Notes
Article history
The research reported here is the product of an HS&DR Evidence Synthesis Centre, contracted to provide rapid evidence syntheses on issues of relevance to the health service, and to inform future HS&DR calls for new research around identified gaps in evidence. Other reviews by the Evidence Synthesis Centres are also available in the HS&DR journal.The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/05/12. The contractual start date was in March 2016. The final report began editorial review in February 2017 and was accepted for publication in July 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Preston et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
The emergency department (ED) setting has long been acknowledged as a complex setting in which to deliver care to older people. The difficulties of delivering care have to be viewed alongside the more general challenges that are facing NHS EDs. In 2013, NHS England set out a strategy for an urgent care system that was:
more responsive to patients’ needs, improves outcomes and delivers clinically excellent and safe care.
This strategy also needs to be viewed alongside the UK government target of 95% of all ED patients being discharged, transferred or admitted within 4 hours of presenting at an ED.
The delivery of safe and appropriate care to older patients in the ED has a number of challenges. Older patients are not a homogeneous group. They encompass a wide age range and are a diverse group in terms of their general health and presenting complaints. The National Service Framework: Older People2 describes older people as being in one of three groups: entering old age (still living an active and independent life), transitional (between healthy active life and frailty) and frail older people (vulnerable as a result of health problems or social care needs).
This review is focused on the delivery of care to this last group (frail older people). Set within the context of increasing demand and pressure on the delivery of care in the ED, frail older people are a group who present a specific challenge to the ED. First, older people are more likely to present to the ED and, second, once they are in the ED, they present a specific set of challenges to the delivery of safe and effective care.
In terms of the volume of demand that older people place on the ED, this is in part a result of the ageing population. There has been an increase in the absolute and relative numbers of older people in the general population as people are living to an older age. The University of Sheffield undertook a rapid review on urgent care for the National Institute for Health Research, which found that frail older people use emergency care more frequently (especially those who are aged > 80 years and those who are acutely unwell or in the last year of life). 3 Gruneir et al. 4 report on the disproportionate use of the ED by older age groups compared with younger age groups. However, this disproportionate use is not inappropriate: both medical and non-medical reasons underpin the reliance of this group on the care provided in EDs. A recent literature review commissioned by the NHS Confederation,5 which examined the evidence on how to improve urgent care for older people, found that demand on the ED from older people is not simply related to their need for urgent and emergency care; it is also related to the care that they receive (or do not receive) elsewhere in the health-care system. Examples of the types of interventions that might reduce demand on EDs include preventing ED admission through ambulatory triage, referring older people directly to a ward, a medical assessment unit or elderly care unit, delivering appropriate care within a home/community setting (a nursing home or their own home) and preventing readmissions when older people are discharged from acute medical care through interventions delivered in the home.
Once older people present to the ED, they present a specific set of challenges in terms of their management and care. Older people are more likely to have long-term conditions and multiple morbidities and they are often taking multiple medications. They may have disabilities that make the fast-moving nature of the ED highly unsuitable. They are also more likely to have dementia, or present with delirium, and this is often alongside the presenting complaint that has required them to seek emergency care. Older patients can also often present non-specifically5 and are therefore difficult to diagnose and treat accordingly. Underlying all of this is that a number of older patients are frail and the ED faces difficulties in identifying those who are frail and delivering appropriate care to them. Once frail older people are in the ED, it becomes critical to manage their presenting complaint in the context of their frailty. A recent Lancet editorial6 outlined the four issues facing EDs in their management of frail older people: (1) timely recognition of frail patients is difficult; (2) there is no standard definition for frailty; (3) frail older people need to be treated in the context of their frailty as opposed to treating them only according to their presenting complaint; and (4) there are a lack of clinical guidelines for treating frail older people in the ED.
Identifying frail older people is highly challenging and this challenge is acknowledged widely in the academic literature: ‘. . . there is no single operational definition of frailty that can satisfy all experts’. 7 There is no set age threshold for when an older person becomes frail; however, Dent et al. 8 suggest that frailty is present in around one-quarter of people aged > 85 years. Carpenter et al. 9 discuss how chronological age is often seen as synonymous with biological age and the majority of research studies consider people aged ≥ 65 years as a homogeneous population. In an evidence review examining discharge interventions, Lowthian et al. 10 found three groups of older people in the literature: (1) patients stratified by age (which varied from ≥ 65 years to ≥ 75 years); (2) vulnerable people within these age categories; and (3) older people who had been screened and were considered to be at high risk.
Some clinicians and academics believe that frailty can be defined using a set of clinical indicators (e.g. patients with multimorbidity or an increased risk of falls). Others believe that frailty is more closely linked to changes in the physiology of older people (accumulated deficits). However, what is widely acknowledged in the literature is the need to manage these patients with their frailty considered alongside their presenting complaint. 8,11 There are numerous reasons for this, such as the need to avoid polypharmacy,12 the need for follow-up care for patients and the high rate of readmission of frail patients. 13 It is known that frail patients have worse outcomes than the general population of older people if they attend the ED. Maile et al. 14 cite 46% mortality for frail older people within a year of them attending the ED.
Therefore, the scope of this review is how best to manage frail older people within the ED. This will allow us to map interventions to identify frail older people and those at high risk of adverse outcomes, study the management of frail older people in the ED and examine the potential for improvements in both patient and health service outcomes.
The research questions for the review were as follows:
-
What is the evidence for the range of different approaches to the management (identification and service delivery interventions) of frail older people within the ED?
-
Is there any evidence of their potential and actual impact on health service and patient-related outcomes, including impacts on other services used by this population and health and social care costs?
Additional research questions included:
-
What specific approaches to the management of frail older people exist within the ED?
-
What evidence is there that these approaches to management within the ED could influence attendance and/or reattendance rates in frail older people, hospital admission and/or readmission rates in frail older people, patient-centred outcomes in frail older people and costs to the health service?
-
What evidence is there that these approaches to management within the ED could influence other health service outcomes (as reported in the literature and as mentioned as important by the clinical academics/topic experts) and is there evidence of any unintended outcomes (such as the displacement of care) as a result of how frail older people are managed in the ED?
Chapter 2 Review methods
This chapter describes the methods utilised in our evidence synthesis. These are:
-
protocol development
-
literature search
-
choice of review methodology
-
study selection
-
study classification
-
data extraction
-
synthesising evidence
-
assessment of the evidence base
-
use of internal and external experts.
Protocol development
The protocol was developed following the suggestion of the review topic by the Health Services and Delivery Research (HSDR) review commissioners. The protocol was developed by the team at the School of Health and Related Research (ScHARR), led by the review author. The protocol was shared with our internal team and our topic experts, as well as with the HSDR team. Suggested changes were made and the final protocol was produced in June 2016. Following this, the review was registered with PROSPERO (reference number CRD42016043260).
Literature search
The review started with the search for evidence and three search iterations were undertaken to efficiently identify relevant evidence for the review. The review team was already aware that the topic had a substantial evidence base in terms of the quantity of evidence, with a number of evidence reviews already published. Therefore, the search strategy had to be designed in light of these considerations and in light of the fact that the aim of the review was to systematically map the current evidence base.
Stage 1: search of evidence retrieved for earlier review and scoping search
An initial search (in May 2016) was undertaken using the evidence base retrieved for the Turner et al. 3 review. These references were filed in an EndNote library (version 8; Clarivate Analytics, Philadelphia, PA, USA) and this was searched using terms for older people and frail older people. The purpose of this search was to provide an initial idea of the size and scope of the available literature and to refine search terms for the database search. The following keywords were searched for in the title of the references: ‘ageing’, ‘aged’, ‘elderly’, ‘frail’, ‘old’ and ‘geriatric’.
Additionally, a search was conducted in May 2016 in MEDLINE (via OvidSP) for reviews and other relevant literature; it was developed using pre-existing search strategies, used for reviews in the same topic area, devised by information specialists at the University of Sheffield. The search was structured using terms for population (frail older people) and setting (ED). The search was not limited by intervention type as an a priori decision about which interventions were to be included could have limited our understanding of the scope of the topic. The search was limited to evidence published from 2005 to 2016 to ensure currency of the included research and limited to English-language-only papers as time constraints meant that it would not have been feasible to translate non-English-language papers. The search was not limited to any specific geographical region as published search filters to identify evidence from specific countries are not always successful. The MEDLINE search strategy is provided in Appendix 1.
Stage 2: search of health and medical databases
The second search, undertaken in July 2016, involved a wider range of health and medical databases. The following databases were searched, with the MEDLINE search adapted appropriately for the different databases:
-
EMBASE via OvidSP
-
The Cochrane Library via Wiley Online Library
-
Web of Science via Web of Knowledge via ISI
-
Cumulative Index to Nursing and Allied Health Literature via EBSCOhost
-
Health Management Information Consortium via OpenAthens
-
PROSPERO.
Stage 3: complementary searching
We also undertook a number of complementary searches (in autumn 2016) to ensure that we had retrieved all relevant evidence for the review. These included scrutiny of reference lists of included papers and relevant reviews. Any relevant papers that were within our date range were obtained and, if they met the inclusion criteria, were included in the review. The reviews used for this exercise are detailed in Appendix 2. In addition, we undertook citation searching of included primary studies that focused on a frail or at-risk population.
Choice of review methodology
Based on our knowledge of the volume of evidence on interventions for older people in the ED and the need to generate a useful review product for the HSDR programme and the ED/frailty community, a systematic mapping review was selected as the most appropriate evidence product. 15 The appropriateness of the mapping review methodology was based on the diverse and diffuse evidence base and the need to ‘collate, describe and catalogue available evidence relating to a topic or question of interest’. 15 The aim of a mapping review is to ‘map out and categorize existing literature from which to commission further reviews and/or primary research by identifying gaps in research literature’. 16
Study selection
Studies were included in the review according to the inclusion and exclusion criteria in Table 1.
| Category | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Population |
|
Aged < 65 years |
| Intervention |
|
Interventions that are delivered wholly outside the ED |
| Outcome | The study had to report either patient or health service outcomes. Qualitative studies that report service user views or experiences of specific interventions would be included | Studies that do not report an outcome of an intervention; for example, a study that reported only the mean age of people being treated in an EFU would not be included. Qualitative evidence providing general experiences of ED care of (frail) older people would not be included, unless relating to a specific intervention |
| Setting | Delivered within the ED or units embedded in the ED | Delivered in community/home settings or ambulatory care |
| When patients are admitted (e.g. medical assessment units and frailty units) | ||
| Study type |
|
|
Screening criteria
We limited the evidence included in our review to that published from 2005 to 2016. The reason for this was related to the volume of evidence in the area and the need to retrieve a manageable evidence base. In addition, earlier evidence would have been identified and included in the many evidence reviews published in this area. Restricting the date ensured that the evidence included was relevant to the current clinical environment.
Notably, the review does not include ‘frail older people’ as an inclusion criteria. Throughout the process of the review, from the development of the protocol onwards, it became clear that identifying papers that had a population of frail older people according to predefined criteria would be challenging. Had we included only evidence from papers in which the authors had defined their population as frail, or their intervention as targeted at frail older people, then we would have limited the review, as scrutiny of titles and abstracts often did not reveal the population included. Therefore, we took the approach at the screening stage to include all studies in which the population was aged ≥ 65 years and then, at a later stage, further divided these studies into those including frail older people and those including a general population of older people.
Screening process
Screening was undertaken by three reviewers (LP, AC and DC). All titles and abstracts retrieved by the searches were entered into EndNote and EndNote was used for screening. All titles and abstracts were screened by one reviewer (either LP or AC), with DC screening 50% of the titles and abstracts screened by LP and 50% of the titles and abstracts screened by AC (i.e. 50% of all titles and abstracts). The decisions made about whether articles should be ‘included’, ‘excluded’ or ‘queried’ were noted in EndNote. Any queries were discussed with a fourth reviewer (JT) until consensus was reached. The inclusion and exclusion criteria were used to guide this discussion. Queries tended to be around the setting of an intervention and whether or not it was delivered in an ED setting. Articles that met the inclusion criteria that were (systematic) reviews were also marked as ‘include’ and background articles were also identified. To check the screening consistency of the two reviewers, a third reviewer screened approximately 50% of the references as detailed above and a kappa coefficient was calculated.
Study classification
Following the screening process, a list of included studies was drawn up. Full-text papers were obtained for all of the included studies and an examination of titles, abstracts and full texts was undertaken. As this review was a systematic mapping review, it was important to classify the evidence in order to develop a better understanding of the evidence base. It became clear that there was not a clear definition of the population of frail older people and so the review would need to include evidence on a wider population of older people (generally aged ≥ 65 years). In addition, this classification allowed the review team to divide articles into two categories: (1) those looking at the identification of frail older people or older people at high risk and (2) those looking at service delivery interventions to better manage older people and frail older people in the ED.
Data extraction
Once the final list of included studies had been determined, data extraction was undertaken by one of four reviewers (AC, LP, DC and FC). As this review was a mapping review, the focus was on extracting data that described interventions and their outcomes, rather than on numerical estimates of effectiveness. Therefore, single data extraction was an appropriate method as it can be undertaken with limited risk to the interpretation of results and findings from individual studies.
A standardised approach was developed and a data extraction form was developed for all of the three types of data extraction undertaken. These were:
-
full data extraction for all studies on population groups defined as frail older people or older people at ‘high risk’ by the study authors
-
brief data extraction for all studies on a population of older people, normally aged ≥ 65 years, without any specific risk criteria
-
brief data extraction for all relevant reviews that met our review inclusion criteria.
All of these data extraction tables were tested and refined by the review team. When it was clear that a conference abstract was related to a study that was published later, the data from these publications were extracted together.
Bearing in mind the complexity involved in defining frailty and the varying views about how it should be measured and applied in clinical care, our approach was to use the definitions of frailty described by study authors, but to also include older patients defined by study authors as being at high risk alongside frail patients. This approach was required partly because of the lack of clear definitions in the literature about which groups were frail and which groups consisted of all older people, for example whether or not the existence of a specific condition (e.g. patients aged ≥ 65 years with a fall) meant that patients were considered to be frail, and partly because of the lack of research into older people with frailty both generally and specifically in terms of their use of Emergency and Urgent Care. 17
Therefore, the approach adopted by this review was to undertake a full data extraction on evidence that was clearly about frail or at-risk older people. However, as it became clear that focusing solely on this evidence would not allow the development of understanding about how different approaches might influence outcomes, a brief data extraction was undertaken on the interventions that targeted a general older population, aged ≥ 65 years. This approach extends what was outlined in the review protocol. The approach described in the review protocol was that ‘where evidence exists for other elderly populations, this may be extracted into evidence tables (depending on the volume of evidence retrieved) but not used in the evidence synthesis’. However, the review used this evidence in a more thorough manner to better map the range of interventions that may potentially be used for older people in the ED.
Synthesising evidence
Data were extracted and tabulated and summary tables were created. These were used to inform the narrative synthesis presented in Chapter 4. Because of the heterogeneity of study interventions and outcomes, it was not possible to undertake any formal meta-synthesis. Data were synthesised by intervention type: interventions to identify patients as being frail or at high risk and interventions that changed the delivery of care to patients (service delivery innovations).
Assessment of the evidence base
This review aimed to map the evidence on interventions to identify and manage frail older people. Mapping reviews seek to characterise an evidence base, not compare interventions on the basis of their effectiveness. Although formal quality assessment is appropriate within the systematic review process to examine whether or not included studies may be at risk of bias, it is not required in a mapping review, as a mapping review does not interpret evidence to inform specific clinical questions or decisions. Indeed, use of a standard tool would not have been possible in this review because of the diversity of the study designs.
Rather than a formal quality assessment, we carried out a bespoke assessment of the evidence base using three distinct methods:
-
an examination of the research designs used and the strengths and limitations of those designs
-
an examination of the self-reported limitations included in the articles relating to frail or high-risk older people
-
an assessment of the relevance of the evidence to the contemporary UK NHS setting.
Use of internal and external experts
Our review used internal and external experts. Within ScHARR, three very experienced professors of emergency medicine, who are also practising ED consultants, advised on the research questions and the protocol and commented on the summary documents for the final report. In addition, we were aided by the Sheffield Teaching Hospitals NHS Foundation Trust Clinical Research Office Online Patient Advisory Panel who read and commented on our plain English summary and scientific summary.
Changes from the protocol
The protocol was developed prior to extensive literature searching and the choice of a mapping review methodology was made by the research team once the volume of evidence, diversity of study designs and heterogeneity of the evidence was clear. The choice of a mapping review impacted on two main areas: how evidence from other systematic reviews was used and how quality assessment was handled.
A more methodical approach to handling evidence from relevant reviews was adopted. Rather than simply mapping reviews against primary studies, as per the protocol, we used relevant reviews (whether systematic or not) as a source of evidence to locate additional papers for this review. In addition, when reviews matched the inclusion criteria for this review, these data were extracted and review findings were summarised in the results.
The review protocol stated that the Cochrane risk-of-bias tool would be used for quality assessment. However, this tool is appropriate only for a selected number of study designs, few of which were used by the studies reported in the review. As stated earlier, formal quality assessment using a validated checklist is not a standard feature of a mapping review. Therefore, we developed criteria to assess the evidence base, which are described in Chapter 4, Assessment of the evidence base.
Chapter 3 Results: included and excluded studies
This chapter details the studies that were included in, and excluded from, the review.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
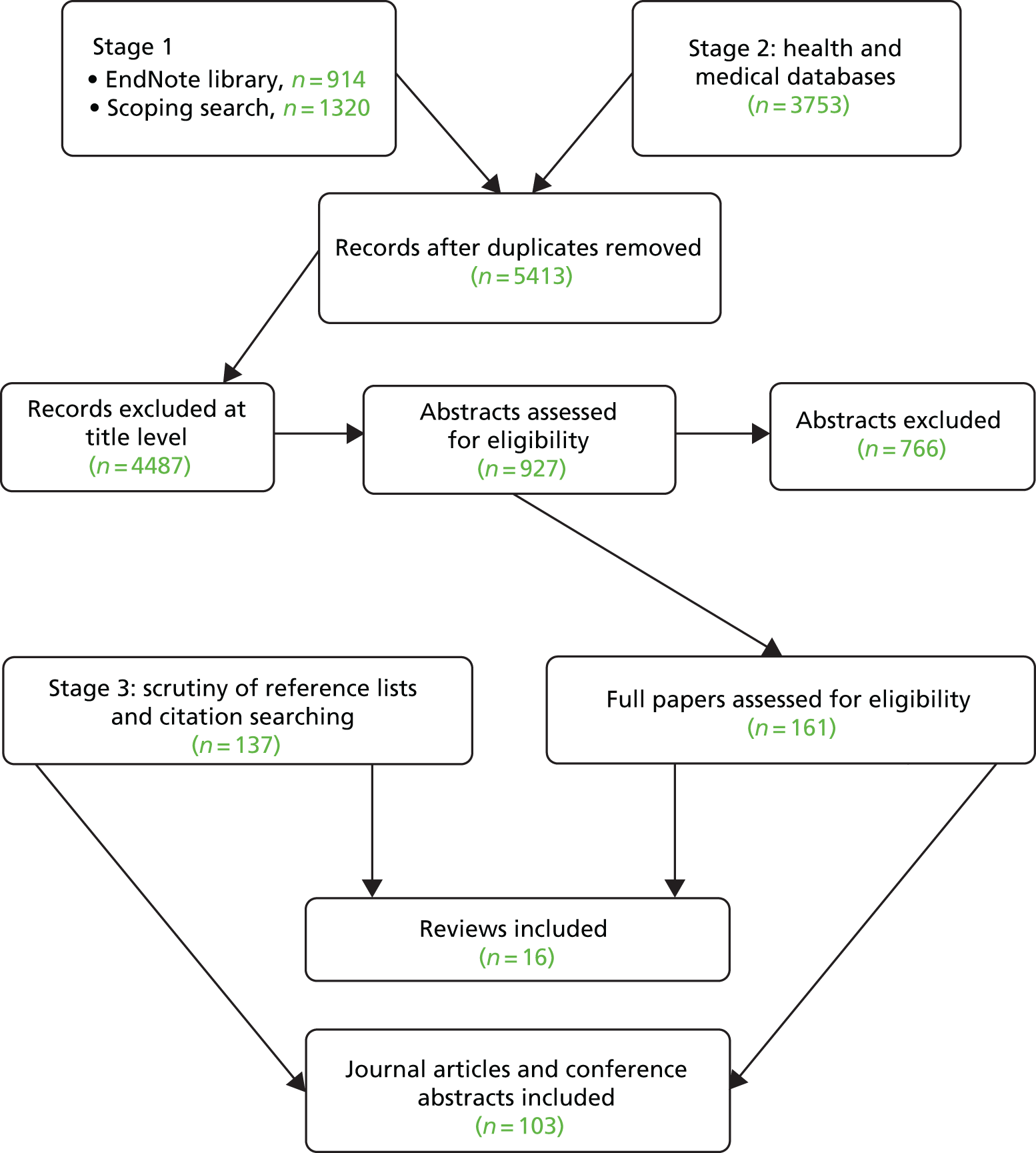
The full papers, conference abstracts and reviews identified as a result of the literature search are described in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram in Figure 1.
FIGURE 1.
Modified PRISMA flow diagram.
Second screening of retrieved references
A kappa coefficient was calculated for the double screening process, demonstrating good agreement between the reviewers [κ = 0.794, 95% confidence interval (CI) 0.665 to 0.929].
Studies included in the review
A total of 103 papers (full journal articles and conference abstracts) and 16 reviews were included in the review. Further details of the characteristics of these studies are provided in Chapter 4.
Studies excluded from the review
A list of the full-text studies and conference abstracts excluded from the review and the reasons for their exclusion is available in Appendix 3.
Chapter 4 Results of the review
This chapter presents the main results from the review, related to:
-
the overall evidence base
-
the characteristics of included studies (identification of frail/at-risk older people and service delivery innovations for this group)
-
a narrative summary of the evidence
-
a patient pathway diagram
-
an assessment of the evidence base.
Characteristics of the overall evidence base
In total, 103 articles,18–120 representing 90 studies, were included in this systematic mapping review. Detailed data extraction tables of included studies are provided in Appendices 2, 4 and 5.
There were 61 full papers,19,21,23,27–29,33,35,36,38–43,49–61,63–65,68,69,71–73,76–82,86,88–90,93,95,101,106,108,110,112–117,119,120 38 conference abstracts18,20,22,25,30,32,34,37,45–48,62,66,67,70,74,75,83–85,87,91,92,94,96–100,102–105,107,109,111,118 and four papers24,26,31,44 classified as ‘other’ (letters to the editor and editorials containing data).
Of the 92 studies reported in the 103 articles/conference abstracts, 32 included a frail or high-risk population21–25,27,29,30,49,50,52–54,61,62,67,68,71–75,78,83,86–90,98,99,102–104,106,112,114,118,119 and 60 included a population of older people. 18–20,23,26,28,31–48,51,55–60,63–66,69,70,76,77,79–82,84–97,100,101,105,107–111,113,115–117,120
Thirty-seven studies18–23,27–60 reported on interventions to identify frail or high-risk older people. These comprised diagnostic tools to screen for frailty-related issues (n = 720,22,27–33), diagnostic tools to screen for frailty (n = 718,34–39), prognostic tools to measure the risk of adverse events in the ED (n = 523,40–43) and prognostic tools to measure the risk of adverse events on discharge (n = 1819,21,44–60).
Interventions to manage older people and frail older people in the ED were reported in 53 studies: 21 examined changes to ED staffing,26,61–85 11 examined changes to the physical infrastructure of the ED,86–97 18 examined changes to how care was delivered24,25,98–117 and other interventions were reported in three studies. 119–121
The majority of the studies were undertaken in the USA (n = 2718,19,35,36,38–40,45,46,48,57,59,64,66–68,70,84,91–94,96,97,113,114,116,119,120), the UK (n = 1420,61,62,72,74,83,86,88,89,95,98,102–106,117) and Australia (n = 1026,44,60,63,73,76–80,82,110). The UK studies were more likely to focus on frail or high-risk older people (n = 11). Other studies were undertaken in Italy (n = 721,27,49,58,90,111,118), Canada (n = 628,37,47,51,52,65), Ireland (n = 534,69,71,75,107), Switzerland (n = 322,33,42,53,54), the Netherlands,32,55 Singapore,112,115 Hong Kong,25,108,109 Spain,87,99 Sweden24,31 and France41,81,85 (all n = 2) and Belgium,56 Germany,50 New Zealand,29,30 South Korea,23 Taiwan100,101 and Turkey43 (all n = 1).
A wide number of study types were utilised. Table 2 gives the study designs and number of studies of each type. No studies on the cost-effectiveness of interventions to identify and manage older people in the ED were located in the evidence base.
| Experimental studies | Observational studies | Unclear |
|---|---|---|
|
|
|
Table 3 highlights that the main group that interventions were targeted at was adults aged > 65 years with no specific condition.
| Age category | Studies (n) |
|---|---|
| ≥ 65 years | 44 |
| ≥ 65 years with trauma/acute condition | 4 |
| ≥ 65 years with fall/chronic condition | 3 |
| ≥ 65 years with positive diagnosis of ‘at risk’ | 3 |
| ≥ 65 years with, or ≥ 70 years without, chronic condition | 4 |
| ≥ 70 years | 5 |
| ≥ 72 years | 1 |
| ≥ 75 years | 11 |
| ≥ 75 years, frail/multiple comorbidities | 2 |
| ≥ 80 years with syndromes described as geriatric | 2 |
| ≥ 85 years | 1 |
| No age category | 10 |
| Total | 90 |
Although it was not possible to undertake a numerical analysis of the mean or median age of the population of older people studied in the review, because of the incomplete reporting of data, it is possible to say that, although interventions tended to be targeted at those aged > 65 years (considered to be older people in the literature), the average age of study participants (and, therefore, those benefiting from interventions) was much higher, generally around 80 years of age.
Studies were categorised as being related to either the identification of frail older people or changes to how ED services were configured or delivered. The classification of the service delivery interventions was based on how studies were reported in the included articles and the elements of service delivery that were researched. Fifty-eight of the studies focused on service delivery interventions and 37 on screening (diagnostic and prognostic). A further breakdown of these categories is given in Table 4.
| Category | Description | Studies (n) | Articles (n) |
|---|---|---|---|
| Screening | Diagnostic tools to identify frailty | 7 | 7 |
| Diagnostic tools to screen for frailty-related issues | 7 | 9 | |
| Prognostic tools to measure risk of adverse events in the ED | 5 | 5 | |
| Prognostic tools to measure risk of adverse events on discharge | 18 | 19 | |
| Service delivery interventions | Individual or team changes to ED staffing | 21 | 26 |
| Changes to the physical infrastructure of the ED | 11 | 12 | |
| Care delivery and assessment interventions (CGA) | 18 | 22 | |
| Miscellaneous | Various | 3 | 3 |
Characteristics of included studies: screening
Thirty-seven studies (40 publications18–23,27–60) dealt with strategies aimed at identifying patients with frailty or distinguishing higher- from lower-risk patients in the ED. The great majority of these studies assessed the diagnostic or prognostic accuracy of tools using a prospective or retrospective cohort design, which is an appropriate design for this type of study. Only one study (published as a conference abstract) used a randomised trial design18 and one was a secondary analysis of data from a randomised trial. 19 Both of these studies were conducted in the USA.
The largest group of studies came from the USA (n = 1218,19,35,36,38–40,45,46,48,57,59), followed by Canada (n = 528,37,47,51,52). Among European countries, the largest numbers of studies were performed in Switzerland (n = 322,33,42,53,54) and Italy (n = 421,27,49,58). The Netherlands (n = 232,55) was the only other European country with more than one included study. The only study included from the UK was a study of a screening tool that was reported in abstract form only. 20 Outside Europe, studies were included from Australia,44,60 New Zealand,29,30 Turkey43 and South Korea. 23
The numbers of patients included in screening studies ranged from 6918 to 2057. 21 Two other studies22,23 recruited > 1000 patients. Most studies recruited patients aged ≥ 65 years, but the average age of patients actually recruited was considerably older, typically in the mid-seventies or older (see data extraction tables in Appendices 4 and 5). The proportions of men and women included varied among the included studies.
Characteristics of included studies: interventions
Fifty-three studies (63 articles24–26,61–120) examined changes made to how ED services were delivered to populations of (frail) older people. These studies tended to investigate changes to the structure of the ED (n = 1186–97), changes to staffing in the ED (n = 2126,61–85) or changes to how care is delivered (n = 1824,25,98–117), such as the introduction of comprehensive geriatric assessment (CGA) or similar assessment-type interventions. There were also a number of unique interventions (n = 3119–121), which are also reported here.
The majority of the studies reported here were observational studies; predominantly before-and-after studies or cohort studies. Three studies reported results from randomised controlled trials (RCTs). 24–26
All of the studies reported either patient or health service outcomes that were derived from patient data, with the exception of one study,120 which reported changes in ED clinician prescribing behaviour. The main patient-related outcome measures were mortality, functional status, frailty and place of residence (own home or residential/nursing care). The main health service outcomes were admissions, readmissions, ED reattendance and length of stay.
The largest group of studies came from the USA (n = 1564,66–68,70,84,91–94,96,97,113,114,116,119,120), followed closely by the UK (n = 1361,62,72,74,83,86,88,89,95,98,102–106,117). Nine studies were undertaken in Australia. 63,73,76–80,82,110
Most studies reported outcomes for patients aged ≥ 65 years, as these patients were considered to be ‘older people’ and, therefore, the target age for identification of frailty or at risk of adverse outcomes. However, when a mean age was reported, this tended to be > 75 years (see Appendix 6; more detailed reporting of age is not possible because of variable reporting in the included articles). The proportion of men and women included varied among the studies.
Detailed analysis of study and intervention characteristics was hindered by the limited data in the included papers, many of which were conference abstracts.
Narrative synthesis of screening papers
The objective of using a diagnostic or prognostic screening tool as a supplement to clinical judgement is to improve the health-care provider’s ability to distinguish older people who are frail or at high risk of adverse outcomes from those who are not. Older people who are identified as frail can then be considered for specific management in the ED. A test to identify older people as frail in the ED setting needs to be both accurate and feasible to apply. The interventions that may be delivered to these groups are described in Diagnostic tools to identify frailty.
The evidence identified in this review showed that screening tests were used on both populations of older adults aged > 65 years and on populations that were already considered to be at high risk. We distinguished between:
-
studies that compared the findings of the test with those of a more comprehensive test (reference standard, i.e. diagnostic accuracy studies); these tended to be related to the identification of frailty or frailty-related issues
-
studies that evaluated the ability of the test to predict adverse outcomes during a period of follow-up (i.e. prognostic studies); these tended to be screening tests to identify older people at risk of adverse events in the ED or adverse events following discharge from the ED.
Further details of all of the studies can be found in the data extraction tables (see Appendices 2, 4 and 5).
Diagnostic tools to identify frailty
We included seven studies (nine publications20,22,27–33) of diagnostic tools to identify frailty (Table 5). These were studies that recruited a sample of older people attending the ED and assessed the accuracy of a screening tool against a reference standard.
| Study | Participants (n) | Tool | Reference standard | Findings |
|---|---|---|---|---|
| Salvi et al.27 | 200 | ISAR | DAI | The ISAR tool had sensitivity of 94% and specificity of 63%. The ISAR tool is a useful screening tool for frailty and identifies patients who are at risk of adverse outcomes after an ED visit as well as those who are likely to benefit from a geriatric intervention |
| Asomaning and Loftus28 | 525 | ISAR | No reference standard | 271 patients (representing 51.6% of those eligible for screening) were screened with the ISAR tool. Low compliance by staff was a barrier to implementation of the tool |
| Boyd et al.29,30 | 139 | BRIGHT | CGA | The BRIGHT tool successfully identifies older adults with decreased function and may be useful in differentiating patients in need of comprehensive assessment |
| Eklund et al.31 | 161 | FRESH | Frailty indicators | Both sensitivity (81%) and specificity (80%) of the FRESH tool were high. The tool is simple and rapid to use, takes only a few minutes to administer and requires minimal use of energy by the patient |
| Wall and Wallis20 | 118 | CFS | Validated frailty scales | Analysis of ROC curves showed that the CFS accurately identified frail patients compared with other well-established frailty scales (AUC 89–91%) at appropriate cut-off points. Its implementation in the ED could increase the proportion of frail patients admitted directly to a geriatric ward |
| Lonterman et al.32 | 300 | ED screening tool | Safety management screening bundle | The ED screening tool has moderate validity compared with the screening bundle and can identify most older ED patients at high risk of adverse outcomes |
| Schoenenberger et al.22,33 | 1547 | EGS | ED diagnosis | Introduction of the EGS was associated with an increase in the detection of potentially overlooked geriatric problems. Adaptations to enhance feasibility and to ensure clinical benefit are needed |
The included studies evaluated a wide variety of screening tools. The Identification of Seniors at Risk (ISAR) tool was the only tool to be evaluated in two studies. 27,28 A diagnostic accuracy study27 reported that the ISAR tool had a sensitivity of 94% and specificity of 63% relative to a frailty measure, the Deficit Accumulation Index (DAI). The area under the receiver operating characteristic (ROC) curve was 0.92, indicating a good performance in identifying frailty based on the DAI definition. However, a study of the implementation of the ISAR tool in a Canadian ED setting found that only 51.6% of eligible patients actually received an ISAR screen. 28 This was attributed to the fast-paced nature of emergency care and lack of staff resources at night.
Other screening tools have been evaluated in single diagnostic accuracy studies. The Brief Risk Identification for Geriatric Health Tool (BRIGHT), developed in New Zealand, is an 11-item tool that showed a good ability to identify older people with ‘decreased function’ relative to a reference standard of CGA. 29,30 The limitations of this study, identified by the authors, include that it was a small, single-centre study and that 18% of patients who completed BRIGHT were lost to follow-up, raising the possibility of follow-up bias. BRIGHT is designed to be suitable for completion by the patient or a carer and used in combination with a particular type of CGA.
The only other fully published study of this type evaluated FRESH, which is a five-item tool (subsequently reduced to four items) that was specifically designed to screen for frailty. 31 FRESH was evaluated using a range of frailty indicators as reference standards and performed well, with both sensitivity and specificity being around 80%. The test takes only a few minutes to administer and requires minimal input from the older person. However, the tool has been evaluated in only one small study to date (n = 161) and the data were not collected during the ED visit but during a subsequent visit to patients at home. 31
Finally, of three diagnostic accuracy studies published only as conference abstracts, one was carried out in a UK setting. 20 This study used the Clinical Frailty Scale (CFS), a rapid and simple case-finding tool, to assess 118 older patients admitted to geriatric wards from the ED. The CFS performed well in comparison with established frailty scales at appropriate cut-off points. The authors suggested that use of the CFS as a triage tool in the ED could increase the proportion of frail older people admitted directly to geriatric wards (i.e. admitted earlier rather than later). However, although this was a study of a relevant population, data were not actually collected in the ED and patient management and outcomes were not evaluated. Thus, the value of this study by itself appears to be limited.
The other two conference abstracts evaluated an ED screening tool32 and an emergency geriatric screen (EGS). 22,33 The ED screening tool performed well, with an area under the curve (AUC) of 0.83 relative to a reference standard, described as a safety management screening bundle. However, few details of either tool were reported in the abstract. The second study used actual ED diagnoses as the reference standard and reported an increase in the detection of potentially overlooked geriatric problems compared with a control period.
Overall, the evidence for the diagnostic accuracy of tools for identifying frail older people is limited. None of the tools has been evaluated extensively using this methodology and differences in terminology make it unclear whether or not different studies are examining the same phenomenon. In addition, individual studies have different methodological features and settings, which may limit their internal or external validity. However, the evidence base using follow-up to evaluate the predictive abilities of these tools is more extensive and the evidence summarised here should be read alongside Prognostic tools for adverse events after discharge.
Diagnostic tools to identify specific frailty-related issues
We identified seven diagnostic accuracy studies of tools to screen for specific frailty-related issues (as distinct from frailty as a general overall condition) in the ED (Table 6). All of the studies evaluated screening for cognitive impairment/dysfunction and most used the Mini Mental State Examination (MMSE) as a reference standard. Two studies did not use a standard diagnostic accuracy design. 18,34 In a randomised trial published as a conference abstract,18 physicians were either informed or not informed of the results of screening for mental status and delirium. The study found that information about screening results did not appear to influence physicians’ decisions in relation to documentation, disposition or management. 18 This is a potentially important finding, but the study was small (69 patients).
| Study (issue) | Participants (n) | Tool | Reference standard | Findings |
|---|---|---|---|---|
| Carpenter et al.18 (geriatric syndromes) | 69 | MMSE/CAM | N/A (RCT of screening) | Screening did not appear to influence the decisions made by physicians |
| Carpenter et al.35 (cognitive dysfunction) | 169 | Ottawa 3DY; Brief Alzheimer’s Screen; SBT; and caregiver-completed AD8 | MMSE | Brief screening instruments such as the SBT can rapidly identify patients at lower risk of cognitive dysfunction |
| Carpenter et al.36 (cognitive dysfunction) | 371 | SIS and caregiver-completed AD8 | MMSE | The SIS was superior to the caregiver-completed AD8 for identifying older adults at increased risk of cognitive dysfunction |
| Eagles et al.37 (impaired mental status) | 260 | Ottawa 3DY | MMSE | Ottawa 3DY is a simple screening tool that has been shown to be feasible for use in the ED |
| Hadbavna et al.34 (cognitive impairment) | 117 | TRST and SIS | N/A | A high proportion of older patients attending the ED met criteria for cognitive impairment. There was considerable variation in the implementation of the screening instruments between nurses, despite training |
| Wilber et al.38 (cognitive impairment) | 352 | SIS | MMSE | The sensitivity of the SIS (63%) was lower than in earlier studies. Further research is needed to identify the best brief mental status test for ED use |
| Wilber et al.39 (cognitive impairment) | 150 | SIS and Mini-Cog | MMSE | The SIS had a sensitivity of 94% and specificity of 86%. The test is short, easy to administer and unobtrusive, allowing it to be easily included in the initial assessment of older ED patients |
Hadbavna et al. 34 also did not use a conventional diagnostic accuracy study design in their study evaluating the six-item screener (SIS) test and triage risk screening tool (TRST). Instead, repeat screening with the SIS was used to confirm whether or not patients met the criteria for cognitive impairment. The authors found that there was considerable variation between nurses in the implementation of screening. 34 This adds to the study of Asomaning and Loftus28 in identifying potential problems in administering screening tools in normal clinical practice.
Prognostic tools for adverse events within the emergency department
We included five studies evaluating the accuracy of screening tools for assessing patients’ risk of adverse events within the ED itself (Table 7). Each study used a different tool, suggesting that there is currently no consensus around which tools to use. Follow-up was limited to the time that the patient was in hospital, with the exception of one study that included a 30-day follow-up. 40 This study40 found that a delirium prediction rule based on age, prior stroke or transient ischaemic attack, dementia, suspected infection and acute intracranial haemorrhage had good predictive accuracy for delirium determined by the confusion assessment method (CAM).
| Study | Participants (n) | Tool | Follow-up | Findings |
|---|---|---|---|---|
| Beauchet et al.41 | 424 | BGA | In hospital | The combination of a history of falls, male sex, cognitive impairment and aged < 85 years identified older ED patients at high risk of a long hospital stay |
| Dundar et al.43 | 939 | REMS/HOTEL | In hospital | The REMS, REMS without age and HOTEL scores cannot be used to identify GED patients requiring hospital admission, but they are of value for predicting in-hospital mortality and intensive care admission |
| Grossmann et al.42 | 519 | Emergency Severity Index | In ED | The Emergency Severity Index level showed good validity for resource consumption, disposition, ED length of stay and survival |
| Kennedy et al.40 | 700 | Delirium prediction rule | 30 days | The delirium prediction rule had good predictive accuracy (area under the ROC curve = 0.77) |
| Lee et al.23 | 1903 | CTAS | In ED | The CTAS is a triage tool with high validity for older patients and is especially useful for categorising severity and recognising those who require an immediate life-saving intervention |
One study carried out in France used a brief geriatric assessment (BGA) method to identify patients in the ED who were at high risk of a long hospital stay. 41 The BGA consisted of six items and the authors concluded that a history of falls, male sex, cognitive impairment and age of < 85 years identified patients at increased risk of a long hospital stay (≥ 13 days). The authors noted that this group of patients would require geriatric care and planning for discharge. Further evidence on the management of patients following geriatric assessment in the ED is presented in Narrative synthesis of service delivery intervention papers.
The other studies in this group evaluated tools for predicting the risk of hospital or intensive care unit (ICU) admission or the need for an immediate life-saving intervention. Emergency Severity Index level 1 had low sensitivity (46.2%) but high specificity (99.8%) for predicting the need for a life-saving intervention. 42 The index level was also correlated with resource consumption, disposition, ED length of stay and survival. The Canadian Triage and Acuity Scale (CTAS) showed both high sensitivity (97.9%) and high specificity (89.2%) for the need for life-saving intervention. 23 The results of a Turkish study evaluating the Rapid Emergency Medicine Score (REMS) and Hypotension, Oxygen saturation, low Temperature, ECG changes and Loss of independence (HOTEL) tools indicated that these tools cannot be efficiently used to identify older ED patients requiring hospital admission. 43 However, the tools had reasonable validity for predicting ICU admission and in-hospital mortality. The HOTEL score was a stronger predictor than REMS or REMS without taking age into account.
These studies focus on the short-term outcomes of older patients attending the ED. The exception is the study by Beauchet et al. ,41 which may be read alongside other studies of geriatric assessment in the ED. The limited number of studies identified makes it difficult to draw conclusions about which tools may be of most value in the setting of the UK NHS.
