Notes
Article history
The research reported here is the product of an HS&DR Evidence Synthesis Centre, contracted to provide rapid evidence syntheses on issues of relevance to the health service, and to inform future HS&DR calls for new research around identified gaps in evidence. Other reviews by the Evidence Synthesis Centres are also available in the HS&DR journal. The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/05/11. The contractual start date was in November 2016. The final report began editorial review in March 2017 and was accepted for publication in July 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Dalton et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Introduction
Mental health care for armed forces personnel in the UK while they are still in service is commissioned by the Defence Medical Services (DMS) (but inpatient mental health services are currently provided by a NHS consortium). Services on discharge are mainly the responsibility of the local NHS [Clinical Commissioning Groups (CCGs)] in terms of payment and provision. However, a few services, including ones that have been initiated by the DMS, may be provided by the DMS for 6 months. The transition of the individual from one service to another may create a reason for reticence to present for help. In the UK, the Armed Forces Covenant exists as a formal commitment and moral obligation to the armed forces community that no one will face disadvantage compared with other citizens in relation to the provision of public and commercial services, and special considerations are appropriate in some cases (e.g. the injured or bereaved). 1
In 2011, it was reported that only 23% of UK veterans suffering symptoms of post-traumatic stress disorder (PTSD) went on to access support services. 2 More recently, it has been reported that half of the armed forces veterans with PTSD now seek help from NHS services, but also that individuals are rarely referred to the correct specialist care. 3
The background to this research arises from current thinking about the anticipated rise in demand for psychological trauma services in the UK, with particular reference to armed forces veterans with PTSD. 4 In 2014, there were 2.8 million ex-service personnel in the UK, and it was envisaged that requirements for specialist support would grow as a result of armed forces restructuring and ever more complex needs arising from recent conflicts. 5,6
Given the transitionary arrangement and the anticipated rise in demand for services, there is a need to explore the adequacy and suitability of current and planned mental health services to treat PTSD to meet the specific requirements of armed forces veterans. Our research maps out key services currently being provided in the UK and evaluates the empirical evidence on the effectiveness of models of care and the effectiveness of available treatments.
Veterans and post-traumatic stress disorder
Definitions of ‘veteran’
In the recent NHS England stakeholder engagement survey questionnaire, a veteran is referred to as follows:
We use ‘veteran’ to mean anyone who has been a serving member of the British armed forces for a day or more. It means the same as ‘ex-service personnel’ . . . when we say ‘veteran’ or when we talk about armed forces’ experiences, this includes reservists as well as regulars.
p. 2 of the questionnaire7
Other definitions exist. For example, in the USA, a veteran is ‘a person who served in the active military, naval, or air service and who was discharged or released under conditions other than dishonourable’ (Title 38 of the Code of Federal Regulations). 8
In our research we aimed to capture definitions of ‘veteran’ in the international research literature and adopt a consistent approach to reporting.
Post-traumatic stress disorder and ‘complex post-traumatic stress disorder’
Post-traumatic stress disorder is an anxiety disorder following very stressful, frightening or distressing events. People with PTSD can experience nightmares and flashbacks; they can feel isolated, irritable and guilty. Various sequelae, such as insomnia and poor concentration, can have a significant impact on day-to-day living. NHS standard treatments for PTSD currently include watchful waiting, psychotherapy, trauma-focused cognitive–behavioural therapy (TFCBT), eye movement desensitisation and reprocessing (EMDR), group therapy and counselling, and medication (antidepressants). 9
Post-traumatic stress disorder is not a static condition. Many people leave the armed forces with undiagnosed PTSD, and the condition often manifests after they have left the service. Expert opinion suggests that veterans will commonly (around 50% of the time) suffer from ‘complex PTSD’ (or complex presentations of PTSD). There is currently no agreed diagnostic code for this condition, and ‘complex PTSD’ is not a universally agreed term in the research literature.
‘Complex PTSD’ is described by field experts as PTSD compounded by comorbidities such as substance misuse and depression. It is linked to multiple (as opposed to single) traumatic events, although it does not always arise from active military service; for example, the condition may result from repeated trauma/sexual abuse in childhood. 10,11 ‘Complex PTSD’ is interpreted by some medical professionals as PTSD with additional syndromes, such as pathological disassociation, emotional dysregulation, somatisation and altered core schemes about the self, relationships and sustaining beliefs. 12 The US Department of Veterans Affairs National Center for PTSD describes ‘complex PTSD’ as a condition arising from repeated trauma over a number of months or years, manifesting as a cluster of symptoms that may require special treatment consideration. 13
Despite the absence of a clear definition and a diagnostic mechanism for ‘complex PTSD’, it appears to be distinguished from PTSD by its link with exposure to multiple traumatic events. Therefore, for the purposes of our work we assumed that PTSD in the veteran population was synonymous with ‘complex PTSD’.
It is thought that the context, severity and complexity of PTSD in armed forces veterans may require different approaches13 (i.e. treatments or models of care) from those offered to the general population; these are, as yet, not fully understood. Veterans appear to have higher levels of adverse childhood events before they join, seem to drink more alcohol than the general population and are more likely to have been exposed to multiple traumatic events that may produce different challenges for treatment when compared with treatment for single events or occasions of sexual/domestic abuse and rape. It is also thought that veterans are more willing to admit to combat-related PTSD as a less-stigmatised form of mental illness. 10
Relevant ongoing research
Current National Institute for Health and Care Excellence (NICE) guidance on the management of PTSD (CG26, March 2005) is being updated and is due for completion in August 2018. 14 Early in 2016, the National Institute for Health Research (NIHR) released a Health Technology Assessment programme call: ‘Treating mental health problems with a history of complex traumatic events’. In response to this call, ongoing work now includes: INterventions for Complex Traumatic Events (INCiTE). 15
Brief overview of current policy context and commissioning for veterans’ mental health in the UK
In England, most NHS health-care services (including mental health services) for veterans are currently commissioned locally by CCGs. NHS England has specific duties (and separate funding) to commission a small number of specialised mental health services (such as online and specialised residential services and specific psychological therapies), prosthetic services, assisted conception, online psychological support for veterans and families, and inpatient PTSD services. 16 A number of third-sector organisations collaborate in service provision.
The NHS England strategic review of commissioning intentions for Armed Forces and their families for 2016/17 reports priorities to improve care for veterans with mental health issues, specifically in relation to (1) people with complex PTSD, including comorbidities linked to substance misuse and (2) when stigma is a barrier to accessing care. 16 Alongside the strategic review, NHS England conducted a stakeholder engagement exercise between January and March 2016, focusing on mental health services for veterans currently provided across 12 sites in the UK. 7,17 The findings of this engagement were published in September 2016. 18 In the final report, there is reference to three pilots for enhanced models of care for veterans’ mental health services conducted between November 2015 and March 2016.
In general, mental health services for veterans in England, Scotland, Wales and Northern Ireland are provided by (1) the mainstream NHS services, (2) bespoke NHS-funded specialist clinics (including those for PTSD), (3) the Veterans and Reserves Mental Health Programme (for those who have been deployed since 1982 and are experiencing mental health problems as a result of military service) via the Ministry of Defence and (4) third-sector organisations, for example Combat Stress, Help for Heroes and Walking with the Wounded. 19 In Scotland, veterans are eligible for priority treatment as determined by their general practitioner (GP),20 and a network of specialist help is currently being established to mirror geographic coverage of the regional health boards. In Northern Ireland, medical and other support services for former full-time and part-time Ulster Defence Regiment (UDR) and Royal Irish Regiment (R IRISH) (home service) soldiers and their families are provided by the charity Aftercare. 21 In Wales, each of its seven local health boards appoints a veteran therapist (VT) with an interest in, or experience of, military mental health problems. This is part of a Welsh government-funded service called Veterans NHS Wales. Referrals to the VT come from health-care staff, GPs, veteran charities and self-referral. 22
Commissioning decisions across the UK are supported by detailed mental and related health-needs assessments across each country; these assessments also outline key messages for research and practice. The most recent reports are available for England in 2015,23 Wales in 201624 and Scotland in 2016. 25 The review for Northern Ireland was published in May 2017 and did not form part of our analysis. 26
Objectives
Against this background, our research sought to explore the adequacy and suitability of current and planned mental health services in the UK to treat PTSD in relation to the specific requirements of armed forces veterans. To do this, we reported what is known about current provision of services in the UK and brought this together with a rapid evidence review to indicate which models of care and which treatments may be effective.
The research answered four research questions, as follows:
-
What services are currently provided in the UK for UK armed forces veterans with PTSD (stage 1 of this report)?
-
What is the evidence of effectiveness of models of care* for UK armed forces veterans with PTSD (as described above), including impact on access, retention, clinical outcomes, patient satisfaction and cost-effectiveness (stage 2 of this report)?
-
What treatments show promise for UK armed forces veterans with PTSD? (stage 3 of this report)?
-
What are the high-priority areas for further research?
*We adopted the working definition of a model of care suggested by the Government of Western Australia Department of Health:27 models of care should outline the best-practice care and services for a patient, population or cohort in their progression through the stages of a condition, injury or event and should aim to ensure that people receive appropriate care at the right time and in the right setting by the right team.
The project is a rapid evidence review. There is no universally accepted definition of this term and a number of other terms have been used to describe rapid reviews incorporating systematic review methodology modified to various degrees. Our intention was to carry out a review using systematic and transparent methods to identify and appraise relevant evidence and produce a synthesis that goes beyond identifying the main areas of research and listing their findings. We foresaw that the process would be less exhaustive and the outputs somewhat less detailed than might be expected from a full systematic review.
Chapter 2 Methods
Scope of the review
We had a limited timeframe (3.5 months) so we adopted a pragmatic approach with regular reviews to adjust the scope and content of our work as necessary.
We conducted the rapid evidence review in four stages:
-
Stage 1: a brief overview of current practice in the UK for the treatment of PTSD in armed forces veterans.
-
Stage 2: a rapid evidence review on models of care for armed forces veterans with PTSD.
-
Stage 3: a rapid metareview evaluating the effectiveness of treatments for PTSD in armed forces veterans.
-
Stage 4: a narrative synthesis of the evidence on potentially effective models of care (stage 2) and treatments (stage 3), using the overview of current practice (stage 1) as a guiding framework, highlighting priority areas for further research.
Inclusion criteria
Population
We included armed forces veterans with PTSD after repeated exposure to traumatic events. We did not generalise to PTSD caused by single trauma events.
Intervention
For stage 2 (see Stage 2: a rapid evidence review on models of care) we included models of care for PTSD in armed forces veterans. As part of the brief from our research commissioners, we were asked to pay specific attention to peer support types of interventions. To help explore the elements of care models, we gathered information on current service provision in the UK (see Stage 1: a brief overview of current practice in the UK).
For stage 3 (see Stage 3: a rapid metareview of treatments) we included treatments for PTSD in armed forces veterans.
Setting
We focused on the NHS across the UK. We considered models of care and treatments in the international literature (e.g. US Department of Veterans Affairs) if deemed applicable to the NHS in the UK.
Comparator
Not applicable.
Outcomes
We identified any outcomes reported in the included studies, but focused on those considered relevant and important by stakeholders.
Study design
For stage 2 we did not restrict by study design. For stage 3 we included only systematic reviews. In stages 2 and 3, systematic reviews were included only if they met the minimum quality criteria for entry to the Database of Abstracts of Reviews of Effects (DARE) produced by the Centre for Reviews and Dissemination. 28
Stage 1: a brief overview of current practice in the UK
We provided a brief overview of arrangements currently in place in the UK for the treatment of PTSD in UK armed forces veterans. Particular attention was paid to peer support-type interventions, including those supported by the third sector. Using a pro forma list of questions (see Appendix 1), we carried out the following activities:
-
We contacted the 12 service providers17 referred to in the NHS England stakeholder engagement survey,7 and we also contacted selected service providers in Scotland, Wales and Northern Ireland to find out what is provided specifically for armed forces veterans in relation to PTSD. We contacted (as appropriate) third-sector organisations involved in the provision of services across the UK.
-
We drew on the knowledge of expert contacts to help with information gathering. Individuals and organisations were identified through existing links and contacts.
Stage 2: a rapid evidence review on models of care
We undertook a rapid evidence review of the effectiveness of models of care for armed forces veterans with PTSD. Although we adhered to the principles of robustness and transparency, our approach was less exhaustive and outputs less detailed than would be the case in a full systematic review.
Searching
The aim of the search was to identify relevant systematic reviews, primary research, guidelines or grey literature on models of care for PTSD in veterans. A search strategy was developed in MEDLINE (via Ovid) and included terms for veterans, PTSD and models of care. No geographical, language, date or study design limits were applied. The MEDLINE strategy was adapted for use in the other resources searched.
The searches were carried out in November/December 2016. The following databases were searched: MEDLINE (including: Epub Ahead of Print, In-Process & Other Non-Indexed Citations); PsycINFO; and PILOTS (Published International Literature on Traumatic Stress database).
In addition, a search for relevant guidelines was undertaken via NHS Evidence, the National Guideline Clearinghouse and the US Department of Veterans Affairs. The research report sections of the following websites were searched to identify additional relevant reports or grey literature:
-
US Department of Veterans Affairs – Health Services Research and Development [www.hsrd.research.va.gov/ (accessed 10 November 2016)]
-
Australian Government Department of Veterans Affairs [www.dva.gov.au/about-dva/publications/research-and-studies (accessed 10 November 2016)]
-
Government of Canada Veterans Affairs Canada [www.veterans.gc.ca/eng/about-us/research-directorate/publications/reports (accessed 11 November 2016)]
-
National Academies of Sciences, Engineering and Medicine [www.nationalacademies.org/hmd/Reports.aspx (accessed 11 November 2016)]
-
Forces in Mind Trust [www.fim-trust.org/reports/ (accessed 8 December 2016)]
-
King’s Centre for Military Health Research [www.kcl.ac.uk/kcmhr/publications/Reports/index.aspx (accessed 8 December 2016)].
The results of the searches for stages 2 (review of models of care) and 3 (metareview of treatments) were imported into EndNote X7 [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA], deduplicated and then screened for inclusion in either review. Full search strategies can be found in Appendix 2.
Study selection
We included any study design relevant to models of care for armed forces veterans with PTSD, but only when it was possible to extract findings separately for this population. Particular attention was paid to peer support-type interventions, including those supported by the third sector. We assessed studies from the international literature when this was deemed relevant to UK armed forces veterans. We prioritised evaluations (when available), followed by descriptive/observational research. We anticipated that not all reviews would be systematic reviews (i.e. using objective and transparent methods to identify, evaluate and summarise all relevant research evidence). Therefore, reviews were included only if they met the minimum quality criteria for DARE. It was mandatory that they demonstrated adequate inclusion/exclusion criteria, literature search and synthesis. In addition, formal quality assessment of primary studies and/or sufficient study details must have been reported. Full details of the DARE process are available. 28
As a result of the short time frame to complete this evidence synthesis, studies were excluded if we were unable to locate a full-text copy by 13 January 2017.
We used EPPI-Reviewer (EPPI-Centre, Social Science Research Unit, Institute of Education, University of London, UK) and EndNote X7.4 to screen titles and abstracts. Study selection was carried out by two reviewers independently, with disagreements resolved by consensus or by a third reviewer when necessary.
Data extraction
Data were extracted on participants, models of care, outcomes (when applicable) and any other characteristics we considered helpful to our work.
We created data extraction tables in Microsoft Word (Microsoft Corporation, Redmond, WA, USA). Data extraction was carried out by one reviewer and checked by a second reviewer, with disagreements resolved by consensus or by a third reviewer when necessary.
Quality assessment
We assessed systematic reviews using the DARE critical appraisal process. Based on the quality criteria used to select studies (see Study selection), a judgement was made on the overall reliability of the review and its findings. For evaluative primary research, we used the EPOC (Effective Practice and Organisation of Care) risk-of-bias tool for controlled studies29 and the CASP (Critical Appraisal Skills Programme) critical appraisal tool for qualitative research. 30 See Post-protocol decisions relating to stage 2 for further details of quality assessment.
Quality assessment was carried out by two reviewers independently, with disagreements resolved by consensus or by a third reviewer when necessary.
Synthesis
We synthesised the evidence narratively and highlighted potentially effective models of care. During the regular reviews, as the project progressed, we made adjustments to the scope and content of the work.
Post-protocol decisions relating to stage 2
Our working definition of ‘models of care’ (see Chapter 1, Objectives) was helpful in shaping initial parameters for stage 2. However, during screening and selection of studies it became clear that the term ‘model of care’ could be interpreted in more than one way. For example, we found studies that described a specific method or mechanism by which an intervention was delivered (e.g. telehealth, smartphone applications, group support) and others that adopted a broader organisational or systems perspective (e.g. integrated care, community outreach). This important distinction turned our thoughts to what might be the most helpful perspective for readers of our rapid evidence synthesis. Given the ongoing UK policy focus to achieve sustainable new models of care (i.e. how services can be optimally organised and structured), we decided to focus on the broader ‘systems’ interpretation. Based on this interpretation, we developed a coding list (see Appendix 3) to help organise the evidence and to shape the data extraction and synthesis going forward. Two reviewers independently assigned codes to individual studies. Disagreements were resolved by consensus or through discussion with a third reviewer.
The number of included studies was much larger than expected. Given the short time frame and resources, we had to make pragmatic decisions at the data extraction stage to ensure that there was sufficient time to adequately synthesise the studies. We therefore chose to data extract in full and critically appraise more robust study designs, conventionally considered to be systematic reviews, randomised controlled trials (RCTs) and controlled trials. We also chose to extract data in full qualitative studies that provide insight from a service user perspective. The remaining studies were predominantly single-group designs, which are typically considered less methodologically robust. These studies had more limited data extraction (e.g. study design, sample size, code and description of model of care, list of outcomes and a summary of authors’ conclusions and recommendations). Although these single-group studies were not formally assessed for methodological quality, we considered the adequacy and clarity of reporting on context, methods and impact.
Stage 3: a rapid metareview of treatments
We undertook a rapid metareview of systematic reviews evaluating the effectiveness of treatments for PTSD in armed forces veterans.
Searching
The aim of the search was to identify relevant systematic reviews of treatments for PTSD in veterans. A search strategy was developed in MEDLINE (via Ovid) and included terms for veterans and PTSD. No geographical, language or date limits were applied. Study design search filters were used in the strategy (when appropriate) to limit retrieval to systematic reviews.
The searches were carried out in November 2016. The following resources were searched: Cochrane Database of Systematic Reviews, DARE and the Health Technology Assessment database. PROSPERO was also searched to identify any ongoing reviews. In addition, searches of MEDLINE, EMBASE, PsycINFO and CINAHL (Cumulative Index to Nursing and Allied Health Literature) were carried out to identify any relevant systematic reviews published since the closure of DARE in 2015.
The results of the searches for stages 2 (review of models of care) and 3 (review of treatments) were imported into Endnote X7, deduplicated and then screened for inclusion in either review. Full search strategies can be found in Appendix 2.
Study selection
We included systematic reviews on treatments for armed forces veterans with PTSD. We assessed reviews from the international literature when this appeared to be relevant to UK armed forces veterans. Systematic reviews were included only if they met the minimum quality criteria for DARE (see stage 2). If, in the course of searching for treatments, we found additional systematic reviews on models of care, we assessed them for inclusion in stage 2 (see Stage 2: a rapid evidence review on models of care).
We used EPPI-Reviewer and Endnote X7.4 to screen titles and abstracts. Study selection was carried out by two reviewers independently, with disagreements resolved by consensus or by a third reviewer when necessary.
Data extraction
Data were extracted on participants, treatments, comparators, outcomes (when applicable) and any other characteristics we considered helpful to our work. Data extraction was carried out by one reviewer and checked by a second reviewer; disagreements were resolved by consensus or by a third reviewer when necessary. We created data extraction tables in Microsoft Word.
Quality assessment
We assessed systematic reviews using the DARE critical appraisal process (see Stage 2: a rapid evidence review on models of care). Quality assessment was carried out by two reviewers independently and disagreements were resolved by consensus or by a third reviewer, when necessary.
Synthesis
We presented a brief narrative overview to highlight potentially effective treatments.
Stage 4: narrative synthesis of all stages
We synthesised the evidence narratively on potentially effective models of care (stage 2) and treatments (stage 3), using the overview of current practice (stage 1) and the models of care coding list (see Appendix 3) as a guiding framework. We adopted a ‘best evidence approach’ (i.e. highlighting the best-quality and most-promising evidence) to inform future research and practice.
Public and patient involvement
As a result of the short timescale for this project, we used findings from the NHS England stakeholder engagement survey as a starting point to represent service user input. 18 We also contacted a veteran (who was also a service user) to provide additional input. We aimed to use this input to help explore patterns in the NHS England public and patient engagement data and to provide supplementary insights, as appropriate.
Advisory group
We called on existing links and contacts to establish an advisory group of people who have a specific interest in this topic area. The advisory group comprised representatives with academic, military and service commissioning experience who we anticipated would be able to help (1) strengthen our background knowledge on policy context and current research and practice, and (2) develop further contacts. Further detail is provided in Acknowledgements, External advice, at the end of this report.
Chapter 3 Results
Stage 1: what services are currently provided in the UK for UK armed forces veterans with post-traumatic stress disorder?
We provide a brief overview of arrangements currently in place in the UK for the treatment of PTSD in armed forces veterans. Information was gathered from the following sources: we sent (by e-mail) a pro forma list of questions (see Appendix 1) to the 12 service providers in England referred to in the NHS England stakeholder engagement survey;17 and we also approached the main contacts for service provision in Scotland, Wales and Northern Ireland. In addition, we contacted selected third-sector organisations known to offer UK-wide coverage. Prior to sending out the questions, we identified a named contact at each organisation who was willing to assist with the information gathering. A number of experts helped us to identify contacts, particularly in the third sector.
We received 17 responses out of 21 service provider contacts (81% response rate) and details are presented in Appendix 4. We spoke with five experts selected to provide key perspectives of importance to our work. These included representation from NHS England (one person), public health/local authority (two people), and academia/clinical practice (two leading academics with experience in military operations and/or clinical practice).
Development of a coding framework on models of care
Using the information gathered from the service providers, we developed a set of codes to represent descriptions of how services were organised and delivered (models of care). The list was expanded and codes were clarified using information from the literature in stage 2. Given our decision to distinguish care delivery mechanisms (models with a narrower focus) from systems-based models, we divided the list into two sections. The list of codes is presented in Appendix 3.
Overview of current service arrangements in the UK for veterans with post-traumatic stress disorder
Most providers report a range of mental health services for veterans, and many are delivered as part of a wider package of interventions across the NHS and third sector. Various models of care are employed to deliver services for veterans. Collaborative working across sectors is commonplace. Peer support and ‘Veterans Champions’ are also in place. Referrals to services occur via many different routes and access via self-referral is available as an option in most cases. Multiple (clinical and non-clinical) professions are involved in the delivery of services and these services are available to veterans beyond the clinical setting. Several organisations mention specific support for veterans with PTSD. This does not necessarily mean that other providers do not provide targeted services for PTSD; rather, it appears that specialist treatment for this condition can be embedded in wider mental health services and assistance for comorbid conditions. Factors affecting the successful implementation of services and treatments for veterans with PTSD appear to be (1) inadequate funding and resources, (2) wider system challenges, (3) lack of research and development and (4) the inherent complexities of the target population. Evaluation of services and treatments appears to be taking place, but sporadically and to varying degrees. Responses were not received on all questions from every provider; therefore, the information set out below reflects where detail was offered to us. The findings are presented grouped by geographical area, reflecting the NHS England document. 17
North of England (four service providers)
What services and treatments are provided/how are clients referred?
Veterans’ mental health services in the north of England are currently provided by NHS foundation trusts (or partnership trusts) in Greater Manchester West; Greater Manchester and Lancashire; Yorkshire and Humberside; and Northumberland, Tyne Wear and Esk Valleys. All except Yorkshire and Humberside report that they have collaborative working arrangements with third-sector organisations, namely Combat Stress, Walking with the Wounded and Royal British Legion. A variety of services and treatments are offered across the area, including specific trauma-focused activity [e.g. TFCBT; prolonged exposure (PE); cognitive restructuring; EMDR] and Improving Access to Psychological Therapies (IAPT) services for those with less complex trauma. Other (more generic) services include case management across health and social care pathways; signposting to other psychological-related problems such as substance misuse; and linkages with services tackling wider determinants of well-being such as housing and financial and social needs. Yorkshire and Humberside offers an outreach service delivered by four specialist therapists trained in mental health and with experience of working with ex-military personnel. Referrals to services occur through many routes, including referral from health-care professionals (GP and other), self-referral, family members and carers, third-sector organisations and prisons. In Greater Manchester and Lancashire, 74% of referrals arrive via non-NHS routes; this site provides specific support for veterans with PTSD and was the location for one of three 6-month NHS England pilots for enhanced models of care in 2015/16 (‘Overcoming the barriers’, a model to address some of the issues that veterans experience when accessing mental health services). 18
Where and how services and treatments are provided/who provides them?
Access to services in the north of England appears to be largely in the community setting. For example, in Greater Manchester and Lancashire, access routes involve a number of community venues as close to home as possible, from football grounds to libraries, but also in the client’s own home where this is more appropriate. Individuals involved in the delivery of services in this part of England include various types of specialist psychological therapist (some with military experience), mental health nurses and counselling staff; others are peer support workers, case managers and those from non-psychological specialisms such as art therapy and employment mentoring.
Midlands (three service providers)
What services and treatments are provided/how are clients referred?
All services are provided by NHS foundation trusts and all have some level of working arrangement with Combat Stress. Geographical coverage is North Essex, East Midlands and West Midlands.
Services and treatments include packages of care reflecting a holistic approach to mental health needs including assistance with housing, employment and social integration, in addition to specialist mental health support. Veteran support groups with input from third-sector organisations are also offered. Other providers report on broader models of care, such as integrated community mental health, early intervention and veterans’ liaison services. Specific psychological therapies are available [including those recommended by NICE such as cognitive–behavioural therapy (CBT) and EMDR]. Referral routes to services include GPs, local authorities and third-sector organisations; referrals to specialist services are through the NHS or criminal justice system. The West Midlands Military Veterans’ Hub (part of South Staffordshire and Shropshire NHS Foundation Trust) takes a proactive approach to recruitment. It asks service users if they wish to be seen by the Veterans Service and automatically notifies the service regarding those who are interested. This service is a collaboration of eight NHS mental health service providers, each with its own ‘Veterans Champion’ to link with existing teams and providers. Veterans First (Essex), which is part of the North Essex Partnership University NHS Foundation Trust, provided two of the three 6-month NHS England pilots for enhanced models of care in 2015/16. 18 One pilot programme was a joint substance misuse and mental health service model; the second was an outpatient service for veterans with moderate to severe PTSD.
Where and how services and treatments are provided/who provides them?
Treatments and services can be accessed at the NHS trusts, in the veteran’s own home or at a location agreed (as appropriate) with the service user.
Delivery of services in this area of England calls on the skills of clinical nurses and psychologists with specialist training in trauma-focused interventions and therapists conversant with CBT and EMDR. Other staff also attend Veterans Awareness training and have access to specialist lead clinicians.
South of England (five service providers)
What services and treatments are provided/how are clients referred?
Services for veterans in the south of England are provided by NHS foundation trusts (or partnership trusts) in all cases except for Surrey. Here, arrangements for veterans are provided by Virgin Care on behalf of Surrey County Council. Some providers report close working arrangements with third-sector organisations. Geographical coverage is London, Berkshire, Avon and Wilshire (South West), Surrey and Sussex. Interventions range from signposting services to comprehensive multidisciplinary assessment, case management and specific trauma-focused services (including NICE-approved CBT and EMDR). Specialist PTSD services are offered at two locations (London Veterans Service and South Central Veterans Mental Health Service delivered by the Berkshire Healthcare NHS Foundation Trust). Surrey Engagement and Veterans Emotional Support (SERVES) offers a range of services including advice and information (signposting to third-sector organisations), drop-in centres, crisis helplines and ‘emotional gyms’. In Sussex, the Sussex Armed Forces Network is led by CCGs in partnership with the NHS Foundation Trust. Partnership working with a range of organisations (including local authorities) facilitates a pathway for veterans covering various sources of help on wider determinants of health (including mental health) and Veterans Champions are trained to work in secondary care. The main sources of referral are self-referral, GPs and other health professionals, IAPT services, third-sector organisations and family members.
Where and how services and treatments are provided/who provides them?
The delivery of services and treatments across the south of England takes place in various settings, including NHS clinics, community outreach, prison inreach, third-sector-run facilities and GP surgeries. People involved in providing services include specialist health professionals (clinical psychologists, clinical nurse specialist, psychiatrists and VTs) and non-clinical staff such as art therapists and social workers.
Scotland
What services and treatments are provided/how are clients referred?
Veterans First Point (V1P) Scotland is the government-funded NHS provider that facilitates a network of NHS–third-sector partnerships to support veterans across Scotland. This service is supported specifically with the help of libor-funding (a commitment by the government to use banking fines to fund services). At present, services include drop-in centres, peer support, psychological therapy, community outreach, prison inreach, occupational therapy, brokerage and identification of individuals with complex needs. An Individual Placement Model is also offered to help promote mental health recovery through work. Self-referral appears to be popular; other referrals occur via existing psychology services.
Where and how services and treatments are provided/who provides them?
In 2016, eight newly funded V1P centres were established and services for veterans continue to develop within each of the following locations, reflecting the Scottish health boards: Ayrshire and Arran, Borders, Fife, Grampian, Highland, Lanarkshire, Lothian (the largest) and Tayside. Services and treatments are provided by peer support workers, occupational therapists, psychological therapists and other clinicians.
Wales
What services and treatments are provided/how are clients referred?
Services and treatments for veterans in Wales are facilitated by Veterans NHS Wales, which is funded by the Welsh Government. Each of the seven local health boards in Wales has an appointed VT. The organisation offers multiple options for treating individuals with PTSD [including TFCBT, EMDR, cognitive processing therapy (CPT) for couples and cognitive and behavioural conjoint therapy]. One-to-one peer mentoring is offered through the service charity ‘Change Step’, while peer mentoring through ‘Care After Combat’ is specifically for veterans released from prison. The organisation also signposts people to various third-sector organisations. Self-referrals are accepted and others arrive from primary and secondary care and third-sector organisations.
Where and how services and treatments are provided/who provides them?
Veterans NHS Wales has 14 mental health professionals with wide-ranging backgrounds, from occupational psychology to social work. All have been trained to deliver EMDR.
There are seven local health boards, each employing between one and four VTs. Services are provided via a ‘hub and spoke’ model (the hub being the University Hospital of Wales in Cardiff).
Northern Ireland
What services and treatments are provided/how are clients referred?
