee J, Arzola C, Hayter M, Friedman Z (2013)145 | 1 | 1 | 2 | |||||||||||||||
| Tallentire VR, Smith SE, Skinner J, Cameron HS (2011)72 | 1 | 1 | 1 | 2 | 2 | |||||||||||||
| Tamuz M, Giardina TD, Thomas EJ, Menon S, Singh H (2011)116 | 1 | 5 | 3 | 1 | ||||||||||||||
| Tell D, Engstrom S, Molstad S (2015)96 | 1 | 1 | ||||||||||||||||
| Teunissen Pim W, Stapel Diederik A, van der Vleuten C, Scherpbier A, Boor K, Scheele F (2009)127 | 1 | |||||||||||||||||
| Thorpe JM, Smith SR, Trygstad TK (2004)181 | ||||||||||||||||||
| Thursky KA, Mahemoff M (2007)194 | ||||||||||||||||||
| Tobaiqy M, McLay J, Ross S (2007)97 | 1 | 1 | ||||||||||||||||
| Ummenhofer W, Amsler F, Sutter PM, Martina B, Martin J, Scheidegger D (2001)128 | 1 | |||||||||||||||||
| Undeland DK, Kowalski TJ, Berth WL, Gundrum JD (2010)114 | 1 | |||||||||||||||||
| Valerio M, Vena A, Bouza E, Reiter N, Viale P, Hochreiter M, Giannella M, Munoz P, Comic study group (2015)65 | ||||||||||||||||||
| van Schaik S, Plant J, O’Brien B (2015)143 | 1 | |||||||||||||||||
| Vivekananda-Schmidt P, Vernon B (2014)100 | 1 | |||||||||||||||||
| Walton MM (2006)78 | 1 | 1 | 2 | 1 | ||||||||||||||
| Weingart SN, Toth M, Sands DZ, Aronson MD, Davis RB, Phillips RS (2003)188 | ||||||||||||||||||
| Welch SA, Novy M, Preisz P, Quinn DI, Whicker SD, Brown SE, Day RO (2000)91 | 1 | 1 | ||||||||||||||||
| Wiener-Ogilvie S, Bennison J, Smith V (2014)117 | 1 | 2 | ||||||||||||||||
| Zaidi ST, Thursky KA (2013)98 | 1 | 2 | 1 | 1 | ||||||||||||||
| Zallman L, Ma J, Xiao L, Lasser KE (2010)113 | 1 | |||||||||||||||||
| Ziglam HM, Morales D, Webb K, Nathwani D (2006)92 | 1 | 1 | ||||||||||||||||
Appendix 3 Details of coding applied to the literature included in the review
In Tables 11 and 13, nodes refer to the number of codes applied to each article, that is, how many codes have been attached to excerpts within the article. This means that the terms nodes and the codes can be used interchangeably. The more nodes attached to each article, the more informative this was for the review as it either provided evidence for a range of CMOCs, or provided in-depth evidence for a smaller subset of CMOCs.
References (in NVivo terminology) relate to the number of text excerpts coded within each article, although many parts of the article have codes applied to them. Similarly to nodes, the more references within each article, the more useful an article has been to inform programme theory.
In Tables 12 and 14, sources refer to the number of articles where a specific node (code) has been applied.
References (in NVivo terminology) relate to the number of text excerpts coded under each node. The more references coded using a specific node, the more useful this node has been to inform programme theory.