Prognostic tools for adverse events after discharge
Eighteen studies (19 publications19,21,44–60) assessed the ability of screening tools to predict adverse outcomes following a patient’s discharge from the ED (Table 8). The studies evaluated a wide range of tools, with follow-up ranging from 28 days to 12 months. The ISAR tool and TRST were most commonly evaluated, with one study44 evaluating a tool derived from the ISAR tool. None of the included studies was performed in the UK. Four studies were published as conference abstracts only. 45–48
| Study | Tool | Follow-up | Findings |
|---|---|---|---|
| Studies of ISAR | |||
| Hegney et al.44 (n = 2139) | Screening tool adapted from the ‘Screening Tool for Elderly Patients’, which in turn was developed from the ISAR tool | 28 days (study used a before-and-after design) | There was a decrease in re-presentations. It is suggested that this is because of increased referral to other community-based services (i.e. diverting patients elsewhere) |
| Salvi et al.49 (n = 200) | ISAR | 6 months | The ISAR tool was a reliable and valid predictor of death, long-term care placement, functional decline, ED revisit or hospital admission at 6 months’ follow-up |
| Singler et al.50 (n = 520) | ISAR | 28 days | The ISAR tool with a cut-off score of ≥ 3 is an acceptable screening tool for use in German EDs |
| Studies of TRST | |||
| Fan et al.51 (n = 120) | TRST | 120 days | The TRST cannot be used as a single diagnostic test to predict whether or not Canadian ED elders will have an ED revisit, hospital admission or long-term care placement at 30 or 120 days |
| Hustey et al.19 (n = 650) | TRST | 120 days | The TRST is a valid proxy measure for assessing functional status in the ED and may be useful in identifying patients who would benefit from referrals or surveillance after discharge |
| Lee et al.52 (n = 788) | TRST | 12 months | The TRST demonstrated only moderate predictive ability and, ideally, a better prediction rule should be sought |
| Studies comparing ISAR with TRST | |||
| Carpenter et al.45 (n = 225) | ISAR and TRST | 3 months | Neither the ISAR tool nor the TRST distinguish older ED patients at high or low risk for 1- or 3-month adverse outcomes |
| Graf et al.53,54 (n = 375) | ISAR, modified ISAR and TRST | 12 months | The screening tools may be useful for identifying older patients who can be discharged from the ED without further geriatric evaluation, thus avoiding unnecessary CGA |
| Salvi et al.21 (n = 2057) | ISAR and TRST | 6 months | Risk stratification of older ED patients with the ISAR tool or TRST is substantially comparable for selecting older ED patients who could benefit from geriatric interventions. The ISAR tool had slightly higher sensitivity and lower specificity than TRST |
| Studies comparing several tools | |||
| Buurman et al.55 (n = 381) | ISAR, TRST, questionnaires of Runciman et al.123 and Rowland et al.124 | 120 days | None of the screening tools was able to discriminate clearly between patients with and without poor outcomes |
| Moons et al.56 (n = 314) | ISAR, TRST, questionnaires of Runciman et al.123 and Rowland et al.124 | 90 days | Repeat visits in older persons admitted to an ED seemed to be most accurately predicted using the Rowland questionnaire, with an acceptable number of false positives. This instrument can be easily integrated into the standard nursing assessment |
| Studies of other tools | |||
| Baumann and Strout57 (n = 929) | ESI | 1 year | When used to triage patients aged > 65 years, the ESI algorithm demonstrates validity. Hospitalisation, length of stay, resource utilisation and survival were all associated with ESI categorisation in this cohort |
| Di Bari et al.58 (n = 1632) | ISAR, Silver Code | 6 months | Prognostic stratification with the Silver Code is comparable with that obtained by direct patient evaluation |
| Dziura et al.46 (n = 250) | Rapid screening assessment | 30 days | Rapid screening assessment provides a rapid and accurate method for identifying older patients in the ED who are likely to return to the ED |
| Eagles et al.47 (n = 504) | TUGT | 6 months | TUGT scores were associated with frailty, functional decline and fear of falling. TUGT scores were associated with falls at the initial ED visit but were not predictive of falls at 3 or 6 months |
| Post et al.48 (n = 250) | GRAY | 30 days | The ED GRAY can be quickly performed in the ED to initially assess disability and identify issues that need to be addressed. Combined with other data, it provides good discrimination of the risk of ED readmission within 30 days |
| Stiffler et al.59 (n = 107) | SHARE-FI | 30 days | The SHARE-FI tool appears to be a feasible method to screen for frailty in the ED |
| Tiedemann et al.60 (n = 397) | Two-item screening tool (falls) | 6 months | The two-item screening tool showed good external validity and accurately discriminated between fallers and non-fallers. The tool could identify people who may benefit from referral or intervention after ED discharge |
The ISAR tool was developed in Canada in the 1990s. 122 It is a self-report screening tool with six questions related to functional dependence, recent hospitalisation, impaired memory and vision and polypharmacy. A score of ≥ 2 (i.e. positive answers to two or more items) is the normal cut-off point for being considered high risk. Two studies in this review evaluated the ISAR tool alone for screening older patients in the ED. 49,50 Both studies concluded that the ISAR tool was a valid and reliable screening tool in their setting. Singler et al. 50 used a cut-off point of ≥ 3 rather than ≥ 2 in their study, which would have the effect of increasing the specificity of the tool. A study of a screening tool derived from the ISAR used a before-and-after design and found a decrease in re-presentation to the ED after introduction of the tool. 44 The authors suggested that this was attributable to an increase in referrals to community-based services, which diverted patients away from attending the ED.
The TRST is a risk-screening tool designed to be applied to patients aged ≥ 75 years in the ED. Like the ISAR tool, it includes six items and a score of ≥ 2 indicates high risk. Three studies in the review evaluated the TRST alone and two of them51,52 cast doubt on the predictive ability of the tool. By contrast, a study in the USA concluded that the TRST was a valid measure for assessing functional status in the ED and may be useful in identifying patients requiring referral or monitoring after discharge. 19 Thus, the evidence base for the TRST when evaluated alone is limited and mixed.
Although evaluation of single screening tools appears most feasible for delivery in the ED and the least burdensome for patients, many studies have compared two or more tools using the same sample of patients. Three studies compared the ISAR tool and the TRST. Salvi et al. 21 and Graf et al. 53,54 both concluded that the tools are useful for risk stratification in the ED and have similar properties. However, Salvi et al. 21 emphasised use of the screening tools to select patients who could benefit from geriatric interventions, whereas Graf et al. 53,54 favoured their use to avoid unnecessary intervention. By contrast, a US study45 found that neither tool successfully distinguished patients at high and low risk for adverse outcomes at 1 and 3 months. Once again, it is difficult to draw firm conclusions from this group of studies.
Two further studies compared the performance of ISAR and TRST with that of two other tools, the Runciman123 and Rowland124 questionnaires. Moons et al. 56 highlighted the value of the Rowland questionnaire for predicting repeat ED visits, whereas Buurman et al. 55 found that none of the screening instruments distinguished between patients with and without poor outcomes over 120 days of follow-up. These similarly designed studies were carried out in Belgium and the Netherlands, respectively, and so their relevance to UK settings is uncertain.
Other screening tools have been evaluated in single studies. We included seven studies of this type, all of which reported positive results. The emergency screening instrument (ESI),57 rapid screening assessment46 and Survey of Health, Aging and Retirement in Europe Frailty Instrument (SHARE-FI)59 are short question-based tools similar to those discussed above. Eagles et al. 47 evaluated the timed up and go test (TUGT) and reported that scores were associated with frailty, functional decline and fear of falling. Limited details of this study are available as it was published as a conference abstract only. Two studies described tools to predict specific frailty-related outcomes: falls60 and ED readmissions. 48 Finally, the Silver Code differs from other risk screening tools by being derived from administrative data. When compared with the ISAR tool, the Silver Code showed a similar ability to predict ED return visits, hospital admission and mortality over 6 months of follow-up. 58 The concept of using administrative data to support initial triage in the ED seems attractive, but in this study the Silver Code was derived retrospectively several months after the patient was enrolled for the study. As noted by the authors, improved processing and flow of administrative data would be necessary for the data to be used for real-time triage in the ED.
Summary of screening papers
The evidence on tools to support the identification and management of patients with frailty in the ED is extensive but inconclusive. The ISAR tool and the TRST are the most extensively evaluated tools, but many other tools are available, including non-question-based tests and, potentially, tools using administrative data. Limitations of the included studies include the small sample sizes, that most were conducted at a single centre and that many were published as conference abstracts with limited details. Contradictory results obtained in different prognostic studies using the same tool reflect the fact that health service use-related outcomes, in particular outcomes such as repeat ED visits and hospital admission, will be influenced by the health and care system as well as by patient factors. Hence, the results of studies performed in one country cannot be readily generalised to another country. The lack of UK studies in this body of evidence limits the relevance of the evidence to NHS settings. There are other studies that examine screening tools for conditions that are common in frail older people; however, these have not been included in the review as they were not identified through the literature searches as they were not specifically limited to a frail or older population.
Narrative synthesis of service delivery intervention papers
This section reports papers that describe changes to how care is delivered to frail and older patients within the ED. The service delivery interventions that are reported here were targeted at both frail older people and a more general population of people aged > 65 years. Differentiating between the groups at whom interventions were targeted was often difficult. Data extraction tables for these service delivery interventions are available in Appendices 4 and 5.
Overall, the intervention reporting was descriptive rather than analytical, with limited data on the feasibility and acceptability of interventions. Therefore, this section aims to map, classify and describe the interventions delivered and the outcomes on which they are reported to have had an impact.
To present the synthesis in a clear and logical manner, interventions were classified as follows:
-
ED staffing initiatives (21 studies reported in 26 articles26,61–85)
-
changes to the physical infrastructure of the ED (11 studies reported in 12 articles86–97)
-
care delivery interventions (18 studies reported in 22 articles24,25,98–117)
-
other interventions (three studies reported in three articles119–121).
Emergency department staffing initiatives
We identified 21 studies (26 publications26,61–85) reporting on instances in which the staffing of the ED had been modified to better meet the needs of an older population. These staffing modifications varied; there were examples of initiatives in which a single individual was located in the ED or added to an existing multidisciplinary team (MDT) or in which a new MDT was established. Differentiating between staffing initiatives and care initiatives (e.g. when CGA was introduced to an ED and delivered by a newly established geriatric liaison nurse) was problematic. The description of the interventions was often brief, reflected in the fact that a number of the studies were reported in conference abstracts only. Details of these interventions are given in Table 9.
| Intervention | Staff | Study, population | |
|---|---|---|---|
| Frail older | General older | ||
| Staffing initiatives: individual | Admissions avoidance geriatrician | Jones and Wallis,61 Jones et al.62 | |
| Aged care pharmacist | Mortimer et al.63 | ||
| Clinical pharmacy specialist | Shaw et al.64 | ||
| EDCCs | Bond et al.65 | ||
| Geriatric nurse practitioner | Argento et al.66 | ||
| Nurse liaison | Aldeen et al.,67 Aldeen et al.68 | ||
| Aged care nurse liaison | Basic and Conforti26 | ||
| Triage nurse | Fallon et al.69 | ||
| Geriatric nurse liaison | Dresden et al.70 | ||
| Staffing initiatives: team | Geriatric medicine liaison | Tan et al.71 | |
| ATOP | Leah and Adams72 | ||
| ASET | Ngian et al.73 | ||
| Geriatric liaison team | Thompson et al.74 | ||
| FITT | O’Reilly et al.75 | ||
| CCT (falls) | Harper et al.76 | ||
| CCT (general) | Arendts et al.77,78 | ||
| Allied health staff (falls) | Waldron et al.79 | ||
| MDT CCT | Corbett et al.80 | ||
| MGT | Launay et al.81 | ||
| CCT | Arendts et al.82 | ||
| Acute care of the elderly service | Bell et al.83 | ||
| Patient liaison service | Berahman et al.84 | ||
Individual initiatives
We identified nine studies (across 11 articles26,61–70) of interventions in which a single clinician was introduced to the ED setting or added to an existing team. A variety of clinicians were introduced (geriatric consultants, pharmacists and nurses) in addition to other roles such as emergency department care co-ordinators (EDCCs).
Jones and Wallis61 and Jones et al. 62 reported on an admissions avoidance consultant geriatrician. The geriatrician worked in conjunction with allied health professionals and also provided follow-up, which was required by one-third of the patients in the cohort. The geriatrician’s role was to provide medication advice and follow-up planning. Outcomes for this intervention were broadly positive compared with ‘hospital averages’. However, the authors cautioned that reducing admissions among more-stable patients may lead to wards having a higher proportion of less-stable patients and, therefore, the outcomes of the admitted patients may appear to be negatively affected by the intervention.
Admissions avoidance was also the primary aim of the matched pairs study reported by Bond et al. 65 EDCCs aimed to reduce admission rates through better linkages with home care and community services. The study did not show any difference in any of the outcomes measured (admission rates, revisit rates or readmission rates) between those who received the EDCC intervention and those who did not, although the design of the study may have contributed to this.
Two studies reported on the role of a geriatric pharmacist. 63,64 A prospective evaluation of an aged care pharmacist was undertaken by Mortimer et al. 63 The aged care pharmacist’s role was to examine medication history, review medication orders and liaise with medical staff about medication-related issues. The aged care pharmacist was effective at reducing medication errors compared with the control group receiving usual care, the intervention was acceptable to patients and there was no difference in terms of re-presentation following discharge between the aged care pharmacist group and the control group. Shaw et al. 64 described a new role of a clinical pharmacy specialist, who delivered medication review and management. The study found that clinical outcomes were not improved as a result of the intervention.
Nursing interventions were also common. Argento et al. 66 reported a pilot study of a geriatric nurse practitioner intervention. The geriatric nurse practitioner provided specific care to older people, with the study finding positive outcomes. As part of the wider Geriatric Emergency Department Innovations through the Workforce, Informatics and Structural Enhancements (GEDI-WISE) programme, one of the innovations was to develop the geriatric assessment and care co-ordination skills of ED nurses, as reported in the study by Aldeen et al. 67 The nurse liaison undertook screening tests, liaised with the wider MDT, created safe discharge plans and followed up patients. Preventable admissions in high-risk patients were reduced (although admissions were increased in those with a less severe presentation, perhaps because of underlying problems being identified). Length of stay in the ED was increased for patients seen by the nurse. Basic and Conforti26 reported on a RCT of an intervention for high-risk older people involving early geriatric assessment by an aged care nurse, who assessed, monitored and referred patients with high-risk criteria. They found that the intervention did not significantly reduce any of their outcomes of interest (admission, functional decline or length of stay), with the authors arguing that this was because the intervention did not influence patient care and management following discharge or have any influence over the care provided once patients had been admitted.
Fallon et al. 69 reported on a triage nurse initiative, which involved screening with the TRST. The intervention was delivered in the ED and patients were admitted to the acute medical assessment unit (AMAU) if it was deemed necessary. The TRST identified patients as being at risk of an adverse outcome. Although the outcomes of these patients are unknown, the study identified characteristics of the frail older population and suggested that geriatric AMAUs may better meet their needs.
Dresden et al. 70 undertook a prospective cohort study of a geriatric nurse liaison intervention (GNLI) involving assessment and care co-ordination in the USA. The GNLI group (n = 829) had significantly improved outcomes compared with the control group (n = 873) with regard to hospitalisation, 30-day readmission rates and length of stay. However, no data were collected past 30 days and no information on ED readmissions was collected.
Team initiatives
We identified 12 studies across 15 publications71–85 that reported team initiatives. Staff interventions also took the form of initiatives that involved the establishment of new MDTs for older patients. Six interventions71–73,83 were identified for frail or high-risk patients.
Three papers77,78,82 reported findings from an Australian study that established a care co-ordination team (CCT) to deliver comprehensive allied health assessment/intervention to older patients to improve patient outcomes. The CCT comprised a minimum of one physiotherapist, occupational therapist or social worker, all of whom had geriatric experience. The intervention included functional assessment to identify patients’ needs and direct them to appropriate care and services. Further details are provided in Table 10.
| Study and type | Sample characteristics and size | Outcome measured | Results |
|---|---|---|---|
| Arendts et al.78 (matched pairs study) |
|
28-day ED reattendance, readmission and mortality | No difference in mortality between the intervention group and the control group. The intervention group had a slightly increased ED reattendance rate and a much higher risk of hospital readmission compared with the control group |
| Arendts et al.77 (non-randomised, prospective pragmatic study) |
|
Hospital length of stay for patients admitted | No difference in length of stay (median 88 vs. 87 hours) in unadjusted (log-rank p = 0.28) or adjusted (IRR 0.97, p = 0.32) analysis |
| Arendts et al.82 (non-randomised, prospective study) |
|
Admission to inpatient beds | 72.0% for the intervention group and 74.4% for the control group – borderline statistical significance (OR 0.88, 95% CI 0.76 to 1.00; p = 0.046) |
The work of the CCT in the same setting was reported by Harper et al. ,76 who looked at the role of the CCT specifically for older falls patients. Patients referred by ED clinicians were given targeted falls support. The study reported the changes over 3 years since the introduction of the CCT, with regression modelling demonstrating a decrease in re-presentation and readmission rates, although these results were not significant. Another falls prevention intervention, also delivered in Australia by allied health professionals, was reported by Waldron et al. 79 A prospective before-and-after study of 313 geriatric falls patients demonstrated that allied health staff significantly increased the proportion of patients reviewed and significantly increased referrals for comprehensive guideline care, with a consequent increase in the average quality-of-care index score.
Patients with multiple diagnoses or aged > 80 years were referred to an ED geriatric medicine liaison service in a pilot study undertaken in Ireland. 71 A MDT approach to assessment, led by a senior geriatrician, dealt with 285 patients over a nearly 3-year period. Although study numbers were relatively small, analysis was undertaken on the data collected, with the finding that mean length of stay was significantly shortened for the ED geriatric medicine patients compared with usual care patients. This did not adversely affect repeat attendances or readmission rates.
An assessment team for older people (ATOP) was established in a UK hospital to meet the needs of an increasingly frail population. 72 The focus of the team was to provide CGA to patients with two or more markers of frailty, with assessment not simply based on age alone. The ATOP consisted of a geriatrician, six senior nurses, a senior social worker and assistant, a senior occupational therapist and assistant and a health-care assistant. The aim of the ATOP was to prevent admissions and, in the 4 months of the study, 178 admissions were prevented in patients who the ED team would otherwise have admitted. A basic cost analysis stated that ‘the potential cost saving from preventing the admission of the 89 patients aged 80 years and above seen in the study period could be more than £500,000’. 72
Seven studies73–75,80,81,83–85 examined interventions delivered to general geriatric populations. An aged care service emergency team (ASET) was established in Australia to reduce missed diagnoses in the ED and prevent inappropriate discharges (and, therefore, ED re-presentations). A study by Ngian et al. 73 examined these discordant cases (i.e. cases in which the ASET had recommended the admission of patients who were considered suitable for discharge by the ED). The study looked at what additional evidence was measured by the ASET and found that it was more likely to measure functional, cognitive and mobility impairments as well as identifying acute medical conditions. The data collected were largely qualitative and did not have a comparator; however, the study demonstrated the additional information that might be useful when planning the discharge or admission of frail older patients.
A conference abstract of a UK study carried out in the John Radcliffe Hospital ED reported findings from a newly established geriatric liaison team undertaking CGA. 74 The limited data reported indicated that, over 6 months, and for the 35 patients studied, the length of stay was reduced by 4.8 hours.
An intervention targeted specifically at frail older people was reported by O’Reilly et al. 75 The frail intervention therapy team (FITT) combined allied health professionals to identify all frail patients who presented to the ED and then deliver MDT assessment to them. To analyse the outcomes of the FITT, data were compared for the first quarter of 2015 and 2016 (after the FITT was established). The study reported an 11.6% increase in patients presenting to the ED, a 59% increase in patients discharged and a 42% increase in patients transferred to a ward in < 9 hours.
The formation of a care co-ordination programme in 2005 in Australia was reported by Corbett et al. 80 This MDT, with an emphasis on allied health professional input, was set up to reduce avoidable admissions and inappropriate re-presentations to the ED. Positive study outcomes confirmed a statistically significant reduction in the proportion of patients admitted as well as improvements in the mean quality-of-life score and user satisfaction following the introduction of the care co-ordination programme.
A brief report of a mobile geriatric team (MGT) was provided by Launay et al. 81,85 The intervention consisted of medical assessment (termed geriatric assessment by the study authors) followed by geriatric (medical) and gerontological (medical and social) discharge recommendations. Although outcomes for a small number of patients were evaluated (n = 168), the study authors reported that only the geriatric recommendations were associated with early discharge from the ED [odds ratio (OR) 4.38; p = 0.046].
In another study, an acute care of the elderly (ACE) service was developed that focused on the establishment of a team (consultant, junior doctor and nurse) to deliver CGA to patients aged > 80 years with complex problems or frailty. 83 Data from 10 months of the service showed that 459 out of 662 inappropriate admissions were avoided.
A patient liaison service to better meet the needs of the older patient was evaluated and reported by Berahman et al. ,84 with the main outcome of the study being the measurement of patient satisfaction with the patient liaison service. Comparing the satisfaction of patients who had and had not received the intervention, there was a non-significant slight trend towards improved scores when a patient liaison was present.
Overall, mapping these studies showed that there were few similarities between them. Staffing interventions that added a single member of staff to an ED tended to focus on improving processes and outcomes related to medication management (whether they were delivered by a pharmacist or by another clinician) and improving care co-ordination, follow-up and linkages between the ED and home. Interventions that added a new team to the ED tended to have more of a focus on frail older people, perhaps indicating that, for care to be focused on the frail older person, a variety of health-care professionals need to be included. There were fewer similarities across all of the studies in the outcomes that were assessed, although avoiding admissions and mortality were most frequently measured.
Changes to the physical infrastructure of the emergency department
Eleven studies (12 articles86–97) reported changes to the ED in terms of the physical infrastructure of the ED. These interventions ranged from the creation of geriatric emergency departments (GEDs) (which will also have included changes to staffing), through to making EDs ‘frail friendly’, making general changes to the ED to benefit all patients but with specific benefits for frail and older people and the establishment of specific units in the ED to meet the needs of frail and older patients. These studies are presented in Table 11.
| Details | Study, population | |
|---|---|---|
| Frail older | General older | |
| Staff and structural changes | Silvester et al.86 | |
| Geriatric/‘frail-friendly’ units | Pareja-Sierra et al.,87 Ellis et al.,88 Conroy et al.89 | |
| GED/senior ED | Salvi et al.90 | Genes et al.,91 Karounos et al.,92 Keyes et al.,93 Wilber et al.94 |
| RAC in the ED | Tang et al.95 | |
| GED incorporating GEDI-WISE | Ng et al.96,97 | |
A UK study by Silvester et al. 86 reported on the redesign of the system of care for older people. This consisted of the formation of a MDT with a clinical systems engineer who facilitated changes in discharge, 7-day working and the designation of a medical assessment unit as a frailty unit with a co-located MDT. Analysis of data over 2 years (before and after the changes) demonstrated a fall in bed occupancy rates, a fall in mortality rates and unchanged rates of readmission.
A key UK study by Ellis et al. 88 evaluated an ACE unit. The four-bedded ACE unit undertook CGA, with the aim of admissions avoidance or direct specialty admission. The study was a non-randomised trial comparing three groups of patients: (1) patients admitted before the ACE unit was set up, (2) patients admitted to the ACE unit and (3) patients admitted to the medical receiving unit outside the hours that the ACE unit was open. The study measured a number of outcomes for patients receiving ACE care and found that there was an increase in same-day discharge, mixed findings on length of stay and no significant findings in terms of 7- and 30-day readmission, 12-month mortality, admission to residential care or living at home.
Another key UK intervention was the establishment of an emergency frailty unit (EFU) within an ED in the UK. 89 The study was a before-and-after study and the outcome measures were admission rate from the ED, readmission following an ED visit, length of stay for admitted patients and total bed-day use. The EFU, which had 8–12 beds and undertook CGA, was staffed by geriatricians, emergency physicians, physiotherapists, occupational therapists and ‘primary care co-ordinators’. Analysis of the pre- and post-intervention data indicated that, although there was a pattern of increased ED attendances over the period of the study, admission rates fell significantly, from 69.6% in 2010 to 61.2% after the EFU was implemented. Readmission rates also decreased (4.7% vs. 3.3% at 7 days; 12.4% vs. 9.2% at 30 days; and 19.9% vs. 26.0% at 90 days). The EFU demonstrated a clear improvement in service delivery outcomes; however, no data on patient outcomes, such as mortality, were collected.
Salvi et al. 90 reported on the patterns of use of a GED (an ED with a six-bed elderly observation unit staffed by geriatricians) by frail older people. Comparing patients who had used the GED (n = 200) with those who had used a conventional ED, the patients using the GED had a small but significantly lower mortality rate.
Pareja-Sierra et al. 87 described the impact of an emergency department observation unit (EDOU) on admissions and length of stay. The EDOU was a small, six-bed unit staffed by geriatricians and targeted at frail older people. The author compared data from before and after the EDOU was set up. Although data were limited, the authors reported that an initial increase in admissions was followed by a decrease in admissions and length of stay.
Genes et al. 91 reported on patient satisfaction with a GED that combined structural enhancements with service delivery changes. Analysing patient satisfaction data from 286 patients (67 of whom were described as geriatric) surveyed both before and after the GED was established, the authors found that, although overall satisfaction scores did not change significantly for either group, the geriatric group saw significant improvements in satisfaction relating to specific aspects of the GED.
Admissions data were analysed by Karounos et al. 92 following the introduction of a GED. Examining data from pre and post introduction of the GED, there were significantly fewer admissions post introduction [2.9% fewer (n = 1130); p < 0.001]. This was a large data set (n = 27,838), although the authors caution that a further analysis on readmissions and costs is required.
Keyes et al. 93 also looked at admissions, length of stay and ED visits following the introduction of a senior ED and compared data with those from before the senior ED was introduced. The senior ED comprised a number of changes including staff education, changes to physical infrastructure and screening. Study outcomes demonstrated that the senior ED was associated with decreased admissions but not with ED return visits or length of stay.
A rapid access centre (RAC), a six-bed consultant-led ward, was introduced to a hospital in the UK in an intervention reported by Tang et al. 95 Data on admissions from the RAC were compared with data on admissions from the ED for two 7-month periods before and after the introduction of the RAC. Simple analysis of data from 441 patients showed that patients admitted from the RAC had a shorter length of stay and were discharged earlier.
Ng et al. 96,97 reported on a GEDI-WISE intervention, the introduction of a GED and a before-and-after evaluation of admission rates. They found that admission rates declined by a statistically significant amount following introduction of the ED, from 58.9% in January 2011 to 50.7% in May 2013.
Wilber et al. 94 reported on a senior ED, which was a 15-bed unit, with assessment by a nurse care co-ordinator, interventions and discharge follow-up. This was a pilot intervention and quality assurance data were analysed from before and after the intervention. Statistically significant results were seen for the outcome of admissions, which significantly decreased (from 55.5% to 51.2%, difference –4.3 percentage points, 95 CI –7.2 to –1.4 percentage points). There was a small but insignificant decrease in length of stay and revisits resulting in admission or observation at 7 and 30 days.
Overall, the interventions reporting changes to the physical infrastructure of the ED were also highly variable. Predictably, in most of the studies reported here, changes to the physical infrastructure were made alongside changes to staffing as part of an overall reconfiguration of how care was delivered. Again, the outcomes measured and reported across the studies were variable; however, the majority of studies reported improvements in admissions-related outcomes, although whether or not these were planned outcomes of the interventions and the wider implications for patients of reduced admissions are not reported.
Care delivery interventions
The studies reported in this section are those that describe and evaluate changes to the whole care package delivered to (frail) older people within the ED. The interventions reported in this section take the form of CGA, which combines interventions to identify frail or at-risk older people and interventions to deliver targeted care to them. ‘Comprehensive geriatric assessment has become the internationally established method to assess elderly people in clinical practice. It is a process of specialist elderly care delivered by a MDT to establish an elderly person’s medical, psychological and functional capability, so that a plan for treatment and follow-up can be developed’. 125
The majority of studies that we identified in this review were descriptive reports of CGA and CGA-type interventions introduced to ED settings. Details of the 18 CGA studies (22 publications24,25,98–117) included in this review are provided in Table 12.
| Study (type); name of the intervention; who delivers it; where it is delivered | Type of study; sample size | Outcome measure(s) | Results (given only when the results are significant) |
|---|---|---|---|
| Ismail et al.98 (frail); CGA; interface geriatrician; ED | Service evaluation; 534 patients | Admissions avoidance | Not significant |
| Pareja99 (frail); CGA; geriatrician; ED medical short-stay unit | Prospective study; 1200 patients | Admissions avoidance | Not significant |
| Chou et al.,100 Liao et al.101 (general); CGA; geriatric team; ED | Prospective cohort study; 137 patients (26 intervention patients) | Admissions, ED revisits | Intervention: more likely to be admitted (50% vs. 22%) and fewer visits to the ED within 1 month (0.81 vs. 1.75 visits) and 6 months (2.2 vs. 4 visits) |
| Scott et al.,102 Wentworth et al.,103 Keelan et al.104 (frail); CGA; OPAL team; ED and clinical decisions unit | Scott et al.:102 service evaluation; 148 patients | LOS, admissions | Not significant |
| Wentworth et al.:103 service evaluation; 990 patients (plus age-matched controls) | LOS, admissions | Not significant | |
| Keelan et al.:104 service evaluation; not provided | Admissions, LOS, 4-hour ED target | Not significant | |
| Hughes et al.105 (general); CGA; OPAL team; ED and clinical decisions unit | Service evaluation | Discharge location and discharge rates, admission location and admission rates, LOS, readmission rates | Not significant |
| Fox et al.106 (frail); CGA; embedded geriatrician; ED | Retrospective feasibility study; 168 patients | LOS, discharge rates, admission rates | No control group |
| Beirne et al.107 (general); ISAR plus CGA; ED | Prospective data analysis; 300 patients | ED reattendance | Not significant |
| Yuen et al.,108 Chui and Kun109 (general); ‘We Care’ CGA; ED | Retrospective study; 2202 patients | Admissions avoidance | Not significant |
| Yuen et al.,108 Chui and Kun109 (general); ‘We Care’ CGA; ED | Retrospective study; 1096 patients | Admissions avoidance | Not significant |
| Nguyen et al.110 (general); synthesised geriatric assessment; ED | Pilot observational convenience study; 25 patients | Time taken to complete SGA | N/A |
| Lo Storto et al.111 (general); CGA; social health triage team | Prospective cohort study; 226 patients | Admissions avoidance | N/A |
| Foo et al.112 (frail); TRST, assessment, intervention; ED | Quasi-RCT; 780 patients (280 intervention and 500 control patients) | Change in functional status (3, 6, 9 and 12 months), ED reattendance, rehospitalisation | Intervention group had significant preservation in function at 12 months (basic ADL −0.99 vs. −0.24, p < 0.01; IADL −2.57 vs. 0.45, p < 0.01). Small but not significant reduction in ED reattendance and hospitalisation for the intervention group |
| Yim et al.25 (frail); ISAR, intervention and CGA-type intervention; ED | RCT then cohort study; RCT 1279 patients, cohort study 1820 patients | Composite outcome of institutionalisation, hospital admission within 1 month, early return or frequent visits to ED or death | |
| Grudzen et al.113 (general); screening, intervention; ED | Retrospective cohort study; 8519 patients | ICU admission rate | Over a 29-month study period, unadjusted ICU admission rate declined from 2.3% to 0.9%. Adjusting for age, sex, ESI score and others, decline was still significant (β –0.0073, 95% CI –0.0105 to –0.0041; p < 0001) |
| Warburton114 (frail); ISAR screening, intervention; community hospital ED | Evaluation research | LOS, ED returns, hospital admissions, multiple ED returns/admissions following the index episode | Reported qualitatively |
| Foo et al.115 (general); geriatric nurse liaison assessment; EDOU | Prospective before-and-after study; 487 patients (315 intervention and 172 control patients) | ED reattendance, hospitalisation | Intervention: lower ED reattendance rate (adjusted IRR 0.59, 95% CI 0.48 to 0.71) and lower 12-month hospitalisation rate (adjusted IRR 0.64, 95% CI 0.51 to 0.79) |
| Eklund et al.24 (frail); continuum of care; ED and community | RCT; 76 control and 85 intervention patients | Functional ability, frailty | Improved degree of ADL independence at 3 and 12 months (OR: 2.37 intervention, 2.04 control). No differences between groups with regard to changes in frailty |
| Mahony et al.116 (general); screening, discharge/admission, follow up; ED | Pilot project – chart review; 894 patients | Not stated | Not significant |
| Wright et al.117 (general); TREAT (geriatrician, CGA, discharge support); ED | Before-and-after retrospective cohort study; 5416 patients before and 5370 patients after, with 593 geriatric admissions | Admissions, LOS |
Median LOS for intervention reduced by 2 days and mean LOS by 18.6% (1.78 days; p < 0.001) Control: median LOS was unchanged and mean LOS reduced by 1.08% (0.11 days; p = 0.065) Intervention: percentage of admissions resulting in same-day discharges increased from 12.26% to 16.23% (OR 1.386, 95% CI 1.203 to 1.597; p < 0.001) following the introduction of TREAT Control: same-day discharge fell from 15.01% to 9.77% (OR 0.613, 95% CI 0.737 to 0.509; p = 0.001)a |
Ismail et al. 98 reported on an interface geriatrician delivering CGA in the UK, which was positively received by staff and patients and led to a non-significant fall in admissions. Three additional UK studies evaluated CGA delivered by an older people assessment and liaison (OPAL) team in Manchester. 102–104 In these very small-scale service evaluations, there were no significant changes in outcomes following the intervention, although the studies reported a non-significant decrease in admissions and in length of stay compared with age-matched control patients or patients not given CGA by the OPAL team. A similar evaluation of a CGA OPAL team elsewhere in the UK reported similar, improved patient outcomes, although these were also non-significant. 105
A study undertaken in Taiwan100,101 of CGA introduced to older people visiting the ED three times in 30 days found that ED revisits were reduced but that the intervention increased admissions. Whether or not this was a positive outcome for patients and the health service overall was not reported.
Identification of at-risk older people followed by CGA was reported in five studies. Beirne et al. 107 reported on the use of the ISAR tool to screen patients, who then received a CGA intervention if they were at risk. A convenience sample of the ‘at-risk’ patients received CGA in the ED with community follow-up. There was a small, insignificant, reduction in ED reattendance in the intervention group. Foo et al. 112 reported on a quasi-RCT undertaken in Singapore that had functional status as its primary outcome measure. Despite the fact that those in the intervention group were frailer than those in the control group, there was a significantly better outcome of functional preservation at 12 months in the intervention group than in the control group. There were also improvements for the control group in terms of avoiding admissions and ED reattendance, but these were not significant. Yim et al. 25 developed a Hong Kong version of the ISAR tool to screen patients and then delivered a CGA-type intervention to those identified as being at high risk. High-risk patients were identified through a cohort study of the Hong Kong ISAR tool and then patients were randomised to the intervention or the control. Limited information on the methods used in the RCT were provided and there were no significant differences between the intervention group and the control group in any of the individual or composite outcomes. Grudzen et al. 113 reported on an intervention that combined screening to identify patients in need of an intervention to prevent inappropriate admissions with appropriate referrals to palliative care services. This was part of the wider GEDI-WISE intervention. With the premise that admission to acute services is not appropriate for patients who require palliative care services, ICU admissions significantly declined.
The development of a screening plus intervention ‘elder alert’ in the USA was described by Warburton. 114 The aim of elder alert was to develop a strategy to identify and manage high-risk ED patients aged > 75 years. This included screening patients using the ISAR tool. Screening was found to be accurate and referral to appropriate management appeared to have a positive impact. Comparing groups of patients showed that screening needed to be followed by an intervention for patient outcomes to be improved. Notable cost savings were projected by the evaluation.
The Hong Kong-based ‘We Care’ CGA programme108,109 delivered CGA with the aim of admissions avoidance. The authors reported positive results, with only 15% of patients admitted; however, they did not compare these data with any other admissions data.
Limited evidence from Ngyuen et al. 110 indicated that a self-administered intervention, the synthesised geriatric assessment, was feasible as it was completed within 20 minutes (n = 25 patients). Lo Storto et al. 111 reported on the introduction of a social health and triage team to deliver CGA and found that inappropriate admissions were avoided, although data to confirm this finding were not provided.
Four studies24,115–117 reported on discharge interventions, which was a smaller number than anticipated. In the study by Foo et al. ,115 additional geriatric assessment prior to discharge was delivered by a geriatric nurse, with interventions delivered as appropriate. Positive outcomes for this assessment were reported in terms of hospitalisation and ED reattendance.
Interventions that started in the ED but that included substantial post-ED follow-up were reported in three studies. 24,116,117 Eklund et al. 24 evaluated the ‘continuum of care’, which was designed to help frail older people to remain in their home environment. The intervention was initiated in the ED by geriatric nurses and followed up in the community by a multiprofessional team. The outcomes studied were frailty and activities of daily living (ADL), with the intervention demonstrating improvements in ADL compared with the control group; there were no differences in frailty scores.
Mahony et al. 116 examined an intervention in which patients were screened by a nurse for palliative care triggers and, if they screened positive, received an intervention that consisted of an assessment of needs, consultation and follow-up. Although the results were not significant, there were small reductions in length of stay, which were attributed to better links with home care services.
A before-and-after cohort study by Wright et al. 117 reported on the UK triage and rapid elderly assessment team (TREAT) intervention, consisting of assessment, CGA and pre- and post-discharge support. This complex intervention saw improvements in a number of outcomes. Median and mean length of stay were significantly reduced. The same-day discharge rate significantly increased for those who had been given the TREAT intervention.
To summarise, the evidence base describing CGA and CGA-type interventions is larger than that for other types of service delivery innovations, which is suggestive of the acceptability and feasibility of these types of interventions. More data on outcomes were provided by study authors, with most of these studies measuring outcomes in terms of either admissions avoidance or ED reattendance. Only one study focused on patient outcomes alone (ADL and frailty). 24 There appears to be a general trend for these interventions to improve admissions avoidance. Notably, there was little evidence on discharge interventions that are delivered in the ED to prevent readmission.
Other interventions
Three additional interventions were identified and are reported in Table 13.
| Details | Study, population | |
|---|---|---|
| Frail older | General older | |
| Silver Code to reduce waiting times | Lovato et al.118 | |
| TUGT assessment to identify ‘at-risk’ falls patients | Huded et al.119 | |
| Prescribing decision support to reduce prescribing errors | Terrell et al.120 | |
Terrell et al. 120 reported a RCT from the USA of computer-aided decision support to reduce prescribing errors for older people by reducing the prescription of potentially inappropriate medicines on discharge from the ED. The intervention was delivered to 32 ED physicians (with 31 acting as a control group). The RCT found that the proportion of potentially inappropriate medicines being prescribed significantly decreased from 5.4% to 3.4%.
A screening intervention to identify patients at a high risk of falls119 and a screening intervention to reduce waiting times118 were identified. Huded et al. 119 reported on the use of the TUGT, which was performed on 443 of 1135 patients by a geriatric nurse. These patients had not presented with falls but those who screened positively were referred to fall prevention interventions.
In the study by Lovato et al. ,118 the Silver Code prognostic tool was demonstrated to result in reduced waiting times for frail older people. On arrival in the ED, patients were allocated a colour code and those who received a specific code were seen more quickly. The observational retrospective data showed that waiting times for frail older people decreased, without waiting times for other groups increasing.
Summary of service delivery interventions
Staffing initiatives tended to take the form of either a specialist geriatric member of staff (doctor, nurse or pharmacist) working in the ED or the development of a geriatric MDT. Roles tended to be in care-co-ordination, assessment or medication management. Differentiating between studies of staff initiatives and the introduction of CGA-type initiatives was not always straightforward and interventions to change the physical infrastructure of the ED were often delivered in addition to a change in staffing.
The evidence for improved outcomes for individual staff interventions was limited. Across a broad range of outcomes there was limited evidence that the interventions had improved patient outcomes. Study authors attribute this to problems with study design and the lack of community follow-up of the ED intervention.
Evidence from MDT-type interventions largely showed beneficial outcomes in terms of reducing avoidable admissions and improving early discharge rates from the ED. The CCT interventions had mixed results, with a borderline improvement in reducing avoidable admissions in one study,78 but a higher risk of ED reattendance and a much higher risk of hospital readmission in another. 82
Structural changes to the ED took the form of the development of GEDs (all studies were from the USA), adapting ED environments to better meet the needs of older or frail patients or establishing units on the ED to meet the needs of these patients. A number of UK studies were reported in this category, with largely positive outcomes in terms of decreased admissions and improved discharge times and rates.
The evidence base for CGA-type interventions was much larger than that for other types of service delivery changes. Of the 18 studies24,25,98–117 that described CGA and assessment interventions in the ED, six reported results that had statistical significance. 24,100,101,112,113,115,117 These results were again highly variable but there was a general trend towards improved outcomes in terms of admissions avoidance.
Narrative summary of relevant systematic reviews
A number of systematic reviews (and other review types) have examined interventions delivered in the ED to frail and older people. Seventeen reviews10,121,122,126–139 are presented below. As with the primary research papers, these have been divided into sections reporting studies on the identification of frail/high-risk populations and studies reporting service delivery interventions. Summary tables of data from these reviews are available in Appendix 2.
Identification of frail or at-risk older people
The review by Sutton et al. 121 focused on screening tools to identify older patients presenting to EDs who are at risk of functional decline. Five separate screening tools were identified: the hospital admission risk profile (HARP), ISAR tool, TRST, complexity prediction instrument (COMPRI) and Evaluation du Risque de Perte d’Autonomie (SHERPA). None of these tools was recommended as a gold standard screening tool. Thiem et al. 126 also examined the same five tools, plus the Index of Functional Decline. They found that, even though the ISAR tool has been examined the most frequently and tested the most widely, even for this tool the evidence is weak or conflicting. The review authors also cautioned that management approaches need to be considered alongside screening tools, as there is no value in identifying frail or high-risk patients unless interventions can be tailored to meet their needs.
In 2012, McNamara et al. 127 examined six screening tools used during triage of older patients to identify those at risk. These tools comprised three ‘general’ tools (Manchester Triage, Emergency Severity Index and the CTAS) and three specific tools [ISAR, TRST and variables indicative of placement (VIP)]. The review found that the ISAR tool and TRST performed best, with good sensitivity, a high negative predictive value, low specificity and a low positive predictive value. The VIP had low sensitivity. The review cautioned that clear distinctions need to be made between those who are in need of acute medical care and those who are in need of discharge follow-on care.
Bissett et al. 128 looked at the functional assessment tools used in ED practice. They identified 14 different assessments, four of which were developed specifically for the ED [TRST, ISAR, Runciman questionnaire123 and Functional Status Assessment of Seniors in Emergency Departments (FSAS-ED)]. The review examined the validity of the tools rather than their outcomes and found that the ISAR tool and TRST were most suitable for fast screening and the Runciman questionnaire123 and FSAS-ED were most suitable for comprehensive screening.
The review by Yao et al. 122 looked at the ISAR tool only, in terms of its predictive validity in identifying adverse outcomes for older patients following an ED visit. The review included 10 studies and found that the ISAR tool is quick to use and inexpensive and recommended its use. However, although it was found to have value in identifying high-risk patients with frailty, it has poor, or poor to fair, predictive validity for adverse health outcomes for patients discharged from the ED.