From the information we received, veterans in Northern Ireland are looked after by the UDR and R IRISH (home service) Aftercare Service, funded by the Ministry of Defence. Services are limited to veterans who have served in either the UDR or R IRISH. This organisation offers access to a specific trauma-focused psychological therapy intervention comprising an initial assessment followed by 10 sessions of one-to-one counselling. The main source of referral is via case workers who have responded to requests for home visits by veterans; other referrals come from GPs, health trusts and third-sector organisations.
Where and how services and treatments are provided/who provides them?
Case workers offer a holistic approach to medical, welfare and benevolence. They also help with completion of referral forms. The specific intervention (above) offered by this organisation is initiated in Belfast, followed by sessions delivered locally to the individual by a network of contract counsellors.
UK-wide third-sector organisations
What services and treatments are provided/how are clients referred?
We contacted four UK third-sector organisations, three of which reported that they deal specifically with mental health/PTSD in armed forces veterans.
The first of these, Combat Stress, claims to be the leading mental health charity for veterans in the UK. The influence of this organisation is reflected in our summary of service provision so far, Combat Stress being the most frequently mentioned collaborator with the NHS. Combat Stress is best known for its stepped-care intervention dealing with three stages of recovery: (1) stabilisation, (2) trauma therapy and (3) reconnecting veterans with their lives. PTSD treatment is the focus of trauma therapy in the second stage. This stage is characterised as the intensive treatment programme (ITP), based on work from the Australian Department of Veterans Affairs. The programme was commissioned by the NHS in 2011 and is free for veterans with severe PTSD. Activity within the ITP is based on TFCBT, psychoeducation and well-being, using group and individual delivery formats, and art therapy is offered throughout. In the third stage, part of reconnecting veterans with their lives involves family member involvement in psychoeducation about PTSD and reducing stigma. The organisation also offers a crisis helpline, community clinics, residential treatment centres and case management for substance misuse.
The organisation PTSD Resolution Ltd offers a model of care incorporating counselling and psychotherapy for veterans with PTSD based on Human Givens therapy. 31
Walking with the Wounded operates the ‘Head Start’ Programme, which is offered to people with mild to moderate common mental health disorders, including PTSD. Specifically for PTSD, the organisation offers access to NICE-recommended approaches such as TFCBT and EMDR.
Help for Heroes does not offer direct clinical interventions, but instead provides a variety of other services to help with recovery and welfare. Part of the organisation ‘Hidden Wounds’ offers free individual support for mental health and associated comorbidities such as adverse drinking habits. Help for Heroes also directly commissions services from the NHS, Walking with the Wounded and Combat Stress.
Referral routes to third-sector organisations appear to be similar to those found among the NHS service providers we contacted. Walking with the Wounded appears to connect with multiple agencies, but most referrals are received via GPs. This organisation has also assisted Public Health England in a national programme of GP training for veteran mental health matters.
Where and how services and treatments are provided/who provides them?
Multidisciplinary teams with wide-ranging clinical, non-clinical and military backgrounds make up the general profile of those who provide third-sector services for veterans. PTSD Resolution has a network of 200 therapists all trained in Human Givens therapy; these therapists are registered and the list is accredited in the UK by the Professional Standards Authority for Health and Social Care. Services and treatments from third-sector organisations are generally delivered in various locations, including an inpatient setting, a community setting and in the person’s own home. Walking with the Wounded has a national network of accredited therapists and guarantees that clients receive support within 10 days of returning consent forms and within 10 miles of their home.
Other service providers
Two other organisations in the north of England were contacted on the basis that they did not appear to fit with either the NHS or third-sector delivery models. The St Johns and Red Cross Defence Medical Welfare Service is available across Greater Manchester hospitals. It does not provide treatment but instead provides support and signposting for veterans across the referral pathway. The service is specifically for veterans aged ≥ 65 years.
Liverpool Veterans appears to be an independent organisation developed by Breckfield and North Everton Neighbourhood Council in conjunction with the Foundation for Art and Creative Technology (FACT). It provides links to services, research and fundraising events for veterans and their families in the Liverpool area. Of particular note is that the organisation signposts individuals with PTSD to Tom Harrison House (a specialist facility for addiction recovery). 32
Factors affecting implementation
Several challenges to the implementation of services and treatments for veterans with PTSD were reported by the service providers we contacted. These are summarised in the following sections.
Funding and resources
Inadequate funding to meet current demand was frequently cited, particularly for trauma services. Availability of appropriate clinicians and venues was also seen to be problematic. Lack of resources was reported to result in lengthy waiting lists for services and treatment in some areas. In Northern Ireland, restriction of eligibility to those only with previous service in the UDR or R IRISH (home service) or a veteran discharged via the Personnel Recovery Unit was seen as a limitation.
Wider system challenges
Perhaps as a consequence of inadequate funding and resources, further challenges to implementation were difficulties in negotiating appropriate longer-term treatments (such as psychotherapy) within the NHS. Service providers also mentioned that NHS IAPT can be slow to provide definitive treatment. As veterans often present in crisis because of pressure from partners, employers or the criminal justice system, such delay is at odds with the pressing needs and expectations that require prompt attention in this population group.
Poor co-ordination of care between agencies was also cited as a hindrance to successful implementation of services and treatments. For example, veterans with comorbid substance misuse were described by one service provider as ‘. . . a football between services’. The difficulty, in their view, appears to be about where to place the veterans’ needs on the continuum of care. Indeed, veterans are often viewed as too risky for well-being services but not unwell enough for secondary psychological services.
Research and development: knowledge base
Inadequate research and treatment development was cited by one service provider as being at odds with the increased drive to deliver evidence-based interventions with appropriate assurances in place. A concern expressed by another service provider was that a particular delivery model delivered by them was not understood sufficiently by commissioners, resulting in the inability to achieve full implementation of the intervention.
Complexities of the client group
Successful implementation of services and treatments for veterans with PTSD is affected, generally, by the fact that this is a highly challenging client group. They are described by service providers as unstable, unreliable and generally hard to engage because of inherent difficulties they tend to experience with help seeking. On referral, clients often arrive with testing social, financial and premorbid disposition. They can also feel let down because of problems already mentioned in relation to long waiting lists, unsatisfactory previous treatment and wider system challenges.
Evaluation of services and treatments
Evaluation of current service provision for veterans is clearly taking place across the UK. However, activity appears to be sporadic and is discharged to varying degrees. NICE evidence-based therapies are being implemented, and several service providers referred to various types of evaluation (past or present).
Ongoing activity includes unspecified projects and research relevant to particular organisations; standard assurance processes such as inspections by the Care Quality Commission and the Friends and Family Test; and general audits of medical services covering clinical governance and client satisfaction. Other providers refer to regular reporting mechanisms providing feedback to NHS England on key performance indicators.
More specific and detailed evaluations were reported by other organisations, such as the 1-year evaluation of the Veterans Wellbeing Assessment and Liaison Service (North East). In Wales, an annual report is published reflecting on services provided by Veterans NHS Wales; a specific evaluation was carried out in 2014 by Public Health Wales on behalf of the Welsh Government. 33 This evaluation contained pre–post intervention clinical measures and patient satisfaction (measured by questionnaires and focus groups with veterans and their partners). In its March 2016 newsletter,34 V1P Scotland reports on the evaluation of its services (‘The Transformation Station’), which is a collaboration between NHS Lothian and Queen Margaret University working with V1P Scotland.
Publications relating to specific programme evaluation using observational study designs were cited by two service providers: PTSD Resolution Ltd and Combat Stress. 35,36 The latter organisation has a large repository of research available on its website.
Collaboration with academic institutions was reported. King’s College London (King’s College Mental Health Research) is currently evaluating the Head Start programme at Walking with the Wounded. Standardised and reliable measures are being used {Patient Health Questionnaire – 9 items (PHQ-9), Generalised Anxiety Disorder-7-item scale (GAD-7), Alcohol Use Disorders Identification Test (AUDIT), PTSD Checklist – Civilian Version (PCL-C), and Work and Social Adjustment Scale (patient-reported outcome measure) [WSAS (PROMS)]} at the start, middle and end of therapy. Client evaluation for West Midlands Veterans Hub takes place through the University of Worcester, with IAPT measures taken to measure client progress.
Stage 2: what is the evidence of effectiveness of models of care for UK armed forces veterans with post-traumatic stress disorder?
We included 61 articles (56 studies) (Figure 1).
FIGURE 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart.
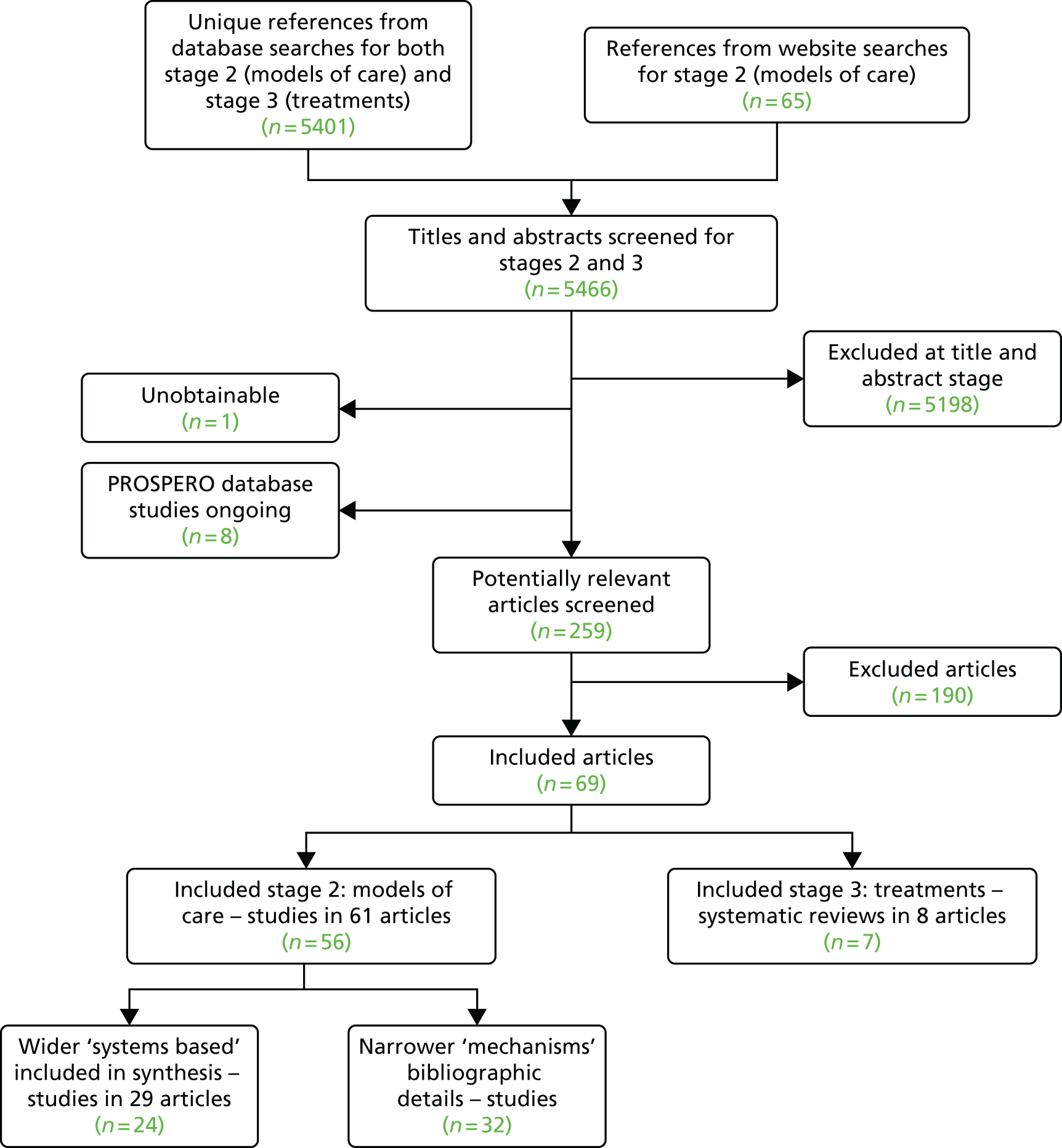
Thirty-two studies reported on types of care delivery with a narrower focus (e.g. delivery mechanisms such as telehealth and triage assessment). We identified these studies using the coding framework developed from stage 1 (see Appendix 3). No further analysis was carried out on these studies as they were not the main focus of our rapid evidence review (see Chapter 2). For completeness, the 32 studies are listed bibliographically in Appendix 5.
We focused on models of care adopting a wider or ‘system-based’ perspective (e.g. integrated care, settings-based delivery, etc.). Twenty-four studies (29 articles) were selected (using the stage 1 coding framework in Appendix 3) (Table 1). Within these studies, three RCTS (four papers) were prioritised to represent evidence from a conventionally more robust study design. 37–40 In addition, a qualitative study41 was identified as potentially important to provide insight from a service user perspective. The four studies underwent full quality assessment. All were connected to the Veterans Health Administration, US Department of Veterans Affairs.
| First author, year, reference | Study design | Partnership, cross-sector, liaison work, co-location | Co-ordinated, integrated, collaborative, networks, multidisciplinary care | Inpatient | Outpatient | Day care | Residential | Primary care | Peer support | Multicomponent treatment programmes | Family systems model | Community outreach | Use of IAPT | Prison inreach | Case management | Stepped-care model | Early intervention | Crisis management |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RCTs (USA) | ||||||||||||||||||
| Schnurr, 2013;37 VA | RCT | ✓ | ✓ | |||||||||||||||
| McFall, 2010;38 and McFall, 2007;39 VA | RCT | ✓ | ||||||||||||||||
| McFall, 2000;40 VA | RCT | ✓ | ||||||||||||||||
| Qualitative study (USA) | ||||||||||||||||||
| Hundt, 2015;41 VA | Qualitative | ✓ | ||||||||||||||||
| Other study designs | ||||||||||||||||||
| Australia | ||||||||||||||||||
| Pietrzak, 2011;42 McGuire, 2011;43 Bredhauer, 201144 | Critical review and analysis (guideline) | ✓ | ✓ | |||||||||||||||
| Forbes, 200845 | Survey | ✓ | ✓ | ✓ | ✓ | |||||||||||||
| Creamer, 200246 | Quasi-experimental observational study | ✓ | ✓ | ✓ | ||||||||||||||
| UK | ||||||||||||||||||
| Burdett, 2016;35 PTSD Resolution charity | Service evaluation | ✓ | ||||||||||||||||
| Murphy, 2015;36 and Murphy, 2016;47 Combat Stress – NHS funded third sector | Observational | ✓ | ✓ | |||||||||||||||
| USA | ||||||||||||||||||
| Ohye, 201548 | Descriptive article | ✓ | ||||||||||||||||
| Sniezek, 201249 | Descriptive article (guest editorial) | ✓ | ✓ | |||||||||||||||
| USA, conducted or funded via VA | ||||||||||||||||||
| Baringer, 1990;50 VA | Before-and-after intervention pilot study | ✓ | ✓ | ✓ | ||||||||||||||
| Brawer, 2011;51 VA | Observational | ✓ | ✓ | |||||||||||||||
| Bohnert, 2016;52 VA | Observational system evaluation | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||||
| Chan, 2007;53 VA | Descriptive article (thesis) | ✓ | ||||||||||||||||
| Donovan, 2001;54 and Donovan, 1999;55 VA | Before-and-after treatment study | ✓ | ||||||||||||||||
| Fontana, 1997;56 VA | Quasi-experimental observational | ✓ | ||||||||||||||||
| Forman, 1990;57 Department of Public Health and Massachusetts Department of Veterans Services | Descriptive article | ✓ | ||||||||||||||||
| Jain, 2014;58 Jain, 2016;59 and Jain, 2015;60 VA | Observational study | ✓ | ✓ | |||||||||||||||
| Joseph, 2015;61 VA | Letter describing programme | ✓ | ||||||||||||||||
| Otis, 2009;62 VA | Before-and-after study (pilot) | ✓ | ||||||||||||||||
| Plagge, 2013;63 VA | Before-and-after | ✓ | ✓ | ✓ | ||||||||||||||
| Randall, 201564 | Observational | ✓ | ||||||||||||||||
| Walter, 2014;65 VA | Non-randomised comparison | ✓ | ✓ | |||||||||||||||
| Total number of studies | 2 | 11 | 5 | 4 | 2 | 5 | 7 | 3 | 4 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | |
The 20 remaining studies (24 articles) used designs typically regarded as less methodologically sound. These were primarily single-group designs, comprising the following: five observational studies (eight articles),36,47,51,52,58–60,64 five descriptive pieces,48,49,53,57,61 four before-and-after studies (five articles),50,54,55,62,63 two quasi-experimental studies,46,56 a critical review/guideline,44 a survey,45 a service evaluation35 and a non-randomised comparison. 65 Although these studies were not formally assessed for methodological quality, they were carefully considered and retained as important contributors to the evidence picture on models of care.
Across the total number of included studies (24 studies, 29 articles) in our review, publication years ranged from 1990 to 2016. Eighteen studies (23 articles) were conducted in the USA37–41,48–65 (17 of these were connected to the Veterans Health Administration, US Department of Veterans Affairs), three studies were conducted in Australia44–46 and two studies (three articles) were carried out in the UK. 35,36,47
Models of care
The majority of studies focused on integrated/collaborative care, or primary care models, to deliver services for veterans with PTSD. Other popular models were settings based, such as residential, inpatient, outpatient or day-care delivery. Multicomponent programmes, partnership working, peer mentoring, family systems models and community outreach were also described. Some studies reported more than one model of care (see Table 1).
Outcomes
Clinical measures related to PTSD were the most frequently reported. Others included intervention access and uptake, service use, and perspectives or satisfaction related to the intervention. Various measurement tools were used.
The next section of this chapter begins with an examination of studies that were subject to full quality assessment. We then provide an overview of the remaining studies. For all studies, we review the setting, the model of care (guided by the stage 1 framework, see Appendix 3) and the outcomes as reported in the studies. When possible, we identify the authors’ conclusions and, for the more robust study designs, we provide our assessment of reliability. We signpost any material differences in coverage between the more robust and less methodologically sound study designs. We conclude with a summary of the evidence, identifying where this best demonstrates effectiveness of models of care for UK armed forces veterans with PTSD.
Evidence from the randomised controlled trials
Three RCTs (four papers)37–40 were included. One RCT was well conducted and was rated as being at a minimal risk of bias; the other two trials had risks of bias which may affect the reliability of their findings. 37 Full details of the RCTs and their quality are presented in Tables 2 and 3.
| Study details (first author) | Stage 1 category and characteristics of models of care as described by authors | Outcomes, measures and summariesa | Commentaryb |
|---|---|---|---|
| Collaborative care | |||
|
Schnurr, 201337 Country: USA Setting: primary care/VA clinic/multiple sites Evaluative/descriptive: evaluation Type of publication: RCT Participants: n = 195 |
Stage 1: co-ordinated, integrated, collaborative, networks, multidisciplinary care; primary care Comparisons: 3CM (collaborative care) including telephone care management vs. usual care 3CM: education and tools for primary care clinicians and staff; telephone care management for patients by a centrally located care manager to answer questions and promote treatment adherence; support from a psychiatrist who supervises care managers by telephone, provides consultation to primary care clinicians and facilitates mental health care referral; content specific to PTSD (not specified) Programme adapted from RESPECT-D for treatment of depression Usual care: not defined All primary care providers received 1-hour training on PTSD (diagnostic criteria, assessment, treatment) |
Outcomes and measures (at baseline, 3 and 6 months): primary outcome – PTSD symptom severity (measured by PDS). Secondary outcomes – depression (Hopkins Symptom Checklist-20), functioning [SF-12 or SF-36 (text and table 2 differ in the paper)], perceived quality of care (5-point scale), utilisation (electronic patient records, clinician consultation, technology codes, VA Decision Support System) and costs (VA Decision Support System, Fee Basis programme) Summary of results as reported by the author: veterans in the 3CM group were more likely to have mental health visits (p = 0.04), antidepressant prescriptions (p = 0.05) and refills (p = 0.03), and higher outpatient pharmacy costs (p < 0.001). Over a 6-month period, no differences were found between 3CM and usual care for PTSD symptoms, depression or functioning. 3CM was associated with a lower perceived quality of PTSD care Treatments within each intervention package were delivered at the provider’s discretion. Summary of authors’ conclusions: careful examination of the way in which collaborative care models to treat PTSD are implemented is needed. Primary care providers need additional support to encourage them to manage PTSD Authors’ research recommendations: not reported |
|
|
McFall, 2010;38 and McFall 200739 Country: USA; multisite VA clinics Single/multiple provider: single provider Evaluative/descriptive: evaluation Type of publication: RCT Participants: n = 943 |
Stage 1: co-ordinated, integrated, collaborative, networks, multidisciplinary care Comparison: IC vs. SCCs IC: individual smoking cessation treatment integrated within mental care for PTSD. Delivered by mental health clinicians (largely psychologists and social workers). Training was provided to those delivering the intervention SCC (usual care): VA smoking cessation clinics Full details of the interventions are provided in the paper |
Outcomes and measures: primary outcomes – 12-month prolonged abstinence from tobacco between 6 and 18 months post randomisation (self-report with bioverification when possible). Secondary outcomes – 7- and 30-day point prevalence abstinence (self-report with bioverification when possible), severity of PTSD (CAPS and PCL), depression (PHQ-9), number of treatment sessions (VA electronic records), use of cessation medications (self-report) Summary of results as reported by the author: IC was more effective than SCC for prolonged abstinence (adjusted OR 2.26, 95% CI 1.30 to 3.91; p = 0.004). Differences in 7-day and 30-day point prevalence abstinence (favouring IC) were largest at 6 months (16.5% vs. 7.2%, p < 0.001; 13.8% vs. 5.9%, p = 0.001, respectively) and remained statistically significant at 18 months. The number of counselling sessions and days of cessation medication explained 39.1% of the treatment effect. Psychiatric status (including improvements in PTSD symptoms in both groups) did not differ between the groups at 18 months’ follow-up The authors reported that a small minority of IC clinicians did not deliver the treatment as designed, which may have led to less favourable IC outcomes. There were no significant differences in adverse events between IC and SCC groups Summary of authors’ conclusions: among smokers with military-related PTSD, integrated care involving smoking cessation treatment and mental health care resulted in greater prolonged abstinence than specialised cessation treatment alone Authors’ research recommendations: not reported |
|
| Community outreach | |||
|
McFall, 200040 Country: USA Single/multiple provider: single provider – large urban VA medical centre Evaluative/descriptive: evaluative Type of publication: RCT Participants: n = 594 |
Stage 1: community outreach Intervention group: mailing followed by direct telephone contact. The mailing included information about locally available PTSD treatment services, an invitation to seek care and details of how participants could respond. Direct telephone contact (by the study co-ordinator 1 month after the mailing) included a 15-minute survey covering treatment history, awareness of mental health resources, barriers to access and willingness to receive further information about specialised services Control group received the telephone survey 6 months after the intervention group received the mailing |
Outcomes and measures: participant enquiries (return of postcards, telephone calls), arrangement of an intake appointment with a mental health provider (verbal agreement with the study co-ordinator), attendance at intake assessment session at the VA centre and attendance at one or more VA treatment follow-up sessions (medical centre electronic records). Outcomes were measured within 6 months of mailing to the intervention group Summary of results as reported by the author: compared with the control group, veterans in the intervention group were significantly more likely to arrange an intake appointment (28% vs. 7%; p < 0.001), attend the appointment (23% vs. 7%; p < 0.001) and to attend at least one follow-up treatment session (19% vs. 6%; p < 0.001). Barriers to accessing treatment were identified as personal obligations, inconvenient clinic hours and receipt of treatment from a non-VA provider Summary of authors’ conclusions: an inexpensive outreach intervention can increase use of mental health services by underserved veterans with PTSD. This model may be useful for other populations with chronic mental illness Authors’ research recommendations: not reported |
|
| First author, year | (1) Was the allocation sequence adequately generated? | (2) Was the allocation adequately concealed? | (3) Were baseline outcome measurements similar? | (4) Were baseline characteristics similar? | (5) Were incomplete outcome data adequately addressed? | (6) Was knowledge of the allocated interventions adequately prevented during the study? | (7) Was the study adequately protected against contamination? | (8) Was the study free from selective outcome reporting? | (9) Was the study free from other risks of bias? |
|---|---|---|---|---|---|---|---|---|---|
| Collaborative care | |||||||||
| Schnurr, 201337 | Low | Low | Low | Low | Low | Low | Unclear | Low | Low |
| McFall, 2010;38 and McFall, 200739 | Low | High | Low | Low | High | High | High | Low | Unclear |
| Community outreach | |||||||||
| McFall, 200040 | Low | Unclear | Unclear | Low | Low | Unclear | High | Low | Unclear |
Models of care covered collaborative primary care-based delivery, integrated mental health care and lifestyle behaviour treatment and community outreach. Outcomes comprised clinical outcomes (including PTSD-related outcomes and smoking abstinence), intervention access and service uptake. All studies were conducted in the USA in the context of the Veterans Health Administration (US Department of Veterans Affairs).
Collaborative/integrated types of care were the focus in two RCTs (three articles). 37–39 The first RCT by Schnurr et al. 37 (195 participants) focused on a three-component model (3CM) (a programme of education and support for primary care clinicians and staff across multiple sites) with additional telephone care management for patients and staff. 3CM included PTSD-specific content, but this aspect was not described in detail. The combined intervention was compared with usual care (not defined), and all interventions were delivered at the provider’s discretion. Results for health care use showed that veterans in the 3CM group had higher numbers of mental health visits, higher numbers of antidepressant prescriptions, higher numbers of refills and higher costs relating to outpatient pharmacy. There were no differences between 3CM and usual care in PTSD symptoms, depression or functioning over a 6-month period, but 3CM was associated with lower perceived quality of PTSD care. This was a well-conducted trial with low risk of internal bias; however, generalisability may be limited to a US Veterans Affairs (VA) population of middle-aged males. The study authors emphasised the need to support primary care providers in managing PTSD; they also suggest that future attention to intervention fidelity (how interventions are delivered in practice) is required. The authors’ conclusion seems reliable.
Another form of collaborative/integrated care was investigated in the second RCT by McFall et al. 38,39 (943 participants). In this study, individual smoking cessation treatment was integrated with mental health care for PTSD and compared with services delivered by VA smoking cessation clinics (usual care). The authors stated that not all treatments were delivered as designed. Integrated care was associated with greater prolonged abstinence from smoking, and also with higher rates of prevalence abstinence at 6 months, which remained statistically significant at 18 months (although this was mediated by the number of counselling sessions and days of cessation medication). Improvements in PTSD symptoms did not differ between the study groups at 18 months and there were no significant group differences in adverse events. The authors suggest that integrated mental health care and smoking cessation in veterans with PTSD is a promising intervention. This conclusion reflects the evidence presented, but some potential bias in the conduct of the trial may limit its reliability. Generalisability beyond older male Vietnam-era veterans with chronic PTSD and co-occurring depression may be limited; mediation or contamination by concurrent intervention was possible; and issues of variable implementation may affect claims to intervention effectiveness.
The remaining RCT conducted by McFall et al. 40 focused on 594 participants receiving community outreach from a large urban US VA medical centre. The intervention group received mailed information about available PTSD treatment and an invitation to seek care, followed by telephone contact and a survey 1 month later. This group was compared with a control group receiving only the telephone survey 6 months after the intervention group mailing. Access to (and uptake of) treatment was higher in veterans in the intervention group; these participants were also more likely to attend follow-up treatment sessions. Barriers to accessing care included personal obligations, inconvenient appointment times and receipt of treatment from elsewhere. The authors suggested that low-cost outreach can increase mental health service use by underserved veterans with PTSD. The reliability of this conclusion may be limited because of potential bias arising in the conduct of the trial. Generalisability beyond male Vietnam veterans in receipt of VA disability benefits for PTSD may be limited.
Qualitative evidence
Service user perspectives on peer support (defined as ‘. . . a model of care in which patients “in recovery” from an illness provide emotional, instrumental, and informational support to patients with the same disorder’) was the focus of a well-conducted qualitative study by Hundt et al. 41 The views of 23 participants were sought on perceived benefits, drawbacks and favoured programme characteristics of peer support (reported primarily as group delivery) when incorporated into existing PTSD programmes at a US VA PTSD clinic. In general, views about peer support were positive at all stages of the care process. Perceived benefits included improved social support and understanding, purpose and meaning (for peer supporters); normalisation of PTSD symptoms; and feelings of hope and therapeutic benefit as a result of talking to others. Peer support also helped to initiate professional treatment. Reported drawbacks were largely related to uneasiness about group dynamics and trusting others. Preferences were expressed for strong leadership and separate peer support provision according to type of conflict, trauma (combat or sexual) and gender. The authors’ conclusion, suggesting that peer support is an acceptable complement to other PTSD treatments, seems reliable. Generalisability to a wide range of veterans (including those beyond the VA system) is plausible. Details of this study and quality assessment are presented in Tables 4 and 5.
| Study details (first author) | Stage 1 category and characteristics of models of care as described by authors | Outcomes, measures and summariesa | Commentaryb |
|---|---|---|---|
| Peer support | |||
|
Hundt, 201541 Country: USA Single/multiple provider: single provider – VA PTSD clinic Type of publication: qualitative study Participants: n = 23 |
Stage 1: peer support Peer support incorporated into existing PTSD programmes Peer support is defined as: |
Outcomes and measures: perceived benefits, drawbacks and desired programme characteristics (one-time qualitative interview in person or by telephone) Summary of results as reported by the author: overall, veterans were positive about peer support. Benefits included improved social support and understanding, the provision of purpose and meaning (for peer supporters), normalisation of PTSD symptoms and feelings of hope, therapeutic gain through the process of opening up to others and helping to initiate professional treatment. A few perceived drawbacks were largely related to uneasiness about peer group dynamics, fears about prejudice and difficulties trusting others. In general, peer support was considered valuable at all points in the care process (before care to increase initiation of treatment, during care to encourage adherence and after care to help maintain skills learned). Strong leadership was considered important and separate peer support groups were preferred according to type of conflict, type of trauma (combat or sexual) and gender Summary of authors’ conclusions: veterans found peer support to be highly acceptable as a complement to existing PTSD treatments, with only a few drawbacks Authors’ research recommendations: future focus on patient satisfaction with peer support and effectiveness; more attention to the most effective structure and format of peer support |
|
| First author, year | (1) Was there a clear statement of the aims of the research? | (2) Is a qualitative methodology appropriate? | (3) Was the research design appropriate to address the aims of the research? | (4) Was the recruitment strategy appropriate to the aims of the research? | (5) Were the data collected in a way that addressed the research issue? | (6) Has the relationship between researcher and participants been adequately considered? | (7) Have ethical issues been taken into consideration? | (8) Was the data analysis sufficiently rigorous? | (9) Is there a clear statement of finding? | (10) How valuable is the research? |
|---|---|---|---|---|---|---|---|---|---|---|
| Peer mentoring | ||||||||||
| Hundt, 201541 | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | Yes | Yes | Contributions to research and practice are reported |
In summary, limited evidence suggests that the most promising model of care is a collaborative arrangement that provides staff and patient support, and additional help to facilitate good care management, resulting in improved uptake of health care by veterans. The positive impact on smoking abstinence of integrated care, incorporating mental health care with smoking cessation treatment, is encouraging but less well substantiated, as is the effect of community outreach on increasing treatment access and uptake. Generalisability of these systems of care outside the VA setting and to younger, female veterans returning from conflicts other than Vietnam may be limited. There appears to be good evidence suggesting that peer support can be an acceptable complement to other PTSD treatments and this type of care delivery may be generalisable to a range of veteran populations. There was no clear evidence of effect for models of care on PTSD symptoms or other mental health outcomes.