| Authors (year) | Nodes | References |
|---|---|---|
| May L, Gudger G, Armstrong P, Brooks G, Hinds P, Bhat R, Moran GJ, Schwartz L, Cosgrove SE, Klein EY, Rothman RE, Rand C (2014)10 | 24 | 69 |
| Charani E, Castro-Sanchez E, Sevdalis N, Kyratsis Y, Drumright L, Shah N, Holmes A (2013)35 | 14 | 57 |
| Livorsi D, Comer A, Matthias MS, Perencevich EN, Bair MJ (2015)70 | 23 | 49 |
| Barlow G, Nathwani D, Myers E, Sullivan F, Stevens N, Duffy R, Davey P (2008)68 | 25 | 46 |
| De Souza V, MacFarlane A, Murphy AW, Hanahoe B, Barber A, Cormican M (2006)63 | 16 | 44 |
| Mattick K, Kelly N, Rees C (2014)43 | 22 | 43 |
| Dallas A, van Driel M, van de Mortel T, Magin P (2014)73 | 19 | 40 |
| Garcia C, Llamocca LP, Garcia K, Jimenez A, Samalvides F, Gotuzzo E, Jacobs J (2011)137 | 18 | 35 |
| Abbo L, Sinkowitz-Cochran R, Smith L, Ariza-Heredia E, Gomez-Marin O, Srinivasan A, Hooton TM (2011)101 | 15 | 32 |
| Cortoos PJ, De Witte K, Peetermans WE, Simoens S, Laekeman G (2008)62 | 14 | 29 |
| Gaur AH, Hare ME, Shorr RI (2005)108 | 11 | 28 |
| Ajemigbitse AA, Omole MK, Osi-Ogbu OF, Erhun WO (2013)56 | 13 | 26 |
| Pulcini C, Williams F, Molinari N, Davey P, Nathwani D (2011)170 | 12 | 23 |
| Liabsuetrakul T, Chongsuvivatwong V, Lumbiganon P, Lindmark G (2003)74 | 16 | 23 |
| Fakih MG, Hilu RC, Savoy-Moore RT, Saravolatz LD (2003)107 | 13 | 23 |
| Jaensch SL, Baysari MT, Day RO, Westbrook JI (2013)123 | 10 | 22 |
| Hong SY, Epstein LH, Lawrence K, Davidson L, Taur Y, Nadkarni L, Doron S (2013)59 | 8 | 21 |
| Dallas A, Magin P, Morgan S, Tapley A, Henderson K, Ball J, Scott J, Spike N, McArthur L, van Driel M (2015)105 | 8 | 20 |
| Chaves NJ, Cheng AC, Runnegar N, Kirschner J, Lee T, Buising K (2014)69 | 12 | 20 |
| Zaidi ST, Thursky KA (2013)98 | 12 | 20 |
| Menendez R, Torres A, Zalacain R, Aspa J, Martin-Villasclaras JJ, Borderias L, Benitez-Moya JM, Ruiz-Manzano J, de Castro FR, Blanquer J, Perez D, Puzo C, Sanchez-Gascon F, Gallardo J, Alvarez C, Molinos L, Neumofail Group (2005)110 | 11 | 20 |
| Chow A, Lye DCB, Arah OA (2015)99 | 11 | 19 |
| Navarro-San Francisco C, Del Toro MD, Cobo J, De Gea-Garcia JH, Vano-Galvan S, Moreno-Ramos F, Rodriguez-Bano J, Pano-Pardo JR (2013)76 | 9 | 19 |
| Doyon S, Perreault M, Marquis C, Gauthier J, Lebel D, Bailey B, Collin J, Bussieres JF (2009)106 | 9 | 19 |
| Tobaiqy M, McLay J, Ross S (2007)97 | 8 | 19 |
| Almatar MA, Peterson GM, Thompson A, Zaidi ST (2014)66 | 12 | 18 |
| Lee TC, Frenette C, Jayaraman D, Green L, Pilote L (2014)89 | 10 | 18 |
| Akici A, Kalaca S, Goren MZ, Akkan AG, Karaalp A, Demir D, Ugurlu U, Oktay S (2004)86 | 7 | 18 |
| Asseray N, Mallaret MR, Sousbie M, Liberelle B, Schaerer L, Borrel E, Rieussec MO, Walter B, Guimier C, Buffet X, Soule H, Croize J, Stahl JP (2002)102 | 12 | 18 |
| Fakih MG, Berschback J, Juzych NS, Massanari RM (2006)88 | 7 | 18 |
| Alweis R, Greco M, Wasser T, Wenderoth S (2014)61 | 12 | 17 |
| Ali MH, Kalima P, Maxwell SR (2006)60 | 8 | 16 |
| Valerio M, Vena A, Bouza E, Reiter N, Viale P, Hochreiter M, Giannella M, Munoz P, Comic study group (2015)65 | 7 | 15 |
| Pacheco GS, Viscusi C, Hays DP, Woolridge DP (2012)161 | 11 | 15 |