The review by Carpenter et al. 129 looked at what might predict short-term adverse outcomes in GED patients and examined the prognostic value of individual risk factors and ED screening instruments. Seven tools were examined: ISAR, TRST, VIP, Silver Code, Mortality Risk Index and Rowland124 and Runciman123 questionnaires. Various predictors of vulnerability were also considered. The review found that adverse outcomes often occurred post discharge and so identification of these outcomes is critical. However, the review found that there were no risk factors or screening instruments that had sufficient prognostic accuracy to distinguish patients at risk.
The findings of these reviews broadly reflect the findings of our mapping of the primary research – that there are a wide number of tools to identify older people at high risk of adverse outcomes following ED and to identify older patients with frailty. There is no clear recommendation on which tools to use in practice – the ISAR tool is used widely and has been extensively evaluated, but the evidence base for use of the tool is not strong.
Service delivery innovations
Looking specifically at the population of cognitively impaired older people, Parke et al. 130 examined screening and service delivery interventions to better manage this population in the ED. They found that the contextual details and characteristics of interventions were poorly reported and that there were no interventions that were effective and the screening tools identified were inconsistently used and it was therefore difficult to measure effectiveness.
Schnitker et al. 131 also examined evidence on interventions for cognitively impaired older people and identified 12 studies of their management in the ED. These 12 studies were categorised into four groups: (1) those designed to improve recognition of cognitive impairment (and subsequent provision of care); (2) those designed to prevent delirium; (3) those designed to manage behavioural or psychological symptoms; and (4) ‘other interventions’. They proposed the routine inclusion of screening and assessment into care practices and stressed the importance of both screening patients quickly to recognise cognitive dysfunction and using risk tools on discharge.
Two reviews examined the use of CGA in the ED. Graf et al. 132 looked at how best to screen to identify eligible patients for CGA as well as the use and value of CGA. They found that routinely using CGA without screening first was too time-consuming and that an approach that screened for high-risk patients who were then given CGA was most effective. The most effective tool was found to be the ISAR tool. CGA was found to be effective at decreasing functional decline, ED readmission and possibly nursing home admission. Conroy et al. 133 looked at whether or not CGA improved outcomes for frail older people who received this intervention at the point of discharge when they had been discharged rapidly. Using formal systematic reviewing methods, the review looked at a number of outcomes and did not find clear evidence for the benefits of CGA at the point of discharge for this specific population. The review highlighted the lack of trial evidence in this population and the limitations of the small amount of trial evidence that does exist.
Fan et al. 134 reviewed interventions to reduce ED utilisation. The scope of their review was wider and looked at community interventions as well as those delivered in the ED. Although the community interventions were generally more effective than those delivered in the ED for reducing ED utilisation, five ED interventions significantly reduced ED utilisation. These interventions were varied and incorporated risk screening, assessments or discharge planning and referral co-ordination.
The review by Lowthian et al. 10 looked at ED-to-community transition strategies. The review identified nine low-quality research studies that examined interventions that tended to consist of ED assessment with community follow-up. The assessments took a number of forms, including use of the ISAR tool, CGA and discharge planning. There was limited evidence of effectiveness with regard to the outcomes of interest, which included unplanned reattendance, admissions or mortality.
In 2015, Karam et al. 135 undertook a review of interventions delivered within EDs in relation to four outcomes (ED revisits, hospitalisations, nursing home admissions and deaths following discharge). Nine studies met the review inclusion criteria. The effectiveness of interventions was found to be related to intervention intensity – the more intensive an intervention, the more frequently it resulted in reduced adverse outcomes. For the less intensive interventions, effectiveness was enhanced when a screening tool for identifying high-risk patients was used. Karam et al. 135 argued that the specific choice of screening tool to use may be less important than how the tool is actually used.
Others
Tran et al. 136 examined interventions to prevent ED returns in a population of older ED patients. The intensive interventions that they examined, alongside risk factors for ED return, resulted in a reduction in short-term ED returns, but this pattern did not hold in the long term. It was not clear whether or not this long-term pattern was anticipated.
Sinha et al. 137 used a systematic review to develop a geriatric emergency practice model to improve patient outcomes. Examining 28 outcome measures, their review included eight model characteristic components that were seen to contribute to improved outcomes. These eight components were evidence-based practice, nursing clinical involvement/leadership, risk screening, focused geriatric assessments, discharge planning within the ED, interprofessional working practices, discharge follow-up and evaluation/monitoring.
Both screening and service delivery interventions were considered in the review by Fealy et al. ,138 who looked at the effectiveness of nursing interventions for older ED attendees. Although no statistically significant effects were found on patient or health service outcomes, improved effectiveness was demonstrated when interventions incorporated post-ED discharge planning and/or referral.
Summary of review-level evidence
The systematic and other types of reviews that we identified in the searches for the review of primary evidence encompassed both screening and intervention studies.
The screening reviews tended to identify the tools that were available and aimed to assess their value and determine whether or not a single tool could be recommended for use in the ED. The evidence for screening tools was found to be very mixed. The ISAR tool and TRST were found to be the best-performing tools for triage,127 frailty screening122 and rapid functional assessments. 128 However, other reviews that examined these tools did not find sufficient evidence to recommend their use. A prognostic review by Carpenter et al. 129 found that there were no risk factors or screening instruments that had sufficient prognostic accuracy to distinguish patients at risk.
In terms of service delivery interventions, there was mixed evidence on the outcomes of CGA. 132,133 There was evidence that specific interventions reduced short-term ED returns, but this did not hold in the long term. 136 Fan et al. 134 identified five ED interventions that reduced ED utilisation, which included elements of the following: risk screening, assessments, discharge planning and referral co-ordination. Karam et al. 135 examined the effect of interventions on ED revisits, hospitalisations, nursing home admissions and deaths following discharge and found that the intensity of an intervention was a greater predictor of effectiveness than the intervention itself and that the choice of which tool to use was less important than how the tool was used.
Focusing on interventions delivered by a specific health-care professional, Fealy et al. 138 examined nursing interventions, none of which was found to be significant in terms of patient or health service outcomes, although outcomes were improved when post-ED discharge planning was incorporated in the intervention.
Focusing on a specific population, Parke et al. 130 and Schnitker et al. 131 examined screening and service delivery interventions to better manage cognitively impaired older people. No specific tools or interventions were found to be effective – the inconsistent application of the screening tools limited any conclusions that could be drawn from the evidence.
Patient pathway diagram
Summarising the evidence from the primary research studies on identifying frail and at-risk older people, interventions to manage them and the identified systematic reviews, a patient pathway diagram (Figure 2) was developed to present the interventions identified and their potential outcomes.
FIGURE 2.
Patient pathway diagram.
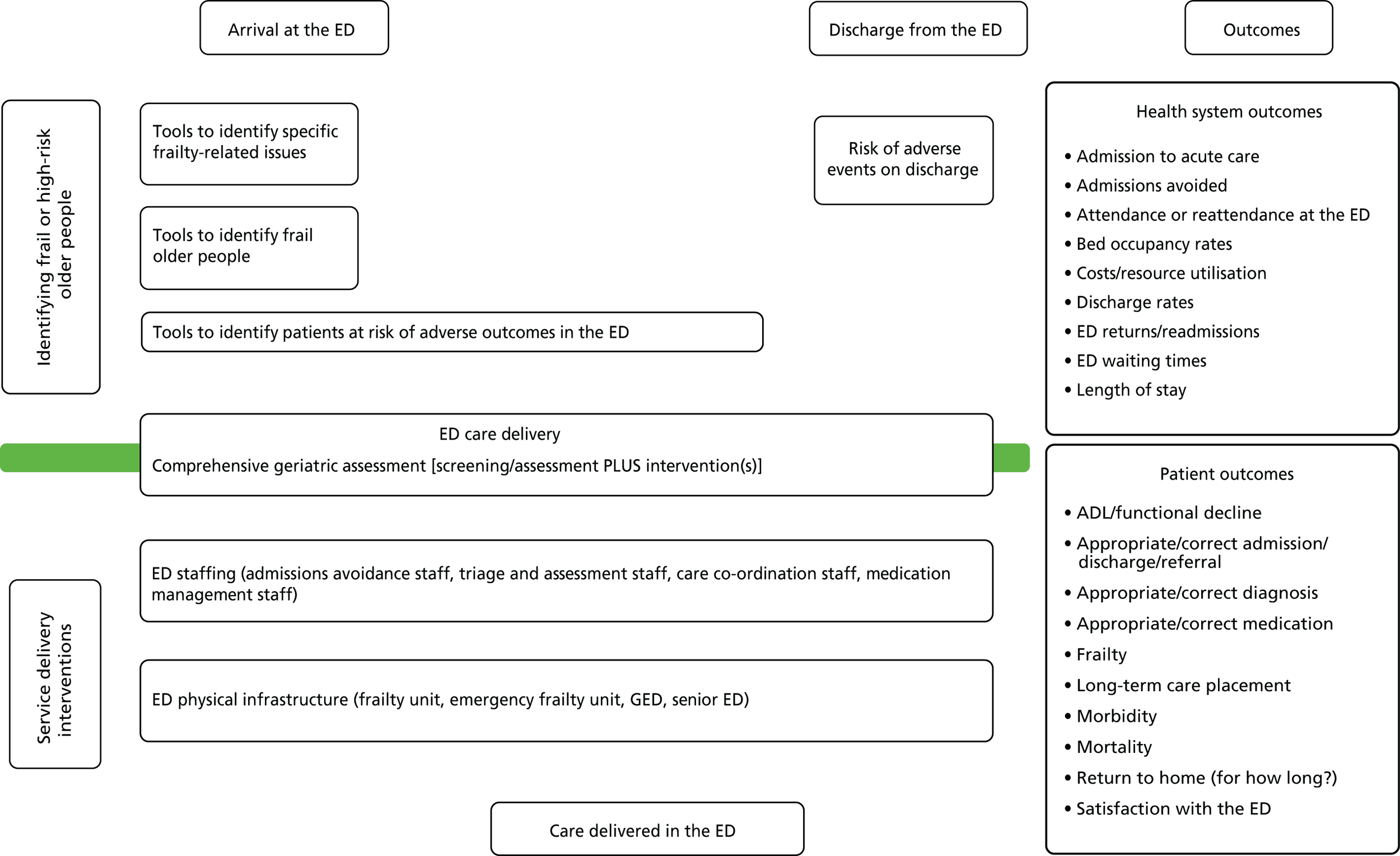
Assessment of the evidence base
This review aimed to map the evidence on interventions to identify and manage frail older people. Mapping reviews seek to characterise an evidence base, not compare interventions on the basis of their effectiveness. Although formal quality assessment is appropriate within the systematic review process, to examine whether or not included studies may be at risk of bias, it is not required in a mapping review, as a mapping review does not interpret evidence to inform specific clinical questions or decisions. Rather, it aims to summarise and map studies and make future research recommendations.
In the case of this mapping review, the use of a single standard tool for quality assessment, such as the Cochrane risk of bias tool, would not have been possible because of the diversity of the study designs. In addition, the use of a set of quality-assessment tools would have been challenging because of the variable reporting of interventions and outcomes in the research.
Rather than a formal quality assessment, we carried out a bespoke assessment of the evidence base using three distinct methods:
-
an examination of the research designs used and the strengths and limitations of those designs
-
an examination of the self-reported limitations included in the articles relating to frail or high-risk older people
-
an assessment of the relevance of the evidence to the contemporary UK NHS setting.
Research designs and their strengths and limitations
The majority of included studies used a prospective observational research design. The screening papers generally measured the accuracy of a tool by gathering follow-up data at a particular time point (that varied across studies) from different sources, including medical records, patient and carer interviews or return visits to the ED. This type of study design was also used in the majority of service delivery intervention studies. These studies, although valuable for descriptive purposes, do not provide direct evidence on the clinical usefulness of a screening tool (in comparison with another tool or an unscreened control group) or the effectiveness of an intervention. The lack of a control group means that it is not possible to determine if the intervention or tool is more clinically effective or cost-effective than usual care.
There are a number of other weaknesses of these study designs that may influence the reliability and validity of their findings. The selection of the study population depends on whether or not patients were exposed to the screening tool or the intervention. Selection bias may therefore influence which patients were given the assessment tool or the intervention. In some studies, for example, the use of a tool was limited to specific times of the day,21 or particular groups were excluded such as those presenting with trauma. 90 This might lead to an under- or over-representation of particular groups of patients and limits the generalisability of findings.
The methods of measuring follow-up outcomes may also introduce bias in studies of this design. Studies may rely on the collection of data that may not have been undertaken consistently. Patients may, for example, return to different ED departments or hospital records may not be consistently coded. The length of follow-up also varied in the included studies, meaning that comparisons between studies may be limited. The number of patients lost to follow-up was also poorly reported but is likely to be very high. This may result in bias if there are differences in follow-up between those who had the outcome being measured and those who did not.
Prospective studies in which data on explanatory and confounding variables are collected before outcomes are known to have an advantage over other study types in determining whether or not outcomes might be associated with the outcome of a tool or the effect of an intervention, as there is less risk of selection or information bias relating to outcomes. In contrast, a retrospective design, used in 12 studies in this review, may affect outcome classification if the exposure to the tool or intervention is known by the person assessing the outcome status (observer bias).
Of the included studies, only a small number used designs that would be appropriate for testing diagnostic accuracy of screening tools or the clinical effectiveness of interventions. The studies that were used to evaluate clinical effectiveness included RCTs, a quasi-randomised study and before-and-after studies.
These research designs are also at risk of bias. Diagnostic accuracy studies in this review may be vulnerable to selection bias if the sample of patients chosen to receive the screening tool or intervention is not random. It may be that the expertise of the individuals using the tools may influence how they are used, leading to measurement bias. The reference standards may also have limitations.
Before-and-after studies offer a valuable method of evaluating clinical effectiveness when a randomised trial may not be feasible. They can provide a historical control against which outcome data may be compared. A weakness of this type of study design is attributing change in outcomes solely to an intervention. It may be that other factors might also influence outcomes, for example staff changes or initiatives in the community for frail older people by a voluntary organisation.
There was a limited attempt to measure the costs of screening and interventions, in terms of either the cost of the intervention or the costs saved as a result of improved outcomes. The nature of many of the interventions reported here is that patients are more appropriately cared for in community settings on discharge, rather than in the acute setting, which is why reduced admissions are a frequently reported outcome. However, there is little evidence on measuring how this ‘care’ is displaced from the ED to the community and the effect that this has on costs.
Compared with service delivery intervention studies more generally, there was a lack of long-term follow-up of individual study participants in the studies reported here. This may be because of the nature of frail older people. Interventions delivered to general older populations, on the other hand, can be followed up over a longer period of time because of their relative better health. The nature of research in the ED means that short-term outcomes are more straightforward to measure. These shorter-term outcomes, such as admissions and length of stay, are outcomes for both the health service and patients. Longer-term patient outcomes (such as mortality) often assumed lesser importance in the reporting of study findings. However, shorter-term outcomes are much more appropriate for an older population, especially given that frail older people are often nearing the end of life. Not only are longer-term outcomes harder to measure, they also assume less importance for this population group, whose outcomes may be better reported in terms of intervention acceptability, for example.
Much of the evidence was not experimental; the majority of the study designs were retrospective or prospective before-and-after cohort studies, with very few trials (either randomised or non-randomised). The sample sizes tended to be small, particularly for the experimental research.
The ED is a challenging place to deliver care, let alone undertake experimental research. The difficulties in undertaking research are reflected in the fact that many of the described interventions are limited in terms of the hours during which they are offered to patients, the staff who are available to deliver them or unintended events (such as outbreaks of infectious diseases), which hamper their evaluation.
There was not much evidence on staff education, which is surprising. When looking at interventions that introduced staff changes, the extent to which staff members had received additional education and training is unclear. The lack of evidence on staff education in this review may in part be related to the outcomes of interest to this review; patient and health service outcomes may be too distal for staff education and the outcomes of interest to staff education interventions, such as increased knowledge and confidence, were outside the scope of this review.
One of the key limitations of the evidence base was the inability to distinguish the frail population from the general population of older adults. Much of the evidence included in the review was not specific to frail older people, instead including a target population aged ≥ 65 years. However, on closer scrutiny, although the interventions tended to be taken up by populations with a mean or median age of ≥ 65 years, in many cases the population was much older. However, the lack of consensus around the definition of frailty makes designing interventions for this population and monitoring their outcomes, and the effectiveness of their outcomes, challenging. In addition to the lack of ‘frail’ population groups, only two studies used changes to frailty as an outcome measure. 24,112
Author-reported limitations
The authors of studies routinely highlighted limitations of their methodology, which led them to caution the extent to which their findings can be generalised and compared with those of other studies. The self-reported limitations of the studies in which frail older people were the focus and full data extraction was undertaken were extracted and a narrative summary of these is given below. A major limitation is the number of conference abstracts that were included in the review; not only is detail missing on the study methods for our assessment of the limitations of the evidence, but conference abstracts rarely contain data on study limitations.
In terms of the sources of data used, data were often collected from routine sources not specific to the studies. 86,88 Authors commented on the seasonal fluctuations in ED attendance,61,106 which may affect the generalisability of the results. There was a general lack of data from outside the ED on participants or service use (community or use in other settings),86 which limited follow-up, and many of the data collected were retrospective. 53
Many of the studies were retrospective or prospective before-and-after studies and there were a limited number of controlled trials. Jones and Wallis61 and Fox et al. 106 noted the lack of a control group, with Silvester et al. 86 and Conroy et al. 89 commenting on the lack of a contemporaneous control group. In addition, a number of authors cautioned that their study had a small sample size;67,71,98,106 that both participants and staff were not blinded (when there was some element of controlling interventions);21,24,112 that not all variables were controlled for;27,78 that the study was conducted at a single centre therefore limiting generalisability;29,33,49,53 and that there may have been some selection bias. 52
The way in which screening and interventions were delivered was cited as a limitation; examples included that the intervention was not delivered 24 hours a day so not all potential participants were included;21,27,49,78,106 only non-urgent attenders were included; the screening tool used was amended for a local setting;78 the difficulty in recruiting patients;112 and unforeseen circumstances, such as an infectious disease outbreak, which may have influenced the study results (before-and-after study). 88
The impact of study findings was limited by the lack of long-term follow-up patient outcome data73,86,89 and the fact that, when there was follow-up, there were high rates of dropout24,29 because of the nature of the population. Two authors also mentioned that study findings would have been enhanced if qualitative data on staff or carer satisfaction with the intervention had been collected. 86,112
In line with the limitations that we identified, there was no clear definition of frail older people27,61 and there was a lack of cost data. 72,89
Relevance of the evidence to the current NHS setting
The consideration of the relevance of the included studies to the NHS setting lies largely in whether or not they have reported research undertaken within the same health system, whether or not the health systems in which the studies were undertaken can be compared with the NHS and whether or not the interventions and screening tools used could be used within the NHS.
In terms of the screening papers, it is noteworthy that only one screening paper20 reported research undertaken in UK EDs. This is in contrast with the depth of research being undertaken in community settings on screening for frailty. In contrast, the intervention papers more widely reported UK research. In particular, interventions for frail populations in the UK combined screening and interventions, perhaps suggesting that it is considered more effective to combine these interventions rather than consider them separately.
In terms of whether or not the included studies could provide models that could be used in the NHS, it is unlikely, given the current NHS landscape, that the GED is a model that would be adopted. Indeed, the current pressures on the ED service make it a challenge (both financial and logistical) to introduce any new interventions and evaluate them.
Chapter 5 Discussion
This mapping review identified > 100 papers from the last 11 years that reported screening or management interventions for older people, including those identified as being frail or at high risk of adverse outcomes in the ED. This large body of evidence was subdivided into interventions for identifying those older people who are frail or who are at risk of adverse outcomes and interventions for managing them. The following sections summarise the overall evidence base and the evidence for the identification and management of frail older people.
The evidence base
This review has summarised a large and heterogeneous evidence base on approaches to the management of frail and older people in the ED. The review has taken an inclusive approach to evidence, looking at conference abstracts, full papers and systematic reviews in an attempt to examine the approaches used and the outcomes that they have (potentially) influenced. The way in which the term ‘frail’ was used by study authors was very variable and the age at which patients were considered to be older also varied. The evidence base in terms of study design and reporting is variable and not particularly robust. However, the aim of this review was not to compare the effectiveness of interventions, but to characterise the full range of interventions reported and their outcomes.
Summary of the evidence for screening
Many screening tools have been evaluated, particularly the ISAR tool and TRST, but few have been validated in a wide range of populations/settings and specifically in UK settings. The evidence demonstrates that screening tools are used for different purposes: to identify those requiring further assessment or, directly, to support management decisions. For example, a tool with a high diagnostic sensitivity for frailty may be useful for identifying people who are unlikely to benefit from further geriatric assessment. Newer tools appear worthy of further evaluation; these include the Silver Code, which uses administrative data available at the time of presentation. The ability of tools to predict patient outcomes such as return to the ED or hospital readmission is likely to be health system specific, as it depends in part on what support is available in the community to support patients to achieve these outcomes. Hence, it follows that results from non-UK settings cannot easily be generalised to the UK. The number and variety of tools used to identify frail and at-risk patients in the ED was reinforced through the findings of the review of systematic reviews. CGA interventions included screening patients for frailty or patients at high risk and then delivering bespoke interventions to this group.
Summary of the evidence for service delivery innovations
The evidence base on changes to service delivery for (frail) older people is large. Even limiting this to evidence from the last 10 years, a wide variety of approaches were identified. The evidence was divided into a number of categories: changes to ED staffing, structural changes, introduction of CGA and CGA-type interventions and other interventions. However, there was significant crossover in the interventions, for example structural changes tended to change what was done to patients, as well as where it was done. This was not a surprising finding, as to isolate and control for specific staff or structural elements in a system as complex as an ED would be a challenging undertaking. The range of outcomes was highly diverse, with an example being that some interventions focused on preventing inappropriate discharges (of patients who required an admission), whereas others focused on preventing inappropriate admissions (in patients who were medically able to be discharged but who, because of their frailty, were likely to be admitted).
Changes to staffing in the ED included the introduction of a specific member of staff or a new team with a specific remit to address an issue pertinent to the care of frail and at-risk older people (e.g. medication management or care co-ordination).
Physical infrastructure changes often incorporated staff changes in addition to those of the physical surroundings of the ED. All of these interventions reported positive outcomes for patients – generally reduced admissions to acute care and improved discharge times and rates. The three categories of physical infrastructure changes that we identified had slightly different mechanisms for how outcomes might be changed. GEDs may be available for all older people; therefore, those who are attending and who are frail or at high risk may need additional screening to identify their needs. Making all EDs frail friendly will have benefits for everyone who attends, but the greatest benefit should be for patients who are frail or at high risk, who may receive additional interventions. Finally, frailty units will require screening of older patients to identify those who are frail or at high risk. McNamara140 discussed the development of GEDs, which have been largely developed in the USA11 but are a proposed solution to the fact that older people have different clinical and social needs from those of the general adult population. However, Maile et al. 14 argued that it is more appropriate and realistic to make EDs ‘frail friendly’, as to develop a specific GED has cost and access implications. It appears that the approach of making EDs more frail friendly, or introducing ‘frail units’ within EDs, has been adopted more widely in the UK than the more radical reorganisation of services to create GEDs.
The interventions focused on CGA and assessment of frail and high-risk older people demonstrated a general trend towards improved admissions avoidance and reduced ED attendance.
The review found some evidence on discharge planning. This took a number of forms: from prognostic screening to identify patients at risk on discharge, to CGA interventions that incorporated discharge planning, to interventions such as the continuum of care, which integrated ED and community follow-up. The aim of these interventions tended to be to prevent readmissions to the ED, which in turn can improve patient outcomes. There is little evidence in this review of evaluation taking place; interventions tended to be reported in terms of study outcomes at a single point in time, with few papers reporting ongoing data collection and evaluation of these data. In addition, there was little evidence of evaluation around satisfaction with interventions from staff or patient/carer perspectives.
A theme running throughout the interventions reported here is that increased engagement with health professionals through service delivery interventions may appear to stimulate demand through increased admissions to acute care (or increased readmissions), which could represent an unintended consequence of interventions. Additional admissions and readmissions may represent increased interaction with the health service, but these patients may well represent the frailest patients and it is not possible, using the data from the studies, to determine whether or not these admissions and readmissions were unexpected. 141 Although this may be an unintended consequence of interventions, interventions may uncover unmet need or lead to older people receiving care in a more appropriate setting, resulting in positive outcomes for individual patients. Only one study looked at interventions for repeat attenders at the ED, even though repeat attendance was an outcome that was frequently measured. Even in the general population including all adults, not just those who are older/frail, readmissions to UK EDs within 1 week of attendance are around 8%. 142
Links with the wider literature
Looking at wider ED interventions, a systematic review by Fan et al. 134 identified seven elements that were common to effective interventions that reduced ED utilisation. These were (1) MDT gerontological expertise, (2) risk screening and geriatric assessment, (3) care planning and management, (4) discharge planning and referral, (5) integrated or enhanced primary care, (6) integration between health and social care and (7) co-ordination. This review has described interventions and outcomes for the first four elements. However, this highlights that interventions to better manage frail older people in the ED also need to consider interventions that are delivered outside the ED, so that only those in real need of ED care for specific presenting complaints (as opposed to underlying frailty) present to the ED. Research focusing on the ED system alone is likely to influence only ED outcomes (as measured in the majority of the studies here). Whether or not these are salient outcomes for patients is another matter.
McCusker et al. 143 developed a checklist of categories for EDs to use to ensure that the care that they deliver is appropriately geriatricised. 9 This checklist, presented in Table 14, highlights the areas in which interventions may be targeted to manage frail older people more effectively. This table has been added to with the evidence that we identified in our mapping review.
| Area | Intervention | Findings from our review |
|---|---|---|
| Education | Education and educational initiatives for staff working in elderly-focused ED care | No evidence of this; however, this may be related to our search strategy |
| Environment | Elder-friendly physical environment and design principles | Frail-friendly EDs, frailty units and GEDs were all identified in this review |
| Staff | Presence of staff with geriatrics expertise – either specialist or general | Addition of single staff members or teams of staff to the ED was identified |
| Screening/assessment/protocols | High-risk screening tools to identify vulnerable elderly adults. Cognitive, functional and mobility assessments. Medication review and reconciliation | In this review we identified diagnostic tools to identify frail patients or patients at high risk because of frailty-related issues and prognostic tools to identify patients at risk of adverse events in the ED and on discharge from the ED. Assessments were carried out as part of CGA. Little evidence on the use of protocols for older adults in the ED was identified |
| Standardised protocols for identification, prevention and management of delirium, falls, functional decline, dehydration, incontinence and pain | ||
| Transitions of care | Discharge planning | We identified evidence on prognostic tools for patients at high risk on discharge, discharge co-ordinators or teams and CGA with community follow-up |
| Community services | Not applicable in this review | |
| Evaluation | Ongoing evaluation of care processes, in particular hospital admission rates, ED and hospital lengths of stay, ED repeat visits and subsequent hospital admission rates and patient, caregiver and provider satisfaction with service | We found little evidence of ongoing evaluation |
Limitations of the review
This review was a systematic mapping review. The review was systematic in how evidence was identified, extracted and synthesised and is transparent and reproducible. When feasible and methodologically necessary, we have undertaken double checking of our work (screening of study results). Although double data extraction was not undertaken, the extraction of verbatim data into extraction tables and the use of descriptive rather than numerical data limits the risk of errors in our interpretation of the evidence.
A systematic mapping review seeks to ‘collate, describe and catalogue available evidence relating to a topic or question of interest’. 15 In identifying > 100 research studies and classifying these according to the intervention delivered and the outcomes considered, we have met the aims of a mapping review. Despite this, the review has a number of limitations.
The search strategy for the review was designed to find evidence on the identification of frailty and high risk in older people and interventions to manage (frail) older people in the ED. The search strategy may have missed evidence relating to specific conditions that, on the whole, affect only older people (e.g. delirium or falls). Such interventions, although targeted at older people, may not be indexed or keyworded as such and, therefore, may not have been identified by the search strategy.
The a priori exclusion of evidence relating to units, such as assessment units and frailty units, may have limited the review; some older patients are diverted straight to an assessment or frailty unit and, therefore, these units have a similar population to the population of older people presenting at the ED.
The arrival of a (frail) older person at an ED is part of a patient pathway. Interventions undertaken in other parts of the patient pathway, such as in the home setting, and admissions avoidance interventions clearly influence how patients use the ED, but were outside the inclusion criteria for this review.
The objectives of the review (as outlined in the study protocol) did include a research question relating to the effectiveness of interventions, although this was not the main aim of the review, which was to map the existing interventions. The review was unable to answer this research question, comparing the effectiveness of interventions. This was because of the variability of interventions identified (population, interventions and outcomes) and the methods through which they were tested (very few controlled studies). To draw any conclusions about the effectiveness of interventions would require much greater similarities between the studies. Despite this, when the evidence permits, we have summarised the evidence for effectiveness of interventions as reported in individual studies, but have not pooled these data.
The results are presented narratively and tabulated numerically when the evidence permits. The aim of a mapping review is not to produce a numerical synthesis of interventions to answer a specific question but rather to present the evidence and, when feasible, identify trends in the evidence.
A limited number of qualitative studies were included in the review, which is of note when summarising the evidence base. The reasons for this are unclear; however, the challenges in following up patients once they had left the ED, as reported in the studies included in the review, may account for the lack of evidence on intervention acceptability and feasibility (which is generally reported qualitatively). The focus of the review was on interventions for identifying and managing frail older people and mapping these interventions and their outcomes. Qualitative evidence of relevance to the review would have needed to be related to these interventions – either service user views on the interventions or service user views on their feasibility and acceptability.
The bespoke assessment of the evidence base allowed an assessment of the study designs, the self-reported study limitations and the applicability of the evidence to the NHS. Although this was not a standard quality-assessment approach, it is appropriate for a mapping review; indeed, the limited evidence provided in many of the studies would have made a standard assessment of risk of bias very difficult to undertake.
In terms of the evidence identified, we were limited by the reporting of the studies; a significant number of the studies were reported in conference abstracts, which contained limited information on interventions and outcomes. In addition, reporting of the results of studies was limited by the difficulty in identifying frail older people in the evidence. In the absence of any clearly defined criteria, we included both studies in which older people had been defined as frail in the literature or were a high-risk group and studies in which people were defined as older, which tended to be based on their age (> 65 years). This proxy for an agreed definition of frailty was the most feasible approach and did not lead to any studies being excluded from the review.
The evidence identified for the mapping review tended to view older people as a homogeneous group and not differentiate between specific population groups, for example older people with trauma or older people with dementia or specific issues that might affect patients in the ED (e.g. recognition of polypharmacy). Service improvements are continually being made for specific populations or issues such as these, but these were not reflected in the evidence that we identified for the review.
Implications for practice
The extent to which a mapping review can have any implications for practice is limited as it does not seek to answer questions about the effectiveness of interventions. The data presented in this review are focused on what interventions have been implemented and reported and the outcomes that they influence. Therefore, any assessment of which are the best interventions to identify and manage frail and high-risk older people cannot be made. It is clear that specific screening tools, namely the ISAR tool and TRST, have been more frequently evaluated. However, the results of these studies may not be relevant to the NHS as they were undertaken outside the UK. The review mapped out a wide variety of interventions. There was evidence from individual studies of some positive findings; however, additional research would need to determine which of these interventions are effective and on which outcomes they have a positive impact. It is also evident that little attention has been paid to the costs and benefits of interventions and these would need to be determined prior to any implementation in a practice setting.
Implications for research
Key priority areas for further research
A number of areas warranting further examination have emerged throughout this review.
There is a lack of UK evidence relating to how to identify frail older people, compared with the volume of evidence on service delivery interventions from the UK. It is unclear whether this is because there is a greater consensus around how to identify older people who are frail or at risk, because older people are treated as a homogeneous group or because of some other reason. Research is needed in the UK on which tools are currently used in practice and how does identifying patients as frail or high risk subsequently link to their treatment and management. It would be useful to have evidence on whether the purpose of identifying frail and older patients is to identify those needing further assessment or to rule out those not needing it. Consensus on a tool to identify frailty needs to consider which aspects of frailty are more important in the ED, for example patients with dementia or delirium may need very different treatment from patients who are prone to falls and identifying them simply as frail or as being at high risk does not reflect these subtleties. The acceptability of tools to patients and the usefulness of tools to clinicians also needs to be examined. This could include a comparison between tools that are question based and those that employ different methods.
Looking at the complexity of the health-care system, it is unclear whether or not interventions to reduce inappropriate admissions are displacing care to elsewhere in the health-care system; the implications of ‘displaced’ care have not been considered. Another issue that has not been addressed in any detail is whether or not the staff member delivering an intervention has any effect on the outcomes or acceptability of the intervention (i.e. whether it is delivered by a doctor, nurse or other health-care professional and whether or not this staff member requires specific geriatric expertise). These models appear to have been evaluated in the literature; however, the reasons for why a specific clinician was chosen remain unclear and whether or not it is thought that this may have influenced the costs and outcomes of an intervention is not reported.
This review did not identify many interventions that were delivered both within and outside the ED. This may be related to our search approach; however, it would be interesting to further examine interventions that combine ED intervention with home follow-up and compare different models of discharge management and follow-up and the cost implications of these interventions. Community screening to identify those older patients at greater risk of admission to hospital or nursing homes may provide an opportunity for patients who present at the ED to be ‘prescreened’ and identified as frail and high risk, so that their care can be managed accordingly. It may be that interventions that divert frail older people away from presenting at the ED may be more effective than trying to improve outcomes for the proportion who will inevitably attend the ED with an acute medical condition.
In terms of service delivery interventions, it has been argued that it is unlikely that the GED model will become widespread11 because of the cost and resource implications required to develop this model. However, there is a precedent with the use of paediatric EDs in the UK. With an ageing population, further exploration of the GED may be of use.
One area that was not covered in this research and will undoubtedly be of interest and importance to patients, carers and the health service are which outcomes are important for patients and how long should we measure these outcomes for. Bearing in mind that many frail patients may be nearing the end of life, how important is it to measure long-term outcomes? The quality of the experience of ED care may well be more important to patients than how quickly they are discharged. Knowing more about which outcomes are important will help us to determine which interventions should be considered.
Key design features of research
A standard evidence review approach has allowed us to discover what evidence is available on the identification and management of frail older people in the ED. The variability in the types of interventions used, the outcomes reported and the standard of reporting more generally has meant that it is not possible to make overarching conclusions about which interventions are more effective. Limited qualitative data were identified on the feasibility and acceptability of interventions, so it would be useful to understand the views of patients, carers and clinicians about the ED more generally and the appropriateness of interventions. One way of doing this would be through a qualitative review or a realist synthesis of evidence, which would allow for disparate types of evidence to understand more about how and why interventions work and would be less restricted by the requirement of this review to focus on interventions and their outcomes.
Data on anything other than patient and health service outcomes were rare; a basic cost analysis was undertaken by Leah and Adams,72 who estimated cost savings from reducing avoidable admissions. Many of the studies reported increased engagement with health services as a beneficial outcome of the intervention, for example an increase in appropriate admissions, consultation with a geriatrician in the ED, increased community follow-up and more people referred for care according to guidelines and protocols. However, there is very little evidence on the cost of these outcomes. Although there may be a cost benefit in reducing admissions, there is no evidence on the displacement of these costs and the increased cost of community-based interventions when inappropriate admissions are avoided. This is specifically the case for older people generally, and frail older people in particular, as their engagement with the health service differs in its cost and frequency from that of the wider population.
Chapter 6 Conclusions
This review is a systematic mapping review that has identified > 100 studies that have investigated the identification and management of frail, older and high-risk patients in the ED. The variability of interventions and outcomes and the nature of and variability in reporting of interventions has made any summary of the evidence, other than a narrative assessment of interventions and outcomes, difficult to make. Any interpretation of causality between interventions and outcomes is challenging as there was little consistency between studies and, in some cases, there were contradictory results resulting from similar interventions.
In this review, we examined the approaches that exist to manage frail older people in the ED. Because of the difficulty in differentiating frail or high-risk older people from older people (aged > 65), the review looked at all evidence from 2005 to 2016 onwards on the management of frail older people, older people at high risk of adverse outcomes and older people aged > 65 years who met our inclusion criteria. Including only papers in which frail older people were a specific, named population would have limited the scope of the review and, as the aim of the review was to map all approaches to the management of frail older people, some of these may have been missed had the population group been limited. However, including the population of those aged > 65 years has meant that, in some cases, the exact nature of frailty has not been considered in the design and implementation of interventions.
The importance of the appropriate delivery of care to frail older people is highlighted by their recent inclusion in the research priority-setting exercise, undertaken by the James Lind Alliance and the Royal College of Emergency Medicine. 144 Included in their top 10 research priorities, published in early 2017, is a priority relating to service delivery, asking ‘Is a traditional ED the best place to care for frail older people?’. The priority-setting exercise presents three alternative models of care: GEDs, geriatric liaison with the ED or the adaptation of current EDs to better meet the needs of older people with frailty. This research priority covers two of the three service delivery intervention categories developed in this review (physical infrastructure and staffing changes) and, arguably, geriatric liaison services cover both staffing and CGA interventions. The final research question, regarding whether or not current services should be made more frail friendly, has not been addressed in our review in terms of specific interventions, but is arguably the philosophy that underpins CGA. 11 The agreement between the findings from our review and the research priority-setting exercise is noteworthy.
Examining this heterogeneous body of evidence was challenging because of the sheer volume of evidence and the difficulty in bringing together very different study types, with different interventions and different methods. The variability in the reporting of these methods and the inclusion of evidence from conference abstracts meant that the data that the report is based on are highly variable. Despite this, we have been able to classify key interventions (both screening and service delivery interventions) for older people in the ED and, when specific issues have arisen for frail older people, have attempted to draw these out. We have considered the variety of outcomes that have been evaluated and have summarised the evidence base, with reference to key literature, including systematic reviews.
This review is unique in that it has brought together evidence from both screening and service delivery innovations and has considered all patient and health service outcomes. The emergent patient pathway diagram (see Figure 2) has represented these interventions and the outcomes that they may potentially influence, to guide the development of future interventions.
It is clear from the literature that improvements in the care of frail older people have the potential to improve both patient and health service outcomes, yet the purpose of this review was not to examine the effectiveness of interventions. The evidence for both screening and service delivery innovations was not sufficiently strong to suggest that specific interventions should be adopted because of their effectiveness and future research needs to determine the outcomes that are of importance to the health service and patients. The research reported in this review establishes that a number of outcomes may be important to both of these groups (patients and the health service), but it is often difficult to unpick these and differentiate whether interventions are targeted at improving patient outcomes, health service outcomes or both.
We know from the published literature that frailty screening is complicated and definitions of frailty vary. There is no set age threshold for frailty and, although most of the interventions in this review were targeted at patients aged > 65 years, they seemed to have been utilised by an older population. It is clear that identifying frail populations will lead to appropriate care being delivered and indeed a number of (mostly UK) interventions reported in this review have taken the approach of combining screening with other interventions to improve outcomes. To meet the needs of frail older people, it is not sufficient to know that screening tools are effective at identifying a population at risk; they need to predict a risk that can be reduced by either delivering or not delivering interventions as appropriate.
Returning to the research questions, the studies included in the review have reported data on the health service outcomes of interest (attendance, reattendance, admissions and readmissions), although the findings from interventions could not be integrated to give any key messages about whether or not outcomes have been influenced. There is less evidence on patient-centred outcomes and a very limited amount of evidence on costs to the health service. We were unable to identify any patterns in unintended outcomes, although studies have reported increased engagement with health services, which may increase admissions. Discharging patients appropriately, rather than admitting those who do not require acute care, may lead to a greater proportion of acute older patients being very frail or unwell. This may lead to the outcomes for acute and older wards appearing to be worse, as a result of decreasing inappropriate admissions. There was no evidence on where patients were ‘displaced’ to if they were discharged early or not admitted. There was also no evidence that interventions increased ED demand. Interventions may lead to previously undiagnosed problems being diagnosed or to patients being labelled as frail or at high risk, which may actually increase health and social service use, improving patient outcomes but increasing costs.
The scope of this review was limited to interventions delivered in the ED. However, the review has put forward that the most effective interventions in terms of positive outcomes for the health service and patients are those that accept the complexity of the social and health needs of frail older people and are designed accordingly. This necessarily means that follow-up outside the ED is a key element of effective interventions.
A systematic review published in 2015 by Lowthian et al. 10 highlights the dearth of research in frail older people in the ED. Despite the recognised challenges of undertaking research with this population, there is little high-quality evidence. They contrasted the findings of their review from 2015 with those of a review undertaken in 2005,145 arguing that there has been little progression in the evidence base since this review.
Complex populations such as frail older people need to be identified in a timely fashion so that appropriate and often complex interventions can be targeted to address their needs. Limiting interventions for this population to the ED alone might demonstrate improvements in outcomes, such as increased discharge rates in the short or medium term, but it may well be the interventions that take place in the community that prevent re-presentations and readmissions in the longer term.
The studies reported in this review have demonstrated that interventions in frail elderly populations result in reduced admission rates; however, this is arguably only a successful outcome if we see a benefit in preventable reduced return ED visits; there is limited value in returning older people to their normal place of residence if they are just going to re-present to the ED again for the same reason. Ideally, evaluations of changes in ED service provision need to collect information about the impact on all relevant service use, both in hospital and in the community, and the associated costs and staffing implications.
Acknowledgements
We would like to thank:
-
Our review advisors Professor Steve Goodacare, Professor Fiona Lecky and Professor Sue Mason for commenting on the protocol, advising on the research questions and reading and commenting on the final report.
-
Surgeon Captain Jason Smith, Consultant in Emergency Medicine and College of Emergency Medicine Professor, for advice when designing the study and writing the protocol.
-
Sheffield Teaching Hospitals NHS Foundation Trust Clinical Research Office Online Patient Advisory Panel for reading and commenting on the Plain English summary and the Scientific summary.
-
Andrew Clegg, Clinical Senior Lecturer and Honorary Consultant Geriatrician, Bradford Teaching Hospitals NHS Foundation Trust, for reading and commenting on the Scientific summary.
-
Andrew Booth, University of Sheffield, for comments on the final report.
Contributions of authors
Louise Preston (Research Fellow, Health Economics and Decision Science) was responsible for screening of the search results, data extraction, analysis and synthesis of the intervention papers and writing up of this section, project management and report writing and editing.