Overview of the remaining included study designs
Twenty studies (24 articles) provided further information on models of care. 35,36,44–65 Various study designs (primarily involving single groups) were used, including quasi-experimental, before-and-after studies, observational designs and descriptive pieces. Sample sizes (when reported) ranged from 6 (patients) to 696,379 (administrative data). These studies were not assessed for methodological quality, but were considered important contributors to the evidence picture and are reviewed below.
Models of care among the less robust study designs can be summarised as integrated care, partnership working, networks and co-located services; settings-based delivery (inpatient, outpatient, residential, day care, primary care); peer support; multicomponent programmes; and a family systems model. Some studies covered more than one model of care. In these cases, we made a judgement as to the most prominent delivery aspect. Comparators (when reported) included usual care (variably defined), different programme intensities or settings and the UK IAPT programme. When measured, outcomes included clinical (e.g. mental health, PTSD diagnosis and symptoms), quality of life, substance misuse, family functioning, service use (including access and uptake), characteristics of successful programmes, patient satisfaction and cost.
Fifteen studies reported in 18 articles were conducted in the USA48–65 (13 of these were delivered in the context of the Veterans Health Administration, US Department of Veterans Affairs); three studies were carried out in Australia,44–46 and two studies (three articles) were carried out in the UK. 35,36,47
The types of care models and an overview of the studies within each are summarised in the following sections. We draw particular attention to studies with an evaluative component.
Integrated care, partnership working, networks and co-located services
These types of care models were the most frequently reported (Table 6 presents details of the models). Two before-and-after studies conducted in the US VA setting reported on benefits for PTSD and pain. 62,63 Of these, Plagge et al. 63 suggested that involving primary care in the delivery of behavioural activation therapy was feasible and potentially effective in treating PTSD and comorbid pain in veterans. Benefits for pain and PTSD were also indicated following the integration of CPT and CBT in Otis et al. 62 Returning to primary care involvement, a VA-based evaluation by Bohnert et al. 52 suggested that same-day integrated mental health services (i.e. delivering services on the same day as initial need is detected) in collaboration with primary care increased the likelihood of PTSD diagnosis and treatment initiation after a positive screen when compared with mental health service delivery in other settings. An observational study by Brawer et al. 51 also drew links to the success of integrating primary care and mental health services on increasing rates of consultation in the VA setting.
| First author, provider (when reported), e.g. VA | Year | Country | Study design (as defined by authors) and sample size | Stage 1 model of care and brief description of model of care | Outcomes (when applicable) | Summary of authors’ conclusions |
|---|---|---|---|---|---|---|
| Australia | ||||||
| Pietrzak,42 McGuire43 and Bredhauer44 | 2011 | Australia |
Critical review and analysis (guideline) N/A |
Stage 1: co-ordinated, integrated, collaborative, networks, multidisciplinary care; and multicomponent treatment programmes PTSD Group Treatment programmes |
N/A |
There are a number of recommendations to provide guidance on the next phase of the group treatment programmes, which, the authors state, are not a radical departure from the model as it currently stands. The authors state that the current model of care is based on best-practice treatment and the programmes are regularly reviewed and accredited. Their recommendations offer suggestions for improvements that would enhance the programmes, provide the ability to compare outcomes from the programmes with outcomes reported in the literature, facilitate knowledge sharing and make economic analysis possible Research recommendations: not reported |
| UK | ||||||
| Burdett;35 PTSD Resolution – UK charity offering services to UK armed forces | 2016 | UK |
Service evaluation (observational data) n = 504 |
Stage 1: co-ordinated, integrated, collaborative, networks, and multidisciplinary care HGT delivered via Practice Research Network (200 therapists) vs. IAPT |
CORE-10 score (brief mental health measure) |
The findings suggested that HGT treatment provided by PTSD Resolution therapists led to improvements in service users’ mental health, but the data did not clarify if this may have been a result of other causes of improvement Research recommendations: further research/evaluation is needed: to clarify reasons for measured improvement in mental health; to conduct an RCT to assess the impact of employment on treatment outcomes; to explore reasons for dropout from outpatient therapy; and to conduct an RCT to evaluate HGT provided by PTSD Resolution therapists |
| USA | ||||||
| Sniezek49 | 2012 | USA |
Descriptive article (Guest editorial) N/A |
Stage 1: co-ordinated, integrated, collaborative, networks, multidisciplinary care; primary care CBWSI. Description of an integrated community based primary care ‘strategy’ |
N/A |
Describes the CBWSI Research recommendations: not reported |
| USA: VA | ||||||
| Baringer,50 VA | 1990 | USA |
Before-and-after intervention pilot study n = unclear |
Stage 1: partnership, cross-sector, liaison work, co-location; co-ordinated, integrated, collaborative, networks, multidisciplinary care; inpatient 28-day inpatient PTSD stabilisation unit co-located with existing treatment unit |
Anger, communication, depression, fear and anxiety, grief, self-esteem, social isolation, stress |
Patient-identified problem areas and the method of determining their severity supplement clinical observation and may serve as a model for other programme evaluations Research recommendations: to measure the influence of the intervention on patient-identified problem areas that are more clearly defined |
| Bohnert,52 VA | 2016 | USA |
Observational system evaluation n = 21,427 |
Stage 1: Co-ordinated, integrated, collaborative, networks, multidisciplinary care; inpatient, outpatient, primary care, day care, residential Same-day primary care mental health integration vs. same-day specialty mental health care vs. primary care |
Rates of PTSD diagnosis and initiation of treatment following positive screen |
Same-day integrated mental health services within primary care increase the likelihood of PTSD diagnosis and treatment initiation after a positive screen Research recommendations: |
| Brawer,51 VA | 2011 | USA |
Observational n = 129 consultations |
Stage 1: co-ordinated, integrated, collaborative, networks, multidisciplinary care; primary care VA PCMHI programme (collaborative care/integrative care) |
Access and continuity of care, rates of consultation, confirmed PTSD, PTSD symptoms |
PCMHI potentially preserves health-care resources and increases continuity of care for veterans Research recommendations: implementation studies of integrated care and further comprehensive evaluations including treatment outcome and cost-effectiveness |
| Chan,53 VA | 2007 | USA |
Descriptive article (thesis) N/A |
Stage 1: co-ordinated, integrated, collaborative, networks, multidisciplinary care Collaborative care depression treatment vs. usual care |
Depression (Hopkins Symptom Checklist-20) and costs |
The thesis describes three studies on collaborative care for depression Research recommendations: more research on factors leading to successful collaborative care for depression, and how to encourage access to care in minority population groups |
| Otis,62 VA | 2009 | USA |
Before-and-after (pilot) n = 6 |
Stage 1: co-ordinated, integrated, collaborative, networks, multidisciplinary care Integrated treatment for chronic pain and PTSD (combination of CPT and CBT) |
Clinical measures: PTSD symptoms, pain, distress, disability |
Participants appeared to benefit from receiving the integrated treatment for pain and PTSD. A RCT is currently being conducted to evaluate the efficacy of this treatment approach Research recommendations: the authors refer to an ongoing RCT |
| Plagge,63 VA | 2013 | USA |
Before-and-after n = 58 |
Stage 1: partnership, cross-sector, liaison work, co-location; co-ordinated, integrated, collaborative, networks, multidisciplinary care; primary care Collaborative approach using BA therapy to treat comorbid pain and PTSD (including collaboration with primary care) physical/exercise therapy, psychotherapy, medication |
Clinical measures: PTSD symptoms, pain, QoL, mental health |
The findings suggested that a collaborative approach that includes BA therapy is a feasible and a potentially effective treatment for comorbid PTSD and chronic pain Research recommendations: |
In other studies, a before-and-after survey conducted by Baringer et al. 50 revealed improvements in a range of patient-identified psychosocial problem areas following a short-term pilot inpatient PTSD stabilisation unit co-located with existing VA treatment provision. A service evaluation in the UK by Burdett and Greenberg35 revealed improvements in veterans’ mental health following human givens therapy31 delivered by a countrywide network of 200 therapists when compared with the UK IAPT programme.
The remaining studies were descriptive. From Australia there was a critical analysis of PTSD group treatment programmes,44 and from the USA there was a thesis on collaborative care depression treatment in the VA setting53 and an editorial describing an integrated community-based primary care strategy (the Community-Based Wounded Warrior Sustainability Initiative). 49
Settings-based models of care
Two quasi-experimental studies compared care delivery across different settings (Table 7). 46,56 In Australia, Creamer et al. 46 indicated that delivery in a less expensive (and less restrictive) day hospital may be equally effective for veterans with PTSD as inpatient or outpatient programmes on a range of psychological and social variables. A similar trend was reported by Fontana and Rosenheck56 in the USA VA setting, favouring less intensive programmes to achieve clinical, satisfaction and cost outcomes. Delivery of care in a local setting matched to the severity of clinical symptoms appeared to be favoured in Australia by Forbes et al. 45 Cognitive reprocessing therapy resulted in greater PTSD symptom relief when delivered to veterans as outpatients compared to those in residential care in the VA-based study by Walter et al,65 although the reliability of this finding may be limited by baseline group differences in PTSD symptom severity. The observational study (using a large administrative data set) in the USA VA system by Randall et al. 64 illustrated that lower rates of hospitalisation and lower demand for specialist care could be achieved by enhancing access to primary care through Primary Aligned Care Teams (PACT). In the UK, Murphy et al. 36,47 used observational data to demonstrate the success of a 6-week residential programme (underpinned by TFCBT), offered by Combat Stress, in terms of long-term benefits on PTSD symptoms and functional assessment.
| First author, provider (when reported), e.g. VA | Year | Country | Study design (as defined by authors) and sample size | Stage 1 model of care and brief description of model of care | Outcomes (when applicable) | Summary of authors’ conclusions |
|---|---|---|---|---|---|---|
| Australia | ||||||
| Creamer46 | 2002 | Australia |
Quasi-experimental observational study n = 202 |
Stage 1: inpatient, outpatient, primary care Inpatient vs. outpatient vs. day hospital PTSD treatment |
PTSD, alcohol use, anxiety and depression, family functioning, anger, general health |
The study lends broad support to the recommendations that treatment services for veterans with PTSD should be delivered in the least restrictive environment Research recommendations: not reported |
| Forbes45 | 2008 | Australia |
Survey (at three time points) n = 4,339 |
Stage 1: inpatient, outpatient, day care, residential Five different models (intensities) of group-based cognitive behavioural treatment: high-intensity inpatient–outpatient programmes, high-intensity residential programmes, moderate-intensity day hospital programmes, moderate-intensity regional day hospital programmes, low-intensity programmes |
PTSD, anxiety, depression, alcohol misuse (self-assessment) |
The study indicated that comparable outcomes were evident across variation in PTSD programme intensity type. There was some suggestion that outcomes are maximised when veterans participate in programme intensity types that match their level of PTSD and comorbidity severity. If matching is not feasible, then the most consistent outcomes seemed to be in the moderate-intensity programmes. Data suggested that delivering treatment in their local environment does not detract from, and may enhance, outcomes for regionally based veterans Research recommendations: findings require confirmation in studies using randomised controlled design and methodology |
| UK | ||||||
| Murphy (1-year follow-up)47 | 2016 | UK |
Observational (1 year follow-up) n = 268/401 (69%) at follow-up |
Stage 1: residential, multicomponent treatment programme Combat Stress Residential PTSD – a national programme including various modalities underpinned by TFCBT |
Clinical outcomes: clinician- and participant-reported PTSD symptoms, participant-reported functional assessment and other self-reported measures |
The findings suggest longer-term benefits of the Combat Stress 6-week residential programme for veterans with PTSD. The findings also suggest the importance of continued support targeted to particular individuals at post treatment to improve longer-term outcomes Research recommendations: a RCT to evaluate the intervention |
|
Murphy (data from 6-month follow-up)36 Combat Stress – NHS funded third sector |
2015 | |||||
| USA – VA | ||||||
| Fontana,56 VA | 1997 | USA |
Quasi-experimental observational n = 785 |
Stage 1: inpatient Comparison of three different models: long-stay specialised inpatient PTSD unit, short-stay specialised evaluation and brief-treatment PTSD units, non-specialised general psychiatric units |
Nine measures of symptoms and social functioning (including PTSD, violent behaviours and thoughts, days of paid work in the last month, social involvement); satisfaction with programme; and costs |
A paucity of evidence of sustained improvement from ‘costly’ long-stay specialised inpatient PTSD programmes and an indication of high satisfaction and sustained improvements in the ‘far less costly’ short-stay specialised evaluation programme and the brief-treatment PTSD programme suggest that systematic restructuring of VA inpatients PTSD treatment could result in the delivery of effective services to a larger number of veterans Research recommendations: not reported |
| Randall,64 VA | 2015 | USA |
Observational n = 696,379 (administrative data) |
Stage 1: primary care PACT primary care model (a version of the ‘patient-centred medical home’) |
Using hospital records: service utilisation |
PACT implementation was followed by an associated lower rate of hospitalisations and specialty care visits, and a higher rate of primary care visits, for veterans with PTSD, indicating enhanced access to primary care Research recommendations: |
| Walter,65 VA | 2014 | USA |
Non-randomised comparison n = 992 |
Stage 1: outpatient, residential Comparing residential with outpatient treatment with cognitive reprocessing therapy |
Clinical measures: PTSD, depression |
Demographic and symptom severity differed between outpatient and treatment samples. Findings suggested that outpatients experienced greater PTSD symptom relief than those in residential treatment, although outpatients began treatment with a lower symptom severity Research recommendations: to examine factors influencing treatment outcome and choice |
Peer support
In rural California, an observational study (reported in three articles) by Jain et al. 58–60 suggested that positive perceptions of peer support delivered in residential- and community-based settings in the VA system can favourably influence attitudes to recovery in veterans with PTSD. Peer support delivered by telephone outreach in the VA setting was also described in a written communication by Joseph et al. 61 (Table 8).
| First author, provider (when reported), e.g. VA | Year | Country | Study design (as defined by authors) and sample size | Stage 1 model of care and brief description of model of care | Outcomes (when applicable) | Summary of authors’ conclusions |
|---|---|---|---|---|---|---|
| USA – VA | ||||||
| Jain,58–60 VA | 2014 2016 2015 | USA |
Observational study n = 55 |
Stage 1: peer support, residential Peer support in rural California |
Characteristics of successful peer support, correlation with recovery attitudes relating to PTSD59 Participant satisfaction60 Descriptive58 |
The findings suggest that positive perceptions of peer support favourably influence attitudes towards recovery for veterans with PTSD who receive support Research recommendations: a systematic study of recovery-orientated approaches to PTSD treatment |
| Joseph,61 VA | 2015 | USA |
Letter describing programme n = 82/143 (57%) received telephone call |
Stage 1: peer support Peer support telephone outreach |
Characteristics of successful implementation, participant engagement with intervention |
Descriptive data of a telephone support outreach programme Research recommendations: to investigate whether or not peer support telephone outreach has the capacity to improve outcomes for veterans |
Multicomponent programmes
A promising multicomponent theory-based VA programme (‘Transcend’: a combination of cognitive–behavioural skills training, substance abuse relapse and peer support) was reported for PTSD and addiction severity outcomes by Donovan et al. (two articles). 54,55 Another VA-based study by Forman and Havas57 described a multicomponent hospital-based treatment and rehabilitation programme covering a wide range of activity (Table 9).
| First author, provider (when reported), e.g. VA | Year | Country | Study design (as defined by authors) and sample size | Stage 1 model of care and brief description of model of care | Outcomes (when applicable) | Summary of authors’ conclusions |
|---|---|---|---|---|---|---|
| USA: VA | ||||||
|
Donovan54 Donavan (descriptive)55 VA |
2001 1999 |
USA |
Before-and-after treatment study n = 46 |
Stage 1: multicomponent treatment programmes ‘Transcend’: group-focused programme incorporating cognitive–behavioural skills training, constructivist theory approaches, substance abuse relapse prevention strategies, peer social support |
PTSD, addiction severity |
The findings suggest that an integrative treatment approach to chronic combat-related PTSD and comorbid substance abuse may be effective Research recommendations: an investigation of intervention impact on social functioning and quality of life (such as improved vocational success, family relationships and community integration) |
| Forman,57 Department of Public Health and Massachusetts Department of Veterans Services | 1990 | USA |
Descriptive article N/A |
Stage 1: multicomponent treatment programmes Hospital-based treatment and rehabilitation programme (includes individual counselling, group process psychotherapy, structured human relations training, substance abuse education and counselling, vocational counselling, family, art and recreational therapy, medical care) |
N/A |
Description of service Research recommendations: not reported |
Family systems model
The ‘Home Base’ three-generational family systems health-care model, codeveloped by a third-sector organisation and a general hospital in the USA, was described by Ohye et al. 48 The application of this clinical model, designed to address three interdependent aspects of family life affected by PTSD (i.e. relationship attachments, impaired family role of the veteran and multiple pathways to treatment) was illustrated by case studies (Table 10).
| First author, provider (when reported), e.g. VA | Year | Country | Study design (as defined by authors) and sample size | Stage 1 model of care and brief description of model of care | Outcomes (when applicable) | Summary of authors’ conclusions |
|---|---|---|---|---|---|---|
| Ohye48 | 2015 | USA |
Descriptive article N/A |
Stage 1: family systems model Family system health-care model ‘Home Base’ Veteran and Family Clinic |
N/A |
Describes the programme Research recommendations: not reported |
In summary, a range of evidence from less robust study designs spanned five different types of care model. The reliability of this evidence is unclear; however, these studies were reviewed principally to enrich the descriptive evidence map. The emphasis of activity appears to lie in integrated care, partnership working, networks and co-located services. This is followed by other services delivered with a settings-based approach. Indications from the VA system are that integrating mental health services in primary care, and the combination of CPT and CBT, may be promising models of care to improve pain and PTSD-related outcomes in veterans. Co-located stabilisation services may also successfully complement VA provision in reducing psychosocial problems. In the UK, a specialist network delivering theory-based treatment may be helpful in improving veterans’ mental health. With the exception of one study in the UK,36,47 which endorsed the value of treatment in the residential setting, all studies (from the USA and Australia) indicated that less expensive, less intensive and locally delivered services (including the provision of day hospitals, patient-centred primary care teams and outpatient cognitive reprocessing therapy) could lead to favourable PTSD-related outcomes, patient satisfaction and reduced hospitalisation. Evidence for multicomponent models and peer support was supported by one study each in the VA system, indicating, respectively, potentially positive outcomes for PTSD and on perceptions influencing veterans’ attitudes to recovery.
Summary of stage 2 results
In terms of where the weight of evidence lies on models of care, there are some parallels between what is reported in the more robust evidence we identified (i.e. the RCTs and qualitative study) and intervention coverage in the less robust study designs. Broadly, collaborative or integrated care arrangements and peer support show promise in both strands of the evidence we reviewed. In addition, mental health care integrated with smoking cessation, and community outreach, may also be effective, as indicated by the more robust study designs. A number of signposts exist to other potentially effective models of care (and specific treatments delivered within those models), but the reliability of this evidence is unclear. The strongest evidence on outcomes appears to be connected to intervention access and uptake, behavioural change and patient satisfaction. Although there was no reported evidence of clinical effect for mental health and PTSD in the more robust study designs, these outcomes were abundantly considered in studies we regarded as less methodologically sound. Most studies were carried out in the US VA setting, which raises questions about generalisability of the delivery models to the UK setting.
Research implications arising from the literature
Research recommendations in the more robust study designs were limited to one study. In the qualitative study by Hundt et al. ,41 the authors suggested future focus on patient satisfaction with peer support and an exploration of the most effective structure and format of peer groups. Various research implications were reported across the less robust study designs. Generally, more robust investigations using RCTs (and with longer follow-up) were called for, as were process measures to explore factors affecting intervention implementation, treatment uptake and outcomes. More research on peer support telephone outreach was proposed. Further focus on patient satisfaction, social functioning and quality-of-life outcomes, improving access to services, understanding age-related treatment effectiveness disparities and intervention cost-effectiveness was also recommended.
Stage 3: what treatments show promise for UK armed forces veterans with post-traumatic stress disorder?
Overview of evidence
Seven systematic reviews (eight articles)66–73 were included in the review of treatments (see Figure 1). Studies of veterans were the focus in four reviews (five articles)67–69,71,72 and in a subset of three reviews looking at PTSD treatments. 66,70,73 The reviews were published between 2007 and 2016, and featured primary studies in veteran populations from 1988 to 2014 (when reported).
Two reviews did not report where primary studies were conducted;66,72 two reviews (three articles) reported studies conducted only in the USA;67–69 and the remaining three reviews featured predominantly USA studies and others from Australia, Europe and Israel. 70,71,73 Population characteristics were variably reported in the reviews, with veteran characteristics being unavailable for two reviews69,73 and the rest reporting some, but not all, aspects of age, gender or exposure. 66–68,70–72 When reported, reviews indicated a greater proportion of male participants, an approximate age range of 25–50 years and combat experience in Operation Iraqi Freedom (OIF), the Gulf War, Croatia or Vietnam. 66–68,70–72
Interventions in the included reviews could be broadly grouped into psychosocial or pharmacotherapy, or an indirect comparison of both. Clinical measures related to PTSD were the most frequently reported, with some reviews also reporting outcome measures for anxiety and depression symptoms. 71–73 Some reviews67–69 reported whether studies or subgroups of studies were conducted in inpatient or outpatient settings, but no other details were reported on how treatment was delivered, who it was delivered by or levels of treatment uptake.
Evidence from the reviews
Findings were reported for psychosocial or pharmacotherapy interventions. The results of the reviews are described below, with consideration of the validity and reliability of the authors’ conclusions. One review72 conducted separate analysis for pharmacotherapy studies and psychotherapy studies, and then combined these results to compare pharmacotherapy with psychotherapy.
Psychosocial interventions
Five reviews (six articles) reported solely on psychosocial interventions (Table 11). 66–70,73 Goodson et al. 69 reported interventions conducted in a VA setting, including exposure-based interventions featuring EMDR, PE and implosive therapy. Exposure-based treatment demonstrated large effect sizes for reducing PTSD symptoms (12 studies). Inpatient interventions, described as multicomponent multidisciplinary treatment programmes, reported a small effect size for reduction in PTSD symptoms (seven studies). Cognitive–behavioural interventions comprised CPT and trauma management and showed reductions in PTSD symptoms with a large effect size favouring treatment (seven studies), but the sample size was unknown. Authors also reported single-study data for miscellaneous interventions. Conclusions suggested that across intervention types, about half of treated individuals would show improvement and, therefore, evidence-based exposure treatments were likely to be effective for combat-related trauma. No assessment of the quality of the studies was carried out and there was a lack of reporting of methods of meta-analysis, which may limit interpretation of the analysis. The conclusions were supported by the evidence analysed. However, as these interventions were conducted within the VA system they may not be generalisable to UK and NHS practice.
| Study details (first author) | Veteran characteristicsa | Intervention(s) (and comparators when reported) | Outcomes and measures | Authors’ conclusions and summary of results (including cost-effectiveness when reported) | Commentary |
|---|---|---|---|---|---|
|
Bisson, 200766 (part of NICE clinical practice guidelines 26 #305) Countries: NR Study designs: two RCTs (part of larger review with 38 RCTs) Date range of studies: years of publication unclear |
All male, Vietnam veterans | Psychological treatments appeared effective for chronic PTSD, with TFCBT having stronger evidence than EMDR. However, results in the veteran population showed these interventions to be less effective compared with other studies in the review. The authors indicated a need for more direct comparisons of psychological treatments in trials and for large-scale (Phase 4) trials |
The review question and inclusion criteria were clear. The authors searched a number of relevant databases and made attempts to identify unpublished studies. This reduces the likelihood that some relevant studies were not included in the review. However, only studies with an English abstract were eligible for inclusion, which might have increased the possibility of language bias. The authors used appropriate methods to minimise bias and error in the study selection, validity assessment and data extraction processes. Although the authors stated that a validity assessment was carried out, the results of this assessment were not reported; this makes it difficult to assess the implications of the assessment for the review conclusions The decision to employ meta-analysis with appropriate use of subgroups and sensitivity analyses appears reasonable. This was a well-conducted review and the authors’ conclusions generally reflect the evidence included in the review. However, as the authors stated, the small sample sizes and methodological problems of some of the included studies should be kept in mind Note: only two out of five included studies on veterans were reported in a sensitivity analysis. The authors did not give reasons for this selection. This review also informed a wider NICE guideline |
||
| Mean age 41.3 (SD 2.84) years | EMDR (vs. waiting list) | Clinician-rated PTSD symptoms (undefined) | Results favoured treatment over waiting list at reducing PTSD symptoms with SMD = –0.97 (95% CI –1.81 to –0.13), based on 1 RCT, n = 25 | ||
| Mean age 34.6 (SD 4.3) years | TFCBT (vs. waiting list) | Results suggested little difference between treatment and waiting list at reducing PTSD symptoms with SMD = –0.22 (95% CI –1.03 to 0.58), based on one RCT, n = 24 | |||
|
Country: USA, n = 20 Study designs: 20 studies; 10 clinical trials, 10 observational (routine clinical care) Date range of studies: years of publication from 2009 to 2014 |
Mean ages 25.8 years to 39.0 years Percentage of females: 0% to 20% Percentage of ethnic minority participants: 5% to 69% Veterans of OEF/OIF/OND (81.7%, active service members 18.3%) receiving outpatient treatment |
Dropout for psychosocial interventions may differ between clinical care and trial settings, likely because of differences in approach and populations. When aiming to retain service users, individual therapies may be best. Authors suggested investigation of treatments with shorter time frames and further research, but it is unclear if this was based on the evidence in the review | Authors outlined a well-defined review question and adequate search methodology. Inclusion criteria were reported. The population was predominantly veterans, but did include active service members, and 15% of participants were subthreshold for PTSD, raising external validity issues. The authors stated that two reviewers selected full papers for inclusion but it is unclear whether or not efforts were made to reduce reviewer error and bias in the other review stages. There are minor inconsistencies in the figures presented. No formal quality assessment was conducted, providing uncertainty as to the quality of evidence. The methods of analysis appear appropriate. However, high heterogeneity is seen (particularly in group therapy studies) and may indicate a lack of reliability in analyses. As the authors pointed out, reasons for dropout are not examined, although they made suggestions as to why differences may occur. Overall, the cautious conclusions are within the limitations of the review | ||
| Psychosocial interventions including PE, CPT, exposure therapy, CBT, seeking safety, writing-based treatment and adaptive disclosure | Pooled dropout ratio |
Pooled dropout across treatments was 36.0% (95% CI 26.90 to 45.00). Average dropout in routine clinical care settings was 42.0% and in clinical trials it was 28.0% (although this difference was not statistically significant) Dropout ratio differed by treatment format (OR = 1.28, 95% CI 1.06 to 1.53): average dropout in individual therapy studies = 31.1% (95% CI 25.1 to 37.2, I2 = 69.4%) and in studies with a group therapy component = 54.4% (95% CI 30.2 to 78.6, I2 = 95.3%) |
|||
|
Goodson, 201169 Country: USA, n = 24 Study designs: 24 studies; 10 controlled trials, 14 open trials Date range of studies: years of publication from 1989 to 2009 |
Combat veterans with PTSD treated in a VA setting. No characteristics of veterans from the individual studies were provided | Treatments in the VA programme were moderately effective at reducing the PTSD symptoms of veterans. Across all 24 studies, an effect size of 0.43 suggests that over half of those treated should show improvement. Evidence-based treatments, particularly those with exposure components, appeared to be most the effective for combat-related PTSD. Authors suggested future research including validation of evidence-based treatment in practice and obtaining outcome data from existing programmes | The review set out a well-defined question, with comprehensive search and clear inclusion criteria. Studies are described in the narrative, though no quality assessment has been conducted. Study details are limited and there are inconsistencies in the report between results presented in the tables and text. Authors pointed out the analysis includes exploratory and non-empirically supported interventions, which could bias effect sizes and this may also reduce external validity of conclusions. The measures pooled in meta-analyses were not described and effect sizes were described with minimal interpretation for their application in the synthesis. Tests of statistical significance were not used to compare different modalities, limiting comparison between types of treatment. Authors indicated that higher-quality studies provided smaller effect sizes. However, this was based on study design alone with no assessment of study quality. Conclusions are supported by the evidence analysed and stated within the remit of VA system services, which limits external validity, particularly with regard to overall ‘PTSD treatment’ meta-analysis | ||
| Exposure-based interventions (EMDR = 4, PE = 3, implosive therapy = 2, group-based exposure = 1, exposure with family therapy = 1, systematic desensitisation = 1) | PTSD symptoms (effect size calculated using Cohen’s d, outcome measures used were not reported) |
Results favoured exposure treatment with a within-group post-treatment effect size of 1.10 (range = –0.58 to 2.20), based on 11 studies, n = 319 Results of between-group analysis favoured treatment with a post-treatment effect size of 0.64 (range = 0.05 to 0.95), based on seven studies, n = 85 For all 12 exposure-based studies; mean n = 21.7, SD 24.0 |
|||
| Inpatient interventions (multicomponent multidisciplinary PTSD treatment programmes = 7) |
Results showed an effect of treatment with a within-group post-treatment effect size of 0.19 (range = –0.54 to 0.74), based on seven studies, n = 1178 Results of between-group analysis favoured treatment with a post-treatment effect size of 0.20, based on one study, n = 51 For all inpatient studies; mean n = 106 (SD 10.5) based on seven studies |
||||
| Cognitive–behavioural interventions (CPT = 1, trauma management therapy = 1) |
Between-group effect size of 1.07, favouring treatment, based on two studies Trauma management therapy showed a within-group effect size of 0.81, based on one study |
||||
| Miscellaneous interventions (spirituality-based intervention = 1, BA = 1, skills-based group = 1) |
Results showed an effect of treatment with a within-group effect size of 0.48 for BA and 0.67 for spirituality-based intervention (one study each) A between-group effect size of 0.56 was found for the spirituality-based intervention (results based on one study) |
||||
| PTSD treatment assessed in controlled trials (including seven exposure-based and all miscellaneous interventions) |
Results showed an effect of treatment with an effect size of 0.49 (95% CI 0.27 to 0.71), based on meta-analysis of 10 controlled trials, n = 429. Studies were shown to be heterogeneous (Q = 6.27; p < 0.001) At follow-up, there was a decreased effect of treatment, with effect size 0.39 (95% CI 0.06 to 0.72), based on a subset of four studies, n=39 |
||||
|
Kitchiner, 201270 Countries: Australia, n = 1; USA, n = 3 Study designs: four RCTs (part of a larger review with 29 studies included) Date range of studies: years of publication (for studies in veterans) 1989 to 2006 |
169 Vietnam and one non-Vietnam veterans with PTSD | Some evidence for effectiveness of group or individually delivered trauma-based psychological interventions for chronic PTSD when the therapist is in the room. Dropout was no higher for interventions than controls across all studies, suggesting a lack of major adverse effects. Authors indicated the need for more research on psychosocial interventions outside the USA and specifically among veteran populations. Future studies should compare active psychosocial treatments, as well as the role of pharmacological treatments in combination with psychosocial therapy. The role of technology that utilises psychosocial therapy in novel formats needs to be developed and evaluated. Further robust trials are needed to assess adverse events, tolerability and cost-effectiveness |
The review question and inclusion criteria were clear. A number of relevant databases were searched and attempts made to locate unpublished studies. Only studies with an English abstract were eligible for inclusion and the authors acknowledged that some other studies may have been missed. Appropriate methods were used to minimise reviewer error and bias. The quality assessment was used to inform the synthesis. Study quality was variable in many studies, which, authors acknowledged, needs to be taken into account when interpreting the results The methods used to conduct the meta-analyses seem appropriate. Over half of the studies were not included in the quantitative synthesis because of variation between studies or missing data. These studies were described but not synthesised and do not contribute to the findings of the review. The conclusions are based on the small number of studies included in the meta-analyses and the authors acknowledged this as a limitation Note: three out of the four studies in the meta-analysis relating to veterans with PTSD were published prior to 1990, which may limit their relevance to current practices. Thirteen other studies were reported in tables but not synthesised |
||
| Trauma-focused interventions (vs. usual care or waiting list) (included EMDR, implosive flooding and CPT) | Self-reported PTSD symptoms (undefined) | Results favoured intervention in reducing self-reported PTSD symptoms with SMD = –0.59 (95% CI –1.09 to –0.10, I2 = 43%) compared with usual care or waiting list, based on four studies, n = 128. The authors reported methodological concerns with each of the included studies | |||
|
Tran, 201673 Countries: Australia, n = 1; USA, n = 7 Study designs: seven studies; two RCTs and five non-RCTs (part of a larger review featuring 16 studies) Date range of studies: veteran studies published from 2006 to 2014 |
Across all studies in the review there was a mean age of 32 to 54 years Percentage of males: 0% to 97% Veteran characteristics were not reported separately |
CPT may be effective for reducing PTSD symptoms, depression or anxiety in potentially vulnerable groups, such as women who have experienced military or childhood sexual trauma. The overall quality of evidence was moderate to low. Future research suggested includes comparison between combinations of therapy with outcomes such as quality of life and remission rate |
The conduct of this review was generally good. The authors clearly reported the review process and made sufficient attempts to minimise error and bias. Appropriate methods of study selection, quality assessment and synthesis are reported. The tentative conclusion seems reliable and is consistent with results from limited data presented for military veterans The authors’ reference to potential effectiveness for female veterans is outside the scope of our rapid evidence synthesis (the study comprised female veterans who had military sexual trauma, not combat trauma) Further results on contextual analysis, for example impact of treatment on health equity and access; patient values and preferences; and cost-effectiveness (though this is restricted to one study with cost information only) are included in the paper |
||
| CPT (vs. waiting list or usual care) | PTSD symptoms measured by CAPS | Reduced clinician-scored symptom severity with MD –21.15 (95% CI –31.33 to –10.97). Meta-analysis MD –16.01 (95% CI –26.71 to –5.31). Results are based on two RCTs (n = 119) and evidence was of low quality | |||
| PTSD symptoms measured by PCL scale | Reduced self-scored symptom severity with MD –5.05 (95% CI –9.30 to –0.8). Results are based on two observational studies (n = 213) and evidence was of very low quality | ||||
| Depression symptoms measured by BDI-II | Reduced depression symptom severity with MD –6.49 (95% CI –11.55 to –1.43). Meta-analysis MD –3.61 (95% CI –8.97 to 1.76). Results are based on two RCTs (n = 119) and evidence was of low quality | ||||
| CPT (vs. EMDR + CPT) | PTSD symptoms measured by PCL | No difference between groups’ change in PTSD symptom severity, CPT 62.53 ± 9.72 and EMDR + CPT 65.82 ± 13.52. Results based on one observational study (n = 34), with very low quality of evidence | |||
| Depression symptoms measured by BDI-II | No difference between groups’ change in depression symptom severity, CPT 25.24 ± 12.81and EMDR+CPT 26.00 ± 13.11. Results based on one observational study (n = 34), with very low quality of evidence | ||||
| Anxiety symptoms measured by BAI | No difference between groups’ change in anxiety symptom severity, CPT 25.88 ± 13.14 and EMDR+CPT 23.47 ± 13.42. Results based on one observational study (n = 34), with very low quality of evidence | ||||
| CPT (vs. PE) | PTSD symptoms measured by PCL | PE was associated with greater improvement in PTSD severity at the end of treatment with MD 12.54 (95% CI 8.27 to 16.81). The result was based on one observational study (n = 263) of very low quality. A further observational study showed no difference between CPT and PE at the end of treatment (n=70) (data not reported in study and quality not reported) |
A review by Kitchiner et al. 70 also investigated trauma-focused interventions. These included EMDR, CPT and implosive flooding, and were compared with usual care or waiting list. The results showed a small but significant decrease in self-reported PTSD symptoms following treatment (four studies, 128 participants). The findings were based on a small number of studies with moderate statistical heterogeneity. The authors concluded that there is some evidence of effectiveness for trauma-based interventions and call for more research into combined therapy as well as tolerability. Of note is the fact that, although half the included studies could not be quantitatively synthesised, they were also not included in the narrative, which, the authors acknowledge, is a limitation. Most of the studies were conducted before 1990, potentially limiting their relevance to current practice. The authors also reported concerns about the methodological quality of the studies.