| Simpson JH, Lynch R, Grant J, Alroomi L (2004)125 | 10 | 15 |
| Feucht CL, Rice LB (2003)162 | 9 | 15 |
| Dobrzanski S, Hammond I, Khan G, Holdsworth H (2002)58 | 9 | 15 |
| Almatar MA, Peterson GM, Thompson A, McKenzie DS, Anderson TL (2015)103 | 8 | 14 |
| Sellman JS, Decarolis D, Schullo-Feulner A, Nelson DB, Filice GA (2004)135 | 9 | 14 |
| Steinke DT, Bain DJ, MacDonald TM, Davey PG (2000)126 | 8 | 14 |
| Patel R, Green W, Martinez MM, Shahzad MW, Larkin C (2015)64 | 8 | 13 |
| Ajemigbitse A, Omole M, Ezike N, Erhun W (2014)85 | 9 | 13 |
| Aydin S, Yaris F, Ozcakir A, Agalar C (2005)202 | 6 | 13 |
| Mincey BA, Parkulo MA (2001)111 | 4 | 13 |
| Levinsky Y, Mimouni FB, Fisher D, Ehrlichman M (2013)186 | 5 | 12 |
| Stone S, Gonzales R, Maselli J, Lowenstein SR (2000)212 | 7 | 12 |
| Tell D, Engstrom S, Molstad S (2015)96 | 9 | 11 |
| Lee MJ, Kim M, Kim NH, Kim CJ, Song KH, Choe PG, Park WB, Bang JH, Kim ES, Park SW, Kim NJ, Oh MD, Kim HB (2015)168 | 7 | 11 |
| Alagha HZ, Badary OA, Ibrahim HM, Sabri NA (2011)201 | 9 | 11 |
| Zallman L, Ma J, Xiao L, Lasser KE (2010)113 | 4 | 11 |
| Thursky KA, Mahemoff M (2007)194 | 8 | 11 |
| Hall KK, Philbrick J, Nadkarni M (2003)160 | 8 | 11 |
| Bowes J, Yasseen AS 3rd, Barrowman N, Murchison B, Dennis J, Moreau KA, Varughese N, Le Saux N (2014)203 | 7 | 10 |
| Guerra CM, Pereira CA, Neves Neto AR, Cardo DM, Correa L (2007)163 | 7 | 10 |
| Roumie CL, Halasa NB, Edwards KM, Zhu Y, Dittus RS, Griffin MR (2005)165 | 2 | 10 |
| Ambroggio L, Thomson J, Murtagh Kurowski E, Courter J, Statile A, Graham C, Sheehan B, Iyer S, Shah SS, White CM (2013)104 | 6 | 9 |
| Baker E, Pryce Roberts A, Wilde K, Walton H, Suri S, Rull G, Webb A (2011)67 | 6 | 9 |
| Seemungal IA, Bruno CJ (2012)211 | 8 | 9 |
| Undeland DK, Kowalski TJ, Berth WL, Gundrum JD (2010)114 | 8 | 9 |
| Coupat C, Pradier C, Degand N, Hofliger P, Pulcini C (2013)205 | 6 | 9 |
| Neumark T, Brudin L, Molstad S (2015)169 | 6 | 8 |
| Flannery MT, McCool MJ (2005)167 | 5 | 8 |
| Allison GM, Weigel B, Holcroft C (2015)57 | 6 | 7 |
| McCarthy RM, Hilmer SN (2013)182 | 4 | 7 |
| Rinke ML, Moon M, Clark JS, Mudd S, Miller MR (2008)166 | 4 | 7 |
| Thorpe JM, Smith SR, Trygstad TK (2004)181 | 4 | 7 |
| Oppenheim MI, Vidal C, Velasco FT, Boyer AG, Cooper MR, Hayes JG, Frayer WW (2002)187 | 6 | 7 |
| Nambiar S, Schwartz RH, Sheridan MJ (2002)164 | 6 | 7 |
| Solomon DH, Van Houten L, Glynn RJ, Baden L, Curtis K, Schrager H, Avorn J (2001)171 | 4 | 7 |
| Harnett SJ, Allen KD (2000)207 | 5 | 7 |
| Flannery DD, Swami S, Chan S, Eppes S (2014)206 | 5 | 6 |
| Deuster S, Roten I, Muehlebach S (2010)184 | 5 | 6 |
| Oshikoya KA, Senbanjo IO, Amole OO (2009)208 | 6 | 6 |
| Ziglam HM, Morales D, Webb K, Nathwani D (2006)92 | 6 | 6 |
| Salomon L, Levu S, Deray G, Launay-Vacher V, Brucker G, Ravaud P (2003)210 | 5 | 6 |
| Coleman JJ, Hemming K, Nightingale PG, Clark IR, Dixon-Woods M, Ferner RE, Lilford RJ (2011)204 | 2 | 4 |
| Weingart SN, Toth M, Sands DZ, Aronson MD, Davis RB, Phillips RS (2003)188 | 3 | 4 |
| Aggarwal S, Mathew J, Singh H, Sharma V (2014)183 | 3 | 3 |
| Codes | Sources | References |