Duncan Chambers (Research Fellow, Public Health) was responsible for screening of the search results, data extraction, analysis and synthesis of the screening papers and writing up of the section on screening of papers.
Fiona Campbell (Research Fellow, Health Economics and Decision Science) was responsible for data extraction and assessment of the evidence base.
Anna Cantrell (Research Associate, Health Economics and Decision Science) designed and ran the literature searches and was responsible for the screening of the search results, data extraction and writing up of the section on search methods.
Janette Turner (Reader in Urgent and Emergency Care Research, Health Services Research) was responsible for screening of the search results and report editing and contributed to ED expertise.
Elizabeth Goyder (Professor of Public Health) was responsible for report editing and project management.
All of the team contributed to writing the review protocol and commented on and edited the final report.
Data sharing statement
All available data can be obtained by contacting the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- High Quality Care for All, Now and for Future Generations: Transforming Urgent and Emergency Care Services in England – Urgent and Emergency Care Review End of Phase 1 Report. Leeds: NHS England; 2013.
- Department of Health and Social Care . National Service Framework: Older People 2001. www.gov.uk/government/uploads/system/uploads/attachment_data/file/198033/National_Service_Framework_for_Older_People.pdf (accessed 6 December 2017).
- Turner J, Coster J, Chambers D, Cantrell A, Phung V, Knowles E, et al. What evidence is there on the effectiveness of different models of delivering emergency care? A rapid review. Health Serv Deliv Res 2015;3. https://doi.org/10.3310/hsdr03430.
- Gruneir A, Silver MJ, Rochon PA. Emergency department use by older adults: a literature review on trends, appropriateness, and consequences of unmet health care needs. Med Care Res Rev 2011;68:131-55. https://doi.org/10.1177/1077558710379422.
- Appleton S, Miller R. What the Evidence Tells us about Improving Urgent Care for Older People. A Literature Review to Support the Independent Commission on Improving Urgent Care for Older People. London: NHS Confederation; 2016.
- Dent E, Hoogendijk EO, Cardona-Morrell M, Hillman K. Frailty in emergency departments. Lancet 2016;387. https://doi.org/10.1016/S0140-6736(16)00177-X.
- Rodríguez-Mañas L, Féart C, Mann G, Viña J, Chatterji S, Chodzko-Zajko W, et al. Searching for an operational definition of frailty: a Delphi method based consensus statement. The Frailty Operative Definition-Consensus Conference Project. J Gerontol A Biol Sci Med Sci 2013;68:62-7. https://doi.org/10.1093/gerona/gls119.
- Dent E, Kowal P, Hoogendijk EO. Frailty measurement in research and clinical practice: a review. Eur J Intern Med 2016;31:3-10. https://doi.org/10.1016/j.ejim.2016.03.007.
- Carpenter CR, Shelton E, Fowler S, Suffoletto B, Platts-Mills TF, Rothman RE, et al. Risk factors and screening instruments to predict adverse outcomes for older emergency department patients: a systematic review. Ann Emerg Med 2014;1. https://doi.org/10.1016/j.annemergmed.2014.07.250.
- Lowthian JA, McGinnes RA, Brand CA, Barker AL, Cameron PA. Discharging older patients from the emergency department effectively: a systematic review and meta-analysis. Age Ageing 2015;44:761-70. https://doi.org/10.1093/ageing/afv102.
- Conroy SP, Turpin S. New horizons: urgent care for older people with frailty. Age Ageing 2016;45:579-86. https://doi.org/10.1093/ageing/afw135.
- Cesari M, Marzetti E, Thiem U, Pérez-Zepeda MU, Abellan Van Kan G, Landi F, et al. The geriatric management of frailty as paradigm of ‘The end of the disease era’. Eur J Intern Med 2016;31:11-4. https://doi.org/10.1016/j.ejim.2016.03.005.
- Salvi F, Morichi V, Grilli A, Giorgi R, De Tommaso G, Dessì-Fulgheri P. The elderly in the emergency department: a critical review of problems and solutions. Intern Emerg Med 2007;2:292-301. https://doi.org/10.1007/s11739-007-0081-3.
- Maile EL, Harrison JK, Chikura G, Russ K, Conroy SP. Ethical issues for older people in the emergency department. Eur Geriatr Med 2016;7:372-8. https://doi.org/10.1016/j.eurger.2016.02.005.
- James KL, Randall NP, Haddaway NR. A methodology for systematic mapping in environmental sciences. Environ Evid 2016;5. https://doi.org/10.1186/s13750-016-0059-6.
- Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J 2009;26:91-108. https://doi.org/10.1111/j.1471-1842.2009.00848.x.
- Banerjee J, Conroy S, O’Leary V, Rawstorne S, Wenman J, Walker A, et al. Quality Care for Older People With Urgent and Emergency Care Needs 2012. www.bgs.org.uk/campaigns/silverb/silver_book_complete.pdf (accessed 6 December 2017).
- Carpenter C, Bassett E, Fischer G. Emergency department geriatric technician case-finding: a randomized controlled trial. Acad Emerg Med 2010;17:S111-S12. https://doi.org/10.1111/j.1553-2712.2010.00743.x.
- Hustey FM, Mion LC, Connor JT, Emerman CL, Campbell J, Palmer RM. A brief risk stratification tool to predict functional decline in older adults discharged from emergency departments. J Am Geriatr Soc 2007;55:1269-74. https://doi.org/10.1111/j.1532-5415.2007.01272.x.
- Wall J, Wallis SJ. Can a frailty scale be used to triage elderly patients from emergency department to geriatric wards?. Age Ageing 2014;43. https://doi.org/10.1093/ageing/afu044.4.
- Salvi F, Morichi V, Lorenzetti B, Rossi L, Spazzafumo L, Luzi R, et al. Risk stratification of older patients in the emergency department: comparison between the Identification of Seniors at Risk and Triage Risk Screening Tool. Rejuvenation Res 2012;15:288-94. https://doi.org/10.1089/rej.2011.1239.
- Schoenenberger AW, Ozguler O, Bieri C, Businger R, Moser A, Haberkern M, et al. Evaluation of an emergency geriatric screening for older patients in the emergency department. Eur Geriatr Med 2013;4:S70-1. https://doi.org/10.1016/j.eurger.2013.07.232.
- Lee JY, Oh SH, Peck EH, Lee JM, Park KN, Kim SH, et al. The validity of the Canadian Triage and Acuity Scale in predicting resource utilization and the need for immediate life-saving interventions in elderly emergency department patients. Scand J Trauma Resusc Emerg Med 2011;19. https://doi.org/10.1186/1757-7241-19-68.
- Eklund K, Wilhelmson K, Gustafsson H, Landahl S, Dahlin-Ivanoff S. One-year outcome of frailty indicators and activities of daily living following the randomised controlled trial: ‘continuum of care for frail older people’. BMC Geriatr 2013;13.
- Yim VWT, Rainer TH, Graham CA, Woo J, Wong TW, Lau FL, et al. Emergency department intervention for high-risk elders: identification strategy and randomised controlled trial to reduce hospitalisation and institutionalisation. Hong Kong Med J 2011;17:4-7.
- Basic D, Conforti DA. A prospective, randomised controlled trial of an aged care nurse intervention within the emergency department. Aust Health Rev 2005;29:51-9. https://doi.org/10.1071/AH050051.
- Salvi F, Morichi V, Grilli A, Lancioni L, Spazzafumo L, Polonara S, et al. Screening for frailty in elderly emergency department patients by using the Identification of Seniors At Risk (ISAR). J Nutr Health Aging 2012;16:313-18. https://doi.org/10.1007/s12603-011-0155-9.
- Asomaning N, Loftus C. Identification of Seniors At Risk (ISAR) screening tool in the emergency department: implementation using the plan–do–study–act model and validation results. J Emerg Nurs 2014;40:357-64. https://doi.org/10.1016/j.jen.2013.08.014.
- Boyd M, Koziol-McLain J, Yates K, Kerse N, McLean C, Pilcher C, et al. Emergency department case-finding for high-risk older adults: the Brief Risk Identification for Geriatric Health Tool (BRIGHT). Acad Emerg Med 2008;15:598-606. https://doi.org/10.1111/j.1553-2712.2008.00157.x.
- Boyd M, Koziol-McLain J, Yates K, Kerse N, McLean C, Pilcher C. Brief screen for high risk older adults in an emergency department. 2007 Society for Academic Emergency Medicine Annual Meeting. Acad Emerg Med 2007;14:S151-2. https://doi.org/10.1197/j.aem.2007.03.1131.
- Eklund K, Wilhelmson K, Landhal S, Ivanoff-Dahlin S. Screening for frailty among older emergency department visitors: validation of the new FRESH-screening instrument. BMC Emerg Med 2016;16. https://doi.org/10.1186/s12873-016-0087-0.
- Lonterman S, Bal Y, Peeters S, Mesman R, Ostelo R. Emergency department screening for older adults at risk of adverse health outcomes: the diagnostic accuracy of the emergency department/geriatric screening tool compared to the safety management system screening bundle. Eur Geriatr Med 2011;2. https://doi.org/10.1016/j.eurger.2011.06.002.
- Schoenenberger AW, Bieri C, Ozguler O, Moser A, Haberkern M, Zimmermann H, et al. A novel multidimensional geriatric screening tool in the ED: evaluation of feasibility and clinical relevance. Am J Emerg Med 2014;32:623-8. https://doi.org/10.1016/j.ajem.2014.03.024.
- Hadbavna A, Drumm B, Hearne N, Moran M, Coughlan T, O’Neill D, et al. Use of a brief cognitive screening instrument in older patients attending emergency department – a pilot study. Eur Geriatr Med 2013;4. https://doi.org/10.1016/j.eurger.2013.07.713.
- Carpenter CR, Bassett ER, Fischer GM, Shirshekan J, Galvin JE, Morris JC. Four sensitive screening tools to detect cognitive dysfunction in geriatric emergency department patients: brief Alzheimer’s Screen, Short Blessed Test, Ottawa 3DY, and the caregiver-completed AD8. Acad Emerg Med 2011;18:374-84. https://doi.org/10.1111/j.1553-2712.2011.01040.x.
- Carpenter CR, DesPain B, Keeling TN, Shah M, Rothenberger M. The Six-Item Screener and AD8 for the detection of cognitive impairment in geriatric emergency department patients. Ann Emerg Med 2011;57:653-61. https://doi.org/10.1016/j.annemergmed.2010.06.560.
- Eagles D, Otal D, Sinha SK, Wells G, Stiell IG. Performance of the Ottawa 3DY Scale as a screening tool for impaired mental status in elderly emergency department patients. CJEM 2014;16. https://doi.org/10.1017/S1481803500003171.
- Wilber ST, Carpenter CR, Hustey FM. The Six-Item Screener to detect cognitive impairment in older emergency department patients. Acad Emerg Med 2008;15:613-16. https://doi.org/10.1111/j.1553-2712.2008.00158.x.
- Wilber ST, Lofgren SD, Mager TG, Blanda M, Gerson LW. An evaluation of two screening tools for cognitive impairment in older emergency department patients. Acad Emerg Med 2005;12:612-16. https://doi.org/10.1197/j.aem.2005.01.017.
- Kennedy M, Enander RA, Tadiri SP, Wolfe RE, Shapiro NI, Marcantonio ER. Delirium risk prediction, healthcare use and mortality of elderly adults in the emergency department. J Am Geriatr Soc 2014;62:462-9. https://doi.org/10.1111/jgs.12692.
- Beauchet O, Launay CP, Fantino B, Lerolle N, Maunoury F, Annweiler C. Screening for elderly patients admitted to the emergency department requiring specialized geriatric care. J Emerg Med 2013;45:739-45. https://doi.org/10.1016/j.jemermed.2012.11.110.
- Grossmann FF, Zumbrunn T, Frauchiger A, Delport K, Bingisser R, Nickel CH. At risk of undertriage? Testing the performance and accuracy of the emergency severity index in older emergency department patients. Ann Emerg Med 2012;60:317-25. https://doi.org/10.1016/j.annemergmed.2011.12.013.
- Dundar ZD, Karamercan MA, Ergin M, Colak T, Tuncar A, Ayranci K, et al. Rapid emergency medicine score and HOTEL score in geriatric patients admitted to the emergency department. Int J Gerontol 2015;9:87-92. https://doi.org/10.1016/j.ijge.2015.02.003.
- Hegney D, Buikstra E, Chamberlain C, March J, McKay M, Cope G, et al. Nurse discharge planning in the emergency department: a Toowoomba, Australia, study. J Clin Nurs 2006;15:1033-44. https://doi.org/10.1111/j.1365-2702.2006.01405.x.
- Carpenter CR, Abboud S, Feng D, Li S, Nadeem O, Hu J, et al. Do prognostic screening instruments predict adverse short-term outcomes among geriatric emergency department patients with dementia or low health literacy?. Acad Emerg Med 2012;19. https://doi.org/10.1111/j.1553-2712.2012.01332.x.
- Dziura JD, Page C, Conner T, Moore C, Cooney LM, Brandt CA, et al. A rapid assessment to predict ED revisits, hospital admissions, or death at 30 days following ED discharge in older individuals. Acad Emerg Med 2013;1. https://doi.org/10.1111/acem.12115.
- Eagles D, Sirois MJ, Perry JJ, Lang E, Daoust R, Lee J, et al. Timed up and go in elderly emergency department patients following minor trauma. Acad Emerg Med 2015;1:S117-18. https://doi.org/10.1111/acem.12644.
- Post LA, Conner T, Moore C, Brandt CA, Cooney LM, Page C, et al. Developing and validating the ED GRAY (Geriatric Readmission Assessment at Yale). Acad Emerg Med 2013;1:S293-4. https://doi.org/10.1111/acem.12115.
- Salvi F, Morichi V, Grilli A, Spazzafumo L, Giorgi R, Polonara S, et al. Predictive validity of the Identification of Seniors At Risk (ISAR) screening tool in elderly patients presenting to two Italian emergency departments. Aging Clin Exp Res 2009;21:69-75. https://doi.org/10.1007/BF03324901.
- Singler K, Heppner HJ, Skutetzky A, Sieber C, Christ M, Thiem U. Predictive validity of the identification of seniors at risk screening tool in a German emergency department setting. Gerontology 2014;60:413-19. https://doi.org/10.1159/000358825.
- Fan J, Worster A, Fernandes CM. Predictive validity of the triage risk screening tool for elderly patients in a Canadian emergency department. Am J Emerg Med 2006;24:540-4. https://doi.org/10.1016/j.ajem.2006.01.015.
- Lee JS, Schwindt G, Langevin M, Moghabghab R, Alibhai SM, Kiss A, et al. Validation of the triage risk stratification tool to identify older persons at risk for hospital admission and returning to the emergency department. J Am Geriatr Soc 2008;56:2112-17. https://doi.org/10.1111/j.1532-5415.2008.01959.x.
- Graf CE, Giannelli SV, Herrmann FR, Sarasin FP, Michel JP, Zekry D, et al. Identification of older patients at risk of unplanned readmission after discharge from the emergency department: comparison of two screening tools. Swiss Med Wkly 2012;141. https://doi.org/10.4414/smw.2011.13327.
- Graf CE, Giannelli SV, Herrmann FR, Sarasin FP, Michel JP, Zekry D, et al. Can we improve the detection of old patients at higher risk for readmission after an emergency department visit?. J Am Geriatr Soc 2012;60:1372-3. https://doi.org/10.1111/j.1532-5415.2012.04026.x.
- Buurman BM, van den Berg W, Korevaar JC, Milisen K, de Haan RJ, de Rooij SE. Risk for poor outcomes in older patients discharged from an emergency department: feasibility of four screening instruments. Eur J Emerg Med 2011;18:215-20. https://doi.org/10.1097/MEJ.0b013e328344597e.
- Moons P, De Ridder K, Geyskens K, Sabbe M, Braes T, Flamaing J, et al. Screening for risk of readmission of patients aged 65 years and above after discharge from the emergency department: predictive value of four instruments. Eur J Emerg Med 2007;14:315-23. https://doi.org/10.1097/MEJ.0b013e3282aa3e45.
- Baumann MR, Strout TD. Triage of geriatric patients in the emergency department: validity and survival with the Emergency Severity Index. Ann Emerg Med 2007;49:234-40. https://doi.org/10.1016/j.annemergmed.2006.04.011.
- Di Bari M, Salvi F, Roberts AT, Balzi D, Lorenzetti B, Morichi V, et al. Prognostic stratification of elderly patients in the emergency department: a comparison between the ‘Identification of Seniors at Risk’ and the ‘Silver Code’. J Gerontol A Biol Sci Med Sci 2012;67:544-50. https://doi.org/10.1093/gerona/glr209.
- Stiffler KA, Wilber ST, Frey J, McQuown CM, Poland S. Frailty defined by the SHARE Frailty Instrument and adverse outcomes after an ED visit. Am J Emerg Med 2016;34:2443-5. https://doi.org/10.1016/j.ajem.2016.09.001.
- Tiedemann A, Sherrington C, Orr T, Hallen J, Lewis D, Kelly A, et al. Identifying older people at high risk of future falls: development and validation of a screening tool for use in emergency departments. Emerg Med J 2013;30:918-22. https://doi.org/10.1136/emermed-2012-201783.
- Jones S, Wallis P. Effectiveness of a geriatrician in the emergency department in facilitating safe admission prevention of older patients. Clin Med 2013;13:561-4. https://doi.org/10.7861/clinmedicine.13-6-561.
- Jones S, Ahsan M, Wallis PJ, Fergusson N, Macnamara A. Admission prevention of the frail elderly by a geriatrician in the emergency department. Age Ageing 2012;41. https://doi.org/10.1093/ageing/afs112.
- Mortimer C, Emmerton L, Lum E. The impact of an aged care pharmacist in a department of emergency medicine. J Eval Clin Pract 2011;17:478-85. https://doi.org/10.1111/j.1365-2753.2010.01454.x.
- Shaw PB, Delate T, Lyman A, Adams J, Kreutz H, Sanchez JK, et al. Impact of a clinical pharmacy specialist in an emergency department for seniors. Ann Emerg Med 2016;67:177-88. https://doi.org/10.1016/j.annemergmed.2015.06.022.
- Bond CM, Freiheit EA, Podruzny L, Kingsly AA, Wang D, Davenport J, et al. The emergency to home project: impact of an emergency department care coordinator on hospital admission and emergency department utilization among seniors. Int J Emerg Med 2014;7. https://doi.org/10.1186/1865-1380-7-18.
- Argento V, Grey W, Donal Conway JF, Skudlarska B. Experiences from a geriatric emergency room: the first 100 cases. Eur Geriatr Med 2010;1. https://doi.org/10.1016/j.eurger.2010.07.009.
- Aldeen AZ, Courtney DM, McCarthy DM, Dresden SM, Gravenor S. GEDI WISE: geriatric-specific assessment intervention in the emergency department is associated with differences between initial and final disposition. Acad Emerg Med 2014;1:S233-4. https://doi.org/10.1111/acem.12365.
- Aldeen AZ, Courtney DM, Lindquist LA, Dresden SM, Gravenor SJ. Geriatric emergency department innovations: preliminary data for the geriatric nurse liaison model. J Am Geriatr Soc 2014;62:1781-5. https://doi.org/10.1111/jgs.12979.
- Fallon A, Armstrong J, Coughlan T, Collins DR, O’Neill D, Kennelly SP. Characteristics and outcomes of older patients attending an acute medical assessment unit. Ir Med J 2015;108:210-11.
- Dresden SM, McCarthy DM, Aldeen AZ, Lindquist LA, Kang R, Gravenor SJ, et al. GEDI WISE: comparative effectiveness of ED based geriatric nurse liaison intervention in preventing hospitalization for geriatric ED patients. Acad Emerg Med 2015;1. https://doi.org/10.1111/acem.12644.
- Tan KM, Lannon R, O’Keeffe L, Barton D, Ryan J, O’Shea D, et al. Geriatric medicine in the emergency department. Ir Med J 2012;105:271-4.
- Leah V, Adams J. Assessment of older adults in the emergency department. Nurs Stand 2010;24:42-5. https://doi.org/10.7748/ns2010.07.24.46.42.c7911.
- Ngian VJ, Ong BS, O’Rourke F, Nguyen HV, Chan DK. Review of a rapid geriatric medical assessment model based in emergency department. Age Ageing 2008;37:696-9. https://doi.org/10.1093/ageing/afn160.
- Thompson S, Phelps A, Sebastian Fairweather D, McCann L. The role of the geriatric assessment in the emergency department in Oxford. Eur Geriatr Med 2010;1. https://doi.org/10.1016/j.eurger.2010.07.009.
- O’Reilly C, Maloney P, Alexander E, Bernard P, O’Riordan Y, Gill D, et al. Frail Intervention Therapy Team: a step in the right direction. Early assessment in the emergency department. Age Ageing 2016;45:ii13-56. https://doi.org/10.1093/ageing/afw159.205.
- Harper KJ, Gibson NP, Barton AD, Petta AC, Pearson SK, Celenza A. Effects of emergency department care coordination team referrals in older people presenting with a fall. Emerg Med Australas 2013;25:324-33. https://doi.org/10.1111/1742-6723.12098.
- Arendts G, Fitzhardinge S, Pronk K, Hutton M. Front-loading allied health intervention in the emergency department does not reduce length of stay for admitted older patients. Int J Clin Pract 2013;67:807-10. https://doi.org/10.1111/ijcp.12153.
- Arendts G, Fitzhardinge S, Pronk K, Hutton M. Outcomes in older patients requiring comprehensive allied health care prior to discharge from the emergency department. Emerg Med Australas 2013;25:127-31. https://doi.org/10.1111/1742-6723.12049.
- Waldron N, Dey I, Nagree Y, Xiao J, Flicker L. A multi-faceted intervention to implement guideline care and improve quality of care for older people who present to the emergency department with falls. BMC Geriatr 2011;11. https://doi.org/10.1186/1471-2318-11-6.
- Corbett HM, Lim WK, Davis SJ, Elkins AM. Care coordination in the emergency department: improving outcomes for older patients. Aust Health Rev 2005;29:43-50. https://doi.org/10.1071/AH050043.
- Launay C, Annweiler C, de Decker L, Kabeshova A, Beauchet O. Early hospital discharge of older adults admitted to the emergency department: effect of different types of recommendations made by a mobile geriatric team. J Am Geriatr Soc 2013;61:1031-3. https://doi.org/10.1111/jgs.12294.
- Arendts G, Fitzhardinge S, Pronk K, Donaldson M, Hutton M, Nagree Y. The impact of early emergency department allied health intervention on admission rates in older people: a non-randomized clinical study. BMC Geriatr 2012;12. https://doi.org/10.1186/1471-2318-12-8.
- Bell C, Hashemi N, Wieland F, Lowrey C, Kaur V. ACE impact: evaluation of an integrated geriatric service. Age Ageing 2014;43. https://doi.org/10.1093/ageing/afu124.29.
- Berahman T, Karounos M, Hochman S, Schultz R, Christensen M, Sadi M, et al. Effects of patient liaison in a geriatric emergency department. J Am Geriatr Soc 2014;62. https://doi.org/10.1111/jgs.12870.
- Launay C, De Decker L, Annweiler C, Beauchet O. Early hospital discharge of older adults admitted to emergency department: effect of the different types of recommendations made by a mobile geriatric team. Eur Geriatr Med 2013;4. https://doi.org/10.1016/j.eurger.2013.07.235.
- Silvester KM, Mohammed MA, Harriman P, Girolami A, Downes TW. Timely care for frail older people referred to hospital improves efficiency and reduces mortality without the need for extra resources. Age Ageing 2014;43:472-7. https://doi.org/10.1093/ageing/aft170.
- Pareja-Sierra T, Hornillos-Calvo M, Rodriguez-Solis J, Sepulveda-Moya DL, Bassy-Iza N, Martinez-Peromingo FJ, et al. Implementation of an emergency department observation unit for elderly adults in a university-affiliated hospital in Spain: a 6-year analysis of data. J Am Geriatr Soc 2013;61:1621-2. https://doi.org/10.1111/jgs.12433.
- Ellis G, Jamieson CA, Alcorn M, Devlin V. An acute care for elders (ACE) unit in the emergency department. Eur Geriatr Med 2012;3:261-3. https://doi.org/10.1016/j.eurger.2012.03.004.
- Conroy SP, Ansari K, Williams M, Laithwaite E, Teasdale B, Dawson J, et al. A controlled evaluation of comprehensive geriatric assessment in the emergency department: the ‘emergency frailty unit’. Age Ageing 2014;43:109-14. https://doi.org/10.1093/ageing/aft087.
- Salvi F, Morichi V, Grilli A, Giorgi R, Spazzafumo L, Polonara S, et al. A geriatric emergency service for acutely ill elderly patients: pattern of use and comparison with a conventional emergency department in Italy. J Am Geriatr Soc 2008;56:2131-8. https://doi.org/10.1111/j.1532-5415.2008.01991.x.
- Genes N, Olmedo R, Abraham G, Grudzen C, Hwang U, Nassisi D, et al. GEDI WISE: improvement in patient satisfaction after implementation of a geriatric emergency department. Acad Emerg Med 2013;1. https://doi.org/10.1111/acem.12115.
- Karounos M, Schultz R, Christensen M, Hwang U, Rosenberg M. Implementation of a geriatric emergency department and its effects on geriatric admissions. J Am Geriatr Soc 2014;62. https://doi.org/10.1111/jgs.1287=0.
- Keyes DC, Singal B, Kropf CW, Fisk A. Impact of a new senior emergency department on emergency department recidivism, rate of hospital admission, and hospital length of stay. Ann Emerg Med 2014;63:517-24. https://doi.org/10.1016/j.annemergmed.2013.10.033.
- Wilber ST, Blake K, Bosley D, Cleveland ML, Cox SR, Holder C, et al. Outcomes of a pilot senior emergency department program. Ann Emerg Med 2013;62. https://doi.org/10.1016/j.annemergmed.2013.07.427.
- Tang K, Lavery P, Maybin C, Amir K. Developing a rapid access unit (RAC) to improve quality of care for elderly patients attending the local emergency department. Age Ageing 2016;45. https://doi.org/10.1093/ageing/afw159.180.
- Ng K, Grudzen CR, Davila C, Winkel G, Richardson LD, Hwang U. GEDI WISE: initial effects on admissions at a hospital with a geriatric emergency department (ED). J Am Geriatr Soc 2014;62. https://doi.org/10.1111/jgs.12870.
- Ng K, Grudzen CR, Davila C, Winkel G, Richardson LD, Hwang U. GEDI WISE: initial effects on admissions at a hospital with a geriatric emergency department. Acad Emerg Med 2014;1:S212-13. https://doi.org/10.1111/acem.12365.
- Ismail S, Fox G, Cracknell A, Burns E. Interface geriatrics and new ways of working: avoiding admissions by implementing early specialist assessment by interface geriatricians in the emergency department (ED). Age Ageing 2014;43. https://doi.org/10.1093/ageing/afu036.61.
- Pareja T. Do geriatric interventions in the emergency department reduce the need of hospital admission of frail older adults?. J Am Geriatr Soc 2008;56:S126-7.
- Chou MY, Chou SL, Liang CK, Liao MC, Hsueh KC, Lin YT, et al. The effectiveness of comprehensive geriatric assessment-based intervention reducing frequent emergency department visits in a tertiary medical center in Southern Taiwan. Eur Geriatr Med 2015;6. https://doi.org/10.1016/S1878-7649(15)30109-1.
- Liao MC, Chen LK, Chou MY, Laing CK, Lin YT, Lo YK, et al. Effectiveness of comprehensive geriatric assessment-based intervention to reduce frequent emergency department visits: a report of four cases. Int J Gerontol 2012;6:131-3. https://doi.org/10.1016/j.ijge.2011.08.003.
- Scott S, Bertram Ralph E, Andrew A, Ray R. Comprehensive geriatric assessment (CGA) in the emergency department by OPAL (older people assessment and liaison): does it prevent admissions?. Eur Geriatr Med 2014;5. https://doi.org/10.1016/S1878-7649(14)70689-8.
- Wentworth L, Briggs S, Keelan R, Ashraf S, Wileman L, Williams J. A comprehensive geriatric assessment in the emergency department reduces admissions and length of stay. Eur Geriatr Med 2015;6:S22-3. https://doi.org/10.1016/S1878-7649(15)30074-7.
- Keelan R, Briggs S, Wentworth L. Comprehensive geriatric assessment in emergency department by OPAL (older people assessment and liaison) can prevent admissions. Future Hosp J 2016;3. https://doi.org/10.7861/futurehosp.3-2-s26.
- Hughes CT, Laghi L, Wyrko Z. Experience of the ‘Older Persons Assessment and Liaison (OPAL)’ service in a teaching hospital in Birmingham, UK. Eur Geriatr Med 2014;5. https://doi.org/10.1016/S1878-7649(14)70686-2.
- Fox J, Pattison T, Wallace J, Pradhan S, Gaillemin O, Feilding E, et al. Geriatricians at the front door: the value of early comprehensive geriatric assessment in the emergency department. Eur Geriatr Med 2016;7:383-5. https://doi.org/10.1016/j.eurger.2016.04.013.
- Beirne A, Carey T, O’Keeffe J, Crowe M, O’Shea D, Tan KM, et al. The role of geriatric medicine in the emergency department. Ir J Med Sci 2012;181. https://doi.org/10.1007/s11845-012-0842-5.
- Yuen TM, Lee LL, Or IL, Yeung KL, Chan JT, Chui CP, et al. Geriatric consultation service in emergency department: how does it work?. Emerg Med J 2013;30:180-5. https://doi.org/10.1136/emermed-2012-201139.
- Chui CPY, Kun E. Geriatric consultation service in emergency department. Eur Geriatr Med 2013;4. https://doi.org/10.1016/j.eurger.2013.07.448.
- Nguyen A, Straney L, Cameron P, Lowthian J. Synthesised geriatric assessment in the emergency department setting: is it NEAT?. Aust Health Rev 2014;38:370-6. https://doi.org/10.1071/AH13217.
- Lo Storto M, Minozzi G, Goat B, Bosisio E, Bazzano S, Seresin C, et al. A social-health triage (SHT) in emergency services (ES) of older patients: a two-year study. Eur Geriatr Med 2011;2:S136-7. https://doi.org/10.1016/j.eurger.2011.06.002.
- Foo CL, Siu VW, Ang H, Phuah MW, Ooi CK. Risk stratification and rapid geriatric screening in an emergency department – a quasi-randomised controlled trial. BMC Geriatr 2014;14. https://doi.org/10.1186/1471-2318-14-98.
- Grudzen C, Richardson LD, Baumlin KM, Winkel G, Davila C, Ng K, et al. Redesigned geriatric emergency care may have helped reduce admissions of older adults to intensive care units. Health Aff 2015;34:788-95. https://doi.org/10.1377/hlthaff.2014.0790.
- Warburton RN. Preliminary outcomes and cost–benefit analysis of a community hospital emergency department screening and referral program for patients aged 75 or more. Int J Health Care Qual Assur Inc Leadersh Health Serv 2005;18:474-84. https://doi.org/10.1108/09526860510619453.
- Foo CL, Siu VW, Tan TL, Ding YY, Seow E. Geriatric assessment and intervention in an emergency department observation unit reduced re-attendance and hospitalisation rates. Australas J Ageing 2012;31:40-6. https://doi.org/10.1111/j.1741-6612.2010.00499.x.
- Mahony SO, Blank A, Simpson J, Persaud J, Huvane B, McAllen S, et al. Preliminary report of a palliative care and case management project in an emergency department for chronically ill elderly patients. J Urban Health 2008;85:443-51. https://doi.org/10.1007/s11524-008-9257-z.
- Wright PN, Tan G, Iliffe S, Lee D. The impact of a new emergency admission avoidance system for older people on length of stay and same-day discharges. Age Ageing 2014;43:116-21. https://doi.org/10.1093/ageing/aft086.
- Lovato E, Minniti D, Piolatto A, Barberis B, Papalia R, Sacco R, et al. Silver Code: a new tool for the management of the frail elderly in emergency department. Results of a year of experimental use. Eur J Public Health 2012;22.
- Huded JM, Dresden SM, Gravenor SJ, Rowe T, Lindquist LA. Screening for fall risks in the emergency department: a novel nursing-driven program. West J Emerg Med 2015;16:1043-6. https://doi.org/10.5811/westjem.2015.10.26097.
- Terrell KM, Perkins AJ, Dexter PR, Hui SL, Callahan CM, Miller DK. Computerized decision support to reduce potentially inappropriate prescribing to older emergency department patients: a randomized, controlled trial. J Am Geriatr Soc 2009;57:1388-94. https://doi.org/10.1111/j.1532-5415.2009.02352.x.
- Sutton M, Grimmer-Somers K, Jeffries L. Screening tools to identify hospitalised elderly patients at risk of functional decline: a systematic review. Int J Clin Pract 2008;62:1900-9. https://doi.org/10.1111/j.1742-1241.2008.01930.x.
- Yao JL, Fang J, Lou QQ, Anderson RM. A systematic review of the identification of seniors at risk (ISAR) tool for the prediction of adverse outcome in elderly patients seen in the emergency department. Int J Clin Exp Med 2015;8:4778-86.
- Runciman P, Currie CT, Nicol M, Green L, McKay V. Discharge of elderly people from an accident and emergency department: evaluation of health visitor follow-up. J Adv Nurs 1996;24:711-18. https://doi.org/10.1046/j.1365-2648.1996.02479.x.
- Rowland K, Maitra AK, Richardson DA, Hudson K, Woodhouse KW. The discharge of elderly patients from an accident and emergency department: functional changes and risk of readmission. Age Ageing 1990;19:415-18. https://doi.org/10.1093/ageing/19.6.415.
- Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet 2013;381:752-62. https://doi.org/10.1016/S0140-6736(12)62167-9.
- Thiem U, Heppner HJ, Singler K. Instruments to identify elderly patients in the emergency department in need of geriatric care. Z Gerontol Geriatr 2015;48:4-9. https://doi.org/10.1007/s00391-014-0852-1.
- McNamara R, Moses M, Cummins F. Appropriate triage of older adults in the ED. Ir J Med Sci 2012;181:S295-6. https://doi.org/10.1007/s11845-012-0842-5.
- Bissett M, Cusick A, Lannin NA. Functional assessments utilised in emergency departments: a systematic review. Age Ageing 2013;42:163-72. https://doi.org/10.1093/ageing/afs187.
- Carpenter CR, Shelton E, Fowler S, Suffoletto B, Platts-Mills TF, Rothman RE, et al. Risk factors and screening instruments to predict adverse outcomes for undifferentiated older emergency department patients: a systematic review and meta-analysis. Acad Emerg Med 2015;22:1-21. https://doi.org/10.1111/acem.12569.
- Parke B, Beaith A, Slater L, Clarke AM. Contextual factors influencing success or failure of emergency department interventions for cognitively impaired older people: a scoping and integrative review. J Adv Nurs 2011;67:1426-48. https://doi.org/10.1111/j.1365-2648.2011.05611.x.
- Schnitker L, Martin-Khan M, Beattie E, Gray L. What is the evidence to guide best practice for the management of older people with cognitive impairment presenting to emergency departments? A systematic review. Adv Emerg Nurs J 2013;35:154-69. https://doi.org/10.1097/TME.0b013e31828c7f4a.
- Graf CE, Zekry D, Giannelli S, Michel JP, Chevalley T. Efficiency and applicability of comprehensive geriatric assessment in the emergency department: a systematic review. Aging Clin Exp Res 2011;23:244-54. https://doi.org/10.1007/BF03337751.
- Conroy SP, Stevens T, Parker SG, Gladman JR. A systematic review of comprehensive geriatric assessment to improve outcomes for frail older people being rapidly discharged from acute hospital: ‘interface geriatrics’. Age Ageing 2011;40:436-43. https://doi.org/10.1093/ageing/afr060.
- Fan L, Lukin W, Zhao J, Sun J, Hou XY. Interventions targeting the elderly population to reduce emergency department utilisation: a literature review. Emerg Med J 2015;32:738-43. https://doi.org/10.1136/emermed-2014-203770.
- Karam G, Radden Z, Berall LE, Cheng C, Gruneir A. Efficacy of emergency department-based interventions designed to reduce repeat visits and other adverse outcomes for older patients after discharge: a systematic review. Geriatr Gerontol Int 2015;15:1107-17. https://doi.org/10.1111/ggi.12538.
- Tran QK, Bayram JD, Boonyasai R, Case M, Connor C, Doggett D, et al. Risk factors and interventions to prevent post emergency department discharge complications among geriatric population: a literature review. Ann Emerg Med 2014;1. https://doi.org/10.1016/j.annemergmed.2014.07.201.
- Sinha SK, Bessman ES, Flomenbaum N, Leff B. A systematic review and qualitative analysis to inform the development of a new emergency department-based geriatric case management model. Ann Emerg Med 2011;57:672-82. https://doi.org/10.1016/j.annemergmed.2011.01.021.
- Fealy G, McCarron M, O’Neill D, McCallion P, Clarke M, Small V, et al. Effectiveness of gerontologically informed nursing assessment and referral interventions for older persons attending the emergency department: systematic review. J Adv Nurs 2009;65:934-45. https://doi.org/10.1111/j.1365-2648.2009.04961.x.
- Kessler C, Williams MC, Moustoukas JN, Pappas C. Transitions of care for the geriatric patient in the emergency department. Clin Geriatr Med 2013;29:49-6. https://doi.org/10.1016/j.cger.2012.10.005.
- McNamara R. Why Should We Have a ‘Geriatric’ Emergency Department? 2016. https://britishgeriatricssociety.wordpress.com/2016/02/12/why-should-we-have-a-geriatric-emergency-department/ (accessed 24 January 2017).
- Carpenter CR, Heard K, Wilber S, Ginde AA, Stiffler K, Gerson LW, et al. Research priorities for high-quality geriatric emergency care: medication management, screening, and prevention and functional assessment. Acad Emerg Med 2011;18:644-54. https://doi.org/10.1111/j.1553-2712.2011.01092.x.
- NHS Digital . Provisional Accident and Emergency Quality Indicators – England, by Provider for October 2016 2016. www.content.digital.nhs.uk/catalogue/PUB23176 (accessed 24 January 2017).
- McCusker J, Verdon J, Vadeboncoeur A, Levesque JF, Sinha SK, Kim KY, et al. The elder-friendly emergency department assessment tool: development of a quality assessment tool for emergency department-based geriatric care. J Am Geriatr Soc 2012;60:1534-9. https://doi.org/10.1111/j.1532-5415.2012.04058.x.
- James Lind Alliance Priority Setting Partnership . Top 10 Emergency Medicine Research Priorities 2017. www.rcem.ac.uk/JLAEMPSP (accessed 24 January 2017).
- Hastings SN, Heflin MT. A systematic review of interventions to improve outcomes for elders discharged from the emergency department. Acad Emerg Med 2005;12:978-86. https://doi.org/10.1111/j.1553-2712.2005.tb00810.x.
- Gupta A. The effectiveness of geriatrician-led comprehensive hip fracture collaborative care in a new acute hip unit based in a general hospital setting in the UK. J R Coll Physicians Edinb 2014;44:20-6. https://doi.org/10.4997/JRCPE.2014.105.
- Edmans J, Bradshaw L, Gladman JR, Franklin M, Berdunov V, Elliott R, et al. The Identification of Seniors at Risk (ISAR) score to predict clinical outcomes and health service costs in older people discharged from UK acute medical units. Age Ageing 2013;42:747-53. https://doi.org/10.1093/ageing/aft054.
- Carpenter CR, Platts-Mills TF. Evolving prehospital, emergency department, and ‘inpatient’ management models for geriatric emergencies. Clin Geriatr Med 2013;29:31-47. https://doi.org/10.1016/j.cger.2012.09.003.
- Emergency Care for the Elderly Patients Who are in the Poorest Health. Stockholm: Swedish Council on Health Technology Assessment; 2013.
- Patterson BW, Khare RK, Courtney DM, Lee TA, Kyriacou DN. Cost-effectiveness of influenza vaccination of older adults in the ED setting. Am J Emerg Med 2012;30:1072-9. https://doi.org/10.1016/j.ajem.2011.07.007.
- Ong BS, Van Nguyen H, Ilyas M, Boyatzis I, Ngian VJ. Medical assessment units and the older patient: a retrospective case–control study. Aust Health Rev 2012;36:331-5. https://doi.org/10.1071/AH11076.
- Lowthian JA, Brand C, Barker AL, Andrianopoulos N, Smith C, Batey C, et al. Managing older patients safely in the time critical environment of an emergency department. Hong Kong J Emerg Med 2012;19:264-71. https://doi.org/10.1177/102490791201900405.
- Lowthian J, Cameron P, Smit D, Newnham H, Hunter P, Brand C, et al. Safe elderly emergency discharge (SEED) project: determining best practice for safe discharge of the older emergency patient. Emerg Med J 2012;29:A12-13. https://doi.org/10.1136/emermed-2012-201246.10.
- Lowthian J, Straney LD, Brand CA, Barker AL, De Villiers Smit P, Newnham H, et al. Unplanned early return to the emergency department by older patients: the Safe Elderly Emergency Department Discharge (SEED) project. Age Ageing 2016;45:255-61. https://doi.org/10.1093/ageing/afv198.
- Wilhelmson K, Duner A, Eklund K, Gosman-Hedström G, Blomberg S, Hasson H, et al. Design of a randomized controlled study of a multi-professional and multidimensional intervention targeting frail elderly people. BMC Geriatr 2011;11. https://doi.org/10.1186/1471-2318-11-24.
- Thomas K. Emergency department: emergency departments for seniors tackle future challenges of geriatric care. Hosp Health Netw 2011;85.
- Legrain S, Tubach F, Bonnet-Zamponi D, Lemaire A, Aquino JP, Paillaud E, et al. A new multimodal geriatric discharge-planning intervention to prevent emergency visits and rehospitalizations of older adults: the optimization of medication in AGEd multicenter randomized controlled trial. J Am Geriatr Soc 2011;59:2017-28. https://doi.org/10.1111/j.1532-5415.2011.03628.x.
- Carey T, O’Keeffe J, Lawlor G, Carlin T, Tan KM, O’Shea D, et al. Development of geriatric specialist expertise in the emergency department. Ir J Med Sci 2011;180. https://doi.org/10.1007/s11845-011-0742-0.
- Mun Tan K, Lannon R, O’Keeffe L, Ryan J, O’Shea D, Hughes G. The role of specialty specific management in improving outcomes of the older adult presenting to the emergency department. Eur Geriatr Med 2010;1:S121-2. https://doi.org/10.1016/j.eurger.2010.07.009.