The veteran studies within the review by Tran et al. 73 focused on comparing CPT with waiting list, usual care or another intervention. When compared with waiting list, CPT significantly reduced clinician-rated PTSD symptom severity (two RCTs, 119 participants) and, to a smaller extent, self-rated symptoms (two observational studies, 213 participants). There was also a reduction in depression symptoms treatment (two RCTs, 119 participants). Comparisons between CPT versus EMDR with concurrent CPT, and CPT versus PE, were based on single observational studies that found mixed effects between CPT and comparisons for PTSD, depression and anxiety symptoms. Authors reported very low to low methodological quality of evidence for these outcomes and sample sizes were generally small. No separate veteran characteristics were reported, making generalisability to other veteran populations uncertain. The authors’ conclusion suggests that CPT may be effective in vulnerable groups, but the quality of evidence is low. The authors’ tentative conclusion seems reliable and is consistent with results from the limited data presented for military veterans. Future research aims included incorporating quality-of-life outcomes as well as investigating combinations of therapy.
A review by Bisson et al. 66 provided single-study data for EMDR and TFCBT in comparison with waiting list. EMDR was reported to significantly reduce PTSD symptoms as rated by a clinician (one RCT, 25 participants), while TFCBT showed no significant difference compared with waiting list (one RCT, 24 participants). Both findings were based on small samples of male Vietnam veterans in their mid-thirties to early forties and should be considered with caution because of the nature of single-study data. The conclusions indicated that, although TFCBT and EMDR appeared effective generally, they were less so for veterans. Future research should focus on more direct comparisons between treatments. The authors did not report the results of the quality assessment of primary studies, making it difficult to assess the reliability of the conclusions.
Goetter et al. 67,68 included psychosocial interventions featuring PE, CPT and exposure therapy in outpatient settings. Within the included studies, there were few females; there was some representation of ethnic minority groups and participant age ranged from mid-twenties to early forties. Veterans had served in different conflicts including OEF (Operation Enduring Freedom), OIF and Operation New Dawn, and 18.3% of participants were still on active service. Dropout varied between research setting (clinical care and clinical trials), with trials experiencing less attrition, although the difference was not statistically significant. When comparing treatment format, a greater likelihood of dropout was found in group therapy settings rather than in individual therapy settings. Although there was a high level of statistical heterogeneity and clinical heterogeneity (particularly in clinical care) in these studies, it suggests that clinical care showed greater dropout than clinical trials, which the authors suggested was because clinical trials provided free treatment, support staff were motivated to retain participants and participants were motivated for treatment, having completed pre-screening. Conclusions suggest that use of individual therapy may encourage treatment completion. Overall, the cautious conclusions are within the limitations of the study. Inconsistencies in figures presented, as well as the lack of quality assessment and high degree of heterogeneity, give rise to concerns about bias and lack of reliability. It is also reported that 15% of participants were at the subclinical threshold for PTSD, which may limit generalisability to other veteran populations.
Pharmacotherapy interventions
Puetz et al. 71 reviewed pharmacotherapy interventions including selective serotonin reuptake inhibitors (SSRIs) (such as fluoxetine and sertraline), antidepressants (such as nefazodone and amitriptyline), antipsychotics (risperidone) and anticonvulsants (such as divalproex) (Table 12). All drug groups were found to reduce PTSD, anxiety and depression symptom severity with moderate effect size. The results were based on 18 studies (773 participants) that included predominantly male participants from Vietnam, Europe and other conflicts, with an average age of 47 years. The authors suggested that this supports the use of pharmacotherapy [in particular SSRIs and tricyclic antidepressants (TCAs)], which showed the largest effect size in reduction of PTSD symptoms. The reliability of the review is affected by moderate to substantial statistical heterogeneity; in addition, the meta-analysis methodology was not clearly reported and may have involved undue weighting of trials with multiple outcomes. Although study quality was assessed, the authors did not apply this to the synthesis, making it difficult to judge the reliability of the evidence.
| Study details (first author) | Veteran characteristicsa | Intervention(s) (and comparators when reported) | Outcomes and measures | Authors’ conclusions and summary of results (including cost-effectiveness when reported) | Commentary |
|---|---|---|---|---|---|
|
Puetz, 201571 Study designs: 18 RCTs Countries: USA, n = 16; Europe, n = 1; Israel, n = 1 Date range of studies: years of publication from 1988 to 2013 |
Included US Vietnam veterans, US mixed-conflict veterans, European veterans and Israeli veterans | Pharmacotherapy reduces PTSD, anxiety and depression symptoms among veterans with PTSD, with moderate but significant therapeutic effects. The results support the use of pharmacotherapy as concurrent treatment for combat-related PTSD, particularly SSRIs and TCAs, to alleviate symptoms. Future research should consider novel class treatments and concurrent assessment of related symptoms | The authors clearly defined the review question and selection criteria, with a comprehensive search. Included study characteristics were clearly described and stratified by outcome. Authors reported a quality assessment, however, this was neither described nor interpreted; the quality rating presented in the characteristics table was not used in the synthesis, lending uncertainty to the quality of the included RCTs. The authors did report varying heterogeneity in outcomes, which indicates a lack of reliability. The methods used to conduct the meta-analyses were not clearly reported, but may have involved undue weighting of trials with multiple outcome measures. This will limit the reliability of the review | ||
| Mean age 47.3 (SD 7.8) years, 98.3% male | Pharmacotherapy interventions including SSRIs (such as fluoxetine and sertraline), TCAs (such as nefazodone and amitriptyline), antipsychotics (risperidone), anticonvulsants (such as divalproex) and novel class drugs | PTSD symptom severity most frequently measured by CAPS and CGI-S | Reduced PTSD symptom severity following pharmacotherapy effect size = 0.38 (95% CI 0.23 to 0.52), not consistently found across studies (I2 = 66.7%). Larger effects were seen for SSRIs and TCAs (effect size = 0.63, 95% CI 0.48 to 0.78) than all other drug therapies (effect size = 0.10, 95% CI –0.05 to 0.25). Results based on 18 studies, 50 effects, n = 773 | ||
| Mean age 47.7 (SD 8.7) years, 98.6% male | Anxiety symptom severity most frequently measured by HAM-A and BAI | Reduced anxiety following pharmacotherapy effect size = 0.42 (95% CI 0.30 to 0.54), found with moderate consistency across studies (I2 = 40.9%). Results based on 6 studies, 28 effects, n = 365 | |||
| Mean age 47.1 (SD 8.8) years, 98.2% male | Depression symptom severity most frequently measured by MADRS and HAM-D | Reduced depressive symptoms following pharmacotherapy with effect size = 0.52 (95% CI 0.35 to 0.70), effect not found consistently across studies (I2 = 76.8%). Results based on 10 studies, 40 effects, n = 550 |
Psychosocial and pharmacological interventions
Stewart and Wrobel72 investigated both psychosocial and pharmacotherapy interventions (Table 13). Most of the participants in the review were veterans of Vietnam, and the remainder were veterans of Croatia and Gulf Wars; no further participant details were reported. The psychosocial interventions studied included CPT, stress management and trauma-focused interventions. The results showed a small decrease in PTSD immediately post treatment (based on nine studies, 1134 participants). A small decrease in depression symptoms was reported immediately post treatment (number of studies and participants was unclear).
| Study details (first author) | Veteran characteristicsa | Intervention(s) (and comparators when reported) | Outcomes and measures | Authors’ conclusions and summary of results (including cost-effectiveness when reported) | Commentary |
|---|---|---|---|---|---|
|
Stewart, 200972 Countries: NR Number of studies in review and designs: 24 studies; study designs NR Date range of studies: publication dates from 1988 to 2006 |
22 studies on Vietnam veterans (up to 25–30 years post combat), other studies on Gulf War veterans (10–15 years post combat) and Croatia veterans (5–10 years post combat) | Conclusions suggest that both pharmacotherapy and psychological interventions reduce both PTSD and depression symptoms in veterans with PTSD. The authors appear to conclude that pharmacotherapy resulted in a greater reduction in PTSD symptoms than psychotherapy in a comparable time frame. Suggestions for future research highlight the need for research in effectiveness of combined therapies that are generalisable to veterans of Iraq and Afghanistan |
The review question was clearly defined and supported by appropriate inclusion criteria, although these were broad for study design and outcomes. The literature search was somewhat limited and was restricted to publications in English, so potentially relevant studies may have been missed. The authors did not state the designs of the included studies and did not state that validity was assessed, which means that the quality of the included studies was unclear. The authors did not state whether or not each stage of the review process was undertaken in duplicate and so reviewer error and bias could not be ruled out. Assumptions of normality and homogeneity of variance were confirmed, but the authors acknowledged that there was variability between study populations and methods and this may have limited the applicability and generalisability of the results. The authors acknowledged the inclusion of a number of patients in the psychotherapy studies who received concurrent pharmacotherapy. They acknowledged that most studies were of populations who had not seen combat for as many as 25 to 30 years, and follow-up was only short term. Sample characteristics were unclear and, therefore, extrapolating conclusions to a specific population is not possible. It was unclear how many studies were included in the analysis of depressive symptoms and how many participants were involved. No direct comparisons between pharmacotherapy and psychotherapy were undertaken Potential for bias in the review, uncertain quality of the included studies and indirect comparison of pharmacotherapy and psychotherapy interventions suggest that the authors’ conclusions should be treated with caution. The recommendation for further research seemed appropriate |
||
| Pharmacotherapy (three TCAs, two MAOIs, three antipsychotics, two serotonergic agents, one anticonvulsant, one SSRI; drugs included risperidone, fluoxetine and imipramine) | PTSD symptoms measured most commonly by CAPS and IES | Results showed a decrease in PTSD symptoms with MD –1.00 (SD 0.46) immediately post treatment. Results based on 11 studies, n = 286 | |||
| Depression symptoms measured most commonly by HAM-D | Results showed a decrease in depression symptoms with MD –0.70 (SD 0.47) immediately post-treatment | ||||
| Psychotherapy (including cognitive processing, time limited, group based, person centred, understanding PTSD, stress management, anger management, Transcend, trauma focused, trauma management) | PTSD symptoms measured most commonly by CAPS and PCL-M | Results showed a decrease in PTSD symptoms with MD –0.52 (SD 0.39) immediately post-treatment. Results based on nine studies, n = 1134 | |||
| Depression symptoms measured most commonly by BDI | Results show a decrease in depression symptoms with MD –0.32 (SD 0.25) immediately post-treatment | ||||
| Pharmacotherapy versus psychotherapy (above categories compared in aggregate) | PTSD symptoms (as previous) | Pharmacotherapy produced a statistically significantly greater decrease in PTSD symptom change from baseline than psychotherapy [p = 0.01, t(22) = –2.74, d = 0.05]. Adjusting for length of time indicated the rate of change in PTSD symptoms as a function of time was significantly different between groups (p = 0.02), with pharmacotherapy having an expected symptom change –0.48 lower than psychotherapy at 1 month | |||
| Depression symptoms (as previous) | Pharmacotherapy produced a statistically significantly greater decrease in depression symptom change from baseline than psychotherapy [p = 0.04, t(15.77) = –2.26, d = 0.16]. Adjusting for length of time indicated the rate of change in depression symptoms as a function of time was marginally significant between groups (p < 0.10). This was also indicated by a random coefficient model |
This review also found evidence in favour of pharmacotherapy. The studies in the review most commonly featured TCAs and antipsychotics (drugs included risperidone, fluoxetine and imipramine) and found a small decrease in both PTSD (based on 11 studies, 286 participants) and, to a lesser extent, depression symptoms immediately post treatment (number of studies and participants was unclear). The authors’ conclusions suggested pharmacotherapy to be an effective treatment for PTSD symptom reduction.
The authors also performed an indirect comparison of the psychotherapy and pharmacotherapy results. The comparison found a statistically significantly greater reduction in PTSD symptoms among pharmacotherapy studies. Further to this, the rate of change in PTSD symptoms over time was seen to be significantly different, with pharmacotherapy studies having an expected symptom change lower than psychotherapy studies at 1 month. Pharmacotherapy studies also produced a greater decrease in depression symptoms than psychotherapy studies over the same period of time, but this difference was not statistically significant.
The authors conclude that pharmacotherapy and psychological interventions independently reduce PTSD and depression symptoms in veterans with PTSD. They also conclude that there is a need for more research into the effectiveness of combined therapies that are generalisable to veterans in Iraq and Afghanistan. Potential biases in the conduct of the review, the uncertain quality and design of the included studies and the fact that the comparison of pharmacotherapy and psychotherapy interventions was indirect suggest that the authors’ conclusions should be treated with caution. Recommendations for further research seem appropriate.
Summary of stage 3 results
The rapid metareview identified seven systematic reviews of varying quality and there were potential biases in reporting or conduct across the reviews. Many reviews lacked quality assessment of primary studies and reporting of outcomes, measures and participant characteristics. The lack of transparency in the reporting of the reviews means that it is unclear whether or not this is the result of an absence of reporting in the primary studies. However, when reported, the quality of the included studies was low. Reviews that include few veteran studies or only single-study data present a problem with bias and reliability and interpretation of findings. Despite methodological issues, there appears to be a broad consensus across the reviews on the effectiveness of treatments, both psychosocial and pharmacological.
Psychosocial interventions were grouped quite broadly, with EMDR and CPT among some of the most commonly featured, alongside trauma based and exposure focused. It is arguable that, despite subgrouping, there was a large overlap between the included interventions of each review. The evidence suggested that psychosocial interventions may be somewhat effective in reducing PTSD symptoms in veterans, while use of individual therapy may help reduce dropout. Further research into reasons why dropout may occur and patient-relevant outcomes (such as quality of life) may inform enhanced practice and provide greater context. Reviews seemed to lack clinical implications, which may be as a result of the limitations of the primary evidence, an important element for understanding generalisability across populations and settings.
Pharmacological interventions were also broadly grouped. Large samples were presented here, supporting the use of pharmacotherapy, with authors often recommending this in adjunct to psychosocial therapy. It is suggested that pharmacotherapy offers a more rapid improvement of symptoms, although there is no evidence of its use in combination with psychotherapy in the reviews presented here; hence this is commonly featured as a research recommendation.
In conclusion, psychosocial and pharmacotherapy treatments may be individually effective in veteran populations for reduction of PTSD symptoms. In particular, CPT and pharmacotherapy are highlighted (although evidence was limited on specific drugs). Limitations of the evidence base preclude more specific conclusions.
Acceptability and adverse events are unknown. Individual settings may reduce dropout compared with group settings, based on poor-quality evidence.
Research implications arising from the literature
Based on the findings of this rapid metareview and recommendations of the included reviews, it is suggested that future research should focus directly on veteran populations with a broader range of outcomes. No data regarding satisfaction, access or uptake across subgroups were found, and this should also be considered. The review authors’ recommendations for future research include more direct comparisons between psychological treatments66 and validation of treatments in practice, as well as use of outcome data from existing programmes. 69 Others indicated a need for a greater variety of outcome measures, such as adverse events, tolerability, cost-effectiveness,70 quality of life and remission rate. 73 Following the indirect comparison of therapies, a suggestion for more research into combined therapies was presented, as well as research that is generalisable to veterans of Iraq and Afghanistan. 72 Finally, a suggestion for future research into therapies in shorter time frames was made by Goetter et al. ,67 although it is unclear if this was based on the evidence in the review.
Stage 4: synthesis
In this section, we bring together findings from three stages of our rapid evidence synthesis on the provision of services in the UK for UK armed forces veterans with PTSD.
In stage 1, our overview of current service delivery arrangements (models of care) across the UK showed a range of activity across NHS and third-sector settings. There has been little formal evaluation of this activity. We examined information received from service providers to develop a coding framework to support subsequent work as follows: (1) to help organise the evidence in our review of effectiveness on models of care and (2) to explore links between current UK practice, and potentially effective treatments and models of care in the literature.
The reliability of findings from our evidence review on models of care in stage 2 was limited as a result of methodological weaknesses in the primary research study designs. The small collection of more robust evidence did, however, indicate some promising associations between popular models of care in UK practice and those identified in the research literature. For example, the potential effectiveness of collaborative care arrangements was supported by a RCT looking at a programme of education and support involving primary care clinicians and staff across multiple sites;37 integrated care (including specialist provision for veterans within general mental health services) showed promise in another RCT evaluating integrated smoking cessation treatment within mental health care;38,39 support for interventions delivered beyond the clinical setting was indicated in a study of community outreach;40 and peer support was viewed as a potentially acceptable complement to other PTSD treatments in one qualitative study. 41 The less methodologically sound study designs also indicated potentially effective care arrangements that are currently provided in practice, but reliable conclusions cannot be drawn from these studies. These arrangements included integrated care, partnership working, networks and co-located services;35,44,49–53,62,63 settings-based models;36,45–47,56,64,65 peer support;58–61 and multicomponent programmes (including behavioural interventions). 54,55,57
A family systems model reported in a less robust study design48 was not seen in the information we received on current UK practice. Conversely, other arrangements reported in practice (such as IAPT, prison inreach, case management, stepped care, early intervention and crisis management) were not represented in the literature.
Stage 3 revealed limited evidence to populate our metareview on treatments, and the reliability of the evidence was generally unclear. This was as a result of poor reporting or conduct of the included systematic reviews, often insufficient detail to determine the quality of primary research and the reporting of aggregate data, making it difficult to provide any meaningful interpretation. Tentative links could be drawn between treatments currently delivered in UK practice and those considered potentially effective in the research literature. In particular, psychosocial interventions (such as EMDR, CPT, TFCBT and exposure-based therapies) delivered in practice were supported by reviews. 66,69,70,72,73 One review67,68 suggested that individually delivered psychosocial therapy may be preferable to group therapy in reducing risk of intervention dropout. Types of pharmacotherapy delivered in UK practice were not well documented in the information offered by service providers. Findings from the metareview suggest general support for the use of SSRIs, TCAs and antipsychotics. 71,72 Other interventions offered in UK practice, such as counselling, art therapy and an intervention based on human givens therapy,31 were absent in our metareview of treatments.
We did not find any evidence, across our overview of current practice and reviews of evidence, to suggest which treatments might most effectively be delivered within which models of care. Largely, this was due to lack of reporting on care delivery settings and contexts in the metareview of treatments.
Similarities between our review of effectiveness on models of care and the metareview on treatments included geographical focus (when reported) being primarily in the USA. Veteran populations in both strands of evidence tended to be older males from the USA who had served in the Vietnam or Iraq wars, although limited detail was generally reported on veteran characteristics. These aspects raise the question of generalisability of this literature to UK veterans in the NHS setting.
Clear differences were noted across the review and metareview. Outcomes in the more robust research from the review of models of care focused on intervention access and uptake, behaviour change and patient satisfaction, but there was little evidence on clinical outcomes. Conversely, the metareview of treatments concentrated entirely on clinical outcomes, primarily PTSD and other mental health problems, such as depression and anxiety. Various outcome measures were used, with little consistency.
Implications for practice and research arising from the three stages of our review are as follows.
-
Practice:
-
the provision of adequate funding and resources to deliver future services
-
address various challenges (outlined in stage 1) emanating from the current wider system of care
-
understand more clearly the complexities of the target population and take account of veterans’ views and needs in future service design.
-
-
Research:
-
more research relevant to the UK setting
-
routine and continuous evaluation of interventions in practice
-
for models of care:
-
more robust research on models of care, with longer follow-up
-
explore a wider range of outcomes including: process (intervention uptake), clinical, patient satisfaction, social functioning, quality of life, disparities in age-related treatment effectiveness, improving access to services by minority populations and cost-effectiveness
-
more research on the format and structure of group peer support and peer support by telephone outreach.
-
-
for treatments:
-
use of direct treatment comparisons
-
investigate the effectiveness of combined therapies (e.g. pharmacological and psychosocial)
-
explore outcomes such as tolerability (including reasons for dropout) and adverse events, quality of life and cost-effectiveness
-
evaluate treatments in veterans from a wide range of conflicts and settings
-
improve the methodological rigour of systematic reviews (including primary study quality assessment).
-
-
Discussion and conclusions
In this final section, we recap on the findings. We draw on public and patient involvement and we offer conclusions from this rapid evidence synthesis. In particular, use of our overview of current UK practice and two rapid evidence reviews helped us to highlight the most promising models of care and treatments for UK armed forces veterans with PTSD. We also summarise the strengths and limitations of our synthesis and of the underlying research that was used to inform its findings. Finally, we present the implications for future health-care practice and for research.
The background to our research arose from current thinking about anticipated rises in demand for psychological trauma services in the UK, with particular reference to armed forces veterans with PTSD. 4 In 2014, there were 2.8 million ex-service personnel in the UK, and it was envisaged that requirements for specialist support would grow as a result of armed forces restructuring and ever more complex needs arising from recent conflicts. 5,6
Needs assessments commissioned by the Forces in Mind Trust74 across England, Wales, Scotland and Northern Ireland established key factors when planning future services for veterans and their families. 23–25 (The review for Northern Ireland was published in May 2017 and did not form part of our analysis. 26) Issues for veterans in Wales and Scotland resonate with three suggested building blocks for future service planning in England, which are: (1) targeted and intelligent use of data and information, (2) implementation of appropriate and sensitive evidence-based services and (3) involvement of veterans and family members. 23
The strategic review of future commissioning for armed forces and their families,16 and the recent NHS England publication of stakeholder views on the 12 specialist mental health services provided for veterans since 2010,17,18 offered further background to our research.
Public and patient involvement
As described in Chapter 2, Public and patient involvement, the short timescale for this project inspired us to seek efficient ways to gather relevant and helpful service user representation to help contextualise our findings. Given that the NHS England stakeholder engagement survey18 (mentioned previously in Discussion and conclusions) focused entirely on views and experiences connected to the present 12 specialist services in England, we considered this a suitable starting point. In the final stages of compiling our report, we drew further insights from a veteran who was recommended to us by one of our expert advisors.
NHS England stakeholder engagement survey: summary of findings relating to veterans
NHS England survey respondents were largely white male veterans aged between 41 and 65 years, and who had previous service in the army. Almost two-thirds of respondents had experienced a mental health problem and some had clearly suffered PTSD, although exact numbers were unclear.
The findings of surveys of veterans who had not yet begun treatment revealed a general lack of awareness (on the part of both patients and GPs) about the availability of the 12 specialist services. Despite this, veterans noted a reluctance to seek help, often because of fear of their condition being misunderstood. They also anticipated problems with being pushed around a poorly co-ordinated system. Difficulties with access (waiting lists and obtaining appointments), continuity of care (including transfer of medical records) and lack of funding were also cited. Early intervention before leaving the armed forces, including advertising of services and adequate health screening prior to discharge, was seen as a way to improve transition to civilian life. Veterans already receiving treatment apparently did so using a combination of NHS and specialist services (though not always one of the 12 providers under review), including those provided by the third sector. In general, patients perceived greater benefits from specialist services than those provided in NHS mainstream settings. Although the above matters were raised only in the context of services provided in England, many of the issues mirrored those raised in the needs assessments of veterans and their families carried out in Scotland and Wales. 24,25 This indicates a consistent pattern of veterans’ mental health-care needs across the UK, with the exception of Northern Ireland, where data are (as yet) unavailable. Veterans’ views about services in England were also reflected in factors affecting service implementation communicated to us by some current UK service providers (e.g. lack of knowledge in primary care about the complex needs of veterans, and the challenges of poorly co-ordinated care).
Views from a veteran and service user
We were fortunate to obtain the views and comments of a veteran and service user on the first draft of our report. Lieutenant Colonel (retired) John Skipper, an army veteran with 35 years’ military service, provided advice and input into the interpretation of our research findings. We drew on John’s account of deployments in worldwide conflicts (including the Falklands, Northern Ireland and Bosnia) and from reflections on his engagement with UK health services following a diagnosis of PTSD. 75,76
He considered our work to be a timely and relevant contribution to current research and practice in the topic area. Indeed, many of his observations resonate with our background research and interpretation of the evidence presented at stages 1, 2 and 3 of this rapid evidence synthesis.
Our reflections on complexities of the veteran population chimed with John’s. The influence of stigma (particularly relevant for veterans living in deprived communities, in his view), reticence to seek help and associations with complex presentations of PTSD compounded by comorbidities (such as substance misuse and criminal activity) were significant. John drew our attention to personal experience of time lapse between his trauma and presentation of PTSD, supporting the case for pre-emptive intervention early in the transition from military to civilian life.
Peer support had featured prominently in John’s military career, and its identification as an area of focus early in our research was welcomed by him. He also considered the intervention to be temporally relevant, especially given the present economic challenges in providing more resource-intensive therapies. John reminded us of the changing nature of conflict and how much additional learning might be gained from conflicts of higher intensity such as the Falklands, Iraq, Afghanistan, Bosnia, Northern Ireland and Sierra Leone, and from the continued effects of world-wide terrorism. We had already gleaned from stages 2 and 3 a clear need for more research in other conflicts and settings.