|---|---|---|
| Social norms and culture | 9 | 20 |
| Hierarchies and informal influences | 1 | 1 |
| Team practices or collective prescribing | 3 | 6 |
| Senior influence and opinion leaders | 34 | 108 |
| Prescribing independence by junior doctors, or lack of | 5 | 13 |
| Trying to prove oneself | 3 | 4 |
| Conscious reliance on others | 1 | 1 |
| Prescribing autonomy or non-interference | 6 | 12 |
| Circumvention to preserve autonomy | 3 | 5 |
| Politics of prescribing | 6 | 18 |
| Role of pharmaceuticals | 5 | 7 |
| Role of infectious disease specialists, pharmacists, etc. | 28 | 45 |
| Role and responsibility as clinician | 8 | 22 |
| Humility | 8 | 9 |
| Prescribing support, or lack of | 10 | 18 |
| Perceptions of antibiotic overuse and resistance prevalence | 15 | 29 |
| Global vs. local problem | 9 | 17 |
| Attitudes towards prescribing tasks | 2 | 2 |
| Patient related | 0 | 0 |
| Patient characteristics | 16 | 31 |
| Managing patient and family expectations | 15 | 40 |
| Operational structures and inefficiencies | 11 | 27 |
| Time and operational pressures | 19 | 29 |
| Interward variability | 4 | 5 |
| Inconsistency of prescribing practices | 2 | 2 |
| Laboratory tests | 10 | 29 |
| Information technology | 12 | 19 |
| Use and perceived usefulness | 4 | 9 |
| Implementation | 3 | 7 |
| Guidelines and recommendations | 0 | 0 |
| Positive perceptions and acceptance | 12 | 18 |
| Patterns of use or non-use | 18 | 26 |
| Outcomes | 3 | 3 |
| Guideline interventions | 2 | 7 |
| Contradicting or unclear guidelines | 12 | 20 |
| Awareness and availability of guidelines | 20 | 43 |
| Translation gap | 2 | 4 |
| Recommendations evolving fast | 1 | 2 |
| Accepted non-compliance | 6 | 8 |
| Scepticism against guidelines | 7 | 17 |
| Contradicting evidence on local ownership | 6 | 10 |
| Personal experience and confidence | 8 | 15 |
| Influence of colleagues and seniors | 8 | 11 |
| Feedback, or lack of, and other learning opportunities | 29 | 53 |
| Diagnostic or clinical uncertainty | 15 | 23 |
| Uncertainty about process or mechanics of prescribing | 5 | 14 |
| Self-awareness and reported confidence | 12 | 20 |
| Risk perceptions or cultures | 9 | 10 |
| Better safe than sorry | 11 | 31 |
| Fear of litigation | 2 | 3 |
| Balancing with side effects or adverse events | 4 | 7 |
| Knowledge or lack of | 20 | 37 |
| Medication errors and inappropriate prescribing | 15 | 19 |
| Gap between theoretical knowledge and real-world prescribing | 9 | 22 |
| Clinical judgement and experience | 23 | 34 |
| Prescribing uncertainty | 2 | 5 |
| Influence of previous clinical experience or rotation | 7 | 8 |
| Differences between prescribers | 27 | 88 |
| Cost considerations | 8 | 15 |
| Attitudes towards certain conditions | 1 | 3 |
| Authors (year) | Nodes | References |
|---|---|---|
| Fiordelli M, Schulz PJ, Caiata Zufferey M (2014)120 | 11 | 45 |
| Hoff TJ (2008)93 | 7 | 32 |
| Bould MD, Sutherland S, Sydor DT, Naik V, Friedman Z (2015)83 | 7 | 30 |
| Tallentire VR, Smith SE, Skinner J, Cameron HS (2011)72 | 10 | 29 |
| Gordon LJ, Rees CE, Ker JS, Cleland J (2015b)84 | 7 | 28 |