- McNicholas A, Fernandez F, Malka A, Cardenas L, Zavilla J, Schwab C. A tier II trauma triage system within the emergency department is effective in identifying injured geriatric patients at risk for ICU admission. Crit Care Med 2010;38. https://doi.org/10.1097/01.ccm.0000390903.16849.8c.
- Flynn DS, Jennings J, Moghabghab R, Nancekivell T, Tsang C, Cleland M, et al. Raising the bar of care for older people in Ontario emergency departments. Int J Older People Nurs 2010;5:219-26. https://doi.org/10.1111/j.1748-3743.2010.00209.x.
- Lee JS, Choi HS, Ko YG, Yun DH. Performance of the Geriatric Nutritional Risk Index in predicting 28-day hospital mortality in older adult patients with sepsis. Clin Nutr 2013;32:843-8. https://doi.org/10.1016/j.clnu.2013.01.007.
- Shanley C, Sutherland S, Tumeth R, Stott K, Whitmore E. Caring for the older person in the emergency department: the ASET program and the role of the ASET clinical nurse consultant in South Western Sydney, Australia. J Emerg Nurs 2009;35:129-33. https://doi.org/10.1016/j.jen.2008.05.005.
- Meurer WJ, Smith BL, Losman ED, Sherman D, Yaksich JD, Jared JD, et al. Real-time identification of serious infection in geriatric patients using clinical information system surveillance. J Am Geriatr Soc 2009;57:40-5. https://doi.org/10.1111/j.1532-5415.2008.02094.x.
- Schumacher JG. Emergency medicine and older adults: continuing challenges and opportunities. Am J Emerg Med 2005;23:556-60. https://doi.org/10.1016/j.ajem.2004.12.011.
- Launay CP, de Decker L, Kabeshova A, Annweiler C, Beauchet O. Screening for older emergency department inpatients at risk of prolonged hospital stay: the brief geriatric assessment tool. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0110135.
- Milne WK, Choo EK, Carpenter CR. Hot off the press: assessing older adult fall risk in the emergency department. Acad Emerg Med 2015;22:121-3. https://doi.org/10.1111/acem.12550.
- Griffiths D, Morphet J, Jones T, Williams A, Innes K, Crawford K, et al. Management of aged care residents in the emergency department. Aust Nurs Midwifery J 2014;21.
- Somes J. Emergency medical care and the older adult. Int Emerg Nurs 2014;22:37-9. https://doi.org/10.1016/j.ienj.2013.03.006.
- Booth D. Geriatric care in the emergency department. J Emerg Nurs 2013;39. https://doi.org/10.1016/j.jen.2013.07.019.
- Mangram AJ, Mitchell CD, Shifflette VK, Lorenzo M, Truitt MS, Goel A, et al. Geriatric trauma service: a one-year experience. J Trauma Acute Care Surg 2012;72:119-22. https://doi.org/10.1097/TA.0b013e318241f0ba.
- Jackson SE. The efficacy of an educational intervention on documentation of pain management for the elderly patient with a hip fracture in the emergency department. J Emerg Nurs 2010;36:10-5. https://doi.org/10.1016/j.jen.2008.08.022.
- Wolfe F. A geriatric ‘gem’ in the emergency department. Perspectives 2006;30:12-5.
- Lees L. A framework to promote the holistic assessment of older people in emergency care. Nurs Older People 2005;16:16-8. https://doi.org/10.7748/nop2005.02.16.10.16.c2294.
- Fernandes CM. Geriatric care in the emergency department. Acad Emerg Med 2005;12:158-9. https://doi.org/10.1111/j.1553-2712.2005.tb00856.x.
- Adams J, Adinaro D, Baumlin K, Aldeen A, Christensen M, Courtney DM, et al. GEDI WISE: geriatric emergency department innovations in care through workforce, informatics, and structural enhancements. Ann Emerg Med 2013;1:S54-5. https://doi.org/10.1016/j.annemergmed.2013.07.433.
- Beauchet O, Launay C, De Decker L, Annweiler C. Mobile geriatric team and length of hospital stay among older inpatients: a case–control pilot study. Eur Geriatr Med 2013;4. https://doi.org/10.1016/j.eurger.2013.07.295.
- Hullick C, Rosen T, Stern ME, Lachs MS. Understanding innovative emergency department interventions for older adults. J Am Geriatr Soc 2010;58. https://doi.org/10.1111/j.1532-5415.2010.02850.x.
- Hwang U, Rosenberg M, Aldeen A, Abraham G, Adams J, Baumlin K, et al. GEDI WISE: geriatric emergency department innovations through workforce, informatics, and structural enhancements. J Am Geriatr Soc 2013;61. https://doi.org/10.1111/jgs.12263.
- Stiffler KA, Finley AM, Midha S, Wilber ST. Assessment of frailty in older emergency department patients. Acad Emerg Med 2011;1. https://doi.org/10.1111/j.1553-2712.2011.01073.x.
- Butler MJ, Biram RWS. Streamlining the elderly patient pathway: who is best suited for admission to an acute medicine for the elderly (AME) unit?. Age Ageing 2012;41. https://doi.org/10.1093/ageing/afs112.
- Carey T, O’Keeffe J, Lawlor G, Tan KM, O’Shea D, Hughes G. Challenges to implementing a new service model for older people in the emergency department. Ir J Med Sci 2011;180:S348-9. https://doi.org/10.1007/s11845-011-0742-0.
- Ellis G, Jamieson CA, Devlin V. Evaluation of an acute care for the elderly unit in the emergency department. Age Ageing 2011;40. https://doi.org/10.1093/ageing/afr002.
- Fernandez M, Bermudez M, Roa-Granthon P, Ramos M, Solano-Jaurrieta JJ. Impact of a geriatric team in the emergency department. Eur Geriatr Med 2014;5:S210-1. https://doi.org/10.1016/S1878-7649(14)70575-3.
- Huq F, Forster B, Collett P. Improving the care of elderly patients: medical assessment units as a new model of care in an Australian state. J Am Geriatr Soc 2010;58. https://doi.org/10.1111/j.1532-5415.2010.02850.x.
- Michael AB, Ijaola F. Frail elderly short stay unit; a model of emergency care for older people. Eur Geriatr Med 2014;5. https://doi.org/10.1016/S1878-7649(14)70570-4.
- Miller DK, Lewis LM, Nork MJ, Morley JE. Controlled trial of a geriatric case-finding and liaison service in an emergency department. J Am Geriatr Soc 1996;44:513-20. https://doi.org/10.1111/j.1532-5415.1996.tb01435.x.
- McCusker J, Dendukuri N, Tousignant P, Verdon J, Poulin de Courval L, Belzile E. Rapid two-stage emergency department intervention for seniors: impact on continuity of care. Acad Emerg Med 2003;10:233-43. https://doi.org/10.1111/j.1553-2712.2003.tb01997.x.
- McCusker J, Verdon J, Tousignant P, Courval LP, Dendukuri N, Belzile E. Rapid emergency department intervention for older people reduces risk of functional decline: results of a multicenter randomized trial. J Am Geriatr Soc 2001;49:1272-81. https://doi.org/10.1046/j.1532-5415.2001.49254.x.
- Baumann MR, Strout TD. Team triage: addressing challenges to emergency department flow. J Healthc Qual 2006;28:W4-3.
- Sanon M, Abraham G, Investigators TGW. Geriatric Emergency Department Innovations through Workforce, Informatics, and Structural Enhancements (GEDI WISE): an acute care for the elderly (ACE) model for elders in the ED. J Am Geriatr Soc 2016;64.
- Taylor JK, Gaillemin OS, Pearl AJ, Murphy S, Fox J. Embedding comprehensive geriatric assessment in the emergency assessment unit: the impact of the COPE zone. Clin Med 2016;16:19-24. https://doi.org/10.7861/clinmedicine.16-1-19.
- Gorichky RR. ED Care coordination: an effective approach for at-risk, frail older adults. J Emerg Nurs 2015;41:438-40. https://doi.org/10.1016/j.jen.2015.06.005.
- Caplan G. Comprehensive geriatric assessment in the emergency department. Australas J Ageing 2015;34.
- Edmans J, Bradshaw L, Franklin M, Gladman J, Conroy S. Specialist geriatric medical assessment for patients discharged from hospital acute assessment units: randomised controlled trial. BMJ 2013;347. https://doi.org/10.1136/bmj.f5874.
- Rogers D. The increasing geriatric population and overcrowding in the emergency department: one hospital’s approach. J Emerg Nurs 2009;35:447-50. https://doi.org/10.1016/j.jen.2009.02.009.
- Koehler BE, Richter KM, Youngblood L, Cohen BA, Prengler ID, Cheng D, et al. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med 2009;4:211-18. https://doi.org/10.1002/jhm.427.
- Biedsoe J, Bossart P, Sugerman P, Bernhisel K, Cheng M, Mataoa T, et al. Appropriately screened geriatric chest pain patients may be appropriate for an emergency department observation unit. Ann Emerg Med 2008;52. https://doi.org/10.1016/j.annemergmed.2008.06.398.
- McCusker J, Ionescu-Ittu R, Ciampi A, Belzile E, Cardin S, Vadeboncoeur A, et al. Geriatric services reduce emergency department (ED) return visits. J Am Geriatr Soc 2005;53.
- Vandewoude MF, Geerts CA, d’Hooghe AH, Paridaens KM. A screening tool to identify older people at risk of adverse health outcomes at the time of hospital admission. Tijdschr Gerontol Geriatr 2006;37:203-9. https://doi.org/10.1007/BF03074806.
- Small C. Frailty in an emergency department: predictors and point prevalence of frailty and pre-frailty in an Irish cohort. Age Ageing 2016;45. https://doi.org/10.1093/ageing/afw159.28.
- Hastings SN, Purser JL, Johnson KS, Sloane RJ, Whitson HE. Frailty predicts some but not all adverse outcomes in older adults discharged from the emergency department. J Am Geriatr Soc 2008;56:1651-7. https://doi.org/10.1111/j.1532-5415.2008.01840.x.
- Department of Health and Social Care . Urgent Care Pathways for Older People With Complex Needs n.d. http://webarchive.nationalarchives.gov.uk/20130124041403/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_080136.pdf (accessed 6 December 2017).
- Birns J, Beaumont D. The Older Person in the Accident &Amp; Emergency Department n.d. www.bgs.org.uk/good-practice-guides/resources/goodpractice/gpgaae (accessed 6 December 2017).
- Comprehensive Assessment of the Frail Older Patient n.d. www.bgs.org.uk/good-practice-guides/resources/goodpractice/gpgcgassessment (accessed 6 December 2017).
- Department of Health and Social Care . Reforming Emergency Care n.d. http://webarchive.nationalarchives.gov.uk/20120106112528/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4058836.pdf (accessed 6 December 2017).
Appendix 1 MEDLINE search strategy
Sample MEDLINE search
-
*Emergency Service, Hospital/
-
*Emergency Medical Services/
-
*Emergency Medicine/
-
(emergency adj2 service*).ab,ti.
-
“emergency care”.ab,ti
-
“urgent care”.ab,ti.
-
“emergency department* ”.ab,ti.
-
“accident and emergency”.ab,ti.
-
casualty.ab,ti.
-
or/1-9
-
*“Aged, 80 and over”/
-
*Health Services for the Aged/
-
*Frail Elderly/
-
*Aged/ or *Aging/
-
(ageing or elderly or geriatric or frail or aged).ti
-
(old or older).ti.
-
or/11-16
-
10 and 17
-
limit 18 to (english language and humans and yr=“2005 –Current”)
Appendix 2 Review-level evidence data extraction table
| Study | Population | Aim | Screening or intervention | Outcome(s) | Summary | Headline message |
|---|---|---|---|---|---|---|
| Tran et al.136 | Geriatric (aged > 60 years) | Identify risk factors and interventions to prevent ED returns |
Examination of risk factors Interventions (bundle of care: nursing screening then interventions outside the ED) |
ED returns | There are risk factors that identify the likelihood of ED return. These are psychosocial (feeling depressed, no primary care practitioner, low primary care use, low socioeconomic status) and medical (digestive disease, cardiovascular disease, high-risk chief complaint) | Intensive bundle of interventions for this high-risk population appeared to be effective in preventing short- but not long-term ED returns |
| Kessler et al.139 | Geriatric | Transitions of care for ED patients | Both | Errors in transitions of care to and from the ED |
Specific challenges include complex medical morbidities, dependence in ADL, polypharmacy and higher frequency of transitions Central to adverse outcomes were communication issues. Communication on admission from nursing homes was limited |
Failed transitions are implicated in morbidity and mortality. Standardised communication and robust metrics could reduce this |
| Sinha et al.137 | Identify process, component and outcome measures in geriatric emergency practice model | Both | Health outcomes, social/health service utilisation outcomes | There were 28 outcome measures and eight model characteristic components. Programmes having more of these components tended to produce better outcomes | Successful models of ED case management have the following characteristics: evidence-based practice model; nursing clinical involvement or leadership; high-risk screening with a validated tool; focused (as opposed to time-intensive) geriatric assessments; care and disposition planning in the ED; interprofessional and capacity-building work practices; post-ED discharge follow-up with patients; and evaluation and monitoring processes | |
| Parke et al.130 | Cognitively impaired, non-institutionalised older people (aged > 65 years) | Effectiveness of interventions to manage cognitively impaired older people in the ED | Both | Detection of cognitive impairment | Contextual details and relevant features of appropriate interventions poorly reported | Cognitive state has been shown to be one predictor of visits to the ED; there are a lot of older people with cognitive impairment receiving care in the ED. Screening tools exist to identify this population; however, they are inconsistently used so difficult to measure effectiveness. No specific interventions were identified to care for this population |
| Graf et al.132 | Older patients | Use and value of CGA in the ED for evaluations of older patients; using ED screening tools to detect high-risk patients needing CGA |
CGA efficiency Screening tools |
CGA in the ED is efficient for decreasing functional decline, ED readmission and possibly nursing home readmission. This review found that the best tool was the ISAR tool (others not validated for screening plus CGA and TRST not accurate enough) | CGA is too time-consuming to use routinely in the ED, even though it has positive outcomes. Other tools to screen for high-risk older people exist. It is better to screen for high risk than carry out age-based screening. High-risk patients can then benefit from CGA and interventions. Advocate a two-stage approach (screening for high-risk patients using the ISAR tool and then CGA) | |
| Conroy et al.133 | Frail older people (aged > 65 years) | Does CGA improve outcomes for frail older people rapidly discharged from acute settings? | CGA (geriatrician led and nurse led) | Mortality, readmissions, subsequent institutionalisation, functional ability, quality of life and cognition | No clear benefit in terms of any outcome | CGA has been shown to have benefits. Limited research on CGA at the point of rapid discharge. Few trials undertaken and they are of poor quality; more trials required |
| Sutton et al.121 | Patients aged > 65 years presenting to the ED of an acute hospital (three included studies included patients aged > 70 years) | Identify, appraise and characterise screening tools to screen for elderly patients at risk of functional decline | Screening | Five screening tools identified: HARP, ISAR, TRST, COMPRI and SHERPA | There is no gold standard tool. No single tool had better predictive validity to recommend its use. Therefore, undertaking an intervention based on the outcome of these screening tools is not advisable | |
| Thiem et al.126 | Elderly patients | Screening instruments for the identification of patients in EDs in need of geriatric care | Screening | TRST, SHERPA, ISAR, COMPRI, HARP and Index of Functional Decline | The ISAR tool is the most frequently studied tool and has been tested most widely; however, the evidence is weak or conflicting. Conflicting evidence also exists for the other tools. In addition, it is important to know how best to manage these patients once they have been screened | |
| Fan et al.134 | The effectiveness of interventions targeting the elderly population at reducing ED utilisation | Primary: ED utilisation | Qualitative appraisal resulted in the identification of seven ‘elements’ that were common to the interventions studied: MDT expertise; integrated/enhanced primary care; integrated social and medical care; risk screening and geriatric assessment; care planning and management; discharge planning and referral co-ordination; and follow-up/regular group visits | Review included hospital- and community-based interventions. A larger proportion of community interventions demonstrated reduced ED utilisation. Five of 20 hospital interventions significantly reduced utilisation. Most were characterised by risk screening and assessment and discharge planning and referral co-ordination. There was evidence of increased ED utilisation in some studies. These negative studies tended to have fewer ‘elements’ than the positive ones. The most effective interventions were those in which linkages were made (either MDT in the ED, links with social care, links to community and primary care) | ||
| Karam et al.135 | Review and update existing literature on interventions within EDs | ED revisits, hospitalisations, nursing home admissions and deaths following discharge | Nine studies met the inclusion criteria. The more intensive an intervention, the more frequently it resulted in reduced adverse outcomes compared with simple referralsAmongst the lowest intensity, referral based interventions, studies that used a validated prediction tool to identify high risk patients more frequently reported improved outcomes than those that did not use such a tool | Interventions were more successful if they extended beyond referral and if they used a validated risk prediction tool to identify potential candidates. . . the specific tool used might not be as important as the actual implementation of one to screen patients and target interventions | ||
| Lowthian et al.10 | People aged > 65 years | The effectiveness of the ED in community transition strategies | Intervention | Unplanned ED re-presentation or hospitalisation, functional decline, nursing home admission and mortality | Nine studies. Interventions tended to comprise assessment in the ED with community follow-up. These assessments included comprehensive geriatric nurse assessment and use of the ISAR tool, as well as discharge planning | The evidence base in this area is limited and the research is not of high quality. There is limited evidence on effectiveness in reducing unplanned ED reattendance, hospital admission or mortality |
| McNamara et al.127 | People aged ≥ 65 years | Which triage tool is the most effective for use with older patients presenting to the ED? | Screening | Six tools were identified. Three general tools, Manchester Triage, Emergency Severity Index and CTAS – Manchester Triage and Emergency Severity Index, undertriage older adults. Three were specific tools: ISAR, TRST and VIP; ISAR and TRST have good sensitivity, a high negative predictive value, low specificity and a low positive predictive value and VIP has low sensitivity | Traditional tools undertriage. Need to differentiate between tools to identify who is in need of acute medical care and tools to identify who is in need of ongoing medical care following discharge | |
| Bissett et al.128 | Older people | Identify functional assessments used in the ED, what psychometric properties analysis has been undertaken and what assessments are recommended for practice | Screening |
14 functional assessments Four were developed for use in the ED to identify patients at risk [TRST, ISAR, Runciman questionnaire and FSAS-ED (FSAS-ED was available only in French)]. Four were recommended for practice with reservations: TRST, ISAR, OARS and FSAS-ED. Most tools used self-report rather than patient observation |
his review did not look at outcomes of the screening tools, but at their validity, etc. ISAR and TRST were suitable for fast screening and FSAS-ED was suitable for comprehensive screening:Where time and personnel are constrained and screening is the only realistic option for functional assessment of older people, the ISAR and TRST are the assessments of choice as they have had the most psychometric testing including positive ratings for clinical utility | |
| Fealy et al.138 | Older persons | Effectiveness of nursing interventions targeted at older attendees of EDs | Screening and intervention | Patient and health service outcomes | Interventions categorised as assessment and screening interventions and referral and follow-up interventions | Benefits in terms of reduced service use and reduced functional decline. No statistically significant effects on patient or health service outcomesAssessment interventions that incorporate a post-ED discharge planning and referral component appear to be more effective |
| Schnitker et al.131 | Older, cognitively impaired patients | Identify practices designed to meet the specific care needs of older, cognitively impaired patients in EDs | Assessment of cognitive function |
12 studies in the ED Four categories of best practice: interventions to improve recognition of cognitive impairment and subsequent provision of care; interventions designed to prevent acute confusion (delirium); interventions to manage behavioural/psychological symptoms; and other interventions |
Routine screening and assessment of cognitive function are not common practice and incorporating this into care practices would be beneficial:There are several short, sensitive screening tools suited to the fast-paced ED environment that will identify cognitive dysfunction in older patientsDischarge risk tools are also beneficial | |
| Carpenter et al.129 | Geriatric patients (aged ≥ 65 years) | The prognostic accuracy of individual risk factors and ED screening instruments to distinguish patients more or less likely to experience short-term adverse outcomes | Screening | Short-term adverse outcomes such as unanticipated ED returns, hospital readmissions, functional decline or death | Seven geriatric prognostic screening instruments: ISAR, TRST, VIP, Silver Code, Mortality Risk Index and Rowland and Runciman questionnaires | Adverse outcomes often occur when older people are discharged from the ED. It would be useful to be able to identify these people and the risk factors that lead to unsatisfactory outcomes:None of the individual predictors of vulnerability or published risk stratification instruments demonstrate sufficient prognostic accuracy to distinguish high risk or low risk subsets of geriatric patients in EDsThere are no significant prognostic differences when nurses administer screening instruments (as opposed to geriatric specialists or research teams) |
| Yao et al.122 | Elderly patients | Evaluate the predictive validity of ISAR in identifying older patients at risk of adverse outcomes after an ED visit | Screening | Adverse outcomes |
10 studies ISAR has poor or poor/fair predictive validity for revisiting the ED, hospital readmission, mortality and composite outcomes |
The ISAR tool is quick and cheap to use so it is useful for screening high-risk patients for frailty who are seen in the ED; however, it has poor to fair predictive validity for adverse health outcomes for patients discharged from the ED:It is not suitable to use the ISAR alone for identifying seniors at risk for adverse outcomes in the ED |
Appendix 3 List of full texts excluded and reasons for exclusion
| Study | Reason for exclusion |
|---|---|
| Gupta146 | Not examining the impact on the ED or ED patient outcomes |
| Edmans et al.147 | Study on whether or not the ISAR tool predicts clinical outcomes and health and social services costs of older people discharged from UK acute medical units |
| Carpenter et al.148 | ‘This article describes recent and ongoing efforts to enhance the quality of emergency care for older adults’ using a variety of management approaches (i.e. this is a descriptive article) |
| Swedish Council on Health Technology Assessment149 | Non-English-language article |
| Patterson et al.150 | Modelling the cost-effectiveness of providing vaccination to > 50 patients in EDs |
| Ong et al.151 | Setting in a medical assessment unit |
| Lowthian et al.152 | Protocol for the SEED project (conference abstract is Lowthian et al.153 and full paper is Lowthian et al.154) |
| Lowthian et al.153 | Review and audit of practices: conference presentation (full paper is Lowthian et al.154) |
| Wilhelmson et al.155 | Intervention protocol for intervention delivered in the community |
| Thomas156 | Discussion piece |
| Legrain et al.157 | Setting is acute geriatric units (with ED visit as a primary outcome) |
| Carey et al.158 | No data on outcomes |
| Mun Tan et al.159 | Interventions take place outside the ED |
| McNicholas et al.160 | Population aged > 60 years; outcomes related to trauma management |
| Flynn et al.161 | Geriatric emergency management nurses as a catalyst for change (no outcomes) |
| Hustey et al.19 | Screening for functional decline in the home setting following an ED admission |
| Lee et al.162 | Predicative value of a tool that is not related to ED management |
| Shanley et al.163 | Descriptive, no data |
| Meurer et al.164 | Outcomes not relevant (infections) |
| Schumacher165 | Opinion/discussion paper |
| Launay et al.166 | Population is geriatric patients hospitalised in acute care medical units after admission to the ED |
| Milne et al.167 | Discussion paper |
| Griffiths et al.168 | Protocol/summary of study on transfer of information between care facilities and the ED |
| Somes169 | Not an intervention |
| Booth170 | Letter to the editor, no data |
| Mangram et al.171 | Specific to trauma ED care |
| Jackson172 | Irrelevant outcomes |
| Wolfe173 | Pain management intervention for elderly hip pain patients |
| Lees174 | No data |
| Fernandes175 | Commentary paper |
| Adams et al.176 | Baseline description of intervention, no outcome data included |
| Beauchet et al.177 | Intervention delivered outside the ED |
| Hullick et al.178 | Descriptive paper (conference abstract) describing innovative interventions for the elderly in EDs via a questionnaire survey |
| Hwang et al.179 | No outcome data |
| Lowthian et al.154 | Not an intervention study |
| Stiffler et al.180 | Tool to assess what proportion of older ED patients are frail; administered post discharge |
| Butler and Biram181 | Development of a short-stay medicine for the elderly ward |
| Carey et al.182 | No data on outcomes |
| Ellis et al.183 | Setting is an acute care for the elderly unit |
| Fernandez et al.184 | Insufficient data |
| Huq et al.185 | Outcomes and setting (medical assessment unit) |
| Michael and Ijaola186 | Development of a frail elderly short-stay unit (conference abstract) |
| Miller et al.187 | Outside the date range |
| McCusker et al.188 | Outside the date range |
| McCusker et al.189 | Outside the date range |
| Baumann and Strout190 | Intervention not specific to older people |
| Sanon et al.191 | Short description of the intervention, no data, conference abstract |
| Taylor et al.192 | Population is those admitted to the emergency assessment unit |
| Gorichky193 | Survey of EDs regarding implementation of an EDCC |
| Caplan194 | Abstract for a conference paper, no data |
| Edmans et al.195 | Effect of specialist geriatric medical management on the outcomes of at-risk older people discharged from AMAUs |
| Rogers196 | Description of an intervention; no data on implementation, uptake or use |
| Koehler et al.197 | Impact of a supplemental care bundle on reducing readmission or ED visits in high-risk elderly inpatients |
| Biedsoe et al.198 | Not an intervention |
| McCusker et al.199 | Study looking at whether or not certain ED and non-ED variables are predictive of a return visit to the ED |
| Vandewoude et al.200 | Screening tool for admission |
| Small201 | No outcomes |
Appendix 4 Brief data extraction table
| Authors, year, country | Study design, population, patient numbers | Intervention/assessment tool | Results | Headline message |
|---|---|---|---|---|
| Wright et al.,117 2014, UK |
Pre and post retrospective cohort study Patients aged > 70 years attending A&E department 5416 participants pre intervention and 5370 patients after intervention, TREAT accepted 593 geriatric admissions |
Admissions avoidance system: TREAT. TREAT combines early A&E senior doctor review, CGA, therapist assessment and supported discharge; post-discharge supported recovery; and a rapid geriatric ‘hot-clinic’. A PACE team provided short-term nursing support immediately following discharge to support TREAT |
Following the TREAT intervention period, LOS was reduced (median LOS reduced by 2 days and mean LOS by 18.6% (1.78 days; p < 0.001). For residual admissions, LOS was unchanged (median LOS) and mean LOS was reduced by 1.08% (0.11 days; p = 0.065) For TREAT patients who were admitted, admissions resulting in discharge on the same day increased from 12.26% to 16.23% (OR 1.386, 95% CI 1.203 to 1.597; p < 0.001). Comparing with the residual population, admissions resulting in discharge on the same day fell from 15.01% to 9.77% (OR 0.613, 95% CI 0.737 to 0.509; p < 0.001) |
TREAT appears to have reduced avoidable emergency geriatric admissions and to have shortened LOS for all emergency geriatric admissions |
| Kennedy et al.,40 2014, USA |
Prospective observational study Individuals aged ≥ 65 years presenting for ED care n = 700 |
Structured mental status assessment and attention tests. Delirium determined using the CAM | 9% had delirium. Delirium patients had worse outcomes than those without (LOS 4 days vs. 2 days, ICU admission 13% vs. 6% and discharge to long-term facility 37% vs. 9%). ED delirium was associated with a higher 30-day mortality rate (6% vs. 1%) and 30-day readmission rate (27% vs. 13%) | Delirium prediction rule created as older age, prior stroke or transient ischaemic attack, dementia, suspected infection and acute intracranial haemorrhage and had good predictive accuracy (area under the ROC curve = 0.77) |
| Yuen et al.,108 2012, Hong Kong |
Retrospective study Older people referred by emergency physician 2202 geriatric patients were referred |
Geriatric consultation programme ‘We Care’. Older patients were referred by the emergency physician and screened by the geriatric consultation team, who provided CGA; they were detoured to acute medical admission via either direct admission to a convalescent hospital for further care or discharge with support of the community nursing service |
Age of patients ranged from 45 to 99 years; 15.3% of cases needed acute medical admission for further management, whereas the rest could be admitted to a convalescent home or discharged home. Majority of patients (98.4%) did not suffer any adverse outcomes in the study period; there was a 1.6% reattendance rate and a 1.6% mortality rate after discharge The most prevalent case mix was chronic pulmonary disease, followed by debilitating cardiac disease and neurological problems. Small proportions of patients suffered from terminal malignancies and non-respiratory infection. Patients having chronic pulmonary disease, diabetes-related problems and non-respiratory infections were statistically more likely to be admitted to a convalescent home or discharged home after geriatric consultation |
‘We Care’ provided CGA to suitable geriatric patients, resulting in an effective reduction in acute geriatric hospital admissions |
| Harper et al.,76 2013, Australia |
Single-centred retrospective data analysis Patients aged ≥ 65 years presenting to the ED with a fall 5162 patients from 2006 to 2009 |
Introduction of multidisciplinary CCT staffed by occupational therapists and physiotherapists to intervene with older patients presenting with a fall. Majority of patients referred from ED doctors. Interventions by the CCT varied between patients, but usually included assessment and falls risk stratification, patient education, functional retraining, supply of equipment and referral to a falls clinic or outpatient allied health services | Statistically significant predictors for being referred to the CCT were increasing age, being female, arriving by ambulance, being transferred from a nursing home and higher socioeconomic category. Arrival by ambulance and a history of previous falls were associated with re-presentation and readmission. A decreasing trend from 2006 to 2009 was seen in rate ratios and ORs via regression modelling for both re-presentation and readmission in patients referred to the CCT | Maturing of the CCT is associated with a decrease in re-presentation and readmission rates. Over time, the CCT attended higher-urgency patients associated with stable admission rates. These associations were not significant and the clinical effectiveness of ED CCTs requires further examination |
| Arendt et al.,77 2013, Australia |
Non-randomised prospective pragmatic study Patients aged ≥ 65 years diagnosed with one or more of six conditions (cerebrovascular insufficiency, fractured neck of femur, cardiac failure, myocardial ischaemia, exacerbation of chronic airways disease and respiratory tract infection) 3572 patients (2121 intervention patients, 1451 comparator patients) |
Early allied health intervention conducted in the ED by the CCT for older people with common diagnoses. The CCT consisted of at least one physiotherapist, occupational therapist or social worker with geriatric experience. Intervention patients received comprehensive allied health assessment/intervention by at least one professional working in the CCT. Comparison patients received no assessment | In 2121 intervention patients and 1451 comparator patients, there was no difference in LOS (median 88 vs. 87 hours) on unadjusted (log-rank p = 0.28a) or adjusted (IRR 0.97; p = 0.32a) analysis | Undertaking allied health assessment in ED earlier than in standard care has no effect on hospital length of stay |
| Grossmann et al.,42 2012, Switzerland |
Prospective, single-centre cohort study Patients aged ≥ 65 years n = 519 |
Emergency Severity Index. Test predictive validity, inter-rater reliability and diagnostic accuracy in older ED patients. Identify reasons for inadequate triage | Emergency Severity Index level was associated with resource consumption (95% CI –0.519 to –0.379; Spearman’s rp = –0.449), disposition (Kendall’s r = –0.452, 95% CI –0.516 to –0.387), ED LOS (Kruskal–Wallis χ2 = 92.5, df = 4; p < 0.001) and mortality (log-rank χ2 = 37.04, df = 3; p < 0.001)ESI sensitivity to predict life-saving interventions was 0.462 (95% CI 0.232 to 0.709) and specificity was 0.998 (95% CI 0.989 to 1.000). There was high inter-rater reliability (Cohen’s weighted κ = 0.934, 95% CI 0.913 to 0.954). Undertriage was reported in 117 cases | Undertriage was a risk for older patients and happened when high-risk situations and vital signs were not assessed appropriately. Another reason may have been that there was only moderate inter-rater reliability between triage nurses and triage experts. Emergency Severity Index level had good validity with resource consumption, disposition, ED LOS and survival |
| Foo et al.,115 2012, Singapore |
Single-centre before-and-after prospective study Patients aged ≥ 65 years 172 control (25 December 2006 to 30 March 2007) and 315 intervention (1 April 2007 to 31 December 2007) group patients |
Geriatric assessment in an EDOU. Intervention group received geriatric assessment by an emergency nurse trained in geriatric care before discharge. The nurse then discussed each patient with an ED physician trained in geriatric care or a geriatric nurse clinician and interventions were initiated as required. Control group received usual EDOU care | 71.7% of patients in the intervention group had hidden needs that required intervention. The intervention group had significantly lower ED reattendance (adjusted IRR 0.59, 95% CI 0.48 to 0.71) and hospitalisation (adjusted IRR 0.64, 95% CI 0.51 to 0.79) rates at 12 months | Older patients admitted to an EDOU are an at-risk group and benefit from geriatric assessment before discharge |
| Waldron et al.,79 2011, Australia |
Prospective before-and-after study Study participants were aged ≥ 65 years presenting to the ED as the result of a fall 313 participants |
Allied health staff in the ED to facilitate the referral pathway, audit and feedback | Allied health staff increased the proportion of patients being reviewed from 62.7% before the intervention to 89% after the intervention (p < 0.001). Referral for comprehensive guideline care took place for only 6/177 patients (3.4%) before the intervention compared with 28/136 patients (20.6%) after the intervention (difference = 17.2%, 95% CI 11% to 23%). The average quality of care index (maximum score 100) increased from 18.6 (95% CI 16.7 to 20.4) to 32.6 (95% CI 28.6 to 36.6) | A multifaceted change strategy was associated with an improvement in allied health in ED prioritising the review of ED fallers as well as subsequent referral for comprehensive geriatric care |
| Mortimer et al.,63 2011, Australia |
Prospective evaluation of a newly established service Patients presenting to the DEM, aged ≥ 65 years with a chronic condition or aged ≥ 70 years without a chronic condition 199 patients (101 intervention patients, 98 control patients) |
Specialist aged care pharmacist for reconciliation of initial medication history, review of medication orders and report of medication-related issues to the Department of Emergency Medicine (DEM) doctor. Control patients received continued management by the DEM doctor | Patients in the intervention group had a significantly longer LOS in the DEM compared with patients in the control group [12 hours 42 minutes (n = 101) vs. 10 hours 5 minutes (n = 98); p < 0.01]. 101 cases were managed by the ACP. Of these, 33 had medication orders from the DEM doctor. 48 errors and/or omissions were identified by the ACP. Patients admitted to a ward (control group, n = 92; intervention group, n = 73) had a second medication reconciliation by the ward pharmacist. 41 errors and/or omissions were identified in 25/66 DEM patients, compared with 2/73 ACP patients. For ACP admitted patients 51/73 had a medication related issue. Only 17/66 controls had a medication related issue. There was no difference in the groups in representation at 2 and 4 weeks | This study supports the integration of an ACP in the ED assessing elderly patients |
| Mahony et al.,116 2008, USA |
Pilot project Patients were aged > 65 years and met the following criteria: uncontrolled chronic pain; multiple organ failure that had been rejected for ICU admission; hospice eligible, requiring relief from symptoms; and a chronic incurable illness requiring access to community resources The nurses conducted 894 consultations |
Two advance practice nurses carried out consultations on elderly patients using the palliative care trigger tool to identify patients with one or more ‘palliative care triggers’. Patients eligible for the study then completed a needs assessment form, which was followed by a consultation. Nurses followed up patients to ensure that they had been linked with home care or hospice services | Of the 894 consultations, 263 patients were referred to home care organisations and 287 to hospice organisations, of whom 83 received home care and 91 received hospice services; 90% of patients were admitted to the medical centre, with 41.9% discharged to skilled nursing facilities, 24.2% discharged home with home care and 19.1% discharged home without home care. The project did not have an impact on rates of subsequent use of the ED. Compared with the pre-project chart review, there were small reductions in the length of hospital stay, from 7.9 to 7 days. Linkage with hospital-based palliative care services was enhanced. There was some evidence to suggest that the provision of palliative care and case management services in an ED was associated with increased patient and family satisfaction with symptom relief and increased uptake of hospital-based palliative care and hospice services. There was a limited impact on the utilisation of acute care for the patients in this study | The presence of palliative care, home care and hospice outreach services in the ED can connect end-of-life elderly patients with relevant services |
| Moons et al.,56 2007, Belgium |
Longitudinal study of admission Patients were aged ≥ 65 years and had been admitted to the ED 314 patients (agreed to participate) – 83 spent < 24 hours in the ED, 74 with complete follow-up after 90 days |
To compare the abilities of four different screening tools to predict return visits of older people after they have been discharged from the ED: ISAR tool; TRST; eight-item questionnaire of Runciman et al.;123 and seven-item questionnaire of Rowland et al.124 | There were 28 readmissions in 25 patients (three patients were readmitted twice). During the first 2 weeks of discharge, 10% (8/80) of the patients revisited the ED after 14 days. At 30 and 90 days, the readmission rates were 15.8% (12/76) and 32.5% (25/77), respectively. When using three or more positive answers as the cut-off scores, the Rowland questionnaire proved to be the most accurate predictive tool, with a sensitivity of 88%, specificity of 72% and negative predictive value of 98% at 14 days after discharge; 30 days after discharge, the sensitivity was 73%, specificity was 75% and negative predictive value was 92%. The ideal cut-off scores, as determined by the ROC curves in this study, were ≥ 2 for the ISAR tool, ≥ 2 for the TRST, ≥ 4 for the Runciman questionnaire and ≥ 3 for the Rowland questionnaire | Repeat visits in older people admitted to an ED seemed to be most accurately predicted using the Rowland questionnaire, with an acceptable number of false positives. This instrument can be easily integrated into the standard nursing assessment |
| Baumann and Strout,57 2007, USA |
Retrospective health record survey methodology and a survival analysis Patients aged ≥ 65 years 929 patients |
Estimate the validity of the Emergency Severity Index (version 3) triage algorithm and the association between the Emergency Severity Index categorisation and 1-year survival, LOS, disposition and resource utilisation | Hospitalisation associated with Emergency Severity Index triage assignment (Kendall’s τb = 0.476, 95% CI –0.524 to –0.425). LOS associated with Emergency Severity Index assignment (Kruskal–Wallis test p = 0.000). Emergency Severity Index categorisation was associated with vital status at 1 year (Kaplan–Meier χ2 67.85, df 4; p = 0.0000). The area under the ROC for Emergency Severity Index predictive ability for hospitalisation was 0.77 (95% CI 0.748 to 0.806). Significant relationship between triage category and resource utilisation (Spearman’s r correlation 0.683, 95% CI 0.716 to 0.647a). Results show statistically significant reduction in the proportion of patients admitted from ED to ward since introduction of the care co-ordination programme. There was also a significant difference in the mean-related quality-of-life score before and after the intervention, and staff and patient satisfaction with the service | When used to triage patients aged > 65 years, the Emergency Severity Index algorithm demonstrates validity. Hospitalisation, LOS, resource utilisation and survival were all associated with Emergency Severity Index categorisation in this cohort |
| Corbett et al.,80 2005, Australia |
Programme effectiveness evaluation Patients aged ≥ 65 years presenting to an ED; able to speak and understand English; able to communicate by telephone after discharge; expected to be discharged back into the community; not exhibiting signs of diminished cognition (as assessed by the care co-ordinator); and requiring discharge planning |
Introduction of a care co-ordination programme that consisted of a multidisciplinary case management approach by a team. The professional mix of the team has included physiotherapy, occupational therapy, speech pathology, nursing and social work. The intervention aimed to provide early interventions to prevent unnecessary admissions from the ED to hospital and inappropriate or unnecessary presentation or re-presentation to the ED. Additionally, it aimed to ensure co-ordination and provision of service and programmes for patients with complex care needs on discharge from the ED to the community. Primary role is co-ordination of services although team can provide services | A multidisciplinary case management approach was effective at reducing the admission rate for patients presenting to the ED. Results from this and other studies demonstrate that the care co-ordination programme provides positive outcomes for all stakeholders; it can be easily integrated into existing ED processes and, therefore, can be considered for inclusion in all ED settings | |
| Fallon et al.,69 2015, Ireland |
Prospective data analysis Participants were aged ≥ 65 years Data from 3071 patients attending the AMAU over 1 year were collected and information on characteristics and outcomes for 1066 older patients was retrieved |
Patients attending the AMAU are initially reviewed by a triage nurse in the ED and referred following assessment if deemed suitable | In 2013, 3071 patients were assessed in the AMAU and one-third (1066/3071, 34.7%) were aged ≥ 65 years. Older people presented more acutely unwell than younger counterparts. The most common presenting complaints were breathing difficulty followed by chest pain. Further common presenting complaints were collapse, dizziness and confusion. Only 314/1067 older patients had a TRST assessment completed in ED triage; 196/314 (62.4%) were identified as being at risk of an adverse outcome. Admission rate (644/1067) for older patients was double that of younger patients | The higher admission rate highlights the increasing complexity of this group. AMAUs that are adapted for frailty have great potential to enhance care for older patients |
| Nguyen et al.,110 2014, Australia |
Pilot observational convenience study Patients aged ≥ 65 years (range 66–96 years, mean 78 years) 25 participants |
SGA | Overall, the time required for completion of the SGA by 90% of this sample was 20 minutes 40 seconds | This pilot study shows that use of the SGA in Australian ED settings is possible within the time requirements of the new Australian NEAT, which requires discharge of patients within 4 hours of arrival. The SGA requires a small fraction of the 4-hour target, allowing an overall net benefit by improving patient outcomes and preventing readmissions |
| Beauchet et al.,41 2013, France |
Prospective cohort study design Elderly (aged 84.0 ± 6.5 years) 424 patients |
To examine whether or not a BGA administered to elderly patients admitted to the ED may predict the risk of a long hospital stay in the geriatric acute care unit | Prediction of LOS with a six-item BGA was possible in the sample of older inpatients admitted to the ED. The risk of a long hospital stay changed depending on the different combinations of the six items on the BGA. The combination of a history of a recent fall, male sex, cognitive impairment and age < 85 years identified the elderly ED patients with the highest risk of a long hospital stay requiring geriatric care and planning for discharge | The combination of a history of falls, male sex, cognitive impairment and age < 85 years identified elderly ED patients at high risk of a long hospital stay |
| Launay et al.,81 2013, France |
Prospective cohort study Participants were aged ≥ 75 years 168 older adults admitted to the ED |