John tabled a possibility that the inconsistent national picture of service provision we found in stage 1 may (in part) be a consequence of devolved health care and consequent variations in practice. The extensive services provided by third-sector organisations are, in his view, a vital complement to those from the NHS; however, lack of evaluation and the need for proper regulation would be critical to assure future best practice. He expressed particular concern about the potential danger of non-evidence-based treatments, especially in undiagnosed patients. We gathered from John’s feedback that a mental health service provided uniquely for veterans may not be paramount. Furthermore, with appropriate training of clinicians and proper signposting, all accredited mental services should have the capacity to treat veterans, and important learning from this may ultimately also benefit civilians who experience trauma. This view is, to some degree, at odds with feedback from the NHS England engagement survey,18 in which some veterans favoured specialist services over mainstream NHS provision.
Our approach to appraising the evidence on models of care in stage 2 (i.e. summarising, rather than labouring over the less methodologically sound study designs) was viewed as refreshing and distinct from other research reports John had reviewed. He was encouraged by some of the best evidence presented, namely the identification of peer support as a potentially effective adjunct to treatment, the essential multidisciplinary approach to address PTSD, and indications that low-intensity interventions closer to home may represent the most promising help.
In relation to treatments, John stressed the importance of delivering complementary treatment plans to patients, stating that pharmacological solutions alone are too often applied in practice without proper attention to the complexities of PTSD and full understanding of the veteran patient. This feedback supported our research implications in stage 3 for the future evaluation of combined psychological/pharmacological interventions. His comments also supported research indications for future direct treatment comparisons (such as CBT and EMDR). In terms of future developments, John alerted us to an ongoing RCT focusing on 3MDR (Military Motion-Assisted Memory Desensitisation and Reprocessing) – a new psychosocial therapy for PTSD funded by the Forces In Mind Trust, the University of Cardiff and Veterans NHS Wales.
Our implications for practice were viewed as appropriate and timely. In John’s view, our findings signify the need for a consistent, properly resourced, well-signposted, multidisciplinary UK-wide approach based on best practice complicit with the Armed Forces Covenant.
The present context
Since the introduction of the Armed Forces Covenant1 (designed to promote fairness and equity for the armed forces community in respect of access to public services), implementation of this formal promise across the UK is seemingly inconsistent; consequently, the pressing need for strengthened relationships between local councils and relevant agencies has been reinforced. 77
In addition to this, commissioning and service provider activity to improve veterans’ health continues to gather pace. As an example from somatic care, November 2016 saw the launch of a new Veterans Trauma Network to deliver comprehensive medical care. 78 Following the NHS England strategic review16 and stakeholder engagement findings,17,18 new contracts for specialist veterans’ mental health services in England are due to commence in April 2017. All this points to encouraging developments to help meet the complex health needs of veterans. Given the anticipated increased demand for services, detailed information available on veterans’ needs and refreshed commissioning activity in 2017, our research is timely.
In this rapid evidence synthesis, we answered our four research questions as follows.
Research question 1: what services are currently provided in the UK for UK armed forces veterans with post-traumatic stress disorder?
We examined information on current activity provided to us by the 12 specialist mental health service providers in England,17 and material from organisations known to us in Scotland, Wales and Northern Ireland (see Appendix 4). Our information-gathering exercise showed a range of services being delivered to veterans, often via partnerships between the NHS and third sector, and facilitated by various models of care. Findings reveal that collaborative arrangements are commonplace, as are partnerships and networks. Pockets of integrated care are evident (e.g. general mental health services with embedded specialist care, or alongside a behavioural intervention); community outreach and peer support also featured. Not all models of care in UK practice appeared in the literature that we subsequently included to address research question 2.
Research question 2: what is the evidence of effectiveness of models of care for UK armed forces veterans with post-traumatic stress disorder, including impact on access, retention, clinical outcomes, patient satisfaction and cost-effectiveness?
The 61 included articles provided a much wider than anticipated evidence base. We focused our analysis on 24 studies (in 29 articles) looking at ‘systems-based’ models of care. Research was situated largely in the USA and on male veterans in the VA setting. Therefore, the generalisability of models of care in the literature to the UK setting and to female veterans is uncertain. The most promising evidence supports the potential effectiveness of collaborative care arrangements (education and support for primary care clinicians and staff across multiple sites)37 and community outreach (a proactive mailed intervention to patients with telephone follow-up)40 for improving intervention access and uptake, integrated care (including smoking cessation treatment for veterans within general mental health services) for increased smoking abstinence, but with no effect on PTSD symptoms,38,39 and peer support41 as an acceptable complement to other PTSD treatments. All these broad types of delivery were seen in our overview of current UK practice. Some of the outcomes measured in the better-quality evidence (e.g. smoking abstinence) may not directly reflect priorities in practice. The remaining studies meeting our inclusion criteria employed designs that are considered methodologically weak. In these studies, multicomponent programmes and settings-based delivery (e.g. primary care, residential care) featured prominently and clinical outcomes were measured more frequently than in the more robust designs. Good-quality research is needed to substantiate any tentative associations arising in these studies.
Research question 3: what treatments show promise for UK armed forces veterans with post-traumatic stress disorder?
The conclusions from our metareview of treatments are restricted by methodological limitations in the seven included systematic reviews, the poor or uncertain quality of the underlying primary research and a lack of clinically meaningful data from which to extrapolate for practice. This means that further robust research is needed to substantiate any tentative conclusions. Although this result is disappointing, ongoing research on treatments for PTSD and complex trauma more generally14,15,79 should extend and enlighten our findings. In the meantime, our metareview suggests that the potentially effective types of treatment currently delivered in practice for reducing clinical symptoms in veterans with PTSD are psychosocial in nature (e.g. EMDR, CPT, TFCBT and exposure-based therapies)66–70,72,73 and pharmacotherapy (e.g. SSRIs, TCAs, anticonvulsants and antipsychotics). 71,72 Other treatments currently delivered in practice, such as counselling and art therapy, were not examined in the systematic reviews included in our metareview.
In conclusion, our rapid evidence synthesis shows tentative support for some models of care and some treatments currently being delivered in UK practice. These are shown in Box 1.
Cost-effectiveness
There was no clear evidence on the cost-effectiveness of models of care or of treatments.
Research question 4: what are the high-priority areas for further research?
A number of implications for research arose from our rapid evidence synthesis as follows.
General
-
More research relevant to the UK setting.
-
Routine and continuous evaluation of how interventions work in practice.
For models of care
-
More robust research on models of care, with longer follow-up.
-
Explore a wider range of outcomes, including process outcomes (intervention uptake), clinical, patient satisfaction, social functioning, quality of life, disparities in age-related treatment effectiveness; improving access to services by minority populations; and cost-effectiveness.
-
More research on the format and structure of group peer support.
-
More research on peer support using telephone outreach.
For treatments
-
Use of direct treatment comparisons.
-
Investigate the effectiveness of combined therapies (e.g. pharmacological and psychosocial).
-
Explore outcomes such as tolerability (including reasons for dropout), adverse events, quality of life and cost-effectiveness.
-
More evaluation of treatments in veterans from a wide range of conflicts and settings.
-
Improve the methodological rigour of systematic reviews (including primary study quality assessment).
-
Report clinically meaningful data.
Implications for health-care practice
We draw specifically here on our summary of public and patient involvement and from factors affecting implementation reported to us by service providers in the UK. Together, these suggest that future practical arrangements to improve veterans’ mental health might helpfully focus on:
-
early intervention to improve transition from military to civilian life
-
improving knowledge and awareness of specialist services available to veterans among primary care (especially GPs) and general mental health services
-
understanding more clearly the complex needs of veterans and account for veterans’ views by involving them in future service design
-
addressing challenges for veterans presented by the wider system of care
-
the provision of adequate funding and resources to deliver future services.
Strengths and limitations of this rapid evidence synthesis
This rapid evidence synthesis was carried out over a short timescale. It provides an overview of current UK practice and highlights the most promising models of care and treatments for UK armed forces veterans with PTSD.
Importantly, this review offers a timely update to commissioners and service providers as they continue to shape the suite of activity for veterans’ health care in the UK. We are confident that our overview of current practice provides sufficient representation across the UK, although accounts of veterans’ needs and the full complement of services within Northern Ireland are less comprehensive than for other countries.
In our reviews of effectiveness, every attempt was made to retrieve all major sources of evidence. The most relevant databases and websites, containing UK and international research relating to veterans’ health, were prioritised for searching. As a result of time constraints in this rapid evidence synthesis, we focused our literature searches carefully, specifically in relation to population group. We acknowledge that relevant evidence may be available from wider literature on armed forces health services and on PTSD/mental health services in general.
The search strategies for both reviews were maximised for sensitivity, as for a full systematic review (see search strategies in Appendix 2). However, for the stage 3 review (on treatments), broad reviews on interventions for PTSD that did not mention veterans or synonyms for veterans in the titles, abstracts or subject headings of the database records would not have been identified by the searches.
For the stage 2 review, we acknowledge the inherent difficulties in defining a ‘model of care’. To help steer our work, we adopted a broad working definition. Using this definition, a comprehensive list of possible search terms for models of care was drawn up by the project team to try to capture the wide variety of models, approaches and ways of delivering care used in the literature. However, there remains the possibility that some terms for models of care that were not known to the project team could have been missing from the search strategy.
The pool of literature on this topic was much larger than originally anticipated. Overall, evidence for potentially effective models of care and treatments is limited in quality and quantity. The magnitude of poorer-quality study designs returned by our searches meant that we needed to take a pragmatic approach to assessment and reporting. When selecting studies for our reviews of effectiveness, we needed to deal with inconsistent terminology, particularly regarding veterans and models of care. This made it difficult, on occasion, to decide on the eligibility of studies for inclusion. To mitigate this, such cases were discussed fully to ensure that consistent judgements were made and steps were taken to help ensure consistent reporting in our work wherever possible. When there was doubt about the value of a study, it was not included. The rapid time frame for the review meant that the detail of some studies was summarised rather than fully documented.
The development of a coding framework to describe models of care, and the subsequent distinction between system-based models and narrower-focused delivery mechanisms, helped us to organise the evidence in a systematic way. As these codes were grounded in the information we received on current UK practice, their subsequent application to help structure our findings and interpretations provides a high level of integrity to our research.
Despite the speed of the process, this rapid evidence synthesis is built on strong foundations. A systematic approach, with clear search strategies, fully documented inclusion and exclusion criteria, decision-making by more than one member of the research team, and appropriately detailed data extraction and quality assessment provides confidence that our conclusions are firmly rooted in the best evidence available. Our interpretation of review findings is strengthened by our decision to draw on relevant recently published public and patient involvement data; expert advisors with academic, military and service commissioning backgrounds; and insights from an armed forces veteran with experience in research methods.
Acknowledgements
We are grateful to all the organisations listed in Appendix 4 that helped us explore current service provision in the UK for armed forces veterans with PTSD.
Contributions of authors
Jane Dalton (Research Fellow, Evidence Synthesis) drafted the protocol and carried out study selection, data extraction, critical appraisal and write up of the report.
Sian Thomas (Research Fellow, Evidence Synthesis) carried out study selection, data extraction, critical appraisal and write up of the report.
Hollie Melton (Research Training Fellow in Systematic Reviews) carried out study selection, data extraction, critical appraisal and write up of the report.
Melissa Harden (Information Specialist) conducted all searching, wrote the search sections of the report and commented on the draft report.
Alison Eastwood (Professor, Evidence Synthesis) oversaw the project, contributed advice and expertise and commented on all drafts of the report.
All authors commented on the protocol.
External advice
We offer our appreciation to Andy Bacon [Lead (Assistant Head) Armed Forces Central Team (NHS England)] for his advice at the early stages of our work and for his comments on the first draft of the report; Professor Jonathan Bisson (Division of Psychological Medicine and Clinical Neurosciences, University of Cardiff) for his advice at the early stage of our work and for helping us to identify suitable public and patient involvement; Dr Charlotte Gath (Consultant in Public Health, Public Health Warwickshire) and Emily Fernandez [Commissioning and Performance Lead (Wider Determinants), Public Health Warwickshire] for their insights from a public health perspective; Professor Neil Greenberg (Professor of Defence Mental Health, King’s College London) for his assistance at the early stages of our work; and Professor Ian Watt (Professor of Primary and Community Care, University of York) for his comments on the first draft of our report.
Our sincere thanks and appreciation are also given to Lieutenant Colonel (retired) John Skipper (army veteran and service user) for his detailed comments on our draft report, for sharing his experiences with us and for helping to provide validation to our interpretation of the findings.
We sought to consult with representatives from other agencies to help us gather further information on the UK public health context, service provision in Northern Ireland and implementation issues regarding the Armed Forces Covenant. These attempts were unsuccessful.
Data sharing statement
All available data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Ministry of Defence . Armed Forces Covenant 2016. www.gov.uk/government/publications/armed-forces-covenant-2015-to-2020/armed-forces-covenant (accessed 25 November 2016).
- Iversen AC, van Staden L, Hughes JH, Greenberg N, Hotopf M, Rona RJ, et al. The stigma of mental health problems and other barriers to care in the UK Armed Forces. BMC Health Serv Res 2011;11. https://doi.org/10.1186/1472-6963-11-31.
- The Five Year Forward View for Mental Health. Leeds: NHS England; 2016.
- Scope to Be Discussed With Evidence Synthesis Team: HS&Amp;DR Project Briefing Document October 2016 2016.
- NHS Healthcare for Veterans. Department of Health and Social Care; 2015.
- Pozo A, Walker C. UK Armed Forces Charities. An Overview and Analysis. London: Directory of Social Change; 2014.
- Developing Mental Health Services for Veterans in England. Oxford: NHS England; 2016.
- Code of Federal Regulation. 38 Parts 0 to 17. Pensions, Bonuses, and Veterans’ Relief. Washington, DC: Office of the Federal Register, National Archives and Records Administration; 2008.
- NHS Choices . Post-Traumatic Stress Disorder (PTSD) 2015. www.nhs.uk/Conditions/Post-traumatic-stress-disorder/Pages/Introduction.aspx (accessed 18 October 2016).
- Bacon A. NHS England 2016.
- Greenberg N. London: King’s College; 2016.
- Coventry P. Centre for Reviews and Dissemination 2016.
- US Department of Veterans Affairs . Complex PTSD 2016. www.ptsd.va.gov/professional/PTSD-overview/complex-ptsd.asp (accessed 18 October 2016).
- Post-Traumatic Stress Disorder: Management. London: NICE; 2005.
- National Institute for Health Research (NIHR) Evaluation, Trials and Studies Coordinating Centre . HTA - 16 11 03: INterventions for Complex Traumatic Events: INCiTE 2017. www.journalslibrary.nihr.ac.uk/programmes/hta/161103/#/ (accessed 1 March 2017).
- Ling A. Armed Forces and their Families Commissioning Intentions – 2016/17. Leeds: NHS England; 2016.
- Developing Mental Health Services for Veterans in England. List of the 12 Mental Health Services. Leeds: NHS England; 2016.
- Developing Mental Health Services for Veterans in England Engagement Report. Leeds: NHS England; 2016.
- Citizens Advice . Healthcare for People Injured in the Armed Forces and Veterans n.d. www.citizensadvice.org.uk/healthcare/armed-forces-and-veterans/healthcare-for-people-injured-in-the-armed-forces-and-veterans/ (accessed 8 November 2016).
- Scottish Government . Have You Served Your Country? Taking Care of Veterans 2008. www.gov.scot/Publications/2008/04/30100639/1 (accessed 8 November 2016).
- Aftercare Service . UDR and R IRISH (HS) Aftercare Service n.d. www.aftercareservice.org/ (accessed 8 November 2016).
- Veterans NHS Wales n.d. www.veteranswales.co.uk/ (accessed 8 November 2016).
- Call to Mind: a Framework for Action. Findings from the Review of Veterans and Family Members Mental and Related Health Needs Assessments. Final Report. London: Forces in Mind Trust; 2015.
- Call to Mind: Wales. Findings from the Reviews of Veterans’ and their Families’ Mental and Related Health Needs in Wales. Final Report. London: Forces in Mind Trust; 2016.
- Call to Mind: Scotland. Findings from the Review of Veterans’ and their Families’ Mental and Related Health Needs in Scotland. Final Report. London: Forces in Mind Trust; 2016.
- Forces in Mind Trust . Call to Mind: Northern Ireland – Findings from the Review of Veterans’ and Their Families’ Mental and Related Health Needs in Northern Ireland. 2017. www.fim-trust.org/wp-content/uploads/2017/06/Call-to-Mind-Northern-Ireland.pdf.
- Government of Western Australia Department of Health . Models of Care 2012. www.agedcare.health.wa.gov.au/home/moc.cfm (accessed 20 October 2016).
- Chambers D, Wade R, Wilson P. Training Manual for Selecting Reviews and Writing Abstracts for the Database of Abstracts of Reviews of Effects (DARE). York: Centre for Reviews and Dissemination, University of York; 2012.
- Suggested Risk of Bias Criteria for EPOC Reviews. EPOC Resources for Review Authors. Oslo: Norwegian Knowledge Centre for the Health Services; 2016.
- Qualitative Research Checklist. 10 Questions to Help You Make Sense of Qualitative Research. Oxford: CASP; 2013.
- The Human Givens Institute . How a Human Givens Therapist Can Help n.d. www.hgi.org.uk/therapist-register/how-human-givens-therapist-can-help (accessed 3 January 2017).
- Tom Harrison House . Military Veteran Addiction Recovery Centre n.d. http://tomharrisonhouse.org.uk/ (accessed 3 March 2017).
- Chick P. A Review of the Veterans NHS Wales Service. Cardiff: Public Health Wales; 2014.
- Newsletter March 2016 (Issue 5). Edinburgh: Veterans First Point Scotland; 2016.
- Burdett H, Greenberg N. A Service Evaluation of PTSD Resolution. Client Outcome Data. London: King’s Centre for Military Mental Health Research; 2016.
- Murphy D, Hodgman G, Carson C, Spencer-Harper L, Hinton M, Wessely S, et al. Mental health and functional impairment outcomes following a 6-week intensive treatment programme for UK military veterans with post-traumatic stress disorder (PTSD): a naturalistic study to explore dropout and health outcomes at follow-up. BMJ Open 2015;5. http://doi.org/10.1136/bmjopen-2014-007051.
- Schnurr PP, Friedman MJ, Oxman TE, Dietrich AJ, Smith MW, Shiner B, et al. RESPECT-PTSD: re-engineering systems for the primary care treatment of PTSD, a randomized controlled trial. J Gen Intern Med 2013;28:32-40. https://doi.org/10.1007/s11606-012-2166-6.
- McFall M, Saxon AJ, Malte CA, Chow B, Bailey S, Baker DG, et al. Integrating tobacco cessation into mental health care for posttraumatic stress disorder: a randomized controlled trial. JAMA 2010;304:2485-93. https://doi.org/10.1001/jama.2010.1769.
- McFall M, Saxon AJ, Thaneemit-Chen S, Smith MW, Joseph AM, Carmody TP, et al. Integrating smoking cessation into mental health care for post-traumatic stress disorder. Clin Trials 2007;4:178-89. https://doi.org/10.1177/1740774507076923.
- McFall M, Malte C, Fontana A, Rosenheck RA. Effects of an outreach intervention on use of mental health services by veterans with posttraumatic stress disorder. Psychiatr Serv 2000;51:369-74. https://doi.org/10.1176/appi.ps.51.3.369.
- Hundt NE, Robinson A, Arney J, Stanley MA, Cully JA. Veterans’ perspectives on benefits and drawbacks of peer support for posttraumatic stress disorder. Mil Med 2015;180:851-6. https://doi.org/10.7205/MILMED-D-14-00536.
- Pietrzak E, Warfe P, Kenardy J, McGuire A, Bredhauer K. Review of PTSD Programs: International Literature Review of Evidence-Based Best Practice Treatments for PTSD. Centre for Military & Veterans’ Health; 2011.
- McGuire A, Bredhauer K, Anderson R, Warfe P. Review of PTSD Group Treatment Programs: Final Report. Centre for Military & Veterans’ Health; 2011.
- Bredhauer K, Anderson R, McGuire A, Warfe P, Waller M, Kanesaraja J. Review of PTSD Group Treatment Programs: Phase 2 In-Depth Quantitative and Qualitative Analyses. Centre for Military & Veterans’ Health; 2011.
- Forbes D, Lewis V, Parslow R, Hawthorne G, Creamer M. Naturalistic comparison of models of programmatic interventions for combat-related post-traumatic stress disorder. Aust N Z J Psychiatry 2008;42:1051-9. https://doi.org/10.1080/00048670802512024.
- Creamer MC, Forbes D, Biddle D, Elliott P. Inpatient versus day hospital treatment for chronic, combat-related posttraumatic stress disorder: a naturalistic comparison. J Nerv Ment Dis 2002;190:183-9. https://doi.org/10.1097/00005053-200203000-00007.
- Murphy D, Spencer-Harper L, Carson C, Palmer E, Hill K, Sorfleet N, et al. Long-term responses to treatment in UK veterans with military-related PTSD: an observational study. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011667.
- Ohye BY, Brendel RW, Fredman SJ, Bui E, Rauch PK, Allard MD, et al. Three-generation model: a family systems framework for the assessment and treatment of veterans with posttraumatic stress disorder and related conditions. Prof Psychol Res Pr 2015;46:97-106. https://doi.org/10.1037/a0037735.
- Sniezek DP. Community-Based Wounded Warrior Sustainability Initiative (CBWSI): an integrative medicine strategy for mitigating the effects of PTSD. J Rehabil Res Dev 2012;49:ix-xix. https://doi.org/10.1682/JRRD.2012.02.0025.
- Baringer E, Silver SM, Steenhusen N, Salamone-Genovese LM. A short-term stabilization unit for PTSD. VA Practitioner 1990;7:53-6.
- Brawer PA, Brugh AM, Martielli RP, O’Connor SP, Mastnak J, Scherrer JF, et al. Enhancing entrance into PTSD treatment for post-deployment veterans through collaborative/integrative care. Translational Behavioral Medicine 2011;1:609-14. https://doi.org/10.1007/s13142-011-0097-0.
- Bohnert KM, Sripada RK, Mach J, McCarthy JF. Same-day integrated mental health care and PTSD diagnosis and treatment among VHA primary care patients with positive PTSD screens. Psychiatr Serv 2016;67:94-100. https://doi.org/10.1176/appi.ps.201500035.
- Chan D. Depression and Comorbid PTSD in Veterans: Evaluation of Collaborative Care Programs and Impact on Utilization and Costs 2007.
- Donovan B, Padin-Rivera E, Kowaliw S. ‘Transcend’: initial outcomes from a posttraumatic stress disorder/substance abuse treatment program. J Trauma Stress 2001;14:757-72. https://doi.org/10.1023/A:1013094206154.
- Donovan BS, Padin-Rivera E. Transcend: a program for treating PTSD and substance abuse in Vietnam combat veterans. National Center for PTSD Clinical Quarterly 1999;8:51-3.
- Fontana A, Rosenheck R. Effectiveness and cost of the inpatient treatment of posttraumatic stress disorder: comparison of three models of treatment. Am J Psychiatry 1997;154:758-65. https://doi.org/10.1176/ajp.154.6.758.
- Forman SI, Havas S. Massachusetts’ post-traumatic stress disorder program: a public health treatment model for Vietnam veterans. Public Health Rep 1990;105:172-9.
- Jain S, Hernandez JM, Lindley SE. Peer support program for veterans in rural areas. Psychiatr Serv 2014;65. https://doi.org/10.1176/appi.ps.650704.
- Jain S, McLean C, Adler EP, Rosen CS. Peer support and outcome for veterans with Posttraumatic Stress Disorder (PTSD) in a residential rehabilitation program. Community Ment Health J 2016;52:1089-92. https://doi.org/10.1007/s10597-015-9982-1.
- Jain S, Joseph K, Holt H, Rosen CS, Lindley SE, Roberts LW, et al. Partnerships for Mental Health: Narratives of Community and Academic Collaboration. Cham: Springer International Publishing; 2015.
- Joseph KM, Hernandez JM, Jain S. Peer support telephone outreach intervention for veterans with PTSD. Psychiatr Serv 2015;66. https://doi.org/10.1176/appi.ps.660903.
- Otis JD, Keane TM, Kerns RD, Monson C, Scioli E. The development of an integrated treatment for veterans with comorbid chronic pain and posttraumatic stress disorder. Pain Med 2009;10:1300-11. https://doi.org/10.1111/j.1526-4637.2009.00715.x.
- Plagge JM, Lu MW, Lovejoy TI, Karl AI, Dobscha SK. Treatment of comorbid pain and PTSD in returning veterans: a collaborative approach utilizing behavioral activation. Pain Med 2013;14:1164-72. https://doi.org/10.1111/pme.12155.
- Randall I, Mohr DC, Maynard C. VHA patient-centered medical home associated with lower rate of hospitalizations and specialty care among veterans with posttraumatic stress disorder [published online ahead of print 2015]. J Healthc Qual 2015. https://doi.org/10.1111/jhq.12092.
- Walter KH, Varkovitzky RL, Owens GP, Lewis J, Chard KM. Cognitive processing therapy for veterans with posttraumatic stress disorder: a comparison between outpatient and residential treatment. J Consult Clin Psychol 2014;82:551-61. https://doi.org/10.1037/a0037075.
- Bisson JI, Ehlers A, Matthews R, Pilling S, Richards D, Turner S. Psychological treatments for chronic post-traumatic stress disorder. Systematic review and meta-analysis. Br J Psychiatry 2007;190:97-104. https://doi.org/10.1192/bjp.bp.106.021402.
- Goetter EM, Bui E, Ojserkis RA, Zakarian RJ, Brendel RW, Simon NM. A systematic review of dropout from psychotherapy for posttraumatic stress disorder among Iraq and Afghanistan combat veterans. J Trauma Stress 2015;28:401-9. https://doi.org/10.1002/jts.22038.
- Goetter EM, Bui E, Ojserkis RA, Zakarian RJ, Brendel RW, Simon NM. A systematic review of dropout from psychotherapy for posttraumatic stress disorder among Iraq and Afghanistan combat veterans. J Trauma Stress 2015;28. https://doi.org/10.1002/jts.22038.
- Goodson J, Helstrom A, Halpern JM, Ferenschak MP, Gillihan SJ, Powers MB. Treatment of posttraumatic stress disorder in U.S. combat veterans: a meta-analytic review. Psychol Rep 2011;109:573-99. https://doi.org/10.2466/02.09.15.16.PR0.109.5.573-599.
- Kitchiner NJ, Roberts NP, Wilcox D, Bisson JI. Systematic review and meta-analyses of psychosocial interventions for veterans of the military. Eur J Psychotraumatol 2012;3. https://doi.org/10.3402/ejpt.v3i0.19267.
- Puetz TW, Youngstedt SD, Herring MP. Effects of pharmacotherapy on combat-related PTSD, anxiety, and depression: a systematic review and meta-regression analysis. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0126529.
- Stewart CL, Wrobel TA. Evaluation of the efficacy of pharmacotherapy and psychotherapy in treatment of combat-related post-traumatic stress disorder: a meta-analytic review of outcome studies. Mil Med 2009;174:460-9. https://doi.org/10.7205/MILMED-D-04-1507.
- Tran K, Moulton K, Santesso N, Rabb D. Cognitive Processing Therapy for Post-Traumatic Stress Disorder: A Systematic Review and Meta-Analysis (CADTH Health Technology Assessment; no. 141). Ottawa, ON: Canadian Agency for Drugs and Technologies in Health; 2016.
- Forces in Mind Trust (FiMT) n.d. www.fim-trust.org/ (accessed 27 February 2017).
- Skipper J. Presentation to CBT4Wales Conference: CBT in a Cold Climate 2014.
- Skipper J. Comments of Draft Report 2017.
- Our Community – Our Covenant. Improving the Delivery of Local Covenant Pledges. London: Forces in Mind Trust; 2016.
- Hettiaratchy S. Better Care Is Coming Out of the Trauma of War 2017. www.england.nhs.uk/2017/01/veterans-trauma-network/ (accessed 27 February 2017).
- National Institute for Health and Care Excellence . Post-Traumatic Stress Disorder (Update) 2016. www.nice.org.uk/guidance/indevelopment/gid-ng10013 (accessed 14 February 2017).
- Centre for Reviews and Dissemination . Search Strategies for DARE 2015. www.crd.york.ac.uk/crdweb/searchstrategies.asp (accessed 1 November 2016).
- Acierno R, Gros DF, Ruggiero KJ, Hernandez-Tejada BM, Knapp RG, Lejuez CW, et al. Behavioral activation and therapeutic exposure for posttraumatic stress disorder: a noninferiority trial of treatment delivered in person versus home-based telehealth. Depress Anxiety 2016;33:415-23. https://doi.org/10.1002/da.22476.
- Battaglia C, Stein KF. A clinical translation of the research article titled ‘building a tobacco cessation telehealth care management program for veterans with posttraumatic stress disorder’. J Am Psychiatr Nurses Assoc 2013;19:92-7. https://doi.org/10.1177/1078390313485907.
- Fortney JC, Pyne JM, Kimbrell TA, Hudson TJ, Robinson DE, Schneider R, et al. ‘Telemedicine-based collaborative care for posttraumatic stress disorder: a randomized clinical trial’: Correction. JAMA Psychiatry 2015;72. https://doi.org/10.1001/jamapsychiatry.2014.1575.
- Fortney JC, Pyne JM, Kimbrell TA, Hudson TJ, Robinson DE, Schneider R, et al. Telemedicine-based collaborative care for posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry 2015;72:58-67. https://doi.org/10.1001/jamapsychiatry.2014.1575.
- Frueh BC, Monnier J, Yim E, Grubaugh AL, Hamner MB, Knapp RG. A randomized trial of telepsychiatry for post-traumatic stress disorder. J Telemed Telecare 2007;13:142-7. https://doi.org/10.1258/135763307780677604.
- Gros DF, Yoder M, Tuerk PW, Lozano BE, Acierno R. Exposure therapy for PTSD delivered to veterans via telehealth: predictors of treatment completion and outcome and comparison to treatment delivered in person. Behav Ther 2011;42:276-83. https://doi.org/10.1016/j.beth.2010.07.005.
- Gros DF, Lancaster CL, Lopez CM, Acierno R. Treatment satisfaction of home-based telehealth versus in-person delivery of prolonged exposure for combat-related PTSD in veterans [published online ahead of print 31 August 2016]. J Telemed Telecare 2016. https://doi.org/10.1177/1357633X16671096.
- Hoerster KD, Jakupcak M, Stephenson KR, Fickel JJ, Simons CE, Hedeen A, et al. A pilot trial of telephone-based collaborative care management for PTSD among Iraq/Afghanistan war veterans. Telemed J E Health 2015;21:42-7. https://doi.org/10.1089/tmj.2013.0337.