| Tamuz M, Giardina TD, Thomas EJ, Menon S, Singh H (2011)116 | 7 | 28 |
| Gordon LJ, Rees CE, Ker JS, Cleland J (2015a)115 | 7 | 27 |
| Belyansky I, Martin TR, Prabhu, AS, Tsirline VB, Howley LD, Phillips R, Sindram D, Heniford BT, Stefanidis D (2011)139 | 10 | 26 |
| Cosby KS, Croskerry P (2004)213 | 9 | 26 |
| Coffey M, Thomson K, Tallett S, Matlow A (2010)140 | 8 | 23 |
| Sutcliffe KM, Lewton E, Rosenthal MM (2004)134 | 6 | 20 |
| Wiener-Ogilvie S, Bennison J, Smith V (2014)117 | 11 | 19 |
| Friedman SM, Sowerby RJ, Guo R, Bandiera G (2010)131 | 6 | 18 |
| Hilliard R, Harrison C, Madden S (2007)77 | 9 | 17 |
| Friedman Z, Hayter MA, Everett TC, Matava CT, Noble LM, Bould MD (2015)82 | 4 | 15 |
| Rosenbaum JR, Bradley EH, Holmboe ES, Farrell MH, Krumholz HM (2004)215 | 7 | 15 |
| Maisonneuve JJ, Lambert TW, Goldacre MJ (2014)121 | 6 | 14 |
| Stack SJ, Watson MJ (2001)216 | 7 | 14 |
| Vivekananda-Schmidt P, Vernon B (2014)100 | 7 | 14 |
| Conte H, Scheja M, Hjelmqvist H, Jirwe M (2015)87 | 4 | 13 |
| Lingard L, Reznick R, Espin S, Regehr G, DeVito I (2002)214 | 5 | 13 |
| Pian-Smith MC, Simon R, Minehart RD, Podraza M, Rudolph J, Walzer T, Raemer D (2009)142 | 3 | 13 |
| Sculli GL, Fore AM, Sine DM, Paull DE, Tschannen D, Aebersold M, Seagull FJ, Bagian JP (2015)90 | 4 | 13 |
| Farnan JM, Johnson JK, Meltzer DO, Humphrey HJ, Arora VM (2008)132 | 6 | 12 |
| Hamui-Sutton A, Vives-Varela T, Gutierrez-Barreto S, Leenen I, Sanchez-Mendiola M (2015)122 | 8 | 11 |
| van Schaik S, Plant J, O’Brien B (2015)143 | 4 | 11 |
| Walton MM (2006)78 | 7 | 11 |
| Kobayashi H, Pian-Smith M, Sato M, Sawa R, Takeshita T, Raemer D (2006)144 | 3 | 10 |
| Sydor DT, Bould MD, Naik VN, Burjorjee J, Arzola C, Hayter M, Friedman Z (2013)145 | 3 | 10 |
| Bongiovanni T, Yeo H, Sosa JA, Yoo PS, Long T, Rosenthal M, Berg D, Curry L, Nunez-Smith M (2015)119 | 5 | 8 |
| Doyle P, VanDenKerkhof EG, Edge DS, Ginsburg L, Goldstein DH (2015)141 | 5 | 8 |
| Reader TW, Flin R, Mearns K, Cuthbertson BH (2007)147 | 4 | 5 |
| Bethune R, Canter R, Abrams P (2012)146 | 2 | 4 |
| Limbert C, Lamb R (2002)109 | 1 | 4 |
| Ummenhofer W, Amsler F, Sutter PM, Martina B, Martin J, Scheidegger D (2001)128 | 3 | 4 |
| Codes | Sources | References |
|---|---|---|
| Teamworking and relationships | 13 | 31 |
| Recommendations | 23 | 63 |
| Other themes | 2 | 2 |
| Performing under stress | 7 | 9 |
| Lack of experience | 2 | 2 |
| Knowledge into practice | 2 | 3 |
| Confirmation bias | 1 | 1 |
| Inappropriate or inadequate supervision | 6 | 11 |
| Good supervision | 1 | 2 |
| Interprofessional working and supervision | 6 | 22 |
| Hierarchies | 25 | 98 |
| Value conflicts | 3 | 8 |
| Senior stepping back | 2 | 8 |
| Responsibility | 11 | 29 |
| Positive aspects | 9 | 20 |
| Negative role modelling | 1 | 1 |
| Less hierarchical relationships | 1 | 4 |
| Language | 2 | 2 |
| Implicit rules | 4 | 5 |
| Identity work | 6 | 20 |
| Hierarchy of assistance | 2 | 7 |
| Guidelines | 1 | 4 |
| Coping strategies | 9 | 17 |
| Circumvention | 1 | 1 |
| Being in the middle | 2 | 3 |
| Discrepancies between seniors and juniors | 6 | 25 |
| Differences | 1 | 3 |
|
8 | 11 |
|
4 | 32 |