MGT providing BGA and then related geriatric or gerontological recommendations. Geriatric recommendations defined as medical recommendations only (recommendations for diagnosis and treatment of polymorbid older adults with disabilities); gerontological recommendations defined as a combination of medical and social recommendations (as above with establishment of formal and adapted home-help services) | 48/168 participants (28.6%) received MGT recommendations (16 geriatric recommendations and 32 gerontological recommendations); 32 participants (19.1%) were discharged early from the ED, including 12 who received a MGT programme. Multiple logistic regression showed that only the geriatric recommendations were associated with early discharge from the ED (OR 4.38; p = 0.046) | Study demonstrated that geriatric recommendations are more effective at reducing length of stay than gerontological recommendations. Gerontological recommendations provide specific social advice, which can take time, thus delaying discharge and explaining the result |
| Arendts et al.,82 2012, Australia |
Prospective non-randomised trial Study participants were aged > 65 years and presented with 1 of 10 common complaints: urinary infection, respiratory tract infection, fall with minor injury, hip or knee pain, back pain, cardiac failure, angina pectoris, syncope, transient ischaemic attack or new-onset confusion or delirium 5265 patients, 3165 in the intervention group and 2100 in the control group |
Early comprehensive allied health input was compared with no allied health input. The service was provided by a CCT consisting of at least one physiotherapist, occupational therapist or social worker with extensive geriatric experience. The CCT undertook comprehensive functional assessment followed by initiation of services to meet identified needs | The admission rate to an inpatient hospital bed from the ED was 72.0% for the intervention vs. 74.4% for the control. The difference was of borderline statistical significant (OR 0.88, 95% CI 0.76 to 1.00; p = 0.046). Subgroup analysis found that patients with musculoskeletal symptoms and angina pectoris in the intervention group had significantly lower admission rates than those in the control group | Early allied health intervention in the ED had a significant but modest impact on admission rates in older patients. Effects appeared to be limited to a small number of common presenting problems |
| Fan et al.,51 2006, Canada |
Prospective, observational cohort study Patients aged > 64 years n = 120 |
TRST to predict resource utilisation defined as ED revisits, hospital admission and long-term care placement at 30 and 120 days after an ED presentation. TRST score of ≥ 2 defined patients as high risk for the above outcomes | This study demonstrates that the TRST is a poor diagnostic test to predict ED revisit, hospital admission or long-term care placement at 30 and 120 days as witnessed by the failure of the likelihood ratio CIs to achieve levels of clinical significance | The TRST cannot be used as a single diagnostic test to predict whether or not Canadian ED elders will have an ED revisit, hospital admission or long-term care placement at 30 or 120 days |
| Argento et al.,66 2010, USA |
Prospective cohort study 100 consultations with patients aged > 65 years |
Geriatric nurse practitioner stationed in ED to provide consultative care to supplement care already provided by ED staff | Of 100 patients assessed, 31% required admission, 16% returned to a nursing home and 5% were referred to a nursing home for ongoing care; 48 patients returned home, of whom 60% had a visiting nurse put in place and 6% were discharged with home hospice | Although the period of the study was short, the advance practice nurse was able to generate consultations and provide geriatric-specific care to elderly ED patients. Further research will focus on quality care initiatives and patient-specific outcomes |
| Carpenter et al.,18 2010, USA |
RCT Adults aged > 65 years, mean age 76 years n = 69 |
Geriatric technicians screened elderly people presenting at the ED (MMSE and CAM ICU). Physicians were either informed or not informed of the results of the screening | A chart review was conducted to assess admission rates, documentation of recognized geriatric syndromes, discharge instructions, and follow-up plansInformed physicians were unaware of abnormal screening results in 71% of patients, including > 50% of delirium patients | Screening did not appear to influence the decisions made by physicians – either in their documentation, disposition or management decisions |
| Carpenter et al.,45 2012, USA |
Prospective consecutive patient trial Patients aged > 65 years 225 patients enrolled, 159 at 1-month follow-up |
Baseline measures included the OARS ADL plus the ISAR tool and TRST. Telephone follow-up was carried out to quantify the composite outcome of reported ED recidivism, hospitalisation, OARS ADL functional decline and interval death | The TRST and ISAR tool labelled 65% and 82% of patients as being at high risk, respectively. At 3 months, 51% reported diminished function, 35% had another ED evaluation and were hospitalised, 2% had been institutionalised and 70% had the composite outcome. Neither TRST nor the ISAR tool predicted 1- or 3-month composite outcomes in either general geriatric patients or those with cognitive impairment or lower health literacy | Neither the ISAR tool nor the TRST distinguish GED patients at high or low risk for 1- or 3-month adverse outcomes |
| Dresden et al.,70 2015, USA |
Prospective cohort study Patients aged > 65 years 829 intervention patients, 873 control patients |
GNLI using ED-based assessment and care co-ordination was implemented for GED patients | GNLI when compared with controls had: higher discharge rate (52.5% vs. 30.0%; RD 22.5%, 95% CI 17.8% to 27.0%); lower inpatient rate (28.6% vs. 48.3%; RD –19.7%, 95% CI –24.2% to –15.2%); no significant change in observation rate (18.9% vs. 21.7%; RD –2.8%, 95% CI –6.5% to 1.1%). ‘Of potential 30-day readmissions, the GNLI group had a higher discharge rate than the control group (46.7% vs. 24.9%; RD 21.8%, 95% CI 11.1% to 32.0%)’. ‘GNLI patients admitted to inpatient or observation had a shorter mean hospital LOS than control patients (88.2 vs. 104.3 hours; difference in mean –16.1 hours, 95% CI –30.9 to –1.3 hours)’ | GNLI in this sample was associated with significant decreases in hospitalisation rate, 30-day readmission rate and hospital LOS. A further study to evaluate ED recidivism after GNLI is needed |
| Dziura et al.,46 2013, USA |
Medical record review Patients aged > 65 years n = 250 |
Rapid screening assessment measuring ED visits in the past 12 months, disability, polypharmacy and age. Disability was assessed using a 12-item questionnaire | 42 participants (17%) experienced at least one 30-day return visit or death. In the multivariable model, previous ED visits (OR 2.6, 95% CI 1.2 to 5.5), greater global disability (OR 1.56, 95% CI 0.99 to 2.5), age (OR 1.04, 95% CI 1.0 to 1.08) and polypharmacy (> 10 medications; OR 1.8, 95% CI 0.9 to 3.9) were associated with a greater likelihood of a 30-day event. The fit of the multivariable model was good (Hosmer–Lemeshow goodness of fit test, p = 0.85) and it provided good discrimination between those having and those not having 30-day events (area under ROC curve = 0.73). The predicted probability of a return visit ranged from 3% to 56% | Rapid screening assessment provides an accurate method to identify in the ED older patients who are likely to have a return visit or to die |
| Eagles et al.,47 2015, Canada |
Substudy of a prospective cohort study. ED following trauma then follow-up at 3 and 6 months Patients aged ≥ 65 years with minor trauma; mean age 76.8 years n = 504 |
Used a standardised test, the TUGT, for assessing mobility in the ED. Assessed the TUGT and its relationship with frailty, functional decline, fear of falling and falls | Significant association between TUGT scores and frailty, functional decline at 3 and 6 months, fear of falling at 0, 3 and 6 months and self-reported falls at 0 months | In a population of community-dwelling older people with trauma, on presentation to the ED the following were associated with TUGT scores: frailty, functional decline and fear of falling. There was an association between the TUGT and falls at the initial visit, but not at 3 or 6 months’ follow-up. These findings suggest that the TUGT can be used to identify patients with frailty who are at risk of further decline |
| Eagles et al.,37 2014, Canada |
Prospective cohort study Patients aged ≥ 75 years n = 260 |
The O3DY is a four-question cognitive screening tool. Abnormalities resulted in a comprehensive cognitive evaluation. Descriptive statistics were used to assess level of implementation, prevalence of altered mental status and sensitivity and specificity compared with the MMSE, using a cut-off point of < 25. Kappa coefficients were calculated | Screening rates were 78.3% overall, 51.8% for physicians and 64.2% for nurses. Strong inter-rater reliability (κ = 0.65, 95% CI 0.51 to 0.80). Physician and nurse sensitivity compared with the MMSE was 78.9% (95% CI 53.9% to 93.0%) and 84.6% (95% CI 64.3% to 95.0%) and specificity was 39.4% (95% CI 23.4% to 57.8%) and 54.2% (95% CI 39.3% to 68.3%). Physicians and nurses reported that the O3DY was easy to learn (98%, 97%), remember (88%, 95%) and use (95%, 97%). Both groups were less sure about patient benefit (30%, 55%) and usefulness to practice (50%, 72%). Patient living situation, level of education, triage location, hospitalisation, admission location and death in 30 days were associated with altered mental status | The O3DY is a simple screening tool for altered mental status that has been shown to be feasible for use in the ED. Implementation will increase the identification of altered mental status in elderly patients presenting to the ED |
| Hadbavna et al.,34 2013, Ireland |
Convenience sample – data from clinical records Patients aged > 65 years n = 117 |
Brief nurse-administered 6-CIT in the ED | Over two-thirds (79/117, 67.5%) required hospital admission. The TRST was used on 48/117 patients (41%) and 37/48 (77%) were identified as being high-risk vulnerable older adults. The initial 6-CIT was positive in 43/117 patients (36.8%). The repeat 6-CIT was performed on 28/43 (65%) of these, with the remainder having been discharged from the ED. All except 4/28 (14%) remained positive. The CAM ICU was positive for delirium in 7/28 patients (25%) screened | ‘A high proportion of older patients attending the ED met the criteria for cognitive impairment. Of those admitted, many met the criteria for delirium. There was considerable variation in the applicability and implementation of the screening instruments between nurses, despite training.’ The ED has the potential to be a location in which to identify patients with undiagnosed dementia |
| Launay et al.,85 2013, France |
Prospective cohort study 168 older adults |
Early MGT combining BGA and standardised recommendations | Of the included patients (n = 168), 48 benefited from recommendations from the MGT (16 geriatric and 32 gerontological). Of the 168 patients, 32 (of whom 12 received MGT recommendations) were discharged early. Of the recommendations, only the geriatric recommendations were associated with ED early discharge (OR 4.38, p = 0.046) | MGT geriatric recommendations were associated with early discharge from the ED, whereas gerontological recommendations were not |
| Lonterman et al.,32 2011, the Netherlands |
Cross-sectional diagnostic cohort study Patients aged ≥ 65 years presenting to the ED n = 300 |
ED/geriatric screening tool compared with safety management system screening bundle (reference standard). Screening tool was administered by nurses (presumably at admission but not explicitly reported) and the screening bundle by researchers | Area under the ROC curve for the screening tool was 0.83 (95% CI 0.78 to 0.88). One of the original eight items could be removed without reducing validity. In both the eight- and seven-item screening tool, the overall misclassification was lowest at a cut-off score of 2 (52% and 47%, respectively). Using a cut-off score of 2, the seven-item screening tool had sensitivity of 64% and specificity of 89% | The screening tool has moderate validity compared with the screening bundle and can be used to identify most elderly ED patients at high risk of adverse outcomes |
| Terrell et al.,120 2009, USA |
RCT 63 emergency physicians (32 intervention and 31 control) Average patient age 74 years |
Computer-assisted decision support to reduce potentially inappropriate medicine prescribing to older adults. Primary outcome was the proportion of visits that resulted in one or more prescriptions for a potentially inappropriate medicine | There were 2647 visits to an intervention physician; at 111 visits an intervention physician attempted to prescribe a potentially inappropriate medicine. Decision support was provided 114 times (107 visits); 49 (43%) of these decision support recommendations were accepted. One or more inappropriate medications were prescribed at 2.6% of intervention ED visits by seniors and 3.9% of control visits. The proportion of all prescribed medications that were inappropriate significantly decreased from 5.4% to 3.4% | There are specific medicines that are inappropriate for older people; however, these continue to be prescribed. As an intervention to improve ED care for older people, computerised decision support reduced the prescription of potentially inappropriate medications on discharge from the ED |
| Tiedemann et al.,60 2013, Australia |
Prospective cohort study (6-month follow-up) Patients aged ≥ 70 years who presented to the ED after falling or with a history of two or more falls in the previous year n = 219 in the development study and n = 178 in the subsequent external validation study |
Final screening tool involved two items: two or more falls in the past year and taking six or more medications. Participants were assessed in the ED at the time of presentation by clinical staff as part of their normal duties | Mean patient age was 81 years; 46% of the development sample and 27% of the validation sample were male. During follow-up, 31% and 35% of participants fell in the development and external validation samples, respectively. Area under the ROC curve for the two-item screening tool was 0.7 (95% CI 0.64 to 0.76), which was similar to that for the FROP-Com and PROFET tools | A simple, two-item screening tool demonstrated good external validity and accurately discriminated between fallers and non-fallers. This tool could identify high-risk individuals who may benefit from onward referral or intervention after ED discharge |
| Beirne et al.,107 2012, Ireland |
Prospective data analysis (1 year) All older attendees to the ED (aged > 72 years) ISAR, n = 7596; convenience sample (ISAR > 2), n = 300 |
Use of the ISAR tool for predicting ED reattendance; CGA | Patients aged ≥ 72 years attending the ED accounted for 20% of all attendances (2003 = 16%). ISAR for 15% of patients and sensitivity for ED reattendance was 77% at 1 month, 80% at 3 months and 79% at 6 months. Comparing patients with ISAR score of > 2 (n = 300) who received CGA, with those who did not, reattendance figures are as follows (21% vs. 24% at 3 months; 27% vs. 33% at 6 months) | In an intervention that combined identification of at-risk older people using the ISAR tool followed by CGA for those scoring ‘at risk, ED reattendance was lower in the CGA group. ‘Appropriate community follow-up’ was also included |
| Berahman et al.,84 2014, USA |
Prospective questionnaire (five questions, scored from 0 to 10) survey about patient satisfaction and overall ED experience when a patient liaison was present and not present Patients aged 65–99 years, mean age 75 years 637 patients (432 with a patient liaison, 205 with no patient liaison) |
Patient liaison programme: ‘interaction with physician and staff in order to address non-medical needs and update them on the status of their ED visit’ | There was no significant difference between the groups for four of the five questions. For the other question (increased satisfaction in how often visited by ED staff), the mean score was 7.83 for the patient liaison group and 7.23 for the non-patient liaison group (p = 0.012) | Trend towards improved satisfaction scores when a patient liaison was present but this was not statistically significant or was barely significant |
| Chou et al.,100 2015, Taiwan; Liao et al.,101 2012, Taiwan |
Appears to be a prospective cohort study (12-month follow-up, results at 6 months reported) Older people who visited the ED three times within 30 days (n = 137, of whom 26 received a CGA-based intervention) |
After initial assessment in the ED, CGA and ‘geriatric interventions’ were performed by a geriatric team | Mean patient age was 80.3 years and 74% were male; there were no demographic differences between the intervention group and the non-intervention group. The intervention group was more likely to be admitted (50% vs. 22%) and made fewer visits to the ED within 1 (0.81 vs. 1.75 visits) and 6 (2.2 vs. 4 visits) months | The CGA-based intervention reduced subsequent ED visits significantly, but a RCT would be required to confirm the findings |
| Chui and Kun,109 2013, Hong Kong |
All patients receiving a geriatric consultation service Prospective cohort study Patients aged 64–99 years, mean age 80.3 years n = 1096 |
‘Program We Care’ (geriatric consultation service) | Following the geriatric consultation, of the 1096 study participants, 508 were transferred for convalescent care, 475 were discharged home with follow-up, 111 were discharged home with follow up and a community nurse referral and 113 required acute medical admission. The total number who reattended the ED within 48 hours was 16 | The aim of the intervention was to reduce acute medical admissions from the ED. Study authors argue that their intervention did reduce admissions; however, no control group or data for comparison |
| Dundar et al.,43 2015, Turkey |
Prospective cohort study (in-hospital follow-up) Patients aged ≥ 65 years admitted with acute medical or surgical complaints n = 939 |
REMS, REMS without age and HOTEL | Median patient age was 74 years and 54% were male. REMS and HOTEL scores differed significantly between patients who were discharged from the ED, those admitted to the ward and those admitted to intensive care. The scores of patients who died in hospital were significantly higher than those of survivors. Area under the ROC curve values for REMS, REMS without age and HOTEL were 0.77, 0.76 and 0.83, respectively | The REMS, REMS without age and HOTEL scores cannot be used to identify GED patients requiring hospital admission, but they are of value for predicting in-hospital mortality and intensive care admission |
| Genes et al.,91 2013, USA |
Before-and-after study comparing 3-month periods before and after implementation of a GED Discharged patients aged < 65 years (n = 219) and ≥ 65 years (n = 67) |
Press Ganey surveys [sic] were reviewed after discharge | Following implementation of the GED, patient satisfaction scores among older patients increased significantly for areas related to information about home care; measures to protect safety; treatment of family and friends; and ancillary testing. Non-significant increases in overall satisfaction, plus satisfaction regarding nurses, doctors, registration and arrival increased | Implementation of a GED increased patient satisfaction scores in people aged ≥ 65 years, but not in younger patients |
| Hughes et al.,105 2014, UK |
Prospective review of patients over a 4-week period Acute admissions presenting to the ED Patients aged ≥ 70 years 547 patients (admitted to ED and clinical decision unit) |
CGA as delivered by an OPAL service | 547 medical patients were admitted to the ED and clinical decision unit; 56% (n = 307) were assessed by the OPAL team and received CGA. Of these, 57% (174/307) returned to their usual place of residence, 8% (25/307) were transferred to a community hospital, 35% (108/307) were transferred to a medical specialty ward, 47% (51/108) were admitted to an elderly care ward and one patient died. In total, 53% (164/307) were discharged within 48 hours of admission. Median LOS was 2 days (range 2 hours to 37 days). Current readmission rate within 1 month of discharge was 14% (42/307) | Older people who received CGA at the point of admission appeared to benefit from improved function at discharge, reduced length of stay and increased probability of returning to their usual place of residence on discharge |
| Karounos et al.,92 2014, USA |
Retrospective review of geriatric admissions, 1 year before and after a GED opened Patients aged > 65 years n = 27,838 |
GED: geriatric-friendly physical attributes; educated staff; geriatric care team (care transitions); dementia screening as standard; and medication review for drug–drug interactions | Outcome measure was geriatric admissions. Before: 13,354 patients, 7065 admitted (52.9%); post: 14,484 patients, 7247 admitted (50%); 1130 fewer admissions (2.9%) (p < 0.001) | Admissions were reduced, possibly because of extra emphasis on transitions of care. Further research is needed to look at rates of revisit and cost savings required |
| Lo Storto et al.,111 2011, Italy |
Prospective cohort study Older patients (age range 65–100 years) attending the ED n = 226 over 2 years |
CGA was performed by a team, including a geriatrician, a nurse and a social worker. When admission to hospital was considered inappropriate, alternatives including home services and/or temporary residential accommodation were proposed | Mean patient age was 80.5 years and 63.7% were female. Hospital admission was considered appropriate for 141 patients and inappropriate for 84, of whom 66 were discharged home after activating home services | The social health and triage team reduced hospital admissions and improved quality of care |
| Ng et al.,96,97 2014, USA |
Before-and-after study using administrative data Patients aged ≥ 65 years attending an ED between January 2011 and May 2013 (GED opened in February 2012 and GEDI-WISE programme began in October 2012) |
No details of screening in the GED were reported | Mean patient age was 77 years (SD 8.6 years). Admission rate declined from 58.9% in January 2011 to 50.7% in May 2013, a change that remained statistically significant after adjustment | There was a decrease in admission rates of patients aged > 65 years following the opening of a GED |
| Post et al.,48 2013, USA | Retrospective chart review to develop a measure of disability for use in the ED, followed by a prospective cohort study (n = 250 patients aged ≥ 65 years) to further refine and validate the measure | The GRAY measure has five screening and 15 follow-up questions covering physical and cognitive disability, stress, depression and isolation. A global score and estimated risk of readmission within 30 days are generated. Not reported where screening takes place | 56 participants (22%) experienced at least one 30-day return visit or death. Greater disability as measured by the ED GRAY global disability was associated with an increased likelihood of an event (OR 1.7 for each 1-point worsening in severity, 95% CI 1.2 to 2.5). In the multivariable model, prior ED visits (OR 2.7, 95% CI 1.4 to 5.2), ED GRAY global score (OR 1.4, 95% CI 1.0 to 2.1) and age (OR 1.03, 95% CI 0.99 to 1.07) were associated with a greater likelihood of a 30-day event. The fit of the multivariable model was good and it provided good discrimination between those having and those not having a 30-day event (area under the ROC curve = 0.70). The predicted probability of a return visit ranged from 3% to 56% | The GRAY measure can be quickly performed in the ED to initially assess disability and identify issues that need to be addressed. Combined with other data, it provides good discrimination of risk of ED readmission within 30 days |
| Grudzen et al.,113 2015, USA |
Review of administrative data from health records and billing data (1 January 2011 to 31 May 2013) All aged ≥ 65 years |
Palliative care elements of GEDI-WISE: GED space, volunteers to help geriatric patients, screening using the ISAR tool (those with a score of > 2 had additional screening including identifying for palliative care) and training to carry out screening as well as additional training in palliative care ED screening tool for the rapid identification of older adults with a high likelihood of re-presentation or readmission, who require palliative care plus a wider model of care GEDI-WISE Because 50% of adults aged > 65 years in the last month of life present to the ED, there is a need for interventions to prevent admissions to intensive care for these adults and redirect them to appropriate palliative care |
Primary outcome = ICU admission rate from the ED for patients aged > 65 years. Also measured ED-initiated palliative care consultations and hospice referrals. Over a 29-month study period, the unadjusted ICU admission rate declined from 2.3% to 0.9%. Adjusting for age, sex, ESI score and others, the decline was still significant (β –0.0073, 95% CI –0.0105 to –0.0041; p < 0001) | Decline in geriatric admissions cannot be attributed to GEDI-WISE because there were additional interventions taking place at the same time, such as the opening of a palliative care unit. However, there was a national increase in ICU admissions so this is against this trend |
| Wall and Wallis,20 2014, UK |
Diagnostic accuracy study People aged ≥ 75 years admitted to wards from the ED over a 2-week period n = 118 |
In this study the CFS was applied after admission to wards to compare the distribution of frail patients in geriatric vs. non-geriatric wards. The CFS was compared with other frailty scales (Edmonton Frailty Scale, PRISMA-7 and ISAR) | There was no statistically significant difference in frailty between patients in geriatric and patients in non-geriatric wards. Analysis of ROC curves showed that the CFS accurately identified frail patients compared with other well-established frailty scales at appropriate cut-off points | The CFS is a rapid and simple case-finding tool. Its implementation in the ED could increase the proportion of frail patients admitted directly to a geriatric ward |
| Lee et al.,23 2011, South Korea |
Diagnostic accuracy study People aged ≥ 65 years presenting to an ED over a 3-month period n = 1903 |
CTAS at admission | Severity (e.g. mortality and ICU admission) increased as CTAS score increased. In total, 94 patients received a life-saving intervention within 1 hour of arriving at the ED. The sensitivity and specificity of a CTAS score of ≥ 2 for identifying patients receiving an immediate intervention were 97.9% and 89.2%, respectively | The CTAS is a triage tool with high validity for elderly patients and is especially useful for categorising severity and recognising those who require an immediate life-saving intervention |
| Hegney et al.,44 2006, Australia |
Before-and-after study Patients aged > 70 years n = 2139 |
Risk screening to refer patients for home and community care services. Screening tool adapted from the ‘Screening Tool for Elderly Patients’, which in turn was developed from the ISAR tool | 2139 older people (of whom 246 were re-presentations and 1102 were admitted). There was a 16% decrease in re-presentation rate from 21% to 5% (χ2 = 15.59; p < 0.001) and a 5.5% decrease in readmission rate from 10.2% to 4.7% (χ2 = 4.61; p < 0.05). There was a decrease in re-presentations of those patients who present three or more times per month (not a significant result) and a decrease in LOS from 6.17 days to 5.37 (privacy restrictions made any substantial data analysis impossible) | There was a decrease in re-presentations. It was suggested that this was because of increased referral to other community-based services (i.e. diverting patients elsewhere)The average number of days started to decrease prior to the introduction of the intervention, which may suggest some other factor(s) than the nurse-led model of discharge planning may have influenced the results |
| Basic and Conforti,26 2005, Australia |
RCT Elderly patients [functional impairment, psychological disability, social disability, active multisystem (2+) disease, discharge from hospital within the last 14 days] Mean age 78.7 ± 6.4 years n = 224 (114 intervention patients, 110 control patients) |
Early geriatric assessment in the form of an aged care nurse intervention – screening using a variety of instruments; liaison with carers and health-care professionals; and organised and assisted in the care of those admitted as inpatients | Our aged care nurse intervention, based in the emergency department and comprising detailed assessment, monitoring and referral, failed to reduce admission of elderly patients to the hospital, LOS, or functional decline during the hospitalisation | Intervention had no effect on admission rates, LOS or functional decline. The authors believe that this was because the intervention did not (1) give timely access to community support or (2) have the ability to change the course of care in hospital. However, impaired function was a strong predictor of outcomes. Delayed impact of nursing interventions |
| Asomaning and Loftus,28 2014, Canada |
Audit of implementation of the ISAR tool Patients aged ≥ 65 years presenting to the ED over two 14-day periods n = 525 |
Use of the ISAR tool by nurses in the ED | 271 patients (51.6% of those eligible) were screened with the ISAR tool, of whom 158 (58%) had a positive result (answered yes to two or more questions). Patients with positive results were more likely to be aged > 79 years, were more likely to be admitted and had a longer LOS than those screening negative | Low compliance by staff was a barrier to implementation of the ISAR tool. Reasons identified included the fast-paced nature of emergency care and lack of staff at night. Strategies to address this included tool adaptation and providing staff with knowledge of ED and inpatient geriatric resources and feedback on completion rates |
| Bond et al.,65 2014, Canada |
Matched paired study using administrative data (four EDs with an EDCC and four without) Seniors aged > 65 years with a discharge diagnosis of fall or musculoskeletal pathology 910 matched pairs (1820 patients; matched on a number of criteria) |
EDCCs to reduce hospital admission rates on index visit (secondary outcomes: LOS, 30-day recidivism, 30-day revisit resulting in admission) through better linkages with home care and community services on discharge | No difference between EDCC and non-EDCC patients in the following: admission rates (OR 0.88, 95% CI 0.69 to 1.12); revisit rates at 30 days (OR 1.19, 95% CI 0.95 to 1.51); and readmission rates at 30 days (OR 1.03, 95% CI 0.73 to 1.46) | ‘This study showed no reduction in senior patients’ admission rates, recidivism at 30 days or hospital LOS when comparing seniors seen by an EDCC with those not seen by an EDCC.’ However, EDCC may have other positive outcomes not measured in this study. Numerous problems with the study design |
| Buurman et al.,55 2011, the Netherlands |
Prospective diagnostic cohort study Patients aged ≥ 65 years discharged from an ED over an 11-month period n = 381 |
ISAR tool, TRST and Runciman and Rowland questionnaires administered after discharge together with an interview to assess functional status at the time of visiting the ED | Mean patient age was 79.1 years. Within 120 days, 14.7% of patients returned to the ED, 17.2% were hospitalised and 2.9% died. The area under the ROC curve was low for all of the screening tools, indicating poor discriminatory power | None of the screening tools was able to discriminate clearly between patients with and without poor outcomes |
| Carpenter et al.,35 2011, USA |
Prospective diagnostic cohort study Patients aged ≥ 65 years attending an ED between June 2009 and March 2010 n = 169 |
O3DY, BAS, SBT and caregiver-completed AD8 compared with MMSE as reference standard. Screening by researchers in the ED | Complete data were collected for 163 patients, of whom 37% had cognitive dysfunction. The SBT, BAS and O3DY each showed 95% sensitivity, compared with 83% sensitivity for the caregiver-completed AD8. The SBT had the highest specificity (65%) followed by the caregiver-completed AD8 (63%). The SBT showed the best overlap with the MMSE | Brief screening instruments such as the SBT can rapidly identify patients at lower risk of cognitive dysfunction |
| Carpenter et al.,36 2011, USA |
Prospective diagnostic cohort study Patients aged ≥ 65 years attending an ED between June 2009 and March 2010 n = 371 |
SIS and AD8 compared with MMSE as reference standard. Screening by researchers in the ED | Of 319 patients who completed cognitive testing, 35% had cognitive dysfunction. The SIS had the highest sensitivity (74%), specificity (77%) and area under the ROC curve compared with either the caregiver- or the patient-completed AD8 | The SIS was superior to the caregiver- or patient-completed AD8 for identifying older adults at increased risk of cognitive dysfunction |
| Di Bari et al.,58 2012, Italy |
Prospective cohort study Patients aged ≥ 75 years attending a GED over an 8-month period n = 1632 |
The ISAR tool was administered at triage in the ED and compared with Silver Code results obtained retrospectively from administrative data | Mean patient age was 84 years and 61% were women; 75% were ISAR positive (answered yes to two or more questions). ISAR and Silver Code scores were moderately correlated (r = 0.35) and had a similar area under the ROC curve for predicting hospital admission. ISAR-positive patients had an increased risk of hospital admission and death and risks also increased with increasing Silver Code risk category. In a 6-month follow-up period, the tools had a similar ability to predict repeat ED visits, hospital admission and death | Prognostic stratification with the Silver Code is comparable with that obtained by direct patient evaluation. The Silver Code predicts ED readmission and future hospitalisations even in patients discharged directly from the ED. The Silver Code is based on data available at the time of accessing the ED and could in principle be used to aid triage, although only as a preliminary step |
| Hustey et al.,19 2007, USA |
Secondary analysis of data from a randomised trial Patients aged ≥ 65 years who attended an ED and were discharged home n = 650 |
TRST administered at triage in the ED | Mean patient age was 74 years and 59% were women. TRST scores were correlated with baseline ADL impairments, IADL impairments and self-reported physical health at all end points. A TRST score of ≥ 2 was moderately predictive of decline in ADL or IADL at 30 and 120 days | TRST provides a valid proxy measure for assessing functional status in the ED and may be useful in identifying high-risk patients who would benefit from referrals for further evaluation or surveillance upon ED discharge |
| Keyes et al.,93 2014, USA |
Four groups: seniors (aged ≥ 65 years) in the ED before the senior ED opened; those in the new senior ED; younger patients (aged 55–64 years) treated before the senior ED opened; and younger patients treated after it opened 12,015 patients (7598 aged > 64 years and 4417 aged 55–64 years); mean age of all patients was 70 years (77.5/76.9 years in the senior groups) |
Effect of senior ED/GED on rates of admission to hospital, LOS and ED return visit within 30 and 180 days. GED comprised a case management approach, which included improved staff education; changes to physical space; and universal screening for common elderly comorbidities | There was no significant difference in time to return within 30 days or average hospital LOS. Risk of being admitted on the index visit was lower for seniors treated in the senior ED than for seniors in the regular ED (relative risk 0.93, 95% CI 0.89 to 0.98) | A new senior ED was associated with decreased admissions but not with ED return visits or LOS. ‘There is evidence from our analysis that care in our senior ED might contribute to fewer admissions on the index visit, but this was not the primary hypothesis of this study.’ We need to be sure that if patients are being discharged early then this is not just increasing the rates of return ED visits. Screening thresholds should allow us to identify those who are at risk of return. There may be an unintended consequence that a GED increases return rates because patients would prefer to be seen in this setting (no evidence for this in this study). Authors argue that the reason for improvements in admission rates is related to the use of social workers |
| Wilber et al.,38 2008, USA |
Prospective diagnostic accuracy study Patients aged ≥ 65 years attending an ED between January 2006 and January 2007 n = 352 |
SIS before or after MMSE (reference standard) administered by a physician in the ED | Mean patient age was 77 years and 63% were women; 111 patients were cognitively impaired based on the MMSE. The SIS had 63% sensitivity and 81% specificity. The area under the ROC curve was 0.77 (95% CI 0.72 to 0.83) | Sensitivity of the SIS was lower in this study than in previous studies therefore unable to recommend it as a brief mental status test in the ED |
| Wilber et al.,39 2005, USA |
Diagnostic accuracy study Patients randomised between screening tests; aged ≥ 65 years attending an ED in autumn 2003 n = 150 |
SIS or Mini-Cog administered by a physician in the ED followed by MMSE (reference standard) | Mean patient age was 75 years and 55% were women. The SIS had sensitivity of 94% (95% CI 73% to 100%) and specificity of 86% (95% CI 74% to 94%). The Mini-Cog had sensitivity of 75% (95% CI 48% to 93%) and specificity of 85% (95% CI 73% to 93%) | The SIS, with a cut-off point of ≤ 4, is short, easy to administer and unobtrusive, allowing it to be easily included in the initial assessment of older ED patients |
| Stiffler et al.,59 2016, USA |
Prospective cohort study Patients aged ≥ 65 years attending an urban ED n = 107 |
SHARE-FI administered in the ED. Patients classified as non-frail, pre-frail and frail | Mean patient age was 79 years and 50% were women. The composite 30-day primary outcome (death, functional decline, repeat ED or hospital admission or nursing home admission) occurred in 19% of non-frail, 44% of pre-frail and 78% of frail patients. Falls occurred in 0%, 6% and 21%, respectively | The SHARE-FI tool appears to be a feasible method to screen for frailty in the ED |
| Eklund et al.,31 2016, Sweden |
Cross-sectional diagnostic accuracy study Older patients attending the ED between October 2008 and June 2010; aged ≥ 80 years or aged 65–79 years with at least one chronic disease and dependence in at least one daily living activity n = 161 |
Five-question FRESH screening tool administered in participants’ homes followed by measurement of eight frailty indicators (reference standard) | Both sensitivity (81%) and specificity (80%) of the FRESH tool were high. A question about repeated visits to the ED did not improve accuracy and was removed, reducing the number of questions to four | The FRESH tool has high clinical value in screening for frailty. It is simple and rapid to use, takes only a few minutes to administer and requires minimal energy use by the person being screened |
| Tang et al.,95 2016, UK |
Observational before-and-after study (two 7-month periods) People aged > 65 years; RAC group (mean age 75 years), comparator group (A&E, mean age 73 years) n = 441 (346 A&E patients, 95 RAC patients) |
RAC: six-bedded consultant-led ward | LOS was 5.6 days when admitted by A&E and 4.1 days when admitted by RAC. This relationship held when looking at groups by diagnosis | Use of RAC led to a shorter LOS and patients were discharged earlier |
| Shaw et al.,64 2016, USA |
Retrospective cohort analysis Patients aged > 65 years 4103 patients, 872 treated in the ED for seniors and 342 of these treated by the clinical pharmacy specialist |
Implementation of the ED for seniors, including a clinical pharmacy specialist, specialised in geriatric training including medication management training, as a key member of the ED team | Compared with other patients, both patients treated in the senior ED and those treated by the clinical pharmacy specialist did not have a reduction in ED return visits at 30 or 90 days, mortality, cost of follow-up care or hospital admissions. The clinical pharmacy specialist identified 45% of patients as having at least one medication-related problem | Although at least one medication-related problem was identified in almost half of patients treated by the clinical pharmacy specialist in the ED for seniors, incorporation of a clinical pharmacy specialist into the ED staff did not improve clinical outcomes |
| Wilber et al.,94 2013, USA |
Retrospective cohort analysis of quality assurance data Patients aged ≥ 65 years 2260 eligible visits in 2012 (comparison group) and 2286 eligible visits in 2013 (intervention group) |
Triage to a 15-bed senior ED, with overflow to a standard ED. Assessment by a registered nurse transitional care co-ordinator, care protocols, education, pharmacy review and call backs on discharged patients | There was a small but not significant decrease in LOS (300 minutes to 296 minutes). There was a significant decrease in admissions (55.5% to 51.2%; difference –4.3 percentage points, 95% CI –7.2 to –1.4 percentage points). There was an increase in patient observations were from 2.2% to 3.9% (difference 1.7 percentage points, 95% CI 0.7 to –2.7 percentage points)Revisits resulting in admission or observation at 7 (4.9 to 4.5) and 30 (13.2 to 12.3) daysa were slightly but not significantly decreased | A pilot senior ED programme reduced admissions without increasing LOS or revisits resulting in admission or observation |
Appendix 5 Full data extraction tables
| Full paper | Authors: Silvester et al.86 | Year: 2014 | Country: UK | |
|---|---|---|---|---|
| Study design | Prospective systems redesign study | |||
| Data source | Routinely collected attendance and admissions data | |||
| Study aim(s) | To conduct a patient flow analysis of older emergency patients to identify and address delays in ensuring timely care without extra resources | |||
| Sample size | ||||
| Setting | GM directorate in an acute hospital (Sheffield Teaching Hospitals NHS Foundation Trust) with 1920 beds | |||
| Frail elderly – definition | ||||
| Study population | Age: not defined | Condition: older people admitted as emergencies | ||
| Intervention | What | Formation of a MDT, including consultant geriatricians, junior doctors, nurses, pharmacists, therapists and clerical staff, with expert clinical systems engineers as the facilitators who introduced a series of changes:
|
||
| Who | MDT, including consultant geriatricians, junior doctors, nurses, pharmacists, therapists and clerical staff, with expert clinical systems engineers as the facilitators | |||
| Duration | 2 years | |||
| Other | ||||
| Comparator group | Analyses of attendance and admissions data for 1 April 2009 to 31 March 2010 to understand profile of attendance to ED and subsequent profile of admissions into GP specialty | |||
| Outcome measures |
|
|||
| Findings | After the changes there was a fall in bed occupancy, a drop in mortality and no change in readmission rates. Statistical analyses showed that the average bed occupancy fell by 20.4 beds (95% CI –39.6 to –1.2;a p = 0.037) after the intervention. The odds of death in hospital reduced by 12% (OR 0.78, 95% CI 0.61 to 1.00; p = 0.056). The absolute reduction in risk of death before vs. after the intervention was 11.4% – 9.15% = 2.25%, which equates to a number needed to treat of 45 and a 19.7% reduction in risk of mortality. The odds of readmission remained unchanged (OR 0.94, 95% CI 0.75 to 1.18; p = 0.61) at 17.1% vs. 16.3% after the changes. Only cost associated with changes were those required for the improvement effort | |||
| Conclusion | Radically redesigning the system of care for older patients led to reductions in bed occupancy and mortality without adversely affecting the readmission rate or requiring additional resources. Radical redesign offers a promising way to meet the needs of patients within existing resources | |||
| Self-reported limitations | The study did not collect quality-of-care data from case note reviews so any specific aspects of care that changed remain unclear. The study focused on in-hospital mortality, but attention to longer-term mortality is warranted. The study did not undertake a qualitative study of patients’ and carers’ experiences of the changes, although anecdotal evidence was positive. No contemporaneous controlled comparisons with GM units in other hospitals or control wards in the same hospital were carried out | |||
| Headline message | Redesigning the system of care for older emergency patients led to reductions in bed occupancy and mortality without affecting readmission rates or requiring additional resources | |||
| Other comments | No definition of frailty in article but do establish a frailty unit | |||
| Conference abstract | Authors: Ismail et al.98 | Year: 2014 | Country: UK | |
|---|---|---|---|---|
| Study design | Service innovation | |||
| Data source | ED records | |||
| Study aim(s) | To reduce unnecessary admissions from the ED by accessing alterative pathways as appropriate | |||
| Sample size | 534 patients | |||
| Setting | ED in Leeds, UK | |||
| Frail elderly – definition | Medically stable frail older people experiencing a change in physical or cognitive function and/or complex comorbidities | |||
| Study population | Age: not defined | Condition: generally frail | ||
| Intervention | What | Two interface geriatricians provide early CGA by consulting in the ED. Following assessment, patients access appropriate alternative pathway: to admission, intermediate care or early geriatric outpatient review | ||
| Who | Interface geriatricians | |||
| Duration | Service has been running for 1 year | |||
| Other | ||||
| Comparator group | Discharge rates for intervention group are compared with previous ED discharge rates for frail older people | |||
| Outcome measures |
|
|||
| Findings |
|
|||
| Conclusion | Service is avoiding unnecessary admissions with their associated risks and costs. Feedback from ED staff, EDAT and patients has been extremely positive | |||
| Self-reported limitations | Conference abstract so none discussed | |||
| Headline message | Interface geriatricians performing early CGA can reduce unnecessary admissions | |||
| Other comments | Small sample size; no information about the number of frail older people presenting to the ED. Promising but would need to be replicated. Conference abstract so no detailed methodological information | |||
| Conference abstract and full paper | Authors: Aldeen et al.67,68 | Year: 2014 | Country: USA | |
|---|---|---|---|---|
| Study design | Prospective, observational | |||
| Data source | Medical records | |||
| Study aim(s) | The aims of this GEDI project were to develop GEDI nurse liaisons by training ED nurses in geriatric assessment and care co-ordination skills, describe characteristics of patients who these GEDI nurse liaisons see and measure the admission rate of these patients | |||
| Sample size | 408 had consultations; 7213 total older adults in ED, 2124 eligible for GEDI consultation | |||
| Setting | ED | |||