- Lindsay JA, Kauth MR, Hudson S, Martin LA, Ramsey DJ, Daily L, et al. Implementation of video telehealth to improve access to evidence-based psychotherapy for posttraumatic stress disorder. Telemed J E Health 2015;21:467-72. https://doi.org/10.1089/tmj.2014.0114.
- Maieritsch KP, Smith TL, Hessinger JD, Ahearn EP, Eickhoff JC, Zhao Q. Randomized controlled equivalence trial comparing videoconference and in person delivery of cognitive processing therapy for PTSD. J Telemed Telecare 2016;22:238-43. https://doi.org/10.1177/1357633X15596109.
- Morland LA, Pierce K, Wong MY. Telemedicine and coping skills groups for Pacific Island veterans with post-traumatic stress disorder: a pilot study. J Telemed Telecare 2004;10:286-9. https://doi.org/10.1258/1357633042026387.
- Morland LA, Greene CJ, Rosen CS, Foy D, Reilly P, Shore J, et al. Telemedicine for anger management therapy in a rural population of combat veterans with posttraumatic stress disorder: a randomized noninferiority trial. J Clin Psychiatry 2010;71:855-63. https://doi.org/10.4088/JCP.09m05604blu.
- Morland LA, Hynes AK, Mackintosh MA, Resick PA, Chard KM. Group cognitive processing therapy delivered to veterans via telehealth: a pilot cohort. J Trauma Stress 2011;24:465-9. https://doi.org/10.1002/jts.20661.
- Morland LA, Raab M, Mackintosh MA, Rosen CS, Dismuke CE, Greene CJ, et al. Telemedicine: a cost-reducing means of delivering psychotherapy to rural combat veterans with PTSD. Telemed J E Health 2013;19:754-9. https://doi.org/10.1089/tmj.2012.0298.
- Morland LA, Mackintosh MA, Greene CJ, Rosen CS, Chard KM, Resick P, et al. Cognitive processing therapy for posttraumatic stress disorder delivered to rural veterans via telemental health: a randomized noninferiority clinical trial. J Clin Psychiatry 2014;75:470-6. https://doi.org/10.4088/JCP.13m08842.
- Rosen CS, DiLandro C, Corwin KN, Drescher KD, Cooney JH, Gusman F. Telephone monitoring and support for veterans with chronic posttraumatic stress disorder: a pilot study. Community Ment Health J 2006;42:501-8. https://doi.org/10.1007/s10597-006-9047-6.
- Rosen CS, Tiet QQ, Harris AH, Julian TF, McKay JR, Moore WM, et al. Telephone monitoring and support after discharge from residential PTSD treatment: a randomized controlled trial. Psychiatr Serv 2013;64:13-20. https://doi.org/10.1176/appi.ps.201200142.
- Strachan M, Gros DF, Ruggiero KJ, Lejuez CW, Acierno R. An integrated approach to delivering exposure-based treatment for symptoms of PTSD and depression in OIF/OEF veterans: preliminary findings. Behav Ther 2012;43:560-9. https://doi.org/10.1016/j.beth.2011.03.003.
- Tuerk PW, Yoder M, Ruggiero KJ, Gros DF, Acierno R. A pilot study of prolonged exposure therapy for posttraumatic stress disorder delivered via telehealth technology. J Trauma Stress 2010;23:116-23. https://doi.org/10.1002/jts.20494.
- Wierwille JL, Pukay-Martin ND, Chard KM, Klump MC. Effectiveness of PTSD telehealth treatment in a VA clinical sample. Psychol Serv 2016;13:373-9. https://doi.org/10.1037/ser0000106.
- Yuen EK, Gros DF, Price M, Zeigler S, Tuerk PW, Foa EB, et al. Randomized controlled trial of home-based telehealth versus in-person prolonged exposure for combat-related PTSD in veterans: preliminary results. J Clin Psychol 2015;71:500-12. https://doi.org/10.1002/jclp.22168.
- Ziemba SJ, Bradley NS, Landry LA, Roth CH, Porter LS, Cuyler RN. Posttraumatic stress disorder treatment for Operation Enduring Freedom/Operation Iraqi Freedom combat veterans through a civilian community-based telemedicine network. Telemed J E Health 2014;20:446-50. https://doi.org/10.1089/tmj.2013.0312.
- Belsher BE, Kuhn E, Maron D, Prins A, Cueva D, Fast E, et al. A preliminary study of an internet-based intervention for OEF/OIF veterans presenting for VA specialty PTSD care. J Trauma Stress 2015;28:153-6. https://doi.org/10.1002/jts.21994.
- Engel CC, Litz B, Magruder KM, Harper E, Gore K, Stein N, et al. Delivery of self training and education for stressful situations (DESTRESS-PC): a randomized trial of nurse assisted online self-management for PTSD in primary care. Gen Hosp Psychiatry 2015;37:323-8. https://doi.org/10.1016/j.genhosppsych.2015.04.007.
- Hobfoll SE, Blais RK, Stevens NR, Walt L, Gengler R. Vets prevail online intervention reduces PTSD and depression in veterans with mild-to-moderate symptoms. J Consult Clin Psychol 2016;84:31-42. https://doi.org/10.1037/ccp0000041.
- Kahn JR, Collinge W, Soltysik R. Post-9/11 veterans and their partners improve mental health outcomes with a self-directed mobile and web-based wellness training program: a randomized controlled trial. J Med Internet Res 2016;18. https://doi.org/10.2196/jmir.5800.
- Erbes CR, Stinson R, Kuhn E, Polusny M, Urban J, Hoffman J, et al. Access, utilization, and interest in mHealth applications among veterans receiving outpatient care for PTSD. Mil Med 2014;179:1218-22. https://doi.org/10.7205/MILMED-D-14-00014.
- Kuhn E, Greene C, Hoffman J, Nguyen T, Wald L, Schmidt J, et al. Preliminary evaluation of PTSD Coach, a smartphone app for post-traumatic stress symptoms. Mil Med 2014;179:12-8. https://doi.org/10.7205/MILMED-D-13-00271.
- Smith B, Harms WD, Burres S, Korda H, Rosen H, Davis J. Enhancing behavioral health treatment and crisis management through mobile ecological momentary assessment and SMS messaging. Health Informatics J 2012;18:294-308. https://doi.org/10.1177/1460458212445349.
- Mott JM, Stanley MA, Street RL, Grady RH, Teng EJ. Increasing engagement in evidence-based PTSD treatment through shared decision-making: a pilot study. Mil Med 2014;179:143-9. https://doi.org/10.7205/MILMED-D-13-00363.
- Watts BV, Schnurr PP, Zayed M, Young-Xu Y, Stender P, Llewellyn-Thomas H. A randomized controlled clinical trial of a patient decision aid for posttraumatic stress disorder. Psychiatr Serv 2015;66:149-54. https://doi.org/10.1176/appi.ps.201400062.
- Schumm JA, Walter KH, Bartone AS, Chard KM. Veteran satisfaction and treatment preferences in response to a posttraumatic stress disorder specialty clinic orientation group. Behav Res Ther 2015;69:75-82. http://doi.org/10.1016/j.brat.2015.04.006.
Appendix 1 Pro forma list of questions to service providers
Appendix 2 Search strategies
Search strategies for the rapid evidence review of the effectiveness of models of care for armed forces veterans with post traumatic stress disorder
MEDLINE [Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R)]
Via Ovid: http://ovidsp.ovid.com/
Date range searched: 1946 to present.
Date searched: 1 November 2016.
Records retrieved: 2227.
Search strategy
-
Veterans/ (12,568)
-
Veterans Health/ (719)
-
Military Personnel/ (34,456)
-
veteran$.ti,ab. (27,569)
-
military.ti,ab. (36,759)
-
(armed adj (force$or service$or personnel)).ti,ab. (4278)
-
(army or soldier$or troop or troops).ti,ab. (21,270)
-
(serviceman or servicemen or service-man or service-men).ti,ab. (1225)
-
(servicewoman or servicewomen or service-woman or service-women).ti,ab. (159)
-
(ex-service$or ex-force$or ex-military).ti,ab. (115)
-
(reservist$or National Guard or (reserve$adj2 (territorial$or force$or volunteer$or home))).ti,ab. (893)
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 (95,591)
-
Stress Disorders, Post-Traumatic/ (25,510)
-
PTSD.ti,ab. (17,118)
-
(stress$adj4 (post-trauma$or posttrauma$or trauma$)).ti,ab. (26,896)
-
13 or 14 or 15 (36,828)
-
12 and 16 (7041)
-
Combat Disorders/ (2847)
-
((combat or battle or war) adj2 (disorder$or stress$)).ti,ab. (1130)
-
operational stress$.ti,ab. (103)
-
((combat or battle or war) adj (neurosis or neuroses or fatigue)).ti,ab. (220)
-
(shell shock$or shellshock$).ti,ab. (118)
-
18 or 19 or 20 or 21 or 22 (3898)
-
12 and 23 (2540)
-
17 or 24 (7665)
-
“Delivery of Health Care”/ (74,408)
-
exp “Delivery of Health Care, Integrated”/ (10,160)
-
Patient-Centered Care/ (14,029)
-
disease management/ (25,683)
-
Case Management/ (9287)
-
models, nursing/ (11,501)
-
“Continuity of Patient Care”/ (16,469)
-
Comprehensive Health Care/ (6335)
-
Patient Care Management/ (2788)
-
exp Patient Care Team/ (60,170)
-
exp Patient Care Planning/ (57,684)
-
Holistic Health/ (7383)
-
Holistic Nursing/ (3019)
-
Hospitals, veterans/ (6235)
-
United States Department of Veterans Affairs/ (6219)
-
(deliver$adj3 (care or healthcare or service$)).ti,ab. (50,137)
-
((system or systems) adj3 (care or healthcare or service$)).ti,ab. (71,733)
-
((organis$or organiz$) adj3 (care or healthcare or service$)).ti,ab. (27,915)
-
((model or models) adj2 (care or healthcare or service$or treatment$or intervention$or therap$)).ti,ab. (26,806)
-
(integrat$adj2 (care or healthcare or service$or program$or approach$)).ti,ab. (27,863)
-
(collaborat$adj3 (care or manag$or healthcare or service$or program$or approach$or working)).ti,ab. (12,675)
-
(patient-centred or patient-centered).ti,ab. (13,147)
-
(medical home or PCMH).ti,ab. (2297)
-
shared care.ti,ab. (1054)
-
(continu$adj2 care).ti,ab. (13,214)
-
((coordinat$or co-ordinat$) adj2 (care or healthcare or service$or program$or approach$)).ti,ab. (10,337)
-
(team$adj2 (care or treatment$or assessment$or consultation$or healthcare or service$or program$or approach$)).ti,ab. (21,699)
-
(multidisciplinary or interprofessional or multispecialty or interdisciplinary or multimodal or multi-disciplinary or inter-professional or multi-specialty or inter-disciplinary or multi-modal).ti,ab. (118,039)
-
(interorgani?ation$or multiprofessional or multiagenc$or interagenc$or inter-organi?ation$or multi-professional or multi-agenc$or inter-agenc$).ti,ab. (5085)
-
(specialty adj2 (care or healthcare or clinic$or service$or program$or approach$or treatment$or therap$or intervention$)).ti,ab. (5571)
-
((case or care) adj management).ti,ab. (14,962)
-
(comanag$or co-manag$).ti,ab. (789)
-
stepped care.ti,ab. (973)
-
holistic.ti,ab. (15,996)
-
or/26–59 (566,945)
-
25 and 60 (1076)
-
exp Telemedicine/ (19,483)
-
exp Telephone/ (18,496)
-
Telecommunications/ (4596)
-
exp Videoconferencing/ (1306)
-
Mobile Applications/ (1421)
-
Therapy, Computer-Assisted/ (5834)
-
Internet/ (59,701)
-
(telemedicine or telehealth or telehealthcare or telecare or telemental or telemanagement or telerehabilitation or telepsychology or teletherapy or tele-medicine or tele-health or tele-healthcare or tele-care or tele-management or tele-mental or tele-rehabilitation or tele-psychology or tele-therapy).ti,ab. (11,881)
-
(telephone$or cell phone$or cellphone or mobile phone$or smartphone$or smart phone$or mobile app$or mobile device$).ti,ab. (60,915)
-
(text messag$or SMS or short messag$service$or texting or messaging).ti,ab. (7844)
-
(teleconferenc$or videoconferenc$or tele-conferenc$or video-conferenc$).ti,ab. (2822)
-
(web-based or internet-based).ti,ab. (26,638)
-
((web or online or on line or internet or computer or digital or e-mail or e-mail or phone or electronic) adj3 (therap$or treatment$or intervention$or program$or platform$)).ti,ab. (29,416)
-
(mobile health or mhealth or e-mental health or mobile technolog$).ti,ab. (2645)
-
or/62–75 (193,044)
-
25 and 76 (299)
-
self care/ (27,976)
-
self administration/ (10,235)
-
self medication/ (4350)
-
Self-Assessment/ (11,254)
-
(selfcare or self care).ti,ab. (13,145)
-
(selfmanag$or self manag$).ti,ab. (12,880)
-
(selfmonitor$or self monitor$).ti,ab. (5983)
-
(selfhelp or self help).ti,ab. (5419)
-
(selftreat$or self treat$).ti,ab. (1407)
-
(selfmedicat$or self medicat$).ti,ab. (3394)
-
(selfdiagnos$or self diagnos$).ti,ab. (570)
-
(selfadminist$or self administ$).ti,ab. (35,495)
-
(selfassess$or self assess$).ti,ab. (11,970)
-
Self-Help Groups/ (8362)
-
or/78–91 (123,524)
-
25 and 92 (159)
-
exp Psychotherapy, Group/ (24,738)
-
(group$adj2 (therap$or psychotherap$or treatment$or intervention$or program$)).ti,ab. (149,929)
-
((family or families) adj2 (therap$or psychotherap$or treatment$or intervention$or program$)).ti,ab. (15,774)
-
94 or 95 or 96 (178,963)
-
25 and 97 (310)
-
biopsychosocial.ti,ab. (4211)
-
(psychopharmacolog$or psychopharmacotherap$).ti,ab. (8052)
-
99 or 100 (12,220)
-
25 and 101 (34)
-
exp Mental Health Services/ (83,986)
-
Community Mental Health Centers/ (2801)
-
Community Psychiatry/ (1773)
-
(mental health adj2 (service$or clinic$or setting$or provider$or program$)).ti,ab. (20,910)
-
(community adj4 (service$or clinic$or setting$or provider$or program$)).ti,ab. (54,269)
-
(community-based adj4 (service$or clinic$or setting$or provider$or program$)).ti,ab. (12,066)
-
outreach.ti,ab. (10,169)
-
103 or 104 or 105 or 106 or 107 or 108 or 109 (153,728)
-
25 and 110 (704)
-
Organizations, Nonprofit/ (3024)
-
Voluntary Health Agencies/ (4073)
-
Charities/ (3551)
-
third sector.ti,ab. (131)
-
(nonprofit or non profit or not-for-profit).ti,ab. (6859)
-
(voluntary adj2 (agenc$or organi?ation$or sector$)).ti,ab. (1531)
-
(charity or charities or charitable).ti,ab. (4705)
-
or/112–118 (20,768)
-
25 and 119 (17)
-
social support/ (59,357)
-
peer group/ (16,566)
-
(support adj2 (group$or network$or peer$or social)).ti,ab. (40,743)
-
(peer$adj2 (intervention$or service$or program$or visit$)).ti,ab. (2102)
-
or/121–124 (97,101)
-
25 and 125 (412)
-
61 or 77 or 93 or 98 or 102 or 111 or 120 or 126 (2304)
-
(letter or editorial or comment).pt. (1,539,706)
-
127 not 128 (2227)
Key
/ = indexing term (MeSH heading)
exp = exploded indexing term (MeSH heading)
$ = truncation
ti,ab = terms in either title or abstract fields
adj = terms next to each other (order specified)
adj2 = terms within two words of each other (any order)
pt = publication type
? = optional wildcard – one or no characters present
PILOTS: Published International Literature on Traumatic Stress
Via Proquest: www.proquest.com/
Date ranged searched: inception to 4 November 2016.
Date searched: 4 November 2016.
Records retrieved: 3462.
Search strategy
(SU.EXACT(“Veterans”) OR SU.EXACT(“Air Force Personnel” OR “Army Personnel” OR “Child Soldiers” OR “Coast Guard Personnel” OR “Commissioned Officers” OR “Enlisted Personnel” OR “Marine Personnel” OR “Military Personnel” OR “Military Police Personnel” OR “Missing in Action” OR “National Guard Personnel” OR “Navy Personnel” OR “Noncommissioned Officers” OR “Peacekeeping Personnel” OR “Reserve Personnel” OR “Resistance Fighters” OR “Special Forces Personnel”) OR TI,AB(veteran* OR military) OR TI,AB((armed NEAR/1 force*) OR (armed NEAR/1 service*) OR (armed NEAR/1 personnel)) OR TI,AB(army OR soldier* OR troop OR troops) OR TI,AB(serviceman OR servicemen OR service-man OR service-men) OR TI,AB(servicewoman OR servicewomen OR service-woman OR service-women) OR TI,AB(ex-service*) OR TI,AB(ex-force*) OR TI,AB(ex-military) OR TI,AB(reservist* OR National Guard OR (reserve* NEAR/2 territorial*) OR (reserve NEAR/2 force*) OR (reserve NEAR/2 volunteer*) OR (reserve NEAR/2 home))) AND ((SU.EXACT(“Integrated Treatment”) OR SU.EXACT(“Client Centered Psychotherapy”) OR SU.EXACT(“Case Management”) OR (SU.EXACT(“Veterans Centers”) OR SU.EXACT(“Veterans Hospitals”)) OR SU.EXACT(“Veterans Organizations”)) OR (TI,AB(deliver* NEAR/3 (care OR healthcare OR service*)) OR (TI,AB((system OR systems) NEAR/3 (care OR healthcare OR service*)) OR TI,AB((organis* OR organis*) NEAR/3 (care OR healthcare OR service*))) OR (TI,AB((model OR models) NEAR/2 (care OR healthcare OR service* OR treatment* OR intervention* OR therap*)) OR TI,AB(integrat* NEAR/2 (care OR healthcare OR service* OR program* OR approach*))) OR (TI,AB(collaborat* NEAR/3 (care OR manag* OR healthcare OR service* OR program* OR approach* OR working)) OR TI,AB(patient-centred OR patient-centered)) OR (TI,AB(“medical home” OR PCMH) OR TI,AB(“shared care”)) OR (TI,AB(continu* NEAR/2 care) OR TI,AB((coordinat* OR co-ordinat*) NEAR/2 (care OR healthcare OR service* OR program* OR approach*))) OR (TI,AB(team* NEAR/2 (care OR treatment* OR assessment* OR consultation* OR healthcare OR service* OR program* OR approach*)) OR TI,AB(multidisciplinary OR interprofessional OR multispecialty OR interdisciplinary OR multimodal OR multi-disciplinary OR inter-professional OR multi-specialty OR inter-disciplinary OR multi-modal))) OR (TI,AB(interorgani?ation* or multiprofessional or multiagenc* or interagenc* or inter-organi?ation* or multi-professional or multi-agenc* or inter-agenc*) OR (TI,AB(specialty NEAR/2 (care OR healthcare OR clinic* OR service* OR program* OR approach* OR treatment* OR therap* OR intervention*)) OR TI,AB((case OR care) NEAR/1 management)) OR (TI,AB(comanag* OR co-manag*) OR TI,AB(“stepped care”)) OR TI,AB(holistic)) OR ((SU.EXACT(“Telemedicine”) OR SU.EXACT(“Computer Assisted Psychotherapy”) OR SU.EXACT(“Videotherapy”)) OR TI,AB(telemedicine OR telehealth OR telehealthcare OR telecare OR telemental OR telemanagement OR telerehabilitation OR telepsychology OR teletherapy OR tele-medicine OR tele-health OR tele-healthcare OR tele-care OR tele-management OR tele-mental OR tele-rehabilitation OR tele-psychology OR tele-therapy) OR TI,AB(telephone* OR “cell phone” OR “cell phones” OR cellphone OR “mobile phone” OR “mobile phones” OR smartphone* OR “smart phone” OR “smart phones” OR (mobile NEAR/1 app*) OR “mobile device” OR “mobile devices”) OR TI,AB(text messag* OR SMS OR short messag* service* or texting or messaging) OR TI,AB(teleconferenc* OR videoconferenc* OR tele-conferenc* OR video-conferenc*) OR TI,AB(web-based OR internet-based) OR TI,AB((web OR online OR on-line OR internet OR computer OR digital OR e-mail OR e-mail OR phone OR electronic) NEAR/3 (therap* OR treatment* OR intervention* OR program* OR platform*)) OR TI,AB(“mobile health” OR mhealth OR “e-mental health” OR mobile technolog*)) OR (SU.EXACT(“Self Help Techniques”) OR TI,AB(selfcare OR self-care OR selfmanag* OR self-manag* OR selfmonitor* OR self-monitor* OR selfhelp OR self help OR selftreat* OR self-treat* OR selfmedicat* OR self-medicat* OR selfdiagnos* OR self-diagnos* OR selfadminist* OR self-administ* OR selfassess* OR self- assess*)) OR (SU.EXACT(“Encounter Group Therapy” OR “Group Psychotherapy” OR “Marathon Group Therapy” OR “Psychodrama” OR “Therapeutic Community” OR “Trauma Focused Group Psychotherapy”) OR SU.EXACT(“Behavioral Couples Therapy” OR “Conjoint Therapy” OR “Family Therapy”) OR TI,AB(group* NEAR/2 (therap* OR psychotherap* OR treatment* OR intervention* OR program*)) OR TI,AB((family OR families) NEAR/2 (therap* OR psychotherap* OR treatment* OR intervention* OR program*))) OR (SU.EXACT(“Psychopharmacology”) OR TI,AB(biopsychosocial OR psychopharmacolog* OR psychopharmacotherap*)) OR (SU.EXACT(“Community Mental Health Centers”) OR TI,AB(“mental health” NEAR/2 (service* OR clinic* OR setting* OR provider* OR program*)) OR TI,AB(community NEAR/4 (service* OR clinic* OR setting* OR provider* OR program*)) OR TI,AB(community-based NEAR/4 (service* OR clinic* OR setting* OR provider* OR program*)) OR SU.EXACT(“Outreach Programs”) OR TI,AB(outreach)) OR ((SU.EXACT(“Nongovernmental Organizations”) OR SU.EXACT(“Voluntary Organizations”)) OR (TI,AB(“third sector”) OR TI,AB(nonprofit or “non profit” or “not-for-profit”)) OR (TI,AB(voluntary NEAR/2 (agenc* OR organi?ation* OR sector*)) OR TI,AB(charity OR charities OR charitable))) OR ((SU.EXACT(“Support Groups”) OR SU.EXACT(“Social Support Networks”) OR SU.EXACT(“Peer Counseling”)) OR (TI,AB(support NEAR/2 (group* OR network* OR peer* OR social)) OR TI,AB(peer* NEAR/2 (intervention* OR service* OR program* OR visit*)))))
Key
SU.EXACT = subject heading
TI,AB = terms in the title or abstract fields
NEAR/2 = terms within two words of each other (any order)
* = truncation
? = wildcard – represents one single character
“ “ = phrase search
PsycINFO
Via Ovid: http://ovidsp.ovid.com/
Date range searched: 1806 to October week 5 2016.
Date searched: 4 November 2016.
Records retrieved: 2102.
Search strategy
-
military veterans/ (9952)
-
exp military personnel/ (14,544)
-
military duty status/ (466)
-
veteran$.ti,ab. (16,396)
-
military.ti,ab. (20,151)
-
(armed adj (force$or service$or personnel)).ti,ab. (1717)
-
(army or soldier$or troop or troops).ti,ab. (12,397)
-
(serviceman or servicemen or service-man or service-men).ti,ab. (444)
-
(servicewoman or servicewomen or service-woman or service-women).ti,ab. (78)
-
(ex-service$or ex-force$or ex-military).ti,ab. (109)
-
(reservist$or National Guard or (reserve$adj2 (territorial$or force$or volunteer$or home))).ti,ab. (685)
-
or/1–11 (46,364)
-
exp posttraumatic stress disorder/ (26,208)
-
PTSD.ti,ab. (24,525)
-
(stress$adj4 (post-trauma$or posttrauma$or trauma$)).ti,ab. (33,779)
-
13 or 14 or 15 (38,912)
-
12 and 16 (7945)
-
((combat or battle or war) adj2 (disorder$or stress$)).ti,ab. (1275)
-
operational stress$.ti,ab. (118)
-
((combat or battle or war) adj (neurosis or neuroses or fatigue)).ti,ab. (516)
-
(shell shock$or shellshock$).ti,ab. (207)
-
or/18–21 (1978)
-
12 and 22 (1190)
-
17 or 23 (8451)
-
health care delivery/ (18,876)
-
integrated services/ (2775)
-
client centered therapy/ (2870)
-
disease management/ (5365)
-
case management/ (2839)
-
“continuum of care”/ (1452)
-
interdisciplinary treatment approach/ (6544)
-
multimodal treatment approach/ (1708)
-
treatment planning/ (4672)
-
holistic health/ (1764)
-
(deliver$adj3 (care or healthcare or service$)).ti,ab. (22,836)
-
((system or systems) adj3 (care or healthcare or service$)).ti,ab. (23,069)
-
((organis$or organiz$) adj3 (care or healthcare or service$)).ti,ab. (10,782)
-
((model or models) adj2 (care or healthcare or service$or treatment$or intervention$or therap$)).ti,ab. (197,32)
-
(integrat$adj2 (care or healthcare or service$or program$or approach$)).ti,ab. (13,619)
-
(collaborat$adj3 (care or manag$or healthcare or service$or program$or approach$or working)).ti,ab. (5305)
-
(patient-centred or patient-centered).ti,ab. (3997)
-
(medical home or PCMH).ti,ab. (667)
-
shared care.ti,ab. (293)
-
(continu$adj2 care).ti,ab. (4434)
-
((coordinat$or co-ordinat$) adj2 (care or healthcare or service$or program$or approach$)).ti,ab. (3892)
-
(team$adj2 (care or treatment$or assessment$or consultation$or healthcare or service$or program$or approach$)).ti,ab. (8461)
-
(multidisciplinary or interprofessional or multispecialty or interdisciplinary or multimodal or multi-disciplinary or inter-professional or multi-specialty or inter-disciplinary or multi-modal).ti,ab. (46,265)
-
(interorgani?ation$or multiprofessional or multiagenc$or interagenc$or inter-organi?ation$or multi-professional or multi-agenc$or inter-agenc$).ti,ab. (4708)
-
(specialty adj2 (care or healthcare or clinic$or service$or program$or approach$or treatment$or therap$or intervention$)).ti,ab. (1881)
-
((case or care) adj management).ti,ab. (5731)
-
(comanag$or co-manag$).ti,ab. (164)
-
stepped care.ti,ab. (582)
-
holistic.ti,ab. (14,723)
-
or/25–53 (183,056)
-
24 and 54 (697)
-
telemedicine/ (3607)
-
exp telephone systems/ (4970)
-
telecommunications media/ (1315)
-
teleconferencing/ (799)
-
exp mobile devices/ (4195)
-
exp electronic communication/ (15,247)
-
computer assisted therapy/ (775)
-
online therapy/ (1981)
-
internet/ (25,981)
-
websites/ (3982)
-
(telemedicine or telehealth or telehealthcare or telecare or telemental or telemanagement or telerehabilitation or telepsychology or teletherapy or tele-medicine or tele-health or tele-healthcare or tele-care or tele-management or tele-mental or tele-rehabilitation or tele-psychology or tele-therapy).ti,ab. (2376)
-
(telephone$or cell phone$or cellphone or mobile phone$or smartphone$or smart phone$or mobile app$or mobile device$).ti,ab. (26,422)
-
(text messag$or SMS or short messag$service$or texting or messaging).ti,ab. (3833)
-
(teleconferenc$or videoconferenc$or tele-conferenc$or video-conferenc$).ti,ab. (1709)
-
(web-based or internet-based).ti,ab. (13,534)
-
((web or online or on line or internet or computer or digital or e-mail or e-mail or phone or electronic) adj3 (therap$or treatment$or intervention$or program$or platform$)).ti,ab. (13,744)
-
(mobile health or mhealth or e-mental health or mobile technolog$).ti,ab. (1286)
-
or/56–72 (88,277)
-
24 and 73 (258)
-
exp self management/ (55,00)
-
drug self administration/ (1799)
-
self medication/ (615)
-
self evaluation/ (8634)
-
self report/ (14,534)
-
self monitoring/ (2705)
-
(selfcare or self care).ti,ab. (7059)
-
(selfmanag$or self manag$).ti,ab. (7186)
-
(selfmonitor$or self monitor$).ti,ab. (5204)
-
(selfhelp or self help).ti,ab. (7348)
-
(selftreat$or self treat$).ti,ab. (361)
-
(selfmedicat$or self medicat$).ti,ab. (1437)
-
(selfdiagnos$or self diagnos$).ti,ab. (271)
-
(selfadminist$or self administ$).ti,ab. (15,229)
-
(selfassess$or self assess$).ti,ab. (6761)
-
self-help techniques/ (3779)
-
self-care skills/ (3811)
-
or/75–91 (75,444)
-
24 and 92 (218)
-
exp group psychotherapy/ (21,025)
-
group intervention/ (1501)
-
group counseling/ (4872)
-
(group$adj2 (therap$or psychotherap$or treatment$or intervention$or program$)).ti,ab. (54,312)
-
((family or families) adj2 (therap$or psychotherap$or treatment$or intervention$or program$)).ti,ab. (28,035)
-
family intervention/ (2582)
-
exp family therapy/ (20,429)
-
or/94–100 (97,322)
-
24 and 101 (430)
-
biopsychosocial approach/ (3261)
-
exp psychopharmacology/ (8635)
-
biopsychosocial.ti,ab. (5739)
-
(psychopharmacolog$or psychopharmacotherap$).ti,ab. (9986)
-
103 or 104 or 105 or 106 (21,786)
-
24 and 107 (57)
-
exp mental health services/ (37,137)
-
(mental health adj2 (service$or clinic$or setting$or provider$or program$)).ti,ab. (31,993)
-
(community adj4 (service$or clinic$or setting$or provider$or program$)).ti,ab. (34,242)
-
(community-based adj4 (service$or clinic$or setting$or provider$or program$)).ti,ab. (7412)
-
outreach programs/ (977)
-
outreach.ti,ab. (5977)
-
exp community services/ (29,021)
-
109 or 110 or 111 or 112 or 113 or 114 or 115 (99,911)
-
24 and 116 (614)
-
nonprofit organizations/ (1960)
-
ngos/ (993)
-
third sector.ti,ab. (176)
-
(nonprofit or non profit or not-for-profit).ti,ab. (5566)
-
(voluntary adj2 (agenc$or organi?ation$or sector$)).ti,ab. (1336)
-
(charity or charities or charitable).ti,ab. (2918)
-
118 or 119 or 120 or 121 or 122 or 123 (10,784)
-
24 and 124 (16)
-
social support/ (30,634)
-
support groups/ (3891)
-
peers/ (9862)
-
(support adj2 (group$or network$or peer$or social)).ti,ab. (51,505)
-
(peer$adj2 (intervention$or service$or program$or visit$)).ti,ab. (2364)
-
126 or 127 or 128 or 129 or 130 (73,308)
-
24 and 131 (420)
-
55 or 74 or 93 or 102 or 108 or 117 or 125 or 132 (2161)
-
(editorial or letter or “review book” or “review media” or “review software other”).dt. (176,536)
-
133 not 134 (2102)
Key
/ = subject heading
$ = truncation
ti,ab = terms in either title or abstract fields
adj2 = terms within two words of each other (any order)
dt = document type
Guideline searches
National Guideline Clearinghouse
Date searched: 15 November 2016.