|
2 | 2 |
| Communication | 7 | 24 |
| Challenging or seeking advice | 23 | 83 |
| Negative case | 3 | 3 |
| Clinical or administrative duties prioritised over learning | 4 | 13 |
| Background | 13 | 21 |
Glossary
- Abductive reasoning
- An analytical process that provides the best explanation (or theory) for a phenomenon, that is, inference to the best explanation.
- Antimicrobial resistance
- The lack of effectiveness of antiviral, antifungal, antibacterial and antiparasitic medicines against microbes.
- Antimicrobial stewardship
- An intervention to promote and monitor the appropriate use of antimicrobials to sustain their effectiveness.
- Context
- The settings, structures, environments, conditions or circumstances that trigger behavioural and emotional responses (i.e. mechanisms) for those affected.
- Context–mechanism–outcome configuration
- A relationship between the building blocks of realist analysis, that is, how mechanisms are triggered under specific contexts to result in particular outcomes.
- Mechanism
- The way in which individuals respond to and reason about the resources, opportunities or challenges offered by a particular programme, intervention or process. Mechanisms are triggered in specific contexts and lead to changes in behaviour.
- Outcome
- The impact or behaviours resulting from the interaction between mechanisms and contexts.
- Programme theory
- A set of theoretical explanations or assumptions about how a particular programme, process or intervention is expected to work.
- Stages in clinical training (in the UK)
- Medical school graduates enter the 2-year foundation programme (foundation years 1 and 2). They then continue as specialty/core trainees or registrars in hospital for 5 years (specialist trainee years 1–5) or in general practice for 3 years. Registrars in their final year are called senior registrars, with consultants being the next level in seniority. Until recently, trainees in their foundation years were called pre-registration house officers and senior house officers. The term ‘junior doctors’ incorporates medical school graduates and those in registrar grades.
- Stages in clinical training (in the USA and Canada)
- Attending physicians have completed clinical training and are responsible for the supervision of fellows (those who have completed residency training) and residents/house officers (those still undergoing specialty training). ‘Internship’ is commonly used to refer to an early stage of residency training.
List of abbreviations
- AMR
- antimicrobial resistance
- ASSIA
- Applied Social Sciences Index and Abstracts
- C
- context
- CDSR
- Cochrane Database of Systematic Reviews
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CMOC
- context–mechanism–outcome configuration
- CPCI-S
- Conference Proceedings Citation Index – Science
- HTA
- Health Technology Assessment
- IMPACT
- IMProving Antimicrobial presCribing for doctors in Training
- KTA
- knowledge to action
- M
- mechanism
- O
- outcome
- PHE
- Public Health England
- PPI
- patient and public involvement
- SCIE
- Science Citation Index Expanded
- WHO
- World Health Organization