| Frail elderly – definition | Individuals were eligible for GEDI consultation if they had an ISAR score of > 2 or it was requested by the ED clinician | |||
| Study population | Age: ≥ 65 years, mean 79.3 years | Condition: ISAR score of > 2 | ||
| Intervention | What |
GNL An intervention for older adults. GEDI-WISE aims to reduce preventable admissions by assessing non-acute care needs in the ED that are related to the patient’s age The GNL liaises with pharmacy, social work, physical therapy, geriatrics, palliative care and hospice services and advises the ED team and the patients primary care provider. A discharge plan is generated and two follow-up telephone calls are made to assess pain, medication concerns, outpatient appointment status, home health-care status and unexpected visits to health-care settings. Outcomes are noted in the patient’s electronic medical record |
||
| By whom | GNL | |||
| Duration | Not reported, but did result in a longer ED stay | |||
| Other | ||||
| Comparator group | Those not receiving the intervention but who attended the ED during the same time period | |||
| Outcome measures | Inpatient admissions | |||
| Findings | GEDI was associated with 13% fewer admissions overall (16% fewer where Emergency Severity Index = 2). This reduction in inpatient admissions was the result of more discharges rather than more observation stays. Increase in discharges did not lead to an increase in representations | |||
| Conclusion |
Older adults with a high triage acuity score (Emergency Severity Index 2 or 3) who were given the GEDI-WISE intervention were more likely to be discharged from the ED than the control group |
|||
| Self-reported limitations | There is no precisely defined comparison group with which the GEDI cohort can be compared with. That observation admissions were not different between the two cohorts suggests that the two groups were similarA second limitation was that GEDI consultation was associated with a statistically significantly longer median ED LOS (1.1 hour longer)The proportion of individuals undergoing the GEDI-WISE intervention has been small relative to the overall number of older adults in the ED (5.7%) and the number of individuals eligible for the intervention (19.2%) | |||
| Headline message | ED nurses undergoing a 3-month training programme can develop geriatric-specific assessment skills. Implementation of these skills in the ED may be associated with fewer admissions of older adults | |||
| Other comments | ||||
| Full paper | Authors: Jones and Wallis61 | Year: 2013 | Country: UK | |
|---|---|---|---|---|
| Study design | Cohort study | |||
| Data source | ED records. Data collected for all patients seen consecutively during four separate blocks each of 2 months’ duration | |||
| Study aim(s) | To investigate the effectiveness of basing a consultant geriatrician in the ED to facilitate admission prevention for older patients | |||
| Sample size | 848 patients seen by a consultant geriatrician | |||
| Setting | ED in Birmingham Heartlands Hospital | |||
| Frail elderly – definition | No clear definition | |||
| Study population | Age: median 85 years, range 58–105 years | Condition: patients deemed by ED staff to be in definite need of admission or to require involvement of the ED geriatrician in the admission decision. Patients aged < 65 years had relevant condition (e.g. Parkinson’s disease) | ||
| Intervention | What | Consultant geriatrician based in the ED; 5.5 clinical sessions per week. Geriatrician also provided elderly care clinic with multidisciplinary support in the medical day hospital for patients discharged from the ED | ||
| By whom | Consultant geriatrician working in collaboration with a team of occupational therapists and physiotherapists | |||
| Duration | 30 days | |||
| Other | ||||
| Comparator group | No | |||
| Outcome measures |
|
|||
| Findings |
Most patients (804/848, 94.8%) either needed admission or needed review by a geriatrician prior to admission. A minority (44/848, 5.2%) were suitable for discharge but needed geriatrician input prior to discharge. ED geriatrician facilitated discharge of 543/848 patients (64%) and facilitated direct admission to the elderly care ward of 174/305 (57%). Minority of remaining patients were admitted elsewhere The ED geriatrician facilitated discharge from the ED (and potential readmission) in 40/76 cases. These patients had a 7-day reattendance rate of 10.1% [86/848, which is higher than the hospital average (6.3% for the > 75 years age group)]. However, all patients were included regardless of problem or frailty |
|||
| Conclusion | ED based consultant geriatrician can facilitate safe admission prevention and can reduce readmission rates for patients recently discharged. Preventing admission required expansion of outpatient services | |||
| Self-reported limitations | None reported | |||
| Headline message | The placement of a consultant geriatrician in the ED is effective in facilitating admission prevention for older patients | |||
| Other comments |
Data collection was spread throughout the year so would include any seasonal fluctuations. No clear definition of frail elderly No control group |
|||
| Full paper | Authors: Eklud et al.24 | Year: 2013 | Country: Sweden | |
|---|---|---|---|---|
| Study design | Randomised non-blinded controlled trial | |||
| Data source | Representative sample of frail older people at high risk of future health-care consumption | |||
| Study aim(s) | To evaluate the effects of the ‘Continuum of Care for Frail Older People’ on functional ability in terms of ADL and frailty | |||
| Sample size | 161 elderly people (76 control group, 85 intervention group) | |||
| Setting | ED in a Swedish hospital | |||
| Frail elderly – definition | Aged ≥ 80 years or 65–79 years with at least one chronic disease and dependent in at least one ADL | |||
| Study population | Age: ≥ 80 years or 65–79 years if has chronic disease or ADL dependency | Condition: ≥ 80 years or 65–79 years with at least one chronic disease and dependent in at least one ADL | ||
| Intervention | What |
‘Continuum of Care for Frail Older People’ intervention, which involved ‘collaboration between a nurse with geriatric competence at the ED, the hospital wards and a multiprofessional team for care and rehabilitation of older people in the municipality with a case manager as the hub’ Usual care for the control group |
||
| Who | Older people seeking care at the ED of a Swedish hospital | |||
| Duration | Follow-up measured at 3, 6 and 12 months | |||
| Other | ||||
| Comparator group | 76 people acted as the control group and 85 as the intervention group; outcomes were tested for confounders because of possibly relevant differences at baseline between groups | |||
| Outcome measures |
|
|||
| Findings |
3- and 12-month follow-up found that the intervention group had a higher OR for improved degree of ADL independence (OR 2.37) compared with the control group (OR 2.04). At 6 months the older people who had decreased their ADL independence in the intervention group had a lower OR (OR 0.52, 95% CI 0.27 to 0.98) than those in the control group No differences between groups with regard to changes in frailty |
|||
| Conclusion | Intervention could potentially reduce ADL dependencies and enable older people to live at home longer or need less help to remain living at home | |||
| Self-reported limitations |
Non-blinded as participants could reveal their group at follow-up and there was an assumption that there would be less attrition if participants had the same research assistant at the follow-ups ADL staircase has fewer IADL items than other international ADL instruments have, but good validity in this age group Some dropouts, main reason deceased |
|||
| Headline message | A continuum of care intervention could reduce dependency in ADL, enabling frail older people to age in place, benefiting both the individuals and society | |||
| Other comments |
Excluded people with severe illness with immediate needs assessment and treatment, dementia and palliative care Good-quality RCT |
|||
| Full paper | Authors: Arendts et al.78 | Year: 2013 | Country: Australia | |
|---|---|---|---|---|
| Study design | Prospective comparative study with matched controls | |||
| Data source | Prospective | |||
| Study aim(s) | Are older patients who are discharged from the ED with support from allied health professionals (care co-ordination team) at increased risk of hospital readmission and/or death? | |||
| Sample size | 1098 patients enrolled to intervention group and matched 1 : 1 with control subjects deemed low risk on risk screening | |||
| Setting | Tertiary referral hospital EDs in metropolitan Perth. One ED was exclusively an adult ED and trauma centre and the other was a mixed adult–paediatric ED | |||
| Frail elderly – definition | Patients with a positive risk screen from the brief initial screening process applied soon after arrival at the ED by a nurse or member of the CCT | |||
| Study population | Age: ≥ 65 years | Condition: varied | ||
| Intervention | What | Patients aged ≥ 65 years presenting to the ED underwent risk screening. Positive screen led to intervention which was comprehensive functional and needs assessment to detmine needs and discharge risk by the CCT. CCT care included referral to post-discharge services | ||
| By whom | CCT (physiotherapist, occupational therapist or social worker with the option to co-opt other allied health, nursing and medical input as required) | |||
| Duration | Patients were followed up at 28 days and 1 year | |||
| Other | ||||
| Comparator group | Intervention group matched 1 : 1 with control subjects deemed to be of low risk on risk screening | |||
| Outcome measures |
|
|||
| Findings | ‘At 28 days, there was a 3% absolute difference in the reattendance rate to the ED (cases 17.9%, controls 14.8%; p = 0.05) and no mortality difference (cases 1.4%, controls 1.3%; p = 0.85)’. Following up at 1 year, cases did have a higher incidence of unplanned hospitalisation but not death [hospitalisation (43.4% vs. 29.5%; p < 0.001) and death (10.7% vs. 10.2%; p = 0.66)] | |||
| Conclusion | Facilitated discharge of selected older adults by a CCT is relatively safe in the short term. Such patients have an increased likelihood of hospitalisation in the year after discharge | |||
| Self-reported limitations |
Matching of cases and controls did not account for confounding variables The CCT did not operate 24 hours a day and so not all patients in the study period were screened for inclusion Screening tool not externally validated and processes, especially discharge, not standardised. Not all relevant outcome measures were included |
|||
| Headline message | Allied health-facilitated discharge of patients with a positive risk screen is associated with a small increase in the risk of early re-presentation. However, these patients are at markedly increased risk of hospitalisation beyond the early discharge period | |||
| Other comments | ||||
| Full paper | Authors: Tan et al.71 | Year: 2012 | Country: Ireland | |
|---|---|---|---|---|
| Study design | Pilot service development | |||
| Data source | Prospective data | |||
| Study aim(s) | To assess the impact of the introduction of a pilot ED GM liaison service on appropriate discharge and LOS | |||
| Sample size | 285 patients | |||
| Setting | ED in university hospital in Dublin | |||
| Frail elderly – definition | No definition provided | |||
| Study population | Age: ≥ 65 years with multiple medical diagnoses or aged > 80 years | Condition: patients with multiple medical diagnoses, frailty, dementia, delirium, falls, syncope and other common presentations in older adults | ||
| Intervention | What | Patients were referred to the ED GM liaison service by senior ED personnel. Patients were then assessed in the ED by a consultant geriatrician or senior trainee geriatrician and physiotherapy, medical social work and occupational therapy input was available when required. GM service also took over care of all patients aged > 80 years every 1 of 9 days | ||
| By whom | Consultant geriatrician or senior trainee geriatrician | |||
| Duration | Data collected over a period of 2 years and 9 months | |||
| Other | ||||
| Comparator group | No | |||
| Outcome measures |
|
|||
| Findings |
The ED referred 285 patients (mean age 83.5 ± 6.8 years) to the ED GM liaison service 139 patients (49%) were discharged from the ED with appropriate follow-up. The 1-month re-presentation rate to the ED after discharge was 22%, with 8% admitted to hospital on subsequent presentation The remainder [146 (51%)] were admitted under the GIM team on call or other specialist services 268 patients aged > 80 years were taken over from the GIM service every 1 of 9 days. This gave a total of 414 inpatients (mean age 84.6 ± 5.5 years) for analysis. Of these patients, 300 (72%) were admitted under GM, 71 (17%) under GIM and 43 (10%) under other specialist services. Overall, 54 (13%) inpatients died during their admission period. The mean LOS of the patients who died was 20.4 ± 25.6 days Comparison of LOS was carried out for 323 patients discharged alive from the GIM and GM services. The mean LOS of 62 patients discharged from GIM care was 33.5 ± 27.7 days compared with 20.3 ± 25.0 days (p < 0.001) for 261 patients under GM care When LOS analysis excluded patients discharged to a nursing home, mean LOS was 25.0 ± 18.6 days for GIM and 15.2 ± 16.3 days (p < 0.0001) for GM. Mean LOS of a patient admitted from home and discharged to a nursing home was 62.9 ± 35.9 days 23% of patients admitted from home under GIM care were discharged to nursing home care compared with 14% of patients under GM care (p = 0.11) There were 320 patients who were discharged for whom there was 1-month follow-up data and this showed GM readmission was 14.7% and GIM was 19.4% (p = 0.37). The readmission rates did not differ significantly. There was 3-month follow-up data for 301 patients and the readmission rate was 17.4% for GM and 20.3% for GIM (p = 0.59) |
|||
| Conclusion | Direct admission of the older, frail adult under the GM service has the potential to reduce LOS without adversely affecting . . . the rate of ED repeat attendances and readmission to hospital. A substantial proportion of older adults could . . . be discharged from the ED with a tailored treatment and follow-up plan | |||
| Self-reported limitations | The numbers analysed were small, leading to reduced statistical strength of the analysis. The reasons for attendance at the ED were also not recorded as it was decided to concentrate on the collection of basic demographic data, readmissions rates and ED repeat attendances. The future developments for the GM service in this department include formalisation of the ED GM liaison service with GM clinical nurse specialist support; an inpatient nursing home liaison service; and an outreach nursing home liaison service in which patients will be reviewed in their place of residence in the nursing home. The ISAR screening tool, which has good predictive validity for clinical outcomes and health services utilisation in the older adult, will be used to select patients suitable for assessment with the ED GM liaison team | |||
| Headline message | The findings suggest that specialty-specific GM management of the older adult presenting to the ED can improve service and patient outcomes | |||
| Other comments | Lack of detail about methodology. No definition of frailty. No comparator group | |||
| Full paper | Authors: Salvi et al.21 | Year: 2012 | Country: Italy | |
|---|---|---|---|---|
| Study design | Prospective observational study with 6 months’ follow-up | |||
| Data source | Hospital records | |||
| Study aim(s) | The aim of this study was to compare the ISAR tool and TRST | |||
| Sample size | 2057 | |||
| Setting | ED in a geriatric hospital | |||
| Frail elderly – definition | ||||
| Study population | Age: ≥ 65 years, mean age 81.7 years, range 65–103 years | Condition: an ISAR score of ≥ 2 (range 0–6) suggests an increased risk for functional decline, repeat ED visits, hospital admissions, institutionalisation and death within 6 months after an ED visit | ||
| Intervention | What | ISAR tool and TRST | ||
| By whom | Nurse | |||
| Duration | Not reported | |||
| Other | ||||
| Comparator group | None | |||
| Outcome measures | Hospital admission and mortality at the index ED access, early (within 30 days) and late ED revisit, hospitalisation and death in 6 months | |||
| Findings |
TRST and ISAR were significantly correlated in terms of predicting hospital admission, mortality and early ED revisit (ISAR 0.68; TRST 0.66), (ISAR 0.74; TRST 0.68), (ISAR 0.63; TRST 0.61) Long term, using 6-month follow-up data, patients had comparable ED return visits (ISAR 0.60; TRST 0.59), hospital admission (ISAR 0.63; TRST 0.60) and mortality (ISAR 0.74; TRST 0.73) |
|||
| Conclusion | ISAR and TRST are comparable in terms of selecting elderly ED patients who need geriatric interventions. ISAR had slightly higher sensitivity and lower specificity | |||
| Self-reported limitations | Under-representation of trauma patients. Exclusion of night time arrivals. This specific ED was unique in its characteristics therefore limiting generalisability. Triage nurse scored both ISAR and TRST. No data on inter-rater reliability. Some relevant outcomes such as functional status/delirium were not included | |||
| Headline message |
Both tools appeared positive in the majority of patients, indicating that the tools lacked specificity |
|||
| Other comments | ||||
| Full paper | Authors: Salvi et al.27 | Year: 2012 | Country: Italy | |
|---|---|---|---|---|
| Study design | Prospective observational study | |||
| Data source | Secondary analysis of prospective observational cohort study | |||
| Study aim(s) | To test the validity of the ISAR screening tool by testing whether or not a CGA-based approach using the ISAR tool was associated with the brief DAI of frailty | |||
| Sample size | 200 | |||
| Setting | Two urban EDs in Italy | |||
| Frail elderly – definition | Frail subjects were defined as those in need of mobility or ADL assistance and/or who were cognitively impaired | |||
| Study population | Age: ≥ 65 years, mean age 80.3 ± 7.4 years, 28.5% aged > 85 years | Condition: not given | ||
| Intervention | What | The ISAR tool was administered following triage to patients (or accompanying family member if patients were cognitively impaired or acutely confused). During the ED visit patients also underwent BGA using the Charlson index for comorbidity, the SPMSQ for cognitive function and the Katz ADL scale | ||
| Who | Trained research assistant | |||
| Duration | Follow-up telephone interviews at 30 days and 6 months to collect data on current Katz ADL dependence, number of ED visits, hospital admissions and mortality | |||
| Other | Not applicable | |||
| Comparator group | No data are available for excluded patients, non-screened patients or patients who refused to participate | |||
| Outcome measures |
|
|||
| Findings |
Consistency of DAI-based frailty definition was tested by verifying the proportion of subjects according to frailty status who had experienced any adverse outcomes (30 days and 6 months) since ED discharge Frail patients experienced more ED revisits within 30 days and 6 months and were more likely to undergo hospital admissions than non-frail patients Frail patients did not have an increased risk of functional decline within 6 months after an ED presentation after adjusting for age, sex and living status Occurrence of a combined outcome of ED revisit, hospital admission, functional decline or death within 6 months was significantly more frequent in frail patients The 6-month mortality rate for frail elderly ED patients was higher than for non-frail patients (hazard ratio 8.68, 95% CI 2.60 to 28.94; p < 0.0001) ISAR score was highly correlated with frailty: the AUC was 0.92 (95% CI 0.88 to 0.96), indicating good performance in identifying frailty according to the DAI-based definition An ISAR cut-off score of 2 had a sensitivity of 0.94 (95% CI 0.88 to 0.97) and specificity of 0.63 (95% CI 0.51 to 0.73) Using a cut-off score of 3 allowed for stricter selection of frail patients: sensitivity was 0.79 (95% CI 0.71 to 0.86) and specificity was 0.93 (95% CI 0.84 to 0.97) |
|||
| Conclusion | The ISAR score is a reliable and valid predictor of death, ED revisit, hospital admissions and functional detail in the 6 months after an ED visit in a complex ED population such as the elderly. The ISAR tool can identify high-risk patients who are more likely to benefit from an integrated clinical approach, longer observation time and appropriate referrals | |||
| Self-reported limitations | ‘Choice of a simple DAI-based definition of frailty’ ‘post hoc analysis of a previously carried out study, therefore the choice of using the Rockwood criteria of frailty was formulated using the available data’. Sample limited to weekday/daytime ED arrival (n = 200). Data were in line with Hastings et al.202 on frailty. Generalisability may be limited due to the setting (two Italian cities) | |||
| Headline message | The ISAR tool is a useful screening tool for frailty and identifies elderly patients at risk of adverse outcomes after an ED visit. The ISAR tool can also be used to select high-risk patients who are more likely to benefit from a geriatric approach or intervention | |||
| Other comments | Small sample, applicability, no data for excluded non-screened patients or for patients who refused to participate | |||
| Full paper and conference abstract | Authors: Graf et al.53,54 | Year: 2012 | Country: Switzerland | |
|---|---|---|---|---|
| Study design | Retrospective cohort study | |||
| Data source | Review of patient records | |||
| Study aim(s) | To assess the ability of two screening tools to predict readmissions after an ED visit in patients aged ≥ 75 years | |||
| Sample size | 375 | |||
| Setting | ED of Geneva University Hospitals, Switzerland | |||
| Frail elderly – definition | Patients aged ≥ 75 years seen by the geriatrics team in the ED | |||
| Study population | Age: mean 84 years (SD 5.7 years) | Condition: orthopaedic problem or trauma (30%), cardiac problem (25%), psychiatric illness (12%) | ||
| Intervention | What | Screening with the ISAR tool, modified ISAR tool and TRST | ||
| By whom | Geriatrics team physician | |||
| Duration | Not provided | |||
| Other | Patients seen between 2007 and 2009 | |||
| Comparator group | N/A | |||
| Outcome measures | Accuracy of screening tools for predicting unplanned readmission at 1, 3, 6 and 12 months | |||
| Findings | The ISAR tool, modified ISAR tool, TRST and a multiple regression model derived from them had similar power to predict readmissions at 1, 3, 6 and 12 months (area under the ROC curve between 0.6 and 0.7). Negative predictive values at 1 month were 89.1% for the ISAR tool and 83.6% for the TRST | |||
| Conclusion | The screening tools studied have limited power to predict readmission risk. They may be useful for avoiding unnecessary interventions in people who screen negative because of their high negative predictive value | |||
| Self-reported limitations | Single-centre study, limited to patients triaged as non-urgent; retrospective data collection | |||
| Headline message | The screening tools may be useful for identifying older patients who can be discharged from the ED without further geriatric evaluation, thus avoiding unnecessary CGA | |||
| Other comments | ||||
| Full paper | Authors: Leah and Adams72 | Year: 2010 | Country: UK | |
|---|---|---|---|---|
| Study design | Descriptive paper | |||
| Data source | Patient records | |||
| Study aim(s) | This article describes the establishment of an ATOP created to address the issues related to providing optimum care for those with complex health and social needs in a district general hospital | |||
| Sample size | 666 | |||
| Setting | ED | |||
| Frail elderly – definition |
The frailty markers were developed locally using the Urgent Care Pathways for Older People with Complex Needs,203 The Older Person in the Accident and Emergency Department204 and the Comprehensive Assessment for the Older Frail Patient205 Frailty markers (two or more) |
|||
| Study population | Age: ranged from 60 to 103 years | Condition: older people attending an ED | ||
| Intervention | What | An ATOP was established in the ED and medical assessment unit at a district general hospital. The focus of the team was to provide CGA. Access to the ATOP was based on a combination of age and needs. ATOP based on Reforming Emergency Care,206 to provide an ‘accessible, patient-centred, integrated, high-quality service delivered without delay or loss of dignity’. Patients screened in the ED/MAU by a member of the ATOP. If patients screen positive for frailty markers they are assessed in a different environment to the ED. Care planning involves patients (and where appropriate, carers). Care planning involves staff within and outside hospital. Nursing assessment and mental health assessments also carried out. Swallow assessments and mobility assessments can be carried out by nurses | ||
| By whom | The ATOP team consists of a physician, a consultant nurse, five clinical nurse specialists, a senior social worker and assistant, a senior occupational therapist and assistant and a health-care assistant | |||
| Duration | Not described | |||
| Other | ||||
| Comparator group | None | |||
| Outcome measures |
|
|||
| Findings | The ATOP prevented admission for 178/666 patients (27%) who other clinicians had decided to admit (either for medical reasons or because they were unsafe to discharge home). Of these 178, 19 reattended and six were admitted (readmissions due to falls and cognitive impairment). ‘As the cost of ‘hotel services’ alone in the hospital is estimated to be £600 per day, the potential cost saving from preventing the admission of the 89 patients aged ≥ 80 years seen in the study period could be > £500,000’ | |||
| Conclusion | In the 4 months of the study period, the ATOP prevented admission of 178 of the 666 patients seen. Of the 178 patients who were not initially admitted to hospital, 19 reattended the hospital and six were admitted. The majority of readmissions were as a result of recurrent falls and issues relating to cognitive impairment. Four patients returned with significant new, but unrelated, health problems, whereas five patients who had chosen to return home against advice also reattended | |||
| Self-reported limitations | The actual cost saving is difficult to establish, as the ATOP may have made extra referrals that would have to be set against this potential saving | |||
| Headline message | A dedicated team with a focus on the needs of frail older adults has proved to be a beneficial addition . . . A more comprehensive assessment process has been successful in preventing some admissions, with consequent improvement in outcomes, a probable financial saving for the trust and quality-of-life benefits for patients | |||
| Other comments | Not an effectiveness study – no comparison group | |||
| Full paper | Authors: Salvi et al.49 | Year: 2009 | Country: Italy | |
|---|---|---|---|---|
| Study design | Prospective observational study | |||
| Data source | Hospital records | |||
| Study aim(s) | This study evaluated the predictive validity of the ISAR tool for elderly patients presenting to an Italian ED | |||
| Sample size | 200 | |||
| Setting | Two urban EDs | |||
| Frail elderly – definition | Acutely ill ED patients aged ≥ 65 years | |||
| Study population | Age: 80.3 years (SD 7.4 years) | Condition: not given | ||
| Intervention | What | ISAR screening tool – assesses risk factors predisposing elderly ED patients to adverse outcomes | ||
| By whom | Nurse | |||
| Duration | Not reported | |||
| Other | ||||
| Comparator group | None | |||
| Outcome measures |
Single outcomes: ED revisit at 30 days and 6 months, frequent ED return, hospital admission and functional decline Composite outcomes: (1) death, long-term care placement, functional decline; (2) death, long-term care placement, functional decline plus any ED revisit or hospitalisation |
|||
| Findings |
The ISAR screen was positive for 141 subjects (70.5%), who had high comorbidity, disability and cognitive impairment ISAR-positive patients had an OR of 4.77 (95% CI 2.19 to 10.42) for undergoing the composite outcome and 3.46 (95% CI 1.68 to 7.15) for experiencing the composite outcome The ISAR tool also predicted ED revisit and frequent use, hospitalisation and functional decline at 6 months and was an independent predictor of 6-month mortality (hazard ratio 6.9, 95% CI 1.65 to 29; p = 0.008) |
|||
| Conclusion | The ISAR tool can be used as a screening test to identify Italian elderly ED patients who have an increased 6-month risk of death, long-term condition placement, functional decline, ED revisit or hospitalisation | |||
| Self-reported limitations | Weekday/daytime convenience sample. Small sample size (200 patients). Limited generalisability (academic EDs located in cities with a lower prevalence of older people or without a GED). Sample size/admission rate at the index ED visit prevented analysis of the performance of the ISAR tool separately | |||
| Headline message | The ISAR tool was confirmed as a reliable and valid predictor of death, long-term condition placement, functional decline, ED revisit or hospital admission during the 6 months after an ED visit. The ISAR tool can be administered by a nurse immediately after triage without any further workload for ED staff. It can indicate high-risk patients who would benefit from an integrated approach, longer observation time and appropriate referral | |||
| Other comments | ||||
| Full paper | Authors: Salvi et al.90 | Year: 2008 | Country: Italy | |
|---|---|---|---|---|
| Study design | Secondary analysis of a prospective observational cohort study | |||
| Data source | ||||
| Study aim(s) | To consider patterns of use for a geriatric emergency service for acutely ill elderly patients compared with a conventional ED in Italy | |||
| Sample size | 200 acutely ill ED patients aged ≥ 65 years from two EDs (CED and GED) | |||
| Setting | A CED and a GED. The CED was in a tertiary care academic hospital. The GED was a hybridised ED with a six-bed observation unit designed for elderly non-trauma patients within an academic-affiliated hospital | |||
| Frail elderly – definition | Frail as suggested by high levels of comorbidity, disability and cognitive impairment | |||
| Study population | Age: ≥ 65 years | Condition: not given | ||
| Intervention | What | GED – ED department staffed by geriatricians for elderly non-trauma patients | ||
| By whom | Geriatricians | |||
| Duration | 30-day and 6-month follow-up telephone interviews were conducted with patients | |||
| Other | ||||
| Comparator group | Patients from a CED | |||
| Outcome measures |
Early (within 30 days) and late (within 6 months) unscheduled ED revisit Frequent ED return 6-month mortality Hospital admission within 6 months 6-month functional decline |
|||
| Findings |
Patient mean age 80.3 ± 7.4 years (28.5% were aged ≥ 85 years) There was no significant difference between patients seen in the GED in terms of triage, comorbidity, admission at time of enrolment, ICU admissions and length of in-hospital stay (although they were older and medically and socially frailer) ED setting was not associated with early, late and frequent ED return rates, hospitalisation or functional decline. Although GED patients tended to be more frail, mortality rates did not differ significantly between the EDs |
|||
| Conclusion | The data suggests a slight superiority for the GED in the acute care of older people, supporting the hypothesis that ED facilities specially designed for older adults may provide better care | |||
| Self-reported limitations | The fact that the INRCA hospital, unlike Azienda Ospedali Riuniti, lacked a resuscitation ward may have introduced a first pre-ED selection bias. Another limitation may be that the study included a convenience sample of 200 elderly ED patients and patients too ill to collaborate and those with cognitive impairment and no available informant were excluded. ‘Nonetheless, the rate of urgent visits in the sample was higher than that in the general Italian ED population (25.5% vs. 8.4%) and was similar in the two EDs, suggesting that the sample was representative of elderly ED patients. Elderly patients are known to use EDs appropriately, because emergent and urgent visits are more frequent than semi-urgent and non-urgent ones‘. Trauma patients were not included. This is a secondary analysis of data therefore the design of the study could be improved | |||
| Headline message | A GED staffed by geriatricians and organised to meet the needs of older patients showed slight superiority, suggesting a benefit of specially designing care for older adults | |||
| Other comments | ||||
| Full paper | Authors: Lee et al.52 | Year: 2008 | Country: Canada | |
|---|---|---|---|---|
| Study design | Prospective, observational study with 1 year of follow-up | |||
| Data source | Medical records | |||
| Study aim(s) | Predictive validity of the TRST to identify return to the ED (high-risk patients) or hospitalisation at discharge at 30, 120 and 365 days. To determine whether different TRST cut-off points to define high-risk patients or whether or not there were different explanatory variables | |||
| Sample size | 788 | |||
| Setting | EDs of three hospitals in Toronto, Canada | |||
| Frail elderly – definition | ||||
| Study population | Age: range 65–101 (mean 76.6) years | Condition: not given | ||
| Intervention | What | TRST identifies older patients at risk for ‘failed’ discharge home from the ED (failed discharge is return to the ED, admission to the hospital or admission to a nursing home within 30–120 days after discharge). The five TRST items are:
|
||
| By whom | Emergency nurse or a patient care co-ordinator | |||
| Duration | 2–5 minutes | |||
| Other | ||||
| Comparator group | None | |||
| Outcome measures | Return to the ED or admission to hospital (within 30, 120 and 365 days after discharge from the ED) | |||
| Findings | 147/788 subjects (18.7%) reached the composite endpoint in 30 days, 245 (31.1%) by 120 days and 346 (43.9%) by 365 days. Mean TRST score was 1.55 (range 0–5). Sensitivity of a TRST score of ≥ 2 was 62% (95% CI 54% to 70%), specificity was 57% (95% CI 53% to 61%) and likelihood ratio was 1.44 (95% CI 1.23 to 1.66). The AUC was 0.61 using a cut-off score of 2 | |||
| Conclusion | The TRST demonstrated only moderate predictive ability and, ideally, a better prediction rule should be sought. Future studies to develop better prediction rules should compare their performance with that of existing prediction rules, including the TRST and ISAR tool, and assess the effect of any new prediction rule on patient outcomes | |||
| Self-reported limitations | TRST forms were completed for 49% of eligible patients, therefore selection bias was possible. This study did not include patients who were admitted to nursing homes after ED discharge. Staff were not blinded to TRST result when making post discharge referrals. Patients who experienced the study outcomes but who returned to another institution may have been missed. It was not established whether or not return ED visits were planned at the time of discharge | |||
| Headline message | The TRST demonstrated only moderate predictive ability and, ideally, a better prediction rule should be sought | |||
| Other comments | ||||
| Full paper | Author: Warburton114 | Year: 2005 | Country: USA | |
|---|---|---|---|---|
| Study design |
Evaluation Quality improvement project with nine Plan–Do–Study–Act cycles in 15 months to assess the Elder Alert screening and referral programme. Outcomes assessed by comparing patient subgroups based on risk status and interventions received. Cost and benefits assessed based on estimated programme outcomes and average costs |
|||
| Data source | The full evaluation of Elder Alert has six components:
|
|||
| Study aim(s) | The purpose of this article was to report preliminary outcome and cost–benefit results for a patient safety quality improvement programme intended to improve outcomes for patients aged ≥ 75 years visiting the ED. The programme uses the ISAR tool to screen and refers patients at high risk for appropriate intervention | |||
| Sample size | 277 | |||
| Setting | Community hospital ED | |||
| Frail elderly – definition | None | |||
| Study population | Age: patients aged ≥ 75 years visiting the ED | Condition: not given | ||
| Intervention | What | ISAR plus intervention | ||
| By whom | ED staff | |||
| Duration | Not reported | |||
| Other | ||||
| Comparator group | 150 who were not screened | |||
| Outcome measures | Outcomes within 30 days of the end of the index care episode (discharged from ED or from hospital if admitted) were compared for the four patient groups (not screened, high risk, screened and receiving all intended services and risk). Outcomes were:
|
|||
| Findings |
Screening tool appears to be accurate – outcomes better for patients screened as low risk than patients not screened (even though the ‘not screened’ group has younger/low risk patients). Referrals have a positive impact – outcomes for patients screened as high risk and receiving complete referrals are better than for patients screened as high risk and receiving partial or no referrals. Screening on its own has a negative effect (worse outcomes for high risk patients receiving no intervention) Using audit data, authors estimated the value of saved visits and days as a result of the Elder alert intervention. Assuming that all eligible patients were screened and all high-risk patients received referrals |
|||
| Conclusion | When completed, screening and referral slightly reduce LOS (for patients admitted at the index ED visit) and reduce returns to the ED and admissions to hospital within 30 days | |||
| Self-reported limitations | None reported | |||
| Headline message | Not all eligible patients were screened and referred however there is evidence that the Elder Alert intervention has a positive outcome on LOS. Low programme costs meant the programme had net benefits. ‘The methods for improvement (the Plan–Do–Study–Act framework; process evaluation; multidisciplinary working; group meetings; outcome assessment) are practical and useful for improving quality and safety in a small community hospital with limited resources’ | |||
| Other comments | ||||
| Full paper and conference abstract | Author: Schoenenberger22,33 | Years: 2013, 2014 | Country: Switzerland | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study design | Prospective controlled study: pre–post design, consecutively presenting patients | |||||||||||||||
| Data source | Original EGS forms and ED discharge reports | |||||||||||||||
| Study aim(s) | To evaluate feasibility of a ‘novel multidimensional EGS tool’ to detect geriatric problems in an ED setting. Study aims were to
|
|||||||||||||||
| Sample size | 338 | |||||||||||||||
| Setting | University hospital ED | |||||||||||||||
| Frail elderly – definition | Not reported | |||||||||||||||
| Study population | Age: ED patients aged ≥ 75 years throughout a 4-month period |
Condition: Main condition leading to ED visitControl, n (%)Screening, n (%)Cardiovascular179 (23.8)188 (23.6)Infectious disease136 (18.1)142 (17.9)Other conditions437 (58.1)465 (58.5) |
Main condition leading to ED visit | Control, n (%) | Screening, n (%) | Cardiovascular | 179 (23.8) | 188 (23.6) | Infectious disease | 136 (18.1) | 142 (17.9) | Other conditions | 437 (58.1) | 465 (58.5) | ||
| Main condition leading to ED visit | Control, n (%) | Screening, n (%) | ||||||||||||||
| Cardiovascular | 179 (23.8) | 188 (23.6) | ||||||||||||||
| Infectious disease | 136 (18.1) | 142 (17.9) | ||||||||||||||
| Other conditions | 437 (58.1) | 465 (58.5) | ||||||||||||||
| Intervention | What | The EGS contains four domains relevant for older ED patients: cognition, falls, mobility and ADL. For each, short validated instruments were selected:
|
||||||||||||||
| By whom | ED physicians | |||||||||||||||
| Duration | < 5 minutes | |||||||||||||||
| Other | 457 patients did not receive EGS and were excluded from the per-protocol analysis (175 for clinical reasons and 282 for logistical reasons) | |||||||||||||||
| Comparator group | Usual care (no geriatric screening/risk prediction tools) | |||||||||||||||
| Outcome measures |
The number of abnormal EGS findings The number of EGS-related diagnoses on the ED discharge reports during screening in comparison with the preceding control period |
|||||||||||||||
| Findings | EGS was performed on 338 (42.5%) of 795 patients presenting during screening and took < 5 minutes to perform in most (85.8%) cases. Of the 338 screened patients, 285 (84.3%) had at least one abnormal EGS finding. In 270 of these patients, at least one abnormal EGS finding did not result in a diagnosis in the EDThere were statistically significant increases in the number of patients with EGS-related diagnoses on ED discharge reports during screening . . . 142 (42.0%) of the 338 screened patients had at least one diagnosis listed within the four EGS domains, significantly more than the 29.3% of patients presenting during the control periodPatients with three or four abnormal EGS findings were more frequently admitted from the ED to an inpatient unit than patients with two or fewer abnormal EGS findings (OR 2.68, 95% CI 1.65 to 4.35; p = 001). EGS predicted nursing home admission after the in-hospital stay (OR for ≥ 3 vs. < 3 abnormal domains 12.13, 95% CI 2.79 to 52.72; p = 0.001) | |||||||||||||||
| Conclusion | This new EGS was demonstrated to be feasible in the ED setting, to identify geriatric problems not previously identified and to predict future care. The study does not demonstrate that geriatric screening in the ED ultimately improves patient outcomes | |||||||||||||||
| Self-reported limitations | The non-randomised pre–post design limited the comparability of the screening and control groups. Generalisability is limited as the EGS was only tested in one centre. Tester reliability was not assessed | |||||||||||||||
| Headline message | The novel EGS is feasible, identifies previously undetected geriatric problems and predicts determinants of subsequent care | |||||||||||||||
| Other comments | Claims to be feasible but was not used in 282 cases for logistical reasons | |||||||||||||||
| Full paper and conference abstract | Author: Boyd29,30 | Years: 2007, 2008 | Country: New Zealand | |
|---|---|---|---|---|
| Study design | Cross-sectional study | |||
| Data source | Assessment forms | |||
| Study aim(s) | To test the ability of the BRIGHT to identify older ED patients with functional and physical impairment by comparing results from the BRIGHT with a CGA undertaken within 10 days of their index visit to the ED | |||
| Sample size | 139 | |||
| Setting | ED in an acute care hospital | |||
| Frail elderly – definition | Not given | |||
| Study population | Age: ≥ 75 years (65 years for Maori and Pasifika elders), mean age 82.5 years | Condition: presenting to the ED with a non-urgent complaint (triage level 3–5) during a convenience sample of 4-hour time blocks over a 12-week period | ||
| Intervention | What | BRIGHT is a self-report tool (patients or carers) comparable with other tools such as the interRAI MDS-HC (interRAI MDS-HC requires staff input.) BRIGHT includes: help with bathing, personal hygiene, dressing the lower body, getting around indoors, difficulty making decisions about everyday activity, shortness of breath, recent falls, perception of general health, memory problems, ability to do ordinary housework and depression | ||
| By whom | Self-administered or with assistance from untrained caregivers or family members | |||
| Duration | Not reported | |||
| Other | ||||
| Comparator group | Results from the BRIGHT were compared with those of a CGA conducted using the interRAI MDS-HC or the interRAI-AC (acute care). After participants’ ED visit, trained assessors (n = 6) conducted a CGA either in the hospital or in the home. The assessors were blinded to participants’ BRIGHT score | |||
| Outcome measures | Primary outcome measures were IADL, CPS and ADL. ROC curves and likelihood ratios were also used to identify an optimal BRIGHT cut-off score | |||
| Findings |
Most (75%) patients did not complete the BRIGHT themselves (assisstance from visitor/staff). CGA was completed for 114 (82%) participants; the average time between the BRIGHT screen and the interRAI full assessment was 3.98 days (SD 4.23 days) For predicting IADL deficit, sensitivity was 0.76 and specificity was 0.79 (cut-off score of ≥ 3) and the area under the ROC was 0.83 (95% CI 0.74 to 0.91). For predicting cognitive performance, sensitivity was 0.70 and specificity was 0.74 (cut-off score of ≥ 4) and the area under the ROC was 0.73 (95% CI 0.62 to 0.84). Both of these results indicated moderate accuracyPositive likelihood ratios for the three outcomes of interest were 3.6, 1.7 and 1.8, respectively. Negative likelihood ratios were 0.3, 0.4 and 0.3, respectively |
|||
| Conclusion | The BRIGHT demonstrated a reasonable ability to identify functional issues in older adults presenting to the ED. This case-finding tool was designed to be used in combination with the interRAI assessment system and to be quickly and efficiently self-administered by older adults or their family caregivers | |||
| Self-reported limitations |
This study was conducted in a single ED with a small sample size 18% of those who completed the BRIGHT were lost to follow-up for the CGA |
|||
| Headline message | The 11-item BRIGHT successfully identifies older adults in the ED with decreased function and may be useful in differentiating elder patients in need of comprehensive assessment | |||
| Other comments | ||||
| Full paper | Author: Ngian73 | Year: 2008 | Country: Australia | |
|---|---|---|---|---|
| Study design | Retrospective observational study | |||
| Data source | ASET electronic databases | |||
| Study aim(s) | To review discordant cases between the ED and the ASET (i.e. where elderly patients deemed for discharge by the ED were subsequently admitted following ASET review). These cases were examined with regard to clinical outcomes. ASET contribution was also reviewed with respect to assessment of cognitive, functional and mobility status as compared with that undertaken in the ED | |||
| Sample size | 1680 referrals were made to ASET; 103 (6.1%) were identified as discordant cases | |||
| Setting | ED | |||
| Frail elderly – definition | Patients needed to fulfil two out of five of the following criteria for ASET referral:
|
|||
| Study population | Age: 83 (± 6.5) years | Condition: the three most commonly reported comorbidities were hypertension (56%), osteoporosis (38%) and ischaemic heart disease (37%) | ||
| Intervention | What | ASET service which is led by doctors. Older patients are assessed by a geriatric team, having been initially assessed by the ED as suitable for discharge. ASET established in order to reduce missed diagnoses, prevent inappropriate discharge and prevent re-presentation of elderly ED attendees | ||