47 results browsed – five relevant.
Search strategy
(“post-traumatic stress” OR “posttraumatic stress” OR PTSD)
NHS Evidence
Date searched: 14 November 2016.
Records retrieved: 11.
Search strategy
-
intitle:PTSD OR intags: PTSD OR inurl:PTSD
18 results browsed – seven relevant.
-
intitle:“post-traumatic stress” OR intags:“post-traumatic stress” OR inurl:“post-traumatic stress”
Six results browsed – five relevant.
-
intitle:“posttraumatic stress” OR intags:“posttraumatic stress” OR inurl:“posttraumatic stress”
One relevant result.
Relevant results from the three searches were deduplicated leaving 11 results in total.
US Department of Veterans Affairs – VA/DoD Clinical Practice Guidelines
www.healthquality.va.gov/index.asp
Date searched: 11 November 2016.
Browsed the clinical guidelines. One relevant guideline found.
Website searches
Australian Government Department of Veterans Affairs
www.dva.gov.au/about-dva/publications/research-and-studies
Date searched: 10 November 2016.
Browsed the research and studies section of the website. Nine relevant reports found.
Forces in Mind Trust
Date searched: 9 December 2016.
Browsed the report section of the website. Ten relevant reports found.
Government of Canada Veterans Affairs Canada
www.veterans.gc.ca/eng/about-us/research-directorate/publications/reports
Date searched: 11 November 2016.
Browsed the research directorate reports section of the website. Four relevant reports found.
King’s Centre for Military Health Research
www.kcl.ac.uk/kcmhr/publications/Reports/index.aspx
Date searched: 8 December 2016.
Browsed the reports list in the reports section of the website. Five relevant reports found.
National Academies of Sciences, Engineering and Medicine
www.nationalacademies.org/hmd/Reports.aspx
Date searched: 11 November 2016.
Browsed the veterans health topic in the publications section of the website. Eight relevant reports found.
US Department of Veterans Affairs – Health Services Research and Development
Date searched: 10 November 2016.
-
Browsed the publications section of the HSR&D Publications section of the US Department of Veterans Affairs.
-
Browsed the HSR&D Research topics section for PTSD.
Fifteen relevant reports found.
Search strategies for the rapid metareview of systematic reviews evaluating the effectiveness of treatments for post-traumatic stress disorder in armed forces veterans
Cochrane Database of Systematic Reviews
Via Wiley Online Library: http://onlinelibrary.wiley.com/
Issue 10 of 12, October 2016.
Date searched: 1 November 2016.
Records retrieved: two.
Search strategy
#1 MeSH descriptor: [Veterans] this term only (655)
#2 MeSH descriptor: [Veterans Health] this term only (21)
#3 MeSH descriptor: [Military Personnel] this term only (730)
#4 veteran*:ti,ab,kw (2903)
#5 military:ti,ab,kw (1832)
#6 (armed next (force* or service* or personnel)):ti,ab,kw (104)
#7 (army or soldier* or troop or troops):ti,ab,kw (837)
#8 (serviceman or servicemen or service-man or service-men):ti,ab,kw (30)
#9 (servicewoman or servicewomen or service-woman or service-women):ti,ab,kw (6)
#10 (ex-service* or ex-force* or ex-military):ti,ab,kw (2)
#11 (reservist* or “National Guard”):ti,ab,kw (22)
#12 (reserve* near/2 (territorial* or force* or volunteer* or home)):ti,ab,kw (9)
#13 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 (4957)
#14 MeSH descriptor: [Stress Disorders, Post-Traumatic] this term only (1267)
#15 PTSD:ti,ab,kw (1701)
#16 (stress* near/4 (post-trauma* or posttrauma* or trauma*)):ti,ab,kw (2587)
#17 #14 or #15 or #16 (2919)
#18 #13 and #17 (535)
#19 MeSH descriptor: [Combat Disorders] this term only (94)
#20 ((combat or battle or war) near/2 (disorder* or stress*)):ti,ab,kw (118)
#21 operational next stress*:ti,ab,kw (9)
#22 ((combat or battle or war) next (neurosis or neuroses or fatigue)):ti,ab,kw (5)
#23 (shell next shock* or shellshock*):ti,ab,kw (3)
#24 #19 or #20 or #21 or #22 or #23 (134)
#25 #13 and #24 (97)
#26 #18 or #25 (544)
#27 #18 or #25 in Cochrane Reviews (Reviews and Protocols) (2)
Key
MeSH descriptor = indexing term (MeSH heading)
* = truncation
ti,ab,kw = terms in either title or abstract or keyword fields
near/2 = terms within two words of each other (any order)
next = terms are next to each other
“ “ = phrase search
Database of Abstracts of Reviews of Effects
Via www.crd.york.ac.uk/CRDWeb/
Date range searched: inception to 31 March 2015.
Date searched: 3 November 2016.
Records retrieved: 23.
Search strategy
-
MeSH DESCRIPTOR Veterans (38)
-
MeSH DESCRIPTOR Veterans health (6)
-
MeSH DESCRIPTOR Military Personnel (50)
-
(veteran*) OR (military) (621)
-
(armed NEAR1 (force* or service* or personnel)) (9)
-
(army or soldier* or troop or troops) (92)
-
(serviceman or servicemen or service-man or service-men) (1)
-
(servicewoman or servicewomen or service-woman or service-women) (1)
-
(ex-service* or ex-force* or ex-military) (0)
-
(reservist* or “National Guard”) (3)
-
(reserve* NEAR2 (territorial* or force* or volunteer* or home)) (0)
-
((territorial* or force* or volunteer* or home) NEAR2 reserve*) (0)
-
#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 (685)
-
MeSH DESCRIPTOR Stress Disorders, Post-Traumatic (138)
-
(PTSD) (105)
-
(stress* NEAR4 (post-trauma* or posttrauma* or trauma*)) (155)
-
((post-trauma* or posttrauma* or trauma*) NEAR4 stress*) (212)
-
#14 OR #15 OR #16 OR #17 (264)
-
#13 AND #18 (33)
-
MeSH DESCRIPTOR Combat Disorders (10)
-
((combat or battle or war) NEAR2 (disorder* or stress*)) (11)
-
((disorder* or stress*) NEAR2 (combat or battle or war)) (1)
-
(operational NEAR1 stress*) (0)
-
((combat or battle or war) NEAR1 (neurosis or neuroses or fatigue)) (0)
-
(shell shock* or shellshock*) (1)
-
#20 OR #21 OR #22 OR #23 OR #24 OR #25 (11)
-
#13 AND #26 (8)
-
#19 OR #27 (33)
-
(*) IN DARE (45,418)
-
#28 AND #29 (23)
-
(*) IN NHS EED (17,613)
-
#28 AND #31 (6)
-
(*) IN HTA (16,640)
-
#28 AND #33 (4)
Key
MeSH DESCRIPTOR = indexing term (MeSH heading)
* = truncation
NEAR2 = terms within two words of each other (order specified)
Health Technology Assessment database
Via www.crd.york.ac.uk/CRDWeb/
Date range searched: inception to 3 November 2016.
Date searched: 3 November 2016.
Records retrieved: four.
See Database of Abstracts of Reviews of Effects for search strategy used.
Additional searches for systematic reviews
Additional searches were carried out to identify systematic reviews since the closure of DARE in 2015. Search strategies developed at the Centre for Reviews and Dissemination for identifying reviews for DARE were used to limit retrieval to systematic reviews. 80
Cumulative Index to Nursing & Allied Health (CINAHL Plus)
Via EBSCOhost www.ebscohost.com/
Date range searched: inception to 31 October 2016.
Date searched: 1 November 2016.
Records retrieved: 71.
Search strategy
S48 S24 AND S47 Limiters – Publication Year: 2014–2016 (71)
S47 S45 NOT S46 (295,149)
S46 PT BOOK REVIEW (36,770)
S45 S25 or S26 or S27 or S28 or S29 or S30 or S31 or S32 or S33 or S34 or S35 or S36 or S37 or S38 or S39 or S42 or S43 or S44 (307,328)
S44 AB systematic* N10 overview* or AB methodologic* N10 overview* or AB quantitative* N10 overview* or AB research* N10 overview* or AB literature* N10 overview* or AB studies N10 overview* or AB trial* N10 overview* or AB effective* N10 overview* (4152)
S43 AB systematic* N10 review* or AB methodologic* N10 review* or AB quantitative* N10 review* or AB research* N10 review* or AB literature* N10 review* or AB studies N10 review* or AB trial* N10 review* or AB effective* N10 review* (98,661)
S42 S41 and S40 (59,677)
S41 AB systematic* or AB methodologic* or AB quantitative* or AB research* or AB literature* or AB studies or AB trial* or AB effective* (1,050,600)
S40 PT review (142,621)
S39 TX electronic* N2 database* or TX electronic* N2 data base* or TX bibliographic* N2 database* or TX bibliographic* N2 data base* (6634)
S38 (MH “Reference Databases+”) or (MH “Reference Databases, Health+”) (48,839)
S37 TX hand N2 search* or TX manual N2 search* or TX database* N2 search* or TX computer* N2 search* (18,143)
S36 TX pooled analy* or TX data N2 pool* (5809)
S35 TX medline or medlars or embase or scisearch or psycinfo or psychinfo or psychlit or psyclit (53,783)
S34 TX synthes* N3 literature* or TX synthes* N3 research or TX synthes* N3 studies or TX synthes* N3 data (6541)
S33 (MH “Literature Searching+”) or (MH “Computerized Literature Searching+”) (7177)
S32 (MH “Literature Review+”) (42,113)
S31 TI review* or TI overview* (146,228)
S30 PT systematic review (52,177)
S29 PT nursing interventions (1483)
S28 AB cochrane or TI cochrane (17,132)
S27 TI meta-analy* or AB meta-analy* (31,524)
S26 TI metaanaly* or AB metaanaly* (585)
S25 (MH “Meta Analysis”) (25,410)
S24 S17 OR S23 (4073)
S23 S12 AND S22 (330)
S22 S18 OR S19 OR S20 OR S21 (547)
S21 TI ((shell N1 shock$) or shellshock*) OR AB ((shell N1 shock$) or shellshock*) (30)
S20 TI ((combat or battle or war) N1 (neurosis or neuroses or fatigue)) OR AB ((combat or battle or war) N1 (neurosis or neuroses or fatigue)) (53)
S19 TI operational N1 stress* OR AB operational N1 stress* (44)
S18 TI ((combat or battle or war) N2 (disorder* or stress*)) OR AB ((combat or battle or war) N2 (disorder* or stress*)) (446)
S17 S12 AND S16 (3983)
S16 S13 OR S14 OR S15 (17,946)
S15 TI (stress* N4 (post-trauma* or posttrauma* or trauma*)) OR AB (stress* N4 (post-trauma* or posttrauma* or trauma*)) (9338)
S14 TI PTSD OR AB PTSD (5505)
S13 (MH “Stress Disorders, Post-Traumatic”) (14,849)
S12 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 (34,395)
S11 TI (reserve* N2 (territorial* or force* or volunteer* or home)) OR AB (reserve* N2 (territorial* or force* or volunteer* or home)) (50)
S10 TI (reservist* or “National Guard”) OR AB (reservist* or “National Guard”) (404)
S9 TI (ex-service* or ex-force* or ex-military) OR AB (ex-service* or ex-force* or ex-military) (51)
S8 TI (servicewoman or servicewomen or service-woman or service-women) OR AB (servicewoman or servicewomen or service-woman or service-women) (130)
S7 TI (serviceman or servicemen or service-man or service-men) OR AB (serviceman or servicemen or service-man or service-men) (140)
S6 TI (army or soldier* or troop or troops) OR AB (army or soldier* or troop or troops) (5602)
S5 TI ((armed N1 (force* or service* or personnel)) OR AB ((armed N1 (force* or service* or personnel)) (729)
S4 TI military OR AB military (10,664)
S3 TI veteran* OR AB veteran* (12,146)
S2 (MH “Military Personnel+”) (11,574)
S1 (MH “Veterans+”) (10,554)
Key
MH = indexing term (CINAHL heading)
* = truncation
TI = terms in the title
AB = terms in the abstract
TX = all text – search of all the database’s searchable fields
“ “ = phrase search
N2 = terms within two words of each other (any order)
PT = publication type
EMBASE
Via Ovid: http://ovidsp.ovid.com/
Date range searched: 1974 to 31 October 2016.
Date searched: 1 November 2016.
Records retrieved: 149.
Search strategy
-
veteran/ (22,605)
-
veterans health / (2230)
-
army/ (21,878)
-
soldier/ (28,570)
-
veteran$.ti,ab. (33,235)
-
military.ti,ab. (41,917)
-
(armed adj (force$or service$or personnel)).ti,ab. (4635)
-
(army or soldier$or troop or troops).ti,ab. (21,419)
-
(serviceman or servicemen or service-man or service-men).ti,ab. (1325)
-
(servicewoman or servicewomen or service-woman or service-women).ti,ab. (167)
-
(ex-service$or ex-force$or ex-military).ti,ab. (120)
-
(reservist$or National Guard or (reserve$adj2 (territorial$or force$or volunteer$or home))).ti,ab. (919)
-
or/1–12 (102,894)
-
posttraumatic stress disorder/ (45,906)
-
PTSD.ti,ab. (21,535)
-
(stress$adj4 (post-trauma$or posttrauma$or trauma$)).ti,ab. (32,413)
-
14 or 15 or 16 (51,213)
-
13 and 17 (9016)
-
((combat or battle or war) adj2 (disorder$or stress$)).ti,ab. (1350)
-
operational stress$.ti,ab. (118)
-
((combat or battle or war) adj (neurosis or neuroses or fatigue)).ti,ab. (216)
-
(shell shock$or shellshock$).ti,ab. (113)
-
19 or 20 or 21 or 22 (1734)
-
13 and 23 (850)
-
18 or 24 (9211)
-
systematic$review$.ti,ab. (117,217)
-
systematic$literature review$.ti,ab. (8478)
-
“systematic review”/ (143,688)
-
“systematic review (topic)”/ (26,161)
-
meta analysis/ (151,314)
-
“meta analysis (topic)”/ (35,770)
-
meta-analytic$.ti,ab. (5747)
-
meta-analysis.ti,ab. (112,370)
-
meta-analysis.ti,ab. (381)
-
metaanalysis.ti,ab. (5356)
-
meta analysis.ti,ab. (112,370)
-
meta-synthesis.ti,ab. (434)
-
metasynthesis.ti,ab. (205)
-
meta synthesis.ti,ab. (434)
-
meta-regression.ti,ab. (5203)
-
metaregression.ti,ab. (687)
-
meta regression.ti,ab. (5203)
-
(synthes$adj3 literature).ti,ab. (2365)
-
(synthes$adj3 evidence).ti,ab. (6731)
-
(synthes$adj2 qualitative).ti,ab. (1218)
-
integrative review.ti,ab. (1272)
-
data synthesis.ti,ab. (10,781)
-
(research synthesis or narrative synthesis).ti,ab. (1410)
-
(systematic study or systematic studies).ti,ab. (10,249)
-
(systematic comparison$or systematic overview$).ti,ab. (2688)
-
(systematic adj2 search$).ti,ab. (18,122)
-
systematic$literature research$.ti,ab. (202)
-
(review adj3 scientific literature).ti,ab. (1322)
-
(literature review adj2 side effect$).ti,ab. (12)
-
(literature review adj2 adverse effect$).ti,ab. (2)
-
(literature review adj2 adverse event$).ti,ab. (12)
-
(evidence-based adj2 review).ti,ab. (2890)
-
comprehensive review.ti,ab. (11,342)
-
critical review.ti,ab. (14,108)
-
critical analysis.ti,ab. (7074)
-
quantitative review.ti,ab. (633)
-
structured review.ti,ab. (792)
-
realist review.ti,ab. (131)
-
realist synthesis.ti,ab. (83)
-
(pooled adj2 analysis).ti,ab. (12,942)
-
(pooled data adj6 (studies or trials)).ti,ab. (2044)
-
(medline and (inclusion adj3 criteria)).ti,ab. (16,488)
-
(search adj (strateg$or term$)).ti,ab. (26,187)
-
or/26–68 (371,133)
-
medline.ab. (95,491)
-
pubmed.ab. (75,334)
-
cochrane.ab. (60,420)
-
embase.ab. (61,687)
-
cinahl.ab. (17,654)
-
psyc?lit.ab. (967)
-
psyc?info.ab. (14,345)
-
lilacs.ab. (4913)
-
(literature adj3 search$).ab. (48,103)
-
(database$adj3 search$).ab. (45,204)
-
(bibliographic adj3 search$).ab. (1961)
-
(electronic adj3 search$).ab. (16,059)
-
(electronic adj3 database$).ab. (22,560)
-
(computeri?ed adj3 search$).ab. (3583)
-
(internet adj3 search$).ab. (3066)
-
included studies.ab. (15,272)
-
(inclusion adj3 studies).ab. (12,104)
-
inclusion criteria.ab. (88,306)
-
selection criteria.ab. (26,431)
-
predefined criteria.ab. (1925)
-
predetermined criteria.ab. (1060)
-
(assess$adj3 (quality or validity)).ab. (71,096)
-
(select$adj3 (study or studies)).ab. (62,732)
-
(data adj3 extract$).ab. (53,541)
-
extracted data.ab. (11,673)
-
(data adj2 abstracted).ab. (6337)
-
(data adj3 abstraction).ab. (1654)
-
published intervention$.ab. (159)
-
((study or studies) adj2 evaluat$).ab. (189,108)
-
(intervention$adj2 evaluat$).ab. (10,713)
-
confidence interval$.ab. (347,680)
-
heterogeneity.ab. (146,768)
-
pooled.ab. (83,220)
-
pooling.ab. (12,028)
-
odds ratio$.ab. (239,358)
-
(Jadad or coding).ab. (165,503)
-
evidence-based.ti,ab. (99,142)
-
or/70–106 (1,408,000)
-
review.pt. (2,202,348)
-
107 and 108 (171,657)
-
review.ti. (385,550)
-
107 and 110 (97,090)
-
(review$adj10 (papers or trials or trial data or studies or evidence or intervention$or evaluation$or outcome$or findings)).ti,ab. (392,491)
-
(retriev$adj10 (papers or trials or studies or evidence or intervention$or evaluation$or outcome$or findings)).ti,ab. (20,124)
-
69 or 109 or 111 or 112 or 113 (734,880)
-
letter.pt. (960,245)
-
editorial.pt. (521,200)
-
115 or 116 (1,481,445)
-
114 not 117 (720,757)
-
(animal/or nonhuman/) not exp human/ (4,996,453)
-
118 not 119 (696,240)
-
25 and 120 (423)
-
limit 121 to yr=“2014 -Current” (149)
Key
/ = indexing term (Emtree heading)
exp = exploded indexing term (Emtree heading)
$ = truncation
ti,ab = terms in either title or abstract fields
adj2 = terms within two words of each other (any order)
pt = publication type
? = optional wildcard – one or no characters present
MEDLINE [Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R)]
Via Ovid: http://ovidsp.ovid.com/
Date range searched: 1946 to present.
Date searched: 1 November 2016.
Records retrieved: 100.
Search strategy
-
Veterans/ (12,568)
-
Veterans Health/ (719)
-
Military Personnel/ (34,456)
-
veteran$.ti,ab. (27,569)
-
military.ti,ab. (36,759)
-
(armed adj (force$or service$or personnel)).ti,ab. (4278)
-
(army or soldier$or troop or troops).ti,ab. (21,270)
-
(serviceman or servicemen or service-man or service-men).ti,ab. (1225)
-
(servicewoman or servicewomen or service-woman or service-women).ti,ab. (159)
-
(ex-service$or ex-force$or ex-military).ti,ab. (115)
-
(reservist$or National Guard or (reserve$adj2 (territorial$or force$or volunteer$or home))).ti,ab. (893)
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 (95,591)
-
Stress Disorders, Post-Traumatic/ (25,510)
-
PTSD.ti,ab. (17,118)
-
(stress$adj4 (post-trauma$or posttrauma$or trauma$)).ti,ab. (26,896)
-
13 or 14 or 15 (36,828)
-
12 and 16 (7041)
-
Combat Disorders / (2847)
-
((combat or battle or war) adj2 (disorder$or stress$)).ti,ab. (1130)
-
operational stress$.ti,ab. (103)
-
((combat or battle or war) adj (neurosis or neuroses or fatigue)).ti,ab. (220)
-
(shell shock$or shellshock$).ti,ab. (118)
-
18 or 19 or 20 or 21 or 22 (3898)
-
12 and 23 (2540)
-
17 or 24 (7665)
-
systematic$review$.ti,ab. (96,659)
-
meta-analysis as topic/ (15,527)
-
meta-analytic$.ti,ab. (5101)
-
meta-analysis.ti,ab,pt. (112,016)
-
meta-analysis.ti,ab. (154)
-
metaanalysis.ti,ab. (1343)
-
meta analysis.ti,ab. (89,076)
-
meta-synthesis.ti,ab. (448)
-
metasynthesis.ti,ab. (203)
-
meta synthesis.ti,ab. (448)
-
meta-regression.ti,ab. (4285)
-
metaregression.ti,ab. (437)
-
meta regression.ti,ab. (4285)
-
(synthes$adj3 literature).ti,ab. (2067)
-
(synthes$adj3 evidence).ti,ab. (6112)
-
integrative review.ti,ab. (1541)
-
data synthesis.ti,ab. (8840)
-
(research synthesis or narrative synthesis).ti,ab. (1451)
-
(systematic study or systematic studies).ti,ab. (9500)
-
(systematic comparison$or systematic overview$).ti,ab. (2506)
-
evidence based review.ti,ab. (1663)
-
comprehensive review.ti,ab. (9872)
-
critical review.ti,ab. (13,037)
-
quantitative review.ti,ab. (574)
-
structured review.ti,ab. (632)
-
realist review.ti,ab. (146)
-
realist synthesis.ti,ab. (109)
-
or/26–52 (228,219)
-
review.pt. (2,210,291)
-
medline.ab. (82,238)
-
pubmed.ab. (60,165)
-
cochrane.ab. (51,665)
-
embase.ab. (52,752)
-
cinahl.ab. (17,105)
-
psyc?lit.ab. (907)
-
psyc?info.ab. (15,280)
-
(literature adj3 search$).ab. (38,960)
-
(database$adj3 search$).ab. (37,818)
-
(bibliographic adj3 search$).ab. (1749)
-
(electronic adj3 search$).ab. (14,328)
-
(electronic adj3 database$).ab. (17,712)
-
(computeri?ed adj3 search$).ab. (3128)
-
(internet adj3 search$).ab. (2372)
-
included studies.ab. (13,532)
-
(inclusion adj3 studies).ab. (10,602)
-
inclusion criteria.ab. (54,859)
-
selection criteria.ab. (27,829)
-
predefined criteria.ab. (1476)
-
predetermined criteria.ab. (875)
-
(assess$adj3 (quality or validity)).ab. (56,562)
-
(select$adj3 (study or studies)).ab. (49,846)
-
(data adj3 extract$).ab. (43,459)
-
extracted data.ab. (11,150)
-
(data adj2 abstracted).ab. (4198)
-
(data adj3 abstraction).ab. (1208)
-
published intervention$.ab. (142)
-
((study or studies) adj2 evaluat$).ab. (138,715)
-
(intervention$adj2 evaluat$).ab. (8231)
-
confidence interval$.ab. (304,749)
-
heterogeneity.ab. (121,995)
-
pooled.ab. (62,890)
-
pooling.ab. (9616)
-
odds ratio$.ab. (200,376)
-
(Jadad or coding).ab. (146,871)
-
or/55–89 (1,064,827)
-
54 and 90 (171,903)
-
review.ti. (340,666)
-
92 and 90 (79,487)
-
(review$adj4 (papers or trials or studies or evidence or intervention$or evaluation$)).ti,ab. (138,414)
-
53 or 91 or 93 or 94 (400,694)
-
letter.pt. (945,544)
-
editorial.pt. (422,191)
-
comment.pt. (687,401)
-
96 or 97 or 98 (1,539,706)
-
95 not 99 (390,874)
-
exp animals/not humans/ (4,333,932)
-
100 not 101 (379,938)
-
25 and 102 (235)
-
limit 103 to yr=“2014 -Current” (100)
Key
/ = indexing term (MeSH heading)
exp = exploded indexing term (MeSH heading)
$ = truncation
ti,ab = terms in either title or abstract fields
adj = terms next to each other (order specified)
adj2 = terms within two words of each other (any order)
pt = publication type
? = optional wildcard – one or no characters present
PsycINFO
Via Ovid: http://ovidsp.ovid.com/
Date range searched: 1806 to October week 4 2016.
Date searched: 1 November 2016.
Records retrieved: 85.
Search strategy
-
military veterans/ (9925)
-
exp military personnel/ (14,525)
-
military duty status/ (463)
-
veteran$.ti,ab. (16,365)
-
military.ti,ab. (20,113)
-
(armed adj (force$or service$or personnel)).ti,ab. (1714)
-
(army or soldier$or troop or troops).ti,ab. (12,388)
-
(serviceman or servicemen or service-man or service-men).ti,ab. (443)
-
(servicewoman or servicewomen or service-woman or service-women).ti,ab. (77)
-
(ex-service$or ex-force$or ex-military).ti,ab. (109)
-
(reservist$or National Guard or (reserve$adj2 (territorial$or force$or volunteer$or home))).ti,ab. (682)
-
or/1–11 (46,300)
-
exp posttraumatic stress disorder/ (26,162)
-
PTSD.ti,ab. (24,474)
-
(stress$adj4 (post-trauma$or posttrauma$or trauma$)).ti,ab. (33,716)
-
13 or 14 or 15 (38,840)
-
12 and 16 (7923)
-
((combat or battle or war) adj2 (disorder$or stress$)).ti,ab. (1273)
-
operational stress$.ti,ab. (118)
-
((combat or battle or war) adj (neurosis or neuroses or fatigue)).ti,ab. (516)
-
(shell shock$or shellshock$).ti,ab. (207)
-
or/18–21 (1976)
-
12 and 22 (1188)
-
17 or 23 (8429)
-
metaanaly*.ti,sh. (70)
-
meta-analy*.ti,sh. (14,782)
-
cochrane*.ti. (166)
-
(review or overview).ti. (139,627)
-
meta analysis/ (3906)
-
meta analysis.md. (15,491)
-
(review adj2 literature).ti. (3827)
-
“literature review”.md. (123,386)
-
“systematic review”.md. (14,982)
-
(synthes* adj3 (literature* or research or studies or data)).ti. (699)
-
pooled analys*.ti,ab. (576)
-
((data adj2 pool*) and studies).ti,ab. (826)
-
((hand or manual* or database* or computer* or electronic*) adj2 search*).ti,ab. (7356)
-
((electronic* or bibliographic*) adj2 (database* or data base*)).ti,ab. (3471)
-
or/25–38 (244,855)
-
(“review software other” or “review media” or editorial or letter or “review book”).dt. (176,419)
-
(electronic collection or encyclopedia).pt. (44,525)
-
(rat or rats or mouse or mice or hamster or hamsters or animal or animals or dog or dogs or cat or cats or bovine or sheep).ti,ab,sh. (300,843)
-
40 or 41 or 42 (477,299)
-
39 not 43 (154,382)
-
24 and 44 (343)
-
limit 45 to yr=“2014 -Current” (85)
Key
/ = subject heading
$ = truncation
* = truncation
ti,ab = terms in either title or abstract fields
adj2 = terms within two words of each other (any order)
sh = subject heading field
md = methodology field
dt = document type
pt = publication type
Appendix 3 Stage 1 list derived from service provider responses
Models of care
-
Case management (e.g. planning, delivery and monitoring of services/treatment tailored to individual/family needs).
-
Community outreach (e.g. mailouts/information provided from treatment centres; efforts to engage directly with veterans).
-
Co-ordinated/integrated/collaborative/networks/multidisciplinary care (e.g. PTSD clinic plus behavioural strategies/pain treatments; ‘Seeking Safety’; geographic therapist networks).
-
Crisis management.
-
Day care (include only if focus of the study is evaluating the delivery process, not evaluating the treatment).
-
Early intervention.
-
Family systems model (e.g. services for veterans and wider family; family group education).
-
Inpatient (include only if focus of the study is evaluating the delivery process, not evaluating the treatment).
-
Multicomponent treatment programmes (include only when components comprise different treatments and/or services).
-
Outpatient (include only if focus of the study is evaluating the delivery process, not evaluating the treatment).
-
Partnership/cross-sector/liaison work/co-location (e.g. co-located treatment units; involvement of multiple providers across specialities and locations).
-
Peer support (e.g. programmes, groups, helplines, ‘buddy’ arrangements delivered by veteran peers).
-
Primary care (include only if focus of the study is evaluating the delivery process, not evaluating the treatment).
-
Prison inreach (e.g. a psychotherapy treatment programme delivered in the prison setting).
-
Residential (include only if focus of the study is evaluating the delivery process, not evaluating the treatment).
-
Stepped care model.
-
Use of IAPT (a model to improve access).
The following were excluded from the above coding, on the basis that these are (narrower) treatment delivery mechanisms/aids, not structures for the organisation of services
-
Advice/information/education.
-
Assessment/triage.
-
Direct service/treatment provision.
-
Group support.
-
Internet/web/online interventions (e.g. where intervention is accessed by patient/participant; reaction to what is available).
-
Mobile/smart app.
-
NICE-supported therapy.
-
One-to-one support.
-
Self help (e.g. self management).
-
Shared decision-making/decision aids (e.g. manuals and decision-making documents/prompts to aid decision-making).
-
Signposting and linkage.
-
Telehealth (e.g. includes videoconferencing; telepsychiatry; telehealth intervention delivered proactively by the service provider to the participant).
-
Theory-based support.