| By whom | ASET consists of an on-call senior geriatrician supervising a geriatric medicine trainee based solely in the ED. The service is supported by on-site nursing and an allied health team comprising a physiotherapist, occupational therapist and social worker | |||
| Duration | Study duration: 30 months | |||
| Other | ||||
| Comparator group | No | |||
| Outcome measures | Clinical outcomes of patients who were deemed safe for discharge but were subsequently admitted | |||
| Findings | There were 65 cases (63.1%) where ASET made additional acute medical diagnoses in referred patients - these were fractures (14%), complicated urinary tract infections (13%), cardiovascular disorders (15%), neurological diseases (16%), delirium (8%) and adverse drug reactions (6%). The average LOS was 14.6 days (range 1–51 days). Eighty four patients (81.5%) were admitted for acute care, with 19 (18.5%) requiring subacute care). 84% of patients were discharged to their usual residence and 15% required new residential care. One patient died | |||
| Conclusion |
Assessment of elderly patients by ASET yielded additional information on functional, mobility and cognitive issues, which were overlooked by the ED. ASET staff were more likely than the ED to document functional, cognitive and mobility impairment, either new or worsening ASET was able to prevent 6.1% of inappropriate discharges from the ED |
|||
| Self-reported limitations | Limitations include that the study audited only those patients who were subsequently admitted from the ED. The study did not follow up patients who were discharged following the ASET review | |||
| Headline message | A physician-led ASET can complement and improve the current ED-based system of evaluating elderly patients, providing a more comprehensive medical assessment incorporating patients’ cognitive, mobility and functional status and preventing inappropriate discharges | |||
| Other comments | ||||
| Full paper | Authors: Foo et al.112 | Year: 2014 | Country: Singapore | |
|---|---|---|---|---|
| Study design | Quasi-RCT | |||
| Data source | Screening tool scores and hospital records | |||
| Study aim(s) | Does risk stratification followed by rapid geriatric screening in an ED reduce patient outcomes of functional decline, ED reattendance and hospitalisation? | |||
| Sample size | 780 (500 control and 280 intervention group patients) (1156 were eligible) | |||
| Setting | ED of a 1500-bed acute care public hospital in Singapore | |||
| Frail elderly – definition | See below | |||
| Study population | Age: the eligibility criteria for inclusion in the study were
|
Condition: not known | ||
| Intervention | What |
TRST to risk stratify, followed by rapid geriatric screening and intervention for at-risk seniors Patients were assessed by the GEM nurse while still in the ED, prior to discharge. Nurse undertook focused geriatric screening (15-question screening form including cognition, mood, continence, visual acuity and hearing, mobility and social issues). In addition, the GEM nurses undertook medication reconciliation and measurement of postural blood pressure With the results of the screening, clinically significant findings were dealt with immediately. Referrals were made including to allied health professionals or to other services. Education and advice were given on discharge. Patients were followed up at 3, 6, 9 and 12 months to ascertain their BADL and IADL scores. Subsequent ED attendance and hospitalisation rates were recorded |
||
| By whom | Nurse | |||
| Duration | 15–30 minutes | |||
| Other | ||||
| Comparator group | Standard care | |||
| Outcome measures | The primary outcome of the study was change in patients’ functional status, measured using BADL and Lawton’s IADL scores. The secondary outcomes were health-care utilisation, as measured by ED reattendance and rehospitalisation | |||
| Findings |
Comparing control and intervention groups the intervention group had higher TRST scores (34.3% vs. 25.4% TRST ≥ 3; p = 0.01) and lower baseline IADL scores (22.84 vs. 24.18; p < 0.01). The most frequent findings were fall risk (65.0%), visual impairment (61.4%) and improper footwear (58.2%) Most of the intervention group had unmet needs (82.9%) but only 62.1% accepted the intervention – 28.2% referred to geriatric clinic and 11.8% admitted Over 80% of patients from both intervention and control groups completed follow up and after adjusting for TRST and baseline IADL scores, the intervention group had significant preservation in function (basic ADL −0.99 vs. –0.24, p < 0.01; IADL –2.57 vs. 0.45, p < 0.01) at 12 months. Reductions in ED reattendance and hospitalisation were not significant BADL scores for both control and intervention group deteriorated over 12 months. IADL scores for the control group also deteriorated over 12 months, the scores for patients in the intervention group actually improved and the difference was statistically significant (0.45 vs. –2.57; p < 0.01) |
|||
| Conclusion | This method of screening was feasible and effective and resulted in positive outcomes through ‘significant and sustained preservation of function over 12 months’ | |||
| Self-reported limitations | A large number of patients who were randomized to the intervention group were unwilling to participate in the intervention. Staff who did the patient follow up were not blinded to allocation group. Data were not collected on patient views of the GEM nurse screening in the ED | |||
| Headline message | Risk stratification and focused geriatric screening in the ED resulted in significant preservation of patients’ function at 12 months. Multidisciplinary assessment as well as strong interdisciplinary collaboration are key components of an effective geriatric emergency service | |||
| Other comments | ||||
| Letter | Authors: Pareja-Sierra et al.87 | Year: 2013 | Country: Spain | |
|---|---|---|---|---|
| Study design | Data analysis (6 years, 2005–11) | |||
| Data source | Not clear if data are prospective or retrospective | |||
| Study aim(s) | To determine the impact on admissions and LOS of an EDOU for elderly adults | |||
| Sample size | 5571 patients admitted to the ED | |||
| Setting | EDOU in a tertiary care urban hospital in Guadalajara, Spain. The EDOU has six beds and is visited by a geriatrician twice a day | |||
| Frail elderly – definition | Aged ≥ 75 years with multiple comorbidities, dementia or physical impairment with acute illness that can be treated in < 72 hours. Admission to the unit was at the discretion of the emergency physician | |||
| Study population | Age: ≥ 75 years, mean age 87.4 years | Multiple comorbidities, dementia or physical impairment with acute illness that can be treated in < 72 hours. Most had moderate to severe physical disability (70%) and mild to moderate cognitive impairment (70%) measured using the Barthel Index and Geriatric Dementia Scale | ||
| Intervention | What | EDOU for elderly adults visited by the geriatrician twice daily, multidimensional geriatric assessment with individualised treatment, referring patients to different outpatient levels of the geriatric service and avoiding unnecessary hospital admissions and avoiding discharge of frail elderly adults without follow-up care | ||
| By whom | Geriatrician | |||
| Duration | 6 years | |||
| Other | Admission to the unit was at the discretion of the emergency physician | |||
| Comparator group | Comparison with data before the EDOU was implemented | |||
| Outcome measures |
|
|||
| Findings | The percentage of individuals requiring admission to the geriatric ward has stabilised initial increase; this has been accompanied by a decrease in mean LOS from 9.9 days in 2006 to 7.6 days in 2011 | |||
| Conclusion | Development and implementation of a geriatric observation unit in the ED for individuals aged ≥ 75 years with a geriatrician on call was effective at preventing admission to the hospital in a large percentage of elderly adults. There was also a decrease in mean LOS | |||
| Self-reported limitations | Other factors could be involved such as better qualification of nursing home medical staff or easier access to geriatric clinics in case of destabilisation or chronic illness | |||
| Headline message | Specialised geriatric assessment in the EDOU provides higher-quality health care, minimising the deleterious effects of hospitalisation in older adults and optimising the use of resources | |||
| Other comments | Very little detail on methodology | |||
| Conference abstract | Authors: Yim et al.25 | Year: 2011 | Country: Hong Kong | |
|---|---|---|---|---|
| Study design | Cohort study | |||
| Data source | Telephone interview for the cohort study; not reported for the RCT | |||
| Study aim(s) | To derive and validate a Hong Kong version of the ISAR screening tool and to use the validated tool to identify people at risk and study the effects of a structured ED intervention | |||
| Sample size | Cohort study 1820; RCT 1279 | |||
| Setting | Three EDs in Hong Kong | |||
| Frail elderly – definition | People identified as high risk based on positive answers to two or more of the six items of the Hong Kong ISAR tool | |||
| Study population | Age: derivation cohort mean 74.5 years (SD 6.2 years); RCT: 75 years (SD 6.8 years) for the control group and 76.3 years (SD 6.8 years) for the intervention group | Condition (additional to frailty): patients aged ≥ 65 years who were about to be discharged from the ED | ||
| Intervention | What | Administration of the validated Hong Kong ISAR tool followed by a structured ED intervention for those identified as high risk (scoring two or more out of six possible positive answers). The intervention consisted of a brief standardised assessment of functional status, mental state and relevant social factors. Referrals to community-based clinics and other agencies were arranged according to individual needs | ||
| By whom | Not specifically reported (presumably researchers) | |||
| Duration | Outcomes measured at 6 months | |||
| Other | ||||
| Comparator group | Usual care in the ED | |||
| Outcome measures | Composite outcome of institutionalisation, hospital admission within 1 month, early return or frequent visits to the ED or death | |||
| Findings |
In the derivation group, the Hong Kong ISAR tool predicted poor outcomes, with a sensitivity of 68.3% and specificity of 49.4%. The area under the ROC curve was 0.62. Corresponding figures for the validation group were 76.1%, 33.3% and 0.59, respectively In the RCT, there were no significant differences between the intervention group and the control group for the composite outcome or any of its components |
|||
| Conclusion | The Hong Kong ISAR tool is suitable for use in an ED setting to identify patients at risk of adverse outcomes; it is more applicable to the local population than the original ISAR tool. However, an ED-based intervention for patients identified as high risk did not improve outcomes at 6 months compared with usual care | |||
| Self-reported limitations | Authors attributed failure of the intervention to a lack of co-ordination among the agencies receiving referrals | |||
| Headline message | An ED-based assessment and referral intervention for elderly patients at high risk of adverse outcomes did not improve outcomes at 6 months | |||
| Other comments | Authors noted that differences between the original and the Hong Kong ISAR tool may indicate differences between health systems in use of the ED by elderly patients. Methods of randomisation, etc., for the RCT were not reported and so the risk of bias is unclear | |||
| Full paper | Authors: Ellis et al.88 | Year: 2012 | Country: Scotland | |
|---|---|---|---|---|
| Study design | Cohort, prospective before-and-after service evaluation | |||
| Data source | Not known | |||
| Study aim(s) | To implement a four-bedded ACE unit in the ED to better undertake rapid and thorough CGA with an outcome of either direct specialty admission or admission avoidance | |||
| Sample size |
749 patients Before: 212 consecutive patients admitted before the opening of the unit; ACE: 210 consecutive patients admitted to the unit; after: 327 patients admitted elsewhere after the opening of the unit |
|||
| Setting | District general hospital in Scotland | |||
| Frail elderly – definition | Aged ≥ 65 years | |||
| Study population | Age: ≥ 65 years; mean age was 80.5 years (before), 81.1 years (ACE) and 80.3 years (after) | Condition (additional to frailty): functional impairment (acute or chronic); cognitive impairment (acute or chronic); falls, ‘off legs’ or other geriatric syndromes; care home patients | ||
| Intervention | What | Rapid and thorough CGA in a discrete, acute care for elders unit | ||
| By whom | Senior geriatricians, nursing staff | |||
| Duration | N/A | |||
| Other | Usual care: standardised screening and assessment tools (functional need, falls risk, cognitive status, mood, pressure area risk or nutritional state, medical acuity), multidimensional assessment by a MDT and proactive discharge planning | |||
| Comparator group | 327 patients admitted after the opening of the unit but admitted to the medical receiving unit (outside the hours of the ACE unit). These were a parallel prospective control group | |||
| Outcome measures |
Primary outcome: same-day discharge Secondary outcomes: percentage access to specialty beds on day of admission, LOS in a non-specialty bed, acute and total LOS, 7-day readmission rates (so called ‘failed discharges’) and 30-day readmission rates (excluding elective admissions). The 12-month outcomes included mortality, admission to residential care and the outcome ‘living at home’ at 12 months (the inverse of death and admission to residential care) |
|||
| Findings |
Patients in the ACE unit were more likely to be discharged immediately (17.1% vs. 1.4% ‘before’ and 7.7% ‘after’; p < 0.0005) Access to specialty beds on the day of admission was significantly different (71% ‘before’, 69% ACE unit, 60% ‘after’; p = 0.019) LOS in a non-specialty bed was not reduced compared with the ‘before’ group (1.0 days vs. 1.2 days; p = 0.09), but was compared with the ‘after’ group (1.0 days vs. 1.6 days; p = 0.0001) LOS was not significantly different [12.2 days ‘before’ vs. 12.7 days ACE unit (p = 0.78) or vs. 11.7 days ‘after’ (p = 0.54)] 7- and 30-day readmission, 12-month mortality, admission to residential care or living at home were not significantly different |
|||
| Conclusion |
ACE unit patients were more likely to be discharged immediately Access to specialty beds on the day of admission was significantly different LOS in a non-specialty bed was not reduced compared with the ‘before’ group but was compared with the ‘after’ group LOS was not significantly different 7- and 30-day readmission, 12-month mortality, admission to residential care or living at home were not significantly different |
|||
| Self-reported limitations | This study has a number of important limitations. First, as an uncontrolled or non-randomised trial, the possibility exists that there are differences between the groups. This criticism cannot be eliminated but should be partly minimised by the prospective and unselected nature of the study. The fact that this was a service evaluation of routinely collected data does not allow patient-specific data such as functional or cognitive outcomes to be compared to evaluate this concern. The patients admitted out of hours may differ in disease severity from those admitted in daytime hours. The only anonymised data that we are able to present here to compare the groups is the proportion of patients classified as category 1 by the ED triage systems. These data do not show any striking differences. Second, and most importantly, the before-and-after design (rather than a randomised controlled design) means that complex interventions such as this can be subject to change in circumstances such as the outbreak of norovirus. This appears to have had a significant impact on the study outcomes and may account for the reduction in the impact seen for the ACE unit | |||
| Headline message |
Having these units embedded in EDs allows for immediate CGA. This can have a positive impact on adverse outcomes for patients. There was an increase in same-day discharge and reduced LOS in non-specialty beds and increased access to specialty beds, with no impact on discharge, readmissions or long-term outcomes Same-day discharge improved in the comparator group, which might reflect an overall change in emphasis on early discharge |
|||
| Other comments | Study was affected by an outbreak of norovirus, which affected study outcomes | |||
| Conference abstract | Authors: Jones et al.62 | Year: 2012 | Country: UK | |
|---|---|---|---|---|
| Study design | Not provided | |||
| Data source | Not provided | |||
| Study aim(s) | To reduce unnecessary admissions and their associated risks by the use of a geriatrician in the ED | |||
| Sample size | 441 | |||
| Setting | ED in Birmingham, UK | |||
| Frail elderly – definition | ‘Frail elderly people’ | |||
| Study population | Age: not given | Condition: not given | ||
| Intervention | What | Assess frail elderly patients who ED staff considered that it was necessary to admit | ||
| By whom | Consultant geriatrician | |||
| Duration | N/A | |||
| Other | During normal working hours | |||
| Comparator group | None | |||
| Outcome measures |
Number discharged 7-day reattendance rate LOS |
|||
| Findings |
260/441 (59%) discharged by geriatrician; 46% of these had outpatient follow-up and 38% a therapist assessment 30/441 patients had already had an acute hospital admission with the same problem within the last 30 days and the geriatrician was able to discharge 16/30 (53%) of these 7-day ED reattendance rate was 9.5% (42/441) (hospital average 7.4%) |
|||
| Conclusion | Based on these results, consultant geriatrician input supported by therapists within the ED is effective in admission avoidance of the frail elderly | |||
| Self-reported limitations | Not provided | |||
| Headline message | Consultant geriatrician reduced admissions as all of the patients were admitted by the ED team | |||
| Other comments | Undertaking admission prevention on more stable patients means that the wards will have a higher proportion of unwell and complex patients, so ward-based outcomes might appear to have worsened as a result of the intervention | |||
| Conference abstracts | Authors: Scott et al.,102 Wentworth et al.103,104 | Years: 2014, 2015, 2016 | Country: UK | |
|---|---|---|---|---|
| Study design | Observational study with age-matched controls | |||
| Data source | Appears to be hospital administrative data | |||
| Study aim(s) | To assess the effect of CGA in the ED on hospital admissions and LOS | |||
| Sample size | 148 (2014); 990 (2015). Numbers refer to people assessed by the OPAL team | |||
| Setting | ED of University Hospital of South Manchester | |||
| Frail elderly – definition | Older patients (aged ≥ 80 years) presenting with ‘geriatric syndromes’ such as frailty or falls | |||
| Study population | Age: average age not reported | Condition: see above | ||
| Intervention | What | CGA performed in the ED | ||
| By whom | OPAL team consisting of a consultant geriatrician, physiotherapist, occupational therapist and discharge facilitator | |||
| Duration | N/A | |||
| Other | ||||
| Comparator group | Age-matched controls not seen by the OPAL team (further details not reported) | |||
| Outcome measures | Hospital admissions and LOS for those admitted | |||
| Findings | Rates of hospital admission were 26% (2014) for patients assessed by the OPAL team compared with 73% for those seen by ED staff alone. Between June 2014 and February 2015, admission rates were 39.2% and 65.6%, respectively. Average LOS for those admitted was 9.3 days (OPAL) and 10.1 days (control). The 4-hour ED target was achieved in 84.9% and 80.7% of patients, respectively | |||
| Conclusion | CGA performed by a specialist team in the ED can avoid unnecessary admissions, reduce LOS and improve patient flow in the ED. Geriatricians have the skills to deal with these complex patients | |||
| Self-reported limitations | None reported, but these are conference abstracts with limited reporting of methods | |||
| Headline message | As above | |||
| Other comments | ||||
| Conference abstract | Authors: Thompson et al.74 | Year: 2010 | Country: UK | |
|---|---|---|---|---|
| Study design | Appears to be an uncontrolled observational study | |||
| Data source | Review of patient records | |||
| Study aim(s) | To assess the impact of geriatric assessment in the ED on patients aged ≥ 65 years | |||
| Sample size | 35 | |||
| Setting | ED of John Radcliffe Hospital, Oxford | |||
| Frail elderly – definition | Patients referred by ED staff for emergency (same-day) assessment by the GLT | |||
| Study population | Age: mean 84 years (range 68–97 years) | Condition: various, including falls (n = 25) and ‘collapse’ (n = 5). Patients assessed by ED staff as definitely needing admission were excluded | ||
| Intervention | What | CGA performed in the ED | ||
| By whom | GLT (no further details reported) | |||
| Duration | N/A | |||
| Other | ||||
| Comparator group | None | |||
| Outcome measures | Outcome of referrals and LOS for those admitted | |||
| Findings | Of 35 patients assessed, 27 (77%) were female. 26 (75%) were discharged home, 7 (20%) were admitted to the acute medical unit and 2 (5%) were admitted to an intermediate care bed.a Of 26 discharged patients, 23 (88%) needed further geriatrics input. This was provided by the MDT in the day hospital (18 patients), in a next-day geriatric clinic (3 patients) and in a falls clinic (2 patients). Average LOS in the ED was reduced by 4.8 hours since GLT input became available (no further details reported) | |||
| Conclusion | Same-day geriatric assessment in the ED has reduced hospital admissions, helped maintain patients in the community and reduced ED LOS | |||
| Self-reported limitations | None reported but this is a conference abstract with limited reporting of methods | |||
| Headline message | As above | |||
| Other comments | Small study, no comparison group data reported. Data are for February–July 2009 | |||
| Conference abstract | Authors: Bell et al.83 | Year: 2014 | Country: UK | |
|---|---|---|---|---|
| Study design | Not provided. Service evaluation | |||
| Data source | Not provided | |||
| Study aim(s) | Development of an ACE service | |||
| Sample size | 662 patients | |||
| Setting | ED observation ward of a district general hospital in London | |||
| Frail elderly – definition | Patients over the age of 80, with complex problems or frailty, but who do not require inpatient care | |||
| Study population | Age: > 80 years | Condition: complex problems or frailty | ||
| Intervention | What | ACE service including CGA | ||
| By whom | Consultant with support from junior doctor and band 6 nurse | |||
| Duration | Study undertaken January–October 2013 | |||
| Other | Based in ED observation ward: in-reach service to the ED and liaison to the acute medical unit. Weekday in-hours resource | |||
| Comparator group | N/A | |||
| Outcome measures | Inappropriate admissions avoided | |||
| Findings |
662 patients were assessed and 459 inappropriate admissions were avoided. CGA and treatment to discharge – extra 4.76 hours Rate of admission reduced from 61.2% to 35.1% |
|||
| Conclusion | ACE service has been beneficial in terms of avoiding admissions and providing timely care | |||
| Self-reported limitations | Not provided | |||
| Headline message | ACE and CGA are effective | |||
| Other comments | ||||
| Conference abstract | Authors: Lovato et al.118 | Year: 2012 | Country: Italy | |
|---|---|---|---|---|
| Study design | Observational retrospective study | |||
| Data source | Administrative data | |||
| Study aim(s) | To evaluate the impact of the SC prognostic tool in reducing waiting times for frail elderly | |||
| Sample size | 7061 | |||
| Setting | ED | |||
| Frail elderly – definition | All aged > 85 years and aged > 75 years with some criteria of risk | |||
| Study population | Age: ≥ 70 years (mean 79.5 years) | Condition: not given | ||
| Intervention | What | SC (four-level triage: white, green, yellow, red) to identify elderly, then a ‘priority green code’ with certain characteristics | ||
| By whom | Not provided | |||
| Duration | N/A | |||
| Other | N/A | |||
| Comparator group | ||||
| Outcome measures | Waiting time (arrival in the ED until medical care) | |||
| Findings |
7061 admitted to medical ward through the ED Green code assigned to 96.4% of patients Mean waiting time with SC was 65.8 (SD 72.55) minutes vs. 95.3 (SD 98.11) minutes without SC, regardless of colour (p = 0.000) |
|||
| Conclusion | Application of SC resulted in reduced waiting times | |||
| Self-reported limitations | None provided | |||
| Headline message | Application of SC reduced waiting times; this did not increase waiting times for other patients | |||
| Other comments | Abstract states that organisational aspects and management of ED were affected too | |||
| Conference abstract | Author: Pareja99 | Year: 2008 | Country: Spain | |
|---|---|---|---|---|
| Study design | Prospective study | |||
| Data source | Not provided | |||
| Study aim(s) | Whether or not specialised geriatric evaluation may reduce rates of hospital admission and iatrogenesis (unnecessary interventions) | |||
| Sample size | 1200 | |||
| Setting | General hospital | |||
| Frail elderly – definition | High-risk older patients | |||
| Study population | Age: mean 86 years | Condition: not given (see Findings) | ||
| Intervention | What | CGA and treatment for acute-mild severity or unstable chronic diseases | ||
| By whom | Geriatrician (in the short-stay unit, having been referred there by medical staff from the ED) | |||
| Duration | N/A | |||
| Other | N/A | |||
| Comparator group | N/A | |||
| Outcome measures | Admission | |||
| Findings |
72% were discharged home (29% were followed up in geriatric clinics, 9% by the home care medical team and 14% by the nursing home primary care doctor) 28% were admitted 18% of the discharged patients needed hospital attention in the following month |
|||
| Conclusion | Frail older people using the ED have different patterns of service use and the traditional disease-oriented model may not meet their health-care needsShort medical units carried out by geriatricians seem to have the potential to increase patient satisfaction, reduce the length of hospital stay and improve the efficiency of the emergency departments | |||
| Self-reported limitations | Not provided | |||
| Headline message | This unit discharged a lot of patients; however, there was no comparator group | |||
| Other comments | The conclusion makes claims that are not substantiated in the results of the study about patient satisfaction and efficiency | |||
| Full paper | Authors: Singler et al.50 | Year: 2014 | Country: Germany | |
|---|---|---|---|---|
| Study design | Prospective cohort study | |||
| Data source | Review of patient records and follow-up telephone interviews | |||
| Study aim(s) | To assess the validity of the ISAR screening tool in a German ED | |||
| Sample size | 520 | |||
| Setting | ED of an urban university-affiliated hospital | |||
| Frail elderly – definition | Patients aged ≥ 75 years attending the ED and living at home or in a long-term care facility | |||
| Study population | Age: mean 82.8 years (SD 5 years) | Condition: not reported but patients expected to die within 24 hours were excluded | ||
| Intervention | What | Screening with the ISAR tool | ||
| By whom | Study nurses | |||
| Duration | N/A | |||
| Other | ||||
| Comparator group | N/A | |||
| Outcome measures | Accuracy of the ISAR tool for predicting a composite end point of death, hospitalisation, repeat ED visit or transfer to a long-term care facility at 28 days | |||
| Findings | Of the 520 patients, 425 patients scored ≥ 2 on the ISAR tool and 315 scored ≥ 3. The primary end point was observed in 250 patients on day 28 and 260 on day 180. The area under the ROC curve for the ISAR score was 0.62 on day 28 and 0.66 on day 180 | |||
| Conclusion | The ISAR tool acceptably identified high-risk elderly patients in the ED. Using a cut-off score of ≥ 3 rather than ≥ 2 gave better overall results | |||
| Self-reported limitations | Patients not recruited 7 days/week; lack of data on clinical utility of the ISAR tool | |||
| Headline message | The ISAR tool with a cut-off score of ≥ 3 is an acceptable screening tool for use in German EDs | |||
| Other comments | ||||
| Full paper | Authors: Conroy et al.89 | Year: 2014 | Country: UK | |
|---|---|---|---|---|
| Study design | Before-and-after study | |||
| Data source | Hospital administrative data | |||
| Study aim(s) | To evaluate the effect of implementing an EFU within an ED | |||
| Sample size | Total ED attendance (number aged ≥ 85 years):
|
|||
| Setting | Large ED in the East Midlands, UK | |||
| Frail elderly – definition | Not specifically defined, but data were collected for ED attendees aged ≥ 85 years | |||
| Study population | Age: average age not reported | Condition: older people attending the ED and likely to be discharged home within 24 hours | ||
| Intervention | What | EFU with between 8 and 12 beds integrated with the main ED and performing CGA with referral to social and community care as required. Geriatricians also provided an in-reach function to the major receiving area of the ED | ||
| By whom | Geriatricians, emergency physicians, physiotherapists, occupational therapists and ‘primary care co-ordinators’ | |||
| Duration | N/A | |||
| Other | ||||
| Comparator group | People attending the ED before implementation of the EFU when standard care for frail older people was delivered in an emergency decisions unit without routine input from specialists in geriatric medicine | |||
| Outcome measures | Primary outcome was admission rate from the ED. Secondary outcomes were readmissions following attendance at the ED, LOS for admitted patients and total bed-day use. Outcomes were assessed for age groups 16–64 years, 65–74 years, 75–84 years and ≥ 85 years | |||
| Findings | ED attendances by older people increased over the study period. Admission rates from the ED of patients aged ≥ 85 years decreased from 69.6% in 2010 to 61.2% after the EFU was implemented. The change was statistically significant (relative risk 0.88, 95% CI 0.81 to 0.95). Readmission rates also decreased (4.7% vs. 3.3% at 7 days; 12.4% vs. 9.2% at 30 days; and 19.9% vs. 26.0% at 90 days). The relative risk for 90-day readmission was 0.77 (95% CI 0.63 to 0.93). Mean LOS in the oldest patients increased from 8.9 days to 11.1 days and total bed-day use from 4385 to 4826 | |||
| Conclusion | CGA can be performed in the ED and early intervention for frail older people may offer benefits for both patients and health services. More robust evaluations are required to assess the generalisability of the findings | |||
| Self-reported limitations | No contemporaneous control group; lack of process data on the number of patients seen by the EFU; lack of patient outcome and service cost data | |||
| Headline message | CGA in the ED was associated with improved discharge rates and reduced readmissions in older people | |||
| Other comments | Admission and readmission rates also fell for younger age groups, which the authors suggested may be because emergency physicians had their time freed up, which allowed them to care for younger patients | |||
| Full paper | Authors: Fox et al.106 | Year: 2016 | Country: UK | |
|---|---|---|---|---|
| Study design | Feasibility study | |||
| Data source | Electronic patient record | |||
| Study aim(s) | To improve the quality of care delivered in the ED to frail older people | |||
| Sample size | 168 patients | |||
| Setting | ED of an urban teaching hospital | |||
| Frail elderly – definition | . . . defined as being from residential care or intermediate care, presenting with confusion as a result of dementia or delirium or admitted with a fall | |||
| Study population | Age: mean 84.9 years (range 70–102 years) | Condition: frail elderly were preferentially but not exclusively chosen for the intervention | ||
| Intervention | What | Geriatrician-led CGA with an all-inclusive CGA document (functional and medical baselines, progress, problems and the plan of care):
|
||
| By whom | Consultant geriatrician (plus MDT – nursing staff, occupational therapist, physiotherapist, social worker) | |||
| Duration | N/A. Delivered between 10:00 and 20:00, 7 days a week | |||
| Other | N/A | |||
| Comparator group | None | |||
| Outcome measures | None | |||
| Findings |
Most patients were dependent for ADL. Over 50% were admitted from their own home, with 41% admitted from institutional care. Over 40% had a confirmed dementia diagnosis and the mean number of comorbid conditions was 2.5. Median time from presentation at triage to consultation with a geriatrician was 1 hour 52 minutes |
|||
| Conclusion | Compared with other research studies in this area, this intervention compares favourably in terms of positive outcomes (discharge, LOS and readmission) | |||
| Self-reported limitations | The main limitations were lack of a control group, the small number of patients seen within the study time frame (168 patients in 31 days), the short length of the study (1 month) and the fact that the study was retrospective | |||
| Headline message | This feasibility study highlighted that older patients were often being assessed by numerous different professionals. This intervention allowed them to be assessed once. There was no comparator group for the intervention | |||
| Other comments | ||||
| Conference abstract | Authors: O’Reilly et al.75 | Year: 2016 | Country: Ireland | |
|---|---|---|---|---|
| Study design | Feasibility study/report of intervention | |||
| Data source | N/A | |||
| Study aim(s) | To identify 100% of frail patients who presented to the ED during core hours and deliver a MDT assessment | |||
| Sample size | 2200 screened for frailty | |||
| Setting | ED of a hospital in Ireland | |||
| Frail elderly – definition | . . . medical conditions often further complicated by functional decline, cognitive deterioration and complex social care needs | |||
| Study population | Age: > 75 years | Condition: frail | ||
| Intervention | What | Screening for frailty then referral to the MDT (FITT) | ||
| By whom | FITT (physiotherapy, occupational therapy, medical social work, speech and language therapy, dietetics and pharmacy) | |||
| Duration | N/A | |||
| Other | N/A | |||
| Comparator group | Comparing data for the first quarter of 2015 (before) and the first quarter of 2016 (after) | |||
| Outcome measures | Discharge directly homeTransfer to ward in < 9 hours | |||
| Findings |
Over 75% of patients screened were deemed to be frail Comparing quarter 1 in 2015 and quarter 1 in 2016: |
|||
| Conclusion | FITT provided earlier intervention to frail adults thus improving hospital experience and patient outcomes | |||
| Self-reported limitations | N/A | |||
| Headline message | FITT can promote safe discharge and transfer with MDT intervention | |||
| Other comments | N/A | |||
| Full paper | Authors: Huded et al.119 | Year: 2015 | Country: USA | |
|---|---|---|---|---|
| Study design | Prospective observational study | |||
| Data source | Prospective | |||
| Study aim(s) | To incorporate TUGT assessments by geriatric nurses into ED assessments in order to identify elderly patients at high risk of falls | |||
| Sample size | 19,511 patients treated in the ED, 1135 evaluated by a geriatric nurse and the TUGT performed on 443 | |||
| Setting | ED of an urban academic level 1 trauma centre with 56 beds | |||
| Frail elderly – definition | Geriatric nurses assessed elderly patients and identified a high-risk population for the TUGT as identified by the GEDI-WISE protocol | |||
| Study population | Age: ≥ 65 years | Condition: | ||
| Intervention | What | Fall-risk screening with the TUGT | ||
| By whom | Geriatric nurses | |||
| Duration | Study ran from 1 April 2013 to 31 May 2014 | |||
| Other | ||||
| Comparator group | No | |||
| Outcome measures |
Positive TUGT Referral interventions Number of patients discharged Number of patients admitted Number of patients under observation |
|||
| Findings |
368 patients experienced a positive result on the TUGT. Interventions for positive results included referral to an ED-based physiotherapist (n = 63, 17.1%), outpatient physiotherapist referral (n = 56, 12.2%) and social work consultation (n = 162, 44%) For those with a positive TUGT score, 74% were discharged home (n = 274) and the remainder were admitted under inpatient or observation status |
|||
| Conclusion |
The ED visit may provide an opportunity for older adults to be screened for fall risk ED nurses can conduct the TUGT, a validated and time-efficient screen, and place appropriate referrals based on assessment results |
|||
| Self-reported limitations | This study shows how it is possible, using a protocol, to measure the risk of falls in elderly patients requiring acute care from the ED for reasons other than falls. The study limitations were single site study and screening delivered by specialised staff already in place. Only a small number of potentially eligible patients were screened. TUGT needs to be adapted to the ED | |||
| Headline message | Identifying and intervening in high fall-risk patients who visit the ED has the potential to improve the trajectory of functional decline in our elderly population | |||
| Other comments | ||||
Appendix 6 Data tables
| Location | Total (n) |
|---|---|
| Australia | 10 |
| Belgium | 1 |
| Canada | 6 |
| France | 2 |
| Germany | 1 |
| Hong Kong | 2 |
| Ireland | 5 |
| Italy | 7 |
| The Netherlands | 2 |
| New Zealand | 1 |
| Singapore | 2 |
| South Korea | 1 |
| Spain | 2 |
| Sweden | 2 |
| Switzerland | 3 |
| Taiwan | 1 |
| Turkey | 1 |
| UK | 14 |
| USA | 27 |
| Total | 90 |
| Type of study | Reference |
|---|---|
| Action research | 114 |
| Audit | 28 |
| Before-and-after cohort study | 117 |
| Cross-sectional cohort | 29,32 |
| Diagnostic accuracy study | 20,23,31,38,39 |
| Evaluation | 80,83 |
| Feasibility study | 75,106 |
| Longitudinal study | 56 |
| Medical record review | 34,46,113 |
| Observational study | 74,102,110 |
| Observational before-and-after study | 95 |
| Pilot project | 116 |
| Prospective before-and-after study | 22,33,44,79,88,89,91,115 |
| Prospective cohort study | 30,35–37,41–43,47,48,50,51,55,58–62,66,70–72,81,85,86,100,105,109,111 |
| Prospective comparative study | 78 |
| Prospective data analysis | 69,99,107 |
| Prospective evaluation | 63 |
| Prospective non-randomised study | 82 |
| Prospective observational study | 21,27,40,49,52,67,90,119 |
| Prospective pragmatic study | 45,77 |
| Prospective questionnaire | 84 |
| Quasi-RCT | 112 |
| RCT | 18,19,24,26,120 |
| Retrospective before-and-after study | 92,96 |
| Retrospective cohort study | 53,57,64,65,76,93,98,108 |
| Retrospective observational study | 73,87,118 |
| Sample size | Reported age of participants (years) | Reference | ||
|---|---|---|---|---|
| Mean (SD) | Median | Range | ||
| 5416 pre, 5370 post | 117 | |||
| Not provided | 86 | |||
| 700 | 40 | |||
| 534 | 98 | |||
| 7213 | 79.3 | 67,68 | ||
| 2202 | 45–99 | 108 | ||
| 848 | 85 | 58–105 | 61 | |
| 5162 | 76 | |||
| 85 intervention, 76 control | 24 | |||
| 2121 intervention, 1451 comparator | 77 | |||
| 2196 (1098 matched pairs) | 78 | |||
| 285 | 83.5 ± 6.8 | 71 | ||
| 2057 | 81.7 | 65–103 | 21 | |
| 200 | 80.3 ± 7.4 | 27 | ||
| 519 | 42 | |||
| 375 | 84 (5.7) | 53,54 | ||
| 315 intervention, 172 control | 115 | |||
| 313 | 79 | |||
| 101 intervention, 98 control | 63 | |||
| 666 | 60–103 | 72 | ||
| 200 | 80.3 (7.4) | 49 | ||
| 200 | 80.3 ± 7.4 | 90 | ||
| 894 | 116 | |||
| 788 | 76.6 | 65–101 | 52 | |
| 314 | 56 | |||
| 929 | 57 | |||
| 277 | 114 | |||
| Not provided | 80 | |||
| 795 screening, 752 control | 82.7 ± 5, 82.6 ± 5.1 | 22,33 | ||
| 139 index visit and 130 follow-up visit | 82.5 ± 5.4, 80 | 29,30 | ||
| 1680 | 83 ± 6.5 | 73 | ||
| 3071 | 69 | |||
| 280 intervention, 500 control | 112 | |||
| 25 | 78 | 66–96 | 110 | |
| 424 | 84 ± 6.5 | 41 | ||
| 5571 | 87.4 | 87 | ||
| 168 | 81 | |||
| 3165 intervention, 2100 control | 82 | |||
| 120 | 51 | |||
| 100 | 66 | |||
| 69 | 76 | 18 | ||
| 225 | 45 | |||
| 829 intervention, 873 control | 70 | |||
| 250 | 46 | |||
| 504 | 76.8 | 47 | ||
| 260 | 37 | |||
| 117 | 34 | |||
| 168 | 85 | |||
| 300 | 32 | |||
| 32 intervention, 31 control | 74 | 120 | ||
| 219 development, 178 validation | 81 | 60 | ||
| 1820 cohort, 1279 RCT | Derivation group, 74.5 (6.2); Control group, 75 (6.8); Intervention group, 76.3 (6.8) | 25 | ||
| 300 | 107 | |||
| 432 intervention, 205 control | 75 | 84 | ||
| 137 | 80.3 | 100,101 | ||
| 1096 | 80.3 | 109 | ||
| 939 | 74 | 43 | ||
| 212 before, 210 intervention, 327 comparator | 80.5, 81.1, 80.3 | 88 | ||
| < 65 years = 219, ≥ 65 years = 67 | 91 | |||
| 547 | 105 | |||
| 441 | 62 | |||
| 13,354 pre, 14,484 post | 92 | |||
| 226 | 80.5 | 111 | ||
| Not provided | 77 (8.6) | 96,97 | ||
| 250 | 48 | |||
| 148 in 2014, 990 in 2015 | 102–104 | |||
| 35 | 84 | 68–97 | 74 | |
| 662 | 83 | |||
| Not provided | 113 | |||
| 118 | 20 | |||
| 7061 | 79.5 | 118 | ||
| 1903 | 23 | |||
| 1200 | 99 | |||
| 2139 | 44 | |||
| 114 intervention, 110 control | 78.7 ± 6.4 | 26 | ||
| 525 | 28 | |||
| 1820 (910 matched pairs) | 65 | |||
| 381 | 79.1 | 55 | ||
| 169 | 35 | |||
| 371 | 36 | |||
| 1632 | 84 | 58 | ||
| 650 | 74 | 19 | ||
| 4417 (55–64 years), 7598 (≥ 65 years) | 77.5, 76.9 | 93 | ||
| 520 | 82.8 (5) | 50 | ||
| 352 | 77 | 38 | ||
| 150 | 75 | 39 | ||
| 109,994 usual care, 53,182 transition, 110,517 intervention | 89 | |||
| 107 | 79 | 59 | ||
| 161 | 31 | |||
| 168 | 84.9 | 70–102 | 106 | |
| 2200 | 75 | |||
| 346 before, 95 after | 73, 75 | 95 | ||
| 19,511 | 119 | |||
| 4103 | 64 | |||
| 2286 intervention, 2260 control | 94 | |||
| Category | Reference | Total, n |
|---|---|---|
| ≥ 65 years | 18,19,21,23,27,28,32,34–36,38–40,42,43,46,48,51,52,55–57,59,64,66,69,70,74,76,77,79,80,84,88,91–96,109–111,113,115,119 | 46 |
| ≥ 65 years with trauma | 45,47 | 2 |
| ≥ 65 years with fall | 65 | 1 |
| ≥ 65 years with chronic condition | 82,116 | 2 |
| ≥ 65 years with acute condition | 49,90 | 2 |
| ≥ 65 years with positive screen for ‘at risk’ | 78,88 | 2 |
| ≥ 65 years, ISAR score > 2 | 25,67 | 2 |
| ≥ 65 years, TRST score > 2, eligible for discharge | 112 | 1 |
| ≥ 65 years with chronic condition, ≥ 70 years without | 63 | 1 |
| ≥ 65 years with chronic condition, ≥ 80 years without | 24,31,71 | 3 |
| ≥ 70 years | 44,60,73,105,117,118 | 6 |
| ≥ 72 years | 107 | 1 |
| ≥ 75 years | 20,29,33,37,41,50,53,58,81,86,114 | 11 |
| ≥ 75 years, frail | 75 | 1 |
| ≥ 75 years, multiple comorbidities | 87 | 1 |
| ≥ 80 years with geriatric syndromes | 83,102 | 2 |
| ≥ 85 years | 89 | 1 |
| No category | 21,26,27,61,62,72,74,85,98,100,106,108,118,120 | 14 |
| Outcome | Reference | |
|---|---|---|
| Frail elderly population | General geriatric population | |
| ADL | 24 | |
| Acute admissions from the ED | 25,71,87,89,90,99,102–104,114 | 26,65,80,82,93,94,96,97,100,115,117 |
| Admission to specialty bed | 88 | |
| Avoided admissions | 61,67,68,72,83,98 | 92,113 |
| Costs | 72 | |
| Discharge rates | 62,71,88,98,99 | 81,85,105,116 |
| Discharges: inappropriate | 73 | |
| ED reattendance | 25,62,71,78,90,112,114 | 65,76,93,94,100,107–109,115 |
| ED waiting times | 98,118 | |
| Frailty | 24 | |
| Functional decline/functional status | 90,112 | 26 |
| In-hospital mortality | 86 | |
| Inpatient bed occupancy | 86 | |
| Institutionalisation | 25 | |
| Intervention acceptability | 110 | |
| Length of stay | 62,71,74,87–89,102–104,106,114 | 26,63,77,93–95,105,116,117 |
| Living at home vs. access to residential care | 88 | |
| Medication errors avoided/problems identified | 63,64 | |
| Mortality (all) | 25,78,88,90 | 108 |
| Outcome of referrals | 74 | |
| Quality-of-life score | 80 | |
| Readmission | 71,78,86–89,99,106,112,114 | 65,76,105 |
| Referred for appropriate care | 79 | |
| Satisfaction with the ED | 84,91 | |
| Total bed-day use | 89 | |
Appendix 7 Example brief data extraction form
| Reference ID, author, year, country | Study design, population, patient numbers | Intervention/assessment tool | Results | Headline message |
|---|---|---|---|---|
Appendix 8 Example full data extraction form
| Reference ID | Author | Year | Country | |
|---|---|---|---|---|
| Study design | ||||
| Data source | ||||
| Study aim(s) | ||||
| Sample size | ||||
| Setting | ||||
| Frail elderly – definition | ||||
| Study population | Age | Condition | ||
| Intervention | What | |||
| Who | ||||
| Duration | ||||
| Other | ||||
| Comparator group | ||||
| Outcome measures | ||||
| Findings | ||||
| Conclusion | ||||
| Self-reported limitations | ||||
| Headline message | ||||
| Other comments | ||||
List of abbreviations
- ACE
- acute care of the elderly
- ADL
- activities of daily living
- AMAU
- acute medical assessment unit
- ASET
- aged care service emergency team
- ATOP
- assessment team for older people
- AUC
- area under the curve
- BGA
- brief geriatric assessment
- BRIGHT
- Brief Risk Identification for Geriatric Health Tool
- CAM
- confusion assessment method
- CCT
- care co-ordination team
- CFS
- Clinical Frailty Scale
- CGA
- comprehensive geriatric assessment
- CI
- confidence interval
- COMPRI
- complexity prediction instrument
- CTAS
- Canadian Triage and Acuity Scale
- DAI
- Deficit Accumulation Index
- ED
- emergency department
- EDCC
- emergency department care co-ordinator
- EDOU
- emergency department observation unit
- EFU
- emergency frailty unit
- EGS
- emergency geriatric screen
- ESI
- emergency screening instrument
- FITT
- frail intervention therapy team
- FSAS-ED
- Functional Status Assessment of Seniors in Emergency Departments
- GED
- geriatric emergency department
- GEDI-WISE
- Geriatric Emergency Department Innovations through Workforce, Informatics and Structural Enhancements
- GNLI
- geriatric nurse liaison intervention
- GRAY
- Geriatric Readmission Assessment at Yale
- HARP
- hospital admission risk profile
- HOTEL
- Hypotension, Oxygen saturation, low Temperature, ECG changes and Loss of independence
- HSDR
- Health Services and Delivery Research
- ICU
- intensive care unit
- ISAR
- Identification of Seniors at Risk
- MDT
- multidisciplinary team
- MGT
- mobile geriatric team
- MMSE
- Mini Mental State Examination
- OPAL
- older people assessment and liaison
- OR
- odds ratio
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RAC
- rapid access centre
- RCT
- randomised controlled trial
- REMS
- Rapid Emergency Medicine Score
- ROC
- receiver operating characteristic
- ScHARR
- School of Health and Related Research
- SHARE-FI
- Survey of Health, Aging and Retirement in Europe Frailty Instrument
- SHERPA
- Evaluation du Risque de Perte d’Autonomie
- SIS
- six-item screener
- TREAT
- triage and rapid elderly assessment team
- TRST
- triage risk screening tool
- TUGT
- timed up and go test
- VIP
- variables indicative of placement