Appendix 4 Respondents table
| Organisation | Services and treatments provided | Referral routes | Who provides services and treatments | Where and how delivered | Evaluation activity | Additional notes (including website information) | Stage 1 code |
|---|---|---|---|---|---|---|---|
| NHS services in England | |||||||
| North | |||||||
| Military Veterans’ Service delivered by Greater Manchester West Mental Health NHS Foundation Trust | ‘Veterans in Mind’ – mental health services for military veterans in Cheshire and Merseyside (excluding Liverpool). Provides clinical services and links to support with housing, financial and social needs. Works in partnership with Combat Stress, particularly for psychological-related problems (including depression, anxiety, substance misuse, trauma, adjustment disorders and personality disorder problems) | GP; health-care professional; third-party organisation; family member or carer; self referral | – | – | – | Website: www.gmw.nhs.uk/military-veterans-services | Partnership, cross-sector, liaison work, co-location; co-ordinated, integrated, collaborative, networks, multidisciplinary care; primary care |
| Military Veterans’ Service (Greater Manchester and Lancashire) delivered by Pennine Care NHS Foundation Trust in Greater Manchester, and in partnership with Lancashire Care NHS Foundation Trust in Lancashire | TFCBT; PE; cognitive restructuring; EMDR; psychodynamic psychotherapy; CAT; ACT; DBT skills; mindfulness skills; couples’ therapy; art psychotherapy; substance misuse and offender case management; stabilisation programme |
74% non-NHS (probation, addiction services, local authorities, social services, prisons, police, MOD, veteran charities) 33% self referrals By telephone, e-mail, fax or website (no GP required) Anybody can refer with client consent (including family) |
Clinical psychologist, psychodynamic psychotherapist, CBT therapist, EMDR therapist, AMHP social worker, RMN, CPN, art psychotherapist, couples’ counsellor, substance misuse and offender case worker, psychological well-being practitioner, employment mentor, peer mentor | Various venues across the commissioned footprint (whole of Greater Manchester and Lancashire), GP surgeries, football grounds, TA centres/barracks, supermarket community rooms, libraries, fire stations, local authority buildings, probation, client home where clinically indicated, etc.; as close to client as reasonably possible | Yes |
Mental health support including depression, alcohol and substance misuse, anger problems and PTSD. Services are overseen by clinical psychologists, well-being practitioners and case managers with knowledge of armed forces culture. In addition, works with third sector – ‘Walking with the Wounded’, ‘Veterans in Communities’ and ‘Inspiration NW’ – to help veterans overcome barriers to access (from website: www.penninecare.nhs.uk/your-services/military-veterans-service/) ‘Overcoming the Barriers’ was one of the 6-month NHS England pilots for enhanced model of care. The model was developed to address barriers that some veterans experience when accessing mental health services |
Partnership, cross-sector, liaison work, co-location; co-ordinated, integrated, collaborative, networks, multidisciplinary care; community outreach; case management; peer mentoring; direct service/treatment provision |
| Veterans’ Outreach Service (Yorkshire and the Humber) delivered by Humber NHS Foundation Trust | Host organisation, working in partnership with Leeds/York Partnership NHS Foundation Trust and Sheffield Health and Social Care Foundation NHS Trust: veterans’ outreach service includes mental health triage/assessment and signposting; four named outreach therapists cover the region. No crisis service | Open referral system (self referral; any statutory/non-statutory organisation) | Includes outreach service, covered by four therapists. All have mental health training and experience working with ex-military personnel | – | – | Website: www.humber.nhs.uk/services/veterans-outreach-service | Partnership, cross-sector, liaison work, co-location; community outreach; signposting and linkage; assessment/triage |
| Veterans’ Wellbeing Assessment and Liaison Service (North East) delivered by Northumberland Tyne and Wear/Esk and Wear Valleys NHS Foundation Trusts |
IAPT services for those with less complex trauma – one-to-one therapy short term, CBT and EMDR and well-being group Veterans’ well-being service – case manages veterans into appropriate care pathway across any health and social care setting Tertiary level regional centre for CBT – sees people including veterans with complex trauma who require longer-term input – CBT and EMDR – other psychologically informed therapies, much more intense therapy and looking at life events Community treatment teams – where associated risk means cannot be seen in primary care biopsychosocial care – psychology, psychiatry, occupational therapy and nursing Veterans’ substance misuse service – to sequence care, helping veterans to manage substance misuse |
Open referral including self referral | Nurse consultant, consultant psychologists, associate specialists, case managers, community nurses, OTs, IAPT practitioners, consultant psychiatrists, support workers, peer support workers | Within community settings predominantly | CQC inspections, 1-year evaluation of Veterans’ Wellbeing Assessment and Liaison Service | Collaborates with Combat Stress and British Legion. Veterans’ Wellbeing and Liaison Service provides a single point of access to a range of mental health services across the North East (from website: www.tewv.clients.wtg.co.uk/site/care-and-treatment/all-services/Veterans’%20Wellbeing%20Assessment%20and%20Liaison%20Service) | Partnership, cross-sector, liaison work, co-location; co-ordinated, integrated, collaborative, networks, multidisciplinary care; use of IAPT; community outreach; case management; peer mentoring; day care; direct service/treatment provision |
| Midlands | |||||||
| Veterans First (Essex) part of North Essex Partnership University NHS Foundation Trust |
North Essex Partnership University NHS Foundation Trust hosts Veterans First, a specialist mental health team for UK armed forces veterans covering the trust area of north Essex Currently providing a full care co-ordination and holistic approach supporting mental health needs, housing, employment, social integration, etc. Three monthly support groups for veterans are also run, which are attended by other veteran organisations, such as Combat Stress, Royal British Legion and Veterans UK to name a few We have an Employment Mentor seconded into the team from the Career Transition Partnership funded by Walking With The Wounded |
GP; self; through the Trust’s Access and Assessment services and other trust specialist services (e.g. Criminal Justice Mental Health Team, other organisations, such as Royal British Legion, Combat Stress, SSAFA, etc.) |
Clinical Nurse Specialist Band 7 – EMDR, trauma-focused therapy We also have two psychologists who work on an honorary basis providing therapy Psychologist #1: registered chartered psychologist (C.Psych. AFBPsS) Accredited CBT therapist EMDR practitioner Psychologist #2: registered chartered counselling psychologist and also a trust specialty doctor who sees a couple of patients a week for EMDR as part of his special interest day |
Treatments are mainly delivered at trust premises, although occasionally in the veteran’s home on a one-to-one basis. No group therapy sessions | – |
Provides information on care pathways, monitors and delivers veterans’ services throughout North Essex. Works with Combat Stress and other third-sector partners (from website: www.nevmhn.org.uk/veterans-first-service.html) Note: this location is one of the 6-month NHS England pilots for enhanced model of care. Two programmes include (1) a joint substance misuse and mental health service model and (2) an outpatient service for veterans with moderate to severe PTSD |
Partnership, cross-sector, liaison work, co-location; co-ordinated, integrated, collaborative, networks, multidisciplinary care; outpatient; primary care; group support |
| Veterans’ Mental Health Services (East Midlands) led by Lincolnshire Partnership NHS Foundation Trust | Psychological therapies, integrated community mental health teams, early intervention services, Veterans Liaison Service | GP, charitable organisations, internal teams, local authorities, police, MOD, A&E departments, prisons | Consultant psychologist and Veteran Liaison Services | Delivered within clinical settings or agreed location, in partnership with service user. A plan of care is formulated and delivered | Current veteran liaison service reports to NHS England on identified key performance indicators. As a trust, we encourage feedback via the NHS Friends and Family test, which is then reported to the trust board | Works with Combat Stress; mentions adult inpatient mental health services for armed forces veterans (from website: www.lpft.nhs.uk/our-services/adult-services/veterans-mental-health-services) | Partnership, cross-sector, liaison work, co-location; co-ordinated, integrated, collaborative, networks, multidisciplinary care; early intervention; primary care; direct service/treatment provision |
| West Midlands Military Veterans’ Hub, part of South Staffordshire and Shropshire NHS Foundation Trust | Veterans Service for all ex-forces covering all mental health difficulties including PTSD. All treatments are as per NICE guidelines (e.g. CBT/EMDR) | All service users across all teams are asked if they have served in the armed forces and whether or not they wish to be seen by the Veterans Service. Automatic notification is sent to the Veterans Service if a service user wishes to be seen. All veterans are seen within 4 weeks of referral. GP referrals go through normal routes, this being the single point of access where service users are screened according to level of risk | All services within the trust should be able to engage with service users with PTSD or other mental health conditions. Some staff have attended veterans awareness training and all have access to the lead nurse for veterans for supervision or consultation | All services engage with veterans throughout catchment area | Client evaluation takes place through the University of Worcester; IAPT measures are taken to measure client progress. The NHS Friends and Family review as per normal satisfaction survey | Collaboration of eight NHS mental health service providers in the West Midlands. Each area has a Veterans’ Champion to oversee, promote and link with existing teams and providers. Works with Combat Stress and CHANGES (social enterprise) to develop inclusive programme for veterans (though those with drug and alcohol issues encouraged to be free of substances before contact) (from website: http://veterans.sssft.nhs.uk/veteranservices/west-midlands-regional-veterans-service) | Partnership, cross-sector, liaison work, co-location; co-ordinated, integrated, collaborative, networks, multidisciplinary care; direct service/treatment provision; NICE- supported therapy |
| South | |||||||
| London Veterans’ Service delivered by Camden and Islington NHS Foundation Trust and South London and Maudsley NHS Foundation Trust |
Our service provides a comprehensive multidisciplinary assessment for mental health for anyone who has served in the British military. We are able to case manage, when appropriate, into mainstream NHS services. We also offer trauma-focused treatment for specific cases. We have a prison inreach programme and also run regular educational courses for veterans about better managing their mental health. We have regular meetings with our closest charity providers to ensure good pathways for the clients and we have been providing training to charities and IAPT services when able We are also currently running the NHS England transition pathways pilot for London and the South East, one of three national services |
Self referral, GP, IAPT, charity sector and by family are our main sources of referrals | Clinical psychologist, clinical nurse specialist, psychiatrist, art therapist, honorary trainee counselling psychologist, assistant psychologists | Our service provides assessment and treatment for those within the M25. Clients mainly come to our central London centre, but we also offer some peripatetic clinics around London. We also have a prison inreach service for those incarcerated | Yes |
Based at St Pancras Hospital, has a section on specialist treatment for PTSD. Website offers self-help strategies on grounding and distraction. Gives information on therapies e.g. TFCBT, EMDR (from website: http://londonveterans.nhs.uk/ Note: both above treatments are included in NICE guidelines |
Partnership, cross-sector, liaison work, co-location; co-ordinated, integrated, collaborative, networks, multidisciplinary care; prison inreach; case management; primary care: direct service/treatment provision; advice/information/education; assessment/triage; self help |
| South Central Veterans’ Mental Health Service delivered by Berkshire Healthcare NHS Foundation Trust | Assessment for all mental health needs and help to access appropriate services. Offers specialist direct treatment for PTSD (‘Traumatic Stress Service’) and liaison/signposting to other agencies for a range of mental health-related conditions (such as alcohol and drug problems) and other services (housing, debt, employment and benefits) | CPE service; self referral; GP; mental health professional | – | – | – |
Website: www.berkshirehealthcare.nhs.uk/ServiceCatInfo.asp?id=119 Traumatic Stress Service: www.berkshirehealthcare.nhs.uk/ServiceCatInfo.asp?id=51 |
Partnership, cross-sector, liaison work, co-location; primary care; direct service/treatment provision; signposting and linkage; assessment/triage |
| South West Veterans’ Mental Health Service delivered by Avon and Wiltshire Mental Health Partnership NHS Trust | Triage; assessment; case management; liaison; signposting; trauma therapy | All referrals accepted. Self, partner, GP, forces charities, defence medical services | Veterans’ therapists; RMNs, social worker; clinical psychologist; also generic IAPT services | Delivered at Royal British Legion pop-in centres, NHS Mental health facilities; Help for Heroes recovery centre; GP surgeries – following NICE guidelines CG2614 | NICE evidence-based therapy; user feedback; monthly reporting to NHS England | Appears to be a signposting service to local charities (from website: www.swveterans.org.uk/ | Partnership, cross-sector, liaison work, co-location; community outreach; case management; primary care; direct service/treatment provision; signposting and linkage; assessment/triage; NICE-supported therapy |
| SERVES delivered by First Steps Surrey (Virgin Care on behalf of Surrey County Council) | Advice and information on common mental health and emotional issues; self-help resources; ‘Emotional Gyms’; signposting; drop-in; crisis helpline; case workers. No one-to-one support | Website access; emotional gyms do not need GP referral | Trained mental health advisors from variety of professions | – | – | Website: www.firststeps-surrey.nhs.uk/serves/ | Case management; primary care; Signposting and linkage; advice/information/education; self help |
| Sussex Armed Forces Network led by Sussex CCGs and Sussex Partnership NHS Foundation Trust | – | – | – | – | – | Joining Forces Training set up to understand specific pathways and services in Sussex for Armed Services community (including mental health). A pathway page is available on the website, covering sources of help for wider determinants of health (including mental health). Mental health section includes how to access full mental health assessment and treatment options for veterans. Works with a range of partners, including local authorities (from website: www.sussexarmedforcesnetwork.nhs.uk/) | Partnership, cross-sector, liaison work, co-location; co-ordinated, integrated, collaborative, networks, multidisciplinary care; peer mentoring; signposting and linkage; advice/information/education |
| NHS services in Scotland | |||||||
|
V1P Scotland Information gathered from V1P newsletters (March, August, December 2016) |
A network of NHS–third-sector partnerships across Scotland; also provides staff training modules for eight new funded V1P centres established in March 2016. Under development, but include drop-in centres; peer support; psychological therapy; outreach service; prison inreach; occupational therapy; Individual Placement Model to promote mental health recovery through work; leisure and art activities; brokerage and identification of clients with complex needs | Self referral; others via existing psychology services | Peer support workers; OTs; psychological therapists and other clinical appointments | Eight new funded V1P centres (2016): Ayrshire and Arran; Borders; Fife; Grampian; Highland; Lanarkshire; Lothian; Tayside |
V1P Scotland Evaluation: The Transformation Station is a collaboration between NHS Lothian and Queen Margaret University, Working with V1P Scotland (March 2016 newsletter) Location-specific service reviews Network teams continue to gather data as part of an evaluation by Queen Margaret University |
Website: www.veteransfirstpoint.org.uk/ | Partnership, cross-sector, liaison work, co-location; co-ordinated, integrated, collaborative, networks, multidisciplinary care; community outreach; prison inreach; peer mentoring; direct service/treatment provision |
| NHS services in Wales | |||||||
| Veterans NHS Wales |
Veterans NHS Wales currently provides an assessment, treatment and signposting service for Armed Forces veterans with PTSD. We offer in-house individual treatment for PTSD with TFCBT, EMDR, CPT for couples and we offer cognitive and behavioural conjoint therapy for PTSD We signpost veterans to the usual veterans’ charities including the Royal British Legion, SSAFA and in Wales we have a peer mentoring service charity called Change Step who offer one-to-one peer mentoring. We also refer to Care After Combat, which also offers peer mentoring for veterans coming out of prison |
Veterans can self refer to our service via our telephone number, e-mail or bespoke website: www.veteranswales.co.uk. We also receive referrals from the usual sources including primary care, secondary care and veterans’ charities | We have 14 mental health professionals with a background in occupational psychology, counselling psychology, mental health nursing, occupational therapy, mental health social work or who have a postgraduate qualification in a psychological therapy (CBT) at diploma to master’s degree level. They all also have training in EMDR | Veterans NHS Wales, funded by Welsh Government, has seven local health boards that all have between one and four VTs, many of whom work part time, on a sessional basis, for the service via a hub and spoke model, with the hub centred in University Hospital of Wales, Cardiff | Yes | Each of the seven local health boards in Wales appoints a VT with an interest or experience of military mental health problems. Referrals to the VT come from health-care staff, GPs, veteran charities and self referral (from website: www.veteranswales.co.uk/ | Partnership, cross-sector, liaison work, co-location; co-ordinated, integrated, collaborative, networks, multidisciplinary care; peer mentoring; primary care; DIRECT service/treatment provision; signposting/linkage; assessment/triage |
| NHS services in Northern Ireland | |||||||
| UDR and R IRISH (HS) Aftercare Service | The UDR and R IRISH (HS) Aftercare Service offer access to a trauma-focused psychological therapy intervention consisting of an initial assessment followed by up to 10 sessions of one-on-one counselling | Clients are referred to our services, in the main, by our own case workers, who conduct domiciliary visits on request. Referrals from a number of additional pathways include Veterans UK, Combat Stress, GP and local health trusts | Our group of caseworkers provide a range of services to our client group including a holistic approach to medical, welfare and benevolence including completion of referral forms | The psychological therapy intervention is delivered by contracted providers. After an initial assessment in Belfast, the remainder of the intervention is provided via a network of counsellors who deliver sessions local to the referred individual | An audit of our medical service provision was undertaken in 2012; this measured clinical governance along with outcomes and client satisfaction |
The NHS Choices website for services in Northern Ireland signposts Veterans to the Northern Ireland Veterans Support Committee c/o UDR and R IRISH (HS) Aftercare Service www.aftercareservice.org/ The UDR and R IRISH (HS) Aftercare Service is a MOD-funded organisation formed in 2007 specifically to address the legacy of the UDR and R IRISH (HS) regiments who served in OP BANNER in Northern Ireland – The services offered are currently limited to eligible clients, i.e. those veterans who served in either the UDR or R IRISH |
Case management; primary care; direct service/treatment provision/assessment/triage |
| Third sector (UK) | |||||||
| Combat Stress |
Three stepped-levels of intervention:
|
Self referral; family members; mental health professionals | Multidisciplinary teams comprising psychiatrists, psychologists, nurses, OTs, art therapists, support workers, community and outreach teams | Community; outreach; inpatient | Published evaluation of ITP (Murphy et al.36). See also ‘Our Research’ section of website for more evaluations |
The leading mental health charity for veterans in the UK. Various services, including 24-hour helpline; community support (clinics); magazine; residential treatment centres; case management for substance misuse (from website: www.combatstress.org.uk/ Commissioned by the NHS in 2011 to provide specialist 6-week ITP free for veterans with severe PTSD |
Co-ordinated, integrated, collaborative, networks, multidisciplinary care; community outreach; stepped care model; multicomponent treatment programme; family systems model; inpatient; residential; crisis management; direct service/treatment provision; telehealth; one-to-one support; group support |
| Help for Heroes | No direct clinical interventions; but array of Sports Recovery, Welfare support, Career recovery and psychological support and onward referral. Directly commission services from NHS, Walking with Wounded and Combat Stress | Self, health professionals, significant others | N/A | We refer people to other organisations such as the NHS, Combat Stress, Walking with the Wounded | N/A | ‘Hidden Wounds’ – free individual support for mental health and associated problems (drinking habits); Help for Heroes also supports Big White Wall (early online intervention service) (from website: www.helpforheroes.org.uk/) | Signposting and linkage |
| PTSD Resolution Ltd | Counselling and psychotherapy, one to one, using HGT | Self referrals, other charities, prisons, probation services, by contacting www.ptsdresolution.org or ringing 0300 302 0551 |
Admin 1 – office worker Admin 2 – office worker 200 therapists all HGT trained, registered and regulated |
Treatment is delivered in the person’s home, a clinic, the therapist’s home clinic, a mutually convenient place or prison as applicable | Yes | A network of counselling therapists throughout the UK to deal with PTSD in veterans with limited resources. Website indicates 78% of PTSD can be resolved to sub-clinical level (from website: www.ptsdresolution.org/) | Co-ordinated, integrated, collaborative, networks, multidisciplinary care; direct service/treatment provision; theory-based support |
| Walking with the Wounded | See our ‘what we do’ booklet and specifically the Head Start programme, which is our mental health programme. Treatment is offered for mild to moderate conditions of common mental health disorders including PTSD akin to the IAPT framework providing step 3 care from 0–18 sessions of private accredited therapy using NICE-recommended approaches to therapeutic helping, specifically TFCBT and EMDR for PTSD | Using an e-referral or hard copy referral form which can found on our website, referrals received from MOD DCMH’s R&VMHP, NHS GPs and NHS Veteran teams × 12, Big White Wall, H4H Hidden Wounds and Combat Stress (collaborative stepped care model). We liaise with all the afore-mentioned to ensure an effective pathway. NHS GPs are our main referrer. We have assisted Public Health England in a national programme of training GPs in veteran mental health matters, particularly read coding and the range of statutory and third-sector services available, with emphasis on sourcing ethical-assured treatment from those in the COBSEO Contact group | Head Start programme manager Bachelor of Arts (Honours) Law and Criminology, MHFA (undefined) (Veterans) and clinical lead Lieutenant Colonel (retired) Bachelor of Science (Honours) CBT, DipHE CHWS, RN(MH) RN(A) CPN Dip, EMDR parts 1, 2 and 3 (former Ministry of Defence nurse consultant) | This is facilitated by a national network of accredited therapists, (BABCP, BACP, EMDR UK etc.). Clients receive support within 10 days of returning their consent and within 10 miles of their home. Thus, treatment is ethical, community-based and near their homes. Therapists are given information on engaging with veterans and some common abbreviations, relevant academic papers, conference dates and a newsletter is sent to the network. We suggest that they undertake the two NHS England e-Learning modules | KCL KCMHR are evaluating the programme with results yet to be published. We use standardised and reliable measures, PHQ-9, GAD-7, AUDIT, PCL-C, and WSAS (PROMS) at the start, middle and end of therapy | Head Start provides choices for mental health support that are complementary to those provided by the NHS and other third-sector organisations (from website: http://walkingwiththewounded.org.uk/how-we-help/wwtw-special-projects/head-start/) | Partnership, cross-sector, liaison work, co-location; co-ordinated, integrated, collaborative, networks, multidisciplinary care; primary care; direct service/treatment provision; NICE-supported therapy |
| Other services | |||||||
| St Johns and Red Cross Defence Medical Welfare Service (available across Greater Manchester Hospitals) | This organisation does not provide treatment. The project in Greater Manchester supports veterans aged ≥ 65 years. No direct support around PTSD. Support through the referral pathway or signpost to sources of professional help | – | – | – | – |
Services are available to all Armed Forces personnel, including Veterans. See also Ex-Forces Action Network, Greater Manchester (supporting ex-service personnel who have had contact with the criminal justice system) (from website: www.dmws.org.uk/the-aged-veterans-project-greater-manchester) www.dmws.org.uk/the-ex-forces-action-network-greater-manchester |
Signposting and linkage |
| Liverpool Veterans | Suggests we look at Tom Harrison House – http://tomharrisonhouse.org.uk/ | – | – | – | – | Appears to be an independent organisation run by Liverpool Veterans HQ (developed by Breckfield and North Everton Neighbourhood Council) in conjunction with FACT. Provides links to services, research and fundraising events for veterans and their families in the Liverpool area (from website: www.liverpoolveterans.co.uk/get-support/health-wellbeing/) | Signposting and linkage |
| Factors affecting implementation of services and treatments for veterans with PTSD reported by service providers contacted | |||||||
|
|||||||
Appendix 5 Treatments delivery mechanisms/aids (rather than structures for the organisation of services)
| First author, year | Title |
|---|---|
| Telehealtha | |
| Acierno, 201681 | Behavioral activation and therapeutic exposure for posttraumatic stress disorder: a noninferiority trial of treatment delivered in person versus home-based telehealth |
| Battaglia, 201382 | A clinical translation of the research article titled ‘building a tobacco cessation telehealth care management program for veterans with posttraumatic stress disorder’ |
| Fortney, 201583,84 | Telemedicine-based collaborative care for posttraumatic stress disorder: a randomized clinical trial |
| Frueh, 200785 | A randomized trial of telepsychiatry for PTSD |
| Gros, 201186 | Exposure therapy for PTSD delivered to veterans via telehealth: predictors of treatment completion and outcome and comparison to treatment delivered in person |
| Gros, 201687 | Treatment satisfaction of home-based telehealth versus in-person delivery of PE for combat-related PTSD in veterans |
| Hoerster, 201588 | A pilot trial of telephone-based collaborative care management for PTSD among Iraq/Afghanistan war veterans. |
| Lindsay, 201589 | Implementation of video telehealth to improve access to evidence-based psychotherapy for posttraumatic stress disorder |
| Maieritsch, 201690 | Randomized controlled equivalence trial comparing videoconference and in person delivery of CPT for PTSD |
| Morland, 200491 | Telemedicine and coping skills groups for Pacific Island veterans with PTSD: a pilot study |
| Morland, 201092 | Telemedicine for anger management therapy in a rural population of combat veterans with posttraumatic stress disorder: a randomized noninferiority trial |
| Morland, 201193 | Group CPT delivered to veterans via telehealth: a pilot cohort |
| Morland, 201394 | Telemedicine: a cost-reducing means of delivering psychotherapy to rural combat veterans with PTSD |
| Morland, 201495 | CPT for posttraumatic stress disorder delivered to rural veterans via telemental health: a randomized noninferiority clinical trial |
| Rosen, 200696 | Telephone monitoring and support for veterans with chronic posttraumatic stress disorder: a pilot study |
| Rosen, 201397 | Telephone monitoring and support after discharge from residential PTSD treatment: a randomized controlled trial |
| Strachan, 201298 | An integrated approach to delivering exposure-based treatment for symptoms of PTSD and depression in OIF/OEF veterans: preliminary findings |
| Tuerk, 201099 | A pilot study of PE therapy for posttraumatic stress disorder delivered via telehealth technology |
| Wierwille, 2016100 | Effectiveness of PTSD telehealth treatment in a VA clinical sample |
| Yuen, 2015101 | Randomized controlled trial of home-based telehealth versus in-person PE for combat-related PTSD in veterans: preliminary results |
| Ziemba, 2014102 | Posttraumatic stress disorder treatment for OEF/OIF combat veterans through a civilian community-based telemedicine network |
| Internet, web, online interventionsb | |
| Belsher, 2015103 | A preliminary study of an internet-based intervention for OEF/OIF veterans presenting for VA specialty PTSD care |
| Engel, 2015104 | Delivery of self training and education for stressful situations (DESTRESS-PC): a randomized trial of nurse assisted online self-management for PTSD in primary care |
| Hobfoll, 2016105 | Vets Prevail online intervention reduces PTSD and depression in veterans with mild-to-moderate symptoms |
| Kahn, 2016106 | Post-9/11 veterans and their partners improve mental health outcomes with a self-directed mobile and web-based wellness training program: a randomized controlled trial |
| Mobile, smart app | |
| Erbes, 2014107 | Access, utilization, and interest in mHealth applications among veterans receiving outpatient care for PTSD |
| Kahn, 2016106 | Post-9/11 veterans and their partners improve mental health outcomes with a self-directed mobile and web-based wellness training program: a randomized controlled trial |
| Kuhn, 2014108 | Preliminary evaluation of PTSD Coach, a smartphone app for post-traumatic stress symptoms |
| Smith, 2012109 | Enhancing behavioral health treatment and crisis management through mobile ecological momentary assessment and SMS messaging |
| Shared decision-making, decision aidsc | |
| Mott, 2014110 | Increasing engagement in evidence-based PTSD treatment through shared decision-making: a pilot study |
| Watts, 2015111 | A randomized controlled clinical trial of a patient decision aid for posttraumatic stress disorder |
| Advice, information, education | |
| Schumm, 2015112 | Veteran satisfaction and treatment preferences in response to a posttraumatic stress disorder specialty clinic orientation group |
| Group Support | |
| Schumm, 2015112 | Veteran satisfaction and treatment preferences in response to a posttraumatic stress disorder specialty clinic orientation group |
| One-to-one support | |
| Gros, 201687 | Treatment satisfaction of home-based telehealth versus in-person delivery of PE for combat-related PTSD in veterans |
| Self help | |
| Engel, 2015104 | Delivery of self training and education for stressful situations (DESTRESS-PC): a randomized trial of nurse assisted online self-management for PTSD in primary care |
Glossary
- Behavioural activation
- A treatment for depression involving the patient and therapist working in parallel to identify current behavioural impact and develop positive solutions [www.nice.org.uk/guidance/cg90/ifp/chapter/treatments-for-mild-to-moderate-depression (accessed 1 February 2017)].
- Cognitive–behavioural therapy
- A talking therapy concentrating on behavioural determinants and skills to cope with different problems [www.mind.org.uk/information-support/drugs-and-treatments/cognitive-behavioural-therapy-cbt/#.WMquXm-ebIU (accessed 1 February 2017)].
- Cognitive processing therapy
- No standard definition could be located. Defined by Wikipedia as ‘a manualized therapy used by clinicians to help people recover from posttraumatic stress disorder (PTSD) and related conditions. It includes elements of cognitive behavioral therapy (CBT) treatments’ [https://en.wikipedia.org/wiki/Cognitive_processing_therapy (accessed 1 February 2017). This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 3.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/3.0/].
- Eye movement desensitisation and reprocessing
- An eight-phase psychotherapy involving eye movement to help patients properly process traumatic memories and assist with coping procedures [www.counselling-directory.org.uk/emdr.html (accessed 1 February 2017)].
- Human givens therapy
- Delivered by registered therapists, this present-centred approach uses various methods to help provide solutions to emotional distress, focusing on unmet needs of the patient [www.counselling-directory.org.uk/human-givens-therapy.html (accessed 1 February 2017)].
- Prolonged exposure
- No standard definition could be located. Defined by Wikipedia as ‘a form of behavior therapy and cognitive behavioral therapy designed to treat post-traumatic stress disorder, characterized by re-experiencing the traumatic event through remembering it and engaging with, rather than avoiding, reminders of the trauma (triggers). Sometimes, this technique is referred to as flooding’ [https://en.wikipedia.org/wiki/Prolonged_exposure_therapy (accessed 1 February 2017). This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 3.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/3.0/].
- Trauma-focused cognitive–behavioural therapy
- A specific form of cognitive–behavioural therapy for people with post-traumatic stress disorder [www.nice.org.uk/guidance/cg123/chapter/Appendix-E-Glossary (accessed 1 February 2017)].
List of abbreviations
- 3CM
- three-component model
- CBT
- cognitive–behavioural therapy
- CCG
- Clinical Commissioning Group
- CPT
- cognitive processing therapy
- DARE
- Database of Abstracts of Reviews of Effects
- DMS
- Defence Medical Services
- EMDR
- eye movement desensitisation and reprocessing
- GP
- general practitioner
- IAPT
- Improving Access to Psychological Therapies
- ITP
- intensive treatment programme
- NICE
- National Institute for Health and Care Excellence
- OIF
- Operation Iraqi Freedom
- PE
- prolonged exposure
- PTSD
- post-traumatic stress disorder
- R IRISH
- Royal Irish Regiment
- RCT
- randomised controlled trial
- SSRI
- selective serotonin reuptake inhibitor
- TCA
- tricyclic antidepressant
- TFCBT
- trauma-focused cognitive–behavioural therapy
- UDR
- Ulster Defence Regiment
- V1P
- Veterans First Point
- VA
- Veterans Affairs
- VT
- veteran therapist
